Notes
Article history
The research reported in this issue of the journal was funded by the EME programme as project number 09/160/06. The contractual start date was in September 2011. The final report began editorial review in June 2014 and was accepted for publication in October 2014. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The EME editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2015. This work was produced by Freeman et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Background
Having a mental health problem can be a frightening, isolating, and even terrifying experience. Seeing things and hearing voices can be disturbing and carry with them stigma and exclusion from ordinary human relationships, employment, and even simple things that are taken for granted like socializing, going out, or making friends.
Ben Gray (p.1)1
When I am psychotic, I feel as though my awareness is happening to me. It’s a passive experience. I’m at the mercy of ‘my’ thoughts and ‘my’ perceptions of people. When I am psychotic, I am almost always paranoid. I perceive the universe itself as hating me.
Roberta Payne (p. 899)2
Psychotic experiences can cause great distress, upset and disruption for patients and their families. Schizophrenia is estimated to cost English society £11.8B per year and the public sector £7.2B. 3 Treatments require major improvement. Many patients do not respond to neuroleptic medication, relapse is common and adherence to these treatments is problematic,4 and the first generation of generic cognitive–behavioural therapy (CBT) approaches show only weak to moderate effects5 and have not been shown to change key causal factors. 6 Part of the problem is likely to be that diagnoses such as schizophrenia actually contain a heterogeneous collection of independent experiences. 7–9 Studying single psychotic experiences has emerged as a way of making progress with the complex problem of schizophrenia spectrum diagnoses. Our focus has been on persecutory delusions, one of the key psychotic experiences.
Persecutory delusions are the unfounded belief that others are deliberately trying to harm the person. 10 In psychosis, persecutory delusions are very frequent,11 are particularly distressing for patients,12 are often acted on13 and are a predictor of admission to psychiatric hospital. 14 Paranoid thinking is associated with increased rates of suicide attempts15 and causes particular problems for carers. 16 In the last 10 years there have been considerable advances in understanding persecutory delusions17 but these are only now beginning to be translated into treatment. The current project is designed to test the effects of taking one key causal factor and targeting it in treatment. This is known as an interventionist–causal model approach: ‘it connects causation with the practical interests of psychiatry, defining causation in terms of “what would happen under interventions”, a question of key interest to those of us whose interest is ultimately in intervening to prevent and treat illness’ (p. 881). 18
Theoretical rationale
We have developed a theoretical model of the development of persecutory delusions. 19,20 Delusions arise from a number of interacting factors, but worry is given a central role in the model. The mechanistic connection is plausible – worry brings unlikely and distressing ideas to mind and keeps them there – and has been established empirically. It has been shown that worry is extremely common in individuals with persecutory delusions, that it is especially associated with more distressing persecutory delusions and that it is a predictor of paranoia persistence. 21–25 Other studies that we have conducted have shown that worry is associated with non-clinical paranoia and predicts its occurrence. 15,26,27 Furthermore, in a longitudinal study of > 2000 people taking part in the Adult Psychiatric Morbidity Survey, worry was shown to predict the new occurrence of paranoid thinking over an 18-month period. 28 Drawing on the theoretical literature for generalised anxiety disorder, we have shown that worry in individuals with persecutory ideation is associated with catastrophising (characterised as the worrier posing internal, automatic questions of the form ‘what if this bad thing happens?’) and positive and negative meta-cognitive beliefs. 21,22,26
The pilot study
On the basis of this work we completed a pilot study examining the impact of a brief cognitive–behavioural worry intervention for patients with persecutory delusions. 29 The aim was to treat the clinical problem of worry in patients with delusions but also to examine the subsequent impact on persecutory delusions. In total, 24 patients with persistent persecutory delusions were recruited. Half were randomised to the four-session intervention in addition to their standard psychiatric care and half were randomised to the control group (standard psychiatric care). Assessments were carried out at baseline, at the end of treatment (1 month) and at follow-up (2 months). There was a large effect size reduction in worry (Penn State Worry Questionnaire; PSWQ)30 and also in the persecutory delusions (Psychotic Symptom Ratings Scale; PSYRATS). 31 One in three patients showed a ≥ 25% reduction in worry and the delusion. Changes in worry were associated with changes in persecutory delusions. However, the trial assessments were not carried out blind and the sample size was small. A more rigorous evaluation was required. It is also of note that in a case series we showed that helping patients with persistent persecutory delusions emotionally process their paranoid experiences (in a three-session intervention) led to reductions in worry and the delusions. 32 The identification of worry as a problem originally arose from discussions between patients in therapy and the first author, which was then empirically established in the later research studies. From the pilot study the main feedback received from patients was that three or four sessions on the topic of worry were too few. Therefore, in the current trial the intervention was lengthened to six sessions.
Research objectives and hypotheses
The main project objective was to rigorously test the clinical efficacy and treatment mechanisms of a brief cognitive–behavioural intervention for worry for patients with current persecutory delusions. We aimed to test the intervention in addition to standard care. A psychological intervention control group was not included in the design; instead, we aimed to show a large treatment effect, greater than would be expected by attention effects alone, and that the treatment worked specifically by reducing worry. The trial hypotheses were:
-
the worry intervention will reduce levels of worry in patients with persecutory delusions
-
the worry intervention will reduce persecutory delusions
-
the improvements will be maintained at follow-up
-
worry will be the mediator of the changes in persecutory delusions.
The secondary objective was to develop the understanding of persecutory delusions, especially in relation to worry. The trial had a strong explanatory component: testing the treatment mechanism. Also embedded within the trial were assessments to increase the knowledge of worry processes in patients with persecutory delusions. The key question here was about how worry interacts with psychotic processes. Further, there is increasing interest in psychological well-being as an outcome measure and therefore we assessed psychological well-being for the first time in this patient group and compared scores against those of a non-psychosis general population group. In addition to the main trial outcome paper, five of these studies have been accepted for publication during the period of the grant, and additional tests of the data set are also planned. The five studies conducted to date are:
-
The interaction of affective with psychotic processes. 33 Built into the baseline assessment was an experimental study testing the effects on psychotic processes of a bout of worry in patients with persecutory delusions. It was hypothesised that a bout of worry, compared with relaxation or a neutral control condition, would exacerbate key psychotic processes: jumping to conclusions (JTC), working memory difficulties and the occurrence of anomalous internal experiences. This had never been examined before.
-
Depersonalisation in patients with persecutory delusions. 34 The results of the experimental study highlighted one particular type of internal anomalous experience: depersonalisation. Therefore, we introduced at the final follow-up time point a full assessment of these experiences, to provide the first estimate of their prevalence in this patient group. It was predicted that depersonalisation experiences would be common in patients with persecutory delusions.
-
How patients with persecutory delusions bring worry to a close. 35 At the end of their trial involvement we asked eight patients in the control group to identify how they brought their worry periods to a close. Potentially, this will inform advice given to patients and ongoing treatment development. An open-ended semistructured interview technique and interpretive phenomenological analysis were used. This is the first research study in which patients with psychosis have been asked about how worry periods end.
-
Jumping to conclusions in patients with persecutory delusions. 36 A key process in delusions is JTC, making a decision on the basis of limited data gathering. We assessed JTC in the baseline assessment, which allowed an examination of factors, including worry, that may potentially drive this reasoning style. Although the trial was focused on altering one key causal factor, we were keen to learn how paranoia related to other causes, that is, to keep the research embedded within a multifactorial model of psychosis. It was predicted that JTC would be associated with the worry-related process of intolerance of uncertainty and lower working memory performance.
-
Persecutory delusions and psychological well-being. 37 Psychological well-being, sometimes also referred to as positive mental health, life satisfaction or happiness, had not been examined in patients with persecutory delusions. However, from patient discussions it was clear that this is an important outcome. We used the most promising well-being measure, the Warwick–Edinburgh Mental Well-being Scale (WEMWBS),38 and collected comparison non-clinical data. It is likely that this measure may be routinely used in mental health services. It was predicted that levels of psychological well-being would be very low in most patients with persecutory delusions.
Chapter 2 Methods
Trial design
The trial was registered (Current Controlled Trials ISRCTN23197625) and the protocol has been published. 39 Patients were randomised to the worry intervention in addition to standard care or standard care alone. The outcome measures were completed at 0 weeks (baseline), 8 weeks (end of therapy) and 24 weeks (follow-up). Enrolment and the assessments were carried out by three graduate psychologists. The trial had received a favourable opinion from a NHS Research Ethics Service Committee (ref. 11/SC/0001). Written informed consent was received from all patients. A Trial Steering Committee and Data Monitoring and Ethics Committee including independent chairs and members were formed.
Participants
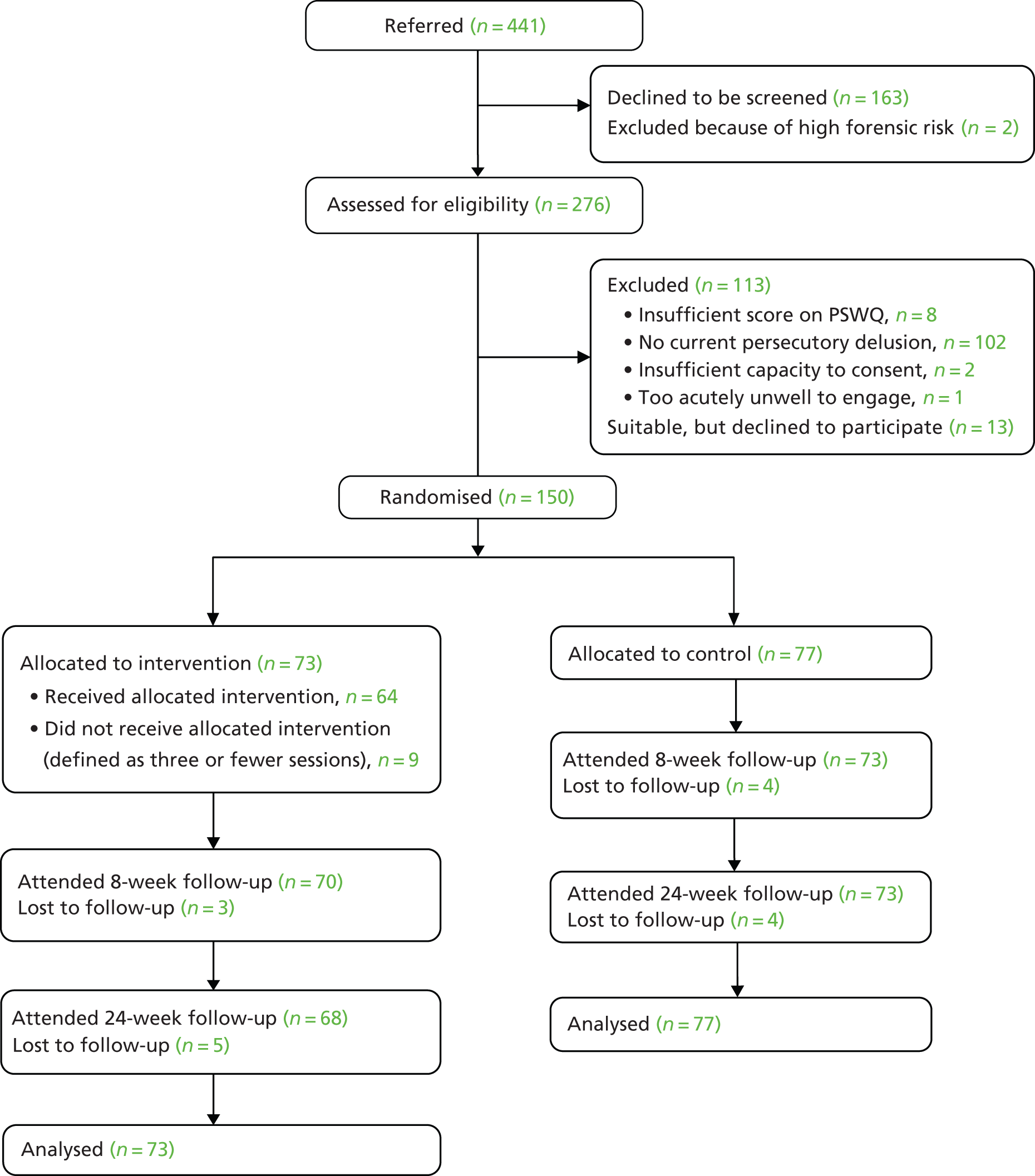
In total, 150 patients with persecutory delusions were recruited. We sought referrals of patients with persecutory delusions from two centres: Oxford Health NHS Foundation Trust and Southern Health NHS Foundation Trust. These large mental health services cover populations of approximately 1.2 million people each. The inclusion criteria were a current persecutory delusion as defined by Freeman and Garety;10 scoring at least 3 on the conviction scale of the PSYRATS;31 that the delusion has persisted for at least 3 months; a clinical diagnosis of schizophrenia, schizoaffective disorder or delusional disorder (i.e. a diagnosis of non-affective psychosis); a clinically significant level of worry, as indicated by a score of > 44 on the PSWQ;40 age between 18 and 65 years; and, when major changes in medication are being made, entry to the study would not occur until at least a month after stabilisation of dosage. Criteria for exclusion were a primary diagnosis of alcohol or substance dependency or personality disorder; organic syndrome or a learning disability; a command of spoken English inadequate for engaging in therapy; and currently having individual CBT. Recruitment took place from November 2011 to September 2013, with the last assessments completed in March 2014. Figure 1 summarises the participant flow through the trial.
FIGURE 1.
Flow diagram of patient recruitment and trial progress.
Randomisation
Randomisation occurred after the baseline assessment was fully complete. Randomisation was carried out using a secret allocation table, generated by the University of Oxford’s Centre for Statistical Medicine (CSM), with four strata and a variable length block structure to ensure that allocations were balanced and could not be predicted by trial staff. Stratification was on the basis of centre (Oxford Health NHS Foundation Trust/Southern Health NHS Foundation Trust) and level of worry (‘moderate’ when 44 ≤ worry score ≤ 62, ‘high’ when 63 ≤ worry score). The trial used a web-based randomisation system, written by the clinical trials software development team in the Oxford Cognitive Health and Neuroscience Clinical Trials Unit and hosted by the Medical Sciences Information Management Unit at the University of Oxford. The deployed software was fully validated using a combination of automated tests and manual checks and the algorithms used were independently checked by the statisticians at the University of Oxford’s CSM.
Blinding
The assessors were blind to patient allocation. All patients were informed of allocation by a trial therapist. Precautionary strategies included consideration of room use and diary arrangements; patients being reminded by the assessors not to talk about allocation; and, after the initial assessment, assessors not looking at clinical notes. If an allocation was revealed then reblinding occurred by using another rater, which happened 11 times. However, if the blind was broken during an assessment session then these ratings were used – two eight-week assessments (both treatment) and four 24-week assessments (three treatment) were therefore carried out unblinded.
Measures
Primary outcomes
-
Penn State Worry Questionnaire. 30 The PSWQ is the most established measure of trait worry style and has been used in non-clinical and clinical populations (see review by Startup and Erickson40). Each of the 16 items is rated on a 5-point scale, with higher scores indicating a greater tendency to worry.
-
Psychotic Symptom Rating Scales delusions subscale. 31 The PSYRATS delusions sbscale is a six-item multidimensional measure. It assesses the conviction, preoccupation, distress and disruption associated with delusions. Symptoms over the last week are rated. Higher scores indicate greater severity.
Secondary outcomes
-
Warwick–Edinburgh Mental Well-being Scale. 38 The WEMWBS is a fourteen-item scale assessing well-being over the past fortnight. Each item is rated on a scale from 1 (none of the time) to 5 (all of the time) and therefore the total score can range from 14 to 70, with higher scores indicating a greater level of well-being. Example items are ‘I’ve been feeling optimistic about the future’, ‘I’ve been feeling useful’, ‘I’ve been feeling relaxed’, ‘I’ve been feeling good about myself’, ‘I’ve been feeling confident’, ‘I’ve been feeling loved’ and ‘I’ve been feeling cheerful’. The scale has high test–test reliability and criterion validity with other well-being scales.
-
Positive and Negative Syndrome Scale (PANSS). 41 The PANSS is a 30-item rating instrument developed for the assessment of patients with schizophrenia. Symptoms over the last week were rated (i.e. currently present). Higher scores indicate the greater presence of psychiatric symptoms.
-
Green et al. Paranoid Thoughts Scale (GPTS). 42 The GPTS is a 32-item measure of paranoid thinking. Part A assesses ideas of reference (e.g. ‘It was hard to stop thinking about people talking about me behind my back’) and part B assesses ideas of persecution (e.g. ‘I was convinced there was a conspiracy against me’). Each item is rated on a 5-point scale, with higher scores indicating a greater level of paranoid thinking. The scale was completed for the period of the previous fortnight.
-
Perseverative Thinking Questionnaire (PTQ). 43 The PTQ is a 15-item questionnaire asking about how a person typically thinks about negative problems (e.g. ‘The same thoughts keep going through my mind again and again’), with each item assessed on a scale from 0 to 4. Higher scores indicate greater levels of repetitive negative thinking.
-
Choice of Outcome in CBT for Psychoses (CHOICE). 44 The CHOICE is a psychosis service user-led outcome measure with 24 items. We used 10 items that we considered reflected positive mental health, to provide validation of the WEMWBS in the persecutory delusions group. The 10 items had high internal reliability in the persecutory delusions group (Cronbach’s alpha = 0.90). The items included self-confidence, the ability to relax, having ways of dealing with distressing experiences, feeling safe and secure and a sense of being in control. Ratings were obtained for the past week. Higher scores indicate a higher sense of well-being.
Moderators
-
Wechsler Abbreviated Scale of Intelligence (WASI). 45 The WASI is a standardised short and reliable measure of intelligence. The Vocabulary and Matrix Reasoning subtests were used to obtain an estimate of intelligence quotient (IQ).
-
Jumping to conclusions: the beads task. 46 Data gathering was assessed with a probabilistic reasoning task that has been extensively used with individuals with delusions. Participants are asked to request as many pieces of evidence (coloured beads) as they would like before making a decision (from which of two hidden jars the beads are drawn). The two jars have beads of two different colours in opposite ratios. The ratio of beads used in the current study was 60 : 40. The key variable is the number of beads requested before making a decision. Requesting two or fewer beads is classified as JTC.
-
Working memory: tasks from the Wechsler Adult Intelligence Scale III (WAIS-III). 47 Three working memory tasks were used: digit span forwards (repeating back series of numbers), digit span backwards (repeating back series of numbers in reverse) and letter–number sequencing (sorting and recalling a series of letters and numbers). The demands on working memory increase across each of the three tasks.
-
Maudsley Addiction Profile. 48 The Maudsley Addiction Profile was developed with a large sample from a substance abuse clinic. Respondents are asked directly about the use over the past month of illicit drugs including cannabis, cocaine powder, crack cocaine, heroin, amphetamines and methadone.
-
Illness and treatment representations. 49 An adapted version of the Illness Perception Questionnaire was used. 50 It assesses four constructs: causes, consequences, cure/control and timeline. This adapted measure was developed based on the results of a previous study which found that illness representations predicted take-up of CBT. 51
Further theoretical variables
-
Intolerance of Uncertainty Scale (IUS). 52 The IUS has 27 items each rated on a scale from 1 to 5. Higher scores indicate greater levels of intolerance of uncertainty. There are four subscales derived from factor analysis:53 desire for predictability (e.g. ‘Unforeseen events upset me greatly’), a tendency to become paralysed in the face of uncertainty (e.g. ‘When I am uncertain I can’t function very well’), distress in the face of uncertainty (e.g. ‘The ambiguities in life stress me’) and inflexible uncertainty beliefs (e.g. ‘Being uncertain means that a person is disorganised’).
-
Worry Stop Rules Checklist (WSRC) (unpublished questionnaire by Kato, MacDonald and Davey, unpublished, University of Sussex). The WSRC is a 19-item measure of the rules that people use to determine whether to continue or stop worrying. Each item is a statement that represents the types of thoughts that people have when deciding whether to continue worrying or not. Each statement is rated on a 5-point scale, from 1 – ‘strongly disagree’ to 5 – ‘strongly agree’. It contains two subscales, an ‘as many as can’ subscale (10 items), which includes items such as ‘I must find a solution to this problem, so keep thinking about it’, and a ‘feel like continuing’ subscale (nine items), which includes items such as ‘Don’t worry about it, things will get better’. Higher scores on the ‘as many as can’ subscale indicate a greater tendency for individuals to continue worrying. Higher scores on the ‘feel like continuing subscale’ indicate a greater tendency for individuals to stop worrying earlier.
-
Catastrophising interview. 54 The catastrophising interview is an experimental assessment of worry. Individuals are asked to specify their main worry and are then asked what worries them about their main worry. This question (‘What worries you about that?’) is repeated for each following answer that the participant gives. The interview is brought to a close when no further responses are elicited or the participant repeats the same or a similar answer (e.g. the person cannot think of any more worrying steps). Each response is counted as a catastrophising step. A greater number of catastrophising steps indicates an increased tendency to perseverate a bout of worry.
-
Meta-Cognitive Beliefs Questionnaire (MCQ-30). 55 The MCQ-30 is a 30-item measure of meta-cognitive beliefs that have been found to be relevant to psychopathology. Each item asks participants to indicate how much they agree with different statements about worry and is rated on a 4-point scale, from 1 – ‘do not agree’ to 4 – ‘agree very much’. The items cluster into five factors measuring cognitive confidence (e.g. ‘I have a poor memory’), positive beliefs about worry (e.g. ‘worry helps me cope’), cognitive self-consciousness (e.g. ‘I am constantly aware of my thinking’), uncontrollability and danger of worry (e.g. ‘when I start worrying I cannot stop’) and need to control thoughts (e.g. ‘I should be in control of my thoughts all the time’). Higher scores indicate that the participant has a greater number of strongly held meta-cognitive beliefs.
-
Beck Anxiety Inventory (BAI). 56 The BAI is a 21-item self-report measure of the severity of physical and emotional symptoms of anxiety over the past week. Each item is rated from 0 – ‘not at all’ to 3 – ‘severely, I could barely stand it’. Higher scores indicate greater anxiety.
-
Anomalous experiences I: Cardiff Anomalous Perceptions Scale (CAPS). 57 In the experimental study the CAPS was adapted into a state measure by asking whether or not any of the perceptual anomalies had occurred in the past 5 minutes, with participants simply responding with a yes or no. A higher number of yes responses represents the reporting of a greater number of perceptual anomalies. The scale covers a variety of anomalies including changes in levels of sensory intensity (e.g. ‘Are sounds much louder than they normally would be?), distortion of own body or the external world (e.g. ‘Have you found the appearance of things or people seeming to change in a puzzling way, e.g. distorted shapes or sizes or colour?’), sensory flooding (e.g. ‘Have you found that sensations happened all at once and flooded you with information?’), temporal lobe experiences (e.g. ‘Have you had the feeling of being uplifted, as if driving or rolling over a road while sitting quietly?’) and hallucinations (e.g. ‘Have you heard noises or sounds when there was nothing about to explain them?’). In the current study we analysed the total score but also tested separately the hallucination items and the non-hallucination perceptual anomalies.
-
Anomalous experiences II: Cambridge Depersonalisation Scale (CDS). 58 We included a second scale in the experimental study to help capture the wide variety of anomalous experiences. The CDS was based on the view that depersonalisation comprises feelings of unreality but ‘also includes emotional numbing, heightened self-observation, changes in body experience, distortions in the experiencing of time and space, changes in the feeling of agency, feelings of having the mind empty of thoughts, memories and/or images, and an inability to focus and sustain attention’ (p. 154). 58 Two studies have shown that the scale assesses five distinct types of anomalous experience. 58,59 We used an adapted state version by asking about the occurrence of such experiences in the past few minutes. We used 19 items from the CDS, as 10 items were not suitable for a state version (e.g. ‘Previously familiar places look unfamiliar, as if I had never seen them before’). Higher scores indicate a greater occurrence of anomalies. We examined the total score but also used four factors from the largest study of the CDS structure:59 unreality of self [e.g. ‘Familiar voices (including my own) sound remote and unreal’], perceptual alterations (e.g. ‘I have the feeling that my hands or my feet have become larger or smaller’), unreality of surroundings (e.g. ‘What I see looks “flat” or “lifeless”, as if I were looking at a picture’) and temporal disintegration (e.g. ‘It seems as if things that I have done had taken place a long time ago’).
-
CDS. 58 Following on from the experimental study, the last 50 patients entering the trial completed the full CDS during the baseline assessment. The CDS is a 29-item measure of the frequency of depersonalisation experiences over the last 6 months. It was developed by Sierra and Berrios58 using an ‘exhaustive review of the descriptive psychopathology of depersonalisation’ (p. 155) as one of the item sources. The scale was developed as a response to the perceived lack of validity and comprehensiveness of existing measures, such as the Dissociation Experiences Scale60 and the Dixon Scale. 61 Each item in the CDS is rated on a 5-point scale, from 0 – ‘never’ to 4 – ‘all the time’, with the scale skewed towards the higher end of frequency. 58 In this study, the 7-point scale used to indicate the duration of the experience was omitted. Higher scores indicate a greater level of depersonalisation. The CDS can be separated into five factors:59 numbing (e.g. ‘When a part of my body hurts, I feel so detached from the pain that it feels as if it were somebody else’s pain’); unreality of self (e.g. ‘Whilst doing something I have the feeling of being a “detached observer” of myself’); perceptual alterations [e.g. ‘I cannot feel properly the objects that I touch with my hands for it feels as if it were not me who were touching it’ (italics as in original)]; unreality of surroundings (e.g. ‘What I see looks “flat” or “lifeless”, as if I were looking at a picture’); and temporal disintegration (e.g. ‘When in a new situation, it feels as if I have been through it before’).
Inter-rater reliability
Inter-rater reliability was tested for the two interviewer-rated outcome assessments, PSYRATS and PANSS, using two-way, mixed, single-measure intraclass correlations (ICCs). Rater 1 completed all assessments in the Oxford Health NHS Foundation Trust and rater 2 carried out the majority of the assessments in the Southern Health NHS Foundation Trust before being replaced with rater 3. Rater 1 attended 23 assessments with rater 2 and their reliability ratings were very good (PSYRATS total ICC = 0.99, PANSS total ICC = 0.83). Rater 1 attended 18 assessments with rater 3 and they also had very good reliability (PSYRATS total ICC = 0.98, PANSS total ICC = 0.75).
Interventions
The aim was to provide the CBT worry reduction intervention in six sessions over 8 weeks. Each session lasted for approximately an hour and took place in a NHS clinics or at the patient’s home. Before therapy began the clinician met the patient for an initial introduction and assessment.
The highly manualised intervention is designed to provide clear and simple messages for patients to take into their day-to-day lives. A set of six session booklets, shared by the patient and therapist, was written. The worry reduction strategies included were indicated in the anxiety literature to be effective at reducing worry and do not challenge the delusion itself. The main techniques were psychoeducation about worry, identification and reviewing of positive and negative beliefs about worry, increasing awareness of the initiation of worry and individual triggers, use of worry periods, planning activity at times of worry and learning to ‘let go’ of worry. Tasks were set between sessions. Whenever patients were agreeable, telephone calls were made or texts were sent between sessions to encourage the trying out of new strategies. In essence, patients were helped to learn that they had understandable positive beliefs about worry (e.g. ‘worry keeps me safe’), which meant that they engaged with this thinking style. They were helped to see the skewed view that worry provides and how it exacerbates fears. The two principal practical techniques to reduce worry were then introduced: the use of worry periods (confining worry to about a 20-minute set period each day) and the planning of activity at peak worry times. Worry periods were implemented flexibly. For example, most patients set up one worry period a day, but a person could choose to have two worry periods a day or, in severe instances, patients instead aimed for a worry-free period. Ideally, the worry period was then substituted with a problem-solving period.
Three clinical psychologists provided therapy, receiving weekly supervision from DF and HS. Therapy sessions were taped when patients gave permission. To assess treatment fidelity, 12 tapes, chosen at random, were rated on the Cognitive Therapy Scale – Revised62 by an independent clinical psychologist experienced in CBT for psychosis. All tapes were rated as providing at least satisfactory cognitive therapy (i.e. an average score of at least three on scale items).
Standard care was delivered according to national and local service protocols and guidelines. This usually consists of the prescription of antipsychotic medication, visits from a community mental health worker and regular outpatient appointments with a psychiatrist. It was recorded using the Client Service Receipt Inventory. 63
Sample size and power calculations
The recruitment target was 150 patients, split equally between the two centres (which was achieved). We were interested in detecting moderate or large effects. A simple two-tailed t-test with 60 people per group would provide 90% power to detect an effect size of 0.60 at a significance level of 0.05. It would have 80% power to detect an effect size of 0.52. In practice, further power would be gained by the use of multiple regression. Therefore, conservatively allowing for 20% dropout, 150 people would need to be recruited to enable full data to be obtained from 120 participants.
Statistical analysis
For the trial outcomes all analyses were carried out using Stata version 13 (StataCorp LP, College Station, TX, USA). All main analyses were carried out at the end of the last follow-up assessment (i.e. there were no interim analyses) and were based on the intention-to-treat principle, with due consideration being given to potential biases arising from loss to follow-up. Random- or mixed-effects models (using Stata’s xtreg command) were fitted to the repeated measures to estimate treatment effects for outcomes, controlling for stratum [treatment centre crossed by initial level of worry (moderate/high)] and the corresponding baseline assessment for the outcome under investigation. We allowed for the presence of missing outcome data under the assumption that the data are missing at random, using the terminology of Little and Rubin. 64 Standardised effect sizes (Cohen’s d) were calculated by dividing the estimated treatment effects by the pooled standard deviation (SD) at follow-up.
Secondary trial analyses to investigate putative meditational mechanisms were carried out using methods similar to those of Baron and Kenny65 but with allowance being made for the repeated measures of both the putative mediator (worry) and the outcome (delusions). This involved the use of the structural equations software package Mplus version 7 (Muthén & Muthén Los Angeles, CA). 66 All statistical testing was two-tailed.
The theoretical studies were analysed as in the following sections.
The interaction of affective with psychotic processes
All analyses were carried out using SPSS version 20 (IBM Corporation, Armonk, NY, USA). To test change after the randomisation condition (worry induction, worry reduction, neutral), analysis of covariance was used, with post-randomisation score as the dependent variable, group as a fixed factor and baseline score as the covariate. When there was a main effect of the group, least significant difference pairwise comparisons for the estimated marginal means were tested.
Depersonalisation in patients with persecutory delusions
All analyses were carried out using SPSS version 20. First, descriptive statistics for the CDS were calculated, to determine the level of depersonalisation in this population. Bivariate Pearson correlation analyses were then run to assess the relationship between participants’ depersonalisation (CDS total and its five component factors) and measures of psychotic and emotional symptoms.
How patients with persecutory delusions bring worry to a close
Eight patients in the control arm were interviewed at the end of their final trial assessment. A semistructured interview schedule was devised following a review of the relevant literature. In the opening question participants were asked about the kinds of things they worry about. Paranoid worries were the focus of the analysis. Participants were then asked to bring to mind a recent time when they had been worried about what they had described and to talk through how their period of worry came to an end. The aim of the interview was to explore the internal and external processes (e.g. cognitive, behavioural and emotional components) that may lead to a period of worry stopping. In line with interpretative phenomenological analysis recommendations,67 questions began open-ended and the interviewers encouraged elaboration with both verbal (e.g. ‘Can you tell me a bit more about that?’) and non-verbal (e.g. nodding) cues. The transcripts were qualitatively analysed using interpretative phenomenological analysis. 67
Jumping to conclusions in patients with persecutory delusions
Analyses were carried out using SPSS version 20.0. The patient group was divided into two: those who demonstrated JTC and those who did not. To test the two primary hypotheses these two groups were then compared using t-tests on the measures of working memory and intolerance of uncertainty.
Persecutory delusions and psychological well-being
A control group of 346 adults from the general population was recruited for comparison with the patient group. Participants were recruited predominantly through the playing of local radio adverts in Oxfordshire (n = 221) and the website of a local newspaper (n = 66). A smaller number of participants were recruited through the local universities (n = 29), by word of mouth (n = 15) or from other sources (n = 15). Analyses were carried out using SPSS version 20.0. The central hypothesis concerned the difference in well-being scores between the persecutory delusions group and the non-clinical group, which was examined using a t-test. Associations between well-being and symptoms scores were tested using Pearson correlation coefficients.
Chapter 3 Results
Demographic and basic clinical data
The demographic data are summarised in Table 1. As in other studies of persistent psychotic experiences, the group has a slightly higher preponderance of men, the average age is around 40 years, the majority are unemployed and the main diagnosis is schizophrenia. All but nine patients were taking antipsychotic medication. Most patients had been in contact with mental health services for many years.
| Variable | Treatment group (n = 73) | Control group (n = 77) |
|---|---|---|
| Age (years), mean (SD) | 40.9 (10.5) | 42.1 (12.2) |
| Male to female ratio | 42 : 31 | 44 : 33 |
| Ethnicity, n | ||
| White | 68 | 69 |
| Black | 1 | 0 |
| Chinese | 0 | 2 |
| Indian | 0 | 3 |
| Other | 4 | 3 |
| Employment status, n | ||
| Unemployed | 55 | 51 |
| Part-time employed | 8 | 6 |
| Full-time employed | 3 | 10 |
| Self-employed | 1 | 2 |
| Retired | 2 | 6 |
| Student | 1 | 2 |
| Housewife/husband | 3 | 0 |
| IQ, mean (SD) | 100.3 (19.0) | 101.8 (18.2) |
| Diagnosis, n | ||
| Schizophrenia | 58 | 53 |
| Schizoaffective disorder | 5 | 6 |
| Delusional disorder | 4 | 6 |
| Psychosis not otherwise specified | 6 | 12 |
| Outpatient to inpatient ratio | 71 : 2 | 76 : 1 |
| Inpatient admission in previous 6 months, n | 10 | 8 |
| Chlorpromazine-equivalent antipsychotic medication dose (mg/day), mean (SD) | 523.2 (394.3) | 475.5 (420.6) |
| Approximate time in contact with services, n | ||
| < 1 year | 5 | 7 |
| 1–5 years | 12 | 17 |
| 6–10 years | 16 | 12 |
| 11–20 years | 18 | 26 |
| > 20 years | 21 | 15 |
Provision of therapy
The mean number of sessions received was 5.5 (SD 1.8). The median number of sessions received was 6. In total, 51 patients attended six sessions. In the interests of flexibility, for a small number of patients the intervention was provided in seven (n = 7) or eight (n = 2) sessions during the 8-week period. Two patients attended no therapy sessions. The remainder of the patients attended one (n = 5), two (n = 1), three (n = 1), four (n = 3) or five (n = 1) sessions. Patient accounts of the therapy are provided in Box 1.
The discussions about preventing worry and reducing worry were extremely helpful to me. It made me see my worry as something real. The breakthrough was that I was able to, with the help of my psychologist, come up with a strategy – that is, when worry gripping me I would say ‘Excuse me worry while I do . . .’ or ‘Excuse me worry I need to interrupt you because . . .’. I sometimes worry about people trying to harm me but now I can interrupt my worry and do something else. I challenge myself to do this because I know it works for me.
Patient 2
I had no confidence in who I was and felt I avoided everyone because of my thoughts and being in company was really frightening. I found the therapy challenging and sometimes very difficult. But it was eye-opening as I didn’t realise how much I worried and where the worry was coming from. To see it on paper made it more straightforward and made my life more clear. I do feel that I now try to take time out whether that’s a cup of tea or going to the shops. Just doing things that I actually enjoy doing and building on them as I was so wrapped up in anxiety I was lost. I am more relaxed at certain times of the day where I was once completely stressed. I still find it hard around people but I feel I can still build on the skills you gave me and if it’s slightly better that’s good.
Patient 3
The therapy was very rewarding. There wasn’t anything I didn’t like. I needed that kind of therapy at the time because if I didn’t have that therapy at that time I wouldn’t be here. It was therapeutic talking about things. I listened to what you had to say and wrote down how I felt. I also tried relaxing to the tape and I ignored people when they were horrible to me. It was hard becoming disciplined but we worked as a team, that’s what I liked about it. You don’t get nowhere in this world if you don’t work as a team. I was having a hard time and you was doing your best to stop me having a hard time. That’s what I call teamwork, I couldn’t have been able to do it by myself, no way. I thought a lot about what I thought the therapy did – it decreased my worrying but in other ways it built my confidence.
Patient 4
It was hard talking about some of the stuff we talked about but it was worth it in the end. The worry period and the voice period helped a lot. Being able to say ‘I’ll worry later’ helped it go out of mind for a bit. I’m worrying less and that is good. Talking about it helps. That’s something I learnt from therapy. Talking helped clear my head and realise that maybe it, my mum poisoning me, wasn’t going to happen. The Worry Intervention Trial therapy was helpful, thank you.
Patient 5
The worst bit was the paranoia – that people were talking about me and me losing my temper and stuff. Going to crowded places was a big deal for me. The therapy helped me a lot to understand my illness better, it helped me deal with it a lot better. It still affects me but I’m in a better place now. I liked being given ways to deal with it, like the worry box. That sticks in my mind the most, it really does help. It makes my day better to set aside time to worry and then having the rest of the day free from it. I hadn’t thought about trying that before. I was a bit cynical about it at first if I’m honest but it really does work. My illness doesn’t seem as daunting now. It’s been a long time now since I had a hospital admission, over a year. That’s down to lots of things – the worry therapy and the help I’ve had from assertive outreach. It’s good to know there’s help there if I need it.
Primary outcome data
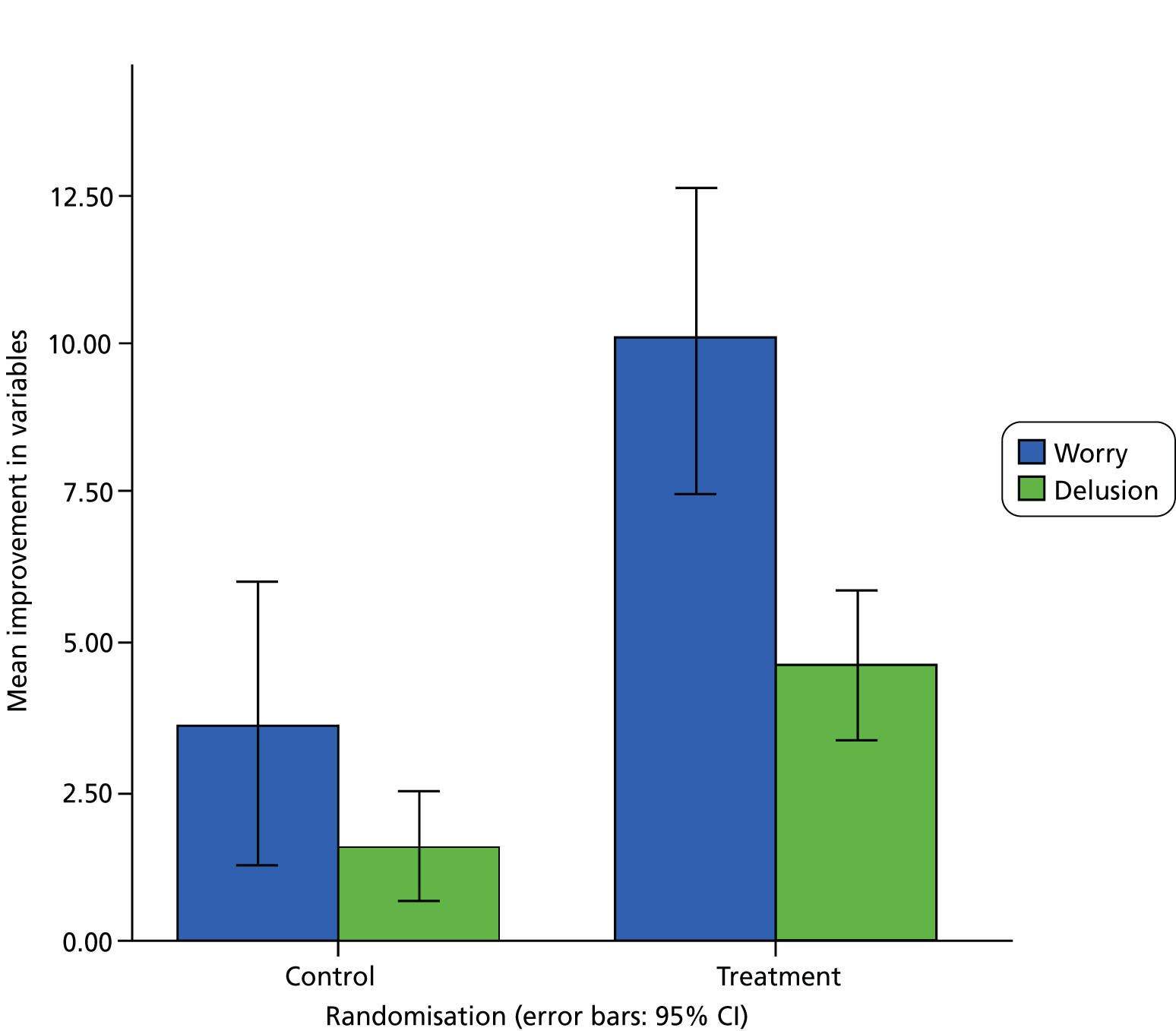
The scores for the outcome measures are summarised in Table 2. Compared with treatment as usual, the CBT intervention led to a highly significant reduction in levels of worry. In a repeated-measures (mixed-model) analysis, the estimated reduction in PSWQ score at 8 weeks as a result of treatment was 6.35 [standard error (SE) 1.56, 95% confidence interval (CI) 3.30 to 9.40; p < 0.001], that is, the reduction in worry was estimated to be 6.35 units more in the patients receiving the CBT intervention than in those in the control condition. There was also a highly significant reduction in levels of persecutory delusions [estimated reduction in PSYRATS scores as a result of treatment = 2.08 (SE 0.73), 95% CI 0.64 to 3.51; p = 0.005]. Change scores are summarised in Figure 2. The treatment by follow-up time interactions were estimated to be –2.43 (SE 1.57; p = 0.121) and +0.86 (SE 0.68; p = 0.205) for PSWQ and PSYRATS scores, respectively, indicating that the treatment effects were smaller for PSWQ at 24 weeks but larger for PSYRATS. However, neither of these interactions approached statistical significance and the models were refined to estimate treatment effects that were assumed to be common to both follow-up times. The resulting treatment effect estimates were 5.15 (SE 1.35, 95% CI 2.50 to 7.79; p < 0.001; Cohen’s d = 0.47) and 2.50 (SE 0.65, 95% CI 1.22 to 3.78; p < 0.001; Cohen’s d = 0.49). We note that there were no significant time trends for either outcome between 8 and 24 weeks (this is relevant for the model for mediation, introduced in Moderation and mediation analyses).
FIGURE 2.
Mean improvement in worry and delusion scores at 8 weeks.
| Measure | Treatment group | Control group | ||||
|---|---|---|---|---|---|---|
| n | Mean | SD | n | Mean | SD | |
| Primary measures | ||||||
| Worry (PSWQ) | ||||||
| 0 weeks | 73 | 64.8 | 8.6 | 77 | 64.5 | 9.5 |
| 8 weeks | 70 | 54.8 | 10.5 | 73 | 61.0 | 12.2 |
| 24 weeks | 68 | 56.1 | 9.7 | 73 | 59.8 | 11.0 |
| Delusion (PSYRATS) | ||||||
| 0 weeks | 73 | 18.7 | 3.0 | 77 | 18.0 | 3.0 |
| 8 weeks | 70 | 14.3 | 4.8 | 73 | 15.9 | 5.1 |
| 24 weeks | 68 | 13.6 | 5.6 | 72 | 16.4 | 4.8 |
| Secondary measures | ||||||
| Delusion distress (PSYRATS distress) | ||||||
| 0 weeks | 73 | 6.4 | 1.4 | 77 | 6.5 | 1.3 |
| 8 weeks | 70 | 5.1 | 1.9 | 73 | 5.8 | 2.1 |
| 24 weeks | 68 | 5.0 | 2.2 | 72 | 6.1 | 1.8 |
| Total symptoms (PANSS) | ||||||
| 0 weeks | 73 | 82.0 | 13.6 | 76 | 79.0 | 13.5 |
| 8 weeks | 69 | 70.7 | 12.4 | 73 | 75.3 | 16.0 |
| 24 weeks | 68 | 71.5 | 15.4 | 71 | 76.3 | 16.7 |
| Paranoia (GPTS) | ||||||
| 0 weeks | 73 | 115.9 | 27.3 | 77 | 110.8 | 27.8 |
| 8 weeks | 70 | 90.0 | 32.2 | 73 | 102.3 | 31.7 |
| 24 weeks | 67 | 92.5 | 32.7 | 73 | 105.6 | 32.4 |
| Rumination (PTQ) | ||||||
| 0 weeks | 70 | 44.3 | 9.7 | 72 | 44.9 | 9.8 |
| 8 weeks | 68 | 37.7 | 9.7 | 70 | 41.0 | 11.7 |
| 24 weeks | 64 | 37.3 | 10.5 | 71 | 42.7 | 10.6 |
| Patient outcomes (CHOICE) | ||||||
| 0 weeks | 71 | 49.4 | 17.3 | 75 | 49.5 | 18.5 |
| 8 weeks | 67 | 64.4 | 17.1 | 69 | 51.7 | 21.1 |
| 24 weeks | 66 | 61.6 | 21.4 | 70 | 52.5 | 22.4 |
| Well-being (WEMWBS) | ||||||
| 0 weeks | 73 | 36.4 | 9.6 | 77 | 34.5 | 9.2 |
| 8 weeks | 68 | 41.5 | 9.1 | 73 | 36.5 | 11.3 |
| 24 weeks | 67 | 40.2 | 10.8 | 73 | 36.6 | 10.5 |
Secondary outcome data
There were significant improvements with the CBT treatment for all of the secondary outcome measures. There were no significant treatment by follow-up time interactions and therefore treatment estimates common to both follow-up times are made. Compared with treatment as usual, there was a reduction in delusion distress with CBT [estimated reduction in PSYRATS distress score = 0.85 (SE 0.25); p = 0.001], a reduction in psychiatric symptoms [estimated reduction in PANSS score = 6.16 (SE 1.69); p < 0.001] and a reduction in levels of paranoia [estimated reduction in GPTS score = 14.68 (SE 4.18); p < 0.001]. There was an improvement in psychological well-being with CBT [estimated improvement in WEMWBS score = 2.40 (SE = 1.11); p = 0.03], a reduction in rumination [estimated reduction in PTQ score = 3.51 (SE 1.43); p = 0.014] and an improvement in patient-chosen outcomes [estimated improvement in CHOICE score = 10.45 (SE 2.42); p < 0.001].
Moderation and mediation analyses
There was no evidence of moderation of treatment effects by centre, level of worry or delusions, intellectual functioning, illicit drug use, illness perceptions, reasoning or working memory (p > 0.05).
The main outcome analysis demonstrated an effect of the CBT treatment on both the putative mediator (worry; GPTS) and the clinical outcome (delusions; PSYRATS). This is necessary, but not sufficient, for the demonstration of mediation. The more difficult challenge is providing a robust demonstration (estimate) of the effect of the putative mediator on the clinical outcome and the corresponding direct effect of the intervention (that not explained by changes in the mediator) on outcome. Our strategy follows that of the well-known procedure advocated by Baron and Kenny,65 but uses statistical models that (1) account for the repeated measures of both mediator and outcome, (2) acknowledge that there is likely to be confounding of the effect of the mediator on the outcome and (3) allow for the fact that the mediator (and outcome) is subject to considerable measurement error. 68 The chosen models were motivated by the finding that there were neither temporal trends in the mediator or outcome between the two follow-up times nor treatment by follow-up time interactions (i.e. the treatment effects were constant over time).
We start with two simple measurement or factor analysis models, one for worry and one for delusions. In each case the loadings for 8 and 24 weeks are constrained to be 1, the intercept term for each time point is constrained to be zero and the variances of the measurement errors (random temporal variations) are equal for the two time points. In the psychometrics jargon, we have assumed that the measurements at the two follow-up times are parallel measures of a stable underlying latent variable (factor). 69 The measurement errors for worry and delusions were allowed to be correlated at 8 weeks and again at 24 weeks.
Following Baron and Kenny,65 we now estimate the effects of the intervention on (1) the worry outcome factor (FW) and (2) the delusions outcome factor (FD) and (3) the effect of FW on FD, allowing for a direct effect of the intervention on the latter. In practice, (1) and (2) were assessed in a joint structural equations model (SEM), allowing for the residual (i.e. not explained by the intervention and baseline covariates) variation in FW and FD to be correlated (as would be expected if mediation were present). For (3) we jointly modelled the effect of the intervention on worry and the effect of worry and the intervention on outcome (this time not allowing the residuals to be correlated).
Confounding is mainly allowed for by including baseline values of both worry and delusions (in addition to the stratifying factors) in all of the above SEM analyses. Note that in the earlier intention-to-treat analyses there is no problem of confounding and the covariates are simply included to increase precision (statistical power). In a mediation analysis (estimating the effects of the mediator on outcome) we are looking at a non-randomised comparison (neither mediator nor outcome are under the direct control of the investigator) and there may, therefore, be confounding. A major source of such confounding is likely to be the correlation between the baseline values of worry and delusions (estimated here to be 0.51).
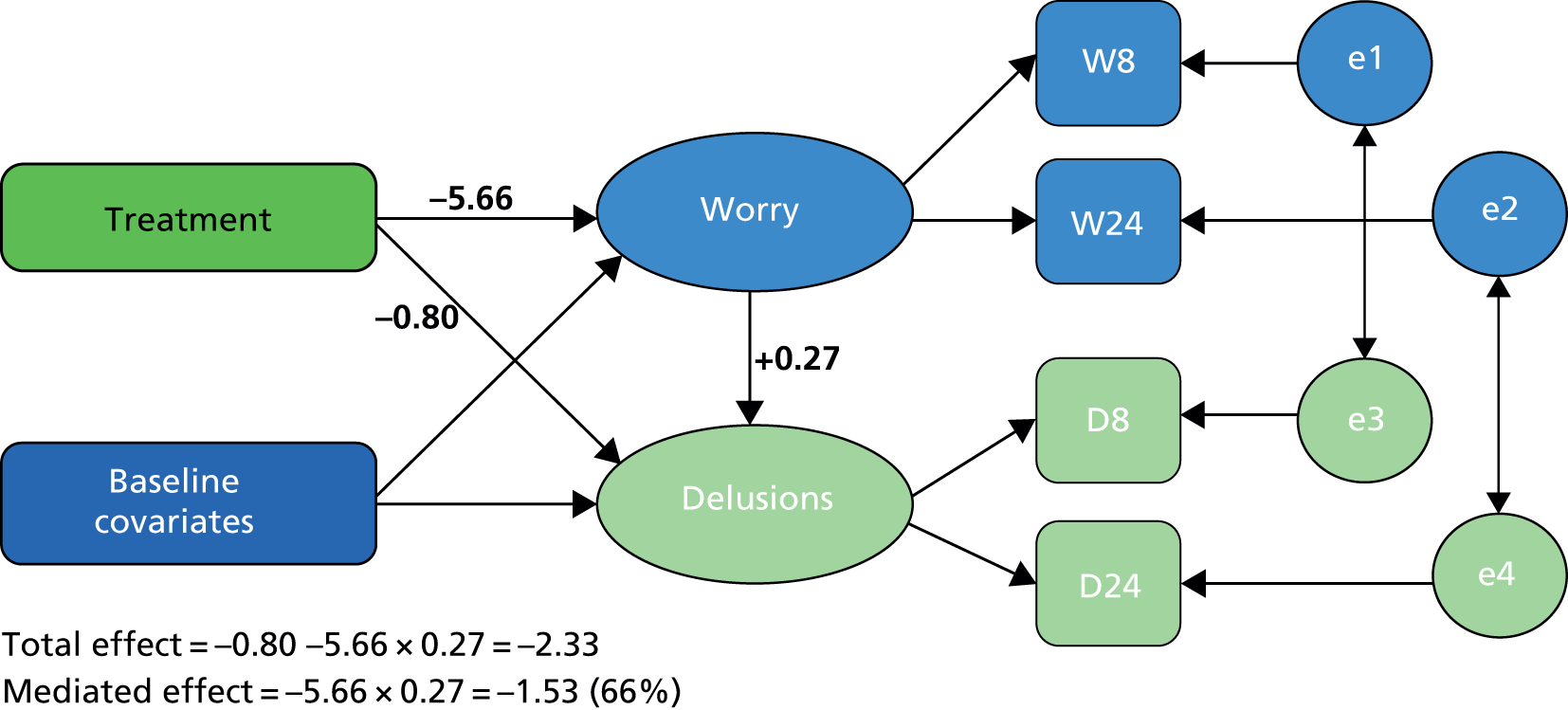
The results of the SEM analyses (Figure 3) are summarised as follows. The effect of the intervention was to reduce FW by 5.66 units (SE 1.32 units, 95% CI 3.08 to 8.24 units; p < 0.11). The total effect of the intervention on FD was a reduction of 2.33 units (SE 0.64 units, 95% CI 1.08 to 3.58 units; p < 0.001). The direct effect of the intervention on FD was a reduction of 0.80 units (SE 0.65 units, 95% CI –0.70 to 2.07 units; p = 0.214). Each unit reduction in the FW produced a 0.27 change in FD (SE 0.06, 95% CI 0.15 to 0.39; p < 0.001). The estimated indirect (mediated) effect of the intervention on FD was a reduction of 1.53 units (SE 0.49 units, 95% CI 0.57 to 2.48 units; p = 0.002). The proportion of the effect of the intervention on outcome (delusions) that is mediated by changes in worry is therefore 1.53/2.33 = 66%. The excellent fit of the SEM to the data is indicated by a chi-square of 20.03 with 17 degrees of freedom (df) (p = 0.273), a root-mean-square error of approximation of 0.035 and a comparative fit index of 0.992.
FIGURE 3.
Summary of the mediation analysis. Rectangles or squares are measured variables. Ellipses or circles are latent variables (including random errors/residuals). Single-headed arrows indicate causal effects, with the main ones of interest in bold. Double-headed arrows reflect correlations. W8 and W24, worry measures; D8 and D24, delusion measures; e1 and e2, random residuals (worry); e3 and e4, random residuals (delusions).
Provision of standard care
In Table 3 the provision of standard care for the 6 months before the trial and the 6 months of the trial is summarised. The standard care provided for each allocation group is comparable. The number of days in hospital data is skewed for the CBT treatment group: one patient was in hospital for 2 years before entering the trial although was discharged 3 months into the trial.
| Variable | Treatment group | Control group | ||||||
|---|---|---|---|---|---|---|---|---|
| n | Mean | SD | Median | n | Mean | SD | Median | |
| 6 months before the trial | ||||||||
| Days in hospital | 73 | 7.4 | 26.8 | 0 | 77 | 2.8 | 9.5 | 0 |
| Psychiatrist meetings | 72 | 2.4 | 3.9 | 2 | 77 | 2.8 | 4.2 | 2 |
| Community psychiatric nurse meetings | 72 | 12.3 | 9.9 | 12 | 76 | 10.5 | 10.1 | 7 |
| Counsellor/therapist meetings | 72 | 1.5 | 6.2 | 0 | 77 | 1.1 | 4.7 | 0 |
| Day-care centre visits | 72 | 0.8 | 4.3 | 0 | 77 | 1.7 | 10.6 | 0 |
| GP meetings | 73 | 3.8 | 4.8 | 3 | 77 | 2.6 | 3.2 | 1 |
| 6 months during the trial | ||||||||
| Days in hospital | 73 | 3.5 | 15.0 | 0 | 77 | 0.2 | 1.6 | 0 |
| Psychiatrist meetings | 65 | 1.6 | 1.9 | 0 | 71 | 1.8 | 2.2 | 0 |
| Community psychiatric nurse meetings | 65 | 11.2 | 11.3 | 3 | 71 | 9.2 | 13.9 | 2 |
| Counsellor/therapist meetings (outside trial) | 61 | 1.0 | 3.6 | 0 | 66 | 1.1 | 3.4 | 0 |
| Day-care centre visits | 65 | 0.4 | 2.6 | 0 | 71 | 1.0 | 6.3 | 0 |
| GP meetings | 65 | 2.6 | 2.6 | 1 | 71 | 2.6 | 2.5 | 1 |
Adverse events
During the trial any adverse event that came to our attention was recorded. Medical notes were also checked at the end of the trial for the following events prespecified as adverse: (1) all deaths, (2) suicide attempts, (3) serious violent incidents, (4) admissions to secure units and (5) formal complaints about therapy. Two patients did not give us permission to check their medical notes at the end of the trial. During the trial there were no deaths, admissions to secure units or formal complaints about therapy. There were six suicide attempts (two in the treatment group and four in the control group). There were two serious violent incidents (one in each allocation group). None of the adverse events was related to therapy or the assessments.
Theoretical study results
The interaction of affective with psychotic processes
The post-randomisation performance of each experimental study group (randomised in the baseline assessment to the worry induction, worry reduction or neutral condition) on the tasks assessing psychotic processes is summarised in Table 4. It can be seen that there are no differences between the groups in performance on working memory or JTC tasks (controlling for baseline scores). However, there are increases in the occurrence of anomalies of experience in the worry induction condition compared with the other two conditions. The only exception for anomalous experiences is that the occurrence of hallucinations is not affected by randomisation condition.
| Task | Worry induction (n = 20) | Neutral condition (n = 22) | Worry reduction (n = 25) | Test of group effect | ||||
|---|---|---|---|---|---|---|---|---|
| Mean | SE | Mean | SE | Mean | SE | F(2,65) | p-value | |
| Working memory | ||||||||
| Forward digit span | 9.0 | 0.5 | 9.6 | 0.5 | 9.6 | 0.4 | 0.5 | 0.618 |
| Backward digit span | 6.2 | 0.4 | 5.8 | 0.3 | 5.8 | 0.3 | 0.5 | 0.637 |
| Letter–number sequencing | 8.2 | 0.4 | 8.7 | 0.4 | 8.4 | 0.3 | 0.6 | 0.563 |
| JTC | ||||||||
| Number of beads | 6.4 | 0.6 | 6.5 | 0.6 | 7.8 | 0.6 | 1.8 | 0.175 |
| Anomalous experiences | ||||||||
| CAPS | 4.7 | 0.5 | 4.3 | 0.5 | 3.3 | 0.5 | 2.3 | 0.107 |
| Hallucinations | 1.2 | 0.2 | 1.1 | 0.2 | 1.3 | 0.2 | 0.3 | 0.777 |
| Non-hallucination anomalies | 2.2a | 0.3 | 1.9a | 0.3 | 0.9b | 0.3 | 5.5 | 0.006 |
| CDS | 5.0a | 0.5 | 2.5b | 0.5 | 2.4b | 0.4 | 10.0 | < 0.001 |
| Unreality | 1.7a | 0.2 | 1.1a,b | 0.2 | 0.7b | 0.2 | 4.8 | 0.012 |
| Perceptual | 0.9a | 0.1 | 0.4b | 0.1 | 0.2b | 0.1 | 6.3 | 0.003 |
| Surroundings | 0.5a | 0.1 | 0.2b | 0.1 | 0.2b | 0.1 | 3.8 | 0.028 |
| Temporal | 1.1a | 0.1 | 0.6b | 0.1 | 0.5b | 0.1 | 4.5 | 0.015 |
Depersonalisation in patients with persecutory delusions
Examining the CDS scores (Table 5) revealed that participants are experiencing high levels of depersonalisation. Viewing the subscales of the CDS separately, and standardising them to a percentage of the maximum possible score available on that subscale, shows that this population is experiencing temporal disintegration-type depersonalisation experiences the most and perceptual alterations-type experiences the least. The depersonalisation total and factor scores all correlated positively with levels of paranoia and worry. It was also found that depersonalisation was associated with delusions, anxiety, perseverative thinking, positive psychotic symptoms and levels of psychotic symptomatology as a whole (Table 6).
| Summary variable | CDS (total) | CDS: numbing | CDS: unreality of self | CDS: perceptual alterations | CDS: unreality of surroundings | CDS: temporal disintegration | PANSS (positive symptom total) |
|---|---|---|---|---|---|---|---|
| Mean score | 36.8 | 7.6 | 8.2 | 3.6 | 2.9 | 5.9 | 21.4 |
| Median score | 36.5 | 6.0 | 7.0 | 3.0 | 3.0 | 6.0 | 22.0 |
| SD | 22.0 | 5.2 | 5.5 | 3.6 | 2.1 | 3.7 | 3.4 |
| Percentiles | |||||||
| 25th | 19.8 | 4.0 | 4.0 | 0.0 | 1.0 | 3.0 | 18.8 |
| 75th | 50.5 | 10.0 | 11.3 | 5.3 | 4.0 | 8.3 | 24.0 |
| Mean score as % of maximum possible | 31.7 | 31.7 | 34.2 | 18.0 | 36.3 | 36.9 | 43.7 |
| Measure | CDS (total) | CDS: numbing | CDS: unreality of self | CDS: perceptual alterations | CDS: unreality of surroundings | CDS: temporal disintegration | |
|---|---|---|---|---|---|---|---|
| PSWQ (total) | r | 0.36 | 0.22 | 0.33 | 0.27 | 0.39 | 0.32 |
| p | 0.01 | 0.12 | 0.02 | 0.06 | 0.01 | 0.02 | |
| BAI (total) | r | 0.51 | 0.51 | 0.42 | 0.42 | 0.37 | 0.44 |
| p | < 0.01 | < 0.01 | < 0.01 | < 0.01 | 0.01 | < 0.01 | |
| PTQ (total) | r | 0.29 | 0.25 | 0.21 | 0.18 | 0.33 | 0.24 |
| p | 0.05 | 0.08 | 0.14 | 0.22 | 0.02 | 0.09 | |
| GPTS (total) | r | 0.33 | 0.25 | 0.29 | 0.32 | 0.21 | 0.38 |
| p | 0.02 | 0.09 | 0.04 | 0.02 | 0.15 | 0.01 | |
| GPTS part A | r | 0.30 | 0.21 | 0.23 | 0.30 | 0.23 | 0.35 |
| p | 0.04 | 0.14 | 0.18 | 0.04 | 0.10 | 0.01 | |
| GPTS part B | r | 0.28 | 0.22 | 0.28 | 0.26 | 0.13 | 0.31 |
| p | 0.05 | 0.13 | 0.05 | 0.07 | 0.35 | 0.03 | |
| PSYRATS (total) | r | 0.51 | 0.46 | 0.49 | 0.38 | 0.37 | 0.46 |
| p | < 0.01 | < 0.01 | < 0.01 | 0.01 | 0.01 | < 0.01 | |
| Hallucinations (PANSS item) | r | 0.26 | 0.25 | 0.33 | 0.11 | 0.07 | 0.24 |
| p | 0.07 | 0.08 | 0.02 | 0.45 | 0.64 | 0.09 | |
| PANSS (positive) | r | 0.19 | 0.13 | 0.22 | 0.09 | 0.11 | 0.19 |
| p | 0.20 | 0.37 | 0.12 | 0.56 | 0.43 | 0.19 | |
| PANSS (total) | r | 0.57 | 0.51 | 0.53 | 0.44 | 0.43 | 0.50 |
| p | < 0.01 | < 0.01 | < 0.01 | < 0.01 | < 0.01 | < 0.01 | |
How patients with persecutory delusions bring worry to a close
Within the transcripts, five superordinate themes were identified relating to the topic of bringing worry to an end. Table 7 details these superordinate themes and the subthemes within them. Participants often described a passive relationship with worry (‘natural drift’), in which they felt unable to do anything about their worry, apart from waiting for it to end. Some participants struggled to notice when they had stopped worrying or how long they had been worrying for (e.g. ‘I just have to wait for it to wear off . . . I know I shouldn’t smoke but I do have cigarettes and a cup of tea, and . . . I just sit and wait for it to . . . wash over me’). Despite often describing their worry as uncontrollable, many participants talked about trying to manage worry with distraction techniques. These were predominantly behavioural in nature, with participants trying to take their mind off worry by doing something else (e.g. ‘Well I had the music on and that helps, so that’s my . . . y’know there’s always got to be a distraction there. If there’s no distraction it permeates my brain constantly’). The superordinate concept of interpersonal support was defined by two subthemes. The first of these encompasses the help that participants received from others (e.g. ‘Well I’d talk with somebody about it. Helped quite a bit . . . helped to get it off my mind really’). The other subtheme describes the opposite to this, when participants felt unsupported by others (e.g. ‘the fact that it keeps on happening and nobody gives a toss. That comes to the forefront every time’). Some participants talked about using their feelings as a guide that worry had ended. In contrast to the ‘feel like continuing’ stop rule, participants seemed to be using their feelings as a communication that worry had ended or had ‘naturally drifted’ [e.g. ‘(How would you notice that it had stopped?) I’d feel happy and I’d go down and do my work like normal’]. Some participants seemed to be trying to reason with themselves when they were worrying to bring worrying to an end (‘reality testing’) (e.g. ‘I say don’t be silly, they can’t do that. But I know they are doing it’).
| Superordinate themes | Subthemes |
|---|---|
| 1. Natural drift | |
| 2. Distraction | |
| 3. Interpersonal support | 3.1 Help from others |
| 3.2 Lack of support from others | |
| 4. Feeling better | |
| 5. Reality testing |
Jumping to conclusions in patients with persecutory delusions
Those patients who jumped to conclusions showed lower levels of intolerance of uncertainty than those who did not, although this was statistically significant only for the presence of inflexible certainty beliefs (Table 8). Patients who jumped to conclusions also reported significantly lower levels of worry but no differences in anxiety or repetitive negative thinking. Worry positively correlated with total IUS score (r = 0.49, p < 0.001). When total IUS score was entered with worry as independent variables in a binary logistic regression, there was a trend for worry scores to predict JTC (B = –0.055, odds ratio = 0.95, p = 0.067), but IUS score did not predict JTC (B = –0.008, odds ratio = 0.99, p = 0.450). A similar pattern was found for the IUS inflexible certainty beliefs score. In a binary logistic regression predicting JTC, there were indications that worry was a predictor (B = –0.051, odds ratio = 0.95, p = 0.078), but the IUS inflexible certainty beliefs did not predict JTC (B = –0.073, odds ratio = 0.93, p = 0.213). Those patients who jumped to conclusions showed poorer working memory performance and had lower IQ scores than those who did not. There were no significant correlations between worry and the working memory tasks (all p > 0.1). In a binary logistic regression with JTC as the dependent variable and letter–number sequencing and worry as the independent variables, both poorer working memory (B = –0.229, odds ratio = 0.80, p = 0.002) and lower levels of worry (B = –0.082, odds ratio = 0.922, p = 0.005) predicted JTC.
| Variable | JTC, mean (SD) | No JTC, mean (SD) | Mean difference | 95% CI | p-value |
|---|---|---|---|---|---|
| IUS total | 81.6 (22.2) | 90.6 (24.4) | 9.1 | –0.9 to 19.0 | 0.074 |
| Desire for predictability | 21.5 (23.9) | 23.9 (6.9) | 2.4 | –0.4 to 5.3 | 0.088 |
| Uncertainty paralysis | 18.4 (5.6) | 20.2 (6.0) | 1.8 | –0.7 to 4.2 | 0.159 |
| Uncertainty distress | 16.5 (4.5) | 17.3 (5.0) | 0.8 | –1.3 to 2.8 | 0.453 |
| Inflexible certainty beliefs | 10.1 (3.4) | 11.9 (4.3) | 1.8 | 0.1 to 3.5 | 0.036 |
| Anxiety | 24.9 (11.1) | 26.4 (14.9) | 1.5 | –3.6 to 6.6 | 0.565 |
| Worry | 60.7 (8.4) | 64.8 (7.6) | 4.2 | 0.9 to 7.4 | 0.012 |
| Preservative thoughts | 44.0 (9.5) | 44.6 (9.6) | 0.6 | –3.4 to 4.7 | 0.757 |
| Forward digit span | 8.9 (1.8) | 9.8 (2.5) | 0.9 | 0.1 to 1.8 | 0.033 |
| Backward digit span | 5.0 (2.1) | 6.2 (2.1) | 1.2 | 0.3 to 2.0 | 0.013 |
| Letter–number sequencing | 6.8 (3.5) | 8.9 (3.1) | 2.1 | 0.7 to 3.5 | 0.003 |
| IQ | 91.4 (16.8) | 102.0 (18.3) | 10.6 | 3.2 to 18.1 | 0.006 |
Persecutory delusions and psychological well-being
The mean WEMWBS score was 35.4 for the persecutory delusions group (SD 9.4, minimum 14, maximum 55, median 35.0) and 50.9 for the non-clinical group (SD 8.4, minimum 24, maximum 70, median 52.0). This mean difference of 15.4 points (95% CI 13.8 to 17.1 points) was statistically significant (t = 18.08, df = 494, p < 0.001). The non-clinical group mean score was almost identical to the WEMWBS original Scottish general population data. 38 In total, 76.6% (n = 115) of the persecutory delusions group were scoring at least 1 SD below the non-clinical control group mean score and 46.7% (n = 70) of the persecutory delusions group were scoring at least 2 SDs below the non-clinical group mean score. This clear difference in scores between the two groups can be seen in Figure 4.
FIGURE 4.
Box plot for well-being scores by group.
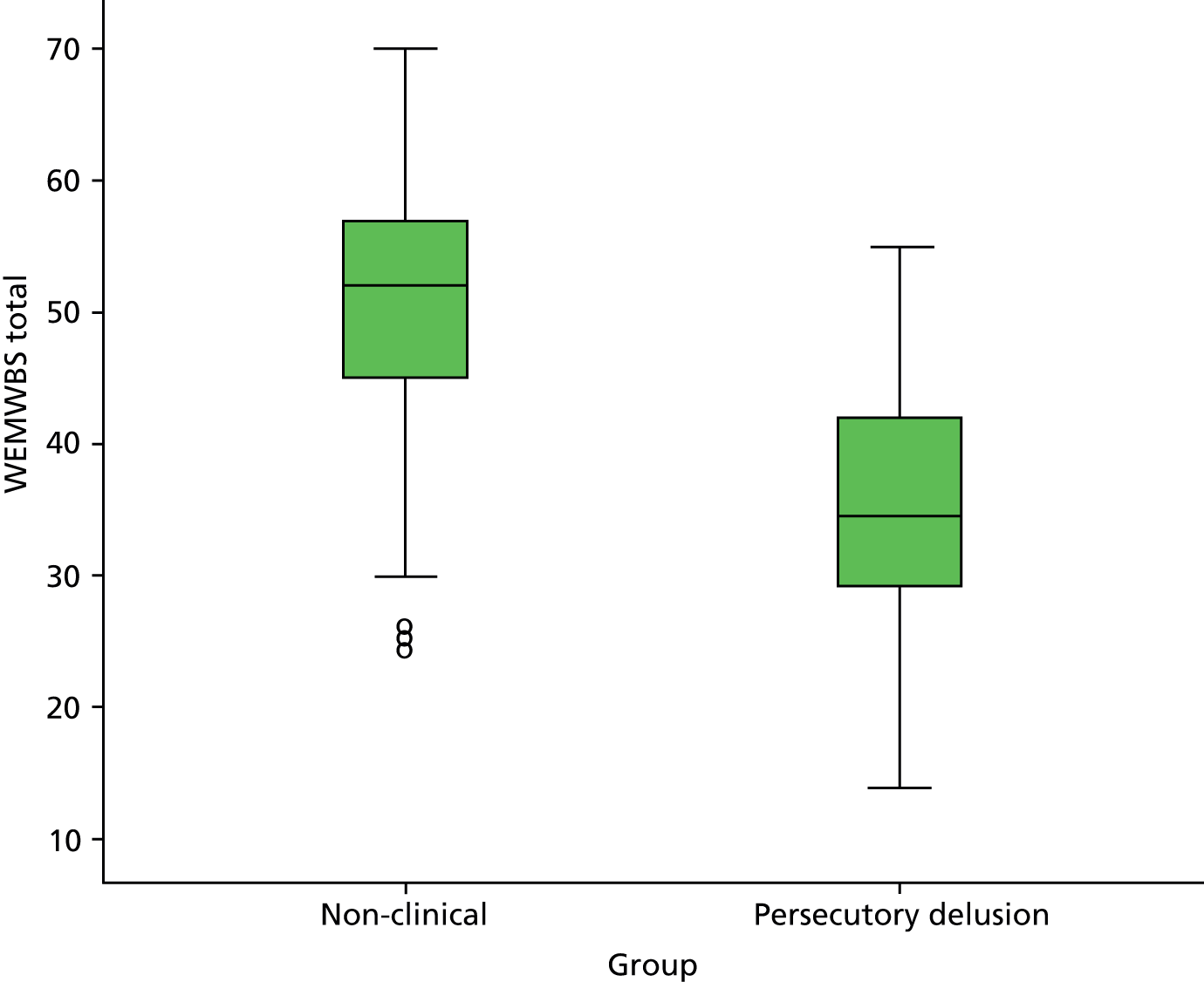
In the persecutory delusions group, lower levels of well-being were associated with higher levels of the persecutory delusion (PSYRATS) (r = –0.44, p < 0.001), paranoia (GPTS) (r = –0.30, p < 0.001) and suspiciousness (PANSS) (r = –0.31, p < 0.001). Lower levels of well-being were also associated with higher PANSS depression (r = –0.46, p < 0.001), PANSS anxiety (r = –0.24, p = 0.003), PANSS hallucination (r = –0.17, p = 0.036), PANSS general (r = –0.34, p < 0.001), PANSS negative (r = –0.28, p < 0.001) and PANSS total (r = –0.32, p < 0.001) scores but not with PANSS positive scores (r = –0.07, p = 0.425). PANSS grandiosity scores were associated within the patient group with a higher level of well-being (r = 0.20, p = 0.013). Within the non-clinical group, lower levels of well-being were associated with higher levels of paranoia (GPTS) (r = –0.44, p < 0.001).
Chapter 4 Conclusions
The main therapy trial
This project concerned improving the treatment of persecutory delusions, a key psychotic experience. The approach taken was to translate one key research finding into treatment. Worry has been identified as a plausible factor in the occurrence of paranoid thinking, and worry is known to be tractable with CBT in anxiety disorders. Traditionally, a fundamental divide has been made between neurosis and psychosis. Worry was studied and treated in emotional disorders, not in psychosis. The irony is that the Worry Intervention Trial (WIT) study, to our knowledge,70 is the largest trial to date of a psychological treatment for patients with clinical worry but it was carried out with patients with diagnoses of psychosis. It was based on a theoretical understanding of the role of worry in delusions, empirical studies indicating an important link and the results of a promising pilot study. The group treated had severe persecutory delusions that had not responded sufficiently to other treatments. Many patients had had their persecutory delusions for many years. The main outcomes were very clear. A brief cognitive–behavioural intervention for worry led to highly significant reductions in both worry and the persecutory delusions. The planned analysis indicated that changes in the worry thinking style led to the majority of the reductions in the delusions. There were also a number of other important outcomes for the patients. Overall levels of psychiatric symptoms reduced, general levels of paranoid thinking reduced and psychological well-being improved. To our knowledge, this is the first study to show changes in psychological well-being with treatment in patients with delusions.
Patients liked the focus on worry, seen in the high uptake of the therapy sessions. It is a problem that they agree that they have. Nonetheless, by reducing preoccupation with threat and increasing activity levels the persecutory delusions were implicitly challenged. Some patients, by being more active with the goal of dealing with worry, learned that they were safer outside. In a future evaluation it would be beneficial to assess changes in activity levels in the intervention group. Only eight patients with persecutory delusions were excluded from entering the trial on the basis of reporting insufficient worry. The intervention was deliberately highly manualised to facilitate later dissemination. The length of therapy is remarkably short to achieve such change in long-standing delusional beliefs. Agreeing to six sessions helps both the patient and therapist to initiate active techniques earlier and it keeps therapy precisely focused. Nevertheless, we do not envisage the worry intervention to be all that patients should receive. The patients still had significant levels of worry and paranoia – benefits need to be enhanced, maintained and assessed over longer periods. We are now beginning to test this intervention in combination with modular interventions targeting other causal factors such as insomnia, negative beliefs about the self, interpersonal sensitivity and reasoning biases. 71–73
There are several main limitations to the study. We did not include a control condition to control for therapist contact. Instead, we set out to achieve large reductions in the delusion based on targeting a putative causal factor and to show that therapy exerted its effects through this mechanistic route. At this stage of evaluation we considered the comparison with treatment as usual as the most important to establish. Although we consider it unlikely that befriending or supportive counselling, for example, would have such effects on worry and delusions, this remains to be tested specifically in this patient group. It would have been beneficial to have a specific measure of clinicians’ competence in the therapy. There are also limitations to the mediation analysis. We did not aim to determine temporal relationships between changes in worry and changes in the delusion. We did not alter significance levels for multiple testing, raising the risk of type I errors. It is also the case that follow-up was only 4 months after the end of treatment, although we consider this appropriate for such a short intervention. In clinical practice it would be sensible to add booster sessions. We did not assess levels of social functioning but it is plausible that this increased as a result of a key intervention technique being scheduling activity at peak worry times. Patient views on the therapy itself were not systematically collected. Finally, it is important to highlight that the test of the intervention – provided by clinical psychologists supervised in a research setting – was carried out in two NHS trusts but depended on referrals to the trial. Therefore, the next step is to evaluate the intervention in routine clinical practice, including a greater number of centres. We envisage developing the intervention booklets for online and app delivery so that the intervention, with mental health professional support, has the possibility for a large degree of self-management. We propose that this test of an amended (i.e. greater self-management element) intervention in a larger number of centres with a larger number of patients is the next research step. The intervention should also be tested in younger and older age groups. It may have the potential to help in the prevention of psychotic disorders.
The theoretical studies
The trial was designed to examine the mechanism of action of treatment and also to learn more about persecutory delusions to feed back into treatment refinement.
In an experimental test, we examined the effects of a bout of worry in these individuals on processes customarily considered as markers of psychosis. Given that worry was known to occur frequently in these patients we wanted to know whether or not it impacted on psychotic processes. The results were very clear. The occurrence of worry did not affect working memory or JTC, but it did lead to an increase in a range of low-level anomalous experiences. Increases in sensations of the unreality of self and surroundings (e.g. feeling of being a detached observer), perceptual alterations (e.g. body feeling very light as it if were floating) and temporal disintegration (e.g. seeming as if things done recently had taken place a long time ago) were all more likely to occur after a period of worry. Worrying less reduced the occurrence of anomalies of sensory intensity (e.g. lights or colours seeming brighter or more intense than usual) and sensory flooding (e.g. difficulty distinguishing one sensation from another). Our assessment covered a wide variety of anomalous experiences and only the occurrence of hallucinations was unaffected. The point of interest learned from the experiment is that a period of worry in these patients creates a range of potentially confusing and puzzling perceptual experiences that are known to predict paranoid thoughts. Worry causes odd subjective states that are known to lead to odd ideas. This is an illustration of an interaction of affective with psychotic processes and adds to our understanding of how worry may contribute to delusional experience. This information can be incorporated into future therapy: clinicians can assess for and normalise the occurrence of such anomalies after a period of worry in patients with persecutory delusions.
Following the experimental study, we carried out a novel study looking at the presence of depersonalisation in patients with persecutory delusions. The results highlight how common depersonalisation experiences are in patients with persecutory delusions: 30 of the 50 patients each reported having ≥ 10 depersonalisation symptoms at least as frequently as ‘often’ over the last 6 months. Our results also support the earlier experimental study, which found a close association of depersonalisation with worry in patients with persecutory delusions. It is plausible that these experiences, triggered by worry, contribute to the occurrence of paranoid thoughts. The primary clinical implication at this stage is that there are grounds for routinely assessing depersonalisation experiences in patients with persecutory delusions. The presence of depersonalisation experiences in patients with persecutory delusions had not previously been recognised.
We also sought to find out what patients with persecutory delusions report are the factors that bring a worry episode to an end. This had never been researched in a qualitative study before. Eight patients with persecutory delusions who reported high levels of worry participated. An open-ended semistructured interview technique and interpretative phenomenological analysis were employed to encourage a broad elaboration of relevant constructs. Analyses revealed one theme that captured participants’ detailed descriptions of their experience of worry and five themes that identified factors important for bringing worry episodes to a close: natural drift, distraction, interpersonal support, feeling better and reality testing. Patients with persecutory delusions report worry being uncontrollable and distressing but are able to identify ways that a period of worry can stop. The present study suggests that building on individuals’ distraction techniques, reality testing ability and social support networks could be of benefit in the refinement of treatment.
Our baseline assessment also enabled an examination of another putative causal factor: a reasoning style of JTC. Two potential contributors to the JTC reasoning style were examined within a large group of patients with current persecutory delusions. JTC was considered in relation to basic information-processing capacity problems and motivational beliefs concerning uncertainty. It is the former for which the most confident conclusions can be drawn. Given the similar findings of two other large studies,74,75 we can now be confident of an association of JTC with working memory. Keeping alternative explanations in mind, gathering data and weighing the evidence all have plausible memory load; pursuing one explanation, gathering confirmatory evidence and reaching a definitive conclusion are likely to reduce demands on memory. Working memory difficulties via the reasoning strategies that they provoke are likely to be a factor in the persistence of delusional beliefs.
Levels of intolerance of uncertainty in the patients with persecutory delusions were high, consistent with the presence of worry in this group at a level comparable to that in patients with anxiety disorders. Against prediction, however, the IUS score was slightly higher in the patients with delusions who did not jump to conclusions than in the patients who did jump to conclusions. Greater intolerance of uncertainty was clearly not associated with JTC, consistent with the study of Dudley et al. 76 As originally proposed by Freeston et al. ,52 intolerance of uncertainty may, at least within a clinical psychosis sample, lead to greater information search before certainty. However, the levels of worry in the group may well explain the association. Caution is needed about overinterpreting this result before replication. This is especially the case as there was no association with the occurrence of general repetitive negative thinking; an experimental study with patients with persecutory delusions showed no change in JTC in the period after a bout of worry;33 and there is little evidence that anxiety disorder groups seek more data during the beads task than non-clinical control subjects. 77 The study provides little evidence that one form of motivational belief – intolerance of uncertainty – is a factor in JTC.
Lastly we researched a new topic in relation to persecutory delusions: psychological well-being. There are many markers of the distress caused by persecutory delusions. The aim of the study was to assess levels of positive mental well-being in a large cohort of patients with current persecutory delusions. The results are striking. Almost half of the persecutory delusions group scored lower than 2 SDs below the mean of the non-clinical group, indicating that they are approximately in the bottom 2% of the population for positive mental well-being. The highest score in the persecutory delusions group was close to the mean of the non-clinical group, in which, by contrast, the highest score was at the top of the scale. The absolute score on the well-being measure for patients with persecutory delusions was clearly low; the average item score for patients indicated that they are reporting positive mental well-being little more than rarely. The individuals with delusions were not in an acute episode but had established paranoid fears that had remained despite treatment with neuroleptic medication. Greater levels of paranoia were associated with lower levels of psychological well-being. Psychological well-being was also associated with levels of anxiety and depression; indeed, the persecutory delusions group score was comparable to that in people with depression. 78 The WEMWBS could be a valuable addition to routine outcome monitoring and is likely to be used increasingly in both evaluations of routine treatments in services and in clinical trials. In the current study we have reported initial scores for patients with positive psychotic symptoms and so for the first time have demonstrated that it is a valid measure to use in a key group using mental health services, that is, those who have psychosis. Agreeing and evaluating the goal of feeling more positive, as assessed by such a scale, is likely to help with patient engagement and collaboration with services. The study was cross-sectional and therefore cannot provide insights into the causes of the low levels of psychological well-being. The data were also collected as part of a clinical trial and not routinely in a service, which will affect their degree of representativeness.
Patient and public involvement
Our view is that this research programme was strongly rooted and guided by patient views, principally by discussions with, and eliciting direct feedback from, patients seen during provision of psychological therapy. The patient involvement in the research was important in four main areas. First, the focus on worry initially arose out of the first author’s discussions with patients during provision of CBT for psychosis, that is, during clinical practice. It became clear that worry was a common and important topic and that worry techniques could well be effective. It was from this work that the research studies followed, establishing the high rates of worry in this patient group and the potential benefits of treating it. Second, the intervention and materials were guided from patient feedback. In particular, on the basis of patient comments the intervention was extended to six sessions and greater provision was made in the materials for providing patient accounts of experiences. Third, during the trial we carried out the qualitative interviews about the experience of worry and stopping bouts of worry; this can now feed back into the intervention materials and suggests ways of potentially enhancing the intervention. Lastly, patient involvement was also important in the work carried out in the trial on psychological well-being. Discussions with patients during CBT had made it clear that this was an important outcome. In the trial we therefore measured well-being for the first time in this patient group, included it as a secondary outcome and collected non-clinical data to provide comparison scores. Judging from our experiences with patients in the trial, and from the high follow-up rates and uptake of therapy, we think that the trial was very well received by participants but it would have been valuable to have included an independent patient-led evaluation of the experience of participating in the trial. In the future we would value time with patients working further on the intervention, for example developing videos of patients recounting their experiences of worry and how to overcome it. We would also wish to receive patient guidance on how to enhance the self-management of the worry intervention (for instance, in developing appropriate digital components such as online or mobile applications).
Summary
The predominant form of treatment for delusions is neuroleptic medication, but this has problems of adherence, side effects and efficacy. Psychological interventions for patients with current delusions are in their infancy, with the early evidence indicating that they have weak to moderate effects. The current trial was carried out as part of a process of substantially improving psychological treatment for persecutory delusions. One key causal factor was targeted in a brief intervention tested with patients with persistent persecutory delusions, typically held for many years. The evaluation was robust: assessments were blind and follow-up rates were very high. The results were striking: this brief intervention reduced worry, paranoia, rumination and overall levels of psychiatric symptoms. Psychological well-being also improved. The hypothesised mechanism of action of the intervention, reducing a worry thinking style, was shown to be the main mediator of treatment change. This supports the theoretical rationale behind the work. Evaluation of the treatment in routine services and with younger and older age groups is now indicated.
Acknowledgements
This project (09/160/06) was awarded by the Efficacy and Mechanism Evaluation (EME) programme and is funded by the UK Medical Research Council (MRC) and managed by the UK NHS National Institute for Health Research (NIHR) on behalf of the MRC–NIHR partnership. Daniel Freeman is supported by a MRC Senior Clinical Fellowship (G0902308). Methodological research by Graham Dunn is supported by the MRC (MR/K006185/1). We thank all of the trial participants; the trial clinical psychologists (Katherine Pugh, Jacinta Cordwell, Helen Mander); the trial research assistants (Emma Černis, Gail Wingham, Katherine Shirvell); the independent members of the Trial Steering Committee (Thomas Craig, Anthony Morrison, John Norrie) and the Data Monitoring and Ethics Committee (Douglas Turkington, Paul French, Sabine Landau); Katie Ashcroft for rating the therapy tapes; and the clinical teams in Oxford Health NHS Foundation Trust and Southern Health NHS Foundation Trust for their support of the trial.
Contributions of authors
Daniel Freeman took the main responsibility for drafting the study protocol and report. All of the authors contributed to the design of the trial and read and approved the final report.
Daniel Freeman was the main lead of the trial and took particular responsibility in Oxford, with David Kingdon leading the research in Southampton.
Graham Dunn had the main responsibility for the trial outcome and mediation analyses.
Helen Startup was the trial co-ordinator.
Daniel Freeman, Helen Startup and David Kingdon provided the training and supervision for the trial therapists and research workers.
Disclaimers
This report presents independent research. The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, MRC, NETSCC, the EME programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the EME programme or the Department of Health.
Publications
Freeman D, Dunn G, Startup H, Kingdon D. The effects of reducing worry in patients with persecutory delusions: study protocol for a randomized controlled trial. Trials 2012;13:223.
Freeman D, Startup H, Dunn G, Černis E, Wingham G, Pugh K, et al. The interaction of affective with psychotic processes: a test of the effects of worrying on working memory, jumping to conclusions and anomalies of experience in patients with persecutory delusions. J Psychiatr Res 2013;47:1837–42.
Freeman D, Startup H, Dunn G, Černis E, Wingham G, Pugh K, et al. Understanding jumping to conclusions in patients with persecutory delusions: working memory and intolerance of uncertainty. Psychol Med 2014;44:3017–24.
Freeman D, Startup H, Dunn G, Wingham G, Černis E, Evans N, et al. Persecutory delusions and psychological well-being. Soc Psychiatry Psychiatr Epidemiol 2014;49:1045–50.
Startup H, Pugh K, Cordwell J, Kingdon D, Freeman D. How do individuals with persecutory delusions bring worry to a close? An interpretative phenomenological analysis [published online ahead of print 31 January 2014]. Behav Cogn Psychother 2014: doi.org/10.1017/S1352465813001136
Černis E, Dunn G, Startup H, Kingdon D, Wingham G, Pugh K, et al. Depersonalisation in patients with persecutory delusions. J Nerv Ment Dis 2014;202:752–8.
Freeman D, Dunn G, Startup H, Pugh K, Cordwell J, Mander H, et al. Effects of cognitive behaviour therapy for worry on persecutory delusions in patients with psychosis (WIT): a parallel, single-blind, randomised controlled trial with a mediation analysis. [published online ahead of print March 2015]. Lancet Psychiatry 2015. http://dx.doi.org/10.1016/S2215-0366(15)00039-5
References
- Gray B. Recovery champions: a personal view on making recovery happen [published online ahead of print 19 August 2013]. Schizophr Bull 2013. http://dx.doi.org/10.1093/schbul/sbt116.
- Payne R. Night’s end. Schizophr Bull 2012;38:899-901. http://dx.doi.org/10.1093/schbul/sbs051.
- Andrews A, Knapp M, McCrone P, Parsonage M, Trachtenberg M. Effective Interventions in Schizophrenia: the Economic Case. A Report Prepared for the Schizophrenia Commission. London: Rethink Mental Illness; 2012.
- Bebbington P, Pilling S, Whittington C, Freeman D, Bentall R, Garety P. Persecutory Delusions. Oxford: Oxford University Press; 2008.
- van der Gaag M, Valmaggia L, Smit F. The effects of individually tailored formulation-based cognitive behavioural therapy in auditory hallucinations and delusions. Schizophr Res 2014;156:30-7. http://dx.doi.org/10.1016/j.schres.2014.03.016.
- Garety P, Fowler D, Freeman D, Bebbington P, Dunn G, Kuipers E. A randomised controlled trial of cognitive behavioural therapy and family intervention for the prevention of relapse and reduction of symptoms in psychosis. Br J Psychiatry 2008;192:412-23. http://dx.doi.org/10.1192/bjp.bp.107.043570.
- Peralta V, Cuesta MJ. Dimensional structure of psychotic symptoms: an item-level analysis of SAPS and SANS symptoms in psychotic disorders. Schizophr Res 1999;38:13-26. http://dx.doi.org/10.1016/S0920-9964(99)00003-1.
- Wigman JTW, Vollebergh WAM, Raaijmakers QAW, Iedema J, van Dorsselaer S, Ormel J, et al. The structure of the extended psychosis phenotype in early adolescence – a cross-sample replication. Schizophr Bull 2009;37:850-60. http://dx.doi.org/10.1093/schbul/sbp154.
- Ronald A, Sieradzka D, Cardno A, Haworth C, McGuire P, Freeman D. Characterization of psychotic experiences in adolescence using the Specific Psychotic Experiences Questionnaire (SPEQ): findings from a study of 5000 16 year old twins. Schizophr Bull 2014;40:868-77. http://dx.doi.org/10.1093/schbul/sbt106.
- Freeman D, Garety PA. Comments on the content of persecutory delusions: does the definition need clarification?. Br J Clin Psychol 2000;39:407-14. http://dx.doi.org/10.1348/014466500163400.
- Sartorius N, Jablensky A, Korten A, Ernberg G, Anker M, Cooper JE, et al. Early manifestations and first-contact incidence of schizophrenia in different cultures. Psychol Med 1986;16:909-28. http://dx.doi.org/10.1017/S0033291700011910.
- Applebaum PS, Robbins PC, Roth LH. Dimensional approach to delusions: comparison across types and diagnoses. Am J Psychiatry 1999;156:1938-43.
- Freeman D, Garety P, Kuipers E, Fowler D, Bebbington PE, Dunn G. Acting on persecutory delusions: the importance of safety seeking. Behav Res Ther 2007;45:89-9. http://dx.doi.org/10.1016/j.brat.2006.01.014.
- Castle DJ, Phelan M, Wessely S, Murray RM. Which patients with non-affective functional psychosis are not admitted at first psychiatric contact?. Br J Psychiatry 1994;165:101-6. http://dx.doi.org/10.1192/bjp.165.1.101.
- Freeman D, McManus S, Brugha T, Meltzer H, Jenkins R, Bebbington P. Concomitants of paranoia in the general population. Psychol Med 2011;41:923-36. http://dx.doi.org/10.1017/S0033291710001546.
- Onwumere J, Smith B, Kuipers E, Freeman D, Bentall R, Garety P. Persecutory Delusions. Oxford: Oxford University Press; 2008.
- Freeman D, Garety P. Advances in understanding and treating persecutory delusions: a review. Soc Psychiatry Psychiatr Epidemiol 2014;49:1179-89. http://dx.doi.org/10.1007/s00127-014-0928-7.
- Kendler KS, Campbell J. Interventionist causal models in psychiatry. Psychol Med 2009;39:881-7. http://dx.doi.org/10.1017/S0033291708004467.
- Freeman D, Garety PA, Kuipers E, Fowler D, Bebbington PE. A cognitive model of persecutory delusions. Br J Clin Psychol 2002;41:331-47. http://dx.doi.org/10.1348/014466502760387461.
- Freeman D. Suspicious minds: the psychology of persecutory delusions. Clin Psychol Rev 2007;27:425-57. http://dx.doi.org/10.1016/j.cpr.2006.10.004.
- Freeman D, Garety PA. Worry, worry processes and dimensions of delusions. Behav Cogn Psychother 1999;27:47-62.
- Startup H, Freeman D, Garety PA. Persecutory delusions and catastrophic worry in psychosis: developing the understanding of delusion distress and persistence. Behav Res Ther 2007;45:523-37. http://dx.doi.org/10.1016/j.brat.2006.04.006.
- Morrison AP, Wells A. Relationships between worry psychotic experiences and emotional distress in patients with schizophrenia spectrum diagnoses and comparisons with anxious and non-patient groups. Behav Res Ther 2007;45:1593-600. http://dx.doi.org/10.1016/j.brat.2006.11.010.
- Bassett M, Sperlinger D, Freeman D. Fear of madness and persecutory delusions. Psychosis 2009;1:39-50. http://dx.doi.org/10.1080/17522430802535031.
- Vorontsova N, Garety P, Freeman D. Cognitive factors maintaining persecutory delusions in psychosis: the contribution of depression. J Abnorm Psychol 2013;122:1121-31. http://dx.doi.org/10.1037/a0034952.
- Freeman D, Pugh K, Antley A, Slater M, Bebbington P, Gittins M, et al. A virtual reality study of paranoid thinking in the general population. Br J Psychiatry 2008;192:258-63. http://dx.doi.org/10.1192/bjp.bp.107.044677.
- Freeman D, Brugha T, Meltzer H, Jenkins R, Stahl D, Bebbington P. Persecutory ideation and insomnia. J Psychiatr Res 2010;44:1021-6. http://dx.doi.org/10.1016/j.jpsychires.2010.03.018.
- Freeman D, Stahl D, McManus S, Meltzer H, Brugha T, Wiles N, et al. Insomnia worry anxiety and depression as predictors of the occurrence and persistence of paranoid thinking. Soc Psychiatry Psychiatr Epidemiol 2012;47:1195-203. http://dx.doi.org/10.1007/s00127-011-0433-1.
- Foster C, Startup H, Potts L, Freeman D. A randomised controlled trial of a worry intervention for individuals with persistent persecutory delusions. J Behav Ther Exp Psychiatry 2010;41:45-51. http://dx.doi.org/10.1016/j.jbtep.2009.09.001.
- Meyer TJ, Miller ML, Metzger RL, Borkovec TD. Development and validation of the Penn State Worry Questionnaire. Behav Res Ther 1990;28:487-95. http://dx.doi.org/10.1016/0005-7967(90)90135-6.
- Haddock G, McCarron J, Tarrier N, Faragher FB. Scales to measure dimensions of hallucinations and delusions: the psychotic symptom rating scales (PSYRATS). Psychol Med 1999;29:879-89. http://dx.doi.org/10.1017/S0033291799008661.
- Hepworth C, Startup H, Freeman D. Developing treatments for persistent persecutory delusions: the impact of an emotional processing and metacognitive awareness (EPMA) intervention. J Nerv Ment Dis 2011;199:653-8. http://dx.doi.org/10.1097/NMD.0b013e318229cfa8.
- Freeman D, Startup H, Dunn G, Černis E, Wingham G, Pugh K, et al. The interaction of affective with psychotic processes: a test of the effects of worrying on working memory, jumping to conclusions and anomalies of experience in patients with persecutory delusions. J Psychiatr Res 2013;47:1837-42. http://dx.doi.org/10.1016/j.jpsychires.2013.06.016.
- Černis E, Dunn G, Startup H, Kingdon D, Wingham G, Pugh K, et al. Depersonalisation in patients with persecutory delusions. J Nerv Ment Dis 2014;202:752-8. http://dx.doi.org/10.1097/NMD.0000000000000185.
- Startup H, Pugh K, Cordwell J, Kingdon D, Freeman D. How do individuals with persecutory delusions bring worry to a close? An interpretative phenomenological analysis [published online ahead of print 31 January 2014]. Behav Cogn Psychother 2014. http://dx.doi.org/10.1017/S1352465813001136.
- Freeman D, Startup H, Dunn G, Černis E, Wingham G, Pugh K, et al. Understanding jumping to conclusions in patients with persecutory delusions: working memory and intolerance of uncertainty. Psychol Med 2014;44:3017-24. http://dx.doi.org/10.1017/S0033291714000592.
- Freeman D, Startup H, Dunn G, Wingham G, Černis E, Evans N, et al. Persecutory delusions and psychological well-being. Soc Psychiatry Psychiatr Epidemiol 2014;49:1045-50. http://dx.doi.org/10.1007/s00127-013-0803-y.
- Tennant R, Hiller L, Fishwick R, Platt S, Joseph S, Weich S, et al. The Warwick–Edinburgh Mental Well-being Scale (WEMWBS): development and UK validation. Health Qual Life Outcomes 2007;5. http://dx.doi.org/10.1186/1477-7525-5-63.
- Freeman D, Dunn G, Startup H, Kingdon D. The effects of reducing worry in patients with persecutory delusions: study protocol for a randomised controlled trial. Trials 2012;13. http://dx.doi.org/10.1186/1745-6215-13-223.
- Startup HM, Erickson TM, Davey GCL, Wells A. Worry and its Psychological Disorders. Chichester: Wiley; 2006.
- Kay SR. Positive and Negative Syndromes in Schizophrenia. New York, NY: Brunner; 1991.
- Green C, Freeman D, Kuipers E, Bebbington P, Fowler D, Dunn G, et al. Measuring ideas of persecution and reference: the Green et al. Paranoid Thought Scales (G-PTS). Psychol Med 2008;38:101-11.
- Ehring T, Zetsche U, Weidacker K, Wahl K, Schönfeld S, Ehlers A. The Perseverative Thinking Questionnaire (PTQ): validation of a content-independent measure of repetitive negative thinking. J Behav Ther Exp Psychiatry 2011;42:225-32. http://dx.doi.org/10.1016/j.jbtep.2010.12.003.
- Greenwood K, Sweeney A, Williams S, Garety P, Kuipers E, Scott J, et al. CHoice of Outcome In Cbt for psychosEs (CHOICE): the development of a new service user-led outcome measure of CBT for psychosis. Schizophr Bull 2010;36:126-35. http://dx.doi.org/10.1093/schbul/sbp117.
- Wechsler D. Wechsler Abbreviated Scale of Intelligence (WASI). San Antonio, TX: Psychological Corporation; 1999.
- Garety PA, Freeman D, Jolley S, Dunn G, Bebbington PE, Fowler DG, et al. Reasoning emotions and delusional conviction in psychosis. J Abnorm Psychol 2005;114:373-84. http://dx.doi.org/10.1037/0021-843X.114.3.373.
- Wechsler D. Wechsler Adult Intelligence Scale-III/Wechsler Memory Scale. Third Edition Technical Manual. San Antonio, TX: Psychological Corporation; 1997.
- Marsden J, Gossop G, Stewart D, Best D, Farrell M, Lehmann P, et al. The Maudsley Addition Profile (MAP). Addiction 1998;93:1857-67. http://dx.doi.org/10.1046/j.1360-0443.1998.9312185711.x.
- Marcus E, Garety P, Weinman J, Emsley R, Dunn G, Bebbington P, et al. A pilot validation of a modified Illness Perceptions Questionnaire designed to predict response to cognitive therapy for psychosis. J Behav Ther Exp Psychiatry 2014;45:459-66. http://dx.doi.org/10.1016/j.jbtep.2014.06.003.
- Weinman J, Petrie KJ, Moss-Morris R, Horne R. The Illness Perception Questionnaire: a new method for assessing the cognitive representation of illness. Psychol Health 1996;11:431-45. http://dx.doi.org/10.1080/08870449608400270.
- Freeman D, Dunn G, Garety P, Weinman J, Kuipers E, Fowler D, et al. Patients’ beliefs about the causes, persistence and control of psychotic experiences predict take-up of effective cognitive behaviour therapy for psychosis. Psychol Med 2013;43:269-77. http://dx.doi.org/10.1017/S0033291712001225.
- Freeston M, Rhéaume J, Letarte H, Dugas M, Ladouceur R. Why do people worry?. Pers Individ Dif 1994;17:791-802. http://dx.doi.org/10.1016/0191-8869(94)90048-5.
- Berenbaum H, Bredemeier K, Thompson R. Intolerance of uncertainty: exploring its dimensionality and associations with need for cognitive closure psychopathology and personality. J Anxiety Disord 2008;22:117-25. http://dx.doi.org/10.1016/j.janxdis.2007.01.004.
- Vasey M, Borkovec TD. A catastrophising assessment of worrisome thoughts. Cogn Ther Res 1992;16:505-20. http://dx.doi.org/10.1007/BF01175138.
- Cartwright-Hatton S, Wells A. Beliefs about worry and intrusions: the meta-cognitions questionnaire and its correlates. J Anxiety Disord 1997;11:279-96. http://dx.doi.org/10.1016/S0887-6185(97)00011-X.
- Beck AT, Epstein N, Brown G, Steer R. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol 1988;56:893-97. http://dx.doi.org/10.1037/0022-006X.56.6.893.
- Bell V, Halligan PW, Ellis HD. The Cardiff Anomalous Perceptions Scale (CAPS). Schizophr Bull 2006;32:366-77. http://dx.doi.org/10.1093/schbul/sbj014.
- Sierra M, Berrios G. The Cambridge Depersonalisation Scale. Psychiatry Res 2000;93:153-64. http://dx.doi.org/10.1016/S0165-1781(00)00100-1.
- Simeon D, Kozin D, Segal K, Lerch B, Dujour R, Giesbrecht T. De-constructing depersonalization. Psychiatry Res 2008;157:303-6. http://dx.doi.org/10.1016/j.psychres.2007.07.007.
- Bernstein EM, Putnam FW. Development reliability and validity of a dissociation scale. J Nerv Ment Dis 1986;174:727-35. http://dx.doi.org/10.1097/00005053-198612000-00004.
- Dixon JC. Depersonalization phenomena in a sample population of college students. Br J Psychiatry 1963;109:371-5. http://dx.doi.org/10.1192/bjp.109.460.371.
- Blackburn I, James I, Milne D, Baker C, Standart S, Garland A, et al. The Revised Cognitive Therapy Scale (CTS-R). Behav Cogn Psychother 2001;29:431-46. http://dx.doi.org/10.1017/S1352465801004040.
- Beecham J, Knapp M, Thornicroft G, Brewin CR, Wing JK. Measuring Mental Health Needs. London: Gaskell; 1992.
- Little RJA, Rubin DB. Statistical Analysis with Missing Data. New York, NY: Wiley; 2002.
- Baron R, Kenny DA. The moderator–mediator variable distinction in social psychological research. J Pers Soc Psychol 1986;5:1173-82. http://dx.doi.org/10.1037/0022-3514.51.6.1173.
- Muthén LK, Muthén BO. Mplus User’s Guide. Los Angeles, CA: Muthén & Muthén; n.d.
- Smith JA, Osborn M, Smith JA. Qualitative Psychology: a Practical Guide to Research Methods. London: Sage; 2008.
- Emsley R, Dunn G, White IR. Modelling mediation and moderation of treatment effects in randomised controlled trials of complex interventions. Stat Methods Med Res 2010;19:237-70. http://dx.doi.org/10.1177/0962280209105014.
- Dunn G. Statistical Evaluation of Measurement Errors: Design and Analysis of Reliability Studies. London: Arnold; 2004.
- Hanrahan F, Field A, Jones F, Davey G. A meta-analysis of cognitive therapy for worry in generalised anxiety disorder. Clin Psychol Rev 2013;33:120-32. http://dx.doi.org/10.1016/j.cpr.2012.10.008.
- Myers E, Startup H, Freeman D. Cognitive behavioural treatment of insomnia in individuals with persistent persecutory delusions. J Behav Ther Exp Psychiatry 2011;42:330-6. http://dx.doi.org/10.1016/j.jbtep.2011.02.004.
- Bell V, Freeman D. A pilot trial of cognitive behavioural therapy for interpersonal sensitivity in individuals with persecutory delusions. J Behav Ther Exp Psychiatry 2014;45:441-6. http://dx.doi.org/10.1016/j.jbtep.2014.06.001.
- Waller W, Freeman D, Jolley S, Dunn G, Garety P. Targeting reasoning biases in delusions. J Behav Ther Exp Psychiatry 2011;42:414-21. http://dx.doi.org/10.1016/j.jbtep.2011.03.001.
- Garety P, Joyce E, Jolley S, Emsley R, Waller H, Kuipers E, et al. Neuropsychological functioning and jumping to conclusions in delusions. Schizophr Res 2013;150:570-4. http://dx.doi.org/10.1016/j.schres.2013.08.035.
- Falcone A, Murray R, Wiffen B, O’Connor J, Russo M, Kolliakou A, et al. Jumping to conclusions, neuropsychological functioning and delusional beliefs in first episode psychosis [published online ahead of print 22 July 2014]. Schizophr Bull 2014. http://dx.doi.org/10.1093/schbul/sbu104.
- Dudley R, Shaftoe D, Cavanagh K, Spencer H, Ormrod J, Turkington D, et al. ‘Jumping to conclusions’ in first-episode psychosis. Early Interv Psychiatry 2011;5:50-6. http://dx.doi.org/10.1111/j.1751-7893.2010.00258.x.
- Jacobsen P, Freeman D, Salkovskis P. Reasoning bias and belief conviction in obsessive–compulsive disorder and delusions. Br J Clin Psychol 2012;51:84-99. http://dx.doi.org/10.1111/j.2044-8260.2011.02014.x.
- Powell J, Hamborg T, Stallard N, Burls A, McSorley J, Bennett K, et al. Effectiveness of a web-based cognitive–behavioural tool to improve mental well-being in the general population. J Med Internet Res 2013;15. http://dx.doi.org/10.2196/jmir.2240.
List of abbreviations
- BAI
- Beck Anxiety Inventory
- CAPS
- Cardiff Anomalous Perceptions Scale
- CBT
- cognitive–behavioural therapy
- CDS
- Cambridge Depersonalisation Scale
- CHOICE
- Choice of Outcome in CBT for Psychoses
- CI
- confidence interval
- CSM
- Centre for Statistical Medicine
- df
- degree of freedom
- FD
- delusions outcome factor
- FW
- worry outcome factor
- GPTS
- Green et al. Paranoid Thoughts Scale
- ICC
- intraclass correlation
- IQ
- intelligence quotient
- IUS
- Intolerance of Uncertainty Scale
- JTC
- jumping to conclusions
- MCQ-30
- Meta-Cognitive Beliefs Questionnaire
- MRC
- Medical Research Council
- NIHR
- National Institute for Health Research
- PANSS
- Positive and Negative Syndrome Scale
- PSWQ
- Penn State Worry Questionnaire
- PSYRATS
- Psychotic Symptom Rating Scales
- PTQ
- Perseverative Thinking Questionnaire
- SD
- standard deviation
- SE
- standard error
- SEM
- structural equations model
- WASI
- Wechsler Abbreviated Scale of Intelligence
- WEMWBS
- Warwick–Edinburgh Mental Well-being Scale
- WIT
- Worry Intervention Trial
- WSRC
- Worry Stop Rules Checklist