Notes
Article history
The research reported in this issue of the journal was funded by the EME programme as project number 13/119/18. The contractual start date was in February 2016. The final report began editorial review in December 2020 and was accepted for publication in March 2021. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The EME editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
Copyright © 2022 Green et al. This work was produced by Green et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaption in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2022 Green et al.
Chapter 1 Introduction
Parts of this report are reproduced or adapted with permission from Green et al. 1 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
Scientific background
Intervention evaluation research in autism spectrum disorder (hereafter ‘autism’) has recently accelerated, with studies across a range of interventions considered in recent National Institute for Health and Care Excellence (NICE) guidance,2 Cochrane Library reviews3 and other reviews. 4–6 The pattern of findings across a number of early childhood interventions is for reproducible moderate-to-good effects on targeted ‘proximal’ or intermediate outcomes, such as improvement in social interaction and communication in the local treatment context. 7–9 However, for an intervention to demonstrate a tangible impact on a child’s life and overall development, the challenge is to show effects beyond the immediate intervention context, for instance that changes are also seen in non-direct treatment contexts, such as in interactions with other people inside or outside the classroom or in the family home setting, or an impact identified on other developmental function or symptom outcomes over time and in a variety of settings. In this regard, there is much less evidence,4,6 despite the fact that without such changes the claim that autism interventions are truly effective is harder to substantiate.
Reinforcing the transmission of targeted ‘proximal’ intervention effects into functional change seen in the wider context pervading the child’s life is, thus, a key current challenge for autism treatment research,6,10 and raises the question why does this appear to be so difficult in autism? The capacity to generalise acquired skills flexibly across different situations, people and environmental contexts – a central feature of skill acquisition in neurotypical development – has often been suggested to be a core difficulty for individuals with autism. In this context, one can consider two different forms or concepts of generalisation, which will be referenced throughout this report. First, the concept of generalisation of specific behaviours (for instance the observation of a specific newly acquired skill or behaviour in one setting that then occurs in another) has been commonly investigated in behavioural learning theory and could be termed ‘homotypic’ generalisation. Second, the concept of a ‘developmental cascade’ from precursor skills through to developmentally related but different subsequent skills (e.g. specific vowel sounds in infant development through to evolved language) is the subject of much study in general developmental science, and might be characterised as ‘heterotypic’ (‘homotypic’ and ‘heterotypic’ being terms originating in the longitudinal epidemiology literature). Although a recent systematic review concludes that the empirical evidence for difficulty in generalisation in the first sense is inconsistent,11 many single-subject design studies using behavioural learning methods have described difficulties that autistic children have in transferring newly taught skills to different settings, people or materials/activities, and it has been an assumption in developmental science, as well as from clinical experience, that there is additional difficulty in generalisation in both senses for autistic children. However, these are assumptions that have not been fully evaluated.
Possible explanations, particularly for the second, heterotypic, form of generalisation, include the autistic child’s well-documented lack of internal symbolic representation, which is likely to interfere with the consolidation and thus transfer of procedural aspects of skill across contexts into different forms of behaviour, independent of the specific context in which the skill was acquired. Another related barrier may be weaknesses in autistic cognitive central coherence, associated with an over-reliance on concrete behavioural prompts or reinforcers, which can lead to fragmented learning dissociated from the social pragmatic context as a whole rather than a more diverse integration of learning with connected understanding in context. There may be further factors related to a general lack of behavioural flexibility in applying new skills across different environments. Plausible approaches to helping overcome some of these generalisation difficulties in autism include embedding the intervention into the social environment through parent mediated and education staff-mediated learning, which may optimise the interpersonal cues and continuity of learning across contexts. 12 This method supports opportunities for incidental or naturalistic learning, by weaving functional social and communication learning into the child’s daily experiences, where skills are acquired. Working with children in naturalistic environments is now often highlighted as best practice for early intervention. 13
Early social communication intervention, delivered through parents, therapists or teachers, is the only early autism intervention with a ‘consider’ recommendation by NICE. 2 The Preschool Autism Communication Trial (PACT)7 tested a clinic-delivered, parent-mediated social communication intervention against regular care in what was, to the best of our knowledge, one of the largest randomised controlled trials (RCTs) in the field. 14 The therapy showed a substantial impact on the targeted immediate outcome of parental communicative synchrony with the child [effect size (ES) 1.22, 95% confidence interval (CI) 0.85 to 1.59)] and also on the child’s communication initiations with the parent (ES 0.41, 95% CI 0.08 to 0.74). The original publication7 demonstrated that PACT was associated with non-significant effects on the Autism Diagnostic Observation Schedule, Second Edition (ADOS-2) social communication domain when considered alone, but subsequent analysis of outcome on the full autism symptom phenotype [measured across both social communication and repetitive behaviour and sensory symptom domains in the ADOS-2 Calibrated Severity Score (CSS)] found a significant intervention effect at the end point, with a log-proportional odds ratio of 0.64. 14 Subsequent follow-up of the PACT7 cohort 6 years after treatment end, when participant mean age was 10.5 years, with blinded assessment of the original randomly allocated groups (80% follow-up completeness on the primary outcome) found evidence suggesting further sustained effect on reduced autism symptom severity on the ADOS-2 (log-odds ES 0.70, 95% CI –0.05 to 1.47), and a significant overall treatment effect when calculated over the treatment and follow-up time period (log-odds ES 0.55, 95% CI 0.14 to 0.91). Non-blind, parent-rated autism symptoms on the Social Communication Questionnaire (lifetime version) (SCQ) (ES 0.40, 95% CI 0.05 to 0.77) and repetitive and sensory behaviours on the Repetitive Behaviour Questionnaire (RBQ) (ES 0.87, 95% CI 0.47 to 1.35) also showed comparable improvement at follow-up. 14
To our knowledge, the PACT intervention was the first study in the field to show that a preschool autism intervention could have downstream developmental effects to reduce child autism symptom severity for a substantial period after treatment end. This PACT treatment7 was 93% clinic delivered and the key outcomes were measured in a research context; there was little measurement of effects within educational or home environments. Consequently, in the Paediatric Autism Communication Trial – Generalised (PACT-G), we aimed to extend the work of the original PACT,7 with the aim of (1) reinforcing the extension of treatment effects within the different naturalistic environments of the child’s early life, in home and educational settings, and (2) responding to moves towards home-based therapy delivery. The intervention was taken into the child’s daily naturalistic home and nursery/school setting, incorporating parent- and education staff-mediated interventions, and embedding individualised strategies within these naturalistic learning contexts.
A further development was the extension of the intervention into the primary school years, up to the age of 11 years. Autism intervention studies to date have been largely limited to preschool (< 5 years) interventions; however, early communication development continues into the school years,15 and social communication skills in the early school-age period are strong predictors for later development. 16 The persisting and significant impairments in social interaction and communication among children with autism argue for a developmentally sustained intervention into middle childhood, utilising the child’s naturalistic learning environments. However, because of the focus of the intervention on early social communication skill development, the cohort of autistic children of school age (> 5 years) receiving the treatment was restricted to those who had no more than a 4 years’ language-equivalent level.
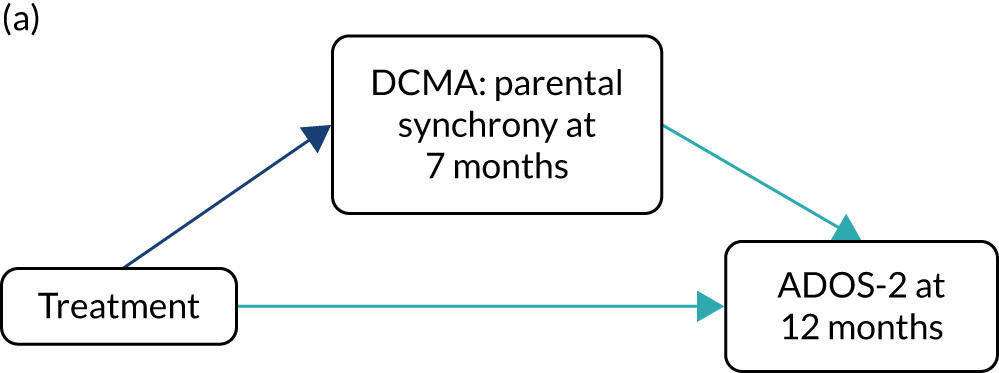
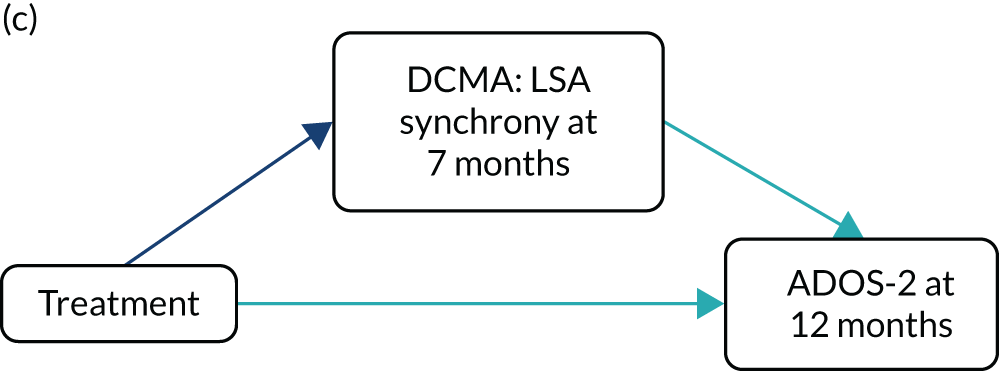
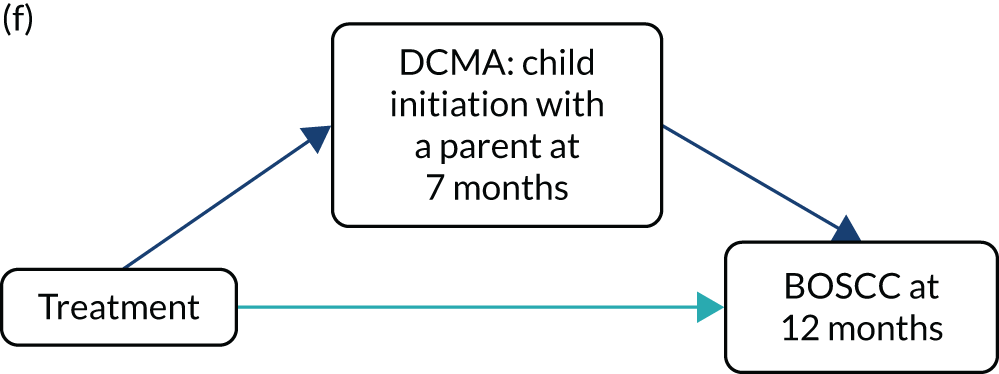
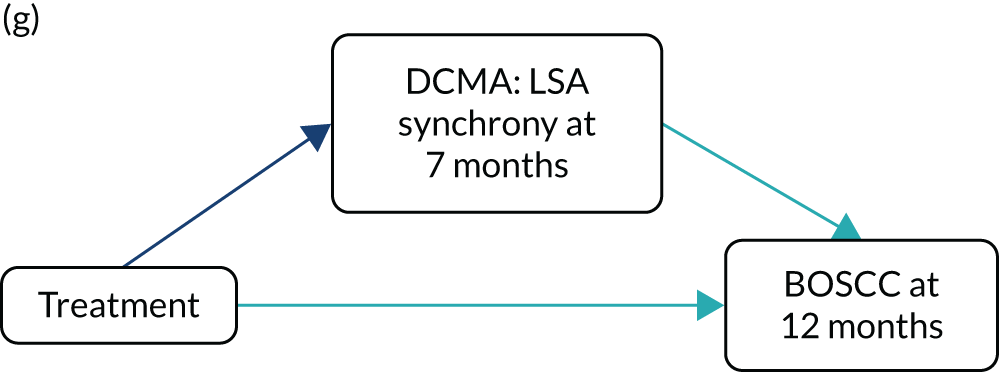
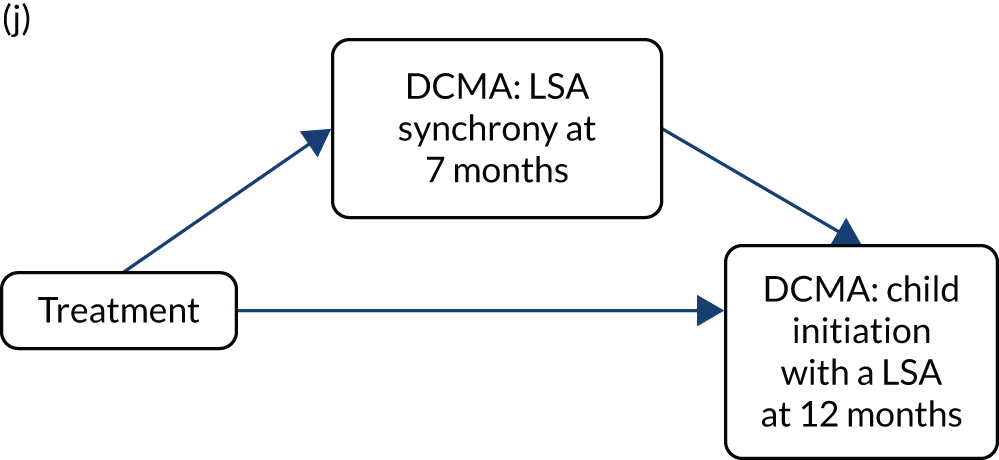
In addition, a mechanism study within PACT-G built on the understanding gained from the mediation analysis in the original PACT. 17 This previous analysis had tested for mediation of primary treatment effects on child autism symptoms (ADOS-G) through the proximal intervention target of improvement in parental synchronous response to child communication, and an increase in child communication initiations with the parent within dyadic communication (both of which were researcher assessed by video-coding blind to intervention group). In this analysis, increases in child initiations with a parent were shown to be strongly (mediated 80%) by the change in parental synchronous response produced by the treatment. These changes in child initiation with a parent then, in turn, were shown to strongly mediate (97%) the change in child autism symptoms. This mediation analysis had supported the theoretical logic model of the PACT7 intervention by showing a causal-effect chain from parent response to child, to child communication with a parent, and from child communication with a parent to a generalised social communication change in child symptoms. A similar mediation effect had been shown previously in the smaller PACT. 18 In the PACT-G mechanism design, we aimed to test whether or not a similar chain of mediation effect would be maintained when measured in the home and educational settings, and whether or not such changes in two parallel naturalistic settings simultaneously might be further additive in mediating an enhanced effect on symptom outcomes in the research context. In addition, the assessment of mediators and outcomes in different simultaneous naturalistic contexts might provide an innovative opportunity to study key mechanisms of child developmental learning across contexts and whether or not different contextual learning might generalise in an additive way to related downstream symptom outcomes.
Background literature on autism intervention
A significant evidence base from RCTs of early interventions for young children with autism has accumulated over the past 15 years. 4,6,19 Many of these interventions aim to ameliorate the impact of core social communication impairments on early social interactions, particularly with parents, who often find their child’s behaviour perplexing and challenging. The tested interventions have varied in design, duration and intensity, and include developmental and behavioural approaches20 that are mediated through parents and delivered directly by therapists, and there is significant study-to-study variation in the effects found. However, robust evidence now exists that some aspects of social communication can be improved for many young children with autism. 4
The most consistent findings are improvements in dyadic interaction between children and their parents or another adult. 7,9,21–25 Although many studies report improvements in language and communication on unblinded parent-report measures,7,14,25–27 findings on observational or standardised measures of communication and language ability are more variable. Thus, some studies report improvements7,14,23,26–28 whereas others do not. 7,21,24 Only a few studies have demonstrated treatment reductions in autism symptom severity,14,27 whereas most have not. 25,26,28 A recent review4 contains a thorough review of this literature in the context of study design and reporting quality.
Despite this promising evidence base, there is wide recognition that the early autism intervention research field faces challenges. 29–31 Even trials demonstrating group-level improvements report modest ESs,4 reflecting, in part, that a significant proportion of participants in many studies do not benefit. There are sparse examples of designs that would better inform ‘personalised medicine’ approaches (i.e. ‘who benefits from which treatments?’), including comparative or equivalence trials, and rigorous examination of which children benefit from these interventions (moderating effects) and how (mediating effects). Only two long-term follow-ups have been conducted to assess maintenance of effects,14,21 and there has generally been a lack of independent replication of substantial findings. In addition, reporting standards have been variable and there has been inadequate measurement of and attention to the critical importance of testing if and how interventions have an impact on everyday functional abilities that extend beyond the proximal intervention context. 11
In an earlier study, we found that a therapist-directed, parent-mediated intervention that uses video-guided feedback to and coaching for parents, following a transactional developmental model,32 resulted in improvements in parental synchrony and child initiations when interacting with each other. We also found moderate ES reductions in overall autism symptom severity on a blinded observational measure at treatment end point (log-proportional odds ES 0.64, 95% CI 0.07 to 1.20), which was sustained at the 6-year follow-up (log-proportional odds ES 0.70, 95% CI –0.05 to 1.47), with an overall log-proportional odds ES of 0.55 (95% CI 0.14 to 0.91; p = 0.004), as was the improvement in child initiations. 14
A qualitative interview study with parents who had received PACT therapy within the previous PACT7 confirmed the largely positive evaluation of the core effects of the therapy on communication, interaction and child progress, as well as emphasising valued improvements in the parents’ sense of the relationship with their child and enhanced parental and family well-being. However, the study revealed practical difficulties for some families in attending therapy sessions within a clinic environment,33 including the inconvenience (travel, child care), unfamiliarity with and lack of preparedness for autism in therapy venues, and challenges with occupying the child during video-feedback sessions and discussion. Delivery of the intervention within the home and educational settings and the use of video telecommunication software aimed to address some of these practical challenges, while also, importantly, in theory, providing a method of enhancing the adoption and generalisation of therapeutic strategies within the child’s family and everyday naturalistic environments. The use of teleconferencing technology was also thought to have the potential to remove practical barriers, as video material of adult–child interactions could be made in either the home or educational setting prior to the session, and then shared and discussed between the therapist and parent/member of education staff through teleconferencing at a later time without the child present. The advantages and disadvantages of these adjustments found in practice are discussed further below.
Interventions for autism in the educational setting
There are a number of programmes delivered within UK educational contexts to support children with autism. 34 The focus of many of these is on enhancing cognition and learning and reducing challenging behaviours. The majority of interventions fall into two broad categories: comprehensive treatment models (CTMs) and focused interventions. CTMs tend to be developmentally focused, multicomponent educational programmes, aiming to improve functioning across cognition, emotional and social development. They are often embedded within the classroom setting itself and delivered by members of staff. 35 A common UK example of a CTM is the Treatment and Education of Autistic and related Communication-Handicapped Children (TEACCH) programme, which incorporates the use of classroom-based visual schedules and prompts. 36 In the USA, Social Communication, Emotional Regulation, and Transactional Support (SCERTS)37 and the Learning Experiences and Alternative Program for Preschoolers and their Parents38 have also been used; these are also occasionally available in UK specialist autism schools. Although these approaches may be based on different conceptual models,39 they share similar general goals of embedding group, class-based support for children with autism within the educational setting.
Focused interventions tend to target specific skills;40 for example, the Picture Exchange Communication System (PECS) is used to support picture exchange as an alternative form of making a child’s needs known. 41 Alternative and augmentative language systems (e.g. Makaton)42 and the use of technology, such as voice output communication aids, are also sometimes available in the UK. A teacher-delivered interactive communication intervention for specific language impairments [the Social Communication Intervention Project (SCIP)]43 is also applicable to high-functioning autistic children in middle childhood. Peer-mediated interventions promote naturalistic peer socialisation and support in the school environment44,45 and have face validity. 46 In contrast to CTMs, the model by which many of these interventions are delivered is through consultation with schools by specialist health professionals (e.g. psychologists, speech and language therapists or trained teachers), but with the aim of collaborating with ‘non-specialists’ in their implementation [e.g. peers and learning support assistants (LSAs)]. 47 Funded LSAs are often allocated for differentiated support and learning in the classroom for individual children. There is a relative lack of high-quality implementation trials of such interventions in educational settings. 34,48
Education provision for children with autism in the UK
In the UK, 71% of children with a diagnosis of autism attend a mainstream educational setting. 49 Despite the benefits of inclusion in mainstream schools (notably the, potentially, wider participation in the educational experience, peer role models, acceptance and opportunities to develop academic, social and emotional skills50) access to specialist professional support and guidance is often very limited. Depending on the level of special educational needs (SEN), pupils receive non-specialist LSA support, but this is highly variable between schools. 51,52 LSA roles are wide-ranging and include supporting children with complex health, medical, behavioural and learning needs. 53 LSAs in special schools are more likely to work in a team with the teacher and support the whole class of children than they are to work one to one with an individual child.
Chapter 2 Study aims
PACT-G had two aims. The first aim was to test whether or not the multicomponent PACT-G social communication intervention protocol, extended from the original PACT7 intervention and implemented in both home and educational settings simultaneously, would show treatment effects on (1) autism symptom outcomes, as measured in an independent research setting (primary outcome), and (2) dyadic social communication, functional adaptation and autism symptoms in the separate home and educational settings (secondary outcomes). These objectives were tested using blinded measures, maximising the ability to detect meaningful change (see Chapter 5, Measures), and were evaluated by analysis at the 12-month trial end point.
The second aim was a mechanism analysis using the experimental trial to investigate aspects of the developmental and cross-context generalisation of specific acquired competencies in autism. We built on the mediation analysis from our previous PACT7 (see Pickles et al. 14) to test the mediation of the generalised treatment effect in the home and educational settings. We tested how effects in naturalistic contexts might combine to enhance transmission of treatment effect to research-assessed symptoms in a standardised test setting. In doing this, we used prespecified measures of mediation that were identified in our previous PACT. 7
Chapter 3 Organisation
Trial organogram
The organisation of the three-site trial is shown in Figure 1, with the trial principal investigators named and their roles given. The full trial team is named and acknowledged in Acknowledgements. The study progress Gantt chart is shown in Table 1.
FIGURE 1.
Trial organogram.

| PACT-G timeline task | Month | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| January | February | March | April | May | June | July | August | September | October | November | December | |
| 2016 | ||||||||||||
| Start of grant | ||||||||||||
| Recruit research associates | ||||||||||||
| Research associates in post (36 months) | ||||||||||||
| Recruit SALTs | ||||||||||||
| SALTs in post (33 months) | ||||||||||||
| Recruit research assistants | ||||||||||||
| Research assistants in post (26 months) | ||||||||||||
| Pilot study | ||||||||||||
| 2017 | ||||||||||||
| Research associates in post (36 months) | ||||||||||||
| SALTs in post (33 months) | ||||||||||||
| Research assistants in post (26 months) | ||||||||||||
| Main trial | ||||||||||||
| 2018 | ||||||||||||
| Research associates in post (36 months) | ||||||||||||
| SALTs in post (33 months) | ||||||||||||
| Research assistants in post (26 months) | ||||||||||||
| Main trial | ||||||||||||
| Video scoring, data checking and entry | ||||||||||||
| 2019 | ||||||||||||
| Research associates in post (36 months) | N/A | N/A | N/A | N/A | N/A | |||||||
| SALTs in post (33 months) | N/A | N/A | N/A | N/A | N/A | |||||||
| Research assistants in post (26 months) | N/A | N/A | N/A | N/A | N/A | |||||||
| Main trial | N/A | N/A | N/A | N/A | N/A | |||||||
| Video scoring, data checking and entry | N/A | N/A | N/A | N/A | N/A | |||||||
| Analysis | N/A | N/A | N/A | N/A | N/A | |||||||
Chapter 4 Pilot feasibility study
PACT-G formally started on 1 February 2016. As per the deliverability project plan from January 2016 (see Appendix 3), the management team was contracted to demonstrate by month 12 that the following success criteria had been met in relation to two stop–go decision points to allow progression to the main trial:
-
Stop–go 1: at the end of the pilot phase of the trial, a minimum of 27 educational settings have been engaged with the educational setting buy-in protocol, with a written Memorandum of Agreement (MoA) from at least 11.
-
Stop–go 2: by the end of the 6-month pilot phase (month 12 of the study), the team will have identified, assessed for eligibility and consented a sufficient number of patients to proceed to treatment in 24 patients (eight in each site).
Stop–go 1: educational engagement
Contact with educational settings
The process for contacting educational settings varied between the sites (Manchester, Newcastle upon Tyne, London), depending on the size and type of provision. Sites mainly approached specialist schools and schools with significant specialist provision with which they were familiar. For most of the younger children recruited to the pilot phase, who had been referred through clinical services, we contacted their nursery or preschool at the point of the family’s consent to seek their engagement in the project.
Table 2 shows each educational setting that was contacted, as well as those where further discussions took place and the outcome of the engagement. A small number of educational settings that were contacted did not want further information. For those educational settings that wanted to learn more about the study, we sent the study information sheet and produced a standard presentation that was given at most educational setting visits. We also collected standardised information from the educational settings, including information about their provision of specialist education, the educational setting size and key staff involved in this service.
| Site | Number initially contacted | Number engaged | Number that signed the MoA |
|---|---|---|---|
| Manchester | 17 | 14 | 10 |
| Newcastle upon Tyne | 10 | 10 | 6 |
| London | 7 | 7 | 2 |
| Total | 34 | 31 | 18 |
Numbers of educational settings contacted, engaged and agreeing to participate
Table 2 shows the number of educational settings at each site that were contacted, the number that received further information and engaged with the study team, and the number that signed the MoA. The results clearly demonstrate our achievement in meeting the success criteria for stop–go 1; we engaged 31 educational settings against a target of 27, and had signed MoAs from 18 educational settings against a target of 11.
Stop–go 2: pilot phase recruitment
Identified families
In total, we contacted 34 families during the pilot phase of the study. We consented and then assessed the children against the prespecified eligibility criteria on three assessments:
-
observed autism symptom severity on the ADOS-2
-
reported autism symptom severity in the parental autism diagnostic interview (preschool-aged children) or parent-rated SCQ (school-aged children)
-
necessary developmental level (i.e. 12 months) on the Mullen Scales of Early Learning (preschool-aged children) or British Ability Scales (school-aged children).
Three families dropped out after consent: one family worried about the impact of participating in an autism study and the potential stigma in the community, one family dropped out because of family pressures and one family could not be contacted to arrange eligibility assessments following initial consent.
Number of families approached, consented and assessed as eligible
Table 3 sets out the number of families contacted at each site, those that consented and the number of participants assessed as eligible and ready to proceed to treatment. A full anonymised recruitment log showing dates of birth and dates of consent is available from the authors.
| Site | Number approached | Number consented | Number assessed as eligible |
|---|---|---|---|
| Manchester | 9 | 8 | 8 |
| Newcastle upon Tyne | 12 | 9 | 8 |
| London | 13 | 10 | 8 |
| Total | 34 | 27 | 24 |
The results indicate our success against the criteria in stop–go 2; we assessed eight patients as eligible in each site.
In November 2016, the team reviewed progress in the pilot feasibility study, with the results being signed off on 3 November in a meeting with the Trial Steering Committee (TSC), that supported trial progression.
Chapter 5 The PACT-G randomised controlled trial
Design
The trial was a three-site, two-group, RCT of the experimental treatment plus treatment as usual (TAU) compared with TAU alone. Children aged 2–10 years with autism were recruited to the trial in the local areas following referral by clinical specialists and education professionals. Consented families were then randomised to three sites around the UK to receive either the PACT-G social communication intervention in addition to TAU (referred to as the PACT-G group) or TAU alone (referred to as the TAU group). Assessments were administered on entry (baseline) to the trial, at the 7-month mid-point and at the 12-month end point. An embedded mechanism study aimed to test specific mediation hypotheses in the trial and to, potentially, use the experimental intervention design with repeated measures to contribute to a general understanding of the generalisation of acquired skills in autism development across both time and setting, and also in terms of downstream predicted developmental cascades to symptom and adaptive outcomes for the child.
Settings
The settings for the trial were family homes, mainstream nurseries and preschools, specialist nurseries, mainstream schools with specialist autism units and specialist SEN/autism school settings, all of which were in Greater Manchester, London or Newcastle upon Tyne.
Study population
The inclusion criteria were as follows:
-
Participants aged 2–10 years.
-
Diagnosis of autism given by referral services.
-
Meeting criteria for autism on the ADOS-2.
-
Scoring ≥ 15 (school aged) or ≥ 12 (preschool aged) on the SCQ – the accepted clinical cut-off points for children at these ages.
-
Children aged ≥ 5 years between P3 and P8 for the English curriculum. (In England, at the time of the study, P scales described targets for children aged 5–16 years with special educational needs. P3 communication skills indicate that a child is beginning to use ‘intentional communication’. P8 was taken to represent an expressive language age-equivalent of approximately 4 years in a typically developing child.)
-
Parents with sufficient English to potentially participate in the intervention and who speak English to their child at least some of the time.
The exclusion criteria were as follows:
-
having a sibling with autism already in the trial
-
participation in the PACT-G pilot phase
-
children aged ≤ 12 months with a non-verbal age-equivalent level
-
epilepsy not controlled by medication
-
children with an identified genetic disorder that would impact on their ability to participate or affect the validity of data
-
severe hearing or visual impairment in parent or child
-
current severe learning disability in the parent or current severe parental psychiatric disorder
-
current safeguarding concerns or other family situation that would affect child/family participation in the trial
-
no agreement to participate from child’s educational setting.
Sample size
The PACT7 showed an ES of 1.22 (95% CI 0.85 to 1.59) on parental synchrony [Dyadic Communication Measure for Autism (DCMA)], which mediated 70% of the ES of 0.41 (95% CI 0.08 to 0.74) on child communication, which in turn mediated 72% of the ES of 0.24 (95% CI 0.59 to 0.11) on symptom outcome (ADOS-2). The intervention strategies in PACT-G were specifically targeted to enhance generalisation of the child communication to increase primary outcome effects in home, educational and research settings. Therefore, we expected the ES for the symptom outcome to be substantially above 0.24 and clinically meaningful.
For PACT-G, power was calculated using the sampsi command in Stata® (StataCorp LP, College Station, TX, USA), for an analysis using analysis of covariance with α = 05, with pre- and post-measures correlated 0.67 (from PACT7). With 110 patients followed up in each group (70/70 preschool-aged and 40/40 school-aged children), 80% power was retained for an ES of 0.28 and 90% power for an ES of 0.33. Allowing for 10% attrition (compared with 4% in PACT7), we proposed to recruit 244 families (rounding up to 82 per site: 52 with preschool-aged children and 30 with school-aged children).
Interventions
The PACT-G intervention is an adaptation and extension of the original, largely clinic-delivered, PACT7 intervention into home and educational settings (93% of original PACT7 sessions were delivered in a clinic setting, whereas all of the PACT-G sessions were delivered in a home setting, in an educational setting or by teleconferencing). PACT7 is a ‘caregiver-mediated’ intervention; in this context, the carers are the parents and education professionals who are the primary recipients of the individualised intervention sessions. PACT-G utilises videos of caregiver–child interaction to provide feedback and guide caregivers to adapt their communication with the child. Therapists support caregivers to adopt evidence-based strategies in their communication so as to enhance child communication development,7,54 and to practise these strategies initially during the 30-minute home practice sessions and eventually throughout the day. Recent research indicates that optimal interaction with a sensitive and responsive communication partner can be effective in increasing communication and social interaction skills in children with autism. 4 In the original PACT,7 this caregiver-mediated approach was found to be effective in increasing the quality of parental communicative responses to the child, which in turn led to increased child-initiated communications with the parent and generalised effects on reduced child autism symptom severity. 7
The PACT-G intervention retains these effective elements, but encourages generalisation of the child’s newly acquired skills into other settings. For instance, the design of PACT-G includes more integration of PACT7 techniques into daily routines and play, and the addition of an adult from the child’s educational setting supports skill development in school. 55,56 The intervention is intended to begin with the caregiver at home and then extend into the child’s educational setting. However, sometimes the contingencies of school term times meant that sessions were coincident in timing. Furthermore, the PACT-G intervention incorporated more recent advances in research17 since the publication of the original PACT. 7 These included focusing on specific strategies to enhance the child’s response to shared attention with objects and play as precursors to the early stages of language development. 57,58 These modifications allow more differentiation of the starting point of the intervention to ensure that it is appropriate for the individual child’s initial level of object play and social engagement.
In common with the original PACT7 therapy, PACT-G therapy takes a staged approach that is based on theoretically informed precursor skills for typical communication development, as well as on addressing atypical communication and language development in autism. 15,59,60 Caregivers are initially encouraged to adopt strategies for establishing essential foundation skills for the child’s communication and language development, including shared attention57 and initiating social communication skills,37 before moving on to strategies that support and enhance the child’s receptive and expressive language development8,58 and reciprocal conversation. 43
In contrast to many manualised intervention programmes, PACT7 and PACT-G do not provide a curriculum or prescribed topic guide for sessions. The manual instead outlines six stages, each with a ‘toolbox’ of strategies that could be used to facilitate development. Therapists are trained to minutely analyse videos of caregiver–child interactions to assess the areas for further development and the potential strengths. 61 Based on these observations, therapists then establish which of the manualised therapy targets are most appropriate for that dyad at that stage of development, and agree these as targets for intervention with the caregiver. Therefore, targets and strategies are individualised for each child, depending on their interactive style. Progress is evaluated and subsequent targets for each dyad are based on that pair’s progress, allowing for a highly individualised intervention approach that accommodates each individual, but can remain within a well-defined framework. This is described further below.
The PACT-G method of video feedback facilitates a collaborative partnership, empowering caregivers. 22,33 A new caregiver–child interaction video is recorded at each session, and the therapist guides the caregiver in observing and analysing the most successful moments of dyadic interaction on video, thereby helping the caregiver to see how their use of strategies promotes and enhances the development of the child’s communication. Insights from this discussion are then used to set individual step-by-step caregiver goals (i.e. strategies they will adopt) within the stages of the manual that are appropriate to the identified individual needs of the child. Between sessions, caregivers are encouraged to practise using these strategies with the child, initially in protected time and later at opportune moments throughout the day. The PACT-G intervention is designed for preschool- and primary school-aged children, from those with little communication or no language to children who use spoken sentences. Progression through the stages of PACT-G is individually differentiated so it is related to both the caregiver and the child’s readiness to progress. Many dyads may remain at the early stages focusing on shared attention, caregiver-adapted responding and child communication initiation; others may progress to later PACT-G stages of language expansion and reciprocal conversation.
The PACT-G intervention manual provides clearly defined stage aims, child outcomes, therapy targets and a range of caregiver strategies. Each of the six stages includes a list of objective measures to determine a dyad’s readiness to progress to the next stage.
Stage 1
‘Establishing shared attention’ helps the caregiver to establish and maintain extended periods of mutual shared attention with the child. 8,57 All dyads complete at least one session at stage 1. For dyads already showing extended periods of mutual shared attention, the focus of the single stage 1 session ensures caregiver understanding of the concept of shared attention and highlights successful strategies that are applied. For dyads at the very earliest stages of development, with fleeting or no shared attention, further sessions at stage 1 are needed and include play with or without toys and caregiver modelling. In stage 1, the caregiver learns to sensitively observe the child’s focus, as well as non-verbal and verbal signals, and thereby to identify opportunities for shared attention.
Stage 2
‘Synchronicity and sensitivity’ emphasises caregiver sensitivity in responding, with a focus on the child’s perspective and experiences. 54 Caregivers are encouraged to closely observe the child to identify opportunities to respond, thereby reducing asynchronous communication (mistimed responses that place a demand on the child) and increasing adult synchronous communication. Caregiver observations from video help them identify and reduce demands, instructions and directive responses, and replace them with synchronous responses to the child’s communicative behaviours and social initiations, commenting on or acknowledging intentions.
Stage 3
‘Focusing on language input’ helps the caregiver to model language that accurately matches the child’s interests and communication competencies. 8,13,58 Caregiver language and non-verbal gestures are carefully monitored and modified to be contingent on the child’s focus and comprehension. The caregiver is assisted to respond to the child’s non-verbal communication and to model complementary verbal responses that express the child’s inferred communication intent.
Stage 4
‘Establishing routines and anticipation’ is a consolidation phase that aims to develop child verbal understanding, anticipation and participation using repetitive rhymes, predictable routine phrases and familiar interactive play. 54
Stage 5
‘Increasing communication functions’ is carried out by eliciting communication acts through the sensitive use of communication ‘teasers’ to provide opportunities for child initiation. For example, the caregiver may make use of pauses and gaps within familiar, predictable play situations that the child fills with social and verbal responses. Communicative teasers entice the child to initiate intentional communication. 17,37 These are gradually extended to pose deliberate problems and/or to introduce ‘sabotage' in situations where the caregiver makes obvious mistakes (e.g. offering an empty cup or unopened snack, or a puzzle/game with pieces missing). A range of pragmatic communication acts can be elicited in this way, including requesting, negating, directing and commenting.
Intervention delivery
Parent sessions
Parents were offered 12 intervention sessions at home over 6 months. This was a reduction from the original PACT,7 in which 18 sessions were offered over 12 months. In the previous trial, the best proximal effect of intervention on parent–child dyadic interaction was achieved by 12 sessions (6–8 months), and this proximal dyadic effect strongly mediated the reduction in 13-month end-point autism symptom severity. Pragmatically, we needed to adopt this reduced session number for each setting in this trial so as to make the treatment in the parallel home and educational settings feasible within a fixed time frame.
Prior to starting the PACT-G programme, a home visit was conducted to introduce the intervention to the parents, understand the family context and set expectations. The PACT-G approach to parent sessions differed from that of the original PACT7 in setting, number of sessions and nature of delivery. The therapy sessions were delivered in the home and, instead of the solely in-person sessions in PACT,7 the therapy sessions alternated between home-based in-person sessions and video conferencing or telephone-delivered consultations, with the delivery style being flexible in accordance with the needs of the family. This approach aimed to promote generalisation of new skills development in the home setting. Other clinical and research experience has indicated that video conferencing session formats were popular with parents. 62
Each parent session began with a discussion and review of the progress made since the last session. The parent and child were then filmed while playing for 10 minutes. Immediately after this, the therapist and parent watched the video, or, during video conferencing sessions, the therapist and parent watched a 1- to 2-minute parent-filmed video of a home-based practice session. The therapist facilitated parents to identify child communications and to adopt PACT-G strategies in their interactions with the child. Parents were assisted to set goals for themselves based on the interaction strategies discussed. The parent and therapist discussed the opportunities to practise these strategies each day at home for half an hour, as in the original PACT. 7
Educational setting sessions
In most cases, therapy in the educational setting began after the parent had commenced therapy at home. The start times and duration of educational setting-based therapy were aimed to fit in two education terms, where possible. In the educational setting, PACT-G sessions were delivered by a LSA or equivalent, nominated by the senior management team. LSAs and other education staff received an initial training session to introduce them to PACT-G therapy. The education-based intervention then consisted of therapist–LSA sessions that mirrored the therapist–parent sessions in the home. Videos recordings of the LSA and the child were used to coach the LSA in the use of PACT-G strategies in a similar procedure to the parent. The LSA was then asked to implement these with the child daily – inside or outside class. There was a maximum of 12 therapist–LSA sessions over 6 months, alternating educational setting visits and video conference or telephone consultations. PACT-G strategies were expected to be integrated in a complementary way with other communication strategies that may already have been in use in the educational setting. This combination of therapist–parent and therapist–LSA sessions resulted in a maximal offer of 24 sessions for PACT-G across home and educational settings.
Collaboration between parent and education staff
The separate therapeutic work with parents and LSAs described above was designed to be supplemented with a schedule of joint parent–LSA meetings [i.e. home–school conversations (HSC)] to support communication and complementary use of strategies across the home and education settings. These meetings used the manualised and validated technique of HSC. 63,64 Meetings were structured around ‘explore’, ‘focus’, ‘plan’ and ‘review’ stages, which allowed the LSA and parent to share experiences to promote generalisation of techniques across settings. HSCs have been shown to be highly effective in motivating parents and education staff. 63,64 HSC sessions were designed to take place in the educational setting and were planned to occur as regularly as possible during the intervention period, in association with therapist’s visits to the educational setting. This allowed for up to six HSC sessions, with the minimum acceptable number set at three per child. Table 4 summarises the intervention procedure over time.
| Session type | Month | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 0 (baseline) | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 (end point) | |
| Researcher assessment |
ADOS-2 BOSCC |
ADOS-2 BOSCC |
|||||||||||
| Parent assessment |
BOSCC DCMA |
BOSCC DCMA |
BOSCC DCMA |
||||||||||
| Intervention with parent |
Initial home visit 12 intervention sessions (home-based sessions and telephone/video conference support sessions) HSC sessions in educational setting |
HSC sessions continue for the period of the educational setting-based intervention. The number will vary depending on term times, but with a minimum number of three sessions | |||||||||||
| School assessment |
BOSCC DCMA |
BOSCC DCMA |
BOSCC DCMA |
||||||||||
| Intervention in educational setting |
Initial LSA in educational setting training visita Up to 12 intervention sessions (educational setting alternating with video conference/telephone support) incorporating HSC meetings with parents |
HSC sessions continue until final assessment | |||||||||||
Training and fidelity of treatment
Training in the PACT-G therapy was conducted centrally by the lead speech and language therapists, who undertook overall co-ordination of the therapy in the trial and organised quarterly across-site therapist meetings. Therapists were regularly supervised by the clinical lead in each site. All therapy sessions were videotaped, and randomly selected tapes of one home and one education in-person session per therapist were independently rated using the PACT-G fidelity rating scale (see Appendix 4) at regular intervals across the trial period. Therapists and research staff were trained in practices that minimise non-compliance and dropout. Arrangements were also made at each site to ensure that PACT-G therapists had no contact with TAU only (control intervention) families. Therapy compliance and receipt of other interventions outside the protocol were monitored.
Treatment as usual
The control intervention was TAU only. We had detailed information on TAU in the preschool population from the group’s previous work on the original PACT and in older children from the PACT 7–11 follow-up study. 65 Data on the services received by all families recruited to PACT-G were collected by the research team.
Avoidance of contamination
There were separate clinical and research leads at each site and separate training and supervision structures. Researchers were housed separately from the staff involved in the delivery of the PACT-G intervention. Mid- and end-point research interviews and assessments were conducted so as to avoid inadvertent divulging of information that could reveal treatment status. The assessment suite and materials used were different in type and location to those used for the therapy intervention in home or educational settings to avoid any familiarity effect for children in the treatment group.
Measures
Primary outcome: ADOS-2
The ADOS-266,67 is a standard autism diagnostic symptom measure with good external validity for long-term outcomes in autism development. The assessment was undertaken during researcher–child interaction using a standardised set of social presses and was video-recorded for later coding to preserve blindness in follow-up assessments. The scoring metrics of ADOS-2 have been modified in line with the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition,68 with social communication and repetitive behaviour symptom domains combined into a unitary total symptom score [social affect (SA) and restricted and repetitive behaviour (RRB) overall total raw score]. ADOS-2 modules are available for different stages of child development and were assigned at baseline accordingly. The same module was used at the end point as the baseline for each child. Recent studies14,69 have demonstrated the ability of the ADOS-2 to measure treatment effects; for instance, in the PACT follow-up study,14 effects were sustained for 6 years after treatment end.
Other measures
Diagnostic inclusion
The Mullen Scales of Early Learning70 or British Ability Scales71 were used depending on the child’s age and ability level. These are standard measures of early development that enable a developmental level of non-verbal abilities to be ascertained for inclusion criteria and allow characterisation of the cohort in relation to other autism treatment trials.
The SCQ72 is a brief (40-item) parent-report screening measure that identifies characteristics associated with autism. Items cover three subdomains: reciprocal social interaction; communication; and restricted, repetitive and stereotyped patterns of behaviour. The ‘lifetime’ version refers to the entire developmental history of the child.
Secondary outcomes
The Brief Observation of Social Communication Change (BOSCC) with a researcher73–75 involved the researcher coding the autism symptoms from videotaped child–adult interactions. It addresses the same autism symptom constructs as the ADOS-2, but is designed to detect clinically meaningful symptom change in treatment studies. Codings combine symptom frequency, severity and atypicality on a 16-item, 0–5 scale (overall range 0–80). The BOSCC is designed to be a standard treatment outcome measure for the autism field and is currently used in large, funded trials in the USA and the European Union. The BOSCC has high-to-excellent inter-rater and test–retest reliability and has convergent validity with measures of communication and language skills. It demonstrated increased sensitivity to change over time compared with the ADOS-2 CSS in an observational study. 75 Three moderate-sized RCTs applying the standard naturalistic BOSCC as an outcome measure reported small and non-significant ESs. 76–78 When applying the standard BOSCC coding scheme to a non-standard, structured parent–child interaction, one study27 found a large, significant intervention effect.
For module 1 BOSCC (non-verbal or minimally verbal children), the recommended protocol consists of 4 minutes of free play followed by 2 minutes of bubble play, which is then repeated with a new set of toys. From this, 4 minutes of free play and 1 minute of bubble play were coded for each of the two segments. For module 2 BOSCC (phrase speech), as there was no recommended administration procedure developed at the start of PACT-G, a play and conversation administration was agreed with the developers in which the children had 4 minutes of free play followed by 2 minutes of conversation, which was then repeated with a new set of toys, before 2 minutes of bubble play.
The BOSCC with a parent and LSA73–75 was a measure of the intervention effect in the naturalistic settings in which the intervention took place. It involved the coding of video-recordings of child–parent play sessions in the home setting (at baseline, 7-month mid-point and 12-month end point) and child–LSA play sessions in the educational setting (baseline, 7-month interim and 12-month end point). BOSCC ratings were made from the same video-capture as for the DCMA (see below) and, to allow this, its administration deviated slightly from the recommended BOSCC protocol. For module 1 BOSCC, each child had 8 minutes of free play with the adult with the same box of toys, followed by 2 minutes of bubble play. From this, 4 minutes of free play and 1 minute of bubble play were coded for each BOSCC segment. For module 2 BOSCC, parent and teacher BOSCCs had 8 minutes of free play with the same set of toys, 4 minutes of conversation, and then 2 minutes of bubble play, based on a prototype ‘verbal’ BOSCC administration using module 1 toys. It became apparent during the trial that the conversation element was too challenging for the majority of module 2 children and it was decided, in discussion with the BOSCC developers, to code the module 2 items from 4 minutes of free play and 1 minute of bubble play in each segment.
The DCMA with parent and with LSA14 was coded from the same videos as for the BOSCC. This measure includes independent codes of adult communication (synchronous response) and child communication (child initiations). The DCMA synchronous response variable is defined as the proportion of the adult’s total communication acts that are synchronous with the child, where a synchronous communication act is a comment or acknowledgement that follows the child’s focus of play, actions, thoughts or intentions. Requests, directions, commands, questions and negations are not considered synchronous, even if related to the child’s focus of attention. The DCMA child initiations variable is defined as the proportion of the child’s total communication acts that are initiations, where initiations are verbal or non-verbal communication acts that serve to start an episode of interaction. This measure had proved sensitive in the original PACT mediation analysis and is used in PACT-G to test treatment effect and mediation in home and educational settings.
The Vineland Adaptive Behavior Scales (VABS) (parent and teacher versions)79 includes domains of communication, daily living skills and socialisation; it has been used widely and measures child functional ability in the home and educational settings.
The MacArthur Communicative Development Inventories (MCDIs) (word and gestures, sentences and grammar),80 the Receptive and Expressive One-word Picture Vocabulary Test (EOWPVT)81 and the Preschool Language Scale-5 (PLS-5)82 are standardised assessments used to measure children’s overall language level to supplement the measures of autism-specific communication included in the BOSCC and ADOS-2.
The Very Early Processing Skills (VEPS)59,60 assesses children’s sociocognitive skills (social responsiveness, joint attention and symbolic comprehension).
The RBQ83 is a 26-item parent questionnaire for assessing repetitive behaviours in children with autism.
The Developmental Behaviour Checklist (DBC) – Parent (2nd edition)84 is a 96-item instrument used for the assessment of behavioural and emotional problems in young people aged 4–18 years with developmental and intellectual disabilities. It includes two subscales, the Disruptive/Anti-social Subscale and the Anxiety Subscales (36 items), and is completed by a parent or carer.
The Strengths and Difficulties Questionnaire (SDQ) – parent and teacher versions85 – is a 25-item brief measure of psychological well-being in 2- to 17-year-olds and is completed by parents and teachers.
The Child Health Utility 9D (CHU9D)86 is a paediatric measure of health-related quality of life. It consists of nine items, rated on five levels (ranging from no problems to severe problems). It is designed to be completed by children aged 7–17 years. Proxy completion by parents on behalf of their child is also possible for younger or children with developmental disabilities.
The Warwick–Edinburgh Mental-Wellbeing Scale (WEMWBS)87 is a self-rated parental well-being questionnaire recommended by the UK Department of Health and Social Care as the preferred measure of mental well-being to incorporate in studies of this kind.
The Tool tO measure Parenting Self-Efficacy (TOPSE)88 is a 48-item, self-reported measure of parenting competence. It is a measure of possible change in parents’ confidence in their ability to make a difference to their child’s development. It was completed at baseline and end-point assessments.
The Child and Adolescent Service Use Schedule (CASUS) and the School Service Use Schedule65 were developed to record therapies and service use accessed throughout the study. Forms were adapted to young populations with autism in PACT7 and PACT 7–11. 6
The Working Alliance Inventory-Short Revised (WAI-SR)89 is a measure of engagement with therapy for parents and LSAs in group only. For parents and LSAs, there is a simple rewording of the client and therapist versions of the Working Alliance Inventory, which has been validated and is now frequently used. It was completed at the 2- and 5-month stages of the intervention.
Demographic, clinical and family language information comprised relevant demographic and clinical information and details of home language(s) spoken with the child. The intervention schedule is summarised in Table 5.
| Time point | Measure |
|---|---|
| Eligibility | ADOS-2 |
| SCQ | |
| Mullen Scales of Early Learning (preschool-aged children) | |
| British Ability Scales (school-aged children) | |
| Baseline | BOSCC – researcher |
| BOSCC/DCMA – parent | |
| BOSCC/DCMA – LSA | |
| VABS – parent interview | |
| VABS – teacher survey | |
| VEPS | |
| EOWPVT | |
| RBQ | |
| WEMWBS | |
| MCDIs (word and gestures; sentences and grammar) | |
| SDQ – parent | |
| SDQ – teacher | |
| TOPSE | |
| CHU9D | |
| Key information and demographics | |
| Clinical information and service use | |
| School Service Use Schedule | |
| Family language interview | |
| Mid-point home/parent | BOSCC/DCMA – parent |
| Status form | |
| Mid-point LSA/school | BOSCC/DCMA – LSA |
| End point | ADOS-2 |
| RBQ | |
| BOSCC – researcher | |
| BOSCC/DCMA – parent | |
| BOSCC/DCMA – LSA | |
| PLS-5 | |
| EOWPVT | |
| VABS – parent interview | |
| VABS – teacher survey | |
| WEMWBS | |
| MCDIs (word and gestures) | |
| DBC – parent (disruptive/antisocial and anxiety subscales) | |
| SDQ – parent | |
| SDQ – teacher | |
| TOPSE | |
| Changes to key information and demographics | |
| School Service Use Schedule | |
| CASUS | |
| CHU9D |
Procedures
Data collection
Research staff confirmed eligibility and obtained consent. Baseline assessments were undertaken prior to treatment assignment.
Randomisation
Randomisation took place using a web-based service hosted at the King’s Clinical Trial Unit. 90 This system was accessed only by trained trial staff who had previously been allocated a username and password. Requests for passwords were sent through the trial manager to the King’s Clinical Trial Unit. Randomisation was at the level of the individual participant, 1 : 1, stratified for site, age group (2–4 years and 5–11 years) and gender imbalance using random block sizes. Once randomised, the system automatically generated and sent an unblinded e-mail confirmation to the therapy lead (for records, blinded copy was sent to the local researcher who made the request and to the Manchester trial manager).
Blinding/concealment
Researchers who administered assessments were blind to participants’ group allocation and every effort was made to maintain blindness throughout the trial: research staff were located separately from therapists, parents were reminded at every meeting with the researchers not to divulge allocation information, staff in the educational settings were given photographs to distinguish therapists from research staff, and, where possible, different school staff signed in therapists and researchers.
To preserve blinding in follow-up visits, the primary outcome and putative mechanisms at the end points were cross-coded from videos by researchers at the other sites who had been trained to high levels of reliability and blinded to intervention allocation. A randomly selected proportion of assessments were double rated for reliability. All other researcher assessments were also blinded; however, parent and teacher questionnaires and interview measures were unblinded. Participant families could not be blinded to allocation. All therapy sessions were video-recorded. Variability due to therapist effects was minimised by frequent clinical supervision and checks of continuing therapist fidelity against the treatment manual; randomly selected sessions for each therapist were formally coded for fidelity over the course of the study by independent clinicians using the model successfully used in the PACT.
Engagement with referrers, schools and families
Extensive information-sharing and engagement activities with clinical teams and local mainstream and specialist educational settings were undertaken to promote clinical referrals and engagement with both home and educational aspects of the intervention. Regular trial newsletters to participating families, schools and nurseries and clinical teams, along with voucher payments to educational settings (schools and nurseries), acted to maintain involvement and adherence. Families received an individualised feedback report on the assessments conducted with their child, copied to school and clinical teams with parental consent, if desired. Parents received a small voucher payment at the end of their participation to thank them for their time and efforts. A local referring clinician for each participant was informed of the study progress and findings, with procedures for clinical support and aftercare beyond the study, should this be necessary.
Memorandum of Agreement with participating educational settings
There has been a recent emphasis on the need for collaborative research partnerships between educational settings and evidence-focused partners. 91,92 To address this call,46 more research teams are utilising MoAs or similar to formalise partnerships with the educational settings that participate in their large-scale trials. 93 Although traditionally used in school–school partnerships to share best practice, there is a clear benefit to developing mutually beneficial links between educational settings and evidence-focused partners. There is a great need for collaboration in these contexts and stakeholders to understand how effective interventions for children with autism can be developed. 54,55,94
A MoA was developed for PACT-G to develop working relationships with participating educational settings. The MoA and accompanying information sheet contained information about the PACT-G intervention, explaining the requirements of the randomised control design of the trial and the need for an appropriate member of staff to be available to attend intervention sessions and participate in research assessments, and providing information on how the educational setting would benefit for taking part.
The decision on who to nominate as the intervention partner was made by the educational setting; however, we theorised that the LSA would best fit this role because of the likelihood that they would spend the most contact time with children out of all education staff and because they had more time in the school day than teachers.
The MoA itself required a signature from a senior member of management and a member of the governing body, when applicable, which meant that ‘buy-in’ was formalised for the educational setting. Evidence shows that the drive for improvement and demonstration of good practice from senior leadership has a downstream positive effect on school culture. 95 Moreover, Goodrich and Cornwell96 suggest that the influence of organisational culture, routines and training plays a substantial role in the quality of care and outcomes.
Data management
All data in the trial were anonymised. Site files were held at each site and a trial master file was held centrally by the trial manager at the University of Manchester. This contained the key linking the anonymised trial name to personal details. The main trial data were entered into the web-based data entry service of King’s Clinical Trials Unit, which has a full audit trail. Appropriate quality control was carried out during the trial and before the database lock, and recorded in a standard operating procedure (SOP). This included data entry checking of:
-
all measures of the first two cases entered by each individual carrying out data entry
-
10% source data verification on data entry for all measures
-
all the primary and secondary outcome data entries, including ADOS-2 and researcher BOSCC data.
Primary analysis of the data was undertaken by the trial statisticians, with senior statisticians masked to treatment allocation. Analyses involving therapy data were not masked and were undertaken in part by the chief investigator’s administrative team. Full data sets were also shared with each site in the collaboration.
Adverse events
Adverse events (AEs) were enquired about systematically by researchers at each meeting with the family. AEs were also collected in parallel by trial therapists, as and when a situation became known to them, and documented separately in a therapy log. As well as recording AEs in a predefined standard format, we included AEs relating to child health, well-being and behaviour; significant issues in the educational setting; and family events such as separation or significant parental ill health. AEs were monitored using a bespoke semistructured interview and documented by the research team post intervention and as they arose during intervention sessions, regardless of the relationship to the study intervention or research procedures. Hospitalisation and bereavement in a family member residing in the home were considered severe AEs. We reported on all serious AEs (any AE which results in death, is life-threatening, requires hospitalisation or prolongs hospitalisation, causes persistent or significant disability, or results in birth defects) and all suspected unexpected serious adverse reactions (serious AEs that are believed to have a causal relationship with the PACT-G treatment). We also recorded events particularly relevant to this trial, such as significant changes in family or school situation. The clinical principal investigators (JG, TC, JP, ALC, HMc, VS, CA, VG) reviewed and agreed all AEs at the end of the study. An unblinded list of AEs by group was prepared by the statistical team and reviewed by the study Data Monitoring and Ethics Committee.
Adherence to allocated treatment, session validity and manual fidelity
Any departures from intended treatment assignment were described. The total numbers of sessions with parents, LSAs and in HSCs were reported, as well as the number of sessions that met the criterion for satisfactory quality. The service use form was used to identify any TAU families who had made use of the PACT treatment outside the trial. Therapists were regularly supervised by the clinical lead at each site.
Intervention manual fidelity
All therapy sessions were video-recorded at regular intervals across the trial period; one in-person session in the home setting and one in the educational setting were randomly selected per therapist for rating (CT, JG and PH), independent of therapy delivery and supervision, using the PACT fidelity rating scale (see Appendix 4). The scale has 16 items, rated 0 or 1, and was used to assess adherence to the PACT-G protocol. The proportion of tapes above the 80% fidelity threshold was reported.
Remote sessions and HSCs were not formally rated because of anticipated difficulties in recording these adequately, but they were informally monitored by the therapy supervisors during therapy supervision. The independent fidelity raters did, however, review a selection of remotely delivered sessions in the home and educational settings, chosen to reflect the range of remote sessions delivered, to assess the acceptability of remote intervention in the different settings.
Session validity from therapist logs
A key component of the PACT-G therapy is the use of video-mediated feedback. However, as the PACT-G therapy was being delivered in both home and educational settings, and often in challenging circumstances, a set of criteria was developed against which therapists could judge the ‘acceptability’ of each session. Detailed therapist logs were maintained through the course of the trial. Information from these was used to collate (1) the number of sessions delivered in each category, (2) the acceptability of these sessions against quality criteria and (3) qualitative notes on treatment setting, barriers to delivery, feasibility and acceptability. A number of ‘exclusion deviations’ were prespecified which, if present, resulted in the session being rated as falling below an acceptability threshold. Criteria for a number of ‘acceptable deviations’ were also prespecified. These were deviations from the content of an ‘ideal’ session that, despite the deviation, the therapist rated as a good enough therapy session to be valid.
The home–school conversation sessions
Home–school conversation sessions were not video-recorded or rated for acceptability or fidelity purposes. However, the number of sessions and session length were recorded. HSCs lasting < 30 minutes were deemed unacceptable as a valid session.
Chapter 6 Patient and public involvement
Patient and public involvement input into original intervention development
Ongoing sequential development of the PACT intervention has been carried out in close collaboration with families and service users. At an early stage, the team co-developed with service users the first user-nominated measure of treatment outcome in autism,97 which helped focus on key parent-nominated priorities. Parent reports on the experience of receiving PACT therapy in the initial stages were evaluated through independently conducted interviews and the results were fed back into the design of the next iteration of the therapy within PACT-G. 33 This feedback, including around clinic visits and home-based practice, informed the design of the home-based aspects in PACT-G.
Patient and public involvement review following the pilot phase
This planned review included input into research design and adaptation of the intervention prior to finalisation of the trial protocol.
Aim
We aimed to involve parents and education staff as service users in the design and piloting of novel aspects of the intervention, including generalisation of the parent training sessions into the home and educational settings and joint working with educational settings.
Methods
At the end of the pilot phase, we carried out a feedback exercise with pilot families and education staff. We interviewed seven parents, five members of nursery/school management and two LSAs to obtain feedback on the participant information sheet (PIS) provided about the study, trial documentation, baseline assessment burden and intervention process. We asked about their experiences of taking part in the intervention and how intervention sessions could be delivered in a way that minimised any additional burden to families or educational settings. Additional feedback from therapists and research staff was also incorporated. This feedback was summarised and fed back to the PACT-G trial team.
Results and subsequent actions
Generally speaking, interviewees spoke positively about their experience of the study. They reported that the research burden was acceptable. A summary of the main points from their feedback is given below. This feedback was shared with the PACT-G trial team and led to multiple changes in our procedures that are also detailed below.
Participant information sheet
The PIS could be easily understood by most; however, one parent commented that she found the PIS to be too long and complicated:
-
We obtained an ethics committee amendment agreement for a short and easy-read version of the PIS. This was offered to parents alongside the full PIS.
Running the research in educational settings
The combination of written and verbal information sources provided to educational settings was appropriate in quantity and accessibility. The research team were advised to make sure that LSAs had all the practical information that they required for intervention delivery, as they did not always attend the initial orientation session. Education staff suggested that the time commitment involved in the study needed to be presented much more clearly from the outset and that it was important for appointments to be booked as far in advance as possible. This was fed back to all trial staff working with educational settings. Education staff also commented that they needed clearer guidance on aspects of research design, such as the inclusion criteria, avoiding group contamination and researcher unblinding:
-
Members of education management teams were encouraged to attend the orientation session, as this provided them with the practical details of the study. A copy of the information sheet was also available for reference and to share with other staff members. We adjusted procedures to ensure that education staff fully understood the time commitment to the study from the earliest stages.
-
Steps were taken to ensure that parents and staff in educational settings understood the different roles of researchers/therapists. A handout was produced for education staff, summarising research design issues and how educational settings can help with these. Posters with photographs of research/therapy personnel were made available so that all staff in educational settings knew who was who to prevent unblinding.
Burden of baseline assessments on parents
The burden of baseline assessments was acceptable to parents. Some thought that the child assessment session was tiring and one parent felt awkward in the play assessment:
-
Research staff recognised that child assessment sessions mean a long day for the child and did what they could to reduce burden (offer breaks, etc.). They also reassured parents that the researchers recognised that some aspects of the play assessments might not seem as natural as usual.
Organising research assessments/therapy sessions
No parents reported problems with organising appointments, but flexibility of therapists in accommodating them was appreciated by a number of parents. Staff in educational settings found this more challenging because of practical and logistical reasons:
-
Therapists booked therapy sessions and research assessments well in advance/at regular times to allow educational settings to organise rooms/staff cover.
Video-conferencing/telephone sessions
Problems were described by parents and LSAs/education management (and by therapists) in terms of making videos (if no other adult was present or if the child did not like being video-recorded), and sending videos [problems with system, parent has limited internet capacity, handing over universal serial buses (USBs) instead of using video-sharing software/education information technology (IT) set-up/difficulty if only one device for looking at video and Skyping (Skype™; Microsoft Corporation, Redmond, WA, USA) simultaneously]:
-
Written information on using technology (Skype/video-sharing) was produced for parents/LSAs.
Home–school conversations
All parents reported HSCs to be easy or fairly easy to arrange and found these to be helpful or very helpful – they liked hearing how their child was getting on in an educational setting and sharing their experiences. Both LSAs who were interviewed had a HSC and found these easy to organise. One LSA found these HSCs to be very informal and was unclear on the objective of the session:
-
LSAs were given an initial explanation about the purpose and format of HSCs and how they are different from the more usual type of education planning meetings they might have been involved in.
Critical reflections on this process
This feedback was very informative and ensured that parents and particularly education staff were fully informed about the commitment required for the research and key aspects of trial design. It also meant that members of the trial therapy team understood how best to support allocated education staff to access and benefit from the therapy sessions.
Patient and public involvement input to the Trial Steering Committee and Local Steering Groups
Two parent representatives were members of the TSC. Both were parents of children with autism and one was a qualified teacher with experience of working in both mainstream and specialist schools. At all meetings, the parent representatives contributed to discussions and provided valuable input on aspects of the trial design and the therapy process. Some specific areas of feedback from the parent service user TSC members that led to changes to procedures included:
-
Discussion around how researchers could sensitively introduce some of the research assessments, which led to SOP researcher guidelines on how to introduce research measures.
-
Ways to keep parents engaged with the trial team to maximise participant retention, especially in the TAU group. This led to the purchase of trial-branded merchandise (coffee cups, magnets, pens, etc.), which kept particpants aware of the trial and acted as a small token of appreciation.
-
Discussion about borderline eligibility issues, such as significant parent mental ill health, child epilepsy and child genetic conditions. This led to a tightening of the eligibility criteria, ensuring that referring clinicians and trial personnel understood the clear and consistent eligibility criteria for participation.
-
Reflections on potential parental experiences of the HSC and some of the parent–education staff dynamics that might affect the delivery and success of these sessions. This resulted in greater awareness among the trial team and increased sensitivity to some of these issues.
Critical reflection
The two patient and public involvement (PPI) representatives contributed in a positive and constructive way that led to increased understanding of the perceptions and experiences of parents and education staff and to material changes to procedures. One of the PPI representatives has since continued to collaborate with the team by acting as a parent representative co-investigator on another National Institute for Health and Care Research (NIHR)-funded trial (the HTA-funded REACH-ASD trial, HTA 17/80/09).
A local PACT-G steering group took place every 6 months throughout the study at the Newcastle upon Tyne site. The group included a parent representative (who had taken part in the previous PACT), two representatives from special needs schools and two referring clinicians, as well as members of the research and therapy team. These meetings shared local knowledge up-to-date information about the whole study to promote recruitment and retention procedures. Important lessons included feedback on acceptable study merchandise; using text messages and e-mails to contact recruited parents who might not answer unrecognised telephone numbers; the value for parents of the research assessment reports; promoting recruitment opportunities with local parent support groups and at multidisciplinary/multiagency events; and sharing methods of providing regular feedback on research procedures with key co-ordinating professionals in both educational settings and clinical services (e.g. the use of study posters to minimise unblinding and sharing examples of best practice to support recruitment and retention). This information was fed back to the PACT-G trial team.
Chapter 7 Analysis
Aims of formal analysis
Objective 1: testing the efficacy of the PACT-G intervention
To test whether or not the extended PACT-G social communication intervention protocol, using targeted enhancement strategies within home and educational settings, showed a treatment effect on:
-
researcher-assessed autism symptom primary outcome
-
dyadic social communication and autism symptoms in home and educational settings.
This objective was tested using a variety of measures to maximise the ability to detect meaningful change (see Chapter 5, Measures) and evaluated by estimation of effects at the trial end point.
Objective 2: mechanism analysis
The mechanism analysis used the experimental trial to illuminate core processes of generalisation of specific, acquired competencies in autism across contexts:
-
We built on the mediation analysis from our previous PACT56 to test mediation of the generalised treatment effect in home and educational setting.
-
We tested whether or not and how effects in naturalistic contexts might combine to enhance transmission of effect to research-assessed symptoms in a standardised test setting.
A statistical analysis plan was written by the trial statisticians (AP and RE) and agreed by the trial principal investigators before approval by the TSC and Data Monitoring Committee prior to completion of data entry, data lock and analysis. All statistical analyses were carried out using Stata or Mplus (Muthén & Muthén, Los Angeles, CA, USA). 98
In accordance with the Consolidated Standards of Reporting Trials (CONSORT) statement for non-pharmacological interventions,99 we report all participant flow. Descriptive statistics summarise recruitment, dropout and completeness of interventions. Analysis was undertaken after all 12-month outcome measures were completed. The main efficacy analysis followed intention-to-treat (ITT) principles. For the primary outcome, baseline measurement was completed to confirm eligibility for randomisation. The proposed primary analysis was a regression of end-point ADOS-2 score, stratified by ADOS-2 module, on baseline ADOS-2, and dummy variables for randomisation stratifiers and treatment assignment. Continuously scored secondary outcomes with both baseline and end-point measures were analysed by joint baseline–end-point regression analyses100 that efficiently recover ITT estimates using data from all participants with any pre- or post-randomisation measurement under the missing at random assumption. When outcomes were unavailable for > 10% of participants, a sensitivity analysis was to be undertaken in which outcome scores were multiply imputed using relevant available auxiliary baseline and follow-up measures and assuming the absence of a treatment effect. There were no planned interim analyses for efficacy or futility. Summary statistics of baseline characteristics are presented by randomised group without formal statistical tests.
Phase 1: objective 1 testing the efficacy of the PACT-G intervention
We tested the primary hypothesis for between-group differences in the outcome ADOS-2 total score using linear regression, stratified by ADOS-2 module, covarying by baseline ADOS-2 total and dummy variables for site, gender and age group. Standard residual diagnostics were applied and, when required, skew-minimising transformations were adopted. An overall ES was calculated pooling stratum-specific estimates for strata defined by the ADOS-2 module, weighted by their precision, and using a 95% CI estimated from 5000 bootstrap replicates. The secondary outcomes were analysed in a similar way but without stratification by the ADOS-2 module. A forest plot of ESs for primary and secondary outcomes is presented (see Figure 8). A test of homogeneity of ES for the ADOS-2 and BOSCC scales is reported. The primary analysis reports a test of homogeneity of effect for the primary outcome in preschool- and school-aged children. Secondary analysis (see Phase 3: moderation and subgroups) is to report an optimal moderation index,101 including bias correction from overfitting to a finite sample.
Phase 2: objective 2 mechanisms evaluation
Mediation analysis17 gave detailed insight into an attenuated transmission or generalisation in the original PACT across changes in person, task and context (see Chapter 1). In PACT-G, we tested for enhanced generalisation into home by keeping parent–child dyadic cues constant but increasing functionally relevant interaction contexts, and into education by introducing education staff (i.e. LSA)–child dyadic interventions and enhancing relevant parent–education staff (i.e. LSA) communication. The mechanism study investigated the mediation process in this model and, through that, aimed to illuminate key basic knowledge about developmental generalisation of acquired skills in autism. Some of the pathways of interest are illustrated in Figure 2. If the efficacy analysis showed significant between-group differences in the mediators [DCMA and/or BOSCC at home (path a) and in education contexts (path c); see Figure 9], then we used parametric regression models to:
-
test for mediation of the intervention on primary symptom outcome (ADOS-2) through DCMA and/or BOSCC at home (paths a, e and f)
-
test for mediation of the intervention on primary symptom outcome through DCMA and/or BOSCC in educational setting (paths c, d and f)
-
test for mediation of intervention on DCMA and/or BOSCC in educational setting through DCMA and/or BOSCC at home (paths a, b and c)
-
use structural equation modelling to examine multiple pathways through DCMA and/or BOSCC at home and in the educational setting to primary symptom outcome (paths a–f).
FIGURE 2.
Key mediation pathways tested in the PACT-G mechanism study.
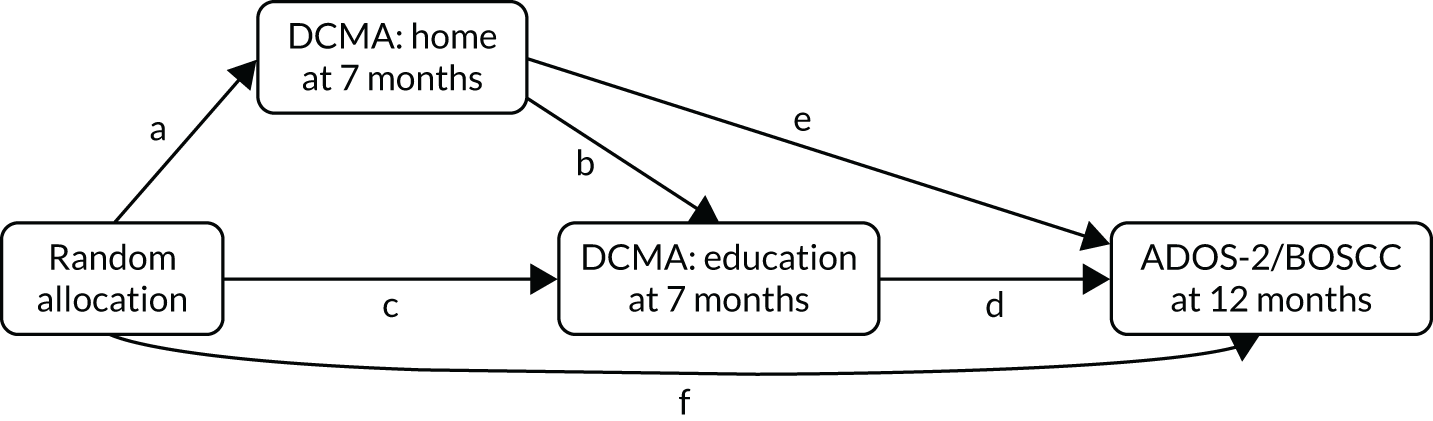
We repeated these four steps using researcher BOSCC as the outcome variable in place of the ADOS-2. As all of the measures are continuous, the indirect effects were calculated by multiplying relevant pathways. Bootstrapping was used to produce valid standard errors for the indirect effects. All analyses were adjusted for baseline measures of the mediators (BOSCC/DCMA), primary outcome (ADOS-2) and putative measured confounders. Mediation analyses are potentially biased by measurement error in mediators and hidden confounding between mediators and outcomes; we built on our previous methodological and applied work in this context to include repeated measurement of mediators and outcomes to account for classical measurement error17 and baseline confounding. 102
Phase 3: moderation and subgroups
We tested whether or not the mediation analysis was consistent across the two age groups by testing for moderation of paths a–f by age group stratifier (including interaction terms or performing a multiple group analysis in the structural equation model). The heterogeneity of autism is well recognised and, therefore, offers numerous potential moderators of treatment effects (e.g. language level, RRB, functional impairment). We planned to examine an extended list of moderators using bias correction/cross-validation methods to identify robust evidence for moderation and a moderation index, both on the overall effect and also along the steps of the mediation.
Primary outcome analysis
The ADOS-2 is a structured researcher-led assessment that maximises ascertainment of both social communicative competency and autism-related atypicality. Both tasks and scoring vary with the child’s verbal ability according to the ADOS-2 module completed, and the same module was used at baseline and end point. Stratified by module (and, for module 1, by child’s level of language to allow for the three items that differ for children with/without words), a module and language-level stratified regression of the end-point ADOS-2 SA plus RRB raw total score included treatment assignment, randomisation stratifiers (dummy variables for site, age group and gender), baseline ADOS-2 score and any other baseline variables found to predict missingness. Residual plots were used to determine whether or not prior transformation of the ADOS-2 scores was required. Using the within-group end-point standard deviation (SD), an ES was calculated for each module stratum. A single estimate pooled across modules was calculated using a weighted mean, where the weights were the inverse of the variance of each stratum-specific estimate. A CI for this pooled estimate was obtained using 1000 bootstrapped samples. The stratified analysis is illustrated below in Figure 3. To be consistent with the treatment main effects analysis, the test of difference in treatment effect by age group was based on the bootstrap p-value over 5000 replicates of the pooled within-ADOS-2 stratum estimate of the treatment difference.
FIGURE 3.
Stratified structure of analysis model. Analysis of primary outcomes: weighted sum of a, b and c (each standardised by within-group variance of outcome). 1m nv, module 1 non-verbal; m1 v, module 1 verbal; m2, module 2.
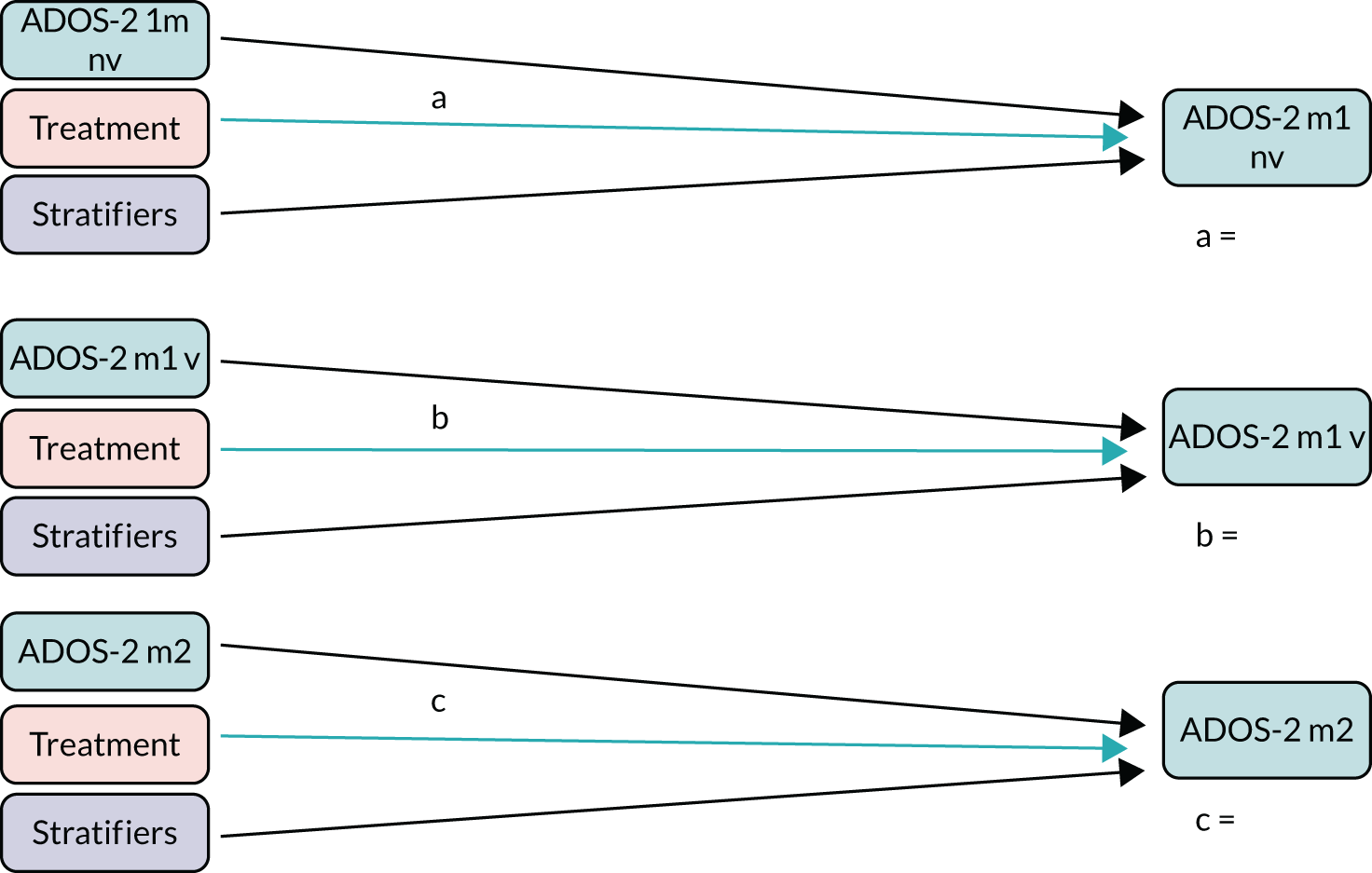
Non-adherence and complier-average causal effect estimator
The total number of therapy sessions meeting the satisfactory quality and fidelity criterion was used to define the dose of PACT-G therapy received (see Table 13). We estimated the effect of each satisfactory therapy session using instrumental variable regression (the model being identified by assuming the exclusion restriction that the offer of treatment does not itself influence the outcome) after accounting for receipt of treatment. The model had two correlated equations, the first for the number of satisfactory sessions received and the second predicting outcome, with treatment received replacing treatment assignment. The distributional form for the number of sessions was examined to determine whether or not this could be assumed Gaussian, or overdispersed Poisson with, the model being estimated using Stata sem or gsem, as appropriate. A dose–response model, assuming a linear dose–response relationship, was used to calculate how many sessions would be required to achieve a criterion level of clinical efficacy – defined here as the ES included in the power calculation, that is, an ES of 0.28.
We defined a more approximate variable for TAU families, where significant use of PACT-like treatment was identified. If this exceeded 10% of TAU participants using PACT, then an extended complier-average causal effect (CACE) model was estimated.
Sensitivity analysis
As per the statistical analysis plan, if missingness of the primary outcomes exceeded 10%, sensitivity analyses were to be carried out using multiple imputation; as missingness was very low (4.4%), no such analyses have been performed.
Analysis and presentation of secondary outcomes
Secondary outcomes with baseline, mid-point and end-point data:
-
the parent BOSCC total
-
the LSA BOSCC total
-
the researcher BOSCC total (no mid-point)
-
parent synchrony from the DCMA
-
LSA synchrony from the DCMA
-
child initiations from the parent DCMA
-
child initiations from the LSA DCMA.
Secondary outcomes with baseline and/or end-point data:
-
Language composite – MCDI receptive and expressive scores, the one-word tests and the PLSs.
-
Anxiety composite – DBC anxiety and emotional subscale of the SDQ. DBC anxiety was collected at the end point only.
-
SCQ – collected at baseline only.
-
Repetitive behaviour composite – parent SCQ and insistence on sameness and sensory motor scores from the RBQ. Parent SCQ was collected at baseline only.
-
Adaptive behaviour composite – VABS composite standard scores from parent and teacher and the prosocial subscale of the SDQ parent and teacher.
-
Parent well-being composite – WEMWBS and TOPSE.
-
Child health-related quality of life – CHU9D.
-
Disruptive behaviour composite – SDQ conduct subscale and disruptive/behaviour problems from the DBC. The DBC was collected at the end point only.
Secondary outcomes are presented either as a single-measure estimate from an analysis of covariance or, where multiple measures contributed, formed into composites and analysed using structural equation modelling (SEM), as illustrated below in Figure 4 for a composite with three baseline and four end-point components.
FIGURE 4.
Structure of SEM-based models for the analysis of composites.

Assessing quality of outcome measures
ADOS-2
All ADOS-2 video coding was completed blind to treatment allocation. Baseline ADOS-2 videos were coded by the research assistant (RA) at the local site (London, Manchester or Newcastle upon Tyne). End-point ADOS-2 videos were coded by the RA at a different site. End-point ADOS-2 videos were allocated for coding balancing for treatment group and site. Consensus meetings were held approximately every 5–6 months, with clinical leads chairing rating discussions (six meetings in total) to maintain coder reliability at all three sites across the coding period.
Dyadic interaction
DCMA: coding team
The team comprised five coders, all based in the UK (SL, CP, LK, FM and LD): three psychology graduates student, one psychology postdoctoral researcher, and one speech and language therapy undergraduate student. The coders were trained (by CA and HMc) in a 6-hour workshop, including introduction to the Behavioral Observation Research Interactive Software (BORIS)103 coding platform and how to export files in Excel (Microsoft Corporation, Redmond, WA, USA). The coders then independently coded two video-recordings to check the level of accuracy of coding against consensus. Coding was completed blind to treatment allocation and time point. Each coder was allocated videos in balanced blocks – each block contained a balance of treatment group (PACT-G plus TAU or TAU only), context (LSA or parent) and time point (baseline, mid-point or end point) for a range of cases. A total of 1396 DCMAs were coded. Consensus meetings were held monthly by telephone conference during the main coding period (six meetings in all), discussing two independently coded videos on each occasion, with written feedback, to maintain reliability. In addition, coding questions were addressed in an ongoing social media group. Thirty-five DCMAs were double-coded for formal reliability.
BOSCC: coding team
There were twenty coders in total: nine module 1 coders based in the UK (SC, LL, NEH, LP, MB, OW, YAK, RR and CH) and 11 coders based in the USA, divided between module 1 (KM, NBu, AJ, GG and AA) and module 2 (AH, KB, RN, MT, AM and NBa). Of the 20 coders, two were psychology/neuroscience undergraduate students and all others were graduates of psychology and/or neuroscience. A UK-based BOSCC trainer (Sue Fletcher-Watson) provided initial training to a cohort of five UK-based coders. SC was also trained to reliability by the BOSCC developers in the USA. SC oversaw initial and ongoing reliability and trained a further four UK coders. The 11 US-based coders had previously been trained to reliability in BOSCC coding by the BOSCC developers and through training by SC on the PACT-G BOSCC tapes. All coders were required to meet reliability with the UK PACT-G coders before commencing coding; reliability was judged as three consecutive tapes within four points of overall total and 12 out of 15 items per segment within 1 point, as per the manual. Coding was completed blind to treatment allocation and time point. Each coder, once trained to reliability, was allocated videos to rate independently in balanced blocks, each block containing a balance of treatment group (PACT-G plus TAU or TAU only), context (LSA, parent or researcher) and time point (baseline, mid-point or end point) for a range of cases. A total of 1840 BOSCCs were coded (Table 6).
| BOSCC | Time point (n) | Total (n) | ||
|---|---|---|---|---|
| Baseline | Mid-point | End point | ||
| Researcher | 238 | N/A | 233 | 471 |
| LSA | 237 | 225 | 223 | 685 |
| Parent | 236 | 221 | 227 | 684 |
The BOSCC videos were coded over a period of 2 years by UK and USA coding teams. During busier coding periods, and following any new coders starting their coding, consensus meetings were held every 2 weeks, in person or online. During times of less intense coding (e.g. two coders coding a few videos per week), consensus meetings were held monthly. These meetings were held to maintain coder reliability across the coding period. BOSCCs were multiple-coded for formal reliability. All coders, in varied pairings and groupings that included combinations of US- and UK-based coders, contributed to this process, with secondary coding being stratified in proportion to the number of videos they had been allocated for primary coding.
For module 1 BOSCC reliability, a total of 63 BOSCCs were coded for formal reliability. Fifty-seven BOSCCs were double-coded by UK-based coders. To check UK–USA consistency, a subset was also allocated for US coding. Thirty BOSCCs were double-coded by US-based coders. Formal reliability was assessed across UK and USA sites and 24 BOSCC videos were quadruple-coded by a UK pair and a USA pair. For module 2 BOSCC, which were all coded in the USA, 48 BOSCCs were double-coded for formal reliability.
Chapter 8 Results
Participant flow
Participant flow is summarised in Figure 5. The first randomisation into the trial occurred on 18 January 2017, and last randomisation on 19 April 2018. The follow-up mid-point assessments ran from 15 August 2017 to 7 December 2018 and the end-point assessments ran from 5 January 2018 to 3 May 2019. Study withdrawal rates were very low and, as shown in Table 7, were predominantly from the TAU group. Although there were small variations in the numbers of mid-point and end-point assessments completed in the different settings, completion rates were very high. Only one participant did not contribute data to the analysis of the primary outcome.
FIGURE 5.
The PACT-G CONSORT flow diagram. a, One family inadvertently received PACT-G treatment.
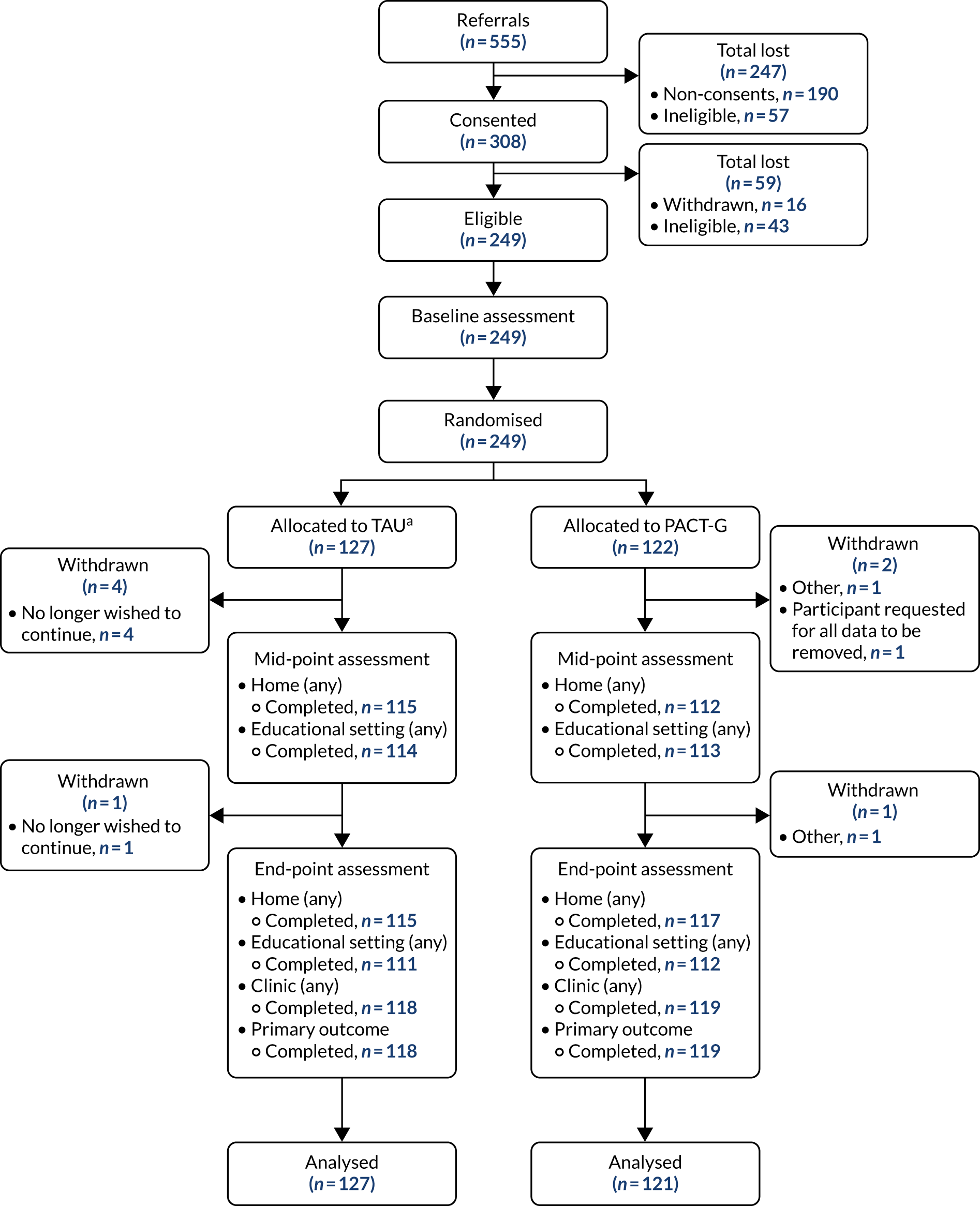
| Withdrawals | Treatment group, n (%) | Overall, n (%) | |
|---|---|---|---|
| TAU | PACT-G | ||
| Did the participant withdraw from the study? | |||
| No | 121 (95.3) | 119 (98.3) | 240 (96.8) |
| Yes | 5 (3.9) | 2 (1.7) | 7 (2.8) |
| Yes, and requested all data to be removed | 1 (0.8) | 0 (0.0) | 1 (0.4) |
| Reason for withdrawal | |||
| Participant no longer wishes to continue | 5 (100.0) | 0 (0.0) | 5 (71.4) |
| Participant moved | 0 (0.0) | 1 (50.0) | 1 (14.3) |
| Participant unhappy with progression of intervention | 0 (0.0) | 1 (50.0) | 1 (14.3) |
Baseline comparability of randomised groups
Table 8 summarises baseline characteristics by treatment group. Participants were predominantly white (60.1%) and male (79.4%) and spoke only English at home (79.4%). There was very little missing baseline demographic information. The participant population was ethnically diverse, in keeping with the large urban context of two of the sites and the mixed urban–rural setting of the third.
| Characteristic | Treatment group, n (%) | Overall, n (%) | |
|---|---|---|---|
| TAU | PACT-G | ||
| Age (years) | |||
| Preschool aged, n (%) | 77 (60.6) | 74 (61.2) | 151 (60.9) |
| School aged, n (%) | 50 (39.4) | 47 (38.8) | 97 (39.1) |
| Preschool age, mean (SD) | 3.9 (0.7) | 4.1 (0.6) | 4.0 (0.6) |
| School age, mean (SD) | 6.9 (1.4) | 7.4 (1.6) | 7.1 (1.5) |
| Sex, n (%) | |||
| Female | 27 (21.3) | 24 (19.8) | 51 (20.6) |
| Male | 100 (78.7) | 97 (80.2) | 197 (79.4) |
| Ethnicity, n (%) | |||
| White | 73 (57.5) | 76 (62.8) | 149 (60.1) |
| Black | 21 (16.5) | 19 (15.7) | 40 (16.1) |
| Asian | 16 (12.6) | 13 (10.7) | 29 (11.7) |
| Mixed | 17 (13.4) | 6 (5.0) | 23 (9.3) |
| Other | 0 (0.0) | 7 (5.8) | 7 (2.8) |
| Second parent in household?, n (%) | |||
| No | 28 (22.0) | 27 (22.3) | 55 (22.2) |
| Yes | 99 (78.0) | 94 (77.7) | 193 (77.8) |
| Languages spoken to child at home, n (%) | |||
| English only | 98 (77.2) | 99 (81.8) | 197 (79.4) |
| Other only | 3 (2.4) | 1 (0.8) | 4 (1.6) |
| English and other | 26 (20.5) | 21 (17.4) | 47 (19.0) |
| Non-verbal IQ, n | 127 | 121 | 248 |
| Mullen – visual standard t, mean (SD) | 25.2 (11.7) | 22.9 (8.0) | 24.1 (10.1) |
| Mullen – visual raw score mean (SD) | 28.3 (7.8) | 28.5 (7.0) | 28.4 (7.4) |
| Mullen – fine motor standard t, mean (SD) | 22.8 (8.6) | 21.8 (7.3) | 22.3 (8.0) |
| Mullen – fine motor raw score mean (SD) | 26.3 (6.9) | 27.2 (6.5) | 26.7 (6.7) |
Tables 9 and 10 present selected baseline measures by age group. With a few exceptions, the children in the older age group scored ≥ 2 SDs below the population mean for the Mullen Scales of Early Learning developmental quotient (DQ) and development of communication. Children in the younger age group showed somewhat lower autism severity than those in the school-aged group, but were nevertheless markedly intellectually and communicatively impaired.
| Baseline | Age group | |
|---|---|---|
| Preschool aged (N = 151) | School aged (N = 97) | |
| Module 1 (non-verbal), n = 110 | 63 | 47 |
| VEPS – social response, median [range] (IQR) | 0 [0–12] (0 –1) | 1 [0–11] (0–3) |
| VEPS – joint attention, median [range] (IQR) | 2 [0–13] (0–5.5) | 2 [0–17] (1–6) |
| Mullen – visual raw score, median [range] (IQR) | 23 [16–34] (20–25) | 26 [16–41] (23–29) |
| > 2 SDs below standard norm, t-score | 97% | 100% |
| Mullen – fine motor raw score median [range] (IQR) | 22 [15–29] (19–24) | 23 [15–44] (20–25) |
| > 2 SDs below standard norm, t-score | 98% | 100% |
| Module 1 (verbal), n = 77 | 52 | 25 |
| VEPS – social response, median [range] (IQR) | 1.5 [0–12] (0–3) | 2 [0–10] (0–3) |
| VEPS – joint attention, median [range] (IQR) | 6 [0–18] (3–9) | 8 [0–15] (6–11) |
| Mullen – visual raw score, median [range] (IQR) | 26.5 [17–44] (24–29.5) | 31 [22–48] (28–34) |
| > 2 SDs below standard norm, t-score | 88% | 96% |
| Mullen – fine motor raw score, median [range] (IQR) | 27 [19–44] (25–28) | 29 [19–46] (28–35.5) |
| > 2 SDs below standard norm, t-score | 92% | 96% |
| Module 2, n = 61 | 36 | 25 |
| VEPS – social response, median [range] (IQR) | 6 [0–12] (2–8) | 3 [0–12] (1–8) |
| VEPS – joint attention, median [range] (IQR) | 12 [0– 18] (7–15) | 10 [0–18] (8–12) |
| Mullen – visual raw score, median [range] (IQR) | 33 [21–50] (30.5–42) | 33 [25–49] (30.5–43) |
| > 2 SDs below standard norm, t-score | 56% | 92% |
| Mullen – fine motor raw score, median [range] (IQR) | 30 [23–44] (28–36) | 33.5 [21–47] (29.5–39.5) |
| > 2 SDs below standard norm, t-score | 67% | 96% |
| All modules | 151 | 97 |
| VEPS – social response, median [range] (IQR) | 1 [0– 12] (0–3) | 2 [0– 12] (0–4.5) |
| VEPS – joint attention, median [range] (IQR) | 6 [0– 18] (1–10) | 6 [0– 18] (2–10) |
| Mullen – visual raw score, median [range] (IQR) | 26 [16– 50] (23–31) | 29 [16– 49] (25–32) |
| > 2 SDs below standard norm, t-score | 84% | 97% |
| Mullen – fine motor raw score, median [range] (IQR) | 26 [15– 44] (22–28) | 27 [15– 47] (23–32) |
| > 2 SDs below standard norm, t-score | 89% | 98% |
| ADOS-2 CSS baseline | Age group, n (%) | |
|---|---|---|
| Preschool aged (N = 150) | School aged (N = 97) | |
| 6 | 48 (32) | 35 (36) |
| 7 | 53 (35) | 26 (27) |
| 8 | 23 (15) | 27 (28) |
| 9 | 13 (7) | 6 (6) |
| 10 | 13 (7) | 3 (3) |
Table 10 shows that, with respect to autism severity, the groups were similar and at a level consistent with the inclusion criteria of severe autism.
Although the same module was used at baseline and at the end point, two items used in the module 1 ADOS-2 algorithm for calculating the ADOS-2 total score for ‘no-words’ children were replaced by different items when the ‘some words’ level of language was achieved, and vice versa if language regressed. Table 11 shows the modules and level of language of participants at baseline and the end point.
| ADOS-2 | Time point, n (%) | |||||
|---|---|---|---|---|---|---|
| Baseline | End point | |||||
| TAU | PACT-G | Overall | TAU | PACT-G | Overall | |
| Module 1 (non-verbal) | 53 (42) | 57 (47) | 110 (44) | 48 (41) | 48 (40) | 96 (41) |
| Module 1 (verbal) | 42 (33) | 35 (29) | 77 (31) | 40 (34) | 42 (35) | 82 (34) |
| Module 2 | 32 (25) | 29 (24) | 61 (25) | 30 (25) | 29 (24) | 59 (25) |
Education provision
The educational settings across both groups of the trial, characterised at baseline, are shown in Table 12. The majority of preschool-aged children recruited to PACT-G attended a mainstream nursery [for both the PACT-G (n = 45) and TAU (n = 48) groups]. These settings consisted of privately owned independent day nurseries and local authority day nurseries. A small number of children in this age group attended a specialist nursery (PACT-G n = 3; TAU group, n = 2). These settings were either charity-led or local authority nurseries. One child attended a child-minding setting (TAU). All of these settings deliver a child-led curriculum within the Early Years Foundation Stage (EYFS). 104
| Education setting | Treatment group (n) | |||||
|---|---|---|---|---|---|---|
| PACT-G | TAU | |||||
| London | Manchester | Newcastle upon Tyne | London | Manchester | Newcastle upon Tyne | |
| Mainstream nursery | 20 | 13 | 12 | 26 | 11 | 11 |
| Specialist nursery | 0 | 3 | 0 | 0 | 1 | 1 |
| Mainstream primary school | 8 | 10 | 7 | 3 | 15 | 7 |
| Mainstream school with SEN/autism resource class/base | 4 | 0 | 0 | 2 | 1 | 1 |
| Special school with mixed disabilities | 1 | 10 | 12 | 3 | 12 | 17 |
| Specialist autism school | 8 | 3 | 10 | 7 | 12 | 5 |
| Childminder | 0 | 0 | 0 | 0 | 1 | 0 |
The majority of school-aged children in the PACT-G (n = 44) and TAU (n = 56) groups attended a special educational setting. These settings were either for children with a range of disabilities or were specialist autism schools. Other children in this age group attended a mainstream primary school (PACT-G group, n = 25; TAU group, n = 25) or a resourced specialist provision within a mainstream primary school (PACT-G group, n = 4; TAU group, n = 4). These children access the national curriculum (key stage standards) and have SEN support at school or have an education, health and care plan in place. 91
Intervention delivery
PACT-G implementation at home
In the PACT-G group, there was a median of 10 [interquartile range (IQR) 8–12; range 2–12] parent sessions per case out of 121 observations. Across the whole trial implementation, 64% of the home sessions were in person and 36% were by video conferencing. Of these sessions, 2% of the in-person sessions and 12% of the online video-conferencing sessions were judged as unacceptable by therapists in their logs, using the set criteria referred to above (see Chapter 5, Session validity from therapist logs). Of these unacceptable sessions, the majority of the online video-conferencing sessions were unacceptable because of the lack of ability to share a home-filmed video; the reasons for unacceptability in the in-person sessions were more varied (Table 13).
| Session details | Home setting | Educational setting | ||
|---|---|---|---|---|
| In person | Video conference/telephone | In person | Video conference/telephone | |
| Total sessions, n (%) | 765 (64) | 424 (36) | 632 (66) | 320 (34) |
| Acceptable sessions, n (%) | 720 (94) | 364 (86) | 591 (94) | 269 (85) |
| Reasons for session being unacceptable, % | ||||
| No targets set | 18 | 0 | 17 | 6 |
| It was not possible for the adult and therapist to watch a video of ACI | 27 | 98 | 17 | 86 |
| Child did not take part in ACI | 17 | 0 | 24 | 0 |
| Sibling interfered in ACI to the extent that it disrupted the session | 17 | 0 | 0 | 0 |
| No therapy feedback | 21 | 0 | 10 | 8 |
| Acceptable session deviations, n (%) | 428 (57) | 94 (22) | 140 (22) | 42 (13) |
| Additional person in during session, % | 13 | 5 | 9 | 5 |
| Technical difficulties experienced, % | 2 | 38 | 18 | 46 |
| Therapist and adult both watched video but not simultaneously, % | 0 | 12 | 0 | 11 |
| Sibling present during session, % | 17 | 3 | 0 | 0 |
| Feedback disrupted by child, % | 44 | 17 | 16 | 7 |
| ACI interrupted, % | 3 | 0 | 7 | 0 |
| Additional full face-to-face sessions instead of remote (i.e. greater dosage), % | 2 | 0 | 6 | 0 |
| Video-conferencing/telephone session carried out in person, % | 2 | 7 | 5 | 22 |
| Review carried out after ACI, % | 2 | 0 | 9 | 0 |
| Missing data because of technical difficulty (but session fully delivered), % | 7 | 8 | 16 | 4 |
| PACT approach required modification (e.g. teaching), % | 6 | 9 | 5 | 4 |
| ACI video short, % | 2 | 2 | 10 | 0 |
PACT-G implementation in educational settings
Professionals delivering PACT-G in educational settings
Initial discussion with each participating educational setting (pre randomisation) allowed them to identify the professional in the education structure who would be best to participate in the trial and deliver the PACT-G therapy as appropriate in their context. The nominated professionals are shown in Table 14. The majority of nominated staff across both groups of the trial were in a teaching assistant/LSA role (PACT-G group, n = 92; TAU group, n = 92). There was also a balance of early years assistants across both arms (PACT-G group, n = 11; TAU group, n = 9). Other nominated adults in educational settings had more senior roles, including teachers (PACT-G group G, n = 7; TAU group, n = 10), SEN co-ordinators (PACT-G group, n = 3; TAU group, n = 9) and nursery managers/deputies (PACT-G group, n = 2; TAU group, n = 1).
| Adult role | Treatment group (n) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PACT-G | TAU | ||||||||||||
| Mainstream nursery | Specialist nursery | Mainstream primary school | Resourced provision within mainstream | Special school with mixed disabilities | Specialist autism school | Mainstream nursery | Specialist nursery | Mainstream primary school | Resourced provision within mainstream | Special school with mixed disabilities | Specialist autism school | Childminders | |
| Teaching assistant/LSA | 27 | 3 | 24 | 1 | 20 | 17 | 27 | 1 | 18 | 2 | 31 | 13 | |
| Teacher | 3 | 3 | 1 | 5 | 4 | 1 | |||||||
| Special education needs co-ordinator | 3 | 9 | |||||||||||
| Nursery manager/deputy manager | 2 | 1 | |||||||||||
| Inclusion manager | 1 | ||||||||||||
| Head of room | 1 | ||||||||||||
| Intervention co-ordinator | 2 | 1 | |||||||||||
| Nursery/early years officer/nurse/practitioner | 9 | 1 | 1 | 5 | 1 | 3 | |||||||
| Speech and language therapist | 1 | ||||||||||||
| Outreach worker | 1 | ||||||||||||
| Childminder | 1 | ||||||||||||
| Communication champion | 3 | 1 | |||||||||||
Change in education professional within therapy
Eighty-five (34.3%) children across the trial experienced a change in the education professional delivering PACT-G between baseline and the mid-point, and 94 (37.9%) children experienced a change in education professional between the mid-point and end point. Twenty-two (20%) children experienced changes at both time points. When this change occurred, the therapist began the PACT-G therapy again with the new education professional. For the purposes of assessing the adequacy of the delivery of the PACT-G therapy, a pragmatic assumption was made that a notional two sessions would be needed for the replacement education professional to achieve minimum familiarity with the method delivery of the therapy and to establish a consistent interaction with the child.
Therapy implementation in education
From 117 observations, a median of 8 (IQR 5–10; range 0–12) teacher sessions were undertaken during the trial. Of those in-educational setting sessions, 66% were in person and 34% were by online video conferencing; 1% of the in-person sessions and 11% of the online video-conferencing sessions were judged as unacceptable by therapists in their logs using the set criteria referred to above (see Chapter 5, Session validity from therapist logs). Reasons for unacceptability showed a similar profile to the home-based sessions as above: the main cause of unacceptability in the online video-conferencing educational-setting sessions was a lack of available video-sharing. Acceptable deviations for educational-setting sessions were noted in 22% of in-person and 13% of video-conferencing sessions, with a similar profile across both in-person and online video-conferencing sessions (see Table 13).
Implementation by stages of PACT-G therapy across home and educational settings
As noted in Chapter 5, Interventions, the PACT therapy proceeds on the basis of manualised sequential stages. All dyads begin at stage 1; the progression that they make depends on child characteristics such as cognitive ability, developmental level and autism severity, as well as the characteristics, progress and adaptations of their carer or LSA as the therapy progresses. Not all dyads are expected to achieve stage 6. As the home and education implementations of PACT-G were separate but involved the same child as the interactive dyadic partner, it is possible to compare the stage progress made for an individual child in each context. Table 15 shows the proportion of children reaching each stage at home and in the educational setting, or at a group level. Although the median stage reached by both parents and LSAs was the same, namely stage 3, a mixed ordinal logistic regression (not prespecified) suggested that parents attained a significantly higher stage than the LSAs (p = 0.014).
| End-point stage | Children reaching each stage, n (%) | |
|---|---|---|
| Parents | LSAs | |
| 1 | 12 (10) | 24 (20) |
| 2 | 29 (24) | 27 (22) |
| 3 | 44 (36) | 42 (34) |
| 4 | 17 (14) | 15 (12) |
| 5 | 15 (12) | 9 (7) |
| 6 | 4 (3) | 4 (3) |
| Total | 121 | 121 |
Intervention manual fidelity
In-person sessions
Ten therapists delivered a total of 1397 in-person intervention sessions during the trial. Fidelity checks were carried out at three time points across the trial: 6, 12 and 18 months from the beginning of the main trial phase. This was to make sure that fidelity was maintained and did not drift during the trial. At each time point, one education session and one in-home session per active therapist was randomly selected to give a representative picture. Of the 45 sessions selected, two could not be rated because of technical difficulties and COVID-19 restrictions, giving 43 sessions (21 in home settings and 22 in educational settings), representing 3.1% of the total in-person sessions delivered in the trial (2.7% in home settings and 3.5% in educational settings). Scores could range from 0 to 16, with a score of 13 (representing > 80% items passed) set as the minimum fidelity threshold. The mean fidelity across all rated sessions was 14.67 (median 15, range 10–16), with the fidelity threshold being met for 37 (86%) sessions and not met for 6 (14%) sessions (Figure 6).
FIGURE 6.
Distribution of fidelity ratings (n = 43; score > 13 represents acceptable fidelity).

Within the overall total, 17 out of 21 (81%) in-home sessions reached an acceptable mean fidelity score of 14.3 (median 15, range 10–16) and 20 out of 22 (91%) education sessions reached an acceptable mean fidelity score of 14.95 (median 16, range 10–16). Table 16 shows that this did not vary substantially by therapist.
| Therapist | Mean fidelity (range; median) |
|---|---|
| 1 | 14.3 (10–16; 15) |
| 2 | 15.5 (14–16; 16) |
| 3 | 15.25 (13–16; 16) |
| 4 | 14.67 (12–16; 15) |
| 5 | 13.8 (11–15; 15) |
| 6 | 15 (14–16; 15) |
| 7 | 15.75 (15–16; 16) |
| 8 | 13.6 (10–16; 14) |
| 9 | 14.5 (13–16; 14.5) |
| 10 | 15.5 (15–16; 15.5) |
Remote sessions (video conferencing or telephone)
Informal fidelity monitoring of a small number (n = 11; 2%) of the remote sessions indicated that, where parents and LSAs had supplied suitable interactive play videos and there were no technical difficulties, the sessions could be of similar quality to face-to-face sessions. However, given the small sample, we can make no inference as to the overall quality of remote session delivery in this trial.
Home–school conversations
The HSC meetings were arranged between a therapist, parent and LSA to facilitate the generalisation of skills across the home and educational settings. HSC meetings were structured around ‘explore’, ‘focus’, ‘plan’ and ‘review’ stages, which allowed the LSA and parent to discuss strategies and techniques that worked well in different settings. The trial had planned up to six HSC sessions per case, with the minimum acceptable number set at three per child. These were to be arranged between the parent and LSA, with the therapist in attendance when possible, particularly for the early sessions.
In the trial period, 281 HSCs were recorded for 125 participants, with an average of 2.2 HSCs per participant. The numbers varied by trial site: London completed 120 HSCs for 42 participants, with an average of 2.9 HSCs per participant; Newcastle upon Tyne completed 42 HSCs for 43 participants, with an average of 1.0 HSC per participant; and Manchester completed 119 HSCs for 40 participants, with an average of 3.0 HSCs per participant.
We have anecdotal information from trial therapists as to the difficulties in arranging HSCs that led to an average below the acceptable minimum planned. Problems included (1) the practical difficulties of organising the sessions in addition to the treatment within school curriculum time, (2) HSCs required further time out of class for the LSAs and (3) the difficulties encountered arranging mutually convenient times between the LSA, the parent and, when necessary, the therapist. The lack of time available for HSCs within the educational setting in the main trial seemed at variance with the results from the feasibility pilot and PPI feedback (see Chapters 4 and 6).
Treatment as usual
Home-based therapy
Parent reports of non-PACT-G treatment received across both trial arms in home and clinic settings during the 12-month trial is shown in Table 17. Home-based therapy consisted of a programme of at least four home-based sessions that were delivered directly to the child in the home [either by the parent or trained therapist, e.g. applied behaviour analysis (ABA)]. Speech and language therapy provision was recorded for a programme of therapy (i.e. more than general advice-giving) and was administered either directly to the child or with the parent in the home or clinic setting.
| Treatment type | Treatment group | |
|---|---|---|
| PACT-G (N = 118) | TAU (N = 117) | |
| Home-based therapy (at least four sessions) | ||
| ABA | 10 | 10 |
| Number of sessions, mean (range) | 65 (5–236) | 89 (15–226) |
| Duration of sessions (minutes), mean (range) | 135 (120–300) | 153 (45–240) |
| CAMHS behaviour management | 1 | 0 |
| Number of sessions | 6 | 0 |
| Duration of sessions (minutes) | 45 | 0 |
| Listening therapya | 1 | 0 |
| Number of sessions | 500 | 0 |
| Duration of sessions (minutes) | 15 | 0 |
| Intensive interaction | 1 | 0 |
| Number of sessions | 12 | 0 |
| Duration of sessions (minutes) | 240 | 0 |
| Speech and language provision in home or clinic settings | ||
| PECS | 1 | 5 |
| Number of sessions | 3 | 6 (range 1–12) |
| Duration of sessions (minutes) | 45 | 47 (range 30–60) |
| Hanen | 0 | 1 |
| Number of sessions | 0 | 8 |
| Duration of sessions (minutes) | 0 | 150 |
| EIBI/verbal behaviour | 1 | 1 |
| Number of sessions | 12 | 60 |
| Duration of sessions (minutes) | 360 | 3 |
| Colourful semantics | 1 | 0 |
| Number of sessions | 2 | 0 |
| Duration of sessions (minutes) | 40 | 0 |
| Unnamed or eclectic therapy package | 30 | 28 |
| Number of sessions, mean (range) | 10 (1–50) | 12 (2–40) |
| Duration of sessions (minutes), mean (range) | 50 (15–90) | 58 (30–120) |
| Video feedback involvedb | 1 | 6 |
| Autism-related parent training courses | ||
| Generic autism awareness/post-diagnostic course | 30 | 34 |
| Number of sessions, mean (range) | 6 (1–12) | 6 (1–20) |
| Duration of sessions (minutes), mean (range) | 144 (60–180) | 134 (60–240) |
| Communication/interaction | 6 | 11 |
| Number of sessions, mean (range) | 2.5 (1–8) | 7 (1–12) |
| Duration of sessions (minutes), mean (range) | 170 (60–420) | 153 (90–300) |
| Alternative and augmentative systems (e.g. Makaton) | 2 | 5 |
| Number of sessions, mean | 1 | 3 (range 1–8) |
| Duration of sessions (minutes), mean (range) | 105 (90–120) | 126 (60–180) |
| Behaviour/sensory processing/emotion regulation | 5 | 2 |
| Number of sessions, mean (range) | 2.8 (1–8) | 7 (1–12) |
| Duration of sessions (minutes), mean | 174 (range 120–240) | 180 |
| Non-specific/other parent training | 8 | 5 |
| Number of sessions, mean (range) | 4.75 (1–10) | 3 (1–7) |
| Duration of sessions (minutes), mean (range) | 197 (120–480) | 135 (120–180) |
Child’s educational setting
Non-PACT-G treatments received in educational settings across both trial groups during the trial reported by the child’s class teacher are shown in Table 18. These treatments were delivered by either professionals external to the education context or staff within the setting. General advice from professionals (e.g. speech and language therapists) or post-assessment feedback sessions were not counted as treatment sessions. The majority of treatment delivered in both arms was an unnamed or eclectic therapy package (PACT-G group, n = 36; TAU group, n = 50). The interventions characterised here, on the whole, were ‘discrete’ rather than ‘comprehensive’; that is, these were bespoke, pragmatic interventions developed as solutions in the naturalistic context of school using the resources available in the setting, rather than a selected intervention ‘package’. Some interventions in this category employed the use of video feedback (PACT-G group, n = 4; TAU group, n = 4).
| Treatment type | Treatment group | |
|---|---|---|
| PACT-G (n = 118) | TAU (n = 117) | |
| SCERTS | 1 | 0 |
| Colourful semantics | 3 | 4 |
| Music therapy | 1 | 1 |
| LEGO® (LEGO System A/S, Billund, Denmark) therapy | 2 | 1 |
| Intensive interaction | 3 | 4 |
| ABA/EIBI/verbal behaviour | 0 | 2 |
| PECS | 12 | 4 |
| Visual supports/TEACCH | 1 | 3 |
| Makaton/sign language | 2 | 0 |
| Unnamed or eclectic therapy package | 36 | 50 |
| Video feedback involved | 4 | 4 |
Use of PECS was reported more frequently in the PACT-G group (n = 12) than in the TAU group (n = 4). There may be under-reporting of the use of PECS as an intervention because specialist school settings use PECS and similar communication systems as an integrated system in the classroom. Thus, it is not necessarily viewed as an intervention per se, but more as a mode of communication in the classroom. Other interventions reported in education contexts were colourful semantics (PACT-G group, n = 3; TAU group, n = 4), intensive interaction (PACT-G group, n = 3; TAU group, n = 4), ABA, (PACT-G group, n = 0; TAU group, n = 2), visual supports/TEACCH (PACT-G group, n = 1; TAU group, n = 3), Makaton (PACT-G group, n = 2; TAU group, n = 0), LEGO therapy (PACT-G group, n = 2; TAU group, n = 1) and music therapy (PACT-G group, n = 1; TAU group, n = 1). One child in the PACT-G group was also reported to be receiving SCERTS. SCERTS and TEACCH are fully integrated approaches to supporting autistic children in their development and education. However, for the purposes of reporting, these have been included as the strategies and principles used specifically in allocated intervention sessions with the child.
Treatment as usual across trial arms
Analysis of non-PACT-G treatment received during the treatment period indicates that home-based therapy programmes were similar across the two trial arms. Ten parents reported home-based intensive ABA; however, the TAU group reported an average of 24 more sessions (PACT-G group, mean 65 sessions; TAU group, mean 89 sessions), with an average duration 18 minutes longer than the PACT-G group (PACT-G group, mean 135 minutes; TAU group, mean 153 minutes). All other types of home-based therapy programmes were received by participants in the PACT-G group, which included intensive interaction (n = 1), listening therapy (n = 1) and a Child and Adolescent Mental Health Services (CAMHS) behaviour management programme (n = 1).
Speech and language provision in the home and other settings was less well defined, with the majority of parents reporting that they accessed an ‘unnamed or eclectic’ programme of therapy (PACT-G group, n = 30; TAU group, n = 28). The delivery of speech and language interventions in this category was varied, with some parents reporting that they attended a clinic or the therapist came to their home to provide bespoke strategies that they could use with their child. These intervention sessions also varied between direct implementation of strategies with the child or giving parents strategies to use with their child; in-clinic sessions varied between individual and group sessions for children.
Other named interventions accessed were, on balance, equivalent across arms and included Hanen (PACT-G group, n = 0; TAU group, n = 1), ABA/early intensive behavioural intervention (EIBI)/verbal behaviour (PACT-G group, pivotal response therapy, n = 1; TAU group, ABA, n = 1) and colourful semantics (PACT-G group, n = 1). More parents in the TAU group than the PACT-G group accessed PECS sessions, although this number was small overall (PACT-G group, n = 1; TAU group, n = 5). Autism parent training courses (independent of group deliverer profession) were also similar across trial arms, for example group-based autism post-diagnostic psychoeducation (PACT-G group, 25%; TAU group, 27%) and communication and interaction-focused training (PACT-G group, 5%; TAU group, 9%).
Assessing quality of outcome measures
ADOS-2
A random sample of 24 ADOS-2 videos was sampled to assess coding reliability (16 module 1 and 8 module 2 videos), including a proportionate balance of preschool- and school-aged children. These were triple-coded blind to treatment allocation (i.e. by all three RAs). The intraclass correlations (ICCs) were 0.80 (95% CI 0.61 to 0.91) for module 1, 0.70 (95% CI 0.38 to 0.90) for module 2 and 0.78 (95% CI 0.62 to 0.88) overall.
DCMA
All coders, in varied pairings, contributed to this process, with the double-coding being stratified in proportion to the number of videos raters had been allocated for primary coding. The ICCs were 0.75 (95% CI 0.53 to 0.89) for parent proportions and 0.78 (95% CI 0.57 to 0.90) for child proportions.
Outcome estimation
Table 19 shows the baseline and end-point ADOS-2 total scores for the participants by treatment group. In both the TAU and PACT-G groups, changes in ADOS-2 scores within module 1 (non-verbal) and module 2 (older) were small; there was modest improvement (i.e. decline in scores) in module 1 (verbal) and more marked improvement in module 2 (young). The pattern was similar across both the SA and RRB subscales. Outcome estimation by trial group is reported below.
| Scale | Baseline | End point | ||||
|---|---|---|---|---|---|---|
| TAU | PACT-G | Overall | TAU | PACT-G | Overall | |
| ADOS-2 total score, n | 127 | 121 | 248 | 118 | 119 | 237 |
| Module 1 (non-verbal), mean (SD) | 21.4 (2.9) | 20.9 (2.5) | 21.2 (2.7) | 20.9 (3.2) | 20.4 (3.4) | 20.6 (3.3) |
| Module 1 (verbal), mean (SD) | 17.6 (3.1) | 17.3 (2.6) | 17.5 (2.9) | 16.8 (4.6) | 16.0 (4.2) | 16.3 (4.4) |
| Module 2 (young), mean (SD) | 15.2 (2.8) | 15.5 (4.0) | 15.3 (3.4) | 11.5 (4.3) | 13.7 (3.6) | 12.6 (4.1) |
| Module 2 (old), mean (SD) | 15.0 (4.4) | 17.7 (3.5) | 16.3 (4.1) | 15.5 (3.2) | 17.3 (3.5) | 16.4 (3.4) |
| ADOS-2 total score, mean (SD) | 18.6 (4.0) | 18.8 (3.6) | 18.7 (3.8) | 17.5 (5.0) | 17.6 (4.5) | 17.6 (4.8) |
| ADOS-2 SA, mean (SD) | ||||||
| Module 1 (non-verbal) | 16.4 (2.7) | 16.1 (2.1) | 16.3 (2.4) | 16.4 (2.5) | 15.7 (2.5) | 16.0 (2.5) |
| Module 1 (verbal) | 13.9 (2.6) | 13.3 (2.5) | 13.7 (2.5) | 12.8 (3.7) | 12.6 (3.2) | 12.7 (3.4) |
| Module 2 (young) | 12.4 (3.0) | 12.1 (2.9) | 12.3 (2.9) | 10.1 (4.2) | 11.3 (3.1) | 10.7 (3.7) |
| Module 2 (old) | 11.8 (3.5) | 13.8 (2.5) | 12.8 (3.2) | 11.8 (2.8) | 13.7 (2.6) | 12.7 (2.8) |
| ADOS-2 SA total score | 14.5 (3.3) | 14.5 (2.8) | 14.5 (3.1) | 13.8 (4.0) | 13.8 (3.3) | 13.8 (3.6) |
| ADOS-2 RRB, mean (SD) | ||||||
| Module 1 (non-verbal) | 5.0 (1.5) | 4.8 (1.6) | 4.9 (1.6) | 4.5 (1.6) | 4.8 (1.5) | 4.6 (1.6) |
| Module 1 (verbal) | 3.7 (1.5) | 3.9 (1.5) | 3.8 (1.5) | 3.9 (1.8) | 3.3 (1.7) | 3.6 (1.8) |
| Module 2 (young) | 2.8 (1.2) | 3.4 (1.4) | 3.1 (1.3) | 1.4 (0.9) | 2.4 (1.5) | 1.9 (1.3) |
| Module 2 (old) | 3.2 (1.7) | 3.9 (1.4) | 3.5 (1.6) | 3.8 (1.6) | 3.7 (1.9) | 3.7 (1.7) |
| ADOS-2 RRB total score | 4.1 (1.7) | 4.3 (1.6) | 4.2 (1.7) | 3.8 (1.9) | 3.8 (1.8) | 3.8 (1.9) |
| RBQ, n | 119 | 115 | 234 | 100 | 105 | 205 |
| RBQ – sensory motor, mean (SD) | 10.9 (5.3) | 9.4 (4.7) | 10.1 (5.1) | 10.2 (5.4) | 9.1 (5.3) | 9.6 (5.4) |
| RBQ – insistence on sameness, mean (SD) | 8.6 (6.4) | 8.3 (5.9) | 8.5 (6.1) | 8.6 (6.2) | 7.8 (5.6) | 8.2 (5.9) |
| SCQ, n | 127 | 121 | 248 | – | – | – |
| SCQ total score, mean (SD) | 23.4 (5.2) | 23.6 (5.4) | 23.5 (5.3) | – | – | – |
The language and communication scores from Table 20 show that, at baseline, > 40% of the sample were at the basal level of the receptive one-word test and almost 50% were at the basal level of the expressive one-word test, with these percentages decreasing by around 8% at the end point in each case. Improvement was also seen in the MCDI measure at the end point. In other secondary outcomes (Table 21), except for education reported VABS composite, all cells show changes in the expected direction.
| Scale | Baseline | End point | ||||
|---|---|---|---|---|---|---|
| TAU | PACT-G | Overall | TAU | PACT-G | Overall | |
| Language scores, n | 127 | 120 | 247 | 118 | 116 | 234 |
| Receptive one word, n at basal level | 57 | 46 | 103 | 42 | 39 | 81 |
| Receptive one word (raw score), mean (SD) | 29.4 (22.5) | 32.1 (19.3) | 30.8 (20.9) | 42.2 (21.9) | 43.2 (20.0) | 42.7 (20.9) |
| Expressive one word, n at basal level | 62 | 58 | 120 | 52 | 49 | 101 |
| Expressive one word (raw score), mean (SD) | 28.2 (19.2) | 32.0 (12.9) | 30.1 (16.4) | 42.0 (21.7) | 42.5 (18.5) | 42.2 (20.1) |
| MCDI, n | 120 | 119 | 239 | 101 | 107 | 208 |
| MCDI words understood, mean (SD) | 202.4 (128.4) | 213.4 (134.7) | 207.9 (131.4) | 260.6 (130.6) | 264.8 (121.9) | 262.8 (125.9) |
| MCDI words understood and said, mean (SD) | 139.1 (141.5) | 152.1 (144.3) | 145.6 (142.8) | 188.7 (156.1) | 175.7 (159.3) | 182.0 (157.5) |
| VEPS, n | 124 | 116 | 240 | – | – | – |
| VEPS social response, mean (SD) | 2.6 (3.4) | 2.7 (3.2) | 2.7 (3.3) | – | – | – |
| VEPS joint attention, mean (SD) | 6.3 (5.4) | 6.1 (5.2) | 6.2 (5.3) | – | – | – |
| VEPS – symbolic total, mean (SD) | 4.1 (5.0) | 3.8 (4.2) | 3.9 (4.6) | – | – | – |
The researcher BOSCCs were collected at baseline and the end point, whereas the BOSCC/DCMAs with the parent and with the LSA were collected at baseline, the 7-month mid-point and the end point. All cells in Table 22 show changes in the expected direction for the BOSCC. On average, the mid-point assessments were completed 7.3 months after randomisation, with a range of 4.7–10.9 months. End-point assessments were completed, on average, 12.2 months after randomisation, with a range of 10.5–15.6 months. Changes in the DCMA were small for the TAU group, but for the PACT-G group there was some improvement for LSAs, and more marked improvement for parents, by the mid-point, with some loss of the gains by the end point.
Primary outcome analysis
Univariate logistic regression was used to detect if any further baseline variables were predictive of missing primary outcome data. No baseline variables were seen to predict missingness beyond those that would already be included in the model (stratifiers and baseline measures of the scale), so no others were included.
The end-point ADOS-2 algorithm score was treated as a continuous variable, with the baseline score as a covariate and randomisation factors included. Three regression relationships were estimated, one for each of the strata defined by the ADOS-2 module [module 1 (non-verbal), module 1 (verbal), module 2] at the end point (Table 23). Regression residual plots were checked within each strata. These showed no evidence of non-normality (see Appendix 1). A single estimate of the treatment effect was obtained by pooling the three stratum-specific ES estimates using the minimum variance estimator. As shown in Table 19, the ITT analysis did not detect an effect of the intervention on the primary outcome of ADOS-2 at the end point. To be consistent with the treatment main effects analysis, the test of difference in treatment effect by age group was based on the bootstrap p-value of > 5000 replicates of the pooled within-ADOS-2 stratum estimate of the treatment difference.
| Scale | Baseline | End point | ||||
|---|---|---|---|---|---|---|
| TAU | PACT-G | Overall | TAU | PACT-G | Overall | |
| Non-verbal IQ | ||||||
| Non-verbal IQ, n | 127 | 121 | 248 | |||
| Mullen – visual standard t-score, mean (SD) | 25.2 (11.7) | 22.9 (8.0) | 24.1 (10.1) | |||
| Mullen – visual raw score, mean (SD) | 28.3 (7.8) | 28.5 (7.0) | 28.4 (7.4) | |||
| Mullen – fine motor standard t-score, mean (SD) | 22.8 (8.6) | 21.8 (7.3) | 22.3 (8.0) | |||
| Mullen – fine motor raw score, mean (SD) | 26.3 (6.9) | 27.2 (6.5) | 26.7 (6.7) | |||
| SNC – standard score, mean (SD) | 55.0 (15.6) | 55.0 (15.6) | ||||
| VABS composite standard score | ||||||
| VABS – parent, n | 127 | 120 | 247 | 111 | 117 | 228 |
| VABS – parent, mean (SD) | 62.2 (10.3) | 61.6 (8.9) | 61.9 (9.6) | 63.9 (12.8) | 62.7 (11.5) | 63.3 (12.2) |
| VABS – teacher, n | 117 | 110 | 227 | 103 | 105 | 208 |
| VABS – teacher, mean (SD) | 58.9 (15.7) | 57.4 (14.1) | 58.2 (14.9) | 58.1 (16.5) | 58.9 (16.5) | 58.5 (16.5) |
| Child Health Utility, n | 116 | 114 | 230 | 103 | 104 | 207 |
| Child Health Utility, mean (SD) | 17.4 (5.4) | 16.7 (5.3) | 17.0 (5.3) | 16.4 (5.3) | 15.5 (4.6) | 15.9 (5.0) |
| Strength and Difficulties total score | ||||||
| SDQ – teacher, n | 123 | 113 | 236 | 104 | 105 | 209 |
| SDQ – teacher, mean (SD) | 17.4 (4.5) | 17.7 (4.8) | 17.5 (4.6) | 17.2 (5.1) | 16.2 (4.7) | 16.7 (4.9) |
| SDQ – parent, n | 118 | 118 | 236 | 102 | 107 | 209 |
| SDQ – parent, mean (SD) | 19.1 (4.4) | 18.3 (4.6) | 18.7 (4.5) | 18.5 (5.3) | 17.2 (5.1) | 17.8 (5.2) |
| WEMWBS, n | 117 | 117 | 234 | 103 | 104 | 207 |
| WEMWBS – total, mean (SD) | 49.6 (9.0) | 48.9 (9.9) | 49.2 (9.5) | 48.8 (9.5) | 50.6 (9.9) | 49.7 (9.7) |
| TOPSE, n | 120 | 113 | 233 | 99 | 106 | 205 |
| TOPSE, mean (SD) | 368.7 (57.2) | 368.5 (53.5) | 368.6 (55.3) | 370.5 (55.5) | 379.8 (53.1) | 375.3 (54.3) |
| Assessment | Baseline | Mid-point | End point | ||||||
|---|---|---|---|---|---|---|---|---|---|
| TAU | PACT-G | Overall | TAU | PACT-G | Overall | TAU | PACT-G | Overall | |
| BOSCC | |||||||||
| Researcher, n | 124 | 114 | 238 | 118 | 115 | 233 | |||
| Researcher, mean (SD) | 39.9 (9.3) | 40.0 (8.3) | 40.0 (8.8) | 37.0 (10.9) | 37.0 (11.2) | 37.0 (11.0) | |||
| LSA, n | 119 | 118 | 237 | 114 | 111 | 225 | 111 | 112 | 223 |
| LSA, mean (SD) | 37.8 (9.8) | 38.7 (10.0) | 38.2 (9.9) | 35.2 (10.1) | 36.8 (11.0) | 36.0 (10.6) | 35.1 (11.5) | 36.4 (11.6) | 35.7 (11.5) |
| Parent, n | 124 | 112 | 236 | 109 | 112 | 221 | 112 | 115 | 227 |
| Parent, mean (SD) | 36.1 (9.4) | 36.7 (8.7) | 36.4 (9.1) | 33.5 (10.1) | 34.9 (10.6) | 34.2 (10.4) | 33.7 (9.8) | 34.4 (11.3) | 34.0 (10.6) |
| DCMA: LSA | |||||||||
| LSA, n | 125 | 119 | 244 | 109 | 113 | 222 | 110 | 114 | 224 |
| LSA synchronous response, mean (SD) | 0.32 (0.14) | 0.31 (0.13) | 0.31 (0.13) | 0.34 (0.12) | 0.46 (0.18) | 0.40 (0.16) | 0.32 (0.12) | 0.44 (0.17) | 0.38 (0.16) |
| Child, n | 125 | 118 | 243 | 109 | 112 | 221 | 109 | 113 | 222 |
| Child initiations, mean (SD) | 0.26 (0.17) | 0.24 (0.19) | 0.25 (0.18) | 0.24 (0.18) | 0.32 (0.22) | 0.28 (0.20) | 0.25 (0.18) | 0.32 (0.21) | 0.29 (0.20) |
| DCMA: parent | |||||||||
| Parent, n | 124 | 121 | 245 | 115 | 112 | 227 | 115 | 115 | 230 |
| Parent synchronous response, mean (SD) | 0.35 (0.11) | 0.33 (0.13) | 0.34 (0.12) | 0.37 (0.14) | 0.47 (0.18) | 0.42 (0.17) | 0.36 (0.13) | 0.43 (0.18) | 0.40 (0.16) |
| Child, n | 124 | 121 | 245 | 114 | 110 | 224 | 113 | 115 | 228 |
| Child initiations, mean (SD) | 0.29 (0.21) | 0.26 (0.20) | 0.28 (0.20) | 0.25 (0.21) | 0.36 (0.25) | 0.30 (0.24) | 0.24 (0.20) | 0.29 (0.22) | 0.27 (0.21) |
| ADOS-2 | Unstandardised effect | Standard error | Standardised effect (95% CI) |
|---|---|---|---|
| Module 1 (non-verbal), n = 96 | –0.45 | 0.59 | –0.13 (–0.48 to 0.21) |
| Module 1 (verbal), n = 82 | –1.18 | 0.81 | –0.27 (–0.63 to 0.09) |
| Module 2, n = 59 | 1.48 | 0.83 | 0.36 (–0.04 to 0.75) |
We mapped the change in the ADOS-2 algorithm scores to the CSS, which allows comparison across ADOS-2 modules. Shown in Figure 7, there was little difference between the distributions expected for the study participants undergoing PACT-G treatment and those undergoing TAU, with expected rates in the non-autism 1–3 range of 2.6% and 2.5%, in the autism 4–5 range of 7.3% and 6.9%, in the autism 6–8 range of 78.3% and 75.5%, and in the high-severity cut-off range of 11.8% and 15.1%, respectively.
FIGURE 7.
Distributions of CSS outcome. Plotted by treatment group at the end point for all participants, as implied by the estimated effect on the ADOS-2 algorithm total score (the mapping of scores was carried out using Stata’s multiple imputation command using nearest neighbour matching of predicted scores and the published 18-stratum total score to the CSS algorithm).

Primary outcome complier-average causal effect estimator
In the PACT-G group, out of 121 observations, there was a median of 10 (IQR 8–12) acceptable parent sessions, with an IQR of 2–12 and, from 117 observations, a median of 8 (IQR 5–10) acceptable LSA sessions, with an IQR of 0–12. An instrumental variable estimator of a CACE was calculated. Treatment receipt was measured as the number of acceptable sessions with a parent and LSA. We report the estimated effect of receiving a total of eight sessions across home or educational settings (the TAU group being considered as receiving no sessions), which was the minimum number of sessions therapists and the research team took to constitute a delivered treatment. The across-strata, pooled CACE estimate for a dose of eight sessions was non-significant (–0.02; p = 0.755). To reach the minimum clinically significant change of 0.28, 112 sessions would be required.
Secondary outcomes
Table 24 shows the effect estimates for all secondary measures and composites.
| Outcome | Estimated treatment effect | 95% CI | p-value |
|---|---|---|---|
| Primary outcome | |||
| ADOS-2 | –0.04 | –0.26 to 0.18 | 0.734 |
| Secondary outcomes | |||
| BOSCC – parent | 0.01 | –0.19 to 0.21 | 0.889 |
| BOSCC – teacher | –0.001 | –0.18 to 0.18 | 0.991 |
| BOSCC – researcher | –0.03 | –0.31 to 0.25 | 0.850 |
| DCMA – parent synchrony | 0.54 | 0.39 to 0.69 | < 0.001 |
| DCMA – LSA synchrony | 0.32 | 0.14 to 0.49 | < 0.001 |
| DCMA – child initiations with a parent | 0.27 | 0.12 to 0.41 | < 0.001 |
| DCMA – child initiations with a LSA | 0.21 | 0.06 to 0.36 | 0.005 |
| Language composite | –0.03 | –0.15 to 0.10 | 0.671 |
| Anxiety composite | –0.01 | –0.54 to 0.52 | 0.978 |
| Repetitive behaviour composite | 0.001 | –0.35 to 0.35 | 0.997 |
| Adaptive behaviour composite | 0.01 | –0.15 to 0.18 | 0.651 |
| Parent well-being composite | 0.44 | 0.08 to 0.79 | 0.016 |
| CHU9D | –0.09 | –0.34 to 0.15 | 0.450 |
| Disruptive behaviour composite | –0.29 | –0.57 to –0.01 | 0.046 |
| ADOS-2 split by age group | |||
| Preschool aged | –0.11 | –0.45 to 0.23 | 0.524 |
| School aged | 0.08 | –0.27 to 0.43 | 0.667 |
| Differencea | –0.19 | –0.67 to 0.30 | 0.447 |
| Outcome | Baseline | End point | ||||
|---|---|---|---|---|---|---|
| TAU | PACT-G | Overall | TAU | PACT-G | Overall | |
| Language composite | ||||||
| MCDI, mean (SD) | ||||||
| Words understood | 202.4 (128.4) | 213.4 (134.7) | 207.9 (131.4) | 260.6 (130.6) | 264.8 (121.9) | 262.8 (125.9) |
| Words understood and said | 139.1 (141.5) | 152.1 (144.3) | 145.6 (142.8) | 188.7 (156.1) | 175.7 (159.3) | 182.0 (157.5) |
| Language scores | ||||||
| Receptive one word, n at basal | 57 | 46 | 103 | 42 | 39 | 81 |
| Receptive one word, mean (SD) | 29.4 (22.5) | 32.1 (19.3) | 30.8 (20.9) | 42.2 (21.9) | 43.2 (20.0) | 42.7 (20.9) |
| Expressive one word, n at basal | 62 | 58 | 120 | 52 | 49 | 101 |
| Expressive one word, mean (SD) | 28.2 (19.2) | 32.0 (12.9) | 30.1 (16.4) | 42.0 (21.7) | 42.5 (18.5) | 42.2 (20.1) |
| PLS | ||||||
| Receptive, mean (SD) | 59.5 (18.9) | 57.7 (13.7) | 58.7 (16.6) | |||
| Expressive, mean (SD) | 59.3 (20.0) | 57.5 (14.9) | 58.4 (17.7) | |||
| Anxiety composite, mean (SD) | ||||||
| SDQ | ||||||
| Teacher emotional | 2.1 (1.9) | 2.2 (2.1) | 2.1 (2.0) | 2.5 (1.9) | 2.2 (1.9) | 2.3 (1.9) |
| Parent emotional | 3.1 (2.1) | 2.5 (2.2) | 2.8 (2.2) | 3.0 (2.2) | 2.6 (2.1) | 2.8 (2.1) |
| DBC | ||||||
| Anxiety subscale | 5.3 (4.1) | 6.2 (4.1) | 5.7 (4.1) | |||
| Repetitive behaviour composite, mean (SD) | ||||||
| SCQ | ||||||
| Parent repetitive | 6.5 (1.8) | 6.4 (1.7) | 6.5 (1.7) | |||
| RBQ | ||||||
| Insistence on sameness | 8.6 (6.4) | 8.3 (5.9) | 8.5 (6.1) | 8.6 (6.2) | 7.8 (5.6) | 8.2 (5.9) |
| Sensory motor | 10.9 (5.3) | 9.4 (4.7) | 10.1 (5.1) | 10.2 (5.4) | 9.1 (5.3) | 9.6 (5.4) |
| Adaptive behaviour composite, mean (SD) | ||||||
| SDQ | ||||||
| Teacher prosocial | 1.6 (1.9) | 1.8 (2.0) | 1.7 (1.9) | 2.2 (2.5) | 2.5 (2.3) | 2.3 (2.4) |
| Parent prosocial | 2.4 (2.1) | 2.6 (2.2) | 2.5 (2.1) | 3.2 (2.4) | 3.5 (2.3) | 3.4 (2.4) |
| VABS | ||||||
| Parent | 62.2 (10.3) | 61.6 (8.9) | 61.9 (9.6) | 63.9 (12.8) | 62.7 (11.5) | 63.3 (12.2) |
| Teacher | 58.9 (15.7) | 57.4 (14.1) | 58.2 (14.9) | 58.1 (16.5) | 58.9 (16.5) | 58.5 (16.5) |
| Parent well-being, mean (SD) | ||||||
| WEMWBS total | 49.6 (9.0) | 48.9 (9.9) | 49.2 (9.5) | 48.8 (9.5) | 50.6 (9.9) | 49.7 (9.7) |
| TOPSE | 368.7 (57.2) | 368.5 (53.5) | 368.6 (55.3) | 370.5 (55.5) | 379.8 (53.1) | 375.3 (54.3) |
| Child health-related quality of life, mean (SD) | ||||||
| CHU9D | 17.4 (5.4) | 16.7 (5.3) | 17.0 (5.3) | 16.4 (5.3) | 15.5 (4.6) | 15.9 (5.0) |
| Disruptive behaviour composite, mean (SD) | ||||||
| DBC | ||||||
| Disruptive | 12.9 (9.8) | 14.7 (9.2) | 13.8 (9.5) | |||
| SDQ | ||||||
| Disruptive subscale | 2.9 (1.5) | 2.8 (1.9) | 2.9 (1.7) | 3.0 (1.7) | 2.4 (1.5) | 2.7 (1.7) |
Significant changes are seen on the parent and LSA DCMA measures, which are the proximal target behavioural mediators of the therapy (Table 22). Similarly, the child initiations, as measured using the DCMA with both parents and LSAs, also show significant effects. The BOSCC measure, an observational measure of autism-specific behaviours, showed no significant change in any of the three settings of interaction with a parent, LSA and researcher. Parent-reported measures of language, anxiety, repetitive and adaptive behaviour, and an overall measure of child health-related quality of life showed no effect. There was significant improvement in parent- and teacher-reported child disruptive behaviour and parental well-being (Table 25).
Overall outcomes
Figure 8 shows the pattern of treatment effect across all planned outcomes, with directions of effects signed with beneficial effects on the right-hand side of the null.
FIGURE 8.
The ESs of the primary and secondary outcomes. rev, reversed.

Adverse events
Table 26 shows AEs collated by treatment group. There were 46 AEs, with six of these classified as serious. Seven events were possibly related to the study, and these were balanced across treatment arms. One serious AE was deemed possibly related to the study: an impact on a parent’s mental health because of the autism diagnostic process and collaborative nature of therapy received.
| Event characteristic | Treatment group, n (%) | Overall, n (%) | |
|---|---|---|---|
| TAU | PACT-G | ||
| Is the event serious? | |||
| No | 20 (90.9) | 20 (83.3) | 40 (87.0) |
| Yes, requires hospitalisation | 2 (9.1) | 2 (8.3) | 4 (8.7) |
| Yes, persistent or significant disability | 0 (0.0) | 2 (8.3) | 2 (4.3) |
| AE-type events (people) | |||
| Reduction in school attendance | 1 (4.5) | 0 (0) | 1 (2.2) |
| Other issues with school | 1 (4.5) | 1 (4.2) | 2 (4.3) |
| Relationship breakdown (parent) | 0 (0) | 5 (20.8) | 5 (10.9) |
| Significant change in child behaviour or well-being | 13 (59.1) | 11 (45.8) | 24 (52.2) |
| Significant family illness | 1 (4.5) | 1 (4.2) | 2 (4.3) |
| Death in immediate family | 1 (4.5) | 1 (4.2) | 2 (4.3) |
| Other personal/family issue | 4 (18.2) | 3 (12.5) | 7 (15.2) |
| Other | 1 (4.5) | 2 (8.3) | 3 (6.5) |
| Relationship to study | |||
| Possibly related | 4 (18.2) | 3 (12.5) | 7 (15.2) |
| Not related | 18 (81.8) | 21 (87.5) | 39 (84.8) |
Mechanism study
In this planned analysis of treatment effect mechanism, we examined several putative mechanisms between randomisation and outcomes in a series of mediation analyses. As in the primary outcome analysis, estimates are made for each ADOS-2 or BOSCC module, which are then combined into a total score using an inverse variance-weighted estimator. The findings are presented with no adjustment for measurement error in the mediator, and the results are displayed as unstandardised effect estimates.
For each analysis, the results show the estimated effect of treatment on the mediator, the estimated effect of the mediator on the outcome, the estimated indirect effect (the product of the preceding two estimates), the direct effect that represents any other pathway from treatment to outcome that does not act through the mediator being considered and the total effect (the sum of the direct and indirect effects). In Tables 27–33, we present the effect estimates, standard errors, 95% CIs and p-values.
The first model examines mediation of treatment to DCMA parent synchrony at 7 months to ADOS-2 at 12 months (Figure 9).
FIGURE 9.
Model pathway from treatment to ADOS-2 outcome.
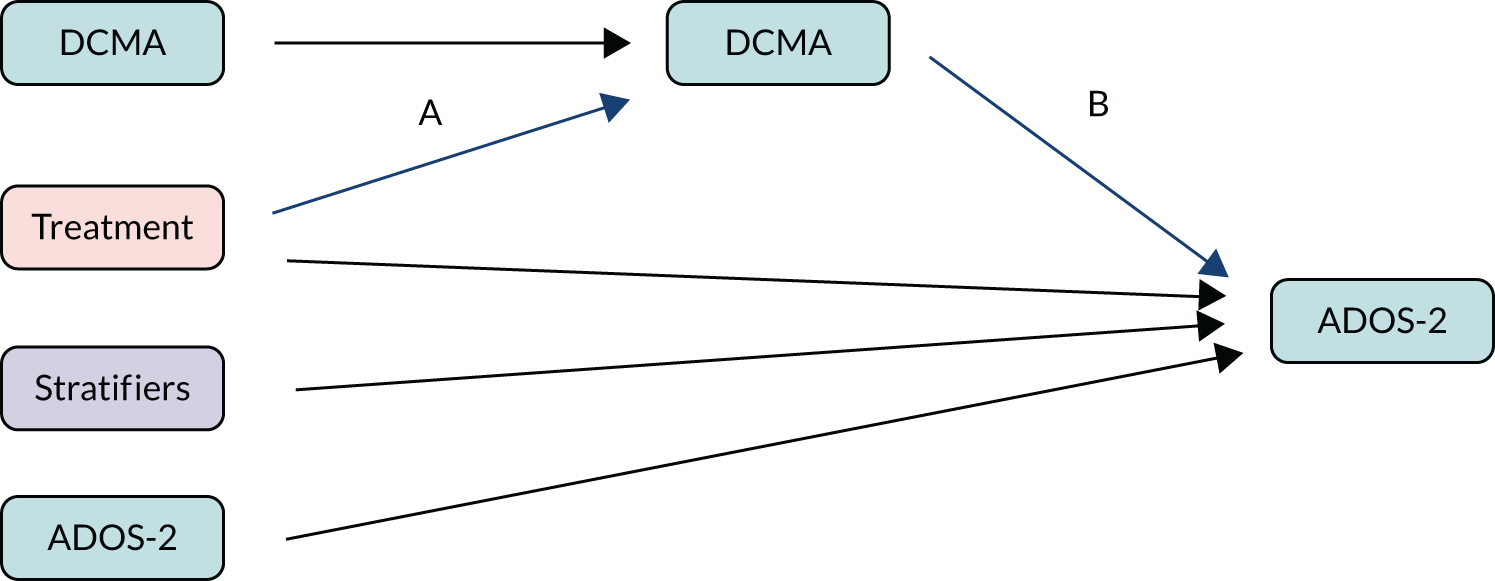
To summarise the findings presented in Table 27, there is no total effect to be mediated (as demonstrated in the primary ITT analysis), but there is a significant effect of treatment on parent synchrony at 7 months (A path) in favour of the PACT-G intervention.
| ADOS-2 | A path (SE); (95% CI); p-value | B path (SE); (95% CI); p-value | Indirect effect (SE); (95% CI); p-value | Direct effect (SE); (95% CI); p-value | Total effect (SE); (95% CI); p-value |
|---|---|---|---|---|---|
| Module 1 (non-verbal), n = 91 | 0.10 (0.03); (0.04 to 0.15); 0.001 | 0.81 (2.29); (–3.68 to 5.30); 0.724 | 0.08 (0.22); (–0.36 to 0.51); 0.727 | –0.52 (0.63); (–1.76 to 0.71); 0.406 | –0.45 (0.59); (–1.60 to 0.71); 0.450 |
| Module 1 (verbal), n = 82 | 0.17 (0.04); (0.10 to 0.24); < 0.001 | 2.85 (2.76); (–2.55 to 8.26); 0.300 | 0.49 (0.49); (–0.46 to 1.45); 0.312 | –1.65 (0.93); (–3.47 to 0.16); 0.074 | –1.18 (0.81); (–2.77 to 0.42); 0.147 |
| Module 2, n = 58 | 0.12 (0.03); (0.06 to 0.18); < 0.001 | –0.93 (4.07); (–8.91 to 7.04); 0.819 | –0.11 (0.49); (1.06 to 0.84); 0.818 | 1.60 (0.96); (–0.29 to 3.49); 0.096 | 1.48 (0.83); (–0.15 to 3.12); 0.075 |
| Overall | 0.12 (0.02); (0.09 to 0.16); < 0.001 | 1.24 (1.62); (–1.93 to 4.40); 0.444 | 1.33 (1.42); (–1.45 to 4.12); 0.347 | –0.32 (0.46); (–1.22 to 0.58); 0.486 | –0.16 (0.41); (–0.97 to 0.65); 0.699 |
We found no association between parent synchrony at 7 months and ADOS-2 at 11 months (B path), and the indirect effect is non-significant, which we concluded was because of the non-significant B paths.
We see the opposite signs for the B path in module 2 than those seen in module 1: an increase in parent synchrony leads to lower ADOS-2 scores in module 2, but to higher ADOS-2 scores in module 1. This leads to the indirect effects having opposite signs between module 2 and module 1, and opposite signs to the direct and total effects, where module 1 showed improvement and module 2 showed worsening.
This direct effect reduced symptom severity in module 1, but increased symptom severity in module 2 [the positive coefficient indicating a worse (higher) score in the PACT-G group]. The negative coefficient for the overall direct effect indicates a reduction in ADOS-2 independent of the mediator, although this effect is non-significant.
In the analysis shown in Table 28, we consider child initiations at 7 months as the mediator, and find that the A path shows significant treatment effect on child initiations at 7 months in module 1 (verbal) and module 2, but not in module 1 (non-verbal). Overall, there is a significant effect in favour of the PACT-G intervention. As with parent synchrony, there is no association between child initiations at 7 months and ADOS-2 at 12 months. There are no significant mediated effects, and the direct effects have the same pattern as with parent synchrony, described previously.
| ADOS-2 | A path (SE); (95% CI); p-value | B path (SE); (95% CI); p-value | Indirect effect (SE); (95% CI); p-value | Direct effect (SE); (95% CI); p-value | Total effect (SE); (95% CI); p-value |
|---|---|---|---|---|---|
| Module 1 (non-verbal), n = 91 | 0.03 (0.03); (–0.03 to 0.09); 0.336 | 1.11 (2.15); (–3.10 to 5.31); 0.605 | 0.03 (0.08); (–0.11 to 0.18); 0.654 | –0.52 (0.59); (–1.68 to 0.65); 0.386 | –0.45 (0.59); (–1.60 to 0.71); 0.450 |
| Module 1 (verbal), n = 82 | 0.14 (0.04); (0.07 to 0.22); < 0.001 | 2.42 (2.52); (–2.52 to 7.36); 0.337 | 0.35 (0.38); (–0.39 to 1.09); 0.356 | –1.45 (0.89); (–3.18 to 0.29); 0.103 | –1.18 (0.81); (–2.77 to 0.42); 0.147 |
| Module 2, n = 58 | 0.10 (0.05); (0.01 to 0.19); 0.033 | –4.56 (2.50); (–9.45 to 0.34); 0.68 | –0.44 (0.31); (–1.04 to 0.16); 0.151 | 1.88 (0.83); (0.26 to 3.50); 0.023 | 1.48 (0.83); (–0.15 to 3.12); 0.075 |
| Overall | 0.08 (0.02); (0.04 to 0.12); < 0.001 | –0.20 (1.37); (–2.88 to 2.48); 0.882 | 1.30 (1.42); (1.48 to 4.08); 0.359 | –0.10 (0.42); (–0.93 to 0.73); 0.820 | –0.16 (0.41); (–0.97 to 0.65); 0.699 |
Table 29 shows that there is a significant effect of treatment on LSA synchrony at 7 months (A path), but there is no association between LSA synchrony at 7 months and ADOS-2 at 12 months (B path). The indirect effect is non-significant because of the non-significant B paths. In this analysis, we see opposite signs for the B path in module 1 (verbal) than in module 1 (non-verbal) and module 2.
| ADOS-2 | A path (SE); (95% CI); p-value | B path (SE); (95% CI); p-value | Indirect effect (SE); (95% CI); p-value | Direct effect (SE); (95% CI); p-value | Total effect (SE); (95% CI); p-value |
|---|---|---|---|---|---|
| Module 1 (non-verbal), n = 96 | 0.10 (0.04); (0.03 to 0.17); 0.007 | –2.82 (1.76); (–6.26 to 0.62); 0.108 | –0.28 (0.20); (–0.68 to 0.12), 0.167 | –0.15 (0.61); (–1.34 to 1.04); 0.805 | –0.45 (0.59); (–1.60 to 0.71), 0.450 |
| Module 1 (verbal), n = 82 | 0.13 (0.03); (0.07 to 0.20); < 0.001 | 3.67 (2.79); (–1.80 to 9.15); 0.189 | 0.49 (0.39); (–0.28 to 1.25); 0.210 | –1.64 (0.87); (–3.35 to 0.07); 0.061 | –1.18 (0.81); (–2.77 to 0.42); 0.147 |
| Module 2, n = 59 | 0.15 (0.03); (0.09 to 0.21); < 0.001 | –0.89 (4.13); (–8.98 to 7.20); 0.829 | –0.14 (0.63); (–1.37 to 1.10); 0.830 | 1.63 (1.08); (–0.49 to 3.75); 0.131 | 1.48 (0.83); (–0.15 to 3.12); 0.075 |
| Overall | 0.13 (0.02); (0.09 to 0.17); < 0.001 | –0.98 (1.40); (–3.72 to 1.77); 0.485 | –0.15 (1.42); (–2.93 to 2.63); 0.915 | –0.24 (0.45); (–1.13 to 0.65); 0.600 | –0.16 (0.41); (–0.97 to 0.65); 0.699 |
The analysis in Table 30 shows a similar pattern to previous findings, demonstrating significant effects of the treatment on child initiations with a LSA at 7 months (A path). As with parent and LSA synchrony, there is no association between child initiations at 7 months and ADOS-2 at 12 months (B path) and, overall, there are no significant mediated effects.
| ADOS-2 | A path (SE); (95% CI); p-value | B path (SE); (95% CI); p-value | Indirect effect (SE); (95% CI); p-value | Direct effect (SE); (95% CI); p-value | Total effect (SE); (95% CI); p-value |
|---|---|---|---|---|---|
| Module 1 (non-verbal), n = 96 | 0.13 (0.05); (0.03 to 0.22); 0.011 | –0.69 (1.31); (–3.26 to 1.89); 0.600 | –0.09 (0.17); (–0.42 to 0.25); 0.608 | –0.39 (0.61); (–1.58 to 0.79); 0.516 | –0.45 (0.59); (–1.60 to 0.71); 0.450 |
| Module 1 (verbal), n = 82 | 0.15 (0.05); (0.05 to 0.24); 0.002 | –0.60 (1.99); (–4.51 to 3.30); 0.762 | –0.09 (0.30); (–0.67 to 0.49); 0.764 | –1.08 (0.87); (–2.78 to 0.62); 0.212 | –1.18 (0.81); (–2.77 to 0.42); 0.147 |
| Module 2, n = 59 | 0.09 (0.05); (0.00 to 0.19); 0.042 | 3.19 (2.64); (–1.98 to 8.36); 0.227 | 0.30 (0.29); (–0.26 to 0.86); 0.292 | 1.18 (0.86); (–0.51 to 2.86); 0.171 | 1.48 (0.83); (–0.15 to 3.12); 0.075 |
| Overall | 0.12 (0.03); (0.07 to 0.18); < 0.001 | –0.10 (1.01); (–2.08 to 1.89); 0.925 | –0.73 (1.42); (–3.51 to 2.04); 0.606 | –0.17 (0.43); (–1.01 to 0.67); 0.695 | –0.16 (0.41); (–0.97 to 0.65); 0.699 |
We repeated these analyses using the same modelling approach, replacing the outcome measures as the BOSCC instead of the ADOS-2. An example is shown in Figure 10. Estimates are shown for each BOSCC module, and then combined into a total score using an inverse variance-weighted estimator.
FIGURE 10.
Model pathway from treatment to BOSCC outcome.

Table 31 shows the results for four different mediators. As these mediators are unchanged, we have already demonstrated that there is a significant treatment effect on each of these (the A paths).
| Mediator at 7 months | A path (SE); (95% CI); p-value | B path (SE); (95% CI); p-value | Indirect effect (SE); (95% CI); p-value | Direct effect (SE); (95% CI); p-value | Total effect (SE); (95% CI); p-value | |
|---|---|---|---|---|---|---|
| Parent synchrony | Module 1, n = 191 | 0.12 (0.02); (0.07 to 0.16); < 0.001 | 0.09 (3.56); (–6.89 to 7.07); 0.980 | 0.01 (0.42); (–0.81 to 0.84); 0.980 | –0.21 (1.12); (–2.39 to 1.98); 0.854 | –0.19 (1.02); (–2.19 to 1.81); 0.854 |
| Module 2, n = 57 | 0.13 (0.03); (0.07 to 0.18); < 0.001 | –10.23 (16.27); (–42.12 to 21.66); 0.529 | –1.30 (2.08); (–5.38 to 2.77); 0.531 | –0.02 (3.86); (–7.60 to 7.55); 0.995 | –1.28 (3.33); (–7.81 to 5.25); 0.700 | |
| Overall | 0.12 (0.02); (0.09 to 0.16); < 0.001 | –0.38 (3.48); (–7.20 to 6.43); 0.912 | –0.21 (0.50); (–1.18 to 0.76); 0.671 | –0.19 (1.07); (–2.29 to 1.91); 0.858 | –0.28 (0.97); (–2.19 to 1.63); 0.773 | |
| Child initiations with a parent | Module 1, n = 191 | 0.07 (0.03); (0.02 to 0.12); 0.003 | –6.82 (3.16); (–13.01 to –0.63); 0.031 | –0.51 (0.29); (–1.08 to 0.07); 0.084 | 0.27 (1.03); (–1.75 to 2.28); 0.796 | –0.20 (1.02); (–2.20 to 1.80); 0.843 |
| Module 2, n = 57 | 0.11 (0.05); (0.02 to 0.20); 0.023 | –18.32 (9.61); (–37.16 to 0.51); 0.057 | –1.98 (1.32); (4.57 to 0.61); 0.133 | 1.19 (3.48); (–5.63 to 8.02); 0.732 | –1.01 (3.42); (–7.73 to 5.70); 0.767 | |
| Overall | 0.08 (0.02); (0.04 to 0.13); < 0.001 | –7.94 (3.00); (–13.82 to –2.06); 0.008 | –0.78 (0.34); (–1.44 to –0.11); 0.022 | 0.34 (0.99); (–1.59 to 2.28); 0.730 | –0.27 (0.98); (–2.18 to 1.65); 0.784 | |
| LSA synchrony | Module 1, n = 191 | 0.11 (0.02); (0.06 to 0.16); < 0.001 | 3.99 (3.22); (–2.33 to 10.30); 0.216 | 0.43 (0.37); (–0.28 to 1.15); 0.235 | –0.62 (1.08); (–2.73 to 1.49); 0.563 | –0.18 (1.02); (–2.17 to 1.82); 0.863 |
| Module 2, n = 57 | 0.17 (0.04); (0.10 to 0.24); < 0.001 | –41.82 (13.45); (–68.18 to –15.45); 0.002 | –6.92 (2.68); (–12.17 to –1.67); 0.010 | 7.58 (4.44); (–1.13 to 16.28); 0.088 | –0.47 (3.86); (–8.03 to 7.09); 0.903 | |
| Overall | 0.13 (0.02); (0.09 to 0.17); < 0.001 | 1.50 (3.13); (–4.64 to 7.64); 0.633 | –0.45 (0.46); (–1.34 to 0.44); 0.324 | –0.17 (1.05); (–2.22 to 1.88); 0.873 | –0.19 (0.98); (–2.12 to 1.73); 0.843 | |
| Child initiations with a LSA | Module 1, n = 191 | 0.12 (0.03); (0.06 to 0.19); < 0.001 | –4.23 (2.38); (–8.90 to 0.44); 0.076 | –0.52 (0.32); (–1.16 to 0.12); 0.109 | 0.29 (1.05); (–1.76 to 2.34); 0.784 | –0.18 (1.02); (–2.18 to 1.82); 0.857 |
| Module 2, n = 57 | 0.14 (0.05); (0.04 to 0.24); 0.008 | –9.30 (9.23); (–27.38 to 8.78); 0.313 | –1.30 (1.39); (–4.02 to 1.42); 0.350 | –0.14 (3.66); (–7.32 to 7.05); 0.971 | –1.37 (3.41); (–8.05 to 5.31); 0.687 | |
| Overall | 0.13 (0.03); (0.07 to 0.18); < 0.001 | –4.55 (2.31); (–9.06 to –0.03); 0.049 | –0.67 (0.37); (–1.40 to 0.06); 0.073 | 0.26 (1.00); (–1.71 to 2.22); 0.800 | –0.28 (0.98); (–2.20 to 1.64); 0.774 | |
We find there are overall effects of child initiations with both the parent and the LSA on the BOSCC score at 12 months. This leads to a statistically significant indirect effect of the treatment through child initiations with the parent (p = 0.022) and weak evidence for an indirect effect of child initiations with the LSA (p = 0.073). All of the direct effects are not statistically significant and, as noted in the primary analysis, there are no statistically significant total effects on the BOSCC.
We tested if there was a mediation of treatment effects between the DCMA measures of parent/LSA synchrony and child initiations at 12 months. The results are shown in Table 32.
| Outcome at 12 months | Mediator at 7 months | A path (SE); (95% CI); p-value | B path (SE); (95% CI); p-value | Indirect effect (SE); (95% CI); p-value | Direct effect (SE); (95% CI); p-value | Total effect (SE); (95% CI); p-value |
|---|---|---|---|---|---|---|
| Child initiations with a parent | Parent synchrony | 0.12 (0.02); (0.08 to 0.16); < 0.001 | 0.46 (0.08); (0.30 to 0.62); < 0.001 | 0.05 (0.01); (0.03 to 0.08); < 0.001 | 0.02 (0.02); (–0.02 to 0.07); 0.341 | 0.08 (0.02); (0.03 to 0.12); 0.001 |
| Child initiations with a LSA | LSA synchrony | 0.11 (0.02); (0.07 to 0.15); < 0.001 | 0.31 (0.09); (0.14 to 0.49); < 0.001 | 0.03 (0.01); (0.01 to 0.06); 0.003 | 0.02 (0.03); (–0.04 to 0.07); 0.508 | 0.05 (0.03); (0.00 to 0.11); 0.048 |
This test demonstrates that there is mediation of the effect of treatment on child initiations with a parent at 12 months through parent synchrony at 7 months, and there is mediation of the effect of treatment on child initiations with a LSA at 12 months through LSA synchrony at 7 months.
One of the assumptions underpinning the analysis approach is the absence of measurement error in the mediator. If present, this could cause a bias in the estimation of the B path and the direct effect, and lead to misleading conclusions. To check this assumption, we extended the structural equation models to allow for measurement error in the mediator by using an approach outlined in Pickles et al. 17 This involves fitting a latent variable model for the repeated measures of the mediator, constraining the factor loadings and measurement error variance across time and ADOS-2 group. We allowed the variance of the factors to vary across ADOS-2 group. The mediator in this model is the latent measure of DCMA at 7 months, which is taken to be a measurement error-free construct. As previously, estimates are shown for each ADOS-2 module, and then combined into a total score using an inverse-weighted estimator. A schematic of the model is shown in Figure 11.
FIGURE 11.
Model allowing for measurement error using repeated measures.

The pattern of results, shown in Table 33, is consistent with those seen previously for the effect of treatment on ADOS-2 mediated through parent synchrony at 7 months. There is no evidence of an association between the mediator and outcome, implying that measurement error was not attenuating this association previously. We display this for one mediation analysis for illustrative purposes.
| ADOS-2 | A path (SE); (95% CI); p-value | B path (SE); (95% CI); p-value | Indirect effect (SE); (95% CI); p-value | Direct effect (SE); (95% CI); p-value | Total effect (SE); (95% CI); p-value |
|---|---|---|---|---|---|
| Module 1 (non-verbal); n = 96 | 1.48 (0.59); (0.31 to 2.64); 0.013 | 0.06 (0.51); (–0.95 to 1.06); 0.909 | 0.09 (0.76); (–1.40 to 1.57); 0.910 | –0.53 (1.02); (–2.53 to 1.46); 0.599 | –0.45 (0.60); (–1.63 to 0.73); 0.457 |
| Module 1 (verbal); n = 82 | 2.14 (0.63); (0.91 to 3.36); 0.001 | 3.36 (8.41); (–13.12 to 19.83); 0.690 | 7.17 (18.95); (–29.97 to 44.31); 0.705 | –8.25 (18.87); (–45.23 to 28.73); 0.662 | –1.13 (0.85); (–2.79 to 0.53); 0.181 |
| Module 2, n = 59 | 1.84 (0.73); (0.40 to 3.28); 0.012 | –2.08 (4.95); (–11.78 to 7.62); 0.674 | –3.83 (10.06); (–23.55 to 15.89); 0.704 | 5.34 (10.18); (–14.62 to 25.30); 0.600 | 1.51 (0.86); (–0.17 to 3.18); 0.079 |
| Overall | 1.80 (0.53); (0.75 to 2.85); 0.001 | 0.05 (0.51); (–0.94 to 1.04); 0.925 | 0.23 (1.17); (–2.06 to 2.53); 0.842 | –0.50 (1.01); (–2.47 to 1.47); 0.620 | –0.16 (0.41); (–0.97 to 0.65); 0.699 |
Figure 12 displays a summary of the mediation analysis findings from Tables 27–33. These need to be understood in relation to the hypothesised chain of effect (found in our previous studies7,14,17,18,54) from the intervention to (1) caregiver adult response to the child in the dyadic context, measured at 7 months; (2) child response to the caregiver adult in that same context, also measured at 7 months; and (3) child response to another adult (researcher) in a generalised research context, measured at 12 months.
In all of these analyses, there was a consistent statistically significant effect of treatment on caregiver synchronous response with the child, indicating that the PACT-G intervention led to a between-group difference effect on the initial target mechanism, as found in our previous studies. The analyses also demonstrated the second hypothesised effect, that is from caregiver synchrony to later child communication initiation, so that the effect on child initiation was mediated through synchrony with the respective partner.
We did not find any evidence of a downstream effect from the mediator to the ADOS-2 outcomes. However, in keeping with our previous work, there was a significant association between child initiation with both the parent and the LSA in home and educational settings, and later symptom change on the BOSCC at 12 months, and a significant indirect effect was estimated through the parent synchrony measure.
Chapter 9 Discussion
Aims
This trial addressed a number of contemporary challenges in autism intervention research. The first was extending a manualised, largely clinic-based treatment within the naturalistic community settings of home and education, and, for added efficiency, including use of remote video-conferencing sessions, in addition to in-person delivery. Second, we introduced parallel home and education therapy for the child, with the aim of reinforcing the child’s developmental learning across contexts and persons. The purpose of this was to address a key difficulty, suggested in many single-subject design studies, that autistic children are thought to have in generalising and implementing acquired skills across contexts11 – a difficulty assumed to place significant limitations on the functional effectiveness of interventions in development. Third, the study extends the intervention into the early school years for children with intellectual disability and autism, whereas most early psychosocial interventions to date have been implemented in the preschool period. In addition, our large and detailed Mechanism study, one that we believe to be by far the most extensive yet in the autism field and perhaps across wider developmental science, provided the opportunity to, for the first time, look in detail at autism symptoms across different contexts and, from our mediation analysis, to investigate processes of generalisation of change through intervention.
This trial addresses current NHS priorities in child development and mental health, for instance the emphasis on therapy delivery within educational contexts in The NHS Long Term Plan. 105 The trial’s focus on autism symptoms as the primary outcome is consistent with our previous work in addressing the core defining characteristics of autism, and supports the mechanistic approach to analysing both proximal and distal effects of intervention and mediation. The data-rich, repeated-measures design provided enhanced power to account for the measurement error in behavioural studies of this kind and allowed mediation/mechanism modelling of the findings.
Strengths and limitations
Validity and measurement
Data from the CONSORT flow diagram (see Figure 5) show highly successful implementation and internal validity in this complex trial. Only one child out of 249 randomised children was lost to end-point analysis under ITT (one participant withdrew from the PACT-G group). Primary outcome analysis was achieved on 118 out of 127 (93%) participants in the TAU group and 119 out of 122 (98%) in the PACT-G group. Overall, attrition was very low, at 8 out of 249 (3.2%) children withdrawing (five in the TAU group and three in the PACT-G group). Data completeness was excellent and did not require imputation strategies. The trial sampling was across three urban/semiurban settings throughout England (i.e. Manchester, London, Newcastle upon Tyne). By using broad inclusion criteria for children with severe autism, we aimed for a broadly representative sampling of autistic children in England.
The intermediate outcome and mechanistic analysis required a very large number of video-interaction captures and structured, blinded video coding. The DCMA coding system of naturalistic social communication between the child and parent or LSA was applied to six captures per participant across the trial, at baseline, mid-point and end point. This resulted in a total of 1610 codings, each taking approximately half an hour of coding time. The BOSCC, a semistructured interactive assessment of child autism symptoms across contexts, was applied to eight captures per participant (home and educational settings at three time points, and the research clinic setting at two time points). This resulted in a total of 2147 codings across the trial, each taking approximately an hour of coding time. Both sets of codings (i.e. DCMA and BOSCC) achieved excellent internal validity and inter-rater reliability. This total of approximately 3500 detailed manualised codings in a repeated-measures design over 1 year, undertaken by UK and US coders, is, we believe, an unprecedented achievement within a developmental science study. Apart from its utility in the mechanism analysis, it represents a unique resource for data-sharing within international autism developmental science. An add-on study using a cohort analysis from these data, additional to our trial protocol, is noted in Appendix 1 as an example of a novel analysis of the comparison of acquired skills in autism development across context and person.
A resulting strength from the mechanistic design and high level of reliable data completion is that this trial has allowed us to successfully address aspects of intervention effects and developmental change in autistic children in a way that we think is unprecedented in autism intervention trials to date.
Intervention adherence
The implementation achieved means of 10 out of 12 (83%) and 8 out of 12 (66%) sessions, delivered through in-person and remote sessions against the intended dose in home and educational settings, respectively; 5.5% of these sessions in home and 5% in education were rated as ‘unacceptable’ (see Chapter 5, Intervention manual fidelity, and Table 13). This compares with a mean 16 out of 18 (89%) session delivery in the original, predominantly clinic-delivered, in-person PACT intervention trial. 7 The figures reflect the challenges of home and, particularly, education environments for delivery of the intervention in PACT-G (for considerations of dosage, see Overall evidence); however, independent fidelity checks on a random sampling of 3.1% of sessions across therapists and time points suggested that delivered sessions that were rated had a similar manual fidelity to the PACT7 fidelity. In addition, six structured collaborative conversations (i.e. HSCs) between parents and LSA were intended per case, with the aim of enhancing the integration of the parallel home and education treatment programmes. However, in practice, the HSC was essentially not achieved, with a mean of 2.2 HSC sessions delivered per case, compared with a prespecified minimum acceptable threshold of three sessions per case.
We have therefore shown that it is possible to deliver an individualised early autism intervention using video feedback in home and educational settings – a finding that is important and relevant in the context of NHS priorities. 105 However, we have also highlighted potential problems with the implementation of and adherence to the intervention, particularly in educational settings. Specific considerations, detailed below in the report, provide important learning for future work of this kind. Feedback from therapists and participants on our online, remotely delivered therapy sessions indicated advantages and disadvantages. Therapists reported that it was often not possible to deliver the full therapy session as planned using the available video-conferencing technology, but also that the video-conferencing sessions were popular with some parents for scheduling reasons. These reflections and experiences are now of greater relevance in the light of the COVID-19 pandemic. 106
Overall evidence
Outcomes estimation
The outcomes estimation for the PACT-G intervention delivered in home and educational settings did not show an effect on child autism symptom severity in the primary outcome research setting or in the home or educational settings. This finding was also seen in the unblinded parent rated measures, where there was no evidence of group difference on the child’s adaptive behaviour, rates of repetitive behaviours or quality of life. Similarly, there was no group difference on the objectively rated language composite.
The more proximal target outcomes of the intervention were, however, achieved in both home and educational settings. These were changes in the quality of adult–child dyadic social communication interaction (adult synchronous response and child communication initiations) with a parent at home and with a LSA (or equivalent) in education. This effect was significant, but at about half the ES on parent–child communication reported in the original PACT. 7 Two other areas where the PACT-G therapy also showed significant positive group difference were in improving parental well-being and reducing child disruptive behaviour. The latter measure is a composite of unblinded ratings by both parents and the teacher, suggesting that the improvement in child disruptive behaviour occurred across home and educational settings.
Mechanism study
The hypothesis of the PACT-G design was that the delivery of the intervention in both home and school contexts in parallel would produce increased opportunities for the autistic child to make overall developmental progress in communication skills, and promote the generalisation of changes in more distal autistic behaviours and skills measured using independently observed symptom outcomes. The mechanism study was designed to test this hypothesis and illuminate the process of generalisation of acquired skills within development. By ‘generalisation’ in this context, as discussed in Chapter 1, we refer both to (1) the generalisation of a newly acquired behaviour or skill from one context into another context of person or environment and (2) the generalisation of an acquired precursor behaviour or skill into a downstream effect on other abilities through a cascading chain of effect across context and through time (what could be termed a ‘homotypic’ vs. a ‘heterotypic’ generalisation).
An example of the heterotypic form of generalisation is intrinsic to the theory behind the PACT-G treatment, and was supported in our mediation analysis from the PACT. 17 Here, a primary targeted enhancement of adult social responsiveness results in an enhancement of child social initiation in a specific dyadic context between them (a chain effect across persons). Then, this child dyadic social initiation generalises into an alteration in child symptoms with another person in another context (generalisation across context, person and developmental skill). To the limited extent that the measure of child symptoms also involves dyadic social initiation from the child, this can be understood as ‘homotypic’ generalisation in the first sense, but for the majority of social affective skills, sensory sensitivities and repetitive and restricted behaviours impacted by PACT treatment, this represented a ‘heterotypic’ generalisation into developmentally related ongoing change. To further test this generalisation model in PACT-G, the trial gathered what is, to the best of our knowledge, an unprecedented quantity of detailed, repeated-measures observational data on functional dyadic communication with parents and LSA, and symptom expression in both home and educational settings, as well as in an independent research setting.
Useful background for considering the results of the PACT-G mechanism study comes from a post hoc analysis of the study cohort using the BOSCC measure to consider independently observed child symptom expression across time and context (see Appendix 1, analysis not specified in the trial protocol). The analysis tracked the expression of autism symptomatology simultaneously across contexts and investigated how change in one context over time may relate to change in the same symptomatology in another context. The analysis found that developmental change in social communication and autism-related behaviours with the parent during the first 7 months of the study was significantly associated with developmental change in the same domains with the LSA in the educational setting over the same period. In addition, these context-specific changes were both independently associated with change in child symptom behaviours in the research context between baseline and the 12-month end point. When changes in both the home and educational settings were modelled together, the home context proved more salient and the education context was no longer significantly associated with symptom change. The analysis suggests, but does not unequivocally prove, ‘generalisation’ or ‘transmission’ from one context to another, as the association could reflect confounding because of intrinsic developmental progression in the child expressed simultaneously in different contexts. The theory of the PACT-G intervention was based on a presumption of the existence of these kinds of generalising developmental effects across contexts in autism, and how they could be enhanced. In this treatment trial, for instance, by introducing an intervention to enhance the rate of change of dyadic developmental skills that are precursors to the symptomatology, we could test the potential causal influences between them.
In the event, the findings of the mechanism analysis in the treatment trial context present a mixed picture. The intervention succeeded in improving the precursor dyadic social interaction in both the parent–home and LSA–education contexts as planned. As in our previous work, this improvement in adult synchronous response mediated the improvement in child dyadic social interaction – with this study thereby extending the results of the previous work in showing the effect both between parent and child at home and between LSA and child in education. However, in contrast to the previous PACT, these improvements in precursor dyadic behaviours did not translate into improvement in child symptom outcomes, in the home or educational settings, or in independent researcher assessment. This lack of generalisation to symptom change is all the more striking given the strong mediation in the original PACT from child communication change to symptom outcome improvement in the researcher context. 17 However, despite the lack of symptom outcome change, the mechanism analysis did provide partial evidence to support the full mediation pathway found in the previous PACT. The improvement in child dyadic social communication with an adult (parent in home and LSA in educational settings) mediated change in 12-month BOSCC symptom outcome (see Table 31) – a pattern that was not found in the ADOS-2 outcome. The full mechanism study findings are illustrated in Figure 12.
Interpretation
Outcome effects and the health literature
The lack of primary treatment effect on symptom outcome in this trial is in the context of a wider literature on the impact of early interventions on autism symptoms. Some previous RCTs of parent-mediated video-feedback-aided interventions (e.g. used in PACT-G and in the original PACT7,14) have found positive symptom outcome effects,14,54,107 but others have not. 69,76,108 A relatively intensive treatment model of parent training combined with child intervention reportedly had significant effects on symptoms using the BOSCC measure, but measurement was not independent of therapy context;27 other relatively intensive approaches have not shown symptom change. 25,26,28 On the other hand, the positive effects of the PACT-G intervention in targeted change in adult-child dyadic communication do replicate a number of previous findings on the effectiveness of video-feedback therapy and similar therapies across demographic and cultural contexts. These include studies of children diagnosed with autism;7,23,25,54,108 infants at familial risk of autism in the USA, the UK107–110 and South Asia;76,111 and in non-autistic populations at psychosocial risk. 112–115
In general terms, the PACT-G result is consistent with the commonly reported finding that autism interventions impact proximal intermediate targets, but rarely achieve change in autism symptoms across context and person. 30 The original PACT was one of the few studies that demonstrated a transmission from proximal effects to wider symptom outcome, and, to the best of our knowledge, the only one to date to do so over a lengthy time period. We discuss possible reasons why PACT-G did not achieve the same result in the subsequent sections.
Outcome effects in the education literature
There have been a number of recent trial reports of interventions within the educational setting that are relevant to PACT-G. The closest in style is a RCT, conducted over 1 year, of an individually delivered social communication and educational attainment-focused intervention (DS1-EI) in specialist autism settings in France (day-care hospitals and medicoeducational institutes). 116 Participants comprised 72 children aged 5–9 years with ‘severe’ autism and intellectual disability. 116 Children in the intervention group received 10 hours per week of one-to-one instruction with a trained teacher (considerably more than attempted in PACT-G). The trial found no significant differences in main clinical outcomes reflecting autism symptoms, but educational attainment was significantly improved for the DS1-EI group and led to more students in the intervention group being included in mainstream classrooms at the 3-year end point. Two other intervention studies reported on the implementation of a more classroom level (CTM) approach. A recent, good-quality cluster-randomised trial from the USA of a classroom-embedded, curriculum-based SCERTS intervention delivered by teachers over a school year117 reported a significant small to moderate treatment effect in improving objectively observed social interaction in the classroom. Although this measure does not constitute an autism symptom outcome, it does reflect aspects of social functioning. There was no treatment effect on an observed ‘instructional participation’ component involving emotional regulation and academic involvement, nor on formal language progress. Unblinded parent and teacher reports suggested effects on child social functioning, communication and executive skills. Kaale et al. 118 had previously reported the 12-month follow-up of a teacher-delivered social communication and joint attention skills (JASPER) intervention in preschool-aged children (n = 61), implemented twice daily for 20 minutes over 8 weeks, predominantly in mainstream school settings. The study reported gains in two out of five proximal social communication outcomes, but no improvements in the core autism outcome [measured with the Social Communication Questionnaire – Current (SCQ-C)]. A previous school-based social communication trial for children with language disorder had similar findings. 43 Another systematic review119 reported some positive effects but was based solely on single case study designs. Overall, this relatively small number of studies shows that RCTs for autism can be conducted in educational settings. Results are mixed, with no effects found on autism symptoms, but improvements in social functioning reported in the curriculum-based SCERTS trial117 and on academic performance in the DS1-EI trial. 116 A briefer social communication classroom-based intervention118 achieved results somewhat similar to PACT-G.
In the education context, our PACT-G LSA-delivered intervention was an individually targeted approach that aimed to build synergy with the parallel home-based therapy for an individual child. It was not embedded in the curriculum as a CTM and was delivered with the individual child outside the classroom. Proximal positive change in objectively rated social initiation with a LSA was seen, but this did not translate into autism symptom change. The section below will reflect on possible reasons for this and how they could be further investigated.
We can conclude that this mode of therapy is feasible (albeit with challenges) in educational settings, was acceptable (and, indeed, welcomed by many school teachers and LSAs), and produced communication change between the autistic children and their communication partners. Informal feedback suggested that the education partners often found the method intuitive and appealing as an approach to working with the child and, although the trial did not demonstrate downstream benefits of this dyadic change on adaptation social competency, it did show a significant, albeit modest, effect on reduction in child disruptive behaviour measured across home and educational settings. This is important because emotional and behavioural difficulties are the norm and not the exception in young children with autism and comprehensive approaches to management and care should address these alongside social communication development. 43 We cannot be sure from this current analysis whether or not the reduction in disruptive behaviour was mediated by the identified changes in dyadic interactions, but disruptive behaviours in the classroom are a major issue in practice for educational settings (nurseries and schools) and have an inevitable impact on classroom integration and curriculum access. In this regard, these findings merit further investigation.
Learning points
Lack of generalisation from dyadic effects to autism symptoms
What might explain the lack of generalising transmission to symptom change compared with that found in the original PACT? We consider dosage, therapy environment, treatment fidelity, and the sensitivity and specificity of measures.
Dosage
The original PACT intervention consisted of 18 in-person, parent-mediated therapy sessions, with a median of 16 sessions delivered. 7 In PACT-G, the dosage of comparable parent-mediated sessions differed in three respects: (1) the therapy was delivered at home and not predominantly in the clinic, (2) the maximum number of sessions offered was 12, with a median of 10 delivered and (3) 36% of these were delivered by video conferencing rather than in-person, with 12% of the video-conferencing sessions deemed inadequate, compared with 2% of the in-person sessions. In the educational setting, a median of 8 out of 12 possible sessions were delivered, 34% of which were by video conferencing, with 11% deemed unacceptable, compared with 1% of the in-person sessions (see Table 13). In education, the LSA therapy partner for the child changed in one-third of cases at mid-point, in another third at the end point, and in one-fifth at both time points.
Thus, although the total number of therapy sessions offered overall in PACT-G was greater than in the original PACT, in PACT-G these sessions were divided between parent- and LSA-mediated components, resulting, for instance, in an effective reduction of 40% in the parent-mediated component delivered in PACT-G, compared with what was delivered in PACT (in which there was no comparable educational component). Positive intermediate effects on proximal dyadic outcomes after 12 sessions in the PACT had originally encouraged this design in PACT-G, along with the constraints of mounting parallel delivery across two settings; but, with hindsight, it is possible that this resulted in insufficient therapy dosage in each setting in this trial to achieve the intended result on symptoms. This effect may have been compounded by the inclusion of video-conferencing delivery in one-third of the sessions, and therapists rated video-conferencing delivery to be more commonly compromised than the in-person sessions in both home and education settings. In the educational setting, findings for a classroom-based implementation of a related social communication therapy43 are somewhat similar to PACT-G (with positive proximal effects not translating to longer-term language and social function measures); insufficient dosage was also postulated as a reason in this trial, which consisted of 80 brief teacher-delivered sessions over 2 months. Dosage of the two comprehensive classroom-embedded interventions discussed above (DS1-EI and SCERTS), which achieved objective educational and social interaction gains, respectively, was in effect all day, every day over a school year116,117 and thus delivered with a very substantially higher dose equivalent than in PACT-G.
Consistent with a dose explanation is the fact that the PACT-G additional data collection and video-conferencing sessions delivered in PACT-G produced about half the effect on parent–child dyadic interaction compared with the PACT (PACT-G ES: parent synchrony 0.54, child initiation 0.27; PACT ES: parent synchrony 1.22, child initiations 0.41). Against a dose explanation is our CACE analysis, which demonstrated that simply increasing the dose, assuming a linear dose–response relationship, would fail to produce an effect. In addition, the strong mediation found in the PACT from child dyadic interaction to autism symptom change, should have implied at least some effect on symptoms from our dyadic measures, whereas the current analysis showed otherwise. An alternative explanation could involve non-linear dose threshold effects on the transmission from dyadic interaction to independently observed symptoms, with the lesser ES on proximal measures not sufficient to mediate a change in the child autism symptomatology outcome. Such non-linear effects are commonly found in other treatment modalities,120 but were not tested here.
Multicomponent complexity
Adaptation of the PACT intervention into PACT-G involved a significant increase in multicomponent complexity. The PACT-G intervention was based on a theoretical assumption that a multicomponent therapy delivered in parallel in two contexts could have an additive effect on child learning and outcomes. The rationale for this, as discussed, was that there would be an additive effect between home-based and education-based components of intervention on overall child outcomes. It is possible, however, that the provision of these therapy experiences with two different adults might, in fact, be confusing and contradictory for the autistic child, particularly because the therapeutic process could be at a slightly different stage in each context (see Table 15). While typically developing children, like adults, are used to synthesising diverse and contradictory experiences, it is possible that the combination of this disjunction along with the lower relative dosage, as above, may have made learning slower and less effective. In addition, the HSCs initially designed to maximise co-ordination between home and education therapy often proved impracticable (see Chapter 8, Home–school conversations). In the context of general child development, the hypothesis of additive effects in multicomponent interventions was tested in a significant meta-analysis of 213 universal multicomponent interventions for social and emotional skills development across community and education. 121 Against this starting hypothesis, this study did not find the expected benefit of multicomponent over single-component programmes, speculating that the former are more challenging to implement and also less likely to ensure that critical components are delivered. In a number of ways, the learning points described above also possibly support this view in the current autism context, which could be a matter of consideration for policy and research planning going forward.
Remotely delivered sessions
PACT-G used remote virtual sessions to complement traditional face-to-face delivery. These sessions constituted 36% of home sessions and 34% of education sessions, usually delivered through video conferencing, but sometimes by telephone. In keeping with NHS guidance that recommends that remote sessions are not used to start treatment, all caregivers in PACT-G had two face-to-face sessions prior to any remote delivery. Online sessions needed to be conducted using a secure and NHS-approved video-call platform. For PACT-G, we needed the additional competency of screen-sharing to allow the caregiver and therapist to watch the therapy video together.
During the period of this trial (2016–19), remote online delivery of interventions was still relatively uncommon and posed some related challenges. The online sessions were more likely to be rated as inadequate by therapists (12% of sessions in the home and 11% in education compared with 1% and 2% respectively for in-person sessions). Given the already reduced dosage in this trial compared with previous work, this suggestion from therapists that remote sessions were not fully productive was a concern. Qualitative feedback from therapists about difficulties often related to technical problems in sharing videos. Therapists also reported that they required more regular and longer supervision to deal with the added aspects of online working, as face-to-face sessions were not the same as remote virtual sessions. This included thinking through therapeutic considerations, such as building a trusted relationship (which is an essential element of effective therapy), more regular summarising of techniques, and thinking through positioning in relation to camera and screen. For future practice, there are also challenges such as unequal access to digital technology; issues about whether or not vulnerable caregivers can and will engage with digital content; and personal preferences, as some caregivers did not find it as supportive to their needs.
However, on the positive side, there are some clear potential advantages for virtual delivery over traditional delivery mechanisms. Online delivery can be more convenient, with sessions arranged flexibly around working schedules and child-care arrangements. The video-recording and therapist sessions can be arranged at different times, enabling parent/caregivers to identify a quiet time to focus on their feedback. Teleconference PACT can be delivered in the comfort of the home/caregiver setting, removing the need for travelling, parking or waiting in waiting rooms. Online remote sessions can be more efficient and reduce stress for both professionals and families, releasing professional time, energy and resources to, for instance, see more children and conduct more sessions from their work or home work base. Remote sessions can feel personal and more representative, with the benefit of observing video footage of the child’s daily interaction in their familiar setting. They can remove logistical and geographical barriers. These advantages have been exemplified during the current COVID-19 pandemic when, for much of the period, remote sessions have been the only available resource for many services and it is likely that this will remain as a feature of future service delivery post pandemic. 122,123
We return to these issues in Recommendations for research.
Therapy environment
The therapy environment in both home and educational settings differed considerably from that of the original PACT. Home delivery can be subject to the distractions and interruptions of everyday family life. This was frequently observed in the fidelity ratings, as just 81% of therapy sessions met the fidelity criteria. Although parent feedback in the original PACT33 showed that some parents would prefer home-based and video-conferencing sessions, in terms of convenience, scheduling and avoiding non-attendance at clinic, such acceptability does not necessarily equate to efficacy. Another evaluation that included home-based intervention delivery gave some support for its effect. 9 Further assessment of the impact of parent-mediated video interventions delivered both online and in the home will be needed to more fully evaluate treatment efficacy and effectiveness for this form of delivery.
The educational setting proved considerably more challenging than initially hoped for this individualised and focused intervention, which required delivery to the child from a consistent adult (see below). The mobility in LSA roles and activities across classrooms and years in education, with 34.3% of trial children experiencing a change in LSA by mid-point, 37.9% a change between mid-point and end point, and 20% experiencing multiple change between these points, may be typical within an education environment at this time, but provides an obvious difficulty for delivery of an individualised therapy predicated on consistency of adult delivery. The proportion of session dose adherence achieved in the educational setting (67% of planned sessions were delivered) was also smaller than that in the home context. Although the manual fidelity of sessions sampled from those actually delivered was comparable to or even higher than that of home sessions, it is at least likely that the child’s experience of those sessions will have been compromised by the changes in therapy partner.
A further consideration is the frequency of opportunities for parents and LSAs to practise the PACT-G intervention strategies. In the original PACT, and in PACT-G, parents were asked to practise the strategies learned in the clinic for 30 minutes per day at home. For PACT-G, the same request was made for parents at home, but in the educational setting this was slightly shorter for pragmatic reasons (30 minutes per day, three times per week). A feature of both PACT and PACT-G was that it was not objectively practicable to test adherence to these requests in either home or education contexts; however, informal feedback in PACT-G indicated that this kind of practice was not easy to achieve for LSAs alongside other curriculum demands and this was sometimes similar for parents at home.
Sample and measurement issues
One of the differences between the original PACT and PACT-G is the inclusion of primary school-aged children. For inclusion in the trial, the children’s ability was capped at the minimally verbal level, meaning that this group’s overall developmental level [Mullen’s developmental quotient (DQ)] was considerably lower than that of the preschool sample (see Table 9 and Appendix 2). About one-quarter of the school-aged sample met the criteria for ADOS-2 module 2, but nearly all these children had a DQ ≥ 2 SD below the mean; one-quarter of the preschool sample also met the criteria for module 2, but only half of these children had a DQ > 2 SD below the mean. The proportions in module 1 were relatively balanced for age group, although the school-aged group contained a slightly larger proportion of children in the module 1 (non-verbal) stratum. In sum, at baseline, the preschool subgroup had a wider range of ability, with a proportion (≈ 10%) who were relatively higher functioning and met the criteria for module 2. The school-aged subgroup had lower cognitive functioning (by definition, given the inclusion criteria) and almost all had a low DQ (≥ 2 SD below the standard t-score). It is notable that this was a cognitive DQ function effect, not an autism symptom severity effect; autism severity measured by the ADOS-2 CSS showed balance across the age groups (see Table 10). The potential impact of a lower DQ combined with age on intervention response may, therefore, be a further consideration, although, as above, there is no simple age cohort effect on the outcome estimates.
The ADOS-2 measurement system had evolved between the original PACT and PACT-G, particularly in relation to the module for minimal verbal development. This necessitated a more complex analysis of the ADOS-2 into three strata for this trial, based on end-point developmental module assignment. Considered by module, the treatment ESs show opposite directions by stratum: module 1 (verbal) showing a moderate positive effect of the PACT-G intervention, module 1 (non-verbal) showing a weak positive effect, and module 2 showing a moderate negative effect of treatment compared with TAU (see Table 11). This same diverging pattern by module is seen in the mechanism analysis, where there are opposite signs between ADOS-2 modules for the ‘B paths’ from mediator to outcome (e.g. see Tables 27–29 and Mechanism study). Although this could have been a chance finding, the consistency of the pattern across the primary outcome and mechanism analyses is striking and suggests a need for further consideration of the direction of treatment effects from this therapy across ADOS-2 module, age and DQ.
Implementation issues within education
The current NHS Long Term Plan105 promotes the importance of the education context for community delivery of child and adolescent mental health interventions. However, this is an emerging field of practice and recent literature highlights some of the implementation barriers for cross-agency work of this kind. 124 As described in Chapter 1, there is a distinction to be made between health interventions delivered in a school context (e.g. PACT-G) and interventions embedded in the classroom curriculum. In a small number of studies (as above), the classroom-based approach seems to produce stronger effects, but the tailored approach to an individual child in school may still be theoretically and practically relevant for targeting individual needs effectively.
However, in a review of the implementation of interventions in education contexts, Lendrum and Humphrey124 describe how the expectation on staff to implement an ever-increasing number of new interventions has resulted in scepticism about the permanence and practicability of interventions. 125,126 This is cautionary about any assumption that school-based delivery of health interventions is straightforward, and emphasises the need for clinicians and researchers to work collaboratively with schools, develop meaningful relationships with them and take into account the social ecology and organisational culture of the school in intervention planning. 13,94
Delivering a RCT design in a complex environment, such as educational settings, inevitably places responsibility and pressure on the individuals delivering the intervention. For example, in our study, LSAs were asked not to disclose information about the components of the intervention that they were delivering to the child to maintain the blindness of the research team. Aspects of the trial such as this are contrary to their usual model of practice and support within a school setting. 127 However, rigorous testing of education-based intervention delivery is essential, and LSAs have reported a desire for further training in their roles, which would increase their profile in the school team, their self-efficacy and their job satisfaction. 128,129
PACT-G does show that delivering a high-quality manualised therapy and rigorous experimental trial design in an educational setting is feasible, although there are real challenges, reflected by a lower sessional adherence of the PACT-G intervention and the HSCs and in the reduced effectiveness shown here in comparison with a clinic-delivered intervention. Practical barriers to implementation include the alteration of the child and staff member’s routine in the educational setting, and the need for flexibility and time when working around other daily education priorities and in their delivery of the day-to-day curriculum. Dingfelder and Mandell130 emphasise that, to be useful to practitioners, such information about training and the resource burden of interventions should be reported alongside outcomes. Some comparative evidence suggests improved outcomes for children receiving an intervention in mainstream preschool settings compared with other types of setting. 130 Our implementation seemed feasible across both settings, and one other study,131 which randomised the same autism intervention between either mainstream or special school settings, found no evidence that this made a difference.
The dual delivery model (parents/carers and LSAs) included the idea that PACT-G would enhance a collaborative approach between home and school, with the clinical team as intermediaries/mediators providing support for both of these implementation contexts. Such home–school collaboration is commonly espoused as an ideal. Future work could explore, in more detail than was possible in this study, how this may best be achieved. The literature on home–school collaboration indicates that the most effective interventions are those characterised by a two-way exchange of information (e.g. parent–teacher action research teams, daily report cards, school-to-home notes)132,133 and shared decision-making in the pursuit of mutually determined goals. However, due consideration needs to be given to the range of contextual factors that may facilitate or impede effective collaboration, including policy/legislation, the relational history between a given family and school, and family and school cultural issues (e.g. congruence of beliefs, values and expectations). 133
Conclusions
PACT-G tested an adaptation of the original, essentially clinic-delivered PACT intervention,14,54,63 into a multicomponent parallel home/education intervention. The rationale was that provision of concurrent parallel intervention for the child, embedded in each of these settings, could have an additive effect on overall developmental progress and symptom reduction, thereby enhancing generalisation of treatment effects in a useful way. Therapy sessions were divided across home and educational settings, with the home-based dosage in practice at 60% of the original PACT, and included remote as well as in-person sessions.
The original PACT had demonstrated a mediated effect between the proximal intervention target of change in parent–child dyadic social communication and the child’s social communication and symptoms in a generalised independent research context,17,18 representing a generalisation of treatment effect in both behavioural and developmental senses across person, time and context (see Chapters 1 and 9). The mechanism study within PACT-G aimed to test this same mediation pathway within the home and educational settings, as well as testing the potential for additive mediated effects on research outcomes.
The results show that the therapy produced significant proximal dyadic social communication change between child and adults in both settings, at about half the ES seen with parents in the original PACT. 14 However, there was no generalised treatment effect on the primary outcome of autism symptoms in the outcome research assessment setting or either treatment setting, and also no effect on parent report of language and parent-/teacher-reported adaptive behaviour. There were, by contrast, significant positive secondary outcome effects with small to moderate ESs on improving parental self-reported well-being and teacher-/parent-reported child disruptive behaviour across home and educational settings.
The mechanism study demonstrated a replication, in both home and educational settings, of the original mediation found in PACT between the intervention effect on parental social communication and improved child dyadic social communication. 17 In addition, there was potential evidence of an overall ‘dose–response’ in the intervention on parental synchrony when compared across the PACT and PACT-G studies. In PACT-G, the intervention achieved 60% of overall session dosage compared with PACT, one-third of which were remote video-conferencing sessions, resulting in about half the proximal ES on parent and child dyadic communication compared with PACT. In the original PACT, this treatment effect on child social communication in the dyad, in turn, strongly mediated the overall treatment effect on child autism symptom outcomes. In PACT-G, there was some evidence of this latter mediation pathway, from the improvements found in child dyadic communication in both home and educational settings to change in child end-point BOSCC symptoms. However, this was not sufficient to lead to an overall treatment group effect on symptom outcome. Thus, although we have evidence of the transmission pathway operating as it did in the PACT, the degree of effect seems insufficient to give an overall symptom change. Given that the PACT-G effect on dyadic child–adult interaction is about half the size of that found in the PACT (see above), we have postulated that there may be a dose-threshold effect here on symptom change (albeit, in the light of our CACE analysis, this would need to have been a non-linear effect). We have also postulated explanations for the reduced power of intervention, in terms of environmental factors in home and school, or the impact of the complexity of the multicomponent delivery method.
Implications for health care
The trial has shown that it is feasible to implement a sophisticated video-feedback therapy not only with parents in the home setting (something we and others have demonstrated previously both for autism and other conditions),76,107,111,120,134 but also in educational settings (something rarely attempted in this way; although see Adams et al. 43). Given that current (i.e. 2021) health-care policy in the UK strongly supports the school-based implementation of mental health interventions, this is important evidence of feasibility. The intervention was found to be acceptable and welcome in both settings and, although there were no improvements seen in child generalised autism symptoms or adaptation, there were demonstrated improvements in parental well-being and child disruptive behaviour, which are both of potential clinical value.
Although we have shown some effects in the education environment, it is important to note that the education component of PACT-G was designed not as an embedded standalone education intervention per se, but rather to extend and complement home-based practice by providing implementation of this health intervention in an educational setting (as in current health policy). We did not collect systematic measures of curriculum access or learning progress, and so cannot evaluate any change there; however, evidence from the comparator education-based interventions discussed116,117 suggests that daily classroom-embedded curriculum-based intervention over a longer period than was the case for PACT-G may be needed to achieve noticeable change in school-based performance.
We note other evidence that multicomponent combined education and community interventions similar to PACT-G in other areas of child development have been found to add considerable complexity, and do not seem to confer an additive effect over a single-component intervention;121,135 indeed, the increased complexity may reduce efficacy. Thus, a judgement on the clinical utility of this implementation in the educational setting will depend on whether or not the improved dyadic social communication and reduced disruptive behaviour, both important goals in their own right, are felt to be of sufficient benefit for the intervention investment. Implementation issues within education suggests additional modifications to PACT-G that could be considered in the future to enhance the embeddedness of the intervention within everyday school contexts.
Within the home setting, the flexible home-based and remote online delivery of the intervention was often welcomed by parents and is in line with many recent trends in health-care delivery, particularly accelerated by the COVID-19 pandemic. However, a caveat must be included as to whether or not intervention efficacy and effectiveness are diluted by these modes of delivery. Potential dosage and other contextual effects on intervention effectiveness are critical to consider in generalised implementation. Simple inference from demonstrated efficacy in a clinic-based setting to other modes of delivery cannot be assumed. Therefore, in the future, it will be prudent to advise a reversion to the full 18-session PACT dosage for home-based therapy (for which there was evidence of good efficacy; see Chapter 1); and carefully monitor any diluting effects on treatment fidelity or efficacy of online delivery (see Recommendations for research).
The mechanism analysis in this trial gives further support to part of the theoretical model of PACT-style video-aided intervention in autism, in that enhancement of parental synchronous responsiveness mediates the improved child dyadic social communication. However, there was no overall treatment effect on the symptom outcome measures. Despite this, we did find evidence for a mediation path from increased child dyadic response to reduced autism symptom severity on the BOSCC measure (although not on ADOS-2), in both home and educational settings. This is partial replication of the mediation model developed from the original PACT for a social communication intervention in autism. The finding supports the premise of early social communication-based intervention in aiming for downstream and generalised developmental effects.
Recommendations for research
Remote intervention
An innovation in this trial was the inclusion of alternate remote video-conferencing therapy delivery of sessions along with in-person delivery. Given the rapid current development towards provision of online therapies of all kinds, in mental health and elsewhere, it will be important to build on this trial in evaluating the efficacy of remote and online delivery. One RCT of fully online PACT delivery is in its early stages, and others are planned, including the blended approach used in PACT-G. These further studies of mode of delivery and dose will be critical going forward. As noted above, it cannot be assumed that the efficacy of any therapy from a clinic context will be preserved in online implementation, and specific dose-finding and online implementation studies will need to be a priority across all interventions, including this one, to ensure that there is not a dilution of already evidenced effects in psychosocial treatments going forward.
Dosage threshold
In the light of the lack of transmission across contexts in this trial compared with the previous PACT intervention, and potential explanation of non-linear dose–response, it will be important to further investigate potential dose-threshold effects in the context of a complex intervention that involves video-delivered therapy across different contexts/settings. This recommendation goes hand in hand with further mechanistically focused and adaptive trials on the active components of autism treatments more generally – essential for the field to incrementally move towards more efficient and effective forms of intervention. It is also widely recognised for psychosocial interventions, including in the autism field, that ‘one size does not fit all’. 136 Building further evidence for individualisation and improving the person-fit of different intervention approaches, and components thereof, will require further large-scale mechanistically informed trials, such as the current one and others that adopt ‘new-generation’, so-called adaptive trial designs, such as Sequential Multiple Assignment Randomised Trials (SMART). 137
Multicomponent therapy in the education context
We have seen that there is only a small literature on rigorous trials of therapy for autism in the education context. Given the increasing focus on the education environment as a locus for treatments for improving mental health and well-being in general and in autism in particular, there needs to be more focus on designing and implementing such mechanistic trials in the UK across health and education. For interventions like PACT-G that rely on effective home–school collaboration, research could usefully focus on how this could be optimised.
Fundamental research in autism social development
PACT-G has acquired large-scale data on dyadic communication and autism symptom behaviours of autistic children across different contexts (e.g. at home with a parent, in education with a LSA, in a research environment with a researcher) and across three time points during a 1-year period in trial conditions. This represents, to our knowledge, a unique data resource internationally that could be used to study aspects of the social development of autistic children over time. One of the key perceived areas of difficulty for autistic children has been the generalisation of acquired and related skills across context, person and time – this data set provides an opportunity to study these aspects of skill development, and the potential for follow-up of this cohort into later development. Video-based child interaction data have been a mainstay of the developmental science investigation into early childhood autism and currently there is active interest in sharing such video material across research groups internationally; this large data set will be potentially of great value in that endeavour, the raw data lending themselves to analysis through methods that are the same as or different from those we have used.
Acknowledgements
Families, clinicians and education
The authors gratefully acknowledge the invaluable contribution of all of the participating families, as well as the participating nurseries and schools and referring clinicians.
PACT-G group, therapy, data collection, trial management and administration
Hilary Beach (Manchester University NHS Foundation Trust), Claire Bennett (University of Manchester), Imogen Crook (University of Manchester), Hannah Danvers (Manchester University NHS Foundation Trust), Kate Dartnall (Manchester University NHS Foundation Trust), Hannah Foote (Guy’s & St Thomas’ NHS Trust), Jessica Graham (Newcastle University), Sarah Jamieson (Cumbria, Northumberland, Tyne & Wear NHS Foundation Trust), Anna Kappa (University of Manchester), Anna Knight (Cumbria, Northumberland, Tyne & Wear NHS Foundation Trust), Jo Lowe (University of Manchester), Ruth Madeley (Cumbria, Northumberland, Tyne & Wear NHS Foundation Trust), Deborah Maskell (University of Manchester), Olivia Mitchell (University of Manchester), Francisca Monteiro (King’s College), London, Cat Papastavrou Brooks (University of Manchester), Amelia Pearson (University of Manchester), Leanne Rogan (Newcastle University), Jessica Rose (Guy’s & St Thomas’ NHS Trust), Lisa Slater (Cumbria, Northumberland, Tyne & Wear NHS Foundation Trust), Susanna Vosper (Manchester University NHS Foundation Trust) and Helen Wilson (University of Manchester).
PACT-G additional data collection and video coding
We gratefully acknowledge the contribution of Alana Barnett, Lydia Johnson-Ferguson, Rachel Lisle, Hafsa Rahman and Hafiza Sadiq. The DCMA coders were Lucy Dempster and Laura Kidd. The UK BOSCC coders were Young Ah Kim, Nicole El Hawi, Chloe Hayes, Leonie Luk, Laurie Preston, Rachel Randle and Owen Waddington. The US BOSCC coders were Alex Francisco Aspuru, Niki Bahri, Nurit Benrey, Katherine Byrne, Gabrielle Gunin, Alison Holbrook, Alapika Jatkar, Kassandra Martinez, Allison Megale, Nicole Rosen and Maira Tafolla.
We gratefully acknowledge invaluable training and outstanding collaboration from Professor Cathy Lord, Dr Alison Holbrook (UCLA), Dr Sue Fletcher Watson (Edinburgh) and Sheri Stegall (Western Psychological Services, USA).
Governance
We sincerely thank the following members of the TSC and support during the work: Professor Stuart Logan (chairperson), Professor Anne O’Hare, Professor Liz Pellicano, Professor Emily Jones, Louisa Harrison and Kellie Bell for their valuable guidance. We also thank the members of the Data Monitoring and Ethics Committee, Professor Paul Ramchandani (chairperson), Professor Amanda Farrin and Professor Jacqueline Barnes, for their helpful contribution.
Sponsor and monitor
Manchester University NHS Foundation Trust, Central Research Office, Nowgen Building, Grafton Street M13 9WL. Telephone: 01612764125.
Trial adoption
By NIHR Clinical Research Network: March 2016.
Final trial protocol
V6, July 2018; available from corresponding author (see Appendix 5 for summary of protocol amendments during the trial).
Trial website
http://research.bmh.manchester.ac.uk/pactg/ (accessed June 2021).
Contributions of authors
Jonathan Green (https://orcid.org/0000-0002-0143-181X) (Professor, Child Psychiatry) conceived and led the design of the study and the application for funding, and was chief investigator. He was responsible for the drafting and revision of the report and for the final report submission.
Kathy Leadbitter (https://orcid.org/0000-0002-0744-2800) (Research Fellow, Psychology) conceived and designed the study, and managed and conducted the trials. She contributed to training, supervision and quality assurance of data collection and observational coding; the interpretation of results; and the writing of the report.
Ceri Ellis (https://orcid.org/0000-0002-8735-9993) (Research Associate, Psychology) contributed to the trial design, data collection, coding, data entry, and the writing and editing of the report. She also provided comments on drafts.
Lauren Taylor (https://orcid.org/0000-0002-1821-6163) (Research Assistant, Psychology) was responsible for overseeing the day-to-day running of the research aspects of the study at the London site. This involved participant recruitment and retention, data collection, data entry and data management.
Heather L Moore (https://orcid.org/0000-0002-2999-8332) (Research Assistant, Psychology) contributed to the design of the study and the evaluation of the feasibility and acceptability of the pilot study, and was responsible for data collection and data entry at the Newcastle upon Tyne site.
Sophie Carruthers (https://orcid.org/0000-0003-1616-415X) (Research Assistant, Psychology) contributed to the acquisition, analysis and interpretation of data; and contributed to the drafting of parts of the report.
Kirsty James (https://orcid.org/0000-0002-2657-8148) (Research Assistant, Statistics) co-analysed the quantitative data for the primary and secondary outcomes of the trial.
Carol Taylor (https://orcid.org/0000-0003-3317-2207) (Research Assistant, Speech and Language Therapy) contributed to the design of the study, contributed to the development of the intervention and its adaptation for schools, evaluated the feasibility and acceptability of the pilot study and contributed to the design. She also assessed and monitored the intervention fidelity and the reliability of measures, and contributed to the writing of the report.
Matea Balabanovska (https://orcid.org/0000-0002-3585-1935) (Research Assistant, Psychology) contributed to data acquisition (a substantial part of the BOSCC data, and other data collected during clinic assessments) and the management of BOSCC coding, including main coding processes, video allocations, reliability calculations and also had a minor contribution to the writing of the report (the breakdown of BOSCC videos).
Sophie Langhorne (https://orcid.org/0000-0003-1293-3310) (Research Assistant, Psychology) contributed to observational coding of DCMA data, quality assurance of observational video-coding data and the writing of the report.
Catherine Aldred (https://orcid.org/0000-0002-9686-8685) (Lecturer, Speech and Language Therapy) contributed to the design of the study, the development of the intervention and its adaptation for schools, older children and online use. She was responsible for the training and supervision of the RAs and therapists, the assessment and monitoring of intervention fidelity, liaising with stakeholders, resolving issues and data collection, and contributed to the writing of the report.
Vicky Slonims (https://orcid.org/0000-0003-3339-2365) (Consultant, Speech and Language Therapy) contributed to the original ideas, as well as the design and planning of the study, the development, delivery, measurement and evaluation of the therapy; and contributed to the interpretation and reporting of results, and the plans for implementation and dissemination.
Victoria Grahame (https://orcid.org/0000-0003-4541-7574) (Consultant, Clinical Psychology) was the clinical lead at the Newcastle upon Tyne site, provided weekly supervision to the therapists and also contributed to writing of this report.
Jeremy Parr (https://orcid.org/0000-0002-2507-7878) (Professor, Paediatrics) was the co-investigator and contributed to the funding application, trial design and delivery, attended local and trial co-investigator meetings, co-supervised the Newcastle upon Tyne research team and contributed to drafts of the final report.
Neil Humphrey (https://orcid.org/0000-0002-8148-9500) (Professor, Education) consulted on the adaptation for education/school settings and on the implementation-related aspects of the study.
Patricia Howlin (https://orcid.org/0000-0002-1804-6053) (Professor, Psychology) advised on study design and implementation, assessed treatment fidelity and contributed to the writing of the final report.
Helen McConachie (https://orcid.org/0000-0002-0713-3987) (Professor, Psychology) contributed to the design and planning of the study, co-led and supervised the coding of adult–child interactions and contributed to the writing of the report.
Ann Le Couteur (https://orcid.org/0000-0001-9991-3608) (Professor, Child Psychiatry) contributed to the conception and design of the research and, as research lead for the Newcastle upon Tyne site, was responsible for the training and supervision of the RAs based in Newcastle upon Tyne. She also contributed to the training of RAs across all sites on some of the research measures, contributed to the interpretation of the study findings and to the writing and reviewing of the content of the final report.
Tony Charman (https://orcid.org/0000-0003-1993-6549) (Professor, Psychology) obtained funding, was involved in designing the study and then read, made revisions to and approved the final version of the manuscript.
Richard Emsley (https://orcid.org/0000-0002-1218-675X) (Professor, Methodology and Statistics) contributed to the design of the trial, co-conducted the statistical analysis and also contributed to reading, evaluating and approving the final report.
Andrew Pickles (https://orcid.org/0000-0003-1283-0346) (Professor, Methodology and Statistics) contributed to the design and implementation of the study and led the majority of the analysis and reporting.
Publication
Green J, Leadbitter K, Ellis C, Taylor L, Moore HL, Carruthers S, et al. Combined social communication therapy at home and in education for young autistic children in England (PACT-G): a parallel, single-blind, randomised controlled trial. Lancet Psychiatry 2022;4:307–20.
Data-sharing statement
We will make data available to the scientific community with as few restrictions as feasible, while retaining exclusive use until the publication of major outputs. All data request should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research. The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the MRC, the EME programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the EME programme or the Department of Health and Social Care.
References
- Green J, Leadbitter C, Ellis B, Taylor L, Moore HL, Carruthers S, et al. Combined social communication therapy at home and in education for young autistic children in England (PACT-G): a parallel, single-blind, randomised controlled trial. Lancet Psychiatry 2022;4. https://doi.org/10.1016/s2215-0366(22)00029-3.
- National Institute for Health and Care Excellence . Autism: The Management and Support of Children and Young People on the Autism Spectrum 2013. http://guidance.nice.org.uk/CG170 (accessed 31 January 2013).
- Oono IP, Honey EJ, McConachie H. Parent-mediated early intervention for young children with autism spectrum disorders (ASD). Cochrane Database Syst Rev 2013;4. https://doi.org/10.1002/14651858.CD009774.pub2.
- Sandbank M, Bottema-Beutel K, Crowley S, Cassidy M, Dunham K, Feldman JI, et al. Project AIM: autism intervention meta-analysis for studies of young children. Psychol Bull 2020;146:1-29. https://doi.org/10.1037/bul0000215.
- Lord C, Wagner A, Rogers S, Szatmari P, Aman M, Charman T, et al. Challenges in evaluating psychosocial interventions for autistic spectrum disorders. J Autism Dev Disord 2005;35:695-708. https://doi.org/10.1007/s10803-005-0017-6.
- Green J, Aldred C, Charman T, Le Couteur A, Emsley RA, Grahame V, et al. Paediatric Autism Communication Therapy-Generalised (PACT-G) against treatment as usual for reducing symptom severity in young children with autism spectrum disorder: study protocol for a randomised controlled trial. Trials 2018;19. https://doi.org/10.1186/s13063-018-2881-3.
- Green J, Charman T, McConachie H, Aldred C, Slonims V, Howlin P, et al. Parent-mediated communication-focused treatment in children with autism (PACT): a randomised controlled trial. Lancet 2010;375:2152-60. https://doi.org/10.1016/S0140-6736(10)60587-9.
- Kasari C, Paparella T, Freeman S, Jahromi LB. Language outcome in autism: randomized comparison of joint attention and play interventions. J Consult Clin Psych 2008;76:125-37. https://doi.org/10.1037/0022-006X.76.1.125.
- Kasari C, Lawton K, Shih W, Barker TV, Landa R, Lord C, et al. Caregiver-mediated intervention for low-resourced preschoolers with autism: an RCT. Pediatrics 2014;134:e72-9. https://doi.org/10.1542/peds.2013-3229.
- Warren Z, McPheeters ML, Sathe N, Foss-Feig JH, Glasser A, Veenstra-Vanderweele J. A systematic review of early intensive intervention for autism spectrum disorders. Pediatrics 2011;127:e1303-11. https://doi.org/10.1542/peds.2011-0426.
- Carruthers S, Pickles A, Slonims V, Howlin P, Charman T. Beyond intervention into daily life: a systematic review of generalisation following social communication interventions for young children with autism. Autism Res 2020;13:506-22. https://doi.org/10.1002/aur.2264.
- Paul R. Interventions to improve communication in autism. Child Adolesc Psychiatr Clin N Am 2008;17:835-56. https://doi.org/10.1016/j.chc.2008.06.011.
- Dunst CJ, Raab M, Trivette CM. Characteristics of naturalistic language intervention strategies. J Speech Lang Pathol Appl Behav Anal 2012;5:8-16. https://doi.org/10.1177/1053815113502235.
- Pickles A, Le Couteur A, Leadbitter K, Salomone E, Cole-Fletcher R, Tobin H, et al. Parent-mediated social communication therapy for young children with autism (PACT): long-term follow-up of a randomised controlled trial. Lancet 2016;388:2501-9. https://doi.org/10.1016/S0140-6736(16)31229-6.
- Wodka EL, Mathy P, Kalb L. Predictors of phrase and fluent speech in children with autism and severe language delay. Pediatrics 2013;131:e1128-34. https://doi.org/10.1542/peds.2012-2221.
- Howlin P, Moss P, Savage S, Rutter M. Social outcomes in mid- to later adulthood among individuals diagnosed with autism and average nonverbal IQ as children. J Am Acad Child Adolesc Psychiatry 2013;52:572-8. https://doi.org/10.1016/j.jaac.2013.02.017.
- Pickles A, Harris V, Green J, Aldred C, McConachie H, Slonims V, et al. Treatment mechanism in the MRC preschool autism communication trial: implications for study design and parent-focussed therapy for children. J Child Psychol Psychiatry 2015;56:162-70. https://doi.org/10.1111/jcpp.12291.
- Aldred C, Green J, Emsley R, McConachie H. Brief report: mediation of treatment effect in a communication intervention for pre-school children with autism. J Autism Dev Disord 2012;42:447-54. https://doi.org/10.1007/s10803-011-1248-3.
- French L, Kennedy EMM. Annual Research Review: Early intervention for infants and young children with, or at-risk of, autism spectrum disorder: a systematic review. J Child Psychol Psychiatry 2018;59:444-56. https://doi.org/10.1111/jcpp.12828.
- Schreibman L, Dawson G, Stahmer AC, Landa R, Rogers SJ, McGee GG, et al. Naturalistic developmental behavioral interventions: empirically validated treatments for autism spectrum disorder. J Autism Dev Disord 2015;45:2411-28. https://doi.org/10.1007/s10803-015-2407-8.
- Kasari C, Gulsrud A, Paparella T, Hellemann G, Berry K. Randomized comparative efficacy study of parent-mediated interventions for toddlers with autism. J Consult Clin Psychol 2015;83:554-63. https://doi.org/10.1037/a0039080.
- Shire SY, Gulsrud A, Kasari C. Increasing responsive parent-child interactions and joint engagement: comparing the influence of parent-mediated intervention and parent psychoeducation. J Autism Dev Disord 2016;46:1737-47. https://doi.org/10.1007/s10803-016-2702-z.
- Shire SY, Chang YC, Shih W, Bracaglia S, Kodjoe M, Kasari C. Hybrid implementation model of community-partnered early intervention for toddlers with autism: a randomized trial. J Child Psychol Psychiatry 2017;58:612-22. https://doi.org/10.1111/jcpp.12672.
- Smith T, Iadarola S, Mandell DS, Harwood R, Kasari C. Community-partnered research with urban school districts that serve children with autism spectrum disorder. Acad Pediatr 2017;17:614-19. https://doi.org/10.1016/j.acap.2017.04.017.
- Wetherby AM, Guthrie W, Woods J, Schatschneider C, Holland RD, Morgan L, et al. Parent-implemented social intervention for toddlers with autism: an RCT. Pediatrics 2014;134:1084-93. https://doi.org/10.1542/peds.2014-0757.
- Dawson G, Rogers S, Munson J, Smith M, Winter J, Greenson J, et al. Randomized, controlled trial of an intervention for toddlers with autism: the Early Start Denver Model. Pediatrics 2010;125:e17-23. https://doi.org/10.1542/peds.2009-0958.
- Gengoux GW, Abrams DA, Schuck R, Millan ME, Libove R, Ardel CM, et al. A pivotal response treatment package for children with autism spectrum disorder: an RCT. Pediatrics 2019;144. https://doi.org/10.1542/peds.2019-0178.
- Rogers SJ, Estes A, Lord C, Munson J, Rocha M, Winter J, et al. A multisite randomized controlled two-phase trial of the Early Start Denver Model compared to treatment as usual. J Am Acad Child Adolesc Psychiatry 2019;58:853-65. https://doi.org/10.1016/j.jaac.2019.01.004.
- Charman T. Editorial: trials and tribulations in early autism intervention research. J Am Acad Child Adolesc Psychiatry 2019;58:846-8. https://doi.org/10.1016/j.jaac.2019.03.004.
- Green J, Garg S. Annual research review: the state of autism intervention science: progress, target psychological and biological mechanisms and future prospects. J Child Psychol Psychiatry 2018;59:424-43. https://doi.org/10.1111/jcpp.12892.
- Lord C, Brugha TS, Charman T, Cusack J, Dumas G, Frazier T, et al. Autism spectrum disorder. Nat Rev Dis Primers 2020;6. https://doi.org/10.1038/s41572-019-0138-4.
- Sameroff A, Sameroff A. The Transactional Model of Development: How Children and Contexts Shape Each Other. Washington, DC: American Psychological Association; 2009.
- Leadbitter K, Macdonald W, Taylor C, Buckle KL. the PACT Consortium . Parent perceptions of participation in a parent-mediated communication-focussed intervention with their young child with autism spectrum disorder. Autism 2020;24:2129-41. https://doi.org/10.1177/1362361320936394.
- Agur M, Hallam R, Barber J, Meagher J, Roberts L, Ross P, et al. A Rapid Evidence Assessment of the Effectiveness of Educational Interventions to Support Children and Young People with Autistic Spectrum Disorder. Cardiff: Welsh Government; 2018.
- National Research Council . Educating Children With Autism 2001.
- Mesibov GB, Shea V, Schopler E, Adams L, Merkler E, Burgess S, et al. The TEACCH Approach to Autism Spectrum Disorders. Boston, MA: Springer; 2005.
- Prizant BM, Wetherby AM, Rubin E, Laurent AC, Rydell PJ. The SCERTS Model: A Comprehensive Educational Approach for Children with Autism Spectrum Disorders. Baltimore, MD: Paul H Brookes Publishing Co., Inc.; 2006.
- Strain PS, Bovey EH. Randomized, controlled trial of the LEAP model of early intervention for young children with autism spectrum disorders. Topics Early Child Spec Educ 2011;31:133-54. https://doi.org/10.1177/0271121411408740.
- Boyd BA, Hume K, McBee MT, Alessandri M, Gutierrez A, Johnson L, et al. Comparative efficacy of LEAP, TEACCH and non-model-specific special education programs for preschoolers with autism spectrum disorders. J Autism Dev Disord 2014;44:366-80. https://doi.org/10.1007/s10803-013-1877-9.
- Wong C, Odom SL, Hume KA, Cox AW, Fettig A, Kucharczyk S, et al. Evidence-based practices for children, youth, and young adults with autism spectrum disorder: a comprehensive review. J Autism Dev Disord 2015;45:1951-66. https://doi.org/10.1007/s10803-014-2351-z.
- Yoder PJ, Lieberman RG. Brief report: randomized test of the efficacy of picture exchange communication system on highly generalized picture exchanges in children with ASD. J Autism Dev Disord 2010;40:629-32. https://doi.org/10.1007/s10803-009-0897-y.
- Lal R. Effect of alternative and augmentative communication on language and social behavior of children with autism. Educ Res Rev 2010;5:119-25.
- Adams C, Lockton E, Freed J, Gaile J, Earl G, McBean K, et al. The Social Communication Intervention Project: a randomized controlled trial of the effectiveness of speech and language therapy for school-age children who have pragmatic and social communication problems with or without autism spectrum disorder. Int J Lang Commun Disord 2012;47:233-44. https://doi.org/10.1111/j.1460-6984.2011.00146.x.
- Koegel L, Matos-Freden R, Lang R, Koegel R. Interventions for children with autism spectrum disorders in inclusive school settings. Cognit Behav Pract 2012;19:401-12. https://doi.org/10.1007/s12098-015-1938-5.
- Kasari C, Locke J, Gulsrud A, Rotheram-Fuller E. Social networks and friendships at school: comparing children with and without ASD. J Autism Dev Disord 2011;41:533-44. https://doi.org/10.1007/s10803-010-1076-x.
- Bond C, Symes W, Hebron J, Humphrey N, Morewood G. Educating persons with autistic spectrum disorder: a systematic literature review. Sch Psychol Int 2016;37:303-20. https://doi.org/10.1177/0143034316639638.
- Naveed S, Waqas A, Amray AN, Memon RI, Javed N, Tahir MA, et al. Implementation and effectiveness of non-specialist mediated interventions for children with autism spectrum disorder: a systematic review and meta-analysis. PLOS ONE 2019;14. https://doi.org/10.1371/journal.pone.0224362.
- Guldberg K. Making a difference in the education of autistic children and young people: the Autism Education Trust (AET) good autism practice guidance, 2019. Good Autism Pract 2019;20.
- Department for Education . Pupils With SCLN in Mainstream Schools 2012. www.gov.uk/government/publications/profiles-of-need-and-provision-for-children-with-language-impairments-and-autism-spectrum-disorders-in-mainstream-schools-a-prospective-study (accessed 12 October 2020).
- Humphrey N. Including pupils with autistic spectrum disorders in mainstream schools. Support Learn 2008;23:41-7. https://doi.org/10.1111/j.1467-9604.2007.00367.x.
- Skipp A, Hopwood V. Deployment of Teaching Positions in Schools 2019. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/812507/Deployment_of_teaching_assistants_report.pdf (accessed 12 October 2020).
- Syme W, Humphrey N. School factors that facilitate or hinder the ability of teaching assistants to effectively support pupils with autism spectrum disorders (ASDs) in mainstream secondary schools. Eur J Spec Needs Educ 2011;11:153-61. https://doi.org/10.1111/j.1471-3802.2011.01196.x.
- Abbot L, Mcconkey R, Dobbins M. Key players in inclusion: are we meeting the professional needs of learning support assistants for pupils with complex needs?. Eur J Spec Needs Educ 2011;26:215-31. https://doi.org/10.1080/08856257.2011.563608.
- Aldred C, Green J, Adams C. A new social communication intervention for children with autism: pilot randomised controlled treatment study suggesting effectiveness. J Child Psychol Psychiatry 2004;45:1420-30. https://doi.org/10.1111/j.1469-7610.2004.00338.x.
- Kasari C, Smith T. Interventions in schools for children with autism spectrum disorder: methods and recommendations. Autism 2013;17:254-67. https://doi.org/10.1177/1362361312470496.
- Dykstra Steinbrenner JR, Watson LR, Boyd BA, Wilson KP, Crais ER, Baranek GT, et al. Developing feasible and effective school-based interventions for children with ASD: a case study of the iterative development process. J Early Intervent 2015;1:23-4. https://doi.org/10.1177/1053815115588827.
- McDuffie AS, Lieberman RG, Yoder PJ. Object interest in autism spectrum disorder: a treatment comparison. Autism 2012;16:398-405. https://doi.org/10.1177/1362361309360983.
- Siller M, Sigman M. Modelling longitudinal change in the language abilities of children with autism: parent behaviors and child characteristics as predictors of change. Dev Psychol 2008;44:1691-704. https://doi.org/10.1037/a0013771.
- Chiat S, Roy P. Early predictors of language and social communication impairments at ages 9–11 years: a follow-up study of early-referred children. J Speech Lang Hear Res 2013;56:1824-36. https://doi.org/10.1044/1092-4388(2013/12-0249).
- Chiat S, Roy P. Early phonological and sociocognitive skills as predictors of later language and social communication outcomes. J Child Psychol Psychiatry 2008;49:635-45. https://doi.org/10.1111/j.1469-7610.2008.01881.x.
- Aldred C, Taylor C, Wan MW, Green J, Siller M, Morgan L. Handbook of Parent-Implemented Interventions for Very Young Children with Autism. New York, NY: Springer Nature; 2018.
- Vismara LA, Young GS, Rogers SJ. Telehealth for expanding the reach of early autism training to parents. Autism Res Treat 2012;2012. https://doi.org/10.1155/2012/121878.
- Humphrey N, Squires G. Achievement For All National Evaluation: Final Report 2011. https://core.ac.uk/download/pdf/4153651.pdf (accessed January 2021).
- Lendrum A, Barlow A, Humphrey N. Developing positive school-home relationships through structured conversations with parents of learners with special educational needs and disabilities (SEND). J Res Spec Educ Needs 2013;15:87-96. https://doi.org/10.1111/1471-3802.12023.
- Barrett B, Byford S, Sharac J, Hudry K, Leadbitter K, Temple K, et al. Service and wider societal costs of very young children with autism in the UK. J Autism Dev Disord 2012;42:797-804. https://doi.org/10.1007/s10803-011-1306-x.
- Lord C, Rutter M, DiLavore PC, Risi S, Gotham K, Bishop S. Autism Diagnostic Observation Schedule (ADOS-2) Manual (Part I): Modules 1–4. Torrance, CA: Western Psychological Services; 2012.
- Gotham K, Pickles A, Lord C. Standardizing ADOS scores for a measure of severity in autism spectrum disorders. J Autism Dev Disord 2009;39:693-705. https://doi.org/10.1007/s10803-008-0674-3.
- Diagnostic and Statistical Manual of Mental Disorders. Arlington, VA: American Psychiatric Association; 2013.
- Estes A, Munson J, Rogers SJ, Greenson J, Winter J, Dawson G. Long-term outcomes of early intervention in 6-year-old children with autism spectrum disorder. J Am Acad Child Adolesc Psychiatry 2015;54:580-7. https://doi.org/10.1016/j.jaac.2015.04.005.
- Mullen EM. Mullen Scales of Early Learning. Circle Pines, MN: American Guidance Service, Inc.; 1995.
- Elliot CD, Smith P. British Abilities Scale-3 (BAS-3). Windsor: NFER-Nelson; 2011.
- Rutter M, Bailey A, Lord C. The Social Communication Questionnaire. Torrance, CA: Western Psychological Services; 2003.
- Carr T, Colombi C, MacDonald M, Lord C. Measuring Respond to Intervention With the Autism Diagnostic Observation Schedule-Change (ADOS-C) n.d.
- Colombi C, Carr T, MacDonald M, Lord C. Developing a Measure of Treatment Outcomes: The Autism Diagnostic Observation Schedule-Change n.d.
- Grzadzinski R, Carr T, Colombi C, McGuire K, Dufek S, Pickles A, et al. Measuring changes in social communication behaviors: preliminary development of the Brief Observation of Social Communication Change (BOSCC). J Autism Dev Disord 2016;46:2464-79. https://doi.org/10.1007/s10803-016-2782-9.
- Divan G, Vajaratkar V, Cardozo P, Huzurbazar S, Verma M, Howarth E, et al. The feasibility and effectiveness of PASS Plus, a lay health worker delivered comprehensive intervention for autism spectrum disorders: pilot RCT in a rural low and middle income country setting. Autism Res 2019;12:328-39. https://doi.org/10.1002/aur.1978.
- Fletcher-Watson S, Petrou A, Scott-Barrett J, Dicks P, Graham C, O’Hare A, et al. A trial of an iPad™ intervention targeting social communication skills in children with autism. Autism 2016;20:771-82. https://doi.org/10.1177/1362361315605624.
- Nordahl-Hansen A, Fletcher-Watson S, McConachie H, Kaale A. Relations between specific and global outcome measures in a social-communication intervention for children with autism spectrum disorder. Res Autism Spectr Disord 2016;29:19-2. https://doi.org/10.1016/j.rasd.2016.05.005.
- Sparrow SS, Cicchetti DV, Balla DA. Vineland Adaptive Behavior Scales. Oxford: NCS Pearson, Inc; 2005.
- Fenson L, Marchman V, Thal D, Dale P, Reznick S, Bates E. MacArthur Communicative Development Inventories: User’s Guide and Technical Manual. Baltimore, MD: Brookes; 2007.
- Brownell R. Receptive and Expressive One-Word Picture Vocabulary Tests (ROWPVT-4, EOWPVT-4). San Antonio, TX: Pearson Education; 2010.
- Zimmerman IL, Steiner VG, Pond E. Preschool Language Scales (PLS-5). San Antonio, TX: Pearson; 2011.
- Honey E, McConachie H, Turner M, Rodgers J. Validation of the repetitive behaviour questionnaire for use with children with autism spectrum disorder. Res Autism Spectr Disord 2012;6:355-64. https://doi.org/10.1016/j.rasd.2011.06.009.
- Einfeld SL, Tonge BJ. Manual for the Developmental Behaviour Checklist: Primary Carer Version (DBC-P) and Teacher Version (DBC-T). Melbourne, VIC: Monash University Centre for Developmental Psychiatry and Psychology; 2002.
- Goodman R. The Strengths and Difficulties Questionnaire: a research note. J Child Psychol Psychiatry 1997;38:581-6. https://doi.org/10.1111/j.1469-7610.1997.tb01545.x.
- Stevens K. Valuation of the Child Health Utility 9D Index. PharmacoEconomics 2012;30:729-47. https://doi.org/10.2165/11599120-000000000-00000.
- Tennant R, Hiller L, Fishwick R, Platt S, Joseph S, Weich S, et al. The Warwick–Edinburgh Mental Well-being Scale (WEMWBS): development and UK validation. Health Qual Life Outcomes 2007;5. https://doi.org/10.1186/1477-7525-5-63.
- Kendall S, Bloomfield L. Developing and validating a tool to measure parenting self-efficacy. J Adv Nurs 2005;51:174-81. https://doi.org/10.1111/j.1365-2648.2005.03479.x.
- Hatcher RL, Gillaspy JA. Development and validation of a revised short version of the Working Alliance Inventory. Psychother Res 2006;16:12-25. https://doi.org/10.1080/10503300500352500.
- King’s College London . King’s Clinical Trials Unit n.d. http://ctu.co.uk/ (accessed 18 October 2020).
- Department for Education . Statements of SEN and EHC Plans: England, 2015 2015. www.gov.uk/government/statistics/statements-of-sen-and-ehc-plans-england-2015 (accessed 1 October 2020).
- Parsons S, Kovshoff H. Building the evidence base through school-research partnerships in autism education: the Autism Community Research Network @ Southampton [ACoRNS]. Good Autism Pract 2019;20:5-12.
- Humphrey N, Hennessey A, Lendrum A, Wigelsworth M, Turner A, Panayiotou M, et al. The PATHS curriculum for promoting social and emotional well-being among children aged 7–9 years: a cluster RCT. Public Health Res 2018;6. https://doi.org/10.3310/phr06100.
- Humphrey N, Safford K, Stacey M, Hancock R. Small-Scale Research in Primary Schools: A Reader for Learning and Professional Development. New York, NY: Routledge; 2013.
- Fullan M. Whole School Reform: Problems and Promises. Chicago, IL: Chicago Community Trust; 2001.
- Goodrich J, Cornwell J. Seeing the Person in the Patient: The Point of Care Review Paper 2008. http://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.737.6944%26rep=rep1%26type=pdf (accessed 16 January 2021).
- Leadbitter K, Aldred C, McConachie H, Le Couteur A, Kapadia D, Charman T, et al. The Autism Family Experience Questionnaire (AFEQ): an ecologically-valid, parent-nominated measure of family experience, quality of life and prioritised outcomes for early intervention. J Autism Dev Disord 2018;48:1052-62. https://doi.org/10.1007/s10803-017-3350-7.
- Muthén LK, Muthén BO. Mplus User’s Guide. Los Angeles, CA: Muthén & Muthén; n.d.
- CONSORT . Non-Pharmacologic Treatment Interventions n.d. www.consort-statement.org/extensions/overview/non-pharmacologic-treatment-interventions (accessed 18 October 2020).
- White I, Thompson S. Adjusting for partially missing baseline measurements in randomized trials. Stat Med 2005;24:99-1007. https://doi.org/10.1002/sim.1981.
- Kraemer HC. Discovering, comparing, and combining moderators of treatment on outcome after randomized clinical trials: a parametric approach. Stat Med 2013;32:1964-73. https://doi.org/10.1002/sim.5734.
- Landau S, Emsley R, Dunn G. Beyond total treatment effects in randomised controlled trials: baseline measurement of intermediate outcomes needed to reduce confounding in mediation investigations. Clin Trials 2018;15:247-56. https://doi.org/10.1177/1740774518760300.
- Friard O, Gamba M. BORIS: a free, versatile open-source event-logging software for video/audio coding and live observations. Meth Ecol Evol 2016;7:1325-30. https://doi.org/10.1111/2041-210X.12584.
- Department for Children, Schools and Families . Department for Children, Schools and Families Departmental Report 2008. www.gov.uk/government/publications/department-for-children-schools-and-families-departmental-report-2008 (accessed 12 October 2020).
- NHS . The NHS Long Term Plan 2019. www.longtermplan.nhs.uk/ (accessed 18 October 2020).
- Solomon D, Soares N, McClain M, Shahidullah J, Mezher K. Interprofessional Care Coordination for Pediatric Autism Spectrum Disorder. Cham: Springer; 2020.
- Green J, Pickles A, Pasco G, Bedford R, Wan MW, Elsabbagh M, et al. Randomised trial of a parent-mediated intervention for infants at high risk for autism: longitudinal outcomes to age 3 years. J Child Psychol Psychiatry 2017;58:1330-40. https://doi.org/10.1111/jcpp.12728.
- Whitehouse AJO, Varcin KJ, Alvares GA, Barbaro J, Bent C, Boutrus M, et al. Pre-emptive intervention versus treatment as usual for infants showing early behavioural risk signs of autism spectrum disorder: a single-blind, randomised controlled trial. Lancet Child Adolesc Health 2019;3:605-15. https://doi.org/10.1016/S2352-4642(19)30184-1.
- Watson LR, Crais ER, Baranek GT, Turner-Brown L, Sideris J, Wakeford L, et al. Parent-mediated intervention for one-year-olds screened as at-risk for autism spectrum disorder: a randomized controlled trial. J Autism Dev Disord 2017;47:3520-40. https://doi.org/10.1007/s10803-017-3268-0.
- Kasari C, Siller M, Huynh LN, Shih W, Swanson M, Hellemann GS, et al. Randomized controlled trial of parental responsiveness intervention for toddlers at high risk for autism. Infant Behav Dev 2014;37:711-21. https://doi.org/10.1016/j.infbeh.2014.08.007.
- Rahman A, Divan G, Hamdani SU, Vajaratkar V, Taylor C, Leadbitter K, et al. Effectiveness of the parent-mediated intervention for children with autism spectrum disorder in south Asia in India and Pakistan (PASS): a randomised controlled trial. Lancet Psychiatry 2016;3:128-36. https://doi.org/10.1016/S2215-0366(15)00388-0.
- Bakermans-Kranenburg MJ, van IJzendoorn MH, Juffer F. Less is more: meta-analyses of sensitivity and attachment interventions in early childhood. Psychol Bull 2003;129:195-21. https://doi.org/10.1037/0033-2909.129.2.195.
- Doria MV, Kennedy H, Strathie C, Strathie S. Explanations for the success of video interaction guidance (vig): an emerging method in family psychotherapy. Fam J 2013;22:78-87. https://doi.org/10.1177/1066480713505072.
- Juffer F, Bakermans-Kranenburg MJ, van IJzendoorn MH. Promoting Positive Parenting: An Attachment-Based Intervention. Hillsdale, NJ: Lawrence Erlbaum Associates, Inc.; 2008.
- Klein Velderman M, Bakermans-Kranenburg MJ, Juffer F, van IJzendoorn MH. Effects of attachment-based interventions on maternal sensitivity and infant attachment: differential susceptibility of highly reactive infants. J Fam Psychol 2006;20:266-74. https://doi.org/10.1037/0893-3200.20.2.266.
- Saint-Georges C, Pagnier M, Ghattassi Z, Hubert-Barthelemy A, Tanet A, Clément MN, et al. A developmental and sequenced one-to-one educational intervention (DS1-EI) for autism spectrum disorder and intellectual disability: a three-year randomized, single-blind controlled trial. EClinicalMedicine 2020;26. https://doi.org/10.1016/j.eclinm.2020.100537.
- Morgan L, Hooker JL, Sparapani N, Reinhardt VP, Schatschneider C, Wetherby AM. Cluster randomized trial of the classroom SCERTS intervention for elementary students with autism spectrum disorder. J Consult Clin Psychol 2018;86:631-44. https://doi.org/10.1037/ccp0000314.
- Kaale A, Fagerland MW, Martinsen EW, Smith L. Preschool-based social communication treatment for children with autism: 12-month follow-up of a randomized trial. J Am Acad Child Adolesc Psychiatry 2014;53:188-98. https://doi.org/10.1016/j.jaac.2013.09.019.
- Sutton BM, Webster AA, Westerveld MF. A systematic review of school-based interventions targeting social communication behaviors for students with autism. Autism 2019;23:274-86. https://doi.org/10.1177/1362361317753564.
- Orsini N, Li R, Wolk A, Khudyakov P, Spiegelman D. Meta-analysis for linear and nonlinear dose-response relations: examples, an evaluation of approximations, and software. Am J Epidemiol 2012;175:66-73. https://doi.org/10.1093/aje/kwr265.
- Durlak JA, Weissberg RP, Dymnicki AB, Taylor RD, Schellinger KB. The impact of enhancing students’ social and emotional learning: a meta-analysis of school-based universal interventions. Child Dev 2011;82:405-32. https://doi.org/10.1111/j.1467-8624.2010.01564.x.
- Esposito M, Dipierro MT, Mondani F, Gerardi G, Monopoli B, Felicetti C, et al. Developing telehealth systems for parent-mediated intervention of young children with autism: practical guidelines. Int J Psychiatr Res 2020;3:1-11. https://doi.org/10.33425/2641-4317.1061.
- Inchausti F, MacBeth A, Hasson-Ohayon I, Dimaggio G. Telepsychotherapy in the age of COVID-19: a commentary. J Psychother Integration 2020;30. https://doi.org/10.1037/int0000222.
- Lendrum A, Humphrey N. The importance of studying the implementation of interventions in school settings. Oxf Rev Educ 2012;38:635-52. https://doi.org/10.2307/41702781.
- Office for Standards in Education . The National Strategies: A Review of Impact 2010. https://dera.ioe.ac.uk/1102/1/The%20National%20Strategies%20a%20review%20of%20impact.pdf (accessed 9 October 2020).
- Lendrum A. Implementing Social and Emotional Aspects of Learning (SEAL) in Secondary Schools in England: Issues and Implications 2010. https://doi.org/10.1037/e734362011-002.
- Basford E, Butt G, Newton R. To what extent are teaching assistants really managed?: ‘I was thrown in the deep end, really; I just had to more or less get on with it’. Educ Manag 2017;37:288-310. https://doi.org/10.1080/13632434.2017.1324842.
- Groom B. Building relationships for learning: the developing role of the teaching assistant. Support Learn 2006;21:199-203. https://doi.org/10.1111/j.1467-9604.2006.00432.x.
- Tillery CY, Werts MG, Roark R, Harris S. Perceptions of paraeducators on job retention. Teach Educ Spec Educ 2003;26:118-27. https://doi.org/10.1177/088840640302600205.
- Dingfelder HE, Mandell DS. Bridging the research-to-practice gap in autism intervention: an application of diffusion of innovation theory. J Autism Dev Disord 2011;41:597-609. https://doi.org/10.1007/s10803-010-1081-0.
- Vivanti G, Dissanayake C, Duncan E, Feary J, Capes K, Upson S, et al. Outcomes of children receiving Group-Early Start Denver Model in an inclusive versus autism-specific setting: a pilot randomized controlled trial. Autism 2019;23:1165-75. https://doi.org/10.1177/1362361318801341.
- Cox DD. Evidence-based interventions using home–school collaboration. School Psychol Q 2005;20. https://doi.org/10.1521/scpq.2005.20.4.473.
- Cowan R, Swearer Napolitano S, Sheridan S. Home–school collaboration. Encycl Appl Psychol 2004;2:201-8. https://doi.org/10.1016/B0-12-657410-3/00776-5.
- Poslawsky IE, Naber FB, Bakermans-Kranenburg MJ, van Daalen E, van Engeland H, van IJzendoorn MH. Video-feedback Intervention to promote Positive Parenting adapted to Autism (VIPP-AUTI): a randomized controlled trial. Autism 2015;19:588-603. https://doi.org/10.1177/1362361314537124.
- Cooper M, Evans Y, Pybis J. Interagency collaboration in children and young people’s mental health: a systematic review of outcomes, facilitating factors and inhibiting factors. Child Care Health Dev 2015;42:325-42. https://doi.org/10.1111/cch.12322.
- Stahmer AC, Suhrheinrich J, Roesch S, Zeedyk SM, Wang T, Chan N, et al. Examining relationships between child skills and potential key components of an evidence-based practice in ASD. Res Dev Disabil 2019;90:101-12. https://doi.org/10.1016/j.ridd.2019.04.003.
- Pallmann P, Bedding AW, Choodari-Oskooei B, Dimairo M, Flight L, Hampson LV, et al. Adaptive designs in clinical trials: why use them, and how to run and report them. BMC Med 2018;16. https://doi.org/10.1186/s12916-018-1017-7.
Appendix 1 Acquisition of social communication over time and across contexts
As described in the protocol and main report, to examine the extent to which change in behaviour in one context, with one interaction partner, was carried through to change in behaviour in other contexts, with another interaction partner, PACT-G recorded naturalistic interaction with the parent and LSA at baseline, mid-point and end point and with the researcher at baseline and end point. These were coded blind to treatment group and assessment point by UK and US video-coding teams (both trained to reliability and meeting reliability criteria obtained from a random sample of multiply-rated tapes stratified by rater). Summary statistics are shown in Table 34 and showed high levels of completeness.
| Group | Baseline | Mid-point | End point | |||
|---|---|---|---|---|---|---|
| TAU | PACT-G | TAU | PACT-G | TAU | PACT-G | |
| Researcher module 1 | 30.8 (6.24), n = 96 | 31.0 (4.90), n = 90 | 28.4 (7.30), n = 90 | 28.3 (7.29), n = 90 | ||
| Researcher module 2 | 35.0 (12.1), n = 28 | 37.9 (9.36), n = 23 | 30.8 (13.2), n = 28 | 32.5 (13.0), n = 25 | ||
| Parent module 1 | 28.0 (6.60), n = 95 | 27.9 (6.24), n = 87 | 27.1 (7.37), n = 79 | 27.1 (7.21), n = 85 | 26.9 (7.55), n = 83 | 26.1 (7.80), n = 89 |
| Parent module 2 | 30.4 (11.9), n = 29 | 33.0 (10.2), n = 25 | 27.3 (9.54), n = 27 | 30.0 (11.7), n = 25 | 24.9 (9.26), n = 29 | 29.5 (11.6), n = 26 |
| LSA module 1 | 29.3 (6.95), n = 91 | 29.4 (6.95), n = 92 | 27.2 (7.24), n = 87 | 27.5 (7.15), n = 85 | 27.1 (8.46), n = 84 | 27.5 (8.36), n = 86 |
| LSA module 2 | 32.6 (11.2), n = 28 | 33.3 (10.4), n = 28 | 28.2 (12.1), n = 27 | 32.8 (13.3), n = 26 | 29.8 (12.3), n = 27 | 31.3 (13.2), n = 25 |
Change in teaching assistant
Changes in the school-based interaction partner during the course of the trial occurred more frequently than expected. Eighty-five (34.3%) children experienced a change in LSA between baseline and the mid-point, and 94 (37.9%) children between the mid- and end point. Twenty-two children experienced changes at both time points.
Structural equation model
Generalisation was examined by fitting models of the form shown in Figure 3. The model was stratified as a two-group model by the BOSCC module and estimated by maximum likelihood. In the light of changes in interaction partner, the model included dummy variables to allow for a mean difference where a change in partner had occurred. The models were estimated in Mplus using maximum likelihood estimation with robust standard errors, and standardised estimates are reported. At the mid-point, the path from parent to LSA is included but the reverse reciprocal was not significantly different from zero and, therefore, not included.
The model was run with the social communication subscale of the BOSCC. The length and setting of the interaction was considered to elicit too few RRBs to make their separate analysis reliable.
FIGURE 13.
Structural equation model fitted to baseline, mid-point and end-point BOSCC data from parent, teacher and researcher. R, researcher; P, parent. Numerical suffix = month from start of therapy. Circles represent latent variables, squares represent observed variables. Light blue arrows represent the paths from intervention to BOSCC assessment, and orange arrows represent the generalisation paths tested. Covariation paths are dashed double-headed curved paths.

Results
Social communication subscale
Parent and researcher
First, we ran the model using only BOSCC data from interactions with a parent and a researcher. This model was just-identified with no residual degrees of freedom [root mean square error of approximation (RMSEA) of 0.000 and comparative fit index (CFI) of 1.00]. With both modules constrained to be equal, the path from the parent mid-point to researcher end point was significant (p < 001), with a coefficient of 0.67 (95% CI 0.51 to 0.82).
Teacher assistant and researcher
Second, for the LSA and researcher bivariate model, with one residual degree of freedom owing to the additional change of teacher variable, the model fit was good, with a RMSEA of 0.051 and a CFI of 0.958. The path from the LSA mid-point to researcher end point was significant (p < 0.001), with a coefficient of 0.49 (95% CI 0.31 to 0.67) for module 1 and a coefficient of 0.48 (95% CI 0.32 to 0.64) for module 2.
Parent, teacher and researcher
For the model combining all three contexts, model fit was good, with a RMSEA of 0.014 and a CFI of 0.997. Direct paths from the parent mid-point to researcher end point, parent mid-point to LSA mid-point, and LSA mid-point to researcher end point are given in Table 35. In addition to the direct path between the parent mid-point and researcher end point, there is an indirect path between the two through the LSA mid-point. The total path from the parent mid-point to researcher end point is also provided in Table 35, which incorporates the direct and indirect path.
| Path | Standardised coefficient | 95% CI | p-value |
|---|---|---|---|
| Direct paths | |||
| Parent mid-point to researcher end point | |||
| Module 1a | 0.86 | 0.47 to 1.26 | < 0.001 |
| Module 2a | 0.82 | 0.40 to 1.23 | < 0.001 |
| Parent mid-point to teaching assistant mid-point | |||
| Module 1a | 1.01 | 0.49 to 1.53 | < 0.001 |
| Module 2a | 0.74 | 0.51 to 0.96 | < 0.001 |
| LSA mid-point to researcher end point | |||
| Module 1a | –0.20 | –0.60 to 0.20 | 0.338 |
| Module 2a | –0.25 | –0.76 to 0.25 | 0.328 |
| Indirect paths | |||
| Parent mid-point to researcher end point (via LSA mid-point) | |||
| Module 1 | –0.20 | –0.61 to 0.21 | 0.347 |
| Module 2 | –0.19 | –0.58 to 0.20 | 0.349 |
| Total paths | |||
| Parent mid-point to researcher end point | |||
| Module 1 | 0.67 | 0.51 to 0.82 | < 0.001 |
| Module 2 | 0.63 | 0.42 to 0.84 | < 0.001 |
Summary
These analyses were set out to explore the extent to which children’s social communication, as measured by the BOSCC, generalised across contexts from interaction with familiar adults (i.e. parent and LSA) to an unfamiliar setting and unfamiliar adult (i.e. the researcher). This was tested using the social communication subscale of the BOSCC. The initial model, considering only two contexts at a time, showed that social communication with a parent generalised to later interaction with a researcher, such that increased social communication skills in interactions with the parent transferred to improved social skills with the researcher. This appeared also to be true for social communication during interactions with a LSA. In each of these analyses, the generalisation arising from the excluded interaction partner may be considered an omitted confounder. A trivariate analysis with all three raters is required to confirm the effects. When all three contexts were included in the same model, although the generalisation of social communication from parent to researcher remained (both directly and overall including the indirect effect), the effect from LSA to researcher was no longer significant. Generalisation was also shown to be significant for the parent mid-point to LSA mid-point. This analysis provides supportive evidence for cross-context generalisation in behavioural change, particularly from the home setting to educational setting. However, although we account for both measurement error and baseline confounding, our analyses have not yet eliminated the possible confounding effects of context general shared developmental change in autism severity as a source of bias. We hope to further develop our analyses of the mechanisms of cross-context and cross-behavioural (DCMA/ADOS-2) change to address this source of developmental confounding.
Appendix 2 Breakdown of Autism Diagnostic Observation Schedule, Second Edition module by developmental quotient
| Baseline | Preschool aged (N = 151) | School aged (N = 97) |
|---|---|---|
| Module 1 (non-verbal), n = 110 | 63 | 47 |
| Visual reception DQ, mean (SD) | 44.7 (12.0) | 27.4 (8.6) |
| Fine motor DQ, mean (SD) | 44.8 (11.4) | 26.5 (8.9) |
| Module 1 (verbal), n = 77 | 52 | 25 |
| Visual reception DQ, mean (SD) | 54.2 (13.2) | 41.0 (16.4) |
| Fine motor DQ, mean (SD) | 56.6 (13.0) | 42.4 (16.0) |
| Module 2, n = 61 | 36 | 25 |
| Visual reception DQ, mean (SD) | 73.9 (21.9) | 48.4 (18.2) |
| Fine motor DQ, mean (SD) | 67.3 (14.4) | 49.2 (15.7) |
| All modules | 151 | 97 |
| Visual reception DQ, mean (SD) | 54.9 (19.0) | 36.2 (16.3) |
| Fine motor DQ, mean (SD) | 54.2 (15.5) | 36.3 (16.2) |
Appendix 3 Deliverability project plan: January 2016
Appendix 4 The PACT-G treatment fidelity rating scale
Appendix 5 Trial protocol amendments
| Old version | New version | Date | Amendment |
|---|---|---|---|
| 1.0 | 2.0 | 6 October 2016 | Addition of parent questionnaires in sections 8.2 and 8.3 |
| 2.0 | 3.0 | 18 November 2016 |
|
| 3.0 | 4.0 | 2 February 2017 |
|
| 4.0 | 5.0 | 1 September 2017 |
|
| 5.0 | 6.0 |
|
A substantive change to the protocol following trial commencement was the alteration of the nominated primary outcome – from BOSCC to ADOS-2 in the final analysis plan. A change to the primary outcome was first proposed in October 2017, following new published data from our group14 and others, indicating that ADOS-2 measurement could be sensitive to change from the intervention, and in our study showing sustained change for 6 years after intervention end. The initial alteration proposed was to use a combined BOSCC/ADOS-2 outcome metric. Following discussion with the funders, this change was modified to using the ADOS-2 measure alone, with BOSCC as a secondary outcome. This change was agreed with the TSC, reflected in the final version of the trial protocol (version 6, July 2018) and in the subsequently published trial protocol paper,6 as well as the final statistical analysis plan, finalised and lodged before data-lock and data analysis (see Chapter 7, Aims of formal analysis).
List of abbreviations
- ABA
- applied behaviour analysis
- ADOS-2
- Autism Diagnostic Observation Schedule, Second Edition
- AE
- adverse event
- BOSCC
- Brief Observation of Social Communication Change
- CACE
- complier-average causal effect
- CASUS
- Child and Adolescent Service Use Schedule
- CFI
- comparative fit index
- CHU9D
- Child Health Utility 9D
- CI
- confidence interval
- CONSORT
- Consolidated Standards of Reporting Trials
- CSS
- Calibrated Severity Score
- CTM
- comprehensive treatment model
- DBC
- Developmental Behaviour Checklist
- DCMA
- Dyadic Communication Measure For Autism
- DQ
- developmental quotient
- DS1-EI
- individually delivered social communication and educational attainment-focused intervention
- ES
- effect size
- HSC
- home–school conversation
- ICC
- intraclass correlation
- IQR
- interquartile range
- ITT
- intention to treat
- LSA
- learning support assistant
- MCDI
- MacArthur Communicative Development Inventory
- MoA
- Memorandum of Agreement
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health and Care Research
- PACT
- Preschool Autism Communication Trial
- PACT-G
- Paediatric Autism Communication Trial – Generalised
- PECS
- Picture Exchange Communication System
- PIS
- participant information sheet
- PLS
- Preschool Language Scale
- PPI
- patient and public involvement
- RA
- research assistant
- RBQ
- Repetitive Behaviour Questionnaire
- RCT
- randomised controlled trial
- RMSEA
- root-mean-square error of approximation
- RRB
- restricted and repetitive behaviour
- SA
- social affect
- SCERTS
- Social Communication, Emotional Regulation, and Transactional Support
- SCQ
- Social Communication Questionnaire (lifetime version)
- SD
- standard deviation
- SDQ
- Strengths and Difficulties Questionnaire
- SEM
- structural equation modelling
- SEN
- special education needs
- SOP
- standard operating procedure
- TAU
- treatment as usual
- TEACCH
- Treatment and Education of Autistic and related Communication-Handicapped Children
- TOPSE
- Tool tO measure Parental Self-Efficacy
- TSC
- Trial Steering Committee
- VABS
- Vineland Adaptive Behavior Scales
- VEPS
- Very Early Processing Skills
- WEMWBS
- Warwick–Edinburgh Mental-Wellbeing Scale