Notes
Article history
The contractual start date for this research was in June 2017. This article began editorial review in March 2023 and was accepted for publication in December 2023. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The Global Health Research editors and publisher have tried to ensure the accuracy of the authors’ article and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this article.
Permissions
Copyright statement
Copyright © 2024 Jamal et al. This work was produced by Jamal et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2024 Jamal et al.
Introduction
Worldwide, about 74% of all deaths are attributed to non-communicable diseases (NCDs), of which more than three-quarters occur in low- and middle-income countries (LMICs). 1 NCD prevention and control has mainly focused on the four conditions responsible for the greatest number of deaths. Known as the ‘Big Four’, cardiovascular diseases (CVDs), followed by cancers, chronic respiratory diseases and diabetes, comprise the highest rates of mortality as they contribute to 33.3 million deaths globally. These NCDs are all driven by modifiable behaviours, namely, unhealthy diets, physical inactivity, tobacco smoking and harmful use of alcohol. 2,3 These behavioural determinants are widely recognised as the main entry points for the prevention and control of NCDs. 4
According to the American Psychiatric Association, mental disorders, also called mental illnesses, are classified as any condition characterised by cognitive and emotional disturbances, abnormal behaviours, impaired functioning or any combination of these. 5 The World Health Organization (WHO) identifies depressive disorders and anxiety disorders, including post-traumatic stress disorder (PTSD), as the two main diagnostic categories comprising common mental health disorders. 6 In 2012, the WHO identified three different categories of risks affecting an individual’s mental health, namely, individual attributes and behaviours, social and economic circumstances and environmental factors. 7 Although the WHO called these factors ‘risks to mental health’, they are similar to the social determinants of mental health that were proposed later by Marmot et al. in 2014. 8 At the individual and behavioural level, poor dietary habits9 and smoking10 were found to be associated with depression. In addition, socioeconomic conditions, such as unemployment and financial hardships, predispose individuals to mental illnesses. 7 According to the WHO, the poorest segment of society is often the most susceptible to poor mental health. 11 The stress that accompanies absolute poverty is a powerful risk factor for mental disorders such as depression and substance dependence. 12
Common mental illnesses and NCDs often coexist. Systematic reviews linked cancer with anxiety disorders13,14 and PTSD. 15 Meta-analyses linked diabetes with a range of mental disorders, including depression and PTSD. 16 Across countries, the odds ratios for the association of heart disease with mood disorders, anxiety disorders and alcohol dependence were found to be 2.1, 2.2 and 1.4, respectively. 17
The exact mechanism linking common mental disorders (CMDs) to NCDs remains to be clearly understood. It has been suggested that they influence each other directly through physiological systems (e.g. neuroendocrine system). For instance, depression is shown to provoke a cascade of events in the hypothalamic–pituitary–adrenal axis, which is normally stimulated in response to stress, leading to insulin resistance and eventually to type 2 diabetes. 18 On the other hand, there is evidence associating individual, social and environmental factors, known to be determinants of mental health, with NCDs. Individual factors that were mentioned earlier to be associated with depression, namely, smoking and poor dietary habits, are known to be the main entry points for the prevention and control of NCDs. 4 Poverty, a social determinant of mental health,19 is shown to exert a similar effect on NCD incidence. In a large-scale population cohort in the UK, it was found that the segment of the population who were more socioeconomically deprived had an increased risk for developing heart disease (incidence rate ratio 1.61, 95% CI 1.58 to 1.64) and did so earlier in life than those from the most affluent group (adjusted difference −3.51 years, 95% CI −3.77 to −3.25). Factors such as health inequity, poor access to basic services such as clean water and electricity, political instability, discrimination and armed conflicts are just examples of environmental determinants of mental health7 that were also found to be associated with higher rates of diabetes and CVDs20 and with an increased incidence of cancer. 21
Physical health outcomes for people living with a chronic physical condition are worse in the presence of a mental illness, including a reduced quality of life and a shortened lifespan. Studies show that mental illness contributes to an increased risk of mortality from CVDs and cancer. 22–24 According to the World Mental Health Surveys, an 8–12% increase in mortality, due to smoking, diabetes, history of myocardial infarction and hypertension, was found among people with common mental health disorders. 17 Figures of myocardial infarctions, a NCD complication, are higher among individuals subjected to stressful situations such as armed conflicts or natural disasters compared to pre-emergency figures. 25
Despite the supportive evidence that links CMDs and their determinants to NCDs, and despite the fact that physical health outcomes get worse for people living with a NCD in the presence of a mental illness, the connection between them is usually overlooked in clinical settings and, to a great extent, in country-level policy-making. This has been attributed to factors such as limited government capacities for policy development, weak health systems and insufficient finances, among other factors. 26,27 In 2005, member states in the WHO European Region endorsed the ‘no health without mental health’ statement owing to mental health’s contribution to years of disability. 28 The WHO’s Global Action Plan (2013–20), to reduce the global burden of non-communicable illnesses and preventable mortality, includes mental disorder prevention and control objectives. 29 However, mental and physical disease prevention initiatives remain essentially separate and independent from one another. 30 The current systematic review aims to address the link between mental illness and NCDs by exploring the aforementioned individual, social and environmental determinants associated with both conditions. It aims to answer the research question: ‘What are the individual, social and environmental determinants that lead to the development of NCDs {CVD, cancers, respiratory diseases [including chronic obstructive pulmonary disease (COPD)] and diabetes mellitus [DM]} among patients with common mental health disorders (depression and anxiety disorders including PTSD)?’ Considering these overlapping determinants may be a practical and effective way of providing integrated prevention programmes to reduce the burden of these conditions as well as the associated disability. This review is part of an entire PhD research work on the social determinants of mental health and how they affect population health.
Methods
This review was conducted in accordance with a published protocol prepared by the authors and published on PROSPERO with a registration number CRD42019157800. 31
The review follows the latest Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 reporting guidelines. 32
Inclusion and exclusion criteria
The current review utilised the population, intervention/exposure, control, outcome and study (PICOS) design format as a systematic and rigorous method for delineating inclusion and exclusion criteria (Table 1). This approach ensures coherence and uniformity in the item selection process. 33 This review included observational studies (case-control, retrospective and prospective cohort studies) only as they can provide valuable evidence for establishing a causal relationship between common mental health disorders and NCDs. Cross-sectional studies were excluded because, unlike cohort studies, they did not measure the incidence of disease and, unlike case-control studies, could not measure the effect of multiple exposures on disease outcome. 34 The exclusion of interventional studies was deemed necessary due to their limited suitability as the primary approach for evaluating the incidence of NCDs. Experimental studies can offer valuable insights into the efficacy of interventions in preventing and managing NCDs. However, in the current review, we did not prioritise examining such aspects.
| Inclusion criteria | Exclusion criteria | |
|---|---|---|
| Participants | Participants ≥ 18 years old With common mental health problem |
Participants < 18 years old Participants with comorbid mental health and NCD conditions Participants with pre-existing NCD Participants with severe mental health illness |
| Exposure | Reports at least one outcome of the following:
|
Reports on any of these: quality of life, satisfaction with life, happiness |
| Control | Participants who do not develop one of the four NCDs | Not applicable |
| Outcome | Incidence of common NCDs (diabetes, cancers, COPD and CVD) | Incidence of illnesses other than common NCDs Comorbidity of NCDs with mental health problem |
| Study design | Observational studies (cohort studies and case-control studies) | Cross-sectional studies Experimental studies Interviews/focus groups/case studies Review articles and meta-analysis Reports (conference abstracts, study registrations, study protocol papers, result reports, policy briefs, book chapters, dissertations and theses, editorials, commentaries and website content) |
In the included studies, CMDs were identified via an established clinician-administered instrument [e.g. Structured Clinical Interview for Diagnostic and Statistical Manual of Mental Disorders (SCID) and the Composite International Diagnostic Interview (CIDI)], clinical records and/or using a validated self-report instrument [e.g. Patient Health Questionnaire-9 item (PHQ-9) and Generalised Anxiety Disorder-7, Hospital Anxiety and Depression Scale]. There are two main references to classify mental disorders: the International Classification of Disease (ICD) published by the WHO and the Diagnostic and Statistical Manual of Mental Disorders (DSM) published by the American Psychiatric Association, the most recent versions of which are ICD-11 and DSM-5, respectively. DSM is primarily used by clinicians for diagnosis, while ICD is primarily used for the coding of diseases in clinical settings and for epidemiological purposes. The listing of conditions differs between the two. For example, the ICD-11 lists depressive disorders under mood disorders, whereas the DSM-5 lists depressive disorders as a separate category. 35,36 The classification of conditions is routinely revised. For example, PTSD was previously classified under anxiety disorders in DSM-4 and is currently listed in DSM-5 under ‘Trauma- and Stressor-Related Disorders’. 37
The incidence of the NCD conditions, on the other hand, was based on either self-report, clinical or biochemical assessments.
We excluded studies that involved participants with comorbid NCDs, given that NCDs were the outcome and each could independently be linked to the incidence of the other. For example, studies have shown that there are biological mechanisms associated with DM that increase the risk for CVD among diabetic patients. 38 Also, we excluded studies that did not involve participants who have CMDs, namely, depression and/or anxiety disorders. Studies reporting on the incidence of NCDs without reporting the exposure (individual, social and/or environmental determinants) leading to the development of NCDs were excluded.
Search criteria
Our searches were restricted to English. There were no geographical restrictions and no time frame limits. One author (ZJ) searched MEDLINE, PsycINFO, EMBASE and CINAHL from database inception to August 2019 using a search strategy developed and validated for the right use of Boolean phrases and medical subject heading (MeSH) terms with the support of a specialist librarian. We searched each database by combining four different concepts related to NCDs along with three different concepts of mental health disorders, namely, ‘cardiovascular diseases’, ‘diabetes’, ‘cancers’, ‘chronic obstructive pulmonary disease’ with ‘anxiety’, ‘depression’ and ‘post-traumatic stress disorder’. The search encompassed the combination of various terms for each concept and included both free text words and MeSH terms, utilising relevant search options corresponding to each resource. A sample of the electronic search strategy is available in Appendix 1.
Study selection
Zeina Jamal imported the retrieved studies into EndNote to remove duplicates. After removing all duplicates, references were then imported to Excel for title and abstract screening. Another reviewer (MR) screened 10% of the titles and abstracts of all potentially eligible articles using a checklist for inclusion and exclusion criteria (Table 1). A list of full-text articles was identified. A third reviewer (AN) was available for mediation throughout the full-text screening and the data extraction phase. Disagreements were resolved via group consensus.
Data extraction
For each article, the first author (ZJ) extracted all data according to a pre-specified template (see Appendix 2). The main variables covered relate to study identifiers, context of the study and aims, data collection details, measurement of main outcome and important findings.
Synthesis
The process of the synthesis was guided by the synthesis without meta-analysis guidelines. 39 For initial syntheses of the studies, they were grouped based on the NCD outcome (Tables 2–5). Based on individual study appraisals of quality, studies were further grouped into categories of high, medium and low quality. All available evidence, regardless of quality of evidence, was initially collated, after which information from high-quality studies only was synthesised. An overview of all relevant exposures (the determinants) across all outcomes was then collated, with subsequent focused synthesis on studies of high quality only. A narrative synthesis, rather than meta-analysis, was used to consider the association between the different determinants in relation to the incidence of the NCD outcomes, given the diverse nature of the latter and the numerous determinants that were studied. Other sources of heterogeneity are described below.
| Study | Country/name of the study | Design | Duration of follow-up | Sample size; % females | Type of assessed MH | Measurement of MH condition | Covariates | Outcome | Measurement of outcome | Association of depression/anxiety with overall incident cancer and with cancer subtypes (95% CI) | Important results/highest risk group | CASP quality assessment |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Gross et al. (2010)40 | Baltimore Epidemiologic Catchment Area Study, USA | Cohort prospective longitudinal | 24 years | 3177; F 61.2% | Depression: (MDE and dysphoric episode) | DIS/DSM-III MDE |
|
Cancer (colon, prostate, lung, skin and breast) | Self-report of cancer diagnosis plus death certificates | DIS/DSM-III MDE HR 1.87 (1.16 to 3.01) for overall cancer DIS/DSM-III MDE HR 4.4 (1.08 to 17.6) for breast cancera DIS/DSM-III MDE (single episode) |
Older age (reference: 45 years): HR 1.03 CI (1.02 to 1.04) for overall cancer Smoking status HR 34.3 CI (4.30 to 273.74) for lung cancer |
Medium |
| HR 6.88 (1.98 to 23.90) for prostate cancerb Dysphoric episode HR 1.69 (1.3 to 2.19) for overall cancer Dysphoric episode HR 2.42 (1.17 to 4.98) for breast cancera Dysphoric episode HR 3.54 (1.55 to 8.10) for colon cancer |
||||||||||||
| Penninx et al. (1998)41 | Established Populations for Epidemiologic Studies of the Elderly, USA | Cohort prospective longitudinal | 10 years | 4825; F 64.6% | Depression (chronic depression) | CES-D scale |
|
Cancer | Medicare hospitalisation records plus death certificates | Chronic depression HR 1.88 (1.3 to 3.14) for overall cancer Chronic depression HR 4.8 (1.01 to 22.79) for uterus, adnexa cancersa |
Not chronically depressed mood X smoking: Ex-smoker HR 1.65 CI (1.29 to 2.1) |
High |
| Current smoker HR 1.96 CI (1.16 to 3.34) Chronically depressed mood X smoking: Ex-smoker HR 2.17 CI (0.68 to 6.88) Current smoker HR 2.8 CI (0.65 to 11.94) |
||||||||||||
| Linkins et al. (1990)52 | Household survey Washington County, USA; | Cohort prospective longitudinal | 12 years | 2264; F 58% | Depression | CES-D scale |
|
Cancer | Examination of records of the Washington County Cancer Register | Depressed mood at initial survey No (reference) Yes RR 1.09 (0.69 to 1.71) |
Depressed mood present Current smokers RR 2.6 CI (1.41 to 4.80) Current smoker 1–14 cigarettes/day RR 0.75 CI (0.10 to 5.46) |
Low |
| 15–24 cigarettes/day RR 2.6 CI (1.11 to 6.07) ≥ 25 cigarettes/day RR 4.47 CI (1.88 to 10.60) Depressed mood present ≥ 25 cigarettes/day RR 18.47 CI (4.58 to 74.41) for cancer sites associated with smokingc |
||||||||||||
| Persky et al. (1987)53 | Western Electric Study, USA | Cohort prospective longitudinal | 20 years | 2017; F 0% | Depression | MMPI |
|
Cancer | Self-report of cancer diagnosis plus death certificates | High D profile proportional Hazards coefficient 0.3188 p = 0.055 |
Age coefficient 0.0885 p < 0.001 Cigarettes (#/day) 0.0129 p = 0.035 |
Low |
| Study | Country/name of the study | Design | Duration of follow-up | Sample size; % females | Type of assessed MH | Measurement of MH condition | Covariates | Outcome | Measurement of outcome | Adjusted association of depression/anxiety with overall incident asthma (95% CI) | Important results/highest risk group | CASP quality assessment |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Brunner et al. (2014)42 | The Coronary Artery Risk Development in Young Adults (CARDIA) Study, USA | Prospective cohort design | 20 years | 3614; F 64.1% | Depression | CES-D scale |
|
Asthma | A new report of asthma medication use and/or self-reported provider diagnosis of asthma | Baseline depression RH 1.26 (1.02 to 1.56) Cumulative exposure to depressiona RH 1.15 (1.02 to 1.29) |
Gender Female RH 1.93 (1.55 to 2.41) BMI (< 25 reference) BMI = 25–29 HR 1.19 (0.95 to 1.50) BMI = 30+ RH 1.41 (1.10 to 1.81) |
High |
| Education (<HS is reference) HS RH 0.74 (0.51 to 1.09) Some college RH 0.64 (0.43 to 0.95) College or more RH 0.66 (0.44 to 0.99) |
||||||||||||
| De La Hoz et al. (2016)43 | World Trade Centre Worker and Volunteer Medical Screening Program, USA | Prospective cohort design | Mean = 4.95 years | 3757; F 16.15% | PTSD | PTSD checklist questionnaire |
|
Asthma | Self-report of new physician-diagnosed asthma | Baseline PTSDb OR 2.41 (1.85 to 3.13) Recovering PTSD OR 1.34 (0.81 to 2.23) Late-onset PTSD OR 3.07 (2.18 to 4.31) Chronic PTSD OR 4.18 (3.06 to 5.72) |
Gender (male as reference) Female OR 1.38 (1.03 to 1.85) Race/ethnicity (white is reference) Latino OR 0.89 (0.69 to 1.16) African American OR 0.62 (0.42 to 0.91) |
Medium |
| Asian OR 1.32 (0.63 to 2.74) Other OR 3.58 (1.52 to 8.46) BMI (normal is reference) Overweight OR 1.1 (0.79 to 1.54) Obese OR 1.42 (1.01 to 2.00) |
| Study | Country/name of the study | Design | Duration of follow-up | Sample size; % females | Type of assessed MH | Measurement of MH condition | Covariates | Outcome | Measurement of outcome | Adjusted association of depression/PTSD with overall incident asthma (95% CI) | Important results/highest risk group | CASP quality assessment |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Boyko et al. (2010)44 | Seattle Epidemiologic Research and Information Centre, Department of Veterans Affairs Puget, Washington, USA | Prospective cohort longitudinal | 3 years | 44,754; F 25.8% | Depression and PTSD | Self-administered PHQ and PTSD checklist civilian version |
|
DM | Self-report of physician diagnosis | PTSD OR 2.07 (1.31 to 3.29) |
Age OR 1.06 (1.05 to 1.08) BMI OR 1.2 (1.17 to 1.23) Race/ethnicity (Caucasian is reference) African American OR 1.46 (1.10 to 1.94) Hispanic OR 1.35 (0.89 to 2.05) |
Low |
| Asian OR 1.67 (1.11 to 2.52) Other OR 1.07 (0.52 to 2.19) Separated from military as of follow-up (No is reference) Yes OR 2.18 (1.61 to 2.93) Component (Reserve/(Guard is reference) |
||||||||||||
| Active duty OR 0.74 (0.56 to 0.98) Depression × gender (Non-depressed men reference)Depressed men OR 1.14 (0.6 to 2.15) Non-depressed women OR 1.63 (1.26 to 2.13) Depressed women OR 0.51 (0.15 to 1.7) |
||||||||||||
| Mezuk et al. (2008)45 | Sound Health Care System, Seattle, Washington | Prospective cohort longitudinal | 23 years | 1071; 79.3% with MDD 61.7% no MDD |
Depression | DIS |
|
DM | Self-report at each wave; excluding diabetes cases that began within 1 year of depression onset and before the age of 30 | Depression (1981–2005)a HR 1.62 (1.03 to 2.55) (1993–2005) HR 2.04 (1.09 to 3.81)b |
Analysis stratified by educational attainmentc College degree or more HR 0.45 (0.11 to 1.80) High school or less HR 2.26 (1.11 to 4.6) |
Medium |
|
MDD x college degree or more (reference)d MDD × high school or less HR 4.1 (1.84 to 9.16) No MDD × college degree or more HR 0.92 (0.27 to 3.15) No MDD × high school or less HR 1.44 (0.82 to 2.55) |
| Study | Country/name of the study | Design | Duration of follow-up | Sample size; % females | Type of assessed MH | Measurement of MH condition | Covariates | Outcome | Measurement of outcome | Adjusted association of depression/PTSD with overall incident asthma (95% CI) | Important results/highest risk group | CASP quality assessment |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| O’Neil et al. (2016)46 | South-Eastern Australia/Geelong Osteoporosis Study | Prospective longitudinal study | Up to 18 years | 860 women | Depression and anxiety | SCID-I/NP |
|
Primary outcome: Occurrence of a CHD event that resulted in hospital Secondary outcome: CVD morbidity/hypertension treatment/IHD incidence and fatality |
Hospital medical records | Primary outcome (incidence yes/no): Baseline depression (OR 3.28, CI 1.36 to 7.9) Baseline anxiety (OR 0.62, CI 0.18 to 2.14) Secondary outcome (all cardiac events): Depression OR 2.74 CI (1.42 to 5.29) Anxiety OR 0.34 CI (0.12 to 0.99) Number of CHD events Depression IRR 1.03 CI (0.40 to 2.63) Anxiety IRR 1.64 CI (0.35 to 7.76) |
Primary outcome: Age OR 1.07 (1.02 to 1.11) Education OR 0.49 (0.27 to 0.87) Secondary outcome: Age OR 1.04 (1.01 to 1.07) Years of smoking OR 1.03 (1.00 to 1.05) Number of CHD events Age IRR 1.07 (1.01 to 1.13) BMI IRR 17.21 (1.26 to 235.46) Alcohol frequency IRR 3.29 (1.40 to 7.73) |
High |
| Balog et al. (2017)47 | Hungarian Epidemiological Panel Survey/Hungary | Prospective longitudinal study | 4 years | 2725; 56.44% | Depression | BDI-S |
|
CVD morbidity including hypertension treatment/CVD event incidence | Self-reported | Depressive symptomatology factor OR 1.15 CI (0.97 to 1.36) | Age OR 1.05 (1.04 to 1.07) BMI OR 1.05 (1.01 to 1.10) |
Low |
|
||||||||||||
| Anda et al. (1993)48 | USA (NHANES follow-up study of 1987) | Prospective longitudinal study | Mean length of follow-up was 12.4 years | Individuals being treated for hypertension (n = 277) and cardio- and/or cerebrovascular incidents (n = 131) for the first time during the follow-up period were compared to participants never treated for CVD (n = 2317) | Depression | General Well-being Questionnaire |
|
Ischaemic heart disease incidence and fatality | Hospital discharge records Cause of death was determined via death records coded against ICD-9 | Fatal IHD Depressed affect No (Ref) Yes RR 1.5 (1.0 to 2.3) Non-fatal IHD Depressed affect No (Ref) Yes RR 1.6 (1.1 to 2.4) |
Additive interaction Non-smoker/Non-depressed (Ref) Depressed affect Adjusted RR 1.31 Smoker only Adjusted RR 1.65 Smoker and depressed Adjusted RR 2.97 |
Medium |
Heterogeneity
Several sources of heterogeneity are present within this systematic review. Studies included utilised different tools for assessing mental disorders, and the results themselves are presented differently [i.e. hazard ratio (HR), relative risk, coefficients etc.). Also, there is some between-study variance in terms of assessing the impact of certain determinants. For example, the impact of smoking was assessed in some studies based on the duration of smoking, while in others on the number of cigarettes smoked per day.
Quality assessment
The Critical Appraisal Skills Programme (CASP) checklists for assessing the quality of cohort49 and case-control studies50 were used. The CASP checklists, devised for use in health-related research, were used for quality assessment of papers as ‘high’, ‘medium’ or ‘low’ quality. CASP is commonly used in qualitative evidence syntheses and is endorsed by the Cochrane Collaboration. 51 All articles were assessed for quality by a reviewer (ZJ), and another reviewer (AN) was available for mediation to arrive at a consensus through discussion using the CASP checklists.
Results
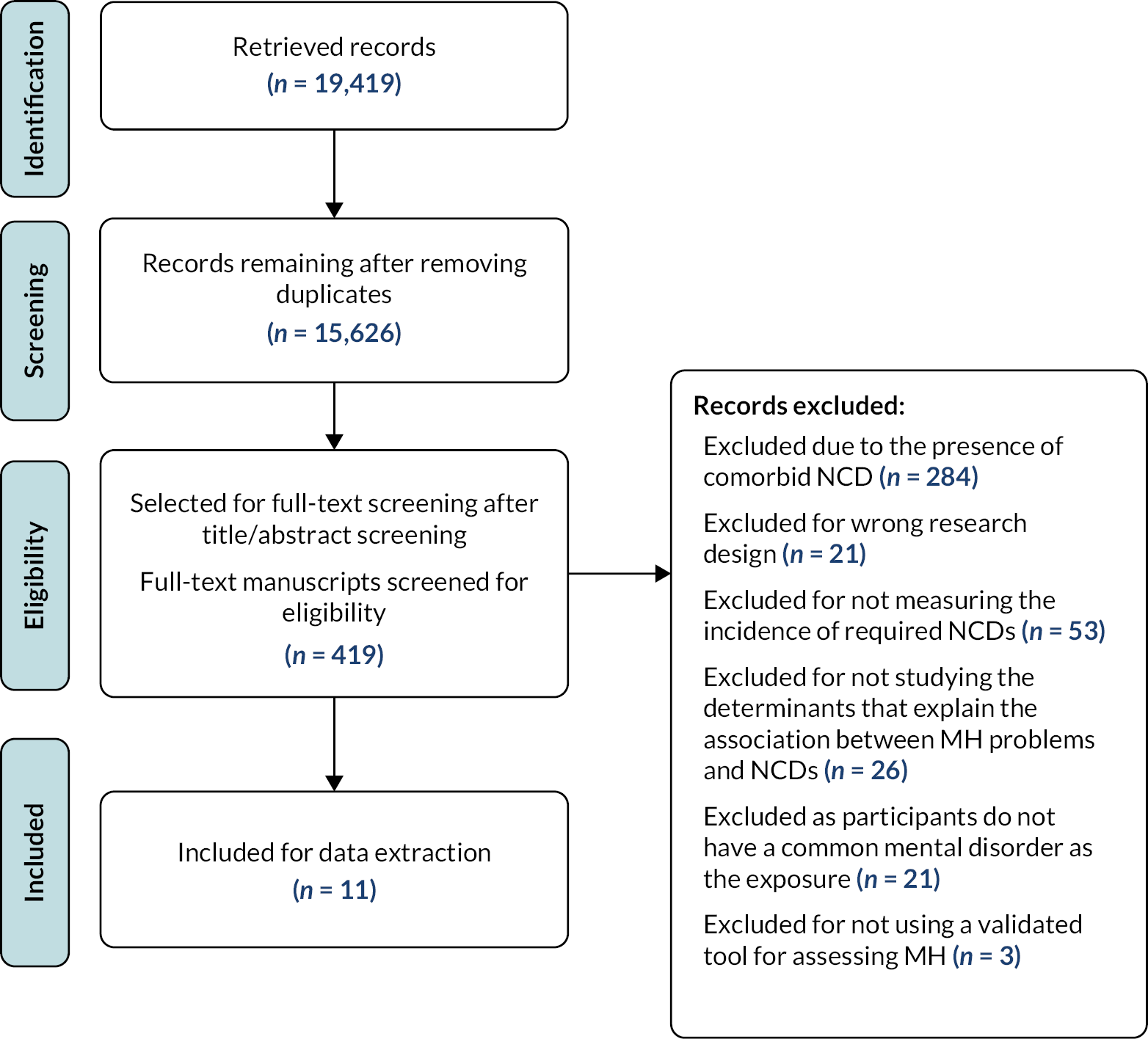
The study selection process is summarised in Figure 1, following PRISMA reporting guidelines. 32 More than 19,000 studies were found in the initial search. A total of 11 studies from 3 countries were included in the final review, with the majority (n = 9) conducted in the USA. All studies were longitudinal prospective studies, presenting outcomes for a total of 71,896 people. Four studies determined the association between depression and cancer, two studies depression with CVD and one study depression with diabetes. One study determined the association between depression and anxiety together with diabetes and another with CVD. No studies were found examining association between CMDs and COPD per se, but two studies addressing asthma were included (one considering depression and the other PTSD). A summary of the included studies is presented in Table 6.
FIGURE 1.
PRISMA flow diagram.
| Study characteristic | Number of studies (N = 11) |
|---|---|
| Countries | |
| USA | 9 |
| Australia | 1 |
| Hungary | 1 |
| Study design | |
| Prospective longitudinal cohort | 11 |
| Sample size | |
| < 1000 | 1 |
| 1000–3000 | 5 |
| ≥ 3000 | 5 |
| CMD | |
| Depression | 8 |
| Anxiety | 1 |
| Both | 2 |
| CMD screening tool | |
| PHQ-9 | 1 |
| Beck’s Depression Inventory (BDI-S) | 1 |
| Diagnostic Interview Schedule (DIS/DSM-III) | 2 |
| Centre for Epidemiological Studies Depression Scale (CES-D) | 3 |
| PTSD checklist | 2 |
| Minnesota Multiphasic Personality Inventory (MMPI) | 1 |
| SCID-I/NP | 1 |
| General Well-Being Schedule | 1 |
| NCD | |
| DM | 2 |
| CVD | 3 |
| Cancer | 4 |
| COPD | 0 |
| (Asthma = 2) CASP quality assessment | |
| High | 3 |
| Medium | 4 |
| Low | 4 |
Cancer
Evidence linking social determinants to cancer incidence: Table 7 summarises evidence grouped per determinant. It suggests that the determinants that showed a significant association were all associated with an increase in cancer incidence; however, one high-quality study and one medium-quality study were available. The latter suggested that age may be associated with cancer incidence; however, smoking status probably is.
| Quality of included studies (results of CASP tool) | |||
|---|---|---|---|
| Social determinants | H | M | L |
| Age | Gross et al. (2010)40 + | Linkins et al. (1990)52 + Persky V. et al. (1987) + |
|
| Smoking status | Penninx et al. (1998)41 + | Gross et al. (2010)40 + | Linkins et al. (1990)52 + |
| Number of cigarettes/day | Linkins et al. (1990)52 + Persky et al. (1987)53 + |
||
Summary of findings from retrieved articles
Four papers studied the effects of individual (smoking, age, gender, alcohol intake, body mass index and ethnicity) and social (marital status, occupational status and socioeconomic status) mental health determinants on cancer incidence (Table 2). None of the included studies adjusted for environmental factors. Follow-up period ranged between 10 and 24 years. Three of the four papers reported a significant association between depression and incident cancer. 40,41,53 Two population-based studies assessed depression at three different time intervals. Both studies revealed a specificity to the association between depression and hormonally mediated cancers, thus supporting the hypotheses about a common biological pathway between depression and cancer. 40,41 Penninx et al. measured chronic depression at three different times (1982, 1985 and 1988) in order to consider if depression is related to temporary stressful life circumstances that may remit shortly after. 41 Unlike baseline depression which was not significantly associated with incident cancer, chronically depressed mood, persistent for 6 years among individuals aged 71 years and above, was associated with an increased HR of 1.88 (95% CI = 1.3 to 3.14) for developing cancer after adjusting for age, sex, alcohol intake, smoking, race, physical disability and hospital admissions. A similar HR of 1.87 (CI 1.16 to 3.01) and 1.69 (CI 1.3 to 2.19) for the development of cancer among persons diagnosed with major depression and dysphoria, respectively, was observed in the study by Gross et al. 40 The association between depression and incident cancer in the study by Persky et al. among male employees was significant (p < 0.05); yet it was only observed when cancer was diagnosed during the first 10 years of follow-up.
The analysis of interaction between smoking, depression and incident cancer showed mixed results in all four studies. Smoking habits were unlikely to be related to the increased cancer risk among chronically depressed individuals. In the study where incident cancer was examined among persons with chronic depression, the HR for non-smokers exceeded that of smokers who are not chronically depressed. Compared with the non-chronically depressed participants, chronically depressed participants were more often females and of older age and less often smokers or excessive drinkers. Also, a more strict cut-off point for CES-D scores was adopted, 20 instead of 16, to yield a higher accuracy for the identification of participants with severe depression among older individuals. 41 In contrast, three studies found a significant association between smoking status and the incidence of cancer among depressed individuals. 40,52,53 The study by Persky et al. found an association between number of cigarettes smoked and cancer risk among employees with depression, with no specification to the type of cancer. In the other two studies, the interaction was observed at cancer sites related to smoking, such as buccal cavity and pharynx cancer52 and lung cancer. 40 As indicated in Table 7, age and smoking status were the only two covariates adjusted for in the study by Linkins et al. which might have resulted in an overestimation of the impact of smoking.
The two studies adjusting for older age found it to be significantly associated with an increased risk for developing cancer. 40,53 Except for ‘never having been married’ which had a protective effect against the development of cancer [HR 0.37 (CI 0.18 to 0.75)],40 none of the remaining covariates in all studies had any significant association with incident cancer among depressed individuals.
Chronic obstructive pulmonary disease and asthma
Evidence linking social determinants to asthma incidence
Available evidence from a medium-quality article suggests that female gender and BMI may be associated with an increased risk of developing asthma, and evidence from the high-quality article confirms that this is probably the case. Evidence from a medium-quality article suggests that being Latino or African, compared to being white, may be associated with decreased likelihood of developing asthma. Finally, based on one high-quality study, educational attainment is probably negatively associated with developing the condition (Table 8).
| Quality of included studies (results of CASP tool) | ||
|---|---|---|
| Social determinants | H | M |
| Female gender | Brunner et al. (2014)42 + | De La Hoz et al. (2016)43 + |
| BMI | Brunner et al. (2014)42 + | De La Hoz et al. (2016)43 + |
| Latino and African ethnicities | De La Hoz et al. (2016)43 – | |
| Educational attainment | Brunner et al. (2014)42 – | |
Summary of findings from retrieved articles
As noted previously, no studies linking depression and/or anxiety with incident COPD per se were identified in the literature. However, asthma is a form of lung disease that shares similar pathophysiological characteristics with COPD. 54 Also, there is evidence linking COPD to incident asthma. A recent longitudinal study of women, followed prospectively for 13 years, found that more than one in three women with asthma developed COPD. Sociodemographic, lifestyle and environmental risk factors were shown to have a significant association with the progression from asthma to COPD. Older age, obesity, cigarette smoking, unemployment, low education attainment and rural residence were all found to play a significant role in the progression to COPD. 55 Some risks associated with the progression from asthma to COPD were also found to be significantly associated with the progression from depression and anxiety to asthma. 42,43 Since there was evidence linking asthma to COPD incidence and since there was also evidence that mental health disorders could play a role in this, it was logical for the research team to include studies that looked at asthma as a disease outcome.
Two longitudinal studies identified in this review investigated the link between mental ill-health and incident asthma. As shown in Table 3, both studies reported significant associations with factors such as gender and obesity as independent predictors of incident asthma. In the multicentre Coronay Artery Risk Development in young adults (CARDIA) study, baseline and chronic depression were significantly associated with incident asthma. 42 The chronicity of PTSD in the study by de la Hoz also had a greater cumulative impact on the incidence of asthma. In a multivariable analysis, lifetime non-smokers with probable PTSD were found to be 2.41 times more likely to develop asthma than non-smokers without PTSD at baseline (OR = 2.41, 95% CI 1.85 to 3.13). The risk increased when participants had probable PTSD at baseline and follow-up visits. Participants with chronic PTSD were more than four times more likely to develop asthma (OR = 4.18, 95% CI 3.06 to 5.72). That the magnitude of association was greater between late-onset or chronic PTSD and incident asthma than with recovering probable PTSD and incident asthma suggests that treating PTSD could potentially reduce risk for asthma. 43
In both studies, incident asthma was defined either by a new report of asthma medication use and/or by self-reported physician diagnosis. Self-report of asthma has been found to be acceptable in epidemiologic studies with respect to physician diagnosis and is not linked to misclassification bias. 56 Misclassification bias is a pervasive systematic error that leads to the inaccurate classification of individuals participating in a study. 57 In other words, individuals who provide self-reports of asthma are prone to exhibit comparable asthma states to those who have received a medical diagnosis, hence suggesting a reasonable degree of accuracy in self-reporting. 58
Diabetes mellitus
Evidence linking social determinants to diabetes mellitus incidence
Table 9 suggests that there is inconclusive evidence linking age, BMI and ethnicity to increased incidence of diabetes, due to low quality of evidence. However, educational attainment may be negatively associated with increased risk for diabetes incidence, as per one medium-quality study.
Summary of findings from retrieved articles
Two studies reporting the incidence of DM as an outcome were included. Mezuk et al. tested prospectively the relationship between depression and type 2 diabetes among residents of East Baltimore. 45 Depression assessed via Diagnostic Interview Schedule (DIS) was collected in 1982, 1993 and 2005. The DIS is a standardised interview protocol conducted by individuals without professional clinical training. Its purpose is to determine diagnoses of major depressive disorder (MDD) and depressive syndrome, as well as ascertain the age at which these disorders first appeared and their recent occurrence, using diagnostic algorithms. 59 The onset of depression was determined as the earliest age when symptoms of depression began. The average age of depression onset was 30.9 years, and that of type 2 diabetes was 55 years. Respondents self-reported diabetes incidence, which may also have underdetected cases of diabetes. On average, it took 16 years for diabetes to develop after the onset of depression. Depression was found to be associated with diabetes onset [HR 1.62 (1.03 to 2.55)] after controlling for age, gender, race, education, social network size and antidepressant use. This association was more evident after controlling for additional sociodemographic characteristics and health behaviours [HR 2.04 (1.09 to 3.81)]. In a stratified analysis, the risk was elevated among those with 12 years of education or less (Table 4). No effect was seen for behavioural factors such as smoking or physical activity; however, that could be due to the actual measures not being sensitive enough to capture an effect. For instance, information on current smoking status was collected and not on number of cigarettes smoked or duration of smoking. For alcohol intake, information was collected on number of days where participants drank in the past month. Survival bias is also another limitation in such a study where the duration of follow-up was 23 years. Survival bias is observed when examining the relationship between a certain exposure during early life and a future health outcome during later stages of life. The presence of bias in the study may introduce a potential distortion in the results, as the examination exclusively focuses on the participants who have survived while neglecting to consider the characteristics of those who did not survive. 60
Diabetes risk was measured in 44,754 members of the US military service followed up for 3 years after assessing depression and anxiety at baseline. 44 Diabetes onset was self-reported, and the survey instrument included sociodemographics, weight, height and military service information. In a univariate comparison of baseline characteristics by diabetes status at follow-up, those with MDD and PTSD, screened using the self-administered PHQ-9 and PTSD checklist, respectively, had higher odds for developing diabetes: unadjusted OR 1.95 (1.23 to 3.11) and unadjusted OR 2.56 (1.78 to 3.67). In the multivariable model, only baseline PTSD, and not depression, was significantly associated with diabetes onset after adjusting for age, sex, BMI, education, race/ethnicity, military service characteristics and mental health conditions OR 2.07 (1.31 to 3.29). The authors suggested that the high occurrence of both conditions at baseline suggests that depression may serve as a surrogate marker for PTSD in other studies not measuring both conditions. Also, participants might have under-reported mental health symptoms due to fear of adverse consequences on their military records. Increased odds for diabetes were seen among participants of older age, higher BMI, non-Caucasians and those separated from the military. Being on active duty seems to have a protective effect against developing diabetes, which could be due to the fact that those selected for deployment pass a medical screening and are usually healthier and more fit. In this study, the interaction between gender and depression with DM onset suggests that gender plays a role in the development of DM. Non-depressed males were found to be at a significantly increased risk for developing DM. There is inconclusive evidence however whether the same association remains when depression ensues.
Cardiovascular diseases
Evidence linking social determinants to cardiovascular disease incidence
High-quality evidence suggests that age and educational attainment are probably associated with a positive and a negative association, respectively, with the incidence of CVD. Smoking status may be associated with an increased risk of CVD, and there is inconclusive evidence linking BMI to an increased incidence of CVD due to low-quality evidence only being available (Table 10).
| Quality of included studies (results of CASP tool) | |||
|---|---|---|---|
| Social determinants | H | M | L |
| Age | O’Neil et al. (2016)46 + | Balog et al. (2017)47 + | |
| BMI | Balog et al. (2017)47 + | ||
| Smoking status | Anda et al. (1993)48 + | ||
| Educational attainment | O’Neil et al. (2016)46 – | ||
Summary of findings from retrieved articles
Three studies examining the effect of depression on CVD incidence were identified, with follow-up periods ranging between 4 and 23 years. A prospective study of 860 women randomly selected from Australian electoral rolls was followed up for 18 years to study the impact of depression and anxiety on events requiring hospitalisation admission confirming coronary heart disease (CHD) incidence (primary outcome) and additional diagnosis of stable/unstable angina and ‘not otherwise defined’ CHD events (secondary outcome). 46 Depression and anxiety diagnosis was conducted by mental health professionals, at baseline and 10 years later, utilising the Structured Clinical Interview for Diagnostic and Statistical Manual of Mental Disorders, fourth edition, non-patient edition, which is the gold standard for assessing such disorders. Depression (OR 3.28, CI 1.36 to 7.9), and not anxiety (OR 0.62, CI 0.18 to 2.14), was found to be an independent risk factor for CHD after adjusting for demographic, anthropometric, health and clinical factors. Neither depression nor anxiety was significantly associated with recurrent cardiac episodes. The association shown between depression and CHD incidence was of greater magnitude than the association seen with other risk factors (Table 5). This suggests a need to set depression as a target in primary prevention of CHD as well as its influence on risk factor behaviours, an approach that could be useful for helping alleviate CVD burden globally.
Another study by Balog et al. examined the concurrent effects of depression and vital exhaustion (described by the authors as loss of energy, increased irritability and general demoralisation) on CVD morbidity in a random sample of 2317 participants from the Hungarian Epidemiological Panel Survey. 47 Greater age and BMI were positive predictors of CVD incidence after 4 years of follow-up, according to the logistic regression model, while depression did not have a significant predictive role. In addition to the relatively short follow-up duration, all information, including that of mental distress, was collected via self-administered questionnaires. Therefore, information pertaining to CVD incidence and/or diagnosis is highly unreliable. Also, survival bias is another limitation in such a case.
Using a subscale from the General Well-Being Questionnaire, depressed affect was assessed in a population sample of 2832 US citizens to examine the association of ischaemic heart disease (IHD). 48 After a mean follow-up period of 12.4 years, depression was found to be associated with an increased risk of fatal and non-fatal incidence of IHD (Table 5) after adjusting for age, sex, race, education, marital status, smoking, total cholesterol, systolic blood pressure, BMI, alcohol use and physical activity. No analysis was run to measure the individual effect of confounding variables on the incidence of IHD. The interaction between depression and smoking indicated a synergistic effect, increasing the relative risk for developing IHD.
Discussion
Findings from the systematic review suggest that the chronicity of depression and PTSD could be associated with increased risk for cancer and asthma onset, respectively, and therefore treating depression and PTSD could prevent progression into the development of the latter NCDs. Moreover, the high association between depression and CHD suggests the need to target depression as primary prevention to prevent the progression into CHD. On the other hand, factors such as educational attainment, number of cigarettes smoked, female gender, older age, elevated BMI and ethnicity may contribute to an elevated risk for developing NCDs among adults with depression and/or PTSD. Therefore, in order to reduce the incidence of NCDs, mental disorders should be identified and treated, and health and prevention strategies focusing primarily on high-risk groups, where factors listed above are present, can and should be adopted.
Our findings are consistent with cohort studies where older age,61 low educational attainment,62 higher BMI63 and smoking status61 were found to be associated with CVD incidence. In the current review, the study by O’Neil has identified depression as an independent risk factor for CVD onset,46 which is also suggested by other longitudinal studies. 64–66 We, therefore, recommend to include depression as a target for primary prevention of CVD.
Ethnicity was found to be associated with the onset of diabetes. Factors identified earlier as being related to CVD incidence, except smoking, were also reported in this review to be associated with diabetes onset. This is in agreement with findings from the literature that linked older age, higher BMI67,68 and low educational attainment69 with incident diabetes. Our results regarding the type of mental disorder associated with type 2 diabetes incidence contradict findings of the literature, however. While numerous research has demonstrated a bidirectional association between depression and type 2 diabetes,70,71 our review indicates that PTSD, and not depression, was found to increase incident diabetes when the effects of depression and PTSD were studied together. A study by Scherrer et al. found that reducing PTSD symptoms lowered the risk of type 2 diabetes72 among participants with PTSD. In the same study, depression remission contributed to lower diabetes onset among participants diagnosed with comorbid PTSD and depression, and not with depression alone. Therefore, there may be further benefit from reducing PTSD symptoms to lower type 2 diabetes risk in populations that are exposed to potentially traumatic events, such as veterans. For other populations exposed to such events, for example, refugees and the general population affected by adverse events, studies are lacking. Therefore, it is difficult at this point to generalise a recommendation as to target PTSD for the primary prevention of type 2 diabetes.
In relation to cancer incidence, three out of four studies demonstrated an association between depression and incident cancer. This is in line with two previous meta-analyses. 73,74 Although not all studies included in this review showed a significant impact of depression on cancer initiation, some trends emerged regarding the extended duration of depression having an important role in a slowly developing health condition such as cancer. This view is shared by Garssen75 who suggested in 2004 specific risk factors among this population, namely, smoking, BMI, age and alcohol intake. This research also found that behavioural factors, namely smoking76 and alcohol intake,77 were associated with increased cancer onset.
Our review showed a significant association between depression and PTSD with incident asthma. In 2005, a review that explored the interaction between depression and asthma as comorbidities suggested that the respiratory tract (mainly the airways) is greatly reactive to the psychological changes of individuals. 78 The findings of our study suggest that depression could lead to asthma onset via this mechanism. Regarding PTSD, our findings are consistent with those in the literature whereby PTSD was found to be positively associated with asthma onset. 79,80 Our study identified risk factors such as female gender, increased BMI and low educational attainment as being related to asthma onset. Therefore, special attention should be given to such population groups in clinical practice and public health interventions that aim to reduce the incidence of asthma.
In addition to the complexity in conducting longitudinal studies to test the causal association between common mental health disorders and NCDs, there appears to be a challenge in relation to the reporting of health conditions. Epidemiological investigations and population-based studies mainly rely on self-reports to obtain information on health outcomes, such as diabetes, given the high cost and low efficiency of clinical diagnosis. 81,82 A number of studies assessing the accuracy of self-reported data, using test characteristics such as sensitivity (the fraction of people who fit the medical criteria for the outcome and self-report a diagnosis, i.e. true positive) and specificity (the fraction of people who have normal measures and do not report a diagnosis, i.e. true negative), gave mixed results. 83–85 Compared to biochemical measurements, self-reported data on diabetes among Chinese adults ≥ 45 years showed low sensitivity and a moderate overall agreement. Factors associated with accurate self-reported data were female sex, older age, high socioeconomic status, better educational attainment and recent utilisation of medical services. 85 Goldman et al. attributed the lack of accuracy in self-reports to several factors, such as undiagnosed diseases, inability to recall, unwillingness to disclose medical information and lack of accessibility to health services. 84 This could further be exacerbated among individuals facing psychological stressors. Depression, for instance, was found to be associated with barriers deterring individuals from utilising medical services. Factors such as mistrust in health providers and the health system,86 loss of income87 and low motivation to seek medical care88 may all result in underdiagnoses leading to under-reporting. Therefore, the above-mentioned issues that feed into under-reporting should be taken into account when conducting future research on this topic.
Another common challenge pertains to the identification of cases of common mental health disorders. There is no single diagnostic tool for such conditions. For instance, several valid and reliable instruments are used by primary care clinicians and researchers to identify cases of depression and anxiety. 89–91 The selection of the appropriate tool depends on factors such as feasibility, administration time and personnel and interest in measuring the severity of the condition or monitoring the response to therapy. These tools tend to under-report cases compared with the clinical psychiatric examination and hinder the ability to compare results from different studies.
Strengths and limitations
This systematic review provides additional evidence on how common mental health disorders are linked to the onset of the four most common NCDs. The particularity of the evidence that emerged has to do with the type of individual studies: the included longitudinal studies provide valuable evidence for establishing a causal relationship between common mental health disorders and NCDs in this specific direction. However, it should be noted that the utilisation of a longitudinal research design does not completely preclude the possibility of other explanations, such as the influence of third variables. Consequently, it does not definitively demonstrate a causal relationship or enable the formulation of causal claims. 92 Other limitations of the current review should be acknowledged. First, our review did not include studies from the grey literature and was limited to literature published in English language only. Second, measures of depression and anxiety varied among studies, with the majority relying on self-report using different screening tools with various cut-off points. This might have caused a misclassification of exposure and, hence, lessened the association between mental disorders and the incidence of NCDs. Third, measures of covariates were different across studies which makes it difficult to compare their effects on the onset of diseases. And finally, the majority of included studies limited their assessment of mental conditions to one point in time which might have been a transient episode. The association found between chronic depression/PTSD and incident NCDs emphasised the importance of assessing the chronicity of mental illnesses and their impact on health.
Conclusion
This study contributed to the existing global body of evidence regarding the factors that are directly linked to the onset of NCDs. As a result, policy-makers and practitioners can utilise the findings to customise interventions that target these specific factors, with the aim of interrupting the cycle between mental health disorders and other NCDs. Interventions need to target those with common mental health disorders and take into account: age (older age groups are more at risk), sex (females are more at risk), educational level (individuals with ˂12 years of education are more at risk) and smoking status (smokers are more at risk). Furthermore, there is an urgent need to conduct studies to understand the linkages between mental health and NCDs in LMICs, given the absence of evidence in those settings and the increasing burden of NCDs and mental health conditions they are experiencing. Finally, research to evaluate public health interventions and to assess the responsiveness of healthcare systems (mainly at the primary care level) is essential to alleviate the burden of those conditions at population level. In summary, this review adds to the body of evidence that prioritising the social determinants of mental health is crucial for enhancing public health outcomes through the implementation of a preventative health promotion strategy. Through this approach, it becomes possible to address the systemic determinants of health that are often overlooked, which can contribute to the development of disease. 93
Reporting community engagement and involvement: Since this was a review article, there was no patient and public involvement in this study.
Equality, diversity and inclusion: Research around mental and physical health multimorbidity is limited, despite the fact that the global burden of mental illnesses and NCDs is high. This review contributes to the existing global body of evidence regarding the factors that are directly linked to the onset of NCDs. Findings can be utilised to inform interventions for high-risk populations worldwide to prevent development of NCDs.
Additional information
Acknowledgements
We would like to acknowledge the support of Mairi Redman for her generous donation of time to assist in abstract screening and Aya Noubani for being available for mediation throughout the full-text screening and the data extraction phase.
CRediT contribution statement
Zeina Jamal (https://orcid.org/0000-0002-5078-3416): Conceptualisation (equal), Data curation (lead), Formal analysis (lead), Investigation (lead), Project administration (lead), Visualisation (lead), Writing – original draft (lead), Writing – editing and reviewing (equal). Alastair Ager (https://orcid.org/0000-0002-9869-544X): Conceptualisation (equal), Investigation (supporting), Supervision (equal), Visualisation (supporting), Writing – editing and reviewing (equal). Rebecca Horn (https://orcid.org/0000-0002-9474-3563): Conceptualisation (equal), Investigation (supporting), Supervision (equal), Visualisation (supporting), Writing – editing and reviewing (equal).
Disclosure of interests
Full disclosure of interests: Completed ICMJE forms for all authors, including all related interests, are available in the toolkit on the NIHR Journals Library report publication page at https://doi.org/10.3310/CTDH4677.
Primary conflicts of interest: The authors declare that they have no competing interests.
Data-sharing statement
Requests for access to data should be addressed to the corresponding author.
Ethics statement
This study is classified as a systematic review, and consequently, ethical approval was not required.
Information governance statement
This is a systematic review, and therefore, the current research did not handle any personal information.
Official Development Assistance (ODA) compliance statement
The research project holds considerable importance in relation to mental health and NCDs due to its direct applicability to the developmental challenges encountered by LMICs. These countries face an immense burden in addressing the challenges posed by mental illness and NCDs, as well as grappling with inadequacies in properly addressing and treating these conditions. Although the main focus of this study was not specifically directed towards LMICs, the findings of this research will have substantial implications for policy formulation and practical implementation in LMIC settings. By gaining a comprehensive understanding of the complex interplay between mental health, NCDs and the determinants influencing them, policy-makers and healthcare professionals can develop more efficacious approaches to prevent, promptly detect and manage these conditions within LMICs.
Department of Health and Social Care disclaimer
This publication presents independent research commissioned by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, MRC, NIHR Coordinating Centre, the Global Health Research programme or the Department of Health and Social Care.
Study registration
The study protocol was registered with PROSPERO (CRD42019157800).
Funding
This article presents independent research funded by the National Institute for Health and Care Research (NIHR) Global Health Research programme (NIHR award ref: 16/136/100) using UK aid from the UK Government to support global health research. The views expressed in this publication are those of the authors and not necessarily those of the NIHR or the UK government. Research is published in the NIHR Global Health Research Journal. See the NIHR Funding and Awards website for further award information.
This article reports on one component of the research award Effect of contributing factors on the incidence of non-communicable diseases among adults with common mental health disorders: a systematic review. For more information about this research please view the award page [https://www.fundingawards.nihr.ac.uk/award/16/136/100]
About this article
The contractual start date for this research was in June 2017. This article began editorial review in March 2023 and was accepted for publication in December 2023. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The Global Health Research editors and publisher have tried to ensure the accuracy of the authors’ article and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this article.
This article was published based on current knowledge at the time and date of publication. NIHR is committed to being inclusive and will continually monitor best practice and guidance in relation to terminology and language to ensure that we remain relevant to our stakeholders.
Copyright
Copyright © 2024 Jamal et al. This work was produced by Jamal et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
List of abbreviations
- BMI
- body mass index
- CASP
- Critical Appraisal Skills Programme
- CHD
- coronary heart disease
- CIDI
- Composite International Diagnostic Interview
- CMD
- common mental disorder
- COPD
- chronic obstructive pulmonary disease
- CVD
- cardiovascular disease
- DM
- diabetes mellitus
- ICD
- International Classification of Disease
- IHD
- ischaemic heart disease
- MeSH
- medical subject heading
- NCD
- non-communicable disease
- PHQ-9
- Patient Health Questionnaire-9 item
- PICOS
- population, intervention/exposure, control, outcome and study design
- PRISMA
- Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- PTSD
- post-traumatic stress disorder
- SCID
- Structured Clinical Interview for Diagnostic and Statistical Manual of Mental Disorders
- WHO
- World Health Organization
References
- World Health Organization . Noncommunicable Diseases 2022. www.who.int/health-topics/noncommunicable-diseases#tab=tab_1 (accessed 23 October 2022).
- Pan American Health Organization . Noncommunicable Diseases 2023. www.paho.org/en/topics/noncommunicable-diseases (accessed 16 September 2023).
- World Health Organization . Noncommunicable Diseases: Fact Sheet 2022. www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases (accessed 20 January 2022).
- World Health Organization . Noncommunicable Diseases 2018. www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases (accessed 23 October 2022).
- American Psychological Association . APA Dictionary of Psychology 2020.
- World Health Organization . Depression and Other Common Mental Disorders: Global Health Estimates 2017.
- World Health Organization . Risks to Mental Health: An Overview of Vulnerabilities and Risk Factors 2012.
- Marmot M, Goldblatt P, Allen J, Bell R, Bloomer E, Donkin A, et al. Review of Social Determinants and the Health Divide in the WHO European Region 2014.
- Pryor L, Da Silva MA, Melchior M. Mental health and global strategies to reduce NCDs and premature mortality. Lancet Public Health 2017;2:e350-1.
- Chaiton M, Cohen JE, Rehm J, Abdulle M, O’Loughlin J. Confounders or intermediate variables? Testing mechanisms for the relationship between depression and smoking in a longitudinal cohort study. Addict Behav 2015;42:154-61.
- World Health Organization . Mental Health in the Eastern Mediterranean Region: Reaching the Unreached 2006.
- Carrà G, Bartoli F, Riboldi I, Trotta G, Crocamo C. Poverty matters: cannabis use among people with serious mental illness: findings from the United States survey on drug use and health, 2015. Int J Soc Psychiatry 2018;64:656-9.
- Watts S, Leydon G, Birch B, Prescott P, Lai L, Eardley S, et al. Depression and anxiety in prostate cancer: a systematic review and meta-analysis of prevalence rates. BMJ Open 2014;4.
- Watts S, Prescott P, Mason J, McLeod N, Lewith G. Depression and anxiety in ovarian cancer: a systematic review and meta-analysis of prevalence rates. BMJ Open 2015;5.
- Arnaboldi P, Riva S, Crico C, Pravettoni G. A systematic literature review exploring the prevalence of post-traumatic stress disorder and the role played by stress and traumatic stress in breast cancer diagnosis and trajectory. Breast Cancer (Dove Med Press) 2017;9:473-85.
- Vancampfort D, Correll CU, Galling B, Probst M, De Hert M, Ward PB, et al. Diabetes mellitus in people with schizophrenia, bipolar disorder and major depressive disorder: a systematic review and large scale meta-analysis. World Psychiat 2016;15:166-74.
- Korff MV, Scott K, Gureje O. Global Perspectives on Mental-Physical Comorbidity in the WHO World Mental Health Surveys. Cambridge: Cambridge University Press; 2009.
- Gragnoli C. Depression and type 2 diabetes: cortisol pathway implication and investigational needs. J Cell Physiol 2012;227:2318-22.
- Compton MT, Shim RS. The social determinants of mental health. Focus 2015;13:419-25.
- Wagner J, Burke G, Kuoch T, Scully M, Armeli S, Rajan TV. Trauma, healthcare access, and health outcomes among Southeast Asian refugees in Connecticut. J Immigr Minor Health 2013;15:1065-72.
- Taylor TR, Williams CD, Makambi KH, Mouton C, Harrell JP, Cozier Y, et al. Racial discrimination and breast cancer incidence in US Black women: the Black Women’s Health Study. Am J Epidemiol 2007;166:46-54.
- Lemogne C, Nabi H, Melchior M, Goldberg M, Limosin F, Consoli SM, et al. Mortality associated with depression as compared with other severe mental disorders: a 20-year follow-up study of the GAZEL cohort. J Psychiatr Res 2013;47:851-7.
- Spiegel D, Bloom JR, Kraemer HC, Gottheil E. Effect of psychosocial treatment on survival of patients with metastatic breast cancer. Lancet 1989;334:888-91.
- Klaassen Z, Wallis CJD, Goldberg H, Chandrasekar T, Sayyid RK, Williams SB, et al. The impact of psychiatric utilisation prior to cancer diagnosis on survival of solid organ malignancies. Br J Cancer 2019;120:840-7.
- Hayman KG, Sharma D, Wardlow RD, Singh S. Burden of cardiovascular morbidity and mortality following humanitarian emergencies: a systematic literature review. Prehosp Disaster Med 2015;30:80-8.
- Banatvala N, Akselrod S, Webb D, Sladden T, Hipgrave D, Schneidman M. Actions needed to prevent noncommunicable diseases and improve mental health. Bull World Health Organ 2019;97:75-75A.
- United Nations General Assembly . Resolution Adopted by the General Assembly on 25 September 2015 2015.
- World Health Organization . Mental Health: Facing the Challenges, Building Solutions 2005.
- World Health Organization . Global Action Plan for the Prevention and Control of Noncommunicable Diseases 2013–2020 2013.
- O’Neil A, Jacka FN, Quirk SE, Cocker F, Taylor CB, Oldenburg B, et al. A shared framework for the common mental disorders and non-communicable disease: key considerations for disease prevention and control. BMC Psychiatry 2015;15:1-6.
- Jamal Z, Ager A, Horn R. A Systematic Review Studying the Effect of Mental Health Determinants on the Incidence of Main NCDs Among Adults With Common Mental Health Disorders. PROSPERO 2019 n.d. www.crd.york.ac.uk/PROSPERO/display_record.php?RecordID=157800 (accessed 14 November 2022).
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Rev 2021;10:1-11.
- Booth A, Cantrell A, Preston L, Chambers D, Goyder E. What Is the Evidence for the Effectiveness, Appropriateness and Feasibility of Group Clinics for Patients with Chronic Conditions? A Systematic Review. Southampton: NIHR Journals Library; 2016.
- Thiese MS. Observational and interventional study design types; an overview. Biochem Med (Zagreb) 2014;24:199-210.
- World Health Organization . ICD-11 for Mortality and Morbidity Statistics 2021. https://icd.who.int/browse11/l-m/en#/http%3a%2f%2fid.who.int%2ficd%2fentity%2f334423054 (accessed 10 October 2021).
- American Psychological Association . The Organization of DSM-5 2021. www.psychiatry.org/psychiatrists/practice/dsm/educational-resources/dsm-5-fact-sheets (accessed 10 October 2021).
- American Psychiatric Association Division of Research . Highlights of changes from DSM-IV to DSM-5: posttraumatic stress disorder. Focus 2013;11:358-61.
- Leon BM, Maddox TM. Diabetes and cardiovascular disease: epidemiology, biological mechanisms, treatment recommendations and future research. World J Diabetes 2015;6:1246-58.
- Campbell M, McKenzie JE, Sowden A, Katikireddi SV, Brennan SE, Ellis S, et al. Synthesis without meta-analysis (SWiM) in systematic reviews: reporting guideline. BMJ 2020;368.
- Gross AL, Gallo JJ, Eaton WW. Depression and cancer risk: 24 years of follow-up of the Baltimore Epidemiologic Catchment Area sample. Cancer Causes Control 2010;21:191-9.
- Penninx BW, Guralnik JM, Pahor M, Ferrucci L, Cerhan JR, Wallace RB, et al. Chronically depressed mood and cancer risk in older persons. J Natl Cancer Inst 1998;90:1888-93.
- Brunner WM, Schreiner PJ, Sood A, Jacobs DR. Depression and risk of incident asthma in adults: the CARDIA study. Am J Respir Crit Care Med 2014;189:1044-51.
- de la Hoz RE, Jeon Y, Miller GE, Wisnivesky JP, Celedón JC. Post-traumatic stress disorder, bronchodilator response, and incident asthma in World Trade Center rescue and recovery workers. Am J Respir Crit Care Med 2016;194:1383-91.
- Boyko EJ, Jacobson IG, Smith B, Ryan MAK, Hooper TI, Amoroso PJ, et al. Millennium Cohort Study Team . Risk of diabetes in U.S. military service members in relation to combat deployment and mental health. Diabetes Care 2010;33:1771-7.
- Mezuk B, Eaton WW, Golden SH, Ding Y. The influence of educational attainment on depression and risk of type 2 diabetes. Am J Public Health 2008;98:1480-5.
- O’Neil A, Fisher AJ, Kibbey KJ, Jacka FN, Kotowicz MA, Williams LJ, et al. Depression is a risk factor for incident coronary heart disease in women: an 18-year longitudinal study. J Affect Disord 2016;196:117-24.
- Balog P, Falger PRJ, Szabó G, Rafael B, Székely A, Konkolÿ Thege B. Are vital exhaustion and depression independent risk factors for cardiovascular disease morbidity?. Health Psychol 2017;36.
- Anda R, Williamson D, Jones D, Macera C, Eaker E, Glassman A, et al. Depressed affect, hopelessness, and the risk of ischemic heart disease in a cohort of U.S. adults. Epidemiology 1993;4.
- Critical Appraisal Skills Programme . CASP Cohort Study Checklist 2018. https://casp-uk.net/wp-content/uploads/2018/01/CASP-Cohort-Study-Checklist_2018.pdf (accessed 25 September 2020).
- Critical Appraisal Skills Programme . CASP (Case-Control Study Checklist) 2018. https://casp-uk.b-cdn.net/wp-content/uploads/2020/10/CASP_RCT_Checklist_PDF_Fillable_Form.pdf (accessed 25 September 2020).
- Noyes J, Booth A, Flemming K, Garside R, Harden A, Lewin S, et al. Cochrane Qualitative and Implementation Methods Group guidance series – paper 3: methods for assessing methodological limitations, data extraction and synthesis, and confidence in synthesized qualitative findings. J Clin Epidemiol 2018;97:49-58.
- Linkins RW, Comstock GW. Depressed mood and development of cancer. Am J Epidemiol 1990;132:962-72.
- Persky VW, Kempthorne-Rawson J, Shekelle RB. Personality and risk of cancer: 20-year follow-up of the Western Electric Study. Psychosom Med 1987;49:435-49.
- Cukic V, Lovre V, Dragisic D, Ustamujic A. Asthma and chronic obstructive pulmonary disease (COPD): differences and similarities. Mater Sociomed 2012;24:100-5.
- To T, Zhu J, Gray N, Feldman LY, Villeneuve PJ, Licskai C, et al. Asthma and chronic obstructive pulmonary disease overlap in women. Incidence and risk factors. Ann Am Thorac Soc 2018;15:1304-10.
- Torén K, Brisman J, Järvholm B. Asthma and asthma-like symptoms in adults assessed by questionnaires. A literature review. Chest 1993;104:600-8.
- Spencer EA, Mahatni KR, Brassey J, Heneghan C. Catalogue of Bias Collaboration. Misclassification Bias 2018. www.catalogueofbiases.org/biases/misclassificationbias (accessed 16 September 2023).
- Brumpton BM, Langhammer A, Ferreira MAR, Chen Y, Mai XM. Physical activity and incident asthma in adults: the HUNT Study, Norway. BMJ Open 2016;6.
- Robins LN, Helzer JE, Croughan J, Ratcliff KS. National Institute of Mental Health Diagnostic Interview Schedule. Its history, characteristics, and validity. Arch Gen Psychiatry 1981;38:381-9.
- Howe CJ, Robinson WR. Survival-related selection bias in studies of racial health disparities: the importance of the target population and study design. Epidemiology 2018;29:521-4.
- Al-Shamsi S, Regmi D, Govender RD. Incidence of cardiovascular disease and its associated risk factors in at-risk men and women in the United Arab Emirates: a 9-year retrospective cohort study. BMC Cardiovasc Disord 2019;19:1-9.
- Dégano IR, Marrugat J, Grau M, Salvador-González B, Ramos R, Zamora A, et al. The association between education and cardiovascular disease incidence is mediated by hypertension, diabetes, and body mass index. Sci Rep 2017;7:1-8.
- Canoy D, Cairns BJ, Balkwill A, Wright FL, Green J, Reeves G, et al. Body mass index and incident coronary heart disease in women: a population-based prospective study. BMC Med 2013;11:1-9.
- Majed B, Arveiler D, Bingham A, Ferrieres J, Ruidavets JB, Montaye M, et al. PRIME Study Group . Depressive symptoms, a time-dependent risk factor for coronary heart disease and stroke in middle-aged men: the PRIME Study. Stroke 2012;43:1761-7.
- Surtees PG, Wainwright NWJ, Luben RN, Wareham NJ, Bingham SA, Khaw KT. Depression and ischemic heart disease mortality: evidence from the EPIC-Norfolk United Kingdom prospective cohort study. Am J Psychiatry 2008;165:515-23.
- Kendler KS, Gardner CO, Fiske A, Gatz M. Major depression and coronary artery disease in the Swedish twin registry: phenotypic, genetic, and environmental sources of comorbidity. Arch Gen Psychiatry 2009;66:857-63.
- Abdullah A, Peeters A, de Courten M, Stoelwinder J. The magnitude of association between overweight and obesity and the risk of diabetes: a meta-analysis of prospective cohort studies. Diabetes Res Clin Pract 2010;89:309-19.
- Lindström J, Tuomilehto J. The diabetes risk score: a practical tool to predict type 2 diabetes risk. Diabetes Care 2003;26:725-31.
- Steele CJ, Schöttker B, Marshall AH, Kouvonen A, O’Doherty MG, Mons U, et al. Education achievement and type 2 diabetes – what mediates the relationship in older adults? Data from the ESTHER study: a population-based cohort study. BMJ Open 2017;7.
- Eaton WW, Armenian H, Gallo J, Pratt L, Ford DE. Depression and risk for onset of type II diabetes: a prospective population-based study. Diabetes Care 1996;19:1097-102.
- Lustman PJ, Clouse RE. Depression in diabetes: the chicken or the egg?. Psychosom Med 2007;69:297-9.
- Scherrer JF, Salas J, Norman SB, Schnurr PP, Chard KM, Tuerk P, et al. Association between clinically meaningful posttraumatic stress disorder improvement and risk of type 2 diabetes. JAMA Psychiatry 2019;76:1159-66.
- Oerlemans ME, van den Akker M, Schuurman AG, Kellen E, Buntinx F. A meta-analysis on depression and subsequent cancer risk. Clin Pract Epidemiol Ment Health 2007;3:29-11.
- McGee R, Williams S, Elwood M. Depression and the development of cancer: a meta-analysis. Soc Sci Med 1994;38:187-92.
- Garssen B. Psychological factors and cancer development: evidence after 30 years of research. Clin Psychol Rev 2004;24:315-38.
- Johnson KC, Hu J, Mao Y. Canadian Cancer Registries Epidemiology Research Group . Passive and active smoking and breast cancer risk in Canada, 1994–97. Cancer Causes Control 2000;11:211-21.
- Smith-Warner SA, Spiegelman D, Yaun SS, van den Brandt PA, Folsom AR, Goldbohm RA, et al. Alcohol and breast cancer in women: a pooled analysis of cohort studies. JAMA 1998;279:535-40.
- Opolski M, Wilson I. Asthma and depression: a pragmatic review of the literature and recommendations for future research. Clin Pract Epidemiol Ment Health 2005;1:1-7.
- O’Toole BI, Catts SV. Trauma, PTSD, and physical health: an epidemiological study of Australian Vietnam veterans. J Psychosom Res 2008;64:33-40.
- Sareen J, Cox BJ, Stein MB, Afifi TO, Fleet C, Asmundson GJG. Physical and mental comorbidity, disability, and suicidal behavior associated with posttraumatic stress disorder in a large community sample. Psychosom Med 2007;69:242-8.
- Wu F, Guo Y, Kowal P, Jiang Y, Yu M, Li X, et al. Prevalence of major chronic conditions among older Chinese adults: the Study on Global AGEing and adult health (SAGE) wave 1. PLOS ONE 2013;8.
- Borrell LN, Dallo FJ, White K. Education and diabetes in a racially and ethnically diverse population. Am J Public Health 2006;96:1637-42.
- Okura Y, Urban LH, Mahoney DW, Jacobsen SJ, Rodeheffer RJ. Agreement between self-report questionnaires and medical record data was substantial for diabetes, hypertension, myocardial infarction and stroke but not for heart failure. J Clin Epidemiol 2004;57:1096-103.
- Goldman N, Lin IF, Weinstein M, Lin YH. Evaluating the quality of self-reports of hypertension and diabetes. J Clin Epidemiol 2003;56:148-54.
- Ning M, Zhang Q, Yang M. Comparison of self-reported and biomedical data on hypertension and diabetes: findings from the China Health and Retirement Longitudinal Study (CHARLS). BMJ Open 2016;6.
- LaVeist TA, Nickerson KJ, Bowie JV. Attitudes about racism, medical mistrust, and satisfaction with care among African American and white cardiac patients. Med Care Res Rev 2000;57:146-61.
- Dohrenwend BP, Levav I, Shrout PE, Schwartz S, Naveh G, Link BG, et al. Socioeconomic status and psychiatric disorders: the causation-selection issue. Science 1992;255:946-52.
- Haviland MG, Pincus HA, Morales LS. Depression and satisfaction with health coverage and medical care in the 1998 NRC Healthcare Market Guide Survey. Adm Policy Ment Health 2003;30:511-22.
- Ferenchick EK, Ramanuj P, Pincus HA. Depression in primary care: part 1 – screening and diagnosis. BMJ 2019;365.
- Mulrow CD, Williams JW, Gerety MB, Ramirez G, Montiel OM, Kerber C. Case-finding instruments for depression in primary care settings. Ann Intern Med 1995;122:913-21.
- Bliese PD, Wright KM, Adler AB, Cabrera O, Castro CA, Hoge CW. Validating the primary care posttraumatic stress disorder screen and the posttraumatic stress disorder checklist with soldiers returning from combat. J Consult Clin Psychol 2008;76:272-81.
- Oxford Bibliographies . Longitudinal Research 2023. www.oxfordbibliographies.com/display/document/obo-9780199846740/obo-9780199846740-0028.xml (accessed 16 September 2023).
- Quijada CS, López-Contreras N, López-Jiménez T, Medina-Perucha L, León-Gómez BB, Peralta A, et al. Social inequalities in mental health and self-perceived health in the first wave of COVID-19 lockdown in Latin America and Spain: results of an online observational study. Int J Environ Res Public Health 2023;20.
Appendix 1 MEDLINE search strategy
| # | Searches | Results |
|---|---|---|
| 1 | TI, AB cardiovascular disease* OR CVD OR heart disease* OR vascular disease* OR cerebrovascular diseases | 415,338 |
| 2 | (MM ‘Cardiovascular Diseases’) OR (MM ‘Pathological Conditions, Signs and Symptoms’) OR (MM ‘Disorders of Environmental Origin’) OR (MH ‘Endocrine System Diseases+’) OR (MH ‘Nutritional and Metabolic Diseases+’) OR (MH ‘Vascular Diseases+’) OR (MH ‘Heart Diseases+’) | 3,753,932 |
| 3 | TI, AB type 2 diabetes OR type ii diabetes or noninsulin dependent or non insulin dependent OR non-insulin dependent OR NIDDM OR adult onset diabetes OR maturity onset OR diabetes mellitus | 415,051 |
| 4 | (MM ‘Diabetes Mellitus, Type 2’) OR (MM ‘Diabetes Complications/DI/ET/PX/EP/CO’) | 102,692 |
| 5 | TI, AB neoplas* OR cancer* OR carcinoma* OR tumor* OR tumour* OR malignan* OR leukaemia OR leukemia OR lymphoma | 3,805,137 |
| 6 | (MM ‘Neoplasms/PX/ET/EP/CO/DI’) OR (MM ‘Carcinogenesis’) | 77,036 |
| 7 | TI, AB COPD OR chronic obstructive pulmonary disease OR lung disease OR pulmonary disease | 238,793 |
| 8 | (MM ‘Pulmonary Disease, Chronic Obstructive/CO/DI/EP/ET/PX’) | 10,078 |
| 9 | (MM ‘Non-communicable Diseases/PX/EP’) OR (MM ‘Communicable Diseases, Emerging/DI/EP/PX/ET/CO’) | 2133 |
| 10 | TI, AB stress disorder OR PTSD OR Post-traumatic OR Posttraumatic OR psychological distress OR emotional distress | 96,438 |
| 11 | (MM ‘Stress Disorders, Post-Traumatic/CO/DI/EP/ET/PX’) | 16,533 |
| 12 | TI, AB anxiety OR phobi* OR panic OR anxio* | 60,099 |
| 13 | (MM ‘Anxiety Disorders+/DI/CO’) | 10,301 |
| 14 | (TI depress*) OR (AB depress*) | 429,598 |
| 15 | (MM ‘Depressive Disorder/CO/EP/PX’) | 15,364 |
| 16 | (MM ‘Mental Health’) | 20,351 |
| 17 | TI (‘follow up’ OR ‘follow-up’) OR AB (‘follow-up’ OR ‘follow up’) | 895,827 |
| 18 | TI longitudinal OR AB longitudinal | 224,732 |
| 19 | S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 OR S9 | 7,384,756 |
| 20 | S10 OR S11 OR S12 OR S13 OR S14 OR S15 OR S16 | 569,216 |
| 21 | S19 AND S20 (publication type: observational study) | 886 |
| 22 | S19 AND S20 (no limiters applied) | 100,223 |
| 23 | S22 AND S18 | 3439 |
| 24 | S22 AND S17 | 9104 |
| 25 | S23 OR S24 OR S21 | 9153 (full text) |
Appendix 2 Data extraction sheet template
| Duration of cohort | Study design | # of cohort/case-control population | Gender (%F) | Age group | Type of MH assessed | MH measurement (validated tool/self-report) | Determinants assessed | Method for assessing determinants | Type of incident NCD | NCD outcome (biochemical assessment) |
|---|---|---|---|---|---|---|---|---|---|---|
