Notes
Article history
The contractual start date for this research was in April 2018. This article began editorial review in March 2023 and was accepted for publication in October 2023. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The Global Health Research editors and publisher have tried to ensure the accuracy of the author’s article and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this article.
Permissions
Copyright statement
Copyright © 2024 Deivanayagam et al. This work was produced by Deivanayagam et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2024 Deivanayagam et al.
Introduction
The challenges Sri Lankans have faced and impact on mental health
Sri Lanka has suffered four decades of violent conflict, a tsunami, terrorist attacks and an economic crisis, with unknown mental health consequences. 1 Some stability over the following decade was shaken by the Easter Sunday bombings of churches and luxury hotels in 2019 by Islamic State of Iraq and Syria (ISIS) terrorists, killing more than 250 people, which led to increased hostility and outbreaks of violence against Muslims. 2 In 2020, Sri Lanka was hit by the coronavirus disease 2019 (COVID-19) pandemic, with more than 600,000 confirmed cases and over 16,000 official deaths in Sri Lanka. 3 The adoption of large tax cuts in 2020 combined with COVID-19 control measures, which included closing borders, lockdowns and school closures, had substantial negative economic impacts and starved social sectors of fiscal resources, resulting in substantial job losses and disrupted social services, and contributed to the worst economic crisis since the 1930s, which from late 2021 led to a scarcity of fuel, food and medicines. 4 The COVID-19 Delta wave in mid-2021 also resulted in over 3000 infections and 150 deaths per day in August 2021 and overwhelmed the hospital system for several months. Hospitals in the country in 2022 reported shortages of essential medicines and other health items, while frequent power outages affect the delivery of health services. 5 The United Nations Office for Coordinated Humanitarian Affairs estimated in April 2022 that 5.7 million people needed humanitarian assistance including food, fuel, cooking gas, essential supplies and medicines in 25 districts across the country. 6 In June 2022, the World Food Programme estimated that 3 in 10 households (6.2 million people) were food insecure, and food inflation was alarmingly high at 57.4%. 7
The mental health impacts of conflict, natural disasters and economic crises have been documented in Sri Lanka and globally. The prevalence of mental health disorders in conflict-affected populations is substantially higher than in the average population: 17.3% versus 5.3% for depressive disorders. 8,9 People living in conflict-affected settings are at increased risk of developing depressive, anxiety and psychotic disorders. 10 The negative mental health consequences of the 2004 Indian Ocean tsunami have been investigated particularly amongst mothers and adolescents in Sri Lanka. 11,12 A 2021 study found that the current crisis has led to high levels of distress among young people. 13 The current economic crisis and accompanying political uncertainties, widespread protests and social disruptions have the potential to adversely affect mental health, though this has not been studied extensively. Worsening public mental health in the context of these multiple crises can additionally strain health systems. 14
Regarding previous prevalence estimates, in 2008, the World Health Organization (WHO) estimated that around 3% of the Sri Lankan population experienced some form of mental ill health. 15 According to 2015 WHO estimates, the prevalence of depressive disorder in Sri Lanka was around 4.1% and anxiety disorder 3.4%. 13 Sri Lanka also has a high suicide mortality rate of 14 per 100,000 in 2019, compared to a global average of 9.2 per 100,000. 16 Higher levels of mental distress are an important risk factor for suicide. 16,17
Barriers to healthcare use and access
People living with mental health difficulties may experience individual, interpersonal, social or structural barriers to help-seeking. The literature consistently highlights that, culturally, social stigma associated with mental health is common in Sri Lanka, whereby negative attitudes lead to people being marginalised in society. 1,13 Patients, carers and families face subsequent social and economic exclusion due to mental health difficulties, depriving them of participating in socioeconomic processes such as work and marriage. 16 Stigma experienced by patients and carers is associated with delays in help-seeking. 17 Lack of knowledge about mental health as a result of these social norms means individuals and carers may not recognise difficulties and in turn may not seek help. If they recognise difficulties, they may avoid seeking help due to stigma, denial or fear of societal repercussions. Even if people recognise that they need support, there is another layer of barriers to obtaining care. Some of these barriers in the context of mental health include language,18 acceptability/appropriateness of care,19 lack of family support,20 availability of medication,21 lack of transport22 and financial barriers. 21 It is possible that several of these factors may have manifested during this challenging time period, for example, the high price of fuel and the lack of availability of medicines, impacting on healthcare use and access. Worldwide systematic reviews also highlight that the rate of healthcare use declined following the COVID-19 pandemic23 and economic downturn. 24
Aims
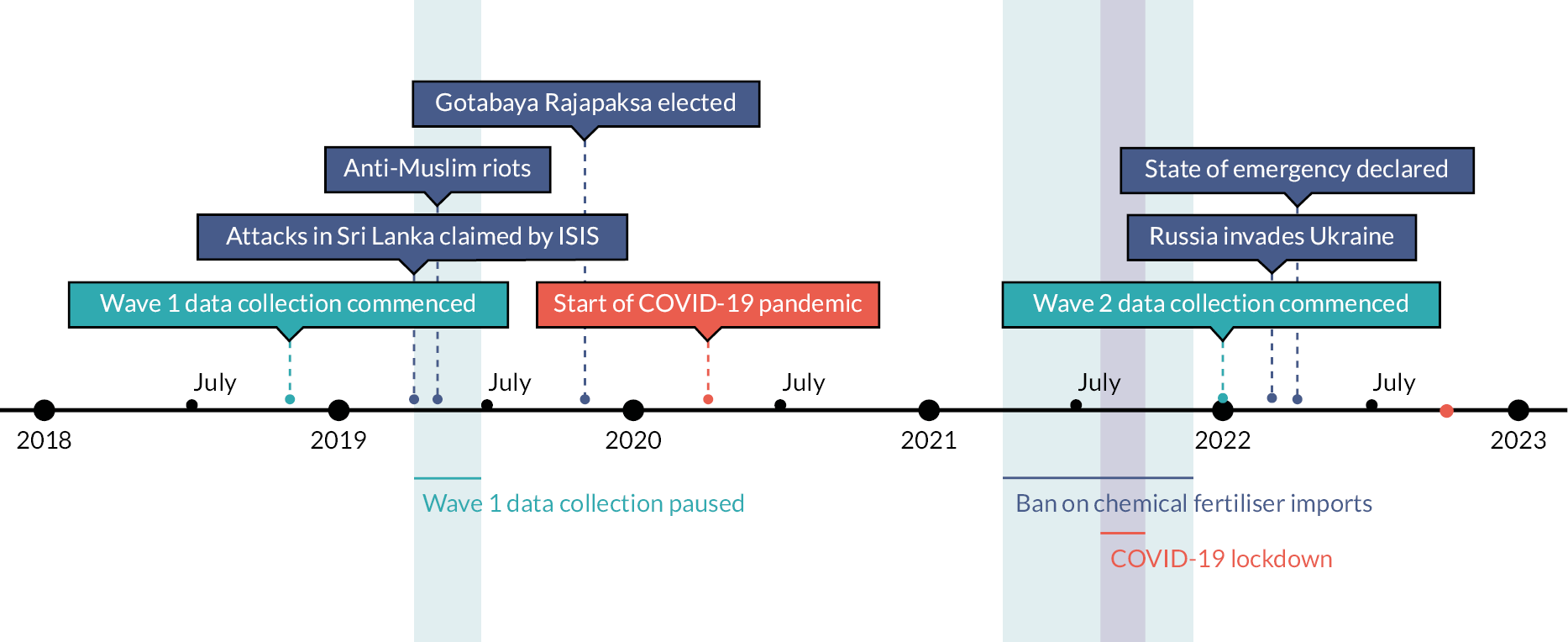
Given the various sociopolitical, health and environmental stressors affecting individuals in Sri Lanka between 2018 and 2022 (Figure 1), there is a need to estimate the prevalence of mental health difficulties, as well as healthcare use and access for people experiencing poor mental health, to inform policy and guide service provision.
FIGURE 1.
A timeline of significant public health and sociopolitical events in Sri Lanka between 2018 and 2022.
Using data from two waves of the nationally representative Sri Lanka Health and Aging Study (SLHAS), this study aimed to assess the changes in the prevalence of mental health conditions, and subsequent changes in rates of healthcare usage and access, among adults in Sri Lanka between 2018 and 2022. Specifically, we aimed to explore whether mental health conditions have changed over time between 2018 and 2022, spanning a period of crisis and unrest, inclusive of the Easter Sunday attacks in 2019, anti-Muslim riots, the COVID-19 pandemic and lockdown measures, as well as the current economic crisis that started in late 2021.
While this study focused on mental health, it formed part of a wider National Institute for Health and Care Research (NIHR) Global Health Research award developing a package of care for the mental health of suvivors of violence against women and adolescents, and a substudy exploring the impact of COVID-19 on a variety of health and well-being topics such as healthcare access, employment, income, food security, social isolation, vaccine uptake, testing, COVID-19 symptom prevalence, social contact and public views about the COVID-19 response.
Research questions
The project aims to answer the following questions:
-
How did the prevalence of (common) mental health difficulties amongst adults in Sri Lanka change between 2018–9 (Wave 1) and 2022 (Wave 2)?
-
How do the rates of healthcare use among those with high mental health difficulties compare to those without high mental health difficulties at Waves 1 and 2?
-
How do the rates of healthcare access (unmet need) among those with high mental health difficulties compare to those without high mental health difficulties in Waves 1 and 2?
-
Are the differences in rates of healthcare use and access between those with differing mental health difficulties dependent upon sociodemographic factors?
Methods
Sample
The SLHAS is a national, longitudinal, cohort study managed by a consortium of the Institute for Health Policy, the University of Colombo, University of Peradeniya, University of Ruhuna and the University of Rajarata, approved by the Ministry of Health (MOH), Sri Lanka. The project uses data from the SLHAS, an ongoing nationally representative study of adults (aged 18 years and older) living in Sri Lanka. Six thousand six hundred and sixty-eight adults participated in Wave 1, the majority of which (4548) also completed the follow-up in Wave 2. This study uses an analytic sample of 4030 respondents who participated in the healthcare use module in both Wave 1 and Wave 2 and held information for at least one mental health measure in both surveys.
SLHAS Wave 1 was conducted from November 2018 to November 2019. Detailed information on the recruitment and sampling strategy can be found as part of recent work using data collected in the SLHAS. 25 Recruited participants were invited to a field clinic near their residence to complete in-person interviews. In April 2019, during Wave 1 of data collection, Sri Lanka was impacted by terrorist attacks, which caused a 6-week disruption of field work leading to non-coverage of several primary sampling units (PSUs), a fall in Muslim response rates, and the inability to survey one predominantly Muslim PSU owing to security conditions. The affected PSU was replaced with a substitute PSU from the same stratum matching by district, sector and level of socioeconomic development. However, it was not possible to match the ethnic profile of the original PSU.
SLHAS Wave 2 data collection took place between August 2021 and August 2022. Participants completed interviews by telephone, with information being collected on COVID history, vaccination, mental health, healthcare use and access, household well-being and public opinion.
Across both waves, participants provided information about themselves and their households.
Measures
Outcome: common mental health difficulties
Common mental health difficulties were captured using the Patient Health Questionnaire (PHQ) and/or the Depression Anxiety Stress Scales (DASS). Following standard interpretations, difficulties were categorised as ‘minimal’, ‘mild’ and ‘moderate to severe’. High mental health difficulties in this study equates to an outcome of a ‘moderate to severe’ score in the PHQ, in DASS, or in both.
Patient Health Questionnaire
The PHQ-9 is a nine-item scale that assesses symptoms of depression used for diagnostic screening purposes in primary care26 All participants in Wave 1 completed the nine-item PHQ-9. In Wave 2, due to concerns around the risk to psychological well-being following telephone interviews, participants completed a modified eight-item PHQ, excluding the item addressing suicide ideation. As such, for comparability, standardised PHQ-8 scores ranging from 0 to 24 were used across both waves. Scores between 5 and 9 were categorised as ‘mild’ depressive symptoms and scores of 10 and above as ‘moderate to severe’ depressive symptoms. 27
Depression Anxiety Stress Scales
The DASS-A and DASS-S are self-report questionnaires made up of seven items exploring anxiety and stress, respectively,28,29 and were administered to individual subsamples (33%) of participants. Those who completed the DASS-A and DASS-S at Wave 1 were administered the same questions in Wave 2. DASS scores ranged between 0 and 42. DASS-A scores of 8–14 denote ‘mild’ anxiety, and scores > 14 ‘moderate to severe’ anxiety; DASS-S scores between 15 and 25 denote ‘mild’ stress, and scores > 25 ‘moderate to severe’ stress. 28
Healthcare use and access
In Waves 1 and 2, participants were asked about the frequency of their inpatient healthcare use and their outpatient healthcare use in the previous 12 months. For this analysis, healthcare use was categorised as ‘none’ and ‘one or more visits’ for inpatients and outpatients. Participants were also asked about their ability to access health care when required. Wave 1 responses consider access to health care in the previous year, and Wave 2 responses consider access in the previous month. Healthcare access responses reflected ‘unmet need’, ‘met need’ and ‘no need’.
Cohort characteristics and covariates
Self-reported sex, age (in 10-year bands), educational attainment (O level + or below O level), socioeconomic status (in quintiles from a household asset-based index),25 ethnicity (Sinhala, Tamil, Muslim, other), religion (Buddhist, Hindu, Muslim, Christian), region of residence (by province) and questionnaire language (Sinhala or Tamil) were recorded at each wave.
Time period
As detailed in the introduction, during the 4-year period 2019–22, several significant events took place, both locally and globally, potentially impacting people living in Sri Lanka. Figure 1 highlights the data collection periods for Waves 1 and 2.
Data analysis
A series of descriptive analyses were conducted to provide an overview of the demographic and socioeconomic characteristics of the cohort, and to quantify the prevalence of mental health difficulties within the cohort at each wave, stratified by socioeconomic subgroups. Subsequent regression analyses examined the changes in prevalence of mental health difficulties over time, again stratified by economic subgroups. Cross-sectional descriptive analyses examined rates of healthcare use and access among those experiencing mental health difficulties in Waves 1 and 2, and regression analyses compared use and access for those experiencing ‘mild’ and ‘high’ mental health difficulties with those experiencing ‘minimal’ mental health difficulties, adjusting for confounding variables in four stages: unadjusted; adjusted for age and sex; further adjustment for education and socioeconomic status; and further adjustment for ethnicity, religion, region and language.
The cohort was weighted to be representative of the population of Sri Lanka, accounting for sampling design and differential non-response within the second wave of data collection.
All analyses were conducted in STATA® Release 17 (StataCorp LLC, College Station, TX, USA). 30
Results
Demographic characteristics
The sociodemographic characteristics of the cohort are presented in Table 1. The cohort comprised of 4030 participants with a mean age of 49.1 years [standard error (SE): 0.25], 51.2% of which were female. The majority of participants were Buddhist (73.8%), and ethnically Sinhalese (78.3).
| Sample descriptives | Common mental health difficulties | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Wave 1 | Wave 2 | ||||||||||||||
| Minimal | Mild | High | Minimal | Mild | High | ||||||||||
| n | % | n | % | n | % | n | % | n | % | n | % | n | % | ||
| Full analytic sample | 4030 | 100 | 2901 | 72.0 | 1014 | 25.1 | 115 | 2.9 | 2112 | 52.4 | 1671 | 41.5 | 247 | 6.1 | |
| Sex | Male | 1948 | 48.3 | 1489 | 76.5 | 422 | 21.7 | 36 | 1.9 | 1000 | 51.4 | 839 | 43.1 | 108 | 5.6 |
| Female | 1082 | 51.7 | 1412 | 67.8 | 591 | 28.4 | 79 | 3.8 | 1112 | 53.4 | 832 | 39.9 | 139 | 6.7 | |
| Age | 18–24 years | 501 | 12.4 | 376 | 75.0 | 115 | 22.9 | 10 | 2.1 | 180 | 59.5 | 110 | 36.4 | 13 | 4.1 |
| 25–34 years | 769 | 19.1 | 588 | 76.5 | 170 | 22.1 | 10 | 1.4 | 423 | 54.9 | 313 | 40.7 | 34 | 4.4 | |
| 35–44 years | 986 | 24.5 | 722 | 73.3 | 234 | 23.8 | 29 | 3.0 | 533 | 54.7 | 381 | 39.1 | 60 | 6.1 | |
| 45–54 years | 699 | 17.3 | 500 | 71.6 | 177 | 25.3 | 22 | 3.1 | 369 | 49.4 | 324 | 43.3 | 55 | 7.4 | |
| 55–64 years | 603 | 15.0 | 400 | 66.3 | 178 | 29.6 | 25 | 4.1 | 322 | 49.9 | 285 | 44.1 | 39 | 6.1 | |
| 65–74 years | 473 | 11.7 | 314 | 66.5 | 139 | 29.5 | 19 | 4.1 | 285 | 48.4 | 258 | 43.7 | 47 | 8.0 | |
| SES | 5 | 913 | 22.7 | 716 | 78.4 | 181 | 19.9 | 16 | 1.8 | 511 | 54.9 | 373 | 40.1 | 47 | 5.1 |
| 4 | 874 | 21.7 | 665 | 76.1 | 185 | 21.2 | 24 | 2.8 | 498 | 54.8 | 366 | 40.3 | 45 | 4.9 | |
| 3 | 817 | 20.3 | 589 | 72.1 | 214 | 26.2 | 13 | 1.7 | 430 | 52.4 | 341 | 41.6 | 49 | 5.9 | |
| 2 | 726 | 18.0 | 508 | 70.0 | 189 | 26.1 | 29 | 3.9 | 392 | 49.9 | 332 | 42.2 | 62 | 7.9 | |
| 1 | 701 | 17.4 | 424 | 60.5 | 244 | 34.9 | 33 | 4.7 | 281 | 48.2 | 258 | 44.2 | 45 | 7.6 | |
| Education | O level+ | 2236 | 55.5 | 1731 | 77.4 | 468 | 21.0 | 36 | 1.6 | 1183 | 52.9 | 928 | 41.5 | 125 | 5.6 |
| Below O level | 1794 | 44.5 | 1169 | 65.2 | 545 | 30.4 | 79 | 4.4 | 929 | 51.8 | 743 | 41.4 | 123 | 6.8 | |
| Religion | Buddhist | 2976 | 73.8 | 2295 | 77.1 | 618 | 20.8 | 62 | 2.1 | 1491 | 50.1 | 1270 | 42.7 | 215 | 7.2 |
| Hindu | 388 | 9.6 | 184 | 47.5 | 181 | 46.7 | 22 | 5.7 | 238 | 61.4 | 143 | 36.9 | 7 | 1.7 | |
| Muslim | 368 | 9.1 | 229 | 62.1 | 121 | 33.0 | 18 | 4.9 | 241 | 65.5 | 118 | 32.2 | 9 | 2.3 | |
| Christian | 298 | 7.4 | 193 | 64.7 | 93 | 31.1 | 13 | 4.2 | 142 | 47.7 | 139 | 46.6 | 17 | 5.7 | |
| Ethnicity | Sinhala | 3156 | 78.3 | 2432 | 77.1 | 659 | 20.9 | 65 | 2.1 | 1577 | 50.0 | 1354 | 42.9 | 225 | 7.1 |
| Tamil | 480 | 11.9 | 228 | 47.5 | 220 | 45.9 | 32 | 6.6 | 286 | 59.6 | 182 | 37.9 | 12 | 2.5 | |
| Muslim | 370 | 9.2 | 229 | 61.9 | 123 | 33.2 | 18 | 4.9 | 242 | 65.3 | 120 | 32.4 | 9 | 2.3 | |
| Other | 24 | 0.1 | 12 | 50.0 | 12 | 50.0 | 0 | 0.0 | 8 | 31.9 | 15 | 61.1 | 2 | 7.0 | |
| Region | WP | 1211 | 30.1 | 907 | 74.9 | 271 | 22.4 | 33 | 2.7 | 673 | 55.4 | 472 | 38.9 | 69 | 5.7 |
| CP | 483 | 12.0 | 334 | 69.0 | 136 | 28.2 | 13 | 2.7 | 257 | 52.8 | 202 | 41.6 | 27 | 5.6 | |
| SP | 540 | 13.4 | 425 | 78.8 | 104 | 19.3 | 11 | 2.0 | 279 | 52.1 | 212 | 39.6 | 45 | 8.3 | |
| NP | 208 | 5.2 | 96 | 46.0 | 93 | 44.5 | 20 | 9.5 | 131 | 62.8 | 75 | 35.8 | 3 | 1.4 | |
| EP | 252 | 6.3 | 151 | 60.1 | 92 | 36.6 | 8 | 3.2 | 170 | 67.8 | 77 | 30.6 | 4 | 1.7 | |
| NWP | 470 | 11.7 | 352 | 74.9 | 104 | 22.1 | 14 | 2.9 | 231 | 49.4 | 208 | 44.5 | 29 | 6.2 | |
| NCP | 247 | 6.1 | 177 | 71.6 | 67 | 27.1 | 3 | 1.3 | 101 | 40.9 | 122 | 49.1 | 25 | 10.0 | |
| Uva | 226 | 5.6 | 157 | 69.8 | 63 | 27.7 | 6 | 2.5 | 89 | 39.8 | 117 | 52.4 | 18 | 7.8 | |
| Sab | 393 | 9.8 | 302 | 76.7 | 83 | 21.2 | 8 | 2.1 | 181 | 45.8 | 186 | 47.1 | 28 | 7.1 | |
| Language | Sinhala | 3234 | 80.3 | 2457 | 76.0 | 707 | 21.9 | 70 | 2.2 | 1641 | 49.7 | 1421 | 43.1 | 238 | 7.2 |
| Tamil | 796 | 19.7 | 444 | 55.8 | 306 | 38.5 | 46 | 5.7 | 471 | 64.6 | 249 | 34.2 | 9 | 1.2 | |
Mental health prevalence
The prevalence of high common mental health difficulties in Wave 1 was 2.9% (n = 115) and 6.1% (n = 247) in Wave 2. During Wave 1, 25.1% of the cohort experienced mild mental health difficulties, and 72.0% experienced minimal difficulties. During Wave 2, 41.5% experienced mild mental health difficulties, while 52.4% experienced minimal difficulties. Prevalence estimates of common mental health difficulties differed by age, sex, ethnicity, SES, education, region and religion, and are presented in Table 1.
Change in prevalence of mental health difficulties over time
Table 2 displays multivariable regression analyses comparing prevalence of mental health difficulties between waves. The levels of high mental health difficulties changed significantly between the two waves [β = 0.23, 95% confidence interval (CI) 0.20 to 0.26; p < 0.05], highlighting the increased prevalence of common mental health distress in Wave 2 compared to in Wave 1. This change in prevalence was greater for women, older people, people in lower SES quintiles, people with below O-level education, non-Buddhist people and non-Sinhala people.
| Cohort size | Common mental health difficulties | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Wave 1 | Wave 2 | ||||||||||||||
| Minimal | Mild | High | Minimal | Mild | High | ||||||||||
| n | n | % | n | % | n | % | n | % | n | % | n | % | |||
| Healthcare use in previous month | Outpatient | None | 4030 | 2298 | 79.2 | 715 | 70.5 | 74 | 64.6 | 1765 | 83.6 | 1325 | 79.3 | 166 | 67.2 |
| Once or more | 604 | 20.8 | 299 | 29.5 | 41 | 35.4 | 348 | 16.5 | 346 | 20.7 | 81 | 32.8 | |||
| Inpatient | None | 4030 | 2655 | 91.5 | 903 | 89.1 | 97 | 84.0 | 1919 | 90.9 | 1481 | 88.6 | 189 | 76.3 | |
| Once or more | 246 | 8.5 | 111 | 10.9 | 18 | 16.0 | 193 | 9.1 | 190 | 11.4 | 59 | 23.7 | |||
| Unmet need for medical care | Previous year | No need | 2708 | 218 | 10.9 | 111 | 17.6 | 6 | 7.2 | – | – | – | – | – | – |
| Met need | 1640 | 82.2 | 434 | 68.8 | 54 | 65.1 | – | – | – | – | – | – | |||
| Unmet need | 137 | 6.9 | 85 | 13.5 | 23 | 27.7 | – | – | – | - | – | – | |||
| Previous month | No need | 4009 | – | – | – | – | – | – | 825 | 39.3 | 647 | 38.8 | 91 | 37.0 | |
| Met need | – | – | – | – | – | – | 1195 | 57.0 | 938 | 56.3 | 134 | 54.4 | |||
| Unmet need | – | – | – | – | – | – | 77 | 3.7 | 81 | 4.9 | 21 | 8.6 | |||
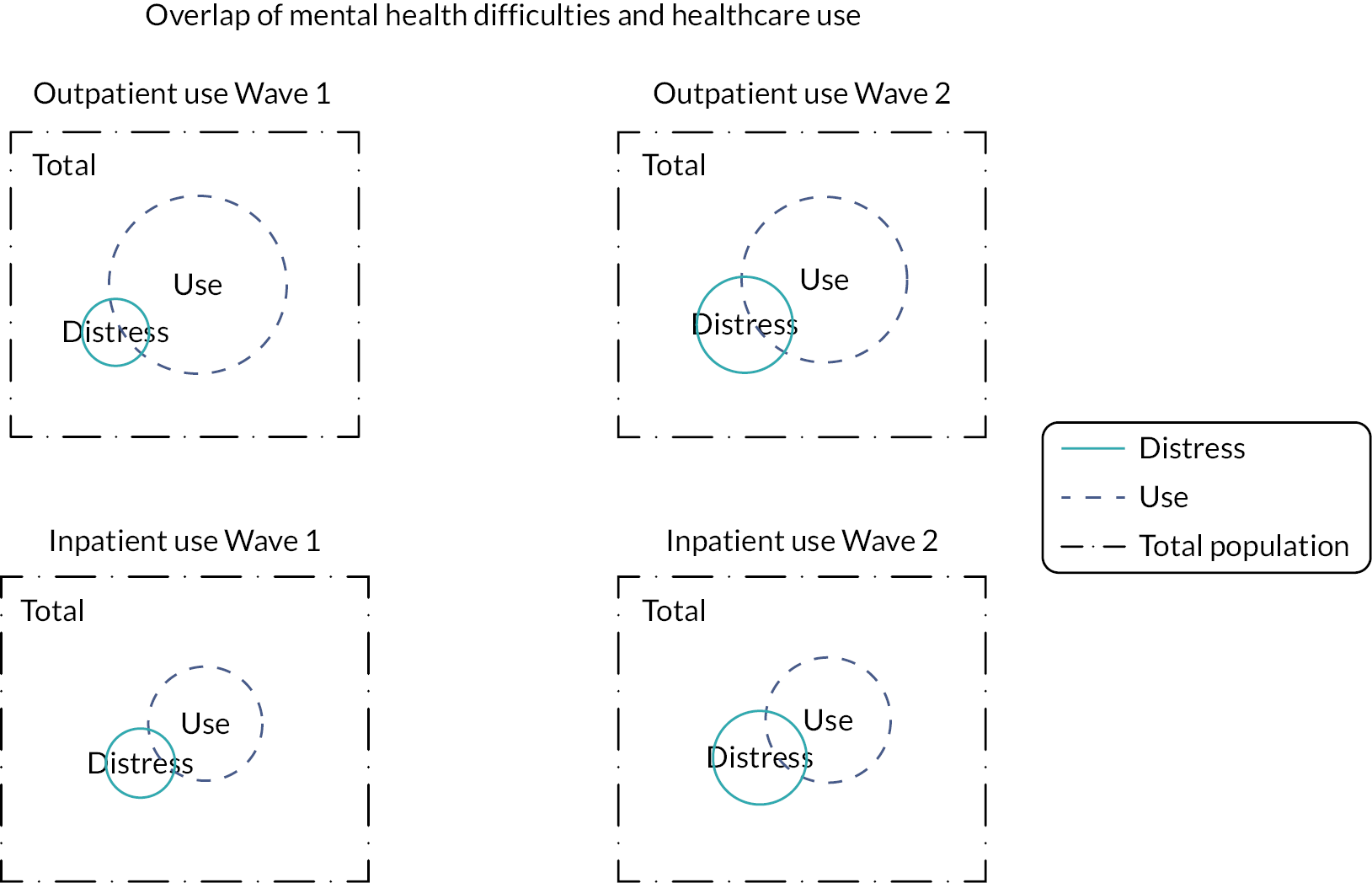
Healthcare use and access
Figure 2 displays the overlap of high mental health difficulties and the use of outpatient and inpatient medical services during Waves 1 and 2. Among the people experiencing high common mental health difficulties, rates of outpatient use in the previous 12 months decreased by 3.1% between waves, from 35.4% to 32.3% in Waves 1 and 2, respectively (see Table 3). However, rates of inpatient use in the previous 12 months increased by 7.7% between waves (Wave 1: 16.0%; Wave 2: 23.7%).
FIGURE 2.
Inpatient and outpatient use of medical care for Sri Lankans reporting ‘moderate to severe’ mental health difficulties in SLHAS 2018–9 and 2021–2.
| Model 1 | Model 2 | Model 3 | Model 4 | |
|---|---|---|---|---|
| Wave 2 mental health difficulties (ref: Wave 1) | 0.23 (0.20 to 0.26) | 0.23 (0.20 to 0.26) | 0.23 (0.20 to 0.26) | 0.23 (0.20 to 0.26) |
| Sex (ref: male) | ||||
| Female | 0.05 (0.01 to 0.08) | 0.04 (0.01 to 0.07) | 0.04 (0.00 to 0.07) | |
| Age (ref: 16–24 years) | ||||
| 25–34 years | 0.00 (–0.08 to 0.08) | 0.00 (–0.08 to 0.07) | 0.00 (–0.08 to 0.08) | |
| 35–44 years | 0.04 (–0.04 to 0.11) | 0.02 (–0.05 to 0.10) | 0.03 (–0.04 to 0.11) | |
| 45–54 years | 0.07 (–0.01 to 0.15) | 0.05 (–0.02 to 0.12) | 0.06 (–0.02 to 0.13) | |
| 55–64 years | 0.10 (0.03 to 0.18) | 0.07 (0.00 to 0.15) | 0.08 (0.00 to 0.15) | |
| 65–74 years | 0.11 (0.03 to 0.19) | 0.08 (0.00 to 0.15) | 0.08 (0.01 to 0.16) | |
| SES quartile [ref: 5 (highest)] | ||||
| 4 | 0.03 (–0.2 to 0.08) | 0.03 (–0.2 to 0.07) | ||
| 3 | 0.06 (0.01 to 0.11) | 0.06 (0.01 to 0.11) | ||
| 2 | 0.11 (0.06 to 0.15) | 0.11 (0.05 to 0.15) | ||
| 1 | 0.16 (0.10 to 0.22) | 0.14 (0.08 to 0.20) | ||
| Education (ref: O level +) | ||||
| Below O level | 0.04 (0.00 to 0.07) | 0.03 (0.00 to 0.07) | ||
| Religion (ref: Buddhist) | ||||
| Hindu | –0.04 (–0.17 to 0.09) | |||
| Muslim | –0.15 (–0.46 to 0.17) | |||
| Christian | 0.04 (–0.04 to 0.11) | |||
| Ethnicity (ref: Sinhala) | ||||
| Tamil | 0.19 (0.04 to 0.34) | |||
| Muslim | 0.24 (–0.09 to 0.57) | |||
| Other | 0.24 (0.06 to 0.42) | |||
| Province (ref: WP) | ||||
| CP | 0.03 (–0.03 to 0.08) | |||
| SP | 0.00 (–0.06 to 0.05) | |||
| NP | 0.03 (–0.07 to 0.13) | |||
| EP | –0.03 (–0.11 to 0.05) | |||
| NWP | 0.03 (–0.03 to 0.09) | |||
| NCP | 0.10 (0.03 to 0.17) | |||
| Uva | 0.08 (0.00 to 0.15) | |||
| Sab | 0.04 (–0.02 to 0.10) | |||
| Language (ref: Sinhala) | ||||
| Tamil | –0.12 (–0.25 to 0.02) | |||
When adjusted for confounders, those experiencing high mental health difficulties were significantly more likely to access outpatient services in both Wave 1 [adjusted odds ratio (aOR) = 2.15, 95% CI 1.27 to 3.63] and Wave 2 (aOR = 1.96, 95% CI 1.34 to 2.85) than those with minimal difficulties (see Table 4). Similarly, those experiencing high mental health difficulties were significantly more likely to use inpatient services than those with minimal difficulties in both waves (Wave 1: aOR = 2.03, 95% CI 1.10 to 3.76; Wave 2: aOR = 2.76, 95% CI 1.80 to 4.22).
| Cohort size | Common mental health difficulties (ref: minimal) [aOR (CI)] | ||||||
|---|---|---|---|---|---|---|---|
| Wave 1 | Wave 2 | ||||||
| n | Mild | High | Mild | High | |||
| Healthcare use in previous month | Outpatient | Model 1 | 4152 | 1.59 (1.29 to 1.96) | 2.09 (1.27 to 3.43) | 1.32 (1.07 to 1.64) | 2.48 (1.62 to 3.36) |
| Model 2 | 1.49 (1.20 to 1.85) | 1.81 (1.10 to 2.99) | 1.30 (1.05 to 1.62) | 2.36 (1.63 to 3.41) | |||
| Model 3 | 1.48 (1.19 to 1.84) | 1.79 (1.08 to 2.96) | 1.30 (1.05 to 1.61) | 2.31 (1.61 to 3.32) | |||
| Model 4 | 1.66 (1.33 to 2.07) | 2.15 (1.27 to 3.63) | 1.19 (0.96 to 1.49) | 1.96 (1.34 to 2.85) | |||
| Inpatient | Model 1 | 4152 | 1.32 (0.98 to 1.77) | 2.06 (1.14 to 3.71) | 1.28 (0.98 to 1.67) | 3.10 (2.04 to 4.71) | |
| Model 2 | 1.31 (0.97 to 1.77) | 2.03 (1.12 to 3.68) | 1.26 (0.96 to 1.65) | 2.97 (1.96 to 4.48) | |||
| Model 3 | 1.27 (0.94 to 1.72) | 1.87 (1.03 to 3.43) | 1.25 (0.95 to 1.63) | 2.85 (1.87 to 4.33) | |||
| Model 4 | 1.32 (0.97 to 1.79) | 2.03 (1.10 to 3.76) | 1.20 (0.91 to 1.58) | 2.76 (1.80 to 4.22) | |||
| Unmet need for medical care | Previous year | Model 1 | 2780 | 0.57 (0.41 to 0.80) | 1.59 (0.53 to 4.73) | – | – |
| Model 2 | 0.54 (0.38 to 0.75) | 1.39 (0.45 to 4.31) | – | – | |||
| Model 3 | 0.56 (0.40 to 0.79) | 1.55 (0.49 to 4.92) | – | – | |||
| Model 4 | 0.72 (0.50 to 1.03) | 2.53 (0.71 to 9.06) | – | – | |||
| Previous month | Model 1 | 4131 | – | – | 1.02 (0.86 to 1.22) | 1.11 (0.76 to 1.60) | |
| Model 2 | – | – | 0.99 (0.82 to 1.18) | 1.01 (0.71 to 1.45) | |||
| Model 3 | – | – | 0.99 (0.83 to 1.19) | 1.02 (0.71 to 1.46) | |||
| Model 4 | – | – | 0.98 (0.82 to 1.18) | 1.02 (0.71 to 1.48) | |||
In addition, while 27.7% of the cohort experiencing high mental health difficulties did not access medical services when required in the 12 months prior to Wave 1, they were not statistically significantly less likely to access services than those with minimal mental health difficulties (aOR = 2.53, 95% CI 0.71 to 9.06). In the month prior to Wave 2 responses, 8.6% of participants experiencing high mental health difficulties did not access needed medical services, again not significantly more than those with minimal mental health difficulties (aOR = 1.02, 95% CI 0.71 to 1.48).
Discussion
This study estimated the changes in prevalence of common mental health difficulties amongst the adult population of Sri Lanka over an extended period of crises. It also estimated the rates of both outpatient and inpatient healthcare use, and unmet need based on issues accessing health care, over the same time period, for those with high mental health difficulties compared to those with mild and minimal difficulties.
Primary findings and concordance with previous research
Prevalence of high mental health difficulties rose significantly over the study period. This rise was not equal across different sociodemographic groups, with a disproportionate increase in mental health difficulties amongst older adults, those in the lowest socioeconomic classes and those not from minority ethnic groups. In addition, the gap between inpatient use for those living with the highest and lowest levels of mental health difficulties widened across the study period, though the outpatient use gap remained stable. Finally, while those with high mental health difficulties reported high levels of unmet need for health care, when compared to those with the lowest levels of mental health difficulty, the difference was not found to be significant, likely due to a restricted sample size.
These results are largely concordant with previous research. Prevalence of mental health difficulties increased throughout the study period, mirroring a qualitative rapid needs assessment in Sri Lanka, which found reduced mental health and psychosocial well-being at the household level since the start of the economic crisis. 31 Globally, studies consistently report a worsening of population mental health following periods of public health crises such as the COVID-19 pandemic;32 economic disruption;33 and exposure to ethnically and politically driven riots and protests. 34 In addition, the overall decrease in use of healthcare services estimated in this study, particularly in terms of outpatient services, is consistent with findings from worldwide systematic reviews focused on rates of healthcare utilisation following the COVID-19 pandemic23 and economic downturn. 24
Increase in prevalence of mental health difficulties
Our results indicate that those groups that were disproportionately affected by an increase in mental health difficulties were also at increased risk of exposure to the health and sociopolitical crises afflicting Sri Lanka during the study period. Older adults were particularly at risk of severe illness as a result of COVID-19,35 those within minority ethnic groups were more likely to be vulnerable during the riots, and those with the lowest socioeconomic statuses were less likely to be able to afford basic housing and food, all of which could contribute to worsening mental health.
Changes in healthcare utilisation
There are a multitude of factors associated with utilisation of outpatient services, including individual, interpersonal and structural barriers – all of which are affected during health and sociopolitical crises. For example, individual awareness of, and self-evaluated importance of, healthcare needs are likely to change during times of economic disruption, especially for those in lower socioeconomic classes with financial barriers to access. 36 Familial and social support networks can be disturbed during periods of mandated social isolation, such as during national lockdowns. 37 In addition, the COVID-19 pandemic led to significant healthcare disruptions, with reduced availability of services, increased wait times and reductions in use of medical services owing to the fear of patients contracting COVID-19. Notably, the gap between outpatient use for those with the highest and lowest mental health difficulties remained stable over the course of the study period, indicating these barriers appear to have affected those with the highest and lowest mental health difficulties equally during this time frame.
Conversely, that gap between inpatient service use for those with high and minimal mental health difficulties increased across the study period. The pathway to utilisation of inpatient services is different to that of outpatient services. Particularly during periods of conflict, and public health crises (e.g. the COVID-19 pandemic), admittance to an inpatient service is a medical necessity, regardless of personal, interpersonal and structural barriers. It is possible that the utilisation gap has widened as a result of an increase in those with high levels of mental health difficulties presenting to inpatient services with advanced symptoms that could have previously been treated at outpatient services. However, there is a bidirectional relationship between inpatient utilisation and mental health distress,38 and further research is necessary to unpick the complex nature of this widening gap.
Unmet need for healthcare services
Utilising healthcare services does not necessarily equate to the fulfilment of healthcare needs. As the particular type of health service accessed by participants cannot be distinguished, there is no certainty that the mental health needs of those with the highest levels of mental health difficulties are being met. Indeed, 27% of those respondents in Wave 1 indicated an unmet need for health care. There are several reasons why the mental health needs of the cohort are not being met. There is significant stigma around the topic of mental health in Sri Lanka, which may contribute to reluctance to disclose mental health difficulties in a healthcare setting. In addition, clinician response to the presentation of mental health-related symptoms may be affected by stigma. Alternatively, somatisation of mental health may lead to the treatment of physical symptoms without addressing the underlying mental health cause. Again, somatisation can affect unmet need twofold: a patient may not be aware of the link between their symptoms and mental health or may feel disclosure of physical symptoms is more likely to lead to effective treatment; and a practitioner may (1) not recognise underlying mental health difficulties, (2) prioritise physical symptoms and/or (3) not be trained in mental health.
Strengths
A key strength of this study is that it utilises a large, nationally representative sample. To our knowledge, this study is the first population prevalence estimate for common mental health difficulties in Sri Lanka across the adult population. Moreover, this study provides longitudinal prevalence estimates, highlighting changes in prevalence between two critical periods for Sri Lankans pre- and post-COVID-19. Furthermore, surveys were completed at critical stages in times when the population was facing significant social, political and economic unrest. Therefore, the surveys have captured mental health difficulties during a particularly challenging period of time for Sri Lankans, when they have experienced significant barriers to meeting their basic needs such as access to food and fuel in 2022.
Limitations
This study explores common mental health difficulties measured by the PHQ and DASS – depression, stress and anxiety; however, it does not provide insight into more complex or less common mental health disorders. Additionally, it was not possible to capture whether people with mental health difficulties used or accessed mental health care, distinct from health care more broadly. Although data on self-reported reasons for using medical care were collected in Wave 1, the reported percentage of visits was too low to include in the analysis, possibly due to systematic under-reporting. Similarly, the differences in questions asked between Wave 1 and Wave 2, and the proportion of people asked, limit conclusions that can be drawn around healthcare use and access. As such, only the prevalence estimates are longitudinal, while the estimates of use and access to medical care are cross-sectional, and therefore could not be compared between time periods.
It is unknown whether negative attitudes towards mental health may have led to underestimation of mental distress in this study. As noted above, due to the COVID-19 pandemic, Wave 1 was undertaken in-person and Wave 2 via telephone, which may have further deterred disclosure of mental health difficulties during this time period. Although this has not yet been analysed among Sri Lankan adults, there is evidence that the PHQ performs well in phone modality. 39 It would be beneficial for future studies to investigate issues related to measuring mental health, applicability and cultural safety of mental health measures.
Equality, diversity and engagement
The sampling design28 prioritised coverage of all demographics including socioeconomically disadvantaged communities by maximising the number of clusters in relation to the overall sample size, explicitly including socioeconomic indicators in the stratification of PSUs within the sampling frame and ensuring that all districts and sectors within districts were covered in the final sample. To include participants from all ethnicities who speak different languages, interviews were carried out by a team of field staff who spoke Sinhala, Tamil and English. If the selected participant spoke a language not spoken by the interviewer, the interview was rescheduled to another time by another interviewer. Following the ISIS terrorist attacks in April 2019, there was a fall in Muslim response rates, and it became unfeasible to survey one predominantly Muslim PSU due to security reasons. Despite replacing this PSU with a substitute from the same stratum matching by district, sector and level of socioeconomic development, it was not possible to match the ethnic profile of the original PSU. During the analysis stage, under-representation of specific ethnic groups or geographical regions in the final sample was directly dealt with by unweighting that took into account these characteristics. Regarding diversity of the research team, there was a range of expertise, spanning epidemiology, social science, public health and statistics. Three of the paper’s authors are early career researchers.
Community engagement and involvement
The SLHAS has maintained contact with its participants by sending all participants a newsletter updating them on progress and developments in the study, and including postcards for participants to send back feedback, which many have. The SLHAS also makes efforts to widely communicate its research findings and publications to the general public via social media and the local news media.
Conclusion and recommendations
This study estimates the prevalence of common mental health difficulties for Sri Lankans and healthcare use and access by demographic features using a nationally representative data set of adults. It found that 2.9% of Sri Lankans experienced high mental health difficulties during 2018–9 and 6.1% in 2021–2. It shows that there was a statistically significant increase in prevalence between 2018–9 and 2021–2. Those groups that were disproportionately affected by an increase in mental health difficulties were also at increased risk of exposure to the health and sociopolitical crises afflicting Sri Lanka. This suggests the need for targeted interventions to support the mental health needs of older adults and socially and racially minoritised population adults.
The study also found an overall decrease in the use of healthcare services, and while those with high mental health difficulties reported high levels of unmet need for health care, when compared to those with the lowest levels of mental health difficulty, the difference was not found to be significant. This is an important study that explores mental health in Sri Lankans during critical time periods where the country experienced the trauma of terrorist attacks, ethnicity-based violence and the COVID-19 pandemic. In addition, the lessons learnt from how mental health and healthcare access and use were measured in this study allows us to strengthen methods for future studies and make them more robust, allowing for longitudinal analyses of healthcare use and access for those experiencing common mental health difficulties.
Additional information
Acknowledgements
Ravindra Prasan Rannan-Eliya and Kishan Patel are joint last authors of this paper. The authors thank their colleagues that facilitated the SLHAS, Dr Alexis Palfreyman, Safiya Riyaz and Kavitha Vijayaraj for support in the design of the tools and training of data collection staff and Professor David Osrin, who was principal investigator of the NIHR Global Health Research Group (17/63/47).
Contributions of authors
Thilagawathi Abi Deivanayagam (https://orcid.org/0000-0002-1130-2333) (NIHR Academic Clinical Fellow in Public Health) contributed to study design and data acquisition, co-ordinated the analysis and drafting process and drafted the manuscript.
Sorcha Ní Chobhthaigh (https://orcid.org/0000-0002-5215-6352) (PhD Student in Public Health) contributed to study design and data acquisition, and drafted the manuscript.
Delan Devakumar (https://orcid.org/0000-0002-8695-6817) (Professor of Global Child Health) contributed to study design and data acquisition.
Kishan Patel (https://orcid.org/0000-0002-5693-6831) (Research Fellow) contributed to study design and data acquisition, performed statistical analysis and drafted the manuscript.
Ravindra Prasan Rannan-Eliya (https://orcid.org/0000-0002-5013-2816) (Executive Director at the Institute of Health Policy, Sri Lanka) conceived, designed and managed the data acquisition.
SLHAS Collaborators conceived, designed and managed the data acquisition.
All authors contributed to editing the manuscript and read and approved the final version of the manuscript.
Disclosure of interests
Full disclosure of interests: Completed ICMJE forms for all authors, including all related interests, are available in the toolkit on the NIHR Journals Library report publication page at https://doi.org/10.3310/HJWA5078.
Primary conflicts of interest: Ravindra Prasan Rannan-Eliya has received grants from the Institute for Health Policy and Swiss National Science Foundation (SNSF).
Data-sharing statement
Any queries on the new data created in the preparation of this article should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review.
Ethics statement
Ethical approval for the SLHAS data collection was obtained from the Sri Lanka Medical Association (ERC/18-022). Data for this study were requested from the Institute of Health Policy, Colombo, Sri Lanka.
Information governance statement
University College London (UCL) is committed to handling all personal information in line with the UK Data Protection Act (2018) and the General Data Protection Regulation (EU GDPR) 2016/679. Under the Data Protection legislation, UCL is the Data Controller.
Funding
This article presents independent research funded by the National Institute for Health and Care Research (NIHR) Global Health Research programme as award number 17/63/47 using UK aid from the UK Government to support global health research. The views expressed in this publication are those of the author(s) and not necessarily those of the NIHR or the UK government. Research is published in the NIHR Global Health Research Journal. See the NIHR Funding and Awards website for further award information.
The SLHAS Wave 1 data collection was supported by the Swiss Agency for Development Cooperation (SDC) and the Swiss National Science Foundation (SNSF) through the Swiss Programme for Research on Global Issues for Development (r4d programme) by the grant ‘Inclusive social protection for chronic health problems’ (Grant number 400640_160374), and the Institute for Health Policy Public Interest Research Fund (Grant number PIRF-2018-02).
Department of Health and Social Care disclaimer
This publication presents independent research commissioned by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, MRC, NIHR Coordinating Centre, the GHR programme or the Department of Health and Social Care.
This article was published based on current knowledge at the time and date of publication. NIHR is committed to being inclusive and will continually monitor best practice and guidance in relation to terminology and language to ensure that we remain relevant to our stakeholders.
This article reports on one component of the research award Mental health prevalence, healthcare use and access between 2018 and 2022 in Sri Lanka: an analysis of survey data. For more information about this research please view the award page (https://www.fundingawards.nihr.ac.uk/award/17/63/47)
About this article
The contractual start date for this research was in April 2018. This article began editorial review in March 2023 and was accepted for publication in October 2023. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The Global Health Research editors and publisher have tried to ensure the accuracy of the author’s article and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this article.
Copyright
Copyright © 2024 Deivanayagam et al. This work was produced by Deivanayagam et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
List of abbreviations
- aOR
- adjusted odds ratio
- DASS
- Depression Anxiety Stress Scales
- NIHR
- National Institute for Health and Care Research
- PHQ
- Patient Health Questionnaire
- PSU
- primary sampling unit
- SE
- standard error
- SLHAS
- Sri Lanka Health and Aging Study
- WHO
- World Health Organization
References
- Siva N. Sri Lanka struggles with mental health burden. Lancet 2010;375:880-1.
- Wijayaratne S. After the violence. J Relig Health 2020;59:428-30.
- World Health Organization . Sri Lanka: WHO Coronavirus (COVID-19) Dashboard 2022. https://covid19.who.int/region/searo/country/lk (accessed 3 October 2022).
- International Monetary Fund . Sri Lanka 2021 Article IV Consultation: Press Release; Staff Report; And Statement by the Executive Director for Sri Lanka 2022. www.imf.org/en/Publications/CR/Issues/2022/03/25/Sri-Lanka-2021-Article-IV-Consultation-Press-Release-Staff-Report-and-Statement-by-the-515737 (accessed 6 October 2022).
- Sarkar S. The devastating health consequences of Sri Lanka’s economic collapse. BMJ 2022;377.
- OCHA . Sri Lanka: Food Security Crisis – April 2022 2022. https://reliefweb.int/disaster/ce-2022-000199-lka (accessed 3 October 2022).
- World Food Programme . WFP Sri Lanka: Situation Report 6 July 2022 2022. https://reliefweb.int/report/sri-lanka/wfp-sri-lanka-situation-report-6-july-2022 (accessed 3 October 2022).
- Tol WA, Barbui C, Galappatti A, Silove D, Betancourt TS, Souza R, et al. Mental health and psychosocial support in humanitarian settings: linking practice and research. Lancet 2011;378:1581-91.
- Steel Z, Chey T, Silove D, Marnane C, Bryant RA, van Ommeren M. Association of torture and other potentially traumatic events with mental health outcomes among populations exposed to mass conflict and displacement. JAMA 2009;302:537-49.
- Gupta J, Falb KL, Carliner H, Hossain M, Kpebo D, Annan J. Associations between exposure to intimate partner violence, armed conflict, and probable PTSD among women in rural Côte d’Ivoire. PLOS ONE 2014;9.
- Wickrama KAS, Wickrama KAT. Family context of mental health risk in Tsunami affected mothers: findings from a pilot study in Sri Lanka. Soc Sci Med 2008;66:994-1007.
- Wickrama KAS, Kaspar V. Family context of mental health risk in Tsunami-exposed adolescents: findings from a pilot study in Sri Lanka. Soc Sci Med 2007;64:713-23.
- Matthias AT, Jayasinghe S. Worsening economic crisis in Sri Lanka: impacts on health. Lancet Glob Health 2022;10.
- World Health Organization . Depression and Other Common Mental Disorders: Global Health Estimates 2017. https://apps.who.int/iris/bitstream/handle/10665/254610/WHO-MSD-MER-2017.2-eng.pdf;jsessionid=3ED73641EBE0B10BFE5C413296330468?sequence=1 (accessed 2 October 2022).
- World Health Organization . Mental Health Update 2008.
- World Health Organization . Global Health Observatory Data Repository 2019. https://data.worldbank.org/indicator/SH.STA.SUIC.P5?name_desc=true (accessed 5 October 2022).
- Fernando SM, Deane FP, McLeod HJ. The delaying effect of stigma on mental health help-seeking in Sri Lanka. Asia-Pacific Psychiatr 2017;9.
- Ohtani A, Suzuki T, Takeuchi H, Uchida H. Language barriers and access to psychiatric care: a systematic review. Psychiatr Serv 2015;66:798-805.
- Saurman E. Improving access: modifying Penchansky and Thomas’s theory of access. J Health Serv Res Policy 2016;21:36-9.
- Mohd Rosnu NS, Singh DKA, Mat Ludin AF, Ishak WS, Abd Rahman MH, Shahar S. Enablers and barriers of accessing health care services among older adults in South-East Asia: a scoping review. Int J Environ Res Public Health 2022;19.
- Raja S, Wood SK, de Menil V, Mannarath SC. Mapping mental health finances in Ghana, Uganda, Sri Lanka, India and Lao PDR. Int J Ment Health Syst 2010;4.
- Syed ST, Gerber BS, Sharp LK. Traveling towards disease: transportation barriers to health care access. J Community Health 2013;38:976-93.
- Moynihan R, Sanders S, Michaleff ZA, Scott AM, Clark J, To EJ, et al. Impact of COVID-19 pandemic on utilisation of healthcare services: a systematic review. BMJ Open 2021;11.
- Sánchez Recio R, Alonso Pérez De Ágreda JP, Rabanaque MJ, Aguilar Palacio I. Understanding the effect of economic recession on healthcare services: a systematic review. Iran J Public Health 2022;51:495-507.
- Rannan-Eliya RP, Wijemunige N, Perera P, Kapuge Y, Gunawardana N, Sigera C, et al. SLHAS Collaborators . Prevalence and associations of hypertension in Sri Lankan adults: estimates from the SLHAS 2018–19 survey using JNC7 and ACC/AHA 2017 guidelines. Glob Heart 2022;17.
- Kroenke K, Spitzer RL, Williams JBW. The PHQ-9. J Gen Intern Med 2001;16:606-13.
- Kroenke K, Spitzer RL. The PHQ-9: a new depression diagnostic and severity measure. Psychiatr Ann 2002;32:509-15.
- Lovibond PF, Lovibond SH. The structure of negative emotional states: comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav Res Ther 1995;33:335-43.
- Osman A, Wong JL, Bagge CL, Freedenthal S, Gutierrez PM, Lozano G. The Depression Anxiety Stress Scales-21 (DASS-21): further examination of dimensions, scale reliability, and correlates. J Clin Psychol 2012;68:1322-38.
- StataCorp . Stata Statistical Software: Release 17 2021.
- Burgess M, Chia J, Francis D, Lamichhane N. Sri Lanka Crisis: Rapid Needs Assessment June 2022 2022. https://resourcecentre.savethechildren.net/pdf/Sri-Lanka-Rapid-Needs-Assessment.pdf/ (accessed 5 October 2022).
- Santomauro DF, Mantilla Herrera AM, Shadid J, Zheng P, Ashbaugh C, Pigott DM, et al. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet 2021;398:1700-12.
- Guerra O, Agyapong VIO, Nkire N. A qualitative scoping review of the impacts of economic recessions on mental health: implications for practice and policy. Int J Environ Res Public Health 2022;19.
- Ni MY, Kim Y, McDowell I, Wong S, Qiu H, Wong IO, et al. Mental health during and after protests, riots and revolutions: a systematic review. Aust N Z J Psychiatry 2020;54:232-43.
- Romero Starke K, Reissig D, Petereit-Haack G, Schmauder S, Nienhaus A, Seidler A. The isolated effect of age on the risk of COVID-19 severe outcomes: a systematic review with meta-analysis. BMJ Glob Health 2021;6.
- Silva M, Resurrección DM, Antunes A, Frasquilho D, Cardoso G. Impact of economic crises on mental health care: a systematic review. Epidemiol Psychiatr Sci 2020;29.
- Williams CYK, Townson AT, Kapur M, Ferreira AF, Nunn R, Galante J, et al. Interventions to reduce social isolation and loneliness during COVID-19 physical distancing measures: a rapid systematic review. PLOS ONE 2021;16.
- Alzahrani N. The effect of hospitalization on patients’ emotional and psychological well-being among adult patients: an integrative review. Appl Nurs Res 2021;61.
- Pinto-Meza A, Serrano-Blanco A, Peñarrubia MT, Blanco E, Haro JM. Assessing depression in primary care with the PHQ-9: can it be carried out over the telephone?. J Gen Intern Med 2005;20:738-42.
Appendix 1
Members of SLHAS collaborators author group and their affiliations
-
Professor Vajira Dissanayake, Dean, Faculty of Medicine, University of Colombo, Colombo, Sri Lanka.
-
Dr Prasadini Perera, Senior Lecturer, Faculty of Allied Health Sciences, University of Peradeniya, Peradeniya, Sri Lanka.
-
Professor HMM Herath, Professor, Faculty of Medicine, University of Ruhuna, Galle, Sri Lanka.
-
Professor Bilesha Perera, Professor, Faculty of Medicine, University of Ruhuna, Galle, Sri Lanka.
-
Dr Nilmini Wijemunige, Fellow, Institute for Health Policy, Colombo, Sri Lanka.
-
Dr Anuji Gamage, Senior Lecturer, Faculty of Medicine, General Sir John Kotelawala Defence University, Rathmalana, Sri Lanka.
-
Dr Shanti Dalpatadu, Senior Fellow, Institute for Health Policy, Colombo, Sri Lanka.
-
Dr Sarath Samarage, Senior Fellow, Institute for Health Policy, Colombo, Sri Lanka.
