Notes
Article history
The contractual start date for this research was in August 2017. This article began editorial review in April 2023 and was accepted for publication in June 2024. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The Global Health Research editors and publisher have tried to ensure the accuracy of the authors’ article and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this article.
Permissions
Copyright statement
Copyright © 2024 Jones et al. This work was produced by Jones et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaption in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2024 Jones et al.
Introduction
Stroke is recognised as a global health challenge. Worldwide, there are approximately 13.7 million new cases of stroke every year. The incidence of stroke is increasing in developing nations including India,1 where stroke is the fourth leading cause of death and the fifth leading cause of disability. 2
In India, people typically experience a first stroke at 58 years of age,3 and there are higher rates of death than in higher income countries; case fatality has been reported to range from 18% to 42%. 4 Of those surviving, many will have disabilities including hemiparesis, speech deficits, cognitive impairment, incontinence, dysphagia, visual impairment and psychological problems. 5
Accurate, early recognition and diagnosis is vital for all stroke patients in order to maximise the benefits of treatment. Healthcare delivery in India has three levels: primary, secondary and tertiary. Primary consists of subcentres and primary health centres. Community Health Centres largely form the secondary tier, while government-funded medical colleges and hospitals, All India Institutes, specialised hospitals and private hospitals form the tertiary level. It is at the tertiary level that most patients seek medical help for stroke. It is well established that patient outcomes are improved when post-stroke care is delivered at the earliest opportunity on a specialist stroke unit and recovery from a disabling stroke greatly depends on early and easy access to tailored, comprehensive and specialist stroke care. 6 However, most people in India live in areas with no access to stroke units or neurological expertise. 7 There is a shortage of available data, but in 2013, it was estimated that there were only 35 hospitals with dedicated stroke units throughout India, and these were mostly situated in private hospitals in urban areas. 8 However, there is a shortage of data on the availability of stroke units and associated resources.
The aim of this study was to undertake a survey of stroke services, stroke workforce and engagement in stroke research across India.
Methods
Design
Structured survey.
Survey tool development
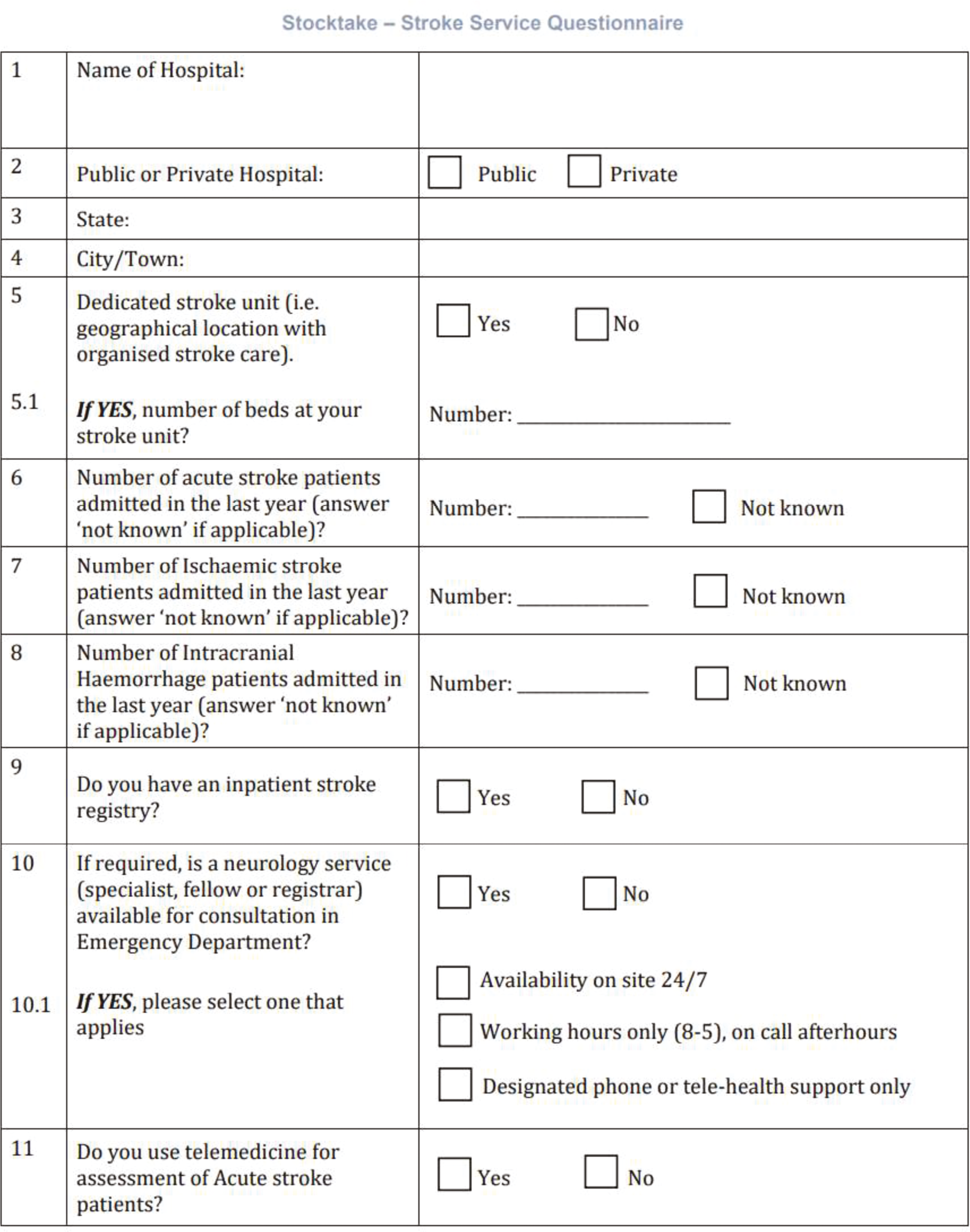
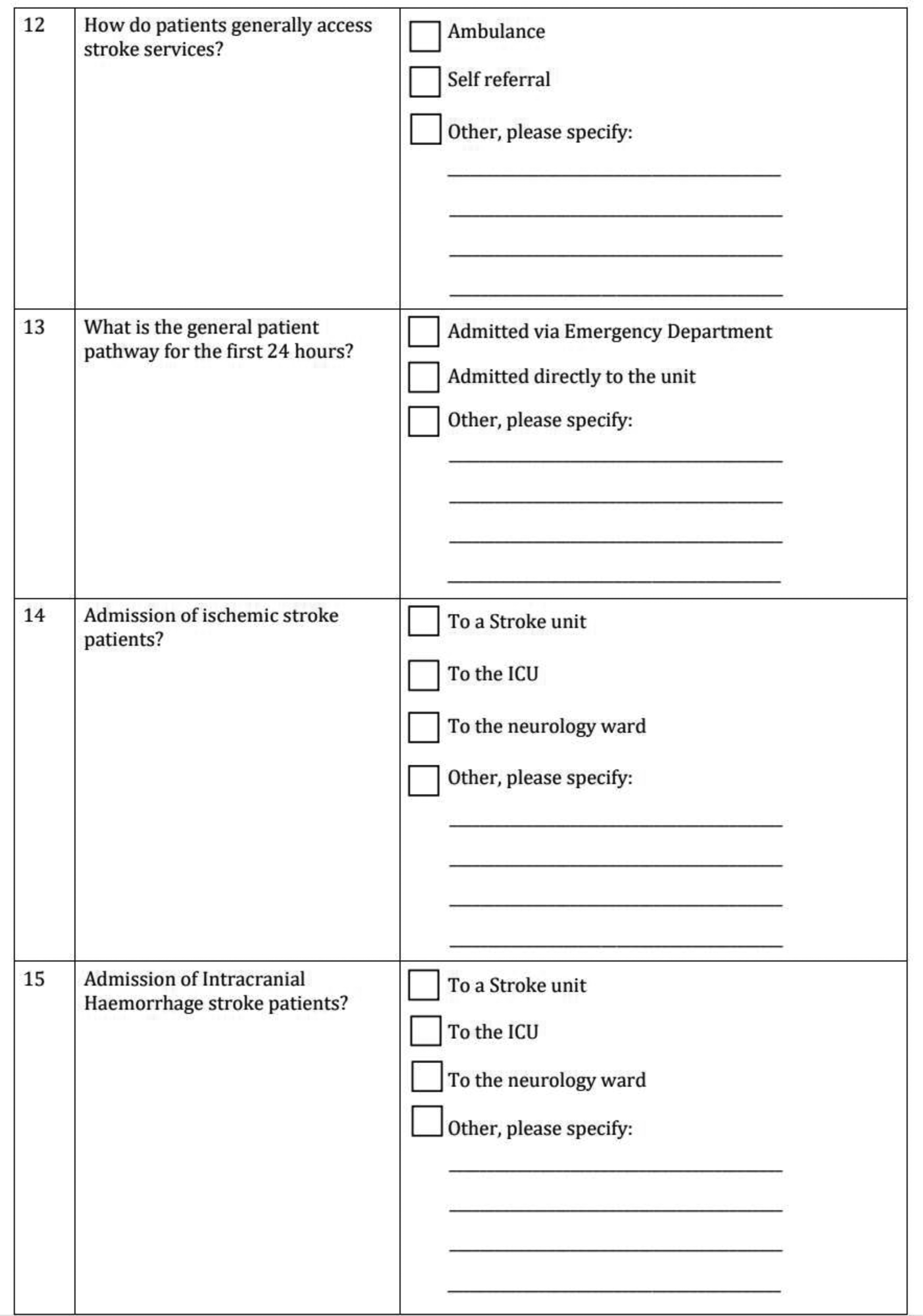
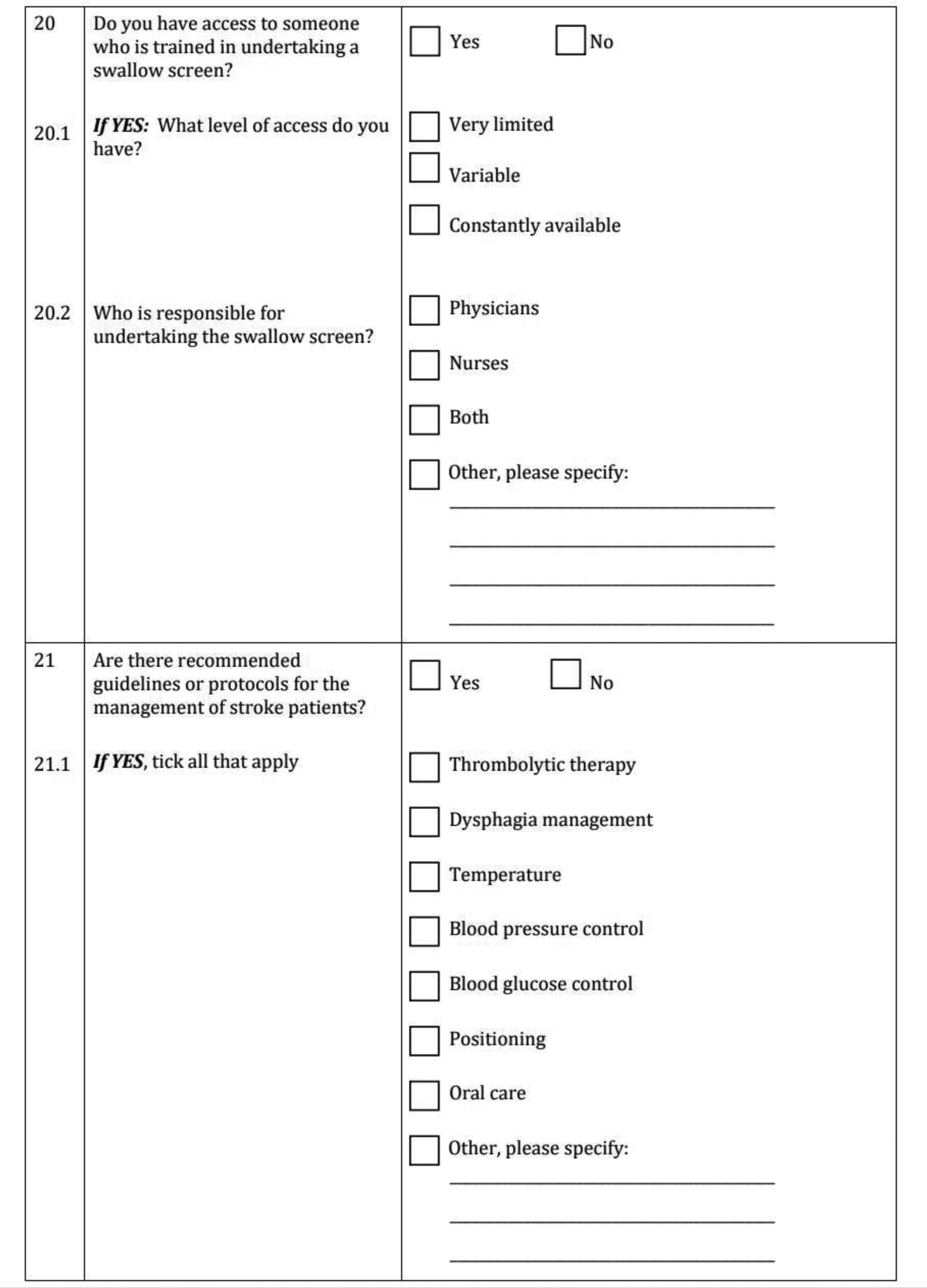
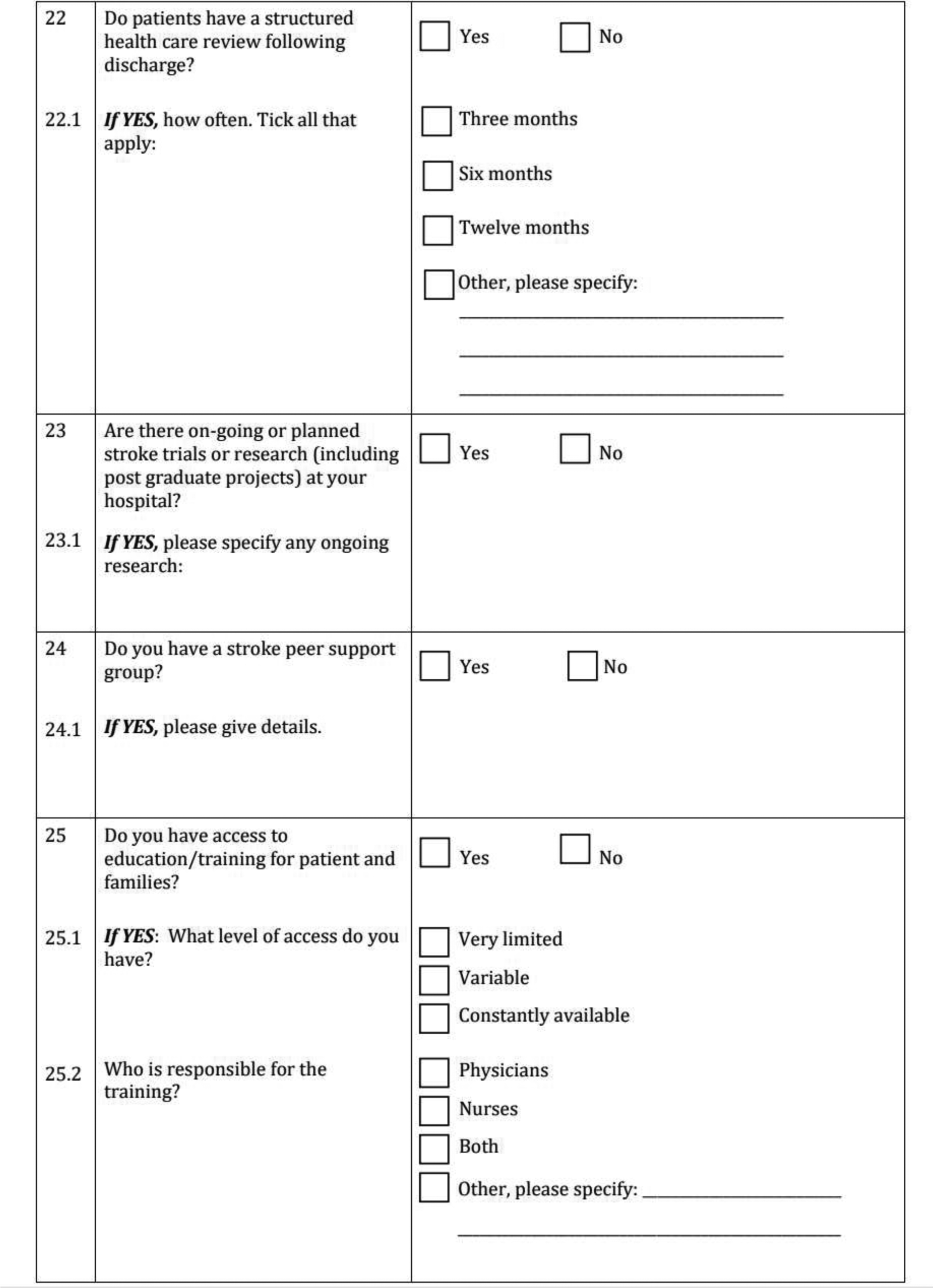
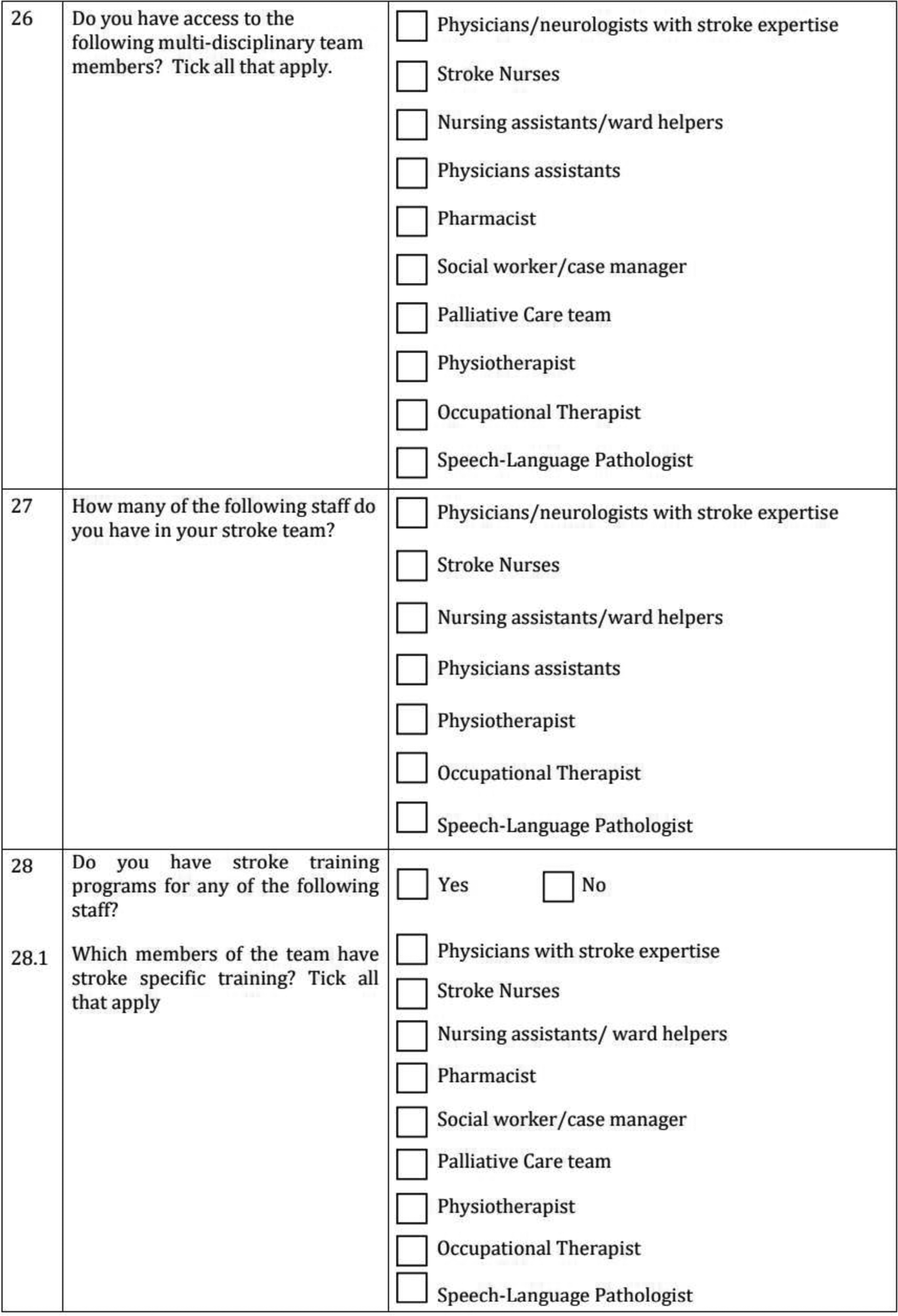
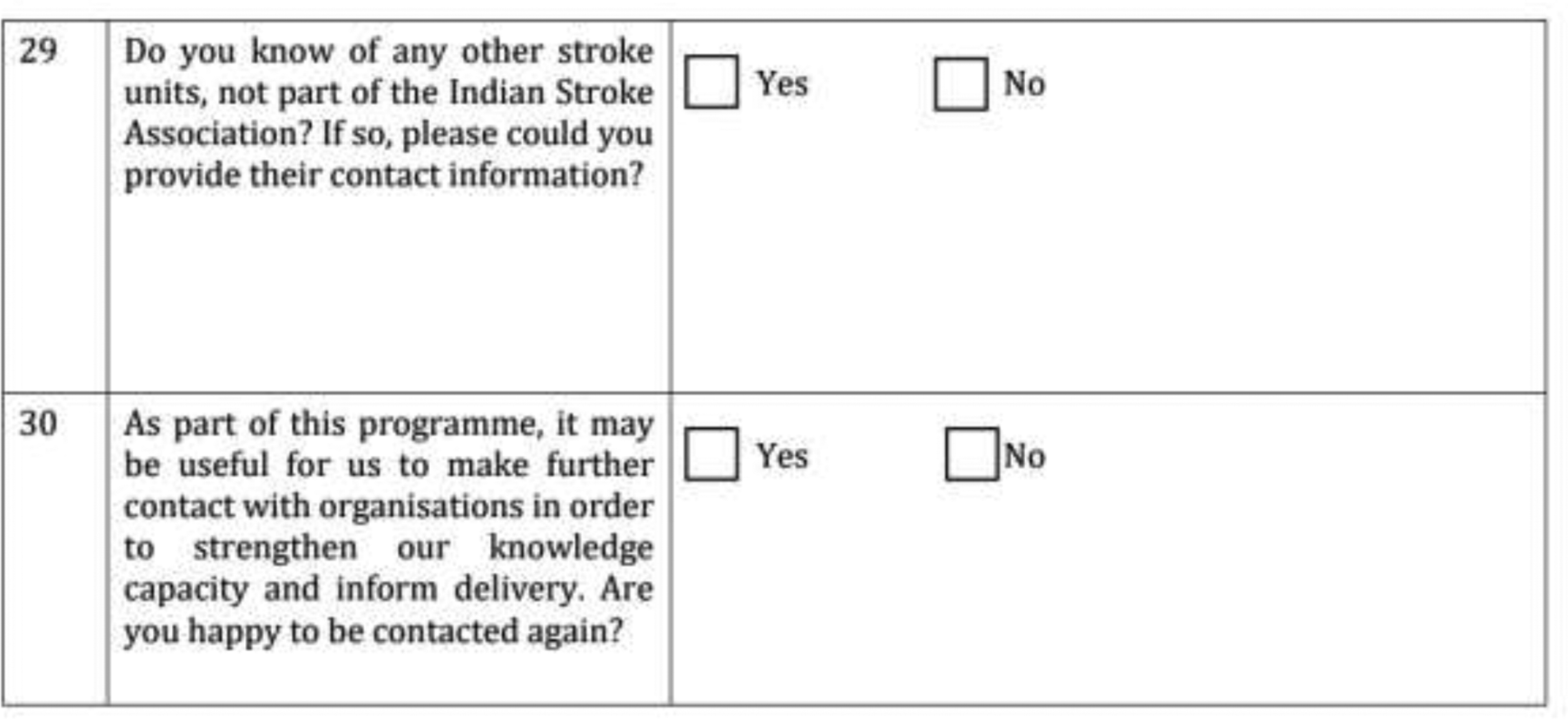
The survey tool was informed by the World Stroke Organization Roadmap to Delivering Quality Stroke Care9 and through discussion with local stakeholders (four neurologists, two nurses and two physiotherapists) around the survey content and format. The tool had 30 mostly closed questions including: information on the respondent’s profession, site characteristics [location, hospital status (private, fee paying) or public], stroke unit availability and capacity, the number of people admitted with ischaemic stroke and primary intracerebral haemorrhage (PICH), available diagnostic services (basic or advanced as defined by the World Stroke Organization Roadmap to Delivering Quality Stroke Care), treatments (thrombolysis and endovascular thrombectomy) and telemedicine. The remaining questions asked about stroke workforce, staff training and education, services to support stroke survivors and their families, and organisational involvement in research.
Setting
Public and private hospitals in India.
Subjects
Respondents comprised physicians, nurses, physiotherapists, researchers and speech and language therapists. In some cases, where more than one representative from a hospital completed the survey tool, the responses from the most senior member of staff were selected and included in the analysis. Only one response was included per hospital.
The survey tool (see Appendix 2) was distributed between December 2017 and August 2019 in paper format to attendees at the Indian National Stroke Conference (New Delhi) and the International Conference on The Essentials of Stroke Care (Kerala). The survey tool was also sent electronically via e-mail to members of the Indian Stroke Clinical Trial (INSTRuCT) network, the Indian Academy of Neurology and Indian Stroke Association.
If the survey tool was not returned within 2 weeks, a maximum of two reminders were sent by e-mail. The survey tool was completed in English and was returned in person at the conferences or via e-mail. Respondents frequently missed out answers to some of the questions. Where possible, we contacted respondents by e-mail for missing information.
Analysis
Data from the survey tools were entered into Excel and imported into IBM SPSS Statistics for Windows, version 26 [IBM Corporation, Armonk, NY, USA (IBM SPSS Statistics from version 19 onwards)]. Analysis was grouped by hospital status (private or public). Descriptive data were summarised using percentages, medians and interquartile ranges (IQR). Where respondents did not answer a question, frequencies and percentages were calculated from the hospitals with complete data. Percentages were calculated from the total number of responding hospitals, unless otherwise stated.
Results
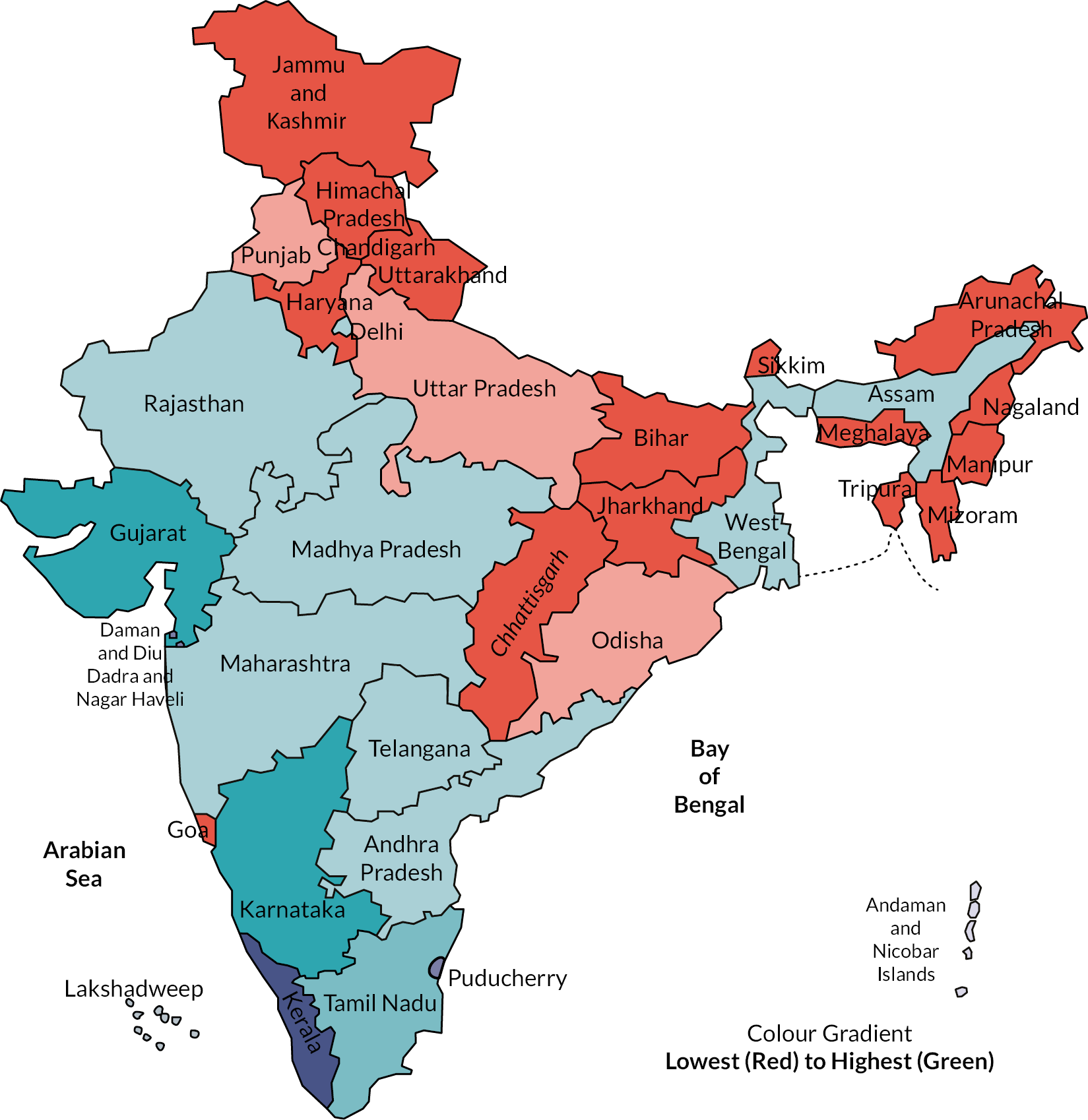
Completed surveys were received from 95 hospitals, representing 15 states and 2 union territories (Table 1 and Figure 1). Nearly half of the survey tools returned (48%) represented hospitals in the state of Kerala.
| States and union territories | Completed survey tools, N = 95 (%) |
|---|---|
| Andhra Pradesh | 3 (3) |
| Assam | 2 (2) |
| Chandigarh | 1 (1.5) |
| Delhi | 2 (2) |
| Gujarat | 7 (7) |
| Karnataka | 10 (11) |
| Kerala | 46 (48) |
| Madhya Pradesh | 2 (2) |
| Maharashtra | 5 (5) |
| Orissa | 1 (1.5) |
| Pondicherry | 1 (1.5) |
| Punjab | 1 (1.5) |
| Rajasthan | 3 (3) |
| Tamil Nadu | 6 (6) |
| Telangana | 2 (2) |
| Uttar Pradesh | 1 (1.5) |
| West Bengal | 2 (2) |
FIGURE 1.
States and union territories represented.
Respondents were physicians (49, 52%), nurses (23, 24%), physiotherapists (5, 5%), researchers (3, 3%), speech and language therapists (2, 2%) and 13 (14%) respondents did not specify their profession. Overall, data were provided for 50 (53%) private and 45 (47%) public hospitals.
Respondents from 58 (61%) hospitals reported that a total of 20,661 stroke patients were treated over a 12-month period (median 300 per hospital; IQR 173–461). Of these, 14,392 (70%) had an ischaemic stroke (median 210; IQR 109–350) and 6269 (30%) had a PICH (median 70; IQR 40–119). Private hospitals treated 12,338 (60%), and public hospitals treated 8323 (40%) stroke patients.
Stroke unit availability
Respondents at 48 (50%) hospitals reported having a dedicated stroke unit. Of these, 36 (75%) were in private hospitals compared to 12 (27%) in public hospitals. Forty-five (47%) hospitals had 596 stroke beds (median 9 beds per hospital; IQR 6–12). Private hospitals had a total of 502 (84%) stroke beds (median 8; IQR 6–13) compared to 94 (16%) (median 10; IQR 4–11) in public hospitals.
Stroke workforce
Eighty-six (91%) hospitals had access to a multidisciplinary team (MDT) defined as a minimum of two physicians/doctors trained in stroke care, four nurses and a physiotherapist10 (see Appendix 3), including all private hospitals who were more likely to have access to larger numbers of staff within the MDT (41, 82% vs. 21, 47%).
Education and training
Private hospitals had more staff with stroke-specific training across all professions (Table 2).
| Staff members with stroke training available | Responses all sites, N = 90 (95%) | Responses private hospitals, N = 49 (98%) | Responses public hospitals, N = 41 (91%) |
|---|---|---|---|
| Physicians with stroke expertise | 58 (64) | 35 (71) | 23 (56) |
| Stroke nurses | 53 (59) | 33 (67) | 20 (49) |
| Physiotherapists | 46 (51) | 28 (57) | 18 (44) |
| Speech and language therapists | 31 (34) | 21 (43) | 10 (24) |
| Pharmacists | 16 (18) | 12 (25) | 4 (10) |
| Nursing assistants/ward helpers | 33 (37) | 22 (45) | 11 (27) |
| Occupational therapists | 26 (29) | 17 (35) | 9 (22) |
| Palliative care team | 13 (14) | 10 (20) | 3 (7) |
| Social workers/case managers | 13 (14) | 10 (20) | 3 (7) |
Neurology services
Of the 93 hospitals with data, 67 (72%) had a neurology service in their emergency department. Private hospitals were more likely to have a neurology service compared to public hospitals (45/50, 90% vs. 22/43, 51%) and these were frequently available 24 hours a day, 7 days a week, in private and public hospital settings (33/45, 73% vs. 15/22, 68%).
Diagnostic services
Of the 89 hospitals with data for diagnostic services, 49 (55%) had access to basic and advanced diagnostic services. Private hospitals were more likely to have basic and advanced diagnostic services (35, 72% vs. 14, 34%) whereas most public hospitals only had access to basic diagnostic services (25, 61%). A telemedicine service was provided by 24/92 (26%) hospitals, and these were more likely to be available in private hospitals (15/48, 31% vs. 9/44, 21%).
Thrombolysis and thrombectomy
Data on the availability of thrombolysis were provided for 91 (96%) hospitals; 64 (70%) delivered thrombolysis to 1525 ischaemic stroke patients over a 12-month period (median 25; IQR 11–35). Thrombolysis was more likely to be available in private compared to public hospitals (42, 88% vs. 22, 51%). Of 89 hospitals that provided data, 38 (43%) had performed endovascular thrombectomy, treating 313 patients over 12 months (median 6; IQR 3–10) and was more likely to be available in private hospitals (31, 69% vs. 7, 16%).
Services to support stroke survivors and their families
Seventy-five (79%) hospitals had a structured healthcare review for patients following discharge. These varied in how often they were carried out: 37 hospitals (49%) reviewed patients every 3 months, 8 (11%) reviewed patients every month, 25 (33%) had variable time intervals ranging from 2 weeks to 12 months and 5 (7%) did not specify review the timeframe. A structured healthcare review was more likely to take place in private hospitals (46, 61% vs. 29, 39%).
Thirty (32%) hospitals reported having a stroke peer support group. A stroke peer support group was more likely in private compared to public hospitals (19/50, 38% vs. 11/44, 25%).
Sixty-four (67%) hospitals provided education and training for patients and their families; availability was more common in private hospitals (42, 66% vs. 22, 34%).
Organisational involvement in research
Data regarding research were provided by 93 hospitals; 38 (41%) hospitals had plans to, or had recently, participated in stroke research including: multicentre randomised controlled trials, and studies based on stroke registries, community health and stroke prevention. Planned or ongoing research was more common in private versus public hospitals (23/48, 48% vs. 15/45, 33%).
Discussion
There are substantial differences between private and public hospitals in the availability of stroke units, diagnostic services and treatments for stroke, structured healthcare review and follow-up. Only half of the hospitals reported having a dedicated stroke unit with a total of 596 beds. This reflects similar findings in the recent ‘State of stroke services across the globe: Report of World Stroke Organization–World Health Organization surveys’, with 12 hospitals in India reporting that 56% of patients had access to a stroke unit. 11 Advanced diagnostic services and treatments were more likely to be provided in private hospitals with access to a more comprehensive range of staff within the MDT, and a greater range of stroke-specific education and training opportunities. A lack of organised stroke unit facilities, and an insufficiency of trained healthcare professionals, continue to be challenges for the provision of stroke care in India,12 particularly in public hospitals.
Of the hospitals with data, almost three-quarters had a neurology service available; these were almost twice as likely to be available in private compared to public hospitals (90% vs. 49%). Previous reports have suggested that across India, on average, there is 1 neurologist per 1,250,000 people (over a third of which are located in metropolitan cities). 13 Despite these challenges, there are many models of stroke care available in low/middle-income countries (LMICs), for example, MDT care led by a stroke neurologist, specialist-led care by neurologists, physician-led care, hub and spoke models incorporating stroke telemedicine, and task sharing involving community health workers. 14 As the burden of stroke increases in LMICs, innovative service delivery models may need to be explored further to determine if these are effective solutions to limited resources and workforce expertise.
In addition to the provision of stroke specialist services, it is well established that stroke survivors whose care is provided by an MDT that specialise in stroke care are more likely to be alive and independent 1 year after stroke. 6 While most hospitals (91%) had access to a MDT, there was wide variation in the type and numbers of team members. There is a recognised shortage of stroke-specialist staff in many countries globally and solutions are needed to train and retain health professionals with stroke-specific knowledge and skills. 15,16 Stroke-specific education and training can provide staff development opportunities and improve outcomes for stroke patients. 17
Accurate early recognition of stroke signs and symptoms as stroke is necessary to maximise the benefits of hyperacute treatment with thrombolysis and/or mechanical thrombectomy, where indicated, and early access to specialist MDT care. 18,19 While the National Programme for Prevention and Control of Cancer, Diabetes and Stroke places emphasis on the importance of a timely stroke diagnosis,8 this survey suggests that diagnostic services were largely only available to patients with access to private health care.
Despite evidence supporting the effectiveness of thrombolysis and thrombectomy, access in India is often limited by availability and cost. 14 In 2013, there were between 35 and 50 stroke units thrombolysing 2000 patients every year in India, a rate of between 1% and 5%. 8,20 Recent research has identified that challenges in the delivery of time-dependent stroke treatments are largely due to pre-hospital delays, affordability, a lack of neurointerventionalists and thrombectomy-capable centres, and the need for improved access to acute stroke imaging modalities. 14,21 While the availability of thrombolysis and thrombectomy is increasing, the lack of emergency medical service provision, delay in patient arrival and diagnosis, and high cost of treatment, remain challenges in the treatment of acute ischaemic stroke patients. 13
Telemedicine is one service that can facilitate the provision of health care to underserved areas and its provision has been growing across India over the last decade. 22,23 Yet, only 26% of hospitals reported the use of telemedicine, with little differences between private and public hospitals. Most telemedicine projects across India were conducted through government and private enterprises rather than within hospital settings. 23 While telemedicine is a growing component of India’s healthcare system, it appears that this is happening largely outside of hospital centres; therefore, there is an important role for telemedicine in stroke in the future, although we acknowledge our survey was conducted pre COVID-19, and the availability of telemedicine may have increased as a result of the pandemic. 24
For stroke patients and their relatives, stroke peer support groups may contribute to positive adjustment by providing them with socialisation, new relationships, shared experiences and hope after disability. 25–27 With most (66%) private hospitals providing stroke education and training for patients and their families (34% in public hospitals), there is room for improvement and opportunity to determine the effectiveness of implementation through research. This could be facilitated by increasing the number of research-active practitioners to enable healthcare organisations to provide better-quality care and improve patient outcomes, while also building research capacity and capability. 28–32
Currently, there is variability in the levels of types of all aspects of stroke unit resources (staff, education, training, facilities and treatment available). The recent World Stroke Organization and National Accreditation Board of Hospitals and Healthcare providers joint Stroke Centre certification programme aims to create the standardised delivery of stroke care across the country, promoting quality and safety of care and improving long-term stroke patient outcomes. 33 Following roll-out of the certification programme, further research is needed to map stroke service provision, including over a wider geographic area and exploring the impact of the programme on key stroke service infrastructure, patient access and outcomes.
Limitations
Our study has several limitations. The hospitals that took part in this study were mainly recruited via two national conferences and the INSTRuCT network. There was a high completion rate from representatives in Kerala; 14 states and 5 union territories were not represented at all and for others we had very few responses. We did not seek to identify all hospitals caring for stroke patients in India and, therefore, we do not know the number of non-identified or non-responding sites and, as such, the findings may not be representative of other hospitals in other regions of India. The survey was distributed at a national (Indian National Stroke Conference) and an International Conference (International Conference on the Essentials of Stroke Care), as well as through the INSTRuCT Network, Indian Stroke Association and Indian Academy of Neurology. It is possible that further responses would have been gained if we had also targeted other organisations such as the Neurological Society of India. In some cases, where more than one representative from a hospital completed the survey tool, the responses from the more senior member of staff were included in the analysis. However, we could not determine with certainty which of these multiple responses were the most accurate. Respondents frequently missed out answers to some of the questions, and although we contacted a number of hospitals for missing information, additional data were not always available. Since the study took place, it is likely that there have been major changes to the availability and delivery of stroke services as a result of the COVID-19 pandemic.
Equality, diversity and inclusion
We sought survey responses from a wide range of respondents who had an overview of stroke services at their respective hospitals in India. Respondents were mainly physicians (52%), followed by nurses (24%), physiotherapists (5%), researchers (3%), speech and language therapists (2%) and unspecified (14%), representing both private and public hospitals. The majority of respondents represented hospitals in the state of Kerala. We did not collect any further data about individual respondents as data collection was focused on hospital stroke services rather than individuals.
Conclusions
Dedicated stroke units, stroke-specific staff, education, training and research opportunities, diagnostic services and specialist treatments were most available within private hospitals; however, there is a paucity of available stroke services data. Further research is needed to map stroke service provision in a wider range of tertiary stroke care providers and stroke units following implementation of the World Stroke Organization and National Accreditation Board of Hospitals and Healthcare providers joint Stroke Centre certification programme and to explore the impact of key stroke service infrastructure and patient access on outcomes.
Additional information
CRediT contribution statement
Stephanie P Jones (https://orcid.org/0000-0001-9149-8606): Formal analysis (lead); Project administration (lead); Validation (lead); Visualisation (equal); Writing – original draft (lead); Writing – reviewing and editing (lead).
Kamran Baqai (https://orcid.org/0000-0002-6190-3241): Formal analysis (supporting); Validation (supporting); Visualisation (equal); Writing – original draft (supporting); Writing – reviewing and editing (supporting).
Rachel Georgiou (https://orcid.org/0000-0002-0920-0602): Conceptualisation (supporting); Data curation (supporting); Funding acquisition (equal); Methodology (equal); Project administration (equal); Writing – reviewing and editing (equal).
Maree L Hackett (https://orcid.org/0000-0003-1211-9087): Conceptualisation (equal); Funding acquisition (equal); Methodology (equal); Supervision (equal); Writing – reviewing and editing (equal).
Catherine E Lightbody (https://orcid.org/0000-0001-5016-3471): Conceptualisation (equal); Data curation (lead); Funding acquisition (equal); Methodology (equal); Project administration (equal); Supervision (equal); Writing – reviewing and editing (equal).
Pallab K Maulik (https://orcid.org/0000-0001-6835-6175): Conceptualisation (equal); Funding acquisition (equal); Methodology (equal); Writing – reviewing and editing (equal).
MV Padma Srivastava (https://orcid.org/0000-0001-7615-9411): Conceptualisation (equal); Funding acquisition (equal); Methodology (equal); Writing – reviewing and editing (equal).
Jeyaraj D Pandian (https://orcid.org/0000-0003-0028-1968): Conceptualisation (equal); Funding acquisition (equal); Methodology (equal); Writing – reviewing and editing (equal).
PN Sylaja (https://orcid.org/0000-0003-4896-8275): Conceptualisation (equal); Data curation (equal); Funding acquisition (equal); Methodology (equal); Writing – reviewing and editing (equal).
Caroline L Watkins (https://orcid.org/0000-0002-9403-3772): Conceptualisation (lead); Funding acquisition (lead); Methodology (lead); Supervision (lead); Writing – reviewing and editing (equal).
Data-sharing statement
All relevant data are provided in the article. Requests for additional data should be submitted to the corresponding author.
Ethics statement
As a survey of existing stroke services in India, this study did not require ethical approval and informed consent was assumed on completion and submission of the survey.
Information governance statement
The University of Central Lancashire is committed to handling all personal information in line with the UK Data Protection Act (2018) and the General Data Protection Regulation (EU GDPR) 2016/679. Under the Data Protection legislation, the University of Central Lancashire is the Data Controller, and you can find out more about how we handle personal data, including how to exercise your individual rights and the contact details for our Data Protection Officer here: (https://www.uclan.ac.uk/legal/data-protection).
Disclosure of interests
Full disclosure of interests: Completed ICMJE forms for all authors, including all related interests, are available in the toolkit on the NIHR Journals Library report publication page at https://doi.org/10.3310/JVNW9009.
Primary conflicts of interest: The authors declare that there are no conflicts of interest.
Department of Health and Social Care disclaimer
This publication presents independent research commissioned by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, MRC, NIHR Coordinating Centre, the Global Health Research programme or the Department of Health and Social Care.
This article was published based on current knowledge at the time and date of publication. NIHR is committed to being inclusive and will continually monitor best practice and guidance in relation to terminology and language to ensure that we remain relevant to our stakeholders.
Funding
This research was funded by the National Institute for Health and Care Research (NIHR) Global Health Research programme (NIHR award ref: 16/137/16) using UK aid from the UK Government to support global health research. The views expressed in this publication are those of the author(s) and not necessarily those of the NIHR or the UK government
This article reports on one component of the research award NIHR Global Health Research Group on Improving Stroke Care, University of Central Lancashire. Other articles published as part of this thread are: [LINKS to other articles]. For more information about this research please view the award page (https://www.fundingawards.nihr.ac.uk/award/16/137/16)
About this article
The contractual start date for this research was in August 2017. This article began editorial review in April 2023 and was accepted for publication in June 2024. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The Global Health Research editors and publisher have tried to ensure the accuracy of the authors’ article and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this article.
Copyright
Copyright © 2024 Jones et al. This work was produced by Jones et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaption in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
List of abbreviations
- INSTRuCT
- Indian Stroke Clinical Trial Network
- LMICs
- low/middle-income countries
- MDT
- multidisciplinary team
- PICH
- primary intracerebral haemorrhage
References
- Khurana D, Padma MV, Bhatia R, Kaul S, Pandian J, Sylaja PN, et al. For ISA Executive Committee . Recommendations for the early management of acute ischemic stroke: a consensus statement for healthcare professionals from the Indian Stroke Association. J Stroke Med 2018;1:79-113.
- Directorate General of Health Services: Ministry of Health and Family Welfare. National Programme for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases and Stroke . Government of India 2019. https://main.mohfw.gov.in/Major-Programmes/non-communicable-diseases-injury-trauma/Non-Communicable-Disease-II/National-Programme-for-Prevention-and-Control-of-Cancer-Diabetes-Cardiovascular-diseases-and-Stroke-NPCDCS (accessed 21 September 2020).
- Sylaja PN, Pandian JD, Kaul S, Padma Srivastava MV, Khurana D, Schwamm LH, et al. Ischemic stroke profile, risk factors, and outcomes in India: the Indo-US Collaborative Stroke Project. Stroke 2018;49:219-22.
- Jones SP, Baqai K, Clegg A, Georgiou R, Harris C, Holland EJ, et al. Stroke in India: a systematic review of the incidence, prevalence and case fatality. Int J Stroke 2021;17:132-40.
- Lloyd J, Pinto AM, Nair S, Tarey S. A qualitative study on palliative needs of stroke patients in an Indian tertiary care setting – doctors’ perspective. Ind J Palliat Care 2019;25:84-91.
- Langhorne P, Ramachandra S. Stroke Unit Trialists’ Collaboration . Organised inpatient (stroke unit) care for stroke: network meta‐analysis. Cochrane Database Syst Rev 2020;4.
- Ganapathy K. Distribution of neurologists and neurosurgeons in India and its relevance to the adoption of telemedicine. Neurol India 2015;63:142-54.
- Pandian JD, Sudhan P. Stroke epidemiology and stroke care services in India. J Stroke 2013;15:128-34.
- Lindsay MP, Norrving B, Furie KL, Donnan G, Langhorne P, Davis S. Global Stroke Guidelines and Action Plan: A Road Map for Quality Stroke Care. Geneva: World Stroke Organization; 2016.
- National Programme for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases & Stroke (NPCDCS) . Guidelines for Prevention and Management of Stroke 2019. mohfw.gov.in (accessed 8 January 2024).
- Owolabi MO, Thrift AG, Martins S, Johnson W, Pandian J, Abd-Allah F, et al. Stroke Experts Collaboration Group . The state of stroke services across the globe: report of World Stroke Organization —World Health Organization surveys. Int J Stroke 2021;16:889-901. https://doi.org/10.1177/17474930211019568.
- Pandian JD, Sebastian IA. Integrated approach to stroke burden: are we doing enough?. Lancet Neurol 2021;20:774-5. https://doi.org/10.1016/S1474-4422(21)00287-8.
- Khurana D, Das B, Kumar A, Kumar A, Khandelwal N, Lal V, et al. Temporal trends in intravenous thrombolysis in acute ischemic stroke: experience from a Tertiary Care Centre in India. J Stroke Cerebrovasc Dis 2017;26:1266-73.
- Pandian JD, Kalkonde Y, Sebastian IA, Felix C, Urimubenshi G, Bosch J. Stroke systems of care in low-income and middle-income countries: challenges and opportunities. Lancet (London, England) 2020;396:1443-51.
- Mehndiratta MM, Singhal AB, Chaturvedi S, Sivakumar MR, Moonis M. Meeting the challenges of stroke in India. Neurology 2013;80:2246-7.
- Kenton EJ, Culebras A, Fayad PB, Goldstein LB, Kaskie B, Leira EC, et al. AAN Vascular Neurology Stroke Practice Resources Workgroup . Impact of stroke call on the stroke neurology workforce in the United States: possible challenges and opportunities. J Stroke Cerebrovasc Dis 2018;27:2019-25.
- Jones SP, Miller C, Gibson JME, Cook J, Price C, Watkins CL. The impact of education and training interventions for nurses and other health care staff involved in the delivery of stroke care: an integrative review. Nurse Educ Today 2018;61:249-57.
- Wardlaw JM, Murray V, Berge E, del Zoppo G, Sandercock P, Lindley RL, et al. Recombinant tissue plasminogen activator for acute ischaemic stroke: an updated systematic review and meta-analysis. Lancet (London, England) 2012;379:2364-72.
- Vidale S, Longoni M, Valvassori L, Agostoni E. Mechanical thrombectomy in strokes with large-vessel occlusion beyond 6 hours: a pooled analysis of randomized trials. J Clin Neurol 2018;14:407-12.
- Wasay M, Khatri IA, Kaul S. Stroke in South Asian countries. Nat Rev Neurol 2014;10:135-43.
- Sundar K, Panwar A, Yagaval DR, Huded V, Sylaja PN. Mission thrombectomy 2020 (MT2020): India’s biggest healthcare challenge yet. J Stroke Med 2021;3.
- Devanbu VGC, Nirupama AY, Taneja N. Telemedicine: new technology, new promises?. Ind J Commun Health 2019;31:437-41.
- Mathur P, Srivastava S, Lalchandani A, Mehta JL. Evolving role of telemedicine in health care delivery in India. Prim Health Care 2017;7:2167-72.
- Sylaja PN, Srivastava MVP, Shah S, Bhatia R, Khurana D, Sharma A, et al. The SARS-CoV-2/COVID-19 pandemic and challenges in stroke care in India. Ann N Y Acad Sci 2020;1473:3-10.
- Ch’Ng AM, French D, Mclean N. Coping with the challenges of recovery from stroke: long term perspectives of Stroke Support Group members. J Health Psychol 2008;13:1136-46.
- Davison KP, Pennebaker JW, Dickerson SS. Who talks? The social psychology of illness support groups. Am Psychol 2000;55:205-17.
- Muller M, Toth-Cohen S, Mulcahey MJ. Development and evaluation of a hospital-based peer support group for younger individuals with stroke. Occupat Therap Health Care 2014;28:277-95.
- Krzyzanowska MK, Kaplan R, Sullivan R. How may clinical research improve healthcare outcomes?. Ann Oncol 2011;22:vii10-5.
- Ozdemir BA, Karthikesalingam A, Sinha S, Poloniecki JD, Hinchliffe RJ, Thompson MM, et al. Research activity and the association with mortality. PLOS ONE 2015;10.
- van Oostveen CJ, Goedhart NS, Francke AL, Vermeulen H. Combining clinical practice and academic work in nursing: a qualitative study about perceived importance, facilitators and barriers regarding clinical academic careers for nurses in university hospitals. J Clin Nurs 2017;26:4973-84.
- Windsor J, Searle J, Hanney R, Chapman A, Grigg M, Choong P, et al. Building a sustainable clinical academic workforce to meet the future healthcare needs of Australia and New Zealand: report from the first summit meeting. Intern Med J 2015;45:965-71.
- Windsor J, Garrod T, Talley NJ, Tebbutt C, Churchill J, Farmer E, et al. The clinical academic workforce in Australia and New Zealand: report on the second binational summit to implement a sustainable training pathway. Intern Med J 2017;47:394-9.
- National Accreditation Board for Hospitals and Healthcare Providers . NABH Stroke Standards Accreditation Programme 2023. https://nabh.co/h-doc (accessed September 2024).
Appendix 1
IMPROVIng Stroke carE in India (IMPROVISE) Collaboration
-
Dr. Jeyaraj D Pandian
-
Principal and Professor
-
Department of Neurology
-
Christian Medical College and Hospital
-
Brown Road, Ludhiana
-
Punjab, 141008, India
-
Dr. MV Padma Srivastav
-
Professor
-
All India Institute of Medical Sciences
-
Department of Neurology, Room no 708, 7th floor
-
All India Institute of Medical Sciences Ansari Nagar, New Delhi 110029, India
-
Dr. PN Sylaja
-
Sree Chitra Tirunal Institute of Medical Sciences and Technology
-
Department of Neurology Sree Chitra Tirunal Institute for Medical Sciences & Technology, Thiruvananthapuram 695011, Kerala, India
-
Professor Dame Caroline Watkins
-
Professor of Stroke & Older People’s Care/Faculty Director of Research and Innovation
-
School of Nursing and Midwifery, University of Central Lancashire
-
Preston, PR1 2HE, United Kingdom
-
Dr Liz Boaden
-
Senior Research Fellow
-
Stroke Research Team
-
School of Nursing and Midwifery, University of Central Lancashire
-
Preston, PR1 2HE, United Kingdom
-
Associate Professor Dominique Cadilhac
-
Head of Translational Public Health Research Stroke and Ageing Research Group
-
Monash University, Level 3 Hudson Institute Building
-
27–31 Wright Street
-
Clayton, VIC 3168, Australia
-
Professor Andy Clegg
-
Professor Health Services Research
-
School of Nursing and Midwifery, University of Central Lancashire
-
Preston, PR1 2HE, United Kingdom
-
Mrs Denise Forshaw
-
Principal Clinical Trials Manager and Deputy Director (Operations and Governance), Lancashire Clinical Trials Unit, University of Central Lancashire
-
Preston, PR1 2HE, United Kingdom
-
Professor Mark Gabbay
-
Director of NIHR NWC CLAHRC
-
Primary Care and Health inequalities
-
University of Liverpool, Institute of Psychology Health and Society
-
University of Liverpool
-
Liverpool, L69 3BX, United Kingdom
-
Ms Rachel Georgiou
-
Senior Research Fellow
-
Stroke Research Team
-
School of Nursing and Midwifery, University of Central Lancashire
-
Preston, PR1 2HE, United Kingdom
-
Dr Jo Gibson
-
Reader in Applied Health Research
-
Stroke Research Team
-
School of Nursing and Midwifery, University of Central Lancashire
-
Preston, PR1 2HE, United Kingdom
-
Professor Maree Hackett
-
Program Head Mental Health, The George Institute for Global Health, Neurological & Mental Health Division
-
Level 10, King George V Building, 83–117 Missenden Road, Camperdown, NSW 2050, Australia
-
Dr Steph Jones
-
Programme Manager
-
Stroke Research Team
-
School of Nursing and Midwifery, University of Central Lancashire
-
Preston, PR1 2HE, United Kingdom
-
Dr Yogeshwar Kalkonde
-
Society for Education, Action and Research in Community Health
-
Gadchiroli, India
-
Dr Liz Lightbody
-
Professor of Stroke Care and Improvement
-
Stroke Research Team
-
School of Nursing and Midwifery, University of Central Lancashire
-
Preston, PR1 2HE, United Kingdom
-
Professor Richard Lindley
-
Professor of Geriatric Medicine, Westmead Clinical School, The University of Sydney, Australia
-
Professorial Fellow, The George Institute for Global Health, United Kingdom
-
Professor of Geriatric Medicine, Blacktown Hospital, The University of Sydney, Australia
-
Principal Investigator, Westmead Applied Research Centre, The University of Sydney, Australia
-
-
Professor Pallab K Maulik
-
Deputy Director and Director of Research, The George Institute for Global Health, India
-
Professor, Faculty of Medicine, UNSW Sydney
-
Professor, Prasanna School of Public Health, Manipal Academy of Higher Education, India
-
Provost's visiting Professor of Mental Health, Imperial College London, United Kingdom
-
-
Professor Sandy Middleton
-
Director, Nursing Research Institute
-
Australian Catholic University and St Vincent’s Health Australia Sydney Level 5, deLacy Building, St Vincent’s Hospital, Sydney
-
390 Victoria Street, Darlinghurst
-
NSW 2010, Australia
-
Dr Gordon Prescott
-
Reader in Medical Statistics and Deputy Director of the Lancashire Clinical Trials Unit
-
Lancashire Clinical Trials Unit
-
University of Central Lancashire, Preston, PR1 2HE, United Kingdom
-
Professor Kate Radford
-
Professor of Rehabilitation Research, Faculty of Medicine & Health Sciences
-
Room B102 Medical School, Queen’s Medical Centre
-
Nottingham, United Kingdom
-
Professor Caroline Sanders
-
Professor of Medical Sociology
-
University of Manchester, School of Health & Sciences
-
The University of Manchester
-
Brunswick Street, Manchester, M139 PT, United Kingdom
-
Professor Doris Schroeder
-
Professor of Moral Philosophy and Director of the Centre for Professional Ethics
-
School of Health, Social Work and Sport
-
University of Central Lancashire, Preston, PR1 2HE, United Kingdom
-
Dr Anil Sharma
-
Clinical Adviser to NIHR Global Health Research Group
-
University of Central Lancashire
-
Preston, PR1 2HE, United Kingdom
-
Dr Chris Sutton
-
Senior Lecturer in Clinical Trial Statistics
-
School of Health Sciences
-
Division of Population Health, Health Services Research and Primary Care
-
The University of Manchester, United Kingdom
-
Professor Marion Walker
-
Professor of Stroke Rehabilitation; Associate Pro Vice-Chancellor (Equality, Diversity and Inclusion), Nottingham University, Queen’s Medical Centre, Nottingham NG7 2UH, United Kingdom
-
Department of Health through the National Institute for Health Research, Room 132, Richmond House, 79 Whitehall, London, SW1A 2NS, United Kingdom
-
Appendix 2
Appendix 3 Hospitals with multidisciplinary team members
| Access to number of MDT members | All sites 95 (100%) | Private hospitals 50 (100%) | Public hospitals 45 (100%) |
|---|---|---|---|
| 0 MDT members | 9 (10) | 0 (0) | 9 (20) |
| 1–5 MDT members | 24 (25) | 9 (18) | 15 (33) |
| 6–10 MDT members | 62 (65) | 41 (82) | 21 (47) |
