Notes
Article history
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as award number NIHR129645. The contractual start date was in January 2021. The draft manuscript began editorial review in April 2023 and was accepted for publication in January 2024. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ manuscript and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this article.
Permissions
Copyright statement
Copyright © 2024 Brimblecombe et al. This work was produced by Brimblecombe et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2024 Brimblecombe et al.
Chapter 1 Context
Policy and practice
Research in relation to young and young adult carers has focused on estimating their prevalence and the outcomes of caring on them. 1 Aside from the United Kingdom (UK) and Australia, few countries have developed policy in relation to young carers. 2 However, some countries, primarily in the Global North, are beginning to increase their awareness of, and support for, young carers (e.g. Canada, New Zealand and Western Europe). Studies based in these countries indicate that comparatively, the role of a young carer is similar across countries and continents. 3 What does vary widely, according to local circumstances, are the tasks and responsibilities of a young carer, which may include domestic tasks, nursing or personal care, management of household or finances, care of siblings or emotional support,4 and the support offered to young carers to mitigate the negative impacts of these tasks and responsibilities. Yet few studies have the voices and perspectives of young carers at their centre, and there is a knowledge gap when it comes to understanding what young carers believe would be most helpful to them in terms of support.
An ongoing controversy concerning the needs of young carers may be a leading cause of this knowledge gap. Because of the ethical concerns of children and young people providing care, providing support for them can suggest an acceptance of their role as a carer. 4 This conflicts with ‘western constructions of childhood,’2 which do not ascribe regular caregiving responsibilities to children.
In England, young carers were first legally acknowledged in the 1995 Carers’ (Recognition and Services) Act5 and, since then, a series of laws and policies have referred to young and young adult carers. (See Appendix 1, Table 7; ‘Key legislation and policy affecting provision for young carers in the UK’ for more detail.) Following several revisions, the current definition used by the Department of Health in the 2014 Care Act6 and 2014 Children and Families Act,7 Section C.6, describes a young carer as follows: ‘a person aged under 18 years, who provides or intends to provide care for another person (of any age), except where that care is provided for payment, pursuant to a contract or as voluntary work.’ Individuals aged 18 years and above are legally considered to be adult carers in the UK; however, in much research and practice, the term ‘young adult carer’ is used frequently to describe a person with caring responsibilities who is between the ages of 16 and 25 years. 8,9
The 1989 Children Act10 placed a duty on local authorities to assess the needs of young carers in their area. Until this point, policy-makers, researchers and welfare professionals in the UK had failed to recognise and account for young carers2 and it was not until The 2004 Children Act11 and 2004 Carers (Equal Opportunities) Act12 that local authorities were given responsibility to proactively identify young carers in their area. These Acts also encouraged the adoption of a whole-family approach to need assessments across adult and children’s services. 13
Following this, the 2014 Children and Families Act7 alongside the 2014 Care Act6 created rights for young carers and their families to be identified, receive an assessment (the Carer’s Assessment of Needs on the first point of contact, and the Transition Assessment if a young carer is turning 18 and has previously received a Carer’s Assessment of Needs) and be supported using a whole-family approach. These Acts stipulated that services working with adults or children with care needs should identify young carers through their work with other family members. Moreover, local authorities were encouraged to join up the work of children’s services and adult services, so that young carers and young adult carers could benefit from service collaboration.
Another part of the 2014 Care Act (Section C.23)6 that impacted provision for young carers was that it required local authorities to consider ‘replacement’ care. This is the option of allowing the young carers’ needs for support to be met by providing services to the care recipient. Under the 2014 Care Act, local authorities are required to prevent a caring role having a negative impact on a young carers’ wellbeing and as such, ‘replacement’ care could reduce caring responsibilities or mitigate potential harm by reducing the young carer role. 6
Statutory guidance accompanying the 2014 Care Act13 acknowledged the possible short-, medium- and long-term effects of caring responsibilities for young people and further outlined how caring roles may impact the development of a child or young person. However, defining what care responsibilities are inappropriate or excessive is a complex and culturally contextualised process. 14 Even if one were to consider a base line for the role of ‘young carer’, many children in the UK undertake domestic and caring responsibilities. Therefore, it is difficult to determine the point at which children are considered to be young carers.
Young carers are an ongoing priority for health and social care policy and practice in England. For example, the 2019 National Health Service (NHS) Long Term Plan15 includes access to preventative health services and support for young carers. Young carers and the organisations that support them have also expressed need for better, more easily accessed services for themselves and the person they support. 16,17 The 2022 Health and Care Act18 introduced measures that aim to support carers further, such as legislating for carers’ involvement when decisions are made around developments to services, and young carers are named as a target population cohort in the NHS England Core20PLUS5, a national approach to support the reduction of health inequalities at both national and system level and improve care for children and young people. 19
Currently, preventing the negative consequences of care provision on young people’s health and wellbeing is a high priority for health and social care policy and practice. Costs associated with the negative consequences of providing care are high,20 and limited resources within health and social care sectors heighten the need to target services and provide appropriate and equitable support. Inequalities in care provision, care need and the impacts of care provision on health make this relevant to current emphases in health and social care practice on reducing health inequalities. 15 In England and Wales, an estimated 5.0 million usual residents aged 5 years and over provided unpaid care in 2021,21 and support for young carers is a key priority in health and social care long-term plans,15 reflecting the expectation that support for carers will remain highly and increasingly important in the future. Appropriate, acceptable and easily accessed support for young carers and the people they care for is therefore likely to remain core to the future needs of the NHS and the social care sector.
Review of the evidence
Impacts on young people of providing care
Previous research has shown that providing care has multiple impacts on young people, including their health and wellbeing,4,22,23 education4,24,25 and employment prospects. 4,20,26 This creates substantial associated costs to individuals, the government and the NHS. 20 Transition into adulthood can be a particular challenge for young carers because their caring responsibilities may be a barrier to employment, vocational training or further education. 27 However, and despite the increased rights to support described above, there are knowledge gaps on how to best support young carers and prevent these impacts. 22 This is especially the case for young adult carers aged 16–25 years; carers and care recipients who currently under-access services and people from underserved population groups such as ethnic minorities families. 28
What is good or not good about existing services? What can be improved?
Recent research findings have illustrated some of the problems with support that is currently available for younger carers and some of the ways in which support has been successful. 24,27 Qualitative research with young carers has shown that they value opportunities for respite. 29 By providing fun and meaningful activities, young carers can experience hiatus from their caring responsibilities and serious concerns. 30 However, when asked how services can best support them, young carers have identified that better support for the person they care for is, or would be, most useful. 4,29
As such, some scholars have highlighted the benefits of services that provide a whole-family approach to support. Ronicle and Kendall, in their 2011 research report, concluded that whole-family approaches had been helpful in reducing the proportion of young people taking on inappropriate caring responsibilities. 31 Moreover, Carers Trust, which supports 24,000 young carers in the UK each year, has noted how young carers and their families have spoken about the benefits of family support workers, who act as a main contact and liaison with several services that young carers and families use. 32 Similarly, Whitley and Wooldridge,33 in their evaluation of Sheffield Young Carers Family Project, found that the 90 families involved in the project indicated a positive experience. They appreciated the one-to-one intervention from family support workers due to the high quality of support provided and their dedicated and proactive nature. On top of this, whole-family social activities (such as group support and parent networking events) were beneficial. For young carers, they offered the opportunity to do fun and exciting activities; for cared for people, these activities facilitated them to speak to other families with a young carer, increasing their informal support networks and reducing isolation. The combination of dedicated family support and opportunities for social activities was a feature that was unique to the programme. As such, demand was high, with more than 30 families on a waiting list for involvement. 33
Outside of the UK, Schlarmann et al. (2011)34 have highlighted the benefits of Germany’s first young carers project, Supakids. Taking a whole-family approach, participants felt that the project allowed them to be ‘as they are’ and meet others in similar situations. Moreover, the service provided a first port of call for a variety of problems, providing a break from life at home. However, as Hafting and colleagues emphasise in their 2019 study, taking a whole-family approach is necessary but not sufficient when identifying young carers in Norway. 35 They found that this was because parents felt ambivalent about revealing information about family matters, which can prevent young carers from receiving further support, while general practitioners (GPs) felt ambivalent about bringing up this potentially sensitive topic of conversation with adult care recipients. Subsequently, services focusing on adults (such as substance misuse services) must recognise their responsibility for the wellbeing of a client’s child or children. 36
Few studies focus on support for young carers provided at schools and educational institutions; however, Eley’s 2004 report provides insight through interviews with 11 young carers in Scotland. Young people in this study felt ambivalent about disclosing their role as a carer for fear of unwanted intrusion in their family life, or reactions from teachers who would consider their caring responsibilities to be an ‘excuse’ for absence or poor performance. As such, although young people were reluctant to be identified, they felt frustrated by their teachers’ lack of awareness. 37 Young people may also yearn for normalcy, impacting their willingness to disclose their identity. 38
An evaluation of the Young Carers in Schools Programme (YCSP) by the charity Coram39 provides insight into the benefits this England-wide initiative offers. Firstly, the introduction of the initiative in schools resulted in increased identification of young carers, which led to an increase in referrals to local agencies and community-based carers services. This gave the young carers opportunities outside of school that they otherwise would not have accessed.
According to respondents of the survey (78% of which were leaders for young carers within schools, and 15% of which were support workers, school managers and family liaison officers), greater awareness of the needs of young carers through the YCSP helped staff to be more flexible and understanding, helping young carers to manage their schoolwork and have a more fulfilled student experience. Schools reported an improvement in academic engagement and attainment, with a higher motivation to learn.
Participants in Coram’s survey also reported that young carers appeared to benefit from participation in group activities and access to a supportive peer group. They reported that young carers were demonstrating widespread improvements in wellbeing, happiness and confidence. 39 The benefits of peer support have also been highlighted by other studies in the UK and Austria, which have investigated the experiences of young carers supporting parents with mental illness. 40,41
Strengthening the resilience of young carers through psychoeducation and support groups has been a benefit identified by Gettings et al. ,42 whose longitudinal feasibility study investigated methods of audio-conferencing to facilitate support groups for siblings of people with a neurodevelopmental disability in the UK. Young carers involved in the study stated how they felt more prepared, as they gained a better understanding of their siblings’ neurodisability. Moreover, the group provided a space where young carers could share difficult thoughts and feelings and reduce their isolation.
The method by which these programmes are delivered could have a major influence on how successful they are in supporting young carers. Although eHealth is becoming a more accessible and reliable means by which vulnerable individuals may seek support and information,43,44 for young adult carers in the UK, in-person support was reported as preferable in the past,8 although this may have changed in the intervening years. Online interventions may include the benefit of anonymity,45 but internet literacy and access can be barriers preventing individuals from reaching the information and help they require, as well as having the potential for being overheard. Moreover, young people involved in previous studies have noted the importance of services in youth-friendly formats46 as well as professional and responsive workers. 47
Studies in the United States (US) and Australia have also suggested that access to skill-building and targeted education programmes may be beneficial for young carers, providing them with the opportunity for self-efficacy and proficiency in the care they provide. 48–50 For example, the YCare protocol piloted by Kavanaugh and colleagues aimed to provide supportive training for young carers, ages 8–16 years. Participants in this study reported a significant increase in their confidence to complete caring tasks correctly, and many noted the benefit of meeting peers in a group training environment. 50
In summary, the literature fails to capture the service landscape for young carers in the UK from the perspective of young carers themselves. Although existing studies have indicated some benefits of particular programmes – such as a whole-family approach, or provision of respite opportunities for young carers – these do not give us a comprehensive idea of how young carers think services could be improved; particularly as many studies are based outside of the UK, are focused on a small geographical area, and/or predate the current rights for young carers and the more recent rise in young carer voluntary sector support organisations. 51
What additional support is needed
Financial support is a prominent area highlighted in the literature, as many young carers have unmet financial needs. In 2013, a longitudinal study of young carers in England found that the average income of a young carer’s family was on average £5000 less than a family with no young carer. 52 Moreover, the study found that young carers were more than four times as likely as non-carers to be in families where no-one was in paid work. Qualitative research with young carers often found that they were aware of the financial constraints their families faced. 29 More recently, Vizard and colleagues53 examined child poverty outcomes among young carers in the UK from 2005 to 2015 and found that in the wake of the financial crisis, recession and the onset of austerity, young carers have fared worse than other young people who did not have caring responsibilities. As such, this strongly suggests that young carers and their families face difficulties directly aggravated by poverty.
One contributing factor of lower family income is the difficulties young carers face with study and employment. Young carers are not included in the list of vulnerable groups who can apply for the 16–19 Bursary Fund, although individual higher education institutions may be willing to give young carers a discretionary bursary. The lower age limit for receipt of a carer’s allowance is 16, which excludes young carers below this age. The benefit also requires the person cared for to be in receipt of a disability-related benefit and for the carer to be providing 35 hours of care per week or more. For those who do qualify, there is an earnings limit for receipt of a carer’s allowance of £132 per week. The benefit specifically excludes carers in full-time education or those who study for more than 21 hours per week. Subsequently, in their interviews of young carers in the US, Keigher and colleagues54 found that young carers unable to seek employment may risk illegal activity (such as drug dealing) or other unstable jobs to make ends meet. 54
Young carers in school or college in the UK have also identified areas in which they require further support, including difficulties making friends who understand their caring role;55 challenges meeting the needs of a course or their homework;56 and bullying. 25 Young carers may also be more likely to miss and be late for school than their non-carer peers. 57 In light of this, as Becker and Becker8 suggest, young carers require the support and understanding of teachers – and from the education system more generally. Of course, although raising awareness and sharing information about young carers among staff and other students may be helpful, Bostock58 reminds us that this needs to be done according to the wishes of the young person, as some are more comfortable with their sensitive information being shared than others.
Another significant unmet need highlighted in the literature is communication within and between support services. Because many services work in isolation, this can lead to delays, miscommunication and the added stress of young carers and their families having to repetitively tell their stories to a wide number of services. Moreover, as Becker and Becker8 have indicated, there is a gap between support offered by youth services and adult services. As such, some young adult carers have suggested that the creation of an interdisciplinary and interprofessional network would aid communication between services in the UK. 59 Leading researchers in the field are also calling for a new agenda for policy development, one that champions greater awareness of the need for interdisciplinary and multi-agency working. 4
With regard to services for the care recipient, which could help reduce caring responsibilities, several studies point to difficulties they may face as a result of shortcomings within the healthcare services for care recipients. For example, according to young carers, they may not be included in decisions regarding the provision of care, or discussions between healthcare professionals and the care recipient. 56 The inclusion of young carers in this way can provide them with education and knowledge to support them in their role as a carer, and furthermore, it can instil confidence that the care recipient is well supported. 50
Turning to studies based outside of the UK, Hamilton and Adamson60 have suggested that identifying gaps in service provision may be difficult for young carers in Australia, as they may have limited time away from their caring responsibilities. Moreover, Moore and colleagues found that many of the young carers in their Australian study reported that the level of care they provided was downplayed either by themselves, their families or the services they accessed. 47 This may be due to stigma attached to the role of a young carer, particular family dynamics, or inadequate needs assessments by local service providers. Smyth and colleagues61 have also highlighted how young carers may not identify as such and therefore remain ‘hidden’ to services and support providers. As such, unidentified support needs may be prevalent among young carers and their families. In light of this, Moore and colleagues recommend a service approach that focuses on the impact of the responsibilities that young carers have, with an understanding that there are multifaceted issues behind these impacts. On top of this, as the needs of care recipients, young carers and their families change, services need to evolve and adapt to ensure an adequate provision of care, delivered at a pace that suited them. 62 This may be relevant to young carers in the UK who have found that their level of caring responsibilities has increased since the COVID-19 pandemic. 63
Through their interviews with young carers and young adult carers in Switzerland, Leu and colleagues45 have emphasised that there should be greater inclusion of the needs of young carers in emotional support and prevention programmes for children and adolescents with ill parents or siblings. From studies speaking to young carers and young adult carers in contexts outside of the UK, services to meet this need could include links to, and communication with, other people with similar experiences29,45,47 or advice from professionals on how to support themselves and practise self-care. 45 Two key components of these relationships, for young carers, is the feeling of trust in the person(s) they are talking to47 and that there is continuity within these relationships, whereby a stronger connection can be built. 62
Overall, studies have identified some of the unmet needs of young carers in the UK but offer little insight with regard to what this support may look like, or how services may be improved. Although it has been suggested that families with young carers may face financial difficulty, the literature, as of yet, has failed to fully investigate young carers’ perspectives about these issues.
Barriers to support
Research literature identifies numerous factors that may prevent young carers and their families from accessing support. These can be grouped into three overlapping categories: first, barriers of communication at the service level; second, barriers of identification (at both the personal and service level); and third, barriers of design, organisation and delivery of services.
Barriers of communication at the service level
Speaking to both young carers and service providers in the UK, Wayman and colleagues16 reported that many young carers did not realise that there were services available to support them nor how to access them. This may be because communication methods do not take into account the diverse needs of young carers, providing information suitable for their age, language abilities, disability (and communication needs), cultural beliefs or understanding. 16,64
Professionals (such as GPs and social workers) may fail to keep young carers informed about the person they care for. 65 Subsequently, young carers have indicated that this can make learning about the needs of a care recipient more challenging, and it can also restrict their ability to identify appropriate support services. 16
Barriers to identification
As previously mentioned, in many contexts the term ‘young carer’ may be one that young people do not identify with, or their role may not be recognised by their families. 29,61,64,66 For instance, young carers may regard their caregiving roles as usual household chores;65,66 for others, ‘young carer’ could have connotations of being a victim, or a ‘do-gooder’, which contrasts with the way that young people see themselves. 29
In the UK, some young carers may only recognise their role following their engagement with services. 67 Moreover, Obadina68 has highlighted that there may be stigma attached to the label of ‘young carer’, or a reluctance of young people and their families to self-identify due to a fear of unwanted intervention from services, fear of being judged, or family break-up. For some, it may harbour feelings of being different to other young people. 69
In their analyses of services accessed by young carers in Wales, Thomas et al. highlighted how identifying young carers may sit outside the remit of professionals, whose priority is the care recipient,56 and there may also be difficulty for some groups of young carers to be recognised as such. Butler and Astbury,69 for example, found that young carers in Cornwall were an ‘invisible population’ often overlooked by services. They noted a low referral rate to new young carers services in the area from GPs and schools, which they suggest is illustrative of a lack of recognition of young carers and their needs. This issue of identifying young carers was highlighted most recently by Warhurst and colleagues,70 whose study found that UK school staff found difficulty in identifying young carers who did not offer information about their caring responsibilities. 70
Barriers at service level – design, organisation and delivery
In a 2022 independent evaluation commissioned by NHS England, young carers noted that services for young carers were inconsistent across the country. 71 This inconsistency may leave many young carers struggling to access sufficient support.
Several studies based in Australia and the UK have highlighted that for individuals with specific needs, mainstream support services for young carers and their families may not be appropriate. First, young carers in a study by McDougall et al. 46 illustrated how mental health services may not be aware of the experiences of young carers and the difficulties they face, so may not be able to provide appropriate support or advice. Second, because young carers have competing responsibilities, they may have little (or no) time to engage with services and support available to them,60 particularly if they have a mental or physical illness or a disability. Third, as highlighted by Shah and Hatton’s UK study,72 services may have a lack of understanding of cultural needs of young carers and their families, including language, dress and etiquette and this may lead to reluctance of families to engage with such services.
In terms of accessing services, barriers at the service level include the cost of services and the transport to reach them, which may be restrictive for families. 60,73 Moreover, as there is no integrated pathway to support, professionals may fail to share information about young carers with other services, which can slow down referral processes and prevent young carers from accessing other resources. 29 A high turnover of staff may also affect access to services, as knowledge of the situations of young carers and their families may be lost through regular transition. Additionally, a high staff turnover can deter service users from accessing services, as they may be reticent to sharing and repeating sensitive and personal information. 16
Young carers and their families may feel discouraged from using services again if they have had previous negative experiences. This may include long waiting lists, unwelcoming environments or a low standard of service. 46 Families may feel frustrated or unable to communicate with service providers16 and these experiences may also inform their advice to others in their local community, who may be deterred from approaching services.
Overall, the literature focusing on barriers at the service level for young carers suggests that a lack of knowledge of young carers and their needs may lead to problems when accessing services. Although many of the studies in this area are UK-focused, many were written at least a decade ago, hence more up-to-date knowledge is required to understand the current experiences of young carers.
Conceptual framework
We drew on a number of theoretical and conceptual frameworks to inform the study. In considering both carer and care recipient views on service acceptability, we adopted Twigg and Atkin’s ‘dual perspective’: that caring takes place in a relationship, that there is a multiplicity of needs and that needs sometimes conflict. 74 We also utilised Purcal et al. ’s 2012 analytical framework which classifies three different possible aims of service support: (1) prevention of a child or young person taking on the caring role or working towards reducing or removing care by the child if that is already taking place; (2) assistance (supporting the carer to carry out their caring); and (3) mitigation (providing help to the young person which addresses negative impacts on them of their caring role). 75 This framework is closely related to Twigg74 and Twigg and Atkin’s76 typology of the ways in which the statutory care system engages with unpaid carers.
In exploring the barriers experienced by young carers and the people helped by them to getting the support they say they need, value and find helpful, we drew on and adapted Andersen’s Behavioral Model of Health Services Use (BMHSU). 77,78 The BMHSU was originally developed to assess and understand under-access in healthcare use, and inequalities in access, for which it has been widely used. 79 It has also been used, although to a lesser extent, in studies of social care. 80,81 Other adaptations of the model have added aspects such as competing priorities (see e.g. Lederle review, 2021) or a greater emphasis on psychosocial factors. 80,82 In the BMHSU, barriers are termed ‘inhibiting’ and ‘impeding’ factors. 79 Individual impeding factors in the models include material circumstances; competing priorities; self-determination (privacy, dignity, independence, willingness to seek or receive help) and psychosocial factors such as fear, mistrust or nervousness. Contextual factors in the model include care policy; care financing (which affects availability, affordability, resources and staffing) and service organisation (e.g. accessibility, approachability, degree of specialisation, integration and communication). A further component of the BMHSU is ‘health literacy’, or in the study ‘service and support literacy’. Depending on the stance taken, whether that be a medical model or public health model perspective, ‘health literacy’, a key component of various iterations of the BMHSU, can be seen as being an individual-level barrier (e.g. individual knowledge, competencies and confidence); an organisational or other contextual-level barrier (e.g. ability of provider and/or governments to provide appropriate and accessible information and to communicate well about available support and services and how they work); or a combination of both. 83 Other components of the model can also be seen also have individual or contextual aspects or both. For example, cost of a service as barrier could be attributed to lack of affordability and/or lack of materials resources.
Chapter 2 Research objectives
The overarching research question was ‘What are the barriers to young and young adult carers accessing carer support services and/or services for the recipient of care, and what interventions and support services are acceptable to these groups and the persons they look after?’
The aims and objectives were to explore the following questions:
-
What types, components or features of services and other support are seen as helpful, valued and acceptable to young people who look after someone at home and the people they support? Conversely, what is found to be less or unhelpful?
-
What additional support is perceived as needed?
-
What are the barriers experienced by young and young adult carers in seeking and accessing services for themselves or the person they support?
-
What are the barriers and facilitators for practitioners in providing support and services perceived as valued, helpful, and needed by young and young adult carers and the people they support?
Chapter 3 Methodology
Engagement, recruitment and outreach
The focus of the research was on young and young adult carers and the people they support. These groups have historically been less likely to access services and other support than others with similar levels of need. 84 Many young carers do not identify as such because of, for example, fear of authorities, lack of engagement with any service or reluctance from families and/or young carers to be identified or labelled because of stigma, guilt and shame and/or because they feel it is not of benefit to their situation, so are unknown to services. 61 We aimed to include particularly marginalised groups of young carers and the people they care for, such as young carers of, and people with, stigmatised conditions such as severe mental illness. People with mental ill health and/or their carers are less likely to seek or access support than people with other conditions68,85 and people with mental illness supported by a young carer are even less likely to be receiving support than people supported by an adult carer. 86 Because of this focus, we initially intended to do pre-focus group/interview engagement activities, for example information meetings to explain the research and address any concerns or questions. These could be linked to existing events. However, because of COVID-19 restrictions during most of the fieldwork period, existing groups were not meeting in person, or at all, nor holding events and it was not the right time or method to attend any online events, so we changed the recruitment strategy accordingly.
In the study, we worked closely with collaborating organisations in four localities. These were young carers organisations that had already done extensive engagement and outreach within their areas and helped us recruit from among the young carers and care recipients they were or had been in contact with, many of whom were from the more marginalised populations in their areas. The young carers organisations also helped recruit from the wider body of organisations and groups within their localities, although not as widely as initially planned.
The engagement and recruitment strategies for the project included:
-
Co-development of recruitment materials and methods with young carer, care recipient and practitioner advisors
-
Young carers project workers’ direct involvement in study recruitment
-
Project workers in each locality working with young carers, care recipients and marginalised groups helping with recruitment and providing support for study participants
-
Providing clear information and reassurance during recruitment and data collection about confidentiality, anonymity and the information being gathered for research purposes only
-
Aiming to ensure that process, format and content of focus groups/interviews were as inclusive as possible. We were flexible about timing of focus groups and interviews. We arranged accessible focus group and interview venues (with options for interviews online or by phone) and arranged transport as needed. Transport was especially important for people with mobility issues and people living in areas where public transport is limited and transport costs high, but in practice the majority of participants in all localities attended by taxi, suggesting this was important to their attendance and inclusion.
Research design
The philosophical approach informing this study is that understanding what support is helpful, less helpful and needed and the barriers to support requires the perspective of those with lived experience,87 in this case the young and young adult carers and the people they support. The study had an in-depth qualitative methodology utilising focus groups, workshops and in-depth semistructured interviews. An explanatory rather than confirmatory framework was needed because not enough was known about experiences of those not receiving services to be able to explore these issues in a survey-type approach. 87 A qualitative approach was well suited to answering the research questions around barriers; what aspects of support are or would be acceptable; and to understand experiences and motivations and how these relate to interactions with, and intentions towards, services. The semistructured approach allowed us to be flexible in how we went about seeking answers to these questions.
While pragmatic considerations (convenience and preferences of individual participants) guided who took part in focus groups, and who took part in interviews, these two methods of data collection had different aims. Both addressed experiences with services, barriers to services use, and what good service provision looks like. However, the focus groups aimed to uncover, or allow to develop, shared understandings within the group, whereas the interviews aimed to encourage more in-depth exploration of personal circumstances, trajectories and experiences. Previous research has found that focus groups may be more effective than face-to-face interviews and questionnaires because people have often not thought about how they feel on the issues to be discussed and opinions may not be formed in isolation. 88 The focus group format can feel less threatening or challenging for some participants89 and younger carers may respond better in group settings. 90,91 However, some potential participants may have been unwilling or unable to join in a focus group and so were offered the option of face-to-face or telephone interviews. In practice, the vast majority of participants in the study chose to take part in a focus group rather than an interview (see Report Supplementary Material 1).
Ethics and informed consent
Ethics approval for the focus groups and interviews was granted by the London School of Economics and Political Science (LSE) Ethics on 21 May 2021 (Ref. 1247).
1. Confidentiality and data security
We adhered to the 2018 Data Protection Act as well as General Data Protection Regulation (GDPR) guidance related to the security of information. Completed paper materials (consent forms) are stored in locked filing cabinets in secure offices at the LSE. Access is by the research team. Interviews were transcribed by a professional transcription service, also adhering to GDPR guidelines, and data have been anonymised. Interview recordings and transcripts are held on a secure folder on the LSE servers accessed from password-protected computers in secure offices at the LSE. Information sheets explained that information would be kept confidential. The exception to confidentiality was that if the participants in interviews or focus groups raised concerns of serious risk of harm to participants or others. In this event we had a policy to aim to talk to the person and potentially take further action as required (see also Safeguarding below). This was also explained in the participant information sheets.
2. Safeguarding
We had in place robust safeguarding procedures for the study, developed with relevant experienced organisations and based on previous materials. This included situations where safeguarding issues might be disclosed and covered both the research and advisory processes. LSE also has a safeguarding procedure. Each key collaborating organisation had its own extensive safeguarding procedure which we and they also adhered to. Researchers carrying out the focus groups and interviews were Disclosure and Barring Service (DBS) checked and had training and experience in conducting research with vulnerable adults and children. Project and support workers also had DBS checks.
Participant information sheets and advisory group information sheets explained the limits to confidentiality (i.e. that everything they told us would be confidential unless they told us something that indicated that they or someone else was at risk of harm, in which case we would discuss this with them before telling anyone else if possible). This was reiterated at the beginning of interviews, focus groups and advisory group meetings and conversations. If potential harm was disclosed, we followed our and others’ procedures. Participant information sheets also included helplines and information about what to do if a participant felt that they or someone they know was at risk of harm. Information sheets were available in age-appropriate versions.
3. Raising potentially sensitive topics
We took a number of measures developed in previous research which carried out interviews with vulnerable children and young people, adapted and built on for this project. These measures were based on our experience of conducting research on potentially sensitive subjects and were refined in conjunction with young carer advisors and with input from Health Research Authority (HRA) research ethics. Focus group facilitators/interviewers have extensive experience and expertise in this area. Experienced support workers were available during and after focus groups and interviews in case anything came up that the young people needed to discuss or wanted additional support with.
4. Consent
We sought informed consent from participants. We followed the HRA guidance on seeking consent for research from children. 92 If the participant was aged under 16 years, we sought assent from the young people themselves and consent from their parent/guardian. For participants aged 16 years or older, we sought consent directly from them. Information sheets to inform consent were distributed. These explained the purpose and nature of the research; what taking part involved and the potential benefits, risks and burdens; confidentiality; anonymisation of data and the voluntary nature of participation. Consent was also discussed with participants before the focus group/Interview began covering key points from the information sheet and consent taken either verbally or in person depending on the format. We liaised with project workers to get informed consent from parents/guardians before the focus group/interview but final consent, taken at the focus group/interview, was from participants. The child could refuse consent even if their parent had agreed consent and this was made clear to both parties. Participants were informed and reminded of the option to withdraw at any point including during the interview/focus group. Information sheets to inform consent were available in age-appropriate versions.
Sampling
The inclusion criteria for the study for young and young adult carers were that they be aged between 9 and 25 years and providing unpaid care. We also aimed to recruit a smaller number of care recipients; the inclusion criteria for care recipient participants were that they be aged 16 years or older and cared for by a young carer (not necessarily a young carer involved in the study). We recruited participants in four different localities in England. The four areas included different young caring situations and marginalised groups and represented different types of geographical and sociodemographic areas within England. All four areas are also internally diverse. Young carers who, at least on some level, identify as such, were common to all four sites, allowing a spread of experiences to be studied. Each locality also had in place strategies and networks to contact ‘hidden’ young carers, another marginalised group, again allowing a range of experiences to be gathered. The additionally marginalised groups in each area varied according to historic and sociodemographic context. These groups were identified by the young carers and other organisations in each locality. They were also, in the main, from population groups known to experience additional barriers to services more generally. Collaborating organisations recruited care recipients to take part through their existing networks, including parent groups, and contact lists for parents of young carers involved in their events and activities, and parents receiving one-to-one support. Siblings who were recipients of care were generally not included in these networks, and because of pandemic-related restrictions on the outreach activities we were limited to approaching potential participants via these organisations.
The four localities are described below:
Locality 1
Large city in the North of England; approximately a fifth of the population is from ethnic minority backgrounds; range of socioeconomic circumstances, with several areas with high levels of deprivation.
Locality 2
County in the South of England with a mix of rural areas, towns and cities. Lower than national average proportion from ethnic minority backgrounds; range of socioeconomic circumstances, with several areas with high levels of deprivation.
Specific additionally marginalised groups: young people providing care and the people they care for who experience stigmatised conditions, such as severe mental ill health and/or substance misuse.
Locality 3
Rural county in the North East of England; high proportion of people from White British backgrounds; range of socioeconomic circumstances, with high levels of deprivation in many areas.
Specific additionally marginalised groups: young people providing care and the people they care for who are rurally isolated; caring for/experiencing severe mental ill health, in some cases with substance misuse.
Locality 4
Coastal area in North West England with high area deprivation, below-average high household income, and much higher-than-average child poverty.
Specific additionally marginalised groups: young people providing care and the people for whom they care who experience stigmatised conditions, such as severe mental ill health and/or substance misuse.
Locality 4 was added to the study part-way through in response to a call for additional workstreams focusing on mental ill health and particular regions that have high mental health needs but are historically underserved by research activity on the topic.
Data collection
We discussed specific approaches to data collection with public advisors, the study steering group, and collaborating organisations in developing the project and before and during data collection. Research materials were also developed together with the project advisors, including information sheets and topic guides. We adapted and refined methods in response to local area circumstances, age, situation and number of participants, and in compliance with COVID-19 regulations at the time. Fieldwork commenced in June 2021 and during that time there was a range of COVID-19 procedures in place that varied geographically and organisationally. This included use of face masks, ventilation and spacing.
Focus groups
Focus groups were co-facilitated by two of the research team and project workers and aimed to discuss participants’ experiences with services, features of services and support needed and barriers to seeking support (research questions 1, 2 and 3). Focus groups were carried out in person, with one exception. Informed consent was sought to audio record the sessions, with assurances of confidentiality. Ground rules such as keeping confidentiality within the group were discussed and agreed with participants, the research team, and project or support workers. Topics for discussion included what aspects of services and other support participants had found helpful, less helpful and could be improved; what additional support was needed: what needs it would meet, what features it would have, and how and by whom it would be delivered; and barriers to getting the support that is needed.
Focus groups took about 2 hours including a break for food, usually pizza. We used a range of methods for the focus groups, co-developed with practitioners and young carer advisors and informed by the available literature. 93 This enabled a range of ways (verbal, visual, written, group, individual) for young carers to talk about their experiences. 93 Data collection methods included group and paired discussions, use of flipchart and stickers, drawing, writing and annotation. Data collection methods were designed to be engaging and interactive. We adapted methods and format according to the age, number and vibe of each group. For example, ice breakers and interim and closing activities were different for different age groups; these were often chosen by the co-facilitators from the care organisations. We also somewhat adapted activities depending on the nature and size of the group. Differences included the degree to which we worked with people individually, or held smaller group discussions within the larger group. The researchers took fieldnotes throughout.
We began the groups with icebreaker activities before we started on the topics and tasks. Following these activities, we began by working as a group to develop a list of all the different types of services and other support that young carers (or care recipients) come into contact with. Participants called out different people or services involved with them and their family, with prompts as needed from the research team (e.g. ‘Is there anyone that comes to your house? Anyone that you see at school? Anyone you see at other places? Anything you do for fun that is important to you?’). The research team made a list on a flipchart that the whole group could see. Some discussion about experiences with these services took place during the making of the list. Once we had the long list of services, we then took participants up to the flipchart, usually in pairs. Each participant had their own set of coloured stickers and during the discussions at the flipchart they were asked to rate services they had been in contact with, using stickers of different colours. The colours indicated whether the service or support had been good, ok but could be better, or bad. For ‘bad’ it was further suggested that this might mean they recommended other young carers to avoid this service. For the parent groups, we used coloured pens rather than stickers and did the rating activity as a group.
This rating exercise then led to discussion with the pair at the flipchart, or sometimes a single person, about what was helpful and unhelpful about services. This was done as a group for parents, though parents also shared information and views individually, for example during a break or while people were working alone on the ‘ideal world’ task. We were able to follow up these ratings with questions like, ‘so you gave this one a bad rating – could you tell me about that?’ The chart was annotated with key points by the researcher at the flipchart. The researcher also took notes, especially where information was personal and not appropriate to record on the flipchart. When points were added to the flipchart, this was discussed with the participant (‘shall I write that down’?). While some participants were at the flipchart, the remainder carried on with other activities, described below.
To explore additional unmet need, participants were guided to individually, or with the research team, annotate a simple representation of a young carer and the person they care for, with their views of the support they or someone else in their situation would receive in an ‘ideal world’, and which currently unmet needs it would help meet. Specifically, they were asked to consider what sort of things would help support young people who look after someone at home. We explained that this could include both help for the young carer and for the person they cared for. Researchers discussed the activity with the young people while they were doing it, asked prompts, and took notes. This was initially going to be a group activity. COVID-19 rules meant we could not do it this way, but we found that participants individually annotating the diagrams with the research team or support workers worked well for participants and gave them options for individual work and discussions. In later sessions, when restrictions were reduced, some participants completed the task in pairs, but each still completing their own sheet.
To explore barriers experienced by young carers and the people they supported, we asked participants to individually, in pairs, or with the research team, write on coloured bricks their views and experiences of barriers to support. Researchers prompted as needed. Each pair or individual then read out two barriers for others in the group to comment on, add to, agree or disagree with, facilitated by the research team.
We finished with a summary and synthesis activity. In this, the research team attempted to summarise key points made in the session by presenting what we understood to be the aspects and components that made up a good and not-so-good support or service, and what additional support was needed. We asked participants to indicate whether they agreed, disagreed or were not sure by holding up green, red and yellow cards, respectively. Participants could also add to the summary verbally or in written form. This gave participants an opportunity to consider whether we had listened properly; had understood correctly; and to establish areas of consensus and dissensus. To end the group, we held a ‘cool down’ activity unrelated to the study topics and reminded participants of the availability of the research team and the attending support workers after the group and the information sheet with helplines.
One-to-one, in-depth semistructured interviews were carried out where participants preferred this alternative. Interviews explored individual experiences of services, needs and barriers to finding or accessing services and other support (research questions 1, 2 and 3). Interviews took place variously by phone, in person in a place convenient and accessible for the participant, and online.
We carried out a total of 21 focus groups across the four areas, one online and the remainder in person. Two focus groups were carried out with adult care recipients and 19 with young carers. There were approximately 6–8 participants per group. The number of participants per focus group was based on typically suggested optimum size94 and on our previous experience holding focus groups with young people. For practical reasons, some groups were bigger or smaller than this in practice. The combined number of participants enabled us to cover a range of experiences, allowing the emergence of principle and subthemes, while remaining manageable within the project. The final sample numbers were determined by the continuing emergence of new themes, or where saturation of themes appears to be reached, as well as practical considerations. We also carried out two in-person interviews with care recipients and eight phone or online interviews with young carers. Focus groups and interviews for young carers and for care recipients took place separately from each other. The resultant sample was 150 participants, of which 17 were care recipients. Participants were aged 9–25 years with a range of caring and life circumstances and sociodemographic characteristics, including ethnicity, gender and social class. Forty of the carer participants were aged 9–11 years, 57 were aged 12–15 years, and 36 were aged 16–25 years. Where known, 25 cared for a sibling, 46 for a parent and 2 for another relative. Some cared for more than 1 person. Reasons for needing care, where known, were mental ill health (N = 26), physical ill health (N = 19), substance misuse (N = 8) and other (N = 5). Other included dementia, neurodiversity and learning disability. Many of the people cared for had more than one care need, for example mental and physical ill health. Care recipient participants were aged 16 years or older and had a range of physical and/or mental care and support needs. All care recipient participants were parents of the young person who cared for them. Although the inclusion criteria for care recipient participants potentially allowed for siblings to take part, in the event only parents were included. This was due to the existing networks and contacts of the collaborating young carers’ organisations; siblings tended not to be involved with the organisations in the same way that parents were. There were in addition ethical concerns from organisations about inviting sibling care recipients to participate, due to the need to identify their sibling as a carer and around ambiguities in who were the care recipients within the family.
Practitioner workshops
We held workshops for practitioners from each of the four study areas. The initial plan was to hold them in person by locality, but we decided to hold them online for flexibility and ease of taking part for participants. This method also meant we could include practitioners from different locations in the same workshops. In the workshops we discussed selected key findings from the focus groups and interviews and explored the applicability of the findings to practice, barriers to putting the findings into practice, and any facilitating factors, or examples from practice where there had been successful approaches addressing the issues under discussion. We wanted to find out how the findings related to current service provision from the perspective of service providers and commissioners. The aims were: (1) to help inform study recommendations and (2) to address research question 4: ‘What are the barriers and facilitators for practitioners in providing support and services perceived as acceptable and appropriate by young carers and the people they support?’
Three workshops were held with 19 practitioners from schools, colleges, young carers organisations, voluntary sector services, mental health services, the NHS, adult social care and social care commissioners (Table 1). The first workshop was attended by five practitioners, the second by eight and the third by six. Each session lasted 90 minutes. We recruited practitioners through local young carer collaborating organisations in the four localities which contacted their wider networks to invite people to the workshops. The choice of types of service to invite was informed by findings from the focus groups and interviews, and by discussion with project advisors and collaborating organisations. A mix of practitioners from different service types was included in each workshop; the full list of the practitioner job roles and service types of those who took part is shown in Table 1.
| Job role | Service type |
|---|---|
| Support worker | Youth development agency |
| Community engagement manager | Young carers support charity |
| One-to-one worker | Young carers organisation |
| One-to-one worker | Young carers organisation |
| Youth participation officer | Young carers organisation |
| Senior practitioner and designated safeguarding lead | Young carers organisation |
| Development manager | Young carers organisation |
| Health development worker | Young carers organisation |
| Young carer practitioner | Voluntary sector family charity |
| Tutor/mentor | Sixth form college |
| Tutor/mentor | Sixth form college |
| School counsellor | Primary school |
| Associate director, engagement and experience | NHS |
| Assistant service manager | Multi-agency support team, local authority |
| Early-help coordinator | Local authority |
| Commissioning officer | Local authority |
| Commissioning officer for children and young people’s mental health | Local authority |
| Key worker | Family centre and advice hub, local authority |
| Managing director | Counselling, psychotherapy and supervision provider |
Following discussion among research team members and with project advisors, we chose the following key themes (aspects of valued or wished-for support), from the analysis of focus groups and interviews, to discuss in the workshops:
-
Signposting and linking to support
-
On-call and ongoing support/changing your mind
-
Support that reduces the young person’s caring responsibilities
-
Support that considers the whole family
-
Someone who listens and understands/building relationships and trust
For each theme we first briefly presented the research findings then invited discussion. At the first two workshops we discussed themes 1–4. For the third workshop theme 1 was replaced with theme 5, as we felt theme 1 had been well covered.
We followed up the presentation of each theme with questions on a slide to prompt discussion, but practitioners were keen to address the issues raised and discussion flowed easily. We were interested in hearing from practitioners on the following types of questions:
-
How does/might this work in practice?
-
What does/would get in the way of you providing that support?
-
What would help address these difficulties?
Chapter 4 Analysis
Overall approach
Transcripts and field notes from the focus groups, interviews and workshops were organised and coded by researchers with the help of NVivo 12 (QSR International, Warrington, UK) software. 95 Analysis of the focus groups and interviews with carers and care recipients took place prior to the practitioner workshops, so that preliminary results could be discussed with the advisory groups and used to inform workshop discussions. The analysis approach was largely deductive and inductive thematic analysis. 96,97 We set out with particular research questions in mind, seeking to discover what acceptable intervention or support looked like, and for who, how this related to what was currently on offer, and what the barriers to access were. Initial codes and themes were also informed by the theoretical frameworks described above. Coding also took place inductively, with categories not pre-set but drawn from the data, allowing the development of themes which had not been anticipated. Within this broad framework, the approach taken varied by the specific research question the analysis was seeking to answer.
What is good or not good about existing services? What can be improved?
The material for analysis of this research question consisted of the annotated flipcharts, notes written by both participants and researchers during the session, notes made by researchers after the session, and transcripts. Material relating to a single focus group or interview was added to a single file and entered into NVivo. The dataset consisted of 21 focus group files and 10 interview files.
In this analysis we aimed to understand how young carers, and their parents, experienced the services and support they received. The analysis focused on seeking answers to the research question: ‘What makes support helpful, how can it be improved?’ We examined what was considered good or not good about existing services, and where it was felt improvements could be made. Material relating to gaps in services, needs that were perceived as not being addressed by services and barriers to accessing services were coded and analysed separately.
For this section of the analysis, material was coded both by the type of service being referred to, and thematically by the aspects of services and support that was considered helpful or unhelpful. The presence or absence of a particular aspect of support was at first coded together (e.g. person was non-judgemental/person was judgemental), partly because views were not always easily categorised as positive or negative, but also because reviewing the different aspects together allowed a more nuanced analysis. Later stages could then pick out and separate recurring themes related to what made a support helpful or less helpful. While some aspects of support were specific to a particular type of service (e.g. care workers in the home), there were also many themes which cut across different service types (e.g. ‘listening and understanding’). Material was coded both in relation to specific service types, so that themes which related to specific service types could be identified, and across service types, to identify cross-cutting themes. The initial themes constituted findings about what aspects of support were valued; what made support valuable and appreciated; what made support unhelpful, or not wanted; and how existing support could be improved. Material within codes was reviewed and code categories were further subdivided or combined as the thematic analysis proceeded. Files were named for the location, age range and other distinguishing features of each group or interview so that context was always apparent. Material within each code retained the link to the original file so that the broader context of excerpts could be reviewed as needed to enhance understanding.
Additional support needs
Analysis of additional support needs began with familiarisation with the data, including reading and rereading the interview transcripts. An initial coding framework was then developed, structured around the conceptual frameworks75,76 and the research question: ‘What additional support is perceived as needed by young and young adult carers aged 9–25 years and the people they support in England and what needs would it meet?’ Initial themes were reduction or removal of caring responsibilities; mitigation and improvement of negative impacts of caring; and assistance with caring role. Each theme had two initial subthemes: (1) the need the support would address and (2) the mode by which it would address it.
We then gathered all data relevant to each theme, including counterexamples and exceptions. Themes were adapted as required in response to the data, and deductive and inductive analysis then used to identify subthemes within the initial themes. Themes and subthemes were iteratively reviewed in relation to the extracts coded and not coded to each theme and subtheme. Iterations of analysis were also informed by discussions on initial themes and subthemes with young carer and practitioner advisors.
Barriers experienced by young carers in seeking and accessing services for themselves or the person they support
After initial familiarisation with the data, an initial coding framework was developed, structured around the conceptual framework77,78 and the research question: ‘What are the barriers experienced by young carers and the people they support in seeking and accessing services and support?’ The initial coding frame had the following overarching themes and subthemes: (1) individual barriers; and subthemes: material circumstances, competing priorities, self-determination and psychosocial; and (2) contextual barriers; and subthemes: care policy and care financing and care organisation.
As above, we then collated all data relevant to each theme, including counterexamples and exceptions. Themes and subthemes were adapted as required. For example, in the conceptual models that informed this analysis (e.g. Andersen’s BMHSU), health literacy has been variously conceived as an individual or as a contextual determinant. In the analysis it became clear that this had both individual and contextual aspects, so subthemes for ‘service and support literacy’ were created under both of those overarching themes with text coded accordingly. Deductive and inductive analysis was subsequently used to identify additional themes and further subthemes within the initial themes. As above, themes and subthemes were iteratively reviewed in relation to the extracts coded and not coded to each theme and subtheme. Iterations of analysis were also informed by discussions on initial themes and subthemes with young carer and practitioner advisors.
Practitioners workshops
Workshop discussions were transcribed verbatim and entered into an NVivo database. The transcripts were coded thematically in three ways. One researcher coded the three transcripts inductively, considering emergent themes. A second researcher coded the transcripts specifically to look for recommendations for practice. A third researcher interrogated the project, using both sets of coding and the original transcripts to develop themes in response to the five highlighted themes from the analysis of young carer and cared-for parent focus groups and interviews, which had guided the practitioners workshops, and other themes relating to the overall research question around which the practitioners workshops were devised: ‘What are the barriers and facilitators for practitioners in providing support and services perceived as acceptable and appropriate by young carers and the people they support?’
Cost analysis
The aim for this part of the analysis was to report economic evidence that could inform the recommendations developed in consultation with young carers and practitioners, which were themselves based on the findings. Economic evidence in this area is extremely rare. We wanted to explore what economic evidence was available and identify possibilities for how future research might be conducted to examine the costs and (economic) benefits of interventions that are supporting young carers.
Based on the recommendations developed for the study, we conducted a targeted, exploratory review of the literature – both academic articles and online reports from the UK social care sector – to identify economic information concerning some of the interventions that were covered by some of the recommendations. We focused on interventions that were likely to be suitable for potential economic analysis, that is that had substantial costs, outcomes and consequences attached to them. We summarised interventions from all sectors that we identified as most relevant, excluding areas that were very broad and where it was unclear what kind of resources the implementation or delivery would involve. We first used our own knowledge, and consultation with experts, to gather key literature. We also used the Economics of Social Care Compendium (ESSENCE) database (https://essenceproject.uk/glossary/). Following this, we undertook a search on Google Scholar for relevant documents published over the last two decades, focusing mainly on studies, reports and articles based on a UK context. We also undertook a general Google search for relevant grey literature, including annual reports from third-sector organisations and undertook snowballing searches of the literature. We extracted data pragmatically focusing on information about the cost, net savings and other considerations relevant for economic analysis.
We held a 1.5-hour online workshop with 10 service managers or chief executives of local voluntary sector provided services in England, policy and practice leads at voluntary sector organisations concerned with providing services and advocating for young carers, as well as local authority commissioners. This included leads of a national network concerned with sharing information and good practice evidence on young carers. All individuals had specific expertise and focus of their work with young carers. The objectives of the workshop were to discuss the findings from the review, including their relevance to the young carers field, identify evidence gaps and discuss what economic research might need to be conducted.
Chapter 5 Results
What is good or not good about existing services? What can be improved?
In the following section, we present results of the analysis relating to research question 1: ‘What types, components or features of services and other support are seen as helpful, valued and acceptable to young people who look after someone at home and the people they support? Conversely, what is found to be less or unhelpful?’ The findings mainly reflect the views of the young and young adult carers who made up the majority of the sample. Where views are those of the care recipients, this is indicated in the quote annotation.
As explained previously, this analysis draws principally on the section of the focus groups and interviews where we discussed the services and supports they had come into contact with. In the focus groups we created, together with participants, a list of services and supports young carers and care recipients were involved with, and then rated and discussed those services. Material from the other sections of the groups and interviews was also brought into the analysis where relevant to the research question.
The themes are presented in two sections. The first section sets out the themes that are specific to a particular service types (these types being: Support for the care recipient; Young carers groups; Mental health services; and Support in schools) while the second section presents themes with relevance across service types (under the broad top-level themes outlining what is helpful or unhelpful): Finding, and linking to other sources of support; Listening and understanding; People you can trust/confidentiality; Involving the young carer in decisions about support; Proactive, persistent or intrusive (a balanced and flexible approach to individual and changing preferences and needs); and the strong recurring theme of the level of each type of support received being ‘Not enough’.
Table 2 shows a list of the services mentioned by participants in the focus groups. The labels largely reflect the language participants used, although some categories have been combined. The purpose of the table is to show the range of services and supports under discussion. Participants did not necessarily know the role or profession of the person they encountered. For example, they were often unclear whether someone who visited them at home was a social worker or had a different role.
| Service | Young carers (N focus groups in which mentioned) | Parents (N focus groups in which mentioned) | Total |
|---|---|---|---|
| School and college-based support | |||
| Young carers group/lead at school | 6 | 0 | 6 |
| Person at school/pastoral/SENCO | 13 | 1 | 14 |
| Time-out room/card at school | 10 | 0 | 10 |
| Family engagement/support worker | 4 | 1 | 5 |
| Teachers | 19 | 0 | 19 |
| School counsellor | 11 | 0 | 11 |
| Other students | 4 | 0 | 4 |
| Free school meals/breakfast club | 9 | 1 | 10 |
| After-school clubs/activities for young carer | 4 | 1 | 5 |
| ‘Worry box’ | 1 | 0 | 1 |
| School behaviour team | 2 | 0 | 2 |
| School nurse | 4 | 0 | 4 |
| Pupil premium | 0 | 1 | 1 |
| University lecturer | 1 | 0 | 1 |
| University counsellor/wellbeing services | 2 | 0 | 2 |
| Young carers and carers groups | |||
| Young carers/carer centre groups and services | 16 | 1 | 17 |
| Parent group by young carers organisation | 0 | 1 | 1 |
| Mental health | |||
| Mental health worker/Therapist for young carers | 9 | 0 | 9 |
| Mental health worker/Therapist for care recipient | 7 | 2 | 9 |
| CAMHS for care recipient (sibling) | 5 | 0 | 5 |
| CAMHS for young carers | 9 | 2 | 11 |
| Family counsellor | 1 | 0 | 1 |
| Crisis team | 1 | 0 | 1 |
| Social care and related | |||
| Social worker for care recipient | 9 | 2 | 11 |
| Paid carers | 13 | 1 | 14 |
| Council carers | 1 | 0 | 1 |
| Social worker for young carer | 6 | 0 | 6 |
| Family support worker | 5 | 1 | 6 |
| Family social worker | 8 | 1 | 9 |
| Social services | 1 | 1 | 2 |
| Multi-agency support team worker | 4 | 1 | 5 |
| Home adaptations/equipment | 2 | 0 | 2 |
| Respite carers | 5 | 0 | 5 |
| Health and related | |||
| Hospital | 5 | 0 | 5 |
| GP/doctor | 8 | 2 | 10 |
| Social prescriber | 0 | 1 | 1 |
| District nurse | 4 | 0 | 4 |
| Pharmacist | 1 | 0 | 1 |
| Occupational therapist | 2 | 1 | 3 |
| Physiotherapist for young carers | 1 | 0 | 1 |
| Speech and language therapist for care recipient | 1 | 0 | 1 |
| Drug and alcohol support for care recipient | 2 | 0 | 2 |
| Autism services for care recipient | 3 | 1 | 4 |
| Autism/ADHD services for young carers | 1 | 0 | 1 |
| Other sources of support/services in contact with | |||
| Family | 16 | 0 | 16 |
| Friends | 11 | 0 | 11 |
| Neighbours | 4 | 0 | 4 |
| Pets | 2 | 0 | 2 |
| Trips | 8 | 0 | 8 |
| Welfare benefits | 5 | 1 | 6 |
| Charities/community support/volunteers | 4 | 2 | 6 |
| Clubs/activities for care recipient | 3 | 0 | 3 |
| Clubs/activities for young carers | 10 | 1 | 11 |
| Support at work for young carers | 1 | 0 | 1 |
| Case worker | 1 | 0 | 1 |
| Transport for care recipient | 1 | 0 | 1 |
| Helplines and online communities/support | 4 | 1 | 5 |
| Police | 0 | 2 | 2 |
| Adult learning | 0 | 1 | 1 |
| Peer support | 1 | 1 | |
| Citizens Advice Bureau | 1 | 1 |
The results of the qualitative analysis are presented in two sections. In the first section, we present findings which are specific to particular service types, namely, support for the care recipient; young carers groups; mental health support and support in schools. The themes are first summarised in Table 3 and then explained in detail and illustrated by quotes.
| Support for the care recipient | |
|---|---|
| Why and how is support for the care recipient helpful for young carers? | Can give young carers a break/time for other things/less worry |
| Emotional support for care recipients gives them someone to talk to/share concerns with and can reduce emotional burden on young carers | |
| Company for care recipients | |
| Some jobs can sometimes be done better by a professional | |
| Practitioners can helpfully mobilise support from family, friends and neighbours | |
| When and how is support for the care recipient unhelpful? | Can cause stress, when new/untrusted, or too rushed |
| Sometimes rude, unfriendly, do not communicate effectively | |
| Young carers groups | |
| What is helpful about young carers groups? | Meeting other young carers, making friends |
| Having fun, doing activities, time out, taking their mind off things | |
| Staff at young carers organisations understand their situation; access to an adult who can listen and understand | |
| Parent care recipients can also receive direct support through young carers organisations | |
| What can be more difficult about attending young carers groups? | Concerns about leaving the care recipient |
| Feelings of anxiety or exclusion on first attending groups; groups are not for everyone | |
| Mental health services | |
| What is helpful about mental health services? | When one can talk to someone who listens and understands; flexible and patient support, and understanding of the young carer role |
| What makes mental health services unhelpful? | Long wait times for support; often felt to not be worth the wait; reputation puts people off seeking support |
| Mental health supporters do not always understand the caring role of young carer | |
| Support in schools | |
| What support do young carers value in schools? | Someone to talk to (and a place to go) |
| Time-out cards can help young carers leave class when they need a break; early-leaving cards to support caring responsibilities | |
| Extra help and flexibility about schoolwork and homework; the right balance of wellbeing and academic support | |
| What is unhelpful for young carers in schools? | When staff are not flexible or understanding |
| Form filling for no apparent purpose | |
In the second section, we present key themes about what makes support helpful or unhelpful which cut across service types. These cross-cutting themes are all important for the key service types presented in the first section, but as they are relevant across services, we discuss them separately. These themes are summarised in Table 4.
| Subtheme | |
|---|---|
| Finding, and linking to, other sources of support | |
| Helpful | Being linked with other services, appropriately, because the person listened |
| Advice about, and help with, welfare benefits and housing issues | |
| Initial support in attending a service for example mental health support, or a meeting | |
| Listening and understanding | |
| Helpful | Someone to talk to |
| Helpful | Takes time, lets the person talk, and choose what to talk about, when they want to and are ready to |
| Validates your feelings and experiences | |
| Adjusting support to meet specific needs and wishes of the individual or family; enabling activities that are important to them | |
| Problem | Parents perceive unlistening support as judgemental |
| Problem | Social workers who don’t understand focus on the wrong things |
| Problem | There is a perception that only extreme cases will get support |
| Trust, confidentiality and perception of risk | |
| Problem | Experiences with, and reputations of, services result in deep mistrust of services (including fear of child protection intervention) |
| Helpful | Someone they get to know |
| Helpful | Someone who will not share what young carer have shared in confidence |
| Helpful | Awareness of young carers and the issues they face |
| Involving the young carer in making plans and decision-making | |
| Helpful | Having the opportunity to ask questions, discuss solutions; relates to services both for themselves, and those for the cared for person |
| Helpful | Choice and flexibility |
| Problem | Involving young carers can sometimes conflict with care recipient’s wishes |
| Proactive, persistent or intrusive | |
| Problem | Some young carers feel pressurised to be involved with/accept support for themselves, and can see it as ‘too much’ or ‘demanding’ |
| Helpful | A balanced and flexible approach to individual and changing preferences and needs |
| Helpful | Holding contacts in places and ways that suit the young carer and family |
| Helpful | Being able to change your mind about wanting, or not wanting, support |
| Not enough support | |
| Problem | Some support would be helpful if it was more frequent/lasted longer |
| Problem | It is unhelpful/distressing when services end with no warning |
Illustrative quotes are used to help explain the themes. These are often taken from researchers’ field notes (made both on the flipchart and separately) and not always from transcripts so they are not necessarily verbatim. As far as possible, quotes are identified according to the type of data collection (focus group or interview) and, where it is a young carers focus group, the age range of all those who took part in that group. All parents referred to are parent recipients of care by a young carer, their child. Some focus groups were specific for young carers of people with mental health or substance misuse problems; they are referred to below as mental health groups. However, participants in other groups also cared for people with mental health and/or substance misuse problems.
What is helpful or unhelpful about specific service types?
A wide range of views were expressed by participants. Table 3 summarises key themes which are related to four specific types of service and support; the themes are then explained and illustrated, with attention paid to where there were differing views.
Support for the care recipient
Young carers appreciated support for the person with care needs, from carers and/or other family and friends. This freed some of their time and helped to alleviate their worry for the person. One participant, for example, wanted the practitioner to focus more on the cared-for parent and less on her (the young carer). Practical support and adaptations that made things easier for the person with care needs at home were appreciated, such as rails, accessible showers or, as in the following example, an alarm, which was provided as part of a local programme:
They asked what she was worried about and she went, ‘Mummy falling’, so they said she said, ‘What happens if I can’t get her up? so they said had we heard about [alarm system]? and it was peace of mind for her at school… if I say to her, ‘Oh, I’m staying at home today,’ she’ll say, ‘Oh be careful, don’t fall.’ Now, she doesn’t say that as much now.
Parent
Some families had a certain amount of help from paid care workers in the home, and a few young carers specifically commented that this gave them more time: ‘it gives me a break when they’re there’.
Respondents were not always clear what professionals’ roles were, but some came only every few weeks to check how things were. Young respondents appreciated it when this gave the care recipient someone to talk to, either to share concerns with, or just for company. Therapeutic impact was appreciated. As one participant commented: ‘they calm him down’.
This one woman that would usually come round, and just be there for my mum, when she was feeling a bit low, and just needed someone to talk to, other than which would usually be me… to kind of have a professional to be there for her as well. So, that was quite positive.
Young carer 16‒25
In other families paid care workers came more regularly, taking on some of the regular caring and housework. This was reported as beneficial, not just for saving the young carer time, but also for the care recipient, because professionals could do some jobs better. One young carer described the paid care worker’s role as doing ‘pretty much everything else I don’t do’ (mental health group). Several carers were discussed in positive terms by both young carers and parent care recipients (‘brilliant’ and ‘really nice’). Good paid care workers listened to what was needed and supported people’s independence, as in this example about help with bathing:
They let me do the top bit so I feel like I’m getting my independence.
Parent
Unfortunately, many young carers in the sample would have liked this sort of support but did not receive it, while some whose families received support would have liked more (see also Additional support needs).
On the other hand, several participants reported bad experiences with support for their relative. Not all support provided to the cared-for person reduced worry for the young person. Unpredictable visit times were awkward and could provoke stress; for example, one young carer (13–19) was sometimes prevented from going to school when the care worker did not turn up on time to relieve them. Another, who cared for a parent with mental health problems, said they (the young carer) often did not let the practitioner in when they turned up at 10 minutes’ notice, because it was so unhelpful.
Young carers described lack of care, low standards and unfriendliness:
They are not very good, they don’t have a lot of training.
Young carer 13‒19
‘Council carers’. Always in a rush; we had to get rid of them. They were supposed to be helping get up in the morning and provide personal care but wasn’t nice.
Young carer 16‒25, from notes
Paid care workers were described several times as ‘rude’. Many respondents talked about changing or ‘getting rid of’ unhelpful care workers. One young person reported that they themselves had higher standards than their parent (the care recipient) and that they pushed for better care on their parent’s behalf. Another had been told by their GP that they did not have a choice; they had to keep a care worker that they felt did more harm than good because they did not speak to the care recipient (mental health group). Others were described as making a mess, or making mistakes, sometimes because of language/communication barriers.
Changes of care worker were more often not by choice however, and constantly changing personnel could add to young carers’ stress:
If someone new is with my mum I get a funny feeling in my stomach if I leave the house as I don’t know if they will be okay.
Young carer 9‒11
Conversely a parent care recipient explained:
My daughter knows who’s coming in to help so she’s not edgy.
Parent
One young carer’s mother explained how they had decided to stop using the care workers for her mother, the young carer’s grandmother:
She’s confused and she’s delusional, so she talks to herself in the mirror, and there are people that she says appear in the house: children, adults, whatever. So I can’t have her being disturbed every morning by somebody different, and rushing in, just to rush out 20 minutes later.
Young carer 16‒25
One parent explained how valuable professional care support could be and put part of the problem down to lack of respect for the profession of caring:
Carers are looked at as, if you can’t get a job go and do caring and it’s wrong because if people see how they help people like me and how they change my life and the effect by doing those ten hours a week for me and what it enabled me to do, it doesn’t just change my life, it changes my daughter’s life and it’s not, all caring isn’t about old people and taking them to the toilet and, but I think caring gets that stigma to it.
Parent
Valued support for the care recipient also came from family, friends and neighbours, and this could take some of the load off a young carer’s shoulders, as this interviewee made clear when asked what helpful support they appreciated:
I think probably my aunty taking her to her house, but even if it’s not that helpful, it’s just nice for her to be gone.
Young carer interviewee
Sometimes steps were taken by paid services to increase support from family, friends and neighbours, when a young person had been listened to, and their situation understood:
Now that I’ve got a social worker and all that, my jobs, the amount of jobs that I usually get have been cut a bit. Yeah because I just couldn’t handle the [school] work from the jobs on my shoulders. So I told [school SENCO (special educational needs coordinator)] about it and she put us on to a social worker and now my Dad’s doing a huge percentage of the jobs so I don’t have to do as much.
This example shows how valuable support involves understanding the situation, and that addressing it is not always about putting in more paid resources.
Young carers groups
Young carers appreciated getting together with others who shared aspects of their experiences as carers. They also appreciated having fun, doing interesting activities, and having ‘time out’ from their day-to-day lives. Comments on attending young carers groups included: ‘fun’, ‘trips’, ‘socialising’, ‘gets me away from everything’, ‘highlight of the week’, ‘everyone’s friendly’ and sometimes ‘you get food’, ‘meeting other people like you, you’re not alone’, ‘meet people in similar situations, who understand you’ and ‘space to hang out with people like you’. Occasionally there were opportunities for trips, which could address multiple needs as one participant explained: ‘Residentials help you take time off and make new friends (that relate with your situation) and learn about the person you care for’ (Young carer 16‒25).
However some worried, when attending residentials, about leaving the person they cared for: ‘It was really good, but then some of the kids, they were like crying, because they weren’t sure whether the people who they were caring for were going to get any support’ (Young carer 16‒25).
Important benefits of young carers groups included the availability of adult supporters for the young person to speak with and being linked to other sources of support. Workers at young carers organisations were generally talked about in positive terms: ‘you can talk about everything’ and ‘they know about young carers’. They were often described as listening and understanding, a theme discussed below.
Young carers groups provided different and multiple types of services to participants. There could be group-based or one-to-one opportunities to share feelings and experiences, with workers, or with peers, as well as diverting activities, socialising and outings. The young participants spoke about the support workers being helpful both for them and for the person they cared for. Some workers visited the family in their own home or came to the child’s school.
Not all participants found all aspects of taking part in groups easy, however, especially at first. Some preferred the one-to-one meetings offered. A young person who had recently joined said: ‘getting used to new people can be tricky’, while another described it as ‘scary’. Others had not yet ‘plucked up the courage’ to attend a group, while a number who had opted not to attend groups offered described themselves as not enjoying meeting new people. But others commented that their group was good at helping if they struggled socially, while another said attending had really helped with their confidence. Some preferred to use spare time to meet with existing friends, but others mentioned having few friends, and appreciated the social aspects of groups. There can be issues in groups that make people uncomfortable, and a couple of participants who had attended a young adult carers group said they found it quite ‘excluding’, and that more could be done to involve new arrivals. Others found groups too noisy, ‘it gets quite out of hand sometimes’ (young carer 12–16) too crowded, or the activities too restrictive. Some had had long waits to be given a place in a group, while in other localities, the young carers organisation managed demand in different ways, such as open-access regular drop-in groups, rather than a waiting list. Demand also varied by area.
One young carers centre also ran parents groups, which, one parent told us, ‘cheers everybody up’ and was felt to be beneficial. Parents appreciated the opportunities to have their voices heard, and to share experiences both for themselves and for their offspring but regretted that support for the young carer was time-limited, as was one-to-one support for the parent. Parents were aware that group work was not for everyone. In one group, a discussion took place about how the group, rather than creating dependency, could help put its members on a new trajectory.
Mental health support
While many participants expressed a need for mental health support, and some were receiving helpful assistance, a greater number reported that the mental health support provided was either unhelpful or unwanted. Many young carers referred to long periods on waiting lists to be seen (many months or even years); a common comment was ‘not worth the wait’. Others said the support from Child and Adolescent Mental Health Services (CAMHS) was ‘terrible’, ‘always on their terms’, ‘harmful’, ‘tell you stuff you know already’ and ‘limited’. Several young people said they felt they needed mental health support but had been turned down by CAMHS or were put off approaching CAMHS because of negative reports from peers, including about long waiting times. A parent commented that if a child was doing fine at school, it could be difficult to qualify for mental health support, while a young interviewee who had difficulty managing their anger felt support was stopped after three sessions because her issue was anger and not self-harm. Participants in one of the young adult carer groups felt CAMHS did not understand the impact of the caring role and could be dismissive. They wished that mental health support could be more available to younger carers, to help them express their anxieties and stresses.
However, some people had received helpful mental health support from CAMHS (‘fantastic’), as well as from other sources, including school and college counsellors, NHS adult mental health self-referral services for over-16s and GPs. In counter to the point above, two young adult carers said CAMHS had specifically addressed their caring responsibilities and how they could be carried out. Examples of mental health services that were seen as helpful included providing proactive and flexible support, someone getting in touch when the school was aware of a family incident (e.g. health crisis for a parent), flexible arrangements to meet (e.g. at school, or in outdoor locations) and a patient approach. ‘They were like really helpful and my CBT [cognitive-behavioural therapy] worker, she took stuff at the pace how I wanted to go’ (Young carer 16‒25 re CAMHS cognitive-behavioural therapy.)
Positive comments often referred to the person being good to talk to, and this is explored further in themes below.
Support in schools
According to the young participants, some schools seemed to provide better support than others. Perhaps through an awareness of this, one school told one of the young carer participants they were happy to carry on offering support even after they had left to go to another school. Young people often found a particular staff member easy and helpful to talk to; the most mentioned job roles were school counsellor, teacher or tutor, and designated young carers support person. Teachers that participants felt supported by were not necessarily ones who (still) taught the child but were individuals with whom a relationship had developed and continued. This was valued. ‘It was just I ended up having a good relationship with her ‘cos she was like always there when I needed to talk, like whether she was busy or not’ (Young carer interviewee re a teacher).
The way that support was provided varied widely. It could be provided via regular support groups for young carers and/or as a drop-in service (sometimes with a therapy dog as an extra bonus). Some young carers were invited to check in with a support person at school every day; sometimes a support worker heard about issues/incidents through other avenues and would come to check on the young person. One participant told us they were often taken out of school for a walk and chat and some of the participants got understanding support from the ‘behaviour team’.
My mum needs support because services say she overshares with me. Sometimes she’s upset and I don’t know what’s wrong and we end up arguing. I have someone I talk to at school twice a week. They are better than the last person I had, we didn’t get on. It doesn’t interrupt my lessons, it’s usually during form time.
Young carer 12‒16
This quote shows that services for care recipients can and sometimes do take account of the carer’s needs as well as those of the care recipient and suggests that there can be good coordination between services. Different approaches suited different people:
At school there were one-to-one sessions but it just wasn’t the same – I (and others) really did not like coming out of lessons to go to a session, or out of break. Meant I missed time with friends. Not good. At the end of the school day would be better. At school, there’s never enough time, and there’s lots of cancellations.
Young carer 16‒25, from notes
Sometimes there was a place, or a person, that the young carer could go to whenever needed. The participants liked having a place to go in school, sometimes referred to as a ‘time- out room’; sometimes (for primary-age children) this was just a corner of a room. Some of these ‘places to go’ were nice places to be. But sometimes the ‘place to go’ was also the ‘isolation room’ or the room where people went when they’d behaved badly, which could be problematic or unpleasant. It was appreciated if there was an understanding staff member present in the room, but this was not always the case, sometimes there was no-one. Some young carers had ‘time-out cards’ which they could show to teachers to be given permission to leave class. Although these were usually seen as a good thing, some participants commented that they were used inconsistently and not all teachers accepted them.
Some people don’t know enough to be helpful (e.g. at school).
Young carer 16‒25
It’s good if teachers all know their situation – can be on their record [it was in some cases]; teachers need to accept Time Out cards with no questions.
Young carer 16‒25
One primary school had an ‘I’d like to talk’ box by the front door, where one could leave notes colour-coded to indicate the level of urgency. This was appreciated, although some said it could be embarrassing when the staff member came to find the pupil in class.
In the focus groups, some young carers noted that they, or their school, did not have the support available that they were hearing about from other participants in the group. However, even where there was this provision, not everyone the young carers encountered at school was perceived as helpful. Some of the reasons for this are explored in the section below. Where feelings about school support were more negative, participants often felt school staff lacked knowledge about young people’s wellbeing in general, and prioritised discipline and grades over student wellbeing (young carer 16–25).
There are two kinds of teachers – some just teach, others really care about children and understand the importance of wider wellbeing.
Young carer 16‒25
Anything that isn’t like easily physical, so like, they’re given training on like if someone bumped their arm, but they’re not given training on like what to do if someone’s really struggling mentally, or how to talk to them about their family, or anything like that.
Young carer 12‒18
In one college focus group it was considered that help was only available to people who, or whose parents, make a fuss. This had included the respondents in that group, but they didn’t think that was a fair system; they felt everyone should be equally supported.
There was help with schoolwork and homework; breakfast clubs were appreciated. Some young carers had passes to give them permission to leave school early, for example, to pick up a sibling:
I’m ok, I don’t need anything, as long as my Mum’s alright. I have a pass at school that lets me leave at 2.30 to look after her but if I don’t have the pass I can’t leave. It’s stupid.
Young carer 12‒16
Unhelpful support in school included multiple form filling. This was a common complaint when that was all that seemed to take place in what the young person described as what was supposed to be a counselling session.
Although in general it was felt that mental health and wellbeing should be prioritised over academic work, there was the occasional mention of the converse view, that perhaps they could have been pushed more academically.
Cross-service themes about what makes support helpful or unhelpful
There were strong themes emerging from the analysis about what makes support helpful or unhelpful. The themes presented below apply across different service types, and emerged during discussions about what it was that made some interactions helpful and others not, or some people helpful and others not. The factors set out below apply across services to people generally in a one-to-one role with the young carer or parent respondent, including social and family support workers, as well as individuals in the service types discussed above.
Finding and linking to other support, information and advice
People described as helpful were often those who, through listening and understanding, could find and get back to the young person or family member with information wanted, or who were able to identify appropriate other sources of support, and help them with accessing and using that support. Young carers and, particularly parents, commented that it was difficult to know what support was available without someone who could tell them about it. There was a strong feeling in one parents group that opportunities were missed and that families came into contact with practitioners (e.g. in health services) who should have been able to inform the family about available support but did not. Several young carers noted that it would have been very helpful for them to have been linked into support earlier, but they had not known it was available.
Social workers were among those in a position to supply sought-after information. One boy’s social worker was ‘[g]ood because you could ask them to find out something and the next week they would get back to you with the answer’ (Young carer 12‒18).
However, an older participant in the same group had less-positive experiences: ‘Need more and better info – get passed around, conflicting info, don’t know what’s available or what need’ (Young carer 12‒18).
Parents made similar comments. A ‘good’ social worker was able to access support regarding, for example, children’s special needs and associated support, holiday schemes and respite for children. Social workers whose support was appreciated helped intervene with landlords, getting housing adaptations in place, and sometimes acted as an advocate to get things done. They could also help young people defend themselves: ‘She used to go to meetings with us, just to basically say how well I was doing’. One young carer of a sibling with autism noted it had been helpful to be linked to other families facing similar difficulties.
In one college-based focus group, participants felt support at college was more useful than support they had received at school specifically because it did help with outside-college issues. However, some school-age participants in other groups also received support for problems outside school. Important information, from social workers and others, included informing people about benefits and how to get them: ‘Having like the carers allowance, or things like that, like that sort of stuff just isn’t really talked about and then it’s hard to find yourself’ (Young carer 12‒18).
Money problems raised included: reduction in carer’s allowance once the child turned 18; being turned down for a carer’s allowance because another family member was already claiming it (which is not supposed to be the criterion, which are instead based on the number of hours for which an individual cares); and being declined Personal Independence Payments (PIP), the decision not to award being subsequently overturned on appeal. There were also some positive comments about PIP assessments.
Linking people to other support had to be done sensitively, however. There was a strong distaste in many cases to being ‘referred on’, when it meant someone new getting in touch, asking participants to tell their story again, sometimes when they didn’t know what organisation they were from, why or how they knew about them, and what, if anything, they were offering. A few individuals described positive experiences of having a practitioner (one was from a young carers organisation) who would support them in attending another service (e.g. a mental health service) for the first time. Parents also referred to the benefits of having a trusted practitioner who would support them in attending meetings and could advocate for them or be a supportive presence.
How linking to useful support could be done sensitively and with the involvement and understanding of the young person or family is related to the themes set out below.
Listening and understanding
Having an adult to turn to and talk to was repeatedly raised as a feature of good service provision. While many participants were happy to discuss their caring situation with peers, others preferred only to speak about that with adults. Being someone the young person wanted to open up to did not seem straightforward, however, and we had many accounts of the young person saying they had not wanted to talk or be questioned, in particular circumstances, or sometimes as a general rule. These issues are a central theme cutting across service interactions. Someone the young person felt they could talk to was highly valued: ‘I pretty much rely on those kinds of people because I can’t talk to my mum about that kind of stuff’ (Young carer 9‒12).
People in various roles with respect to the young person could take the role of ‘someone to talk to’, those most commonly mentioned were school staff and young carer workers from groups in or outside school. Other people taking this role included social workers [‘we do fun stuff, it calms me down’ (Young carer 12–14)], family workers [‘easy to talk to’ (Young carer 12–14)], paid care workers who came to the home, GPs, family members, friends of the family, and neighbours. Participants had different preferences and opinions as to whether they liked to see someone that was there for the whole family or just for them, and young carers also often said they wanted someone for the cared-for person to talk to.
Many young carers lived in complicated family situations and many had, or their parents had had, poor experiences with services in the past. Some families had conflicting perceptions of needs for support, and roles, between individuals in the family. A strong theme across all groups and most interviews was that a feature of helpful and appreciated support was when someone listened to them and understood them. This was a feature of appreciated support from services including schools, social work and young carers organisations.
Whether or not a particular worker was good at listening, understanding and being helpful was often said to be ‘down to the individual’. This could be because of personality, experience, skills, or the amount of effort the worker put in, or time they had. Descriptions of helpful support were often set against descriptions of what had been unhelpful. In one young carers group discussion about ‘good social workers’ and ‘bad social workers’, the difference was described as being due to:
Just overall lack of communication. The social worker doesn’t take enough care in exactly what that person needs, and then because of that the young person doesn’t want to communicate, because there’s no trust, and then the communication falls down, and then nothing happens… And the ones who can’t be bothered to take out some of their own time they’ve got to make sure like the person that they’re supposed to be helping is actually getting help, so they’re just doing the basic minimum and then doing something to just get the job… as long as you’re still getting like your pay cheque.
Young carer 12‒16
Good listening was described in different ways: you can ‘talk about what you want to talk about’; they ‘listen to you, complement you’ (both referring to young carers support workers) ‘lets me speak’ (regarding a young carer worker at primary school). In another group, specifically for young people who cared for someone with mental health or substance misuse issues, a social worker was described as being ‘a good one’ because they allowed the young carers to speak about issues regarding the cared-for person. A ‘good’ worker also validated feelings and experiences about caring: ‘allows you to be angry’ and ‘discusses facts: “I know your mum does this, I’m annoyed with her too”’.
However, ‘lets me speak’ was different from feeling obliged to do so: ‘Some are nice and listen, others aren’t so good, make you take the lead in conversation, which is difficult’ (Young carer re CAMHS).
It is a feature throughout these results that different approaches work for different people, leading to a conclusion that person-centred, flexible and listening approaches are needed. Good support was described as changing, based on having listened to what the respondent said. This could include decisions on where and when contacts would take place, it could include providing access or equipment that might enable someone to do something that made a difference to them. One participant said a support worker had been trying to source a bike for them, for example, and another had helped acquire a laptop. Choice and flexibility about what was offered, for example at a young carers centre, was valued: ‘Gives you things to do, but they’re optional’.
A lack of listening was linked to less helpful support. One social worker ‘doesn’t always pay attention’, while another ‘makes decisions for you, doesn’t listen’. Speaking to someone who did understand was described as ‘a relief’. However, some practitioners were described as listening, but not understanding. Some participants described being upset by being asked to explain more and feeling unable to; there was a common theme about a lack of understanding about the young carers’ situation.
CAMHS was sometimes described as not understanding and making unhelpful suggestions as a result. Examples given that were considered ‘ridiculous’ included: to take a bath when feeling sad (the young carer did not have a bath at home); to have a cup of tea; to do the washing up as a distraction from feeling anxious; not to cry or frown when feeling sad (young carers in one group aged 12–14 years). Our participants often said that CAMHS provided support, signposting or advice which was not what was needed, and that this was because they had not listened properly to what the young carer told them. Some respondents described CAMHS as being ‘mean’ or ‘unpleasant’ and said that the service could do more harm than good. Two respondents had the following exchange:
It’s a bit of luck on who you get.
Yeah, like the one where you go ‘Oh, that’s really nice,’ and like understands everything, but then there’s the rest… well, they understand, but they don’t understand like properly.
Not being taken seriously led to not being understood. For example, one young person felt that preventative action could have been taken if the family’s raising of concerns had been taken seriously by the first GP they had been trying to access support through. Lack of understanding was also linked to lack of knowledge or consideration of the issue, participants felt. Young carers sometimes had a wealth of experience both of services and of the person they cared for. One group of young adults were critical of social services, which they described as often rude, lacking training, unfriendly and uninformed about how much young carers do: ‘Rarely, you get an understanding person but it’s uncommon’ (Young carer 16–25).
Sibling young carers, usually where a parent was also caring, often felt their role and its impacts were dismissed, as did those caring for a parent with a mental health or substance misuse problem: ‘You’re not an official/professional carer so you’re not supported… The role is not acknowledged’ (Young carer 16‒25).
This young person felt he did ‘therapy’ with his mother. She spoke to him about difficult things, but he wasn’t given any support to deal with it.
Parent participants concurred that helpful supporters listened to what was important to the family and tried to make the support offered fit:
They will always work round life as much as they can, or say, well let’s leave it for next week but I’ll give you a ring, so they’ll still like log in with you but they might, you might not have a session but they’ll still log in just to make sure you’re alright.
Parent
For parent respondents, not listening and understanding was sometimes linked to being judgemental and making assumptions about the family, or about their parenting. Parents also referred to not being believed by the social worker sometimes because, they felt, the story told by other parties, such as ex-partners, were believed over their own.
Not listening sometimes meant not understanding the severity of the situation and need for support. One parent had tried to convey their need to social services: ‘I said to this lot, “You’re not listening,” I said “The only way my sons are going to get help, is if I go and kill myself”… and I stormed out the meeting’.
Following this, a search party had been sent to look for her, as she had wanted to calm down before going home, reinforcing her view of the need for extreme threats in order to get support. Other parents also expressed their perception that they could get help only if they were ‘a drug addict’, alcoholic, suicidal or accused of mistreating their children.
One parent group discussed the need for social workers to be taught empathy; they felt some newly qualified workers were well meaning but had little life experience, meaning they did not understand those with different lives. They felt the problem was a combination of training, personality and ‘the system’.
Parents, as well as, frequently, young carers themselves, described schools and services as not understanding:
When you say ‘My child is a young carer,’ to school, half of the time they’re like, ‘What?’
Parent
Most services do not consider the issue of young carers; they do not understand it.
Parent
One of the focus groups consisted of a pre-existing group of parents who had been meeting regularly, organised by the young carers organisation, and they appreciated the listening and understanding they received in the group both from peers and staff.
Trust, confidentiality and perception of risk
Many young carers, as well as parents, referred to a ‘good’ support person being someone they could trust, and a ‘bad’ support person being someone they could not trust. Many children, young people and parents in the study were distrustful of services and had deep reservations about talking to people outside the family.
If they come to see you and you don’t know them, they could use the information against you.
Young carer 9–11
I wouldn’t talk if they came home because they can search you up.
Young carer 9–11
Young carers described some visits as ‘intimidating’ or ‘concerning’; identifying them as connected to child protection procedures. However, the explicit fear of child protection intervention was a theme more likely to be raised in parents groups. Parent participants talked of feeling frightened of social workers because ‘they have power to take your children away’, and this could also lead to feeling frightened of seeking help in general:
Advice needs to be available somewhere where you don’t feel in danger of your child being taken away.
Parent
Feels like the system is there to see when you fail; you think someone is there to help you, but then you see they are keeping tabs, waiting for you to slip up.
Parent
Parents in one group laughed at the idea of a social worker for ‘the whole family’, feeling that their own needs were not considered in contacts with social workers.
Sometimes trusting someone was down to having someone the family, or the individual, had got to know. Participants who were reluctant to share their stories with services said that talking to someone outside the family would be ok if it was ‘someone you knew really well’ (Young carer 9–11).
Young carers participating in the study often had positive things to say about individual social workers (parents less so) often, again, contrasted with less helpful support in that role. ‘I think the helpful ones always leave too soon, but the ones that don’t know anything stay way too long’ (Young carer 12–16).
Young people who had difficulty trusting practitioners sometimes developed a bond with a particular person; these could be valuable relationships, but progress (e.g. improved mental health) often meant the relationship had to end. One young carer described this process in relation to a therapist with whom contact had ceased following her improved mental state; she was very sad about the contact ending and missed her therapist.
Breaches of confidentiality and sharing of information/awareness
Many participants gave a negative rating to a school staff member or a social or family worker because of breaches of confidentiality: ‘Can’t trust them, they will tell the head and get you referred’ (Young carer, mental health group re school tutor).
Here, being referred is presented as a negative outcome, speaking to the theme of risk perception. ‘Not trustworthy. You put trust in them and then they tell other teachers and don’t help’ (Young carer 11‒15 re class teacher).
A perceived breach of confidentiality could lead to disengagement from services: ‘They told other people when I didn’t want them to’ (Young carer 12‒16 re social worker).
As a result of one breach of confidentiality, the young person stopped communicating with the social worker. Conversely, young carers in one group were very positive about a particular school counsellor and agreed: ‘You can trust her; [but] teachers will tell other people/other teachers’ (Young carer 9‒11).
Distrust of school staff could also be expressed by parents: ‘You put trust in them and then they tell other teachers and don’t help’ (Parent re school family support worker).
But teachers could also be a trusted person: ‘Won’t go ‘round telling everyone’ (Young carer mental health group re class teacher) and ‘You can trust Mr … Head of year’.
And parents also had school staff they could trust: ‘Can trust them, really seem to care’ (Parent).
Conversely, sharing of information could be fine if it was discussed with the young person first. A positive rating was given to a member of school staff who: ‘[u]ses the info you give her but not until/unless she needs to and it’s in private’ (Young carer 9‒11).
Good examples given by young carer participants were when the staff asked if it was alright to share aspects of conversations they had had with the young carer’s parent; or when the practitioner had ideas of other useful referrals/connections but checked with the young carer before going ahead.
While there was a strong desire for confidentiality, young people also appreciated it if there was a certain level of awareness of their situation, as long as this awareness was combined with understanding. At school or college, where this could support helpful interactions and allowances: ‘I would like college to know what I am going through a bit more… Only my main college tutor knows, and she allows me to leave things earlier’ (Young carer interviewee).
Conversely:
School can be a bit of lottery though, I had one maths tutor that just didn’t get that I was a young carer, I got really stressed and stopped going to his class. I am having to take extra maths classes now.
Young carer in focus group discussion
There were mixed feelings about how much awareness young carers wanted other people to have about their caring situation; some reacted strongly against the idea of some other people knowing (e.g. a Scouts group and some school staff). This seemed to be partly because there were some spheres where the young carers just did not want to have that persona, or have to talk about it, but in other cases, it was because they did not like people to know about their young carer status if they did not understand it. ‘It is personal and I don’t want to share if people keep asking’ (Young carer 12‒16).
Young carers did not want people to know personal details of their lives, when they had not shared it themselves, or approved the sharing of the information, but they did want people to be understanding of some of the repercussions, for example, to do with attendance, homework, or, sometimes, behaviour or becoming upset.
As has been seen, participants were keen that there should be greater understanding of young carers. They felt there was poor understanding of what was involved and that there should be better understanding in professions such as teaching, the police, nurses and other health staff. To some extent the sharing of information about individual cases could help support this, but this would need to be done through discussion with the individuals involved about what was appropriate and useful to share.
Involving the young carer in making plans and decisions
A theme which intersects with the appreciation of practitioners who listen, understand and can be trusted, is that of involving the young carer in decisions that affect both them and the people they care for. Both young carers and parents, unsurprisingly, appreciated it when decisions about referrals concerning them were discussed with them. They also appreciated it, when they wanted to know more about the cared-for person’s condition and supports, if these were discussed with them.
Frequent comments from participants related to people getting in touch and decisions being made, that they did not feel they had been involved in: ‘When younger than sixteen he really felt he had been shut out of care, even though he was caring. He wasn’t consulted or included in discussions’ (Research notes re young sibling carer, 16‒25).
Participants appreciated having their role taken into account by services supporting the care recipient. This was mentioned, for example, in relation to positive ratings for a PIP assessment, a GP and a pharmacist. Young carers appreciated being kept informed about changes in medication and care for the care recipient, and having these explained.
The role of young carers in relation to siblings with care needs where there was also a parent providing care, was especially likely to be overlooked. One participant felt that he was not allowed to provide care in the way he wanted. His sister, with autism, had activities arranged by their social worker, but he was not included in these. He felt that, for many activities she would get more from the experience if he went with her, that she would participate better and feel less anxious. He said that his attendance was never thought of, even for something such as the cinema, and usually activities were arranged without him.
Several participant young carers voiced frustration at having information about the care recipient’s condition withheld from them (with confidentiality sometimes cited as the reason), or of professionals taking the (parent) care recipients’ account as the correct one, without listening to the young carer’s version of the story. Conversely, another participant, whose sister had special needs, was encouraged to ask questions by the service working with her. This was appreciated. One young person knew that her mother whom she helped care for preferred her not to be too involved and therefore withheld information, but the young person said she would prefer to be informed. Her conclusion was that it would be better for a professional to take the roles her mother was uncomfortable about the young carer helping with (in this case, taking medication). Another young carer objected to being told to go upstairs and stay out of the way whenever a person came to help her mother.
An important aspect of involving the young carer relates to services for the care recipient considering the wellbeing of the young carer. But several young carers described services which could have taken their role and needs into account, but did not. Social workers and care workers (at least sometimes identified as being for the care recipient) were often identified as being ‘dismissive’ of the young carer. This was agreed by participants in a young adult carer group: ‘Good ones will help get you through stuff, most only think of the person they care for’ (Young carer 16‒25).
Young adult carers in one group made involvement of young carers a key message for the government if it wanted to improve support for young carers:
Listen to young carers and recognise when they need help and help them!
Young carer 16‒25
We’re the best judges of our needs, ask us instead of trying to guess.
Young carer 16‒25
Proactive, persistent or intrusive; changing your mind
In this section the focus is on a theme to which many of those above are related – the difficult balance in adapting a level of persistence from services to individual needs and feelings – the right level of proactiveness, without being intrusive. As this level could be different for each family or each person, services need to be flexible in their approach.
In a focus group for young carers of people with mental health conditions, a helpful social worker was described as one who does not make demands, fits around the family rather than the reverse; doesn’t tell them what they have to do, and when they have to accept their visit. Appointments made at inconvenient times could cause problems and stress and it was not appreciated when people appeared to turn up ‘uninvited’ or ‘randomly’. However, there were differences of opinion on this point in another group. While some said that people who do not say when they are coming is unhelpful, others felt that random visits could help show services what was really going on at home (young carer, mental health group 12–18). Some of these ‘random’ visits may have been stipulated as part of child protection or child in need plans.
Flexibility in approach/person-centred/on-call or calls you
A theme across several focus groups was of support that was ‘helpful, but sometimes too much’. ‘Too much’ here could mean too intense, too persistent, too pushy or goes on too long. In one group most participants agreed that they kept being offered help they did not need: ‘Good that they help, but it’s sometimes too much – you don’t need help but it doesn’t stop’ (Young carer mental health group 9‒18 re social worker).
One described support at a young carers centre as ‘good, but sometimes too much’. Another interviewee who had recently attended a group (online) for the first time described how nervous they had been. She said: ‘[b]ut they, like, encourage you a lot to do it, and it’s a bit pressuring’ (Young carer interviewee, re young carers centre).
In another group, two young carers made a similar point, that a social worker, or family worker, was ‘too demanding’, they kept referring the carers to people they did not want to go to and/or when they were too tired after school (Young carer in mental health group 12–18). Some said they had been referred to groups or activities they did not want, and one participant said he had been referred to something even after saying no (Young carer in mental health group 12–18).
Parents also sometimes described support as ‘too much’. A parent commented that support could be ‘[d]ifficult to get rid of if don’t suit you, if it isn’t working. Formal complaints sometimes work, sometimes don’t (but I don’t actually want to go down the complaints route)’ (Parent).
Other comments from young people showed that some workers trod this line between being proactive or over-persistent carefully. Some groups provided opportunities for one-to-one chats within the group setting, which was valued. One young carer (9–11) said how important they thought it was that the worker checked in with them personally to see how they were doing with the group.
Workers from some young carers centres would regularly call round to check on people, which could be appreciated:
When she’s on the phone she always says, do you have anything that you need to speak about? And like if it’s not that, she just like rings every so often to check up, and she offers like me to go to either a one-on-one session or like a group session, to discuss like how I’m feeling, and things like that, just vent really. And then they offer you to go on activities and things.
Young carer interviewee
This young person had not yet taken up the offer of one-to-one support but appreciated that someone was checking in. This was a repeated theme. Providing flexible support that could meet young carers’ changing circumstances and feelings sometimes involved this ‘checking in’ while at other times the option of making contact was given to the young person. Some young carers valued having a number to call if needed.
This young person had a support worker they could call if they needed to, and who would also call them: ‘She [support worker]’s good because I can contact her if I need help with anything, like if I need a break or if I need someone to talk to I can contact her’ (Young carer interviewee).
This idea of ‘on-call support’ was discussed in several groups, often as something that was lacking: ‘There’s no support in between crises’ (Parent).
A few people did feel they have some sort of support person they could call when needed, while others said they would call emergency services if there was a crisis.
Opportunities to change your mind
We have seen that having an adult to talk to was highly valued by young carers, and that this needed to be someone who could listen and understand and could be trusted. Listening and understanding were valued in themselves, and were also identified as a way for helpful, tailored support to be put in place. However, many attempts by adults to open dialogue were not appreciated, and feeling able to talk to someone about issues was not easy for some participants:
Sometimes I don’t want to open up.
Young carer aged 12‒16
It depends who the person is.
Young carer aged 12‒16
Getting the level of proactivity or persistence right enabled people to be able to change their mind about receiving support. There were several accounts of offers of services being turned down, either by the young carer, or by the care recipient. One teenage young carer told us that the support workers were helpful, but the young carer did not feel they could open up to the support worker, leading the worker to conclude the young person did not need them, when they felt they did.
Conversely another young person described turning down support because they did not see themselves as a carer, but they were given the opportunity to change their mind later, which they did. Another young carer interviewee had also been given the option to change their mind, and the option of going back to their contact at the young carers organisation when they needed to:
I think it’s just like the offer – the support – even if you decide you like – even if I decide I don’t need it right now, it’s always an option. Like they said, if you ever do need us, just contact us. And I think that’s really good cos they don’t think, oh well they don’t need it, so they disregard it completely. It’s always an option.
Young carer interviewee
Similarly, a parent in one focus group found it valuable that support from the NHS community mental health service could be accessed when she needed it without referral:
Yeah, it’s a limited amount but you get, I think it’s eight or ten sessions and then they review, but then they can add on sessions which they did with me but I know I can still ring [named counsellor] if I wanted to now and speak to [named counsellor] even though it’s between sessions.
Parent
There were examples of both care recipients and young carers changing their mind about wanting a carer to come to the house, being initially reluctant.
He assessed me, I got a package, and then I felt embarrassed… and so I stopped the package, and then they referred me this year… I’ve hit myself in the head, do you know what I mean? I’ve like give(n) myself a wobble and said look, it’s not fair on your children.
Parent
This parent eventually accepted the support offered, despite her reluctance, seeing the potential benefit for her children.
The opportunity to revisit a previous ‘no’ needs to be available, at the same time as not overdoing repeated contacts that some young people, as well as some parents, objected to as over-persistent or intrusive. In one group (young carers 16–18), the problem was summarised as staff being unavailable but, conversely, that they will not stop giving support/contacting you when you no longer want it.
Not enough support
Although we have seen that ‘support’ was not always appreciated, that sometimes support was offered when it was not felt needed, and that it could be ‘too much’, a huge theme in the analysis was that there was not enough of the support people appreciated. When asked how support could be improved the answer was often that there needed to be more of it.
Young carers groups and activities, for example, should be available more often (one boy whose group ran once per fortnight felt this was not enough), others ‘would like to be able to do this more often’ (Young carer 12–16) and ‘a bit more often and more activities’ (Young carer 12–16). And even during the group: ‘There’s not always enough support in young carers because there is so many young carers’ (Young carer 12‒16).
Special activities or outings, one young carer noted, could be difficult to schedule, given everyone’s different responsibilities.
Sometimes, even where a worker had identified the needed support, service constraints prevented this being put in place or continuing. One young adult noted that a social worker used to take the care recipient out, realising this was the best help that could be given, but the social worker was taken off their case, allegedly for being ‘too involved’ (Young carer 16–25).
There were many comments regarding support at school and college along the lines of workers not having enough time:
Helpful but too busy.
Young carer 9‒12 re school support person
They are very accomplished but can be very busy.
Young carer 13‒19
There was an awareness of stretched resources:
So many teachers just don’t have the time. I mean like a Head of Year is looking after like what, 700 kids.
Young carer 12‒18
And similarly for family support and social workers:
Liked when they came although didn’t come often enough to help much.
Young carer 12‒16
Really nice, tries to help, makes me feels better, I would like to see her more.
Young carer mental health group 9‒18, re social worker who visited school twice per week
Good when do come but could contact more.
Young carer 12‒16
Could be improved if they stayed longer.
Young carer 9‒12 re social worker for mother
I’m not sure they do much to help my mum. They just turn up and check things but that’s it.
Young carer 12‒16
Helped with mum when feeling down but only stayed 3 weeks.
Young carer 9‒12 re family support worker
Equally, regarding activities for a care recipient:
He seems better, happier after. But better if they did more with him whilst he was there and that he went more often.
Young carer 12‒16 re sibling
And we have seen that people were deterred from trying to get mental health support because they knew there was not enough available:
Well, like mental health support, I think at my school it’s …not really accessible, because there’s no clear way to like get in and some people who were meant to get in didn’t get the letters, and there’s too many people in it.
Young carer 12‒18
Support often ended before the person receiving it wanted it to. Sometimes the ending did not appear to have been warned of in advance. Similar comments were made by parents where helpful support, including mental health support and support groups for themselves, as well as support for their children, sometimes did not continue for as long as they would like. One interviewee described having told their child’s school that they were not coping (during lockdown due to the pandemic) and was referred to a family intervention project. She said:
They got involved with me, straightaway, and then they did work with me, and then they turned round and said oh no, we’ve got to leave you now because you’re coping very well now. So, because I was coping – but I wasn’t – they stopped.
Parent
‘Not enough’ could also mean not enough at the right time: support sometimes came too late and was not then welcome; the opportunity to talk to someone needed to be there at the time the young person wanted to talk; and/or waiting lists could mean participants did not get help at the time they needed it.
Parents in one group also perceived as ‘arbitrary boundaries’ those where children were moved on from helpful services because they reached a certain age bracket.
One parent reported having been told they should have had family support but because of staff redundancies the family received what was described as ‘child protection’ intervention instead. Parents in another group talked about service silos leading to lack of accessible and sufficient support. They were constantly being told by services that it is ‘not their issue’ and that the onus is on parents to navigate services. These service issues contribute to ‘not enough’ support being received and underline the importance of a practitioner who will help people to navigate services, as discussed in the ‘finding and linking’ theme above.
Many of the themes presented in this chapter are interlinked, and aspects of the themes are reflected in the chapters to follow which set out what support is wished for but not received, and about barriers to accessing and using support. Helpful support received by some services highlight missing support elsewhere, while reported barriers to access highlight where access has been helpfully facilitated. The themes and their significance for policy and practice are brought together with the results from other chapters in the discussion.
What additional support is needed
In this section, findings are presented from the focus groups and interviews where answers were sought to research question 2: ‘What additional support is perceived as needed by young and young adult carers and the people they support and what needs such support would meet?’
Drawing on Purcal’s75 and Twigg’s76 frameworks, the findings are structured around three main themes: (1) prevent, reduce or remove caring responsibilities (the superseded carer); (2) mitigate the effects of providing care and, going beyond that, improve the affected aspects of young carers lives (carer as co-client); and (3) assist the carer in their caring role (carer as resource). Quotes included in the findings mainly represent annotations from young carers, from adult care recipients on the simple representation of a young carer and the person they care for, and also researcher’s annotations while discussing points to clarify or expand on them. In some cases, quotes are from recordings of focus groups or interviews. All quotes are anonymised.
‘A bit less care – a bit less looking after to do’: Young carers and their families say they need support that reduces young people’s caring responsibilities
Participants in the study identified three main needs that required the reduction or removal of caring responsibilities. These needs, or subthemes, were (1) to enable them to pursue their own personal goals and interests; (2) to have less or shared responsibility; and (3) to improve the life of the care recipient.
Pursuing personal goals and interests
Reductions in their care provision would mean more time, but also more physical and emotional energy, for the young person to pursue personal goals and interests. This included education. Having someone to check on the cared-for person while the young person was at school, for example, meant they could attend school and concentrate while there. Having support for the person at home would mean the carer could go to after school clubs, and many expressed interest in pursuing activities and hobbies. Less caring would also enable greater social participation and connection. This could be with non-cared-for family members but was mainly with friends. For example:
Someone in the house (I can go out to the park).
Young carer annotation
Someone to sit with my mum while I go out with my friends.
Young carer annotation
Free time with friends.
Young carer annotation
A further goal identified by participants that a reduction in care could address was to have some time to and for themselves. This was described by one young carer as ‘to be able to do what I like when I want without worrying about my dad’. This could be on a regular basis or for specific activities, for example, to have some ‘space away’, or a ‘get-away/residential so that I can relax & know they’re safe but also relax myself’ (young carer annotation).
Care recipients helped by a young carer also expressed the need and desire for better support for themselves so that the young carer did less and had time for themselves:
Even if it was just one week a year the difference that would make because…. then she didn’t even have to do anything, she wouldn’t even [help me get dressed] in a morning so that week was just for her.
Care recipient interview
More, and more easily accessed, information about available support and services that they might be eligible for was identified as needed by care recipients, to access the care they needed. The following quotes demonstrate what this information might include:
Help with services that I should be entitled to.
Care recipient annotation
What services [are] available.
Care recipient annotation
Better awareness on how to access the relevant support.
Care recipient annotation
Shared or less responsibility
A reduction or removal of care provided by young carers would reduce the responsibility felt by the participants in this study, something that caused a great deal of anxiety and stress. One young carer described the role this reduction would meet as follows: ‘outside help [would] ease my load of work and mental health’. Care in an emergency – ‘a person to call when parent is sick’ and ‘support if needed 24/7’ – was an aspect of this.
Improving the life of the care recipient
Mental or physical health support for the person they cared for to prevent that person being physically and/or mentally unwell, or improve their health, was a key unmet need identified by young carers. This would help by reducing their caring role and the stresses and strains of living with someone with, for example, mental ill health. It was also strongly related to a desire for the person they cared for to feel happier, or in less physical pain:
For my mum not to have depression and for life to be easier.
Young carer annotation
Seeing my mum happy and energetic all the time would give me a lot of motivation to be happier.
Young carer annotation
Would like my sister to walk and talk > be good if she has people to help her do this.
Young carer annotation
Mode of addressing ‘reduce or remove’ needs
In describing the type of services and support needed to bring about a reduction of their physical and/or emotional caring, the young people identified several sources of alternative support for the care recipient, although in a number of cases young people did not know where the support would come from, only that they needed more help and to provide less care. For example, ‘people coming to help’, ‘an extra helper’, ‘more help from other people’ or ‘extra support for her needs’ (young carer annotations). Where identified, mode of reducing care by young carers included social care services such as paid care workers, respite care, aids and adaptations, mental health support, activities outside the home or help from family.
Social care services
As the following annotations by young carers show, this could be to help with personal care, supervision or support to enable them to leave the house:
Carers – wash hair.
Young carer annotation
Having contact every day to make sure she doesn’t black out and fall.
Young carer annotation
A care worker to take her out and understand her more.
Young carer annotation
Aids and adaptations
Increased accessibility within the house and in the external environment for the person with care needs through, for example, aids and adaptations, were also key to reducing young caring, as well as increasing independence for the care recipient. This could be (more affordable) specialist equipment such as wheelchairs, alarms, or it could be street or home adaptations. Some examples from the young carer annotations are to ‘fix the high kerbs’ or have ‘house adaptations for physical/mobility needs’. This would enable the cared for person to ‘get around the house so she doesn’t struggle’ (young carer quote in discussion around the task).
Mental health or addiction support
Mental health support was an important part of what was needed to reduce or replace often intensive emotional care by the young carer:
More help for my mum so I don’t have to take all the emotional baggage.
Young carer annotation
More people to talk to when she is upset or sad.
Young carer annotation
Care recipients also expressed the need for mental health services and support for themselves as the following annotations by people receiving care from a young person show:
Support for mental health issues as a result of chronic conditions.
Care recipient annotation
Counselling ‒ for parents and child.
Care recipient annotation
Help to deal with addiction and substance misuse was also mentioned by young carers:
Regular group + people to talk to help her stop drinking.
Young carer annotation
Help support with drug/alcohol abuse.
Young carer annotation
Practical support
Young carers also expressed a need for practical support to reduce their domestic responsibilities and time spent on housework, shopping, and care of younger siblings. This included:
Support with housework.
Young carer annotation
People who help clean and cook.
Young carer annotation
Outside help for cleaning/chores to ease my parents’ pains and illnesses.
Young carer annotation
Somebody to look after my sister while I care for my mum.
Young carer annotation
Activities outside of the house
Replacing or superseding the young carer, giving them a break and improving the life of the care recipient could also come about, in part at least, by improving the social connectedness of the care recipient and their ability to participate in activities outside of the house. In the views of young carers, this included support networks or ‘support groups for people going through the same thing’ (young carer annotation). It also included ‘trips for the cared for person’, ‘support to go outside’ and ‘motivat[ion] so go out more’ (young carer annotations).
Care recipients also expressed the need for more social connectedness and support groups for themselves:
It’s lonely being ill, it’d be nice if there was groups that you could meet other people.
Care recipient interview
I want to do more social things for my age…just to meet other parents, like who’s in the same situation as me. I don’t want to go to these old people’s stuff! [Laughs]. Like, you know like they have these day centres for old people – I don’t want to go to like things like that. I wouldn’t mind having day centres for my age.
Care recipient interview
Paid work was another component of participation in activities outside of the house as expressed by young carers – ‘help her to get her job’ (young carer annotation) – and adult care recipients: ‘more support to get disabled people a job’; ‘I’d much rather be out doing your job or doing something, I miss working’ (care recipient interview).
Family support for the care recipient
Support did not necessarily need to come solely through statutory services, or even through statutory services at all. Alongside the need for social and community connection and emotional support for the care recipient, many young people expressed a need for more help from other family members:
More family members to help.
Young carer annotation
Dad should help.
Young carer annotation
Young carers say they need support that helps with some of the impacts of caring and/or their other life issues
‘Mitigation’ involves services and support for young carers that aims to address, and in our framework to also improve, some of the areas of young carers’ lives that caring has negatively impacted. Young carers identified four domains where support was needed to mitigate negative impacts: their mental health and wellbeing; education; social connections and relationships with family. For some participants, these appeared to be areas where unpaid caring had had negative effects, education being perhaps the clearest example. In others, there was a more complex mix of care provision leading to, or worsening, a young person’s mental health, for example, and other issues that existed for the young person outside of their caring role. This highlights the importance of recognising the context in which young caring takes place for individuals and supporting them accordingly.
Mitigating mental health and wellbeing impacts
Support for their mental health, wellbeing, and stress levels was the aspect of their lives that many young carers mentioned in their annotations, as the following examples show:
Help with my emotions.
Young carer annotation
Mental health help.
Young carer annotation
Being able to talk to more people about problems.
Young carer annotation
Stress release like to ring someone and after school some person.
Young carer annotation
A mental health service that is provided to young carers to help them express home struggles and worries.
Young carer annotation
Mental health support for young people could come from the NHS or voluntary or community sector mental health services. It could also come from school: ‘young carers should get access to school counselling’ (young carer annotation) and/or from young carer organisations. Other methods of supporting mental health and wellbeing were also mentioned such as stress balls, squeeze pillows and emotional support animals. Young carers expressed an unmet need for a time out space, rage or calm room, which they felt would help with their mental health, wellbeing and stress:
Time out of class when stressed about home or cared for person.
Young carer annotation
I would like to have a time out pass at school because I think it would help me.
Young carer annotation
People that can take me out lesson to have a calm down with.
Young carer annotation
A frequently mentioned gap in support was someone available to talk to, as the following quotes show:
Having people to talk to when needed.
Young carer annotation
Having someone to talk to outside of your home, outside of your family.
Young carer annotation
Have someone to talk to about my situation.
Young carer annotation
Someone who understands properly what happens at home.
Young carer annotation
Not all young people wanted someone to talk to:
It could be good for other people, but I don’t really like to express what’s happening. I just like to keep it to myself.
Young carer annotation
I feel like some things should be kept to yourself.
Young carer annotation
Schools, as well as mental health services and young carer organisations, were often mentioned as a place where they would like someone to talk to:
Someone in school that young carers can talk to.
Young carer annotation
It would help if I could speak to someone at school about what’s happening at home.
Young carer annotation
Care recipients’ views echoed those of the young carers: they also felt that the young people that helped support them needed more mental health support, including in schools.
Mitigating educational impacts
Another domain where ‘mitigate and improve’ support was needed was for young carers’ education. This could be help with their schoolwork and homework, especially where parents could not help, or the young person had no time or space to do it at home. Or it could be more flexibility over homework as the following two young carer annotations show: ‘longer homework dates if teacher noticed something isn’t right’ and ‘less homework for young carers or a better understanding of home life’. However, young carers were aware that there was a difficult balance for schools between mitigating the effects on young carers’ stress and mental health and on their educational attainment.
Mitigating social disconnection
Social connection and ability to participate socially was often disrupted in young carers’ lives in the study and many expressed a need for help with making friends and for helping friends be more understanding of their situation. One way to facilitate development of friendships is through removing or reducing their caring role, as described above. It could also be part of mitigatory support. Young carers talked about the need for:
Friends to connect with and feel close to.
Young carer annotation
Meeting new friends.
Young carer annotation
Have friends that understand.
Young carer annotation
Feel confident to say I am a young carer [with friends].
Young carer annotation
Family relationships can also be disrupted by caring in the family and young carers expressed the need for better relationships with family as well. For example, ‘free family therapy to work out rules, because the parental relationship often flips’ (young carer annotation).
Young carers say they need support that assists with their caring role
‘Carer as resource’ support models and policies aim to assist the carer in their caring role, including ensuring that it is sustainable. For young carers in the study, subthemes related to unmet need for assistance included peer support; information; and awareness, recognition and understanding.
Peer support
This was a key unmet need subtheme for young carers in the study, and was identified as an aspect of support that was helpful when received as reported above. Peer support may have a particular salience for young carers because of the importance of peer support to children and young people in general98 and because their non-carer friends sometimes found it difficult to understand about their caring or the disability or illness of the person they cared for. Peer support was also important because of fear of disclosure of private and potentially sensitive family or personal information to people who did not have similar experiences. ‘Meeting others like myself’, ‘friends who are carers’ and ‘people who are in a similar situation who can understand’ (all young carer annotations) would mean they did not have to explain themselves and potentially be judged, a main perceived benefit of peer support. Peers could be an important source of emotional support and someone to listen or talk to. They could also be a source of information, as the following young carer annotation illustrates: ‘getting help from other young carers to deal with my brother’. While most of the young carers in the study attended voluntary sector or school young carer groups, others did not. For those that did not, some felt that they would like a regular young carer group run by young carer organisations, in or after school, or simply to ‘know other young carers at school’ (young carer annotation).
Information and advice
Information and advice was another aspect of support that young carers perceived might assist them in their caring role. This included information about the care recipient’s care needs, how needs might change, and how best to support them, as the following examples show:
Info on situations/conditions.
Young carer annotation
Finding information for how to best support them.
Young carer annotation
Learning more things to help my mum.
Young carer annotation
Learning basic first aid and how to lift someone heavier than you.
Young carer annotation
This environment can give lessons to help you with the person you care for.
Young carer annotation
As the young carers describe below, being kept informed about the care recipient’s treatment would also help the young person in their caring role:
Being able to know my mum is safe when she is in hospital.
Young carer annotation
For the doctor or someone to talk to me about my mum’s health.
Young carer annotation
A further gap was information about support for young carers:
More info about available support.
Young carer annotation
A web page on help for young carers.
Young carer annotation
Recognition, understanding and awareness
Recognition, understanding and awareness of young caring, as well as inclusivity within services, were additional unmet needs. Young people felt that these qualities could assist them in their caring role. This meant their views being believed and respected:
Being able to tell someone that you think someone needs to be looked after.
Young carer annotation
Other people shouldn’t tell me what to do – we are the experts who know the people we care for.
Young carer annotation
Young carers also felt that greater recognition, awareness and understanding of young carers, including how caring affected young people, were needed in schools and other services. This included:
Teachers knowing I’m a young carer.
Young carer annotation
School know I’m a young carer and share it with the right people.
Young carer annotation
It also meant the school needed to understand what young caring involves and what support young carers might need, as the following examples illustrate:
Teachers that understand that I’m a young carer.
Young carer annotation
Schools being informed about carers & how to help them.
Young carer annotation
Someone who understands properly what happens at home.
Young carer annotation
Moreover, it was felt that schools had a role to play in increasing awareness and understanding among their students:
I used to have some friends a couple of months ago where I used to say to them I care for my brother but they don’t really know full on what I do for my caring role and they used to pick on me….In a way I kind of wish they take it further in school like they talk about young carers in school.
Young carer quote from discussion
Take it on board to tell kids at school what a young carer is.
Young carer annotation
Wider public awareness and understanding about young carers and about people with health conditions and disabilities was another unmet need identified by young carers and care recipients in the study. Reducing this could help in young people’s caring role. The young carers explained this as follows:
More people understanding that people are young carers.
Young carer annotation
Family/friends that don’t judge.
Young carer annotation
People don’t stare in supermarkets etc. staff and public.
Young carer annotation
People to understand and appreciate people that have disabilities.
Young carer annotation
Care recipients echoed this:
Services need to know there is a young carer, and what this means.
Care recipient annotation
Make life easier for disabled people – shouldn’t be such a battle to get services for vulnerable people.
Care recipient annotation
I think my wish for anybody in my position is for people to listen…that’s the most difficult part for me is when people look at you and you’re not, you don’t look ill. It’s hard because they don’t see the pain and then you get this stigma where everybody just thinks, oh she’s alright, look she’s out with her daughter but they might not realise the pain that I’m in…. You’d be amazed at what people say and yes, they’re ignorant people, that’s the way I look at them but your child also hears it.
Care recipient interview
Multiple roles
Support or services for young carers need to have multiple functions, supporting both the young carer and care recipient, reducing, mitigating and/or assisting the caring role. The support that several young carers described as needed could be considered multifunction and whole family: providing help for the person they care for (and so reducing their caring role and improving the life of the care recipient) and help for themselves. The following quotes are some examples:
This place can help you and the person you care for!
Young carer annotation
Help us as well as helping him.
Young carer annotation
Like I don’t think it should be just me who gets to speak to somebody. I feel like maybe my mum could be able to speak to someone too.
Young carer quote from discussion
Care recipients also felt that support for the family as a whole was needed, but often lacking:
The service would look at the family as a whole.
Care recipient annotation
A family support worker who works with myself & children, helps with everything.
Care recipient annotation
Barriers
Using Andersen’s BMHSU and recent adaptations to it, this results section is structured around the two main initial themes and their subthemes: (1) individual barriers (impeding factors) and (2) contextual barriers (impeding factors). Quotes are mainly from written text by the young carers or from the adult care recipients or, in some cases, from recordings of focus groups or interviews. All quotes are anonymised.
Young carers and the people they support experience individual barriers to seeking and accessing the services and support they need, value and find helpful
Five main subthemes were identified by participants under the theme of individual impeding factors. These were ‘material resources’; ‘competing priorities’; ‘psychosocial factors’; ‘self-determination’; and ‘service and support literacy: individual’.
Lack of material resources
A barrier frequently mentioned by young carers and care recipients was material resources. For example, ‘financial difficulties’ (young carer annotation), ‘Mum’s got no money to get things’ (young carer annotation) or ‘financial limitations’ (care recipient annotation). Expanding on this further, one young carer wrote that ‘young carers can suffer from money problems as their parents might struggle to find jobs’.
The cost of the service and support they needed was the most frequently mentioned barrier under this subtheme, as well as the cost potentially being off-putting to parents as the following quote illustrates: ‘parents might not think you need help [and therefore might not want to pay for it if it costs]’ (discussion in young carers focus group). Costs of getting there or costs of accessing the service online (costs of internet) were also mentioned.
Competing priorities
Competing priorities were often just expressed as not having enough time to seek support; this was mentioned by both young carers and care recipients. Competing priorities related to school and schoolwork: ‘time – also have after schools clubs, school, homework’, ‘school pressure’. Several young carers were impeded from seeking or accessing support by their caring responsibilities:
Worrying on how others will be [if leave them to access support for self].
Young carer annotation
Duty to take care of parents [so can’t access things for self].
Young carer annotation
Because [young carer] doesn’t like leaving me, she won’t go on overnight stays without me.
Care recipient interview
A further competing priority that acted as a barrier to service receipt was the person’s mental or physical health. In one example, the parent of a young carer explained that the young carer’s mental health meant she found it difficult to attend groups and talk to other people and several young carers said that their anxiety, including social anxiety, prevented them from attending things like young carer or other support groups. The following young carer annotation is indicative: ‘Anxiety stopping me from trying to get hold of service’.
For care recipients, ‘having multi-health issues [meant that] accessing and going to all the services is draining’ (care recipient annotation) and that they needed to prioritise their health.
Psychosocial factors
Psychosocial barriers included nervousness or anxiety, fear or mistrust and embarrassment and fear of judgement. Several young carers said that feeling nervous, worried or anxious about accessing support would get in the way of people getting that support. Other said that fear was or would be a barrier. Specifically, a fear of the consequences: ‘if tell someone might be bad consequences’ (young carer annotation); ‘consequences for talking’ (young carer annotation); and ‘fear about children being taken away’ (young carer annotation). This was linked to lack of trust in the services, which was also mentioned as a barrier by young carers and care recipients. A further strand of mistrust was a concern about having care workers in the house who ‘might steal things’ or ‘damage my house’ (both young carer annotations).
Another psychosocial impeding factor was embarrassment or fear of judgement. Several participants in the study expressed that it was hard and ‘embarrassing to admit needing help’ (young carer annotation) and that this was a barrier. ‘Worry about being judged’ was part of this (young carer annotation). It was also hard to accept help as this quote from a care recipient interview shows:
‘I did have it [support package] at first, and then I got embarrassed so I stopped it myself…I had an assessment, he assessed me, I got a package, and then I felt embarrassed and so I stopped the package’.
As shown in What is good or not good about existing services? What can be improved?, the care recipient subsequently overcame this barrier and re-accessed support, showing how opportunities to change a young carer’s mind can help overcome initial feelings of embarrassment about seeking help.
Self-determination
In the BMHSU versions that include it,82 self-determination incorporates privacy, dignity and independence and underlines the importance of being able to have choice but also the inherent conflicts in a dyadic carer-care recipient relationship. It is highly related to psychosocial barriers such as embarrassment or fear of being judged. Dignity was sometimes described in this study in terms of ‘pride’. The following quote expands on this. In the interview with a care recipient, she was asked what got in the way of her getting the support she needed:
Pride I think, because you don’t want to feel that you can’t do things yourself. That sounds awful but I’d been a carer for my husband…so to then become the person that needs caring for is quite hard because you also know what it feels like to be a carer and that is hard because you can’t help it, there’s nothing you…To get into the position to realising that I was going to need help it was a big turning point for me.
Care recipient interview
The care recipient or young carer declining or being reluctant to accept services or support was seen as a further potential barrier. The following young carer annotations illustrate this reluctance:
I think that my mum doesn’t accept more support.
People refusing help.
Not thinking you need help.
Service and support literacy: individual
As described above, ‘service and support literacy’ can be conceptualised as being an individual barrier and/or an organisational or other contextual barrier. In this section, we have included lack of confidence as an individual barrier. Other aspects which are more contextual barriers are reported on below. Several young carers expressed lack of confidence as a barrier, including ‘confidence to speak out’, ‘confidence in communicating in an assertive way’ and ‘digital confidence’ (young carer annotations).
Young carers and the people they support experience contextual barriers to seeking and accessing the services and support they need, value and find helpful
In the BMHSU, contextual factors include three main themes: care policy, care financing and care organisation. Some subthemes, such as availability, affordability, or accessibility cut across these overarching themes.
Care policy and care financing
In the study there were three main contextual subthemes under ‘care policy’ or ‘care financing’ which acted as barriers: availability; affordability; and accessibility.
This could be no availability at all in their local area or limited availability resulting in long waiting times. This was often attributed to lack of social care funding. Limited availability also referred to services that existed but were not well aligned with support preferences, as the following quote describes:
Like, you know like they have these day centres for old people – I don’t want to go to like things like that. I wouldn’t mind having day centres for my age.
Care recipient interview
Lack of resources and staffing was perceived as being part of this. One care recipient described in an interview how she had had the funds to pay for a care worker, but
‘there isn’t enough carers to do it because, especially since COVID, there’s so many more people that are needing carers…there’s not enough carers there to get round people.
Care recipient interview
Cost of the service – lack of affordability – was mentioned by several young carers and care recipients as a possible barrier. This included for services, extra support in school, and community activities such as yoga or mindfulness that might help with care needs. This subtheme was linked to the material resources subtheme above.
‘Accessibility’ referred to physical accessibility barriers, including ‘accessibility of buildings’ (care recipient annotation), but in particular not being able to get to the service or support because there was no provision nearby – several mentioned this – and because transport was non-existent, impractical or unaffordable, mentioned by several more. Two examples are below:
She [care recipient] used to go to [name of group for children on the autism spectrum]…But it was like a 40 minute drive there and back. So, it was hard getting there….She did like it.
Young carer interview
I did [get offered counselling], but I said that I didn’t really want to take it because it was travelling to the place to get it…I don’t have a, you know, I can’t really get there… [It’s] not that far but [place name] is probably about a 40-minute drive.
Young carer interview (There was no public transport)
Care organisation
There were certain aspects of inaccessibility that were more aptly categorised under the theme of care organisation because they related to the way the service or support was provided or how it interacted with the people who needed it, and because the solution arguably lies with organising more than policy or financing. Subthemes under the organisation theme were ‘approachability’ and ‘service and support literacy: contextual’, both linked.
The subtheme of lack of approachability as a barrier included two aspects. First, a lack of understanding from services. This could be difficulty in young carers or those they care for expressing themselves in the way the service or support was receptive to; feeling that people are or would be judgemental; and ‘people not listening’ (young carer annotation). The second aspect of inapproachability was staff: ‘unfriendly’, ‘unhelpful’, or ‘unkind’ staff.
According to the BMHSU, ‘health’ literacy, or ‘service and support literacy’ in the analysis, at contextual level can be defined as ability of providers and/or governments to provide appropriate and accessible information and to communicate well about available support and services and how they work. These were frequently mentioned barriers in the analysis. The following annotations show some aspects of this:
Not knowing who to call, who to ask, no support, no point of contact.
Care recipient annotation
User-unfriendly instructions.
Young carer annotation
Understanding what different services do.
Young carer annotation
Stress not knowing what will happen. Procedures, policies.
Young carer annotation
Information about services sometimes did not mention people like them, for example:
Not knowing or thinking of self as YC and info often mentions YC.
Young carer annotation
Lack of representation [within services and support].
Young carer annotation
Services’ inability to communicate in diverse ways was a further potential barrier as the following young carer annotations illustrate. Barriers to access included being, for example, ‘deaf, blind, English not first language ‒ not everyone can see or read’, or having ‘disability issues e.g. hearing/visual’. One care recipient expanded on this as follows:
There’s like – there is groups like Samaritans and stuff like that, but when you’re deaf…How can I speak to anybody when I can’t hear them?
Care recipient interview
There were also communication barriers related to neurodiversity:
It’s mainly my autism because…when I’m talking to someone in person I don’t know, I would usually only freeze up and say yes or no to questions, and I won’t make direct eye contact because my eyes would be going in that direction. But if I get to know that person, I would open myself up a bit.
Young carer interview
Practitioners workshops
The following section presents findings from the workshops with practitioners (N = 19) to discuss barriers and facilitators to, and ways of, implementing in practice the findings on what supported is valued, found helpful and is perceived as needed by young carers and their families.
Practitioners engaged eagerly in the discussion and spoke positively about having the opportunity to reflect on practice, share ideas and learn from each other, and from the research findings. Practitioners valued meeting other professionals who encountered young carers and there was a desire from practitioners for more opportunities to work together across service types, share problems and approaches to addressing them, and develop service solutions. Attending practitioners recognised and validated the issues raised as important by our young carer and parent research participants. Their considerations are discussed below and summarised as barriers and facilitators in Table 5. Quotes are taken verbatim from transcripts.
| Barriers | Facilitators and good practice examples |
|---|---|
| Effective signposting and linking to services | |
| Insufficient staff training and understanding | Having built up a relationship with the person already |
| Accompanying to appointments; help complete applications | |
| Advocacy instead of signposting | |
| Families may not know what support they are entitled to (e.g. welfare benefits) | Knowing what services are available; local services directory kept updated; one-stop shop for information |
| Practitioners need access to knowledge about services and supports, including benefits, but these change; local services close or change purpose | |
| Capacity constraints of the services being signposted to (funding, resources, waiting lists); access barriers, not meeting eligibility criteria, being at the boundary between child/adult services | Not everyone needs an assessment; helpful support can sometimes be quickly provided |
| On-call and ongoing support | |
| An additional drain on services | If used, ongoing support approaches need to be included in contracts, so workers do not end up doing it in unpaid time |
| Checking in, even a year later | |
| Transitions: support can be lost on leaving school | Exit and ‘maintenance of support’ planning |
| Empowering families to actively seek support, including from their informal networks and local communities; help them build friendships | |
| Responsibility falls back on under-resourced schools because of high thresholds for access to social and mental health services (also when services are unsuccessful in providing accepted support) | Support for universal services (e.g. in schools) can be a way to provide ongoing support |
| Limited number of sessions when time is needed to build trust | Providing more counselling in schools and other services, and a place to go |
| Service silos; different areas of expertise | Joint commissioning between adult and children’s services |
| Support that reduces the young person’s caring responsibilities | |
| Building support networks, including informal sources | |
| Childcare role of young carers not always acknowledged | Addressing over-burden within the family for example advocate for the young carer to do less childcare of siblings |
| Lack of awareness and consideration of possibility of young carer from adult services | Adult mental health workers can ask: are you a parent? Helping GPs be aware and ask questions for example when a family with a young carer does not attend an appointment |
| Young carer assessments are seldom done | Assessments that ask: do I need to do a referral to adult social services? |
| Lack of staffing capacity of some young carers organisations | Helping families to have a plan in place for who to call and when (including in an emergency) to try to move some burden of responsibility away from the young carer |
| It may be that young carers are eligible for support but the care recipient does not meet the criteria to be eligible for support for themselves | |
| Support that considers the whole family | |
| Family group conferencing | |
| Professional networks that cross professions, to help connect between different sectors, share ideas and develop solutions | |
| Whole-family workshops and networking events – several families, children and parents, form a community; peer support | |
| Young carer assessments as a way of working out what is happening and what is needed for the whole family | |
| Schools that offer support to parents as well as the child when a young carer is identified | |
| Issues around confidentiality; care recipients often do not want children to know about their health problems | Consulting and engaging with care recipient about what information is helpful to share |
| Whole-family respite trips | |
| Very high threshold for adult mental health and substance misuse services (both for parents and for young adult carers) | Giving priority to situations where a child is involved |
| Schools are now providing more and more whole-family support; teachers, teaching assistants and leaders do not have enough time | Getting specialist counsellors into schools, that can consider the whole family |
| Mental health issues are becoming less stigmatised meaning earlier, more preventative support is possible | |
| Specialist skills, be it for working with young carers, or for working with whole families | |
| Complicated family networks can be a source of problems as well as strengths | |
| Discovering and meeting the needs of young carers who are home-educated | |
| Someone who listens, understands/building relationships and trust | |
| Fear of service involvement | Better communication about services being there to help |
| Stigma associated with accessing support | Emphasising universal services; put up posters about help on offer in schools |
| Listening to the young person, being led by them – what do they want/need? Not making assumptions about best plan | |
| Planning together with families | |
| Planning together with other professionals | |
| Providing transport where needed; not always taxis, helps develop independence | |
| Being clear about what is on offer from a particular service, and when it will end; prepare for ending | |
| Short-termism in commissioning | ‘Listening commissioners’ to facilitate flexible and creative responses; have someone from commissioning on service steering groups |
| Insufficient awareness and understanding of good practice | Whole-school training in listening skills and other sharing of good practice |
| Need to make staff aware (in schools) vs. not breaking confidentiality | Enabling young people to make decisions about disclosing information, when they are ready; discuss before sharing information more widely |
| Involving young carers in discussion and decisions about needs and solutions | |
| Parents with mental health problems often think it is better to keep knowledge about the condition from their children | Finding ways to share appropriate information on the care recipient’s condition; workshops on mental health can be reassuring |
| Including the child in (part of) discussions around child protection concerns – in an age-appropriate way | |
| Including the young carer in the care recipient’s recovery plan – they may be the one most likely to spot changes in parent’s behaviour or wellbeing | |
| Stigma about accessing support in schools | Providing choice about how to access support including outside school options, for example youth information and counselling services |
| ‘Check it out’ sessions for young people to try for example counselling or a young carers group; they can bring someone trusted along | |
Signposting and linking to support
Practitioners agreed that effectively linking people to useful support was often more complicated than simply letting them know it exists: ‘[s]ticking it on a website is probably not going to work’.
For signposting to be appropriate and helpful, the young person needed to be able to talk openly. This required a context of trust and was easier when a relationship with that person already existed. The likelihood of a young person engaging with a service they were referred on to could be increased, if initial introductions were handled together with someone they already trusted:
I think sometimes when a young person has built up that trust with you, knowing that then you’ve got a trusting relationship with the other professional, that other agency just really, really helps them as well.
This was also seen as a helpful strategy for adult care recipients:
We’ve got experience of a fabulous staff member who’s left us now, who did all the substance misuse work, who would literally walk through the door with an adult.
Hands-on and practical approaches were shared:
We can maybe go to their house and we can get on a bus or a tram with them and help them get to their appointment.
Support was also provided by completing paperwork together with the person seeking support. Helping people find out about and apply for the various grants and benefits could be crucial, and there was frustration at this being so difficult:
A lot of the time it’s so complicated… [they need] somebody to be able to advocate on their behalf and support them to – making sure they are getting everything that they’re entitled to, which will ease those financial worries.
The point was made that sometimes signposting might be used when advocacy was more appropriate:
It’s about you, as a practitioner, having the right training and guidance to be able to do some of that stuff yourself, to advocate for that young person in a meeting at school about the fact that I don’t want your detention because I’m late. And I might need to look at my phone because my mum’s poorly.
Assessment was cited as the way to find out what young carers were doing and what they needed. However, in the context of the challenges of service capacity it was also suggested that sometimes help was relatively simple to provide, and a young carer could be gently encouraged to make use of existing school resources without the need for an assessment. Where appropriate, this would address an issue raised in What is good or not good about existing services? What can be improved? about participants disliking filling in forms which appeared to have no purpose or did not lead to any support.
Practitioners appreciated the importance of adapting approaches to the individual:
We all intake information in a particular way that’s personal to us. So on our referral form, we would really ask young people about what works for them and then work with referrers to try and give that information in a way that’s very personalised and adapted to that individual.
There was acknowledgement that more could be done, if capacity allowed, to keep updated local service directories, or a ‘one-stop shop’ for the public, and to be clear about what was on offer: ‘I’m thinking, is there something we could be doing more to actually tag certain activities that might be supporting actual young carers?’.
On-call and ongoing support/changing your mind
The issue of young carers and their families turning down, or not accessing, support that might be beneficial, was familiar to practitioners, who discussed ways to allow people to change their minds. For example, one practitioner said they could not keep people on the waiting list forever, but would say ‘we’ll just hold that for a few months and put the ball in your court. Have a little think about it’. In response to this discussion, one practitioner wanted to emphasise strongly the importance of universal services in schools: ‘Because they will be there before, they’ll be there during and they’ll be there after’.
As well as finding ways to re-offer support and to ‘check in’, the importance of enabling families to access support from other sources, including informal sources and from friends, was acknowledged.
We discussed the idea raised in focus groups that it would be good to have an ‘on-call’ number, so that carers could get in touch when needed, even if perhaps they had turned down support previously. Some agencies already felt they provided this type of support, for a while at least; another thought it was a good idea, but saw dangers if it was not properly commissioned, funded and included in contracts:
It would need to be properly funded and there would need to be some kind of a rota arrangement and proper handover and that kind of thing. Because it could cause harm to the support workers, but also could cause harm to the young people if there wasn’t a good connection between information sharing.
Some practitioners felt that it seemed like a good idea in principle but considerations of the feasibility of offering ongoing support were usually bound up with capacity issues:
We’re a very, very small team covering a huge area. But empowering that family to recognise, if things are starting to slip or go downhill, actively seeking out that help, whether it is through school or the GP or the local mental health service.
Some practitioners had more philosophical objections based on the wish to foster resilience:
It’s an issue that’s faced by everybody, this need for ongoing support when it’s needed and easy to access. That is massively challenging and I suppose one of the ways that we’ve tried to address that around parental mental illness is to really just try to empower the family to support one another, whilst also connecting the young people with their communities.
Nevertheless, there was also a challenge to the idea that it was resource-intensive to leave ‘cases’ open, by allowing future follow-up if needed. This sort of availability could go hand-in-hand with empowerment:
In my experience, usually, over the course of that year, it’s very rare that we have people phoning up all the time. Sometimes you might think, as a worker, maybe that’s leaving it open to people wanting to contact you all the time. But I think if you’ve been very clear in those sessions about what they’d like to achieve and understand that that has been achieved through the course of them sessions, then it’s nice just them knowing that they’ve got you at the other end of the telephone.
Support that reduces the young person’s caring responsibilities
There was agreement that some adult services did not consider the child’s caring role: ‘When adult mental health services are working with the family, I find that often the children are invisible’.
In one workshop, participants talked about conversations that did take place between children’s and adult’s services around how adult social care services can meet needs of the young carer. Assessments that started with the young carer, one participant told us, included a question: ‘Do I need an assessment to adult social services?’
In one group, family group conferences were discussed as a solution to identifying support which reduced young people’s caring responsibilities. Empowering families to make use of other resources, including peer support, continued to be a theme in this discussion. We were told how one service worked with young carers and their family to identify their support networks (family, friends and neighbours) and make sure the young carer knew where to go if a service was not available.
Some practitioners felt that reducing caring was not always the key goal:
We can’t take their caring role away completely, and nor would we want to, because that’s the thing that’s part of them. But it’s just being able to build that resilience so that they can cope, and if things are going wrong, they know where to go in the future.
This service set up safety plans with young carers so that in emergencies, responsibility could be moved away from the young person:
That’s really been effective in a lot of cases where that young person would be trying to manage things…they’ve got a little child-friendly step-by-step plan and then a written plan with emergency contacts.
These plans included access to a local authority all-hours emergency contact, which could also be accessed by the care recipient via an alarm system.
Reducing the young carer’s responsibilities was raised in relation to childcare; it was commented that young carers often end up spending a lot of time looking after siblings (where the care recipient is the parent) and that sometimes services could intervene:
It is about having those difficult open conversations sometimes with them as a family. Because that young person might not want to upset the person that they care for by saying, ‘I don’t want to do that,’ or, ‘I’m not comfortable.’ And that’s our role, as advocate, then, to help them with that.
Support that considers the whole family
The need for, and challenges of, working with the whole family were recognised, alongside an acknowledgement that not all practitioners needed to take this approach, and some could work effectively with individuals.
I really believe strongly in both/and, both family work and direct work with young carers. Young carers need that space away from their parents as well. So that would be my last message, I think, really.
Assessments were again cited by one participant as an essential way to do this:
If you don’t do a young carers’ assessment, you’re not working whole family, you’re not able to work holistically. Because if you’re not physically doing the young carers’ assessment, how do you know what the young carer is doing? And therefore, are there any hidden needs for that adult?
One service provider told us about a project for parents with mental health problems, where they invited a group of families to attend a workshop together. There were fun activities alongside facilitation for parents and children to hear from each other. The children, separately, made videos about their situation which the parents watched; this could have a powerful effect on parents (‘they were gobsmacked!’). Parents were supported to consider what was and what was not appropriate for children to know and do, and how they, as parents, might support each other.
We have seen in other chapters how there could be conflicts within the family, or differences of opinion about needs and possible solutions. This was another way family group conferencing could help; although often used with families in crisis, in one site, the approach was now being used by trained facilitators working at a more preventative level:
It’s a really restorative way of getting a family around a table – not a table, they don’t use tables. But the idea is to get them as a group when they’ve identified, whether it’s a neighbour, friends, anybody they want at the meeting. And it’s basically owned by the family, the family come up with their own plan, and it’s usually there has to be a referral from a practitioner, but people in schools can refer in.
The way the model was being used seemed to address some of the concerns our young carer and parent participants had raised about everyone in the family being supported to have their needs and views considered:
This model is working really well for children/young people that don’t meet that threshold where it’s lower down and they want to bring the family together to come up with a plan. But the children are all given their own advocates, so it’s really well supported.
The approach could help identify what was important to individuals in the family, and how particular needs or wishes could be met, including things as simple as enabling a child to attend a sports club by having a relative cover caring duties.
Not all practitioners had access to such a service however, and eligibility barriers were cited; family group conferencing was not always available to use in a preventative way due to different local resource-use decisions. However, there was much agreement that, with the right resources and training, the approach would be beneficial to use in-house, for example in young carers’ services, to enable families to discuss needs and options and ‘take ownership’ of solutions. It was agreed that training a family group conferencing specialist for each agency working with young carers was a good idea. A word of caution from one participant was that you had to make sure the right individuals were trained: ‘I know our young carers workers here are amazing with lots and lots of skills. And there’s a but, and that but is it doesn’t necessarily mean that they’re skilled in working with families’.
Someone working with the whole family needed also to manage expectations:
Sometimes … the expectations are that somebody come into the family home and care for the mam 24/7. That’s not going to happen, it isn’t. It might be a wish…So it’s about being able to break that down.
Other services appeared to provide similar support where they brought in the whole family to discuss issues and solutions, sometimes with other services too, but ‘[w]e would always have a meeting with the family present. We would never do a professionals-only meeting’.
One school aimed to put support in place for parents and guardians when they identified that a child was a young carer. Schools were seen as increasingly bearing the brunt of lack of sufficient other services, now needing to support whole families:
I’ve noticed that schools seem to be taking on more and more and more of that sort of whole-family support. I’ve noticed that it is that you are the first port of call, really, and the schools are just taking on masses of support. There isn’t those services out there and it all tends to fall on schools. As I say, I don’t know how you do it.
Someone who listens, understands/building relationships and trust
In this section, we concentrate on three key challenges; navigating issues around being the trusted individual versus being the person with the right expertise; people’s fear of service involvement; and involving the young carer in approaches to support. Young people often developed trusted relationships with particular practitioners, and that could be crucial to support being effective but could also create challenges.
Service silos or service expertise?
We had heard stories from young carers and parents about people who they had built helpful relationships with being ‘taken off their case’ or otherwise prevented from providing help in a way both parties wanted. We heard the same from practitioners:
In my role, there was a student who wanted me to have that conversation with his mum as well. And I was told by the staff, ‘That’s out of your job role, you shouldn’t be doing that.’ So it’s a really challenging one because it’s what’s allowed within the remit of the job and whether pastoral or staff should be doing that. I don’t know.
There was not a straightforward solution here though, as there may be legitimate concerns about having the relevant capabilities and training:
I think their argument was I’m not a counsellor, I’m not trained in being a mediator in those kinds of conversations necessarily. Therefore, they felt it was beyond my pay scope but also beyond my job description.
This practitioner had struggled with whether they should bring in someone they perceived to be better qualified to address the situation (which was not what the young carer wanted) or to deal with it herself, which appeared to be the only option:
That’s a thing that I really struggled with. In the end, I did have a meeting but I don’t know if I overstepped the barrier there by having a meeting with this kid’s mum. But there wasn’t anyone in the college who could or would do that, you know?
Practitioners concurred that sometimes the person designated a particular role (e.g. school young carers lead) was not necessarily the person the young carer connected with, and that some flexibility about young carers’ preferences was needed in order to find solutions. However, a need for people with specialist understanding and skills for working with young carers was also expressed, for example regarding support provided by colleges and Sixth Forms.
Fear of service involvement
Communication was mentioned as a ‘huge barrier’ to engagement in services; good communication was needed to build relationships, convey the acceptability of services, and explain that they were about support not surveillance. Practitioners understood that some families had a fear of social services, even if they felt that those fears could be misplaced: ‘That might be from their past experiences of their social care, maybe like when that adult was a child, when things were maybe very different’.
Practitioners had also experienced the need for parental consent being a barrier to putting support in place for a child, due to parental reluctance.
While these points could appear to put blame on parents, some practitioners acknowledged where practitioners, and services, needed to rethink how they presented themselves and communicated with families, as we will now see.
Involving the young person and their family
One participant talked about, when there were child protection concerns, involving the child in those conversations in school, to demystify the processes: ‘Being honest and open and involving the child, young person, with the process is absolutely the way forward’.
There was a discussion around practitioners needing to listen more:
As adults, we often think we know what needs to happen. And it’s so far removed to what the child or family actually want. I think as professionals we see a huge picture and actually it might be something as simple as, I don’t know, coming to school at 9:05. That might be all that’s required, but I think as professionals, over the years it’s been instilled in us to do to families rather than let them. I think that it’s key that the families and the young carers take control and we should be the ones then – I think that in itself, there are some professionals that will really struggle with that.
This could, it was felt, be straightforward:
Yes, it’s like we generally overcomplicate things whereas, like you say, it’s a simple question, ‘What do you need?’. And it might not be a massive referral to someone that they don’t want to speak to…. sometimes it’s as simple as, ‘She loves reading but we don’t live near a library and we can’t afford books.’ ‘Well, we’ve got a ton of books.’ ‘Brilliant.’ ‘I’ll pop some in the post.’ And sometimes it’s not simple, but it’s the way you ask things and the way you involve the young carer and the family, absolutely.
Practitioners described successful approaches, being clear and open with the young person, and being led by them in thinking about aims and solutions:
We’re very clear with young people when they start about what it’s going to involve. It’s all completely young person-led, they kind of set themselves some achievable goals. Anything that they’d like to work on in those six one-to-one sessions.
But limited numbers of sessions were recognised as barriers given the difficulty of relationship building:
Sometimes it will take us two, three sessions just to build up that trust before they even feel capable or confident enough to talk about their caring role. That can be really, really difficult and a massive challenge.
An organisation in one site described involving young carers in service design, working closely with commissioners. They explained that this was possible only because nobody else was bidding for that particular contract, and this meant the organisation could involve both young people and commissioners in developing a creative and flexible approach. This way of working together with commissioners to develop a service was described as ‘less performance managed’ and more cooperative. Another service had involved young carers in ‘co-production’ work, considering how Care Quality Commission quality markers for supporting carers in general practice could be improved to be more relevant to young carers.
Another practitioner recommended the close involvement of commissioners:
Just a little bit of advice around something like that. If you’ve got a great service like that, that is reducing responsibility of care, have a steering group and have somebody from commissioning sat on that steering group, because then they can really, really hear.
Commissioners who get to listen to young carers may be better able to support the provision of appropriate services.
Another aspect of involving young carers was in giving them appropriate and useful information about the care recipient’s condition. Although parents sometimes tried to keep information about the illness from children (particularly in relation to mental illness), practitioners said research suggested having greater understanding of conditions could be reassuring for young carers:
It’s a way of reducing the need by actually just empowering families to be able to talk together and to understand each other’s needs and to understand what works.
Following discussion of our results, and discussion between the attending practitioners, a strong take-home message was the need to listen to young carers and their families:
I guess the central message is asking a young person and asking their family what they want. There’s a million and one things that professionals could do or could signpost to, but if it’s not relevant to their family, if it’s not what they want, I guess that’s the biggest barrier, isn’t it?
Summary
Table 5 summarises practitioners’ perceptions of the barriers and facilitators to addressing the five key themes we took to the workshops relating to what young carers and parents say are, or would be, characteristics of valuable services. Involving young carers in discussion and decision about needs and solutions is included as a sixth theme. This was also a strong theme from the work with young carers and parents and was a theme across the discussions with practitioners. In Table 5, where the facilitator at least partially addresses a mentioned barrier, they appear on the same row.
A further implication of the above findings is that services would benefit from practitioners having more opportunities to meet and discuss; one case study area already had a professionals meeting a couple of times per year. Other areas attending said they would like to do the same. These may have been a particularly engaged group of practitioners, given that they were prepared to give time to being involved in the research and attending a discussion group. We do not see this as a limitation per se. Nevertheless, it might be important to speak to some of the practitioners who are struggling to provide the sort of listening, understanding, person-centred and flexible support that appears to be needed, to see if there are additional barriers we have not identified.
Cost analysis
Results from the scoping of the economic evidence for the selected recommendations is presented in Appendix 2, Table 8. The following section presents the results from the review and the economic evaluation workshop.
Co-developed support planning
Co-developed support planning refers to assessment and care planning that is done in partnership with the young carer (and their family). It is an individualised interview, and its principles are outlined in the 2014 Care Act6 which sets out that the process should be person-centred and that outcomes should be considered holistically, reflecting peoples’ wishes and feelings, their needs, values and aspirations.
We identified one source with cost information from a 2015 Think Local Act Personal report,99 which was produced to support the implementation of the 2014 Care Act. It presents costs in four categories by which support planning can be delivered: in-house by social work teams; in-house by a discreet team; outsourced process of assessment and support planning; and outsourced process of support planning only. The information refers to adult social care. The report also concludes that evidence on cost-effectiveness is patchy but that some views and experiences from local authorities suggest that separating out support planning from assessment, and outsourcing the support planning to user-led organisations can be cost-effective, as it might achieve better outcomes by encouraging creativity in planning and drawing more fully on informal support and community resources. Outcomes might be measured using tools such as the Personal Outcomes Evaluation Tool. The report acknowledges that data available about the costs of support planning is lacking and that little detail is presented by local authorities. However, the report presents a summary of costs across a number of local authorities. Averages seem to range widely from £101 for a standard support plan carried out in-house by a community care worker, to £328 for a more complex support plan carried out by a social worker. The report explains that these costs are based on an estimated cost per hour, based on current average salaries for social workers and support workers. These costs are similar to those quoted for outsourced support plan services, which range between £10 and £18 per hour. However, at our workshop, these estimates were considered to be very low in comparison to current costs. This suggests that the report may not include many of the relevant salary – oncosts and overheads. In addition, the source is dated, and salaries have increased since 2014–15. 99
At the workshop, it was discussed that the costing information was not sufficiently relevant, and the actual costs were underestimated substantially. It was discussed that the actual hourly rates were much higher than those reported in the source. In addition, the ongoing support costs would be much higher than reported in the source, and for most young carers the ongoing cost of support planning exceeded the costs of the assessments substantially. It was also discussed that the hourly rates strongly varied between regions, which also needed to be considered. Furthermore, the variation between individual young carers was likely to be even higher than reflected by the cost ranges in the report. The challenges of implementing support plans with the young carer and families could be substantial (e.g. when the person cared for did not have full recognition of their situation).
An evaluation of a training intervention to increase user and carer involvement in mental healthcare planning, highlighted the challenges of implementing high-quality, co-developed care planning. 100 Costs included the costs of healthcare professionals’ time to attend the training, the trainers’ time to deliver the training, consumables and room hire. Unit costs were applied where relevant and costs refer to cost year 2015/2016. Costs of delivering the intervention were set against any gains in quality-adjusted life-years (QALYs). Overall, the training intervention was associated with a net loss of £54.00 [95% confidence interval (CI) −£193.00 to £84.00], with a net QALY loss of –0.014 (95% CI −0.034 to 0.005), meaning it was not cost-effective.
Whole-family approach
A whole-family approach refers to a range of interventions that specifically work with the family as a whole, rather than just the child. Examples include family-focused assessment and care planning, family group conferencing, Team Around the Child and KidsTime workshops.
We identified three studies that included information about costs and benefits of interventions that followed a whole-family approach. The cost of conducting a family assessment in CAMHS prior to an intervention taking place was £700 per child. 101 The Early Intervention Foundation published a report in 2018 which found that the costs of family group conferencing in the borough of Camden were between £1200 and £1500. 102 An evaluation of KidsTime workshops by the London-based Anna Freud Centre, found that an average costs of a monthly workshop at their three sites in Camden, Hackney and Islington, was about £14,000 per year,103 although the report does not state how many families benefit from the service in total. A further evaluation by Spierling and colleagues in 2019101 found that KidsTime workshops cost £2000 per family, per year, on average but this evaluation did not specify the year in which data were collected. A report by the Institute for Public Care104 using data from cases from 2011 to 2013 showed that costs for providing Team Around the Child interventions ranged from £2302 to £15,175 per case. While the eligibility for interventions was not restricted to families in which parents had long-term care needs, most interventions were provided to this population and thus are relevant to young carers. Estimated benefits that were reported in the Institute for Public Care ranged widely, from £10,900 to under £1.4M. Net benefits ratios, ranging from potential cost savings of £5 to £91 for every £1 spent, were calculated based on individual family stories and did not use robust methodologies. They referred to averting costly long-term consequences such as child removal and instances where a child may require ‘looked-after’ care arrangements over their childhood period. However, the report did not include counterfactual examples. For example, what would have happened without the intervention and assumed zero additional cost occurred after the intervention.
At the workshop, individuals discussed that a challenge to costing family assessments was that they were done very differently in different localities, organisations and services. Moreover, there was no guidance or standards on how family assessments should be done. This also meant that such assessments often took place initially without the knowledge of parents’ problems. It could take several weeks of working with parents and children, establishing a trusting relationship, before the presenting issues were ascertained. Difficulties in identifying young carers was considered an important barrier to targeted whole-family approaches.
A key challenge towards establishing economic evidence is that most benefits occurred in the future and that it was difficult to establish those as part of regular evaluations with relatively short time periods. For example, there is evidence highlighting the large costs to the government and society if children or young people caring for someone with mental health problems are left unsupported during their childhood. This includes the costs to adult mental health services, as often young carers need support because of the emotional impact of caring. 26,55
The issue of costs and benefits occurring to different departments was discussed, as it was mainly children services paying for whole-family interventions. Adult services potentially benefitted from this, through potential cost savings (although those were difficult to evidence). Silo budgeting was a key barrier to establishing the economic case for interventions in this area. It was also discussed that the lack of organisational and senior manager buy-in was driving up the costs of implementing interventions substantially.
Signposting and information
Since signposting and information could refer to a wide range of services, we focused on social prescribing, which has been scaled most widely in recent years in England although we were unable to identify evidence that referred specifically to young carers.
We identified two sources which reported on costs and/or benefit of social prescribing schemes. 105,106 The 2020 Unit Costs of Health and Social Care referred to the Rotherham Social Prescribing pilot, for which the average cost of receiving social prescribing, through referral to funded voluntary and community sector organisations, was £570 per person. Estimated cost savings per person ranged between £265 and £385 and referred to reductions in the use of accident and emergency and other health service use (it is expected that as people are referred to and access more appropriate services earlier on, they are less likely to use more intensive and costly health services). Estimated return on investment, which is calculated by dividing benefits (‘returns’) by the costs of the service or support, ranged from a negative return of £0.5 per £1 pound spent, to a positive return of £3.4 per £1 spent. All the costs included in this report were updated to 2019/2020 levels, by using Prospective Payment System inflators.
At the workshop, it was discussed that most evidence on social prescribing referred to adults and that there are many other (potentially more appropriate) ways to signpost and provide information to young carers. Quantifying the benefits of signposting and information would be extremely challenging, and it was not possible to assume that benefits for adults applied to young carers, who had very different health and wellbeing needs. It was discussed that the lack of knowledge about appropriate support could have devastating consequences. While recently collected data from the school census could potentially address some of the existing evidence gaps, generally conducting economic evaluation in this area was considered very challenging due to the many ways by which signposting and information provision could be conducted. It was also discussed that providing information is quite different to signposting to services, and as such, these approaches might need to be considered separately in the analysis.
Designated (lead) person in schools
A designated person in school refers to a teacher or other professional employed by the school who is responsible for managing the school’s provision for young carers and their families and serves as a main contact for providing advice and support.
We identified one briefing paper from Barnardo’s charity,107 which made the case for having a designated mental health support team in every school, and a report by Pro Bono Economics on the cost and returns of a Place2Be counselling programme. 108 For the Place2Be cohorts spanning 2016–2021, the average cost per child was £1100, the estimated net benefit was £7700, and the estimated return was £8 for every £1 spent. Benefits referred to long-term economic benefits linked to improvements in children’s mental health (measured with the Strengths and Difficulties Questionnaire), such as highly hourly wage and increase chance of employment, reduction in truancy and exclusion.
At the workshop, the group discussed that having a designated person in schools was highly valued among young carers and that understanding the economic case would be very useful. The choice of designated person varies between schools, and currently there is little agreement as to the specific roles and responsibilities of this person. Depending on roles there were likely to be additional activities that had costs attached to them, such as organising young carers groups or activities. The group debated whether the designated person would come from existing school resources, since it was part of what school should be delivering, or whether additional resources were needed to ensure that schools were able to support the person to do the role well. This might include introducing a pupil’s premium for young carers (similar to a premium linked to special educational needs). Furthermore, there was no agreement on whether the designated person would get additional payments for taking on this role, and whether there were costs of additional training that needed to be considered. From an economic perspective, there would be opportunity cost attached to having a designated person since the time spent on this role and activities could not be spent on other things that would generate value to the person and school. The benefits of having a dedicated lead could be substantial if it led or is linked to comprehensive support that enables the young person to stay in school. With regard to current provision and implementation challenges, this strongly varied between localities. For example, in regions such as Cambridgeshire, every secondary school had a designated lead. Challenges to the implementation of a lead person role included staff turnover and existing school priorities on safeguarding and special education needs.
Chapter 6 Discussion
The findings add to the previously very limited body of research on how to best support young carers and the people they care for. The study adds to previous evidence on support for young carers and updates these findings to the period after the implementation of new rights for young carers and the increase in young carer voluntary sector support organisations in England. It thus reflects what support is offered, valued and missing in the current service and policy landscape. Crucially, the study provides evidence on what support is needed and valued and how current services can be improved and augmented from the perspective of the potential receivers of support: young and young adult carers and the people they care for. The perspectives of commissioners and deliverers of support also contributed to this picture.
We heard from 133 young carers and 17 parents who were care recipients during this research, resulting in a wealth of material relating to people’s experiences with services. As a group, young carers and their families had been in contact with a wide range of services and support and could identify what had worked well and what had worked less well, although there was a big range within the sample in terms of services received with some young carers only in contact with one service, usually schools. Participants also identified the kind of support that was needed but often missing. Those participants who did receive these types of support valued and appreciated it. The findings thus reinforce the value of these types or aspects of support in reducing caring, dealing with some of the consequences of caring and improving lives and life chances. Discussions with practitioners underlined the importance and salience of selected themes for efforts to improve support and address unmet need, with exceptions and/or acknowledgement of the complexity, as discussed below. The young carers advisory group further validated the themes and findings.
Summary of findings and relation to previous literature
Young carers and the people they care for value having someone they trust to talk to. This person would listen, understand and be non-judgemental and would not share private information inappropriately and without consulting with them first. Mistrust and concerns about negative consequences were often considerable, as has also been found in previous research56 and building trusting relationships was important and valued where it occurred. The difficulties of encouraging trust of services following previous betrayals of trust has been found elsewhere. 109 Here, we were able to hear from young carers who had developed trusting relationships with a practitioner, even sometimes when previous or other experiences had been negative. Practitioners concurred with the importance of this trusted relationship to young carers but recognised the challenges in making these available. They also talked about ways in which some of these challenges had been overcome, for example by having the time to build relationships, good communication about the service’s purpose, listening to the young person and co-planning support with them. Young carers said that this trusted person could be a named person or role in school or college or a school counsellor; a key worker in a young carers organisation; a social worker or family support worker; or their GP.
Young carers and their family also wanted clear, early, accessible information about what to expect and not expect from a service or person. This might include information about length of the waiting list for that service and clarity about roles – what is the social worker or support person there to do, and how a service or person can and cannot help. The expected number of sessions was also helpful to know, and people wanted to be told about when information might need to be shared with others and for what purposes. Being transparent, and consulting with the young person, about the sharing of information helps build trust. Clear and well-managed endings were important. This included flagging in advance when a service was getting near the end, or for services which ran for a fixed period, or fixed number of sessions, explaining this from the beginning when support was first offered and nearer the time. Information could helpfully be given on why the support was ending, what would happen next, and where they could go when they needed similar help in the future. Linking to other support or new workers when existing staff leave was also needed, and valued when received.
To meet young carers’ and care recipients’ needs, a wide range of support might be required. Information, advice and support to access wider resources and the formal and informal support that might be available, and information on how to access it, was therefore also needed. Previous research has pointed to difficulties young carers have experienced in finding out about available support services. 110 Information should be accessible and therefore in a variety of formats. Nicholls and colleagues found that young carers appreciated information from a variety of sources, both from the care recipient, and from leaflets, for example, which they felt could be trusted. 59 In the study, with a larger sample of young carers in a variety of situations, these themes also appeared. However, information alone was rarely seen to be enough. Our qualitative and group-based approach led to discussions and accounts about how linking to useful support had been achieved successfully. Support to access these wider services and support was perceived as needed and valued by young carers and care recipients, if received, and practitioners felt that linking to other services by an already-trusted practitioner could increase likelihood of take-up and engagement with the service.
Useful practice included helping with introductions to services, attending sessions or appointments with the young carer or care recipient, and checking in after first sessions to address any barriers and concerns. Practitioners felt that advocacy could also play an important role. Information and help with access was wanted for a wide range of services, including young carers support, social care, mental health and welfare benefits. Help linking with, or mobilising, informal support could also be valuable, such as from other family members and community facilities. Information about the care recipient’s health conditions and treatment was also valued by the young carers. Confidentiality and privacy are important, and care recipients in the study generally did not want this information shared. However, generic information about, for example, severe mental health or addiction, was found to be helpful by young carers when received. Research, with small samples, in some specific populations has highlighted the importance of knowledge, advice and feedback, including about the care recipients’ condition. The importance of information about the care recipient’s condition has been found in relation to young carers of people with mental health conditions111 and with care recipients receiving cancer treatment;59 trusted information about the care recipients’ condition and treatment could be reassuring and help reduce anxiety for young carers and promote joint coping within the family.
Heterogeneity in the young carer population and in caring experiences and circumstances means that not all young carers and their families want, need or value the same support. Choice, flexibility and co-development of plans and solutions are key. This meant involving young carers in decisions and plans; a flexible approach to support decided with the young person; and allowing young carers and their families repeated chances to accept support from services. Timing was very important to the young carers and the people they support, and they were not always ready to access support when it was offered or needed to return to support as circumstances or life stage changed. Practitioners had experienced changes in readiness or circumstances by young carers and care recipients and in some cases had been able to keep waiting list places open for longer, for example. Many young carers and the people they support expressed the desire for on-call or ongoing support. Some young carers organisations operated on this basis either formally or informally. However, others felt that it was either not feasible, because of staff capacity issues and length of service contracts, and/or not desirable because it could potentially be disempowering.
Support that reduces young people’s practical and emotional caring responsibilities was needed. It was also valued when received, although it often was not, making this a considerable unmet need. Reduced caring responsibilities would enable young people to have more time for other things in their lives such as education, social participation and hobbies, and to have less stress and sense of responsibility. In some cases, it was also perceived that support provided by others would improve the health, happiness, independence and lives of the care recipient. Support needed varied but could come, it was felt, from paid caregivers, adult mental health services, other family members, community groups, social connections and activities, or aids and adaptations. It could involve long-term reductions, short breaks and/or emergency or crisis support for the person with care needs. Previous research from the UK and other countries has also found that young carers expressed the need for more support for the person they care for29,47,111 and a break from their caring role. 3,8,29,47,59 Some of these findings, that young carers want to do less caring, date from over 15 years ago and are still being replicated today, despite huge changes in rights and awareness. Those changes in rights include that children should not provide ‘inappropriate and excessive’ care, nor care that risks an impact on their wellbeing, education or life chances. 117 However, experiences continue, as reported in our research and the current review of the 2014 Children and Families Act entitled ‘A Failure of Implementation’. 112
Relatedly, we found that support that considers the whole family – the young carer, other family members that are or may be carers, and the care recipient – was needed. While practitioners recognised the value of whole-family working, both practitioners and young people felt there was also effective support that could be given working with specific individuals only, and some young people valued having a practitioner that was ‘just for them’. Practitioners also recognised the challenges involved in providing support for the whole family such as eligibility criteria mismatches, differences of opinion within the family, and different commissioning systems for children’s and adult services. Practitioners described some whole-family practice examples that they felt had worked well, including KidsTime workshops (https://ourtime.org.uk/kidstime-workshops/) or family group conferencing.
In the absence of support that reduced or removed caring responsibilities, or in addition to it, support that helps with some of the impacts of caring and/or young carers’ other life issues was identified as needed and was valued when received. This included timely, helpful, accessible and young-carer-aware mental health support. Emotional and educational support were also identified as important to young carers in previous research. 47,113 Our research shows that support is also needed to help mitigate the effects of caring on social connection; relationships with family; and ability to take part in hobbies and activities, as well as more time to do these things. Support that helps with the impacts of caring and other life issues would also involve greater understanding at school, such as flexibility of deadlines for schoolwork and homework, although there was a recognition of the difficult balance to be reached between making allowances for the situation at home and supporting the young person’s educational progress. Opportunities to take a break at school were greatly valued as were systems where this did not involve publicly having to explain the reason a break was needed. Examples given were having a ‘time out’ or ‘young carer’ card which afforded them these special considerations. Peer support from other young carers was valued in the main as were activities that were fun and provided a break, and activities were often provided by young carer organisations or sometimes by young carers clubs in schools. Peer support has been found to be useful in other studies. 59
Greater awareness, recognition and understanding of young carers, what young carers do and about disability and mental and physical illness would be helpful to young carers. Although there were some examples where schools, for example, or other students had shown good awareness and understanding, this was felt to be a gap in support needed by both young carers and care recipients. Greater awareness and understanding was needed by school staff and other students. Other services, in particular children’s mental health services, needed to be more understanding of the interaction between mental ill health and caring responsibilities. A greater societal awareness of disability and of caring, it was felt, would help ease some of the impacts of providing care and of being disabled.
Young carers and the people they care for expressed several barriers to accessing the support they needed and valued. The support needed may not available. Recent studies have also shown that services for young carers are inconsistent across the country71 and that this inconsistency may leave many young carers struggling to access sufficient, or the right types of, support. 107 We found that services not being accessible or approachable were further barriers. There may not be enough information about a service and how it works and/or it may be that information is not available or communicated in accessible, user-friendly formats. Barriers of communication or approachability have also been found in some other studies. 16,64
Other perceived barriers identified in the study were service boundaries and lack of links between services. Young carers’ and care recipients’ lack of time and competing priorities such as school or caring responsibilities (for the young carers) and their mental or physical health could get in the way of needed and valued support as also found in an Australian study. 60 Feelings of fear, mistrust, nervousness, embarrassment, fear of judgement or lack of confidence in seeking help were further barriers and ones that services could help overcome. Lack of transport might prevent some carers and care recipients from accessing services, exacerbated by centralised, rather than local, hubs. Lack of understanding about young carers, especially those caring for someone with mental ill health or substance misuse, acted as a substantial barrier for some young carers in our study. We already know that people with mental ill health and/or their carers are less likely to seek or access support than people with other conditions. 68,85
A short summary of our findings is also available in an animation which was co-produced with young and young adult carer project advisors: ‘Reducing barriers and improving support for young carers’ (REBIAS-YC).
Our findings, especially those about prevention, have economic implications. Provision of care by young adult carers costs the state an estimated billion pounds annually. 20 In this study, we also sought to investigate the economic implications of selected findings. We summarised economic evidence and views from experts concerning selected findings from the study. We found that recent, relevant and high-quality economic evidence on interventions supporting young carers is very limited. None of the evidence we identified related specifically to young carers. Costs of interventions per person ranged from £121 to £778 for co-developed support planning and review (although this estimate was almost certainly too low); £1200 to more than £15,000 for family interventions; £265 to £385 for social prescribing; and £1100 for having a designated person at school. Return on investment ranged from £5 to £91 per £1 spent on whole-family approaches; £0.5 per £1 spent (suggested a negative return on investment) to £3.40 per £1 spent for social prescribing; and £8 per £1 spent for a designated person at school. Most of the returns related to a societal perspective, thus including benefits to the government (e.g. a reduction in healthcare requirements or criminal justice expenditure) and to individuals (such as in the form of income gains).
Findings from this evidence scoping are broadly in line with a 2008 report by Crossroads and The Princess Royal Trust,114 which estimated average cost of an intervention supporting young carers of £2500 per person and an average return on investment of £6.72 (which referred to a societal perspective). Potential cost-offsets in the report were linked to the expected prevention of adverse outcomes such as truancy, or removal of children from the family. However, it is difficult to say from this kind of evidence whether realising those cost savings is likely. Key components of interventions in this 2008 report were similar to the support covered by our report and included: reducing the burden of caring; providing additional support at school; promoting mental and physical health; addressing substance misuse and improving self-esteem. The general economic argument for investing in support for this population is very strong. There is increasing knowledge and understanding of the potential economic benefits of supporting young carers, and the large costs of leaving this population unsupported. 115 For example, the long-term costs for a child with a mother who experiences depression has been estimated at £11,600, which is linked to an increased likelihood of the child, as an adult, being unemployed, earning lower wages, smoking and adulthood depression. 108
Strengths and limitations
The strengths of this study are that we talked in-depth to more than 130 young and young adult carers of different ages, gender, ethnicity, socioeconomic status, geographic location and home and caring circumstances whose voices and opinions are not often heard. This included children and young people caring for people with stigmatised conditions, who are even less-often heard and who have particular difficulties accessing support. This enabled us to gain a rich and deep understanding of what support is needed and valued from a diversity of perspectives. However, a potential limitation is that some voices are still missing. As described elsewhere in this report, we were not able to engage with, or recruit, young carers from Roma and Traveller communities or asylum seeker or migrant young carers. Recruiting those groups involves a great deal of pre-engagement, which COVID-19 restrictions during most of the fieldwork period hampered. It may be that hearing from these young carers requires a dedicated project and the involvement of peer researchers from those communities. Another possible limitation is that, again partly because of COVID-19 measures during the study, we mainly recruited through young carers organisations. However, this was balanced by recruitment through schools and extensive outreach and engagement by the collaborating organisations prior to the project starting. A further strength is the participation in this study not just of young carers but also the people they care for and the practitioners who are responsible for commissioning, providing or delivering services to both groups. This gave us a broader and richer insight. A possible limitation is that care recipients could be recruited only through existing groups, although again this is partly mitigated by pre-existing outreach ad engagement with these care recipients. One result was that all care recipient participants were parents of a young carer; siblings receiving care from a young carer were not included, as explained in the Methodology section.
In the practitioner workshops, there was not sufficient time to discuss all of the themes. Themes were selected following discussion among research team members and with project advisors, including our young carer advisors, on what were considered to be the key priority themes on which to get practitioners’ input. There will inevitably be some bias in this selection process – a potential limitation – and not all themes have therefore received triangulation with practitioners’ perspectives.
There is potential for perceptions (perhaps unconscious) of a power imbalance between ourselves and participants, due to age and perceived status, as well as the use of incentives to take part, to affect the research process, and potentially the findings. However, the voluntary nature of participation was emphasised on several occasions together with reassurance that there were no wrong answers. As described above, the format of the sessions was informal, with icebreakers and a support worker in attendance. It was made very clear that activities were optional and participants could step out at any point. It was also made clear that receiving the payment voucher was not dependent on any answer given or not given, nor affected by them leaving the session early. Many participants said that they welcomed the opportunity to talk to the research team and other young carers. The team were aware that data collection and analysis may have been influenced by our position as researchers bringing our own personal life experiences, social position, and ontological, philosophical, and political views. While not a limitation as such, we recognise that it is important to be aware of and reflect on these potential sources of bias and assumptions and we worked carefully, as a team and with the two advisory groups, to continually challenge any assumptions.
Lastly, although there were some limitations, COVID-19 measures and procedures could have limited the in-person data collection more than it did. Talking to the young people in person was crucial to establishing rapport, creating an informal atmosphere and enabling the young people to speak to us individually and privately. Others had a mistrust of telephone or Zoom methods and/or would have been overheard, or worried about being overheard. The research team and partner organisations’ responsive approach and flexibility helped minimise potential limitations. In fact, many of the COVID-19-adapted methods were kept once restrictions were lifted due to their effectiveness in gathering data.
Recommendations for future research
The findings updated and have added to the previously very limited body of research on how to best support young carers and the people they care for from the perspective of young and young adult carers and the people they support. This was augmented by the perspectives of practitioners responsible for delivering this support. More research in this area and from these perspectives would broaden and further enrich this understanding of what support is needed. While we heard from a diverse range of carers, including those who face additional barriers to accessing support, future research could usefully include other voices, for example, extremely marginalised groups of young carers such as those from Roma and Traveller communities or from refugee and migrant communities. Including the perspectives of practitioners in the study enabled us to hear about barriers and facilitators to implementing the support that young carers and their families say they need and value. More research is however needed to further investigate how to implement this type of support in a sustainable manner, what the barriers are, and how these can be overcome. Other findings from the study might also benefit from further investigation. These include timing of support, co-production of support plans, whole-family approaches and building the knowledge, understanding and skills of professionals who come into contact with young carers and their families.
Future research could also valuably include economic evaluation of the support needed by young carers set against the costs of not providing it. There are several key challenges that need to be considered when designing any future economic evaluation:
-
There is currently very little standardisation of practice and interventions, which means that information on costs and benefits need to be generated together with contextual factors and key mechanisms, so that findings allow for the drawing of conclusions about generalisability.
-
Implementing interventions in this area is likely to be challenging, which means that costs of implementation might not offset the benefits, at least in the short term. This means that implementation evaluations, which investigate costs and outcomes under real-world-conditions, are likely to be important. The REBIAS-YC study has already established some of the factors that are likely to drive costs or outcomes, and these are important to consider in economic analysis.
-
Many of the economic benefits are likely to be long term. This means follow-up periods need to be long enough to capture those; and/or techniques such as decision modelling might be needed to extrapolate short-term to long-term benefits.
-
Processes of identifying and engaging with young carers and their families can require substantial time and resources. While it is difficult to measure this in exact terms it is important to include sufficient time and resources in the analysis, as not having them might have substantial adverse consequences (as findings of the REBIAS-YC study have shown).
-
Since many interventions require multi-agency/sector involvement, costs and benefits might not be equally distributed among sectors; this might need to be considered when deciding which costs to include and how to present findings.
Methods recommended in recent guidance116 on evaluating complex interventions – including participatory approaches, and the use of mixed-method approaches for gathering and analysing qualitative and quantitative data – are likely to be particularly suitable in this area. This includes the use of stakeholder- and theory-informed approaches (e.g. Theory of Change) to set out an evaluation framework outlining expected short-, medium- and long-term outcomes and consequences, as well to identify contextual factors and key mechanisms expected to lead to economic impacts.
In terms of methodology, the study benefitted greatly from four core elements: (1) hearing what is needed from the perspectives of the people who would receive this support; (2) hearing also from the practitioners that are or would be commissioning, or delivering this support so enabling both triangulation and an understanding of implementation barriers and successes; (3) involvement of young carer advisors and social care practitioners in the project from the outset; and (4) in-depth engagement and recruitment building on, and enacted by, the involvement of trusted organisations that had understanding of the local context and established networks. We recommend that any future research on this topic includes these elements.
Implications for decision-makers
The findings shed light on how current services can be improved and augmented. Many of the aspects that young carers say they need, want and value are already in current legislation – the 2014 Care Act6 and the 2014 Children and Families Act7 in particular. For example, that children should not undertake ‘inappropriate or excessive caring roles that may have an impact on their development’ with impact on development referring to when a young person’s caring role risks impacting their ‘emotional or physical wellbeing and their prospects in education and life’. 117 There is also a requirement for local authorities to take action to support young and young adult carers’ employment, education, health and wellbeing needs. 7 Explicitly in legislation is the option of needs being met and negative consequences prevented by provision of services to the care recipient. 118 The whole-family approach is also embedded in current legislation and guidance (e.g. No Wrong Doors,119 whole-family assessments, Think Family and the Disabled Parent Protocol). Where legislation and guidance exist, the implication for decision-makers is to address implementation barriers, several of which were identified in the study. In other cases, legislation or guidance may need to be created or updated. The planned revision of No Wrong Doors is welcome in this context.
Specifically, the following are the main implications for commissioners, policy-makers and other decision-makers:
-
There needs to be more funding overall, and more targeted funding and allocation of resources nationally and locally for adult social care and mental health services to fulfil the requirements of the 2014 Care Act to prevent children undertaking inappropriate or excessive caring roles and prevent impacts on young carers’ wellbeing, education and life prospects.
-
Funding also needs to be directed at practitioners and organisations working with young carers and the people they care for to have time to provide the support young carers say they need and value and to have time to build trusted relationships.
-
Commissioning practices could also be more of a facilitator of the type of flexible, holistic, co-produced, responsive and whole-family support that is needed and valued.
-
Commissioning of services and support in schools, adult and children’s social care, young carers organisations and mental health services could be done in ways that enable continuity of valued support and flexibility of support.
-
Flexible support, that responds to changes in needs and strengths over time, and as people’s readiness to access support, and their circumstances change is needed. More flexible support will enable greater implementation of whole-family working.
-
Decision-makers should facilitate wider implementation of whole-family agreements, assessment and practice across and within adult and children’s social care, mental health, and the voluntary and community sector. This could include wider implementation of the Disabled Parent Protocol, whole-family memoranda of understanding, designated lead professionals and/or whole-family practices.
While legislation and guidance already cover rights to some of the support needed, key changes or additions could include:
-
Policy or guidance around having a person(s) available in schools for young carers to talk to about their caring situation or if they are in need of extra help.
-
A national statutory requirement to incorporate measures to enable a whole-family approach in adult mental health recovery plans where it is currently lacking.
-
Decision-makers could also enable a wider roll-out of good practice on co-developing support plans with young carers, based on their needs, strengths, wishes and priorities in the sessions available to them; and more use of active linking to wider support, accompanying people to meetings or appointments, and advocacy. One initiative outlined in the NHS Long Term Plan15 was the roll-out of ‘top tips’ for general practice developed by young carers, which include access to preventative health and social prescribing, and timely referral to local support services. They estimate that up to 20,000 young carers will benefit from this more proactive approach by 2023/2024; we await the results with interest.
A further implication for decision-makers is the need for the provision of more, and more accessible and multiformat, information. As well as this being perceived in the study as needed, and valued when received, lack of information was also identified as a barrier to seeking or accessing support. Advocacy to help people negotiate the system might be beneficial but better communication is key. Information could be provided about the system for contacting the right person in schools and other organisations. Information could also be provided about the care recipient’s mental or physical illness and treatment, either specifically, where possible and while respecting privacy of care recipient, and/or generally, especially for more stigmatised conditions such as severe mental illness or addiction. Information could also be provided, and discussions held, about waiting list times, what the service can offer, when, and what happens when it ends; when a person might need to share information with others, what for, and what the process is; how to re-contact a service if circumstances or readiness to access support change; and what support is available locally and what they might be entitled to and eligible for.
Lastly, decision-makers need to recognise that young carers are young people first and that the impacts of the care they provide, the context they provide it in, and the support that they need and value, varies.
Equality, diversity and inclusion
Participant representation
We took several steps to optimise participation and inclusivity. This entailed extensive outreach and engagement work by partner organisations before the project began and during the active recruitment phases. Recruitment materials were co-developed with public advisors (young carers and social care practitioners) to ensure they were age-appropriate, culturally sensitive and appealing to a wider range of carers. Young carer project workers were directly involved in study recruitment. Recruitment of a wider range of young carers was facilitated by this trusted relationship and the local knowledge of key target groups. A barrier to participation for some young carers can be parental consent. The experienced project workers facilitated this process. As described elsewhere, methods and research materials were co-designed with young carers and practitioners working with young carers, increasing active participation in the research data collection. Research materials were also designed to be age-appropriate and culturally sensitive. The research team were experienced in working with vulnerable adults and children, and learnt further skills from the social care practitioner team member who had extensive experience in working specifically with the study target groups. This helped improve inclusivity and accessibility. Project workers in each locality working with young carers, care recipients and marginalised groups co-facilitated focus groups and provided support where needed.
Participants were made aware they could step out of the focus group at any time, with a support worker available to accompany them. Project workers also helped organise ‘cool down’ activities and ‘ice breakers’. Before each session began, participants were invited to consider and agree ‘group rules’ which would help them feel comfortable and willing to share information in the session. Group rules were jointly made by participants, supporting staff and the research team and all agreed to abide to them. Clear information and reassurance about confidentiality, anonymity and the use of the information being gathered was provided during recruitment and data collection. We were flexible about timing of focus groups; arranged accessible focus group and interview venues (with options for interviews online or by phone); and arranged transport as needed. The provision of transport was important to participation in all localities. We offered to cover the costs of replacement care and/or support workers to attend; neither were however used. We also offered the option to have information sheets in easy read, languages other than English and the use of an interpreter for interviews. In the event neither were needed to enable participants to engage in the research. Information and consent forms were also read and further explained to participants when needed.
As a result of these activities and actions, we were able to recruit young carer participants from a wide range of experiences and communities. This included young carers from ethnic minorities; neurodiverse or disabled young carers; those supporting care recipients around mental health and substance misuse; urban and rural, small town and city young carers; and carers of different ages, genders, socioeconomic status and home and caring circumstances. We also gained participation from a range of care recipients, although the latter not as diverse as the young carer sample but also not as large. Young and young adult carers and the people they support are already an under-represented group. We also recruited from particularly under-researched groups, such as from under-represented geographical regions such as the North West of England, or care types such as caring for someone with severe mental health or addiction. Accurate statistics on the young carer population are difficult to obtain. However, we were not aiming to be representative of the young carer population as a whole but instead to ensure we had participation from young and young adult carers with a wide range of experiences and circumstances. This we achieved. As described elsewhere, we were not able to recruit from very under-represented groups of young carers such as Roma and Traveller or asylum seekers and migrants. While these are a small proportion of the population, we would have liked to have included them and hope that future research will be able to do so, perhaps by ensuring researchers from these communities as part of the research team.
Reflections on the research team and wider involvement
The research team comprised academic researchers, voluntary sector social care practitioners who are often under-represented in social care research teams, and young carer advisors, who are also often under-represented. There was a range of experience and expertise across the research team and different expertise and experiences complemented each other with, for example, the social care practitioners being more expert in working with the study target groups and public advisors, and the study lead being more experienced in leading academic research studies. There were two research assistants linked to the project at different times. They contributed skills around literature review and additional ways of engaging with young carer advisors, including utilising technology for this purpose, as well as bringing new perspectives. Within their time allocation on the project, junior members of the team were encouraged to observe and take part in all aspects of the study including advisory processes, data collection, analysis and outputs. The research team were experienced in working with vulnerable adults and children and learnt further skills from the social care practitioner team member who had extensive experience in working specifically with the study target groups. Although none of the research team had direct experience of being a young or young adult carer, it was assisted by the young carers advisory group and a study steering group who did bring that experience and perspective.
The young carer advisors in the project included carers who were disabled, neurodiverse and those from ethnic minorities and under-represented socioeconomic statuses, as well as representing a wide range of caring circumstances and geographical areas. The role of public involvement is described in more detail in the section on public involvement below.
Public involvement
Aim of public involvement in our study
The aim of public involvement in the study was to ensure that from the start, and throughout, the research was co-produced with the people for whom it was intended that the research findings would have the most impact. This was young and young adult carers, the people they care for, and health and social care practitioners from the statutory and voluntary and community sectors who are involved in identifying, supporting and funding services for them. Their expertise and voice were important in ensuring the study was relevant to the experiences of young carers and their families.
Public involvement methods
Engagement and outreach activities were a key element of the study, enabled by the active engagement of young carer organisations in the study’s four localities. Their extensive local knowledge and established networks, both with young carers and other professionals, were key in reaching the number of participants who engaged in the research through focus groups, and practitioner workshops. They were particularly important in engaging with more marginalised groups in their areas and enabling us to recruit from the wider body of organisations and groups within their localities.
We used a number of advisory and reference groups to inform the study as well as a range of methods. The groups included:
-
Young carers advisory group: Young and young adult carers were recruited from the four localities; each young person had been a recipient of services provided by the local young carers organisation. The advisors represented a range in terms of gender, ethnicity, socioeconomic circumstances and caring situation, as well as geographical area and type. The group were recruited in February 2021 with the first meeting held online in March 2021 to co-design the focus group topic guides. The second (hybrid) meeting reviewed and sought the young people’s reflections on the findings, co-designed research materials for practitioner workshops, and established which job roles to invite. The third meeting, held online, helped co-produce the research briefing paper to be used in the dissemination events and to discuss who best to share the findings with. A further in-person meeting in January 2023 helped co-produce other outputs such as the animation (REBIAS-YC). Each advisory group member received a voucher for their participation and all expenses were paid for face-to-face meetings, including two meetings at the London School of Economics. Project workers from the four locality young carers services supported the recruitment and engagement of the advisory group. They were known and trusted by the young advisors and were able to make the local arrangements to support the young people to engage.
-
Study steering group: This included social care professionals working with young carers and their families as well as policy-makers and other academics. These were recruited from outside the four localities to inform the development of the study, including feedback on materials and the findings. The steering group met in February 2021, May 2022, and February 2023.
-
Young carers organisations group: The four locality based young carers organisations have been highly involved in recruiting and supporting young carer advisors; recruiting and supporting research participants; and co-producing the study’s research and action events. The research and action events took place in March 2023.
In addition to the above groups, we also had the following additional support for public involvement:
-
The social care practitioner co-investigator who was able to bring her knowledge to research material design, methods, analysis and outputs. Her expertise in the active participation of young people in service design and delivery, as well as research, was of particular note. She also led on the development and delivery of the research and action events.
-
We held a workshop in January 2023 to discuss cost implications of our findings with young carer professionals. (See also Cost analysis.)
Practitioner involvement in engagement and recruitment of participants, especially of more marginalised groups, was core to the study and fundamental to its success. The study’s collaborating organisations have developed a range of strategies to reach young carers and their families, which the study used and built on.
These included:
-
Co-development of recruitment materials and recruitment
Materials for the study were co-produced with the young carers advisory group, young carers organisations group and the social care practitioner co-applicant. Their feedback informed the content and presentation of the materials, including the participant information and consent sheets, and the questions we asked in the focus groups and the way we asked them. As a result, we made changes to wording and presentation of the information sheet and consent form and to the question wording, prompts and methods used in the focus groups.
-
Culturally sensitive and targeted materials
Young carers, while they share the experience of undertaking caring responsibilities, are from a diverse range of communities, family structures and cultures. To ensure that the focus groups and materials were accessible to as many young carers as possible, we benefitted from the advice and support of young carer project workers in the four localities. Their local knowledge of individual young carers, and of the wider communities within which they live, enabled them to support participants to engage. However, this approach has its own limits, being reliant on the four locality young carers projects to recruit as wide a range of young carers and families as possible. We explore this limitation further in the section on outcomes below.
-
Working closely with relevant organisations such as local community organisations and family support services in each of the four areas
The four young carers organisations met regularly to share their expertise and to plan recruitment in each locality. The meetings also helped co-design the focus groups and plan which venues, times and participant groups would participate. This local community and young carer knowledge meant that the focus groups, while using a similar format and materials, happened in a space and place where young carers and care recipients felt confident and comfortable to speak about their experiences and to discuss issues including barriers to support.
-
Locally based social care practitioners contribute to outreach and engagement activities
Locally based social care practitioners (project workers) were an important part of the study, both in terms of reach into communities but also in their knowledge and expertise in working with young carers and families. The presence of local project workers helped to develop a safe space, as they were able to support engagement and offer support if any of the issues triggered a response from participants. At the same time, the focus groups were led by the research team and emphasis was placed on safety and encouraging participants to express both what worked and what had not worked, or what had been difficult encounters with support services, including their own young carers service. The continued involvement of the locally based project workers enabled the dissemination events to be co-produced and led by young carers, fitting in with our overall public involvement aim: of young carers’ voices being central to the development and delivery of the study.
-
Providing clear information and reassurance about the information being gathered
The information provided to participants was co-designed with young carer advisors, and the social care practitioner co-applicant who has experience of developing young people-friendly materials and resources, and other social care practitioners. The information sheet and consent letter were agreed by the participating young carers services who were able to explain the information to participants individually and as a group where appropriate. The information being explained by a trusted professional benefitted the study as the participants, and parents where consent was required, were confident to ask questions and to participate in the focus groups/interviews with a clear understanding of what was going to happen and that they could at any point withdraw from the study. The young carers services deal with issues of confidentiality on a regular basis and confidentiality agreements are part of the consent to engage with the services and this familiarity benefited the study.
-
Safeguarding procedure
The safeguarding expertise of the local young carers services complemented the research team’s experience around confidentiality and consent from a research perspective. This enabled us to have in place effective safeguarding procedures. This included the presence of project workers who acted as support for the young people and families, in case any of the material being discussed was upsetting or potentially triggering.
Reflections on public involvement outcomes
Where public involvement had a positive impact
The positive outcomes of the public involvement plan and work has been the central role it played in enabling young carers’ voices and expertise to inform the project from planning, development of study materials and methods, through to leading the dissemination events.
As a result of discussion and advice from our public advisors, we made substantial and highly beneficial changes to the recruitment strategies, study materials (information sheets, topic guides) and research methods. For example, we included a wider range of potential services and support in our focus group activities and interview prompts; used more interactive data collection methods; used a combination of group, paired and individual activities; and made use of ‘warm up’, interim and ‘cool down’ fun activities as part of the focus groups. Public involvement was also key to safeguarding and supporting the young carer advisors and the young carer and care recipient participants; a considerable strength of our approach. Public involvement also had a positive impact on the dissemination methods and content, for example, deciding who to share findings with, how to share them, and in the co-design and leading by young and young adult carers of key study outputs.
The involvement of young carers social care professionals and young carers enhanced the study’s equality, diversity and inclusion. Participation in the focus groups and events we held was wide ranging and broadly representative of the local areas and young carers sector. This included young carers from ethnic minorities backgrounds; disabled young carers, young carers with special educational needs (SEND) or ill health; those supporting care recipients around mental health and substance misuse; urban and rural young carers. Key to this was the link with locally based community organisations with reach into the communities that the research study was aimed at. However, it was not only the reach but also the skill and expertise in supporting participants to engage in the focus groups, the advisory group and in the research and action events that highlighted good practice in engaging with vulnerable service users, in particular young people. Also key to this was the young carer advisors’ input into recruitment strategies, and research methods.
By fostering a real sense of being heard, being valued and listened to, the public involvement work has led to an open, honest and constructively critical set of findings which can be used to influence practice in the funding, commissioning, development and delivery of support services to young carers and their families.
As a research team, we have also learnt a great deal about how to approach and support public involvement from working with young carer and practitioner advisors which we hope to take forward into any future projects and which we have shared (anonymously) with colleagues.
Where public involvement had a limited impact
While there were substantial benefits of public involvement during the study, there were areas where we were not able to undertake all elements of our public involvement plan. In some cases, this was exacerbated by external circumstances. COVID-19 was one example, as described elsewhere in the report. In another example, we had hoped to engage with specific communities who experience multiple disadvantage such as the Roma community and refugee and asylum-seeking communities. Within one locality, there is an established Roma community, but we were unable to undertake a focus group specific to this community as part of the study. The local young carers service engaged with community organisations within the local Roma community, speaking with professionals that work within the community and other services that have been able to involve young Roma people and families. We had hoped to recruit young Roma carers through this outreach and community engagement, but this was not possible. The feedback we received from the community organisations highlighted the issues that face external agencies who wish to work with the Roma community. The distrust of external agencies, with voluntary organisations also being seen in the same light as statutory services; the extended family structure of the community and cultural norms mean that young caring is often not identified or acknowledged. By reaching out to work within the community, rather than expecting the community to come to us, we had hoped to research the issues they face. It would have informed the study about the experience of young Roma people who are not accessing locally based young carers services.
A further limit to the impact of public involvement is that all of the advisors were receiving, or had received, support from the local young carers service. This has meant that the study is mostly informed by those who have already been identified and received support from a young carers service, although both young carer advisors and young carer practitioners were able to share thoughts about other young carers they knew who were not in contact with services and/or their own experiences before coming into contact with a young carers service. The advisors were also able to inform us about their experiences before they were in touch with services or identified as young carers.
The way(s) public involvement will support dissemination of the results
Public involvement has, and will, support dissemination in several ways, also described above. First, the young carer and practitioner advisors have commented on the results, ‘sense-checking’ them and ensuring that they are relevant and useable in practice. Second, they have informed who the findings will be shared with and how. Third, they have helped co-design the briefing paper content and format. Fourth, they have co-designed other outputs such as the animation. A key element of public involvement in dissemination in this study is the research and action events in each of the four localities. This is an opportunity to present the findings back to the communities we researched. Research and action events were held in March 2023. The events are based on a similar model to that delivered by the social care practitioner co-investigator following a research project in 2018. The events will bring together research participants and people whom the research can influence into taking action on the findings. This will include commissioners, policy- and decision-makers, funders and other statutory services who play a role in the identification and support of young carers and their families. As with other elements of the study dissemination, young carers will co-produce the events and will take a lead role in running the events and in particular the focus on drawing out the practical actions in response to the research findings. It is this important link between research and practical action, based on the evidence, that has been at the heart of the REBIAS-YC project.
Learning from public involvement will also form part of the presentation of findings at research conferences and within academic papers produced as a result of the research.
Communities of practice
Background
‘Communities of practice are groups of people who share a concern, a set of problems, or a passion about a topic and who deepen their knowledge and expertise in this area by interacting on an ongoing basis’. 120 Proponents of communities of practice, such as Millen et al. 121 or Wenger et al. 120 argue that they have multiple benefits for individuals (e.g. through professional development, knowledge acquisition and increasing confidence); the community of practice itself (e.g. through opportunities to share ideas and improved problem solving and decision-making); and the organisation as a whole (e.g. as a way of benefiting from past experience rather than ‘reinventing the wheel’, enabling benchmarking and fostering innovation).
There are many examples of communities of practice models being applied across different types of organisation and sector, including health and social care. 122–124 However, although we identified one review about communities of practice for family carers of people with Alzheimer’s disease,125 we did not find any published examples of them being used specifically with young carers or practitioners working with young carers.
Communities of practice have benefited from technological advances which have increased the speed and reliability of internet connections and the number of platforms over which individuals can meet (e.g. Zoom and Microsoft Teams). Online, or virtual, communities of practice have been shown to be helpful in reducing professional isolation among health and social care professionals, particularly in rural areas where opportunities for in-person training and professional networking are more difficult. 126 Unsurprisingly, the COVID-19 pandemic has created increased interest in online communities of practice. 127
While most published accounts are overwhelmingly positive, there have also been some criticisms. Key to this have been concerns about power and ownership. While communities of practice were originally presented as spontaneous, self-organising and fluid processes, characterised by small groups working in the same workplace or in close proximity,128 many host organisations have taken responsibility for creating communities of practice and controlling the way they operate. This may mean that power and ownership are vested in the host organisation rather than the community of practice itself. 129 Nicolini et al. 130 took a different stance on this topic by highlighting the risk that communities of practice could perpetuate power imbalances by defending experts’ self-interest or by delegitimising the knowledge of non-members.
Methods and participants
The design for the communities of practice evolved as the study progressed. This was primarily influenced by the COVID-19 pandemic which ended the plan for face-to-face meetings in partner organisations. Instead, we retained the plan of establishing three different communities of practice to capture different job roles, but switched them to an online format. The three communities of practice consisted of:
-
carer workers engaged in direct work with young carers, offering one-to-one or group support for young carers or undertaking young carer assessments
-
practitioners in other roles, such as early-help services or widening participation
-
commissioners and managers.
We also decided to reschedule the communities of practice so that, instead of taking place at the same time as the main data collection, they would take place once it was almost completed. This was to help focus the discussions on topics that we knew from our findings were salient for young carers, care recipients and practitioners. Two meetings were held within the research team to discuss how emerging themes from the interviews with young carers, care recipients and practitioners could inform the communities of practice. This resulted in an outline plan shown in Figure 1.
FIGURE 1.
Communities of practice flowchart.
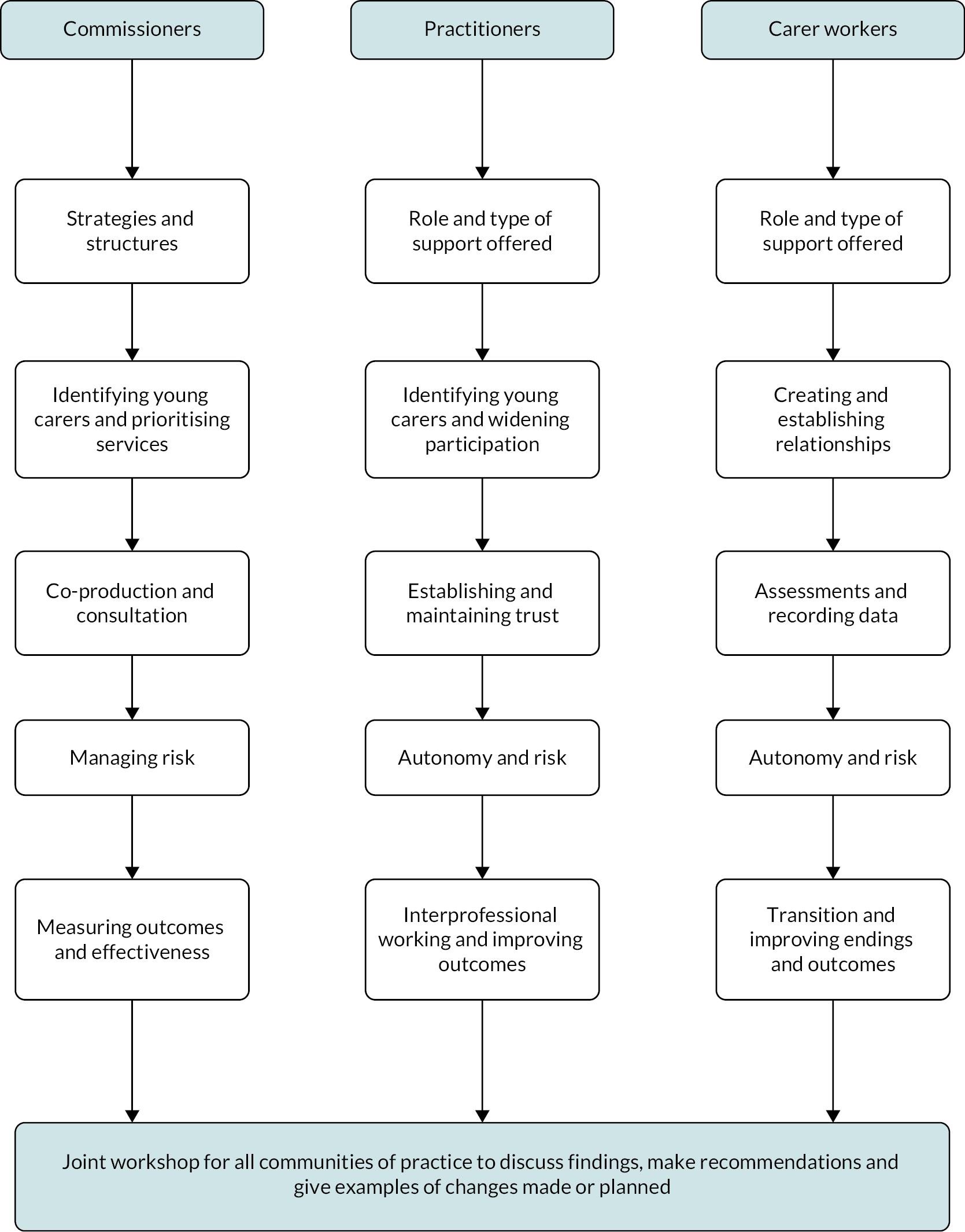
Recruitment took place in three ways. The first was via forums that were in touch with individuals and organisations working with young carers. These included the Young Carers Alliance and Making Research Count (a collaborative research dissemination initiative). The second was through the use of web searches to identify different organisations supporting young carers. The organisations contacted were selected to achieve variation in geographical location and type of organisation. The third was via social media on Twitter. While this resulted in multiple likes and retweets, not one person taking part in the communities of practice was recruited this way.
As shown in Figure 1, the format for the communities of practice consisted of five online meetings lasting 45–60 minutes, followed by a hybrid final meeting combining all the groups and to which participants in the practitioners’ workshops were also invited.
Table 6 shows the number of participants in each community of practice and their job roles.
| Community of practice | Job rolesa | Number of people involved |
|---|---|---|
| Carer workers | Assessment worker, carer support advisor, cognitive behavioural therapist, senior key worker, senior practitioner, service coordinator, service manager, wellbeing coordinator | 13 |
| Commissioners and managers | Commissioning and contracts manager, commissioning officer, chief executive, manager, market oversight manager, senior manager, service lead | 12 |
| Practitioners | Development worker, early-help consultant, education and family support worker, head of engagement, operations manager, project worker, senior access development officer, senior project officer, social work student, specialist support worker, widening participation manager, widening participation officer | 13 |
| Total | 38 |
There was some role overlap between the groups. Participants came from all sectors, including local authorities, national and local voluntary organisations, the NHS, and higher education. Each group held 5 online meetings, resulting in 126 attendances spread across 38 individuals. A final hybrid event bringing all the groups together was held in October 2022. Excluding the research team, this was attended by 30 people, 21 online and 9 in person. In addition, six individual or dyad interviews took place to discuss individual services with people who were unable to attend the meetings or to discuss individual services.
Discussion themes
Improving recognition of young carers
Non-recognition was an unmet need identified by young carers and a barrier to support and improving recognition was a major theme of much of the discussions. There was a strong consensus that many young carers were not receiving any support and that improvements should be made to improve the recognition of under-represented young carers, such as young carers who were refugees, neurodiverse young carers and young carers living in poverty, which included young carers from deprived coastal communities as well as those in more urban settings. It was also felt that carers aged 18–25 years often fell between services for young carers and adult social care. One participant ran a social support group for young carers in this age group which was mainly dependent on local funding. While it was recognised that initiatives such as the schools census would help with the recognition of young carers, it was suggested that this would not pick up young carers who were home-schooled.
Assessments
Many of the participants used the Multidimensional Assessment of Caring Activities (MACA-YC18) and Positive and Negative Outcomes of Caring Questionnaire (PANOC-YC20) in their assessments. 131 They were generally positive about these measures but highlighted that they were not always suitable for younger age groups. Many participants used artefacts such as a dolls house to make the process of assessment easier and there was a lot of mutual interest in how they could be used to improve the assessment process.
Providing a range of support
An important part of the discussions was the different roles undertaken by those who provided intensive support, for example for young carers experiencing mental health problems, and those who were involved in social activities. It was recognised that it was important to provide a spectrum of support. There were also debates around the advantages and disadvantages of time-limited interventions, especially when it came to managing demand for services.
Working with other professionals
An important part of participants’ roles was their work helping raise awareness of young carers among other professionals. The ultimate aim was to improve other professionals’ confidence and self-efficacy in working with young carers, but there was also frustration at repeatedly turning up to forums such as open days and having to repeat the same messages from their last visit.
Funding challenges
This was a major theme, especially because of the financial constraints on local authorities. It was widely agreed that insecure funding was a major barrier to developing quality services. It also had implications for workforce development as many care workers were on insecure funding and this led to churn in terms of recruitment and retention as workers left young carer services for more secure jobs.
Communities of practice as a way of sharing knowledge
One of the advantages of online meetings was the opportunity for participants to meet other practitioners from different parts of the country. This gave them the chance to share experiences and recognise the similarities and differences that they faced as practitioners. For example, one practitioner from a rural area highlighted the lack of public transport as a problem facing young carers, particularly when it came to attending social or group activities. By contrast, practitioners from London found that young carers were often reluctant to travel because of fear of knife crime. It was striking how often participants used the chat function in meetings to share experiences, including one moving moment when a member shared experiences of a safeguarding review involving a young carer. There were also examples where participants working in higher education were able to give advice about the systems in universities aimed at improving the numbers of young carers and other under-represented groups in higher education. The hybrid event was less successful at attracting in person attendances, highlighting how the COVID-19 pandemic has changed the way in which professionals interact.
Chapter 7 Conclusions
In the study we heard from 133 young and young adult carers aged 9–25 years with diverse sociodemographic characteristics and caring and life circumstances, from four different localities across England. We also heard from 17 adult care recipients from those localities. In these conversations, we sought to understand what support is seen as helpful, valued and acceptable and what additional support is needed by young and young adult carers, and by the recipients of care, and the barriers to accessing and taking up this support. The main aspects of support and services were felt needed, were often lacking, but were found to be helpful when received were:
-
someone trusted available to talk to
-
clear, early, accessible information about what to expect and not expect from a service or person
-
choice, flexibility and co-development with the young carer of plans and solutions
-
information, advice and support to access wider resources
-
support that reduces young people’s practical and emotional caring responsibilities
-
support that helps with some of the impacts of caring and/or people’s other life issues
-
greater awareness, recognition and understanding of young carers, what young carers do and about disability and mental and physical illness
The main barriers for young carers and their families in accessing this support are that the support needed is not available or is not accessible or approachable; or that there is not enough information about the service and how it works and/or that information is not available or communicated in accessible, user-friendly formats. Service boundaries and lack of links between services were further barriers. Young carers’ and care recipients’ lack of time and competing priorities or their mental or physical health could also get in the way of needed and valued support. Feelings of fear, threat, mistrust, nervousness, embarrassment or lack of confidence were further barriers that services could help overcome. Lack of transport prohibited some carers and care recipients from accessing services, exacerbated by centralised, rather than local, hubs. Finally, lack of understanding about young carers, especially when caring for someone with mental ill health or substance misuse, acted as a substantial barrier to accessing support for some young carers in this study.
Discussions with practitioners on the main findings above showed that barriers to implanting needed and valued support included insufficient staff training and understanding; lack of information about wider support and services; capacity constraints within all sectors including schools; too few sessions to build trust; service silos; issues with young carer, care recipient and whole family assessments including differential threshold; and fear of service involvement and stigma. Facilitators and good practice examples included relationship building; active linking to services and advocacy; tiered or multilevel support; exit and ‘maintenance of support’ planning, including empowering families to actively seek support; universal services; joint commissioning between adult and children’s services; improving informal and statutory assessments, especially in mental health, crisis planning, and building informal and formal support networks; and better communication, listening and planning. Whole-family good practice included family group conferencing, intersectoral professional networks, whole-family workshops and networking events, and schools or young carers organisations being able to offer support to parents as well as the child when a young carer is identified. Lastly, professionals and services would benefit from professionals having more opportunities to meet and discuss barriers and facilitators and share good practice.
Additional information
Acknowledgements
We thank the many young and young adult carers and receivers of care who generously shared their experiences of services and other support with us. We hope that we have adequately reflected their views and voices here. We also very much appreciate the practitioners who shared with us their practice of supporting young carers and their families and some of the barriers and facilitators.
We are grateful to our young carer advisory group for supporting the study throughout and greatly improving it, ably supported by expert support workers. In alphabetical order young carer advisors were Brendon, Chloe, Jemima Dinning, Luca Vizor, Morgan Cooper, Rebecca, Thomas Atkin-Withers and Yusraa Bibi Khan. We also thank our study steering group. We are very grateful to the young carer organisations who helped recruit and facilitate the data collection and supported the young carer participants to take part.
Lastly, as Principal Investigator, I would like to thank my research team for making it such a successful, enjoyable and rewarding project.
Contributions of authors
Nicola Brimblecombe (https://orcid.org/0000-0002-6147-5726) Principal Investigator; Assistant Professional Research Fellow. Contributed to the inception of the work, design, methodology, data collection and analysis, public involvement activities, project outputs, had project oversight and lead the write-up of the final report.
Madeleine Stevens (https://orcid.org/0000-0003-3540-3494) Co-Investigator; Assistant Professional Research Fellow. Contributed to the inception of the work, design, methodology, data collection and analysis, public involvement activities, project outputs and write-up of the final report.
Sara Gowen (https://orcid.org/0000-0003-3102-3777) Social Care Practitioner Co-Investigator; Managing Director Sheffield Young Carers. Public involvement lead, contributed to the inception of the work, data collection, project outputs and write-up of the final report.
Jo Moriarty (https://orcid.org/0000-0003-1574-1242) Co-Investigator; Research Fellow. Communities of practice lead, design and implementation, project outputs and write-up of the final report.
Robin Skyer (https://orcid.org/0000-0003-0018-050X) Research Assistant on the project. Contributed to public involvement activities, data collection and analysis, literature and policy review, project outputs and write-up of the final report.
Annette Bauer (https://orcid.org/0000-0001-5156-1631) Consultant to the project; Assistant Professional Research Fellow. Designed, lead and conducted the cost analysis, contributed to write-up of the final report.
Camille Bou (https://orcid.org/0000-0003-0444-1121) Research Assistant on the project. Contributed to public involvement activities, literature review and write-up of the final report.
Disclosure of interests
Full disclosure of interests: Completed ICMJE forms for all authors, including all related interests, are available in the toolkit on the NIHR Journals Library report publication page at https://doi.org/10.3310/ABAT6761.
Primary conflicts of interest: Sara Gowen received salary as Managing Director of Sheffield Young Carers. Annette Bauer received funding from the Austrian Ministry of Health Department for Science and Research as co-investigator of a study on supporting children of parents with mental illness. Camille Bou received funding from the NIHR School for Social Care Research for a PhD Studentship about young adult carers. Nicola Brimblecombe, Madeleine Stevens, Jo Moriarty, and Robin Skyer declare no conflicts of interest.
Data-sharing statement
This is a qualitative study and therefore the data generated is not suitable for sharing beyond that contained within the report. Further information can be obtained from the corresponding author.
Ethics statement
Ethical approval was granted by LSE Ethics Committee on 11 May 2021 (REC ref. 1247).
Information governance statement
London School of Economics and Political Science is committed to handling all personal information in line with the UK Data Protection Act (2018) and the General Data Protection Regulation (EU GDPR) 2016/679. Under the Data Protection legislation, London School of Economics and Political Science is the Data Processor, and we process personal data in accordance with their instructions. You can find out more about how we handle personal data, including how to exercise your individual rights here https://info.lse.ac.uk/staff/divisions/Secretarys-Division/Information-Rights-and-Management/Making-Requests-For-Your-Information-Subject-Access-Requests
Department of Health and Social Care disclaimer
This publication presents independent research commissioned by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by the interviewees in this publication are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, MRC, NIHR Coordinating Centre, the HSDR programme or the Department of Health and Social Care.
This monograph was published based on current knowledge at the time and date of publication. NIHR is committed to being inclusive and will continually monitor best practice and guidance in relation to terminology and language to ensure that we remain relevant to our stakeholders.
Disclaimers
This article presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care.
References
- Leu A, Guggiari E, Phelps D, Magnusson L, Nap HH, Hoefman R, et al. Cross-national analysis of legislation, policy and service frameworks for adolescent young carers in Europe. J Youth Stud 2022;25:1215-35.
- Becker S. Global perspectives on children’s unpaid caregiving in the family: Research and policy on ‘young carers’ in the UK, Australia, the USA and Sub-Saharan Africa. Global Social Policy 2007;7:23-50.
- Nagl-Cupal M, Daniel M, Koller MM, Mayer H. Prevalence and effects of caregiving on children. J Adv Nurs 2014;70:2314-25. https://doi.org/10.1111/jan.12388.
- Joseph S, Sempik J, Leu A, Becker S. Young carers research, practice and policy: an overview and critical perspective on possible future directions. Adolesc Res Rev 2020;5:77-89. https://doi.org/10.1007/s40894-019-00119-9.
- Her Majesty’s Government . Carers’ (Recognition and Services) Act 1995 n.d. https://www.legislation.gov.uk/ukpga/1995/12/introduction/enacted (accessed 13 October 2023).
- Her Majesty’s Government . Care Act 2014 n.d. http://www.legislation.gov.uk/ukpga/2014/23/contents/enacted/ (accessed 13 October 2023).
- Her Majesty’s Government . Children and Families Act 2014 n.d. https://www.legislation.gov.uk/ukpga/2014/6/contents/enacted (accessed 13 October 2023).
- Becker F, Becker S. Young Adult Carers in the UK: Experiences, Needs and Services for Carers Aged 16-24. Princess Royal Trust for Carers; 2008.
- Sempik J, Becker S. Young Adult Carers and Employment. London: Carers Trust; 2014.
- Her Majesty’s Government . Children Act 1989 n.d. https://www.legislation.gov.uk/ukpga/1989/41/ (accessed 13 October 2023).
- Her Majesty’s Government . The Children Act 2004 n.d. https://www.legislation.gov.uk/ukpga/2004/31/ (accessed 13 October 2023).
- Her Majesty’s Government . Carers (Equal Opportunities) Act 2004 n.d. https://www.legislation.gov.uk/ukpga/2004/15/ (accessed 13 October 2023).
- House of Commons . Care Act 2014. Explanatory Notes 2015. https://www.legislation.gov.uk/ukpga/2014/23/pdfs/ukpgaen_20140023_en.pdf (accessed 13 October 2023).
- Gowen S, Hart C, Sehmar P, Wigfield A. ‘It takes a lot of brain space’: understanding young carers’ lives in England and the implications for policy and practice to reduce inappropriate and excessive care work. Child Soc 2022;36:118-36. https://doi.org/10.1111/chso.12488.
- NHS . The NHS Long Term Plan 2019. https://www.longtermplan.nhs.uk/publication/nhs-long-term-plan/ (accessed 13 October 2023).
- Wayman S, Raws P, Leadbitter H. There’s Nobody is There–no One Who Can Actually Help? The Challenges of Estimating the Number of Young Carers and Knowing How to Meet Their Needs. London: The Children’s Society; 2016.
- Brimblecombe N, Stevens M, King D, Knapp M. The role of formal care services in supporting young people who provide unpaid care in England. J Youth Stud 2022;25:1-16.
- Her Majesty’s Government . Health and Care Act 2022 n.d. https://www.legislation.gov.uk/ukpga/2022/31/ (accessed 13 October 2023).
- NHS England . Core20PLUS5 – An Approach to Reducing Healthcare Inequalities 2022. https://www.england.nhs.uk/about/equality/equality-hub/national-healthcare-inequalities-improvement-programme/core20plus5/ (accessed 13 October 2023).
- Brimblecombe N, Knapp M, King D, Stevens M, Cartagena Farias J. The high cost of unpaid care by young people: health and economic impacts of providing unpaid care. BMC Public Health 2020;20. https://doi.org/10.1186/s12889-020-09166-7.
- Office for National Statistics . Unpaid Care, England and Wales: Census 2021 2023. https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/healthandwellbeing/bulletins/unpaidcareenglandandwales/census2021#unpaid-care-in-england-and-wales (accessed 13 October 2023).
- Scottish Government . Young Carers: Review of Research and Data. Scottish Government 2017. https://www.gov.scot/binaries/content/documents/govscot/publications/research-and-analysis/2017/03/young-carers-review-research-data/documents/00514848-pdf/00514848-pdf/govscot%3Adocument/00514848.pdf (accessed 13 October 2023).
- Lacey RE, Xue B, McMunn A. The mental and physical health of young carers: a systematic review. Lancet Public Health 2022;7:e787-96. https://doi.org/10.1016/S2468-2667(22)00161-X.
- Me-We . Enabling Young Carers to Pursue Their Goals in Life and Reach Their Full Potential: Converting Research Findings into Policy Actions 2019. https://carers.org/downloads/resources-pdfs/me-we/enabling-young-carers-to-pursue-their-goals-in-life-and-reach-their-full-potential.pdf (accessed 13 October 2023).
- Cheesbrough S, Harding C, Taylor L, Public K, Jo W, Young A. London: Department of Education; 2017.
- Sempik J, Becker S. Young Adult Carers and Employment. Carers Trust London; 2014.
- Leadbitter H, Goold L. Shaping our Future. The Childrens Society; 2020.
- Department of Health & Social Care . Carers Action Plan 2018-2020 - Supporting Carers Today 2018. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/713781/carers-action-plan-2018-2020.pdf (accessed 13 October 2023).
- Moore T, McArthur M. We’re all in it together: supporting young carers and their families in Australia. Health Soc Care Community 2007;15:561-8. https://doi.org/10.1111/j.1365-2524.2007.00719.x.
- Richardson K, Jinks A, Roberts B. Qualitative evaluation of a young carers’ initiative. J Child Health Care 2009;13:150-60.
- Ronicle J, Kendall S. Improving Support for Young Carers--Family Focused Approaches 2011. https://anti-bullyingalliance.org.uk/sites/default/files/uploads/attachments/Ronicle%20%26%20Kendall%20%282010%29%20family%20focused%20interventionpdf_0.pdf (accessed 13 October 2023).
- Phelps D. Commissioning Services for Young Carers and Their Families. London: Carers Trust; 2012.
- Whitley J, Wooldridge R. Sheffield Young Carers Project – Family Project Evaluation. Ecorys; 2017.
- Schlarmann JG, Metzing-Blau S, Schnepp W. Implementing and evaluating the first german young-carers project: intentions, pitfalls and the need for piloting complex interventions. Open Nurs J 2011;5:38-44. https://doi.org/10.2174/1874434601105010038.
- Hafting M, Gullbrå F, Anderssen N, Rørtveit G, Smith-Sivertsen T, van Doesum K. Overcoming clinician and parent ambivalence: general practitioners’ support of children of parents with physical or mental illness and/or substance abuse. Front Psychiatry 2019;9.
- Advisory Council on the Misuse of Drugs . Hidden Harm: Responding to the Needs of Children of Problem Drug Users 2003. https://lx.iriss.org.uk/sites/default/files/resources/130.%20Hidden%20Harm%20-20Responding%20to%20the%20Needs%20of%20Children%20of%20Problem%20Drug%20Users.pdf (accessed 13 October 2023).
- Eley S. ‘If they don’t recognize it, you’ve got to deal with it yourself’: gender, young caring and educational support. Gend Educ 2004;16:65-7. https://doi.org/10.1080/0954025032000170345.
- McGibbon M, Spratt T, Davidson G. Young carers in Northern Ireland: perceptions of and responses to illness and disability within the family. Br J Soc Work 2019;49:1162-79.
- Mesie J. A Better Relationship with Learning: An Evaluation of the Young Carers in Schools Programme. Coram; 2018.
- Gellatly J, Bee P, Kolade A, Hunter D, Gega L, Callender C, et al. Developing an intervention to improve the health related quality of life in children and young people with serious parental mental illness. Front Psychiatry 2019;10.
- Matzka M, Nagl‐Cupal M. Psychosocial resources contributing to resilience in Austrian young carers—a study using photo novella. Res Nurs Health 2020;43:629-39.
- Gettings S, Franco F, Santosh PJ. Facilitating support groups for siblings of children with neurodevelopmental disorders using audio-conferencing: a longitudinal feasibility study. Child Adolesc Psychiatry Ment Health 2015;9:1-15.
- Eccleston C, Blyth FM, Dear BF, Fisher EA, Keefe FJ, Lynch ME, et al. Managing patients with chronic pain during the COVID-19 outbreak: considerations for the rapid introduction of remotely supported (eHealth) pain management services. Pain 2020;161:889-93.
- Stevens M, Cartagena Farías J, Mindel C, D’Amico F, Evans-Lacko S. Pilot evaluation to assess the effectiveness of youth peer community support via the Kooth online mental wellbeing website. BMC Public Health 2022;22. https://doi.org/10.1186/s12889-022-14223-4.
- Leu A, Frech M, Jung C. Young carers and young adult carers in Switzerland: caring roles, ways into care and the meaning of communication. Health Soc Care Community 2018;26:925-34.
- McDougall E, O’Connor M, Howell J. ‘Something that happens at home and stays at home’: an exploration of the lived experience of young carers in Western Australia. Health Soc Care Community 2018;26:572-80.
- Moore T, McArthur M, Noble-Carr D. Different but the same? Exploring the experiences of young people caring for a parent with an alcohol or other drug issue. J Youth Stud 2011;14:161-77. https://doi.org/10.1080/13676261.2010.522561.
- Coles AR, Pakenham KI, Leech C. Evaluation of an intensive psychosocial intervention for children of parents with multiple sclerosis. Rehabilitation Psychology 2007;52.
- Cunningham LC, Shochet IM, Smith CL, Wurfl A. A qualitative evaluation of an innovative resilience‐building camp for young carers. Child Fam Soc Work 2017;22:700-10.
- Kavanaugh MS, Cho Y, Fee D, Barkhaus PE. Skill, confidence and support: conceptual elements of a child/youth caregiver training program in amyotrophic lateral sclerosis–the YCare protocol. Neurodegener Dis Manag 2020;10:231-41.
- Aldridge J. Where are we now? Twenty-five years of research, policy and practice on young carers. Crit Soc Policy 2018;38:155-65.
- Hounsell D. Hidden from View: The Experiences of Young Carers in England. London: The Children’s Society; 2013.
- Vizard P, Obolenskaya P, Burchardt T. Child poverty amongst young carers in the UK: prevalence and trends in the wake of the financial crisis, economic downturn and onset of austerity. Child Indic Res 2019;12:1831-54.
- Keigher S, Zabler B, Robinson N, Fernandez A, Stevens PE. Young caregivers of mothers with HIV: need for supports. Child Youth Serv Rev 2005;27:881-904.
- Cree VE. Worries and problems of young carers: issues for mental health. Child Fam Soc Work 2003;8:301-9.
- Thomas N, Stainton T, Jackson S, Cheung WY, Doubtfire S, Webb A. ‘Your friends don’t understand’: invisibility and unmet need in the lives of ‘young carers’. Child Fam Soc Work 2003;8:35-46. https://doi.org/10.1046/j.1365-2206.2003.00266.x.
- Lovell H, Cleaver K. The needs of young carers and the role of the school nurse. Br J Sch Nurs 2015;10:441-5.
- Bostock A. Ensuring that young carers have the support they need in school. Br J Sch Nurs 2012;7:406-7.
- Nicholls W, Patterson P, McDonald FEJ, Hulbert-Williams NJ. Unmet needs in young adults with a parent with a chronic condition: a mixed-method investigation and measure development study. Scand J Caring Sci 2017;31:191-200. https://doi.org/10.1111/scs.12320.
- Hamilton MG, Adamson E. Bounded agency in young carers’ lifecourse-stage domains and transitions. J Youth Stud 2013;16:101-17.
- Smyth C, Blaxland M, Cass B. ‘So that’s how I found out I was a young carer and that I actually had been a carer most of my life’. Identifying and supporting hidden young carers. J Youth Stud 2011;14:145-60. https://doi.org/10.1080/13676261.2010.506524.
- Millenaar JK, van Vliet D, Bakker C, Vernooij-Dassen MJFJ, Koopmans RTCM, Verhey FRJ, et al. The experiences and needs of children living with a parent with young onset dementia: results from the NeedYD study. Int Psychogeriatr 2014;26:2001-10.
- Health, Disability, and Unpaid Care: Census 2021 in England and Wales. ONS; 2023.
- McAndrew S, Warne T, Fallon D, Moran P. Young, gifted, and caring: a project narrative of young carers, their mental health, and getting them involved in education, research and practice. Int J Ment Health Nurs 2012;21:12-9.
- Mills H. Meeting the Needs of Black and Minority Ethnic Young Carers. Barnardo’s; 2003.
- Warren J. Young carers: Conventional or exaggerated levels of involvement in domestic and caring tasks?. Child Soc 2007;21:136-46.
- National Centre for Social Research . Identification Practice of Young Carers in England – Review, Tips and Tools 2019. https://carers.org/downloads/resources-pdfs/identification-practice-of-young-carers-in-england/identification-practice-of-young-carers-in-england-review-tips-and-tools.pdf (accessed 13 October 2023).
- Obadina S. Parental mental illness: effects on young carers. Br J Sch Nurs 2010;5:135-9. https://doi.org/10.12968/bjsn.2010.5.3.47459.
- Butler AH, Astbury G. The caring child: an evaluative case study of the Cornwall Young Carers project. Child Soc 2005;19:292-303.
- Warhurst A, Bayless S, Maynard E. Teachers’ perceptions of supporting young carers in schools: identifying support needs and the importance of home–school relationships. Int J Environ Res Public Health 2022;19.
- Medforth N. Our unified voice to implement change and advance the view of young carers and young adult carers.’ an appreciative evaluation of the impact of a national young carer health champions programme. Soc Work Public Health 2022;37:581-98.
- Shah R, Hatton C. Caring Alone: Young Carers in South Asian Communities. Barnardo’s; 1999.
- Olsen R. Families under the microscope: parallels between the young carers debate of the 1990s and the transformation of childhood in the late nineteenth century. Child Soc 2000;14:384-94.
- Twigg J. Caring for Frail Elderly People: Policies in Evolution. Vol 19. Paris, France: OECD; 1996.
- Purcal C, Hamilton M, Thomson C, Cass B. From assistance to prevention: categorizing young carer support services in australia, and international implications. Soc Policy Adm 2012;46:788-806. https://doi.org/10.1111/j.1467-9515.2011.00816.x.
- Twigg J, Atkin K. Carers Perceived: Policy and Practice in Informal Care. Buckingham, UK: Open University Press; 1994.
- Andersen R, Newman JF. Societal and individual determinants of medical care utilization in the United States. Milbank Q 2005;83:95-124. https://doi.org/10.1111/j.1468-0009.2005.00428.x.
- Andersen R, Davidson P, Baumeister S. Changing the U.S. Health Care System: Key Issues in Health Services Policy and Management. New Jersey, US: Jossey-Bass; 2013.
- Lederle M, Tempes J, Bitzer EM. Application of Andersen’s behavioural model of health services use: a scoping review with a focus on qualitative health services research. BMJ Open 2021;11:e045018-13. https://doi.org/10.1136/bmjopen-2020-045018.
- Travers JL, Hirschman KB, Naylor MD. Adapting Andersen’s expanded behavioral model of health services use to include older adults receiving long-term services and supports. BMC Geriatr 2020;20:1-16. https://doi.org/10.1186/s12877-019-1405-7.
- Floridi G, Carrino L, Glaser K. Socioeconomic inequalities in home-care use across regional long-term care systems in Europe. J Gerontol B Psychol Sci Soc Sci 2021;76:121-32. https://doi.org/10.1093/geronb/gbaa139.
- Bradley EH, McGraw SA, Curry L, Buckser A, King KL, Kasl SV, et al. Expanding the Andersen model: the role of psychosocial factors in long-term care use. Health Serv Res 2002;37:1221-42. https://doi.org/10.1111/1475-6773.01053.
- Sørensen K, van den Broucke S, Fullam J, Doyle G, Pelikan J, Slonska Z, et al. (HLS-EU) Consortium Health Literacy Project European . Health literacy and public health: a systematic review and integration of definitions and models. BMC Public Health 2012;12. https://doi.org/10.1186/1471-2458-12-80.
- Reducing Health Inequalities through New Models of Care: A Resource for Vanguards. UCL Institute of Health Equity; 2018.
- Rose HD, Cohen K. The experiences of young carers: a meta-synthesis of qualitative findings. J Youth Stud 2010;13:473-87. https://doi.org/10.1080/13676261003801739.
- Department of Health . Developing Services for Carers and Families of People With Mental Illness 2002.
- Bryman A. Social Research Methods. Oxford: Oxford University Press; 2016.
- Hildebrandt E. Focus groups and vulnerable populations. Insight into client strengths and needs in complex community health care environments. Nurs Health Care Perspect 1999;20:256-9.
- Kitzinger J. Qualitative research: introducing focus groups. BMJ (Clinical Research ed.) 1995;311:299-302.
- Gorin S, Baginsky M, Moriarty J, Manthorpe J. ‘She made you feel like there’s hope’: gaining a better understanding of how children negotiate their relationships with social workers from their own accounts. Br J Soc Work 2021;51:3135-52. https://doi.org/10.1093/bjsw/bcaa148.
- Stewart DW, Shamdesani PM. Focus Groups: Theory and Practice. SAGE Publications Ltd; 2015.
- Health Research Authority (HRA) . Research Involving Children 2021. https://www.hra.nhs.uk/planning-and-improving-research/policies-standards-legislation/research-involving-children/ (accessed 13 October 2023).
- Moore T, McArthur M, Noble-Carr D. Little voices and big ideas: lessons learned from children about research. Int J Qual Methods 2008;7:77-91. https://doi.org/10.1177/160940690800700205.
- Bloor M. Focus Groups in Social Research. London: SAGE Publications Ltd; 2001.
- QSR International Pty Ltd . NVivo (Version 12) 2018. https://www.qsrinternational.com/nvivo-qualitative-data-analysis-software/home (accessed 13 October 2023).
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77-101. https://doi.org/10.1191/1478088706qp063oa.
- Braun V, Clarke V. One size fits all? What counts as quality practice in (reflexive) thematic analysis?. Qual Res Psychol 2021;18:328-52. https://doi.org/10.1080/14780887.2020.1769238.
- Coleman N, Sykes W, Groom C. Peer Support and Children and Young People’s Mental Health: Research Review. London: Department for Education; 2017.
- Think Local Act Personal . Delivering Care and Support Planning 2015. https://www.thinklocalactpersonal.org.uk/_assets/Resources/SDS/TLAPCareSupportPlanning.pdf (accessed 15 February 2023; 13 October 2023).
- Lovell K, Bee P, Bower P, Brooks H, Cahoon P, Callaghan P, et al. Training to enhance user and carer involvement in mental healthcare planning: the EQUIP research programme including a cluster RCT. Programme Grants for Applied Research 2019;7:1-140. https://doi.org/10.3310/pgfar07090.
- Henner Spierling K, Tahta-Wraith K, Kulikowska H, Cunnane D. Family Therapy - New Intervention Programs and Researches. IntechOpen; 2019.
- Early Intervention Foundation . Family Group Conferencing, Camden 2018. https://www.eif.org.uk/resource/family-group-conferencing-camden (accessed 15 February 2023; 13 October 2023).
- Anna Freud Centre . Evaluation Report for the Evaluation of Kidstime Workshops (2010-2011) 2014. https://www.ucl.ac.uk/evidence-based-practice-unit/sites/evidence-based-practice-unit/files/pub_and_resources_project_reports_kidstime_report.pdf (accessed 15 February 2023; 13 October 2023).
- Institute of Public Care . Review of Team Around the Family Arrangements Final Report 2013. https://ipc.brookes.ac.uk/files/publications/Swansea_TAF_Review_Final_Report_December_2013.pdf (accessed 13 October 2023).
- Curtis L, Burns A. Unit Costs of Health and Social Care 2020. PSSRU; 2020.
- Dayson C, Bashir N. The Social and Economic Impact of the Rotherham Social Prescribing Pilot: Main Evaluation Report. Sheffield: Sheffield Hallam University; 2014.
- Rice B. The Case for a Mental Health Support Team in Every School. Barnardo’s; 2022.
- Gomez R. Place2Be’s One-to-One Counselling Service in UK Primary Schools: An Updated Cost-Benefit Analysis 2022. https://www.place2be.org.uk/media/esfjzc3f/pro-bono-economics-report-place2be-2022.pdf (accessed 13 October 2023).
- Grant G, Repper J, Nolan M. Young people supporting parents with mental health problems: experiences of assessment and support. Health Soc Care Community 2008;16:271-81. https://doi.org/10.1111/j.1365-2524.2008.00766.x.
- Stevens M, Brimblecombe N. What can the experiences of young adult carers tell us about what can make services more helpful for them and their families?. J Youth Stud 2021;25:1182-98. https://doi.org/10.1080/13676261.2021.1945562.
- Elf M, Skärsäter I, Krevers B. ‘The web is not enough, it’s a base’ – an explorative study of what needs a web-based support system for young carers must meet. Inform Health Soc Care 2011;36:206-19. https://doi.org/10.3109/17538157.2011.553298.
- House of Lords Select Committee . Children and Families Act 2014: A Failure of Implementation 2022.
- Md. Nawi NH, Megat Ahmad PH, Malek DA, Cosmas G, Ibrahim H, Voo P, et al. Structural relationship between emotional and social support for young adult carers towards intergenerational care of the multi-ethnic elderly. Qual Ageing Older Adults 2017;18:188-200. https://doi.org/10.1108/QAOA-05-2017-0015.
- Crossroads, The Princess Royal Trust for Carers . Economic Evaluation of Young Carers’ Interventions 2008. http://docs.scie-socialcareonline.org.uk/fulltext/026360.pdf (accessed 13 October 2023).
- Zechmeister-Koss I, Strohmaier C, Hölzle L, Bauer A, Goodyear M, Christiansen H, et al. Economic evaluation of family-focused programs when parents have a mental health problem: methodological considerations. Value Health 2022;26:704-11. https://doi.org/10.1016/j.jval.2022.11.016.
- Skivington K, Matthews L, Simpson SA, Craig P, Baird J, Blazeby JM, et al. A new framework for developing and evaluating complex interventions: update of Medical Research Council guidance. BMJ 2021;374. https://doi.org/10.1136/bmj.n2061.
- Department of Health . Care and Support Statutory Guidance: Issued under the Care Act 2014 2014.
- Her Majesty’s Government . Care Act 2014 Explanatory Notes 2014. http://www.legislation.gov.uk/ukpga/2014/23/notes/contents (accessed 13 October 2023).
- Directors of Children’s and Adult Social Services . No Wrong Doors: Working Together to Support Young Carers and Their Families 2016. https://www.local.gov.uk/sites/default/files/documents/no-wrong-doors-working-to-27d.pdf (accessed 13 October 2023).
- Wenger E, McDermott R, Snyder WM. Cultivating Communities of Practice. Massachusetts, US: Harvard Business School Press; 2002.
- Millen DR, Fontaine MA, Muller MJ. Understanding the benefit and costs of communities of practice. Commun ACM 2002;45:69-73.
- Le May A. Communities of Practice in Health and Social Care. New Jersey, US: Wiley-Blackwell; 2008.
- Adedoyin AC. Deploying virtual communities of practice as a digital tool in social work: a rapid review and critique of the literature. Soc Work Educ 2016;35:1-14. https://doi.org/10.1080/02615479.2016.1154660.
- Shaw L, Jazayeri D, Kiegaldie D, Morris ME. Implementation of virtual communities of practice in healthcare to improve capability and capacity: a 10-year scoping review. Int J Environ Res Public Health 2022;19. https://doi.org/10.3390/ijerph19137994.
- Romero-Mas M, Gómez-Zúñiga B, Cox AM, Ramon-Aribau A. Designing virtual communities of practice for informal caregivers of Alzheimer’s patients: an integrative review. Health Informatics J 2020;26:2976-91. https://doi.org/10.1177/1460458220950883.
- McLoughlin C, Patel KD, O’Callaghan T, Reeves S. The use of virtual communities of practice to improve interprofessional collaboration and education: findings from an integrated review. J Interprof Care 2018;32:136-42. https://doi.org/10.1080/13561820.2017.1377692.
- McLaughlan T. Facilitating factors in cultivating diverse online communities of practice: a case of international teaching assistants during the COVID-19 crisis. Int J Inf Learn Technol 2021;38:177-95. https://doi.org/10.1108/IJILT-05-2020-0074.
- Lave J, Wenger E. Situated Learning: Legitimate Peripheral Participation. Cambridge, UK: Cambridge University Press; 1991.
- Roberts J. Limits to communities of practice. J Manage Stud 2006;43:623-39. https://doi.org/10.1111/j.1467-6486.2006.00618.x.
- Nicolini D, Pyrko I, Omidvar O, Spanellis A. Understanding communities of practice: taking stock and moving forward. Acad Manag Ann 2022;16:680-718. https://doi.org/10.5465/annals.2020.0330.
- Joseph S, Becker S, Becker F, Regel S. Assessment of caring and its effects in young people: development of the multidimensional assessment of caring activities checklist (MACA-YC18) and the positive and negative outcomes of caring questionnaire (PANOC-YC20) for young carers. Child Care Health Dev 2009;35:510-20. https://doi.org/10.1111/j.1365-2214.2009.00959.x.
- Department of Health . Mental Health Act 1983 Code of Practice 2015.
- HM Government . The Young Carers (Needs Assessments) Regulations 2015 2015.
- Department of Health and Social Care . People At The Heart Of Care. Adult Social Care Reform White Paper 2021.
- Department for Education . Keeping Children Safe in Education 2023 2023.
- Macleod SH, Elliott L, Brown R. What support can community mental health nurses deliver to carers of people diagnosed with schizophrenia? Findings from a review of the literature. Int J Nurs Stud 2011;48:100-20. https://doi.org/10.1016/j.ijnurstu.2010.09.005.
- Kane CF, DiMartino E, Jimenez M. A comparison of short-term psychoeducational and support groups for relatives coping with chronic schizophrenia. Arch Psychiatr Nurs 1990;4:343-53. https://doi.org/10.1016/0883-9417(90)90024-F.
- Brooker C, Falloon I, Butterworth A, Goldberg D, Graham-Hole V, Hillier V. The outcome of training community psychiatric nurses to deliver psychosocial intervention. Br J Psychiatry 1994;165:222-30. https://doi.org/10.1192/bjp.165.2.222.
- Addington J, McCleery A, Addington D. Three-year outcome of family work in an early psychosis program. Schizophr Res 2005;79:107-16. https://doi.org/10.1016/j.schres.2005.03.019.
- Forster A, Brown L, Smith J, House A, Knapp P, Wright JJ, et al. Information provision for stroke patients and their caregivers. Cochrane Database Syst Rev 2012;11.
- O’Brien BC, Harris IB, Beckman TJ, Reed DA, Cook DA. Standards for reporting qualitative research: a synthesis of recommendations. Acad Med 2014;89:1245-51. https://doi.org/10.1097/ACM.0000000000000388.
Appendix 1
| Title (and country in which legislation/policy is applicable) | Provision for young carers |
|---|---|
| The 1983 Mental Health Act Code of Practice (England)132 |
|
| The 1989 Children Act10 (England, Northern Ireland, Scotland, Wales) |
|
| The 1995 Carers’ (Recognition and Services) Act5 (England, Scotland, Wales) |
|
| The 2004 Children Act11 and 2004 Carers (Equality of Opportunity) Act12 (England, Wales) |
|
| The 2014 Care and Support Act6 (England) |
|
| The 2014 Care and Support Act statutory guidance13 (England) |
|
| The 1989 Children Act (as modified by the 2014 Children and Families Act)7 (England) |
|
| No Wrong Doors: working together to support young carers and their families (2015) (England)119 | Promoted collaboration between adult and children’s social care services and enhanced partnership working with health and third sector partners. Recommended that the following key principles underpin practice:
|
| Young Carers (Needs Assessments) Regulations 2015 (England)133 |
|
| Carers Action Plan 2018–2019 (England) |
|
| NHS Long Term Plan 201915 (England) |
|
| People at the Heart of Care: Adult Social Care Reform White Paper 2021 (England)134 |
|
| The 2022 Health and Care Act18 (England) |
|
| Keeping Children Safe in Education 2022 – Statutory guidance for schools and colleges (England)135 |
|
| NHS England, Core20PLUS5 202219 (England) |
|
Appendix 2
| Area description | Evidence on costs | Evidence on benefits |
|---|---|---|
| Co-developed support planning | See Lovell et al. 2019100 for costings re. training intervention for health professionals in community mental health teams. Personalised care and support planning summary guide (Think Local Act Personal, 2015, Appendix 1): |
Lovell et al.100 co-developed and co-delivered a training intervention which aimed to enhance service user and carer involvement in care planning. There were high levels of satisfaction with the training, but there was no evidence that the costs or health benefit differed between the intervention and the control. Costs included the costs of healthcare professionals’ time to attend the training, the trainers’ time to deliver the training, consumables and room hire. Unit costs were applied where relevant and costs refer to cost year 2015/2016. Costs of delivery were set against any gains in QALYs. Overall, the training intervention was associated with a net loss of £54, with a net quality-QALY loss of −0.014. |
|
||
| Whole-family approach (including family conferences, disabled parent protocol, memoranda of understanding, KidsTime) | Evaluation of the KidsTime programme delivered by the Anna Freud Centre in Hackney, Camden and Islington in 2010 and 2011: Average annual cost of a monthly workshop in each site was about £14,000 per year, which included staff costs (drama facilitator and family workers), venue hire and transportation costs for attendees103 Henner Spierling et al. (2019)101 found that the annual costs per family in England to take part in a monthly KidsTime workshop was approximately £2000. An initial assessment, prior to any intervention taking place by CAMHS cost £700 per child. Early Intervention Foundation, 2018:101 Camden borough estimated that a standard family group Conference costs about £1200–£1500 including the review but not the referral process. Institute of Public Care (2013)104 reviewed a Team Around the Family programme in Swansea (costings refer to a single case/family): |
KidsTime provides a context where issues around mental health can be discussed without a family/parent being exposed. Families can hear both positive and ‘corrective’ responses from others. Groups also allow for a range of activities and exercises.103 Early Intervention Foundation, 2018:102 Families reported feeling empowered by the family group conference process and described ways in which it had helped boost their confidence and self-esteem. Early Intervention Foundation, 2018:102 reported that 79% of families who had an early-help family group conference did not receive further early help or social work intervention within 12 months of closure. This percentage was similar (83%) for those families receiving formal early-help casework. Whitley (2017):33 Sheffield Young Carers Family Project – the 90 families involved in the project indicated a positive experience. There was a combination of dedicated family support and opportunities for social activities. While not about young carers, a review by MacLeod et al. (2011)136 of interventions for carers of people diagnosed with schizophrenia reported that people experiencing whole-family interventions reported reduced depression,137 improved general health,138 and improved wellbeing.139 |
|
||
| Signposting and information for example community navigators, link workers, health champions, social prescribing | Unit Costs of Health and Social Care,105 Rotherham Social Prescribing pilot: commissioned by NHS Rotherham as part of a GP-led Integrated Case Management Pilot and delivered by Voluntary Action Rotherham. The pilot was funded for two years from April 2012 to March 2014, at a total cost of £1M. This consisted of grants given to twenty-four VCOs, which delivered 31 distinct social prescribing services. A total of 1607 patients were referred to the service and the five most common types of referral were: |
Total NHS cost reductions by the end of the pilot was £552,000; a return on investment of 50 pence for each pound. There were also potential cost reductions of £415,000 in the first year of post-referral when the service was running at full capacity105 If the benefits identified were sustained over a longer period, the authors estimated that costs of delivering the service for a year would be recouped after 18–24 months. Moreover, for each year of delivery, they estimated that five-year cost reductions could be as high as £1.9M, a return on investment of £3.38 for each pound. Even if the benefits of the pilot dropped off each year at a rate of 33%, they could still lead to total cost reductions of £807,000, a return-on-investment of £1.41 for each pound105 There is evidence that information improves patient/carer knowledge, patient satisfaction and reduces patient depression scores.140 |
|
||
| The average cost per person per year was £177, with VCO excluded. Including VCO grants, the average cost was £398 per person per year. For a person referred on to funded VCOs, the average cost was £570. (All costs have been updated to 2019/2020 levels using Prospective Payment System inflators).105 Total health and social care costs over 1 year for patients whose carers received intervention were significantly lower (−£4043, 95% CI −£1595 to −£6544).140 |
||
| Designated person in schools | The Place2Be counselling programme, offered in primary schools in England, costs £1100 per child on average per year but it generates about £8 in benefits for every £1 spent.108 | The Place2Be counselling programme generates benefits of £36M each year. Children receiving one-to-one counselling had an average 3.5-point reduction in their SDQ score, of which the authors reported that an average 2.1-point score reduction is likely to be attributable to the Place2Be programme.108 |
List of abbreviations
- BMHSU
- Behavioral Model of Health Services Use
- CAMHS
- Child and Adolescent Mental Health Services
- CI
- confidence interval
- DBS
- Disclosure and Barring Service
- GDPR
- General Data Protection Regulation
- GP
- general practitioner
- HRA
- Health Research Authority
- NHS
- National Health Service
- PIP
- Personal Independence Payments
- QALY
- quality-adjusted life-year
- REBIAS-YC
- reducing barriers and improving support for young carers
- YCSP
- Young Carers in Schools Programme
Notes
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/ABAT6761).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
