Notes
Article history
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as award number 16/138/31. The contractual start date was in January 2021. The draft manuscript began editorial review in December 2022 and was accepted for publication in July 2023. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ manuscript and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this article.
Permissions
Copyright statement
Copyright © 2024 Newbould et al. This work was produced by Newbould et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2024 Newbould et al.
Chapter 1 Introduction
Box 1 provides a summary of Chapter 1 of this report.
Summary of key points
-
In England, the National Health Service (NHS) Long Term Plan endorsed digital ambitions for primary care, promising that patients would be able to choose digital-first options. The 2019 GP contract also included requirements for online consultations by April 2020 and video consultations by April 2021.
-
Digital First Primary Care is when a patient’s first contact with a GP is via a digital route. Digital First Primary Care might be accessed by a patient online, through a computer or a smartphone.
-
Approaches vary by provider, but the principles remain the same: a patient inputs their symptoms and concerns through a digital platform and then is given an appropriate response, which could include guidance for self-care, a suggested telephone, video or face-to-face practice appointment.
-
At the time of scoping for the project, in 2019, uptake of digital primary care was modest across England. The COVID-19 pandemic saw a rapid change in modes of service delivery in general practice, with all GP surgeries having to rapidly adapt their services to provide non-face-to-face consultations. At the time of writing, it is reported that under a third of consultations were remote.
-
There have been various shifts in policy focus in England in relation to the use of digital approaches during the pandemic. Initially, there was a directed shift to appointments via telephone or, to a lesser extent, video. As restrictions began to ease, this position changed with the increased use of face-to-face appointments.
-
These changes have taken place amidst an extremely challenging climate for general practice in England with workforce shortages and increased workloads.
What is Digital First Primary Care?
This rapid evaluation has conceptualised Digital First Primary Care as described below:
Digital First Primary Care is when a patient’s first contact with primary care is through a digital route, either through a laptop or smartphone. The patient enters details of the issue which they wish to consult a health professional about, either by completing a form or by entering a free-text narrative. The patient will then be contacted by the practice, usually on the same day, about their issue.
Practices which use this approach also provide a mechanism for access for those unable to use the digital route. Patients telephone the practice and a member of practice staff enters the information into the digital interface and the request is dealt with by the practice in the same way as it would be if the patient entered the information digitally.
Most practices enable patients to order repeat medication online; we would not define this as Digital First Primary Care, as the purpose of contact is not to see or speak to a health professional, rather to obtain medication.
The term, Digital First Primary Care, originated from an NHS programme during the COVID-19 pandemic where it was defined as follows:1
Digital First Primary Care is the name of a programme which supports the transformation of primary care by promoting the implementation, understanding and improvement of digital tools within general practice. 1
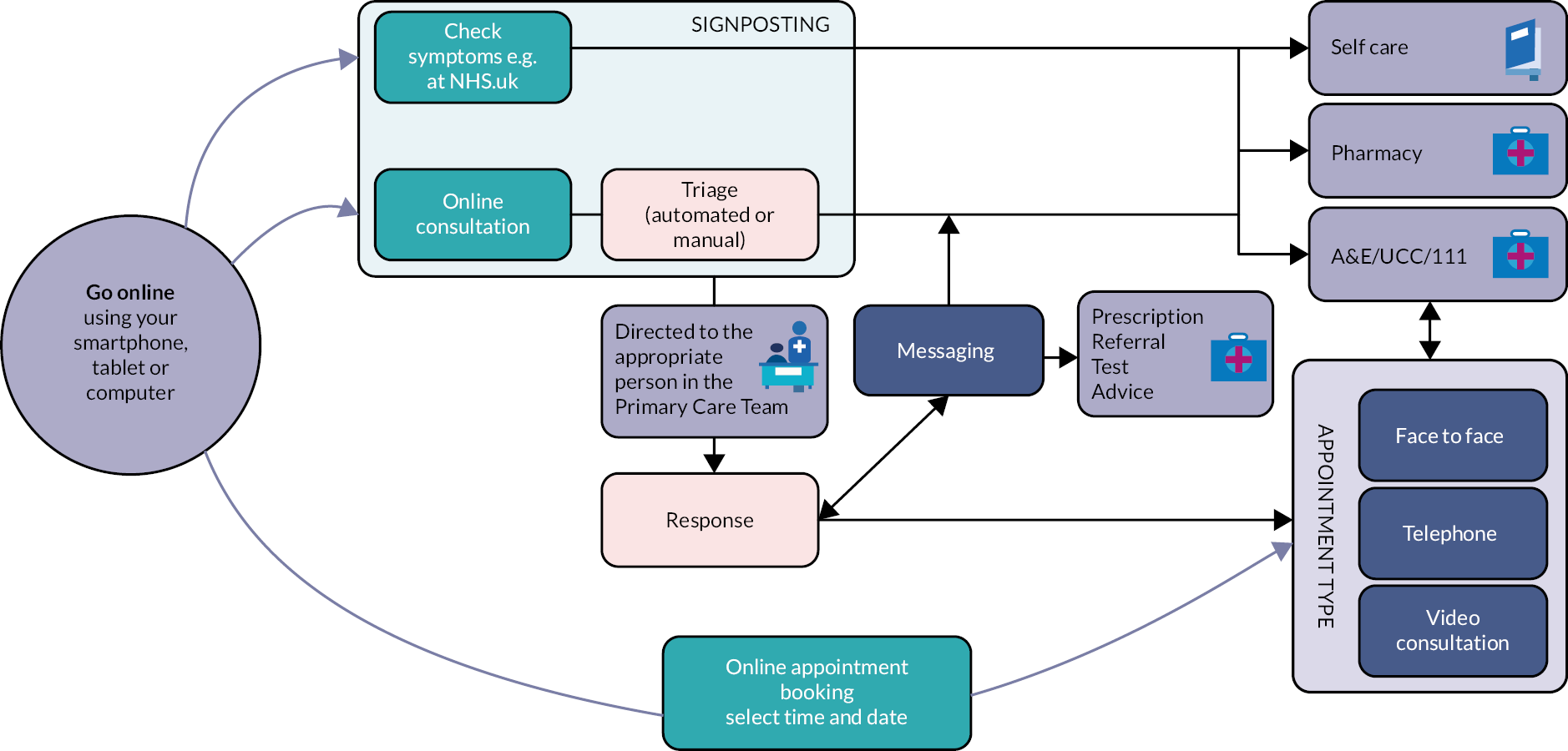
Figure 1, produced by NHS England, outlines the various patient pathways, from when a patient first contacts their practice digitally to the holding of a consultation. 1
Most general practices offer Digital First Primary Care by purchasing the approach from a commercial provider, although practices may also create the approach themselves. The design of Digital First Primary Care platforms varies by commercial provider, although the main principles are the same. The patient inputs their symptoms and concerns through a digital platform, such as a computer or smartphone, either via a set of questions within a digital algorithm or through a free-text submission. Once the information is entered, the patient is then given an appropriate response, which could be from a staff member within the practice or automatically generated by the algorithm for example an online message. This response could, for example, offer guidance for self-care, advice to attend an accident and emergency service (if the problem is deemed to be a serious one that cannot wait), a message back from a professional or a suggested telephone, video or face-to-face appointment with a general practitioner (GP) or other member of the practice team. Most models enable swift responses from practices back to patients, usually on the same day, and if a consultation is required, this is usually on the same day too. These approaches have been advocated by NHS England to enable clinicians to prioritise the care of patients in the most need. 2
Digital First Primary Care can, therefore, lead to a conventional general practice consultation style, such as a telephone consultation or face-to-face consultation, or a less traditional consultation, such as the health professional messaging the patient. Yet, the consultation is framed by the information the health professional receives ahead of the consultation, submitted through the digital route. Digital First Primary Care approaches may also enable practices to more easily provide video consultations.
Table 1 outlines the principles of the Digital First Primary Care consultation as compared to a traditional general practice system.
| Traditional appointment system | Digital First Primary Care | |
|---|---|---|
| First contact with the practice | Telephone or in-person at GP reception | Through digital platform |
| Triage and assessment | N/A (patient booked directly for appointment by reception team) | Either through digital algorithm or reviewed by health professional and digital message from the practice; patient may be referred to other services, such as self-care or pharmacy |
| Contact with health professional | Telephone or in-person | Message from health professional (digital), telephone consultation, face-to-face consultation or video consultation with health professional from the practice |
Accessing services via a digital route may mean that a patient’s experience of care differs from that of a patient accessing the practice via an alternative route, such as by telephone or by visiting a surgery. For example, messages about a person’s care might be exchanged between the patient and professional or the clinician may conduct the consultation having prior written information from the patient, for example discussing a patient’s diabetes having already received their blood-sugar readings via message, which would not be possible if the patient had not accessed care digitally.
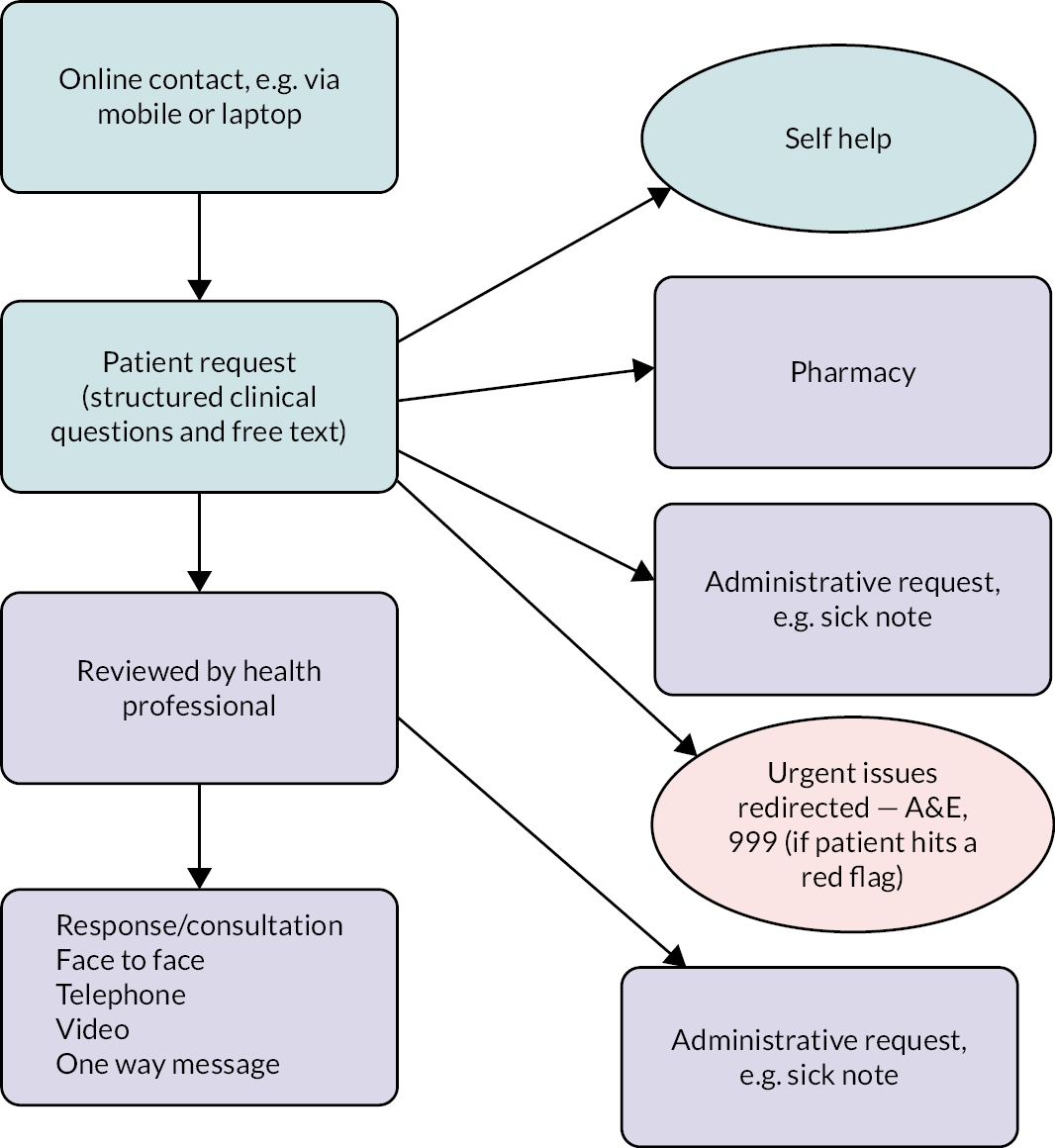
The exact nature of the Digital Frist Primary Care patient pathway depends upon the provider used, but most use either a free-text approach or an algorithm approach, Figures 2 and 3 illustrate examples of patient pathways from initial contact with the practice to the outcome, using two different approaches to Digital First Primary Care.
FIGURE 2.
Example of a Digital First Primary Care patient pathway: free-text approach.
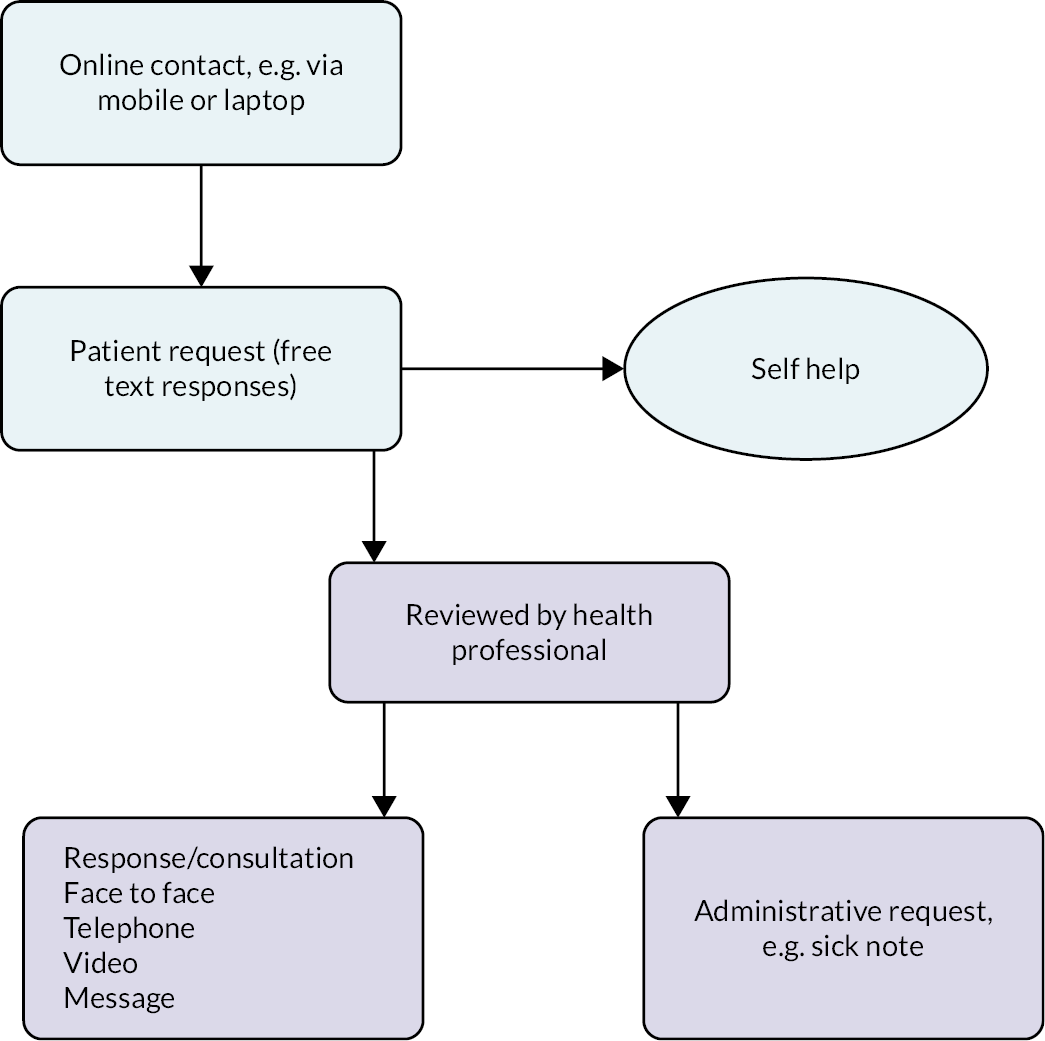
FIGURE 3.
Example of a Digital First Primary Care patient pathway: algorithmic approach.
A ‘free-text approach’ (see Figure 2) is where a patient enters the nature of their problem in the system in their own words. The patient then receives an automated response to say they will hear back from the surgery. The response is then reviewed by a healthcare professional and the response is either dealt with by the administrative team at the surgery, for example a sick note, or a response is provided by a health professional in the form of a message or consultation, by a variety of means.
An alternative approach is an algorithm approach (see Figure 3) where the patient completes an online form which asks a series of questions. The form gives the patient options to choose from, for example the part of the body that the problem is in, the duration of time they have had it. After the query has been submitted a response is automatically generated and immediately sent to the patient. This could include self-help, if the problem is deemed as not requiring a primary care health professional, or to contact a pharmacist. If the problem is considered urgent, a message is sent telling the patient to dial 999 or attend an accident and emergency department immediately. Alternatively, patients are sent a message to say a health professional from the practice will contact them.
It should be noted that the figures outline examples of ‘typical’ patient pathways for patients using these Digital First Primary Care approaches; however, the ways in which the systems have been implemented and are used in practice may vary across general practices. For example, they may have different staff responsible for dealing with requests within a practice or some practices may use messaging or photos more than others.
English policy context
Scoping for this project began in July 2019, at a time when general practices throughout England were struggling with rising demand from patients with complex health needs, more work being transferred from secondary to primary care and increasing difficulty in recruiting and retaining GPs. 3,4 The General Practice Forward View (2016) aimed to help GP practices reduce and better manage their workload and the increased use of digital technologies was advocated. 4 The digital ambition for primary care was further endorsed in the NHS Long Term Plan (2019), which set out a target that, within the next 10 years, the NHS would offer a ‘Digital First’ option in primary care for most patients,5 with the aim that this would enable ‘longer and richer face-to-face consultations with clinicians where patients want or need it’. 5 More specifically, the plan set out a milestone that every patient in England would be able to access a Digital First Primary Care offer by 2023/24. 5 The 5-year framework for GP contract reform also reflected this policy shift towards digital approaches, including a requirement that practices should ensure that all patients have the right to Digital First Primary Care, including online consultations, by April 2020 and consultations via video by April 2021, with the aim to provide this access as quickly as possible. 6
Despite the increasing policy shift towards digital approaches, most GP surgeries were not operating in this way in early 2020, with an analysis of primary care data suggesting that 13–15% of consultations were conducted remotely in January 2020. 7 Wider studies suggest that factors such as a lack of training, inadequate technology and concerns about issues such as inequity of access, safety and workload limited the use of alternative approaches to face-to-face consultations, as well as low patient uptake in practices where digital approaches had been adopted. 8–10
The impact of COVID-19 on Digital First Primary Care
The COVID-19 pandemic saw a rapid change in modes of service delivery in general practice, with all GP surgeries having to rapidly adapt their services to provide non-face-to-face consultations, which could be supported by digital platforms. At the time of scoping for this project in 2019, the uptake of digital primary care was modest across England. In response to the COVID-19 outbreak, general practices had to quickly adapt their ways of working to reduce footfall in GP surgeries, protecting patients and staff from infection. 11
It was noted by providers that there was a dramatic increase in the adoption of Digital First approaches in primary care in response to COVID-19, although there are no publicly available data. Data are available, however, on the use of other forms of consultation. An analysis by The Health Foundation suggested that remote consultations increased from < 20% to > 50–60% of all consultations at the peak of the first national lockdown. 7 This trend appears to have continued, with further analysis conducted by the Health Foundation demonstrating that March 2021 saw the highest number of telephone appointments ever, at 11.4 million compared to 3.5 million in March 2019. 12 More recently, in 2022, the British Medical Association (BMA)13 reported that the ratio of face-to-face versus remote appointments has changed alongside the waves of COVID-19. In 2022, under one-third of consultations were remote, with September having the highest number of face-to-face appointments since before the pandemic. 14
When looking at specific types of digital approaches, evidence from the Health Foundation examining data from practices using one specific provider, suggested that patient preference for consultation via SMS/online messaging increased from 26% of requests before the pandemic to over a third in 2020 and 2021 and that a telephone consultation was the most popular patient preference. 15 While the majority of requests were initiated online (rather than by telephone or in person) before the pandemic, this continued to rise from 60% in June 2019 to 71.8% during 2021. 15 In addition, between March and June 2020, the use of video by patients to communicate with GP surgeries increased 50-fold compared to before the pandemic,11 although, compared to other forms of digital communication, the use of video was low and this remains the case more widely, accounting for around only 0.6% of consultations at the time of writing. 14
The impact of COVID-19 on policy and guidance in England
There have been various shifts in policy focus in relation to the use of digital approaches during the pandemic. In March 2020, all practices were written to by NHS England informing them that ‘all practices are now being advised to change face-to-face appointments booked online to triage appointments via telephone or video’. 16 Then, in a speech delivered in late July 2020, the then Health and Social Care Secretary, Matt Hancock, specified that ‘from now on, all consultations should be teleconsultations unless there’s a compelling clinical reason not to’. 17 To support this, NHS Digital provided guidance to practices about approved online consultation suppliers that could be used immediately, to enable practices to swiftly implement digital approaches.
As the easing of COVID-19 restrictions started to take place, a shift in policy and media narrative towards the availability and delivery of face-to-face appointments was noticeable. 16–18 Digital First Primary Care systems were widely procured and adopted at practice and system level during COVID-19 and made available via a Digital First Online Consultation and Video Consultation (DFOCVC) framework. A policy objective (from the NHS Long Term Plan) was therefore expedited by COVID-19. Yet, the use of online consultation and video systems remains highly variable across general practices in England due to population demographics, practice contexts and staff digital skills.
Further guidance was issued to practices in May 2021 detailing that video, online and phone consultations could be maintained, but that GP practices should ensure they offered face-to-face appointments and that patient preferences for face-to-face care should be respected,16 reversing the previous position of offering telephone or online triage before face-to-face appointments.
Later in 2021, this was followed by a plan from NHS England and NHS Improvement designed to improve access to GP appointments for patients. 17 The plan acknowledged longstanding issues around patients access to care and the subsequent need for changes in access as a result of COVID-19 and highlighted emerging challenges for practices in achieving an ideal blend of face-to-face and remote appointments. In response to these challenges, the plan laid out a range of actions to be taken to support general practice and improve access. This included a new £250 million Winter Access Fund in England, which detailed that practices that were deemed to not be providing appropriate levels of face-to-face care would not be able to access the additional funding and instead offered support to improve. 17
More recently, 2022/23 priority and operational planning guidance from NHS England and NHS Improvement asked healthcare systems to support primary care networks (PCNs) and practices to deliver the commitment to ensure that all patients have the right to be offered Digital First Primary Care by 2023/24, which would enable them to reach the right service, whether remotely or face-to-face. 18
During summer 2022, a new Digital Health and Care plan was published by the Department of Health and Social Care and NHS England, which set out priorities for digital transformation, consolidating previous commitments and ambitions. This included the development of the NHS app and website to support patient access to services, and the use of digital to support the management of long-term conditions. This noted that patients would not have to use digital services: for those who cannot or prefer not to access services digitally, traditional services would stay in place. 19
More widely, the multiple changes in emphasis and policy throughout this period were not well received by GPs. Following the guidance to return to offering face-to-face appointments, the BMA GP committee chair stated that: ‘NHSE and the Government owe practices a huge debt of gratitude, not a public rebuke for ultimately doing what they were instructed to do’ while the Chair of the Royal College of GPs explained that ‘it needs to be down to individual GP practices to be able to decide how they deliver services, based on their knowledge of their patient population’. 20
While some of the changes may only have been thought to be temporary – in place to support primary care to be able to continue providing patient care during the pandemic – it is likely that Digital First Primary Care approaches will be used to a greater extent than before the pandemic, with a blend of approaches supported in government policy. In the future, practices will likely offer a range of options and will operate in different ways, linked to their practice circumstances, set-up and the needs of their practice population. Notably, the term ‘Digital First Primary Care’ is a term that continues to evolve, as do the digital approaches adopted in general practice, such as the use of online consultations and triage systems.
Patients with multiple long-term conditions in England
In England, approximately a quarter of adults (depending on which conditions are included) have two or more long-term conditions. 21 People with multimorbidity are higher users of healthcare services, with estimates suggesting that their care needs account for over half of NHS costs, and they often have a lower quality of life and poorer life expectancy. 21,22 Continuity of care is particularly important in this patient group, given their frequent interactions with the health service. Continuity of care can help to reduce the number of times a patient needs to re-tell their story, improve relationships and trust with healthcare providers and give patients greater involvement in their own care. 23
The 2022 GP Patient Survey included questions related to digital use, and the data can be broken down by patients with long-term conditions and individuals with caring responsibilities. 24 While nearly two-thirds of both groups found it easy to use their GP practice website to find information or access services, over 40% of both groups had not used online GP services (e.g. booking appointments, ordering repeat medication or having an online consultation). Almost no patients from these groups (1–2%) had an online consultation for their last appointment, although over 40% had spoken to someone on the phone. 24
The issue of multimorbidity is prominent and is receiving consideration in NHS policy and guidance. Throughout the NHS Long Term Plan,5 multimorbidity is a key theme, with aims for the NHS to be more joined-up in its care, breaking down barriers to support people with long-term conditions. The recent Health and Care Act (2022) built on this,25 introducing significant changes to how health services are organised and delivered to support the delivery of more integrated and co-ordinated care. This is of importance in addressing challenges for those with multimorbidity who often require support from multiple organisations simultaneously, and should enable organisations to meet patient needs in a more joined up way.
The recent stocktake of primary care in the English NHS, in the form of the Fuller review,26 set out a vision for integrating primary care and bringing together general practice with other parts of the system to improve patient care. The vision was centred around three essential offers, one of which referred explicitly to providing more proactive, personalised care, including to those with multiple long-term conditions. 26 It highlighted that digital- and technology-based approaches offered solutions in providing access to and delivery of care for those who wish to use it, potentially freeing up more time for face-to-face support for those who need it most. 26
More widely, multimorbidity was also identified as a major strategic priority for the NIHR in 2021,27 with the Academy of Medical Sciences in 2018 calling for more research to address the challenge. 28
Context within English general practice at the present time
The changes described have taken place amidst an extremely challenging climate for general practice in England, with workforce shortages and increasing workload which were apparent even before the pandemic. The number of full-time equivalent, fully qualified GPs has fallen since 2015 yet GP appointment numbers are higher than they were before COVID-19,29 and the average number of patients GPs are responsible for has risen. 13 A provider poll carried out in August 2022 showed that 90% of the primary care providers who responded agreed or completely agreed that they were finding it difficult to recruit staff. 30 Yet the number of healthcare professionals in total (excluding GPs) has increased by over 6000 during the last year, in line with the government’s target to increase the number of health professionals working in general practice. 5,31 This could be linked, in part, to the Additional Roles Reimbursement Scheme, introduced in 2019 as part of the GP contract framework, to support the recruitment of 26,000 additional staff working in general practice by 2023/24 and aid an increase in the number of annual appointments in general practice. 32,33
Relatedly, the latest GP work–life survey highlighted that a third of GPs plan to leave direct patient care within 5 years, with GPs reporting the greatest stress from a range of factors including increasing workloads, long working hours and increasing patient demands. 34 Further, as a result of the pandemic, primary care professionals have been working in an uncertain and ever-shifting environment,35 and the impacts of COVID-19 on primary care were considerable,12 with the whole system now seeking to recover.
More widely, these pressures have been accompanied by negative media coverage and a narrative that general practice is ‘closed’, and less willing to see patients face-to-face. A statement from the chair of the BMA’s GP committee discussed ‘anti-GP’ rhetoric in the media following a media campaign about GP face-to-face appointments in England. 36 This was supported by a recent study, which found that newspaper coverage of remote consulting was highly negative, that remote consultations had become associated with poor practice and that some papers were ‘leading the war’ on general practice. 37
Aims of this study
This rapid evaluation originally had one distinct aim: to understand the experiences of those with multiple long-term conditions of Digital First Primary Care, from the perspectives of patients, their carers and healthcare professionals. However, due to recruitment challenges and a lack of uptake to the study from general practice, largely due to COVID-19 pressures, the focus instead was amended to the experiences of healthcare professionals and stakeholders. As a result, minor amendments were made to the research questions.
As a result of the scoping work, where relevant literature on the use of Digital First Primary Care by patients with multiple long-term conditions was engaged with and a workshop with patients [members of the BRACE patient and public involvement (PPI) group] was held, four research questions were identified by which to address this aim. 1
-
What is the experience of Digital First Primary Care for health professionals and stakeholders (including academics, policy makers and Digital First Primary Care providers), both before and during the COVID-19 pandemic?
-
What is the impact of Digital First Primary Care on the nature of consultations, from the perspective of health professionals and stakeholders, for patients with multiple long-term conditions and their carers? This includes aspects of communication, timeliness of care and continuity of care.
-
What, if any, are the advantages or disadvantages of Digital First Primary Care for health professionals when providing care for patients with multiple long-term conditions?
-
What lessons can be learnt from staff and stakeholders for future service delivery for patients with multiple long-term conditions in primary care? Are there individual groups within the community where there is particular learning for future service provision?
While in Chapter 1 we have set out a definition of Digital First Primary Care, it should be noted that, within the literature and during interviews with health professionals and stakeholders, firm distinctions and definitions were often not used.
Chapter 2 Locating the study within the wider literature
Box 2 provides a summary of Chapter 2 of this report.
Summary of key points
-
We explored key literature related to the use of Digital First Primary Care, including for patients with long-term conditions.
-
Digital First Primary Care has been subject to much research over the last decade, starting with research into telephone triage and moving towards the assessment of digital approaches as these became more commonly used.
-
While these studies identified positive aspects of using Digital First Primary Care, such as patient convenience, other evidence is mixed across studies, for example relating to GP workload.
-
While Digital First Primary Care has been the focus of much recent research, this has often not included a specific exploration of how digital approaches impact patients with multiple long-term conditions. Studies that have included patients with multiple long-term conditions specifically have identified some positive experiences of using Digital First Primary Care. However, challenges do exist, such as digital literacy, impersonal interactions and difficulties picking up on non-verbal cues. It is likely that the type, number and complexity of long-term conditions influence patients’ use and experience of Digital First Primary Care; however, there is very little research into this area.
To locate this study within the existing research and evidence on the use of Digital First Primary Care by patients, specifically those with multiple long-term conditions, we have reviewed the literature relating to this topic. Due to the complexities in the definition of Digital First Primary Care, noted in Chapter 1, a broad and inclusive approach was taken when examining the wider literature. At the start of the study, we undertook an initial pragmatic and rapid review of the relevant studies (see Box 3 for further information). While we acknowledge that there is a large literature base on the use of digital approaches in healthcare (including for specific conditions), we focused on key literature to provide context to our study, rather than providing a full systematic review of the literature.
-
Search terms used: digital, Digital First Primary Care, digital triage, COVID-19, long-term conditions and multi-morbidity.
-
Search engines used: PubMed and Google Scholar.
-
Additional searches: the reference lists of identified articles were screened for further potentially interesting references.
-
Years searched: 2011–present.
-
Searches conducted: at three points during the study (start, middle and towards the end).
-
Inclusion criteria: articles detailing the use of Digital First Primary Care in a general practice setting, either pre, during or after the COVID-19 pandemic, particularly those related to multiple long-term conditions.
-
Exclusion criteria: Articles not in the English language, studies conducted outside of the UK.
-
The findings from the identified literature were written-up in a thematic way to identify context and learning that applied to each of the research questions.
Here, we present a brief overview of the key literature related to the use and impact of Digital First Primary Care for patients (including those with long-term conditions) and healthcare professionals.
Impact of Digital First Primary Care on patients
Digital First Primary care could impact patients in a range of ways, as identified by multiple studies on this topic. Here, we discuss the impacts on patients in general and later in this section we discuss its use and impacts specifically for patients with multiple long-term conditions.
Some studies found that patient satisfaction could be high with regards to digital methods of engaging with GP practices; patients valued having multiple routes to communicate with their practice and appreciated the convenience of digital engagement (e.g. no need to travel and ability to minimise the amount of work missed). 38–43 However, other studies found more mixed evidence in relation to patient satisfaction, which could be due to differences in the digital literacy of patients and the complexity of the patient’s issue (see later). 43–45 The method of data collection for studies which explored this issue can also be a challenge (e.g. collecting data online only may skew data collection towards the views of the digitally literate, who may have more favourable views). 40
There was mixed evidence on how comfortable and confident patients felt discussing their symptoms remotely. One study found that patients had concerns around whether they could communicate their symptoms effectively remotely,40 but another found that patients may feel more confident doing this remotely. 44
There were some challenges identified in the literature for patients using digital methods of engagement with their practice. These included concerns over privacy/confidentiality, language barriers, a less holistic assessment of the patient, a heightening of inequalities, less continuity of care and the reduced quality of patient–clinician interactions. 43,44 There could also be issues with staff phoning patients at different times than they had originally specified. 42,44 One study found that one of the key issues raised by patients was the importance of respecting their time and understanding how appointments fit in with their lives. 42
Digital First Primary Care specifically for patients with long-term conditions
Few studies have been conducted that include an exploration of how Digital First Primary Care has been used specifically by patients with long-term conditions, highlighting variations in its uptake, benefits and challenges. While the focus of our study is on multiple long-term conditions, very little literature was identified in relation to this group of patients. Therefore, here, we summarise the findings from key studies exploring the use and impact of Digital First Primary Care both for patients with single and multiple long-term conditions.
The evidence is mixed as to the uptake of Digital First Primary Care for patients with multiple long-term conditions. A 2018 study found that patients with multiple long-term conditions showed higher rates of accessing alternatives to face-to-face consultations (although this group has a higher use of any type of consultation in general) than those without multiple long-term conditions. 9 However, an evaluation of Babylon GP at Hand, a primary care practice in North West London that offered Digital First approaches to primary care, found that users were likely to be healthier and that patients with more complex needs were less likely to use the service (with only 29% of users reporting that they had a long-term condition). 46 The low number of patients with long-term conditions using the service was speculated by the authors to be due to a cautionary note sent to potential users stating that those needing more frequent face-to-face appointments would need to travel to a surgery which may not be local to them; this may well have deterred those with long-term conditions from using the service.
Studies have found some benefits for patients with long-term conditions when utilising Digital First Primary Care approaches. Both the evaluation of Babylon GP at Hand and a study that explored the use of remote primary care consultations for people with dementia (and their carers) found that there was quicker access to care. 46,47 A 2021 rapid literature review exploring how patients and healthcare professionals experienced remote consultations found that they allowed for better monitoring of patients than in-person appointments. This was found to be particularly beneficial for patients with long-term conditions who could more conveniently complete tasks such as medication adjustments from home. 44 The study of patients with dementia also noted the benefits of the reduced risk of contracting and transmitting infectious diseases, such as COVID-19, when engaging remotely with primary care,47 which is particularly beneficial as patients with long-term conditions are often at high risk of worse outcomes from infectious diseases.
The literature also highlights the challenges patients with long-term conditions may face when engaging with their practice digitally. There may be difficulties in accessing care digitally for those with long-term conditions. For example, a 2021 rapid literature review found that staff reported a reduction in cases of certain chronic conditions, which may mean that these conditions were not being managed as well as they should. 44 In addition, a 2022 Nuffield Trust report found potential issues for patients with more complex health conditions as the availability of online support can increase demand for GP services overall, often for minor illnesses that do not require GP input, meaning less availability of consultations for patients with long-term conditions. 38 Other barriers to using remote consultation approaches were mentioned in the study exploring the views of dementia patients/carers, although many of these could apply to all patients, not just those with long-term conditions. These included interactions feeling impersonal, challenges with technology, hearing/memory challenges, the inconvenience of GPs not calling at the arranged time and difficulty in voicing concerns and in healthcare professionals picking up on non-verbal indicators of health (particularly physical health). 47
It is likely that the type, number and complexity of long-term conditions will influence patients’ use and experiences of Digital First Primary Care. For example, the evaluation of Babylon GP at Hand found that experiences varied according to the type of long-term condition, with patients with physical mobility problems reporting worse experiences and those with breathing problems reporting better experiences. 46
Impact on primary care staff
Primary care practice staff are also impacted by the introduction of Digital First Primary Care approaches and have opinions about its use. Here, we describe some of the benefits and challenges healthcare professionals may face when supporting patients both with and without long-term conditions.
Some studies found staff to be positive about the introduction of a new digital system, feeling confident in patients using it and that it could complement existing services. 38,39,41 As with patient impact, there is also the benefit of reduced transmission of infectious diseases, such as COVID-19, due to less footfall in the practice. 44 Some of the benefits of remote consulting were found to be prioritising patients with poorly controlled conditions, greater control over the working day for GPs and patients being more direct in describing their issue and raising fewer problems during phone consultations. 48 Video consultations were thought to be particularly useful for dynamic patient assessments, assessing children, training patients/carers in at-home procedures (e.g. wound care) and connecting with elderly/vulnerable patients. Using text messaging was thought to be effective for fitness to work notes, prescription information and risk assessment questionnaires for patients with long-term conditions. 48
There are also some important concerns from the perspective of staff, such as uncertainties about integrating new digital systems with existing processes and greater difficulties in healthcare professionals making clinical decisions when consulting remotely. 39,44 A challenge of the new ways of triaging patients included reaching out to vulnerable patients, for example those without a carer or homeless patients. 49
Studies have found mixed evidence on whether staff workload changes as a result of introducing digital systems,44,45 although many do note an increased staff burden and unintended consequences on workload in primary care or elsewhere. For example, one study found that most e-consultations resulted in phone or face-to-face appointments, which GPs felt duplicated their workload. 8 A 2019 rapid evidence review found that, while there was some evidence that Digital First services could reduce the burden on primary care, this differed across studies, depending on the outcomes of interest and the type of digital approach used. 50 In a 2021 mixed-methods study which explored GPs’ experience of triaging patients during the pandemic, GPs reported that telephone triage took longer than expected and felt similar to conducting a remote consultation, and this may result in confusion for the patient as to the purpose of the triage call. There may also be a risk of over-referring for face-to-face appointments (rather than remote) due to concerns over missing something a patient may be presenting with. 49 The Nuffield Trust published a report in 2022 on the practical challenges related to remote consultations and identified that remote consultations took longer than face-to-face consultations and there were greater referrals to other services. 38
There are also some concerns over patient safety. For example, studies identified challenges in picking up non-verbal cues from patients when conducting remote consultations, difficulties in building trust and rapport during shorter remote consultations, feelings of fatigue due to dealing with higher clinical risk, potential problems with missed or delayed diagnoses and safeguarding issues. 38,48,49 A longitudinal exploration of remote consulting during the pandemic found that telephone consultations required additional (and careful) questioning as complex cases which previously would have been seen in person were being managed by phone. 48
Summary
In summary, while Digital First Primary Care has been subject to previous research, this has often not included a specific focus on patients with long-term conditions. In particular, there is a significant gap in understanding its use and impact for patients with multiple conditions and the views of carers. For those studies that do include patients with multiple long-term conditions, this is often a secondary consideration rather than the core focus of the study (as outlined in this chapter). In addition, most studies focused on experiences of remote consultations as opposed to exploring the entire Digital First Primary Care pathway, starting from the initial (digital) contact with a GP practice. Therefore, our study is well placed to fill this gap in understanding and evidence from the perspective of healthcare professionals and stakeholders on the use of Digital First Primary Care specifically for patients with multiple long-term conditions.
Chapter 3 Methods
Box 4 provides a summary of Chapter 3 of this report.
Summary of key points
-
The original aim of this rapid evaluation was to understand the experiences of those with multiple long-term conditions of Digital First Primary Care from the perspectives of patients, their carers and healthcare professionals. Due to pressures within the general practices recruited, largely due to COVID-19, it was not possible to recruit patients and carers to the study. Instead, the study focused on the experiences of healthcare professionals and stakeholders. We completed a qualitative evaluation comprised of four linked work packages (WPs):
-
WP1. Locating the study within the wider context, engaging with literature, as well as co-designing the study approach and research questions with patients.
-
WP2. Interviews with health professionals working across general practice and expert topic stakeholders from policy organisations, academia and policy.
-
WP3. Analysis of data, generation of themes and testing findings with patients.
-
WP4. Synthesis, reporting and dissemination
-
-
We undertook a purposive sampling strategy to select general practices from two digital providers, GP federations and super-partnerships to identify NHS members of staff. A convenience sampling approach was used to recruit stakeholders.
-
Despite not applying an explicit theoretical framework, our analysis was guided by empirical literature on Digital First Primary Care both pre and post the COVID-19 pandemic.
General approach
Original approach
The original aim of this study was to understand the experiences of those with multiple long-term conditions of Digital First Primary Care from the perspectives of patients, their carers and healthcare professionals.
Our general approach to meet this aim was a qualitative evaluation comprised of four WPs: (1) contextually embed the study within the relevant literature and co-design the study with patients; (2) conduct interviews with NHS staff and patients and carers; (3) analysis of data; and (4) synthesis of learning and reporting.
Modified approach
General practices did not have the time, resources or capacity to recruit patients to the study, so we were unable to conduct interviews with patients/carers.
Following the initial study conception, the team reviewed and refined the research questions with respect to the on-going challenges and changes occurring in general practice and more widely. For example, our research questions were not only amended due to recruitment challenges, but also to include the topic of COVID-19. Table 2 illustrates the adaptation of the research questions for the study.
| Research questions at conception of the study (2019–2020) | Research questions addressed in the current study |
|---|---|
| Question 1: What is the experience of Digital First Primary Care for patients with multiple long-term conditions, their carers and health professionals? | Question 1: What is the experience of Digital First Primary Care for health professionals and stakeholders (including academics, policy makers and Digital First Primary Care providers), both before and during the COVID-19 pandemic? |
| Question 2: What is the impact of Digital First Primary Care on the nature of consultations for carers/patients with multiple long-term conditions and health professionals, which includes aspects such as the health professional(s) spoken to, timeliness of care and continuity of care? | Question 2: What is the impact of Digital First Primary Care on the nature of consultations, from the perspective of health professionals and stakeholders, for patients with multiple long-term conditions and their carers? This includes aspects of communication, timeliness of care and continuity of care. |
| Question 3: What, if any, are the advantages or disadvantages of Digital First Primary Care for patients with multiple long-term conditions and their carers? | Question 3: What, if any, are the advantages or disadvantages of Digital First Primary Care for health professionals when providing care for patients with multiple long-term conditions? |
| Question 4: What lessons can be learnt from staff, patients’ and carers’ views for future service delivery for patients with multiple long-term conditions in primary care? Are there individual groups within the community where there is particular learning for future service provision? | Question 4: What lessons can be learnt from staff and stakeholders for future service delivery for patients with multiple long-term conditions in primary care? Are there individual groups within the community where there is particular learning for future service provision? |
Protocol sign-off
The study topic was identified and prioritised for rapid evaluation in 2019 through the BRACE Centre’s approach to identifying innovations through horizon scanning. An initial topic specification (first stage protocol) was prepared (September 2020) and, once approved by NIHR HSDR, was used as the basis for writing the full research protocol (March 2021, published on the NIHR HSDR webpage), which drew on the findings from mapping the published and grey literature alongside stakeholder and PPI engagement (WP1). A revised protocol, version 3.0, was published following amendments to the approach.
Ethical approval
An application for ethical review to the University of Birmingham’s Humanities and Social Sciences Ethical Review Committee was made by the project team and approval was obtained in August 2021 (approval number ERN_13-1085AP43, ERN_21-1233). The project team received confirmation from the Health Research Authority (HRA) that this study was to be categorised as a service evaluation and therefore approval by the HRA or the NHS Research Ethics Committee was not required. In addition, clarification was sought from the Head of Research Governance and Integrity at the University of Birmingham, who confirmed that the project should be categorised as service evaluation.
The methods used in the first, second and third WPs are described in the following paragraphs.
Description of the methods used to engage with patients from the BRACE Patient and Public Involvement group
A workshop with patients (five members of the BRACE PPI group) was held online in September 2020 to shape the research questions and share learning from the literature on the introduction, implementation and use of Digital First Primary Care services. During the workshop, members expressed a wish that the study team focus more on the impact of the COVID-19 pandemic on the roll-out of Digital First Primary Care services, and on the impact of greater digital use in general practice more generally and how this affects access to and continuity of care. As a result, the authors ensured the interview topic guides for participants were amended to include these areas.
Focus on patients with multiple long-term conditions
Our evaluation focused on people living with multiple long-term conditions, forming part of the BRACE Centre’s overarching analysis of service innovations and how they are experienced by and impact on people living with multiple long-term conditions. 51 We used the definition from the National Institute for Health and Care Excellence (NICE) which defines multimorbidity as ‘the presence of two or more long-term health conditions which can include’:
-
Defined physical and mental health conditions, such as diabetes or schizophrenia.
-
Ongoing conditions, such as learning disability.
-
Symptom complexes, such as frailty or chronic pain.
-
Sensory impairment, such as sight or hearing loss.
-
Alcohol and substance misuse. 52
As part of this evaluation, we considered how any comorbidities a patient with multiple long-term conditions has may influence their use and experience of Digital First Primary Care (e.g. fatigue caused by the health condition or treatment side effects).
A note on the logistical challenges of recruiting GP practices
Throughout the duration of this study, we faced significant challenges in recruiting GP practices. This resulted in a change to the original protocol to enable the completion of the study. This section describes the challenges faced and subsequent changes to the research protocol. The project was initially conceived as a 6-month project but, ultimately, was completed over a period of 22 months due to a pause (during the pandemic) and challenges to recruitment.
The original aim of the study was to recruit six GP practices, conducting interviews with one to two GPs, one to two other healthcare professionals and three patients per practice (12–24 staff interviews and 18 patient interviews in total). While we recruited more than the intended practices to the study (8 in total), there were significant challenges with recruitment, and it took much longer than expected (8 months). Most practices did not respond to repeated recruitment requests, hence, we lack reasons for non-participation. Those who did respond mentioned the significant workload, staffing pressures and demand challenges they were facing (often related to COVID-19), which meant that they felt they the lacked capacity to participate. We attempted multiple methods of recruitment to bring GP practices on board, including at least weekly e-mail and telephone reminders. We also attempted to recruit practices via multiple sources, including direct contact from the research team (contacting 179 practices in total), recruitment via an open invitation from a Digital First Primary Care provider to all practices using their service, as part of their monthly newsletter, a purposeful approach via a GP super-partnership to all practices in their group and direct contact to practices who had participated in previous research studies known to the research team (see further detail later in this chapter).
To encourage recruitment, we offered flexibility in the timing and length of interviews and offered support in conducting the patient database search to identify patients/carers to approach to take part in an interview. Given the cited pressures on primary care, we had to reflect on when the right point was to stop contacting individual practices as we did not want to pressurise already-stretched staff. We also had to decide when to try alternative recruitment methods (the initial aim was to just recruit via direct researcher contact rather than via providers/super-partnerships) to ensure that we kept to the timelines for the study. For the practices recruited to the study, we were unable to recruit patients/carers for interviews as practices were unable to dedicate the resources needed to conduct the patient database search, despite offers of payment of service-support costs to participating practices. One practice was able to conduct the search but was unable to find the time for a GP to review the list of patients, a requirement before the letters could be posted. COVID-19 presented particular challenges in this respect; in previous studies the PI had been able to attend practices and help staff to prepare envelopes and stick on stamps. The lack of patient/carer views on Digital First Primary Care is a significant limitation of this study and it is important that this is the focus of future research studies (see Discussion and conclusions).
To mitigate some of these recruitment challenges, we made an amendment to our research design to include interviews with key Digital First Primary Care stakeholders, such as policy makers, think tanks, third sector organisations, academics, Digital First Primary Care providers and health professionals working in other roles [such as within Clinical Commissioning Groups (CCGs)/integrated care systems]. This helped to address gaps in knowledge about the development and implementation of Digital First Primary Care and provided a better understanding of the challenges of making digital policy-related changes within primary care. As several of the stakeholders were also practising health professionals, it also enabled the views of professionals from a greater number of practices to be included in the study.
As it appears that Digital First Primary Care is here to stay,53 it is important that we understand how its use impacts the care received by different patient groups, including those with multiple long-term conditions. Given the limited exploration of this topic in the literature so far, the authors have added to current understanding in this area and provide lessons for future practice (see Discussion and conclusions).
Sampling and recruitment of general practices delivering Digital First Primary Care
Two commercial providers of Digital First Primary Care (Provider A and Provider B) agreed to participate in our study and assist with the identification of practices using their approach. At the time of writing this report, we were unable to locate publicly available information to determine how many commercial providers were providing Digital First Primary Care services in England and how many practices and GPs were using these services.
Providers varied in the approach they were happy to take in terms of recruitment, so it was necessary for the research team to be flexible. One provider (Provider A) supplied the study team with a list of practices operating a Digital First approach for 6 months or more for the research team to contact directly. Provider B preferred a different approach, by which they sent recruitment material to a randomly selected sample of 150 practices using their Digital First approach on behalf of the research team. Due to recruitment challenges, the research team also contacted a super-partnership which shared recruitment material across their 45 practices. Practices across the super-partnership used both Provider A and B’s Digital First Primary Care platforms.
Our initial approach was to use a maximum variation sampling strategy to identify general practices, 54 for example with varied list sizes, locations (urban or rural) and including areas of high deprivation and with ethnic diversity. However, due to the recruitment challenges outlined, it was necessary to adopt a convenience sampling strategy.
Two study team members (MS and LH) approached all 179 practices from the list provided by Provider A as well as interested practices from the super-partnership via (1) an electronic invitation via e-mail sent to practice managers (or central practice e-mail addresses if the practice manager e-mail was unavailable) explaining the purpose of the study and their potential involvement, followed up by (2) weekly telephone calls to arrange meetings with primary care staff to discuss the study, concluding with (3) a final e-mail reminder for practices who had not responded within the 6–8 week timeframe. Despite approaching 179 practices for Provider A, only 2 were recruited.
For Provider B, an e-mail invitation was drafted by the research team and sent to a sample of randomly selected practices by the provider. Practices interested in taking part in the study were asked to get in contact with a member of the research team to arrange interviews. Initially, 50 invitations were sent out, followed by another 100. However, no practices were recruited via this method. Due to these recruitment challenges, the research team approached a GP super-partnership, whereby an e-mail invitation was sent out to the 45 practices in the partnership on behalf of the research team. This approach was successful and resulted in five practices being recruited to the study. In addition, members of the research team approached practices they had recruited to other research studies to see if they would like to take part in the study. This resulted in one further practice being recruited to the study. This meant a total of eight practices were recruited. All practices within our sample were using Digital First Primary Care in some capacity prior to the COVID-19 pandemic. A summary of the practice recruitment is provided in Table 3. Due to the challenges with recruitment, it took place over an 8-month period (January to August 2022) to ensure that we recruited enough practices to collect sufficient data.
| Recruitment source | Total number of practices invited | Number recruited | Provider |
|---|---|---|---|
| Provider A contact list: contacted directly by researcher | 179 | 2 | Provider A |
| Provider B-led recruitment: newsletter from provider | 150 | 0 | – |
| GP super-partnership-led recruitment: partnership e-mail on behalf of researchers | 49 | 5 | Either current or previous Provider B user |
| Practices involved in previous research: approached by researchers | 3 | 1 | Provider B |
| Total | 381 | 8 | – |
Sampling and recruitment of patients and carers
To identify patients with multiple long-term conditions, practice staff (and central administrators as part of the super-partnership) were asked to run a search of patient records to identify suitable patients. The research team worked with practices to refine their search depending on the clinical system used. The following inclusion criteria were used:
-
Aged 18 years and over.
-
Living with at least two long-term health conditions (in accordance with NICE guidance).
-
Have accessed Digital First Primary Care services recently.
The practices were asked to send invitations to up to 100 patients at a time who met the above search criteria in order to recruit up to four patients per practice. The intention was for practices to send a study invitation on behalf of the research team and the patients/carers to return a form to the research team if they wanted to participate in an interview. However, due to capacity challenges in the recruited practices, seven of the practices were unable to develop and run a patient search on their database. In the eighth practice the patient search was conducted but GP staff were not available to review the list of patients, a requirement of the study, within the timeframe of the project.
Other approaches to recruit patients and carers to this project, outside of general practice, were considered by the BRACE team in consultation with the steering group and PPI group. However, due to COVID-19 and pressures within other organisations, and the time constraints of the project, this was not possible.
Recruitment of health professionals and expert stakeholders
The study team invited any primary care clinician and allied health professional who was involved in using the Digital First Primary Care approach when managing patients living with multiple long-term conditions for an interview. A senior clinician or practice manager was identified across each practice to act as a gatekeeper to identify relevant staff to take part in interviews. A gatekeeper was defined as a person who could act as an intermediary between a researcher and potential participants with the authority to deny or grant permission for access to potential research participants. 55,56 The gatekeeper facilitated the identification of key individuals involved in the design, implementation, governance or use of Digital First Primary Care platforms for patients with multiple long-term conditions.
Staff were provided with a participant information sheet (see project documents) and completed interviews online (MS Teams/Zoom). Each respondent was provided with the participant information sheet in advance (see project documents). Interviewees had the opportunity to ask questions about the study and signed a consent form (see project documents) prior to participating in the interview, including whether they consented to the recording of the interview. Participants were informed that they were entitled to withdraw from the study at any time and were given information about how to find out more about the study and how to raise any concerns about its conduct.
The evaluation team originally planned to complete 2–4 interviews across each practice (1–2 GPs and 1–2 other health professionals, 12–24 interviews total). However, due to the previously mentioned recruitment and capacity challenges within primary care, 14 interviews were conducted with staff. These were held with 10 GPs and 4 nurses. The interviews lasted between 20 and 60 minutes.
Expert stakeholders were defined as participants that had regional or national level expertise in Digital First Primary Care, including those who may have critical oversight at a level beyond individual practices, for example GP federations and CCGs, decision-makers at a national level, those who work in academia, policy think tanks or commercial companies. The sampling was purposive, identifying participants with topic knowledge of Digital First Primary Care from the groups outlined. Potential participants were identified from the scoping of the published literature, grey literature, policy documents and organisations identified during the scoping work. Snowball sampling was also used – at the end of each interview, participants were asked ‘is there anyone else with topic knowledge in this area that you think we should speak to?’. E-mail invitations to participate in an interview, with information sheets, were sent to 30 contacts, 14 interviews were conducted with 15 participants. No explicit declines were received. The interviews lasted 30–75 minutes.
Fieldwork was completed in parallel across general practices and expert stakeholders (March to September 2022) by three members of the research team with experience of undertaking interviews and qualitative data analysis (lead by JN with MS and LH). JN, MS and LH were responsible for all communication and data collection; a small number of recordings of interviews completed by LH and MS with primary care staff for were reviewed by JN.
A topic guide for use with NHS staff was developed, adapted (as a result of changes to theresearch questions) and used by researchers as an aide-memoire during the interviews (see Appendix 1). The main themes covered by the topic guide were: reasons for implementing and using a digital platform; staff training (if any); the benefits and drawbacks of Digital First Primary Care; the impact on managing patients living with multiple long-term conditions; the impact on practice workload and staff satisfaction levels. A topic guide for stakeholders was developed covering similar topics with specific questions on their perceptions about the benefits and drawbacks of Digital First Primary Care for patients and submitted as an amendment for ethical approval.
The interviews were audio-recorded (subject to consent being given), transcribed verbatim by a professional transcription service, anonymised and kept on the University of Birmingham’s research data server in compliance with the General Data Protection Regulation 2018 and the Data Protection Act 2018.
The study did not formally aim to achieve data saturation, but participant samples were regularly reviewed during the data collection phase, while a purposive approach was taken to target specific stakeholders that were under-represented (i.e. nurses).
Characteristics of sites and participants
Eight practices were recruited representing a broad variation across locations, ethnic diversity, practice size, proportion of patients aged ≥ 65 years and level of deprivation (see Table 4). The reasons for declining participation included COVID-19 pressures and a lack of capacity due to staffing challenges. The researchers conducted fieldwork with practices from April to August 2022.
| Practice ID | Size (small < 6000 patients; medium 6000–12,000 patients; large ≥ 12,000 patients) |
Location | Percentage of non-White British patients by practice (%) | Percentage of patients ≥ 65 years old registered with practice (%) | Deprivation (1 = high, 10 = low) | Specific example of digital facilitation |
|---|---|---|---|---|---|---|
| A | Medium | Rural | 1.4 | 31.6 | Low (score = 8) | One of several practices that is part of a vertical integration set-up with the local acute hospital. Using Provider A, introduced pre pandemic. |
| B | Large | Semi-rural | 7.2 | 17.1 | Low (score = 8) | Part of a nationwide super-partnership. Using Provider B, introduced pre pandemic alongside other digital platforms. |
| C | Large | Urban | 5.5 | 20.1 | Low (score = 10) | Part of a nationwide super-partnership. Using Provider B, introduced pre pandemic alongside another digital platform. |
| D | Large | Rural | 22.1 | 17.2 | High (score = 2) | Part of a nationwide super-partnership. Previously used Provider B but had moved away from it in favour of another digital platform. |
| E | Large | Rural | 3.7 | 27.3 | Low (score = 9) | Part of a nationwide super-partnership. Previously used Provider B but had moved away from it in favour of another digital platform. |
| F | Large | Rural | 15.3 | 16.5 | High (score = 2) | Part of a nationwide super-partnership. Previously used Provider B but had moved away from it in favour of another digital platform. |
| G | Medium | Urban | 55.5 | 8.3 | High (score = 3) | Using Provider B, introduced pre pandemic alongside another digital platform. |
Description of practice staff interviewed
We invited 19 potential participants and interviewed 10 GPs and 4 nurses across 8 practices (see Table 5). The interview lengths ranged from 30 to 75 minutes. The interviews were conducted via video conference or telephone.
| Characteristics | Number of participants (total = 14) | |
|---|---|---|
| Gender | Female | 6 |
| Male | 8 | |
| Role in practice | GP | 10 |
| Nurse | 4 | |
Description of stakeholder interview participants
In total, 15 stakeholders were interviewed, across 14 interviews, between June and September 2022. The interview lengths ranged from 28 minutes to 1 hour.
In summary, we took an empirically led approach to the data collection and analysis for this rapid evaluation, including repeated discussion across the whole project team and PPI members. Our approach supported engagement with the data in a timely fashion while simultaneously keeping abreast of ongoing developments with Digital First Primary Care in general practice by speaking to stakeholders. In the following chapter, we present our findings in relation to the context in which Digital First Primary Care has been implemented and its benefits and challenges for patients living with multiple long-term conditions, from the perspective of our participants.
Analysis and interpretation
Data analysis
Between April and September 2022, the data gathered through interviews were analysed. To aid the process of analysing and interpreting the data, the team (JN, MS, LH, KD) held twice-monthly video call meetings for the duration of the project to discuss the project’s progress and emerging findings. Furthermore, the team undertook four online half-day workshops (September 2020, August 2022, October 2022 and November 2022). The purpose of these meetings was to discuss the data in the context of findings from mapping the relevant literature (WP1), identify any unexplored gaps in the data and develop a theoretically informed line of argument to answer the research questions.
The interview analysis was informed by the Gale et al. framework method for the analysis of qualitative data in multi-disciplinary health research. 58 This method of analysis is a systematic method of categorising and organising data while continuing to make analytical and interpretive choices transparent and auditable. There are seven stages to the analysis.
-
Transcription of interviews.
-
Familiarisation with the interview/observation/documentary material.
-
Coding.
-
Developing a working analytical framework.
-
Applying the analytical framework.
-
Charting data in a framework matrix.
-
Interpreting the data.
Stage 1. Transcription. All interviews with staff and expert stakeholders were transcribed verbatim through a professional, outsourced transcribing company.
Stage 2. Familiarisation with the material. The members of the study team established familiarity with the data by each reading three transcripts (one each conducted by JN, MS and LH) and discussing their learning at twice-monthly meetings, while the data collection was still ongoing (April to September 2022). During meetings, the team members were able to discuss and share their preliminary thoughts and impressions of the early findings.
Stage 3. Coding and Stage 4. Developing a working analytical framework. Stages 3 and 4 of the analysis took place in tandem. The study team applied a deductive approach, having developed pre-defined codes focusing on the specific areas of interest identified from our scoping of the relevant literature. These were reviewed, refined and added to. NVivo 12 was used to assist with the coding of data. An analytical coding framework was agreed upon (September 2022) by all study team members (see Appendix 2). The codes were categorised under broad themes.
Stage 5. Applying the analytical framework. The working analytical framework was then applied by indexing (KD, MS, LH) across all interview transcripts, that is the systematic application of codes from the agreed analytical framework to the whole dataset and subsequent transcripts using the existing categories and codes. Stakeholder and staff interviews were treated as one dataset.
Stage 6. Charting codes. The team developed a narrative-led framework based on the summaries of each code (once the analytical framework had been applied to all transcripts) to ensure that all the research questions were answered. This process was led by two researchers within the project team (MS, LH) with input from the other team members. The narrative-led framework was structured according to the research questions. As a result, codes were merged to develop preliminary themes.
Stage 7. Interpreting the data. The project team held an analysis workshop in August 2022 to finalise the development of themes, which was followed by another workshop in November 2022 to refine interpretation following an internal review. The main purpose was to understand the application of Digital First Primary Care across primary care and identify differences across the data, incorporating theoretical concepts for the purposes of critique relational to our research questions and mapping connections across our themes. Once all members of the study team had agreed on the final themes, writing up of the findings commenced.
Analysis and reflecting on findings with key experts and patients
The study team completed their analysis across WPs, bringing together the key themes from the data collection across different stakeholder groups. This was achieved rapidly by holding a workshop (after data analysis and write up, in November 2022) to bring together the knowledge and data collected throughout the project. As a result, one researcher (JN) developed a set of draft lessons for policy makers concerning the future care of patients with multiple long-term conditions in primary care and recommendations for further research which were developed further with the whole team (LH, KD, MS) (see Discussion and conclusions).
These draft lessons and recommendations were tested with members of the BRACE PPI group. In summary, our approach supported engagement with the data in a timely fashion while retaining the wider context discussed within the interviews.
Chapter 4 Results
Box 5 provides a summary of Chapter 4 of this report.
Summary of key points
-
It is important to recognise the context in which Digital First Primary Care is implemented. Primary care continues to face significant sustained pressure due to higher patient demand combined with staff shortages and pressure from secondary care, leading to staff burnout.
-
The main reason practices introduced Digital First Primary Care was to manage patient demand and reduce the need for unnecessary face-to-face appointments. The COVID-19 pandemic saw the rapid introduction of Digital First Primary Care approaches (to reduce viral transmission), which was not always as well thought through as it may have been pre-pandemic.
-
The introduction of Digital First Primary Care was frequently cited by interviewees as leading to an increase in patient demand. To manage this, some practices reported reducing the time the system was available for use (e.g. closing it down over the weekend).
-
Health professionals and stakeholders reported that Digital First Primary Care provided some benefits to patients with multiple long-term conditions. This included being able to speak to a healthcare professional more quickly, reducing unnecessary face-to-face appointments and supporting patients’ preferences. However, they felt there could also be drawbacks for this patient group, including challenges with digital forms or algorithms, poorer quality interactions and relationships with healthcare professionals and concerns over patient safety. Mixed views were found on whether Digital First Primary Care helped to improve continuity of care.
-
The interviewees felt that Digital First Primary Care may be particularly useful for patients with certain types of long-term health conditions (e.g. diabetes, cardiovascular conditions, mental health conditions and hearing loss). Younger patients, those working full-time and/or those who do not have English as a first language (if translation is available within the system) could also benefit from Digital First Primary Care. Health professionals and stakeholders reported that patient groups who may benefit less from Digital First Primary Care included those who are older/frail and those who do not have access to digital technology (or the skills to use it).
-
The interviewees reported that carers of patients with long-term conditions may benefit from Digital First Primary Care as they can have greater communication with healthcare professionals and be more actively involved in the patient’s care. However, there are some concerns about confidentiality, privacy and consent when it comes to carers accessing medical information. Some participants also noted that carers can lose the added support and in-depth discussion that a face-to-face appointment provides.
-
With regards to healthcare professionals, Digital First Primary Care can offer advantages in terms of better information sharing and communication across staff and patients, improved relationships with patients and greater efficiencies and flexibility. However, others felt that Digital First Primary Care was detrimental to the clinician–patient relationship, creating some inefficiencies. There were also concerns raised over the confidence staff have in their own clinical decision-making when using Digital First Primary Care and the issue of increased (unmanageable) patient demand.
Wider context in which Digital First Primary Care is being implemented
As described in Chapters 1 and 3, the fieldwork for the evaluation was undertaken during an extremely challenging period for general practice. Here, we will briefly discuss the points raised by the interviewees related to the wider context in which Digital First Primary Care was being implemented. While this is not exclusively relevant to patients with multiple long-term conditions, these contextual challenges will particularly impact patients who see a GP more frequently, which includes those with multiple long-term conditions.
Workforce recruitment and retention challenges within primary care were frequently mentioned by participants. Staff shortages and difficulties filling vacancies were a key issue across general practice in relation to both clinical and non-clinical staff, with shortages of working GPs highlighted as a particular issue. The interviewees reflected on how the number of GPs was falling, with fewer entering primary care and some retiring or leaving for other reasons. This challenge aligns with national data from the BMA, who note that the number of GPs in England has grown very little since 2015. 13 Linked to this, a reliance on locums in the absence of being able to recruit permanent staff to practices was reported by participants.
So if you go pre-COVID, there were a range of things that were making life more difficult for GPs. The population was getting older. The population was increasing. The number of GPs was decreasing.
Interview 7, researcher
For those working in general practice, challenges were reported with staff working in busy and pressured environments, putting a strain on the workforce and causing staff burnout. This burnout of healthcare professionals following the COVID-19 pandemic has also been reported more widely.
… I have worked in the NHS my whole career and I have never worked so hard. Yesterday I got in at half past six, I did prescriptions while eating my sandwich over lunch because we had so many of them, and I got out of the building at half seven last night and I categorically did not stop from the moment I got in the door to the moment I left – and that’s really a new way of working – the pressure is intense. I mean, I think that’s probably the defining feature at the moment and the thing that’s going to decide what happens next, is the fact that there’s intense pressure, breaking pressure at the moment in the service … I can’t get patients seen.
Interview 2, GP
In terms of the wider healthcare system, pressures in secondary care, particularly following the pandemic, were also having an impact on primary care and increasing the demands on services. Some participants reflected on how an increasing amount of work was coming out of hospitals and into primary care, with GPs having to take on work that they may not feel qualified to do and manage patients they felt should be cared for in secondary care. This challenge of the pressure of secondary care impacting primary care has also been identified in other studies (e.g. Baird et al. 201859).
… There’s huge frustration with waiting times and secondary care, with additional workload being placed on primary care because of waiting times in secondary care, and having to manage patients who really need to be managed in secondary care, but because they can’t get an appointment yet or they have months to wait.
Interview 9, Digital First Primary Care company stakeholder and GP
For many participants, managing increasing patient demand was a challenge. While participants reported that demand had subsided during the pandemic as patients contacted health services less frequently (despite some needing care), demand was now felt to be rapidly increasing to levels which were unsustainable. High demand is a challenge identified from national data analysis by the BMA, for example, appointments in the winter of 2021 (very shortly before recruitment for this study started) reached ‘record highs’. 13
It [demand] dipped initially when everyone – it’s hard to remember back to March 2020 – everyone was terrified to do anything – so it definitely dipped a little bit – then it’s increased, then it sort of steadied, but it’s increased – demand is higher than it ever was pre COVID now – I’m just spread across everywhere!
Interview 27, GP
Despite interviewees reporting that patients can be satisfied with receiving care remotely, external influences – such as the media and changes in policy, particularly those aspects focused on seeing patients face-to-face – were mentioned to have contributed towards a challenging environment for practices. Several participants felt that the criticism from media outlets around patients receiving consultations remotely had been demoralising and frustrating for GPs. This challenge has also been noted nationally and is not unique to our study. For example, the BMA called for action from the Health Secretary to reduce negative media against primary care due to concerns over further exacerbating the issues with staff recruitment and retention. 60
I guess probably towards the end of last year I think when there was lots of negative media coverage where there were some very vocal patients, very demanding about face-to-face appointments but the vast majority [of patients], in my experience now, are happy to consult remotely.
Interview 9, Digital First Primary Care company stakeholder and GP
How Digital First Primary Care is implemented and used within primary care
Digital First Primary Care was conceptualised differently across practices, including those embedded within the same super-partnership, which subsequently altered how Digital First Primary Care platforms were introduced. The most common characteristic of the implementation of Digital First Primary Care was that every initial contact made by any patient, including those living with multiple long-term conditions, with a healthcare professional in general practice was via a digital medium, such as an online platform directed by answering a series of questions. Subsequent interactions with a patient after this initial contact could then be online (e.g. messaging via a Digital First Primary Care platform), by phone, in-person or, rarely, by video.
The primary rationale that practices reported for introducing Digital First Primary Care (other than governmental policy mandating its use during the pandemic) was to manage patient demand and reduce the need for face-to-face appointments for every patient query. Hence, it was not solely about improving access for patients to general practice services. While remote care was beneficial in preventing COVID-19 transmission during the pandemic, many aspects of Digital First Primary Care have been retained since the pandemic as a result of the other potential benefits it offered.
As mentioned in Chapter 1, there are multiple different Digital First Primary Care systems available for practices to use, each offering slightly different approaches. Some practices in our sample considered switching Digital First Primary Care providers to better suit the needs of the practice and their patients (e.g. to better integrate with existing digital systems or to have better triaging ability or increased accessibility for patients). Others changed Digital First Primary Care platforms as a result of governance decisions within their super-partnership. Some participants questioned the lack of available and robust evidence on the advantages and drawbacks of the different Digital First Primary Care providers’ systems, which made it difficult for general practices to make decisions about which platforms to adopt given their workforce composition, the administrative support available and the needs of their patients.
Some of that sort of bedding down after all the franticness of COVID, would be quite helpful. And I think I would choose to prioritise that rather than the next new tech thing, because I’m worried about layering on too much stuff, and then the whole thing just collapsing.
Interview 18, national policy-maker
The introduction of Digital First Primary Care was sometimes accompanied by the application of other digital approaches, including platforms which enabled practice staff to text message patients. Using these additional digital approaches, patients could reply to the practice by providing a response to a request (e.g. providing an image) but were unable to initiate contact themselves (unlike with Digital First Primary Care systems). In addition, staff from several practices discussed how they were able to embed Digital First Primary Care as part of another digital system to create a more user-friendly platform that could be bespoke for each practice. This also allowed the incorporation of more information relevant to patient self-management; for instance, signposting patients to relevant health-related and self-help websites.
With the onset of the COVID-19 pandemic, staff across general practice were faced with a scenario where there was very little time between being aware of the widespread introduction of Digital First Primary Care and its implementation, with little information and training offered to support implementation.
I think that it’s almost like there was no [Digital First Primary Care system] and then suddenly there is, so we created a tsunami of workload.
Interview 4, GP
The volume of enquiries submitted using Digital First Primary Care varied across our sample. Monday was often reported as being the busiest day of the week due to a backlog of enquiries sent by patients over the weekend. Most patient queries were addressed within 24–48 hours of submission. Even where practices were using Digital First Primary Care prior to the pandemic, its application was scaled up dramatically when the pandemic ensued. This is reflected in national data analyses during the pandemic which indicate large increases in the number of remote consultations across the country. 7
So on a Monday we’ll do 60 and then the other days we’ll make capacity for 30 on each of those days and I think that’s been pretty stable in terms of the numbers coming through.
Interview 19, GP
One of the most significant methods adopted by general practices to manage the high (often unmanageable) number of Digital First Primary Care enquiries from patients was to alter when the service was available for patients to access. Hence, practices adopted an approach of both a planned and ad hoc reduction of hours when Digital First Primary Care was available; for example, during times of high pressure or during weekends and bank holidays to ease the pressure on Monday mornings. Instead, patients needed to contact the practice by phone during these times. However, some argued that this approach only reduces the number of patients the practice is aware of, it does not mean these patients no longer need care, and so the demand for health care may not actually change overall.
But we cap it [number of Digital First Primary Care queries from patients] at a certain point. So, past 40 to 45, just from a safety point of view where … unless something urgent, you know, that is contact by reception or the hospital or somebody will contact us just so that because initially we didn’t have a cap and we were getting severe burnout from all clinicians.
Interview 17, GP
There was an absence of standardisation regarding Digital First Primary Care availability even where practices were part of the same super-partnership. For example, one practice may receive nearly all their patient contact digitally, while others only have the Digital First Primary Care system available for a certain period during the day (e.g. 9–11 a.m.), whereas others may have a designated number of Digital First Primary Care consultations scheduled for a given day or week completed by a single GP. Altering the hours of access was seen as an effective method to allocate work across clinical and non-clinical staff working in the practice, as well as remotely, which was felt to help prevent staff burnout and improve patient safety.
The introduction and use of Digital First Primary Care during the COVID-19 pandemic
All practices within our sample were using Digital First Primary Care in some capacity prior to the COVID-19 pandemic; however, its use was not widespread, and practices were quite pragmatic about its application relevant to clinician expertise and administration support to underpin the roll out of the system. Some practices took steps to work with the providers of Digital First Primary Care to prepare staff for roll out, as well as patients with respect to engagement. For example, some clinicians cited how they worked with Digital First Primary Care providers to manage new workflows and adapt their working culture and behaviour to make the best use of Digital First Primary Care post implementation.
[I’m] not really sure how it was introduced, as in how it came about to the practice, but it was just introduced to us – I think we had a training session on it, at a whole practice meeting, and just an explanation on what could be used, and how they were triaged, for reception and stuff.
Interview 3, nurse
However, this was not the case for all practices, where, as mentioned earlier, the introduction of Digital First Primary Care during the pandemic was often more rushed in order to quickly reduce footfall in the practice, with less time and capacity available to consider the optimal way of introducing the new approach.
We needed to kind of find a way of managing the situation we were in with COVID … This wouldn’t have happened if COVID hadn’t happened … it’s shoved everyone kind of five years on almost in terms of this technology. So it was a way of trying to manage what was going on and try to manage patients, how to give them some access in a way that made sense really.
Interview 2, GP
During the height of the pandemic, and more recently, staff felt that more patients were finding telephone and video consultations more acceptable but understood that this was heavily dependent on the digital literacy of patients and the health issue at hand (see Impact of Digital First Primary Care on patients). Other studies have found similar preferences for digital/remote consultations among patients (e.g. Clarke et al. 202215). The introduction of Digital First Primary Care also meant fewer patients entering general practices physically, which helped manage COVID-19 infections and protected staff working in the practice.
Impacts of Digital First Primary Care on patients with multiple long-term conditions
Several advantages and disadvantages for patients were described in relation to the use of Digital First Primary Care. However, there are two points to note when outlining these findings. The first is that this data was only collected from GP staff and stakeholders; therefore, the impacts described here are those that are perceived to have occurred by these individuals (rather than being described directly by patients themselves). Secondly, some of these impacts do not specifically relate to patients with multiple long-term conditions, they also apply to patients more generally. However, we highlight specific information in relation to patients with multiple long-term conditions where available.
Advantages of using Digital First Primary Care for patients with multiple long-term conditions, as reported by interviewees
Patients can speak to a healthcare professional more quickly
A key advantage described by almost all interviewees of Digital First Primary Care for patients, including those with multiple long-term conditions, is that they were able to speak to a GP more quickly as a GP would get back to them within 1–2 days, rather than waiting in long telephone queues. This was thought to help improve patients access to care.
Quicker access to a clinician was also mentioned specifically in relation to patients with multiple long-term conditions. For example, the Digital First Primary Care system can help to flag patients with multiple long-term conditions, so that they are contacted by a clinician more quickly.
I think maybe it is slightly quicker, because they’re booked an appointment, triaged at reception generally, but if it’s an [Digital First Primary Care enquiry], then you already know their history, so you know if they need to be seen quicker, because they’ve put the history of the presenting complaint at the time, and they’ve also put … their medical history, so you know whether they need to be seen sooner than somebody … that doesn’t have a long-term condition.
Interview 3, nurse
The interviewees felt this was particularly beneficial for patients with well-controlled long-term conditions who could be reviewed more quickly and more conveniently remotely (see the following section for further information).
… If that is a really well-controlled [long-term condition], that takes down the amount of appointment time that they need, then we can review them much quicker. And so I think for convenience for patients, that’s quite nice. If they are well-controlled, they don’t have any symptoms, that sometimes means they don’t actually have to come in and don’t need a face-to-face appointment – we can review their medication over the phone.
Interview 3, nurse
Reduced need for unnecessary or inconvenient face-to-face appointments
The interviewees felt that a particular benefit for patients with multiple long-term conditions in relation to Digital First Primary Care was that in some practices, health information and readings (e.g. blood sugar levels, blood pressure readings) could be submitted by the patient at home, rather than needing to be seen in-person. As mentioned, this is particularly helpful for patients with well-managed long-term conditions where in-person assessments are often not necessary. For these patients, using Digital First Primary Care can reduce the length of appointments and reduce the need for an in-person appointment and staff felt it was more convenient for patients.
And I feel the same when you do blood pressure diary on a [Digital First Primary Care system], so for hypertension, again, that’s the same. So many patients, even more so now, post pandemic, have their own blood pressure machine. And they’re like, do I have to come in, because I’ve got one at home, and they can just fill that in, and it can be added to their notes, and we can review them that way.
Interview 3, nurse
While the use of Digital First Primary Care could avoid unnecessary in-person appointments for those with multiple long-term conditions, it still allowed clinicians to regularly keep in touch with these patients to check their stability (e.g. via messaging systems). This was useful both for patients with well-managed long-term conditions and patients that need to be more closely monitored, for example, those who were elderly or frail and at greater risk of deterioration.
…There can be good benefits in terms of … providing those sort of like regular review questionnaires. And then an extension to that, some of them remote monitoring type work, so you can have those regular check-ins, as a practice, with that cohort of patients with long-term conditions, and then pick up perhaps more quickly if they’re deteriorating or actually they’re quite stable, and they don’t need intervention, and that can help that process.
Interview 18, national policy-maker
Digital First Primary Care was considered to be particularly beneficial for patients who needed a quick answer to a simple issue and for less complex issues, for example sick notes, repeat prescriptions or letters, that did not require patients to be seen in person. This included patients with multiple long-term conditions where a specific problem is straightforward to deal with.
So for example, for fit notes, it does work really well. So before people could book an appointment for a fit note, now we can just send it to them via text message or via email, or you can write [Digital First Primary Care message] back … I’ve done five this morning, that’s saved five GP appointments, face-to-face appointments.
Interview 20, GP
Stakeholders discussed the benefit of patients not having to physically go to the practice, for example carers did not need to get frail patients to the practice and patients working away from home could more easily speak to a health professional.
Digital First Primary Care could better identify and support patients’ preferences for the format of communication with the practice and it could be more convenient for them. For example, patients could request an in-person appointment or could submit queries and review the clinician’s response in their own time, they were not pressured to do it at a certain time.
… patients who didn’t have English as a first language actually really liked the online consult forms because they could get their children to do it for them and they could really think about, or take their time, because they could use Google Translate and other things rather than having the pressure of a real-time consultation, which was more difficult.
Interview 5, researcher
Continuity of care
The views of participants on the impact on continuity of care for patients living with multiple long-term conditions were mixed. The benefits to continuity of care will be discussed here and the negatives in the following section.
A small number of participants discussed how Digital First Primary Care allowed for greater sharing of and access to medical information. This could allow GPs who were not familiar with a patient to get a better understanding of the patient’s history, even if they had not seen that patient before, which could support continuity of care. This benefit was also mentioned specifically in relation to patients with long-term conditions, whereby any clinician caring for the patient would have access to information about all conditions the patient had in one place ahead of the consultation.
I do believe that these [Digital First Primary Care systems] … improves continuity of care. And why I say that is because with a lot of these digital technology, you can cover a lot of information. So if you’ve got a diabetic patient with also heart disease, cholesterol, but also if they used to see it, and again if you’ve got one app that will do it all, but if you see the app with their peak flows and symptoms … and you’ve got the digital glucometer that measures the BMs, and it saves to the patient records, and you’ve got, say cholesterol, they deliver their blood pressure pulse, exercise symptoms, and all that is populating the system, that can be one focus consultation to do the actual review. Because you don’t need to gather all these and get it in. You can also, when you’ve gotten information, decide whether they need any further blood tests or any other tests, so you can arrange all these prior to that, instead of getting them in, arranging it, and then needing to bring them back in for review.
Interview 12, CCG role and GP
Some clinicians discussed how enhancing continuity of care with the introduction of Digital First Primary Care was dependent on the type of digital platform chosen and how a practice had decided to implement said platform with other care co-ordination processes (see Figures 2 and 3 in Chapter 1 for examples of different Digital First Primary Care pathways). For instance, some Digital First Primary Care provider systems were reported to allow for a patient to request that their enquiry be passed to a specific GP who knows them to support continuity of care. This was a feature that was reported to be particularly useful for patients with multiple long-term conditions, as they could request the GP (or other healthcare professional) that understands and is familiar with their clinical history. However, such an approach had only been established recently, it was not available in all Digital First Primary Care systems and was not often introduced at the time of implementation, nor during the height of the pandemic where continuity of care was difficult to achieve (see Disadvantages for patients with multiple long-term conditions, as reported by interviewees).
Because the GP has to actively allocate a request to a staff member who’s going to deal with it, if the person doing the allocation is good, they will consider which GP usually deals with this patient if the patient is a regular, OK always go to her, diabetic – always go to the diabetes nurse – if it’s this patient really needs to talk to that doctor then we always allocate it to that doctor. So that, I think the process, the internal workflow process makes continuity easier to do, but we also asked patients whether they wanted to see a specific doctor and we allowed them to name the doctor, so we record that.
Interview 28, Digital First Primary Care company stakeholder
Types of long-term conditions to which the use of Digital First Primary Care may be better suited
The interviews included an exploration of which long-term conditions may be better suited to using Digital First Primary Care approaches. While the interviews aimed to explore how patients with multiple long-term conditions experienced Digital First Primary Care, most interviewees struggled to think of combinations of conditions where Digital First Primary Care may be particularly beneficial. However, individual long-term conditions were discussed by the interviewees and are outlined here.
Diabetes was reported by multiple participants to be well-suited to being managed remotely, as patients could submit home glucose readings and be sent electronic reminders of when their regular review is due.
So if someone is capable with technology, that is now able to manage their diabetes without having to take time off work and go to the GP practice because they can do it all through their app, and they understand their sugars and so on …
Interview 11, CCG role and GP
Cardiovascular conditions, including asthma, chronic obstructive pulmonary disease and hypertension were also reported by the interviewees to be well-suited to Digital First Primary Care. Again, this was because patients could complete tests and reviews at home, such as peak flow readings for asthma or blood pressure readings. Clinicians could then review these data and take action if required.
I suppose COPD [chronic obstructive pulmonary disease] would maybe a good review group because you could easily send out [Digital First Primary Care system] links or tell patients maybe, oh, why don’t you click on the website? There’s an [Digital First Primary Care system] link to do an asthma or COPD review. Then obviously it comes back there’s a concern. We can obviously contact you if it’s fine. We’ll just carry on with your inhalers.
Interview 17, GP
For patients with mental health conditions, assessment questionnaires could be completed remotely ahead of an in-person appointment, which could save time and provide the clinician with information before the consultation. Engagement with patients with mental health conditions could also be improved by using digital approaches, for example not needing to attend the GP practice could reduce anxiety and it was reported that messages sent to patients via text could result in better engagement. One respondent also reported that patients with drug/alcohol addiction may prefer digital forms of engagement and, thus, be more responsive to these methods.
I’ve had patients with severe anxiety and agoraphobia who suddenly feel able to contact and ask for help.
Interview 19, GP
Patients who were deaf or hard of hearing may benefit from Digital First Primary Care as correspondence could be written, which could be more beneficial than in-person verbal discussions.
I’ve got a deaf patient who can contact us for help through [Digital First Primary Care platform] whereas Phonepoint and even face-to-faces were difficult. So it’s improved access for groups of people who otherwise wouldn’t have contacted us …
Interview 19, GP
As mentioned, patients who may struggle to leave their home, such as those with dementia or physical disability, could also benefit from Digital First Primary Care, as they did not need to attend the practice in-person.
I know of instances where carers of older people with dementia … love digital because it means they don’t have to get there, either somebody in to care for their spouse while they go to the doctor or get their spouse up and dressed and out to the doctors because the partner needs a medical appointment, so they’re able to do that on the phone; it just makes it easier.
Interview 5, researcher
Groups of patients who may benefit from using Digital First Primary Care
In addition to specific long-term health conditions that may benefit from Digital First Primary Care, the interviewees also discussed other groups of patients who may benefit from Digital First Primary Care. This included patients who work full time and/or struggle to take time off work to attend an in-person appointment. Younger patients may also prefer Digital First Primary Care and so use it more, for example due to its convenience and their familiarly with digital ways of working. Their health issues may also more frequently be simpler to deal with and, thus, better suited to remote management. For patients whose first language is not English, some Digital First Primary care systems allowed electronic messages to be translated online.
… People with language issues, so let’s say they don’t speak English well enough to make a request, we found several people who were doing, just because they were using a smartphone, they could type the request in Polish, have google translate … and so actually if you’re doing it on a smartphone, it would have probably made things easier, it’s automatically translated.
Interview 28, Digital First Primary Care company stakeholder
Disadvantages for patients with multiple long-term conditions, as reported by interviewees
Format of digital forms
Some Digital First Primary Care approaches used an algorithm approach, in which a digital set of online questions helped clinicians to assess and triage a patient’s care needs. It was reported by participants that patients with multiple long-term health conditions may struggle to navigate these algorithmic approaches, as the questions may be irrelevant or not ask about something important. For example, the questions may not provide information on the impact the issue is having on the patient’s quality of life. In addition, the questions often only asked about one health problem, when patients with multiple long-term conditions may need care for more than one problem.
I think if you have multiple conditions, it’s probably harder to navigate [a Digital First Primary Care system] because it just keeps opening up new bits for you to fill out … But sometimes patients also don’t know how to, like, where should I put this? There’s not the section for it. Or they have to put something in a section in order to go to the next section. So, when you ring up, they’re like, no, no, I don’t have a headache, but I just couldn’t get past the section in order to write something on the next bit … So, sometimes you read it and you’re like this is nothing like what you’ve told me … So, just checking, do you have a headache or neck pain or anything? They’re like, no, no, no, no, no.
Interview 17, GP
When a patient submits an enquiry via a Digital First Primary Care system, the system can interpret the inputted data to recommend next steps, such as consulting a GP, visiting a pharmacist, or calling 111 or 999. For a patient with multiple long-term conditions, the outcome of a digital form may be to call 111/999 which the patient, who knows their condition(s) very well, may know is not necessary. The interviewees reported that this can mean patients purposively entering the wrong information into the form, so that they were able to submit their enquiry to their GP, rather than be directed elsewhere. This then required the GP to go over the information and history again in the appointment to ensure that the information they have is correct.
I myself have got elderly parents and when I’ve had to use [Digital First Primary Care system] to get through the practice, which is actually the only way you can get through to their practice, I found it tricky to use inasmuch as it kept telling me to call 999 or call 111 whereas I really actually knew that I didn’t need to do that. So I almost ended up sort of fabricating something in order just to get through to the place where I wanted to get to.
Interview 4, GP
The participants noted that the digital forms were also very simplistic, often only providing yes/no response options which do not offer the nuanced detail a GP needs to make informed decisions. GPs were often unable to follow-up with the patient to clarify responses via the digital system. Relatedly, these forms were often long and could result in lots of information (not all of it relevant) that a GP needed to read through, which could be difficult and time consuming to digest. As before, this can result in the patient needing to repeat their story again when they meet with their GP and could create inefficiencies. This issue was often exacerbated the more complex a patient or condition was, meaning it was likely to be worse for patients with multiple long-term conditions.
I think because long-term conditions are always very complex. And most of the time the conditions interrelate. You can’t just sperate one thing from another, it’s all connected. And I think it’s always used up a lot of information. I think [Digital First Primary Care system] is quite good if you need something very simple like for example someone wants a pill check … but for long-term conditions, there’s a lot of information that is needed and I don’t think that’s particularly easy to get out of an [Digital First Primary Care system].
Interview 21, nurse
Patients themselves may also not share all the information a GP needs via a digital form, despite having the opportunity to do so, such as photos. This may mean that a follow-up appointment was needed in-person to fully understand what the problem was.
Like you think well, if it’s a rash, take a photo of it and submit it, but it’s not mandatory. You can skip it … you have to then say, look, can you please send the photograph? I’ll do it via [Digital First Primary Care system] and then we’ll start again.
Interview 17, GP
Interactions and relationships between staff and patients
The use of digital mechanisms to communicate with patients could result in poorer quality interactions with patients and disrupt the patient–clinician relationship. For example, staff noted that patients may feel less able to share their concerns when not interacting with their GP face-to-face. Patients may also feel less reassurance when speaking with a GP remotely, for example they cannot see the clinician’s body language or facial expressions. Staff also noted that patients may not feel as listened to or have as much trust in healthcare professionals when interacting with them remotely. Staff also felt that some patients may miss the face-to-face contact and be frustrated that they were seen remotely or could not get through to speak to a person when using digital channels.
One of the disadvantages is the lack of being able to give appropriate information for some people and of course they would feel that they are unable to voice their problem effectively unless they’re physically in front of somebody to explain precisely what has been going on.
Interview 24, GP
It can be more difficult for clinicians to pick up on patients’ body language or behaviour changes when conducting remote appointments, with some noting concerns about ‘losing something’ when not seeing the patient in-person regularly. Clinicians may also find it more challenging to build rapport and relationships with patients when conducting appointments remotely, with interactions feeling more transactional. This may be a particular challenge for new staff members and/or with new patients, which may have subsequent implications for patient safety (see the following section).
You can’t do a holistic assessment as you would when someone walks in usually, you are, when someone walks in in a face-to-face appointment, you are doing multi-level thinking and processing which I realise from all my experience, I’ve realised that we do a lot of processing without trying, without intending to, so we’re assessing the patient as you’re looking at them. You’re kind of eyeballing them, the notes, the meds everything, whereas in [Digital First Primary Care system], it’s not so easy to do that
Interview 20, GP
Patient safety
Importantly, there were notable concerns regarding patient safety when providing care for patients, including those with multiple long-term conditions, remotely. The GPs in our sample felt that clinicians working remotely were more reluctant to explore the nuanced complexities of patient aliments via a remote consultation and, as a result, these patient queries were frequently conducted in clinic as part of a face-to-face consultation. One interviewee noted that this issue may be worsened when the GP is not familiar with a patient beforehand.
… I mean the guy was reading some out when he was talking to me: ‘Unfortunately the patient died of appendicitis’ was one quote and you think in this day and age a patient died of appendicitis? It would not have happened pre-pandemic because abdominal pain would have been seen in the surgery. You occasionally see these horrific examples in the tabloids and you don’t know whether they’re true or not, whatever. So I’m worried about safety.
Interview 8, researcher
In addition, digital consultations with patients with complex needs placed a significant burden on individuals to use the correct language and terminology to present their symptoms in a manner which permits a clinician to make a diagnosis. This increases the risk of potentially missing something serious, especially when care has not been optimally joined up.
Continuity of care
As mentioned, whilst some interviewees expressed positive outcomes related to continuity of care when using Digital First Primary Care, others did not feel the same way. The respondents shared concerns that increased communication using online, telephone and video formats, as opposed to face-to-face communication, had a significant impact on continuity of care. In addition, depending on the type of Digital First Primary Care system used, patients could be allocated randomly to clinicians rather than to the clinician who knows them well.
… it’s people like my dear departed mother-in-law who just, she was so complicated with all her bag of tablets and the different things wrong with her that really only one doctor in the practice had got their head round the complexity of her. And of course she didn’t have the skills or the confidence to plough her way through the hurdles [to reach this GP], so that’s one thing.
Interview 8, researcher
In particular, the use of Digital First Primary Care during the pandemic was noted as a time of a lack of continuity of care, whereby patients were allocated to clinicians on an ad hoc basis. This practice worked well during quieter periods of the pandemic but was thought to be unsustainable by clinicians.
Continuity started to go a bit out the window [during the pandemic] and everybody got very frustrated with it, and you ended up with re-work then because you’d say, ‘Well I think you’d better go back to your ordinary GP to deal with that and we’ll get them to contact you’ and there was a lot of inefficiencies.
Interview 10, locum GP
Types of long-term conditions the use of Digital First Primary Care may be less well suited to
There were several long-term-condition situations that the interviewees noted may be less suited to support via Digital First Primary Care methods, including the following.
-
Some patients with mental health conditions who are better suited to in-person consultations to discuss the issue face-to-face, especially if it is a newly presenting issue.
-
Patients with learning difficulties who may struggle to understand how to use the online system and/or not have the language skills to explain the problem in writing or over the phone.
-
While some interviewees noted that Digital First Primary Care can be beneficial for patients who are deaf or hard of hearing when communication is written, others noted that video consultations can pose difficulties with lip reading and consulting over the phone can be a challenge with these patients.
-
While some interviewees reported that diabetes could be well-managed via digital mechanisms, others disagreed, as patients require blood tests and foot checks which need to be conducted in-person.
-
Staff felt that patients who were blind or partially sighted may struggle to use Digital First Primary Care approaches as much of the information is provided in a written format.
-
There were concerns that respiratory conditions seen remotely meant that the clinician could not check on the patient’s breathing or whether an inhaler was being used correctly.
-
Conditions affecting dexterity, for example Parkinson’s, as patients may struggle to use online systems.
-
Patients with drug/alcohol addiction who may benefit from in-person support.
The challenging ones are the mental health ones because … it’s very hard to do a mental health [Digital First Primary Care enquiry], especially if they’ve written ‘I feel suicidal’, ‘I feel down’. I know there’s safety mechanisms in there from the [Digital First Primary Care system] to tell the patient you know to seek help or advice if there’s any immediate risk but it’s very hard to respond back because with mental health you need to discuss a lot more and if they need a medication change, you can’t just change a medication. I could type a whole essay but by the time I’ve typed a whole essay out, I could just call them, it’s quicker.
Interview 20, GP
Other patient groups that may be less well-suited to using Digital First Primary Care
In addition to specific long-term conditions, other groups of patients who Digital First Primary Care may not work so well for were also mentioned. Most interviewees mentioned that older patients, particularly those who were frail, and/or those without access to the required technology, may struggle to interact with the practice digitally. These patients may also prefer to interact with the practice in-person. Although some interviewees noted that, since the pandemic, some older patients were more adept at using digital technology.
I think perhaps there are significant numbers of the elderly who just don’t have access to a computer and who are cognitively impaired and both of those things would impede your access to [Digital First Primary Care system] really. So there has to be a phone option, there has to be another way in for now.
Interview 2, GP
There may also be language barriers to engaging with practices digitally. This may be relevant for patients whose first language was not English, particularly if the chosen Digital First Primary Care platform did not offer translation options. In addition, as mentioned previously, there can be challenges for patients who cannot read or write, or who do not have the language skills to explain their problem sufficiently. This challenge may affect a significant proportion of patients, as it is estimated that over 16% of adults in England have poor literacy skills. 61
People who don’t speak very good English are kind of reluctant to use [Digital First Primary Care system]. So I think they tend to come less through that avenue.
Interview 4, GP
Caring for children remotely can also be a challenge. For example, parents may be less reassured when consultations are consulted remotely. The participants noted certain conditions in children that were not suited to a remote appointment.
As there were groups of patients who are unable or do not want to engage with the practice remotely, all staff interviewees reported that patients could phone the surgery and their data be entered into the Digital-First system by a member of the administrative team. Some interviewees also noted that they educated patients on the digital options available to them and encouraged their use.
I think as clinicians, some of us have gone through an [Digital First Primary Care system] with a patient, like if we’ve seen them face-to-face and they’ve said it’s difficult to get an appointment. I personally have myself gone through to help an elderly patient to show easy it is to do an [Digital First Primary Care platform] with them, in the hope that may make it more accessible for them.
Interview 3, nurse
The impact of Digital First Primary Care on carers of those with multiple long-term conditions
For those with multiple long-term conditions, carers can be a key source of support and will be involved in their care coordination, and so may also be impacted by Digital First Primary Care. The participants discussed the impact of Digital First Primary Care approaches for carers of those with multiple long-term conditions, both in terms of the benefits and challenges it offered. As with the previous section on patient impacts, this section represents the perceived impacts on carers as described by practice staff and stakeholders, rather than those described directly by carers.
Advantages for carers using Digital First Primary Care, as reported by interviewees
Digital First Primary Care approaches provided a way for carers of those with multiple long-term conditions to reach a clinician more easily and conveniently. For example, carers do not need to wait in a telephone queue, attend the practice in-person or support a frail patient to get to the practice. Digital First Primary Care also provided a platform for the carer to directly share any concerns or questions they may have, which could be particularly important for those with multiple long-term conditions. This gives carers the opportunity to become more involved in the care of a patient and, in parallel, could support clinicians to understand a situation or concern more easily and quickly. This also has the benefit of ensuring that carers are fully aware of the issues that have been discussed in a consultation and the information given to patients.
… a lot of sort of frail or patients or people who otherwise aren’t very good at articulating for themselves, they will have a relative or carer who is able to do that for them. So often I will [have] quite a lot of contact with a carer or relative who is able to send me a message and often they’re very articulate and they can say ‘I’m concerned about this. I think they need this treatment’ and something, and I can say ‘Yeah, let’s do that’ rather than sort of have a kind of very long consultation in which we come to the same conclusion.
Interview 11, CCG role and GP
Digital First Primary Care approaches could be particularly useful to enable those who live further away or with full time work commitments to become more involved in conversations and decisions about the care and support of a patient, as it enabled people to access systems when it worked best for them and without the need to wait in telephone queues. This communication included making contact with the practice on behalf of patients.
… But they were very elderly, or whatever, the issue of contacting us digitally … most of them would do it through their carer or their family member, and their family member could be the other end of the country. So we got that a lot in our area because it’s quite an affluent area. We even got emails from Australia and from America about people’s parents.
Interview 10, locum GP
Further, numerous participants described how carers could support patients to use Digital First Primary Care, broadening accessibility and enabling them to use technology to communicate directly with clinicians. Although, this required carers to be digitally confident or have access to the internet or required technology to do so.
I think some of the older population, like if they’ve got children or relatives, they will fill out the questionnaires for them or they’ll book appointments online for them so it supports their engagement.
Interview 25, nurse
The use of Digital First Primary Care approaches by formal carers in care homes was also reported by participants. Two examples given described how care homes had appointed a designated individual to make requests on behalf of their patients, enabling the easier management and discussion of a number of patients virtually, which could aid the care of patients with multiple long-term conditions.
Disadvantages for carers using Digital First Primary Care, as reported by interviewees
Several potential disadvantages of Digital First Primary Care for carers were shared by the participants. A few concerns were raised about the logistics associated with using such digital approaches, primarily in relation to consent and confidentiality. The participants described how healthcare professionals were unable to discuss healthcare issues with a carer if a patient had not provided the appropriate permissions for them to do so. Once these permissions had been obtained, this was felt to no longer be an issue.
I see the major issues are consent and making sure we’ve got consent from the patient to liaise with said person. I’ve been lucky in that I think all the ones that I have dealt with, there’s been very clear consent on the notes to be able to deal with these people and liaising with them has been just like a normal [Digital First Primary Care enquiry].
Interview 22, GP
As one healthcare professional reported, it could be easier to gauge permission from the patient for the involvement of carers in consultations during face-to-face interactions compared to doing so remotely. This may be particularly relevant for informal, family member carers where a patient may not wish for the carer to know certain aspects of their medical history.
I guess there’s sort of more complexity in the sense that you have to be sure of the patient’s consent to discuss information with a carer, whereas if they walked into a room together that’s kind of implied the patient is happy for the carer to be aware.
Interview 11, CCG role and GP
Related to confidentiality, the participants reported challenges associated with remote consultations being overheard by others. For example, it could be difficult for clinicians to know who else might be in the room when a patient was discussing issues or concerns on the phone, or if speakerphone had been enabled. This is also connected with safeguarding concerns.
The problem with it – and especially if it’s telephone – you don’t really know who’s in the room and you don’t know who’s controlling the situation. And that, to me, is more problematic, especially for a safeguarding and for that sort of safety element, it is really nice when you do pull people in where you can say ‘I’m going to be doing an examination, is it OK if you leave the room or we’re going to go through …’ and you get that one on one time, you don’t know if you’re getting a one on one time over the phone or even a video, because there can be people out of sight, so that’s the downside of technology.
Interview 16, GP
There could also be practical challenges for carers using Digital First Primary Care, for example, instances where carers required a patient’s login details to access online platforms, without which they had to call the practice. There can also be confusion from the clinician’s side around whether the details entered into the Digital First Primary Care system are those of the patient or carer.
While some participants felt that Digital First Primary Care improved the communication between carers and healthcare professionals, others felt that these approaches potentially removed the opportunity for carers to communicate with clinicians and receive the support that a face-to-face consultation may have provided. This may be particularly important for those caring for patients with multiple long-term conditions where in-person support and the discussion of complex issues could be beneficial. Attending appointments in person offered healthcare professionals a window in which to check how a carer was, as well as the patient – the impact of not being able to do this during the COVID-19 lockdowns was noted.
I think a lot of carers were really struggling during COVID and I think they missed that personal face-to-face communication they get when they come in and get support and that sort of thing… their support mechanisms stopped during the pandemic, everything just stopped …
Interview 21, nurse
The impact of Digital First Primary Care on healthcare professionals caring for patients with multiple long-term conditions
The introduction of Digital First Primary Care approaches, by its nature, changed the way in which healthcare professionals work, both individually and with each other, and changed the nature of the healthcare professional–patient relationship. Digital First Primary Care was reported by the participants to both support and hinder these aspects in different ways. Staff noted in particular the importance of developing strong relationships with patients with multiple long-term conditions given their complexity and greater need for continuity of care.
Advantages for healthcare professionals using Digital First Primary Care
Information sharing and communication
While some interviewees felt that Digital First Primary Care had not impacted care co-ordination (rather, it just changed the way co-ordination was achieved), others noted that Digital First Primary Care supported the collection of more information about a patient and greater information sharing and communication across healthcare professionals. This included sharing information across staff in different settings, as well as with colleagues within the same GP practice. Hence, Digital First Primary Care allowed clinicians to have all of a patient’s history to develop a detailed account of the illness at hand and the patient could be triaged/prioritised more effectively to the appropriate health professional (although, this depended on how complete the online form was in the first place, see Impact of Digital First Primary Care on patients).
… so I’ve been doing my diabetic clinic this morning … I’ve had one patient that I need the doctor to review so I’ve put it onto [Digital First Primary Care system] straightaway and put in capital letters and I’ve flagged it that it’s an urgent … for the doctor that deals with the diabetics. And he will then pick that up later this afternoon or possibly tomorrow morning and then he’ll ping that back into my box for me to contact the patient. So, yeah, it’s saved me leaving the room, going and knocking on, disturbing whatever he’s doing. So, yeah, from that point of view, selfishly and for the patient journey, I think that’s much better than how it was before.
Interview 1, nurse
Better information sharing could also allow for a more immediate exchange of information between practitioners and patients to ascertain any deterioration in patients’ well-being more quickly. One respondent noted the particular benefit to healthcare professionals in the community, such as district nurses and paramedics being able to raise issues about a patient through a Digital First Primary Care system, which could support communication and team-working across staff in different organisations.
… as an example, district nurses visiting patients at home concerned about the condition of their skin or legs, if they see anything they can communicate via the system, and we can make a plan together. Again, we do very similar work with paramedics; some things they can think is delivered to us, and we communicate, and it just eases the ways of working as a wider team, really. And it also improves the record keeping, you can go back and reflect on it.
Interview 12, CCG role and GP
Digital First Primary Care allowed all staff within a GP practice to have access to the same information, notes and history, which helped to ensure that there was no missing data or misinterpretation. Furthermore, GPs felt that Digital First Primary Care could reduce the risk of human error when uploading information, documents or images onto patient records.
I think it makes it easier, because we’ve all got exactly the same history. You know that everyone sees things differently, everyone writes things differently, but also patients’ history changes from day to day. They add things in and take things away, but actually we’re all dealing with the same initial contact, because we’ve all seen that initial [Digital First Primary Care notes], and we know what they’re first presenting complaint was… so we’re working off the same rule.
Interview 3, nurse
Relationships between staff and patients
From the staff point of view, the use of Digital First Primary Care could support the development of good relationships between staff and patients. For example, as Digital First Primary Care could improve access to care for patients, patients may be more satisfied with their care and, thus, have better relationships with their clinicians. In addition, one interviewee noted that once a relationship has been built with a patient, it could be sustained well remotely without the need for face-to-face consultations.
I think … we build a better relationship with a patient in some respects because of the accessibility, and because of the quickness, they then are happier.
Interview 3, nurse
Greater efficiencies and flexibility
There may be benefits for clinicians using Digital First Primary Care in terms of greater efficiencies. For example, using Digital First Primary Care could mean that more patients are seen in a shorter space of time, such as by sending messages to patients rather than arranging face-to-face appointments, or Digital First Primary Care systems automatically interpreting the data provided by patients. One participant reported that workload can reduce 10–20% if digital approaches are used properly, but inefficiencies can be created when they are not.
Say it takes you one or two minutes to type up a consultation, if you’ve got a 10 minute appointment, that’s 10 to 20% of the appointment time. Similarly you save the time of the patient actually coming into the room so for some patients that might be less than a minute but for other patients it might more than a minute so again that’s another potentially 10% of your appointment time saved just by the efficiency of having a remote consultation.
Interview 19, GP
The use of Digital First Primary Care may also gave healthcare professionals more control over their day, as tasks were completed remotely, allowing staff to take breaks during the day.
I think it [Digital First Primary Care] does feel very different … so I did my first year GP with face-to-face, you know, waiting room full of patients, pressure of they’re going to be late … they’re all sat there and that feels really pressured and getting up and going to get them and all the rest of it, whereas that virtual space means that I’m in control of my own time, I can prepare myself before I do my consultation, all my screens can have various things up on them, I can have books open on my desk, so I can portray a very different environment in my room that they can’t see and that feels quite empowering for my side.
Interview 16, GP
Disadvantages for healthcare professionals using Digital First Primary Care
Clinician–patient relationship
Despite some of the positive aspects that could arise for healthcare professionals when using Digital First Primary Care, others noted challenges, particularly in relation to the clinician–patient relationship. The majority of GPs felt that the medium of communication associated with Digital First Primary Care, such as e-mail and telephone, inhibited the ability of clinical staff to generate a rapport with patients and meant that the relationship could be seen as transactional. This was reported to make it more difficult to develop strong relationships with some patients, with the use of Digital First Primary Care being viewed as impersonal.
I think it’s [Digital First Primary Care] very much more impersonal. There is very little rapport building. I can write a token sentence at the start saying ‘I’m very sorry to hear this’ but that’s quite formulaic. There is none of that rapport building. So I would imagine patients would say, assuming they’ve got a response from a new doctor, I would image they’d say there is no rapport there. I think they can probably say whether it was a polite response, an informative response, but that’s going to be very objective rather than that emotional and subjective response.
Interview 22, GP
In particular, the participants noted the challenge of being less able to pick up on non-verbal cues and behaviour changes when interacting with patients remotely, such as their mobility, appearance and facial expressions. This also links to the challenges in implementing continuity of care mentioned earlier in this chapter, as if a patient sees a different health professional at each appointment, clinicians may not be able to notice behavioural changes. This challenge could be exacerbated if the patient was not seen in-person.
… you won’t get the full picture of somebody if you only oversee them digitally. And it’s everything. It is really, you hear how people walk down the corridor … If I don’t get up and get them, I can hear their footsteps … and if I know it’s somebody who normally runs and they’re shuffling that gives me a huge clue before they’ve even come through the door. Do they grab hold of the chair and lower themselves down slowly which would tell me their arthritis is in really bad shape, or do they just come in and sit down … Does a person smell? Do they smell of urine? Are they incontinent? Are they brushing their hair or whatever? It all puts together a picture of people.
Interview 6, researcher and GP
Confidence in clinical decision-making
Non-face-to-face approaches could make clinicians less confident in their clinical decision-making which could lead to greater numbers of in-person follow-up appointments or longer consultation lengths. Relatedly, there may be issues with safety (see Impact of Digital First Primary Care on patients) and litigation against clinicians due to errors made when consulting remotely (see later in this section).
One other thing that’s been really surprising for me is that how much longer it’s taking me to feel confident in a clinical decision when I’m consulting over the telephone and I can’t see somebody.
Interview 6, researcher and GP
Confidence in decision-making was noted as a particular challenge for less experienced healthcare professionals who may need greater support when making remote clinical decisions for patients. Delivering care remotely also offered less opportunity for shadowing other professionals. This could be particularly difficult if the less experienced staff member needed to build a relationship with a patient from scratch. Relatedly, some GPs we interviewed felt that certain patient requests required quite careful interpretation and decision-making and would be best suited to a more experienced GP who was comfortable diagnosing remotely.
… I don’t think we realised just how much people learn from what used to be called ‘sitting with Nelly’ … not necessarily sitting with the expert all the time but having the expert in the next door room … you also have that vicarious learning of immediately seeing how the more experienced doctor or practitioner managers the patient that you’ve just spent 20 minutes taking history from. And that is fundamentally the unit of learning in medicine and also in advanced nurse practitioner work … so I’m massively worried about training.
Interview 8, researcher
Clinicians were also concerned, if they did not see the patient face-to-face, about whether they were covered from a legal perspective. As healthcare professionals may not feel confident in their clinical decision-making, they may prefer to see a patient face-to-face for some appointments, such as when prescribing, or just to check in on the patient more generally.
I think the concern is the medico-legal aspect of have you done a thorough assessment on the phone/video? … it’s a lot of thinking to make sure … you’ve covered everything and you have to go above and beyond in terms of your history-taking and your thinking whereas actually if they’re in the room, you would be like ‘this is not going to be an issue ever’.
Interview 20, GP
Creating inefficiencies
While some participants felt that Digital First Primary Care offered greater efficiencies and time savings, others noted the greater burden using Digital First Primary Care could place on healthcare professionals. For example, the extra time and capacity needed to review Digital First Primary Care enquiries and triage them appropriately, or Digital First Primary Care creating greater patient demand.
It was originally designed for somebody to be dedicated to look at an [Digital First Primary Care enquiry] and decide this is a clinical or for a doctor or for a nurse, an administrative pathway, a physiotherapy pathway. If we had all the different pathways effectively manned in the primary health care setting, and a team dedicated to review and deal with the [Digital First Primary Care enquiries] and read them as they came through and forward them to the appropriate area. This kind of facility never really existed in general practice and you need to have almost a hub of telephonists who are manning the [Digital First Primary Care enquiries] as they come through.
Interview 24, GP
Caring for patients with multiple long-term conditions via Digital First Primary Care posed challenges in terms of creating inefficiencies. This was because patients seen remotely by a clinician often needed to go to the practice for a face-to-face appointment, particularly for long-term conditions which needed regular in-person review. Some participants also noted that consultations conducted by phone were as long as face-to-face ones and did not save any time. This created an added burden for both staff and the patient.
… it [Digital First Primary Care] doesn’t take away the need for them to have an appointment because so many long-term condition reviews need to be done face-to-face. So if anything, it’s just an added thing for them, and for us, to do … You know, like diabetes – they need to have a face-to-face diabetes review, and check their bloods and stuff, so if they’re then pulling an [Digital First Primary Care enquiry] saying I need a review, then essentially, you’ve just added something for reception to triage, for them to have to fill in themselves, when actually they still need to be seen.
Interview 3, nurse
Some participants noted that the lack of integration of Digital First Primary Care with patient record systems led to practice administration staff undertaking burdensome tasks of entering patient data on multiple databases.
If it would work really like neatly with their current, like EMIS, then software so it can … you know sometimes patients say I used this cream in the past, can I have it again? What cream? … When was it, what year? Just making it that bit smarter, talking to each other better rather than just a PDF slammed in the middle of their notes.
Interview 20, GP
Increasing patient demand
It was reported by some healthcare professionals that the introduction of Digital First Primary Care led to an increase in demand from patients as it was easier to get in contact with the practice. Staff noted that this resulted in patients submitting an enquiry via Digital First Primary Care for issues that were likely to be quickly resolved by themselves.
If you’ve got real problems with capacity to deal with the demand as it is at the moment, your demand is likely, in some ways, to go up a bit because you’re giving people an easier route to get in and that’s why people turn it off.
Interview 10, locum GP
However, not all interviewees agreed with this theory, with a small number noting that it was a misconception that making access easier led to increased demand.
There’s a common trope that online consultations and easy access to general practice has led to more and more trivial presentations to us and patients coming to us at an earlier stage in their illness rather than trying to self-care or wait it out. And this has become, it’s hard to fight this narrative, and actually the data does not back this up.
Interview 11, CCG role and GP
For some, the higher demand meant that care became less accessible for all patients and that GP time was not dedicated to the patients most in need of it. While some practices tried to get around this issue by restricting the times Digital First Primary Care was available (see How Digital First Primary Care is implemented and used within primary care), this may have made it more difficult for patients to access care.
I think it’s incredibly easy access to the point where I think that I also want to be accessible to people, but I don’t necessarily want to be accessible to them if their child’s just vomited once or had a fever once. So it seems to have driven out a lot of kind of common-sense almost … and actually the problem is there’s very little that I can say that is helpful other than say ‘Let’s just see how things go and let’s see how things go for the next twenty four to forty eight hours’. I feel like it’s skewed towards the worried well.
Interview 4, GP
Summary of the main findings of the study
In this section the main findings of the study are summarised, ahead of the Discussion and conclusions.
The aim of this evaluation was to explore the experiences of Digital First Primary Care for patients with multiple long-term conditions from the perspectives of health professionals and stakeholders. Here, we provide an overview of the key study findings.
Overall, the COVID-19 pandemic led to the rapid adoption of Digital First Primary Care on a larger scale than pre pandemic. The roll out was done at speed and there was little opportunity for healthcare professionals to reflect on the impact on patient groups, such as those with multiple long-term conditions. Nor has much consideration been given to the impacts that the widespread use of these approaches may have on the healthcare professionals who provide care for those with multiple long-term conditions.
Choosing a Digital First Primary Care provider and implementing the change could be a challenge for practices, and the way in which a practice implemented the Digital First Primary Care approach could adversely impact those with multiple long-term conditions for example in assisting or hindering continuity of care. The introduction of Digital First Primary Care was frequently cited by participants as leading to an increase in patient demand. To manage this, multiple practices reported reducing the time the system was available for use (e.g. closing it down over weekends).
Patients with multiple long-term conditions could face additional challenges with the use of Digital First Primary Care compared to other patients. These challenges included navigating Digital First Primary Care systems, particularly digital questionnaires which followed algorithmic approaches and restricted the opportunity for descriptive narrative and speaking with a professional who knew them and their conditions well. Alternatively, Digital First Primary Care could offer additional benefits to patients with multiple long-term conditions, such as greater convenience and easier completion of simple tasks, such as repeat prescriptions. However, these benefits were, in part, determined by the nature and severity of the patient’s condition(s).
The presence of multiple long-term conditions was not the only factor which could impact upon the ease of use of a Digital First Primary Care approach. Other factors noted by the interview respondents included patients for whom English was not their first language, literacy skills, confidence in navigating online services (often perceived by the participants to be correlated with the age of the patient) and the availability of technology to engage with the practice this way.
There were differing views from the participants as to the extent to which Digital First Primary Care helped to manage staff workload. For some it did, particularly for straightforward tasks such as sick notes. But for other conditions or patient groups, the efficiency of the system was often questioned, for example for use with patients with multiple long-term conditions where the digital form may not fully or accurately inform the health professional about the problem, leading to inefficiencies.
Several participants noted a preference from staff to see patients face-to-face, particularly those with multiple long-term conditions. For many, a face-to-face consultation was not just seen as a transactional consultation but a chance to assess the patient more holistically. Some felt that once a relationship between a healthcare professional and a patient with multiple long-term conditions had been established, other forms of consultation could be used, for example a telephone consultation or messaging via a Digital First Primary Care platform.
The participants identified benefits of Digital First Primary Care to carers of those with multiple long-term conditions, particularly the ability to be more involved in consultations with healthcare professionals and the care of the patient. However, some concerns around confidentiality and privacy were raised. Carers’ experiences of Digital First Primary Care have, until now, been relatively overlooked, and this represents an area where further research could be of benefit.
Chapter 5 Discussion and conclusions
Box 6 provides a summary of Chapter 5 of this report.
Summary of key points
-
Despite patients with multiple long-term conditions making up a high proportion of those who consult with a GP, relatively little consideration had been given by the interview respondents to the experience of Digital First Primary Care in this group.
-
There remain debates within the literature about the extent to which Digital First Primary Care impacts on staff workload. Within our study, some participants felt that the use of Digital First Primary Care approaches reduced workload, whereas others felt that it increased it.
-
The push for greater access to general practice, and the corresponding focus on seeing and speaking to a patient rapidly, appears at times to have occurred at the expense of some of the other aspects of general practice care which were felt to be valued by patients and health professionals working with those with multiple long-term conditions. These include continuity of care (particularly during the COVID-19 pandemic) and an established doctor–patient relationship which enables effective two-way communication.
-
In this study, Digital First Primary Care could be seen to compromise continuity of care. The impact on this depended largely on how surgeries implemented the Digital First Primary Care approach and if their system enabled continuity of care to be encouraged or achieved.
-
For stakeholders and health professionals in our study, the overwhelming view was that Digital First Primary Care approaches to primary care could be useful for the management of patients with multiple long-term conditions but should not be a substitute for face-to-face consultations.
-
The participants in this evaluation revealed the impact they felt that Digital First Primary Care had on carers of those with multiple long-term conditions and the opportunities it afforded carers for greater involvement in primary care consultations, an issue which future research with carers could potentially explore further.
-
Stakeholder and health professionals reported that Digital First Primary Care approaches could work better for some patients with multiple long-term conditions than others. For example, experienced patients who were able to record and monitor their symptoms themselves and were confident about their care and able to seek health professional input when it was required.
-
As outlined in this report, the research team experienced considerable challenges recruiting general practices to participate in the study. Practices often mentioned the pressures on primary care due to COVID-19, increased patient demand and staff recruitment and retention issues. It is critically important for the future of general practice that research continues to be conducted within this group. The authors note that primary care is not supported to conduct research in the same way as secondary care, which has greater research infrastructure.
-
Lessons for the future use of Digital First Primary Care approaches for patients with multiple long-term conditions for practices, PCNs and integrated care systems are noted.
-
The strengths and limitations of the study are outlined.
Discussion of the findings
In this section of the report, the key findings from this rapid evaluation are examined in greater detail and in the context of previous research. The implications for practice are also explored, and the strengths and weaknesses of the approach are noted.
Digital First Primary Care and the COVID-19 pandemic
A key finding in this evaluation is that Digital First Primary Care approaches were rapidly rolled out during the COVID-19 pandemic and dramatically changed the way in which general practice operated. Digital First Primary Care was implemented at a rapid pace, at a time of immense pressures on staff, which meant there was little time for consideration of the impacts on groups of patients, including those with multiple long-term conditions. These approaches were originally designed to manage patient demand in general practice and began with use for only ‘on the day’ and more urgent problems rather than for routine care for patients with multiple long-term conditions. Today, they are used for all patients whether they have an acute problem or long-term conditions.
Many participants in this study felt that the pressures on primary care services were worse than they had ever been, with issues such as increased demand, challenges in secondary care capacity and problems of staff retention and recruitment being widely cited. It was clear from the data that health professionals were experiencing considerable pressures at the present time, and the fall in fully qualified GPs and the increase in the number of patients a GP was responsible for has had an impact on professionals. 13,29 There remains debate within the literature about the extent to which Digital First Primary Care impacts on staff workload, with one large study identifying an increase in staff workload as a result of the introduction of telephone-first approaches (the forerunner to Digital First Primary Care) and a smaller study noting that GPs felt there was duplication of work when many digital-first consultations resulted in telephone or face-to-face appointments. 8,62 Within our study, some participants felt that the use of Digital First Primary Care approaches reduced workload, whereas others felt that it increased it. Increases in workload could be due to greater demand, as healthcare professionals are more accessible to patients. It was reported that Digital First Primary Care could increase workload particularly in relation to certain groups of patients, such as those with multiple long-term conditions, as the information from online forms was often not adequate and the health professional was required to have an in-person consultation with the patient anyway. In such circumstances the reading of the digital form generated more work for health professionals.
Digital First Primary Care for patients with multiple long-term conditions
In England, approximately a quarter of adults have two or more long-term conditions. 21 Despite patients with multiple long-term conditions making up a high proportion of those who consult with a GP, relatively little consideration had been given by the interview respondents to the experience of Digital First Primary Care in this group. The digital-first systems appear to be designed with a ‘typical’ patient in mind with a single issue, rather than more complex patients with multiple conditions. One report noted that care for those with two or more conditions accounts for a large proportion of NHS costs, including over half of the costs of primary and secondary care, and three-quarters of the costs of primary care prescriptions. 22 Despite this, the participants struggled to think of combinations of multiple long-term conditions which might impact a patient’s experience of Digital First Primary Care.
The participants noted that they felt that Digital First Primary Care might work better for some groups of patients with multiple long-term conditions than others. The so called ‘expert patient’ who is experienced in managing their condition, is proactive in seeking professional advice when they need it and is confident in managing and monitoring their condition at home might be comfortable with a more Digital First Primary Care approach to the management of multiple long-term conditions. However, for some groups of patients with multiple long-term conditions, this reliance on them to articulate and be proactive was a challenge. For example, patients who struggle with memory due to their condition, those with learning difficulties and those who find accessing Digital First Primary Care challenging due to issues with their dexterity. The recent Fuller review set out a vision for integrating primary care and explicitly for the delivery of ‘more proactive personalised care with support from multidisciplinary team of professionals to people with more complex needs, including, but not limited to, those with multiple long-term conditions.’26 While our data suggested that more personalised care for those with multiple long-term conditions would be valued, it also showed the importance of building a relationship between patients and healthcare professionals. This may be built up over both acute and ongoing illness episodes.
The health professionals and stakeholders who we interviewed reported that patients could struggle with Digital First Primary Care approaches, particularly digital questionnaires which follow algorithmic approaches, and this restricted the opportunity for descriptive narratives. It was noted in such circumstances that patients may alter what is entered into the system to ensure the enquiry would not be redirected to an emergency response. If patients are unable to truthfully enter symptoms into the system this may undermine patient confidence in the Digital First Primary Care system.
For patients who were not able to access the practice through digital means, all practices in the study had telephone lines which were a route of access available to patients wishing to request a consultation with a health professional. However, it should be noted that the availability of a telephone line did not necessarily equate to good access for those not using a digital route. For example, practices varied in terms of the number of telephone lines they had available and sufficient administrative staff who were available to answer telephones, meaning it could take longer to contact the practice by telephone than by a digital route. The authors note that there is a difference between an alternative to Digital First Primary Care being available to patients within a surgery, and that service being equitable. While some surgeries managed all enquiries within one system, whether they come by telephone or a digital route, other practices manage digital and telephone queries as separate streams of work. As a result, differences may include the speed within which a health professional is spoken to.
Impact of Digital First Primary Care on healthcare professionals caring for patients with multiple long-term conditions
The push for greater access to general practice, and the corresponding focus on seeing and speaking to a patient rapidly, appeared at times to have occurred at the expense of some of the other aspects of general practice care which were valued for patients and health professionals working with those with multiple long-term conditions. These included continuity of care (particularly during the COVID-19 pandemic) and an established doctor–patient relationship which enabled the clinician and patient to have effective communication. For the participants in our study, the overwhelming view was that Digital First approaches to primary care were useful for professionals and stakeholders when it came to patients with multiple long-term conditions, but not at the expense of face-to-face consultations. For example, health professionals may find Digital First Primary Care approaches helpful for accessing patient-reported data on their condition, such as at-home blood pressure readings, or to discuss how a patient is getting on with a new medication. But they were not a substitute for face-to-face consultations where a physical examination may be required, or when the health professional may wish to obtain a more holistic view of the patients’ well-being.
Our findings suggest that Digital First Primary Care may benefit some patients more than others. Patients who are comfortable monitoring their own condition and contacting health professionals through digital routes when needed may find their care is enhanced with the greater use of digital approaches facilitating more regular contact with health professionals. However, patients who are not digitally literate or who struggle to describe their condition or symptoms through a written format may be disadvantaged by the widespread use of digital approaches. A recent editorial highlighted this point, emphasising that while digital technologies can facilitate care for some, there can be a barrier to others due to language, cognitive or hearing challenges. 63
Recent research has demonstrated the complexities of a number of practice- and patient-level factors in relation to remote consultations. Greenhalgh et al. noted how the interactions between individual, organisational and system-level factors influenced how remote consultation services were established and delivered at a local level. 64 Within the practices included in this study there was great variation in the circumstances in which Digital First approaches had been adopted and the attitudes of staff towards it. Previous work exploring use of video consultations in general practice has shown that clinicians often varied in their willingness to engage with digital innovations. 65 The challenge, particularly during the COVID-19 pandemic, was that professionals had to engage with digital approaches, even if they would previously have shied away from their use. A study of health professionals during COVID-19 identified concerns regarding clinical risk when consulting remotely. 48 This issue was raised in this research and may be particularly concerning for patients with multiple long-term conditions where understanding the nature of a patient’s different conditions and their concerns may be particularly important.
Continuity of care is a concept which has been shown for some time to be particularly important for patients with multiple long-term conditions, for example for outcomes for patients with dementia and for patients without specific long-term conditions. 43,66 Digital First Primary Care approaches have been introduced in primary care as a way to manage demand and to ensure patients are seen or spoken to more rapidly than under a traditional appointment system. However, for staff and for patients with multiple long-term conditions, timeliness of access to a professional may be less important than a consultation with a professional who is known to them and knows their multiple conditions. A previous study concluded that there was little evidence of the impact of improved access on continuity of care and noted that for health professionals, relational continuity was an important element of their role. 67 For several health professionals and stakeholders in our study, this move to Digital First Primary Care compromised continuity of care. This depended largely on how surgeries implemented the Digital First Primary Care approach and if their system enabled continuity of care to be encouraged or achieved. It should be noted that the concept of continuity of care has been widely debated and interpreted as continuity of care between one health professional and the patient, between a small team of healthcare professionals and the patient or episodic continuity of care (where continuity is achieved for a single health problem). There was little evidence in our data that practices were able to prioritise continuity of care, of any of these conceptual models. Even in the practices in our study which had a system in place to try to increase continuity of care for patients, this was not reported to be a priority in practice.
Linked to continuity of care was the associated workload for healthcare professionals when cases were passed from professional to professional. In these cases, multiple professionals spent time reviewing the Digital First Primary Care information, but then passed it to someone else to review who then would deal with it. If several healthcare professionals consider a patient’s case it takes more collective resource than a single face-to-face consultation with one healthcare professional who knows the patient and their conditions well.
A recent literature review noted the difficulties for health professionals in making clinical decisions without seeing a patient face to face. 44 This was echoed in the findings of this rapid review which has highlighted the impacts on clinical staff of working with a Digital First Primary Care approach. Professionals had to work in a largely different way than they had trained for, for example without any reliance on non-verbal cues and body language. This can be challenging for health professionals and the implications for patient safety and litigation have been noted in this report. The workload and intensity of work was also noted, with a greater volume of patients being spoken to per day compared with traditional approaches.
Impact of Digital First Primary Care on carers of those with multiple long-term conditions
This evaluation revealed the impacts Digital First Primary Care may have on the carers of those with multiple long-term conditions and the opportunities this affords carers for greater involvement in primary care consultations. The impacts on the carers of those with multiple long-term conditions in relation to Digital Frist Primary Care do not appear to have been considered to a great extent in the existing literature, and we suggest this might be an area for further study collecting data directly from patients and carers and an area of interest to national health and carer organisations, citizen panels and the Department of Health and Social Care.
Conducting a rapid evaluation in primary care
As outlined in this report, the research team experienced significant challenges in this study with the recruitment of patients and carers. The research team were experienced in studies of general practice, through the BRACE evaluation centre as well as other work. The principal investigator had conducted research in primary care for the last 13 years, recruiting through general practices. While recruitment to research in primary care has always been a challenge, noted in previous work of BRACE, the challenges at this point were unprecedented. Practices often mentioned the pressures on primary care due to COVID-19, including the vaccination roll-out, increased patient demand and staff recruitment and retention issues. It is critically important for the future of general practice that research continues to be conducted with this group. It was noted by the researchers that at a time of great pressures on the service, finding additional time to participate in research was a real challenge. The logistics of discussing the research with practice staff prior to obtaining consent to participate was also difficult and time consuming. The authors note that primary care is not supported to conduct research in the same way as secondary care, which has greater research infrastructure. If the issues of general practice recruitment are widespread, and we understand from informal discussions that this is the case, this may be an issue of critical importance to the profession and to the research community more widely.
Future research on Digital First Primary Care
Due to significant challenges of recruitment, the research team were unable to seek the views of patients and their carers in this research. As noted, this is a weakness of this study and staff, or stakeholder, perceptions of the views of patients and carers are no substitute for the views of patients and carers themselves. The authors see important future work in obtaining the views of patients and their carers and comparing those alongside the views of health professionals and stakeholders obtained in this study. It may be necessary for such a study to avoid recruiting participants through general practice, due to the challenges outlined in this report.
The participants in this study struggled to identify clusters of multiple long-term conditions which may be particularly impacted by Digital First approaches. Future work should explore this issue further; a list of conditions or combinations of conditions which may be adversely impacted would enable general practice staff to target particular help to groups of patients.
This report highlights how general practice has changed considerably since the COVID-19 pandemic and there remains little understanding of the implications of widespread Digital First Primary Care approaches on staff and patients. In particular, the impact of the use of these approaches on workload and the resulting impact on staff morale and retention. A multi-methods longitudinal study would be beneficial in this area, alongside an economic analysis.
The findings of this research suggest that particular groups of patients, such as those with difficulties with literacy or for whom English is not their first language, may find Digital First Primary Care approaches particularly challenging to access and engage with. Other groups who lack access to digital technology, such as those living in areas of deprivation or with chaotic lifestyles, may also be adversely impacted by the increased use of Digital First approaches in primary care. More research, particularly with patients and carers, is required to understand these challenges and the ways in which they can be overcome. As communication between a patient and general practice increasingly relies on digital approaches there is concern that it may widen health inequalities further. While all the practices included in this study had options for patients to telephone the practice, rather than make contact digitally, access by telephone may be more challenging and take longer than via digital routes; more research is needed to understand if this is the case and the implications of this.
Future direction of Digital First Primary Care within general practice
At the time of writing, November 2022, the impact of COVID-19 on the healthcare system remains unclear as winter pressures begin to be felt within the system. The legacy of COVID-19 on general practice is largely unknown, but participants in the study were clear that general practice would not revert to only a face-to-face medium in the future. There is a need for practices to consider the impacts Digital First Primary Care has on different groups within the practice population, for example those with multiple long-term conditions.
What lessons can be learnt for future practice of Digital First Primary Care for patients with multiple long-term conditions?
Here we address our final research question by considering the lessons which can be learnt for the future use of Digital First Primary Care approaches for patients with multiple long-term conditions across a range of stakeholders. The lessons at general-practice level may also be useful for other groups.
Implications for individual general practices
It was evident that the type of Digital First Primary Care approach used by a practice may impact on how suitable the approach is for patients with multiple long-term conditions and the health professionals who care for them. In particular, the use of rigid algorithmic approaches were reported to be challenging for patients with multiple long-term conditions to complete satisfactorily and for health professionals to process, as they fail to take account of nuance in symptoms. As a result, digital-first providers need to have greater consideration of how patients living with long-term and complex conditions engage with and use digital-first systems from the point of contact through to submitting information about their condition. Digital-first providers may require more in-depth consultation with this group of patients to reconsider or adapt algorithms insofar they are designed to capture patient narratives more accurately. A recent article noted that the negative impacts of online consultations could be mitigated through system design, for example the use of a free-text format. 45 It is a finding in this report that, although practices might use the same Digital First Primary Care provider, the ways in which practices implement and use these approaches vary greatly. Practices have adapted approaches to suit their population, staffing model and, increasingly, capacity. It might be helpful for practices to review how Digital First Primary Care approaches work for patients with multiple long-term conditions, and the healthcare professionals who work with them. This may include practices which enhance the provision of continuity of care or enable at-home monitoring to be discussed during the consultation. Adapting practices may lead to improvements in care for patients and efficiencies in workload for the health professionals who care for them.
The practice of turning Digital First Primary Care access routes to primary care on and off should be carefully considered and could have adverse impacts on patients. The aim of this approach was articulated as reducing demand for GP surgeries at times when they were struggling with too many requests. Yet, some participants in this study felt there was no evidence that demand was in fact reduced, with patients using telephone routes if Digital First Primary Care ones were not available. It should be noted that turning off Digital First Primary Care routes may only serve to cause frustration and confusion to patients and reduce their confidence in primary care. Future work with patients and carers could usefully explore this point further.
The presence or not of multiple long-term conditions may impact upon how a patient experiences Digital First Primary Care but it should be noted that other factors are important to consider, for example if the patient’s first language is English and if they have the digital literacy to use and adopt technology (in the interviews this was often correlated with the age of a patient, although this may not be the case in practice). Practices may wish to seek to adapt their Digital Frist Primary Care system dependent upon the population the practice serves to assist them in using the system, for example the practices in our study had enabled online translation functions to ease use of the online form for patients for whom English was not their first language.
Digital First Primary Care puts the onus on the patient to articulate their problem well through written means, either through the submission of a free-text approach or through the navigation of an algorithmic approach. This can be more challenging for some patients than others, for example those with learning difficulties.
In addition to individual practices these findings may be applicable to the BMA and RCGP as they seek to support their members in the use of digital approaches in primary care. Implications for consideration at PCN and Integrated Care System level.
The participants often described challenges when choosing which provider to use and a lack of capacity, at individual practice level, to comprehend the options and strengths and weaknesses of different approaches. There may be economies of scale in terms of expertise and buying power with providers for practices commissioning Digital First Primary Care approaches at PCN or Integrated Care System level.
The ways in which practices use Digital First Primary Care was shown to vary considerably in this study. There may be shared learning across practices within PCNs and Integrated Care Systems as to the factors which can assist the use of Digital First Primary Care for groups of patients, for example those with multiple long-term conditions.
Historically, the choice of Digital First Primary Care provider has often not been made by individual practices but at CCG level, who would offer to fund a particular provider’s approach. It should be noted that frequent changing of the Digital First Primary Care provider could be challenging to health professionals and patients. With the abolition of CCGs, at the time of writing, it is unclear how the commissioning of future services will be configured. Going forward, PCNs will need to decide whether adopting a single Digital First provider for all practices in their network is a sustainable model given the heterogeneity of patient needs and patient populations.
Implications for policy-makers
It is clear from the interviews conducted as part of this study that general practices are experiencing the impact of COVID-19 and the pressures of demand. While Digital First Primary Care approaches to primary care were first introduced to aid demand management, several of our participants felt that general practice was struggling now more than ever. The frequent changes in policy on digital approaches versus face-to face-consultations served to further demoralise primary care staff, with several participants feeling that as soon as they modified their service provision to be in line with one guidance policy, another was introduced. Future guidance on Digital First Primary Care should seek to support practices and support local decisions based on the needs of the population served, staffing and resources.
There is little current monitoring of the use of digital services in general practice. The most frequently reported metric is the number of patients signed up to digital services, but this does not record the volume of digital contacts in general practice. A greater knowledge of the types of services being used in general practice may assist policy-makers in providing information and support on digital systems to practices and provide leverage to work with providers to ensure that services are meeting the needs of all patient groups. Further, given the scale of digital tools being used in general practice, policy makers need to ensure that they capture the experiences of patients and understand how such tools affect their experience of accessing and receiving care. This could be achieved by including more specific questions about patients’ experience of using digital systems as part of the GP Patient Survey. Additional questions within this large survey may also enable the further scrutiny of inequalities and the impacts of these on experiences of Digital First Primary Care.
Strengths and weaknesses of the approach
Digital First Primary Care has become a popular approach used by general practice during and since the COVID-19 pandemic, so this project has focused on an issue of central importance to primary care at the current time and contributes to the discussion of how general practice adapts to this period post the COVID-19 pandemic. The focus of this rapid evaluation was on the impacts on patients with multiple long-term conditions, from the perspectives of stakeholders and health professionals, of Digital First Primary Care. Information on the impacts on patients with multiple long-term conditions was largely not present in the published literature. The findings also identify issues for the carers of patients with multiple long-term conditions, as noted by stakeholders and health professionals, a group often neglected in previous research.
The key weakness of this study was that the research team were not able to obtain the views of patients with multiple long-term conditions and their carers. The research team recruited fewer healthcare professional interviewees (n = 14) than had originally been planned. The study is limited to eight general practices and the use of two digital providers. The participants were not able to identify specific combinations of multiple long-term conditions for which Digital First Primary Care was a challenge.
Due to the challenges of recruiting general practice staff, additional interviews were conducted with stakeholders who also worked in general practices. Despite seeking to do so, the researchers were not able to include the views of a range of allied health professionals within primary care in this study. GPs formed the majority of participants interviewed; however, this may reflect the fact that the majority of Digital First Primary Care approaches were led by GPs. Several of the general practices recruited to the study were from one super-partnership. Therefore, their experiences may be aligned compared to other practices who are not within a super-partnership. Fortunately, the research team were experienced in qualitative approaches and primary care research and were, therefore, able to adapt the approach as needed when faced with recruitment challenges.
Despite the recruitment challenges faced, we believe we have collected useful data and distilled learning on the experiences, advantages and disadvantages of using Digital First Primary Care approaches for patients with multiple long-term conditions. The interviews with stakeholders provide insights into the current national primary care context and digital-related policy. The findings from this study remain timely given the ongoing Digital First Primary Care implementation and policy challenges, as well as the pressures on primary care.
Conclusions
Despite a large volume of the consultations in general practice taking place with patients with multiple long-term conditions, the roll-out of Digital First Primary Care, particularly during the COVID-19 pandemic, did not specifically address the needs of patients with multiple long-term conditions. Nor has there been consideration of the use of these approaches by the health professionals who care for patients with multiple long-term conditions. This includes the efficiency of the system and the ways in which it addresses the needs of this patient population.
The findings of our rapid evaluation suggest that those interviewed feel there may be benefits associated with Digital First Primary Care approaches for the carers of those with multiple long-term conditions, a group which up until now have been largely absent from the literature on Digital First Primary Care approaches. Future work should seek to include the views of Digital First Primary Care of patients with multiple long-term conditions and their carers, which was not possible in this study due to challenges with capacity within general practice. This study highlights how general practice has developed and adapted swiftly over the last few years and how little is known about the impacts of Digital First Primary Care. A mixed methods longitudinal study or economic evaluation of its impacts could be potential ways to understand the impacts of these changes more comprehensively.
Equality, diversity and inclusion
Participant representation
Within this evaluation, we aimed to ensure that the participants interviewed were representative of general practices within England and with respect to primary-care expertise more widely.
Site characteristics
We recruited eight general practices from a range of regions across England, representing different working relationships with other practices local to their area, Integrated Care Systems/Integrated Care Boards and trusts, and varied in their urban/rural characteristics, deprivation scores, ethnicity and workforce size (see Chapter 3).
Strategies to improve representation
Within the study we undertook a range of strategies to try and ensure that our study was inclusive. We aimed to purposively sample using a range of criteria (e.g. clinician type, role within primary care-related organisation, knowledge on topic area for expert stakeholders) to ensure that our sample was as inclusive and representative as possible. We offered different modes of interview (telephone, Microsoft Teams, Zoom) scheduled around participants’ working commitments to reduce the burden and to ensure accessibility for as many people as possible. We offered the option for members of the research team to support practices to prepare invitation packs to be sent to patients.
Further efforts are needed to ensure that studies of primary care are as representative as they can be in future, for example approaching practices who provide care across a range of different models (federations, super-partnerships, vertically integrated with NHS Trusts, as well as PCNs) and hold different contracts (e.g. general medical services, alternative provider medical services, personal medical services). There were limited opportunities in our study to reach out further due to the pressures placed on primary care workforces and the timescales of our study.
Participant characteristics
Despite efforts to include a range of health professionals from primary care, many of our participants were male and/or spoke English as a first language. Notably, we did not purposely sample for gender, ethnicity, language nor length of time working in general practice. In addition, our sample is over-represented by GPs and under-represents nurses and allied health professionals working in primary care. However, this may in part reflect the central role GPs play when using Digital First Primary Care in practice. However, our sample of stakeholders was diverse in that the participants came from a range of primary-care related organisations, academic institutions and policy bodies. Notably, we were unable to recruit and interview patients living with multiple long-term conditions. We did not collect data relating to staff’s personal demographics for example age and ethnicity as we focused on their professional characteristics.
Research topics relating to equality, diversity and inclusion
Our study had a clear focus on the provision of care for patients living with multiple long-term conditions with respect to service research and staff and patient engagement with Digital First Primary Care, and an analysis of staff accounts of implementing and delivering care using digital means.
Reflections on the research team and wider involvement
Research team
Overall, our team included researchers from academic university settings and a not-for-profit research organisation. The research team was small (n = 4) but had experiences of using qualitative mixed methods to collect data and working in many different disciplines (sociology, applied health research, public health and social policy). The team members differed in seniority from senior researcher (PI) to researchers earlier in their careers. The research team comprised a mix of backgrounds in relation to age, gender and ethnicity.
The team held bi-monthly project meetings throughout and weekly data collection and analysis meetings during the second half of the project to ensure that all members of the team were well-supported. Members of the team have been involved in a range of aspects regarding the project, from conception to data collection and analysis and the dissemination of findings (see Contributions of Authors). All the researchers were supported by the principal investigator (JN) and senior members of the BRACE team.
Wider involvement
In addition to the research team, our evaluation also included input from our BRACE steering group, executive team, and PPI group, who were actively involved throughout the project (including project design and analysis). Our PPI panel included six members (representing a range of lived experience, age, gender and ethnicity). Our PPI panel members have experience of living with a range of complex and long-term conditions, and all have experience of navigating and/or working within the healthcare system. Through online meetings, workshops and e-mail, the PPI members were involved throughout all stages of the research, including shaping the research questions, developing interview guides and interpreting the findings.
Additional information
Patient and public involvement
During the scoping stage of the study, a workshop to discuss the evaluation design and shape the research questions was held with members of the BRACE Health and Care panel, which included members of the BRACE PPI panel. As a result of the workshop, several changes were made to the protocol, including having more of a focus on access to digital approaches in primary care. The evaluation protocol was also reviewed by two members of the BRACE PPI panel.
Through online meetings, workshops and via e-mail, members of the group have continued to be involved, including by sharing feedback on how best to recruit participants, developing interview guides and interpreting and providing feedback on the findings. Discussion regarding the challenges of recruiting both patients and staff were discussed extensively at each BRACE steering group meeting (n = 3), with representatives from the PPI panel. The steering group, alongside the PPI panel, put forward suggestions of how the team could bolster recruitment, in particular by approaching super-partnerships and federations. A ‘Plain English’ summary of the final report has also been reviewed by two members of the BRACE PPI panel. We will seek the advice of the BRACE PPI panel regarding how best to communicate the findings of the evaluation to patient and public audiences.
The initial protocol for this study included further patient and public involvement with a plan to undertake interviews with patients and/or carers to understand their experiences of using Digital First Primary Care approaches. However, due to challenges in recruitment this was not possible.
Acknowledgements
We would sincerely like to thank all the participants in this study and our contacts at practices who helped to coordinate some of the interactions with interviewees. We would also like to thank everyone who gave their time to support the project, including stakeholders from the two digital providers the study focused on and from the super-partnership. We recognise that the point during which we conducted this study was a time of extreme pressure on primary care; therefore, we are very grateful that, despite this, staff still found time to support and contribute to our study.
We would also like to thank our BRACE colleagues and members of the BRACE steering group, Health and Care panel and User Involvement group for their constructive feedback and input throughout the study: Professor Russell Mannion and Professor Judith Smith (both University of Birmingham) for undertaking a critical review of the draft of the report; Cathy Dakin and Ann Evans (BRACE Centre senior research administrators) for providing varied and valued support throughout; and two members of our User Involvement group for reviewing our Plain language summary of the report. Particular thanks to Dilwyn Sheers (NHSE), Geraldine M Clarke, Richard Brine and Emma Vestesson (The Health Foundation) who have discussed the project during its lifetime with the PI (JN).
Contributions of authors
Jennifer Newbould (https://orcid.org/0000-0002-2602-6984) (Research Leader) was the principal investigator for the study. She conducted the scoping work for this project and conceived the content and design of the study, led the data collection, conducted stakeholder interviews and led the overall data analysis. She led the writing of Chapter 5 and contributed to all other chapters. She provided a critical review of the final report and is the guarantor and corresponding author.
Lucy Hocking (https://orcid.org/0000-0002-8319-962X) (Senior Analyst) was the project manager for this study and contributed to the conception and design of the study, the data collection with practices and the overall data analysis and interpretation. She contributed to the final report, leading the writing of Chapter 2, co-writing and then leading Chapter 4 and supporting the writing of Chapter 5.
Manbinder Sidhu (https://orcid.org/0000-0001-5663-107X) (Associate Professor) contributed to the conception and design of the study, the data collection with practices and the overall data analysis and interpretation. He also contributed to the final report, leading the writing of Chapter 3, co-writing Chapter 4 and supporting the writing of Chapter 5.
Kelly Daniel (née Singh) (https://orcid.org/0000-0002-4513-1026) (Evaluation Fellow) contributed to the overall data analysis and interpretation. She also contributed to the final report, leading the writing of Chapter 1, supporting the writing of Chapters 2 and 5 and co-writing Chapter 4.
All authors contributed to integrating the findings of the study. Jennifer Newbould made critical revisions to the report for important intellectual content and approved the final manuscript. All authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the article are appropriately investigated and resolved.
Disclosure of interests
Full disclosure of interests: Completed ICMJE forms for all authors, including all related interests, are available in the toolkit on the NIHR Journals Library report publication page at https://doi.org/10.3310/AWBT4827.
Primary conflicts of interest: None
Data-sharing statement
Data from the interviews will be accessible to the participants who took part in this rapid evaluation following GDPR, RAND Europe and University of Birmingham data protection guidelines upon request. All requests should be sent to the corresponding author in the first instance. To protect the anonymity of interviewees, the data are not publicly available. Further information can be obtained from the corresponding author.
Ethics statement
Ethical approval was obtained from the University of Birmingham Humanities and Social Sciences Ethical Review Committee in September 2021 (ERN_13-1085AP35, see project documents).
Information governance statement
The University of Birmingham is committed to handling all personal information with regard to all qualitative data in line with the UK Data Protection Act (2018) and the General Data Protection Regulation (EU GDPR) 2016/679.
Department of Health and Social Care disclaimer
This publication presents independent research commissioned by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by the interviewees in this publication are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, MRC, NIHR Coordinating Centre, the HSDR programme or the Department of Health and Social Care.
This monograph was published based on current knowledge at the time and date of publication. NIHR is committed to being inclusive and will continually monitor best practice and guidance in relation to terminology and language to ensure that we remain relevant to our stakeholders.
Disclaimers
This article presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care.
References
- NHS England . Digital First Primary Care n.d. https://www.england.nhs.uk/gp/digital-first-primary-care/ (accessed 8 July 2022).
- Bakhai M, Croney M, Waller L, Henshall N, Felstead C. Using Online Consultations In Primary Care: Implementation Toolkit 2020. https://www.england.nhs.uk/wp-content/uploads/2020/01/online-consultations-implementation-toolkit-v1.1-updated.pdf (accessed 3 October 2023).
- Primary Care Workforce Commission . The Future of Primary Care: Creating Teams for Tomorrow 2017. https://napc.co.uk/wp-content/uploads/2017/09/Future_of_primary_care.pdf (accessed 3 October 2023).
- NHS England . General Practice Forward View 2016. https://www.england.nhs.uk/gp/gpfv/ (accessed 3 October 2023).
- NHS . The NHS Long Term Plan 2019. https://www.longtermplan.nhs.uk/wp-content/uploads/2019/08/nhs-long-term-plan-version-1.2.pdf (accessed 3 October 2023).
- NHS England, British Medical Association . Investment and Evolution: A Five-Year Framework for GP Contract Reform to Implement the NHS Long Term Plan 2019. https://www.england.nhs.uk/wp-content/uploads/2019/01/gp-contract-2019.pdf (accessed 3 October 2023).
- Watt T, Firth Z, Fisher R, Thorlby R, Kelly E. Use of Primary Care During the COVID-19 Pandemic 2020. https://www.health.org.uk/news-and-comment/charts-and-infographics/use-of-primary-care-during-the-covid-19-pandemic (accessed 8 July 2022).
- Edwards HB, Marques E, Hollingworth W, Horwood J, Farr M, Bernard E, et al. Use of a primary care online consultation system, by whom, when and why: evaluation of a pilot observational study in 36 general practices in South West England. BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2017-016901.
- Atherton H, Brant H, Ziebland S, Bikker A, Campbell J, Gibson A, et al. The potential of alternatives to face-to-face consultation in general practice, and the impact on different patient groups: a mixed-methods case study. Health Serv Deliv Res 2018;6:1-200. https://doi.org/10.3310/hsdr06200.
- Atherton H, Brant H, Ziebland S, Bikker A, Campbell J, Gibson A, et al. Alternatives to the face-to-face consultation in general practice: focused ethnographic case study. Br J Gen Pract J R Coll Gen Pract 2018;68:e293-300. https://doi.org/10.3399/bjgp18X694853.
- Clarke G, Pariza P, Wolters A. How Has COVID-19 Affected Service Delivery in GP Practices That Offered Remote Consultations Before the Pandemic? n.d. https://www.health.org.uk/news-and-comment/charts-and-infographics/how-has-covid-19-affected-service-delivery-in-gp-practices (accessed 8 July 2022).
- Fraser C, Fisher R. How Has the COVID-19 Pandemic Impacted Primary Care? 2021. https://www.health.org.uk/news-and-comment/charts-and-infographics/how-has-the-covid-19-pandemic-impacted-primary-care (accessed 8 July 2022).
- British Medical Association . Pressures in General Practice Data Analysis. The British Medical Association Is the Trade Union and Professional Body for Doctors in the UK 2022. https://www.bma.org.uk/advice-and-support/nhs-delivery-and-workforce/pressures/pressures-in-general-practice-data-analysis (accessed 11 November 2022).
- NHS Digital . Appointments in General Practice 2022. https://digital.nhs.uk/data-and-information/publications/statistical/appointments-in-general-practice (accessed 11 November 2022).
- Clarke GM, Dias A, Wolters A. Access to and Delivery of General Practice Services: A Study of Patients at Practices using Digital and Online Tools. The Health Foundation; 2022.
- NHS England and NHS Improvement . GP Access Letter n.d. https://www.england.nhs.uk/wp-content/uploads/2021/05/B0497-GP-access-letter-May-2021-FINAL.pdf (accessed 4 July 2024).
- NHS England and NHS Improvement . Our Plan for Improving Access for Patients and Supporting General Practice 2021. https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2021/10/BW999-our-plan-for-improving-access-and-supporting-general-practice-oct-21.pdf (accessed 3 October 2023).
- NHS England and NHS Improvement . 2022/23/Priorities/and/Operational/Planning/Guidance 2022. https://www.england.nhs.uk/publication/2022-23-priorities-and-operational-planning-guidance/ (accessed 3 October 2023).
- Department of Health and Social Care, NHS England . A Plan for Digital Health and Social Care 2022. https://www.gov.uk/government/publications/a-plan-for-digital-health-and-social-care (accessed 3 October 2023).
- Iacobucci G. GPs should return to offering face-to-face appointments without prior triage, says NHS. BMJ 2021;373. https://doi.org/10.1136/bmj.n1251.
- Stafford M, Deeny SR, Dreyer K, Shand J. Multiple long-term conditions within households and use of health and social care: a retrospective cohort study. BJGP Open 2021;5. https://doi.org/10.3399/BJGPO.2020.0134.
- Stafford M, Thorlbyy R, Fisher R. Understanding the Health Care Needs of People With Multiple Health Conditions. The Health Foundation; 2018.
- Engamba SA, Steel N, Howe A, Bachman M. Tackling multimorbidity in primary care: is relational continuity the missing ingredient?. Br J Gen Pract 2019;69:92-3. https://doi.org/10.3399/bjgp19X701201.
- Ipsos MORI . GP Patient Survey 2022. https://www.gp-patient.co.uk/ (accessed 11 November 2022).
- UK Government . Health and Care Act 2022 2022. https://www.legislation.gov.uk/ukpga/2022/31/enacted (accessed 11 November 2022).
- Fuller C. Next Steps for Integrating Primary Care: Fuller Stocktake Report 2022. https://www.england.nhs.uk/publication/next-steps-for-integrating-primary-care-fuller-stocktake-report/ (accessed 3 October 2023).
- National Institute of Health and Care Research . Multiple Long-Term Conditions (Multimorbidity): Making Sense of the Evidence 2021. https://doi.org/10.3310/collection_45881 (accessed 3 October 2023).
- The Academy of Medical Sciences . Multimorbidity: A Priority for Global Health Research 2018. https://acmedsci.ac.uk/policy/policy-projects/multimorbidity (accessed 3 October 2023).
- Beech J, Fraser C, Fisher R, Vestesson E. Understanding Activity in General Practice: What Can the Data Tell Us? 2022. https://www.health.org.uk/news-and-comment/charts-and-infographics/understanding-activity-in-general-practice-what-can-the-data-tell-us (accessed 11 November 2022).
- Care Quality Commission . The State of Health Care and Adult Social Care in England 2021 22 2022. https://www.cqc.org.uk/sites/default/files/2022-10/20221024_stateofcare2122_print.pdf (accessed 3 October 2023).
- Nuffield Trust . NHS Staffing Tracker 2022. https://www.nuffieldtrust.org.uk/nhs-staffing-tracker/general-practice/ (accessed 11 November 2022).
- Baird B, Lamming L, Bhatt R, Beech J, Dale V. Integrating Additional Roles into Primary Care Networks. London: The Kings Fund; 2022.
- British Medical Association, NHS England . Update to the GP Contract Agreement 2020 21–2023 24 2020. https://www.england.nhs.uk/publication/investment-and-evolution-update-to-the-gp-contract-agreement-20-21-23-24/ (accessed 3 October 2023).
- Torjesen I. One in three GPs intends to quit within five years, survey finds. BMJ 2022;377.
- Burn E, Locock L, Fisher R, Smith J. Organising Care in a Time of Covid-19: Implications for Leadership, Governance and Policy. London: Palgrave Macmillan Cham; 2021.
- British Medical Association . ‘Anti-GP’ Media Rhetoric Risks Fuelling Climate of Abuse, Says BMA 2021. https://www.bma.org.uk/bma-media-centre/anti-gp-media-rhetoric-risks-fuelling-climate-of-abuse-says-bma (accessed 11 November 2022).
- Mroz G, Papoutsi C, Greenhalgh T. UK newspapers ‘on the warpath’: media analysis of general practice remote consulting in 2021. Br J Gen Pract 2022;72:e907-15. https://doi.org/10.3399/BJGP.2022.0258.
- Rosen R, Leone C. Getting the Best Out of Remote Consulting in General Practice – Practical Challenges and Policy Opportunities. London: Nuffield Trust; 2022.
- Cowie J, Calveley E, Bowers G, Bowers J. Evaluation of a digital consultation and self-care advice tool in primary care: a multi-methods study. Int J Environ Res Public Health 2018;15. https://doi.org/10.3390/ijerph15050896.
- Anderson J, Walsh J, Anderson M, Burnley R. Patient satisfaction with remote consultations in a primary care setting. Cureus 2021;13. https://doi.org/10.7759/cureus.17814.
- Scott J, Hill M. Improving Quality and Tackling Inequalities: Emerging Insights About Video Consultations. Q Community; 2020.
- Healthwatch, National Voices, Traverse . The Doctor Will Zoom You Now: Getting the Most Out of the Virtual Health and Care Experience 2020. https://www.healthwatch.co.uk/report/2020-08-18/doctor-will-zoom-you-now-getting-most-out-virtual-health-and-care-experience (accessed 8 July 2022).
- The Patients Association . Pandemic Patient Experience 2020. https://www.patients-association.org.uk/blog/pandemic-patient-experience (accessed 8 July 2022).
- Verma P, Kerrison R. Patients’ and physicians’ experiences with remote consultations in primary care during the COVID-19 pandemic: a multi-method rapid review of the literature. BJGP Open 2022;6. https://doi.org/10.3399/BJGPO.2021.0192.
- Darley S, Coulson T, Peek N, Moschogianis S, van der Veer SN, Wong DC, et al. Understanding how the design and implementation of online consultations affect primary care quality: systematic review of evidence with recommendations for designers, providers, and researchers. J Med Internet Res 2022;24. https://doi.org/10.2196/37436.
- Ipsos MORI, York Health Economics Consortium . Evaluation of Babylon GP at Hand: Final Evaluation Report 2019.
- Tuijt R, Rait G, Frost R, Wilcock J, Manthorpe J, Walters K. Remote primary care consultations for people living with dementia during the COVID-19 pandemic: experiences of people living with dementia and their carers. Br J Gen Pract 2021;71:e574-82. https://doi.org/10.3399/BJGP.2020.1094.
- Murphy M, Scott LJ, Salisbury C, Turner A, Scott A, Denholm R, et al. Implementation of remote consulting in UK primary care following the COVID-19 pandemic: a mixed-methods longitudinal study. Br J Gen Pract 2021;71:e166-77. https://doi.org/10.3399/BJGP.2020.0948.
- Lackey S, Schmidtke KA, Vlaev I. A mixed-methods study describing behavioral factors that influenced general practitioners’ experiences using triage during the COVID-19 pandemic. BMC Fam Pract 2021;22. https://doi.org/10.1186/s12875-021-01469-x.
- Rodgers M, Raine G, Thomas S, Harden M, Eastwood A. Informing NHS Policy in ‘Digital-first Primary Care’: A Rapid Evidence Synthesis. Southampton: NIHR Journals Library; 2019.
- Sussex J, Smith J, Wu FM. Service innovations for people with multiple long-term conditions: reflections of a rapid evaluation team. Health Soc Care Deliv Res 2024;12.
- National Institute of Health and Care Research . Multimorbidity: Clinical Assessment and Management 2016. https://www.nice.org.uk/guidance/ng56 (accessed 11 November 2022).
- Paddison C, McGill I. Digital Primary Care: Improving Access For All?. London: Nuffield Trust; 2022.
- Ritchie J, Lewis J, McNaughton Nicholls C, Ormston R. Qualitative Research Practice: A Guide for Social Science Students and Researchers. Thousand Oaks, CA: SAGE Publications Ltd; 2014.
- Andoh-Arthur J. SAGE Research Methods Foundation. London: SAGE Publications Ltd; 2020.
- Johl SK, Renganathan S. Strategies for gaining access in doing fieldwork: reflection of two researchers. Electron J Bus Res Methods 2010;8:25-34.
- Office for Health Improvement & Disparities . National General Practice Profiles 2022. https://fingertips.phe.org.uk/profile/general-practice/data#page/12/ati/7/are/M81034 (accessed 24 November 2022).
- Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol 2013;13. https://doi.org/10.1186/1471-2288-13-117.
- Baird B, Charles A, Honeyman M, Maguire D, Preety D. Understanding Pressures in General Practice. London: The Kings Fund; 2016.
- British Medical Association . Dial Down the Negative and Critical Commentary Against GPs or the NHS Will Lose Even More Doctors, BMA Tells Health Select Committee 2022. https://www.bma.org.uk/bma-media-centre/dial-down-the-negative-and-critical-commentary-against-gps-or-the-nhs-will-lose-even-more-doctors-bma-tells-health-select-committee (accessed 22 November 2022).
- National Literacy Trust . Adult Literacy n.d. https://literacytrust.org.uk/parents-and-families/adult-literacy/ (accessed 23 November 2022).
- Newbould J, Abel G, Ball S, Corbett J, Elliott M, Exley J, et al. Evaluation of telephone first approach to demand management in English general practice: observational study. BMJ 2017;358. https://doi.org/10.1136/bmj.j4197.
- Pope C. Remote care – good for some, but not for all?. J Health Serv Res Policy 2023;28:147-8. https://doi.org/10.1177/13558196231172715.
- Greenhalgh T, Rosen R, Shaw SE, Byng R, Faulkner S, Finlay T, et al. Planning and evaluating remote consultation services: a new conceptual framework incorporating complexity and practical ethics. Front Digit Health 2021;3. https://doi.org/10.3389/fdgth.2021.726095.
- Greenhalgh T, Shaw S, Wherton J, Vijayaraghavan S, Morris J, Bhattacharya S, et al. Real-world implementation of video outpatient consultations at macro, meso, and micro levels: mixed-method study. J Med Internet Res 2018;20. https://doi.org/10.2196/jmir.9897.
- House of Commons, Health and Social Care Committee . The Future of General Practice: Fourth Report of Session 2022–23 2022.
- Palmer W, Hemmings N, Rosen R, Keeble E, Williams S, Imison C. Improving Access and Continuity in General Practice: Practical and Policy Lessons. London: Nuffield Trust; 2018.
Appendix 1 Interview topic guide for health professionals and stakeholders
Topic guide for health professionals
-
Reasons for changing to a Digital First Primary Care approach and proportion of consultations through Digital First Primary Care, including the impact and legacy of COVID-19 on how practices use Digital First Primary Care.
-
– Describe how the Digital First Primary Care approach was introduced?
-
– Who was involved? How were decisions made and against what criteria?
-
– Explain the reasoning behind the provider selected to deliver primary care services?
-
– How many consultations are being delivered using this new platform? How has this changed from pre, during and, more lately, as a result of the pandemic?
-
-
Have members of staff received any training on delivering Digital First Primary Care?
-
– What training did they receive? How many hours?
-
– Attitudes towards training? Is further/repeat training required? If yes, describe the nature of training desired?
-
-
Are there particular groups of patients the Digital First Primary Care approach favours? Are there groups which don’t use it? (With particular focus on underserved communities.)
-
– Repeat users?
-
– Those who do not engage? Those who had reservations and are now frequent users?
-
– Younger cohort? Those living with long-term conditions?
-
-
Are there particular conditions, or combinations of conditions, that the Digital First Primary Care approach favours or is less appropriate for?
-
– Impact on the nature of relationships developed and rapport generated amongst certain patients?
-
– How do consultations across groups differ?
-
-
Are there particular advantages/disadvantages of the approach for patients with multiple long-term conditions?
-
– Better understanding of needs and enhanced engagement?
-
-
Differences in workflow with the use of Digital First Primary Care (e.g. impacts on demand, perceptions of re-consultation rates, impacts on DNAs and on homes visits).
-
Impacts on the GP practice (e.g. change in registered number of patients, prescribing, staffing, work pattern, work location, issues of staff retention and recruitment).
-
Staff satisfaction/challenges.
-
– Staff job satisfaction changed since introduction?
-
– Greater pressure to do with greater number of contacts across different platforms?
-
-
Perceptions of impacts on patient care (e.g. are diagnoses made more quickly, is the patient pathway more or less efficient, do the notes ahead of patient contact aid or hinder the consultation)—with a particular focus on patients with multiple long-term conditions.
-
Is there anything else we have not covered that you would like to tell me about?
Topic guide for stakeholders
-
Can you tell me about your role?
-
– Do you have a dual role? Are you a practising clinician?
-
– Have you done particular work in digital primary care?
-
-
Thinking about digital approaches in primary care what are your views on using these in primary care at the current time?
-
– Prompt: pros/cons
-
-
Are there particular advantages/disadvantages of digital-first approaches in primary care for patients with multiple long-term conditions?
-
– Prompt: pros/cons
-
-
Thinking from the perspective of patients, how do digital approaches to primary care impact on patients with multiple long-term conditions?
-
– Speed of access to see or speak to a clinician?
-
– Which clinician is seen?
-
– Continuity of care?
-
-
Thinking from the perspective of health professionals, how do digital approaches to primary care impact on the care they can provide to patients with multiple long-term conditions?
-
– Speed of access to see or speak to a clinician?
-
– Which clinician is seen?
-
– Continuity of care?
-
-
Are there particular conditions, or combinations of conditions, that the Digital First Primary Care approach favours or is less appropriate for?
-
– Older patients? Those without access to digital means?
-
-
We know that some patients with multiple long-term conditions will want to consult with their carers. Do digital approaches present challenges to this?
-
– How are these overcome?
-
-
Thinking more generally about Digital First Primary Care now and less about those with multiple long-term conditions, do you feel Digital First Primary Care impacts on patient care? In what ways?
-
– Are diagnoses made more quickly, is the patient pathway more or less efficient, do the notes ahead of patient contact aid or hinder the consultation?
-
-
What do you think has been the impact of COVID-19 on digital approaches to primary care?
-
Thinking about where we are in the pandemic now, how do you see the future for general practice with the use of digital approaches?
-
– Will the balance change? Will face-to-face become the norm or is digital here to stay?
-
-
Is there anything else that we have not covered that you would like to add?
Appendix 2 Coding framework for staff and stakeholder interviews
| Staff interview broad coding themes | Expert stakeholders broad coding themes |
|---|---|
| Role of interviewee | Role of interviewee |
| How and when Digital First Primary Care was introduced, including the rationale for doing so | General practice culture and context |
| Alternative to using digital system (e.g. phone) and other Digital First Primary Care systems used | Views on using digital approaches in primary care at this time |
| Number of Digital First Primary Care-based consultations and changes over time | Digital First Primary Care policy, including recent changes around face-to-face vs. digital consultations |
| Availability of digital system (e.g. times of day) | Insights on Digital First Primary Care from a clinical perspective |
| Changes in the use of Digital First Primary Care during COVID-19 | How using Digital First Primary Care impacts on the care healthcare professionals can provide to patients with multiple long-term conditions (including access, continuity) |
| How the practice uses Digital First Primary Care, how it is managed and how it impacts on demand | Impacts of using digital approaches to primary care on patient care more generally (not those with multiple long-term conditions) and how it impacts on demand |
| Description of the patient journey when using Digital First Primary Care | Health conditions Digital First Primary Care is more and less appropriate for |
| General practice culture and context | The advantages and disadvantages of using Digital First Primary Care for patients with multiple long-term conditions |
| Staff training on Digital First Primary Care | Impact of using Digital First Primary Care on patients with multiple long-term conditions (including access, continuity) |
| Patient views and expectations about Digital First Primary Care | If digital approaches present challenges to patients with carers and solutions for overcoming these |
| How Digital First Primary Care approaches work for patients in general and for those with multiple long-term conditions | Impact of COVID-19 on digital approaches to primary care |
| How the digital approach helps or hinders care co-ordination | Future for primary care in relation to Digital First Primary Care |
| The advantages and disadvantages of using Digital First Primary Care for patients with multiple long-term conditions | Any other information not covered by another code |
| Health conditions Digital First Primary Care is more and less appropriate for | |
| How Digital First Primary Care helps or hinders the health-care provider–patient relationship | |
| How Digital First Primary Care impacts access to primary care | |
| How Digital First Primary Care impacts carers | |
| How Digital First Primary Care impacts patient care | |
| Groups of patients who are not engaging with Digital First Primary Care and how this is managed | |
| Future plans or ways of working related to Digital First Primary Care | |
| Any other information not covered by another code |
List of abbreviations
- BMA
- British Medical Association
- CCG
- Clinical Commissioning Group
- GP
- general practitioner
- HRA
- Health Research Authority
- NHS
- National Health Service
- NICE
- National Institute for Health and Care Excellence
- PCN
- primary care network
- PPI
- patient and public involvement
- WP
- work package