Notes
Article history
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as project number NIHR128359. The contractual start date was in January 2020. The final report began editorial review in April 2021 and was accepted for publication in February 2022. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
Copyright © 2023 Evans et al. This work was produced by Evans et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaption in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2023 Evans et al.
Chapter 1 Background and rationale
One in six children aged 5–19 years in England has a probable mental disorder,1 and a recent National Assembly inquiry found a 100% increase in demand for mental health services in Wales between 2010 and 2014. 2 With resources stretched and young people often waiting lengthy periods to be seen, increasing numbers of children and young people (CYP) are seeking help or have had help sought on their behalf during mental health crises. During such periods of crisis, it is vital that effective and timely evidence-based care is provided. Crisis care for CYP has become a policy priority both nationally2,3 and internationally,4 with substantial funding allocated to the development of crisis services. 5 The needs of young people in crisis can be met through designated clinical services [e.g. local Child and Adolescent Mental Health Services (CAMHS) teams and/or dedicated CAMHS crisis teams] and in emergency departments, but also through non-clinical services provided through a range of organisations.
In the UK, the landscape of crisis care delivery has shifted substantially in recent years, with particular investments being made in dedicated community crisis teams that aim to provide care close to home and avoid the need for hospital admission. 6 However, little is known about how these teams are organised and experienced, their effectiveness or how they are integrated within local systems, and concerns continue to be expressed regarding their adequacy. 7 In the context of local services, community crisis teams work alongside community CAMHS teams and sometimes other types of specialist CAMHS, such as those providing assertive outreach, emergency departments and paediatric wards. In the larger ecology of service provision, crisis responses are also provided through general NHS provision (e.g. in emergency departments, in schools and universities, by the police, through social services, via the third sector and through internet- or telephone-based counselling services).
Despite the prioritisation of crisis care for CYP, no up-to-date data are available on types of service responses and their organisation, the experiences of young people, their families and staff, and outcomes for CYP. Previous reviews have focused specifically on the provision of designated clinical services for those in mental health crisis,8–10 neglecting the diverse settings where young people are likely to access initial crisis support outside the mental health system (e.g. schools, online networks and social media, crisis helplines, emergency departments, third-sector organisations, the criminal justice system). However, given that CAMHS are unable to meet the needs of the large numbers of children in crisis each year, it is likely that (in the UK context) a substantial proportion of crisis responses occur outside NHS services. Non-NHS settings may be more frequent points of access to crisis support for young people, making it important to understand how these systems interact with designated mental health services, how these different response types are experienced by young people and their families and what their outcomes are. For example, a recent report11 revealed that the police account for the largest number of referrals to children’s services of 16- and 17-year-olds, whereas the second highest source of referral for those aged < 18 years is education. There have also been increasing reports of mental health problems and self-harm from teachers12 and from third-sector organisations in front-line contact with children and adolescents. 13
International policy guidance has consistently stressed the importance of a joined-up systems approach in providing support to CYP, advocating cohesive working between health, education, social services, youth work and the third sector. 4 Recent guidance from the National Assembly for Wales7 recommends that schools should form community hubs of cross-sector and cross-professional support for children’s emotional and mental well-being. Therefore, a research approach that isolates clinical responses to mental health crises would risk excluding valuable data. By including evidence from wider social contexts, broader lessons may be learned about what CYP experiencing mental health crisis find particularly helpful.
Why is the research important?
This project was designed to meet a priority health need about which there is expressed and sustained interest, that is the mental health of CYP between the ages of 5 and 25 years. This is an area of international importance4 and is a priority for future UK mental health research. 14 One in six (12.8%) children aged 5–19 years in England has a mental health difficulty,1 with services struggling to meet demand as need rises. 3,7 A particular concern is the provision of safe, accessible and effective care for young people who need urgent help during a mental health crisis. This is in the context of a significant number of CYP experiencing mental health crises each year, characterised by serious self-harm and/or other behaviours that present major risks to the self and/or others. There was a 68% increase in self-harm incidence among girls aged 13–16 years in England between 2011 and 2014. 15 There are a number of organisations that might respond to CYP at these times of mental health crisis, including children’s mental health services, hospital emergency departments, pastoral or counselling staff in schools, third-sector organisations and the police. The aim of this review was to investigate the evidence underpinning such responses. Since the development of the initial proposal for this study, the world has been affected by the COVID-19 pandemic. Initial studies have found that the mental health of CYP has been affected by the stress associated with the impact of both COVID itself and lockdowns, particularly in CYP with specific additional vulnerabilities, such as those with pre-existing mental health conditions or those being quarantined because of infection/fear of infection. 16 However, this study predated the COVID pandemic and did not draw on any of the COVID-related literature.
In England, out-of-hours and crisis services for young people are a policy priority,3,17 with model service specifications including expectations that NHS trusts provide round-the-clock home-based crisis care. 18 InWales, crisis care is also a priority,19 with new CAMHS investment including money for urgent mental health interventions. 5,20 Intensive ‘hospital at home’ services have featured in Scottish guidance,21 and in Northern Ireland calls have been made for similar investments. 22,23 Responding appropriately to young people in crisis has also featured in recent national Crisis Care Concordats. 24,25 This is, therefore, a high-priority area that falls clearly within the remit of the Health and Social Care Delivery Research programme in addressing the four areas of quality, access, organisation and outcomes.
In the context of such high levels of need and in view of the urgency of this issue, it is vital that the care being provided to CYP in crisis is evidence based and effective. Evidence from this synthesis created knowledge of immediate use to NHS managers, practitioners, carers and others involved in the care of CYP. The project was designed to have an affect on services and practice by presenting its findings in accessible ways to health education and social services, the public, practitioners and educators.
Why is the research needed?
Despite the national and international prioritisation of crisis care for CYP, to our knowledge, no up-to-date data were available on the following aspects of the existing range of crisis responses: service organisation; effectiveness; and young people’s, their family members’ and staff members’ experiences. National guidance has been developed, stating what ought to be present in dedicated services of this type, drawing on what young people want. This includes care that is immediately accessible, provided by the right professional and is understandable. In addition, care should be provided in settings that are acceptable and not in hospital, whenever possible, and should be characterised by continuity. 6 However, we did not know how far these standards were being met and what their evidence base was. This contrasted sharply with what was known about crisis services for adults with mental health difficulties, which have been subjected to recent national audit26 and quality inspection27 and the evidence for which has recently been updated. 28,29
A number of alternative services provide responses for young people in crisis or distress outside the NHS. For instance, school and university counselling services (e.g. Place2Be school services) and online platforms provide online counselling and well-being support (including moderated peer-support forums, 7 days per week, until 10 p.m.) for CYP. Often these counselling services involve the integration of services across statutory and third sectors. 30 Given the increasing emphasis on cohesive working across systems, there was a need to consider the international evidence for all forms of crisis support provided across social, education and third-sector organisational contexts.
Initial search and the need for an evidence update
An initial search of the existing literature across MEDLINE and PsycINFO® was conducted to establish the feasibility of conducting a full systematic review of the relevant evidence prior to funding being agreed. Three systematic reviews were found that informed this study; however, these reviews also revealed a gap for a new updated review and synthesis. Shepperd et al. 31 brought together evidence for alternatives to inpatient mental health services for CYP and mapped current provision at the time. In this review,31 ‘crisis care’ was included alongside other types of non-hospital care for young people with ‘complex mental health needs’. Hamm et al. 10 limited their review to emergency department interventions, whereas Janssens et al. 8 reviewed the organisation of mental health emergency care for CYP, noting a lack of clarity around terminology. The authors of these three reviews, along with others,9 made a case for advancing the evidence base in a context in which descriptions of provision are unclear and research is both underdeveloped and of variable quality.
The Cochrane review of Crisis Intervention for People with Severe Mental Illnesses28 excludes CYP, but does, however, contain a helpful definition of ‘crisis services’:
Any type of crisis-orientated treatment of an acute psychiatric episode by staff with a specific remit to deal with such situations, in and beyond ‘office hours’. This can include mobile teams caring for patients within their own homes, or non-mobile residential programmes based in home-like houses within the community.
Murphy et al. 28
Although this definition emphasises clinical service provision by those ‘with a specific remit’ to deal with psychiatric crisis, we derived a broader definition of crisis care, which is inclusive of non-clinical environments. For this review, we considered a crisis service for CYP to be:
The provision of a service in response to extreme psychosocial distress, which for CYP may be provided in any location such as an emergency department, a specialist or non-specialist community service, a school, a college, a university, a youth group, or via a crisis support line.
Our search for evidence also uncovered additional studies of relevance, including evaluations in emergency departments. 32–34 In addition, our search extended to the National Institute for Health and Care Research database, where we uncovered National Institute for Health and Care Research-commissioned studies investigating mental health crisis services for adults (e.g. Paton et al. 29 and Lloyd-Evans et al. 35) and different ways of providing mental health care for young people (e.g. Tulloch et al. 36).
In conclusion, with one in six (12.8%) children aged 5–19 years in England having a probable mental disorder, the demand for services was increasing and growing numbers of CYP were seeking help during their mental health crises. New models of crisis services for CYP are continually being developed across the UK and internationally, and there was a need to consider the evidence for all forms of crisis support provided across social, education and third-sector organisational contexts, and how they interact with existing services. Therefore, an up-to-date evidence synthesis was required, taking into account new evidence published since the previous reviews,8–10 as well as incorporating UK-only grey literature relating to the organisation, provision and experience of mental health crisis responses for CYP.
Chapter 2 Working with stakeholders and defining parameters
This chapter describes the approach taken with stakeholders, including members of the public with personal experience of CYP experiencing mental health crisis and receiving care. Our engagement with patients and the public reflects commitments and experiences demonstrated in other studies on which members of this project team have worked (e.g. Hannigan et al. ,37 which provided an evidence synthesis into ‘risk’ for young people in mental health hospitals and which actively involved young people as stakeholders in shaping the study’s progress). Reporting of this section is completed with reference to GRIPP2-SF standards. 38 GRIPP2-SF standards require reporting of how public and patient involvement has informed all parts of a project, including its aim, methods and outcomes.
We worked with Liz Williams, who identifies herself as a carer of young adults with mental health issues, and Mair Elliot, who identifies herself as an expert patient, in the initial development of the project proposal. This is clearly an area of importance for people who want to access services for CYP in psychological crisis. Both Liz Williams and Mair Elliot have been co-investigators on this study and have contributed to several critical stages of the project where their expertise was most important, including the creation of search terms, selection of papers, synthesis and plan for the dissemination of findings. Discussions about the focus of the project were also held with clinical colleagues working in local CAMHS during the development of the proposal.
The project was supported by a Stakeholder Advisory Group (SAG), which was established during the project set-up phase. The SAG included professionals from a range of sectors that respond to CYP in mental health crisis, including professionals from an emergency department, a secondary school, social services and specialist CAMHS, parents with the lived experience of using mental health services for their family members and members of the third-sector organisation Place2Be (London, UK), which provides mental health support to children in schools. The SAG was independently chaired by Professor Michael Coffey from Swansea University (Swansea, UK).
The full membership of the SAG is found in Report Supplementary Material 1, and over the life of the study the combined project team and SAG met at three strategic time points (i.e. in person in Cardiff, and then via two further virtual meetings convened using videoconferencing because of the COVID pandemic restrictions). In the first meeting, the terms of reference (see Report Supplementary Material 2) were discussed and then agreed with the SAG, and the SAG were invited to review our search terms and assist with the generation of others, including identifying suitable databases and sources of UK-only grey literature. The notes of the meeting can be found in Report Supplementary Material 3. The second (virtual) meeting took place at the completion of evidence searching, providing an opportunity to share work in progress (see Report Supplementary Material 4). The final (virtual) meeting was scheduled towards the commencement of the whole-project synthesis and report-writing phase, with a focus on sharing preliminary findings and discussing plans for dissemination and maximising impact (see Report Supplementary Material 5). Following discussion during the first stakeholder meeting, the project title was changed from CAMHS crisis to child and adolescent mental health (CAMH) crisis.
Defining the project’s search parameters
At the first SAG meeting, candidate database search strategies and search terms developed by the project team for CYP were presented and discussed, and candidate definitions of the terms ‘crisis’ and ‘mental health’ were distributed and discussed at length with the purpose of refinement (see Report Supplementary Material 6). The decision was made not to search by specific services (e.g. schools, police) at this point and to have a four-arm search.
Arm 1: children and young people
The additional terms discussed at the SAG for this arm focused on trying to identify studies in which our population group may have been referred to by terms more related to setting than the terminology already identified as relevant to defining CYP. The SAG was concerned that CYP, particularly within educational, juvenile and other settings, may be missed. Additional suggestions that were discussed were the words and phrases ‘pupil’, ‘student’, ‘undergraduates’, ‘learner’, ‘apprentice’, ‘young offender’ and ‘adults aged 18–25 years’. A particular mention was made of adverse childhood experiences and whether or not this could be incorporated into this arm. The suggestions were evaluated by an information specialist (EG) and reported back to the project team. The words that were included within the final search strategy were ‘pupil’, ‘student’ and ‘young offender’. Other terms were considered to be too broad (e.g. ‘learner’ and ‘apprentice’), problematic to search given the constraints of the databases (e.g. ‘age 18–25 years’ and ‘minor’) or would already be retrieved through the use of existing key terms (e.g. ‘adverse childhood experiences’ and ‘children in care’).
Arm 2: crisis
At the outset, the decision was made not to search for specific crisis events, as it was felt that this potentially could have led to an endless list of presenting clinical situations and that certain crisis events, not thought of, could be missed. Our strategy was to use the keywords ‘crisis’ or ‘crises’ in arm 2 and ‘mental health’ or ‘psych*’ in arm 3. However, when the search strategy was being tested to ensure that all recognised relevant papers were being retrieved, Elizabeth Gillen found that several already-identified key papers were missing. This was because these papers used the term ‘rapid response’ and ‘suicide’ to define the crisis event with no mention of the terms ‘crisis’ or ‘mental health’. After discussion at a later project team meeting, it was felt that the terms ‘suicide’ and ‘self-harm’ were so synonymous with a crisis that they should be included as specific examples in the mental health arm. The term ‘rapid response’ was then added to arm 2.
Arm 3: mental health
The general use of a mental health arm was discussed at length, as the SAG was concerned that this could make the search very medicalised and that the project needed a strategy to ensure the retrieval of non-health sector articles. It was recognised, however, that without this third arm the search would be unwieldy. A discussion followed that, although in practice episodes of crisis happen in many sectors, it is likely that any write-up of research undertaken in the area would refer to mental health in some capacity and so this arm was included and expanded on, as detailed above. To address the concerns, and to increase the sensitivity of our search, a fourth arm was introduced that encapsulated alternative terminology that could be used to define a mental health crisis, which could then be combined with arm 1 to provide us with a second search methodology.
Arm 4: mental health and crisis
Positional operators were used within our new arm 4 to retrieve articles using alternative terminology to describe a mental health crisis. The terms discussed with the SAG included the terms ‘severe’, ‘extreme’, ‘intense’, ‘emergency’, ‘critical incident’, ‘urgent’, ‘distress’ and ‘trauma’. ‘Trauma’ was removed, as it was felt that this term would retrieve too many irrelevant records related to physical trauma. Following further discussions, it was decided to proceed with four of these terms (i.e. ‘emergency’, ‘critical incident’, ‘urgent’ and ‘distress’) in proximity to the terms ‘mental’ and ‘psych*’. Trials combining this new arm with arm 1 showed the strategy to be successful in increasing the sensitivity of our search, pulling in alternative literature, without excessively compromising precision or making the search unmanageable.
Finding UK-only grey literature
Websites to search, which had already been identified by the project team, were circulated (see Report Supplementary Material 7), and in the first meeting SAG members were invited to identify additional online sites.
Feedback from young people
One member of the project team (RL) met with young people from the Advice Leading to Public Health Advancement (ALPHA) group. The ALPHA group is a research advisory group that works for the Centre for Development, Evaluation, Complexity, and Implementation in Public Health Improvement (School of Social Sciences, Cardiff University, Cardiff, UK). The ALPHA group comprises young people aged 14–25 years who provide advice to health-based researchers. The purpose of meeting with members of the ALPHA group was to obtain advice from these young people about search terms, UK organisations and services, and sources of support available to them, and to determine the most suitable methods of sharing the findings from this evidence synthesis. Table 1 presents the breakdown of the 11 participants by age and gender.
| Participant age (years) | Gender | |
|---|---|---|
| Male (n) | Female (n) | |
| 14 | 0 | 0 |
| 15 | 0 | 1 |
| 16 | 0 | 1 |
| 17 | 1 | 3 |
| 18 | 1 | 2 |
| 19 | 0 | 0 |
| 20 | 0 | 2 |
The activity was broken up to tasks. Task 1 was about generating further search terms. For this task, we split the ALPHA members into two groups. We asked each group to spend 10 minutes at each station discussing the topics, then moving onto the next station until all four stations have been met with both groups. We used this technique as it allows for ALPHA members to have open discussions in their group and work collaboratively to answer the questions. It also allows for the other group to analyse the previous group’s findings, either by agreeing and providing further feedback or by disagreeing and providing suitable alternatives. Table 2 and Figures 1 and 2 contain a summary of the key points discussed at each station.
| Station | Findings |
|---|---|
Describe the following terms and how they may affect someone:
|
Physical structure and chemical make-up of the brain can affect mental health (e.g. people with adverse childhood experiences are more disposed to mental disorders, as their brain has changed to adapt to their environment) |
| General attitude, good and bad, emotional well-being, logical thinking and ability to think clearly, emotional responses, ability to cope | |
| A point where you need to heal, danger, inability to do or solve, feeling trapped, isolating yourself, panic attacks | |
| Stops your ability to function, cause distress, negative effect on well-being, psychological, emotions | |
| Anxiety, depression, bipolar disorder, eating disorder, schizophrenia, psychosis, multiple personality disorder, body dysmorphia, substance abuse | |
| Suffering in any way: mental and physical, impairment of function, chronic stress, relationship breakdown, isolating yourself | |
| What places do young people go when they are in crisis? |
|
| What resources do young people use when in crisis? |
|
| Suggestions on where to look for grey literature? |
|
FIGURE 1.
Responses for what places do young people go when they are in crisis.
FIGURE 2.
Responses for what resources do young people use when in crisis.
As a part of this study and evidence synthesis, the study team wanted to know the most suitable methods and approaches for sharing these findings. The findings were to be aimed and CYP and parents/carers to provide advice or guidance on services to access at time of emotional crisis. For this second task, we asked ALPHA members to remain in the same groups and answer the following questions:
-
Who should we share this information with?
Responses: teachers, local authorities, helping, parents, in school counsellors, NHS and young people.
-
What information to include?
Responses: specific relatable information tailored for the correct audience (e.g. posters in school for young people); main study findings with accessible information, including useful services and more specific services.
-
Where should this information be shared?
Responses: these posters can be in hotspot areas in the schools, such as back of toilet doors. If feasible, targeted adverts on Instagram (Meta Platforms, Inc., Cambridge, MA, USA) or Facebook (Meta Platforms, Inc., Menlo Park, CA, USA).
-
Why do we need to share this information?
Responses: increased awareness and use of services; young people will feel comfortable knowing where they can go to access information.
-
What is the best approach for sharing this information?
Responses: ParentMail (IRIS Software Group Ltd, Slough, UK), ParentPay (IRIS Software Group Ltd, Slough, UK), posters at school, animation video to showcase main findings, parents evening, e-mail/letter and social media.
We asked ALPHA members whether or not it was a good idea to present the findings from this systematic review in an animation video format. We received a mixed response to this question, as some ALPHA members thought that it was a good idea and a useful way of sharing the information, whereas others were unsure. Some ALPHA members felt that there are too many information animation videos and producing another one would not have the desired impact and, therefore, suggested using a different platform for sharing this information, such as either a poster or a whole-school approach.
Chapter 3 Methods and description of included reports
The methods used in this evidence synthesis and the materials finally included are described in this chapter. The protocol for the evidence synthesis was registered with the International Prospective Register of Systematic Reviews (PROSPERO CRD42019160134) at the commencement of the project. For the purposes of this review, guidance for undertaking reviews in health care published by the Centre for Reviews and Dissemination39 was followed. To incorporate stakeholder views, methods informed by the EPPI-Centre (Evidence for Policy and Practice Information and Co-ordinating Centre)40,41 were used. To ensure rigour, the reporting of this evidence synthesis follows the PRISMA (Preferred Reporting Items for Systematic Reviews) statement. 42
Aims and objectives
The aim of this project was to synthesise international evidence relating to the organisation and effectiveness of services that respond to CYP in crisis, and the evidence relating to the experiences of people using and working in these services.
Detailed objectives were to critically appraise, synthesise and present the best-available international evidence. Specifically, we looked at:
-
the organisation of crisis services for CYP aged 5–25 years, across education, health, social care and the third sector
-
the experiences and perceptions of CYP, their families and staff with regard to mental health crisis support for CYP aged 5–25 years
-
determining the effectiveness of current models of mental health crisis support for CYP
-
determining the goals of crisis intervention.
Inclusion criteria
We used PICOS/PiCo framework to guide the inclusion criteria on population (P), intervention/phenomena of interest (I), comparators (C), outcome (O), study design (S) and context (Co).
Population
This evidence synthesis considered all relevant evidence specifically relating to support for CYP (aged 5–25 years) in emotional/mental health crisis.
For the purposes of the current study, CYP will included individuals within the age range of 5–25 years. A number of mental health services for CYP in the UK and internationally now cater for this age range. Imposing an age limit of 18 years would, therefore, have risked excluding valuable studies concerning those aged 18–25 years.
Intervention and phenomena of interest
This evidence synthesis considered all relevant evidence on the:
-
organisation of services relating to crisis support
-
effectiveness of current models/interventions that provide support to CYP in mental health crisis
-
views and experiences of CYP, families and staff
-
goals of services.
Building on the definition used in Crisis Intervention for People with Severe Mental Illnesses,28 for this proposed review a crisis response for CYP was defined as follows:
The provision of a service in response to extreme psychosocial distress, which for children and young people may be provided in any location such as an emergency department, a specialist or non-specialist community service, a school, a college, a university, a youth group, or via a crisis support line.
Comparators
No comparators were used in the study.
Outcomes
The following outcomes were considered: the organisation of crisis services and their effectiveness (i.e. all outcomes as described across the primary studies), the experiences of CYP and their families, and the goals of crisis services.
Context
All records were considered with regard to the organisation of crisis services, their effectiveness and the experiences of CYP and their families in any setting, including virtual.
Study design/types of evidence
Types of evidence sought included both quantitative and qualitative research, and UK-only grey literature. Reports published in the English language since 1995 were considered.
Exclusion criteria
The following exclusion criteria were used:
-
usual care provided at emergency departments with no specific mental health component
-
standard CAMHS care
-
under-fives
-
CYP not in mental health crisis
-
evidence relating to adult mental health services, where there is no designated provision for young people
-
evidence relating to general/non-crisis/long-term support
-
studies that included participants who are children and adults, but the average age of the participants was > 25 years
-
crisis was a group crisis experience, such as a mass shooting or stabbing in an educational establishment or a natural disaster
-
care not at actual point of crisis.
Developing the search strategy
The focus of the search strategy was to achieve high sensitivity without overcompromising precision and making the search results unwieldy. To ensure that all relevant literature was obtained, a comprehensive search strategy was designed. The search strategy took into consideration the discussions around the research question during the first combined project team and SAG meeting (see Chapter 2).
Preliminary searching
Preliminary database searching using MEDLINE and PsycINFO were carried out as part of an initial scoping exercise undertaken during preparation of the proposal for funding, with material from this drawn for Chapter 1. The preliminary keywords that were used to inform these searches included ‘child’ OR ‘adolescent’ AND ‘CAMHS’ OR ‘mental health’ AND ‘crisis’. This search strategy was further developed, taking into account relevant synonyms and alternative spellings. The text words contained in the title and abstract and the index terms used to describe the articles retrieved were then analysed and used to develop more comprehensive and detailed searches.
Comprehensive searching
The preliminary search terms were presented and discussed at the first combined project team and SAG meeting (see Chapter 2). As a result of this process, Elizabeth Gillen developed a comprehensive search strategy.
As a means of testing and refining this search strategy before applying it across multiple databases, records retrieved across MEDLINE and PsycINFO were first screened by Deborah Edwards to ensure relevance and to assess that the strategy was neither too broad nor too narrow.When the project team was satisfied with the search strategy, the strategy was then tailored across all databases, with searches run from database inception and undertaken between February and April 2020 (updated in January 2021). The final search strategies are displayed in Appendix 1.
The 17 databases searched were:
-
MEDLINE ALL (on the Ovid platform)
-
PsycINFO (on the Ovid platform)
-
EmCare (on the Ovid platform)
-
Allied and Complimentary Medicine Database (on the Ovid platform)
-
Health Management Information Consortium (on the Ovid platform)
-
Cumulative Index to Nursing and Allied Health Literature
-
Education Resources Information Center (on the ESBCOhost platform)
-
Applied Social Sciences Index and Abstracts (on the ProQuest platform)
-
Sociological Abstracts (on the ProQuest platform)
-
Social Services Abstracts (on the ProQuest platform)
-
ProQuest Dissertations & Theses database (PQDT) Open (on the ProQuest platform)
-
Criminal Justice Abstracts (on the National Criminal Justice Reference Service)
-
Scopus
-
Web of Science (WoS)
-
OpenGrey
-
Cochrane Central Register of Controlled Trials
-
Electronic Theses Online Service (EThOS).
To identify UK-only grey literature documents, a number of supplementary searches were undertaken. Members of the SAG advised the project team as to which relevant websites to search (see Chapter 2). (A full list of the websites searched, along with the search terms utilised, can be found in Report Supplementary Material 8.) Members of the SAG were also asked to inform the research team of any other reports they were aware of that might be relevant to the evidence synthesis.
Searches were also conducted using Google as described by Mahood et al. 43 The first 10 pages of each Google output were screened using the terms:
-
young people, mental health crisis
-
children, mental health crisis.
To identify published reports that had not yet been catalogued in electronic databases, recent editions of Pediatric Emergency Care, Psychiatric Services, Journal of the American Academy of Child and Adolescent Psychiatry and Crisis: The Journal of Crisis Intervention and Suicide Prevention were hand-searched. These journals were selected because of the large number of outputs identified in database searches from these journals. Reference lists of included studies were scanned and forward citation tracking was performed using WoS.
Primary research records retrieved from database searches
All records retrieved from the 17 database searches were imported or entered manually into EndNote (Clarivate Analytics, Philadelphia, PA, USA) and duplicates were removed. The total number of hits retrieved for each database is displayed in Table 3.
| Database searched | Number of references retrieved |
|---|---|
| MEDLINE ALLa | 11,756 |
| PsycINFO | 10,077 |
| EmCare | 4447 |
| HMIC | 663 |
| CINAHL | 5210 |
| AMED | 191 |
| ERIC | 1940 |
| ASSIA | 1037 |
| Sociological Abstracts | 701 |
| Social Services Abstracts | 564 |
| Scopus | 10,593 |
| WoS | 9277 |
| Cochrane | 872 |
| OpenGrey | 220 |
| EThOS | 320 |
| PQDT Open | 116 |
| Criminal Justice Abstracts | 10 |
| Total | 57,994 |
Primary research records identified from supplementary searching
All primary research citations identified as potentially relevant from the supplementary searches (see Table 4) were entered manually into EndNote. A total of 31 records were identified.
| Source | Number of citations |
|---|---|
| Reference lists of included studies | 23 |
| Forward citation tracking of included studies | 7 |
| 0 | |
| SAG | 0 |
| Organisational websites | 1 |
| Hand-searching | 0 |
| Total | 31 |
Removing irrelevant records
The next stage was to remove irrelevant records by searching for keywords within the title using the search feature within the EndNote software. The keywords used to identify papers that did not meet the evidence synthesis inclusion criteria were agreed by the project team. The results for each keyword were screened by Deborah Edwards to ensure that they were, in fact, irrelevant before removing them. All records that remained at the end of this process were exported as an XML (extensible markup language) file and imported to Covidence™ (Melbourne, VIC, Australia).
Examples of the types of keywords that were used were as follows:
-
asthma
-
armed
-
abortion
-
adult*
-
baby
-
cancer
-
child abuse
-
cultural crisis
-
culture
-
diabetes
-
disaster
-
economic crisis
-
epilepsy
-
fertili*
-
financial crisis
-
first aid
-
gun
-
HIV/AIDS
-
hostage
-
hurricane
-
infant
-
maternal
-
migrant
-
military
-
mother*
-
neonat*
-
politic*
-
postpartum
-
predictor*
-
prison
-
refugee
-
screening
-
soldier
-
sexual abuse
-
validity
-
war.
Title and abstract screening
Two members of the review team independently assessed each record for relevance using the information provided in the title and abstract and the software package Covidence. A third reviewer resolved any disagreements. The full texts of all records that appeared to meet the inclusion criteria, or in cases in which a definite decision could not be made based on the title and/or abstract alone, were retrieved.
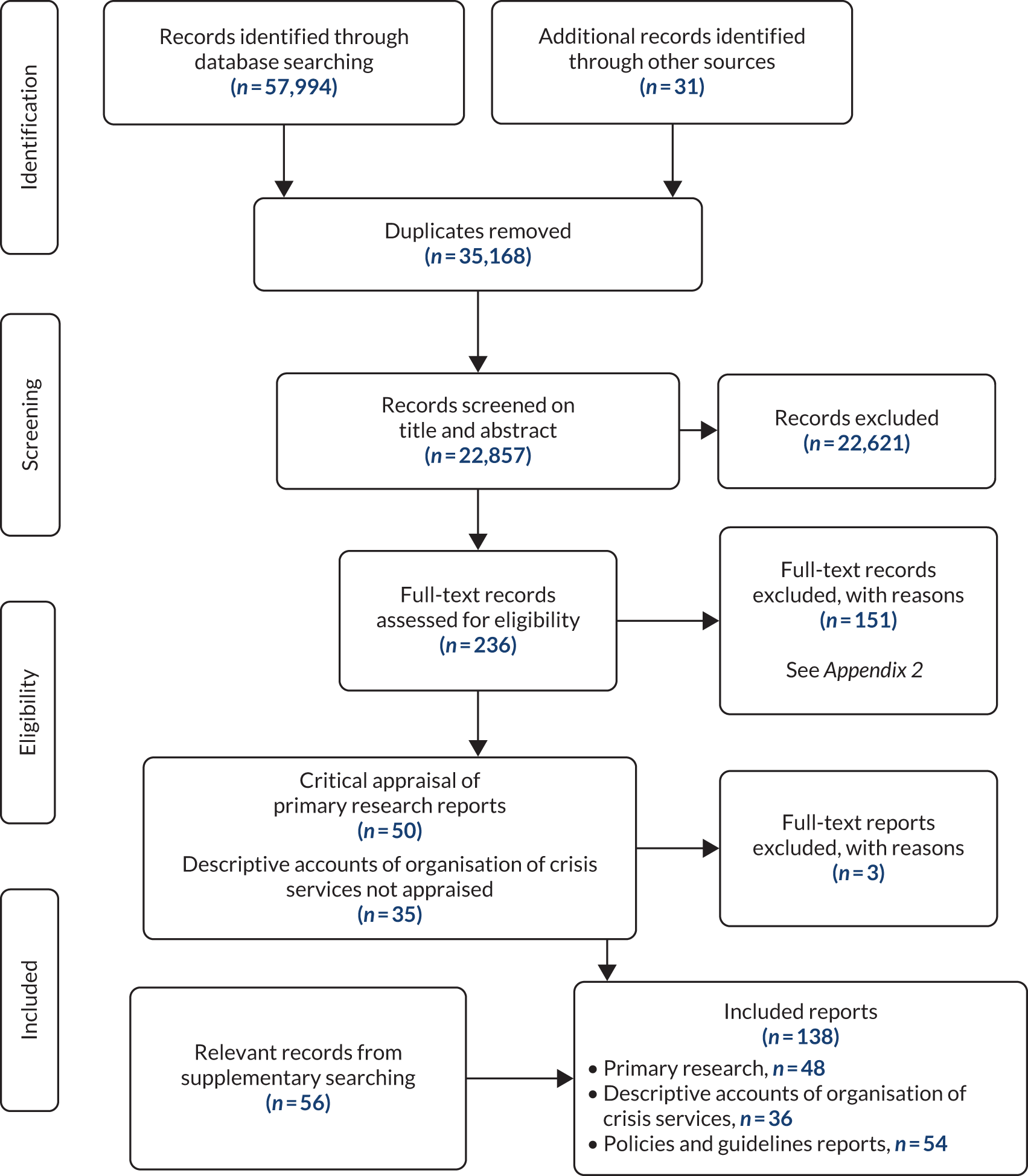
Full-text screening
A purposely designed form was used to screen each retrieved report. The form was piloted on 10 reports before being used independently by two reviewers to complete the full-text screening. Disagreements were resolved through discussion with a third reviewer. All English-language items relating to the objectives were included at this stage. Figure 3 shows the flow of records through each stage of the evidence synthesis process in the PRISMA flow chart. 42
FIGURE 3.
A PRISMA flow chart.
UK-only grey literature identified from supplementary searching
Sixty-nine literature records were identified as being potentially relevant from across all supplementary searches (see Table 5) and these records were all entered manually into EndNote. The UK-only grey literature identified was read by two members of the project team and considered against the topic inclusion criteria, with disagreements resolved as above. Thirteen records were excluded (see Report Supplementary Material 9), leaving a total of 56 records being assessed as relevant to the evidence synthesis (see Appendix 3).
| Source | Number of citations |
|---|---|
| Organisational websites | 64 |
| 5 | |
| SAG | 0 |
| Total | 69 |
Reports included in the evidence synthesis
One hundred and thirty-eight reports were included in the evidence synthesis and consisted of primary research (n = 48), descriptive accounts of the organisation of crisis services (n = 36) and UK-only grey literature (n = 54).
Quality appraisal
The methodological quality of all the research reports was assessed following searching and screening using a design-specific checklist (see Table 6). Alternative tools, which reflected the specific design and methods used in individual research outputs, were used as necessary when suitable Critical Appraisal Skills Programme (CASP) tools were not available. This was independently undertaken by two reviewers and any disagreement was resolved through discussion with a third reviewer.
| Study design | Checklist |
|---|---|
| RCT | CASP checklist for RCTs:44 11 items (‘yes’, ‘no’, ‘can’t tell’) |
| Quasi-experimental study | JBI checklist for quasi-experimental studies (non-randomised experimental studies):45 nine items (‘yes’, ‘no’, ‘unclear’, ‘not applicable’) |
| Prospective cohort study | Scottish Intercollegiate Guidelines Network Methodology Checklist 3: Cohort Studies:46 14 items (‘yes’, ‘no’, ‘can’t say’, ‘does not apply’) |
| Retrospective cohort study | Scottish Intercollegiate Guidelines Network Methodology Checklist 3: Cohort Studies:46 eight items (‘yes’, ‘no’, ‘can’t say’, ‘does not apply’) |
| Descriptive cross-sectional study | SURE checklist:47 12 items (‘yes’, ‘no’, ‘can’t tell’) |
| Qualitative study | CASP checklist for qualitative studies:44 10 items (‘yes’, ‘no’, ‘can’t tell’) |
Based on critical appraisal, the following three reports48–50 were excluded:
-
A qualitative study by Rossi and Cid48 was excluded because the data analysis was not sufficiently rigorous and it was concluded that there were insufficient data to be able to extract from.
-
A quasi-experimental study by McBee-Strayer et al. 49 was excluded because overall assessment of the quality of the study was rated as ‘unacceptable’.
-
A quasi-experimental study by Blumberg50 was excluded because the overall assessment of the quality was rated as ‘unacceptable’.
The descriptive accounts of organisation/models of crisis services and the UK-only grey literature were not subjected to quality appraisal.
For the CASP, Joanna Briggs Institute and Specialist Unit for Review Evidence checklists, an overall score is generated reflecting the number of items answered ‘yes’. For Scottish Intercollegiate Guidelines Network Methodology Checklist 3: Cohort Studies,46 the overall assessment reflects how well the study has sought to minimise the risk of bias or confounders. The final ratings are classified as high quality (described as the majority of criteria met with little or no risk of bias and the results are unlikely to be changed by further research), acceptable (described as most of the criteria met with some flaws in the study and an associated risk of bias, and the conclusions may change in the light of further studies) or low quality (described as either most of the criteria not met or significant flaws relating to key aspects of study design, and conclusions are likely to change in the light of further studies).
The authors46 of the checklist suggest that retrospective designs should not receive a rating higher than acceptable, as they are generally regarded as a weaker design.
Data extraction, analysis and synthesis
When multiple research reports from the same study were identified (i.e. 47 research reports covering 40 research studies), data were extracted and reported as a single study. The demographic data were extracted directly into tables based on study design following guidance from the Centre for Reviews and Dissemination. 39 The data extracted included the aim of the research, nature of the crisis, type and location of treatment, participant details, recruitment, age, gender, ethnicity, intervention or programme, data sources, outcomes and outcome measures. This process was conducted by one of the team of reviewers (JC, NE or RL), with each being responsible for a different study design, and then this process was independently checked for accuracy and completeness by a second reviewer (DE). A record of corrections was kept.
The full texts of all the reports and the electronic versions of all UK-only grey literature were uploaded into the software package NVivo 12 (QSR International, Warrington, UK) to aid the extraction, analysis and synthesis of the content. The data analysis and synthesis for each of four objectives was conducted separately and is presented as separate chapters.
The first objective was to critically appraise, synthesise and present the best-available evidence on the organisation of crisis services for CYP aged 5–25 years, across education, health, social care and the third sector. To answer objective 1, a narrative approach was employed that involved the development of thematic summaries,40,51,52 synthesising the data relating to the organisation of crisis services from primary research, descriptive accounts and UK-only grey literature documents. Thematic summaries are ‘summaries of findings of their included studies that have been arranged into themes’. 53 Natural groups of studies that investigated the same areas were brought together into meaningful sections and the final thematic summaries were written by one researcher and checked by a second. This objective is presented in Chapter 4.
The second objective was to explore the experiences and perceptions of CYP, their families and staff with regard to mental health crisis support for 5- to 25-year-olds. A thematic synthesis53 was performed on qualitative data extracted from primary research studies, wider research reports and stakeholder consultations with service providers and/or young people and their families (which were part of a wider body of work). Using NVivo, inductive data-driven codes, led jointly by Rhiannon Lane and Deborah Edwards, were generated through line-by-line reading of each document in line with each of the research objectives. The codes were then grouped into themes and subthemes by one researcher (RL) and checked by a second (DE). The confidence in the synthesised findings from the qualitative research to address objective 3 was assessed by two reviewers (DE and NE) using the CERQual (Confidence in the Evidence from Reviews of Qualitative research) approach. 54,55 This objective is presented in Chapter 5.
The third objective was to determine the effectiveness of current models of mental health crisis support for CYP. Owing to the heterogeneity of the included intervention studies, meta-analyses could not be performed and so thematic summaries, as described above, were conducted. Outcome data were extracted as they were presented across the primary research reports using NVivo. The purpose of this was to group data for each outcome and not to code the extracts in any detail. The confidence in the synthesised findings from the quantitative data was assessed by two reviewers (DE and JC) using the GRADE (Grading of Recommendations Assessment, Development and Evaluation) approach. 56 This objective is presented in Chapter 6.
The fourth and final objective was to determine the goals of crisis intervention. To address this objective, thematic summaries, as described above, were employed to bring together data across the primary research, descriptive accounts of the organisation of crisis services and UK-only grey literature documents that related to the goals of crisis services. This was led by Ben Hannigan and was checked by Deborah Edwards and Nicola Evans. This objective is presented in Chapter 7.
Description of reports
Forty-eight reports, covering 42 research studies, were deemed suitable for inclusion in the evidence synthesis. Demographic information on the characteristics of included research studies is displayed in Appendices 4–9. Thirty-six additional reports, covering 39 descriptive accounts of the organisation services, were also included (see Report Supplementary Material 10).
Country of origin
The majority of the research reports were conducted within the USA (25 studies across 30 reports32,34,57–84), followed by Canada (eight studies across nine reports85–93), the UK (n = 394–96) and Australia (n = 291,92), and one study from each of the following countries: Ireland,97 the Netherlands,98 New Zealand99 and Sweden. 100 The descriptive accounts of the organisation of crisis services were mainly from the USA (19 descriptions across 15 reports33,101–114) and Canada (n = 10115–124). Three reports125–127 were from Australia and one report from each of the following countries: Germany,128 Switzerland,129 the Netherlands130 and the UK. 131
Study designs and methods
For the research studies, there were 31 quantitative studies (reported across 37 reports32,34,57–69,71–75, 77–89,92,93,98,132) and 11 qualitative studies. 70,76,90,91,94–97,99,100,133 The quantitative studies included a prospective cohort study (n = 132), retrospective cohort studies (n = 1234,62,65–68,71,72,74,75,87,89), quasi-experimental studies (four studies across six reports82,83,86,92,93,132), randomised controlled trials (RCTs) (four studies across eight reports57,61,64,78–81,84) and descriptive cross-sectional studies (n = 1058–60, 63,69,73,77,85,88,98).
Participant characteristics
Participants across the research studies were:
-
CYP experiencing, or who had experienced, a crisis (31 studies across 34 reports32,34,58–63,65–75,77,82–84,86,87,89,91–95,97,98,100,132)
-
CYP experiencing crisis and their family members (two studies across six reports57,64,78–81)
-
family members/parents of CYP experiencing crisis (n = 276,88)
-
caregivers and siblings of CYP experiencing crisis (n = 190)
-
family and close friends bereaved by suicide of a CYP (n = 1133)
-
youth counsellors (n = 1134)
-
staff members from project sites (n = 194)
Participant group sizes for CYP ranged from two134 to 253262 participants. One qualitative study91 had a large number of participants (n = 1449), but data from only one-third of these participants were analysed.
Some studies did not identify the ages of the CYP, labelling them as adolescents,34 young people,134 child psychiatry patients,71 elementary school students77 or high school students. 60,69,73,77 Three studies71,94,100 included young people aged > 16 years only (i.e. 16–24 years,100 16–25 years94 and 18–25 years70).
The majority of research studies included a mix of male and female CYP. One study included only males58 and a further study (across two reports) included only females. 82,83 A further seven studies34,66,71,77,90,94,99 did not report gender.
Outcomes across effectiveness studies
Symptoms of depression
Levels of depression were reported in three studies (across four reports57,78,82,83) and were measured using the Beck Depression Inventory,82,83 the Brief Symptom Inventory,78 the anxiety and depression subscale of the Child Behaviour Checklist (CBCL),78 the Hopelessness Scale for Children of the Youth Self-Report Scale78 or the Centre for Epidemiological Studies Depression Scale (CES-D). 57
Psychiatric symptoms
Psychiatric symptoms or symptomatology was addressed in three studies (across four reports64,79,87,98) and were measured using the Global Severity Index of the Brief Symptom Inventory,64,79 the functioning subscale on the Childhood Acuity Psychiatric Illness Scale (CAPI)87 or the Health of the Nation Outcome Scales for Children and Adolescents (HoNOSCA). 98
Behaviour
Three studies (across four reports57,61,64,79) investigated internalising and externalising behaviour using the CBCL. The internalising behaviours measured reflected mood disturbance (including anxiety and depression) and social withdrawal. The externalising behaviours reflected conflict with others and violation of social norms.
Psychosocial functioning
Psychosocial functioning was investigated in four studies (across five reports61,64,79,86,87) and was measured using the Child and Adolescent Functional Assessment Scale,61 the Children’s Global Assessment Scale (CGAS),86 youth and/or caregiver reports on the social competence subscales of the CBCL,61,64,79 youth reports on the antisocial friends and conventional involvement of friends subscale of the Family, Friends, and Self Scale (FFS)64,79 and through tracking school attendance. 64,79 Greenham and Bisnaire87 measured the levels of functioning of those with psychiatric symptoms using the functioning subscale on the CAPI.
Hospitalisation rates
Nine studies (across 12 reports32,64,68,74,75,79,80,84,86,89,92,93) investigated the effectiveness of a number of different crisis-based interventions or assessment processes on hospitalisation rates. These interventions/processes were explored at the time of the crisis,68,86 within 72 hours of the crisis,75 within 30 days of the crisis,68,89 at 1-month follow-up,84 at 2-month follow-up,86,93 at 3-month follow-up,32 at 6-month follow-up,86,93 up to 1-year follow-up64,79,80 or at an unspecified time frame. 74,92
Costs
Costs were addressed in seven studies. 58,65,67,72,74,81,93 The types of analysis that were conducted included cost savings (n = 658,65,67,72,74,93), cost-effectiveness (n = 281,93), cost-efficiency74 and opportunity costs. 67 Five studies58,65,67,72,74 reported significant cost savings and one study93 found no significant differences. Of the studies reporting cost savings, four58,67,72,74 out of the five58,65,67,72,74 studies reported that these savings were reflective of reduced lengths of stay (LOSs).
Discharge destination and referral pathways
The destination to which CYP were discharged or referred on to was reported across 11 studies,32,58,59, 61,63,65,74,85,87,92,98 and are reported as follows:
-
home (biological or foster family) or the residence they were previously living in (n = 5;58,59,61,74,87 and, when reported, the percentage of those discharged ranged from 65%65 to 86%61)
-
residential treatment facilities (n = 2;59,65 2%65 and percentage not reported59)
-
outpatient mental health services (n = 3;32,63,98 and, when reported, the percentage ranged from 43%32 to 90%63)
-
hospital/inpatient psychiatric units (n = 10;32,58,59,61,63,65,74,85,87 and, when reported, the percentage ranged from 8%61 to 35%32)
-
no further specialised treatment needed (n = 2;85,98 with the percentage ranging from 16.7%98 to 82%85)
-
other services, which included outpatients or other psychiatric facilities (n = 1;65 12.2%65).
Emergency department visits post discharge
Repeat emergency department visits post intervention were addressed in nine studies32,34,62,66,72,74,75,86,89 at the following time points post discharge: within 72 hours,74,75 within 1 month,32 within 30 days,66,89 within 6 months,86 within 12 months34,72 or within 18 months. 62
Family functioning/empowerment
Six studies (across seven reports33,61,64,79,82–84) addressed family functioning or empowerment. This was measured using the Family Adaptation and Cohesion Scales – Version II (FACES II),61 the Family Adaptation and Cohesion Scales – Version III (FACES III),64,79,82,83 caregiver self-reports on the Global Severity Index of the Brief Symptom Inventory,64,79 the Family Empowerment Scale84 or the Conflict Behaviour Questionnaire. 57
Length of stay
Two studies59,87 provided descriptive information regarding LOS across the inpatient crisis programmes/interventions and ten studies58,65,67,71,72,74,75,86,89,132 investigated the impact of a variety of interventions on LOS.
Completed suicide and suicide attempts
Four studies32,57,78,86 investigated the incidence of attempted or completed suicide at different follow-up points post intervention.
Suicidality
Five studies (across six reports32,57,82,83,86,87) reported on levels of suicidality measured using the Harkavy–Asnis Suicide Scale (HASS),57,82,83 the risk factors subscale of the CAPI,87 the Spectrum of Suicidal Behaviour Scale (SSBS)86 and the Reasons for Living Inventory for Adolescents. 84
Post-discharge use of services/resources
Four studies (across six reports57,82,83,86,89,93) investigated the effects of interventions on resources and/or patient treatment accessed post discharge.
Self-esteem/self-concept
Three studies (across five reports61,64,79,82,83) investigated the impact of the intervention on levels of self-esteem64,79,82,83 or self-concept. 61 The instruments used included the Rosenberg Self-esteem Scale,82,83 the self-esteem subscale of the FFS64,79 and the Piers–Harris Children’s Self-Concept Scale. 61
Impulsivity
One experimental study (across two reports82,83) investigated the impact of the intervention on levels of impulsivity using the Impulsiveness Scale.
Satisfaction with mental health crisis services/programmes
Aspects of satisfaction with mental health crisis services/programmes were reported in nine studies64,74,75,77,84,85,88,92,132 and one organisational report. 96 Five studies64,74,84,92,132 looked at client satisfaction defined as satisfaction with the mental health crisis service/programme by patients, their parents or guardians, which was measured using Lubrecht’s Family Satisfaction Survey (LFSS),64 the Client Satisfaction Questionnaire,61 a telehealth satisfaction survey74 or satisfaction questionnaires developed specifically for the studies. 92,132
Health-care staff satisfaction with mental health crisis services/programmes
Four studies74,75,85,96 investigated health-care staff satisfaction with the service. Satisfaction was measured with a telehealth satisfaction survey74 or with satisfaction questionnaires developed specifically for the studies. 75,85,96
Satisfaction with clinicians who delivered the mental health crisis service/programme
Satisfaction with the clinicians who delivered the mental health crisis service/programme was explored in two descriptive cross-sectional studies. 77,88 Satisfaction was measured using a satisfaction questionnaire developed specifically for the study77 or using an adapted version of the Quality of Care Parent Questionnaire. 88
Results of quality appraisal
Randomised controlled trials
The methodological quality of each of the four RCTs (reported across eight reports57,61,64,78–81,84) was judged against the relevant 11 quality criteria used in the CASP checklist and each is summarised in Table 7. Five reports64,78–81 reported on different elements of the same multisystemic therapy (MST) intervention and were appraised as one study. Only one study57 scored highly, answering ‘yes’ to all the questions on the checklist. Two studies61,84 did not provide enough information to determine if true randomisation had taken place (question 2), stating that randomisation had been performed, but no further details were provided. In one study,61 not enough information was provided to determine whether or not all participants had been accounted for at the end of the trial (question 3). Two studies57,84 blinded recruitment and assessment staff (question 4). For one study,64,78–81 the experimental and control groups were not treated identically because of the nature of the intervention and control (question 6). All of the studies reported results for all the outcomes (question 7). Only one study57 reported confidence intervals (CIs) with regard to the precision of the estimate of the treatment effect (question 8). Owing to the way the sample was recruited, it was difficult to say whether or not the results were generisable across two studies (question 9). 61,64,78–81 It was not evident whether or not the benefit of the intervention was worth the harms and costs in one study57 (question 11).
| Study and country | Location of intervention | Type of intervention | Question | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | |||
| Asarnow et al.;57 USA | ED | Crisis services/interventions initiated within the ED | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Evans et al.;61 USA | Home | Home- or community-based programme | Y | CT | CT | N | N | Y | Y | N | CT | Y | CT |
| Henggeler et al.,64,79 Huey et al.,78 Schoenwald et al.80 and Sheidow et al.;81 USA | Home | Home- or community-based programme | Y | Y | Y | N | Y | N | Y | N | CT | Y | Y |
| Wharff et al.;84 USA | Paediatric ED | Crisis services/interventions initiated within the ED | Y | CT | Y | Y | Y | Y | Y | N | Y | Y | Y |
Quasi-experimental studies
The methodological quality of each of the four quasi-experimental cohort studies (reported across six reports82,83,86,92,93,132) was judged against the nine quality criteria used in the Joanna Briggs Institute checklist and each is summarised in Table 8. When multiple reports existed for the same study, these were appraised as one study. Three studies82–83,86,92–93 scored highly, with one pilot study132 included that had a lower score. For one study,92 there were some differences between the study group and matched comparison group (question 2). Another study86 did not delineate between the control group and the experimental group in terms of loss to follow-up (question 6), but, overall, this was low (3% at 2 months and 8% at 6 months). For one other study,132 all carers who were able to be contacted took part in the survey and differences between groups were taken into account in the analysis.
| Study and country | Location of intervention | Type of intervention | Question | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |||
| Roberts et al.;92 Canada | Telepsychiatry suite in remote EDs | Telepsychiatry | Y | N | Y | Y | Y | Y | Y | Y | Y |
| Rotheram-Borus et al.;82,83 USA | ED | Crisis services intervention initiated within the ED | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Greenfield et al.86 and Latimer et al.;93 Canada | Paediatric ED and then outpatient department | Outpatient mental health programme | Y | Y | Y | Y | Y | U | Y | Y | Y |
| Nagarsekar et al.;132 Australia | Paediatric ED | Assessment approach with the ED | Y | Y | U | Y | N | Y | Y | Y | Y |
Cohort studies
The methodological quality of each of the 13 cohort studies32,34,62,65–68,71,72,74,75,87,89 was judged against the relevant quality criteria derived from the Scottish Intercollegiate Guidelines Network Methodology Checklist 3: Cohort Studies46 and each is summarised in Table 9. All 13 studies were judged to be of acceptable quality, indicating that some flaws in the study design were present with an associated risk of bias. For two studies,34,67 it was not possible to determine if the two groups being studied were from the same source population and for a further one study74 the two groups were from different populations (criterion 2). The retrospective cohort study conducted by Maslow et al. 66 did not have a comparison cohort (criterion 2). Four studies66,75,84,89 did not identify any confounders and in one further study34 it was not possible to determine this information (criterion 13). Only three of the studies62,68,75 provided CIs as part of the statistical analysis (criterion 14). Although the study by Greenham and Bisnaire87 was a retrospective study, 89.8% of parents/guardians gave informed consent for the use of their clinical information for research purposes. Three studies34,71,89 utilised both retrospective and prospective samples, with the retrospective data used as the control group.
| Study and country | Location of intervention | Type of intervention | Criterion | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | Rating | |||
| Wharff et al.;32 USA | PED | Crisis services/interventions initiated within the ED | Y | Y | Y | N/A | 55.4% | Y | Y | N/A | Y | Y | Y | Y | N | N | A |
| Greenham and Bisnaire;87 Canada | Inpatient unit | Inpatient care | Y | N | Y | N/A | N/A | N/A | Y | N/A | N/A | Y | Y | N/A | Y | N | A |
| Fendrich et al.;62 USA | Community | Mobile crisis service | Y | Y | N/A | N/A | N/A | N/A | Y | N/A | N/A | Y | Y | N/A | Y | Y | A |
| Holder et al.;65 USA | PED | Implementation of a dedicated mental health team in the ED | Y | Y | N/A | N/A | N/A | N/A | Y | N/A | N/A | Y | Y | N/A | Y | N | A |
| Mahajan et al.;67 USA | PED | Implementation of a dedicated mental health team in the ED | Y | CS | N/A | N/A | N/A | N/A | Y | N/A | N/A | Y | Y | N/A | Y | N | A |
| Rogers et al.;72 USA | Inpatient unit | Inpatient care | Y | Y | N/A | N/A | N/A | N/A | Y | N/A | N/A | Y | Y | N/A | Y | N | A |
| Uspal et al.;75 USA | PED | Implementation of a dedicated mental health team in the ED | Y | Y | N/A | N/A | N/A | N/A | Y | N/A | N/A | Y | Y | N/A | N | Y | A |
| Lee et al.;89 Canada | PED | Assessment approach with the ED | Y | Y | Y | N/A | 11% | CS | Y | N/A | Y | Y | Y | N/A | N | N | A |
| Martin;68 USA | Community | Mobile crisis service | Y | Y | N/A | N/A | N/A | N/A | Y | N/A | N/A | Y | Y | N/A | Y | Y | A |
| Thomas et al.;74 USA | Telepsychiatry suite in remote ED | Telepsychiatry | Y | N | N/A | N/A | N/A | N/A | Y | N/A | N/A | Y | Y | N/A | Y | N | |
| Maslow et al.;66 USA | Outpatient clinic | Outpatient mental health programme | Y | N/A | N/A | N/A | N/A | N/A | Y | N/A | N/A | Y | Y | N/A | N | N | A |
| Reliford and Adebanjo;71 USA | PED | Telepsychiatry | Y | Y | N/A | N/A | N/A | N/A | Y | N/A | N/A | Y | Y | N/A | Y | N | A |
| Greenfield et al.;34 Canada | Outpatient clinic | Outpatient mental health programme | Y | CS | N/A | N/A | N/A | N/A | Y | N/A | N/A | Y | Y | N/A | CS | N | A |
Descriptive cross-sectional studies
The methodological quality of 10 descriptive cross-sectional studies58–60,63,69,73,77,85,88,98 was judged against the 12 quality criteria used in the Specialist Unit for Review Evidence tool47 and each is summarised in Table 10. Five studies60,63,69,73,77 failed to clearly state the study design. All studies addressed clearly focused questions apart from one73 in which it was unclear. All studies selected participants fairly and all provided details on participant characteristics, apart from Walter et al. 77 who provided details of students attending schools in general rather than of those in crisis. Two studies63,98 did not provide adequate details of their methods of sampling and in a further two studies77,85 it was unclear whether or not the outcome measures were appropriate. One evident weakness of most studies was description of statistical methods, which was good in only four studies. 77,85,88,98 Results were well described in all 10 studies. 58–60,63,69,73,77,85,88,98 One study77 failed to provide information on participant eligibility. No studies reported any sponsorship/conflict of interest and three studies60,63,73 failed to identify limitations.
| Study and country | Location of treatment | Type of treatment | Question | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | |||
| Michael et al.;69 USA | High school | Assessment approach with educational settings | N | Y | Y | Y | Y | Y | Y | N | Y | Y | N | Y |
| Sale et al.;73 USA | High school | Assessment approach with educational settings | N | U | Y | Y | Y | Y | Y | N | Y | Y | N | N |
| Capps et al.;60 USA | High school | Assessment approach with educational settings | N | N | Y | Y | Y | Y | Y | N | Y | Y | N | N |
| Walter et al.;77 USA | Elementary and high school | Assessment approach with educational settings | N | Y | Y | Y | N | U | Y | Y | N | Y | N | Y |
| Baker and Dale;58 USA | RTC | Crisis programmes | Y | Y | Y | Y | Y | Y | Y | U | Y | Y | N | Y |
| Baker et al.;59 USA | RTC | Crisis programmes | Y | Y | Y | Y | Y | Y | Y | U | Y | Y | N | Y |
| Dion et al.;85 | Canada Psychiatric ED at a children’s hospital | Crisis services/interventions initiated within the ED | Y | Y | Y | Y | Y | U | Y | Y | Y | Y | N | Y |
| Lee and Korczak;88 Canada | PED | Outpatient mental health programmes | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | N | Y |
| Gillig;63 USA | Outpatient clinic | Adolescent crisis service | N | Y | U | Y | Y | Y | N | N | Y | Y | N | N |
| Muskens et al.;98 the Netherlands | Home | Home-based programme | Y | Y | Y | Y | Y | Y | N | Y | Y | Y | Y | Y |
Qualitative studies
The methodological quality of each of the 11 qualitative studies70,76,90,91,94–97,99,100,133 were judged against the 10 quality criteria used in the CASP qualitative checklist44 and are summarised in Table 11. Only one study100 discussed whether or not the relationship between researcher and participants had been adequately considered, indicating an overall weakness in reporting this concept. Across four studies,90,91,96,99 not enough information was provided to state definitively whether or not the research design was appropriate to the aims of the research (question 3). The recruitment strategy was unclear for two studies91,94 (question 4). Three studies76,96,97 did not state whether or not they had ethics approval (question 7). Six studies90,91,94–97 failed to identify whether or not the data analysis was sufficiently rigorous, with a lack of in-depth description (question 8).
| Question | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Study and country | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
| Bolger et al.;97 Republic of Ireland | Y | Y | Y | Y | Y | N | N | N | Y | Y |
| Haxell;99 New Zealand | Y | Y | CT | Y | Y | N | Y | CT | Y | Y |
| Idenfors et al.;100 Sweden | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Garcia et al.;94 UK | Y | Y | Y | CT | Y | N | Y | CT | Y | Y |
| Liegghio and Jaswal;90 Canada | Y | Y | CT | Y | Y | N | Y | CT | Y | Y |
| Liegghio et al.;91 Canada | Y | Y | CT | CT | Y | N | Y | CT | Y | Y |
| Narendorf et al.;70 USA | Y | Y | Y | Y | Y | N | Y | Y | Y | Y |
| Nirui and Chenoweth;133 Australia | Y | Y | Y | Y | Y | N | Y | Y | Y | Y |
| Walter et al.;76 USA | Y | Y | Y | Y | Y | N | N | Y | Y | Y |
| NICCY;95 Northern Ireland | Y | Y | Y | Y | Y | N | Y | CT | Y | Y |
| RCEM;96 UK | Y | Y | CT | Y | Y | N | N | CT | Y | Y |
Chapter 4 Organisation of crisis services
This chapter addresses the first objective, which was to present the best-available evidence on the organisation of crisis services for CYP aged 5–25 years, across education, health, social care and the third sector.
An overview of the different types of crisis services/responses that have been described across the included literature was presented to the SAG at the second meeting (see Report Supplementary Material 4). After discussion, it was decided to categorise the different types of crisis services/responses as follows: triage/assessment-only approaches, digitally mediated support approaches, and intervention approaches and models (see Report Supplementary Material 11).
Triage/assessment-only approaches
Twenty-three reports60,67,69,71,73,74,85,88,89,110,115–117,119–121,123,124,130,132,136,227 described different triage/assessment-only approaches for CYP experiencing crisis (see Report Supplementary Material 11) and three UK-only grey literature documents95,135,141 each presented a case example. Approaches included CYP presenting in crisis to the following types of services: emergency departments, educational settings, telephone triage and out-of-hours mental health emergency services.
Emergency departments
Eight reports89,110,115–117,119,123,124 described mental health assessment tools for paediatric emergency department clinicians, which included the HEADS-ED,110,116,117 HEARTSMAP89,119,123,124 and a Mental Health Assessment Triage Tool. 115 Four reports88,120–122 described urgent follow-up models after initial assessments had taken place at the emergency department. Two reports67,85 described the addition of involving trained mental health workers within a medical emergency department setting. Another report132 described Kids Assessment Liaison for Mental Health (KALM), which sought to build extra capacity for an emergency department medical officer to complete the assessment and to link with an on-call psychiatrist regarding an assessment and management plan. A further two reports71,74 described videoconference-based psychiatric emergency consultation programmes (i.e. telepsychiatry). One further report110 described the enhanced care co-ordination model for all CYP aged 0–21 years presenting with mental health concerns. The model involves a comprehensive needs assessment, a review of the CYP’s current use of services, and a package of medical and behavioural health follow-up with support for the family. 110
A case example95 described a 24 hours per day, 7 days per week (24/7), service that used a model in which the crisis response home treatment team worked together with Rapid Assessment Interface Discharge professionals. CYP were assessed by mental health practitioners in emergency department within 2 hours and then linked with onward support. 95 Another case example135 described a crisis service that provided assessments in the emergency department within 4 hours and appropriate follow-up care, which was available beyond normal office hours. The aim of the service was to prevent admission, and support could be provided for up to 6 weeks. 135
Educational settings
Four reports60,69,73,136 investigated CYP who presented within educational settings, of which three60,69,73 explored the use of the Prevention of Escalating Adolescent Crisis Events (PEACE) protocol within US high schools. This protocol involved an in-school facility in which high school-aged children could be assessed by psychology services before referral on to appropriate mental health services. The fourth report136 presented an urgent evaluation service for students, which aimed to provide ambulatory psychiatric evaluation within school hours, offering same-day assessment, co-ordination of care and linkage to the emergency department within the same hospital if required.
Telephone triage
Two reports102,110 described crisis telephone services within the USA in which onward referrals were made to appropriate services. One case study110 described a triage approach that responded to CYP presenting with mental health crises. This allowed for all referrals to access care via a single point of access telephone number between 9 a.m. and 9 p.m. The response time was determined by the location of the CYP and so ranged between 4 and 24 hours. Further assessment was carried out by either a consultant or the crisis team.
Out-of-hours mental health services
One report130 described an out-of-hours mobile crisis team for child care/custody protection services, as well as mental health-care providers in the region. One case study130 described a street triage model that enabled police officers to seek immediate consultation, advice or face-to-face support from a specialist mental health practitioner in making an assessment between 6 p.m. and 2 a.m. about anyone they encountered with an apparent mental health crisis. This triage model was for all ages and was not specifically for CYP. The aims of this model were to reduce the use of Section 136 Mental Health Act 1983137 and to provide more appropriate response to people’s mental health needs. (In England and Wales, Section 136 of the Mental Health Act 1983137 refers to powers that police have to move a person from a public space, when they appear to be suffering from mental disorder, to a place of safety.)
Digitally mediated approaches
Six reports99,101,104,109,118,127 described the organisation of digitally mediated approaches for CYP who were experiencing crisis (see Report Supplementary Material 12). One further UK-only grey literature document138 presented two case examples describing digitally mediated approaches. Approaches included telephone support/counselling services, text-based support/counselling services, telephone and text support/counselling services and online mutual-help groups.
Telephone support/counselling
One report101 described a telephone-based approach for CYP experiencing crisis, with which follow-up, emergency support and telephone tracing for those feeling suicidal were made available. The case example138 described Childline139 and the Samaritans,140 which provide support for people in mental health crises, particularly those who feel suicidal, with Childline in particular aimed at CYP aged < 19 years. Although both Childline139 and the Samaritans140 offer support via telephone and e-mail, Childline139 also has a live webchat facility.
Text-based support/counselling
Three reports99,104,109 described text-based support for CYP experiencing any type of crisis. All three reports99,104,109 involved possible onward referrals or further support following initial contact. The case example138 described a 24-hour text messaging service for young people in crisis called SHOUT. SHOUT used artificial intelligence to assist the prioritisation of messages before young people making contact were assigned to a volunteer.
Telephone and text support/counselling
One report127 described a joint telephone and text-based support service for university students in crisis with possible onward referrals to general practitioner (GP) medical services and university support services.
Online mutual-help groups
One report118 described peer-run online support for young people experiencing mental health issues, including suicidality. Responses were provided by trained volunteers within 24 hours of posting.
Intervention approaches and models
Fifty-one reports described intervention approaches and models in response to CYP experiencing crisis (see Report Supplementary Materials 13–15). In addition, six UK-only grey literature documents141–146 presented case examples that described a range of intervention approaches and models. The different intervention approaches and models included inpatient services, outpatient mental health programmes, mobile crisis services, crisis services or interventions initiated within emergency departments, increasing paediatric mental health expertise in the emergency department, home- or community-based crisis programmes, school–hospital partnerships, multicomponent or multiagency services, crisis programmes located within residential treatment centres (RTCs) and generic crisis services.
Inpatient services
Eight reports70,72,87,106,108,128,129,131 described inpatient models of care in response to CYP experiencing crisis. There was a number of theoretically informed therapeutic approaches employed, including psychoanalytic therapy,128,129 solution-focused brief therapy131 and motivational therapy,131 as well as a broader approach to brief crisis intervention. A case example141 described a purpose-built inpatient unit that also contained a dedicated S136 facility alongside the specialist intensive care and generic wards. Section 136 of the Mental Health Act 1983 (2008) gives the police the authority to remove people from a public place of they believe that they need immediate help and are suffering from a mental disorder. The police then transport the person to a place of safety.
Outpatient mental health programmes
Seven reports34,63,66,86,92–93,110 explored outpatient mental health programmes. One study110 involved an outpatient crisis programme for CYP with high levels of mental health risk or behavioural difficulties experiencing a crisis. Three studies34,86,93 involved rapid response outpatient models for adolescents presenting to paediatric emergency departments following suicide attempts. One study63 described an adolescent crisis service within an outpatient clinic for those in rural areas and a further study66 described an integrated paediatric mental health outpatient clinic that was designed to enhance capacity for urgent assessments.
Mobile crisis services
Four reports62,68,113,114 described mobile crisis services. One report113 explored a mobile crisis intervention service, which involved rapid deployment to home or community locations, warm telephone lines (i.e. a crisis line run by peers), crisis stabilisation, crisis safety planning and short-term treatment. Two reports62,114 described emergency mobile psychiatric services that provide crisis stabilisation and support, screening and assessment, suicide assessment and prevention, and a brief solution-focused intervention. One of these reports114 was a description of the programme and the other62 examined whether or not the programme was associated with reduced behavioural health emergency department visits for those who had used the service. One study68 described a mobile response team for CYP at risk of endangering themselves or others. All services provided referral and linkage to ongoing care within community or inpatient settings.
Crisis services or interventions initiated within the emergency department
Two reports105,110 explored crisis services initiated within emergency departments. One report105 described a paediatric psychiatry crisis service that included post-discharge monitoring for those experiencing suicidality, including onward referral to outpatient services. The other publication described a response model110 for CYP presenting to the emergency department in psychiatric crisis. In this model, referral for additional mental health services could be provided, including long-term crisis stabilisation treatment (up to 6 months).
Three reports considered family-based crisis interventions (FBCIs). 32,84,107 FBCIs are interventions conducted in the emergency department that look to stabilise suicidal adolescents within a single visit so that they may return home safely with their families. One report107 presented a detailed description of the intervention and a further two reports32,84 explored the feasibility and safety of FBCIs32 and detailed the efficacy outcomes. 84 Six reports33,57,82,83,111,147 explored Family Intervention for Suicide Prevention (FISP). FISP was designed to be used during emergency department visits and sought to deliver an intervention improving outcomes for suicidal youths and enhance motivation for follow-up treatment. Two reports33,83 presented in-depth descriptive details of the intervention and a further three57,82,111 reports described a RCT that tested the effectiveness of the intervention across different periods of follow-up.
Increasing paediatric mental health expertise in the emergency department
In the specific context of the emergency department, two reports65,75 described services with the goal of increasing the availability of specialist mental health staff as a route to responding more effectively to CYP’s crises. The first report65 involved additional training for psychiatric professionals in an emergency department for those presenting in crisis. The second report75 described the implementation of a dedicated mental health team within an emergency department for children presenting with psychiatric complaints (excluding self-inflicted injuries).
Home- or community-based crisis programmes
Two reports61,103 described three models of intensive in-home services: (1) home-based crisis intervention (HBCI), (2) enhanced HBCI (HBCI+) and (3) crisis case management (CCM). One of these reports103 described the three services and a further report61 sought to determine the effectiveness and compare all three models across a range of outcomes for children in psychiatric crisis. Home-based MST for CYP presenting to emergency departments or inpatient services with psychosis, or with suicidal or homicidal ideation or threat, was the focus of six reports. 64,78–81,112 One of these reports112 described the adaptation of MST for use in youths presenting with psychiatric emergencies and a further five reports64,78–81 tested the effectiveness of MST compared with hospitalisation across a range of outcomes and different periods of follow-up.
The case examples142,143,146 described a number of different approaches to home-based crisis care within the UK. The first case example142 set out CYP mental health local transformation plans, including the development of a number of intensive home treatment services in the UK. The service was designed to help CYP at risk of admission by providing direct care through daily visits at home. The service also aimed to support other non-specialist professionals who care for CYP in crisis by providing consultation, for example in emergency departments. The publication by the National Collaborating Centre for Mental Health on ‘All Age Crisis Care’143 provided a description of a CAMHS home treatment team as an example of positive practice. Young people who had been identified as requiring an inpatient admission were offered care at home, and the team then worked to discharge them as soon as possible and to provide them and their family with practical support. 143 Five areas from the east of England provided information on their current crisis service, their responses to mental health crises of CYP and three case examples that detailed home-based services. 146 One home treatment team was designed as a hospital avoidance service in which the home treatment team provided a service to CYP aged 2–18 years with complex needs who would otherwise have been admitted to hospital, or to CYP discharged early. An intensive community outreach service offered intensive home-based care following a rapid assessment. This service was aimed at CYP aged 11–17 years with severe, enduring or complex mental illness, or at those who found engaging with services difficult. Both mental and physical health needs were addressed by this service. The aims of these services were to reduce costs associated with inpatient care and to keep the CYP as close to home as possible. A tertiary service provided CYP aged 12–18 years with additional support alongside other involved providers at transitional points, such as following discharge after self-harm, before a planned admission or following discharge from inpatient care, or to avoid admission.
Four reports125,126,141,143 provided descriptions of services that were organised and located within CAMHS. The reports described the safety first assessment intervention (SFAI), which provides an assessment and family-focused intervention delivered by CAMHS clinicians working within an intensive care and assessment team for high-risk CYP. The focus of the SFAI is to assist the young person and their family to achieve both physical and emotional safety. 125,126 One report presented a description of the SFAI and a further report described the safety first model that underpins the intervention. A case example presented within the Care Quality Commission report, A Safer Place to Be,141 also described how safety planning was integrated into existing processes, including liaising with police to avoid the application of Section 136 Mental Health Act 1983. 137,141 The report by the National Collaborating Centre for Mental Health, All Age Crisis Care143 provided a description of a CAMHS Crisis, Liaison and Intensive Home Treatment Team as an example of positive practice. The focus of this service was to provide comprehensive mental health and risk assessments to CYP in crisis, including follow-up support, intervention options and transition to adult services. The service collaborated with CYP, their families or carers and relevant professionals to co-produce personalised crisis care plans. This collaborative model was also described as being used for future service developments.
School–hospital partnerships
One report77 evaluated the implementation of a school–hospital partnership using a model of multitiered systems of support to deliver crisis management in acute mental health crisis.
Crisis programmes located within residential treatment centres
Two reports58,59 described an on-campus crisis residence programme as an alternative to hospital treatment for boys aged 5–17 years who were experiencing a psychiatric crisis while residing in a RTC.
Multicomponent or multiagency services
Three reports113,148,149 described the use of multicomponent approaches to crisis care. The Ventura County Children’s Crisis Continuum is a continuum of services providing three levels of care:113 (1) a mobile crisis team offering de-escalation and safety planning at home or in the community, (2) a crisis stabilisation unit providing a brief admission of < 24 hours for assessment and safety planning and (3) a crisis resolution team offering therapeutic treatment for a few months for two CYP at a time. The Solar community crisis resolution team offer both a working hours and an out-of-hours service 7 days per week. 149 The service aims to triage CYP within 1 hour of referral and to complete assessments with 4 hours in which both home and community treatment are offered. Ribbers et al. 148 described a crisis and transition services model that was an emergency department diversion programme that provided transitional clinical care and offers safety planning, lethal means restriction counselling, 24-hour crisis support and care co-ordination. Other services variably included in-home individual and family therapy, psychiatric evaluation and medication management, and family peer support.
A case example from the HoNOSCA crisis team described a multiagency team that offered wraparound 24/7 care to CYP in crisis at their homes. 143 Another case example144 offered a range of different approaches, including out of hours, self-referral ‘havens’, targeted intervention for vulnerable CYP, a day service, and a specific out-of-hours and weekend crisis service offering assessments, home visits and a residential unit for up to 10 days. The final case example145 provided 24/7 multiagency crisis response teams, all-age Rapid Assessment Interface Discharge teams, intensive home treatment teams, access to safe zones, enhanced community support over 7 days and 72-hour crisis beds.
Generic crisis services
One report94 provided information on three generic services that contained components addressing crisis care. The first generic service was a city centre providing early intervention in crisis that took referrals from GPs and CAMHS and self-referrals for CYP aged 13–25 years with a range of mental health problems. Another generic service was for CYP aged 16–25 years experiencing distress/crisis with referrals accepted from professionals, families and friends, and self-referrals. A large variety of interventions was provided for those experiencing distress/crisis, including drop-in support with attending other services, intensive support and child care for 24–48 hours. A third generic service involved self-referral support and catering for CYP aged 16–21 years already using other services. The service provided a rapid response to those suffering from crisis, with onward referral and signposting to other agencies, with referrals also accepted from the organisation’s support workers.
Organisation of crisis services: thematic summaries
The second part of this chapter presents a series of thematic summaries for the organisation of crisis services/responses as described across the descriptive reports and the UK-only grey literature documents. For details of the methods of the narrative approach to thematic summaries see Chapter 3, Data extraction, analysis and synthesis. Four thematic summaries were developed based on the included literature: (1) recommendations for initial assessment in the emergency department, (2) the importance of providing home- or community-based crisis support, (3) places of safety and (4) general characteristics of a crisis response.
Recommendations for initial assessment in the emergency department
Several recommendations relating to initial assessment in the emergency department were evident in the literature, including:
-
national development of all-age liaison psychiatry services in accident and emergency departments3
-
assessments to be undertaken in a separate age-appropriate area of the emergency department, thereby reducing the impact of the environment on CYP’s mental health135,143,150,151
-
assessment undertaken by professionals with expertise with this client group135,150–152
-
assessment to be conducted in a non-judgemental manner and to be developmentally appropriate135
-
both a physical health and a mental health assessment to be included150,154
-
alternative locations for crisis assessments to be identified, such as crisis cafes. 143
In line with National Institute for Health and Care Excellence guidance,150 after being assessed in the emergency department, CYP (especially those who have harmed themselves) normally require admission to an inpatient paediatric or medical ward for a full physical and psychosocial assessment. 150,152–154 Sometimes admission is required because of safeguarding or social concerns. 135 However, the Royal College of Emergency Medicine disputes this practice because of the lack of evidence of its benefit. 152 It is also important that clear follow-up pathways are developed with multidisciplinary CAMHS input. 135,151,154
It is considered essential that all emergency department staff have the appropriate skills and understanding about the mental health needs of CYP,135,154 especially those who are vulnerable because of family instability and mental health stigma. 135,151 Specialist liaison professionals can be available to offer support, supervision and advice to emergency department staff,135,151,154 and where this is not available contact with local on-call mental health services has been suggested. 135 Paediatric liaison teams provide crisis assessments within acute hospital settings and this can include short stays, including multidisciplinary interventions, to avoid admission for inpatient psychiatric care. 146 However, although liaison improves links between CAMHS and emergency department staff, the commissioning and provision of these services in acute settings in some regions in the UK has been reported to be varied. 155
The importance of providing home- or community-based crisis support
It is recognised that the first port of call if a CYP needs help for a mental health crisis should be in the home or the community and that admission to hospital should be avoided if possible. 24,145,156 If CYP do need to be admitted, then this should be as close to home as possible so that local teams can maintain contact with families and carers,24,145 unless they are factors in the crisis. 24 Families are acknowledged as being able to make an important contribution to the planning and provision of care to CYP in crisis. 145,157,158
In the UK, services can follow the CYP from hospital to home, such as the tier 3.5 or tier 3 + teams,146 crisis care home treatment teams146 or intensive outreach services,159 which are designed to support early discharge from hospital by offering intensive home treatments with the goal of preventing re-admission. Alternatively, intensive home treatment is designed to help avoid admission by providing a home-based intervention. 17,146,157,160
With regard to CAMHS, a recent NHS benchmarking exercise identified that only 40% of CAMHS networks currently have community-based crisis response services. 146 There are several different models available, such as clinic based, assertive outreach, home treatment155 or intensive community treatment,21,146,155,161 which are provided by professionals with appropriate training in risk assessment,153 who receive supervision162 and adhere to best practice principles. 163
From the literature in this chapter, examples of innovations in crisis care include locating a CAMHS in an emergency department that operates 7 days per week from 8 a.m. to 11 p.m. to ensure that CYP can be seen in a timely manner by specialists,164 a CAMHS-operated telephone support service,164 ‘crisis plans’ or ‘crisis cards’ so that CYP and their families know what to do in a crisis situation164 and Saturday morning clinics for CYP on the waiting list. 164 Services also needed to ensure that an assertive approach to follow-up of those who do not attend appointments was undertaken. 146 It has been suggested that CAMHS should use their webpages to inform CYP and families of what support is available to them, including information on support available in a crisis, which should contain details of out-of-hours services. 165
Places of safety
In the UK, all people experiencing mental health disturbances (including CYP) to a degree that might be harmful to themselves or others can be moved to a ‘place of safety’ by the police. Section 135 or 136 of the Mental Health Act 1983 for England and Wales137,162 gives police the authority to act in these situations and move the person to an appropriate location.
The creation of dedicated Section 136 facilities for CYP is recommended,141,145,166 as long as this is linked with other facilities with adequate staffing. 158 These facilities should have separate entrances, have sufficient staff who are appropriately trained, have been checked through the national Disclosure and Barring Service, and have access to additional support should de-escalation or restraint be required. 158 Such facilities can be located across a variety of settings and include adolescent mental health inpatient units, hospitals, paediatric wards or any other suitable places. 158,167 An example of one such place of safety is a designated under-sixteens safe space attached to one local inpatient CAMHS unit. The safe space is staffed by experienced professionals, in a suitable environment, who can access a dedicated on-call consultant psychiatrist as required. The safe space has resulted in a dramatic reduction in the numbers of CYP being inappropriately held in police custody. 141 There are some specific suites for CYP in emergency departments,155,158,167 but these are not widespread. 155
The inappropriateness of the places of safety that are sometimes used for CYP, such as adult mental health facilities24,141,158 and police cells,24,25,159,162,168,169 has been widely reported. Police cells should be used in only very exceptional circumstances when the immediate safety of a CYP requires it. 24 In these instances, a protocol needs to be developed between relevant services to guide practice in that situation. 155
Several recommendations exist for the exceptional situations in which CYP are detained under Section 136 in a police cell:
-
an assessment should be carried out by professionals suitably qualified and experienced in working with CYP167
-
a review should be undertaken, ideally with an multiagency approach of the CYP’s care, within 7 days158
-
the detention should be reported as a ‘serious untoward incident’ for governance purposes. 25,141,158
Ideally, the police would work proactively with mental health-care professionals (HCPs) to plan how the needs of CYP presenting in mental health crises are collaboratively addressed. 20,155 Whenever CYP have been detained under Sections 135/136 of the Mental Health Act, these data should routinely be collated and reported for quality assurance and monitoring. 158
In some areas of the UK, where no specific places of safety are identified,3 it is acknowledged that there is a need for a clear pathway for those CYP detained under the Sections 135/136 of the Mental Health Act137,143 other than a police station. This pathway needs to be age appropriate and used only as a short-term measure (up to 72 hours) while a longer-term plan for that CYP is developed. 141,145,158,159 It is acknowledged that there might be a difference in what can be considered suitable in an emergency compared with longer-term care. 170 Sometimes the police do not know how to access mental health care and it has been suggested that there needs to be some form of advanced agreement about how police can access the facility or pathway. 135,141,155,162,167
General characteristics of a crisis response
Providing a timely response
It is recognised that responses to CYP in crisis should be timely so that CYP do not need to wait for help. 3,14,24,146,154,158,171 However, the independent report carried out by the Mental Health Taskforce reported that fewer than half of CYP services have a dedicated crisis team. 17 The Youth Commission for Mental Health recommended that CYP should not be turned away from hospitals or other services when at a crisis point for their mental health and that hospitals should have a crisis support team. 172 The amount of time a CYP in mental health crisis may need to wait for an assessment from specialist professionals varies greatly. 146,154,156,157,167,173–176 A general principle is that CYP should be seen quickly and easily. 176 This varies from within a few hours of initial request146 to the same day,146 but is mandated as being within 4 weeks. 174
Age-appropriate care
Whenever possible, those responsible for the care and treatment of CYP should be CAMHS specialists. In exceptional cases when a young person is admitted to an adult psychiatric ward, clinical staff should have regular access to, and make use of, a CAMHS specialist for advice and consultation. 162 The Mental Health Crisis Care Concordat sets out that the views of CYP should be sought in the setting and maintenance of quality standards for crisis services to ensure that they are age appropriate and suitable for their needs and that each child and young person should have access to an advocate. 24 However, access to appropriate and timely psychiatric liaison from specialist CAMH services is not always available, with some CYP placed inappropriately on general paediatric or adult wards. 3 The Welsh Government recommends that admitting a child/young person aged > 16 years to an adult mental health ward outside working hours in a crisis/emergency situation should be considered only after a risk assessment of the presenting concerns is carried out and admission is deemed appropriate because of risk of self to others and/or a need for a place of safety. 167
In evaluating the Mental Health Crisis Care Concordat for England, Gibson et al. 166 suggest that a CYP-focused model of crisis care is urgently needed to address the lack of crisis services for CYP, especially with regard to the local availability of appropriate inpatient care. To better support people of all ages at risk of experiencing a mental health crisis, in 2017 the Department of Health and Social Care launched a £15M scheme ‘Beyond Places of Safety’ to support services for those needing urgent and emergency mental health care, including CYP. 14 In Wales,20 recommendations include ensuring that arrangements for the holding of designated beds for CYP admitted in crises are in place and sustainable. It is also acknowledged that services also need to ensure that CYP aged 16–17 years do not fall between paediatric and adult services. 155
Providing a single point of access
A clear pathway with a single point of access is advocated. 20,177,178 Emergency departments across the UK offer a 24/7 single point of access to CYP following self-harm or a mental health crisis. 152,154–156 Access to services remains poor and the number of CYP attending emergency departments for a psychiatric condition has continued to rise. Although this mirrors the general rise in ED attendance, more CYP presenting at emergency departments receive a psychiatric diagnosis, with some struggling to access services until they reach crisis point. 179
Accessibility
Ideally, specific pathways for CYP in crisis need to be developed to avoid CYP presenting to the emergency department and/or being admitted to paediatric wards. 145 It is widely agreed that services should be located at a place suitable for and accessible to CYP, and available at a time that suits CYP14,135,145,146,156,158,160,167,172,180 to enable a swift and comprehensive assessment of the crisis issue. 3 Crisis care should include facilities to conduct risk assessments 24/7, along with practical support and interventions to reduce risk from a confident and well-trained multiagency team. 135,145,156 Suggested locations include face-to-face appointments in locations in which the CYP feels safe,146 including the use of safe zones (i.e. locations staffed by the third sector where CYP can go to receive support, advice or interventions that is away from a stressful or triggering environment),14,145,156 dedicated safe spaces within the emergency department (i.e. a quiet and welcome environment that is monitored by staff with mental health training)172 or at CYP’s homes. 14,158
Crisis and out-of-hours services should incorporate specialist advice, support, consultation by telephone and direct face-to-face assessment and management when necessary. 167 Support services that offer out-of-hours services are available in a variety of methods (e.g. face to face, telephone and online), including those appealing to CYP, such as mobile applications. 138,145,146,163,172,180,181 It is also felt that attempts need to be made to appropriately advertise the availability of such services so that CYP know about them,172 and that such platforms might also be useful in promoting health more generally. 163 Even with online and telephone support, there needs to be a process of triaging to ensure that an appropriate intervention or pathway is offered to CYP138 and that people working in these services are trained to deal with CYP in crisis. 155
Help and support can also be provided in educational settings14,145,171,173,181 or through voluntary organisations,145,181 as well as via the internet145,181 or telephone contact,145,146 and at times of the day that ensure that CYP do not need to take time off school. 172 Higher education institutions in the UK draw from a range of initiatives to support young people in crisis, including in-house support services171 and outsourced or external service provision. 14,171,173 Such provision could include a 24/7 counselling or support service,14 online self-help services14 and crisis lines for signposting to out-of-hours support,14,171 crisis telephone lines,14 counselling14 or referral and liaison with external mental health services,171,173 which includes emergency services and subsequent hospital admission171 or urgent response services. 171
Availability
Crisis services for CYP should ideally offer out-of-hours availability. 17,145,146,156,158,160,172,177,178,180,182,183 The Welsh Government recommends that health boards should prioritise the resources available in CAMHS to ensure that community intensive treatment teams or comparable services have access to sufficient CAMHS expertise in managing the demands of young people for extended hours. 167 In 2016, a recommendation of the Mental Health Taskforce was that, for CYP, NHS England should develop an equivalent model of care to the current crisis resolution and home treatment teams for adults, which should be available around the clock, with a community-based mental health response, providing intensive home treatment as an alternative to acute inpatient admission. 17 Compared with adult services, however, the small numbers of CYP presenting in crisis in a local area may mean that the cost of providing 24/7 CAMHS care would be proportionally very high. 154 The lack of a 24/7 CAMHS workforce is ameliorated to some extent by use of social care, paediatricians and adult mental health professionals, but does mean that CYP might have a wait of up to 5 days to receive definitive care planning, which is seen as unacceptable. 154
Although out-of-hours cover is provided across some CAMHS,146 there is a wide variation in service provision155 and most CAMHS routinely provide crisis services during normal office hours. 154 Although the availability of 24-hour access is welcomed, it is difficult to provide because of insufficient workforce154 and limited capacity. 167
The provision of home-based crisis care that is available 24/717,160,177 should be made available to all CYP regardless of age and ethnic backgrounds. 3,145,153,154,160,166
By 2023/24, NHS England177 states that there will be 100% coverage of 24/7 mental health crisis care provision for CYP, which combines crisis assessment, brief response and intensive home treatment functions. This follows on from NHS England’s earlier recommendation in Implementing the Five Year Forward View for Mental Health178 that Clinical Commissioning Groups should commission improved access to 24/7 crisis resolution and liaison mental health services that are appropriate for CYP. In Transforming Children and Young People’s Mental Health Provision: A Green Paper,14 it is suggested that the savings made from reducing and minimising hospital stays should be reinvested to improve local community response for CYP presenting in crisis and that there should be improved access to intensive home treatment with support from their local community team. 14
Responsive and needs led
One report179 suggests that, because access to routine CYP’s mental health services is poor, CYP struggle to access services until they reach a crisis point. It is helpful to conceptualise crises in CYP as a psychosocial response to a contextual stressor, such as a safeguarding, physical health or mental health stressor. 146 As a consequence, services that are provided to CYP in crisis should be responsive and targeted to CYP’s individual needs145,146 and at a level of intensity that is appropriate using the stepped-care approach. 145 A key characteristic of crisis provision is an assertive approach that often involves creativity to connect with CYP. 146,158 This can be achieved either through mobilising resources around the CYP in the community or by linking with a third-sector provider or an emergency department. 158 It has been recommended that the location of any intervention should be as close to home as possible, including if inpatient care is required. 24,160
Evidence based
It is acknowledged that interventions provided to CYP should be evidence based so that limited resources are used effectively and to ensure the best-possible outcomes. 3,14,142,145 It is important that training for health professionals providing crisis services should also be evidence based. 20,154
Multiagency working
Health-only responses are not likely to resolve a CYP crisis,145,154 as they are often wide-ranging in nature, resulting from problems at home or school, experience of trauma, families being under stress or family breakdown. Therefore, services need to draw on a multiagency approach,14,145,146,153,156,158,175,183 and involve health, social care, education and the third sector. 14,181 A co-ordinated response,3,20 preferably with a 24-hour community-based service available17,183 and a follow-up plan,20,145 is considered important. In Wales, it has been suggested that a country-wide triage model could allow HCPs to work with Welsh police forces and be situated in police control rooms to provide advice when CYP present in crisis. 20
Suitably qualified/experienced professionals
It is acknowledged that assessments of CYP in crisis ideally should be carried out in a timely fashion by professionals who themselves are competent in this skill. 24,146,153,154 Professionals should have appropriate training to achieve competence in this area. 145,156,167,173,175 It has also been suggested that professionals with specialist skills and knowledge in the care of CYP with mental health needs should provide training, advice and consultation to paediatric wards, emergency departments and social services145,153,167,175,184 and should develop protocols for the assessment and care of CYP in crisis. 153
Crisis planning
The development of a crisis plan is suggested as useful for CYP at risk of further episodes of mental health crisis. 135,157,171,185 Crisis plans need to be developed proactively in collaboration with CYP,135,166,171,186 their families135,153,187 and other relevant professionals,24,185 and should be available if required in the case of crisis. 135
Such a plan needs to contain information on how to recognise early warning signs of a relapse or crisis,157 who to contact153 and how to access support during crises, including out of hours,153,171,185 or to prevent admission to hospital. 157 Crisis plans should contain self-management strategies. 184
Summary
This evidence synthesis has shown that there are a number of different approaches to crisis care that all have applicability to the UK provision. These approaches include triage/assessment only, digitally mediated support approaches, and intervention approaches and models. Triage/assessment approaches include responses to CYP who present in times of crisis to emergency departments, to educational settings, to telephone triage and to out-of-hours psychiatric emergency services. Digitally mediated support approaches are facilitated through telephone and/or text-based responses or online technology. Finally, a wide variety of different intervention approaches and models have been described, including treatment that is started in the emergency department and then moved to outpatient services, inpatient care through hospitals or RTCs, home-based programmes, CAMHS, treatment involving telepsychiatry or via a community resource (e.g. mobile outreach through) and school–hospital partnerships and generic walk-in crisis services provided by voluntary organisations.
Four themes emerged from the thematic summaries of the descriptive reports and UK-only grey literature documents. These themes are recommendations for initial assessment in the emergency department, the importance of providing home- or community-based crisis support, places of safety and general characteristics of a crisis response. The first theme, with recommendations for initial assessments in an emergency department, includes assessments being undertaken in separate age-appropriate areas by skilled professionals with expertise in CYP who have received appropriate training. Guidance relating to how initial assessments are carried out in the emergency department also focuses on risk assessments and broadly follows National Institute for Health and Care Excellence guidelines. 150 The importance of follow-up pathways is emphasised.
The importance of providing home- or community-based crisis support is the focus of the second theme. When possible, crisis care should be offered as close to where CYP live as possible, therefore, either in the home or in community-based locations, recognising that families make an important contribution to the planning and provision of care. The third theme is around places of safety. This shows that places of safety need to be appropriately staffed with experienced and trained professionals, ideally in a dedicated space so that the use of adult mental health facilities and police cells can be avoided. The final theme addresses general characteristics of a crisis response. This highlights that, in general, crisis services should provide a timely response, be age appropriate, have a single point of access, be accessible and available 24/7, be responsive and needs led, involve multiagency working, be staffed by suitably qualified and experienced professionals, and involve crisis planning and risk assessment using evidence-based practice.
Chapter 5 Experiences and perceptions of crisis support
The second objective of this evidence synthesis was to explore the experiences and perceptions of CYP aged 5–25 years, their families and staff with regard to mental health crisis support. This chapter presents a thematic synthesis of qualitative data from primary research studies, wider research reports and stakeholder consultations with service providers and/or young people and their families that was part of a wider body of work. For details of the methods of the thematic synthesis, see Chapter 3, Data extraction, analysis and synthesis. Four themes were identified: (1) barriers to and facilitators of seeking and accessing appropriate support, (2) what CYP want from crisis services, (3) CYP’s and their families’ experiences of crisis services, and (4) service provision.
Barriers to and facilitators of seeking and accessing appropriate support
Six qualitative studies,70,76,97,99,100,133 qualitative data from within two wider research reports94,95 and four stakeholder consultations with service providers and/or young people as part of a wider body of work20,146,172,188 contributed to this theme, which addressed the barriers to and facilitators of seeking and accessing appropriate support. Seven subthemes were identified, which were (1) service eligibility, (2) knowing where to go when in crisis, (3) access to mental health services and professionals, (4) support from others during times of crisis, (6) external factors that influence access and (7) transitions across services.
Service eligibility
Participants in one study70 described how having diagnostic-specific eligibility criteria in place for free or reduced-cost care had prevented them previously accessing the service. Other services had a threshold, such as suicidality, before offering a service to CYP. 76 Families of CYP who had accessed a crisis helpline felt that their definition of crisis was not the same as that of the call handlers and as a result felt dismissed by the service. 76 Across the UK, it was noted that those with less severe mental health problems were not eligible for specialist CAMHS and, consequently, these CYP felt that there was nowhere to turn to other than the emergency department when they needed help. 188
Knowing where to go when in crisis
Being unsure as to what relevant services exist, where to locate them and how to access them was found to prevent CYP from getting help. 100 Some CYP had heard of mental health services but did not know what they provided or how to get in touch with them. Although services may have had a web presence, with details of a mobile psychiatric team,100 this was too vague and more information about how the service worked was wanted. The lack of direct telephone numbers made it difficult to make contact or several attempts were needed to navigate through a web of services before accessing the right one. 70,100 Friends and relatives of those who had taken their own lives commented that they had been unaware of how to manage or help people at risk of suicide before it had become an issue for them. 133 Stakeholders in the UK felt that this lack of information for family members could be one of the reasons why there was an increase in use of the emergency department when CYP were experiencing crisis. 146 Knowing of friends and/or family members who had already accessed services was also described by some interviewees as an important means of finding out what support was available. 70 Some CYP initiated initial contact via walk-in crisis services or hotlines, or through meetings that had been previously scheduled if they were already known to mental health services. 76 The lack of information for parents/carers was highlighted as a factor that potentially had an impact on the increased use of emergency departments. 146
Access to mental health services and professionals
Children and young people frequently described wanting easier access to inpatient and outpatient mental health services and specialist professionals. 94,97,146 Suggestions included more informal walk-in/drop-in services without having to have an appointment,94,97 24/7 provision,94,146 and clear and single points of access. 146 Some CYP described wanting immediate help, as they found that they had to wait too long for appointments after initial contact was made and felt that their condition deteriorated as a result. 95,100,146 One report146 explored what parents would like to happen when CYP were experiencing crisis, and responses included timely support, service cohesiveness and ease of access. Parents reported wanting to be able to access appropriate and timely support or advice at all times, including out of hours. Having a single point of access to services was noted as helpful, as opposed to having numerous different services with different means of accessing these. 146
Support from others during times of crisis
Having someone to talk to in times of crisis, whether this was a friend or family member, was seen as important. 97,100 Some CYP felt that talking to someone in confidence outside the family, such as a teacher, school counsellor, community nurse, emergency department staff, priest or GP, who could be trusted and provide a non-judgemental atmosphere, was also crucial. 97,99
However, some CYP described feelings of hopelessness and being unable to confide in others. 97,133,172 Some CYP did not want help at times when they felt suicidal, and young men in particular identified that they struggled to open up to others. 97 From the perspective of family and friends of those who had taken their own lives, people reported that the CYP had found it difficult disclosing the details of their emotional state to their GP, partly because of the short consultation time, their lack of relationship with the GP or the GP’s perceived insufficient knowledge. 133
Some families felt that one of the key facilitators that enabled them to access support was existing relationships with professionals, such as school personnel, police, parole officers, counsellors and child protection agencies. 76 Having support from significant people in their lives (family, friends, teachers, etc.) was seen as being key to accessing support for some, particularly during times of poor mental health and diminished capacity, making it difficult for individuals to actively seek help on their own behalf. 70,100 Parents, and other family members, in particular, were important, as they could provide practical help and accompany CYP to their appointments. Parents were also able to provide information, as well as signpost to appropriate services and community resources. 70
External factors that influence access
The external factors that influenced a child or young person’s and/or their parents’ ability to access crisis services included financial concerns and difficulties with transportation. Financial concerns were evident in US studies for those who were not covered by insurance or who had poor financial resources. 70,76
It was reported by CYP that transportation to the crisis service in some instances was provided by the police, other service providers, secure transport companies and family members or significant people in their lives,70,76 and in other cases CYP walked or took public transport. 70 For some, not having access to transportation was considered a barrier70,76 and parents with a child displaying challenging behaviour who did not have their own transport described avoiding public transport because of the inherent difficulties with it. 76
Transitions across services
In a study70 that looked at uninsured young adults, other social service organisations, such as domestic violence counsellors, homeless services, criminal justice and substance use services, facilitated access to help by providing referrals or transport. However, it was often reported that there was a lack of continuity in mental health service provision following a young person’s discharge from the criminal justice system where mental health care had been provided. 70 Another study76 described lack of communication and collaboration between child welfare, school systems and mental health providers as a common barrier exerting an effect on service quality. Findings from interviews with young people told of a young person being ‘shuttled around groups’ and ultimately taking their own life. 172 In other studies,146 youths stated that they did not want to be ‘passed around’ services when they are in crisis. Where specific crisis intervention teams had been created, there was an improvement in their willingness to collaborate with specialist CAMHS, accident and emergency services, and paediatric services, and this resulted in noticeable differences. 20 Where investment had been made into specific crisis services (e.g. emergency liaison, crisis outreach), the collaboration between CAMHS, emergency department and crisis care was improved and, therefore, more accessible. 20,146 Parents viewed the sharing of information between agencies and sectors as important, enabling all involved professionals to have access to the same information about young people and their families. This helped avoid having to repeatedly keep providing the same information. 146
What children and young people want from crisis services
Two primary studies,97,99,100 qualitative data from one wider research report94 and two reports of consultations with stakeholder service providers and/or young people as part of a wider body of work146,164 contributed to this theme, which explored what young people want from crisis services. Four subthemes were identified: (1) importance of lived experience and peer support, (2) services specifically for young people, (3) attributes of health professionals and (4) need for different forms of support and pathways to services.
Importance of lived experience and peer support
Some young people identified the importance of peers, who have experienced mental health difficulties in the past, working alongside HCPs and counsellors in any service. Moreover, being able to meet up and share with others who had had similar experiences was crucial. 97 Peer support in schools and youth work settings was also seen as important, along with more training for teachers in mental health issues so that teachers could become more aware of how best to support young people when in mental health crisis. 94
Services specifically for young people
Many CYP felt that there should be services catering specifically to them. 94,97,146 Specific types of crisis support were also needed, and older youths felt that it would be helpful if there were services targeted specifically at 16- to 25-year-olds that are ‘young people-friendly’ in design and approach. 94 In one area, there was a request for services for the under-fourteens because there was no crisis care for this group. 146
Attributes of health professionals
Parents wanted health professionals to understand that a crisis for a young person was also a crisis for parents. 146 CYP felt that when they are in crisis they would like a choice of workers so that they can build rapport with someone. 94 CYP wanted those caring for them to be sensitive94 and compassionate to their needs,146 to listen to what they say146 and to exhibit transparency. 146 CYP also wanted to be seen as a ‘real person’ and to feel understood. 146 Skilled support was also highlighted as being important, specifically the ability to ask the right questions, to navigate the system and to be clear on next steps. 146 Many CYP wanted drop-in crisis services to be staffed by youth workers with knowledge of mental health. 94 Others had concerns that staff within other crisis services were not sufficiently trained to help those with mental health issues, especially in the emergency department. 146,164 A potential solution suggested by CYP with experience of crisis services was for them to become involved in staff training94,146 so that a more sensitive service could be provided. 94
Need for different forms of support and pathways to services
The need for different forms of support and pathways to services was identified by CYP, including through telephone,94,97,100,146 text99,146 and e-mail. 100 Those who preferred to use the telephone to make contact said that they would want to have access to a direct number, as being passed back and forth was found to be frustrating. 100 Others wished for an out-of-hours telephone helpline staffed by skilled counsellors who also knew the available local services to signpost people to. 94 Those CYP who wanted to remain anonymous felt that being able to access staff this way would be helpful. 97 Texting services were seen as positive, and CYP described what they liked about them, which included immediate support, convenience, comfort, anonymity, having control, low cost, a distraction from rumination and negative thinking, and having the ability to store and refer back to the messages at a later date. 99
Parents felt that the telephone counselling services that their children had used did not provide timely services and that the duration of crisis counselling via a hotline was found not to be long enough. 133 There were some occasions when there was a mismatch between what a telephone hotline was offering and what parents wanted. 76 Hotline services worked well when parents could transport their children to the mental health centre or other location for assessment. However, hotline services were not helpful in resolving an immediate crisis with a child’s violent or dangerous behaviour and parents were often told to phone the police. 76 On other occasions, some families reported that hotline responders told them to ‘call back during business hours’. 76
Children and young people’s, and their families’, experiences of crisis services
Five primary studies70,76,97,100,133 and qualitative data from within seven wider reports20,94,95,146,153,172,188 contributed to this theme, which addressed young people’s and their families’ experiences of crisis services. Four subthemes were identified: (1) lack of support before crisis is reached; (2) assessment, management and follow-up in the emergency department; (3) processes leading to inpatient admission and experience of inpatient care; and (4) views of CAMHS and crisis teams.
Lack of support before crisis is reached
A general lack of support before crisis is reached was described by CYP. 94,95,133,172 This included being moved around services,95,172 not being taken seriously by GPs who often put CYP concerns down to age or hormones95,172 and HCPs being dismissive of the urgency of the situation and prioritising other issues. 172 Long wait times for mental health appointments after making initial contact with GPs70,95 and a lack of information for parents/carers on where to go if their child was in mental health crisis146 have also been reported by CYP and their families. In this context, the emergency department often became the default option for CYP when faced with a mental health crisis, particularly in instances of self-harm and/or overdose. 20,95,188 Calls have been made for crisis services to work with young people who feel that they are at risk of falling into crisis, helping them to develop strategies and access resources at an earlier point. 94
Stakeholders in the UK acknowledged that CYP often experience difficulties in accessing support from specialist CAMHS and/or primary care. 20,76,188 In some cases, it is because CYP are not considered eligible188 or because there are gaps in the availability or accessibility of appropriate care,76,188 in particular out of hours or crisis responses. 188
Assessment, management and follow-up in the emergency department
Family and friends of those who had taken their own lives felt that there had been a lack of appropriate hospital management of people with suicidal behaviour, with care often involving the patient just being given medication. 133 Parents and CYP reported that there were often long wait times in the emergency department, including during the triage process, often resulting in delays in receiving specialist mental health support. 76,95,100,146 Other negative experiences that CYP reported with regard to emergency department visits included the lack of suitability of the environment (specifically the noise, brightness and large numbers of people),146 the lack of mental health professionals 24/7,146 no privacy146 and poor attitudes of staff. 94,97,146 CYP, their friends and their families, and other stakeholders in the UK frequently raised concerns about the level of follow-up care after discharge from emergency department following a crisis. 20,95,97,133 However, some CYP described that staff were supportive and understanding in the emergency department. 97,153
Processes leading to inpatient admission and experience of inpatient care
The processes leading to admission when a child/young person was in mental health crisis were found to be overly complicated, lengthy and frustrating for both the child/young person themselves and their families. 70 This process may have occurred in community mental health centres, criminal justice locations or in emergency departments. The apparent lengthy wait appeared to be linked to the need for agencies to share information and for practitioners to be able to access previous medical records. The experience of receiving care, however, was reported by CYP as being positive,153 including CYP finding health-care practitioners to be positive and reassuring, and treatment relating to self-harming behaviour and the prescribing of medication to be effective. However, other CYP felt that they were being treated like a patient rather than a person. 94
Views of CAMHS and crisis teams
There were mixed views from CYP about CAMHS, with some finding them exceptional95 after an initial wait and others not pleased with their service. 133 The use of crisis plans as a contingency agreement was not common, even though it was felt that these plans were important. 146 Where crisis plans existed, they were insufficiently detailed, suggesting such interventions as calling the case manager, crisis hotline or police. 76
A further area in which views were expressed was in relation to the naming of ‘crisis services’. Some CYP reported that the term ‘crisis’ may deter some CYP from receiving help, as they felt that it assumes that they were already on a pathway to crisis, as opposed to actually being in crisis. 94
Service provision
Three primary studies,76,90,91 qualitative data from within one wider research report94 and four reports of consultations with stakeholders, service providers and/or young people as part of a wider body work20,96,141,146 contributed to this theme, which addressed young people’s and their families’ experiences of crisis services. Five subthemes were identified: (1) inappropriate admissions to adult wards, (2) availability of a crisis team outside traditional office hours, (3) geographical boundary issues and variable service provision across different regions, (4) CAMHS and (5) police involvement and places of safety.
Inappropriate admissions to adult wards
When experiencing crisis, some CYP were sometimes admitted to adult or paediatric wards. 20,94,146 Front-line crisis mental health practitioners noted that, although considered inappropriate,20,146 when CYP needed admission, successful adaptations could sometimes be made for accommodation on adult mental health wards. Service providers from the UK in the report by Garcia et al. 94 described an example of a third-sector organisation that worked with adult mental health services to raise awareness of what the third sector can offer, and to connect with all young persons on adult wards during their admission. 94
Availability of a crisis team outside traditional office hours
It was acknowledged that demand also presents during evenings and weekends, and at these times crises could be exacerbated because of insufficient services. 20 The lack of availability of a crisis team and/or specialist CAMHS outside traditional office hours was frequently reported and, as a consequence, the emergency department was often the first port of call for CYP experiencing a crisis. 20,96,146,164 However, when CAMHS experts were available, this was seen by both service providers and CYP to be helpful. 96 The tension for commissioners was described as providing accessibility where demand dictates, without being wasteful with underused resources. 20 Young people often reported that they had to wait a long time to be seen out of hours. 146
Geographical boundary issues and variable service provision across different regions
Other barriers identified by both stakeholders and CYP across the UK were about accessing a service when the CYP originated from a different locality from where the service was sited,20,94 or where the CYP was 16–17 years and the age appropriateness of a service was unclear. 146 Although some areas had crisis services for CYP, availability in different areas was variable, with some services operating within office hours only. 146 Some CYP were admitted into hospital as a strategy to avoid breaching emergency department waiting times targets. 146 Referral onto statutory services by third-sector organisations was difficult when the child/young person lived outside the district and so involvement of a GP was sometimes necessary to facilitate this process. 94 Different processes to manage safeguarding were described, with some processes involving liaison nurses checking the reason for the CYP’s attendance at emergency departments. 146
CAMHS
Stakeholders in the UK presented a variety of views regarding CAMHS provision. It was felt that there needed to be fully supported community mental health provision for CYP to reduce the need for inpatient care and to reduce LOS. 20,141 It was also felt that developing community-based resources,141,146 such as assertive outreach,20 and early intervention were critical to reduce the need for admission into crisis beds. 20 Emergency department clinical leads and emergency department mental health departmental leads from across the UK reported that CYP did not have access to CAMHS in the emergency department and the only way that a child/young person could be assessed by CAMHS was for them to be admitted. 96
Police involvement and places of safety
Analysis of memos from police encounters with CYP in mental health crisis, and interviews with caregivers and siblings, revealed that the main reason for contact was to de-escalate situations such as self-harming, harming others and aggression. In such cases, the child/young person would be escorted to the emergency department for further mental health assessment. 90,91 Families of CYP admitted to a mental health ward stated that police officers had been involved as part of the crisis response to homes or schools, although families did not like the use of police in these situations. 76
InWales, UK police representatives reported that, despite an increase in the frequency of police having to manage mental health crises with CYP, there was optimism that increased resources would become available following government investment and through the introduction of the Mental Health Crisis Care Concordat. 20 The Mental Health Crisis Care Concordat is a national agreement setting out how services and agencies will work together to support people in crisis. This approach helps to address police concerns about their lack of suitable resources and appropriate training to be able to effectively help CYP in mental health crises. 20 One suggestion of how this could be applied is the introduction of a mental health practitioner in police control rooms to advise officers when they are faced with a CYP in crisis. 20
The police also have a role to play when CYP need a place of safety, and staff have raised concerns about the lack of appropriate facilities, suggesting that alternatives are needed. 141,146 Staff were aware that in some instances CYP were reviewed in police cells, although the police did seek alternatives, such as in residential units or emergency departments, where available. 141 In one area, it was reported that 41 CYP had been detained in police cells over the previous year. 141 Although this is ordinarily regarded as an unsuitable environment, there is an acknowledgement that there is a difference between what a suitable environment is for CYP in an emergency situation and what a suitable environment is in the longer-term provision. 141
Confidence in the evidence
The qualitative findings were assessed for confidence using the CERQual approach and 27 synthesis summary statements were generated, which are presented in Table 12. Of the 27 synthesis summary statements, only two were judged as having a high degree of confidence. The remaining statements were judged as having a moderate (n = 15), low (n = 3) or very low (n = 7) degree of confidence. Report Supplementary Material 16 includes the detail of how the CERQual statements were generated, along with the details derived from ungraded summary statements obtained via reports of consultations with stakeholders, service providers and/or young people as part of a wider body of work.
| Summary of evidence synthesis finding | Studies contributing to evidence synthesis finding | CERQual confidence |
|---|---|---|
|
Synthesis 1: barriers to and facilitators of seeking and accessing appropriate support
Service eligibility |
||
| Various thresholds of eligibility exist making access to specialist services difficult | Studies 6 and 8; consultations with stakeholders188 | M |
| Knowing where to go when in crisis | ||
| Many CYP and their friends and relatives state that they do not know where to turn when they are experiencing mental health crises | Studies 1, 7 and 8 | M |
| Access to mental health services and professionals | ||
| CYP want easier and more immediate access to specialist services | Studies 1, 2, 4 and 5; consultations with CYP146 | M |
| Support from others during times of crisis | ||
| Some CYP want someone to talk to, whereas others find it too difficult to talk at the time of a crisis | Studies 1–3 and 6–8; consultations with CYP172 | M |
| Where CYP have support from significant people in their lives, this assists them to access crisis services | Studies 1, 6 and 8 | M |
| External factors that influence access | ||
| Some CYP feel that their ability to access crisis services is affected by external factors, such as finance and transport | Studies 6 and 8 | M |
| Transitions across services | ||
| Clear pathways between different services are seen as helpful, but a lack of communication and collaboration is often described, with CYP often slipping through the gaps | Studies 6 and 8; consultations with stakeholders and CYP20,146,172 | L |
| Synthesis 2: what CYP want from crisis services | ||
| Importance of lived experience and peer support | ||
| Some CYP feel that peer support and involving those with lived experience of mental health crisis within services is important | Studies 2 and 4 | M |
| Services specifically for young people | ||
| Some CYP feel that services should cater specifically for them and be targeted at specific age groups | Studies 2 and 4; consultations with CYP146 | M |
| Attributes of health professionals | ||
| CYP would like the health professionals they engage with during times of crisis to be understanding, sensitive, compassionate, have good listening skills and to be skilled and knowledgeable in mental health issues | Study 4 and consultations with CYP146 | VL |
| Need for different forms of support and pathways to services | ||
| The need for different forms of support and pathways to services is identified by CYP, including through telephone, text and e-mail | Studies 1–4; consultations with CYP146 | H |
| Access to telephone crisis support is preferred via a direct line, with out-of-hours availability and staffed by trained counsellors | Studies 1, 2 and 4 | H |
| CYP report that texting provides immediate support and anonymity, and CYP like having the ability to store and refer back to the messages at a later date | Study 3 | M |
| Parents report that telephone counselling services are not always seen as providing timely or appropriate advice | Studies 6 and 7 | M |
| Synthesis 3: children’s and young people’s, and their families’, experiences of crisis services Lack of support before crisis is reached | ||
| CYP feel that there is a general lack of support before crisis is reached | Studies 4, 5, 7 and 8; consultations with CYP172 | M |
| Long wait times for specialist services and a lack of information result in the ED being the default option when CYP are in mental health crisis | Studies 5 and 8; consultations with stakeholders and CYP20,188 | VL |
| Stakeholders acknowledge that CYP often have difficulties accessing support from specialist CAMHS and/or primary care for mental health problems before crisis is reached | Study 6; consultations with stakeholders and CYP20,188 | VL |
| Assessment, management and follow-up in the ED | ||
| A number of concerns have been raised by CYP and their families, and stakeholders, with regard to the assessment, management and level of follow-up care of CYP who present in crisis to an ED | Studies 1, 2, 5 and 7; consultations with stakeholders and CYP20,146,153 | M |
| Some CYP find the noisy and busy environment of ED unhelpful with lack of privacy and poor staff attitudes adding to the unsuitability | Studies 2 and 4; consultations with CYP146 | M |
| Processes leading to inpatient admission and experience of inpatient care | ||
| The processes leading to admission when a CYP is in crisis are described as being lengthy, overcomplicated and frustrating, and there are mixed views from CYP regarding their experiences of inpatient care | Studies 4 and 8; consultations with CYP153 | M |
| Views of CAMHS and crisis teams | ||
| There are mixed views from CYP about CAMHS and crisis services | Studies 4, 5 and 7 | M |
| CYP feel that crisis plans lack sufficient detail | Study 6 | VL |
|
Synthesis 4: service provision
Inappropriate admissions to adult wards |
||
| Where CYP have been inappropriately admitted to adult or paediatric wards, service providers feel that sometimes adaptations could be made | Study 4; consultations with service providers20,146 | VL |
| Stakeholders and service providers in the UK express a number of concerns with regard to inadequate crisis care outside of traditional office hours, but when available this is seen as helpful | Studies 4 and 11; consultations with stakeholders and providers20,146,164 | L |
| Geographical boundary issues and variable service provision across different regions | ||
| Stakeholders and service providers in the UK express a number of concerns with regard to variable service provision in terms of location and age entry criteria | Study 4; consultations with stakeholders and service providers20,146 | VL |
| CAMHS | ||
| Stakeholders feel that the need for crisis beds could be reduced by ensuring adequate community resources, such as assertive outreach and early intervention services; however, admission is required from ED for a CYP to have a CAMHS assessment | Study 11; consultations with stakeholders20,96,141,146 | VL |
| Police involvement and places of safety | ||
| Although some families report that they do not like police involvement, they find that it helps to de-escalate situations | Studies 9 and 10 | L |
Summary
A thematic synthesis of the qualitative data identified four themes with regard to the experiences of crisis support from the perspective of CYP and their families, stakeholders and service providers (see Table 12). These themes were (1) barriers to and facilitators of seeking and accessing appropriate support, (2) what CYP want from crisis services, (3) CYP’s and families’ experiences of crisis services and (4) service provision.
The first theme revealed a number of barriers to and facilitators of seeking and accessing appropriate support. One of the barriers identified is that various thresholds of eligibility exist, making access to specialist services difficult (moderate CERQual rating). Another barrier is that many CYP and their friends and relatives state that they do not know where to turn when they are experiencing mental health crises (moderate CERQual rating). Several external factors influence access, and some CYP feel that their ability to access crisis services is affected by finance and transport (moderate CERQual rating). Transitions across services, in particular clear pathways between different services, are seen as helpful, but a lack of communication and collaboration is often described, with CYP often slipping through the gaps (low CERQual rating). CYP say that they want easier and more immediate access to mental health services and mental health professionals (moderate CERQual rating). Support from others during times of crisis is identified as a facilitator; however, although some CYP want someone to speak to, other CYP find it too difficult to talk at the time of a crisis (moderate CERQual rating). CYP are assisted to access crisis services when have support from significant people in their lives (moderate CERQual rating).
The second theme explored what CYP want from crisis services. Some CYP feel that peer support and involving those with lived experience of mental health crisis within services is important (moderate CERQual rating). In addition, CYP feel that services should cater specifically for them and be targeted at specific age groups (moderate CERQual rating). Others describe the attributes that they would like the health professionals who they engage with during times of crisis to have, which include being understanding, sensitive, compassionate, having good listening skills and being skilled and knowledgeable in mental health issues (very low CERQual rating). The need for different forms of support and pathways to services is identified by CYP, including through telephone, text and e-mail (high CERQual rating). Access to crisis support via telephone is preferred via a direct line, with out-of-hours availability and staffing from trained counsellors (high CERQual rating). However, parents report that telephone counselling services are not always seen as providing timely or appropriate advice (moderate CERQual rating). CYP report that texting provides immediate support and anonymity, and they like having the ability to store and refer back to the messages at a later date (moderate CERQual rating).
Children and young people’s, and their families’, experiences of crisis services was the focus of the third theme. CYP feel that there is a general lack of support before crisis is reached (moderate CERQual rating). Stakeholders acknowledge that CYP often experience difficulties in accessing support from specialist CAMHS and/or primary care for mental health problems before a crisis is reached. (very low CERQual rating). Long wait times for specialist services and a lack of information result in the emergency department being the default option when CYP are in mental health crisis (very low CERQual rating). A number of concerns are raised by CYP and their families and stakeholders with regard to the assessment, management and level of follow-up care of those CYP who present in crisis to an emergency department (moderate CERQual rating). Some CYP find the noisy and busy environment of the emergency department unhelpful, with a lack of privacy and poor staff attitudes adding to its unsuitability (moderate CERQual rating). The processes leading to admission when a child or young person is in crisis are described as being lengthy, overcomplicated and frustrating, and there are mixed views from CYP regarding their experiences of inpatient care (moderate CERQual rating). There are also mixed views from CYP about CAMHS and crisis services (moderate CERQual rating) and some CYP feel that crisis plans lack sufficient detail (very low CERQual rating).
The fourth theme was concerned with service provision. When CYP have been inappropriately admitted to adult or paediatric wards, service providers feel that sometimes adaptations could be made (very low CERQual rating). Stakeholders and service providers in the UK express a number of concerns with regard to inadequate crisis care outside traditional office hours, but when available this is seen as helpful (low CERQual rating). Geographical boundary issues and variable service provision across different age groups and across different regions are concerns expressed by stakeholders and service providers in the UK (very low CERQual rating). Stakeholders feel that the need for crisis beds could be reduced by ensuring adequate community resources, such as assertive outreach and early intervention services; however, admission is required from emergency department for CYP to have CAMHS assessments (very low CERQual rating). With regard to police involvement, although some families report that they do not like police involvement, some families find that police involvement helps to de-escalate situations (low CERQual rating). Service providers have raised concerns regarding the lack of appropriate facilities in police cells as places of safety and feel that alternatives are needed (ungraded as there is no primary research).
Chapter 6 Effectiveness of intervention approaches or models of mental health crisis support
The third objective of this study was to determine the effectiveness of current models of mental health crisis support for CYP. We have used this phrase (mental health crisis support) to encapsulate all intervention approaches or models. This chapter presents the analysis of the data from quantitative research studies that explored the effectiveness of the following intervention approaches or models: crisis services/interventions initiated within the emergency department (five studies across seven reports32,57,82–85,96), home-or community-based programmes (three studies across six reports64,78–81,98), inpatient care (two studies72,87), crisis programmes within RTCs (one study across two reports58,59), outpatient mental health programmes (three studies across four reports34,66,86,88), mobile crisis services (two studies62,68), telepsychiatry (two studies74,92), implementing a dedicated mental health team in the emergency department (two studies65,75), assessment-only approaches within the emergency department (three studies67,89,132) and assessment approaches within educational settings (two studies across four reports60,69,73,77). As there was too much heterogeneity across the studies with regard to the interventions, a meta-analysis was not performed and all findings are, therefore, presented as a series of thematic summaries.
The outcome data from the RCTs and observational studies were assessed for confidence using the GRADE approach. Owing to heterogeneity of the different interventions within similar settings, outcome data were available for results that arose from single studies only and guidance was followed on undertaking the GRADE for data of this type. 189 Report Supplementary Material 17 includes the detail of how the GRADE evidence profiles were generated. The RCTs were all downgraded from a rating of high to moderate and the observational studies from a rating of low to very low. Table 13 presents an overall summary of findings and describes the effectiveness of current models of mental health crisis support across the different settings.
| Outcome | Findings | Study | Certainty of the evidence (GRADE) |
|---|---|---|---|
| Effectiveness of crisis services/interventions initiated within the ED | |||
| Symptoms of depression | ↓ (two studies) | Asarnow et al.57 | Moderatea |
| Rotheram-Borus et al.82,83 | Very lowb | ||
| Behaviour | – (one study) | Asarnow et al.57 | Moderatea |
| Hospitalisation rates | ↓ (two studies) | Wharff et al.32 | Very lowb |
| Wharff et al.84 | Very lowb | ||
| Repeat ED visits post discharge | – (one study) | Wharff et al.32 | Very lowb |
| Family functioning | ↑ (one study) | Asarnow et al.57 | Moderatea |
| Family empowerment | ↑ (one study) | Wharff et al.84 | Very lowb |
| Family adaptability | – (one study) | Rotheram-Borus et al.82,83 | Very lowb |
| Family cohesion | – (one study) | Rotheram-Borus et al.82,83 | Very lowb |
| Linkage to outpatient services | ↑ (one study) | Asarnow et al.57 | Moderatea |
| Number of outpatient visits attended | ↑ (two studies) | Asarnow et al.57 | Moderatea |
| Rotheram-Borus et al.82,83 | Moderatea | ||
| Attend for any outpatient treatment | ↑ (one study) | Rotheram-Borus et al.82,83 | Very lowb |
| Complete outpatient treatment | ↑ (one study) | Rotheram-Borus et al.82,83 | Very lowb |
| Referral to intensive outpatient care | ↑ (one study) | Wharff et al.32 | Very lowb |
| Number of completed suicides and suicide attempts | – (two studies) | Asarnow et al.57 | Moderatea |
| Wharff et al.32 | Very lowb | ||
| Impulsivity | – (one study) | Rotheram-Borus et al.82,83 | Very lowb |
| Self-esteem | – (one study) | Rotheram-Borus et al.82,83 | Very lowb |
| Suicidality | ↓ (one study) | Rotheram-Borus et al.82,83 | Very lowb |
| – (two studies) | Wharff et al.84 | Moderatec | |
| Asarnow et al.57 | Moderatea | ||
| Client satisfaction | ↑ (one study) | Wharff et al. 201984 | Moderatec |
| Health-care staff satisfaction with mental health crisis services/programmes | Mixed responses (two studies) | Dion et al.85 | N/A |
| RCEM 201896 | N/A | ||
| Home- or community-based programmes | |||
| Symptoms of depression | ↓ (one study) | Huey et al.78 | Moderatec |
| Psychiatric symptoms | ↓ (two studies) | Muskens et al.98 | N/A |
| Henggeler et al.64,79 | Moderatec | ||
| Behaviour | ↓ (one study) | Evans et al. 200361 | Moderatec |
| – (one study) | Henggeler et al.64,79 | Moderatec | |
| Psychosocial functioning | – (two studies) | Evans et al.61 | Moderatec |
| Henggeler et al.64,79 | Moderatec | ||
| Hospitalisation rates | ↓ (two studies) | Henggeler et al.64,79 | Moderatec |
| Schoenwald et al.80 | Moderatec | ||
| Cost-effectiveness | ↑ (one study) | Sheidow et al.81 | Moderatec |
| Remain in community post treatment | ↑ (two studies) | Evans et al.61 | Moderatec |
| Schoenwald et al.80 | Moderatec | ||
| Family adaptability | ↑ (two studies) | Henggeler et al.64 | Moderatec |
| Evans et al.61 | Moderatec | ||
| Family cohesion (youth report) | – (two studies) | Henggeler et al.64 | Moderatec |
| Evans et al.61 | Moderatec | ||
| Family cohesion (parental report) | ↑ (one study) | Henggeler et al.64 | Moderatec |
| Family structure | ↑ (one study) | Henggeler et al.64 | Moderatec |
| Number of completed suicides and suicide attempts | ↓ (one study) | Huey et al.78 | Moderatec |
| Self-esteem | – (two studies) | Evans et al.5 | Moderatec |
| Henggeler et al.64,79 | Moderatec | ||
| Self-concept | ↑ (one study) | Evans et al.61 | Moderatec |
| Client satisfaction | ↑ (one study) | Henggeler et al.64 | Moderatec |
| Inpatient care | |||
| Psychiatric symptoms | ↓ (one study) | Greenham and Bisnaire87 | Very lowb |
| Psychosocial functioning | ↑ (one study) | Greenham and Bisnaire87 | Very lowb |
| Costs | ↓ (one study) | Rogers et al.72 | Very lowb |
| Suicidality | ↓ (one study) | Greenham and Bisnaire87 | Very lowb |
| LOS | ↓ (one study) | Rogers et al72 | Very lowb |
| Repeat ED visits post discharge | – (one study) | Rogers et al.72 | Very lowb |
| Crisis programmes within RTCs | |||
| Costs | ↓ (one study) | Baker and Dale58 | N/A |
| LOS | ↓ (one study) | Baker et al.59 | N/A |
| Outpatient mental health programmes | |||
| Psychosocial functioning | – (one study) | Greenfield et al.93 | Very lowb |
| Hospitalisation rates | ↓ (one study) | Greenfield et al.93 | Very lowb |
| Cost-effectiveness | ↑ (one study) | Latimer et al.93 | Very lowb |
| Repeat ED visits post discharge | – (three studies) | Greenfield et al.34 | Very lowb |
| Greenfield et al.93 | Very lowb | ||
| Maslow et al.66 | Very lowb | ||
| LOS in ED | – (one study) | Greenfield et al.93 | Very lowb |
| Post-discharge use of services/resources | – (one study) | Greenfield et al.93 | Very lowb |
| Access to additional resources | ↑ (one study) | Greenfield et al.93 | Very lowb |
| Number of suicide attempts | – (one study) | Greenfield et al.93 | Very lowb |
| Suicidality | – (one study) | Greenfield et al.93 | Very lowb |
| Parental satisfaction | ↑ (one study) | Lee and Korczak88 | N/A |
| Mobile crisis services | |||
| Hospitalisation rates | – (one study) | Martin68 | Very lowb |
| Repeat ED visits post discharge | ↓ (one study) | Fendrich et al.62 | Very lowb |
| Telepsychiatry | |||
| Hospitalisation rates | – (one study) | Roberts et al.92 | Very lowb |
| ↓ (one study) | Thomas et al.74 | Very lowb | |
| Costs | ↓ (one study) | Thomas et al.74 | Very lowb |
| Referral pathways | – (one study) | Roberts et al.92 | Very lowb |
| Repeat ED visits post discharge | – (one study) | Thomas et al.74 | Very lowb |
| LOS | ↓ (two studies) | Roberts et al.92 | Very lowb |
| Thomas et al.74 | Very lowb | ||
| Parental satisfaction | High levels | Roberts et al.92 | N/A |
| Thomas et al.74 | Very lowb | ||
| Staff satisfaction | ↑ (one study) | Thomas et al.74 | Very lowb |
| Implementation of a dedicated mental health team in the ED | |||
| Hospitalisation rates | ↓ (two studies) | Uspal et al.75 | Very lowb |
| Holder et al.65 | Very lowb | ||
| LOS | ↓ (two studies) | Uspal et al.75 | Very lowb |
| Holder et al.65 | Very lowb | ||
| Returning to home environment | ↑ (one study) | Holder et al. 65 | Very lowb |
| Repeat ED visits post discharge | – (one study) | Uspal et al.75 | N/A |
| Costs | – (one study) | Holder et al.65 | Very lowb |
| Health-care staff satisfaction with mental health crisis services/programmes | ↑ (one study) | Uspal et al.75 | Very lowb |
| Assessment approach within the ED | |||
| Repeat ED visits post discharge | – (one study) | Lee et al.89 | Very lowb |
| LOS | ↓ (one study) | Mahajan et al.67 | Very lowb |
| – (two studies) | Lee et al.89 | Very lowb | |
| Nagarsekar et al.132 | Very lowb | ||
| Costs | ↓ (one study) | Mahajan et al.67 | Very lowb |
| Client satisfaction | – (one study) | Nagarsekar et al.132 | Very lowb |
| Triggering recommendations for further community services | Successful | Lee et al.89 | N/A |
| Assessment approaches within educational settings | |||
| Number of completed suicides and suicide attempts | None reported | Michael et al.69 | N/A |
| Sale et al.73 | N/A | ||
| Capps et al.60 | N/A | ||
| Referral pathways | Variety of referral destinations | Michael et al.69 | N/A |
| Sale et al.73 | N/A | ||
| Capps et al.60 | N/A | ||
| Acute levels of care avoided | Walter et al.77 | N/A | |
| Staff satisfaction | High | Walter et al.77 | N/A |
Crisis services/interventions initiated within the emergency department
Symptoms of depression
Two experimental studies (across three reports57,82,83) investigated symptoms of depression. Adolescents in a specialised emergency department programme conducted by Rotherham-Borus et al. 82,83 reported significantly lower levels of depression when assessed after the emergency room intervention (post-discharge assessment) than those who received standard care (mean Beck Depression Inventory score: intervention 12.6 ± 11.0 vs. control 15.9 ± 10.0; p < 0.01). For the emergency department-based FISP intervention conducted by Asarnow et al. ,57 there were significant improvements in levels of depression from baseline to follow-up post intervention [total CES-D score p < 0.05; odds ratio (OR) for severe depression 0.24, 95% CI 0.14 to 0.41].
Behaviour
One experimental study57 investigated behaviour. The study by Asarnow et al. 57 found that the FISP intervention did not lead to significant improvements in internalising and externalising behaviour (CBCL total problems in clinical range OR 0.52, 95% CI 0.30 to 0.90; p = 0.02).
Hospitalisation rates
Two experimental studies32,84 explored hospitalisation rates. Wharff et al. 32 conducted a pilot study of a FBCI for suicidal adolescents and their families and reported that none of the patients for whom data were collected at the 1-day follow-up required inpatient hospitalisation. At the 3-month follow-up, 12.7% of patients reported that they had been hospitalised since the initial emergency room visit, and of these patients only two (3.6%) were hospitalised because of suicidal complaints. Adolescents in the pilot cohort were significantly less likely to be hospitalised than those in the comparison group (36% vs. 5%; p < 0.0001). The same intervention was then tested by Wharff et al. 84 in a RCT, and adolescents who had received FBCI were significantly less likely to be hospitalised than those who received treatment as usual (TAU) (FBCI 38% vs. TAU 68%) (OR 3.4, 95% CI 1.7 to 6.8; p < 0.005).
Discharge destination
One experimental study that explored a FBCI, which was conducted by Wharff et al. ,32 looked at discharge destination. Wharff et al. 32 found that CYP in FBCI were significantly more likely to be referred to intensive outpatient than those in the TAU comparison group (FBCI 21% vs. TAU 5.3%; p < 0.001). 32
Emergency visits post discharge
An experimental study conducted by Wharff et al. 32 looked at the number of emergency visits post discharge. 32 No significant differences were reported in CYP needing another crisis evaluation since their initial visit to the emergency department between CYP receiving FBCI (13%) and CYP receiving TAU (4%) (p = 0.07).
Family functioning/empowerment
Three experimental studies (across four reports57,82–84) explored family functioning/empowerment. Wharff et al. 84 investigated the effectiveness of FBCI for suicidal adolescents and their families. Significantly higher ratings of family empowerment were reported post test by parents in the FBCI group than parents who received TAU (mean change in Family Empowerment Scale score: intervention group 2.7 ± 3.8, control group 1.0 ± 3; p < 0.005), which were maintained at the 1-month follow-up period (p < 0.001). Another study conducted by Rotherham-Borus et al. 82,83 reported that there were no significant differences in levels of family adaptability (p > 0.05) or family cohesion (p > 0.05) between receiving specialised emergency department care or standardised emergency department care at initial follow-up83 or 18 months later. 82 For an emergency department-based FISP intervention conducted by Asarnow et al. ,57 there were significant improvements in levels of family functioning from baseline to follow-up post intervention (p < 0.001).
Completed suicide and suicide attempts
Two experimental studies looked at the number of completed suicides and suicide attempts. 32,57 In a study conducted by Asarnow et al. ,57 for those receiving the FISP within an emergency department, it was reported that this did not lead to significant decreases in suicide attempts [intervention group n = 4 (6.4%), control group n = 5 (6.5%), OR 1.0, 95% CI 0.3 to 3.8]. Wharff et al. 32 reported on the implementation of a specialised family-based intervention conducted within the emergency department (FBCI) and found no incidence of attempted or completed suicide within 3 months of the intervention.
Suicidality
Three studies (across four reports57,82–84) explored suicidality. In a study by Rotheram-Borus et al. ,82,83 adolescents who took part in a specialised emergency department intervention had significantly lower mean scores for levels of suicide intent at post-discharge assessment than adolescents who received standard care (mean scores on the HASS: intervention group 1.4 ± 2.38, control group 2.1 + 2.86; p < 0.05). The emergency department-based FISP intervention conducted by Asarnow et al. 57 found no significant differences in levels of suicide intent at follow-up post intervention [mean scores on the HASS: intervention group 13.6 ± 13.3, control group 12.1 ± 12.2; adjusted odds ratio (aOR) (note that baseline suicide attempts were adjusted for site, gender, age and baseline CES-D, and that the follow-up analyses included additional variables of time to follow-up, baseline suicide attempts and baseline CBCL total problem score) 1.7, 95% CI –2.7 to 6.2] or suicidal behaviour (mean scores on the HASS: intervention group 3.2 ± 4.8, control group 3.6 ± 4.7, aOR –0.3, 95% CI –1.9 to 1.3). Findings from a study by Wharff et al. 84 indicated that all participating adolescents, whether in the intervention or control groups, reported lower levels of suicidality at post test and at 1-month follow-up than at baseline assessment. Further analysis did not find any significant differences between the groups (mean change in the Reasons for Living Inventory for Adolescents: intervention group 0.07 ± 0.44, control group 0.15 ± 0.45; p = 0.24).
Post-discharge use of services/resources
Two experimental studies (across three reports57,82,83) looked at post-discharge use of services/resources. One of the goals of the emergency department intervention (FISP) conducted by Asarnow et al. 57 was to link paediatric suicidal patients with follow-up mental health treatment. The findings showed that patients who received FISP were significantly more likely than those in the control group to be linked to outpatient treatment after discharge [intervention group 92%, control group 76%, aOR (adjusted for baseline score for the same outcome, days between baseline and follow-up, site, age, gender, CBCL total problems and CES-D) 6.2, 95% CI 1.8 to 2; p = 0.004] and to receive significantly more outpatient treatment visits (intervention group 5.3 ± 7.0, control group 3.1 ± 5.5, aOR 2.0, 95% CI 1.3 to 3.2; p = 0.003). The aim of the specialised emergency department intervention conducted by Rotheram-Borus et al. 82,83 was to assess the impact of the intervention on outpatient treatment adherence. Those CYP who received the specialised programme were significantly more likely than those who received standard care condition to return to the clinic for any outpatient treatment following their discharge from the emergency department (intervention group 95.4%, control group 82.7%, χ2 5.56, degrees of freedom 1; p = 0.018). However, there was no significant difference in the number of treatment sessions attended by both groups (intervention group 5.73 ± 3.40, control group 4.67 ± 3.71; p = 0.079). Logistic regression analysis was conducted to determine which variables predicted adherence to outpatient treatment. Higher suicidal behaviour scores (OR 1.30, 95% CI 0.00 to 0.46; p < 0.05) and higher self-esteem were significant predictors of completing treatment. It was also determined that those in specialised care intervention were three times more likely to complete outpatient treatment than youths in the standard care condition (OR 3.11, 95% CI 1.20 to 16.98; p < 0.02). Baseline suicidal ideation (OR 1.09, 95% CI 1.00 to 7.43; p < 0.05) was also associated with treatment completion, with the more ideation the CYP reported, the more likely they were to complete treatment. 82,83
Self-esteem/self-concept
One study (across two reports82,83) explored self-esteem. The introduction of a specialised emergency department programme in the study by Rotheram-Borus et al. 82,83 had no significant impact on levels of self-esteem immediately post discharge (mean score on the Rosenberg Self-esteem Scale: intervention group 29.0 ± 5.61, control group 27.6 ± 5.32; p > 0.05).
Impulsivity
One study (across two reports82,83) explored impulsivity. Rotherham-Borus et al. 82,83 reported that the introduction of a specialised emergency department programme had no significant impact on levels of impulsivity (mean score on the Impulsiveness Scale: intervention group 10.8 ± 4.69, control group 11.7 ± 4.37; p > 0.05).
Client satisfaction
One experimental study84 looked at client satisfaction. Wharff et al. 84 compared a family-based intervention conducted in the emergency department (FBCI) with usual care. Post test, parents/guardians whose CYP had been randomised to FBCI reported significantly higher levels of patient satisfaction than their usual care counterparts (mean score on the Client Satisfaction Questionnaire: intervention group 30.4 ± 2.4, control group 28.6 ± 3.3; p < 0.001).
Health-care staff satisfaction with mental health crisis services/programmes
Two descriptive cross sectional studies85,96 investigated health-care staff satisfaction with the service. Dion et al. 85 explored the emergency department staff satisfaction with the crisis intervention programme, which was collected in terms of both numeric data and open-ended responses highlighting satisfaction with all aspects of the programme, apart from availability of crisis intervention workers and, in particular, coverage during weekends and nights. Frequently reported strengths included reduction of emergency department physician workload, skills of the crisis intervention worker at managing and assessing patients, prompt access to mental health services and crisis intervention workers’ awareness of community resources. The Royal College of Emergency Medicine conducted a national survey with all of its members regarding the services and quality of care that CYP in the emergency department receive (93/240 members responded). 96 Sixty-two per cent of respondents reported that they felt that emergency department services for CYP presenting with an acute mental health problem were ‘poor’ or ‘awful’, with wide variability in availability of CAMHS and other specialist services, particularly at evenings and weekends. 96
Summary
What this evidence synthesis has shown is that crisis services/interventions initiated within the emergency department are effective in reducing depression (very low to moderate GRADE rating) and improving family functioning (moderate GRADE rating) or family empowerment (very low GRADE rating) between recruitment and follow-up periods. Mixed findings are reported regarding the number of outpatient visits attended, with one61 out of two studies reporting that those in the intervention group attended more outpatient treatment sessions (moderate GRADE rating). Mixed findings are also reported for suicidality, with only one82,83 study (across two reports) out of three studies reporting that the intervention was effective in reducing levels of suicidality (very low to moderate GRADE rating). CYP receiving crisis services initiated within the emergency department are more likely to be linked or referred to intensive outpatient care (moderate GRADE rating), to attend for outpatient treatment (very low GRADE rating) or to complete outpatient treatment (very low GRADE rating) and are less likely to be hospitalised (very low GRADE rating). CYP receiving crisis services initiated within the emergency department also report greater satisfaction with services than those in a control group (moderate GRADE rating). No differences are reported for behaviour (moderate GRADE rating), family adaptability (very low GRADE rating), family cohesion (very low GRADE rating), impulsivity (very low GRADE rating), self-esteem (very low GRADE rating), likelihood of repeat emergency department visit post discharge (very low GRADE rating) and number of completed suicides or suicide attempts between recruitment and follow-up periods (very low to moderate GRADE rating). Health-care staff are satisfied with some aspects of mental health crisis services/programmes that they provide, but are generally dissatisfied around the lack of out-of-hours availability.
Home- or community-based programmes
Symptoms of depression
One experimental study, conducted by Huey et al. ,78 investigated symptoms of depression. A significant linear time effect (p < 0.001) for reduction of depression symptoms (across all measures) was found for those CYP receiving home-based MST at the time of crisis up to 1 year post treatment.
Psychiatric symptoms
One descriptive cross-sectional study98 and one experimental study (reported across two reports64,79) investigated psychiatric symptoms. Muskens et al. 98 investigated changes in the type and severity of mental health symptoms from admission to 2 and 4 months post discharge following a period of intensive home treatment combined with admission to psychiatric high and intensive care. A 53% reduction on mean HoNOSCA total scores after 4–5 months of treatment was observed (mean HoNOSCA total scores: admission 18.82 ± 5.18, 2 months 13.03 ± 5.06, 4 months 9.4 ± 5.16; p < 0.01). There were no significant moderating effects found for gender, age, primary diagnosis, clinical admission, home treatment time, additional therapy and medication. 98 Henggeler et al. 64,79 investigated differences in emotional distress in those receiving home-based MST compared with those who received usual services (i.e. emergency hospitalisation) at the point of crisis. Henggeler et al. 64,79 reported that CYP in both groups demonstrated clinically significant reductions in emotional distress over time (p > 0.05). 64 For those CYP in the MST condition, levels of emotional distress sharply declined during the first few weeks of treatment, levelled during treatment and improved slightly during follow-up. Those CYP in the emergency hospitalisation condition demonstrated a steady improvement in symptoms that levelled off during follow-up. 79
Behaviour
Two experimental studies (across three reports61,64,79) investigated behaviour. The study by Evans et al. 61 investigated the effectiveness of three models of intensive in-home services. Significant reductions in both internalising behaviour and externalising behaviour scores were reported from admission to 6 months post discharge for all programmes (p < 0.05). Henggeler et al. 64 compared MST with usual services (i.e. emergency hospitalisation) and found that at the time of completion of MST at 4 months, MST was significantly more effective than emergency hospitalisation at decreasing youths’ externalising behaviour (mean scores on the CBCL externalising caregiver report: MST 63.7 ± 12.4, hospitalisation 64.3 ± 14.2, p < 0.05; mean scores CBCL externalising teacher report: MST 67.8 ± 15.1, hospitalisation 38.0 ± 13.0, p < 0.05). However, these differences were no longer significant at 12–16 months’ follow-up. 79 Henggeler et al. 64,79 also reported that caregiver and teacher reports for internalising problems for the youths were similar between treatment conditions and that no significant differences were observed for internalising behaviours at any time point (p > 0.05).
Psychosocial functioning
Two experimental studies (across three reports61,64,79) investigated psychosocial functioning. Henggeler et al. 64 investigated differences in psychosocial functioning between youths receiving home-based MST and youths receiving usual services (i.e. emergency hospitalisation) at the point of crisis. At the time of MST completion, youths in the MST condition spent significantly fewer days out of school than their counterparts in the hospitalisation condition (mean days: MST 14 ± 36.8 days, hospitalisation 37 ± 58 days; p < 0.05). However, at 12–16 months post recruitment, it was reported that these group differences were no longer statistically significant, with both groups of youths having spent significantly fewer days in a regular school setting than at baseline. 79 There were also no significant differences in psychosocial functioning as measured by the CBCL social youth report (p > 0.05), the CBCL social caregiver report (p > 0.05) or the FFS (p > 0.05) between those in the MST condition and those in emergency hospitalisation condition. 64 Evans et al. 61 found no significant changes in social competency scores from admission to discharge or post 6 months discharge across three models of intensive home services. In a study of HBCI by Evans et al. ,61 data from the Child and Adolescent Functional Assessment Scale were not included in the final analysis because of the poor quality of the responses obtained at follow-up.
Hospitalisation rates
One experimental study (across three reports64,79,80) investigated hospitalisation rates. Henggeler et al. 64 demonstrated that home-based MST resulted in only 44% of youths being hospitalised within the 1-year study time period. Overall, youths in the home MST intervention had 72% fewer days in hospital than those in the control group. 80 Between the time when the control group was discharged from hospital and when the MST group had completed their treatment (at approximately 4 months), 13% of those in the control group had been re-hospitalised for an average of 8.5 days. 79 It was found that MST was significantly effective (p < 0.001) in preventing admission to hospital for 75% of youths assigned to the MST arm of the study during the 2-week period following referral. 80
Costs
One experimental study81 compared the costs of an intervention with usual care to determine whether or not the intervention was cost-effective. Sheidow et al. 81 calculated insurance expenditures for those in receipt of MST or usual services to determine whether or not MST was cost-effective and showed significant savings from the time treatment was started to when it was completed 4 months later [mean ± standard deviation (SD): MST US$8236 ± US$6680, usual care US$11,725 ± US$5065; p = 0.004]. However, from the period when treatment finished to the 12-month follow-up point, costs were comparable (mean ± SD: MST US$11,709 ± US$13,396, usual care US$13,451 ± US$16,351; p = 0.556). Risk-adjusted models of costs were also calculated and adjusted for the youth’s age, the caregiver’s age, caregiver’s educational level, number of caregivers in the household and a variable representing the interaction between the treatment duration, the treatment and differences in symptoms levels, as measured by the Global Severity Index. This analysis showed that MST demonstrated better short-term cost-effectiveness for each of the clinical outcomes than usual care (i.e. inpatient care followed by community aftercare). 81
Discharge destination
Two experimental studies61,80 looked at discharge destination and destination following discharge from home-based programmes and found that between 57%80 and 86%61 of CYP were able to continue living within the community, depending on the type of intervention. Evans et al. 61 explored the difference across three different home-based interventions and found that there was no significant difference between each of the models in relation to CYP remaining in the community (CCM, 78.4%; HBCI, 83%; HBCI+, 85.7%). Schoenwald et al. 80 demonstrated that CYP receiving home-based MST spent fewer days in out-of-home placements than CYP in the hospitalisation comparison group (MST group 644 days, comparison group 1490 days; no further statistical analysis). CYP receiving home-based MST also had fewer days in foster care, supervised independent living, group home, RTC, hospital care and detention, but more days in therapeutic foster care (no statistical details provided).
Family functioning/empowerment
Two experimental studies (across three reports61,64,79) explored family functioning. Henggeler et al. 64 investigated the effects of home-based MST compared with usual services (i.e. emergency hospitalisation) and found that family functioning significantly improved for the youths in the MST condition. More specifically, youths reported significant greater family adaptability than those in the hospital condition from baseline to 12–16 months’ follow-up (p < 0.039), but no changes in levels of family cohesion (p > 0.05). Families in the MST condition had become more structured, whereas families in the hospitalisation condition had become less structured (p < 0.009). 64 Caregiver reports of family cohesion showed significant treatment effects (p < 0.001) in that family cohesion significantly increased for those in the MST condition and significantly decreased for those in the hospitalisation condition (p < 0.004). 64 Over time, youths receiving MST reported a slight increase in adaptability, whereas youths receiving emergency hospitalisation reported a slight decrease in family adaptability, resulting in a significant linear between-group effect. Youth reports of family cohesion differed significantly between groups, with emergency hospitalisation families evidencing no significant change and MST youths reporting a steady decrease during MST treatment followed by a rise in family cohesion (i.e. a U-shape effect). A further report79 from the same study showed that caregiver reports of cohesion were generally stable, with only a slight linear increase over baseline among MST families but no significant between-group differences in patterns. In the study conducted by Evans et al. ,61 for those children receiving home-based care across three different programmes (i.e. HBCI, HBCI+ and CCM), all reported significant gains from admission to discharge in family adaptability (p < 0.01). With regard to family cohesion, only those children in the HBCI and HBCI+ groups showed significant gains (p < 0.05). Families of children who received HBCI or HBCI+ services also showed significant admission to discharge gains in cohesion (using the FACES II), although these gains were not noted for families of children assigned to CCM (main effect for admission to discharge p > 0.05).
Completed suicide and suicide attempts
One experimental study conducted by Huey et al. 78 looked at the number of completed suicides and suicide attempts. The results indicated that both MST and psychiatric hospitalisation were significantly associated with a reduced incidence of attempted suicide, as rated by the youths themselves (p < 0.001) and their caregivers (p < 0.001). However, MST was significantly more effective than psychiatric hospitalisation at reducing attempted suicide over the course of 16 months following recruitment. Results also indicated that age (p < 0.05), gender (p < 0.01) and ethnicity (p < 0.01) each moderated the effects of MST on caregiver-rated attempted suicide incidence. 78
Self-esteem/self-concept
Two studies (across three reports61,64,79) explored self-esteem. In a study by Henggeler et al. ,64 differences in self-esteem were explored for youths receiving home-based MST compared with youths who received usual services (i.e. emergency hospitalisation) at the point of crisis. For those in the MST condition, there were no significant differences in levels of self-esteem from baseline to completion of the MST (mean scores on the FFS: baseline 2.57 ± 0.9, completion of MST 2.55 + 1.1). 64 At the time of completion of MST, youths who were in the hospitalisation condition reported significant improvements in self-esteem compared with youths in the MST condition (mean scores on the FFS: MST 2.55 ± 1.1, hospitalisation 2.73 ± 0.9; p < 0.05). 64 However, at the 1-year follow-up time point, these treatment effects were no longer observed (mean scores on the FFS: MST 2.50, hospitalisation 2.22; p > 0.05). 79 In the study conducted by Evans et al. ,61 children assigned to each of three models of intensive home services showed significant improvement in self-concept from admission to discharge (p < 0.05) and these improvements were still present at 6 months post discharge (p < 0.01).
Client satisfaction
One experimental study64 looked at client satisfaction. Evans et al. 64 compared home-based MST with usual services (i.e. emergency hospitalisation). Youths who received MST and their caregivers reported significantly greater treatment satisfaction at the time MST was completed compared with those who received emergency hospitalisation (mean score on the LFSS: youth MST 15.7 ± 4.4, youth hospitalisation 13.3 ± 4.2, p = 0.007; caregiver MST 17.6 ± 3.2, caregiver hospitalisation 16.5 ± 3.4, p-value not reported) and at 1-year follow-up (mean score on the LFSS: youth MST 15.5 ± 4.5, youth hospitalisation 12.0 ± 4.6, p-value not reported; caregiver MST 17.9 ± 3.4, caregiver hospitalisation 16.4 ± 3.9, p = 0.044).
Summary
Effectiveness of home- or community-based programmes was the focus of three studies (across seven reports61,64,78–81,98). The findings showed that home- or community-based programmes were effective in reducing depression (moderate GRADE rating), psychiatric symptoms (moderate GRADE rating) and the number of completed suicides and suicide attempts (moderate GRADE rating) between recruitment and follow-up periods, improving self-concept (moderate GRADE rating), family adaptability (moderate GRADE rating) and family cohesion (parents’ perspective) (moderate GRADE rating), and were more cost-effective. Mixed findings were reported for behaviour, with one out of two studies reporting that the intervention was effective in reducing levels of internalising and externalising behaviour (moderate GRADE rating). CYP receiving these services were more likely to remain in the community after treatment (moderate GRADE rating), less likely to be hospitalised (moderate GRADE rating) and reported greater satisfaction with services than those in the control groups (moderate GRADE rating). No differences were reported for psychosocial functioning (moderate GRADE rating), self-esteem (moderate GRADE rating) and family cohesion (CYP perspective) (moderate GRADE rating) between recruitment and follow-up periods.
Inpatient care
Psychiatric symptoms
One experimental study87 investigated psychiatric symptoms. During admission to an inpatient crisis stabilisation programme, Muskens et al. 87 reported significant reductions in the severity of psychiatric symptoms regardless of the type of services received [mean change in score: crisis group 10.4 ± 9.3, assessment group 10.7 ± 7.8, transition group 9.8 ± 11.5; p > 0.05 for both univariate and multivariate analysis of variances (ANOVAs)].
Psychosocial functioning
One experimental study87 investigated psychosocial functioning. During admission to an inpatient crisis stabilisation programme, Greenham and Bisnaire87 demonstrated improvements regardless of the type of services received (mean change in score: crisis group 5.3 ± 9.1, assessment group 5.8 ± 9.5, transition group 4.8 ± 11.2; p > 0.05 for both univariate and multivariate ANOVAs).
One experimental study conducted by Rogers et al. 72 investigated costs. There were significant cost savings after the CARES (Child & Adolescent Rapid Emergency Stabilization) programme was established, which the authors felt was reflective of a reduction in LOS. Specifically, the average charge for patients significantly decreased (from US$1472.20 before CARES to US$903.15 after CARES, i.e. a decrease of US$569.05; p < 0.0001) and the total cost per patient also significantly decreased (from US$1472.20 before CARES to US$903.15 after CARES, i.e. a decrease of US$569.05; p < 0.0001). However, there were no significant differences in the payments per patient (before CARES US$923.88 vs. after CARES US$812.29, i.e. a decrease of US$111.59; p < 0.06).
Emergency visits post discharge
One experimental study conducted by Rogers et al. 72 looked at the number of emergency visits post discharge. 72 No significant differences in the recidivism rate [i.e. single visits or more than one visit per year for those who had been inpatients before and after the introduction of the CARES inpatient programme (χ2 = 0.089; p = 0.766)] were found.
Length of stay
Two experimental studies72,87 investigated LOS. Greenham and Bisnaire87 reported that the median LOS in an inpatient crisis stabilisation programme and assessment service was 4 days, with a mean of 6.2 ± 6.9 days. Another study conducted by Rogers et al. 72 evaluated LOS before and after the introduction of the CARES unit and found that LOS was significantly shorter post CARES than with the former emergency department provision [mean LOS: pre CARES 19.7 ± 32.6 hours, post CARES 10.8 ± 19.9 hours (a reduction of 47.3%); p < 0.001].
Suicidality
One experimental study conducted by Greenham and Bisnaire87 explored suicidality. During admission to an inpatient crisis stabilisation programme, reductions in levels of suicide risk were demonstrated regardless of the type of services received (mean change in score: crisis group 11.4 ± 10.0, assessment group 12.6 ± 9.1, transition group 7.7 ± 7.9; p > 0.05 for both univariate and multivariate ANOVAs). 87
Summary
Two studies72,87 explored the effectiveness of specific inpatient programmes for CYP requiring crisis care. The evidence synthesis72,87 found that specific inpatient programmes were effective in reducing psychiatric symptoms (moderate GRADE rating) and suicidality (moderate GRADE rating), and improving psychosocial functioning (moderate GRADE rating) between recruitment periods and follow-up. These inpatient programmes could also decrease LOS (moderate GRADE rating) and, subsequently, costs (moderate GRADE rating) at the time of the crisis. No differences were reported in the rate of emergency department visits for up to 1 year post discharge (moderate GRADE rating).
Outpatient mental health programmes
Psychosocial functioning
One experimental study86 conducted by Greenfield et al. 86 investigated psychosocial functioning. No significant differences were reported in levels of psychological and social functioning after the introduction of a rapid response outpatient model at 2 months’ follow-up (mean score on the CGAS: intervention group 13.12 ± 14.6, control group 13.48 ± 15.5; p > 0.05) and at 6 months’ follow-up (mean score on the CGAS: intervention group 14.86 ± 15.29, control group 13.26 ± 17.52; p > 0.05).
Hospitalisation rates
One experimental study (reported across two reports86,93) explored hospitalisation rates. A rapid response outpatient model was effective in reducing hospitalisation rates (defined as hospitalisation at least once at any hospital for reasons related to suicidality). Adolescents in the intervention group were 71% less likely than adolescents in the comparison group to be hospitalised immediately after assessment in the emergency department for suicidality [intervention group 11% vs. comparison group 40%, RR (relative risk) 29, 95% CI 0.18 to 0.46; p < 0.001] and 59% less likely to be hospitalised over the 6 months after an emergency assessment in the emergency department for suicidality (intervention group 18% vs. comparison group 43%, RR 0.41, CI 0.28 to 0.61; p < 0.001). 86,93
Costs
One experimental study93 investigated costs. Latimer et al. 93 investigated cost savings from the treating hospital’s perspective and a societal perspective for those receiving a rapid response treatment intervention compared with those without a rapid response in the control group. There were no significant differences (difference of US$1886; p = 0.11) in hospital costs per person between the intervention (US$2114, range £134 to US$46,273) and the control (US$4000, range US$150 to US$127,998). There were also no significant differences (difference of US$991; p = 0.67) in societal viewpoint costs per person between the intervention (US$10,785, range US$1424 to US$107,406) and the control ($11,775, range US$559 to US$164,134). The point estimates indicated that the intervention would save the treating hospital approximately US$1208 and society approximately US$636 for every additional point improvement on the CGAS functional scale, compared with the control intervention. However, the control intervention would save the treating hospital approximately US$13,780 and society approximately US$7238 for every additional point improvement on the Suicide Severity Scale compared with the intervention. 93
Emergency visits post discharge
Three experimental studies34,66,86 looked at the number of emergency visits post discharge. Greenfield et al. 86 reported no significant differences within the 6-month follow-up period after the introduction of a rapid response outpatient team and initial presentation to the emergency department (p > 0.05). In addition, Greenfield et al. 34 reported no significant differences within 12 months after the introduction of a specialised outpatient service with an emergency room follow-up team (p > 0.05). A further study conducted by Maslow et al. 66 reported on the first year after opening an integrated paediatric mental health outpatient clinic for acute mental health crisis. Examination of electronic health data indicated a reduction in the rate of emergency department visits within 30 days after patients’ initial contact with the clinic (reporting 333 emergency department visits in 30 weeks before vs. 172 emergency department visits in the 30 weeks after). However, no further statistical analysis was conducted to confirm this finding.
Length of stay
One experimental study conducted by Greenfield et al. 86 investigated LOS. No significant differences were reported in LOS in the emergency department after the introduction of a rapid response outpatient model at recruitment (mean days: intervention group 6.6 ± 5.6, control group 3.9 ± 3.8; p > 0.05), at 2 months’ follow-up (mean days: intervention group 7.1 ± 6.1, control group 4.1 ± 3.9; p > 0.05) and at 6 months’ follow-up (mean days: intervention group 7.8 ± 9.9, control group 5.1 ± 6.8; p > 0.05).
Completed suicides and suicide attempts
One experimental study conducted by Greenfield et al. 86 looked at the number of completed suicides and suicide attempts. 86 No significant differences in the numbers of suicide attempts made were reported during the 6-month follow-up period, excluding those at the time of recruitment, as a result of the implementation of a rapid response outpatient team (p < 0.05).
Suicidality
One experimental study conducted by Greenfield et al. 86 explored suicidality. No significant differences were reported in levels of suicidality after the introduction of a rapid response outpatient model at 2 months’ follow-up (mean scores on the SSBS: intervention group –1.64 ± 1.26, control group –1.63 ± 1.27; p > 0.05) and at 6 months’ follow-up (mean scores on the SSBS: intervention group –1.40 ± 1.26, control group –1.54 + 1.21; p > 0.05). 86
Post-discharge use of services/resources
One experimental study (reported across two reports86,93) looked at post-discharge use of services/resources. Resource use during the 6-month follow-up period after the introduction of an outpatient rapid response model for those presenting in crisis to an emergency department was investigated and was found to be similar for those in the intervention and control groups for the majority of services. However, those from the control group, on average, had more meetings with outpatient psychotherapists (mean number of meetings: intervention group 0.06 ± 0.47, control group 0.44 ± 1.60; p < 0.01) and social workers (mean number of meetings: intervention group 0.13 ± 6, control group 0.57 ± 1.91; p < 0.01) than those from the experimental group. Time from first telephone contact with a health professional following discharge from an emergency department varied from 1.5 days [interquartile range (IQR) 1.0–6.0 days] for the patients in the experimental group to 4 days (IQR 1.0–7.5 days) for patients in the control group. Time to first appointment was 6 days (IQR 1.0–11.0 days) for the patients in the experimental group and 10 days (IQR 5.0–17.0 days) for patients in the control group. 86,93
Satisfaction with clinicians who delivered the mental health crisis service/programme
One descriptive cross sectional study88 explored satisfaction with clinicians who delivered the mental health crisis service/programme. Lee and Korsak88 explored parents’ satisfaction with an outpatient urgent care clinic consultation. It was noted that there was a significant association between parental satisfaction and the degree to which parents felt listened to by consultants (p < 0.05), the amount learned from the consultation, and time between referral and consultation and appointment length (p < 0.05). Over 52% of parents implemented consultant recommendations, with a significant association between satisfaction and adherence (p < 0.05).
Summary
The effectiveness of outpatient mental health programmes was explored in three studies (across four reports66,86,93,120). This evidence synthesis found that CYP receiving outpatient mental health programmes were less likely to be hospitalised than CYP in a control group (very low GRADE rating) and could experience quicker access to additional resources (very low GRADE rating). An association also exists between parental satisfaction and increased adherence to outpatient treatment (very low GRADE rating). No differences were reported for psychosocial functioning (very low GRADE rating), in the number of emergency department visits for up to 1 year post discharge (very low GRADE rating), LOS in the emergency department before discharge to a rapid outpatient service (very low GRADE rating), number of suicide attempts (very low GRADE rating), suicidality (very low GRADE rating) and post-discharge use of resources (very low GRADE rating).
Mobile crisis services
Hospitalisation rates
One experimental study conducted by Martin68 investigated hospitalisation rates. There were no significant differences in the percentage of CYP who were hospitalised within 30 days of attending a mobile crisis intervention or a walk-in hospital-based crisis intervention (OR 1.01, 95% CI 0.54 to 1.92). 68 However, regardless of service provision, CYP aged 6–11 years were 298% more likely to be hospitalised within 30 days after a crisis stabilisation than CYP aged 15–17 years (OR 3.98, 95% CI 1.66 to 9.51; p < 0.002).
Emergency visits post discharge
One experimental study conducted by Fendrich et al. 62 looked at the number of emergency visits post discharge. It was reported that youths who had attended an emergency mobile crisis service for a behavioural health need (defined as one in which any psychiatric diagnosis was provided during an emergency department service encounter) had significant reductions in further visits to the emergency department in the next 18 months compared with youths in a comparison sample (incident rate ratio 0.75, 95% CI 0.66 to 0.85; a reduction of 25%).
Summary
Two studies62,68 investigated the effectiveness of mobile crisis services and reported that CYP receiving mobile crisis services were less likely to attend emergency department post discharge than CYP in a control group (very low GRADE rating), but that there were no differences in the rates of hospitalisation (very low GRADE rating).
Telepsychiatry
Hospitalisation rates
Two experimental studies74,92 investigated hospitalisation rates. Roberts et al. 92 explored outcomes between telepsychiatry or face-to-face emergency consultations for CYP from rural and remote communities, finding that there were no differences in admissions (telepsychiatry, n = 18; face to face, n = 5; p > 0.05). However, Thomas et al. 74 reported that CYP who received telepsychiatry as opposed to usual care were significantly less likely to be admitted to hospital [aOR (adjusted for patient variables, but no further details provided) 0.59, 95% CI 0.40 to 0.86; p < 0.001).
Costs
One experimental study conducted by Thomas et al. 74 investigated costs. The use of telepsychiatry consultations was compared with usual care and total patient charges were significantly lower for those who received telepsychiatry consultations than those who received usual care (US$3493 vs. US$8611; p < 0.001). A cost-efficiency analysis concluded that although telepsychiatry was more expensive than usual care, the improved efficiency of telepsychiatry resulted in lower charges and shorter LOSs. 74
Discharge destination
One experimental study92 looked at discharge destination. Roberts et al. 92 explored outcomes between telepsychiatry and face-to-face emergency consultations for CYP from rural and remote communities, finding that there were no differences in referral pathways (telepsychiatry, n = 37; face to face, n = 32; p > 0.01).
Emergency visits post discharge
One experimental study conducted by Thomas et al. 74 looked at the number of emergency visits post discharge. 74 No significant differences in the 72-hour emergency department visit return rate were reported among patients who received a telepsychiatry emergency consultation (85%) compared with those who received usual care (90%) (p > 0.05).
Length of stay
Two experimental studies investigated LOS. 71,74 Reliford and Adebanjo71 demonstrated a significantly reduced monthly LOS in the paediatric emergency department for those who did not need admission (pre intervention 285 hours, post intervention 193 hours; p = 0.032). However, there was no significant difference in monthly LOS for those who required admission (pre intervention 168.5 hours, post intervention 161.7 hours; p > 0.05). The second study conducted by Thomas et al. 74 showed a significant reduction in monthly LOS in the paediatric emergency department (pre intervention 5.5 hours, post intervention 8.3 hours; p = 0.001).
Client satisfaction
Two experimental studies74,92 looked at client satisfaction and reported high patient or parent/guardian satisfaction with telepsychiatry emergency assessments in terms of overall acceptability (i.e. user friendliness of the technology) and efficiency (i.e. time saved from not having to travel). Parents and guardians expressed appreciation for not having to travel to access main services, which saved them time and money, and stated that they would use the service again. 74,92
Health-care staff satisfaction with mental health crisis services/programmes
One experimental study74 investigated health-care staff satisfaction with a telepsychiatry service. Thomas et al. 74 conducted a survey both before and after the introduction of telepsychiatry. Satisfaction survey scores significantly increased on questions regarding the process for evaluating and managing patients with mental health concerns (p < 0.05), family satisfaction (p < 0.05), making appropriate disposition decisions (p < 0.05) and process safety (p < 0.05). No change occurred in faculty members’ levels of comfort around, or when assessing, patients with mental health concerns (p > 0.05).
Summary
The effectiveness of telepsychiatry initiatives was reported across two studies. 74,92 Telepsychiatry initiatives were effective in decreasing LOS (very low GRADE rating) and costs (very low GRADE rating). Parents reported high levels of satisfaction (very low GRADE rating) and levels of staff satisfaction were improved (very low GRADE rating). No differences were reported in the rate of repeat visits to the emergency department (very low GRADE rating) or in referral pathways after the introduction of telepsychiatry (very low GRADE rating). Mixed findings were reported for the rate of hospitalisation with one74 out of two studies reporting that telepsychiatry was effective at reducing the likelihood that a person would be hospitalised (very low GRADE rating).
Implementation of a dedicated mental health team in the emergency department
Hospitalisation rates
Two experimental studies65,75 explored hospitalisation rates. Uspal et al. 75 reported that there were no significant increases in admission rates (pre intervention 23% vs. post intervention 22%; p < 0.01) or the 72-hour return rate (pre intervention 2.1% vs. post intervention 3.6%; p < 0.01) after the implementation of a dedicated mental health team in the emergency department. Holder et al. 65 found that as a result of introducing additionally trained psychiatric professionals fewer CYP were admitted to a paediatric treatment unit (p < 0.005). However, there was a significant increase in the number of CYP discharged to a psychiatric hospital post intervention as opposed to pre intervention (p < 0.05).
Costs
One experimental study65 investigated costs. Holder et al. 65 implemented a programme that added CYP psychiatrists and psychiatric social workers to the paediatric emergency department, but did not find any significant differences in cost before and after its introduction (before US$602 vs. after US$588, i.e. a decrease of US$14; p = 0.451). The authors concluded that this was attributable to the costs of the additional staff, even though LOS had decreased.
Discharge destination
One experimental study conducted by Holder et al. 65 looked at discharge destination. Introducing additionally trained psychiatric professionals to a paediatric emergency department significantly increased the number of CYP returning to the home environment after the initial crisis (pre addition 65% vs. post addition 65.2%; p < 0.05). 65
Emergency visits post discharge
One experimental study conducted by Uspal et al. 75 looked at the number of emergency visits post discharge. No significant differences in the 72-hour emergency department return rates were reported after the introduction of a dedicated mental health team based in the paediatric emergency department (p = 0.13). 75
Length of stay
Two experimental studies65,75 investigated LOS. Holder et al. 65 reported a significant reduction in LOS from triage to discharge (mean LOS: pre intervention 14.7 hours, post intervention 12.1 hours; p < 0.001) and the other study conducted by Uspal et al. 75 found a significant reduction in overall LOS in the paediatric emergency department [mean LOS: pre intervention 332 (95% CI 309 to 353) minutes, post intervention 244 (95% CI 233 to 254) minutes; p < 0.01].
Health-care staff satisfaction with mental health crisis services/programmes
One experimental study investigated health-care staff satisfaction within a paediatric emergency department. Findings from the retrospective cohort study conducted by Uspal et al. 75 reported that those working within a paediatric emergency department after the introduction of a dedicated CYP mental health team reported significant improvements:
-
Staff felt that the system supported making appropriate disposition decisions regarding discharge plans or on admissions for patients with acute mental health concerns (p < 0.05). 75
-
Staff were satisfied with the paediatric emergency department process for evaluating and managing patients with mental health concerns and felt that the system was safe for patients (p < 0.05). 75
-
Families were satisfied with the paediatric emergency department processes for evaluating and managing patients (p < 0.05). 75
However, there were no significant differences in the levels of comfort around patients or in assessing patients with acute mental health concerns before and after the introduction of the intervention (p > 0.05). 75
Summary
When a dedicated mental health team was implemented in the emergency department, CYP were less likely to be hospitalised (very low GRADE rating) and more likely to return to a home environment (very low GRADE rating). LOS were also decreased (very low GRADE rating). No differences were reported in the 72-hour return rate to the emergency department (very low GRADE rating) or in the costs of implementing the service (very low GRADE rating).
Assessment approaches within the emergency department
Hospitalisation rates
One experimental study conducted by Lee et al. 89 explored hospitalisation rates. Lee et al. 89 used a tool known as HEARTSMAP to assess and manage CYP within the paediatric emergency department and reported that it was reliable at identifying CYP requiring psychiatric admission. During pilot implementation, 62 patients received HEARTSMAP assessments. Of the 62 patients, 46 (74%) received a recommendation for emergency department psychiatry assessment, 39 (63%) were evaluated by psychiatry and 13 (21%) were admitted. For those patients hospitalised for further psychiatric care, either at their index visit or at their return visit within 30 days, all (100%) were initially identified by HEARTSMAP at the index visit as requiring emergency department psychiatric consultation. 89
Costs
One experimental study conducted by Mahajan et al. 67 investigated costs. Costs were described as an average cost per hour of occupied emergency department room as a result of the addition of a full-time psychiatric social worker who evaluated all CYP with mental health needs. A reduced LOS for those CYP who presented to the emergency department with a mental health crisis was reported and the associated cost savings were calculated to be US$10,651. Opportunity costs of extended LOS of visits for mental disorders (VMD) in the emergency department after the addition of a full-time psychiatric social worker were also calculated to establish the average revenue foregone had a non-VMD emergency department patient occupied the same room.With average LOS longer for VMD than non-VMD visits, lost revenue due to extended LOS for VMD was estimated at $201,173.30. 67
Length of stay
Three experimental studies67,89,132 investigated LOS. Mahajan et al. 67 described the addition of a full-time psychiatric social worker as part of a child guidance model and found that the overall LOS in the emergency department was significantly reduced (pre 259.49 ± 171.12 minutes vs. post 216.39 ± 152.95 minutes, mean difference of 43.10 minutes; p = 0.001). The time taken for physician disposition to be undertaken (pre 169.31 ± 140.83 minutes vs. post 218.10 ± 171.02 minutes, mean difference of 48.79 minutes; p = 0.00) and for triage were also significantly reduced (pre 45.67 ± 40.72 minutes vs. post 41.56 ± 35.83 minutes, mean difference of 4.11 minutes; p = 0.08)67 as a result of the addition of a full-time psychiatric social worker.
Another study, conducted by Nagarsekar et al. ,132 implemented KALM, which sought to build in extra capacity for an emergency department medical officer to complete the assessment and then to link with an on-call psychiatrist regarding an assessment and management plan. There was no significant difference (p = 0.1407) in median LOS for those on the KALM pathway [4.13 hours (minimum 0.46 hours, maximum 11.55 hours)] compared with those on the TAU pathway [5.09 hours (minimum 0.21 hours, maximum 19.12 hours)]. The National Emergency Access Target stipulates that a patient should be treated and leave the emergency department within 4 hours. Fewer patients breached the National Emergency Access Target when the KALM pathway (56%) was used, but differences were not significant (OR 0.68, 95% CI 0.36 to 1.31; p = 0.252) when compared with those in the TAU pathway (64%).
Lee et al. 89 found that the introduction of the assessment-based approach HEARTSMAP did not have any significant effect on LOS in the paediatric emergency department (median minutes: pre HEARTSMAP 288 minutes, post HEARTSMAP 297 minutes; p = 0.89).
Emergency visits post discharge
One experimental study conducted by Lee et al. 89 looked at the number of emergency visits post discharge. No significant differences in the 30-day emergency department return rate were reported after the introduction of HEARTSMAP in the paediatric emergency department (p > 0.05).
Post-discharge use of services/resources
One experimental study conducted by Lee et al. ,89 in which the HEARTSMAP assessment tool was implemented in a paediatric emergency department, looked at post-discharge use of services/resources. 89 In addition to HEARTSMAP, an emergency outpatient follow-up service was created for families with unmet mental health needs (i.e. the ‘LINK’ clinic). All CYP for which HEARTSMAP triggered recommendations for further community services accessed resources within 30 days. The resources included access to social workers, primary care providers, private psychiatry, private counselling, private psychology, school counselling, substance misuse/detox services, youth clinics, non-urgent community mental health services and urgent community mental health services.
Client satisfaction
One experimental study132 looked at client satisfaction. Nagarsekar et al. 132 assessed how satisfied carers were with the newly implemented KALM pathway compared with the TAU pathway. There were no significant differences between the two care pathways. However, the number of carers answering the survey for the KALM pathway was small (n = 16) and so findings should be treated with caution. 132
Summary
Carrying out assessment approaches within the emergency department was successful at triggering recommendations for further community services, which were accessed; however, there were no differences in the 30-day return rate to the emergency department (very low GRADE rating). Mixed findings were reported for LOS, with one67 out of three studies67,89,132 reporting a reduced LOS (very low GRADE rating). There were also no differences in client satisfaction with the newly implemented KALM pathway compared with the TAU pathway (very low GRADE rating).
Crisis programmes within residential treatment centres
Costs
One descriptive cross-sectional study conducted by Baker and Dale58 investigated costs. The daily cost of total treatment across the entire sample at a crisis programme within a RTC was US$300 per day for a total of 2628 days, compared with US$550 per day for a total of 2628 days if the sample of boys had been treated in a nearby hospital (thereby saving US$650,000). However, hospital stays were, on average, 15 days longer and on accounting for this scenario the savings were calculated to be US$1,490,250.
Length of stay
One descriptive cross-sectional study (reported across two reports58,59) investigated LOS. Baker et al. 59 reported that the LOS for youths admitted to a crisis residence programme varied depending on from where they had been referred (biological family 4.17 ± 4.08 weeks, foster homes 3.77 + 3.01 weeks, RTC 6.68 weeks). Baker and Dale58 reported that LOS was significantly shorter (on average by 15 days) for youths treated at a crisis residence for their first crisis than for those treated in hospital (mean LOS: crisis residence 24.30 ± 20.72 days, hospital 39.04 ± 33.18 days; p < 0.04), despite this group being more at risk.
Assessment approaches within educational settings
Discharge destination
Three descriptive cross-sectional studies60,69,77 looked at discharge destination. Both Michael et al. 69 and Capps et al. 60 focused on students’ risk of harm following assessment using the PEACE protocol. Both studies60,69 reported that decisions on referral options were based on the severity of the crisis or family preference and included comprehensive school mental health services that offered assessment support and a counselling centre (ranging from 26%60 to 33%69) or community mental providers (ranging from 14.3%69 to 26.9%60). Michaels et al. 69 also reported that around 12% of students who were felt to be a significant risk of self-harm were hospitalised after the initial assessment (either straight away or within 2 weeks). Walter et al. 77 investigated the outcomes of a school–hospital partnership that delivered crisis interventions to students and found that in 26% of encounters the partnership was able to avoid referrals to more acute levels of care.
Completed suicide and suicide attempts
Three descriptive cross-sectional studies60,69,73 that implemented the PEACE protocol, including initiation of a response/safety plan, looked at the number of completed suicides and suicide attempts. All studies found that there were no completed suicides or suicide attempts that necessitated medical intervention immediately after (i.e. within the same day) the protocol administration was completed. 60,69,73
Satisfaction with clinicians who delivered the mental health crisis service/programme
One descriptive study77 explored satisfaction with clinicians who delivered a mental health crisis service/programme.Walter et al. 77 explored a school–hospital partnership that sought to provide multitiered levels of support. Walter et al. 77 reported high levels of school staff satisfaction with the ways in which crisis services were provided by programme clinicians and across the different aspects of support offered.
Summary
Assessment approaches within educational settings were reported across four studies. 60,69,73,77 No completed suicides or suicide attempts were reported within educational settings when assessment approaches were introduced (GRADE rating not applicable). A variety of referral destinations were noted and in some cases referrals to more acute levels of care were avoided. Moreover, levels of staff satisfaction were high (GRADE rating not applicable).
Overall summary
The overall summary of findings is presented in Table 13. The quality of evidence reporting the effectiveness of approaches or models of crisis support was variable, ranging from moderate to very low. The areas where the evidence was moderate and, therefore, worthy of consideration for clinical application were in the following sections: improvement of family functioning following a crisis service or intervention initiated in the emergency department, increased referral for the CYP to intensive outpatient care after being seen in emergency department, increased satisfaction with crisis services, reduction in psychiatric symptoms and improvement of psychosocial functioning, and no increase in rate of attendance for crisis care after being seen in emergency department.
Much of the evidence about effectiveness was drawn from outside the UK in different service settings and, consequently, might not be directly applicable to UK services. In the UK, the preference is for emergency departments not to be the first point of contact for people in mental health crises.
Chapter 7 Goals of crisis interventions
The fourth objective was to determine the goals of crisis intervention. This chapter addresses this objective by presenting a number of thematic summaries of the goals of crisis services from primary research (n = 48), descriptive accounts of the organisation of crisis services (n = 36) and UK-only grey literature documents (n = 54). For details of the methods of the narrative approach to the development of the thematic summaries, see Chapter 3, Data extraction, analysis and synthesis. Seven distinct goals have been described across the included literature and these have been categorised as:
-
to keep CYP in their home environment as an alternative to admission
-
to assess need and to plan
-
to improve CYP’s and/or their families’ engagement with community treatment
-
to link CYP and/or their families to additional mental health services as necessary
-
to provide peer support
-
to stabilise and manage the present crisis over the immediate period
-
to train and/or supervise staff.
Five services, however, did not provide any explicit, or implicit, description of their goals. 76,90,97,100,133 Crisis care was provided with little information provided on the service per se, but these papers described the following:
-
Young people with suicidal ideas being seen in the emergency department. 97
-
Young people’s experiences of using a variety of inpatient, community or emergency department services. 90,100
-
An investigation involving interviews with family members and close friends of people who had taken their own lives. 133
-
A study examining young people’s and family members’ comprehension of crises. 48
-
A project recruiting families of children admitted to hospital. 76
The goals of crisis intervention
To keep children and young people in their home environment as an alternative to admission
Twelve services described in 22 reports32,34,58,59,61,63,64,68,78–81,84,93,98,103,107,110,112,113,122,148 explicitly have the goal of keeping CYP in their own homes and avoiding admission to psychiatric hospital.
Examples include services that aim to reduce inappropriate admission, defuse crises and also reduce frustration among community and emergency department staff in securing access,122 along with single-session FBCI delivered in the emergency department, aiming to improve mutual understanding of CYP’s suicidal behaviour and avoid admission. 32,84,107 Other services with the goal of avoiding admission include WAARM, which provides immediate access to home care for CYP initially seen in the emergency department and a service consisting of five sessions of family-based interventions along with ‘rapid response’ follow-up following a paediatric emergency department visit. 110 The emergency room follow-up team is an outpatient crisis service, beginning with the receipt of referrals from the emergency department and involving initial contact within 24 hours of presentation, with the purpose of avoiding admission. 34,93 The crisis and transition services model diverts CYP from the emergency department for home-based care. 148 MST is a family-based strengths-oriented intervention that has also been proposed and tested as an alternative to hospital admission for CYP experiencing severe emotional distress,64,78–81,112 with other services including short-term intensive home-based care mobilised within 24 hours of receipt of referral and offered for typical periods of 4–6 weeks. 61,103 Avoiding hospitalisation, and the dislocations this brings, has also been the goal of services providing intensive residential services in the community. 58,59 In addition, solution-focused intensive home treatment and psychiatric high and intensive care (combining work on improving relationships, reducing self-harming behaviour and reintegration into school, work and leisure) involves up to 4 months of home-based care, potentially following a purposefully short hospital admission. 98 The HBCI combines crisis resolution, relationship-building and skills-teaching, including in contexts where cultural competency is important. 61,103 Other community programmes with hospital-avoidance goals include multidisciplinary crisis intervention, combining family therapy, psychiatric care and school consultation. In resource-limited rural settings, outpatient-based services have been proposed as an alternative to admission. 63 Two different mobile crisis services were described, which respond wherever in the community the need arises and also have the explicit goal of helping CYP remain at home. 68,113
To assess need and to plan
Forty-five services described in 61 reports32–34,57,60–62,66,68,69,72–75,77–84,87–89,92,93,98,102–120,122–126,129–132,136,147–149,171 either explicitly identify the goals of assessing the needs of CYP and their families and/or planning interventions, or infer to them as necessary precursors to providing care and treatment.
In emergency department, triage involving the use of specific assessment tools or scales by nurses was described. 115 The ‘HEADS interview’ is a professional-led interview approach that focuses on home, education (eating), activities/ambition, drugs and drinking, sexuality, and suicide and depression. 116,117 Variants include HEADS-ED (a clinician-rating tool),87,110 HEADDS (an assessment tool)96 and the online HEARTSMAP tool, which are designed to support comprehensive assessment by emergency department clinicians informing recommendations for onwards intervention outside the emergency department environment based on staff members’ estimations of urgency. 119,123,124 Examples were also reported of an emergency department diversion service in which assessment and safety planning are key,148 and of mental health teams being located in emergency departments75 as a way of enabling expert mental health assessment (including in remote emergency departments). Two different examples were described of telepsychiatry supporting remote assessment. 74,92 To support the goal of enabling expert child psychiatrist assessment following emergency department visits, a combination of a telephone and face-to-face appointments have also been used. 122 Another service involves mental health professionals visiting and assessing CYP within hours of their arrival in emergency department after a suicide attempt. The aim of this approach is to promote longer-term inpatient treatment. 129 Another innovation involves the use of a ‘soap opera’-format video in the in emergency department. The video is shown to CYP who have attempted suicide, and their families, by therapists as a precursor to the shared planning of responses to future suicide-eliciting circumstances. 82,83,111
Specific clinical interventions introduced into the emergency department context, which presuppose assessments of need and care planning, include the family systems approach underpinning the FISP. 33,57,147 These interventions include the goal of decreasing the risks of repeat suicidal behaviour by promoting the uptake of follow-up appointments. FBCI is a further emergency department-based approach, which has the single-session goal of assessing, safety planning and intervening through the construction of what is described as a ‘joint crisis narrative’. 32,84,107
Brief assessment-oriented hospital-based services include the children’s comprehensive psychiatric emergency programme, which combines brief inpatient stabilisation and/or outpatient care following a thorough assessment. 106 Other examples involving the use of short-stay hospital beds for the purposes of initial assessment include a service beginning with interdisciplinary assessment87 and the CARES unit, which provides short-stay assessment and stabilisation. 72 Further examples of suites of services combining inpatient and outpatient care, beginning with assessment, are the comprehensive assessment and response training system108 and a programme potentially beginning with up to 2 weeks of admission (if needed) for assessment, initial planning and treatment followed by intensive home treatment. 98 One further model involves the use of an evaluation centre, through which triage assessments and outpatient care are provided. 66
Services offering alternatives to emergency department interventions for CYP in crisis also exist. The goal of meeting mental health crisis needs, beginning with the triage of referred CYP, is a component of an inclusive mental health service for all 0- to 19-year-olds provided by the Solar community crisis resolution team. 149 Out of a variety of initiatives described in a single publication,110 all involve some aspect of assessment:
-
The Lifespan paediatric behavioural health emergency services brings together combinations of hospital-based and community crisis responses, with suites of integrated services, including a telephone triage line for the rapid assessment of need called KidsLink.
-
The Nationwide Children’s Hospital created the outpatient crisis programme, which provides outpatient urgent assessments within 72 hours of presentation.
-
The Allina Health system provides an acute response model (WAARM), which provides expert mental health assessment in the children’s emergency department to reduce waits for urgent interventions and time spent in the emergency department.
-
The enhanced care co-ordination initiative involves expert mental health assessment within 48 hours of paediatric emergency department discharge and linking to follow-up.
Multiple examples exist of specific models or intervention approaches that begin with crisis assessment and/or planning components (including outside the hospital environment). The HBCI is a model of home-based crisis care set up to prevent hospital admission, beginning with care initiated within 24 hours of referral and extending for a period of 4–6 weeks,12 to which HCBI+ adds training in cultural competence. 61,103 The safety first model approach emphasises community-based support to promote safety and begins with formulation and collaborative planning. The service operates on a ‘safety not cure’ ethos and begins with assessment in the home and family environment. 125,126 A further model begins with the addressing of ‘disorganisation’ in families through systemic functional analysis. 131 MST begins with a comprehensive plan underpinned by the use of an ‘ecological framework’, which locates the young person in their family, peer and neighbourhood environment. 64,78–81,112 Another example from a mobile crisis service is the emergency mobile psychiatrics service, which also begins with stabilisation, support and assessment, followed by care for up to 45 days. 62,114
In the case of schools and universities, the PEACE protocol is a school-based approach to self-harm, suicide assessment and response planning. 60,69,73 The multitiered system of support programme is another tiered school-based approach, beginning with the training of staff to identify crisis and extending to clinical assessment and planning. 77 Reports also exist of universities developing specific crisis responses, which begin with stabilising and assessment and, when necessary, referring on. 171 Moreover, there was a report of a model for school-aged young people in which triaging and assessment of safety concerns is offered as an alternative to visits to the in emergency department. 136
The model of providing same-day mental health professional assessment and treatment planning was commonly reported. Telephone referral from emergency department (or community) staff was reported,105 along with urgent outpatient assessment within 72 hours of emergency department attendance88,120 or proactive telephone contact followed by an appointment in the case of CYP presenting to emergency department. 73,86,93 The emergency room follow-up team is a service receiving referrals for assessment and intervention following emergency department presentation, beginning with contact with the family within 24 hours. 34
Examples of telephone, text and internet services as vehicles for the direct assessment of CYP in crisis exist and include the screening, assessment and support services programme, which takes calls from concerned adults or directly from CYP in crisis, with telephone operators then able to direct people onward for face-to-face assessment as necessary. 102 Similar services exist for students, underpinned by the idea that out-of-hours telephone contact, involving safety assessment and crisis planning with people associated with the university, is less stigmatising than contact with external agencies. 102 Two text-based services were also described, providing assessment and safety planning. 104,109 In addition, internet-based services provide both information and message boards for CYP to share their concerns, with the content monitored by peer volunteers trained in suicide prevention. 118
Other crisis response models providing assessment and planning include mobile services offering outreach after hours. 130 One mobile crisis response is part of a combined suite of services also including 24-hour stabilisation, a crisis residential team and outpatient care, with safety planning the goal of the mobile team. 113 The mobile response team aims to prevent admission by offering rapid stabilisation and safety planning. 68
To improve children and young people’s and/or their families’ engagement in community treatment
A specific goal identified in 10 crisis response services described in 16 reports32,33,57,61,82–84,103,107,110,111,113, 125,126,129,147 is to improve the engagement of CYP and/or their families in community treatment.
Examples include the FISP,33,57,147 HBCI,61,103 FBCI,32,84,107 KidsLink,110 WAARM,110 the enhanced care co-ordination initiative,110 an emergency department-based innovation involving the use of videotape, with the explicit purpose of improving adherence to follow-up,82,83,111 the Ventura County Children’s Crisis Continuum,113 the safety first model125,126 and an inpatient crisis unit for adolescents and young adults service, which seeks to overcome resistance to ongoing support. 129
To link children and young people and/or their families to additional mental health services
Forty services in 52 reports32,33,57,61,62,66,68,69,72,73,75,77,82–84,86–89,93,98,102–107,109–111,113,114,116–127,129,132,136,147–149,171 have one of their stated goals as connecting CYP and families to ongoing mental health support.
Emergency department-based services described goals such as the arrangement of post-emergency department follow-up, with examples including referral to a variety of inpatient, outpatient and community care services. 121,122,132,148 More specifically, the literature described:
-
the FISP in seeking to link young people in the emergency department with ongoing care33,57,147
-
the FBCI, including the creation of a joint crisis narrative and identifying what needs to be carried out to avoid future crises32,84,107
-
a family treatment approach that involves the use of a ‘soap opera’-style video and includes the facilitation of outpatient follow-up82,83,111
-
a model of locating a dedicated mental health team in the emergency department, which looks to support young people and families to access ongoing support75
-
a model that combines triage and outpatient services, which seeks to connect young people to community services66
-
a paediatric psychiatry crisis service that refers suicidal CYP for additional therapy either to one of the subspecialty clinics within the outpatient department or to an outside agency. 105
Rapid response outpatient models described the goal of connecting young people to ongoing care, with one model involving referring patients with ‘urgent’, but not ‘emergent’, needs from the emergency department to a follow-up service that is able to respond within 3 days. 88,120 A second model was also described in which all emergency department assessments for crisis are followed by immediate referral to a rapid response outpatient team, which then initiates telephone contact and ongoing care. 86,93 Publications that focused on assessment in the emergency department also described a focus on discharge and disposition arrangements, such as the HEADS-ED intervention110,116,117 and HEARTSMAP. 89,119,123,124
Outside the emergency department, a number of services with mobile, hospital and community components describe linking young people and families to ongoing services as part of their goals. Mobile crisis services aim to provide links to ongoing care after a period of crisis stabilisation. 62,68,113,114 Crisis services located in the community also describe the goal of linking young people and their families to ongoing support in either hospital or community settings. As part of the systematic family-based SFAI, therapists work purposefully with support networks in the community. 125,126 Likewise, the screening, assessment and support services intervention is a crisis telephone line that links callers to hospital or community crisis care. 102 Services that provide home-based programmes, such as the HBCI model, aim to avoid hospitalisation, including through connecting young people and families to existing mental health services, whereas the HBCI+ adaptation also ensures that staff are culturally competent. 61,103 Enhanced care co-ordination linking young people onward was described in a US initiative,110 as was the linking work provided by the WAASH model. 110 CCM has the goal of assessing in the home and linking young people and their families to existing services. 61,103 Integrated services were also described, where a goal arising from short hospital admission and intensive home-based care is to increase motivation for therapy. 98 Two-way communication between urgent care providers and rural outpatient clinics was also described, enabling decisions to be made on onward care and support. 63 In an inclusive mental health service, crisis care is provided as one component, with the goal of integrating this with ongoing services. 149
Descriptions exist of inpatient care linking young people to ongoing services. For example, the children’s comprehensive psychiatric emergency programme provides immediate crisis care plus connects young people and families onward to additional services. 106 Onward referral to other mental health services was also described elsewhere. 129 Evaluations described inpatient services that include the goal of mobilising resources in the community during preparation for discharge. 87 The comprehensive assessment and response training system unit provides crisis stabilisation, but also aims to connect young people to ongoing services in either community or hospital settings. 72
Services provided in educational settings, including examples organised using telephone and text responses, include the option of opening up routes for onward referral and long-term support. 77,127,171 The PEACE protocol, used in the high-school setting, supports systematic assessments of risk and helps guide decision-making, and includes the option in individual plans of action to mobilise external services or to arrange follow-ups. 60,69,73 A service running as an alternative to the emergency department for school students in crisis has the goal of linking young people to ongoing services. 136
Support-based crisis response services involving the use of technology similarly include goals of linking young people to other services where necessary. For example, a website and online message board service in which messages are monitored by trained volunteers who make onward referrals as needed,118 and text-based services that include, in their goals, the direction of people who make contact towards longer-term help. 104,109
To provide peer support
Two services in two reports101,118 described the goal of providing peer support. One report101 described Teen Line, which is a telephone service in which carefully selected, trained and supported high-school student volunteers respond to calls received by other young people in crisis. 101 Another report118 described an internet-based service in which young people are able to read information and also participate in an online message board addressing ‘suicide’. Messages are monitored by trained peers and serve as a means of providing and receiving support. 118
To stabilise and manage crisis
A stated goal of 35 crisis response services cited across 50 reports32–34,57,60–62,64,66,68–70,72,73,75,77–84,86–88,93,98, 102,103,105–107,110–114,120,122,125,126,129–132,136,147–149,171 is to stabilise and manage the young person’s crisis in the immediate period, using combinations of emergency department-based interventions, hospital care and care on an outpatient or community basis.
Responses located in the emergency department setting with the clear aim of immediately stabilising and managing a crisis include services linked to the goal of avoiding admission. 122 FISP aims to directly minimise the risk of suicidal behaviour. 33,57,147 The FBCI, as a single-session intervention, aims to assess and stabilise, with a focus on safety planning and non-judgemental collaboration. 32,84,107 The soap opera-style videotape approach aims to immediately plan for foreseeable suicide-eliciting scenarios in the future,82,83,111 whereas rapid response models to follow-up from the emergency department have been used to stabilise and manage the crisis. 34,86,88,93,120 Led by emergency department medical officers, one model begins with the structured assessment of need to inform decision-making. 132 The location of a mental health team in the emergency department is also described in a service that has the goal of working with the emergency department medical team to de-escalate crises and promote safety. 75 The crisis and transition services programme aims to stabilise crises while aiding transition to community services. 148
Three services described in a single descriptive paper,110 that is, KidsLink,WAARM and the enhanced care coordination initiative, all centre on the provision of responses to stabilise. 110 Triage within an evaluation centre receiving referrals from the emergency department and other sources is described in a service in which safety planning and suicide risk reduction are initial goals. 66 Crisis services as part of an all-inclusive approach to young people’s mental health care aims to offer rapid management of crisis. 149 In a further service, crisis workers have options to refer to either inpatient or intensive community care, with the aim of providing an immediate response. 102 Multiple descriptions62,68,113,114,130 are also found of mobile crisis services that aim to stabilise and manage the immediate crisis.
Specific models of intervention include examples explicitly identifying the initial aim of managing the crisis or, for example, providing ‘containment’. 131 Other service goals include ensuring physical, emotional and relational safety, including through partnerships with wider networks, as with the safety first model. 125,126 Brief stabilisation is also the goal of models preventing hospital admission, such as the HBCI and HBCI+ approaches61,103 (i.e. services offering daily contact105 and MST64,78–81,112).
In hospital settings, acting swiftly to respond to crisis following a suicide attempt has been identified as a goal so that young people do not trivialise their self-harm attempt. 129 The options to provide inpatient care as a stabilisation response or to immediately refer for community care are also described in an integrated model. 106 The MST approach, when used in the inpatient setting, has the goal of resolving crisis, using an ecological approach that locates the individual in their broader context. 112 The CARES programme describes its goals as one of rapid stabilisation in a residential unit. 72 Short admissions, when necessary, combined with intensive home treatment is also described in services that set out to reduce self-harming behaviour using specific psychological and medical therapies. 98 Crisis stabilisation, in hospital and over a short period, is also the goal of services in which risk reduction is a key aim,87 along with providing a level of immediate care beyond what can be achieved in the community. 70
Services with goals to immediately stabilise and manage exist in education settings. 60,69,73,77,136,171 The PEACE protocol60,69,73 is an in-school facility in which high school-aged children can be assessed by psychology services before referral on to appropriate mental health services (see Chapter 4, Educational settings). The PEACE protocol receives referrals from anyone in the school system and aims to guide interventions tailored to the level of risk. The multitiered system of support model is a comprehensive school-based programme with a tiered approach, at the top of which is a crisis intervention component to manage acute need. 77 Services for university students in the UK include initial responses from staff aiming at stabilising the crisis,171 whereas the urgent evaluation service offers a rapid response to the management of crisis in school students as an alternative to emergency department presentation. 136
To train and supervise staff
Ten services described in 14 reports61,82,83,85,103,110–112,115,119,122,125,126,132 include the goal of training and supervising of staff. More specially, this includes:
-
the training of emergency department staff in the use of a triage tool115
-
the training of emergency department medical officers in the use of an assessment tool132
-
the education of staff in the emergency department, crisis and wider primary care, and school system in the use of a rapid response model122
-
the education and training for emergency department staff to use HEARTSMAP (i.e. a tool used to inform assessments and decision-making)119
-
an emergency department-based model combining a video and family therapy, which includes the goal of training emergency department, mental health and other staff as part of the overall service82,83,111
-
the training of emergency department staff as part of a well-resourced emergency department service offering crisis intervention85
-
training and supervision as part of the community-based SFAI approach125,126
-
the home-based HBCI approach, which begins with 4 days of training in the homebuilder’s model for staff103
-
increasing the clinical supervision offered to therapists, with this being provided by child psychiatrists as part of providing community-based MST112
-
the training of school crisis teams to use a standardised risk assessment and the education of paediatricians about a crisis hotline (i.e. KidsLink). 110
Summary
In this evidence synthesis, we have elicited what the goals of a crisis service should be and, in brief, these are to (1) keep CYP in their home environment; (2) facilitate the assessment of the child or young person’s needs, offering a stabilisation of the crisis; (3) improve CYP and their family’s engagement with community treatment; and (4) link CYP to ongoing mental health services, as necessary, using peer support when possible. Some crisis services include training and/or supervision of others as part of their function. The goals have been identified from policy and empirical evidence, most of which were generated outside the UK. Nevertheless, the goals resonate with practice in the UK, with the key goals of stabilising the immediate crisis and identifying ongoing mental health support being common drivers for crisis services.
Chapter 8 Discussion and conclusions
This project was conducted using EPPI-Centre methods of engaging with stakeholders through a number of routes. The SAG and the two co-applicants who identified themselves as experts by experience, that is, current or previous users of mental health services, helped with the identification of key search terms, with the location of UK-only grey literature documents, with the sense-making of our findings and with dissemination strategies. For the evidence synthesis overall, comprehensive searching was conducted across 17 databases. Supplementary searching included online searches using Google, targeted interrogation of organisational websites and of journal tables of content, scanning reference lists of included studies and forward citation tracking.
One hundred and thirty-eight publications were used to inform this evidence synthesis, which included 39 descriptive accounts of the organisation of crisis services (across 36 reports), 42 primary research studies (across 48 reports) and 54 UK-only grey literature documents.
For the purpose of this evidence synthesis, CYP were defined as those aged between 5 and 25 years. There was some debate in the design of this study on the age boundaries; however, we felt that children aged < 5 years were unlikely to have a mental health crisis and when challenges in their behaviour existed this would be addressed by health visiting and equivalent services. There was a number of options for the upper age limit for this evidence synthesis. We were aware from clinical colleagues that some services operate to aged 16 years and others to aged 18 years, and we were aware of the emergence of ‘youth’ mental health services that often span ages 14–25 years. With the aim of being as inclusive as possible, for the purposes of this evidence synthesis, we selected 25 years as the upper age limit to capture any research on services or models for youth.
As a defining boundary, we considered a crisis response to be the provision of a service in the context of extreme psychosocial distress, which for CYP may be provided in any location, such as an emergency department, a specialist or non-specialist community service, a school, a college, a university, a youth group or via a crisis support line.
In this evidence synthesis, we have elicited what the goals of a crisis service should be and, in brief, these are to (1) keep CYP in their home environment; (2) facilitate the assessment of the child or young person’s needs, offering a stabilisation of the crisis; (3) improve CYP and their family’s engagement with community treatment; and (4) link CYP to ongoing mental health services, as necessary, using peer support when possible. Some crisis services include training and/or supervision of others as part of their function. Despite multiple approaches to the organisation and provision of mental health crisis care (see Chapter 4), there was moderate evidence that CYP and their families did not know how to access such services, and may not have been eligible because of threshold criteria. Even when accessing services, some CYP were not able to talk while they were in crisis and there was high-quality evidence94,97,100 that alternative methods of communicating, such as text, telephone and online provision, were welcomed. There was moderate evidence that CYP would like access to peers at this time or to be able to access age-appropriate services that is available out of hours. Attendance at the emergency department was the default service, given the lack of alternatives, and this was described as stressful for the CYP and experienced as noisy, busy and generally unsuitable. There was evidence to suggest that much of the care provided in the emergency department was effective, including improvement of family functioning following a crisis service or intervention initiated in the emergency department, increased referral for the CYP to intensive outpatient care after being seen in the emergency department, increased satisfaction with crisis services, reduction in psychiatric symptoms and improvement in psychosocial functioning, and no increase in rate of attendance for crisis care after being seen in the emergency department.
One of the dilemmas posed by this review is that, philosophically, emergency departments are not designed to manage crises for mental health for any age; however, in this review, we found that actually there was a significant number of innovative models located in emergency departments that were both effective and acceptable for CYP experiencing such a presentation. The challenge is to develop services that are available prior to a crisis and in an accessible and available location, providing service outside office hours, with appropriately skilled professionals, to reduce the use of emergency departments for this purpose. This review specifically looked at the international literature to learn from models beyond the UK. It was surprising that most of the studies retrieved through this review originated from the USA. Comparisons between health-care provision in the USA and in UK are difficult because of the different ways in which health care is both commissioned and delivered. There was also a lack of studies that described how different services were integrated, particularly so in relation to the UK and, therefore, this was not commented on. Subsequently, direct applicability of findings from the review to the UK is not possible, but there are principles about practice that can be adapted and used to inform service development. In the UK, as a general principle, it is not advocated that emergency departments become a key service to support CYP in mental health crisis; however, where this needs to happen, owing to limited services elsewhere, there are evidence-based practices and processes elicited from this review that could be embraced.
Of the 27 synthesis summary statements that were assessed for confidence using the CERQual approach, only two were judged as having a high degree of confidence. When a synthesised review finding is assessed as being ‘high confidence’, then this indicates that this should be seen as a reasonable representation of the evidence relating to the phenomenon of interest. The statements of high confidence for this evidence synthesis related to what CYP wanted from crisis services, which was centred around the need for different forms of support and pathways to services. This included support through telephone (via a direct line, with out-of-hours availability and staffed by trained counsellors), as well as via text and e-mail. Despite the availability of evidence from CYP and their families about acceptability, much of this was not rated as being of good quality and, therefore, ought not be used to inform developments.
Implications for practice and service development
In considering implications for practice and service development following this evidence synthesis, we were mindful that the included literature was predominantly from outside the UK, in countries such as the USA where the model of health-care delivery is quite different from that in the UK. In addition, we considered the strength of evidence as well as contextual issues to make recommendations that could be relevant and applicable to the UK. The GRADE and CERQual assessments presented in earlier chapters are explicitly drawn on in this section and with particular weight given to the two summary statements for which there was a high degree of confidence and, for the 14 summary statements for which there was a moderate degree of confidence, cautious recommendations are offered.
Key implications
-
A high degree of confidence existed in the synthesised evidence relating to crisis responses using telephone, text and e-mail, and in the synthesised evidence relating to direct line telephone access with round-the-clock support from trained staff.When taken together, the evidence has important implications for future service commissioning. It is suggested that in the development or review of crisis services, the inclusion of text, telephone and e-mail could be helpful as a component of a 24-hour service model.
-
Several of the synthesis statements that were rated as having a moderate degree of confidence related to the barriers to and facilitators of seeking and accessing appropriate support. As CYP and families did not know how to access crisis care, better signposting and information using family-friendly language possibly co-produced with CYP and avoiding the use of jargon on how to locate the right service are important. Addressing the thresholds of eligibility that exist that make access to specialist services and professionals difficult and making crisis services easier to access for those with financial or transport issues are also priority areas for CYP and families.
-
A moderate degree of confidence was found in the synthesised evidence relating to CYP feeling that peer support and involving those with lived experience of mental health crisis within services was important, or CYP feeling that services should cater specifically for them and be targeted at specific age groups. When new services are being commissioned or existing services developed, it might be helpful to include representatives from a panel of CYP to advise on aspects of service design to address age appropriateness of facilities.
-
What this evidence synthesis has identified, with a moderate degree of confidence, is that, because of long wait times for specialist services, services provided by emergency departments are a central component to mental health crisis care for CYP. This is offered as a recommendation with caution, given the unique structure and function of the NHS compared with health services overseas, but an acknowledgement that there might be aspects to be drawn from the evidence that could inform operating processes in UK emergency departments where CYP present with mental health crises. We acknowledge that the quality of evidence from intervention studies was low. Therefore, caution is recommended before applying this for service development, but these are issues that might need considering in service developments and design of future research projects. It is clear is that crisis care and assessment initiated within the emergency department can result in a number of positive outcomes for CYP. To strengthen this, services need to be developmentally appropriate, staff in emergency department need a level of expertise with this client group, and the environment needs to offer privacy and a calm environment. The emergency department also needs to be networked with outpatient care, where there is transparency about eligibility and 24-hour availability. The emergency department environment itself could benefit from creating a separate area to address the concerns about the noisy and busy environment, the lack of privacy and poor staff attitudes. Admission processes could be streamlined.
-
Services should consider pathways in and out of crisis, as there was evidence, with a moderate degree of confidence, of a general lack of support before crisis was reached, as well as with the assessment, management and level of follow-up care of those CYP who presented in crisis to an emergency department. Mental health support networks could be strengthened to increase the possibility of CYP being able to access early and appropriate support within their community to prevent episodes of crisis. Accessible community-based early intervention support with shorter waiting times is, therefore, important. This has relevance for the UK context, with investment in preventative and supportive services offering care in a way that might reduce the chance of a CYP experiencing a mental health crisis.
-
School-, community- and home-based crisis programmes also appeared to be associated with a number of positive outcomes for CYP. However, it is important that a variety of different modes of crisis support (e.g. telephone, e-mail, text based, in person) are available so that CYP can access these in the way that is most convenient for them.
Implications for future research
-
With most of the research evidence being generated in the USA, and only three research studies included in this evidence synthesis being completed in the UK, a clear case exists for the commissioning of new, high-quality studies investigating the organisation, delivery and effectiveness of the range of existing services that provide crisis responses to CYP in the UK.
-
Given that the importance of out-of-hours support for CYP in crisis was highlighted by a number of stakeholders, further research could usefully explore the precise types of support that would be most useful in out-of-hours situations, including whether or not this would need to be available 24/7 and what form it would take (e.g. a drop-in centre, telephone support or face to face).
-
Further research needs to identify precisely which kinds of community support would be most effective in preventing CYP from reaching mental health crisis.
-
A number of different types of crisis intervention models have been shown to be associated with positive outcomes for CYP and, therefore, it would be helpful to (1) identify whether or not particular interventions/models are more effective for different subgroups of CYP and (2) explore the distinct needs of particular subgroups of CYP when in crisis.
-
Much of the evidence about acceptability from CYP and their families was not of good quality and so further good-quality research into this aspect is justified.
Limitations
In advance of conducting this evidence synthesis, we had anticipated that there would be a body of empirical research that reported on a range of social, education and health innovations relating to supporting CYP in mental health crisis in both the UK and overseas. However, the validity of the results is limited by the methods of the included studies, as there was a lack of high-quality research from well-conducted RCTs. The literature that informed this evidence synthesis was largely drawn from the USA. There were papers from other countries, but there was a paucity of UK-based empirical research and so generalisability to a UK audience is limited. Reported in the literature was a wide range of types of intervention within each setting. As a result, it is not possible to conduct a meta-analysis or to make comparisons about these and determine their efficacy and, therefore, only general conclusions are made. A decision was made to include UK-only policy and guidance, but this was prior to the discovery that most research evidence that met our criteria for inclusion was from outside the UK. Therefore, this might be considered a limitation of the scope of the evidence synthesis. The age range for this evidence synthesis attempted to capture research that was relevant for CYP up to age 18 years and also to capture emerging literature that might have been available for youths (i.e. age 18–25 years). There were three studies71,94,100 that reported only for young people over the age of 16 years and so the evidence was predominantly children and early adolescents.
Acknowledgements
The team are grateful to all members of the SAG and particularly to the group’s independent chairperson Dr Michael Coffey for their time, energy and expertise.
Contributions of authors
Nicola Evans (https://orcid.org/0000-0001-5154-0478) (Reader) contributed to the development of the protocol; screened, selected, appraised and synthesised reports; and wrote for and edited the final report.
Deborah Edwards (https://orcid.org/0000-0003-1885-9297) (Research Fellow) contributed to the development of the protocol; screened, selected, appraised and synthesised reports; and wrote for and edited the final report.
Judith Carrier (https://orcid.org/0000-0002-2657-2280) (Reader) contributed to the development of the protocol; screened, selected, appraised and synthesised reports; and wrote for and edited the final report.
Mair Elliott (https://orcid.org/0000-0002-0472-436X) (Public and Patient Project Member) contributed to the development of the protocol, screened reports and commented on the final report.
Elizabeth Gillen (https://orcid.org/0000-0002-3700-3913) (Subject Librarian) contributed to the development of the protocol, searched for reports, and wrote for and edited the final report.
Ben Hannigan (https://orcid.org/0000-0002-2512-6721) (Professor of Mental Health Nursing) contributed to the development of the protocol; screened, selected, appraised and synthesised reports; and wrote for and edited the final report.
Rhiannon Lane (https://orcid.org/0000-0002-4964-2472) (Research Associate) contributed to the development of the protocol; screened, selected, appraised and synthesised reports; and commented on the final report.
Liz Williams (https://orcid.org/0000-0001-5936-2987) (Public and Patient Project Member) contributed to the development of the protocol, screened reports and commented on the final report.
Data-sharing statement
All available data can be obtained by contacting the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care.
References
Appendix 1 Final search strategies
MEDLINE
Date searched: February 2020 (updated January 2021).
Date range searched: from database inception.
Search strategy
| # | Search term | Result |
|---|---|---|
| 1 | exp Adolescent/ | 1,994,329 |
| 2 | exp Child/ | 1,881,002 |
| 3 | exp Young Adult/ | 812,513 |
| 4 | exp Students/ | 124,926 |
| 5 | adolescen*.tw | 269,263 |
| 6 | teen*.tw | 29,733 |
| 7 | child*.tw | 1,351,093 |
| 8 | “young person”.tw | 1024 |
| 9 | “young adult*”.tw | 91,753 |
| 10 | “young people”.tw | 26,245 |
| 11 | “young patient*”.tw | 28,302 |
| 12 | youth*.tw | 71,671 |
| 13 | Juvenile*.tw | 79,683 |
| 14 | p?ediatric*.tw | 339,038 |
| 15 | student*.tw | 270,751 |
| 16 | pupil*.tw | 28,442 |
| 17 | “young offender*”.tw | 474 |
| 18 | OR 1-17 | 4,157,532 |
| 19 | exp Crisis Intervention/ | 5611 |
| 20 | crisis.tw | 48,352 |
| 21 | crises.tw | 10,317 |
| 22 | “rapid response”.tw | 5862 |
| 23 | OR 19-22 | 65,249 |
| 24 | exp Mental Health/ | 36,655 |
| 25 | exp Mental Disorders/ | 1,216,222 |
| 26 | exp Psychology, Adolescent/ | 13,386 |
| 27 | exp Psychology, Child/ | 13,244 |
| 28 | exp Adolescent Psychiatry/ | 2811 |
| 29 | exp Child Psychiatry/ | 5551 |
| 30 | exp Community Psychiatry/ | 2008 |
| 31 | exp Mental Health Services/ | 93,977 |
| 32 | exp Community Mental Health Centers | 3205 |
| 33 | mental*.tw | 343,355 |
| 34 | psych*.tw | 794,644 |
| 35 | camhs.tw | 359 |
| 36 | exp Suicide/ | 61,612 |
| 37 | exp Self-Injurious Behavior/ | 69,276 |
| 38 | suicid*.tw | 75,153 |
| 39 | “self-harm”.tw | 5117 |
| 40 | “self-injur*”.tw | 4582 |
| 41 | OR 24-40 | 1,944,932 |
| 42 | 18 AND 23 AND 41 | 4773 |
| 43 | (mental adj5 emergenc*).tw | 1360 |
| 44 | (psych* adj5 emergenc*).tw | 4795 |
| 45 | (mental adj3 “critical incident*”).tw | 6 |
| 46 | (psych* adj3 “critical incident*”).tw | 28 |
| 47 | (mental adj3 urgent).tw | 55 |
| 48 | (psych* adj3 urgent).tw | 130 |
| 49 | (mental adj3 distress).tw | 2344 |
| 50 | (psych* adj3 distress).ti | 5164 |
| 51 | OR 43-50 | 13,476 |
| 52 | 18 AND 51 | 5088 |
| 53 | 42 OR 52 | 9600 |
PsycINFO
Date searched: February 2020 (updated January 2021).
Date range searched: from database inception.
Search strategy
| # | Search term | Result |
|---|---|---|
| 1 | adolecen*.tw | 254,388 |
| 2 | teen*.tw | 22,597 |
| 3 | child*.tw | 703,951 |
| 4 | “young person”.tw | 1306 |
| 5 | “young adult*”.tw | 49,386 |
| 6 | “young people”.tw | 28,017 |
| 7 | “young patient*”.tw | 1863 |
| 8 | youth*.tw | 99,634 |
| 9 | Juvenile*.tw | 27,204 |
| 10 | p?ediatric*.tw | 39,336 |
| 11 | student*.tw | 582,787 |
| 12 | pupil*.tw | 26,765 |
| 13 | “young offender*”.tw | 1400 |
| 14 | Students/ | 23,477 |
| 15 | OR 1-14 | 1,415,340 |
| 16 | Crisis Intervention/ | 3492 |
| 17 | Crises/ | 5392 |
| 18 | Crisis Intervention Services/ | 1422 |
| 19 | crisis.tw | 33,294 |
| 20 | crises.tw | 8634 |
| 21 | “rapid response”.tw | 781 |
| 22 | OR 16-21 | 40,364 |
| 23 | Mental Health/ | 63,465 |
| 24 | Mental Disorders/ | 82,887 |
| 25 | Adolescent Psychiatry/ | 4847 |
| 26 | Adolescent Psychology/ | 4021 |
| 27 | Child Psychiatry/ | 6655 |
| 28 | Child Psychology/ | 4280 |
| 29 | Community Psychiatry/ | 863 |
| 30 | Mental Health Services/ | 33,881 |
| 31 | Community Mental Health/ | 2021 |
| 32 | Emergency Services Psychiatric/ | 1153 |
| 33 | mental.tw | 421,441 |
| 34 | psych*.tw | 1,232,205 |
| 35 | camhs.tw | 600 |
| 36 | Suicide/ | 26,556 |
| 37 | Self-Injurious Behavior/ | 3909 |
| 38 | suicid*.tw | 64,162 |
| 39 | self-harm.tw | 5388 |
| 40 | self-injur*.tw | 6368 |
| 41 | OR 23-40 | 1,489,794 |
| 42 | 15 AND 22 AND 41 | 6056 |
| 43 | (mental adj5 emergenc*).tw | 1209 |
| 44 | (psych* adj5 emergenc*).tw | 5761 |
| 45 | (mental adj3 “critical incident*”).tw | 11 |
| 46 | (psych* adj3 “critical incident*”).tw | 87 |
| 47 | (mental adj3 urgent).tw | 35 |
| 48 | (psych* adj3 urgent).tw | 188 |
| 49 | (mental adj3 distress).tw | 2306 |
| 50 | (psych* adj3 distress).ti | 4933 |
| 51 | OR 43-50 | 14,076 |
| 52 | 15 AND 51 | 3749 |
| 53 | 42 OR 52 | 9555 |
EmCare
Date searched: February 2020 (updated January 2021).
Date range searched: from database inception.
Search strategy
| # | Search term | Result |
|---|---|---|
| 1 | exp child/ | 607,961 |
| 2 | exp adolescent/ | 326,461 |
| 3 | exp young adult/ | 61,127 |
| 4 | exp student/ | 153,306 |
| 5 | adolescen*.tw | 135,560 |
| 6 | teen*.tw | 14,730 |
| 7 | child.tw | 474,785 |
| 8 | “young person”.tw | 721 |
| 9 | “young adult*”.tw | 37,853 |
| 10 | “young people”.tw | 17,616 |
| 11 | “young patient*”.tw | 8505 |
| 12 | youth*.tw | 47,404 |
| 13 | juvenile*.tw | 13,672 |
| 14 | p?ediatric*.tw | 141,558 |
| 15 | student*.tw | 158,682 |
| 16 | pupil*.tw | 7478 |
| 17 | “young offender*”.tw | 433 |
| 18 | OR 1-17 | 1,121,095 |
| 19 | exp crisis intervention/ | 1783 |
| 20 | crisis.tw | 17,506 |
| 21 | crises.tw | 3373 |
| 22 | “rapid response”.tw | 1810 |
| 23 | OR 19-22 | 22,301 |
| 24 | exp mental health/ | 93,023 |
| 25 | exp mental disease/ | 624,707 |
| 26 | exp child psychiatry/ | 5487 |
| 27 | exp child psychology/ | 2975 |
| 28 | exp social psychiatry/ | 884 |
| 29 | exp mental health service/ | 23,268 |
| 30 | exp community mental health/ | 2490 |
| 31 | mental*.tw | 163,139 |
| 32 | psych*.tw | 349,034 |
| 33 | camhs.tw | 339 |
| 34 | exp suicide/ | 20,791 |
| 35 | exp automutilation/ | 6698 |
| 36 | self-harm.tw | 3174 |
| 37 | self-injur*.tw | 2311 |
| 38 | OR 24-37 | 866,519 |
| 39 | 18 AND 23 AND 38 | 1749 |
| 40 | (mental adj5 emergenc*).tw | 850 |
| 41 | (psych* adj5 emergenc*).tw | 2175 |
| 42 | (mental adj3 “critical incident*”).tw | 5 |
| 43 | (psych* adj3 “critical incident*”).tw | 22 |
| 44 | (mental adj3 urgent).tw | 37 |
| 45 | (psych* adj3 urgent).tw | 67 |
| 46 | (mental adj3 distress).tw | 1444 |
| 47 | (psych* adj3 distress).ti | 2192 |
| 48 | OR 40-47 | 7609 |
| 49 | 18 AND 48 | 2192 |
| 50 | 39 OR 49 | 3851 |
Health Management Information Consortium
Date searched: February 2020 (updated January 2021).
Date range searched: from database inception.
Search strategy
| # | Search term | Result |
|---|---|---|
| 1 | exp children/ | 19,989 |
| 2 | exp young people/ | 10,769 |
| 3 | exp students/ | 3889 |
| 4 | adolescen*.tw | 3988 |
| 5 | teen*.tw | 1590 |
| 6 | child*.tw | 30,745 |
| 7 | “young person”.tw | 158 |
| 8 | “young adult*”.tw | 1000 |
| 9 | “young people”.tw | 5373 |
| 10 | “young patient*”.tw | 69 |
| 11 | youth*.tw | 2123 |
| 12 | juvenile*.tw | 560 |
| 13 | p?ediatric*.tw | 2602 |
| 14 | student”.tw | 6632 |
| 15 | pupil*.tw | 621 |
| 16 | “young offender*”.tw | 335 |
| 17 | OR 1-16 | 50,150 |
| 18 | exp Crisis Intervention/ | 121 |
| 19 | exp Crisis intervention services/ | 198 |
| 20 | crisis.tw | 2891 |
| 21 | crises.tw | 328 |
| 22 | “rapid response*”.tw | 128 |
| 23 | exp rapid response teams/ | 44 |
| 24 | OR 18-23 | 3310 |
| 25 | 17 AND 24 | 475 |
| 26 | (mental adj5 emergenc*).tw | 103 |
| 27 | (psych* adj5 emergenc*).tw | 181 |
| 28 | (mental adj3 “critical incident*”) | 0 |
| 29 | (psych* adj3 “critical incident*”) | 2 |
| 30 | (mental adj3 urgent).tw | 11 |
| 31 | (psych* adj3 urgent).tw | 12 |
| 32 | (mental adj3 distress).tw | 165 |
| 33 | (psych* adj3 distress).tw | 492 |
| 34 | OR 26-33 | 916 |
| 35 | 17 AND 34 | 177 |
| 36 | 25 OR 35 | 647 |
Cumulative Index to Nursing and Allied Health Literature
Date searched: February 2020 (updated January 2021).
Date range searched: from database inception.
Search strategy
| # | Search term | Result |
|---|---|---|
| 1 | (MH “Child”) | 419,380 |
| 2 | (MH “Adolescence+”) | 484,604 |
| 3 | (MH “Young Adult”) | 228,337 |
| 4 | (MH “Students+”) | 125,959 |
| 5 | TI adolescen* | 83,532 |
| 6 | AB adolescen* | 88,970 |
| 7 | TI teen* | 9117 |
| 8 | AB teen* | 10,721 |
| 9 | TI child* | 258,851 |
| 10 | AB child* | 323,474 |
| 11 | TI “young adult*” | 14,862 |
| 12 | AB “young adult*” | 24,894 |
| 13 | TI “young person” | 60 |
| 14 | AB “young person” | 630 |
| 15 | TI “young people” | 5969 |
| 16 | AB “young people” | 13,261 |
| 17 | TI “young patient*” | 1598 |
| 18 | AB “young patient*” | 4523 |
| 19 | TI youth* | 22,604 |
| 20 | AB youth* | 34,713 |
| 21 | TI juvenile* | 5729 |
| 22 | AB juvenile* | 6357 |
| 23 | TI p#ediatric* | 70,729 |
| 24 | AB p#ediatric* | 84,378 |
| 25 | TI student* | 72,977 |
| 26 | AB student* | 122,062 |
| 27 | TI pupil* | 1505 |
| 28 | AB pupil* | 3994 |
| 29 | TI “young offender*” | 200 |
| 30 | AB “young offender*” | 238 |
| 31 | OR 1-30 | 1,199,847 |
| 32 | (MH “Crisis Intervention”) | 3668 |
| 33 | TI crisis | 9364 |
| 34 | AB crisis | 13,752 |
| 35 | TI crises | 732 |
| 36 | AB crises | 13,752 |
| 37 | TI “rapid response*” | 945 |
| 38 | AB “rapid response*” | 1282 |
| 39 | OR 32-38 | 25,349 |
| 40 | (MH “Mental Health”) | 34,042 |
| 41 | (MH “Mental Disorders+”) | 524,045 |
| 42 | (MH “Adolescent Psychiatry”) | 1209 |
| 43 | (MH “Child Psychiatry”) | 1777 |
| 44 | (MH “Adolescent Psychology”) | 3655 |
| 45 | (MH “Child Psychology”) | 2879 |
| 46 | (MH “Community Mental Health Nursing”) | 1873 |
| 47 | (MH “Community Mental Health Services”) | 9725 |
| 48 | (MH “Mental Health Services+”) | 74,351 |
| 49 | TI mental* | 64,876 |
| 50 | AB mental* | 128,126 |
| 51 | TI psych* | 109,573 |
| 52 | AB psych* | 229,195 |
| 53 | TI camhs | 133 |
| 54 | AB camhs | 360 |
| 55 | (MH “Suicide+”) | 29,100 |
| 56 | (MH “Injuries, Self-Inflicted”) | 2356 |
| 57 | TI suicid* | 19,120 |
| 58 | AB suicid* | 21,513 |
| 59 | TI “self harm” | 1677 |
| 60 | AB “self harm” | 2928 |
| 61 | TI “self injur*” | 1479 |
| 62 | AB “self injur*” | 2022 |
| 63 | OR 40-62 | 825,803 |
| 64 | 31 AND 39 AND 63 | 2040 |
| 65 | TI mental N5 emergenc* | 437 |
| 66 | AB mental N5 emergenc* | 802 |
| 67 | TI psych* N5 emergenc* | 948 |
| 68 | AB psych* N5 emergenc* | 1489 |
| 69 | TI mental N3 “critical incident*” | 4 |
| 70 | AB mental N3 “critical incident*” | 9 |
| 71 | TI psych* N3 “critical incident*” | 4 |
| 72 | AB psych* N3 “critical incident*” | 18 |
| 73 | TI mental N3 urgent | 14 |
| 74 | AB mental N3 urgent | 59 |
| 75 | TI psych* N3 urgent | 22 |
| 76 | AB psych* N3 urgent | 74 |
| 77 | TI mental N3 distress | 372 |
| 78 | AB mental N3 distress | 1468 |
| 79 | TI psych* N3 distress | 3386 |
| 80 | OR 65-79 | 8034 |
| 81 | 31 AND 80 | 2702 |
| 82 | 64 OR 81 | 4624 |
Allied and Complimentary Medicine Database
Date searched: February 2020 (updated January 2021).
Date range searched: from database inception.
Search strategy
| # | Search term | Result |
|---|---|---|
| 1 | exp Child/ | 18,046 |
| 2 | exp Adolescent/ | 5872 |
| 3 | exp Students/ | 3434 |
| 4 | adolescen*.tw | 7622 |
| 5 | teen*.tw | 293 |
| 6 | child*.tw | 24,295 |
| 7 | “young person”.tw | 37 |
| 8 | “young adult*”.tw | 1660 |
| 9 | “young people”.tw | 684 |
| 10 | “young patient*”.tw | 155 |
| 11 | youth*.tw | 1270 |
| 12 | juvenile*.tw | 407 |
| 13 | p?ediatric*.tw | 3416 |
| 14 | student*.tw | 8312 |
| 15 | pupil*.tw | 209 |
| 16 | “young offender”.tw | 13 |
| 17 | OR 1-16 | 37,804 |
| 18 | crisis.tw | 512 |
| 19 | crises.tw | 77 |
| 20 | “rapid response”.tw | 29 |
| 21 | OR 18-20 | 587 |
| 22 | exp Mental Health/ | 2000 |
| 23 | exp Mental Disorders/ | 28,631 |
| 24 | exp Adolescent psychology/ | 51 |
| 25 | exp Child psychology/ | 90 |
| 26 | exp Community mental health service/ | 842 |
| 27 | exp Mental health services/ | 1695 |
| 28 | mental.tw | 16,759 |
| 29 | psych*.tw | 56,174 |
| 30 | camhs.tw | 9 |
| 31 | exp Suicide/ | 1281 |
| 32 | exp Self injurious behaviour | 256 |
| 33 | suicide*.tw | 1655 |
| 34 | “self-harm”.tw | 82 |
| 35 | “self-injur*”.tw | 330 |
| 36 | OR 22-35 | 76,269 |
| 37 | 17 AND 21 AND 36 | 51 |
| 38 | (mental adj5 emergenc*).tw | 25 |
| 39 | (psych* adj5 emergenc*).tw | 61 |
| 40 | (mental adj3 “critical incident*”).tw | 0 |
| 41 | (psych* adj3 “critical incident*”).tw | 0 |
| 42 | (mental adj3 urgent*).tw | 1 |
| 43 | (psych* adj3 urgent*).tw | 4 |
| 44 | (mental adj3 distress).tw | 67 |
| 45 | (psych* adj3 distress).tw | 795 |
| 46 | OR 38-45 | 930 |
| 47 | 17 AND 46 | 137 |
| 48 | 37 OR 47 | 187 |
Education Resources Information Center
Date searched: February 2020 (updated January 2021).
Date range searched: from database inception.
Search strategy
| # | Search term | Result |
|---|---|---|
| 1 | TI adolescen* OR teen* OR child* OR “young person” OR “young adult*” OR “young people” OR “young patient*” OR youth* OR juvenile* OR p#ediatric* OR student* OR pupil* OR “youth offender*” | 940,015 |
| 2 | AB adolescen* OR teen* OR child* OR “young person” OR “young adult*” OR “young people” OR “young patient*” OR youth* OR juvenile* OR p#ediatric* OR student* OR pupil* OR “youth offender*” | 355,288 |
| 3 | OR 1-2 | 966,788 |
| 4 | TI crisis OR crises OR “rapid response*” | 3803 |
| 5 | AB crisis OR crises OR “rapid response*” | 11,586 |
| 6 | OR 4-5 | 13,386 |
| 7 | TI mental* OR psych* OR camhs OR suicide* OR “self-harm” OR “self-injur*” | 41,082 |
| 8 | AB mental* OR psych* OR camhs OR suicide* OR “self-harm” OR “self-injur*” | 120,360 |
| 9 | OR 7-8 | 127,708 |
| 10 | 3 AND 6 AND 9 | 1048 |
| 11 | TI mental N5 emergenc* | 9 |
| 12 | AB mental N5 emergenc* | 77 |
| 13 | TI mental N3 (“critical incident*” OR urgent OR distress) | 16 |
| 14 | AB mental N3 (“critical incident*” OR urgent OR distress) | 103 |
| 15 | TI psych* N3 (“critical incident*” OR urgent OR distress) | 332 |
| 16 | AB psych* N3 (“critical incident*” OR urgent OR distress) | 1127 |
| 17 | TI psych* N5 emergenc* | 46 |
| 18 | AB psych* N5 emergenc* | 151 |
| 19 | OR 11-18 | 1518 |
| 20 | 3 AND 19 | 952 |
| 21 | 10 OR 20 | 1972 |
Applied Social Sciences Index and Abstracts
Date searched: February 2020 (updated January 2021).
Date range searched: from database inception.
Search strategy
| # | Search term | Result |
|---|---|---|
| 1 | MAIN SUBJECT EXACT (“Adolescents”) | 25,366 |
| 2 | MAIN SUBJECT EXACT (“Children”) | 51,450 |
| 3 | MAIN SUBJECT EXACT (“Young adult”) | 9892 |
| 4 | MAIN SUBJECT EXACT (“Students”) | 23,077 |
| 5 | ti (adolescen* OR teen* OR child* OR “young person” OR “young adult*” OR “young people” OR “young patient*” OR youth* OR juvenile* OR p*ediatric OR student* OR pupil* OR “young offender*” | 197,417 |
| 6 | ab (adolescen* OR teen* OR child* OR “young person” OR “young adult*” OR “young people” OR “young patient*” OR youth* OR juvenile* OR p*ediatric OR student* OR pupil* OR “young offender*” | 318,691 |
| 7 | OR 1-6 | 346,143 |
| 8 | MAIN SUBJECT EXACT (“Crisis Intervention”) | 688 |
| 9 | MAIN SUBJECT EXACT (“Crisis”) | 227 |
| 10 | MAIN SUBJECT EXACT (Crisis Management”) | 71 |
| 11 | ti (crisis OR crises OR “rapid response*”) | 4085 |
| 12 | ab (crisis OR crises OR “rapid response*”) | 10,582 |
| 13 | OR 8-12 | 12,668 |
| 14 | MAIN SUBJECT EXACT (“Mental Health Care”) | 11,881 |
| 15 | MAIN SUBJECT EXACT (“Psychiatric disorders”) | 5721 |
| 16 | MAIN SUBJECT EXACT (“Adolescent psychiatry”) | 418 |
| 17 | MAIN SUBJECT EXACT(“Child psychiatry”) | 514 |
| 18 | MAIN SUBJECT EXACT (“Community psychiatric nursing”) | 83 |
| 19 | MAIN SUBJECT EXACT (Community mental health services) | 3291 |
| 20 | MAIN SUBJECT EXACT (“Mental health services”) | 9989 |
| 21 | ti (mental* OR psych* OR camhs) | 49,405 |
| 22 | ab (mental* OR psych* OR camhs) | 112,609 |
| 23 | MAIN SUBJECT EXACT (“Suicide”) | 4465 |
| 24 | ti (suicide* OR “self-harm” OR “self harm” OR “self-injur*” OR “self injur*) | 10,201 |
| 25 | ab (suicide* OR “self-harm” OR “self harm” OR “self-injur*” OR “self injur*) | 15,950 |
| 26 | OR 14-25 | 141,857 |
| 27 | 7 AND 13 AND 26 | 544 |
| 28 | ti (mental N/5 emergenc*) | 132 |
| 29 | ab (mental N/5 emergenc*) | 314 |
| 30 | ti (psych* N/5 emergenc*) | 44 |
| 31 | ab (psych* N/5 emergenc*) | 174 |
| 32 | ti (mental N/3 (“critical incident*” OR urgent OR distress)) | 190 |
| 33 | ab (mental N/3 (“critical incident*” OR urgent OR distress)) | 884 |
| 34 | ti (psych* N/3 (“critical incident*” OR urgent OR distress)) | 22 |
| 35 | ab (psych* N/3 (“critical incident*” OR urgent OR distress)) | 102 |
| 36 | OR 28-35 | 1622 |
| 37 | 7 AND 36 | 441 |
| 38 | 27 OR 37 | 960 |
Sociological Abstracts
Date searched: February 2020 (updated January 2021).
Date range searched: from database inception.
Search strategy
| # | Search term | Result |
|---|---|---|
| 1 | MAIN SUBJECT EXACT (“Adolescents”) | 27,118 |
| 2 | MAIN SUBJECT EXACT (“Children”) | 39,326 |
| 3 | MAIN SUBJECT EXACT (“Young adults”) | 8902 |
| 4 | ti (adolescen* OR teen* OR child* OR “young person” OR “young adult*” OR “young people” OR “young patient*” OR youth* OR juvenile* OR p*ediatric OR student* OR pupil* OR “young offender*” | 134,124 |
| 5 | ab (adolescen* OR teen* OR child* OR “young person” OR “young adult*” OR “young people” OR “young patient*” OR youth* OR juvenile* OR p*ediatric OR student* OR pupil* OR “young offender*” | 266,404 |
| 6 | OR 1-5 | 290,185 |
| 7 | MAIN SUBJECT EXACT (“Crisis Intervention”) | 336 |
| 8 | ti (crisis OR crises OR “rapid response*”) | 14,637 |
| 9 | ab (crisis OR crises OR “rapid response*”) | 38,885 |
| 10 | OR 7-9 | 45,629 |
| 11 | MAIN SUBJECT EXACT (“Mental Health Services”) OR MAIN SUBJECT EXACT (“Community Mental Health Centres”) OR MAIN SUBJECT EXACT (“Mental Health”) OR MAIN SUBJECT EXACT (“Community Mental Health”) | 14,454 |
| 12 | ti (mental* OR psych* OR camhs) | 21,006 |
| 13 | ab (mental* OR psych* OR camhs) | 63,754 |
| 14 | MAIN SUBJECT EXACT (“Suicide”) | 3319 |
| 15 | ti (suicide* OR “self-harm” OR “self harm” OR “self-injur*” OR “self injur*) | 5419 |
| 16 | ab (suicide* OR “self-harm” OR “self harm” OR “self-injur*” OR “self injur*) | 8669 |
| 17 | OR 11-16 | 80,940 |
| 18 | 6 AND 10 AND 17 | 517 |
| 19 | ti (mental N/5 emergenc*) | 16 |
| 20 | ab (mental N/5 emergenc*) | 85 |
| 21 | ti (psych* N/5 emergenc*) | 27 |
| 22 | ab (psych* N/5 emergenc*) | 101 |
| 23 | ti (mental N/3 (“critical incident*” OR urgent OR distress)) | 109 |
| 24 | ab (mental N/3 (“critical incident*” OR urgent OR distress)) | 435 |
| 25 | ti (psych* N/3 (“critical incident*” OR urgent OR distress)) | 2 |
| 26 | ab (psych* N/3 (“critical incident*” OR urgent OR distress)) | 49 |
| 27 | OR 19-26 | 727 |
| 28 | 6 AND 27 | 171 |
| 29 | 18 OR 28 | 679 |
Social Services Abstracts
Date searched: April 2020 (updated January 2021).
Date range searched:
Search strategy
| # | Search term | Result |
|---|---|---|
| 1 | MAIN SUBJECT EXACT (“Adolescents”) | 15,154 |
| 2 | MAIN SUBJECT EXACT (“Children”) | 23,483 |
| 3 | MAIN SUBJECT EXACT (“Young adults”) | 3598 |
| 4 | ti (adolescen* OR teen* OR child* OR “young person” OR “young adult*” OR “young people” OR “young patient*” OR youth* OR juvenile* OR p*ediatric OR student* OR pupil* OR “young offender*” | 83,569 |
| 5 | ab (adolescen* OR teen* OR child* OR “young person” OR “young adult*” OR “young people” OR “young patient*” OR youth* OR juvenile* OR p*ediatric OR student* OR pupil* OR “young offender*” | 117,890 |
| 6 | OR 1-5 | 131,762 |
| 7 | MAIN SUBJECT EXACT (“Crisis Intervention”) | 620 |
| 8 | ti (crisis OR crises OR “rapid response*”) | 2361 |
| 9 | ab (crisis OR crises OR “rapid response*”) | 6549 |
| 10 | OR 7-9 | 7866 |
| 11 | MAIN SUBJECT EXACT (“Mental Health Services”) | 7433 |
| 12 | MAIN SUBJECT EXACT (“Community Mental Health Centres”) | 781 |
| 13 | MAIN SUBJECT EXACT (“Mental Health”) | 13,119 |
| 14 | MAIN SUBJET EXACT (“Community Mental Health”) | 1325 |
| 15 | ti (mental* OR psych* OR camhs) | 17,027 |
| 16 | ab (mental* OR psych* OR camhs) | 35,736 |
| 17 | MAIN SUBJECT EXACT (“Suicide”) | 1577 |
| 18 | ti (suicide* OR “self-harm” OR “self harm” OR “self-injur*” OR “self injur*) | 2781 |
| 19 | ab (suicide* OR “self-harm” OR “self harm” OR “self-injur*” OR “self injur*) | 4454 |
| 20 | OR 11-19 | 45,980 |
| 21 | 6 AND 10 AND 20 | 410 |
| 22 | ti (mental N/5 emergenc*) | 35 |
| 23 | ab (mental N/5 emergenc*) | 116 |
| 24 | ti (psych* N/5 emergenc*) | 12 |
| 25 | ab (psych* N/5 emergenc*) | 20 |
| 26 | ti (mental N/3 (“critical incident*” OR urgent OR distress)) | 70 |
| 27 | ab (mental N/3 (“critical incident*” OR urgent OR distress)) | 345 |
| 28 | ti (psych* N/3 (“critical incident*” OR urgent OR distress)) | 0 |
| 29 | ab (psych* N/3 (“critical incident*” OR urgent OR distress)) | 17 |
| 30 | OR 22-29 | 547 |
| 31 | 6 AND 30 | 149 |
| 32 | 21 OR 31 | 544 |
Scopus
Date searched: February 2020 (updated January 2021).
Date range searched: from database inception.
Search strategy
| # | Search term | Result |
|---|---|---|
| 1 | TITLE (adolescen* OR teen* OR child* OR “young person” OR “young adult*” OR “young people” OR “young patient*” OR youth* OR juvenile* OR paediatric* OR pediatric* OR student* OR pupil* OR “young offender” | 1,707,464 |
| 2 | ABS (adolescen* OR teen* OR child* OR “young person” OR “young adult*” OR “young people” OR “young patient*” OR youth* OR juvenile* OR paediatric* OR pediatric* OR student* OR pupil* OR “young offender” | 3,033,729 |
| 3 | OR 1-2 | 3,569,657 |
| 4 | TITLE (crisis OR crises OR “rapid response*” | 84,062 |
| 5 | ABS (crisis OR crises OR “rapid response*” | 214,600 |
| 6 | OR 4-5 | 257,464 |
| 7 | TITLE (mental* OR psych* OR camhs OR suicid* OR “self-harm” OR “self-injur*” | 744,496 |
| 8 | ABS (mental* OR psych* OR camhs OR suicid* OR “self-harm” OR “self-injur*” | 1,652,030 |
| 9 | OR 7-8 | 1,954,700 |
| 10 | 3 AND 6 AND 9 | 4477 |
| 11 | TITLE (mental W/5 emergenc*) | 628 |
| 12 | ABS (mental W/5 emergenc*) | 1744 |
| 13 | TITLE (psych* W/5 emergenc*) | 3235 |
| 14 | ABS (psych* W/5 emergenc*) | 5776 |
| 15 | TITLE (mental W/3 distress) | 717 |
| 16 | ABS (mental W/3 distress) | 3380 |
| 17 | TITLE (psych* W/3 distress) | 6769 |
| 18 | TITLE (mental W/3 (“critical incident*” OR urgent)) | 25 |
| 19 | ABS (mental W/3 (“critical incident*” OR urgent)) | 120 |
| 20 | TITLE (psych* W/3 (“critical incident*” OR urgent)) | 77 |
| 21 | ABS (psych* W/3 (“critical incident*” OR urgent)) | 356 |
| 22 | OR 11-21 | 19,877 |
| 23 | 3 AND 22 | 4408 |
| 24 | 10 OR 23 | 8683 |
Web of Science
Date searched: February 2020 (updated January 2021).
Date range searched: from database inception.
Search strategy
| # | Search term | Result |
|---|---|---|
| 1 | TOPIC (adolescen* OR teen* OR child* OR “young person” OR “young adult*” OR “young people” OR “young patient*” OR youth* OR juvenile* OR p$ediatric* OR student* OR pupil* OR “young offender” | 3,159,103 |
| 2 | TOPIC (crisis OR crises OR “rapid response*” | 209,757 |
| 3 | TOPIC (mental* OR psych* OR camhs OR suicid* OR “self-harm” OR “self-injur*” | 1,588,843 |
| 4 | 1 AND 2 AND 3 | 3162 |
| 5 | TOPIC (mental NEAR/5 emergenc*) | 1573 |
| 6 | TOPIC (psych* NEAR/5 emergenc*) | 5627 |
| 7 | TOPIC (mental NEAR/3 distress) | 3075 |
| 8 | TOPIC (psych* NEAR/3 distress) | 7645 |
| 9 | TOPIC (mental NEAR/3 “critical incident*”) | 14 |
| 10 | TOPIC (psych* NEAR/3 “critical incident*”) | 41 |
| 11 | TOPIC (mental NEAR/3 urgent) | 93 |
| 12 | TOPIC (mental NEAR/3 urgent) | 242 |
| 13 | OR 5-12 | 17,724 |
| 14 | 1 AND 13 | 4288 |
| 15 | 4 OR 14 | 7263 |
Cochrane Central Register of Controlled Trials
Date searched: February 2020 (updated January 2021).
Date range searched: from database inception.
Search strategy
| # | Search term | Result |
|---|---|---|
| 1 | MeSH descriptor: [Adolescent] explode all trees | 100,693 |
| 2 | MeSH descriptor: [Child] explode all trees | 1236 |
| 3 | MeSH descriptor: [Young Adult] explode all trees | 258 |
| 4 | MeSH descriptor: [Students] explode all trees | 4080 |
| 5 | (adolescen* OR teen* OR child* OR “young adult” OR “young person” OR “young people” OR youth* OR juvenile* OR paediatric* OR pediatric* OR student* OR “young offender*”): ti, ab, kw (word variations have been searched) | 265,016 |
| 6 | OR 1-5 | 303,485 |
| 7 | MeSH descriptor: [Crisis Intervention] explode all trees | 152 |
| 8 | (Crisis OR crises): ti, ab, kw (word variations have been searched) | 3348 |
| 9 | MeSH descriptor: [Hospital Rapid Response Team] explode all trees | 13 |
| 10 | (“rapid response”): ti, ab, kw (word variations have been searched) | 355 |
| 11 | OR 7-10 | 3696 |
| 12 | MeSH descriptor: [Mental Health] explode all trees | 1379 |
| 13 | MeSH descriptor: [Mental Disorders] explode all trees | 70,204 |
| 14 | MeSH descriptor: [Psychology, Adolescent] explode all trees | 252 |
| 15 | MeSH descriptor: [Psychology, Child] explode all trees | 256 |
| 16 | MeSH descriptor: [Adolescent Psychiatry] explode all trees | 1379 |
| 17 | MeSH descriptor: [Child Psychiatry] explode all trees | 12 |
| 18 | MeSH descriptor: [Community Psychiatry] explode all trees | 15 |
| 19 | MeSH descriptor: [Mental Health Services] explode all trees | 6480 |
| 20 | MeSH descriptor: [Community Mental Health Services] explode all trees | 711 |
| 21 | MeSH descriptor: [Community Mental Health Centres] explode all trees | 112 |
| 22 | (mental* OR psych* OR camhs): ti, ab, kw (word variations have been searched) | 168,895 |
| 23 | MeSH descriptor: [Suicide] explode all trees | 1139 |
| 24 | MeSH descriptor: [Self-Injurious Behavior] explode all trees | 1342 |
| 25 | (suicid* OR “self harm” OR “self-harm” OR “self injur*” OR “self-injur*”): ti, ab, kw (word variations have been used) | 5891 |
| 26 | OR 12-25 | 198,618 |
| 27 | 6 AND 11 AND 26 | 411 |
| 28 | (mental NEAR/5 emergenc*: ti, ab, kw (word variations have been searched) | 110 |
| 29 | (psych* NEAR/5 emergenc*: ti, ab, kw (word variations have been searched) | 418 |
| 30 | (mental NEAR/3 “critical incident*”): ti, ab, kw (word variations have been searched) | 0 |
| 31 | (psych* NEAR/3 “critical incident*”): ti, ab, kw (word variations have been searched) | 3 |
| 32 | (mental NEAR/3 urgent): ti, ab, kw (word variations have been searched) | 7 |
| 33 | (psych* NEAR/3 urgent); ti, ab, kw (word variations have been searched) | 26 |
| 34 | (mental NEAR/3 distress): ti, ab, kw (word variations have been searched) | 259 |
| 35 | (psych* NEAR/3 distress): ti, ab, kw (word variations have been searched) | 489 |
| 36 | OR 28-35 | 1274 |
| 37 | 6 AND 36 | 394 |
| 38 | 27 OR 37 | 774 |
OpenGrey
Date searched: April 2020 (updated January 2021).
Date range searched: from database inception.
Search strategy
(crisis OR crises) AND (child* OR adolescen* OR teen* OR student* OR “young person” OR “young adult*” OR “young people” OR “young patient*” OR youth* OR juvenile* OR paediatric* OR pediatric OR pupil* OR “young offender*”)
Two hundred and twenty references found.
Electronic Theses Online Service and ProQuest Dissertations & Thesis database Open
Date searched: February 2020 (updated January 2021).
Date range searched: from database inception.
Search strategy
A series of basic keyword searches were compiled to search both EThOS and PQDT Open using the agreed terms used in the previous searches describing both population and crisis.
EThOS: 320 references found.
PQDT Open: 116 references found.
Criminal Justice Abstracts
Date searched: February 2020 (updated January 2021).
Date range searched: from database inception.
Search strategy
A series of basic keyword searches were compiled to search Criminal Justice Abstracts using the agreed terms used in the previous searches describing both population and crisis.
Zero references found.
Appendix 2 Table of studies excluded from the review
| Study | Reason for exclusion |
|---|---|
| Adams 190 | Not about intervention or care |
| Al et al. 191 | Focus on family crisis and child safety, rather than child crisis |
| Anderson et al. 192 | Evaluation of a skills training programme, not a model of crisis care |
| Archbold 193 | Mental health consultation and support for GPs – not crisis |
| Archbold 194 | Mental health consultation and support for GPs – not crisis |
| Asarnow et al. 195 | Follow-up treatment with participants recruited within 3 months of suicide attempt |
| Balkin et al. 196 | Characteristics of young people presenting to an acute psychiatric hospital |
| Besier et al. 197 | Not about intervention or care |
| Biddle et al. 198 | Examined students who participated in a student assistance programme and their drug-/alcohol-related behaviours and school suspensions |
| Boyer et al. 199 | Characteristics of children and adolescents presenting to a psychiatric ED over a 6-year period |
| Brock et al. 200 | Not about intervention or care at point of crisis |
| Brown et al. 201 | Unavailable |
| Buffini and Gordon 202 | Although 42% of participants were aged between 18 and 24 years, there were no separate data presented for this age group |
| Caffy et al. 203 | Explored the increasing time between presentation at the ED of a patient with a primary psychiatric complaint and their disposition |
| Campo 204 | Discussion paper |
| Canto et al. 205 | Review article |
| Cappelli et al. 206 | Satisfaction and outcomes of routine ED practice |
| Chun et al. 207 | Discussion paper |
| Chun et al. 208 | Discussion paper |
| Clossey et al. 209 | Not related to young people in crisis, but children with severe behavioural problems |
| Cloutier et al. 210 | Description of clinical presentations and expectations of young people attending the ED for mental health concerns |
| Cordell and Snowdon 211 | Clinical characteristics of those presenting receiving crisis treatment in a multiprogramme, multiservice agency serving vulnerable youth in both community and residential settings |
| Crisp et al. 212 | Peer support mental health training for universities |
| Currier and Allen 213 | Not related to young people in crisis |
| Currier et al. 214 | Mean age of participants was 32.7 years |
| D’Oosterlinck et al. 215 | Not about intervention or care |
| Dieppe et al. 216 | Development of an ED triage tool |
| Dixon Dieppe et al. 217 | An outreach service for young homeless people, but was not about point-of-crisis care |
| Donaldson et al. 218 | Follow-up treatment involving treatment of suicidal behaviour, not a model of crisis response |
| Donaldson et al. 219 | Follow-up treatment involving treatment of suicidal behaviour, not a model of crisis response |
| Doulas and Lurigio 220 | Discussion paper |
| Doulas and Lurigio 221 | Evaluation of a crisis intervention team training programme for police officers |
| Doupnik and Fu 222 | Commentary |
| Doupnik et al. 223 | Discussion paper |
| Duarté-Vélez et al. 224 | Follow-up treatment after discharge from the ED |
| Edelsohn and Gomez 225 | Discussion paper |
| Ellem et al. 226 | Participants were not in mental health crisis |
| Epstein 227 | Critical stress de-briefing after an incident |
| Ermer 228 | Not a model of crisis care |
| Evans et al. 229 | Conference presentation: full study publication retrieved |
| Evans et al. 230 | Conference presentation: full study publication retrieved |
| Evans et al. 231 | Baseline statistical data only: full study publication with follow-up retrieved |
| Flomenhaft and Voronoff 232 | Not about intervention or care |
| Forrest 233 | News article |
| Foster 234 | Literature review |
| Frosch et al. 235 | Focus on characteristics related to repeated attendance at the ED |
| Frosch et al. 236 | Focus on prior mental health service use in ‘suicide attempters’ |
| Futo 237 | Discussion paper |
| Gadancheva et al. 238 | Characteristics of adolescents with mental health crisis presenting to EDs |
| Gibson et al. 239 | Discussion of use of different psychological services for adolescents with mental health problems, not about the moment crisis |
| Goldstein and Findling 240 | Discussion paper |
| Gould et al. 241 | Survey regarding use of a helpline, not all surveyed had experienced a crisis |
| Gould et al. 242 | Adults |
| Grady et al. 243 | Not about intervention or care |
| Grimes et al. 244 | Young people with serious emotional disturbance |
| Grover and Lee 245 | Discussion of a paediatric behavioural health unit, but no therapeutic approach and treatment not described |
| Grudnikoff et al. 246 | Characteristics and disposition of adolescents with a mental health crisis presenting to an ED |
| Grupp-Phelan et al. 247 | Follow-up treatment after discharge from the ED, not a model of crisis response |
| Grupp-Phelan et al. 248 | Identifying young people with risk factors for suicide |
| Halamandaris and Anderson 249 | Discussion paper |
| Hackfeld et al. 250 | Not an evaluation of a crisis service |
| Halsall et al. 251 | Not an evaluation of a crisis service |
| Hanson 252 | Participants had disruptive behavioural disorders in a school setting |
| Harrison 253 | Not a model of crisis care |
| Hart et al. 254 | Participants were not in the moment of crisis |
| Haruvi Catalan et al. 255 | Not about intervention or care |
| Hazell 134 | Description of a model of standard ED care |
| He et al. 256 | Focuses on factors predicting admission to hospital for youths in state custody |
| Henggeler et al. 257 | No statistics, the aim was to highlight service and treatment issues prior to the full RCT |
| Herbert 258 | Unavailable |
| Hopson and Kim 259 | Discussion paper |
| Huggett et al. 260 | A mobile application and a paper-based pocket guide companion for young people with mental health issues |
| Hutt-Macleod et al. 261 | Not an evaluation of a crisis service |
| Iyer et al. 262 | Not about intervention or care |
| Jacobsen et al. 263 | Discussion of an intervention for inpatient care |
| Jabbour et al. 264 | Protocol for research study |
| James et al. 265 | Discussion about the role of school resource officers |
| Jorm et al. 266 | Discussion of increase in rates of mental health crisis in CYP |
| Kalafat et al. 267 | Mean age of participants was 32.6 years |
| Kalb et al. 268 | Not an evaluation of a crisis service |
| Kamradt 269 | Insufficient details reported (a brief mention of a mobile crisis team with a wraparound service) |
| Kennedy et al. 270 | Characteristics of young people attending an ED-based crisis intervention programme and very brief description of the intervention programme |
| Leiter 271 | Unavailable |
| Leon et al. 272 | Evaluating the use of psychiatric hospitalisation by RTCs |
| Leverett et al. 273 | Specifically, on sequelae of trauma |
| Lightburn et al. 274 | Description of innovative practices, insufficient detail on individual programmes |
| Mascayano et al. 275 | Early-onset psychosis programme |
| McKay and Shand 276 | Description of standard CAMHS care |
| McNamara et al. 277 | Skill-based application for use following discharge from an acute care setting |
| Mendez 278 | Not an evaluation of a crisis service |
| Meyer et al. 279 | Paediatric intensive care unit treatment, not about mental health crisis |
| Mier et al. 280 | Description of college-based counselling services with a very brief section on crisis care |
| Miller and Barber 281 | Discussion paper |
| Milne et al. 282 | Evaluating the accuracy of an automated triage system of an online peer support forum |
| Mokkenstorm et al. 283 | Evaluation of an online suicide prevention crisis chat service. Includes all ages. Young people not reported separately |
| Monahan et al. 284 | Not an evaluation of a crisis service |
| Montreuil et al. 285 | De-escalation approaches in mental health settings and the use of restraint and seclusion |
| Morris et al. 286 | Families in crises pending children being placed in care |
| Morrison 287 | Critical incident stress management, not individual crisis |
| Mroczkowski and Havens 288 | Discussion article with brief overviews of programmes from across USA and Canada |
| Narendorf et al. 289 | Prior experiences of using other mental health services since diagnosis |
| Navarro et al. 290 | Not an evaluation of a crisis service |
| Newman 291 | Not about intervention or care |
| Newton et al. 292 | Characteristics of young people attending EDs with mental health problems and the associated costs |
| Newton et al. 293 | Characteristics of young people attending EDs with mental health problems |
| Newton et al. 294 | Association of patient and ED mental health visit characteristics with wait time and LOS |
| Nickerson and Zhe 295 | Survey of school psychologists of a broad range of crisis, such as terrorist attacks and natural disasters |
| Nolan et al. 296 | Not an evaluation of a crisis service |
| Noronha 297 | Unavailable |
| O’Reilly et al. 298 | Mental health first aid training |
| Ougrin et al. 299 | Not an evaluation of a crisis service |
| Owen and Charles 300 | Not an evaluation of a crisis service |
| Owens et al. 301 | Study of families and completed suicides |
| Painter 302 | Not an evaluation of a crisis service |
| Parsons 303 | Discussion paper |
| Parsons 304 | Theoretical paper |
| Pazaratz 305 | Residential treatment programme established to deal with adolescent drug users |
| Pazulinec 306 | Discussion paper |
| Peake 307 | Not about young people in crisis |
| Perez 308 | Unavailable |
| Pfeiffenberger et al. 309 | Care needs of children of adults who accessed crisis services |
| Pikard et al. 310 | Characteristics, diagnosis and referral patterns to a CAMH urgent consult clinic |
| Pilowsky and Kates 311 | Crisis as in developmental/attachment crisis |
| Pineda and Dadds 312 | Not an evaluation of a crisis service |
| Porter 313 | Not an evaluation of a crisis service |
| Pycroft et al. 314 | Not an evaluation of a crisis service |
| Reder and Quan 315 | Availability of social workers to the ED |
| Reinhardt et al. 316 | Review article |
| Rhodes et al. 317 | Highlighted key aspects of ED management of paediatric suicide-related behaviours as priorities for performance measure development |
| Rice 318 | Not an evaluation of a crisis service |
| Rice et al. 319 | Follow-on treatment/care after crisis has been dealt with |
| Rickwood et al. 320 | Not an evaluation of a crisis service |
| Rittner 321 | Not an evaluation of a crisis service |
| Roberts and Yeager 322 | Juvenile drug abuse: assessment and treatment |
| Rogers et al. 323 | Review of ED attendance |
| Rudd et al. 324 | Not an evaluation of a crisis service |
| Ruth et al. 325 | Factors leading to immediate hospitalisation of CYP after a psychiatric emergency |
| Shankar et al. 326 | Discussion about preventing adolescent suicide |
| Spirito et al. 327 | Follow-up treatment after discharge from the ED, not a model of crisis response |
| Starling et al. 328 | Characteristics of children presenting to a paediatric ED with mental health problems |
| Sullivan and Riveria 329 | Characteristics of children and adolescents presenting to a psychiatric ED |
| Taylor and Gibson 330 | Not a model of crisis care |
| Thompson 331 | Predictors that influenced help-seeking behaviour for depression, anxiety and suicidal thoughts among young people |
| Thompson et al. 332 | Not an evaluation of a crisis service |
| Urgelles et al. 333 | Emergency prevention and management intervention, but emergencies were family emergencies |
| Van Der Linden et al. 334 | Young people and adults and no disaggregated results |
| Vichta et al. 335 | Young people in the study were not described as being in crisis |
| Witkon et al. 336 | Case example of domestic abuse involving a 12-year-old girl and the involvement of social services |
| Woolston 337 | Theoretical discussion paper |
| Wright et al. 338 | Description of standard CAMHS care |
| Yu et al. 339 | Patient and treatment characteristics of paediatric mental health ED visits associated with alcohol and other drug use |
| Zakirova et al. 340 | Theoretical discussion paper |
Appendix 3 Table of policies, guidelines and reports
| Study | Focus |
|---|---|
| Healthy London Partnership 154 | CYP in mental health crisis |
| Local Government Association 144 | CYP in mental health crisis |
| Healthy London Partnership 155 | CYP in mental health crisis |
| National Collaborating Centre for Mental Health 143 | Mental health crisis care |
| Specific sections for CYP | |
| Royal College of Emergency Medicine 152 | Mental health crisis care |
| Specific sections for CYP | |
| Royal College of Emergency Medicine 96 | CYP in an ED |
| Specific sections on mental health crisis | |
| Royal College of General Practitioners, Royal College of Paediatrics and Child Health and Royal College of Psychiatrists 175 |
CYP mental health Brief mention on CYP in mental health crisis |
| Royal College of Paediatrics and Child Health 135 | CYP in an ED |
| Specific sections on mental health crisis | |
| Fellow-Smith et al. 158 | CYP in mental health crisis |
| Mental Health Foundation 151 | CYP in mental health crisis |
| Centre for Mental Health 187 | CYP mental health |
| Specific sections on mental health crisis | |
| Wilkins et al. 138 | CYP mental health |
| Specific sections on mental health crisis | |
| Care Quality Commission 164 | CYP mental health |
| Specific sections on mental health crisis | |
| Care Quality Commission 141 | CYP in mental health crisis |
| Care Quality Commission 186 | Mental health |
| Specific sections on CYP in mental health crisis | |
| Care Quality Commission 188 | CYP mental health |
| Specific sections on CYP in mental health crisis | |
| Williams et al. 171 | Young people’s mental health |
| Specific sections on mental health crisis | |
| Faculty of Child and Adolescent Psychiatry and Royal College of Psychiatrists 159 | CYP mental health |
| Specific sections on mental health crisis | |
| Royal College of Psychiatrists 153 | CYP in mental health crisis |
| Garcia et al. 94 | Mental health in CYP |
| Specific sections on mental health crisis | |
| Clarke et al. 173 | Young people’s mental health |
| Specific sections on mental health crisis | |
| National Institute for Health and Care Excellence 150 | Mental health in CYP |
| Specific sections on mental health crisis | |
| National Institute for Health and Care Excellence 184 | Mental health in CYP |
| Specific sections on mental health crisis | |
| National Institute for Health and Care Excellence 185 | Mental health in CYP |
| Specific sections on mental health crisis | |
| National Institute for Health and Care Excellence 157 | Mental health in CYP |
| Specific sections on mental health crisis | |
| National Institute for Health and Care Excellence 160 | Mental health in CYP |
| Specific sections on mental health crisis | |
| Mental Health Taskforce 17 | Mental health |
| Specific sections on CYP in mental health crisis | |
| NHS England 177 | Mental health |
| Specific sections on CYP in mental health crisis | |
| NHS England 182 | General health |
| Specific sections on CYP in mental health crisis | |
| NHS England 178 | Mental health |
| Specific sections on CYP in mental health crisis | |
| East of England Clinical Networks 146 | CYP in mental health crisis |
| Specific sections on mental health crisis | |
| HM Government 24 | Mental health crisis care |
| There are specific sections on CYP | |
| Department of Health and Social Care and Department of Education 14 | Mental health in CYP |
| Specific sections on mental health crisis | |
| Department of Health and Social Care 162 | Mental health in CYP |
| Specific sections on mental health crisis | |
| National Audit Office 179 | CYP mental health |
| Specific sections on mental health crisis | |
| House of Commons Health Committee 168 | CYP mental health |
| Specific sections on mental health crisis | |
| London Strategic Clinical Network 156 | Acute care for CYP |
| Specific sections on mental health crisis | |
| NHS England 142 | CYP mental health |
| Specific sections on mental health crisis | |
| HM Government 181 | Mental health crisis care |
| There are specific sections on CYP | |
| Department of Health and Social Care and Department of Education 174 | CYP in mental health crisis |
| NHS England and the Department of Health and Social Care 3 | Mental health in CYP |
| Specific sections on mental health crisis | |
| Gibson et al. 166 | CYP in mental health crisis |
| Irvings and Barnes 145 | CYP in mental health crisis |
| Welsh Government 176 | Mental health |
| Specific sections on CYP in mental health crisis | |
| Welsh Government 183 | Mental health |
| Specific sections on CYP in mental health crisis | |
| Welsh Government and Partners 25 | Mental health |
| Specific sections on CYP in mental health crisis | |
| Welsh Government 169 | Mental health |
| Specific sections on CYP in mental health crisis | |
| National Assembly for Wales. Children, Young People and Education Committee 7 | CYP in mental health crisis |
| Welsh Assembly Government 170 | CYP mental health |
| Specific sections on mental health crisis | |
| Scottish Government 21 | Mental health |
| Specific sections on CYP in mental health crisis | |
| Scottish Government 180 | Mental health |
| Specific sections on CYP in mental health crisis | |
| Children & Young People’s Mental Health Taskforce 163 | Mental health in CYP |
| Specific sections on CYP in mental health crisis | |
| Children & Young People’s Mental Health Taskforce 165 | Mental health in CYP |
| Specific sections on mental health crisis | |
| Youth Commission on Mental Health 172 | Mental health in CYP |
| Specific sections on mental health crisis | |
| Department of Health, Social Services and Public Safety 161 | Mental health in CYP |
| Specific sections on mental health crisis |
Appendix 4 Characteristics of randomised controlled trials included in the review
| Study | Recruitment and participant characteristics | Intervention, outcomes of interest and outcome measures |
|---|---|---|
| Asarnow et al.
57
USA Aim To evaluate the FISP designed to increase motivation for follow-up treatment, support, coping and safety, augmented by care linkage telephone contacts after discharge Nature of crisis Suicide attempt or ideation Type of treatment Specialised ED intervention Location of treatment ED or inpatient units |
Participants
Youths aged 10–18 years (n = 181, rr 86%) and their parents Intervention, n = 89; control, n = 92 Recruitment From two EDs (April 2003–August 2005) Age (years), mean ± SD Overall: 14.7 ± 2.0 Intervention: 14.8 ± 2.1 Control: 14.6 ± 1.9 Gender Female: intervention, 66%; control, 72% Ethnicity White non-Hispanic: intervention, 35%; control, 32% African American: intervention, 14%; control, 12% Hispanic: intervention, 35%; control, 32% Other: intervention, 35%; control, 32% |
Intervention
FISP vs. usual care FISP: an ED-level staff training designed to improve usual ED care and the quality of the ED environment in which the other intervention components were delivered Outcomes of interest Primary outcome: rates of outpatient mental health treatment after discharge Secondary outcomes: suicide attempts, levels of suicidality, depression, family functioning and behaviour Outcome measures Baseline and 2 months after discharge Routinely collected data Service Assessment for Children and Adolescents (modified) DISC-IV, HASS, CES-D, CBCL, CBQ |
| Henggeler et al. 64,79 | Participants | Intervention |
| Huey et al.
78
Schoenwald et al. 80 Sheidow et al. 81 USA Aim To determine whether or not MST, modified for use with youths presenting psychiatric emergencies, can serve as a clinically viable alternative to inpatient psychiatric hospitalisation |
Adolescents aged 12–17 years and their families (n = 116, rr 87%; three dropped out before starting) Intervention, n = 57; control, n = 56 Recruitment Referral for hospitalisation was initiated by personnel from community child service agencies (mental health, juvenile justice, social welfare, schools), probate court and caregivers. After initial assessment, crisis caseworkers assisted the MST team to meet with the family to determine study eligibility |
MST vs. hospitalisation MST: a family-centred home-based intervention that targets the multiple systems in which the youth and family are embedded. Treatment is delivered in home or community settings by a therapist who is available 24/7 Psychiatric hospitalisation: admission to an inpatient unit for stabilisation, psychiatric evaluation and the establishment of an aftercare plan |
| Nature of crisis | Age (years), mean ± SD | Outcomes of interest |
| Suicidal ideation, homicidal ideation, psychosis or threat of harm to self or others Type of treatment MST Location of treatment Homes |
12.9 ± 2.1 Gender Female: 35% Ethnicity African American: 65% White: 33% Asian American: 1% Hispanic: 1% |
Hospitalisation, resource use
64,79,80
Placement outcomes 79,80 Discharge destination 80 Caregiver and youth satisfaction with services 64 Cost-effectiveness 81 Changes in status from admission to discharge/follow-up for the following clinical outcomes: Behaviour, psychosocial functioning, emotional distress and self-esteem 64,79 Depressive affect (depression, anxiety, hopelessness) 78 Suicidal ideation and suicide attempts 78 Family functioning and family relations 64,79 Outcome measures Baseline, when control group were discharged from hospital, at completion of MST (around 4 months’ follow-up), 6 months’ follow-up and at 1-year follow-up (post treatment) Global Severity Index of the BSI, 64,79 FACES III, 64,79 CBCL, 64,79 depression subscale of the BSI, 78 self-esteem subscale of the FFS, 64,79 hopelessness subscale of the YSR, 78 suicidal ideation using items from YSR, BSI and YRBS, 78 suicide attempts using items from CBCL and YRBS 78 and LFSS 79 Days in foster care, group homes, RTCs, juvenile justice facilities and mental health or substance abuse inpatient facilities were aggregated to index out-of-home placements 79,80 Medicaid costs 81 |
| Evans et al. 61 | Participants | Intervention |
| USA Aim To examine the efficacy of three models of intensive in-home services (HBCI, HBCI+ and CCM) as alternatives to hospitalisation for children experiencing a psychiatric crisis Nature of crisis Psychiatric crisis, including dangerousness to self and others, suicide ideation and aggression Type of treatment Intensive in-home services Location of treatment Homes |
CYP aged 5–17 years (n = 279, rr 89.4%) and their families. Of these, 13 children enrolled twice during the study period and 49 (17.6%) failed to successfully complete HBCI, n = 90; HBCI+, n = 85; CCM, n = 63 Recruitment Those who were at risk for inpatient admission or other out-of-home placement as a result of a psychiatric crisis. Assessed by clinicians at participating hospitals Age (years), mean ± SD 12.3 ± 3.6 Gender Females: 47.1% Ethnicity Hispanic: 58.8% African American: 33.6% White: 5.5% Other: 2.1% |
Three models of intensive in-home services that were intensive short-term interventions, lasting approximately 4–6 weeks, conducted in homes HBCI is based on the HOMEBUILDERS® model of family preservation developed for a child welfare population. Counsellors trained in this model carry caseloads of two families concurrently. The goal of this programme is to keep children in their home environment through resolving the immediate crisis, teaching caregivers communication and other relevant skills, helping families improve relationships and linking the child and family to needed services HBCI+ has the same programmatic goal as HBCI and offers the same services. In addition to the counsellor, the intervention team in this model used a bilingual, bicultural family advocate who established a parent support group and provided individualised parent support and advocacy CCM is an adaptation of the existing intensive CCM that does not offer clinical treatment services in the home. The programme goal was to assess needs, provide concrete services and link the child and family to needed services to keep children in their natural environments. Case managers carried maximum caseloads of eight families (four families in crisis and four requiring generic case management services) Outcomes of interest Percentage of children maintaining at home/community Self-concept, family functioning, behaviour and social competencies Discharge destination Outcome measures Baseline, post treatment and 6-month follow-up Routinely collected data PHSCS, FACES II, ISSB and CBCL |
| Wharff et al. 84 | Participants | Intervention |
| USA Aim To examine the efficacy of FBCI Nature of crisis Suicidality Type of treatment Specialised ED intervention Location of programme Paediatric ED |
Adolescents aged 13–19 years (n = 142, rr 49%) Intervention, n = 68; control, n = 71; withdrawn, n = 3 Recruitment Those presenting to the ED with suicidality (January 2012–May 2014) Age (years), mean ± SD Intervention: 15.4 ± 1.3 Control: 15.6 ± 1.5 Gender Female: intervention, 74%; control, 70% Ethnicity Black: intervention, 4%; control, 8% White: intervention, 62%; control, 70% Latino: intervention, 9%; control, 10% Asian: intervention, 4%; control, 1% Mixed: intervention, 21%; control, 15% |
FBCI: participants received a standard psychiatric evaluation followed by an emergency psychiatry intervention. The FBCI was designed to sufficiently stabilise suicidal adolescents within a single ED visit and delivered by social workers in a 60- to 90-minute session. The session helped the adolescent and family develop a joint crisis narrative of the problem and taught them cognitive–behavioural skill-building, therapeutic readiness, psychoeducation about depression and safety planning TAU: participants received a standard psychiatric evaluation and clinical/discharge recommendations Outcomes of interest Primary outcomes: suicidality, family empowerment Secondary outcomes: client satisfaction and recidivism (hospitalisation post discharge, crisis assessment post discharge) Outcome measures Baseline and 1-month follow-up RFL-A, FES, CSQ-8 Recidivism via two self-reported questions (i.e. ‘since your initial visit to the ED, has your child required another crisis evaluation?’ and ‘has your child been psychiatrically hospitalised again?’) |
Appendix 5 Characteristics of included quasi-experimental studies
| Study | Recruitment and participant characteristics | Intervention, outcomes of interest and outcome measures |
|---|---|---|
| Roberts et al. 92 | Recruitment | Intervention |
| Canada Aim To examine physician and patient satisfaction with emergency psychiatric consult through telepsychiatry, and to compare clinical characteristics and outcome of telepsychiatry emergency consultations with face-to-face emergency consultations of children and adolescents from rural and remote communities Nature of crisis Suicidal, anxiety, aggression and psychosis Location of programme Remote |
Children and adolescents aged < 18 years who were assessed by the CAMHUCC at a university hospital from November 2015 to November 2016 and who completed the telepsychiatry satisfaction questionnaire The MCG consisted of 60 patients who had a face-to-face assessment in the clinic over the same 12-month period Participants Children and adolescents aged < 18 years (n = 120) Intervention, n = 60); MCG, n = 60 Age (years), mean ± SD 14 ± 0.36 Gender Female: 67% Ethnicity (% Aboriginal) Intervention, 50%; MCG, 6.7% (p < 0.001) |
Telepsychiatry assessment and brief intervention The CAMHUCC has a telepsychiatry suite, linked through the Ontario Telemedicine Network, allowing telepsychiatry assessment for patients and direct consultation to the ED physicians in remote emergency rooms and clinics within 24 hours of patient presentation Outcomes Patient satisfaction Referral pathways Hospitalisation Discharge destination Outcome measures AOQ: patient satisfaction Routinely collected |
| Rotheram-Borus et al. 82,83 | Participants | Intervention |
| USA Aim To compare standard emergency room treatment with a specialised emergency room programme, and to evaluate the impact of a specialised emergency room care intervention over the subsequent 18 months Nature of crisis Suicide attempts Type of programme Assessment approach |
Adolescents aged 12–18 years (n = 140) Standard emergency room care, n = 75; specialised emergency room care, n = 65 Recruitment A consecutive series of adolescent suicide attempters and their families presenting to the emergency room from March 1991 to August 1992 received the standard emergency room care. Those presenting from September 1992 to February 1994 received the specialised emergency room programme |
Specialised emergency room programme Three changes were introduced: 1. Staff training workshops 2. A ‘soap opera’-style videotape, which aimed to set realistic treatment expectations and to provide families with a better understanding of adolescent suicidality and the course of outpatient therapy 3. A family therapy session [after discharge from the emergency room all attempters were referred to the adolescent suicidal disorders clinic for a standardised outpatient six session family treatment programme (i.e. SNAP)] |
|
Location of programme
ED |
Age (years), mean ± SD
Standard emergency room care: 15.3 ± 1.6 Specialised emergency room care: 15.0 ± 1.4 Gender Female: 100% Ethnicity Latino: standard emergency room care, 85.3%; specialised emergency room care, 89.2% |
Outcomes of interest
Depression, suicidality, impulsivity, self-esteem and family functioning Outcome measures Baseline: Pierce Suicidal Intent Scale and Hamilton Rating Scale for Depression Post-discharge assessment: weekly logs, including attendance of at least one treatment session, completion of SNAP treatment and the total number of treatment sessions attended; AOQ for attitude towards treatment; HASS; BDI; FACES III; RSES; and Junior 16 3-, 6-, 12- and 18-month follow-up: HASS, BDI, FACES III and Junior 16 |
| Greenfield et al. 86 | Recruitment | Intervention |
| Latimer et al.
93
Canada Aim To study the clinical outcomes of suicidal adolescents who were treated within a rapid response outpatient model in a setting in which a 10-day wait was usually required before outpatient treatment could be started, 86 and to investigate the cost- effectiveness of a rapid response team compared with usual care for treating suicidal adolescents 93 Nature of crisis Suicide attempts Location of programme Paediatric A&E and then outpatient department |
Suicidal adolescents admitted to an ED during the study period (December 1996–October 1998) Participants Adolescents aged 12–17 years (n = 286) Intervention, n = 158; control, n = 128 Age (years), mean ± SD Intervention: 14 ± 1.59 Control: 14 ± 1.46 Gender Female: intervention, 72%; control, 66% Ethnicity White: intervention, 70%; control, 72% Black: intervention, 8%; control, 4% Hispanic: intervention, 4%; control, 4% Other: intervention, 18%; control, 20% |
Rapid response outpatient team Assessed by on-call paediatrician as needing as immediate psychiatric consultation. For the intervention group, the on-call psychiatrists had access to the rapid response outpatient team. Psychiatrists in both groups either admitted the patient or discharged them from the ED with subsequent referral to the intervention or control condition Intervention: rapid response outpatient team that contacted the patient and family. Interventions were aimed at reframing misconceptions, maladaptive behaviours, and communicating patterns Control: no access to the rapid response outpatient team. Psychiatrists could follow the patient as an outpatient, or refer to a hospital-based outpatient psychiatric clinic, a non-hospital-based community health facility or a private mental health worker Outcomes Psychosocial functioning, suicide attempts, level of suicidality 86 Time to first contact with HCP and first appointment 86 Hospitalisation and ED return rates 86,93 LOS 86 Resource use: inpatient and outpatient services 93 |
|
Costs and cost-effectiveness 93 Outcome measures Baseline 2-month follow-up and 6-month follow-up: CGAS, 86 SSBS 86 and routinely collected data Research interview at 2 and 6 months after ED assessment 86 Hospital service costs (ED visits, outpatient visits, inpatient stays and rapid response team) based on financial and activity reports of the hospitals, supplemented by information from hospital financial officers and data supplied by trial research team, and estimated using standard methods 93 Fees paid to physicians and unit costs of drugs were obtained from the Quebec Health Insurance Board 93 Costs of private visits with a psychiatrist or other HCPs were obtained from professional boards 93 |
||
| Nagarsekar et al. 132 | Recruitment | Intervention |
| Australia Aim To investigate an innovative pathway that builds capacity of ED medical officers to manage children and adolescents with mental health problems Nature of crisis Mental health problems, including deliberate self-harm, suicidal behaviour, emotional dysregulation or situational crisis Location of programme Paediatric ED |
Children and adolescents presenting for mental health problems in an ED (September–December 2017) Participants Children and adolescents aged 8–17 years Age (years) < 11: intervention, 10%; control, 6% 12–15: intervention, 60%; control, 69% > 16: intervention, 30%; control, 25% Gender Female: intervention, 66%; control, 66% Ethnicity Not stated |
A clinical pathway called the KALM pathway was implemented in the ED to build in extra capacity for an ED medical officer to complete the assessment and to link with an on-call psychiatrist regarding assessment and management plan Control TAU Outcomes LOS Carer satisfaction Outcome measures Clinical and demographic data were collected for all eligible ED presentations from the ED patient management systems Carer survey administered by CAMHS clinicians as part of routine follow-up telephone calls within 48 hours of the ED presentation |
Appendix 6 Characteristics of prospective cohort studies included in the review
| Study | Location of programme/setting, recruitment and patient characteristics | Design, outcomes of interest and outcome measures |
|---|---|---|
| Wharff et al. 32 | Location of programme | Design |
| USA Aim To explore the safety and feasibility of FBCI in a population of adolescents presenting with suicidal complaints in a large urban paediatric emergency room Nature of crisis Suicidal attempt Type of intervention FBCI Specialised ED interventions |
Paediatric ED Recruitment Suicidal adolescents presenting consecutively to the paediatric ED at Boston Children’s Hospital over 18 months (January 2001–June 2002) Compared retrospectively with suicidal adolescents who presented consecutively to the same ED over 18 months (January 1999–June 2000) Participants Prospective cohort: intervention adolescents aged 13–18 years (n = 67, rr 67%) Retrospective cohort: control adolescents (n = 150) Age (years), mean ± SD Intervention: 15.6 ± 1.5 Control: ns Gender Female: intervention, 76%; control, 74% Ethnicity White: intervention, 65%; control, 64.7% Black: intervention, 11%; control, 17.3% Hispanic/Latino: intervention, 11%; control, 11% Biracial: intervention, 3%; control, 1.3% Asian: intervention, 2%; control, 2.7% Other: intervention, 3%; control, 4.0% |
Prospective cohort study (over 18 months) compared with data collected retrospectively (over 18 months) Outcomes Suicide attempts Referral pathways Hospitalisation post discharge Emergency department visits post discharge Outcome measures 1-day follow-up, 1-week follow-up, 2-week follow-up, 1 month follow-up and 3-month follow-up Data were obtained through a medical record review of routinely collected data |
Appendix 7 Characteristics of retrospective cohort studies included in the review
| Study | Patient characteristics and recruitment | Type of programme, data sources, outcomes of interest and outcome measures |
|---|---|---|
| Greenham and Bisnaire 87 | Participants | Type of programme |
| Canada Aim To describe characteristics and outcomes of youths aged 7–17 years who received inpatient psychiatric and mental health services along different clinical pathways of a new service delivery model Nature of crisis Suicidal ideation Location of programme Inpatient psychiatry unit at the Children’s Hospital of Eastern Ontario |
Youths CSS, n = 96; IAS, n = 90; TCS, n = 25 Recruitment Consecutive admissions to the programme over a 1-year period from October 2000 to October 2001. The majority (65%) of youths were admitted through the ED or from an off-service bed on another medical/surgical ward (21%) Age (years), mean ± SD CSS: 14.8 ± 2.0 IAS: 14.9 ± 1.8 TCS: 15.3 ± 1.2 Gender Female: CSS, 64%; IAS, 70%; TCS, 80% Ethnicity ns |
Inpatient crisis stabilisation and assessment programme Data sources Discharge summary notes in the medical chart Outcomes LOS and discharge destination Suicide risk, symptoms and psychosocial functioning Outcome measures Routinely collected data CAPI |
| Fendrich et al. 62 | Participants | Type of programme/intervention |
| USA Aim To evaluate a mobile crisis service intervention implemented in Connecticut with the aim of examining whether or not the intervention was associated with reduced behavioural health ED use among those in need of services Nature of crisis Behavioural health need (as one in which any psychiatric diagnosis was provided during an ED service encounter) |
Client sample using the MCS: youths aged 4–18 years (n = 2532) Comparison sample using the ED: youths aged 4–18 years (n = 3961) Recruitment Clients anywhere in the state can access mobile crisis services by dialling a specifically assigned number that connects to a call specialist at a call centre. All those receiving services during the fiscal year 2014 Age (years), mean ± SD MCS: 12.20 ± 3.38 ED: 12.60 ± 3.65 |
Emergency mobile crisis service Data sources All data pertaining to ED use in this study were based on paid Medicaid claims. Deidentified data were made available from Beacon Health Options, the behavioural health administrative service organisation for the state Medicaid agency (the Connecticut Department of Social Services) Data from clients receiving mobile crisis services were obtained from the provider information exchange system that is maintained by the Connecticut Department of Children and Families |
|
Location of programme
Community based |
Gender
Female: MCS, 51%; ED, 45% Ethnicity Non-Hispanic white: MCS, 33%; ED, 39% Non-Hispanic black: MCS, 20%; ED, 12% Hispanic: MCS, 40%; ED, 29% Other: MCS, 7%; ED, 20% |
Outcomes
Behavioural health ED visits during an 18-month follow-up period Outcome measures Routinely collected data |
| Holder et al. 65 | Participants | Type of programme/intervention |
| USA Aim To assess improvement in the ED LOS and costs after implementation of an ED programme that added board-certified psychiatrists and trained psychiatric social workers to the paediatric ED Nature of crisis Children in crisis with mental health disorders/behavioural reasons Location of programme Paediatric ED |
Before July 2010, patients treated had limited access to evaluations by staff with mental health expertise CYP aged 5–18 years Pre programme, n = 1237; post programme, n = 1983 Recruitment All paediatric psychiatric visits of children aged 5–18 years who were seen and discharged from the Greenville Memorial Hospital ED from January 2007 to June 2013 Age (years), mean ± SD Pre programme: 14.9 ± 3.1 Post programme: 14.3 ± 3.1 Gender Female: pre programme, 46.2%; post programme, 47.3% Ethnicity White: pre programme, 72.7%; post programme, 71.3% African American: pre programme, 20.4%; post programme, 21.2% Hispanic: pre programme, 4.2%; post programme, 3.7% Other: pre programme, 2.8%; post programme, 3.8% |
Addition of trained psychiatric professionals Standard PED with psychiatric crisis team Data sources Existing electronic data on the study population Outcomes LOS, cost savings and discharge destination Outcome measures Routinely collected data Costs (not reported) |
| Mahajan et al. 67 | Participants | Type of programme/intervention |
| USA Aim To evaluate the impact of the child guidance model on the ED LOS and ED costs on children with VMD Nature of crisis Suicidal/homicidal ideation, behavioural problems and violent/psychotic behaviour Location of programme Paediatric ED |
Children (n = 1031), of whom 54% (n = 561) were evaluated by the child guidance model team Recruitment All children who attended the paediatric ED for mental disorders over a 1-year period from June 2002 (i.e. since the initiation of the child guidance model) Age (years), mean ± SD 12.5 ± 3.4 Gender Female: 33% Ethnicity ns |
Child guidance model Standard paediatric ED with psychiatric crisis team (full-time social worker) Data sources Review of medical records in 2002 Outcomes LOS, cost savings and opportunity costs Outcome measures Routinely collected data Costs obtained from the Institute for Strategic Financial Analysis (an internal hospital department that tracks and analyses facility costs) |
| Rogers et al. 72 | Participants | Type of programme |
| USA Aim To determine how the CARES unit influenced LOS and costs for psychiatric patients in the paediatric ED Nature of crisis Acute psychiatric emergencies Location of programme Crisis stabilisation unit (inpatient) |
CYP aged 5–17 years (n = 1719) presenting 1 year before CARES (October 2006–October 2007) were compared with CYP (n = 1863) presenting 1 year after (October 2007–October 2008) Setting/recruitment Patients who presented to the paediatric ED with an acute psychiatric emergency Age (years), mean ± SD Pre CARES: 12.9 ± 3.1 Post CARES: 13.2 ± 2.9 Gender Female: pre CARES, 48.2%; post CARES, 48.1% Ethnicity White: pre CARES, 42.9%; post CAREs, 43.2% African American: pre CARES, 36.1%; post CARES, 34.3% Hispanic: pre CARES, 18.7%; post CARES, 20.5% |
CARES programme Data sources Medical charts Outcomes LOS, cost savings and recidivism rate (ED visits) Outcome measures Routinely collected data Costs were obtained using the EPSi™ decision support application (Allscripts Healthcare Solutions, Inc., Chicago, IL, USA) |
| Uspal et al. 75 | Recruitment | Type of programme |
| USA Aim To improve the quality of care for patients with psychiatric complaints at a tertiary care children’s hospital’s ED using Lean methodology Nature of crisis Psychiatric complaints (self-inflicted injuries excluded) Location of programme Paediatric ED |
Patients attending the paediatric ED who were identified as having a mental health complaint on or before arrival to the paediatric ED. New process was implemented in March 2011. The pre-implementation period was March 2010–March 2011 and the post-implementation period was March 2011–March 2012 Participants All children with a primary discharge diagnosis code consistent with a mental health diagnosis Age (years), mean ± SD Pre intervention: 13.5 ± 3.4 Post intervention: 13.8 ± 3.4 Gender Female: pre intervention, 65%; post intervention, 51% Ethnicity White: pre intervention, 69%; post intervention, 65% Black: pre intervention, 8%; post intervention, 11% Other/refused: pre intervention, 23%; post intervention, 24% |
Dedicated mental health team based in the paediatric EDStandard paediatric ED with psychiatric crisis team Data sources Electronic medical records Outcomes Primary outcome: LOS Secondary outcomes: hospitalisation rates, ED 72-hour return rate and faculty satisfaction Outcome measures Routinely collected data Faculty surveys were conducted on ED mental health care before and after implementation |
| Martin 68 | Participants | Type of programme |
| USA Aim To determine if a mobile crisis intervention has comparable or lower youth hospitalisation outcomes than hospital-based crisis intervention Nature of crisis Serious risk of psychiatric hospitalisation Location of programme Community |
Youth aged from 4 to 17 years (n = 897) served by the psychiatric emergency services (n = 584) and the MRT (n = 313) Recruitment No details provided Age (years) 0–5: MRT, 2%; paediatric ED, 1% 6–11: MRT, 27%; paediatric ED, 13% 12–14: MRT, 42%; paediatric ED, 34% 15–17: MRT, 29%; paediatric ED, 52% |
Mobile crisis intervention programme compared with a hospital-based crisis intervention Data sources Data were gathered from the MRT client database and the Contra Costa County Children’s Mental Health database Outcomes Psychiatric hospitalisation at time of crisis and psychiatric hospitalisation within 30 days after crisis stabilisation Outcome measures Routinely collected data |
|
Gender
Female: MRT, 51%; paediatric ED, 54% Ethnicity Caucasian: MRT, 58%; paediatric ED, 58% African American: MRT, 28%; paediatric ED, 24% Filipino: MRT, 0.6%; paediatric ED, 0.5% East Asian: MRT, 1%; paediatric ED, 8% Latin American: MRT, 1%, paediatric ED, 3% Mexican American/Chicano: MRT, 10%; paediatric ED, 8% Other non-white: MRT, 0.3%; paediatric ED, 2% Southeast Asian: MRT, 0.6%; paediatric ED, 1% Unknown: paediatric ED, 2% |
||
| Lee et al. 89 | Recruitment | Type of programme |
| Canada Aim To evaluate the impact of HEARTSMAP on the paediatric ED flow and system utilisation Nature of crisis Acute psychiatric consultation (including depression, anxiety, suicidal ideation, self-harm, substance abuse, mood, eating, and behavioural and psychotic disorders or their permutations) Location of programme Paediatric ED |
Retrospective sample: a random sample of mental health-related paediatric ED visits of patients aged < 17 years. Using an administrative database containing records of all BCCH paediatric ED visits, mental health-related presentations were identified from chief complaints and discharge diagnoses Prospective sample: youths aged < 17 years who were identified by the triage nurse as presenting at the paediatric ED for a mental health-related complaint and placed in the mental health assessment room Participants CYP aged < 17 years Retrospective sample, n = 104; prospective sample, n = 70 Age (years), mean Retrospective sample, 13.5; prospective sample, 12.9 Gender Female: retrospective sample, 66%; prospective sample, 72% |
HEARTSMAP (an emergency psychosocial assessment and management tool) Data sources Medical records A retrospective (pre-implementation) cohort served as the control group Outcomes LOS, receiving psychiatric consultation in paediatric ED, admission, return to the EDwithin 30 days, admittedwithin 30 days,wait time to see a physician and resource use post discharge Outcome measures Routinely collected data |
| Greenfield et al. 34 | Recruitment | Type of programme |
| Canada Aim To determine the impact of an outpatient psychiatric ERFUT on the hospitalisation rate of youths in crisis (mostly suicidal adolescents) Nature of crisis Suicide attempt Location of programme Outpatients |
Suicidal adolescents admitted to ED during the study period (dates not provided) Participants Retrospective sample (year prior to creation of ERFUT): n = 412 Prospective sample (third year that ERFUT was fully functional): n = 568 No further participant details provided |
Specialised outpatient service ERFUT Outcomes Hospitalisations, ED visits post discharge, suicidality, psychosocial functioning and mortality Outcome measures Routinely collected data and data from the coroner’s office 4 years later to identify any patient deaths during the intervening years |
| Thomas et al. 74 | Participants | Type of programme |
| USA Aim To evaluate a videoconference-based psychiatric emergency consultation programme (telepsychiatry) Nature of crisis Psychiatric emergency behavioural health complaint that was not immediately life-threatening Location of programme Remote |
In early 2015 before implementation, usual care was received by 268 (54%) paediatric patients After implementation of telepsychiatry, consultation was received by 226 (46%) paediatric patients Parents/guardians, n = 156; HCPs, n = 195 Recruitment Paediatric patients who presented in 2015 at a network ED with a primary presenting complaint of an acute behavioural health condition Age (years), mean ± SD Telepsychiatry: 13.1 ± 2.7 Usual care: 13.3 ± 2.5 Gender Female: telepsychiatry, 57%; usual care, 63% Ethnicity Caucasian: telepsychiatry, 77%; usual care, 69% Other: telepsychiatry, 23%; usual care, 31% |
Telepsychiatry compared with usual care Data sources Electronic medical record. The psychiatric emergency service staff also abstracted specific text fields from encounter records into a de-identified version of the REDCap database (Vanderbilt University, Nashville, TN, USA) Outcomes LOS, re-admission to ED within 72 hours, costs, hospitalisations and satisfaction with telepsychiatry Outcome measures Routinely collected data Telehealth satisfaction survey Costs (billing data for facility charges came from the hospital finance office and data for provider fees came from the faculty practice plan) |
| Maslow et al. 66 | Recruitment | Type of programme |
| USA Aim To describe and evaluate an integrated paediatric evaluation centre designed to prevent the need for treatment in emergency settings by increasing access to timely and appropriate care for acute mental health Nature of crisis |
Patients who had attended the evaluation centre in 2016 and all patients with a visit for social work in the interval from September 2015 (when the clinic opened) to January 2017 Participants CYP aged 2–22 years (n = 641) with 1447 completed appointments Age (years), mean ± SD |
An integrated paediatric mental health outpatient clinic Data sources Retrospective referral and waitlist data gathered by the care management team and use of reports for all patients seen by ED and evaluation centre providers. Analysis using electronic health records from the health system, including data on ED visits and clinic visits |
| Acute mental health needs Location of programme Outpatient clinic Reliford and Adebanjo 71 USA Aim To evaluate data regarding child psychiatry fellow use of telepsychiatry Nature of crisis Those presenting to a paediatric ED in need of psychiatric care Location of programme Paediatric ED |
13.01 + 3.84 Gender ns Ethnicity ns Recruitment CYP aged 3–18 years presenting to a paediatric ED (during study period) in need of psychiatric care Pre implementation of telepsychiatry: July 2016–December 2016 Post implementation of telepsychiatry: July 2017–December 2017 No further details provided |
Outcomes
ED visit frequency post discharge Outcome measures Routinely collected data Type of programme Telepsychiatry Data sources Prospective real-time questionnaire that each child psychiatry fellow filled out at the end of their weekend call LOS measured from patient’s registration time through time of discharge Data from study period compared with retrospective data Outcomes LOS, physician use of telepsychiatry, clinical evaluation time, travel time and reasons for refusal of telepsychiatry Outcome measures Routinely collected data AOQ |
Appendix 8 Characteristics of descriptive cross-sectional studies included in the review
| Study | Patient characteristics | Location of programme, recruitment, outcomes of interest and outcome measures/questionnaires |
|---|---|---|
| Michael et al. 69 | Patient characteristics | Location of programme |
| USA Aim To further describe the PEACE protocol (a crisis risk assessment tool) after its initial pilot year (2012–13) and to report the results from the 2013–14 year Nature of crisis Suicidality and homicidally Type of programme Risk assessment and decision-making tool within a school mental health programme |
High school students (n = 42) who were involved in 68 separate crisis events Recruitment Referrals to the assessment, support and counselling centre for crisis events during 2013–14. The centre services three districts. Referrals are made by professional school counsellors and administrators, peers and students Gender Female: 52% Ethnicity Caucasian: 90.5% Non-Caucasian: 9.5% Age 9th grade: 33% 10th grade: 14% 11th grade: 36% 12th grade: 17% |
High school Outcomes Suicide attempts, referral pathways, and umber and types of referrals Outcome measures PEACE protocol (revised and extended) Routinely collected data |
| Sale et al. 73 | Patient characteristics | Location of programme |
| USA Aim Describes the development and implementation of a school mental health programme in western rural North Carolina Nature of crisis Suicidality and homicidally |
High school students (n = 20) who were involved in 33 separate crisis events Recruitment Referrals to the assessment, support and counselling centre for crisis events in one high school during 2012–13. Students were referred by parents and school personnel |
High school Outcomes Suicide attempts, referral pathways, and number and types of referrals Outcome measures PEACE protocol (revised and extended) Routinely collected data |
|
Type of programme
Risk assessment and decision-making tool within a school mental health programme |
Gender
Female: 65% Ethnicity Caucasian: 100% Age 9th grade: 50% 10th grade: 20% 11th grade: 20% 12th grade: 10% |
|
| Capps et al. 60 | Patient characteristics | Location of programme |
| USA Aim To describe the results of a replication of the PEACE protocol implemented during the 2016–17 school year Nature of crisis Suicidality, homicidality and self-injury Type of programme Risk assessment and decision-making tool within a school mental health programme |
High school students aged 13–18 years (n = 58) involved in 78 separate crisis events Recruitment Referrals to the assessment, support and counselling centre for crisis events during 2016–17. The centre serviced three districts. Referrals were made by professional school counsellors and administrators, peers and students Gender Female: 55.1% Transgender: 1.3% Age (years), mean ± SD 15.42 ± 1.22 Ethnicity Caucasian: 87.2% Non-Caucasian: 12.8% |
High school Outcomes Suicide attempts, referral pathways, and number and types of referrals Outcome measures PEACE protocol Routinely collected data |
| Walter et al. 77 | Patient characteristics | Location of programme |
| USA Aim To test the ‘real-world’ implementation of a multitiered system of support model of mental health services for elementary through to high school students in urban communities Nature of crisis Emotional distress, suicidal thoughts or behaviours and dysregulated behaviours Type of programme School–hospital partnership |
Students (n = ns) who were involved in 491 crisis encounters Recruitment Crisis intervention services were delivered by programme clinicians to individual students in an acute mental health crisis who were referred by school staff No further details reported for those in crisis |
Elementary and high school Outcomes Per cent referred for acute level care, wait time for crisis services and average wait time for crisis services Outcome measures/questionnaires Routinely collected data |
| Baker and Dale 58 | Patient characteristics | Location of programme |
| USA | Boys (n = 81) aged 5–17 years | Crisis programme within a RTC |
| Aim | Recruitment | Outcomes |
| To document the incidence, frequency and timing of psychiatric crises of youths in residential treatment and to determine whether or not the on-campus crisis residence functioned as an effective alternative to hospitalisation Nature of crisis Psychiatric crisis (including suicide attempt, fire-setting and violence) Type of programme Short-term CIP The crisis residence |
All boys who were treated at the crisis residence between January 1995 and December 1997, referred from the agency’s (The Children’s Village) own RTC and other agency programmes, such as adoption and foster care Gender Male: 100% Age (years) Range: 5.03–16.15 Ethnicity African American: 56.7% Hispanic: 32.2% White: 7% Missing data: 4% |
LOS, cost savings, discharge destination, proportion hospitalised within 1 month of treatment and satisfaction Outcome measures Routinely collected data Costs (no details of data source) |
| Baker et al. 59 | Participants | Location of programme |
| USA | Youths (n = 103) aged 5–17 years | RTC |
| Aim | Recruitment | Outcomes |
| To provide descriptive information regarding two groups of young people entering a hospital diversion programme for young persons in psychiatric crisis: (1) those who entered the programme from a RTC and (2) those who entered the programme as an outside referral (typically young persons living with their own family or a foster family) Nature of crisis Suicidality and homicidally Type of programme/intervention Short-term CIP The crisis residence |
All youths who were treated at the crisis residence (within a RTC – The Children’s Village) in fiscal year 2001–2. Patients were referred from three sources: (1) the agency’s (The Children’s Village) own RTC and other agency programmes, such as adoption and foster care; (2) local and out-of-state social service agencies and departments of mental health; and (3) insurance companies and managed care organisations Age (years), mean ± SD RTC sample: 14.61 ± 2.1 Outside referral sample: 13.52 ± 2.9 Gender Male: RTC sample, 100%; outside referral sample, 42.3% Ethnicity Ethnic minority: RTC sample, 93.8%; outside referral sample, 84.3% |
Discharge destination and LOS Outcome measures Routinely collected data |
| Dion et al. 85 | Participants | Location of programme |
| Canada | ED medical staff (n = 124, rr 70%) | PED at a children’s hospital |
| Aim | Recruitment | Outcomes |
| To explore how capable ED staff feel in managing paediatric mental health issues and what they value in ED crisis intervention Nature of crisis Suicidality and homicidally Type of programme CIP |
ED medical staff working on the CIP with the Children’s Hospital of Eastern Ontario Patient characteristics CYP assessed in PED from April 2005 to March 2006 (n = 784) classified as having at least one risk behaviour/clinical symptom in the moderate/severe range on the CAPI (93.1%) Age (years), mean ± SD 14.0 + 2.36 Gender Female: 52.8% Ethnicity ns |
Staff satisfaction and discharge destination Outcome measures AOQ |
| Lee and Korczak 88 | Participants | Location of programme |
| Canada | Parents of CYP (n = 124, rr 71%) | ED at a children’s hospital |
| Aim | Recruitment | Outcomes |
| To explore parental satisfaction with a paediatric crisis clinic Nature of crisis Suicidality and aggressive behaviour Type of programme Urgent referral model |
The parents of CYP referred for CAP consultation and seen at the paediatric crisis clinic from May 2007 to April 2008 Patient characteristics ns Age (years), mean ± SD 12.2 ± 3.2 Gender Female: 37% Ethnicity ns |
Parental satisfaction Outcome measures Adapted from the Quality of Care Parent Questionnaire |
| Gillig 63 | Participants | Location of programme |
| USA Aim To report on 48 adolescents who were admitted consecutively for emergency hospitalisation evaluation Nature of crisis Suicidality, homicidally and self-harm Type of programme/intervention Adolescent crisis service |
Adolescents (n = 48) aged 12–18 years Recruitment Consecutive admissions to an urgent care centre for emergency hospitalisation evaluation. Evaluations were requested by members of the community (e.g. police, urgent care physicians, nurses, teachers and family) Age (years) Mode: 16.5 Gender Female: 54% |
Hospital outpatients Outcomes Discharge destination Outcome measures Routinely collected data |
| Muskens et al. 98 | Participants | Location of programme |
| The Netherlands Aim To investigate treatment outcome of IHT, combined with HIC, by measuring the clinical outcome of adolescents with severe psychiatric crisis Nature of crisis Severe psychiatric crisis (including severe depression, food refusal, disabling obsessive–compulsive disorder, psychosis and suicidal) Type of programme IHT with and without admission to HIC unit |
Children and adolescents aged 11–18 years Recruitment Those admitted with severe psychiatric symptoms in need of acute and intensive treatment Age (years), mean ± SD 14.8 ± 0.3 Gender Female: 52% Ethnicity ns |
Home Outcomes Type and severity of mental health symptoms and discharge destination Outcome measures Baseline, 2-month follow-up, 4-month follow up HoNOSCA |
Appendix 9 Characteristics of included qualitative studies
| Study | Participant characteristics and recruitment | Design, methodology, data collection methods and data analysis | Thematic findings of interest |
|---|---|---|---|
| Idenfors et al.
100
Sweden Aim To explore young people’s views of professional care before first contact for DSH, and factors that influenced the establishing of contact Nature of crisis DSH (e.g. self-poisoning, cutting, attempted jump, hitting) |
Participants
Young people aged 16–24 years presenting with DSH (n = 10) Recruitment From the ED, psychiatric emergency services, the child and adolescent psychiatry clinic or a psychiatric ward Age (years) Mean: 20 Range: 17–24 Gender Female: 60% Ethnicity ns |
Design
Qualitative descriptive Methodology ns Data collection methods Interviews Data analysis Qualitative content analysis |
Six categories were created, four of which were relevant to this review: 1. Lack of knowledge about where to turn 2. Need for many possible routes to professional care 3. The importance of immediate help 4. A need for a more flexible, available and varied health care |
| Bolger et al.
97
Ireland Aim To review the clinical presentation of, and A&E department clinical response to, 14- to 20-year-olds in suicidal crisis in inner city Dublin and to carry out a 6-month follow-up of these young people Nature of crisis Suicidal behaviour or ideation |
Participant characteristics
Young people aged 14–20 years (n = 31, rr 35%) Recruitment Young people who had attended the A&E from June 2001 to May 2002 with suicidal behaviour or ideation Age (years) 14–16: 32% 17–20: 68% Gender Female: 29% Ethnicity ns |
Design
Qualitative descriptive as part of a wider mixed-methods study Methodology ns Data collection methods Interviews 6 months after A&E attendance Data analysis ns |
Respondents were asked their opinions on what support or services would have been helpful to them at the time of their episode of suicidal behaviour |
| Haxell
99
New Zealand Aim To report on the experiences of texting a 24-hour crisis helpline for young people Nature of crisis ns |
Participant characteristics
Youthline New Zealand counsellors (n = 22) Young person users of the service (n = 2) Recruitment Youthline New Zealand crisis text service. Those who had either used or provided the service participated in semistructured interviews regarding their experiences in making use of the texting service No further participant details reported |
Design
Qualitative descriptive as part of a wider mixed-methods study Methodology ns Data collection methods Interviews and text message conversations with young people Data analysis Analysis of Youthline New Zealand text message conversations with young people |
Reponses to the question that asked about the experiences in making use of the texting service were reported under three headings: 1. Accessibility 2. Friendliness 3. Relevance |
| Garcia et al.
94
UK Aim To look at the work of eight voluntary organisations working with young people with mental health and emotional problems, and to find out how these organisations work to ensure that their services deliver what young people want, particularly as identified on the ‘wish list’ Nature of crisis Severe distress, including those self-harming and/or with an intention to commit suicide or who had previously made a suicide attempt |
Participant characteristics
In-depth consultation: young people aged 16–25 years (n = 200) Interviews or focus groups: young people aged 16–25 years (n = 32) Staff members from project sites (n = 31) Recruitment Staff from eight different voluntary organisations selected young people who were currently using the service, or who had done in the past, with mental health and emotional problems No further participant details reported |
Design
Qualitative descriptive Methodology ns Data collection In-depth consultation, interviews or focus groups Data analysis ns |
In-depth consultation
Wish list for services Interviews or focus groups Themes of relevance included: • delivering a successful • service • providing choice • providing accessible services • providing support at all stages |
| Northern Ireland Commissioner for Children and Young People
95
UK Aim This report looks at the adequacy of mental health services and support for CYP using a rights-based perspective |
Participant characteristics
Young people aged 14–25 years with learning difficulties (n = 15) or drug/ alcohol issues (n = 17) Recruitment Engagement with young people was carried out in partnership with three organisations known to work with the groups of young people who met the criteria for inclusion |
Design
Qualitative descriptive as part of a wider study Methodology ns Data collection Interviews Data analysis Thematic analysis |
Thematic areas were
Waiting too long for help Experiences of facilities/services |
|
Nature of crisis
ns |
Age (years) Learning disability: mean 21; range 17–25 Drug and alcohol: mean 19; range 14–25 Gender Female: learning disability, 46%; drug and alcohol, 41% |
||
| Walter et al.
76
USA Aim To gain a rich understanding of the circumstances surrounding the admission of children to hospitals, qualitative interviews elicited parents’ experiences of the crisis and community-based services preceding their child’s admission Nature of crisis Violent behaviour directed at self or others, threats to harm self or others and running away |
Participant characteristics
Families of children aged 6–12 years (n = 12) Setting/recruitment Participants were recruited from a convenience sample of families with children aged ≤ 12 years who were admitted to or residing at state mental hospitals in Kansas from November 2004 to January 2005 Age (years) Range: 6–12 Gender Female: 34% Ethnicity Caucasian: 92% |
Design
Qualitative descriptive as part of a wider case study evaluation Methodology ns Data collection methods Interviews with family members (n = 13) Data analysis Coding of transcripts with the development of themes |
Four themes emerged, of which three were relevant to the review: • The crisis response • Screening and admission • Prior community-based services |
| Nirui and Chenworth
133
Australia Aim To explore the kind of experiences that ‘suicidees’ had when seeking support from health-care services in the period leading up to their death, as perceived by close family and friends, and to find out what type of support was considered helpful to those at risk of suicide, from the point of view of family and close friends Nature of crisis Suicide |
Participant characteristics
People bereaved by suicide (i.e. family and close friends of young people) (n = 15) Recruitment Advertisements Purposive and snowball sampling. Participants mainly recruited from support groups for people affected by suicide Age (years) Mean: 25 years Gender Female (80%) Ethnicity ns |
Design
Qualitative descriptive (interpretivist) Methodology ns Data collection methods Interviews Data analysis Inductive analysis Constant comparison of codes and coding clusters |
Four themes emerged, of which two were relevant to the review • Perceptions of the role of the general medical practitioner in suicide prevention and support for people associated with suicide • Awareness and effectiveness of support services |
| Narendorf et al.
70
USA Aim To explore pathways to crisis service use for uninsured young adults who accessed emergency psychiatric treatment Nature of crisis Suicidal ideation or attempt, anxiety, depression, anger or aggression and psychotic symptoms |
Participant characteristics
Young people aged 18–25 years who had a current diagnosis of bipolar disorder, a recurrent major depressive disorder or a schizophrenia spectrum disorder (n = 55) Recruitment Young people who were admitted to an inpatient short-term stabilisation unit following a visit to a crisis emergency centre from July 2013 to March 2014. Young people were enrolled until saturation reached Age (years), mean ± SD 21.5 ± 2.3 Gender Female: 46% Ethnicity African American: 27% White: 27% Hispanic: 20% Multiracial: 20% Asian/American Indian: 5% |
Design
Qualitative descriptive Methodology ns Data collection methods Interviews Data analysis Analytic process based on techniques used in grounded theory |
The overall themes identified could be classified in relation to three broad dimensions that formed the pathway to crisis services. Two of these dimensions were relevant to this review: • Dimension 2 ◦ Translating intention into action by presenting to the psychiatric emergency centre ◦ Individual barriers and facilitators ◦ Systematic barriers • Dimension 3 ◦ The influence of natural supports and other social service providers and systems across the entire process ◦ Natural supports ◦ Service systems |
| Liegghio and Jaswal
90
Canada Aim To explore police encounters in child and youth mental health Nature of crisis Harming self or others, accused of committing a criminal act and needing physical interventions, such as restraint |
Participant characteristics
Caregivers (n = 7) and siblings (n = 7) of CYP aged 13–21 years Recruitment Recruitment occurred through a community-based children’s mental health service from January to August 2011 Purposive sampling was used to identify a non-random selection of caregivers with a child aged between 12 and 22 years old identified as having a mental health issue and siblings Characteristics of CYP in crises not provided |
Design
Qualitative descriptive as part of a wider mixed- methods study Methodology ns Data collection methods Interviews (n = 14) and focus groups (n = 2) Data analysis An inductive process consisting of a thematic content analysis and based on the principles of grounded theory |
Two themes emerged, one of which was relevant to this review: • De-escalate a high conflict situation involving a distressed child/sibling |
| Liegghio et al.
91
Canada Aim To present preliminary work in its early stages examining the issue of policing and police encounters in CYP with mental health problems Nature of crisis Leaving the home without permission/missing, destroying property, verbal and physical aggression towards family members (parents and siblings) and/or saying or making suicidal gestures |
Participant characteristics
CYP (n = 1449) Recruitment All CYP who had experienced police involvement at the time of intake into a community-based CYP mental health agency Age (years) 2–9: 7.7% 10–13: 24.4% 14–17: 63.8% 18–24: 5.1% Gender Female: 38% Ethnicity ns |
Design
Qualitative descriptive Methodology ns Data collection methods Qualitative memos collected between January 2009 and 2011 by the intake department (n = 567) Data analysis Owing to time and resource constraints, only one-third of the complete set of qualitative memos were analysed Thematic content analysis |
Coding of the memos resulted in a list of main reasons and circumstances for which CYP accessing mental health services had police involvement |
| Royal College of Emergency Medicine
96
UK Aim To explore what kind of facilities and expertise was available for CYP presenting to ED with mental health problems Nature of crisis All presenting to an ED |
Participant characteristics
Representatives from EDs in UK (n = 93, rr 38%) Recruitment All ED clinical leads and all known ED mental health departmental leads who were available at the annual Royal College of Emergency Medicine conference No participant details presented |
Design
Qualitative descriptive as part of a wider study Methodology ns Data collection Open-ended questions on online survey Data analysis ns |
Opened-ended comments presented alongside survey data under the following headings: • Availability of services and waiting times • Needs for admission |
Glossary
- Grey literature
- For the purpose of this evidence synthesis, the term grey literature covers UK-only government/organisational publications or policy/guidance documents providing relevant information.
- Record
- The title or abstract (or both) of a report indexed in a database or website.
- Report
- A (paper or electronic) document supplying information about a particular study or crisis service. For the purposes of this evidence synthesis, the term report covers journal articles and grey literature.
- Study
- An investigation, such as a randomised controlled trial, that includes a defined group of participants and one or more interventions and outcomes. A study might have multiple reports.
List of abbreviations
- 24/7
- 24 hours per day, 7 days per week
- ALPHA
- Advice Leading to Public Health Advancement
- ANOVA
- analysis of variance
- aOR
- adjusted odds ratio
- CAMH
- child and adolescent mental health
- CAMHS
- Child and Adolescent Mental Health Services
- CAPI
- Childhood Acuity Psychiatric Illness Scale
- CARES
- Child & Adolescent Rapid Emergency Stabilization
- CASP
- Critical Appraisal Skills Programme
- CBCL
- Child Behaviour Checklist
- CCM
- crisis case management
- CERQual
- Confidence in the Evidence from Reviews of Qualitative research
- CES-D
- Centre for Epidemiological Studies Depression Scale
- CGAS
- Children’s Global Assessment Scale
- CI
- confidence interval
- CYP
- children and young people
- EPPI-Centre
- Evidence for Policy and Practice Information and Co-ordinating Centre
- EThOS
- Electronic Theses Online Service
- FACES II
- Family Adaptation and Cohesion Scales – Version II
- FACES III
- Family Adaptation and Cohesion Scales – Version III
- FBCI
- family-based crisis intervention
- FFS
- Family, Friends, and Self Scale
- FISP
- Family Intervention for Suicide Prevention
- GP
- general practitioner
- GRADE
- Grading of Recommendations Assessment, Development and Evaluation
- HASS
- Harkavy–Asnis Suicide Scale
- HBCI
- home-based crisis intervention
- HBCI+
- enhanced home-based crisis intervention
- HCP
- health-care professional
- HoNOSCA
- Health of the Nation Outcome Scales for Children and Adolescents
- IQR
- interquartile range
- KALM
- Kids Assessment Liaison for Mental Health
- LFSS
- Lubrecht’s Family Satisfaction Survey
- LOS
- length of stay
- MST
- multisystemic therapy
- OR
- odds ratio
- PEACE
- Prevention of Escalating Adolescent Crisis Events
- PQDT
- ProQuest Dissertations & Thesis database
- PRISMA
- Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- RCT
- randomised controlled trial
- RTC
- residential treatment centre
- SAG
- Stakeholder Advisory Group
- SD
- standard deviation
- SFAI
- safety first assessment intervention
- SSBS
- Spectrum of Suicidal Behaviour Scale
- TAU
- treatment as usual
- VMD
- visits for mental disorders
- WoS
- Web of Science
Notes
-
Notes from Stakeholder Advisory Group meeting held in January 2020
-
Notes from Stakeholder Advisory Group meeting held in May 2020
-
Notes from Stakeholder Advisory Group meeting held in March 2021
-
Full list of websites searched along with the search terms utilised
-
Characteristics of additional reports that describe the organisation of crisis services
-
CERQual qualitative evidence profile
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/BPPT3407).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
