Notes
Article history
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as project number 17/99/19. The contractual start date was in September 2019. The final report began editorial review in October 2022 and was accepted for publication in February 2023. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ manuscript and would like to thank the reviewers for their constructive comments on the final manuscript document. However, they do not accept liability for damages or losses arising from material published in this manuscript.
Permissions
Copyright statement
Copyright © 2024 Cavallaro et al. This work was produced by Cavallaro et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2024 Cavallaro et al.
Chapter 1 Background
Parts of this chapter have been reproduced from the published papers by Cavallaro et al. 1 and Cavallaro et al. 2 These are open-access articles distributed in accordance with the Creative Commons Attribution 4.0 Unported (CC BY 4.0) licence, which permits others to copy, redistribute, remix, transform and build upon this work for any purpose, provided the original work is properly cited, a link to the licence is given and an indication of whether changes were made. See: http://creativecommons.org/licenses/by/4.0/.
Chapter outline
This chapter describes the context of adolescent pregnancy and the health visiting services available in England. It briefly describes the implementation of the Family Nurse Partnership (FNP) in England and reviews the literature on its effectiveness. It concludes with a description of the rationale for the present study and study objectives.
Adolescent pregnancy and adverse outcomes
Each year, approximately 3% of babies (~16,000 in 2020) are born to mothers aged < 20 years in England and Wales. 3 Adolescent mothers are more likely to experience adversity, be less engaged with education and employment and have rapid repeat pregnancies compared with older mothers. 4–7 For their children, young maternal age is associated with a higher incidence of preterm birth, low birthweight8,9 and a greater risk of child maltreatment and associated adverse long-term consequences, including poorer physical health and social, emotional and cognitive outcomes. 10–12 These adverse maternal and child outcomes of adolescent pregnancy, due to social adversity, disruption to education and employment and child-rearing practices, are of major importance to public health research and the NHS. 13,14 Programmes supporting adolescent mothers, such as the FNP, are therefore likely to remain a priority for the NHS and local authorities (LAs). 15
Understanding how best to target services to the most vulnerable mothers is key to improving the health of these mothers and their children. Evidence to help improve targeting is being called for by service providers, who need to understand the value of interventions in the context of their target populations and local services in order to inform commissioning and justify spending. 16
The Family Nurse Partnership and early years health visiting in England
Health visiting in England is delivered as part of the Healthy Child Programme. All families with children should receive a minimum of five visits from 28 weeks of pregnancy until the age of two and a half. 17,18 These mandated assessments allow health visitors to identify families in need of additional support and offer more intensive support, including additional health visitor contacts and referrals to other, more intensive, programmes. This model of proportionate universalism, an approach combining universal service provision accessible to all with more intensive services proportional to the level of need, has been recommended as key to reducing health inequalities in the UK. 19
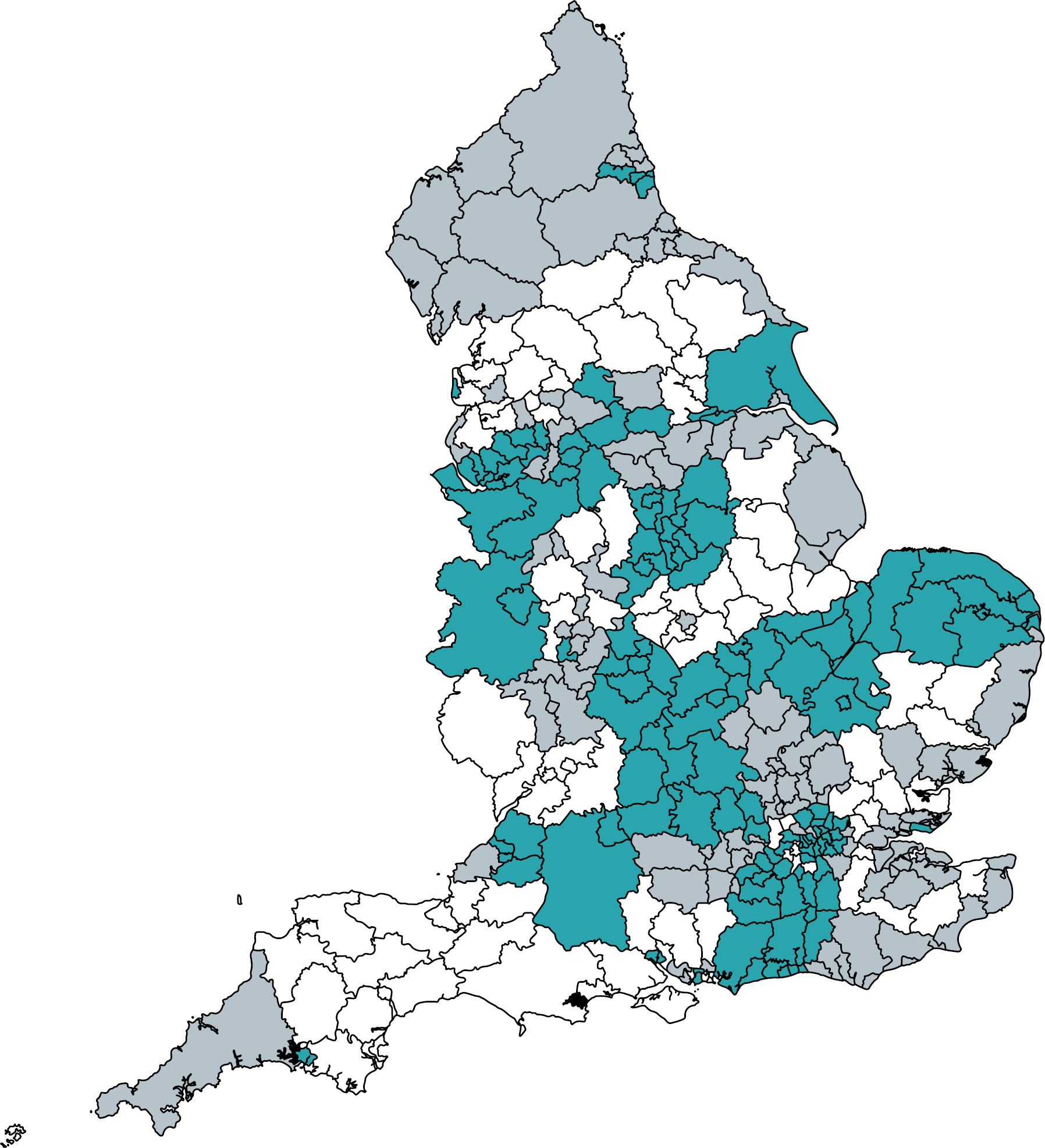
Several intensive health services aiming to reduce inequalities between adolescent and older mothers have been trialled; of these, FNP, an intensive home visiting programme supporting young first-time mothers, has a strong evidence base from several randomised trials in the USA and is recommended within the UK government’s Healthy Child Programme. 19,20 Mothers enrolled in the FNP receive up to 64 home visits by a dedicated Family Nurse from early pregnancy until the child’s second birthday. The FNP aims to improve birth outcomes, child health and development and promote economic self-sufficiency among young mothers. 21 Although a randomised trial of the FNP in England found no evidence of benefit on smoking in pregnancy, birthweight, hospital admissions before age 2 or second pregnancy within 2 years, improved cognitive development outcomes were reported, and there remains strong support for the programme locally (see Literature review – evidence of effect of Family Nurse Partnership programmes on maternal and child outcomes). 20–23 The Building Blocks 2- to 6-year follow-up reported no evidence of effect on maltreatment outcomes but evidence of improved school readiness, measured by a Good Level of Development in the early years foundation stage profile (EYFSP) and improved educational achievement at Key Stage 1. 24 The FNP has been commissioned in > 130 English LAs since 2007 (Figure 1).
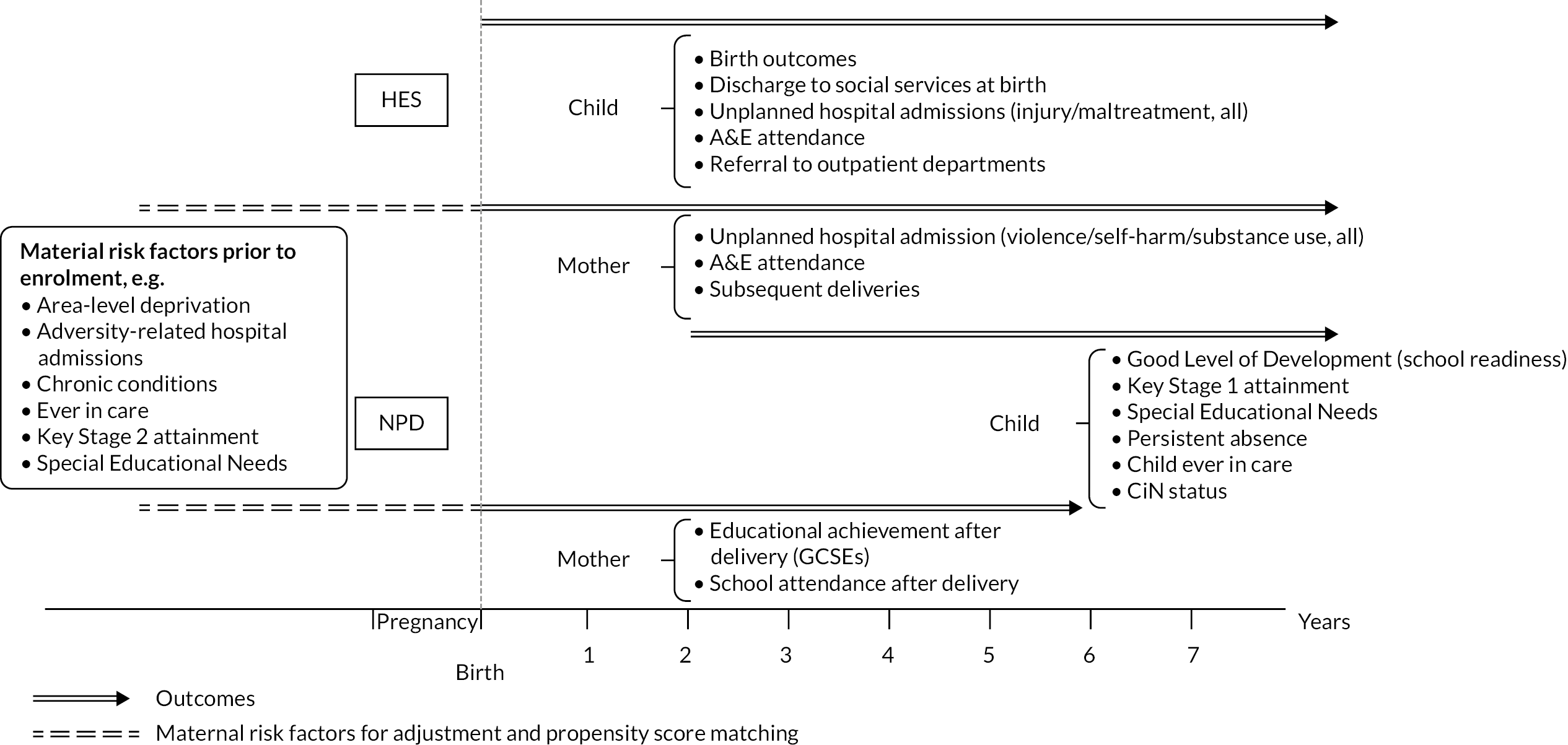
FIGURE 1.
Family Nurse Partnership site activity status in March 2019 among all FNP sites active during the study period (2010–9), by English LA.
Literature review – evidence of effect of Family Nurse Partnership programmes on maternal and child outcomes
Review approach
We conducted a literature review of the effect of FNP programmes on maternal and child outcomes using a combination of PubMed searches for ‘FNP’ or ‘Nurse Family Partnership’ (the original programme name in the USA) and identifying additional references through manual review of reference lists of previously identified papers from the USA, UK and other trials.
The evidence base for the FNP spans multiple countries and includes randomised controlled trials as well as a few non-randomised studies. Findings from this review were synthesised by the country in which the research was conducted, given differences in context and the importance of context (usual care) for the effect of interventions.
USA randomised trials
Most of the literature on the effectiveness of the FNP stems from three randomised trials of the Nurse Family Partnership (NFP) conducted in the USA by David Olds and colleagues, including over 20 peer-reviewed articles. The trials were conducted in Elmira, New York (enrolment 1978–80), Memphis, Tennessee (enrolment 1990–1) and Denver, Colorado (enrolment 1994–5). A wide range of maternal and child outcomes were examined, with up to 20 years of follow-up.
Overall, the evidence from the three USA trials indicates a positive effect on some – but not all – maternal and child health and educational outcomes. Often, the positive effect was observed in a subsample of particularly vulnerable mothers but not in the entire cohort. The Elmira trial found a one-third reduction in all accident and emergency (A&E) admissions among children up to age 2 and ages 2–4; however, no effect was observed on all hospital admissions ages 2–4. 25,26 Although a reduction in mean A&E and hospital admissions for injury/maltreatment of 55% was reported in the second year of life, no such effect was detected for injury/maltreatment in ages 0–1 or 2–4. No effect was observed on this outcome for up to 2 years in the Memphis trial. 27 The Elmira trial was the only NFP trial to examine child abuse/maltreatment reports and found a 40% reduction in such reports up to age 15 (although this benefit was not evident before the age of 4 years). 26,28
All three USA trials examined the effect of the NFP on child development and educational achievement. Results were mixed in the Elmira trial, with no effect up to age 4 for the whole sample and no effect on intellectual functioning at age 3 or 4 among children identified as maltreated. 26,29 There was no difference in intellectual functioning at age 3 or 4 among children of women smoking ≥ 10 cigarettes per day at enrolment; however, they did have higher intelligence quotient (IQ) scores (4.86 points on average) at this age than children of smoking mothers in the control arm. 30 The evidence in favour of a positive effect of the FNP was stronger in the Memphis and Denver trials, although these effects were concentrated in the subgroup of mothers with low psychological resources at enrolment (composite score including mental health, sense of mastery and intelligence scores), and even among this group, the positive effects were limited to only a few outcomes by age 6 and/or age 9 in the Denver trial. 31–36 Child mortality was only examined in the Memphis trial, which found no evidence of effect up to age 19 for all-cause mortality but a reduction in preventable-cause mortality in the NFP arm (0% vs. 1.6% in one control group, p = 0.04). 37
The effect of the NFP on maternal outcomes was weaker than on child outcomes. The Elmira trial found evidence of a 50% reduction in child abuse perpetration reports up to 15 years after giving birth. 28,38 There was evidence of 0.5 fewer subsequent births 15 years after the first birth among unmarried women of low socioeconomic status only in the Elmira trial but no evidence at 18 years in the Memphis trial or at 4 years in the Denver trial. However, there was evidence that NFP increased the subsequent birth interval by 5–28 months in all three trials (among the unmarried, low-socioeconomic subgroup in Elmira only). 32,34,38,39 There was no evidence of an effect on maternal educational qualifications beyond 6 months31,34,40,41 or on experience of domestic violence in the three trials (weak evidence of a decrease in the Denver trial). 28,34,42 Evidence was mixed regarding the effect on drug use or impairment. 34,38,42 The effect of NFP on maternal mortality was only examined in the Memphis trial, with no evidence of a difference in all-cause mortality but weak evidence of a 1% reduction for mortality from external causes at 20 years. 37
A more recent trial of 5670 Medicaid-eligible nulliparous pregnant mothers recruited between 2016 and 2020 in South Carolina found no evidence of an effect on birth outcomes (preterm birth, low birthweight, small for gestational age and perinatal death). 43
England Building Blocks randomised trial
One randomised controlled trial of the FNP (the Building Blocks trial) was conducted in England, enrolling approximately 1600 expectant mothers in 2009–10. 44 The Building Blocks trial found no evidence of effect on the four primary outcomes – smoking in late pregnancy, birthweight, second pregnancy within 24 months of first birth and rates of A&E attendance or hospital admissions within 24 months of birth. Some secondary outcomes suggested small positive impacts of the FNP in the first 2 years of life, including maternally reported child cognitive and language development. Safeguarding concerns recorded in primary care records were higher for mothers enrolled in the FNP.
Results for follow-up to age 6 showed no difference for most maltreatment outcomes between the trial arms, including referrals to social services, children referred as Children in Need (CiN), duration for which children were assessed as in Need, children with a child protection plan (CPP) or who were Looked After. 24 However, children in the FNP arm spent on average 2 months less time in care than children in the usual care arm. There was no evidence of a difference in children not attending a hospital outpatient appointment, attending A&E for injury or ingestion or being admitted to hospital for the same causes.
Nonetheless, there was evidence of FNP’s impact on some – but not all – child development and educational outcomes. There was no difference in Special Educational Needs (SEN) provision up to age 6 or educational attendance for ages 2–4. Children of FNP mothers were more likely to achieve a Good Level of Development at school entry (age 5) than in the usual care arm, with a greater beneficial impact on total point score (across 17 learning goals) observed for children of younger mothers. At Key Stage 1, children in the FNP arm were more likely to reach the expected level for reading; no other differences were observed for Key Stage 1 outcomes. The beneficial effects of the FNP were stronger among boys than girls (reading and writing), among younger mothers at enrolment (mathematics and writing) and among mothers not in employment, education or training at the time of enrolment (writing).
Other randomised trials in Germany, the Netherlands and Canada
Several other trials have been conducted in high-income countries. The VoorZorg trial in the Netherlands, enrolling in 2007–9, reported a reduction in child abuse/maltreatment reports by age 3 in the FNP arm, as well as a reduction in some types of interpersonal violence at 32 weeks of pregnancy and 24 months after birth. 45,46 A trial of a FNP-based model in Germany (Pro Kind) reported improved child development among high-risk women only, but no evidence of a difference in subsequent births within 2 years. 47 The follow-up trial evaluating outcomes at age 7 reported fewer behavioural problems in children, less child-abusive parenting, fewer maternal mental health problems and higher maternal life satisfaction in the intervention arm. 48 Some positive effects on mother–daughter interactions were also reported for a small subsample who agreed to participate in video recording. 49
One randomised controlled trial in Canada has not yet published results on primary outcomes but has reported preliminary findings on a number of secondary outcomes, with a reduction in prenatal cannabis use and a modest reduction in cigarette use in smokers associated with the intervention but no reduction in rates of prenatal cigarette and alcohol use. 50
Non-randomised studies in Australia, Scotland and the USA
Non-randomised studies in the USA and Australia have reported reduced preterm births, child maltreatment, infant death and subsequent births among FNP participants compared with controls, as well as higher high school attainment and different patterns of A&E attendance. 51–56 These studies adjusted for confounders through propensity score matching, frequency matching and entropy balancing, although due to limited maternal characteristics, the potential for residual confounding remains. The Australian study compared participants to eligible women who were not referred to and never participated in the programme, thereby also being subject to likely residual confounding. One prospective cohort study in Scotland has not yet reported results. 57
Other evidence
A randomised controlled trial of group FNP in England, administering 44 FNP sessions to groups of 8–12 expectant mothers, found no evidence of effect on parenting or maternal sensitivity or on secondary outcomes [except for a higher proportion of mothers breastfeeding at 6 months, odds ratio (OR) 3.2; 95% confidence interval (CI) 0.99 to 10.6]. 58
Synthesis
The available evidence on the effectiveness of the FNP is summarised in Appendix 1.
The three USA trials of FNP showed mixed but overall positive impacts on child health and development outcomes and some maternal outcomes, similar to the more recent Netherlands trial. These results contrast with the Building Blocks trial in England, which showed no evidence of impact of FNP on most child outcomes, with the exception of some cognitive outcomes. There are two main contributing explanations for the difference in results observed in England compared with the USA and the Netherlands: first, there are likely important differences in usual care contexts between different countries. The social safety net is likely to be stronger in England than in the USA, with better access to services for adolescent mothers not enrolled in FNP (including the minimum five mandated health visiting contacts, universal health care free at the point of care, services provided through free Children’s Centres, etc.), which may explain the lack of association for most outcomes in England. For example, the mothers in the control arm of the Building Blocks trial received an average 16 health visiting contacts up to the child’s second birthday. Nonetheless, the usual care group in the Netherlands trial probably had access to similar or better levels of care than in England, with 9–11 home visits before the child’s second birthday, as well as support from child welfare and mental health organisations,59 indicating that there are important factors (beyond access to services) shaping the effect of FNP.
Second, there are notable differences in the eligibility criteria for FNP in England compared with other countries. The main eligibility criterion for enrolment in FNP in England is maternal age: adolescents who are aged up to 19 at last menstrual period (LMP), and who are first-time mothers, are eligible for enrolment as long as they live in a LA with a FNP site and are enrolled before 28 weeks of pregnancy. From November 2016, a few FNP sites extended their eligibility criteria to enable enrolment after 28 weeks gestation and among mothers aged 20–24 at LMP with other markers of vulnerability, recognising that mothers in these groups could also benefit. 60 Eligibility criteria for the Building Blocks trial (nulliparous, age ≤ 19, living in the catchment area of a local FNP team, < 25 weeks of pregnancy)44 are therefore aligned with the practice in English FNP sites at that time. Young age is the main eligibility criteria for FNP in England, based on the ease of identifying the youngest adolescent mothers, associations between adolescent motherhood and social adversity, disrupted education and employment13,61 and other factors contributing to poor birth and health outcomes among their children. 5,6,62
In contrast, additional socioeconomic criteria such as unemployment, low educational level or low income are used in combination with maternal age in other countries,27,35,63 based on logic models of how the original NFP was expected to provide benefits. 64 As a result, the population of young mothers enrolled in trials in other countries are a more selected and vulnerable group than in England, who may stand to benefit more from the FNP (as evidenced by greater effectiveness in socioeconomically deprived groups demonstrated in the USA trials). 32,36,38
Rationale for the present study
Usual care available to adolescent mothers is likely to have declined between the Building Blocks trial study period and after the introduction of austerity measures in England – in particular, health visitor budgets have decreased since responsibility for commissioning health visiting services shifted from the NHS to local government in England in 2015. 65 Furthermore, evidence from the USA trials suggests that the youngest, most disadvantaged mothers are likely to benefit most from FNP. 22 Adequately powered subgroup analyses are needed to examine whether some groups of families benefit from FNP more than others. In addition, constrained conditions under which trials are conducted often do not match the complexity of real-world implementation of programmes. 66
Linkage of existing administrative records provides a cost-efficient means of evaluating services as they are implemented in the real world by bringing together data from different sectors on a range of outcomes. They also allow for a sufficiently large sample size for subgroup analyses. Our population-based study aims to use longitudinal linked observational data between the health, education and social care sectors to evaluate the effects of FNP on outcomes of eligible mothers and their children up to age 7 to generate evidence on the factors that may influence effectiveness and programme engagement (including participant characteristics, setting, provider and programme delivery). 67,68 Evaluating outcomes for approximately 30,000 FNP families and up to 1 million controls built on the results of the Building Blocks trial24,44 will provide increased statistical power to detect smaller differences, differences in rarer outcomes and subgroup differences for which the Building Blocks trial was underpowered. Use of these data for the real-world evaluation of FNP is important and necessary to inform the targeting and commissioning of services by generating evidence on which groups of mothers and their children benefit from the real-world implementation of FNP in England.
Research aims and objectives
We aimed to evaluate the real-world, ongoing implementation of FNP in England on the outcomes of mothers participating in FNP and their children. Specifically, our objectives were to:
-
determine the rate of and characteristics associated with enrolment in FNP among young mothers across LAs in England
-
determine the effect of FNP on maternal and child outcomes, including identifying which families benefit the most from FNP
-
identify contextual and programme factors that might influence the effects of FNP.
Chapter 2 Methods
Parts of this chapter have been reproduced from the published papers by Cavallaro et al. 1 and Cavallaro et al. 2 These are open-access articles distributed in accordance with the Creative Commons Attribution 4.0 Unported (CC BY 4.0) licence, which permits others to copy, redistribute, remix, transform and build upon this work for any purpose, provided the original work is properly cited, a link to the licence is given and an indication of whether changes were made. See: http://creativecommons.org/licenses/by/4.0/.
Chapter outline
This chapter begins with a description of the study participants and data sources. It then describes the data linkages and manipulations performed for this study: linkage of FNP data to Hospital Admissions Data [Hospital Episode Statistics (HES)], creation of the cohort of FNP mothers and controls, creation of the child cohort and linkage of the FNP-HES mother and baby cohort to education and social care records [National Pupil Database (NPD)]. Lastly, it defines the outcome and exposure variables used, and the analyses conducted, in this study.
Study design and participants
We created a retrospective cohort of all first-time mothers aged 13–19 years at LMP with live births in England between 1 April 2010 and 31 March 2019 and their first-born child(ren), using individual-level, linked, longitudinal data from routinely collected hospital, education and social care records. We also constructed a similar cohort of all first-time mothers aged 20–24 at LMP because some FNP sites implemented modified inclusion criteria to include young mothers up to this age. The cohort was created through linkage of hospital records (HES), education and social care records (NPD) and FNP programme data for mothers and their children. Our approach built on previous linkage of education and health records and validated methods of linking hospital records for mothers and babies. 69–71
Data sources
Hospital Episode Statistics – Hospital Admissions Data
Hospital records for mothers aged 13–24 years and their children in England were extracted from records of births and deliveries in HES. HES is a data warehouse containing details of all hospital admissions (from 1997), outpatient appointments (from 2003) and A&E visits (from 2010) at NHS hospitals in England. 72 HES data have been extensively used in research. In addition to the birth record, we linked information from hospital admissions and A&E attendances for mother and child (including up to 11 years before delivery for the mother; see Appendix 2, Figure 16).
Information captured in HES includes administrative data [including admission dates, NHS trust, general practitioner (GP) code]; demographic information (including age, sex, ethnicity) and clinical information (diagnoses and procedures). A unique ‘Hospital Episode Statistics Identifier (HESID)’ is assigned to enable episodes of care for the same individual to be combined (this has recently changed to a ‘Token Person ID’). Diagnoses are coded by professional coders in hospitals using International Classification of Diseases, 10th Revision (ICD-10) codes (International Classification of Disease, version 10); procedures are coded using Office of Population, Censuses and Surveys Classification of Surgical Operations and Procedures, version 4 codes (OPCS-4). 73,74 Based on previous methodological work, we linked delivery records for mothers and birth records for their children within HES to create a mother–baby HES cohort. 69
National Pupil Database – education and social care data for mothers enrolled or not in Family Nurse Partnership and their children
The HES cohort of mother–baby pairs were linked to education and social care records from the Department for Education for both mothers and children in FNP and comparison groups (including information before delivery for mothers). Information on assessments, attainment and progression at each Key Stage is available for all pupils in state schools in England, alongside eligibility for free school meals (FSM), information about SEN provision and information about absences and exclusions. NPD, including social care data, has been extensively used in research. 75
For both mothers and their children in the cohort, we linked HES data to the following NPD databases:
-
The Spring School Census (formerly PLASC), the Early Years Census, the Pupil Referral Unit (PRU) Census and Alternative Provision – including pupil-level information from 2002 (for the School Census) for pupils aged 2–19+ on SEN, FSM eligibility and information about absences and exclusions.
-
The CiN Census – including information on referrals to children’s social services, assessments carried out upon these children and whether the children became the subject of a CPP, from 2008. 76
-
The Children Looked After (CLA) return – including information on all Looked After children and recent care leavers in England, from 2005. 77,78
For mothers only, we linked to Key Stages 2 and 4 data, which include teacher assessments and/or test results in Year 6 (age 11) and Year 11 (age 16). We also linked to Key Stage 5 data (Year 12–13, ages 17–18) but did not use these data due to small numbers. For children only, we linked to the Early Years Census and EYFSP. These data include whether the child achieved a Good Level of Development at school entry (age 5), which we used as a proxy for school readiness, as well as Key Stage 1 assessment data (age 7).
A Unique Pupil Number (UPN) is used by the Department for Education (DfE) for linkage of CLA and CiN with the NPD. The UPN is usually assigned at first entry to a maintained school or nursery, typically around the age of 4–5. Therefore, it is not possible to link the NPD to CLA or CiN data for children who receive social care services only before they enter nursery/school or for some adopted children (who can be provided with a new UPN). 79 It is not mandatory to return UPN in CLA or CiN beyond age 16. UPN was replaced by an anonymised Pupil Matching Reference in the data that we had access to.
Family Nurse Partnership information system – Family Nurse Partnership service data for mothers enrolled in Family Nurse Partnership
The HES cohort was linked to the Family Nurse Partnership information system (FNP IS) to obtain information on participation in FNP for mothers who were enrolled in FNP. The FNP IS supports the implementation of the FNP programme in England, originally provided by NHS Digital under contract to the FNP National Unit on behalf of Public Health England. Data are reported in real time and are used locally by FNP teams and nationally by the FNP National Unit to monitor programme delivery and support quality improvement.
Data collected in the FNP IS include information from the mother and child collected at enrolment (by 28 weeks gestation at the latest, including mother’s age, marital status, living arrangements, education, employment, social care); 36 weeks gestation (including maternal health, alcohol, drugs and smoking); birth (including birthweight and gestational age) and at regular intervals until 24 months after birth (including child health and development, social care and other maternal baseline variables). Information on each visit is also collected (including date, length of visit, family nurse seen and referrals to other services). The FNP IS became functional in 2009, and data quality was reported to be high from 2010 onwards. FNP data have been used in previous research. 80
The FNP IS contains maternal and child identifiers at enrolment/birth: name, sex, date of birth, postcode, GP code and NHS number. When mothers graduate from the FNP (mostly at the child’s second birthday, but sometimes earlier), pseudonymised data are retained only by the FNP National Unit, and identifiers are held solely on secure servers at NHS Digital.
The time span covered by each data source (including look-back, study and follow-up periods) is described in Appendix 2, Figure 16.
Linkage Family Nurse Partnership-Hospital Episode Statistics
Linking mothers enrolled in Family Nurse Partnership to Hospital Episode Statistics
Linkage between data from the FNP IS and HES was conducted using deterministic linkage via NHS Digital (see Appendix 2, Tables 21 and 22). Of the 32,040 mothers in our FNP cohort who gave birth between April 2010 and March 2019, 31,560 (98.5%) were linked to a record in HES.
Characteristics of unlinked mothers
Appendix 2, Table 24, describes the characteristics of the 31,560 FNP mothers who linked to a HESID and the 480 FNP mothers who either did not link to a HESID (n = 10) or who linked to a likely incorrect HESID and were subsequently excluded (n = 470). Compared to mothers who linked to a HESID, unlinked mothers seemed to be a slightly more vulnerable group: they were less likely to be living with their mother (with or without their partner present) or to have any GCSEs at enrolment and more likely to have missing data. They had a lower mean number of FNP visits (26, compared with 35 for FNP mothers who linked to a HESID). They were more likely to be of black, South Asian or mixed/other ethnicity and living in London.
Description of linkage quality
Of the 31,560 FNP mothers included in our linked study cohort, 31,450 (99.7%) linked to HES via the FNP-HES linkage key at match rank 1 or 2, indicating high-quality links. Only 0.3% (n = 85) of mothers linked at match rank > 2, indicating less-certain links. Twenty-five mothers (< 0.1%) were linked to HES manually (see Appendix 2, Figure 17).
To check for potential false matches between FNP and HES, we assessed the agreement between information recorded separately in both data sources for all FNP mothers in our cohort who linked to at least one HES admitted patient care (APC) record (see Appendix 2, Table 25). Agreement between both data sources was generally high.
Identification of local authorities and enrolment dates for each Family Nurse Partnership site
Mothers aged 13–19
There is a complex history of FNP sites in England, with site openings, closures, mergings and splits throughout the study period. In addition, the catchment area of FNP sites may have changed over time (e.g. a site may have been decommissioned for one LA in its catchment area but continue to operate in another).
We used FNP IS data to identify the first and last month-year in which expectant mothers aged 13–19 at LMP were enrolled in each FNP site based on the enrolment dates recorded in each participant’s record. We calculated start and end dates separately for each lower-tier LA in each FNP site in order to allow for changes in catchment area over time. We used the lower-tier LA recorded in FNP participants’ HES records because FNP IS records only upper-tier LA of residence at enrolment. Lower-tier LA was also used to identify the catchment area for each FNP site (e.g. the Hampshire FNP site included only a subset of lower-tier LAs in Hampshire). Inconsistencies were resolved through detailed consultation with the FNP National Unit, including consultation of site records. Nonetheless, some misclassification in catchment areas or activity dates remains likely, particularly before the FNP became commissioned by LA in October 2015, when Primary Care Trust level commissioning (with potentially non-overlapping boundaries compared with LAs) meant slight changes in catchment areas may have occurred at this time.
Activity dates and lower-tier LAs included in the catchment area for 122 FNP sites are included in Appendix 2, Table 26).
Mothers aged 20–24
As some sites had changed their eligibility criteria during the study period to allow some mothers aged up to 24 to be enrolled, we also planned to include mothers aged ≥ 20 in our analysis. We used FNP IS data to identify LAs that had extended their eligibility criteria to allow for recruitment of older mothers. We classified LAs as having extended criteria if at least 10 mothers aged 20–24 at LMP and giving birth up to 31 March 2019 were enrolled in the FNP. As with mothers aged 13–19, we defined site activity dates as the first and last month-year in which mothers aged 20–24 were enrolled in each site. We did not calculate different activity dates for lower-tier LAs in each site due to small sample sizes and because all but one site only included one lower-tier LA in their catchment area; see Appendix 2, Table 27).
Description of Hospital Episode Statistics cohorts
Mothers aged 13–19
This study cohort included all 130,415 mothers aged 13–19 at LMP who had their first live birth between 1 April 2010 and 31 March 2019 and whose first antenatal booking appointment as recorded in HES (or estimated date of 28 weeks gestation, if missing) occurred on a date when the FNP was active in their LA of residence (Figure 2). Of these, 99,150 (76%) were never enrolled in FNP.
FIGURE 2.
Identification of FNP participants and comparison group among cohort of mothers aged 13–19. Note: numbers have been rounded to the nearest 5 in accordance with NHS Digital’s statistical disclosure rules for subnational analyses; totals may not be equal to the sum of component categories. ANC, antenatal care.
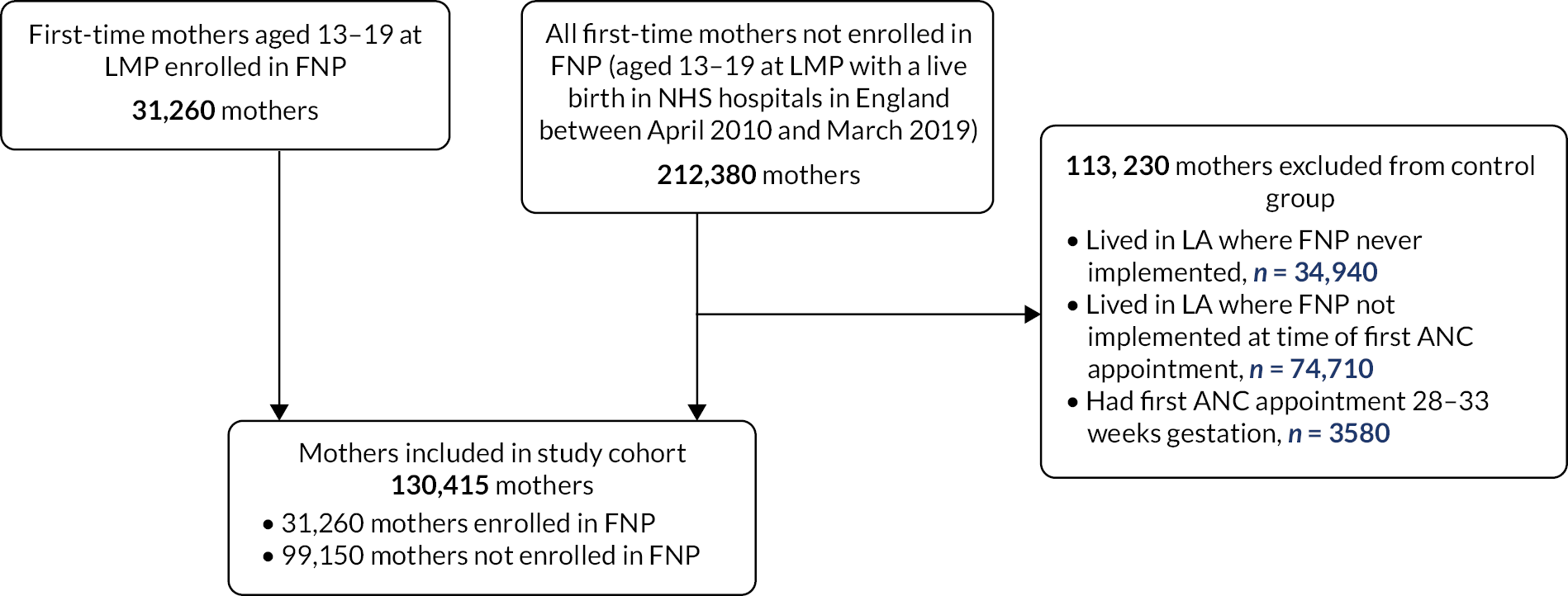
Date at LMP was estimated by subtracting gestational age at birth from the date of childbirth or subtracting 40 weeks (the median gestational age at birth among mothers aged 13–19 in our cohort) from the date of childbirth for the 13% of mothers with missing gestational age at birth. Mothers whose antenatal booking appointment occurred between 28 and 33 weeks gestation were excluded as they would not have met the eligibility criteria for the FNP (see Figure 2). This means we may have excluded a small number of eligible mothers within the few sites that allowed enrolment after 28 weeks from November 2016. Since we observed a spike in the number of mothers with a recorded gestational age at booking appointment of 33 weeks or more, we considered these to be data errors (6% of mothers) and recoded them to 28 weeks so that they could be retained within the cohort.
The creation of the study cohort of mothers aged 20–24 is described in Appendix 2, Figure 18.
Identification of Hospital Episode Statistics child cohort
We used two linkage keys to identify the children of mothers included in the study cohort: first, a FNP-HES mother–baby linkage key provided by the FNP IS, and second, a mother–baby linkage key based on a previously developed algorithm using de-identified HES data. 69
Among the 31,425 FNP mothers in our cohort, 31,260 aged 13–19 and 165 aged 20–24 years, 31,125 (99%) were linked to a baby HESID (see Appendix 2, Figure 18). Among the 1025 mothers in our cohort with multiple births, 80 (78%) had at least two recorded baby HESIDs, 220 (21%) had only one recorded baby HESID and 5 (0.5%) had no recorded baby HESIDs. Where only one baby HESID was recorded for a multiple birth, the identified child was retained in the child study cohort.
Hospital Episode Statistics – National Pupil Database linkage
Description of linkage
Linkage of all mothers and children in the study cohort to NPD education modules was performed by the DfE, following extraction of identifier information (including full name and postcode history) by NHS Digital. DfE used a matching algorithm requiring agreement (full or ‘fuzzy’) on names, date of birth and postcode; matching to NPD was not completed for names and date of birth only or on names and postcodes only (see Appendix 2, Table 28). Subsequent linkage to social care data was performed by DfE via the Pupil Matching Reference number.
Linkage of maternal Hospital Episode Statistics records to National Pupil Database
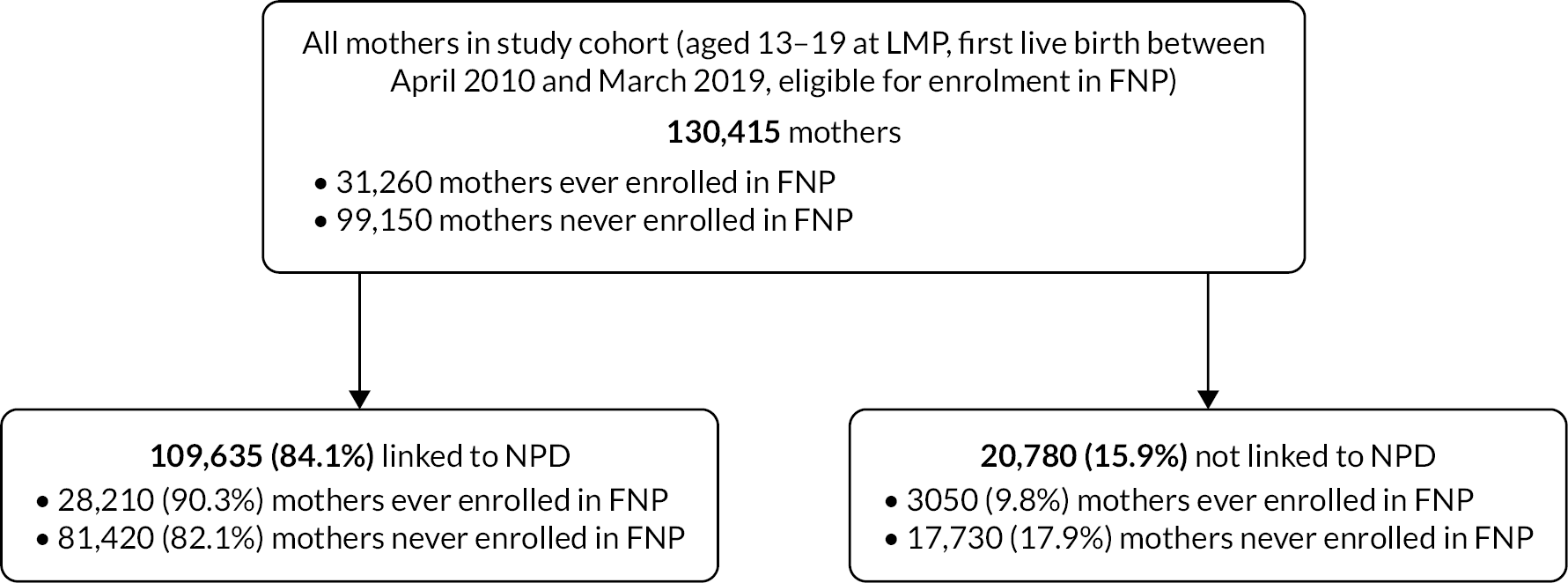
Of the 130,415 mothers aged 13–19 included in the study cohort, 109,635 (84.1%) were linked to a record in NPD (Figure 3). Mothers who were enrolled in FNP were slightly more likely to link (90%) compared with mothers who were not enrolled (82%). Overall, 98% of linked mothers linked at match strength 1, indicating fully confident matches.
FIGURE 3.
Description of linkage of the NPD and HES – mothers in cohort. Note: numbers have been rounded to the nearest 5 in accordance with NHS Digital’s statistical disclosure rules for subnational analyses.
Linkage of child Hospital Episode Statistics records to National Pupil Database
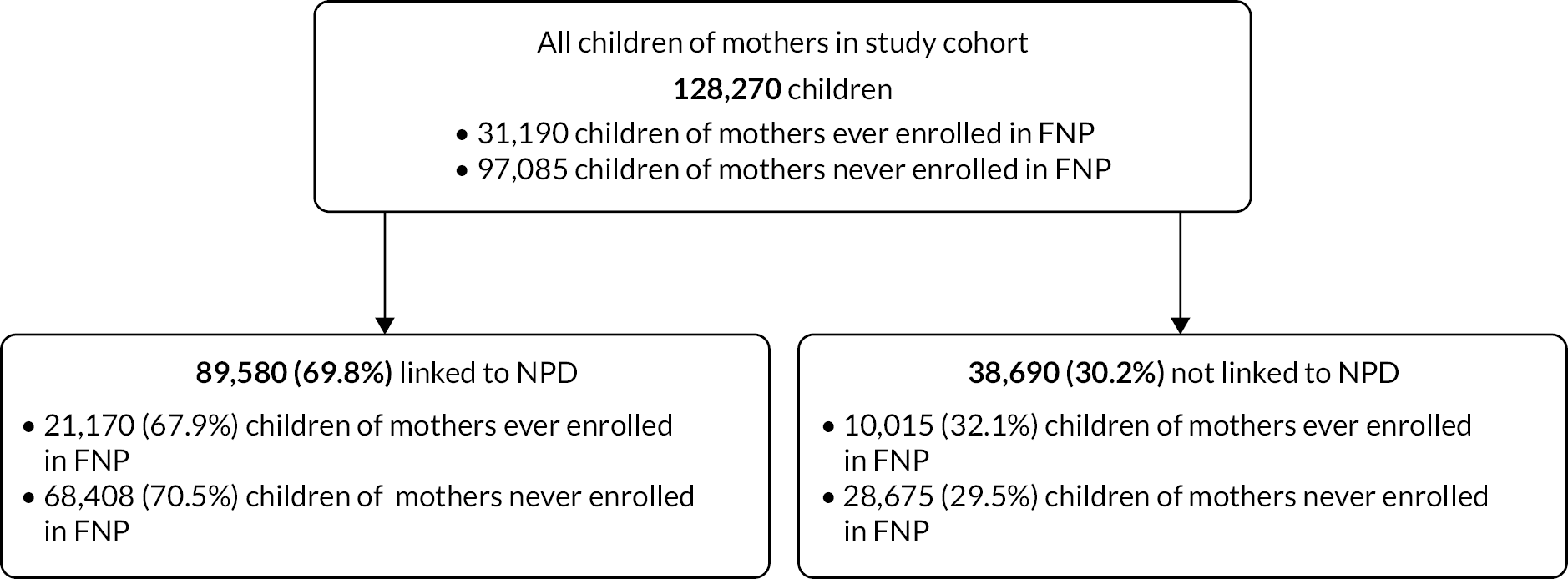
Among 128,270 children of mothers aged 13–19, 89,580 (69.8%) were linked to a record in NPD (Figure 4). Children born to FNP mothers were slightly less likely to link to NPD (68%) than those born to mothers not enrolled in FNP (71%). Overall, 97% of linked children linked at match strength 1, indicating fully confident matches.
FIGURE 4.
Description of linkage of the NPD to HES – children in cohort. Note: numbers have been rounded to the nearest 5 in accordance with NHS Digital’s statistical disclosure rules for subnational analyses.
Characteristics of unlinked mothers and children
There were some differences in the characteristics of mothers in the study cohort who were and were not linked to NPD (see Appendix 2, Table 29). Mothers who did not link to NPD were much less likely to be of white ethnicity (65% vs. 87% among all mothers who linked) and more likely to live in the most deprived quintile (52% vs. 47%) and to have reached 20 weeks of pregnancy at antenatal booking appointment (8% vs. 5%). However, unlinked mothers were less likely than linked mothers to have vulnerability indicators relating to a history of hospital admissions – those related to mental health, adversity and chronic conditions, as well as A&E attendance.
The FNP data gave more insight into the characteristics of those who did and did not link (see Appendix 2, Table 30). FNP mothers who did not link to NPD were more likely to be living alone or in care at enrolment and to attend their antenatal booking appointment after 10 weeks of pregnancy. However, they were less likely to be recorded as CiN, having a CPP or being a child in care during pregnancy.
There were also some differences in the characteristics of children in the study cohort who did and did not link to NPD (see Appendix 2, Table 31). Children who did not link to NPD were more likely to be born from 2016 onward, less likely to have a mother of white ethnicity and slightly more likely to live in less deprived areas.
Definition of outcome variables
Study outcomes and data sources for this study are described in Figure 5 and Table 1. We selected outcomes for the FNP evaluation based on the FNP logic model,64 with some caveats outlined below.
FIGURE 5.
Family Nurse Partnership evaluation – data sources and outcomes.
| Domains | Outcomes | Years after birth | HES | NPDa |
|---|---|---|---|---|
| Child outcomes (up to age 7) | ||||
| Indicators of child maltreatment |
Unplanned hospital admissions for any injury or maltreatment-related diagnosisb | 0–7 | ✓ | |
| Discharge to social services at birth | 0 | ✓ | ||
| CLA | 4/5–7 | ✓ | ||
| CiN status | 4/5–7 | ✓ | ||
| CPP | 4/5–7 | ✓ | ||
| Healthcare use | Unplanned hospital admissions (any diagnoses) | 0–7 | ✓ | |
| A&E visits (any diagnoses) | 0–7 | ✓ | ||
| Referral to outpatient departments (uptake and non-attendance) | 0–7 | ✓ | ||
| Education | School readiness measured by a Good Level of Development in EYFSP at school entry (reception)86 | 5 | ✓ | |
| Achieved expected levels at Key Stage 1 assessment | 7 | ✓ | ||
| SEN provision | 5–7 | ✓ | ||
| FSM (eligible, applies for and receives) | 5–7 | ✓ | ||
| Persistent absence (absent for ≥ 10% possible sessions) | 5–7 | ✓ | ||
| Maternal outcomes (up to 7 years following delivery) | ||||
| Maternal adversity | A&E attendances (any diagnoses) | 0–7 | ✓ | |
| Unplanned hospital admissions (any diagnoses and for violence, self-harm or drug/alcohol abuse)87 | 0–7 | ✓ | ||
| Reproductive outcomes | Subsequent deliveries within 18 months of index birth | 0–2 | ✓ | |
| Education | Key Stage 4 assessmentc (5 A*–Cs at GCSE or equivalent) | 0–2 | ✓ | |
| School attendance after birthd | 0–2 | ✓ | ||
Indicators of child maltreatment
We assessed the effect of FNP on indicators of child abuse and neglect, as measured by the percentage of mothers whose baby was discharged from hospital to social services at birth, whose child had at least one unplanned hospital admission for injury or maltreatment-related diagnoses or who died (up to age 2 or 7) or whose child was ever recorded as a Child in Need, as having a CPP, or being a Child Looked After (at age 4–5 years). ICD-10 code lists for injury or maltreatment-related diagnoses were based on previously published lists81,82 and are included in Appendix 3. As the UPN for linking education and social care data is usually assigned at school entry, social care data for children only involved with social care prior to school entry cannot be linked. Therefore, we only examined CPP, Child in Need and CLA status after school starting age (4–5 years). Thresholds for CiN status vary across the country: only assessments that have been ‘accepted’ are recorded within the data. The CiN data exclude some disabled children (those who are not receiving services from LAs) and children who are receiving support from LAs through early help services. 83 We did not have the primary need code in our data, and some children referred to social care services will be referred for reasons other than child maltreatment (e.g. child disability).
The potential for surveillance bias to distort the effect of early life interventions on child maltreatment has been extensively discussed, and nurse home visiting has been shown to result in increased contact with nurses, potentially leading to lower thresholds for referral to social care services for families enrolled in FNP than families who are not enrolled. 29,44,45 This bias in ascertainment of maltreatment may dilute or reverse the association between FNP participation and maltreatment. Conversely, it has also been hypothesised that a nurse’s closeness to participants may delay reporting of suspected maltreatment. 45 We examined CiN referral source, aiming to determine whether the proportion of referrals initiated by health visitors differed between children of mothers enrolled and not enrolled in FNP.
Child health, developmental and educational outcomes
We firstly described rates of preterm birth (< 37 weeks of pregnancy) and low birthweight (< 2500 g) between groups. We also described A&E attendance and unplanned hospital admissions for any diagnosis. These were reported as descriptive outcomes since the direction of effect could be interpreted positively or negatively (FNP participation might reduce the need for emergency care or alternatively increase appropriate care seeking). Nonetheless, they represent important outcomes for understanding the effects of FNP on care-seeking behaviour.
For children reaching school age, we examined the effect of the FNP on school readiness as measured by the percentage of each group achieving a Good Level of Development as recorded within the EYFSP (level 2 + across the combined five areas of learning at school entry) at age 5, persistent absence (absent for ≥ 10% of possible school sessions), achieving expected levels at Key Stage 1 (age 7) for Mathematics, Reading and Writing and recorded as having SEN provision. We also examined FSM eligibility (pupils are recorded as eligible if a claim for FSM has been made by them or on their behalf by their parents). We also calculated the percentage of children in each group recorded in the EYFSP as having attended nursery.
Maternal outcomes
For mothers, we evaluated unplanned hospital admissions for adversity-related reasons (violence, self-harm and drug/alcohol abuse) or for mental health-related diagnoses after delivery (see Appendix 3). As with child outcomes, A&E attendance and unplanned hospitalisations for any diagnoses were reported as descriptive outcomes. We also examined the effect of FNP participation on subsequent pregnancies within 18 months of the first live birth. We examined subsequent births within 18 months (rather than pregnancies within 24 months as measured in the Building Blocks trial) because 18-month birth intervals are associated with the highest risks of adverse outcomes for women and babies. 84,85 Amongst mothers who had not previously had the opportunity to take GCSEs (i.e. were < 16 at the start of the academic year in which they reached 20 weeks of pregnancy), we evaluated the percentage in each group who achieved 5 A*–C grades including English/Maths at GCSE level (or equivalent), in the 2 years after delivery. We did not evaluate A-level outcomes as these data were available for < 1% of mothers. Amongst mothers who would still have been school age in the year following the academic year in which they reached 20 weeks of pregnancy (i.e. those aged < 15 at the start of the academic year in which they reached 20 weeks of pregnancy), we evaluated the percentage in each group who were enrolled in school up to Year 11 during the 7 years following birth. We did not evaluate school outcomes past Year 11 or the proportion of mothers sitting GCSEs after Year 11, due to small numbers.
Follow-up cohorts
Outcome data were available for up to 7 years after delivery, but eligibility for each outcome depended on the child’s age. We therefore described outcomes (1) at birth, (2) in the 2 years following delivery and (3) in the 7 years following delivery. We describe the cohorts used for each set of outcomes in Table 2.
| Follow-up cohort | Number of mothers | Number of children | ||||
|---|---|---|---|---|---|---|
| Total | 13–19 years | 20–24 years | Total | 13–19 years | 20–24 years | |
| Birth outcomes (Births 2010–9) |
134,880 | 130,415 | 4465 | 132,660 | 128,270 | 4390 |
| FNP mothers | 31,425 | 31,260 | 165 | 31,350 | 31,190 | 165 |
| Non-FNP mothers | 103,445 | 99,150 | 4305 | 101,300 | 97,085 | 4230 |
| 2-year follow-up (Births 2010–7) |
110,555 | 110,555 | – | 108,675 | 108,675 | – |
| FNP mothers | 25,690 | 25,690 | – | 25,630 | 25,630 | – |
| Non-FNP mothers | 84,860 | 84,860 | – | 83,040 | 83,040 | – |
| 7-year follow-up (Births 2010–2) |
27,250 | 27,250 | – | 27,015 | 27,015 | – |
| FNP mothers | 4385 | 4385 | – | 4375 | 4375 | – |
| Non-FNP mothers | 22,865 | 22,865 | – | 22,640 | 22,640 | – |
Definition of exposure variables
The main exposure of interest in this evaluation was enrolment in the FNP, regardless of the number of FNP visits received. Enrolment in the FNP was identified by linkage of a mother in HES to a FNP IS record.
The main maternal risk factors in this study are described in Table 3. We used 20 weeks of pregnancy as the reference point since 93% of all mothers attend an antenatal booking appointment by this stage. 88 We selected exposures based on maternal vulnerability risk factors known to be associated with poor infant outcomes and available within HES delivery records: maternal age, ethnic background and area-level deprivation [Index of Multiple Deprivation (IMD) quintile]. 89 We also considered maternal unplanned hospital admissions in the 2 years prior to 20 weeks gestation: mental health-related admissions (excluding self-harm and substance misuse); adversity-related admissions (violence, self-harm or substance misuse) and chronic condition admissions were identified based on published lists of ICD-10 diagnostic codes (see ICD-10 code lists for maternal hospital admissions related to adversity, mental health and chronic conditions). 87,89–91 Having at least one A&E attendance and repeated A&E attendances within 2 years prior to 20 weeks gestation was also considered as a risk factor. We also considered risk factors recorded in social care and education data. Seasonality of birth (quarter-year) was included based on evidence from the Building Blocks trial of associations, for example, with Key Stage 1 attainment. 24
| Maternal risk factor | Categorisation |
|---|---|
| Date of delivery | Year/quarter-year |
| Maternal age at birth | 13–15, 16–17, 18–19, 20 years |
| Ethnicity | White, black, South Asian, mixed/other or unknown |
| Area-level deprivation at birth | Quintile of the IMD |
| Region of residence | South-East, London, North-West, East of England, West Midlands, South-West, Yorkshire and the Humber, East Midlands, North-East |
| Gestational age at booking | < 10 weeks, 10–20 weeks, 20 + weeks |
| History of hospital attendances in the 2 years before 20 weeks of pregnancy: | Unplanned hospital admissions for adversity-related diagnosesa Unplanned hospital admissions for mental health-related diagnosesa Any hospital admission for chronic condition-related diagnosesa Any A&E attendance Repeated A&E attendance (4 + A&E attendances) Did not attend ≥ 1 outpatient appointment |
| History of Social Care contacts before 20 weeks of pregnancy | Ever had a CPP Ever a CLA |
| Educational risk factors before 20 weeks of pregnancy | Ever recorded as having SEN provision Ever recorded as having FSM (eligible, applies for and receives) Ever in the most deprived IDACI decile Ever excluded from school, in a PRU or alternative provision Ever persistently absent (≥ 10% of possible sessions) Achieved expected levels at Key Stage 2 Mathematics/Englishb Achieved 5 A*–Cs at GCSE levelc |
Analyses
Descriptive analyses
We described maternal risk factors at the time of pregnancy, previous health and educational risk factors (see Table 3) and pregnancy outcomes for all mothers in our cohort according to enrolment in FNP. We further described maternal risk factors at enrolment and during pregnancy among mothers enrolled in the FNP (using risk factors collected in FNP IS, such as living arrangements and intimate partner violence).
Enrolment rate and maternal risk factors associated with enrolment in the Family Nurse Partnership (Objective 1)
We restricted the enrolment analysis to mothers giving birth between April 2010 and March 2017 for those aged 13–19 at LMP in order to use the same cohort for Objectives 2 and 3 (ensuring at least 2 years of follow-up for all mothers and their children in the cohort). We calculated enrolment rates as the percentage of FNP participants among eligible first-time adolescent mothers living in a LA with an active FNP site at the time of first antenatal appointment before 28 weeks of pregnancy, including by site and maternal risk factor (see Table 3). We also calculated the percentage enrolment for all first-time adolescent mothers in England (including areas not offering the FNP). Multilevel logistic regression models with mothers nested within FNP sites were used to calculate crude and adjusted ORs of enrolment. Multivariable models included all maternal risk factors; multicollinearity was assessed using Spearman correlation coefficients. To examine variation in maternal risk factors for enrolment, we stratified the analysis by site characteristics: we classified FNP sites with enrolment rates in the top quartile as ‘high-enrolment sites’ and those with enrolment rates in the bottom quartile as ‘low-enrolment sites’. We stratified the multivariable models according to high-/low-enrolment site, region and financial year of delivery and tested for interactions between these strata and each maternal risk factor. We explicitly classified mothers not linking to NPD as ‘unlinked’ in relevant variables to retain them in the models.
Lastly, we built crude and adjusted funnel plots of the percentage enrolled in each FNP site according to the size of the eligible adolescent mother population, separately for mothers aged 13–17 and 18–20 at childbirth, to assess the extent to which variation in enrolment rates across sites was likely to be due to chance. The outer limits on the plots define the range of percentages that are within three standard deviations (SDs) of the national average. If the observed variation was due to chance alone, we would expect only one in 500 sites to have a percentage that is outside these limits.
We conducted a secondary analysis for first-time mothers aged 20–24 at LMP living in LAs with FNP sites enrolling these older mothers. We used the FNP data to identify LAs that had extended their eligibility criteria as those where at least 10 mothers aged 20–24 at LMP and giving birth up to 31 March 2019 were enrolled in the FNP. We included mothers whose first antenatal appointment (or estimated date of 28 weeks gestation, if date missing) occurred from the month of enrolment of the first mother aged 20–24 in the local site.
We calculated the percentage enrolment as the percentage of FNP participants among the eligible study cohort, by site and across all sites. Multilevel logistic regression models of mothers nested within FNP sites were used to calculate crude and adjusted ORs of enrolment (adjusting for all risk factors). The two least-deprived IMD quintiles were grouped to account for smaller numbers. Sample size of FNP participants was too small for analyses stratified by time, region and high/low enrolment in this age group.
Effect of the Family Nurse Partnership on maternal and child outcomes (Objective 2)
We firstly described the outcomes of interest according to maternal risk factors and enrolment in the FNP.
We then compared outcomes for mothers ever enrolled in FNP, and their children, versus those never enrolled, using two analysis strategies to account for measured confounders related to FNP enrolment and outcomes. Propensity score matching aims to minimise bias, while adjustment for confounders aims to minimise variance.
Propensity score matching
Propensity score matching is a quasi-experimental approach to evaluation that is used in contexts where a randomised controlled trial is not possible. Randomisation ensures that intervention and control arms are comparable at baseline. In observational data, however, intervention and control groups are often not comparable at baseline (e.g. due to family nurses prioritising the more vulnerable mothers for enrolment). Propensity score matching aims to mimic the randomisation process by ensuring that groups being compared have similar baseline characteristics by matching mothers with similar underlying needs who were or were not enrolled in the intervention.
To derive propensity scores in this study, we first constructed regression models with FNP participation as the outcome based on all available pre-enrolment maternal characteristics. 92 The predicted probability of enrolment from the model (the propensity score) reflects the probability of each mother in our cohort being enrolled in the FNP, taking into account, for example, maternal age, deprivation and history of mental health conditions. Mothers with similar propensity scores in the control and intervention arms were then matched to create balanced groups for analysis.
We explored both logistic and probit models for propensity score generation and chose the model that provided the best fit. Since we know that drivers of enrolment in the FNP vary by area, we used a multilevel structure to allow for clustering of mothers (level 1) within sites (level 2), allowing intercepts to vary for each site. 93 We included as predictors all available maternal characteristics associated with enrolment up to 28 weeks gestation (at which point the vast majority of mothers have been enrolled) listed in Table 3, as well as additional risk factors (including ‘did not attend’ hospital outpatient appointments within 2 years before 20 weeks gestation and year and quarter-year of childbirth). We explored interactions, as we hypothesised that predictors of enrolment might vary according to maternal age and by year of delivery (based on our results for Objective 1).
Since there was some missing data on maternal predictors of enrolment (e.g. ethnicity and educational/social care predictors for the mothers who could not be linked to NPD), we explored two options for handling missing data in the propensity score model. First, we explicitly modelled the missing data categories (i.e. ‘Unknown’ ethnicity and ‘Not linked to NPD’). Secondly, we used a missingness pattern information approach. 94 This means that we separately calculated propensity scores for the group of mothers with complete data (including all maternal variables as predictors), the group of mothers with missing data on both gestational age at booking and educational/social care variables (excluding these variables as predictors) and the groups of mothers with complete data on educational/social care variables but missing gestational age at booking (and vice versa). Matching takes place on the entire cohort using the propensity scores that have been derived in this way. Using the missingness pattern information approach, we assume that none of the following scenarios apply: (1) maternal/child outcomes affect missingness of the confounder; (2) outcome and missingness have shared unmeasured common causes and FNP enrolment, and missingness have shared unmeasured common causes and (3) the confounder and FNP enrolment both affect missingness, and the confounder is associated with outcome in the subgroup with missing data. 94 Our final strategy for handling missing data was determined by comparing the balance between FNP and non-FNP mothers in our matched cohort.
Once propensity scores had been generated for each enrolled and non-enrolled mother, matched groups were formed by matching mothers enrolled in the FNP to eligible non-participants within the same FNP site area with a similar propensity score. We explored using both nearest neighbour matching and calliper matching with a range of calliper widths. The selected approach was determined by inspecting the overlap in the distribution of propensity scores between mothers who were and were not enrolled in FNP and the balance of risk factors in the matched cohort. 92 To check the balance, we used standardised differences (effect sizes of 0.2, 0.5 and 0.8 are considered to be small, medium and large effect sizes, respectively). 95 We also inspected the coverage of the matched cohort in terms of the number of FNP mothers for whom a match could be found.
We explored one-to-one matching both with and without replacement, assuming that matching with replacement would minimise exclusion of mothers in the higher propensity score range. In order to determine which strategy to use, we inspected the number of times each non-FNP mother was selected as a match. We did not conduct propensity score analysis for mothers aged 20–24 due to small numbers and differing eligibility criteria and geographic range. The matching process was conducted separately for each follow-up cohort (i.e. for mothers with 2 years of follow-up and for mothers with 7 years of follow-up) to allow for equal numbers of FNP and non-FNP mothers in each group. Where mothers had given birth to multiple babies, we randomly selected one child per mother to analyse; this allowed us to keep balanced numbers in each group.
The effect of FNP was estimated by evaluating outcomes for mothers who received the intervention (i.e. who were enrolled in FNP) compared to the outcomes the same mothers would have experienced had they not received the intervention (in causal language, the average effect of the treatment on the treated). This effect was estimated as the difference in outcomes between matched groups. To estimate this difference, we calculated relative risks (RRs) with 95% CIs based on generalised linear models. We used a doubly robust approach, meaning that within the matched cohort, we adjusted for maternal risk factors. RRs presented from the propensity score analysis are therefore adjusted RRs.
All analyses were conducted in Stata V17. 96
Subgroup analyses
Interactions were used to investigate effect modification for selected outcomes according to maternal age, area-level deprivation, ethnicity, maternal history of adversity and mental health conditions, and maternal history of social care, based on previous evidence suggesting the youngest and most disadvantaged mothers are most likely to benefit from the FNP. We also explored interactions by year of delivery and region. We then presented RRs for each stratum of maternal exposure. Outcomes selected for evaluation were those with sufficient numbers to be analysed in subgroups: child unplanned admissions for maltreatment or injury up to age 2, a Good Level of Development at age 5 (school readiness), maternal unplanned admissions for any diagnosis in the 2 years following birth and subsequent births within 18 months.
Sensitivity analyses
In the main analysis, we restricted matching within the same LA and time period in which FNP was offered within that LA (i.e. to eligible, unenrolled mothers). 97 Secondary analyses relaxed this restriction, aiming to achieve more closely matched groups (with potentially smaller numbers matched) by matching:
-
within the same LA but in different time periods, allowing matches to eligible families before FNP was offered in that LA
-
within the same time period but in different LAs, allowing matches to eligible families in LAs that did not offer FNP.
Multivariable regression
We conducted unmatched regression analyses using generalised linear models to estimate RRs, adjusting for all maternal risk factors listed in Table 3. Models of best fit for each outcome were selected based on AIC.
Contextual factors associated with benefitting from Family Nurse Partnership (Objective 3)
Description of attrition, fidelity targets and dosage in the Family Nurse Partnership
Since we knew that a small number of mothers who enrolled in the FNP did not receive any visits and that some received only a small number of visits, we described attrition, mean visit length and total time spent engaging with the programme. We defined dosage in the FNP among enrolled mothers by calculating the number of completed visits relative to FNP fidelity targets (Table 4). For this analysis, we first restricted the cohort to FNP mothers aged 13–19 who had linked with HES and who gave birth before the end of January 2018 (we had information on visits until January 2020), allowing 2 years for mothers to complete the programme.
| Programme phase | Frequency of visits (maximum) | Target percentage of visits | Attrition targeta |
|---|---|---|---|
| Pregnancy | Weekly for first 4 weeks, then every fortnight until birth (maximum = 14, for those enrolled at the target 16 weeks of pregnancy) | 80% or more | < 10% |
| Infancy (up to the child’s first birthday) | Weekly for first 6 weeks, then fortnightly in infancy (maximum = 28) | 65% or more | < 20% |
| Toddlerhood (child age 1–2 years) | Fortnightly for first 10 months, then monthly in toddlerhood (maximum = 22) | 60% or more | < 10% |
We calculated the proportion of visits completed as the actual number of visits completed divided by the expected number of visits for each mother. Some mothers may choose to leave the programme early (e.g. if they are returning to work and no longer have time for the visits or if they feel they will no longer benefit from visits). We, therefore, determined the expected number of visits by calculating the actual time spent in the programme using dates of enrolment, dates of completion and any leaving and returning dates recorded. We then determined the number of visits that should have occurred within this period based on the frequency of visits for each stage of the programme described in Table 4. 98 This was repeated for each programme stage (pregnancy, infancy up to the child’s first birthday and toddlerhood from age 1–2 years). This means that a mother who left early, but who had received all her visits before her leaving date, would be categorised as having 100% expected visits completed. The very small proportion of visits recorded as being < 15 minutes (0.2%; 2145 out of 1,010,890 visits, of which 565 visits were in the pregnancy stage, 960 in the infancy stage and 620 in the toddlerhood stage) were retained within this analysis. Further information on the data cleaning for this analysis is provided in Appendix 4.
Participant, programme and nurse characteristics associated with dosage in the Family Nurse Partnership
We first described individual and programme characteristics associated with dosage in the FNP, according to maternal risk factors prior to enrolment included in Table 3 and additional risk factors recorded in FNP IS (e.g. engagement of partner or parent in the FNP visits and nurse characteristics) and FNP site- or LA-specific characteristics. We evaluated which risk factors were associated with meeting the fidelity target (see Table 4) for each stage of the programme.
To evaluate the impact of these factors on dosage in the FNP, we modelled whether or not fidelity targets were met according to individual and programme characteristics. We repeated this analysis for each stage of the programme.
Effect of contextual factors and dosage on outcomes
To determine whether meeting fidelity targets and other contextual factors (i.e. individual and programme characteristics) were associated with selected outcomes, we compared outcomes according to whether each mother had met the fidelity target for each stage of the programme, for example, comparing outcomes for mothers who had completed the target number of visits in pregnancy with those who were enrolled but did not complete the target number of visits (see Table 4). We included variables for each stage of the programme, meaning that we compared outcomes for mothers who met the fidelity target for toddlerhood with those who were present at toddlerhood but did not meet the target and with enrolled mothers who had left before toddlerhood. Outcomes included in this analysis were those included in the subgroup analysis for Objective 2: child unplanned admissions for maltreatment or injury up to age 2, a Good Level of Development at age 5 (school readiness), maternal unplanned admissions for any diagnosis in the 2 years following birth and subsequent births within 18 months. As with the multivariable regression used in Objective 2, we used generalised linear models with a multilevel structure to allow for mothers nested within FNP sites. We included maternal risk factors and nurse/programme characteristics as covariates, as we expected these to be related to both engagement and outcomes.
Qualitative analysis
Following feedback from the Study Steering Committee and from the Family Nurses with whom we discussed the findings from this study, we decided that qualitative analysis describing the experiences of family nurses and parents would provide additional context to the quantitative analysis included in this report. This qualitative work is ongoing, but we report initial findings from the first three interviews in boxes within relevant results sections.
The interviews were semistructured and took place virtually during October and November 2022. The interviews were video recorded, transcribed and analysed by a researcher under supervision at the University of Kent. The interviewees comprised a parent (Annie), a FNP supervisor (Betsy) and a FNP nurse (Carol). Annie has two children, now aged 11 and 7, and resides in South-West England. The practitioners are employed by a LA in the same region.
A thematic analysis was completed which broadly followed the approach documented by Braun and Clarke. 100 This included reading and rereading the interview transcripts, coding each segment of each transcript, using the codes to generate themes; reviewing and revising the themes, providing distinct ‘… definitions and names for each theme’ and collating a concise summary to illustrate participants’ lived experiences.
Changes from protocol
We were unable to evaluate mortality in this study due to the large discrepancies between recording of deaths in the different data sources. Date and cause of death were obtained from the Office for National Statistics (ONS) via routine linkage between HES and civil registration (deaths) data performed by NHS Digital. In-hospital deaths are recorded in HES. For mothers enrolled in FNP and their children, deaths are also recorded in the FNP IS. Of the 115 child deaths recorded in the FNP data, < 10 were captured in the ONS mortality data and 60 were captured in HES. There were < 10 child deaths captured in the ONS data and 25 in HES that were not recorded in the FNP data. Due to the small numbers involved, small differences in the numerator could substantially alter inferences; therefore, we do not report mortality for children or mothers.
To further assess the robustness of findings to the analysis approach and to evaluate any potential differences in results due to the use of real-world data, we had planned to use our cohort to replicate findings observed in the Building Blocks trial, by deriving trial outcomes for a group of families in the administrative data cohort who were similar to those enrolled in the trial. Since Building Blocks recruited between June 2009 and June 2010 (and our cohort starts with births in April 2010), we were unable to replicate the trial cohort exactly, but we had planned to conduct a supplementary analysis restricted to mothers aged 13–19 who delivered between April and June 2010 in the 18 Building Block sites (see Appendix 2, Table 26). Only 185 mothers who were enrolled in the FNP gave birth within one of the Building Blocks sites between April 2010 (when our data began) and June 2010 (when recruitment in the Building Blocks trial ended). Since the usual care context began to change around this time period (due to a reduction in the health visiting workforce and a move away from GP attachment), evaluating outcomes for mothers meeting the Building Blocks criteria, but during later years, would not have been appropriate. 65 Therefore, we did not perform a sensitivity analysis for this group. We had planned to conduct propensity score analysis for the group of mothers aged 20–24 at LMP but did not due to small numbers. We had planned to conduct multiple imputations as a sensitivity analysis for the multivariable regression analysis but chose not to due to the large amount of other results from sensitivity analyses presented. We included some additional outcomes (FSM and CPPs in the child) that were not described in the original protocol. 1
Chapter 3 Results
Parts of this chapter have been reproduced from the published papers by Cavallaro et al. 1 and Cavallaro et al. 2 These are open-access articles distributed in accordance with the Creative Commons Attribution 4.0 Unported (CC BY 4.0) licence, which permits others to copy, redistribute, remix, transform and build upon this work for any purpose, provided the original work is properly cited, a link to the licence is given and an indication of whether changes were made. See: http://creativecommons.org/licenses/by/4.0/.
Chapter outline
This chapter begins with a description of the study cohort, providing a comparison of the characteristics of mothers who were and were not enrolled in the FNP. We then present the findings from Objective 1, which aimed to determine which groups of adolescent mothers receive FNP across LAs in England. For Objective 2, we describe child and maternal outcomes for the study cohort, providing an unadjusted comparison of outcomes for those who were or were not enrolled in the FNP (and according to maternal risk factors). We then present findings from the propensity score analysis (with sensitivity analyses) and from our multivariable logistic regression analysis. We show findings for subgroups according to maternal risk factors. Lastly, we present results from Objective 3, which aimed to evaluate the contextual factors associated with benefiting from the FNP.
Description of study cohort
Description of mothers in study cohort
Mothers who were enrolled in FNP were strikingly different from those who were never enrolled (Table 5). FNP mothers were younger, more likely to be admitted to hospital for adversity-related diagnoses or to attend A&E in the 2 years prior to 20 weeks of pregnancy and more likely to have their booking appointment after 20 weeks of pregnancy. FNP mothers were also more likely to have been in care or have a CPP, more likely to be recorded as having SEN provision, FSM and be in the most deprived quintile according to Income Deprivation Affecting Children Index (IDACI), more likely to have been excluded or be persistently absent and less likely to achieve 5 A*–Cs at General Certificate of Secondary Education (GCSE) level (but more likely to have achieved expected levels at Key Stage 1). Further information on the FNP cohort for mothers aged 13–19 based on data from the FNP IS is provided in Appendix 5, Table 33. Similar patterns were seen for mothers aged 20–24 (see Appendix 5, Tables 34 and 35).
| All mothers | Mothers enrolled in FNP | Mothers never enrolled in FNP | ||||
|---|---|---|---|---|---|---|
| N | % | N | % | N | % | |
| Total | 130,415 | 100 | 31,260 | 100 | 99,150 | 100 |
| Maternal age at delivery (years) | ||||||
| 13–15 | 2685 | 2.1 | 1450 | 4.6 | 1235 | 1.2 |
| 16–17 | 26,065 | 20.0 | 10,370 | 33.2 | 15,690 | 15.8 |
| 18–19 | 72,465 | 55.6 | 15,805 | 50.6 | 56,660 | 57.1 |
| 20a | 29,205 | 22.4 | 3635 | 11.6 | 25,565 | 25.8 |
| Ethnicity | ||||||
| White | 109,820 | 84.2 | 26,330 | 84.2 | 83,485 | 84.2 |
| South Asian | 3695 | 2.8 | 670 | 2.1 | 3030 | 3.1 |
| Black | 4650 | 3.6 | 1470 | 4.7 | 3180 | 3.2 |
| Mixed/other | 6840 | 5.2 | 1685 | 5.4 | 5155 | 5.2 |
| Unknown | 5410 | 4.1 | 1110 | 3.5 | 4300 | 4.3 |
| Area-level deprivation (quintile of IMD) | ||||||
| Least deprived | 6810 | 5.2 | 1445 | 4.6 | 5360 | 5.4 |
| 2 | 10,410 | 8.0 | 2305 | 7.4 | 8105 | 8.2 |
| 3 | 17,855 | 13.7 | 4115 | 13.2 | 13,735 | 13.9 |
| 4 | 32,550 | 25 | 7890 | 25.2 | 24,660 | 24.9 |
| Most deprived | 62,630 | 48 | 15,340 | 49.1 | 47,290 | 47.7 |
| Unknown | 160 | 0.1 | – | – | – | – |
| History of admissions/attendances with diagnoses within 2 years prior to 20 weeks of pregnancy | ||||||
| Adversity (violence, self-harm, substance misuse) | 5475 | 4.2 | 2295 | 7.3 | 3185 | 3.2 |
| Mental health (exc. self-harm/substance misuse) | 3340 | 2.6 | 1400 | 4.5 | 1935 | 2.0 |
| Repeat A&E attendances (≥ 4) | 21,105 | 16.2 | 6860 | 21.9 | 14,245 | 14.4 |
| Total linked to NPD (social care and education risk factors before 20 weeks of pregnancy available) | 109,360 | 83.9 | 28,145 | 90.0 | 81,210 | 81.9 |
| Ever excluded, in PRU or alternative provision | 32,945 | 25.3 | 10,560 | 33.8 | 22,390 | 22.6 |
| Ever recorded as persistently absent in a term | 40,600 | 31.1 | 15,090 | 48.3 | 25,510 | 25.7 |
| Ever in care | 6955 | 5.3 | 3235 | 10.3 | 3720 | 3.8 |
| Ever had recorded CPP | 3885 | 3.0 | 1990 | 6.4 | 1895 | 1.9 |
| Educational attainment (GCSEs)b | 100,270 | 76.9 | 23,785 | 76.1 | 76,485 | 77.1 |
| Achieved 5 A*–C GCSEs inc. Eng/Maths | 19,920 | 18.4 | 3975 | 14.2 | 15,945 | 19.8 |
| Total linked to Key Stage 2 data | 104,375 | 80.0 | 27,010 | 86.4 | 77,360 | 78.0 |
| Achieved expected level at Key Stage 2 (Maths) | 56,930 | 43.7 | 14,175 | 45.3 | 42,755 | 43.1 |
| Total linked to NPD Census (FSM, SEN available) | 108,365 | 83.1 | 27,995 | 89.6 | 80,365 | 81.1 |
| Ever recorded as having SEN provision | 56,475 | 43.3 | 17,150 | 54.9 | 39,325 | 39.7 |
| Ever recorded as having FSM | 61,315 | 47.0 | 18,525 | 59.3 | 42,795 | 43.2 |
Objective 1 – which groups of adolescent mothers receive Family Nurse Partnership across local authorities?
Parts of this section have been reproduced from the published paper on FNP enrolment by Cavallaro et al. 2 This is an open-access article distributed in accordance with the Creative Commons Attribution 4.0 Unported (CC BY 4.0) licence, which permits others to copy, redistribute, remix, transform and build upon this work for any purpose, provided the original work is properly cited, a link to the licence is given and an indication of whether changes were made is given. See: http://creativecommons.org/licenses/by/4.0/.
Key messages
-
Only 23.2% (95% CI 23.0% to 23.5%) were enrolled in the FNP (25,680 of 110,520 eligible mothers).
-
Enrolment rates varied substantially across 122 sites (range: 11–68%), and areas with greater numbers of first-time adolescent mothers achieved lower enrolment rates.
-
Mothers aged 13–15 were most likely to be enrolled (52%; adjusted OR 2.65, 95% CI 2.39 to 2.94 compared with 18- to 19-year-olds) but accounted for only 2% of all eligible mothers.
-
Only 26% of adolescent mothers with markers of vulnerability (including living in the most deprived areas and previous mental health-related hospital admissions) were enrolled.
Enrolment among mothers 13–19
We restricted the study cohort to eligible mothers aged 13–19 giving birth between April 2010 and 2017. Among all 110,520 eligible mothers, 25,680 (23.2%; 95% CI 23.0% to 23.5%) were enrolled in the FNP. This percentage ranged across 122 FNP sites, from 11% in Cumbria to 68% in Wandsworth (Figure 6). Appendix 2, Table 26, describes the 136 LAs, enrolment dates and FNP enrolment rates by FNP site.
FIGURE 6.
Percentage enrolment in the FNP among eligible mothers aged 13–19, living in a LA with an active FNP site at the time of first antenatal appointment, by LA – England, births between 1 April 2010 and 31 March 2017. Note: the 122 FNP sites active during the study period covered 136 LAs (numbers and geographic boundaries of sites and LAs changed over the study period). Different sites were active for different periods within the 2010–7 cohort; the FNP was never commissioned in 15 LAs (see Figure 1).
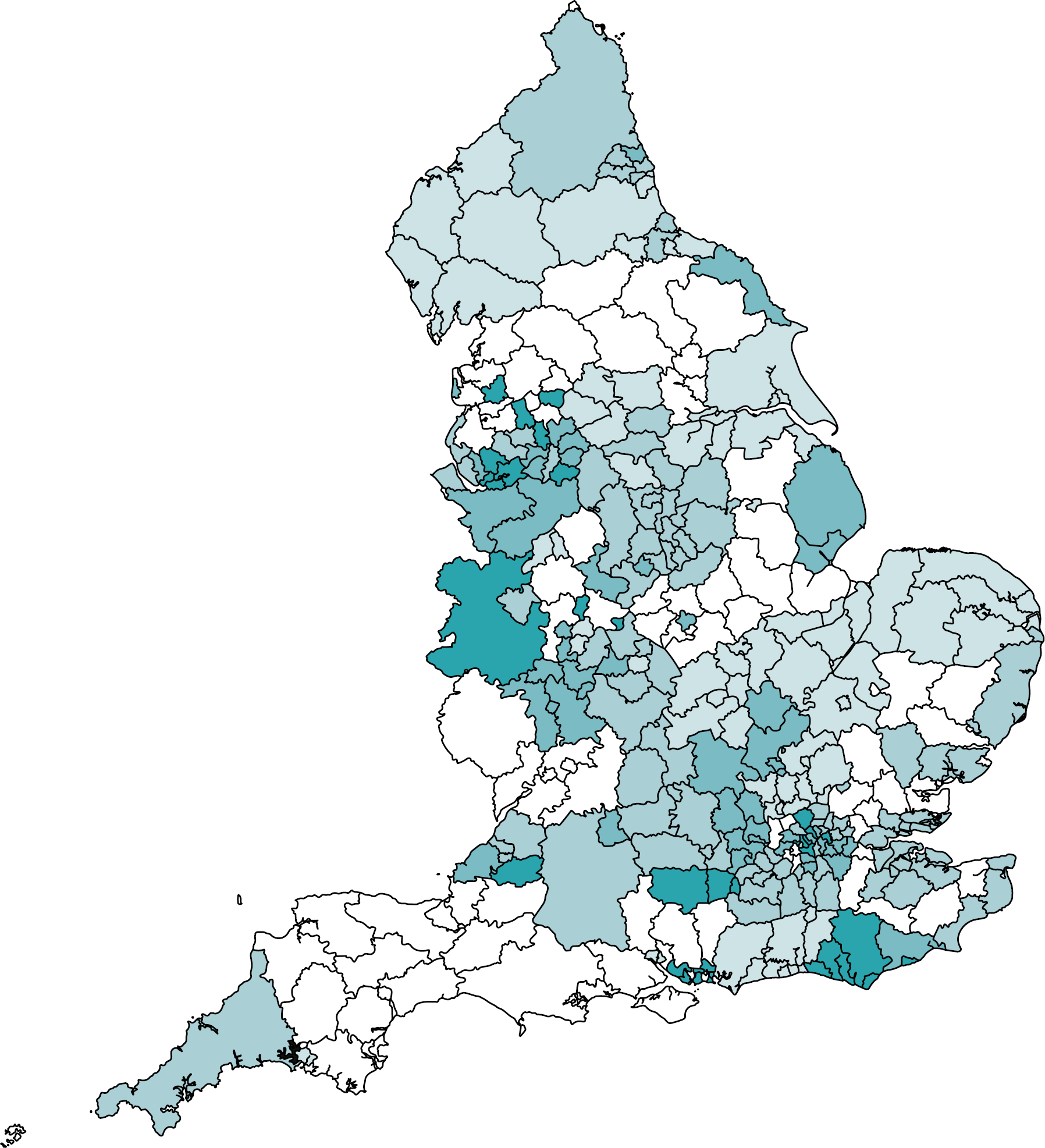
Overall, 12.5% (95% CI 12.4% to –12.7%) of all (25,680–204,690) first-time mothers aged 13–19 giving birth in England between March 2010 and April 2017 were enrolled in the FNP.
Risk factors for enrolment among mothers aged 13–19
Most eligible first-time mothers aged 13–19 in LAs with active FNP sites were white (85%), aged 18–19 at the time of birth (55%) and living in the most deprived quintile (49%) (Table 6). Five per cent of first-time adolescent mothers had ever been Looked After before 20 weeks of pregnancy, 32% had ever been persistently absent and 63% had attempted but not achieved 5 A*–C GCSEs. Characteristics of eligible mothers were similar between LAs that commissioned or had never commissioned FNP (see Appendix 5, Table 36). Overall, 66% of adolescent mothers in the eligible population had at least one vulnerability marker.
| N eligible mothers | N enrolled in FNP | % enrolled in FNP | Crude OR (95% CI) | Adjusted OR (95% CI)a | |
|---|---|---|---|---|---|
| Total | 110,520 | 25,675 | 23.2 | – | – |
| Maternal age at birth | |||||
| 13–15 | 2380 (2.2) | 1240 | 52.1 | 4.62 (4.24 to 5.02) | 2.65 (2.39 to 2.94) |
| 16–17 | 22,725 (20.6) | 8720 | 38.4 | 2.50 (2.42 to 2.59) | 1.80 (1.72 to 1.87) |
| 18–19 | 61,090 (55.3) | 12,875 | 21.1 | 1 (ref) | 1 (ref) |
| 20b | 24,325 (22.0) | 2840 | 11.7 | 0.48 (0.46 to 0.50) | 0.56 (0.53 to 0.59) |
| Ethnicity | |||||
| White | 93,730 (84.8) | 21,845 | 23.3 | 1 (ref) | 1 (ref) |
| South Asian | 3170 (2.9) | 535 | 16.9 | 0.55 (0.49 to 0.61) | 0.74 (0.67 to 0.83) |
| Black | 3970 (3.6) | 1195 | 30.1 | 1.18 (1.09 to 1.28) | 1.31 (1.21 to 1.43) |
| Mixed/other | 5695 (5.2) | 1335 | 23.4 | 0.89 (0.83 to 0.95) | 0.97 (0.90 to 1.04) |
| Unknown | 3950 (3.6) | 770 | 19.5 | 0.69 (0.63 to 0.75) | 0.84 (0.77 to 0.92) |
| IMD (quintile) | |||||
| Least deprived | 5550 (5.0) | 1135 | 20.5 | 0.80 (0.74 to 0.87) | 0.85 (0.78 to 0.92) |
| 2 | 8565 (7.7) | 1820 | 21.2 | 0.91 (0.86 to 0.98) | 0.95 (0.88 to 1.01) |
| 3 | 14,835 (13.4) | 3330 | 22.4 | 1 (ref) | 1 (ref) |
| 4 | 27,520 (24.9) | 6430 | 23.4 | 1.07 (1.02 to 1.13) | 1.02 (0.97 to 1.08) |
| Most deprived | 53,905 (48.8) | 12,820 | 23.8 | 1.19 (1.14 to 1.25) | 1.07 (1.01 to 1.12) |
| Unknown | 145 (0.1) | 145 | 100 | – | – |
| Unplanned admission/attendance within 2 years before 20 weeks of pregnancy | |||||
| Mental health (excluding substance misuse and self-harm) | 2420 (2.2) | 955 | 39.5 | 2.20 (2.03 to 2.40) | 1.41 (1.27 to 1.57) |
| Adversity-related (self-harm, substance misuse, violence) | 4460 (4.0) | 1770 | 39.7 | 2.34 (2.20 to 2.50) | 1.24 (1.13 to 1.36) |
| Any chronic conditionc | 9580 (8.7) | 3170 | 33.1 | 1.74 (1.66 to 1.83) | 1.16 (1.09 to 1.25) |
| A&E attendance | 68,965 (62.4) | 17,815 | 25.8 | 1.48 (1.43 to 1.53) | 1.29 (1.25 to 1.34) |
| Gestational age at antenatal booking appointment | |||||
| Before 10 weeks | 29,390 (26.6) | 6810 | 23.2 | 1 (ref) | 1 (ref) |
| 10–20 weeks | 40,640 (36.8) | 9540 | 23.5 | 0.93 (0.90 to 0.97) | 0.90 (0.87 to 0.94) |
| 20 weeks or more | 6095 (5.5) | 1515 | 24.9 | 0.93 (0.87 to 0.99) | 0.77 (0.71 to 0.82) |
| Unknown | 34,390 (31.1) | 7815 | 22.7 | 0.92 (0.89 to 0.96) | 0.81 (0.78 to 0.85) |
| Ever had a CPP or was Looked After before 20 weeks of pregnancy | |||||
| No CPP or Looked After | 85,890 (77.7) | 19,860 | 23.1 | 1 (ref) | 1 (ref) |
| Looked After | 5540 (5.0) | 2445 | 44.1 | 2.60 (2.46 to 2.76) | 1.92 (1.81 to 2.04) |
| CPP, but not Looked After | 1685 (1.5) | 800 | 47.5 | 2.95 (2.67 to 3.26) | 1.62 (1.46 to 1.80) |
| Ever recorded as having SEN provision before 20 weeks of pregnancy | |||||
| No | 45,270 (49.1) | 9190 | 20.3 | 1 (ref) | 1 (ref) |
| Yes | 46,990 (50.9) | 13,790 | 29.3 | 1.61 (1.56 to 1.66) | 1.22 (1.18 to 1.27) |
| Ever recorded as receiving FSM before 20 weeks of pregnancy | |||||
| No | 41,455 (44.9) | 8050 | 19.4 | 1 (ref) | 1 (ref) |
| Yes | 50,805 (55.1) | 14,930 | 29.4 | 1.69 (1.63 to 1.74) | 1.20 (1.16 to 1.24) |
| Educational attainment before 20 weeks of pregnancy d | |||||
| Did not achieve 5 A*–C GCSEs | 69,345 (80.3) | 16,365 | 23.6 | 1 (ref) | 1 (ref) |
| Achieved 5 A*–C GCSEs | 16,960 (19.7) | 3320 | 19.6 | 0.77 (0.73 to 0.80) | 1.05 (1.00 to 1.10) |
| Ever excluded, in PRU, or alternative provision before 20 weeks of pregnancy | |||||
| No | 65,240 (70.1) | 14,640 | 22.3 | 1 (ref) | 1 (ref) |
| Yes | 27,870 (29.9) | 8620 | 30.7 | 1.55 (1.51 to 1.61) | 1.05 (1.01 to 1.08) |
| Ever persistently absent in a term (≥ 10% possible sessions) before 20 weeks of pregnancy | |||||
| No | 57,760 (62.0) | 10,533 | 18.1 | 1 (ref) | 1 (ref) |
| Yes | 35,360 (38.0) | 12,725 | 35.8 | 2.71 (2.63 to 2.80) | 1.44 (1.39 to 1.50) |
The percentage of eligible mothers enrolled in the FNP was highest (52%) among those aged 13–15 years than 20 years old at childbirth (12%), although 13- to 15-year-olds accounted for only 2% of eligible mothers. The percentage of eligible adolescent mothers enrolled increased slightly from 21% in the least deprived quintile to 24% in the most deprived. Forty per cent of adolescent mothers with a history of mental health- or adversity-related admissions were enrolled, as well as 44% of mothers ever Looked After. Overall, 26% of adolescent mothers with any vulnerability marker were enrolled.
Results from the adjusted model (see Table 6) showed that younger mothers were prioritised for enrolment [the OR decreased from 2.65 (95% CI 2.39 to 2.94) in 13- to 15-year-olds to 0.56 (95% CI 0.53 to 0.59) in mothers aged 20, compared to 18- to 19-year-olds]. Other risk factors included ever been a CLA (OR 1.92, 95% CI 1.81 to 2.04), ever had a CPP (OR 1.62, 95% CI 1.46 to 1.80) and ever identified as having SEN provision (OR 1.22, 95% CI 1.18 to 1.27).
Stratified analyses according to site enrolment level, English region and year of delivery among mothers 13–19
Low-enrolment FNP sites included 51% of all eligible mothers in their catchment areas but enrolled ≤ 21% of mothers in their catchment area, while high-enrolment sites included 9% of all eligible mothers and enrolled > 36% of mothers in their area (see Appendix 5, Table 37).
The effect of age and ethnicity on enrolment was more pronounced in low-enrolment sites (see Appendix 5, Table 38). The association between enrolment and age, ethnicity and deprivation varied across regions (see Appendix 5, Table 39). The age gradient appeared in all regions but was particularly pronounced in the South-West, East Midlands and South-East. In five of nine regions, mothers living in the most deprived areas were more likely to be enrolled than those in the middle quintile of deprivation. Conversely, London was the only region in which enrolment was higher in the least deprived areas (OR 1.68, 95% CI 1.08 to 2.63, compared with the middle quintile).
Risk factors for enrolment also varied over time (see Appendix 5, Table 40), in part due to changes in regional distribution of active sites.
Funnel plots of variation in enrolment rates
A substantial proportion of FNP sites’ enrolment rates fell outside the funnel plot limits, indicating that much of the variation in enrolment rates across sites for younger mothers (aged 13–17 at childbirth) was unexplained by chance (Figure 7). There was even more unexplained variation among mothers aged 18–20 at childbirth, as indicated by the majority of FNP sites falling outside the funnel plot limits. Among both age groups, adjusted enrolment rates were lower than expected in sites with larger numbers of eligible adolescent mothers (see Appendix 5, Figure 27).
FIGURE 7.
Unadjusted funnel plots of variation in FNP enrolment rates among eligible first-time mothers aged 13–19 across FNP sites, by maternal age, births between April 2010 and March 2017.
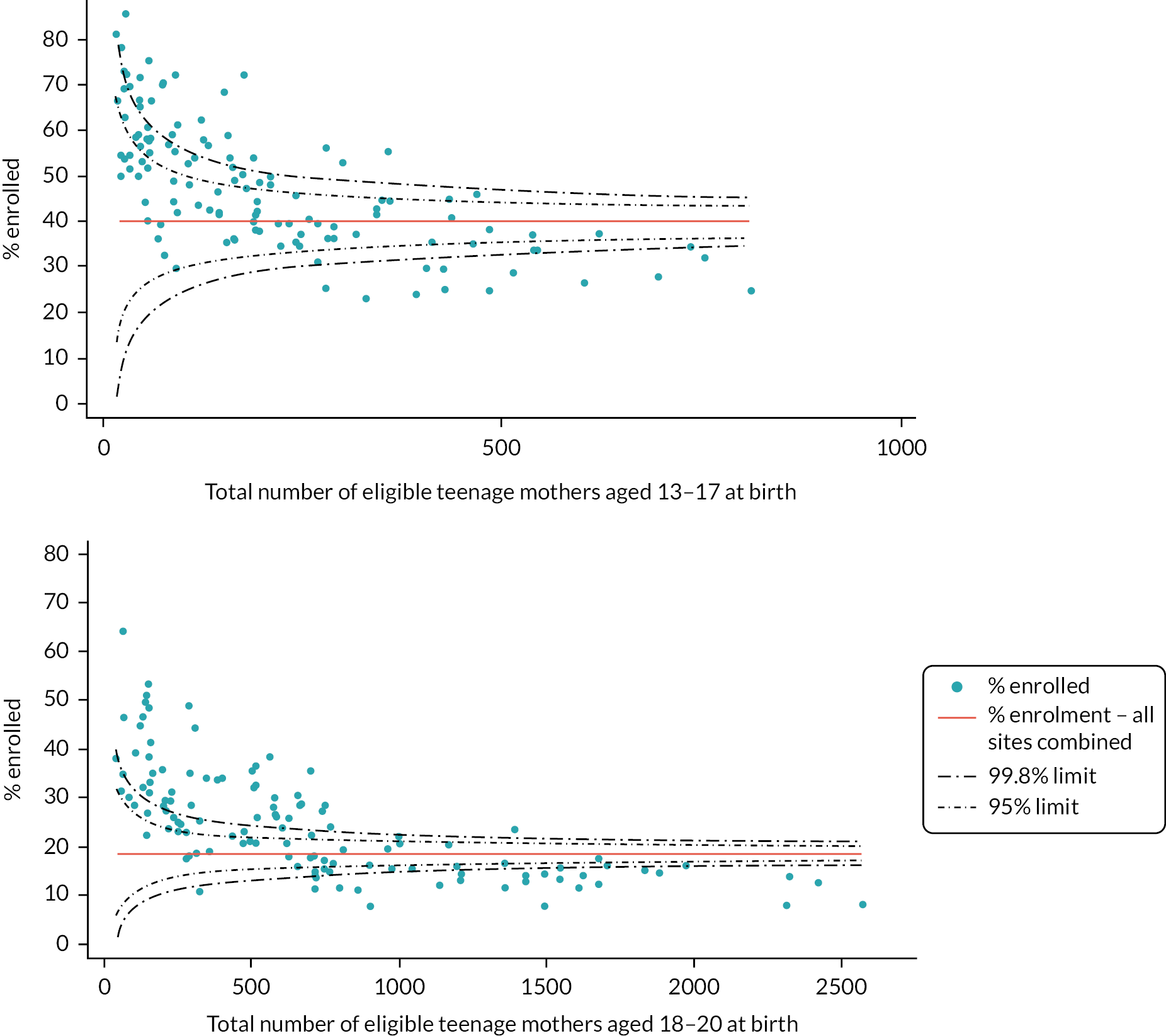
Objective 2 – what was the effect of Family Nurse Partnership enrolment on maternal and child outcomes?
Key messages
-
We found no evidence of an association between FNP and indicators of child maltreatment, except for an increased rate of unplanned admissions for maltreatment/injury-related diagnoses up to age 2 for children born to FNP mothers.
-
There was weak evidence that children born to FNP mothers were more likely to achieve a Good Level of Development (school readiness) at age 5 than those born to mothers who were not enrolled.
-
Mothers enrolled in FNP were less likely to have a subsequent delivery within 18 months of the index birth than those not enrolled.
Descriptive analysis of outcomes of interest according to maternal risk factors
Birth, child and maternal outcomes varied substantially according to maternal risk factors (see Appendix 6). For example, children were more likely to be admitted to hospital for maltreatment or injury if they were born to younger mothers, those living in more deprived areas, those with a history of hospital admissions for adversity or mental health-related admissions, those with contact with social care services as a child and those with lower levels of education.
Descriptive (unadjusted) analysis of outcomes of interest according to enrolment in Family Nurse Partnership
Indicators of child maltreatment (unadjusted)
Over a fifth (22%) of children in our cohort were ever classified as a CiN by age 7, 4.5% had a CPP and 2.0% were Looked After at some point during this period. Children born to mothers in the FNP were more likely to have been discharged from hospital to social care services at birth and more likely to have ≥ 1 admission to hospital for maltreatment or injury-related diagnoses within 2 and 7 years of birth than those born to mothers who were not enrolled (Table 7). Children of mothers enrolled in the FNP were more likely to have a referral to social care services in the 7 years following birth than those of mothers who were not enrolled.
| All children in cohort | Children of mothers ever enrolled in FNP | Children of mothers never enrolled in FNP | ||||
|---|---|---|---|---|---|---|
| N | % | N | % | N | % | |
| Total with information on birth outcomes | 130,415 | 31,260 | 99,150 | |||
| Discharge to social services at birth | 630 | 0.5 | 255 | 0.8 | 375 | 0.4 |
|
Total with 2 years follow-up for health outcomes
(Births between April 2010 and March 2017) |
108,675 | 25,630 | 83,040 | |||
| ≥ 1 unplanned admission for maltreatment or injury | 5790 | 5.3 | 1700 | 6.6 | 4090 | 4.9 |
| Mean no. unplanned injury/maltreatment-related admissionsa (SD) | 1.2 (0.7) | 1.2 (0.6) | 1.2 (0.7) | |||
|
Total with 7 years follow-up for health outcomes
(Births between April 2010 and March 2012) |
27,015 | 4375 | 22,640 | |||
| ≥ 1 unplanned admission for maltreatment or injury | 3175 | 11.8 | 600 | 13.7 | 2575 | 11.4 |
| Mean no. unplanned injury/maltreatment-related admissionsa (SD) | 1.3 (0.9) | 1.3 (0.8) | 1.3 (0.9) | |||
|
Total with 7 years follow-up for social care outcomes
(Births between April 2010 and March 2012) |
17,605 | 3250 | 14,355 | |||
| Ever Looked After | 355 | 2.0 | 85 | 2.6 | 270 | 1.9 |
| Mean no. episodes of careb (SD) | 1.1 (0.3) | 1.1 (0.3) | 1.1 (0.3) | |||
| Ever had a CPP | 790 | 4.5 | 165 | 5.1 | 625 | 4.3 |
| Ever had a CiN referral | 3890 | 22.1 | 835 | 25.7 | 3055 | 21.3 |
| Mean no. CiN referralsc (SD) | 1.6 (1.0) | 1.6 (1.1) | 1.6 (1.0) | |||
| Mean no. CiN referrals made by health visitorc (SD) | 0.0 (0.2) | 0.0 (0.2) | 0.0 (0.2) | |||
Child health, developmental and educational outcomes (unadjusted)
Low-birthweight babies and preterm births were more prevalent in mothers who were enrolled in FNP compared to those who were not (Table 8). Children born to mothers in the FNP were more likely to have ≥ 1 unplanned admission for any diagnosis and were more likely to attend A&E in the 2 and 7 years following birth. The mean number of admissions was similar across groups.
| All children in cohort | Children of mothers ever enrolled in FNP | Children of mothers never enrolled in FNP | ||||
|---|---|---|---|---|---|---|
| N | % | N | % | N | % | |
|
Total with information on birth outcomes
(Births between April 2010 and March 2019) |
130,415 | 31,260 | 99,150 | |||
| Total with information on gestational age at birth | 121,005 | 28,075 | 92,935 | |||
| Preterm birth (< 37 weeks) | 9940 | 8.2 | 2650 | 9.4 | 7295 | 7.8 |
| Total with information on birthweight | 121,815 | 28,350 | 93,460 | |||
| Low birthweight (< 2500 g) | 9395 | 7.7 | 2515 | 8.9 | 6880 | 7.4 |
|
Total with 2 years follow-up
(Births between April 2010 and March 2017) |
108,675 | 25,630 | 83,040 | |||
| ≥ 1 unplanned admission (any diagnosis) | 40,140 | 36.9 | 10,360 | 40.4 | 29,780 | 35.9 |
| ≥ 1 A&E attendance | 77,725 | 71.5 | 19,570 | 76.3 | 58,155 | 70.0 |
| ≥ 1 outpatient referral | 55,630 | 51.2 | 14,310 | 55.8 | 41,320 | 49.8 |
| Did not attend ≥ 1 outpatient appointment | 19,745 | 18.2 | 5485 | 21.4 | 14,260 | 17.2 |
|
Total with 7 years follow-up
(Births between April 2010 and March 2012) |
27,015 | 4375 | 22,640 | |||
| ≥ 1 unplanned admission (any diagnosis) | 13,195 | 48.8 | 2225 | 50.8 | 10,975 | 48.5 |
| ≥ 1 A&E attendance | 23,555 | 87.2 | 3985 | 91.0 | 19,570 | 86.4 |
| ≥ 1 outpatient referral | 20,450 | 75.7 | 3460 | 79.1 | 16,990 | 75 |
| Did not attend ≥ 1 outpatient appointment | 11,150 | 41.3 | 2010 | 45.9 | 9145 | 40.4 |
| Total with information on nursery attendance | 25,140 | 4135 | 21,010 | |||
| Attended nursery between ages 2 and 4 | 24,090 | 95.8 | 3955 | 90.4 | 20,135 | 95.8 |
| Total with information on school readiness at age 5 (EYFSP) | 24,585 | 4035 | 20,545 | |||
| Good Level of Development (across all five domains) | 14,445 | 58.5 | 2325 | 53.1 | 12,120 | 59.0 |
| GLD: Communication and Language | 18,595 | 75.6 | 3010 | 74.6 | 15,585 | 75.9 |
| GLD: Physical Development | 20,340 | 82.7 | 3325 | 82.4 | 17,010 | 82.8 |
| GLD: Personal, Social and Emotional Development | 19,345 | 78.7 | 3130 | 77.6 | 16,215 | 78.9 |
| GLD: Literacy | 15,090 | 61.4 | 2435 | 60.3 | 12,655 | 61.6 |
| GLD: Maths | 16,630 | 67.6 | 2685 | 66.5 | 13,945 | 67.9 |
| Total with information at Key Stage 1 | 24,530 | 4040 | 20,490 | |||
| Expected level of development at KS1 (Maths) | 16,015 | 65.3 | 2580 | 63.9 | 13,435 | 65.6 |
| Expected level of development at KS1 (Writing) | 14,215 | 57.9 | 2255 | 55.9 | 11,960 | 58.4 |
| Expected level of development at KS1 (Reading) | 16,255 | 66.3 | 2635 | 65.3 | 13,620 | 66.5 |
| Total with information on SEN provision and FSM | 24,925 | 4105 | 20,820 | |||
| Ever recorded as having SEN provision | 6175 | 24.8 | 1120 | 27.8 | 5060 | 24.3 |
| Ever recorded as having FSM | 11,780 | 47.3 | 2290 | 56.8 | 9485 | 45.6 |
| Total with information on persistent absence | 25,155 | 4135 | 21,020 | |||
| Ever persistently absent | 14,700 | 58.4 | 2555 | 63.3 | 12,145 | 57.8 |
Children born to FNP mothers were less likely to achieve an expected level of development at school entry and less likely to achieve expected levels of development in Reading, Writing and Maths at Key Stage 1.
Maternal outcomes (unadjusted)
Mothers who were enrolled in the FNP were more likely than those who were not to have an unplanned admission to hospital for an adversity-related diagnosis or any diagnosis and more likely to attend A&E within 2 and 7 years of delivery (Table 9). Amongst mothers who gave birth before they started Year 11, mothers enrolled in the FNP were less likely than those who were not to achieve 5 A*–Cs and GCSEs.
| All mothers in cohort | Mothers enrolled in FNP | Mothers never enrolled in FNP | ||||
|---|---|---|---|---|---|---|
| N with outcome | % | N with outcome | % | N with outcome | % | |
|
Total with 2 years follow-up for health outcomes
(Deliveries between April 2010 and March 2017) |
110,555 | 25,690 | 84,860 | |||
| ≥ 1 unplanned admission for adversity-related diagnoses | 1890 | 1.7 | 695 | 2.7 | 1195 | 1.4 |
| Mean no. unplanned adversity-related admissionsa (SD) | 1.3 (1.1) | 1.4 (1.2) | 1.3 (1.1) | |||
| ≥ 1 unplanned admission for mental health-related diagnoses (excluding substance misuse and self-harm) | 2900 | 2.6 | 1075 | 4.2 | 1825 | 2.1 |
| Mean no. unplanned mental health-related admissionsa (SD) | 1.5 (1.5) | 1.6 (1.5) | 1.5 (1.4) | |||
| Unplanned admission for any diagnosis | 18,975 | 17.2 | 5210 | 20.3 | 13,765 | 16.2 |
| Mean no. unplanned admissionsa (SD) | 1.6 (1.4) | 1.7 (1.6) | 1.6 (1.3) | |||
| ≥ 1 A&E attendance | 54,700 | 49.5 | 14,470 | 56.3 | 40,230 | 47.4 |
| Mean no. A&E attendancesa (SD) | 2.5 (2.7) | 2.8 (3.3) | 2.3 (2.5) | |||
| Subsequent delivery within 18 months | 10,230 | 8.8 | 2325 | 8.5 | 7905 | 8.9 |
| Total with information on educational attainment b | 8145 | 4225 | 3915 | |||
| Mother achieved 5 A*–C inc. Eng/Maths at KS4 | 820 | 10.1 | 405 | 9.6 | 415 | 10.6 |
| Total with information on school enrolment up to Year 11 c | 2035 | 4290 | 18,800 | |||
| School enrolment | 1675 | 82.3 | 960 | 81.8 | 710 | 82.9 |
|
Total with 7 years follow-up for health outcomes
(Deliveries between April 2010 and March 2012) |
27,250 | 4385 | 22,865 | |||
| ≥ 1 unplanned admission for adversity-related diagnoses | 1535 | 5.6 | 345 | 7.9 | 1190 | 5.2 |
| Mean no. unplanned adversity-related admissionsa (SD) | 1.6 (1.6) | 1.7 (2.0) | 1.5 (1.4) | |||
| ≥ 1 unplanned admission for mental health-related diagnoses (excluding substance misuse and self-harm) | 2095 | 7.7 | 440 | 10.0 | 1655 | 7.2 |
| Mean no. unplanned mental health-related admissionsa (SD) | 1.9 (2.4) | 2.1 (3.0) | 1.9 (2.1) | |||
| Unplanned admission for any diagnosis | 11,585 | 42.5 | 2090 | 47.7 | 9495 | 41.5 |
| Mean no. unplanned admissionsa (SD) | 2.4 (2.9) | 2.5 (3.2) | 2.3 (2.8) | |||
| ≥ 1 A&E attendance | 22,065 | 81.0 | 3790 | 86.5 | 18,275 | 79.9 |
| Mean no. A&E attendancesa (SD) | 5.2 (6.7) | 6.3 (8.5) | 5.0 (6.2) | |||
Propensity score matching
The best-fitting model for the propensity score was a multilevel probit model, with mothers clustered in FNP sites. We included as predictors all available maternal risk factors up to 28 weeks gestation (at which point the vast majority of mothers had been enrolled) listed in Table 3. We also included interactions between maternal age and year of delivery and maternal age and gestational age at booking. We explicitly modelled the missing data categories for unknown ethnicity and mothers who did not link to NPD, as this provided a better balance between groups than using the missingness pattern information approach. There was a good overlap of propensity scores between FNP and non-FNP mothers, meaning that there were many mothers who were not enrolled in the FNP who had similar risk factors to those who were enrolled (see Appendix 7, Figure 28).
The most balanced groups were achieved by using one-to-one matching without replacement with a calliper width of 0.01. Using this approach, the mean difference in propensity scores between groups was < 0.001. The standardised differences of key maternal risk factors were small (effect sizes of 0.2, 0.5 and 0.8 are considered to be small, medium and large effect sizes, respectively; see Appendix 7, Table 48). 95 However, since FNP mothers tended to have higher propensity scores (median = 0.39) than non-FNP mothers (median = 0.31), there were a small number of FNP mothers for whom we were unable to find a match (see Appendix 7, Figure 29). When matching the entire cohort of mothers aged 13–19 giving birth between 2010 and 2019, we were able to include 94.9% of mothers in the matched analysis. For the cohort with 2 years of follow-up (births between April 2010 and March 2017), we matched 95.7% of FNP mothers, and for the cohort with 7 years of follow-up (births between April 2010 and March 2011), we matched 99.9% of FNP mothers. The comparatively lower match rates for the later years were due to a smaller number of untreated mothers for these years. Using matching with replacement may have increased the proportion of matched mothers further but would have led to increased imbalance between groups.
Outcomes within matched cohort
Indicators of child maltreatment
There was an increased risk of unplanned admissions for maltreatment/injury-related diagnoses in the 2 years following birth amongst children of mothers who were enrolled in the FNP compared with those who were not (RR 1.15, 95% CI 1.07 to 1.24). There was weak evidence that FNP was associated with an increased risk of a hospital record indicating discharge to social services at birth (RR 1.23, 95% CI 1.00 to 1.51; p-value 0.046) and a decreased risk of a CPP up to 7 years after birth (RR 0.84, 95% CI 0.71 to 1.00; p-value 0.049). There were no other differences between groups in any of the indicators of child maltreatment that were evaluated (Table 10, Figure 8). Due to small numbers, we did not calculate RRs for the percentage of CiN referrals from health visitors.
FIGURE 8.
Indicators of child maltreatment: adjusted RRs and 95% CIs comparing outcomes for mothers enrolled in the FNP vs. mothers who were not enrolled, for mothers aged 13–19 and giving birth in an area in which FNP was offered at the time of pregnancy.

FIGURE 9.
Child health, developmental and educational outcomes: adjusted RRs and 95% CIs comparing mothers enrolled in the FNP vs. mothers who were not enrolled, for mothers aged 13–19 and giving birth in an area in which FNP was offered at the time of pregnancy. KS1, Key Stage 1.
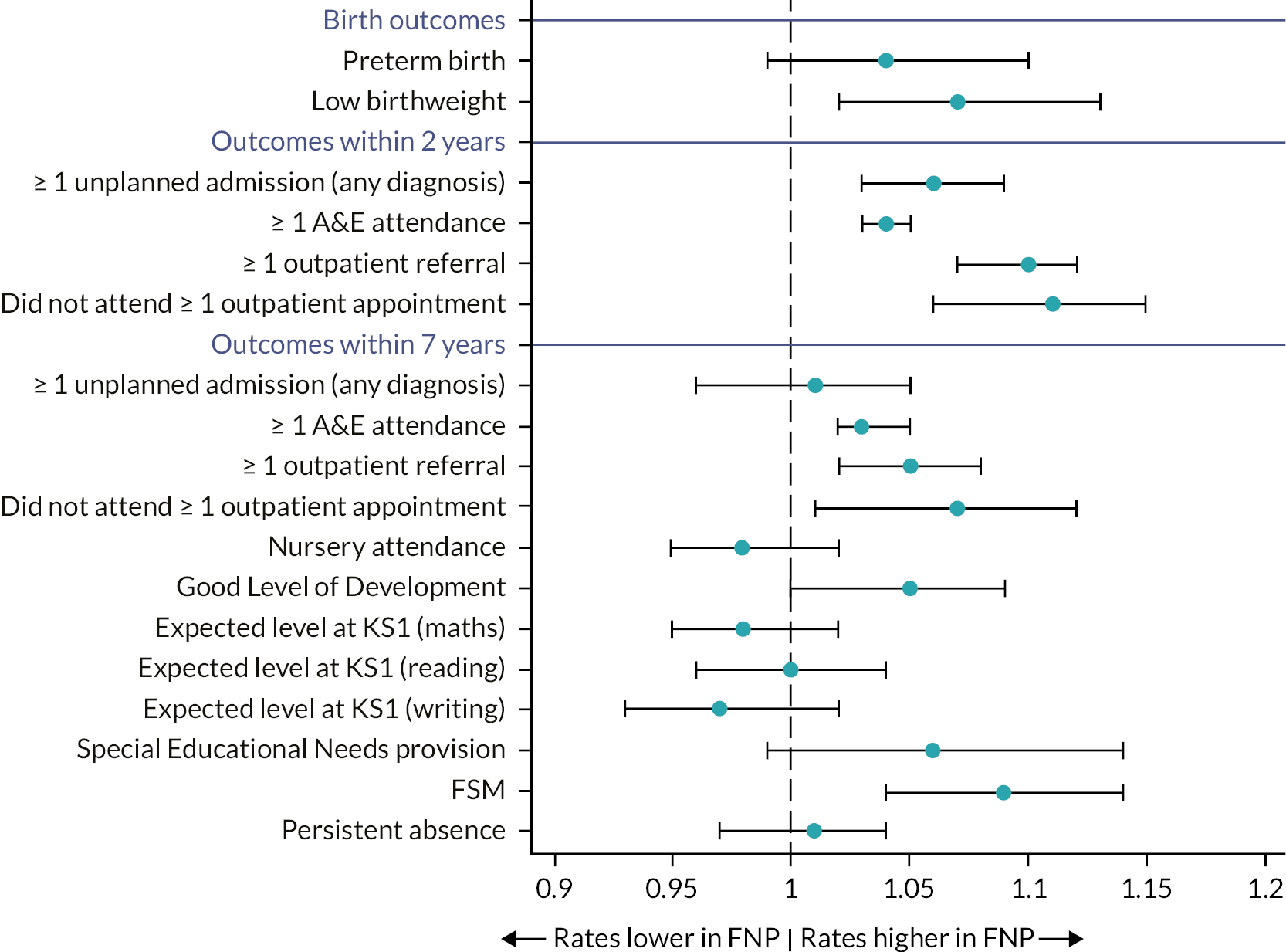
FIGURE 10.
Maternal outcomes: adjusted RRs and 95% CIs comparing outcomes for mothers enrolled in the FNP vs. mothers who were not enrolled, for mothers aged 13–19 and giving birth in an area in which FNP was offered at the time of pregnancy. a, Among mothers who were aged < 16 at the start of the academic year in which they reached 20 weeks gestation. b, Among mothers who were aged < 15 at the start of the academic year in which they reached 20 weeks gestation.
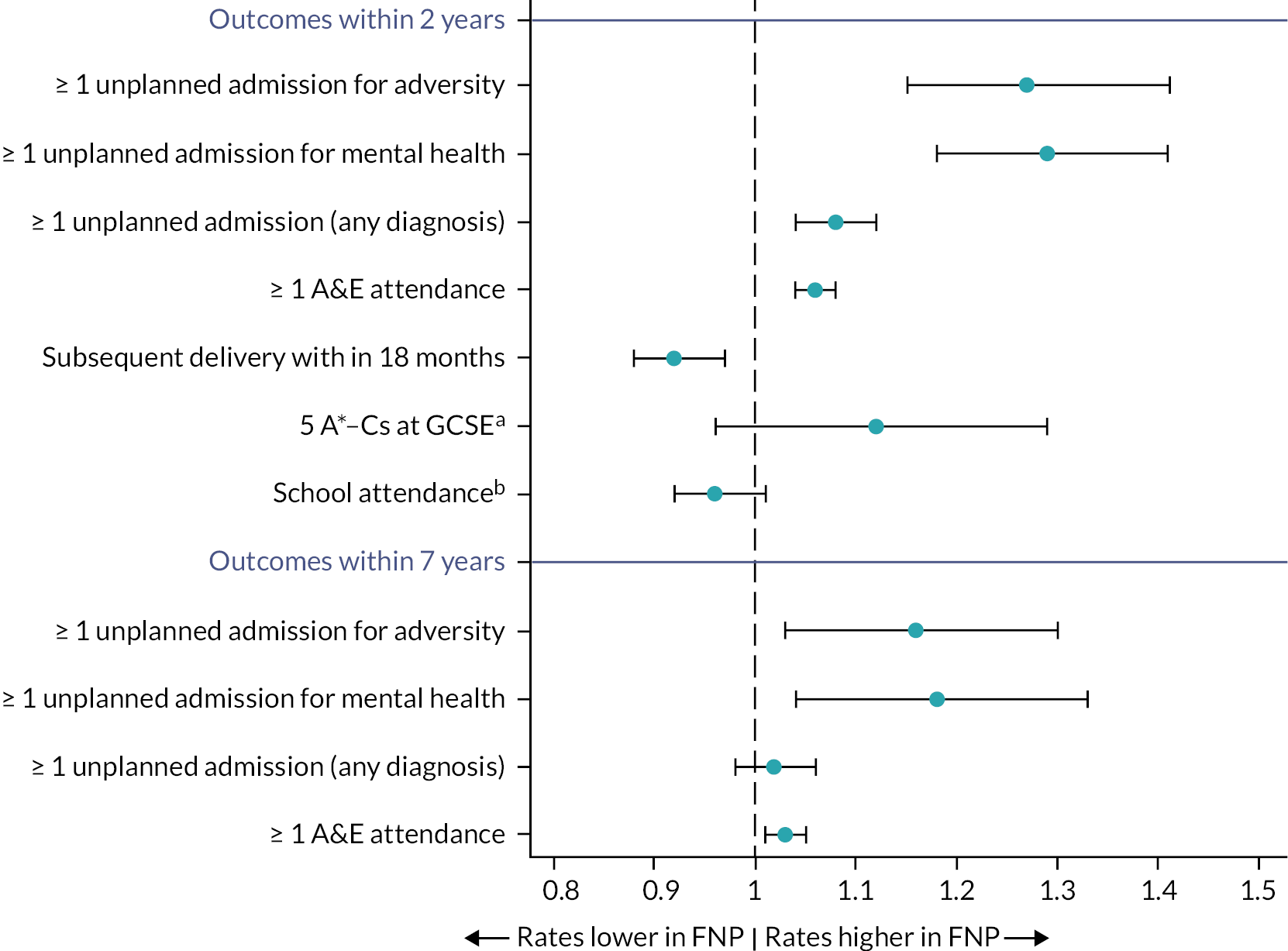
| N (%) in mothers enrolled in FNP (treated) | N (%) in mothers never enrolled in FNP (untreated) | AdjustedRR (95% CI)a | |
|---|---|---|---|
| Birth outcomes (Births between April 2010 and March 2019) |
|||
| Total with information at discharge | 28,995 | 28,710 | |
| Discharge to social services | 215 (0.7) | 180 (0.6) | 1.23 (1.00 to 1.51) |
| Child outcomes – within 2 years (Births between April 2010 and March 2017) |
|||
| Total with information on health outcomes within 2 years | 24,240 | 23,790 | |
| ≥ 1 unplanned admission for maltreatment or injury | 1605 (6.6) | 1385 (5.7) | 1.15 (1.07 to 1.24) |
| Child outcomes – within 7 years Births between April 2010 and March 2012 |
|||
| Total with information on health outcomes within 7 years | 4330 | 4310 | |
| ≥ 1 unplanned admission for maltreatment or injury | 595 (13.6) | 575 (13.2) | 1.03 (0.93 to 1.14) |
| Total with information on social care outcomes within 7 years | 3215 | 2965 | |
| CLA | 85 (2.6) | 85 (2.9) | 0.91 (0.68 to 1.21) |
| CPP | 165 (5.1) | 180 (6.1) | 0.84 (0.71 to 1.00) |
| CiN referral | 830 (19.0) | 785 (18.0) | 0.99 (0.91 to 1.07) |
Child health, developmental and educational outcomes
There was an increased risk of low birthweight amongst mothers who were enrolled in the FNP versus those who were not (RR 1.07, 95% CI 1.02 to 1.13). There was also an increased risk of unplanned admission for any diagnoses (in the 2 years following birth) and for A&E attendances (in the 2 and 7 years following birth).
There was weak evidence that children born to FNP mothers were more likely to achieve a Good Level of Development (school readiness) at age 5 (RR 1.05, 95% CI 1.00 to 1.09) than those born to mothers who were not enrolled. Children in the FNP arm were also more likely to be recorded as having FSM (see Table 11, Figure 9).
| N (%) in mothers enrolled in FNP (treated) | N (%) in mothers never enrolled in FNP (untreated) | Adjusted RR (95% CI)a | |
|---|---|---|---|
| Birth outcomes (Births between April 2010 and March 2019) |
|||
| Total with information on gestational age at birth | 26,485 | 27,375 | |
| Preterm birth (< 37 weeks of gestation) | 2465 (8.4) | 1375 (8.0) | 1.04 (0.99 to 1.00) |
| Total with information on birthweight | 26,740 | 27,625 | |
| Low birthweight (< 2500 g) | 2345 (7.9) | 2240 (7.6) | 1.07 (1.02 to 1.13) |
| Child health outcomes – within 2 years (Births between April 2010 and March 2017) |
|||
| Total with information on health outcomes within 2 years | 24,240 | 23,790 | |
| ≥ 1 unplanned admission for any diagnosis | 9705 (39.7) | 9110 (37.3) | 1.06 (1.03 to 1.09) |
| ≥ 1 A&E attendance | 13,435 (54.9) | 12,235 (50.0) | 1.04 (1.03 to 1.05) |
| ≥ 1 outpatient referral | 5110 (21.1) | 4455 (18.7) | 1.10 (1.07 to 1.12) |
| Did not attend ≥ 1 outpatient appointment | 1990 (46.0) | 1860 (43.2) | 1.11 (1.06 to 1.15) |
| Child health outcomes – within 7 years (Births between April 2010 and March 2012) |
|||
| Total with information on health outcomes within 7 years | 4330 | 4310 | |
| ≥ 1 unplanned admission for any diagnosis | 2200 (50.5) | 2225 (51.0) | 1.01 (0.96 to 1.05) |
| ≥ 1 A&E attendance | 3945 (90.5) | 3800 (87.2) | 1.03 (1.02 to 1.05) |
| ≥ 1 outpatient referral | 18,460 (75.5) | 17,285 (70.7) | 1.05 (1.02 to 1.08) |
| Did not attend ≥ 1 outpatient appointment | 3430 (78.7) | 3265 (74.9) | 1.07 (1.01 to 1.12) |
| Child developmental/educational outcomes – within 7 years (Births between April 2010 and March 2012) |
|||
| Total with information on nursery attendance | 4090 | 4040 | |
| Nursery attendance | 3915 (89.8) | 3870 (88.8) | 1.00 (0.99 to 1.01) |
| Total with information on EYFSP | 3990 | 3955 | |
| Good Level of Development (school readiness)b | 2295 (57.5) | 2190 (55.4) | 1.05 (1.00 to 1.09) |
| Total with information on Key Stage 1 attainment | 4270 | 4260 | |
| Expected levels at KS1 (maths) | 2550 (58.5) | 2485 (57.0) | 0.98 (0.95 to 1.02) |
| Expected levels at KS1 (reading) | 2600 (59.6) | 2490 (57.1) | 1.00 (0.96 to 1.04) |
| Expected levels at KS1 (writing) | 2225 (51.0) | 2180 (50.0) | 0.97 (0.93 to 1.02) |
| Total with information on SEN/FSM | 4060 | 4010 | |
| SEN provision | 1105 (25.3) | 1025 (23.5) | 1.06 (0.99 to 1.14) |
| FSM | 2265 (51.9) | 2035 (46.7) | 1.09 (1.04 to 1.14) |
| Total with information on absence | 4090 | 4040 | |
| Persistent absence | 2530 (61.9) | 2450 (60.6) | 1.01 (0.97 to 1.04) |
Maternal outcomes
Mothers who enrolled in the FNP were more likely to have unplanned admissions for adversity-related diagnoses, mental health conditions or any diagnoses and A&E attendances in the 2 and 7 years following birth, compared to those who were not enrolled (see Table 12, Figure 10). However, these mothers were less likely to have a repeat pregnancy within 18 months of the index birth (RR 0.92, 95% CI 0.88 to 0.97).
| N (%) in mothers enrolled in FNP (treated) | N (%) in mothers never enrolled in FNP (untreated) | Adjusted RR (95% CI)a | |
|---|---|---|---|
| Maternal outcomes – 2 years (Births between April 2010 and March 2017) |
|||
| Total with information on health outcomes within 2 years | 24,455 | 24,455 | |
| ≥ 1 unplanned admission for adversity-related diagnoses | 605 (2.5) | 485 (2.0) | 1.27 (1.15 to 1.41) |
| ≥ 1 unplanned admission for mental health-related diagnoses | 950 (3.9) | 745 (3.0) | 1.29 (1.18 to 1.41) |
| ≥ 1 unplanned admission for any diagnosis | 4860 (19.9) | 4520 (18.5) | 1.08 (1.04 to 1.12) |
| ≥ 1 A&E attendance | 13,610 (55.7) | 12,750 (52.1) | 1.06 (1.04 to 1.08) |
| Subsequent delivery within 18 months | 2065 (8.4) | 2270 (9.3) | 0.92 (0.88 to 0.97) |
| Total eligible for and with information on GCSEs | 2825 | 2765 | |
| 5 A*–Cs at GCSE level | 330 (11.7) | 255 (9.2) | 1.12 (0.96 to 1.29) |
| Total eligible for and with information on school enrolment | 770 | 680 | |
| School enrolment | 620 (80.5) | 570 (83.8) | 0.96 (0.92 to 1.01) |
| Maternal outcomes – 7 years (Births between April 2010 and March 2012) |
|||
| Total with information on health outcomes within 7 years | 4360 | 4360 | |
| ≥ 1 unplanned admission for adversity-related diagnoses | 345 (7.9) | 300 (6.9) | 1.16 (1.03 to 1.30) |
| ≥ 1 unplanned admission for mental health-related diagnoses | 435 (10.0) | 385 (8.8) | 1.18 (1.04 to 1.33) |
| ≥ 1 unplanned admission for any diagnosis | 2080 (47.7) | 2040 (46.8) | 1.02 (0.98 to 1.06) |
| ≥ 1 A&E attendance | 3775 (86.6) | 3665 (84.1) | 1.03 (1.01 to 1.05) |
Subgroup analyses
Although there was variation in the association between FNP and outcomes across subgroups, there were no statistically significant interactions between enrolment in FNP and maternal age, ethnicity, area-level deprivation, maternal contact with social care services, child sex or year of delivery (see Figures 11–14, Appendix 7, Appendix 8, Figures 31–34). However, we did observe a significant interaction between region and subsequent births within 18 months (p = 0.0018). The reduction in subsequent births associated with FNP was seen most strongly in the South-West, South-East and London (see Appendix 8, Figure 33).
FIGURE 11.
Child unplanned admissions for maltreatment/injury in the 2 years following birth: subgroup analysis presenting adjusted RRs and 95% CIs comparing mothers enrolled in the FNP vs. mothers who were not enrolled, for mothers aged 13–19 and giving birth in an area in which FNP was offered at the time of pregnancy.
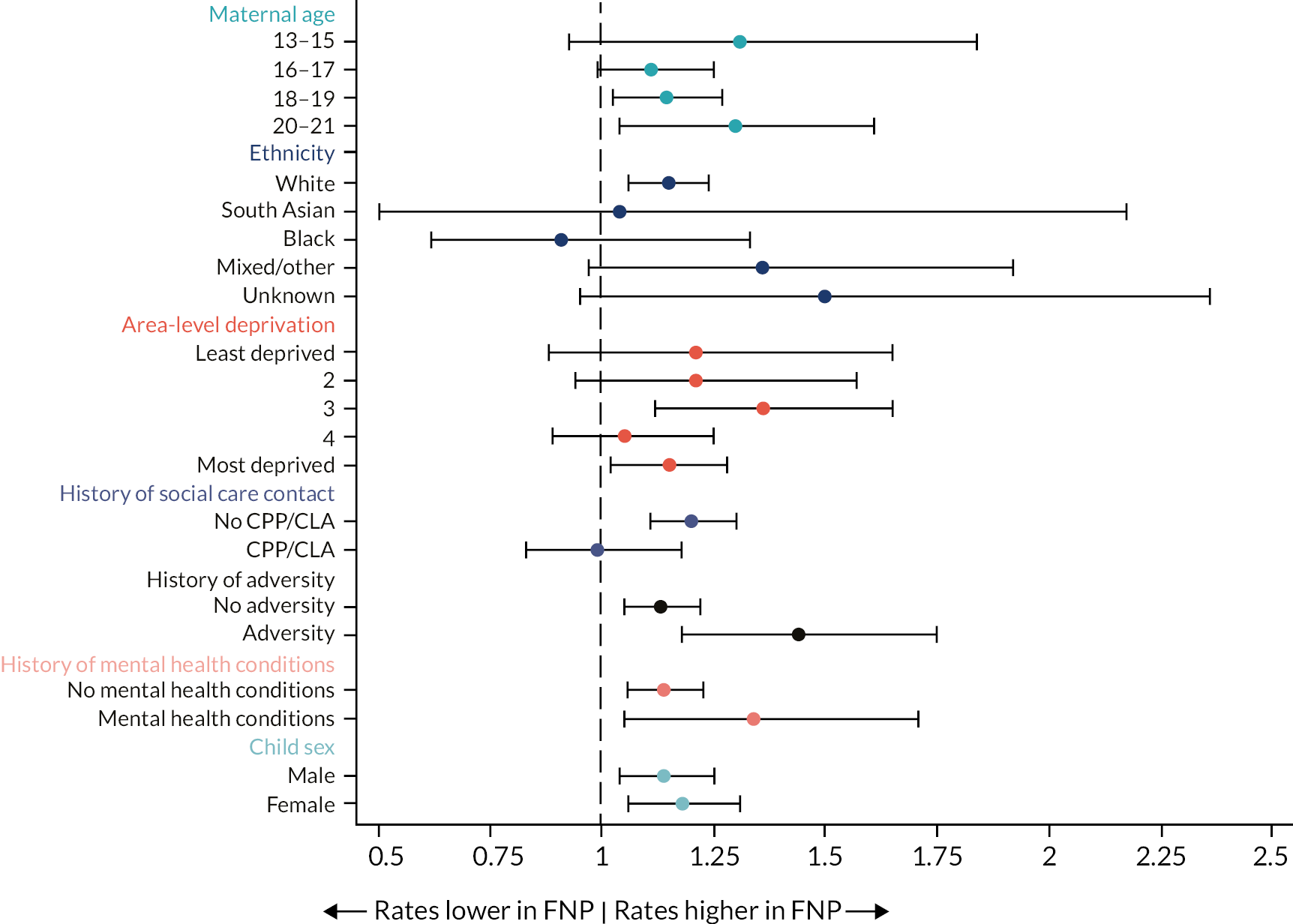
FIGURE 12.
Good level of development: subgroup analysis presenting adjusted RRs and 95% CIs comparing mothers enrolled in the FNP vs. mothers who were not enrolled, for mothers aged 13–19 and giving birth in an area in which FNP was offered at the time of pregnancy.
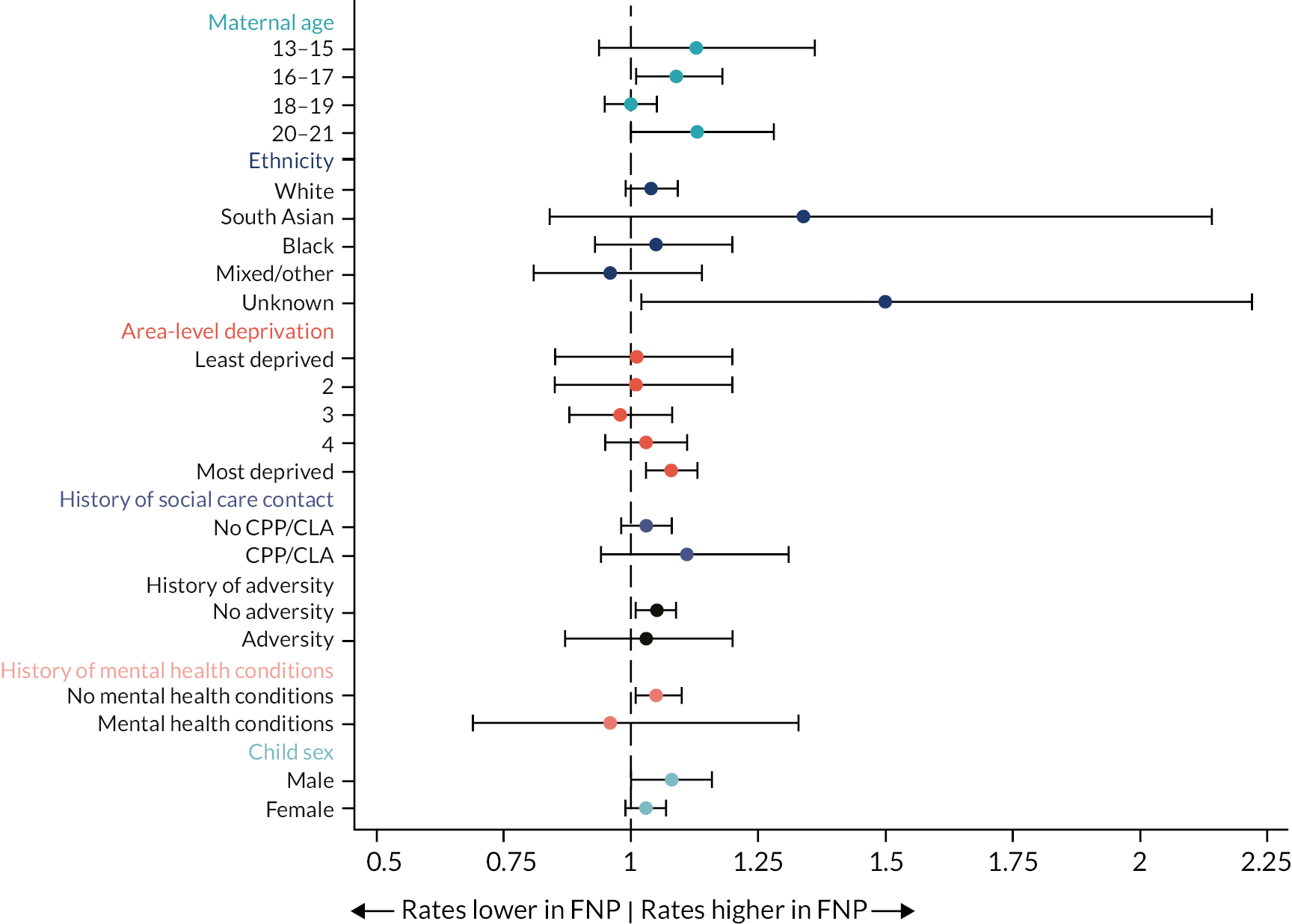
FIGURE 13.
Subsequent delivery within 18 months: subgroup analysis presenting adjusted RRs and 95% CIs comparing mothers enrolled in the FNP vs. mothers who were not enrolled, for mothers aged 13–19 and giving birth in an area in which FNP was offered at the time of pregnancy.

FIGURE 14.
Maternal unplanned admissions for any diagnosis in the 2 years following delivery: subgroup analysis presenting adjusted RRs and 95% CIs comparing mothers enrolled in the FNP vs. mothers who were not enrolled, for mothers aged 13–19 and giving birth in an area in which FNP was offered at the time of pregnancy.
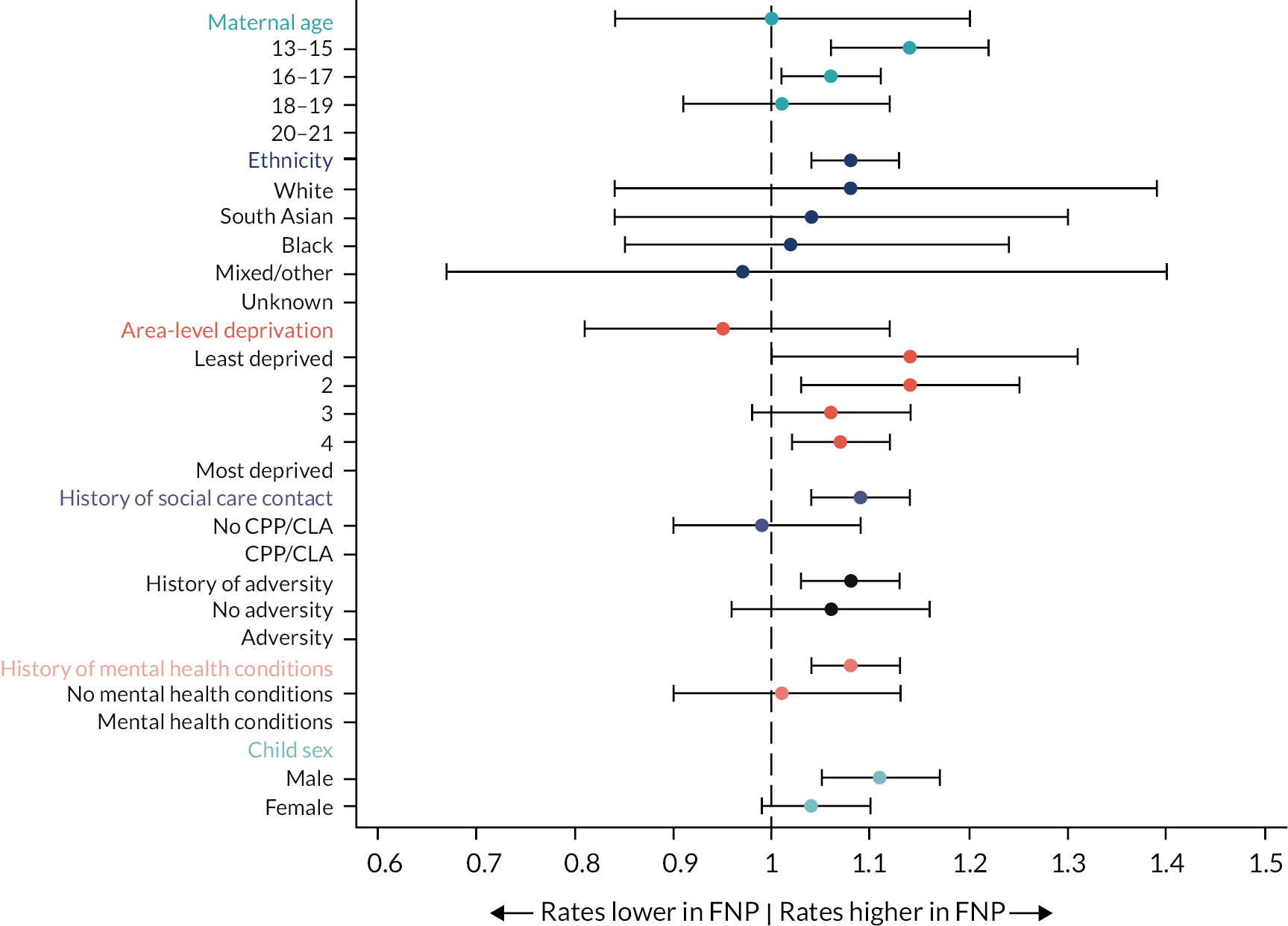
Sensitivity analyses
We performed two sensitivity analyses where the approach to propensity score matching was changed to allow matching (1) within the same LA but in different time periods (comparing FNP mothers with similar mothers before FNP was offered in that LA) and (2) within the same time period but in different LAs (comparing FNP to similar mothers living in different LAs). It was more difficult to find closely matched groups within these sensitivity analyses since the characteristics of mothers differed over time and between LAs that did or did not offer the FNP. We therefore also present results from a matching with replacement strategy, aiming to retain a higher coverage of FNP mothers (see Appendix 2, Table 31). Results from these sensitivity analyses did not differ substantially from those of the main analysis.
Multivariable regression (adjusted) analyses
Effect estimates from the sensitivity analyses using multivariable regression (see Appendix 9, Tables 55–57) were broadly similar to those from the main propensity score analysis, with some differences between groups being attenuated.
Objective 3 – which programme and contextual factors influence the effect of Family Nurse Partnership?
Key messages
-
Fifty-eight per cent of mothers enrolled in FNP completed the programme, and 42% left early.
-
Mothers enrolled in FNP received an average of 38 visits and 42 hours of contact time with a family nurse.
-
Fifty-nine per cent of mothers in pregnancy, 65% in infancy and 61% in toddlerhood met targets for the expected number of visits.
-
Younger mothers and those with a history of unplanned hospital admissions for mental health, adversity or chronic health conditions, received a greater number of visits; other contextual factors, including nurse characteristics and area-level characteristics, had little effect on the number of visits received.
-
Meeting the target for the number of expected visits in pregnancy was associated with a reduction in subsequent births within 18 months; meeting the target in infancy and toddlerhood was associated with an increase in the number of children with unplanned hospital admissions for maltreatment/injury up to age 2.
Description of attrition, fidelity targets and dosage in the Family Nurse Partnership
Of the 31,260 mothers aged 13–19 at LMP enrolled in FNP and giving birth between 2010 and 2019, with linkage to HES (see Figure 2), 28,155 gave birth before January 2018 and were included in this analysis. Of these, 28,120 had at least one visit recorded, 16,305 (58%) completed the programme and 42% left early (slightly higher than the target attrition rate of 40%). A small number of clients had some interrupted periods of enrolment where they left the programme and returned later on (see Appendix 4).
On average, mothers received a total of 38 visits during their enrolment in the FNP (Table 13), corresponding to an average 42 hours of contact time with a family nurse.
| Full programme | Pregnancy | Infancy | Toddlerhood | |
|---|---|---|---|---|
| Number of mothers who started each stage | 28,155 | 28,155 | 25,975 | 20,015 |
| Attritiona (%) | 11,850 (42.1) | 2180 (7.7) | 5855 (22.5) | 3760 (18.8) |
| Number of mothers who were in each stage for > 2 weeks | 28,155 | 28,155 | 25,905 | 19,990 |
| Mean time in the stage (SD), weeks | 94.9 (41.3) | 20.3 (6.4) | 46.0 (13.1) | 45.2 (14.6) |
| Median time in the stage (IQR), weeks | 118 (63–128) | 21 (16–25) | 52 (52–52) | 52 (46–53) |
| Mean number of visits (SD) | 35.9 (17.0) | 9.8 (3.6) | 10.3 (3.3) | 13.3 (6.5) |
| Median number of visits (IQR) | 38 (24–49) | 10 (8–12) | 10 (8–13) | 14 (9–18) |
| N that met targetb (%) | 7745 (27.5) | 16,695 (59.2) | 16,945 (65.4) | 12,115 (60.6) |
| Number of mothers with visit data recorded | 28,120 | 28,085 | 25,635 | 19,695 |
| Mean visit length (SD), hoursc | 1.2 (0.2) | 1.2 (0.2) | 1.1 (0.2) | 1.1 (0.2) |
| Median visit length (IQR), hoursc | 1.0 (1.0–1.3) | 1.2 (1.0–1.5) | 1.1 (1.0–1.2) | 1.0 (1.0–1.2) |
| Mean total time spent with a nurse (SD), hours | 42.1 (21.4) | 12.1 (5.1) | 21.5 (9.0) | 15.4 (8.0) |
| Median total time spent with a nurse (IQR), hours | 43 (27–57) | 12 (9–15) | 22 (16–27) | 15 (10–20) |
At each stage of the programme, there is a target number of visits that mothers should receive, and fidelity to these targets is measured (see Table 4). Mothers are expected to receive at least 80% of the maximum number of visits during pregnancy, 65% during infancy and 60% during toddlerhood. FNP also has targets for attrition: no more than 10% during pregnancy, 20% during infancy and 10% during toddlerhood.
Pregnancy stage
The majority of FNP mothers (25,925; 92%) remained in the programme for the full pregnancy (see Table 13). Eight per cent of mothers dropped out before delivery, and a small number left during pregnancy but returned later (see Appendix 4). For mothers giving birth before January 2018, the FNP fidelity target of < 10% attrition during pregnancy was met.
The maximum possible number of visits during pregnancy is 14 (for those enrolled at 16 weeks of pregnancy), and the average number of visits in our cohort was 10. A total of 16,695 (59%) mothers met the target of 80% of visits completed during pregnancy. The distribution of visits is summarised in Appendix 9.
Infancy stage
Of the 25,975 mothers who were still in the programme at the start of the infancy stage, 19,860 (77%) completed the infancy period in full; 70 mothers were in the infancy period for < 2 weeks, and a small number restarted the programme during the infancy period (i.e. left during pregnancy and returned during infancy). Overall, attrition during infancy was 23% (5855), slightly exceeding the 20% target.
For the infancy period, the maximum possible number of visits is twice that of pregnancy (28). In our cohort, the average number of visits in this stage received remained similar to those received in pregnancy (10 visits). A total of 16,945 (65%) met the target of 65% of visits completed for this stage. The distribution of visits is summarised in Appendix 9.
Toddlerhood stage
Of the 20,015 participants remaining in the programme at the toddlerhood stage, 16,175 (81%) completed the toddlerhood stage in full; 25 mothers were in the toddlerhood stage for < 2 weeks, and a small number of mothers left and returned during the toddlerhood stage. Overall attrition was 19% (3760), higher than the 10% target.
For the toddlerhood stage, the maximum possible number of visits is 22. The average number in our cohort was 14 visits, and 12,115 mothers (61%) met the 60% fidelity target (see Table 13). The distribution of visits is summarised in Appendix 9.
Participant, programme and nurse characteristics associated with dosage in the Family Nurse Partnership
There was substantial variation in whether sites met delivery targets for each stage of the programme, illustrated by the lack of overlap in CIs in Figure 15.
FIGURE 15.
Percentage of mothers meeting fidelity targets for the number of expected visits in pregnancy, infancy and toddlerhood, according to FNP site, for births between April 2010 and January 2018 to mothers aged 13–19 at LMP. The solid line indicates the fidelity target.
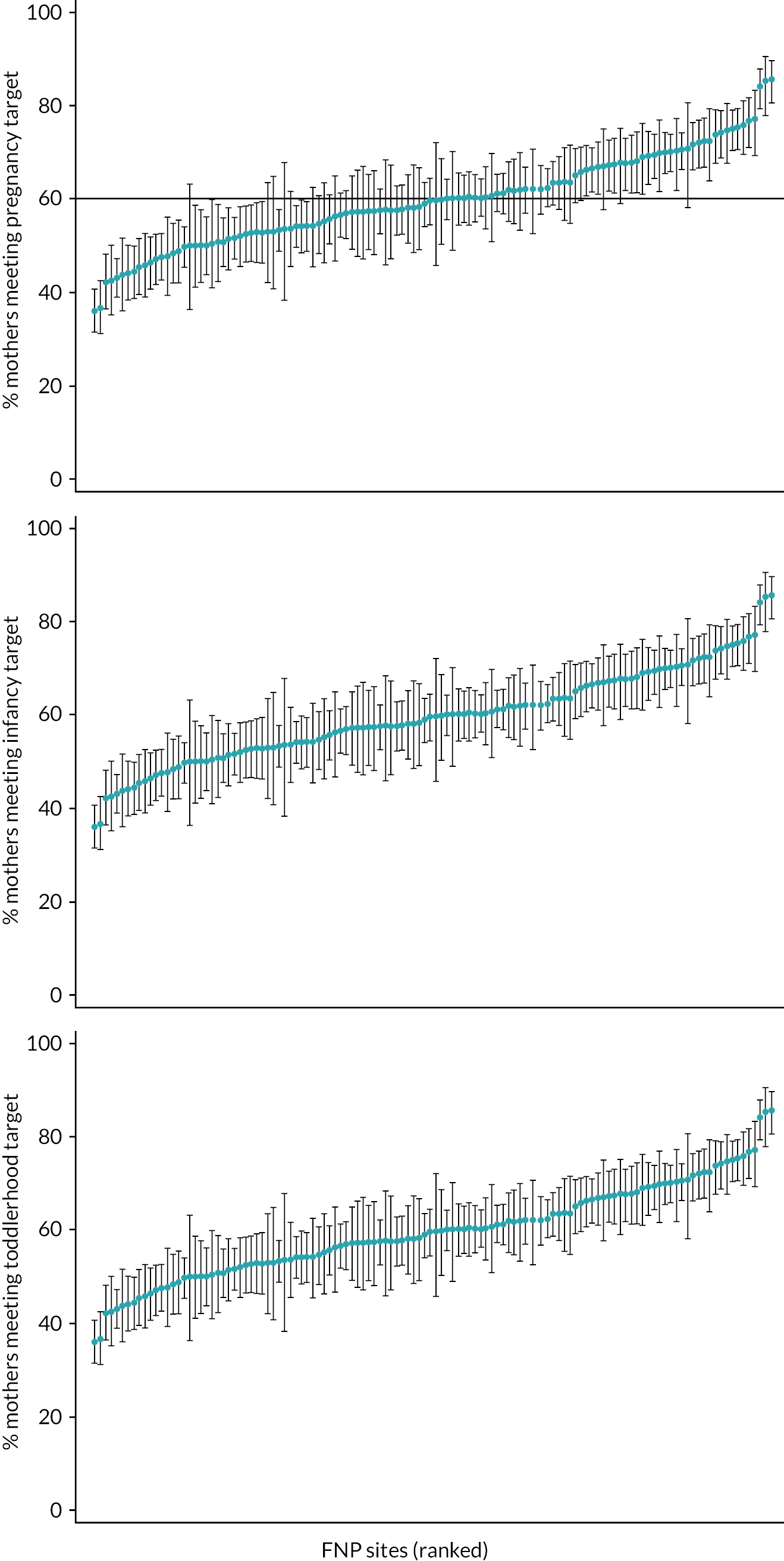
Younger mothers and those with a history of unplanned hospital admission for mental health, adversity or chronic health conditions received a greater number of visits over their time in the programme (see Appendix 10, Table 58). There was little variation in the average number of visits or proportion of mothers meeting fidelity targets according to nurse characteristics (see Appendix 10, Table 59). However, we did see some patterns according to the number of visits with a partner present: mothers whose partner was present for 10–50% of visits tended to receive more visits than those whose partner was never present or those whose partner was present for > 50% of visits. A similar pattern was seen with the presence of parents.
When adjusting for all these maternal factors (Table 14), the greatest drivers of meeting fidelity targets in the pregnancy stage were maternal age (RR 1.13, 95% CI 1.08 to 1.19 comparing mothers aged 13–15 with those aged 18–19), having a history of adversity (RR 1.06, 95% CI 1.02 to 1.09 compared to mothers with no history of adversity), being a CiN at enrolment (RR 1.18, 95% CI 1.14 to 1.21 compared to mothers not CiN at enrolment) and having a CPP at enrolment (RR 1.20, 95% CI 1.14 to 1.26). Mothers who had ever been recorded with persistent absence or who had been excluded were less likely to meet targets, and those who had achieved 5 A*–C GCSEs prior to enrolment were more likely to meet targets (see Table 14).
| N mothers (% of all mothers) |
N who met pregnancy target (% of group) |
Adjusted RR (95% CI)a |
|
|---|---|---|---|
| Total | 27,360 (100) | 16,610 (60.7) | – |
| Maternal age at birth | |||
| 13–15 | 1315 (4.8) | 930 (70.7) | 1.13 (1.08 to 1.19) |
| 16–17 | 9225 (33.7) | 5735 (62.2) | 1.04 (1.02 to 1.07) |
| 18–19 | 13,715 (50.1) | 8145 (59.4) | 1.00 (ref) |
| 20b | 3105 (11.3) | 1800 (58.0) | 0.97 (0.93 to 1.00) |
| History of adversity-related admissions with diagnoses within 2 years prior to 20 weeks of pregnancy | 1950 (7.1) | 1285 (65.9) | 1.06 (1.02 to 1.09) |
| Ever in care prior to 20 weeks of pregnancy | 2695 (9.9) | 1770 (65.7) | 1.08 (1.05 to 1.11) |
| Ever excluded, in PRU or alternative provision prior to 20 weeks of pregnancy | 9140 (33.4) | 5450 (59.6) | 0.94 (0.92 to 0.96) |
| Ever recorded as persistently absent in a term prior to 20 weeks of pregnancy | 13,385 (48.9) | 8165 (61.0) | 0.97 (0.95 to 0.99) |
| Educational attainment before weeks of pregnancy | |||
| Did not achieve 5 A*–C GCSEs | 17,245 (63.0) | 10,200 (59.1) | 1.00 (ref) |
| Achieved 5 A*–C GCSEs | 3560 (13.0) | 2200 (61.8) | 1.03 (1.01 to 1.06) |
| Too young for GCSEs | 3825 (14.0) | 2535 (66.3) | 1.05 (1.01 to 1.09) |
| CiN status at enrolment | 1630 (6.0) | 1185 (72.7) | 1.18 (1.14 to 1.21) |
| CPP at enrolment | 780 (2.9) | 590 (75.6) | 1.20 (1.14 to 1.26) |
| % of visits with partner present, median (IQR) | 13 (2–34.4) | 14.3 (2.5–35.7) | 1.00 (1.00 to 1.00) |
| IMD 2015 quintiles (LA level) | |||
| Least deprived | 6875 (25.1) | 4025 (58.5) | 1.00 (ref) |
| 2 | 6845 (25.0) | 4115 (60.1) | 1.01 (0.94 to 1.08) |
| 3 | 4625 (16.9) | 2855 (61.7) | 1.05 (0.98 to 1.12) |
| 4 | 5945 (21.7) | 3560 (59.9) | 1.02 (0.94 to 1.09) |
| Most deprived | 3070 (11.2) | 2050 (66.8) | 1.09 (1.02 to 1.17) |
The greatest driver of meeting fidelity targets during the infancy and toddlerhood stages was having met the targets in the previous stages of the programme (Tables 15 and 16). The area-level factors we explored (% of mothers in the area who were adolescents, ethnic distribution, % of preterm births, % of mothers smoking at delivery and rates of referrals to children’s social care or CPPs) did not have a significant association with meeting fidelity targets, except for LA-level deprivation, where mothers in the most deprived LAs were more likely to have the expected number of visits.
| N mothers (% of all mothers) | N who met infancy target (% of group) | Adjusted RR (95% CI)a | |
|---|---|---|---|
| Total | 25,635 (100) | 16,845 (65.7) | – |
| Met pregnancy target | |||
| No | 9405 (36.7) | 4420 (47.0) | 1.00 (ref) |
| Yes | 16,230 (63.3) | 12,425 (76.6) | 1.56 (1.50 to 1.61) |
| Maternal age at birth | |||
| 13–15 | 1270 (5.0) | 935 (73.6) | 1.07 (1.02 to 1.11) |
| 16–17 | 8695 (33.9) | 5730 (65.9) | 1.00 (0.98 to 1.03) |
| 18–19 | 12,760 (49.8) | 8330 (65.3) | 1.00 (ref) |
| 20b | 2905 (11.3) | 1850 (63.7) | 0.98 (0.95 to 1.01) |
| History of admissions with diagnoses within 2 years prior to 20 weeks of pregnancy | |||
| Chronic condition (any, exc. mental health) | 3295 (12.9) | 2285 (69.3) | 1.02 (1.00 to 1.05) |
| Repeated A&E visits | 5490 (21.4) | 3720 (67.8) | 1.04 (1.01 to 1.06) |
| Ever in care prior to weeks of pregnancy | 2535 (9.9) | 1810 (71.4) | 1.05 (1.01 to 1.08) |
| Ever had recorded CPP prior to 20 weeks of pregnancy | 1390 (5.4) | 990 (71.2) | 1.03 (1.00 to 1.07) |
| Ever recorded as having SEN prior to 20 weeks of pregnancy | 13,950 (54.4) | 9365 (67.1) | 1.04 (1.02 to 1.06) |
| Ever excluded, in PRU or alternative provision prior to 20 weeks of pregnancy | 8545 (33.3) | 5565 (65.1) | 0.97 (0.95 to 0.99) |
| Ever recorded as persistently absent in a term prior to 20 weeks of pregnancy | 12,585 (49.1) | 8260 (65.6) | 0.97 (0.95 to 0.99) |
| Educational attainment before 20 weeks of pregnancy | |||
| Attempted but did not achieve 5 A*–C GCSEs | 16,115 (62.9) | 10,480 (65.0) | 1.00 (ref) |
| Gained 5 A*–C GCSEs | 3310 (12.9) | 2215 (66.9) | 1.03 (1.00 to 1.05) |
| Too young for GCSEs | 3645 (14.2) | 2510 (68.9) | 1.01 (0.98 to 1.04) |
| CiN at enrolment | 1560 (6.1) | 1165 (74.7) | 1.08 (1.04 to 1.11) |
| CPP at enrolment | 755 (2.9) | 595 (78.8) | 1.11 (1.07 to 1.17) |
| % of visits with partner present, median (IQR) | 13.3 (2.4–34.1) | 14.3 (3.2–35.3) | 1.00 (1.00 to 1.00) |
| IMD 2015 quintiles (LA level) | |||
| Least deprived | 6440 (25.1) | 3925 (60.9) | 1.00 (ref) |
| 2 | 6385 (24.9) | 4100 (64.2) | 1.03 (0.97 to 1.09) |
| 3 | 4365 (17.0) | 2925 (67.0) | 1.07 (1.00 to 1.14) |
| 4 | 5570 (21.7) | 3755 (67.4) | 1.06 (1.00 to 1.12) |
| Most deprived | 2870 (11.2) | 2140 (74.6) | 1.09 (1.01 to 1.17) |
| N mothers (% of all mothers) |
N who met toddlerhood target (% of group) |
Adjusted RR (95% CI)a |
|
|---|---|---|---|
| Total | 19,655 (100) | 11,900 (60.5) | – |
| Met pregnancy target | |||
| No | 6835 (34.8) | 3300 (48.3) | 1.00 (ref) |
| Yes | 12,820 (65.2) | 8600 (67.1) | 1.16 (1.13 to 1.19) |
| Met infancy target | |||
| No | 5805 (29.5) | 1945 (33.5) | 1.00 (ref) |
| Yes | 13,850 (70.5) | 9955 (71.9) | 1.98 (1.90 to 2.07) |
| Ethnicity | |||
| White | 16,610 (84.5) | 10,235 (61.6) | 1.00 (ref) |
| South Asian | 410 (2.1) | 255 (62.2) | 1.01 (0.94 to 1.08) |
| Black | 950 (4.8) | 470 (49.5) | 0.88 (0.81 to 0.94) |
| Mixed/other | 1035 (5.3) | 550 (53.1) | 0.91 (0.85 to 0.97) |
| Unknown | 645 (3.3) | 390 (60.5) | 1.01 (0.95 to 1.07) |
| Repeated A&E visits within 2 years prior to 20 weeks of pregnancy | 4015 (20.4) | 2530 (63.0) | 1.05 (1.03 to 1.07) |
| Ever recorded as having SEN prior to 20 weeks of pregnancy | 10,560 (53.7) | 6520 (61.7) | 1.04 (1.01 to 1.07) |
| Ever recorded as having FSM prior to 20 weeks of pregnancy | 11,340 (57.7) | 6950 (61.3) | 1.05 (1.03 to 1.08) |
| Ever recorded as persistently absent in a term prior to 20 weeks of pregnancy | 9745 (49.6) | 5880 (60.3) | 0.98 (0.96 to 1.00) |
| Number of benefits received at enrolment | |||
| 0 | 11,115 (56.6) | 6525 (58.7) | 1.00 (ref) |
| 1 | 4350 (22.1) | 2755 (63.3) | 1.04 (1.02 to 1.07) |
| 2 | 2400 (12.2) | 1470 (61.3) | 1.01 (0.98 to 1.04) |
| 3 | 1305 (6.6) | 840 (64.4) | 1.05 (1.01 to 1.10) |
| 4 + | 485 (2.5) | 315 (64.9) | 1.04 (0.98 to 1.10) |
| % of visits with partner present, median (IQR) | 13.8 (3–33.3) | 15 (3.8–35) | 1.00 (1.00–1.00) |
Effect of programme and contextual factors and dosage on outcomes
Within the group of mothers enrolled in FNP, none of the additional participant, programme or nurse characteristics (see Appendix 10, Table 59) were associated with child unplanned admissions for maltreatment or injury up to age 2, a Good Level of Development at age 5 (school readiness), maternal unplanned admissions for any diagnosis in the 2 years following birth or subsequent births within 18 months.
However, we observed that meeting the target for the number of expected visits in pregnancy was associated with a reduction in subsequent births within 18 months (RR 0.87, 95% CI 0.78 to 0.97 compared with mothers who did not meet the target in pregnancy, Table 17). Meeting the target in infancy and toddlerhood was associated with an increase in the number of children with unplanned hospital admissions for maltreatment/injury up to age 2 (Table 17).
| Child unplanned hospital admissions for maltreatment/injury up to age 2 | Good Level of Development (school readiness) | Maternal unplanned admissions for any diagnosis in the 2 years following birth | Subsequent live births within 18 months of the index child | |
|---|---|---|---|---|
| RR (95% CI) | RR (95% CI) | RR (95% CI) | RR (95% CI) | |
| Met target in pregnancy (80%) | 0.90 (0.90 to 1.03) | 0.97 (0.92 to 1.02) | 1.00 (0.94 to 1.06) | 0.87 (0.78 to 0.97) |
| Met target in infancy (65%) | 1.27 (1.12 to 1.43) | 0.98 (0.93 to 1.04) | 1.02 (0.94 to 1.10) | 0.90 (0.79 to 1.03) |
| Met target in toddlerhood (60%) | 1.21 (1.09 to 1.35) | 0.98 (0.92 to 1.04) | 1.00 (0.94 to 1.07) | 0.97 (0.82 to 1.14) |
Chapter 4 Discussion and implications of evaluation findings
Parts of this chapter have been reproduced from the published papers by Cavallaro et al. ,1 Cavallaro et al. 2 and Cavallaro et al. 101 These are open-access articles distributed in accordance with the Creative Commons Attribution 4.0 Unported (CC BY 4.0) licence, which permits others to copy, redistribute, remix, transform and build upon this work for any purpose, provided the original work is properly cited, a link to the licence is given and an indication of whether changes were made. See: http://creativecommons.org/licenses/by/4.0/.
Chapter outline
This chapter brings together the findings from the three objectives of this study in order to provide an understanding of the context in which the FNP has been delivered over the past decade in England and to summarise our findings on the real-world implementation of the programme and the factors that may influence effectiveness.
For each objective, we summarise the main results, compare these with previous literature and discuss the implications of our findings. Where relevant, we report initial findings from a qualitative analysis of the FNP (see Qualitative analysis). We then explore the strengths and limitations of the study as a whole. Lastly, we suggest recommendations for policy and practice and further research.
Objective 1 – which groups of adolescent mothers receive Family Nurse Partnership across local authorities?
While eligibility criteria suggest all first-time adolescent mothers are eligible for the FNP, the service has been rationed to ~ 25–30% of adolescent mothers since the rollout in 2010, as sufficient funding for all was not made available. 102 To inform commissioning and targeting of the FNP, we quantified the variation in enrolment rates across 122 FNP sites in England, comparing maternal vulnerability indicators between eligible mothers who were and were not enrolled in FNP and evaluating site characteristics associated with enrolment.
Summary of main results
This study fills an important evidence gap in coverage and targeting of intensive home-visiting services such as FNP within England. We show the most vulnerable mothers are being targeted for FNP, especially the youngest adolescents and those with prior contact with children’s social care. However, our findings indicate insufficient commissioning of FNP relative to local needs: only 23% of eligible mothers in FNP catchment areas were enrolled (2010–7), and areas with the greatest numbers of adolescent mothers had lower enrolment rates. Overall, 26% of eligible mothers aged 13–19 with vulnerability markers associated with adverse outcomes were enrolled, including 52% of those aged 13–15, 44% of those ever recorded as being Looked After and 40% of those with prior mental health- or adversity-related hospital admissions. These groups represent mothers and infants at significantly greater risk of low birthweight, unplanned hospital admissions for injury and infant mortality. 89 We did not find any differences in the populations of mothers in areas that did and did not commission FNP.
Comparison with existing evidence
To our knowledge, this is the first study examining enrolment in a targeted intensive home-visiting programme for expectant mothers. Two previous studies have shown high variation in acceptance rates for universal home visiting between sites, with higher acceptance rates among higher-risk mothers. 103,104 In a similar targeted home-visiting intervention for vulnerable families in Canada (Families First), unenrolled mothers were more vulnerable than enrolled mothers – contrary to our findings – illustrating that it can be difficult to enrol the most vulnerable groups. 105
Interpretation
Budget cuts since the inception of the FNP in England in 2007 mean that the programme, costing approximately £3000 per client per year, has been offered to a more select group of mothers over time. 80,106 This study demonstrates FNP places are not commissioned proportionately to the number of adolescent mothers within local areas, contrary to the stated aims of prioritising ‘areas with […] the highest numbers of eligible population’. 107 Pregnant adolescents living in areas with many adolescent mothers are less likely to receive support than those in areas with few adolescent mothers, with important implications for equity.
Young age is the main eligibility criterion for FNP in England, based on ease of identification, associations with social adversity, disrupted education and employment13,61 and other factors contributing to poor health outcomes among their children. 5,6,62 Unlike some other countries, FNP eligibility criteria in England do not include low educational level or unemployment,27,35,64 which is informed by evidence of higher effectiveness in socioeconomically deprived groups in the US. 32,36,38 In our analysis, only half of mothers aged 13–15 living in areas in which FNP was commissioned were enrolled. Given strict caseload limits (maximum 25 mothers per Family Nurse), many sites in England have explicit policies of prioritising younger adolescent mothers. Overall, 74% of eligible mothers with vulnerability markers were not enrolled in FNP, indicating opportunities for improving policy and commissioning to address vulnerable mothers’ needs, with important and unexplained variation in who is offered intensive services across England.
There are several explanations and implications of this. First, FNP teams may prioritise mothers with additional vulnerabilities not captured in administrative data we used (homelessness or community mental health service use; Box 1), but it is likely that family nurses do not have the full picture of family vulnerability when prioritising services, and some vulnerabilities (such as family violence) may be disclosed only after a trusting relationship is built with their family nurse or health visitor. 108–110 This underscores the need for effective universal services which can identify those at greatest need for intensive services.
Second, there is uncertainty regarding which vulnerable mothers are most likely to accept and benefit from intensive support. Given insufficient funding to offer the programme to all eligible mothers, family nurses and referring providers need standardised, real-time information on vulnerabilities for all mothers to support decision-making and better target the FNP, alongside effective communication between health visitors and family nurses. Ongoing work on defining vulnerabilities by the FNP National Unit will support sites to determine priority criteria for their local context.
Third, vulnerable mothers may have higher refusal rates. Although FNP’s fidelity target is to enrol 75% of mothers offered FNP, aggregate site data suggest not all sites meet this target. We were unable to determine whether under-representation of some groups, for example, South Asian adolescent mothers, was because they were less likely to be offered a place to accept it or both. FNP teams report that most mothers who decline feel socially well-supported, although some decliners are especially vulnerable (e.g. involved with social care services). 111 Last, more vulnerable mothers may be unknown to midwifery services due to presenting to a booking appointment after 28 weeks (or because of moves between LAs in pregnancy). Individual-level information on who is approached and who accepts would help inform strategies to increase uptake among especially vulnerable mothers.
Betsy and Carol reported that persistence is vital in order to recruit the young women onto the programme and to keep them involved; ‘[y]ou need to be really tenacious and keep trying to engage them’. Betsy recognises that the ‘young people … are very mistrusting a lot of the time [because] they’ve been let down so many times in their lives’.
Annie was hesitant to engage with the FNP programme at first. ‘I ignored all her phone calls, all her text messages … she must have tried to contact me in excess of 20 times’. Nevertheless, the FNP nurse was persistent, and she was creative in offering Annie different options for appointments, including meeting Annie at work. This was important for Annie due to her past experiences with practitioners. Annie reported that practitioners either ‘dabble a little bit and then they leave again’ or when ‘you miss a couple of appointments … then no one ever, sort of, comes back’.
Equally, Betsy is improving the referrals process and the service through her own persistence with external organisations: ‘We needed to really market FNP as much as possible, so we did lots and lots of presentations with midwives [and] social workers’.
AcceptanceThere is an acceptance from Betsy and Carol that the system within which they are working is imperfect. Their comments are indicative of a service where there is an increasing number of young people who require support; and where there are increasing numbers of children with a CPP or a CiN plan.
Betsy reported that when she is triaging young parents to provide them with a FNP nurse ‘[t]here’ll be lots of information that you can’t see but there has to be some kind of threshold that we use’. This is because ‘I only have what I have’. Claire said: ‘I think it’s just as it happens. I think I just got the highest [number of children on child protection and child in need plans] at the moment … but … it, kind of, goes up and down…’
DedicationBetsy is dedicated to the programme and her staff. She reported that choosing who will receive support is ‘a big responsibility … and sometimes you, you have to just choose one’. The repetition of ‘who do I, who do I, choose’ and ‘so that’s a, that’s a difficult, that’s a difficult choice to make’ demonstrates her dedication to the young parents in the programme.
Objective 2 – what is the effect of Family Nurse Partnership enrolment on maternal and child outcomes?
For this objective, we aimed to determine the effect of the FNP on maternal and child outcomes, including identifying which families benefit the most from the FNP.
Summary of main results
Cohort description
We identified a number of pre-pregnancy maternal risk factors for indicators of child maltreatment, including younger maternal age, living in more deprived areas, having a history of adversity- or mental health-related hospital admissions, having later first contact with antenatal services, having been referred to social care services as a child, having SEN provision, being persistently absent from school or excluded and having lower educational attainment. Our findings add to previous research that describes the association between having a history of adversity- or mental health-related hospital admissions and increased hospital admissions in infancy by linking additional maternal data on education and social care risk factors and identifying novel risk factors that are important for first-time adolescent mothers. 89 Some of the most important risk factors for child maltreatment in this population are maternal histories of being in care or being excluded from school.
Mothers enrolled in the FNP were much more likely to have these risk factors than those who were not enrolled, and FNP enrolment therefore works as a composite indicator of vulnerability.
Indicators of child maltreatment
There was no difference in CiN or CLA according to enrolment in the FNP, but there was weak evidence that FNP was associated with a reduction in the percentage of children with a CPP (RR 0.84, 95% CI 0.71 to 1.00; p-value = 0.049). We saw an increased risk of unplanned admissions for maltreatment/injury in the 2 years after birth in children born to mothers enrolled in FNP (RR 1.15, 95% CI 1.07 to 1.24, compared to children born to mothers not enrolled in FNP), which did not persist at 7 years after birth.
Other child health/development/education outcomes
We found that FNP was associated with an increase in the number of children with ≥ 1 unplanned admission for any diagnosis up to age 2 and the number of children with ≥ 1 A&E attendance by age 2 and 7. We also found evidence of a small increase in children achieving a Good Level of Development (school readiness) at age 5 in the FNP group (RR 1.05, 95% CI 1.01 to 1.09; p-value = 0.031). There was no evidence that this advantage persisted at Key Stage 1, nor was there any evidence of a difference between groups in SEN provision. FNP was also associated with an increase in the percentage of children registered for FSM (RR 1.09, 95% CI 1.04 to 1.14).
Maternal outcomes
Mothers who were enrolled in the FNP were less likely to have a rapid repeat pregnancy resulting in a subsequent birth within 18 months of the index birth (RR 0.83, 95% CI 0.88 to 0.97). This association varied by region, with strongest associations seen in the South-East, South-West and London. There was no evidence of a difference between groups in the numbers of mothers obtaining 5 A*–C equivalents, including Maths and English at GCSE level or in school enrolment following birth.
Mothers enrolled in the FNP were more likely to have an unplanned admission to hospital for diagnoses relating to adversity (substance misuse, self-harm or violence) or mental health conditions than those who were not enrolled. This association persisted until 7 years following delivery, though the size of the association decreased over time.
Comparison with existing evidence
We were able to use data for almost all eligible mothers ever enrolled in the FNP since 2010 in England, excluding 1360 mothers who did not agree for their data to be used for research. Although we cannot know what the characteristics of the declining mothers are, the high coverage of our cohort means that our results are likely highly generalisable to the eligible population. We were able to link 99% of FNP mothers to a health record, and 98% of these to their baby’s health record.
Linked education data were available for 83% of mothers aged 13–19 (who were born between 1991 and 2006). These linkage rates are similar to those of other studies linking with NPD: 83% of Millennium Cohort Study children (born 2000–1) and 85% of Case Register Interactive Search Child and Adolescent Mental Health children (CRIS CAMHS, children referred between 2008 and 2013) were linked to the NPD. 112 In the study, mothers who could not be linked to NPD were more likely to be older, less likely to be white, more likely to be living in the most deprived areas and less likely to have had hospital admissions in the 2 years prior to 20 weeks of pregnancy. Similar differences in the characteristics of linked and unlinked individuals have been observed in another evaluation of linkage between HES and NPD, which found that the most deprived pupils and those in ethnic minority groups were less likely to link. 71 Such differential linkage is widespread and represents a problem of inequality, whereby particular groups and ethnicities are excluded from research based on analyses of linked administrative data or are less likely to link to information on risk factors or outcomes, meaning they are more likely to have their needs underestimated. 113
Numbers of children classified as CiN in our cohort (22%) was similar to those observed in the Building Blocks trial, which found that 21.5% of children were ever classified as CiN. Since we cannot identify children who were in contact with children’s social care services only before school entry (due to the way in which identifiers are assigned in the DfE data), these estimates likely underestimate true numbers of referrals. Other studies have shown that a large proportion of CiN occurs in preschool children: based on information from a Freedom of Information request, Bilson et al. estimated that 14% of children born between 2009 and 2010 were CiN before their fifth birthday. 114 Based on model estimates using data from the NPD, Jay et al. estimate that 25% of children are ever classed as CiN before age 16. 115
Rates of CPPs were lower in our cohort (4.5% overall and 5.1% in the FNP group) than in the Building Blocks trial (6.8% in the FNP arm and 6.6% in the usual care arm), and rates of CLA were also lower (2.0% in our cohort overall and 2.6% in the FNP group compared with 3.6% in the FNP arm and 3.3% in the usual care arm of the trial). Numbers of CLA in our study population were higher than those observed in the general population, including children born to older mothers. For example, a study of the cumulative incidence of CLA using NPD data found that 1.5% of children born in 2004–6 were ever Looked After by age 6, with increasing rates over time. 78 This may be due to the inclusion of all children recorded as CLA in our data, irrespective of the primary need code.
Our findings of no difference in CiN or CLA between groups mirror those of the Building Blocks 2–6 evaluation, which also found no difference in the timing or first referral, duration or primary need for CiN. 24 The Building Blocks evaluation did find that CLA in the FNP arm were in care for a shorter period of time compared with children in the usual care arm. We did not evaluate duration of periods of care in this study.
In the study, we found that 75% of children had an unplanned hospital admission or A&E attendance in the 2 years following birth (37% had an unplanned hospital admission and 72% had an A&E attendance). This was comparable to rates seen in the Building Blocks trial, where 81% of the FNP arm and 77% of the usual care arm had an unplanned hospital admission or A&E attendance. 99
The proportion of children achieving a Good Level of Development (school readiness) in our cohort was 58%, which was the same as reported in the FNP arm of the Building Blocks trial. 24 Percentages of children reaching the expected standard at Key Stage 1 for Reading and Maths were also similar (65% and 63% compared with 65% and 62%, respectively). Key Stage 1 Writing results were less comparable, due in part to increases in rates of children reaching the expected levels over time, as described in detail in the Building Blocks 2–6 report. 24
Our finding of a reduction in rapid repeat pregnancies in mothers enrolled in the FNP differs to findings from the Building Blocks trial, which observed no evidence of an effect on subsequent pregnancies within 24 months of the first birth. This may in part be due to differences in definitions: we only captured pregnancies that resulted in a live birth (as abortion data were not available and early miscarriages are not well captured in hospital data). We chose the 18-month time period based on evidence that shorter birth-to-pregnancy intervals are associated with the highest risks of adverse outcomes for women and babies and after discussions with our Patient and Public Involvement (PPI) group, who felt that a second birth within 2 years was a positive event for many young mothers. 84 Nevertheless, 17% of mothers had a second child within 24 months in our cohort, compared with 21% of mothers having a repeat pregnancy within 24 months (based on inpatient data only) in the Building Blocks trial.
There are differences in the population of mothers and their social circumstances when enrolling in versions of the FNP that have been implemented in different countries. 22 These differences in underlying risks of maltreatment and in how it is detected and responded to may determine the likelihood that families might benefit from the programme in a particular setting. While there may be benefits in some settings, our findings support previous results in England of no impact on child maltreatment outcomes, and there is no evidence to suggest that benefits from the FNP will appear as children get older.
Interpretation
We found no evidence of an association between FNP and the majority of the outcomes that we evaluated. Our findings are likely to be affected by residual confounding, whereby mothers enrolled in FNP were at higher risk of adverse outcomes than those who were not enrolled, even when matching on pre-pregnancy health, education and social care characteristics. Where differences between groups were observed, interpretation of outcomes captured in administrative data is challenging and complex. 24 For example, our finding of an increased risk of unplanned admissions for injury/maltreatment in the FNP group could represent more injuries in this group but could also reflect more appropriate care-seeking, particularly for minor injuries. Family nurses encourage mothers to have their child seen by a clinician when necessary, and this is particularly likely to be apparent during the 2-year period in which family nurses are visiting families. We also saw increased rates of A&E attendances, outpatient attendances and unplanned admissions for any reason, which may represent appropriate care-seeking behaviour by parents. However, findings from the Elmira trial of the NFP showed a substantial reduction in visits to the physician for injuries or ingestions and in visits to the emergency department associated with the intervention, which, combined with other findings, was interpreted as reflecting a reduction in underlying maltreatment. 25 Therefore, the increased risk of unplanned admissions for injury/maltreatment in the FNP group in the study could genuinely represent an underlying increased risk of maltreatment. This, in turn, might be due to residual unmeasured confounding since mothers enrolled in FNP had more indicators of adversity than mothers who were not enrolled.
Our finding of weak evidence of a reduction in the number of CPPs associated with FNP (and similar directions of non-significant associations for CiN and CLA) reinforces the complexity of understanding the mechanisms underlying these outcomes. Firstly, this finding should be interpreted with some caution given the borderline p-value (0.049) in the context of evaluating a large number of outcomes. Secondly, others have argued that given the ethical, clinical and legal mandate that family nurses have to ensure that children are protected through linkages with appropriate services, increased rates of social care contacts might well be expected in mothers enrolled in the FNP, reflecting earlier and more comprehensive surveillance. 29,116 Family nurses are in a unique position to identify early problems and start processes for safeguarding, which may explain the increased rates of discharge to social services at birth. Indeed, families in the FNP arm of the Building Blocks trial had higher rates of safeguarding procedures noted in the primary care record (13.6%) than families in the usual care arm (8.0%). 99 However, the Building Blocks 2–6 trial found no evidence of surveillance bias when evaluating thresholds for referrals to social care: rates of children who needed no further assessment after being referred were similar between arms. 24 In the study, we measured CiN and CLA in school-age children, who would not have still been seen by the family nurse and who would therefore be less likely to have been affected by surveillance bias.
We observed a higher prevalence of preterm births and low birthweight babies in the FNP group compared with mothers who were not enrolled. These are important birth outcomes, as they are associated with a disproportionate amount of healthcare use (due in part to an increased risk of chronic disease), childhood mortality and poor short- and long-term health and educational outcomes. 117,118 However, the inclusion of low birthweight as one of the primary outcomes of the Building Blocks trial was questioned, as it was not an outcome that the NFP claimed to affect and not one for which previous replicated effects had been observed. 22,23 Home visiting occurs too late to be able to influence preconception health, which is an important predictor of adverse birth outcomes. 119 Indeed, there is little evidence in general for the effect of home visiting on pregnancy outcomes, including from the NFP. 43,120,121 The apparent increased risk of all-cause hospital admissions that we observed in the FNP group may therefore be influenced in part by the higher prevalence of adverse birth outcomes in this group, which are associated with increased unplanned hospital admissions in the first years of life. 122
Our finding of an association between FNP enrolment and a small increase in the number of children achieving a Good Level of Development (school readiness) at age 5 supports similar findings from the Building Blocks 2–6 trial and fewer maternally reported developmental concerns at age 2 in the FNP arm of the original Building Blocks trial. 24 The Good Level of Development is not particularly sensitive to fine changes as a measure of school readiness, and so the underlying association may be even more substantial. 123 Building Blocks 2–6 also found an effect of FNP on Key Stage 1 outcomes, which was not replicated in this study.
Evidence suggests that a large number of families who meet the criteria for FSM do not apply for the benefit. 124 Our finding that mothers enrolled in the FNP were more likely to have children registered for FSM may therefore indicate that family nurses are able to help mothers access the support that is available to them (which includes needing to claim the underlying welfare benefits that form the basis for FSM eligibility) and to overcome recognised barriers such as inadequate information about the claiming process. FSM eligibility is a robust indicator of social disadvantage, and we show that almost half of children born to adolescent mothers are registered (compared with 14% of children nationally who were in school in 2015–6). 125,126 Given the associations between socioeconomic disadvantage, adolescent motherhood and adverse child outcomes, strategies to address the root causes of social disadvantage are also required in order to reduce inequalities and improve outcomes for mothers and their children.
Despite controlling for higher rates of pre-pregnancy unplanned admissions to hospital for diagnoses relating to adversity (substance misuse, self-harm or violence) or mental health conditions in mothers enrolled in FNP, we found that this group continued to have higher rates of these admissions, and A&E attendances, in the 2 and 7 years after giving birth. Part of this may be due to increased self-reflection and self-efficacy as a result of the programme: family nurses work with mothers to explore the trauma that many of them have experienced in the past and to become more insightful about their own needs. Cuts to mental health services have made making appropriate referrals difficult, which may lead to mothers ending up in A&E. We could only measure the most severe problems, as we only identified cases that resulted in a hospital admission record. We did not have data on primary care, which could have provided more information on outcomes that were not severe enough to result in a hospital admission. In our cohort as a whole, 6% of mothers had an unplanned admission to hospital for adversity-related diagnoses, and 8% of mothers had an unplanned admission for mental health-related diagnoses in the 7 years following delivery. Capturing measures of domestic violence is challenging, as mothers may choose not to report violence for fear that a child may be taken away or only make disclosures after a trusting relationship is built with their family nurse or health visitor. 108–110 We are therefore likely to have underestimated the extent of these conditions, meaning that there are many more mothers who are in need of continued support for their health after birth. Others have argued the importance of taking a long-term view of the health of vulnerable mothers, and our findings highlight that vulnerable mothers as well as their children continue to need support for many years after giving birth. 127
Of the younger mothers in our cohort who had not completed their education before becoming pregnant, 10% were able to go on to achieve 5 A*–C grades at GCSE level. While these rates are lower than national figures (around 60%), this still represents a substantial achievement for young mothers who are balancing the responsibilities of caring for a new baby and studying for their exams. However, these findings highlight the structural barriers and challenges that adolescent mothers will face as they become young adults and move into the world of employment. More needs to be done to halt this cycle of poverty and income inequality and to improve the life chances of young mothers. 5
Our finding of a reduction in the number of subsequent deliveries within 18 months should be interpreted cautiously. As we could not measure abortions or miscarriages in this study, we do not know how many mothers in each group became pregnant but chose, or were unable, to continue their pregnancy. However, birth spacing is key for both promoting maternal education and engagement in the workforce and preventing harm to the mother and child, and we show that it may be possible for the programme to influence birth spacing and therefore the maternal life course. This is an important finding: national surveys in England have shown that only 12% of pregnancies in mothers aged 16–19 are planned, highlighting the need for primary prevention strategies to avoid unwanted pregnancies. 128 Previous research has also shown that the effects of adolescent motherhood persist for previous adolescent mothers giving birth again in their 20s, meaning that strategies to improve the life changes of reproductive choices for young women about the timing of their pregnancies could have lasting effects. 12
Objective 3 – what contextual and programme factors influence the effect of Family Nurse Partnership?
For this objective, we aimed to identify contextual and programme factors that might influence FNP programme effect.
Summary of main results and comparison with previous evidence
Overall, 58% of mothers enrolled in the FNP giving birth between April 2010 and January 2018 completed the programme, and 42% left early. Compared with targets, attrition was slightly lower in pregnancy (8%) but higher in infancy (23%) and toddlerhood (19%). These attrition rates are also higher than were observed in the Building Blocks trial (4% in pregnancy, 10% in infancy and 8% in toddlerhood), possibly reflecting a trial effect whereby FNP nurses involved in the trial might have felt more expectation to retain mothers in the programme. Alternatively, this could reflect changes in practice over time and increased flexibility in recent years, allowing mothers to leave the programme early.
The mean number of visits received by mothers across the programme was 36 (median 38). This is similar to that reported in Building Blocks (mean = 39 visits). Across the programme stages, the median number of visits was 10 in pregnancy, 10 in infancy and 14 in toddlerhood, compared with 10, 19 and 13, respectively, in Building Blocks. Overall, mothers enrolled in FNP received an average of 42 hours of contact time with a family nurse throughout the programme.
Approximately 60% of mothers met the fidelity targets for the number of completed visits in pregnancy, 65% in infancy and 60% in toddlerhood. This was slightly higher than fidelity targets reported in the Buildings Blocks trial, which reported 58% in pregnancy, 53% in infancy and 44% in toddlerhood. This may be due to differences in the way that the expected number of visits was calculated in each study, taking into account the time period in which a mother was enrolled (and therefore the number of visits for which she could possibly receive).
Overall, only 28% of mothers met the fidelity targets across all stages of the programme. This could reflect an unrealistic time commitment for mothers or practical problems in arranging visits to suit both mothers and nurses (who have maximum caseloads of 25 mothers). Following the publication of the Building Blocks trial and qualitative research suggesting that mothers wanted more flexibility within the programme, the FNP National Unit made the decision to allow greater flexibility in the appropriate number of visits per mother, which is now decided locally (‘dialling up’ or ‘dialling down’ according to a nurse-client assessment of need), along with the optimal time for graduation. 129,130 It is not yet clear how these recent changes to the programme will impact longer-term outcomes: more information on why a mother leaves the programme is needed to evaluate these changes.
We show that the most vulnerable and youngest mothers tended to have greater numbers of visits and were more likely to meet the fidelity targets than those who did not have these risk factors. After adjusting for these characteristics, mothers who met the target for the number of expected visits in pregnancy were less likely to have a subsequent birth within 18 months than those who did not meet the target; children born to mothers who met the target in infancy and toddlerhood were more likely to have unplanned hospital admissions for maltreatment/injury up to age 2 than those who did not meet the targets in these stages.
Interpretation
Our finding that the most vulnerable and youngest mothers received a greater dosage of visits and were more likely to meet fidelity targets than those who did not have these risk factors suggests that even before the introduction of the Accelerated Design and Programme Testing (ADAPT) sites, family nurses were making decisions about where to prioritise their time and resources and were able to provide more intensive support to those they felt most needed it. These findings make evaluating the impact of dosage of the FNP problematic since the most vulnerable mothers receive more visits but are also independently more likely to experience worse outcomes. However, our findings for unplanned hospital admissions for maltreatment/injury and subsequent births mirror those of Objective 2 comparing mothers enrolled or not enrolled in FNP: mothers who had more visits were more likely to have children with unplanned hospital admissions for maltreatment/injury up to age 2 but less likely to have a subsequent pregnancy within 18 months. For a Good Level of Development and maternal hospital admissions, we found no evidence of a difference in outcomes for mothers who met the fidelity targets and those who did not. An experimental design, combined with more detailed information on why mothers leave the programme, could be used to further evaluate the impact of the number of visits on outcomes. This may be especially relevant in the context of limited resources and previous evidence suggesting that ‘less is more’ for interventions aiming to enhance parental sensitivity and promote attachment. 131
Findings from the qualitative analysis emphasise that the length of the programme is important to both mothers and Family Nurses (Box 2).
The reason that the programme commences at 16 weeks’ gestation and ceases when the child is 2 years old is because the FNP nurses get to know their clients well which is essential in ‘affect[ing] change’ – Betsy.
The length of the programme was important for Annie because it enabled her to develop a trusting relationship with her FNP nurse: ‘It was lovely to be able to have that relationship with someone, you know, always, someone that I could text or call if I needed to’. However, it was difficult when the support came to end: ‘I cried so much when I said goodbye [to the FNP nurse]’.
Nevertheless, the duration of the programme ‘… can be really, really frustrating when there's suddenly poor engagement [from parents]’ – Betsy.
Strengths and limitations
Strengths
A major strength of this study was the use of a population-based cohort of all first-time adolescent mothers giving birth in English NHS hospitals, linked to routine education and social care records. This provided us with a large sample size for analysing subgroups and increased statistical power for detecting small differences. Linking 99% of FNP mothers to HES gave us a highly generalisable cohort of FNP mothers enrolled between April 2010 and March 2019. Using propensity scores derived from observed data on maternal histories recorded in health, education and social care data, we were able to create closely matched groups for > 95% of the FNP mothers in our cohort. The unmatched mothers were captured in a sensitivity analysis using matching with replacement and in the multivariable regression analysis.
Another strength was our use of objective measures of indicators of maltreatment and child development. However, these blunt measures could be supplemented by multimethod approaches in order to give a more nuanced interpretation of outcomes, as is being done for the evaluation of the German Pro Kind intervention, which will use a combination of interviews, observations and administrative data. 132 We also spent a significant amount of time talking to FNP teams, including observing a home visit, in order to understand the perspectives of family nurses and the mothers and families they represent. This enhanced our ability to interpret the results we observed in the data.
Limitations
The potential sources of bias and the steps we took to try to minimise these are summarised in Table 18 and the following sections.
| Bias | Description | Impact on effect estimates |
|---|---|---|
| Indication bias due to FNP nurses deciding which mothers to approach (unmeasured confounding) | Family nurses prioritise the more vulnerable mothers among those meeting eligibility criteria, and so those enrolled may have been more likely than those not enrolled to experience adverse outcomes. | Underestimation of the effect of the intervention. |
| Misclassification bias of eligibility for FNP | In analyses, mothers may have been assigned to different groups than the ones they should be in because eligibility was incorrectly defined. | Bias in either/both directions: random misclassification is likely to underestimate the intervention effect, but bias in misclassification may under or overestimate intervention effect. |
| Consent bias for enrolment in FNP | Mothers who were offered the intervention but who declined may have been different to those who were not offered the intervention. | Bias in either/both directions. Those who were offered the intervention but who declined may be a mixture of the most vulnerable and the least vulnerable mothers. |
| Linkage bias | Linkage error (e.g. missed links or false linksa) could mean that subgroups of the population were differentially excluded from the analysis cohort or had missing data on variables obtained through linkage. Missed links can also lead to misclassification bias (see above). | Bias in either/both directions. It is difficult to ascertain the direction of effect, particularly when there are multiple complex linkages and when the impact of linkage errors works in opposite directions. |
| Measurement bias | Usual care for mothers not enrolled was not captured; surveillance bias might mean that problems in the FNP group were more likely to be detected. | Bias in either direction. Mothers not enrolled in FNP may have had more/less health visiting contacts than usual; FNP nurses may have been more likely to pick up on areas of need (ascertainment/surveillance bias). |
Indication bias due to unmeasured confounders
The main limitation of our analyses was that the administrative data we used did not capture information on all relevant maternal characteristics associated with enrolment, and there were important differences in the characteristics of mothers enrolled in FNP and those who were not, meaning that mothers enrolled in FNP were more vulnerable than the comparison group. For some outcomes, including a Good Level of Development, the findings in the propensity-score-matched cohort reversed those of the unadjusted comparison: while the crude analysis of this outcome showed lower rates in mothers enrolled in FNP, the adjusted comparisons showed higher rates. This suggests that the propensity score matching (and multivariable regression analyses) was able to account for some confounders. However, the higher rates of low birthweight and maternal unplanned admissions after birth in the FNP arm could indicate that residual confounding remains.
Although we used a large number of pre-enrolment maternal characteristics from health, education and social care data for our propensity score matching, it was only possible to evaluate the balance between propensity score-matched groups in terms of these measured characteristics. For measured characteristics, we can only know if groups were balanced on the presence of a characteristic (e.g. a history of hospital admissions for adversity) but not on the nature or severity of that characteristic. This means that although the groups looked comparable in terms of measured characteristics, we likely did not fully account for important unmeasured differences between those that did and did not receive FNP: a phenomenon known as the treatment paradox. 133 For example, some important vulnerabilities (such as family violence) may not be disclosed until a trusting relationship has been built with providers and may not be captured in administrative data at all. 109,110,134 Our approach was restricted by data that were systematically collected by services and the quality of recording of that data.
Characterising usual care provided to mothers not enrolled in Family Nurse Partnership
Usual care for adolescent mothers differs substantially between LAs and over time (including varying numbers of health visitor contacts and additional services for adolescent mothers). 135,136 Health visitors are under-resourced, which makes it likely that not all adolescent mothers are receiving the standard of care that should be expected. 65 Although national data on health visiting are collected, this is not yet well completed nor disaggregated by maternal age. 137–139 We did not have any information on midwifery care and therefore were unable to identify areas in which mothers received care from specialist teenage pregnancy midwives. Bespoke data collection was not feasible within the timeframe of this study; we were therefore unable to include a quantitative measure of usual care in our models, limiting the precision of our intervention effect estimates.
We did not have access to information on additional services that mothers might have accessed as a result of interactions with the family nurse, including, for example, housing services. If mothers not enrolled in FNP had access to high levels of support from other teams in the community, it may be difficult to identify an incremental effect on outcomes for those enrolled in FNP. 23
Misclassification bias (defining our intervention and comparison groups)
In order to make comparisons with mothers who had not been enrolled in FNP but who were eligible, we needed to define the population of adolescent mothers who would have been eligible for the FNP but who were not enrolled due to living in an area in which the FNP was not offered at the time of their pregnancy. If information on recruitment dates was inaccurate, misclassification bias could occur if mothers were categorised as being eligible for the FNP when they were not or vice versa. Site activity dates and geography were key to defining these populations, but this information was not readily available. FNP sites merged and split over time, site boundaries moved and sites discontinued or joined the FNP at different times.
We used extensive data quality checks for LA-specific site activity dates and geographic coverage with the FNP National Unit to minimise misclassification of unenrolled eligible mothers. However, we may have overestimated unenrolled eligible mothers and therefore underestimated some enrolment rates. Conversely, birth ascertainment in HES (97% of total births in English hospitals according to the ONS)69 means some mothers may have been wrongly excluded from the denominator. Neither under- nor over-ascertainment of unenrolled eligible mothers is likely to have biased the analysis of predictors of enrolment, since they should not be associated with risk factors.
Missing data on gestational age at booking appointment (32%) and birth (13%) required us to make some assumptions to determine eligibility for the FNP. Some mothers with missing gestational age at first antenatal appointment may have booked after 28 weeks but were retained in our cohort (2.6% were excluded due to known booking appointment after 28 weeks vs. 7% expected based on primary care records – S Syed, personal communication). We cannot know whether the 0.5% of children who were discharged to social services at birth were reunited with their birth mothers; inclusion of these children in the analysis of outcomes in the 2 and 7 years following birth might have led to a small bias in either direction (as these babies may not have been exposed to their birth mothers during follow-up).
Consent bias due to lack of information on mothers who declined the intervention
It was not possible to identify eligible mothers who were offered enrolment but declined. As a result, these mothers were included in the comparison of mothers who had never been enrolled in the FNP. This could lead to consent bias: if mothers who declined were more vulnerable than those who accepted, it might lead us to underestimate the intervention effect. FNP sites had limited aggregate information on these mothers. Some sites reported that although a small number were particularly vulnerable mothers (e.g. involved with social care services), the majority of mothers who declined were those with strong social support.
Missing data due to linkage error
Eight-three per cent of mothers aged 13–19 in our cohort were linked to NPD. Some unlinked mothers would genuinely not have been captured in NPD due to attending an independent school or a school in a different country. Other mothers may not have been linked due to inconsistencies between identifiers recorded in both data sources. HES records for a small number of FNP mothers who did not link to HES would mistakenly have been treated as belonging to the comparison group, which again may lead to misclassification bias. The extent to which these missed links lead to bias depends on how the unlinked records are dealt with in analysis: in this study, all mothers/babies were retained in the analysis (but we could only measure educational outcomes for those who linked). 140 Determining the potential direction of bias is complex, particularly when successive linkages are performed (such as FNP data linked to health data, then to educational data). We identified groups of mothers who were more at risk of linkage bias or missing data by comparing the characteristics of FNP mothers who did and did not link with HES and NPD records (see Appendix 2, Tables 24 and 29).
Data approval and access delays
It took 4 years from data applications being submitted to the final linked data set being available for analysis (see Appendix 10). Lengthy application processes and delays in receiving administrative data have been widely documented elsewhere. 141–144 Cross-sectoral data linkage adds other delays, including in data providers sending identifier information to trusted third parties for linkage and in migrating data to a single trusted research environment. These delays impeded analysis time: linked data were finally available 1 month before our initial grant endpoint, an insufficient period within which to deliver results based on extensive administrative data cleaning, assessment of linkage quality, construction of study cohorts and optimisation of quasi-experimental approaches. This was exacerbated by problems with the secure server on which the data were hosted, which meant that there were many days when the data were not accessible.
Other limitations
We did not consider costs in this study. The Building Blocks trial found that the FNP costed on average an additional £1812 (95% CI −£2814 to £5557) per mother compared to usual care and that there were only minor differences across trial arms, with largest drivers of costs being hospital inpatient stays. 80 Costs associated with the involvement of other professionals interacting with family nurses, education, social care and primary care costs have never been considered.
In our analysis of the number and duration of visits, we did not account for the content or other factors (e.g. continuity of care) that might influence the effectiveness of the programme. We were unable to report on mortality due to discrepancies in recording of deaths between data sources.
Our PPI was limited by difficulties in engaging FNP graduates. Although the participants who attended our focus group were enthusiastic about remaining involved, the practicalities of keeping in touch with young mothers who have changing priorities over time meant that we struggled to retain mothers through the course of the study. Difficulty in engaging FNP graduates was also described in the Building Blocks 2–6 trial. 24
We designed the study to describe a wide range of outcomes, due in part to the fact that the primary outcomes specified in the original Building Blocks trial were challenged and to enable us to compare the findings from the study with other evaluations of the FNP. 22,23,116 A limitation of this approach is that the large number of comparisons made could generate spurious results since 1 in 20 findings will be by chance when using 95% CIs. Therefore, the few statistically significant findings that we observed out of the many that were evaluated should be considered in the context of patterns of effect (rather than relying on p-values) and the extent to which they align with previous studies.
Patient and public involvement
In the process of designing the study, we engaged with two groups of mothers (some who had participated in FNP, some who had not). We discussed the use of administrative data for research (including concepts that mothers were not previously familiar with, such as de-identification and data linkage), linkage of health and education data without explicit consent and the use of these data specifically for evaluating the FNP. Workshop participants were supportive of the proposed study and fed back that linking health and education data for mothers and their children was a good idea. Participants strongly agreed with sharing their data so that services could be improved and future mothers could benefit and wanted to know how their data had been used to benefit others. Mothers were strongly supportive of taking into account maternal education and area, and wider family support for the FNP, in order to understand whether the programme worked. 145 We incorporated these opinions into the study plan by planning to evaluate whether the linkage of FNP differs by area and by maternal risk factors.
This Study Steering Committee included a former adolescent mother, who was consulted throughout the study period. When it was not possible for her to attend meetings, we organised separate meetings to present the same findings and discuss progress. Towards the end of the study, our lay member withdrew from being involved in the study due to changes in family circumstances. Our committee also initially included one mother who had completed the FNP but later dropped out. In order to increase the level of involvement in the study, we contacted FNP sites via the FNP National Unit to recruit mothers participating in FNP part way through the study and approached two additional mothers (one current and one former FNP participant), who both agreed to join the study. However, communication was challenging as it was difficult to find a time that fitted their schedule. The former FNP participant eventually contacted us to say she no longer had the time to be involved, and we stopped receiving replies from the current FNP participant (whose baby was very young), reflecting the challenges of effective PPI with this target population.
We ran a training day for parents interested in learning more about administrative data research in October 2019 at Great Ormond Street Hospital, which was well attended by parents. On the training day, we gave an overview of what is meant by administrative data research and data linkage, with examples from specific data sets, including those used in this study (HES). We discussed the appropriateness of linking data on mothers and children for purposes such as this study. Participants were strongly supportive of the data being used in this way and fed back that they found the training extremely useful and interesting.
Parent participants will help coproduce information on the study for the FNP and institutional websites, help with interpretation of results and identify the most appropriate methods of dissemination.
Equality, diversity and inclusion
This study included all mothers and their children who were ever enrolled in FNP and was therefore representative of the population receiving the intervention. However, we do not have information on the characteristics of mothers who are not approached for or decline to enrol in FNP, and we do not know the extent to which FNP is inclusive of all mothers who stand to benefit. We aimed to fill gaps in evidence on whether the effect of FNP varied across different subgroups and present results of the intervention effect stratified by ethnicity, age and deprivation.
Our research team did not include those from groups who are generally under-represented in our field of study, but there was a range of experience and expertise across the research team. We provided development opportunities for more junior members of the team, including providing opportunities for teaching and supervision experience and supporting a promotion application. We attempted to include members of the public who were representative of the eligible population of adolescent mothers across a geographic range in England, although this proved to be challenging in practice.
Conclusions
Our findings support previous evaluations of FNP in England, which show no impact on child maltreatment outcomes and no evidence to suggest that further benefits will appear as children get older but are in contrast to qualitative research describing the positive impacts of the programme. There remains uncertainty about whether intensive home visiting is effective for reducing child maltreatment because of the potential for bias relating to the selection of the most vulnerable mothers into FNP on the basis of unmeasured characteristics (which could mask beneficial effects), the lack of information about usual care for adolescent mothers not enrolled in FNP (which could introduce bias to the null) and the challenges of interpreting outcomes captured in administrative data. The findings in this report should therefore be interpreted with three main considerations.
First, we could only control for the fairly crude maternal risk factors associated with enrolment in FNP that are captured in administrative data. The increased rates of maternal unplanned admissions post pregnancy for adversity and mental health-related diagnoses in the FNP group could indicate that there may be additional residual confounding due to bias by indication, even after propensity score matching. Given that we know that mothers enrolled in FNP had more indicators of vulnerability at enrolment than the comparison group, such residual confounding could have limited our ability to detect beneficial effects of the programme. The weak evidence for small improvements in school readiness as measured by a Good Level of Development in the EYFSP and reductions in the number of rapid repeat pregnancies may therefore reflect larger positive effects of the programme. However, these outcomes should still be considered in the context of being the only ‘positive’ effects amongst the many outcomes that were evaluated. The importance of these small effects should be examined alongside other population-level interventions aiming to improve child health and development outcomes.
Second, the increased rates of unplanned admissions and A&E attendances in the mother and child associated with FNP may reflect appropriate care-seeking as a result of advice and support from family nurses rather than residual confounding. Babies born to mothers enrolled in the FNP were more likely to be born preterm and with low birthweight; these are health conditions which are influenced by pre-conception health, and babies with these conditions would be expected to have appropriately increased rates of hospital contacts throughout childhood. Increased rates of admissions in the mother could also be interpreted as demonstrating that family nurses can have a long-term effect on maternal health care-seeking behaviours.
Third, FNP might have positive effects on a range of other outcomes that are not captured in administrative data (Box 3). This study was not able to identify effects on changes in self-reported parental mental health, sense of self, well-being, confidence, behaviour and parent–child engagement and interaction, including for fathers. Nuances in behaviour change are difficult to measure: for example, a mother may not give up smoking completely but may change how she smokes by not smoking in the home and not allowing others to smoke in the home. Existing qualitative work demonstrates overwhelming support for the programme from mothers who have been enrolled and from family nurses who can see the changes and impact that the intensive service has provided for the families they have worked with. 99,130 Mothers often stay in touch with their family nurses after graduation and can reflect on how the programme has helped them transition, become confident as a parent, and be a more responsive parent. 130 There have been no dissenting voices as to the overall efficacy of the programme, and each mother reported it had been helpful in some way – either ‘life changing’ or serving to consolidate existing skills and qualities. 99 However, there is a lack of conclusive, systematic evidence supporting interventions for preventing child maltreatment more generally. 146–149 Evidence is stronger for benefits at later follow-up: ‘sleeper’ effects may mean that benefits of interventions need time to emerge as parents become more practiced and confident in positive parenting strategies over time. 150 Expecting to detect effects of home visiting that starts in pregnancy on birth outcomes and on relatively insensitive child development measures may also be unreasonable in the context of the social disadvantage, discrimination and other challenges that adolescent mothers face before, during and after pregnancy. 151
Despite reductions in adolescent pregnancies over recent decades, there remains a significant population of young and vulnerable mothers in England who need intensive support. Currently, the majority of these mothers are not receiving support from FNP, as it is not offered in all areas, and is only offered to around one in four mothers in areas in which it is commissioned. There is strong support for FNP locally, and FNP practitioners report that mothers participating in the programme develop more reflective parenting and awareness of their child’s needs. Without better evidence, removing support for young mothers could be harmful, especially in the context of increasing social disadvantage and widespread health visitor shortages that are already putting pressure on other services. 152 However, there remains uncertainty about which elements of intensive interventions are most effective, for whom and when and whether it is better to commission highly intensive services for a small portion of the target population or to extend and enhance universal services to better support all adolescent mothers.
For Annie, participating in the FNP programme when she was pregnant with her eldest child was life changing. Firstly, the FNP nurse helped Annie to develop her parenting practices which ‘is completely different to how I was raised’. Annie reported that her parents have commented on that. Secondly, Annie was able to explore healthy and unhealthy relationships in order to ‘make that decision to say actually, you know, enough is enough’. Annie reported that she is now in a loving, stable relationship. Thirdly, the FNP nurse supported Annie to advance her career. Annie is now a qualified midwife and health visitor; Annie is currently ‘specialis[ing] in safeguarding’. This has enabled Annie to reflect on ‘how far we’ve come and how very, very, very different it could be’.
Lack of understandingAnnie discussed the fact that long-term, qualitative outcomes that are important to parents are unlikely to be reflected in data: ‘The stuff that I have achieved can’t be broken down by data’.
ValueAnnie commented that ‘she was probably the first and only person that truly believed in me and my ability’ and she ‘treated me like the adult that I was, really’. This included supporting Annie to make her own decision and advocate for herself. Annie reported that she did not want to attend Baby Groups and that ‘she [the FNP nurse] never forced it’.
Holistic approachThe FNP programme implements a holistic approach with parents and practitioners. For parents, the FNP nurses support them to identify ‘what they would like to achieve … and how they can get to where they want to get to’ – Betsy.
The FNP nurses achieve this by using a strengths-based approach and providing the parents with boundaries: ‘You want to find every opportunity to give affirmations because … that really does build their confidence and help them to feel pride in achieving’ – Betsy. ‘I think having that … therapeutic relationship, where it’s boundaried … [and] consistent; something they might not have had in their, … their life’ – Carol.
The approaches were necessary for Annie: ‘She really worked to your strength[s and] she was not judgmental at all’.
Implications for policy and practice
Delivering interventions to high-risk families
To reduce social inequalities, effective interventions need to be available to all those who meet eligibility criteria. In 2010–7, most adolescent mothers at the highest risk of adverse outcomes were not receiving FNP, and we have few data on the support that they did receive during and after pregnancy. Eligible adolescent mothers living in areas with many births to adolescent mothers were least likely to receive FNP support. Moreover, adolescent mothers with similar vulnerabilities in areas where FNP was not commissioned were unlikely to have had access to equivalent intensive support. Our recommendations for delivering interventions to high-risk families are:
-
Commissioning of interventions to adolescent mothers should aim to provide adequate support to meet the needs of all adolescent mothers (not just a subset of them) through increased provision of intensive services in line with local needs and the availability of other local services. For example, commissioning could be linked to the expected number of adolescents giving birth in an area; local priorities and other factors influencing local commissioning should be routinely recorded so that different commissioning strategies can be evaluated.
-
Information about the maternal characteristics associated with outcomes should inform targeting in the context of insufficient commissioning of the programme.
-
Other groups of mothers who have been shown to be at equally high risk for adverse child outcomes to adolescent mothers, such as those living in deprived areas and those with a history of unplanned hospital admissions for adversity or mental health conditions, should also be considered for intensive support (as they are in FNP ADAPT sites). 60,89
-
Decisions about the appropriate level of care for each family (including ‘dialling up and dialling down’ the intensity of support) should be based on continuous evaluations of who is most likely to benefit, supported by a more complete recording of vulnerabilities antenatally and real-time linkage of routine health and social care data. 89,153 This could add to primary prevention strategies aiming to improve reproductive choices for women about the timing of their pregnancies.
Improving data to support quasi-experimental research studies
There remains uncertainty about whether intensive home visiting is effective for reducing child maltreatment because of the potential for bias relating to the selection of the most vulnerable mothers into FNP on the basis of unmeasured characteristics (which could mask beneficial effects) and the lack of information about usual care for adolescent mothers not enrolled in FNP (which could introduce bias to the null). Understanding variations in usual care provision among both mothers enrolled in FNP and controls is also necessary to better estimate the incremental effect of FNP and account for any unexpected variation in usual care during the evaluation period. Such information would allow more nuanced interpretation of results, including, for example, if the programme worked better in one local area than another. Our recommendations for improving the available data to support evaluations of complex interventions using administrative data are:
-
More complete recording of the characteristics that are used to prioritise mothers for enrolment in each site (including start and end dates of these prioritisation characteristics) and other important maternal characteristics for adjustment purposes.
-
Detailed recording of programme metadata, including site activity dates and geography and criteria being used by FNP teams in order to correctly define eligible groups of mothers who were and were not enrolled or eligible for the intervention. These programme characteristics should be available in an easily searchable central repository.
-
Individual-level or aggregate data on characteristics of all mothers-to-be offered enrolment and those who declined versus those who accepted enrolment.
-
Improved, high-quality data on usual care, that is, community health contacts of all eligible women at the individual level (including, e.g. public health or teenage pregnancy midwife services, number and type of health visitor contacts, number of children’s centres). These data could be captured in the Community Services Dataset, but the completeness of this data set is variable over time and across areas. 137,139
Recommendations for research
Development of the intervention
-
More research is needed to understand which elements of intensive interventions are most effective, for whom and when and to help inform decisions about whether it is better to commission highly intensive services for a small portion of the target population or to extend and enhance universal services to better support all adolescent mothers. For example, research could evaluate the effectiveness of enhanced midwifery support in pregnancy delivered by specialist teenage pregnancy midwives.
-
Research is needed to understand the spillover effects of the programme on non-FNP mothers. 154 While the FNP may enhance other services (e.g. as trained family nurses take on other roles) by dissemination of trauma-informed approaches and understanding of the teenage brain, qualitative data also suggest that professionals are concerned about the licensed nature of FNP and not being able to share freely with wider health visiting colleagues or use it to change practice across services. 111 We do not yet know if FNP diverts resources away from the usual care that an adolescent mother should receive or if there are any other unintended harms of the programme. 155
-
There is ongoing work in the ADAPT sites to tailor the programme more closely to individual mothers and families. Further robust evaluation is needed of modifications to the FNP, including the changes included in the ADAPT sites and including outcomes for mothers aged 20–24 (who we could not assess in this study due to small numbers enrolled with sufficient follow-up).
-
Better understanding is needed of how the programme and outcomes are affected by different modes of delivery, such as those that were implemented during the COVID-19 lockdown. 156 An evaluation of the FNP during lockdown in Scotland found that all survey respondents reported continuing home visits during lockdown, though some mothers were not comfortable receiving home visits. Mothers reported invaluable support and felt their family nurses provided stability, advice and care, particularly those who became socially isolated.
Improvement of delivery, including targeting
-
Research is needed to find ways to support achieving continuity of care and to support learning and wider sharing with health visiting colleagues, which would allow FNP to change practice across the service.
-
Availability of more accurate individual- or household-level deprivation measures (including those available through Unique Property Reference Numbers) would improve our ability to create closely matched groups, provide enhanced information on the social support available within a household and help more effective targeting and follow-up of the many young mothers experiencing socioeconomic disadvantage. 157
Measuring the right outcomes
-
We have reported initial findings from a qualitative study of the experiences of parents and practitioners involved in FNP, and further findings from this work will inform our understanding of the mechanisms of effect of FNP and for which outcomes we are most likely to see effects. This is particularly important in the context of quasi-experimental research studies, where bias and/or data limitations are likely to influence findings.
-
Better measures of changes from enrolment in maternally reported well-being, confidence, mental health, parent–child interaction and child behaviour would allow us to understand more nuanced effects of the programme not routinely captured in administrative data.
-
Future research should also consider outcomes for fathers, who have not been considered to date in evaluations of FNP and who are hard to capture in administrative data. 158
-
Research is needed to understand whether FNP can mediate outcomes for those with adverse birth conditions (e.g. preterm birth and low birthweight) and whether there are any residual (‘sleeper’) effects for subsequent children.
-
More research is needed to understand whether the FNP has an effect on mortality for mothers and children, rates of abortions and the reasons for hospital admissions, including malnutrition.
-
Future studies should quantify the total costs of FNP compared to usual care, including non-contact time of family nurses and additional resources used by FNP mothers and their children.
Design of future studies
-
A randomised controlled trial is needed to further evaluate the impact of the number of FNP visits or contacts on outcomes, including self-reported outcomes and other measures of child development, for example, Language Environment Analysis (LENA). 159 As a trial will also have its challenges, including attrition, recruitment and standardisation of usual care, experimental designs should also have a strong qualitative component to extend the contextual explanation of variation, for example, across localities.
-
Other ways to analyse the data and avoid excluding high-risk mothers from analysis could be explored, for example, using target trial emulation. 160
-
Linkage to primary care and the Maternity Services Dataset could enable investigation of a wider range of risk factors.
-
Routine linkage of education, social care and health data should be used to enable more efficient evaluations of early interventions. 161 Some organisations have called for the collection of a unique identifier in data for all children’s services to enable services to work in a more joined-up way, which could be used to facilitate research in the future. 162,163
Additional information
Acknowledgements
The authors would like to thank members of our Advisory Group from the Building Blocks trial team (Mike Robling, Rebecca Cannings-John and Fiona Lugg-Widger) for their advice on the design and interpretation of this study. MR, RCJ and FLW contributed to the discussion of potential biases relating to the study. We would also like to thank Linda Wijlaars for her help requesting and extracting the data and Emma Howarth for her input to the protocol.
We would like to thank members of our Study Steering Committee (Jane Barlow, Lorna Fraser, Emily Petherick, Marni Brownell, Loretta McGurry and Romy Labrosse) for their helpful input, advice and suggestions throughout the course of the study.
The authors would also like to thank the FNP National Unit for their help in establishing the linked dataset and interpreting the results, including Lynne Reed, Alisa Swarbrick, Andreea Calin, Sarah Tyndall and Alex Stevenson. We would also like to thank the FNP nurses and clinical leads who provided valuable insight into the results and the discussion, including Cheryl Beirne, Alison Goodall, Amanda Malthouse, Nicole Hobson and Christine Anderson. We would also like to thank Cheryll Adams and Alison Morton from the Institute of Health Visiting for their input.
We would like to thank Sue Hillsden from the FNP National Unit for her help identifying catchment areas and activity dates for FNP sites. We thank Nicole Hobson from the FNP National Unit, as well as Debbie Bougard, Karen Arkle, Caroline Scott, Mel Green, Lydia Ottavio, Catherine Dent, Charde Thompson, Anna Parry and Kristin Vreugdenhil from FNP teams, for their help with understanding referral processes and sharing aggregate enrolment data from their sites.
We would like to thank Jenny Woodman, Matt Jay, Anne McKay and Pip O’Byrne for their extremely valuable contributions to our interpretation of results and discussion within the report. We would also like to thank the UCL Great Ormond Street Institute of Child Health Statistics Group for their helpful advice on developing the propensity score matching approach.
Contributions of authors
Francesca Cavallaro (https://orcid.org/0000-0002-9641-8780) did the analysis and contributed to writing the report.
Amanda Clery (https://orcid.org/0000-0002-7366-9982) did the analysis and contributed to writing the report.
Ruth Gilbert (https://orcid.org/0000-0001-9347-2709) contributed to the design of the study, interpretation of results and to writing the report.
Jan van der Meulen (https://orcid.org/0000-0002-9451-2335) contributed to the design of the study, interpretation of results and to writing the report.
Sally Kendall (https://orcid.org/0000-0002-2507-0350) contributed to the design of the study and interpretation of results.
Eilis Kennedy (https://orcid.org/0000-0002-4162-4974) contributed to the design of the study and interpretation of results.
Catherine Phillips (https://orcid.org/0000-0002-9964-3684) conducted the qualitative interviews.
Katie Harron (https://orcid.org/0000-0002-3418-2856) did the analysis, designed the study and wrote the report.
Disclosure of interests
Full disclosure of interests: Completed ICMJE forms for all authors, including all related interests, are available in the toolkit on the NIHR Journals Library report publication page at https://doi.org/10.3310/BVDW6447.
Primary conflicts of interest: No competing interests.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety and plan NHS services. Patient data should be kept safe and secure to protect everyone’s privacy, and it is important that there are safeguards to make sure that they are stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Data-sharing statement
All requests for the anonymised individual-level data from HES and NPD used in this report should be submitted for review to NHS Digital and DfE and may be granted subject to completion of a data-sharing agreement. All other enquiries should be sent to the corresponding author.
This work was produced using statistical data from ONS. The use of the ONS statistical data in this work does not imply the endorsement of the ONS in relation to the interpretation or analysis of the statistical data. This work uses research datasets that may not exactly reproduce National Statistics aggregates.
Ethics and governance
Support for this study has been obtained from the Nottingham Research Ethics Committee (ref 18/EM/0014), the Department for Education (ref DR190430.02) and the Confidentiality Advisory Group (ref 18/CAG/0013). A Study Steering Committee oversaw the study and ensured it was conducted to rigorous standards. Support for the qualitative study was obtained from the University of Kent.
Department of Health and Social Care disclaimer
This publication presents independent research commissioned by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by the interviewees in this publication are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, MRC, NIHR Coordinating Centre, the HSDR programme or the Department of Health and Social Care.
This monograph was published based on current knowledge at the time and date of publication. NIHR is committed to being inclusive and will continually monitor best practice and guidance in relation to terminology and language to ensure that we remain relevant to our stakeholders.
Publications
Cavallaro F, Gilbert R, Van der Meulen J, Kendall S, Kennedy E, Harron K. Intensive home visiting for adolescent mothers in the Family Nurse Partnership in England 2010–2019: a population-based data linkage cohort study using propensity score matching. BMJ Public Health 2024;2:e000514. https://doi.org/10.23889/ijpds.v7i3.1831
Disclaimers
This manuscript presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care.
References
- Cavallaro FL, Gilbert R, Wijlaars L, Kennedy E, Swarbrick A, van der Meulen J, et al. Evaluating the real-world implementation of the Family Nurse Partnership in England: protocol for a data linkage study. BMJ Open 2020;10.
- Cavallaro FL, Gilbert R, Wijlaars LP, Kennedy E, Howarth E, Kendall S, et al. Characteristics of enrolment in an intensive home-visiting programme among eligible first-time adolescent mothers in England: a linked administrative data cohort study. J Epidemiol Commun Health 2022;76:991-8.
- Office for National Statistics (ONS) . Birth Characteristics 2019 2022. www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/livebirths/datasets/birthcharacteristicsinenglandandwales (accessed 5 October 2022).
- Crawford C, Cribb J, Kelly E. Teenage Pregnancy in England 2013. https://ifs.org.uk/publications/teenage-pregnancy-england (accessed 5 January 2023).
- Wellings K, Palmer MJ, Geary RS, Gibson LJ, Copas A, Datta J, et al. Changes in conceptions in women younger than 18 years and the circumstances of young mothers in England in 2000–12: an observational study. Lancet 2016;388:586-95.
- Bellis MA, Hughes K, Leckenby N, Perkins C, Lowey H. National household survey of adverse childhood experiences and their relationship with resilience to health-harming behaviors in England. BMC Med 2014;12.
- Rigsby DC, Macones GA, Driscoll DA. Risk factors for rapid repeat pregnancy among adolescent mothers: a review of the literature. J Ped Adoles Gynecol 1998;11:115-26.
- Restrepo-Méndez MC, Lawlor DA, Horta BL, Matijasevich A, Santos IS, Menezes AMB, et al. The association of maternal age with birthweight and gestational age: a cross-cohort comparison. Paediatr Perinat Epidemiol 2015;29:31-40.
- Cunnington AJ. What’s so bad about teenage pregnancy?. J Fam Plann Reprod Health Care 2001;27:36-41.
- Stier DM, Leventhal JM, Berg AT, Johnson L, Mezger J. Are children born to young mothers at increased risk of maltreatment?. Pediatrics 1993;91:642-8.
- Gonzalez A, MacMillan HL. Preventing child maltreatment: an evidence-based update. J Postgrad Med 2008;54:280-6.
- Jutte DP, Roos NP, Brownell MD, Briggs G, MacWilliam L, Roos LL. The ripples of adolescent motherhood: social, educational, and medical outcomes for children of teen and prior teen mothers. Acad Pediatr 2010;10:293-301.
- Wiggins M, Oakley A, Sawtell M, Austerberry H, Clemens F, Elbourne D. Teenage Parenthood and Social Exclusion: A Multi-Method Study – Summary Report of Findings 2005. https://discovery.ucl.ac.uk/id/eprint/10003007/1/Wiggins2005TeenageParenthood.pdf (accessed 5 October 2022).
- Lawlor D, Shaw M, Johns S. Teenage pregnancy is not a public health problem. BMJ 2001;323.
- Buck D, Gregory S. Improving the Public’s Health: A Resource for Local Authorities. London: The King’s Fund; 2013.
- Booth CM, Tannock IF. Randomised controlled trials and population-based observational research: partners in the evolution of medical evidence. Br J Cancer 2014;110:551-5.
- Cowley S, Whittaker K, Malone M, Donetto S, Grigulis A, Maben J. What makes health visiting successful – or not? 1. Universality. J Health Visit 2018;6:352-60.
- Public Health England . Best Start in Life and Beyond: Improving Public Health Outcomes for Children, Young People and Families. Guidance to Support the Commissioning of the Healthy Child Programme 0 to 19: Health Visiting and School Nursing Services 2018. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/716028/best_start_in_life_and_beyond_commissioning_guidance_2.pdf (accessed 5 October 2022).
- Marmot M. Fair Society, Healthy Lives: The Marmot Review 2010. www.instituteofhealthequity.org/resources-reports/fair-society-healthy-lives-the-marmot-review/fair-society-healthy-lives-full-report-pdf.pdf (accessed 5 October 2022).
- Robling M, Bekkers M-J, Bell K, Butler CC, Cannings-John R, Channon S, et al. Effectiveness of a nurse-led intensive home-visitation programme for first-time teenage mothers (building blocks): a pragmatic randomised controlled trial. Lancet 2016;387:146-55.
- Olds DL, Hill PL, O’Brien R, Racine D, Moritz P. Taking preventive intervention to scale: the nurse–family partnership. Cogn Behav Pract 2003;10:278-90.
- Olds D. Building evidence to improve maternal and child health. Lancet 2016;387:105-7.
- Barlow J, Barnes J, Sylva K, Fonagy P, Fearon P. Questioning the outcome of the Building Blocks trial. Lancet 2016;387:1615-6.
- Robling M, Lugg-Widger F, Cannings-John R, Sanders J, Angel L, Channon S, et al. The Family Nurse Partnership to reduce maltreatment and improve child health and development in young children: the BB:2–6 routine data-linkage follow-up to earlier RCT. Public Health Res 2021;9.
- Olds DL, Henderson CR, Chamberlin R, Tatelbaum R. Preventing child abuse and neglect: a randomized trial of nurse home visitation. Pediatrics 1986;78:65-78.
- Olds DL, Henderson CR, Kitzman H. Does prenatal and infancy nurse home visitation have enduring effects on qualities of parental caregiving and child health at 25 to 50 months of life?. Pediatrics 1994;93:89-98.
- Kitzman H, Olds DL, Henderson CR, Hanks C, Cole R, Tatelbaum R, et al. Effect of prenatal and infancy home visitation by nurses on pregnancy outcomes, childhood injuries, and repeated childbearing. A randomized controlled trial. JAMA 1997;278:644-52.
- Eckenrode J, Ganzel B, Henderson CR, Smith E, Olds DL, Powers J, et al. Preventing child abuse and neglect with a program of nurse home visitation: the limiting effects of domestic violence. JAMA 2000;284:1385-91.
- Olds D, Henderson CR, Kitzman H, Cole R. Effects of prenatal and infancy nurse home visitation on surveillance of child maltreatment. Pediatrics 1995;95:365-72.
- Olds DL, Henderson CR, Tatelbaum R. Prevention of intellectual impairment in children of women who smoke cigarettes during pregnancy. Pediatrics 1994;93:228-33.
- Olds DL, Kitzman H, Cole R, Robinson JA, Sidora K, Luckey DW, et al. Effects of nurse home-visiting on maternal life course and child development: age 6 follow-up results of a randomized trial. Pediatrics 2004;114:1550-9.
- Olds DL, Kitzman H, Hanks C, Cole R, Anson E, Sidora-Arcoleo K, et al. Effects of nurse home visiting on maternal and child functioning: age-9 follow-up of a randomized trial. Pediatrics 2007;120:e832-45.
- Kitzman H, Olds DL, Knudtson MD, Cole R, Anson B, Smith JA, et al. Prenatal and/or infancy nurse home visiting and 18-year outcomes of a randomized trial. Pediatrics 2019;144.
- Olds DL, Robinson J, Pettitt L, Luckey DW, Holmberg J, Ng RK, et al. Effects of home visits by paraprofessionals and by nurses: age 4 follow-up results of a randomized trial. Pediatrics 2004;114:1560-8.
- Olds DL, Robinson J, O’Brien R, Luckey DW, Pettitt LM, Henderson CR, et al. Home visiting by paraprofessionals and by nurses: a randomized, controlled trial. Pediatrics 2002;110:486-96.
- Olds DL, Holmberg JR, Donelan-McCall N, Luckey DW, Knudtson MD, Robinson J. Effects of home visits by paraprofessionals and by nurses on children: follow-up of a randomized trial at ages 6 and 9 years. JAMA Ped 2014;168:114-21.
- Olds DL, Kitzman H, Knudtson MD, Anson E, Smith JA, Cole R. Effect of home visiting by nurses on maternal and child mortality: results of a 2-decade follow-up of a randomized clinical trial. JAMA Ped 2014;168:800-6.
- Olds DL, Eckenrode J, Henderson CR, Kitzman H, Powers J, Cole R, et al. Long-term effects of home visitation on maternal life course and child abuse and neglect. Fifteen-year follow-up of a randomized trial. JAMA 1997;278:637-43.
- Olds DL, Kitzman H, Anson E, Smith JA, Knudtson MD, Miller T, et al. Prenatal and infancy nurse home visiting effects on mothers: 18-year follow-up of a randomized trial. Pediatrics 2019;144.
- Olds DL, Henderson CR, Tatelbaum R, Chamberlin R. Improving the life-course development of socially disadvantaged mothers: a randomized trial of nurse home visitation. Am J Public Health 1988;78:1436-45.
- Kitzman H, Olds DL, Sidora K, Henderson CR, Hanks C, Cole R, et al. Enduring effects of nurse home visitation on maternal life course: a 3-year follow-up of a randomized trial. JAMA 2000;283:1983-9.
- Olds DL, Kitzman HJ, Cole RE, Hanks CA, Arcoleo KJ, Anson EA, et al. Enduring effects of prenatal and infancy home visiting by nurses on maternal life course and government spending: follow-up of a randomized trial among children at age 12 years. Arch Pediatr Adolesc Med 2010;164:419-24.
- McConnell MA, Rokicki S, Ayers S, Allouch F, Perreault N, Gourevitch RA, et al. Effect of an intensive nurse home visiting program on adverse birth outcomes in a medicaid-eligible population: a randomized clinical trial. JAMA 2022;328:27-3.
- Robling M, Bekkers MJ, Bell K, Butler CC, Cannings-John R, Channon S, et al. Effectiveness of a nurse-led intensive home-visitation programme for first-time teenage mothers (Building Blocks): a pragmatic randomised controlled trial. Lancet 2016;387:146-55.
- Mejdoubi J, van den Heijkant SC, van Leerdam FJ, Heymans MW, Crijnen A, Hirasing RA. The effect of VoorZorg, the Dutch nurse–family partnership, on child maltreatment and development: a randomized controlled trial. PLOS ONE 2015;10.
- Mejdoubi J, van den Heijkant SCCM, van Leerdam FJM, Heymans MW, Hirasing RA, Crijnen AAM. Effect of nurse home visits vs. usual care on reducing intimate partner violence in young high-risk pregnant women: a randomized controlled trial. PLOS ONE 2013;8:e781-85.
- Sierau S, Dahne V, Brand T, Kurtz V, von Klitzing K, Jungmann T. Effects of home visitation on maternal competencies, family environment, and child development: a randomized controlled trial. Prev Sci 2016;17:40-51.
- Kliem S, Sandner M. Prenatal and infancy home visiting in Germany: 7-year outcomes of a randomized trial. Pediatrics 2021;148.
- Conti G, Poupakis S, Sandner M, Kliem S. The effects of home visiting on mother–child interactions: evidence from a randomized trial using dynamic micro-level data. Child Abuse Negl 2021;115.
- Catherine NL, Gonzalez A, Boyle M, Sheehan D, Jack SM, Hougham KA, et al. British Columbia Healthy Connections Project Scientific Team . Improving children’s health and development in British Columbia through nurse home visiting: a randomized controlled trial protocol. BMC Health Serv Res 2016;16.
- Segal L, Nguyen H, Gent D, Hampton C, Boffa J. Child protection outcomes of the Australian Nurse Family Partnership Program for Aboriginal infants and their mothers in Central Australia. PLOS ONE 2018;13.
- Carabin H, Cowan LD, Beebe LA, Skaggs VJ, Thompson D, Agbangla C. Does participation in a nurse visitation programme reduce the frequency of adverse perinatal outcomes in first-time mothers?. Paediatr Perinat Epidemiol 2005;19:194-205.
- Rubin DM, O’Reilly AL, Luan X, Dai D, Localio AR, Christian CW. Variation in pregnancy outcomes following statewide implementation of a prenatal home visitation program. Arch Pediatr Adolesc Med 2011;165:198-204.
- Matone M, O’Reilly AL, Luan X, Localio AR, Rubin DM. Emergency department visits and hospitalizations for injuries among infants and children following statewide implementation of a home visitation model. Matern Child Health J 2012;16:1754-61.
- Flowers M, Sainer S, Stoneburner A, Thorland W. Education and employment outcomes in clients of the Nurse–Family Partnership. Public Health Nurs 2020;37:206-14.
- Thorland W, Currie DW. Status of birth outcomes in clients of the Nurse–Family Partnership. Matern Child Health J 2017;21:995-1001.
- Lugg-Widger FV, Robling M, Lau M, Paranjothy S, Pell J, Sanders J, et al. Evaluation of the effectiveness of the Family Nurse Partnership home visiting programme in first time young mothers in Scotland: a protocol for a natural experiment. Int J Pop Data Sci 2020;5.
- Barnes J, Stuart J, Allen E, Petrou S, Sturgess J, Barlow J, et al. Results of the First Steps study: a randomised controlled trial and economic evaluation of the Group Family Nurse Partnership (gFNP) programme compared with usual care in improving outcomes for high-risk mothers and their children and preventing abuse. Public Health Res 2017. http://ncbi.nlm.nih.gov/books/NBK464661/ (accessed 5 October 2022).
- Mejdoubi J, van den Heijkant S, Struijf E, van Leerdam F, HiraSing R, Crijnen A. Addressing risk factors for child abuse among high risk pregnant women: design of a randomised controlled trial of the nurse family partnership in Dutch preventive health care. BMC Public Health 2011;11.
- Family Nurse Partnership National Unit & Dartington Service Design Lab . FNP ADAPT: Using Evidence, Pragmatism and Collaboration to Change the FNP Programme in London 2020. www.fnp.nhs.uk/media/1359/fnp_adapt_report_web.pdf (accessed 5 October 2022).
- Lawlor D, Shaw M, Johns S. Teenage pregnancy is not a public health problem. BMJ 2001;323:1428-9.
- Crawford C, Cribb J, Kelly E. Teenage Pregnancy in England 2013 n.d. https://ifs.org.uk/publications/teenage-pregnancy-england (accessed 4 January 2024).
- Mejdoubi J, van den Heijkant SC, van Leerdam FJ, Crone M, Crijnen A, HiraSing RA. Effects of nurse home visitation on cigarette smoking, pregnancy outcomes and breastfeeding: a randomized controlled trial. Midwifery 2014;30:688-95.
- Cannings-John R, Lugg-Widger F, Lau M, Paranjothy S, Pell J, Sanders J, et al. Evaluation of Family Nurse Partnership: Methods and Process of Evaluation – Appendix 1: Logic Model 2020. www.gov.scot/publications/evaluation-family-nurse-partnership-scotland-methods-paper-process-success-linkages/pages/13/ (accessed 5 October 2022).
- Bryar RM, Cowley DSA, Adams CM, Kendall S, Mathers N. Health visiting in primary care in England: a crisis waiting to happen?. Br J Gener Pract: J Royal Coll Gener Pract 2017;67:102-3.
- Kennedy-Martin T, Curtis S, Faries D, Robinson S, Johnston J. A literature review on the representativeness of randomized controlled trial samples and implications for the external validity of trial results. Trials 2015;16.
- Ogilvie D, Cummins S, Petticrew M, White M, Jones A, Wheeler K. Assessing the evaluability of complex public health interventions: five questions for researchers, funders, and policymakers. Milbank Q 2011;89:206-25.
- Booth CM, Tannock IF. Randomised controlled trials and population-based observational research: partners in the evolution of medical evidence. Br J Cancer 2014;110:551-5.
- Harron K, Gilbert R, Cromwell D, van der Meulen J. Linking data for mothers and babies in de-identified electronic health data. PLOS ONE 2016;11.
- Harron KL, Doidge JC, Knight HE, Gilbert RE, Goldstein H, Cromwell DA, et al. A guide to evaluating linkage quality for the analysis of linked data. Int J Epidemiol 2017;46:1699-710.
- Libuy N, Harron K, Gilbert R, Caulton R, Cameron E, Blackburn R. Linking education and hospital data in England: linkage process and quality. Int J Pop Data Sci 2021;6.
- Herbert A, Wijlaars L, Zylbersztejn A, Cromwell D, Hardelid P. Data resource profile: hospital episode statistics admitted patient care (HES APC). Int J Epidemiol 2017;46:1093-1093.i.
- International Classification of Diseases (ICD) . International Classification of Diseases, 10th Revision, Clinical Modification (ICD-10-CM) 2011. https://cdc.gov/nchs/icd/icd-10-cm.htm (accessed 5 October 2022).
- Health and Social Care Information Centre . OPCS-4 Classification of Interventions and Procedures 2019. https://digital.nhs.uk/data-and-information/information-standards/information-standards-and-data-collections-including-extractions/publications-and-notifications/standards-and-collections/dcb0084-opcs-classification-of-interventions-and-procedures#:~:text=this%20information%20standard-,OPCS%2D4%20is%20a%20statistical%20classification%20for%20clinical%20coding%20of,data%20collections%20for%20secondary%20uses (accessed 10 May 2022).
- McGrath-Lone L, Harron K, Dearden L, Nasim B, Gilbert R. Data resource profile: children looked after return (CLA). Int J Epidemiol 2016;45:716-17.
- Department for Education, National Statistics . Characteristics of Children in Need: 2018–2019 2019. www.gov.uk/government/statistics/characteristics-of-children-in-need-2018-to-2019 (accessed 5 October 2022).
- Department for Education . Children Looked After by Local Authorities in England: Guide to the SSDA903 Collection 1 April 2019 to 31 March 2020 – Version 1.2 2019. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/839236/CLA_SSDA903_2019-20_Guide_Version_1.2.pdf (accessed 5 October 2022).
- McGrath-Lone L, Dearden L, Nasim B, Harron K, Gilbert R. Changes in first entry to out-of-home care from 1992 to 2012 among children in England. Child Abuse Negl 2016;51:163-71.
- Grath-Lone LM, Woodman J, Gilbert R. Safeguarding children and improving their care in the UK. Lancet 2015;386.
- Corbacho B, Bell K, Stamuli E, Richardson G, Ronaldson S, Hood K, et al. Building Blocks trial group . Cost-effectiveness of the Family Nurse Partnership (FNP) programme in England: Evidence from the building blocks trial. J Eval Clin Pract 2017;23:1367-74.
- Schnitzer PG, Slusher PL, Kruse RL, Tarleton MM. Identification of ICD codes suggestive of child maltreatment. Child Abuse Negl 2011;35:3-17.
- Gilbert R, Fluke J, O’Donnell M, Gonzalez-Izquierdo A, Brownell M, Gulliver P, et al. Child maltreatment: variation in trends and policies in six developed countries. Lancet 2012;379:758-72.
- Emmott EH, Jay MA, Woodman J. Cohort profile: Children in Need Census (CIN) records of children referred for social care support in England. BMJ Open 2019;9.
- World Health Organization (WHO) . Report of a WHO Technical Consultation on Birth Spacing. Geneva, Switzerland 13–15 June 2005 2007. https://apps.who.int/iris/bitstream/handle/10665/69855/WHO_RHR_07.1_eng.pdf?sequence=1 (accessed 5 October 2022).
- Conde-Agudelo A, Rosas-Bermúdez A, Kafury-Goeta AC. Birth spacing and risk of adverse perinatal outcomes: a meta-analysis. JAMA 2006;295:1809-23.
- Department for Education, National Statistics . Early Years Foundation Stage Profile Results in England, 2018 2018. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/748814/EYFSP_2018_Main_Text.pdf (accessed 5 October 2022).
- Herbert A, Gilbert R, González-Izquierdo A, Li L. Violence, self-harm and drug or alcohol misuse in adolescents admitted to hospitals in England for injury: a retrospective cohort study. BMJ Open 2015;5.
- NHS Digital . Maternity Services Monthly Statistics November 2019, Experimental Statistics – Gestational Age at Booking Appointment 2020. https://digital.nhs.uk/data-and-information/publications/statistical/maternity-services-monthly-statistics/november-2019/analysis (accessed 5 October 2022).
- Harron K, Gilbert R, Fagg J, Guttmann A, van der Meulen J. Associations between pre-pregnancy psychosocial risk factors and infant outcomes: a population-based cohort study in England. Lancet Pub Health 2021;6:e97-105.
- Hardelid P, Dattani N, Gilbert R. Programme Board of the Royal College of Paediatrics and Child Health . Estimating the prevalence of chronic conditions in children who die in England, Scotland and Wales: a data linkage cohort study. BMJ Open 2014;4.
- Pearson RJ, Jay MA, Wijlaars LPMM, De Stavola B, Syed S, Bedston SJ, et al. Association between health indicators of maternal adversity and the rate of infant entry to local authority care in England: a longitudinal ecological study. BMJ Open 2020;10.
- Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multiv Behav Res 2011;46:399-424.
- Li F, Zaslavsky AM, Landrum MB. Propensity score weighting with multilevel data. Stat Med 2013;32:3373-87.
- Blake HA, Leyrat C, Mansfield KE, Seaman S, Tomlinson LA, Carpenter J, et al. Propensity scores using missingness pattern information: a practical guide. Stat Med 2020;39:1641-57.
- Austin PC. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med 2009;28:3083-107.
- Stata . Stata Statistical Software: Release 17 2021.
- Arpino B, Cannas M. Propensity score matching with clustered data. An application to the estimation of the impact of caesarean section on the Apgar score. Stat Med 2016;35:2074-91.
- Martin C, Marryat L, Miller M, Ormston R, Gordon J. The Evaluation of the Family Nurse Partnership Programme in Scotland: Phase 1 Report – Intake and Early Pregnancy Scottish Government Social Research 2011. www.gov.scot/publications/evaluation-family-nurse-partnership-programme-scotland-phase-1-report-intake-early-pregnancy/documents/ (accessed 3 August 2022).
- Robling M. The Building Blocks Trial. Evaluating the Family Nurse Partnership Programme in England: A Randomised Controlled Trial 2015. www.cardiff.ac.uk/__data/assets/pdf_file/0009/504729/Building-Blocks-Full-Study-Report.pdf (accessed 15 January 2019).
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77-101.
- Cavallaro FL, Cannings-John R, Lugg-Widger F, Gilbert R, Kennedy E, Kendall S, et al. Lessons learned from using linked administrative data to evaluate the Family Nurse Partnership in England and Scotland. Int J Population Data Sci 2023;8.
- Harron K, McGrath-Lone L, Mason S, Gilbert R. Using Linked Administrative Data for Monitoring and Evaluating the Family Nurse Partnership in England: A Scoping Report 2016. http://repository.tavistockandportman.ac.uk/1448/ (accessed 5 October 2022).
- Sword WA, Krueger PD, Watt MS. Predictors of acceptance of a postpartum public health nurse home visit: findings from an Ontario survey. Can J Public Health 2006;97:191-6.
- Alonso-Marsden S, Dodge KA, O’Donnell KJ, Murphy RA, Sato JM, Christopoulos C. Family risk as a predictor of initial engagement and follow-through in a universal nurse home visiting program to prevent child maltreatment. Child Abuse Negl 2013;37:555-65.
- Chartier MJ, Brownell MD, Isaac MR, Chateau D, Nickel NC, Katz A, et al. Is the families first home visiting program effective in reducing child maltreatment and improving child development?. Child Maltreat 2017;22:121-31.
- Bell K, Corbacho B, Ronaldson S, Richardson G, Hood K, Sanders J, et al. Building Blocks Trial Group . Costs and consequences of the Family Nurse Partnership (FNP) programme in England: evidence from the Building Blocks trial. F1000Res 2019;8.
- 0-5 Transfer Team . Transfer of 0–5 Children’s Public Health Commissioning to Local Authorities: Equality Analysis 2015. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/417429/Equality_analysis.pdf (accessed 5 October 2022).
- Feder GS, Hutson M, Ramsay J, Taket AR. Women exposed to intimate partner violence: expectations and experiences when they encounter health care professionals: a meta-analysis of qualitative studies. Arch J Med 2006;166:22-37.
- McTavish JR, Kimber M, Devries K, Colombini M, MacGregor JCD, Wathen N, et al. Children’s and caregivers’ perspectives about mandatory reporting of child maltreatment: a meta-synthesis of qualitative studies. BMJ Open 2019;9.
- Lewis NV, Feder GS, Howarth E, Szilassy E, McTavish JR, MacMillan HL, et al. Identification and initial response to children’s exposure to intimate partner violence: a qualitative synthesis of the perspectives of children, mothers and professionals. BMJ Open 2018;8.
- Sanders J, Channon S, Gobat N, Bennert K, Addison K, Robling M. Implementation of the Family Nurse Partnership programme in England: experiences of key health professionals explored through trial parallel process evaluation. BMC Nurs 2019;18.
- Downs J, Setakis E, Mostafa T, Hayes R, Hotopf M, Ford T, et al. Linking strategies and biases when matching cohorts to the National Pupil Database. IJPDS (2017) Issue 1, Vol 1:348 Proceedings of the IPDLN Conference (August 2016). Int J Pop Data Sci 2017;1.
- Grath-Lone LM, Libuy N, Etoori D, Blackburn R, Gilbert R, Harron K. Ethnic bias in data linkage. Lancet Digit Health 2021;3.
- Bilson A, Martin KEC. Referrals and child protection in England: one in five children referred to children’s services and one in nineteen investigated before the age of five. Br J Soc Work 2016;47:793-811.
- Jay MA, De Stavola B, Dorsett R, Thomson D, Gilbert R. Model estimates of cumulative incidence of children in need status and referral to children’s social care. OSF 2022. https://osf.io/6ecrz/ (accessed 5 October 2022).
- Olds D. Improving the report of the Building Blocks 2–6 study. BMJ Open 2022;12. https://bmjopen.bmj.com/content/12/2/e049960.responses#improving-the-report-of-the-buildling-blocks-2-6-study (accessed 5 October 2022).
- Saigal S, Doyle LW. An overview of mortality and sequelae of preterm birth from infancy to adulthood. Lancet 2008;371:261-9.
- Libuy N, Gilbert R, Mc Grath-Lone L, Blackburn R, Etoori D, Harron K. Gestational age at birth, chronic conditions and school outcomes: a population-based data linkage study of children born in England. Int J Epidemiol 2022;52:132-43.
- Barker M, Dombrowski SU, Colbourn T, Fall CHD, Kriznik NM, Lawrence WT, et al. Intervention strategies to improve nutrition and health behaviours before conception. Lancet 2018;391:1853-64.
- Goyal NK, Teeters A, Ammerman RT. Home visiting and outcomes of preterm infants: a systematic review. Pediatrics 2013;132:502-16.
- Liu N, Li P, Wang J, Chen D, Sun W, Zhang W. Effects of home visits for pregnant and postpartum women on premature birth, low birth weight and rapid repeat birth: a meta-analysis and systematic review of randomized controlled trials. Fam Pract 2019;36:533-43.
- Harron K, Gilbert R, Cromwell D, Oddie S, Guttmann A, van der Meulen J. International comparison of emergency hospital use for infants: data linkage cohort study in Ontario and England. BMJ Qual Saf 2018;27:31-9.
- Teager W, McBride M. An Initial Assessment of the 2-year-old Free Childcare Entitlement: Drivers of Take-up and Impact on Early Years Outcomes. Early Intervention Foundation; 2018.
- Sahota P, Woodward J, Molinari R, Pike J. Factors influencing take-up of free school meals in primary- and secondary-school children in England. Public Health Nutr 2014;17:1271-9.
- Taylor C. The reliability of free school meal eligibility as a measure of socio-economic disadvantage: evidence from the millennium cohort study in Wales. Br J Educ Stud 2018;66:29-51.
- Gov.uk . Schools, Pupils and Their Characteristics 2022. https://explore-education-statistics.service.gov.uk/find-statistics/school-pupils-and-their-characteristics (accessed 17 August 2022).
- Guttmann A, Blackburn R, Amartey A, Zhou L, Wijlaars L, Saunders N, et al. Long-term mortality in mothers of infants with neonatal abstinence syndrome: a population-based parallel-cohort study in England and Ontario, Canada. PLOS Med 2019;16.
- Wellings K, Jones KG, Mercer CH, Tanton C, Clifton S, Datta J, et al. The prevalence of unplanned pregnancy and associated factors in Britain: findings from the third National Survey of Sexual Attitudes and Lifestyles (Natsal-3). Lancet 2013;382:1807-16.
- Dartington Service Design Lab, Family Nurse Partnership National Unit . FNP ADAPT: Using Evidence, Pragmatism and Collaboration to Change the FNP Programme in England 2020 n.d. www.fnp.nhs.uk/media/1359/fnp_adapt_report_web.pdf (accessed 18 August 2022).
- Owens R. Digging Down and Scaling Up: A Psychosocial Exploration of the Family Nurse Partnership. Sussex: University of Sussex; 2020.
- Bakermans-Kranenburg MJ, van IMH, Juffer F. Less is more: meta-analyses of sensitivity and attachment interventions in early childhood. Psychol Bull 2003;129:195-21.
- Kliem S, Sandner M, Lohmann A, Sierau S, Dähne V, Klein AM, et al. Follow-up study regarding the medium-term effectiveness of the home-visiting program “Pro Kind” at age 7 years: study protocol for a randomized controlled trial. Trials 2018;19.
- Cheong-See F, Allotey J, Marlin N, Mol BW, Schuit E, Riet GT, et al. Prediction models in obstetrics: understanding the treatment paradox and potential solutions to the threat it poses. Int J Obstet Gynaecol 2016;123:1060-4.
- Feder GS, Hutson M, Ramsay J, Taket AR. Women exposed to intimate partner violence: expectations and experiences when they encounter health care professionals: a meta-analysis of qualitative studies. Arch Intern Med 2006;166:22-37.
- Bennett V. Continuing the Mandation of the Universal Five Health Visiting Checks. Public Health England; 2017.
- Robling M, Cannings-John R, Channon S, Hood K, Moody G, Poole R, et al. What is usual care for teenagers expecting their first child in England? A process evaluation using key informant mapping and participant survey as part of the Building Blocks randomised controlled trial of specialist home visiting. BMJ Open 2018;8.
- Fraser C, Harron K, Barlow J, Bennett S, Woods G, Shand J, et al. Variation in health visiting contacts for children in England: cross-sectional analysis of the 2–2½ year review using administrative data (Community Services Dataset, CSDS). BMJ Open 2022;12.
- Public Health England . Health Visitor Service Delivery Metrics: 2019 to 2020 2021. www.gov.uk/government/statistics/health-visitor-service-delivery-metrics-2019-to-2020 (accessed 5 October 2022).
- Woodman J, Harron K, Hancock D. Which children in England see the health visiting team and how often?. J Health Vis 2021;9:282-4.
- Doidge JC, Harron KL. Reflections on modern methods: linkage error bias. Int J Epidemiol 2019;48.
- Morris H, Lanati S, Gilbert R. Challenges of administrative data linkages: experiences of Administrative Data Research Centre for England (ADRC-E) researchers. Int J Pop Data Sci 2018;3.
- Dattani N, Hardelid P, Davey J, Gilbert R. Accessing electronic administrative health data for research takes time. Arch Dis Child 2013;98:391-2.
- Taylor JA, Crowe S, Espuny Pujol F, Franklin RC, Feltbower RG, Norman LJ, et al. The road to hell is paved with good intentions: the experience of applying for national data for linkage and suggestions for improvement. BMJ Open 2021;11.
- Cavallaro F, Lugg-Widger F, Cannings-John R, Harron K. Reducing barriers to data access for research in the public interest – lessons from COVID-19. BMJ Opin 2020. https://blogs.bmj.com/bmj/2020/07/06/reducing-barriers-to-data-access-for-research-in-the-public-interest-lessons-from-covid-19/ (accessed 5 October 2022).
- Harron K. “It Did Mean a Lot”: What Public Engagement With Teenage Mothers Taught Us about Our Research 2019. https://blogs.ucl.ac.uk/public-engagement/2019/05/07/engaging-with-teenage-mothers/ (accessed 5 January 2023).
- Mikton C, Butchart A. Child maltreatment prevention: a systematic review of reviews. Bull World Health Organ 2009;87:353-61.
- Vlahovicova K, Melendez-Torres GJ, Leijten P, Knerr W, Gardner F. Parenting programs for the prevention of child physical abuse recurrence: a systematic review and meta-analysis. Clin Child Fam Psychol Rev 2017;20:351-65.
- Euser S, Alink LRA, Stoltenborgh M, Bakermans-Kranenburg MJ, van IJzendoorn MH. A gloomy picture: a meta-analysis of randomized controlled trials reveals disappointing effectiveness of programs aiming at preventing child maltreatment. BMC Public Health 2015;15.
- Chen M, Chan KL. Effects of parenting programs on child maltreatment prevention: a meta-analysis. Trauma Violence Abuse 2016;17:88-104.
- van der Put CE, Assink M, Gubbels J, Boekhout van Solinge NF. Identifying effective components of child maltreatment interventions: a meta-analysis. Clin Child Fam Psychol Rev 2018;21:171-202.
- Moniz MH, Low LK, Stout MJ. Intensive nurse home visiting program and adverse birth outcomes. JAMA 2022;328:23-4.
- Wilkinson E. Health visitor shortages are risking child health and piling pressure on other services. BMJ 2022;378.
- Dheensa S. Recording and Sharing Information about Domestic Violence Abuse in the Health Service 2020. www.standingtogether.org.uk/blog-3/recording-and-sharing-information-about-dva-in-the-health-service-report (accessed 5 October 2022).
- Francetic I, Meacock R, Elliott J, Kristensen SR, Britteon P, Lugo-Palacios DG, et al. Framework for identification and measurement of spillover effects in policy implementation: intended non-intended targeted non-targeted spillovers (INTENTS). Implement Sci 2022;3.
- Lorenc T, Oliver K. Adverse effects of public health interventions: a conceptual framework. J Epi Com Health 2014;68:288-90.
- Morrison K, Doi L, Hughes T, Woodier N. Coronavirus (COVID-19) Family Nurse Partnership Insights: Evaluation Report 2021. www.research.ed.ac.uk/en/publications/coronavirus-covid-19-family-nurse-partnership-insights-evaluation (accessed 13 September 2022).
- Geospatial Commission . Unlocking the Power of Location. The UK’s Geospatial Strategy, 2020 to 2025 2020. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/894755/Geospatial_Strategy.pdf (accessed 10 May 2022).
- Lut I, Harron K, Hardelid P, O’Brien M, Woodman J. ‘What about the dads?’ Linking fathers and children in administrative data: a systematic scoping review. Big Data Soc 2022;9.
- Richards JA, Xu D, Gilkerson J, Yapanel U, Gray S, Paul T. Automated assessment of child vocalization development using LENA. J Speech Lang Hear Res 2017;60:2047-63.
- Moreno-Betancur M, Lynch JW, Pilkington RM, Schuch HS, Gialamas A, Sawyer MG, et al. Emulating a target trial of intensive nurse home visiting in the policy-relevant population using linked administrative data. Int J Epidemiol 2022;52:119-31.
- McGrath-Lone L, Libuy N, Harron K, Jay MA, Wijlaars L, Etoori D, et al. Data resource profile: the education and child health insights from linked data (ECHILD) database. Int J Epidemiol 2021;51. https://doi.org/10.1093/ije/dyab149.
- RCPCH . NHS Number As a Unique Identifier for Children – Position Statement 2021. www.rcpch.ac.uk/resources/nhs-number-unique-identifier-children-position-statement (accessed 13 September 2022).
- Freeguard G, Britchfield C. Missing Numbers in Children’s Services. How Better Data Could Improve Outcomes for Children and Young People. Institute for Government 2020. www.instituteforgovernment.org.uk/sites/default/files/publications/missing-numbers-childrens-services.pdf (accessed 13 September 2022).
Appendix 1 Summary of literature review of effectiveness of Family Nurse Partnership on birth, child and maternal outcomes
| Overall study | Reference | Subgroups | Birth outcomes | Child outcomes | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Smoking in late pregnancy | Birth-weight | Child abuse/maltreatment reports | Child in care/removed from home | CiN/CPP | A&E or hospital admissions for injury/maltreatment | All hospital admissions | All A&E attendances | Outpatient referrals | Child development outcomes | Educational achievement | School attendance | Death | |||
| Elmira NY RCT (USA) | Olds (1986) | Age and smoking | − | ± | |||||||||||
| Olds (1986) | Poor, unmarried | (−) 2 years | − 2 years | − 2 years | (+) 2 years | ||||||||||
| Olds (1994) | Age and poor and unmarried | 0 2–4 years | 0 2–4 years | 0 2–4 years | − 2 to 4 years | 0.2–4 years | |||||||||
| Eckenrode (2000) | N/A | − 15 years | |||||||||||||
| Eckenrode (2017) | Domestic violence | − 15 years | |||||||||||||
| Eckenrode (2010) | Poor, unmarried | 0, 19 years | |||||||||||||
| Olds (1995) | Maltreated | 0, 4 years | 0, 4 years | 0, 4 years | 0, 4 years | − 4 years | 0, 3/4 years | ||||||||
| Olds (1994) | Smoking | 0, 2 months/2 years + 3/4 years |
|||||||||||||
| Memphis TN RCT (USA) | Kitzman (1997) | Schooling and PIH and LPR | 0 | 0, 2 years | |||||||||||
| Olds (2004) | LPR | + 6 years | ± 6 years | ||||||||||||
| Olds (2007) | HPR/LPR | + 9 years | (−) 9 years | ||||||||||||
| Olds (2010) | N/A | (+) 12 years | |||||||||||||
| Olds (2014) | N/A | ± 20 years | |||||||||||||
| Kitzman (2019) | LPR and gender | + 18 years | + 18 years | ||||||||||||
| Denver CO RCTa (USA) | Olds (2002) | LPR | − | + 2 years | |||||||||||
| Olds (2004) | LPR | + 4 years | |||||||||||||
| Olds (2014) | LPR | ± 6/9 years | 0, 6/9 years | ||||||||||||
| Orange County pilot RCT (USA) | Nguyen (2003) | N/A | −? | ||||||||||||
| Voor Zorg RCT (NL) | Mejdoubi (2014) | Smoking | − | 0 | |||||||||||
| Mejdoubi (2015) | Gender and ethnicity | − 3 years | |||||||||||||
| Pro Kind RCT (DE) | Jungmann (2009) | N/A | 0 | 0 | 0, 6 months | ||||||||||
| Sierau (2016) | Risk status | + 2 years | |||||||||||||
| Building Blocks RCT (England) | Robling (2016) | Deprivation and empl./edu. and life skills | 0 | 0 | + 2 years | 0, 2 years | + 2 years | 0, 2 years | + 2 years | ||||||
| OH case-control (USA) | Donovan (2007) | Race | − 1 year | ||||||||||||
| OK retrosp. Cohort (USA) | Carabin (2005) | Married and pregnancy risk | ± | − 1 year | |||||||||||
| PA retrosp. Cohort (USA) | Matone (2012) | N/A | − | ||||||||||||
| Matone (2012) | N/A | ± 2 years | |||||||||||||
| Australia cohort | Segal (2018) | Age and parity | − up to 7 years | − up to 7 years | − up to 7 years | ||||||||||
| South Carolina RCT (USA) | McConnell (2022) | Age, edu, mental health; non-Hispanic Black | 0 | ||||||||||||
| Legend | |||||||||||||||
| Effect observed on whole sample | Effect observed in subgroup only | No effect | 0 | Increased | + | Decreased | − | ||||||||
| Mixed evidence | ± | Weak evidence increase | (+) | Weak evidence decrease | (−) | ||||||||||
| Overall study | Reference | Subgroups | Child abuse perpetration | A&E or hospital admissions for violence/self-harm/drugs/alcohol | All A&E and hospital admissions | Domestic violence | Drug use/impairment | Death | Subsequent live births | Subsequent stillbirths | Subsequent birth interval | Educational qualifications |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Elmira NY RCT (USA) | Olds (1988) | Age and poor and unmarried | 0, 4 years | + 4 years | + 6 months 0, 4 years |
|||||||
| Olds (1997) | Poor and unmarried | −15 years | −15 years | −15 years | + 15 years | |||||||
| Eckenrode (2000) | N/A | −15 years | 0, 15 years | |||||||||
| Eckenrode (2017) | Domestic violence | − 15 years | ||||||||||
| Memphis TN RCT (USA) | Kitzman (1997) | Schooling and PIH and LPR | − 2 years | |||||||||
| Kitzman (2000) | HPR | 0, 4.5 years | 0, 4.5 years | + 4.5 years | 0, 4.5 years | |||||||
| Olds (2004) | LPR | 0, 6 years | 0, 6 years | − 6 years | + 6 years | 0, 6 years | ||||||
| Olds (2007) | HPR/LPR | 0, 9 years | (−) 9 years | −9 years | + 9 years | |||||||
| Olds (2010) | N/A | 0, 12 years | ± 12 years | |||||||||
| Olds (2014) | N/A | ± 20 years | ||||||||||
| Olds (2019) | LPR | 0, 18 years | ||||||||||
| Denver CO RCTa (USA) | Olds (2002) | LPR | − 2 years | 0, 2 years | ||||||||
| Olds (2004) | LPR | (−) 4 years | 0, 4 years | 0, 4 years | + 4 years | 0, 4 years | ||||||
| Voor Zorg RCT (NL) | Mejdoubi (2013) | N/A | −32 weeks preg ± 2 years |
|||||||||
| Pro Kind RCT (DE) | Sierau (2016) | Risk status | 0, 2 years | 0, 2 years | ||||||||
| Building Blocks RCT (England) | Robling (2016) | Deprivation and employment/edu and life skills | (+) 2 years | 0, 2 years | ||||||||
| PA retrosp. Cohort (USA) | Rubin (2011) | Age and urban/rural | −2 years | |||||||||
| USA entropy balanced cohort | Flowers (2019) | Age | ± 1 year | |||||||||
| Legend | ||||||||||||
| Effect observed on whole sample | Effect observed in subgroup only | No effect | 0 | Increased | + | Decreased | − | |||||
| Mixed evidence | ± | Weak evidence increase | (+) | Weak evidence decrease | (−) |
Appendix 2 Additional information on creating the linked cohort
Defining the linked cohort
Figure 2 describes the definition of our cohort of mothers enrolled in the FNP giving birth between 1 April 2010 and 31 March 2019, and their linkage to HES. Of 34,480 FNP mothers in our cohort, 1360 were removed due to patient opt outs of data use in research. We also excluded 670 mothers enrolled in the FNP for their second delivery (e.g. following a previous stillbirth), as well as 310 mothers with FNP pregnancies ending in miscarriage or stillbirth (to ensure comparability with mothers not enrolled in the FNP, since miscarriages are not always captured in routine hospital data), and 105 not meeting age or residential eligibility criteria.
The linkage of FNP mothers to HES records for the remaining 32,040 mothers was performed by NHS Digital. As a first step, the 11% of FNP mothers with missing NHS number in FNP IS data were matched to the NHS Personal Demographics Service spine, using a multistep deterministic algorithm based on first name, last name, date of birth, gender and postcode (see Table 3). Following NHS number retrieval for cohort members with missing NHS number through this linkage, the proportion of all mothers with missing NHS number was reduced from 11% to 2%.
As a second step, all 32,040 FNP mothers were linked to HES using the standard NHS Digital linkage algorithm (see Table 4). This is a multistep deterministic linkage algorithm, based on four identifier variables (NHS number, date of birth, gender and postcode). Records matching on match rank 1 have exact agreement on all identifier variables; match ranks 2–8 subsequently allow for partial or no match on some variables, and are therefore less certain matches. Records matching at a given match rank are subsequently removed from the pool of possible matches for subsequent steps.
The availability of valid identifiers was high for FNP mothers included in the linkage (n = 32,040), with at most 2.5% missing a valid postcode and 2% missing a valid NHS number (see Table 5). Among the 505 mothers who did not link to any HESID in NHS Digital’s algorithm (n = 35) or who were removed after linkage (n = 470), availability was high for first name, surname, date of birth and gender; however, 8% were missing a valid NHS number and 4% were missing a valid postcode.
Of the 32,040 mothers included in the linkage attempt, 32,005 (99.9%) were linked to a HESID via NHS Digital’s algorithm (see Figure 1). We excluded 115 of these mothers due to their linked HESIDs not including any records in HES APC, since this indicates a likely error in the way that HESIDs have been assigned internally. Similarly, we excluded 310 mothers with no hospital admission record within one year of giving birth, and 5 with discrepancies in maternal date of birth recorded in HES and FNP IS.
Manual linkage was attempted for the remaining 35 mothers not linked through the NHS Digital algorithm; 15 of these were linked to HES based on agreement on mother’s month-year of birth, month-year of delivery, birthweight and LA of residence at the time of birth. A further 10 mothers with missing maternal HESID but available baby HESID were linked to a HESID using the HES mother–baby linkage key. Ten mothers could not be linked manually. The total linkage rate was therefore 31,560 of 32,040 FNP (98.5%) mothers in our cohort.
Characteristics of linkage and unlinked mothers are shown in Table 6.
Agreement between information captured in FNP IS and HES was generally high, with 99% agreement for maternal month-year of birth, delivery month-year and on maternal age at birth (see Table 7). Agreement was lower for information on birth outcomes, with higher percentages of mothers missing information in at least one data source (e.g. over 30% missing for gestational age at booking appointment, number of babies and sex of baby). Disagreement was high for gestational age at booking appointment (within 2 weeks), with one-third of linked mothers having different information recorded. Of note, 11% of FNP mothers would be considered to be resident in the catchment area of a different FNP site than the one they were registered in at the time of birth, based on the LA of residence recorded in their HES delivery record (or within 12 months of delivery, where missing).
FIGURE 16.
Time periods and ages of cohort members included in the study. Shaded boxes indicate age of member during study period (blue); look-back period for health data (grey); follow-up (light blue); and age of child during follow-up (green). The look-back period is the earliest of age 11 (for Key Stage 2 results), or 5 years prior to delivery (in HES).
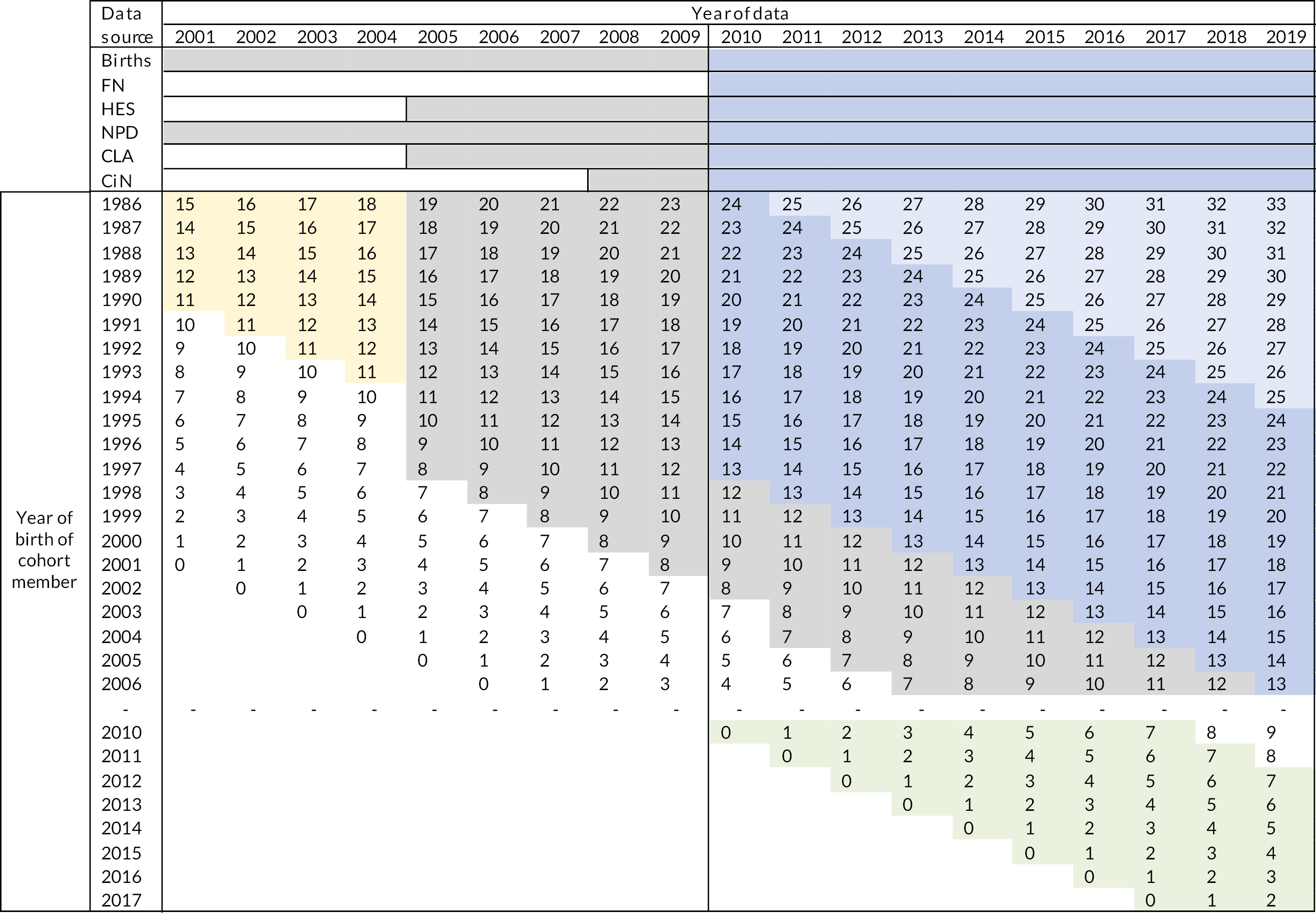
FIGURE 17.
Description of FNP cohort and linkage to HES.
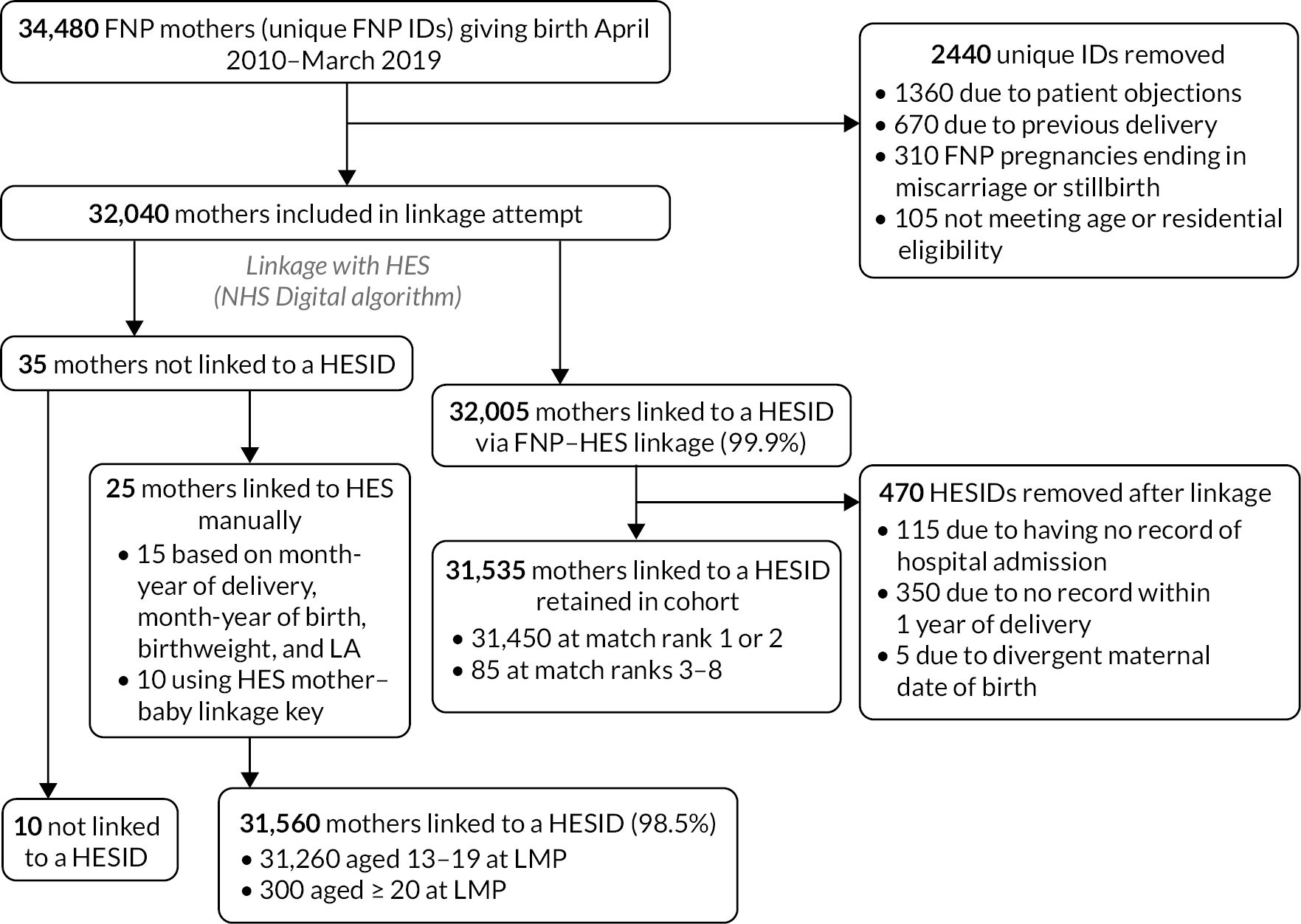
Agreement between data sources was lower for mothers who linked with a match rank higher than 2. This likely reflects lower-quality data in FNP or HES for these mothers, which was also related to more difficulty in linkage. Agreement for maternal month-year of birth was 65% and, as a result of this, agreement was also lower for maternal age at birth (75%), although month-year of delivery agreed for all these mothers. Agreement was lower for ethnicity among mothers linking at match rank > 2 than among all mothers. There were slightly lower rates of agreement for birth outcomes, due primarily to a higher proportion with missing data in at least one data source.
Mothers aged 20–24
We restricted the 20- to 24-year-old cohort to the 4465 mothers aged 20–24 at LMP living in the catchment area of the 10 FNP sites enrolling ≥ 10 mothers in this age group between November 2016 and March 2019 (see Figure 3). Of these, 4305 (96%) were never enrolled in FNP. We included mothers whose first antenatal appointment (or estimated date of 28 weeks gestation, if date missing) occurred from the month of enrolment of the first mother aged 20–24 in the local site. One hundred and sixty-five mothers aged 20–24 were enrolled in the FNP within these 10 sites; an additional 135 mothers were enrolled in the FNP in sites enrolling < 10 mothers in this age group or before November 2016 and were excluded from analyses.
| Match rank | First and last name | Date of birth | Gender | Postcode |
|---|---|---|---|---|
| 1 | Exact | Exact | Exact | Exact |
| 2 | Soundex | Exact | Exact | Exact |
| 3 | Partial | Exact | Exact | Exact |
| 4 | Partial | Exact | Exact | |
| 5 | Exact | Exact | Exact | |
| 6 | Exact | Exact | Exact | |
| 7 | Partial | Exact | Exact | |
| 8 | Exact | Exact | Exact |
| t | NHS number | Date of birth | Gender | Postcode | |
|---|---|---|---|---|---|
| 1 | Exact | Exact | Exact | Exact | |
| 2 | Exact | Exact | Exact | ||
| 3 | Exact | Partial | Exact | Exact | |
| 4 | Exact | Partial | Exact | ||
| 5 | Exact | Exact | |||
| 6 | Exact | Exact | Exact | Where NHS does not contradict the match and date of birth is not 1 January and postcode is not in the ‘ignore’ list | |
| 7 | Exact | Exact | Exact | Where NHS does not contradict the match and date of birth is not 1 January | |
| 8 | Exact |
| First name (%) | Surname (%) | NHS number (%) | Date of birth (%) | Gender (%) | Postcode (%) | |
|---|---|---|---|---|---|---|
| Mothers – all (n = 32,040) | 0 | 0.03 | 2.0 | 0.01 | 0 | 2.5 |
| Mothers – unlinked (n = 505) | 0 | 0.2 | 7.5 | 0.4 | 0 | 3.8 |
Linking mothers to their babies in Hospital Episode Statistics
Among the 31,425 FNP mothers in our cohort (31,260 aged 13–19 and 165 aged 20–24 years), 91% were linked to their first baby through a baby HESID recorded in the FNP-HES linkage key (see Appendix 2, Figure 19). This proportion is somewhat low because some mothers drop out before birth (9% of mothers had no recorded baby FNP ID). Where baby HESID was missing in the FNP-HES mother–baby linkage key, we used the de-identified HES mother–baby linkage key to link an additional 2615 (8%) of FNP mothers in our cohort to a baby HESID.
| Total | Linked mothers | Unlinked mothers | ||||
|---|---|---|---|---|---|---|
| N | % | N | % | N | % | |
| N (row %) | 32,040 | 100.0 | 31,560 | 98.5 | 480 | 1.5 |
| Year of delivery | ||||||
| 2010 | 2085 | 6.5 | 2055 | 6.5 | 25 | 5.6 |
| 2011 | 1925 | 6.0 | 1870 | 5.9 | 55 | 11.0 |
| 2012 | 2925 | 9.1 | 2870 | 9.1 | 60 | 12.1 |
| 2013 | 4130 | 12.9 | 4075 | 12.9 | 50 | 10.8 |
| 2014 | 3640 | 11.4 | 3600 | 11.4 | 40 | 8.5 |
| 2015 | 5180 | 16.2 | 5115 | 16.2 | 65 | 13.5 |
| 2016 | 5360 | 16.7 | 5275 | 16.7 | 85 | 17.7 |
| 2017 | 3275 | 10.2 | 3225 | 10.2 | 50 | 10.8 |
| 2018 | 2815 | 8.8 | 2785 | 8.8 | 30 | 6.7 |
| 2019 | 710 | 2.2 | 695 | 2.2 | 15 | 3.1 |
| Maternal age at birth | ||||||
| 13–15 | 265 | 0.8 | 260 | 0.8 | < 8 | < 1.7 |
| 16–17 | 11,705 | 36.5 | 11,525 | 36.5 | 180 | 37.1 |
| 18–19 | 15,960 | 49.8 | 15,735 | 49.9 | 225 | 46.9 |
| 20 and above | 3990 | 12.4 | 3925 | 12.4 | 65 | 13.5 |
| Missing | 120 | 0.4 | 115 | 0.4 | < 8 | < 1.7 |
| Ethnicity | ||||||
| White | 26,490 | 82.7 | 26,190 | 83.0 | 300 | 62.9 |
| Asian | 755 | 2.4 | 730 | 2.3 | 25 | 4.8 |
| Black | 1640 | 5.1 | 1585 | 5.0 | 55 | 11.7 |
| Mixed/other | 2195 | 6.9 | 2145 | 6.8 | 50 | 10.4 |
| Missing | 960 | 3.0 | 910 | 2.9 | 50 | 10.2 |
| Region | ||||||
| East Midlands | 2880 | 9.0 | 2825 | 9.0 | 55 | 11.0 |
| East of England | 2595 | 8.1 | 2575 | 8.2 | 20 | 4.4 |
| London | 5030 | 15.7 | 4870 | 15.4 | 160 | 32.9 |
| North-East | 2185 | 6.8 | 2170 | 6.9 | 15 | 3.3 |
| North-West | 5130 | 16.0 | 5060 | 16.0 | 70 | 15.0 |
| South-East | 4605 | 14.4 | 4550 | 14.4 | 55 | 11.0 |
| South-West | 1860 | 5.8 | 1840 | 5.8 | 20 | 4.4 |
| West Midlands | 3960 | 12.4 | 3915 | 12.4 | 50 | 10.0 |
| Yorkshire and The Humber | 3800 | 11.9 | 3760 | 11.9 | 40 | 7.9 |
| Relationship status (enrolment) | ||||||
| In a relationship with biological father | 22,710 | 70.9 | 22,400 | 71.0 | 310 | 64.2 |
| In a relationship with other partner | 1005 | 3.1 | 990 | 3.1 | 10 | 2.5 |
| Single | 7370 | 23.0 | 7255 | 23.0 | 110 | 23.1 |
| Missing | 960 | 3.0 | 910 | 2.9 | 50 | 10.2 |
| Living arrangements (enrolment) | ||||||
| Mother (with or without partner) | 16,995 | 53.0 | 16,790 | 53.2 | 205 | 42.3 |
| Partner (with or without others, not mother) | 6175 | 19.3 | 6065 | 19.2 | 105 | 22.3 |
| Relatives/other adults | 3130 | 9.8 | 3095 | 9.8 | 35 | 7.7 |
| Alone | 1860 | 5.8 | 1830 | 5.8 | 30 | 6.5 |
| Foster carers/group home/other | 2920 | 9.1 | 2865 | 9.1 | 55 | 11.0 |
| Missing | 960 | 3.0 | 910 | 2.9 | 50 | 10.2 |
| Has any GCSEs (enrolment) | ||||||
| No | 10,270 | 32.1 | 10,120 | 32.1 | 150 | 31.5 |
| Yes | 20,795 | 64.9 | 20,515 | 65.0 | 280 | 58.1 |
| Missing | 975 | 3.0 | 925 | 2.9 | 50 | 10.4 |
| Care leaver (during pregnancy) | ||||||
| No | 30,140 | 94.1 | 29,720 | 94.2 | 420 | 87.3 |
| Yes | 1185 | 3.7 | 1170 | 3.7 | 15 | 2.9 |
| Missing | 715 | 2.2 | 670 | 2.1 | 45 | 9.8 |
| CiN, CPP or CLA (during pregnancy) | ||||||
| No | 26,510 | 82.7 | 26,145 | 82.8 | 365 | 76.0 |
| Yes | 4815 | 15.0 | 4745 | 15.0 | 70 | 14.2 |
| Missing | 715 | 2.2 | 670 | 2.1 | 45 | 9.8 |
| Drug and alcohol use during pregnancy (2 weeks before enrolment) | ||||||
| No | 29,165 | 91.0 | 28,770 | 91.2 | 395 | 82.3 |
| Yes | 1535 | 4.8 | 1510 | 4.8 | 25 | 4.8 |
| Missing | 1345 | 4.2 | 1280 | 4.1 | 60 | 12.9 |
| Gestational age at booking appointment | ||||||
| Before 10 weeks | 19,255 | 60.1 | 19,000 | 60.2 | 250 | 52.3 |
| 10–20 weeks | 10,955 | 34.2 | 10,770 | 34.1 | 180 | 37.9 |
| 20 weeks or more | 1045 | 3.3 | 1030 | 3.3 | 15 | 2.7 |
| Missing | 790 | 2.5 | 755 | 2.4 | 35 | 7.1 |
| Mean number of FNP visits | 34.9 | 35.0 | 25.8 | |||
| Mothers linked with match rank ≤ 2 | Linked mothers with match rank > 2 or linked manually | |||
|---|---|---|---|---|
| N | % | N | % | |
| N (%) | 31,450 | 100.0 | 110 | 0.3 |
| Maternal month-year of birth | ||||
| Agree | 31,265 | 99.4 | 70 | 64.8 |
| Disagree | 25 | 0.1 | 35 | 34.3 |
| Missing in at least one source | 160 | 0.6 | 0 | 0.9 |
| Delivery month-year | ||||
| Agree | 31,255 | 99.4 | 110 | 100 |
| Disagree | 195 | 0.6 | 0 | – |
| Missing in at least one source | 0 | – | 0 | – |
| Maternal age at birth (years) | ||||
| Agree | 31,135 | 99.0 | 80 | 75.0 |
| Disagree | 205 | 0.7 | 25 | 24.1 |
| Missing in at least one source | 110 | 0.4 | 0 | 0.9 |
| Ethnicity | ||||
| Agree | 27,715 | 88.1 | 85 | 78.7 |
| Disagree | 2830 | 9.0 | 20 | 17.6 |
| Missing in at least one source | 910 | 2.9 | 5 | 3.7 |
| Gestational age at booking appointment (within 2 weeks) | ||||
| Agree | 11,770 | 37.4 | 30 | 28.7 |
| Disagree | 10,575 | 33.6 | 40 | 47.0 |
| Missing in at least one source | 9110 | 29.0 | 35 | 34.3 |
| Number of babies | ||||
| Agree | 21,925 | 69.7 | 65 | 61.1 |
| Disagree | 35 | 0.1 | 0 | – |
| Missing in at least one source | 9495 | 30.2 | 40 | 38.9 |
| Sex of baby | ||||
| Agree | 20,255 | 64.4 | 55 | 52.8 |
| Disagree | 725 | 2.3 | 5 | 2.8 |
| Missing in at least one source | 10,475 | 33.3 | 50 | 44.4 |
| Low birthweight | ||||
| Agree | 24,090 | 76.6 | 80 | 75.0 |
| Disagree | 470 | 1.5 | 0 | 0.9 |
| Missing in at least one source | 6890 | 21.9 | 25 | 24.1 |
| Gestational age at birth (within 1 week) | ||||
| Agree | 23,135 | 73.6 | 80 | 75.9 |
| Disagree | 730 | 2.3 | 0 | 0.9 |
| Missing in at least one source | 7590 | 24.1 | 25 | 23.2 |
| FNP site | ||||
| Agree | 28,095 | 89.3 | 90 | 82.4 |
| Disagree | 3360 | 10.7 | 20 | 17.6 |
| Delivery date within FNP site dates | ||||
| Agree | 30,315 | 96.4 | 105 | 95.4 |
| Disagree | 965 | 3.1 | 0 | – |
| Missing in at least one source | 175 | 0.6 | 5 | 3.7 |
FIGURE 18.
Identification of FNP participants and comparison group among cohort of mothers aged 20–24. Note: numbers have been rounded to the nearest 5 in accordance with NHS Digital’s statistical disclosure rules for subnational analyses; totals may not be equal to the sum of component categories. ANC, antenatal care.
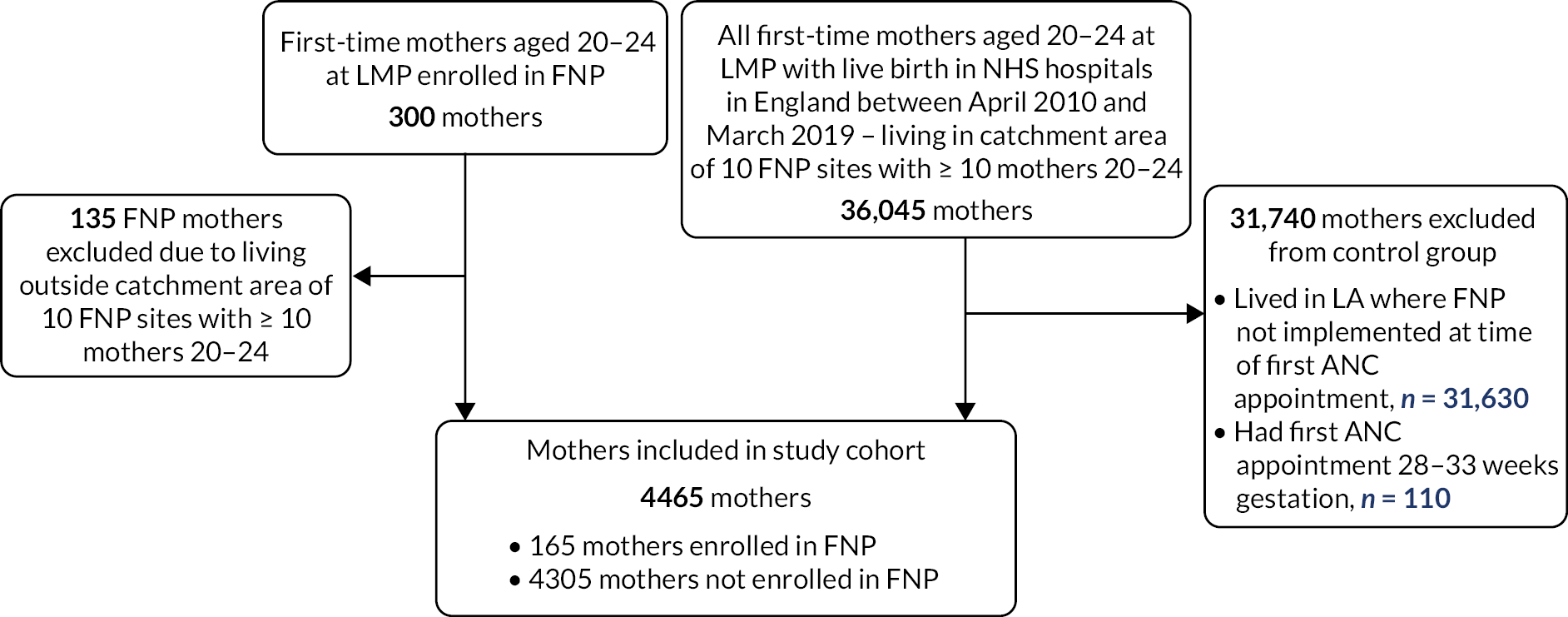
Among the 103,455 mothers in our cohort who were not enrolled in the FNP, 100,720 (97%) were linked to a baby HESID through the de-identified HES mother–baby linkage key. Overall, 131,850 of the 134,880 mothers in our study cohort (97.8%) were linked to a baby HESID for their first birth (see Appendix 2, Figure 19). This percentage was slightly lower (97.3%) among mothers aged 20–24 than those aged 13–19 (97.8%).
We identified 1025 mothers in our cohort with a multiple birth (0.8% of the 134,880 mothers in our cohort), through recording in FNP IS, or in the mother or baby delivery record in HES. This rate is within the range of 0.65% multiple maternities among mothers aged under 20 and 0.99% among mothers aged 20–24 reported by the ONS in 2019. 3 Among these 1025 mothers with multiple births, 80 (78%) had at least two recorded baby HESIDs, 220 (21%) had only one recorded baby HESID, and 5 (0.5%) had no recorded baby HESIDs. Where only one baby HESID was recorded for a multiple birth, the identified child was retained in the child study cohort.
FIGURE 19.
Linkage of mothers in study cohort to their first child(ren). Note: numbers have been rounded to the nearest 5 in accordance with NHS Digital and DfE’s statistical disclosure rules for subnational analyses; some mothers enrolled in FNP who had a multiple birth may have had one baby identified through the FNP-HES linkage key and another through the de-identified mother–baby linkage key; numbers in subcategories for mothers enrolled in FNP do not add up to the total.
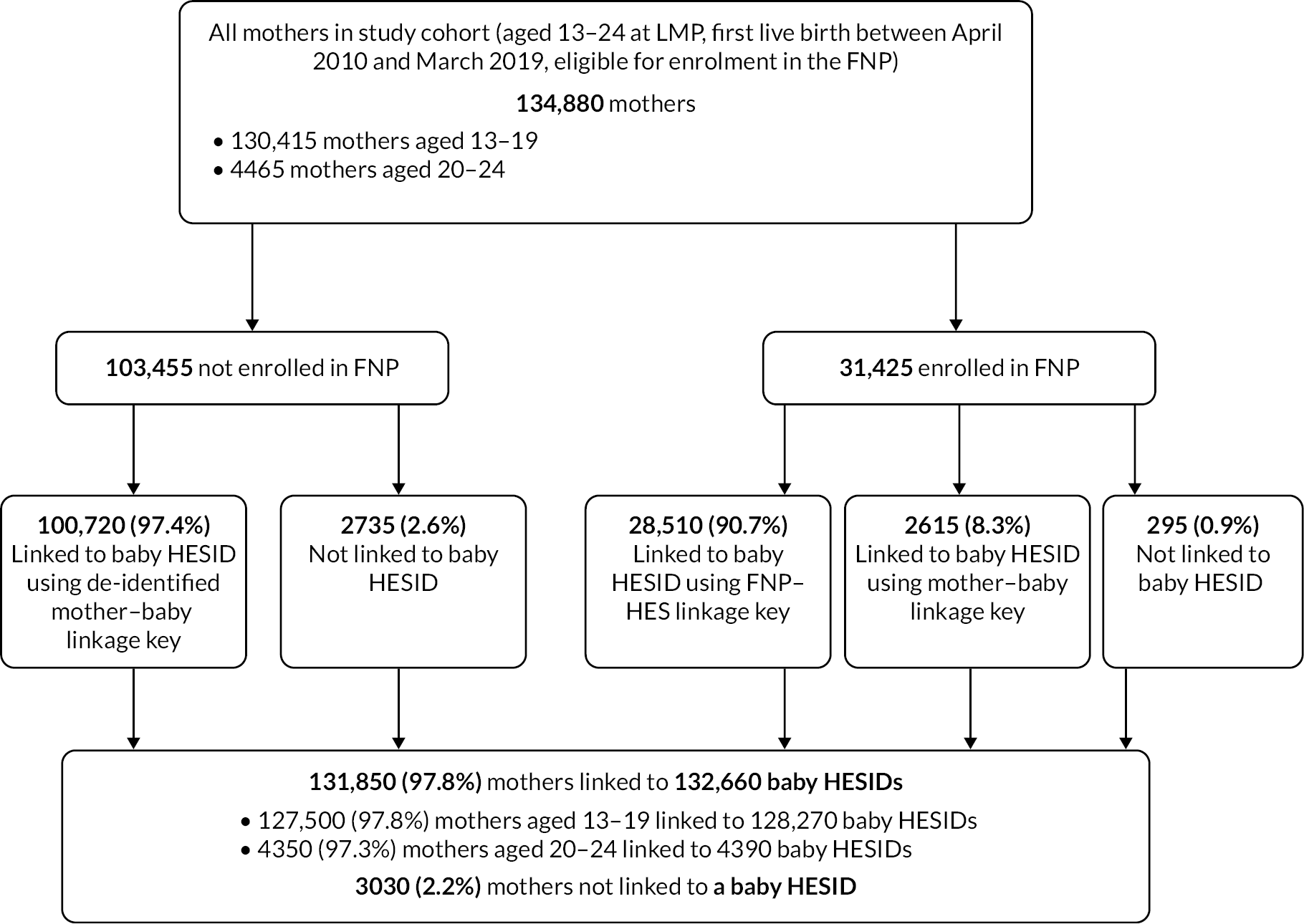
| FNP site name | Lower-tier LA(s) | Start datea | End datea |
|---|---|---|---|
| North-East | |||
| Durham and Darlington | Darlington, County Durham | August 2009 | October 2015 |
| Sunderlandb | Sunderland | August 2009 | March 2019 |
| South Tyneside | South Tyneside | January 2010 | January 2018 |
| Middlesbrough | Middlesbrough, Redcar and Cleveland | March 2012 April 2012 | November 2015 March 2018 |
| Hartlepool | Hartlepool, Stockton-on-Tees | February 2012 April 2012 | February 2017 December 2017 |
| Northumberland | Northumberland | March 2014 | September 2016 |
| Newcastle upon Tyne | Newcastle-upon-Tyne | April 2014 | September 2016 |
| North Tyneside | North Tyneside | March 2014 | March 2016 |
| Gateshead | Gateshead | February 2010 | March 2019 |
| North West | |||
| Manchesterb | Manchester | August 2009 | September 2016 |
| Blackpool | Blackpool | August 2009 | March 2019 |
| Cumbriab | Allerdale, Barrow-in-Furness, Carlisle, Copeland, Eden, South Lakeland | August 2009 | August 2016 |
| Liverpoolb | Liverpool | August 2009 | March 2019 |
| Knowsley | Knowsley | August 2009 | March 2019 |
| Wirral | Wirral | August 2009 | March 2019 |
| Bolton | Bolton | November 2011 | March 2019 |
| Wigan | Wigan | December 2011 | March 2019 |
| Cheshire West | Cheshire West and Chester | February 2012 | March 2019 |
| Cheshire East | Cheshire East | September 2012 | March 2019 |
| Oldham | Oldham | August 2014 | March 2019 |
| Stockport | Stockport | August 2014 | March 2019 |
| Rochdale | Rochdale | August 2014 | February 2017 |
| Bury | Bury | December 2014 | March 2019 |
| Halton | Halton | July 2014 | March 2019 |
| Salford | Salford | December 2014 | March 2019 |
| St Helens | St Helens | December 2014 | March 2019 |
| Trafford | Trafford | January 2015 | March 2017 |
| Blackburn with Darwen | Blackburn with Darwen | May 2015 | April 2016 |
| Lancashire | Burnley, Preston | April 2015 | April 2017 |
| Sefton | Sefton | December 2014 | September 2016 |
| Tameside | Tameside | March 2015 | March 2019 |
| Warrington | Warrington | April 2015 | March 2019 |
| Yorkshire and Humber | |||
| Barnsleyb | Barnsley | August 2009 | November 2015 |
| Calderdale | Calderdale | August 2009 | February 2016 |
| Hullb | Kingston upon Hull, city of | August 2009 | June 2017 |
| Leedsb | Leeds | August 2009 | April 2016 |
| Doncaster | Doncaster | August 2009 | March 2016 |
| Kirklees | Kirklees | August 2009 | March 2019 |
| Sheffield | Sheffield | August 2009 | February 2016 |
| Bradford and Airedale | Bradford | February 2010 | March 2019 |
| Rotherham | Rotherham | November 2011 | December 2016 |
| Wakefield | Wakefield | November 2011 | March 2019 |
| North and North East Lincolnshire | North East Lincolnshire, North Lincolnshire | March 2012 | April 2017 |
| East Riding | East Riding of Yorkshire | June 2013 | March 2019 |
| North Yorkshire | Scarborough | June 2013 | December 2014 |
| East Midlands | |||
| Derby Cityb | Derby | August 2009 | March 2019 |
| Nottingham City | Nottingham | August 2009 | March 2019 |
| Northamptonshireb | Corby, Daventry, East Northamptonshire, Kettering, Northampton, South Northamptonshire, Wellingborough | August 2009 | March 2019 |
| Derbyshire | Amber Valley, Bolsover, Chesterfield, Derbyshire Dales, Erewash, High Peak, North East Derbyshire, South Derbyshire | October 2011 | March 2019 |
| Leicester City | Leicester | September 2011 | May 2017 |
| Nottinghamshire | Ashfield, Bassetlaw, Broxtowe, Gedling, Mansfield, Newark and Sherwood, Rushcliffe | October 2012 | March 2019 |
| Lincolnshire | Boston, East Lindsey | August 2014 | February 2016 |
| West Midlands | |||
| Walsallb | Walsall | August 2009 | September 2016 |
| Stoke-on-Trent | Stoke-on-Trent, Newcastle-under-Lyme | August 2009 | October 2016 |
| Coventryb | Coventry | August 2009 | March 2019 |
| Birminghamb,c | Birmingham | January 2013 | May 2016 |
| Sandwell | Sandwell | August 2009 | January 2017 |
| Telford and Wrekin | Telford and Wrekin | August 2009 | March 2019 |
| Solihull | Birmingham, Solihull | August 2009 | March 2019 |
| Warwickshire North | North Warwickshire, Nuneaton and Bedworth | November 2010 | March 2019 |
| Dudley | Dudley | February 2013 | March 2019 |
| Staffordshire – Cannock and Tamworth | Cannock Chase, Tamworth | March 2013 | August 2016 |
| East Staffordshire | East Staffordshire | March 2013 | April 2017 |
| Shropshire | Shropshire | November 2014 | March 2019 |
| Wolverhampton | Wolverhampton | November 2014 | July 2017 |
| Warwickshire South and Rugby | Rugby, Stratford-on-Avon, Warwick | November 2010 | March 2019 |
| Worcestershire | Bromsgrove, Malvern Hills, Redditch, Worcester, Wychavon, Wyre Forest | September 2015 | April 2018 |
| East of England | |||
| South-East Essexb | Thurrock, Basildon, Castle Point, Rochford | August 2009 February 2015 | October 2016 February 2017 |
| Peterborough and Cambridgeshire | Peterborough, Cambridge, East Cambridgeshire, Fenland, Huntingdonshire, South Cambridgeshire | January 2010 December 2011 | March 2019 |
| Norfolk | Breckland, Broaland, Great Yarmouth, King’s Lynn and West Norfolk, North Norfolk, Norwich, South Norfolk | January 2010 | March 2019 |
| Hertfordshire | Broxbourne, Dacorum, East Hertfordshire, Hertsmere, North Hertfordshire, St Albans, Stevenage, Three Rivers, Watford, Welwyn Hatfield | September 2011 | February 2016 |
| Suffolk | Ipswich, Suffolk Coastal, Waveney | October 2010 August 2013 | March 2018 May 2018 March 2019 |
| North Essex | Braintree, Colchester, Harlow, Tendring | November 2014 | November 2016 |
| Bedford and Bedfordshire | Bedford, Central Bedfordshire | January 2015 | January 2017 |
| Luton | Luton | September 2015 | August 2017 |
| Southend | Southend-on-Sea | August 2009 | March 2019 |
| London | |||
| Southwarkb | Southwark | August 2009 | March 2019 |
| Tower Hamletsb | Tower Hamlets | August 2009 | March 2019 |
| Islington | Islington | August 2009 | March 2019 |
| Lambethb | Lambeth | August 2009 | March 2019 |
| Ealing | Ealing | August 2009 | March 2019 |
| Waltham Forest and Redbridge | Redbridge, Waltham Forest | August 2009 October 2013 | March 2019 |
| West Central London | Hammersmith and Fulham, Kensington and Chelsea, Westminster | February 2010 | March 2019 |
| Lewisham | Lewisham | January 2010 | March 2019 |
| Barking and Dagenham | Barking and Dagenham | November 2010 | November 2015 |
| Croydon | Croydon | October 2010 | March 2019 |
| Haringey | Haringey | July 2010 | March 2019 |
| Barnet | Barnet | November 2011 | March 2019 |
| Hounslow | Hounslow | July 2011 | March 2019 |
| Enfield | Enfield | November 2013 | March 2019 |
| Newham | Newham | September 2013 | March 2019 |
| Sutton | Sutton | January 2014 | June 2017 |
| Brent | Brent | June 2014 | July 2016 |
| Greenwich | Greenwich | April 2014 | March 2019 |
| Hackney | Hackney, City of London | May 2014 | March 2019 |
| Bromley and Bexley | Bexley, Bromley | September 2014 October 2014 | August 2016 March 2019 |
| Camden | Camden | January 2015 | July 2018 |
| Wandsworth | Wandsworth | May 2015 | March 2019 |
| Merton | Merton | September 2013 | March 2019 |
| South East | |||
| Berkshire Eastb | Bracknell Forest, Slough, Windsor and Maidenhead | August 2009 | February 2016 |
| East Sussex – East | Hastings, Rother | August 2009 | November 2015 December 2015 |
| Milton Keynes | Milton Keynes | August 2009 | October 2016 |
| Southampton | Southampton | August 2009 | March 2019 |
| Medway | Medway | August 2009 | December 2015 |
| Oxfordshire | Cherwell, Oxford, South Oxfordshire, Vale of White Horse, West Oxfordshire | February 2010 | March 2019 |
| East Sussex – West | Eastbourne, Lewes, Wealden | November 2010 March 2011 December 2011 | June 2015 November 2015 December 2015 |
| West Sussex | Adur, Arun, Chichester, Crawley, Horsham, Mid Sussex, Worthing | September 2011 | March 2019 |
| Portsmouth | Portsmouth | November 2011 | March 2019 |
| Kent North | Gravesham, Swale, Thanet | February 2012 December 2014 | March 2017 June 2018 |
| Berkshire West | West Berkshire, Reading, Wokingham | November 2012 | June 2016 |
| Brighton and Hove | Brighton and Hove | October 2012 | March 2016 |
| Buckinghamshire | Aylesbury Vale, Chiltern, South Buckinghamshire, Wycombe | July 2012 | March 2019 |
| Kent South | Dover, Maidstone, Shepway, Tonbridge and Malling | February 2013 December 2014 | October 2017 June 2018 |
| Surrey | Elmbridge, Epsom and Ewell, Guildford, Mole Valley, Reigate and Banstead, Runnymede, Spelthorne, Surrey Heath, Tandridge, Waverley, Woking | November 2014 | March 2019 |
| Hampshire | Basingstoke and Deane, Fareham, Gosport, Hart, Havant, Rushmoor | March 2015 April 2015 August 2015 January 2016 | April 2017 March 2018 August 2018 March 2019 |
| South West | |||
| Plymouth | Plymouth | August 2009 | March 2019 |
| Cornwall and Isles of Scillyb | Cornwall, Isles of Scilly | August 2009 | November 2017 |
| Swindon | Swindon | August 2009 | March 2019 |
| Bath and North East Somerset | Bath and North East Somerset | February 2013 | March 2019 |
| Bristol and South Gloucestershire | Bristol, city of, South Gloucestershire | May 2014 | March 2019 |
| Bristol and North Somerset | North Somerset | August 2014 | August 2015 |
| Wiltshire | Wiltshire | November 2014 | March 2019 |
| FNP site name | Lower-tier LA(s) | Start date | End date |
|---|---|---|---|
| North West | |||
| Knowsley | Knowsley | March 2017 | March 2019 |
| Yorkshire and Humber | |||
| Bradford and Airedale | Bradford | February 2017 | March 2019 |
| London | |||
| Barnet | Barnet | November 2017 | March 2019 |
| Ealing | Ealing | May 2017 | March 2019 |
| Haringey | Haringey | January 2018 | March 2019 |
| Lambeth | Lambeth | February 2017 | March 2019 |
| Lewisham | Lewisham | November 2016 | March 2019 |
| South East | |||
| Portsmouth | Portsmouth | November 2016 | March 2019 |
| South West | |||
| Bath and North East Somerset | Bath and North East Somerset | August 2017 | March 2019 |
| Cornwall and Isles of Scilly | Cornwall, Isles of Scilly | November 2016 | November 2017 |
Linking mothers and babies in the study cohort to National Pupil Database
| Match strength | Check(s) |
|---|---|
| 1 (Full confident match) | Full match on names, date of birth, and postcode |
| 2 (Very confident match) | Full match on names, plus combinations of at least two other variables or either fuzzy names/date of birth typo/postcode sector and three other variables |
| 3 (Confident match on a number of variables including fuzzy matching of names/date of birth typo or postcode sector) | Match on either fuzzy names/date of birth typo/postcode sector plus combinations of at least two other variables |
| 4 (Manually checked match on a smaller range of variables and looser fuzzy matching on names/partial postcode) | Lower level of fuzzy matching on names plus combinations of other variables |
| All mothers | Linked mothers | Unlinked mothers | ||||
|---|---|---|---|---|---|---|
| N | % | N | % | N | % | |
| Total (row %) | 134,880 | – | 112,305 | 83.3 | 22,575 | 16.7 |
| Enrolled in FNP | 31,425 | 23.0 | 28,330 | 25.2 | 3095 | 13.7 |
| Maternal age at birth | ||||||
| 13–15 | 2685 | 2.0 | 2395 | 2.1 | 290 | 1.3 |
| 16–17 | 26,065 | 19.3 | 22,805 | 20.3 | 255 | 14.4 |
| 18–19 | 72,465 | 53.7 | 60,970 | 54.3 | 11,495 | 50.9 |
| 20–21 | 30,295 | 22.5 | 24,190 | 21.5 | 6110 | 27.1 |
| 22–25 | 3375 | 2.5 | 1945 | 1.7 | 1425 | 6.3 |
| Maternal year of birth | ||||||
| 1989 | 330 | 0.2 | 250 | 0.2 | 75 | 0.3 |
| 1990 | 3895 | 2.9 | 3110 | 2.8 | 785 | 3.5 |
| 1991 | 8200 | 6.1 | 6865 | 6.1 | 1335 | 5.9 |
| 1992 | 12,275 | 9.1 | 10,120 | 9.0 | 2160 | 9.6 |
| 1993 | 15,260 | 11.3 | 12,535 | 11.2 | 2725 | 12.1 |
| 1994 | 17,080 | 12.7 | 14,135 | 12.6 | 2940 | 13.0 |
| 1995 | 17,680 | 13.1 | 14,650 | 13.0 | 3030 | 13.4 |
| 1996 | 18,025 | 13.4 | 15,040 | 13.4 | 2985 | 13.2 |
| 1997 | 15,985 | 11.9 | 13,250 | 11.8 | 2730 | 12.1 |
| 1998 | 12,630 | 9.4 | 10,610 | 9.4 | 2020 | 8.9 |
| 1999 | 7810 | 5.8 | 6675 | 5.9 | 1135 | 5.0 |
| 2000 | 3695 | 2.7 | 3250 | 2.9 | 450 | 2.0 |
| 2001 | 1465 | 1.1 | 1315 | 1.2 | 150 | 0.7 |
| 2002 | 420 | 0.3 | 385 | 0.3 | 40 | 0.2 |
| 2003 | 105 | 0.1 | 95 | 0.1 | – | – |
| 2004 | 20 | 0.0 | – | – | – | – |
| Ethnicity | ||||||
| White | 112,280 | 83.2 | 97,635 | 86.9 | 14,645 | 64.9 |
| South Asian | 4205 | 3.1 | 2500 | 2.2 | 1710 | 7.6 |
| Black | 5045 | 3.7 | 3395 | 3.0 | 1650 | 7.3 |
| Mixed/other | 7245 | 5.4 | 4650 | 4.1 | 2595 | 11.5 |
| Unknown | 6105 | 4.5 | 4125 | 3.7 | 1980 | 8.8 |
| Area-level deprivation | ||||||
| Least deprived | 6890 | 5.1 | 6125 | 5.5 | 765 | 3.4 |
| 2 | 10,735 | 8.0 | 9330 | 8.3 | 1410 | 6.2 |
| 3 | 18,690 | 13.9 | 15,805 | 14.1 | 2880 | 12.8 |
| 4 | 33,900 | 25.1 | 28,030 | 25.0 | 5870 | 26.0 |
| Most deprived | 64,505 | 47.8 | 52,890 | 47.1 | 11,615 | 51.5 |
| Unknown | 165 | 0.1 | 125 | 0.1 | 40 | 0.2 |
| Admission with diagnoses within 2 years before 20 weeks of pregnancy | ||||||
| Mental health (excluding substance misuse and self-harm) | 3425 | 2.5 | 3055 | 2.7 | 365 | 1.6 |
| Adversity-related | 5540 | 4.1 | 4925 | 4.4 | 615 | 2.7 |
| Any chronic condition | 12,245 | 9.1 | 10,885 | 9.7 | 1360 | 6.0 |
| Any A&E attendance | 84,785 | 62.9 | 73,130 | 65.1 | 11,655 | 51.6 |
| Non-attendance at ≥ 1 outpatient appointment | 38,755 | 32.7 | 32,870 | 32.7 | 5890 | 33.1 |
| Gestational age at booking | ||||||
| Before 10 weeks | 36,095 | 26.8 | 31,730 | 28.3 | 4365 | 19.3 |
| 10–20 weeks | 49,225 | 36.5 | 40,905 | 36.4 | 8320 | 36.9 |
| 20 weeks or more | 7480 | 5.5 | 5680 | 5.1 | 1800 | 8.0 |
| Unknown | 42,080 | 31.2 | 33,990 | 30.3 | 8090 | 35.8 |
| All mothers | Linked mothers | Unlinked mothers | ||||
|---|---|---|---|---|---|---|
| N | % | N | % | N | % | |
| Total | 31,425 | – | 28,330 | 90.2 | 3095 | 9.8 |
| Living arrangements at enrolment | ||||||
| Alone | 1810 | 5.8 | 1585 | 5.6 | 225 | 7.3 |
| Foster carers/group home/other | 2845 | 9.1 | 2510 | 8.9 | 335 | 10.8 |
| Mother (with or without partner) | 16,750 | 53.3 | 15,490 | 54.7 | 1260 | 40.7 |
| Partner (with or without others, not mother) | 6035 | 19.2 | 5160 | 18.2 | 875 | 28.3 |
| Relatives/other adults | 3080 | 9.8 | 2785 | 9.8 | 295 | 9.5 |
| Unknown | 905 | 2.9 | 795 | 2.8 | 110 | 3.6 |
| Relationship status at enrolment | ||||||
| In a relationship with biological father | 22,310 | 71.0 | 20,105 | 71.0 | 2205 | 71.2 |
| In a relationship with other partner | 990 | 3.2 | 915 | 3.2 | 75 | 2.4 |
| Single | 7220 | 23.0 | 6510 | 23.0 | 710 | 22.9 |
| Unknown | 905 | 2.9 | 795 | 2.8 | 110 | 3.6 |
| Alcohol/drug use at enrolment | ||||||
| No | 28,650 | 91.2 | 25,840 | 91.2 | 2805 | 90.6 |
| Yes | 1500 | 4.8 | 1360 | 4.8 | 140 | 4.5 |
| Unknown | 1275 | 4.1 | 1130 | 4.0 | 150 | 4.8 |
| Care leaver during pregnancy | ||||||
| No | 29,605 | 94.2 | 26,720 | 94.3 | 2885 | 93.2 |
| Yes | 1155 | 3.7 | 1030 | 3.6 | 125 | 4.0 |
| Unknown | 665 | 2.1 | 580 | 2.0 | 85 | 2.7 |
| CiN, CPP, or Looked After during pregnancy | ||||||
| No | 26,035 | 82.8 | 23,425 | 82.7 | 2610 | 84.3 |
| Yes | 4725 | 15.0 | 4325 | 15.3 | 400 | 12.9 |
| Unknown | 665 | 2.1 | 580 | 2.0 | 85 | 2.7 |
| Gestational age at booking appointment | ||||||
| Before 10 weeks | 18,915 | 60.2 | 17,180 | 60.6 | 1730 | 55.9 |
| 10–20 weeks | 10,730 | 34.1 | 9590 | 33.9 | 1145 | 37.0 |
| 20 weeks or more | 1030 | 3.3 | 890 | 3.1 | 140 | 4.5 |
| Unknown | 750 | 2.4 | 670 | 2.4 | 80 | 2.6 |
| All babies | Linked babies | Unlinked babies | ||||
|---|---|---|---|---|---|---|
| N | % | N | % | N | % | |
| Total (row %) | 132,660 | – | 89,580 | 67.5 | 43,080 | 32.5 |
| Baby year of birth | ||||||
| 2010 | 9945 | 7.5 | 9220 | 10.3 | 725 | 1.7 |
| 2011 | 13,485 | 10.2 | 12,595 | 14.1 | 890 | 2.1 |
| 2012 | 15,485 | 11.7 | 14,500 | 16.2 | 990 | 2.3 |
| 2013 | 16,385 | 12.4 | 15,225 | 17.0 | 1160 | 2.7 |
| 2014 | 15,885 | 12.0 | 14,565 | 16.3 | 1320 | 3.1 |
| 2015 | 17,655 | 13.3 | 15,150 | 16.9 | 2505 | 5.8 |
| 2016 | 16,515 | 12.4 | 8315 | 9.3 | 8200 | 19.0 |
| 2017 | 13,375 | 10.1 | 10 | 0.0 | 13,365 | 31.0 |
| 2018 | 11,520 | 8.7 | – | – | – | – |
| 2019 | 2405 | 1.8 | – | – | – | – |
| Maternal ethnicity | ||||||
| White | 110,530 | 83.3 | 77,385 | 86.4 | 33,145 | 76.9 |
| South Asian | 4120 | 3.1 | 2360 | 2.6 | 1760 | 4.1 |
| Black | 4925 | 3.7 | 3105 | 3.5 | 1815 | 4.2 |
| Mixed/other | 7075 | 5.3 | 4045 | 4.5 | 3030 | 7.0 |
| Unknown | 6015 | 4.5 | 2685 | 3.0 | 3325 | 7.7 |
| Area-level deprivation | ||||||
| Least deprived | 6810 | 5.1 | 4455 | 5.0 | 2355 | 5.5 |
| 2 | 10,590 | 8.0 | 6935 | 7.7 | 3650 | 8.5 |
| 3 | 18,430 | 13.9 | 12,005 | 13.4 | 6425 | 14.9 |
| 4 | 33,285 | 25.1 | 22,170 | 24.7 | 11,110 | 25.8 |
| Most deprived | 63,390 | 47.8 | 43,925 | 49.0 | 19,465 | 45.2 |
| Unknown | 165 | 0.1 | 90 | 0.1 | 70 | 0.2 |
Appendix 3 International Classification of Diseases, 10th Revision code lists
International Classification of Diseases, 10th Revision code lists for maternal hospital admissions related to adversity, mental health and chronic conditions
Code lists were derived from the following studies:
-
Harron K, Gilbert R, Fagg J, Guttmann A, van der Meulen J. Associations between pre-pregnancy psychosocial risk factors and infant outcomes: a population-based cohort study in England. Lancet Public Health 2021;6(2):e97–105.
-
Herbert A, Gilbert R, González-Izquierdo A, Li L. Violence, self-harm and drug or alcohol misuse in adolescents admitted to hospitals in England for injury: a retrospective cohort study. BMJ Open 2015;5(2):e006079.
-
Hardelid P, Dattani N, Gilbert R. Estimating the prevalence of chronic conditions in children who die in England, Scotland and Wales: a data linkage cohort study. BMJ Open 2014;4(8):e005331.
-
Pearson RJ, Jay MA, Wijlaars LPMM, De Stavola B, Syed S, Bedston SJ, Gilbert R. Association between health indicators of maternal adversity and the rate of infant entry to Local Authority care in England: a longitudinal ecological study. BMJ Open 2020;10(8):e036564.
Unplanned maternal hospital admissions with any of the ICD-10 codes in the following respective categories were considered to be adversity-related or mental health-related. Mothers with any hospital admissions relating to a chronic condition were considered to have a chronic condition.
| Group | Description | ICD10 code |
|---|---|---|
| Adversity-related admissions | ||
| Violence | Maltreatment syndromes | T74 |
| Effects of other deprivation (extreme neglect) | T73 | |
| Perpetrator of neglect and other maltreatment syndromes | Y06, Y07 | |
| Assault by bodily force and sexual assault | Y04, Y05 | |
| Other types of assault | X85–Y03, Y08–Y09 | |
| Events of undetermined intent | Y20–Y34 | |
| Examination and observation following other inflicted injury | Z04.5 | |
| Examination and observation for other reasons: request for expert evidence | Z04.8 | |
| Self-harm | Sequelae of intentional self-harm | Y87.0 |
| Intentional self-poisoning by and exposure to … drugs | X60–X63 | |
| … other and unspecified drugs, medicaments and biological substances | X64 | |
| … alcohol | X65 | |
| … organic solvents and halogenated hydrocarbons and their vapours | X66 | |
| … other gases and vapours | X67 | |
| … pesticides | X68 | |
| … other and unspecified chemicals and noxious substances | X69 | |
| Intentional self-harm by … hanging, strangulation and suffocation | X70 | |
| … drowning and submersion | X71 | |
| … firearm discharge | X72–X74 | |
| … explosive material | X75 | |
| … smoke, fire and flames, or steam, hot vapours and hot objects | X76–X77 | |
| … sharp/blunt objects | X78–X79 | |
| ... jumping from a high place | X80 | |
| … jumping or lying before a moving object, or crashing a motor vehicle | X81–82 | |
| … other specified means | X83 | |
| … unspecified means | X84 | |
| Substance misuse | Mental and behavioural disorders due to psychoactive substance use | F11–F16, F19 |
| Finding of drugs not normally found in blood | R78.1–R78.5 | |
| Poisoning by drugs, medicaments and biological substances | T36–T50 (not T50.6) | |
| Poisoning, undetermined intent | Y10–Y14 | |
| Drug rehabilitation | Z50.3 | |
| Drug abuse counselling and surveillance | Z71.5 | |
| Drug use | Z72.2 | |
| Mental and behavioural disorders due to use of volatile solvents | F18 | |
| Accidental poisoning by and exposure to noxious substances | X40–X44, X46–X49 | |
| Poisoning by chemical or noxious substance, undetermined intent | Y16–Y19 | |
| Special epileptic syndromes (related to alcohol, drugs, etc.) | G40.5 | |
| Blood-alcohol and blood-drug test | Z04.0 | |
| Alcohol-induced pseudo-Cushing syndrome | E24.4 | |
| Mental and behavioural disorders due to use of alcohol | F10 | |
| Degeneration of nervous system due to alcohol | G31.2 | |
| Alcoholic polyneuropathy | G62.1 | |
| Alcoholic myopathy | G72.1 | |
| Alcoholic cardiomyopathy | I42.6 | |
| Alcoholic gastritis | K29.2 | |
| Alcoholic liver disease | K70 | |
| Alcohol-induced acute pancreatitis | K85.2 | |
| Alcohol-induced chronic pancreatitis | K86.0 | |
| Maternal care for (suspected) damage to fetus from alcohol | O35.4 | |
| Finding of alcohol in blood | R78.0 | |
| Poisoning: antidotes and chelating agents, not elsewhere classified | T50.6 | |
| Toxic effect of alcohol | T51 | |
| Accidental poisoning by exposure to alcohol | X45 | |
| Poisoning by exposure to alcohol, undetermined intent | Y15 | |
| Evidence of alcohol involvement determined by blood alcohol level | Y90 | |
| Evidence of alcohol involvement determined by level of intoxication | Y91 | |
| Alcohol rehabilitation | Z50.2 | |
| Alcohol abuse counselling and surveillance | Z71.4 | |
| Alcohol use | Z72.1 | |
| Mental health conditions/behavioural disorders (excluding those falling under adversity or chronic conditions) | ||
| Organic, including symptomatic, mental disorders | F00–F09a | |
| Schizophrenia, schizotypal and delusional disorders | F20–F29 | |
| Mood [affective] disorders | F30–F39 | |
| Neurotic, stress-related and somatoform disorders | F40–F48 | |
| Behavioural syndromes associated with physiological disturbances and physical factors | F50–F59b | |
| Disorders of adult personality and behaviour | F60–F69c | |
| Mental retardation | F70–F79 | |
| Disorders of psychological development | F80–F89 | |
| Behavioural and emotional disorders with onset usually occurring in childhood and adolescence | F90–F98 | |
| Sedatives, hypnotics and antianxiety drugs | Y47 | |
| Psychotropic drugs, not elsewhere classified | Y49 | |
| Chronic conditions (except those falling under mental health conditions) | ||
| Cancer/blood disorders | Neoplasms | C00–C97, D00–D02, D05–D09, D12, D13, D14.1–D14.4, D15, D20, D32–D35, D37– D48, D63.0, E34.0, E88.3, G13.0, G13.1, G53.3, G55.0, G63.1, G73.1, G73.2, G94.1, M36.0, M36.1, M49.5, M82.0, M90.6, M90.7, N08.1, N16.1, Y43.1–Y43.3, Y84.2, Z08, Z51.0–Z51.2, Z54.1, Z54.2, Z85, Z86.0, Z92.3 |
| Immunological disorders | D80–D84, G53.2, Q98.0 | |
| Anaemia and other blood disorders | D50, D56.0–D56.2, D56.4, D56.8, D56.9, D57.0–D57.2, D57.8, D58, D61.0, D61.9, D64, D66, D67, D68.0–D68.2, D68.4–D68.9, D69, D70–D76, M36.2–M36.4, M90.4, N08.2, Z86.2 | |
| Chronic infections | HIV | B20–B24, F02.4, R75, Z21 |
| Tuberculosis | A15–A19, E35.0, K23.0, K67.3, K93.0, M01.1, M49.0, P37.0 | |
| Other | A50, A81, B18, B37.1, B37.5, B37.6, B37.7, B38.1, B39.1, B40.1, B44.0, B44.7, B45, B46, B48.7, B50.0, B50.8, B51.0, B51.8, B52.8, B52.0, B55, B57.2–B57.5, B58.0, B59, B67, B69, B73, B74, B78.7, B90–B94, F02.1, K23.1, K93.1, M00, N33.0, P35.0– P35.2, P35.8, P35.9, P37.1 | |
| Respiratory | Asthma and chronic lower respiratory disease | J41–J47 |
| Cystic fibrosis | E84, P75 | |
| Injuries | S17, S27, S28, T27, T91.4 | |
| Congenital anomalies | Q30–Q37, Q79.0 | |
| Other | G47.3, J60–J70, J80–J86, J96.1, J98, P27, Y55.6, Z43.0, Z93.0, Z94.2 | |
| Metabolic/endocrine/digestive/renal/genitourinary | Diabetes | E10–E14, G59.0, G63.2, I79.2, M14.2, N08.3, O24, Y42.3 |
| Other endocrine | E00, E03.0, E03.1, E07.1, E22.0, E23.0, E25, E26.8, E29.1, E31, E34.1, E34.2, E34.5, E34.8, G13.2, G73.5, Y42.1 | |
| Digestive | K20, K21.0, K22, K23.8, K25–K28, K29.0, K29.1, K29.3–K29.9, K31, K50–K52, K55, K57, K59.2, K63.0–K63.3, K66, K72–K76, K80–K83, K85.0, K85.1, K85.8, K85.9, K86.1–K86.9, K87.0, K90, M07.4, M07.5, M09.1, M09.2, T86.4, Z43.2–Z43.4, Z46.5, Z90.3, Z90.4, Z93.2–Z93.5 | |
| Renal/genitourinary | D63.8, G63.8, G99.8, I68.8, M90.8, N08.4, N00–N05, N07, N11–N15, N16.0, N16.2, N16.4, N16.5, N16.8, N18, N19, N20–N23, N25, N26, N28, N29, N31, N32, N33.8, N35, N36, N39.1, N39.3, N39.4, N40–N42, N70–N74, N80–N82, N85, N86, N87, N88, P96.0, T82.4, T83.1, T83.2, T83.4–T83.9, T85.5, T86.1, Y60.2, Y61.2, Y62.2, Y84.1, Z49, Z93.6, Z94.0, Z99.2 | |
| Congenital anomalies of the digestive/renal/genitourinary system | Q38.0, Q38.3, Q38.4, Q38.6–Q38.8, Q39, Q40.2, Q40.3, Q40.8, Q40.9, Q41, Q42, Q43.1, Q43.3–Q43.7, Q43.9, Q44, Q45, Q50.0, Q51, Q52.0–Q52.2, Q52.4, Q54.0– Q54.3, Q54.8, Q54.9, Q55.0, Q55.5, Q56, Q60.1, Q60.2, Q60.4–Q60.6, Q61, Q62.0– Q62.6, Q62.8, Q63.0–Q63.2, Q63.8, Q63.9, Q64, Q79.2–Q79.5, Q87.8, Q89.1, Q89.2 | |
| Injuries | S36, S37, S38, S39.6, S39.7, T06.5, T28, T91.5 | |
| Other/unspecified | E66, G63.3, G99.0, M14.5, N92, Z86.3, Z93.8 | |
| Musculoskeletal/skin | Musculoskeletal/connective tissue | G55.1–G55.3, G63.5, G63.6, G73.7, J99.0, J99.1, L62.0, M05, M06, M07.0–M07.3, M07.6, M08, M09.8, M10–M13, M14.0, M14.6, M14.8, M30–M35, M40–M43, M45– M48,M50–M54, M60–M62, M63.8, M80.1–M80.9, M81.1–M81.9, M82.1, M82.8, M84.0–M84.2, M84.8, M84.9, M85, M86.3–M86.6, M89, M90.0, M91–M94, N08.5, Y45.4 |
| Skeletal injuries/amputations | S13, S22.0–S22.2, S22.5, S23, S32, S33, S68.3, S68.4, S68.8, S77, S78, S87, S88, S97, S98.0, S98.2–S98.4, T02, T04, T05, T20.3, T20.7, T21.3, T21.7, T22.3, T22.7, T23.2, T23.3, T23.6, T23.7, T24.3, T24.7, T25.2, T25.3, T25.6, T25.7, T29.3, T29.7, T30.3, T30.7, T31.2–T31.9, T32.2– T32.9, T87.3–T87.6, T91.2 T91.8, T92.6, T93.1, T93.4, T93.6, T94.0, T94.1, T95.0, T95.1, T95.4, T95.8, T95.9, Y83.5, Z89.1, Z89.2, Z89.5–Z89.8, Z97.1 | |
| Chronic skin disorders | L10, L11.0, L11.8, L11.9, L12–L14, L28, L40–L45, L57, L58.1, L59, L87, L88, L90, 3 L92, L95, L93, L98.5, M09.0, Q80, Q81, Q87.0–Q87.5, Q89.4 | |
| Congenital anomalies | Q18.8, Q65.0–Q65.2, Q65.8, Q65.9, Q67.5, Q68.2, Q68.3–Q68.5, Q71–Q73, Q74, Q75.3–Q75.9, Q76.1–Q76.4, Q77, Q78, Q79.6, Q79.8, Q82.0–Q82.4, Q82.9, Q86.2, Q89.7–Q89.9 | |
| Neurological | Epilepsy | F80.3, G40.0–G40.4, G40.6–G40.9, G41, R56.8, Y46.0–Y46.6 |
| Cerebral palsy | G80–G83 | |
| Injuries of brain, nerves, eyes or ears | S05–S08, S12, S14, S24, S34, S44, S54, S64, S74, S84, S94, T06.0–T06.2, T26, T90.4, T90.5, T91.1, T91.3, T92.4 | |
| Chronic eye conditions | H05.1–H05.9, H13.3, H17, H18, H19.3, H19.8, H21, H26, H27, H28.0–H28.2, H31, H32.8, H33, H34, H35, H40, H42.0, H43, H44, H47, H54.0– H54.2, H54.4, T85.2, T85.3, Z44.2 | |
| Chronic ear conditions | H60.2, H65.2–H65.4, H66.1–H66.3, H69.0, H70.1, H73.1, H74.0–H74.3, H75.0, H80, H81.0, H81.4, H83.0, H83.2, H90.0, H90.3, H90.5, H90.6, H91, Z45.3 | |
| Perinatal conditions | P10, P21.0, P52, P57, P90, P91.1, P91.2, P91.6 | |
| Congenital anomalies of neurological or sensory systems | Q00–Q07, Q10.4, Q10.7, Q11–Q12, Q13.0–Q13.4, Q13.8, Q13.9, Q14–Q16, Q75.0, Q75.1, Q85, Q86.0, Q86.1, Q86.8, Q90–Q93, Q95.2, Q95.3, Q97, Q99 | |
| Other | F02.2, F02.3, G00–G09, G10–G12, G13.8, G14, G20–G23, G24.1–G24.9, G25–G30, G31.0–G31.1, G31.8, G31.9, G32–G37, G43–G46, G47.0–G47.2, G47.4–G47.9, G50– G52, G53.0, G53.1, G53.8, G54, G55.8, G56–G58, G59.8, G60, G61, G62.0, G62.2– G62.9, G64, G70, G71,G72.2–G72.9, G73.0, G73.3, G90–G93, G94.2, G94.8, G95, G96, G98, G99.1, G99.2, I60–I67, I68.0, I68.2, I69, I72.0, I72.5, T85.0, T85.1, Y46.7– Y46.8, Z98.2 | |
| Cardiovascular | Congenital heart disease | Q20–Q26, Q89.3 |
| Other | I00–I28, I31–I39, I41, I42.0–I42.5, I42.7–I42.9, I43.0, I43.1, I43.2–I43.8, I44.1–I44.7, I45.1–I45.9, I46–I51, I52.8, I70–I71, I72.1–I72.4, I72.8, I72.9, I73–I77, I79.0, I79.1, I79.8, I81–I82, I98–I99, M03.6, N08.8, Q27, Q28, S26, T82.0–T82.3, T82.5–T82.9, T86.2, Y60.5, Y61.5, Y62.5, Y84.0, Z45.0, Z50.0, Z94.1, Z95 | |
| Codes indicating non-specific chronic conditions | - | R62, R63.3, Z43.1, Z51.5, Z75.5, Z93.1, Z99.3 |
International Classification of Diseases, 10th Revision code lists for child maltreatment and healthcare utilisation-related outcomes
Code lists were derived from the following studies:
-
Gilbert R, Fluke J, O’Donnell M, Gonzalez-Izquierdo A, Brownell M, Gulliver P, et al. Child maltreatment: variation in trends and policies in six developed countries. Lancet 2012;379(9817):758–72. https://doi.org/10.1016/S0140-6736(11)61087-8
-
Syed S, Ashwick R, Schlosser M, Gonzalez-Izquierdo A, Li L, Gilbert R. Predictive value of indicators for identifying child maltreatment and intimate partner violence in coded electronic health records: a systematic review and meta-analysis. Arch Dis Child 2021;106:44–53.
-
Robling M, Lugg-Widger F, Cannings-John R, Sanders J, Angel L, Channon S, et al. The Family Nurse Partnership to reduce maltreatment and improve child health and development in young children: the BB:2–6 routine data-linkage follow-up to earlier RCT. Public Health Res 2021;9(2). URL: https://journalslibrary.nihr.ac.uk/phr/phr09020/#/abstracthttps://www.journalslibrary.nihr.ac.uk/phr/phr09020/#/abstract
Unplanned hospital admissions with any of the ICD-10 codes in the following respective categories were considered to be maltreatment or injury related:
| Group | Description | ICD-10 code | Age restriction |
|---|---|---|---|
| Maltreatment and injury-related | |||
| Injury and ingestion | Injuries to the head (includes open wounds, fractures, crushing and dislocation) | S00–S09 | N/A |
| Injuries to the neck | S10–S19 | N/A | |
| Injuries to the thorax | S20–S29 | N/A | |
| Injuries to the abdomen, lower back, lumbar spine and pelvis | S30–S39 | N/A | |
| Injuries to the shoulder and upper arm | S40–S49 | N/A | |
| Injuries to the elbow and forearm | S50–S59 | N/A | |
| Injuries to the wrist and hand | S60–S69 | N/A | |
| Injuries to the hip and thigh | S70–S79 | N/A | |
| Injuries to the knee and lower leg | S80–S89 | N/A | |
| Injuries to the ankle and foot | S90–S99 | N/A | |
| Injuries involving multiple body regions | T00–T07 | N/A | |
| Injuries to unspecified part of trunk, limb or body region | T08–T14 | N/A | |
| Effects of foreign body entering through natural orifice | T15–T19 | N/A | |
| Burns and corrosions | T20–T32 | N/A | |
| Frostbite | T33–T35 | N/A | |
| Poisoning by drugs, medicaments and biological substances | T36–T50 | N/A | |
| Toxic effects of substances chiefly non-medicinal as to source (sting, alcohol, solvents, etc.) | T51–T65 | N/A | |
| Other and unspecified effects of external causes (effects of radiation, heat and light, hypothermia, electric shock, asphyxiation, food deprivation) | T66–T78 | N/A | |
| Accidental poisoning by and exposure to noxious substances | X40–X49 | N/A | |
| Maltreatment | Maltreatment syndromes | T74 | N/A |
| Neglect and abandonment | Y06 | N/A | |
| Other maltreatment | Y07 | N/A | |
| Effects of other deprivation (hunger, thirst, exhaustion due to exposure or excessive exertion) | T73 | N/A | |
| Assault | X85–Y05 Y08–Y09 | N/A | |
| Maltreatment markers for infants < 1 year | Intracranial injuries | S06 | < 1 year |
| Long-bone fractures | S42.2–S42.4, S42.7–S42.8, S52, S72, S82, T10, T12 | < 1 year | |
| Maltreatment markers for children ≤ 4 years | Traumatic brain injuries | S06, S09.7–S09.8, T90.5 | ≤ 4 years |
| Retinal haemorrhage | H35.6 | ≤ 4 years | |
| Rib fractures | T29–T32 | ≤ 4 years | |
Appendix 4 Additional information on methods for Objective 3
In order to calculate the denominator (time at risk) for fidelity target calculations, we first cleaned the dates used in these calculations, including enrolment dates, completion dates, leaving and returning dates. A nurse will record a completion date if the client has come to the end of the programme (which will most likely be at the child’s second birthday, although may be sooner if agreed, such as in ADAPT sites). A leaving date is recorded if the client leaves the programme earlier than is planned, which should be recorded alongside one of the following reasons: client moves out of programme area, the child is no longer with the client (e.g. moved into care), death (maternal, fetal or infant). If a client becomes uncontactable or refuses the programme, they will be recorded as inactive, and a leaving date is also recorded.
Issues with completion dates
Prior to cleaning, 20,560 (73.0%) of the 28,155 mothers enrolled in the FNP had a completion date recorded. Of these, 18,245 had more than one completion date recorded. Most (10,450; 57.3%) of these were duplicated dates and were deleted. For the remaining 7795 individuals, we chose the latest completion date recorded closest to the last visit date recorded.
Seven thousand six hundred and fifteen completion dates were recorded earlier than expected (i.e. before the child’s second birthday). Four thousand four hundred and sixty of these had a leaving date recorded on the same day as the completion date, and for these, we retained the leaving date. For the remaining 3155 with no leaving date recorded, the majority (2855; 90.5%) left when the child was aged 21–24 months old. Only 300 had completion dates when the child was younger than 21 months. There was evidence that these clustered around ADAPT sites, where early completion was possible.
Four thousand six hundred and thirty-five mothers had a completion date that was more than 1 month after the last visit. For these, we truncated the completion date to 1 month after the last visit, as we assumed the mothers had effectively left the programme following their last visit.
Four thousand four hundred and five clients had a completion date more than 1 month after the child’s second birthday. Most of these (4170, 94.7%) had a 24-month visit recorded. Since we assumed that these mothers had left the programme at this point, we updated the completion date for all of these to the child’s second birthday.
Two hundred and twenty clients had no completion date, but a leaving date when the child was 23 months old or older. These were considered to have completed at the child’s second birthday and completion dates were updated to the leaving date.
Two hundred and thirty-five clients had no completion or leaving date. Sixty-five of these had visit dates up until the child’s second birthday. For these, we updated the completion date to the final visit date. For the remaining 170, we created a leaving date at 2 weeks after the final visit date.
After cleaning, 16,305 clients (57.9%) had a completion date.
Issues with leaving and returning dates
Of the 28,155 mothers enrolled in the FNP, 12,145 (43.1%) had at least one leaving date recorded and 4870 (17.3%) had at least one returning date. The combinations of these dates were cleaned to ensure that there were no duplicates and that they could fit into a logical sequence. Four thousand one hundred and seventy had leaving and returning dates on the same day, no completion date and no visits recorded after the returning date, therefore we kept only the leaving date. There were individuals with small numbers of other errors included leaving and returning dates which were after the completion dates (N = 320), leaving and returning dates on the same day, or duplicated dates.
Nine thousand one hundred and twenty (32.4%) FNP participants had no completion dates, and their leaving dates were more than 1 month after their final visit date, suggesting inactivity. For the 3985 of these with no leaving reason, we updated their leaving date to be 1 month after their final visit. This was to account for the opportunity for FNP nurses to attempt to contact the mother before they dropped out of the programme. For the 5135 with a leaving reason, we updated their leaving date to be 2 weeks after their final visit. This was to account for the fact that if the nurses know why the mother left, they are less likely to attempt to schedule further visits.
After cleaning, 12,035 (42.7%) of those enrolled in the FNP had a leaving date, and only 300 (1.1%) had a returning date.
FIGURE 20.
Flow of participants through the full FNP programme, from enrolment to completion.
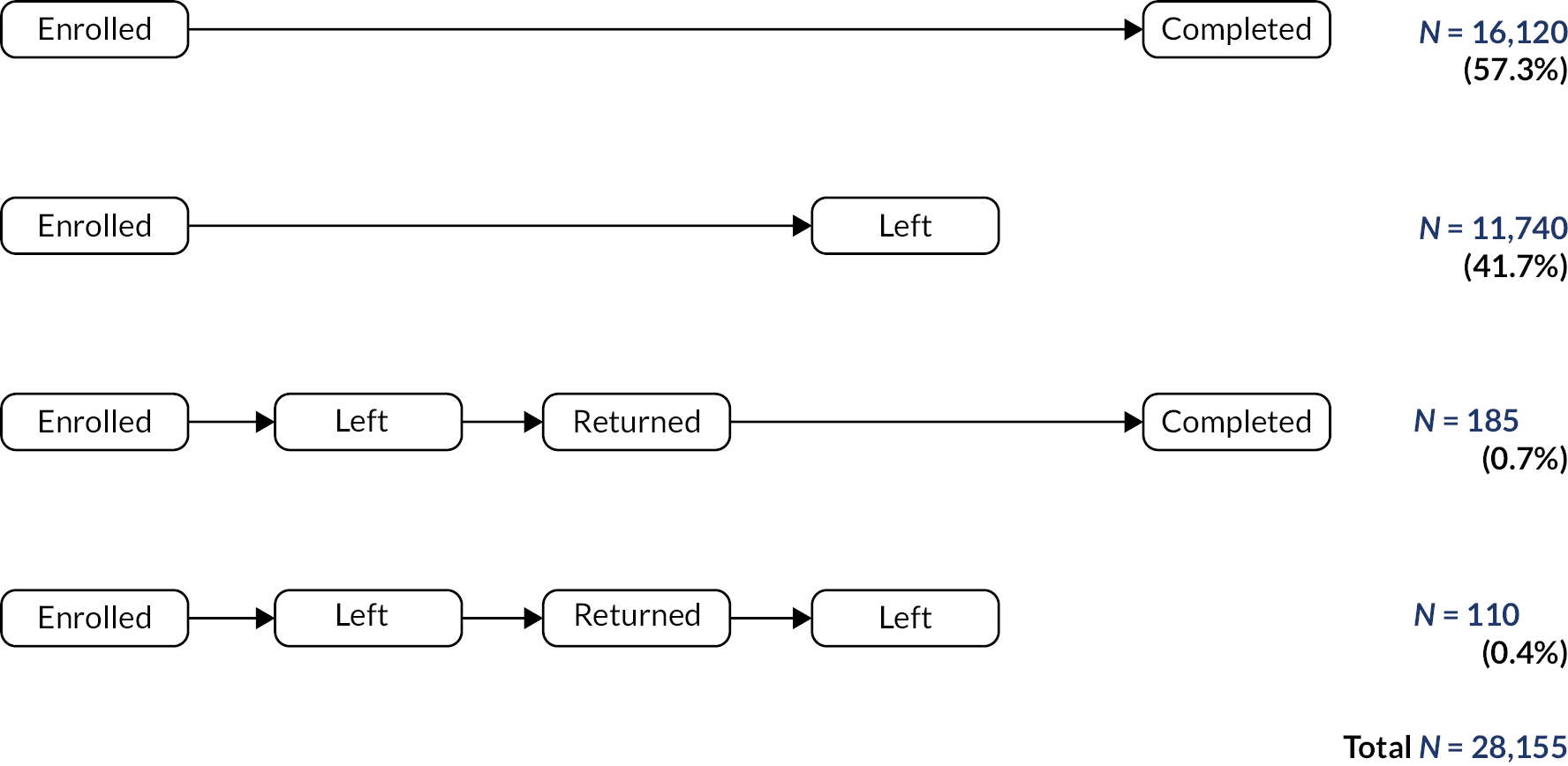
FIGURE 21.
Flow of participants through the pregnancy stage of the programme.
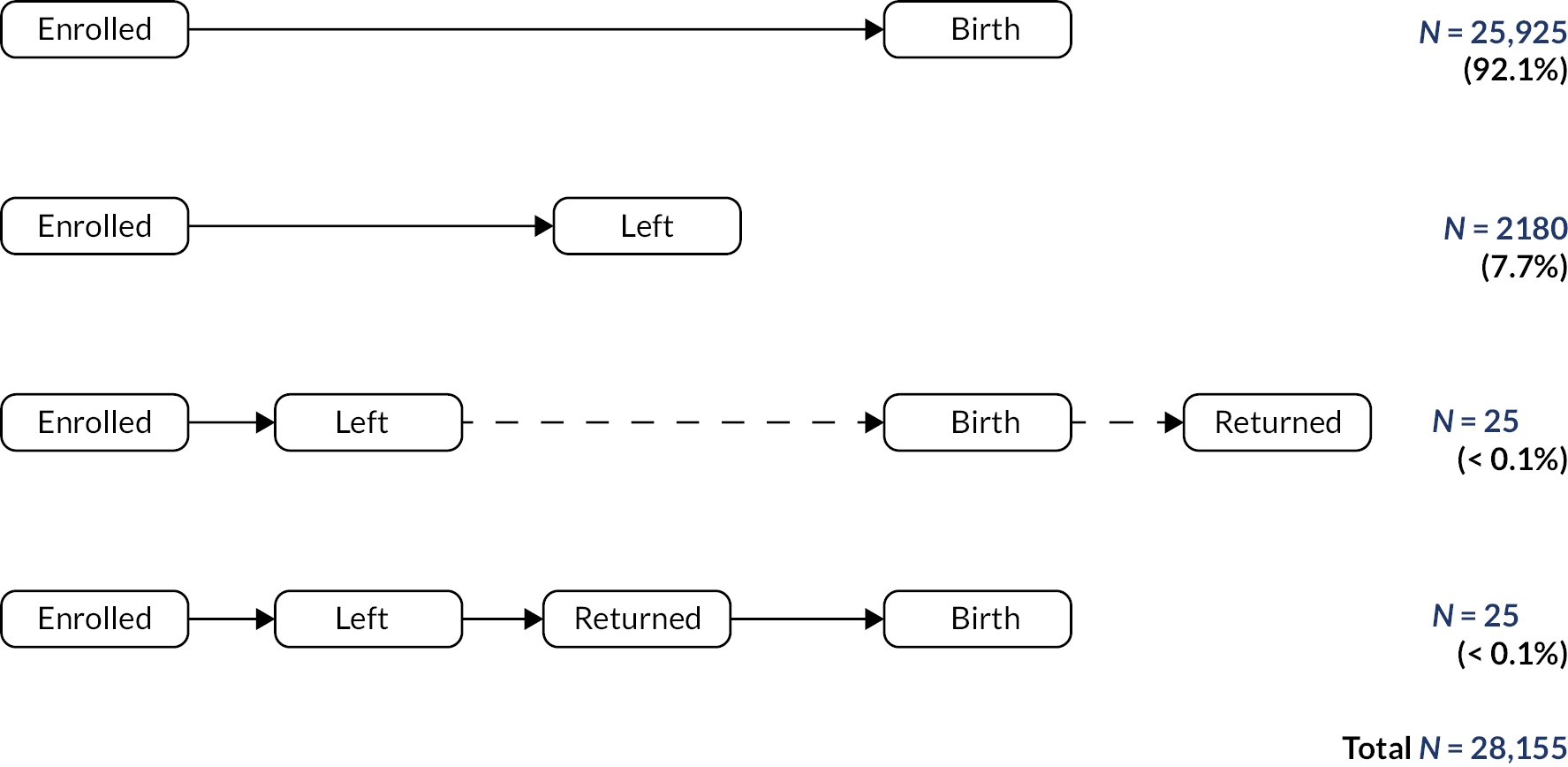
FIGURE 22.
Flow of participants through the infancy stage of the programme.
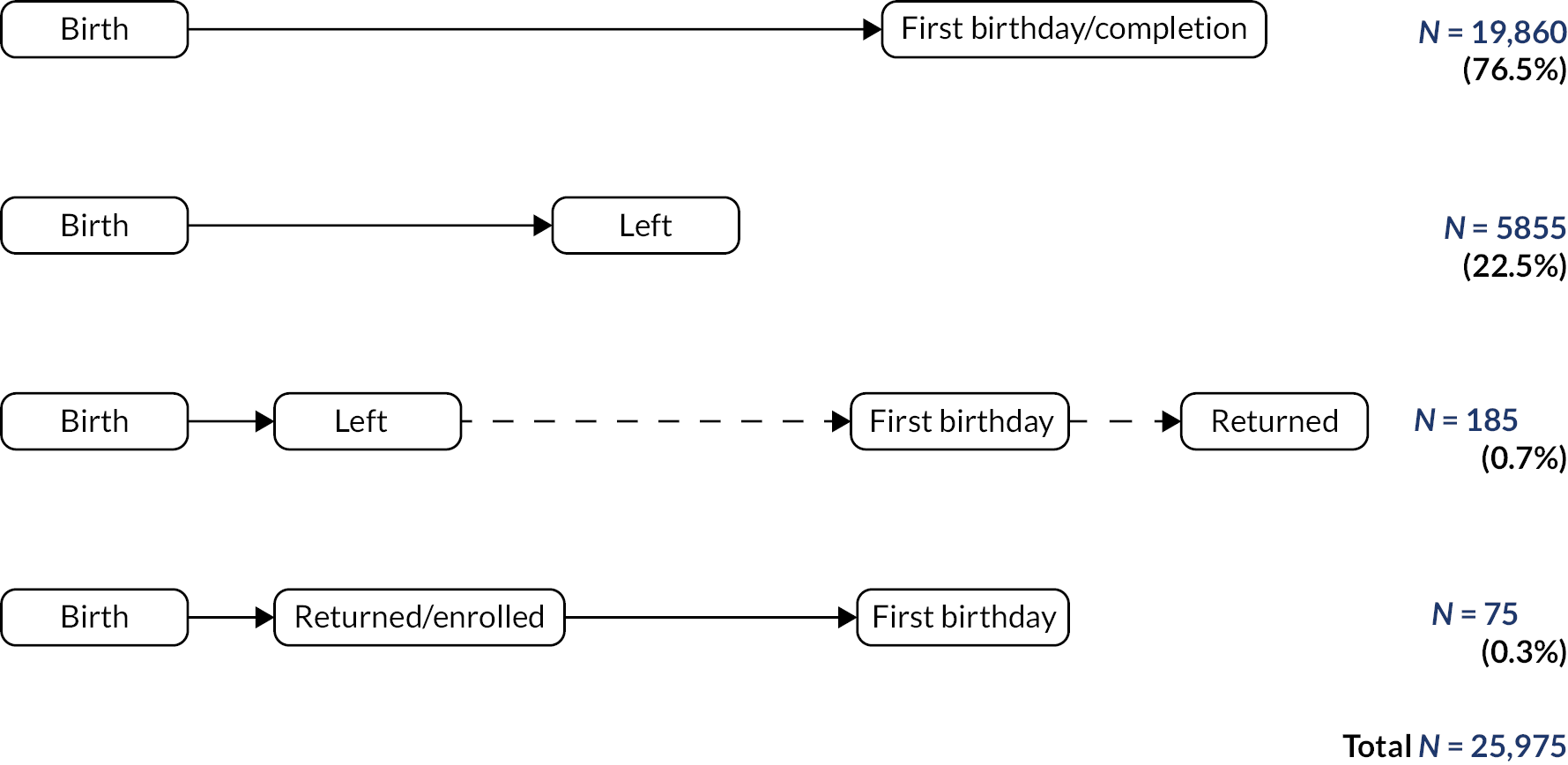
FIGURE 23.
Flow of participants through the toddlerhood stage of the programme.
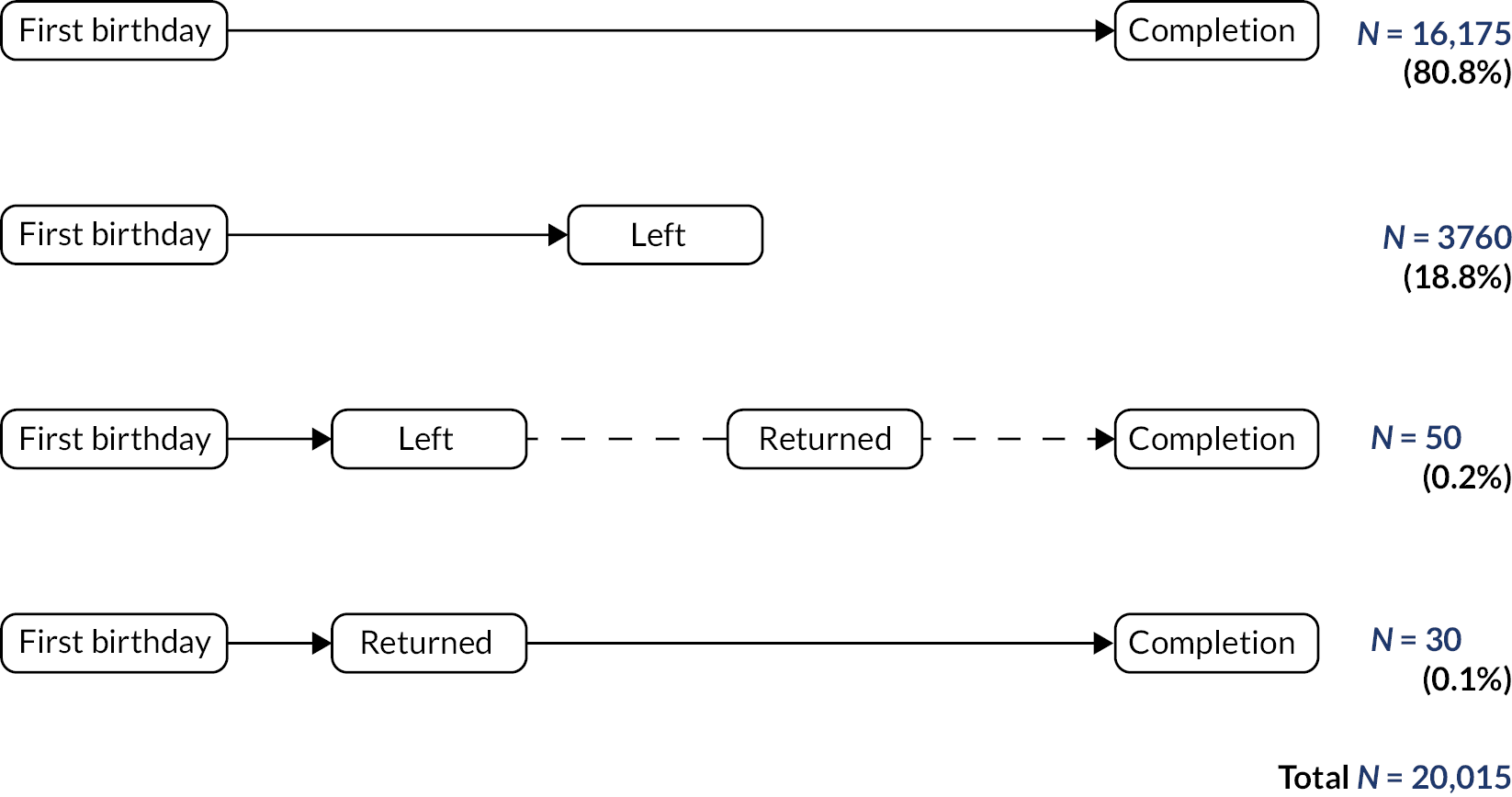
Appendix 5 Additional information on results for Objective 1: enrolment in the Family Nurse Partnership
| FNP site name | LA(s) | Start date | End date | N enrolled | N eligible | % enrolled | Median monthly caseload | Maximum monthly caseload |
|---|---|---|---|---|---|---|---|---|
| Total | – | – | – | 25,675 | 110,520 | 23.2 | – | – |
| North East | ||||||||
| Durham and Darlington | County Durham, Darlington | August 2009 | October 2015 | 560 | 3065 | 18.3 | 143 | 212 |
| Gateshead | Gateshead | February 2010 | March 2019 | 185 | 885 | 20.9 | 56 | 71 |
| Hartlepool | Hartlepool, Stockton-on-Tees | February 2012 April 2012 | February 2017 December 2017 | 225 | 985 | 22.8 | 80 | 111 |
| Middlesbrough | Middlesbrough, Redcar and Cleveland | March 2012 April 2012 | November 2015 March 2018 | 180 | 960 | 18.8 | 51 | 107 |
| Newcastle upon Tyne | Newcastle upon Tyne | April 2014 | September 2016 | 90 | 380 | 23.7 | 60 | 79 |
| North Tyneside | North Tyneside | March 2014 | March 2016 | 90 | 195 | 46.2 | 56 | 75 |
| Northumberland | Northumberland | March 2014 | September 2016 | 90 | 360 | 25 | 58 | 76 |
| South Tyneside | South Tyneside | January 2010 | January 2018 | 215 | 815 | 26.4 | 60 | 86 |
| Sunderland | Sunderland | August 2009 | March 2019 | 315 | 1615 | 19.5 | 94 | 122 |
| North West | ||||||||
| Blackburn with Darwen | Blackburn with Darwen | May 2015 | April 2016 | 55 | 100 | 55 | 34 | 57 |
| Blackpool | Blackpool | August 2009 | March 2019 | 245 | 1045 | 23.4 | 68 | 133 |
| Bolton | Bolton | November 2011 | March 2019 | 240 | 880 | 27.3 | 94 | 123 |
| Bury | Bury | December 2014 | March 2019 | 80 | 160 | 50 | 54 | 73 |
| Cheshire East | Cheshire East | September 2012 | March 2019 | 210 | 530 | 39.6 | 94 | 114 |
| Cheshire West | Cheshire West and Chester | February 2012 | March 2019 | 215 | 675 | 31.9 | 75 | 123 |
| Cumbria | Allerdale, Barrow-in-Furness, Carlisle, Copeland, Eden, South Lakeland | August 2009 | August 2016 | 205 | 1875 | 10.9 | 53 | 86 |
| Halton | Halton | July 2014 | March 2019 | 90 | 220 | 40.9 | 64 | 87 |
| Knowsley | Knowsley | August 2009 | March 2019 | 255 | 740 | 34.5 | 62 | 95 |
| Lancashire | Burnley, Preston, | April 2015 | April 2017 | 105 | 215 | 48.8 | 80 | 100 |
| Liverpool | Liverpool | August 2009 | March 2019 | 430 | 1965 | 21.9 | 116 | 149 |
| Manchester | Manchester | August 2009 | September 2016 | 530 | 2540 | 20.9 | 146 | 192 |
| Oldham | Oldham | August 2014 | March 2019 | 95 | 310 | 30.6 | 61 | 88 |
| Rochdale | Rochdale | August 2014 | February 2017 | 95 | 275 | 34.5 | 52 | 84 |
| Salford | Salford | December 2014 | March 2019 | 85 | 250 | 34 | 63 | 78 |
| Sefton | Sefton | December 2014 | September 2016 | 45 | 170 | 26.5 | 24 | 37 |
| St Helens | St Helens | December 2014 | March 2019 | 105 | 200 | 52.5 | 44 | 89 |
| Stockport | Stockport | August 2014 | March 2019 | 100 | 185 | 54.1 | 52 | 88 |
| Tameside | Tameside | March 2015 | March 2019 | 70 | 195 | 35.9 | 62 | 79 |
| Trafford | Trafford | January 2015 | March 2017 | 20 | 65 | 30.8 | 26 | 30 |
| Warrington | Warrington | April 2015 | March 2019 | 75 | 145 | 51.7 | 69 | 79 |
| Wigan | Wigan | December 2011 | March 2019 | 205 | 895 | 22.9 | 79 | 116 |
| Wirral | Wirral | August 2009 | March 2019 | 345 | 1335 | 25.8 | 103 | 125 |
| Yorkshire and Humber | ||||||||
| Barnsley | Barnsley | August 2009 | November 2015 | 275 | 970 | 28.4 | 89 | 107 |
| Bradford and Airedale | Bradford | February 2010 | March 2019 | 430 | 2415 | 17.8 | 110 | 183 |
| Calderdale | Calderdale | August 2009 | February 2016 | 155 | 935 | 16.6 | 51 | 84 |
| Doncaster | Doncaster | August 2009 | March 2016 | 285 | 1850 | 15.4 | 73 | 128 |
| East Riding | East Riding of Yorkshire | June 2013 | March 2019 | 60 | 400 | 15 | 33 | 60 |
| Hull | Kingston upon Hull, city of | August 2009 | June 2017 | 345 | 2060 | 16.7 | 103 | 127 |
| Kirklees | Kirklees | August 2009 | March 2019 | 345 | 1950 | 17.7 | 80 | 138 |
| Leeds | Leeds | August 2009 | April 2016 | 400 | 3360 | 11.9 | 127 | 171 |
| North and North East Lincolnshire | North East Lincolnshire, North Lincolnshire | March 2012 | April 2017 | 175 | 1130 | 15.5 | 69 | 88 |
| North Yorkshire | Scarborough | June 2013 | December 2014 | 40 | 110 | 36.4 | 16 | 35 |
| Rotherham | Rotherham | November 2011 | December 2016 | 200 | 920 | 21.7 | 69 | 93 |
| Sheffield | Sheffield | August 2009 | February 2016 | 380 | 2135 | 17.8 | 95 | 191 |
| Wakefield | Wakefield | November 2011 | March 2019 | 290 | 1235 | 23.5 | 106 | 147 |
| East Midlands | ||||||||
| Derby City | Derby | August 2009 | March 2019 | 415 | 1350 | 30.7 | 106 | 185 |
| Derbyshire | Amber Valley, Bolsover, Chesterfield, Derbyshire Dales, Erewash, High Peak, North East Derbyshire, South Derbyshire | October 2011 | March 2019 | 355 | 1775 | 20 | 95 | 166 |
| Leicester City | Leicester | September 2011 | May 2017 | 210 | 970 | 21.6 | 71 | 95 |
| Lincolnshire | Boston, East Lindsey | August 2014 | February 2016 | 65 | 200 | 32.5 | 47 | 58 |
| Northamptonshire | Corby, Daventry, East Northamptonshire, Kettering, Northampton, South Northamptonshire, Wellingborough | August 2009 | March 2019 | 375 | 3000 | 12.5 | 96 | 129 |
| Nottingham City | Nottingham | August 2009 | March 2019 | 435 | 1815 | 24 | 124 | 179 |
| Nottinghamshire | Ashfield, Bassetlaw, Broxtowe, Gedling, Mansfield, Newark and Sherwood, Rushcliffe | October 2012 | March 2019 | 370 | 1500 | 24.7 | 170 | 294 |
| West Midlands | ||||||||
| Birmingham | Birmingham | January 2013 | May 2016 | 450 | 2235 | 20.1 | 89 | 238 |
| Coventry | Coventry | August 2009 | March 2019 | 290 | 1610 | 18 | 87 | 115 |
| Dudley | Dudley | February 2013 | March 2019 | 240 | 645 | 37.2 | 108 | 139 |
| East Staffordshire | East Staffordshire | March 2013 | April 2017 | 85 | 210 | 40.5 | 30 | 44 |
| Sandwell | Sandwell | August 2009 | January 2017 | 395 | 2020 | 19.6 | 84 | 167 |
| Shropshire | Shropshire | November 2014 | March 2019 | 95 | 175 | 54.3 | 69 | 106 |
| Solihull | Birmingham, Solihull | August 2009 | March 2019 | 290 | 855 | 33.9 | 80 | 115 |
| Staffordshire – Cannock and Tamworth | Cannock Chase, Tamworth | March 2013 | August 2016 | 155 | 380 | 40.8 | 74 | 106 |
| Stoke-on-Trent | Newcastle-under-Lyme, Stoke-on-Trent | August 2009 | October 2016 | 325 | 2155 | 15.1 | 109 | 170 |
| Telford and Wrekin | Telford and Wrekin | August 2009 | March 2019 | 215 | 975 | 22.1 | 54 | 76 |
| Walsall | Walsall | August 2009 | September 2016 | 340 | 1835 | 18.5 | 100 | 126 |
| Warwickshire North | North Warwickshire, Nuneaton and Bedworth | November 2010 | March 2019 | 200 | 765 | 26.1 | 49 | 94 |
| Warwickshire South and Rugby | Rugby, Stratford-on-Avon, Warwick | November 2010 | March 2019 | 175 | 790 | 22.2 | 58 | 82 |
| Wolverhampton | Wolverhampton | November 2014 | July 2017 | 90 | 295 | 30.5 | 63 | 82 |
| Worcestershire | Bromsgrove, Malvern Hills, Redditch, Worcester, Wychavon, Wyre Forest | September 2015 | April 2018 | 95 | 315 | 30.2 | 60 | 91 |
| East of England | ||||||||
| Bedford and Bedfordshire | Bedford, Central Bedfordshire | January 2015 | January 2017 | 90 | 265 | 34 | 44 | 81 |
| Hertfordshire | Broxbourne, Dacorum, East Hertfordshire, Hertsmere, North Hertfordshire, St Albans, Stevenage, Three Rivers, Watford, Welwyn Hatfield | September 2011 | February 2016 | 215 | 1455 | 14.8 | 74 | 104 |
| Luton | Luton | September 2015 | August 2017 | 60 | 140 | 42.9 | 38 | 63 |
| Norfolk | Breckland, Broaland, Great Yarmouth, King’s Lynn and West Norfolk, North Norfolk, Norwich, South Norfolk | January 2010 | March 2019 | 545 | 3140 | 17.4 | 155 | 210 |
| North Essex | Braintree, Colchester, Harlow, Tendring | November 2014 | November 2016 | 135 | 430 | 31.4 | 72 | 103 |
| Peterborough and Cambridgeshire | Cambridge, East Cambridgeshire, Fenland, Huntingdonshire, Peterborough, South Cambridgeshire | January 2010 December 2011 | March 2019 | 440 | 2375 | 18.5 | 142 | 182 |
| South-East Essex | Basildon, Castle Point, Rochford, Thurrock | August 2009 February 2015 | October 2016 February 2017 | 145 | 585 | 24.8 | 27 | 65 |
| Southend | Southend-on-Sea | August 2009 | March 2019 | 170 | 625 | 27.2 | 45 | 67 |
| Suffolk | Ipswich, Suffolk Coastal, Waveney | October 2010 August 2013 | March 2018 May 2018 March 2019 | 285 | 870 | 32.8 | 91 | 133 |
| London | ||||||||
| Barking and Dagenham | Barking and Dagenham | November 2010 | November 2015 | 185 | 655 | 28.2 | 45 | 71 |
| Barnet | Barnet | November 2011 | March 2019 | 175 | 360 | 48.6 | 60 | 80 |
| Brent | Brent | June 2014 | July 2016 | 75 | 270 | 27.8 | 38 | 49 |
| Bromley and Bexley | Bexley, Bromley | September 2014 October 2014 | August 2016 March 2019 | 90 | 270 | 33.3 | 49 | 61 |
| Camden | Camden | January 2015 | July 2018 | 30 | 55 | 54.5 | 10 | 19 |
| Croydon | Croydon | October 2010 | March 2019 | 200 | 1010 | 19.8 | 69 | 97 |
| Ealing | Ealing | August 2009 | March 2019 | 220 | 720 | 30.6 | 55 | 70 |
| Enfield | Enfield | November 2013 | March 2019 | 110 | 385 | 28.6 | 46 | 78 |
| Greenwich | Greenwich | April 2014 | March 2019 | 110 | 360 | 30.6 | 70 | 86 |
| Hackney | Hackney | May 2014 | March 2019 | 85 | 300 | 28.3 | 41 | 54 |
| Haringey | Haringey | July 2010 | March 2019 | 200 | 725 | 27.6 | 58 | 91 |
| Hounslow | Hounslow | July 2011 | March 2019 | 155 | 435 | 35.6 | 53 | 76 |
| Islington | Islington | August 2009 | March 2019 | 175 | 470 | 37.2 | 34 | 63 |
| Lambeth | Lambeth | August 2009 | March 2019 | 270 | 950 | 28.4 | 72 | 107 |
| Lewisham | Lewisham | January 2010 | March 2019 | 280 | 950 | 29.5 | 84 | 105 |
| Merton | Merton | September 2013 | March 2019 | 45 | 135 | 33.3 | 25 | 33 |
| Newham | Newham | September 2013 | March 2019 | 90 | 425 | 21.2 | 47 | 68 |
| Southwark | Southwark | August 2009 | March 2019 | 270 | 840 | 32.1 | 73 | 86 |
| Sutton | Sutton | January 2014 | June 2017 | 60 | 160 | 37.5 | 25 | 45 |
| Tower Hamlets | Tower Hamlets | August 2009 | March 2019 | 275 | 645 | 42.6 | 79 | 109 |
| Waltham Forest and Redbridge | Redbridge, Waltham Forest | August 2009 October 2013 | March 2019 | 220 | 1085 | 20.3 | 48 | 73 |
| Wandsworth | Wandsworth | May 2015 | March 2019 | 65 | 95 | 68.4 | 49 | 73 |
| West Central London | Hammersmith and Fulham, Kensington and Chelsea, Westminster | February 2010 | March 2019 | 220 | 725 | 30.3 | 47 | 70 |
| South East | ||||||||
| Berkshire East | Bracknell Forest, Slough, Windsor and Maidenhead | August 2009 | February 2016 | 335 | 855 | 39.2 | 96 | 114 |
| Berkshire West | Reading, West Berkshire, Wokingham | November 2012 | June 2016 | 170 | 610 | 27.9 | 66 | 84 |
| Brighton and Hove | Brighton and Hove | October 2012 | March 2016 | 125 | 270 | 46.3 | 52 | 89 |
| Buckinghamshire | Aylesbury Vale, Chiltern, South Buckinghamshire, Wycombe | July 2012 | March 2019 | 225 | 620 | 36.3 | 93 | 128 |
| East Sussex – East | Hastings, Rother | August 2009 | November 2015 December 2015 | 245 | 795 | 30.8 | 72 | 107 |
| East Sussex – West | Eastbourne, Lewes, Wealden | November 2010 March 2011 December 2011 | June 2015 November 2015 December 2015 | 250 | 620 | 40.3 | 95 | 118 |
| Hampshire | Basingstoke and Deane, Fareham, Gosport, Hart, Havant, Rushmoor | March 2015 April 2015 August 2015 January 2016 | April 2017 March 2018 August 2018 March 2019 | 190 | 360 | 52.8 | 145 | 179 |
| Kent North | Gravesham, Swale, Thanet | February 2012 December 2014 | March 2017 June 2018 | 215 | 1045 | 20.6 | 83 | 101 |
| Kent South | Dover, Maidstone, Shepway, Tonbridge and Malling | February 2013 December 2014 | October 2017 June 2018 | 170 | 660 | 25.8 | 58 | 101 |
| Medway | Medway | August 2009 | December 2015 | 265 | 1280 | 20.7 | 75 | 118 |
| Milton Keynes | Milton Keynes | August 2009 | October 2016 | 165 | 995 | 16.6 | 42 | 67 |
| Oxfordshire | Cherwell, Oxford, South Oxfordshire, Vale of White Horse, West Oxfordshire | February 2010 | March 2019 | 475 | 1730 | 27.5 | 131 | 180 |
| Portsmouth | Portsmouth | November 2011 | March 2019 | 290 | 665 | 43.6 | 111 | 155 |
| Southampton | Southampton | August 2009 | March 2019 | 225 | 1200 | 18.8 | 81 | 98 |
| Surrey | Elmbridge, Epsom and Ewell, Guildford, Mole Valley, Reigate and Banstead, Runnymede, Spelthorne, Surrey Heath, Tandridge, Waverley, Woking | November 2014 | March 2019 | 110 | 420 | 26.2 | 58 | 83 |
| West Sussex | Adur, Arun, Chichester, Crawley, Horsham, Mid Sussex, Worthing, | September 2011 | March 2019 | 265 | 1490 | 17.8 | 101 | 118 |
| South West | ||||||||
| Bath and North East Somerset | Bath and North East Somerset | February 2013 | March 2019 | 100 | 175 | 57.1 | 51 | 67 |
| Bristol and South Gloucestershire | Bristol, city of, South Gloucestershire | May 2014 | March 2019 | 150 | 560 | 26.8 | 91 | 124 |
| Bristol and North Somerset | North Somerset | August 2014 | August 2015 | 30 | 80 | 37.5 | 20 | 27 |
| Cornwall and Isles of Scilly | Cornwall | August 2009 | November 2017 | 470 | 2105 | 22.3 | 130 | 167 |
| Plymouth | Plymouth | August 2009 | March 2019 | 225 | 1310 | 17.2 | 61 | 99 |
| Swindon | Swindon | August 2009 | March 2019 | 340 | 920 | 37 | 96 | 132 |
| Wiltshire | Wiltshire | November 2014 | March 2019 | 85 | 285 | 29.8 | 51 | 65 |
| All mothers enrolled in FNP | Mothers aged 13–19 | Mothers aged 20–24 | ||||
|---|---|---|---|---|---|---|
| N | % | N | % | N | % | |
| Total | 31,425 | 31,260 | 165 | |||
| Living arrangements at enrolment | ||||||
| Alone | 1810 | 5.8 | 1785 | 5.7 | 25 | 15.3 |
| Foster carers/group home/other | 2845 | 9.1 | 2825 | 9.0 | 20 | 12.9 |
| Mother (with or without partner) | 16,750 | 53.3 | 16,710 | 53.4 | 45 | 27.0 |
| Partner (with or without others, not mother) | 6035 | 19.2 | 5990 | 19.2 | 50 | 29.4 |
| Relatives/other adults | 3080 | 9.8 | 3055 | 9.8 | 20 | 12.9 |
| Missing | 905 | 2.9 | – | – | – | – |
| Relationship status at enrolment | ||||||
| In a relationship with biological father | 22,310 | 71.0 | 22,215 | 71.1 | 100 | 60.1 |
| In a relationship with other partner | 990 | 3.1 | – | – | – | – |
| Single | 7220 | 23.0 | 7165 | 22.9 | 55 | 33.7 |
| Missing | 905 | 2.9 | – | – | – | – |
| Care leaver during pregnancy | 1155 | 3.7 | 1140 | 3.6 | 15 | 8.0 |
| CiN, CPP or CLA during pregnancy | 4725 | 15.0 | 4710 | 15.1 | 15 | 9.2 |
| Alcohol or drug use in 2 weeks before enrolment | 1500 | 4.8 | – | – | – | – |
| All mothers | Mothers enrolled in FNP | Mothers never enrolled in FNP | ||||
|---|---|---|---|---|---|---|
| N | % | N | % | N | % | |
| Total | 130,415 | 100 | 31,260 | 100 | 99,150 | 100 |
| Maternal age at delivery (years) | ||||||
| 13–15 | 2685 | 2.1 | 1450 | 4.6 | 1235 | 1.2 |
| 16–17 | 26,065 | 20.0 | 10,370 | 33.2 | 15,690 | 15.8 |
| 18–19 | 72,465 | 55.6 | 15,805 | 50.6 | 56,660 | 57.1 |
| 20a | 29,205 | 22.4 | 3635 | 11.6 | 25565 | 25.8 |
| Ethnicity | ||||||
| White | 109,820 | 84.2 | 26,330 | 84.2 | 83,485 | 84.2 |
| South Asian | 3695 | 2.8 | 670 | 2.1 | 3030 | 3.1 |
| Black | 4650 | 3.6 | 1470 | 4.7 | 3180 | 3.2 |
| Mixed/other | 6840 | 5.2 | 1685 | 5.4 | 5155 | 5.2 |
| Unknown | 5410 | 4.1 | 1110 | 3.5 | 4300 | 4.3 |
| Area-level deprivation (quintile of IMD) | ||||||
| Least deprived | 6810 | 5.2 | 1445 | 4.6 | 5360 | 5.4 |
| 2 | 10,410 | 8.0 | 2305 | 7.4 | 8105 | 8.2 |
| 3 | 17,855 | 13.7 | 4115 | 13.2 | 13,735 | 13.9 |
| 4 | 32,550 | 25 | 7890 | 25.2 | 24,660 | 24.9 |
| Most deprived | 62,630 | 48 | 15,340 | 49.1 | 47,290 | 47.7 |
| Unknown | 160 | 0.1 | – | – | – | – |
| Region | ||||||
| North East | 10,195 | 7.8 | 2160 | 6.9 | 8035 | 8.1 |
| North West | 18,820 | 14.4 | 5035 | 16.1 | 13,785 | 13.9 |
| Yorkshire and Humber | 21,045 | 16.1 | 3730 | 11.9 | 17,315 | 17.5 |
| East Midlands | 13,000 | 10.0 | 2815 | 9.0 | 10,185 | 10.3 |
| West Midlands | 17,160 | 13.2 | 3905 | 12.5 | 13,255 | 13.4 |
| East of England | 11,710 | 9.0 | 2565 | 8.2 | 9150 | 9.2 |
| London | 15,300 | 11.7 | 4740 | 15.2 | 10,560 | 10.7 |
| South East | 16,365 | 12.5 | 4510 | 14.4 | 11,855 | 12.0 |
| South West | 6820 | 5.2 | 1805 | 5.8 | 5015 | 5.1 |
| Year of delivery | ||||||
| 2010 | 10,030 | 7.7 | 2045 | 6.5 | 7985 | 8.1 |
| 2011 | 13,620 | 10.4 | 1860 | 6.0 | 11,760 | 11.9 |
| 2012 | 15,820 | 12.1 | 2865 | 9.2 | 12,960 | 13.1 |
| 2013 | 16,810 | 12.9 | 4070 | 13.0 | 12,735 | 12.8 |
| 2014 | 16,225 | 12.4 | 3590 | 11.5 | 12,635 | 12.7 |
| 2015 | 17,955 | 13.8 | 5110 | 16.3 | 12,845 | 13.0 |
| 2016 | 16,745 | 12.8 | 5260 | 16.8 | 11,485 | 11.6 |
| 2017 | 12,135 | 9.3 | 3145 | 10.1 | 8985 | 9.1 |
| 2018 | 9185 | 7.0 | 2660 | 8.5 | 6525 | 6.6 |
| 2019 | 1890 | 1.4 | 650 | 2.1 | 1240 | 1.2 |
| History of admissions/attendances with diagnoses within 2 years prior to 20 weeks of pregnancy | ||||||
| Adversity (violence, self harm, substance misuse) | 5475 | 4.2 | 2295 | 7.3 | 3185 | 3.2 |
| Violence | 475 | 0.4 | 200 | 0.6 | 280 | 0.3 |
| Self-harm | 4055 | 3.1 | 1755 | 5.6 | 2305 | 2.3 |
| Substance misuse | 4960 | 3.8 | 2065 | 6.6 | 2895 | 2.9 |
| Mental health (exc. self-harm/substance misuse) | 3340 | 2.6 | 1400 | 4.5 | 1935 | 2.0 |
| Mental health (inc. self-harm/substance misuse) | 6550 | 5.0 | 2690 | 8.6 | 3860 | 3.9 |
| Chronic condition (any, exc. mental health) | 11,565 | 8.9 | 3770 | 12.1 | 7800 | 7.9 |
| A&E attendances | 82,320 | 63.1 | 21,985 | 70.3 | 60,335 | 60.8 |
| Repeat A&E attendances (≥ 4) | 21,105 | 16.2 | 6860 | 21.9 | 14,245 | 14.4 |
| Did not attend at least one outpatient appointment | 37,575 | 32.7 | 11,030 | 38.3 | 26,545 | 30.9 |
| Gestational age at antenatal booking appointment | ||||||
| Before 10 weeks | 35,280 | 27.1 | 8390 | 26.8 | 26,890 | 27.1 |
| 10–20 weeks | 47,985 | 36.8 | 11,530 | 36.9 | 36,455 | 36.8 |
| 20 weeks or more | 7315 | 5.6 | 1925 | 6.2 | 5395 | 5.4 |
| Unknown | 39,830 | 30.5 | 9420 | 30.1 | 30,415 | 30.7 |
| Total linked to NPD (social care and education risk factors before 20 weeks of pregnancy available) | 109,360 | 83.9 | 28,145 | 90.0 | 81,210 | 81.9 |
| Ever excluded, in PRU or alternative provision | 32,945 | 25.3 | 10,560 | 33.8 | 22,390 | 22.6 |
| Ever recorded as persistently absent in a term | 40,600 | 31.1 | 15,090 | 48.3 | 25,510 | 25.7 |
| Ever in care | 6955 | 5.3 | 3235 | 10.3 | 3720 | 3.8 |
| Ever had recorded CPP | 3885 | 3.0 | 1990 | 6.4 | 1895 | 1.9 |
| Educational attainment (GCSEs)b | 100,270 | 76.9 | 23,785 | 76.1 | 76,485 | 77.1 |
| Achieved 5 A*–C GCSEs inc. Eng/Maths | 19,920 | 18.4 | 3975 | 14.2 | 15,945 | 19.8 |
| Total linked to Key Stage 2 data | 104,375 | 80.0 | 27,010 | 86.4 | 77,360 | 78.0 |
| Achieved expected level at Key Stage 2 (Maths) | 56,930 | 43.7 | 14,175 | 45.3 | 42,755 | 43.1 |
| Achieved expected level at Key Stage 2 (English) | 69,610 | 53.4 | 17,525 | 56.1 | 52,090 | 52.5 |
| Total linked to NPD Census (FSM, SEN and IDACI available) | 108,365 | 83.1 | 27,995 | 89.6 | 80,365 | 81.1 |
| Ever recorded as having SEN provision | 56,475 | 43.3 | 17,150 | 54.9 | 39,325 | 39.7 |
| Ever recorded as having FSM | 61,315 | 47.0 | 18,525 | 59.3 | 42,795 | 43.2 |
| Ever in bottom IDACI decile | 39,090 | 30.0 | 11,565 | 37.0 | 27,525 | 27.8 |
| All mothers | Mothers enrolled in FNP | Mothers never enrolled in FNP | ||||
|---|---|---|---|---|---|---|
| N | % | N | % | N | % | |
| Total | 4465 | 100 | 165 | 100 | 4305 | 100 |
| Maternal age at delivery (years) | ||||||
| 20–21 | 1095 | 24.5 | 80 | 48.5 | 1015 | 23.6 |
| 22–25 | 3375 | 75.5 | 85 | 51.5 | 3290 | 76.4 |
| Ethnicity | ||||||
| White | 2460 | 55.1 | 85 | 53.4 | 2375 | 55.1 |
| South Asian | 510 | 11.4 | 15 | 8.0 | 495 | 11.5 |
| Black | 395 | 8.8 | 25 | 16.0 | 370 | 8.6 |
| Mixed/other | 405 | 9.1 | 20 | 12.3 | 385 | 8.9 |
| Unknown | 695 | 15.6 | 15 | 10.4 | 680 | 15.8 |
| Year of delivery | ||||||
| 2016 | – | – | – | – | – | – |
| 2017 | 1435 | 32.1 | 50 | 30.3 | 1385 | 32.2 |
| 2018 | 2465 | 55.2 | 85 | 51.5 | 2380 | 55.3 |
| 2019 | 565 | 12.7 | 25 | 15.2 | 540 | 12.5 |
| History of admissions/attendances with diagnoses within 2 years prior to 20 weeks of pregnancy | ||||||
| Adversity | 60 | 1.4 | 10 | 7.4 | 50 | 1.2 |
| Violence | 10 | 0.2 | – | – | – | – |
| Self-harm | 40 | 0.9 | 10 | 4.9 | 35 | 0.8 |
| Substance misuse | 55 | 1.3 | 10 | 7.4 | 45 | 1.0 |
| Mental health (exc. self-harm/substance misuse) | 85 | 1.9 | 10 | 7.4 | 75 | 1.7 |
| Mental health (inc. self-harm/substance misuse) | 110 | 2.5 | 15 | 9.2 | 95 | 2.2 |
| Chronic condition (any, exc. mental health) | 400 | 8.9 | 35 | 21.5 | 360 | 8.4 |
| Repeat A&E attendances (≥ 4) | 595 | 13.3 | 45 | 28.8 | 550 | 12.8 |
| A&E attendances | 2465 | 55.1 | 130 | 80.4 | 2330 | 54.2 |
| Did not attend at least one outpatient appointment | 1185 | 32.2 | 75 | 51.8 | 1110 | 31.4 |
| Gestational age at antenatal booking appointment | ||||||
| Before 10 weeks | 815 | 18.3 | 30 | 18.4 | 785 | 18.3 |
| 10–20 weeks | 1240 | 27.7 | 50 | 31.9 | 1185 | 27.6 |
| 20 weeks or more | 165 | 3.7 | 10 | 6.1 | 155 | 3.6 |
| Unknown | 2245 | 50.3 | 70 | 43.6 | 2175 | 50.6 |
| Total linked to NPD (social care and education risk factors before 20 weeks of pregnancy available) | 2655 | 59.5 | 115 | 69.7 | 2545 | 59.1 |
| Ever excluded, in PRU or alternative provision | 505 | 11.3 | 40 | 24.2 | 465 | 10.8 |
| Ever in care | 85 | 1.9 | 25 | 15.2 | 60 | 1.4 |
| Total linked to NPD Census (FSM, SEN and IDACI available) | 2605 | 58.3 | 110 | 67.5 | 2500 | 58.1 |
| Ever recorded as having SEN provision | 1180 | 26.4 | 85 | 51.5 | 1095 | 25.4 |
| Ever recorded as having FSM | 1240 | 27.8 | 90 | 54.5 | 1150 | 26.7 |
| Ever in bottom IDACI decile | 900 | 20.2 | 50 | 30.3 | 850 | 19.7 |
| Educational attainment (GCSEs)a | 2660 | 59.5 | 115 | 69.9 | 2545 | 59.1 |
| 5 A*–C GCSEs inc. Eng/Maths | 920 | 34.5 | 20 | 19.3 | 895 | 35.2 |
| Did not achieve 5 A*–C GCSEs inc. Eng/Maths | 1740 | 65.5 | 90 | 80.7 | 1650 | 64.8 |
| Linked to Key Stage 2 data | 2465 | 55.2 | 105 | 63.6 | 2365 | 54.9 |
| Achieved expected level at Key Stage 2 (Maths) | 1535 | 34.4 | 45 | 27.3 | 1490 | 34.6 |
| Achieved expected level at Key Stage 2 (English) | 1805 | 40.4 | 55 | 33.3 | 1750 | 40.7 |
| N (%) eligible mothers | N enrolled in FNP | % eligible who were enrolled | N (%) mothers in LAs where FNP was never commissioned | |
|---|---|---|---|---|
| Total | 110,520 | 25,675 | 23.2 | 100,455 |
| Maternal age at birth | ||||
| 13–15 | 2380 (2.2) | 1240 | 52.1 | 2160 (2.2) |
| 16–17 | 22,725 (20.6) | 8720 | 38.4 | 20,040 (19.9) |
| 18–19 | 61,090 (55.3) | 12,875 | 21.1 | 56,310 (56.1) |
| 20 | 24,325 (22.0) | 2840 | 11.7 | 21,945 (21.8) |
| Ethnicity | ||||
| White | 93,730 (84.8) | 21,845 | 23.3 | 88,895 (88.5) |
| South Asian | 3170 (2.9) | 535 | 16.9 | 2325 (2.3) |
| Black | 3970 (3.6) | 1195 | 30.1 | 2705 (2.7) |
| Mixed/other | 5695 (5.2) | 1335 | 23.4 | 3905 (3.9) |
| Unknown | 3950 (3.6) | 770 | 19.5 | 2620 (2.6) |
| IMD (quintile) | ||||
| Least deprived | 5550 (5.0) | 1135 | 20.5 | 8460 (8.4) |
| 2 | 8565 (7.7) | 1820 | 21.2 | 12,825 (12.8) |
| 3 | 14,835 (13.4) | 3330 | 22.4 | 18,065 (18.0) |
| 4 | 27,520 (24.9) | 6430 | 23.4 | 25,630 (25.5) |
| Most deprived | 53,905 (48.8) | 12,820 | 23.8 | 34,890 (34.7) |
| Unknown | 145 (0.1) | 145 | 100 | 580 (0.6) |
| Admission with diagnoses within 2 years before 20 weeks pregnancy | ||||
| Mental health (excluding substance misuse and self-harm) | 2420 (2.2) | 955 | 39.5 | 1950 (1.9) |
| Adversity-related (self-harm, substance misuse, violence) | 4460 (4.0) | 1770 | 39.7 | 3910 (3.9) |
| Any chronic condition | 9580 (8.7) | 3170 | 33.1 | 8105 (8.1) |
| A&E attendance | 68,965 (62.4) | 17,815 | 25.8 | 61,255 (61.0) |
| Gestational age at antenatal booking appointment | ||||
| Before 10 weeks | 29,390 (26.6) | 6810 | 23.2 | 25,840 (25.7) |
| 10–20 weeks | 40,640 (36.8) | 9540 | 23.5 | 36,325 (36.2) |
| 20 weeks or more | 6095 (5.5) | 1515 | 24.9 | 10,180 (10.1) |
| Unknown | 34,390 (31.1) | 7815 | 22.7 | 28,105 (28.0) |
| Linkage with education/social care data in the NPD | ||||
| Linked to NPD | 92,260 (83.5) | 22,980 | 24.9 | 84,385 (84.0) |
| Not linked to NPD | 17,405 (15.7) | 2570 | 14.8 | 14,970 (14.9) |
| Linked to NPD but not to NPD census | 855 (0.8) | 125 | 14.6 | 1100 (1.1) |
| Ever had a CPP or was Looked After before 20 weeks of pregnancya | ||||
| No CPP or Looked After | 85,890 (77.7) | 19,860 | 23.1 | 79,965 (79.6) |
| CPP, but not Looked After | 1685 (1.5) | 800 | 47.5 | 14,970 (14.9) |
| Looked after (and CPP) | 5540 (5.0) | 2445 | 44.1 | 4690 (4.7) |
| Education risk factors before 20 weeks of pregnancy | ||||
| Ever recorded as having SEN provisiona | 46,990 (42.5) | 13,790 | 29.3 | 36,645 (36.5) |
| Ever recorded as receiving FSMa | 50,805 (46.0) | 14,930 | 29.4 | 36,820 (36.7) |
| Ever in IDACI bottom decilea | 32,495 (29.4) | 9220 | 28.4 | 19,280 (19.2) |
| Did not achieve 5 A*–C GCSEsb | 69,345 (62.7) | 16,365 | 23.6 | 64,420 (64.1) |
| Ever excluded, in PRU, or alternative provisiona | 28,105 (25.2) | 8620 | 30.7 | 24,485 (24.4) |
| Ever persistently absent in a term (≥ 10% possible sessions)a | 35,535 (32.2) | 12,725 | 35.8 | 32,275 (32.1) |
| Percentage of eligible mothers enrolled (quartiles) | N FNP sites | N mothers enrolled in FNP | N eligible mothers | Median monthly caseload | Median maximum monthly caseload |
|---|---|---|---|---|---|
| Low-enrolment sites (≤ 21%) | 30 | 9610 | 56,020 | 87 | 126 |
| 21–28% | 30 | 6840 | 28,470 | 67 | 95 |
| 28–36% | 30 | 5170 | 16,530 | 61 | 86 |
| High-enrolment sites (36–67%) | 30 | 4070 | 9500 | 58 | 84 |
| High–enrolment sites (≥ 36%) | Low–enrolment sites (≤ 21%) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N eligible mothers | N enrolled in FNP | % enrolled in FN | Crude OR (95% CI) | Adjusteda OR (95% CI) | N eligible mothers | N enrolled in FNP | % enrolled in FNP | Crude OR (95% CI) | Adjusteda OR (95% CI) | |
| Total | 9495 | 4065 | 42.8 | – | – | 56,020 | 9605 | 17.1 | – | – |
| Maternal age at birth | ||||||||||
| 13–15 | 150 (1.6) | 105 | 70 | 3.62 (2.53 to 5.19) | 2.14 (1.39 to 3.29) | 1,295 (2.3) | 585 | 45.2 | 4.66 (4.16 to 5.23) | 2.60 (2.25 to 3.01) |
| 16–17 | 1785 (18.8) | 1145 | 64.1 | 2.59 (2.32 to 2.90) | 1.92 (1.68 to 2.19) | 11,755 (21.0) | 3610 | 30.7 | 2.52 (2.40 to 2.65) | 1.78 (1.67 to 1.89) |
| 18–19 | 5345 (56.3) | 2200 | 41.2 | 1 (ref) | 1 (ref) | 30,650 (54.7) | 4610 | 15 | 1 (ref) | 1 (ref) |
| 20b | 2215 (23.3) | 615 | 27.8 | 0.53 (0.48 to 0.59) | 0.61 (0.55 to 0.69) | 12,320 (22.0) | 800 | 6.5 | 0.39 (0.36 to 0.42) | 0.47 (0.44 to 0.51) |
| Ethnicity | ||||||||||
| White | 7775 (81.9) | 3425 | 44.1 | 1 (ref) | 1 (ref) | 48,735 (87.0) | 8555 | 17.6 | 1 (ref) | 1 (ref) |
| South Asian | 500 (5.3) | 175 | 35 | 0.61 (0.49 to 0.75) | 0.78 (0.62 to 0.99) | 1,670 (3.0) | 160 | 9.6 | 0.44 (0.37 to 0.52) | 0.63 (0.53 to 0.75) |
| Black | 310 (3.3) | 135 | 43.5 | 0.98 (0.77 to 1.25) | 1.09 (0.84 to 1.42) | 1370 (2.4) | 290 | 21.2 | 1.13 (0.99 to 1.30) | 1.31 (1.13 to 1.53) |
| Mixed/other | 475 (5.0) | 190 | 40 | 0.82 (0.67 to 0.99) | 0.93 (0.75 to 1.14) | 2585 (4.6) | 400 | 15.5 | 0.77 (0.69 to 0.86) | 0.85 (0.75 to 0.95) |
| Unknown | 435 (4.6) | 140 | 32.2 | 0.57 (0.47 to 0.71) | 0.72 (0.58 to 0.90) | 1660 (3.0) | 200 | 12 | 0.61 (0.53 to 0.71) | 0.78 (0.66 to 0.91) |
| IMD (quintile) | ||||||||||
| Least deprived | 745 (7.8) | 265 | 35.6 | 0.77 (0.64 to 0.93) | 0.80 (0.66 to 0.98) | 2410 (4.3) | 300 | 12.4 | 0.79 (0.68 to 0.90) | 0.84 (0.73 to 0.97) |
| 2 | 1040 (11.0) | 425 | 40.9 | 0.98 (0.84 to 1.16) | 1.00 (0.84 to 1.19) | 4395 (7.8) | 620 | 14.1 | 0.89 (0.80 to 0.99) | 0.93 (0.83 to 1.03) |
| 3 | 1540 (16.2) | 640 | 41.6 | 1 (ref) | 1 (ref) | 7465 (13.3) | 1160 | 15.5 | 1 (ref) | 1 (ref) |
| 4 | 2490 (26.2) | 1080 | 43.4 | 1.10 (0.97 to 1.26) | 1.03 (0.90 to 1.18) | 13,100 (23.4) | 2210 | 16.9 | 1.11 (1.02 to 1.20) | 1.06 (0.98 to 1.15) |
| Most deprived | 3650 (38.4) | 1630 | 44.7 | 1.20 (1.05 to 1.36) | 1.07 (0.93 to 1.23) | 28,625 (51.1) | 5295 | 18.5 | 1.25 (1.16 to 1.35) | 1.12 (1.04 to 1.21) |
| Unknown | 25 (0.3) | 25 | 100 | – | – | 25 (0.0) | 25 | 100 | – | – |
| Admission with diagnoses within 2 years before 20 weeks of pregnancy | ||||||||||
| Mental health (excluding substance misuse and self-harm) | 260 (2.7) | 160 | 61.5 | 2.19 (1.70 to 2.84) | 1.22 (0.89 to 1.68) | 1170 (2.1) | 365 | 31.2 | 2.25 (1.98 to 2.55) | 1.46 (1.25 to 1.72) |
| Adversity-related | 420 (4.4) | 270 | 64.3 | 2.55 (2.07 to 3.13) | 1.27 (0.96 to 1.68) | 2245 (4.0) | 705 | 31.4 | 2.33 (2.12 to 2.55) | 1.20 (1.05 to 1.38) |
| Any chronic condition | 945 (10.0) | 540 | 57.1 | 1.88 (1.64 to 2.16) | 1.30 (1.07 to 1.57) | 4700 (8.4) | 1195 | 25.4 | 1.76 (1.64 to 1.88) | 1.14 (1.02 to 1.27) |
| A&E attendances | 6010 (63.3) | 2805 | 46.7 | 1.55 (1.42 to 1.69) | 1.31 (1.19 to 1.44) | 33,925 (60.6) | 6525 | 19.2 | 1.47 (1.40 to 1.54) | 1.27 (1.21 to 1.34) |
| Gestational age at antenatal booking appointment | ||||||||||
| Before 10 weeks | 2190 (23.1) | 950 | 43.4 | 1 (ref) | 1 (ref) | 15,375 (27.4) | 2700 | 17.6 | 1 (ref) | 1 (ref) |
| 10–20 weeks | 3745 (39.4) | 1650 | 44.1 | 1.01 (0.91 to 1.13) | 0.99 (0.88 to 1.12) | 19,430 (34.7) | 3300 | 17 | 0.92 (0.87 to 0.98) | 0.88 (0.82 to 0.93) |
| 20 weeks or more | 830 (8.7) | 345 | 41.6 | 0.97 (0.82 to 1.16) | 0.84 (0.69 to 1.02) | 2555 (4.6) | 390 | 15.3 | 0.79 (0.70 to 0.89) | 0.63 (0.55 to 0.71) |
| Unknown | 2730 (28.8) | 1120 | 41 | 0.89 (0.79 to 1.01) | 0.79 (0.69 to 0.91) | 18,660 (33.3) | 3215 | 17.2 | 0.95 (0.89 to 1.02) | 0.82 (0.77 to 0.88) |
| Linked to NPD | ||||||||||
| Linked to NPD | 7860 (82.8) | 3600 | 45.8 | 1 (ref) | 1 (ref) | 47,410 (84.6) | 8800 | 18.6 | 1 (ref) | 1 (ref) |
| Not linked to NPD | 1555 (16.4) | 440 | 28.3 | 0.44 (0.38 to 0.49) | 0.71 (0.60 to 0.84) | 8190 (14.6) | 765 | 9.3 | 0.43 (0.40 to 0.46) | 0.88 (0.80 to 0.97) |
| Linked to NPD but not to NPD census | 85 (0.9) | 20 | 23.5 | 0.38 (0.23 to 0.63) | 0.66 (0.39 to 1.10) | 420 (0.7) | 40 | 9.5 | 0.46 (0.33 to 0.63) | 0.78 (0.56 to 1.09) |
| Ever had a CPP or was looked after before 20 weeks of pregnancy | ||||||||||
| No CPP or Looked After | 7210 (75.9) | 3155 | 43.8 | 1 (ref) | 1 (ref) | 44,470 (79.4) | 7595 | 17.1 | 1 (ref) | 1 (ref) |
| Looked After (CPP) | 545 (5.7) | 350 | 64.2 | 2.28 (1.90 to 2.74) | 1.63 (1.33 to 1.98) | 2640 (4.7) | 970 | 36.7 | 2.79 (2.57 to 3.03) | 2.07 (1.89 to 2.26) |
| CPP, but not Looked After | 190 (2.0) | 120 | 63.2 | 2.06 (1.53 to 2.77) | 1.08 (0.78 to 1.48) | 720 (1.3) | 275 | 38.2 | 3.04 (2.61 to 3.54) | 1.63 (1.38 to 1.92) |
| Not linked to NPD | 1555 (16.4) | 440 | 28.3 | 0.48 (0.42 to 0.54) | –c | 8190 (14.6) | 765 | 9.3 | 0.48 (0.44 to 0.52) | –c |
| Ever recorded as having SEN before 20 weeks of pregnancy | ||||||||||
| No | 3615 (38.1) | 1425 | 39.4 | 1 (ref) | 1 (ref) | 24,000 (42.8) | 3570 | 14.9 | 1 (ref) | 1 (ref) |
| Yes | 4245 (44.7) | 2175 | 51.2 | 1.60 (1.46 to 1.75) | 1.25 (1.13 to 1.39) | 23,405 (41.8) | 5230 | 22.3 | 1.65 (1.57 to 1.73) | 1.22 (1.15 to 1.28) |
| Not linked to NPD | 1555 (16.4) | 440 | 28.3 | 0.56 (0.49 to 0.65) | –c | 8190 (14.6) | 765 | 9.3 | 0.56 (0.52 to 0.61) | –c |
| Linked to NPD but not to NPD census | 85 (0.9) | 20 | 23.5 | 0.50 (0.30 to 0.82) | –c | 420 (0.7) | 40 | 9.5 | 0.60 (0.43 to 0.82) | –c |
| Ever recorded as receiving FSM before 20 weeks of pregnancy | ||||||||||
| No | 3370 (35.5) | 1330 | 39.5 | 1 (ref) | 1 (ref) | 22,330 (39.9) | 3055 | 13.7 | 1 (ref) | 1 (ref) |
| Yes | 4490 (47.3) | 2270 | 50.6 | 1.54 (1.40 to 1.69) | 1.15 (1.04 to 1.28) | 25,080 (44.8) | 5740 | 22.9 | 1.84 (1.75 to 1.93) | 1.24 (1.17 to 1.31) |
| Not linked to NPD | 1555 (16.4) | 440 | 28.3 | 0.56 (0.49 to 0.65) | –c | 8190 (14.6) | 765 | 9.3 | 0.61 (0.56 to 0.67) | –c |
| Linked to NPD but not to NPD census | 85 (0.9) | 20 | 23.5 | 0.49 (0.30 to 0.81) | –c | 420 (0.7) | 40 | 9.5 | 0.66 (0.48 to 0.91) | –c |
| Ever in IDACI bottom decile before 20 weeks of pregnancy | ||||||||||
| No | 5540 (58.3) | 2445 | 44.1 | 1 (ref) | 1 (ref) | 31,310 (55.9) | 5235 | 16.7 | 1 (ref) | 1 (ref) |
| Yes | 2320 (24.4) | 1160 | 50 | 1.22 (1.10 to 1.36) | 0.99 (0.88 to 1.11) | 16,100 (28.7) | 3565 | 22.1 | 1.38 (1.31 to 1.45) | 1.05 (1.00 to 1.12) |
| Not linked to NPD | 1555 (16.4) | 440 | 28.3 | 0.47 (0.41 to 0.54) | –c | 8190 (14.6) | 765 | 9.3 | 0.49 (0.45 to 0.53) | –c |
| Linked to NPD but not to NPD census | 85 (0.9) | 20 | 23.5 | 0.41 (0.25 to 0.67) | –c | 420 (0.7) | 40 | 9.5 | 0.52 (0.38 to 0.72) | –c |
| Educational attainment before 20 weeks of pregnancy | ||||||||||
| Did not achieve 5 A*–C GCSEs | 5830 (61.4) | 2660 | 45.6 | 1 (ref) | 1 (ref) | 35,715 (63.8) | 6130 | 17.2 | 1 (ref) | 1 (ref) |
| Achieved 5 A*–C GCSEs | 1615 (17.0) | 595 | 36.8 | 0.69 (0.61 to 0.77) | 0.92 (0.81 to 1.04) | 8470 (15.1) | 1150 | 13.6 | 0.76 (0.71 to 0.81) | 1.06 (0.98 to 1.14) |
| Not linked to NPD | 1555 (16.4) | 440 | 28.3 | 0.44 (0.39 to 0.50) | –c | 8190 (14.6) | 765 | 9.3 | 0.47 (0.44 to 0.51) | –c |
| Had not attempted GCSEs | 500 (5.3) | 370 | 74 | 3.53 (2.86 to 4.35) | 1.47 (1.13 to 1.90) | 3645 (6.5) | 1560 | 42.8 | 3.62 (3.37 to 3.89) | 1.58 (1.44 to 1.73) |
| Ever excluded, in PRU, or alternative provision | ||||||||||
| No | 5460 (57.5) | 2320 | 42.5 | 1 (ref) | 1 (ref) | 33,555 (59.9) | 5470 | 16.3 | 1 (ref) | 1 (ref) |
| Yes | 2480 (26.1) | 1300 | 52.4 | 1.50 (1.36 to 1.65) | 1.04 (0.93 to 1.16) | 14,275 (25.5) | 3370 | 23.6 | 1.58 (1.51 to 1.66) | 1.03 (0.97 to 1.08) |
| Not linked to NPD | 1555 (16.4) | 440 | 28.3 | 0.50 (0.44 to 0.57) | –c | 8190 (14.6) | 765 | 9.3 | 0.50 (0.46 to 0.55) | –c |
| Ever persistently absent in a term (≥ 10% possible sessions) | ||||||||||
| No | 5140 (54.1) | 1925 | 37.5 | 1 (ref) | 1 (ref) | 29,320 (52.3) | 3590 | 12.2 | 1 (ref) | 1 (ref) |
| Yes | 2805 (29.5) | 1700 | 60.6 | 2.64 (2.40 to 2.90) | 1.47 (1.31 to 1.66) | 18,510 (33.0) | 5250 | 28.4 | 2.87 (2.73 to 3.01) | 1.44 (1.36 to 1.53) |
| Not linked to NPD | 1555 (16.4) | 440 | 28.3 | 0.62 (0.54 to 0.70) | –c | 8190 (14.6) | 765 | 9.3 | 0.70 (0.65 to 0.76) | –c |
FIGURE 24.
Adjusted ORs and 95% CIs comparing FNP enrolment by maternal age, stratified by region.
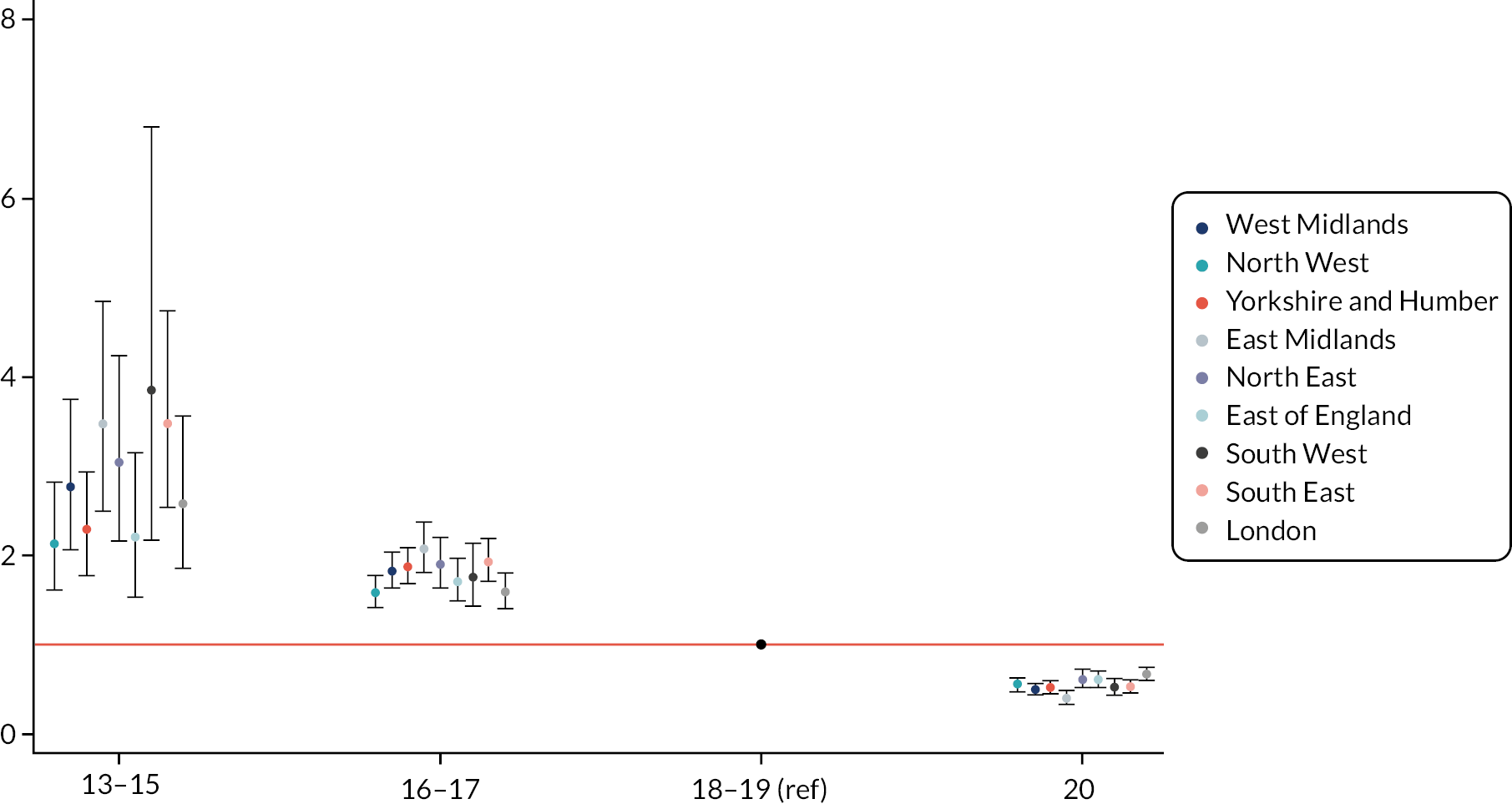
FIGURE 25.
Adjusted ORs and 95% CIs comparing FNP enrolment by ethnic group, stratified by region.
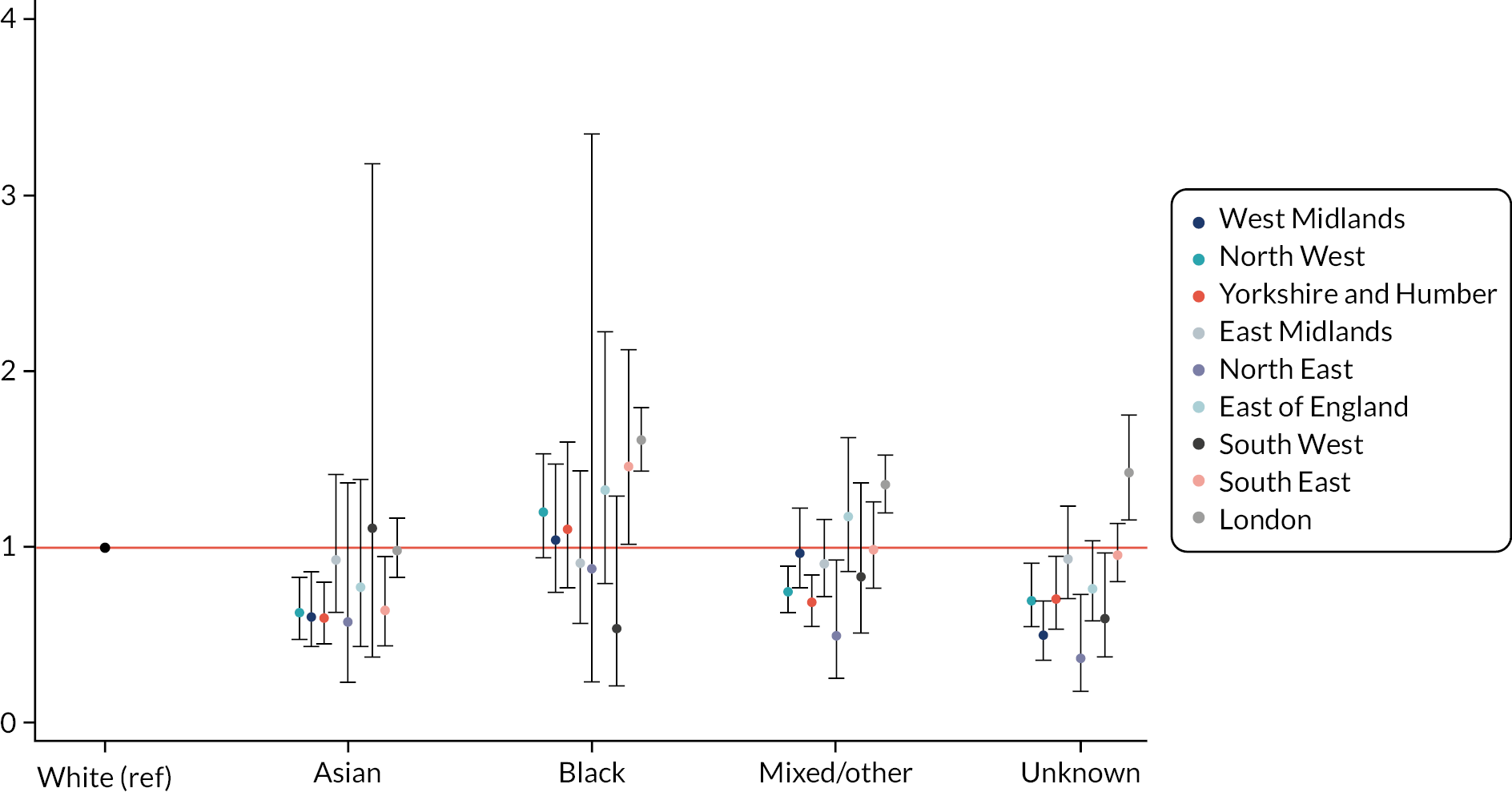
Risk factors for enrolment in the Family Nurse Partnership for mothers aged 20–24 at last menstrual period
Of the 4470 mothers aged 20–24 at LMP living in a LA where 20- to 24-year-old mothers were recruited at the time of their first antenatal appointment, 165 were enrolled in the FNP, accounting for 3.7% (95% CI 3.1% to 4.2%) of eligible mothers (see Table 12). This percentage varied between 2.2% in Cornwall and 10.9% in Haringey.
FIGURE 26.
Adjusted ORs and 95% CIs comparing FNP enrolment by area-level deprivation (quintile of IMD), stratified by region.
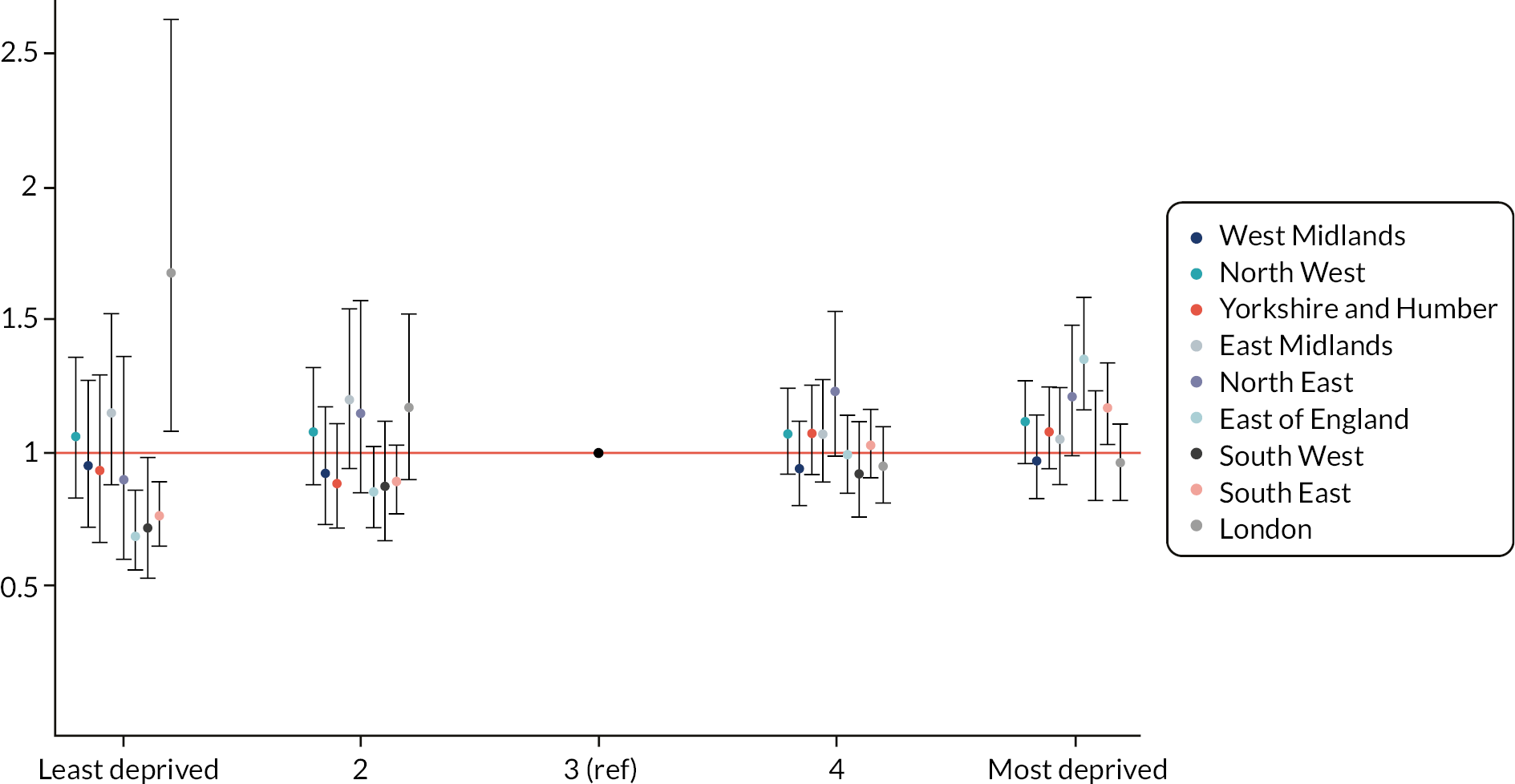
| N eligible mothers | N enrolled in FNP | % enrolled in FNP | Crude OR (95% CI) | Adjusteda OR (95% CI) | |
|---|---|---|---|---|---|
| Total | 4470 | 165 | 3.7 | – | – |
| Maternal age at birth | |||||
| 20–21 | 1095 (24.5) | 80 | 7.31 | 1 (ref) | 1 (ref) |
| 22–25b | 3375 (75.6) | 85 | 2.52 | 0.32 (0.23 to 0.43) | 0.41 (0.29 to 0.58) |
| Ethnicity | |||||
| White | 2460 (55.1) | 85 | 3.46 | 1 (ref) | 1 (ref) |
| South Asian | 510 (11.4) | 15 | 2.94 | 0.87 (0.47 to 1.63) | 1.20 (0.62 to 2.33) |
| Black | 395 (8.8) | 25 | 6.33 | 2.07 (1.24 to 3.45) | 1.71 (0.97 to 3.01) |
| Mixed/other | 405 (9.1) | 20 | 4.94 | 1.54 (0.91 to 2.62) | 1.57 (0.90 to 2.77) |
| Unknown | 695 (15.6) | 15 | 2.16 | 0.71 (0.41 to 1.22) | 1.15 (0.64 to 2.07) |
| IMD (quintile) | |||||
| Least deprived or 2c | 410 (9.2) | 10 | 2.44 | 1.04 (0.49 to 2.17) | 1.20 (0.55 to 2.63) |
| 3 | 835 (18.7) | 20 | 2.4 | 1 (ref) | 1 (ref) |
| 4 | 1345 (30.1) | 40 | 2.97 | 1.29 (0.75 to 2.23) | 1.06 (0.60 to 1.87) |
| Most deprived | 1875 (42.0) | 85 | 4.53 | 2.08 (1.24 to 3.47) | 1.45 (0.83 to 2.52) |
| Admission with diagnoses within 2 years before 20 weeks of pregnancy | |||||
| Adversity-related | 60 (1.3) | 10 | 16.67 | 6.64 (3.43 to 12.88) | 2.20 (0.90 to 5.35) |
| Mental health (excluding substance misuse and self-harm) | 85 (1.9) | 10 | 11.76 | 4.51 (2.37 to 8.58) | 0.76 (0.31 to 1.89) |
| Any chronic condition | 315 (7.1) | 30 | 9.52 | 3.44 (2.25 to 5.26) | 1.86 (1.02 to 3.39) |
| A&E attendance | 2465 (55.2) | 130 | 5.27 | 3.57 (2.40 to 5.30) | 2.41 (1.57 to 3.68) |
| Gestational age at antenatal booking appointment | |||||
| Before 10 weeks | 815 (18.3) | 30 | 3.7 | 1 (ref) | 1 (ref) |
| 10–20 weeks | 1240 (27.8) | 50 | 4 | 1.03 (0.64 to 1.65) | 0.98 (0.60 to 1.61) |
| 20 weeks or more | 165 (3.7) | 10 | 6.1 | 1.53 (0.72 to 3.23) | 1.90 (0.84 to 4.32) |
| Unknown | 2245 (50.3) | 70 | 3.1 | 0.82 (0.51 to 1.32) | 0.77 (0.46 to 1.28) |
| Linked to NPD | |||||
| Linked to NPD | 2610 (58.5) | 110 | 4.2 | 1 (ref) | 1 (ref) |
| Not linked to NPD | 1810 (40.5) | 50 | 2.8 | 0.54 (0.38 to 0.77) | 2.41 (1.22 to 4.75) |
| Linked to NPD but not to NPD census | 50 (1.1) | – | – | 0.72 (0.17 to 3.08) | 2.79 (0.58 to 13.35) |
| Ever had a CPP or was looked after | |||||
| No CPP or Looked After before 20 weeks of pregnancy | 2560 (57.3) | 90 | 3.5 | 1 (ref) | 1 (ref) |
| Looked After before 20 weeks of pregnancy | 85 (1.9) | 25 | 29.4 | 10.53 (6.12 to 18.10) | 6.60 (3.58 to 12.18) |
| CPP before 20 weeks of pregnancy, but not Looked After | 15 (0.3) | – | – | 4.52 (0.99 to 20.68) | 1.78 (0.35 to 9.01) |
| Ever recorded as having SEN provision | |||||
| No | 1430 (32.0) | 30 | 2.1 | 1 (ref) | 1 (ref) |
| Yes | 1180 (26.4) | 85 | 7.2 | 3.81 (2.46 to 5.90) | 2.04 (1.24 to 3.35) |
| Ever recorded as receiving FSM | |||||
| No | 1370 (30.7) | 25 | 1.8 | 1 (ref) | 1 (ref) |
| Yes | 1240 (27.8) | 90 | 7.3 | 4.37 (2.74 to 6.96) | 2.86 (1.72 to 4.76) |
| Ever in IDACI bottom decile | |||||
| No | 1710 (38.3) | 60 | 3.5 | 1 (ref) | 1 (ref) |
| Yes | 900 (20.2) | 50 | 5.6 | 1.64 (1.09 to 2.45) | 0.77 (0.48 to 1.22) |
| Educational attainment | |||||
| Did not achieve 5 A*–C GCSEs prior to 20 weeks of pregnancy | 1740 (39.0) | 90 | 5.2 | 1 (ref) | 1 (ref) |
| 5 A*–C GCSEs gained prior to 20 weeks | 915 (20.5) | 20 | 2.2 | 0.43 (0.27 to 0.69) | 0.97 (0.56 to 1.67) |
| Ever excluded, in PRU, or alternative provision | |||||
| No | 2155 (48.3) | 75 | 3.5 | 1 (ref) | 1 (ref) |
| Yes | 505 (11.3) | 40 | 7.9 | 2.14 (1.43 to 3.22) | 1.03 (0.65 to 1.65) |
FIGURE 27.
Adjusted funnel plots of variation in FNP enrolment among eligible first-time adolescent mothers across FNP sites, by maternal age at birth. (a) Mothers aged 13–17 at birth; (b) mothers aged 18–20 at birth), births between April 2010 and March 2017. Note: adjusted percentages of eligible mothers enrolled adjust for all maternal risk factors (maternal age at birth, ethnicity, area-level deprivation quintile, any unplanned mental health-related, adversity-related, and chronic condition-related hospital admission in 2 years before 20 weeks of pregnancy, and any A&E attendance in 2 years before 20 weeks of pregnancy).
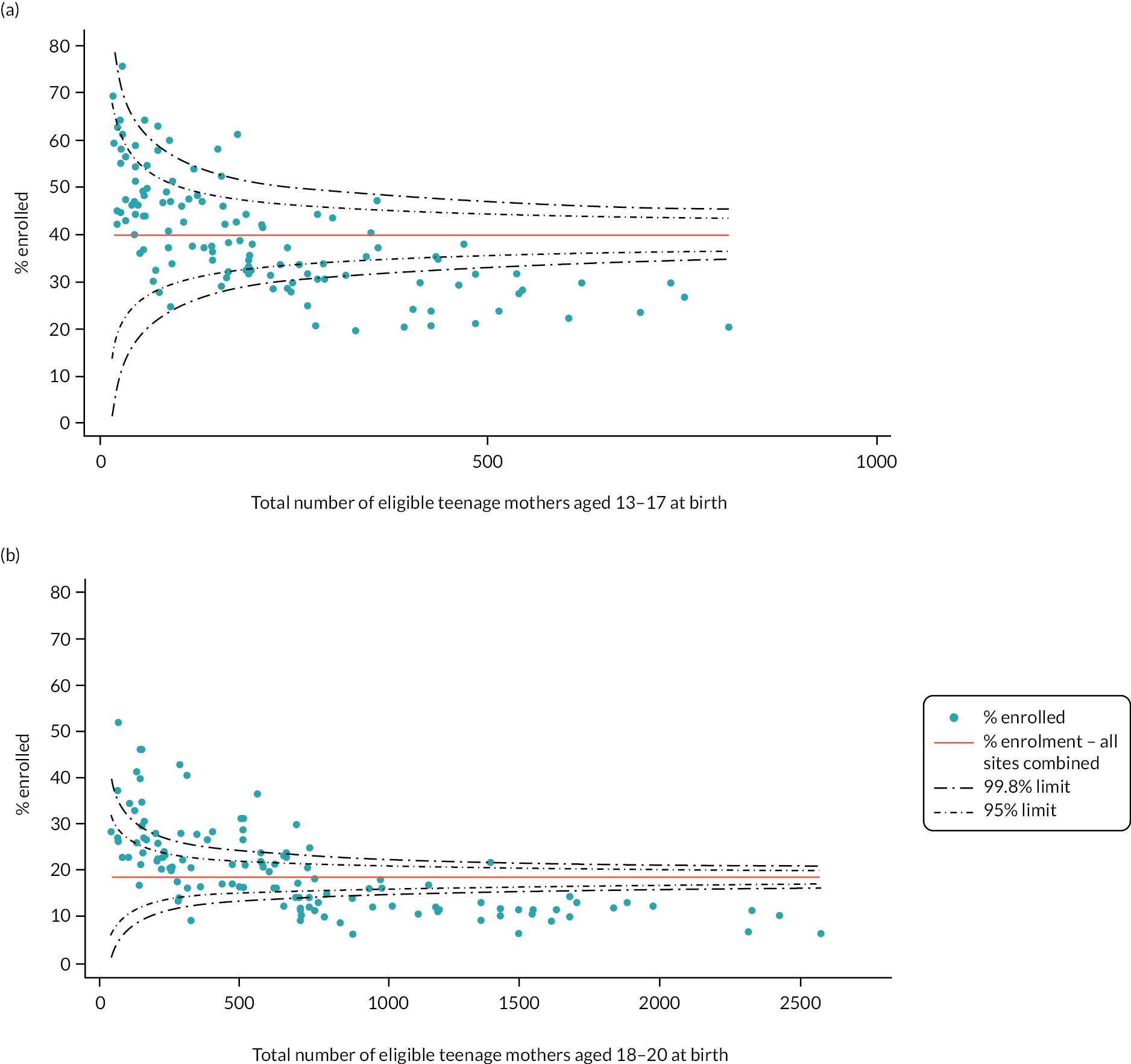
Similar to the 13–19 age group, older mothers were less likely to be enrolled than younger ones. Women with recent A&E attendances were also more likely to be enrolled than those without recent A&E attendances [OR 2.4 (95% CI 1.6 to 3.7)]. Mothers who were Looked After had 6.6 (95% CI 3.6 to 12.2) times higher odds of being enrolled in the FNP, and mothers ever recorded as having SEN provision and receiving FSM had 2–3 times higher odds of being enrolled in the FNP.
Appendix 6 Maternal and child outcomes according to maternal risk factors at enrolment or 20 weeks of pregnancy
| Discharge to social services at birth | Unplanned admission for maltreatment or injury – 2 years | Social care data | Ever Looked After | Ever CPP | Ever had a CiN referral | Unplanned admission for maltreatment or injury – 7 years | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | N with outcome | % | Total | N with outcome | % | Total | N with outcome | % | N with outcome | % | N with outcome | % | Total | N with outcome | % | |
| Total | 128,270 | 630 | 0.5 | 108,675 | 5790 | 5.3 | 17,605 | 355 | 2.0 | 1840 | 2.1 | 3890 | 22.1 | 27,015 | 3175 | 11.8 |
| FNP participation | ||||||||||||||||
| No | 97,085 | 375 | 0.4 | 83,040 | 4090 | 4.9 | 14,355 | 270 | 1.9 | 1345 | 2.0 | 3055 | 21.3 | 22,640 | 2575 | 11.4 |
| Yes | 31,190 | 255 | 0.8 | 25,630 | 1700 | 6.6 | 3250 | 85 | 2.6 | 495 | 2.3 | 835 | 25.7 | 4375 | 600 | 13.7 |
| Maternal age (years) | ||||||||||||||||
| 13–15 | 2645 | 55 | 2.0 | 2345 | 140 | 6 | 360 | 15 | 3.6 | 60 | 3.2 | 120 | 33.5 | 585 | 80 | 13.8 |
| 16–17 | 25,630 | 205 | 0.8 | 22,345 | 1355 | 6.1 | 3765 | 125 | 3.4 | 570 | 3.1 | 1120 | 29.7 | 5825 | 760 | 13.0 |
| 18–19 | 71,150 | 305 | 0.4 | 59,950 | 3215 | 5.4 | 9720 | 185 | 1.9 | 950 | 1.9 | 2065 | 21.2 | 14,740 | 1745 | 11.8 |
| 20a | 28,845 | 65 | 0.2 | 24,030 | 1080 | 4.5 | 3760 | 35 | 0.9 | 255 | 1.3 | 585 | 15.6 | 5870 | 590 | 10.1 |
| Ethnicity | ||||||||||||||||
| White | 108,110 | 535 | 0.5 | 92,255 | 5100 | 5.5 | 15,290 | 320 | 2.1 | 1675 | 2.2 | 3485 | 22.8 | 23,260 | 2825 | 12.1 |
| South Asian | 3620 | 15 | 0.4 | 3100 | 115 | 3.7 | 430 | – | – | 20 | 0.9 | 60 | 14.4 | 670 | 55 | 8.3 |
| Black | 4545 | 35 | 0.8 | 3880 | 170 | 4.4 | 740 | 15 | 2.0 | 60 | 1.9 | 135 | 18.2 | 1190 | 110 | 9.2 |
| Mixed/other | 6675 | 25 | 0.4 | 5560 | 245 | 4.4 | 785 | 15 | 2.2 | 60 | 1.5 | 165 | 21.1 | 1310 | 135 | 10.2 |
| Unknown | 5315 | 25 | 0.5 | 3880 | 160 | 4.1 | 355 | – | – | 20 | 0.7 | 45 | 12.6 | 585 | 50 | 8.6 |
| Area-level deprivation | ||||||||||||||||
| Least deprived | 6725 | 25 | 0.4 | 5475 | 260 | 4.7 | 745 | – | – | 40 | 0.9 | – | – | 1105 | 115 | 10.5 |
| 2 | 10,265 | 40 | 0.4 | 8435 | 430 | 5.1 | 1170 | – | – | 85 | 1.2 | 190 | 16.2 | 1820 | 215 | 11.9 |
| 3 | 17,610 | 85 | 0.5 | 14,620 | 755 | 5.2 | 2140 | 40 | 1.8 | 200 | 1.7 | 415 | 19.5 | 3320 | 345 | 10.4 |
| 4 | 31,955 | 150 | 0.5 | 27,000 | 1420 | 5.3 | 4305 | 70 | 1.6 | 430 | 1.9 | 855 | 19.9 | 6705 | 770 | 11.5 |
| Most deprived | 61,550 | 325 | 0.5 | 52,995 | 2915 | 5.5 | 9235 | 230 | 2.5 | 1080 | 2.5 | – | – | 14,050 | 1725 | 12.3 |
| Maternal history of admissions with diagnoses within 2 years prior to 20 weeks of pregnancy | ||||||||||||||||
| Adversity | 5405 | 90 | 1.7 | 4405 | 375 | 8.5 | 630 | 30 | 4.6 | 145 | 4.1 | 240 | 38.3 | 1000 | 155 | 15.7 |
| Violence | 475 | 20 | 4 | 400 | 40 | 9.8 | 75 | – | – | 15 | 4.2 | 30 | 39.2 | 125 | 15 | 12.1 |
| Self-harm | 4000 | 70 | 1.8 | 3235 | 290 | 9 | 440 | 15 | 3.9 | 100 | 3.8 | 165 | 37.4 | 700 | 120 | 17.4 |
| Substance misuse | 4895 | 75 | 1.5 | 3980 | 335 | 8.4 | 555 | 25 | 4.7 | 130 | 4 | 210 | 38 | 885 | 140 | 15.6 |
| Mental health (exc. self-harm/substance misuse) | 3290 | 60 | 1.9 | 2380 | 230 | 9.7 | 215 | – | – | 50 | 2.7 | 70 | 33.3 | 365 | 65 | 17.4 |
| Mental health (any) | 6460 | 110 | 1.7 | 5075 | 435 | 8.6 | 650 | 30 | 4.6 | 155 | 3.7 | 245 | 37.7 | 1045 | 175 | 16.9 |
| A&E visits | 81,010 | 485 | 0.6 | 67,860 | 4130 | 6.1 | 10,210 | 245 | 2.4 | 1305 | 2.3 | 2535 | 24.8 | 15,870 | 2075 | 13.1 |
| Repeated A&E visits (≥ 4) | 20,750 | 230 | 1.1 | 16,750 | 1390 | 8.3 | 2005 | 75 | 3.7 | 415 | 3 | 655 | 32.8 | 3315 | 575 | 17.4 |
| Did not attend ≥ 1 outpatient appointment | 36,945 | 280 | 0.8 | 30,400 | 1930 | 6.3 | 4260 | 125 | 3 | 635 | 2.6 | 1120 | 26.3 | 6660 | 870 | 13.1 |
| Gestational age at booking | ||||||||||||||||
| Before 10 weeks | 34,850 | 115 | 0.3 | 29,020 | 1635 | 5.6 | 4130 | 75 | 1.8 | 475 | 1.9 | 910 | 22 | 6565 | 795 | 12.1 |
| 10–20 weeks | 47,480 | 190 | 0.4 | 40,200 | 2150 | 5.3 | 6940 | 135 | 2 | 685 | 2.1 | 1510 | 21.8 | 10,335 | 1225 | 11.8 |
| 20 weeks or more | 7245 | 55 | 0.8 | 6035 | 295 | 4.9 | 1130 | 20 | 1.9 | 115 | 2.4 | 265 | 23.6 | 1725 | 200 | 11.5 |
| Unknown | 38,695 | 270 | 0.7 | 33,420 | 1715 | 5.1 | 5405 | 125 | 2.3 | 565 | 2.1 | 1200 | 22.2 | 8390 | 960 | 11.4 |
| Social care and educational characteristics before 20 weeks of pregnancy | ||||||||||||||||
| CL A | 6835 | 225 | 3.3 | 5450 | 435 | 7.9 | 615 | 55 | 9.1 | 195 | 4.5 | 265 | 43.2 | 1015 | 145 | 14.2 |
| CPP | 3820 | 100 | 2.6 | 2450 | 175 | 7.1 | 35 | – | – | 35 | 1.9 | 15 | 42.9 | 90 | 10 | 13.5 |
| SEN | 55,535 | 415 | 0.8 | 46,190 | 2855 | 6.2 | 5650 | 190 | 3.4 | 1015 | 2.6 | 1695 | 30 | 8940 | 1195 | 13.4 |
| FSM | 60,365 | 375 | 0.6 | 50,020 | 2960 | 5.9 | 5965 | 170 | 2.9 | 995 | 2.4 | 1665 | 28 | 9345 | 1200 | 12.8 |
| Bottom IDACI decile | 38,490 | 245 | 0.6 | 32,005 | 1870 | 5.8 | 4795 | 115 | 2.4 | 645 | 2.4 | 1245 | 26 | 7280 | 915 | 12.6 |
| Excluded, in PRU or alternative provision | 32,470 | 300 | 0.9 | 27,460 | 1745 | 6.4 | 3630 | 150 | 4.2 | 720 | 3.1 | 1165 | 32.1 | 5720 | 775 | 13.6 |
| Persistently absent in a term | 40,010 | 285 | 0.7 | 34,825 | 2120 | 6.1 | 6100 | 190 | 3.1 | 855 | 2.9 | 1680 | 27.6 | 9270 | 1235 | 13.3 |
| Did not achieve 5 A*–C GCSEs prior to 20 weeks | 80,555 | 425 | 0.5 | 68,280 | 3840 | 5.6 | 12,045 | 265 | 2.2 | 1375 | 2.3 | 2815 | 23.4 | 17,800 | 2180 | 12.2 |
| Did not achieve expected levels at KS2 Maths | 46,680 | 335 | 0.7 | 40,135 | 2405 | 6 | 6850 | 190 | 2.8 | 925 | 2.7 | 1795 | 26.2 | 10,245 | 1330 | 13 |
| Did not achieve expected levels at KS2 English | 34,210 | 295 | 0.9 | 30,005 | 1865 | 6.2 | 5495 | 160 | 2.9 | 790 | 3.1 | 1485 | 27 | 8110 | 1075 | 13.2 |
| Preterm birth (< 37 weeks) | Low birthweight (< 2500 g) | Hospital data | ≥ 1 unplanned admissions for any diagnosis | ≥ 1 A&E attendance | ≥ 1 outpatient referral | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | N with outcome | % | Total | N with outcome | % | Total | N with outcome | % | N with outcome | % | N with outcome | % | |
| Total | 119,840 | 10,040 | 7.8 | 120,640 | 9615 | 7.5 | 108,675 | 40,140 | 36.9 | 77,725 | 71.5 | 55,630 | 51.2 |
| FNP participation | |||||||||||||
| 0 | 91,680 | 7280 | 7.5 | 92,210 | 6990 | 7.2 | 83,040 | 29,780 | 35.9 | 58,155 | 70.0 | 41,320 | 49.8 |
| 1 | 28,160 | 2760 | 8.8 | 28,430 | 2625 | 8.4 | 25,630 | 10,360 | 40.4 | 19,570 | 76.3 | 14,310 | 55.8 |
| Maternal age | |||||||||||||
| 13–15 | 2420 | 285 | 10.7 | 2455 | 260 | 9.9 | 2345 | 835 | 35.6 | 1685 | 71.8 | 1260 | 53.7 |
| 16–17 | 23,640 | 2290 | 8.9 | 23,905 | 2090 | 8.2 | 22,345 | 8665 | 38.8 | 16,315 | 73.0 | 11,590 | 51.9 |
| 18–19 | 65,320 | 5475 | 7.7 | 65,985 | 5320 | 7.5 | 59,950 | 22,170 | 37.0 | 42,880 | 71.5 | 30,585 | 51.0 |
| 20a | 28,460 | 1990 | 6.9 | 28,295 | 1945 | 6.7 | 24,030 | 8465 | 35.2 | 16,840 | 70.1 | 12,190 | 50.7 |
| Ethnicity | |||||||||||||
| White | 101,515 | 8500 | 7.9 | 102,120 | 7895 | 7.3 | 92,255 | 35,270 | 38.2 | 66,135 | 71.7 | 47,775 | 51.8 |
| South Asian | 3315 | 310 | 8.6 | 3305 | 385 | 10.7 | 3100 | 970 | 31.3 | 2240 | 72.2 | 1595 | 51.5 |
| Black | 4130 | 360 | 7.9 | 4195 | 400 | 8.8 | 3880 | 1065 | 27.4 | 2840 | 73.2 | 1760 | 45.4 |
| Mixed/other | 6040 | 535 | 8,0 | 6125 | 580 | 8.7 | 5560 | 1730 | 31.1 | 4055 | 73.0 | 2670 | 48.0 |
| Unknown | 4835 | 330 | 6.2 | 4890 | 355 | 6.7 | 3880 | 1105 | 28.5 | 2450 | 63.2 | 1830 | 47.2 |
| Area-level deprivation | |||||||||||||
| Least deprived | 6280 | 495 | 7.3 | 6370 | 415 | 6.2 | 5475 | 1885 | 34.4 | 3670 | 67.0 | 2855 | 52.1 |
| 2 | 9550 | 750 | 7.3 | 9655 | 650 | 6.3 | 8435 | 3060 | 36.3 | 5885 | 69.8 | 4375 | 51.9 |
| 3 | 16,325 | 1360 | 7.7 | 16,525 | 1185 | 6.7 | 14,620 | 5365 | 36.7 | 10,120 | 69.2 | 7590 | 51.9 |
| 4 | 29,730 | 2540 | 8.0 | 29,980 | 2360 | 7.4 | 27,000 | 9905 | 36.7 | 19,155 | 70.9 | 13,705 | 50.8 |
| Most deprived | 57,810 | 4875 | 7.9 | 57,970 | 4980 | 8.1 | 52,995 | 19,860 | 37.5 | 38,770 | 73.2 | 27,025 | 51.0 |
| History of admissions with diagnoses within 2 years prior to 20 weeks of pregnancy | |||||||||||||
| Adversity | 5075 | 555 | 10.2 | 5100 | 510 | 9.4 | 4405 | 2090 | 47.4 | 3485 | 79.2 | 2660 | 60.4 |
| Violence | 440 | 55 | 11.4 | 445 | 60 | 12.5 | 400 | 195 | 48.6 | 305 | 76.9 | 245 | 61.3 |
| Self-harm | 3750 | 395 | 9.9 | 3770 | 350 | 8.8 | 3235 | 1525 | 47.1 | 2570 | 79.4 | 1975 | 61.1 |
| Substance misuse | 4590 | 495 | 10.1 | 4615 | 455 | 9.3 | 3980 | 1900 | 47.7 | 3150 | 79.1 | 2410 | 60.6 |
| Mental health (exc. self-harm/substance misuse) | 3090 | 365 | 11.1 | 3115 | 345 | 10.5 | 2380 | 1185 | 49.9 | 1925 | 80.9 | 1525 | 64.1 |
| Mental health (any) | 6065 | 665 | 10.3 | 6100 | 610 | 9.5 | 5075 | 2435 | 48.0 | 4025 | 79.4 | 3100 | 61.1 |
| Chronic condition (any, exc. mental health) | 14,350 | 1605 | 11.2 | 14,430 | 1395 | 9.7 | 12,515 | 5975 | 47.7 | 9885 | 79.0 | 7515 | 60.0 |
| A&E visits | 75,670 | 6790 | 8.4 | 76,190 | 6510 | 8.0 | 67,860 | 27,770 | 40.9 | 52,125 | 76.8 | 36,775 | 54.2 |
| Repeated A&E visits (≥ 4) | 19,310 | 2025 | 9.8 | 19,430 | 1915 | 9.2 | 16,750 | 8270 | 49.4 | 14,260 | 85.1 | 10,175 | 60.7 |
| Did not attend ≥ 4 1 outpatient appointment | 34,290 | 3440 | 9.3 | 34,560 | 3240 | 8.8 | 30,400 | 12,285 | 40.4 | 23,080 | 75.9 | 16,755 | 55.1 |
| Gestational age at booking | |||||||||||||
| Before 10 weeks | 34,845 | 2925 | 8.4 | 34,745 | 2685 | 7.7 | 29,020 | 11,550 | 39.8 | 21,095 | 72.7 | 15,205 | 52.4 |
| 10–20 weeks | 47,455 | 3530 | 7.4 | 47,345 | 3620 | 7.6 | 40,200 | 14,860 | 37.0 | 28,785 | 71.6 | 19,995 | 49.7 |
| 20 weeks or more | 7240 | 750 | 10.3 | 7220 | 690 | 9.5 | 6035 | 2115 | 35.1 | 4150 | 68.7 | 2960 | 49.0 |
| Unknown | 30,300 | 2835 | 7.3 | 31,330 | 2615 | 6.8 | 33,420 | 11,615 | 34.8 | 23,695 | 70.9 | 17,470 | 52.3 |
| Social care and educational characteristics before 20 weeks of pregnancy | |||||||||||||
| CLA | 6305 | 660 | 9.7 | 6345 | 685 | 10.0 | 5450 | 2235 | 41.0 | 4080 | 74.9 | 3220 | 59.1 |
| CPP | 3535 | 395 | 10.3 | 3560 | 430 | 11.2 | 2450 | 990 | 40.5 | 1845 | 75.4 | 1585 | 61.6 |
| SEN | 51,580 | 4705 | 8.5 | 51,940 | 4670 | 8.4 | 46,190 | 18,070 | 39.1 | 34,065 | 73.7 | 1455 | 59.4 |
| FSM | 56,100 | 4970 | 8.2 | 56,525 | 5045 | 8.4 | 50,020 | 19,360 | 38.7 | 36,840 | 73.7 | 24,790 | 53.7 |
| Bottom IDACI decile | 35,895 | 3120 | 8.1 | 36,105 | 3275 | 8.5 | 32,005 | 12,305 | 38.5 | 24,030 | 75.1 | 26,520 | 53.0 |
| Excluded, in PRU or alternative provision | 30,070 | 2735 | 8.4 | 30,275 | 2815 | 8.7 | 27,460 | 10,910 | 39.7 | 20,505 | 74.7 | 16,670 | 52.1 |
| Persistently absent in a term | 36,880 | 3240 | 8.1 | 37,245 | 3145 | 7.9 | 34,825 | 13,615 | 39.1 | 25,420 | 73.0 | 14,485 | 52.7 |
| Did not achieve 5 A*–C GCSEs prior to 20 weeks | 74,775 | 6350 | 8.5 | 75,185 | 6360 | 8.5 | 79,890 | 25,850 | 38.1 | 49,215 | 72.5 | 35,105 | 51.7 |
| Did not achieve expected levels at KS2 Maths | 43,560 | 3855 | 8.8 | 43,800 | 3940 | 9.0 | 46,680 | 15,360 | 38.3 | 29,015 | 72.3 | 21,070 | 52.5 |
| Did not achieve expected levels at KS2 English | 32,020 | 2845 | 8.9 | 32,175 | 2905 | 9.0 | 34,210 | 11,695 | 39 | 21,785 | 72.6 | 15,900 | 53.0 |
| Nursery attendance | SEN | FSM | Persistent absence | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | N | % | Total | N | % | Total | N | % | Total | N | % | |
| Total | 66,085 | 63,625 | 96.3 | 30,865 | 7920 | 25.7 | 30,865 | 14,575 | 47.2 | 31,150 | 17,695 | 56.8 |
| FNP participation | ||||||||||||
| No | 52,480 | 50,465 | 96.2 | 25,655 | 6450 | 25.1 | 25,655 | 11,665 | 45.5 | 25,900 | 14,525 | 56.1 |
| Yes | 13,605 | 13,160 | 96.7 | 5210 | 1470 | 28.2 | 5210 | 2910 | 55.9 | 5250 | 3170 | 60.4 |
| Maternal age | ||||||||||||
| 13–15 | 1465 | 1385 | 94.6 | 670 | 185 | 28.0 | 670 | 390 | 58.1 | 670 | 395 | 59.1 |
| 16–17 | 13,930 | 13,280 | 95.3 | 6610 | 1755 | 26.5 | 6610 | 3745 | 56.6 | 6660 | 4110 | 61.7 |
| 18–19 | 36,200 | 34,935 | 96.5 | 16,835 | 4380 | 26.0 | 16,835 | 7840 | 46.6 | 17,000 | 9590 | 56.4 |
| 20a | 14,490 | 14,020 | 96.8 | 6750 | 1600 | 23.7 | 6750 | 2605 | 38.6 | 6815 | 3595 | 52.8 |
| Ethnicity | ||||||||||||
| White | 57,295 | 55,395 | 96.7 | 26,950 | 6950 | 25.8 | 26,950 | 12,775 | 47.4 | 27,150 | 15,480 | 57.0 |
| South Asian | 1745 | 1660 | 95.4 | 720 | 175 | 24.1 | 720 | 260 | 36.2 | 740 | 415 | 56.2 |
| Black | 2350 | 2215 | 94.2 | 1230 | 280 | 22.9 | 1230 | 650 | 52.8 | 1255 | 675 | 54.0 |
| Mixed/other | 3005 | 2740 | 91.1 | 1345 | 355 | 26.4 | 1345 | 645 | 48.0 | 1375 | 800 | 58.1 |
| Unknown | 1690 | 1615 | 95.7 | 620 | 160 | 25.4 | 620 | 250 | 40.1 | 630 | 325 | 51.3 |
| Area-level deprivation | ||||||||||||
| Least deprived | 3150 | 3070 | 97.4 | 1320 | 280 | 21.1 | 1320 | 415 | 31.4 | 1330 | 670 | 50.4 |
| 2 | 5020 | 4875 | 97.1 | 2185 | 485 | 22.2 | 2185 | 735 | 33.5 | 2210 | 1130 | 51.1 |
| 3 | 8775 | 8545 | 97.4 | 3930 | 875 | 22.2 | 3930 | 1535 | 39.0 | 3955 | 2210 | 55.8 |
| 4 | 16,310 | 15,700 | 96.3 | 7635 | 1905 | 25.0 | 7635 | 3385 | 44.3 | 7710 | 4380 | 56.8 |
| Most deprived | 32,785 | 31,395 | 95.8 | 15,775 | 4370 | 27.7 | 15,775 | 8500 | 53.9 | 15,925 | 9295 | 58.4 |
| History of admissions with diagnoses within 2 years prior to 20 weeks of pregnancy | ||||||||||||
| Adversity | 2425 | 2350 | 96.9 | 1135 | 350 | 31.0 | 1135 | 650 | 57.4 | 1150 | 695 | 60.4 |
| Violence | 235 | 225 | 97.0 | 125 | 45 | 34.9 | 125 | 80 | 63.5 | 130 | 80 | 63.3 |
| Self-harm | 1720 | 1665 | 96.9 | 795 | 250 | 31.4 | 795 | 435 | 54.7 | 800 | 485 | 60.7 |
| Substance misuse | 2175 | 2110 | 97.0 | 1010 | 305 | 30.1 | 1010 | 570 | 56.6 | 1020 | 610 | 59.7 |
| Mental health (exc. self-harm/substance misuse) | 1095 | 1060 | 97.2 | 410 | 125 | 31.1 | 410 | 220 | 54.3 | 420 | 250 | 59.4 |
| Mental health (any) | 2680 | 2600 | 97.1 | 1195 | 365 | 30.6 | 1195 | 675 | 56.4 | 1210 | 725 | 59.9 |
| Chronic condition (any, exc. mental health) | 7065 | 6855 | 97.0 | 3130 | 910 | 29.1 | 3130 | 1635 | 52.2 | 3165 | 1895 | 59.9 |
| A&E visits | 40,610 | 39,230 | 96.6 | 18,345 | 4925 | 26.8 | 18,345 | 9145 | 49.9 | 18,505 | 10,815 | 58.4 |
| Repeated A&E visits (≥ 4) | 9275 | 8945 | 96.4 | 3825 | 1155 | 30.2 | 3825 | 2050 | 53.6 | 3870 | 2380 | 61.5 |
| Did not attend ≥ 1 outpatient appointment | 17,355 | 16,665 | 96.0 | 7575 | 2070 | 27.4 | 7575 | 3965 | 52.4 | 7665 | 4660 | 60.8 |
| Gestational age at booking | ||||||||||||
| Before 10 weeks | 17,565 | 17,105 | 97.4 | 7795 | 1955 | 25.1 | 7795 | 3410 | 43.7 | 7840 | 4435 | 56.6 |
| 10–20 weeks | 24,675 | 23,800 | 96.4 | 12,035 | 3115 | 25.9 | 12,035 | 5660 | 47.0 | 12,135 | 6860 | 56.6 |
| 20 weeks or more | 3720 | 3480 | 93.5 | 1890 | 525 | 27.8 | 1890 | 930 | 49.2 | 1915 | 1115 | 58.4 |
| Unknown | 20,120 | 19,240 | 95.6 | 9145 | 2325 | 25.4 | 9145 | 4580 | 50.1 | 9260 | 5280 | 57.0 |
| Social care and educational characteristics ever before 20 weeks of pregnancy | ||||||||||||
| CLA | 2855 | 2765 | 96.9 | 1140 | 355 | 31.3 | 1140 | 695 | 60.8 | 1150 | 675 | 58.6 |
| CPP | 775 | 750 | 96.5 | 120 | 50 | 39.3 | 120 | 80 | 64.8 | 125 | 85 | 66.7 |
| SEN | 26,840 | 25,950 | 96.7 | 10,850 | 3455 | 31.9 | 10,850 | 6205 | 57.2 | 10,935 | 6580 | 60.2 |
| FSM | 28,580 | 27,605 | 96.6 | 11,245 | 3330 | 29.6 | 11,245 | 6735 | 59.9 | 11,335 | 6795 | 59.9 |
| Bottom IDACI decile | 19,090 | 18,405 | 96.4 | 8525 | 2395 | 28.1 | 8525 | 4915 | 57.7 | 8605 | 5130 | 59.6 |
| Excluded, in PRU or alternative provision | 16,515 | 15,960 | 96.6 | 6890 | 1950 | 28.3 | 6890 | 3985 | 57.8 | 6945 | 4270 | 61.5 |
| Persistently absent in a term | 22,355 | 21,565 | 96.5 | 10,635 | 2860 | 26.9 | 10,635 | 5840 | 54.9 | 10,720 | 6470 | 60.4 |
| Did not achieve 5 A*–C GCSEs prior to 20 weeks | 43,375 | 41,980 | 96.8 | 20,915 | 5735 | 27.4 | 20,915 | 10,560 | 50.5 | 21,050 | 12,325 | 58.6 |
| Did not achieve expected levels at KS2 Maths | 25,420 | 24,600 | 96.8 | 12,030 | 3825 | 31.8 | 12,030 | 6625 | 55.1 | 12,110 | 7145 | 59.0 |
| Did not achieve expected levels at KS2 English | 19,385 | 18,735 | 96.7 | 9445 | 3100 | 32.8 | 9445 | 5395 | 57.1 | 9510 | 5745 | 60.4 |
| Good Level of Development | Key Stage 1 | KS1 Maths | KS2 Writing | KS2 Reading | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Total | N | % | Total | N | % | N | % | N | % | |
| Total | 45,200 | 26,005 | 57.5 | 30,315 | 19,235 | 63.4 | 17,005 | 56.1 | 19,590 | 64.6 |
| FNP participation | ||||||||||
| No | 36,505 | 21,170 | 58.0 | 25,195 | 16,080 | 63.8 | 14,260 | 56.6 | 16,360 | 64.9 |
| Yes | 8695 | 4830 | 55.6 | 5115 | 3150 | 61.6 | 2745 | 53.6 | 3230 | 63.2 |
| Maternal age | ||||||||||
| 13–15a | 1005 | 510 | 50.5 | 655 | 375 | 57.5 | 335 | 51.4 | 385 | 58.7 |
| 16–17 | 9605 | 5210 | 54.3 | 6470 | 3895 | 60.2 | 3370 | 52.1 | 3915 | 60.5 |
| 18–19 | 24,705 | 14,260 | 57.7 | 16,560 | 10,535 | 63.6 | 9345 | 56.4 | 10,750 | 64.9 |
| 20a | 9885 | 6025 | 61.0 | 6630 | 4425 | 66.8 | 3955 | 59.6 | 4540 | 68.5 |
| Ethnicity | ||||||||||
| White | 39,525 | 22,775 | 57.6 | 26,505 | 16,810 | 63.4 | 14,820 | 55.9 | 17,075 | 64.4 |
| South Asian | 1090 | 615 | 56.5 | 705 | 475 | 67.6 | 430 | 61.3 | 490 | 70.0 |
| Black | 1650 | 995 | 60.2 | 1205 | 775 | 64.3 | 715 | 59.2 | 830 | 69.0 |
| Mixed/other | 1925 | 1045 | 54.3 | 1295 | 780 | 60.5 | 700 | 54.2 | 800 | 61.8 |
| Unknown | 1005 | 575 | 57.0 | 605 | 395 | 65.0 | 335 | 55.7 | 395 | 65.5 |
| Area-level deprivation | ||||||||||
| Least deprived | 2025 | 1230 | 60.9 | 1295 | 840 | 64.9 | 750 | 58.0 | 875 | 67.7 |
| 2 | 3380 | 2080 | 61.5 | 2155 | 1415 | 65.7 | 1255 | 58.2 | 1440 | 66.8 |
| 3 | 5975 | 3555 | 59.5 | 3870 | 2525 | 65.2 | 2245 | 58.0 | 2575 | 66.6 |
| 4 | 11,140 | 6485 | 58.2 | 7480 | 4820 | 64.4 | 4290 | 57.4 | 4915 | 65.7 |
| Most deprived | 2025 | 1230 | 60.9 | 1295 | 840 | 64.9 | 750 | 58.0 | 875 | 67.7 |
| History of admissions with diagnoses within 2 years prior to 20 weeks of pregnancy | ||||||||||
| Adversity | 1625 | 880 | 54.3 | 1115 | 670 | 60.2 | 585 | 52.6 | 700 | 63.0 |
| Violence | 165 | 85 | 52.1 | 120 | 75 | 63.1 | 65 | 53.3 | 85 | 68.0 |
| Self-harm | 1140 | 625 | 54.9 | 780 | 470 | 60.1 | 405 | 51.7 | 485 | 62.3 |
| Substance misuse | 1450 | 805 | 55.3 | 995 | 605 | 60.7 | 530 | 53.4 | 625 | 63.0 |
| Mental health (exc. self-harm/substance misuse) | 645 | 350 | 53.9 | 400 | 235 | 58.0 | 215 | 53.0 | 250 | 62.2 |
| Mental health (any) | 1750 | 960 | 54.7 | 1175 | 700 | 59.4 | 620 | 52.6 | 730 | 62.2 |
| Chronic condition (any, exc. mental health) | 4680 | 2620 | 56.0 | 3075 | 1875 | 61.0 | 1655 | 53.8 | 1940 | 63.1 |
| A&E visits | 27,415 | 15,575 | 56.8 | 18,015 | 11,320 | 62.8 | 9955 | 55.3 | 11,575 | 64.3 |
| Repeated A&E visits (≥ 4) | 5965 | 3305 | 55.4 | 3760 | 2235 | 59.5 | 1985 | 52.8 | 2300 | 61.3 |
| Did not attend ≥ 1 outpatient appointment | 11,450 | 6385 | 55.8 | 7430 | 4555 | 61.3 | 4040 | 54.4 | 4730 | 63.7 |
| Gestational age at booking | ||||||||||
| Before 10 weeks | 11,945 | 7105 | 59.5 | 7685 | 4965 | 64.6 | 4470 | 58.2 | 5065 | 65.9 |
| 10–20 weeks | 17,370 | 10,105 | 58.2 | 11,820 | 7625 | 64.5 | 6680 | 56.5 | 7750 | 65.6 |
| 20 weeks or more | 2680 | 1440 | 53.7 | 1845 | 1130 | 61.1 | 1005 | 54.4 | 1145 | 62.1 |
| Unknown | 13,205 | 7350 | 55.7 | 8960 | 5515 | 61.5 | 4845 | 54.1 | 5630 | 62.8 |
| Social care and educational characteristics ever before 20 weeks of pregnancy | ||||||||||
| CLA | 1785 | 910 | 51.0 | 1110 | 625 | 56.1 | 545 | 48.9 | 645 | 57.9 |
| CPP | 310 | 150 | 48.1 | 120 | 55 | 46.6 | 55 | 45.8 | 60 | 52.5 |
| SEN | 17,110 | 8610 | 50.3 | 10,640 | 5835 | 54.8 | 4970 | 46.7 | 5930 | 55.7 |
| FSM | 17,865 | 9585 | 53.7 | 11,035 | 6520 | 59.1 | 5735 | 52.0 | 6700 | 60.7 |
| Bottom IDACI decile | 12,715 | 7050 | 55.5 | 8405 | 5175 | 61.6 | 4500 | 53.6 | 5255 | 62.5 |
| Excluded, in PRU or alternative provision | 10,765 | 5765 | 53.6 | 6775 | 3990 | 58.9 | 3455 | 51.0 | 4050 | 59.8 |
| Persistently absent in a term | 15,580 | 8655 | 55.5 | 10,445 | 6370 | 61.0 | 5615 | 53.7 | 6475 | 62.0 |
| Did not achieve 5 A*–C GCSEs prior to 20 weeks | 30,325 | 16,750 | 55.2 | 20,595 | 12,505 | 60.7 | 11,000 | 53.4 | 12,835 | 62.3 |
| Did not achieve expected levels at KS2 Maths | 17,540 | 8680 | 49.5 | 11,840 | 6335 | 53.5 | 5575 | 47.1 | 6620 | 55.9 |
| Did not achieve expected levels at KS2 English | 13,495 | 6380 | 47.3 | 9300 | 4870 | 52.4 | 4100 | 44.1 | 4895 | 52.6 |
| Outcomes at 7 years | ≥ 1 Unplanned admission for any diagnosis | ≥ 1 A&E attendance | ≥ 1 Outpatient referral | Did not attend ≥ 1 outpatient appointment | |||||
|---|---|---|---|---|---|---|---|---|---|
| Total | N | % | N | % | N | % | N | % | |
| Total | 27,015 | 13,195 | 48.8 | 23,555 | 87.2 | 12,385 | 45.8 | 11,150 | 90 |
| FNP participation | |||||||||
| No | 22,640 | 10,975 | 48.5 | 19,570 | 86.4 | 10,200 | 45.1 | 9145 | 89.7 |
| Yes | 4375 | 2225 | 50.9 | 3985 | 91.1 | 2185 | 49.9 | 2010 | 92.0 |
| Maternal age | |||||||||
| 13–15 | 585 | 295 | 50.4 | 515 | 88.0 | 280 | 47.9 | 260 | 92.9 |
| 16–17 | 5825 | 2960 | 50.8 | 5105 | 87.6 | 2725 | 46.8 | 2570 | 94.3 |
| 18–19 | 14,740 | 7215 | 48.9 | 12,905 | 87.6 | 6750 | 45.8 | 6090 | 90.2 |
| 20a | 5870 | 2730 | 46.5 | 5030 | 85.7 | 2630 | 44.8 | 2230 | 84.8 |
| Ethnicity | |||||||||
| White | 23,260 | 11,690 | 50.3 | 20,370 | 87.6 | 10,735 | 46.2 | 9685 | 90.2 |
| South Asian | 670 | 290 | 43.3 | 570 | 85.1 | 315 | 47.0 | 245 | 77.8 |
| Black | 1190 | 435 | 36.6 | 1030 | 86.6 | 515 | 43.3 | 505 | 98.1 |
| Mixed/other | 1310 | 560 | 42.7 | 1130 | 86.3 | 580 | 44.3 | 505 | 87.1 |
| Unknown | 585 | 225 | 38.5 | 450 | 76.9 | 240 | 41.0 | 210 | 87.5 |
| Area-level deprivation | |||||||||
| Least deprived | 1105 | 515 | 46.6 | 930 | 84.2 | 485 | 43.9 | 380 | 78.4 |
| 2 | 1820 | 865 | 47.5 | 1560 | 85.7 | 845 | 46.4 | 685 | 81.1 |
| 3 | 3320 | 1570 | 47.3 | 2840 | 85.5 | 1490 | 44.9 | 1300 | 87.2 |
| 4 | 6705 | 3295 | 49.1 | 5825 | 86.9 | 3050 | 45.5 | 2740 | 89.8 |
| Most deprived | 14,050 | 6945 | 49.4 | 12,385 | 88.1 | 6505 | 46.3 | 6040 | 92.9 |
| History of admissions with diagnoses within 2 years prior to 20 weeks of pregnancy | |||||||||
| Adversity | 1000 | 585 | 58.5 | 910 | 91.0 | 555 | 55.5 | 500 | 90.1 |
| Violence | 125 | 75 | 60.0 | 110 | 88.0 | 70 | 56.0 | 65 | 92.9 |
| Self-harm | 700 | 420 | 60.0 | 640 | 91.4 | 395 | 56.4 | 345 | 87.3 |
| Substance misuse | 885 | 525 | 59.3 | 805 | 91.0 | 490 | 55.4 | 440 | 89.8 |
| Mental health (exc. self-harm/substance misuse) | 365 | 220 | 60.3 | 330 | 90.4 | 220 | 60.3 | 175 | 79.5 |
| Mental health (any) | 1045 | 625 | 59.8 | 950 | 90.9 | 585 | 56.0 | 515 | 88.0 |
| Chronic condition (any, exc. mental health) | 2705 | 1575 | 58.2 | 2455 | 90.8 | 1485 | 54.9 | 1330 | 89.6 |
| A&E visits | 15,870 | 8390 | 52.9 | 14,330 | 90.3 | 7845 | 49.4 | 7085 | 90.3 |
| Repeated A&E visits (≥ 4) | 3315 | 2040 | 61.5 | 3110 | 93.8 | 1890 | 57.0 | 1710 | 90.5 |
| Did not attend ≥ 1 outpatient appointment | 6660 | 3485 | 52.3 | 5935 | 89.1 | 3340 | 50.2 | 3225 | 96.6 |
| Gestational age at booking | |||||||||
| Before 10 weeks | 6565 | 3390 | 51.6 | 5700 | 86.8 | 3000 | 45.7 | 2775 | 92.5 |
| 10–20 weeks | 10,335 | 5080 | 49.2 | 9040 | 87.5 | 4550 | 44.0 | 4240 | 93.2 |
| 20 weeks or more | 1725 | 800 | 46.4 | 1495 | 86.7 | 770 | 44.6 | 725 | 94.2 |
| Unknown | 8390 | 3930 | 46.8 | 7320 | 87.2 | 4070 | 48.5 | 3415 | 83.9 |
| Social care and educational characteristics ever before 20 weeks of pregnancy | |||||||||
| CLA | 1015 | 550 | 54.2 | 895 | 88.2 | 560 | 55.2 | 470 | 83.9 |
| CPP | 90 | 45 | 50.0 | 75 | 83.3 | 50 | 50.0 | 50 | 100.0 |
| SEN | 8940 | 4590 | 51.3 | 7890 | 88.3 | 4320 | 48.3 | 4065 | 94.1 |
| FSM | 9345 | 4755 | 50.9 | 8245 | 88.2 | 4390 | 47.0 | 4285 | 97.6 |
| Bottom IDACI decile | 7280 | 3635 | 49.9 | 6490 | 89.1 | 3450 | 47.4 | 3265 | 94.6 |
| Excluded, in PRU or alternative provision | 5720 | 2925 | 51.1 | 5080 | 88.8 | 2705 | 47.3 | 2610 | 96.5 |
| Persistently absent in a term | 9270 | 4740 | 51.1 | 8225 | 88.7 | 4345 | 46.9 | 4120 | 94.8 |
| Did not achieve 5 A*–C GCSEs prior to 20 weeks | 17,800 | 8930 | 50.2 | 15,650 | 87.9 | 8280 | 46.5 | 7660 | 92.5 |
| Did not achieve expected levels at KS2 Maths | 10,245 | 5130 | 50.1 | 8995 | 87.8 | 4800 | 46.9 | 4540 | 94.6 |
| Did not achieve expected levels at KS2 English | 10,245 | 4125 | 50.9 | 7130 | 87.9 | 3875 | 47.8 | 3605 | 93.0 |
| Health outcomes up to 2 years following birth | ≥ 1 unplanned admission for adversity-related diagnoses | ≥ 1 unplanned admission for mental health-related diagnosis | ≥ 1 unplanned admission for any diagnosis | ≥ 1 A&E attendance | Subsequent delivery within 18 months of index birth | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | N | % | N | % | N | % | N | % | N | % | |
| Total | 111,195 | 1905 | 1.7 | 2915 | 2.6 | 19,075 | 17.2 | 55,020 | 49.5 | 10,270 | 8.7 |
| FNP enrolment | |||||||||||
| Yes | 25,860 | 1205 | 1.4 | 1835 | 2.1 | 13,830 | 16.2 | 40,450 | 47.4 | 7935 | 8.8 |
| No | 85,335 | 705 | 2.7 | 1085 | 4.2 | 5245 | 20.3 | 14,570 | 56.3 | 2335 | 8.5 |
| Maternal age | |||||||||||
| 13–15 | 2390 | 105 | 4.4 | 85 | 3.5 | 435 | 18.1 | 1270 | 53.2 | 90 | 3.8 |
| 16–17 | 22,855 | 525 | 2.3 | 700 | 3.1 | 4160 | 18.2 | 12,065 | 52.8 | 1970 | 8.2 |
| 18–19 | 61,470 | 985 | 1.6 | 1595 | 2.6 | 10,655 | 17.3 | 30,510 | 49.6 | 5965 | 9.2 |
| 20a | 24,485 | 290 | 1.2 | 540 | 2.2 | 3830 | 15.7 | 11,175 | 45.6 | 2240 | 8.5 |
| Ethnicity | |||||||||||
| White | 94,285 | 1705 | 1.8 | 2710 | 2.9 | 16,840 | 17.9 | 47,225 | 50.1 | 8755 | 8.8 |
| South Asian | 3190 | 40 | 1.2 | 40 | 1.2 | 505 | 15.8 | 1500 | 46.9 | 475 | 14.3 |
| Black | 4000 | 65 | 1.6 | 40 | 1.0 | 575 | 14.3 | 2165 | 54.1 | 275 | 6.5 |
| Mixed/other | 5740 | 85 | 1.5 | 110 | 1.9 | 910 | 15.8 | 2930 | 51.0 | 535 | 8.9 |
| Unknown | 3980 | 10 | 0.2 | 15 | 0.4 | 250 | 6.3 | 1200 | 30.2 | 230 | 5.3 |
| Area-level deprivation | |||||||||||
| Least deprived | 5580 | 95 | 1.7 | 175 | 3.1 | 940 | 16.8 | 2550 | 45.7 | 390 | 6.6 |
| 2 | 8615 | 165 | 1.9 | 235 | 2.7 | 1485 | 17.2 | 4140 | 48.1 | 630 | 6.8 |
| 3 | 14,935 | 230 | 1.5 | 415 | 2.8 | 2515 | 16.9 | 7325 | 49.0 | 1245 | 7.7 |
| 4 | 27,665 | 475 | 1.7 | 735 | 2.7 | 4705 | 17.0 | 13,635 | 49.3 | 2530 | 8.6 |
| Most deprived | 54,250 | 935 | 1.7 | 1355 | 2.5 | 9400 | 17.3 | 27,280 | 50.3 | 5460 | 9.6 |
| History of admissions with diagnoses within 2 years prior to 20 weeks of pregnancy | |||||||||||
| Adversity | 4480 | 390 | 8.7 | 500 | 11.2 | 1515 | 33.8 | 3160 | 70.5 | 525 | 11.0 |
| Violence | 405 | 35 | 8.4 | 35 | 8.9 | 145 | 35.2 | 300 | 73.9 | 45 | 10.8 |
| Self-harm | 3295 | 320 | 9.7 | 405 | 12.3 | 1135 | 34.5 | 2340 | 71.0 | 385 | 11.0 |
| Substance misuse | 4050 | 365 | 9.0 | 470 | 11.6 | 1380 | 34.1 | 2835 | 70.1 | 470 | 10.8 |
| Mental health (exc. self-harm/substance misuse) | 2430 | 230 | 9.4 | 460 | 19.0 | 1015 | 41.8 | 1800 | 74.1 | 325 | 11.8 |
| Mental health (any) | 5165 | 425 | 8.3 | 670 | 12.9 | 1830 | 35.4 | 3670 | 71.0 | 610 | 10.8 |
| Chronic condition (any, exc. mental health) | 9645 | 525 | 5.4 | 920 | 9.5 | 3400 | 35.2 | 6815 | 70.7 | 1070 | 10.2 |
| A&E visits | 69,400 | 1570 | 2.3 | 2495 | 3.6 | 14,570 | 21.0 | 40,455 | 58.3 | 6940 | 9.4 |
| Repeated A&E visits (≥ 4) | 17,040 | 695 | 4.1 | 1210 | 7.1 | 5435 | 31.9 | 12,945 | 76.0 | 2100 | 11.5 |
| Did not attend ≥ 1 outpatient appointment | 31,120 | 805 | 2.6 | 1315 | 4.2 | 6920 | 22.2 | 18,255 | 58.6 | 3315 | 10.0 |
| Gestational age at antenatal booking appointment | |||||||||||
| Before 10 weeks | 29,570 | 520 | 1.8 | 900 | 3.0 | 5395 | 18.2 | 15,065 | 50.9 | 2950 | 9.3 |
| 10–20 weeks | 40,865 | 705 | 1.7 | 1020 | 2.5 | 6770 | 16.6 | 20,055 | 49.1 | 3515 | 8.1 |
| 20 weeks or more | 6145 | 115 | 1.8 | 160 | 2.6 | 920 | 15.0 | 2820 | 45.9 | 505 | 7.8 |
| Unknown | 34,620 | 570 | 1.6 | 835 | 2.4 | 5995 | 17.3 | 17,075 | 49.3 | 3300 | 9.1 |
| Social care and educational characteristics ever before 20 weeks of pregnancy | |||||||||||
| CLA | 5575 | 305 | 5.5 | 395 | 7.1 | 1460 | 26.2 | 3625 | 65.0 | 735 | 12.3 |
| CPP | 2500 | 100 | 4.0 | 150 | 6.0 | 590 | 23.5 | 1540 | 61.6 | 340 | 12.0 |
| SEN | 47,260 | 1030 | 2.2 | 1600 | 3.4 | 8965 | 19.0 | 25,250 | 53.4 | 5005 | 10.0 |
| FSM | 51,110 | 1090 | 2.1 | 1610 | 3.1 | 9385 | 18.4 | 26,925 | 52.7 | 5515 | 10.2 |
| Bottom IDACI decile | 32,690 | 650 | 2.0 | 910 | 2.8 | 5910 | 18.1 | 17,180 | 52.5 | 3425 | 9.8 |
| Excluded, in PRU or alternative provision | 28,035 | 785 | 2.8 | 1005 | 3.6 | 5630 | 20.1 | 15,655 | 55.8 | 3065 | 10.4 |
| Persistently absent in a term | 35,560 | 815 | 2.3 | 1095 | 3.1 | 6690 | 18.8 | 18,885 | 53.1 | 3265 | 8.8 |
| Did not achieve 5 A*–C GCSEs prior to 20 weeks | 69,370 | 1230 | 1.8 | 1950 | 2.8 | 12,525 | 18.1 | 35,365 | 51.0 | 7060 | 9.7 |
| Did not achieve expected levels at KS2 Maths | 41,030 | 755 | 1.8 | 1180 | 2.9 | 7360 | 17.9 | 21,160 | 51.6 | 4255 | 9.9 |
| Did not achieve expected levels at KS2 English | 30,700 | 560 | 1.8 | 860 | 2.8 | 5470 | 17.8 | 15,905 | 51.8 | 3440 | 10.8 |
Appendix 7 Additional information on Objective 2: propensity score generation and matching
FIGURE 28.
Overlap in the distribution of propensity scores between mothers who were and were not enrolled in FNP.

FIGURE 29.
Propensity scores for all FNP mothers and those included in the matched cohort for analysis.

FIGURE 30.
Standardised differences comparing maternal risk factors in the propensity-score-matched cohort of all mothers aged 13–19 giving birth between April 2010 and March 2019. Note: The final matched cohort used a calliper width of 0.01.
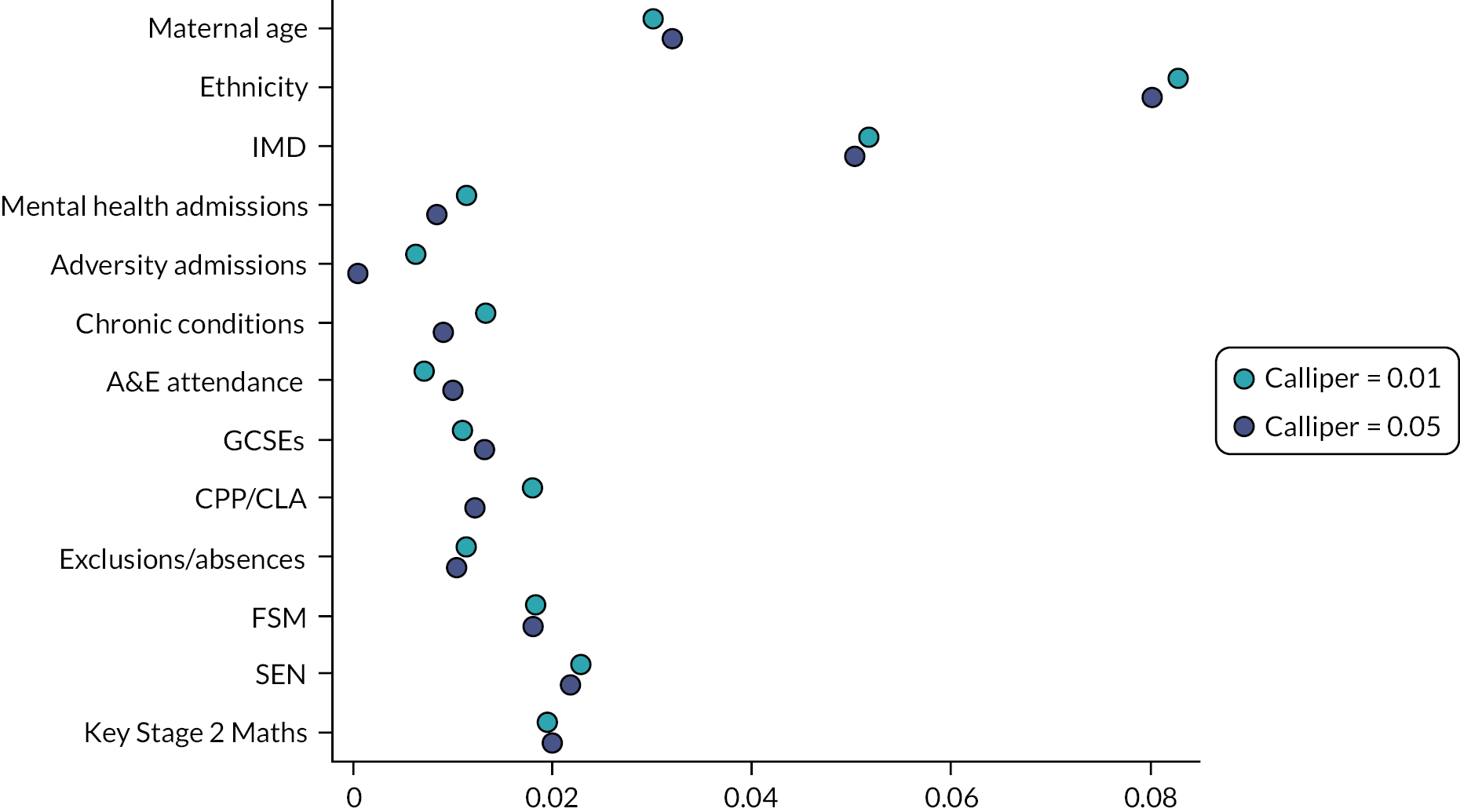
| Mothers enrolled in the FNP (treated) | Mothers never enrolled in the FNP (untreated) | |||
|---|---|---|---|---|
| N | % | N | % | |
| Total | 29,505 | 29,505 | ||
| Maternal age | ||||
| 13–15 | 955 | 3.2 | 970 | 3.3 |
| 16–17 | 9290 | 31.5 | 9460 | 32.1 |
| 18–19 | 15,650 | 53 | 15,745 | 53.4 |
| 20–21 | 3610 | 12.2 | 3325 | 11.3 |
| Ethnicity | ||||
| White | 24,810 | 84.1 | 25,635 | 86.9 |
| South Asian | 645 | 2.2 | 525 | 1.8 |
| Black | 1380 | 4.7 | 1040 | 3.5 |
| Mixed/other | 1595 | 5.4 | 1395 | 4.7 |
| Unknown | 1075 | 3.6 | 910 | 3.1 |
| Area-level deprivation | ||||
| Least deprived | 1395 | 4.7 | 1230 | 4.2 |
| 2 | 2210 | 7.5 | 2170 | 7.4 |
| 3 | 3950 | 13.4 | 3740 | 12.7 |
| 4 | 7495 | 25.4 | 7195 | 24.4 |
| Most deprived | 14,455 | 49.0 | 15,165 | 51.4 |
| Year of delivery | ||||
| 2010 | 2010 | 6.8 | 2295 | 7.8 |
| 2011 | 1850 | 6.3 | 1965 | 6.7 |
| 2012 | 2815 | 9.5 | 2890 | 9.8 |
| 2013 | 3890 | 13.2 | 4075 | 13.8 |
| 2014 | 3460 | 11.7 | 3640 | 12.3 |
| 2015 | 4695 | 15.9 | 4790 | 16.2 |
| 2016 | 4755 | 16.1 | 4520 | 15.3 |
| 2017 | 2970 | 10.1 | 2665 | 9.0 |
| 2018 | 2480 | 8.4 | 2200 | 7.5 |
| 2019 | 575 | 1.9 | 470 | 1.6 |
| Quarter of delivery | ||||
| January–March | 7355 | 24.9 | 7330 | 24.8 |
| April–June | 7260 | 24.6 | 7250 | 24.6 |
| July–September | 7465 | 25.3 | 7420 | 25.1 |
| August–December | 7420 | 25.2 | 7505 | 25.4 |
| History of admissions with diagnoses within 2 years prior to 20 weeks of pregnancy | ||||
| Adversity | 1825 | 6.2 | 1780 | 6.0 |
| Violence | 160 | 0.5 | 150 | 0.5 |
| Self-harm | 1365 | 4.6 | 1320 | 4.5 |
| Substance misuse | 1640 | 5.6 | 1615 | 5.5 |
| Mental health (exc. self-harm/substance misuse) | 1150 | 3.9 | 1085 | 3.7 |
| Mental health (any) | 2185 | 7.4 | 2115 | 7.2 |
| A&E visits | 20,480 | 69.4 | 20,575 | 69.7 |
| Repeated A&E visits (≥ 4) | 6125 | 20.8 | 5945 | 20.1 |
| Did not attend ≥ 1 outpatient appointment | 10,140 | 37.5 | 9760 | 35.7 |
| Gestational age at antenatal booking appointment | ||||
| Before 10 weeks | 7925 | 26.9 | 8355 | 28.3 |
| 10–20 weeks | 10,930 | 37 | 10,620 | 36 |
| 20 weeks or more | 1775 | 6.0 | 1435 | 4.9 |
| Unknown | 8875 | 30.1 | 9095 | 30.8 |
| Linked to NPD | ||||
| Linked to NPD | 26,275 | 89.1 | 26,395 | 89.5 |
| Not linked to NPD | 3075 | 10.4 | 2990 | 10.1 |
| Not linked to NPD census | 150 | 0.5 | 120 | 0.4 |
| Social care and educational characteristics before 20 weeks of pregnancy | ||||
| Ever in care | 2580 | 9.8 | 2485 | 9.4 |
| Ever had recorded CPP | 1470 | 5.6 | 1355 | 5.1 |
| Ever recorded as having SEN | 15,790 | 60.1 | 15,660 | 59.3 |
| Ever recorded as having FSM | 17,050 | 64.9 | 17,055 | 64.6 |
| Ever in bottom IDACI decile | 10,640 | 40.5 | 10,580 | 40.1 |
| Ever excluded, in PRU or alternative provision | 9495 | 36.1 | 9465 | 35.9 |
| Ever recorded as persistently absent in a term | 13,515 | 51.4 | 13,880 | 52.6 |
| KS2 Maths | ||||
| Did not achieve expected level at KS2 | 12,010 | 47.5 | 12,205 | 48.0 |
| Achieved expected level at KS2 | 13,275 | 52.5 | 13,250 | 52.1 |
| KS2 English | ||||
| Did not achieve expected level at KS2 | 8910 | 35.2 | 9190 | 36.1 |
| Achieved expected level at KS2 | 16,380 | 64.8 | 16,270 | 63.9 |
Appendix 8 Additional information on Objective 2
| All children in cohort | Children of mothers ever enrolled in FNP | Children of mothers never enrolled in FNP | ||||
|---|---|---|---|---|---|---|
| N | % | N | % | N | % | |
|
Total with information on birth outcomes
(Births between April 2010 and March 2019) |
130,415 | 31,260 | 99,150 | |||
| Total with information on gestational age at birth | 121,005 | 28,075 | 92,935 | |||
| Preterm birth (< 37 weeks) | 9940 | 8.2 | 2650 | 9.4 | 7295 | 7.8 |
| Total with information on birthweight | 121,815 | 28,350 | 93,460 | |||
| Low birthweight (< 2500 g) | 9395 | 7.7 | 2515 | 8.9 | 6880 | 7.4 |
|
Total with 2 years follow-up
(Births between April 2010 and March 2017) |
108,675 | 25,630 | 83,040 | |||
| ≥ 1 unplanned admission (any diagnosis) | 40,140 | 36.9 | 10,360 | 40.4 | 29,780 | 35.9 |
| Mean no. unplanned admissionsa (SD) | 1.9 (1.9) | 1.9 (1.9) | 1.9 (1.8) | |||
| ≥ 1 A&E attendance | 77,725 | 71.5 | 19,570 | 76.3 | 58,155 | 70.0 |
| Mean no. A&E attendancesa (SD) | 3.0 (2.8) | 3.3 (3.0) | 2.9 (2.7) | |||
| ≥ 1 outpatient referral | 55,630 | 51.2 | 14,310 | 55.8 | 41,320 | 49.8 |
| Mean no. referralsa | 2.3 (2.6) | 2.4 (2.5) | 2.3 (2.6) | |||
| Did not attend ≥ 1 outpatient appointment | 19,745 | 18.2 | 5485 | 21.4 | 14,260 | 17.2 |
| Mean no. Did not attenda | 2.0 (1.7) | 2.1 (1.9) | 2.0 (1.6) | |||
|
Total with 7 years follow-up
(Births between April 2010 and March 2012) |
27,015 | 4375 | 22,640 | |||
| ≥ 1 unplanned admission (any diagnosis) | 13,195 | 48.8 | 2225 | 50.8 | 10,975 | 48.5 |
| Mean no. unplanned admissionsa (SD) | 2.3 (3.2) | 2.5 (3.8) | 2.3 (3.1) | |||
| ≥ 1 A&E attendance | 23,555 | 87.2 | 3985 | 91.0 | 19,570 | 86.4 |
| Mean no. A&E attendancesa (SD) | 4.9 (4.7) | 5.5 (5.3) | 4.8 (4.6) | |||
| ≥ 1 outpatient referral | 20,450 | 75.7 | 3460 | 79.1 | 16,990 | 75 |
| Mean no. referralsa | 4.0 (4.3) | 4.2 (4.6) | 3.9 (4.2) | |||
| Did not attend ≥ 1 outpatient appointment | 11,150 | 41.3 | 2010 | 45.9 | 9145 | 40.4 |
| Mean no. Did not attenda | 3.0 (3.1) | 3.2 (3.5) | 2.9 (3.1) | |||
| Total with information on nursery attendance | 25,140 | 4135 | 21,010 | |||
| Attended nursery between ages 2 and 4 | 24,090 | 95.8 | 3955 | 90.4 | 20,135 | 95.8 |
| Total with information on school readiness at age 5 (EYFSP) | 24,585 | 4035 | 20,545 | |||
| Good Level of Development (across all five domains) | 14,445 | 58.5 | 2325 | 53.1 | 12,120 | 59.0 |
| GLD: Communication and Language | 18,595 | 75.6 | 3010 | 74.6 | 15,585 | 75.9 |
| GLD: Physical Development | 20,340 | 82.7 | 3325 | 82.4 | 17,010 | 82.8 |
| GLD: Personal, Social and Emotional Development | 19,345 | 78.7 | 3130 | 77.6 | 16,215 | 78.9 |
| GLD: Literacy | 15,090 | 61.4 | 2435 | 60.3 | 12,655 | 61.6 |
| GLD: Maths | 16,630 | 67.6 | 2685 | 66.5 | 13,945 | 67.9 |
| Total with information at Key Stage 1 | 24,530 | 4040 | 20,490 | |||
| Expected level of development at KS1 (Maths) | 16,015 | 65.3 | 2580 | 63.9 | 13,435 | 65.6 |
| Expected level of development at KS1 (Writing) | 14,215 | 57.9 | 2255 | 55.9 | 11,960 | 58.4 |
| Expected level of development at KS1 (Reading) | 16,255 | 66.3 | 2635 | 65.3 | 13,620 | 66.5 |
| Total with information on SEN provision and FSM | 24,925 | 4105 | 20,820 | |||
| Ever recorded as having SEN provision | 6175 | 24.8 | 1120 | 27.8 | 5060 | 24.3 |
| Ever recorded as having FSM | 11,780 | 47.3 | 2290 | 56.8 | 9485 | 45.6 |
| Total with information on persistent absence | 25,155 | 4135 | 21,020 | |||
| Ever persistently absent | 14,700 | 58.4 | 2555 | 63.3 | 12,145 | 57.8 |
| N (%) in mothers enrolled in FNP (treated) | N (%) in mothers never enrolled in FNP (untreated) | Adjusted a RR (95% CI) | |
|---|---|---|---|
| Child developmental/educational outcomes – within 7 years (Births between April 2010 and March 2012) |
|||
| Total with information on nursery attendance | 4090 | 4040 | |
| Nursery attendancei | 3915 (89.8) | 3870 (88.8) | 1.00 (0.99 to 1.01) |
| Total with information on EYFSP | 3990 | 3955 | |
| Good Level of Development (school readiness) | 2295 (57.5) | 2190 (55.4) | 1.05 (1.00 to 1.09) |
| GLD: Communication and Language | 2980 (74.7) | 2930 (74.1) | 1.01 (0.98 to 1.04) |
| GLD: Physical Development | 3290 (82.5) | 3220 (81.4) | 1.01 (0.99 to 1.04) |
| GLD: Personal, Social and Emotional Development | 3095 (77.6) | 3040 (76.9) | 1.01 (0.99 to 1.03) |
| GLD: Literacy | 2400 (60.2) | 2290 (57.9) | 1.04 (1.00 to 1.08) |
| GLD: Maths | 2655 (66.5) | 2570 (65.0) | 1.03 (0.99 to 1.07) |
FIGURE 31.
Subgroup analysis: child unplanned admissions for maltreatment/injury up to age 2: adjusted RRs and 95% CIs comparing mothers enrolled in the FNP vs. mothers who were not enrolled, for mothers aged 13–19 and giving birth in an area in which FNP was offered at the time of pregnancy by region and year of delivery.
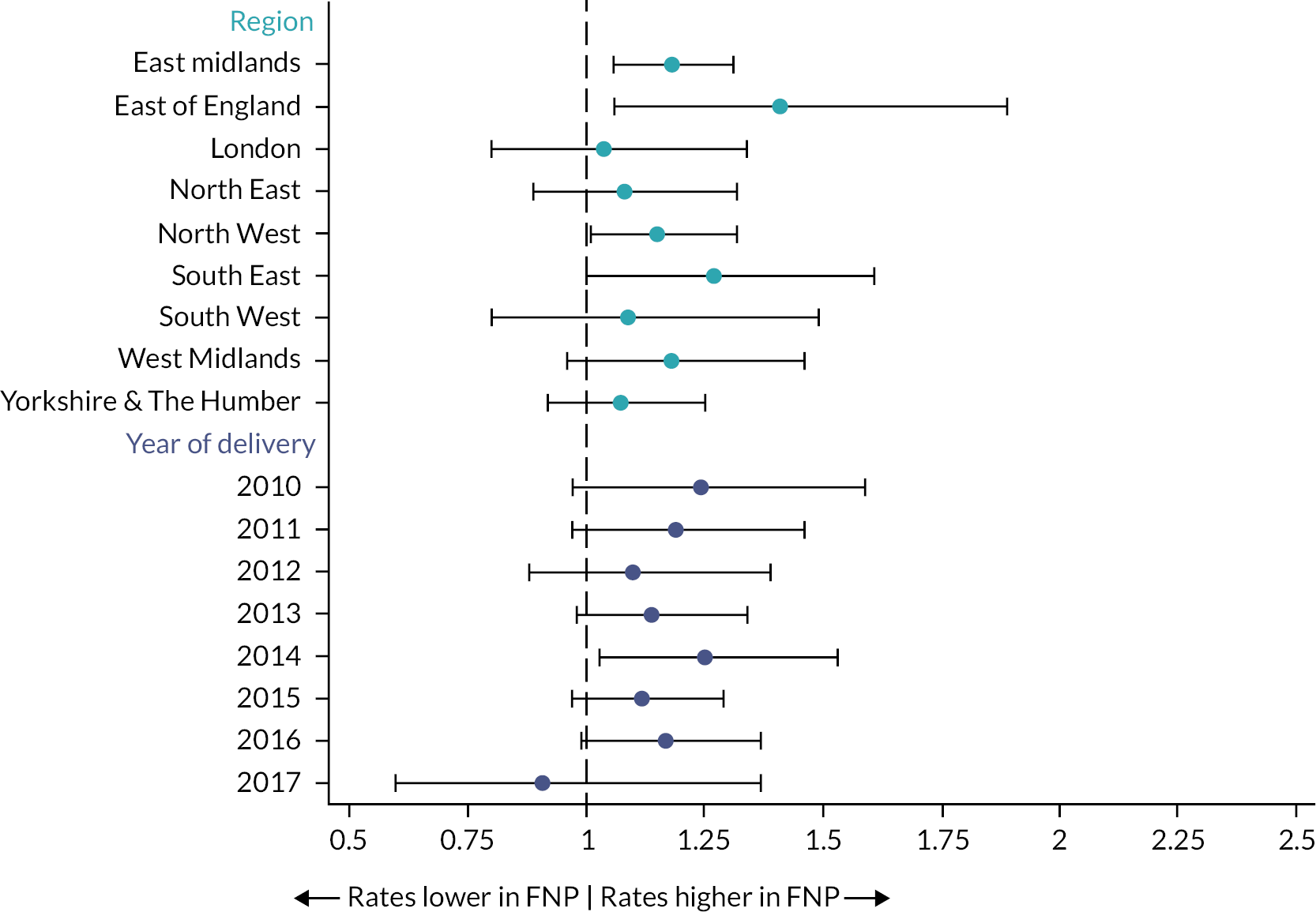
FIGURE 32.
Subgroup analysis: Good Level of Development (school readiness): adjusted RRs and 95% CIs comparing mothers enrolled in the FNP vs. mothers who were not enrolled, for mothers aged 13–19 and giving birth in an area in which FNP was offered at the time of pregnancy by region and year of delivery. Note: A Good Level of Development was not stratified by year of delivery since it was only assessed for children who were born before 2013 (to allow long enough follow-up).

FIGURE 33.
Subgroup analysis: subsequent births within 18 months: adjusted RRs and 95% CIs comparing mothers enrolled in the FNP vs. mothers who were not enrolled, for mothers aged 13–19 and giving birth in an area in which FNP was offered at the time of pregnancy by region and year of delivery.
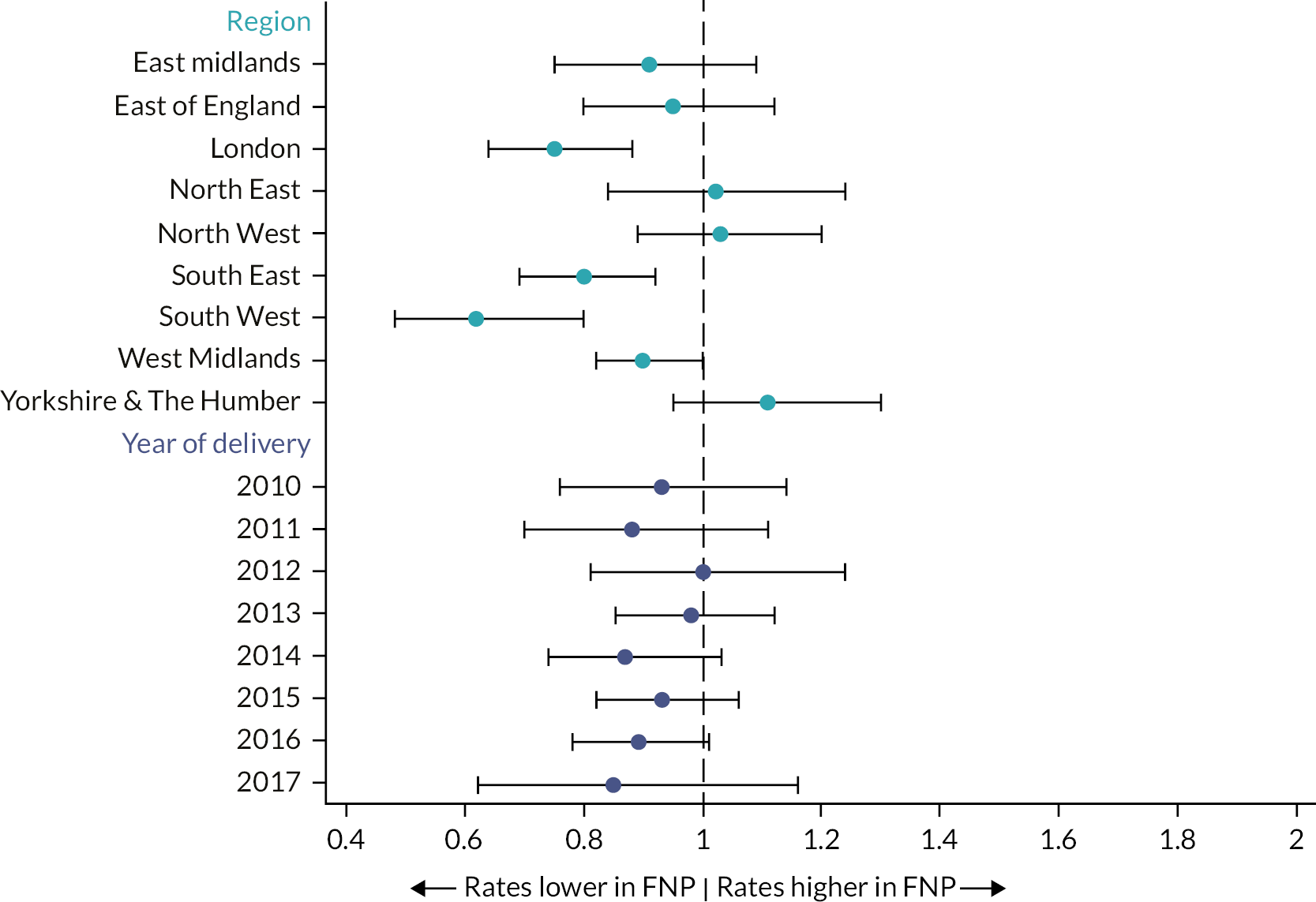
FIGURE 34.
Subgroup analysis: maternal unplanned admissions for any diagnosis in the 2 years following delivery: adjusted RRs and 95% CIs comparing mothers enrolled in the FNP vs. mothers who were not enrolled, for mothers aged 13–19 and giving birth in an area in which FNP was offered at the time of pregnancy by region and year of delivery.

| Subgroup | Child unplanned admission for maltreatment or injury within 2 years | Good level of development (school readiness) at age 5 | Subsequent delivery within 18 months | Maternal admission for any diagnosis within 2 years |
|---|---|---|---|---|
| RR (95% CI) | RR (95% CI) | RR (95% CI) | RR (95% CI) | |
| Maternal age | ||||
| 13–15 | 1.31 (0.93 to 1.84) | 1.13 (0.94 to 1.36) | 1.20 (0.74 to 1.95) | 1.00 (0.84 to 1.20) |
| 16–17 | 1.11 (0.99 to 1.25) | 1.09 (1.01 to 1.18) | 0.88 (0.80 to 0.96) | 1.14 (1.06 to 1.22) |
| 18–19 | 1.15 (1.03 to 1.27) | 1.00 (0.95 to 1.05) | 0.96 (0.88 to 1.05) | 1.06 (1.01 to 1.11) |
| 20–21 | 1.30 (1.04 to 1.61) | 1.13 (1.00 to 1.28) | 0.83 (0.71 to 0.97) | 1.01 (0.91 to 1.12) |
| Ethnicity | ||||
| White | 1.15 (1.06 to 1.24) | 1.04 (0.99 to 1.09) | 0.95 (0.89 to 1.01) | 1.08 (1.04 to 1.13) |
| South Asian | 1.04 (0.50 to 2.18) | 1.34 (0.84 to 2.14) | 1.08 (0.77 to 1.53) | 1.08 (0.84 to 1.39) |
| Black | 0.91 (0.62 to 1.33) | 1.05 (0.93 to 1.20) | 0.71 (0.53 to 0.94) | 1.04 (0.84 to 1.30) |
| Mixed/other | 1.36 (0.97 to 1.92) | 0.96 (0.81 to 1.14) | 0.70 (0.54 to 0.91) | 1.02 (0.85 to 1.24) |
| Unknown | 1.50 (0.95 to 2.36) | 1.50 (1.02 to 2.22) | 0.60 (0.39 to 0.90) | 0.97 (0.67 to 1.40) |
| Area-level deprivation | ||||
| Least deprived | 1.21 (0.88 to 1.65) | 1.01 (0.85 to 1.20) | 0.66 (0.48 to 0.92) | 0.95 (0.81 to 1.12) |
| 2 | 1.21 (0.94 to 1.57) | 1.01 (0.85 to 1.20) | 0.93 (0.72 to 1.19) | 1.14 (1.00 to 1.31) |
| 3 | 1.36 (1.12 to 1.65) | 0.98 (0.88 to 1.08) | 0.84 (0.71 to 1.00) | 1.14 (1.03 to 1.25) |
| 4 | 1.05 (0.89 to 1.25) | 1.03 (0.95 to 1.11) | 0.90 (0.80 to 1.01) | 1.06 (0.98 to 1.14) |
| Most deprived | 1.15 (1.02 to 1.28) | 1.08 (1.03 to 1.13) | 0.97 (0.90 to 1.04) | 1.07 (1.02 to 1.12) |
| Social care contact | ||||
| No CPP or CLA | 1.20 (1.11 to 1.30) | 1.03 (0.98 to 1.08) | 0.93 (0.87 to 1.00) | 1.09 (1.04 to 1.14) |
| CPP or CLA | 0.99 (0.83 to 1.18) | 1.11 (0.94 to 1.31) | 0.89 (0.78 to 1.02) | 0.99 (0.90 to 1.09) |
| History of adversity | ||||
| No | 1.13 (1.05 to 1.22) | 1.05 (1.01 to 1.09) | 0.93 (0.87 to 0.99) | 1.08 (1.03 to 1.13) |
| Yes | 1.44 (1.18 to 1.75) | 1.03 (0.87 to 1.20) | 0.82 (0.68 to 0.99) | 1.06 (0.96 to 1.16) |
| History of mental health conditions | ||||
| No | 1.14 (1.06 to 1.23) | 1.05 (1.01 to 1.10) | 0.93 (0.87 to 0.99) | 1.08 (1.04 to 1.13) |
| Yes | 1.34 (1.05 to 1.71) | 0.96 (0.69 to 1.33) | 0.79 (0.61 to 1.04) | 1.01 (0.90 to 1.13) |
| Child sex | ||||
| Male | 1.14 (1.04 to 1.25) | 1.08 (1.00 to 1.16) | 0.92 (0.85 to 1.00) | 1.11 (1.05 to 1.17) |
| Female | 1.18 (1.06 to 1.31) | 1.03 (0.99 to 1.07) | 0.92 (0.85 to 1.01) | 1.04 (0.99 to 1.1) |
| Region | ||||
| East Midlands | 1.18 (1.06 to 1.31) | 1.11 (0.95 to 1.29) | 0.91 (0.75 to 1.09) | 0.98 (0.89 to 1.07) |
| East of England | 1.41 (1.06 to 1.89) | 0.96 (0.83 to 1.10) | 0.95 (0.80 to 1.12) | 1.04 (0.92 to 1.18) |
| London | 1.04 (0.80 to 1.34) | 1.07 (0.97 to 1.18) | 0.75 (0.64 to 0.88) | 1.11 (0.94 to 1.30) |
| North East | 1.08 (0.89 to 1.32) | 0.99 (0.87 to 1.13) | 1.02 (0.84 to 1.24) | 1.08 (0.93 to 1.27) |
| North West | 1.15 (1.01 to 1.32) | 1.17 (0.96 to 1.42) | 1.03 (0.89 to 1.02) | 1.15 (1.03 to 1.27) |
| South East | 1.27 (1.00 to 1.61) | 1.03 (0.92 to 1.15) | 0.80 (0.69 to 0.92) | 1.03 (0.90 to 1.17) |
| South West | 1.09 (0.80 to 1.49) | 1.11 (1.02 to 1.21) | 0.62 (0.48 to 0.80) | 1.09 (0.95 to 1.26) |
| West Midlands | 1.18 (0.96 to 1.46) | 0.99 (0.92 to 1.07) | 0.90 (0.82 to 1.00) | 1.04 (0.96 to 1.13) |
| Yorkshire and The Humber | 1.07 (0.92 to 1.25) | 1.02 (0.93 to 1.12) | 1.11 (0.95 to 1.30) | 1.14 (1.05 to 1.24) |
| Year of delivery | ||||
| 2010 | 1.24 (0.97 to 1.59) | 0.93 (0.76 to 1.14) | 1.02 (0.89 to 1.18) | |
| 2011 | 1.19 (0.97 to 1.46) | 0.88 (0.70 to 1.11) | 1.04 (0.92 to 1.18) | |
| 2012 | 1.10 (0.88 to 1.39) | 1.00 (0.81 to 1.24) | 1.16 (1.04 to 1.29) | |
| 2013 | 1.14 (0.98 to 1.34) | 0.98 (0.85 to 1.12) | 1.05 (0.94 to 1.17) | |
| 2014 | 1.25 (1.03 to 1.53) | 0.87 (0.74 to 1.03) | 1.11 (1.03 to 1.21) | |
| 2015 | 1.12 (0.97 to 1.29) | 0.93 (0.82 to 1.06) | 1.09 (1.00 to 1.18) | |
| 2016 | 1.17 (0.99 to 1.37) | 0.89 (0.78 to 1.01) | 1.09 (1.00 to 1.18) | |
| 2017 | 0.91 (0.60 to 1.37) | 0.85 (0.62 to 1.16) | 0.89 (0.74 to 1.06) | |
Appendix 9 Additional information on Objective 2: sensitivity analyses
Sensitivity analysis 1: Propensity score matching within the same LA but in different time periods, allowing matches to eligible families before FNP was offered in that LA.
For this sensitivity analysis, fewer FNP mothers could be matched using the main analysis strategy of matching without replacement. For births outcomes (births between April 2010 and March 2019, 18,400/31,100 FNP mothers (59.2%) could be matched. For outcomes in the 2 years after birth (births between April 2010 and March 2017), 14,935/25,545 (58.5%) of FNP mothers could be matched. For outcomes in the 7 years after birth, 3375/4365 (77.3%) of FNP mothers could be matched. Due to this lower coverage, we also present results using a matching with replacement strategy. When this strategy was used, 100% of mothers in each cohort could be matched.
FIGURE 35.
Sensitivity analysis 1: overlap in the distribution of propensity scores between mothers who were and were not enrolled in FNP (top figure); propensity scores for all FNP mothers and those included in the matched without replacement cohort for analysis (bottom figure).
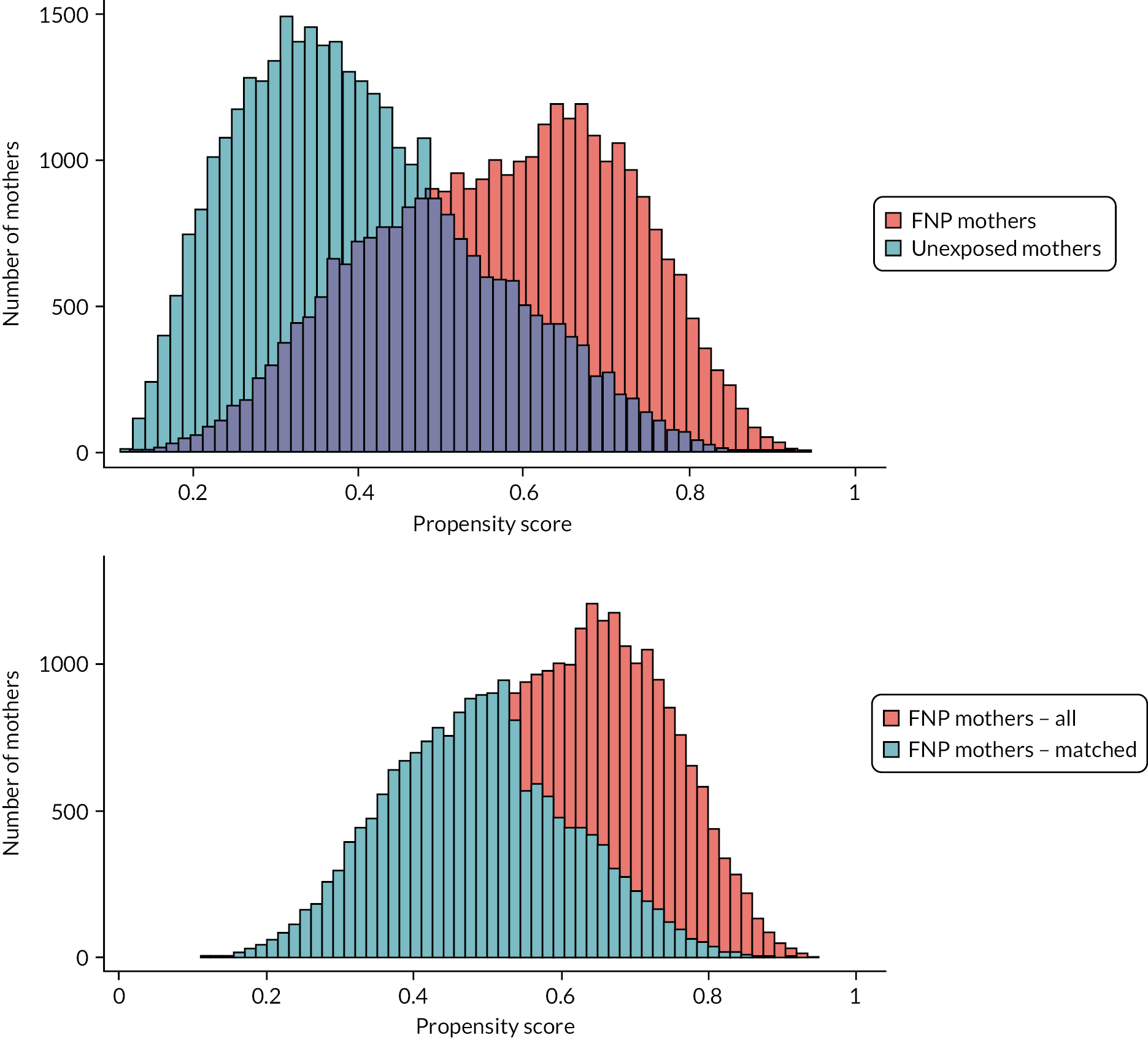
Sensitivity analysis 2: Propensity score matching within the same time period but in different LAs, allowing matches to eligible families in LAs that did not offer FNP.
For this sensitivity analysis, fewer FNP mothers could be matched using the main analysis strategy of matching without replacement (but more were matched than in Sensitivity analysis 2). For births outcomes (births between April 2010 and March 2019), 23,405/31,100 FNP mothers (75.3%) could be matched. For outcomes in the 2 years after birth (births between April 2010 and March 2017), 17,985/25,545 (70.4%) of FNP mothers could be matched. For outcomes in the 7 years after birth, 4360/4365 (99.9%) of FNP mothers could be matched.
FIGURE 36.
Sensitivity analysis 2: overlap in the distribution of propensity scores between mothers who were and were not enrolled in FNP (top figure); propensity scores for all FNP mothers and those included in the matched without replacement cohort for analysis (bottom figure).
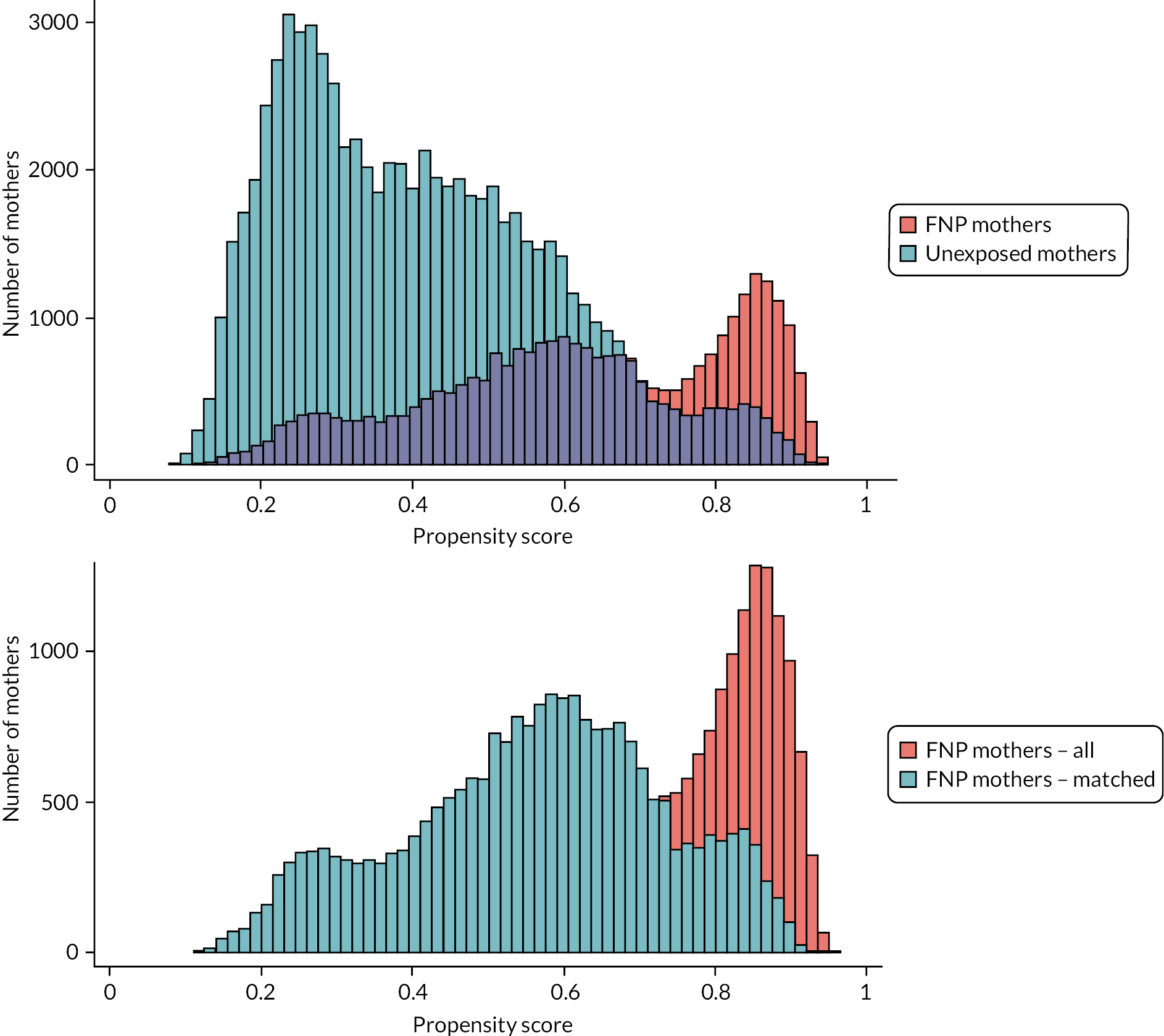
FIGURE 37.
Sensitivity analyses: RRs and 95% CIs for indicators of child maltreatment comparing mothers enrolled in the FNP vs. mothers who were not enrolled, for mothers aged 13–19 in the propensity-score-matched cohort. Note: Sensitivity analysis 1 compares mothers within the same LA but in different time periods; sensitivity analysis 2 compares mothers within the same time period but in different LAs.
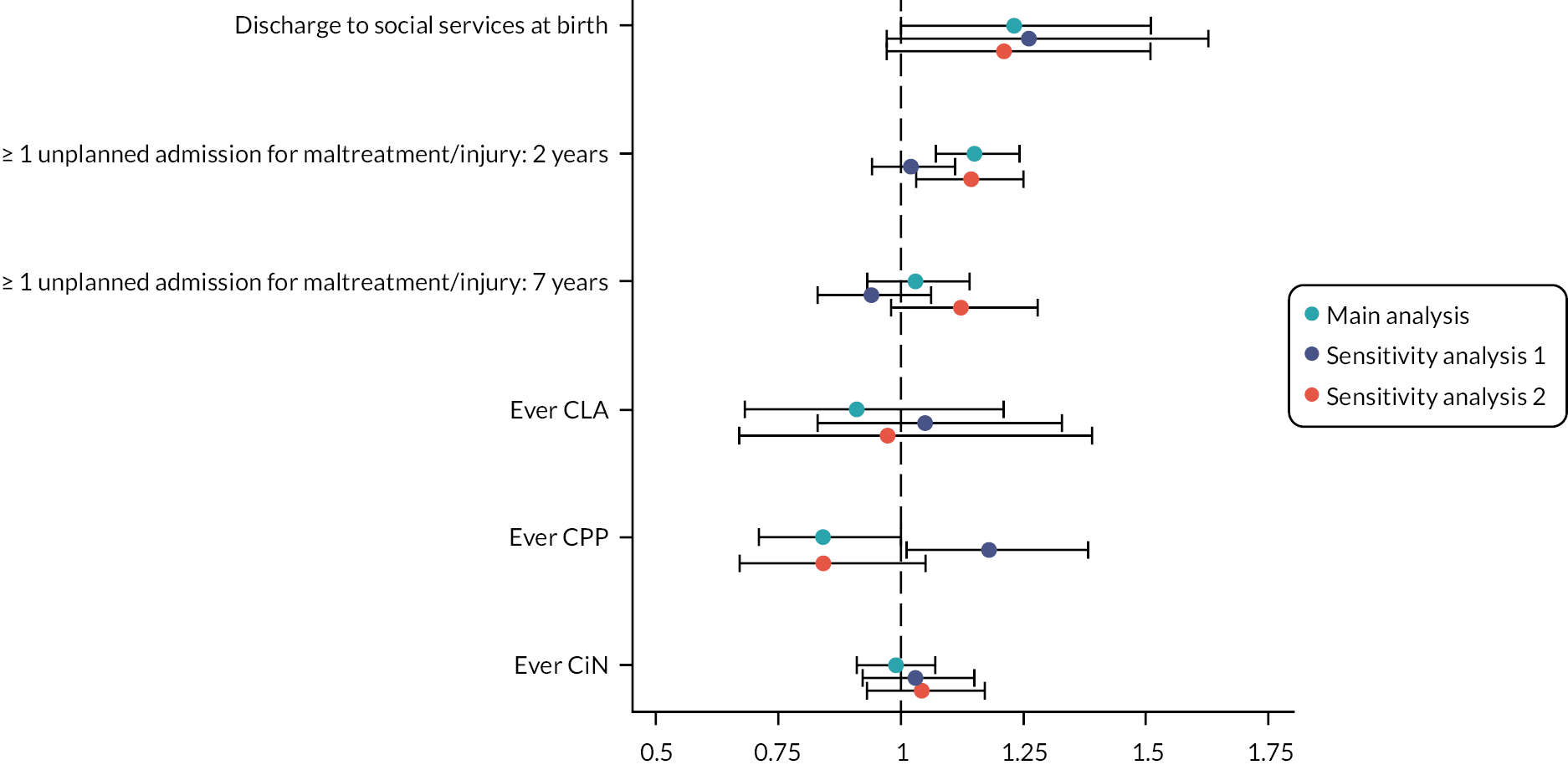
FIGURE 38.
Sensitivity analyses: RRs and 95% CIs for child health, developmental and education outcomes comparing mothers enrolled in the FNP vs. mothers who were not enrolled, for mothers aged 13–19 in the propensity-score-matched cohort. Note: Sensitivity analysis 1 compares mothers within the same LA but in different time periods; sensitivity analysis 2 compares mothers within the same time period but in different LAs. KS1, Key Stage 1.
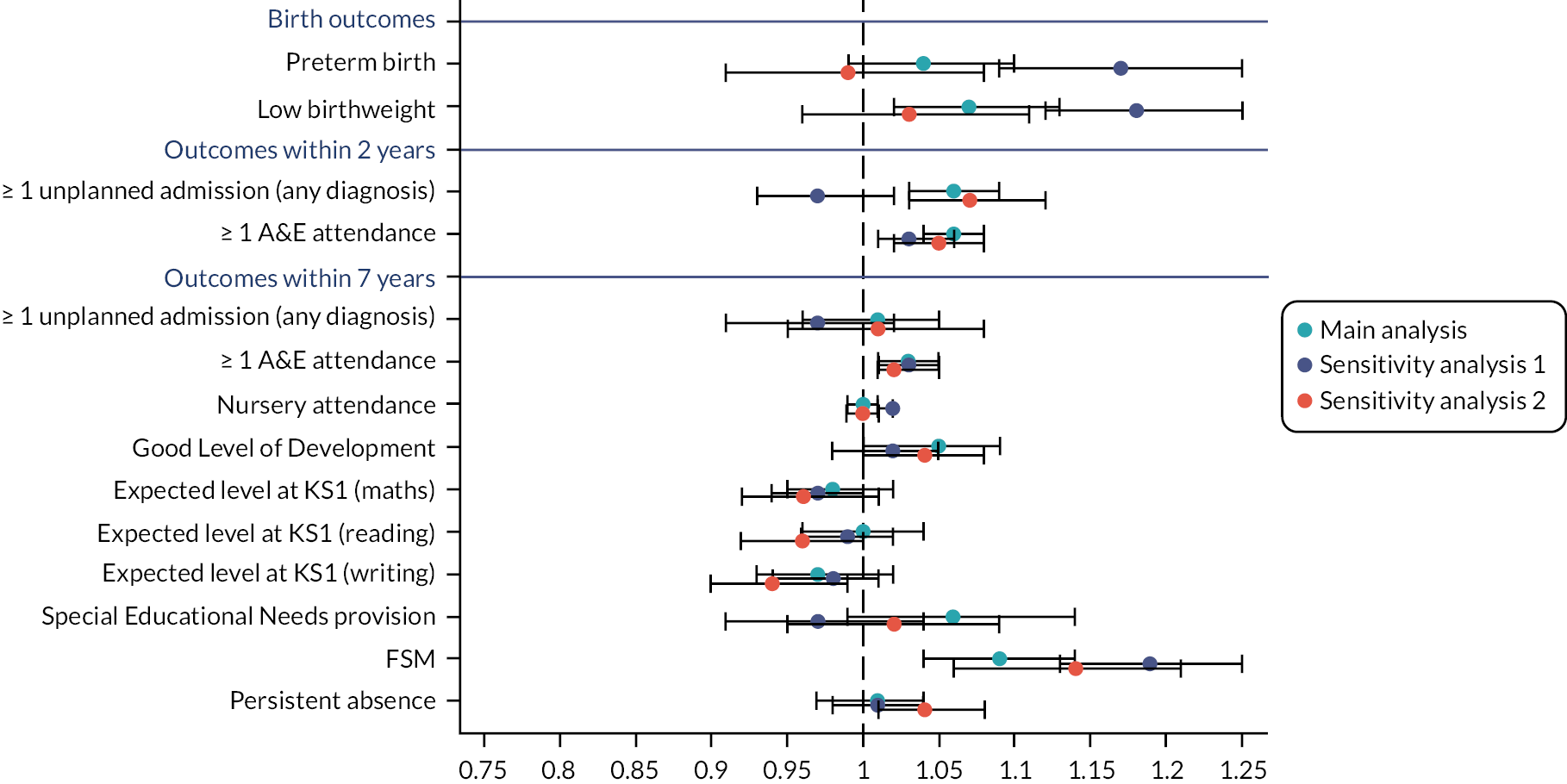
FIGURE 39.
Sensitivity analyses: RRs and 95% CIs for maternal outcomes comparing mothers enrolled in the FNP vs. mothers who were not enrolled, for mothers aged 13–19 in the propensity-score-matched cohort. Note: Sensitivity analysis 1 compares mothers within the same LA but in different time periods; sensitivity analysis 2 compares mothers within the same time period but in different LAs.

| Sensitivity analysis 1 | Sensitivity analysis 2 | |||
|---|---|---|---|---|
| Propensity score matching without replacement | Propensity score matching with replacement | Propensity score matching without replacement | Propensity score matching with replacement | |
| Birth outcomes (Births between April 2010 and March 2019) |
||||
| Discharge to social services | 1.26 (0.97 to 1.63) | 1.12 (0.92 to 1.35) | 1.21 (0.97 to 1.51) | 1.31 (0.93 to 1.85) |
| Child outcomes – within 2 years (Births between April 2010 and March 2017) |
||||
| ≥ 1 unplanned admission for maltreatment or injury | 1.02 (0.94 to 1.11) | 0.98 (0.91 to 1.05) | 1.14 (1.03 to 1.25) | 1.05 (0.92 to 1.20) |
| Child outcomes – within 7 years (Births between April 2010 and March 2012) |
||||
| ≥ 1 unplanned admission for maltreatment or injury | 0.94 (0.83 to 1.06) | 0.93 (0.84 to 1.04) | 1.12 (0.98 to 1.28) | 1.12 (0.98 to 1.27) |
| CLA | 1.05 (0.83 to 1.33) | 0.92 (0.73 to 1.14) | 0.97 (0.67 to 1.39) | 0.96 (0.65 to 1.4-) |
| CPP | 1.18 (1.01 to 1.38) | 1.24 (1.05 to 1.47) | 0.84 (0.67 to 1.05) | 0.77 (0.61 to 0.97) |
| CiN referral | 1.03 (0.92 to 1.15) | 1.02 (0.92 to 1.13) | 1.04 (0.93 to 1.17) | 1.00 (0.89 to 1.13) |
| Sensitivity analysis 1 | Sensitivity analysis 2 | |||
|---|---|---|---|---|
| Propensity score matching without replacement | Propensity score matching with replacement | Propensity score matching without replacement | Propensity score matching with replacement | |
| Birth outcomes (Births between April 2010 and March 2019) |
||||
| Preterm birth (< 37 weeks of gestation) | 1.17 (1.09 to 1.25) | 1.18 (1.12 to 1.26) | 0.99 (0.91 to 1.08) | 1.08 (0.98 to 1.20) |
| Low birthweight (< 2500 g) | 1.18 (1.12 to 1.25) | 1.21 (1.17 to 1.26) | 1.03 (0.96 to 1.11) | 1.11 (1.01 to 1.22) |
| Child health outcomes – within 2 years (Births between April 2010 and March 2017) |
||||
| ≥ 1 unplanned admission for any diagnosis | 0.97 (0.93 to 1.02) | 0.96 (0.92 to 1.00) | 1.07 (1.03 to 1.12) | 1.05 (1.00 to 1.10) |
| ≥ 1 A&E attendance | 1.06 (1.04 to 1.08) | 1.07 (1.05 to 1.08) | 1.04 (1.02 to 1.06) | 1.04 (1.02 to 1.06) |
| ≥ 1 outpatient referral | 1.09 (1.05 to 1.12) | 1.10 (1.06 to 1.14) | 1.05 (1.01 to 1.09) | 1.04 (1.00 to 1.08) |
| Did not attend ≥ 1 outpatient appointment | 1.08 (1.02 to 1.14) | 1.06 (1.02 to 1.11) | 1.12 (1.05 to 1.20) | 1.08 (0.99 to 1.17) |
| Child health outcomes – within 7 years (Births between April 2010 and March 2012) |
||||
| ≥ 1 unplanned admission for any diagnosis | 0.97 (0.91 to 1.02) | 0.97 (0.92 to 1.03) | 1.01 (0.95 to 1.08) | 1.02 (0.95 to 1.09) |
| ≥ 1 A&E attendance | 1.03 (1.01 to 1.05) | 1.04 (1.02 to 1.05) | 1.03 (1.01 to 1.05) | 1.03 (1.00 to 1.05) |
| ≥ 1 outpatient referral | 1.02 (0.99 to 1.05) | 1.03 (1.00 to 1.05) | 1.06 (1.02 to 1.10) | 1.06 (1.02 to 1.10) |
| Did not attend ≥ 1 outpatient appointment | 1.00 (0.94 to 1.06) | 0.98 (0.93 to 1.03) | 1.10 (1.03 to 1.18) | 1.10 (1.02 to 1.18) |
| Child developmental/educational outcomes – within 7 years (Births between April 2010 and March 2012) |
||||
| Nursery attendance | 1.02 (1.01 to 1.02) | 1.01 (1.01 to 1.02) | 1.00 (0.99 to 1.01) | 1.00 (0.99 to 1.01) |
| Good Level of Development (school readiness) | 1.02 (0.98 to 1.05) | 1.01 (0.98 to 1.05) | 1.04 (1.00 to 1.08) | 1.05 (1.00 to 1.09) |
| Expected levels at KS1 (maths) | 0.97 (0.94 to 1.00) | 0.97 (0.94 to 1.00) | 0.96 (0.92 to 1.01) | 0.97 (0.93 to 1.01) |
| Expected levels at KS1 (reading) | 0.99 (0.96 to 1.02) | 0.98 (0.95 to 1.00) | 0.96 (0.92 to 1.00) | 0.97 (0.93 to 1.01) |
| Expected levels at KS1 (writing) | 0.98 (0.94 to 1.01) | 0.96 (0.92 to 0.99) | 0.94 (0.90 to 0.99) | 0.95 (0.90 to 1.00) |
| SEN provision | 0.97 (0.91 to 1.04) | 0.97 (0.92 to 1.02) | 1.02 (0.95 to 1.09) | 1.00 (0.93 to 1.09) |
| FSM | 1.19 (1.13 to 1.25) | 1.12 (1.07 to 1.19) | 1.14 (1.06 to 1.21) | 1.14 (1.07 to 1.22) |
| Persistent absence | 1.01 (0.98 to 1.04) | 1.00 (0.98 to 1.03) | 1.04 (1.01 to 1.08) | 1.04 (1.00 to 1.08) |
| Sensitivity analysis 1 | Sensitivity analysis 2 | |||
|---|---|---|---|---|
| Propensity score matching without replacement | Propensity score matching with replacement | Propensity score matching without replacement | Propensity score matching with replacement | |
| Maternal outcomes – 2 years (Births between April 2010 and March 2017) |
||||
| ≥ 1 unplanned admission for adversity-related diagnoses | 1.27 (1.14 to 1.41) | 1.28 (1.16 to 1.41) | 1.14 (0.97 to 1.34) | 1.08 (0.86 to 1.35) |
| ≥ 1 unplanned admission for mental health-related diagnoses | 1.22 (1.02 to 1.34) | 1.20 (1.09 to 1.31) | 1.26 (1.11 to 1.44) | 1.19 (1.01 to 1.40) |
| ≥ 1 unplanned admission for any diagnosis | 1.06 (1.01 to 1.10) | 1.03 (0.99 to 1.07) | 1.04 (0.98 to 1.10) | 1.03 (0.96 to 1.10) |
| ≥ 1 A&E attendance | 1.03 (1.01 to 1.06) | 1.05 (1.03 to 1.07) | 1.05 (1.02 to 1.08) | 1.06 (1.03 to 1.09) |
| Subsequent delivery within 18 months | 0.87 (0.81 to 0.94) | 0.91 (0.86 to 0.96) | 0.94 (0.87 to 1.01) | 0.96 (0.88 to 1.06) |
| 5 A*–Cs at GCSE level | 1.16 (1.02 to 1.32) | 1.20 (1.09 to 1.32) | 0.93 (0.81 to 1.08) | 1.03 (0.86 to 1.22) |
| School attendance | 1.05 (0.99 to 1.11) | 1.01 (0.97 to 1.04) | 1.04 (0.97 to 1.11) | 1.01 (0.94 to 1.09) |
| Maternal outcomes – 7 years (Births between April 2010 and March 2012) |
||||
| ≥ 1 unplanned admissions for adversity-related diagnoses | 1.11 (1.00 to 1.24) | 1.14 (1.03 to 1.26) | 1.12 (0.95 to 1.33) | 1.15 (0.96 to 1.37) |
| ≥ 1 unplanned admission for mental health-related diagnoses | 1.08 (0.96 to 1.21) | 1.08 (0.97 to 1.19) | 1.05 (0.91 to 1.22) | 1.06 (0.91 to 1.24) |
| ≥ 1 unplanned admission for any diagnosis | 1.07 (1.02 to 1.11) | 1.06 (1.02 to 1.11) | 1.04 (0.99 to 1.10) | 1.05 (0.99 to 1.10) |
| ≥ 1 A&E attendance | 1.03 (1.01 to 1.05) | 1.02 (1.01 to 1.04) | 1.02 (1.00 to 1.05) | 1.02 (1.00 to 1.05) |
| Main analysis: propensity score matched with doubly robust analysis | Sensitivity analysis: multivariable regression | Sensitivity analysis: propensity score matched comparison | |
|---|---|---|---|
| RR (95% CI) | RR (95% CI) | RR (95% CI) | |
| Birth outcomes (Births between April 2010 and March 2019) |
|||
| Discharge to social services | 1.23 (1.00 to 1.51) | 1.17 (0.98 to 1.39) | 1.20 (0.96 to 1.49) |
| Child outcomes – within 2 years (Births between April 2010 and March 2017) |
|||
| ≥ 1 unplanned admission for maltreatment or injury | 1.15 (1.07 to 1.24) | 1.20 (1.14 to 1.27) | 1.15 (1.07 to 1.24) |
| Child outcomes – within 7 years (Births between April 2010 and March 2012) |
|||
| ≥ 1 unplanned admission for maltreatment or injury | 1.03 (0.93 to 1.14) | 1.11 (1.03 to 1.20) | 1.03 (0.93 to 1.14) |
| CLA | 0.91 (0.68 to 1.21) | 1.01 (0.84 to 1.21) | 0.91 (0.67 to 1.22) |
| CPP | 0.84 (0.71 to 1.00) | 0.96 (0.80 to 1.15) | 0.84 (0.71 to 1.00) |
| CiN referral | 0.99 (0.91 to 1.07) | 1.02 (0.94 to 1.11) | 0.99 (0.91 to 1.07) |
| Main analysis: propensity score matched with doubly robust analysis | Sensitivity analysis: multivariable regression |
Sensitivity analysis: propensity score matched comparison | |
|---|---|---|---|
| RR (95% CI) | RR (95% CI) | RR (95% CI) | |
| Birth outcomes (Births between April 2010 and March 2019) |
|||
| Preterm birth | 1.04 (0.99 to 1.10) | 1.04 (0.99 to 1.09) | 1.05 (0.99 to 1.10) |
| Low birthweight | 1.07 (1.02 to 1.13) | 1.07 (1.02 to 1.12) | 1.08 (1.03 to 1.14) |
| Child outcomes – within 2 years (Births between April 2010 and March 2017) |
|||
| ≥ 1 unplanned admission for any diagnosis | 1.06 (1.03 to 1.09) | 1.07 (1.05 to 1.1) | 1.06 (1.04 to 1.09) |
| ≥ 1 A&E attendance | 1.04 (1.03 to 1.05) | 1.04 (1.03 to 1.05) | 1.04 (1.03 to 1.05) |
| ≥ 1 referral to outpatient department | 1.10 (1.07 to 1.12) | 1.09 (1.07 to 1.11) | 1.10 (1.08 to 1.12) |
| ≥ 1 did not attend outpatient appointment | 1.11 (1.06 to 1.15) | 1.10 (1.06 to 1.13) | 1.11 (1.06 to 1.16) |
| Child outcomes – within 7 years (Births between April 2010 and March 2012) |
|||
| ≥ 1 unplanned admission for any diagnosis | 1.01 (0.96 to 1.05) | 1.05 (1.01 to 1.09) | 1.00 (0.96 to 1.05) |
| ≥ 1 A&E attendance | 1.03 (1.02 to 1.05) | 1.04 (1.03 to 1.06) | 1.03 (1.02 to 1.05) |
| ≥ 1 referral to outpatient department | 1.05 (1.02 to 1.08) | 1.06 (1.04 to 1.09) | 1.05 (1.02 to 1.08) |
| ≥ 1 did not attend outpatient appointment | 1.07 (1.01 to 1.12) | 1.08 (1.03 to 1.13) | 1.07 (1.02 to 1.13) |
| Nursery attendance | 1.00 (0.99 to 1.01) | 1.00 (1.00 to 1.01) | 1.00 (0.99 to 1.01) |
| Good Level of Development (school readiness) | 1.05 (1.00 to 1.09) | 1.02 (0.99 to 1.06) | 1.04 (0.99 to 1.09) |
| Expected levels at KS1 (maths) | 0.98 (0.95 to 1.02) | 0.96 (0.93 to 0.98) | 0.98 (0.95 to 1.02) |
| Expected levels at KS1 (reading) | 1.00 (0.96 to 1.04) | 0.96 (0.94 to 0.99) | 1.00 (0.97 to 1.04) |
| Expected levels at KS1 (writing) | 0.97 (0.93 to 1.02) | 0.93 (0.91 to 0.97) | 0.97 (0.93 to 1.02) |
| SEN provision | 1.06 (0.99 to 1.14) | 1.07 (1.01 to 1.13) | 1.07 (1.00 to 1.14) |
| FSM | 1.09 (1.04 to 1.14) | 1.08 (1.04 to 1.13) | 1.10 (1.05 to 1.15) |
| Persistent absence | 1.01 (0.97 to 1.04) | 1.00 (0.98 to 1.03) | 1.02 (0.98 to 1.06) |
| Main analysis: propensity score matched with doubly robust analysis | Sensitivity analysis: multivariable regression |
Sensitivity analysis: propensity score matched comparison | |
|---|---|---|---|
| RR (95% CI) | RR (95% CI) | RR (95% CI) | |
| Maternal outcomes – 2 years Births between April 2010 and March 2017 |
|||
| ≥ 1 unplanned admission for adversity-related diagnoses | 1.27 (1.15 to 1.41) | 1.30 (1.18 to 1.43) | 1.26 (1.13 to 1.40) |
| ≥ 1 unplanned admission for mental health-related diagnoses | 1.29 (1.18 to 1.41) | 1.35 (1.25 to 1.46) | 1.29 (1.17 to 1.42) |
| ≥ 1 unplanned admission for any diagnosis | 1.08 (1.04 to 1.12) | 1.07 (1.04 to 1.11) | 1.08 (1.03 to 1.13) |
| ≥ 1 A&E attendance | 1.06 (1.04 to 1.08) | 1.06 (1.04 to 1.07) | 1.06 (1.04 to 1.08) |
| Subsequent delivery within 18 months | 0.92 (0.88 to 0.97) | 0.92 (0.88 to 0.97) | 0.92 (0.86 to 0.98) |
| 5 A*–Cs at GCSE level | 1.12 (0.96 to 1.29) | 1.02 (0.90 to 1.16) | 1.25 (1.06 to 1.48) |
| School attendance | 0.96 (0.92 to 1.01) | 1.00 (0.96 to 1.05) | 0.96 (0.91 to 1.00) |
| Maternal outcomes – 7 years Births between April 2010 and March 2012 |
|||
| ≥ 1 unplanned admission for adversity-related diagnoses | 1.16 (1.03 to 1.30) | 1.17 (1.05 to 1.30) | 1.16 (1.01 to 1.32) |
| ≥ 1 unplanned admission for mental health-related diagnoses | 1.18 (1.04 to 1.33) | 1.15 (1.04 to 1.26) | 1.15 (1.00 to 1.32) |
| ≥ 1 unplanned admission for any diagnosis | 1.02 (0.98 to 1.06) | 1.05 (1.01 to 1.09) | 1.02 (0.97 to 1.06) |
| ≥ 1 A&E attendance | 1.03 (1.01 to 1.05) | 1.04 (1.02 to 1.05) | 1.03 (1.01 to 1.05) |
Appendix 10 Additional results for Objective 3
FIGURE 40.
Distribution of visits for each stage of the programme, for mothers giving birth between April 2010 and January 2018 aged 13–19 at LMP.
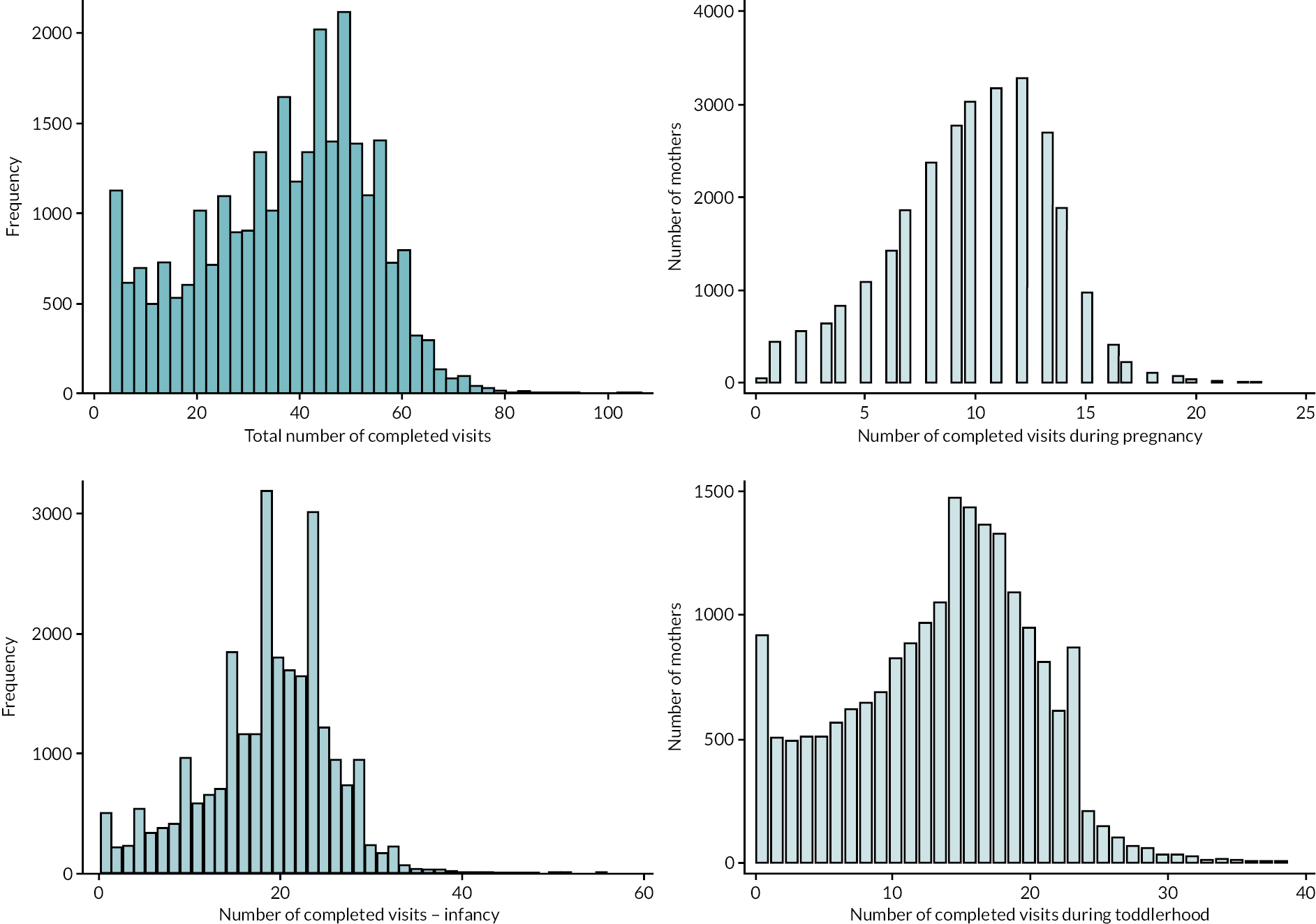
| Full programme | Pregnancy stage (up to birth) |
Infancy stage (0–1 year) |
Toddlerhood stage (1–2 years) |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | Number of visits | Total | Met 80% target | Total | Met 65% target | Total | Met 60% target | ||||||
| N | % | Mean (SD) | Median (IQR) | N | N | % | N | N | % | N | N | % | |
| Total | 28,150 | 100 | 35.9 (17.0) | 38 (24–49) | 28,150 | 16,695 | 59.3 | 25,900 | 16,940 | 65.4 | 19,990 | 12,115 | 60.6 |
| Maternal age at delivery (years) | |||||||||||||
| 13–15 | 1345 | 4.8 | 39.0 (16.7) | 41 (28–51) | 1345 | 935 | 69.5 | 1285 | 940 | 73.2 | 985 | 610 | 61.9 |
| 16–17 | 9485 | 33.7 | 36.5 (17.1) | 39 (24–49) | 9485 | 5765 | 60.8 | 8785 | 5760 | 65.6 | 6785 | 4110 | 60.6 |
| 18–19 | 14,150 | 50.3 | 35.5 (17.1) | 38 (23–48) | 14,150 | 8190 | 57.9 | 12,910 | 8380 | 64.9 | 10,030 | 6095 | 60.8 |
| 20a | 3170 | 11.3 | 35.0 (16.8) | 37 (22–48) | 3170 | 1805 | 56.9 | 2925 | 1860 | 63.6 | 2185 | 1300 | 59.5 |
| Ethnicity | |||||||||||||
| White | 23,820 | 84.6 | 36.3 (17.1) | 39 (24–49) | 23,820 | 14,140 | 59.4 | 21,875 | 14,510 | 66.3 | 16,925 | 10,435 | 61.7 |
| South Asian | 605 | 2.2 | 34.4 (16.7) | 37 (23–48) | 605 | 355 | 58.7 | 550 | 355 | 64.5 | 415 | 260 | 62.7 |
| Black | 1305 | 4.6 | 34.0 (15.9) | 35 (22–46) | 1305 | 755 | 57.9 | 1235 | 695 | 56.3 | 955 | 475 | 49.7 |
| Mixed/other | 1505 | 5.3 | 33.6 (16.3) | 36 (22–46) | 1505 | 900 | 59.8 | 1395 | 835 | 59.9 | 1040 | 550 | 52.9 |
| Unknown | 915 | 3.3 | 35.3 (17.3) | 38 (23–48) | 915 | 540 | 59.0 | 845 | 545 | 64.5 | 650 | 395 | 60.8 |
| Area-level deprivation | |||||||||||||
| Least deprived | 1250 | 4.4 | 36.5 (17.1) | 39 (24–50) | 1250 | 790 | 63.2 | 1140 | 775 | 68.0 | 905 | 555 | 61.3 |
| 2 | 2035 | 7.2 | 36.8 (16.7) | 39 (25–49) | 2035 | 1250 | 61.4 | 1870 | 1285 | 68.7 | 1475 | 880 | 59.7 |
| 3 | 3710 | 13.2 | 36.1 (17.2) | 39 (24–49) | 3710 | 2250 | 60.6 | 3370 | 2275 | 67.5 | 2620 | 1600 | 61.1 |
| 4 | 7060 | 25.1 | 35.9 (17.0) | 38 (24–49) | 7060 | 4150 | 58.8 | 6530 | 4270 | 65.4 | 4975 | 2990 | 60.1 |
| Most deprived | 13,945 | 49.5 | 35.7 (17.1) | 38 (23–49) | 13,945 | 8150 | 58.4 | 12,845 | 8230 | 64.1 | 9900 | 5995 | 60.6 |
| Unknown | 155 | 0.6 | 38.5 (17.7) | 41 (27–51) | 155 | 105 | 67.7 | 145 | 105 | 72.4 | 115 | 90 | 78.3 |
| Region | |||||||||||||
| East Midlands | 2470 | 8.8 | 35.0 (16.7) | 38 (23–47) | 2470 | 1330 | 53.8 | 2240 | 1395 | 62.3 | 1840 | 960 | 52.2 |
| East of England | 2305 | 8.2 | 36.0 (17.6) | 38 (23–50) | 2305 | 1335 | 57.9 | 2115 | 1470 | 69.5 | 1570 | 995 | 63.4 |
| London | 4115 | 14.6 | 33.1 (17.1) | 34 (20–47) | 4115 | 2295 | 55.8 | 3775 | 2225 | 58.9 | 2790 | 1585 | 56.8 |
| North East | 2060 | 7.3 | 34.9 (17.9) | 37 (23–48) | 2060 | 1200 | 58.3 | 1800 | 1205 | 66.9 | 1360 | 825 | 60.7 |
| North West | 4305 | 15.3 | 37.7 (17.1) | 41 (27–50) | 4305 | 2715 | 63.1 | 3965 | 2615 | 66.0 | 3190 | 2005 | 62.9 |
| South East | 4055 | 14.4 | 38.2 (17.3) | 42 (26–51) | 4055 | 2590 | 63.9 | 3750 | 2720 | 72.5 | 2970 | 2025 | 68.2 |
| South West | 1590 | 5.6 | 36.1 (16.3) | 38 (25–48) | 1590 | 855 | 53.8 | 1480 | 930 | 62.8 | 1165 | 675 | 57.9 |
| West Midlands | 3665 | 13.0 | 34.8 (15.9) | 37 (23–47) | 3665 | 2145 | 58.5 | 3435 | 2155 | 62.7 | 2555 | 1410 | 55.2 |
| Yorkshire and The Humber | 3585 | 12.7 | 36.8 (16.8) | 39 (25–49) | 3585 | 2220 | 61.9 | 3345 | 2225 | 66.5 | 2545 | 1635 | 64.2 |
| Year of delivery | |||||||||||||
| 2010 | 2045 | 7.3 | 37.6 (17.0) | 41 (28–49) | 2045 | 1025 | 50.1 | 1900 | 1035 | 54.5 | 1665 | 1105 | 66.4 |
| 2011 | 1860 | 6.6 | 35.8 (17.7) | 40 (23–49) | 1860 | 870 | 46.8 | 1690 | 1000 | 59.2 | 1405 | 905 | 64.4 |
| 2012 | 2865 | 10.2 | 39.9 (17.5) | 44 (30–52) | 2865 | 1865 | 65.1 | 2650 | 1865 | 70.4 | 2265 | 1510 | 66.7 |
| 2013 | 4070 | 14.5 | 40.0 (17.1) | 44 (30–52) | 4070 | 2585 | 63.5 | 3765 | 2665 | 70.8 | 3210 | 2170 | 67.6 |
| 2014 | 3590 | 12.8 | 38.0 (16.6) | 41 (28–50) | 3590 | 2190 | 61.0 | 3330 | 2255 | 67.7 | 2755 | 1715 | 62.3 |
| 2015 | 5110 | 18.2 | 35.0 (16.2) | 37 (24–47) | 5110 | 3175 | 62.1 | 4720 | 3180 | 67.4 | 3470 | 1935 | 55.8 |
| 2016 | 5260 | 18.7 | 31.9 (16.3) | 32 (19–45) | 5260 | 3105 | 59.0 | 4805 | 3065 | 63.8 | 3070 | 1665 | 54.2 |
| 2017 | 3145 | 11.2 | 32.5 (16.5) | 34 (19–45) | 3145 | 1775 | 56.4 | 2865 | 1785 | 62.3 | 2020 | 1060 | 52.5 |
| 2018 | 200 | 0.7 | 28.7 (16.3) | 30 (14–41) | 200 | 100 | 50.0 | 175 | 95 | 54.3 | 125 | 50 | 40.0 |
| Season of birth | |||||||||||||
| January–March | 6675 | 23.7 | 35.6 (17.0) | 38 (23–48) | 6675 | 3870 | 58.0 | 6100 | 4060 | 66.6 | 4675 | 2830 | 60.5 |
| April–June | 7020 | 24.9 | 36.0 (16.9) | 39 (24–49) | 7020 | 4125 | 58.8 | 6505 | 4235 | 65.1 | 5020 | 3025 | 60.3 |
| July–September | 7245 | 25.7 | 36.1 (17.2) | 39 (24–49) | 7245 | 4355 | 60.1 | 6655 | 4295 | 64.5 | 5175 | 3165 | 61.2 |
| October–December | 7210 | 25.6 | 36.1 (17.0) | 38 (24–49) | 7210 | 4340 | 60.2 | 6645 | 4345 | 65.4 | 5115 | 3090 | 60.4 |
| History of admissions within 2 years prior to 20 weeks of pregnancy | |||||||||||||
| Adversity | 2010 | 7.1 | 37.3 (17.9) | 39 (24–50) | 2010 | 1290 | 64.2 | 1855 | 1310 | 70.6 | 1375 | 880 | 64.0 |
| Violence | 175 | 0.6 | 35.4 (18.9) | 36 (20–48) | 175 | 105 | 60.0 | 160 | 110 | 68.8 | 110 | 70 | 63.6 |
| Self-harm | 1540 | 5.5 | 37.4 (17.8) | 40 (25–50) | 1540 | 1000 | 64.9 | 1425 | 1005 | 70.5 | 1050 | 680 | 64.8 |
| Substance misuse | 1810 | 6.4 | 37.4 (17.9) | 39 (25–50) | 1810 | 1160 | 64.1 | 1670 | 1185 | 71.0 | 1245 | 800 | 64.3 |
| Mental health (exc. self-harm/substance misuse) | 1160 | 4.1 | 37.6 (17.5) | 41 (25–50) | 1160 | 775 | 66.8 | 1080 | 805 | 74.5 | 790 | 520 | 65.8 |
| Mental health (any) | 2325 | 8.3 | 37.4 (17.8) | 40 (25–50) | 2325 | 1505 | 64.7 | 2150 | 1530 | 71.2 | 1600 | 1030 | 64.4 |
| Chronic condition (any, exc. mental health) | 3600 | 12.8 | 36.9 (17.6) | 39 (24–50) | 3600 | 2245 | 62.4 | 3330 | 2305 | 69.2 | 2485 | 1575 | 63.4 |
| A&E visits | 19,635 | 69.7 | 35.9 (17.3) | 38 (23–49) | 19,635 | 11,615 | 59.2 | 18,020 | 11,850 | 65.8 | 13,760 | 8390 | 61.0 |
| Repeated A&E visits (≥ 4) | 6050 | 21.5 | 36.0 (17.7) | 38 (23–49) | 6050 | 3600 | 59.5 | 5545 | 3740 | 67.4 | 4095 | 2585 | 63.1 |
| Did not attend at least one outpatient appointment | 9775 | 37.7 | 35.2 (17.4) | 37 (22–48) | 9775 | 5720 | 58.5 | 8900 | 5855 | 65.8 | 6635 | 4025 | 60.7 |
| Gestational age at antenatal booking appointment | |||||||||||||
| Before 10 weeks | 7505 | 26.7 | 36.7 (17.1) | 39 (25–50) | 7505 | 4335 | 57.8 | 6890 | 4565 | 66.3 | 5385 | 3330 | 61.8 |
| 10–20 weeks | 10,450 | 37.1 | 36.5 (16.9) | 39 (25–49) | 10,450 | 6315 | 60.4 | 9735 | 6340 | 65.1 | 7575 | 4535 | 59.9 |
| 20 weeks or more | 1705 | 6.1 | 33.5 (17.4) | 36 (20–47) | 1705 | 1065 | 62.5 | 1525 | 995 | 65.2 | 1150 | 700 | 60.9 |
| Unknown | 8490 | 30.2 | 35.1 (17.0) | 38 (23–48) | 8490 | 4980 | 58.7 | 7745 | 5040 | 65.1 | 5880 | 3550 | 60.4 |
| Linked to NPD | |||||||||||||
| Linked to NPD | 25,185 | 89.5 | 36.1 (17.0) | 39 (24–49) | 25,185 | 14,930 | 59.3 | 23,185 | 15,210 | 65.6 | 17,970 | 10,900 | 60.7 |
| Not linked to NPD | 2835 | 10.1 | 34.5 (17.4) | 37 (21–48) | 2835 | 1685 | 59.4 | 2590 | 1650 | 63.7 | 1915 | 1155 | 60.3 |
| Not linked to NPD census | 135 | 0.5 | 36.6 (17.7) | 39 (23–49) | 135 | 75 | 55.6 | 125 | 80 | 64.0 | 105 | 60 | 57.1 |
| Social care and educational characteristics before 20 weeks of pregnancy | |||||||||||||
| Ever in care | 2760 | 11.0 | 35.5 (17.9) | 37 (21–49) | 2760 | 1770 | 64.1 | 2545 | 1810 | 71.1 | 1715 | 1100 | 64.1 |
| Ever had recorded CPP | 1530 | 6.1 | 35.0 (17.8) | 35 (22–49) | 1530 | 980 | 64.1 | 1405 | 1000 | 71.2 | 945 | 580 | 61.4 |
| Ever recorded as having SEN | 15,275 | 60.7 | 36.3 (17.2) | 39 (24–49) | 15,275 | 9195 | 60.2 | 14,095 | 9430 | 66.9 | 10,720 | 6625 | 61.8 |
| Ever recorded as having FSM | 16,490 | 65.5 | 36.0 (17.2) | 38 (23–49) | 16,490 | 9850 | 59.7 | 15,190 | 9995 | 65.8 | 11,555 | 7090 | 61.4 |
| Ever in bottom IDACI decile | 10,235 | 40.6 | 35.3 (17.0) | 37 (23–48) | 10,235 | 5995 | 58.6 | 9405 | 5945 | 63.2 | 7150 | 4290 | 60.0 |
| Ever excluded, in PRU or alternative provision | 9395 | 37.3 | 35.4 (17.4) | 38 (22–49) | 9395 | 5460 | 58.1 | 8615 | 5585 | 64.8 | 6495 | 3910 | 60.2 |
| Ever recorded as persistently absent in a term | 13,745 | 54.6 | 36.5 (17.0) | 39 (25–49) | 13,745 | 8190 | 59.6 | 12,705 | 8300 | 65.3 | 9905 | 5980 | 60.4 |
| GCSE attainment for those eligible | 3620 | 17.0 | 36.1 (16.4) | 39 (25–49) | 3620 | 2195 | 60.6 | 3315 | 2215 | 66.8 | 2655 | 1535 | 57.8 |
| KS2 Maths (achieved expected levels) | 12,590 | 50.0 | 36.1 (16.8) | 39 (24–49) | 12,590 | 7415 | 58.9 | 11,570 | 7545 | 65.2 | 9135 | 5425 | 59.4 |
| KS2 English (achieved expected levels) | 15,550 | 61.7 | 35.9 (16.8) | 38 (24–48) | 15,550 | 9100 | 58.5 | 14,300 | 9235 | 64.6 | 11,220 | 6610 | 58.9 |
| Full programme | Pregnancy (up to birth) |
Infancy (0–1 year) |
Toddlerhood (1–2 years) |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | Number of visits | Total | Met 80% target | Total | Met 65% target | Total | Met 60% target | ||||||
| N | % | Mean (SD) | Median (IQR) | N | N | % | N | N | % | N | N | % | |
| Total | 28,150 | 100 | 35.9 (17.0) | 38 (24–49) | 28,150 | 16,695 | 59.3 | 25,900 | 16,940 | 65.4 | 19,990 | 12,115 | 60.6 |
| English as primary language | |||||||||||||
| No | 1350 | 4.8 | 33.5 (15.7) | 35 (22–46) | 1350 | 835 | 61.9 | 1275 | 765 | 60.0 | 920 | 490 | 53.3 |
| Yes | 26,035 | 92.5 | 36.9 (16.5) | 39 (25–49) | 26,035 | 15,785 | 60.6 | 24,375 | 16,090 | 66.0 | 18,935 | 11,550 | 61.0 |
| Unknown | 770 | 2.7 | 7.7 (11.9) | 2 (1–7) | 770 | 75 | 9.7 | 250 | 85 | 34.0 | 135 | 75 | 55.6 |
| Marital status | |||||||||||||
| Married/civil partnership | 730 | 2.6 | 34.5 (16.4) | 37 (23–47) | 730 | 425 | 58.2 | 670 | 425 | 63.4 | 495 | 310 | 62.6 |
| Co-habiting | 5325 | 18.9 | 36.8 (16.6) | 39 (25–49) | 5325 | 3245 | 60.9 | 4975 | 3330 | 66.9 | 3830 | 2370 | 61.9 |
| Separated/divorced | 65 | 0.2 | 34.8 (16.6) | 37 (28–48) | 65 | 35 | 53.8 | 60 | 35 | 58.3 | 45 | 25 | 55.6 |
| Single – never married | 21,255 | 75.5 | 36.8 (16.5) | 39 (25–49) | 21,255 | 12,905 | 60.7 | 19,940 | 13,060 | 65.5 | 15,475 | 9335 | 60.3 |
| Unknown | 780 | 2.8 | 8.1 (12.4) | 2 (1–8) | 780 | 80 | 10.3 | 260 | 90 | 34.6 | 140 | 80 | 57.1 |
| % of visits with partner present | |||||||||||||
| 0 | 6825 | 24.2 | 27.1 (17.8) | 27 (11–42) | 6825 | 3375 | 49.5 | 5520 | 3045 | 55.2 | 3545 | 1840 | 51.9 |
| 1–9.9 | 5745 | 20.4 | 41.7 (13.1) | 43 (33–51) | 5745 | 3715 | 64.7 | 5730 | 3990 | 69.6 | 4930 | 3015 | 61.2 |
| 10–29.9 | 7295 | 25.9 | 39.2 (15.1) | 41 (29–50) | 7295 | 4505 | 61.8 | 7105 | 4795 | 67.5 | 5745 | 3570 | 62.1 |
| 30–49.9 | 3965 | 14.1 | 39.1 (15.6) | 41 (29–50) | 3965 | 2510 | 63.3 | 3810 | 2565 | 67.3 | 3050 | 1910 | 62.6 |
| ≥ 50 | 4290 | 15.2 | 33.9 (18.9) | 37 (18–49) | 4290 | 2590 | 60.4 | 3725 | 2550 | 68.5 | 2685 | 1745 | 65.0 |
| % of visits with parent present | |||||||||||||
| 0 | 8880 | 31.5 | 29.0 (18.1) | 29 (13–44) | 8880 | 4505 | 50.7 | 7350 | 4300 | 58.5 | 4945 | 2735 | 55.3 |
| 1–9.9 | 8175 | 29 | 42.3 (13.0) | 43 (34–51) | 8175 | 5355 | 65.5 | 8160 | 5800 | 71.1 | 7065 | 4485 | 63.5 |
| 10–29.9 | 6515 | 23.1 | 38.4 (15.6) | 40 (28–50) | 6515 | 4095 | 62.9 | 6305 | 4135 | 65.6 | 4970 | 3040 | 61.2 |
| 30–49.9 | 2380 | 8.5 | 37.0 (16.7) | 40 (24–50) | 2380 | 1505 | 63.2 | 2245 | 1500 | 66.8 | 1680 | 1055 | 62.8 |
| ≥ 50 | 2165 | 7.7 | 32.1 (19.1) | 34 (16–48) | 2165 | 1235 | 57.0 | 1820 | 1205 | 66.2 | 1290 | 760 | 58.9 |
| Living arrangement | |||||||||||||
| Alone | 15,085 | 53.6 | 37.0 (16.2) | 39 (26–49) | 15,085 | 9135 | 60.6 | 14,185 | 9195 | 64.8 | 11,225 | 6710 | 59.8 |
| Foster carers/group home/other | 5440 | 19.3 | 36.4 (16.5) | 39 (24–49) | 5440 | 3310 | 60.8 | 5070 | 3355 | 66.2 | 3885 | 2375 | 61.1 |
| Mother (with or without partner) | 2770 | 9.8 | 36.8 (17.0) | 39 (24–49) | 2770 | 1680 | 60.6 | 2570 | 1705 | 66.3 | 1970 | 1210 | 61.4 |
| Partner (with/without others, not mother) | 1620 | 5.8 | 36.5 (17.0) | 38 (25–49) | 1620 | 930 | 57.4 | 1520 | 975 | 64.1 | 1170 | 720 | 61.5 |
| Relatives/other adults | 2470 | 8.8 | 36.0 (17.4) | 37 (22–49) | 2470 | 1565 | 63.4 | 2305 | 1625 | 70.5 | 1605 | 1020 | 63.6 |
| Unknown | 770 | 2.7 | 7.7 (11.9) | 2 (1–7) | 770 | 75 | 9.7 | 250 | 85 | 34.0 | 135 | 75 | 55.6 |
| Housing type | |||||||||||||
| Owned | 5245 | 18.6 | 37.2 (15.7) | 40 (27–49) | 5245 | 3150 | 60.1 | 4915 | 3310 | 67.3 | 3960 | 2345 | 59.2 |
| Rented: private | 6000 | 21.3 | 35.7 (16.7) | 38 (23–48) | 6000 | 3525 | 58.8 | 5585 | 3525 | 63.1 | 4250 | 2545 | 59.9 |
| Rented: housing association | 3600 | 12.8 | 38.1 (16.4) | 40 (27–50) | 3600 | 2270 | 63.1 | 3410 | 2280 | 66.9 | 2730 | 1660 | 60.8 |
| Rented: council | 9410 | 33.4 | 37.0 (16.5) | 40 (25–49) | 9410 | 5765 | 61.3 | 8840 | 5770 | 65.3 | 6865 | 4245 | 61.8 |
| Unknown | 3895 | 13.8 | 30.0 (19.6) | 31 (13–46) | 3895 | 1985 | 51.0 | 3155 | 2055 | 65.1 | 2185 | 1320 | 60.4 |
| Number of benefits received at enrolment | |||||||||||||
| 0 | 15,475 | 55 | 36.5 (16.3) | 39 (25–49) | 15,475 | 9475 | 61.2 | 14,480 | 9500 | 65.6 | 11,215 | 6590 | 58.8 |
| 1 | 6050 | 21.5 | 36.8 (16.8) | 40 (25–49) | 6050 | 3580 | 59.2 | 5660 | 3690 | 65.2 | 4390 | 2785 | 63.4 |
| 2 | 3365 | 12 | 36.9 (16.8) | 39 (25–50) | 3365 | 2050 | 60.9 | 3160 | 2110 | 66.8 | 2425 | 1485 | 61.2 |
| 3 | 1835 | 6.5 | 37.2 (17.0) | 40 (25–50) | 1835 | 1115 | 60.8 | 1725 | 1145 | 66.4 | 1325 | 855 | 64.5 |
| 4 + | 650 | 2.3 | 37.7 (16.9) | 41 (26–50) | 650 | 400 | 61.5 | 615 | 410 | 66.7 | 490 | 320 | 65.3 |
| Unknown | 775 | 2.7 | 7.8 (12.0) | 2 (1–7) | 775 | 75 | 9.7 | 255 | 85 | 33.3 | 135 | 80 | 59.3 |
| CiN status at enrolment | |||||||||||||
| No | 25,745 | 91.4 | 36.6 (16.4) | 39 (25–49) | 25,745 | 15,430 | 59.9 | 24,085 | 15,685 | 65.1 | 18,735 | 11,300 | 60.3 |
| Yes | 1635 | 5.8 | 39.1 (17.4) | 41 (26–52) | 1635 | 1185 | 72.5 | 1560 | 1170 | 75.0 | 1120 | 735 | 65.6 |
| Unknown | 775 | 2.7 | 7.9 (12.1) | 2 (1–7) | 775 | 80 | 10.3 | 255 | 85 | 33.3 | 135 | 80 | 59.3 |
| CPP at enrolment | |||||||||||||
| No | 26,595 | 94.5 | 36.6 (16.5) | 39 (25–49) | 26,595 | 16,025 | 60.3 | 24,895 | 16,255 | 65.3 | 19,350 | 11,695 | 60.4 |
| Yes | 780 | 2.8 | 38.8 (17.8) | 40 (24–52) | 780 | 590 | 75.6 | 755 | 595 | 78.8 | 500 | 340 | 68.0 |
| Unknown | 775 | 2.7 | 7.9 (12.1) | 2 (1–7) | 775 | 80 | 10.3 | 255 | 85 | 33.3 | 135 | 80 | 59.3 |
| Alcohol or drug use in the 2 weeks prior to enrolment | |||||||||||||
| No | 25,655 | 91.1 | 37.0 (16.2) | 39 (25–49) | 25,655 | 15,745 | 61.4 | 24,230 | 15,940 | 65.8 | 18,755 | 11,350 | 60.5 |
| Yes | 1380 | 4.9 | 38.3 (16.4) | 40 (27–50) | 1380 | 855 | 62.0 | 1325 | 860 | 64.9 | 1025 | 640 | 62.4 |
| Unknown | 1120 | 4 | 8.5 (13.5) | 2 (1–7) | 1120 | 95 | 8.5 | 345 | 135 | 39.1 | 210 | 125 | 59.5 |
| Characteristics of family nurses | |||||||||||||
| Nurse age (years) | |||||||||||||
| 21–29 | 1235 | 4.4 | 35.3 (15.6) | 37 (24–47) | 1235 | 710 | 57.5 | 1185 | 705 | 59.5 | 895 | 485 | 54.2 |
| 30–39 | 4525 | 16.1 | 35.3 (16.2) | 37 (24–47) | 4525 | 2675 | 59.1 | 4220 | 2695 | 63.9 | 3190 | 1810 | 56.7 |
| 40–49 | 10,580 | 37.6 | 36.1 (16.7) | 39 (24–49) | 10,580 | 6395 | 60.4 | 9760 | 6405 | 65.6 | 7530 | 4515 | 60.0 |
| 50–59 | 5935 | 21.1 | 36.7 (17.2) | 39 (25–50) | 5935 | 3545 | 59.7 | 5505 | 3715 | 67.5 | 4270 | 2640 | 61.8 |
| 60–69 | 305 | 1.1 | 31.6 (16.0) | 35 (18–44) | 305 | 125 | 41.0 | 275 | 145 | 52.7 | 215 | 105 | 48.8 |
| Unknown | 5570 | 19.8 | 35.8 (18.4) | 39 (22–50) | 5570 | 3245 | 58.3 | 4955 | 3275 | 66.1 | 3895 | 2560 | 65.7 |
| Nurse gender | |||||||||||||
| Male | 200 | 0.7 | 33.0 (17.4) | 33 (19–48) | 200 | 110 | 55.0 | 180 | 125 | 69.4 | 120 | 80 | 66.7 |
| Female | 22,380 | 79.5 | 36.0 (16.7) | 38 (24–49) | 22,380 | 13,335 | 59.6 | 20,770 | 13,540 | 65.2 | 15,970 | 9480 | 59.4 |
| Unknown | 5570 | 19.8 | 35.8 (18.4) | 39 (22–50) | 5570 | 3245 | 58.3 | 4955 | 3275 | 66.1 | 3895 | 2560 | 65.7 |
| Nurse ethnicity | |||||||||||||
| White | 20,770 | 73.8 | 36.4 (16.6) | 39 (25–49) | 20,770 | 12,480 | 60.1 | 19,285 | 12,735 | 66.0 | 14,935 | 8925 | 59.8 |
| South Asian | 210 | 0.7 | 29.8 (16.5) | 30 (16–44) | 210 | 110 | 52.4 | 185 | 120 | 64.9 | 120 | 70 | 58.3 |
| Black | 1335 | 4.7 | 30.9 (16.4) | 32 (18–43) | 1335 | 705 | 52.8 | 1215 | 670 | 55.1 | 840 | 460 | 54.8 |
| Mixed/other | 270 | 1 | 33.3 (15.4) | 32 (22–45) | 270 | 155 | 57.4 | 260 | 145 | 55.8 | 195 | 100 | 51.3 |
| Unknown | 5570 | 19.8 | 35.8 (18.4) | 39 (22–50) | 5570 | 3245 | 58.3 | 4955 | 3275 | 66.1 | 3895 | 2560 | 65.7 |
| Nurse health visiting qualification | |||||||||||||
| No BSc HV | 9805 | 34.8 | 35.8 (16.6) | 38 (24–48) | 9805 | 5780 | 58.9 | 9125 | 5865 | 64.3 | 6945 | 4120 | 59.3 |
| BSc HV | 12,780 | 45.4 | 36.1 (16.7) | 38 (24–49) | 12,780 | 7665 | 60.0 | 11,820 | 7800 | 66.0 | 9145 | 5440 | 59.5 |
| Unknown | 5570 | 19.8 | 35.8 (18.4) | 39 (22–50) | 5570 | 3245 | 58.3 | 4955 | 3275 | 66.1 | 3895 | 2560 | 65.7 |
| N mothers (% of all mothers) |
N who met pregnancy target (% of group) |
Adjusted RR (95% CI)a |
|
|---|---|---|---|
| Total | 27,360 (100) | 16,610 (60.7) | – |
| Year of delivery | |||
| 2010 | 1970 (7.2) | 1020 (51.8) | 1.00 (ref) |
| 2011 | 1785 (6.5) | 865 (48.5) | 0.92 (0.84 to 1.01) |
| 2012 | 2795 (10.2) | 1855 (66.4) | 1.22 (1.10 to 1.35) |
| 2013 | 3975 (14.5) | 2575 (64.8) | 1.18 (1.07 to 1.31) |
| 2014 | 3515 (12.8) | 2185 (62.2) | 1.14 (1.03 to 1.27) |
| 2015 | 4975 (18.2) | 3165 (63.6) | 1.17 (1.05 to 1.30) |
| 2016 | 5130 (18.8) | 3085 (60.1) | 1.09 (0.97 to 1.22) |
| 2017 | 3025 (11.1) | 1760 (58.2) | 1.05 (0.93 to 1.17) |
| 2018 | 190 (0.7) | 100 (52.6) | 0.95 (0.81 to 1.13) |
| N mothers (% of all mothers) |
N who met infancy target (% of group) |
Adjusted RR (95% CI)a |
|
|---|---|---|---|
| Total | 25,635 (100) | 16,845 (65.7) | - |
| Year of delivery | |||
| 2010 | 1865 (7.3) | 1030 (55.2) | 1.00 (ref) |
| 2011 | 1670 (6.5) | 990 (59.3) | 1.07 (1.00 to 1.15) |
| 2012 | 2630 (10.3) | 1855 (70.5) | 1.15 (1.07 to 1.23) |
| 2013 | 3740 (14.6) | 2655 (71.0) | 1.15 (1.07 to 1.24) |
| 2014 | 3310 (12.9) | 2240 (67.7) | 1.11 (1.04 to 1.19) |
| 2015 | 4675 (18.2) | 3165 (67.7) | 1.10 (1.02 to 1.18) |
| 2016 | 4755 (18.5) | 3045 (64.0) | 1.04 (0.97 to 1.12) |
| 2017 | 2815 (11.0) | 1765 (62.7) | 1.02 (0.94 to 1.11) |
| 2018 | 175 (0.7) | 95 (54.3) | 0.89 (0.74 to 1.06) |
| Season | |||
| January–March | 6025 (23.5) | 4030 (66.9) | 1.00 (ref) |
| April–June | 6445 (25.1) | 4215 (65.4) | 0.97 (0.95 to 1.00) |
| July–September | 6590 (25.7) | 4275 (64.9) | 0.95 (0.93 to 0.98) |
| October–December | 6575 (25.6) | 4325 (65.8) | 0.96 (0.94 to 0.99) |
| N mothers (% of all mothers) |
N who met toddlerhood target (% of group) |
Adjusted RR (95% CI)a |
|
|---|---|---|---|
| Total | 19,655 (100) | 11,900 (60.5) | - |
| Year of delivery | |||
| 2010 | 1625 (8.3) | 1070 (65.8) | 1.00 (ref) |
| 2011 | 1375 (7.0) | 885 (64.4) | 0.92 (0.86 to 0.98) |
| 2012 | 2235 (11.4) | 1490 (66.7) | 0.86 (0.81 to 0.91) |
| 2013 | 3150 (16.0) | 2130 (67.6) | 0.86 (0.82 to 0.91) |
| 2014 | 2725 (13.9) | 1695 (62.2) | 0.81 (0.76 to 0.86) |
| 2015 | 3440 (17.5) | 1915 (55.7) | 0.71 (0.66 to 0.76) |
| 2016 | 3010 (15.3) | 1630 (54.2) | 0.70 (0.64 to 0.76) |
| 2017 | 1970 (10.0) | 1030 (52.3) | 0.68 (0.62 to 0.74) |
| 2018 | 125 (0.6) | 50 (40.0) | 0.55 (0.44 to 0.69) |
| Season | |||
| January–March | 4580 (23.3) | 2770 (60.5) | 1.00 (ref) |
| April–June | 4950 (25.2) | 2985 (60.3) | 0.97 (0.94 to 1.00) |
| July–September | 5090 (25.9) | 3110 (61.1) | 0.98 (0.95 to 1.00) |
| October–December | 5035 (25.6) | 3040 (60.4) | 0.96 (0.93 to 0.99) |
Appendix 11 Timeline for data access
| October 2017 | Application submitted to DfE for NPD data Application submitted to NHS Digital for linkage between FNP, HES and NPD |
| December 2017 | Application submitted to CAG, confidentiality advisory group/National Research Ethics |
| January 2018 | Ethics approval confirmed |
| February 2018 | CAG provisional approval |
| Delays due to security assurances for DfE not being in place: NHS Digital could not release identifiers for linkage | |
| November 2018 | Amendment submitted to NHS Digital removing request for DfE data (due to delays in security assurances being confirmed). Amendment submitted to CAG to remove DfE data |
| January 2019 | CAG amendment approved New DARS application submitted |
| June 2019 | DfE assurances now in place Amendment submitted to CAG to allow linkage with education data (as per original CAG application) |
| July 2019 | CAG approval for second amendment received We were advised by NHS Digital to wait until the first application (without education data) had been approved before we submitted an amendment (for the education data) |
| September 2019 | Grant started |
| November 2019 | NHS Digital approval for linkage of HES and FNP data |
| July 2020 | Linked HES – FNP data received from NHS Digital |
| August 2020 | Amendment submitted to allow linkage with education data |
| March 2021 | NHS Digital approval of linkage with education data |
| September 2021 | Linkage with education data completed |
| October 2021 | Linked education and social care data available on the ONS SRS |
| December 2021 | HES and FNP data imported into the ONS SRS |
List of abbreviations
- A&E
- accident and emergency
- APC
- admitted patient care
- CiN
- Child in Need
- CLA
- Child Looked After
- CPP
- child protection plan
- DfE
- Department for Education
- EYFSP
- early years foundation stage profile
- FNP
- Family Nurse Partnership
- FNP IS
- Family Nurse Partnership information system
- FSM
- free school meals
- GCSE
- General Certificate of Secondary Education
- GP
- general practitioner
- HES
- Hospital Episode Statistics
- HESID
- Hospital Episode Statistics Identifier
- ICD-10
- International Classification of Diseases, 10th Revision
- IDACI
- Income Deprivation Affecting Children Index
- IMD
- Index of Multiple Deprivation
- IQ
- intelligence quotient
- LA
- local authority
- LMP
- last menstrual period
- NFP
- Nurse Family Partnership
- NPD
- National Pupil Database
- ONS
- Office for National Statistics
- OPCS-4
- Office of Population, Censuses and Surveys Classification of Surgical Operations and Procedures, version 4
- PPI
- patient and public involvement
- PRU
- Pupil Referral Unit
- SEN
- Special Educational Needs
- UPN
- Unique Pupil Number
