Notes
Article history
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as award number 16/117/04. The contractual start date was in September 2018. The draft manuscript began editorial review in March 2023 and was accepted for publication in November 2023. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ manuscript and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this article.
Permissions
Copyright statement
Copyright © 2024 O’Doherty et al. This work was produced by O’Doherty et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2024 O’Doherty et al
Chapter 1 Introduction
Background and context
Evidence suggests that one in five women and one in 25 men in England and Wales have experienced sexual violence and abuse since the age of 16 years. 1 Sexual violence is defined as any sexual act, or attempt at a sexual act, or an act directed at a person’s sexuality, involving coercion, by any person regardless of their relationship with the subjected individual. It includes, but is not restricted to, rape, sexual assault, child sexual abuse (CSA), sexual harassment, rape within marriage and relationships, forced marriage, so-called honour-based violence, female genital mutilation, trafficking, sexual exploitation and ritual abuse. 2 Before the COVID-19 pandemic, fewer than one in six victims of rape reported to the police. In the year ending September 2022, the number of sexual offences recorded by the police (199,021) was the highest level recorded within a 12-month period, and showed a 22% increase when compared with the number of offences recorded by the police for the year ending March 2020. 3
Sexual violence and abuse is a serious public health concern, for which the range of immediate and long-term physical and mental health effects are well-documented. 4,5 Physical health consequences for women include unwanted pregnancy, sexually transmitted infections (STIs), painful sex, chronic pelvic pain and vaginal bleeding. 5,6 For men, these include genital and rectal injuries and erectile dysfunction. 7 The mental health effects of sexual violence are substantial. The incidence and severity of post-traumatic stress disorder (PTSD) is common among women and men who have experienced sexual violence and abuse. 8,9 Other mental health consequences include anxiety, depression, self-harm and suicidality, alcohol and drug abuse as well as eating disorders. 4 Furthermore, experiencing mental health problems is associated with an increased risk of other long-term health conditions including hypertension, cardiovascular disease and gastrointestinal problems. 10 The significant health burden of sexual violence and abuse has wider economic costs to society, reaching more than £12 billion per year (2015/16). 11
Although a wealth of evidence underpins the substantial negative effects of sexual violence and abuse, much less is understood about the longer-term health and well-being outcomes for survivors. In light of this, there has been a call for dedicated longitudinal research on the health effects of sexual violence. 4 Notably, a recent 3-year follow-up study in South Africa reported that women survivors were 60% more likely to acquire human immunodeficiency virus (HIV) infection in that time compared with control group women who had not been raped. 12 However, the longitudinal exploration of survivor’s health and well-being remains limited. More broadly, there are key gaps in sexual violence research with men survivors13 and survivors who have a disability. 14 Additionally, there is a lack of research that has examined sexual violence and abuse exposure and chronic mental health problems, and comorbidity of health outcomes15 and understanding sexual health and well-being outcomes beyond measuring STI acquisition only. 16
Why is research on sexual assault referral centres needed?
Providing accessible and an evidence-based response to survivors is critical. The World Health Organization (WHO) recommended that an initial response should include providing survivors with medico-legal and health services at the same time through holistic care, in the same location and preferably by the same health practitioner. 17 In the USA, many states now offer Sexual Assault Nurse Examiner programmes or Sexual Assault Response Teams to provide the recommended services. This type of support has been modelled in Australia, Canada and the UK. 18 In England and other parts of the UK, investment in sexual assault referral centres (SARCs) has grown considerably, especially as a ‘best practice’ response for survivors after incidents of sexual assault or rape. 19 Sexual assault referral centres are intended to coordinate all of the care and support needs for survivors of any age and gender, regardless of whether the survivor is a recent or non-recent victim, and to support survivors with the opportunity to make a police report if they choose to do so. As highlighted in the National Service Specification for SARCs,19 which outlines the aims and service standards of SARCs, the core services provided at SARCs include crisis emotional support by dedicated crisis workers, a forensic medical examination (FME; or nurse-led examination) to enable the collection of evidence needed to prosecute alleged perpetrators, provision of emergency contraception and HIV post-exposure prophylaxis, referral to sexual health centres and other healthcare services, referral for mental healthcare needs such as counselling and to an Independent Sexual Violence Advisor (ISVA), particularly if navigating the criminal justice system (CJS). Thus, SARCs operate within a wider landscape of Sexual Assault and Abuse Services (SAAS), across several systems and government organisations including health, social care and criminal justice partners. As stated in the Specification, an effective SARC does not simply provide services to survivors, but rather helps them understand what options are available and facilitate their choices with care.
There are approximately 50 SARCs in England, including a number of specialist paediatric sites. 20 While NHS England (NHSE) is responsible for the commissioning of the public health element within SARCs, the police and/or police and crime commissioners are responsible for commissioning forensic medical examination services. SARCs operate with considerable variation in areas where they are located, such as in hospitals or community settings, and the organisational model in which their services are delivered, for example, individual SARCs can be led by the police, private organisations, the NHS or charities. 19,21 To date, little is known about how effective and cost-effective SARCs are in addressing the physical and mental health outcomes for child and adult survivors. There is also a lack of evidence about whether the varying models in which SARCs operate has an effect on their effectiveness to support survivors. There are sparse data focusing on survivors’ access to mental health care after reaching a SARC18 and how service users of ethnic minority backgrounds, as well as sexual and gender minority communities, might experience care and support from SARCs.
Research objectives
Aims
-
To evaluate the evidence for psychosocial interventions for survivors of sexual violence and abuse.
-
To examine SARC models of service delivery by exploring work practices, workforce and technology factors and the integration of SARCs in the broader context of a health and community response to sexual violence and abuse.
-
To undertake a 1-year follow-up study in a cohort of survivors of sexual violence and abuse to explore the effect of different SARC models of service delivery, access to health care and other SAAS on PTSD, depressive symptoms, quality of life (QoL), substance misuse, violence re-exposure, sexual health and costs.
-
To identify the effect of delivering post-crisis trauma-focused counselling interventions in the voluntary sector compared with the NHS on health and other outcomes.
-
To engage young SARC service users (age range: 13–17 years) and explore impacts of exposure to sexual violence and abuse on their lives and quality of care and support from SARCs.
-
To draw on the cohort sample using maximum variation sampling to ensure a broad range of subgroups represented, supplemented by a community sample and to conduct a qualitative investigation of the experiences at SARCs and outcomes of SARCs and barriers and facilitators to access.
Research questions
-
For individuals who have experienced sexual violence and abuse, do psychosocial interventions reduce PTSD and other poor health outcomes? What are providers’ experiences of delivering such psychosocial interventions? What are the experiences of survivors and supporters in accessing such psychosocial interventions?
-
What are the implications of four inter-related aspects of SARCs – the everyday work they do, the workforce, the technology and the organisation – for the delivery of SARC services? What is the work of SARCs including the types of interventions delivered? Who is the SARC workforce? What are the technologies that enable SARCs to get work done? What is the organisational context of SARCs and to what extent are SARCs embedded within the overall response by statutory and voluntary sector organisations to the needs of survivors of sexual violence and abuse?
-
What are the health and cost trajectories of those who attend SARCs? How can these be compared for different SARC models of service delivery and access to health and SAAS?
-
What is the effect of receiving post-crisis counselling in the voluntary sector when compared with that provided through the NHS?
-
What are the experiences of children and young people (CYP) of receiving care and support from SARCs?
-
What are the experiences of access to SARCs by survivors from marginalised or minority populations?
Chapter 2 Project governance
Project steering group
A Study Steering Committee (SSC) independently chaired by Professor Roger Ingham had oversight of the multidisciplinary evaluation of sexual assault referral centres for better health (MESARCH) project. The Committee held 10 sessions at 6-monthly junctures over the project lifecycle, used to gather progress updates from the project team including review of the 6-monthly progress reports submitted to the National Institute for Health and Care Research (NIHR) and the funder’s response. These sessions assessed adherence to the study protocol and discussed amendments; assessed barriers to progress; enabled access to guidance and the range of expertise available through the members, who linked us with resources and networks; and enabled space for problem-solving, reflection and celebrating the ‘big’ and ‘small’ achievements of the project. The membership is listed in our protocol22 and included two members of our Lived Experiences Group/patient and public involvement (PPI) (see Patient and public involvement) and at least one representative was in attendance at all Committee sessions. The NIHR was notified of meeting minutes and actions arising from meetings with the SSC and Data Monitoring and Ethics Committee (DMEC; see Ethics). The SSC was also available to provide independent advice as required outside of the scheduled SSC meetings.
Ethics
Oversight and approvals
Approvals were granted by research ethics committees and the Health Research Authority before any data collection. Approval dates and reference numbers are provided in the Ethics Statement at the end of the report. In addition, five NHS SARC sites and one onward referral NHS agency confirmed site capacity and capability. Amendments to the study protocol and documentation were discussed with the SSC, and approval was sought and obtained from the relevant ethics committees. These amendments are outlined in V3.3 of the protocol. 22 The DMEC met on three occasions over the project course with the purpose of monitoring data collection and analyses across all studies, risks to the project and making recommendations on the ethical considerations where appropriate.
Ethical considerations
We now outline key ethical considerations that were made across the studies that involved primary data collection (SARC process evaluation, cohort study, embedded qualitative study and the CYP’s study). In the presentation of findings and quotes, we have ensured that participants are not identifiable. Where we had permission to use direct quotes from participants, we have used pseudonyms (chosen by participants or the research team) or quotes have been attributed to an unidentifiable label. In addition to the project team receiving regular training for conducting interviews with survivors of sexual violence and abuse, we developed a safety protocol drawing on safety and distress protocols from our previous published work, and based on the expertise of the MESARCH team, members of our Lived Experiences Group (LEG) and SSC, staff at Coventry Rape and Sexual Abuse Centre, and informed by the Charter of Survivors Voices. 23 The safety protocol outlined different procedures the project team would follow in relation to key risks. The procedures are as follows:
Promoting the safety of participants
Project team interviewers were trained to ensure that if a person expressed a concern about their current safety or well-being, then they were ready to ask about safety and support the interviewee or participant to seek the help they need. Equally, the interviewer was trained to enquire and respond if there was a concern based on other cues, such as behaviours of the respondent or indirect expressions of fear or worry or risk of self-harm or suicidality, as well as environment cues such as background noise or activity. Interviewers were trained in revisiting the contract set out at the beginning of the research about exceptions to maintaining confidentiality. The safety protocol also outlined an approach to discuss safety planning with a participant when they disclosed information and processes for recording disclosures of risk. As part of monitoring the safety and well-being of participants, we used a RAG (red, amber, green) system of different categories (see Appendix 1, Table 22). The ‘red’ category incidents involved considering whether we had to break confidentiality to promote safety through mandatory reporting. The decision to break confidentiality did not occur in the project.
Responding to a participant’s distress
We were mindful that there could be situations where a participant could be distressed at any stage of the research. This occurred during 5–10% of interviews. The researchers informed participants that the research could be concluded at any time and were prepared to signpost them to local or national services or connect them with their crisis worker, ISVA or Children and Young People’s Independent Sexual Violence Advisor (ChISVA) for further support. Although we did not ask participants to share details about the nature of the sexual abuse they experienced, the questions included in the interviews were carefully developed to avoid blaming or stigmatising language. Interviewers were mindful of triggers that could cause distress or embarrassment. Interviewers also reminded participants that they could choose which questions they felt comfortable to answer. Researchers were also trained in responding to participants experiencing a flashback during participation in the research and in monitoring whether negative effects were arising directly from the study over time.
New disclosures and data being subpoenaed by the criminal justice system
The project was committed to not jeopardising any criminal proceedings. We explained to participants before the research interviews and throughout the research process that if their case was going through the CJS, then there was a possibility that the project could be asked to provide information submitted by a participant to the research if requested by the courts. If participants had a live case and chose to talk about the incident(s), researchers were trained to remind participants of the commitments of the research and offered to direct the discussion to another part of the interview. New (first) disclosures or disclosures of new information about a live case would require the team to pass on the information to the police; however, we had no instance of having to take this action.
Maintaining safety for researchers
It was important that researchers made their role clear to participants that the purpose of the study was intended for research and not for treatment, signposting them to appropriate services and responding to safeguarding concerns and disclosures appropriately. The researchers communicated with participants and potential participants using their professional details and names, through the project phones and by email rather than providing any personal contact details. The research team was also prepared to respond to potential instances where a participant might frequently contact the project team and/or request to speak with a specific team member. We had no instances of this occurring.
During COVID-19, remote interviews continued to be conducted as researchers worked from home. To support staff members involved in contacting participants and conducting interviews, all communication and planned calls continued to be documented in a shared calendar and tracking system so that all project team members were aware of when contact occurred. The staff members continued to have weekly check-ins and regular opportunities for debriefing. In March 2021, LEG representatives and SSC members recognised the growing effects of conducting the research on those interviewing participants and engaging with data including screening a large number of studies for evidence reviews. The LEG and SSC recommended the introduction of regular supervision for staff members. In response, external clinical supervision was implemented every 6 weeks from May 2021 to ensure the staff members were well supported throughout the project.
Data management
A comprehensive data management plan was developed for our studies involving data collection. We regularly monitored our processes regarding where and for how long personal data and anonymised data sets were stored, as well as who had access to these data. To manage the personal data and safety notes of participants in our 1-year cohort study, a secure tracking system was developed for use by staff members who were interviewing participants, enabling accurate recording and tracking of participants’ personal data (such as their contact details), when they were due follow-up interviews, and information about safety concerns (this included the RAG system) and any actions implemented.
Patient and public involvement
Background
Patient and public involvement refers to involving patients, members of the population directly or indirectly affected by the target problem and/or members of the public in the research process. In MESARCH, we worked with survivors of sexual violence and abuse. While a research context could be empowering and beneficial to survivors in their recovery from trauma,24,25 negative engagement could lead to re-traumatisation. 23 The use of PPI to shape how research with survivors is carried out can lead to high-quality practice and positive experiences for participants. However, previous research suggests that there is considerable scope for improving the quality of PPI in sexual violence and abuse research. 23,26,27 Our research aimed to advance practice in this area.
Methodology
Drawing on principles of co-production, we worked in partnership with those with lived experience of sexual violence and abuse, referred heretofore as ‘the MESARCH LEG’. MESARCH reflects the shift to research being carried out collaboratively with members of the public who share decision-making rather than models of lay consultation and tokenistic involvement. 28,29 Several theoretical positions underpinned our approach. First, we value a multiplicity of knowledge and have afforded great weight to experiential knowledge within the research process thus creating opportunities for epistemic justice, a concept coined by philosopher and feminist Miranda Fricker30 where voices that are often silenced or marginalised are amplified. Second, building and maintaining strong relationships with the LEG was central to our approach to lived experience involvement, premised on theories of relational engagement, dialogical ethics and an ethics of care, and reflecting the significance of the human and socially interactive element of engagement. 31–33 Lastly, drawing on the concepts of citizenship and democracy, the active and meaningful involvement of those with lived experience of sexual violence and abuse in our research promotes the empowerment of survivors. 34 This is particularly relevant in relation to involving survivors of sexual violence and abuse who will have experienced disempowerment through abuse, communities and institutions. To ensure good practice in involving survivors of abuse and trauma in our research, we worked closely with Survivors’ Voices (a survivor-led organisation that harnesses the expertise of people affected by abuse), drawing on their Charter, which details principles and good practice for good survivor engagement in research. 23 We were also guided by the Rape Crisis National Service Standards, adapting a set of quality service standards to meet the needs of survivors of sexual violence and abuse. 35 These principles provide a framework against which we have monitored the extent to which our research is trauma-informed and achieves authentic survivor focus.
Methods
Our LEG was supported by a dedicated public engagement officer to enable a co-design and co-production approach across the project. LEG members were recruited through survivor support groups, delegates at conferences, participants on related research studies and recommendations from other researchers. Over the lifecycle of the project, the group included 11 members participating at different times and brought 794 hours of expertise into the project. Members of the LEG were diverse across sex, age, ethnicity, sexuality, education, employment and life opportunities. They brought a wide range of professional and lived expertise as well as various engagement with the CJS, NHS, therapies and third-sector services. We consistently worked to expand diversity as members moved on and new members joined, recognising the association between diversity and gains being achieved across the research.
The involvement of the LEG in the project was guided by a terms of reference document that was co-produced and regularly reviewed. Involvement was enhanced through formal meetings (8) administered through the lead university, participation of two LEG members in SSC meetings (10) to provide a lived experience perspective and contribute to the oversight of the project, and ongoing communication through other means as and when it was required. The work of the LEG was fully resourced by the NIHR covering people’s time, travel, childcare expenses and conference attendance. We also engaged with survivor support groups, organisations led by survivors, specialist sexual violence and abuse organisations and key stakeholders to further embed PPI across the project.
Patient and public involvement activity across the project lifecycle
Patient and public involvement was embedded across all aspects of the project, from its design and delivery to the interpretation and sharing of the findings (see Figure 1).
FIGURE 1.
Embedding lived experience and ‘experts-by-experience’ across the MESARCH project. CYP, children and young people; ISVA, independent sexual violence adviser; LEG, lived experiences group; PPI, patient and public involvement.
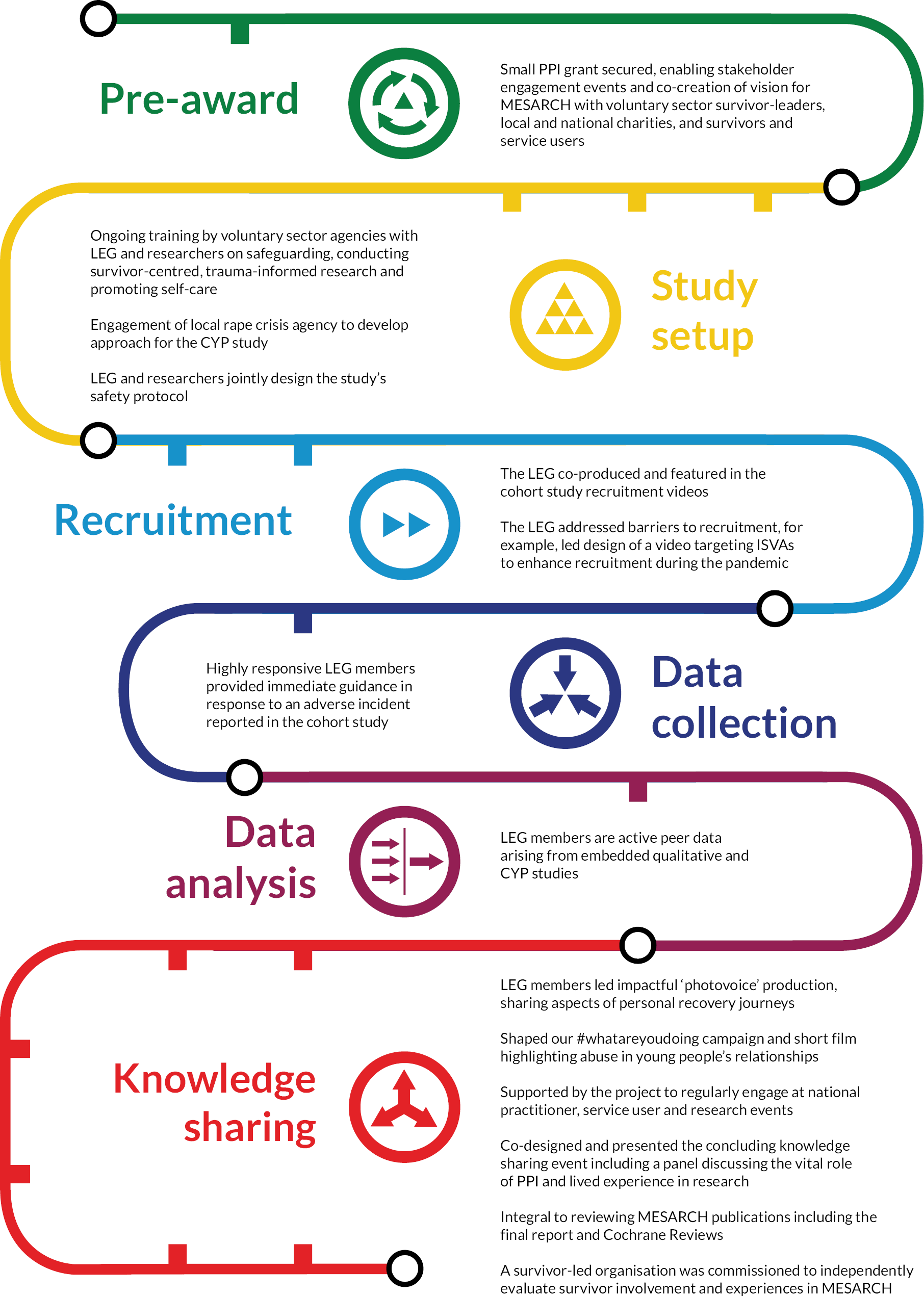
Pre-award
We held a stakeholder event to integrate perspectives from a wide array of third-sector organisations and administered a survey, in collaboration with a charity that supports survivors of sexual trauma, to gather views on research aims and methods. The results shaped our choice of primary outcome, use of incentives and plan for examining post-crisis care. We secured a PPI grant, which enabled us to co-create a vision for the project with survivors and service users; we built partnerships with the charity sector; and we created a leadership team to include survivorship alongside academic and practice-based experience.
Study set-up
From the outset and throughout the project, high-quality training that met gaps in skills and knowledge for teams was critical. The research team and LEG participated in five bespoke training sessions delivered by survivor-led organisations, specialist sexual violence organisations and members of the LEG. The training sessions addressed safeguarding issues; deepened the ability to understand trauma and respond in a research setting; enhanced the research skills of the LEG to enable them to work effectively with the research team; and promoted well-being and self-care. We worked with the LEG and sexual violence and abuse charities to optimise not only how we engaged with target service users and survivor participants but also the quality of participation experiences. This included developing and refining the safety protocol (see Ethics), the interview schedules for the cohort study and embedded qualitative study and the participant facing documentation. Initiation of the CYP study led to connecting with a local sexual violence and abuse charity where the young people (age range: 13–24 years) worked with us to design and develop the methods for the CYP study through a series of workshops.
Recruitment
There are particular challenges to reaching survivors for research purposes, even where that research offers the prospect of improved health and well-being through psychosocial interventions to the individual. 36 When the research is ‘observational’, there is a less apparent benefit to participation. Extensive groundwork and reflection was needed to co-produce a narrative for engagement with survivors and draw people safely and ethically to the research. The LEG was central to identifying and resolving moral questions and dilemmas about the undertaking the research, in addition to some of the more pragmatic details of connecting with survivors safely, and achieving participation and retention rates needed from a scientific viewpoint. Our recruitment videos, co-designed and featuring LEG members, are a good example of a practical response to mitigating the challenges brought about by research in this sphere (see http://mesarch.coventry.ac.uk/join-1000-voices-for-change/). LEG members actively used their collective voice to reduce barriers ISVAs might have faced in referring people to this study (e.g. Is MESARCH safe? Is it in the interest of my clients?).
Data collection
Having hugely influenced the content of interviews and the areas we assessed (e.g. adding suicidality, self-harm and eating problems outcomes and helping to select appropriate measures), the LEG worked towards closely monitoring how participants were experiencing the interviews and were active in resolving problems (see Ethics for details of adverse events).
Data analysis
Although the contribution in this arena was not quite as developed as that in others (because of the analysis tending to come late in the project lifecycle), LEG members have been integral to analysis for our CYP study (see Chapter 7) and our diverse survivor voices work where we tried to engage those hardest-to-reach (see Chapter 8). In these activities our LEG colleagues have fulfilled the definitions of peer or co-researchers, meaning they worked jointly and in partnership with researchers on research tasks using their lived experience to inform their work. 37,38
Knowledge sharing
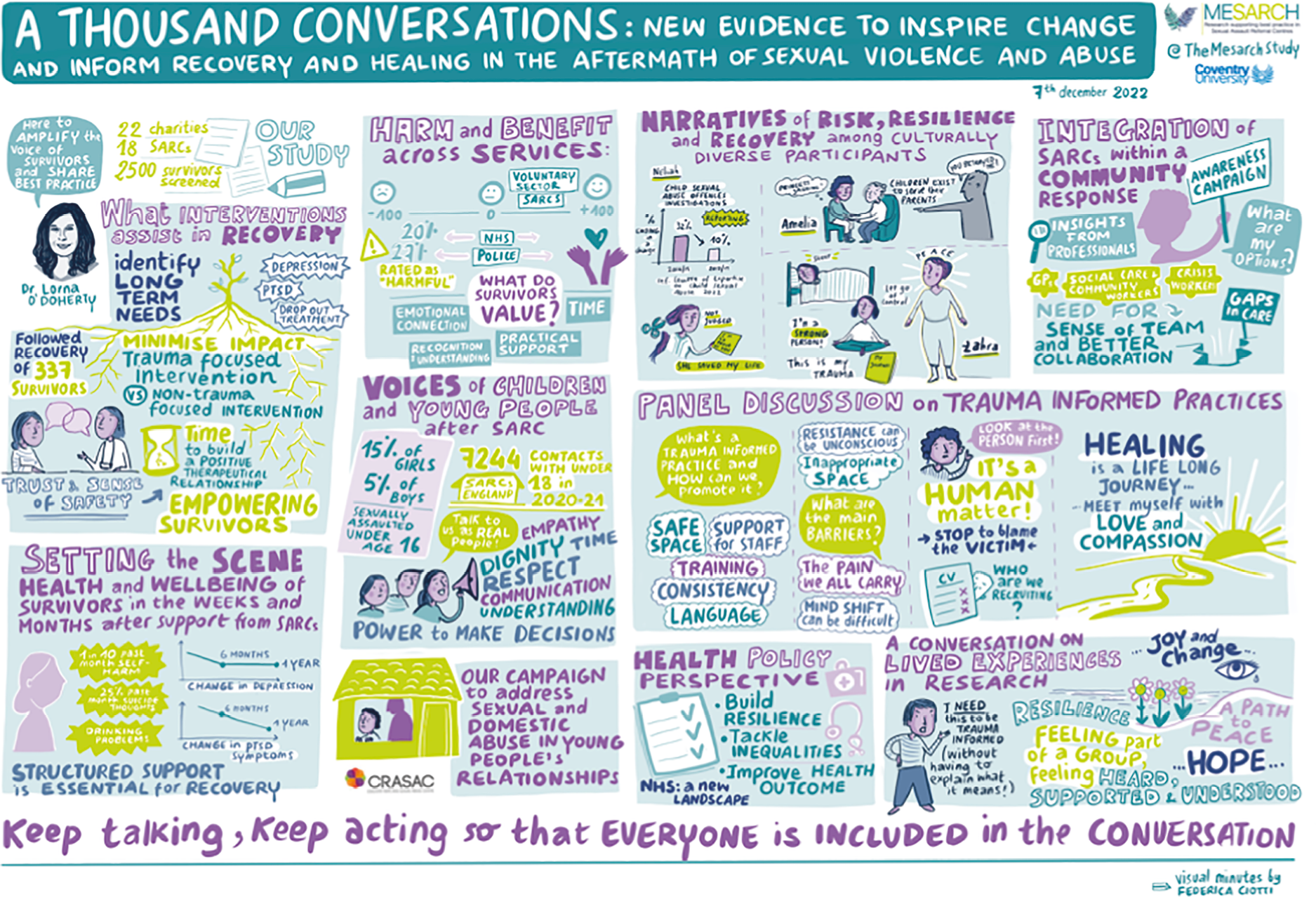
The LEG has been heavily involved in sharing knowledge and insights gained from the research, for example, shaped plain language statements across outputs such as our Cochrane Reviews (see Chapter 3). Other examples include a fully-supported LEG-led production in the form of ‘photovoice’ where members presented photos to convey recovery journeys (https://vimeo.com/547572348/2709483bd8). The end of our project knowledge-sharing event (7 December 2022; see Figure 2) was co-designed and co-delivered by the LEG and researchers (http://mesarch.coventry.ac.uk/whats-our-project-creating/). The LEG also shaped our ‘#whatareyoudoing’ campaign highlighting the problems of sexual and domestic abuse in young people’s relationships39 partly funded by NIHR as part of MESARCH, and raised this work as important at the NHSE survivor forum.
FIGURE 2.
Visual minutes from the MESARCH knowledge-sharing event.
Impact and evaluation of PPI
The overall impact of the LEG/PPI work summarised in Figure 1 on the research has been tremendous and is understood to explain the low incidence of adverse events and known harms arising from the research. This expertise was also part of operational success. There were also direct and unanticipated positive benefits for the LEG members themselves as captured in the testimony of one member (see Appendix 1, Box 43). LEG members also told us that being part of the group has contributed to recovery by enabling safe exposure to triggers. The conversations and interactions (online, by email, in person and in-print) that were part of the everyday work of the project normalised talking about sexual violence and abuse. Members have also commented on how being involved in MESARCH and being heard by MESARCH amplifies individual voices and provides a platform for creating change and being part of influencing better responses to others affected by abuse. PPI also enhanced the research team’s confidence to undertake this work, deepening our understanding in relation to trauma and abuse, and our LEG members’ commitment to the project was hugely motivating for overcoming the challenges encountered during the project. Our work with the PPI group has also inspired future research around understanding long-term physical health outcomes for survivors of sexual violence and abuse, and influencing the implementation of trauma-informed practice across the NHS (considering clinical services beyond mental health); building a toolkit of methods for doing better research in this field; and growing the evidence base on novel interventions for survivors that reflect survivors’ individual needs and preferences.
In an effort to identify any gaps in our PPI provision in MESARCH, we commissioned an independent, survivor-led organisation to evaluate it. 40 A summary of the conclusion reached by Survivors’ Voices is provided in Box 1.
In the MESARCH team approach, we found key features of trauma-informed research: careful attention to creating a safe environment, genuine care for survivors and a commitment to authentic and empowering involvement that amplified the voices of survivors.
Using the evaluation tools of the Survivor Charter and Involvement Ladder, we have gathered clear evidence of trauma-informed practice in the approach of the MESARCH team. This enabled and supported survivors to make a vital contribution to the project, as both participants and co-producers, centering lived experience at the heart of the research. Key strengths were a strong attention to creating a safe environment and demonstrating genuine care for survivor well-being, built on trustworthy relationships. Their commitment to authentic engagement, involving survivors as both participants and co-producers, empowered survivors and researchers. This meant the team could successfully amplify the voices of survivors, bringing the validity and impact of lived experience to trauma, abuse and violence research.
Chapter 3 Evidence synthesis
We conducted two complementary Cochrane Reviews to synthesise the evidence of the effects of psychosocial interventions on mental health and well-being for survivors of sexual violence and abuse. The term ‘psychosocial’ used in this research refers to ‘interpersonal or informational activities, techniques, or strategies that target biological, behavioural, cognitive, emotional, interpersonal, social, or environmental factors with the aim of improving health functioning and well‐being’. 41 This includes the types of interventions that may be offered to survivors by SARCs and by other services in the voluntary sector, the NHS or privately. The first review combined published randomised trials from various parts of the world that examined the effects of interventions designed to support adults in the aftermath of rape, sexual assault or abuse. The second review combined qualitative studies of adult and child survivors of sexual violence and abuse to develop a picture of service users’ (and family members’) experiences of interventions, as well as the perspectives of the professionals who delivered them.
The reviews are referred to as published articles that include detailed descriptions of the methodologies used, 73 studies analysed across both reviews and the findings. 36,42
Our findings underscore the importance of access to psychosocial interventions in the aftermath of sexual violence and abuse as a range of psychosocial interventions were effective at improving the mental health and well-being of survivors in the short term. These include traditional trauma-focused approaches such as those recommended by National Institute for Health and Care Excellence (NICE) guidance43 [e.g. cognitive behavioural therapy (CBT) and Eye Movement Desensitisation Reprocessing (EMDR)], which showed the strongest effects for mental health; non-trauma-focused approaches; and several emerging areas such as Reconsolidation of Traumatic Memories (RTM), trauma-sensitive or trauma-informed yoga, Lifespan Integration and cognitive training (e.g. neurofeedback). Although survivors said that they often found interventions difficult, they also appreciated that they needed to work through trauma, which, they said, resulted in a wide range of benefits. These included positive effects on their physical health, mood, understanding of trauma, and interpersonal relationships, and enabled them to re-engage with a wide range of valued life domains.
Survivors highlighted a range of features associated with the context in which interventions were delivered that had an impact on how they accessed and experienced interventions. This included organisational features, such as staff turnover, that could influence survivors’ engagement with interventions; the setting or location in which interventions were delivered; and the characteristics of those delivering the interventions. Therefore, listening to survivors and providing appropriate interventions at the right time for individuals can make a significant difference to their health and well-being. These findings provide support for NHSE’s aim to provide lifelong support for survivors of sexual violence and abuse, with SARCs being a vital option as a first point of care. Our Cochrane Reviews have been translated for a range of audiences and are accessible here: www.coventry.ac.uk/research/areas-of-research/centre-for-intelligent-healthcare/mesarch/.
Chapter 4 Process evaluation of sexual assault referral centres
Background
NHS England’s strategic direction for SAAS was launched in 2018 and aimed to advance the support to victims and survivors of sexual violence and abuse across England enabling people to recover, heal and rebuild their lives. 44 SARCs are a vital first point of care within this strategy. Service Specification 30 identifies the core services that should be delivered within SARCs including assessment, FMEs, and health and well-being interventions. 19 Nevertheless, SARCs in England vary considerably in the types of organisations that lead them, the staff members who work within them, and the care and support services that they provide. SARCs are further differentiated based on whom they support with some providing care to adults, some to children and others to survivors of all ages. Within this context, we know very little about how staff experience this work and its variation, although we do know that this work can have an emotional toll. 45 Furthermore, while rates of access to SARCs in England and service users’ characteristics have been reported elsewhere,46 understanding about survivors’ experiences of SARC services has been limited. One small study reported that SARCs were experienced as a safe haven, calming and welcoming, and where survivors felt supported and understood. 47 In light of these gaps, the first aim of this study was to identify key issues and concerns associated with the work of SARCs, their workforce and the use of technologies. SARC service delivery was severely affected by the COVID-19 pandemic, which also witnessed shifts in the type and incidence of sexual violence and abuse. Given that our research coincided with the COVID-19 pandemic period, we were able to examine the effect of COVID-19 pandemic on SARC service delivery and document the innovation that occurred. These findings are reported elsewhere.
Sexual assault referral centres act as an initial point of contact; therefore, it is vital that the care and support provided to survivors of sexual violence and abuse is of the highest possible standard and that there is continuity of care beyond SARCs. SARCs in England sit within a large and complex network of organisations and professionals that reflect the widespread needs of survivors at different stages, receiving referrals from these organisations and professionals, and referring SARC clients to them. While inter-agency and inter-professional collaboration has been explored for some years across professions such as social work,48 knowledge regarding collaboration across professionals in the SAAS context is limited. A small amount of relevant research has been conducted in the USA,49–51 but only one example has been described in a European context,52 and none in England. Furthermore, survivors’ perspectives have been largely absent in this research. 51 Therefore, a second aim of this research was to explore the integration of SARCs in the broader context of a health and community response to sexual violence and abuse, drawing on perspectives of both professional and service user stakeholders.
Methods
Study design overview
The main component of this study was a process evaluation of SARCs. A process evaluation is broadly recognised as a method that seeks to understand the work of an intervention, how that intervention is delivered and its effect, alongside contextual factors that may affect outcomes. 53 In completing this process evaluation, we undertook qualitative investigation of professional and survivor voices regarding SARC service delivery and integration of SARCs within the SAAS pathway. From the mapping of all SARC sites in England, we identified several diverse sites to undertake the qualitative enquiry. Data used to map SARCs were collected between March and July 2019. These data were supplemented with national SARC indicators of performance (SARCIPs) data supplied by NHSE54 and gathered from SARCs between April 2018 and April 2019. Data were collected from professionals and survivors participating in the qualitative study between July 2019 and July 2021. We also drew upon qualitative data gathered with survivors as part of the linked cohort study (see Chapter 5) between September 2019 and May 2022.
Changes to protocol
We planned to use Normalisation Process Theory, an effective approach when exploring a new intervention or service. 55 However, when it came to applying Normalisation Process Theory to our data, the services, staff and integration of SARCs were not newly implemented. Therefore, we sought an alternative theoretical approach to capture the importance of effective integration between different organisations and professionals, and drew upon theory related to inter-professional collaboration.
Theoretical approach
Bronstein’s theory of interdisciplinary collaboration48 has been applied extensively across other fields and in two studies exploring integration within Dutch and United States (US) models of SARC provision. 49,52 Coordination and collaboration have been hypothesised to be linked with the effectiveness of Sexual Assault Responses Teams in the USA. 50 These studies point to the theory’s relevance to capturing interdisciplinary collaboration and integration for SARCs in England. Bronstein defines interdisciplinary collaboration as a process that facilitates the achievement of goals that cannot be achieved by individual professionals. 48 Bronstein’s model comprises five components: interdependence, newly created professional activities, flexibility, collective ownership of goals and reflection on process. Interdependence refers to the dependence between and reliance upon different professionals in working together to achieve their own goals and requirements. Newly created professional activities are collaborative acts, programs or structures that can help achieve more than that if undertaken independently by professionals. Flexibility captures deliberate acts of role blurring in which professionals working together can achieve greater efficiency and effective working. Collective ownership of goals relates to a shared responsibility among professionals to achieve goals with a commitment to client-centred care. Finally, reflection on process relates to professionals acknowledging their collaborative roles and evaluating how to effectively achieve and strengthen these relationships. Bronstein argues that inter-professional collaboration can be affected by several characteristics including professional role (e.g. clear and well-defined roles), structural characteristics (e.g. manageable workloads), personal characteristics (e.g. how collaborators perceive each other) and history of collaboration (e.g. prior experiences of collaboration). Previous research has highlighted challenges to inter-professional collaboration, for example, perceived power imbalances and different professional focus/orientations between staff members;49 these challenges will be explored in the context of this research.
Sampling, recruitment and participants
We mapped SARCs across England using data collected from SARC managers through an online survey (36/48 sites returned data) and SARCIPs data. We produced a data set, which allowed sampling of sites for the qualitative process evaluation and the cohort study (see Chapter 5).
Using this data set, we recruited a stratified random sample of seven SARCs from all 48 sites, with strata defined according to service delivery model (police-led, NHS-led, charity-led or private sector); size (small, medium and large) and level of integration of services (on-site, embedded ISVA service or not).
At each site, we invited a range of professionals based at the SARC to participate in an audio-recorded interview. We also approached professionals external to the SARCs whose organisations were part of inward and onward referral pathways. We recruited directly through the UK Association of Forensic Nurses to ensure representation of Forensic Nurse Examiners (FNEs) within the sample. We also invited survivors who had attended these SARC sites through the staff. We undertook 72 interviews with professionals (see Appendix 2, Table 23). Five interviews were conducted with survivors initially. We subsequently recognised the wealth of qualitative data being gathered as part of our cohort study in reference to accessing care at SARCs (see Chapter 5). The qualitative data from our cohort study provided data from a further 293 survivors who accessed 21 SARCs including the eight SARCs where we undertook the in-depth evaluation of SARC services.
Analysis
Thematic analysis (TA) was the chosen process for analysing the two sources of data: in-depth interviews with survivors and professionals (n = 77) and data arising from asking open-ended questions about care during the baseline cohort study interviews (n = 293). Specifically, Braun and Clarke’s Reflexive TA approach was applied. 56–58 This method adopts a flexible and organic approach to coding and subsequent theme development, and it is considered theoretically independent. Primarily, inductive coding was undertaken, being led by the content of the data, with semantic coding used (the data are considered to represent the explicit meaning of the data). The standard TA method was followed including familiarisation and initial code development, clustering of codes to initial preliminary themes, theme development and subsequent finalising of the thematic themes. 56 Coding was undertaken by four members of the team, and during the initial coding phase, regular meetings were undertaken to inform, develop and refine the coding book. Once all the initial coding was completed, one team member checked all codes for quality purposes and to ensure that the data fitted to the code label. This process also refined codes into preliminary themes. The analysis then focused on key themes that explained the research questions in ensuring that these themes were distinct and closely aligned to the data.
Results
Overall, and as set out in the qualitative data presented in Chapter 5, survivors identified accessing SARCs as a positive approach in their recovery journey. Recovery journeys are rarely linear or uniformly positive, but survivors relayed that their encounters with SARCs (and other specialist services) fulfilled what survivors want from services and professionals in the aftermath of abuse. 59,60 In light of the experiences of professionals as well as those of SARC service users, the following sections explore key issues, concerns and strengths associated with the environment and organisational characteristics of SARCs, examining the ‘work’ they do, the workforce, technologies used, and finally SARC integration within the wider community response to sexual violence and abuse. The sections also pay particular attention to the interdisciplinary collaboration across profession(al)s within SARCs, and between SARCs and other agencies, focusing specifically on the key elements of Bronstein’s model.
What is the work of SARCs including the types of interventions delivered?
Sexual assault referral centres provide a vital early or the first point of care for survivors and providing a frontline response to survivors constitutes the majority of their work. There is a standard care offering at SARCs based on Service Specification 30. 19 In the research, survivors focused on the elements of core services that were salient for them. Crisis support was strongly valued by participants – the emotional support, information and options presented, and the referrals made. ‘[SARC staff] tried their hardest not to cause me any more distress, of course there was distress and it was uncomfortable, but not their fault’ – the FME is an extremely demanding experience, and for one participant, akin to ‘having a post-mortem while you were still alive’. ISVA support, which may be provided directly through SARCs, was also highly valued, particularly in relation to practical support through investigative and criminal justice proceedings and the techniques to support recovery. Counselling, increasingly offered through SARCs, was considered a largely positive experience, although wait-lists to access counselling, and the restrictions on the number of sessions meant that some survivors ‘felt I was getting somewhere and then it has to stop, I didn’t think it was good enough that it stopped’.
Another core function of SARCs is access to other services; SARCs opened a range of referrals for clients. However, drawbacks were ‘I was getting bombarded with a lot of people calling me … I had five or six agencies calling me the day after, my phone didn’t stop ringing’ and the consequence of this as ‘I had to keep going over and over my story’. It was highlighted how survivors find it difficult to navigate the services and suggests the value of SARC and ISVAs working closely to assist this understanding: ‘I think victims and survivors find it really difficult to understand the landscape of what’s going on out there in terms of the case, who’s providing what’. (ISVA service delivery manager)
While service specifications set out the core areas of delivery for SARCs,19 variation arose with different leadership models, commissioning arrangements, geography and the needs of the local community. Participants commonly identified typical journeys through SARC services. They also noted divergence from primary routes. Access needs and how people engaged with the services varied with individuals’ circumstances (e.g. specific or complex needs, location); the time since the trauma occurred (e.g. non-recent abuse or CSA); and external factors such as being on wait-lists for therapeutic care and the status/progression of criminal justice proceedings. The research also documented the effects of the COVID-19 pandemic, which saw a step-change in access and service provision and witnessed clear evidence of collaboration within and between the services as commented on by this FNE: ‘you can’t deliver a service like this without being a close-knit team’.
While standard care requirements are set out for SARCs by NHSE, there is much scope for additional work to enhance provision and access. The research documented examples of SARC teams working creatively to ensure that their services could accommodate the range of needs of clients from different communities/locally including those whose access to services had been delayed, non-linear or complicated by different factors. One police officer demonstrated reflection on process in how they worked with their local SARC: ‘I attend the SARC a lot because if there’s been an operational issue, even though it may be north of the county, I will get invited, and then [SARC manager] and I and others will sit down and go, “ok, how can we deal with [this], what can we do going forward to make sure that this doesn’t happen again?”’ Teams developed new initiatives such as in-house emotional support or counselling; acting as a holding contact point while clients awaited access to other SAAS and other forms of care (e.g. community mental health, longer-term counselling); and enabling video interviewing/live link technologies. SARC staff expressed a commitment to clients, ‘we’re here, checking in, or there’s always someone here twenty-four seven … people do call us and say, “I’m suicidal” or ‘I don’t know where to turn to, I haven’t heard from this person”’. They wanted to ensure that their services could support people at any point after sexual violence and abuse, and they saw a role for being a point of contact for survivors of CSA and informing survivors about options for reporting and referrals to ISVA and third-sector support. SARCs expressed that efforts should be made to address public perception that SARC support means police involvement. They demonstrated how self-referral to services was fostered and also noted the ongoing difficulties for self-referring survivors in terms of physically reaching their services in some areas of the country (by contrast, those who report to the police are usually transported to SARCs by police officers). SARC staff operated in line with trauma-informed care; professionals were keen to see that choice was exercised in key areas such as reporting mechanisms as noted by this crisis worker: ‘I think it’s really important to allow people that opportunity to validate what’s happened to them … to try and re-balance, regain some power in a situation where they’ve felt powerless and to have that choice’. Staff highlighted the longer-term storage of forensic data and anonymous submissions to police intelligence as an underutilised service.
In terms of people’s access, there was widespread endorsement of anonymous locations and for sites where survivors can provide alternative reasons for being there (e.g. hospital site). The staff members were aware that co-location with police forces was challenging for survivors. SARC buildings ranged from purpose-built to adapted, and survivor-centred design features were strongly supported. One such example was entering and exiting the space through alternative doors to signal the beginning and end of the SARC journey (at services where clients generally do not return for other care and support). Staff reported a range of issues with SARC estates from lack of physical and confidential spaces for client support and administrative work and shared entrance/common corridors. Forensic rooms were perceived as overly clinical and suggestions were made by professional and survivor participants to address this through features such as wall/ceiling decorations. The staff members reported efforts to ensure that the SARC was welcoming CYP, that furniture was comfortable and that coverings provided to survivors were appropriate (e.g. participants cited instances of gowns being transparent). SARC teams expressed concerns about reaching clients in remote areas. The shift to greater use of digital services and remote care in response to the COVID-19 pandemic had the effect of mitigating some of the geographical barriers affecting survivors’ access to SARCs and ISVA care. Many survivors also identified a preference for remote contact with providers, feeling ‘more relaxed’ and that ‘the distance of a telephone call is better for me’ when talking about difficult topics.
Who is the SARC workforce?
Across service delivery models, staff roles generally seen at SARCs were SARC manager/deputy and an administrative member/team, crisis workers and FMEs/FNEs. Flexibility in roles at SARCs was common ‘my role covers a lot of areas’, for example, managers and administrators trained as crisis workers. Depending on the degree of integration at the site, ISVAs enacted their roles in flexible ways, as core staff at a SARC; employed by the voluntary sector but co-located at a SARC; with largely visiting/remote role; or based physically at a voluntary sector organisation. Thus, many models could be drawn upon to suit the landscape, for example, some sexual health services have ISVAs. NHS SARCs tended to employ clinical staff directly, whereas private sector SARCs made greater use of staff banks. With SARCs increasingly offering short-term psychosocial interventions, counsellors were also integrated into the staff of SARCs, frequently on a part-time/co-located basis. Finally, several roles were noted to lend themselves to specialisation, with some sites training crisis workers and ISVAs to specialise in the care of particular groups, for example, CYP, individuals with learning disabilities. Within the scope of the current research, we focus on two prominent workforce issues: (1) the nature of the crisis worker’s role and related training and (2) challenges to effective interdisciplinary SARC teams.
The crisis worker’s main purpose is to support clients of the service. However, the role involves a diverse range of task and balancing the sensitivities of cases and needs and expectations of vulnerable clients with the constraints of what can be provided:
One morning I might be helping with a forensic medical, and in the afternoon we might be doing call-ups for email enquiries, and reaching out to people that have accessed that way. I think it’s an incredibly difficult role to learn, if I’m honest, because it’s so varied and wide. There are some repetitions within it that are very quick and easy [to learn] … but there’s other stuff that makes it much trickier, like around geographical location. So understanding what services are purchased in relation to paediatric FMEs in a geographical location, which means that if somebody is ringing from [name of city] and they [want to] come in, do we see them or not? Or there’s understanding and learning what the service offers outside of the area as well as in the area.
Crisis worker
Without prior experience of the region, crisis workers’ practice might suffer. Training varied from across sites with most involving formal learning components, for eample, safeguarding, and a period of shadowing: ‘my first client interaction that I shadowed, it was kind of a steep learning curve because it’s not like anything else’ (crisis worker).
Shadowing, and training more broadly, was noted to be variable and rely on standards set by providers. The crisis worker’s role has not attracted much attention within the research literature beyond the toll it places on individuals,45 an issue also recognised in our research. While the role was consistently valued by service users for whom the crisis worker is the first SARC professional they encounter, ‘I found it helpful that I received emotional support from [the crisis worker] when I got there because it was scary and going with the police’ (survivor), professional participants viewed the role as lacking incentivisation (e.g. opportunities for progression).
‘When a client or when a victim is at the SARC and you’ve got [private company who run forensic services], and you’ve got the police, and you’ve got a crisis worker, surely all three agencies should be working together because we’re supporting that one person’. (SARC manager) – meeting the client’s needs was a shared goal for staff at SARCs and there was frequent reference to ‘we are quite a tight knit group’ (ISVA). However, in terms of the challenges to effective interdisciplinary SARC teamsthe nature of staff contracts was a common workforce concern (subcontracting of SARC roles, on-call/zero hours contracts, staff employed by different providers). A crisis worker participant contrasted the scenario of where FNEs are employed directly by SARC and the experience of working with FNEs/FMEs contracted on an on-call basis: ‘the other doctors, you only see them every now and then, so you don’t really build up the same rapport with them, and obviously they all work slightly different … try and suggest the way that you would do it normally, just to try and make it easier and quicker, because obviously we want to put the victims first, so we want to make it easier for them … I do think that it’s so much better when you work together’. Implicit here is that placing survivors ‘first’ requires effective teams and staff who are familiar with each other and the setting. While all participants agreed that consistency in staffing was important for team-working and reducing isolation, flexible contracting was desirable for some professionals balancing other livelihoods and commitments. SARC managers did have particular concerns about crisis workers in this regard: ‘[crisis workers] do an amazing job but I think they do just feel a little bit disconnected from the service’.
Despite the workforce concerns that were voiced across the staff members and SARCs included in the study, we found very high levels of intra-SARC interdependence, particularly among crisis workers and FNEs. There was strong recognition of the importance of clear communication and inter-professional respect, supporting each other to reduce the impact of their work, and a commitment to providing an integrated service to the client. Simple examples such as gathering information from their clients together and sharing information between professionals as appropriate benefited clients in not having to repeat information or re-tell about their experiences and evidenced newly created professional activities. Collective ownership of goals in pursuit of client-centred care represents a key aspect of effective interdisciplinary collaboration. 48 Reflecting the impact of this care, one survivor commented: ‘I felt safe with the doctor, I felt safe with [crisis worker name] who was in the room. I didn’t feel that anything bad was gonna happen’.
What are the technologies that enable SARCs to get work done?
This section focuses on two key issues: (1) use of remote/digital services in providing care and (2) challenges emerging in information sharing across the services. The advent of the COVID-19 pandemic meant that SARCs used digital technologies to facilitate service delivery, including triaging of clients before they attended the SARC. Staff reported that they carefully determined the appropriateness of remote care for different clients. Some benefits to triaging were realised in that clients spent less time at the SARC once they arrived. Survivors reported both positive and negative responses to the increased use of digital technologies, highlighting the need for developing remote services as part of a suite of options and tools. The second key issue related to information sharing. Different IT systems for different organisations meant that SARC staff members spent considerable time making manual referrals through online systems or secure email systems, which added considerably to workload:
I referred a lady to adult social services because I felt her needs would be met with [social care provider]. But I couldn’t go direct with [social care provider]; I had to go through adult social services, and they have to make the referral. And I was told on that phone call that “somebody would be contacting you.” And today, I’ve not had a contact, and it’s been about two weeks, so that’s something that I am going to have to chase up. So that is quite time consuming.
ISVA
This work, described by one SARC staff member as their ‘nagging work’, was frequently highlighted with regard to sharing information with partner organisations. Survivors experienced interruptions or delays in access to onward care:
I haven’t received any care, I got told I’d have sexual health screening, that hasn’t been sorted or anything, I had to go to the doctor’s about getting an examination done, they were supposed to help sort that out, but they didn’t.
Survivor
To what extent are SARCs embedded within the overall response to the needs of survivors of sexual violence and abuse?
The most important external partnerships for SARCs included the police, sexual health, ISVAs, third sector and social care. For example, our data suggested well-established and collaborative relationships between SARC staff and police officers. Single point-of-contact officers in police forces worked directly with SARC managers to develop pathways for survivors and training by SARCs to ensure police officers understood local provision and access. Collaboration with third-sector organisations was more challenged: ‘with any multi-agency working, we all seem to work parallel with each other quite often and not come together at the top to deliver’ (crisis worker). There was a strong sense that collaboration was driven by individual senior members of staff at the SARC and/or the partner organisation and involved local implementation. Positive relationships at senior levels trickled down and fostered positive cross-working, seen to ultimately benefit survivors. Examples of cross-working included co-delivery of training and sharing of resources and space. Professionals expressed a wish for change. For some, implementing a more consistent SARC model was the answer, with more services under ‘one-roof’ such as integrated ISVA and sexual health services. Others recognised existing high-quality provision in these areas within their communities and that pathways and relationships should be strengthened. Another example was Achieving Best Evidence interviews, with some believing these should be conducted consistently at SARCs while others saw SARCs as a place solely for acute crisis care and considered that survivors may not wish to return to these locations. Participants pointed out that SARCs have all evolved in different ways in the communities they serve and, in expressing how the sector needs to develop in the future, emphasised the need for simplification and better approaches to supporting clients with complex needs.
The role of SARCs is vital, but there was real concern about the invisibility of SARC services. Survivors relied on the police and others to learn about SARCs, ‘I wouldn’t have known about them if it hadn’t been for the detective’ (survivor). In response to the lack of public awareness about SARCs, there were several examples of teams initiating outreach services in their communities, often targeting groups seen to experience even greater barriers to receiving help (e.g. men, minority communities). Gaps in knowledge about service provision by SARC extended to important professional groups: ‘there are so many more people that need to know about the SARC’ (crisis worker). GPs were identified as a professional group lacking awareness of SARC services, with referrals from GPs being infrequent. This SARC manager talked about the difficulties of engaging with GPs:
Probably in defence of GPs, they have just got so much demands on their time and they don’t have free time, so we’ve put on training events especially for GPs. We do the open days, we try and target GPs … some of them are just not aware of what we’re doing, they’re really out of date, the information that they are giving clients.
From the perspective of a survivor: ‘GPs have got such little understanding …. They don’t take it in. And then they’re like, we don’t know who you can speak to … they just don’t know what the right support is’.
Discussion
Summary of main findings
This work highlights the excellence in care and support being provided within SARCs, as such, the value of SARCs in the provision of care and support to survivors is supported. The contribution of SARC provision to the care pathway, extends beyond provision of forensic services, importantly fulfilling an early role in coordinating care for survivors. However, this research also documents the challenges that SARCs, and the SAAS sector as a whole, experience in addressing survivors’ needs. Drawing on 77 interviews (72 professionals, 5 survivors) and 293 survivor responses, the novelty of this qualitative enquiry is evident in the breadth of participants spanning both inward and onward referral routes, as well as SARC staff themselves, along with the voices of survivors in sharing about the care and support they received.
In addressing the first aim of this work, findings have highlighted key issues and concerns associated with the work of SARCs, their workforce and the use of technologies. In doing so, this research documents the high level of dedication of SARC staff and captures their commitment to client-centred care and an ethos consistent with trauma-competent practice. 60 This commitment of professionals at SARC was further evidenced in their response to the COVID-19 pandemic, where they effectively utilised technology to ensure that care could be continued while enabling greater flexibility and choice for survivors. Appreciating several distinct roles are involved in producing the range of care and options for survivors, our findings emphasised crisis workers as vital to a survivor’s care journey at SARC. Attention to the crisis worker role is fundamental in further developing the workforce of SARCs.
We found evidence of effective interdisciplinary collaboration spanning across Bronstein’s five components of interdependence, newly created professional activities, flexibility, collective ownership of goals and reflection on process both within SARCs and across the sector. Despite being hampered by the complexity of how different services are contracted, SARC staff worked hard to achieve cohesive teams and ensure that an excellent service is provided for their clients. We saw many examples of work that reflected good quality inter-professional collaboration, specifically inter dependence and collective ownership of goals in delivering client-centred care. Matthew and Hulton called for research to identify whether there is a link between effective SARC collaborative practice and survivors’ experiences of SARC services. 51 This research answers that call with our findings showing high levels of effective inter professional collaboration found between SARC staff (specifically between crisis workers and FMEs/FNEs), and subsequent positive endorsement of SARCs by survivors.
However, there were factors that can hamper inter-professional working within SARC settings. The ways in which professional roles at SARC are commissioned can lead to short-term teams and unstable working hours of staff, whereby collective ownership of goals in pursuit of client-centred care is difficult to achieve. In comparison, consistent teams enabled strong inter-professional working and evidenced best practice. This generated cultures of transparency and respect, more compassionate support and offered a high-quality experience of care for survivors.
Across the sector, and moving beyond the SARC setting, the second aim of the research was to explore the integration of SARCs in the broader context of a health and community response to sexual violence and abuse. In doing so, our research gave a positive picture of interdisciplinary collaboration across the wider sector across criminal justice, health and third-sector organisations. Professionals across these sectors clearly engaged in collective ownership of goals48 in recognising the importance of effective, and cohesive care and support for survivors. This runs counter to US research where research noted cross-system coordination being non-existent or lacking consistency, with subsequent challenges to the effectiveness of SARC provision and integration. 61 However, barriers remain, primarily in the form of inefficient communication systems for sharing information. Effective information sharing systems were highlighted as being critical to enabling strong inter-professional working and importantly contributed to efficient working practices, reducing the workload burden of SARC staff.
However, this study has demonstrated challenges to optimising the access to and fully realising the benefits of SARC services, specifically relating to the invisibility of SARCs. SARCs need to be more apparent as a care option for those in crisis, particularly if the person experienced rape, sexual assault or abuse recently. This includes wider community awareness (e.g. families, workplaces, friends of survivors) given patterns of disclosure in personal/social networks. 62 It is paramount that public awareness of SARCs is prioritised, for example, through investment in public awareness campaigns. This is particularly important for groups of survivors who are underrepresented at SARCs and experience barriers to accessing them. NHSE made efforts to address this problem with a campaign in 2022 targeting specific groups including black and Asian women, men, and survivors from lesbian, gay, bisexual, transgender and/or queer (LGBTQ+) communities with a focus on youth across these groups. A broader campaign was also run in South-East England targeting all ages.
Strengths and limitations
The study’s originality resides in the breadth of the experiences brought to bear on questions about the role and effectiveness of SARC services, with input from 35 SARC professionals and 37 stakeholders outside of SARCs as well as the voices of 293 survivors who have accessed 21 SARCs in England. While prior work49–52 has explored aspects of the work captured, this study benefited from the large-scale nature of data collection which allowed triangulation of experiences of multiple informants. There were important gaps in representing those inside SARCs (medical examiners). The study also lacked GPs and social workers, two professional groups that are integral to early intervention in sexual violence and abuse.
Implications for health care
Enhancing the visibility of SARCs among professionals
The findings highlight the need for awareness-raising work to be continued and further developed, in reaching survivors across all parts of England. However, gaps in awareness of SARCs, specifically highlighted in GPs, critically need to be addressed. For example, current heavy GP workloads may mean that more traditional methods of awareness raising in professional groups at a local level will not be effective. Instead, more thought should be given to developing collaborative relationships at higher levels (e.g. Integrated Care Boards, British Medical Association, General Medical Council, Royal College of General Practitioners), with a clear pathway to facilitating GPs and SARCs to develop local collaborative relationships. In summary, survivors need to be able to make informed and empowered choices about their crisis care and thereafter. Professionals being able to signpost survivors to SARCs provides survivors the option to benefit from specialist knowledge and referral pathways, at minimum. Our findings also suggested that the physical visibility of SARCs needs further attention, for example, Walker et al. 47 recognised a need to balance accessibility and discretion in locating SARCs.
Valuing and developing collaboration
In other words, strong collaborative relationships between SARC staff and other agencies translated into high-quality care and support for survivors. As highlighted in the National Service Specification, SARCs are a mainstream provision, linked to other care pathways and must achieve strong partnerships across health and social care, the specialist sexual violence and abuse services in the voluntary sector and the CJS. However, the effectiveness of this collaboration and partnership was affected by two issues. Firstly, the nature of relationships between SARCs and their partner organisations frequently relied on individual relationship building. Bronstein highlights personal characteristics as a factor that can strengthen inter-professional collaboration, where professionals who view each other with trust, respect, understanding and engage in informal communication can engage in much more successful collaborations. 48 We interviewed many professionals who exemplified this good practice, in the way in which they worked with other individuals. This translated into effective and efficient working that assisted over-burdened service delivery. However, the sustainability of these benefits is threatened by staff changes. Decision-makers may want to consider how relationships between agencies can be developed sustainably.
Secondly, inefficient information sharing substantially increased the workloads of professionals. There is a need for significant financial investment which simplifies information sharing. uncovered a bestWhile it is unlikely that a simple solution exists, decision-makers need to consider how IT interfaces between organisations could be facilitated and also promote reflection on/reviews of referral pathway processes that may be unnecessarily complex. This is particularly key given that it has an impacton survivors when their care is disrupted, delayed or stopped due to issues with information sharing.
The commissioning process for SARC staff and the contracting of SARC services (and services in the wider sector) did not always support staff to collaborate effectively. We consider that a secure workforce should be an aim for commissioners in this area. Our work has not uncovered a best practice model to achieve this (e.g. one SARC model of staffing that should be promoted), and we also recognise that commissioning processes and local existing services means that it is not practical to recommend wholesale change of commissioning processes. However, at a local level, two key aims should be focused upon. The first is that commissioning should be undertaken more collaboratively across all relevant sectors (e.g. public health, criminal justice, local government) so that there is more coherence to the way in which services are contracted across local regions. Secondly, commissioners and integrated care boards should review these structures, and specifically, the processes between organisations with a view to simplification and to reduce barriers that aggravate workloads.
Recommendations for research
Given the gaps in including informants from social work and general practice, future research could examine the specific challenges these professional groups perceive in participating in a community response to sexual violence and abuse. Furthermore, while this research has identified excellent practice in relation to collaboration, continued research attention is needed to evaluate these practices to ensure that this captures the complexity of how SARC services are delivered both nationally and internationally. Overall, we hope to have highlighted the dedication and creativity of staff delivering client-centred care and support in the SAAS sector, which was reflected in survivors’ experiences of high standards of care across the sector.
Chapter 5 Health and well-being of survivors after accessing sexual assault referral centres
Some text in this chapter has been reproduced from O’Doherty et al. 63 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
Background
A cohort study formed a key part of the evaluation of SARCs. It is the most comprehensive study of health and well-being in a British SARC population, being the first to follow up health and well-being outcomes in adult cohort, and is one among the small number of prospective longitudinal studies internationally involving survivors of rape, sexual assault and abuse. 12,64,65 It takes access to SARCs as the starting point for the cohort. It aims to describe the health and service use journeys of survivors in the year after SARCs and examines how the mental health needs of survivors were met in voluntary sector and NHS settings. The study uses a multilevel modelling framework to explore risk factors for burden of PTSD symptoms at baseline and reduction in symptoms during the year after, to determine whether SARC service models and subsequent care influence outcome and to identify whether participant-level factors moderate outcome.
Methods
Study design overview
The study design and methods have been published in a protocol study. 63 This was a cohort study of mental, physical, sexual health and cost outcomes over 1 year in adult survivors of rape, sexual assault and abuse who had received care through SARCs in England. Quantitative measures were implemented at baseline (≥ 4 weeks after index SARC access) and at 6 and 12 months post baseline. The study also gathered qualitative responses at each time point related to quality of care. Recruitment commenced in September 2019 and the last 12-month interview was conducted in December 2022.
Changes to protocol
The main deviation from the protocol (V3.3)22 is that loss-to-follow-up was even greater than anticipated. We interviewed only 223 people at 12 months instead of the projected 270 people. We did, however, reach the target sample size at baseline. Our cohort underwent several changes before V3.3 to cope with challenges to recruitment and these are tabulated in the study protocol. Briefly, the most significant amendments to our original protocol were reduction in the target sample size from 750 to 338 and reduction in the follow-up of 2 years to 12 months (each due to the difficulties reaching a trauma population). The COVID-19 pandemic triggered a change in inclusion criteria: eligibility no longer required service users to present in person at SARC services, and we also began to admit self-referrals into the research (as opposed to requiring referral by a professional). Early consultations with our SSC and LEG (see Chapter 2) after the study launch led to additions/changes in measures; for example, we added assessments of eating problems, suicidality, self-harm, drug use and capability. We also changed the minimum age for entry into the cohort study from 16 to 18 years because care pathways are different for those under 18 years, and it was seen as a better approach to focus on young people separately (see Chapter 7).
Sampling, recruitment and procedures
Using data supplied by NHSE and based on our process evaluation study (see Chapter 4), we divided all SARCs in England into strata based on service delivery model, size and level of integration of services. Next, we randomly selected sites from strata and approached them to participate. In line with our planned site recruitment, 15 SARC sites joined the research. We also recruited 22 of their onward referral partners, mainly ISVA services, because the primary recruitment model relied on referral of SARC service users to research by ISVAs. The requirement to recruit this number of SARC referral partners was unanticipated; we intended to have more of the major SARC sites nationally where ISVAs are employed by SARCs and deliver care on-site and therefore make referral to the research more seamless. However, several of these sites were already participating in another NIHR-funded study. 66
Recruitment of individuals was undertaken in three phases; the first involved SARC staff screening service users for eligibility. People were considered eligible if they were service users at SARC, aged ≥ 18 years and had presented in person at any of the 15 participating sites. After 23 March 2020, the research welcomed survivors who accessed SARC services remotely as well as self-referrals, these being participants who had not necessarily accessed one of the originally recruited 15 SARC sites. The main implication of this was that we could not collect service use data about participants from those sites; in most cases, we asked the participants for the information, where appropriate and safe to do so (e.g. What date did you access the SARC? Who was the perpetrator of the offence?).
Returning to the main model of recruitment, people were excluded by services if, in exercising their own judgement, the responsible member of SARC staff conducting screening anticipated a service user may be too unsafe to participate or may encounter difficulties in providing informed consent due to severe mental health, cognitive or learning problems. We also excluded those who were incarcerated, as conducting follow-up assessments in prisons was outside the scope of the project.
Sexual assault referral centre staff completed a screen form for all those aged ≥ 18 years presenting to the service, recording basic demographic data, and offence and referral characteristics and indicating whether the person was eligible or not, with any reasons for exclusion indicated. These screen forms were assigned a study identification number, containing no identifying information, and passed onto the project team to provide an indication of the characteristics of the pool of service users pre-enrolment. SARCs routinely refer on to other agencies, and nearly all survivors are offered access to ISVAs; thus, our approach was to train ISVAs (working inside SARCs and in the voluntary sector) to invite their clients referred from SARCs to consider joining the research. We co-produced recruitment materials with our LEG (e.g. video),67 which the ISVAs shared with their clients. ISVAs gained consent to pass on the person’s name and phone number and preferences for safe/convenient contact to the research team. Study identification numbers were passed on not only from the SARC to the research team but also from the SARC to ISVA services. Thus, when a person consented to be in the research, we were able to link the person to the service data we held. This minimised the number of questions (including sensitive questions) that we needed to ask. A trained project team member established contact within 1 week of receiving the consent from the ISVA or SARC or in a small number of instances, other recruited sites/settings such as sexual health, and contact was made in line with service users’ preferences. Once contact was made by the research team, we followed our recruitment and safety protocols, explaining the study purpose and gaining full consent (see Chapter 2). When consent to participate was established, baseline data were collected and the person was enrolled in the cohort study. Follow-up was undertaken according to participants’ preferences 6 and 12 months after the baseline interview.
Sample size
The primary outcome of interest for evaluating service user journeys after accessing a SARC was PTSD, measured using the Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5). 68 Our interpretation of models based on the PCL-5 focused on what constitutes a minimal clinically important difference (MCID) for PTSD. Stefanovics et al. concluded that differences of approximately 0.5 of a standard deviation (SD) could be deemed clinically important both cross-sectionally and for within-person change. 69 As this study involved neither randomisation nor placebo control, the analyses focused on changes in PTSD symptoms between baseline and follow-up. We considered the recommendations of Stefanovics et al. in terms of quantifying the change-score group-difference we would expect that separates an effective treatment from an ineffective one. Based on guidelines,68 we anticipated this MCID of 0.5 SD to approximate to a 10-point difference on the PCL-5 change-score; however, Stefanovics et al. propose that an SD-based approach is more robust, and we also recognised that the magnitude of change on the raw-scale metric would be influenced by the length of time between baseline and follow-up. To allow for four levels in a predictor variable (e.g. four types of SARC service provider); up to 10 covariates; two time points; an expected small-to-moderate Cohen’s f, which corresponds to the MCID for our primary outcome variable; and an α error probability of 0.05, 270 participants were required at study completion to achieve a power (1−β error probability) of 0.90. Based on previous studies,64,65 our pilot research and early patterns of recruitment and retention, we estimated attrition at 20% by the 12-month follow-up, requiring a baseline target of 338 individuals. Participants who did not complete a 6-month follow-up were still eligible to complete 12-month follow-up measures.
Data collection and outcomes
The form used by SARC staff to screen service users for the research provided initial data on gender, age, ethnicity, offence characteristics including nature of the relationship to the perpetrator and time since the offence occurred; referral into SARC and indicators of vulnerability at the point of service access (e.g. history of mental health problems, disability, substance use). At baseline, we collected additional detailed sociodemographic information. Baseline data were gathered using computer-assisted telephone interviews by staff trained in survivor-centred research practice (see Chapter 2). We enquired about adverse childhood experiences (ACEs) using the World Health Organization’s ACE International Questionnaire, which measures exposure to 13 adverse experiences under the age of 18 years. 70 We screened for lifetime intimate partner violence as well as in the year up to baseline using the Afraid/Controlled/Threatened/Slapped or physically hurt Screening Measure tool. 71 All other measures applied at baseline focused on standardised timeframes and were used to assess change in survivors’ health and well-being journeys over the year period (see Table 2). Sexual health will be reported elsewhere. Our approach to measuring costs is outlined in the economic evaluation (see Chapter 6). After enquiring about service use at each timepoint, we asked participants to rate the extent to which four different sectors/services (SARC; voluntary sector; NHS; policing and justice) had been beneficial, neutral or harmful to their health and well-being using a scale that extended from minus 100 (maximum harm) to plus 100 (maximum benefit).
Qualitative methods
In addition to the quantitative measures and scales indicated above, interviews also included open-ended questions about participants’ experiences of care and support in the context of four different sectors. This produced an extensive longitudinal qualitative data set to complement the quantitative data. One of the study aims was to explore how survivors experienced mental health care in the NHS compared to the voluntary sector. As there was so much overlap and movement of participants between voluntary and statutory mental health services, it was not possible to examine this aim quantitatively. Thus, we applied Braun and Clarke’s Reflexive TA approach56–58 (see Chapter 4) to examine our longitudinal qualitative data set.
Statistical methods
Descriptive and unadjusted analyses
Baseline sociodemographic, offence and trauma-related characteristics for the sample were summarised using means and SDs for continuous variables and using ns and proportions for nominal and ordinal-level variables. Using the chi-squared test of independence and the independent t-test, we assessed for any differences in the baseline characteristics between participants who were lost to follow-up from the study at 12 months and those who were retained. We also calculated the levels for the main outcome measures for the three time points, tabulated using means and SDs for continuous variables and using ns and proportions for categorical variables. Paired-sample t-tests were used to examine within-group differences in PTSD levels between baseline and the first year. Cohen’s d was calculated to establish effect size. It is calculated based on the difference between two mean values and expressed in SD units to determine how many SDs lie between the two mean values. We used boxplots to represent the data on harm and benefit of services for four different sectors. SPSS V28 (IBM Corporation, Armonk, NY, USA) was used to conduct all descriptive analyses. 72
A multilevel modelling framework
Unless otherwise stated, risk factors (and auxiliary variables) were selected from the baseline wave of data collection (see Box 2).
Our research focused on exploring risk factors for PTSD symptoms measured at baseline and reduction in symptoms during the year following the baseline assessment. Because of the repeated-measures nature of these data, with up to three measurements for each participant, we employed linear mixed-effects models to describe heterogeneity in longitudinal patterns of change. Therefore, we used the lme() function from the nlme package73 in R statistical software (The R Foundation for Statistical Computing, Vienna, Austria)74 using Rstudio75 (see Report Supplementary Material 1). A mixed-effects model partitions variance in PTSD symptoms into within-participant and between-participant variances. Fixed effects describe the average pattern of change in symptoms across the year (typically a linear or more complex polynomial), while random effects represent variation around this population mean trajectory – for instance, the extent to which a particular individual aligns with higher- or lower-than-average at baseline (intercept variability) and observes a reduction in symptoms at a slower or faster rate than the average for the sample (slope variability).
-
Organisational level:
-
ISVA (SARC or non-SARC).
-
Type of SARC (charity-led/police-led/NHS-led/private sector).
-
-
Service experience:
-
Service utilisation (not only baseline).
-
Perceived harm/benefit of policing and justice response (not only baseline).
-
Status of criminal justice proceedings at baseline (open case/self-closed/police-closed).
-
-
Characteristics of the individual and factors relating to the offence:
-
Burden of ACEs (count variable).
-
Long-term mental health problems (yes/no).
-
Time between trauma and visit to SARC (up to 10 days/11 days to 1 year/1 year or longer).
-
Perpetrator type (relationship, if any, between victim and perpetrator) [partner/childsexual abuse (CSA)/acquaintance/stranger/other – refers to perpetrator as person in position of authority or other family perpetrator, but not CSA or partner].
-
Educational attainment of survivor (< A-level/A-levels/> A-levels).
-
Financial problems – ease with which participant could find £100 (impossible/difficult/not a problem).
-
Inability to work, for example, due to disability (yes/no).
-
Following the estimation of the unconditional model described above, we incorporated a succession of risk factors to determine whether each, in turn, was associated with either intercept or slope differences. For this, we focused on the maximal sample of those participants providing any PCL-5 data at any wave. We fit a univariable mixed-effects model for each risk factor. By introducing a main effect of each risk factor as well as an interaction between this factor and time, we derived parameters for both baseline symptom level and symptom change. Parameters represented mean differences in each quantity for categorical risk factors, and a symptom difference for a 1-unit increase in X for any continuous risk factors (e.g. total ACE score). As multi-category risk factors could yield a large number of separate parameters in these models, we used Wald tests to produce a pair of Omnibus tests – one representing the null hypothesis for a lack of association between X as a whole and the baseline symptom level, and the other for the association between X and the slope.
Each of the risk factor models mentioned above was subsequently subjected to two covariate adjustments. Firstly, we adjusted for any baseline auxiliary variable that was found to be related to either dropout or the timing of the post-baseline data collection waves. These comprised (1) religion (yes/no), (2) sex (male/female), (3) ethnicity (white/global majority) and (4) sexual orientation (heterosexual/other). Secondly, for all participant-level characteristics, we further adjusted for two organisational-level variables, namely ISVA type and SARC type.
Diagnostics/reflections on bias
Model diagnostics were used to determine the adequacy of fit of the chosen mean-trajectory by comparing observed and predicted values form the model. QQ plots enabled us to assess the adequacy of the normality assumption, which pertains to both level-2 random effects and level-1 occasion level residuals. In addition, we were mindful about two aspects of the data that might lead to bias, and we have described our approach to these aspects (see Report Supplementary Material 1).
Results
Characteristics of the setting and flow of participants through the study
Overall, 337 people were recruited into the cohort study. It was later determined that two of these individuals, referred into the research by ISVAs and participating up to the 12-month interview, had not actually accessed a SARC; their data were excluded from analyses. Figure 3 shows the flowchart forparticipants in the different stages of the study commencing with screening for eligibility at SARCs.
FIGURE 3.
Flow of participants through different stages of the MESARCH cohort study.
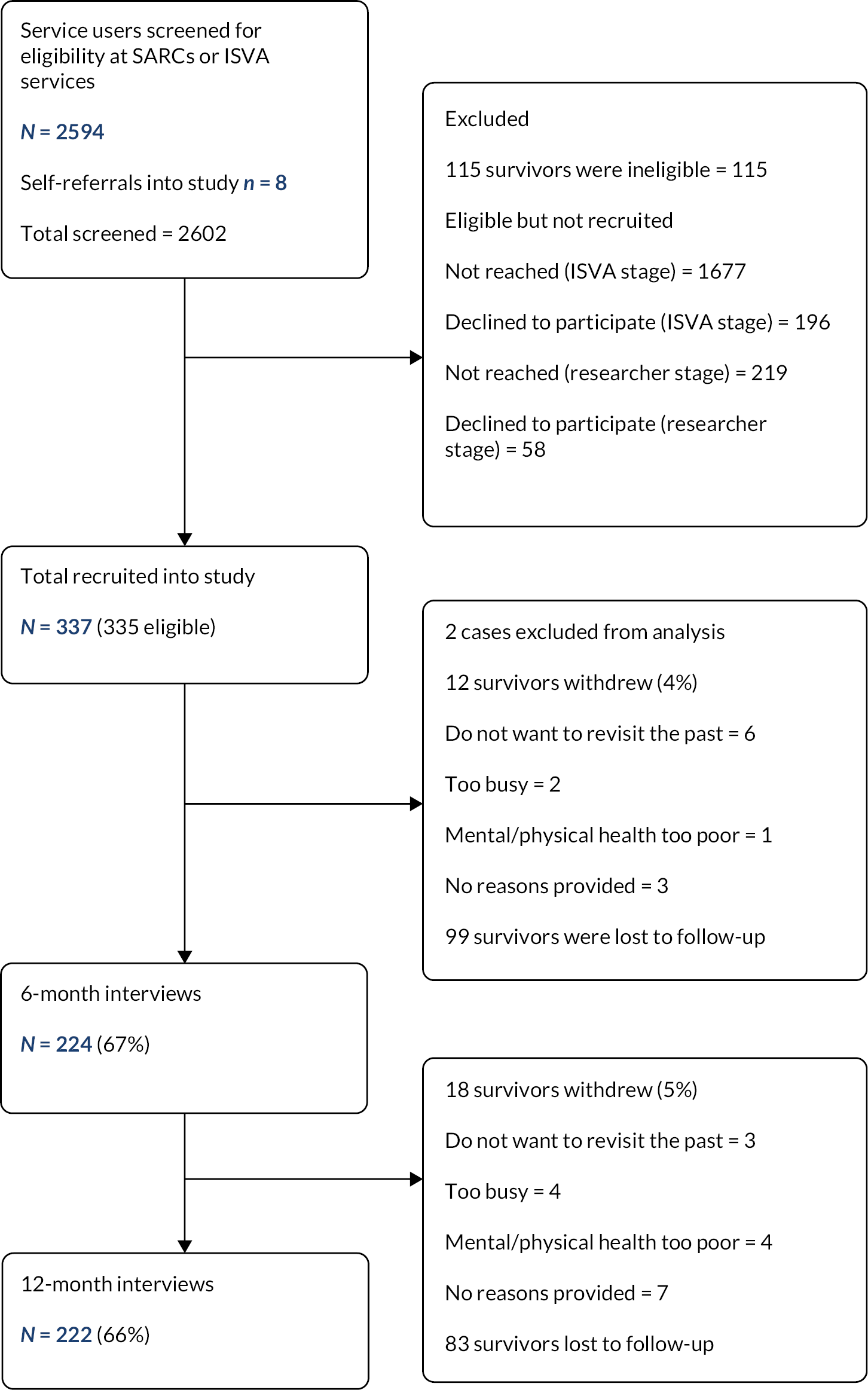
The sample of 335 people had accessed care at 21 different SARCs featuring all four of the models of service delivery under investigation: 67 participants (42%) had attended or otherwise accessed care from a SARC led by private sector companies (10 sites); 115 (34%) accessed care at NHS-led SARCs (five sites); 139 participants (20%) had accessed a police-led SARC (four sites); and 14 participants (4%) had accessed charity-led SARCs (two sites). Six of these sites (affecting experiences of 141 service users) had integrated ISVA services, whereas accessing any of the other 15 SARCs (affecting 194 service users) would have required service users to utilise ISVA care in settings external to the SARC (usually charity sector, but we did have some ISVA services located in sexual health).
There was a high variability in the cluster sizes (i.e. the number of participants linked to each of the 21 sites) ranging from 1 to 104, with an average of 16. This variability was due to varying levels of commitment to the research by SARCs but mainly, by the ISVAs on whom we relied for referrals. Occasionally, a participant self-referred to the research (n = 8), and for one of these individuals, the SARC they attended had not been formally recruited into the project, thus adding a site. Another situation arose when an ISVA referred a person in the usual manner, but we determined that the person had actually accessed a SARC in a different geographic location (i.e. location of the offence/reporting). Five individuals joined the study in this way, generating five additional SARC sites. Thus we had 21 regions/sites altogether, six of which were generated through service users joining rather than the team recruiting the SARC and its referral partners first. The most effective model from a research recruitment perspective was a committed ISVA team co-located at the SARC. The perception in the charity sector that the research was only concerned with SARC practice and related outcomes may have been a barrier to engaging with the project. All agencies were remunerated for recruitment (on a per-client-referred basis).
There was a high degree of variability across the sample in the period between a person’s access to a SARC and participation into the study. For 8% of the sample, a year or more had lapsed since they attended SARC. Given how difficult it is to involve people from a trauma population in research, especially observation research, we had not applied an upper limit on time since SARC access. The duration range was 3 days (for a person who had accessed SARC 3 days earlier for a video-recorded interview) to 5 years (for someone who self-referred to the research). The median duration was 104 days, which was more in line with what we anticipated at the outset, considering most people not being approached at the SARC, waiting for them to be referred to an ISVA service, and for the ISVA to introduce the research at a time they felt was appropriate for their client. Then, it took some time for the research team to undertake the baseline interview.
The first baseline interview was conducted on 18 September 2019, and the final person was recruited on 3 November 2021; the final 12-month follow-up was conducted on 21 December 2022. Baseline interviews took, on average, 1 hour 21 minutes (range: 30 minutes to 3 hours 10 minutes), and most of them were conducted as computer-assisted telephone interviews. The average duration of 6- and 12-month interviews was 67 (range: 20–135) and 64 (range: 15–120) minutes, respectively.
At 6 months, we reached 224 participants, and at 1 year, we reached 222 participants. Thus, overall, the study lost a third of the sample at each time point. However, some individuals not interviewed at 6 months did participate again at 12 months. While we had high levels of loss-to-follow-up at both follow-up time points, intentional withdrawal from the study was low at 9% (see Figure 2 for explanations on why people exited the study). We recorded one adverse event (see Appendix 1, Table 22).
Characteristics of the sample
Baseline characteristics of the total group of participants who accessed SARCs are presented in Table 1. At the time of the baseline interview, participants were aged 18–75 years; 50% of the sample was aged 18–29 years, with one in five participants aged ≥ 45 years. Women constituted the majority of the sample. Overall, 28 men were included in the study; no participants were transgenders, and five people were non-binary or gender-fluid. Overall, 15% of the sample identified as having an ethnic or cultural background other than ‘white’ and included people of dual heritage. Ninety-three per cent of the sample was British, and 95% were residents of the UK. A third had a religious affiliation, that is, Christianity (76), Islam (8) and other religions or beliefs (24). The sample was diverse on indicators of deprivation or opportunity: just under half of people were working full- or part-time and around a half had no financial difficulties. Five per cent of people were in supported accommodation or living in an unstable housing situation. Forty-five per cent of participants (152) had children aged under 18 years.
| Total (n = 335)a | Retained (n = 222) | Lost to follow-up (n = 113) | p-value | |
|---|---|---|---|---|
| n (%) or mean (SD) | ||||
| Age, in years | 32 (11) | 33 (12) | 32 (11) | t (331) = 0.668, p = 0.504 |
| Women (cis-gender) | 302 (90) | 198 (89) | 104 (92) | X2 (1, N = 335) = 0.683, p = 0.446 |
| Sexual identity is heterosexual | 248 (74) | 158 (71) | 90 (80) | X2 (1, N = 335) = 2.797, p = 0.94 |
| Racially minoritised groups | 50 (15) | 34 (15) | 16 (14) | X2 (1, N = 335) = 0.79, p = 0.779 |
| Dual or mixed heritage | 17 | |||
| Black | 16 | |||
| Asian | 10 | |||
| Chinese | 3 | |||
| Other ethnicities | 4 | |||
| Divorced or separated | 70 (21) | 46 (21) | 24 (21) | X2 (1, N = 335) = 2.797, p = 0.94 |
| Education to A-level or above | 220 (66) | 148 (67) | 72 (64) | X2 (1, N = 335) = 0.289, p = 0.591 |
| Earnings as main source of income | 156 (47) | 109 (49) | 47 (42) | X2 (1, N = 335) = 1.696, p = 0.193 |
| Not in work | 98 (29) | 55 (25) | 43 (38) | X2 (1, N = 335) = 6.38, p = 0.012 |
| Unable to work due to illness or disability | 74 | |||
| Looking for work | 24 | |||
| High economic disadvantageb | 57 (17) | 29 (13) | 28 (24) | X2 (1, N = 335) = 7.279, p = 0.007 |
| Longstanding disability/illness limits activity | 153 (46) | 106 (48) | 47 (42) | X2 (1, N = 335) = 1.143, p = 0.285 |
| Long-term mental health problems | 149 (45) | 107 (48) | 42 (37) | X2 (1, N = 335) = 3.689, p = 0.055 |
| Ever attempted suicide | 140 (53) | 89 (50) | 51 (61) | X2 (1, N = 263) = 2.775, p = 0.096 |
| Ever self-harmed | 161 (61) | 112 (62) | 49 (58) | X2 (1, N = 266) = 0.247, p = 0.619 |
| Offence characteristics | ||||
| Access to SARC | ||||
| Within 10 days of sexual assault | 147 (44) | 90 (41) | 57 (51) | X2 (2, N = 334) = 3.583, p = 0.167 |
| > 10 days but within 1 year of assault | 82 (25) | 56 (25) | 26 (23) | |
| > 1 year since the sexual assault | 105 (31) | 76 (34) | 29 (26) | |
| Offence/perpetrator | ||||
| CSA | 43 (13) | 29 (13) | 14 (13) | X2 (4, N = 329) = 2.543, p = 0.637 |
| IPV | 82 (25) | 54 (24) | 28 (26) | |
| Acquaintance | 129 (39) | 87 (39) | 42 (39) | |
| Stranger | 61 (19) | 39 (18) | 22 (20) | |
| Otherc | 14 (4) | 12 (5) | 2 (2) | |
| Forensic medical exam at index visitd | 126 (38) | 75 (34) | 51 (46) | X2 (1, N = 332) = 4.128, p = 0.042 |
| Status of case | ||||
| Conviction of the perpetrator | 1 (< 1) | 1 (< 1) | 0 | X2 (1, N = 334) = 0.106, p = 0.745e |
| Live investigation | 187 (56) | 122 (55) | 65 (58) | |
| Not reported or support withdrawn | 82 (25) | 55 (25) | 27 (24) | |
| Case closed by police or CPS | 64 (19) | 43 (19) | 21 (19) | |
| Trauma history | ||||
| 4 or more ACEsf | 259 (77) | 174 (78) | 85 (76) | X2 (1, N = 334) = 0.264, p = 0.607 |
| Exposure to contact CSA (ACE)g | 189 (60) | 131 (62) | 58 (57) | X2 (1, N = 313) = 0.784, p = 0.376 |
| Witnessed IPV in childhood (ACE) | 167 (51) | 106 (48) | 61 (55) | X2 (1, N = 330) = 1.552, p = 0.212 |
| Ever IPV (ACTS) | 249 (79) | 169 (80) | 80 (78) | X2 (1, N = 315) = 0.175, p = 0.675 |
| Past year IPV (to baseline) (ACTS) | 108 (34) | 67 (32) | 41 (40) | X2 (1, N = 314) = 1.989, p = 0.158 |
Poor mental health was highly visible in the sample. ‘Long-term mental health problems’ (see Table 1) reflects the proportions of participants identified by SARC or ISVA services as having a pre-existing mental health problem or condition at the time they accessed SARC. If this was missing at referral, we obtained it in the interviews based on medication and psychiatric histories. The proportions for ever having attempted suicide or self-harmed were similarly high at 53% and 61%, respectively. Eight per cent of the sample had attempted suicide in the month before the interview, and 16% self-harmed in that period. It is noteworthy that nearly 70% of those with longstanding illness or disability that limited activity also had long-term mental health problems.
In terms of offence characteristics, 13% of participants had reached the SARC for help after exposure to sexual abuse during childhood; a quarter of people wanted to seek help for sexual violence perpetrated by partners or ex-partners; and the majority (60%) of people in the study sought help after assault by strangers or acquaintances. Only under 5% had been victimised as adults by family members other than partners or by persons in positions or trust or authority. While most people reached SARCs through referrals by the police, over a fifth of participants had contacted SARCs themselves. The rest of the referrals were by the charity/voluntary sector (6%) and a small number from general practice, sexual health, mental health, education and social services.
The burden of trauma across the life course is summarised in Table 1. The mean number of ACEs was 6 (range: 0–13) across the 334 participants who answered the questions, and nearly four-fifths indicated exposure to four or more adverse experiences. As indicated above, more than 13% of people sought help in relation to CSA; however, our research found that more than half of the sample had exposure to contact sexual abuse in childhood. Exposure to domestic abuse in the household during childhood was another commonly endorsed ACE, affecting half the sample. Nearly 80% told us they experienced domestic abuse at some point in adulthood including a third in the year up to baseline. We examined whether individuals retained (n = 222) and lost (n = 113) at the 12-month follow-up differed on any of the baseline characteristics. A greater proportion of those lost to follow-up were out of work than those who were retained. Table 2 presents the mean levels on the various assessments of health and well-being in the sample at each time point. For our primary outcome measure, that is, the PCL-5, 71% of participants had scores above the cut-off of 33 for ‘probable PTSD’ at baseline. This rate persisted at 6 months (69%) before reducing to 55% at 12 months. This reflected a mean difference (reduction) of 9 points on the PCL-5 [95% confidence interval (CI) 6.6 to 11, Cohen’s d = 0.53] equating to a MCID change based on the guidance used for the study. Although there were trends towards better health across the measures, the most visible change was on PTSD. Modelling of changes on other outcomes will be reported elsewhere.
| Outcome | Measure | Baseline | 6 months | 12 months | |||
|---|---|---|---|---|---|---|---|
| N | Mean (SD) or n (%) | N | Mean (SD) or n (%) | N | Mean (SD) or n (%) | ||
| Post-traumatic stress disorder (PTSD) | PCL-5a (Weathers et al.)68 | 329 | 44.0 (16.7) | 224 | 41.0 (16.6) | 222 | 35.0 (17.3) |
| Quality of life | World Health Organization Quality of Life Scale (WHO QoL-BREF)b (Skevington et al.)76 | ||||||
| Physical | 329 | 54.9 (21.7) | 224 | 54.3 (22.0) | 220 | 58.4 (22.4) | |
| Psychological | 329 | 43.4 (21.0) | 224 | 48.2 (19.2) | 220 | 49.7 (18.7) | |
| Social | 327 | 58.5 (24.0) | 224 | 59.3 (23.3) | 219 | 64.3 (23.4) | |
| Environmental | 329 | 66.2 (18.0) | 223 | 63.4 (17.2) | 220 | 67.0 (16.6) | |
| Depression | Centre for Epidemiological Studies Depression Scale Revised (CES-D)a (Cole et al.)77 | 322 | 16.8 (7.1) | 217 | 15.2 (7.3) | 216 | 15.2 (6.9) |
| Alcohol use | Alcohol Use Disorders Identification Test (AUDIT)a (Bush et al.)78 | 319 | 3.4 (2.9) | 307 | 3.2 (2.9) | 210 | 3.0 (2.9) |
| Drug use | Drug Use Disorders Identification Test (DUDIT)a (Berman et al.)79 | 316 | 3.0 (6.4) | 308 | 2.9 (6.5) | 210 | 3.2 (7.5) |
| Eating problems (binge eating) | Binge Eating Disorder Screener-7 (BED-7) screen (Herman et al.)80 | 311 | 79 (25.4%) | 201 | 45 (22.4%) | 202 | 42 (20.8%) |
| Eating problem (anorexia/bulimia) | SCOFF screen (Morgan et al.)81 | 312 | 108 (34.6%) | 106 | 52 (49.1%) | 93 | 47 (50.5%) |
| Anxiety | Generalised Anxiety Disorder-7 (GAD-7)a,c (Spitzer et al.)82 | 208 | 11.0 (5.7) | 206 | 10.4 (5.5) | ||
Direct assessments by survivors about quality of care
Survivors’ assessments of harm and benefit of different sectors for meeting the needs of survivors
The research identified levels of harm and benefit derived across sectors in relation to meeting health and social care needs after sexual violence and abuse. Overall, there was no difference in participants’ evaluations of benefit and harm between the SARCs and voluntary sector (see Table 3).
| Types of services accessed/counted | Number of respondentsa | Minimum | Maximum | Median | Mean | SD | |
|---|---|---|---|---|---|---|---|
| Sexual assault referral centres | Immediate remote and in person crisis care, forensic services, sexual health care, emergency contraception and pregnancy testing, referrals to (on-site or off site) ISVAs and other services, some aftercare and follow-up | 292 | −100 | 100 | 90 | 75.6 | 33.6 |
| Policing and justice | Any contact about the case with police officers, CPS, HM Courts and Tribunals Service | 270 | −100 | 100 | 50 | 29.6 | 68.3 |
| Voluntary sector services | ISVA care provided through the charities, brief and long-term counselling services, support groups, domestic violence services, drug and alcohol, helplines people may have accessed over the course of the study period | 264 | −100 | 100 | 90 | 72.0 | 40.9 |
| NHS care | GP and other primary care, IAPT, sexual health, crisis and community mental health, A&E, in-patient care, psychiatry | 257 | −100 | 100 | 75 | 51.9 | 56.1 |
The figures below provide further insight into the distribution of participants’ scores. We have presented median scores given the non-normal distribution of people’s responses. The median score is visible in the figures by the black horizontal line, indicating that 50% of the ratings lie above the line and 50% below it. In Figure 4, half the participants rated SARC care above 90 on our scale, with only four people of 292 rating SARCs as having harmful effects. Similarly, participants rated the voluntary sector positively, with 50% of people having a score of > 90, and 11 people identified harm (see Figure 5). The ratings by survivors for the responses by the NHS and policing were extremely polarised. For NHS care, half of the scores were rated above 75, which indicates many people gained a high degree of benefit; however, 15% of observations were experienced as ‘harmful’ to survivors (see Figure 6). With regard to police and justice, 50% of responses were rated above 50, suggesting many people found benefit through their experience of interacting with the police (see Figure 7). However, a quarter of survivors rated the police and justice response as harmful.
FIGURE 4.
Evaluating sexual assault referral centres care in meeting needs of survivors.
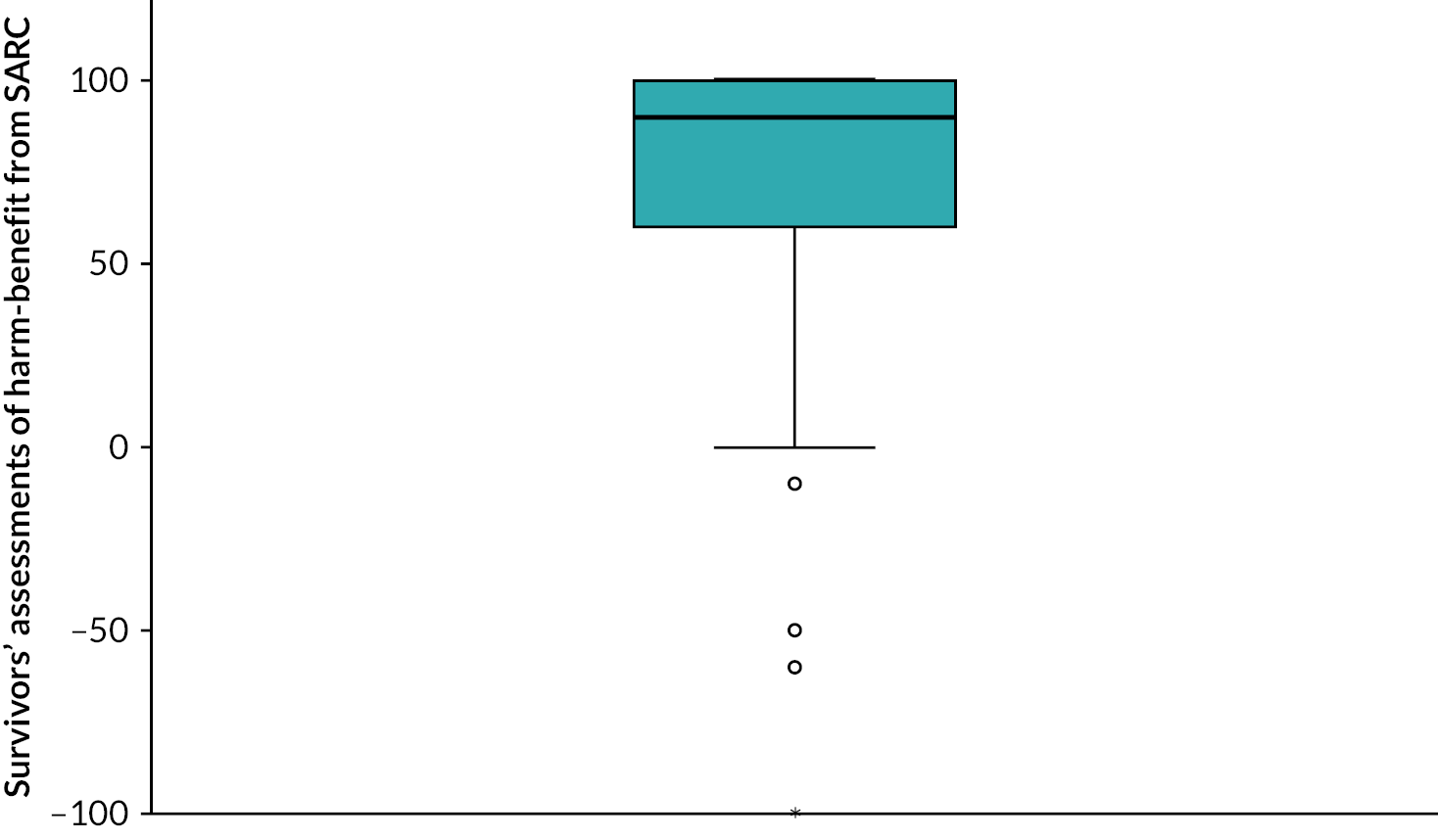
FIGURE 5.
Evaluating voluntary sector care in meeting the needs of survivors.
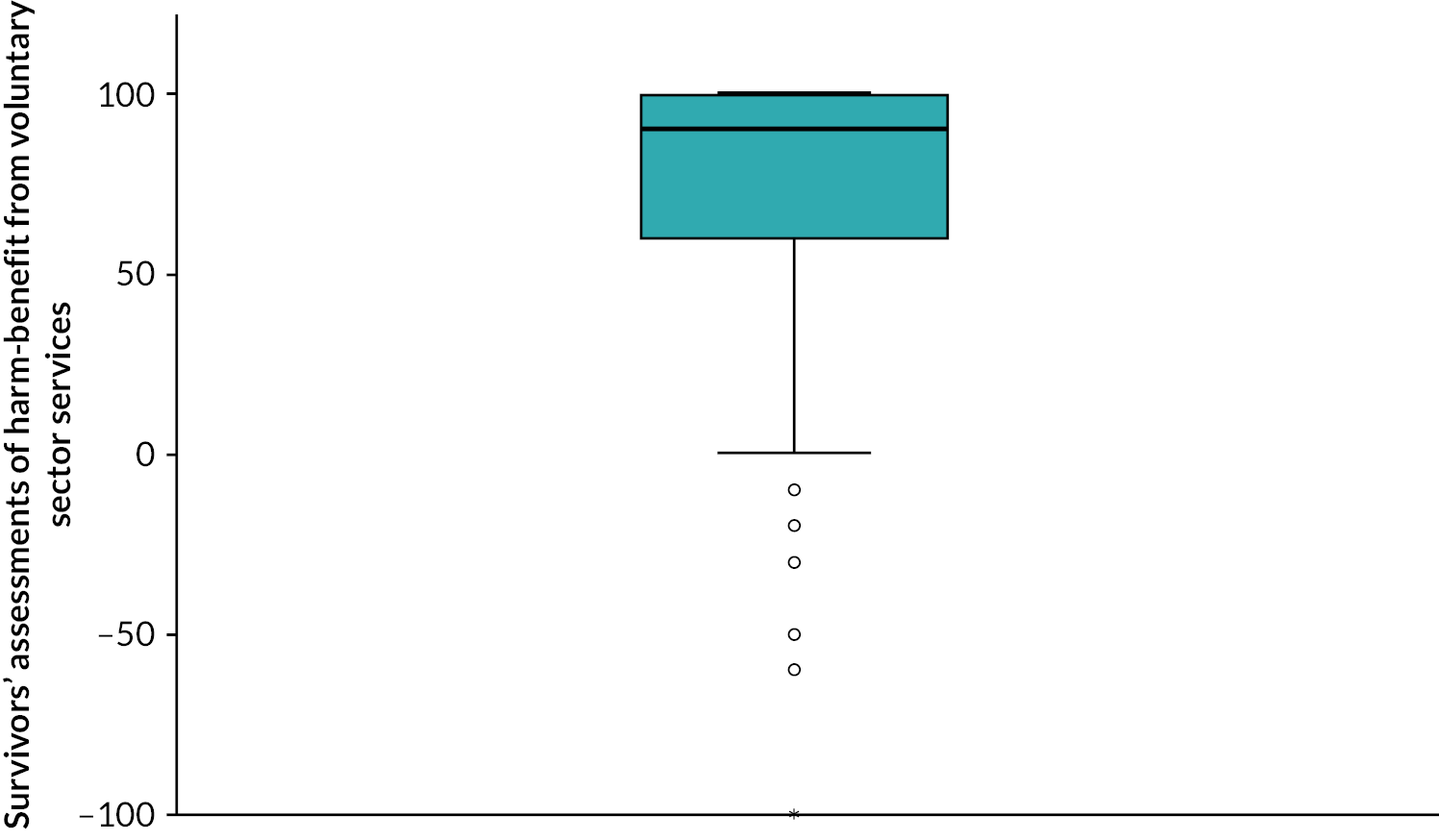
FIGURE 6.
Evaluating NHS care in meeting needs of survivors.
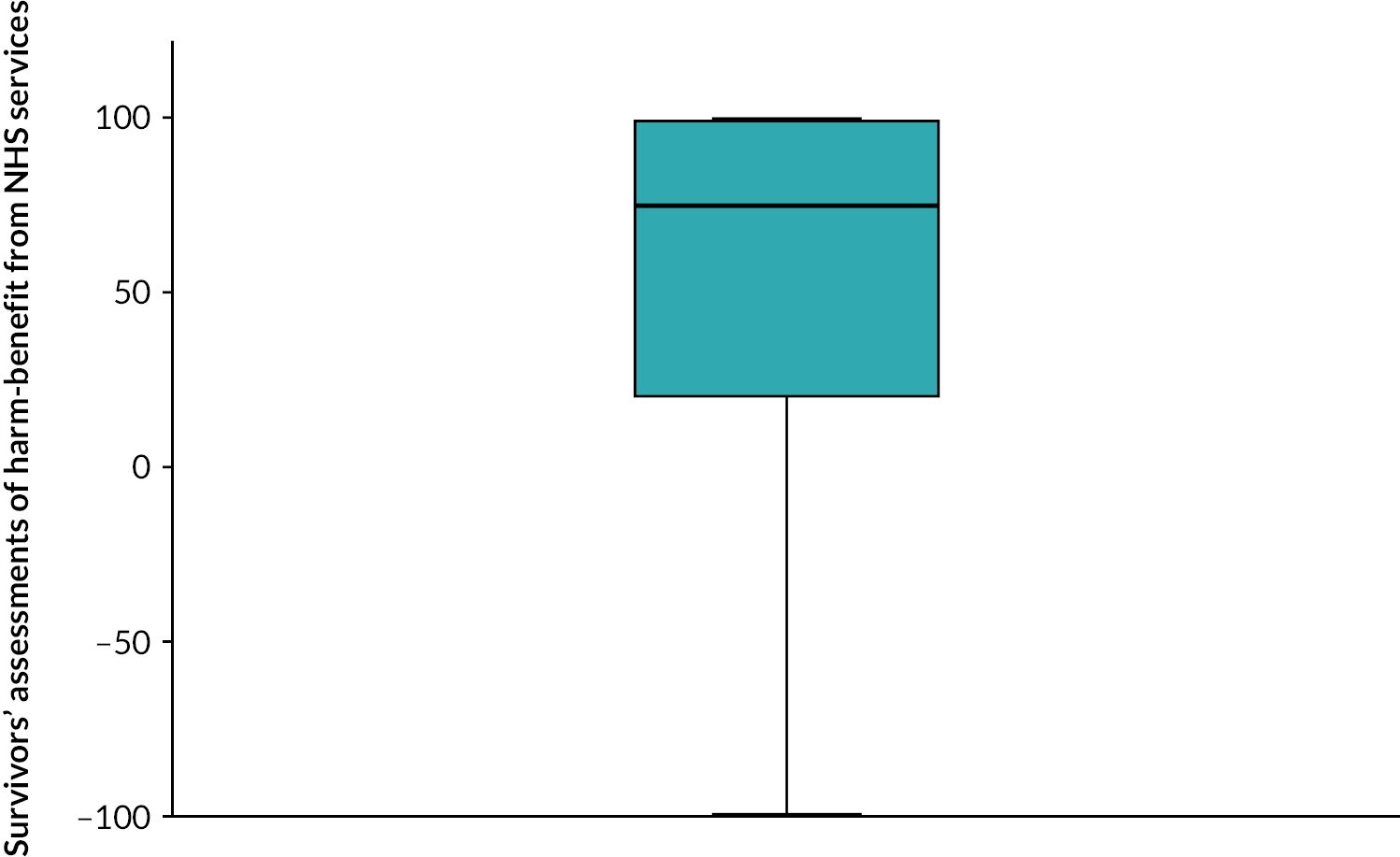
FIGURE 7.
Evaluating policing and justice care in meeting the needs of survivors.
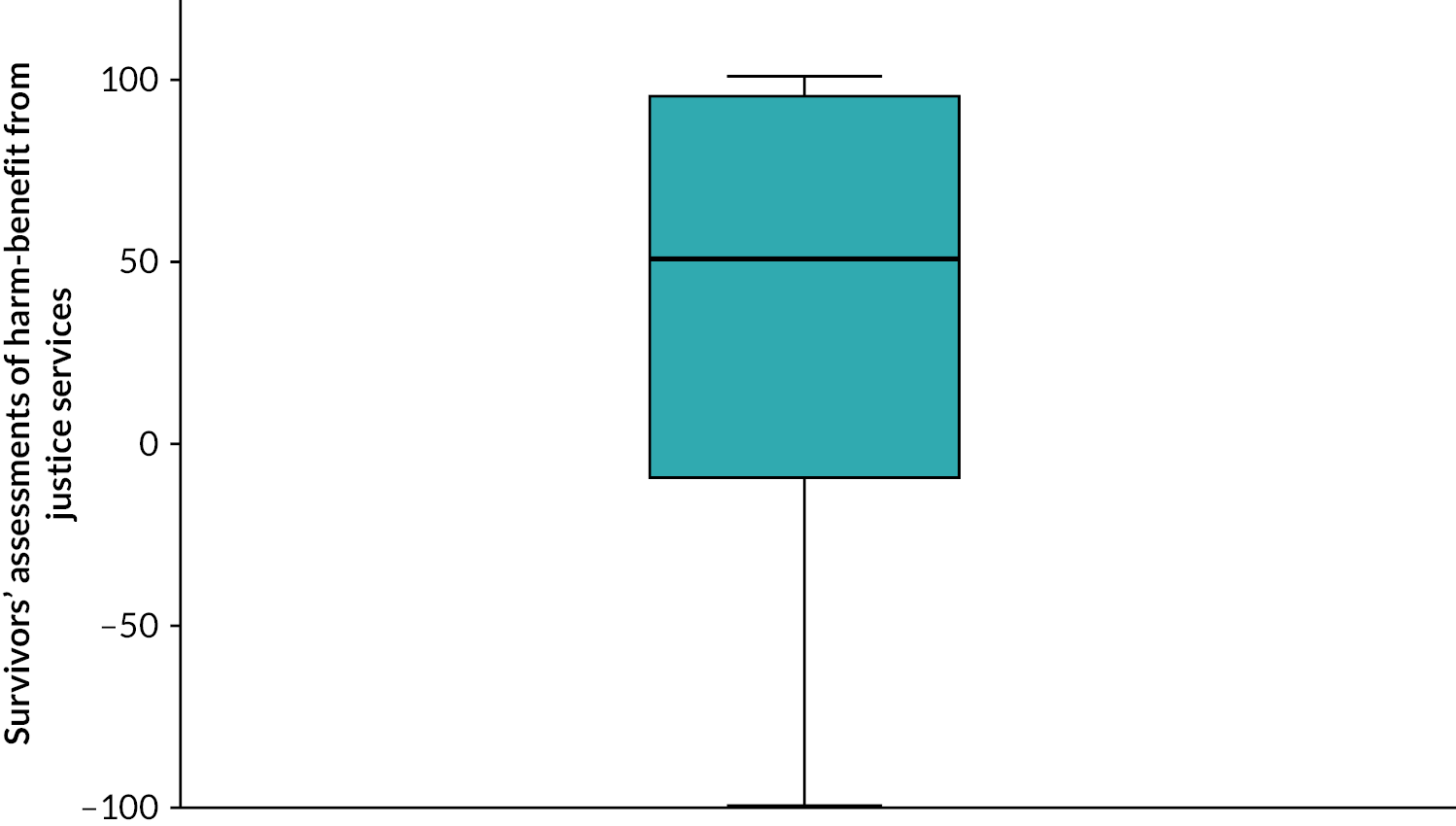
Survivors’ assessments of care for mental health in the NHS and voluntary sector
One of the aims of the study was to explore how survivors fared in the NHS compared to the voluntary sector in having their mental health needs met. As there was so much overlap and movement between voluntary and statutory mental health services, it was not possible to examine this quantitatively. The findings described above provide some context to this question, already highlighting widespread satisfaction with care from the voluntary sector. We observed that many participants also had positive opinions about the NHS, with nearly half of the people gaining considerable benefits. However, harm was more apparent in this context. Barriers to accessing mental health care receive attention in Chapter 8. Here, the research focuses on people’s feedback about specific aspects of mental health care, comparing two highly distinct settings.
With regard to counselling interventions in the voluntary sector, following the pattern for the sector overall, the majority of participants were positive about mental health care. They reported it as helpful in improving how they were feeling, and they were provided tools and techniques for coping with and managing symptoms, which contributed to their recovery:
[Counselling] teaches me how to control emotions I get, how to handle them, how the brain works, mindfulness and different things you can do to help yourself. I felt like I was being understood and not like I had anything to be ashamed of. I didn’t appreciate anything about myself; I get a lot more good days, she’s definitely made a massive difference. I can’t thank her enough, I really appreciate it.
I have one session a week, I think we’ve done about 8 sessions – the transformation has been very quick. I had to set aims that I didn’t think would happen, the aims have been low; aims such as walking around the neighborhood and being able to sleep without the lights in two weeks. I have always really been afraid of the dark. For the last year and half I have slept with the lights on, but now I can sleep in the dark and even go for a walk with my dog at night (in safe places).
A variety of therapeutic approaches and personalisation of care was a feature of the mental health care offered by the voluntary sector. This participant had a particularly positive experience of art therapy:
It was one of the highlights of my year. I really liked it. Each week we focused on a different medium of art. The people who facilitated it [an artist and a counsellor] did it perfectly. They created space for us women, for us to gently interact, it wasn’t too much.
The long waiting lists and caps on the number of sessions are barriers to recovery after sexual violence and abuse. There were some instances where care had been extended:
I really didn’t want to finish (the counselling) so he gave me 10 more [initially given 10 sessions] which was really good.
More commonly survivors could access only a finite number of sessions. Survivors appreciated the immediate support, for example, crisis counselling, where it was provided, and interim support, such as check-in phone calls, provided while waiting for longer-term support. However, long waiting lists to access therapeutic support in the voluntary sector were often mentioned by survivors in addition to limited flexibility in appointment times, meaning that some survivors were unable to access timely support that fully met their needs:
I’ve rung twice a few weeks ago, was told it would be March this year when I would get counselling but as I hadn’t heard anything I called them. They said ‘you won’t get seen until August’. I said ‘someone in your organisation told me it would be March’. They said they would get back to me after they had checked, but they didn’t. I feel like I’ve waited long enough. I also think they should be flexible with the time of when you end up having counselling so it’s outside of working hours. I wouldn’t want to have to explain why I need to take 2 hours off [counselling time and travel time] each week to my boss. They should be flexible.
Experiences of mental health care from the NHS were more mixed. There were many participants who had positive experiences:
The therapy for PTSD completely changed my life. I don’t break down and cry every day and I can go out and not think about it. I could cope with arguments with my partner and not have flashbacks. It just means I don’t have flashbacks any more.
However, for other participants, the mental health care they received did not adequately meet their needs. Care was experienced as too generalised for survivors of trauma with complex needs:
It is impossible to get the care I need on the NHS and I don’t have money for private. Certain therapies are not available. All you get is the short-term: CBT, DIT, EMDR. I tried all of these. Things that could help me [Gestalt] are not available and I can’t afford them so I am not going to get the treatment I need.
Participants were often unable to access the mental health care they needed within the NHS, even if they were in considerable distress:
I was suicidal and I had plans. They decided I wasn’t in need of any help and closed the case or the only support offered was medication.
As with the voluntary sector, survivors also experienced long waiting lists to access therapeutic support from the NHS. Of particular concern were the experiences within the NHS of harmful professional attitudes that replicated rape myths and re-traumatised survivors. These problematic responses from professionals were not reported by participants in relation to the voluntary sector where organisations are more likely to be specialised sexual assault services.
Overall, there were positive experiences of mental health care across both sectors and both sectors face capacity problems. However, the feedback from survivors suggests that there is greater scope within the voluntary sector for providing care that adequately meets the needs of survivors because of the variety and flexibility of support provided. Mental health care from the NHS was often too difficult to access or was inappropriate for the often-complex needs of survivors (see Chapter 8).
Main model
Missing data patterns and amount of available data
The missing at random assumption, on which the maximum likelihood approach to missing data is pinned (not to mention the more ubiquitous multiple imputation), pertains to beliefs about the difference between responders and non-responders – something that cannot be refuted using the observed data alone. Nevertheless, it can be helpful to investigate relationships between patterns and missingness and both model-variables and auxiliary variables. This research uses a string of zeros and ones to describe missingness patterns. For example, ‘000’ is attributed to individuals with all missing data for PCL-5, ‘110’ is attributed to those who missed the final wave and ‘111’ is attributed to those with complete data.
When studying the observed data, we have gatherd some evidence of an association between PCL-5 score and missingness, but the pattern is far from clear. Our a priori belief might have posited that those with more severe symptoms at baseline would be less likely to remain in the study – this is not what the data present. For example, Table 4 shows participants who were lost to follow-up after the first wave tended to have lower symptom scores rather than higher symptom scores at baseline, and there were no overall differences related to the number of measures people completed (see Table 5).
| Missingness pattern | n | Wave 1 (0 months) | Wave 2 (6 months) | Wave 3 (12 months) | |||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | ||
| 111 | 182 | 44.6 | 16.8 | 40.7 | 17.0 | 34.9 | 16.8 |
| 100 | 72 | 41.5 | 16.6 | – | – | – | – |
| 101 | 37 | 39.8 | 16.3 | – | – | 35.3 | 19.3 |
| 110 | 38 | 49.7 | 15.5 | 42.2 | 14.3 | – | – |
| Other | 6 | – | – | 54.0 | 2.7 | 50.0 | 25.5 |
| Number of measures | n | Wave 1 (0 months) | Wave 2 (6 months) | Wave 3 (12 months) | |||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | ||
| 1 | 75 | 41.5 | 16.6 | 53.0 | 2.8 | 32.0 | – |
| 2 | 76 | 44.8 | 16.6 | 42.5 | 14.3 | 36.2 | 19.7 |
| 3 | 182 | 44.6 | 16.8 | 40.7 | 17.0 | 34.9 | 16.8 |
Unconditional mixed-effects models
Figure 8 shows all available data on PCL-5, with each line representing the observed data from one participant. While there is a sense of a downward trend in symptoms across the follow-up period, there is substantial heterogeneity in both scores at baseline and the nature of this trend in terms of its magnitude and sign. Furthermore, by plotting follow-up data in terms of months-since-baseline rather than by wave, there was variation in the timing of subsequent waves, particularly for the final wave.
FIGURE 8.
Plot of all the repeated-measures data for the PCL-5.
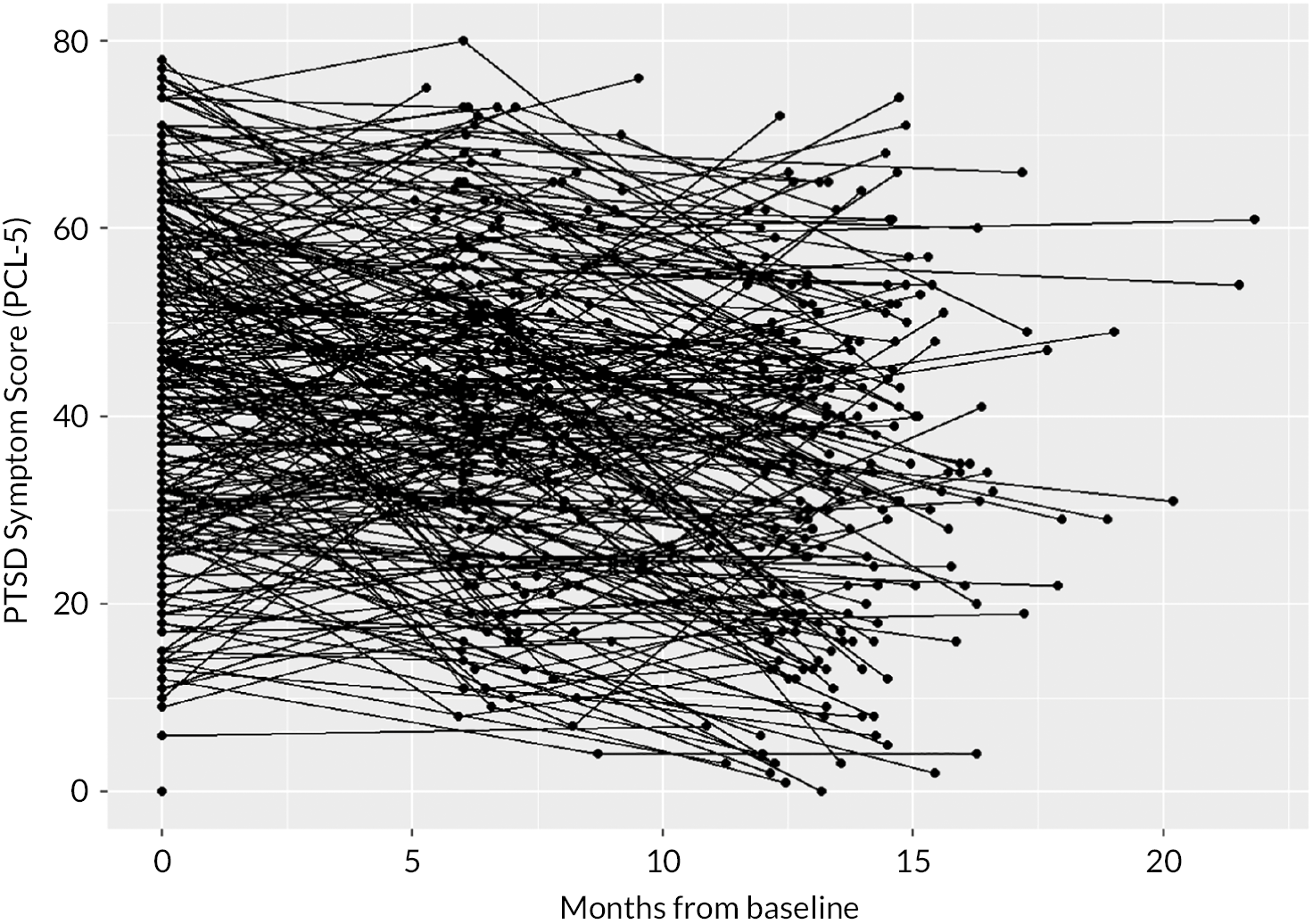
Table 6 shows fixed- and random-effect estimates obtained from a trio of random intercept/slope linear mixed-effects models.
| Predictors | PCL-5 (complete sample) | PCL-5 (2 + Measures) | PCL-5 (maximal sample) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Estimate | 95% CI | p-value | Estimate | 95% CI | p-value | Estimate | 95% CI | p-value | |
| (Intercept) | 44.9 | 42.5 to 47.3 | < 0.001 | 44.9 | 42.9 to 46.9 | < 0.001 | 44.2 | 42.4 to 46.0 | < 0.001 |
| Time year | −8.5 | −10.6 to −6.4 | < 0.001 | −8.1 | −10.0 to −6.2 | < 0.001 | −7.8 | −9.6 to −5.9 | < 0.001 |
| Random effects | |||||||||
| σ2 | 89.55 | 90.61 | 90.68 | ||||||
| τ00 | 196.75 ID | 189.71 ID | 189.32 ID | ||||||
| τ11 | 73.83 ID.time_yr | 79.02 ID.time_yr | 78.37 ID.time_yr | ||||||
| ρ01 | −0.31 ID | −0.29 ID | −0.29 ID | ||||||
| ICC | 0.69 | 0.68 | 0.68 | ||||||
| N | 182 ID | 258 ID | 333 ID | ||||||
| Obs | 546 | 698 | 773 | ||||||
When we focused initially on the complete-case sample of 182 participants, we observed an estimated mean symptom score of 44.9 points at baseline and an average improvement (i.e. reduction) of 8.5 points across the 1-year follow-up.
The baseline random effect has a variance of 196.8 (τ00) corresponding to an SD of 14.0 indicating that we would anticipate 95% of the participants to have symptom scores between 16.8 (i.e. 44.9 − 1.96 × 14.0) and 73.0 (i.e. 44.9 + 1.96 × 14.0) at the first wave. The variance in slope is also substantial (τ11 = 73.8) corresponding to an SD of 8.6 indicating that we would anticipate 95% of the participants to have an improvement in the range of 25.3 to −8.3 across the year of follow-up. The other role of the random-effect SDs here is that they link back to the original power calculation and the quantification of the MCID. The MCID for symptoms scores at baseline is at 14.0 × 0.5 = 7 points on the PCL-5, and the MCID for improvement across the year is approximately 4.25. Finally, it is worth commenting on the correlation between the two random effects (ρ01 = −0.31), which is modest in size, and negative. Thus, there is a tendency for the variance in score to decrease over time, or in other words, greater improvements are observed among participants who entered the study with a greater burden of symptoms.
Changes are subtle if we move to the right in the table and introduce the participants who provided an incomplete set of PCL-5 measurements. We can observe the average yearly improvement reducing slightly to 7.8 points, which is to be expected given the previous observation that participants providing one measurement had slightly lower scores at baseline, and the observation above that there is a negative correlation between baseline scores and the rate of improvement.
Multivariable models
In the multivariable models that follow, we consider each factor of interest and estimate its association with the baseline and change in PCL-5 (i.e. intercept and slope random effects in multilevel-model terminology). This is achieved by introducing the risk factor as both a main effect and an interaction with time. To aid interpretation, we present parameter estimates in terms of two models – a ‘baseline model’ and a ‘slope model’; however, all estimates are obtained from a single linear mixed-effects model with the relevant interaction terms.
For all models presented, a series of covariates has been included; however, their own parameter estimates are not shown. The primary goal of model adjustment here is to address potential bias problems due to variation in the timing of response and loss-to-follow-up. The specific adjustments made for each risk factor are listed in the table footnote. Finally, results are shown for the sample of participants providing at least one measure of PCL-5 across the three waves. The analysis sample for each risk factor varies slightly because of a minor amount of missing data, and this is also summarised in the footnote.
Organisational-level factors
There is little evidence here to suggest a relationship between PTSD as measured by the PCL-5 and either the type of ISVA or the type of SARC. However, we will describe the information shown in the first table (see Table 7) to aid the interpretation of the subsequent tables, which are in the same format.
| Predictor | Baseline model | Slope model | ||||
|---|---|---|---|---|---|---|
| Estimates | 95% CI | p-value | Estimates | 95% CI | p-value | |
| ISVA locationa | 0.471 | 0.334 | ||||
| ISVA off-site | 0.0 (ref) | 0.0 (ref) | ||||
| ISVA on-site | −1.8 | −6.6 to 3.0 | −2.6 | −7.8 to 2.6 | ||
| Type of SARCb | 0.208c | 0.445c | ||||
| Police-led | 0.0 (ref) | 0.0 (ref) | ||||
| Charity-led | 0.6 | −9.8 to 11.0 | −9.9 | −22.1 to 2.2 | ||
| NHS-led | 0.1 | −6.4 to 6.5 | −3.5 | −10.3 to 3.4 | ||
| Private sector | 4.1 | −1.0 to 9.2 | −2.3 | −7.7 to 3.0 | ||
For the first model (ISVA location) we observed that, on average, survivors who attended a ‘SARC ISVA’ were estimated to be 1.8 points lower on the PCL-5 at baseline with a 95% CI from −6.6 points (i.e. 6.6 points lower) to + 3.0 points (i.e. 3 points higher). In terms of slope, survivors attending a SARC ISVA had a 2.6-point greater reduction in PCL-5; however, once again, the 95% CI was wide and the range of values consistent with a benefit of ISVA location, a detriment or the null.
It merits mention that, for these models, we are treating the pair of outcomes baseline and slope as bivariate dependent variables and that it might be more relevant to condition on the baseline symptom level when examining risk factors for change. To facilitate this, we switched over to a structural equation modelling framework, which permits regressions rather than residual covariances between random effects. These models showed that we were not missing an important part of the message by using the models shown below.
To conclude the section of organisational-level factors, the table also contains a second model – that for SARC type. Again, there is little evidence against the null as shown by the pair of large p-values. There does appear to be a large slope effect (−9.9 points) for the charity-led SARC; however, there were very few survivors attending a SARC of this type (hence, the very wide confidence limits).
Service experience
The service use variable considered here is a composite, derived from data from all three waves (see Table 8). We derived an average value for each participant, with the denominator depending on the number of variables collected [three for those with complete data, two for those with one missing wave and one for those with one variable (usually only the baseline measurement)]. The resulting scale was markedly skewed and was log-scaled, which rendered it normal in appearance. While normality in independent variables is not necessary for inferential purposes, it can be beneficial for improving the linearity of associations.
| Predictor | Baseline model | Slope model | ||||
|---|---|---|---|---|---|---|
| Estimates | 95% CI | p-value | Estimates | 95% CI | p-value | |
| Service utilisationa | < 0.001 | 0.509 | ||||
| Service use (log-scaled) | 4.5 | 2.6 to 6.4 | 0.7 | −1.4 to 2.9 | ||
| Perceived harm/benefit of policing and justice responseb | 0.975d | 0.576d | ||||
| Neutral perception | 0.0 (ref) | 0.0 (ref) | ||||
| Negative perception | 1.1 | −5.1 to 7.2 | 2.3 | −4.0 to 8.7 | ||
| Positive perception | 1.0 | −4.1 to 6.1 | 1.6 | −3.7 to 6.9 | ||
| N/A | 0.3 | −6.0 to 6.6 | 4.5 | −2.0 to 11.0 | ||
| Status of criminal case at the first wavec | 0.285e | 0.633e | ||||
| Case remains open | 0.0 (ref) | 0.0 (ref) | ||||
| Case self-closed | −2.8 | −7.2 to 1.6 | 2.0 | −2.5 to 6.5 | ||
| Case police-closed | −3.2 | −7.9 to 1.6 | −0.3 | −5.2 to 4.7 | ||
There is strong evidence (p < 0.001) of a positive association between service use and symptom level at baseline. A 1-unit increase in the log of service use count is associated with a 4.5-point higher symptom score at baseline (95% CI 2.6 to 6.4). Given the nature of this variable, with some data collected from waves after baseline, we must be cautious in our interpretation here; however, it is clear that a greater symptom burden is associated with a greater level of service use, which does not feel contentious.
Aside from service use, there is little/no evidence of either perceived harm/benefit nor baseline status of criminal case as being associated with baseline symptom level, and little evidence of any service experience factor being related to improvement in symptoms across the year.
Characteristics of the individual and the offence
We observed several factors from this third and final domain to be strongly related to baseline PTSD symptom level as measured by the PCL-5 (see Table 9). Firstly, each additional ACE is associated with a 1.4-point greater score of symptoms at baseline (95% CI 0.8 to 1.9; p < 0.001) and evidence of mental health issues with a 7.6-point difference. There is weak evidence (p = 0.087) that a delay of at least 11 days is associated with an approximately 4.5-point greater symptom score, and there is a similar level of evidence in support of an association for perpetrator type, where it appears that where the perpetrator is the survivor’s partner (or ‘other’), the baseline score is greater. There is strong evidence (p = 0.009) and an apparent dose-response for symptoms being lower for those with greater financial resources, and finally there is strong evidence (p < 0.001) that being unable to work is associated with a 10-point higher baseline score. With regard to the slope model, there is little worthy of note. It is evident that the main determinant of improvement, at least when quantified in this way, is symptom burden at baseline. While there is some evidence here that improvement is greater for those with more ACEs, the structural equation model showed that this was being driven by the strong association between ACEs and baseline symptoms.
| Predictor | Category of predictor | Baseline model | Slope model | ||||
|---|---|---|---|---|---|---|---|
| Estimates | 95% CI | p-value | Estimates | 95% CI | p-value | ||
| Burden of ACEsa | Per additional ACE | 1.4 | 0.8 to 1.9 | < 0.001 | −0.6 | −1.3 to 0.0 | 0.054 |
| Long-term mental health problemsa | No evidence | 0.0 (ref) | < 0.001 | 0.0 (ref) | 0.152 | ||
| MH issues present | 7.6 | 4.0 to 11.1 | −2.8 | −6.7 to 1.0 | |||
| Time between trauma and SARCb | Up to ten days | 0.0 (ref) | 0.087e | 0.0 (ref) | 0.236e | ||
| Duration 11 days – 1 year | 4.6 | −0.0 to 9.1 | 0.4 | −4.3 to 5.2 | |||
| Duration > 1 year | 4.4 | −0.5 to 9.3 | −3.6 | −8.5 to 1.3 | |||
| Perpetrator type (relationship, if any, between survivor and perpetrator)c | Partner | 0.0 (ref) | 0.024f | 0.0 (ref) | 0.722f | ||
| Child sexual abuse | −2.6 | −8.9 to 3.7 | 1.1 | −5.6 to 7.8 | |||
| Acquaintance | −6.6 | −11.2 to −2.0 | −0.7 | −5.5 to 4.1 | |||
| Stranger | −6.4 | −12.0 to −0.9 | 3.0 | −2.9 to 8.9 | |||
| Other | 2.3 | −6.8 to 11.5 | −1.1 | −10.3 to 8.1 | |||
| Educational attainment of survivord | Less than A-levels | 0.0 (ref) | 0.113e | 0.0 (ref) | 0.867e | ||
| A-level education | 0.4 | −4.0 to 4.8 | −1.2 | −5.8 to 3.4 | |||
| > A-level education | −3.8 | −8.2 to 0.6 | −0.9 | −5.5 to 3.7 | |||
| Financial problemsa | £100 impossible to find | 0.0 (ref) | 0.009e | 0.0 (ref) | 0.784e | ||
| £100 difficult to find | −3.1 | −8.4 to 2.2 | 2.1 | −3.8 to 8.0 | |||
| £100 not a problem to find | −7.3 | −12.4 to −2.2 | 1.6 | −4.2 to 7.4 | |||
| Inability to work (e.g. due to disability)a | Able to work | 0.0 (ref) | < 0.001 | 0.0 (ref) | 0.370 | ||
| Unable to work | 10.0 | 5.7 to 14.2 | −2.2 | −7.1 to 2.6 | |||
Discussion
Summary of main findings
The cohort study fulfils two major goals of the MESARCH project. Firstly, it addresses questions about the effectiveness of SARCs and the onward pathway of care, adding longitudinal findings to several existing mixed-methods in this field. 21,47,83,84 Second, it enables analysis of health and well-being journeys for survivors of sexual violence and abuse after contact with services. We are not aware of any other UK-based study that has followed-up a sample of survivors of rape, sexual assault and sexual abuse. There are some longitudinal data available in relation to young survivors in the UK, with smaller samples and shorter timescales,85 and a small number of international studies with adults,86–89 with the South Africa longitudinal study conducted by Abrahams et al. being the closest in terms of design. 12,64,65
Participants in our cohort were SARC service users aged ≥ 18 years. They were largely similar to SARC service users nationally,90 although this shifted somewhat in the wake of the COVID-19 pandemic where people accessed SARCs remotely, the time to care profile shifted and likely interacted with how the COVID-19 pandemic led to reductions in some forms of sexual violence and abuse (stranger and acquaintance assaults), increases in other areas (partner-perpetrated and online forms) and a pattern of non-recent survivors, such as survivors of CSA, coming forward for help. 91 Our research captured this varied picture and recruited people approximately 100 days after they had accessed a SARC. Cohort participants were predominantly women (90%) and belonged to non-minoritised ethnicities (85%), and their age ranged from 18 to 75 years.
Survivors reported a high burden of lifetime trauma. Although suffering from ACEs is not deterministic, having four or more ACEs is related to an increased likelihood of experiencing chronic health conditions such as cancer, cardiovascular disease, type 2 diabetes, respiratory diseases and poor mental health. 92 Notably in our study, three-quarters of participants had four or more ACEs, contrasting sharply with rates of approximately 10–15% reported in population-based studies. 92 Nearly half of the survivors had pre-existing mental health problems at the point of accessing SARC, more than half had lifetime experience of attempted suicide, 56% had been prescribed psychotropic medications. Although our sample had a good spread on socio demographic factors, 17% faced major daily financial problems. For offence-related factors, there was weak evidence that a delay of more than 10 days to SARC was associated with more PTSD symptoms, and a similar level of evidence in support of an association for perpetrator type where it appears that when the perpetrator was the survivor’s partner/family the baseline score was greater. The profile of perpetrators differed from ONS data93 on experiences of sexual violence and abuse nationally with a greater proportion of abuse among SARC service user by strangers and acquaintances over partners. ONS data suggest that nearly half of the sexual violence and abuse cases is committed by partners. This signals an access issue for survivors of domestic-perpetrated sexual abuse.
Sexual assault referral centres and third-sector agencies achieved consistently high standards of care for survivors across sub-studies, and harmful encounters were at a minimum. This was in stark contrast to the NHS and police, where the frequency of harmful experiences affected 15% and 25% of people who rated these sectors, respectively, and our qualitative studies have generated many insights into how to improve care in these settings.
Post-traumatic stress disorder proportions and means at entry to our study were consistent with data cited at baseline in international intervention studies with survivors of sexual violence and abuse. 36 Seventy per cent of participants had ‘probable PTSD’ and achieved important reductions at follow-up (9 points on the PCL-5 equivalent to > 0.5SD, which was our threshold for judging a minimal clinically meaningful difference). 69 We found an important triad of risk between ACEs, long-term mental health problems and socio-economic deprivation, and these were the main predictors of PTSD at baseline.
A third of the original cohort was lost-to-follow-up at 1 year, consistent with treatment studies in the field. 71,86 While those retained and lost differed on degree of socio-economic deprivation, people with more trauma symptoms at baseline were not more likely to leave the study. We consider this to be an important observation and reflect the impact of our trauma-informed research practice (see Chapter 2). The service use is described more fully in our economic evaluation (see Chapter 6), but there was strong evidence of a positive association between frequency of service use and symptom level at baseline. This was also consistent with the ACEs-related research on costs. 92
We observed a trend towards improvements on health measures for the sample over the year of the study. While examining in-depth aspects of health in our sample beyond PTSD is outside the scope of this research, we present the QoL data as an example of what is emerging from our work. When using the final timepoint for comparison, the MESARCH cohort sample was found to have poor QoL across three of the four domains on the WHOQoL-BREF relative to the general population. 94 In their study assessing the QoL in people with a variety of illnesses, Skevington and McCrate94 reported the following scores for the WHOQoL-BREF for the control group (a sample of more than 1300 participants who were considered ‘well’): Physical 76.49 (vs. 58 in MESARCH sample); Psychological 67.82 (vs. 49); Social 70.52 (vs. 64); Environment 68.20 (vs. 67). It is noteworthy that there was no difference on environment-related QoL in our sample that connects with important themes of access to health care and safe environments, which we highlight about in Chapter 8.
This study did not detect differences in outcomes on PTSD at 1 year by SARC service model accessed or on accessing a SARC-provided ISVA. This was an important finding and core part of our investigation. Although there was a trend towards benefit from charity-led SARCs over those led by the police, NHS and private sector organisations, we had too few service users accessing charity-led SARCs to have confidence in this finding. Without a control group, we cannot demonstrate causality; however, it is promising to observe improvements among those that have accessed the SARC care pathway. The main predictor of PTSD at 12 months was the baseline score. With 55% of people still exhibiting PTSD symptoms over a year later that would interfere with their daily functioning, there is still a gap in survivors accessing the right care for their recovery. This is crucial to address to avoid future costs of violence, especially given what our Cochrane Reviews have demonstrated in terms of the efficacy of interventions. There is also wide evidence from our qualitative work of a range of novel and alternative treatments and therapies seen as acceptable and beneficial to survivors that may offer cost-effective ways of promoting good health and recovery for survivors. A high ACE profile doubled the odds of meeting the PTSD diagnostic threshold at baseline, this reduced to 1.5 at 6 months and was absent at 1 year. This is a promising sign that the effects of childhood trauma may be alleviated through appropriate care and support.
Strengths, limitations and implications of this work for health care and research are addressed in detail in Chapter 9.
Chapter 6 Economic evaluation
Introduction
The impacts and economic costs associated with sexual violence and abuse for individuals, families, communities and societies are wide-ranging and substantial. 95–97 There is a paucity of evidence on the outcomes of different interventions and programmes targeted at addressing sexual violence and abuse and on the costs associated with such violence. 98,99 Economic evidence is vital to ensure scarce public resources are used optimally. 100 Although the literature is limited in volume, there has been some recent consideration of appropriate methods for economic evaluations in this area. 99,101
Economic evaluations aim to inform decisions by comparing the costs and outcomes of health interventions, to ensure scarce resources are used in the best ways possible to improve health and well-being. 102 Decision-makers need to make difficult decisions around which programmes and interventions should be funded. Very few economic evaluations of interventions and services focused on survivors of sexual violence and abuse have been undertaken, and those that are published are often limited in their scope. 101
The aim of this component was to compare the costs and outcomes associated with different organisational aspects of SARC service delivery. If some SARC models are more strongly associated with reducing PTSD and improving QoL and other mental, physical and sexual health outcomes than others, there are likely to be important cost implications for the healthcare sector, for the wider public sector and for society as a whole.
Methods
Resource use and costs
For the initial analysis, a UK NHS/Personal Social Services perspective was adopted when conducting the economic analysis; accordingly, only direct costs to the health service, social care and SARCs were deemed to be relevant. This was followed by a wider analysis, focusing on public sector resource use as a whole. Resource use data were collected prospectively to estimate the costs associated with different models of SARC service delivery. This included services attended after initial attendance at a SARC, to capture the whole service pathway experienced by survivors.
The resource use monitored included (1) the cost of service use within SARCs (e.g. consultations, treatment); (2) NHS and social care resource use after initial attendance at SARCs (e.g. GP visits, sexual health visits, contacts with social workers). This was distinct from the resource use within the NHS SARCs; (3) third-sector resource use after initial attendance at SARCs (e.g. counselling, information and advice); and (4) wider public sector resource use, for example, in relation to housing and other social welfare systems.
Relevant unit costs for health resource use and treatments were identified from established national sources103,104 (see Report Supplementary Material 2). The total cost associated with each service pathway, at different follow-up points, was estimated using a micro-costing method where unit costs were assigned to the number of utilised resources. 105 As healthcare costs are substantially skewed, 95% CIs around mean differences were estimated using the bootstrap method. 103 All costs are expressed in UK currency (£) for 2021/2. As necessary, costs were inflated using the Hospital and Community Health Services Pay and Prices Index. 103 Discounting of costs and outcomes was not required as the study was concerned with a 12-month period. As no information was publicly available on the costs associated with services in terms of different types of SARCs (police, NHS, charity and private-led services), we assumed that there was no difference in the costs associated with resource use such as consultations across the various SARC types (NHS-led, private etc.). There is currently considerable debate about the cost burden on different sectors, but no definitive data are available on actual cost differences. However, all costs were varied extensively in the sensitivity analyses.
Health outcomes
The primary clinical outcome for the MESARCH study was participant-reported PTSD symptoms, collected using the PCL-5 (see Chapter 5). Self-reported health-related QoL was assessed via the EuroQol-5 Dimensions, five-level version (EQ-5D-5L) questionnaire, completed by participants at baseline and follow-up points. The EQ-5D instrument is a preference-based measure consisting of five dimensions: mobility, self-care, usual activities, pain/discomfort and anxiety/depression. 106 The EQ-5D instrument was selected as it is recommended by the National Institute of Health and Care Excellence (NICE) and has been used for patients experiencing PTSD and in other similar contexts. 107,108 Following NICE guidance utility values were calculated by mapping the 5L descriptive system data onto the 3L value set. 109 The mapping function developed by van Hout et al. 110 was used for the analysis, to allow consistency with NICE recommendations. The mapping function uses data obtained from a survey of the UK population to derive a utility-based value. Following the trapezium rule, the generated score was used to calculate quality-adjusted life-years (QALYs) gained at 12 months, to inform analysis of costs and utility. 111
The ICEpop CAPability measure for Adults (ICECAP-A) instrument was used to measure capability/ wellbeing. The instrument consists of the following five attributes: stability (an ability to feel settled and secure), attachment (an ability to have love, friendship and support), autonomy (an ability to be independent), achievement (an ability to achieve and progress in life) and enjoyment (an ability to experience enjoyment and pleasure). 112 This instrument was included, as there has been wide recognition of the limitations of EQ-5D and other health-related QoL measures in the context of mental health conditions. 113,114 The capability approach is concerned with the evaluation of a person’s ability to achieve ‘functionings’ in life that are important to them. Such ‘functionings’ can range from basic considerations, such as being nourished, to more complex aspects, such as self-respect. Overall, the capability approach attempts to capture a more comprehensive picture of individuals when evaluating programmes or services, rather than just limiting the space to health alone. 115
Changes to protocol
We had originally planned to undertake a cost-effectiveness analysis of different SARC models (based on organisational structure) in terms of the primary clinical outcome which was reduction in trauma symptoms (PTSD-based PCL-5). However, our analysis of the clinical outcome data demonstrated that significant clinical differences in terms of SARC organisational structures were not evident (see Chapter 5). It was therefore judged appropriate to conduct a full economic evaluation in the form of a cost–utility analysis only, focusing on cost per QALY gained. The data are initially presented as a descriptive analysis of costs and outcomes (in the form of an extended cost-consequence analysis), followed by a full economic evaluation in the form of a cost–utility analysis. This allows assessment of service use and costs for participants. It was originally planned to develop a decision-analytic model to evaluate the longer-term impacts of the different types of service delivery on costs and outcomes. However, this was not judged to be appropriate, based on the results of the cohort study, which did not indicate meaningful clinical differences based on SARC organisational structures.
Base case analysis
To compare the costs and benefits of different SARC service delivery models, a within-study analysis was undertaken. A descriptive analysis of the service use and costs associated with different SARC models was undertaken as the first step (a cost-consequence analysis). This involved analysing the service pathways followed by those accessing services. We assessed costs and outcomes in a disaggregated manner for SARC pathways to provide information on the costs and outcomes associated with each model. The main analysis was based on the reported health-related QoL, examining changes at 6 and 12 months. The secondary analysis examined changes in capability.
As shown in the previous chapter, analyses of clinical outcomes demonstrated that there were no significant differences in terms of the primary clinical outcome, which was a reduction in trauma symptoms (PTSD-based PCL-5) based on SARC type. Hence, a cost-effectiveness analysis based on the primary clinical outcome for the study was not deemed appropriate. A full economic evaluation in terms of a cost–utility analysis was performed to compare the cost per QALY gained at 12 months for different SARC types. Following an assessment of the level of missing data, a complete case analysis was undertaken for the cost–utility analysis, and only participants who returned the resource use and EQ-5D question elements at all time points were included in the analysis. It was not possible to employ multiple imputation methods because of the extent of missing data and a complete case analysis needed to be undertaken to explore changes in resource use and costs over time. 116 A similar approach as that outlined in Chapter 5 was adopted to analyse differences in characteristics between participants at baseline.
Sensitivity analyses
A series of one-way deterministic sensitivity analyses were carried out to assess the impact of the assumptions and estimated values included in the base case analysis. Uncertainties around costs and outcomes were analysed, and plausible ranges were specified using information from the study and from the literature. To account for uncertainty due to sampling, a probabilistic sensitivity analysis was undertaken involving a non-parametric bootstrapping approach, applied to derive paired estimates of mean differences in costs and utility values. The paired estimates were presented on scatterplots for the cost–utility analysis on the cost-effectiveness planes. STATA (StataCorp LP, College Station, TX, USA; version 17117) was used to perform the analyses.
Results
Overall, 335 participants were recruited at baseline. Baseline interviews were conducted nearly 100 days after participants had accessed SARCs. Overall, 328 participants (97.9%) completed the NHS resource use questions at baseline. Data on NHS resource use at all time points (baseline, 6 and 12 months) were obtained from only 180 participants (53.7%; see Table 10).
| Charity-led | NHS-led | Police-led | Private sector-led | Total | |
|---|---|---|---|---|---|
| Baseline | |||||
| None | 5 (35.71%) | 31 (26.96%) | 29 (43.28%) | 38 (27.34%) | 103 (30.75%) |
| At least one service | 9 (64.29%) | 82 (71.3%) | 38 (56.72%) | 96 (69.06%) | 225 (67.16%) |
| Missing | 0 (0%) | 2 (1.74%) | 0 (0%) | 5 (3.6%) | 7 (2.09%) |
| 6 months | |||||
| None | 6 (42.86%) | 40 (34.78%) | 23 (34.33%) | 37 (26.62%) | 106 (31.64%) |
| At least one service | 5 (35.71%) | 34 (29.57%) | 23 (34.33%) | 55 (39.57%) | 117 (34.93%) |
| Missing | 3 (21.43%) | 41 (35.65%) | 21 (31.34%) | 47 (33.81%) | 112 (33.43%) |
| 12 months | |||||
| None | 4 (28.57%) | 55 (47.83%) | 22 (32.84%) | 41 (29.5%) | 122 (36.42%) |
| At least one service | 2 (14.29%) | 22 (19.13%) | 21 (31.34%) | 47 (33.81%) | 92 (27.46%) |
| Missing | 8 (57.14%) | 38 (33.04%) | 24 (35.82%) | 51 (36.69%) | 121 (36.12%) |
| All time points | |||||
| Reported | 8 (57.14%) | 50 (43.48%) | 33 (49.25%) | 64 (46.04%) | 180 (53.73%) |
| Not reported | 6 (42.86%) | 65 (56.52%) | 34 (50.75%) | 75 (53.96%) | 155 (46.27%) |
| Total | 14 | 115 | 67 | 139 | 335 |
In total, 318 participants (94.9%) completed the EQ-5D-5L questionnaire at baseline, dropping to 213 participants by 12 months (63.6%; see Table 11). Complete EQ-5D data at all time points were obtainable for only 170 participants (50.8%).
| Charity-led | NHS-led | Police-led | Private sector-led | Total | |
|---|---|---|---|---|---|
| Baseline | |||||
| Reported | 12 (85.71%) | 111 (96.52%) | 64 (95.52%) | 131 (94.24%) | 318 (94.93%) |
| Not reported | 2 (14.29%) | 4 (3.48%) | 3 (4.48%) | 8 (5.76%) | 17 (5.07%) |
| 6 months | |||||
| Reported | 11 (78.57%) | 73 (63.48%) | 44 (65.67%) | 87 (62.59%) | 215 (64.18%) |
| Not reported | 3 (21.43%) | 42 (36.52%) | 23 (34.33%) | 52 (37.41%) | 120 (35.82%) |
| 12 months | |||||
| Reported | 6 (42.86%) | 78 (67.83%) | 42 (62.69%) | 87 (62.59%) | 213 (63.58%) |
| Not reported | 8 (57.14%) | 37 (32.17%) | 25 (37.31%) | 52 (37.41%) | 122 (36.42%) |
| All time points | |||||
| Reported | 6 (42.86%) | 63 (54.78%) | 31 (46.27%) | 70 (50.36%) | 170 (50.75%) |
| Not reported | 8 (57.14%) | 52 (45.22%) | 36 (53.73%) | 69 (49.64%) | 165 (49.25%) |
| Total | 14 | 115 | 67 | 139 | 335 |
Health outcomes
The analysis of the primary clinical outcome showed that there was no statistically significant difference based on SARC model type in terms of a clinically significant reduction in PTSD symptoms (see Chapter 5). Hence, this section focuses on describing the data on health-related QoL (HRQoL) collected during the study. The mean EQ-5D value at baseline was similar across all SARC types at baseline and improved over the 6- and 12-month periods, although remaining below population norms118,119 (see Table 12).
| Charity-led | NHS-led | Police-led | Private sector-led | Overall | |
|---|---|---|---|---|---|
| Baseline | 0.686 (0.644 to 0.729) | 0.749 (0.714 to 0.785) | 0.639 (0.567 to 0.71) | 0.686 (0.644 to 0.729) | 0.70 (0.674 to 0.727) |
| 6 months | 0.793 (0.707 to 0.879) | 0.743 (0.697 to 0.79) | 0.706 (0.633 to 0.779) | 0.676 (0.613 to 0.739) | 0.711 (0.677 to 0.745) |
| 12 months | 0.763 (0.622 to 0.904) | 0.751 (0.708 to 0.795) | 0.698 (0.611 to 0.784) | 0.726 (0.671 to 0.78) | 0.73 (0.698 to 0.763) |
The analysis of mean QALY gain over the 12-month period was slightly higher for participants in police-led SARCs, but there was no statistically significant difference between the SARC models in terms of QALY gain (see Table 13). The results for the ICECAP-A instrument (will be reported elsewhere) showed that capability increased over the 12 months for the study participants.
| Charity-led | NHS-led | Police-led | Private sector-led | Overall | |
|---|---|---|---|---|---|
| QALY gained at 12 months | −0.004 (−0.083 to 0.074) | 0.004 (−0.028 to 0.036) | 0.025 (−0.019 to 0.069) | 0.014 (−0.021 to 0.048) | 0.011 (−0.008 to 0.031) |
Sexual assault referral centre and Independent Sexual Violence Advisor service use
As shown in Table 14, a wide range of services were accessed in all SARCs at baseline (in addition to FMEs, where appropriate). Data on SARC service use were available for 325 participants (97.0%). A similar level of service access was reported across SARCs. SARC service provision reduced over time, with very few participants reporting access to SARC services at 6 and 12 months. Table 15 shows the high level of access to ISVAs by participants in the study with 4056 contacts across the three time points, suggesting around five contacts per participant per timepoint.
| SARC service type | Charity-led SARC | NHS-led SARC | Police-led SARC | Private sector-led SARC | Total |
|---|---|---|---|---|---|
| FME | 6 | 34 | 11 | 75 | 126 |
| Brief advicea | 21 | 159 | 101 | 191 | 472 |
| Structured supportb | 4 | 0 | 1 | 22 | 27 |
| SARC-based counsellingc | 0 | 105 | 106 | 78 | 289 |
| Immediate sexual health (screening) | 6 | 28 | 10 | 69 | 113 |
| Comprehensive sexual health | 1 | 4 | 2 | 4 | 11 |
| Participants with data | 14 | 111 | 67 | 133 | 325 |
| Contacts per participant | 2.71 | 2.97 | 3.45 | 3.3 | 3.19 |
| NHS service type | Charity-led SARC | NHS-led SARC | Police-led SARC | Private-led SARC | Total | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | 6 months | 12 months | Baseline | 6 months | 12 months | Baseline | 6 months | 12 months | Baseline | 6 months | 12 months | ||
| ISVA contactsa | 74 | 42 | 38 | 1004 | 479 | 193 | 264 | 201 | 272 | 878 | 401 | 210 | 4056 |
| Number of participants with data | 14 | 11 | 6 | 111 | 74 | 77 | 67 | 46 | 43 | 132 | 92 | 89 | 762 |
| Contacts per participant | 5.29 | 3.82 | 6.33 | 9 | 6.47 | 2.51 | 3.94 | 4.37 | 6.33 | 6.65 | 4.36 | 2.36 | 5.32b |
NHS resource use and costs
Of the 335 participants interviewed at baseline, 225 reported accessing NHS care at their baseline interview (i.e. distinct from any health care accessed in their SARC visit). As shown in Table 16, the main form of care accessed was related to GP visits, followed by sexual health centre visits. A high proportion of the contacts related to mental health services and when the range of mental health services are combined, the rate of access was similar to primary care. Service use after the initial SARC visit was similar across the different models of SARCs. Overall, reported use of NHS services had decreased at 6 months. Once again, reported service usage mainly related to GP services, with continued access of mental health services. NHS service use further decreased by 12 months. The examination of costs associated with NHS service access across all time points showed that costs were similar across models (complete case analysis; see Table 17).
| NHS service type | Charity-led SARC | NHS-led SARC | Police-led SARC | Private-led SARC | Total | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | 6 months | 12 months | Baseline | 6 months | 12 months | Baseline | 6 months | 12 months | Baseline | 6 months | 12 months | ||
| Accident and emergency | 2 | 0 | 0 | 6 | 3 | 0 | 9 | 3 | 2 | 13 | 5 | 6 | 49 |
| Community mental health | 5 | 0 | 0 | 25 | 4 | 13 | 34 | 7 | 9 | 67 | 8 | 19 | 191 |
| General practitioner | 13 | 5 | 2 | 147 | 24 | 11 | 91 | 16 | 13 | 130 | 38 | 27 | 517 |
| Improved access to psychological therapy | 0 | 0 | 0 | 25 | 3 | 4 | 11 | 1 | 3 | 8 | 1 | 6 | 62 |
| Mental health crisis team | 2 | 0 | 0 | 21 | 3 | 1 | 25 | 5 | 1 | 14 | 1 | 5 | 78 |
| NHS counselling | 4 | 0 | 0 | 21 | 4 | 0 | 4 | 3 | 0 | 19 | 8 | 0 | 63 |
| Other (clinics for physical health injury) | 0 | 0 | 0 | 5 | 1 | 1 | 25 | 1 | 0 | 12 | 3 | 1 | 49 |
| Outpatient mental health | 4 | 0 | 0 | 47 | 3 | 2 | 42 | 3 | 0 | 27 | 4 | 0 | 132 |
| Primary care nurse | 0 | 0 | 0 | 2 | 1 | 0 | 6 | 1 | 3 | 1 | 1 | 2 | 17 |
| Sexual health services | 6 | 1 | 0 | 76 | 5 | 1 | 28 | 1 | 0 | 184 | 4 | 9 | 315 |
| NHS 111 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 1 | 0 | 2 | 1 | 2 | 8 |
| Pharmacy help | 0 | 0 | 0 | 0 | 0 | 0 | 4 | 0 | 0 | 9 | 1 | 1 | 15 |
| NHS walk-in clinic | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 2 |
| Drug and alcohol | 0 | 0 | 0 | 59 | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 0 | 61 |
| Number of participants with data | 14 | 11 | 6 | 113 | 74 | 77 | 67 | 46 | 43 | 134 | 92 | 88 | 765 |
| Contacts per participant with data | 2.57 | 0.55 | 0.33 | 3.85 | 0.69 | 0.43 | 4.19 | 0.93 | 0.72 | 3.63 | 0.83 | 0.89 | 2a |
| NHS-led | Police-led | Private sector-led | Overall |
|---|---|---|---|
| 1635.9 (213.84–4981.67) |
1792.04 (310.95–4821.53) |
1911.4 (405.05–5725.51) |
1737.82 (321.37–5563.76) |
Third-sector and broader public sector costs
Reported resource use for other public sector services is detailed below. A wide range of services were accessed by participants at all time points, with reported levels of use decreasing over time. For policing and criminal justice services, contacts with police officers were the main contacts reported at all time points (see Table 18). For third-sector and other public sector resource use, see Report Supplementary Material 2. A broad range of services were accessed, with reported use decreasing over the time points.
| Police and criminal justice use | Charity-led SARC | NHS-led SARC | Police-led SARC | Private-led SARC | Total | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | 6 months | 12 months | Baseline | 6 months | 12 months | Baseline | 6 months | 12 months | Baseline | 6 months | 12 months | ||
| Police officer | 99 | 30 | 17 | 821 | 377 | 140 | 390 | 241 | 49 | 1025 | 376 | 154 | 3719 |
| Victim support (not covered elsewhere) | 0 | 1 | 1 | 0 | 7 | 4 | 10 | 2 | 0 | 21 | 34 | 21 | 101 |
| CPS | 0 | 0 | 0 | 0 | 7 | 0 | 0 | 4 | 0 | 7 | 6 | 2 | 26 |
| HMCTS | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 16 | 0 | 6 | 3 | 2 | 28 |
| Other | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 17 | 6 | 3 | 328 |
| Number of participants with data | 14 | 11 | 6 | 112 | 74 | 77 | 67 | 46 | 43 | 133 | 91 | 88 | 762 |
| Contacts per participant with data | 7.07 | 2.82 | 3 | 7.29 | 5.28 | 1.87 | 5.97 | 5.72 | 1.14 | 8.09 | 4.67 | 2.07 | 5.5a |
Cost-utility analysis
The results of the cost–utility analysis are presented in Table 19. The police-led model resulted in slightly more QALYs but was slightly more costly than the NHS-led model. However, the differences in costs and outcomes were not statistically significant (95% level).
| NHS-led (n = 63) | Police-led (n = 31) | Private sector-led (n = 69) | Overall (n = 169) | |||||
|---|---|---|---|---|---|---|---|---|
| Mean cost (£) (95% CI) | Mean QALY gain (95% CI) | Mean cost (£) (95% CI) | Mean QALY (95% CI) | Mean cost (£) (95% CI) | Mean QALY gain (95% CI) | Mean cost (£) (95% CI) | Mean QALY gain (95% CI) | |
| Base case values | 2258.41 (164.47 to 17620.62) | 0.004 (−0.028 to 0.036) | 2788.36 (110.00 to 25783.08) | 0.025 (−0.019 to 0.069) | 2729.06 (184.00 to 11766.75) | 0.014 (−0.021 to 0.048) | 2526.76 (183.62 to 17620.62) | 0.011 (−0.008 to 0.031) |
As a secondary analysis, broader societal costs were explored (see Report Supplementary Material 2). This assessed costs incurred by participants and their families. Impacts on participants and their families were substantial. For example, respondents reported important effects on their employment and productivity.
Sensitivity analysis
For details of the deterministic sensitivity analysis, see Report Supplementary Material 2. For the probabilistic sensitivity analysis, the results of 5000 bootstrap replications were plotted on a cost-effectiveness plane for the cost–utility analysis (see Figure 9 and Report Supplementary Material 2). This analysis suggested that there was uncertainty around the differences in costs and outcomes between the SARC models, as replicates were distributed almost equally across all quadrants (in terms of both effectiveness and cost). Accordingly, there is uncertainty around whether different SARC models are more or less costly than the alternative models and whether they are more or less effective.
FIGURE 9.
Cost-effectiveness plane (NHS vs. private-led SARCs).
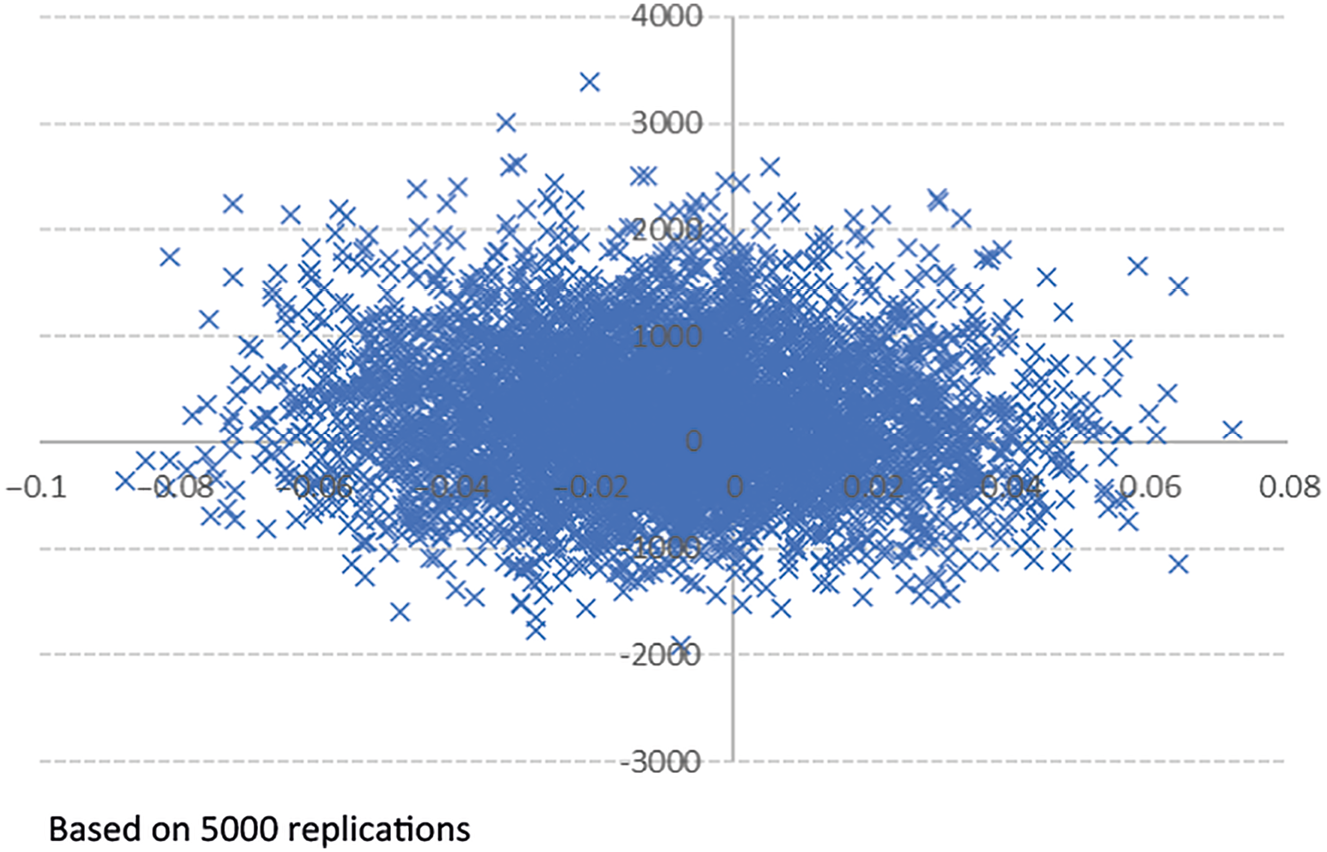
Discussion
Summary of main findings
The data collected in the study suggested that participants accessed a wide range of healthcare services and other public sector services in the period between attending SARCs and joining the study, but over time, service use decreased. The analyses undertaken suggested that the QALY gain and costs between SARC models were similar. The cost-effectiveness plane constructed to incorporate uncertainty around each point estimate in the results shows that there is considerable uncertainty around any estimated differences in costs and outcomes. This is similar to the findings presented in Chapter 5, which suggested that there was little evidence to suggest a relationship between PTSD as measured by the PCL-5 and the SARC type.
However, this study has only focused on those who have accessed SARCs. The lack of a comparator arm means that it is not possible to assess how resource use and QALY gains compare for survivors who did not access such services. Those who experience rape or sexual assault have a higher risk of developing PTSD and that PTSD is more likely to be of a longer duration. 120 Although economic evidence is limited, it is suggested that there are high levels of public sector service use for those who have experienced sexual violence121 and for those experiencing PTSD. 122 This study revealed that there were also substantial economic impacts on participants and their families (e.g. time off work). The results of this analysis suggested that access to services and costs were similar across SARC models. Participants reported improvements in HRQoL over the 12-month period under consideration, although this remained below population norms. 118,119 The absence of a comparator arm means that it is not possible to compare HRQoL for those accessing SARCs with those who did not access SARC services. Although the research base is limited, there is evidence to suggest that a high proportion of those who develop PTSD, are likely to face long-term impacts on HRQoL. 123
Strengths and limitations
This is the first analysis of health outcomes and resource use for those accessing SARCs in England. Detailed data on resource use and health outcomes were collected. The analysis also considered the broader costs for participants and their families associated with experience of sexual violence. Given the limited literature focusing on the economic evaluation of services and programmes to address sexual violence and abuse, the study provides useful data to inform decision-making in this area.
The main limitation of the analysis was the level of missing data on resource use and QoL at all time points. Accordingly, multiple imputation methods could not be employed because of the extent of missing data and a complete case analysis needed to be undertaken. 116 Excluding those who did not complete the resource use questionnaire at all timepoints may have introduced bias and some level of inefficiency. The bias may be based on the finding that certain groups (including more disadvantaged groups) were more likely to be lost-to-follow-up. Furthermore, among those who were retained, the resource use section of the interview was the section more often omitted by field workers in situations where the person reported lacking time or that the interview was too difficult for them to complete. In this sense, the study may have underestimated service use. Caution is also needed in interpreting the level of service use at baseline; while it covers a period of approximately 3 months (median was 104 days), there was a high variability in the timeframe between SARC access and the baseline interview. Another limitation was that the follow-up was only for 12 months, which may not have allowed longer-term impacts to be fully captured.
Recommendations for research
The data collected in the study suggested that participants needed to access a wide range of healthcare, third-sector and other public sector services. There is a gap in understanding about the extent to which SARC service users access voluntary sector care and support in the aftermath of sexual violence and abuse. The study reports on important aspects of resource use in the voluntary sector for SARC service users, specifically, charity-led SARC services and voluntary sector-provided ISVAs. However, a full analysis of the voluntary sector resource use by SARC service users (e.g. helplines, support groups, counselling, advocacy services, domestic violence services) was beyond the scope of the current research. This is a gap our research will fill in future analyses. There is a need for greater understanding of the costs and outcomes for SARC users compared with those who do not access SARC services, which was not possible in this study. It is also important to assess the longer-term service use and health outcomes for those who access SARC services (beyond 12 months). In addition, there is a need to analyse health outcomes and costs for different population groups, which was beyond the scope of this component of the study.
Conclusion
The analyses revealed that costs and outcomes were similar across SARC models. The sensitivity analyses found that there were uncertainties around the estimates, suggesting that further data are needed with improved completion rates. Further research is needed to compare costs and outcomes for those who access SARC services compared with those who do not access such services.
Chapter 7 Children and young people’s experiences of sexual assault referral centres and recovery journeys
Background
It is estimated that at least 15% of girls and young women and 5% of boys and young men in England and Wales are sexually abused before the age of 16 years. 124 It is likely that far more children are sexually abused when compared with the number of cases that are identified by official agencies. The little research that has explored access to SARCs by CYP has predominantly reported trends in data such as the referral sources and per cent reported across regions in England,125–127 or the impact of the nature of the abuse. 128
In 2021–2, 8213 CYP accessed a SARC in England and Wales,126 most (87%) were girls and young women and only 14% were from black, Asian, mixed or other non-white ethnic backgrounds, which is far below the proportion of children from these backgrounds in state schools and nurseries and supported by local authority children’s services due to sexual abuse. Over the 3 years for which data have been available, SARCs’ under-reach to children from minority ethnic backgrounds has remained consistent. During 2021–2, the police constituted two-thirds of referrals of CYP to SARC, followed by 22% from local authority children’s services. All other referrals from health, education or voluntary sector accounted for only 1% each. Self-referrals or referrals from family and friends accounted for 5%, and another 5% of referrals came from other sources.
There is very limited empirical research that explores the role of SARCs in CYP’s recovery from sexual violence and abuse. To date, only one prospective cohort study has explored the mental and sexual health outcomes of 13–17 year olds who attended SARC in a 2-year period. 129 This study observed that the presence of a psychiatric morbidity 4–5 months post-SARC attendance was associated with baseline psychosocial vulnerability (defined as previous social services involvement, mental health service use, self-harm or sexual abuse) but not assault characteristics. Khadr et al. recommended that CYP require comprehensive support to address high levels of pre-existing vulnerability and psychological comorbidity and to prevent re-victimisation. 129
In our Qualitative Evidence Synthesis (see Chapter 3), no studies specifically focused on children’s experiences of SARC. 42 However, a small number have explored experiences of therapeutic services and interactions with professionals outside of the SARC context. 130 Notably, ‘The Making Noise Project’ explored CYP’s experiences of support among those who experienced sexual abuse in the family environment. 131 Of 53 children, 10 reported that they attended a SARC; however, there were limited details about their experiences with SARCs.
In light of the limited evidence base about the role of SARCs in CYP’s recovery from sexual violence and abuse, this was, to the best of our knowledge, the first qualitative study to explore CYP’s experiences of SARCs and their recovery after SARC.
Methods
Study design overview
We conducted semi-structured interviews with CYP about their experiences of attending a SARC and what their recovery looked like afterwards. Qualitative inquiry was important to enable CYP to articulate their own experiences. A focused approach to study recruitment was used (see below), recruiting CYP who attended one of two paediatric SARCs in two geographical regions in England. These were sites where the team had built relationships to work closely with three linked third-sector organisations, ensuring that CYP were supported before, during and after the study.
Changes to protocol
The intended sample size of 40 as proposed in Protocol V3.3 was not fulfilled. Challenges to recruitment are discussed later in this chapter.
Theoretical approach
Our theoretical approach was underpinned by the United Nations Convention on the Rights of the Child,132 whereby all children have the right to make their voices heard in matters that concern them, while having the right to protection from harm and exploitation. 133 We recognised the importance of ensuring that the research did not lead to children experiencing further harm, in light of the potentially long-term and wide-ranging detrimental impacts of experiencing sexual abuse during childhood,134–136 while not wanting to exclude CYP from the research opportunity. 131,137 The approach was also informed by theoretical developments in the sociology of childhood138 viewing children as those able to make meaningful contributions towards issues that affect them, rather than being ‘objects’ of enquiry,139 thus researching with children, as has been acknowledged in inter-related fields. 140
This study was underpinned by Critical Realism141 acknowledging that individuals or societies socially construct independent worlds and there are different yet valid perspectives about ‘reality’. 142 Critical Realism recognises that there is an independent reality as well as a subjective interpretation of it,143 which is influenced by individuals’ interpretation of this reality at individual and social levels.
Sampling and recruitment
Recruitment relied on SARCs and third-sector organisations identifying eligible participants and connecting them to the research team. When appropriate, the professional introduced the study to the CYP and provided the leaflet, participant information sheet (PIS) and directed them to the recruitment video. With the consent of CYP interested in participating (and the parents of those aged 13–15 years), contact details were securely shared with the research team who contacted CYP to discuss the study further. Those who agreed to participate (and the parents of those aged 13–15 years) provided informed consent. Eligible individuals were 13–17 years old in person SARC service users between August 2019 and December 2022. CYP were not approached if the assault occurred ˂ 1 month ago and/or if, in exercising clinical judgement, the professional at SARC or third-sector agency anticipated the CYP might encounter difficulties in providing informed consent or understanding the interview content due to mental or physical health issues, cognitive impairment, learning disability or poor English language skills. CYP were not approached if they were known to be in an unstable or unsafe situation. We were prepared to overcome barriers to participation, for example, through the use of interpreters. It was discussed with third-sector organisations that it might be appropriate for them to provide additional support to CYP as someone who was present in the research interview if the CYP requested, or being available for a debrief or follow-up support afterwards. Two SARCs and three third-sector organisations passed on details for 31 CYP, and we enrolled 12. The first CYP research interview occurred on 3 August 2021, and the final interview was conducted on 27 January 2023. Of the 19 we did not enrol, some no longer wished to participate (n = 6), some arranged the interviews but later changed their minds (n = 3) and we received no responses or communication from others (n = 10).
Recruitment challenges and strategies
The study initiation was delayed due to COVID-19. As the SARCs were NHS-based, NHS studies that were not yet ‘live’ or not primarily focused on COVID-19 were not allowed to progress. Furthermore, the third-sector organisations initially had no capacity to assist due to the impacts of COVID-19 pandemic on their services. Once the SARCs and third-sector organisations had capacity, the research team conducted training sessions to equip sites in their understanding of participant eligibility. The research team worked with organisations to identify strategies and appropriate times for them to facilitate conversations about the research with CYP. There were occasions when SARCs and third-sector organisations regularly shared contact details; however, there were often periods when this was less frequent. This meant that recruitment was slow, as there was a small pool of individuals from which we could approach at any given point in time. Some CYP were quickly enrolled into the study while it took longer to enrol others.
Recruitment challenges also related to the service landscape of third-sector services. While one organisation experienced major staffing shortages exacerbated by COVID-19 pandemic, staff found it helpful to meet with the research team every 6 weeks to discuss recruitment progress. As another organisation had staff members join their team at various junctures, we attended their team meetings at different time points to explain the research opportunity. In the final year of recruitment, a third-sector organisation had capacity to assist, enabling a wider pool of CYP to be approached.
Participants
One boy (cis-gender) participated along with 11 adolescent girls (cis-gender). At entry to the study, three were aged 13–15 years, two were aged 17 years and seven had just turned 18 years. At access to SARC, seven were aged 13–15 years and five were aged 16 or 17 years. Ethnicities included White British (n = 9), Indian British (n = 1), Black British (n = 1) and White British and Black Caribbean heritage (n = 1). While no CYP was known to have a physical disability, two were neurodiverse (attention-deficit hyperactivity disorder and autism diagnoses). At the time of participating, all CYP attended secondary school or 6th form/college. Eleven participants lived with non-abusive parents and one lived independently. All CYP were referred to SARC by the police and seven had a FME. Some also received remote support from the SARC. At the time of accessing SARC, the time since the index offence took place varied among the sample: ˂ 7 days (n = 3), between 7 days and 6 months (n = 4), more than 7 months (n = 1), and over 12 months (n = 4). We spoke to CYP for 2 months to 3 years after they interacted with the SARC.
Information provided by SARC indicated that across our sample, the index offences involved nine rapes and three sexual assaults and the perpetrator included a family member (n = 4), peer (n = 7), and someone in a position of authority (n = 1). Criminal justice outcomes included one withdrawal (due to the perpetrator being re-interviewed), eight cases were dropped by the Crown Prosecution Service or police and three were under police investigation. There were no recorded prosecutions in our sample.
‘Conversations’ with children and young people
We conducted interviews that we referred to as ‘conversations’. We were mindful about language as we did not want CYP to compare the research to a ‘police interview’ as the research was not about them providing an account of the abuse experiences. We also wanted dialogue that was accessible and comfortable. By adopting qualitative participatory methods, we wanted CYP to have the opportunity to articulate their experiences in their own voice. 144,145 CYP were encouraged to challenge misrepresentations, clarify and interpret comments they and/or others made, thus increasing collaboration. All CYP chose to engage in dialogue during the ‘conversation’, and one young person additionally shared a drawing, as she felt this better demonstrated aspects of her journey. Conversations lasted for 30–85 minutes (mean: 49 minutes).
Analytical approach
We adopted Braun and Clarke’s Reflexive TA approach,56–58 which can be used across a range of research questions, sample sizes and data collection methods. 146 The approach complemented our Critical Realist perspective. 141 We used Braun and Clarke’s six phases of TA: (1) familiarisation with the data, (2) coding, (3) generating initial themes, (4) developing and reviewing themes, (5) refining, defining and naming themes and (6) writing-up. 56 Analysis was recursive, enabling movement back and forth between phases. Transcripts were coded by hand. GC and FL who were involved in speaking with CYP remained reflexive throughout the research, considering how preconceptions, values and beliefs impacted how the study was conducted, and how data were interpreted and presented. 147 The iterative process of collecting and analysing data meant that GC and FL checked the correspondence between the developing analysis and the perspectives of CYP during conversations, as well as exploring unexpected findings. 148 GC, FL, ELW and one expert-by-experience (see Chapter 2 for lived experiences methodology) coded the transcripts, generated themes and refined them and drafted the study write-up.
Results
Children and young people explained how their experiences at SARC and subsequently with third-sector organisations, statutory health, education and CJS impacted their recovery. We firstly present key findings that were specific to CYP’s experiences of SARC, followed by key themes related to CYP’s recovery journeys overall.
Children and young people’s experiences of SARCs
Children and young people had positive experiences at SARC, acknowledging its key role in enabling holistic care through conducting FMEs, providing medical care that provided reassurance, and offering referrals to organisations for further support. Many CYP told us that they did not have prior awareness of what a SARC was until they disclosed to a trusted individual and reported to the police. One young person had prior awareness through social media, where they had learned of others’ experiences of what SARCs were like:
I had heard of it before. I got most of the information actually from Tik Tok, where others were all telling their own stories, but both good and bad. I would say my experience is better than a lot of the ones I’d heard of.
Serenity
Children and young people reported that although they had been anxious when they first attended the SARC, the staff made them feel comfortable and welcomed: ‘At the start I felt a bit nervous, I didn’t obviously know what was going on properly. I didn’t really want everyone to look at me … but then by the end I felt a bit more comfortable’. (Ben)
Children and young people appreciated SARC staff communicating clearly to them before and throughout the FME:
They explained it very well what was going to happen … like the whole swabs and how it’s going to work. She said to me, ‘It’s not going to hurt but you might feel a little bit uncomfortable’.
Aurora
I had a full body examination done for bruises and marks. I had a couple of STD tests. I had another internal examination for bruising on the cervix. They’d show me what they were using, and they let me know every step of the way what they were doing.
Serenity
Children and young people valued having opportunities to make decisions during the FME:
They gave me the option for the support worker to stay in the room as well, like behind the curtain to talk to you, to distract you, so that was really good, that helped.
Somaya
The SARCs in our study were based in hospitals, and the CYP had mixed opinions about how suitable this was. Some appreciated the hospital environment, as it provided a sense of anonymity. Others thought it felt clinical and could have been more welcoming:
When I kind of turned up to the SARC, it made me nervous because it just gave me hospital- prison vibes. I think I would give it more kind of homely, I know obviously they have to be like professional and medical, but I don’t know if there was something more kind of welcoming.
Lola
Children and young people highlighted the importance of being able to take literature from SARC home that they could read when they felt in a better place to engage with it. They also valued receiving a care pack ‘It’s like a massive relief the way they told me that I can go home with this really good quality stuff. And I could relax myself, I could clean myself.’ (Serenity)
The service provision landscape after SARCs
Children and young people believed their recovery was impacted by the service landscape in which support services were provided post-SARC; this led to many experiencing continued poor mental health and further trauma symptoms. Long waiting lists for counselling delayed CYP accessing support. Some suggested that time spent on waiting lists could be better managed by services, so that their mental health did not worsen. One CYP has been presented as an example of this.
There was this lady that would call me once a month when I was on the waiting list. That happened 4 or 5 times and she sent me workbooks. They had lots of quotes, powerful messages and activities to do, like naming things you’ve achieved since what happened to you, getting you to think about positives. I found them helpful.
Lola
Some CYP described how they accessed support through digital apps, which they engaged with at their own pace particularly while waiting for counselling. CYP often found these apps themselves and thought they could help them manage physical and mental health impacts associated with their trauma.
For some, long waiting lists for counselling from third-sector organisations led to them starting counselling provided by their school. However, this still had its limitations:
I think they said that it would be a long wait, I think it was like a year and a half. However, the school gave me counselling, but they couldn’t be very helpful because I was in my last year, and I didn’t know the counsellor and I didn’t even do that for long because I was in the last year of school.
Somaya
Those who had positive experiences of support often felt that its duration was too short. This was particularly difficult when CYP had developed positive relationships with those supporting them. CYP felt frustrated about being unable to share details about the abuse with their therapist when their case was going through the CJS. Thus, long waiting lists, short-term support and criminal justice guidance impacted their health and well-being.
Children and young people felt that there should be considerable financial investment into services to educate people about sexual abuse and support those who had experienced it:
I think there needs to be more funding put into recovery groups for people who have been through this kind of thing. People who have been through this kind of thing need a way to rebuild their identity and give them that sense of community. More projects that work around the stigma of boys who have been sexually assaulted. Projects to educate people and then, projects to help rebuild people and their self-esteem after this has happened.
Clara
Organisations and systems working together
Children and young people emphasised the importance of professionals working well together within and between organisations at SARC and post-SARC, as this had implications on the support and care they received.
The staff seemed to work well as a team. They understood each other and the comfortableness I felt, or I could see with them, was put onto me. I felt like I could very much trust them. They were very patient with me. They really understood how it was for me.
Serenity
One young person explained how a staff member in school worked with a third-sector organisation to ensure she had a safe space to engage in virtual therapy sessions during school hours. Working together in this way enabled her to receive support seamlessly. CYP highlighted the importance of joint working within education settings, particularly when the topic of sexual violence and abuse was part of the school curriculum.
The well-being officer was messaging my teachers for me, she was like, ‘Oh she’s feeling a bit like this today, maybe not do this, or maybe not pick on her as much in class, like don’t get her to put her hand up all the time’. She helped me to work with my teachers, especially as I do health and social, and we had to learn about sexual abuse.
Yolanda
Many described the critical role of their ChISVA who provided them with updates and explained criminal justice processes because of their good relationships with other organisations such as the police. CYP felt that their ChISVA fulfilled their role as their advocate.
However, CYP told us how there were missed opportunities for support even when professionals tried to work with other agencies.
I remember there was one time I was with my detective. She casually said in conversation, ’Oh you should tell your social worker this, this and this’ and I was just like, ’What social worker?’ And she was like, ’When I set up your case, I arranged for a social worker to be in contact with you. You should have had one from the start’. I was like, this whole time she thought I had a social worker because she had said to them, ’You need to go do this’. And nothing ever happened.
Clara
Children and young people emphasised the importance of inter-agency communication by professionals following a disclosure of sexual abuse. Aurora shared how her teacher responded by following safeguarding processes, but it was not communicated how quickly her parents and the police would be notified.
Obviously knowing about the whole sexual assault she [teacher] couldn’t keep it to herself. And I think that she had to call safeguarding and obviously safeguarding had to call the police and then she called my mum about it. I knew that she would have to tell someone because obviously I’m under 18. But I didn’t realise it was going to be like, super, super quick.
Aurora
Children and young people valued healthcare professionals working together so they did not have to explain their experience of assault multiple times. Somaya shared how the SARC communicated with her GP, but as the GP did not acknowledge her sexual abuse when prescribing her medication, this led to her feeling as though the GP was not concerned with her overall health.
SARC had told my GP. It says on like my history or something now. They just kind of without questions sort of prescribed the medication. Like they could have asked me and gave me the option and like tried to check my overall health or tried to like support before prescribing. I don’t know, like if they maybe like cared about my overall health rather than just being like, ‘Oh this is for you’.
Somaya
Children and young people expected professionals to work together to help them build their support system by signposting them to other local services, ranging from housing to sexual health. However, CYP and their parents sometimes found it overwhelming and confusing when many services contacted them at once. Thus, CYP recommended a more joined-up approach between organisations.
Principles underpinning a ‘trauma-informed’ approach
Children and young people’s healing was influenced primarily by their experience of interacting with professionals. CYP provided examples of positive interactions and ones that felt damaging. CYP described the following principles that can be seen to be promoted in ‘trauma-informed’ approaches to supporting survivors.
Feeling empowered through having choice and control
Feeling empowered through having choice and control was important to CYP, as the abuse had taken this away from them. This involved professionals making them aware of opportunities where they could make decisions. One CYP appreciated making decisions about how they made contact with their ChISVA. For example, if their ChISVA sent them a text message, they could decide when to reply, without feeling pressured to respond immediately. CYP also reported that having options about how they could engage with services (face to face or remotely) enabled greater accessibility.
Within therapeutic settings, CYP valued flexibility and options in how they communicated their feelings, often in creative ways, which could also be used as a tool outside of the therapy room: ‘I think it’s sometimes when you can’t find the right words for something, sometimes just like an image can show that and portray that rather than describing it in detail’. (Lola)
As part of feeling empowered, CYP valued clear communication particularly while navigating the CJS. A lack of communication often led to CYP feeling as though they were not valued.
There would be like months where I wouldn’t hear anything, which is obviously very natural. But there would be things going on behind the scenes and I don’t think sometimes that information was passed on soon enough.
Cece
Not being judged or blamed
Children and young people valued interactions where they did not feel judged or blamed for the abuse. This was conveyed through what professionals said and how they communicated ‘Just being able to know that you can go to someone with your problems and your feelings and just know that you’re not gonna be judged for it and they’re here to help you’. (Bel)
Children and young people described examples within criminal justice processes where language came across as blaming or judging them.
A lot of the letter I felt was blaming it on me. Basically, at one point they just said, there just wasn’t enough evidence and I was happy with that. But then they went on to sort of blame me and was like, ‘You could’ve …’ They went on to say like, ‘You didn’t …’ Basically I didn’t seem upset enough.
Sophie
Children and young people explained how interactions with professionals could be confusing because the tone and approach could vary depending on the purpose of the interaction.
I would have liked a bit more warning that the police interview wouldn’t be the same as the small talks at home. It was the same guy that came round to my house that did the interview and he was completely different and it was really formal. They were acting like I was lying because of how they were asking stuff. But then he came round again to our house and he was lovely again and he was like, ‘we wanted to let you know that we believe you’. It was all fine, but obviously in that moment it was so different.
Lola
Being treated as a whole person
Children and young people emphasised the importance of being treated as a whole individual, particularly by those providing therapeutic support. While they wanted to be understood for what they had experienced, they did not want to be defined by the abuse. It was important that their resilience and strength was acknowledged even when they were struggling.
You get the vibe that she sees the whole person, like she sees everything that I’ve been through, actually the good, the bad, the lows, the highs. So she knows I’m not just a negative person, but actually when I’m struggling and when I’m not.
Sophie
Children and young people valued services treating them as a whole person through the way in which they promoted CYP’s actual and felt safety, such as providing them with taxis to access the service.
Ideal characteristics or qualities of professionals
Children and young people identified key qualities that they believed professionals should have, all stemming from the principles identified by CYP which could be described as ‘trauma-informed’. While CYP felt that professionals could be trained in these, they recognised these could be inherent qualities within a person, which should be considered when recruiting professionals into job roles.
Empathy
Children and young people said that professionals should listen and show empathy, not just in their words but through their body language. CYP felt they could distinguish between those who showed authentic compassion and those who did not. Experiencing genuine empathy and compassion had a long-lasting impact for CYP.
It’s like everything from the tone of voice to the body language to the actual words that are spoken. You really just have to show it. It’s those people skills. It felt comfortable and friendly whilst also giving that professional level of support. She’s one of the biggest impacts on my life, I will never forget her.
Clara
However, there were damaging implications on health and decisions about pursuing justice when empathy was not conveyed.
The way they would like look at me sometimes or the way they word it, it made me feel like is this really all worth it? Just simple things like looks and phrases, lack of communication, it twists the mind. Especially after these events, you overthink a lot and it’s dangerous for some people.
Serenity
Providing a personalised response
While CYP recognised that professionals had high caseloads, they believed this should not compromise genuine engagement with individuals and building trust. This required professionals to be organised, invest in meaningful relationships with CYP, and work with other professionals who had more established relationships with CYP. CYP felt this would lead to providing personalised support, bespoke to the individual.
It doesn’t feel like you’re just talking to a textbook. It’s not generic, it’s not full of buzzwords. It’s personal. My ChISVA didn’t sound like a talking textbook, she sounded like a real person and it felt like I was talking to a friend.
Clara
Children and young people valued professionals tailoring support and being creative in their communication particularly if they had a disability. When support was not tailored, this negatively affected their engagement with the support.
With my autism I need specific questions to answer because I didn’t really know how to explain my feelings and she would just sit there in silence for ages at a time. It was really awkward. I could never get anything out. I never felt welcome there. It just never helped.
Serenity
As part of this, CYP felt that the type of therapeutic support available to them through services should be varied, recognising that some therapy types might suit some people more than others and this would facilitate engagement in therapy.
Knowledge and expertise
Children and young people believed that as part of providing a personalised response, professionals should be trained in understanding the nature of sexual abuse and its impacts, and were aware of factors that could impact healing, such as difficult relationships at home, the level of ongoing contact they had with the perpetrator, or experiencing domestic abuse. CYP valued reassurance about professionals’ level of understanding. Some described the negative impact of professionals or systems not consistently showing awareness of the wider context in which abuse occurs, particularly in relation to the CJS.
This system isn’t very inclusive. It’s not very accessible and a lot of ethnic minorities and young black girls are subject to sexual violence at a young age and you have people in the system who don’t understand those backgrounds, don’t understand the sociology behind them and how they ended up being the victims of what they were. I think it’s just leading to a lack of justice being provided. There’s not an understanding of the lives of the people that are involved.
Clara
Children and young people felt it was critical that healthcare professionals particularly had general training about sexual violence and abuse when working with any young person, even if they were not aware that they had experienced sexual violence and abuse. This was important in the context of conducting general medical consultations and examinations. Others felt that professionals did not always fully appreciate the devastating effects of all forms of abuse, which led to its minimisation. CYP recommended the importance of professionals receiving specific training.
Calm and resilient
Children and young people often remarked that professionals should be calm and resilient, while recognising that professionals needed support to hold others’ trauma. CYP reported that the calm and resilient nature of professionals could also be influenced by the physical environment in which they provided support, which could be beneficial particularly if young people were accessing support from challenging home environments.
Just have a calm environment where it grows onto them. Because it’s the worst when you’re feeling like panicked and overwhelmed.
Yolanda
Children and young people’s recovery outcomes
Children and young people shared how abuse impacted their lives and how their experiences of accessing support helped to improve these effects. Factors such as being unable to access support or re-victimisation exacerbated these effects. One important outcome was CYP gaining understanding of sexual violence and abuse and how it affected them, knowing it was not their fault and they were not to blame. By receiving appropriate support, CYP found it beneficial to recognise and confront what happened to them.
When your family blame you, your school blame you, it feels like it is your fault, but then when somebody finally goes, ‘it wasn’t your fault what happened’ you kind of feel at peace with yourself.
Ashleigh
This led to CYP experiencing improvements in their physical and mental health, their education, interpersonal relationships and being able to re-engage in a wide range of areas in their lives. CYP valued being provided with tools and techniques they could use once formal support ended.
I think the support has made me more capable of looking after myself. I can notice more in myself, I can identify my emotions and the real reasons behind them. I think I’m more calm. Before I would have outbursts a lot and I’d get really angry quite quickly.
Yolanda
Recovery is ongoing
Children and young people explained how their healing was ongoing, and this was not the same for everyone. CYP recognised that there were time points when they felt ready to start receiving support and times where they did not. Some felt tensions between not feeling ready to engage with support, while being afraid that support may no longer be available if they did not take it up. Although CYP knew their rights to access support at another point, some felt unable to ask for that support again if they had previously refused it. CYP also highlighted the significance of being prepared for formal support to end and having a sense of closure as part of their recovery:
We really got on and then it sort of feels a bit like a break up that you’re never gonna see her. But then, when she sent the letter that was nice because it sort of put it all together, like how much we’d done and accomplished.
Lola
Motivation to make changes for others
Children and young people’s experiences of SARC and support post-SARC motivated them to engage with opportunities where they could be heard. Some support services provided CYP opportunities to participate in a consultation group once formal support ended, where they could influence service delivery. This enabled CYP to remain connected with services and make changes for others.
Children and young people told us that they felt motivated to participate in our research study for a number of reasons. Because of CYP’s positive experiences with services, they wanted to ensure that others received positive support.
I feel like my motivation has just been to help others. When it happened I was in a very down place and I’m now a much happier, more creative, just independent person now. I want people to know that it’s not gonna be like horrible for the rest of their lives.
Polly
For others, negative experiences of support or areas where they felt could have been improved fuelled their motivation to ensure changes were made for CYP in the future:
I hate the thought of someone I know to go through this and have the same experience, where actually one small change would have made the broader difference. I’m keen to give my opinion because I wish things were different for me in some areas.
Sophie
I know that I will be at least making some difference and I’m giving my time, my thoughts and my energy to this research. I want to campaign for change. My own experiences of the criminal justice system made me passionate about helping people.
Clara
Discussion
Summary of main findings
This study is the first of its kind to explore CYP’s experiences of SARCs and their journeys post-SARC. Our findings demonstrated the uniqueness of recovery in this group of survivors. Recovery was influenced by how quickly CYP accessed support, its content and duration, the location and context of care and how well services worked together. Healing was also affected by life events that CYP experienced which included sexual re-victimisation. Re-exposure to abuse served to aggravate trauma symptoms and undermine engagement with services.
Children and young people had positive experiences of SARCs and valued their role in offering them a FME and connecting them with onward support services. As the majority of CYP in the study did not have prior knowledge of SARC, this raises questions about SARC awareness among younger populations and the importance of professionals’ awareness of SARCs when responding to disclosures of sexual violence and abuse. Among the majority of those we spoke to, SARCs played a role in responding to recent sexual offences, which relied on CYP disclosing abuse. In light of the costs to the NHS of delayed disclosures of sexual violence in childhood and lifelong impacts for survivors,149 it is paramount that professionals are prepared to recognise and manage disclosures effectively.
Children and young people felt that their recovery was impacted by the limitations associated with the broader service provision landscape of services accessed post-SARC. Accessing delayed and short-term support was the norm. There continues to be an urgent need to invest in resources for services to minimise the negative health and well-being impacts for young survivors that are exacerbated by not receiving timely and long-term support. Our findings support other research that has shown young survivors managing their own mental health and well-being while waiting for support. 130 While adequate resourcing of services may take time, CYP in the study suggested that there were benefits of services managing waiting list times such as providing psychoeducation.
Children and young people identified principles that were key to their recovery which could be described as principles underlining a ‘trauma-informed’ response to supporting survivors. 44 Recovery outcomes not only were dependent on timely support but were also impacted by CYP’s interactions with professionals at SARCs and across sectors, including specialist sexual violence services, statutory health, education, social services and the CJS. Thus, trauma-informed principles and certain qualities associated with professionals such as showing empathy and compassion, not judging CYP, providing a personalised response and empowering CYP, all play a role in CYP achieving long-term gains in the aftermath of sexual violence and abuse. These principles and qualities reinforce key messages from our qualitative evidence synthesis (see Chapter 3) about what factors impacted survivors’ engagement with interventions and recovery outcomes.
Notably, the lack of a ‘trauma-informed’ approach was associated with poor or delayed healing. Therefore, early intervention and a consistent trauma-informed approach across professionals could prevent long-term negative health and well-being impacts for young survivors. Further exploration is needed to distil what ‘trauma-informed’ practice looks like across sectors that are specialist SAAS agencies and those that are not (e.g. education and NHS services) and how professionals can be trained. This supports observations that demonstrate that adult survivors’ contact with support services alone does not reduce trauma symptoms; rather, it is the quality of services and survivors’ assessments of their interactions with professionals that appear relevant in promoting recovery. 150
The study also observed that when the opportunity is provided, CYP valued being part of informing and developing services to help others. For some, this aspect played a key role in their recovery journey. As noted by Bovarnick et al. ,151 choosing appropriate levels of participation for CYP’s engagement is important going forward, carefully considering how opportunities will empower CYP, whose needs their involvement serves and whether participation can be enacted ethically and meaningfully.
Strengths and limitations
This study provided detailed and novel insights into how SARCs and onward services impacted CYP’s recovery. However, it replicated some of the problems of access to services, with the voices of young participants from black communities and diverse cultural communities, of individuals with physical disabilities and of boys and young men, largely missing in this study. There were also limitations in representing SARC services with only two paediatric services involved. We hope that reflections and learnings from our qualitative study of diverse adult survivors (see Chapter 8) can speak to some of the risk and access issues affecting members of subpopulations missed in the current study.
Implications for health care
It is paramount that a ‘trauma-informed’ approach is adopted across universal and specialist settings, as professionals may unknowingly interact with individuals who have experienced sexual violence and abuse. Therefore, attention should be provided to equipping professionals through training. As delays to receiving support can negatively impact CYP’s health and well-being, urgent investment is needed to resource services adequately. In addition, services should consider ways to manage opportunities while CYP are on waiting lists for therapeutic support which could be beneficial to their recovery. There is also a need for greater education about the role of SARCs and onward support services among any professional a young survivor may interact with, to build CYP’s support network.
Recommendations for research
-
Involving groups that have been under-represented at SARCs is vital to gain increased understanding about barriers to accessing support and how services can be tailored to better meet needs.
-
Further research needs to distil what ‘trauma-informed’ practice means in different sectors and identify barriers to its implementation.
-
The voices of CYP should be part of informing research studies throughout their lifecycle and in the development of services. These opportunities should be safe and trauma-informed spaces.
Chapter 8 Access to sexual assault referral centres among racially minoritised and other disadvantaged survivors
Background
People with minority characteristics may be more likely to experience sexual violence and abuse than other members of the general population. For example, a Centers for Disease Control and Prevention (CDC) (2010) survey (conducted in the USA) found that lesbian and bisexual women are more likely to be victims of rape, physical violence and/or stalking by an intimate partner in their lifetime than heterosexual women. 152 Similarly, in a study of minority stress by Lefevor et al. , non-binary gender individuals were harassed, sexually abused and subjected to traumatic events at higher rates than either cis-gender or binary transgender people; approximately half of non-binary individuals reported one of these experiences. 153 Other population characteristics that may interact with risk for sexual violence and abuse include mental health, disabilities and socioeconomic deprivation. There is a high prevalence of recent sexual and domestic violence in those with severe mental health problems. 154 Studies have also highlighted the risks faced by neurodiverse people155 and those with learning disability. 156 Despite the potential for higher rates of victimisation in some groups, evidence suggests that they may be under-represented among those seeking support for sexual violence and abuse. 157–159
Men, people who identify as LGBTQ+, people from ethnic minority backgrounds, people involved in sex work and older adults are often under-represented among those accessing SAAS including SARCs160 relative to estimates of abuse in different sub-populations. As many as 1 in 20 men are known to have experienced sexual assault since the age of 16 years,93 but may experience gendered barriers to getting help. 90 While an audit of service users at St Mary’s SARC in Manchester, UK, showed over-representation of black and dual-heritage service users, individuals from other ethnic minorities, especially those from Asian backgrounds, were under-represented. 161
Given this under-representation of minority groups within SAAS and SARCs relative to the risk some of these groups face, there is a need to better understand some of the barriers they may face in accessing support. Barriers are likely to include fears about encountering homophobia, transphobia, racism or other forms of discrimination from those who provide services and shame or guilt associated with help-seeking and minority stress. 162 There is also a need to understand the recovery journeys of people with different types of characteristics, so that support services can draw on this understanding of what different types of people may find helpful and be as inclusive and welcoming as possible to anyone who has experienced rape, sexual assault or sexual abuse. This chapter therefore sets out the methods and findings from a qualitative investigation of the experiences and recovery journeys including barriers and facilitators to service access, of members of the MESARCH cohort as well as people recruited from outside of SARC services.
Methods
Study design overview
This qualitative study was embedded within the wider cohort study presented in Chapter 5 and involved interviews with individuals who had and had not accessed SARCs following exposure to sexual violence and abuse at some point in their lives. It employs a story telling approach to gather data with participants and applies narrative analysis. This chapter is underpinned by narrative constructionism; this is an interpretive and socio-cultural approach that positions those participating in research as meaning-makers who use narratives to make sense of and communicate about their experiences. These narratives are seen to have been passed down and co-constructed through participants’ social and cultural worlds. 163 This chapter sets out to explore people’s actions and efforts to help themselves in relation to the occurrence of abuse and violence and the impacts on their lives, in particular, where individuals hold identities associated with marginalisation or ‘minoritisation’. 164 This could relate to identifying as a member of a minority cultural or ethnic group, identifying as transgender, having chronic or long-term mental health problems, involved in sex work through coercion or choice or being homeless. Thus, approaching ‘narratives’ as the cultural and social resources available to participants and upon which they construct the ‘big’ and ‘small’ tales of their lives and experiences of trauma and abuse and help-seeking is viewed as an appropriate orientation for this work.
We acknowledge that without clear explanation, terms such as ‘story’, ‘tale’ and ‘story telling’, which are central to narrative methods could be unhelpful, even harmful, in this context. Indeed, ontological relativism, the basis for viewing knowledge in this study, conceptualises psychosocial phenomena as multiple and ‘created’. This may seem at odds with survivors’ expressed need for being believed and a ‘positivist’ stance that a single truth related to individuals’ victimisation exists. Our research takes the position that all participants are believed, with full understanding of the role of ‘being believed’ in survivors’ healing and recovery. People’s stories are not constructed within a vacuum, this form of narrative enquiry enables the participant to share their experiences in the order of importance that matters most to them. 165,166 This also enables the researcher to look at the whole person and not just that part of a person’s life that is under investigation. 165,166 We also believed narrative enquiry would minimise reductionism and draw attention to power dynamics related to gender, sexuality, race and socioeconomic status operating in everyday life that may affect help-seeking. For us, storytelling is used as a way to gather powerful accounts and authentic voices that centre the survivor as the ‘story-teller’ and the researchers and MESARCH LEG member (or experts-by-experience) as story analysts. Use of the constructionist approach enables the study to advance one of its key aims: to access the critical personal, socio-cultural and political narratives about people’s capacities to keep themselves safe and seek help (e.g. from SARCs) in the aftermath of exposure to trauma and abuse as well as those narratives that influence their recovery journeys while conferring anonymity and contributing to ‘future-forming’ research. 167
Changes to protocol
The study was unable to recruit in the community to the projected target of 20 (Group 2: culturally and linguistically diverse people who had never accessed SARCs) due to the particular barriers of stigma, silencing and abuse faced by marginalised individuals and groups. We engaged with eight willing community-based organisations; these agencies reflected on the difficulties in engaging with their target communities and how they run outreach programmes using workshops about confidence-building and group activities for many months before issues related to safety and abuse can be raised. Despite the challenges, the MESARCH cohort study did recruit 15% of survivors from a range of cultural, ethnic or linguistic backgrounds; therefore, we focused our efforts to understand about barriers for these individuals, expanding beyond our target number of 10 (Group 1). We experienced no difficulties recruiting the planned 20 participants for our third group (Group 3 were individuals in the cohort study with minority characteristics other than cultural or linguistic diversity (e.g. LGBTQ+ identity, people with a disability, men, older people).
Theoretical approach
Reflecting the specific aims of this study, intersectionality168 was employed as a theoretical framework for guiding design, data collection and analysis. It is a valuable lens for interpreting the experiences of people, intentionally accounting for a relational web of factors that may help or hinder their safety, access to helping resources and recovery. This web of factors includes gender and sexual identities, ethnicity, socio-economic status, nationality and immigration and a range of other protected characteristics such as mental health, age and disability. Another important and linked theoretical underpinning is the potential for survivors to be marginalised or ‘othered’ within their own communities. 169 Survivors may be isolated for having poor mental health, for example, or discouraged from seeking help for their health concerns. Similarly, domestic and sexual violence and abuse may be seen as private family matters: victims and survivors attempting to exit abusive relationships or seek help, especially from outside of that community, may be seen to bring shame on families/communities. Othering may also apply where minority populations are treated as ‘them’ by institutions made up of ‘us’ (e.g. inadequate policing responses to a report of a rape by a gay man or by a non-English-speaking migrant woman). Many people who participated in MESARCH would say, in reference to the abuse and what occurred afterwards, that they experienced events that had life-changing consequences. Narratives may serve to rebuild a person’s ‘shattered sense of identity and meaning’,170 and thus, the research was also concerned with capturing these narratives.
Participants and settings
All participants for this story telling and narrative analysis study were aged ≥ 18 years at the time of their qualitative interview.
This part of the MESARCH project set out to engage three sub groups of survivors:
-
Survivors that had accessed a SARC and self-identified as being from any cultural, ethnic or linguistic minority community in England (Group 1).
-
Survivors in the community who self-identified as being from any cultural, ethnic or linguistic minority community in England but had not accessed SARCs (Group 2).
-
Survivors that had accessed SARCs and considered themselves to be from any other minority (e.g. LGBTQ+ community or had a disability) or held a characteristic that may lead to experiencing marginalisation or vulnerability in this context (e.g. men survivors; homeless individuals; those with long-term mental health problems such as psychosis or complex PTSD) (Group 3).
The SARC sample (i.e. Groups 1 and 3) was drawn from the MESARCH cohort study using maximum variation sampling to represent a range of characteristics. The setting of the MESARCH cohort study is described in Chapter 5. Group 2 consisted of people from minoritised groups who had not accessed SARCs and were likely to have experienced delayed help-seeking. 171 This group was more difficult to recruit. We relied on voluntary sector organisations that provide support after sexual assault, rape or abuse and/or those with community ethnic minorities outreach services aimed at engaging seldom heard populations.
Recruitment and consent
See Chapter 2 for a discussion of the ethical principles governing the MESARCH project.
Group 1 and Group 3
It was explained to all participants joining the cohort study that they may be approached following completion in the cohort study to participate in a further interview as part of our embedded qualitative study. It was explained that this would employ an unstructured approach (as distinct from the relatively structured cohort interviews) to hearing about the person’s views and experiences. Participants were also reminded of this after the 12-month cohort interview to provide people the opportunity decline further contact. If people had actively withdrawn from the study (see Chapter 5 for flow of participants through the study), then we did not reach out to them again. Groups 1 and 3 were contacted initially by email or in line with their preferences for contact and provided with a PIS and a new consent form for the qualitative study. Interviewees were offered a range of ways of engaging with the qualitative study and most chose a video meeting. This had not been done for the cohort study (all phone interviews), and for those who had previously engaged with our research, a video link provided an important opportunity for further rapport-building with the research more broadly. This led to several MESARCH participants attending the MESARCH conference (see Chapter 2). Before starting the interview, the main pillars of consent were checked (explaining voluntary nature of participation and rights to withdraw, conditions upon which confidentiality may be breached and use of data). For Groups 1 and 3, we selected 10% of the MESARCH cohort sample (n = 337; see Chapter 5 for a breakdown of baseline sociodemographic characteristics of the full MESARCH sample), examining each individual case at baseline until we had achieved a comprehensive mix of experiences.
Group 2
To recruit Group 2, we engaged with staff at eight charities/voluntary sector agencies in London, the West Midlands and East of England. The staff members then approached their clients and services users, inviting them to contact the researchers.
The MESARCH project operates an empowerment model of engagement with survivors and aimed to be trauma-informed, prioritising survivors’ perspectives, needs and choices. This was even more critical with Group 2. For example, we needed to recognise that survivors of abuse are not a homogeneous group, and that some survivors face more oppression and silencing than others. Relative to other survivors, people eligible for our Group 2 may be more isolated and socially and economically disempowered and at greater risk of negative responses (e.g. disbelief, racist and victim-blaming attitudes, threats by family or community in relation to disclosure) and/or their help-seeking may be influenced by practices and attitudes that normalise violence against women and children. We considered a wide range of ways of enabling safe and empowering participation for these survivors. We minimised any references to sexual violence and abuse and used the features of story telling to enable participants to share as much or as little as they wished, and to start and end the story of their help-seeking journey wherever felt right for them. Potential participants were provided the opportunity to have an interpreter and/or a support worker present at the interview and/or access to therapeutic or support sessions afterwards (provided by the agency through which the participant was recruited). Once contact was established, we provided an information sheet and asked potential participants to complete the consenting process. If needed, this was verbally translated before the interview. Interviews were offered through a range of modalities. At the conclusion of the interview, we gathered some basic sociodemographic information from Group 2 participants, matching the variables presented for Groups 1 and 3 (see Findings below).
The ‘conversation’
We generally referred to a ‘conversation’ over an ‘interview’ as the former may be experienced as less formal and daunting for participants. An interview schedule was used to guide interviews, adapted to each context and group as appropriate, for example, asking about SARC experiences in Groups 1 and 3 but minimising reference to specific service types in Group 2; however, overall a story telling approach was adopted. The guide was carefully designed and pilot-tested to minimise any potential distress for the participants. Story-telling and biographical-narrative interviews are different from semi-structured interviews. Story-telling is linked to broad narratives, interested in exploring in-depth lived experiences, including contexts, identities, different stages of life and ways of sharing personal and collective experiences. 172 This encouraged survivors to tell the story of their help-seeking journey. We undertook 35 hours of data collection with an average interview duration of 51 (range: 13–113) minutes. At the conclusion of interviews, we offered debriefing, an honorarium of £20 in the form of a shopping voucher and offered to cover any expenses incurred such a childcare. All participants in this qualitative study consented to audio-recording of interviews, and these were transcribed verbatim before pseudonymisation and analysis (see Chapter 2 for handling of data).
Analysis
Narrative analysis captures a range of methods that have in common their focus on stories. 173 Visual narrative analysis (focus on how and when an image was created), structural narrative analysis (focus on how stories are told and linguistic features used) and personal narrative analysis (focus on evolving personal life biographies) are all examples of types of narrative analysis. We selected dialogical narrative analysis174,175 because it promotes examining what is told in the story (its content) and how a story is put together in terms of the narrative resources that are deployed. 163 Further, dialogical narrative analysis considers what occurs as a result of telling the story (its effects). Smith refers to narrative as a ‘practical medium and the primary medium for action’ (p. 213)163 making it consistent with the goal of many MESARCH participants: After a history of assault, I think I was more frustrated by it. I just wanted to do something productive and so I contacted SARC about the project. I feel the research is empowering me. I don’t feel the shame I used to feel about. It’s a heavy weight to hold on your own; having this dialogue in a way that will help others is just very good and the wider project’s goals for impact. It is reasonable to blend narrative methods and in fact dialogical narrative analysis blends performative narrative analysis (how the interviewer and interviewee perform a story together and why something is said in an interview) with thematic narrative analysis (what the content of stories is). Story-telling in combination with dialogical narrative analysis potentially achieves a range of functions that are consistent with intersectionality as a theoretical framework for interpreting the findings. 168 They allow us to approach and understand about the various ways in which survivors might experience oppression, risk, barriers and delayed care based on multiple, and often minority, identities.
Stages of the analysis
-
We followed steps of dialogical narrative analysis set out by Smith. 163 (1) We conducted ‘indwelling’ – the notion of becoming familiar with the stories through multiple readings, and also thinking of each participant as a person with a story to tell. (2) We identified the big stories (those that take time to tell, contain substantial detail and reflection over major life events or experiences) and small stories (the mini, side-stories that people tell in relation to everyday things) within the transcripts. (3) Next, we identified narrative themes or patterns running through individual stories by attending to what is repeated and significant for the story-teller, using colour coding for different themes and making notes in the margins. Over-coding was avoided, as it tends to break down the text too much for narrative analysis to be effective. (4) Identifying the structure of the story or stories was about establishing how it was constructed. It can be considered visually by plotting time and the trajectory of the story, for example, a story about moving through the criminal justice process may be depicted as a positive curve (e.g. getting closer to a trial date) or a decline (e.g. going from having high hopes about getting justice to a notification about the case being closed by the police, with little explanation, followed by the conclusion of support from the ISVA). Smith163 also includes a series of guiding questions to extend the dialogical narrative analysis further, for example, identity questions (How do people tell stories about who they were or who they may become?) and function questions (How might this story or telling it be useful to the survivor?).
-
Narrative analysis attends to the particular by looking at the data as a coherent whole. To achieve this, we created core stories176 for each participant in the embedded qualitative study, critically, maintaining the participant’s own words throughout and removing extraneous material. We moved fragments of themes together and integrated events into a temporally organised whole with a thematic thread.
-
The final step in our narrative analysis was for the four researchers and two Lived Experiences Group members to move from story analysts to story tellers through the co-production of composites. 167 This involved the researchers reading and re-reading the core stories, and identifying and discussing common themes, plots and threads across the core stories. We examined these themes, plots and threads for linkages with our research question as well as allowing these to emerge inductively (e.g. connections between cultural background and risk). We clustered stories or themes within stories, tacking together sections of participants’ stories and importantly, retaining the ‘soul of the narrative’ (p. 21). 177
Typologies of narratives arose from the study that communicate the central points about the oppression, barriers, gaps and opportunities discussed by participants; we shared stories and created composites that emphasised temporality and captured common themes in survivor journeys of recovery and healing. Given the wealth of data available, our follow-up on this research will share composites that convey what the telling of stories within the MESARCH project can ‘do’ for survivors, as part of discovering the functional dynamics central to dialogical narrative analysis.
Results
Characteristics and experiences of participants in the embedded qualitative study
The study involved a total of 41 participants: 20 who fulfilled the inclusion criteria for Group 1 and 14 for Group 3. Seven participants were recruited from non-SARC community settings. See Table 20 for an overview of the characteristics of the participants. Core stories were developed for all 41 individuals, and all but one were integrated into the findings presented here. This individual requested that no direct quotes be included for them. The narrative sample diverged from the cohort study (see Chapter 5) on the characteristics shown in Table 20: there was greater minoritisation in the narrative sample as planned. However, the narrative sample was higher for education, and there was no difference on earnings as the main source of income. The community sample (Group 2) constituted six women and one man. All seven participants described themselves as having Asian heritage, from a range of ethnicities including Indian, Bangladeshi and mixed Chinese-Indian. Religious affiliations were Islam, Sikhism, Buddhism, Hinduism and Spiritualism. All participants in Group 2 reported multiple forms of abuse and violence from multiple perpetrators. Sexual violence and abuse had occurred in the context of domestic abuse (100%) and forced marriage, and many of the women had endured honour-based abuse from their families and communities in the UK and overseas. The research also documented testimonials of violent forms of reproductive control and one participant told of persecution over their sexuality from their family in their country of origin.
| Sample characteristics | N (%) or mean (SD) Total (n = 41) |
|---|---|
| Age (years) | 37 (13) |
| Gender | |
| Women (cis-gender) | 35 (86) |
| Men (cis-gender) | 5 (12) |
| Non-binary | 1 (2) |
| Sexual orientation is heterosexual | 25 (61) |
| Ethnic minority groups | 20 (49) |
| Dual or mixed heritage | 7 (17) |
| Black | 3 (7) |
| Asian | 7 (17) |
| Chinese | 2 (5) |
| Other ethnicity | 1 (3) |
| No religion affiliation | 18 (44) |
| Divorced or separated | 12 (29) |
| Education to A-level or above | 30 (78) |
| Earnings as main source of income | 19 (46) |
| In work | 20 (50) |
| Unable to work due to illness or disability | 12 (30) |
| Looking for work | 2 (5) |
| Students | 5 (12.5) |
| Not looking for work | 1 (2.5) |
| Longstanding disability/illness limits activity | 26 (63) |
| Long-term mental health problems | 28 (68) |
Main narrative findings
The 41 core stories developed with survivors shared many narrative plots and arcs central to addressing questions about barriers to access to SARCs, other SAAS, NHS care and justice-related services. We first present typologies of risk in relation to sexual violence and abuse (three sub-themes) (see Table 21), these were not intentionally examined but were a pertinent feature of participants’ narratives, intersecting in important ways with identities about mental health, prior trauma, cultural heritage and social disadvantage. Second, we present typologies that foreground the most significant and urgent access issues identified by our sample (eight sub-themes). We also showcase aspects of best practice in enabling vulnerable and/or minority community survivors access SARCs and other settings. Finally, typologies about recovery and healing are presented. Twelve sub-themes address what defines, promotes and prevents recovery in this context.The narrative study provided in-depth data to complement findings from the process evaluation, and the reporting of clinical outcomes in the cohort study.
Typology of narratives about risk
As survivors recounted their experiences following sexual abuse, a perpetual cycle of repeated exposures to increasingly severe and complex risky situations emerged. In this typology, each composite compiles how the cycle of risk manifested, and what risks survivors described themselves experiencing through their journey thus far.
Gender-based violence: the curse of being a woman
A large sub-sample of our narratives were voices of individuals from a racial minority background. As women reflected on their journey, a core collection of stories emerged around the oppression of women due to historical patriarchal values, and gendered double standards that were socio-culturally reinforced. A prominent theme across the narratives was forced marriages. Within forced marriages, women experienced a severe decline in both mental and physical health. For some, this also involved migrating to a new country, but for most, it was leaving one chaotic environment for another. Women described as being bound, living in a daily hell where they were raped, beaten, berated and, in some cases, physically abused by their in-laws.
Throughout the narratives women transitioned from beliefs that were ego-syntonic to ego-dystonic. Women described being conditioned from an early age about what it means to be a woman in their culture. Such beliefs became ego-syntonic because this was the only one they had ever known, and it was seen across generations before them; hence, oppression was their perceived norm strongly reinforced by family and the wider community. There were powerful accounts of forced marriages and of the atrocities that occurred within the marriages. Across all of the stories, there were turning points, where women began to resist the harmful socio-cultural norms and make a bid for freedom. Though freedom was sought, the road to freedom was one met with multiple experiences of re-victimisation. The composite ‘Mehar’ illustrates this through a story entitled ‘The curse of being a woman’ (see Box 3). Belonging to a culture that oppresses women, Mehar’s life was dictated from the very beginning, her life was to be handed to a man of her parents’ choice, and she would dedicate her life to pleasing him. Her fate was sealed from birth, forced to endure multiple gender-based abuses in her early years, in preparation for adulthood.
[I remember, as] a child, [I was being] mould[ed] to accept abuse, both parents would say, ‘She’s gonna be beaten all her life’. What a mantra to have in your head, I’m gonna be beaten all my life.
Daughters are born, but you’re not part of the family because you’ve got to move on to another family. Being born a girl, it just wasn’t very valued. What is freedom? We are born into families where we are supposed to be subservient to our parents. Children exist to serve the parents, and respect only works one way. [My dad] says these things are cultural. We have to do what our parents tell us to do for the honour of our parents in the community. You know the culture we have grown up is very patriarchal … The rules are different for boys [and] girls. When we were young we were told that we would be married off at a very early age and we wouldn’t have a choice…
I was very heavily sedated, heavily guarded by the family, I was transported to India and kept there for 2 years against my will and forced to marry someone. My dad said to me, ‘if you think about running away, I will find you, I’ll kill you, and I’ll go to prison’. I totally believe that he would do that. So I was forced to marry a stranger and things went into a snowball after that. I moved to England and I was forced to support his … sponsor his visa to England. All [I was] told is you have to please the husband. I was raped by my husband, it was daily rape for eight and a half years of my life. I didn’t used to eat for days, I was underweight, depressed, getting beaten, I [had] to go to my in-laws at the weekend to do all their work …
I eventually ended up leaving him. My family had disowned me at that point. My mental health had deteriorated, I couldn’t see a way out of it. I went into a catalogue of addictions like alcohol … eating painkillers left, right and centre to numb the pain. I had so many episodes of overdosing. This is what honour-based abuse does to you, you get bound by tradition in the after effects of trauma because your parents don’t teach you to be independent. I wish my dad had left his core belief and value systems at Heathrow Airport.
The culture of silence ‘everything that happens is a secret’
This theme captures how silence was more than just being made voiceless. Silence was a systematic disempowerment, resulting in a loss of autonomy. For some individuals from culturally diverse backgrounds in the study, tools that are central to help-seeking (like family support) are often absent. Being silenced operated at multiple levels and subsequently increased the risk of polyvictimisation among survivors within our study. The composite ‘Umang’ captures a story entitled ‘Silence is really not golden’ (see Box 4), where Umang reflects on their experiences of silence. The reflection situates silence in their early experiences, and silencing as precipitating abuse, and dampening chances of help. Taboos about dating, sex, and consent existed in childhood and adolescence, with conversations around sex and dating rarely occurring. There were limited points of reference for survivors to draw on to understand about healthy relationships. They reflected on how silence was reinforced by culture, family members and the wider society, leaving them feeling powerless but also ashamed when sexual abuse occurred. Finally, they reflected on how women of colour are seen in culturally diverse societies and why this coupled with a culture of silence increases the risk of sexual abuse, as well as other forms of abuse.
I guess, culturally it’s not something that we’d ever discussed, we’re not taught about [sex] education when we’re growing up. We’re not taught about consent. We’re not taught about abuse. It’s always perceived to be something that couldn’t or wouldn’t happen to us because of how we are quite reserved as people, like the culture that I come from; just the topic of sex and anything – one massive taboo. We were virtually forced to go to our uncles we don’t even know, we were forced to hug people we don’t even know. That’s apparently part of culture, and that’s what I mean by my mum and dad’s relationship. I did not see any consent around the whole … I’ve not been taught, I’ve not been taught consent around my own body … When I was about 14, I was also taken advantage of by my Arabic teacher. As soon as I told my mum, guess who got told off? ‘Why is he doing that to you? What for? Why? What have you done?’ Instead of questioning the actual situation, she questioned this. Literally minimising my voice. The education is always keep things to yourself. I’m ashamed that it happened. I felt that heaviness on my shoulder because my family is thinking, oh I’m doing whatever I want, succeeding, going ahead with following my dreams. When actually, it’s far beyond that. It is just far beyond that. I will never tell my family because they would not talk to me for years. I would be the one blamed for it because they are narrow minded and ignorant.
I shouldn’t feel shame for something that wasn’t my choice. But it’s a shame because I know how other people are going to perceive me now. That’s the shame that stopped me from telling people that I probably should have told, who would have wanted to help and support me in that time. [Recently] I went to the local [place of worship] and spoke to one of the priests, I explained the situation with them [about domestic violence] … The backlash from that was, ‘you have to make it work, you know, he’s a man, you have to give him attention, you have to cook for him, you have to clean for him’. And I thought, one problem with the whole culture is, you know, brushing things under the carpet and making things seem that everything will be fine if you try a little harder. You know, we make domestic violence or sexual abuse look like it’s nothing, it’s a trivial matter.
I wonder why it happened, I’d love to know … People sexualise [girls] as exotic; ‘Oh you look like Princess Jasmine’; men always sa[y] quite inappropriate things. I sometimes wonder whether [being dual heritage] did make a difference … Another part [is] I think that young black girls are sexualised a fair bit more at young ages … and I think it is [partly] because of that sexualisation, and objectification that [this] happens disproportionately to black girls.
Lifetime trauma: lifelong cycles of trauma
This theme represents cycles of trauma and abuse affecting many participants in the MESARCH project and to an even great extent in our narrative study sample. Survivors indicated cycles of violence, wherein their early life trauma led to deteriorating mental health which exacerbated risks for further abuse. The composite of ‘Madison’ is entitled ‘Cycles of trauma’, which captures abuse in childhood coupled with unmet mental health needs and how this exacerbated subsequent abuse and experiences of multiple victimisation (see Box 5). The cycle of trauma connects with sub-themes of homelessness, addiction and repeated patterns of abusive relationships.
I had quite a chaotic childhood. I had complex trauma [from] an unstable family background. I don’t have like a proper family because of my childhood abuse. My father didn’t sexually abuse me but systematically hit my mother [during my childhood]. I really didn’t have anywhere to turn. I got to the point of breakdown with post-traumatic stress and flashbacks and then that escalated into psychosis and being really, really unwell despite all the efforts to maintain my mental health.
Over the years I’ve been a victim of multiple sociopaths and psychopaths. These are the sorts of people that I’ve attracted as a result of the abuse I’ve suffered. I’ve found that when you’ve been in a life-threatening situation where you are told to perform sexual acts and you do it, then it’s very difficult to avoid coercion in any kind of future relationships and control because you’ve been in that situation.
Unfortunately, I ended up running away when I was 15 from an abuser and ended up getting abused by a police officer. So that’s how that started. And then as an adult, there’s been a couple of experiences. This was just the tip of iceberg. I ended up being in a homeless accommodation in the same town I am still living in today. And that is one of the roughest places you can be.
We lost our house. We lost all our possessions. Pretty much everything. Just to get away from it. They [local council] put me in an accommodation with a woman who used to be a prostitute, funnily enough, and she tried to pressure me into all sorts. And at that point, the only way I could cope was with prescription medication, which was 220 milligrams of antidepressants, gabapentin, propranolol, and diazepam, and alcohol, and cocaine … I couldn’t drink [in the] morning [because of work], so cocaine did the job, and I could just function. My addiction was taking off, days off sick were getting a little bit more. Then it got to the point where home life was crumbling. It became this vicious cycle.
I’ve become a person that just exists. My physical health isn’t good either and I think it all stems from the abuse. I just think the whole thing has systemically battered me.
Typology of narratives about access to care for survivors
Victims and survivors not recognising abuse or lacking access to information
This access typology draws together the many narratives relating to how survivors’ minimal ‘awareness’ of abuse could delay help-seeking. Achieving awareness of coercive behaviours can be particularly problematic because of the insidious nature of domestic abuse and the subtle and exploitative ways in which perpetrators enact abuse (see Box 6).
I just wish there was more help initially when people go through sexual abuse, that there was kind of more help around what a healthy relationship is and more information about what constitutes saying no. Because obviously we have a stereotypical thing, where it’s like you literally shout ‘No, no, no, no’, but you don’t talk much about like the freeze response or like you’ve given him what he wanted because you’re scared. I think there need to be more conversations around coercion and stuff like that because that’s a big concept that I struggled with for many years. I said no initially, but then I got so scared so I just went along with it and I think that would help so many more victims if that was more talked about, rather than just the stereotypical stranger in an alleyway and you’re shouting ‘No!’ We have such a black and white view of what rape is. But even like the media and stuff portray it differently now because it’s not just black and white. So we are getting there but I think it’s important for victims to realise that if what happened to them didn’t fit in that box, doesn’t mean that it didn’t happen.
Participants’ accounts highlight the vital role of communities in making information about abuse available. People may seek such information at critical turning points in their lives when they may struggle to name the abuse but identify that they are unsafe and at risk (see Box 7). Such information must go beyond addressing the ‘black and white’ forms of abuse such as physical violence to encompassing hidden forms as identified in Box 7.
When I was 17, I knew this marriage stuff was looming, but I always believed I would have a choice in it. My dad and his brother took me to Yorkshire, and there I met the man who was going to be my husband. I wasn’t allowed to be alone with him, and we were literally there for half an hour. The transaction, the deal had already been done. ‘What do you think?’ asked my dad on the way home. ‘No’ was my response. My dad’s words were, ‘That’s the man you’re going to marry, whether you like it or not.
That’s when I most wanted a professional in my life, or a poster to say I can just talk to somebody. It was just like I can’t tell anybody about it. I was thinking where am I going to run away to anyway? I haven’t got a qualification to my name. So, I went through with it. I did it at 17 years old, and it was surreal: 4 days of wedding but I felt like I wasn’t there.
Individuals (formally and informally) and organisations across communities being able to ask about abuse when suspected and providing appropriate responses, which includes linking victims and survivors to sources of help were cornerstones of access in this research. The research identifies many instances of workplaces (see Box 8) and university staff supporting survivors to make sense of their difficulties and the abuse, and providing information and referrals.
I was moved to England and I was forced to sponsor his visa to England. I was still under threats and blackmail from my family for the first few years of that marriage. I was coerced to have children, because it would restore honour. I had two sons from this marriage. He was alcoholic and abusive throughout this marriage, and it took me 6 years to finally get out of it. The incident that really changed things was that we were moving in slow-moving traffic, he was driving me to work, and leant over and opened the door and almost pushed me out. If it wasn’t for the seatbelt, he would have thrown me into traffic. That shook me. I went into work crying, and the matron there, called me in her office and she asked me what had happened. I broke down because judging from the way my parents treated me and the way I was blackmailed and emotionally threatened by my parents that nobody will help me, I had a feeling that if I asked for help, I wouldn’t be helped. The matron, she calmed me down and she told me, ‘there’s help for all this. Go to your GP, there’s domestic violence services, get your paperwork out, bring it to work and store it there, we’ll keep it safe for you’. So, I did that and took all my boys’ birth certificates, passports and everything and I just left them in the office, and I called my doctor and I told her what was happening and she put me through to domestic violence services. A few weeks after that, I found out that my ex-husband was going to take the boys to India. We had a major blow out because he was asking for the passports. Luckily, someone from the Public Protection Unit had called me and arranged to put markers on the house, so that if there’s any incident and I call 999, then the police know it’s priority. So, I called the police after that, and they came and they got us. I broke free from the marriage and ended up in refuge provision for a month with my sons.
These mechanisms of citizens ‘knowing’ are particularly relevant where there is low ‘visibility’ of abuse, for example, where abuse occurs in family settings, or environments and communities where abuse is silenced. Abuse thrives when helping resources are relatively distal for an individual or community, for example, linguistically diverse communities may struggle to engage with awareness-raising campaigns, posters and pamphlets when not designed with their needs and barriers in mind. Box 9 identifies the potential of sustained campaigns against abuse and in relation to articulating less well-defined aspects of abuse. It also draws attention to the multiple ways in which agencies across the third sector can support disclosure and access to justice and SAAS at a critical turning point.
One day, I saw something, or I heard something, or I saw an advert that described grooming which alerted me to his behaviour. It wasn’t until that point – my late twenties, probably early thirties – before I understood exactly what grooming was. It all made sense.
Before I reported it to the police, I spoke to [the] NSPCC. I’d spoken to several charitable services over the phone for advice. I reported it to the police via the NSPCC. They made the call on my behalf, which helped a lot as it was someone else taking that responsibility for me, and there was no turning back now. I had taken inspiration and courage from a quote in Lemony Snicket’s book, The Ersatz Elevator, ‘If we wait until we’re ready, we’ll be waiting for the rest of our lives’, which helped me make that decision. I was absolutely devastated about making that phone call. I felt guilty about reporting them, but I needed some closure to the abuse that I suffered, over 20 years of it. I needed closure and that was the only way that I was going to do it, because if I didn’t cut him off myself, after a period of time, after I’d healed myself and moved on, he would creep back into my life again. I visualise the sequence like a recurring line on an electrocardiogram monitor.
Potential entry points to care for sexual violence and abuse missed
Many participants alluded to recognising that what was happening was ‘abuse’ but experiencing considerable barriers to escaping the situation. Picking up at a later point in the narrative To Forced Marriage and Beyond, our participant reflects on not being asked about abuse in an antenatal setting even when they were presented on a third pregnancy loss and in poor health (see Box 10). This signals missed opportunities for enabling access to care for sexual violence and abuse/exiting domestic abuse.
So that felt right, ‘I’ll have children. I’ll have somebody to love, and somebody to love me back, because how else am I going to get through this life?’ I was well underweight because I was malnourished; I miscarried three times. Nobody from health asked did I feel safe at home. And it was only on my third miscarriage, I was lying there, and I thought, ‘I need to get out’, but I wasn’t just leaving him, and the in-laws, and the extended in-laws, I was leaving my mum and dad. I was going to be leaving my brothers and my sisters, and my millions of cousins and aunties and uncles. I knew I was going to have to walk away from them all. So, I did.
The participant in Box 11 explains about why being asked is so important, and why spontaneous disclosure without the question being asked is unlikely. These cases show that some signs of abuse may be more opaque than others (e.g. miscarriage or mental health problems) but this study shows that even when the signs of physical violence were apparent, health professionals may have avoided enquiring.
I look back now and I think actually all the times I went to the GP and said my anxiety meds aren’t working and I kept going on different tablets. Had someone asked me then, maybe I would have said something. But I needed someone to ask me the question. I needed someone to ask me the question. When you have all your choices taken off you by someone, even making a decision like that, you feel like you can’t.
There was one occasion when I went to hospital because I was covered in bruises on my arm. Finger print bruises. In my head I’d [talked] myself into thinking it was a side effect of my medication, my new tablets. They couldn’t find anything wrong with me, they didn’t understand why the bruises were there. They didn’t think it was a side effect, I was just a bit dehydrated. No one asked how I got the bruises. I was hoping someone would ask me so I could tell them. It was hand-shaped, like fingerprints … no one did. I think there was multiple missed opportunities there.
With the GP, I can understand because they didn’t see me again, it was COVID. It was over the phone so they’re going off what I’m telling them. But with those bruises, I think maybe they did. I think a lot of people are scared to ask, although it’s part of their job. It’s always better to ask the question, put a lifeline out there.
The following narrative identifies a range in the experience of quality of responses from health providers (see Box 12). Many opportunities arise ‘to put a lifeline out there’ as survivors seek help for the direct effects of abuse as well as other health-related issues over the course of experiencing domestic abuse. It draws attention to the value of health professionals being able to ask and offer support. Professionals do not always recognise the communication difficulties experienced by people who have been exposed to abuse, ‘Unless I’m asked specific questions, I wouldn’t know how to communicate because for so many years I’d been told to basically keep my mouth shut and told what to say and how to act’.
Discussing bits and pieces that happened, after with GPs, was quite difficult. You’re trying to say that you’re unwell and you can feel it in your body. Like you just feel uncomfortable in your own skin. You always get this bog-standard response of ‘we’re not qualified in that area, to deal with those issues’. And that’s always really disheartening because their response is speak to the police. It’s on you and it’s just on you. You have to go search for that help. That was the response that seemed to happen a lot. And then, after a while, you just stop asking because, what’s the point?
While I was with him, I had to go [to sexual health services] twice because he cheated a lot. So, he gave me chlamydia twice. Even back then, and this was before the incident, they clearly could see something from the outside of the relationship. I remember both times, they said, ‘If you ever need to come in and talk, or if you want to come back for a check-up later on, that’s absolutely fine’. One of them gave me her name, ‘Book an appointment with me and I will be here’. Like, there was just so much more effort. They were brilliant.
Same for the hospital. I had a miscarriage, and we ended up going to a hospital and they were amazing. There was one lady there. She actually pulled me into a room. I hated just him touching me, and she must have noticed because she pulled me aside and she was like, ‘Just need to talk to Macy about, you know, medication. I’m just going to take her into this side room’. She asked, ‘Is there domestic abuse going on?’ I just looked at her and I remember, just sort of like, holding back tears. ‘We can get you out, with your daughter, if that’s what you want’. I remember thinking, that is all I want and I wanted to say it, but I just couldn’t get the words out, but they were incredible.
Related to the difficulties survivors of trauma may experience in communication and decision-making, the final composite voice (see Box 13) shared in this section centres on the vital role and capacity of the NHS to open access to care.
My GPs have all been really brilliant. When I came out of emergency services, I got a phone call from him [GP], and he just said to me, ‘I’m allowed to override the Hippocratic Oath in your situation because I’ve been sent the medical and physical reports from A&E and your life is in serious danger and if you haven’t gone to the police by such and such a time this afternoon, I have been guided and I have the authority from the legal medical practice to go on your behalf to safeguard your life, but it would be better coming from you’. At the time, I was like, ‘Grrrrr, I hate you!’ But, I guess, in the long run, he was doing me a big favour and other people. You know, they care. They care. They’re more medical, I mean, mental health, that’s their interest as well, but not as much as like psychotherapists and everything, that’s my personal experience of my GPs.
I would say that mental health services have professional experience of people who’ve been through severe trauma which enables them to actually open up the field of decision making. So having been in a vulnerable position where even making simple decisions has been almost impossible and having been coerced and controlled, the mental health services have done the opposite. They have actually opened up the field of decision-making, helped me see how I can be part of that decision-making process regarding what medications to take, what activities to fill my day with, and I would say that that’s consistent as an inpatient and as an outpatient.
Racial discrimination as blocking access to safety, justice and dignity
Most participants from culturally diverse backgrounds in this study did not raise racial discrimination enacted towards them as a barrier to accessing SARCs or other forms of care and support after sexual violence and abuse. However, among those that did, the implications of negative and even discriminatory responses for safety, well-being and progress after abuse exposure were profound.
The longer composite we present for ‘Simran’ (see Appendix 3, Box 44) highlights the extreme demands facing those who flee domestic abuse, all the more marked when a person is trying to keep children safe, is isolated, has no access to resources and lacks the language skills to manage a complex, high-risk situation. While Simran’s story highlights many elements of risk and recovery (see later sections), our interest here is in the participant’s difficulties in accessing what they needed initially. Simran’s story demonstrates an increasing degree of disempowerment resulting from early interactions with the police, other professionals (e.g. social workers, interpreters) and settings (e.g. hotels and short-term accommodation). It aggravates the poor state of her mental health and a lack of trust in institutions and services meant when the opportunity for accessing justice more formally did arise, Simran was unable to participate in this process. Simran was far-removed from a SARC, sharing her sense of isolation in day-to-day life: ‘I didn’t know a doctor and I never went to any temple. I didn’t know how to go’.
She struggled to communicate to the police about the domestic violence and abuse, let alone the sexual violence exposure. She was also relying on her child to communicate about their situation to the police, and thus, she experienced many constraints on what she could disclose.
There is a strong access theme throughout concerning Simran’s daughter’s education and which was clearly a priority for Simran: engagement around her GCSEs and A-level examinations was severely disrupted by the abuse and the upheaval of escaping abuse, and temporary accommodation persisting over years. Overall, this composite shows that examining access in an intersectional framework is critical. Understanding racial disparities in access to care (and other opportunities) requires that we consider power dynamics associated with race, such as gender and socioeconomic status, which may also have operated here. Simran shares about the lack of safety in the refuge environment and how little control they had over who accessed their space: ‘People used to knock on our door and my daughter used to be scared. We used to get so scared that flashbacks started coming and there wasn’t any lock controlled by us, there’s only one they [refuge staff] control, and we used to think anyone can come and we didn’t sleep at all, both me and my daughter’. Simran’s mental health needs are substantial, but progress towards therapeutic interventions was clearly slow, and she reported being on a waiting list for counselling.
This study intentionally engaged with individuals from a range of different minoritised populations. Participants drew attention to important steps taken by agencies to improve access and experiences of service users: ‘It was really, really helpful to have someone there that I could ask the questions [of] and just to talk it all through. It’s with an ISVA that deals with people that are LGBTQ+. I’m married to a woman so I fall into that category. I suppose you feel a bit more comfortable knowing that the person on the end of the phone understands. They’re comfortable with who you are as well as what you’re saying. I don’t feel like I’ve been treated differently, and I think that is a really good thing. I can’t fault any of the help that I’ve had; I think everyone has been brilliant, they’ve made me feel comfortable, they’ve made me feel safe, and they’ve made me feel believed’.
Social disadvantage: I’m not worth nothing, I’m not worth the bother
Capturing the essence of the interplay between sociodemographic status and access to health care, therapeutic care and justice, we present Fay’s full narrative (see Appendix 3, Box 45). While Fay does find herself at the SARC soon after contacting the police and accessed some services, thereafter, there is a sense that the care pathway does not hold her on it particularly effectively: ‘I had to have the Hep C, Hep B injections and I had another blood test as well. I should have had a follow-up last June but never got a follow-up phone call to say, ‘Please can you come in, so I’ve not had a follow-up from that’.
She does not believe her case has been adequately investigated. She is experiencing a lot of pain but finds it hard to access the physical and mental health care she needs and feels unsupported. She believes the GP can do only so much. The final part of her narrative alludes to being an older woman: ‘I think the older you are, the more difficult [it is] because I feel that maybe some people are like ‘Oh nobody’s going listen to me, I’m not worth nothing, I’m not worth the bother!’
Mental health: ‘personality disorder used as a bit like a weapon’
The research has identified mental health diagnoses and longstanding or complex mental health problems as one of the most significant barriers to care and justice for sexual violence and abuse across our sample. Box 14 introduces this issue with the person pointing out that their mental health was a greater concern in terms of accessing justice than their cultural background (Black British with Afro-Caribbean heritage). This extract presents concerns about being believed in the CJS and also about how the process of pursuing justice could aggravate their mental health condition.
I did have like worries about my mental health more than worries about my cultural background, to be honest. I think the bonding with the [ethnic minorities] counsellor was just like a nice add-on kind of thing, but I definitely had more worries about my mental health playing a part with all of it … I have been diagnosed with bipolar disorder in 2018. It’s still quite fresh. The assault happened in 2019, so I was still getting used to medication and getting used to the disorder and everything. Still quite fresh with talking to a psychiatrist and my GP. That was something I did bring to the ISVA actually: I was worried about if we did go to trial, would I be able to handle it mentally. Also, if it went to trial, would they rip me apart for having bipolar disorder, and not believing me because I have bipolar disorder. I went to my GP not long after the assault and was kind of like, ‘Look, this has happened to me. I think I may need like some extra mental health support just in case, because I’m not sure if I can deal with it. Or if I will deteriorate because of the assault and everything’.
Across the sample, we detected that mental health was less of a barrier to accessing frontline services such as SARCs and helpline services in the voluntary sector (e.g. MIND, SHOUT and the Samaritans) than it was to progressing cases through the CJS and accessing appropriate forms of mental health care. Many participants of the MESARCH study and those invited into this qualitative study were living with complex PTSD and/or had diagnosed ‘personality disorders’. Such individuals struggled to seek for appropriate care, with Jane’s core narrative (see Appendix 3, Box 46) being illustrative of the many doors that close on survivors with complex mental health.
Cultural narratives influencing reporting of sexual violence and abuse
Here, we address how dominant social, political and cultural narratives presented in the media about justice for sexual offences can interact with the pursuit of justice and influence how people think about help-seeking. Box 15 highlights the benefits of SARCs as an alternative or conduit to the police. It shows the ‘work’ undertaken by survivors in balancing the costs of reporting with the costs of not reporting.
I literally Googled and was just like, ‘What do I do? I’ve been like raped and stuff, what do I do? What are my next steps?’ I think it just gave me like options of what local clinics and stuff, and then when I phoned, they booked me into that one. I hadn’t even heard of SARCs before that. I guess in my head – this is quite silly – but I used to watch a lot of Law-and-Order SVU. In my head I was like, ‘You go straight to the police and they do all the paperwork, all the tests and all of that’. And I was kind of like, ‘I don’t really want to go to the police right now’.
I literally went to the SARC the very next morning, and it was like a surprisingly nice experience, they would be welcoming and kind, and I was like being offered way too much food so it was quite sweet. You don’t know what to expect when you’re going through that experience, definitely. But yeah, it was really good. They gave me the options, if I wanted to take it to the police there and then. And also, the sexual health referral, like on the day, or if I wanted to refer myself. So I accepted all that. Had the swabs done and everything.
I didn’t want to report for a very long time. I guess because I’d seen the stats already of how it’s dealt with and how you’re very unlikely to get a trial and stuff, and how it’s unlikely to go further than a trial and everything. And then when I went to the ISVA, she was telling me like almost the pros and cons, and letting me make that decision, just kind of telling me, ‘Well, this is exactly what would happen’, and it was kind of like a really long experience, and would kind of get like … I already know, if it did get to trial, you do get dragged through the mud almost. And I was like, ‘I’m not sure if I want to do that, I’m not sure if that’s good for me and my mental health’. But then the more I was thinking about it, the more I was [thinking] that I can’t let this happen to someone else as well.
Then it didn’t go to trial or anything, they didn’t fit into it. I was disappointed about it for a long time. But then I was also like, well, I’ve seen the stats and barely anyone [does]. I was like, ‘Well, what can I do?’
Another participant also explains the work and mental navigating that survivors need to do in the lead-up to reporting. In this instance (see Box 16), accessing EMDR through the NHS changed my life completely and provided them the strength to report the abuse. This was particularly needed given their expectations of a negative police response.
EMDR (Eye movement desensitisation reprocessing) made me feel okay enough to be able to report it to the police, something I always wanted to do was to obviously report it, but I wanted to make sure I was strong enough to finish the case, go from start to finish. It’s been great, I can’t fault the police whatsoever. I never really used to like the police, not for any particular reason, but I’ve read a lot online. You hear bad stories about the police. So I didn’t go in with a particularly good outlook, but I thought I’ll try it, see what happens, because it’s a historical thing, I don’t know if they can prove it. It’s just my word against his.
The police have been absolutely wonderful, they’ve kept me informed. Every couple of weeks, if I’ve not heard anything, they’ll give me a message or they’ll give me a ring. I’ve always had a point of contact. Even the interview process was easy to do: they told me where to go, it wasn’t in a big scary police station; it was in a housing estate. No one would know where you’re going. I always felt very well informed of what could or could not happen which I really appreciated.
We also gathered evidence of providers grappling with how to guide and respond to queries from their clients about accessing justice (see Box 17).
I think when I went to [rape crisis centre] the first time, it was kind of said to me that there’s not much point you reporting it to the police because of how low the conviction rate is. Although obviously conviction rates are really low and we see it every day, I think that completely put me off reporting it, because I felt, well, if they’re even saying it what’s the point kind of thing. But even if nothing happens, reporting it means a file is open. I wish that I was supported more with the whole police thing. Because by the time that I reported it in 2021, I didn’t have any evidence on me, so it couldn’t really go anywhere. But if I had supplied stuff back then, because I did have, like the texts and stuff, I could have provided more evidence then than I did in 2021.
Shifting societal and institutional responses to child sexual abuse facilitate access
While crime data can be discouraging, including such aspects as the low conviction rates for sexual offences there is another perspective on the public response to abuse that arose in this research. Steve’s narrative (see Appendix 3, Box 47) provides a survivor’s perspective on how shifts in social responses to sexual abuse have enabled him to take steps towards justice and alleviate some of the burden on him mentally and socially that he had experienced over decades.
Accessing the right care and therapies
Within the ‘access’ typologies, we consider not only survivors’ capacities to reach frontline care such as primary care and SARCs but also people’s access to appropriate therapeutic options in the NHS and voluntary sector services. Participants referred to the difficulties accessing crisis care and the limitations experienced with helplines (see Box 18).
I phoned the Samaritans and then there’s a waiting time for the Samaritans, and like music, you don’t need that when you’re in that situation. Much as they’re there to chat, they don’t really help, they just signpost you. You get fed up of being signposted, you just want actually some real action. Not, ‘Oh, go to this number or go to that number’, be put in another queue, be put on another waiting list. That doesn’t help. That just makes you even worse. But the crisis team, as a service, they were just like, ‘No. Can’t help you, you need to be referred by your doctor’, and it’s a Friday evening, you’ve got to wait until Monday. So, you can’t be suicidal on a Friday night, you got to wait until Monday morning to then get referred by your doctor? It doesn’t work like that, a crisis is a crisis.
We gathered widespread data across the cohort study, and this qualitative study regarding the perceived mismatch between therapy offering and needs. The research gives a sense of services struggling to consistently and effectively provide care for sexual violence and abuse and mental health needs. This is apparent at the primary care level where guidance is sought and in psychiatry services that may lack trauma-informed practice (see Box 19).
They didn’t really give me much help, they were kind of like, ‘Oh well, you’ve already been in contact with the rape counselling and then you don’t have another appointment with your psychiatrist until this time, and like maybe you can phone in to talk to the nurse for a bit?’ and I was like, ‘Well, I don’t want to talk to the nurse, I want to have like a proper appointment where I can sit down and discuss my fears’. So I kind of felt a bit let down. I did have one recent experience that really knocked me off. I moved into my new flat, in a completely different area so they had to give me a new psychiatrist, and a different doctor. My new psych nurse, like in our first get to know each other, basically just went, ‘Oh, by the way, have you ever been like assaulted or abused in the past?’ I was just like, ‘What? Surely that’s not the way that you word things to everyone, and surely you can understand that could be quite triggering for people?’ I was like, ‘Yes, I have!’ Then she was like, ‘Oh, can you tell me about it?’ No care, no care, just very clinical. I think that is like one of the big issues with psychiatrists anyway, and it did really like knock me off. I don’t know how to tell her she’s not doing a good job at this.
Typology of narratives about recovery and healing
Reading of the narrative interview transcripts has highlighted three core narratives that broadly map people’s experiences of recovery. These include narratives aligned to a sense that ‘I cannot’; narratives aligned with the sense that ‘I am recovering’; and narratives aligned with the sense that ‘I feel recovered’. Each of these core narratives is set out below and the sub-narratives that participants drew on to explain where they are in their recovery journeys are identified.
‘I cannot recover’
Participants whose journeys aligned with this core narrative identified a number of factors and experiences that contributed to the challenges in recovery (see Table 21). These include experiences after rape, sexual assault or sexual abuse that continue to make a survivor feel unsafe, such as having to live in or near the place where the assault took place, or not knowing if the perpetrator was still around and able to reach them. There is also a strong connection between having trauma from childhood, complex trauma, poor physical and mental health and lack of recovery within these narratives. A sense that there is broader societal support for the perpetrator also comes through as damaging to recovery.
Societal support for the perpetrator
A number of narratives draw out the sense that perpetrator behaviour can be considered normal and not warrant intervention by the authorities as indicated in Box 20 below where the participant reports on the response of some of her friends when she disclosed to them that she had been raped.
They [friends] kept saying, ‘Oh, that don’t surprise me’, of what the perpetrator did and then it goes, ‘Oh one of his friends said, ‘He’s done something to other people in the past,’ which made me feel sick to my stomach. Was like, it felt like they were, er, what’s the word, supporting him, the perpetrator and not understanding what happened behind those closed doors. Especially when he was in the house share and nobody was there, like I couldn’t do anything. It made me feel very vulnerable, like it still does to this day.
The societal support for perpetrator behaviour is echoed when another participant (see Box 21) talked about a course she had been offered to reduce her risk of being a victim again in the future. It illustrates the tendency for society to place the responsibility for not being raped or sexually assaulted on women (although, of course, not all victims are women), rather than on perpetrators and their behaviour.
I remember someone at some point saying about some course I could identify red flags or predators, and I just thought, ‘Wait, what! Why do I have to do that work?’ I thought he was my friend. Like nothing about him gave me the impression that he was a predator.
They’re implying that you’re some kind of idiot who just lets predators in your door. I just remember thinking, ‘Why does that programme even exist? Like, why are we making women sit through these programmes that make them feel like they’re stupid for having let this person into their lives because actually predators are really clever, and they find ways to do it’. It’s the men we need to work on. They’re the ones who need to go on the courses. [Pause] We can work out which ones are the predators and put a sticker on them. They’re the problem, not us. I just … Yeah, I remember when they offered me that, just being like, ‘Hello?’
Complex trauma and physical illness
Participants whose narratives featured a lack of recovery often talked about having complex trauma, rooted in experiences of childhood abuse or childhood trauma. They talked about the effect on their physical and mental health (see Fay’s narrative in Appendix 3, Box 45). Participants with these experiences found it difficult to access services that responded to complex needs; a 6- or 12-week programme is identified as incapable of addressing this complexity (see Box 22).
You know, these 12-week … not even 12-week, 6-week courses, you know. I don’t know how they expect someone with trauma to get everything out in those 6 weeks. You know, because you’re only in there for 50 minutes and by the time you’re settled in, and ready to talk and something comes up, they’ve got to leave. For me it just stirred up a whole bag of emotions, just spinning around like a washing machine.
There’s many parts to my personality now that I just don’t understand. I don’t understand me anymore. I don’t know. I just … I mean my days are getting shorter and shorter because sometimes I suffer insomnia as well. Through the night, you’re going over what has happened, and the event, so consequently during the day I might want to have a little sleep, and I can actually sleep in my chair sometimes. My energy levels are completely bust. I just don’t do very much. I get up eventually. I have a shower. By the time I’ve done that, I’m exhausted. Come downstairs, have something to eat and then I need another rest because I’ve done that. I’ve exerted myself doing that.
I think I’m a burden on everyone. I think sometimes it will be simpler if I wasn’t here, and they could get on with their lives and not have to worry about me. Sometimes, you know, because I live with chronic pain every day, sometimes you just think, why? You know, why do I have to live like this?
Physical or visual reminders of the abuse or the abuser
Another feature of narratives focused on the lack of recovery of the participant was related to being reminded of the abuse visually. One example of this was where a participant describes moving back to be near her family hoping for their support with caring for her children, only to be confronted with her abuser again (see Box 23). For another participant, smartphones sending reminders of old photos could cause flashbacks. Participants faced many situations, not necessarily unsafe situations, which served as reminders of past abuse and could trigger a response and obstructed recovery.
My first marriage broke down and I went back to the family, village where I was brought up, back into the pit of depravity, I suppose, thinking that would be a good move with my two daughters because my family had shown some kind of interest in helping me, which didn’t happen. I was out of … They were in control again, and I wasn’t in control of my own life, or my children’s lives. So the depression got really bad.
Obviously this family member [who had committed the abuse when she was a child] was in the village as well, so I bumped into him quite often. And I’d have this slight numbing effect whenever I … Well, if I saw him I wouldn’t ever speak to him or, you know, be near him if I could help it. I’d turn and go the other way or do something like that, but just the image of him, and that’s like flashbacks all the time … places, smells, things like that, they’re all triggers. It takes you right back to times that were hard, that were difficult for me.
‘I am recovering’
Within the narratives, there are stories about the long and ongoing process of recovery. Many people talked about having achieved some sense of recovery or having made progress in that direction. There was a sense of hopefulness that recovery would come and that a range of factors were identified as important or linked to the process. For example, moving to get away from the location where an assault had occurred was identified as helpful and is linked to the narratives about being reminded of abuse or the abuser above. People also talked about their efforts in engaging with the internal process of tackling mental health problems, and a growing sense of passion for seeking justice and seeing justice as part of a bigger societal picture. Having good support from others in their lives was also important. People also discussed various types of physical activity or exercise as being helpful for recovery.
Justice and its relationship with healing
For many survivors of sexual violence and abuse there is no court process, as many cases do not pass the threshold of evidence required. Some of the participants had had cases where the justice system was involved, however, and that was playing an important role in their recovery (see Steve’s narrative in Appendix 3, Box 47). For others, there was a sense that getting justice was part of an important statement about the wider issue of violence against women and sexual violence and abuse in society: ‘It’s not just my battle to fight either. It’s not just about me and my body that he actually stripped of dignity, and it was just so atrocious, but it’s actually an offence against the state’. There was a sense that people were putting life (and recovery) on hold while waiting for their case to go through the justice system, as illustrated in Box 24.
I have desires to travel, I have desires to do these things, but I’m aware I’ll have to be in the UK during this time, I’d like to have my own community and support around me during the time. I definitely put things on hold. I was a kind of person who would always want adventure and to do these fun things and I’m just the kind of person who is like doing like the safest, most stable thing possible. I’d love to get to a point where I feel okay to take risks and I feel okay to do the crazy things that I used to do and know that I would be able to like fall back on myself and that like I’ll be fine. So that’s my aspiration.
The journey I’m on at the moment … I think because I have this investigation, I have court dates, that type of thing, it’s very much like split in the back of my brain. I haven’t really felt it and that works really well for me, and I’m going to have to deal with it formally in the future and I think it’s a really good idea not to think about it beforehand. So, my approach has been for the whole last year, erm, uh, back of the brain, don’t think about it. Deal with it later. And that’s okay, I think. Like it’s going to be shit down the line and then I’m going to dig it out and then it’ll be fine.
Struggling with mental health problems and getting support
Everyone described the impact of their assault on their mental health and well-being and generally struggling with the ups and downs as part of the recovery journey. Getting the right support could be difficult. Examples from some of the narratives are provided in Boxes 25 and 26.
I do still think about it to this day. Since then, I’ve suffered with anxiety and depression just constantly. It’s alright at the moment, but I wouldn’t say it’s the best and I wouldn’t say it’s the worst. I felt that it has massively affected me, it’s affected my mental health to this day. It’s almost two and a half years since it happened, but it still affects my mental health today.
I tried to do talking therapies, but what they instantly wanted to do was not trauma therapy but behavioural therapy (CBT) for the anxiety and the depression, so I just cancelled that because they could never actually solve what I was actually thinking of and go for the trauma. I’m still waiting on the trauma therapy. They said they’d call or email me when it’s available. I’ve had no email and I’ve had no call, but I’ll still wait for that one.
I’ve been in therapy for about 5 years now. [The medication] has its ups and downs, trying to find the correct, um, like counselling that you need to do and kind of thing, but it’s been quite good and very supportive.
My mental health in the beginning [following the sexual assault] wasn’t as bad because I was kind of convincing myself that nothing happened, it wasn’t that bad, because I was quite intoxicated when it [the sexual assault] happened. I was trying to convince myself every possible way that it wasn’t what it was, it was fine. Then it started to give me really bad flashbacks and PTSD on top of my already severe and anxious, like severe depression and anxiety that I’ve had. I was unable to leave my room … I was trapped in that room for a very long time. I never have … like I have never had good sleeps like just with it. Mentally I’m doing a lot better. I still get the help … I still have all the contacts if I need any help but I’m doing a lot better.
One participant described a sense of a mismatch between her body and her brain while trying to recover from her experience of sexual abuse and assault. She describes some of the lasting effects including the impact on her ability to build relationships, make decisions and getting into drug-taking (see Box 27).
The frustration for me is that it feels like my brain is somehow stuck in the past but also, like, well it’s just not quite matched up with my body. My body’s telling me something, like, ‘You need to rest now’. And I’m still so restless that I need to kind of pace myself or do excessive exercise or I’m so tired that I just stay in bed for days and days on end. My body’s telling me one thing, my brain is telling me something a little bit different sometimes, and I’ve found that mismatch to be quite challenging. I’ve found that when you’ve been in a life-threatening situation where you are told to perform sexual acts and you do it, then it’s very difficult to avoid coercion in any kind of future relationships and control because you’ve been in that situation. I won’t go into the details of [date of assault] but it was over a forty-eight hour period. It makes you lose confidence in your own decision making. I’ve found decision making quite hard, even just basic decision making and then you let other people take over and I guess that’s why I got into the drug scene briefly.
Using mind–body connecting activity as therapy (e.g. yoga, meditation)
A number of participants whose narratives aligned with having made some progress in recovery and who had hope for recovery talked about having found various forms of mind–body connecting activity and physical activity as helpful, including running marathons, yoga, meditation and art therapy. Excerpts from their stories illustrating this are provided (see Boxes 28–31).
I do yoga, an online yoga class … which I find quite good for grounding. Yeah, I’m finding the yoga’s actually really, really helpful. It’s just, I’ve had the same teacher, it’s … I get it free because I’m on benefits, but it’s through those WEA courses online. They’re really good but the tutor’s very, very good and um, yeah I think it is, I’m finding that quite helpful. Um, yeah, I think mostly feel safe.
Sometimes … I get, like, not flashbacks, but just like vivid memories really or things will just make me think of stuff, and I will have nasty nightmares about stuff that happened. So, that could definitely kind of give me a wobble. I feel good. I have like ups and downs. It feels like hard work sometimes to stay okay but I have lots of things I do and ways of managing to cope and just to generally kind of keep me feeling okay and it really helped. I think a lot of it has just been the way I think about things. I think I never thought of myself as a strong person, and it helped me to realise, I am. I just kind of being able to like, feel that in my body and think I am strong just kind of helps me. I exercise regularly, I run and do workouts, yoga, meditate and keep a journal. They’re all things that kind of help me feel okay or help me if I’m not feeling okay.
The complaints and that aside, I’ve been okay. I’ve tried to find my focus again in things that I enjoy. I like running, triathlons and stuff like that. I’ve set myself some pretty big goals for this year. It’s to help me focus and give me that sense of purpose, to be driven towards a new achievement, which has really helped in my recovery. I don’t want or need pills to make me feel better, I just want to celebrate what I can do, be the very best I can be.
I’m doing a half marathon, two marathons, 6 months apart, and in between, I’ve got a couple of events already booked, a half IronMan, in July, which will be amazing as I’ve never done anything as crazy as that before. I am keeping myself busy with all these challenges and that is what drives me to becoming a better version of myself.
I ended up having art therapy with [specialist provider of sexual violence support services] in the end, and they were really, really good. I think after the sort of initial experience, I was a bit wary bringing up the dissociative identity disorder as a main issue, and I figured maybe I could work through it without that being at the forefront of the therapy. I could do the work outside of the sessions as well and so if I had anything that I didn’t – maybe I thought she wouldn’t understand or I, I didn’t want to bring it up, then I could do that outside. So we did the sessions on Zoom, so if I wanted to then I could show her the work or email her photos and things. The collaging was, was my favourite. I had a real aversion to watercolours because I found them difficult for a good artist to paint with, but we worked through that which was really cool. We started doing painting because I’ve always been quite afraid of mess, so that really, really nice to overcome that. I think it helped with the DID because it helped personalities that expressed themselves without necessarily needing to speak particularly when I didn’t have anyone to speak to so that was really useful in those alone times. But it helped with everything as well.
Accepting that recovery is a process, and there are ups and downs
Another feature of stories that conveyed recovery expressed a sense of hope for the future, and an acceptance that recovery would take time and include both better times and difficult times. These participants wanted to keep working at their recovery journey. Examples of these hopeful narratives are provided (see Boxes 32 and 33).
I just wanna continue on that journey and be a little bit more stable, a little less emotional. I don’t know if that will ever happen for me because these are things that affect your life, but I’d like to contain it a bit more. And for me, I know what the end goal is. I want to work. You know, once I have gone through all I need to go through because there’s a lot I’ve got to unpack, I want to help other people like me. I wanna work in a children’s CSE [child sexual exploitation] home. I want to help other people and turn my misery into something good. I’m currently in the process of writing a book, bit of an autobiography of my past experiences, trauma and currently under a publisher.
I’d say everything in my life has changed [since the assault]. But it still is not something I’ve forgotten. Things will remind me of it. It’s harder than I thought it would be to brush those moments off. I’ve moved away from uni by design to get out of that environment, but like it’s still with me mentally and I guess it’s changed the way that I kind of carry myself and I know that, although I was doing really well on my anxiety before that, then after that it’s just been like a massive spike and I’ve had to build from there again.
I’m definitely not healed from it. I don’t know if that’s anything in my soon future. Um, I think that I’m happy to like openly accept it, like say it happened. And like if it’s like in conversation like I’m not going to shy away from it. Um, but I think there’s still part of me that feels like if I had done something different, like it would have never happened. I know that’s not how I should feel, but, but yeah, I think things – things are starting to change, and I think one of I guess the biggest tools in that is social media. I’ve found a lot of helpful resources, which is surprising but I would say I’m hopeful that everyone’s [better] equipped.
Supportive partners and other relationships
The importance of positive supportive relationships in recovery was discussed by most people. In particular, new partners featured within people’s narratives (see Box 34). People often talked about supportive friends and family members, and an example of the contribution of parenting to thriving in the years after exposure to sexual violence and abuse has been provided (see Box 35).
But then I met my ex and he was a really gentle person and I actually think that was a huge part of my healing journey. Actually, I think it was one of the most significant things that happened to me, was getting into a really loving, kind, nurturing … patient relationship with someone who was just … when it came to things like consent he was all over that. To feel like I’d met someone who knew. Despite his flaws and the reason why we broke up, like … made me feel like … I have like autonomy again of like … what I was doing.
My son – I’m very focused on him, he’s doing really well. I’m so proud of him. People say, ‘You’re a single parent, you do really well for yourself and he’s thriving as well’. Those positive words, to hear that from other people, is really uplifting. It’s me and my son in the future and he’s my rock. He is … if I didn’t have him, I probably wouldn’t be here today. I’m also very grateful that I didn’t take my own life those years ago as I wouldn’t have achieved any of the things I have done so far.
Moving away
Lastly, in relation to those in the process of recovery, participants often referred to having to move away from the location where the assault or abuse had occurred to aid recovery. This maps onto to similar comments about barriers to recovery (see ‘I cannot recover’ above). Boxes 36–38 provide examples drawn from three narratives of recovery.
I tried to make the area and the flat (where assault happened) a place where I could feel happy and reclaim that space, but actually what I realised over the months is that I wasn’t able to do that, so I did need to vacate. I would say that was the kind of real crash, well, more like a sense of, ‘Right, I really do need to get out’, because being in the area was just haunting me. When I vacated, which was in March 2021, so six months later, I got to the point of breakdown with post-traumatic stress and flashbacks and then that escalated into psychosis and being really, really unwell despite all the efforts to maintain my mental health. I kept going to recovery meetings like various sorts of twelve step meetings online, mental health groups. So, I was checking in at every turn, but then there did come a point where I thought, ‘Right, I just need to get out, I’m leaving’.
I didn’t move, I did want to move but finances obviously don’t allow that. So I’ve had to literally change the décor of my house, everything, to try and avoid the reminders. I’ve basically redecorated, moved everything around of that side to try and basically forget it, it still hasn’t fully worked but it’s at least something.
I am still holding out hope, it’s just that I might try again with the doctor and ask for therapy or see if I can go private.
As I grew up, I sort of carried on at the mental health services at school as well and at university, and then eventually managed to move out of the family home where the abuse has taken place so that was a huge step in terms of being able to process things in a space of safety. I think having that safety mentally sort of allowed loads of repressed memories to come up. That’s when I realised I wanted and was able to get help properly. I started by approaching [name of SARC] that helped me access [specialist provider of sexual violence support services] and they were brilliant. They were really, really helpful. I also later on went to [provider of ISVA services].
‘I feel recovered’
For some participants, they were able to tell a story of more complete recovery. They still expressed experience of trauma and having been on a journey but felt that they had reached a positive place that they could call recovery. In addition to the factors described by those participants above, additional features of these narratives included commentary about recent societal progress in talking about sexual violence, a further range of therapies and support and getting good, consistent support from a range of sources (see Table 21).
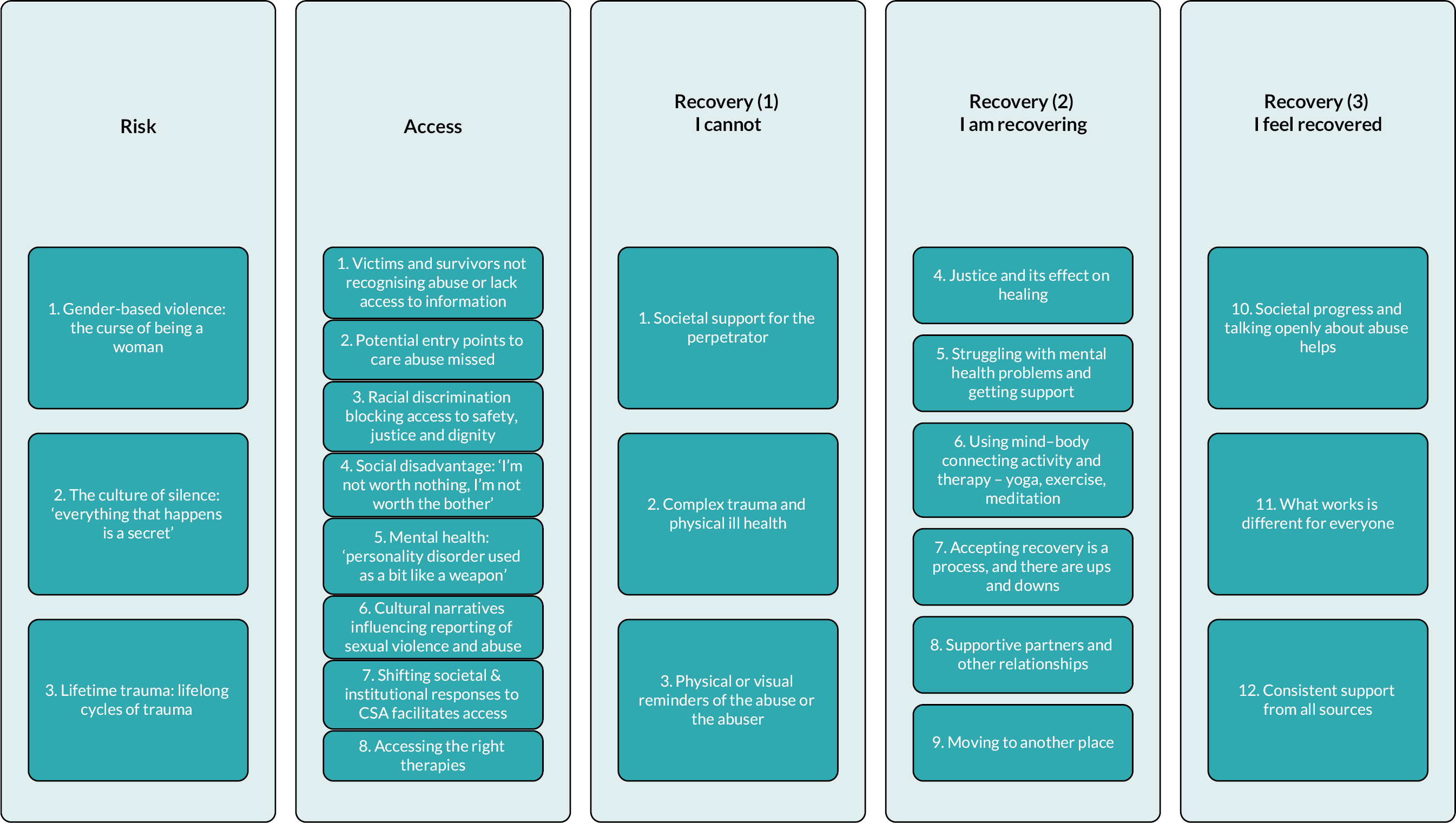
|
Societal progress, talking openly and online help
One participant talked about the experience of a growing openness in society to discuss the issue ofCSA and found this very helpful for recovery (see full core story in Appendix 3, Box 47). Similarly, the growth in online information to support self-help and learning was identified as beneficial by another participant and a source of empowerment (see Box 39).
I don’t think I would have recovered as well if I didn’t do my own research and my own self help, but obviously the internet can be a dodgy place and you can end up making yourself feel worse. But I think trying to increase my self-awareness around what happened to me and the effects, like reading into the complex PTSD side of things and stuff, constantly working on yourself, has really helped me get to where I am today. Because what I was like after that incident compared to now is two different people and, like I said, it wasn’t because of therapy or anything. It was a lot because of my own work that I put into it. I think having sort of good resources online and stuff is really helpful.
What works is different for everyone
What was noticeable about the narratives we gathered from participants was how every person’s path to recovery differed. In addition to the commentary about meditation, yoga, exercise and art therapy outlined above, other helpful therapies and strategies included EMDR (see Box 40), spirituality and religion, forgiveness (see Box 41) and a type of visualisation meditation (see Box 42).
I ended up having EMDR therapy through; it was free, so it was through the NHS. It was great to have access to that, it changed my life completely. Absolutely completely changed my life. Since my EMDR therapy, I’m fine to talk about everything, it’s not a problem really. Nowhere near as much as it used to be. After the first session, it was really difficult and it bought up all the memories again that you try and forget, but the way they make you, that your brain sort of starts working, instead of being like ‘this triggers me’ you know, you see it out and about and instead of triggering you, you think of yeah, there’s that thing. You carry on with your day, I don’t fully understand how I did it. They talked you through, you know you’ve talked through a particular scenario, not even the worst part of your experience, it could have been any part, and you just let your brain take you where it took you. It was really strange, after two or three sessions seeing that particular scenario that you go over and over, seeing how your brain changes. I was already feeling so much difference. That therapy, it was before the COVID-19 pandemic so two and a half years ago and even still I feel okay.
That was also sort of a similar time when I decided that I was going to forgive my dad, and I called off the police investigation, and actually, I just managed to close quite sort of that chapter and start working on the forgiveness and forgiving my mum as well and having more of a relationship with her. So for my mental health, that was definitely the best thing. I think outside of the space created by church, there is so much encouragement, and rightfully so, for people to come forward to report these things to make sure that justice is served and that we get justice for what’s happened to us. I feel maybe a teeny bit guilty saying it because I know that other women struggle with the coming forward, but for me, it’s been so much easier and so much more valuable to actually just let go of it and forget about it and I know that’s a privilege that I have that other people don’t have. But for me, it’s been the right thing, definitely.
My mental health team dropped me after the [trainee] left. But luckily there was the ‘spiritual lady’. I don’t know what else to call her. She did things alternatively like visualisation techniques with you. Basically, it was like meditation. Understanding that I can distance myself. Like, if I’m with a group of people and I don’t feel comfortable, at any point, if there were any actions, words, anything like that, I can still pour love to those people without emptying my cup. Like, you are allowed to have connections, from a distance. You’re allowed to take two minutes to yourself. When you’re sat in a group full of people and you know, you’re suddenly in a panic or a whirlwind, you’re allowed to sit there and just go, sorry guys. I’m just out of this conversation for a minute. Um, and just visualise, yourself. It’s things like visualisation, like light coming from your feet up to your head. Like, just your inner lightbulb, where you’re protected, and no one can hurt you.
Consistent support from all sources
A final feature of the recovery narratives among those who seemed to feel the greatest sense of recovery was the consistency of support they had received from a range of individuals and support services. This is illustrated in Steve’s narrative (see Appendix 3, Box 47). Positive, skilled responses from a range of people, support organisations and the wider system can contribute to a sense of strong support, even when criminal justice proceedings are slow or non-existent. There’s a sense of sharing the burden within these narratives, such that the recovery and healing journey is not done alone but in collaboration with range of professionals and agencies, with family and friends and with colleagues and communities.
Discussion
Summary of main findings
Our analysis of the 41 participants’ narrative data has been presented across three different typologies. We identified narratives relating to (1) narratives relating to risk of experiencing sexual violence and abuse; (2) accessing support in the aftermath of sexual assault or abuse; and (3) narratives relating to recovery aligned to lack of recovery, progress in recovery and hope for the future, and feeling a sense of recovery.
We purposively sampled people from minoritised and underserved communities from our wider cohort study and included a sample of people from outside of our cohort recruited through third-sector organisations to include voices of those who have not accessed support through SARCs. These analyses likely represent the largest scale qualitative investigation to date of the experiences of such a diverse range of minoritised groups’ experiences and journeys in the aftermath of rape, sexual assault and sexual and domestic abuse.
Our findings highlight the fact that recognition of what constitutes rape and abuse may act as a barrier to seeking help, and that many forms of sexual violence and abuse can occur in a complex web of community and family norms which serve to hide the abuse and create additional barriers to seeking help and support, including the opportunity to escape from abusive domestic situations. The health and social care workforce needs to be culturally-competent in understanding when they might need to ask questions, and to do so in safe ways. Disseminating information about how to access support in safe ways to people in all communities who may be suffering or at risk is needed to support better access. Professionals also need to be trained to be confident in intervening when a victim/survivor may not feel able to take the first step, but they are in danger.
In Simran’s story (see Appendix 3, Box 44) it is clear how the structure of the system inadvertently acted in a discriminatory way to block her and her child’s access to safety, justice and the right support to recover. There are additional experiences shared that draw out the positives of a LGBTQ + focused response, and the potential negative influences of intersections of social disadvantage, older age and pre-existing mental health conditions can have. Together these serve to highlight the need for outreach and services that take account of these characteristics. This is particularly pertinent where we have evidence that some minoritised groups may be at greater risk of sexual violence. 152–154
It was interesting that although we did not set out to explore risk of victimisation, our participants presented narratives around risk. In addition to the risk of re-victimisation that experiencing abuse can bring, the risk narratives also drew out some of the ethnically and culturally minoritised experiences of people for whom that characteristic was relevant. Risks included the taboo nature of discussing relationships and sex and deeply entrenched patriarchy as well as cultural practices such as forced marriage and honour-based violence.
Changes in societal (and therefore professional) understandings and attitudes towards victims/survivors of sexual violence was cited by participants as helpful in relation to both access to support and their ongoing recovery journey. There was recognition that people are more open to talking about this issue than in the past, and a greater tendency towards believing survivors and aiming to be trauma-informed. Accompanying this societal change is burgeoning information available to people on the internet which was included in one of the recovery narratives of our participants. The availability of online information and psychoeducation for support can empower survivors to take control of their recovery journey. Continued pervasive societal norms that act in support of perpetrator behaviour was also cited, however, as detrimental to recovery journeys. Hence, our data reflect helpful societal progress, but the need to continue to push to further this empowering and supportive agenda. These findings align with recent discussion in the academic literature about the need to understand better the structural and social causes of sexual and domestic violence in our attempts to prevent it and support those who are victims of it. 178
There were challenges identified in relation to accessing the right kind of care, with many of our participants talking about unsuccessful attempts at therapy and inadequate offers of care that did not suit their needs. Ultimately our narratives where there is hope of recovery demonstrate a level of acceptance that recovery will be a long road, and that a range of different therapies and mind and body connecting activity (such as yoga and meditation) may be useful for that process. These findings reflect those from our two Cochrane Reviews to some extent, which provide emerging evidence of benefit from less traditional interventions and therapies such as trauma-informed yoga (see Chapter 3 of this report). 36,42 Similar to our qualitative Cochrane Review which found that interventions led to a wide range of benefits,42 the narratives of our participants showed recovery as having a range of different outcomes that they viewed as beneficial including reductions in anxiety and flashbacks and the ability to engage in activities that they enjoyed doing such as physical activity and volunteering.
Narratives of access and of recovery encompassed the particular challenges there are for those who have complex trauma to deal with. These are often individuals who have experienced a number of ACEs including abuse and neglect, who have a pre-existing mental health condition and who may be experiencing domestic as well as sexual violence. They may have been victimised many times and be at risk of re-victimisation. They may also have children to take care of. Services are not set up to provide the tailored, bespoke, multi-faceted and multidisciplinary care that survivors with these patterns of abuse need. The narratives of our participants show this poor response to complex cases is likely contributing to the lack of recovery experienced.
Strength and limitations
Large-scale qualitative inquiry into the support and recovery experiences of survivors of sexual violence is challenging to accomplish. A strength of this study is that it has achieved the collation of detailed narratives of these experiences from a large sample of SARC service users as well as survivors who have not accessed SARC. The sample likely represents the most diverse to date in terms of its representation of cultural, linguistic and ethnic groups. It includes people of different genders and sexual orientation, and a range of ages, and levels of socio-economic status and education. It highlights the hope there is for recovery across these diverse groups, but also the gaps in support that exist for those experiencing complex trauma and from the most underserved communities. A further strength of this study is the way it complements the more traditional cohort and health economic analysis of outcomes, valuing multiplicity of knowledge and giving weight to experiential knowledge. Its inclusion within the research process has created opportunities for epistemic justice where silenced or marginalised voices are amplified. 30 As one participant put it, I wanted to really have a voice because I felt in other areas, when I was speaking up before about how I was feeling, it was getting diminished or just ignored. We acknowledge that a limitation was that we reached far fewer participants from non-SARC support contexts than intended. Those we have reached provided detailed narratives and provided insights into the complexity of intersecting forms of marginalisation, how these interact with sexual violence and abuse risk, and the nature of barriers to service access. This part of the study further illustrated the resilience of individuals and communities in the aftermath of abuse, and the creative and personal ways in which people navigate life after trauma.
Implications for health care
Health and care and support services have an important role to play in the recovery of survivors of sexual violence and abuse. Getting a good response from services matters and can contribute to good recovery. The response of wider society matters too though (e.g. see our #whatareyoudoing campaign39), and efforts to improve cultural and societal norms that may contribute to sexual violence and abuse and create the context for recovery are needed as well. Better outreach and training for staff to support those still in abusive environments to escape abuse and get support are needed. Support for those experiencing complex trauma histories, multiple victimisation with complex mental health and personal circumstances are also needed to avoid exacerbating health inequalities and meet the needs of the most vulnerable survivors.
Recommendations for research
Future research should focus in more depth on those with the most complex needs and who do not make it to care through SARCs. Given that minoritised groups are often least likely to access support in the aftermath of sexual violence via SARCs, it is not yet clear whether SARCs are the best care option for all.
Chapter 9 Discussion
This section overviews the key findings from across the MESARCH project studies; considers limitations of the project overall; sets out overarching implications for SARCs, and for health care more broadly; and makes recommendations for future research.
Main findings
Given the breadth and complexity of this 4.5-year project (2018–23), we have presented the key mixed-methods findings according to a typical SARC pathway. 179
Pre-SARC
A primary focus of this research was to understand what promotes or deters access to SARCs. Through sharing their personal narratives and experiences, participants shaped where and when their story starts, with most of them taking us far into the past. This lifespan lens underscores how, for many survivors, risk for sexual violence and abuse begins early in life. 180 This risk is reinforced by power dynamics connected with race, gender, socioeconomic status, religion, sexuality and disability, shown by our research team and others. 14,178,181–184
Our qualitative study identified gender-based violence rooted in gender inequality as a risk factor, especially poignant among the racially minoritised community sample of non-SARC attendees. Another theme concerned ‘silencing’. We gathered widespread accounts of risk arising from a lack of early education and everyday discourse about relationships, intimacy and sex. 185 When sexual violence and abuse did occur, the milieu of customary silence rendered survivors ‘voiceless’ and unable to draw on, otherwise available, informal support networks, and certainly not formal support. While there was a clear historical context for silencing among many of our older participants and a clear minoritisation context for many of the culturally diverse participants, silencing and shame about abuse was ever-present in narratives irrespective of time, place or people’s backgrounds. The absence of tools for talking about abuse and seeking help, and the debilitating context of shame was exploited and could perpetuate the abuse. The final area of risk concerns a triad of trauma, poor mental health and insecurity. Individual and composite narratives bear witness to life struggles as people strived to exit cycles of: (1) escaping abuse leading to unstable, unsafe living conditions; and (2) escaping chaotic, risky living thrusting people back into risk/victimisation; and all this occurring in a context of long-term mental health problems, which included substance misuse among the most minoritised participants in our samples. A central tenet is that trauma itself is a risk factor that continues to compound and shape risk (and recovery).
Our quantitative analysis on risk and mental health burden at entry to our cohort study effectively triangulated these qualitative findings. Consistent with the findings of other studies of people affected by sexual assault and abuse and attendees at SARCs,83,186 45% of participants joining the study had a prior history of mental health problems. For survivor-level factors, pre-existing mental health problems were associated with a 7.6-point difference on baseline PTSD compared to those without long-term mental health difficulties; each additional ACE was associated with a 1.4-point greater score on PTSD symptoms; there was strong evidence and an apparent dose-response for PTSD symptoms being higher for those with fewer financial resources with a 7.3-point difference, and strong evidence that being ‘unable to work’ was associated with a 10-point higher baseline PTSD score.
As such, it is critical that we adopt an intersectional framework for considering the implications of MESARCH findings for two reasons. Firstly, we need it to make sense of their complexity; we are witnessing layers of interconnecting power dynamics at play in the lives of survivors that relate to gender, race, socioeconomic status and disability (especially if we consider the burden of mental health as frequently the basis for survivors being unable to work). Secondly, there is the sheer scale of individuals affected by these risks and ‘dynamics’ and thus any measures to address disparities in access across the SARC pathway; enhance treatment options; build workforce resilience, skills and competencies; and achieve effective lifelong care must draw on a framework that centralises parity. Bearing in mind that the quantitative data are provided by participants who have managed to access help, it is concerning to consider the risk profile in communities and subgroups who are unable or prevented from getting help.
We do not wish to lose sight of the fact that abuse crosses all sociodemographic lines,187 and our sample included many individuals and communities without traditional risk factors – two-thirds were educated to A-level or above, approximately half reported few or no financial problems and many people were in work and the vast majority of participants was not racially minoritised. Yet, our careful ‘categorisation’ and analysis of the sample’s characteristics revealed a burden of childhood trauma (ACEs) that was noteworthy. Nearly four in every five participants in the study indicated four or more ACEs, widely considered as a threshold beyond which people are at risk of poor long-term mental and physical health outcomes. 188–190
Sexual assault referral centres: access and experiences of care
We now move beyond discussing risk to presenting insights into people’s experiences of accessing SARCs and then the care and support obtained in that setting. Rich data, from across the project, extend our understanding about access to SARCs as well as to the wider context of health, voluntary sector and social care services and justice, addressed further on (see Figure 10).
FIGURE 10.
Socio-ecological organisation of barriers to accessing sexual assault referral centres pathways.
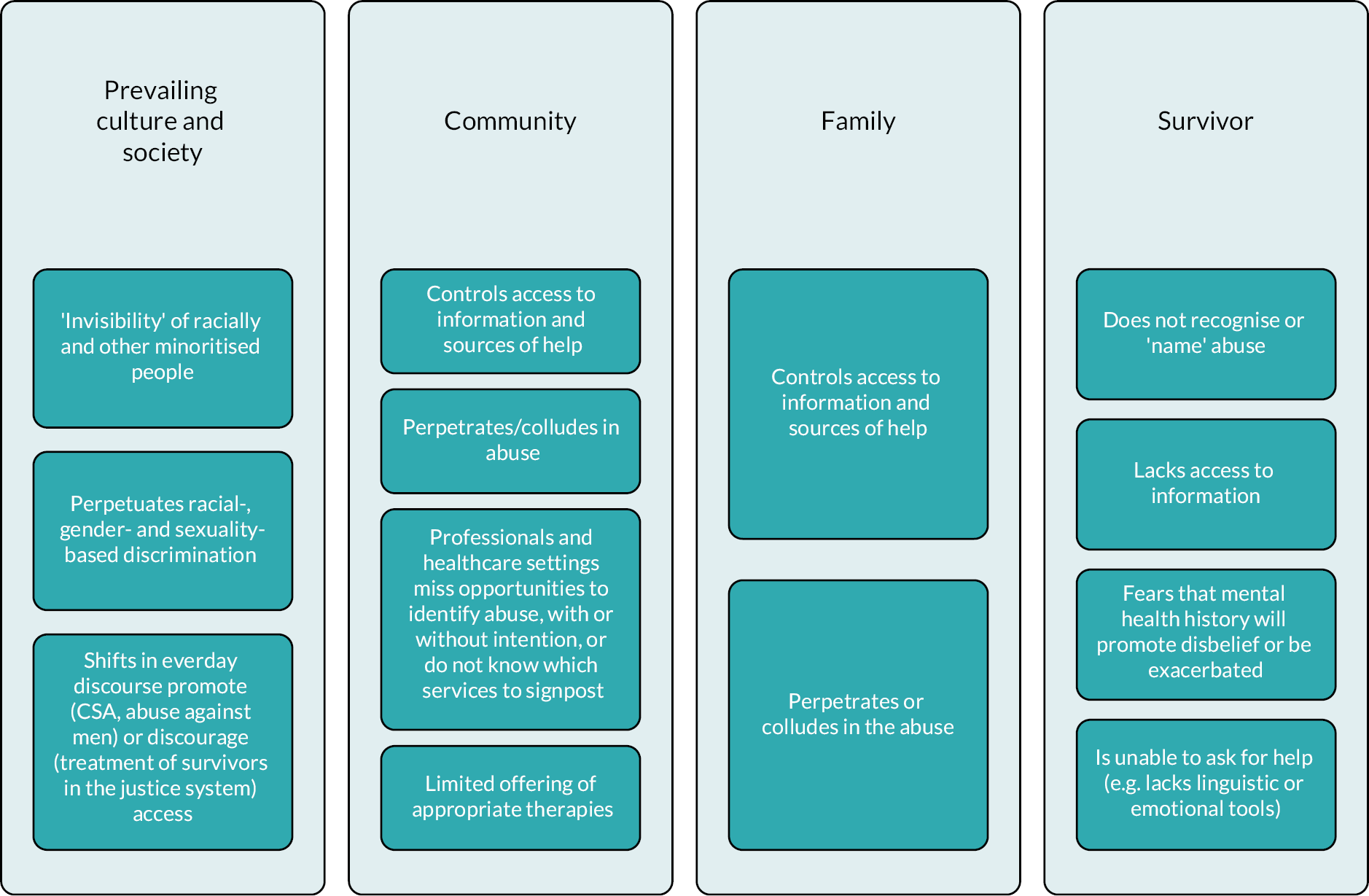
Survivors in this project had accessed 21 SARCs and delays and barriers to accessing SARC resided at individual, family and community levels, such as people not knowing about SARCs, not being ready to seek help, not being able to: After the incident that happened to me, I was in shock for 4 days. Those in our community sample who had experienced severe partner, family and/or community abuse and control (e.g. arranged or forced marriages) rarely perceived options. They were mainly focused on surviving and escaping abuse such that meeting wider needs from sexual abuse (e.g. sexual health care, specific crisis emotional support and forensic care) were not priorities and were neglected for long periods with pervasive long-term effects. Overall, nearly 45% of the recruited sample had accessed SARCs in the first 10 days since the sexual assault down from a pre-COVID-19 pandemic level of 60%, and the most typical perpetrator type was ‘acquaintance’ (40%), followed by partner-perpetrated sexual violence and abuse (25%) and strangers (20%); 13% of people in the sample had sought help in relation to exposure to CSA. Approximately 40% of people had a FME.
The delivery of health care and support by SARCs was consistently evaluated by survivors as exemplary. This finding was consistent across our cohort study, process evaluation and narrative study of minoritised groups. Our findings revealed no indicators of systemic harm, and half of the survivors accessing SARCs rated them as 90 or above for benefit in meeting needs arising from exposure to sexual violence and abuse. While behind every number there is a person and the research has examined individual-level responses, just four individuals reported SARCs had been harmful to them. This was the lowest rate of harm detected across any sector in this research. Our SARC process evaluation emphasised the importance of cohesive regional partnerships between SARCs and multiple statutory and voluntary sector agencies. This was also observed and articulated by survivors with regard to their satisfaction with on-site care, referrals and follow-up. We view SARCs as a vital gateway to recovery and it is often survivors’ first encounter with care in relation to sexual violence and abuse. As such, it is crucial that SARCs provide a safe, individualised response that facilitates the person to continue on the care pathway, as our research shows that there are multiple factors that can derail a person from continuing this journey.
Post-SARC: access and experiences of care
One of the main features of care after SARC was the ISVA service, a professional to advocate for and support survivors through the criminal justice process. Depending on the local model, some survivors continued care with a SARC-provided ISVA; for others, they were referred to an ISVA provided by the voluntary sector. ISVAs were integral to an effective pathway, and for the most part, survivors did not report difficulties accessing ISVA services and adapted during the COVID-19 pandemic to receiving that care online. 191 Furthermore, survivors reported high levels of satisfaction with the support provided by ISVAs. In the study, there were more than 4000 contacts with ISVAs; at baseline, 85% had an ISVA falling to 40% at 1 year in line with the reduction in open cases from 56% to 20%. Participants expressed difficulties when ISVA care was withdrawn in response to case closure and there appears to be variation nationally in the extent to which ISVAs can be accessed or maintained independent of criminal proceedings. The problem of access was much greater in relation to counselling services in the voluntary sector. Capacity issues did not affect SARCs to the same degree, and many survivors accessed other forms of support at SARCs (e.g. information and advice, structured emotional support sessions) to assist them in the time they were on waiting lists.
Young people did express concerns, especially young people from minoritised backgrounds: ‘This system isn’t very inclusive. It’s not very accessible and a lot of ethnic minorities and young black girls are subject to sexual violence at a young age and you have people in the system who don’t understand those backgrounds, don’t understand the sociology behind them and how they ended up being the victims of what they were. I think it’s just leading to a lack of justice being provided. There’s not an understanding of the lives of the people that are involved’.
The findings of the study suggested that participants accessed a wide range of healthcare and other public sector services (with GP visits and police contacts comprising the highest number of reported contacts). Although service use was higher among our participants at baseline (representing a period of nearly 100 days since participants had accessed a SARC), this decreased over time, for example, NHS contacts reduced from almost four contacts at baseline to less than one contact per person at 12 months (covering to the previous 6 months). While a full embedding of the wider health and social care access experiences within wider literature is beyond the scope of this research, we observed survivors’ mental health as a primary barrier to access in all settings. 192,193 For example, in the NHS, survivors struggled to be provided with psychological care specific to sexual abuse, when they had co-existing mental health diagnoses, because the latter was focused upon. There were parallels here with survivors in domestic abuse services, where there were gaps in care for the sexual abuse that had been perpetrated by partners. 6 Another common scenario was being unable to access therapies on the NHS seen as appropriate for complex trauma. Yet another was NHS referral ‘loops’ – patterns of GP referral to mental health, and discharge back to GPs, who were often seen to be ill-equipped or unwilling to support mental health needs of survivors. 186 Formal mental health expertise to identify and support mental health concerns remains limited within the SARC skill mix; the MiMoS project found that staff lacked clarity about pathways into the mental health services together with high thresholds for accepting service users and long waiting lists. 66 As we did with SARCs, we explored survivors’ experiences of harm and benefit in different sectors post-SARC. The findings from the voluntary sector services replicated what we found for SARC – a median of 90, suggesting that half of the people rated maximum benefit scores across a rich landscape of support provision for survivors. The median score for the NHS was 75, with a notably higher proportion of survivors indicating that they experienced a harmful response from the NHS. Coping and recovery for survivors occur in a justice context,194 and while this study captures widespread evidence of positive action, police and justice lagged considerably behind in its harm-benefit profile. While 50% of participants indicated benefit scores more than 50, a quarter of the sample indicated they derived harm from their interactions and experiences: ‘The whole investigation process has been just as traumatic as the abuse, or in another way, worse’. While health care and other support services have come a long way towards providing safe, effective and compassionate care for survivors, society continues to grapple with its poor performance in meeting justice needs. While an in-depth discussion of findings on these aspects is beyond the scope of this research, the next section distils some of the key findings on the factors influencing recovery.
Effectiveness of SARC pathways for survivors of sexual violence and abuse
Central to our endeavour was to understand what impinges on outcomes for survivors. There were many outcomes assessed in the cohort study; here, we summarise the quantitative evidence for a reduction in trauma symptoms (PTSD-based PCL-5) as our primary outcome, complemented by survivors’ voices on recovery journeys. People entered the cohort study with a high trauma load – 70% scored above the diagnostic threshold for PTSD. There was strong evidence of associations between PTSD at baseline and past trauma burden (e.g. ACEs), health profiles (chronic mental health problems) and socioeconomic factors (e.g. economic deprivation). The study also found weak evidence that sexual violence perpetrated by partners, family members and people in positions of trust aggravated PTSD and there was a small effect of time since trauma (more time to SARC, more trauma detected at baseline).
At 1 year, the sample as a whole had achieved a MCID (mean reduction in 9 points > 0.5 SD69); however, 55% were still above the diagnostic threshold. There was no evidence for differences in PTSD at 1 year related to models of SARC service delivery participants had accessed (i.e. charity, police, NHS, private sector provision). Cost-utility analyses also identified no significant difference in cost per QALY gained between these different models of SARC service delivery. Similarly, we did not detect an effect of the ISVA model (i.e. SARC ISVA or non-SARC ISVA). Although intensity/frequency of service use was associated with trauma at baseline, we detected no effect of level of service use over the year or did we detect an effect of harm-benefit from the police/justice response on the PTSD outcome. Thus, the only predictor for PTSD at 1 year was the baseline burden of PTSD, which has been shown to be strongly determined by several well-defined pre-offence characteristics, and to some extent, non-recent sexual violence and abuse and proximity to the perpetrator. Our research also suggests that those with the highest trauma at baseline had the greatest improvement. Furthermore, while those with four or more ACEs had twice the odds of probable PTSD at baseline, this reduced (OR 1.5) at 6 months and effectively was null (OR 1.01) at 1 year. It would be promising if 12–18 months of care and support could dilute the effect of the ACE profile.
Showing clear parallels with our study, Khadr et al. reported based on a study of young survivors that the presence of a psychiatric morbidity 4–5 months post-SARC was associated with baseline psychosocial vulnerability (defined as previous social services involvement, mental health service use, self-harm or sexual abuse), but not assault characteristics. 129 Khadr et al. recommended that CYP require comprehensive support to address high levels of pre-existing vulnerability and psychological comorbidity, and prevent re-victimisation. Our own CYP study observed that recovery and healing was influenced by how quickly CYP accessed support, its content and duration, the location and context of care, how well services worked together (aligning with findings from our process evaluation) and CYP’s interactions with professionals at SARCs and across sectors.
Our process evaluation and narrative analysis helped contextualise these quantitative findings. On the whole, SARCs working with ISVA services is suggested to be an effective gateway to care for survivors: ‘I feel that the support I’ve had from the ISVA service, from SARC, has given me a better outlook on life’. A vast array of other factors interacting at different levels played a role in survivors’ healing journeys (see Figure 11). Some overlapped with ‘access’ barriers and enablers (see Figure 10). Finding therapeutic fit for presenting issues and, importantly, past or complex traumas and this being available within statutory health services was a gap that arose post-SARC. Furthermore, perceiving that justice had prevailed and holding a belief that the police were thorough, respectful, communicative and honest about the investigation was important in recovery and healing.
FIGURE 11.
Socio-ecological organisation of recovery in the context of the sexual assault referral centres pathway.
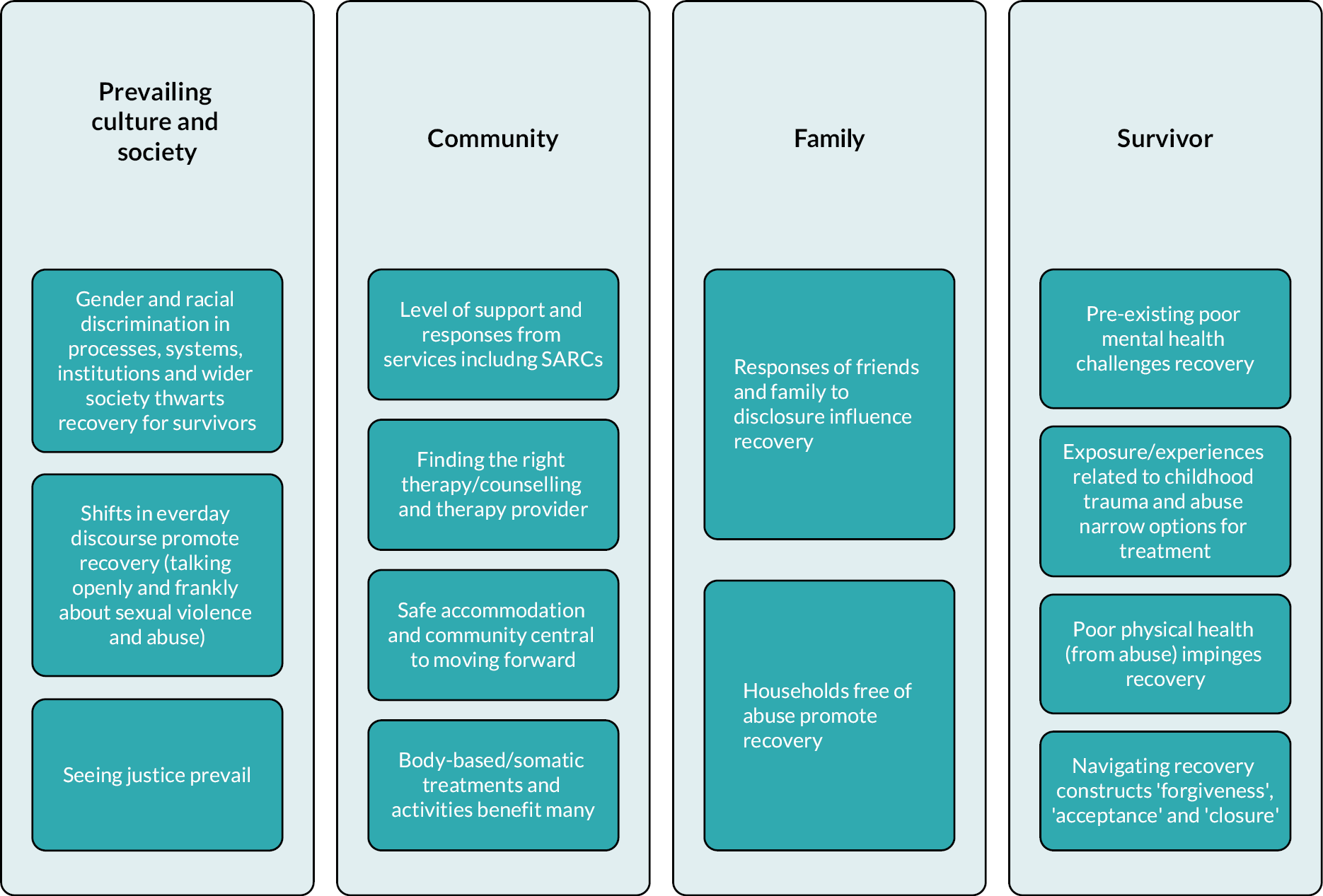
Effectiveness of SARC pathways for children and young people
Our CYP study showed that the holistic care and support provided by SARCs played a critical role in young survivors’ recovery. Their access to support at SARC relied on professionals referring them to SARC once they disclosed the abuse. Improvements in young survivors’ physical and mental health, education, interpersonal relationships and re-engaging in a wide range of areas of their lives was affected by how quickly they accessed support, its content and duration, the location and context of care. CYP’s readiness to access support was impacted by factors such as re-exposure to abuse, living situations or the quality of relationship with a professional. This mirrors findings in the context of CYP experiencing domestic abuse where readiness to engage in support involves a complex interplay of individual, relational and contextual factors. 195 Notably, when young survivors in this study experienced cohesiveness of support between professionals across and beyond the SARC pathway, they had an increased sense of safety. Importantly, interactions with professionals that lacked a ‘trauma-informed’ approach at any stage of their recovery was associated with poor or delayed healing. This supports findings that show how accessing a service in itself does not necessarily improve trauma symptoms. Rather, it is the quality of services and survivors’ interactions with professionals that lead to long-lasting positive effects. 131,150
Effectiveness of psychosocial interventions for survivors of sexual violence and abuse
Sexual assault referral centres represent a gateway to pathway of care for survivors that ideally opens up options to various psychosocial interventions. These may be accessed through NHS services, including Talking Therapies, for anxiety and depression programme (formerly, Improving Access to Psychological Therapies, IAPT) and community mental health, where many of the traditional trauma-focused interventions are offered. Such therapies are also available in the voluntary sector, which additionally offered survivors in our studies a wide range of arts-based, body-based, counselling and social interventions. There are many examples of people accessing therapies through private routes due to being unable to access support they felt they needed or access that in a timely way. Our Cochrane Review, synthesising findings from 36 randomised controlled trials from various parts of the world, found a large reduction in PTSD symptoms and depression at post-treatment following psychosocial interventions compared with controls. 36 Our review also suggested that CBT with a trauma focus such as Prolonged Exposure and Cognitive Processing Therapy and other exposure-based therapies (e.g. EMDR) probably benefit survivors of sexual violence and abuse over non-trauma-focused intervention. However, trauma-focused interventions may result in higher treatment non-completion and some survivors may continue to experience a high symptom load post-treatment. In response to the limits of trauma-focused interventions, there have been calls for more effective approaches to the management of PTSD,196 especially for sexual violence and abuse exposure. 197 One contribution of our review is the synthesis of several novel treatments across a range of promising new areas such as RTM; trauma-sensitive or trauma-informed yoga; Lifespan Integration (LI); and neurofeedback. Some of these treatments have been shown to be effective among survivors of other types of trauma (e.g. RTM),198 while other therapies have scarce evidence in any population.
Strengths
This mixed-methods, multi-study project is the most wide-ranging analysis of health and experiences of care among survivors of sexual violence and abuse in the UK to date. It adds to the contribution made by Hughes et al. 66 on SARC service users’ mental health and alcohol and drug use needs by examining quality of care and service provision in four sectors over 1 year. There is an absence of longitudinal research in the UK investigating the health and well-being of survivors over time. We undertook recruitment, baseline assessments and two follow-ups with survivors in the context of NHSE’s model for the provision of SAAS in England generating not only an evaluation of SARCs, but the entire care pathway. Notwithstanding that this subpopulation represents the ‘tip of the iceberg’ in terms of wider experiences of survivors of sexual violence and abuse in the general population, we have demonstrated a safe, effective and feasible approach to understanding survivors’ experiences over time.
A major contribution of this work lies in our best practice approach to PPI, which opens new opportunities for undertaking research with trauma populations. 199 An external evaluation by Survivors’ Voices identified ‘clear evidence of trauma-informed practice in the approach of the MESARCH team which enabled and supported survivors to make a vital contribution to the project, as both participants and co-producers, centering lived experience at the heart of the research’. Key strengths were strong attention to creating a safe environment and demonstrating genuine care for survivor well-being, built on trustworthy relationships; commitment to authentic engagement, involving survivors as both participants and co-producers, which empowered survivors and researchers; successful amplification of the voices of survivors, bringing the validity and impact of lived experience to trauma, abuse and violence research.
Our project contained many other innovative features including the breadth of its methods, which enabled people from many different backgrounds to engage with us and participate. Further diversity of contributions, which extend the relevance of our findings, includes our qualitative work with CYP to understand about access to SARC and recovery. Our process evaluation gathered views of professionals regarding the work of SARCs across the sector, reflecting both inward and onward referral points. We also ensured a focus on racially minoritised survivors in our small non-SARC community sample and also through the use of maximum variation sampling within our cohort. We gathered life narratives from a whole range of minoritised groups including socially disadvantaged people, those unable to work and living in insecure housing; we spoke to people with complex trauma, people with different disabilities, physical health conditions as well as including men, LGBTQ+ survivors and linguistically diverse people through interpreters.
Our Cochrane Review of trials represents the most comprehensive analysis to date on the efficacy of psychotherapies and other psychosocial interventions for survivors of sexual violence and abuse in adulthood. 36 Through both professionals’ and survivors’ contributions, our research showcases the breadth of the crisis response, and clinical, advocacy, police and support work occurs across sectors and the resilience, technical skill, knowledge and collaboration professionals demonstrate in enabling access to care, justice and recovery for their clients and services users.
Our research has been translated into efforts to prevent violence and abuse and its sequelae, for example, our #whatareyoudoing campaign (https://whatareyoudoing.coventry.domains). With a short film39 about domestic and sexual abuse in a young couple’s relationship as a centrepiece, it has received widespread endorsement from survivors, practitioners and policy makers.
Limitations
One of the key limitations relates to the composition of our sub-study samples, which reflects the challenges of conducting research with survivors of sexual violence and abuse. While recruiting ISVA/third-sector services and relying on them to refer survivors to our research for our adult and children’s studies was the most optimal approach to us and enabled the research to be conduct safely, we do recognise that commitment by site was highly variable. Recruitment challenges meant that our adult cohort study sample size had to be re-calculated, and revisions were made to the study protocol. We also acknowledge that our adult cohort study did not have a control group (non-SARC population) for comparison, which limits a conclusion that access to SARC and other health or therapeutic care explained the reduction observed in PTSD. We could reach participants from a non-SARC population in the narrative study. These participants provided detailed insight into their experiences of services, but the numbers were low. Although we captured a large number of survivors beyond medico-legal services/SARCs through our Cochrane Reviews good support, one key limitation of our primary research is the lack of applicability beyond SARC settings and users, and it is known that most people who are victims of sexual violence and abuse do not access SARCs.
The study was delivered through the COVID-19 pandemic and had a number of implications. The COVID-19 pandemic impacted the extent to which services were able to commit to supporting the project in its recruitment of service users, due to the demands on services and the workforce. Furthermore, the COVID-19 pandemic changed the landscape of service provision and there were difficulties in disentangling what support participants had actually received from SARCs. Importantly, we had to adjust the inclusion criteria for the adult cohort study to include remote services use when our intention had been to only recruit those who presented at SARCs in person. This will have likely influenced the research in ways we are yet to discover, for example, it is conceivable remote models diluted potential benefits of the SARC pathway.
As outlined in Chapter 7, we experienced a number of challenges in recruiting to the children’s study. One of the key limitations is that the voices of young participants from diverse cultural communities, of individuals with physical disabilities and of boys and young men, were largely missing in this study. Furthermore, the study only represented two paediatric SARC services and is therefore not representative of the wider youth population accessing SARCs in England.
There were limitations associated with the data we collected. In our process evaluation, we were unable to gain depth in respect of forensic integrity and equipment as being beyond the scope and expertise of the team. Yet, this is recognised as a key issue for the sector and criminal justice journeys. An important and novel contribution of our cohort study was to gather comparative data on the experiences of benefit and harm across several sectors. We faced challenges in how to best measure perceived harm and benefit of services as part of a telephone interview. The approach we used was highly subjective, with the parameters being interpreted differently by participants.
There was a high level of missing data on resource use at all timepoints as the section was often omitted where participants were finding the interview difficult. As a result, this limited the type of analysis we were able to conduct, with a complete case analysis being undertaken. By excluding those who did not have complete data in relation to these measures at all timepoints, we note that there may be bias in the results. Finally, we are aware that the 12-month follow-up in the present study did not allow longer-term impacts to be fully captured in our study. We had terminated the 12-month follow-up owing to the cost associated with the COVID-19 pandemic and the wider difficulties of recruiting from a trauma population.
Equality, diversity and inclusion
In the Cochrane Reviews, process evaluation and main cohort study our representation of important population characteristics was restricted to some extent to those included within existing studies, employed in sexual assault services, and who have accessed SARCs. In saying that, the 36 studies of the Cochrane Review included 60% global majority and/or minoritised survivors, 15% of our cohort sample comprised individuals from racially minoritised groups, and we had considerable diversity across disability, mental health and socioeconomic status. We took several steps to expand the reach of our work, for example, in the representations in our videos and other recruitment materials. Because it is known that minoritised groups may be at greater risk of sexual violence and abuse and are under-represented in SARCs, we conducted our narrative study with intentional recruitment through maximum variation sampling to reach minoritised people (including people who have not accessed SARC). We worked consistently with our LEG to expand diversity of that group and the participants in the sub-studies. Our LEG comprised people with a range of ethnic and linguistic backgrounds, ages, genders and sexual orientations, educational level and work backgrounds. Recognising the marginalisation and inequalities experienced by survivors of abuse, especially survivors of CSA, we applied ourselves consistently to growing the skills, opportunities and experiences of our LEG colleagues through training, development and engagement (see Chapter 2). Our research team (e.g. field workers) comprised people from a range of different ethnic, cultural and linguistic backgrounds, bringing a diversity of life experience to the day-to-day work of the study. However, we would be more focused on building the survivor leadership of future projects in this field as well as the cultural and ethnic diversity at the leadership level.
Implications for health care
-
Our findings are strong evidence of good practice at SARCs in England.
-
Sexual assault referral centres are a safe, effective point of care for survivors of sexual violence and abuse, offering a gateway to other SAAS, the NHS and police.
-
Sexual assault referral centres must recognise the vulnerability affecting their service users – lifetime traumas, pre-existing mental health ill-health and social disadvantage – which predicted high trauma symptoms in the weeks and months after SARC.
-
Survivors with risk factors associated with PTSD warrant tailored support and follow-up to ensure they are able to access onward care (e.g. sexual health).
-
Early (pre-offence) interventions among vulnerable CYP may be vital to improve safety and reduce risks of sexual violence and abuse exposure.
-
We did not detect evidence that models of SARCs and ISVA services differentially affected service user health outcomes.
-
Enhancing care and support for survivors comes from sharing best practice and building and maintaining strong alliances with police forces, ISVA services and voluntary sector partners, health and social care; agencies should continuously review and refine local care pathways, which include survivor and service user stakeholders.
-
Our findings lend strong support for access to ISVAs with specialisms around supporting particularly vulnerable or minoritised groups given the difficulties reported by these subgroups in accessing justice and other support.
-
Sexual assault referral centres continue to lack visibility among victims and survivors of sexual violence and abuse relative to voluntary sexual violence services and outreach to minoritised groups may improve this.
-
Widespread satisfaction among survivors in relation to provision in the voluntary sector with the exception of waiting lists for access to psychological therapies.
-
Mainstay psychological therapies for PTSD provide benefits for survivors but do not meet the needs of all survivors. Resourcing the voluntary sector further may increase access to alternatives, as we found high levels of satisfaction and recovery in response to a range of novel and inexpensive therapies (e.g. require fewer sessions), treatments and activities that may lack an established scientific evidence base.
-
It is the responsibility of practitioners and therapists to make decisions about treatments appropriate to the circumstances of clients, in consultation with them and their families, carers or guardians.
-
All healthcare settings need to work towards implementing trauma-competent practices as we found evidence of inadequate and even harmful responses in primary care and mental health.
-
Steps to address health disparities and enhance access to the SARC/SAAS care pathway must be designed and delivered within a health inequalities and intersectional framework given the prominence of silencing by perpetrators, families, communities, professionals, services, institutions and wider society.
-
The findings call for cohesive commissioning strategies that recognise the value of partnerships in promoting optimal access and care experiences for survivors.
-
Recognising the distinction between PTSD and complex PTSD when considering suitable trauma treatment is important, as complex PTSD may be less amenable to trauma-focused approaches. It underscores the value of a wide range of treatment options and alternatives to frontline therapies. Many such alternative treatments could have relevance to clinical and policy decisions because they are often shorter and therefore less costly, easier to deliver, may be deliverable online, are more feasible for survivors to access, and scalable.
Recommendations for research
-
The main research recommendation arising from the Cochrane Reviews, which is supported by the primary qualitative findings, is to build the evidence base for a variety of novel (and not necessarily trauma-focused) and potentially cost-effective (e.g. shorter delivery, computer-based or online) treatments and therapies, thereby expanding options for people to heal after abuse.
-
We advocate that all and any future research with adult and child survivors of sexual violence and abuse in any context is conducted in line with principles and methods required for trauma-informed research practice. In particular, future research must engage, build and support a team of experts-by-experience; this enhances the experience of the research for participants and researchers, and increases the feasibility and scientific quality of research. Toolkits and guidance on best practice methodological approaches to achieving this are timely.
-
A contribution of this work is to inform the literature on HRQoL and resource use in a sexual violence and abuse population. Additional research is needed to compare the costs of pathways and PTSD burden among those who access SARC with survivors who do not.
-
Further research needs to distil what ‘trauma-informed’ practice looks like across sectors, and develop models of translation.
Concluding remarks
This mixed-methods multi-workstream programme of research, capturing the data of 6901 participants from a diverse range of backgrounds across its reviews, screening/service level data and primary research, represents the most substantive investigation to date into the health and well-being, and recovery experiences of survivors of sexual violence and abuse. It provides clear evidence of the positive impact of SARCs in England, in terms of support and aftercare provided to survivors. There is also clear evidence that ISVA and third-sector support is beneficial for the vast majority of survivors and that good inter-agency collaboration contributes to effective care and support provided.
There is more work to do, however, to improve the response of some NHS services and of the response provided by police, where they are involved. There is room for improvement in the time taken for survivors to access therapeutic treatment and support and for the range of available types of support and treatment to be increased. There are also clear gaps in the provision of support for people who have experienced complex trauma and who may experience additional barriers to accessing treatment and support due to membership of one or more marginalised groups. More tailored, culturally-competent outreach and service provision is required to help address health disparities related to experience of sexual and domestic violence. Action is also required to continue to improve cultural and societal norms that support and perpetuate sexual violence and abuse and create a challenging context within which survivors must work to recover. The findings of this research set out a clear pathway for developing and offering effective support and care to survivors of sexual violence and abuse for NHSE and its partners and stakeholders, in the future.
Additional information
We would especially like to thank the survivors who took part in the study, whose collective voice and courage is central to this work. We would like to thank all the SARCs and third-sector staff and agencies for their tremendous support in recruiting survivors to the study. Particular thanks go to The Survivors Trust for their efforts in supporting recruitment and to Fay Maxsted OBE for her ongoing support and contribution as a panelist at our final knowedge sharing event. Thanks also go to the professionals from SARCs and other agencies who contributed to the process evaluation of SARCs. We are grateful for and humbled by the immense contribution and commitment to this work by our Patient and Public Involvement Group (Lived Experiences Group) members. The expertise of Dale ‘Banksy’ Banks, Kayleigh Coulton, Gilllian Finch, Geraldine, Nicola Herbert, Rosie Stone and other members was vital and underpins the research. We give our thanks to the survivor-led organisations Survivors’ Voices and Little Ro for expertly undertaking the independent evaluation of Patient and Public Involvement across MESARCH and to Concetta Perôt (consultant and Survivors’ Voices co-founder) for training the team on research with trauma survivors and facilitating panels on lived experience at our knowledge-sharing events. We wish to thank our Study Steering Committee, ably chaired by Professor Roger Ingham, for expert advice and support throughout the life of this project. We are thankful for the all guidance and support that we received from our Data Monitoring and Ethics Committee, chaired by Professor Anne Spencer.
We are also grateful to the NIHR HSDR team for their funding and huge support throughout this project, and to the NIHR reviewers for the [anticipated] detailed and expert feedback, which has helped the report considerably. We wish to thank the Sexual Assault and Abuse Services Programme team at NHSE for their support in this work, in particular, enabling us to reach and recruit SARC sites, assisting our understanding of the policy context for this research and promoting knowledge transfer from the project.
Our thanks go to our Coventry University colleague Joanne Lloyd for supporting the operational aspects of MESARCH from award through to completion; to Dr Maxine Whelan for her contribution to the quantitative systematic review, and to Dr Cain Clark for his advice on sample size calculations. Lastly, we wish to recognise the valuable contributions of Dr Alison Hipwell, Sri Padma Sari, Sarah West, Sara Arouch, Kathleen Hill, and Gail Westerman to data collection, entry, cleaning and preparation.
Contributions of authors
Lorna J O’Doherty (https://orcid.org/0000-0003-0816-9321) (Professor, Trauma, Mental Health and Recovery) was the principal investigator and conceived of and led the study. Lorna oversaw all aspects of the research delivery, analysis and interpretation of findings and is lead author of the final report.
Grace Carter (https://orcid.org/0000-0001-7244-037X) (Research Fellow, Abuse, Trauma and Forensic Psychology) led all ethics submissions and the children and young people’s (CYP) study. Grace conducted the qualitative systematic review; co-led recruitment and data collection for the cohort study; participated in the analysis of the SARC process evaluation study; and contributed to the final report.
Emma Sleath (https://orcid.org/0000-0002-3333-5742) (Associate Professor, Forensic Psychology) contributed to the conception and design of the study, led the SARC process evaluation and contributed to the final report.
Katherine Brown (https://orcid.org/0000-0003-2472-5754) (Professor, Behaviour Change in Health) contributed to the conception and design of the study, was heavily involved in the cohort study and led the embedded qualitative study and contributed to the final report.
Sarah Brown (https://orcid.org/0000-0002-5859-4214) (Adjunct Professor, Forensic Psychology) contributed to the conception and design of the study, led the two Cochrane Reviews, was involved in analysis of the SARC process evaluation study, advised on the CYP study and contributed to the final report.
Eleanor Lutman-White (https://orcid.org/0000-0003-0219-7567) (Research Fellow, Social Work) co-led recruitment and data collection for the cohort study, conducted qualitative data analysis for the SARC process evaluation and the CYP study and contributed to the final report.
Louise Jackson (https://orcid.org/0000-0001-8492-0020) (Associate Professor, Health Economics) contributed to the conception and design of the study, led and conducted the health economics evaluation, and contributed to the final report.
Jon Heron (https://orcid.org/0000-0001-6199-5644) (Associate Professor, Medical Statistics) led the statistical analysis, writing and interpretation for the cohort study and contributed to the final report.
Priya Tek Kalsi (https://orcid.org/0009-0000-5344-5183) (Public Engagement Officer) led all aspects of Patient and Public Involvement and specifically was the liaison for our Lived Experiences Group, responsible for ensuring optimal involvement of survivors in MESARCH. Priya was heavily involved in recruiting sites for all sub-studies, and to this end, the training of ISVAs and other professionals and she contributed to the final report.
Olufunmilola C Ladeinde (https://orcid.org/0009-0008-0992-8725) (Research Assistant, Psychology) conducted recruitment and data collection and data management for the cohort study and CYP study, as well as analysis of the CYP study, recruitment for the embedded qualitative study and contributed to the final report.
Dianne Whitfield (https://orcid.org/0009-0004-8389-1052) (Voluntary sector leader, psychotherapist) contributed to the conception and design of the study and reviewed the support provision to participants over the life of the project, provided support, supervision and training on well-being and self-care to the teams and commented on the final report.
Rachel Caswell (https://orcid.org/0000-0002-9246-2581) (NHS Consultant in Sexual Health and HIV Medicine) contributed to the conception and design of the study, advised on sexual health within the cohort study, and commented on the final report.
Millicent Gant (https://orcid.org/0009-0006-3426-3978) (SARC Manager, Police) contributed to the conception and design of the study, informing and facilitating recruitment of SARCs, and advised on the policing and SARC context of the research and aspects of the economic evaluation. Millie enabled the cohort pilot study, and commented on the final report.
Gemma Halliwell (https://orcid.org/0000-0003-1094-0007) (Voluntary sector leader and researcher) conducted the qualitative systematic review, developed knowledge-sharing materials, contributed to the data collection and analysis of the cohort study and contributed to the final report.
Riya Patel (https://orcid.org/0000-0001-6572-5924) (Research fellow, Health Psychology) contributed to the design and delivery of the embedded qualitative study and undertook the analysis, and contributed to the final report.
Gene Feder (https://orcid.org/0000-0002-7890-3926) (Professor, Primary Care) contributed to the conception and design of the study, providing insights across the project from a primary care perspective. Gene participated in the Cochrane Reviews, interpretation of findings from the cohort study and commented on the final report.
Disclosure of interests
Full disclosure of interests: Completed ICMJE forms for all authors, including all related interests, are available in the toolkit on the NIHR Journals Library report publication page at https://doi.org/10.3310/CTGF3870.
Primary conflicts of interest: All authors received funding through the NIHR HS&DR funding 16/117/04 for the MESARCH study. Grace Carter declares that she is a committee member of the Violence Against Women and Girls Research Network. Emma Sleath declares that she was awarded funding for the NIHR RfPB project – DREAMS project. Sarah Brown declares that she has contracts with the Centre of Expertise on Child Sexual Abuse; is a nominated worker of the Independent Inquiry into Child Sexual Abuse Research Team, Fellow and Chair; and, from May 2023 onwards, is a board member (as Past-Chair) of the National Organisation for the Treatment of Abuse and member and fellow of the Association for the Treatment of Abuse. Gene Feder declares that his salary was supported by the UK Prevention Research Partnership (Violence, Health and Society; MR-VO49879/1), an initiative funded by UK Research and Innovation Councils, the Department of Health and Social Care (England) and the UK devolved administrations and leading health research charities, and that he participates on a Data Monitoring and Ethics Committee for a falls prevention trial.
Patient data statement
This work uses data provided by patients and collected by NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that data are stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review. We will make data available to the scientific community with as few restrictions as feasible, while retaining exclusive use until the publication of major outputs.
Ethics statement
The cohort pilot study received ethical approval from Coventry University Research Ethics Committee (Project ID: P75698 approved on 25 October 2018) and West Midlands Black Country Research Ethics Committee (REC reference: 18/WM/0376). The SARC process evaluation study and the cohort study received ethical approval from Coventry University Research Ethics Committee (Project ID: P86669, approved 9 May 2019) and East Midlands Derby Research Ethics Committee and NHS Health Research Authority (REC reference: 19/EM/0198, approved 30 July 2019). The qualitative study (which was embedded within the cohort study) was later approved by Coventry University Research Ethics Committee (Project ID: P125800, approved on 18/2/2022) and East Midlands Derby Research Ethics Committee (REC reference: 19/EM/0198, approved 8 February 2022). The children and young people’s study received ethical approval from Coventry University Research Ethics Committee (Project ID: P94373, approved on 7 February 2020); and West Midlands Black Country Research Ethics Committee and NHS Health Research Authority (REC reference: 20/WM/0097, approved on 4 June 2020).
Information governance statement
Coventry University is committed to handling all personal information in line with the UK Data Protection Act (2018) and the General Data Protection Regulation (UK and EU GDPR). Under the Data Protection legislation, Coventry University is the Data Controller, and you can find out more about how personal data are handled, including how to exercise your individual rights and the contact details for the Data Protection Officer here: https://www.coventry.ac.uk/gdpr-and-data-protection/key-contacts/.
Department of Health and Social Care disclaimer
This report presents independent research commissioned by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by the interviewees in this publication are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, MRC, NIHR Coordinating Centre, the HSDR programme or the Department of Health and Social Care.
This monograph was published based on current knowledge at the time and date of publication. NIHR is committed to being inclusive and will continually monitor best practice and guidance in relation to terminology and language to ensure that we remain relevant to our stakeholders.
Publications
Brown S, Carter G, Halliwell G, Brown K, Caswell R, Howarth E, Feder G, et al. Survivor, family and professional experiences of psychosocial interventions for sexual abuse and violence: a qualitative evidence synthesis. Cochr Datab Syst Rev 2022;10(10):CD013648. https://doi.org/10.1002/14651858.CD013648.pub2
O’Doherty L, Carter G, Lutman-White E, Caswell R, Jackson L, Feder G, et al. Multi-disciplinary Evaluation of Sexual Assault Referral Centres for better Health (MESARCH): protocol for a 1-year cohort study examining health, well-being and cost outcomes in adult survivors of sexual assault attending SARCs in England. BMJ Open 2022. https://doi.org/10.1136/bmjopen-2021-057449
O’Doherty L, Whelan M, Carter GJ, Brown K, Tarzia L, Hegarty K, et al. Psychosocial interventions for survivors of rape and sexual assault experienced during adulthood. Cochr Datab Syst Rev 2023;10(10):CD013456. https://doi.org/10.1002/14651858.CD013456.pub2
O’Doherty L, Carter G, Lutman-White E, Etwaria R. Bringing Survivor Involvement into the Mainstream. In Winder B, Blagden N, Lievesley R, Swaby H, Hocken K, Banyard P, Harper CA, editors. Sexual Crime. Palgrave Macmillan, Cham; 2024. https://doi.org/10.1007/978-3-031-46626-7_2
Disclaimers
This article presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care.
References
- Office for National Statistics . Violent Crime and Sexual Offences: Intimate Personal Violence and Serious Sexual Assault 2015. www.ons.gov.uk/peoplepopulationandcommunity/crimeandjustice/compendium/focusonviolentcrimeandsexualoffences/2015-02-12/chapter4violentcrimeandsexualoffencesintimatepersonalviolenceandserioussexualassault (accessed 14 March 2023).
- Krug EG, Mercy JA, Dahlberg LL, Zwi AB. The world report on violence and health. Lancet 2002;360:1083-8.
- Office for National Statistics . Crime in England and Wales: Year Ending September 2022 2023. www.ons.gov.uk/peoplepopulationandcommunity/crimeandjustice/bulletins/crimeinenglandandwales/yearendingseptember2022 (accessed 14 March 2023).
- World Health Organization . Global and Regional Estimates of Violence Against Women: Prevalence and Health Effects of Intimate Partner Violence and Non-Partner Sexual Violence 2013.
- Campbell JC. Health consequences of intimate partner violence. Lancet 2002;359:1331-6.
- Campbell J, Jones AS, Dienemann J, Kub J, Schollenberger J, O’Campo P, et al. Intimate partner violence and physical health consequences. Arch Intern Med 2002;162:1157-63.
- Tewksbury R. Effects of sexual assaults on men: physical, mental and sexual consequences. Int J Men’s Health 2007;6:22-35.
- Guina J, Nahhas RW, Kawalec K, Farnsworth S. Are gender differences in DSM-5 PTSD symptomatology explained by sexual trauma?. J Interpers Violence 2016;34:4713-40.
- Liu H, Petukhova MV, Sampson NA, Aguilar-Gaxiola S, Alonso J, Andrade LH, et al. World Health Organization World Mental Health Survey Collaborators . Association of DSM-IV posttraumatic stress disorder with traumatic experience type and history in the World Health Organization world mental health surveys. JAMA Psychiat 2017;74:270-81.
- Pietrzak RH, Goldstein RB, Southwick SM, Grant BF. Prevalence and Axis I comorbidity of full and partial posttraumatic stress disorder in the United States: results from Wave 2 of the National epidemiologic survey on alcohol and related conditions. J Anxiety Disord 2011;25:456-65.
- Heeks M, Reed S, Tafsiri M, Prince S. The Economic and Social Costs of Crime.2nd edn. Research Report 99. London: Home Office; 2018.
- Abrahams N, Mhlongo S, Dunkle K, Chirwa E, Lombard C, Seedat S, et al. Increase in HIV incidence in women exposed to rape. AIDS 2021;35:633-42.
- Weare S, Pattinson B, Hulley J. A Review of the National Male Survivors Helpline and Online Service: Project Report. Lancaster: Lancaster University; 2019.
- Basile KC, Breiding MJ, Smith SG. Disability and risk of recent sexual violence in the United States. Am J Public Health 2016;106:928-33.
- Ellsberg M, Arango DJ, Morton M, Gennari F, Kiplesund S, Contreras M, et al. Prevention of violence against women and girls: what does the evidence say?. Lancet 2015;385:1555-66.
- O’Driscoll C, Flanagan E. Sexual problems and post-traumatic stress disorder following sexual trauma: a meta-analytic review. Psychol Psychother 2016;89:351-67.
- World Health Organization . Guidelines for Medico-Legal Care for Victims of Sexual Violence 2003.
- Stefanidou T, Hughes E, Kester K, Edmondson A, Majeed-Ariss R, Smith C, et al. The identification and treatment of mental health and substance misuse problems in sexual assault services: a systematic review. PLOS ONE 2020;15.
- NHS England . National Service Specification for Sexual Assault Referral Centres. Incorporating NHS Public Health Functions Agreement 2023–24 2023.
- NHS England . Sexual Assault and Abuse n.d. www.england.nhs.uk/commissioning/sexual-assault-and-abuse/#sarcs (accessed 14 March 2023).
- Lovett J, Regan L, Kelly L. Sexual Assault Referral Centres: Developing Good Practice and Maximising Potentials. Home Office Research Study No 285. London: Home Office; 2004.
- O’Doherty L, Sleath E, Carter G, Heron J, Jackson L, Caswell R, et al. Multi-Disciplinary Evaluation of Sexual Assault Referral Centres for Better Health (MESARCH): Study Protocol Version 3.3 2022. https://www.fundingawards.nihr.ac.uk/award/16/117/04 (accessed 26 February 2024).
- Perôt C, Chevous J. Turning Pain into Power: A Charter for Organisations Engaging Abuse Survivors in Projects, Research and Service Development 2018. http://survivorsvoices.org/wp-content/uploads/2018/10/Survivors-Charter-Final-V1-for-Piloting-Oct-2018.pdf (accessed 14 March 2023).
- McClain N, Amar AF. Female survivors of child sexual abuse: finding voice through research participation. Issues Ment Health Nurs 2013;34:482-7.
- Yuen B, Billings J, Morant N. Talking to others about sexual assault: a narrative analysis of survivors’ journeys. J Interpers Violence 2019;36:NP9714-37.
- Kennedy S, Bewley S, Chevous J, Perôt C, Vigneri M, Bacchus LJ. A systematic review that evaluates the extent and quality of involving childhood abuse survivors in shaping, conducting and disseminating research in the UK. Research for All 2022;6:1-25.
- Chevous J. Survivors Voices: Survivor Involvement in Research Ladder (Pilot Draft 2). urvivor Voices; 2018.
- Beresford P. User involvement in research and evaluation: liberation or regulation?. Soc Pol Soc 2002;1:95-105.
- INVOLVE . Briefing Notes for Researchers: Involving the Public in NHS, Public Health and Social Care Research 2012.
- Fricker M. Epistemic Injustice: Power and the Ethics of Knowing. Oxford: Oxford University Press; 2007.
- Palmer VJ, Weavell W, Callander R, Piper D, Richard L, Maher L, et al. The Participatory Zeitgeist: an explanatory theoretical model of change in an era of coproduction and codesign in healthcare improvement. Medical Humanities 2019;45:247-57.
- Richard L, Piper D, Weavell W, Callander R, Iedema R, Furler J, et al. Advancing engagement methods for trials: the CORE study relational model of engagement for a stepped wedge cluster randomised controlled trial of experience-based co-design for people living with severe mental illnesses. Trials 2017;18.
- Tronto J. Caring democracy: markets, equality, and justice. New York: New York University Press; 2013.
- Rose D. Patient and public involvement in health research: ethical imperative and/or radical challenge?. J Health Psychol 2013;19:149-58.
- Rape Crisis . Rape Crisis National Service Standards 2018. https://rapecrisis.org.uk/about-us/national-service-standards/#:~:text=The%20Rape%20Crisis%20National%20Service%20Standards%20%28RCNSS%29%20are,of%20all%20forms%20of%20sexual%20violence%20and%20abuse (accessed 13 March 2023).
- O’Doherty L, Whelan M, Carter GJ, Brown K, Tarzia L, Hegarty K, et al. Psychosocial interventions for survivors of rape and sexual assault experienced during adulthood. Cochr Datab Syst Rev 2023;2023. https://doi.org/10.1002/14651858.CD013456.pub2.
- Beresford P. The role of service user research in generating knowledge-based health and social care: from conflict to contribution. Evid Pol 2007;3:329-41.
- Yang C, Dibb Z. Peer Research in the UK. London: Institute for Community Studies powered by the Young Foundation; 2020.
- MESARCH . What Are You Doing? [video] 2022. www.youtube.com/watch?v=Qib1Tmkezsg (accessed 17 October 2023).
- Chevous J, Etwaria R. A Better Way: An Independent Review of Survivor Involvement in the MESARCH Project. Survivors’ Voices and Little Ro; 2023.
- Institute of Medicine . Psychosocial Interventions for Mental and Substance Use Disorders: A Framework for Establishing Evidence-Based Standards 2015.
- Brown S, Carter GJ, Halliwell G, Brown K, Caswell R, Howarth E, et al. Survivor, family and professional experiences of psychosocial interventions for sexual abuse and violence: a qualitative evidence synthesis. Cochr Datab Syst Rev 2022;10.
- NICE . Post-Traumatic Stress Disorder: NICE Guideline 2018.
- NHS England . Strategic Direction for Sexual Assault and Abuse Services: Lifelong Care for Victims and Survivors: 2018 – 2023 2018.
- Massey K, Horvath Miranda AH, Essafi S, Majeed-Ariss R. Staff experiences of working in a Sexual Assault Referral Centre: the impacts and emotional tolls of working with traumatised people. J Forens Psychiat Psychol 2019;30:686-705.
- Majeed-Ariss R, Karsna K, White C. The nature of child sexual abuse among boys and girls attending Saint Mary’s Sexual Assault Referral Centre in Greater Manchester. Child Abuse Rev 2019;28:431-41.
- Walker T, Majeed-Ariss R, Riley R, White C. Women’s experiences of attending an English sexual assault referral centre: an exploratory study. J Forens Psychiat Psychol 2020;31:123-36.
- Bronstein LR. A model for interdisciplinary collaboration. Soc Work 2003;48:297-306.
- Cole J. Structural, organizational, and interpersonal factors influencing interprofessional collaboration on sexual assault response teams. J Interpers Violence 2018;33:2682-703.
- Greeson MR, Soibatian C, Houston-Kolnik JD. The influence of community sociocultural context on creating an effective, coordinated response to sexual assault. Psychol Women Quart 2018;42:445-60.
- Mathews PA, Hulton L. Interprofessional collaboration practice: are you doing it well? Individual perceptions within Sexual Assault Response Team (SART). J Interprofess Educ Pract 2020;19.
- Zijlstra E, Lo Fo Wong S, Teerling A, Hutschemaekers G, Lagro-Janssen A. Challenges in interprofessional collaboration: experiences of care providers and policymakers in a newly set-up Dutch assault centre. Scand J Caring Sci 2018;32:138-46.
- McGill E, Marks D, Er V, Penney T, Petticrew M, Egan M. Qualitative process evaluation from a complex systems perspective: a systematic review and framework for public health evaluators. PLOS Med 2020;17.
- NHS England . Sexual Assault Referral Centres: Indicators of Performance (SARCIPs) Adult and Children and Young People – User Guide 2018–2019 2018.
- May CR, Cummings A, Girling M, Bracher M, Mair FS, May CM, et al. Using normalization process theory in feasibility studies and process evaluations of complex healthcare interventions: a systematic review. Implement Sci 2018;13.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77-101.
- Braun V, Clarke V. Reflecting on reflexive thematic analysis. Qual Res Sport Exer Health 2019;11:589-97.
- Braun V, Clarke V. One size fits all? What counts as quality practice in (reflexive) thematic analysis?. Qual Res Psychol 2021;18:328-52.
- Feder GS, Hutson M, Ramsay J, Taket AR. Women exposed to intimate partner violence: expectations and experiences when they encounter health care professionals: a meta-analysis of qualitative studies. Arch Intern Med 2006;166:22-37.
- Tarzia L, Bohren MA, Cameron J, Garcia-Moreno C, O’Doherty L, Fiolet R, et al. Women’s experiences and expectations after disclosure of intimate partner abuse to a healthcare provider: a qualitative meta-synthesis. BMJ Open 2020;10.
- Greeson MR, Campbell R. Coordinated community efforts to respond to sexual assault: a national study of sexual assault response team implementation. J Interpers Violence 2015;30:2470-87.
- Ahrens CE, Aldana E. The ties that bind: understanding the impact of sexual assault disclosure on survivors’ relationships with friends, family, and partners. J Trauma Dissociat 2012;13:226-43.
- O’Doherty L, Carter G, Lutman-White E, Caswell R, Jackson LJ, Feder G, et al. Multi-disciplinary evaluation of sexual assault referral centres (SARCs) for better health (MESARCH): protocol for a 1-year cohort study examining health, well-being and cost outcomes in adult survivors of sexual assault attending SARCs in England. BMJ Open 2022;12. https://doi.org/10.1136/bmjopen-2021-057449.
- Abrahams N, Seedat S, Lombard C, Kengne AP, Myers B, Sewnath A, et al. Study protocol for a longitudinal study evaluating the impact of rape on women’s health and their use of health services in South Africa. BMJ Open 2017;7.
- Abrahams N, Mhlongo S, Chirwa E, Lombard C, Dunkle K, Seedat S, et al. Rape survivors in South Africa: analysis of the baseline socio-demographic and health characteristics of a rape cohort. Global Health Action 2020;13.
- Hughes EDJ, Knights N, Price H, Rutsito S, Stefanidou T, . The effectiveness of sexual assault referral centres with regard to mental health and substance use: a national mixed-methods study: the MiMoS Study. Health Soc Care Deliv Res 2023;11:1-117.
- MESARCH . Welcome to the MESARCH Project [video] 2019. www.youtube.com/watch?v=ScJCYgpw-gM (accessed 17 October 2023).
- Weathers FW, Litz BT, Keane TM, Palmieri PA, Marx BP, Schnurr PP. The PTSD Checklist for DSM-5 (PCL-5) 2013. www.ptsd.va.gov/professional/assessment/adult-sr/ptsd-checklist.asp (accessed 8 February 2023).
- Stefanovics EA, Rosenheck RA, Jones KM, Huang G, Krystal JH. Minimal clinically important differences (MCID) in assessing outcomes of post-traumatic stress disorder. Psychiatr Q 2018;89:141-55.
- World Health Organization . Adverse Childhood Experiences International Questionnaire (ACE-IQ) 2018. www.who.int/publications/m/item/adverse-childhood-experiences-international-questionnaire-(ace-iq) (accessed 8 February 2023).
- Hegarty K, Spangaro J, Kyei-Onanjiri M, Valpied J, Walsh J, Chapman J, et al. Validity of the ACTS intimate partner violence screen in antenatal care: a cross sectional study. BMC Publ Health 2021;21.
- IBM Corp . IBM SPSS Statistics for Windows, Version 28.0: Released 2021.
- Pinheiro J, Bates D. R Core Team . Nlme: Linear and Nonlinear Mixed Effects Models. R Package Version 3.1-157 2022. https://CRAN.R-project.org/package=nlme (accessed 13 March 2023).
- R Core Team . R: A Language and Environment for Statistical Computing 2022.
- R Studio Team . Integrated Development Environment for R 2022.
- Skevington SM, Lotfy M, O’Connell KA. The World Health Organization’s WHOQOL-BREF quality of life assessment: psychometric properties and results of the International field trial – a report from the WHOQOL Group. Qual Life Res 2004;13:299-310.
- Cole JC, Rabin AS, Smith TL, Kaufman AS. Development and validation of a Rasch-derived CES-D short form. Psychol Assess 2004;16:360-72.
- Bush K, Kivlahan DR, McDonell MB, Fihn SD, Bradley KA. The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Arch Intern Med 1998;158:1789-95.
- Berman AH, Bergman H, Palmstierna T, Schlyter F. Evaluation of the drug use disorders identification test (DUDIT) in criminal justice and detoxification settings and in a Swedish population sample. Eur Addict Res 2005;11:22-31.
- Herman BK, Deal LS, DiBenedetti DB, Nelson L, Fehnel SE, Brown TM. Development of the 7-item binge-eating disorder screener (BEDS-7). Prim Care Compan CNS Disord 2016;18.
- Morgan JF, Reid F, Lacey JH. The SCOFF questionnaire: assessment of a new screening tool for eating disorders. BMJ 1999;319:1467-8.
- Spitzer RL, Kroenke K, Williams JBW, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med 2006;166:1092-7.
- Brooker C, Edmondson A, Hughes L. The contribution of mental health services to a new strategic direction for sexual assault and abuse services. J Forensic Leg Med 2019;64:45-8.
- Majeed-Ariss R, Walker T, Lee P, White C. The experiences of sexually assaulted people attending Saint Mary’s Sexual Assault Referral Centre for a forensic medical examination. J Forensic Leg Med 2019;66:33-7.
- Bentivegna F, Patalay P. The impact of sexual violence in mid-adolescence on mental health: a UK population-based longitudinal study. Lancet Psychiatry 2022;9:874-83.
- Campbell R, Sprague HB, Cottrill S, Sullivan CM. Longitudinal research with sexual assault survivors: a methodological review. J Interpers Violence 2011;26:433-61.
- Short NA, Lechner M, McLean BS, Tungate AS, Black J, Buchanan JA, et al. Health care utilization by women sexual assault survivors after emergency care: results of a multisite prospective study. Depress Anxiety 2021;38:67-78.
- Strizzi JM, Mortensen EL, Hegelund ER, Wimmelmann CL, Folker AP, Flensborg-Madsen T. Experience of sexual violence and satisfaction with life: a 20-year prospective cohort study. J Sex Aggress 2022;28:316-30.
- Loutfy MR, Macdonald S, Myhr T, Husson H, Du Mont J, Balla S, et al. Prospective cohort study of HIV post-exposure prophylaxis for sexual assault survivors. Antivir Ther 2008;13:87-95.
- Sleath E, Hughes E, Brooker C, Musto A, Tek Kalsi P, Tocque K, et al. Sexual Assault Referral Centres (SARCs): Providing Care and Support for People Following Exposure to Rape, Sexual Assault and Abuse. Coventry: Coventry University; 2021.
- O’Doherty L, Weare S, Carter G, Hudspith L, Sleath E, Munro V, et al. Justice in COVID-19 for Sexual Abuse and Violence: Impacts of the COVID-19 Pandemic on Criminal Justice Journeys of Adult and Child Survivors of Sexual Abuse, Rape and Sexual Assault. Coventry: Coventry University; 2022.
- Bellis MA, Hughes K, Ford K, Ramos Rodriguez G, Sethi D, Passmore J. Life course health consequences and associated annual costs of adverse childhood experiences across Europe and North America: a systematic review and meta-analysis. Lancet Public Health 2019;4:e517-28.
- Office for National Statistics . Sexual Offences Prevalence and Victim Characteristics, England and Wales 2021. www.ons.gov.uk/peoplepopulationandcommunity/crimeandjustice/datasets/sexualoffencesprevalenceandvictimcharacteristicsenglandandwales (accessed 14 March 2023).
- Skevington SM, McCrate FM. Expecting a good quality of life in health: assessing people with diverse diseases and conditions using the WHOQOL-BREF. Health Expect 2012;15:49-62.
- Krahé B. Violence against women. Curr Opin Psychol 2018;19:6-10.
- Vyas S, Meinhart M, Troy K, Brumbaum H, Poulton C, Stark L. The economic cost of violence against women and girls in low- and middle-income countries: a systematic review of the evidence. Trauma Viol Abuse 2021;24:44-55.
- Oliver R, Alexander B, Roe S, Wlasny M. The Economic and Social Costs of Domestic Abuse. London: Home Office; 2019.
- Oosterbaan V, Covers MLV, Bicanic IAE, Huntjens RJC, de Jongh A. Do early interventions prevent PTSD? A systematic review and meta-analysis of the safety and efficacy of early interventions after sexual assault. Eur J Psychotraumatol 2019;10.
- Ferrari G, Torres-Rueda S, Michaels-Igbokwe C, Watts C, Jewkes R, Vassall A. Economic evaluation of public health interventions: an application to interventions for the prevention of violence against women and girls implemented by the ‘what works to prevent violence against women and girls?’ global program. J Interpers Violence 2019;36:NP11392-420.
- Leight J, Deyessa N, Sharma V. Cost-effectiveness analysis of an intimate partner violence prevention intervention targeting men, women and couples in rural Ethiopia: evidence from the Unite for a Better Life randomised controlled trial. BMJ Open 2021;11.
- Ranganathan M, Heise L, Peterman A, Roy S, Hidrobo M. Cross-disciplinary intersections between public health and economics in intimate partner violence research. SSM: Populat Health 2021;14.
- Drummond MF, Sculpher MJ, Claxton K, Stoddart GL, Torrance GW. Methods for the Economic Evaluation of Health Care Programmes. Oxford: Oxford University Press; 2015.
- Jones K, Burns A. Unit Costs of Health and Social Care 2021. Canterbury: Personal Social Services Research Unit, University of Kent; 2021.
- NHS England . Reference Costs 2020 21 2021.
- Neumann P, Ganiats TG, Russell LB, Sanders GD, Siegel JE. Cost-Effectiveness in Health and Medicine. Oxford: Oxford University Press; 2016.
- Brooks R. EuroQolthe current state of play. Health Pol 1996;37:53-72.
- Dams J, Rimane E, Steil R, Renneberg B, Rosner R, König H-H. Health-related quality of life and costs of posttraumatic stress disorder in adolescents and young adults in Germany. Front Psychiatry 2020;11.
- Dams J, Rimane E, Steil R, Renneberg B, Rosner R, König H-H. Reliability, validity and responsiveness of the EQ-5D-5L in assessing and valuing health status in adolescents and young adults with posttraumatic stress disorder: a randomized controlled trial. Psychiatr Q 2021;92:459-71.
- National Institute for Health and Care Excellence (NICE) . Position Statement on Use of the EQ-5D-5L Value Set for England (Updated October 2019) 2019.
- van Hout B, Janssen MF, Feng Y-S, Kohlmann T, Busschbach J, Golicki D, et al. Interim scoring for the EQ-5D-5L: mapping the EQ-5D-5L to EQ-5D-3L value sets. Value Health 2012;15:708-15.
- Manca A, Hawkins N, Sculpher MJ. Estimating mean QALYs in trial-based cost-effectiveness analysis: the importance of controlling for baseline utility. Health Econ 2005;14:487-96.
- Al-Janabi H, Flynn TN, Coast J. Development of a self-report measure of capability wellbeing for adults: the ICECAP-A. Qual Life Res 2012;21:167-76.
- Brazier J, Connell J, Papaioannou D, Mukuria C, Mulhern B, Peasgood T, et al. Parry Group . A systematic review, psychometric analysis and qualitative assessment of generic preference-based measures of health in mental health populations and the estimation of mapping functions from widely used specific measures. Health Technol Assess 2014;18:vii-viii.
- Franklin M, Enrique A, Palacios J, Richards D. Psychometric assessment of EQ-5D-5L and ReQoL measures in patients with anxiety and depression: construct validity and responsiveness. Qual Life Res 2021;30:2633-47.
- Mitchell PM, Venkatapuram S, Richardson J, Iezzi A, Coast J. Are quality-adjusted life years a good proxy measure of individual capabilities?. PharmacoEcon 2017;35:637-46.
- Jakobsen JC, Gluud C, Wetterslev J, Winkel P. When and how should multiple imputation be used for handling missing data in randomised clinical trials: a practical guide with flowcharts. BMC Med Res Methodol 2017;17.
- StataCorp . Stata for Windows, Version 17 2021.
- Janssen MF, Szende A, Cabases J, Ramos-Goñi JM, Vilagut G, König HH. Population norms for the EQ-5D-3L: a cross-country analysis of population surveys for 20 countries. Eur J Health Econ 2019;20:205-16.
- Janssen MF, Pickard AS, Shaw JW. General population normative data for the EQ-5D-3L in the five largest European economies. Eur J Health Econ 2021;22:1467-75.
- Kessler RC, Aguilar-Gaxiola S, Alonso J, Benjet C, Bromet EJ, Cardoso G, et al. Trauma and PTSD in the WHO world mental health surveys. Eur J Psychotraumatol 2017;27.
- Barbosa EC, Brant R. Lifetime Cost of Sexual Violence in Essex. Violence Abuse and Mental Health Network; 2022.
- von der Warth R, Dams J, Grochtdreis T, König H-H. Economic evaluations and cost analyses in posttraumatic stress disorder: a systematic review. Eur J Psychotraumatol 2020;11.
- Avanceña AA-OX, Kahn JG, Marseille EA-O. The costs and health benefits of expanded access to MDMA-assisted therapy for chronic and severe PTSD in the USA: a modeling study. Clin Drug Investig 2022;42:243-52.
- Karsna K, Kelly L. The Scale and Nature of Child Sexual Abuse: Review of Evidence. Barkingside: Centre for Expertise on Child Sexual Abuse; 2021.
- Karsna K. Child Sexual Abuse in 2020/21: Trends in Official Data. Barkingside: Centre for Expertise on Child Sexual Abuse; 2022.
- Karsna K, Bromley P. Child Sexual Abuse in 2021/22: Trends in Official Data. Barkingside: Centre of Expertise on Child Sexual Abuse; 2023.
- Karsna K, Majeed-Ariss R. Characteristics and Experiences of Children and Young People Attending Saint Mary’s Sexual Assault Referral Centre, Greater Manchester: A Review of 986 Case Files. Barkingside: Centre for Expertise on Child Sexual Abuse; 2019.
- Morgan L, Khadr S, Bewley S. Child sexual assault reported to an acute sexual assault referral centre in London. Arch Dis Child 2017;102:165-9.
- Khadr S, Clarke V, Wellings K, Villalta L, Goddard A, Welch J, et al. Mental and sexual health outcomes following sexual assault in adolescents: a prospective cohort study. Lancet Child Adoles Health 2018;2:654-65.
- Allnock D, Beckett H, Soares C, Warrington C, Hagell A, Starbuck L. Learning from the Experts: Understanding the Mental Health and Emotional Wellbeing Needs of Those Who Experience Sexual Abuse During Adolescence. Luton: University of Bedfordshire; 2022.
- Warrington C, Beckett H, Ackerley E, Walker M, Allnock D. Making Noise: Children’s Voices for Positive Change after Sexual Abuse: Children’s Experiences of Help-Seeking and Support After Sexual Abuse in the Family Environment. Luton: University of Bedfordshire; 2017.
- UNICEF UK . The United Nations Convention on the Rights of the Child 1989. https://downloads.unicef.org.uk/wp-content/uploads/2010/05/UNCRC_PRESS200910web.pdf?_ga=2.78590034.795419542.1582474737-1972578648.1582474737 (accessed 17 February 2023).
- Øverlien C, Holt S. Responding to Domestic Violence: Emerging Challenges for Policy, Practice and Research in Europe. London: Jessica Kingsley; 2017.
- Felitti VJ, Anda RF. The Hidden Epidemic: The Impact of Early Life Trauma on Health and Disease. Cambridge: Cambridge University Press; 2009.
- Finkelhor D, Jenkins Tucker C. A holistic approach to child maltreatment. Lancet Psychiat 2015;2:480-1.
- Fisher C, Goldsmith A, Hurcombe R, Soares C. The Impacts of Child Sexual Abuse: A Rapid Evidence Assessment. London: Independent Inquiry into Child Sexual Abuse (IICSA); 2017.
- Warrington C. Young Person-Centred Approaches in CSE: Promoting Participation and Building Self-Efficacy: Frontline Briefing. Dartington: Research in Practice; 2017.
- Prout A, James A. Constructing and Reconstructing Childhood: Contemporary Issues in the Sociological Study of Childhood. London: Falmer Press; 1990.
- Powell MA, Smith AB. Children’s participation rights in research. Childhood 2009;16:124-42.
- Morris A, Hegarty K, Humphreys C. Ethical and safe: research with children about domestic violence. Res Ethics 2012;8:125-39.
- Willig C. Social Constructionist Psychology: A Critical Analysis of Theory and Practice. Buckingham: Open University Press; 1999.
- Wiltshire G. A case for critical realism in the pursuit of interdisciplinarity and impact. Qual Res Sport Exerc Health 2018;10:525-42.
- Hu X. Methodological implications of critical realism for entrepreneurship research. J Crit Real 2018;17:118-39.
- Fargas-Malet M, McSherry D, Larkin E, Robinson C. Research with children: methodological issues and innovative techniques. J Early Childh Res 2010;8:175-92.
- Goddard C, Mudaly N. The ethics of involving children who have been abused in child abuse research. Int J Child Rights 2009;17:261-81.
- Clarke V, Braun V. Thematic analysis. J Posit Psychol 2017;12:297-8.
- Mauthner NS, Doucet A. Reflexive accounts and accounts of reflexivity in qualitative data analysis. Sociology 2003;37:413-31.
- Dixon-Woods M, Shaw RL, Agarwal S, Smith JA. The problem of appraising qualitative research. Qual Saf Health Care 2004;13:223-5.
- Adisa O, Hermolle M, Ellis F. Denial, Disbelief and Delays: Examining the Costs on the NHS of Delayed Child Sexual Abuse Disclosure in England and Wales. Suffolk: Survivors in Transition; 2023.
- Dworkin ER, Schumacher JA. Preventing posttraumatic stress related to sexual assault through early intervention: a systematic review. Trauma Viol Abuse 2018;19:459-72.
- Bovarnick S, Peace D, Warrington C, Pearce JJ. Being Heard: Promoting Children and Young People’s Involvement in Participatory Research on Sexual Violence: Findings from an International Scoping Review. Bedford: University of Bedfordshire; 2018.
- Black M, Basile KC, Breiding MJ, Smith SG, Walters ML, Merrick MT, et al. The National Intimate Partner and Sexual Violence Survey (NISVS): 2010 Summary Report. Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention; 2011.
- Lefevor GT, Boyd-Rogers CC, Sprague BM, Janis RA. Health disparities between genderqueer, transgender, and cisgender individuals: an extension of minority stress theory. J Counsel Psychol 2019;66:385-95.
- Khalifeh H, Oram S, Osborn D, Howard LM, Johnson S. Recent physical and sexual violence against adults with severe mental illness: a systematic review and meta-analysis. Int Rev Psychiat 2016;28:433-51.
- Manning D, Majeed-Ariss R, Mattison M, White C. The high prevalence of pre-existing mental health complaints in clients attending Saint Mary’s Sexual Assault Referral Centre: implications for initial management and engagement with the Independent Sexual Violence Advisor service at the centre. J Forensic Leg Med 2019;61:102-7.
- Olsen A, Majeed‐Ariss R, Teniola S, White C. Improving service responses for people with learning disabilities who have been sexually assaulted: an audit of forensic services. Br J Learn Disab 2017;45:238-45.
- Ali N, Butt J, Phillips M. Improving Responses to the Sexual Abuse of Black, Asian and Minority Ethnic Children. Barkingside: Centre of Expertise on Child Sexual Abuse; 2021.
- Brown K, Bayley J, Baxter A. Evaluation of the Blue Sky Centre SARC. Coventry: Centre for Technology Enabled Health Research, Coventry University; 2014.
- Clarke J, Hyde A, Caswell RJ. A service evaluation of current practices in the assessment of mental-health and referral for support following disclosure of sexual violence. Int J STD AIDS 2023;34:62-6.
- Love G, Michele GD, Giakoumidaki C, Sánchez EH, Lukera MF, Cartei V. Improving access to sexual violence support for marginalised individuals: findings from the lesbian, gay, bisexual and trans* and the black and minority ethnic communities. Crit Rad Soc Work 2017;5:163-79.
- McLean IA. Re-audit of clients from ethnic and local communities in Greater Manchester attending St Mary’s Sexual Assault Referral Centre. J Forensic Leg Med 2007;14:131-7.
- Harvey S, Mitchell M, Keeble J, Nicholls CM, Rahim N. Barriers Faced by Lesbian, Gay, Bisexual and Transgender People in Accessing Domestic Abuse, Stalking, Harassment and Sexual Violence Services. Cardiff: Welsh Government Social Research; 2014.
- Smith B. Analysing Qualitative Data in Psychology. London: SAGE Publications Ltd; 2016.
- Selvarajah S, Deivanayagam TA, Lasco G, Scafe S, White A, Zembe-Mkabile W, et al. Categorisation and minoritisation. BMJ Glob Health 2020;5.
- Carson AM, Fairbairn GJ. The whole story: towards an ethical research methodology. Nurse Res 2002;10:15-29.
- Nelson A, McClintock C, Perez-Ferguson A, Shawver MN, Thompson G. Storytelling narratives: social bonding as key for youth at risk. Child Youth Care Forum 2008;37:127-37.
- Willis R. The use of composite narratives to present interview findings. Qual Res 2018;19:471-80.
- Crenshaw K. Demarginalizing the intersection of race and sex: a black feminist critique of antidiscrimination doctrine, feminist theory and antiracist politics. Univ Chicago Legal Forum 1989;1989.
- Grillo R. An excess of alterity? Debating difference in a multicultural society. Ethnic Rac Stud 2007;30:979-98.
- Crossley ML. Narrative psychology, trauma and the study of self/identity. Theor Psychol 2000;10:527-46.
- Hulley J, Bailey L, Kirkman G, Gibbs GR, Gomersall T, Latif A, et al. Intimate partner violence and barriers to help-seeking among black, Asian, minority ethnic and immigrant women: a qualitative metasynthesis of global research. Trauma Viol Abuse 2022;24:1001-15.
- Atkinson R. The Life Story Interview. Thousand Oaks, CA: SAGE Publications Ltd; 1998.
- Riessman CK. Narrative Methods for the Human Sciences: Narrative Methods for the Human Sciences. Thousand Oaks, CA: SAGE Publications Ltd; 2008.
- Frank A. Letting Stories Breathe. A Socio-Narratology. Chicago, IL: University of Chicago Press; 2010.
- Frank A. Varieties of Narrative Analysis. Thousand Oaks, CA: SAGE Publications Ltd; 2012.
- Emden C. Conducting a narrative analysis. Collegian 1998;5:34-9.
- Riessman CK. Narrative Analysis. Newbury Park, CA: SAGE Publications Ltd; 1993.
- Bedera N, Haltom T. Virtual issue: sexual violence. Soc Probl 2023;1:1-3.
- NHS England . Commissioning Framework for Adult and Paediatric Sexual Assault Referral Centres (SARC) Services 2015.
- Reese E, Haden CA, Baker-Ward L, Bauer P, Fivush R, Ornstein PA. Coherence of personal narratives across the lifespan: a multidimensional model and coding method. J Cognit Develop 2011;12:424-62.
- Acierno R, Resnick HS, Kilpatrick DG. Health impact of interpersonal violence 1: prevalence rates, case identification, and risk factors for sexual assault, physical assault, and domestic violence in men and women. Behav Med 1997;23:53-64.
- Ledingham E, Wright GW, Mitra M. Sexual violence against women with disabilities: experiences with force and lifetime risk. Am J Prev Med 2022;62:895-902.
- Mitra M, Mouradian VE, Diamond M. Sexual violence victimization against men with disabilities. Am J Prev Med 2011;41:494-7.
- Sigurvinsdottir R, Ullman SE. The role of sexual orientation in the victimization and recovery of sexual assault survivors. Violence Vict 2015;30:636-48.
- Santelli JS, Grilo SA, Choo T-H, Diaz G, Walsh K, Wall M, et al. Does sex education before college protect students from sexual assault in college?. PLOS ONE 2018;13.
- Brooker C, Durmaz E. Mental health, sexual violence and the work of Sexual Assault Referral Centres (SARCs) in England. J Forensic Leg Med 2015;31:47-51.
- Dartnall E, Jewkes R. Sexual violence against women: the scope of the problem. Best Pract Res Clin Obstetr Gynaecol 2013;27:3-13.
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: the Adverse Childhood Experiences (ACE) study. Am J Prev Med 1998;14:245-58.
- Hughes K, Bellis MA, Hardcastle KA, Sethi D, Butchart A, Mikton C, et al. The effect of multiple adverse childhood experiences on health: a systematic review and meta-analysis. Lancet Public Health 2017;2:e356-66.
- Korotana LM, Dobson KS, Pusch D, Josephson T. A review of primary care interventions to improve health outcomes in adult survivors of adverse childhood experiences. Clin Psychol Rev 2016;46:59-90.
- Sleath E, Lutman-White E, Carter G, Brown S, O’Doherty L. The impact of COVID-19 on recovery after sexual violence and abuse: voices of help-seeking survivors and those individuals working within specialist support services in England n.d.
- Kantor V, Knefel M, Lueger-Schuster B. Perceived barriers and facilitators of mental health service utilization in adult trauma survivors: a systematic review. Clin Psychol Rev 2017;52:52-68.
- Lewis SJ, Arseneault L, Caspi A, Fisher HL, Matthews T, Moffitt TE, et al. The epidemiology of trauma and post-traumatic stress disorder in a representative cohort of young people in England and Wales. Lancet Psychiat 2019;6:247-56.
- Ellison L, Munro VE. Taking trauma seriously: critical reflections on the criminal justice process. Int J Evid Proof 2016;21:183-208.
- Howarth E, Moore TH, Stanley N, MacMillan HL, Feder G, Shaw A. Towards an ecological understanding of readiness to engage with interventions for children exposed to domestic violence and abuse: systematic review and qualitative synthesis of perspectives of children, parents and practitioners. Health Soc Care Commun 2019;27:271-92.
- Kitchiner NJ, Lewis C, Roberts NP, Bisson JI. Active duty and ex-serving military personnel with post-traumatic stress disorder treated with psychological therapies: systematic review and meta-analysis. Eur J Psychotraumatol 2019;10.
- Regehr C, Alaggia R, Dennis J, Pitts A, Saini M. Interventions to reduce distress in adult victims of sexual violence and rape: a systematic review. Campbell Syst Rev 2013;9:1-133.
- Gray R, Budden-Potts D, Bourke F. Reconsolidation of traumatic memories for PTSD: a randomized controlled trial of 74 male veterans. Psychother Res 2019;29:621-39.
- O’Doherty L, Carter G, Lutman-White E, Etwaria R. Sexual Crime, Victims and Survivors. Springer Nature; n.d.
Appendix 1
| Red, amber, green (RAG) categories and number of incidents | Description of incident | Action taken | Outcome |
|---|---|---|---|
| Red (one incident) A person was in immediate risk of harm, including children and young people not participating in the project, requiring contacting the police or immediate report to child protection services or services to protect vulnerable adults. Response required instant attention from the safeguarding lead and senior academic staff made decisions about breaking confidentiality and providing contact information to the police/child protection/other service as appropriate |
There was a single adverse incident reported within the cohort study. Although not entirely aligned with our definition of a ‘Red’ incident, we considered the potential adverse impact on the study and the individual sufficient to escalate. An ISVA notified the research team that a client they supported had related to their counsellor that questions asked during the MESARCH baseline interview were experienced as traumatising. These related to the topic of sexual health |
The PI and a number of co-investigators, project team members, safeguarding lead, the SSC chair and LEG members engaged in an emergency consultation. The response involved removing two sexual health items from the interview and ensuring that the questions were better placed in the interview. The team reviewed lead-in explanations which emphasised the voluntary and sensitive nature of questions before asking them | The actions were communicated to the ISVA and the participant. The participant appreciated the actions that had been taken and was happy to remain in the study and completed the two subsequent interviews |
| Amber (22 incidents) Concerns were raised about participants or where survey responses were indicative of potential harm. Items were discussed as part of weekly status meetings. As a team we considered what support the person had in place and the appropriateness of making subsequent contact with the person to offer a supportive response |
Participant revealed stalking and harassment by ex-partner in recent months | Interviewer followed-up and ensured they had support available and provided the 24 hour domestic abuse helpline | Participant had support in place and details for helpline and emergency response |
| Participant revealed recent self-harm and suicidality behaviours | Interviewer discussed formal and informal sources of support with participant and provided details of organisations that could provide further support | With their consent, interviewer followed- up with participant later that week and participant had been able to reach out for support | |
| Participant rang interviewer while upset assuming they were a mental health support centre but then hung up when interviewer explained who they were | Interviewer and senior staff including safeguarding lead discussed a response. Interviewer sent a message to participant and asked if it would be helpful to contact their ISVA | Interviewer spoke with the participant the next day and ascertained that participant had since received the support they needed from a support worker | |
| Green Experiences were judged by the research team as consistent with what would normally be expected in a situation of a survivor of sexual trauma participating in research. Given how the vast majority of people entered the study, it was assumed the person had support in place if they wanted this and knew how to access help if needed. However, as part of debriefing with all participants at the end of each research interview, details of national and local support services were shared with the participants |
|||
The project created a safe, level playing field across all who were involved, where everyone was equal and academic qualifications were not relevant in our exchanges. This enabled LEG members to give honest, real opinions in a non-judgemental, supportive environment. The research team expressed a real desire to discover whether what they planned to do and how they planned to do it held real authenticity within the LEG. The way in which they made the group feel at ease and respected when asking for LEG help and advice empowered the LEG members to speak with a freedom of opinion and allowed them to speak about their traumatic experiences openly in the hope that finally someone wanted to listen and not just hear but take what they were saying and use their responses in a practical way that could go on to help others who are in the same situation. This working ‘together’ empowered LEG members to participate using their real selves and live voices in the making of film, social media and marketing campaigns and finally meeting delegates and presenting and speaking up and out at the final conference.
When you find your freedom of voice as a survivor, you are anxious to try and help the next person in your situation. As a result of the stigma of sexual abuse and rape, rarely do we as a group speak out for fear of shame and lack of self-worth. Rarely are we listened to and valued; instead, we are usually pitied or not believed. Never do we find ourselves in a position where the experience of sexual abuse renders us the expert, when in fact we are. Personally, participating in this research study improved my mental health and personal confidence. It has allowed me to articulate difficult feelings that I would not normally bring to anyone’s attention with calm measured behaviour resulting in positive outcomes. Working with the project I have experienced the biggest forward jump in my well-being and recovery because I sought professional help in my darkest days. It has been on both sides a time of respect, education, empowerment, joy and laughter – LEG groups should be mandatory if the desired outcome is to truly help survivors.
Appendix 2
| Case study site (N = 8) | Service delivery model, size and integration of ISVA service | Professional informants (N = 72) | Survivor informants (N = 298a) |
|---|---|---|---|
| A | Private sector, small, ISVA service not integrated | 4 SARC professionals 9 non-SARC professionals |
2 qualitative interviews 17 cohort interviewees |
| B | Police-led, large, integrated ISVA service | 9 SARC professionals 3 non-SARC professionals |
1 qualitative interview 57 cohort interviewees |
| C | NHS-led, small, ISVA service not integrated | 5 SARC professionals 1 non-SARC professional |
0 qualitative interviews 0 cohort interviewees |
| D | Private sector, medium, ISVA services not integrated | 4 SARC professionals 5 non-SARC professionals |
1 qualitative interview 4 cohort interviewees |
| E | Charity-led, small, ISVA service not integrated | 4 SARC professionals 4 non-SARC professionals |
0 qualitative interviews 1 cohort interviewee |
| F | Charity-led, large, ISVA service not integrated | 3 SARC professionals 6 non-SARC professionals |
1 qualitative interview 10 cohort interviewees |
| G | NHS-led, medium, ISVA service not integrated | 2 non-SARC professionals | 0 qualitative interviews 6 cohort interviewees |
| H | NHS-led, large, ISVA service not integrated | 6 SARC professionals 3 non-SARC professionals |
0 qualitative interviews 80 cohort interviewees |
| Non-case study sites (n = 13) | Multiple models | No professional interviews | 118 cohort interviewees |
| FNEs | Not associated with sites | 4 nurses | N/A |
Appendix 3
Core stories
Before, I was so happy I will go to this country, I will make my daughter’s future. [By] three months I was like a slave … my husband telling my daughter she needs to do household chores, she can’t study. They cut the Wi-Fi so she couldn’t access any of the course online or anything. My daughter had a really, really rough time. My daughter was trying to study because she was in GCSEs. She was trying to study, but she couldn’t understand anything because of the environment she had at home: all the time, fighting. I was so worried about my mental health, ‘If I have something happen to me, what will happen to my daughter?’
One day, my daughter wanted to get a haircut done but she wasn’t allowed so my husband told her off and then we had a big argument. It was during lockdown. We left home and we didn’t know where we will go. We were very scared. We had nothing. We were wearing simple things. We had limited money. Me and my daughter went to the police station. I didn’t know what to say because my English was limited. My daughter started, ‘We came from India’, and police said, ‘That thing happens with the Indian families, it’s not a new thing’. So they sat with us 5 minutes and they said ‘You go home!’
The day we left for good, I had an appointment at the police station for 2 o’clock. They were waiting for interpreters because I can’t speak in English very well, so we waited for a translator until 5 o’clock. The translator didn’t come but they had a three-way translation for me. My husband came back home, he didn’t find us and he rang when we were in the police station and we were so scared [about] what he can do. They asked questions, but I can’t remember what the questions were. I was told ‘You will need to go home’. I said, ‘I can’t go back home. I will be in danger’, but they asked, ‘When you will go home? No one will tell you anything, just go home!’ They gave me a domestic violence number. They told me I had to make my own way.
There was no bed space in the refuge. We went to a hotel. I was crying the whole two days. I was feeling like panic attack type things, and I couldn’t answer any phones. My daughter was answering all the phones. I didn’t know what was happening to me, I was so confused because I didn’t know where to go, and my daughter was telling me ‘Don’t cry, don’t cry’. My daughter was giving me comfort.
We paid two days with our money but on the third we were asked to check-out. We stayed in the hotel reception five hours until the social worker came and paid for 8 more days. It was hard because the social worker used to force us, ‘Look you have money, pay your money!’ All I had in total was £300. My daughter had GCSE exams. She had no phone and I was thinking I would buy a phone for her from the £300.
Afterwards, the social worker took us to the refuge. We were given £48 for a week and we used it to get all shopping done. I had nothing in the kitchen. Nothing I could make because the house wasn’t Indian. We got food from food bank and it was some kind of Indian food and drink. We stayed in a flat and people used to knock on our door and my daughter used to be scared. We used to get so scared that flashbacks started coming and there wasn’t any lock controlled by us, there’s only one they control, and we used to think anyone can come and we didn’t sleep at all, both me and my daughter. I started going to one of the support groups but that group closed. I was isolated again, and me and my daughter were so isolated, fearful, I didn’t know what will happen to my daughter. I was more worried about my daughter. I didn’t know a doctor and I never went to any temple. I didn’t know how to go. After three months, they provided us with a house and then we slept well.
The SV charity involved an ISVA and a DV agency. I needed a letter for my visa because I was on a sponsored visa. The ISVA called the police a couple times and then the police gave the letter. After 3 months, police approached me; they were asking whether I want to give a statement. My mental health wasn’t good, and I didn’t want to go back to the experience I had gone through with the police. I didn’t want to give that statement at that moment.
I am happy with the house but I received a letter that I have to leave the building in April and now again, I’m feeling ‘Where I will go again?’ I’m very confused and I am still scared of police. When I was in India, I never went to police, never had anything to do with police and here I still have fear of police, I have fear of – my English is not very good – if I say anything and it was interpreted in a different way, I’m so fearful. I won’t say anyone to go to police.
I am on the waiting list for counselling. I don’t realise what happens to me but my daughter says I am alert. I don’t feel like going anywhere, I don’t feel like doing anything. My daughter goes to school, and I’m all by myself. My friend, she is a very good friend but I could not disclose the address I was living in. I don’t want her to know where I am living and to tell. If she goes back home to India, she might tell someone and the whole village might know; I don’t want shame brought to the family.
Because of this notice to leave my house, I couldn’t sleep and I went to the GP. I told them I can’t sleep and the GP asked why and then I told my situation, ‘My house, I will be homeless’. The GP involved someone. I felt very supported when this lady, from the doctor, when she rang me, and she told if you tell this thing to the support worker, and so I told support worker and then they extended me 56 days more. So I felt supported at that time. My daughter is saying now at least we have the school holidays so, you know, the transfer won’t affect her studies. But if we had to go in June, it will be A levels … I still prefer if the GP was a female because I can tell more and she can understand more than males, and I prefer to speak Hindi.
Where do I start? After the incident that happened to me, I was in shock for 4 days; I just couldn’t believe that it had happened.
How it all came about [was this]: the person who was in my shared house actually moved to that shared house so they weren’t that far from me, I started looking after her as well because her partner was in and out of prison and she was cutting herself and I was giving her support, patching her up at the same time. I think it’s easier to find someone else to look after rather than trying to sort your own problems out. The bloke who done it to me, I met him in that house. The chap who did it to me, he was an actual heroin addict but I didn’t know this at the time, I didn’t know how bad he was. We all got talking, and the next time I came down she wasn’t in but this chap was so, then after my friend left, when the young girl left the house, they turned around and said ‘Oh, you’re still welcome to come down, it’d be good to see you, you’re very good to talk to and you listen as well’. I was like a shoulder to cry on I suppose. But I think one of them just took it a little bit too far, thought that I wanted a relationship and things like that which I didn’t. It’s like any bloke that I do meet, what I’ve been saying is I don’t want a relationship, I do not want to go down that road again.
I didn’t really get in touch with anybody for 4 days. I did eventually call the police and they came and [took] a statement as to what had happened. I saw them nearly half 12/1 o’clock. Then they said that somebody will be picking me up at 3 o’ clock to take me to this clinic. I was taken to SARC where I had to have all the forensic swabs done and all the rest of that. That was a little bit daunting, I was in too much pain. I hadn’t even showered: I thought well if I don’t shower then at least that way they’ve still got [evidence].
When I asked them, ‘What happens now?’ all they said was, ‘Oh well, he’s in prison, we’ve got him in custody and we’ve got him on remand, and he’s denying it’. ‘All the tests show [is] that you had sex’ and I said ‘Yes, non-consensual sex’ because I didn’t want it, I was forced, so that’s rape. I then had an appointment [at the] sexual health clinic. Then I had another swab taken, well they tried to, I was explaining that ‘I’m really, really sore, but it feels sore further up’, like internal pain or like internal bruising, if that’s what you call it. And then, I had to have the Hep [Hepatitis] C, Hep [Hepatitis] B injections and I had another blood test as well. I should have had a follow-up last June but never got a follow-up phone call to say, ‘Please can you come in, so I’ve not had a follow-up from that’.
I then had to move out; the police asked me where would you like to move because we were both living on the same street, ‘Why should I leave?’ It did not make sense. I had to move again.
The police said about doing another statement by video link. I said ‘Yeah, I’m quite happy to do that’. That was the only time it was mentioned. I was waiting for that to happen, and they turned around and said I [had] refused it. I thought to myself well, how can I have refused it if I said yes to it? I think they’re trying to brush it under the carpet as if it didn’t happen or put the file back in the box and put it back on the shelf, it’s as if they just didn’t want to do the paperwork.
They were going to [give me an ISVA] but no, nothing happened. They said that they had to close it because there was not enough and I’m thinking ‘Excuse me, I had bruises on my legs, I’ve taken photos of the bruises’.
I’ve been in pain since it happened with my hips, [lower] back, with my thighs; I’ve had a lot of nerve pain and bone and joint pain on both hips. It has impacted my life because I can’t walk as far as I used to, I have to stop and start walking again. It’s just really, really impacted on my life in that way.
It was just horrible, it really was. I didn’t know what to do next. I didn’t know who to ring; there was not even a victim support officer where I could actually go and speak to someone. Even my mental health doctor, consultant, has actually sent me back, like discharged me and sent me back to my own GP. The GP can only do so much. Alright, yes, they’ve done a brief letter. I did get a nice letter done from the doctors from where it happened. They’re really good and that helped me to get moved out of that property into the property that I’m in now. I’ve asked for another letter to be done, and I had to pay for the letter as well. I then sent that off to the housing association.
II RecoveryI literally can’t live my life at all. I’ve literally had no support and it’s impacted my mental health as well and my well-being and I just can’t seem to, how can I explain it, move forward. It’s still all in my head and I just can’t get my head around it. Well basically, I can’t even get closure on it. Nobody’s telling me what’s happened, whether he has been deported or whether he’s still in the UK. It feels like I’m always looking over my shoulder. The recovery’s been really slow; I have been trying to be more positive, to try and get back to the place where I can feel comfortable and sometimes I’m not very comfortable around men. I think once I get this move then I think I might start feeling myself again; be closer to my family, they’re looking for me for somewhere. I want to get back into my volunteering. I’m still on the books at [charity organisation] because I’d been helping out in like a contact centre. I left that area because of what happened with my husband – it was like verbal abuse, emotional abuse and sexual abuse as well. I had to leave, I just couldn’t cope anymore, my mental health was going through the roof.
I think the older you are, the more difficult [it is] because I feel that maybe some people are like ‘Oh nobody’s going listen to me, I’m not worth nothing, I’m not worth the bother!’ Do you know what I mean? I feel that as you get older, you do find things a lot harder to even register what’s happened. Sometimes you don’t know where to look, you don’t know who’s going be your first point of call to call someone, because you’re that shocked that it’s actually happened in the first place.
I didn’t report for five days after the assault and then I ended up calling 111 and they said, ‘You need to speak to a SARC’. They gave me the number of the SARC, and I rang them, and they were really, really good. We had a conversation and they called me back. There was a forensic examiner on the phone and a crisis worker. They went through what had happened. I said, ‘I’ve got mental health’. They said, ‘We’re not judging on your mental health, it’s got nothing to do with that’. They arranged for me to go in quite quickly. So, I had a forensic examination which was obviously really hard work, but they were very supportive. A few days later, I did get the police involved and I feel now that was a mistake.
Two very young officers came to my flat in the evening which I thought was inappropriate; I wasn’t offered female officers. I think as soon as I told them, ‘I’ve got mental health issues’, it their attitude changed towards me. They said, ‘Well if this does go to court, yeah, your records, your mental health records will be shown to the courts’. Those two police officers, they never, ever looked at the photographs from the SARC. They never looked at any of those things. I felt they had an agenda after they saw me; they did find the guy that assaulted me, but they basically just gave him a telling off, that was what I felt. They just disregarded what I had to say.
We [ISVA and survivor] did a decision review with the police because we felt the original decision wasn’t appropriate. I got video recorded later down the line, which really upset me because I couldn’t remember some of the stuff from the assault. I felt that one of the female officers was very judgmental. She asked me questions about my previous sexual experiences, which I refused to answer because it’s none of her business. We had some information back from the sergeant who was looking into the investigation. He made out that if it had been slightly worse, maybe … But how can you rate an injury I had, you know, internal bruising, as bad or worse? That just really made me angry. We could have met with him afterwards and I was like, ‘Not a chance. I’ve had enough of the police’, if you see what I mean. I was just like, ‘No, it’s not going to help me’. Do you know what I mean? So, I was like, ‘No’.
I have a diagnosis of emotionally unstable personality disorder, and that at times that was used as a bit like a weapon or that was a barrier for me to access certain support. I felt it was used in a sort of negative way. The SARC referred me for counselling services but when I said that I had complex mental health, the woman counsellor said, ‘Well we only really deal with people with anxiety and depression’. She started to obsess about my mental health when I started sessions with her on the phone. I said, ‘Actually I’m not here to talk about [mental health], it’s to do with the sexual assault’. It was as if you couldn’t actually access that service if you had a complex mental health diagnosis, and in the end, I stopped it, because I felt it was making it more detrimental.
I don’t have any support from mental health services at all now. So, they just say, ‘If things get really bad you’ve got to go to A and E’. But A and E’s not the best place, I’ve been there before, for a mental health crisis and it’s not helpful.
I’ve spoken to the police. I did say to the police, I want it to go to court if it can, if they’ve got enough evidence. Obviously, this happened 40 years ago, when I was between 8 and 16. I’ve buried it for such a long time. I still feel really angry about it. There’s no way to describe the anger I feel, that he took away part of my soul and heart. He took my childhood away.
Obviously, [speaking to the police] brought everything back up.
My parents didn’t want to know, when I spoke to them about it. I grew up in the age of where everything was hidden. So, I kept this totally from everybody until 2021.
I heard that he was put in prison; that gave me the courage to come forward. That’s how this process started.
II SupportI feel in a very good place at this moment in time. I feel that the support I’ve had from different organisations has been really helpful. Listening and tried to explain to me that I wasn’t at fault. My mechanism before, to shut everything out; I’ve still got that sort of mechanism. But, I can bring things up now without really being upset about it.
I feel the police have been really helpful. The lady that’s been dealing with the case has been really helpful, in the sense of, explaining everything … Having gone to the police when I did, it has released so much pressure from me, in the sense of letting people in. The only thing I feel, probably that everybody else in my situation feels, it takes longer than you anticipate. The process of the police talking to suspects. It’s not the police’s fault. It’s just the way the system works. I was probably a bit naïve, in the sense of thinking, once I’d made a statement, everything else would [have] fallen in place a lot quicker. Saying that, I feel that the support I’ve had from ISVA service, from SARC, has given me a better outlook on life. With the help that I’ve been having, through the different organisations, it’s helped me, tremendously, and knowing that they’re there.
III Reactions from family, friends and society todayYears ago, when I was talking about it, it wasn’t heard. I wasn’t heard. Looking back over the last couple of years of going through the process, it seems to be that it’s only been brought to light, in the sense of more people are being listened to. So, I feel, in that representation, we are being heard a lot more and taken seriously, which I have never felt before. It has been a lot more open. It’s more accessible. You’re not afraid to talk about it. I feel that I’ve got to a better place now, where I feel that if I need to talk to somebody, say, friends, for instance or work colleagues, even. I’m not ashamed, I’m not ashamed to talk about it. I’ve been very fortunate with my work. They’ve been really good and helpful. I feel that without them, it would have been a lot more difficult. With everybody being on-board, it has been a lot better. HR has been really good. So’s my son and my best mate. He’s been an absolute rock as well.
[W]hat gets me really upset at times is if I’m watching television and abuse comes on the television without, without any warning. For instance, when they were talking about Prince Andrew and then, when they say things … there are television programmes that it’s actually got the subject in that perhaps, I didn’t realise that it had. Then, I start watching it. Then it comes on. Or they show perhaps something’s happened again in the wider world. Then, I feel really, feel really bad.
IV RecoveryI feel that the police are doing all that they can. So, I feel that he’s not actually controlling now. Because they’ve got to do everything the right way. So, I feel knowing that the system is being used correctly, that I know that if and when things do process forward, I know that, everything has been dealt with properly. So, I feel a lot happier. I feel anxious. I don’t feel depressed with it. I feel uptight, because obviously, it’s taken a lot longer than I anticipated. But, by coming forward as well, it’s helping not only myself but if I could help somebody else in the process, then I feel it’s all been worthwhile as well. Because there is a lot of us out there, that’s not either come forward or hasn’t been heard. I just get a bit upset. Not to the point where I’m crying, anymore. Not at the moment. Perhaps when the case goes forward might feel differently. Although I want the case to go forward, nobody knows how you’re going to react. So, yes, and obviously when he used to trap … He trapped me in the shower when we were on holiday as well. I feel that all those things, they’re still in the back of my mind but it’s [come into] the open, people know about it, and gradually, people have a better understanding of my personality. My best mate said to me the other day that he understands now why sometimes I was the way I was, in the sense of my moods and shying away. I’ve known Peter since the age of 7 years and we’ve grown up [together]. We’re best of mates. I’ve let him down, loads of times, and it’s because sometimes I feel like I haven’t been able to get it out of my mind. I’ve kept it a secret for such a long time. I am coping with it now, a lot better than I have done for a very long time.
I’m sorting my life out: I’d run the London Marathon back in ’97 for Childline; I kept my running vest and it’s only now that I got it out, I’ve taken it to a shop, and I’ve had it framed, so that I can put it on the wall. I’ve got to that stage now, where I can face it. I feel a lot freer than I have done for a long time.
I’m in a really good place, in the sense that I know everybody is playing a part. Everybody’s working behind the scenes. So, it’s up to me, in the sense of, having the help and understanding how I feel and how to deal with it. Rather than locking it all away and not telling anybody. That’s given me the strength, knowing that people are out there, helping me. And listening to me. Whereas before nobody was listening. I know now, that people are listening and that’s given me the courage to fight this in a different way, mentally. I’m starting a course with (voluntary sector organisation). I still feel I want to talk about it. I still feel I need to talk about it. I did say to the police, when I was being interviewed, I thought I would take this to the grave with nobody knowing. And now, I can take it to my grave knowing that people know, the whole family knows and I’m happy about that. Once the due process has [been] gone through, whether it does or it doesn’t go to court, no matter what the outcome is, then, I can really draw a line under it.
I can feel free for the rest of my life.
List of abbreviations
- ACE
- adverse childhood experience
- CBT
- cognitive–behavioural therapy
- ChISVA
- Children and Young People’s Independent Sexual Violence Advisor
- CJS
- criminal justice system
- CSA
- child sexual abuse
- CYP
- children and young people
- DMEC
- Data Monitoring and Ethics Committee
- EMDR
- Eye Movement Desensitisation Reprocessing
- EQ-5D-5L
- EuroQol-5 Dimensions, five-level version
- FME
- forensic medical examination/examiner
- FNE
- Forensic Nurse Examiner
- GP
- general practitioner
- HIV
- human immunodeficiency virus
- HRQOL
- health-related quality of life
- ICECAP-A
- ICEpop CAPability measure for Adults
- ISVA
- Independent Sexual Violence Advisor
- LEG
- Lived Experiences Group
- LGBTQ+
- lesbian, gay, bisexual, transgender and/or queer
- MCID
- minimal clinically important difference
- MESARCH
- multidisciplinary evaluation of sexual assault referral centres for better health
- NHSE
- NHS England
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health and Care Research
- PCL-5
- Posttraumatic Stress Disorder Checklist for DSM-5
- PIS
- participant information sheet
- PPI
- patient and public involvement
- PTSD
- post-traumatic stress disorder
- QALY
- quality-adjusted life-year
- QOL
- quality of life
- RAG
- red, amber, green
- RTM
- Reconsolidation of Traumatic Memories
- SAAS
- Sexual Assault and Abuse Services
- SARC
- sexual assault referral centre
- SD
- standard deviation
- SMD
- standardised mean difference
- SSC
- Study Steering Committee
- STIs
- sexually transmitted infections
- TA
- thematic analysis
A note on terminology
We use the term ‘sexual violence and abuse’ throughout the report to refer to exposure to rape, sexual assault or sexual abuse. We use the term ‘survivor’ of abuse to refer to any person in the research who has experienced sexual violence or abuse. This term is used as a shorthand with full understanding that not everyone who is a victim-survivor of sexual violence and abuse recognises or would describe themselves in this way. We sometimes use ‘victim’, especially if the term has been selected by the individual themselves. ‘Client’ and ‘service user’ are used in some instances when referring to statutory and third or voluntary sector services. We have not used participants’ actual names but have, instead, use pseudonyms to refer to the survivors who participated in our research. When referring to professionals, we provide a description of their main role or job title, where needed, but only in an unidentifiable manner.
Notes
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/CTGF3870).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
