Notes
Article history
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as award number NIHR128349. The contractual start date was in September 2020. The draft manuscript began editorial review in February 2023 and was accepted for publication in September 2023. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ manuscript and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this article.
Permissions
Copyright statement
Copyright © 2024 Allen et al. This work was produced by Allen et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2024 Allen et al.
Chapter 1 Background
The overall aim of this research on temporary doctors (generally termed locums) was to provide evidence on the extent, quality and safety of medical locum practice and the implications of medical locum working for health service organisation and delivery in primary and secondary care in the English NHS.
The use of locum doctors in the NHS is widely believed to have increased, and there have been widespread and sustained concerns among policy-makers, healthcare providers, professional associations and professional regulators about the quality/safety, cost and effective use of locum doctors. There was little prior research on locum practice/performance or working arrangements to confirm those concerns or to inform the development of working arrangements for locums which would assure safety and the quality of care.
Locum doctors in the National Health Service in England
The numbers of doctors working as locums in the NHS in England are thought to have grown substantially over the last decade, although there has been surprisingly little empirical data published on the NHS medical workforce to substantiate this trend. Nevertheless, between 2009 and 2015, the use of locums in NHS hospitals was reported to have almost doubled1 and between 2015 and 2019 the number of locums working in primary care was reported to have increased by 250%. 2 In 2018, 8810 doctors were registered with the General Medical Council (GMC) as working primarily as a locum, representing 3.6% of all registered doctors, though it is believed that many other doctors undertake some locum work alongside more conventional permanent employment. 3
Locum doctors are essential for maintaining continuity of service and providing flexibility in service capacity and provision. Healthcare organisations use them to cover gaps in rotas due to unplanned absence or recruitment and retention problems, and also to fill service gaps in underserved or shortage specialties and areas. However, rising locum numbers and particularly the associated increase in cost have led to a growing concern among policy-makers, employers and professional associations about locum use. 4–6 Medical agency staff were estimated to have cost the NHS £1.1 billion in 2015–6,7 and a locum pay cap was introduced in 2015 to curb expenditure. 8
Before undertaking this research, we had already undertaken an international review of the empirical and ‘grey’ literature on locum doctors and the quality and safety of patient care,9 in accordance with Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines, including a comparative analysis of the use of locums in five countries. Our analyses showed that locums were regarded as necessary, as they allow healthcare organisations to maintain adequate staffing levels and flexibility, but also potentially problematic, in that their use may have adverse effects on continuity of care, patient safety, team functioning and costs. This literature also suggested that there was often a lack of robust systems for managing/overseeing locum doctors including inadequate pre-employment checks and induction, unclear line management structures, poor supervision and reporting of performance, and a risk that locums with performance problems move from organisation to organisation.
National Health Service Employers, NHS England and NHS Improvement have all produced guidance on locum working and employment for NHS organisations, locum agencies and locums themselves. 10–12 However, evidence suggests that some basic requirements (such as adequate induction and familiarisation with organisational systems and procedures) are often lacking, communication, especially about locum performance between organisations and locum agencies, is poor, and locum doctors often are not included in or given access to systems for clinical governance and professional development. 13–15
Some insights into these issues arose from the introduction of medical revalidation in the UK from 2012 onwards. Revalidation requires all doctors to demonstrate that they are up to date and fit to practise through participating in regular, annual appraisals and securing a 5-yearly revalidation recommendation to the GMC from a senior doctor in their employing organisation [known as a responsible officer (RO)]. Research on the implementation of revalidation highlighted the lack of robust arrangements for clinical governance for locum doctors. 14 Locums had difficulties in arranging annual appraisals and collecting the portfolio of supporting information about their practice that was required for revalidation [e.g. patient and colleague feedback, details of adverse events and complaints/compliments, records of continuing professional development (CPD) etc.]. As a result, their rates of deferral were higher than for any other group of doctors apart from trainees. 16 A review commissioned by the GMC highlighted a number of concerns and recommended that the GMC and UK health departments should reform the arrangements for overseeing locum doctors. 16
Theoretical context
Internationally, there has been an increasing shift towards non-standard forms of work such as temporary work17 and more people have ‘portfolio’ careers which involve them working for shorter periods or concurrently across different organisations, often without a conventional employment relationship. 2
This research is grounded in three main existing bodies of literature/theory: that related to temporary workers in organisations and the causes/consequences of precarious employment;18–20 the wider literature on the sociology of the medical profession and particularly theories concerned with restratification and intraprofessional hierarchy and the nature and construction of professional identity;21–23 and theories concerned with social identity and intergroup relations, group identity and behaviours. 24,25 The peripatetic nature of locum working may mean that locums practise on the periphery of healthcare organisations and of the profession, and may consequently have a weaker connection to organisational and professional norms and values. This raises questions about how locum doctors’ professional autonomy and identity are constructed and legitimised relationally, how group identities and intergroup relationships are constructed and enacted and the nature of intraprofessional group relationships and behaviours.
Our earlier qualitative research on the experiences of and attitudes towards locum doctors, involving interviews with locum doctors, locum agency staff and representatives of healthcare organisations who use locums,15 showed that locums were often perceived to be inferior to permanently employed doctors in terms of quality, competency and safety. Despite their relatively high occupational status as medical professionals, locum doctors experienced many of the difficulties seen in research on temporary workers in other sectors, such as marginalisation, stigmatisation and limited access to opportunities for training and development. Our findings suggested that the treatment and use of locums could have important potential negative implications for team functioning and patient safety.
The quality and safety of locum doctors
Some high-profile examples of locum failures in care over recent years have contributed to widespread concerns about the quality and safety of locum doctors. 26–29 Locum doctors are often perceived negatively by patients,4 other healthcare professionals5 and NHS leaders. 6 They are often regarded as less professional30 or as untrustworthy ‘outsiders’ who lack commitment and have poor intentions towards the organisation. 31,32
However, empirical evidence that locum doctors provide care which is of a lower quality or less safe than permanent doctors is very sparse. 9 But we do know that locum doctors are more likely to be the subject of complaints, more likely to have those complaints subsequently investigated and more likely to be subject to sanctions by the GMC. 33
Locum doctors may present a greater risk to quality and safety because they often work in unfamiliar teams and settings, and are less likely to receive proper oversight and necessary support from colleagues and employing organisations. 33 The presence of locums in the work environment has been described as an ‘error-producing condition’. 34 On the other hand, the shift towards locum working may represent a wider societal change in attitudes to careers and work–life balance and may provide employers with greater flexibility in staffing and greater externality of perspectives from locums who work across multiple organisations, while it may give locums reduced work pressures/risk of burnout, increased autonomy and new career opportunities/flexibility.
Our recent review found only eight empirical studies comparing locum and permanent doctor practice and performance (three of which were from the UK), generally with small sample sizes and weak methodologies. The most substantial study we identified was from the USA and compared 30-day mortality, costs of care, length of stay and 30-day re-admissions for a random sample of 1,818,873 Medicare patients treated by locums or permanent physicians between 2009 and 2014. There were no significant differences in 30-day mortality rates between patients treated by locums compared with permanent doctors. However, cost of care and length of stay were significantly higher when patients were treated by locums. Furthermore, in subgroup analyses, significantly higher mortality was associated with treatment by locums when patients were admitted to hospitals that used locums infrequently, perhaps due to hospitals being unfamiliar with how to support locums. Only locum doctors who provided 60 days or more of care were included in the analysis, meaning that shorter-term locums, who might have had less opportunity to become familiar with the organisation, may have been excluded. 35 Overall, we concluded that there is limited empirical evidence to support the many commonly held assumptions about the quality and safety of locum working.
Conceptual framework
Our recent international review of the literature on locum working9 identified eight key factors through which locum working may affect the quality and safety of patient care and which may also provide the basis for mechanisms or interventions designed to improve the quality and safety of locum working. These factors are summarised in Table 1, and we have used this framework to structure and guide our research and analysis.
| Theme | Theme description |
|---|---|
| Governance and patient safety | Locums are on the fringes of governance. Gaps in the oversight of locums continue to be a patient safety risk for example background checks. The short-term nature of locum work means that locums are less likely to take part in clinical governance activities, such as audits and CPD. |
| Policies, procedures and continuity of care | Locums are less likely to be aware of contextual issues and local policies and procedures that are relevant to providing safe and effective care, especially if they do not receive adequate induction and briefing when they take up a locum role in a new/unfamiliar organisation. Locums are not prepared for practice in the same way as permanent staff – for example, inductions are often poor or absent, meaning locums are unable to carry out their duties safely and efficiently. Other risks include not knowing how to escalate concerns, and being placed in challenging environments where staffing is an issue. Procedures may be less likely to be carried out when a locum is on duty. The use of locums presents a patient safety issue and may have a negative impact on continuity of care. |
| Impact on the healthcare team – scope of practice | Locums (particularly short-term locums) can place burden on other members of the healthcare team, such as nurses and junior doctors, who could be expected to perform outside of their scope of practice to compensate for a locum’s lack of contextual/local knowledge/competencies. |
| Impact on the healthcare team – workload | Locum working can increase workload for other members of the healthcare team, for example, extra support for the locum who is unlikely to be familiar with policies and protocols and patients returning to see their regular doctor. |
| Information exchange – patients | The quality and quantity of patient information may be reduced when locums are employed, as locums are less likely to be familiar with the patient group and how to report and hand over information about patients to other healthcare professionals. |
| Information exchange – locum practice | The quality and quantity of information exchange about locum doctor practice are poor, meaning that potentially relevant information about locum practice may not be shared with their regulator, employing agency or organisation where they are employed. |
| Professional isolation and peer support | Locums may become professionally isolated and may be less likely to establish/maintain their professional networks and to have good informal networks of peers to turn to for advice, support or social interaction. |
| Professional motivation and commitment | Locums’ moral purpose and vocational commitment are often called into question, and it is suggested that they may be more motivated by financial rewards/incentives than other doctors, and less committed to medicine as a vocation. |
Research aim and research questions
The overall aim of our research was to provide evidence on the extent, quality and safety of medical locum practice and the implications of medical locum working for health service organisation and delivery in primary and secondary care in the English NHS. Our three main research questions were:
-
What is the nature, scale and scope of locum doctor working in the NHS in England? Why are locum doctors needed, what kinds of work do they undertake and how is locum working organised?
-
How may locum doctor working arrangements affect patient safety and the quality of care? What are the mechanisms or factors which may lead to variations in safety/quality between locum and permanent doctors? What strategies or systems do organisations use to assure and improve safety and quality in locum practice? How do locum doctors themselves seek to assure and improve the quality and safety of their practice?
-
How do the clinical practice and performance of locum and permanent doctors compare? What differences in practice and performance exist and what consequences may they have for patient safety and quality of care?
Chapter 2 Overview of the study
The research aim and questions outlined at the end of the last chapter of this report were addressed through four main work packages. In this section, we provide a brief description of each work package and how it relates to the remaining chapters of the report. We also describe some important aspects of the research process including our project advisory group and patient and public involvement (PPI) arrangements and provide details of ethical approval for the research.
Overview of work packages and the structure of this report
The study was organised into four main work packages designed to address the three main research questions outlined above, as follows:
Work package 1 (addressing research questions 1 and 2) involved a survey of medical directors/medical staffing leads in NHS trusts in England and a survey of general practices in England. The two surveys examined the nature, scale and scope of locum doctor working, why locums were needed, what work they undertook and how their work was organised, and sought views on the performance of locum doctors and a range of issues concerning governance and oversight of practice. The findings from these two surveys are reported in Chapters 5 and 6 of this report.
Work package 2 (addressing research questions 1, 2 and 3) involved a combination of semistructured interviews and focus groups conducted across 11 healthcare organisations in both primary and secondary care in the NHS in England. We developed and used three interview schedules (for interviews with locum doctors; people who worked with locums in healthcare organisations; and patients and members of the public). The findings from this work package are reported in Chapters 7 and 8 of this report.
Work package 3 (addressing research question 1) involved the collection and analysis of existing routine quantitative data sets on locum doctor working in the NHS in England. We used quarterly workforce returns from all general practices in England to NHS Digital to examine locum working in primary care. We used weekly locum usage returns from all NHS trusts in England to NHS Improvement to examine locum working in secondary and community services. The findings from this work package are reported in Chapters 3 and 4.
Work package 4 (addressing research question 3) involved the collection and analysis of existing, routine quantitative data sets on doctors’ practice/performance which identify whether doctors are locum or permanent staff and so allow us to compare the practice/performance of locums and permanent doctors. We used the Clinical Practice Research Datalink (CPRD) linked to Hospital Episode Statistics (HES) to examine these issues in primary care. We sought to undertake a similar analysis in secondary care, using electronic patient record (EPR) data from two NHS hospitals: Salford Royal Hospital and the Bradford Royal Infirmary. However, we encountered a number of problems both in securing data extraction from the two hospitals' EPR systems and in identifying locum and permanent staff activity in the data sets, which severely limited our ability to examine these issues in secondary care. The findings from this work package are reported in Chapters 9 and 10.
Project advisory group
We convened a project advisory group which met regularly throughout the research and provided a valued sounding board for the research team as we developed and undertook fieldwork and data analysis and reported on our findings. We are very grateful to all members of the project advisory group, which was chaired initially by Dr Paul Twomey, medical director for NHS England in the northern region, and then after his retirement by Dr Yasmin Khan who succeeded him in that position.
Patient and public involvement
We established a PPI forum with four patient members. The chair of our PPI forum was also a member of our project advisory group. The PPI forum were involved regularly in project design and planning, and gave us feedback and guidance on research materials and outputs (e.g. study protocol, participant information sheets, survey tools, interview schedules, emerging findings). Our PPI group coproduced our patient interview schedule, two members of our PPI forum led the patient focus groups and all were involved in analysis of patient interviews. We are grateful to our PPI group and their input throughout our project. We hope they will continue to provide invaluable support for developing strategies for sharing the findings of the research with the wider community and the public.
Ethical approval
The study sponsor was the University of Manchester. The study received ethical approval from the Health Research Authority on 8 December 2020 [Integrated Research Application System (IRAS) project ID: 278888; Research Ethics Committee (REC) reference: 20/NW/0386].
Chapter 3 The use of locum doctors in general practices in England: analysis of routinely collected workforce data
Sections of this chapter have been reproduced from Grigoroglou et al. 36 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) licence, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
Aims
In this chapter, we quantify general practice locum use in England for the period 2017–9 as an aggregate and by Clinical Commissioning Group (CCG) by age group, country of qualification and gender, for the entire general practitioner (GP) locum workforce of England and we make comparisons with other types of GPs (partners who share ownership and leadership of a practice; salaried GPs who work in a practice for a fixed salary; registrars who are GP in training; and GP retainers who are supported by NHS England to stay in practice often with caring or family responsibilities). We also examine which practice and population characteristics explain variability in locum use at the general practice level for the whole primary care population of England.
Methods
Data
We accessed several data sources to extract individual-level information on full-time equivalent (FTE) working hours (1 FTE = 37.5 hours/week), type of GP (i.e. locum GP, GP partner, salaried GP, GP registrar, junior GP and GP retainer), type of locum GP (i.e. long-term of infrequent locum) and GP characteristics (age, gender, country of qualification). General practice-level information was extracted on population age and gender, quality of care, morbidity burden, patient satisfaction, rurality, deprivation, single-handed practices and healthcare regulators rating for each general practice in England. Definitions and sources for all data are provided in Appendix 1.
Practitioner-level information from NHS Digital was extracted from practices at the last day of each reporting quarter, with 12 quarters available between 31 December 2017 and 30 September 2020. We restricted the time period window, as there were differences in the methodology used by practices to report locum data prior to December 2017. For the period of analysis, some practices did not provide valid or complete records, and this resulted in some data being recorded as missing or estimated. Even though we excluded these records from the analyses, coverage was very high with approximately 95% of all practices providing valid workforce data in December 2019. FTE for locum GPs was derived as an average of the total number of hours worked in each month over the reporting quarter. 37
From NHS Digital,38 we obtained information on achievement indicators for all long-term conditions in the UK’s Quality and Outcomes Framework (QOF), which we used to calculate morbidity burden and performance for each general practice in our data set. The QOF is a national pay-for-performance scheme in primary care that was introduced in 2004 with the aim to improve quality of care and linked financial awards to performance on achievement indicators. Lower-layer super output area (LSOA)-level deprivation, as measured by the Index of Multiple Deprivation (IMD) 2019,39 was available for all LSOAs (geographically defined neighbourhoods of 1500 people on average) and we assigned LSOA deprivation scores to practices based on the practice’s postcode. The IMD is a relative measure of deprivation for all 32,844 LSOAs in England where each LSOA is assigned a score on a continuous scale (i.e. 0–100) and a higher score corresponds to greater deprivation. We extracted data on patient satisfaction for all practices from the GP Patient Survey, data on rural/urban classification based on practices’ location40 and practice overall inspection ratings from the Care Quality Commission (CQC). All data were matched on practice unique identifiers [i.e. organisation data service (ODS)] and year. Data were publicly available and did not require ethical board review.
Statistical analysis
We plotted total locum FTE against total FTE for all types of GPs over time for the whole of England. We used violin plots to compare the age and FTE distribution of locums and other GP types, and by gender. We plotted cumulative FTE by gender and country of qualification for all GP types. We calculated the average rate of general practice locum use in 2019 defined as total locum FTE as a proportion of the total GP FTE and visualised geographical variation in locum use at the CCG level with the use of spatial maps.
We used mean-dispersion negative binomial models with robust standard errors to model locum FTE, with fixed-effect predictors for region (as categorical, to account for between-region variations) and time (as continuous, to account for time trends). We used the natural logarithm of the annual total GP workforce FTE count as offset. We control for several practice characteristics in all models: deprivation, practice CQC ratings, the proportion of practice’s female population, the proportion of practice’s patients aged over 65 years, single-handed practices, rurality, QOF performance, QOF morbidity burden, patient satisfaction and practice workload defined as list size over total GP FTE. We used one set of negative binomial regression models to investigate the relationship between locum FTE and practice and population characteristics over time (2018–9) and one set of models to investigate the relationship cross-sectionally (2019).
Stata v16.1 was used for the principal data cleaning, management and analyses. For the two primary sets of analyses, we used the nbreg command with the exposure option and the incidence rate ratio (IRR) specification. Practices with < 1000 patients were omitted from the regression analyses because these practices are opening, closing or serving specific populations.
Results
Variation in locum use
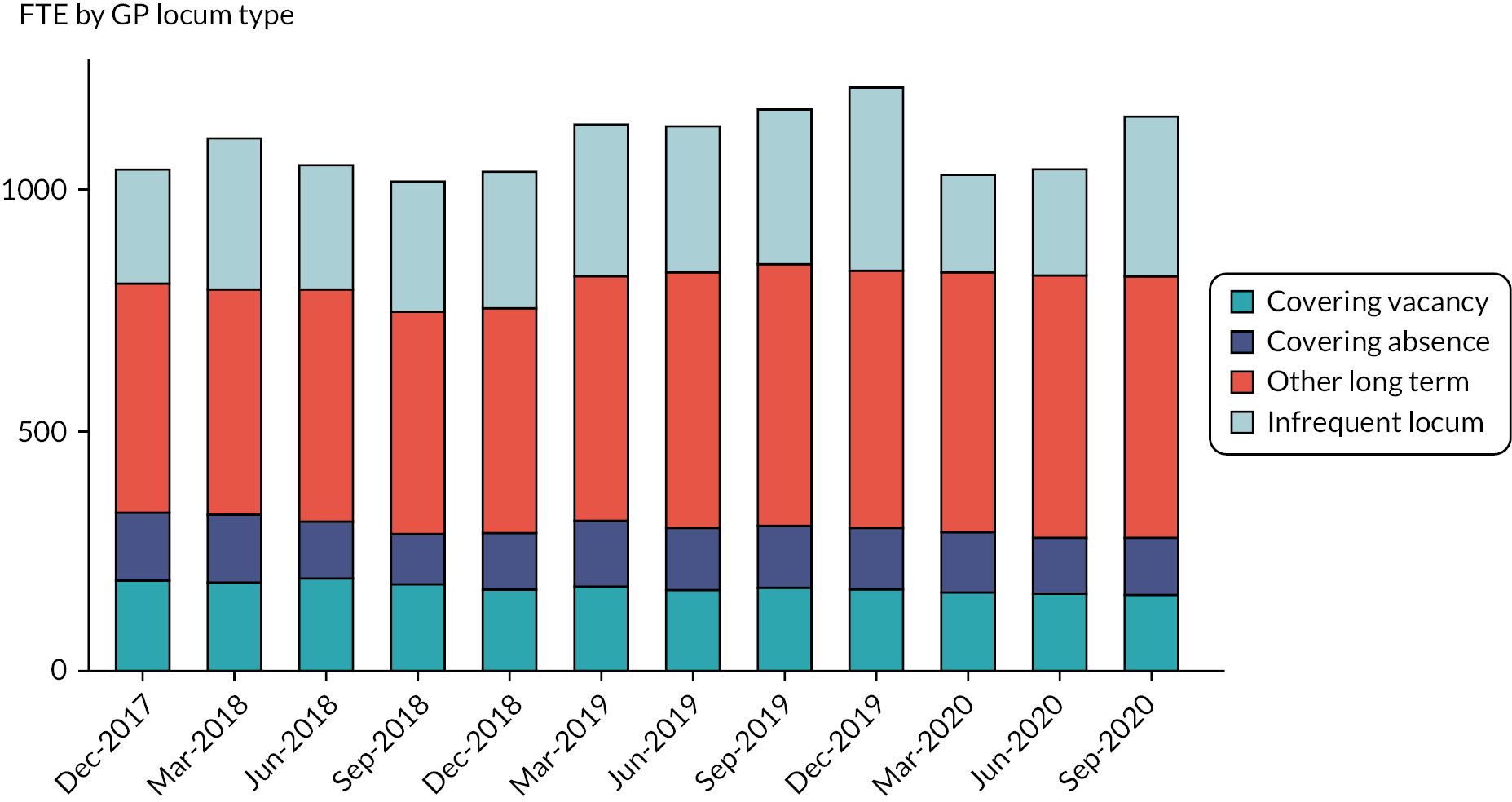
Over time, reported mean locum use in England varied from 3.15% (1045.8 FTE) in December 2017 to 3.31% (1157 FTE) of total GP FTE in September 2020 (Figure 1). The proportion of practices that reported at least some locum use varied from 37.4% and 40.8% in 2018 and 2019, respectively. Most locums (74%) worked in long-term positions compared with infrequent locums (26%) (Figure 2). Long-term locum use remained stable over the study period, though there was a substantial 47% reduction in infrequent locum use between the first and the second quarter of 2020, indicating the impact of the COVID-19 pandemic.
FIGURE 1.
Variation in FTE by GP type over time, December 2017–September 2020.

FIGURE 2.
Variation in locum type over time, December 2017–September 2020.
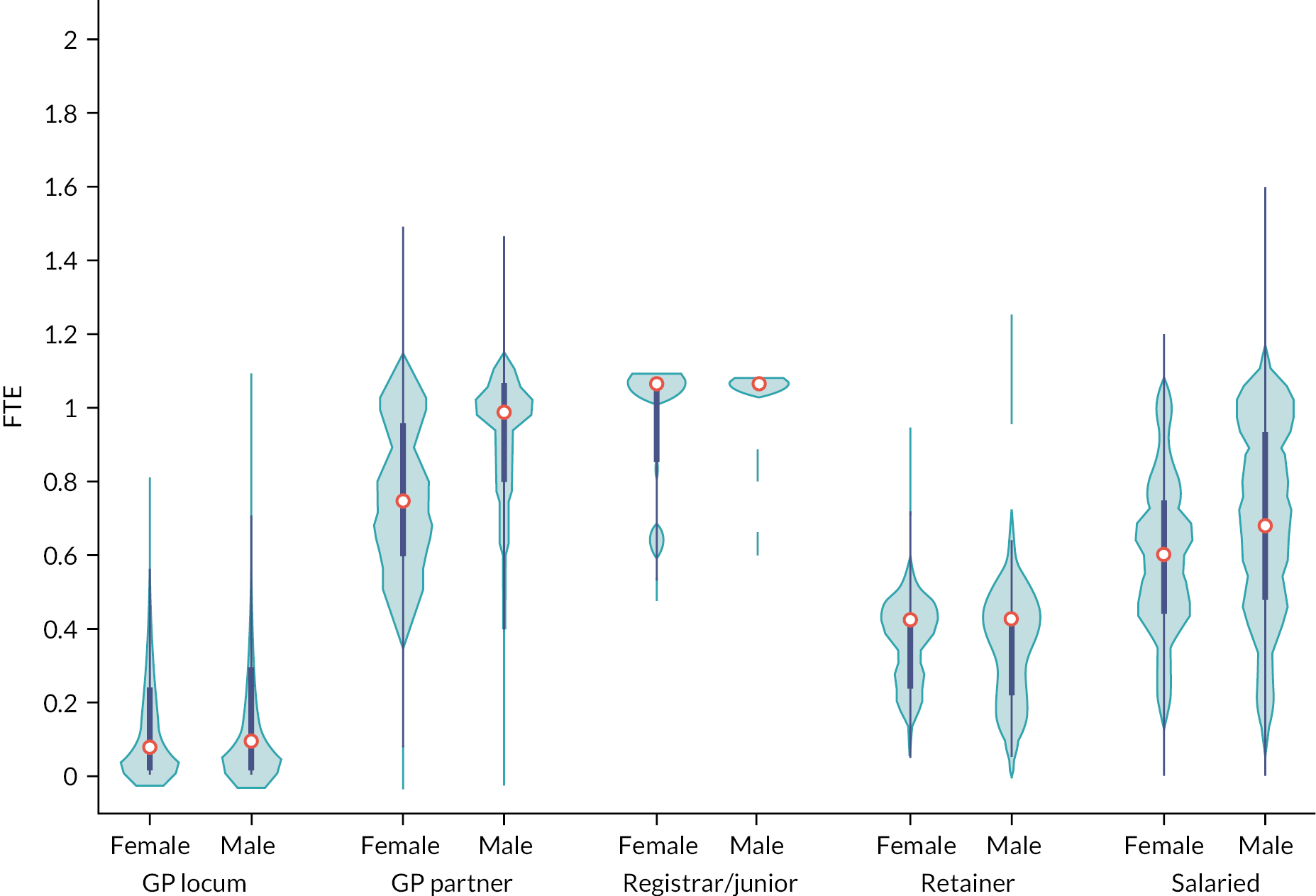
Violin plots depicting the FTE distribution of locums and other types of GPs are presented in Figure 3. Median locum FTE in December 2019 was 0.09 FTE (0.7 sessions in a practice where 1 FTE = 8 sessions) and we observed a similar distribution in FTE for both male and female locums in contrast to other GP types (e.g. GP partners/salaried GPs) where we observed large variation in the distribution of FTE between genders.
FIGURE 3.
Full-time equivalent distribution of GPs in December 2019, by type and gender.
Locum characteristics
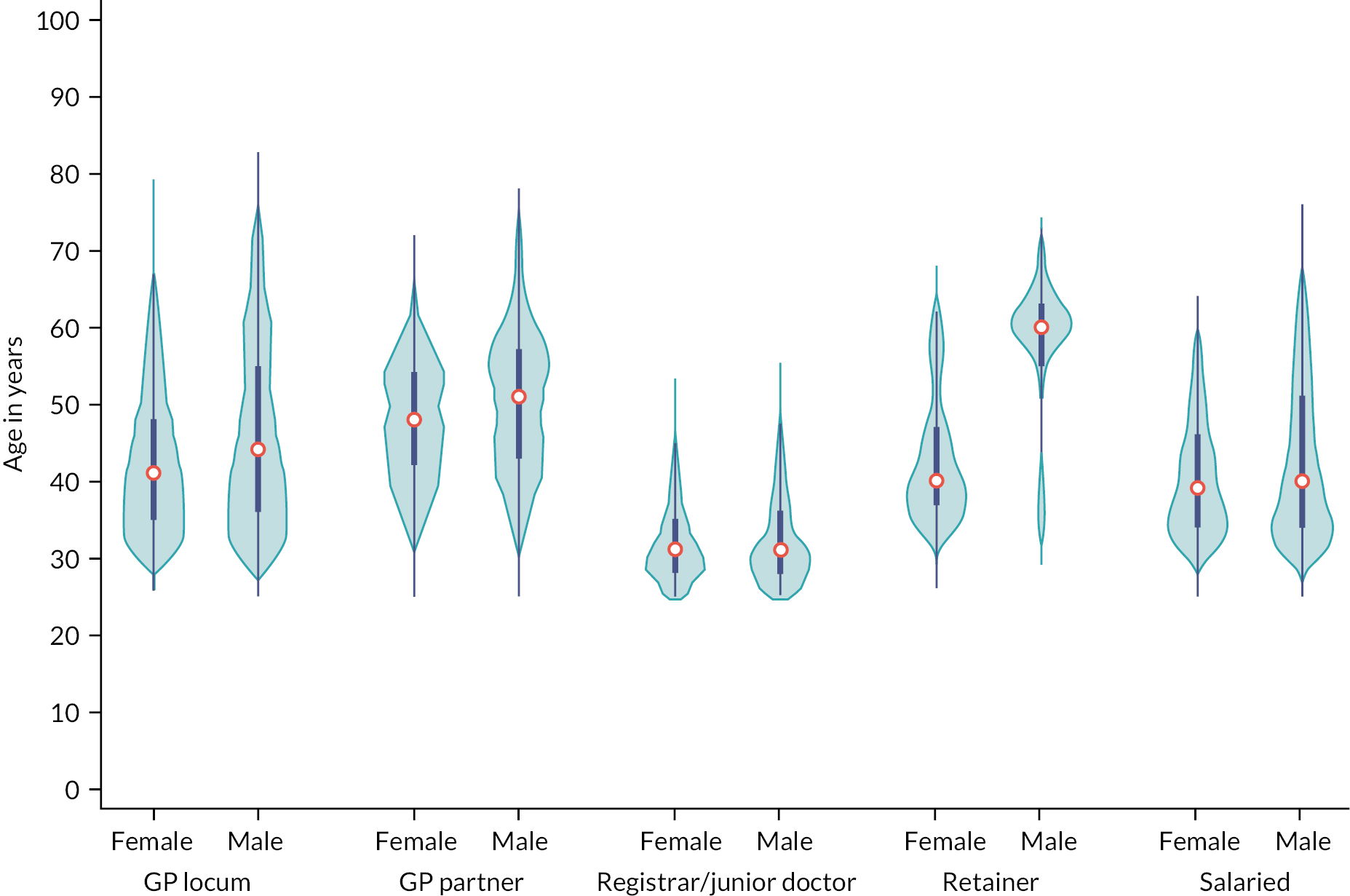
Locum workforce characteristics in terms of age are presented in Figure 4. In December 2019, the age distribution of locums shared similar characteristics with the age distribution of both male and female salaried GPs. Median age of female locums was 41 years [interquartile range (IQR) 35–48] and median age of male locums was 44 years (IQR 37–55). The median age for GP partners, junior doctors, GP retainers and salaried GPs was 49, 31, 42 and 39 years, respectively.
FIGURE 4.
Age distribution of GPs in December 2019, by type and gender.
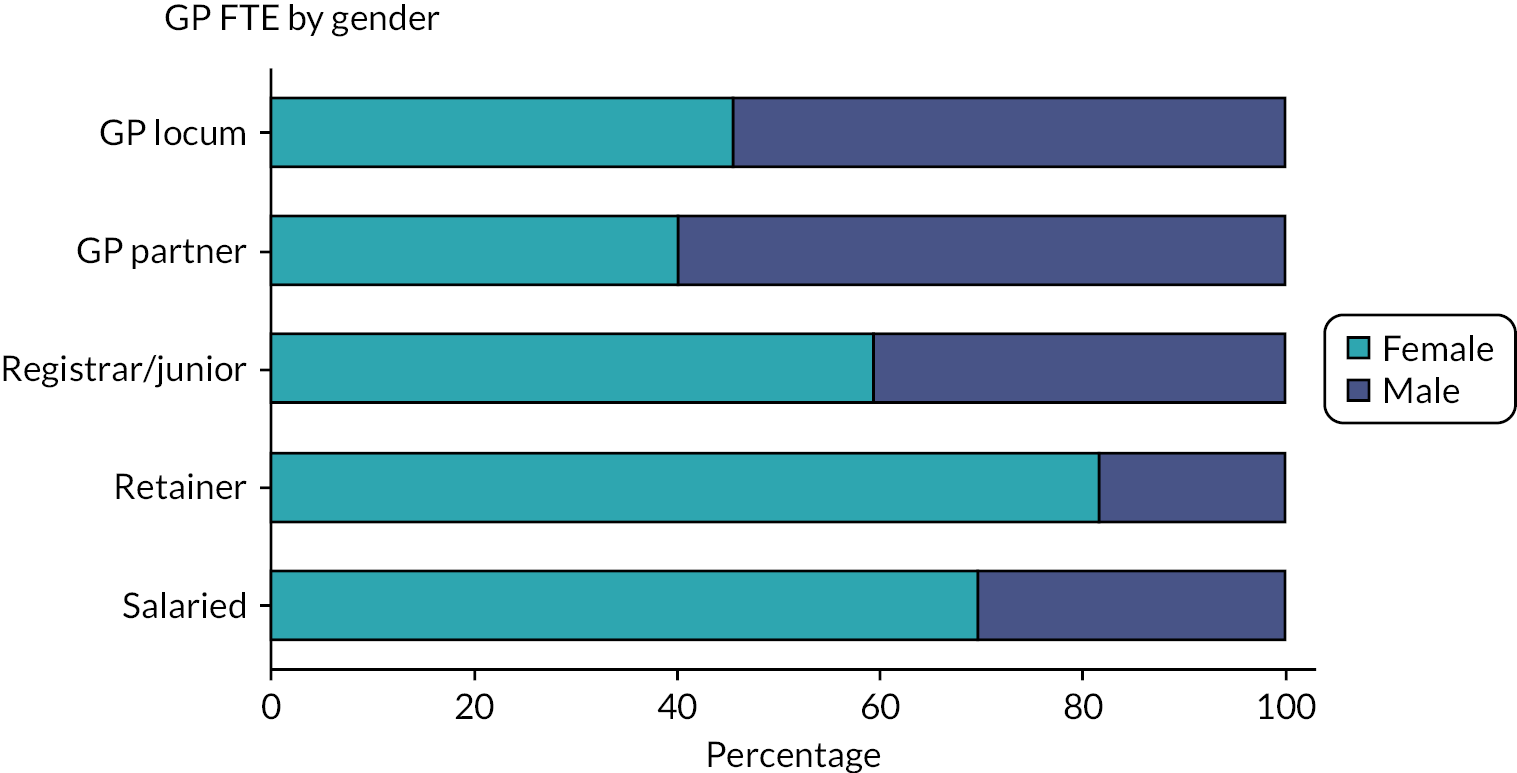
Locum workforce characteristics in terms of gender are presented in Figure 5. Male locums accounted for 54.5% of total locum FTE. This was similar to GP partners who were mostly males (60%) but in contrast to registrars/junior doctors (40.6%), GP retainers (18.5%) and salaried GPs (30.5%) who were mostly females.
FIGURE 5.
Gender breakdown by GP type, December 2019.
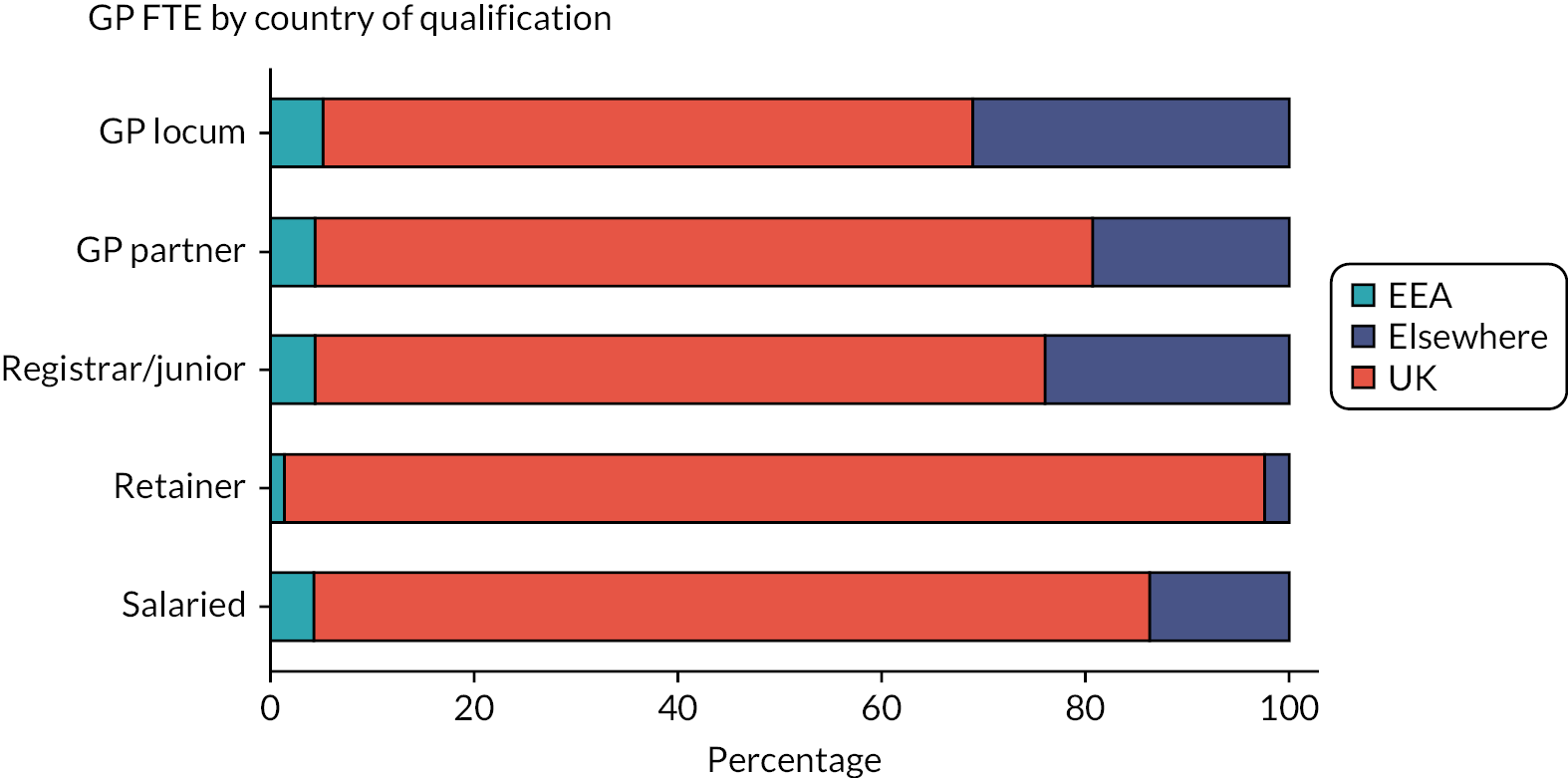
Locum workforce characteristics in terms of country of qualification are presented in Figure 6. Most locums obtained their degree in the UK (63.8%), although this proportion was smaller compared with other types of GPs (82% for salaried GPs and 76% for partner GPs).
FIGURE 6.
Country of qualification breakdown by GP type, December 2019.
Geographic variation of locum use
We present variability in mean locum use at the CCG level across regions in 2019 in Appendix 1, Figure 28, with dark-shaded areas indicating higher locum use and light-shaded areas indicating lower locum use. Locum use varied substantially between regions (from 0.4% to 13.7%) with locum use accounting for 2.5% of total GP FTE in the North East and 7.4% in London. Descriptive statistics on locum FTE, population size estimates, number of practices, census information, deprivation and QOF population achievement for all English regions in 2019–20 are reported in Table 2. In Table 24, Appendix 1 we provide a table with 10 CCGs with the highest use of locums and 10 CCGs with the lowest use of locums in 2019.
| England | North East and Yorkshire | South West | East of England | North West | South East | Midlands | London | |
|---|---|---|---|---|---|---|---|---|
| Locum GP FTE, yearly mean (95% CI) | 192.1 (125 to 259.2) | 136.9 (118.9 to 154.8) | 137.8 (130.2 to 145.3) | 155.1 (147.1 to 163.2) | 165.1 (159.6 to 170.7) | 165.6 (152.5 to 178.6) | 254.8 (234.3 to 275.4) | 329.5 (323.5 to 335.5) |
| Total GP FTE, yearly mean (95% CI) | 4564.1 (1967.4 to 6639.6) | 5457.9 (2754.6 to 8154.1) | 3628 (1849.7 to 5396.3) | 3718.0 (1911.5 to 5497.5) | 4408 (1805.9 to 6983) | 4869 (2238.4 to 7471.5) | 6317.2 (2937.3 to 9699.3) | 4471.7 (1696.9 to 7254.1) |
| Locum use (%)a | 4.2 | 2.5 | 3.8 | 4.2 | 3.7 | 3.4 | 4 | 7.4 |
| General practice population | 57,653,853 | 8,788,992 | 5,477,907 | 6,692,664 | 7,057,650 | 9,178,676 | 10,780,976 | 9,676,986 |
| Practices, n | 6422 | 991 | 539 | 655 | 951 | 856 | 1268 | 1162 |
| Single-handed practices, n | 693 | 73 | 5 | 59 | 119 | 52 | 120 | 107 |
| Practice list size, median (IQR) | 7522 (4692–11,124) | 7708.8 (4913.3–10,884.5) | 8760.8 (5996.8–12,481.5) | 8997 (6065–12,868.5) | 6410.3 (4212.3–9315.8) | 9845.3 (6367.4–13,180) | 7333.5 (4591.8–10,829.6) |
7311.5 (4858–10,554) |
| IMD 2019,b median (IQR) | 21.9 (12.5–35.5) | 29.3 (15.7–46.8) | 18.2 (11.4–26) | 16.6 (9.2–24.5) | 32.5 (17.3–52.8) | 14.2 (7.6–22.5) | 25 (14.3–39.8) | 22.1 (13.6–30.7) |
| Practice female pop, median (IQR) (%) | 3778 (2315–5611) (50) | 3851 (2428.5–5437.8) (50) | 4392.5 (3035.8–6365.5) (50.1) | 4529 (3018.3–6510.8) (50.3) | 3165.8 (2088–4686) (49.4) | 4956.4 (3228.6–6670.6) (50.3) | 3639.3 (2250.3–5441.9) (49.6) | 3617.3 (2380.3–5248.5) (49.5) |
| QOF data | ||||||||
| Population achievement, %, median (IQR) | 82.2 (79.7–84.4) | 83.1 (80.8–85) | 82.6 (80.1–84.3) | 82.5 (80.1–84.6) | 82.6 (80.2–84.7) | 81.8 (79.4–83.9) | 82.5 (79.8–84.6) | 80.6 (78–83.2) |
| Morbidity burden %, median (IQR) | 67 (55–77.3) | 75.7 (67.1–83.2) | 73.2 (64.9–80.4) | 64.8 (56.3–73) | 74.2 (65.5–82.2) | 64.2 (56.5–73.5) | 71 (62.4–79.4) | 50.6 (43.2–57.2) |
| Rural, % | 15.4 | 17.2 | 32.5 | 27.1 | 5.3 | 21.4 | 18 | 0.1 |
Results from regression analyses
After adjusting for practice and population characteristics, large variability in locum FTE between regions persisted (Table 3). Using Midlands as the reference category, practices in London had the highest locum FTE [IRR = 1.369, 95% confidence interval (CI) 1.180 to 1.588], and practices in the North East and Yorkshire had the lowest locum FTE (IRR = 0.711, 95% CI 0.626 to 0.843).
| Model A, analyses over time, sample size = 12,545 practice X year observations | Model B, cross-section analyses, sample size = 6117 practices | |
|---|---|---|
| Rurality (0 = urban, 1 = rural) | 1.250 (1.095–1.428) | 1.300 (1.085–1.559) |
| IMD 2019 | 1.002 (0.999–1.006) | 1.005 (1.000–1.009) |
| QOF practice performance | 1.005 (0.991–1.017) | 1.009 (0.991–1.026) |
| Single-handed practice | 4.611 (4.101–5.184) | 4.618 (3.928–5.428) |
| QOF morbidity burden | 1.384 (0.963–1.991) | 1.255 (0.801–1.996) |
| Percentage of female population | 0.967 (0.959–0.981) | 0.970 (0.946–0.994) |
| Proportion of practice population aged ≥ 65 years | 0.970 (0.950–0.984) | 0.971 (0.958–0.988) |
| Practice workload (total GP FTE/list size) | 1.001 (1.001–1.002) | 1.001 (1.001–1.002) |
| CQC ratings (reference group is Outstanding) | Reference group | Reference group |
| Inadequate | 2.108 (1.370–3.246) | 2.687 (1.451–4.974) |
| Requires improvement | 1.229 (0.949–1.592) | 1.198 (0.822–1.744) |
| Good | 1.343 (1.103–1.637) | 1.267 (0.947–1.696) |
| Year (reference year is 2018) | Reference year | – |
| 2019 | 1.055 (0.970–1.148) | – |
| Constant | 0.041 (0.011–0.142) | 0.020 (0.004–0.111) |
Care Quality Commission ratings appeared to be a strong predictor of locum FTE, where practices rated as having inadequate (IRR = 2.108, 95% CI 1.370 to 3.246) and good services (IRR = 1.343, 95% CI 1.103 to 1.637) had higher locum FTE than practices that were rated as having outstanding services. Single-handed practices had substantially higher locum FTE (IRR = 4.611; 95% CI 4.101 to 5.184) compared with group practices. For practices in rural locations, locum FTE was 25% higher than for practices located in urban areas (IRR = 1.250; 95% CI 1.095 to 1.428). Practices with a higher proportion of female population had 3.3% lower locum FTE (IRR = 0.967; 95% CI 0.959 to 0.981) than practices that had a higher proportion of male population. A larger patient population in the over-65 age group was associated with 3% lower locum FTE (IRR = 0.970, 95% CI 0.950 to 0.984). Finally, patient satisfaction was very weakly associated with locum FTE, while deprivation, QOF quality of care, QOF morbidity burden and practice workload did not appear to have any discerning effect on practice locum FTE. Partial results from the overtime and cross-section regression models are reported in Table 3 and the full results are reported in Appendix 1, Table 25.
Discussion
Summary
This work describes a methodological approach to capture and monitor the scale and scope of the GP locum workforce in English primary care. Our findings suggest that between December 2017 and September 2020, the proportion of GP locum work in the NHS has remained relatively stable, despite widespread perceptions that the number of locum GPs has risen. 3 Regarding regional variation and the characteristics of locums, we describe the intensity of locum use in general practice and how this varies across regions, as well as important information about the composition of the GP locum workforce. We identified substantial geographical variation in locum use between and within regions suggesting differences in the distribution of locums in England. Our comparisons of locums with other GP types showed that locums were more mobile, younger males of whom most had qualified in the UK, although a large percentage had qualified elsewhere. Most locums were employed in long-term positions and on average they did relatively few sessions. Our regression analyses showed that practice characteristics such as rurality, CQC ratings and whether the practice was single handed were stronger predictors of higher locum FTE than population characteristics.
Strengths and limitations
This analysis was conducted at the population level and allowed us to quantify and examine the scale and characteristics of the GP locum workforce compared with other types of GPs for the first time across general practices in England. We explored whether variation in practice and population characteristics explain variability in locum FTE to account for different health needs across different practice populations. The study has national scope and comprehensive coverage of the primary care population (95% of all general practices).
We used publicly available routinely collected data from NHS Digital. However, other databases on workforce report different estimates on the number of locum GPs. The GMC register and the National Association of Sessional GPs estimate approximately 17,000–18,000 GPs with a locum licence in England in 2017,3,41 while the NHS Digital data report only 5040 employed locum GPs in December 2017. There may be several reasons why these differences exist, one being that the NHS Digital data show a picture of the actual GP workforce at each time point rather than the prospective workforce that other databases report. Locum headcounts may overestimate locum use as some locum GPs may also be simultaneously permanently employed.
Second, the GP workforce data collected by NHS Digital have been subjected to changes in data sources and methodology over the years and also include estimates for practices where data are incomplete or have not been submitted. We restricted our time period to exclude data prior December 2017 when the infrequent locum category was first reported in the collection and excluded estimates for those practices that did not submit valid data. Third, the locum data are believed to be under-reported when compared with other types of GPs, mainly due to the infrequent locum category for which reporting may be lower than long-term locum data. In September 2020, NHS Digital switched from quarterly to monthly data collections of the GP workforce data; however, the transition to monthly collection led to a decrease in the number of FTE for infrequent locums. For this reason, the data collections were reverted to quarterly to allow practice managers to report infrequent locum data in time. 37
Interpretation of findings
Previous international evidence shows that the numbers of locums continue to rise,3,42,43 but our findings suggest that this may not be the case for GPs in England. Previous reports from the GMC and the National Association of Sessional GPs showed that the proportion of GPs with a locum GP contract had increased from 30% to 39% of all licensed GPs from 2013 to 2016 and was equivalent to approximately 18,000 GPs in 2018. 3
One recent study examined the geographical variation in the distribution of the GP workforce, including GP locums, across the 13 Health Education England regions using data from NHS Digital but did not make specific comparisons between locums and other types of GPs. 44 Our comparisons can provide a review of the locum workforce at a more granular level which is also particularly relevant to NHS organisations (e.g. CCGs). To our knowledge, no other studies to date have examined contextual factors and their association with locum use in general practices.
The accurate monitoring of the GP workforce may help policy-makers and commissioners to understand current challenges in primary care, including capacity and composition of the GP workforce and inform workforce planning. This can be particularly useful to meet local healthcare needs with sufficient resources for training and deployment of GPs which will help ensure that the targets set out in the NHS long-term plan are met. 45 For example, this research highlights elevated locum GP employment in practices in rural areas and those with inadequate CQC inspection ratings. These types of practices may face substantial challenges in recruiting and retaining permanent GPs and we could hypothesise that relatively high and sustained levels of locum use may be an indicator of wider problems which are affecting recruitment and retention.
Furthermore, this work lays the foundation for future analysis of other existing routine primary care data sets that contain information on service utilisation and patient outcomes. Additional work is needed to identify whether there exist differences in the clinical practice and performance between locum doctors and permanent doctors and also what consequences these may have for patient safety and quality of care. Future work should also aim to identify career intentions of locum GPs and what factors influence the choice to work as a locum. Furthermore, it will be important to understand what implications these career intentions and the observed locum workforce characteristics have on future workforce planning. As more data become available, the impact of COVID-19 on the use of the GP locum workforce should be examined.
Locum GPs have an important role in the delivery of primary care services, particularly in the delivery of out-of-hours care and in helping to address short-term workforce shortages. Despite expectations that locum GP numbers are rising, we found that locum use in primary care has remained stable over time though the use of locums seems to vary substantially across different practice types and areas of the country.
Chapter 4 The use of locum doctors in National Health Service trusts in England: analysis of routinely collected workforce data and electronic patient records
Aims
In this chapter, we use data from NHS Improvement to quantify and describe locum use, and its variation, for all acute, ambulance, community and mental health NHS trusts in England from January 2019 to December 2021. We describe the rate at which NHS trusts were able to fill locum shifts and whether NHS trusts find their locum workforce via their own NHS staff banks or via locum agencies. We explore regional variations for these measures and identify NHS trusts with the highest and lowest locum usage in 2019. Finally, we examine whether some NHS trust and population characteristics explain variability in locum use at the trust level.
Methods
Data
National Health Service trust temporary staff employment data
In England, NHS Improvement is responsible for setting out rules which trusts are expected to follow on temporary staff expenditure. The rules have a strong focus on providing support to trusts to reduce their expenditure and to move towards a sustainable model of temporary staffing. To fulfil this responsibility and support trusts, NHS Improvement collects information from all NHS trusts on their employment of temporary staff. These data are not published and were secured for research through a bespoke data-sharing agreement.
We analysed data on locum use for all NHS trusts in England between January 2019 and December 2021. Data record the weekly number of shifts that were filled by bank or agency locums for each acute, ambulance, community and mental health trust in England. A shift is defined as the period between the doctor commencing and finishing their work, but the duration of shifts is not collected. Bank staff are defined as staff who are usually sourced in-house or from temporary staff banks such as NHS Professionals, which is the largest of these banks supplying temporary staff to NHS trusts. 46 Agency staff are defined as staff who are not on the payroll of the NHS organisation offering employment and are sourced from a third-party agency.
National Health Service Improvement data record information on the number of shifts filled by temporary staff in all staff groups, but we focus on the medical and dental group which includes the aggregate number of shifts, done by all doctors and dentists. The data contain the total number of shifts that were filled by bank staff, the total number of shifts filled by agency staff and the total number of shifts requested by each trust in every reporting week, grouped for doctors and dentists. A detailed table of all the variables in the NHS Improvement data is provided in Appendix 2.
National Health Service trust characteristics
We collected monthly data on all trusts’ substantive employees represented as FTEs and trust annual job turnover data for the medical and dental staff group using the NHS Workforce Statistics database. 47 Trust type information and trust overall inspection ratings were obtained from the CQC, which rates NHS trusts as outstanding, good, requiring improvement or inadequate. 48 Trust-level deprivation was derived using hospital admissions data from NHS Digital and aggregating inpatient postcode deprivation for each trust. 49 Trust-level vacancy rates were obtained in the form of advertised FTE roles for medical and dental staff, available from the NHS Vacancy Statistics from NHS Digital. 50 These trust characteristics were linked to temporary staffing data using unique trust identifiers and are discussed in detail in Appendix 2.
Outcome measures
Locum intensity
Our primary outcome measured locum intensity for each NHS trust in every reporting week. To calculate locum intensity, we combined bank and agency shifts to obtain the total number of shifts reported at trust level in every reporting week. We adjusted this weekly total by the size of the permanent medical and dental workforce in each trust, specifically, the total number of locum shifts was divided by permanent doctor FTE, including dentists (i.e. FTE of NHS and Community Health Hospital Doctors, Consultants, Associate Specialists, Specialty Doctors, Specialty Registrars, Foundation Doctors/Postgraduate Doctors) to give the locum intensity. The annual mean locum intensity was calculated over 12 months of data. A locum intensity of 0.25 indicates that the trust-filled 0.25 locum shifts per week per FTE permanent doctor. We report locum intensity in this way because we do not know the length of the reported locum shifts and therefore cannot directly convert them into FTE. If we assume that one FTE permanent doctor typically works five shifts per week and that shift length for permanent doctors and locum doctors is broadly equivalent, then a locum intensity of 0.25 means that 5% of medical staffing in that week was provided by locums.
Proportion of agency shifts
Our second outcome measured trusts’ reliance on agency staff, which are more costly than bank staff. We divided the number of agency shifts by the total number of filled shifts for every trust in every reporting week. An annual mean proportion of agency shifts was then calculated for each trust over 12 months of data.
Proportion of unfilled shifts
Our third outcome measures shifts that the trust was unable to fill. The total number of shifts requested by each trust in every week was provided by NHS Improvement. The number of filled shifts was subtracted from the number of shifts requested to obtain the number of unfilled shifts for each trust in each week. We calculated the proportion of unfilled shifts by dividing unfilled shifts by shifts requested. An annual mean proportion of unfilled shifts was calculated for each trust over 12 months of data. Trusts occasionally reported a higher number of shifts filled than requested. In these cases, we adjusted the number of shifts requested to reflect the number of total shifts filled in that week. These adjustments were made 811 times out of 11,450 (7.1%) trust-week observations in 2019.
A worked example of the algorithm that we used in each calculation is illustrated below:
-
To obtain the mean locum intensity for Manchester University NHS Foundation trust in 2019, we combined the number of bank and agency shifts to calculate the total number of filled shifts out of the number of shifts requested. For every reporting week in 2019, we divided the total number of shifts that week by the permanent doctor FTE reported for the month in which that week fell. For example, in the week commencing 7 January 2019, Manchester University NHS Foundation trust reported 205 agency shifts and 283 bank staff shifts. We divided the total number of shifts (i.e. 488) by the reported permanent doctor FTE in January (i.e. 4378.8) to obtain a locum intensity value of 0.11, suggesting that for every one full-time doctor, the trust had 0.11 locum doctor shifts that week. That would equate to 2.2% [(0.11/5)*100] of care provided by locums in that week if we assume five shifts per FTE.
-
We calculated the proportion of shifts filled by agency staff by dividing the total number of agency shifts by the total number of all shifts (agency and bank) for each trust in every reporting week. For example, the proportion of agency shifts for Manchester University NHS Foundation trust in the week commencing 7 January 2019 was (205/488)*100 = 42%.
-
We also had information on the number of shifts that each trust requested in every reporting week. For the same week, Manchester University NHS Foundation trust requested 574 bank and agency shifts but failed to fill 86 of these giving an unfilled rate of 15% [(86/574)*100].
Our analysis data set contained information on locum intensity, proportion of agency shifts, proportion of unfilled shifts and trust characteristics for 229 acute, mental health, ambulance and community health trusts in 2019. Of these, three acute trusts and one ambulance trust did not report data on monthly doctor FTE, and one acute trust and seven ambulance trusts reported zero weekly locum returns in every reporting week. Eight ambulance, one acute, one mental health and one community trust reported zero agency shifts in every reporting week. We also explored variation in the three outcomes over time, with 224 and 221 trusts reporting bank and agency shift data to NHS Improvement, in 2020 and 2021, respectively.
Analysis
National Health Service trust temporary staff employment data
Our first set of analyses was descriptive, and we used ordered bar charts to show the distribution of locum intensity, proportion of agency shifts and proportion of unfilled shifts for all trusts in 2019–21. Violin plots showed the geographic variation in each outcome across regions. We used spatial maps to illustrate the distribution of each outcome across all Sustainability and Transformation Partnerships (STPs), local partnerships aiming to improve health and quality of care in the areas they serve. Analysis from 2019 to 2021 uncovered whether trusts reported changes over time in locum intensity, proportion of agency shifts and proportion of unfilled shifts, a period including a majority of the COVID-19 pandemic in England.
Our second set of analyses was inferential and employed three mean-dispersion negative binomial regressions to model locum intensity, proportion of agency shifts and proportion of unfilled shifts in 2019. Each model used robust standard errors with fixed-effects predictors for region (as categorical, to account for between-region variation). Our dependent variables were: the mean number of total shifts (offset: natural logarithm of annual mean total permanent doctor FTE); the mean number of agency shifts (offset: natural logarithm of the annual mean total shifts); and the mean number of unfilled shifts (offset: natural logarithm of annual mean total shifts requested). Our choice of negative binomial models over standard Poisson models was based on the presence of overdispersion in the three outcomes. We controlled for CQC inspection rating, trust type (NHS general acute trusts, NHS specialist trusts, mental health trusts and ambulance trusts), trust size (quintiles of trust permanent doctor FTE), turnover and vacancy rates and regional effects.
The final data set consisted of 197 trusts out of 229 trusts in 2019 with complete data for all covariates (8.6% of missing data). We performed a sensitivity regression analysis excluding 25 ambulance and community trusts as these trusts tend to employ very small numbers of doctors relative to acute and mental health NHS trusts. The exclusion of ambulance and community trusts allowed us to examine the effects of deprivation, which could only be measured for acute and mental health NHS trusts. Stata v16.1 was used for the principal data cleaning, management and analyses. We used the nbreg command with the exposure option.
Results
Overall locum use
In 2019, total unadjusted locum use for all trusts in England was 2,004,485 shifts, of which 909,029 (45.3%) were bank shifts and 1,095,455 (54.7%) were agency shifts. Trusts requested 2,316,302 shifts with a trust mean of 208 per week [standard deviation (SD) = 258.3]. The completeness of the data was good with 99% of all trusts reporting at least some locum use in any week.
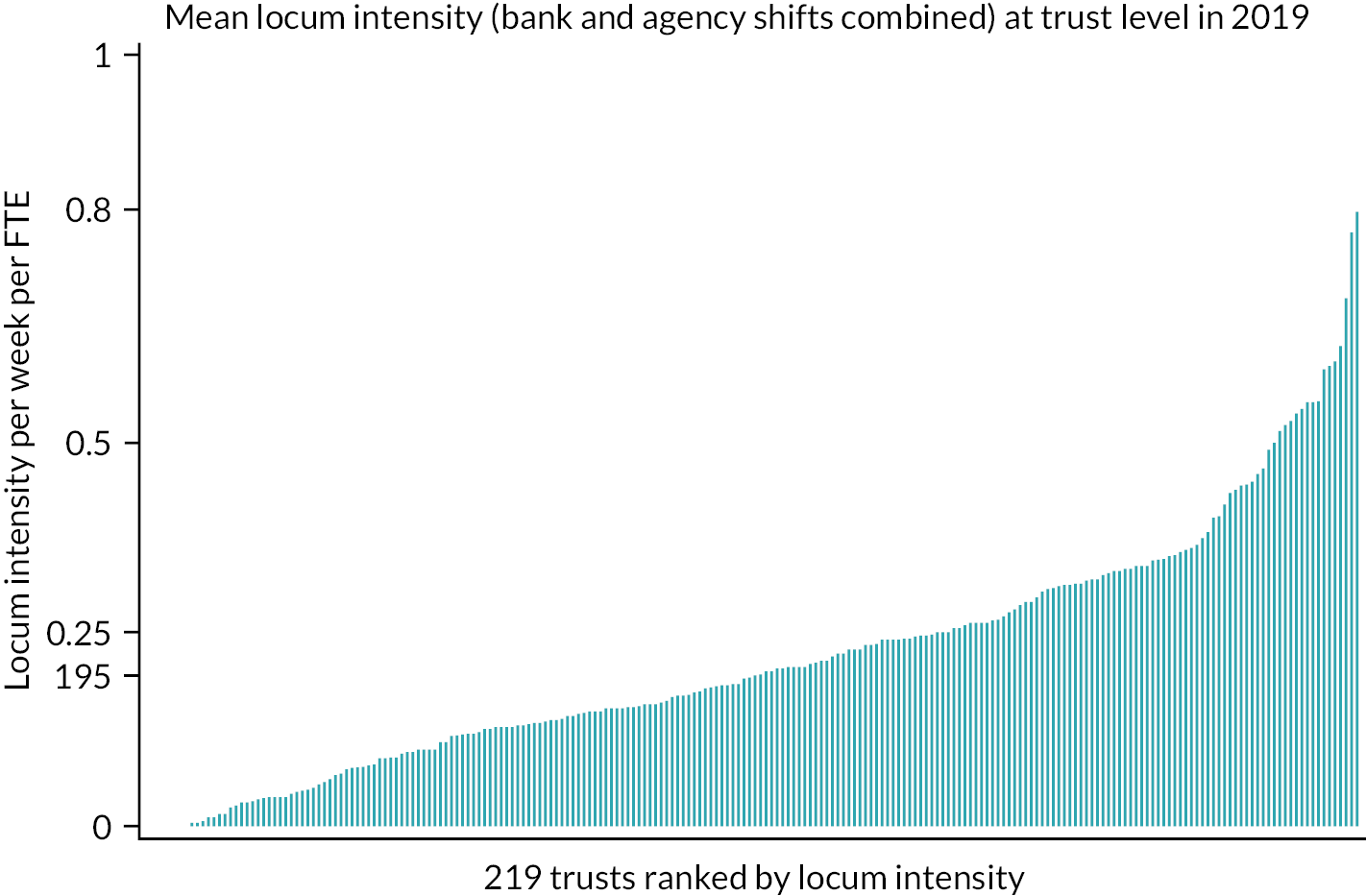
Locum intensity
Figure 7 plots the ranked mean locum intensity in 2019 for 219 NHS trusts in England showing significant variation in locum use across trusts. Mean locum intensity was 0.22 (SD = 0.16) (median = 0.195; 25th–75th centile = 0.11–0.31), indicating 0.22 locum shifts per permanent doctor FTE. Assuming five shifts per FTE, the locum intensity is equivalent to 4.4% of medical staffing provided by locums (25th–75th centile = 2.2–6%). Four ambulance trusts, three acute trusts and one community trust were not included in this analysis as they reported very low or zero permanent doctor FTE and therefore adjustments in their locum intensity could not be performed. The ranked rates of locum intensity in 2020 and 2021 are presented in Appendix 2, Figures 29 and 32. We report the 10 trusts with the highest and lowest reported locum intensity in 2019 in Appendix 2, Table 26.
FIGURE 7.
Locum intensity in 2019, NHS trust level.
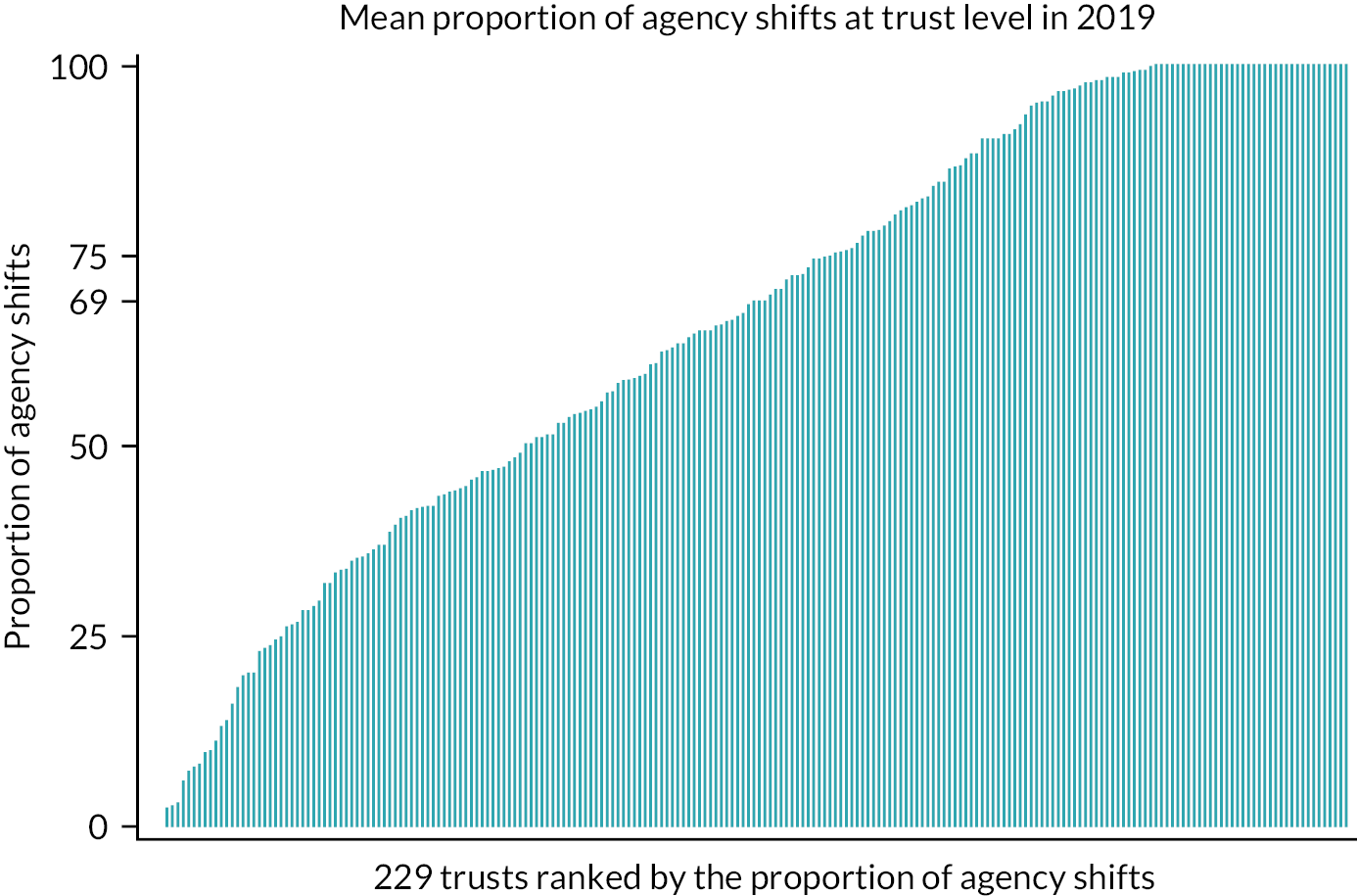
Proportion of agency shifts
The proportion of locum shifts filled by locum agency staff (rather than from staff banks) ranked from low to high at the trust level is depicted in Figure 8. The use of agency shifts varied substantially across trusts in 2019 with a mean of 66.1% (SD = 28.5%; median = 68.9%; 25th–75th centile = 43.5–95.8%). Half of trusts51 reported 100% of shifts filled by agency staff at some point in 2019, of which 24 trusts reported that shifts were filled entirely by agency staff in every week. Eight ambulance, one acute, one mental health and one community trust reported zero agency shifts in every reporting week in 2019. We present the ranked proportion of agency shifts for 2020 and 2021 in Appendix 2, Figures 30 and 33.
FIGURE 8.
Proportion of agency shifts in 2019, NHS trust level.
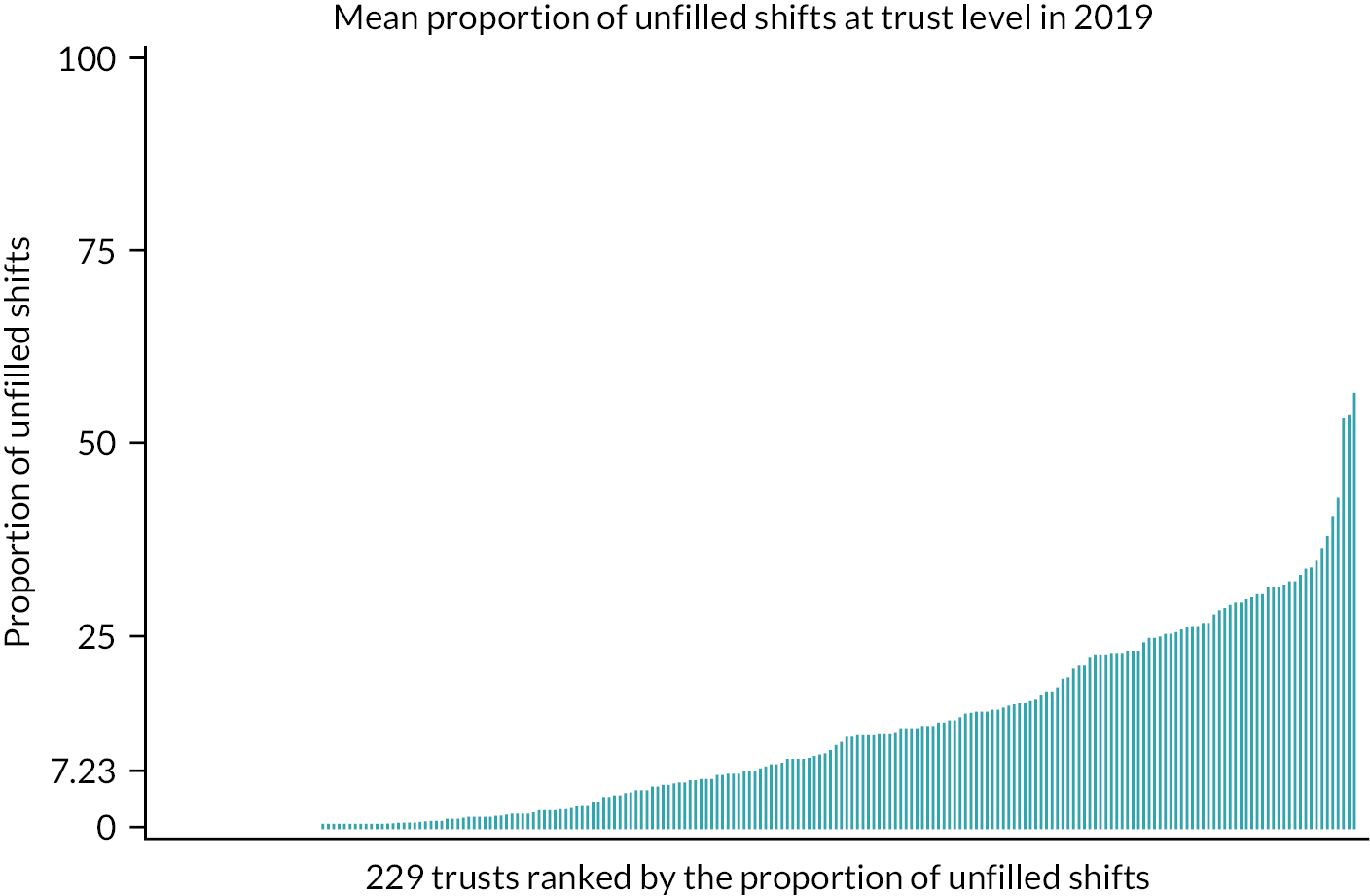
Proportion of unfilled shifts
In Figure 9, trusts are ranked from low to high on their proportion of unfilled shifts. Overall, trusts were able to fill the majority of their requested shifts either via bank or agency staff, but we observed substantial variation. The mean proportion of unfilled shifts was 11.3% (SD = 11.9%; median = 7.23%; 25th–75th centile = 0–18.1%). Seven ambulance and one acute trust did not request any shifts at any point in 2019. The ranked proportions of unfilled shifts for 2020 and 2021 are presented in Appendix 2, Figures 32 and 34.
FIGURE 9.
Proportion unfilled shifts in 2019, NHS trust level.
Regional variation in locum use
In Table 4, we present descriptive statistics on outcomes and trust characteristics at the regional level for 2019. Figure 9 shows regional variation in outcomes at the trust level in 2019. At the regional level, median locum intensity varied substantially from 0.13 in the South West of England to 0.26 in the Midlands (Table 4 and Figure 10). We also observed large variation in the proportion of agency shifts across regions. Trusts in London filled the lowest proportion of shifts using agency staff with a median of 44.8%, while trusts in the East of England filled the highest with a median of 78.1% (Table 4 and Figure 11). Trusts in the East of England filled requested shifts more successfully with unfilled shifts of 3.25%, whereas trusts in London had unfilled shifts of 11.6% (Table 4 and Figure 12). Regional variation for the three outcomes in 2020 (Figures 35–37) and 2021 (Figures 38–40) is presented in Appendix 2.
FIGURE 10.
Regional variation in locum intensity, 2019. Figure includes data from 222 NHS trusts in 2019, adjusted for permanent doctor FTE.
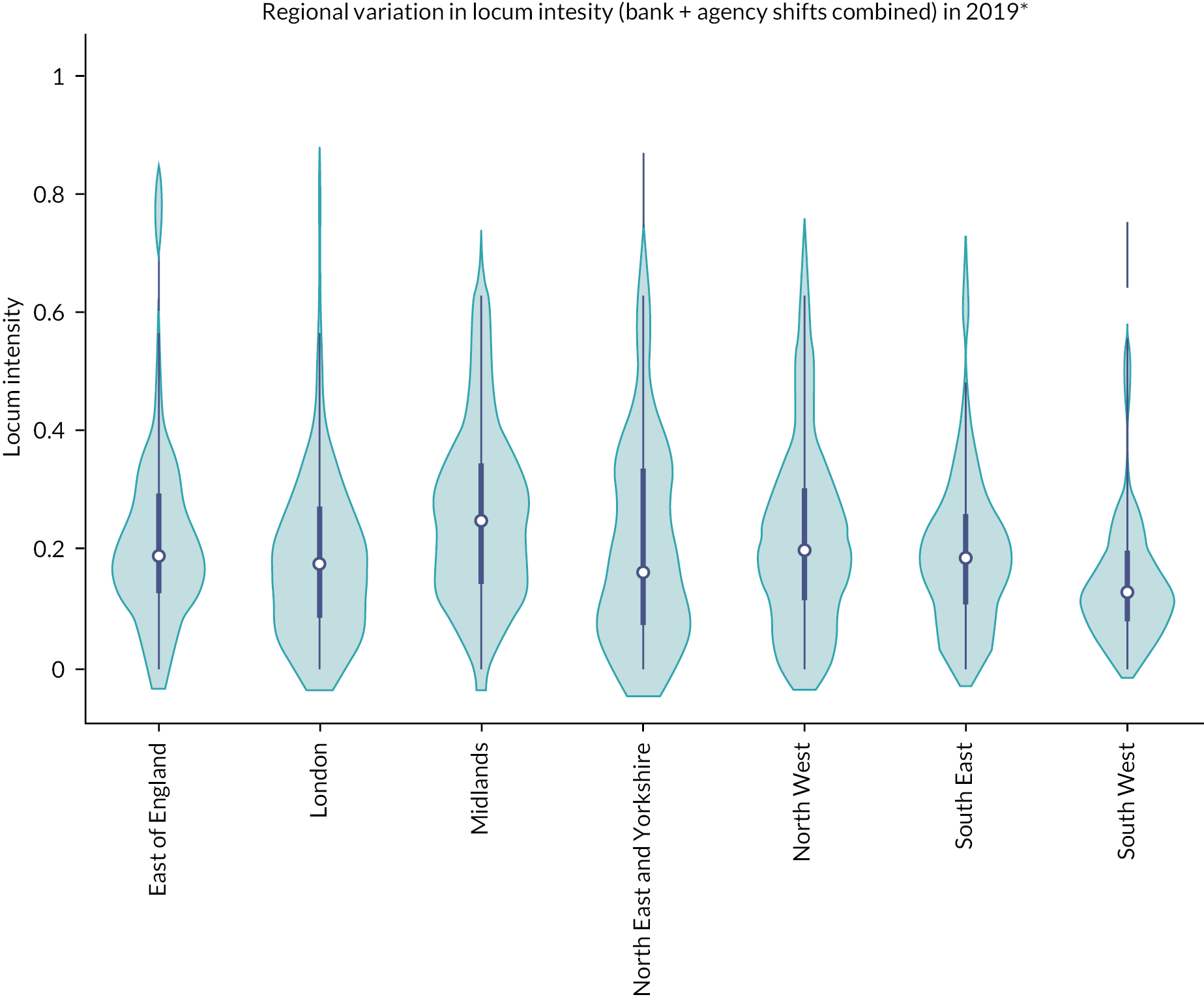
FIGURE 11.
Regional variation in the proportion of agency shifts, 2019. Figure includes data from 229 NHS trusts in 2019.
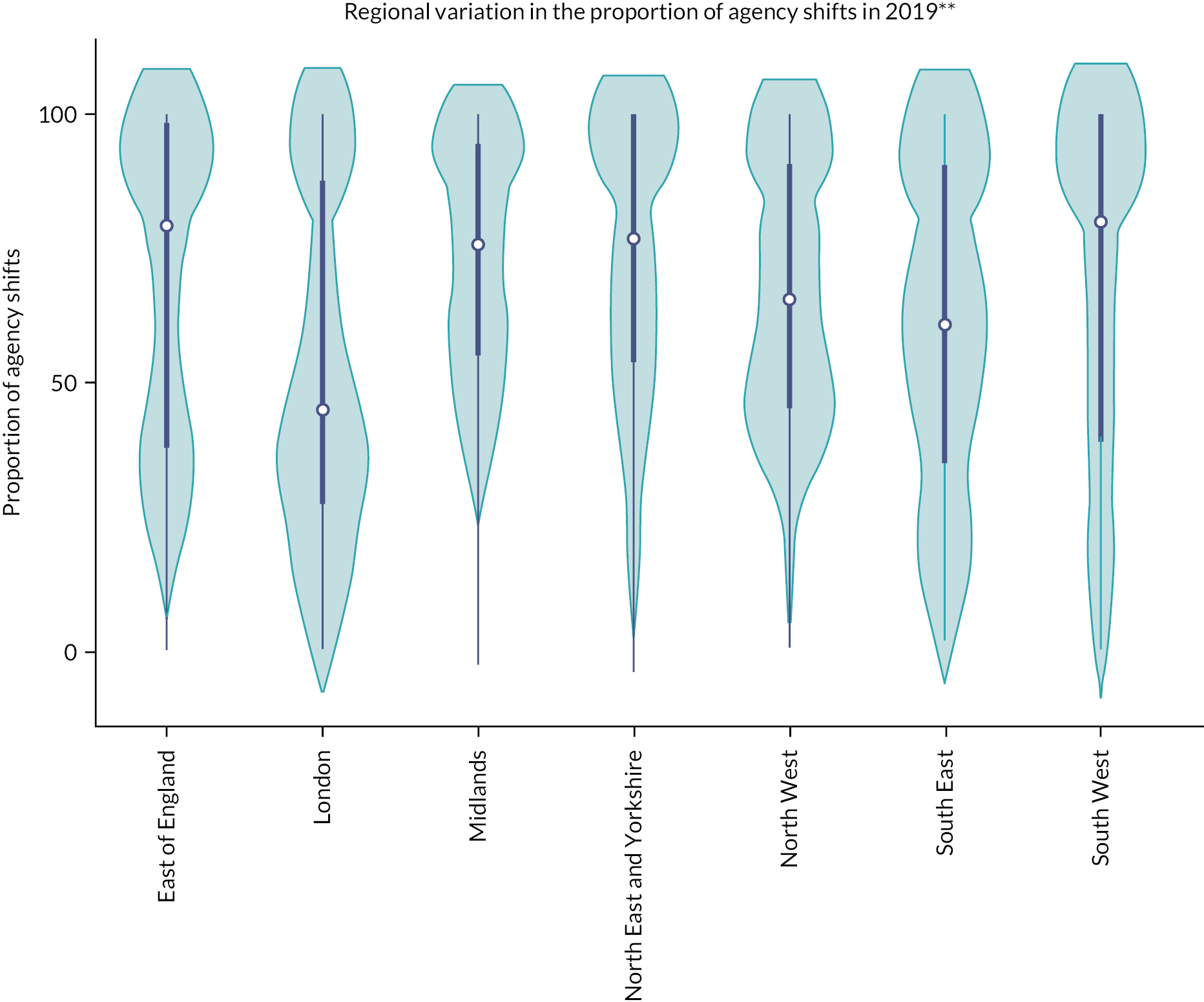
FIGURE 12.
Regional variation in the proportion of unfilled shifts, 2019. Figure includes data from 229 NHS trusts in 2019.
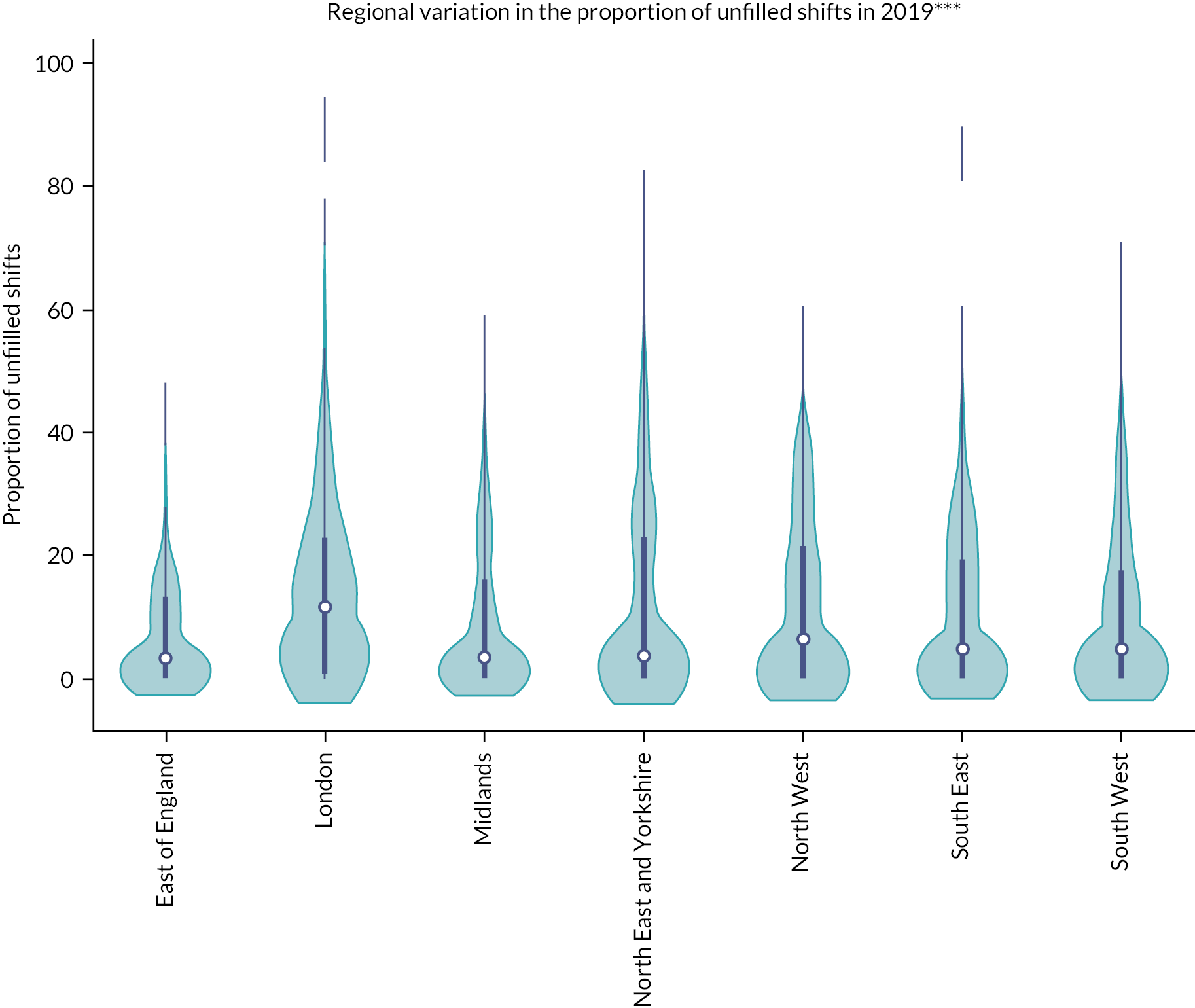
| East of England | London | Midlands | North East and Yorkshire | North West | South East | South West | |
|---|---|---|---|---|---|---|---|
| Locum intensity | 0.19 | 0.18 | 0.26 | 0.17 | 0.21 | 0.19 | 0.13 |
| Proportion of agency shifts (%) | 78.1 | 44.8 | 75.6 | 74.7 | 65.3 | 60 | 77.9 |
| Proportion of unfilled shifts (% of requested shifts) | 3.25 | 11.6 | 3.5 | 3.9 | 6.5 | 4.8 | 5 |
| Full-time doctor FTE | 803.3 | 869.1 | 569 | 715.5 | 612.6 | 1013 | 701.1 |
| Trust types | |||||||
| NHS general acute trusts (n) | 16 | 18 | 20 | 22 | 20 | 17 | 17 |
| Acute – NHS specialist trusts (n) | 1 | 5 | 3 | 1 | 6 | 1 | – |
| Mental health trusts (n) | 4 | 10 | 12 | 9 | 6 | 5 | 6 |
| Community health (n) | 3 | 2 | 4 | 1 | 2 | 5 | – |
| Ambulance service (n) | 1 | 1 | 2 | 2 | 1 | 2 | 1 |
We investigated spatial variation within and between regions using spatial maps at the STP level (see Appendix 2, Figures 41–43). Substantial variability was observed for all three outcomes both within and between regions. High levels of locum intensity were concentrated in the Midlands, the North East and Yorkshire and the North West. The South East and South West ranked among the lowest in terms of locum intensity. High proportions of agency shifts were observed in areas in the Midlands, the East of England and the North East and Yorkshire. London had by far the lowest proportion of agency shifts. The proportion of unfilled shifts was high in areas in London, the Midlands and the South West and low in the East of England.
Results from regression analyses
The regression analyses results using the three different outcomes are presented in Table 5. The results are reported as IRRs for the coefficients of interest. Sensitivity analyses, where we excluded ambulance and community trusts and examined the effects of deprivation on our three outcomes were nearly identical to the results from the main analyses. Deprivation did not appear to have any discernible effect on any of the three outcomes. The results from the sensitivity analyses are provided in Appendix 2, Table 27.
| Locum intensity | Agency shifts | Unfilled shifts | |
|---|---|---|---|
| Trust-level aggregate FTE (reference group is quintile 1) | Reference group | Reference group | Reference group |
| Quintile 2 | 0.784 (0.527 to 1.676) | 0.945 (0.734 to 1.218) | 0.936 (0.449 to 1.952) |
| Quintile 3 | 0.496 (0.299 to 0.825) | 0.937 (0.675 to 1.301) | 1.848 (0.735 to 4.645) |
| Quintile 4 | 0.611 (0.349 to 1.072) | 0.883 (0.617 to 1.264) | 1.878 (0.704 to 5.011) |
| Quintile 5 | 0.347 (0.187 to 0.644) | 0.796 (0.530 to 1.195) | 2.447 (0.826 to 7.251) |
| Trust type (reference group is NHS general acute trust) | Reference group | Reference group | Reference group |
| NHS specialist trust | 0.285 (0.174 to 0.468) | 1.510 (1.086 to 2.100) | 0.233 (0.091 to 0.598) |
| Mental health trust | 0.966 (0.628 to 1.486) | 1.576 (1.198 to 2.073) | 1.062 (0.508 to 2.221) |
| Ambulance service | 55.43 (20.56 to 149) | 0.033 (0.008 to 0.147) | 3.894 (0.453 to 33.14) |
| Community service | 1.443 (0.780 to 2.670) | 0.962 (0.641 to 1.445) | 1.360 (0.471 to 3.930) |
| CQC ratings (reference group is good and outstanding) | Reference group | Reference group | Reference group |
| Inadequate and requiring improvement | 1.495 (1.191 to 1.877) | 1.044 (0.907 to 1.201) | 1.193 (0.789 to 1.804) |
| Trust-level substantive doctor turnover rates | 1.015 (1.009 to 1.021) | 1.001 (0.997 to 1.003) | 0.995 (0.987 to 1.003) |
| Trust-level vacancy rates (FTE) | 1.000 (0.999 to 1.001) | 0.999 (0.999 to 1.001) | 0.999 (0.997 to 1.001) |
| Region (reference region is London) | Reference group | Reference group | Reference group |
| South West | 0.575 (0.361 to 0.915) | 1.447 (1.098 to 1.907) | 0.687 (0.316 to 1.493) |
| South East | 0.701 (0.472 to 1.041) | 1.349 (1.047 to 1.736) | 0.524 (0.252 to 1.092) |
| Midlands | 1.041 (0.714 to 1.520) | 1.425 (1.126 to 1.804) | 0.548 (0.276 to 1.086) |
| East of England | 0.813 (0.533 to 1.240) | 1.525 (1.167 to 1.993) | 0.402 (0.182 to 0.890) |
| North West | 1.045 (0.705 to 1.550) | 1.327 (1.035 to 1.701) | 0.855 (0.412 to 1.773) |
| North East and Yorkshire | 0.754 (0.495 to 1.150) | 1.449 (1.120 to 1.875) | 0.575 (0.269 to 1.230) |
| Constant | 0.030 (0.152 to 0.601) | 0.436 (0.283 to 0.671) | 0.117 (0.038 to 0.357) |
| Sample size | 220 | 214 | 214 |
Locum intensity
Results indicate that in 2019 trust size was a strong predictor of locum intensity. Using quintile 1 (i.e. small trust size) as the reference group, our results showed significant reductions in locum intensity for medium and very large trusts with IRRs of 0.496 (95% CI 0.299 to 0.825) for quintile 3, and 0.347 (95% CI 0.187 to 0.644) for quintile 5. As an example of interpretation, comparing quintile 1 and quintile 3 suggests a locum intensity 50.4% lower for the medium size trusts. NHS specialist trusts had a 71.5% lower locum intensity (IRR = 0.285; 95% CI 0.174 to 0.468) than NHS general acute trusts. Ambulance service trusts had 55 times higher locum intensity than NHS general acute (IRR = 55.43; 95% CI 20.56 to 149). However, this result is an artefact of the very low numbers of permanent doctors employed by ambulance trusts when compared with other trusts. CQC ratings were strongly associated with higher locum intensity with trusts rated as inadequate or required improvement having 49.5% (IRR = 1.495; 95% CI 1.191 to 1.877) higher mean locum intensity than trusts rated good or outstanding. Staff turnover rates had negligible effects on locum intensity (IRR = 1.015; 95% CI 1.009 to 1.021). Trusts in the South West had 40.25% lower locum intensity than trusts in London (IRR = 0.575; 95% CI 0.361 to 0.915).
Proportion of agency shifts
National Health Service specialist trusts and mental health trusts had 51% (IRR = 1.510; 95% CI 1.086 to 2.100) and 57.6% (IRR = 1.576; 95% CI 1.198 to 2.07) higher proportion of agency shifts than NHS general acute trusts. Ambulance service trusts had 96.7% lower proportion of agency shifts (IRR = 0.033; 95% CI 0.008 to 0.147) than NHS general acute trusts. Trusts in the East of England had the highest proportion of agency shifts compared with trusts in London (IRR = 1.525; 95% CI 1.167 to 1.993).
Proportion of unfilled shifts
National Health Service specialist trusts had 76.7% higher proportion of unfilled shifts when compared with NHS general acute trusts. Trusts in the East of England had 59.80 lower rates of unfilled shifts when compared with trusts in London (IRR = 0.402; 95% CI 0.182 to 0.890).
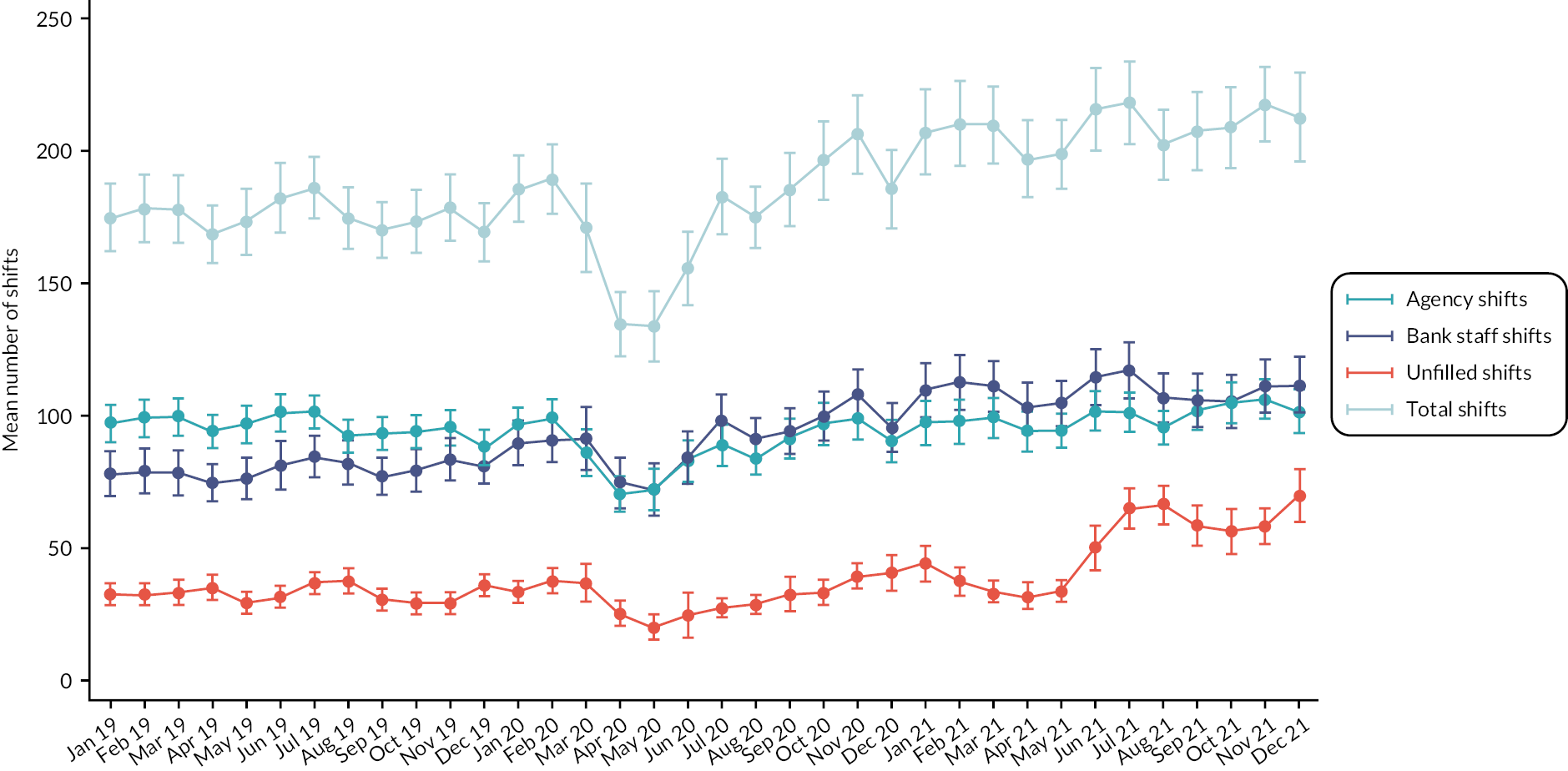
Locum use during the COVID-19 pandemic
Figure 13 shows the mean agency, bank, unfilled and total shifts per week at the trust level in 2019–21. Over time, the trust-level mean was 188.5 shifts per week (SD = 205.8), of which 95.2 (SD = 108.6) were agency shifts and 93.3 (SD = 135.8) were bank staff shifts and the mean of unfilled shifts across all trusts was 38.5 (SD = 85.2). Pre pandemic, we observed a small variability in the mean number of agency, bank and unfilled shifts. In March 2020, there was a steep decline (approximately 18%) in agency and bank shifts per trust as very few trusts reported locum use between March and April. In the third quarter of 2020, we observed an increase (approximately 15%) in agency and bank shifts per trust. In 2021, there was a steep steady increase in the mean number of unfilled shifts from 33.9 to 50.1 (47.8% increase) between May and June, which was sustained throughout 2021 and reached a peak of 69.2 unfilled shifts per trust in December 2021.
FIGURE 13.
Variation in mean number of locum shifts over time, 2019–21.
Discussion
Summary
This study provides evidence on the extent of locum use and factors associated with locum use in NHS trusts in England for the period 2019–21. Our findings show that, on average, 4.4% of medical staffing in NHS trusts in 2019 was provided by locum medical staffing. Trusts with lower CQC ratings, acute trusts and smaller trusts had higher locum intensity. We observed moderate variability in locum use across regions and greater variability in the proportion of shifts filled by agency locums. During 2021, the proportion of shifts that were unfilled reached a 3-year high. Our findings can help inform NHS organisations about the extent of their locum use and can provide important information about the effective planning of the NHS workforce.
Strengths and limitations
The main strength of this study is the national scope and coverage of every NHS trust of England. For the first time, using routinely collected data on locum use, we quantified the extent of locum use, sourced from agencies or banks, across all NHS trusts for the period 2019–21. We also explored whether trusts were able to cover sufficiently for staff shortages and identified drivers of locum use at the trust level for the whole of England. We reveal the impact of COVID-19 on locum use in NHS trust. Our analyses allowed us to control for measured trust and population characteristics.
However, this study has some important limitations which should be considered when interpreting the key findings. First, the NHS Improvement data do not reveal information on locum use by specialty and there may be substantial variations across specialties which we could not identify. Second, although NHS Improvement collects data on the number of locum shifts, it does not collect the shift duration or locum FTE which would allow a more straightforward comparison with permanent doctor FTE. We had to assume that shift lengths for permanent and locum doctors were broadly equivalent in order to estimate the proportion of medical staffing provided by locum doctors. Third, there may also exist variability in locum use between locums of different types (e.g. infrequent or long-term locums) or durations apart from the agency/bank categories, which has been observed in general practice. 36 Some locums may be employed for several months52 often to cover a vacancy which has not been filled, while others may cover short-term absences such as illness for as little as one or two shifts and we did not have that information. Fourth, the data set has no information on how well NHS trusts use their locum workforce such as the provision of adequate induction, training, supervision and feedback in accordance with National Health Service England (NHSE) guidance. Prior work15 suggests that locum performance is driven more by organisational attributes such as these than by the characteristics of the locum doctors themselves.
Interpretation of findings
The use of locum doctors is important because of the high level of spending it entails and because of concerns about the quality and safety of locum staffing arrangement. 9 Our study shows that the actual level of locum use, as a proportion of overall medical staffing, is relatively low on average, but varies considerably, with some trusts having much higher use of locums and some trusts relying overly on more expensive agency locums rather than using staff banks.
Some of this variation may be explained by organisational characteristics. For instance, larger trusts may be more able to cover workforce gaps within their own staff without needing locums, and specialist/tertiary trusts may find it easier to recruit and provide attractive workplaces compared with general acute trusts. Mental health trusts may face particular staffing shortages, which may explain the high level of agency locum use.
Our results show significantly higher locum intensity in trusts with worse CQC ratings (inadequate or requires improvement). It may be that these trusts find it harder to recruit and fill workforce gaps, but it could also be hypothesised that sustained high levels of locum use may impact quality and safety and hence affect CQC ratings.
The introduction of the first UK lockdown brought significant reductions in the numbers of both bank and agency locum doctors employed across NHS trusts, due to cancellations in elective care. However, shortly after, trusts started employing more locums likely in an effort to tackle excessive workload and increasing demand for healthcare services during the pandemic. Furthermore, in 2021, we observed an increase in the mean number of shifts filled by bank compared with the previous years and this was accompanied with a stable trend in agency shifts and an increase in the number of unfilled shifts. This suggests that trusts were meeting the increased demand with bank staff, which is in line with the new agency rules enacted by NHS Improvement in 2019 that aim to reduce reliance on agency staff. 53 Despite the increase in the mean number of total shifts, trusts appeared to be less able to fill the number of shifts they were requesting over the second half of 2021. This may suggest a persisting high workload for permanent doctors that trusts were unable to address with the use of locum doctors over that period.
Chapter 5 The use of locum doctors: findings from a national survey of National Health Service trusts in England
Aims
This chapter explores the use of locum doctors in NHS trusts in England through a national survey of NHS trusts. Locum working has benefits for individual doctors and organisations but there are concerns about the impact of locum working on continuity of care, patient safety, team function and cost. 9,54,55 The aim of this study was to conduct a national survey of NHS trusts to explore locum work, and better understand why and where locum doctors were needed; how locum doctors were engaged, supported, perceived and managed; and any changes being made in the way locums are used.
Methods
Questionnaire design
The survey was developed with input from stakeholders including a medical director, a research director, a senior leader in medical staffing, the chair of our PPI forum, a GP locum and a managing director of a locum agency. Drafts of the survey were sent out via e-mail and stakeholders responded with comments, and where possible in-depth discussions were conducted with stakeholders to gain further feedback. The research team discussed the comments received and made appropriate changes.
The study was approved by the Health Research Authority – National Research Ethics Service England, and the initial page of the survey stated that by completing the survey participants were agreeing to take part in the study.
An 89-question custom-built online open survey56 was generated using Qualtrics software. 57 We collected information about why locums were needed, how locums were recruited, supported, perceived and managed, how the work of locums compared with permanent doctors, experiences of locum agencies, familiarity with the NHSE guidance for supporting locums and how concerns about locums were dealt with. We also sought the views of NHS trusts about the advantages and disadvantages of locum work and how they see locum doctor work changing in the future. A copy of the survey is provided in Appendix 3.
For the purposes of this survey, we defined a locum doctor as a doctor in a temporary or fixed-term placement, engaged through a locum agency, internal locum bank or directly contracted by a healthcare organisation.
Survey distribution
This was a survey of 191 NHS trusts in England. Prior to distribution, we e-mailed ROs to make them aware of the research and to encourage engagement. A RO is accountable for the local clinical governance processes in their particular healthcare organisation, focusing on the conduct and performance of doctors. RO duties include evaluating a doctor’s fitness to practise, and liaising with the GMC over relevant procedures. 58 The survey was initially sent to trust ROs in England and periodic reminders were sent to non-responders. Due to a low initial response rate, we contacted non-responding trusts by telephone to identify appropriate contacts at each trust. The survey was then sent to each of the contacts provided, which included R&D departments, medical staffing departments and medical directors. The electronic link to the survey was active for 7 months between June and December 2021 to allow trusts the time to respond during the pandemic.
Survey analysis
We analysed numeric and Likert scale data from survey respondents using frequency tables. Comparisons between NHS trusts who responded to the survey and all other NHS trusts in England were performed using t-tests. Since most survey responses were not normally distributed, non-parametric tests were used. Differences were investigated using Mann–Whitney U-tests.
Three free-text questions were analysed using thematic analysis;59,60 these questions asked about the advantages and disadvantages of locum agencies, the advantages and disadvantages of locums and the future of locum work. Employing an inductive approach – coding and theme development – involved identifying patterns of shared meaning across responses and was driven by the content of the comments rather than a priori themes. The written responses mostly consisted of short sentences which provided additional contextual detail to the quantitative questions. The written responses were read and reread to become familiar with the content, and notes were made of any potential codes for each question by identifying recurring words or units of meaning. 61 Responses to the three free-text questions were combined and mapped into overarching themes which encompassed the main issues highlighted in the data (a list of these themes and illustrative quotes are shown in Table 9). One further free-text question, which asked for opinions about the NHS England and Improvement guidance about supporting locum doctors, was not included in the thematic analysis as it was specific to the guidance. Illustrative comments are included to provide contextual detail to the quantitative question asking about trusts familiarity with the guidance.
Respondent characteristics
We surveyed a total of 191 NHS trusts and we received 98 usable responses (response rate 51%); of these, 89 completed the whole survey and 9 answered half or more of the questions. The responses included 66 (67%) acute hospitals, 26 (27%) mental health and 6 (6%) community health providers. The survey was completed by 35 (36%) Medical Directors and/or ROs (including Deputies and Associates), 54 (55%) medical staffing (e.g. Temporary Staffing Manager, Head of Medical Workforce), 3 (3%) clinical staff and 4 (4%) other roles (e.g. Medical Human Resources Business Partner). One respondent did not complete the question about their job role. Compared with all other trusts in England, there was no significant difference in CQC ratings, reported extent of locum usage, permanent doctor FTE or deprivation, suggesting the responses were broadly representative of NHS trusts generally.
Results
The need for locums
How often trusts use locums
Over three-quarters of trusts always or most of the time used locums and only one trust reported that it made no use of locums. We asked trusts how long locums were typically engaged for at their organisation. Trusts used locums for all different engagement lengths, but locums were most frequently needed for medium-term (1–3 months) and long-term (3 months–1 year) lengths of time, and less frequently short term (1 week–1 month). Acute trusts used locums more frequently for very short (one session to under a week) and short-term lengths of time compared with mental health trusts (p < 0.001) and community health providers (p < 0.001).
Reasons for locum use
Trusts reported the main reason for using locums was because of difficulties recruiting doctors (Table 6). Acute trusts needed locums to cover planned medical workforce gaps more frequently compared with community health provider trusts (p = 0.008), to cover absences due to short-term ill health more frequently compared with mental health providers (p = 0.002) and to provide additional capacity to meet demand or need more frequently compared with mental health trusts (p < 0.001) and community providers (p = 0.021).
| Often | Sometimes | Rarely | Never | Σ2 | |
|---|---|---|---|---|---|
| Trust typea | |||||
| Because of difficulties recruiting doctors | 69 (71.1) | 21 (21.7) | 6 (6.2) | 1 (1.0) | 2.25 |
| Because of difficulties retaining doctors | 12 (12.4) | 38 (39.2) | 39 (40.2) | 8 (8.3) | 1.12 |
| To cover planned medical workforce gaps, for example maternity/paternity leave, holiday or sabbatical | 28 (28.9) | 52 (53.6) | 15 (15.5) | 2 (2.1) | 6.88* |
| To cover absences due to short-term ill health | 43 (44.3) | 31 (32.0) | 22 (22.7) | 1 (1.0) | 8.20* |
| To cover absences due to long-term ill health | 25 (25.8) | 50 (51.6) | 20 (20.6) | 2 (2.1) | 4.03 |
| To provide additional capacity to meet demand or need | 34 (35.1) | 38 (39.2) | 21 (21.7) | 4 (4.1) | 16.40** |
Factors important to trusts when selecting locums
Most trusts felt that all factors (availability, experience, cost, training and familiarity) were at least moderately important when selecting a locum with greater importance placed on availability and experience and less importance placed on cost and familiarity with the organisation.
How the need for locum doctors is met
The most frequent method for engaging locums was locum agencies. Nearly all respondents used locum agencies that were ‘framework suppliers’ (on a national procurement list selected by Crown Commercial Services) and three-quarters of trusts felt that locum agencies matched their needs and provided accurate information about locums. Trusts also frequently used internal locum banks and doctors who have previously worked for the organisation. The use of Doctors Direct (NHS Professionals) and digital platforms such as Locum Nest were much less frequent. Digital platforms were used significantly more by acute trusts compared with community providers (p = 0.023) and mental health providers (p < 0.001). Internal locum banks were used significantly more by acute trusts compared with community providers (p < 0.001) and mental health providers (p < 0.001).
National Health Service England and improvement guidance about supporting locums
Familiarity with the NHS England and Improvement guidance about supporting locum doctors varied across trusts. Over half of respondents were either very or somewhat familiar but less than half of trusts were either slightly or not at all familiar.
In free-text comments, some respondents were positive about the guidance and reported that they followed the guidance in their organisation.
At [name of trust] we apply the principles of the guidance in providing our agency locum doctors with a service induction when they start from the clinical service where they are working. Prior to them starting we provide them with a welcome providing information of where the post is, access to parking along with who their contacts are whilst in post.
Trust 31
Other respondents emphasised that they follow the guidance where possible or that focus is given to certain aspects of the guidance.
Working short term has specific challenges. We are committed to have systems in place to support the professional development and governance of the Locum doctors. We have a dedicated Medical Lead to support and supervise the practice of the Locum Drs. Particular attention is given in pre-employment checks, occupational health and induction.
Trust 77
Respondents reported that the way medical staffing was organised and the cost of using locums can be barriers to implementing the guidance within their organisations.
The organisation does not have a temporary staffing team it also outsources the medical bank management however this is under review. Therefore best practice is not always adhered to at [Trust name].
Trust 87
Others felt that the guidance was unrealistic, contradicted other guidance requirements and did not recognise differences between trusts. It was also felt that these issues were exacerbated by current staffing pressures.
It’s perfect world stuff, the reality is it’s the Wild West and we are desperate to get people.
Trust 27
Difficult to do when we have to provide medical care and the substantive medical workforce are demanding locum cover … they do not read the guidance VS the GMC/CQC guidance.
Trust 53
I think it’s too generalised and doesn’t understand that each organisation works differently and not 1 size fits all.
Trust 25
Respondents commented that the guidance would benefit from being updated.
The guidance was put together in October 2018 so it is dated -query around some of the content around appraisals etc.
Trust 68
Application of the guidance
We asked trusts how frequently they followed different aspects of the guidance when locums were working in their organisation (Table 7). Key procedures such as verifying documentation and induction were conducted more frequently compared with, for example, providing feedback. Most trusts said they would report concerns about locums but support with annual appraisals (where appropriate) and revalidation was less frequent.
| Always | Often | Sometimes | Rarely | Never | Σ2 | ||
|---|---|---|---|---|---|---|---|
| Trust typea | |||||||
| When a locum doctor is placed in our organisation, we… | Verify documentation (e.g. GMC registration and licence to practise, Healthcare Professional Alert Notices, identity, language, health clearance) | 84 (90.3) | 7 (7.5) | 1 (1.1) | 0 | 1 (1.1) | 1.78 |
| Provide an induction to enable them to carry out the work they are being engaged to do, including access to buildings and appropriate IT systems | 65 (69.9) | 20 (21.5) | 7 (7.5) | 1 (1.1) | 0 | 1.34 | |
| Complete an end-of-placement/exit report | 6 (6.5) | 13 (14.0) | 36 (38.7) | 30 (32.3) | 8 (8.6) | 6.87* | |
| Provide peer/colleague feedback for the locum doctor at the end of the placement | 6 (6.5) | 14 (15.1) | 46 (49.5) | 23 (24.7) | 4 (4.3) | 1.07 | |
| Support the locum doctor’s appraisal preparation | 15 (16.1) | 17 (18.3) | 36 (38.7) | 19 (20.4) | 6 (6.5) | 2.74 | |
| Provide an annual appraisal for the locum doctor, if appropriate to do so (in light of the nature and duration of the placement) | 28 (30.1) | 17 (18.3) | 19 (20.4) | 20 (21.5) | 9 (9.7) | 9.27* | |
| Provide access to professional development activities | 22 (23.6) | 22 (23.6) | 34 (36.6) | 15 (16.3) | 0 | 2.74 | |
| Encourage locum doctors to attend multidisciplinary team meetings | 44 (47.3) | 29 (31.2) | 17 (18.3) | 3 (3.2) | 0 | 8.71* | |
| Inform the locum doctor and locum agency or RO (where relevant) about serious untoward incidents they have been involved in (even if they are no longer employed at my organisation) | 79 (85.0) | 9 (9.7) | 5 (5.4) | 0 | 0 | 0.41 | |
| Inform the locum doctor and locum agency or RO (where relevant) about complaints they have been involved in (even if they are no longer employed at my organisation) | 69 (74.2) | 21 (22.6) | 3 (3.2) | 0 | 0 | 1.0 | |
| Support the locum doctor to engage with revalidation systems within my organisation | 35 (37.6) | 16 (17.2) | 19 (20.4) | 16 (17.2) | 7 (7.5) | 4.67 | |
Trusts experiences of locum doctors
We asked trusts how care provided by locums compares with care provided by permanent doctors, in a number of areas (Table 8). Overall, care provided by locums was largely viewed as about the same as care provided by permanent doctors. Some trusts reported that care was worse, in particular in relation to continuity of care, but also adherence to organisational policies and guidelines, administrative errors and reporting of adverse advents. Mental health trusts were significantly more likely than acute trusts to report that workload for the permanent healthcare team was worse when care was provided by locums rather than permanent doctors.
| Much better | Somewhat better | About the same | Somewhat worse | Much worse | Σ2 | ||
|---|---|---|---|---|---|---|---|
| Trust typea | |||||||
| In your experience, when care is provided by locums rather than permanent doctors what effect, if any, do you think it has on the following aspects of care? | Adherence to organisational policies and guidelines (e.g. prescribing guidelines) | 1 (1.1) | 2 (2.2) | 60 (65.9) | 27 (29.7) | 1 (1.1) | 0.32 |
| Providing continuity of care | 1 (1.1) | 1 (1.1) | 44 (48.4) | 42 (46.2) | 3 (3.3) | 3.40 | |
| Avoiding drug-prescribing errors | 1 (1.1) | 1 (1.1) | 75 (82.4) | 14 (15.4) | 0 | 2.58 | |
| Avoiding administrative errors | 1 (1.1) | 0 | 62 (68.1) | 26 (28.6) | 2 (2.2) | 1.68 | |
| Keeping clear and accurate patient notes/clinical records | 1 (1.1) | 2 (2.2) | 73 (80.2) | 14 (15.4) | 1 (1.1) | 1.25 | |
| Reporting of adverse events or untoward incidents | 0 | 2 (2.2) | 63 (69.2) | 22 (24.2) | 4 (4.4) | 0.26 | |
| Appropriateness of referrals | 0 | 1 (1.1) | 71 (78.0) | 18 (19.8) | 1 (1.1) | 0.05 | |
| The functioning of the healthcare team | 1 (1.1) | 3 (3.0) | 70 (76.9) | 14 (15.4) | 3 (3.3) | 3.15 | |
| Workload for permanent members of staff in the healthcare team | 4 (4.0) | 16 (17.6) | 54 (59.3) | 17 (18.7) | 0 | 14.77** | |
Perspectives on locum doctors and locum agencies
We asked trusts about the advantages and disadvantages of engaging locum doctors and locum agencies and how they see locum doctor work changing in the future (Table 9). Maintaining workforce capacity and the advantage of a flexible workforce to deliver short-term and long-term service was one of the main advantages reported by respondents. Using agencies also provided assurance that compliance checks were in place; however, compliancy checks were not always done resulting in delays in locums being recruited.
| Theme | Illustrative quotes |
|---|---|
| Workforce capacity and flexibility | ‘Helps us fill our gaps by accessing doctors that we do not have access to, particularly at short notice’. (Trust 19) ‘Locums provide cover to support the permanent workforce when gaps arise, which could otherwise compromise patient care and safety’. (Trust 19) ‘Advantage is a flexible workforce has helped us over the last 2-years to overcome the difficulties in staffing levels and activity’. (Trust 83) ‘Locum doctors work is flexible, it gives the doctor the chance to see many aspects of medicine without the requirement of a long term commitment, however the organisation employing the doctor in the future will need to support the doctor’s requirements and take on RO responsibilities, revalidation and appraisal etc’. (Trust 6) |
| Compliance | ‘Assurance that they have already had all appropriate background checks and connection through a single RO makes communication easier’. (Trust 46) ‘Full compliance not always complete at the time of putting the medic forward creating delays from CV approval’. (Trust 10) |
| Lack of alternative options | ‘No option in the current climate’ (Trust 21) ‘Used as a last resort’ (Trust 36) ‘exhausted all other options’ (Trust 49) ‘Needs must! Not enough doctors so no choice’ (Trust 39) ‘a necessary evil’ (Trust 14) ‘I would like to see this become an exception to support short and immediate staffing issues and not become a reliance to solving NHS recruitment gaps’ (Trust 46). ‘We would like to reduce our reliance on locums, but this is a hard slog in terms of agreeing new establishments and recruiting permanent staff’ (Trust 7). ‘I would like to see all locum doctors working via a national NHS locum bank with fixed rates so there is no bargaining for increases in rates and playing Trusts off against each other’ (Trust 42). |
| Cost and control |
‘They will just keep getting more expensive’. (Trust 40)
‘Becoming more expensive, working relationships worsen’. (Trust43) ‘I would like to see a shift in culture of being realistic regarding rates of pay. This can almost feel that the NHS is being held to ransom to deliver patient care and maintain patient safety. I understand this is the case regarding supply and demand due to the pandemic’. (Trust 31) ‘You need to have eyes in the back of your head and micro manage the appointment otherwise you will be overcharged on pay and commission rate. They will also cut corners on due diligence and checks’. (Trust 42) ‘Agencies drive up rates and use the top of the above capped rate as the new baseline, i.e. no one will work within the capped rates’. (Trust 54) ‘[Locum agencies] play the market and prices are always high and negotiations are time consuming and energy sapping’. (Trust 55) ‘Expensive and operate a monopoly over cost as they control the flow of doctors and compete with each other for placing a doctor, offering higher rates to entice new business’. (Trust 83) ‘Agencies sometimes manipulate messages and information for their own gain, making things frustrating when we’re working with tight timescales (e.g. keeping us chasing about a specific locum who will never actually start, in order for them to not lose the booking)’. (Trust 44) |
| Familiarity and continuity of care |
‘Lack of familiarity and engagement with the department and organisation’. (Trust 16)
‘They fill the staffing gap but we would really prefer our own internal locums rather than external locums for continuity and org knowledge’. (Trust 35) ‘There is a huge difference between using an unknown doctor from an agency and using one of our own current or former doctors via our Medical Bank. We always prefer to use Bank for that reason. Bank is usually (but not always) cheaper’. (Trust 48) ‘Better to have a long-term locum rather than occasional shifts as this allows for understanding the policies of the organisation, team work and continuity of care’. (Trust 33) ‘Would be nice to see further development of passport between Trusts, so that info can be handed over, particularly across the ICS. Would also be good to provide a shadowing/placement process for locums new to the NHS – we have concerns about taking on a locum for their first ever shift in the NHS’. (Trust 19) |
| Organisational development | ‘Disadvantages: when the primary driver is financial as is invariably the case, their assumptions and reason for being there is framed in their minds in that way. It does not support a developmental approach either personally or with the team. If we were to be more hospitable and offer the “NHS” privileges of training and time for study etc. and all the other trust support for being a substantive member of staff, then what is the point of being within the NHS? We will have permanent staff and that is not conducive to building a stable workforce which is the requisite for workforce development, flexibility in services and the meeting of the transformation agenda. Additionally, locums are seldom interested in service improvement, do audits of any worth or take part in quality improvement. Being financially driven these are not seen as important enough. Finally, self-development is not seen as a priority which comes through reflection and a deep understanding of |
|
their practice and if not in the same place for long enough to develop good relationships that they trust to give them difficult information, this is very limited’ (Trust 55)
‘The bottom line is that it inhibits the development of teams, reduces continuity of care, probably doesn’t work for the locum in terms of career development, makes organisational development more difficult and is way more expensive’. (Trust 27) |
|
| Reliability |
‘Service instability due to locum doctor leaving with short notice’. (Trust 24)
‘Short-term cancellations resulting in staffing gaps which could lead to patient safety risks’. (Trust 45) ‘Quality not always reliable, service provision is not always as good as that we would usually get from a substantive doctor especially at higher grades’. (Trust 62) |
In the written responses, many trusts reported that they did not want to use locums, particularly due to cost, but they did not feel there was any alternative, especially given current workforce challenges. Respondents did not envisage a reduction in the use of locums due to current staffing pressures across all NHS organisations. Respondents wanted the cost of locums to reduce but did not see this happening and felt that, as a consequence, working relationships would deteriorate. It was felt that agencies control the market and drive up costs through competition. Costs were often above capped rates; commission rates were seen as exploitative and trust in locum agencies was low. Some respondents perceived locums as incentivised by money and some perceived that they were not invested in service improvement and self-development. Respondents felt that their organisations would like to reduce their reliance on locum agencies by increasing the use of locums from internal banks.
Respondents reported in the free-text responses that lack of familiarity with the organisation was a disadvantage and there was a preference for using internal banks rather than agencies or one-off shifts to ensure continuity of care, greater familiarity with internal systems and better investment in the organisation. The use of locums was seen as having a negative impact on organisational development and that locums were not invested or motivated to contribute to service and quality improvement. It was felt that offering better support and incentives for locums could result in further instability in the permanent workforce. To address the risk of taking on locums who have not worked at the organisation before, respondents suggested that improved communication between trusts is required and better systems for supporting doctors in their placements.
As reported in the written responses, the quality and consistency of locums and locum agencies were sometimes perceived as unreliable. Some respondents felt that locum agencies provided quality doctors; however, more respondents felt that the quality of locum doctors provided by agencies was unreliable. Locums can leave at short notice which leads to gaps and service instability and patient safety risks.
Dealing with concerns about locums
We asked trusts what happens when there is a low-, medium- or a high-level concern about a locum doctor. We defined low-level concerns as: causing no harm to patients or staff and the doctor was not at any personal risk, medium-level concerns have potential for serious harm to patients, staff or the doctor was at personal risk and high-level concerns are when patients, staff or the doctor had been harmed. The action that trusts reported they would take increased depending on the severity of the concern (Table 10). The higher the severity of the concern, the more likely that the locums and locum agencies would be informed. It was common for contracts to be ended early when there were concerns and locums to not be used again.
| Always | Most of the time | About half the time | Sometimes | Never | Σ2 | ||
|---|---|---|---|---|---|---|---|
| Trust typea | |||||||
| Low-level concern | The locum doctor is informed | 45 (50.6) |
29 (32.6) |
10 (11.2) |
5 (5.6) |
0 | 5.01 |
| Reported to the locum agency | 37 (41.6) |
24 (27.0) |
9 (10.1) |
19 (21.4) |
0 | 1.51 | |
| Reported to the GMC | 8 (9.0) |
8 (9.0) |
2 (2.3) |
38 (42.7) |
33 (37.1) | 2.86 | |
| The locum contract is ended early | 10 (11.2) |
7 (7.9) |
6 (6.7) |
53 (59.6) |
13 (14.6) | 1.48 | |
| We would not use that locum again | 15 (16.9) |
10 (11.2) |
7 (7.9) |
45 (50.6) |
12 (13.5) | 1.80 | |
| Medium-level concern | The locum doctor is informed | 66 (74.2) |
21 (23.6) |
1 (1.1) |
1 (1.1) |
0 | 4.87 |
| Reported to the locum agency | 62 (69.7) |
21 (23.6) |
3 (3.4) |
3 (3.4) |
0 | 0.24 | |
| Reported to the GMC | 22 (24.7) |
18 (20.2) |
6 (6.7) |
37 (41.6) |
6 (6.7) |
1.11 | |
| The locum contract is ended early | 24 (27.0) |
23 (25.8) |
9 (10.1) |
32 (36.0) |
1 (1.1) |
6.00* | |
| We would not use that locum again | 25 (28.1) |
28 (31.5) |
8 (9.0) |
25 (28.1) |
3 (3.4) |
4.81 | |
| High-level concern | The locum doctor is informed | 83 (93.3) |
6 (6.7) |
0 | 0 | 0 | 0.49 |
| Reported to the locum agency | 84 (94.4) |
5 (5.6) |
0 | 0 | 0 | 3.01 | |
| Reported to the GMC | 60 (67.4) |
14 (15.7) |
5 (5.6) |
10 (11.2) |
0 | 1.58 | |
| The locum contract is ended early | 59 (66.3) |
14 (15.7) |
2 (2.3) |
14 (15.7) |
0 | 6.59* | |
| We would not use that locum again | 56 (62.9) |
20 (22.5) |
1 (1.1) |
10 (11.2) |
2 (2.3) |
5.48 | |
Discussion
We found that the use of locums was an integral part of trust working. Trusts need locums for all different lengths of engagement and very few trusts make no use of locums. The use of locums is driven mainly by workforce issues like recruitment, staff sickness and planned workforce gaps. Trusts face challenges with recruitment of doctors, which is reflected in recruitment and retention challenges nationally;62 this results in trusts often needing locums long term and having to source locums mainly from agencies at high cost. We found, as others have, that there was poor awareness, ambiguity and confusion about the national guidance for locums from NHS England and who was responsible for following it. 16 Trusts focused on processes such as verifying documentation and completing induction, but less was done with regard to feedback and appraisal. This is corroborated by findings from a recent survey of agency locums which recommended that organisations provide greater support for locums to obtain evidence for appraisal and revalidation. 63
Overall, care provided by locums was viewed as about the same or somewhat worse as care provided by permanent doctors, particularly in areas like adherence to organisational policies and guidelines, continuity of care and avoiding administrative errors. One reason for this could be that mistakes are more likely to be made in environments that are unfamiliar. 63 Causes of administration errors in hospitals such as inadequate communication and local working conditions may impact more on locums who are unfamiliar with organisational systems. 64 Locum doctors may also be more likely to make mistakes if permanent staff are unable to support them due to the increased supervisory demands that may be required when locums are unfamiliar with the organisation65 or because of negative perceptions or discrimination. 63 While some trusts felt that continuity of care was worse when care was provided by a locum, it should be recognised that continuity of hospital care requires more than personal continuity at the patient interface. There is a collective organisational responsibility for continuity of care, and team structures and organisational systems should be considered when evaluating continuity of care. 66
In their written responses, respondents felt that lack of familiarity and high cost was a disadvantage, but these were not rated as important when recruiting, suggesting trusts are unable to prioritise familiarity and cost because of high demand to fill gaps. Respondents felt that locum agencies match their needs and provide accurate information about locums; however, there were low opinions of locum agencies in relation to cost. Trusts would like to reduce the reliance on locum agencies and make greater use of internal locum banks in order to reduce costs and increase familiarity with the organisation. The problem of locum cost was linked to challenges in motivating permanent staff and protecting their contractual advantages. Offering locums NHS ‘privileges’ afforded to permanent staff was perceived to be in direct conflict with building a stable workforce. This may result in the limitation of support opportunities for locums. Research has found that locums were perceived as money oriented, were treated differently than permanent staff and were often excluded from additional support processes. 15
Some respondents expressed concern that short-term placement of locums did not allow for building relationships and knowledge of the systems that contributes to self and organisational development. Other research has found that permanent staff in accident and emergency (A&E) would expect temporary staff to have less vested interest in a department, particularly if they know they are not going to return. 65 Targets have already been set for trusts to reduce their use of agency locums and increase the use of internal locum banks. 53 This allows for more regular and familiar locums which increases trust and allows for greater investment in temporary staff in the short and long term.
The results from this survey highlight the precarity of locum work. Locum contracts can be ended early following even low-level concerns, and locums may have less access to communities of practice within trusts for providing appropriate governance, leadership and support, meaning remedying performance problems may be more difficult. Similarly, another study found that short training rotas limited the ability of medical trainees to engage in communities of practice in order to engage in activities and form mutual relationships. 67 This may, in part, explain why locums are more likely to have formal complaints about them to the professional regulator than permanent doctors. 32
This is the largest survey of the use of locum doctors in the NHS. The survey had good regional coverage and was completed by different types of trust and different staff types. The response rate was relatively high for an online survey, and responding organisations appeared to be largely similar to non-respondents in various respects; however, it is possible that non-respondents may differ systematically in some way.
The extent to which the views and perceptions collected in the survey are useful depends partly on the representativeness of the respondents (see above) and on how insightful their perspectives are. Medical directors and leads in medical staffing would be expected to have a good overview of locum work and systems for managing locum engagement; however, we cannot be certain if all respondents, particularly those in other roles, would have enough experience and knowledge to answer all questions accurately. In addition, each response represents the views of just one person in the organisation and may differ from those of others in the same organisation.
Locum doctors are an important resource for NHS trusts enabling them to maintain workforce capacity and provide patient services. However, there are also a number of potential issues relating to the ways that locum work is organised, the way locums are supported and the quality of care provided by locums. Further research is required to consider empirically the clinical practices and performance of locum and permanent doctors, and to recommend how locum work can be arranged by trusts to provide safe care to a high standard.
Chapter 6 The use of locum doctors: findings from a national survey of general practices in England
Aims
This chapter reports on the use of locum doctors in general practice in England, through a national survey of general practices. Locum working has benefits for individual doctors and for organisations, but there are concerns about the impact of locum working on continuity of care, patient safety, team function and cost. 9,54 The aim of this study was to conduct a national survey of general practices to explore locum working. We sought information about why and where locum doctors were needed; how locum doctors were engaged, supported, perceived and managed; and any changes being made in the way locums are used.
Methods
Survey design
The study received research ethics approval from the National Research Ethics Service in England. It was explained on the first page of the survey that agreement to take part was implicit through completion.
Stakeholders who were included in the development of the survey included: a medical director, a research director, a medical staffing senior manager, chair of our Patient and Public Involvement and Engagement (PPIE) group, a locum GP and a locum agency managing director. E-mail drafts of the survey were distributed to stakeholders, to which they replied with feedback and further review and conversations with stakeholders about their input were performed as necessary. Stakeholder feedback was reviewed by the project team and the survey was adapted accordingly.
An online bespoke questionnaire56 consisting of 89 questions was produced using Qualtrics software. 57 Information was gathered about why locums were required, how they were recruited, supported, perceived and managed, how locums work compared with the work of permanent doctors, perspectives of locum agencies, familiarity with the NHS England and Improvement guidance for supporting locums and how practices resolved issues concerning locums. Perspectives were sought regarding the advantages and disadvantages of locums and any future change in locum work (see Appendix 4 for a copy of the survey).
We defined a locum doctor as a doctor in a temporary or fixed-term placement, engaged through a locum agency, GP chambers or locum bank, or directly contracted by a healthcare organisation.
Survey distribution
The survey was distributed via the National Institute for Health and Care Research (NIHR) Local Clinical Research Network (LCRN). LCRNs help increase opportunities for participants to take part in research. This method has been used before and secured a good response rate. 68 The survey link was distributed via e-mail to the 14 LCRNs in England who, in turn, sent it to practices in their region. Practices were selected for inclusion based on different criteria within each LCRN. Some LCRNs sent the survey link only to practices which had opted to take part in research. Other LCRNs sent it to all practices in their area. In most cases, the surveys were e-mailed to practices, but in one region it was distributed via a newsletter and in another only to practices which had expressed interest in taking part. We asked each LCRN how many practices the survey had been distributed to in their area; this totalled 3745 general practices out of 6822 practices in England. 69 Due to the pandemic and to allow practice time to respond, the electronic link to the survey was live from June to December 2021. LCRNs were prompted to send periodic reminders.
Survey analysis
The survey was analysed using frequency tables to describe numeric and Likert scale data. t-tests were performed to compare respondents with all other practices in England. Non-parametric tests were used because the majority of survey responses did not show normal distribution. Associations between responses and practice size and frequency of locum use in practices were investigated using Spearman’s correlation coefficient.
Thematic analysis was used to analyse the written responses to three questions [(1) the advantages and disadvantages of locum agencies; (2) the advantages and disadvantages of locum work; and (3) the future of locum work]. 59,60 Patterns of shared meaning were identified utilising an inductive approach where coding and theme development is based in the information found in the responses. Respondent’s free-text comments were brief and are used to supplement the findings from associated quantitative questions. Familiarisation with the free-text data was achieved through iterative reading and for each question possible codes were noted, taking account of repeated words or meaning. 61 All written comments were reviewed holistically and overarching themes were mapped, encompassing the key messages across the data (see Box 1 for a list of these themes and key sample quotes). Thematic analysis was not used with one question, asking for perspectives about the NHSE guidance about supporting locums; instead, key descriptive comments were included as examples to provide context to the quantitative question enquiring about practice familiarity with the guidance.
Respondent characteristics
We surveyed a total of 3745 practices and we received 605 usable responses (response rate 16.2%). The responses included 23 (3.8%) from single-handed practices, 203 (33.6%) from small practices (2–5 GPs), 238 (39.3%) from medium practices (6–10 GPs) and 141 (23.3%) from large practices (more than 10 GPs). The survey was completed by 205 (33.9%) GP partners, 14 (2.3%) salaried GPs, 9 (1.5%) in other clinical roles (e.g. advanced nurse practitioner), 323 (53.4%) practice managers, 39 (6.5%) non-clinical managers and 14 (2.3%) administrators. Compared with all other practices in England, responding practices were slightly larger both in terms of practice list size and number of GPs employed (for further details comparing responding practices and all other practices in England, see Appendix 4).
The authors acknowledge that the aim and methods for Chapter 6 are similar to those in Chapter 5. These surveys were conducted alongside each other and asked very similar questions of both NHS acute trusts and GP practices.
Results
The need for locums
How often practices use locums
Over half of practices always or often used locums and very few practices made no use of locums. Practices with more GPs employed used locums less frequently than practices with fewer GPs employed, r(563) = 0.15, p < 0.001.
We asked practices how long locums were typically engaged for at their practice. Practices used locums for all different engagement lengths, but locums were most frequently engaged on a very short-term basis. A quarter of practices needed to engage locums on a long-term basis, but a third reported never engaging locums long term.
Reasons for locum use
The main reasons practices reported using locums were to cover planned medical workforce gaps, to provide additional capacity to meet demand and to cover absences due to short-term ill health (Table 11). Practices with fewer GPs employed were significantly more likely to need locums due to difficulties recruiting doctors and less likely to need locums to cover absences due to long-term ill health. Practices with higher frequency of locum use were significantly more likely to need locums for all reasons.
| Often | Sometimes | Rarely | Never | Associations (correlation coefficient) | ||
|---|---|---|---|---|---|---|
| Number of GPs employeda | Frequency of locum useb | |||||
| Because of difficulties recruiting doctors | 154 (26.2) | 128 (21.8) | 116 (19.8) | 189 (32.2) | 0.09* | 0.54** |
| Because of difficulties retaining doctors | 45 (7.7) | 81 (13.8) | 170 (29.0) | 291 (49.6) | −0.06 | 0.33** |
| To cover planned medical workforce gaps | 285 (48.6) | 222 (37.8) | 56 (9.5) | 24 (4.1) | −0.04 | 0.25** |
| To cover absences due to short-term ill health | 108 (18.4) | 222 (37.8) | 165 (28.1) | 92 (15.7) | −0.06 | 0.15** |
| To cover absences due to long-term ill health | 62 (10.6) | 148 (25.2) | 215 (36.6) | 162 (27.6) | −0.18** | 0.19** |
| To provide additional capacity to meet demand or need | 169 (28.8) | 210 (35.8) | 109 (18.6) | 99 (16.9) | 0.02 | 0.50** |
Factors important to practices when selecting locums
We asked practices what factors were important when selecting a locum to work at their practice. Most felt that all factors (availability, experience, cost, training and familiarity) were at least moderately important with slightly greater importance placed on availability and experience and slightly less importance placed on cost and familiarity. Practices with higher frequency of locum use rated availability as significantly more important compared with practices with lower locum use r(584) = 0.17, p < 0.001.
How the need for locum doctors is met
We asked practices about their methods for engaging locums. The most frequent method was the use of doctors who had previously worked for the practice, followed by word of mouth/personal recommendations. The use of Locum Chambers and digital platforms like Locum Nest was much less frequent. Locum Chambers is a model of working where locums are part of a local community of GP locums, who pool together resources to create a holistic support package for their work, supporting each other and the practices where they all work.
The use of locum agencies varied across practices with just under 40% using them often or sometimes but over a third never using them. Practices did not feel that locum agencies consistently matched their needs or provided accurate information. Practices with more GPs employed were significantly less likely to have their needs met by locum agencies r(338) = 0.18, p < 0.001 and report that they were provided with accurate information from locum agencies about locums r(338) = 0.22, p < 0.001. Practices with higher frequency of locum use reported that they were significantly more likely to have their needs met by locum agencies r(367) = 0.19, p < 0.001.
National Health Service England and Improvement guidance about supporting locums
Most practices were not familiar with the NHS England and Improvement guidance about supporting locum doctors. Some felt that it was not applicable to them, not a priority or they did not have the time to consider it.
I rarely have time to read guidance like this, with so much paperwork being sent to us about more critical issues
Practice 141
Some practices followed the guidance or aspects of it, and some had their own policies for supporting locums.
I have not read it – we are used to having locums and I have been a PM for 13 years, so I feel I/we know what we are doing and support our locums well – we follow our Locum policy
Practice 67
There were some positive perspectives on the guidance, with some respondents reporting that it was effective in controlling locum rates and encouraging doctors to take permanent posts.
I think the vision to bring down the rates paid for locum doctors is important as this pushes more into salaried positions and helps provide more stability for both the clinician and practice
Practice 75
Whereas others felt that the guidance was unrealistic, impractical or needed updating.
It is very ivory towers and idealistic, but not practical in real terms
Practice 7
Application of the guidance
We asked practices to tell us how frequently they followed different aspects of the guidance when locums were working in their practice (Table 12). Key procedures such as verifying documentation and induction were conducted more frequently compared with, for example, providing feedback or supporting appraisal. Most practices said they would report concerns or complaints about locums.
| Always | Often | Sometimes | Rarely | Never | Associations (correlation coefficient) | |||
|---|---|---|---|---|---|---|---|---|
| Number of GPs employeda | Frequency of locum useb | |||||||
| When a locum doctor is placed in our organisation, we… | Verify documentation (e.g. GMC registration and licence to practise, Healthcare Professional Alert Notices, identity, language, health clearance) | 516 (94.7) | 17 (3.1) | 7 (1.3) | 2 (0.4) | 3 (0.6) | −0.05 | 0.05 |
| Provide an induction to enable them to carry out the work they are being engaged to do, including access to buildings and appropriate IT systems | 443 (81.3) | 60 (11.0) | 33 (6.1) | 6 (1.1) | 3 (0.6) | −0.01 | −0.03 | |
| Complete an end-of-placement/exit report | 31 (5.7) | 49 (9.0) | 143 (26.2) | 170 (31.2) | 152 (27.9) | 0.05 | −0.02 | |
| Provide peer/colleague feedback for the locum doctor at the end of the placement | 51 (9.4) | 84 (15.4) | 178 (32.6) | 136 (25.0) | 96 (17.6) | 0.11* | 0.04 | |
| Support the locum doctor’s appraisal preparation | 49 (9.0) | 70 (12.8) | 167 (30.6) | 136 (25.0) | 123 (22.6) | 0.03 | 0.11* | |
| Provide an annual appraisal for the locum doctor, if appropriate to do so (in light of the nature and duration of the placement) | 46 (8.4) | 30 (5.5) | 100 (18.4) | 176 (32.3) | 193 (35.4) | 0.00 | 0.09* | |
| Provide access to professional development activities | 84 (15.4) | 96 (17.6) | 169 (31.0) | 106 (19.5) | 90 (16.5) | −0.09* | 0.07 | |
| Encourage locum doctors to attend multidisciplinary team meetings | 126 (23.1) | 96 (17.6) | 132 (24.2) | 106 (19.4) | 85 (15.6) | −0.11* | 0.03 | |
| Inform the locum doctor and locum agency or RO (where relevant) about serious untoward incidents they have been involved in (even if they are no longer employed at my organisation) | 386 (70.8) | 48 (8.8) | 46 (8.4) | 37 (6.8) | 28 (5.1) | −0.03 | 0.03 | |
| Inform the locum doctor and locum agency or RO (where relevant) about complaints they have been involved in (even if they are no longer employed at my organisation) | 375 (68.9) | 67 (12.3) | 41 (7.5) | 30 (5.5) | 32 (5.9) | −0.01 | 0.06 | |
| Support the locum doctor to engage with revalidation systems within my practice | 119 (21.8) | 88 (16.1) | 146 (26.8) | 102 (18.7) | 90 (16.5) | 0.02 | 0.06 | |
Practice experiences of locum doctors
We asked practices how the care provided by locums compared with care provided by permanent doctors in a number of areas (Table 13). Generally, care provided by locums was viewed as about the same as or worse than care provided by permanent doctors. Practices with more GPs employed were significantly more likely to report that adherence to organisational policies and guidelines, providing continuity of care, and reporting of adverse events or untoward incidents was worse when care was provided by locums rather than permanent doctors.
| Much better | Somewhat better | About the same | Somewhat worse | Much worse | Associations | ||
|---|---|---|---|---|---|---|---|
| Number of GPs employedb | Frequency of locum usec | ||||||
| Correlation coefficient | |||||||
| Adherence to organisational policies and guidelines | 8 (1.5) | 24 (4.5) | 238 (44.8) | 236 (44.4) | 25 (4.7) | 0.15** | 0.04 |
| Providing continuity of care | 7 (1.3) | 9 (1.7) | 131 (24.7) | 274 (51.6) | 110 (20.7) | 0.21** | 0.11* |
| Avoiding drug-prescribing errors | 8 (1.5) | 17 (3.2) | 405 (76.3) | 87 (16.4) | 14 (2.6) | 0.04 | 0.08 |
| Avoiding administrative errors | 9 (1.7) | 13 (2.5) | 295 (55.6) | 192 (36.2) | 22 (4.1) | 0.08 | 0.02 |
| Keeping clear and accurate patient notes/clinical records | 13 (2.5) | 69 (13.0) | 373 (70.2) | 69 (13.0) | 7 (1.3) | 0.07 | 0.03 |
| Reporting of adverse events or untoward incidents | 11 (2.1) | 21 (4.0) | 374 (70.4) | 112 (21.1) | 13 (2.5) | 0.12* | 0.06 |
| Appropriateness of referrals | 9 (1.7) | 8 (1.5) | 285 (53.7) | 197 (37.1) | 32 (6.0) | 0.05 | −0.05 |
| The functioning of the healthcare team | 9 (1.7) | 18 (3.4) | 325 (61.2) | 168 (31.6) | 11 (2.1) | 0.06 | 0.05 |
| Workload for permanent members of staff in the healthcare team | 20 (3.8) | 45 (8.5) | 178 (33.5) | 212 (39.9) | 76 (14.3) | 0.06 | −0.02 |
Perspectives about locum doctors and locum agencies
We asked practices about the advantages and disadvantages of engaging locum doctors and locum agencies and how they see locum doctor working changing in the future (Table 14). Maintaining workforce capacity was one of the main advantages reported by respondents. Locums filled gaps in the rota and provided cover for sickness, holidays and maternity, which in turn allowed practices to meet patient demand, maintain appointment levels and relieve workload challenges. This was particularly important for short-term and short-notice cover. Some also felt that locums brought a new perspective and fresh ideas to a practice based on their experiences in a range of different settings. However, some practices noted that locums were not always available when required at short notice.
| Theme | Illustrative quotes |
|---|---|
| Workforce capacity and flexibility | ‘They provide access to large numbers of locums and offer greater flexibility regarding availability and choice of locums’. (GP practice 102) ‘Obvious advantages are to maintain appointment levels and support workload challenges in the event of an absent permanent GP’. (GP practice 20) ‘Can be cost effective if you have a robust administrative team to support GP admin work. Lack of financial support for paying sick leave, mat leave etc. and the need to bring in a locum doctor to cover their work when off makes locums a more attractive prospect (as in some cases a salaried doctors’ fees may end up costing a practice up to 30% more than the base salary you’d pay a locum)’. (GP practice 75) ‘Locums can bring their own expertise which can be utilized by the practice as they often have “other roles in the NHS”, e.g. minor ops, MSKAP conditions’. (GP practice 119) |
| Familiarity | ‘You end up with another new locum who doesn’t know the practice or the patients. New locums take time as there is paperwork and IT set-up to do, checking CVs and certificates, etc. You don’t know what you’re getting, how quickly they work, whether they’re good or whether they create more work for the GPs to come back to’. (GP practice 171) ‘If you are able to have the same GPs come back to you for the next periods … they become more familiar with surgery policies etc. and are increasingly autonomous in their work’. (GP practice 99) ‘We have a very good, stable group of locums that we use on a regular basis to help ease workload pressures, when other permanent members of the staff are away’. (GP practice 69) ‘Very good to have a regular locum who you [and the] practice know and the patients become comfortable with’. (GP practice 140) |
| Continuity of care | ‘Having regular locums’ helps with patient services and continuity of care for patients’. (GP practice 218) ‘Can be more difficult when trying to achieve continuity and they often work at a slower pace’. (GP practice 27) ‘Good to see patients for acute on the day conditions, not so great for long term problems and conditions’. (GP practice 138) |
| Cost | ‘Signing up most regional locums to mainly one agency reduces competition between individual locums and results in high locum rates, and high locum rates in turn affect the affordability of locums and reduce the likelihood of locums ever again joining the work force as salaried GPs or GP partners’. (GP practice 102) ‘Many [locum] GPs are charging astronomical fees which are not appropriate for the work they are doing, yet often surgeries have no choice. I think this can create ill feeling’. (GP practice 104) ‘I think more and more GP’s will turn to locum work rather than regular work as the money is better and the terms of work are better as they can take time off when they want and do the hours they prefer. They are under a lot less pressure than a regular GP’. (GP practice 2) ‘I hope that locums would be regulated with regard to charges, as demand often means that practices do not have any choice with regard to how much they have to pay locums. Locums can, therefore, earn much more than GP partners or salaried GP’s and specify clinic sizes and times worked, which does not encourage them to take permanent posts in practices’. (GP practice 119) |
| Increased workload | ‘Some locums just defer work telling patients to call back another day or prescribe in a way we don’t’. (GP practice 168) ‘Disadvantages: non clinical workload, issues passed down the line for later & not sorted out, increased clinical and nonclinical burden on permanent team, expense, adherence to protocols, medicines optimisation, referrals, lack of familiarity with local services can increase workload for GPs, limits to workload (e.g. no visits, no duty Dr, no cover, won’t work alone), continuity, permanent Drs “picking up the pieces”’. (GP practice 61) |
| Investment and quality | ‘They have no loyalty to the surgery or patients’. (GP practice 67) ‘Some locums are very good and work hard’. (GP practice 2) ‘But in most other respects e.g. continuity of care, working within the MDT, being aware of local policies etc., being able to help with admin in the practice, they are not as good’. (GP practice 136) ‘they are a sticking plaster only really’. (GP practice 55) ‘I consider different regulation is needed, and doctors who want to do locums should have also a regular job–perhaps one day a week based in one place–to understand better general practice, continuity of care, team work, sharing workload, importance of coding, of electronic health records and problem lists maintenance’. (GP practice 77) |
Respondents emphasised in the free-text responses the advantages of flexibility in the use of locums. They can be used as and when needed and contracts can be ended easily when they are no longer required. Some practices saw it as more cost-effective to have short-term cover without the longer-term financial commitment of a permanent member of staff. Some thought locum agencies were efficient in sourcing locums and doing all necessary pre-employment checks and paperwork required.
On the other hand, locum’s lack of familiarity with the practice, the area, the patients and local referral pathways was a disadvantage for practices, as reported in the written responses. It was time consuming for practices to get a new locum setup on all the practice systems. Not knowing the locum resulted in uncertainty about the quality of their work, their efficiency and whether they would create more workload. When the locum was familiar with the practice, this was seen to benefit continuity of care for patients. However, on the whole, locum use was considered to have a negative impact on continuity of care, and this was thought to be particularly problematic for patients with long-term or complex conditions.
Cost was one of main disadvantages reported about locum agencies in the written responses. Some respondents felt that locum agencies control the market and drive up rates. For some, the use of locum agencies to source a locum was a last resort due to the additional costs. The view that locums were expensive contributed to a negative view of locums and created tensions between locums and permanent staff. High locum pay rates were also considered to be a reason why locums would not join the permanent workforce. Respondents felt that the use of locums would continue to increase because of the higher pay, lower workload and greater autonomy and control. To encourage locums to take up permanent posts, some respondents wanted to see stricter regulation of locum pay and access to pensions. Another suggestion was the use of a pool of locums employed locally to reduce costs and improve familiarity and continuity of care.
Respondents reported in the free-text comments that locums generated increased workload for other practice staff, particularly administrative work. The way that locums negotiate terms and conditions was felt to result in them not always performing the full range of duties, for example, not doing administrative work. Other perceived reasons for increased workload included high referral rates, differences in prescribing practices and locums asking patients to return for another appointment. Sometimes patients would refuse to see a locum or would return to see their regular GP after seeing a locum because they were dissatisfied.
For some, locums were a last resort and did not present a long-term solution to staffing problems. As detailed in the written responses, there was a perception that locums were not invested in the practice and were not team players; examples of this included not contributing to quality improvements and achieving targets. In order for locums to have a better understanding of general practice, some wanted locums to have a permanent position either before or during their locum work and felt that this would provide locums with a community of practice and would improve team working and shared workload.
Dealing with concerns about locums
We asked practices to tell us what happened when there were low-, medium- or high-level concerns about a locum doctor in their practice. We defined low-level concerns as: causing no harm to patients or staff and the doctor was not at any personal risk, medium-level concerns have potential for serious harm to patients, staff or the doctor was at personal risk and high-level concerns are when patients, staff or the doctor had been harmed. The action that practices reported they would take to deal with concerns increased depending on the severity of the concern (Table 15). The higher the severity of the concern, the more likely that they said locums and locum agencies would be informed. Practices reported that it was common for contracts to be ended early when there were concerns and locums to not be used again.
| Always | Most of the time | About half the time | Sometimes | Never | Associations (correlation coefficient) | |||
|---|---|---|---|---|---|---|---|---|
| Number of GPs employeda | Frequency of locum useb | |||||||
| Low-level concern | The locum doctor is informed | 262 (51.8) | 131 (25.9) | 32 (6.3) | 73 (14.4) | 8 (1.6) | 0.06 | 0.05 |
| Reported to the locum agency | 153 (30.2) | 91 (18.0) | 26 (5.1) | 125 (24.7) | 111 (21.9) | 0.13* | 0.08 | |
| Reported to the GMC | 35 (6.9) | 20 (4.0) | 20 (4.0) | 136 (26.9) | 295 (58.3) | 0.11* | −0.05 | |
| The locum contract is ended early | 58 (11.5) | 49 (9.7) | 30 (5.9) | 231 (45.7) | 138 (27.3) | 0.05 | 0.02 | |
| We would not use that locum again | 136 (26.9) | 115 (22.7) | 47 (9.3) | 166 (32.8) | 42 (8.3) | −0.04 | −0.03 | |
| Medium-level concern | The locum doctor is informed | 414 (81.8) | 63 (12.5) | 12 (2.4) | 12 (2.4) | 5 (1.0) | 0.02 | 0.02 |
| Reported to the locum agency | 308 (60.9) | 81 (16.0) | 23 (4.6) | 35 (6.9) | 59 (11.7) | 0.06 | 0.09 | |
| Reported to the GMC | 111 (21.9) | 83 (16.4) | 47 (9.3) | 158 (31.2) | 107 (21.2) | −0.01 | −0.00 | |
| The locum contract is ended early | 188 (37.2) | 120 (23.7) | 51 (10.1) | 120 (23.7) | 27 (5.3) | −0.03 | 0.01 | |
| We would not use that locum again | 280 (55.3) | 101 (19.7) | 35 (6.9) | 76 (15.0) | 14 (2.8) | −0.06 | −0.03 | |
| High-level concern | The locum doctor is informed | 485 (95.9) | 9 (1.8) | 5 (1.0) | 1 (0.2) | 6 (1.2) | −0.04 | 0.01 |
| Reported to the locum agency | 433 (85.6) | 16 (3.2) | 8 (1.6) | 4 (0.8) | 45 (8.9) | 0.03 | 0.03 | |
| Reported to the GMC | 377 (74.5) | 45 (8.9) | 20 (4.0) | 41 (8.1) | 23 (4.6) | −0.01 | −0.03 | |
| The locum contract is ended early | 398 (78.7) | 45 (8.9) | 16 (3.2) | 30 (5.9) | 17 (3.4) | −0.04 | −0.02 | |
| We would not use that locum again | 422 (83.4) | 35 (6.9) | 11 (2.2) | 22 (4.4) | 16 (3.2) | −0.04 | −0.00 | |
Discussion
We found that the use of locums was a common and necessary part of practice working. Locums were needed for all different lengths of time and practices not using locums were rare. The use of locums was motivated by workforce issues such as recruitment, providing capacity to meet demand and planned workforce gaps. However, we found, as others have, that there was poor awareness, ambiguity and confusion about the national guidance for locums from NHSE and who was responsible for following it. 16 While we do not know the extent to which practices use their own bespoke guidance for supporting locums, lack of familiarity with the national guidance could result in locums receiving less support and integration into the practice and could be a barrier for locums to work effectively. Practices focused on key processes such as registration checks and induction, but much less was done with regard to engagement, feedback and appraisal. The pressures of the current workforce and workload crisis in practices70 may affect practices’ ability to provide the time and resource to support locums in these ways. Not including locums in systems for feedback and support with appraisal could result in locums feeling marginalised and excluded,15 which in turn does not contribute towards goals of improved patient safety and collaboration. 71
We found that practices generally thought that the quality of care provided by locums was the same as or worse than that provided by permanent GPs, particularly in areas such as continuity of care, adherence to policies and guidelines and making appropriate referrals. Common operational problems which afflict GPs (like difficulties with computer systems, problems with equipment and challenges with the co-ordination of care)72 may affect locums more because of their lack of familiarity with practice systems and processes. While practices felt that continuity of care was worse when care was provided by a locum, it should be recognised that traditional ideas of relational continuity have already been eroded and replaced, in part, by managerial and informational continuity. 54,73
Practices preferred not to use locum agencies and would rather recruit known and trusted locums to maintain familiarity with practice processes, systems and patients. There were on the whole low opinions of locum agencies particularly in relation to cost and there was a general perception that locums were expensive. While we found that practices wanted to see greater control of locum pay caps and reduced incentives for locum work, it is important to note that broader discontent with GP pay and conditions74 may have contributed to the current recruitment and retention challenges. 75
Job demands–resources theory suggests that adding temporary staff should reduce demand and increase resources for permanent staff;76 however, practices reported that the use of locums can result in increased workload for permanent staff, particularly in non-clinical and administrative roles. Certain tasks may not be done by locums because they are unfamiliar with the work setting, it is expensive to pay them to do administrative work or they are not there to follow up, so other staff are required to pick up the work.
The precarity of locum work and its consequences also deserves consideration. Locum contracts can be terminated early following even low-level concerns. One reason for this is that locums may have less access to communities of practice within general practice for providing appropriate governance, leadership and support,67 and remedying performance problems may be more difficult. 9 This may, in part, explain why locums are more likely to have formal complaints about them to the professional regulator than permanent doctors. 33
The response rate was relatively high for an online survey; there was a significant difference in locum FTE, practice list size, GP headcount, locum FTE adjusted for GP FTE (locum use), deprivation and CQC ratings between responding practices and all other practices in England. This could be a consequence of sampling research active practices via the LCRN. Our results should be interpreted with caution because of these differences between survey respondents and the population.
The views and perceptions collected in this survey will vary depending on both the representativeness of the respondents and their awareness of the topics covered. GP partners and practice managers would be expected to have a good understanding of locum work and management, but respondents in other roles may not have sufficient experience and knowledge to answer all questions accurately. Responses are also the views of just one person in the practice and may differ from the views of others in the same practice.
While these findings show that locum working is a common part of English general practice and a necessary and important resource which enables practices to staff and provide services, it raises a number of concerns about the robustness of arrangements for locum working and about aspects of the quality of care. Further research is needed to compare empirically the clinical practices and performance of locum and permanent GPs, and to suggest how practices (and others such as primary care networks and the newly created integrated care systems) can organise locum working in ways that assure the quality and safety of care.
Chapter 7 Locum doctors in the National Health Service: qualitative findings on quality and safety
Aims
This chapter reports on research undertaken to provide evidence on the quality and safety of locum practice and the implications of locum working for health service organisations in primary and secondary care in the English NHS. This research addresses a gap in the empirical evidence base on how locum doctor working arrangements affect quality and safety and outlines factors which might lead to variations in care.
Our aim was to understand what factors might lead to variations in quality and safety between locum and permanent doctors; what strategies or systems organisations used to assure and improve safety and quality in locum practice; and how locum doctors themselves sought to assure and improve the quality and safety of their practice.
Methods
To develop this analysis, we drew on an exploratory, interview-based study of locum doctor working with 130 participants, including locums, patients, permanently employed doctors, nurses and other healthcare professionals with governance and recruitment responsibilities for locums. This strategy has meant we have an understanding of the issue from multiple sources.
This study involved professionals working on a permanent or temporary basis and patients who had experience of being treated by locums. Qualitative data were collected between March 2021 and April 2022.
Our original plan was to use intelligence from our surveys and stakeholders included in our project advisory group to identify a small number of case study sites where we could carry out extensive fieldwork. Our study commenced in March 2020; consequently, data needed to be collected virtually and with minimal impact on organisations responding to the pandemic. To reduce the burden on our research sites, we broadened our approach and instead utilised purposive, snowball and convenience sampling. Fifty-one of our interviews (Table 16) were drawn from eleven sites including three CCGs, one community interest company providing primary care services, one research and development organisation connecting academics with the health sector, five NHS trusts and one arm’s length body of the Department of Health and Social Care providing expertise to the NHS on resolving concerns. Seventy-nine of our participants, representing mostly locums and patients who were not affiliated with a single organisation were categorised as ‘other’.
| Site no. | Site type | Number of participants interviewed |
|---|---|---|
| 1 | CCG | 2 |
| 2 | CCG | 1 |
| 3 | CCG | 1 |
| 4 | NHS Trust | 5 |
| 5 | NHS Trust | 13 |
| 6 | NHS Trust | 8 |
| 7 | NHS Trust | 2 |
| 8 | NHS Advisors | 2 |
| 9 | Other | 79 |
| 10 | NHS Trust | 12 |
| 11 | NHS R&D organisation | 3 |
| 12 | Community Interest Company | 2 |
| Total | 130 | |
Participants were recruited using intelligence from stakeholders including our project advisory group, locum agencies, Locum Chambers and locum recruitment organisations and through disseminating details of the study through networks. Patients were purposively sampled through patient and public contributor forums. We sought to recruit a maximum variety sample of participants through organisations varying on dimensions including size, complexity, geographic location and self-reported or measured levels of locum use.
We were interested in interviewing international medical graduates (IMGs) as issues around racism and discrimination were raised by some of our participants. We also knew from our quantitative work that locums were more likely to be IMGs. Consequently, we approached organisations supporting ethnic minority doctors in the UK to promote the study and recruit participants. We sought participation through organisations including Melanin Medics and the British Association of Physicians from an Indian Origin. We also promoted participation through the CQC and their networks who were involved in a study of ethnic minority-led GP practices, which included representation from organisations such as British Islamic Medical Association and Black and Minority Ethnic medics.
Three semistructured interview guides were developed for use with locums, people working with locums and patients (see Appendix 5). Our previous review of the literature relating to quality and safety and locum work9 informed the interview schedule as well as the initial coding and thematic development; however, as this is an empirically under-researched phenomena, analysis was also exploratory and not restricted to fit our existing framework. 77 Each schedule was intended to explore locum doctor working arrangements with a particular focus on understanding how locum doctor working may affect the safety and quality of care and what strategies or systems organisations and individuals used to assure or improve quality and safety. While our interviews were guided by an interview schedule, participants were encouraged to talk about anything they felt relevant to locum doctor working and quality and safety and were asked open questions about what they felt were relevant issues. Our interview topic guide covered: why locum doctors were needed, why doctors worked as locums, governance and support, experiences of working as, working with, or being treated by locums, what happens when things go wrong or right, advantages and disadvantages, the impact of the pandemic and policies and initiatives used to support locums.
Three authors (JF, GS and KW) conducted 88 semistructured interviews with healthcare professionals including locums, permanently employed doctors; nurses and other health professionals; medical directors/clinical leaders; ROs and appraisers; leads for medical staffing and clinical governance and practice managers (Tables 16 and 17 for more details about participants). Data were collected using video-conferencing software (n = 126) or over the phone (n = 4).
| Characteristic | Professionals (n = 88) | Patients (n = 42) | |
|---|---|---|---|
| Mean agea (SD) | 46 (11.0)b | 59 (14.4)a | |
| Gender (women) | 49 (56) | 24 (57) | |
| Ethnicity | White English | 45 (51)c | 30 (71)a |
| Any other white background | 12 (14)c | 4 (10)a | |
| Mixed/multiple ethnic group | 3 (3)c | 1 (2)a | |
| Asian/Asian British | 15 (17)c | 2 (5)a | |
| Any other Asian background | 2 (2)c | 0a | |
| Black/African/Caribbean/Black British | 2 (2)c | 1 (2)a | |
| Other ethnic group | 1 (1)c | 0a | |
Two female members, JF (BSc, MSc, PhD) and GS (BSc, MA, PGCE, PhD), and one male KW (BSc, PhD) member of the research team conducted the interviews and JF and GS conducted the focus groups with members of the PPI forum. At the time of the study, JF was a Lecturer in Healthcare Management, GS was a Research Associate and KW was a Professor of Health Policy and Management. JF, GS and KW are all experienced healthcare researchers with years of experience carrying out mixed-methods and qualitative research projects and analysing qualitative data. None of the researchers knew the participants prior to the interviews taking place, except for two of the healthcare professional participants who were friends of JF and GS. Prior to the interviews and focus groups being conducted, the interviewers briefly introduced themselves and their backgrounds.
Our analytic strategy was informed by insights from team members with an in-depth understanding of the research field and qualitative methodology. The three interviewers were from non-clinical backgrounds and worked as academics and researchers. The study team considered the ways in which their interactions with participants might be influenced by their own background, experiences and prior assumptions. We had previously published a narrative review of locum working and implications for quality and safety and a qualitative paper which highlighted the stigmatisation and marginalisation experienced by locums.
The primary aim of this research was to question the assumption that locum working had negative implications for quality and safety. Issues we discussed when drawing conclusions from the data concerned whether our previous knowledge would negatively bias our interpretations. We also questioned whether participants who held negative perspectives about locum working were more likely to come forward for interview and whether locums would be willing to talk openly about their experiences given potential reprisals in the medical profession for the disclosure of mistakes. One way we attempted to reduce bias was to ensure that we explicitly incorporated a wide range of different perspectives, so that the viewpoint of one group was never presented as if representing the sole truth about locum working. We also regularly met with our Project Advisory Group that included locum doctors to share our findings and check our assumptions. The lead researcher also frequently met with a senior locum doctor to discuss findings and interpretations. Our objective was to be as fair and balanced as possible while also staying true to our findings.
We developed themes using reflexive thematic analysis (RTA)78 and adopted a constructionist epistemology, in that while we acknowledged the importance of recurrence in generating themes, meaning and meaningfulness were the central criteria in the coding process. 78 The analysis followed Braun and Clarke’s six-phase approach which involved: familiarisation with the data by reading and rereading the transcripts; coding the data set and collating all relevant data extracts; generating initial themes by examining the codes and collated data to identify significant broader patterns of meaning across the data set; reviewing themes by questioning whether themes answered the research question and told a convincing story of the data and combining, splitting and discarding themes as necessary; defining and naming themes by developing a detailed analysis of each theme; and finally the analytical write-up which positioned the analysis in relation to existing literature. 61
Reflexive thematic analysis acknowledges the researcher’s active role in knowledge production and the researcher’s subjectivity as the analytic resource. 78 RTA acknowledges that codes and themes represent the researcher’s interpretations of patterns of meaning across the data set and that no two researchers will interpret the data set in the same way and, as such, does not require that other researchers verify or check for coding reliability. It was acknowledged and understood that there will be interpretive variability between researchers based on differences in their knowledge and skills, theoretical assumptions and differences in how they responded to the data set. Interpretive analysis was based on the flexible and organic interplay between the data set and the theoretical assumptions and skills of the researcher. In this sense, we take the approach to qualitative research described as ‘Big Q’79 as we did not come to our findings through a qualitative positivist lens. Big Q qualitative research describes the use of qualitative tools and techniques, particularly around data generation within a non-positivist framework informed by qualitative research values. 80
In addition, at the end of each interview or focus group, we asked participants to reflect on what they had discussed and identify topics they felt were particularly significant to the research question and areas that the research team should pay particular attention to. Participants were asked to summarise and provide an overview of their ‘key messages’. This meant that the coding was guided by what participants felt was relevant as well as what was deemed as key by the researchers. Themes were discussed by the whole team in weekly meetings as well as at our project advisory group and during collaborative analysis sessions with our PPI group. Regular meetings were also held by the three researchers collecting the qualitative data to discuss analysis. Themes featured in the report were discussed and agreed by the qualitative researchers collectively. Input was sought from the wider team at weekly meetings and through regular meetings with our PPI forum, thereby drawing on the combined insights of those with close involvement with data collection and members of the team with wider perspectives of healthcare quality and safety. We also held several half-day analysis sessions where we discussed and questioned themes and interpretations.
After we developed our themes, we used an abductive approach to position our findings against a background of existing theory and knowledge. This provided a way of constructing empirically based theorisations without confining theory to pre-defined concepts. 81 Our approach integrated inductive data-driven coding with deductive theory-driven interpretation; aiming to find a middle ground between inductive and deductive methods and the most logical solution and useful explanation for phenomena. 81
Results
Characteristics of participants
Of the 130 participants interviewed, 88 were working in health care and 42 were patients. Participant characteristics are summarised in Table 17. The mean number of years of qualification for doctors who participated was 23.2 (SD = 11.0) and ranged from 1 to 48 years. Of the 59 doctors interviewed, 33 worked as locums, while 25 worked on a permanent basis and one worked as a locum in additional to permanent work. Of the permanent doctors, 10 had previously done locum work, 6 were working in primary care, 18 in secondary care and 1 in both sectors. Of the locum doctors, 19 were working in primary care, 12 in secondary care and 2 in both sectors.
In 2020, 38% of all licensed doctors in the UK were from an ethnic minority background. 82 The number of doctors from an ethnic minority background in our sample is 4% lower than the doctor population as a whole. Of the 59 doctors we interviewed, 20 (33.9%) were from ethnic minority backgrounds, while 34 (57.6%) were from a white background. Five doctors chose not to disclose their ethnicity (8.5%). Twelve doctors who took part were IMGs, and had been working in the UK for an average of 15.8 years (SD = 6.27). For seven of the IMG doctors, English was not their first language.
The ethnic breakdown of our locum sample more closely reflected the doctor population; of the 30 locums who reported their ethnicity, 18 (60%) were from White English or other white backgrounds, while 12 (40%) identified as ethnic minorities. The 24 permanently employed doctors who declared their ethnicity were largely in senior leadership positions (consultants, ROs, GP partners); 16 (66.7%) were White English or other white background, and 8 (33.3%) were from ethnic minority backgrounds. This is perhaps reflective of the fact that the ethnic diversity of the medical profession as a whole is not matched by diversity at senior leadership levels. 83
The ethnic breakdown of our patient population was largely reflective of the wider population in the UK where 82% of the population identify as white and 18% belong to an ethnic minority group. 84 In our sample, 34 (81%) patients identified as white, while 8 (19%) patients identified as belonging to an ethnic minority group.
In 2019, of NHS staff whose ethnicity was known, four out of five (79.2%) were white, and one in five (20.7%) were from all other ethnic groups. 85 The ethnic diversity of our qualitative sample of participants who represented professionals working as or with locums was more balanced; 57 (64.8%) were from a white background, while 31 (35.2%) where from ethnic minority groups. This is probably because of the number of doctors in the sample.
The gender breakdown of our doctor respondents was broadly reflective of the general doctor population,82 with women being slightly over-represented. Thirty-one (52.5%) participants were women, while twenty-eight (47.5%) were men. Women were slightly over-represented in our project as a whole.
We interviewed a broad range of participants from primary and secondary care as well as locum agencies. Healthcare organisation and participant details are listed in Table 18.
| Healthcare organisation type | Participant roles | Total |
|---|---|---|
| Primary care | GP × 6 Managing Director Non-Clinical Partner Nurse Practice Manager × 4 |
13 |
| Secondary care | Assistant Psychologist Clinical Director Clinical Lead Clinical Pharmacist Consultant × 9 Deputy Medical Director × 2 Director of Patient Experience Medical Director × 2 Medical Staffing × 6 Nurse × 3 RO × 5 Senior Manager × 3 |
37 |
| Primary care | Locum | 19 |
| Secondary care | Locum | 12 |
| Primary and secondary care | Locum | 2 |
| Locum agencies | Locum Agency RO × 4 Director |
5 |
| Other | Advisor to NHS × 2 | 2 |
Interviews ranged in length from 23 to 171 minutes with the average interview being 59 minutes. Interviews were transcribed verbatim by a professional transcription company and organised into codes and themes using the software package NVivo (QSR International, Warrington, UK). 86
Thematic framework
Our findings are presented under seven broad and inter-related themes that examine how locum work relates to and impacts quality and safety. Themes were identified by their overall ability to answer the research question and how numerous the occurrences were of each theme across the data set. Frequency of the theme did not necessarily determine its importance; rather, the inclusion of a theme was determined by how relevant it was to the research questions. Themes were also guided by our previous narrative review on quality and safety and locum doctors9 as well as the ‘key messages’ participants had identified in their interviews.
The first theme describes how contextual familiarity was regarded as vital for quality and safety. The second theme discusses the impact of variations in familiarity and preparedness to with locums on efficiency and workload. The third theme continues to explore notions of familiarity and knowing and the implications of continuity and discontinuity for patient care. The fourth theme is about the balance between locum and permanent staff and what happens when organisations become overly reliant on locums. The fifth theme highlights the impact of perceptions of locums on how they were treated and viewed. The sixth theme continues to elaborate on the consequences of locum perceptions and how this is related to blame and defensive practice. In our final theme, we describe how locums and organisations engage with governance mechanism and activities. The themes are listed below:
-
Familiarity and continuity: knowing who, where and how:
-
Locum understanding of the local population and staff, as well as how to access equipment/policies/pathways and how to carry out duties safely in unfamiliar environments.
-
-
Efficiency, empowerment and displaced work:
-
The impact of locum working on the workloads of permanent staff and how this related to the organisational preparedness to empower locums to do their job safely and effectively.
-
-
Continuity and discontinuity:
-
The positive and negative implications for continuity and discontinuity for patient care and how safety information was received and shared when doctors were transient.
-
-
Balance of staffing and stability:
-
What happens to quality improvement and organisational and staff development when organisations become more reliant on locums.
-
-
Collegiality, involvement and inclusion:
-
The implications for quality and safety when locums are/are not treated like other staff.
-
-
Defensive practice, hedging and avoidance:
-
How temporary working impacts defensive practice and how locums attempt to practice safely and avoid complaints in complex and unfamiliar environments.
-
-
Governance:
-
How responsibility for the oversight of locum doctors was organised and shared across organisations and how systems of governance worked for doctors who did not have a simple employed relationship with a single organisation.
-
Additional examples of participant quotations to illustrate each theme are provided in Appendix 5.
Familiarity and continuity: knowing who, where and how
Locum doctors faced distinct disadvantages in comparison to permanently employed doctors when they were unfamiliar with both the organisation and patients. Knowing the patients and staff, where to locate equipment and resources and how to escalate concerns and carry out processes was important for delivering care safely. The importance of local knowledge about patients and their communities was described by patients, locums and permanent staff. Familiarity increased with continuity of exposure, providing stability for teams and patients. Recruiting from the same pool of doctors and longer-term locum placements allowed for trusting relationships to be developed and also meant that locums were able to become familiar with the organisation and its staff, local policies, procedures and referral pathways, organisational layout and IT systems, as well as which services they could access.
And the locums we use now are people that we know. So you come on shift and its all regular locums that you’ve met before and you’ve worked with before … So it’s made a huge difference. You know what their skills are, you know what they’re capable of, you know that you trust them.
Interview 11, Clinical Director, Secondary Care
Locum participants described often working in unfamiliar environments, sometimes with minimal induction and varying levels of support. Organisational reluctance to invest in induction left not only patients vulnerable but also locums, who described being ‘set up to fail’. Induction was important given the large degree of variation in policies and procedures between organisations. Not knowing how to navigate IT systems, refer patients, order tests, find equipment and escalate problems, or locate who to go to for support could lead to operational failures or inadequacies and errors in locating information, supplies or equipment needed for patient care.
I was very rapidly discovering was every practice is different to the next practice by up to 500 different guidelines, policies, pathways and procedures … We can’t just be a bad GP in these positions enforced underperformance …
Interview 63, Locum GP, Primary Care
The absence of normal recruitment processes (involving meeting a doctor, carrying out an interview and following up on references) meant that recruiters were reliant on limited information on which to base their hiring decisions; meaning the knowledge and experience of locum doctors were not always formally assessed. Permanent staff with recruitment responsibilities described how the information provided by locum agencies and the format of CVs and references made it difficult to determine competency, scope of practice and suitability for a role. However, staff shortages and a requirement to meet safe staffing ratios meant that organisational leaders had little recourse of action if they were unsure about a doctor’s capability, which caused anxiety and frustration. This suggests that the provision of health care superseded ensuring safety standards and necessitated accepting one of two objectionable alternatives – accepting gaps in staffing that may jeopardise patient safety or accepting unknown staff that may jeopardise patient safety.
If a locum turns up and I have serious doubts about their ability to do the job to the required standard, I don’t have any recourse … And therefore I’m in a position where either I accept this locum or I don’t. There’s not much in the way of middle ground. Not accepting them is a really unpalatable choice because if I say look, I’m sorry, I don’t think you’re up to this, I think you should go home, that leaves me with a gap.
Interview 30, Consultant and Responsible Officer, Secondary Care
Other consequences of not knowing an organisation and its patients were risks to doctors’ professional reputation and registration and locum participants felt mistakes and complaints were more likely in unfamiliar environments. Doctors working as locums wanted to provide high-quality care but found some organisations were not adequately prepared to safely engage, include or support locums. Some locum participants described avoiding working in unfamiliar, chaotic or unsupportive organisations and restricted the number of organisations they worked in order to build relationships and familiarity and practice more safely.
The biggest sort of safety aspect that sticks in my mind, is that it is unbelievably frustrating to have to learn a whole new set of patients from day to day. And again, like I say, at the start, when I was signed up to four different hospitals, plus the locum agencies, I very quickly realised that not only is it the fact that you don’t know the patients from day to day, if you’re chopping and changing site the whole time, then store cupboard are laid out differently, ways of contacting relevant staff members are different, you’ve got to recognise what code to put in to bleep someone that’s different at every single site … So that’s why, pretty quickly in my F3 year, I decided, no, no, this is the hospital I’m going to work at, and I’m just going to stick with this hospital the whole of the way through, essentially. And that’s helped a lot with regards to that idea of consistency and knowing how to do what you need to do, essentially.
Interview 23, Locum, Secondary Care
International medical graduates faced additional difficulties adjusting to unfamiliar NHS systems and cultures when they first began working in the NHS. Locum doctors who trained outside of the UK described struggling to adapt and the added challenges of being naïve to the system; these locums described needing time and support to adjust. However, there were variations in terms of how organisations integrated and supported locum doctors who were IMGs; with some organisations providing additional supervisory support, while others expected locums, regardless of NHS experience, to ‘hit the ground running’. This meant that IMGs were particularly vulnerable to making mistakes. One participant described how they avoided using IMG locums without NHS experience; however, staff shortages meant that sometimes doctors with limited or no NHS experience were contracted.
I think when you get a lot of overseas … We try not to appoint many that haven’t got NHS experience but I remember when I was at the [hospital name] there were some when we were desperate and it’s just the, kind of … We expect them to come in as a locum and hit the ground running, provide a service and go … they were working at … kind of, put themselves down at a certain grade and they’d done that certain grade over in their home country but then they’ve come over here and there’s misinterpretation. They weren’t probably working at that level …
Interview 22, Medical Staffing, Secondary Care
I did actually study medicine abroad, so when I came to do F1 I was totally naïve to the system … I think there’s definitely challenges like with being overseas, you kind of feel a bit like a fish out of water in a way.
Interview 13, Locum, Secondary Care
Participants with recruitment responsibilities and ROs described difficulty in establishing level of qualification and competence when locums had trained outside of the UK. There was some uncertainty about the quality and safety of the practice of IMGs, as it was difficult to establish a clear picture of their clinical competency and capability and whether there were any governance concerns. While there was a reliance on GMC registration and licence to practise for assurance, it was recognised that governance systems were not completely failsafe and that there was some potential for doctors who were not appropriately trained to enter the system or for doctors to work beyond their scope of practice. For locum Ros, this was a challenge in that they were governing these doctors from a distance.
I have to say that our system is not tight, it’s not fool proof, and I find that we do accept doctors, for instance, from abroad, with no experience of the NHS, and actually with very little clinical experience, but to whom the GMC has given a Licence to Practise, and it therefore comes back onto us as the agency to decide whether the doctor is competent to be placed in an NHS position … There is also a very small sub-section of, dare one say, suspicious doctors who come from abroad, on whose governance we don’t have a clear picture other than nothing adverse has been declared, but conversely, we don’t know whether there are positive aspects of governance that should have been declared but are not. There’s a very small number of doctors, and then if they are accepted for registration and their compliance is correct, we fall back onto management of concerns as they may arise. But we are aware, or I am aware, of the very rare, but occasional possibility of either an incompetent doctor, or a dangerous doctor, or a fraudulent doctor that gets into the system. It is rare, it is rare.
Interview 47, Locum Agency RO
Locums managed the risk related to working in unfamiliar environments in a number of ways including avoiding organisations considered chaotic or unsafe or working below their grade. Some locums described working below their capability and experience to avoid having responsibility in unfamiliar organisations where they may not be supported or included in the team. Better networked locums were able to draw on their community to find out which organisations to avoid, while others learnt through experience
Most locums take jobs, locum work below their grade. So a person who’s at a registrar level would take a locum work as an SHO, because they don’t know the trust that well. And when they do that, they already are … have learning at a registrar level. But because they’ve taken a lower level job, and because they’re locum, they’re not included in part of the team at all.
Interview 55, Locum, Secondary Care
Efficiency, empowerment and displaced work
Employing locums meant vital services could be delivered despite staff shortages; however, variations in familiarity, workload and types of work locums did have potential negative impacts on efficiency, quality improvement and working relationships. Depending on contextual factors, such as how prepared an organisation was to empower locums to work safely and efficiently, how familiar the locum was with the team or organisation, length of placement or what terms and conditions the locum or organisation had negotiated, there were differences in terms of the types of work locums did, or were able to do, in comparison to permanent staff. These factors were related to how much additional work was created for permanent staff when locums were employed; for example, organisations with good processes of recruitment and induction, who used locums who were familiar with the organisations systems and processes, produced less work for other staff.
Regardless of their level of qualification and experience and support (or lack of) provided by the organisation, it was recognised that locums were unlikely to be able to perform to the best of their ability in unfamiliar settings and it was likely that they would need to depend on other staff for accessing IT systems, locating information or equipment and understanding policies and differences between hospitals for example. Unfamiliarity with organisational layout, and multiple inconsistent policies and procedures meant that locums felt that their performance could be negatively impacted. Inductions of variable quality were employed to mitigate unfamiliarity, but the responsibility for this fell on busy staff who described this as distracting from their own work, especially when the locum churn was high.
It can become a little bit like Groundhog Day can’t it, how do you keep your resilience up and keep engaged of having the same conversation, the same teaching every time … So you turn up to your shift, it’s busy. Let’s say you’re working on the acute medical unit, you’ve got 20 patients to clerk, there’s an empty shift and you’ve got a different locum. How do I get into the changing room, how do I do this, how do I do that? Oh, I’ve explained this so many times, you know. And do you get some of that, is some of it about resilience and some of it about you use up your usefulness, I don’t know. And again, that’s where it comes down to seeing this person as a person. They are a person, so it doesn’t matter how many times you hold the door open for someone, you continue to hold the door open for them and it just becomes part of what we do. And so it should be the same for these people we’re working with that just see them as the person rather than the locum.
Interview 19, Deputy Medical Director and Responsible Officer, Secondary Care
Locums were not always empowered to do their job efficiently and effectively because of lack of access to or restrictions on computer systems for example. Not providing locums with ready access to systems meant that they were not able to fully function in organisations until access had been arranged, which could take some time. This was particularly problematic for locums working on a short-term basis. Consequently, work that required access to systems, such as prescribing and referring, was sometimes carried out by other members of staff. Locums described having to rely on others as uncomfortable and stressful, particularly when it was perceived that locums were paid significantly more. There was a concern that relying on others could lead to care that was delayed, partially completed or not completed at all. This was also potentially divisive for working relationships between permanent and temporary staff. A workaround for a lack of access to computer systems for ordering tests and prescribing was to use the login credentials of other staff, meaning that prescriptions could not be traced back to individual doctors, which was a governance issue.
I did some A&E shifts in [hospital name]. But it was a logistical nightmare. It’s a different computer system. And by the time … I find it really tricky. As a locum, you’re there for one shift, you’re there for eight hours or 12 hours, however long it happens to be. By the time I found the toilets and the computer log in and managed to order an x-ray, it takes more than eight hours to do all those things. So I personally found it very, very stressful and didn’t like it. I felt like I asked too many questions, felt a bit helpless and hopeless. They probably thought I was similar as well. And so, yeah, never went back again, frankly. So I tend not to work in hospitals I haven’t worked in before.
Interview 53, Locum, Secondary Care
Continuity and discontinuity
Traditional notions of relational continuity were widely regarded as a thing of the past. Patient participants recognised that they were unlikely to be seen by the same doctors at a practice or in an acute setting, regardless of whether the organisation employed locums. Relational and management continuity was seen as difficult in all organisations due to the fragmented ways in which organisations were structured and changes in how doctors worked. Participants spoke about how continuity was generally no longer held by an individual doctor but in a computer system maintained by multiple doctors. Given that relational continuity was no longer the norm, good-quality management continuity was seen as essential. However, there were concerns that there were inconsistencies in terms of recording and sharing information and that the technological infrastructure was not robust enough to ensure continuity of information. Furthermore, locum unfamiliarity with varying local policies and procedures could increase the likelihood of information being incorrectly recorded or shared. A lack of continuity, both relationally and managerially, placed the onus on patient and carers to keep track of their condition and maintain good records. Patients and carers sometimes held the most complete story about what had happened previously; however, this also meant a reliance on memory and health literacy. Having to relay their history to the locum was frustrating for patients who expressed concern about who was ultimately accountable for their care.
Is it the individual and the continuity, or is it, you know, something else? And I think at the back of my mind … well, at the forefront of my mind, I desperately want it to all be about seeing the GP and having continuity, and them knowing me and my family inside out. But I do think we’re at the stage where that’s kind of like a media construct of a GP, it’s like a country practice version of a GP. And it hasn’t existed for like five decades. And we moved to this system where you see whoever you see, whether they’re just another GP in the practice or a locum or whatever. And the theory was that it shouldn’t matter who you see because what matters is the recording and the system and the process. But as I think we’ve all vividly described, we’re all on the same page really that the systems behind what we have now aren’t good enough. And that’s what the issue is rather than anything else.
Patient 2, Focus Group B
Locum participants reported that care could sometimes ‘slip through the net’ or be delayed because of discontinuity and unfamiliarity with systems and processes. There was a perception that patients were unlikely to come into direct harm because of locum working due to safety netting and the rest of the team compensating where there were deficits in knowledge for example. However, indirect consequences due to inefficiencies included, for example, delayed treatment or discharge or referral to the wrong service. A locum working ad hoc shifts described how a lack of continuity impacted handover and caused difficulties communicating information about patients delaying discharge.
So more often than not it’s when you step in for the back end of a week, and you’ll find these plans that the consultant, for example, implemented a plan on Monday, and then left it to a locum, or for example, left it to a junior on the Tuesday to enact, and then a locum on the Wednesday, and then you’ve stepped into their boots. And occasionally its things that do slip through the net … So it’s all delaying, particularly at the minute, delaying patient discharge is the big thing that’s rife with all the pressures and all the rest of it.
Interview 23, Locum, Secondary Care
While lack of familiarity was largely regarded as having negative outcomes, discontinuity was sometimes beneficial for patients as locums provided ‘fresh perspectives’ and could change the trajectory of their care. For patients, there were potential advantages of discontinuity as locums enabled a second or different opinion. Not having previous experience of patients meant that locums did not have pre-conceptions and could come to their problems afresh. The discontinuity locums introduced could be beneficial for patients as new perspectives led to different routes of treatment or management. Discontinuity introduced by locums could disrupt organisational cultures because locums did not have a relationship with the patient and were not perhaps as constrained by the practice culture or as familiar with policies. However, non-compliance, perhaps due to unfamiliarity, with organisational processes or meeting the expectations of the patient could be detrimental for locums in terms of their employment and reputation and potentially detrimental for patients.
I remember coming in to one of my hospitals … and they were giving a child phosphate. And I said to them, but that’s not how we do it anymore, there’s been a change in practice. And they looked at me as though I was completely bonkers … Then I discovered that one of the consultants, another one, not the one I’d spoken to, was aware of it, and together we got on top of it, and I helped them put together a new protocol. But it was finding the right people to support me. Because the first person I went to batted it away … So, it all depends on whether you can find the person that’s open to change.
Interview 56, Locum, Secondary Care
The discontinuity locums introduced could also be beneficial to organisations as locums brought new perspectives and their experience of seeing many types of practice in multiple organisations. However, this systems knowledge and experience was not always capitalised on. Opportunities to share were typically not invited or rejected if offered, meaning organisations did not take up opportunities to learn from the locum. Locums were sometimes reluctant to challenge the status quo because they recognised their status as a newcomer and a temporary member of team, and reflected on experiences when offering alternative solutions had not been welcomed in the past. This was not only with regard to general functioning of the organisation, in terms of processes that might be improved, but also when locums challenged the treatment of individual patients, which had potential consequences for patient safety.
Unfortunately what I’ve found, which again goes back to communication issues and ego problems, is that people don’t want to hear what the locum has to say in terms of like how things might be improved … there’s not that openness. And it’s also that, I think it’s an attitude thing as well, to think that the locum has nothing to really add. You’re only here to see our appointments, it doesn’t really matter what quality of care you offer.
Interview 70, Locum GP, Primary Care
If you see something being done that doesn’t seem quite right, it’s very hard to say something. Obviously, if it was dangerous, you would but you see sometimes, and you think, there’s a better way of doing that, but it’s not my job to tell them, because I’m only there for a bit, and I don’t want to upset the status quo.
Interview 56, Locum, Secondary Care
Balance of staffing and stability
The balance between locum and permanent staff had implications for quality and safety and efficiency of service delivery. Organisations that were heavily reliant on locums were likely to have gaps in medical leadership, meaning that quality improvement was slower or less likely to happen and that team working and trusting relationships between staff were harder to establish. Some participants felt that the balance between locums and permanent doctors was shifting and expressed concern about the long-term impact on the workforce, the perception of the profession and quality and safety. There was a perception that some organisations were heavily reliant on locums in order to maintain service delivery and locums had become ‘almost a workforce’ as they outnumbered permanent staff in some departments and organisations. One participant described how it was now uncommon to have a substantive medical workforce.
Locum work, my view on it is they’re there to fill a gap. They shouldn’t be relied upon to deliver a service Monday to Friday, day in, day out, week in, week out. And unfortunately my trust see it as that, though, that’s my worry that they feel they’re not just plugging a gap, they’re almost as a workforce …
Interview 84, Lead GP, Primary Care
A&E are obviously used to working with locums, they do it regularly, so it tends to be easier to locum there because there are so many other locums. I don’t know if there’s any permanent staff.
Interview 53, Locum, Secondary Care
The balance of permanent staff and locums was regarded as significant for a number of reasons. Locums were employed to deliver immediate services but were typically less likely to be invested in the team and organisational leadership and development and consequentially less involved in long-term planning, clinical governance and quality improvement. Service development, good governance and quality improvement were perceived as more likely when there were permanent staff to lead and facilitate this. Departments that were disproportionately locum dependent were perceived to be in danger of stagnation and lack of progression; for example, the implementation of new guidance tended not to happen or was slower and more difficult to implement.
So, we have some GP surgeries, which are frankly in a state of crisis at the moment … And any sense of stability is long gone out the door. So, when you get those practices … it probably takes two years to turn a practice around, and that’s with a substantive workforce. You’ve zero chance of doing it if your key players are coming and going because no one will lead, or no one will manage.
Interview 85, Medical Director, Primary Care
Well-functioning established teams were regarded as better able to incorporate a small number of locums without being significantly impacted by discontinuity, whereas GP practices run by locums, or small teams in smaller organisations were regarded as being vulnerable to instability and inertia when the majority of services were delivered by different locums. The expectation on permanent staff to continue service improvement without consistent medical leadership and support was regarded as ‘too big an ask’.
I think there’s much more service development and quality improvement with permanent staff. Again, there will clearly be exceptions to this, but locums tend to turn up, they do the shift, they go home. Whereas when you really want to drive improvements in patient care, it’s the permanent staff who do that. If you get a department that is disproportionately locum dependent, then it stagnates, it doesn’t progress … it’s really hard to expect that one person who’s trying to keep the whole service afloat and to a certain extent monitor the locums work and drive change and improvement. It’s just too big an ask.
Interview 30, Responsible Officer, Secondary Care
Locum participants also recognised that having ‘an NHS run by locums’ was detrimental to quality and safety and some avoided organisations that were locum dependent for this reason. A locum GP described their experience of working in an organisation run solely by locums and reported a target-driven culture based on maximising revenue and where follow-up was not carried out. Another locum GP avoided working in practices that were mostly run by locums and described ‘a total lack of continuity’ and a feeling of being vulnerable because of the impact of the lack of clinical leadership on quality and safety. A different locum felt that locums needed to be used ‘judiciously’ because of implications for continuity, quality and safety and efficiency; this participant wondered whether patients attending practices with a high proportion of locums would be more likely to attend A&E because of the lack of follow-up, for example. However, this participant recognised that they would not know what happened to patients because of their transient relationship with the practice.
I worked in a practice where there was one full time GP and everyone else was a locum, so a patient might see six different doctors for one problem over a period of six weeks or something. So if it’s like that and there’s a total lack of continuity …
Interview 59, Locum GP, Primary Care
A medical director articulated the difficulties in balancing temporary and permanent staff in an organisation that was struggling to recruit doctors. This organisation relied on locums in order to maintain service delivery and the medical director described frustration about a lack of supportive mechanisms for organisations that had no other choice but to rely on a temporary workforce in order to provide services. There was a perception that overuse of the locum workforce would be attributed to poor leadership, rather than a consequence of recruitment and retention problems.
What support or protection do organisations get when our staffing levels drop down that low to say, actually, we can’t deliver this service safely, or we’re trying to do it to the best of our ability … if I have locums coming in, suppose tonight, suppose the whole of my A&E department is staffed with locum doctors and something goes wrong, they’re going to say to me, what on earth were you doing, staffing the whole of your A&E department with locums. Well, where would you like me to start? You know, I don’t do it out of badness, you do it out of how do I keep the service running to the best of my ability.
Interview 32, Medical Director and Responsible Officer, Secondary Care
Collegiality, involvement and inclusion
Without exception, locum participants described negative attitudes and perceptions which had a bearing on how collegial colleagues were, and which in turn impacted involvement and inclusion in organisations in a variety of ways. Perceived disparities between pay, workload and organisational and team commitment between locums and permanent staff could be sources of resentment and influenced how locums were treated and viewed. The perception from some permanent staff that they were doing the same or more work for ‘a lot less’ pay threatened collegiality and could be damaging to working relationships and locum well-being. Exclusion from organisational and team processes not only had the potential to increase risk to patient safety, when information was not shared with locums, for example, but could also be damaging to the safety and well-being of locums themselves. Resentment played out in locums being scapegoated when things went wrong and excluded from organisational functions that were necessary for team function, learning and the delivery of safe care. Locums described a lack of collegiality which resulted in lack of support and during the pandemic some felt that they were exposed to greater risk than permanent staff. While there were some examples of inclusive and supportive practice, collegiality towards locums was sometimes motivated by a high need for locums and problems recruiting, meaning that some permanent staff felt a need to mask their resentment in order to fill gaps and not deter locums.
I guess like any temporary post really, you struggle to invest in them, don’t necessarily see them as being part of the team. Not very positive about them, particularly junior staff, particularly in the acute trusts. We’d have locums refusing to come back because of the treatment of the midwives … I’m not a midwife, but if you’re trying to birth a baby together, you’re reliant aren’t you, you’ve got each other doing a physical procedure, your hands in, it’s high risk. The mum might die, the baby might die, you really rely on each other, it’s very, very intensive.
Interview 86, Clinical Lead, Secondary Care
Locum work was judged differently because of perceptions around higher rates of pay and greater expectations were placed on locums, for example, a perception that locums could replace ‘like for like’ and ‘hit the ground running’ when they entered an organisation. A consequence of this was that locums were sometimes expected to work with minimal support and supervision, despite potential training and support needs, or deficits in organisational knowledge.
Not having supervision, not having anyone who you can go to about problems or just about having a rubbish time. I think that is a real problem.
Interview 36, Locum, Secondary Care
I think it’s the fact that you are a trainee, and there is someone who has to look after you, that kind of gives a bit of protection in terms of your learning, which you don’t get as a locum, obviously, ‘cause you don’t have a supervisor … In some ways you are expected to work very independently as a locum, I think. You can ask for help obviously, but I do think that there is kind of an expectation that you kind of just get things done.
Interview 13, Locum, Secondary Care
While different rates of work were tolerated from permanent staff due to an understood variability in complexity of patients and flow, there was less acceptance when it came to locums who were expected to see a greater number of patients faster. While some participants described their organisations as being welcoming and supportive, explicit and open hostility was described by one medical director who had witnessed staff being less than compassionate towards a locum doctor.
It is tricky, it is hard. I think I’d hate to be a hospital doctor thinking, gosh, I’m stuck here forever and these guys are just coming and going, living the dream, doing what they want to do whenever they want to do it. And that does build resentment and sort of breaks down that teamwork that you really need if you want them to learn more and be colleagues really. But I don’t know how you’d change that attitude other than maybe they earn less from being a locum. But I don’t think you’d fill the posts.
Interview 53, Locum, Secondary Care
Defensive practice, hedging and avoidance
Participants described instances of defensive practice or hedging-type defensive medicine which involved providing services (e.g. tests, referrals) usually to reduce perceived litigation or other adverse outcome. For locums, adverse outcomes could include a higher risk of complaints and potential termination of contract at short notice. Some locum participants described practising defensively to keep patients on side and prevent complaints because of the precarious nature of the locum contract and pervasive negative perceptions from patients and other healthcare professionals. Locum participants argued that locums were more likely to practise defensively because they were attempting to practise as safely as possible in complex environments where they were professionally isolated and may not be familiar or supported. Rationing resources was regarded as benefitting the organisation but not the patient or locum; this meant that some patients actively sought out locums who were regarded to be less constrained by the organisation. There was a perception that locums deflected some of their responsibilities because they were disempowered to make decisions, while others felt that some locums were simply avoiding work and evaded responsibility for patients by pushing work onto others or into the future, by which time they will have moved on.
I think decision-making can be very, very difficult as a locum. And also if the patient comes with some demands of sleeping pills, or painkillers, or things, anything. Then putting your foot down is difficult because the patients are more likely to complain about locums than about the partners. So often locums will be softer, and some patients actually know to get an appointment with locums because they can get the antibiotic they want, or whatever they want, kind of thing.
Interview 83, Locum GP, Primary Care
Well, the way things are now and how difficult it is to see any doctor, I’d see anybody … So when you get offered something, you take it. Even though it might mean it’s a complete waste of time, you see somebody who really doesn’t feel able or willing to treat you and advises you to come back and see a regular doctor, you’d do anything because you’re not being offered a choice even to have an appointment.
Patient 2, Focus Group A
In addition, locums described a sense of professional isolation as well as the perception that the ‘system will crush you’ if a mistake is made. Locums described how easily they could be scapegoated, meaning that some locums were reluctant to make decisions and deferred responsibility to others in the organisation. Participants gave examples of overly cautious management including, for example, carrying out more tests or referring patients for second opinion more than necessary and this was sometimes attributed to locums lacking confidence in their own abilities to diagnose without getting a range of investigations done.
And the irritation of partners is that a locum refuses to do this, they over-refer, they make sure that they’ve covered all the options so that nobody can come back to them and say, you didn’t do this right. And the errors will happen. I think that there is a defensiveness in medicine, which is increasing and really harming people. There is nothing else that you can take from the whole Bawa Garba incident other than the system will crush you if you make a mistake, if you don’t deal with an acute problem you can go to jail.
Interview 38, Locum, Primary and Secondary Care
Governance
The governance practices in relation to locums varied widely and were not generally regarded as being as robust in comparison to permanently employed doctors. Responsibility for locum doctors was sometimes unclear in terms of who was accountable for organising, providing or supporting governance mechanisms, such as performance feedback, supervision and oversight, educational opportunities and CPD, appraisal and involvement in quality improvement. While some organisations included locums in their governance activities, others regarded locum work as transactional, where the locum was there to provide a finite service and the organisation assumed no responsibilities for their performance, development or oversight. There were concerns that governance structures were modelled on and designed for permanently employed doctors, meaning locums were not fully integrated into them or able even to access informal and formal governance mechanisms.
Transience and distance meant judgements about clinical ability and systems such as appraisal and revalidation were reliant on information from actors who might have limited knowledge of the locum and their performance. Locum doctors revalidate in the same way as any other doctor, but they may experience challenges in finding a RO or collecting supporting information, particularly if the locum works for a locum agency. NHS ROs are more likely to be familiar with the organisation and the doctors who work there. Locum agencies’ ROs may carry out their role for a number of designated bodies (the employer or agency for which the doctor does the majority of their work). There is a risk that locum agency ROs have less direct involvement in the locum agency systems and with the board or governing body. ROs relied on concerns being escalated in order to keep patients safe, manage concerns, support doctors and make revalidation decisions. However, this became more difficult for locum ROs, as they were unlikely to meet the locums or their appraisers or colleagues. A locum’s relationship with their RO, appraiser, colleagues and patients could be more distant and removed from the usual social exchanges and mutual engagement that occur between colleagues working within an organisation, meaning it was difficult for others to make fully informed judgements about a doctor’s fitness to practice. Agency ROs described not knowing the locum doctors they were responsible for in the same depth as when they had performed the RO role in the NHS, where they knew the doctors personally; ‘they don’t know me and I don’t know them’. Locums could be unfamiliar to colleagues and contact could be limited and others in the organisation were less likely to have a detailed view of the competencies and capabilities of locum doctors. As a consequence, the level of oversight ROs and other colleagues had of locums was likely to be reduced in some circumstances and particularly when locums were very transient.
I think it’s a remote world. It’s like a cloud, you know, it’s like the cloud. We talk about the cloud when it comes to storing information. And I think locum world is a bit like that … And I don’t know the doctors anywhere like as much as I did when I was an RO in the NHS, I knew them all personally. If I used to have a problem, I used to get them in my office there and then, chat it all through, sort it. Can’t do that in locum world, it might take me four days to get hold of the doctor, some of them won’t respond immediately. I always will have a telephone conversation with them. They don’t know me and I don’t know them.
Interview 51, Locum Agency RO
Similar governance and information-sharing problems were described by locum agencies and NHS organisations; both described difficulties in sharing and gathering feedback. When concerns were raised, participants described receiving little or no response or assurances about whether governance information that had been shared across organisations was acted upon and participants were often uncertain as to what happened to the information they shared. Communication difficulties, in part due to the fluid nature of locum working, meant that robust oversight was less likely for doctors moving between organisations.
It would give you more confidence if you heard back. And sometimes I’ll pick up the phone and you try to do the best you can to make sure this information gets passed on. But I just have this nagging doubt that I’m not always convinced it does.
Interview 30, Responsible Officer, Secondary Care
It’s been bothering me for a little while that sometimes when you request for information from other responsible officers you don’t always get a response. Which, kind of, leaves a bit of an unknown, especially when you’re then coming up towards a revalidation decision, you know. It’s not a fool-proof mechanism.
Interview 48, Director of Quality, Locum Agency
To improve the flow of information between organisations, NHS England introduced a system to allow the organisation to share information about locums and doctors moving between designated bodies. The Medical Practice Information Transfer (MPIT) form is designed to support the transfer of information about a doctor’s practice to and from the doctor’s RO. However, organisations did not always complete or return MPIT forms, and one RO indicated that their locum agency did not use their resources in perusing them.
There is now a system in place, that the GMC introduced and we’ve instituted over the last year really called the MPIT, it’s an official form, official GMC form … so somebody signs on with us, a new doctor and connects as a designated body, we send the previous responsible officer this form, basically saying, is there any history with this doctor and their answer is either yes or no. The returns on these forms are not reliable because I would think 50 per cent of the ones, I send off don’t get returned yet but the system is, we got it running pretty much straightaway but I think there is a number of departments in places where the form goes into some address that maybe a person who can’t address it and it doesn’t get … the returns are pretty poor. Now we don’t chase them up because administratively it’s a difficult thing to do with our resources.
Interview 47, Locum Agency RO
Continuity of governance was difficult due to the transient nature of locum work and issues of information flow between organisations. There was a perception that some locums attempted to circumvent governance and revalidation systems by moving between agencies. It was highlighted that some agencies have higher governance standards than others and some locums avoided these agencies because of this. To mitigate this, one agency had a policy on discouraging connections in the period close to revalidation and deferring revalidation for some locums to allow time for gathering evidence. There was also a perception from some locum agency ROs that while the majority of doctors were excellent, there was a percentage of locum doctors that were isolated doctors with potential performance issues who were likely to be most in need of supportive organisational and professional support.
You have to accept that whilst within the agency world, 80 per cent of the doctors we place are excellent, and have no problems, and do a great job, perhaps 20 per cent are those that have shaken down to that 20 per cent in the agency world, because they’ve not succeeded in the NHS, they’ve not got a substantive place, they are lost souls. And they are less able to cope with the vicissitudes of busy clinical life and professional life within a large organisation such as the NHS.
Interview 47, Locum Agency RO
There was concern that governance structures were modelled on and designed for permanently employed doctors, meaning locums were not fully integrated into or able to access informal and formal governance mechanisms. There was broad consensus that locums were less likely to be involved in learning processes in organisations, including routine learning opportunities and communications and learning from mistakes. Locums were not included in in-house learning activities for a number of reasons; there was a perception among some participants that locums were primarily employed to deliver services and cover staff shortages; consequently, some organisations did not assume responsibility for providing learning, largely due to additional cost. Barriers to inclusion in organisational learning also included the additional administrative burden in already pressured environments, the transient nature of the locum workforce and variability between organisations in terms of ability to maintain accurate and current e-mail distribution lists. Resentment around pay and workload and othering was also a factor described by some participants, which meant that learning was sometimes perceived to be exclusive to permanent staff and responsibility for learning was assumed by the locum.
The trust doesn’t consider us to have any responsibility for them in regards to development or career progression.
Interview 7, Medical Staffing, Secondary Care
Locum attendance at in-house non-mandatory training and inclusion in routine communications and team meetings was variable and typically optional for both locums and organisations and, in part, dependent on the motivation and discretion of the organisation and the locum. In some organisations, locums were welcome to attend training (particularly if they were working on a longer-term basis), though sometimes with the proviso that they would not be paid for doing so. However, in organisations that were less inclusive, locum participants described hearing about changes relevant to their practice (e.g. significant changes to policy or practice) by chance or through word of mouth.
They don’t want to pay you for induction, they are not interested in you coming to any of their meetings or MDTs, and they will certainly not have any kind of CPD engagement with you unless you happened to be there and they happened to have it on already and it didn’t make a difference if you were there or not.
Interview 35, Locum GP, Primary Care
Locums did not typically have established relationships or access to support in comparison to permanent doctors. There were also ingrained negative perceptions relating to locum working. As a consequence, locums were likely to be blamed as individuals without taking into account systemic antecedents to problems, such as lack of induction, supervision or support, whereas permanent doctors who made mistakes were described as receiving remediation and support. Problems or mistakes were not typically addressed productively and collaboratively by organisations, meaning locums were sometimes denied the opportunity to learn when things went wrong. Locums did not always receive feedback essential to their practice and learning and end-of-placement feedback was not always provided. Worryingly, participants described instances of locum contracts being ended when there were problems, without the reasons why being communicated with the locum or other required parties. Lack of communication and feedback had implications for locums in terms of equipping them with the necessary information to carry out their role safely and effectively.
We had a big incident actually which was a consultant who tried to blame a locum for something that went wrong … And it was quite clear that it wasn’t the locum that caused the problem … and it’s so much easier just to blame the locum and then brush it all under the carpet because you can just end the locum’s appointment. Whereas actually, if there’s a problem with a substantive appointment, one problem with the NHS is, it’s very difficult to get rid of hopeless individuals.
Interview 24, Locum, Secondary Care
Discussion
This qualitative study provides some profound and concerning insights into the implications of locum working for patient safety and quality of care. The ways in which locums were recruited, inducted, deployed and supported by organisations impacted quality and safety. Our findings indicated that regardless of their level of experience, it was unlikely that doctors would be able to function optimally in unfamiliar environments; and organisations who were inexperienced with locums, or had poor supportive infrastructure and governance mechanisms, were unlikely to enable high-quality safe services. Providing more comprehensive support for locums is essential if quality and safety are to be improved.
Many of the challenges confronting locum doctors were by no means unique to temporary doctors. Problems of productivity,87 inefficient working environments,72 defensive practice,88 difficulty raising safety concerns,89 fear of being held accountable for wider systemic failings,90 barriers to supervision91 and disorganised organisational processes hindered effective governance92 and are perennial issues faced by many in the profession. However, our findings suggest that these challenges were often exacerbated when doctors worked as locums. While it would be inaccurate to suggest that locums were generally less competent or skilled than permanently employed doctors, working as a locum could have longer-term consequences for doctors in terms of their professional development and practice. Participants described the impact of unfamiliarity and peripheral involvement in teams, organisational structures, professional development and formal and informal governance as detrimental for patient safety and quality of care. Unfamiliarity, professional isolation, stigmatisation and disempowering working conditions meant that care could be delayed, inefficient or inappropriate.
Our findings shed light on how temporary doctors fit into the enduring debate93 around how responsibility between organisational systems and individual professionals is distributed. Our findings indicate that a lack of transparency and blame stifled learning and that shared learning was often not fully harnessed. Blaming locums when things go wrong and punishing or disciplining individuals (in the case of locums, this often took the form of ending their contract) who make errors in contexts that are not designed to incorporate temporary workers may divert attention from understanding inadequately designed, poorly functioning systems or indeed the individual practice of other doctors. Locums represent a subsection of the medical profession for whom the wider paradigm shift from individual blame to a systems approach to errors94 appeared to not wholly apply. Our findings suggest that locums, particularly when they worked on a short-term basis, were often not regarded as a part of the organisation, and therefore the system, and not afforded the same protections as permanent staff when things went wrong. However, while our findings highlight multiple systemic barriers to safely integrating temporary doctors, exclusively attributing quality and safety issues to systems obscures the individual as an important aspect of safety. Our research has highlighted quality and safety issues that were described as practice specific to some locums, such as the abdication of responsibility for patients when on short-term placements, and not taking responsibility for team, departmental or organisational quality improvement when on longer-term placements, for example. While we should take into account systemic factors that impede locums from performing safely, we should expect high standards of healthcare professionals, be cognisant of individual agency and recognise the distinction between blaming someone and holding them responsible. 95
Strategies used to support safety largely involved increasing continuity and familiarity for both organisations and locums who reported that quality and safety were improved when locums were familiar with the teams and systems in which they worked and organisations were familiar with the locums and how to support them. The challenges for adapting to new environments and the importance of high-quality induction have been recognised for junior doctors. 96 Some organisations in an effort to enable and empower locums use strategies such as improved induction and removing barriers so that locums were included and had access to support and CPD; however, the implementation of this was varied. Organisations preferred, in the first instance, to recruit from the same pool of doctors – using their own staff banks and locums with whom they had established relationships. Locums attempted to foster familiarity by working in known organisations and sometimes worked below their competence to mitigate risks associated with working in unfamiliar or unsupportive environments, which, at a time of doctor shortages, is a cause for concern.
Furthermore, participants reported avoiding organisations because of lack of support, hostile or unwelcoming teams, chaotic systems and poor working conditions. Filling absences and vacancies is crucial for patient safety; however, poor doctor cover in specific areas has been attributed to a lack of willing or available locums. 90 Consequently, organisations should reflect on how they might maintain consistent positive relationships with locums and consider contextual factors, such as working conditions, support and relationships, learning and development and job satisfaction, which have been found to impact locum retention in our study and doctor retention more generally. 62,97 Creating more supportive work environments and targeting interventions that improve doctors’ health and well-being could reduce the risk of medical negligence claims and contribute to improved patient safety. 98
Cultivating continuity to improve patient care was a strategy used by some organisations and locums and was a significant factor in fostering team stability and improving quality and safety – supporting the extensive literature purporting the benefits of continuity. 99,100 Conversely, disruptive discontinuity was cited as an opportunity for highlighting areas of improvement and was sometimes positive for patient care, which reflects positive patient outcomes on second opinions in other research. 101 However, akin to whistle-blowers in the NHS,102 locums recognised their precarity and vulnerability when offering second opinions, sharing improvement ideas or voicing safety concerns, meaning opinions were not always offered and concerns were not always raised. Organisations should reflect on their safety cultures103 and how open they are to hearing locum voices. 104 If organisations are to improve, then it is important that organisations and the individuals working within them actively search for where improvements can be made and highlight these issues for the benefit of everyone’s learning, rather than seeking comfort by disengaging and failing to address issues.
Given that some locums were not scaffolded by organisational and governance structures, belonging to a Locum Chamber provided access to supportive networks and was potentially beneficial for improving quality and safety for both locum GPs and organisations. Locum Chambers provided infrastructure such as communities of practice, pastoral, professional and educational support and clinical governance information. Locum Chambers also facilitated feedback between locums and organisations to improve mutual learning, which our research found could be problematic for both locums and organisations. Locums who were well networked and informed about local health economies were better able to avoid poorly functioning organisations. However, there were concerns that less-well-networked locums, such as inexperienced or locums who had graduated in other countries, may be more likely to find themselves in unsafe organisations with limited support, which could be detrimental to both patients and locums. Indeed, the regulator has called for comprehensive support to be provided to doctors new to the UK whose role is likely to be isolating, such as locums. 105
The NHS relies heavily on locums and a significant proportion of these locums are IMGs. 33 However, GMC registration and licence to practise do not necessarily assure safe practice; yet it is clear from our research that locums and patient safety are disadvantaged when doctors are unfamiliar with systems, patients and organisations. Our findings indicated that, regardless of where they trained, locums are not always adequately inducted into organisations or considered in formal and information governance structures. The regulator recognises that IMGs experience difficulties in adapting to NHS systems and understanding the ethical and professional standards expected of them. 106 However, locums do not have the same recruitment, induction, support, supervision or oversight, feedback and remediation if things go wrong. Short-term locum positions were not designed to assess whether each new locum possesses the appropriate professional capabilities – a process which would take several weeks. Instead, employing organisations must assume new starters are appropriately trained, meaning patient safety may be at risk.
Governing has been described as a complex interplay of social, political and cultural relationships, knowledge asymmetries and forms of power within and beyond the organisation. 107 These factors shape governance activities, and our findings would suggest that governance activities differ based on contractual status and organisational policies and norms. The governance practices in relation to locums varied widely and were not generally regarded as being as robust in comparison to permanently employed doctors. Systemic problems, including overwork and under-resource,108 were widely recognised and were often used by participants as good reasons for bad practice. For example, participants reported that providing feedback to locums sometimes generated significant additional workload for permanent staff, especially when the locum turnover was high. This research has highlighted that much still needs to be done to develop governance systems which promote and protect the interests of patients and create an environment which supports locum doctors in meeting their professional obligations.
Locums are a growing group in the medical workforce, but are not well represented in research. This is the largest qualitative study to explore locum working and quality and safety. One limitation of the study is that participants were all working in England and, as such, caution should be taken when generalising the findings. To understand more about the impact of locum working on quality and safety of patient care, further research in other countries and contexts would be useful. The sample may have been skewed towards locums, people who work with locums and patients who had more negative perceptions and views of locums; however, patients’ views were overall positive and the perspectives of the sample align with previous research. As our research collection took place during the pandemic when locum work was reduced, this may have affected the findings. We were also unable to conduct the case study research including observations, which would have strengthened our findings and moderated some of the challenges in interviews, such as recall bias.
Our findings indicated that the way in which doctors who worked on a temporary basis were integrated into organisations posed some significant challenges and opportunities for patient safety and quality of care and that both organisations and locums had a part to play in improvement. Doctors working as locums are a heterogeneous group with differing backgrounds, experiences, skills and capabilities that likely reflect the variability seen in the wider population of doctors. Locums are working in the same pressured and imperfect systems as other health workers; it is vital that systemic problems are not mistaken for people problems and important to recognise that locum is not a type of doctor but a way of working. Our findings are a call to action for organisations to take stock of how they engage, support and work with locums and ask both locums and organisations to reflect on whether their practices support a collective approach to patient safety and quality of care.
Chapter 8 Patient perceptions and experiences of locum doctor care
Aims
This chapter reports on research undertaken to understand patient perceptions and experiences of locum doctor working in order to find ways to improve the quality and safety of patient care when temporary doctors were employed.
Methods
In this chapter, we have drawn on and foreground our findings from exploratory focus groups and one-to-one interviews with patients to explore how locum working impacted patient perceptions and experiences. However, we have also drawn on our entire data set to understand the implications of locum working for patient experience by including perceptions from multiple sources to provide a holistic view.
Recruitment
Patients were purposively sampled through patient and public contributor forums. Our PPI chair recommended that we recruit through Research for the Future and NIHR Clinical Research Network (CRN) which is an initiative to help recruit people to take part in health and care research using a ‘consent for approach’ model. Participants were paid £25 in vouchers or by bank transfer for their participation.
Data collection
Two authors (GS and JF) and two members of our PPI forum (MS and MM) carried out 5 focus groups with 30 participants. Focus groups involved between four and eight participants per group. GS and JF also carried out one-to-one interviews with 12 participants. Data were collected using video-conferencing software (n = 15) or over the phone (n = 2). Forty-one participants spoke about their own experiences as a patient; one participant was a carer who spoke about their experiences with the person they care for and also their own experiences as a patient (see Appendix 6 for additional participant quotations).
Analysis
Collaborative data analysis
For a description of the qualitative methods, please see Chapter 7, which details the initial stages of analysis.
It was important that our PPI forum were involved in analysing the data they had collected. We discussed with our PPI forum how they would like to approach this and took guidance from our PPI chair who is a highly experienced contributor in health services research. For our patient focus groups and interviews, we involved our PPI forum in a collaborative analysis session where we examined themes identified by the research team and discussed broader patterns of meaning. We presented extracts from the transcripts under theme headings and provided short descriptive summaries of what these extracts related to; we explored these interpretations with our PPI forum and incorporated views and ideas. We decided to take this approach as our PPI chair advised that this would be efficient and maximise PPI input without having to burden PPI forum members with the lengthy process of reading and coding the full transcripts. During the session, we reviewed each theme to determine whether they told a convincing story of the data, and one that answered the research questions and made changes according to points emphasised by our PPI group. Involving the PPI forum in the analysis offered a form of triangulation to enhance rigour, challenge and alternative interpretations of the findings. 51 Collaborative data analysis meant that alternative views were sought and that our findings were more relevant to the needs and preferences of patients. Strategies used with our PPI collaborators to enhance quality included debriefing to provide an external check on the research process, theme examination, triangulation of researchers and PPI co-researcher perspectives and use of reflexivity, which involved recording decisions, rationales and reflections.
Results
Our findings are presented under four themes that examine patient experiences of locum care from the perspective of patients and staff: how patients perceive locum doctors and how this differed from their perception of permanent doctors; patients’ awareness of whether their care was delivered by locums and whether they should know this; how locum working impacts continuity of care for patients and the implications of reduced continuity; and how communication and practice differ when doctors work as locums and the implications for patient outcomes.
Patient perceptions
Clinical acumen, enthusiasm for the role and the quality of supporting infrastructure were generally regarded by participants as more indicative of a doctor’s performance than employment status. Participants spoke about the variability in practice and personality between different doctors regardless of whether they worked as a locum or not. Participants who attended regularly were knowledgeable about the different GPs at the practice and knew who to avoid and who they preferred. Participants spoke about a false dichotomy between locum and permanent GPs and described positive and negative experiences of both. It was also recognised that the systems and environments that doctors worked in could potentially impact the locum’s ability to perform as well as their local knowledge and familiarity with patients, systems and care pathways.
That I think locums are no different than regular doctors and they find themselves sometimes in a difficult position because they are thrown into unknown place and they have to figure it out quickly. And as I said, they sometimes lack this confidence that a regular doctor has, just from being in single place for a number of years … locums shouldn’t be treated any differently than regular doctors, they’ve completed their education, their training, they want to help, they want to be professional, et cetera. Just perhaps the patients should be more tolerant.
Interview 78, Patient
You’ve got doctors which want to do their job and you’ve got doctors that are just there to get their pay check and clear off at the end of the day. It don’t matter whether they’re a locum or whether they’re full time.
Focus Group B, R8
Perceptions of locums as ‘less than’
In the main, participants did not distinguish between locums and permanently employed doctors in terms of clinical ability. However, some participants perceived locums to be less capable, less committed to their careers and as doctors who locummed because they struggled to find a permanent job. The implications of these attitudes included patient avoidance and lack of trust.
When you mention the word locum doctor, it gives the impression of somebody who’s there temporarily. Somebody who’s not a specialist. Somebody who may be travelling. Somebody who’s not committed to a career say as a GP. And often, they do have portfolio careers when they do more than one thing in the field. So that’s my general impression of a locum.
Focus Group A, R5
Somebody who can’t find full time employment … To me, if they wanted to be doctors, they would be looking for a permanent position either as a GP or in a hospital situation. I’m never happy with them, but that’s my view. It’s they’re not unemployable in that respect, but they don’t seem to fit into one category?
Focus Group C, R1
Patient awareness
Participants were not always aware, in both primary and secondary care, whether their doctor was a locum. Participants mostly spoke about their experiences of seeing a locum at their GP practice, as they were more likely to be familiar with practice staff compared with a secondary care setting. Some participants felt that it was difficult to distinguish who was who at their practice when there were lots of doctors with different working patterns. The fact the doctor was a locum could be communicated by practice receptionists, and sometimes in an apologetic way.
I do get to see a regular GP. But if have to do a telephone appointment, especially if it’s an emergency type one, then I am advised over the phone that it’s a locum. And I have an occasion I’ve been and my regular doctor hasn’t been available and then they’ve said, oh, I’m sorry, the locum’s going to see you today.
Focus Group B, R3
There were differing opinions among participants about whether patients should be informed whether the doctor was a locum. Some participants felt it was important, particularly for those with long-term conditions or mental health problems, to be given information about who they were seeing, especially if they have not seen that doctor before.
That’s very important. Like as a patient, it should be explained under the charter of the service, what the whole purpose is of your treatment, wherever you’ll be seen by a junior doctor. So wherever you’ll be seen by a locum, or wherever you’ll be seen by another specialist. So I think it’s very important, you know, for either trusts or the NHS, to make people aware about what the service is, in the first instance.
Interview 95, Patient
I think when it’s long term patients, as it mostly is with mental health, I think they do need to know that it’s a locum, because it will be a long term relationship usually.
Interview 86, Clinical Lead Secondary Care
Participants perceived that locums and organisations may be reluctant to disclose to patients their doctor was a locum because of the recognised negative perceptions around locum working and the potential implications for consultations and doctor/patient relationships. There were also concerns that patients might not want to be seen by a locum.
I: Do you think that you should be told when you’re seeing a locum?
R: No, no, not necessarily, as I said, I don’t have a problem with that, but I think that some people may be prejudiced and may be, you know, throw a tantrum or something.
Interview 78, Patient
Why would you badge it with locum because I think if the reality is if you do use the word locum, I think most patients are familiar with the word locum and they’ll see it in a negative way as this is somebody that’s not going to know me, this is somebody that’s not going to be as close to my history and it’ll put those barriers up almost immediately.
Interview 27, Medical Director
Sometimes patients don’t react in the best way to knowing that it’s a locum doctor. Oh no, I want to see a ‘real’ doctor, and that is really difficult to manage from the agency doctor point of view ’cause that makes them feel not welcome, it makes them feel like they’re second class citizens, if you like, when absolutely they’re not. That’s difficult to manage from a patient point of view as well.
Interview 25, Medical Staffing, Secondary Care
While some patient participants felt that patients should know when a doctor was working as a locum, the general consensus among participants who were doctors or working in health care was that patients did not need to know. Participants perceived that patients in secondary care were less aware and concerned about whether the doctor was a locum. Participants felt that patients did not need to know their doctor was a locum because the standards of safety, patient care and governance processes should be the same regardless of the doctor’s contract. Some participants perceived that patients were not concerned if they were seen by a locum, as long as care was delivered by a doctor who was qualified and capable.
I: Do you think patients should know or need to know?
R: No, I don’t think they should or be told. I think the system ought to be robust and safe enough that it doesn’t matter.
Interview 30, Responsible Officer, Secondary Care
I: Do you think patients should know or need to know?
R: I would say if we’ve got the right governance in place and we’ve got the same level of assurance that they are safe, they are a quality practitioner and that they are up to date with what they need to be, I’m not sure patients do need to know ’cause there’s no difference in terms of they’ve got the required skillset, they’ve got the required training, they’ve got the required knowledge, I’m not sure there is a need to know.
Interview 25, Medical staffing, Secondary care
Continuity of care
Traditional notions of continuity of care and a family GP were recognised as a thing of the past. This was perceived to be a consequence of how modern general practice was structured and how GPs approached their working lives, with more GPs choosing to work flexibly.
I desperately want it to all be about seeing the GP and having continuity, and them knowing me and my family inside out. But I do think we’re at the stage where that’s kind of like a media construct of a GP, it’s like a country practice version of a GP. And it hasn’t existed for like five decades.
Focus Group B, R2
Accessing care
Participants described their experiences of making appointments and typically not being offered choice about which doctor they saw. Access to a doctor and seeing someone rather than no one meant that participants felt they did not have the option of choosing who they saw. For some participants, access was more important than continuity.
You can never book an appointment with your doctor at our surgery. It’s as simple as that. So you’ve got a choice, you have a locum or you don’t see a doctor.
Focus Group B, R2
I would much rather see a locum than not be able to see anybody at all.
Focus Group C, R2
I personally don’t think that continuity is as important as some people make it out to be … access is king …
Interview 35, Locum GP
Relational, management and information continuity
Participants generally spoke about continuity of care in two ways: relational continuity, which was defined as an ongoing therapeutic relationship with a regular doctor, and management and information continuity, which was described as the continuity of their clinical management including record keeping and sharing of information. Participants spoke about how continuity was generally no longer held by an individual doctor but in their patient records which were maintained electronically by multiple doctors and sometimes across organisations. Given that relational continuity was no longer the norm, good-quality management continuity was seen as essential. However, there were concerns that there were inconsistencies in terms of recording and sharing information and that the technological infrastructure was not robust enough to ensure continuity of information. Participants recognised that they were unlikely to be seen by the same doctor at a practice, regardless of whether the practice employed locums, and relational and information and management continuity was regarded as difficult in all practices.
I don’t even think our general GPs are familiar anymore … These days I don’t even see a regular GP. I end up with them on the end of a telephone … I’ve never seen the same person and yes, well, a few of them were locums. None of them know me.
Focus Group C, R3
Have they read the notes? Do they know me? What continuity am I going to have with this person? How long are they there? Are they there for a week, a month, six months, whatever? Is it worth trying to get a relationship with them?
Focus Group C, R4
One thing that occurred to me is that the whole business of continuity of care seems to be focused on continuity of doctors’ notes … I think one thing I would say is that if I want continuity of care, I want continuity of information passing …
Focus Group D, R4
Serious or chronic conditions and acute or minor illnesses
Continuity of care was described differently and had more importance to participants when they were seeking care for complex, serious or long-term problems. Participants were more amenable to seeing a locum doctor for minor and acute illnesses that were unlikely to require follow-up. There was concern that a lack of relational and management and information continuity could have a negative impact on patient outcomes for patients with serious or chronic conditions and a perception that the absence of continuity placed additional responsibility on the patient to be an accurate reporter of their history.
I do have a concern though and maybe even a fear that you don’t have the continuity. When you have a rare condition, the one thing you want is continuity or faith in somebody understands the neurological condition that you have, in my case. And that continuity hasn’t been there. And it worries me when I see a locum, they only … they can only look at the records and sometimes they’re not as up-to-date as the last time you went to see the consultant. So it concerns me that you’ve got to spend time going over stuff that, you know, you expect an experienced doctor or a regular doctor that you see, if they’re not available, then you’ve got to go over stuff. And sometimes you forget, oh, I should have mentioned this, should have mentioned that, which is relevant. And it’s a fear really and a concern that there isn’t … because you’ll never see the same locum again. And they’re not accountable, they come and they go.
Focus Group A, R5
I think for some patients, especially patients with a background of dementia, or patients who are acutely delirious, I think it can be quite confusing when you get a different doctor day upon day, and even from the simple tasks like doing a cognitive score, one of the questions is, do you know what my job is? And a patient is more likely to give an accurate answer if they’ve seen you for the last two days already, as compared to if it’s the first time you’ve walked in the room.
Interview 23, Locum Secondary Care
Participants with long-term or mental health conditions described the importance of continuity of care and having trusting and knowing relationships with their doctor and the implications for their care when this relationship was absent. These participants reported delaying seeking non-urgent care when their regular GP was not available. Participants who avoided making appointments with doctors they did not know or trust were concerned that locums would not know their history and this could have negative implications for their care.
Unless it was a real, real emergency, I’d wait till my regular GP was in … I just had to wait ’til he’d come back off sabbatical, I think that’s what they said, they said he’s on a sabbatical and he won’t be back for four to six weeks … until I knew my doctors were back, I wouldn’t make an appointment.
Interview 74, patient
Whenever I try and make an appointment, they do say that you can be seen by a different GP, but I insist I’d rather be seen by my regular GP, who’s aware of my treatment, who’s aware of my plans. So I insist and I request that, otherwise I don’t want to be making an appointment … I don’t feel comfortable, or there’s trust issues …
Interview 95, Patient
Participants found it frustrating when they had to recount their detailed medical history to a locum doctor. Locums were regarded as particularly disadvantaged if they had no previous experience of a patient and their medical history and would need to read the notes before or during the consultation, which was frustrating for patients and gave the impression they were not being listened to.
I prefer to see a doctor who knows me because my medical history is complicated. And I think you haven’t got time to look at everything. You know, I’m diabetic, I’ve got fibromyalgia, I’ve got arthritis, I have sleep apnoea. All connected with each other but you’re not seen as a whole. And that’s upsetting … that’s my experience is that if they say a locum, I just think they’re not going to get the full picture, it’s easy to dismiss. Whereas when you see a regular doctor who knows your history, I feel at least I’m being listened to more.
Focus Group B, R1
A participant questioned the cost-effectiveness and efficiency of seeing a locum and having to explain their history compared with a shorter appointment with a familiar doctor.
If I go in and take up 40 minutes of a locum’s time trying to get my point across, telling him the answers to all these things he’s asking, how many patients could he have seen? Four patients. If I go and see my long-term regular doctor, we could probably get it done in ten to 15 maybe. I don’t know. I think there’s definitely … there’s an investigation or something needs to be looked at with regards to time management, patients seen and cost effectiveness.
Interview 76, patient
Participants described being happy to see a locum doctor for acute minor problems but were reluctant for complex, long-term or serious health conditions. This was, in part, because of time pressure as participants did not think the locum would know their medical history or have the time within the appointment to understand it. Others were concerned that the locum would not be there for any follow-up and had concerns about how the problem would be documented on the system.
I’ve got no problem with being seen by a locum for a one-off first event. It’s when it’s an ongoing thing I’d much rather see my own GP … I think that locums are only ever able to scrape the surface and I think that’s a shame, and actually because of the nature of their appointments they don’t have time to find out enough. And therefore, I think that they should just be dealing with first visits or minor complaints. I don’t think they should be standing in for the GPs with people with serious health conditions.
Focus Group C, R2
One participant responded to the consensus that locums should consult on minor issues by questioning how this would impact on the locum’s learning and development.
Are they actually going to learn enough if they’re just doing repetitive simple things?
Focus Group C, R3
Communication and practice
Locum working was described as influencing how doctors communicated and practised, which could have positive or negative implications for patient care and outcomes. Defensive practice was described by patients, locums and participants who worked with locums. However, there were also positive outcomes for patients when they were treated by locums who were able to provide fresh insights and new perspectives.
Defensive communication and practice
Locums described having to approach their consultations differently when they worked as locums for a number of reasons; locums were aware that they could be perceived negatively; as a result, locums described having to work harder to establish trust with patients. Locums were also aware that they were more likely to be complained about by patients, which could have implications for their employment. These factors influenced consultations and communication and potentially patient care and outcomes with some locums describing practising defensively in order to avoid patient complaints.
It’s like being an actress sometimes doing our job, you know, you have to put it all on in some ways … I think when I’ve been a long-term doctor, a long-term salaried GP, you can see that they trust you from the outset because you’ve helped them before I think and it all went well. I think so. So yeah, you probably have to try that bit harder as a locum, you know, you have to give them some eye contact and listen to them while you’re looking in their eyes, that kind of thing, to build up some kind of idea that you are genuinely interested in their problem.
Interview 90, Locum GP
Being risk-averse and practising defensive medicine usually means more tests, more referrals, whereas holding risk tends to be disadvantageous for you as a locum because what’s the benefit to you of not doing that. You’re benefiting the system by rationing resource, the patient won’t thank you, and again as a locum, you don’t need to have the patients coming out singing your praises, but it certainly helps.
Interview 35, Locum GP
And the irritation of partners is that a locum refuses to do this, they over-refer, they make sure that they’ve covered all the options so that nobody can come back to them and say, you didn’t do this right. And the errors will happen.
Interview 38, Locum Primary and Secondary Care
I often wonder with particularly with junior locums whether they’ve got the confidence to make a decision or whether they just go out the room and have a word with the senior GP or what have you.
Focus Group C, R4
Organisational freedom and constraint
Some participants perceived locum practice as being less constrained by the organisation in comparison to permanent doctors. This autonomy had a number of benefits for participants, including locum GPs being able to spend more time with patients and/or order medications and referrals that other doctors in the organisation may not have ordered because of financial constraints for example.
So that doctor, through that line of questioning and not having any sort of prior history … may have, you know, had a chance to look at my notes beforehand, ordered the right tests and didn’t feel constrained in that practice about what tests that they could order. And someone subsequently … because when you get referred to hospital, the consultant said that that doctor was very much on the ball. And, of course, that’s a change to lifelong medication. And literally within a month of the medication kicking in, it transformed my life.
Focus Group A, R1
I was in A&E for a good six hours and they said right, we’re going to send you home in care of the GP. Which is a fair comment but I still couldn’t see, my blood sugar was still raising in the thirties. And lo and behold who walks in but this locum who introduces himself to me that I’ve spoken to on the phone. And said, what they doing? I said, well nothing, they’re going to send me home and refer me to you. He said, well we’re going nowhere. Either they give you a dose of insulin or they give you a litre of fluids to try and flush out your sugar. Now that … I was just blown out of this world, that one the guy had turned up and number two he was going to over-rule the A&E. So, yes, that is a positive side to it.
Focus Group C, R1
While some participants described a lack of organisational constraint, some participants reported how organisational controls and a lack of autonomy meant that they felt disempowered to make decisions. One locum described how their decisions were checked by another GP, which compromised their professional integrity and contributed to negative patient perceptions.
There’s a huge variation. Some practices will review every single referral decision you take before they allow you to send a referral through. So after my clinic I literally go and sit in with the GP and explain every case that I want to send the referrals to, and which referral and why. If they say no, I have to then go back to the patient and try and explain that; then the patient says something, and then I go back to the partner; then I go back to the patient. Which is really, really very soul destroying for you because the patient’s like, somebody else is making the decisions, so who are you, you know; so there is no kind of value for you there.
Interview 83, Locum GP
New perspectives
Participants spoke about how locums had provided a fresh perspective on their condition that their regular GP may not have considered. Locums not having preconceived ideas about a patient or knowing their history may be an advantage for some patients, as the locum may not be building on a previous treatment plan, but instead coming to the problem with a fresh perspective and considering something new. In this sense, a lack of continuity was a positive.
In my case, continuity was damaging because there’s kind of an assumption that if you know the person and you know the personality, then when they come in with certain issues, you dismiss it because, well, it’s just them isn’t it, I know what they’re like, they’ll exaggerate slightly, they’ll do this. And actually sometimes seeing a locum or somebody who doesn’t know you makes them just look at the medical stuff, just look at the factual stuff. And in my instance, that was life-changing. You know, that was literally life-changing because I got somebody who didn’t dismiss it, who didn’t sort of go, well, it’s just him and his problem he comes to the GP practice regularly, you know. So I think we can invest too much in this kind of … version of, you know, see the same GP for all your life and everything’s magically okay. It really isn’t.
Focus Group B, R2
I have benefited from some locum doctors in the past because they’ve brought a fresh pair of eyes and perspective on it … So, it’s not always a bad thing having a different person in front of you …. there has been that element of they brought something fresh to the table to look at or they’ve been aware of a different way of treating something to what your GP previously said. But then there’s the follow-up session again because then you’re back to that, you’re not going to see them again. It’s mainly the inconsistency that gives you the uncertainty.
Focus Group E, R1
Discussion
This is the first study of its kind to explore patient perceptions and experiences of receiving care from locum doctors. Generally, participants regarded the standard of care given by locums to be equivalent to permanent doctors and the new perspectives offered by locums as beneficial. However, some perceived locums to be inferior in comparison to permanent doctors and the temporary nature of their roles as negatively impacting care, particularly when continuity was considered important.
While patients experienced variability in practice between different doctors, regardless of whether the doctor worked as a locum, it was reported that patient care and patient outcomes could be different when they were seen by a locum. Locum working impacted patient consultations, relationships and communication in a number of ways. Locums described practising defensively, approaching consultations differently and working harder to build trust with patients; however, good bedside manner does not necessarily equate to good patient care. Overtreatment and inefficiency place additional demands on the NHS. 109 Our research has found that locum doctors were likely to prescribe antibiotics, for example. It may be that for locums action was better than inaction when it came to building trust with patients. Patients also described defensive practice and experiences of doctors who they perceived as not fully functional due to their temporary and peripheral involvement in the organisation and their care. Unfamiliarity with patients as well as the organisation and its policies and procedures meant that locums could have a partial knowledge of a patient’s care and history and how best to proceed.
Differences in clinical decision-making reported by locums in this study and elsewhere110 and evidence indicating that continuity results in better outcomes for patient’s99 raise the question as to whether patients should know when care will be provided by a locum. There was a perception among some participants that patients did not need to know when their doctor was a locum because the standards of safety, patient care and governance processes should be the same regardless of the doctor’s contract. However, we know from this and earlier research15,111 that systems of governance and standards of safety were not applied in the same way across permanent and temporary staff. Knowledge and application of NHS England guidance were limited, and participants reported that typically only mandatory and essential governance processes were followed. Without the obligation to apply standards of governance when locums are employed, variation is likely to continue.
Doctors reported that they communicated and practised differently and more defensively when they worked as locums. The precarious nature of locum work15 could mean that locums were vulnerable, which could have implications for how doctors behaved and communicated with patients. Clinical decision-making was described as changing when doctors worked as locums, which could have both positive and negative implications for patients. Some patients benefitted from having consultations with locums where new insights led to diagnosis that improved quality of life. The benefit of having a partial knowledge of organisational procedures meant that locums were free from organisational constraints and their lack of patient and organisational knowledge could bring fresh perspectives.
Locums are qualified and trained doctors but were sometimes perceived to be less experienced, less capable, unable to find permanent work and less committed than permanent doctors. This lack of trust meant some participants in our study avoided seeing locums or delayed accessing care when their regular doctor was unavailable. A lack of trust from the outset can result in negative perceptions of continuity of care, poorer outcomes for the patient and could result in increased complaints. 112 A meta-summary of patient experiences when seeing multiple clinicians found that patients experience continuity as security and confidence rather than seamlessness. 113 We found that locums were sometimes perceived as overly cautious or lacking in confidence, which could weaken the notion of continuity and result in less satisfying outcomes for patients.
A general lack of relational and management and information continuity in general practice was a concern and it was felt that the temporary nature of locum work may cause additional inconsistency in record keeping and information transfer. Patients were concerned that the communication processes and the systems for recording and accessing of patient notes were not sufficiently robust when locums were working in unfamiliar environments with unfamiliar patients. We know that when information transfer and technology for accessing health records are insufficient, patient outcomes are negatively affected and patient confidence in professionals is reduced. 114,115
Unprecedented demand and changes in modern-day general practice70 have meant improving patient access to GP appointments has been a primary focus. 116 However, international evidence in support of continuity of care has been published over decades and confirms continuity of care as a significant factor for improving patient outcomes. 117,118 Continuity of care was valued by some patients in our study, and we found, as others have, that the importance of continuity to patients depended on the severity of the issue or condition. Patients preferred to see their regular GP when discussing serious or long-term health conditions, as repeating information about their condition risked important information being omitted and relied on patient memory and health literacy. 119 If continuity of care is reduced, it may be that patients and their carers have a more complete picture of their history than the doctors involved in their care. Previous research has shown that patients want to be actively involved in the communication, monitoring and self-management of their care and that an active involvement in information transfer can ensure a sense of continuity. 113 In developed healthcare systems, there has been a move towards a patient partnership model, where patients are seen as central to their care and the decisions to be made. 120,121 Patient involvement in their care and participation in decision-making is an important feature in what patients feel encompasses continuity of care. 122,123 We found that patients want their role and ideas to be acknowledged, they want to be heard and have their views listened to. They want the opportunity to provide relevant history of their conditions without having to repeat information to different doctors. One set of tools that might help patients in their interactions with different clinicians are patient-completed checklists which provide useful prompts for patients and support effective conversation between patient and clinician. 124 However, this approach is likely to rely on a certain amount of health literacy and may exacerbate health inequalities.
Our findings suggest that locum working and the ways in which locums are perceived can have implications for patient experience. Locums enable access and service delivery at a time of workforce shortages and can provide new ideas and fresh perspectives, which should be recognised and welcomed. While access to care is important, efforts could be made to identify when and how continuity can be provided for patients who might benefit most, such as those with serious or chronic conditions. Defensive practice was described as a consequence of negative perceptions, undermined trust and precarious contracts. Consideration should be given to how to improve the perception of locums and how they could be better supported by when things go wrong.
Strengths and limitations
This is the largest qualitative study to explore locum working and quality and safety and the first study of its kind to explore patient perceptions and experiences of receiving care from locums. However, it is not without limitations. It is possible that our sample may have been skewed towards patients who had negative perceptions and experiences of locums, although patient perspectives were generally positive. We found that patients with long-term and serious conditions were more likely to want continuity of care; however, we did not sample for patients with long-term conditions, meaning we may not have captured the views of patients who were most impacted by locum working. Also, some questions were related to participants’ previous experiences, for which they needed to recall past situations. As a result, bias may have been introduced due to the unreliability of memory.
Chapter 9 Consultation patterns and differences in the clinical practice and performance of locum and permanent doctors in primary care in the United Kingdom
Aims
In this chapter, we use the CPRD to quantify and compare general practice consultation rates by locum GPs and permanent GPs, for all participating practices in the UK from April 2010 to March 2022. Moreover, we describe the variation of locum use over time and by geography. In more detailed analyses of patient-level data, we evaluate the association between locum consultation rates and important quality and safety outcomes while controlling for available patient and general practice characteristics.
Methods
Data
Clinical Practice Research Databank GOLD is a large, computerised database of anonymised primary care medical records. It contains complete electronic health records (EHRs) for over 14 million patients in general practices using the Vision system, with the healthcare events (diagnoses, treatments, referrals, tests and prescriptions) recorded using coding systems. 125 The database is broadly representative of the UK population, although larger practices are over-represented and the data have been shown in numerous validation studies to be generally of high quality. 126,127 Practices need to meet pre-specified data entry quality criteria to be defined as ‘up to research standard’, and for each study year, our main sample included all CPRD practices that were classed as such for the whole year in all UK countries.
We also obtained CPRD-linked HES data. The national HES data contain details of all admissions to NHS hospitals in England, including information on deaths in hospital. 49 Area deprivation, as measured by the latest update of the IMD (i.e. 2015), was available at the 2011 LSOA level. The IMD measures deprivation at area level based on domains, such as income, employment, health, housing and general environment and is the most complete and widely used approach to quantify relative deprivation and affluence for small areas in England. The IMD is assigned to every small area in England and ranks them from 1 (most deprived) to 32,844 (least deprived). 39
Linkage of CPRD GOLD data to the HES and IMD databases is available for those individual patients who are registered at practices in England and who have consented to data linkage. Our cohort was eligible for linkage to HES and IMD, and we provided pseudonymised patient identifiers to CPRD so that linkage could be performed. CPRD used a deterministic linkage algorithm to perform linkage between data sets on behalf of the research team. The algorithm was based on a patient’s exact NHS identification number, sex, date of birth and residential postcode and linked data were subsequently provided to the research team.
Analyses
Study design: retrospective cohort
Stata v17 was used for the principal data cleaning, management and analyses and an α level of 1% was used throughout. 128 However, statistical significance is not very informative in analyses of data sets of this size and we focus on the clinical significance of the effect sizes rather than p-values. 128
We conducted a retrospective cohort study of GP consultations of non-temporary patients at 914 general practices in the whole UK, between 1 April 2010 and 31 March 2022. After initial assessment and comparisons of patterns of locum work in the two databases available from CPRD (CPRD GOLD and CPRD Aurum), we identified that in CPRD GOLD locum GPs are captured more accurately. Previous estimates110 suggest that the proportion of consultations accounted for by locums is more similar to the proportion of care that we identified in CPRD GOLD than CPRD Aurum. This may be attributed to the relatively new nature of CPRD Aurum and the use of a different clinical information system (i.e. EMIS) for practices that participate in CPRD Aurum. More details on the differences between CPRD GOLD and CPRD Aurum are provided in Appendix 7, Table 28.
We used two sets of analyses of consultation data from 1 April 2010 until 31 March 2022, in annual bins of financial years (1) for all UK countries, including England, Scotland, Wales and Northern Ireland (practice-level analyses), and (2) only for England for the second set of analyses (patient-level analyses). Although the database is representative of the UK in terms of age, gender and deprivation, it is only broadly geographically representative since it collects data from practices using the Vision clinical system, and clinical system usage is geographically clustered in the UK. 129 Consultation information was aggregated within each financial year, for each active patient (registered for at least 1 day during the respective year). Patients who had a recorded year of death before the beginning of the period of study were excluded from the analyses. Moreover, patients who had a consultation following their date of death as recorded within CPRD and patients whose record was accessed for administrative purposes were excluded from the analyses. Some well-established measures of prescribing safety were included based on validated indicators aimed at reducing rates of hazardous prescribing. 130
Practice-level analyses
For the first set of analyses, we identified and grouped consultations based on the variable ‘consultation type’ that were completed by GPs, including locum GPs, identified by the ‘staff role’ variable across all CPRD participating practices between 1 April 2010 and 31 March 2022. The complete list of codes used to identify GPs and consultations in CPRD GOLD is provided in Appendix 7, Tables 29 and 30, respectively. We aggregated consultation-level information into three consultation types by all GPs and GP locums, at the general practice level for the period 2010–21 (Appendix 7, Table 31). The consultation types were (1) all consultation types; (2) face-to-face consultations; and (3) telephone and online consultations. We also describe consultations by day of the week for locums and permanent GPs. We conducted additional data quality checks to identify the consistency of the appearance of locum staff role codes in the data across all practices and all years in Appendix 7, Table 32.
In CPRD GOLD, a large number of practices did not participate in every year of our analyses, and particularly the sample of English practices in CPRD GOLD reduced substantially over time (Table 19 and Appendix 7, Table 33). To evaluate the effects of changes in the composition of the database due to fewer practices from England participating in GOLD over time, we conducted sensitivity analyses with only those practices that contributed data across the entire study period from all UK countries. Due to the very low number in emergency, out-of-hours and home visit types of consultations, and the low reliability of data for these types of consultations, we decided to exclude them from the analyses.
| All consultations | F2F consultations | Telephone and online consultations | Total patients | Total practices | ||||
|---|---|---|---|---|---|---|---|---|
| Year | GPs | Locum | GPs | Locum | GPs | Locum | ||
| 2010 | 20,500,102 | 2,159,880 | 18,732,124 | 2,031,389 | 1,773,391 | 128,721 | 4,184,690 | 870 |
| 2011 | 20,742,566 | 2,292,757 | 18,848,827 | 2,148,948 | 1,899,022 | 144,025 | 4,241,700 | 876 |
| 2012 | 21,178,931 | 2,369,278 | 19,080,750 | 2,201,442 | 2,102,590 | 168,024 | 4,245,588 | 854 |
| 2013 | 20,651,224 | 2,241,345 | 18,436,232 | 2,061,195 | 2,219,187 | 180,292 | 4,127,214 | 836 |
| 2014 | 19,136,449 | 2,154,292 | 16,964,052 | 1,969,834 | 2,176,674 | 184,698 | 3,836,633 | 789 |
| 2015 | 16,578,552 | 1,917,670 | 14,682,494 | 1,757,568 | 1,900,072 | 160,299 | 3,392,982 | 716 |
| 2016 | 14,374,307 | 1,665,777 | 12,769,293 | 1,546,654 | 1,607,684 | 119,227 | 2,895,826 | 621 |
| 2017 | 12,798,872 | 1,482,806 | 11,391,487 | 1,377,101 | 1,409,998 | 105,760 | 2,603,629 | 559 |
| 2018 | 11,891,748 | 1,407,405 | 10,619,499 | 1,310,867 | 1,273,273 | 96,605 | 2,443,610 | 524 |
| 2019 | 10,986,944 | 1,311,192 | 9,719,650 | 1,214,468 | 1,268,258 | 96,822 | 2,290,261 | 500 |
| 2020 | 8,931,093 | 1,002,210 | 5,910,979 | 676,680 | 3,024,265 | 326,557 | 1,789,703 | 461 |
| 2021 | 6,498,899 | 756,969 | 4,421,649 | 527,265 | 2,078,320 | 230,096 | 1,551,491 | 422 |
Patient-level analyses
For the second set of analyses, we conducted analyses of all CPRD GOLD GP consultations of non-temporary patients at 407 general practices in England between 1 April 2010 and 31 March 2022. We restricted our sample to include only practices in England, as data on the IMD as well as some key patient outcome, such as emergency admissions and A&E visits, were only available for patients located in England. Within each financial year, we randomly selected one consultation for each patient, and aligned all the outcomes and covariates to that specific event date for the patient. This allowed us to give equal weights to patients and limit the potential for confounding introduced by patients with very poor health who may be visiting numerous times within a year. Our exposure was a binary variable indicating whether the consultation was by a permanent GP or a GP locum. We were able to identify permanent GPs and GP locums through the staff role field which is available for every consultation. The exposure was aligned to patient outcomes using a unique consultation ID.
In terms of the model covariates, we used Read codes to identify the presence of comorbidities by using relevant keywords and codes, across all clinical diagnoses, medication prescribed, vaccination history, diagnostic testing and clinical referrals for each patient in 2010, which was our baseline year. This approach was used to define the validated Cambridge Multimorbidity Score131 for each patient in our cohort. This score includes numerous conditions to calculate an index with the application of appropriate weights for each condition (cancer, dementia, chronic obstructive pulmonary disease, alcohol problems, epilepsy, painful condition, constipation, heart failure, psychosis/bipolar disorder, anxiety/depression, diabetes, atrial fibrillation, stroke and trans-ischaemic attack, chronic kidney disease, coronary heart disease, connective tissue disorders, hypertension, irritable bowel syndrome, hearing loss, asthma).
Additional information on patient age, gender, years registered with the practice, practice list size, patient urban/rural location and region was obtained. We employed multilevel mixed-effects logistic regression models to quantify the association between the exposure of interest (locum/permanent GP) and the outcomes of interest, controlling for all available covariates. Analyses were conducted at the patient level, accounting for the nested structure of the data: patients within general practices, within regions. We included random effects for practices and fixed effects for regions. We also described all outcomes and key covariates of interest at the patient-level over time.
Outcome measures for patient-level analyses
Practice revisit within 7 days
Our primary outcome was general practice revisit within 7 days of a consultation event with a permanent or locum GP. We identified consultation events within CPRD for each patient in each year, and we calculated the time in days between two consecutive consultation events. We generated a binary variable indicating whether the patient had a follow-up consultation within 7 days.
Antibiotic prescriptions
Antibiotic prescriptions were classified using the British National Formulary (BNF) sections. We identified all consultation events with an antibiotic prescription completed by a locum or permanent GP and created a binary variable indicating whether an antibiotic was prescribed during the consultation.
Opioid prescriptions
Opioid prescriptions were classified using the BNF sections. We identified all consultation events with an opioid prescription completed by a locum or permanent GP and created a binary variable indicating whether an opioid was prescribed during the consultation. More details on the specific drugs used to classify opioids are provided in Appendix 7 (see Table 34).
Hypnotics prescriptions
Opioid prescriptions were classified using the BNF sections. Benzodiazepines and z-drugs were used in the analyses. We identified all consultation events with a hypnotic prescription completed by a locum or permanent GP and created a binary variable indicating whether a hypnotic was prescribed during the consultation. More details on the specific drugs used to classify hypnotics are provided in Appendix 7 (see Table 34).
Accident and emergency visits
Accident and emergency visits were measured using the HES A&E data. We identified all A&E visits within 7 days of a consultation event completed by a locum or permanent GP and created binary variables indicating whether an A&E visit was recorded on the same day or within 1–7 days of the consultation event.
Emergency admissions
Emergency admissions were identified in HES Admitted Patient Care by selecting codes relevant to emergency admissions. We identified all emergency admissions within 7 days of a consultation event completed by a locum or permanent GP and created binary variables indicating whether an emergency admission was recorded on the same day or within 1–7 days of the consultation event. More details on the classification of emergency admissions are provided in Appendix 7 (see Table 34).
Ambulatory Care Sensitive Conditions admissions
Classification of Ambulatory Care Sensitive Condition (ACSC) hospital admissions for the study used the International Classification of Diseases, 10th edition (ICD-10) and included all hospital admissions with primary diagnosis related to one of the nine ACSCs that are incentivised in the UK’s QOF. The nine QOF incentivised conditions included: asthma, coronary heart disease, chronic obstructive pulmonary disease, diabetes epilepsy, heart failure, hypertension and stroke. We identified all ACSC admissions following a consultation event completed by a locum or permanent GP and created binary variables indicating whether an ACSC was recorded on the same day or within 1–7 days of the consultation.
Tests
We identified all consultation events with a test ordered by a locum or permanent GP and created a binary variable indicating whether a test was ordered during the consultation event.
Referrals
We identified all consultation events with a referral of any type completed by a locum or permanent GP and created a binary variable indicating whether a referral was ordered during the consultation event.
Prescribing safety indicators
We adapted 10 indicators of prescribing safety developed for PINCER, a pharmacist-led intervention to improve prescribing safety by identifying patients at risk of potentially hazardous prescribing events. 132,133 These indicators are associated with potentially harmful outcomes such as gastrointestinal (GI) bleeding, asthma, heart failure and stroke.
Results
Practice-level analyses
The number of practices across all UK countries who participated in CPRD GOLD varied from 870 in 2010, to 716 in 2015, to 422 in 2021. Over time, data were available for 914 distinct general practices in the UK, of which 511 practices were located in England and its regions, 234 practices were located in Scotland, 127 were located in Wales and 42 were located in Northern Ireland. Of these, only 381 practices contributed data throughout the whole of the study period, of which only 42 were located in England and these are reported in Table 33. Our final cohort consisted of 8,133,324 patients with 184,269,687 recorded consultations.
We provide descriptive statistics for the different types of consultations by type of GP (permanent or locum) and over time in Table 20. We calculated the proportion of consultations done by locums in 2019, as a proportion of all consultations done by all GPs, in every practice in every year and provide descriptive statistics in Table 21. Our reference year was 2019, as that was the year before the onset of the COVID-19 pandemic which brought substantial disruptions in the delivery of NHS services and is generally considered a period of instability within the NHS. This process was followed for all types of consultations. Descriptive statistics for the different consultation types using only practices that contributed data throughout the period of study are provided in Appendix 7 (see Table 35).
| Percentiles (%) | All locum consultations (%) | F2F locum consultations (%) | Telephone and online locum consultations (%) |
|---|---|---|---|
| 5 | 0 | 0 | 0 |
| 25 | 1.3 | 1.3 | 0 |
| 50 | 6.7 | 7 | 1.7 |
| 75 | 17.7 | 18.4 | 15 |
| 95 | 56.6 | 58.3 | 98.6 |
| Mean (SD) | 13.8 (19.1) | 14.3 (19.5) | 15.1 (27.3) |
| Number of patients at risk (%) (N = 13,696,455 consultation events) |
||
|---|---|---|
| Permanent GPs | Locums | |
| Practice revisits within 7 days | 1,008,934 (8.18) |
94,204 (6.89) |
| Antibiotic prescriptions | 1,114,621 (9.04) |
144,724 (10.58) |
| Strong opioid prescriptions | 278,819 (2.26) |
31,535 (2.31) |
| Hypnotics prescription | 105,928 (0.86) |
10,488 (0.77) |
| Same day emergency admissions | 20,048 (0.16) |
2120 (0.16) |
| Same day A&E visits | 37,861 (0.31) |
4723 (0.35) |
| Same day ACSC admissions | 19,084 (0.15) |
2,030 (0.15) |
| Emergency admissions within 1–7 days | 18,217 (0.15) |
1929 (0.14) |
| A&E visits within 1–7 days | 48,545 (0.39) |
6132 (0.45) |
| ACSC admissions within 1–7 days | 18,876 (0.15) |
1989 (0.15) |
| Referrals | 534,873 (4.34) |
53,758 (3.93) |
| Tests | 395,795 (3.21) |
37,770 (2.76) |
| Means and SDs for patient and practice characteristics (N = 13,696,455 consultation events) | ||
| Patient characteristics | ||
| Cambridge multimorbidity score | 0.46 (0.89) | 0.37 (0.79) |
| Age | 46 (23.7) | 42 (23.1) |
| Female | 0.55 (0.50) | 0.56 (0.50) |
| Years registered with the practice | 16.4 (13.5) | 14.8 (12.6) |
| Deprivation quintile | 2.79 (1.4) | 2.97 (1.41) |
| Practice characteristics | ||
| Rurality | 1.16 (0.37) | 1.13 (0.33) |
| List size | 7020 (3493) | 6712 (3604) |
Our practice-level analyses were descriptive and violin plots to depict the variation in the proportion of all, face-to-face (F2F) and telephone/online locum consultations over time are presented in Figures 14–16. Violin plots can be interpreted as box plots (including the median as a marker and a box indicating the IQR), overlaid with the density of the distribution for enhanced visualisation. The median rate of locum consultations as a proportion of all GP consultations varied from 5.5% in 2010 to 6.7% in 2021. For F2F consultations, the median rate varied from 5.9% in 2010 to 6% in 2021. Variation was more pronounced for telephone consultations, where the median rate varied from 0.7% in 2010 to 6.6% in 2021. The results from the sensitivity analyses using only practices that contributed to CPRD throughout the study period are provided in Appendix 7 (see Figures 44–46).
FIGURE 14.
All locum consultations as a proportion of all GP consultations.
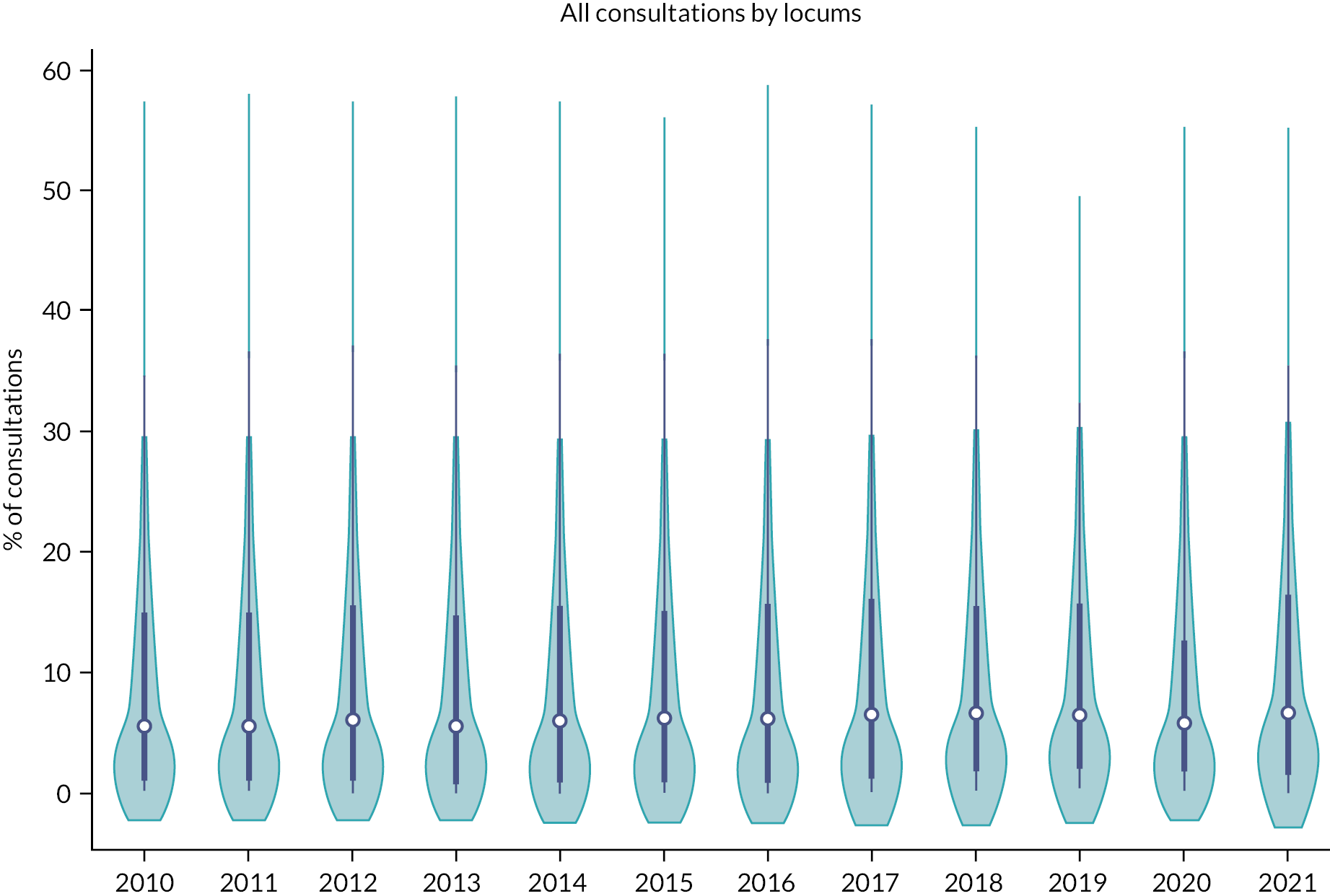
FIGURE 15.
Locum F2F consultations as a proportion of all GP F2F consultations.
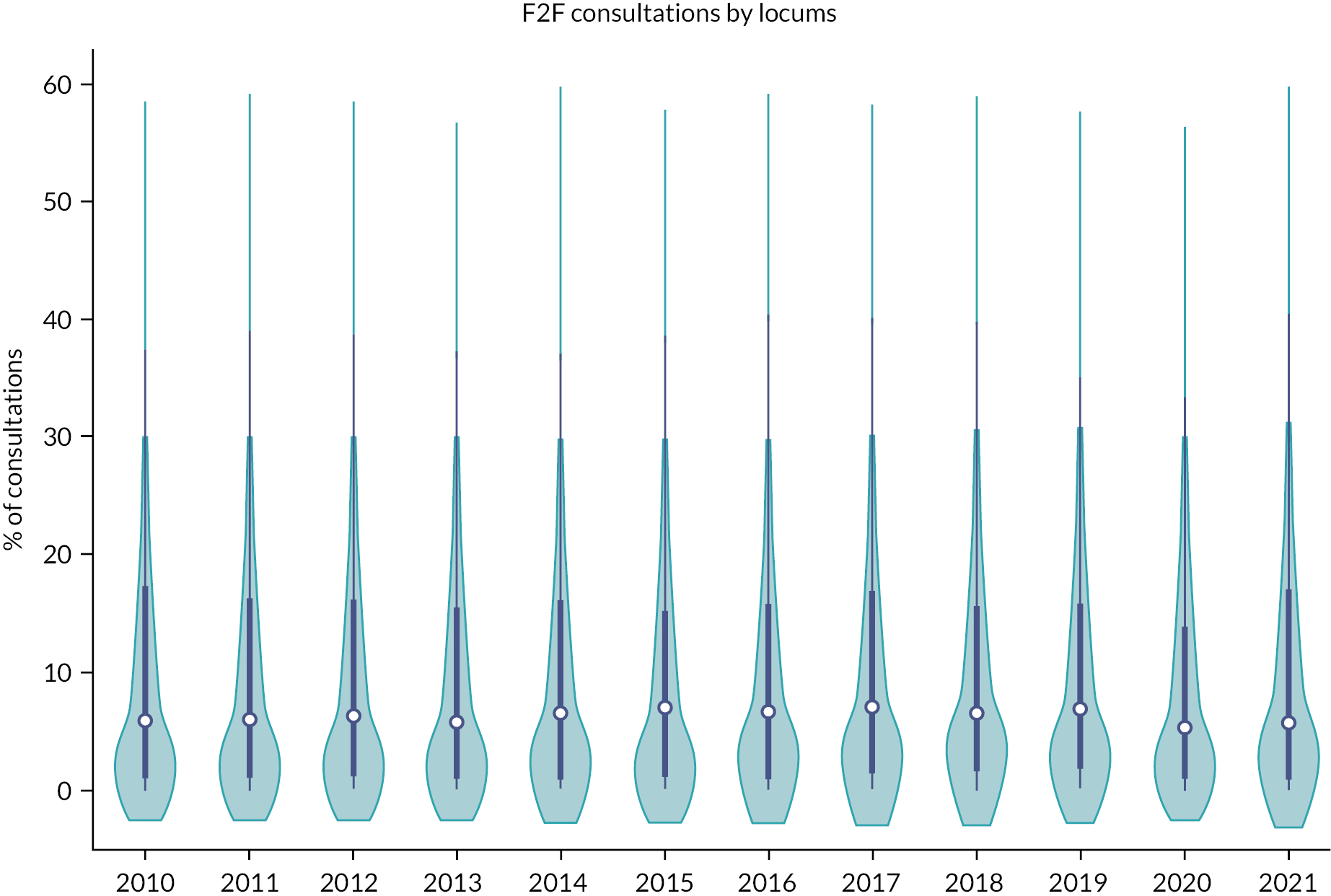
FIGURE 16.
Locum telephone and online consultations as a proportion of all GP telephone and online consultations.
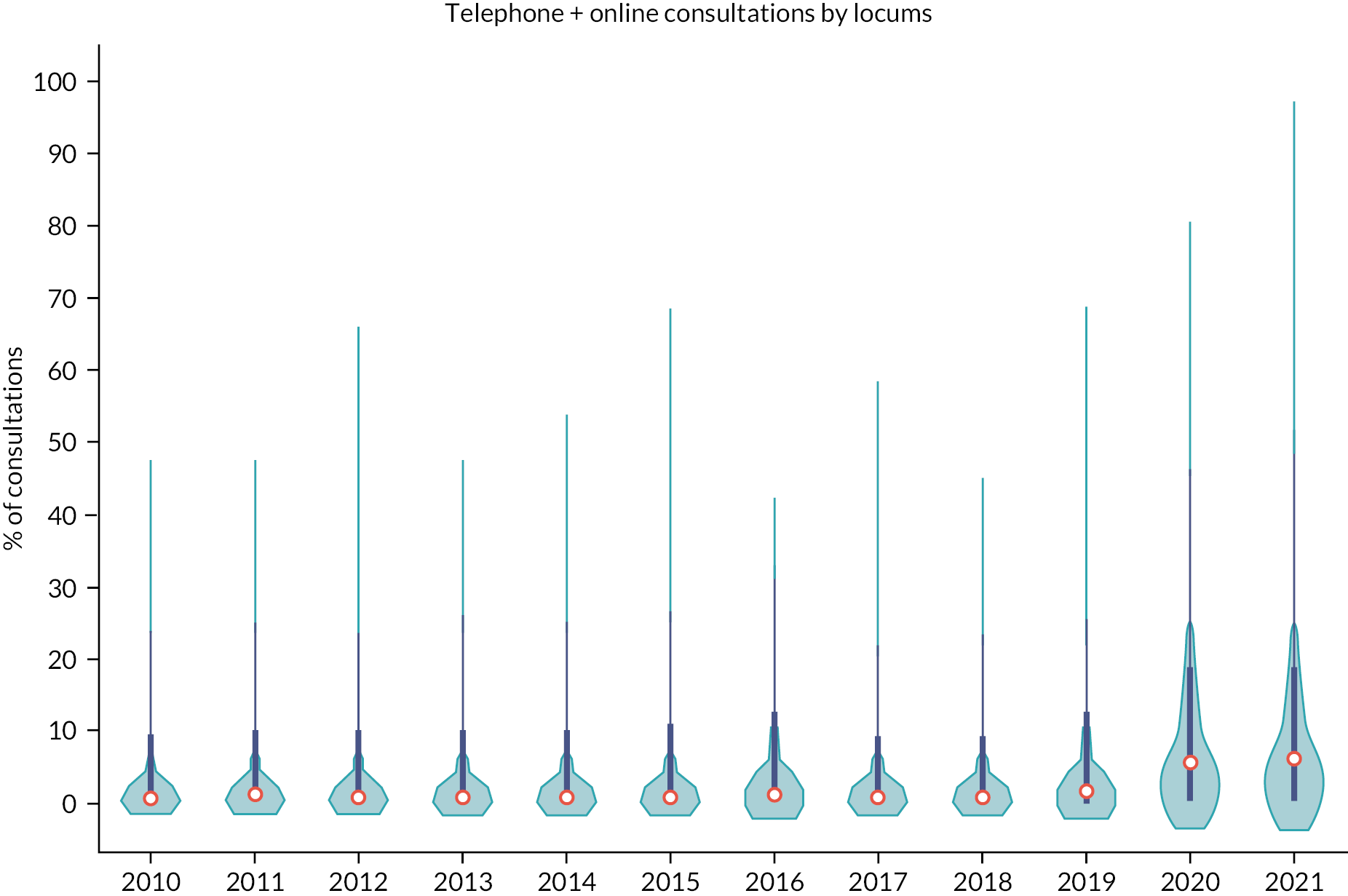
Regional variation in all, F2F, and telephone/online locum consultations aggregated for the period 2010–21 for all UK countries as well as the English regions is depicted in Figures 17–19. Practices in Wales, Scotland and the South West of England had the largest proportion of care provided by locums and practices in the Midlands, East of England and the North East had the lowest. These findings were similar for F2F consultations but for telephone consultations, practices in the Northern Ireland, Wales and Scotland had by far the largest proportion of care provided by locums. The regional variation results from the sensitivity analysis using only practices that contributed data throughout the period of study are presented in Appendix 7 (see Figures 47–49).
FIGURE 17.
Regional variation in the proportion of locum consultations in 2010–21.
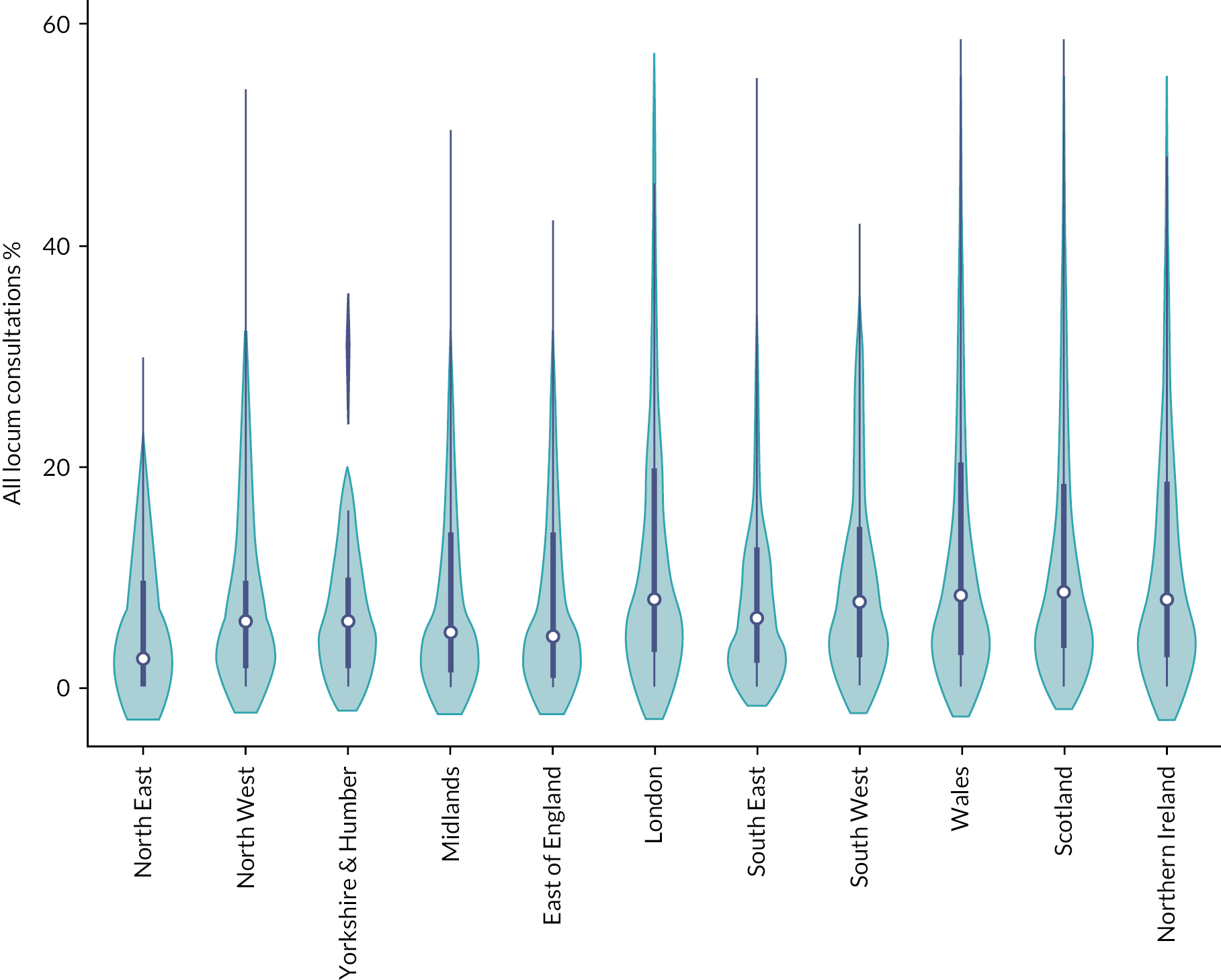
FIGURE 18.
Regional variation in the proportion of F2F locum consultations in 2010–21.
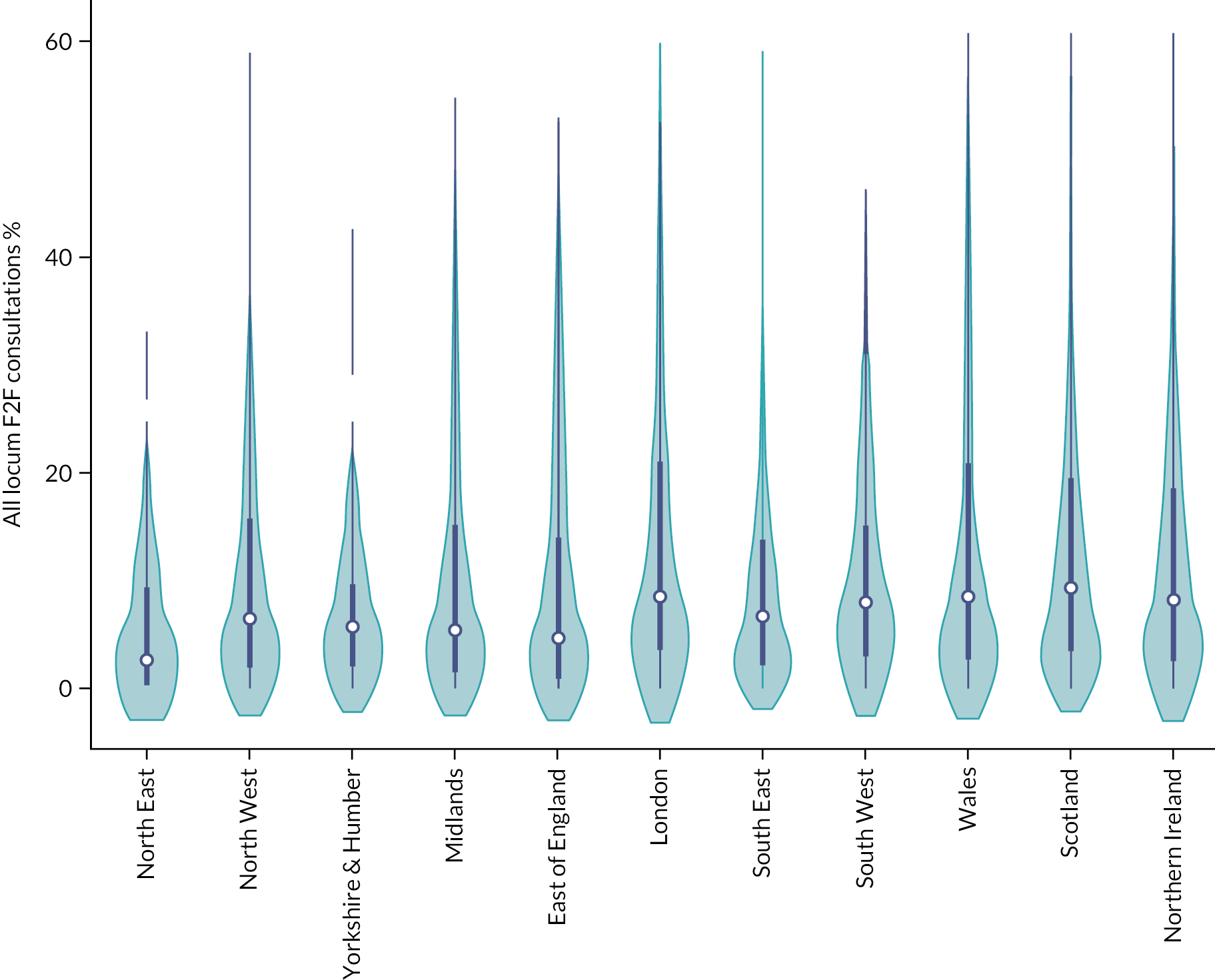
FIGURE 19.
Regional variation in the proportion of telephone and online locum consultations in 2010–21.
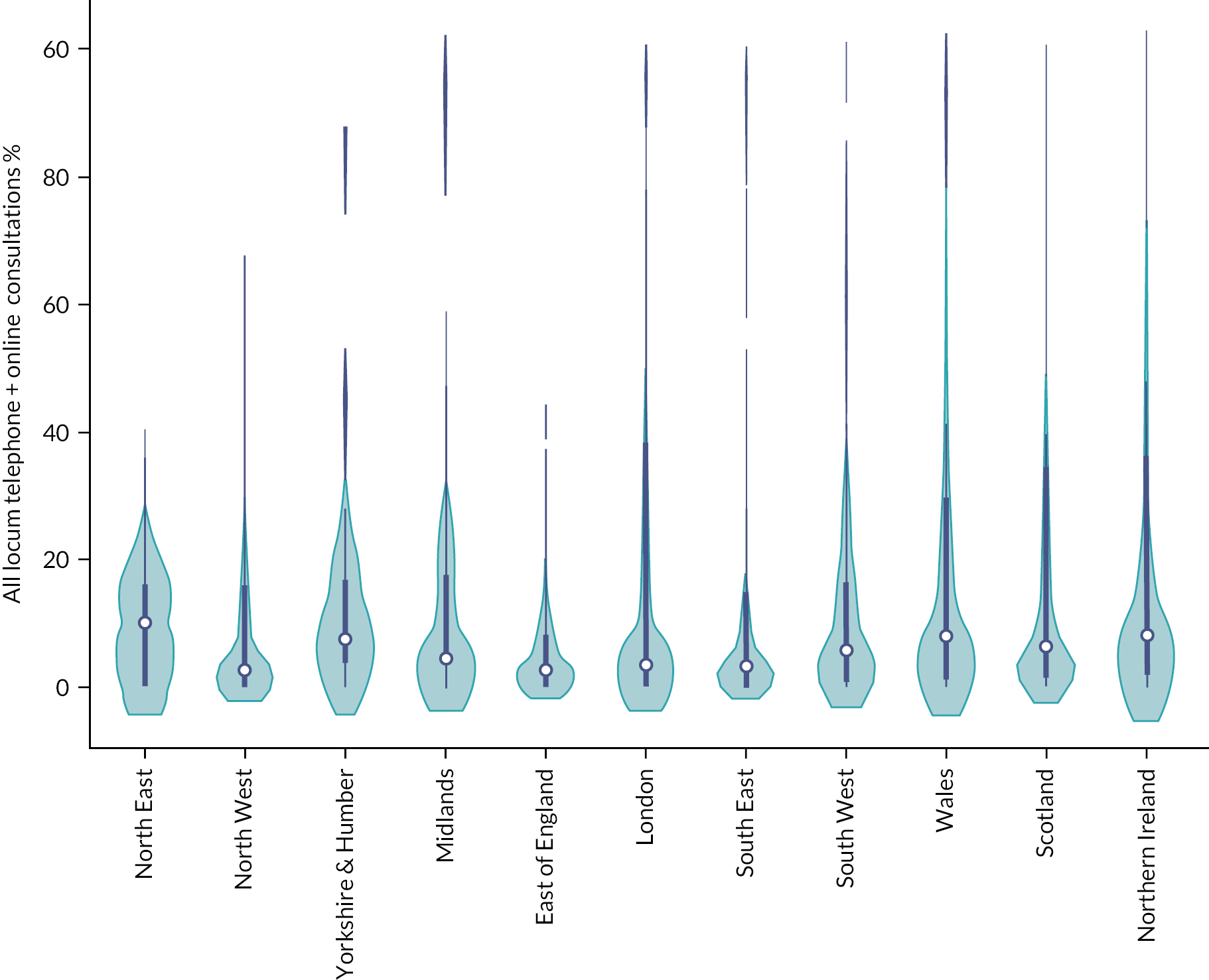
In Figure 20, we show the total number of consultations completed by all GPs and locums by day of week aggregated over 2010–21, and in Figure 21, we show the mean proportion of locum consultations by day of week, over 2010–21. Locum GPs appeared to do more work during the week where they provided on average 15% of total care. The proportion of care provided by locums during the weekend was 14%. The results from the sensitivity analysis using only practices that contributed data throughout the period of study are presented in Appendix 7 (see Figures 50 and 51).
FIGURE 20.
Total consultation volume by GP type and day of week, aggregated over 2010–21.
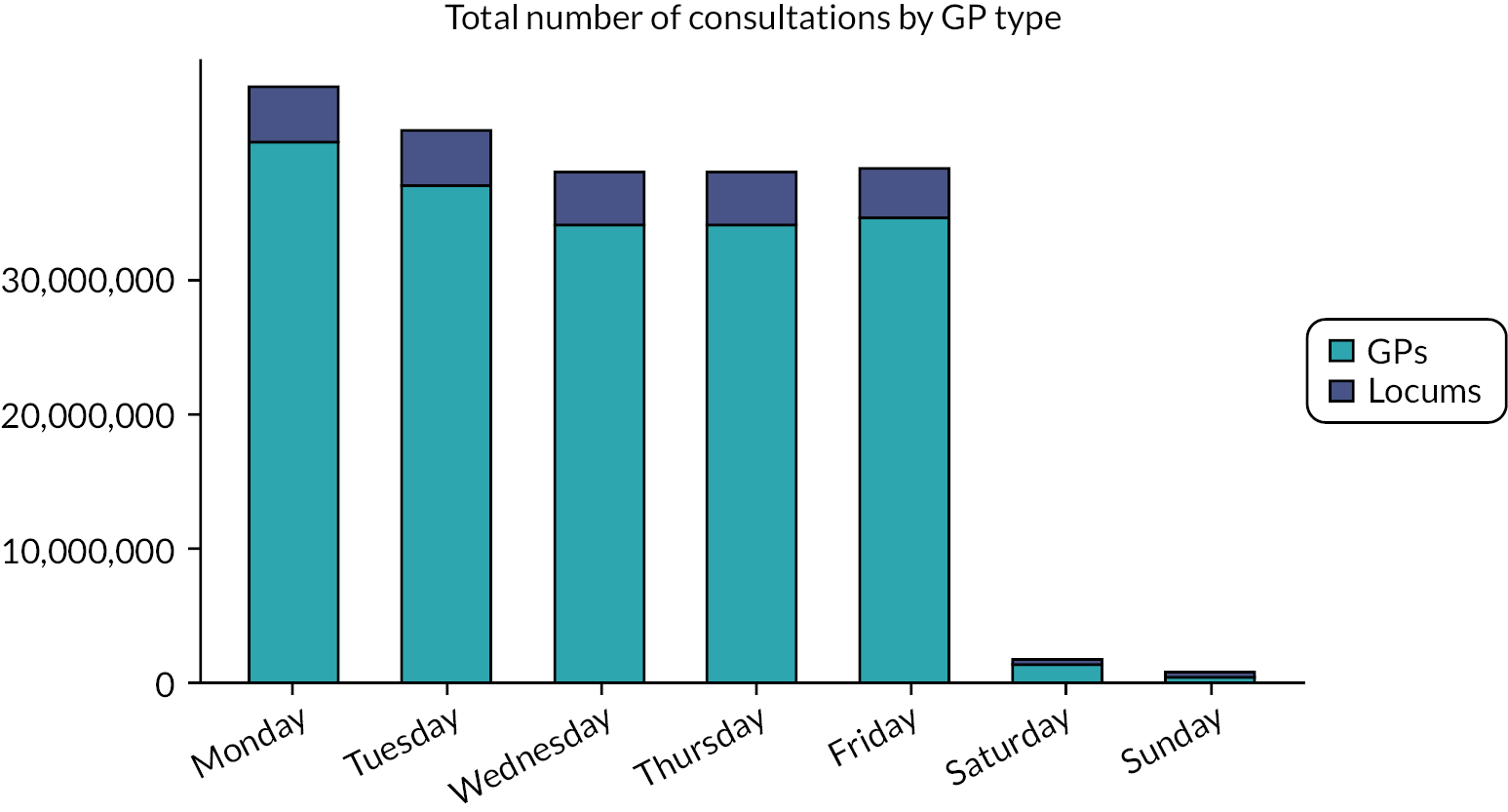
FIGURE 21.
Mean proportion of GP locum consultation by day of week, over 2010–21. Note: Bar labels show the average number of GP consultations done in each day across 870 UK practices.
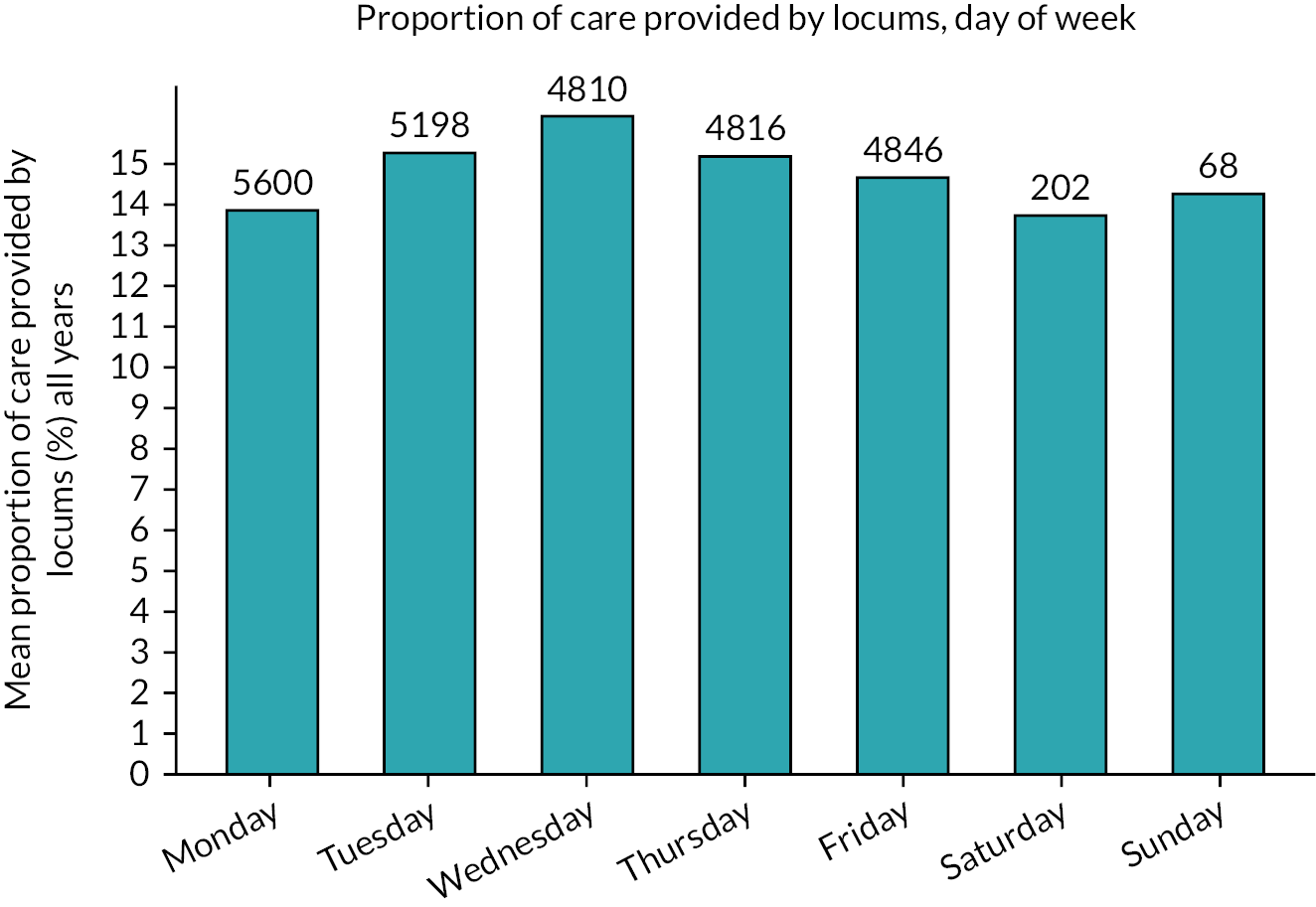
Patient-level analyses
The number of practices in England participating in CPRD GOLD varied from 487 in 2010, to 228 in 2015, to 42 in 2021. Of these, only 42 practices contributed data throughout the whole of the study period. Our final cohort consisted of 3,591,367 patients with 13,696,455 recorded consultations between 407 practices across all years. For the second set of models, our cohort consisted of 547,146 patients with 7,623,205 recorded consultations, which varied by indicator and included patients from 407 practices across all years. We provide descriptive statistics for the outcome and some important practice and patient characteristics in Table 22. In Table 23, we summarise the numerators and denominators that allowed us to calculate the proportion of consultations that were exposed to potentially hazardous prescribing for each indicator. The numerator is the number of consultations that were exposed to each type of potentially hazardous prescribing, and the denominator is the number of consultations of patients at risk of exposure to the hazardous prescribing indicator.
| Number of consultations at risk for potentially hazardous prescribing (N = 7,623,305 consultation events) |
NP Exposed to potentially hazardous prescribing, Permanent GP Numerator (% of denominator) |
DP At risk of potentially hazardous prescribing, Permanent GP Denominator |
NL Exposed to potentially hazardous prescribing, Locum GP Numerator (% of denominator) |
DL At risk of potentially hazardous prescribing, Locum GP Denominator |
|---|---|---|---|---|
| Potential harm: GI bleed | ||||
| Prescription of an oral non-steroidal anti-inflammatory drug (NSAID), without co-prescription of an ulcer-healing drug, to a patient aged ≥ 65 years (Indicator A) (N = 454,929) |
237,867 (56.5) | 420,760 | 19,926 (58.3) | 34,169 |
| Prescription of an oral NSAID, without co-prescription of an ulcer-healing drug, to a patient with a history of peptic ulceration (Indicator B) (N = 2907) |
1376 (52.6) | 2617 | 171 (59) | 290 |
| Prescription of an antiplatelet drug without co-prescription of an ulcer-healing drug, to a patient with a history of peptic ulceration (Indicator C) (N = 3537) |
765 (23.1) | 3309 | 57 (27.4) | 228 |
| Prescription of warfarin or direct oral anticoagulant (DOAC) in combination with an oral NSAID (Indicator D) (N = 222,986) |
4567 (2.2) | 207,655 | 308 (2) | 15,331 |
| Prescription of warfarin or DOAC and an antiplatelet drug in combination without co-prescription of an ulcer-healing drug (Indicator E) (N = 35,421) |
15,856 (47.7) | 33,260 | 976 (45.2) | 2161 |
| Prescription of aspirin in combination with another antiplatelet drug (without co-prescription of an ulcer-healing drug) (Indicator F) (N = 265,499) |
124,950 (50.2) | 249,148 | 8328 (51) | 16,351 |
| Potential harm: Exacerbation of asthma | ||||
| Prescription of a non-selective beta-blocker to a patient with asthma (Indicator G) (N = 163,368) |
11,183 (7.4) | 150,611 | 1165 (9.1) | 12,757 |
| Prescription of a long-acting beta-2 agonist inhaler (excluding combination products with inhaled corticosteroid) to a patient with asthma who is not also prescribed an inhaled corticosteroid (Indicator H) (N = 5,917,201) |
50,239 (0.09) | 5,407,846 | 3293 (0.06) | 509,355 |
| Potential harm: Heart failure | ||||
| Prescription of an oral NSAID to a patient with heart failure (Indicator I) (N = 551,110) |
2610 (0.05) | 551,110 | 195 (0.003) | 551,110 |
| Potential harm: Stroke | ||||
| Prescription of antipsychotics for > 6 weeks in a patient aged ≥ 65 years with dementia but not psychosis (Indicator J) (N = 6347) |
5601 (93.8) | 5972 | 335 (89.3) | 375 |
| Effects of locum consultations on patient outcomes | |
|---|---|
| Practice revisits | 0.88 (0.88 to 0.89), < 0.001 (0.003) |
| Antibiotic prescriptions | 1.21 (1.21 to 1.22), < 0.001 (0.004) |
| Strong opioid prescriptions | 1.08 (1.06 to 1.09), < 0.001 (0.007) |
| Hypnotic prescriptions | 0.97 (0.95 to 0.99), < 0.002 (0.010) |
| Emergency admissions, same day | 0.94 (0.89 to 1.02), < 0.127 (0.033) |
| Emergency admissions within 1–7 days | 1.00 (0.96 to 1.06), < 0.854 (0.026) |
| A&E visits, same day | 1.02 (0.98 to 1.07), < 0.331 (0.028) |
| A&E visits, within 1–7 days | 1.05 (1.02 to 1.08), < 0.001 (0.015) |
| ACSC admissions, same day | 1.00 (0.92 to 1.05), < 0.677 (0.033) |
| ACSC admissions, within 1–7 days | 0.99 (0.94 to 1.04), < 0.890 (0.025) |
| Referrals | 0.850 (0.84 to 0.86), < 0.001 (0.004) |
| Tests | 0.80 (0.80 to 0.81), < 0.001 (0.005) |
| Effects of locum consultations on potentially hazardous prescribing indicators | |
| Indicator A | 1.12 (1.08 to 1.16), <0.001 (0.020) |
| Indicator B | 1.44 (0.94 to 2.22), < 0.547 (0.331) |
| Indicator C | 1.35 (0.72 to 2.54), < 0.349 (0.434) |
| Indicator D | 0.77 (0.64 to 0.93), < 0.007 (0.074) |
| Indicator E | 1.07 (0.79 to 1.44), < 0.675 (0.163) |
| Indicator F | 0.99 (0.92 to 1.08), <0.852 (0.042) |
| Indicator G | 0.99 (0.91 to 1.09), < 0.894 (0.047) |
| Indicator H | 0.89 (0.85 to 0.93), < 0.001 (0.021) |
| Indicator I | 0.96 (0.81 to 1.13), < 0.613 (0.081) |
| Indicator J | 0.49 (0.19 to 1.23), < 0.128 (0.230) |
Clinical practice analyses
In the first set of models investigating various clinical practice indicators, we randomly selected one consultation event for each patient within each financial year, aligning all the patient outcomes and covariates to that specific event date. This allowed us to give equal weights to patients and limited the potential for confounding introduced by higher-need patients who may be visiting numerous times within a year. Our exposure was a binary variable indicating whether the consultation was by a permanent GP or a locum GP. We were able to identify permanent GPs and locum GP through the staff role field which is available for every consultation. This approach was used for practice revisits; prescribing of antibiotics, strong opioids and hypnotics; tests and referrals; and hospital outcomes.
Prescribing safety analyses
In the second set of models investigating the PINCER prescribing safety indicators, for each indicator, we identified all consultation events with patients who could be exposed to potentially hazardous prescribing, because of a specific diagnosis or prescription on the day of the consultation (i.e. index event). These events were split into consultations by locum or permanent GPs. Second, for each index consultation event, we looked at consultation events during a pre-specified time window (which varied across indicators; Appendix 7, Table 36) leading up to the index event, to identify pre-existing prescriptions or conditions that would trigger a potentially hazardous prescribing outcome when combined with the index event. For each index consultation event, a binary variable indicated whether potentially hazardous prescribing was triggered. This allowed us to operationalise rates of potentially hazardous prescribing events for both locum and permanent GPs. Our exposure was again a binary variable indicating whether the consultation involved a permanent GP or a locum GP and we aligned patient covariates to the index consultation event using unique patient IDs.
For example, for indicator A we identified consultations for patients who were over 65 years, at which they were prescribed a NSAID. We then identified those patients who were not also prescribed the recommended proton-pump inhibitor (PPI) or H2 receptor antagonist at the consultation or in the preceding 3 months. The operational definitions for the PINCER prescribing safety indicators are provided in Appendix 7, Table 36.
Our regression models in Table 23 show that a consultation with a locum was 12% less likely to lead to a practice revisit within 7 days [odds ratio (OR) = 0.88, 95% CI 0.87 to 0.88]. A consultation with a locum was 22% more likely to involve a prescription for an antibiotic (OR = 1.22, 95% CI 1.21 to 1.22), 8% more likely to involve a prescription for an opioid (OR = 1.08, 95% CI 1.06 to 1.09) and 4% less likely to involve a prescription for a hypnotic (OR = 0.96, 95% CI 0.94 to 0.98). In terms of hospital-related outcomes, a consultation with a locum was 4% more likely to be followed by an A&E visit on the same day (OR = 1.04, 95% CI 1.01 to 1.08) and 5% more likely to be followed by an A&E visit between the 1st and the 7th day (OR = 1.05, 95% CI 1.02 to 1.08), but there was no impact on emergency admissions or ACSC emergency admissions. Consultations with locums were also 15% less likely to involve a referral (OR = 0.85, 95% CI 0.84 to 0.86) and 19% less likely to involve a test being ordered (OR = 0.81, 95% CI 0.80 to 0.82).
When comparing prescribing safety indicators for permanent and locum GPs, a consultation with a locum GP was 11.2% (OR = 1.12, 95% CI 1.08 to 1.16) more likely to involve the prescription of an oral NSAID, without co-prescription of an ulcer-healing drug, to a patient aged ≥ 65 years. But a consultation with a locum GP was 22.8% (OR = 0.77, 95% CI 0.64 to 0.93) less likely to involve the prescription of warfarin or a direct oral anticoagulant in combination with an oral NSAID, and 11.2% (OR = 0.89, 95% CI 0.85 to 0.93) less likely to involve the prescription of a long-acting beta-2 antagonist inhaler to a patient with asthma who is not also prescribed an inhaled corticosteroid. We did not find any significant differences between permanent and locum GPs across all other prescribing safety indicators.
We plotted the effects and the CIs of locum consultations on performance outcomes in Figure 22 and on prescribing safety outcomes in Figure 23 which enable comparisons across outcomes.
FIGURE 22.
Coefficient plot for locum consultations across all outcomes. Note: Results are expressed as OR and corresponding CIs. When the corresponding CIs cross the dashed vertical line, coefficients are not statistically significant.
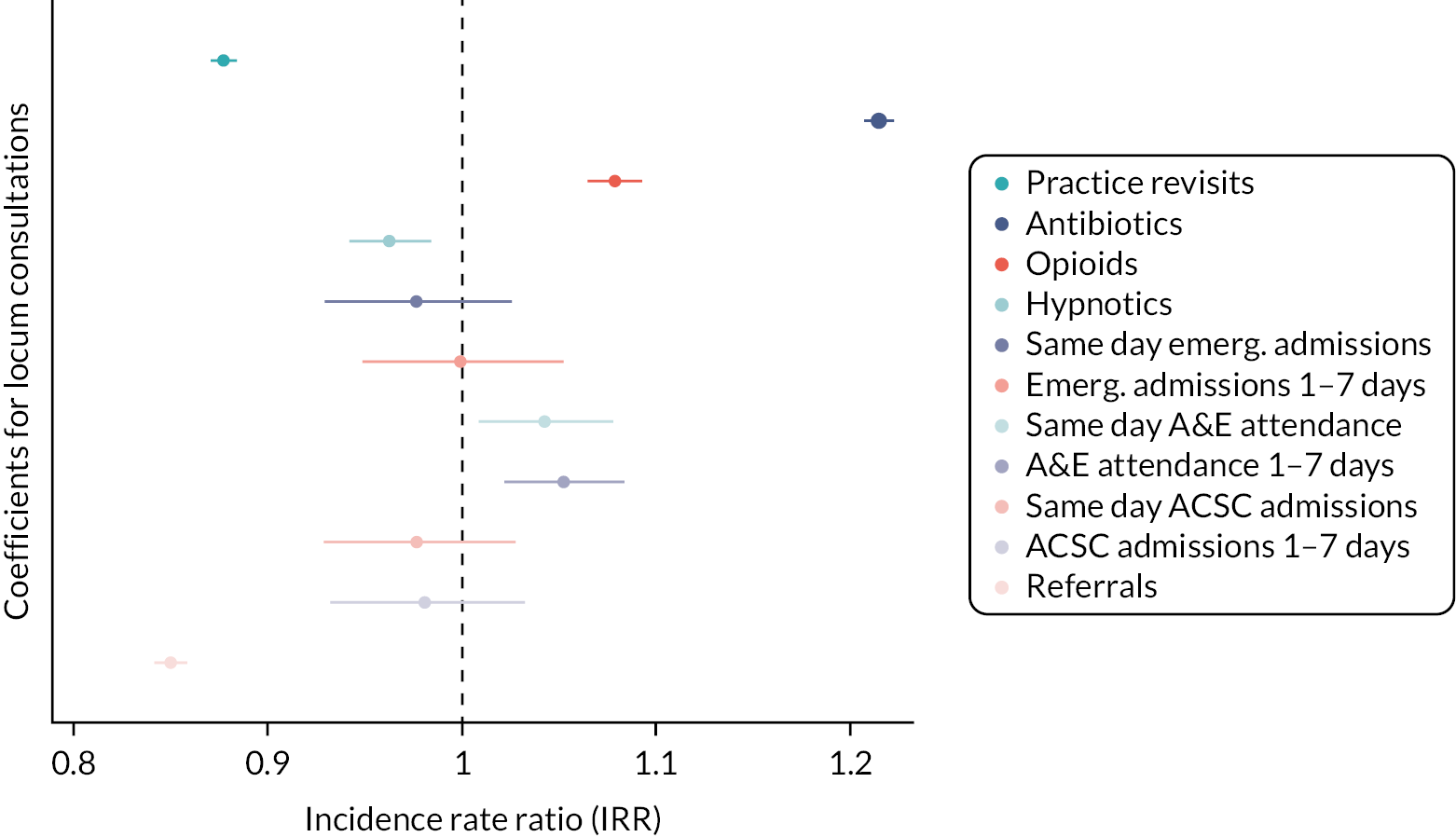
FIGURE 23.
Coefficient plot for locum consultations across all prescribing safety outcomes. Note: Results are expressed as OR and corresponding CIs. When the corresponding CIs cross the dashed vertical line, coefficients are not statistically significant.
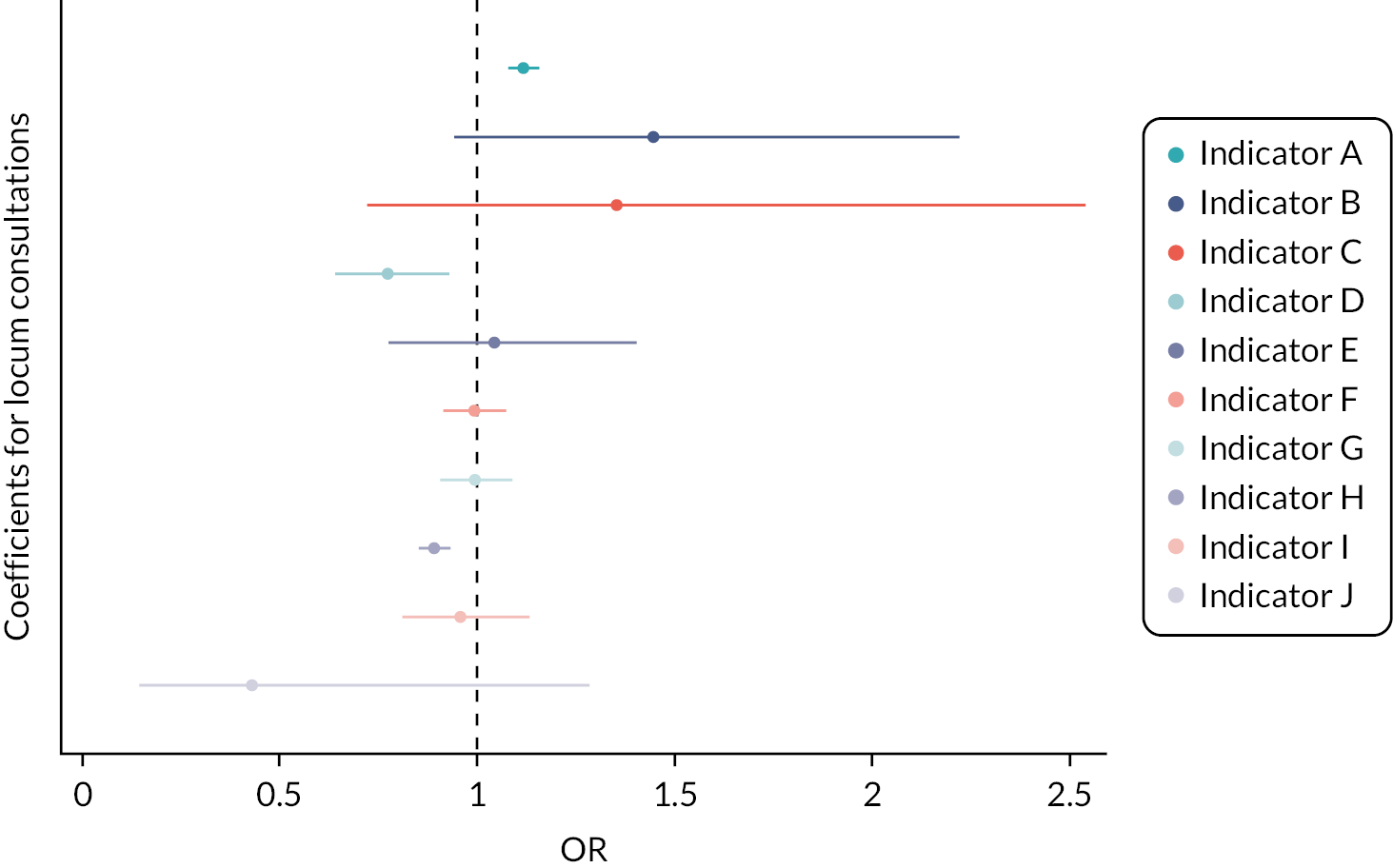
The full output from regressions in Table 23 is presented in Appendix 7, Tables 37 A–C and 38 A and B. We find that patients with increased multimorbidity had higher odds for a practice revisit within 7 days (OR = 1.20, 95% CI 1.19 to 1.20), a same day emergency admission (OR = 1.35, 95% CI 1.36 to 1.37), an emergency admission within 1–7 days (OR = 1.37, 95% CI 1.35 to 1.39). Patients with high multimorbidity also had higher odds of a same day A&E visit (OR = 1.19, 95% CI 1.17 to 1.20), an A&E visit within 1–7 days (OR = 1.19, 95% CI 1.18 to 1.20), a same day ACSC admission (OR = 1.34, 95% CI 1.32 to 1.36) and an ACSC admission within 1–7 days (OR = 1.38, 95% CI 1.36 to 1.39). The odds of an increase in the outcome reduced with deprivation, with the largest difference for opioid prescriptions, hypnotic prescriptions and emergency admissions observed between the 4th and the 5th quintile of deprivation. As deprivation reduced, we also saw an increase in the likelihood of practice revisits, A&E visits, ACSC admissions and tests, with the largest differences observed between the 3rd and the 4th quintile. Higher odds for antibiotics and referrals were observed with increased deprivation.
In Appendix 7, Figure 52, we show the mean and 95% CIs for all non-hospital outcomes (practice revisits, antibiotic prescriptions, opioid prescriptions, hypnotic prescriptions, referrals and tests) at the practice level by locum and permanent GPs in 2010–21. Over time, we observed small variability for practice revisits, hypnotics, referrals and tests; however, in 2020 there were sharp increases for practice revisits and a sharp decline for referrals, hypnotics and tests. We also observed a steady decline in the prescription of antibiotics and opioids over time. Differences between locums and permanent GPs were present for most outcomes and most noticeable for practice revisits and antibiotic prescriptions. In Appendix 7, Figure 53, we show the mean and 95% CIs for all hospital outcomes at the practice level by GP type over 2010–21. Overall, the six outcomes followed a modest increase over the study period and the differences between locums and permanent GPs were minimal. We repeated the analyses of patient outcomes and prescribing safety indicators, excluding all consultations with GP retainers and GP registrars as their clinical practice and prescribing behaviour may differ from permanent GPs. Overall, the results from these analyses were very similar to our primary analyses.
Discussion
Summary
This study provides evidence on the extent of locum use in the UK primary care and evidence on the effects of locum working on patient outcomes for the period 2010–21. Our findings suggest that locum GPs provided around 10% of GP consultations (median = 6.7%, mean = 13.8%) and this figure remained relatively stable over time.
We observed moderate variability in the proportion of care provided by locum GPs across English regions and across the four UK countries. Locums appeared to do more consultations during weekdays compared with the weekend. In terms of the effects of GP consultations on patient outcomes, our primary outcome showed that patients were less likely to revisit their practice within 7 days following a consultation with a locum GP. For secondary outcomes, the largest effects were for antibiotics, referrals and tests, where locum GPs completed more antibiotic prescriptions, but completed fewer referrals and ordered fewer tests when compared with permanent GPs. On the PINCER prescribing safety indicators, again the results are mixed. On most indicators, there is no significant difference between locum and permanent GPs – and the differences we do observe on three indicators are not large and move in different directions. There certainly seems to be no basis to argue that locum GPs differ significantly from permanent GPs on these indicators.
Our findings provide useful insight on the extent of locum use in the UK primary care and have implications for the differences in the clinical practice and performance of locum doctors working in general practices in England.
Strengths and limitations
This is the largest longitudinal study of locum consultation rates in UK primary care. However, there are important limitations. First, any study of this nature is limited by the reliability and accuracy of the data in the patient’s electronic record. We are confident about the reliability of the recorded patient contact data and patient characteristics. However, less is known about the accuracy of the information on type of consultation, as primary care staff may be inclined to record F2F as the default option. If so, our data will have overestimated F2F consultations. 9 Second, we could not assess the recording of the staff role linked to each consultation. Practice managers may sometimes assign locum GPs a staff role value of a permanent GP. This may be more common with long-term locum GPs who tend to work in practices for prolonged periods. Third, CPRD collects data from practices using the Vision clinical information system and recording activity may differ for practices using other systems, although we would not expect that potential variation to affect our findings. Fourth, sex, age and years worked in practice are GP characteristics which are unavailable within CPRD, and we therefore could not control for these characteristics in our regression analyses. Fifth, our comparisons of the distribution of locum work during the week are limited by the complex working arrangements in general practice in the weekend. It may be that weekend work is the responsibility of a trust or consortium of GPs, which complicates comparisons of weekend working. Finally, CPRD GOLD is representative in terms of deprivation and population characteristics,125 collecting of data is available from a single clinical information system (Vision) and therefore contributing practices are not uniformly distributed across English regions, while its market share is in decline. 129 Thus, generalisability to every English region could not be achieved.
Interpretation of findings
The unique contribution of this study is the investigation of distribution and trends in the delivery of consultations by GP locums and the differences in patient outcomes when care is delivered by locums and permanent GPs. Our finding that the amount of care provided by locum GPs has been relatively stable over time confirms the finding in our previous study using NHS Digital data. 36 However, there are differences in the amount of care provided by locums between these two studies, which we attribute to CPRD measuring consultations and NHS Digital measuring FTE. We hypothesise that locums spend more of their time providing consultations than permanent GPs. Our qualitative work revealed that sometimes practice managers may record locums as permanent GPs, and some types of locum GPs, such as long-term locums, may be working long enough in a practice to be considered permanent members of staff. Therefore, the figure that we found in the analyses of NHS Digital data is likely underestimating the proportion of care provided by locum GPs.
In CPRD, recording is considered more accurate, as consultation events are central to how data are organised in the Vision computer system. However, in CPRD, it is not currently possible to identify a member of staff who has worked in multiple roles in a practice or in multiple roles across practices. It may be that salaried GPs are employed simultaneously as locum GPs in other practices and we would not be able to account for that as each member of staff has a staff ID which is unique to that practice. Despite these issues, our analyses can help with the understanding of the NHS workforce and can provide important information about the planning of the delivery of primary care services in the UK.
This work also provides evidence on differences in clinical practice and performance between locum doctors and permanent doctors which may have consequences for patient safety and quality of care. A consultation with a locum was less likely to lead to a practice revisit within 7 days. Locums were more likely to prescribe antibiotics and opioids, but less likely to order tests and referrals and prescribe hypnotics. A consultation with a locum was more likely to lead to an A&E attendance on the same day or within 1–7 days. Previous evidence suggests that the way locum doctors are recruited, employed and used by organisations may pose a higher risk of harm to patients, but our findings provided mixed results. In some areas, locum GPs performed worse and this may suggest that they need additional support from practices with improved induction and communication about practices’ approaches to prescribing and continuity of care. Recording of locum working across general practices should be improved and information should be linked across clinical systems and databases as this would help verify the findings of this chapter. Locum GPs face substantial challenges, with large variability between practices and areas, more acutely unwell and unfamiliar patients, limited communication, feedback and support and professional isolation. If local healthcare needs are to be met, locum GPs need sufficient resources for training and effective integration, which would be aligned with the aims set out in the NHS Long Term Plan. 45
Chapter 10 The use of locum doctors in National Health Service trusts in England: analysis of electronic patient records
Aims
In this chapter, we report on research intended to explore the use of locum doctors and their practice and performance in a NHS trust. Our original research proposal and protocol outlined how we aimed to undertake feasibility work by gaining access to EPR data from Salford Royal NHS Foundation Trust. This was to be used first, to identify locum and permanent doctors and compare their activity levels and, second, to compare these two groups in terms of patient quality and safety. In doing so, we would have comparable analysis for both primary care, from our CPRD work shown in Chapter 9, and secondary care.
However, despite having a previous working relationship with Salford Royal NHS Foundation Trust, having them represented on our Project Advisory Group and their NHS Digital Exemplar status, we encountered several significant challenges with this aspect of the proposal. These challenges meant we sought EPR data from elsewhere as an alternative (Bradford Teaching Hospitals NHS Foundation Trust). A number of the same challenges were found with the Bradford EPR, but access to some data was secured. However, ultimately due to these challenges, we were only able to undertake some much more limited feasibility work using Bradford EPR data.
In this chapter, we explain the processes followed, first with Salford Royal and then with Bradford, and we explain the data we were able to receive from the Bradford EPR. We then describe and present the analysis we performed using these data. The aim of this analysis is to first determine if locums can be identified, and then progress to comparing locums with permanent doctors.
Methods
Our engagement with Salford started with understanding more about the process for accessing their EPR and what data it contained. This began with contacting the Research and Innovation team, the Business Intelligence and Informatics team and the Data Science team. Alongside discussion about the EPR and its contents, we also engaged with the Salford Temporary Staffing Manager and IT Training Manager to learn more about the processes in place for when a locum doctor is employed, specifically how locums gain access to the EPR and how locums are identified within the EPR.
Through our engagement, we identified two main challenges to our research aims. Firstly, the Salford EPR was organised to meet the operational needs of the hospital and was not set up in a way that would facilitate its use for research. In particular, this meant that documentation and data dictionaries were either limited or did not exist, with the information needed to understand the data held within various team members at Salford. Alongside this, Salford did not have any EPR data within a Trusted Research Environment we could access, meaning EPR data would need to be transferred to the University of Manchester systems for analysis, which would require a protracted information governance process. Secondly, from the Temporary Staffing team we learnt that when locums are employed, they are given system login credentials which would identify them as locums. However, these credentials were also used for permanent staff who had forgotten their details and were also reused for different locums on a rotational basis. These issues meant there was not a robust way to identify locums in the EPR and access to the EPR was not possible. We therefore pursued an alternative source for EPR data.
Our engagement with Bradford Teaching Hospitals NHS Foundation Trust fared better and led to accessing an extract from their EPR, although some challenges remained. As with Salford, the Bradford EPR did not contain doctor identifiers which would distinguish between locums and permanent doctors. All doctors with EPR access are given unique identifiers which allow their activity to be tracked over time, but these identifiers are of the same type for all doctors. To identify locums would require linkage between staff records and the EPR, which Bradford were unable to perform. Access to some EPR data was granted via the Connected Yorkshire initiative and their online Trusted Research Environment. We used these EPR data to determine whether locums could be identified by their working patterns and how frequently they appear.
Data
Bradford electronic patient record
An extract of EPR data was obtained from Bradford Teaching Hospitals NHS Foundation Trust under a bespoke data-sharing agreement. The extract is from the Orders table, one of many tables which, when combined, form the full EPR. The data within the Orders table relate to 20 million electronic medication prescribing and administration orders processed for 221,312 patients between September 2017 and November 2021. For each order, we know when it was created and what it was for, that is, the medication, dose and administration method. We also have anonymised identifiers for the patient the order was for and the doctor who created it. However, doctor IDs did not distinguish between permanent or locum doctors. For our analysis, determining if locums can be identified by working patterns, the data were collapsed to count the number of patients seen and orders created by each doctor for each week between September 2017 and November 2021. In this case, a patient is counted as seen if an order is created for them.
Analysis
Descriptive analysis was performed on the collapsed Bradford EPR data. We plotted the mean number of patients seen and orders created per doctor for each week of data. We calculated the total number of patients seen and orders created per doctor over the entire period, and presented the distribution of doctor workload across these measures of activity.
To identify working patterns for doctors, we focus on a 52-week period from 24 September 2017 to 16 September 2018. This period was selected to avoid the impact of COVID-19 and also a change in how the EPR was implemented: see Appendix 8, Figure 54 describing the whole period.
We calculated the number of doctors (unique IDs) who created an order in each week of the data, as a measure of the size of the active workforce over time. We also calculated the number of active weeks for each doctor as a measure of their length of activity for the 52-week period.
As doctor IDs did not distinguish between permanent doctors and locums, we attempted to identify short-term locums as doctors who are active for 4 weeks or less during the 52-week period. We do not identify a doctor as locum if they are only active at the beginning or end of our period, as these may represent longer periods of activity which we do not observe. We compare these short-term locums to all other doctors on the average number of patients seen and orders created per active week.
Results
In Figure 24 we present the mean patients seen and orders created per active doctor per week for 52 weeks from 24 September 2017 to 16 September 2018. For example, in the week beginning 24 September 2017, doctors who were active created orders for a mean of 6.6 patients. For these figures, active doctors are those who saw at least one patient in a given week. The mean number of patients seen was 7.7 and the mean number of orders created was 86.
FIGURE 24.
Mean patients seen and orders created per active doctor per week.
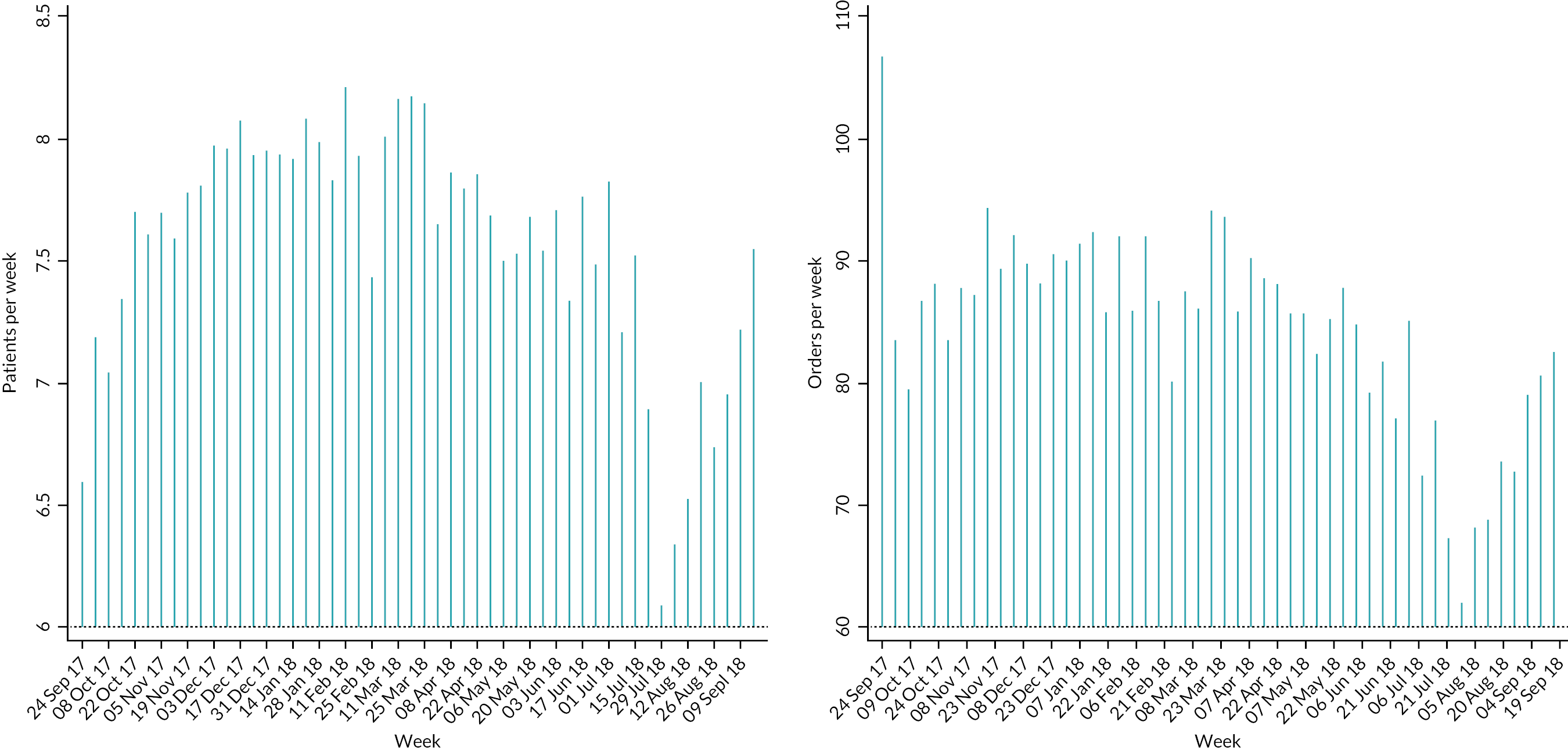
Between 24 September 2017 and 16 September 2018, there were 1461 doctors who were active in at least 1 week. Over all 52 weeks, the total number of patients seen and orders created per doctor is presented in Figure 25. Doctors created orders for a median of 78 (mean of 168) patients and created a median of 564 (mean of 1860) orders. There was significant variation in these values, with some doctors having extremely high levels of activity (e.g. the 95th percentile is 9000 orders created over 52 weeks). This distribution suggests that approximately 70 doctors created on average 170 orders every week, with many doctors creating almost no orders. This seems unlikely to represent true activity levels and may be driven by a mismatch between the doctor IDs within the EPR and with the doctors carrying out the activity. For example, the IDs associated with very high levels of activity may be used by multiple doctors.
FIGURE 25.
Total patients seen and orders created per doctor, September 2017–September 2018. Note: Dashed line for median, solid line for mean.

Doctors were active between 1 and 52 weeks during the period analysed. Figure 26 presents how many weeks doctors were active. For example, from 1461 doctors, 130 of these were active for only 1 week, which represents 8.9% of doctors. These findings suggest that a significant proportion of doctors are only active for a relatively low number of weeks (<10 weeks). This distribution is unusual and raises concerns about the validity of the data and doctor IDs. We do not observe a large group of doctors active for around 44 weeks, which would be expected for those working in full-time permanent positions. Furthermore, that the number of doctors’ active does not vary much between 10 and 52 weeks is also a concern. Some of these unusual patterns might be explained, partially, by junior doctors and their rotations on and off placements.
FIGURE 26.
Count and percentage of doctors by number of weeks active, September 2017–September 2018.
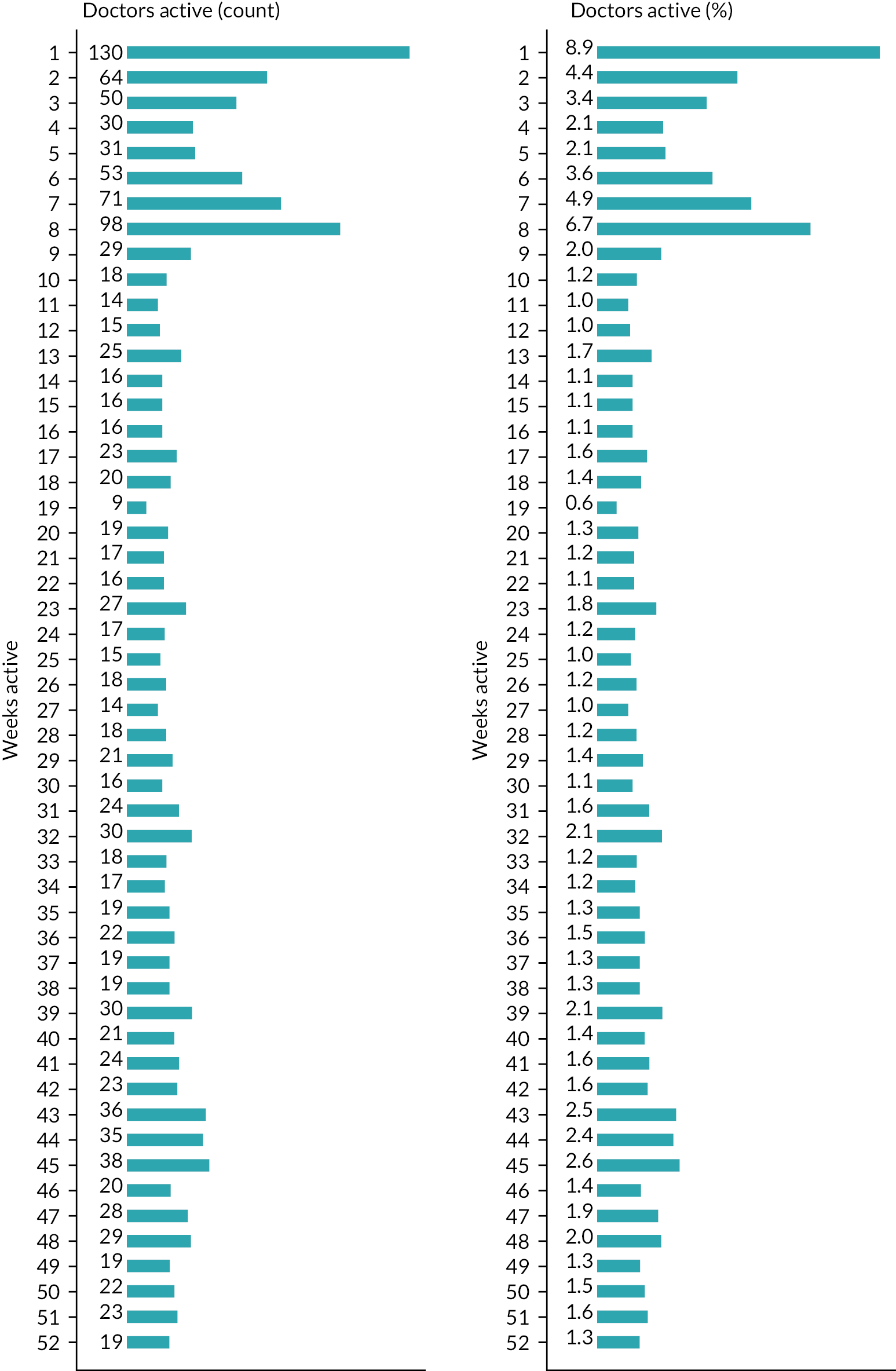
To investigate further and attempt to identify short-term locums, we focus on only those doctors who created an order in 4 weeks or fewer, and the active weeks for these doctors are shown in Figure 27 (274 doctors in total). For example, the first distribution shows doctors who were active for only 1 week, and in which single week they were active. For these doctors, we see a large proportion active in weeks 1 and 2. This is expected and likely capturing some doctors who were active before our observation period: similar patterns are observed for doctors working 2, 3 and 4 weeks.
FIGURE 27.
Count of doctors active in each week, doctors who are active for 1–4 weeks only.
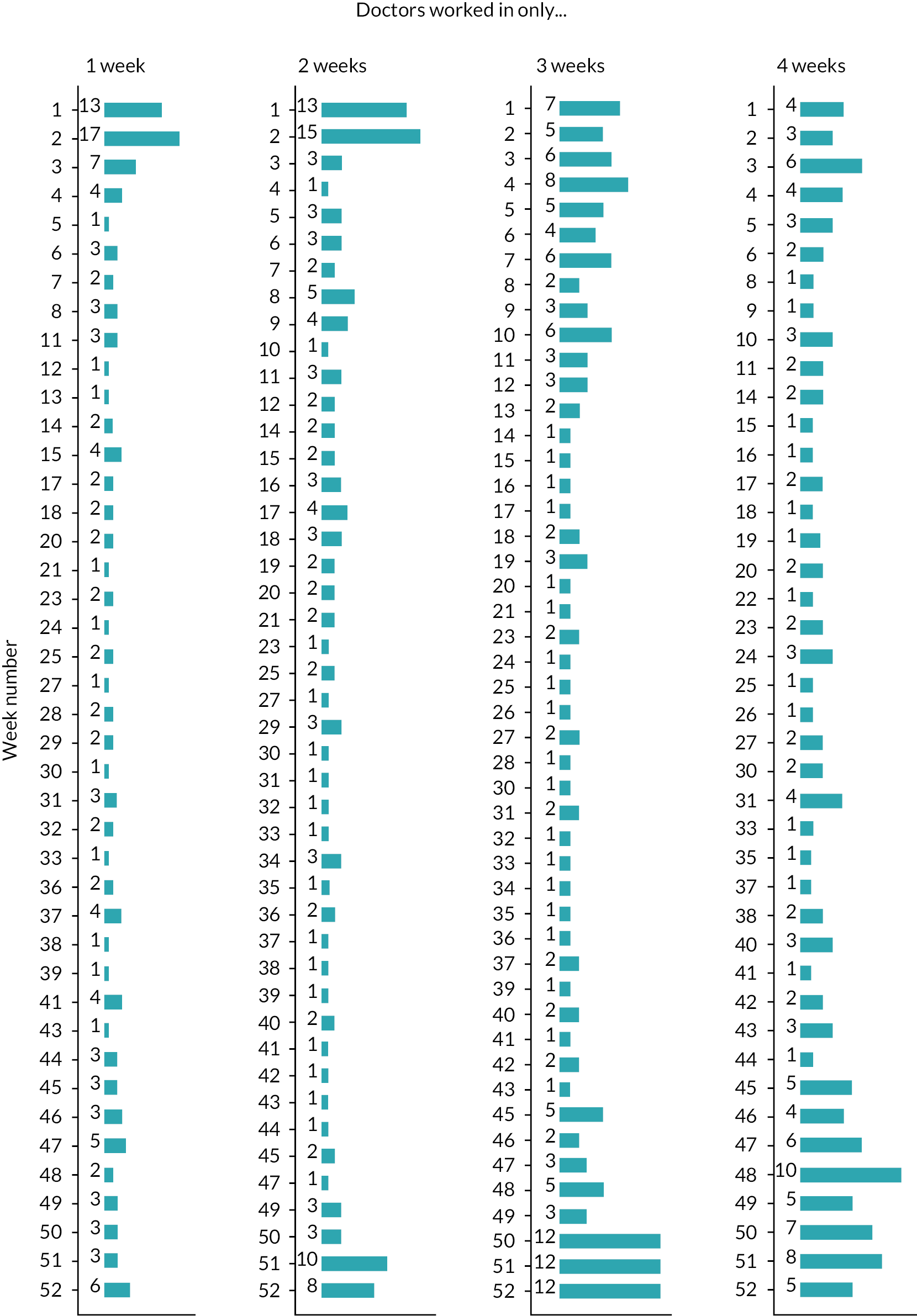
Excluding doctors who work at the beginning and end of the period yields 163 doctors who have working patterns which are consistent with a short-term locum and may identify them as potential locums. These doctors work no more than 4 weeks in a 52-week period and do not work at the beginning or end of this period. The beginning and end periods are defined as:
-
weeks 1, 2 and 52 for doctors working in 1 week only
-
weeks 1, 2, 51 and 52 for doctors working in 2 weeks only
-
weeks 1, 2, 3, 50, 51 and 52 for doctors working in 3 weeks only
-
weeks 1, 2, 3, 4, 49, 50, 51 and 52 for doctors working in 4 weeks only.
These potential locums, on average, created orders for 1.8 patients and created 15 orders per week in the limited weeks they were active. This is a much lower level of activity than doctors we do not identify as potential locums, who doctors created orders for 7.6 patients and created 85 orders per week.
Over the 52 weeks in total, doctors identified as potential locums created orders for 494 patients and created 4133 orders in all the weeks they were active. These numbers represent approximately 0.15% and 0.20% of the total over the period.
The very low levels of activity, both per week and in total, suggest that these doctors are: (1) locums who create orders very rarely; (2) locums who create more orders but these are associated with other doctor IDs; or (3) not locums, perhaps temporary IDs which are used for other purposes. Given the lack of confidence in the ability to identify locums using EPR data, we do not progress with our further aims of comparing locum and permanent doctors on quality and safety.
Discussion
Summary
Accessing any EPR data was challenging and ultimately we concluded that the EPR data we received from Bradford could not be used to robustly identify locums, and so it was not then possible to go on to explore differences in practice and performance (e.g. in test ordering, prescribing or other behaviours). This was due to irregularities in how the working patterns of doctors could be described by doctor ID and the frequency in how these IDs were used.
Strengths and limitations
Access to Bradford EPR is a strength of this study, as it presents the opportunity to understand more about how hospital EPRs can be used for research. We attempted to access EPR data from Salford Royal Hospital but faced significant barriers which ultimately prevented access. The EPR data at Salford Royal were managed by a data team whose purpose was focused on the operational needs of the hospital, and not capable of providing data for research in the timescales needed.
Our analysis of the Bradford EPR is limited as we were unable to identify locums directly via staff employment records, which would have greatly increased the confidence of the identification and allowed for a more robust analysis of their activity. Without better locum identification, we had to rely on looking at working patterns. Locum working patterns should be characterised by short and intermittent presence in the EPR data. However, our attempts have likely also identified some part-time doctors and doctors who are permanent but create orders in the EPR less frequently. The time period we could analyse was also shortened, only 52 weeks, due to the impact of COVID-19 and how the EPR was implemented in Bradford over our observation period.
However, the analysis shows the wealth of potential information contained within EPRs if they can be better used for research. To answer our research questions on the quality and safety of locum doctors, we feel a robust linkage between EPR and electronic staff records (ESRs) would be needed.
Chapter 11 Discussion and conclusions
Introduction
In this chapter, we bring together the main findings from all four of our work packages alongside the existing evidence which was briefly reviewed and summarised in Chapter 1. In so doing, it is worth restating the overall aim of the research and our research questions, which were outlined at the end of Chapter 1. The overall aim of this research on temporary doctors (generally termed locums) was to provide evidence on the extent, quality and safety of medical locum practice and the implications of medical locum working for health service organisation and delivery in primary and secondary care in the English NHS. Our three research questions were:
-
What is the nature, scale and scope of locum doctor working in the NHS in England? Why are locum doctors needed, what kinds of work do they undertake and how is locum working organised?
-
How may locum doctor working arrangements affect patient safety and the quality of care? What are the mechanisms or factors which may lead to variations in safety/quality between locum and permanent doctors? What strategies or systems do organisations use to assure and improve safety and quality in locum practice? How do locum doctors themselves seek to assure and improve the quality and safety of their practice?
-
How do the clinical practice and performance of locum and permanent doctors compare? What differences in practice and performance exist and what consequences may they have for patient safety and quality of care?
We therefore organise this discussion chapter around these three main research questions, while seeking to relate our findings to the wider policy context and to the existing literature. We do not repeat content covered in Chapters 3–10 on the study methodology, data sources or limitations as this has already been presented.
We set out briefly in Chapter 2 the theoretical context for this research – grounded in a wider literature on the medical profession, our prior qualitative research on the experiences of locum doctors, and our earlier review of the literature which provided a framework of eight factors which could affect the quality and safety of locum doctor working. While we do not in this discussion and conclusions chapter revisit this wider framing for the research, we would observe that the findings summarised below are very much consistent with our earlier work and that of others which highlights the liminal space occupied by locum doctors – at the boundaries of or on the periphery of organisations and in the space in between them, and the consequences of this both for locums themselves and for quality and safety of health care.
The nature, scale and scope of locum doctor working in the National Health Service in England
There has been extensive policy concern and much media coverage of the use of locum doctors in the NHS, suggesting that there has been a substantial increase in the use of locum doctors over time, and this is often conflated with concerns about the costs of locum doctors and particularly the high costs charged to the NHS by locum agencies in some shortage areas or specialties. But our research presents a rather more nuanced picture of relatively stable locum use over time. We have not studied locum costs.
In primary care, we found from our analysis of NHS Digital workforce returns that just over 3% of medical staffing was provided by locums and that it had not changed much over the time period 2017–20. However, our analysis of CPRD data for the longer time period of 2010–21 suggested that about 6% of general practice medical consultations were undertaken by locums in 2010 and that this had risen slightly to about 7.1% in 2021. We think there are two main explanations for this discrepancy. First, locums generally only undertake consultations while permanent GPs do a lot of other non-consultation clinical and administrative tasks – the NHS Digital workforce returns measure staff numbers in FTE, while the CPRD data measure numbers of consultations. Second, the NHS Digital workforce returns from general practices may under-report the numbers of locum doctors, and there have been concerns about the quality and completeness of the data. But both data sources suggest a relatively low – and stable – rate of locum use in primary care.
In NHS trusts (mostly secondary care and mental health), our analysis of NHS Improvement returns from NHS trusts indicated that about 4.4% of medical staff FTE was provided by locum doctors. With a much shorter time series from 2019 to 2021, it is rather more difficult to draw any conclusions about the secular trend, although in that time period the rate of locum use was fairly stable – dropping as expected in the first phase of the COVID pandemic in early to mid-2020, and then recovering. We found NHS trusts making more use of bank (rather than agency) locums over the time period, and an increase in the reported numbers of unfilled shifts, which would indicate increasing unmet need.
It may be that the number of doctors working as locums in England has increased as research from the GMC has suggested, but that this comes in part from an increased tendency for some doctors in training to take time out from the training pathway and while doing so to do some locum work. It may also be that more doctors are doing some locum work alongside either full- or part-time working in a permanent role in the NHS. But overall, our data do not seem to suggest a substantial increase in the overall use of locum doctors in the NHS over time.
However, those overall national rates of locum use hide a great deal of variation between organisations which is important to consider. In primary care, we found the NHS Digital workforce returns showed the rate of locum use by CCG varied from 1% to almost 31%. Among NHS trusts, the reported rate of locum use varied from < 1% to almost 16%.
So what might lie behind these variations? Our qualitative work suggested that there were some particularly problematic specialties in which workforce shortages were acute, such as psychiatry. Our multivariate quantitative analyses suggested that there was some variation by region/geography which might reflect workforce capacity or shortage in some parts of England. But they also showed that both smaller general practices and smaller NHS trusts made more use of locums, which might plausibly suggest that larger organisations are more able to cope with workforce gaps without having to resort to locums. In both primary care and NHS trusts, there was an association between CQC ratings and locum use, with organisations with lower CQC ratings making more use of locums. Great caution should be exercised in interpreting this as a causative relationship, in either direction, but it is an important finding. Finally, we did not find an association between locum use and measures of deprivation for the population served, either in primary care or for NHS trusts.
Our surveys of general practices and of NHS trusts showed both some similarities in their reasons for needing locums and ways of using them, as well as some notable differences. Both gave as common reasons for using locums the need to cover either planned or unplanned absences or gaps in staffing – mainly leave and sickness absence – and both reported using them to provide additional workforce capacity when it was needed. However, NHS trusts were much more likely to report needing locums because of difficulties recruiting doctors.
We also found some interesting differences in where general practices and NHS trusts sourced locum doctors from. Practices said they made much less use of locum agencies and tended to use trusted locums who were familiar to the practice, while NHS trusts made much more use of locum agencies and staff banks, and within that there was a lot of variation, in that some NHS trusts made much more use of locum agencies rather than staff banks. Overall, NHS trusts sourced about a third of their locums from staff banks according to our analysis of NHS Improvement returns.
Should we conclude that the use of locum doctors in either primary care or NHS trusts can be an indicator of concern? Our qualitative research certainly found that respondents thought an over-reliance on locums (however that might be defined) could be a ‘red flag’. Respondents suggested that the consistent use of high levels of locums was both a concern in itself, because of the implications for quality and safety (which we turn to later in this discussion) and a potential indicator of wider organisational problems in the general practice or NHS trust. They thought that a service ‘run on locums’ was to be avoided. This suggests that for organisational leaders and other stakeholders (primary care networks, CCGs, integrated care systems etc.) and for regulators such as CQC and the GMC, being able to analyse and understand rates of locum use could be very helpful.
This leads us to reflect on the quality and value of the quantitative data we have used for our research. In both primary care and NHS trusts, we have made use of existing routine data sources, though we do not think those data sets have been used previously to study locum use. In both cases, more extensive analysis and feedback/reporting would be likely to help improve data quality. But in addition, collecting more data or collecting it differently would also be worth considering. For example, the NHS Improvement data set provides a high level of granularity by time, with weekly returns, but it does not collect the specialty or clinical area in which locums are being used, or the reason why they are needed. It is a data set which was really designed to address the policy concerns about the level and cost of locum use in NHS trusts. Similarly, the NHS Digital workforce returns for general practice make a distinction between short-term/ad hoc locums and other/longer-term locums but do not define those terms clearly, and do not collect any information about the reasons for locum use. The returns also collect some potentially useful detailed information on individual doctors which could be used to study and report on locum working, but the published data are aggregated at practice level. We have not, in this study, sought to access the NHS ESR system which covers almost all NHS trusts and has detailed staffing and payment records for over a million NHS employees, but this could be a very useful source of data for future analysis and reporting for NHS trusts.
The use of locum doctors is clearly an important and enduring component of the medical staff workforce in the NHS, and a way to provide flexibility and capacity in medical staffing. However, we should note that it is only one of a number of ways in which organisations can achieve increased flexibility and capacity – for example, through flexible rostering and contracts for medical staff, and improved working conditions. Indeed, our qualitative fieldwork suggests that doctors who choose to work as locums are often doing so because of the working environment they have encountered in permanent staff positions, and in order to achieve a greater degree of control over their own workload and work–life balance than they were able to achieve (or were offered) in a permanent staff position. They trade the loss of security and increased precarity of being a locum in order to get greater autonomy and personal control.
The extent to which locum working increases workforce capacity is somewhat open to question. It is clear from our research that individual practices or organisations are using locum working as a way to fill short-term workforce capacity gaps, provide additional capacity when it is needed, and to deal with longer-term workforce gaps predominantly associated with recruitment problems. But at a macro level, if doctors move from permanent staffing positions into locum work for some of the reasons outlined above, this is probably a zero-sum game – it does not increase the overall workforce capacity of the NHS. It may be that some doctors who move to work as locums would otherwise have exited the workforce entirely, and it may be that some doctors who have left clinical practice come back into practice because of the opportunity to work as a locum. But in those cases, there might be other, better ways to improve retention, or to encourage return to clinical practice.
How locum doctor working arrangements affect patient safety and the quality of care
National Health Service England has published detailed guidance for healthcare providers, locum agencies and revalidation management services on supporting organisations engaging with locums and doctors on short-term placements. The scope of the guidance is not stated explicitly but it clearly applies to all NHS organisations which use locums (it uses examples in both primary care and in NHS trusts) and is relevant to others, such as independent healthcare providers. It sets out a range of advice on areas such as pre-employment checks, induction, appraisal and revalidation, dealing with concerns, end-of-placement reports, etc. As far as we know, there has not previously been work to followup systematically on the operationalisation and implementation of the guidance since it was published in 2018.
Our surveys of NHS trusts and general practices suggest that awareness of the guidance was very mixed – and particularly poor among respondents from general practice. Those who were aware of it in NHS trusts generally viewed it quite favourably, but some commented that it set out an ideal model which was hard to follow in practice. Among general practices, it was often seen as less relevant to their needs and to the setting of an individual general practice. Self-reported compliance with the guidance was generally high in areas like pre-employment checks and induction, but much less good in areas like end-of-placement reporting and supporting the locum with appraisal and revalidation.
Our qualitative research confirmed and extended the survey findings. For example, we found that giving locums a proper induction was viewed by locums as really important to their subsequent ability to perform in their role, and that issues not covered properly in their induction hampered them and could add to the workload of other members of the clinical team. But in our qualitative interviews with respondents who work with locums, we often found an unrealistic expectation that locums should come into the organisation and be able to start work immediately – to ‘hit the ground running’ – and that they should devote all their time to clinical work as that was what they were being paid – and paid well – to do. Locums themselves reported taking steps – like working in fewer organisations and avoiding some organisations, working at a lower level/grade and limiting their scope of practice – to deal with the problems of being inadequately inducted and supported.
This was part of a wider negative and stigmatising narrative which often cast locums as less professional, less committed, less competent, less reliable and more financially motivated than permanent medical staff. By ‘othering’ locum doctors in this way, it was easier both to justify treating them differently (and less well) than other staff and to explain problems or difficulties with quality and safety as being attributable to locums and locum working. In short, it was easy to blame locums when things went wrong, and they were often either not there to defend themselves or not able to do so. The position of locum doctors was by definition precarious – they could be removed or have a placement ended easily.
We found in some of our quantitative analyses that locum doctors in general practice were more likely than permanent staff to have trained outside the European Economic Area (EEA), and there was among some respondents a marked distrust of doctors who had trained outside the UK. They were blamed for not having enough experience of working in the NHS (an alternative view would be that they would be welcomed for coming to the UK and adding to the medical workforce capacity) and some respondents questioned the equivalence of their training and prior experience to UK training and NHS placements. Overall, we think there was an element of racism underlying some of these attitudes and beliefs.
We would contrast this with the attitudes of patients to locum doctors, which were generally more accepting of locum working, and which valued access to seeing a doctor in a timely fashion over whether the doctor was a locum or not. Patients thought that traditional notions of relational continuity were not consistent with their own experiences of care, and some valued the fresh perspectives on their condition which came from seeing a different doctor.
It is clear from our research that locum working can have adverse consequences for the quality and safety of care, but that such consequences were probably more likely to result from the organisational setting and the working arrangements than they were from the locum doctors themselves and their competence, clinical practice or behaviours. It is also clear that there is great variation in the characteristics both of organisations which use locums and of locums themselves.
In simple terms, we found that some organisations were using locums poorly and often extensively, because of long-standing and endemic workforce shortages or problems. Others were using locums more selectively and effectively, as part of a wider workforce strategy aimed at creating sustainable capacity and flexibility and alongside other approaches. Locum doctors are also very heterogeneous. Some have made the positive choice to locum for reasons of work–life balance or personal circumstance, some are locuming at the end of their medical career as an alternative to complete retirement, some are taking a break from medical training pathways to pursue other professional or personal interests and using locum working as a flexible way to sustain their income while doing so. We heard from our respondents concerns about some doctors working as locums because they could not get a permanent position, or because they had persistent problems in relation to their clinical performance or working relationships which made it difficult for them to sustain a permanent position. It must be said that description did not fit any of the locum doctors we interviewed, but doctors in that position were probably less likely to be willing to be interviewed.
One of the concerning findings from our research was that when problems related to locum doctors’ practice arose, they were not dealt with well. Firstly, organisations often did not provide feedback either to locum doctors themselves or to locum agencies at the end of placements. Secondly, when a problem arose, organisations often dealt with it by simply ending the locum placement early or not renewing it, without raising it with either the doctor or the locum agency. Thirdly, the formal mechanism for raising a problem with the locum doctor’s RO simply did not work. It relies on the RO in the organisation where the locum was placed finding out about the problem, and passing information on via the MPIT form to the locum doctor’s RO (who could be at the locum agency or at another designated body where the locum doctor works). This long chain of communication is not designed to deal with locum doctors or others who do not have a conventional employed relationship and whose relationship with employers or designated bodies is more distant and transient. Moreover, even if a problem does get flagged and there is a need for some kind of intervention – training, mentoring, clinical supervision or whatever – it is very difficult to secure that remediation without the locum doctor moving into a permanent job with an employer which has the capability and willingness to provide it.
This raises some questions about the role and operation of locum agencies and alternative models of organisation. Locum agencies are generally designated bodies – that is, they have a RO who provides or oversees appraisal and revalidation for the locums that are connected to the agency, though many locum agencies outsource this function. But in practice, it is difficult for locum doctors to assemble the portfolio of information needed for appraisal and revalidation, and locum agency ROs have virtually no first-hand knowledge of locum doctors’ practice and often do not meet with them F2F at all. In addition, locum doctors may work with multiple agencies but the RO has no way of knowing about their work with other agencies, and locum agency ROs have little scope to do anything about problems by way of remediation. Many of these problems were discussed when medical revalidation was being designed and implemented, and were also highlighted in research on medical revalidation, but they remain unresolved. The emergence of Locum Chambers – collective membership organisations run by locums themselves – may provide some solutions. At present, locum agencies are not regulated by the CQC and one route to reform could be to have a system of licensing or regulation for agencies alongside that for healthcare providers, and to use that to promote compliance with NHS England and GMC guidance.
Overall, the qualitative fieldwork highlighted the importance and value of treating locum doctors decently and affording them the support that would normally be given to permanent members of staff. Locums were more likely to want to work in organisations which afforded them that kind of support, and were more able to do their job properly, and that meant work was less likely to be displaced to other members of the clinical team, and problems related to the quality and safety of care were less likely to arise.
How the clinical practice and performance of locum and permanent doctors compare
From our surveys of NHS trusts and general practices, respondents generally reported that on a range of areas of clinical practice they thought locum doctors performed about the same as or worse than permanent doctors. It is notable that the areas where they tended to think locums performed worse were things like continuity of care, and adherence to guidelines and protocols, which are, as we have already discussed, more influenced by the organisational setting and arrangements like induction than by the locum doctor’s own clinical expertise and fitness to practice.
We were able to explore differences in practice in primary care directly through our quantitative analysis of the CPRD data set, and this provided some very interesting but quite mixed findings which should be interpreted with great caution. For example, our multivariate analysis found that patients who saw a locum doctor were less likely to make a return visit to the general practice within 7 days than those who had seen a permanent doctor. We could hypothesise that a return visit can indicate that a problem was not resolved at the first visit; or we could argue that return visits are a sign of effective follow-up and safety-netting decisions at the first visit. We found that locum doctors and permanent doctors had some differences in prescribing behaviour, but they were mixed (locums prescribed antibiotics and opioids more frequently but hypnotics less frequently than permanent doctors). Locum doctors were less likely to make referrals and to order tests. In terms of hospital events following a consultation with a locum, patients were more likely to visit A&E within 7 days, but there was no difference for hospital admission. Our qualitative fieldwork may help us to understand some of these differences, and suggests that they arise more from the complex interplay of the organisational setting and working arrangements for locums than from particular clinical practice characteristics of locum doctors per se.
We were not able to make a similar quantitative analysis of differences in the hospital setting between locum doctors and permanent doctors as we had planned, despite our efforts to do so using data from the EPR systems from two hospitals. There were three main difficulties. First, extracting data from the EPR system proved impossible at one hospital and difficult at the second. Second, in the limited data set we extracted, we could not reliably identify locum and permanent doctors by their user identifier, because of the way that such identifiers were assigned and used. Temporary user identifiers were sometimes used by permanent staff (who had forgotten their staff ID, for example) and were sometimes reused. We experimented with limited success with identifying locum doctors indirectly by analysing temporariness in the longitudinal data set. Third, and perhaps most importantly, even if we could attribute entries in the EPR, such as test orders, prescribing orders, to individual doctors, because of the way clinical teams work to provide care, it would be difficult to know that particular order was initiated by the doctor who entered it on the EPR or by another member of the clinical team. Overall, we concluded that hospital EPRs are potentially a hugely valuable source of routine data for research, but they have been designed for operational purposes which means data access/extraction, data definitions and data quality are all problematic.
Equality, diversity and inclusion
Inequalities between different ethnic groups are a critical issue in the UK workforce. Black and minority ethnic workers are more likely to be in temporary and insecure work. 134 Indeed, our study found that locum doctors in general practice were more likely than permanent staff to be IMGs. There has been a very limited amount of prior research relating to locum doctors, and consequently, how locum working relates to protected characteristics. Our findings indicated a marked distrust among some respondents of locum doctors who had trained outside of the UK. Overall, we think there was an element of racism underlying some of the attitudes towards these locums. The NHS Medical Workforce Race Equality Standard group could consider IMG locums and locums from ethnic minority backgrounds in their future analysis as locum doctors are not yet considered in the same way as Specialty and Associate Specialist and Locally Employed doctors, who face similar challenges to locums. 83
Our findings indicated that IMGs may not be as well networked as doctors who trained in the UK. This was important because less-well-networked locums may be more likely to find themselves in unsafe organisations with limited support, which could be detrimental to both patients and locums. Future research could go further in examining how ethnicity and place of graduation intersect with employment status, particularly given the significant rise in the number of IMGs. 82 Further research could identify how IMGs can be best supported when they work as locums.
We were interested in speaking to individuals who had experience of being a patient of a locum doctor and used the NIHR organisation ‘Research for the Future’ to recruit the majority of our participants. The project benefited from patient involvement as this was the first project of its kind to focus on patient experiences of being treated by locum doctors and provided invaluable information about how patient experience could be improved when locum doctors are working.
Our quantitative work was very limited in its capacity to comment on equality, diversity and inclusion due to the lack of routine recorded data such as ethnicity or first language. We were able to observe where GPs qualified from NHS digital data but only in very broad groups: UK, EEA and outside EEA. Equivalent data were not available for hospital doctors or for CPRD. We were able to comment on how the use of locums varied with deprivation, finding no relationship.
Accessibility
Our PPI forum (made up of two men and two women) collaborated with us in the design and development of materials used to recruit patient participants to the study to ensure our materials were inclusive and accessible. We offered a range of ways to participate, including providing written accounts, telephone or video calls and individual or group interviews.
The research team
Our research team comprised of five men and two women. We are all from white backgrounds and two of our group are not from the UK. Race inequality continues to be a perennial problem in all areas of higher education, including staffing, admissions and employment. We acknowledge the lack of diversity in our team.
There was a range of experience and expertise across the research team with more senior members mentoring and supporting more junior members. Development opportunities were provided and the research team were involved in mentorship both within the university and externally through Health Services Research UK. The research team also benefitted from attending national and international conferences and presenting study findings. The team have also been supported in developing their writing skills and writing for publication.
Patient and public involvement
Patient and public involvement was embedded in this study from inception to dissemination. The aim of PPI in this study was to collaborate with patients, carers and the public to improve the quality, relevance and outcomes of our research. The ethos of our PPI approach was collaboration and co-production. Our PPI forum included four people with lived experience of health conditions and caring responsibilities. Our PPI forum chair was involved from the development of our application to the dissemination of our findings. Our forum members met at regular intervals throughout the project to coproduce the research, offering advice, commenting on and developing research materials and undertaking research with research participants. Our PPI forum made a significant contribution to the qualitative aspects of our project but were less involved in our quantitative work packages. While our PPI chair provided thoughts at our advisory group, with hindsight, we could have involved our forum in our other quantitative work packages to get a sense of what was important to patients and understand their reflections on the findings.
Our intention was to recruit participants through our case study sites, but as this project began at the beginning of the pandemic, this proved difficult. Recruitment of patients and carers for interviews and focus was slow initially. We sought advice from our PPI forum who recommended the organisation Research for the Future, which proved to be very successful. We sought participants who had lived experience of being treated by locums; in hindsight, we could have sought the opinions of carers too. Two members of our PPI forum were trained in qualitative interview methods by JF and collected data by leading focus groups with 30 patients. Our PPI forum contributed towards qualitative analysis by discussing findings and reviewing, refining, defining and naming themes. We will continue working with our forum to disseminate our findings.
Conclusions
Locum doctors are a key component of the medical workforce in the NHS and provide necessary flexibility and additional capacity for healthcare organisations and services. We found that the extent of reliance on locum doctors varied considerably, but that an over-reliance on locums for service provision was undesirable. Some differences in practice and performance between locum and permanent doctors were found, but these seemed often to arise from organisational characteristics. We found patients were more concerned with the clinical expertise and skills of the doctor they saw than whether they were a locum or not. Organisational arrangements for locum working could be improved in many respects, and there were in particular problems with the way any concerns about locum doctors were managed.
Additional information
Acknowledgements
We thank everyone who contributed to and supported our research, and especially members of our Project Advisory Group and PPI Forum for their invaluable help and support throughout the project. We thank all research participants, including those who responded to our two national surveys of NHS trusts and general practices in England and those who were interviewed and participated in focus groups.
Contributions of authors
Thomas Allen (https://orcid.org/0000-0002-2972-7911). (Senior Research Fellow in Health Economics). Led work packages 3 and 4. He worked with CG on the quantitative research design/methodology, data access, analysis, interpretation and reporting. He contributed particularly to drafting Chapters 3, 4, 9 and 10.
Darren Ashcroft (https://orcid.org/0000-0002-2958-915X). (Professor of Pharmacoepidemioogy). Contributed expert advice and support to contributed expert advice and support to quantitative research design, data analysis, interpretation and reporting in work packages 3 and 4. He contributed particularly to drafting Chapters 3, 4, 9 and 10.
Jane Ferguson (https://orcid.org/0000-0002-8129-8376). (Lecturer in Healthcare Management). Led work packages 1 and 2. She contributed to survey design, administration and analysis in work package 1 and led qualitative research design, fieldwork and data analysis in work package 2. She contributed particularly to drafting Chapters 5, 6, 7 and 8.
Christos Grigoroglou (https://orcid.org/0000-0003-1621-8648). (Research Fellow in Health Economics). Led on data analysis and reporting in work packages 3 and 4. He worked with TA on quantitative research design/methodology, data access, analysis, interpretation and reporting. He contributed particularly to drafting Chapters 3, 4, 9 and 10.
Evan Kontopantelis (https://orcid.org/0000-0001-6450-5815). (Professor of Data Science & Health Services Research). Contributed expert advice and support to research design, data analysis, interpretation and reporting in work packages 3 and 4. He contributed particularly to drafting Chapters 3, 4, 9 and 10.
Gemma Stringer (https://orcid.org/0000-0001-9325-3362). (Research Fellow in Health Services Research). Led on the survey design, administration and analysis in work package 1 and was involved in qualitative research design, fieldwork and data analysis for work package 2. She contributed particularly to drafting Chapters 5, 6, 7 and 8.
Kieran Walshe (https://orcid.org/0000-0002-0696-480X). (Professor of Health Policy & Management). Was the lead applicant and principal investigator for the project. He led on the overall project design and contributed to all work packages and chapters. He contributed particularly to drafting Chapters 1, 2 and 11.
All project team members contributed comments and edits to all chapters in the report.
Disclosure of interests
Full disclosure of interests: Completed ICMJE forms for all authors, including all related interests, are available in the toolkit on the NIHR Journals Library report publication page at https://doi.org/10.3310/CXMK4017.
Primary conflicts of interest: NIHR grant for this project; none others declared.
Patient data statement
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it is important that there are safeguards to make sure that they are stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review.
Ethics statement
The study sponsor was the University of Manchester. The study received ethical approval from the Health Research Authority on 8 December 2020 (IRAS project ID: 278888; REC reference: 20/NW/0386).
Information governance statement
The University of Manchester is committed to handling all personal information in line with the UK Data Protection Act (2018) and the General Data Protection Regulation (EU GDPR) 2016/679. Under Data Protection legislation, for data used in this project for which the University of Manchester is the Data Controller, you can find out more about how we handle personal data, including how to exercise your individual rights and the contact details for our Data Protection Officer here www.manchester.ac.uk/discover/privacy-information/data-protection/. For CPRD data used in this project under Data Protection legislation, the University of Manchester is the Data Processor; the Medicines and Healthcare Products Regulatory Agency is the Data Controller and we process personal data in accordance with their instructions. You can find out more about how we handle personal data, including how to exercise your individual rights and the contact details for CPRD’s Data Protection Officer here https://cprd.com/data-protection-and-processing-notice. Data from the Clinical Practice Research Datalink (CPRD) were obtained under licence from the UK Medicines and Healthcare products Regulatory Agency (MHRA). The data are provided by patients and collected by the NHS as part of their care and support. Hospital Episode Statistics (HES) data are subject to Crown copyright (2022) protection, reused with the permission of The Health and Social Care Information Centre, all rights reserved. The CPRD study protocol was approved by CPRD’s Independent Scientific Advisory Committee (ISAC) (reference: 20_000246). We would like to acknowledge all the data providers and general practices who make anonymised data available for research.
Department of Health and Social Care disclaimer
This publication presents independent research commissioned by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by the interviewees in this publication are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, MRC, NIHR Coordinating Centre, the HSDR programme or the Department of Health and Social Care.
This monograph was published based on current knowledge at the time and date of publication. NIHR is committed to being inclusive and will continually monitor best practice and guidance in relation to terminology and language to ensure that we remain relevant to our stakeholders.
Disclaimers
This article presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care.
References
- Moberly T. Number of locums has doubled since 2009. BMJ 2016;355. https://doi.org/10.1136/bmj.i6207.
- National Health Service Digital . General Practice Workforce, Final 31 March 2019, Experimental Statistics 2019. https://digital.nhs.uk/data-and-information/publications/statistical/general-practice-workforce-archive/final-31-march-2019 (accessed 1 June 2019).
- General Medical Council . What Our Data Tells Us About General Practitioners Working for the NHS in England and Scotland 2018. www.gmc-uk.org/-/media/documents/what-our-data-tells-us-about-gps_pdf-74830685.pdf (accessed 8 July 2022).
- Nutt T. Don’t Talk About the Money?. London; 2017.
- Morgan M, McKevitt C, Hudson M. GPs’ employment of locum doctors and satisfaction with their service. Fam Pract 2000;17:53-5. https://doi.org/10.1093/fampra/17.1.53.
- Lind S. Stop Denigrating GP Locums, ‘Livid’ GP Leader Tells. NHS England; 2017.
- National Health Service Improvement . Agency Controls: Expenditure Reduced by £1 Billion and New Measures 2017. https://improvement.nhs.uk/news-alerts/agency-controls-1-billion-saving-and-new-measures/ (accessed 8 February 2021).
- Rimmer A. Locum pay rates have risen despite hourly rate cap. BMJ 2017;356. https://doi.org/10.1136/bmj.j135.
- Ferguson J, Walshe K. The quality and safety of locum doctors: a narrative review. J R Soc Med 2019;112:462-71. https://doi.org/10.1177/0141076819877539.
- McKeown A, Griffin A. Locum Appraisal, Revalidation and Governance Report. London: University College Education; 2016.
- Chapman R, Cohen M. Supporting Organisations Engaging With Locums and Doctors in Short-Term Placements: A Practical Guide for Healthcare Providers, Locum Agencies and Revalidation Management Services 2018. www.england.nhs.uk/wp-content/uploads/2018/10/supporting_locum_agencies_and_providers.pdf (accessed 17 March 2021).
- National Health Service Improvement . Reducing Reliance on Medical Locums: A Practical Guide for Medical Directors 2016. https://improvement.nhs.uk/resources/reducing-reliance-medical-locums-practical-guide-medical-directors/ (accessed 24 May 2021).
- Archer J, Bloor K, Bojke C, Bryce M, Ferguson J, Gutacker N, et al. Evaluating the Development of Medical Revalidation in England and Its Impact on Organisational Performance and Medical Practice: Overview Report. Manchester: University of Manchester, University of York and University of Plymouth; 2018.
- Walshe K, Boyd A, Bryce M, Luscombe K, Tazzyman A, Tredinnick-Rowe J, et al. Implementing medical revalidation in the United Kingdom: findings about organisational changes and impacts from a survey of Responsible Officers. J R Soc Med 2017;110:23-30. https://doi.org/10.1177/0141076816683556.
- Ferguson J, Tazzyman A, Walshe K, Bryce M, Boyd A, Archer J, et al. ‘You’re just a locum’: professional identity and temporary workers in the medical profession. Sociol Health Illn 2021;43:149-66. https://doi.org/10.1111/1467-9566.13210.
- General Medical Council . Taking Revalidation Forward: Improving the Process of Re-Licensing for Doctors. Sir Keith Pearson’s Review of Medical Revalidation 2017. www.gmc-uk.org/-/media/documents/Taking_revalidation_forward___Improving_the_process_of_relicensing_for_doctors.pdf_68683704.pdf (accessed 26 July 2022).
- Organisation for Economic Co-operation and Development . OECD Employment Outlook 2015 2015. https://doi.org/10.1787/empl_outlook-2015-en (accessed 9 October 2020).
- Organisation for Economic Co-operation and Development . OECD Employment Outlook 2002: Taking the Measure of Temporary Employment 2002. https://doi.org/10.1787/empl_outlook-2002-5-en (accessed 10 October 2020).
- Casey C, Alach P. ‘Just a temp?’: women, temporary employment and lifestyle. Work Employ Soc 2004;18:459-80. https://doi.org/10.1177/0950017004045546.
- Boyce AS, Ryan AM, Imus AL, Morgeson FP. ‘Temporary worker, permanent loser?’ A model of the stigmatization of temporary workers. J Manage 2007;33:5-29. https://doi.org/10.1177/0149206306296575.
- Freidson E. The reorganization of the medical profession. Med Car Rev 1985;42:11-35. https://doi.org/10.1177/107755878504200103.
- Freidson E. Professionalism: The Third Logic. Cambridge: Polity Press; 2001.
- Waring J. Restratification, hybridity and professional elites: questions of power, identity and relational contingency at the points of ‘professional–organisational intersection’. Sociol Compass 2014;8:688-704. https://doi.org/10.1111/soc4.12178.
- Haslam AS, Platow MJ, van Knippenberg D, Ellemers N. Social Identity at Work: Developing Theory for Organizational Practice. New York: Hove Psychology Press; 2003.
- Tajfel H, Turner JC. The Social Psychology of Intergroup Relations. Monterey, CA: Brooks/Cole; 1979.
- Care Quality Commission . Investigation into the Out-of-Hours Services Provided by Take Care Now 2010. www.cqc.org.uk/sites/default/files/documents/20100714_tcn_report_part_1.pdf (accessed November 2021).
- National Health Service Professionals . Patient Safety: Addressing Temporary Worker Clinical Standards, Governance and Compliance 2011. www.nhsprofessionals.nhs.uk/-/media/tbscg/project/nhs/article/guides/301white-paper-325052011final.pdf (accessed 15 May 2021).
- The Royal College of Surgeons of England . Locum Surgeons: Principles and Standards 2011. www.rcseng.ac.uk/library-and-publications/rcs-publications/docs/locum-surgeons-principles-and-standards/ (accessed 18 July 2021).
- Kirkup B. Reading the Signals. Maternity and Neonatal Services in East Kent – The Report of the Independent Investigation 2022. www.gov.uk/government/publications/maternity-and-neonatal-services-in-east-kent-reading-the-signals-report (accessed 25 October 2022).
- Campbell JL, Roberts M, Wright C, Hill J, Greco M, Taylor M, et al. Factors associated with variability in the assessment of UK doctors’ professionalism: analysis of survey results. BMJ 2011;343. https://doi.org/10.1136/bmj.d6212.
- McKevitt C, Morgan M, Hudson M. Locum doctors in general practice: motivation and experience. Br J Gen Pract 1999;49:519-21.
- Chan T, Sabir K, Sanhan S, Sherbino J. Understanding the impact of residents’ interpersonal relationships during emergency department referrals and consultations. J Grad Med Educ 2013;5:576-81. https://doi.org/10.4300/jgme-d-12-00211.1.
- General Medical Council . What Our Data Tells Us About Locum Doctors 2018. www.gmc-uk.org/-/media/documents/what-our-data-tells-us-about-locum-doctors_pdf-74371150.pdf (accessed 26 July 2022).
- Dean B, Schachter M, Vincent C, Barber N. Causes of prescribing errors in hospital inpatients: a prospective study. Lancet 2002;359:1373-8. https://doi.org/10.1016/S0140-6736(02)08350-2.
- Blumenthal DM, Olenski AR, Tsugawa Y, Jena AB. Association between treatment by locum tenens internal medicine physicians and 30-day mortality among hospitalized Medicare beneficiaries. JAMA 2017;318:2119-29. https://doi.org/10.1001/jama.2017.17925.
- Grigoroglou C, Walshe K, Kontopantelis E, Ferguson J, Stringer G, Ashcroft DM, et al. Locum doctor use in English general practice: analysis of routinely collected workforce data 2017–2020. Br J Gen Pract 2022;72:e108-17. https://doi.org/10.3399/BJGP.2021.0311.
- National Health Service Digital . General Practice Workforce, England: Data Quality Statement. 2019. https://files.digital.nhs.uk/A4/F765EA/GPW%20DQStatement.pdf (accessed 20 October 2021).
- National Health Service Digital . Quality and Outcomes Framework, Achievement, Prevalence and Exceptions Data, 2018–19 2019. https://digital.nhs.uk/data-and-information/publications/statistical/quality-and-outcomes-framework-achievement-prevalence-and-exceptions-data/2018-19-pas (accessed 9 December 2021).
- Ministry of Housing, Communities and Local Government . The English Indices of Deprivation 2019. www.gov.uk/government/statistics/english-indices-of-deprivation-2019 (accessed 20 October 2021).
- Bibby P, Shepherd J. Developing a New Classification of Urban and Rural Areas for Policy Purposes – The Methodology. Department for Environment, Food and Rural Affairs; 2004.
- National Association of Sessional GPs . Locum GP Workforce Numbers Out for the Count 2014. www.nasgp.org.uk/news/locum-gp-workforce-figures-out-for-the-count/ (accessed 29 November 2021).
- Staff Care . Survey of Temporary Physician Staffing Trends 2017. www.staffcare.com/locum-tenens-blog/advice/2017-survey-temporary-physician-staffing-trends/ (accessed 29 November 2021).
- Zimlich R. The rise of locum tenens among primary care physicians. Med Econ 2014;91.
- Spooner S, Gibson J, Checkland K, McBride A, Hodgson DE, Hann M, et al. Regional variation in practitioner employment in general practices in England: a comparative analysis. Br J Gen Pract 2020;70:e164-71. https://doi.org/10.3399/bjgp20X708185.
- National Health Service England . The NHS Long Term Plan 2019. www.longtermplan.nhs.uk/wp-content/uploads/2019/08/nhs-long-term-plan-version-1.2.pdf (accessed 21 October 2021).
- National Health Service Professionals . About NHS Professionals 2022. https://rg-sitecore-512680-cd.azurewebsites.net/about-nhsp (accessed 11 October 2022).
- National Health Service Digital . NHS Workforce Statistics 2020. https://digital.nhs.uk/data-and-information/publications/statistical/nhs-workforce-statistics (accessed 9 September 2022).
- Care Quality Commission . Using CQC Data 2020. www.cqc.org.uk/about-us/transparency/using-cqc-data (accessed 3 March 2022).
- National Health Service Digital . Hospital Episode Statistics 2020. https://digital.nhs.uk/data-and-information/data-tools-and-services/data-services/hospital-episode-statistics (accessed 19 September 2022).
- National Health Service Digital . NHS Vacancy Statistics 2021. https://digital.nhs.uk/data-and-information/publications/statistical/nhs-vacancies-survey (accessed 4 April 2022).
- Burke NN, Stewart D, Tierney T, Worrall A, Smith M, Elliott J, et al. Sharing space at the research table: exploring public and patient involvement in a methodology priority setting partnership. Res Involv Engagem 2023;9. https://doi.org/10.1186/s40900-023-00438-1.
- British Medical Association . Locum Working for SAS Doctors 2022. www.bma.org.uk/pay-and-contracts/contracts/sas-doctor-contract/locum-working-for-sas-doctors (accessed 8 October 2022).
- National Health Service Improvement . Agency Rules 2019. www.england.nhs.uk/publication/agency-rules/ (accessed 18 October 2022).
- Jeffers H, Baker M. Continuity of care: still important in modern-day general practice. Br J Gen Pract 2016;66:396-7. https://doi.org/10.3399/bjgp16X686185.
- Jennison T. Locum doctors: patient safety is more important than the cost. Int J Surg 2013;11:1141-2. https://doi.org/10.1016/j.ijsu.2013.09.014.
- Eysenbach G. Improving the quality of Web surveys: the Checklist for Reporting Results of Internet E-Surveys (CHERRIES). J Med Internet Res 2004;6. https://doi.org/10.2196/jmir.6.3.e34.
- Provo . Qualtrics Software. XM Ed. 2011. www.qualtrics.manchester.ac.uk (accessed 12 October 2022).
- National Health Service England . Responsible Officer FAQs 2023. www.england.nhs.uk/professional-standards/medical-revalidation/ro/ro-faqs/#:~:text=As%20a%20responsible%20officer%20you,the%20GMC%20over%20relevant%20procedures (accessed 23 November 2023).
- Braun V, Clarke V, Boulton E, Davey L, McEvoy C. The online survey as a qualitative research tool. Int J Soc Res Methodol 2020;24:641-54. https://doi.org/10.1080/13645579.2020.1805550.
- Braun V, Clarke V. Reflecting on reflexive thematic analysis. Qual Res Sport Exerc Health 2019;11:589-97. https://doi.org/10.1080/2159676x.2019.1628806.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77-101. https://doi.org/10.1191/1478088706qp063oa.
- Lock FK, Carrieri D. Factors affecting the UK junior doctor workforce retention crisis: an integrative review. BMJ Open 2022;12. https://doi.org/10.1136/bmjopen-2021-059397.
- General Medical Council . Understanding the Experiences of Locum Agency Locums: A Qualitative and Quantitative Research Study 2021. www.gmc-uk.org/about/what-we-do-and-why/data-and-research/research-and-insight-archive/understanding-the-experiences-of-locum-agency-locums (accessed 25 June 2022).
- Keers RN, Williams SD, Cooke J, Ashcroft DM. Causes of medication administration errors in hospitals: a systematic review of quantitative and qualitative evidence. Drug Saf 2013;36:1045-67. https://doi.org/10.1007/s40264-013-0090-2.
- Bajorek Z, Guest D. The impact of temporary staff on permanent staff in accident and emergency departments. J Organ Eff 2019;6:2-18. https://doi.org/10.1108/joepp-09-2018-0074.
- Krogstad U, Hofoss D, Hjortdahl P. Continuity of hospital care: beyond the question of personal contact. BMJ 2002;324:36-8. https://doi.org/10.1136/bmj.324.7328.36.
- Amery C, Griffin A. Exploring communities of practice in the NHS: a core medical trainee experience. Future Healthc J 2020;7:e1-5. https://doi.org/10.7861/fhj.2019-0034.
- Odebiyi B, Walker B, Gibson J, Sutton M, Spooner S, Checkland K. Eleventh National GP Worklife Survey. Policy Research Unit in Commissioning and the Healthcare System (PRUComm) 2021. https://prucomm.ac.uk/assets/uploads/Eleventh%20GPWLS%202021.pdf (accessed 7 August 2022).
- National Health Service Digital . Patients Registered at a GP Practice 2022. https://digital.nhs.uk/data-and-information/publications/statistical/patients-registered-at-a-gp-practice/may-2022 (accessed 7 August 2022).
- Marshall M, Ikpoh M. The workforce crisis in general practice. Br J Gen Pract 2022;72:204-5. https://doi.org/10.3399/bjgp22X719213.
- Wei H, Corbett RW, Ray J, Wei TL. A culture of caring: the essence of healthcare interprofessional collaboration. J Interprof Care 2020;34:324-31. https://doi.org/10.1080/13561820.2019.1641476.
- Sinnott C, Moxey JM, Marjanovic S, Leach B, Hocking L, Ball S, et al. Identifying how GPs spend their time and the obstacles they face: a mixed-methods study. Br J Gen Pract 2022;72:e148-60. https://doi.org/10.3399/BJGP.2021.0357.
- Murphy M, Salisbury C. Relational continuity and patients’ perception of GP trust and respect: a qualitative study. Br J Gen Pract 2020;70:e676-83. https://doi.org/10.3399/bjgp20X712349.
- Lok P. Junior doctors in England threaten to take industrial action over pay. BMJ 2022;377. https://doi.org/10.1136/bmj.o1458.
- Atkins R, Gibson J, Sutton M, Spooner S, Checkland K. Trends in GP incomes in England, 2008–2017: a retrospective analysis of repeated postal surveys. Br J Gen Pract 2020;70:e64-70. https://doi.org/10.3399/bjgp19X706073.
- Bakker AB, Demerouti E. Job demands–resources theory: taking stock and looking forward. J Occup Health Psychol 2017;22:273-85. https://doi.org/10.1037/ocp0000056.
- Gioia DA, Corley KG, Hamilton AL. Seeking qualitative rigor in inductive research: notes on the Gioia methodology. Organ Res Methods 2012;16:15-31. https://doi.org/10.1177/1094428112452151.
- Braun V, Clarke V. One size fits all? What counts as quality practice in (reflexive) thematic analysis?. Qual Res Psychol 2021;18:328-52. https://doi.org/10.1080/14780887.2020.1769238.
- Kidder LH, Fine M. Qualitative and quantitative methods: when stories converge. New Dir Prog Eval 1987;1987:57-75. https://doi.org/10.1002/ev.1459.
- Braun V, Clarke V. Toward good practice in thematic analysis: avoiding common problems and be(com)ing a knowing researcher. Int J Transgend Health 2023;24:1-6. https://doi.org/10.1080/26895269.2022.2129597.
- Tavory I, Timmermans S. Abductive Analysis: Theorizing Qualitative Research. University of Chicago Press; 2014.
- General Medical Council . Equality, Diversity and Inclusion: Targets, Progress and Priorities for 2022 2022. www.gmc-uk.org/-/media/documents/equality--diversity-and-inclusion---targets---progress-and-priorties_pdf-89470868.pdf (accessed 25 August 2022).
- National Health Service England . Medical Workforce Race Equality Standard (MWRES): WRES Indicators for the Medical Workforce 2020 2021. www.england.nhs.uk/wp-content/uploads/2021/07/MWRES-DIGITAL-2020_FINAL.pdf (accessed 4 November 2022).
- Office for National Statistics . Census 2021 Results 2022. https://census.gov.uk/census-2021-results (accessed 8 November 2022).
- National Health Service Digital . NHS Workforce 2020. www.ethnicity-facts-figures.service.gov.uk/workforce-and-business/workforce-diversity/nhs-workforce/latest (accessed 10 November 2022).
- QSR International Pty Ltd . NVivo. Version 12 Ed 2018. https://lumivero.com/products/nvivo/ (accessed 8 September 2022).
- Moffatt F, Martin P, Timmons S. Constructing notions of healthcare productivity: the call for a new professionalism?. Sociol Health Illn 2014;36:686-702. https://doi.org/10.1111/1467-9566.12093.
- Ries NM, Jansen J. Physicians’ views and experiences of defensive medicine: an international review of empirical research. Health Policy 2021;125:634-42. https://doi.org/10.1016/j.healthpol.2021.02.005.
- Taylor DJ, Goodwin D. Organisational failure: rethinking whistleblowing for tomorrow’s doctors. J Med Ethics 2022;48:672-7. https://doi.org/10.1136/jme-2022-108328.
- British Medical Association . Caring, Supportive, Collaborative: A Future Vision for the NHS 2021. www.bma.org.uk/media/2035/bma-caring-supportive-collaborative-survey-report-sept-2018.pdf (accessed 13 October 2022).
- Rothwell C, Kehoe A, Farook SF, Illing J. Enablers and barriers to effective clinical supervision in the workplace: a rapid evidence review. BMJ Open 2021;11. https://doi.org/10.1136/bmjopen-2021-052929.
- Spendlove Z. Medical revalidation as professional regulatory reform: challenging the power of enforceable trust in the United Kingdom. Soc Sci Med 2018;205:64-71. https://doi.org/10.1016/j.socscimed.2018.04.004.
- Aveling EL, Parker M, Dixon-Woods M. What is the role of individual accountability in patient safety? A multi-site ethnographic study. Sociol Health Illn 2016;38:216-32. https://doi.org/10.1111/1467-9566.12370.
- Karsh BT, Holden RJ, Alper SJ, Or CK. A human factors engineering paradigm for patient safety: designing to support the performance of the healthcare professional. Qual Saf Health Care 2006;15:i59-65. https://doi.org/10.1136/qshc.2005.015974.
- Parker J, Davies B. No blame no gain? From a no blame culture to a responsibility culture in medicine. J Appl Philos 2020;37:646-60. https://doi.org/10.1111/japp.12433.
- Thomas N, McGrann E, Zammit L, Eaton P, White W, Lingam C, et al. Junior doctor-designed induction booklet to improve future junior doctor experience in a new post. Future Healthc J 2019;6. https://doi.org/10.7861/futurehosp.6-2s-s17.
- Long L, Moore D, Robinson S, Sansom A, Aylward A, Fletcher E, et al. Understanding why primary care doctors leave direct patient care: a systematic review of qualitative research. BMJ Open 2020;10. https://doi.org/10.1136/bmjopen-2019-029846.
- Bradfield OM, Bismark M, Scott A, Spittal M. Vocational and psychosocial predictors of medical negligence claims among Australian doctors: a prospective cohort analysis of the MABEL survey. BMJ Open 2022;12. https://doi.org/10.1136/bmjopen-2021-055432.
- Skarshaug LJ, Kaspersen SL, Bjørngaard JH, Pape K. How does general practitioner discontinuity affect healthcare utilisation? An observational cohort study of 2.4 million Norwegians 2007–2017. BMJ Open 2021;11. https://doi.org/10.1136/bmjopen-2020-042391.
- Freeman G, Hughes J. Continuity of Care and the Patient Experience. London; 2010.
- Meyer ND, Singh H, Graber ML. Evaluation of outcomes from a national patient-initiated second-opinion program. Am J Med 1138;128:1138.e25-33. https://doi.org/10.1016/j.amjmed.2015.04.020.
- Blenkinsopp J, Snowden N, Mannion R, Powell M, Davies H, Millar R, et al. Whistleblowing over patient safety and care quality: a review of the literature. J Health Organ Manag 2019;33:737-56. https://doi.org/10.1108/JHOM-12-2018-0363.
- DiCuccio MH. The relationship between patient safety culture and patient outcomes: a systematic review. J Patient Saf 2015;11:135-42. https://doi.org/10.1097/PTS.0000000000000058.
- Wu F, Dixon-Woods M, Aveling EL, Campbell A, Willars J, Tarrant C, et al. The role of the informal and formal organisation in voice about concerns in healthcare: a qualitative interview study. Soc Sci Med 2021;280. https://doi.org/10.1016/j.socscimed.2021.114050.
- General Medical Council . Fair to Refer? 2019. www.gmc-uk.org/about/what-we-do-and-why/data-and-research/research-and-insight-archive/fair-to-refer (accessed 28 July 2022).
- Kehoe A, Rothwell C, Hesselgreaves H, Carter M, Illing J. Evaluation of GMC Welcome to UK Practice. University of Newcastle; 2019.
- Brown A, Dickinson H, Kelaher M. Governing the quality and safety of healthcare: a conceptual framework. Soc Sci Med 2018;202:99-107. https://doi.org/10.1016/j.socscimed.2018.02.020.
- Anderson M, O’Neill C, Clark JM, Street A, Woods M, Johnston-Webber C, et al. Securing a sustainable and fit-for-purpose UK health and care workforce. Lancet 2021;397:1992-2011. https://doi.org/10.1016/s0140-6736(21)00231-2.
- Warriner D, Malhotra A, Apps A. An epidemic of overdiagnosis and overtreatment: getting to the heart of the problem. J R Soc Med 2017;110:390-1.
- Borek AJ, Pouwels KB, van Hecke O, Robotham JV, Butler CC, Tonkin-Crine S. Role of locum GPs in antibiotic prescribing and stewardship: a mixed-methods study. Br J Gen Pract 2022;72:e118-27. https://doi.org/10.3399/BJGP.2021.0354.
- Tazzyman A, Ferguson J, Hillier C, Boyd A, Tredinnick-Rowe J, Archer J, et al. The implementation of medical revalidation: an assessment using normalisation process theory. BMC Health Serv Res 2017;17. https://doi.org/10.1186/s12913-017-2710-5.
- General Medical Council . The State of Medical Education and Practice in the UK 2014. www.gmc-uk.org/SOMEP_2014_FINAL.pdf_58751753.pdf (accessed 4 April 2022).
- Haggerty JL, Roberge D, Freeman GK, Beaulieu C. Experienced continuity of care when patients see multiple clinicians: a qualitative metasummary. Ann Fam Med 2013;11:262-71. https://doi.org/10.1370/afm.1499.
- Waibel S, Henao D, Aller MB, Vargas I, Vazquez ML. What do we know about patients’ perceptions of continuity of care? A meta-synthesis of qualitative studies. Int J Qual Health Care 2012;24:39-48. https://doi.org/10.1093/intqhc/mzr068.
- Preston C, Cheater F, Baker R, Hearnshaw H. Left in limbo: patients’ views on care across the primary/secondary interface. Qual Health Care 1999;8:16-21. https://doi.org/10.1136/qshc.8.1.16.
- National Health Service England and National Health Service Improvement . NHS Operational Planning and Contracting Guidance 2017–19 2016. www.england.nhs.uk/wp-content/uploads/2016/09/NHS-operational-planning-guidance-201617-201819.pdf (accessed 17 July 2021).
- Sidaway-Lee K, Gray DP, Evans P. A method for measuring continuity of care in day-to-day general practice: a quantitative analysis of appointment data. Br J Gen Pract 2019;69:e356-62. https://doi.org/10.3399/bjgp19X701813.
- Sandvik H, Hetlevik Ø, Blinkenberg J, Hunskaar S. Continuity in general practice as predictor of mortality, acute hospitalisation, and use of out-of-hours care: a registry-based observational study in Norway. Br J Gen Pract 2022;72:e84-90. https://doi.org/10.3399/BJGP.2021.0340.
- von Bultzingslowen I, Eliasson G, Sarvimaki A, Mattsson B, Hjortdahl P. Patients’ views on interpersonal continuity in primary care: a sense of security based on four core foundations. Fam Pract 2006;23:210-9. https://doi.org/10.1093/fampra/cmi103.
- Ocloo J, Garfield S, Franklin BD, Dawson S. Exploring the theory, barriers and enablers for patient and public involvement across health, social care and patient safety: a systematic review of reviews. Health Res Policy Syst 2021;19. https://doi.org/10.1186/s12961-020-00644-3.
- Ocloo J, Matthews R. From tokenism to empowerment: progressing patient and public involvement in healthcare improvement. BMJ Qual Saf 2016;25:626-32. https://doi.org/10.1136/bmjqs-2015-004839.
- Nair KM, Dolovich LR, Ciliska DK, Lee HN. The perception of continuity of care from the perspective of patients with diabetes. Fam Med 2005;37:118-24.
- Harrison A, Verhoef M. Understanding coordination of care from the consumer’s perspective in a regional health system. Health Serv Res 2002;37:1031-54. https://doi.org/10.1034/j.1600-0560.2002.64.x.
- Harris K, Russ S. Patient-completed safety checklists as an empowerment tool for patient involvement in patient safety: concepts, considerations and recommendations. Future Healthc J 2021;8:e567-73. https://doi.org/10.7861/fhj.2021-0122.
- Herrett E, Gallagher AM, Bhaskaran K, Forbes H, Mathur R, van Staa T, et al. Data resource profile: Clinical Practice Research Datalink (CPRD). Int J Epidemiol 2015;44:827-36. https://doi.org/10.1093/ije/dyv098.
- Herrett EL, Thomas SL, Smeeth L. Validity of diagnoses in the general practice research database. Br J Gen Pract 2011;61:438-9. https://doi.org/10.3399/bjgp11X583092.
- Khan NF, Harrison SE, Rose PW. Validity of diagnostic coding within the General Practice Research Database: a systematic review. Br J Gen Pract 2010;60:e128-36. https://doi.org/10.3399/bjgp10X483562.
- Lin M, Lucas H, Shmueli G. Too big to fail: large samples and the p-value problem. Inf Syst Res 2013;24:906-17. https://doi.org/10.1287/isre.2013.0480.
- Kontopantelis E, Stevens RJ, Helms PJ, Edwards D, Doran T, Ashcroft DM. Spatial distribution of clinical computer systems in primary care in England in 2016 and implications for primary care electronic medical record databases: a cross-sectional population study. BMJ Open 2018;8. https://doi.org/10.1136/bmjopen-2017-020738.
- Rodgers S, Taylor AC, Roberts SA, Allen T, Ashcroft DM, Barrett J, et al. Scaling-up a pharmacist-led information technology intervention (PINCER) to reduce hazardous prescribing in general practices: multiple interrupted time series study. PLOS Med 2022;19.
- Payne RA, Mendonca SC, Elliott MN, Saunders CL, Edwards DA, Marshall M, et al. Development and validation of the Cambridge Multimorbidity Score. CMAJ 2020;192:E107-14. https://doi.org/10.1503/cmaj.190757.
- Avery AJ, Rodgers S, Cantrill JA, Armstrong S, Cresswell K, Eden M, et al. A pharmacist-led information technology intervention for medication errors (PINCER): a multicentre, cluster randomised, controlled trial and cost-effectiveness analysis. Lancet 2012;379:1310-9. https://doi.org/10.1016/S0140-6736(11)61817-5.
- Spencer R, Bell B, Avery AJ, Gookey G, Campbell SM. Royal College of General Practitioners . Identification of an updated set of prescribing – safety indicators for GPs. Br J Gen Pract 2014;64:e181-90. https://doi.org/10.3399/bjgp14X677806.
- Aziz SA, Richardson J. The Living Hours Index 2: Exploring the Ethnicity Hours Gap 2022. www.livingwage.org.uk/sites/default/files/Living%20Hours%20Index%20Nov%2022.pdf (accessed 6 July 2022).
- National Health Service England . GP Patient Survey 2021. www.england.nhs.uk/statistics/2021/07/08/gp-patient-survey-2021/ (accessed 8 October 2021).
Appendix 1 Additional material for Chapter 3: the use of locum doctors in general practices in England: analysis of routinely collected workforce data
Data definitions
General practitioners workforce statistics data
The general practice data show numbers and details of GPs, Nurses, Direct Patient Care and Admin/Non-Clinical staff working in General Practice in England, along with information on their practices, staff, patients and the services they provide (available from https://digital.nhs.uk/data-and-information/publications/statistical/general-and-personal-medical-services).
All data are extracted quarterly from the National Workforce Reporting System (NWRS). This is an online system in which GP practices record and update staff details. Practices are asked to ensure that the information about their staff is up to date at the end of each quarter and NWRS automatically extracts the information. Furthermore, practices may make changes to individual records as appropriate, if they find mistakes in entries for the previous quarter. The NWRS has inbuilt validations to reduce data input errors and data are extracted every quarter, at the end of March, June, September and December, but for the October and November 2020 collections the data were extracted monthly at the end of each month. However, in the October and November collections, NHS Digital identified a number of data quality issues that caused a cautious interpretation of the data.
In particular, there was a shortfall in the GP locum data and NHS Digital included some estimations on FTE GP locum figures based on the previous quarter’s data. NHS Digital published only FTE figures for all practice staff, while they developed a methodology to account for missing headcount data. 2
However, the transition to a monthly collection in the autumn of 2020 led to a more wide-reaching decrease in the quality and completeness of the data, as practice managers did not record sufficient information on infrequent locums and the publication series was reverted to quarterly collections in December 2020. For this reason, we did not use the 2020 data in our regression analyses. The monthly series was preserved for transparency purposes, and it is advised that figures from these releases are not used in any further analysis and are not included in time-series tables. 2
In terms of recorded information for locums, the following definitions are used by NHS Digital to capture locums working in general practices:
-
Long term locums (covering vacancy/absence/other): Are defined as those locums who work regularly at the Practice to cover long periods of time, such as maternity leave, long-term sickness or work regularly (e.g. every Monday).
-
Infrequent locums: They are defined as GP locums who do not regularly work at a practice, may cover very few sessions and are typically employed on an ad hoc basis. Infrequent locum records were added to collecting tools in December 2017. The amount and detail of the data held by practices on infrequent locums are limited and the data collected for each infrequent locum reflect this, consisting solely of the total number of hours the infrequent locum worked at the practice during the reporting period, from which a weekly average FTE is calculated. Infrequent locums may not be working at the affected practice at the exact extraction date, but their inclusion improves the quality of the data collected for the period by providing valuable information about their usage.
However, the amount and detail of the FTE data held by practices on infrequent locums are limited and the data collected for each infrequent locum reflect this, consisting solely of the total number of hours the infrequent locum worked at the practice during the reporting period, from which a weekly average FTE is calculated. The infrequent locum data are considered to be of usable quality from the December 2017 release onwards, so it is advised that locum data are comparable from December 2017 onwards.
To conclude, we consider that data on FTE from December 2017 onwards are considered more reliable than that from earlier periods, as it followed the release after December 2016 of the improved guidance which emphasised the importance of recording locum data accurately and clarified how to do so and also it was the first time that infrequent locum data were added to the time series.
English indices of deprivation
Area deprivation was measured by the latest update of the IMD (i.e. 2019) and was available at the 2011 LSOA level. The IMD is a complete and commonly used method to quantify deprivation and affluence for small areas in England. The IMD measures levels of deprivation for all 32,844 LSOAs in England on a continuous scale of deprivation and most of the indicators are based on 2012 statistics. It represents a combined score of deprivation out of a total of 37 separate indicators which are grouped into 7 domains, income, employment, education and skills, health and disability, crime, barriers to housing and services, and living environment, thus reflecting a different domain of deprivation experienced by individuals living in an area. The overall IMD is calculated as a weighted mean across the seven domains and different weights are applied to each domain and the measure is standardised on the scale of 0–100. The IMD represents every small area in England and ranks them from 1 (most deprived area) to 32,844 (least deprived area).
Spatial maps
From the Office for National Statistics (ONS) open geography portal, we obtained. Digital vector boundaries for the 2019 CCGs, generalised to 20 m and clipped to the coastline to reduce size and improve visualisation. We inputted the vector boundaries in Stata using the shp2dta command and calculated the centroid for each CCG in the British National Grid format. The centroids were converted from British National Grid easting and northing to longitude and latitude in degrees.
Sex and population estimates
From NHS Digital, we obtained monthly general practice population counts for 2018 and 2019 at the general practice level (available from https://digital.nhs.uk/data-and-information/publications/statistical/patients-registered-at-a-gp-practice). The patients registered at a GP practice database is a monthly publication showing counts of patients at NHS Regions, Regional Local Offices, STP CCG and GP practice by gender and age. Data are collected at an aggregate level from GP practices by age and gender. The data are used by many NHS and local authority organisations as a denominator for other local analyses and are considered essential to maintaining this level of information. Data are extracted as a monthly snapshot in time from the GP Payments system maintained by NHS Digital.
Health regulators ratings
Health regulators ratings were obtained from the CQC (available from www.cqc.org.uk/about-us/transparency/using-cqc-data). CQC uses a statistical surveillance tool called Intelligent Monitoring (IM) to assess performance indicators based on routinely collected and available data about providers. The IM system for general practices contains 33 performance indicators concerning patient satisfaction, the management of chronic conditions, prescribing, disease prevalence and emergency hospital admissions. Together, these indicators are intended to support inspections with information on which practices to inspect and on which aspects of care to focus on. Performance indicators are aggregated into ratings of potential risk based on expected indicator values. Each year the CQC inspects general practices, and awards each of them one of four rating levels (‘outstanding’, ‘good’, ‘requires improvement’ or ‘inadequate’) in five domains (‘safe’, ‘effective’, ‘responsive’, ‘caring’ and ‘well led’), along with an ‘overall’ rating that summarised the domain ratings. From the CQC, we obtained published inspection ratings and corresponding inspection dates for 6587 of 6909 GP practices in 2018 (i.e. 95.3% of all practices in the GP workforce data set in 2018) and 6392 of 6606 practices in 2019 (i.e. 96.8% of all practices in the GP workforce data set in 2019) that were inspected between January 2017 and December 2019. Over the inspection cycle, some practices were reinspected and their ratings updated. Only the rating from the first inspection was used in this study, as subsequent ratings were likely to have been influenced by the previous inspection process and outcomes. Data on the most recent practice inspections are freely available online.
Patient satisfaction
The GP Patient Survey is an independent survey run by Ipsos MORI (London, UK) on behalf of NHS England (available from www.gp-patient.co.uk). The survey is sent out to over 2 million people across England and focuses on patient experiences of their local GP practice and other local NHS services, and it includes questions about general health. The survey includes questions about a number of issues. For example, how easy or difficult it is to make an appointment at your practice, patient satisfaction with opening hours and the quality of care received from the GP and practice nurses. To capture patient satisfaction, we use responses for the ‘Overall, how would you describe your experience of your GP Practice’. This is the only item relevant to experience that is consistent for all years. From the overall experience questions, we extracted data on the proportion of patients in each practice who responded that their experience was Very Good; Fairly Good; Not Bad Not Good; Fairly Poor and Very Poor. 135
Quality of primary care and practice morbidity burden (Quality and Outcomes Framework)
To quantify ‘health-need’ from chronic condition registers, we used administrative data from the QOF, for the financial year 2018–9 to 2019–20 (available from https://digital.nhs.uk/data-and-information/publications/statistical/quality-and-outcomes-framework-achievement-prevalence-and-exceptions-data). The pay-for-performance scheme, which was introduced in 2004, rewards clinicians for recording and managing numerous clinical domains, mostly chronic conditions. Although it has been downsized in recent years and has been withdrawn completely in Scotland, it has been at the heart of the GP contract for many years and there is evidence that the withdrawal of incentives does not affect recording practices, not in the short term at least.
In 2019–20, 21 clinical domains were included in the scheme: atrial fibrillation, asthma, cancer, coronary heart disease, chronic kidney disease (aged 18 or over only), chronic obstructive pulmonary disease, diabetes both types (aged 17 or over), heart failure, hypertension, osteoporosis (aged 50 or over), palliative care, cardiovascular disease primary prevention, peripheral artery disease, rheumatoid arthritis (aged 16 or over), stroke and obesity (aged 16 or over), dementia, depression (aged 18 or over), epilepsy (aged 18 or over), learning disability (18 or over) and severe mental illness. We used a subset of these conditions as only 14 had clinical indicators linked to them in both data years. The data range refers to the relevant financial year (1 April–31 March) and it is matched to the relevant GP Workforce publication (i.e. QOF 2019–20 data are matched to GP Workforce data from the financial year 2019–20).
Although access to health care is free in the UK, not all people in the UK are registered with primary care and not all general practices participate in the QOF. However, over 95% of the UK population is estimated to be registered with a practice, and over 95% of registered patients attend practices participating in the QOF. A total of 6873 English practices participated in the QOF in 2019–20 and for each of these practices we extracted the denominators from the condition registers. Unfortunately, there is no way to capture multimorbidity with these data, since the QOF is organised in condition silos and a multimorbid patient would be reported under all relevant conditions in the scheme. The total numbers for each of the three groups were also aggregated at the CCG level, with 135 entities covering the whole of English Primary Care.
To capture QOF performance, we used the percentage of patients receiving the intervention for the relevant population across QOF indicators as the main measure of quality. This measure is defined as PA=∑ Ni∑ (Di+Ei) where the numerator represents the sum of all patients who have actually received the care (Ni) described in the relevant indicator (indicator i), and the denominator represents the sum of the number of patients from the appropriate disease register who are eligible to receive the care described in the relevant QOF indicator (Di) and the sum of the number of patients who have been exception reported for the relevant QOF indicator is (Ei). This measure reflects the proportion of patients for whom a practice achieved a quality indicator rather than the number of QOF points scored. This measure also gives a more accurate indication of the rate of the provision of an intervention as the denominator for this measure covers all patients to whom the indicator applies, regardless of exception status (i.e. indicator exceptions and indicator denominator).
Indicators included in the composite measure of quality of care
We extracted data indicator’s numerator, indicators and exceptions for 15 conditions including atrial fibrillation, asthma, cancer, coronary heart disease, chronic obstructive pulmonary disease, dementia, depression, diabetes, heart failure, hypertension, osteoporosis, peripheral arterial disease, rheumatoid arthritis, serious mental illness and stroke and were aggregated into a single score. These indicators have been revised many times over the years, but their underlying aim has remained the same. Furthermore, some indicators were dropped while others were revised for the duration of the QOF. If an indicator was dropped from the scheme, we calculated population achievement for each year from the remaining indicators. If an indicator was revised, we did the revision based on the time span that measurement or treatment was taken or provided (e.g. for some indicators the time span was specified for 15 months but after the revision the time span was reduced to 12 months).
| CCGs with the highest locum use in England | Locum use (%)a | IMD | Sum of general practice population | Practices, n | Practice list size, median (IQR) |
|---|---|---|---|---|---|
| CCGs with the lowest locum use in England | Locum use (%)a | IMD | General practice population | Practices, n | Practice list size, median (IQR) |
| NHS Southend CCG | 14.32 | 27.99 | 189,709 | 27 | 5299 (3069–7853) |
| NHS Thurrock CCG | 13.49 | 23.47 | 180,236 | 27 | 5527 (3278–9743) |
| NHS Barking and Dagenham CCG | 12.80 | 34.12 | 229,789 | 35 | 5703 (4610–8250) |
| NHS Hounslow CCG | 11.96 | 19.69 | 327,295 | 42 | 7199 (5129–8558) |
| NHS City and Hackney CCG | 9.34 | 34.28 | 325,553 | 41 | 7028 (4989–10,364) |
| NHS Leicester City CCG | 9.17 | 32.43 | 417,669 | 55 | 5946 (4053–9507) |
| NHS Waltham Forest CCG | 9.11 | 28.57 | 316,977 | 38 | 7017 (4975–9128) |
| NHS Sandwell and West Birmingham CCG | 8.42 | 41.24 | 577,116 | 81 | 4854 (3248–8592) |
| NHS Blackburn with Darwen CCG | 7.73 | 44.59 | 177,606 | 23 | 5515 (4730–10,719) |
| NHS Knowsley CCG | 7.57 | 54.41 | 167,033 | 25 | 5213 (3754–8758) |
| NHS Vale of York CCG | 0.41 | 13.33 | 362,253 | 26 | 9356 (6068–17,312) |
| NHS Bassetlaw CCG | 0.54 | 25.073 | 118,775 | 9 | 12,024 (3504–18,798) |
| NHS Wirral CCG | 0.52 | 35.43 | 337,781 | 45 | 5935 (4449–8543) |
| NHS Morecambe Bay CCG | 0.71 | 25.27 | 349,905 | 32 | 6374 (4414–9917) |
| NHS South Tyneside CCG | 0.97 | 39.41 | 158,221 | 21 | 6539 (4493–8095) |
| NHS Halton CCG | 0.99 | 50.84 | 132,916 | 12 | 9487 (8251–13,561) |
| NHS North Staffordshire CCG | 1.14 | 21.79 | 218,016 | 31 | 7151 (4300–9142) |
| NHS Trafford CCG | 1.21 | 15.83 | 243,278 | 30 | 4854 (3248–8592) |
| NHS Stafford and Surrounds CCG | 1.26 | 18.43 | 149,477 | 14 | 5515 (4730–10,719) |
| NHS Fylde and Wyre CCG | 1.29 | 22.05 | 178,576 | 17 | 5213 (3754–8758) |
| Model A, analyses over time | Model B, cross-section analyses | |
|---|---|---|
| Rurality (0 = urban, 1 = rural) | 1.250 (1.095 to 1.428), < 0.001 (0.085) | 1.300 (1.085 to 1.559), < 0.004 (0.120) |
| IMD 2019 | 1.002 (0.999 to 1.006), < 0.096 (0.002) | 1.005 (1.000 to 1.009), < 0.046 (0.002) |
| QOF practice performance | 1.005 (0.991 to 1.017), < 0.479 (0.007) | 1.009 (0.991 to 1.026), < 0.298 (0.009) |
| Single-handed practice | 4.611 (4.101 to 5.184), < 0.001 (0.276) | 4.618 (3.928 to 5.428), < 0.001 (0.381) |
| QOF morbidity burden | 1.384 (0.963 to 1.991), < 0.079 (0.257) | 1.255 (0.801 to 1.996), < 0.320 (0.287) |
| Percentage of female population | 0.967 (0.959 to 0.981), < 0.001 (0.006) | 0.970 (0.946 to 0.994), < 0.015 (0.012) |
| Proportion of practice population aged ≥ 65 | 0.970 (0.950 to 0.984), < 0.001 (0.009) | 0.971 (0.958 to 0.988), < 0.001 (0.007) |
| Practice workload (total GP FTE/list size) | 1.001 (1.001 to 1.002), < 0.001 (0.001) | 1.001 (1.001 to 1.002), < 0.003 (0.001) |
| CQC ratings (reference group is practices rates as providing outstanding services) | Reference group | Reference group |
| Inadequate | 2.108 (1.370 to 3.246), < 0.001 (0.464) | 2.687 (1.451 to 4.974), < 0.001 (0.844) |
| Requires improvement | 1.229 (0.949 to 1.592), < 0.118 (0.163) | 1.198 (0.822 to 1.744), < 0.346 (0.229) |
| Good | 1.343 (1.103 to 1.637), < 0.003 (0.136) | 1.267 (0.947 to 1.696), < 0.111 (0.188) |
| Patient satisfaction Very good (reference group is the percentage of patient with very good satisfaction) |
Reference group | Reference group |
| Fairly good | 1.008 (1.003 to 1.014), < 0.001 (0.003) | 1.016 (1.008 to 1.024), < 0.001 (0.004) |
| Not good, not poor | 1.026 (1.017 to 1.035), < 0.001 (0.005) | 1.022 (1.009 to 1.037), < 0.001 (0.007) |
| Fairly poor | 1.032 (1.019 to 1.046), < 0.001 (0.007) | 1.033 (1.014 to 1.054), < 0.001 (0.010) |
| Very poor | 1.010 (0.992 to 1.027), < 0.268 (0.009) | 1.010 (0.987 to 1.033), < 0.392 (0.012) |
| Region (reference region is Midlands) | Reference group | Reference group |
| London | 1.369 (1.180 to 1.588), < 0.001 (0.104) | 1.330 (1.080 to 1.640), < 0.008 (0.142) |
| East of England | 1.100 (0.944 to 1.283), < 0.222 (0.086) | 1.080 (0.869 to 1.344), < 0.486 (0.120) |
| North East and Yorkshire | 0.711 (0.626 to 0.843), < 0.001 (0.055) | 0.811 (0.666 to 0.990), < 0.040 (0.082) |
| North West | 0.916 (0.793 to 1.059), < 0.237 (0.067) | 0.921 (0.750 to 1.130), < 0.432 (0.096) |
| South East | 0.918 (0.793 to 1.062), < 0.248 (0.068) | 1.014 (0.828 to 1.243), < 0.890 (0.105) |
| South West | 1.105 (0.932 to 1.309), < 0.250 (0.096) | 1.080 (0.845 to 1.382), < 0.535 (0.136) |
| Year (reference year is 2018) | Reference year | – |
| 2019 | 1.055 (0.970 to 1.148), < 0.210 (0.045) | – |
| Constant | 0.041 (0.011 to 0.142), < 0.001 (0.026) | 0.020 (0.004 to 0.111), < 0.001 (0.018) |
FIGURE 28.
Geographical distribution of locum use in 2019. Locum use is defined as mean locum FTE as a proportion (%) of total GP FTE. Population is divided into quintiles depending on levels of locum use. A higher level of the measure in the key represents higher locum use in the locality.
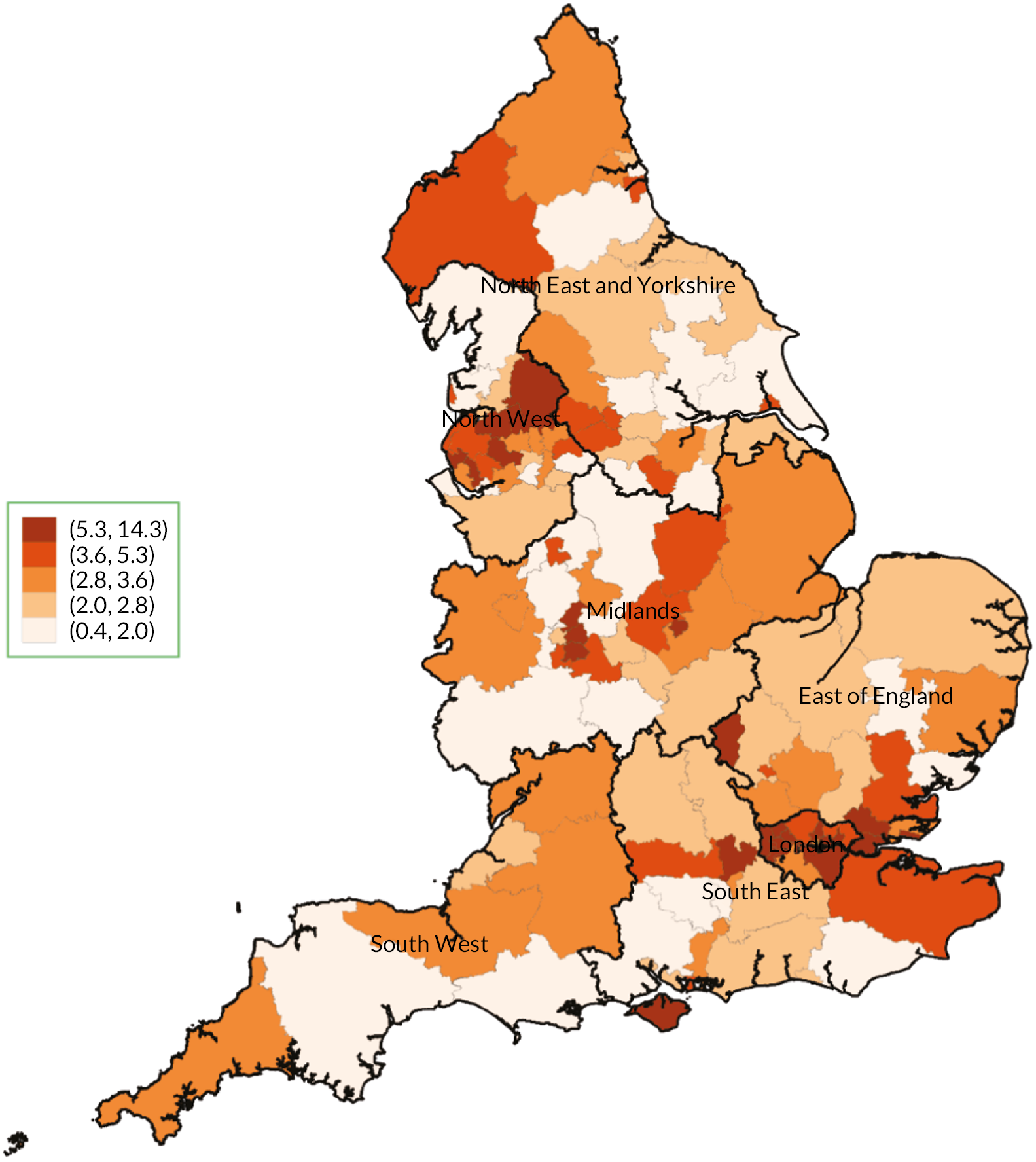
Appendix 2 Additional material for Chapter 4: the use of locum doctors in National Health Service trusts in England:analysis of routinely collected workforce data and electronic patient records
Data definitions
National Health Service workforce statistics database
National Health Service Digital collects monthly NHS Hospital and Community Health Service (HCHS) workforce statistics for staff in NHS trusts and CCGs in England. The data are recorded within the ESR, which is a payroll and human resources system and contains staff records for NHS-employed staff in England since 2008. Data are available as headcount and FTEs and for all months from September 2009 onwards and they represent an accurate summary of the validated data extracted from the NHS ESR system. We downloaded monthly data collections available from NHS Digital from December 2017 to December 2021 (available from https://digital.nhs.uk/data-and-information/publications/statistical/nhs-workforce-statistics). For each month and each NHS trust, we calculated the average total FTE across all available doctor categories in the NHS workforce database and matched the data to NHS improvement data for each trust in each month. The database also included monthly NHS trust level turnover data which were used in the negative binomial regression.
National Health Service vacancy statistics
From NHS Digital, we obtained trust level vacancy rates for the period January 2019–December 2019 (available from https://digital.nhs.uk/data-and-information/publications/statistical/nhs-vacancies-survey). The series refers to vacancy FTE from providers which are available on a quarterly basis but recorded on a monthly basis. This monthly rate is defined as the total number of unfilled posts reported at the end of each respective reporting month. A vacancy is defined as a post that is unfilled by permanent or fixed-term staff. Some vacant posts may be filled by agency or temporary staff, but these posts are still considered vacancies. The number of vacancies is the difference between the number of reported FTE permanent or fixed-term staff in post and planned workforce levels (i.e. the total funded or budgeted establishment on a FTE basis). 50
Health regulators ratings
Health regulators ratings were obtained from the CQC. Each rating is based on the assessment of the evidence against the key lines of enquiry in the assessment framework for healthcare services and, for relevant non-specialist acute trusts, the use of resources assessment framework. The trust level ratings refer to the trust’s overall quality, based on findings under five key quality questions that CQC inspects (safe, effective, caring, responsive and well led). Where applicable, the CQC also awards a combined rating at the trust level, based on the findings of the five trust-level quality ratings plus a use of resources rating. Each year the CQC inspects NHS trusts, and awards each of them one of four rating levels (‘outstanding’, ‘good’, ‘requires improvement’ or ‘inadequate’) in five domains (‘safe’, ‘effective’, ‘responsive’, ‘caring’ and ‘well led’), along with an ‘overall’ rating that summarised the domain ratings. From the CQC, we obtained published inspection ratings and corresponding inspection dates for all 229 NHS trusts in 2019 that were inspected between January 2019 and December 2019. Over the inspection cycle, some NHS trusts were reinspected and their ratings updated. Only the rating from the first inspection was used in this study, as subsequent ratings were likely to have been influenced by the previous inspection process and outcomes. Data on the most recent practice inspections are freely available online from www.cqc.org.uk/about-us/transparency/using-cqc-data.
English indices of deprivation
Area deprivation was measured by the latest update of the IMD (i.e. 2019) and was available at the 2011 LSOA level. The IMD is a complete and commonly used method to quantify deprivation and affluence for small areas in England. The IMD measures levels of deprivation for all 32,844 LSOAs in England on a continuous scale of deprivation and most of the indicators are based on 2012 statistics. It represents a combined score of deprivation out of a total of 37 separate indicators which are grouped into 7 domains, income, employment, education and skills, health and disability, crime, barriers to housing and services, and living environment, thus reflecting a different domain of deprivation experienced by individuals living in an area. The overall IMD is calculated as a weighted mean across the seven domains and different weights are applied to each domain and the measure is standardised on the scale of 0–100. The IMD represents every small area in England and ranks them from 1 (most deprived area) to 32,844 (least deprived area). These area measures were assigned to trust based on trusts’ location. Trusts in our analysis are allocated an IMD score based on the mean IMD score of all admitted patients using data from HES admitted patient care database 2017.
Spatial maps
From the ONS open geography portal, we obtained digital vector boundaries for the 2019 STPs, generalised to 20 m and clipped to the coastline to reduce size and improve visualisation. We inputted the vector boundaries in Stata using the shp2dta command and calculated the centroid for each CCG in the British National Grid format. The centroids were converted from British National Grid easting and northing to longitude and latitude in degrees.
| Trusts with the highest locum intensity in England | Locum intensitya | Trusts with the lowest locum intensity in England | Locum intensitya |
|---|---|---|---|
| North East London NHS Foundation Trust | 0.795 | Royal Papworth Hospital NHS Foundation Trust | 0.001 |
| Bedfordshire Hospitals Foundation Trust | 0.768 | Cambridgeshire Community Services NHS Trust | 0.002 |
| Rotherham Doncaster And South Humber NHS Foundation Trust | 0.684 | The Newcastle Upon Tyne Hospitals NHS Foundation Trust | 0.004 |
| Oxford Health NHS Foundation Trust | 0.621 | Moorfields Eye Hospital NHS Foundation Trust | 0.009 |
| Dudley and Walsall Mental Health Partnership NHS Trust | 0.602 | Alder Hey Children’s NHS Foundation Trust | 0.010 |
| North Cumbria University Hospitals NHS Trust | 0.595 | North Tees and Hartlepool NHS Foundation Trust | 0.014 |
| George Eliot Hospital NHS Trust | 0.591 | University Hospitals Bristol and Weston NHS Foundation Trust | 0.014 |
| North Cumbria Integrated Care NHS Foundation Trust | 0.551 | Sheffield Children’s NHS Foundation Trust | 0.022 |
| United Lincolnshire Hospitals NHS Trust | 0.548 | Leeds Community Healthcare NHS Trust | 0.025 |
| Pennine Acute Hospitals NHS Trust | 0.548 | Imperial College Healthcare NHS Trust | 0.029 |
| Locum intensity | Agency shifts | Unfilled shifts | |
|---|---|---|---|
| Trust-level aggregate FTE (reference group is quintile 1) | Reference group | Reference group | Reference group |
| Quintile 2 | 0.499 (0.369 to 0.676), < 0.001 (0.077) | 1.044 (0.811 to 1.344), < 0.735 (0.134) | 2.189 (0.967 to 4.960), < 0.060 (0.913) |
| Quintile 3 | 0.465 (0.321 to 0.676), < 0.001 (0.088) | 1.044 (0.760 to 1.434), < 0.787 (0.169) | 3.076 (1.179 to 8.023), < 0.022 (1.504) |
| Quintile 4 | 0.486 (0.329 to 0.716), < 0.001 (0.096) | 0.937 (0.671 to 1.311), < 0.708 (0.160) | 2.572 (0.937 to 7.063), < 0.067 (1.325) |
| Quintile 5 | 0.248 (0.157 to 0.390), < 0.001 (0.057) | 0.859 (0.574 to 1.287), < 0.462 (0.177) | 3.783 (1.237 to 11.572), < 0.020 (2.158) |
| Trust type (reference group is NHS non-specialist trust) | Reference group | Reference group | Reference group |
| NHS specialist trust | 0.254 (0.176 to 0.366), < 0.001 (0.047) | 1.600 (1.153 to 2.220), < 0.005 (0.268) | 0.321 (0.119 to 0.866), < 0.025 (0.162) |
| Mental health trust | 0.991 (0.643 to 1.233), < 0.487 (0.147) | 1.556 (1.180 to 2.052), < 0.002 (0.219) | 1.015 (0.457 to 2.256), < 0.971 (0.414) |
| CQC ratings (reference group is trusts that provide good and outstanding services) | Reference group | Reference group | Reference group |
| Inadequate and requiring improvement | 1.626 (1.365 to 1.938), < 0.001 (0.145) | 1.039 (0.899 to 1.201), < 0.601 (0.077) | 1.329 (0.855 to 2.066), < 0.206 (0.299) |
| IMD (reference group is quintile 1, where 1 is the most deprived) | |||
| Quintile 2 | 1.072 (0.818 to 1.406), < 0.610 (0.148) | 1.077 (0.859 to 1.349), < 0.520 (0.124) | 0.585 (0.308 to 1.111), < 0.101 (0.191) |
| Quintile 3 | 1.138 (0.855 to 1.514), < 0.375 (0.166) | 1.182 (0.936 to 1.494), < 0.159 (0.141) | 0.494 (0.248 to 0.986), < 0.046 (0.174) |
| Quintile 4 | 1.153 (0.855 to 1.554), < 0.350 (0.175) | 1.198 (0.933 to 1.539), < 0.156 (0.153) | 0.948 (0.448 to 2.008), < 0.890 (0.363) |
| Quintile 5 | 1.038 (0.741 to 1.455), < 0.827 (0.179) | 1.169 (0.882 to 1.550), < 0.278 (0.168) | 0.628 (0.286 to 1.381), < 0.247 (0.252) |
| Region (reference region is London) | Reference group | Reference group | Reference group |
| South West | 0.468 (0.328 to 0.668), < 0.001 (0.085) | 1.595 (1.198 to 2.123), < 0.014 (0.233) | 1.258 (0.510 to 3.103), < 0.618 (0.580) |
| South East | 0.746 (0.531 to 1.048), < 0.092 (0.130) | 1.498 (1.136 to 1.975), < 0.006 (0.211) | 0.578 (0.262 to 1.273), < 0.174 (0.233) |
| Midlands | 0.980 (0.718 to 1.337), < 0.896 (0.155) | 1.481 (1.149 to 1.908), < 0.001 (0.192) | 0.795 (0.371 to 1.700), < 0.553 (0.308) |
| East of England | 0.815 (0.579 to 1.147), < 0.240 (0.142) | 1.632 (1.233 to 2.161), < 0.001 (0.234) | 0.419 (0.177 to 0.988), < 0.047 (0.184) |
| North West | 0.917 (0.646 to 1.301), < 0.627 (0.163) | 1.289 (0.964 to 1.724), < 0.101 (0.191) | 1.176 (0.508 to 2.724), < 0.704 (0.504) |
| North East and Yorkshire | 0.703 (0.491 to 1.005), < 0.053 (0.128) | 1.450 (1.084 to 1.941), < 0.001 (0.215) | 0.753 (0.299 to 1.901), < 0.549 (0.356) |
| Constant | 0.381 (0.221 to 0.656), < 0.001 (0.105) | 0.339 (0.219 to 0.524), < 0.001 (0.075) | 0.065 (0.017 to 0.247), < 0.001 (0.045) |
FIGURE 29.
Mean locum intensity (bank and agency shifts combined) at trust level in 2020. Dashed line indicates the median (0.170) locum intensity per week per FTE across 216 NHS trusts in 2020. Eight trusts were excluded from due to very small or zero denominators (i.e. permanent doctor FTE).

FIGURE 30.
Mean proportion of agency shifts at trust level in 2020. Dashed line indicates the median (62.9%) proportion of agency shifts per week across 224 NHS trusts in 2020.

FIGURE 31.
Mean proportion of unfilled shifts at trust level in 2020. Dashed line indicates the median (8.12%) unfilled shift rate per week across 224 NHS trusts in 2020.
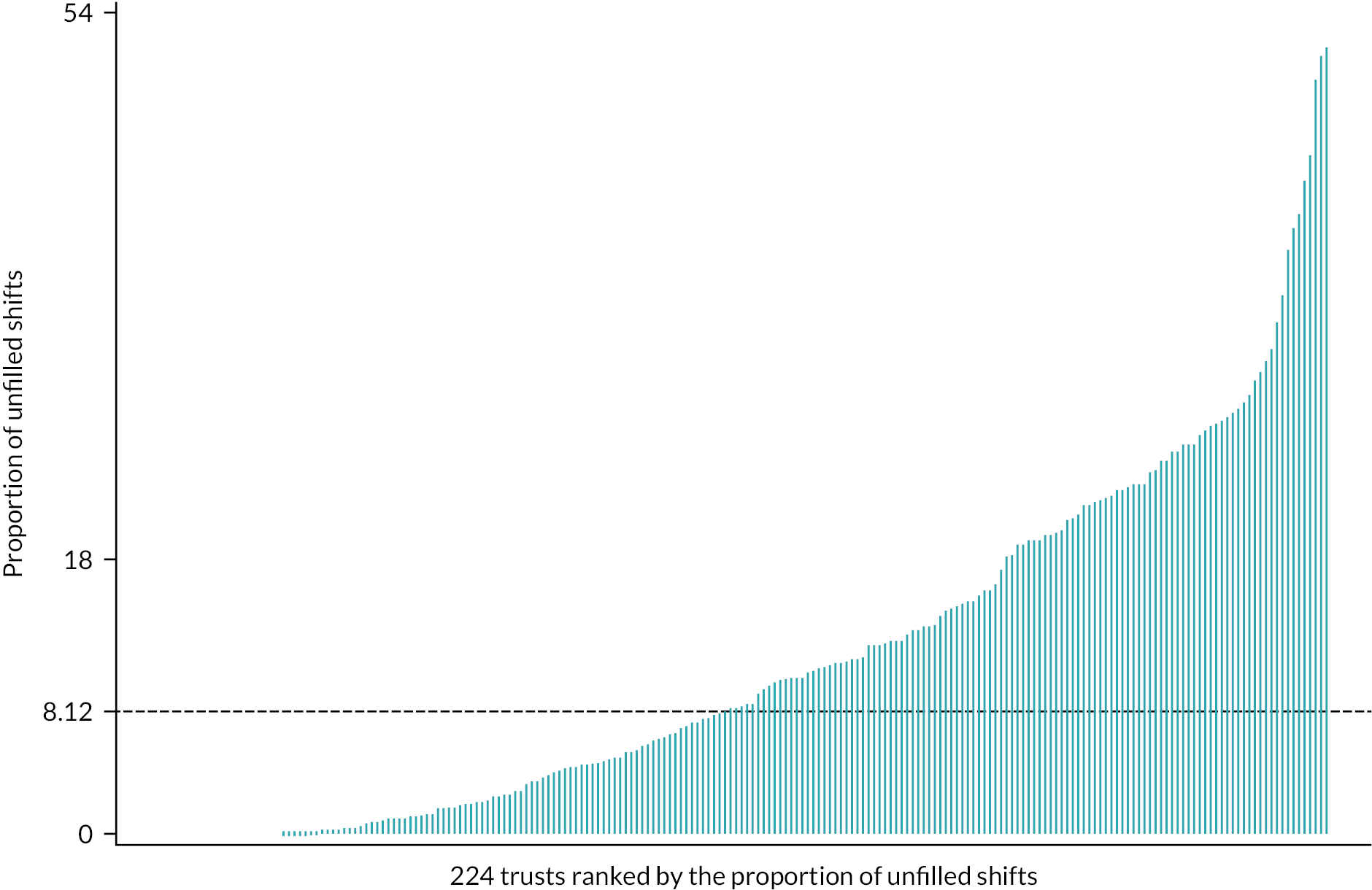
FIGURE 32.
Mean locum intensity (bank and agency shifts combined) at trust level in 2021. Dashed line indicates the median (μ = 0.193) locum intensity per week per FTE across 208 NHS trusts in 2021. Thirteen trusts were excluded from the analyses due to very small or zero denominators (i.e. permanent doctor FTE).
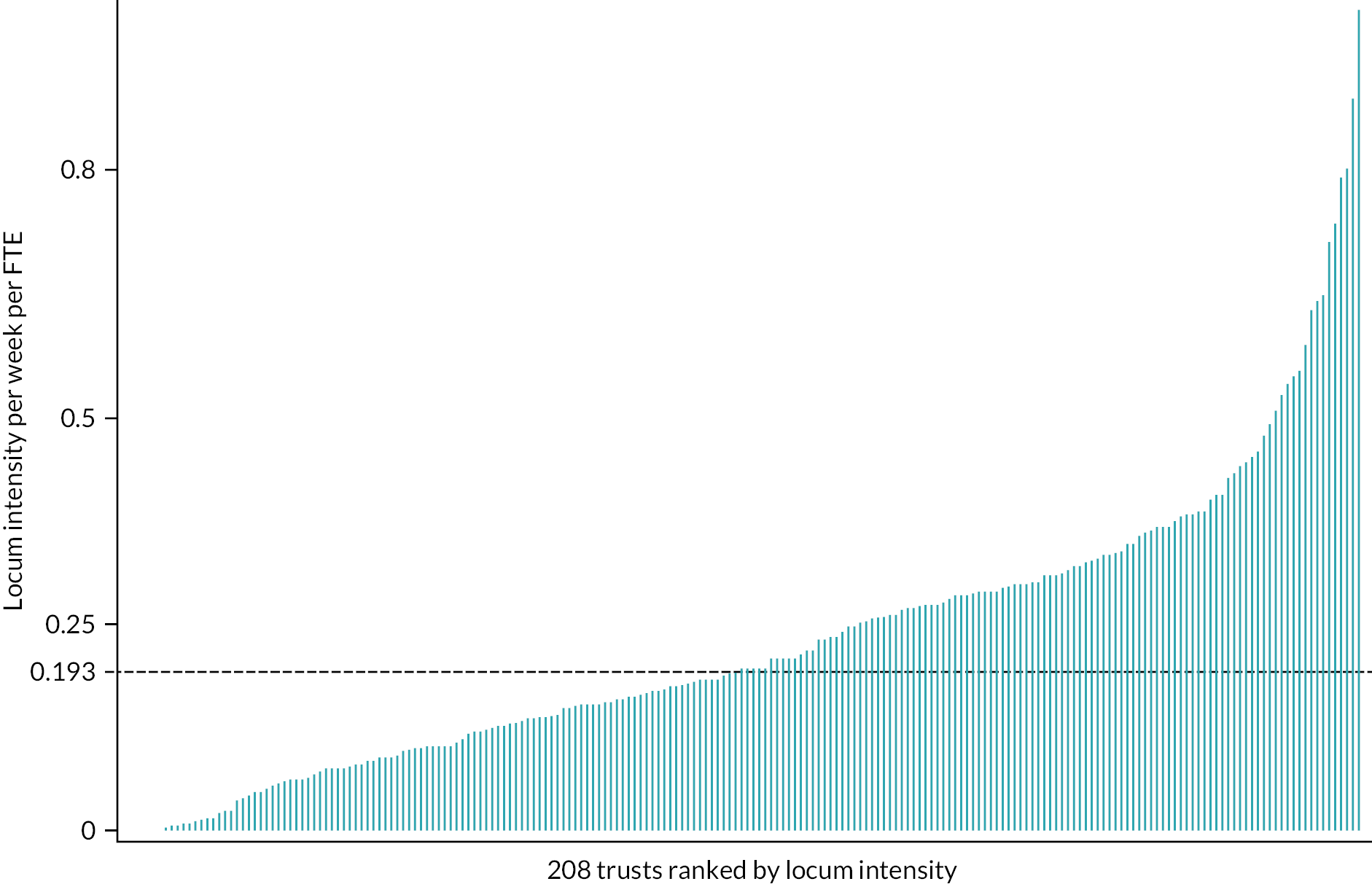
FIGURE 33.
Mean proportion of agency shifts at trust level in 2021. Dashed line indicates the median (μ = 55.7%) proportion of agency shifts per week across 221 NHS trusts in 2021.

FIGURE 34.
Mean proportion of unfilled shifts at trust level in 2021. Dashed line indicates the median (μ = 12%) unfilled shift rate per week across 221 NHS trusts in 2021.
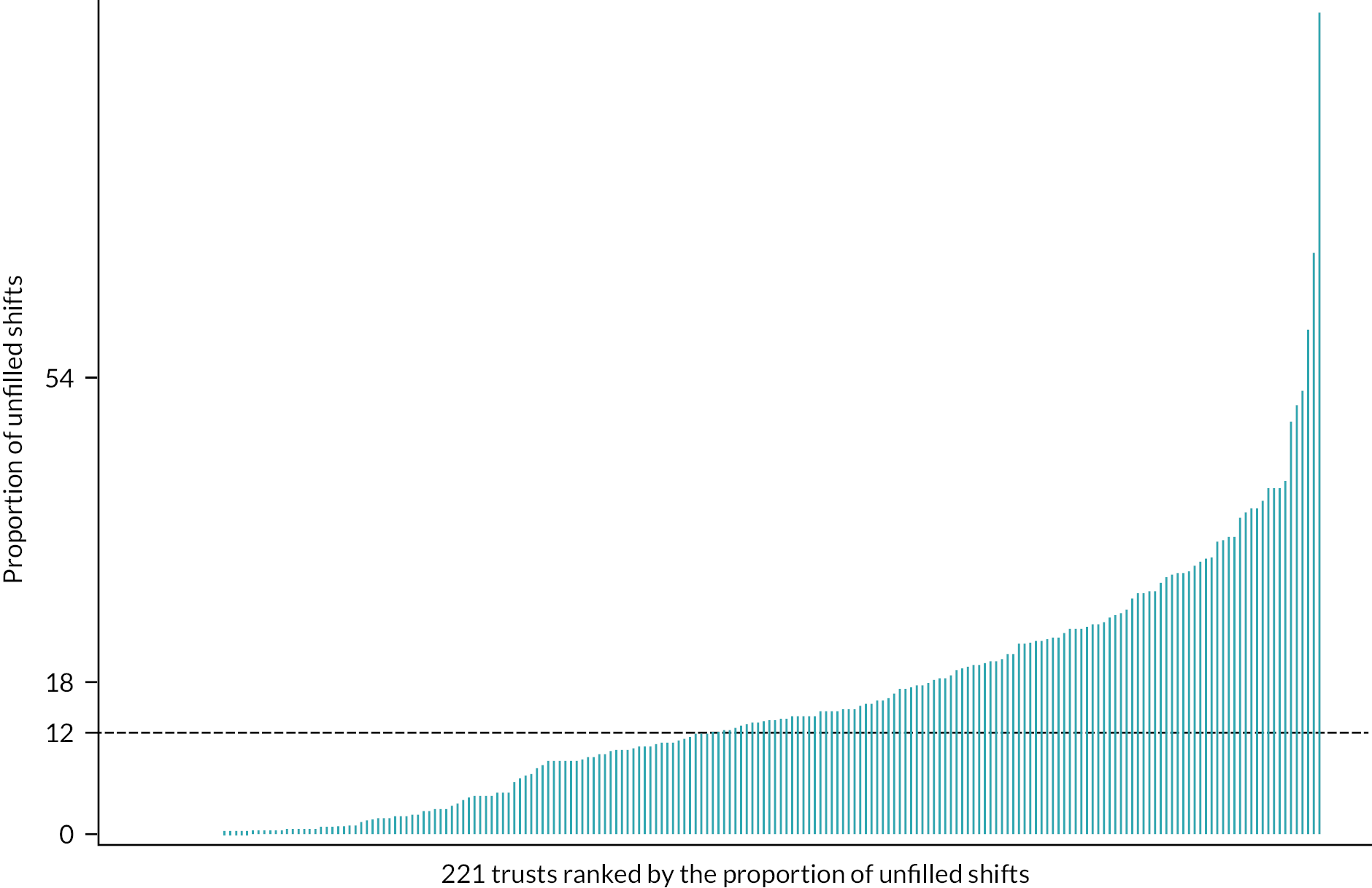
FIGURE 35.
Regional variation in locum intensity (bank and agency shifts combined) at trust level in 2020. Figure includes data from 218 NHS trusts in 2020, adjusted for substantive doctor FTE.
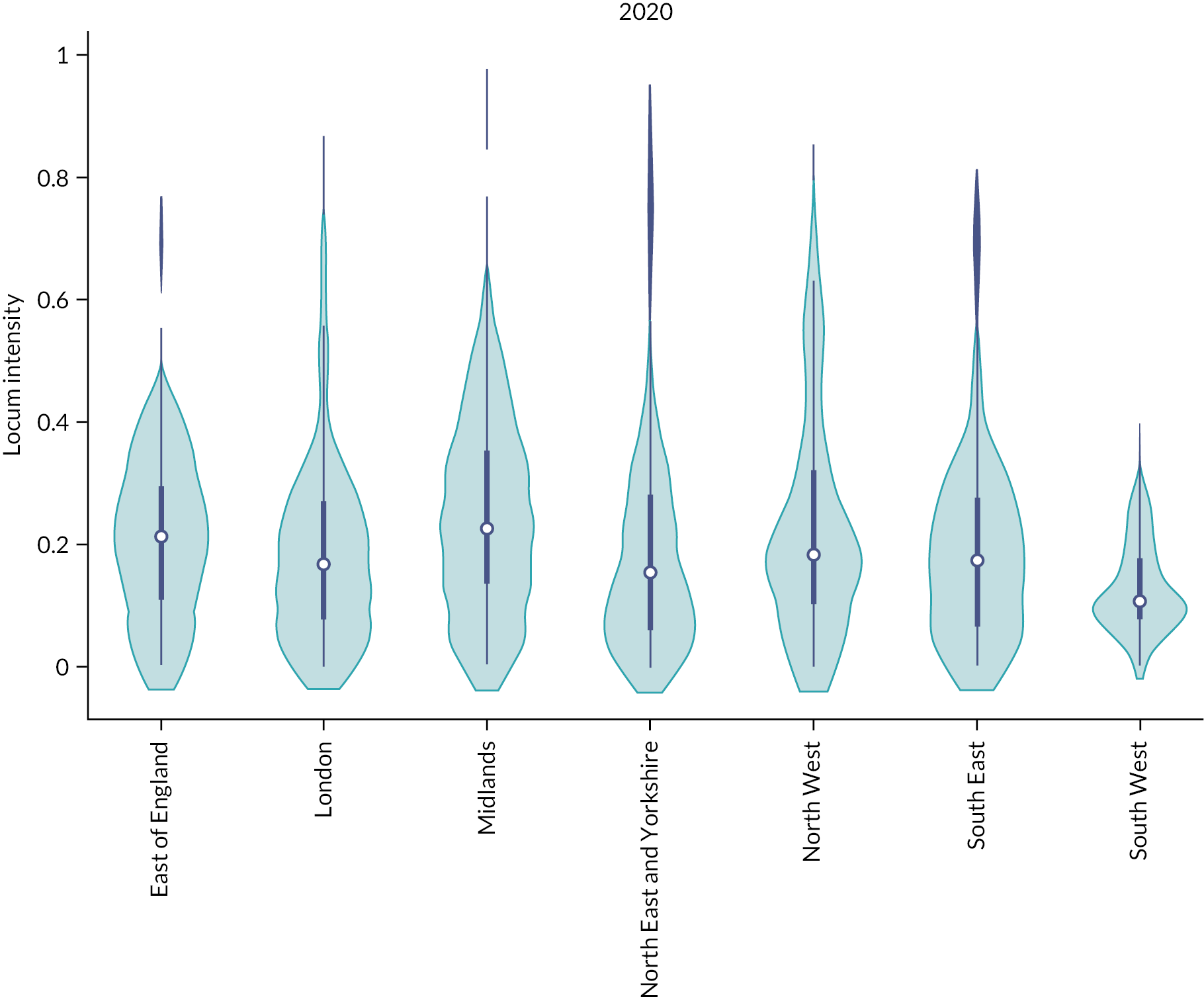
FIGURE 36.
Regional variation in the proportion of agency shifts at trust level in 2020. Dashed line indicates the median (μ = 55.7%) proportion of agency shifts per week across 221 NHS trusts in 2021. The thick blue line represents the IQR (25th–75th centile). The thin line represents the rest of the distribution with upper/lower adjacent values. The white dot represents the median. The distribution shape of the data is based on a kernel density estimation where wider sections of the plot represent a higher chance that members of the population of interest will take on a given value and where thinner section represents lower chance. Eleven trusts were excluded from the analyses due to non-availability of data for permanent doctor FTE.
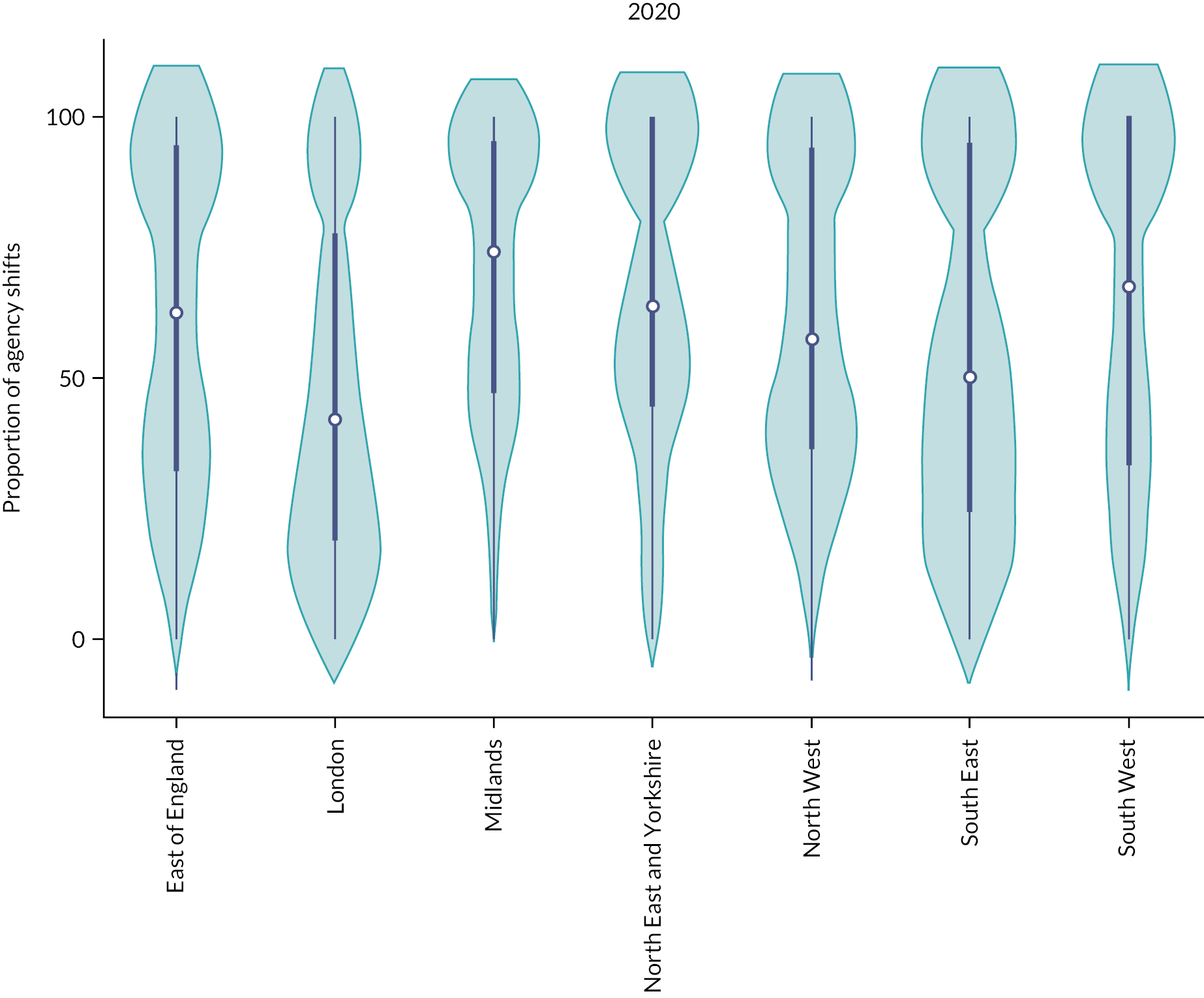
FIGURE 37.
Regional variation in the proportion of unfilled shifts at trust level in 2020 (figure includes data from 224 NHS trusts in 2020). The thick blue line represents the IQR (25th–75th centile). The thin line represents the rest of the distribution with upper/lower adjacent values. The white dot represents the median. The distribution shape of the data is based on a kernel density estimation where wider sections of the plot represent a higher chance that members of the population of interest will take on a given value and where thinner section represents lower chance. Eleven trusts were excluded from the analyses due to non-availability of data for permanent doctor FTE.
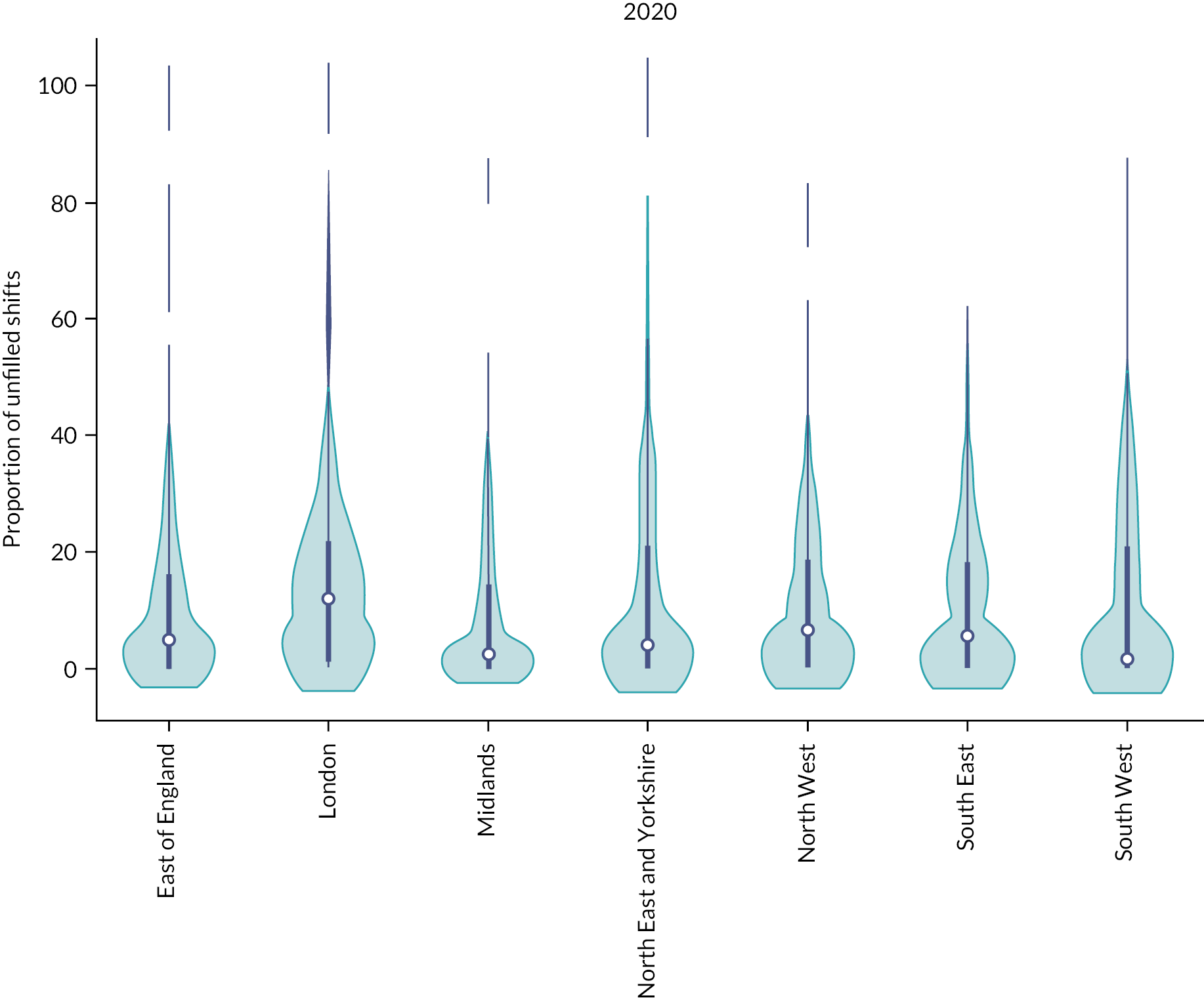
FIGURE 38.
Regional variation in locum intensity (bank and agency shifts combined) at trust level in 2021. Figure includes data from 210 NHS trusts in 2021, adjusted for substantive doctor FTE. The thick blue line represents the IQR (25th–75th centile). The thin line represents the rest of the distribution with upper/lower adjacent values. The white dot represents the median. The distribution shape of the data is based on a kernel density estimation where wider sections of the plot represent a higher chance that members of the population of interest will take on a given value and where thinner section represents lower chance. Eleven trusts were excluded from the analyses due to non-availability of data for permanent doctor FTE.
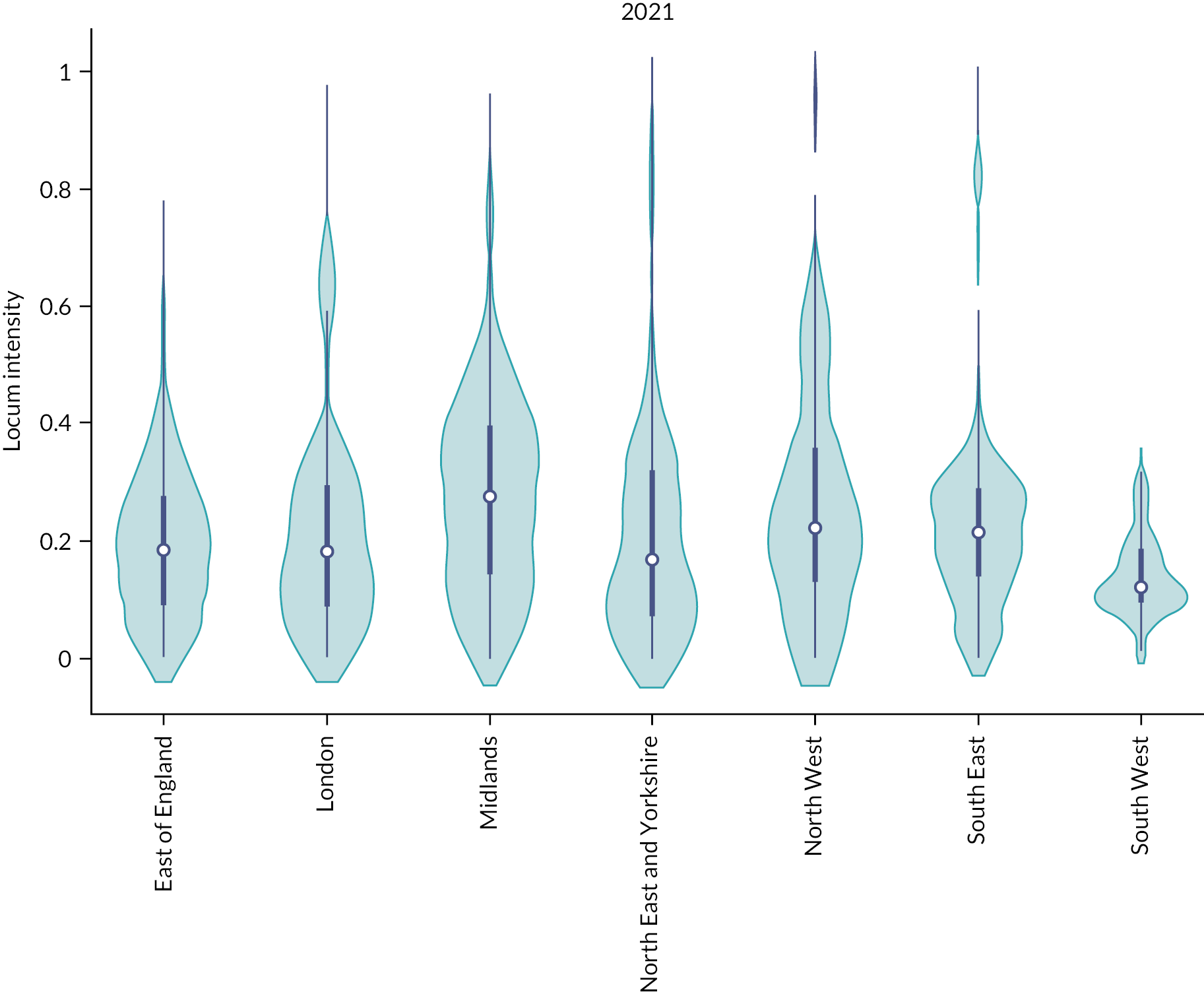
FIGURE 39.
Regional variation in the proportion of agency shifts at trust level in 2021. Figure includes data from 221 NHS trusts in 2021.
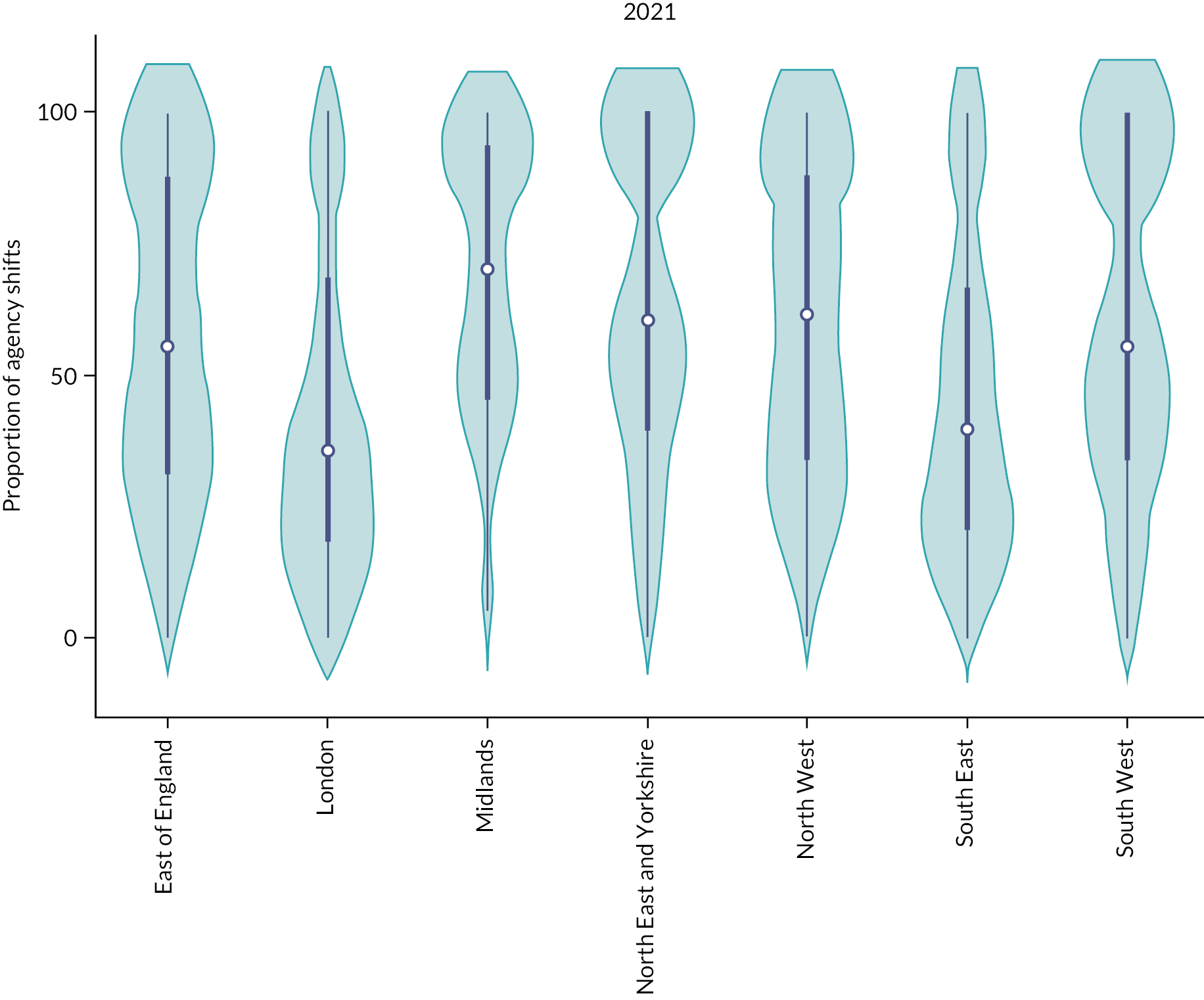
FIGURE 40.
Regional variation in the proportion of unfilled shifts at trust level in 2021. Figure includes data from 221 NHS trusts in 2021. The thick blue line represents the IQR (25th–75th centile). The thin line represents the rest of the distribution with upper/lower adjacent values. The white dot represents the median. The distribution shape of the data is based on a kernel density estimation where wider sections of the plot represent a higher chance that members of the population of interest will take on a given value and where thinner section represents lower chance. Eleven trusts were excluded from the analyses due to non-availability of data for permanent doctor FTE.
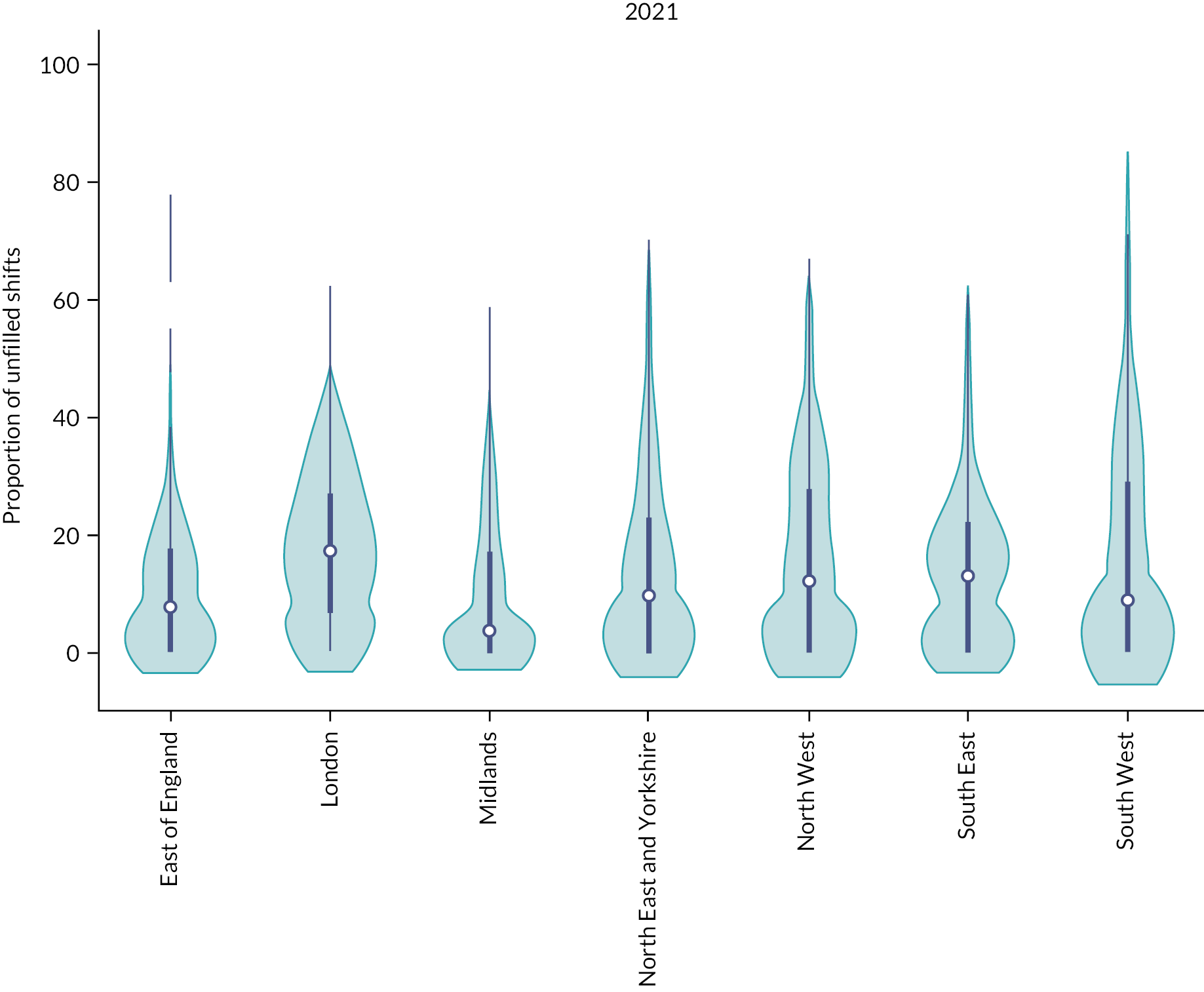
FIGURE 41.
Spatial map of locum intensity at the STPs level, England 2019.

FIGURE 42.
Spatial map of agency shifts at the STPs level, England 2019.
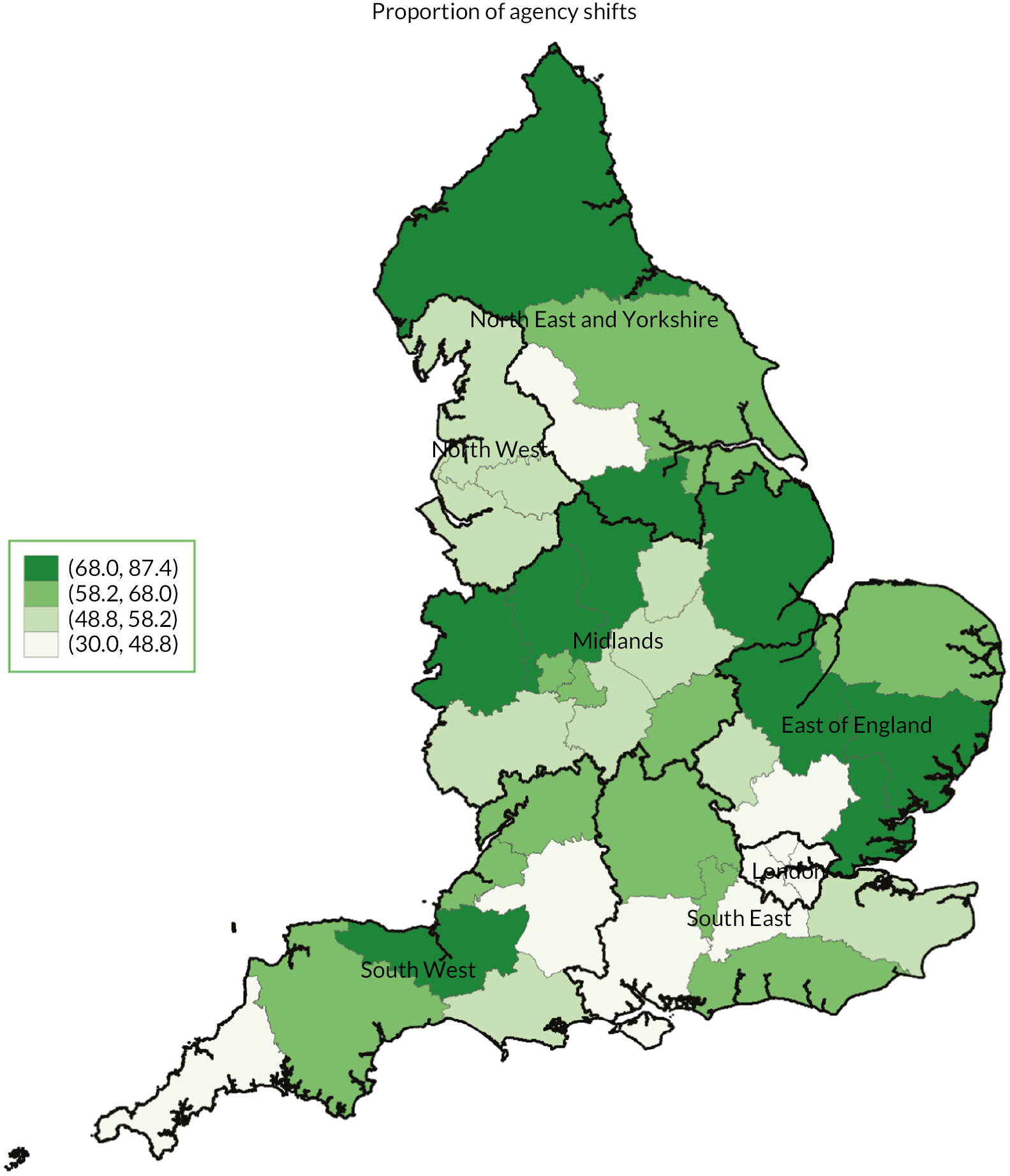
FIGURE 43.
Spatial map of unfilled shifts at the STPs level, England 2019.

Appendix 3 Additional material for Chapter 5: The use of locum doctors: findings from a national survey of National Health Service trusts in England
Secondary care survey
A national survey of the use of locum doctors in the English NHS V1 12 April 2021.
This national survey about the nature, scale and scope of locum usage and management of locum doctors in English NHS has been funded by the National Institute for Health Research. We appreciate that trusts receive many questionnaires, but the findings of this survey will provide for the first time a comprehensive data set on the use and management of locum doctors and will provide a key input into policy-making and we therefore need your help. We are committed to using findings from this survey to inform and improve governance and working arrangements for locums. Your contributions will help inform future decisions about how locum employment is organised. We are asking a representative, such as the Medical Director/RO/Medical Staffing Lead, at all NHS trusts in England to complete this survey. We are interested in views about why locums are needed, the governance of locums, the safety of locum working and how their work is organised by employers. If you don’t know the answer to a question, please don’t let that stop you from answering as much as you can. You may wish to consult with a colleague who you feel can help to answer the questions.
Statement of confidentiality
Everything you say in this questionnaire will remain confidential. There is an ID number on the questionnaire so that we know who has replied and do not send out reminders unnecessarily. To ensure anonymity, please be assured we will not report data on individual NHS trusts. Any information that would permit identification of an individual or an organisation will be held strictly confidential, will be used only for the purposes of this study, and will not be disclosed or released to other persons or used for any other purpose.
Please note that by completing the survey, you are agreeing to take part in this study.
After your responses have been entered onto a secure computer database, the survey will be securely stored in accordance with data protection regulations and destroyed after 5 years.
If you would like to know more about the study, please contact the research team at the University of Manchester: Dr Jane Ferguson: jane.ferguson@manchester.ac.uk; Dr Gemma Stringer: gemma.stringer@manchester.ac.uk.
The questionnaire will take around 15 minutes to complete.
You can stop any time you like and finish the questionnaire later.
Click on the arrow below to start the questionnaire.
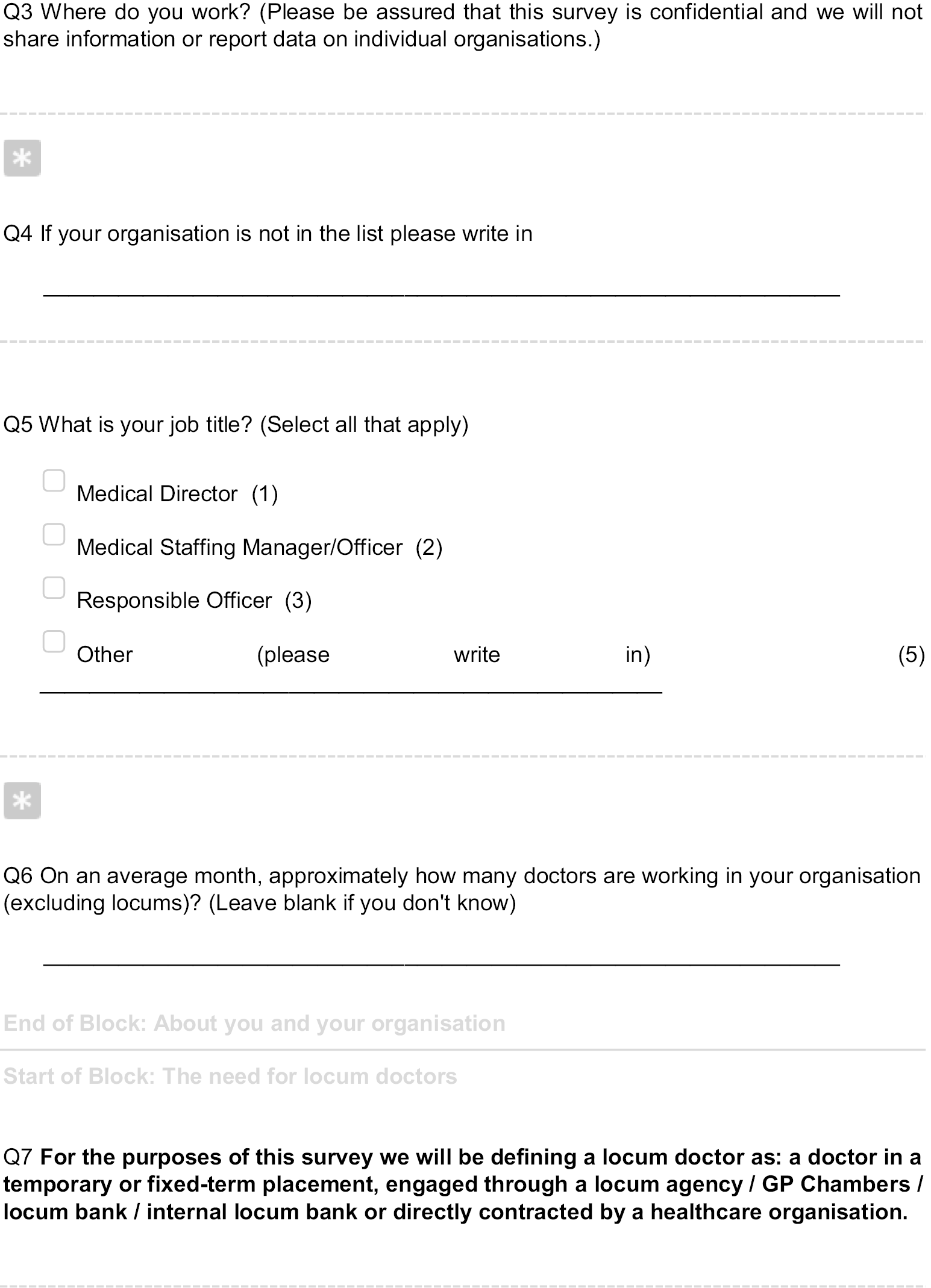
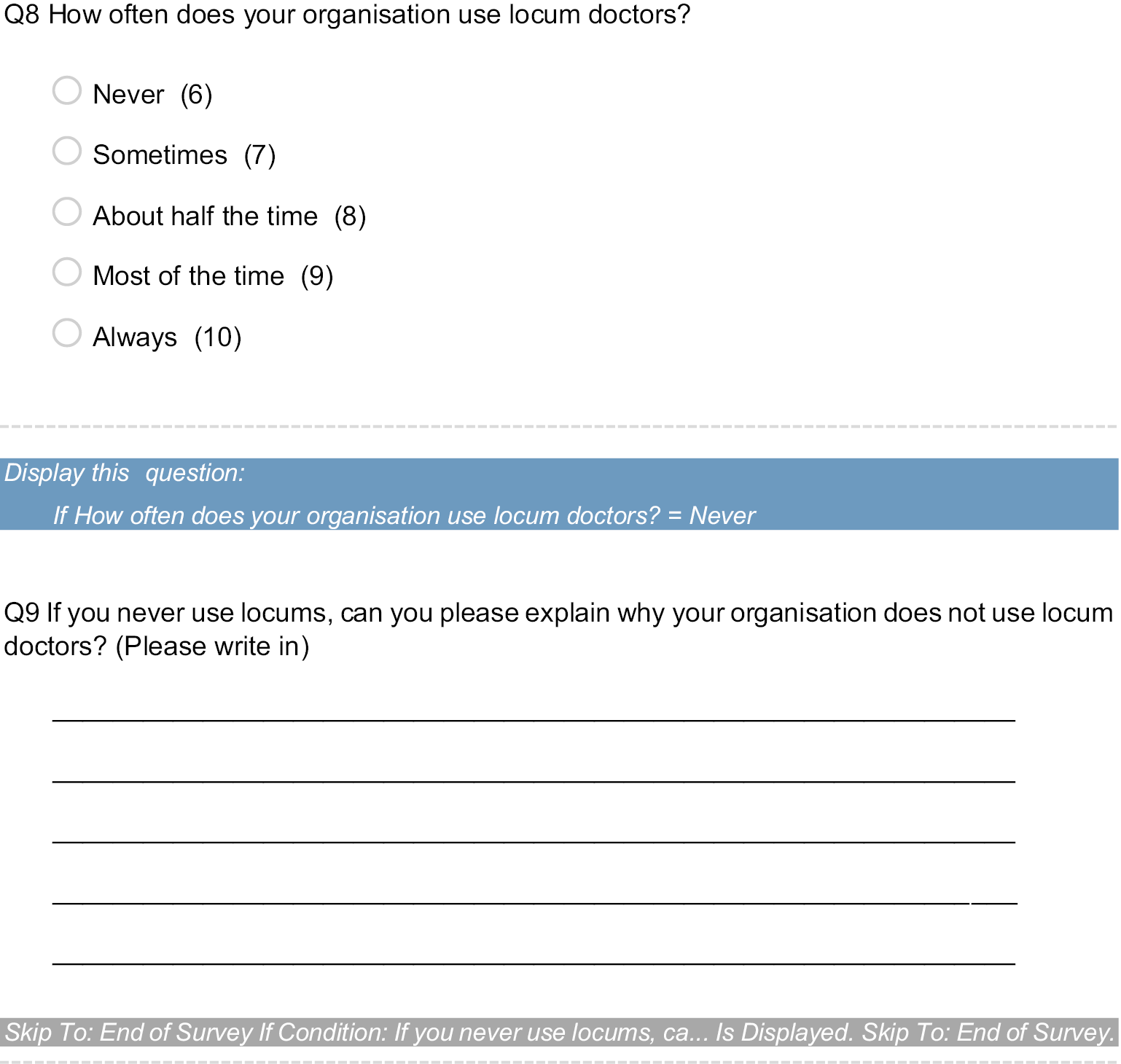
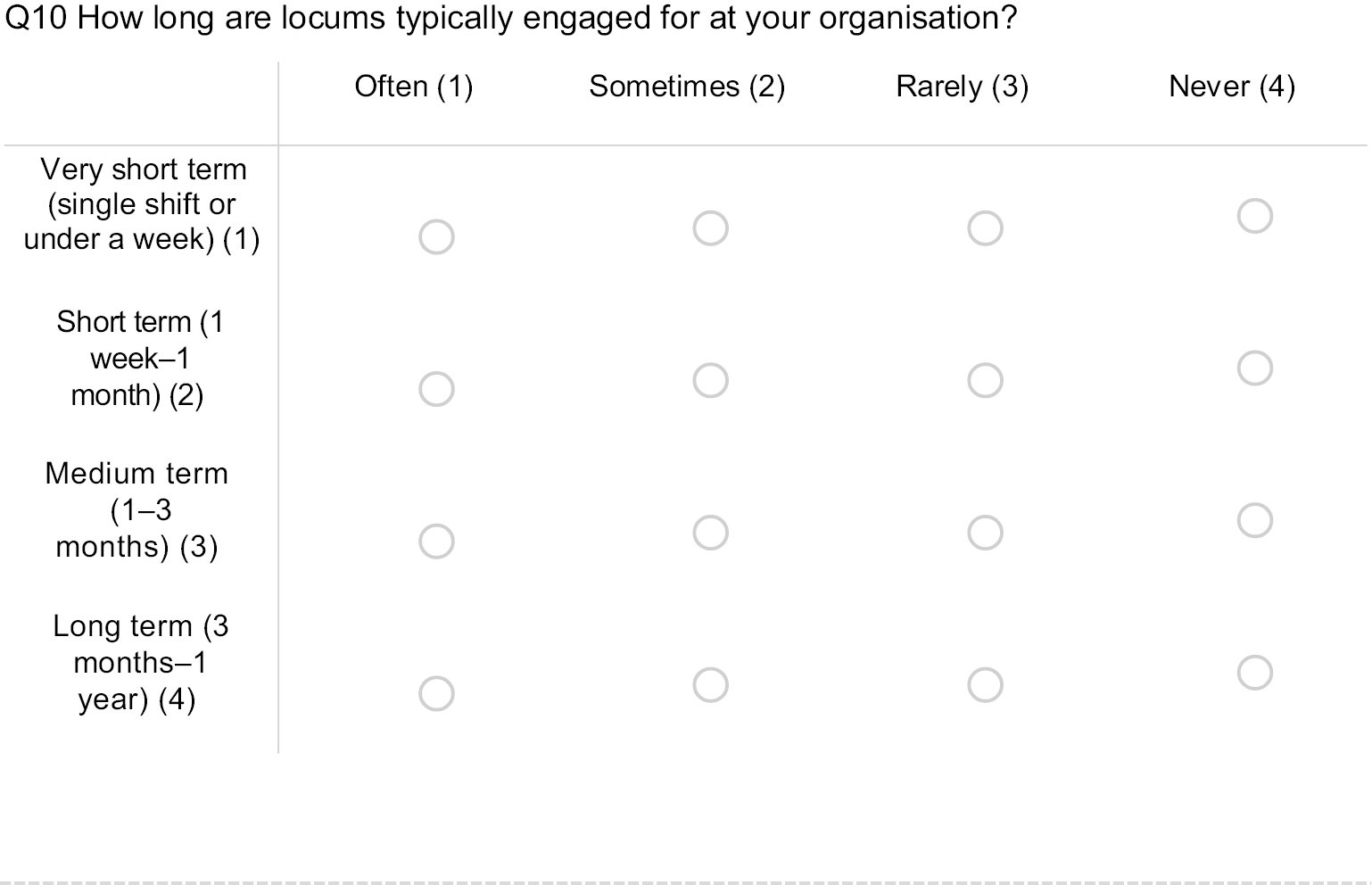
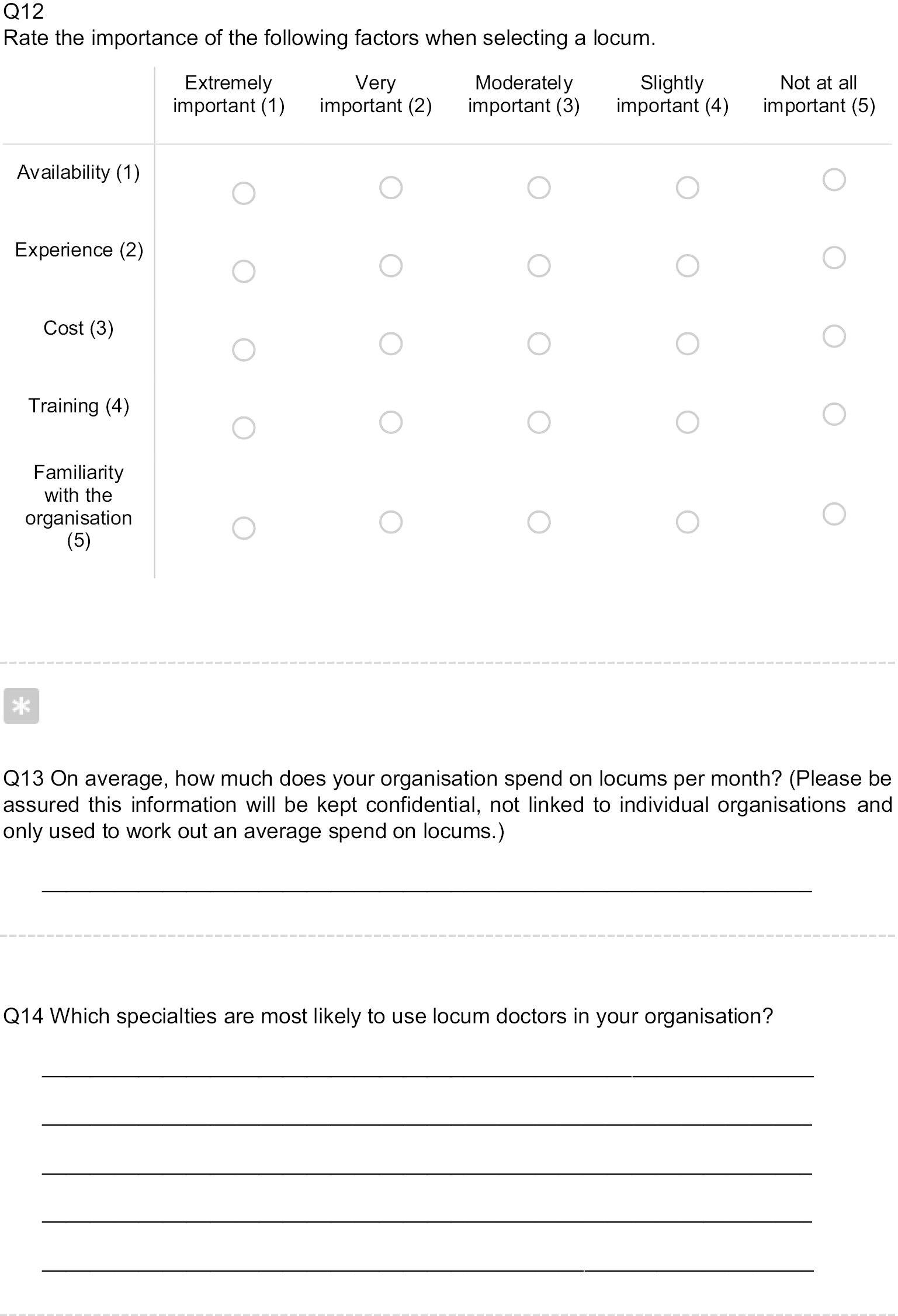
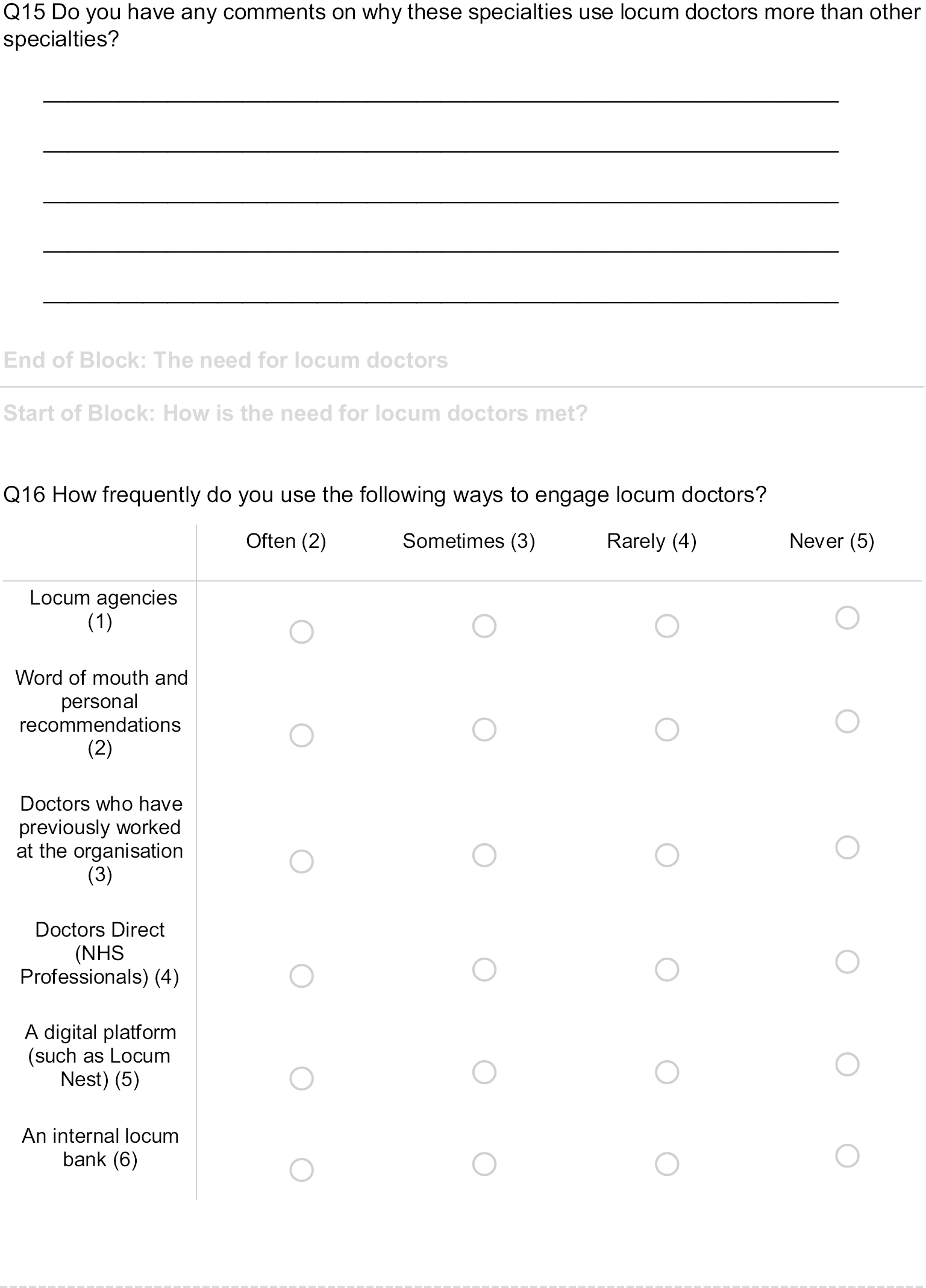
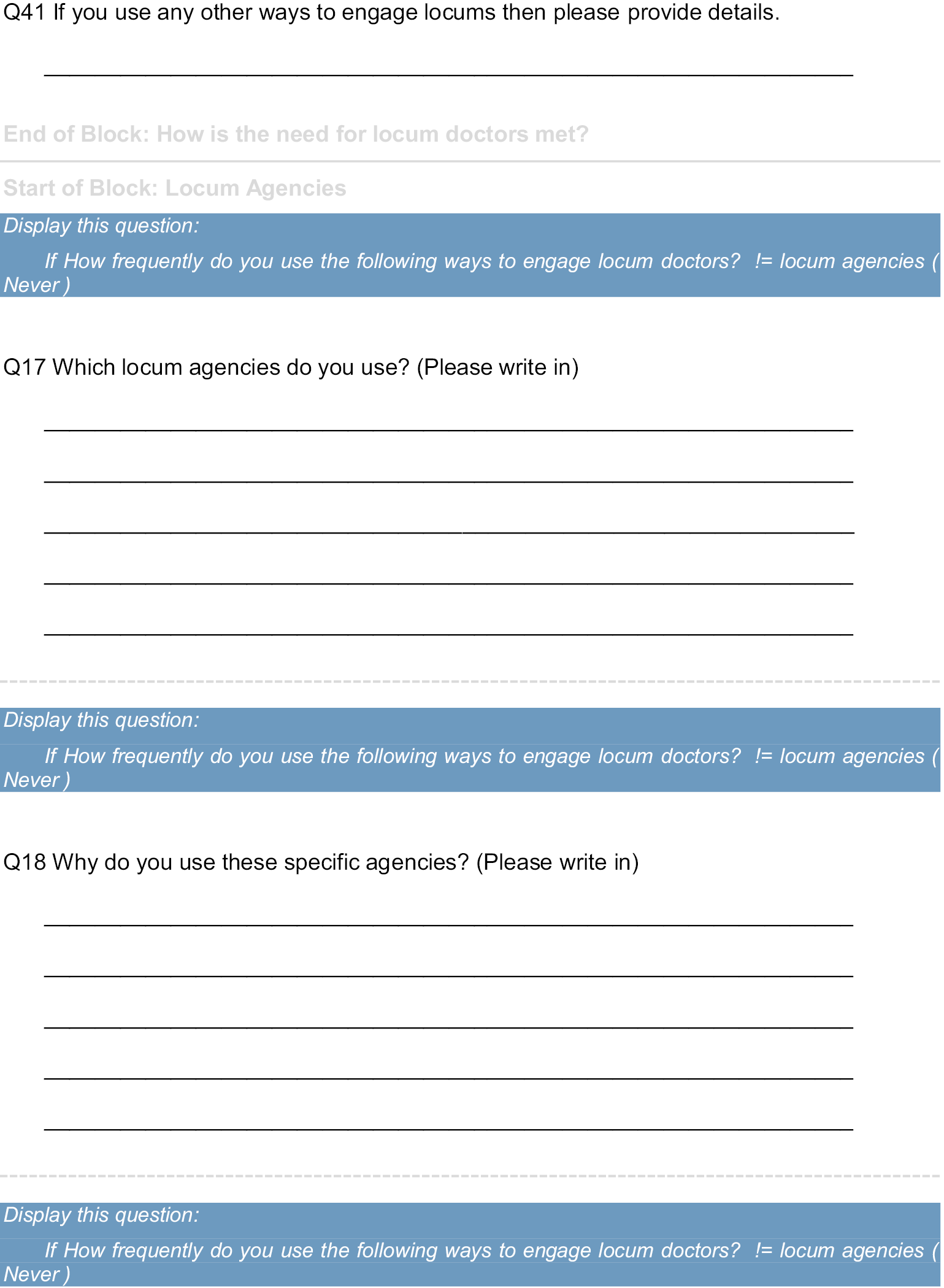



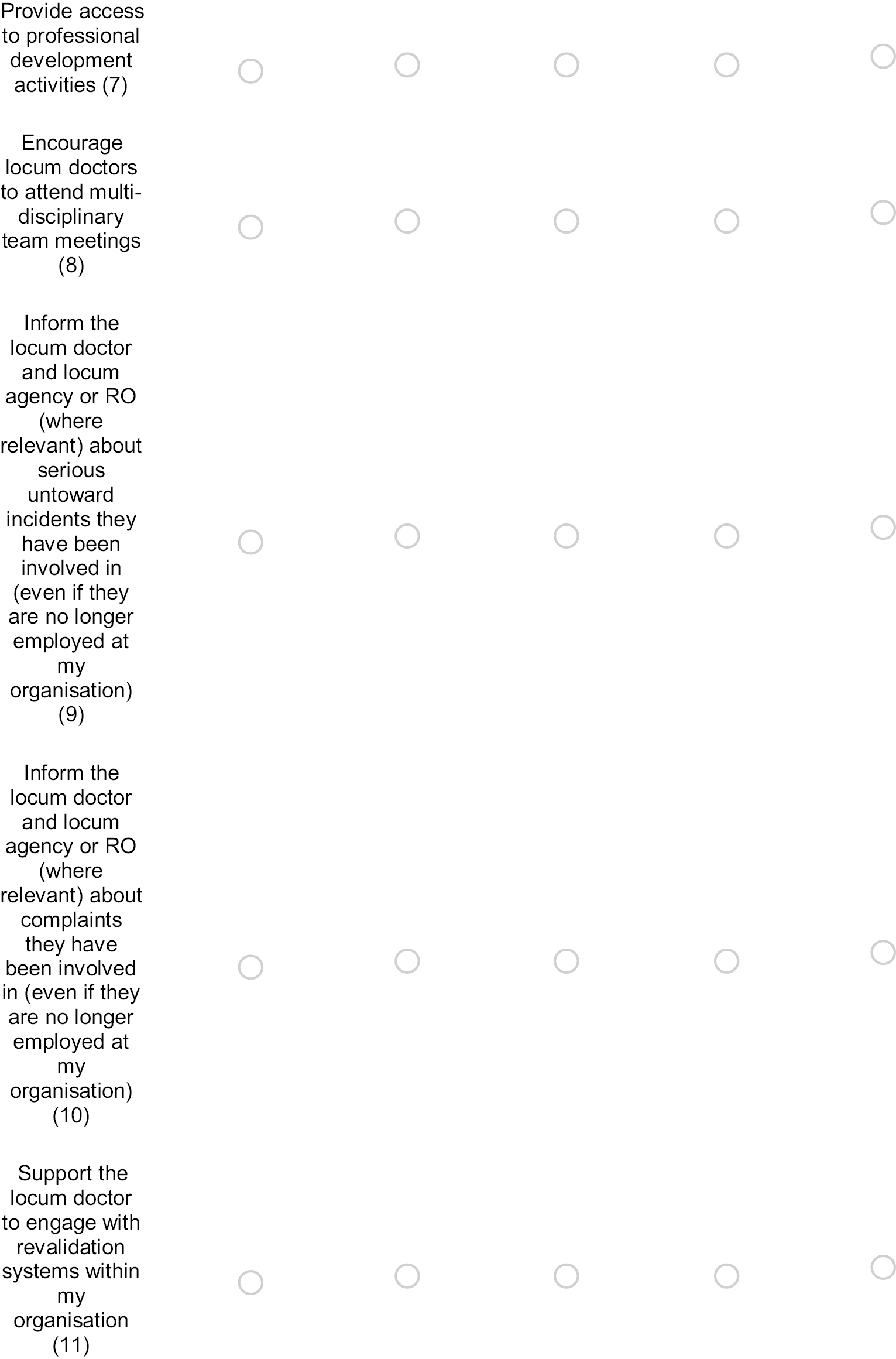
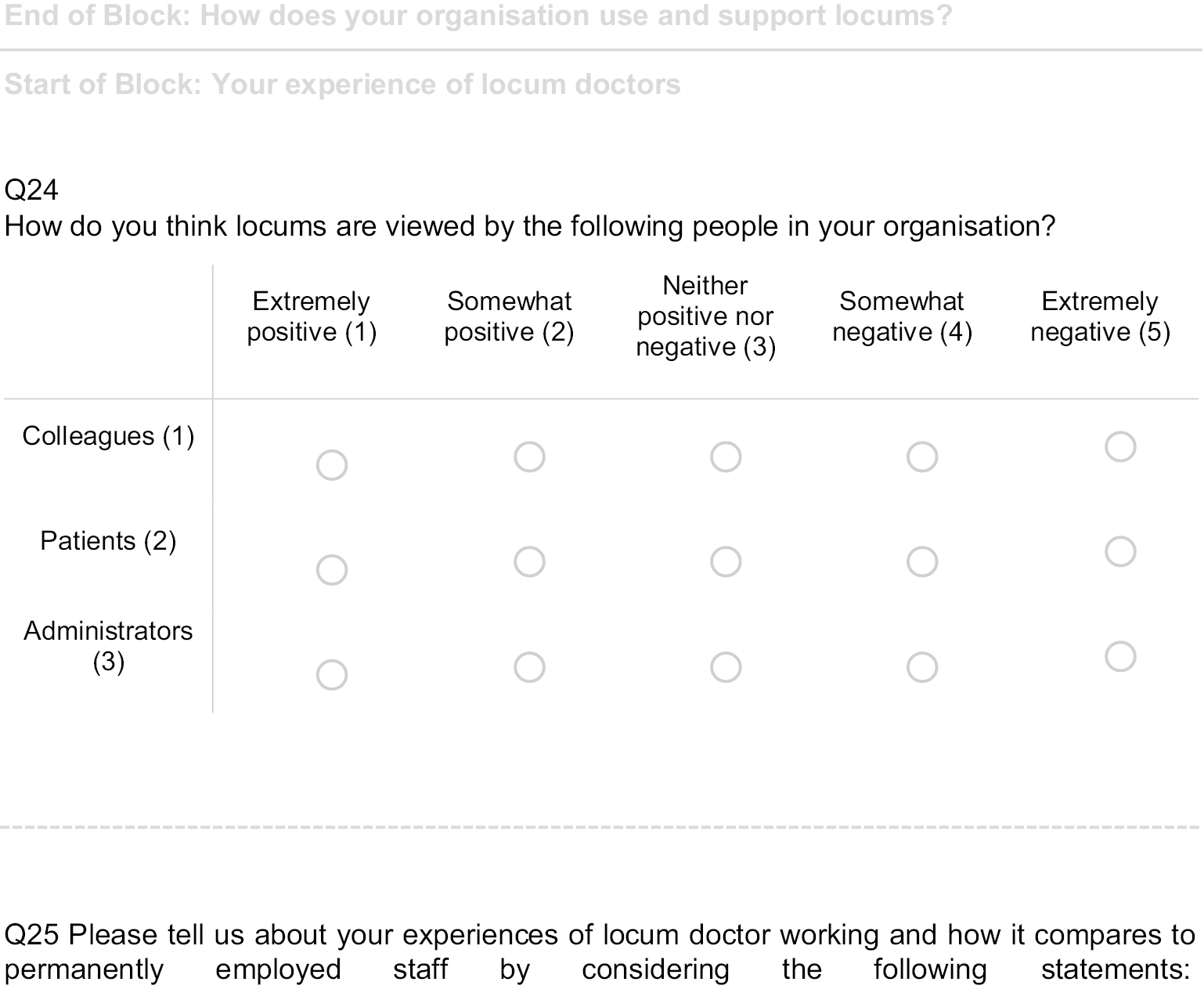
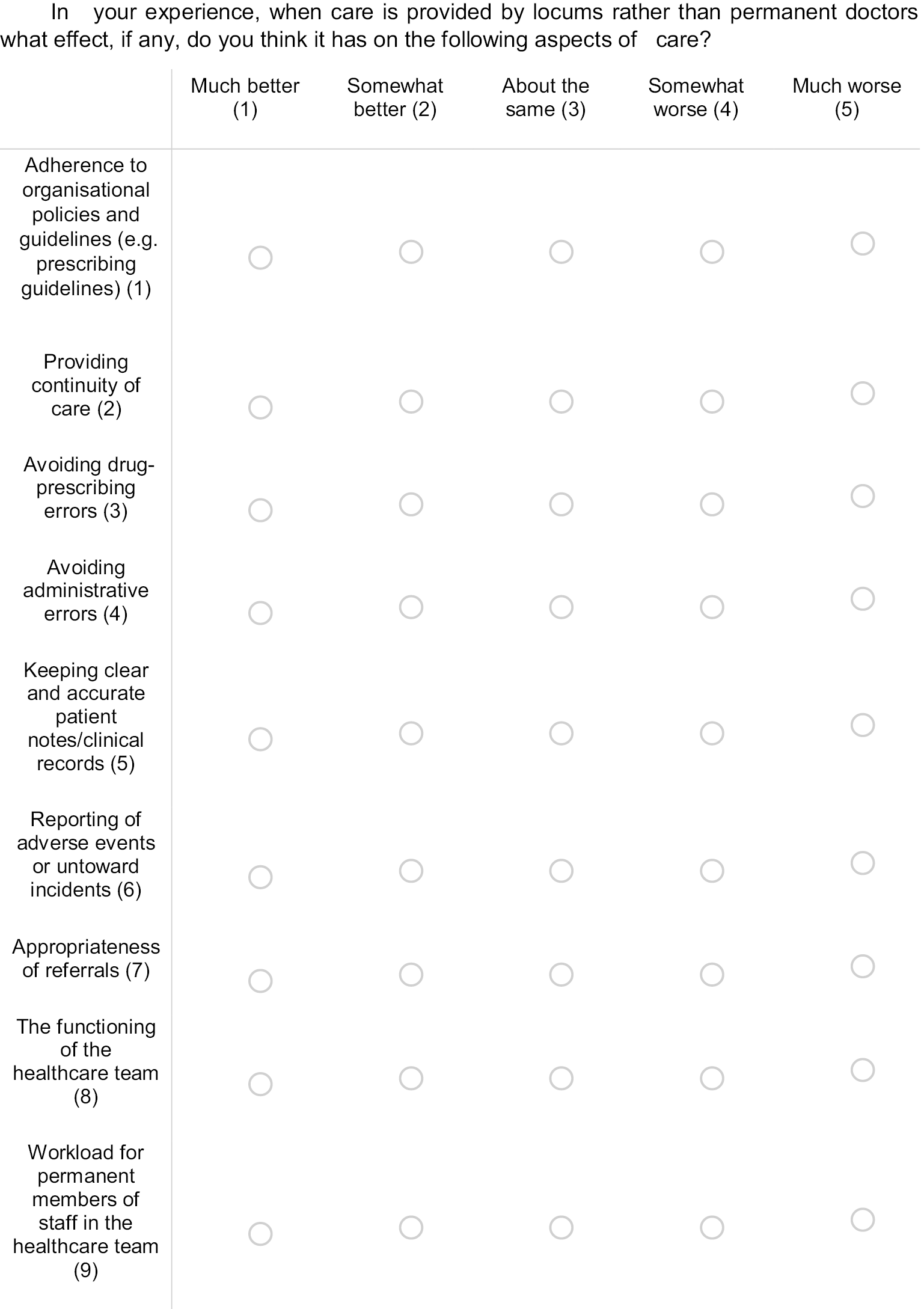
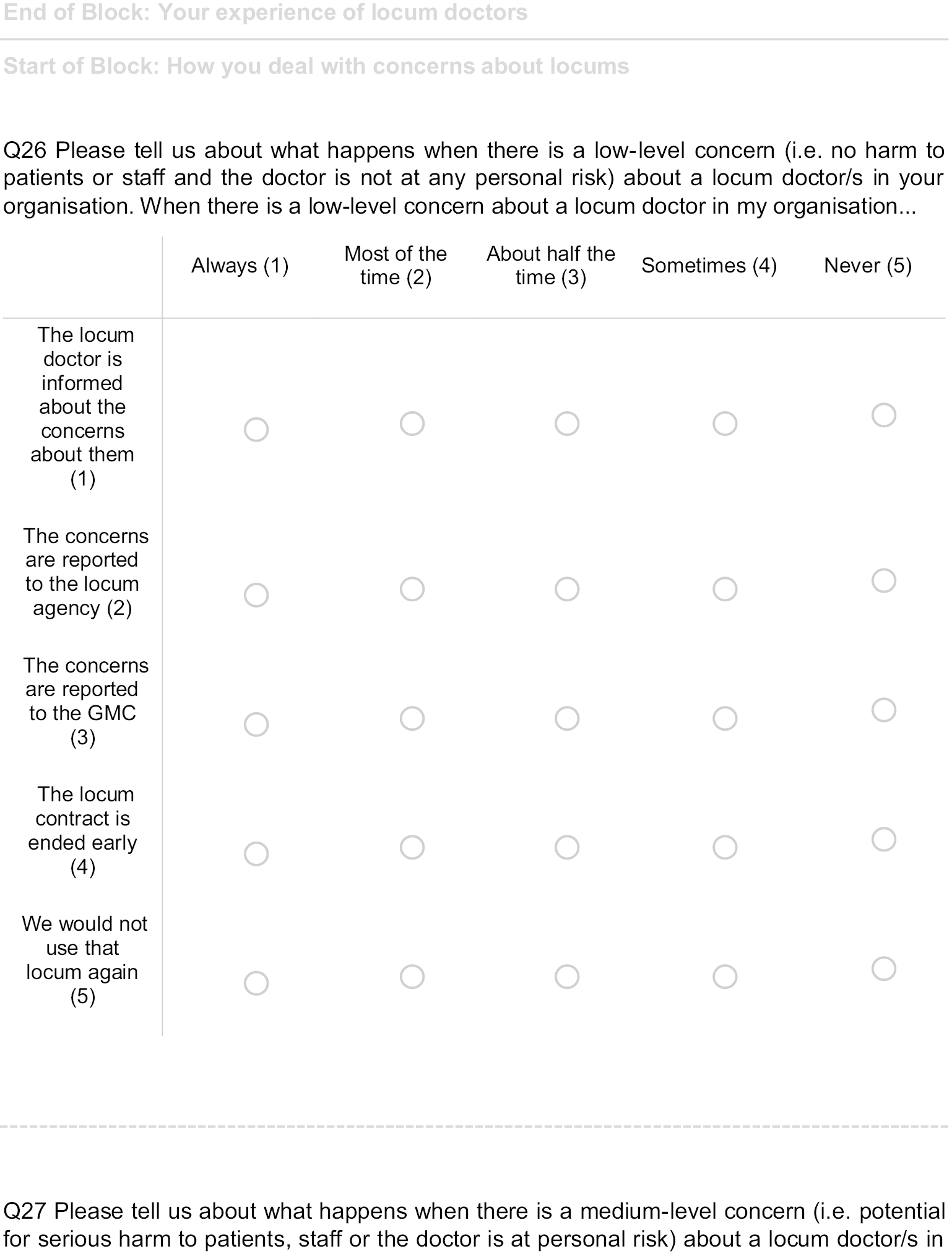
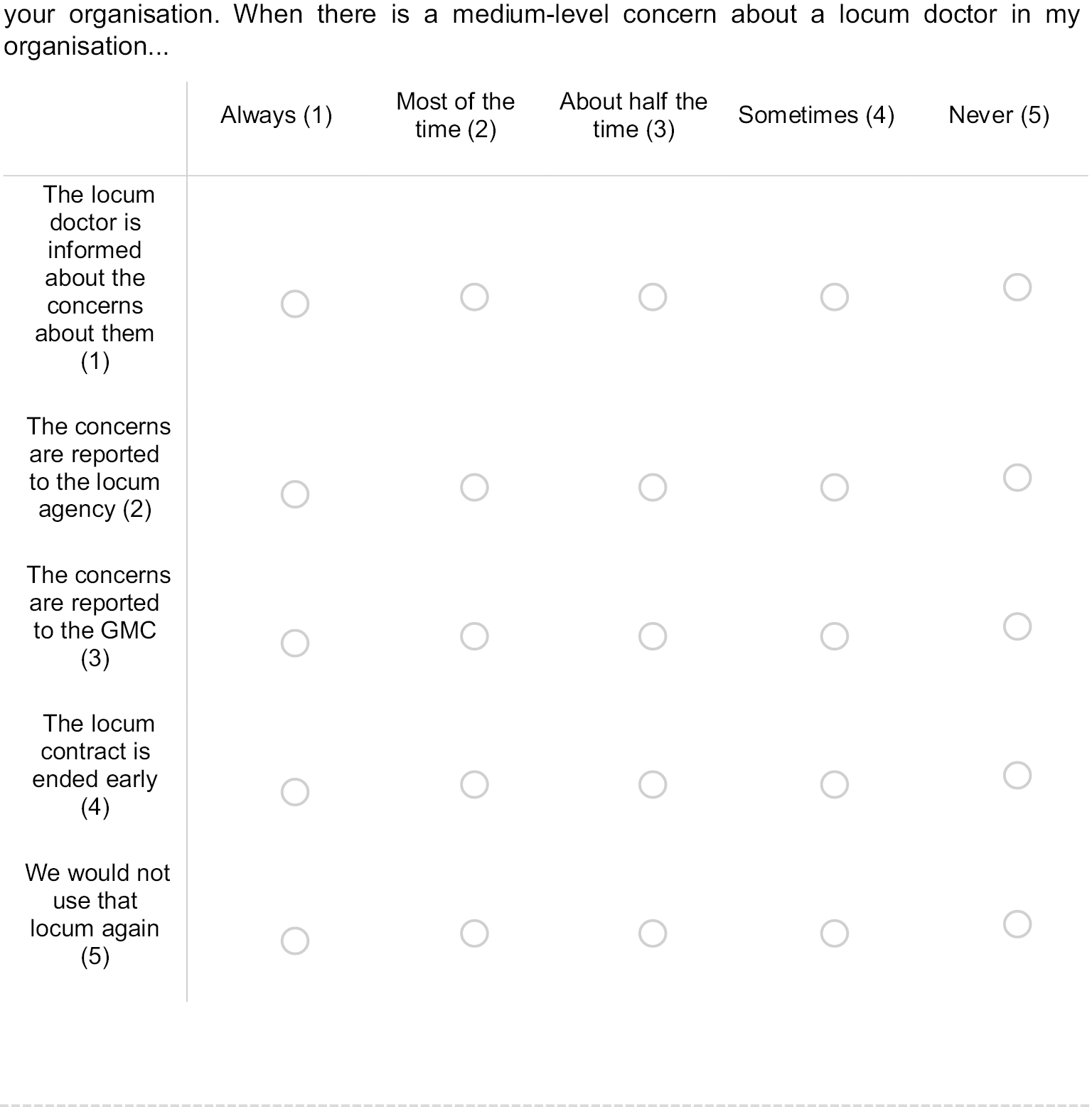
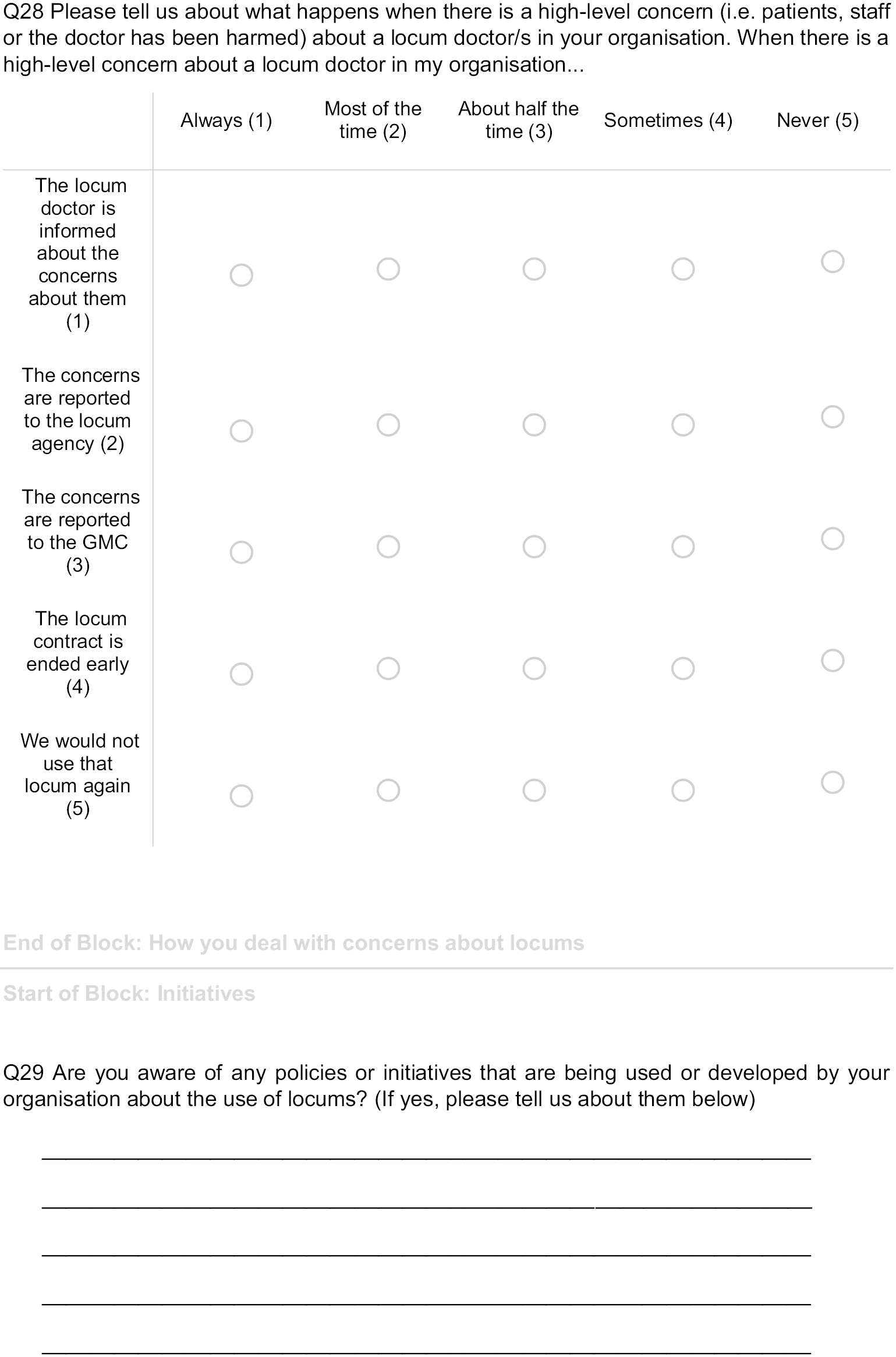
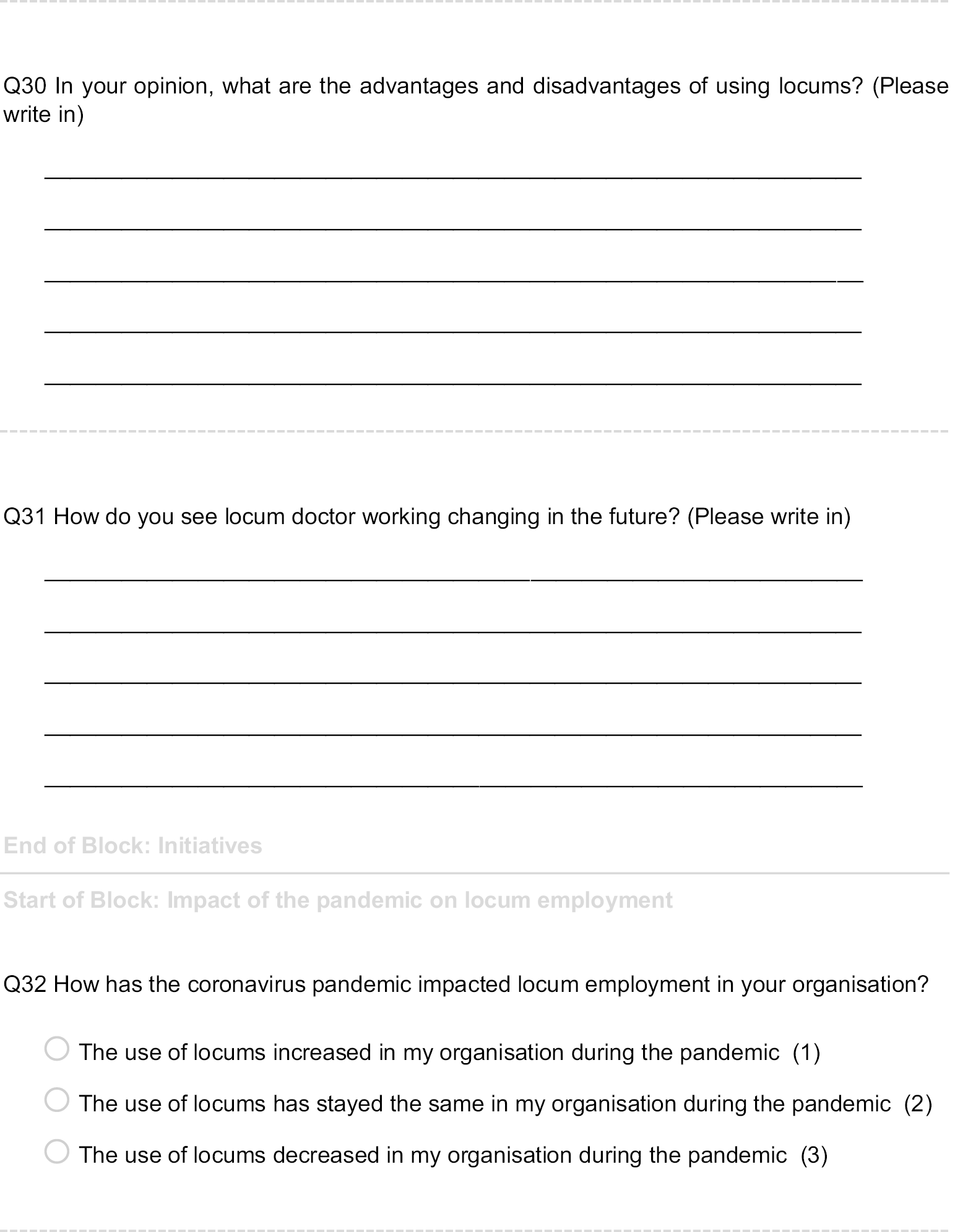
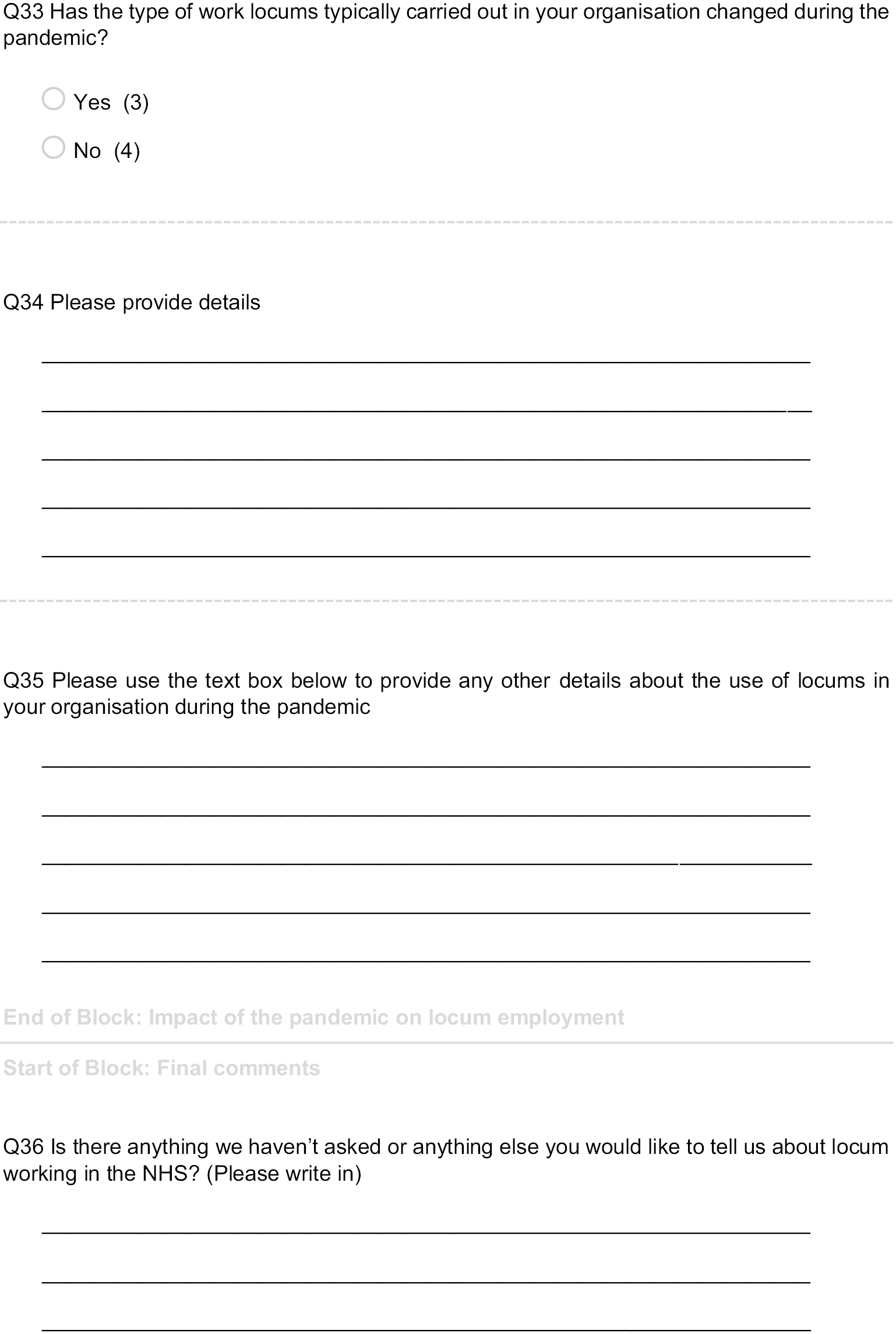
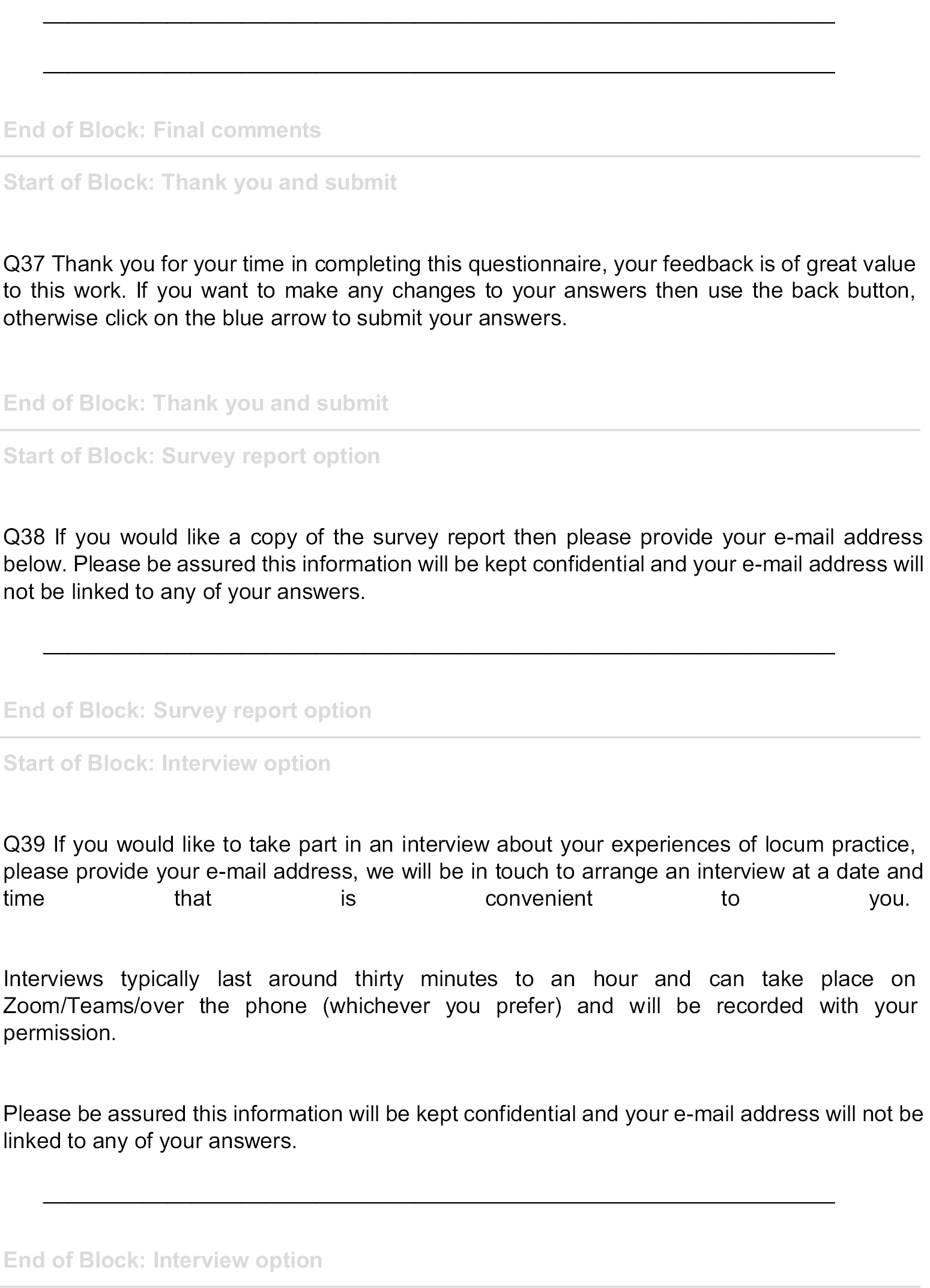
Appendix 4 Additional material for Chapter 6: The use of locum doctors: findings from a national survey of general practices in England
Primary care survey
A national survey of the use of locum doctors in the English NHS V1 12 April 2021.
This national survey about the nature, scale and scope of locum usage and management of locum doctors in English NHS has been funded by the National Institute for Health Research. We appreciate that practices receive many questionnaires, but the findings of this survey will provide for the first time a comprehensive data set on the use and management of locum doctors and will provide a key input into policy-making and we therefore need your help. We are committed to using findings from this survey to inform and improve governance and working arrangements for locums. Your contributions will help inform future decisions about how locum employment is organised. We are asking a representative, namely the practice manager or GP partner, at all GP practices in England to complete this survey. We are interested in views about why locums are needed, the governance of locums, the safety of locum working and how their work is organised by employers. If you don’t know the answer to a question, please don’t let that stop you from answering as much as you can. You may wish to consult with a colleague who you feel can help to answer the questions.
Statement of confidentiality
Everything you say in this questionnaire will remain confidential. We ask for your ODS code on the questionnaire so that we know who has replied and do not send out reminders unnecessarily. To ensure practice anonymity, please be assured that we will not report data on individual practices. Any information that would permit identification of an individual or a practice will be strictly confidential, will be used only for the purposes of this study, and will not be disclosed or released to other persons or used for any other purpose.
Please note that by completing the survey, you are agreeing to take part in this study.
After your responses have been entered onto a secure computer database, the survey will be securely stored in accordance with data protection regulations and destroyed after 5 years.
If you would like to know more about the study, please contact the research team at the University of Manchester:
Dr Jane Ferguson jane.ferguson@manchester.ac.uk
Dr Gemma Stringer gemma.stringer@manchester.ac.uk
The questionnaire will take around 15 minutes to complete.
You can stop any time you like and finish the questionnaire later.
Click on the arrow below to start the questionnaire.
Start of Block: About you and your practice
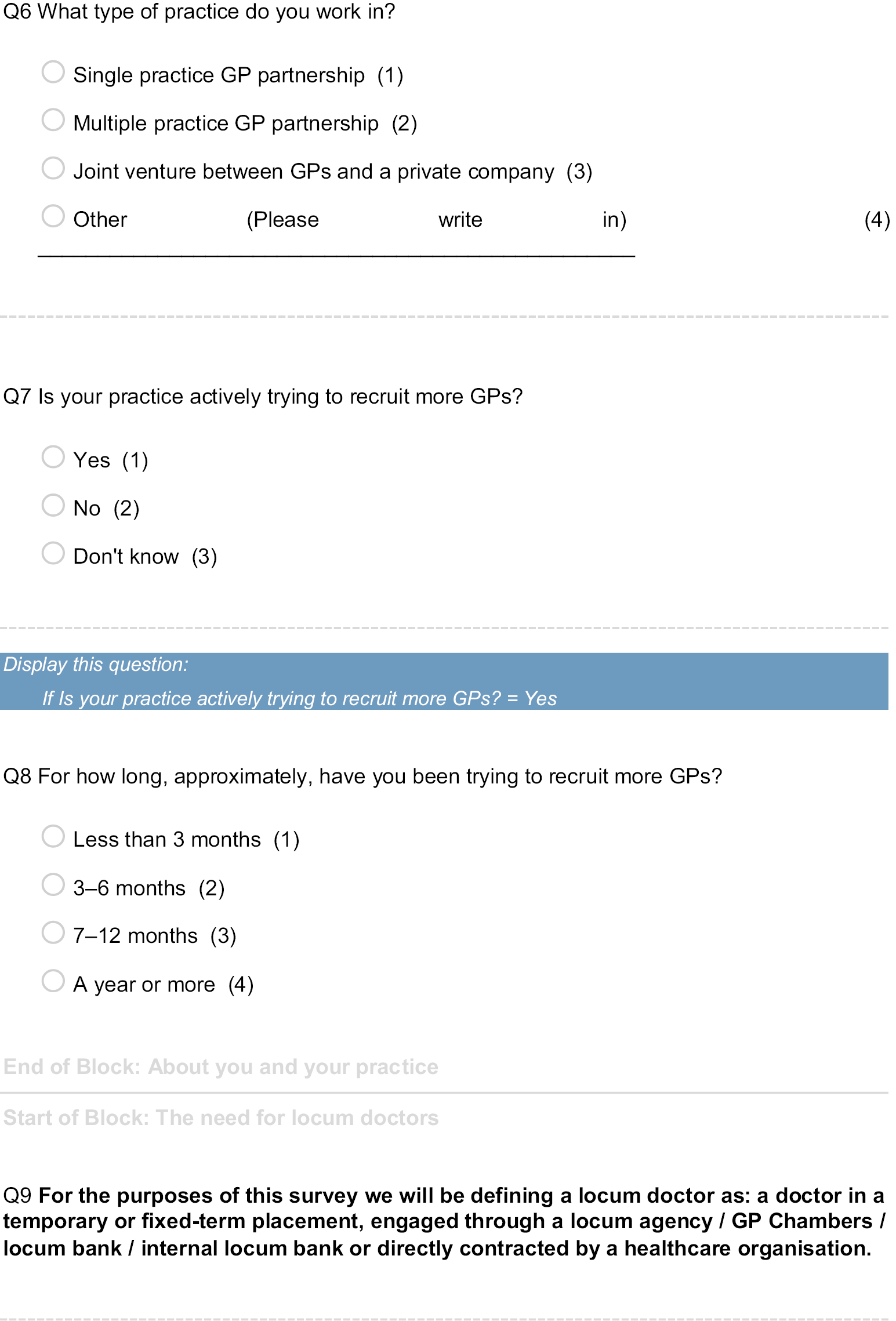
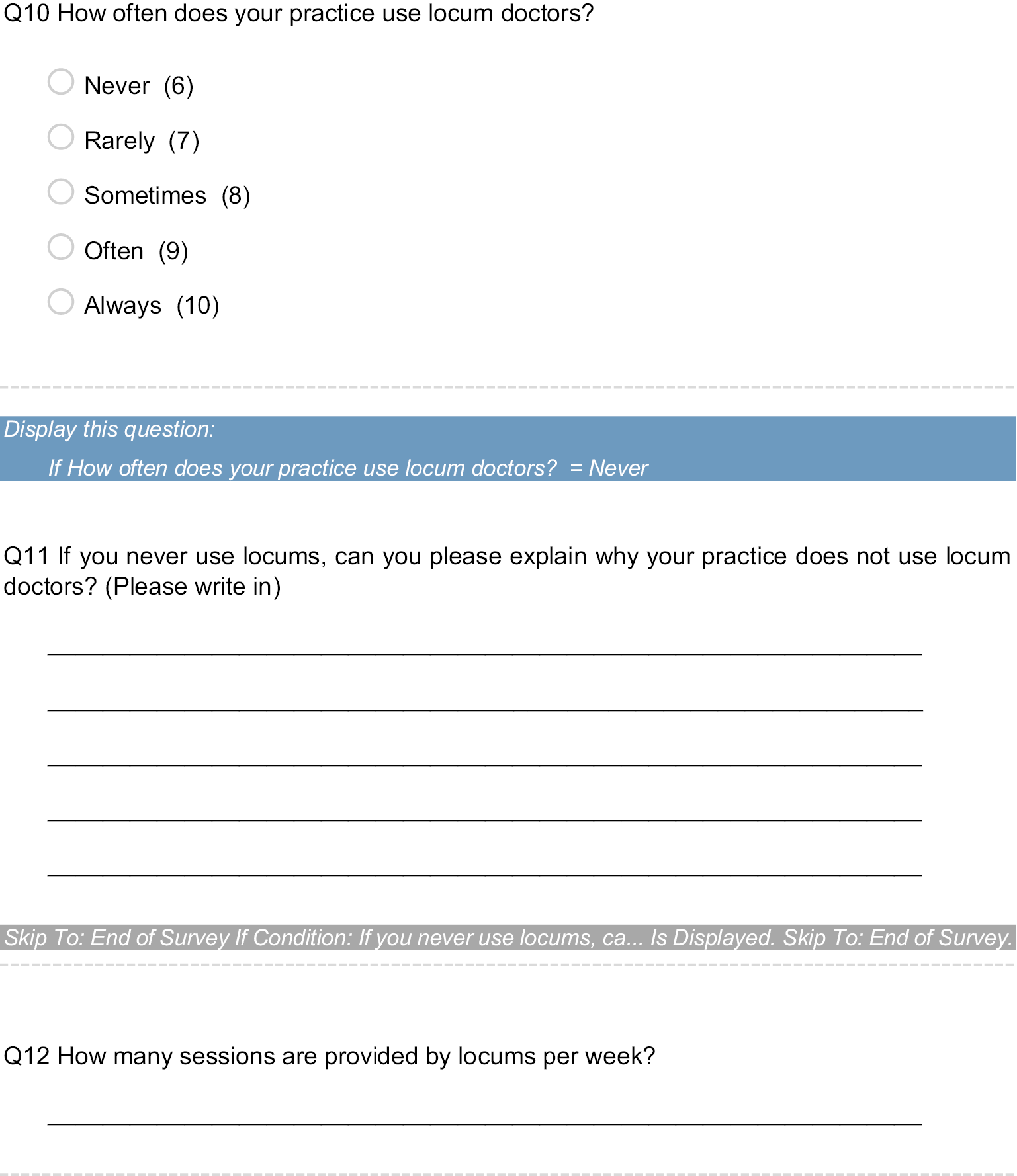

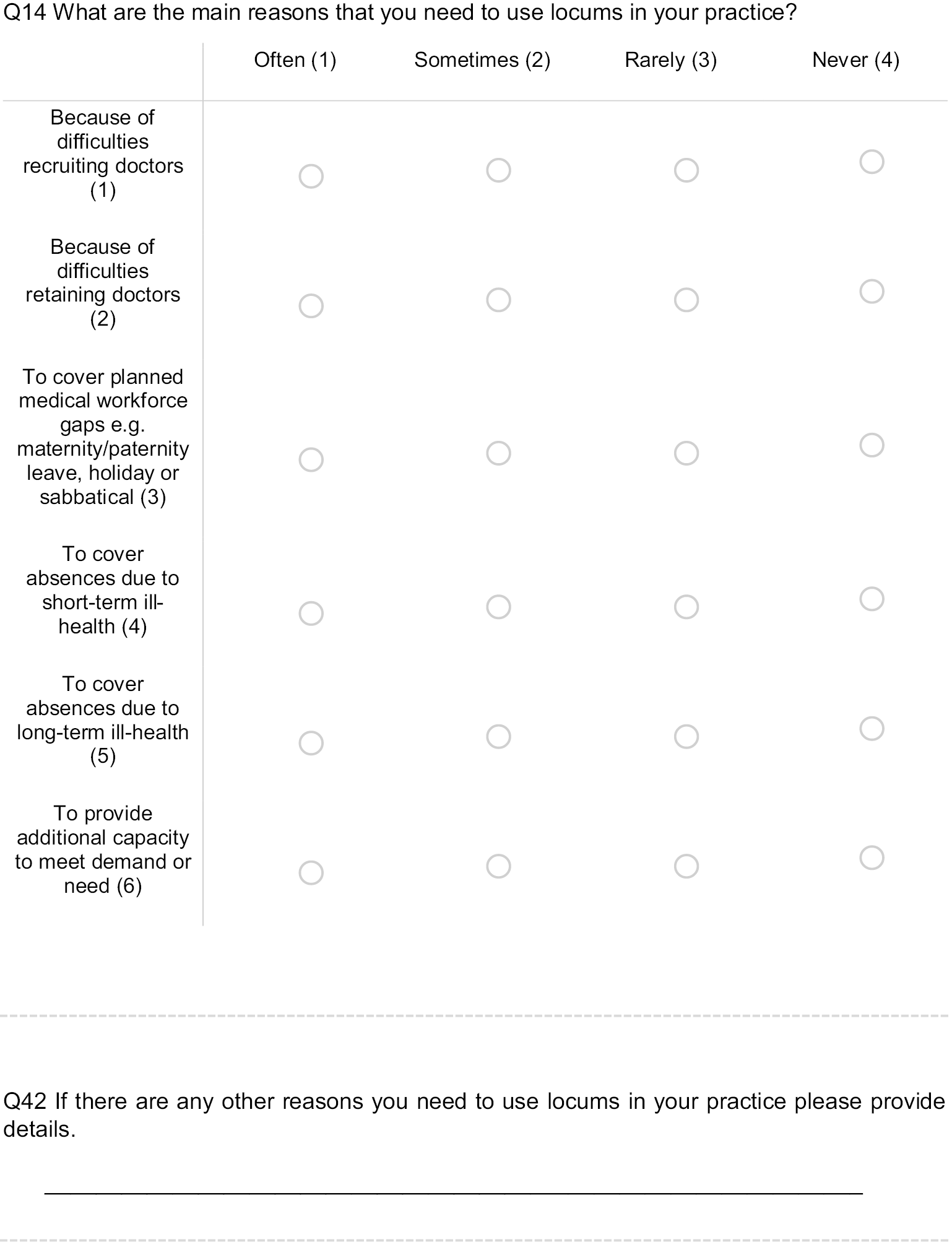
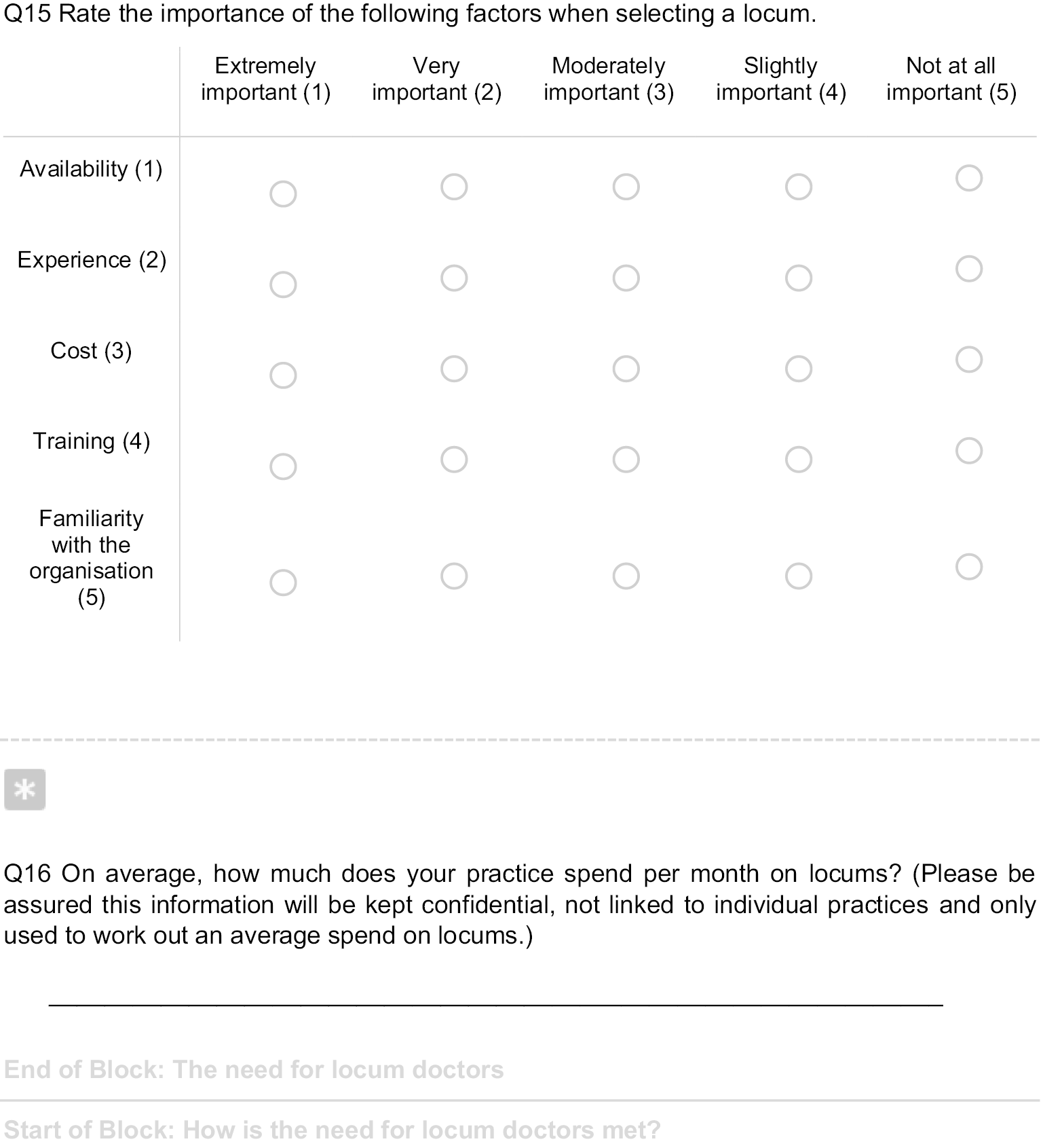
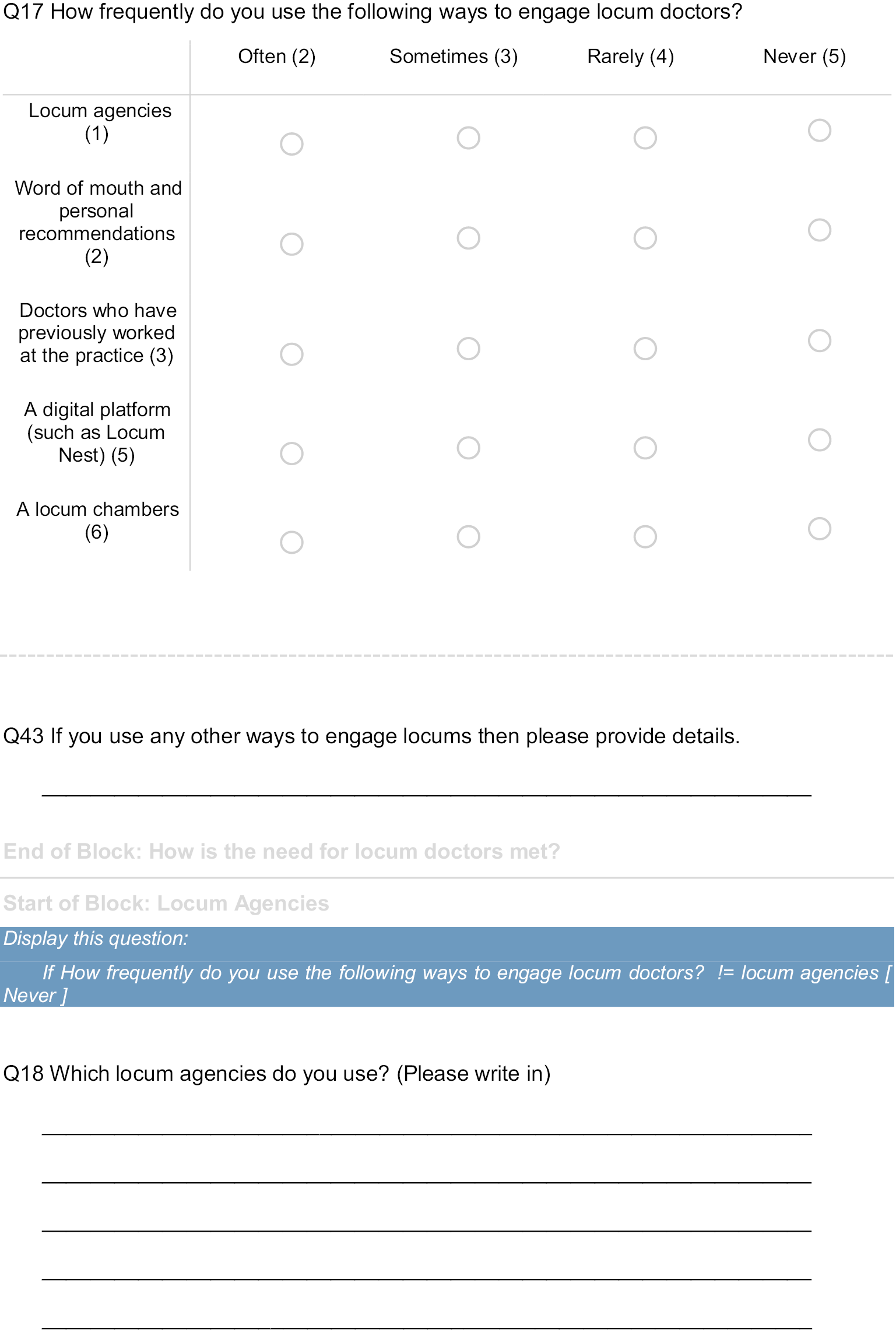
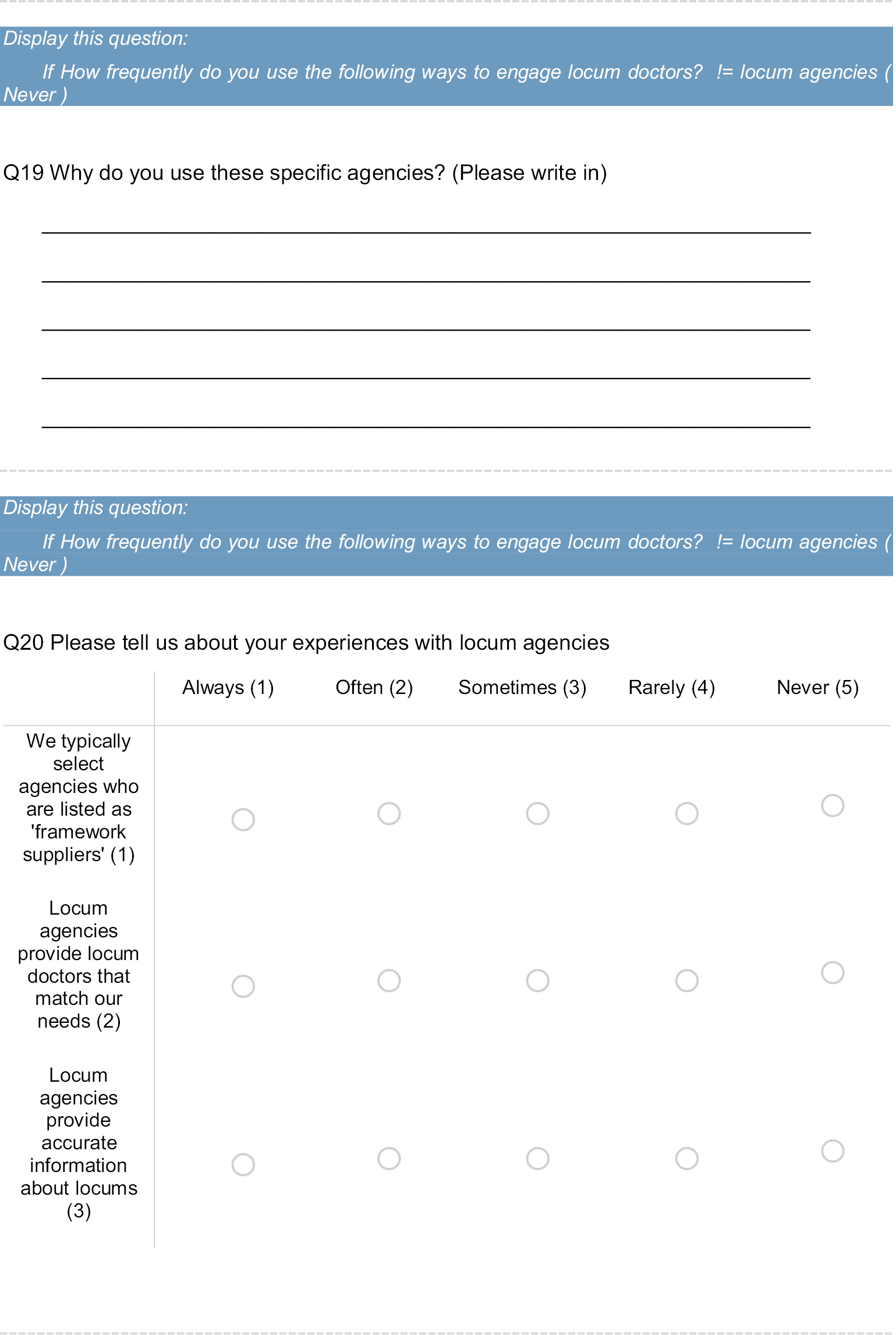
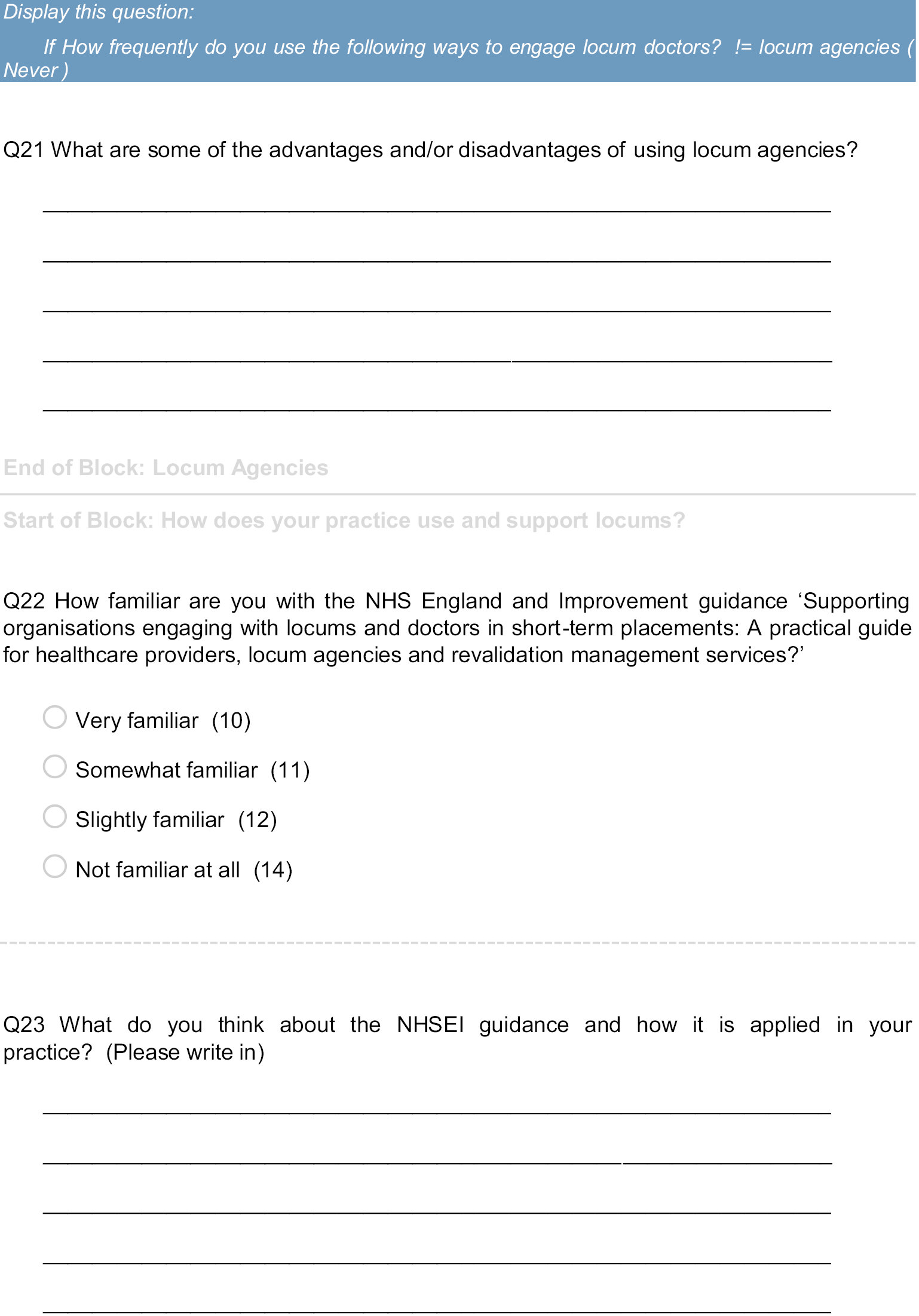
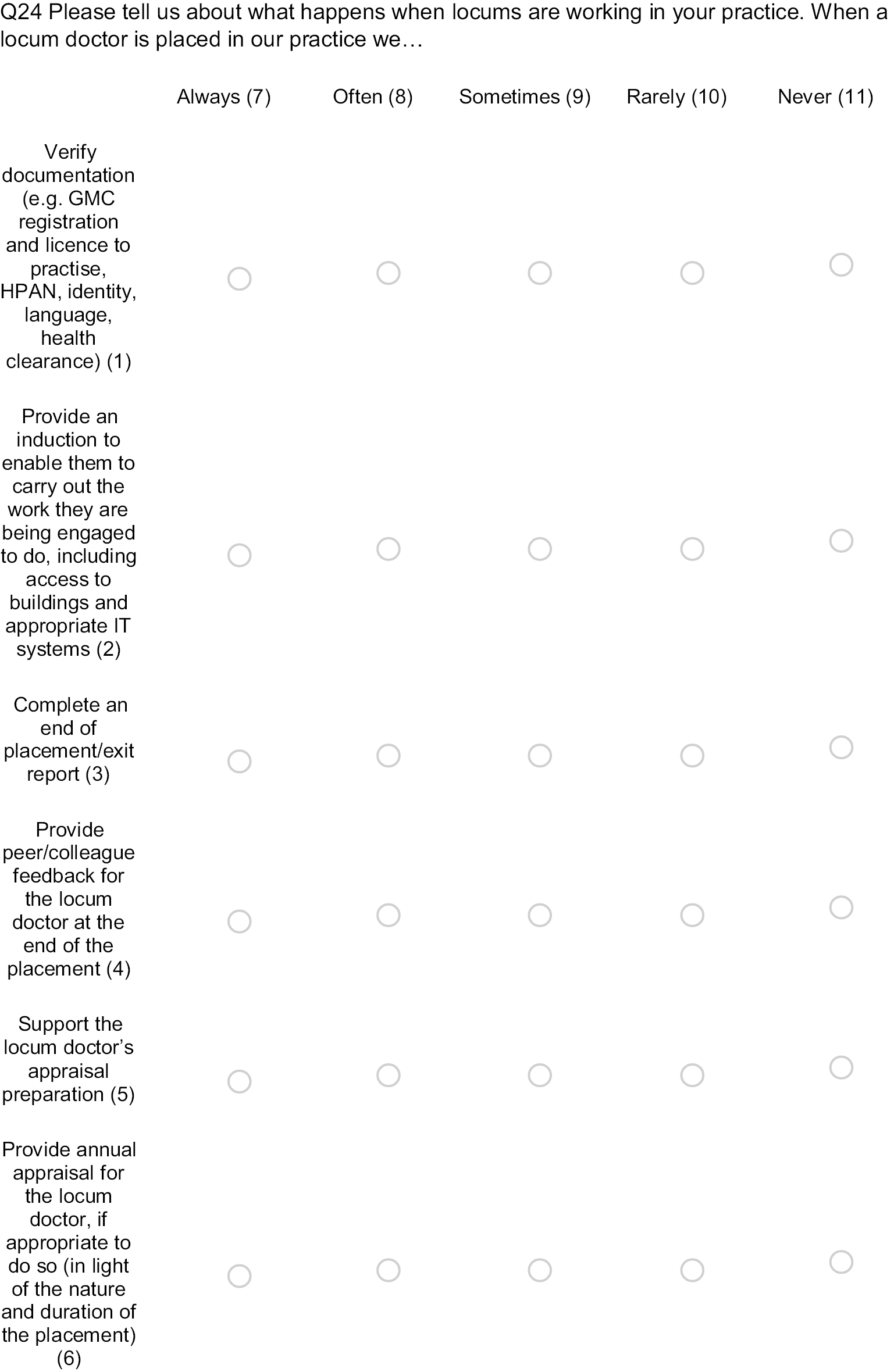
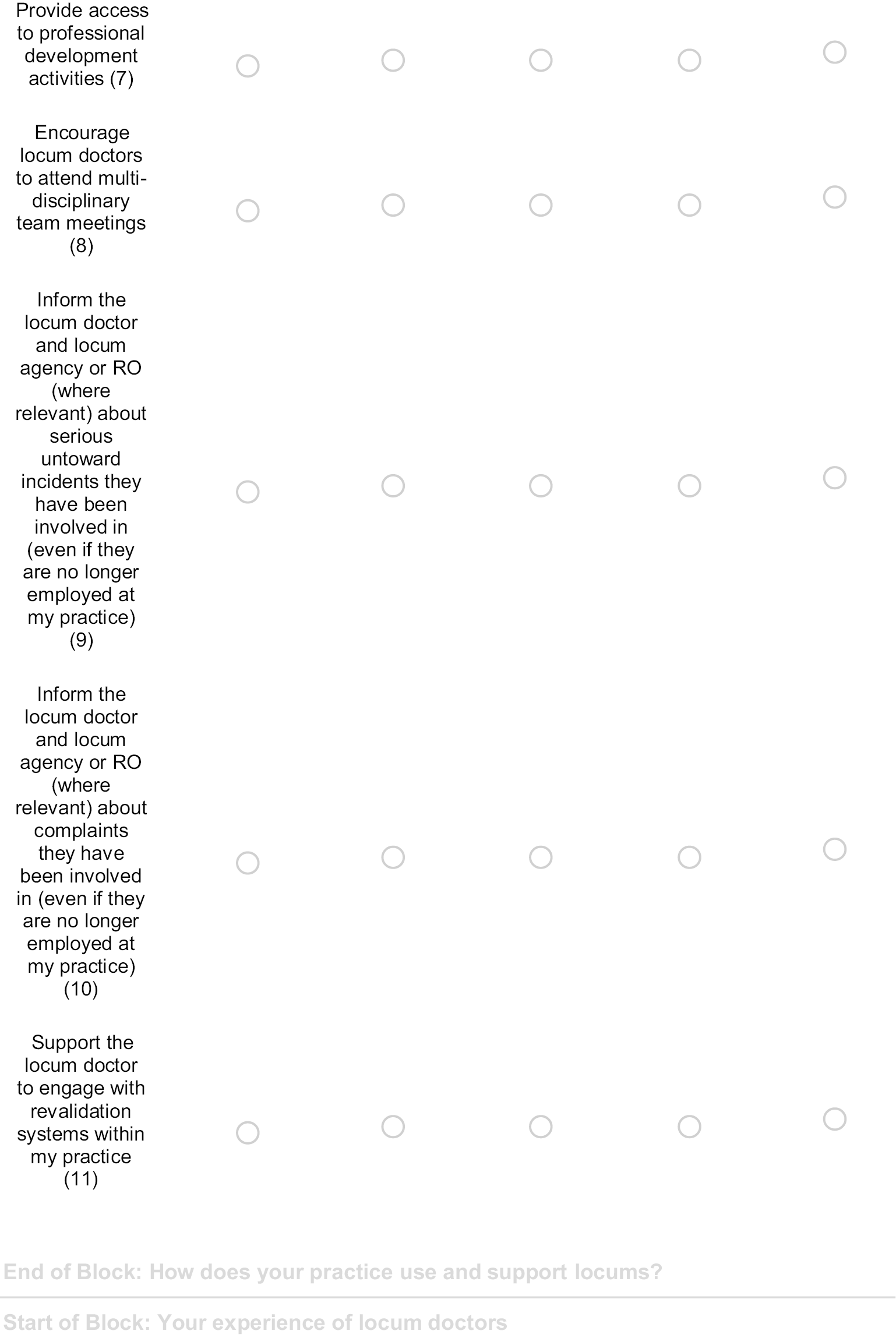
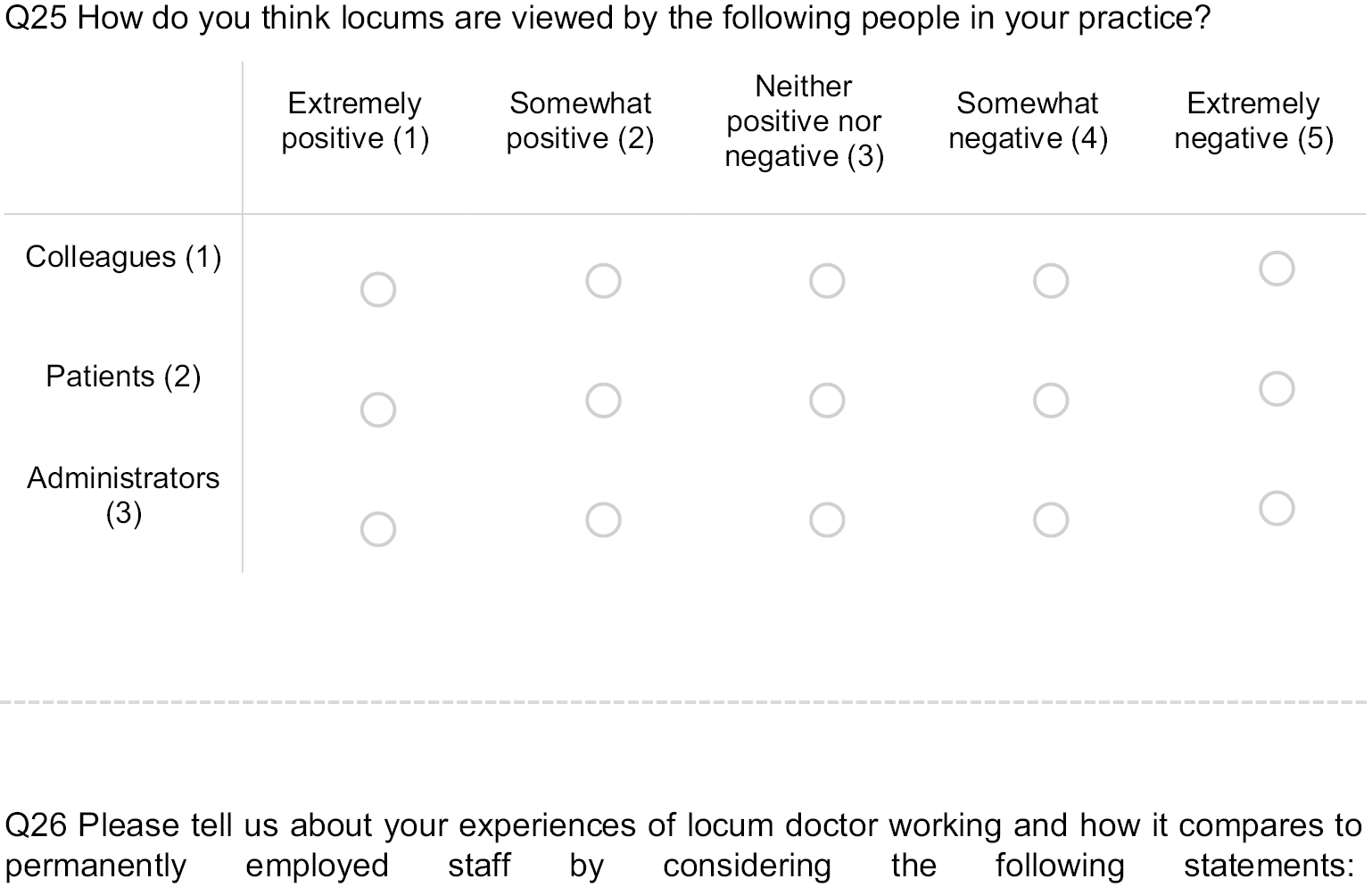


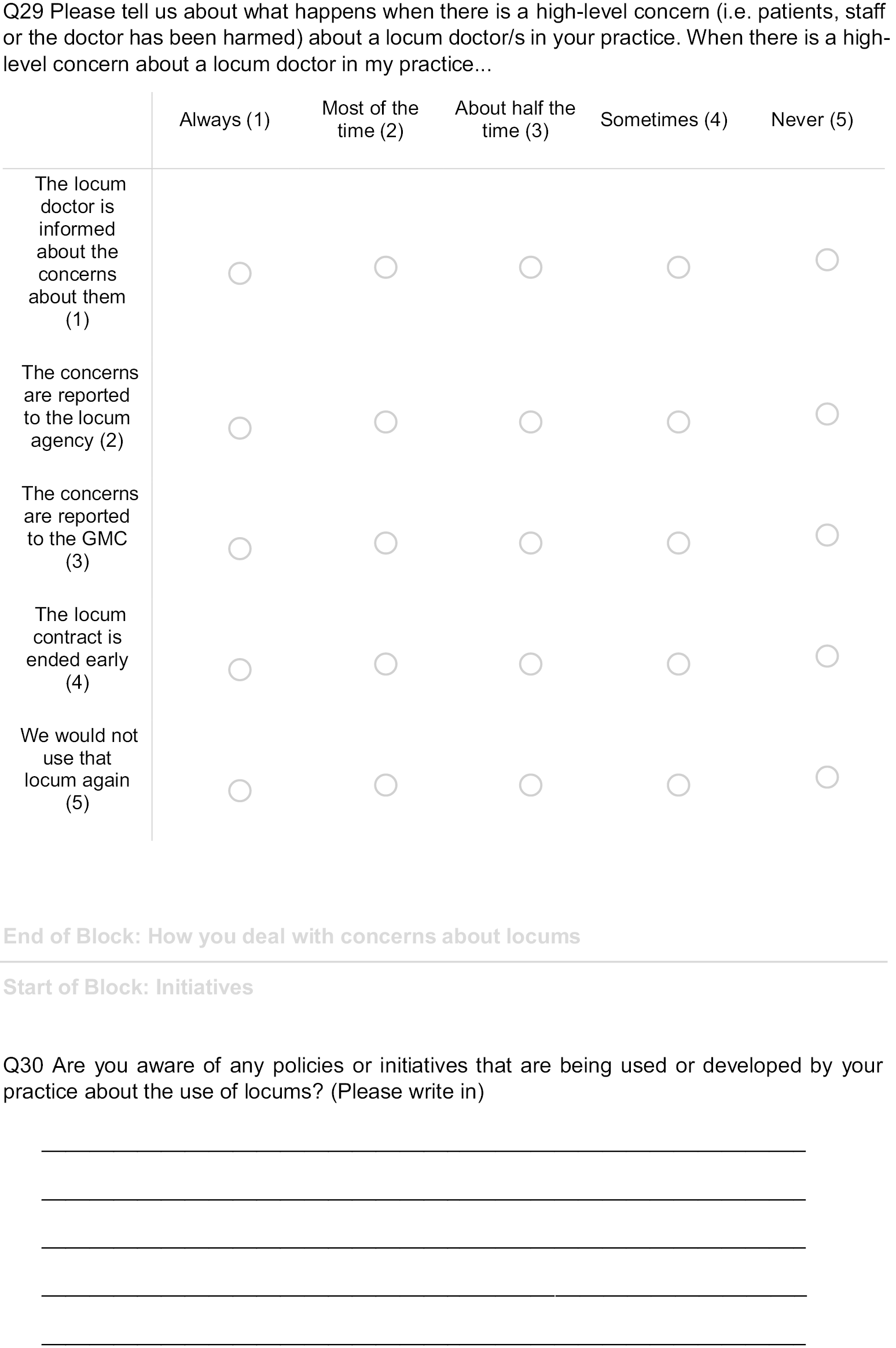
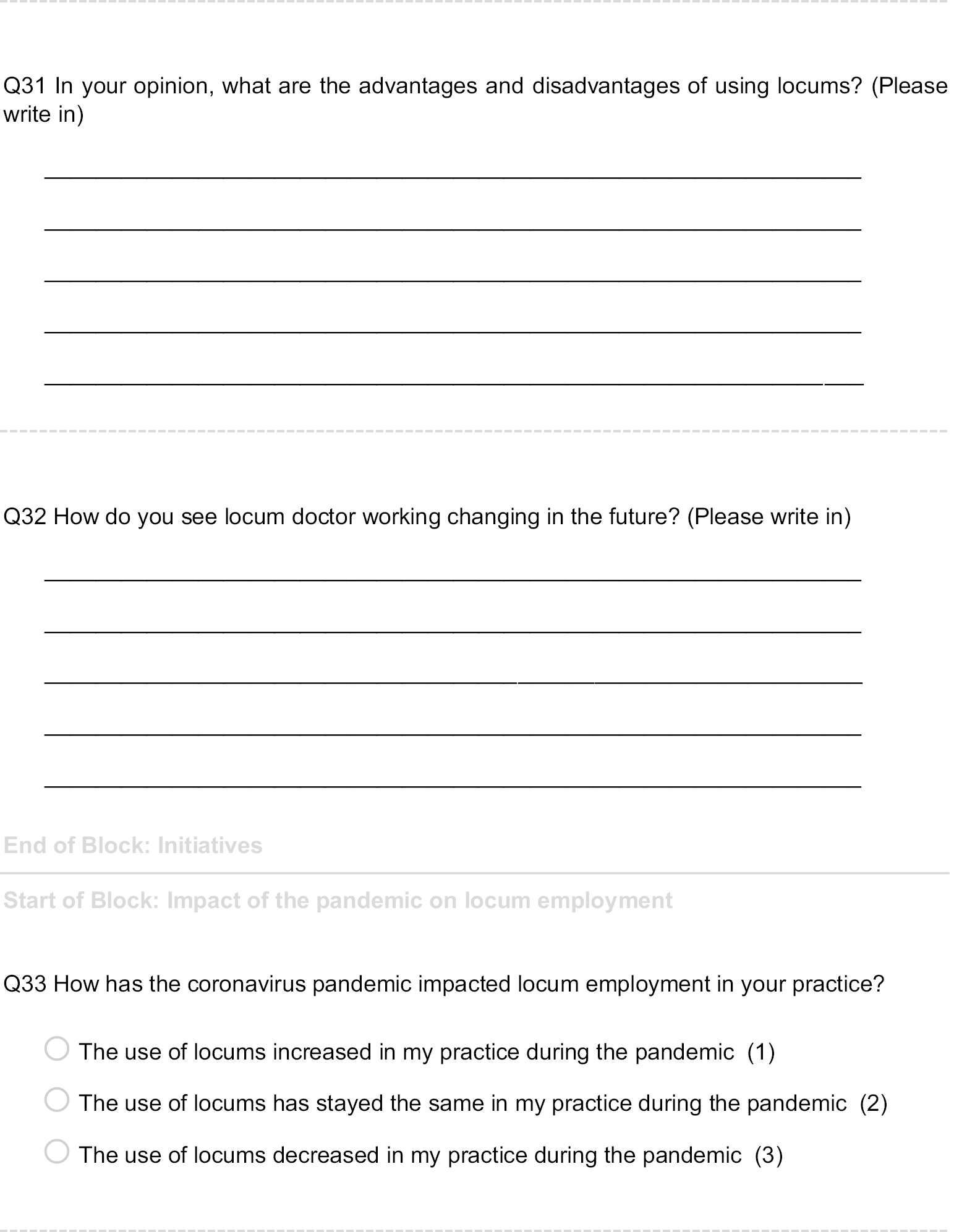
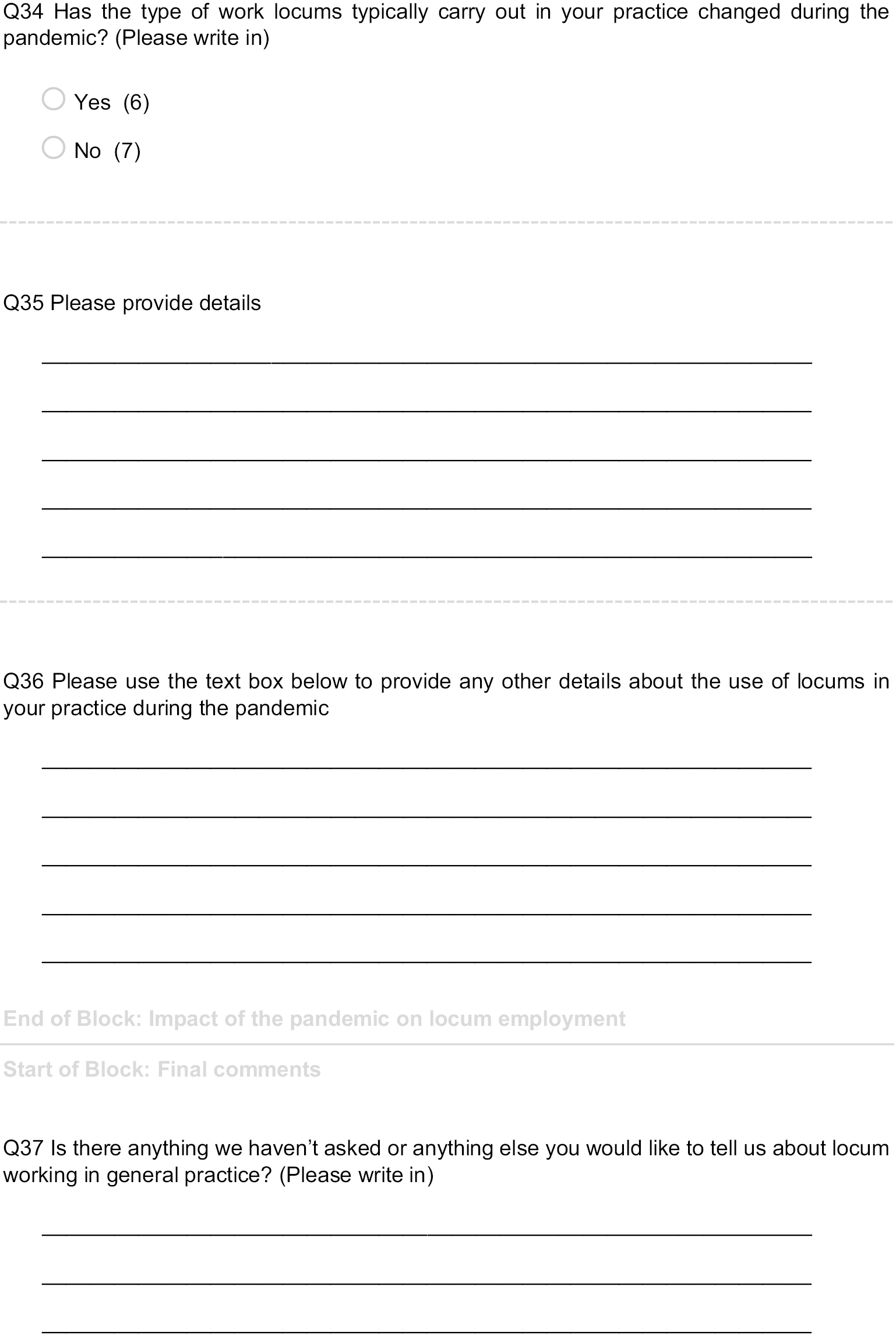
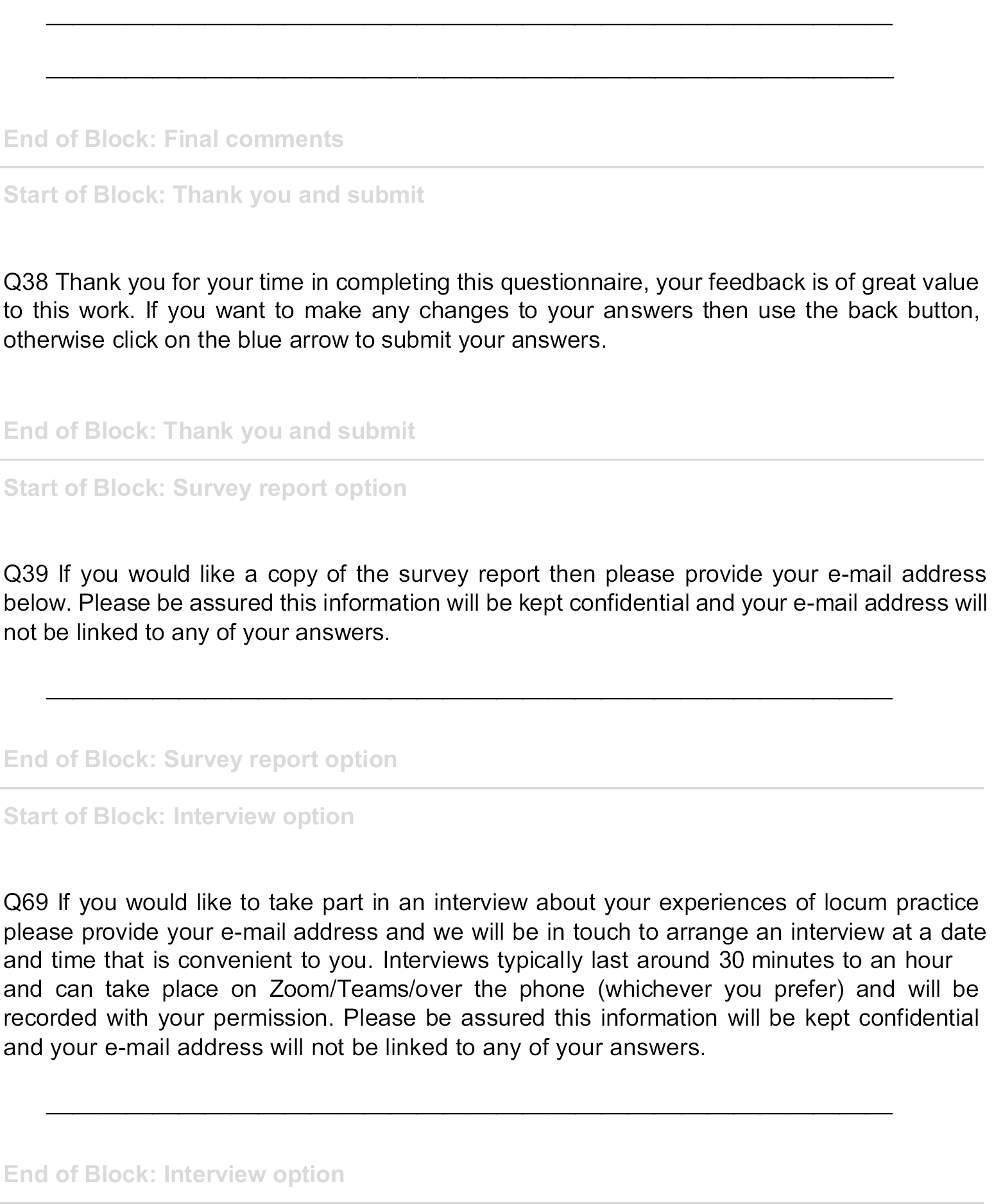
Appendix 5 Additional material for Chapter 7: Locum doctors in the National Health Service: qualitative findings on quality and safety
Interview schedules
Focus group patient and carer schedule
Note to facilitators: Please refer back to these notes just before the group is due to meet to refresh your memory.
One member of the project PPI forum will lead the group and ask the questions, while a member of the University of Manchester research team, Jane Ferguson or Gemma Stringer, will support the interviewer. Jane or Gemma will take responsibility for the recruitment of participants, issuing participants with participant information sheets and consent forms, taking consent from focus group participants, handling the recording equipment, making field notes and transferring sound files.
Remember to take a note of the date and case study site that the focus group is related to and record on the audio.
It is important to remember that you are seeking to explore the viewpoint of the group. You should try to get everyone involved in the discussion; however, this does not mean that everyone must have the same view. You need to explore both majority and minority views.
Before the group assembles
Jane or Gemma will ensure participants have received and completed the relevant paper work before the focus group meets, for example participant information sheets and consent forms, P20 forms so they can claim payment. They will test the recording equipment to make sure it is working and that the sound is recording at an acceptable level.
Preparing to start the session
If the focus group is taking place by a platform such as Zoom or MS Teams, to encourage discussion, ask all participants to keep their microphones and cameras on wherever possible. To facilitate discussion virtually, focus groups will be kept to a maximum of four participants.
Once people are settled, check with the group whether they all know each other. If not, start by going round the group and getting everyone to introduce themselves.
Make sure that everyone is comfortable before you start and that everyone can see and hear each other. Read out the statement on confidentiality:
Opinions expressed will be treated in confidence among project staff for the purpose of understanding patient and carer experiences and views of locum doctors. All responses will remain anonymous. Please don’t refer to any individual patients or doctors by name or name a specific hospital or practices. Also, please don’t describe any serious unsafe practices that led to serious harm that haven’t already been dealt with through the proper channels as we will be obliged to report it.
Check that there are no objections to the use of the audio recorder; then Jane or Gemma will switch it on.
Introduction to the session
Start off by reiterating the purpose of the focus group:
I’m very grateful to you all for sparing time to talk about your views and experiences of locum doctors and how locum working might impact care. The purpose of this focus group is to better understand patients’ and carers experiences of locum doctors and their views of locum working. This understanding will help to find ways to improve the working arrangements for locum doctors and the quality and safety of patient care that they provide. I would like to concentrate on discussing what you think about locums before going on to discuss any experiences you might have had. There are no right or wrong opinions; this discussion is confidential and we would like you to feel comfortable saying what you really think and how you really feel.
Perceptions of locum working
What comes to mind when you think about locum doctors?
Prompt: What do you think a locum doctor is? (i.e. how would you define one).
Accessing care
Do the group think patients and carers generally know when they are seeing a locum?
Prompt: How did you know they were a locum?
-
Do you think you should be told when the doctor is a locum? If so, why?
-
Have you ever made another appointment with your regular doctor after seeing a locum? If so, why/why not?
-
Have you ever refused an appointment because it was with a locum? If so, why?
-
Have you ever not gone to the doctor because your regular doctor wasn’t available? If so, why/why not?
-
Are there particular circumstances when you would prefer to see your regular doctor or permanently employed doctor rather than a locum? Which circumstances would you be happy to see a locum, and when would you rather see your regular doctor?
Critical incident question: experiences of locum doctors
The overall aim of this research is to better understand the quality and safety of locum practice and how locum working might affect care. Can you describe a time, whether it be positive or negative, when care was provided by a locum?
Do you think there are any differences in how care is provided when permanent staff are employed in comparison to when locums are employed? Can you describe any differences and what these differences have meant for you or the person you were caring for?
Prompt: If there was a problem, what happened next? How was it dealt with?
Challenges and opportunities
Why do you think some organisations are more reliant on locums than others?
What challenges do you think a locum doctor might face?
What would a good consultation with a locum look like?
Because they might not know you, are there any key questions the locum should ask?
How do you think locums should be supported to provide safer care?
What do you think should change to make care safer for patients when locums are delivering care?
Anything else
Has taking part in this focus group changed how you think about locum doctors/changed how you might make appointments in the future?
If there is anything we haven’t covered that you would like to talk about?
Summarise the discussion and check in with participants if there are any key issues that study team should focus on.
Ending the session
Finally, thank participants for their time and reiterate that the discussion is confidential.
Jane or Gemma will submit the recording to the transcription service.
Locum doctor interview schedule.
Thank you for agreeing to take part in this project. I’d like to confirm that you have read the participant information sheet and check whether you have any questions about the study? This interview/focus group should last approximately 1 hour. We’d like to remind you that the information collected from interviews and focus groups will be kept strictly confidential, and your responses will be pseudonymised, so you will not be identifiable in any published data. Any discussions that take place during the study are confidential. However, if you were to tell us something that could put someone at risk of harm, or reveal unsafe practice that has not been reported through the usual procedures, the researcher might be professionally obliged to report the incident through the normal risk management procedures. Information that indicates harm to patients or professional misconduct will be disclosed by the research team as part of a safeguarding process, in accordance with established good research practice and with the University of Manchester’s own policy on whistleblowing and public interest disclosure. If this happens, the interview will be stopped and we will discuss with you what we intend to do.
Narrative question
Could you spend 5–10 minutes telling me about your career?
What are your plans for the future?
Prompt: Can you tell me more about your decision to become a locum doctor?
Finding work and induction
How do you find work? For example do you work with an agency? Word of mouth? How do you choose the agencies you work for?
Tell me about the places you work in? How do you choose them?
Are you typically offered induction? Are you typically offered a paid induction?
Tell me about your experiences of induction, for example are you provided with details of where things are, who people are, login details and/or more complete induction processes
What does a good induction look like?
What should be included in induction to make it safer/easier for you to work?
Experiences of locum working
What would you say the key differences were between working permanently and working as a locum?
Prompts: What are the advantages and disadvantages of locum work for you? What are the advantages and disadvantages of locum work for patients?
What have been your pre-COVID and during the pandemic experiences of being a locum?
Do patients know you are a locum? Do you tell them?
How do patients usually respond to you as a locum?
How do staff respond?
Are you usually included in multidisciplinary team (MDT) activities, meetings and/or educational activities?
What types of staff training if any are you offered? For example statutory/mandatory, for example information governance; general professional basics, for example safeguarding and basic life support; general CPD opportunities.
Who do you revalidate through? Do you feel well supported in this? Has this been impacted by the pandemic?
For a provider where you have not worked before do you undertake any preparatory work?
How are you supported in your clinical work? For example peer clinical advice and/or navigating the local system.
Prompt: Who do you usually go to if you need support?
What would happen if there was a clinical problem with your work?
What has happen if there was a general problem with your work?
Do you get to hear about complements and complaints?
What happens when you reach the end of placement? Do you get feedback?
Critical incident question
The overall aim of this research is to provide evidence on the quality and safety of medical locum practice and the implications of medical locum working for health service organisation and delivery. Can you describe a time, whether it be positive or negative, when working as a locum, or how your work was organised by the organisation you worked for, had implications for the quality and safety of care?
Probes for critical incident question
What happened next?
Who was involved?
What did the organisation do?
What was the outcome?
How did that make you feel?
Why did this situation happen in this way?
What could have made the action more effective?
Locum working and the pandemic
What has been the impact of the pandemic on your work as a locum?
Initiatives
Are you aware of any policies or initiatives that are being used or developed to improve how locums are used by organisations?
What would you like to see included in any initiatives?
Anything else?
Is there anything else you’d like to add or anything that we haven’t covered?
Professionals interview schedule
Thank you for agreeing to take part in this project. I’d like to confirm that you have read the participant information sheet and check whether you have any questions about the study? This interview should last approximately 1 hour. We’d like to remind you that the information collected from interviews will be kept strictly confidential, and your responses will be pseudonymised, so you will not be identifiable in any published data. Any discussions that take place during the study are confidential. However, if you were to tell us something that could put someone at risk of harm, or reveal unsafe practice that has not been reported through the usual procedures, the researcher might be professionally obliged to report the incident through the normal risk management procedures. Information that indicates harm to patients or professional misconduct will be disclosed by the research team as part of a safeguarding process, in accordance with established good research practice and with the University of Manchester’s own policy on whistleblowing and public interest disclosure. If this happens, the interview will be stopped and we will discuss with you what we intend to do.
How does your job relate to locum working?
Tell me about what you do and how your job relates to locums? For example do you have hiring responsibilities, governance responsibilities; do you work alongside locums?
(Depending on the nature of the involvement with locum doctors) Can you describe the process of recruitment/induction/governance/integration with the team?
Perceptions of locum working
When you think about locums, what comes to mind?
Why do you think doctors choose to work as locums?
Would you say there were different ‘types’ of locum?
Have you ever worked as a locum? If so, why?
Would you ever work as a locum? Why? Why not?
How do staff respond to locums?
Why are locums needed where you work?
Why are locums needed in your organisation?
Where are they most likely to work?
Does the need for locums differ across specialties? Why?
What types of work do they usually do?
Patients and locums
How do patients respond to locum doctors?
Do patients know when they’re seeing a locum?
Do you think patients should know or need to know?
Do locums typically find out if patients complement them or complain about them?
Critical incident question
The overall aim of this research is to provide evidence on the quality and safety of medical locum practice and the implications of medical locum working for health service organisation and delivery. Can you describe a time, whether it be positive or negative, when locum working, or how a locum was engaged by your organisation, has had implications for the quality and safety of care?
Do you think there are any differences in how services are delivered when permanent staff are employed in comparison to when locums are employed? Can you describe any differences and the implications?
What happens when things go wrong or right?
If there is a problem with a locum, what happens next?
Prompt: What happens if there is a complaint or a serious untoward incident (SUI) involving a locum? What do you do in this situation?
Would you say there are any typical issues when it comes to locum working? What are they?
Does the locum typically find out if they were involved in a SUI?
Prompts: Who deals with this?
What benefits do locums bring to your organisation?
How do you capture their knowledge and share it with others?
Governance and support for locums
How does your organisation support locums?
What sort of support do you think locums should have?
Are locums included in CPD where you work?
Do locums attend MDT meetings and events?
Impact of the pandemic
How has the pandemic impacted on locum working where you work?
Initiatives
Are you aware of any policies or initiatives that are being used or developed to improve how locums are used by organisations?
What would you like to see included in any initiatives?
Anything else?
Is there anything else you’d like to add or anything that we haven’t covered?
Thank you for taking part
Additional participant quotations
| Theme | Example quotes |
|---|---|
| Familiarity and continuity: knowing: who, where and how | Every geographical area has different health conditions that affect that community. So if you were in a predominantly black community, strokes will probably be high in the elderly community. If you’re in a South Asian community, diabetes is very common and so is blood pressure. So we just need to be mindful of knowing the local knowledge. Because some of these locums come in and they’re like, oh, I’ve travelled 40 miles to get here and I haven’t got a clue and this is my second time I’ve come in this area. I’m like, and you’re supposed to understand what are the dynamics and all the issues. Because sometimes GPs say things without realising. Like they’ll say, oh, have you thought of this? And you’re like, we don’t have that in this area … So they need to have local knowledge what is available, what is affordable, what are the income levels, what is the deprivation like of that area. Sometimes they make suggestions and they’re not suitable for the patient because it’s not part of their lifestyle or their local area. (Patient 6, Focus Group A) |
| Often, as a consultant, I haven’t seen their CV, I haven’t been involved in appointing them for this locum shift. So look, I’m going to assume that they’ve got GMC registration. I’m going to assume that they’ve got negligence liability insurance. And I’m going to assume that they’ve been vetted and therefore, even though I’ve got grave misgivings about their ability, the system has put them in a position whereby they’re here. And whether I like it or not it is by far the path of least resistance for me to suck it up and let them get on with it. (Interview 28, Consultant, Secondary Care) | |
| The biggest sort of safety aspect that sticks in my mind, is that it is unbelievably frustrating to have to learn a whole new set of patients from day to day. And again, like I say, at the start, when I was signed up to four different hospitals, plus the locum agencies, I very quickly realised that not only is it the fact that you don’t know the patients from day to day, if you’re chopping and changing site the whole time, then store cupboard are laid out differently, ways of contacting relevant staff members are different, you’ve got to recognise what code to put in to bleep someone that’s different at every single site … So that’s why, pretty quickly in my F3 year, I decided, no, no, this is the hospital I’m going to work at, and I’m just going to stick with this hospital the whole of the way through, essentially. And that’s helped a lot with regards to that idea of consistency and knowing how to do what you need to do, essentially. (Interview 23, Locum, Secondary Care) | |
| I think when you get a lot of overseas … We try not to appoint many that haven’t got NHS experience, but I remember when I was at the [hospital name] there were some when we were desperate and it’s just the, kind of … We expect them to come in as a locum and hit the ground running, provide a service and go … they were working at … kind of, put themselves down at a certain grade and they’d done that certain grade over in their home country but then they’ve come over here and there’s misinterpretation. They weren’t probably working at that level … (Interview 22, Medical Staffing, Secondary Care) | |
| Lots of the doctors who have trained overseas, who come to the UK – particularly doctors who don’t have English as their first language – describe culture being the most difficult thing to get to grips with in the UK. And this is not just locums, it’s across the board. The way in which our system treats its staff and its patients and the expectations of, you know, everybody on everybody else, is unique to the UK, I think. And it’s unwritten and it’s not really described and it’s nuanced and it’s a flipping minefield, you know? I absolutely take my hat off to anybody who even tries to navigate it when they’re not an NHS native, if you like. And that’s very, very difficult and it definitely plays out a bit with locums as well, because, again, it’s a little bit back to why are they a locum, but people who, for whatever reason, haven’t been able to get a permanent or a long-term contract will locum. And I don’t blame them; that’s what I’d do. But if they haven’t got a really good handle on that culture and the way to navigate it, I think it’s just absolutely riddled with potholes for them to fall into. (Interview 28, Consultant, Secondary Care) | |
| It’s very different in different places, but there’s a bit of a spectrum of how much you are engaged day to day and how much they’ll engage with you, which arguably should be the other way round, should be the less you are there, the more they should engage with you to try and make you feel secure and be as good as you can be, because sometimes you’re set up to fail. (Interview 35, Locum GP, Primary Care) | |
|
I’ve not had any induction which I actually think is an issue … I got absolutely torn apart by a consultant one morning because I had referred a patient to the wrong bit of the hospital, they were getting admitted and they were like, oh we should have done this. I was like I didn’t know that, if you’re not going to tell me these things then … (Interview 36, Locum, Secondary Care)
I always went in as a SHO because I didn’t know the hospitals, and of course, quickly when they realised that I worked as a more senior grade, they wanted me to work more senior. (Interview 56, Locum, Secondary Care) |
|
| Efficiency, empowerment and displaced work | I don’t know if it’s a sort of, brave act or just a bit stupid but I’ve worked alongside people who’ve shown up and they are like, I’ve not worked in the region before. And I’m just like, okay, so … you try and do, sort of, a quick induction but I’ve worked shifts before where people haven’t had IT logins, so they’re spending the first two or three hours of their shift on the phone to IT to try and get setup with the computers. And that can be particularly difficult, particularly as a lot of trusts move towards more online systems, so not just electronic prescribing, but electronic observations, all clinic letters going online, all notes going online sometimes. So, it can be quite a hindrance if people aren’t familiar with the systems or already setup. And, obviously, there’s the information governance issue that means that you can’t just log someone in under your account, if you like, just get started. So, it’s that time spent of someone trying to get used to the systems and get access to the systems that is a bit of time being wasted. (Interview 57, Locum, Secondary Care) |
|
And sometimes, you’re having to ask other staff to order it for you. Can you order bloods on, da, da, da, da, ’cause I can’t get in the system? … Because you might have to wait on someone else to look something up for you, and you haven’t got time to do that. So, you just revert to what you know, if you see what I mean? Oh well, I used to do that in that hospital, so this is what I’m doing in this one, because I can’t get to see how it’s done. But, as I say, that’s one of my reasons for working at a level down, so that there’s always somebody there who’s ultimately responsible, if you get what I mean? (Interview 56, Locum, Secondary Care)
I: Can you trace the prescribing or a referral or, you know, whatever tests that’s been ordered back to a locum? … Would they know it was you who’d prescribed from your ID card? |
|
| R: No, you’d just go in as locum X or locum number one and it wouldn’t be … yeah. What’s annoying as well is that when I’m using these cards, there’s certain things as a consultant, it has to be consultant-only prescription and I can’t prescribe things. Even simple opioids which, you know, as an anaesthetist, I would prescribe all the time, I wasn’t allowed to prescribe. And so I had to get one of the trainees to do it, which was a bit of a … which is unreasonable considering, you know, I’m paid significantly more than them, why … it should be the responsibility of an employer to make sure that I’m competent, I can do my job. But then they’ve got to … you know, to get the most out of me, they need to give me the resources that I need to do the job. There’s no point in appointing somebody and then telling them they can’t do anything, which is what happens. (Interview 24, Locum, Secondary Care) | |
| You build, frustration amongst substantive staff because they’re having to pick up pieces, they’re having to give access to systems. They might have to put themselves in a slightly compromised position by lending a login or something like that. And that all feeds into that thing of they’re getting paid more, they’re doing less, they’re making more work for all of us, which is not really ultimately what the purpose of locum work is at all. It’s filling in gaps and I say it is a very beneficial service. But unique to medicine I think it is very challenging. (Interview 54, Locum, Secondary Care) | |
| Continuity and discontinuity | I do have a concern though and maybe even a fear that you don’t have the continuity. When you have a rare condition, the one thing you want is continuity or faith in somebody understands the neurological condition that you have, in my case. And that continuity hasn’t been there. And it worries me when I see a locum, they only … they can only look at the records and sometimes they’re not as up-to-date as the last time you went to see the consultant. So it concerns me that you’ve got to spend time going over stuff … And sometimes you forget, oh, I should have mentioned this, should have mentioned that, which is relevant. And it’s a fear really and a concern that there isn’t … because you’ll never see the same locum again. And they’re not accountable, they come and they go. (Patient 5, Focus Group A) |
| Dr Bloggs has always done things this way and, oh my g*d, he never does this or he never does that … I’ve worked in practices and I’m a bit of an outlier in terms of things like prescriptions for antibiotics, fit notes and hypnotics, diazepam and zopiclone, I’m very much an outlier, an outlier in a good sense because I’m very strict about these things, whereas it’s the easiest thing in the world to dash off a prescription or a sick note and be done with it, but I scrutinise it. And as a result, I’ve become enormously unpopular amongst some circles because the patients then grumble, that feeds through to management and they’re breathing down my neck, and when there’s a culture of appeasement and just doing what the easiest thing is around the patients, then it does upset the apple cart to have an awkward person like me almost putting a finger up and saying this is how we should properly do it. (Interview 58, Locum GP, Primary Care) | |
| I think it’s in the things that go unsaid, you know, like you don’t get asked to come to teaching, you’re not really included in certain discussions about how things are done. And I think as a locum, you end up, even if you don’t move hospitals that much necessarily, but you work on different wards and you see people do things in different ways, and sometimes certain things work better than other things, but for some reason there’s no like, it’s very difficult to have a conversation with someone and be like, oh, you know, have you thought about doing this, and getting anything of that? It’s usually just kind of like, oh this is how we do things and we’re too busy to consider changing thing or whatever. (Interview 13, Locum, Secondary Care) | |
| I remember coming in to one of my hospitals … and they were giving a child phosphate. And I said to them, but that’s not how we do it anymore, there’s been a change in practice. And they looked at me as though I was completely bonkers … Then I discovered that one of the consultants, another one, not the one I’d spoken to, was aware of it, and together we got on top of it, and I helped them put together a new protocol. But it was finding the right people to support me. Because the first person I went to batted it away … So, it all depends on whether you can find the person that’s open to change. (Interview 56, Locum, Secondary Care) | |
| We’ve seen some cases though where a locum’s come in to fill in for somebody where they’ve absolutely identified a bag load of problems with the practice of the individual that they’re covering for. So actually they can be very good at highlighting deficiencies that have probably been concealed or circumnavigated for years. And so that makes it more challenging … when you can identify not necessarily just as a whistle-blower but you can see where there are suboptimal things happening that you then have the challenge of raising when you’re a newcomer, your status and tenure is different from your peers and you’re the new kid on the block coming in sort of saying things that clearly are going to be challenging to hear. (Interview 34, NHS Advisor) | |
| I think where we should be learning from agency doctors is these doctors are travelling around other trusts in the country and so there’s some learning for the organisation to be had on how things work elsewhere, what sort of models are in place, and where we can pull on that. I think there’s some really valuable knowledge, but I just don’t think anybody sees them as a permanent part of the organisation, so you can’t plan with an agency consultant, because your plan is always to recruit into that post on a permanent basis, and with some of the agency doctors you’d love to recruit them into that post, but that’s not what they want. That is not their agenda. (Interview 91, Medical Education Manager, Secondary Care) | |
| Balance and stability | It’s not the most efficient form of medicine. And it’s not, neither for patients nor for doctors and the practices, or the NHS as a whole. So, you know, but I think … I think it’s something, having an NHS run by locums would not be desirable … They need to be used judicially in practices. I think practices that use them all the time, and I’m working in one that does that, I just don’t think they’re going to work efficiently. I don’t know what happens to all the patients in this practice; there’s a lot of them and there’s very few doctors, so, I don’t know whether they all turn up at A&E and urgent care, but then again, I don’t see that because I just go in and do a job and leave at the end of the day and I don’t know, I don’t see any of the stats, figures, feedback, or whatever. (Interview 81, Locum GP, Primary Care) |
| I think there’s much more service development and quality improvement with permanent staff. Again, there will clearly be exceptions to this, but locums tend to turn up, they do the shift, they go home. Whereas when you really want to drive improvements in patient care, it’s the permanent staff who do that. If you get a department that is disproportionately locum dependent, then it stagnates, it doesn’t progress. Things like implementation of new NICE guidance, for example, that sort of thing tends not to happen or happen less well, less quickly. So a big well-functioning, I’m talking more about the sort of consultant level, specialty doctor level, a big well-functioning established team can easily carry a couple of locums without, I think, there being any impact at all. Whereas a small team perhaps one of the small medical specialties where you might only have one permanent neurologist in a small DGH and the other capacity of the service is being delivered by a string of locums, then it’s really hard to expect that one person who’s trying to keep the whole service afloat and to a certain extent monitor the locums work and drive change and improvement. It’s just too big an ask. (Interview 30, Responsible Officer, Secondary Care) | |
| I worked in a practice where there was one full time GP and everyone else was a locum, so a patient might see six different doctors for one problem over a period of six weeks or something. So if it’s like that and there’s a total lack of continuity, and I have to say that those practices I tend not to work in for my own satisfaction and just safety actually. Because there’s a safety quality aspect from the locum but there is also a big one from the practice perspective. So I as a locum if I feel the practice is not aligned with how I like … I have a certain standard of how safe and decent I think a practice is in terms of the quality of their notes, the staffing levels, their systems, and if it doesn’t meet that then I won’t work there, and I have been in a practice like that. (Interview 59, Locum GP, Primary Care) | |
| What support or protection do organisations get when our staffing levels drop down that low to say, actually, we can’t deliver this service safely, or we’re trying to do it to the best of our ability … There’s always a real focus on our nurse staffing and how we make sure that we staff our wards effectively, and yet doctors for some reason are just meant to be able to spread themselves out thinner and thinner and thinner and thinner, and it just doesn’t seem … it doesn’t seem right, doesn’t feel like there’s any sort of support or safety net as it were for the organisations. Because ultimately this is about our patients, I appreciate that, it’s about safety of our patients, but actually … if I have locums coming in, suppose tonight, suppose the whole of my A&E department is staffed with locum doctors and something goes wrong, they’re going to say to me, what on earth were you doing, staffing the whole of your A&E department with locums. Well, where would you like me to start? You know, I don’t do it out of badness, you do it out of how do I keep the service running to the best of my ability. (Interview 32, Medical Director and Responsible Officer, Secondary Care) | |
| Collegiality, involvement and inclusion | One of the partners once commented, when I said, I think we should make the locums more welcome because of, at that time we were struggling to recruit another salaried, and I said it would be good for our image if we can be nice to the locums, just ’cause I know how they all talk and there’s this WhatsApp group, where they’re all in one WhatsApp group together, and word spreads. And then one of the responses from one of the partners was, well, actually, I don’t see why they should get that privilege of teamwork and the luxury of being part of the team and welcomed at the practice, because they’re the ones who have chosen to locum so it comes as part and parcel of that. They shouldn’t get that privilege of having that team support, and that teamwork. (Interview 97, Salaried GP, Primary Care) |
| I’ve worked in another practice where, because they live on locums and they live on ad hoc locums, you’re a piece of dirt under the shoe. You don’t get gloves, you didn’t have aprons, you didn’t have a face visor, you didn’t have safety specs, you have to ask for a mask. Not only are you not treated as a service provider, you’re not treated as a colleague, someone with knowledge. You’re not treated safely. I mean, not just … I’ve been to practices as a locum during the pandemic where there’s been no PPE for the locum at all. I’ve spoken to colleagues who have been told, no, the PPE is for the regular staff. (Interview 44, Locum GP, Primary Care) | |
| You can be in a department and really nobody regards you as anything other than just … well anything really, you just get on with your work until of course something goes wrong and then you’re the one whose … sometimes we do get problems, like for instance, I had an anaphylaxis and I was in … it was actually the same hospital that I said, nobody would speak to me in the department but it could easily have been one of a number of hospitals … I got an anaphylaxis which was a bit of a crisis to start with … when you have a crisis, the first thing you do is call for help and all the absolute standard resuscitation programmes and stuff. That was just not happening at all and nobody would come down from the department … Nobody would come down … the attitude was, well it’s a bl**dy locum, what do they think they’re doing, they don’t know what they’re talking about. That’s a preconceived thing but ultimately, it’s communication because if people came and talked to you or if you’re in theatre and somebody came along to say hello even, you’ve just come, I’ve heard about you, you’re here for a month or so, so you know who these people are. (Interview 47, Locum, Secondary Care) | |
| I think sometimes those doctors will experience a level of hostility from teams. I’ll give an example, if I had a locum registrar working in obstetrics and gynaecology, I think it is likely that the midwives would have a view about that locum doctor that almost they need to prove themselves. Rather than, that’s great, we’ve got this really experienced doctor and until they make a mistake, we will treat them like a member of our team who has worked for years. And I think that is a very real scenario that would play out in a number of settings. And I think there is an expectation that somebody comes in and hits the ground running and is able to, for example, navigate round all of our clinical systems. Well, if they’ve never used our clinical systems and have always worked with others, it is unreasonable to expect that they would be able to do so on day one. But I’m not sure that locums are necessarily shown that level of compassionate understanding that there might be a bit of upskilling needed. Nor, indeed, that actually had that locum chosen not to come to us, we would’ve been in the worse situation where we would’ve had no-one. (Interview 27, Medical Director, Secondary Care) | |
| Defensive practice, hedging and avoidance | I think there are locums who are really committed and, you know, would work as well as a long term doctor in the practice, and there are locums who can just not make any decisions, still see the patient and then you have to still deal with the problem the next day or the day after. So, yeah, there are different kinds, so there are very conscientious locums and there are people who are not so conscientious … Sometimes, I think sitting on the fence can be an issue with the locum role, because it’s quite easy to say, well, we’ll do some bloods and then see you again. But I’m not there to look at those bloods and I’m not there to discuss what way we go, so it can be an inappropriate use of NHS resources, you know, wasting money on unnecessary blood tests and things when you don’t need that really. (Interview 1, GP and CCG Medical Director, Primary Care) |
| One of the difficulties about locuming is, if you run into problems, you’re it. You don’t really know the practice well. I don’t actually know the hospitals where I’m working well because they’re not the ones I worked with as a partner. And, yeah, you’ve just got to use your own resources and you are a bit on your own. And that’s why locums probably refer a lot, do a lot of investigations, and safety-net lots, and sometimes inappropriately all of these things, but that’s partly the situation they’re in. (Interview 81, Locum GP, Primary Care) | |
| Well most of the locums that I know will just say, okay, there’s already somebody else who’s made a decision, it’s not my job to make a decision I just follow through. If things go wrong, call the senior person and be done with it, that’s the end of my role. Actually doing something to protect a patient is not important for a locum because the risk is too high. The GMC’s at risk, you don’t want to do anything. (Interview 55, Locum, Secondary Care) | |
| Governance | And of course, governance is modelled on doctors working within the NHS, that they are meeting colleagues in the corridor all the time, that they’re having contact with other substantive colleagues, and that there is this internal governance system, informal as well as formal. Whereas, in the agency world, I never meet the doctor. Well, I do actually, I make sure I do, but mostly we don’t meet the doctors. And it is therefore virtually impossible for me to make any judgement of a doctor’s clinical ability. Can I even make that judgement over their language ability? It sometimes is quite difficult. (Interview 47, Locum Agency RO) |
|
Some of the locums come asking for feedback, even when you’ve known them only a few hours, and sometimes the assessment won’t be appropriate because you are trying to justify the quality of work after only for a few hours. (Interview 15, Consultant, Secondary Care)
The feedback, say, will tell the responsible officer but did they … I didn’t get any more feedback. I’ve never had a form back where they’ve said, I’ve discussed this with Doctor X, they felt like this, or their comeback is that this happened in their opinion. (Interview 11, Clinical Director, Secondary Care) |
|
| Now in terms of governance of these doctors, you know, the obvious issue that you may also be very well aware of, locum doctors move from one agency to the other at very short notice. And they may do that for their convenience, they may do that to skip the requirements of governance, so feel that, you know, they may get away with an easier appraisal or less exacting standards. And they do that all the time. So that does happen. It used to be more frequent in the past but now it’s much less. We don’t encourage people to join at very short notice before their revalidation date. So what we do is, if somebody does join us at very short notice, we do a blanket deferral for those doctors for about three months because we have … we want to know more about where the doctor is in terms of his appraisal and revalidation. (Interview 49, Locum Agency RO) | |
| Our approach at the Trust has been to give them the same training opportunities as a doctor in training, to pay them on the same pay scales, to add them into the same rotas, to give them a supervisor in the same way that you would get a supervisor if you were a trainee. So all of those things, we try and treat them identically to a trainee. The only exception is that they wouldn’t go to the deanery training opportunities in perhaps the same way. But any local teaching that’s taking place in the department they get invited to. All of those things, we try and treat them the same. (Interview 26, Medical Director, Secondary Care) | |
| But the biggest challenge I find is actually being able to find out who they are. It’s a very fluid workforce and unfortunately in terms of distribution lists with practices it’s very straightforward, who are your partners, who are your salaried GPs, it’s very hard to work out who your locums are in an area. I’ve been to NHS England about this as well because of data sharing and all the governance and so on, we’re not able to have the list of locums assigned to our area, so inevitably we do miss out on communications unfortunately. (Interview 2, Locum GP, Primary Care) | |
|
I: Do you feel as though you get to hear about things that are important for you to do your job?
R: No, not massively, to be honest with you. No. I get like, the Trust’s, you know, weekly newsletter which is pretty useless, quite frankly. But that’s it. Because a lot of things that you need are really important, you hear more from word of mouth more than anything else … there’ll be some changes and you’ll be like, oh, I didn’t know that, for example, because I haven’t been there for a month. (Interview 52, Locum, Secondary Care) |
|
|
So, something simple like being added to a mailing list isn’t an option, I’m still not on their mailing list. I said, you’re already sending an email out to people, why can’t you add me to your mailing list? I don’t understand … why wouldn’t you want your locums to know what’s going on? (Interview 70, Locum GP, Primary Care)
I think for some, there will be services that will not even bother to involve the locum ’cause they’re like, they’re here for three or four weeks, they can, you know. And there will be no feedback given which is also awful because there should be an opportunity to improve, I would want to know if my performance was having a negative impact. (Interview 27, Medical Director, Secondary Care) |
|
| It might just be an email from one of the lead medics who was on call or working that shift just to say that they had some safety issues and concerns with this locum. It would just be a case with it being a temporary workforce we would probably just stop that agency doctor working or that locum working and then we’ll just inform the agency … but we put that on the agencies to inform them. I suppose it’s not great, really. It’s not great for any sort of co-learning and development but again it comes back to the perception of a locum, you know, they’re here just to fill a gap and provide a service and if they’re not providing that service then we just remove our responsibility for them. Whereas if that was obviously a doctor that was working here or a substantive doctor we would give them that feedback and put measures in place to make sure that they’re getting all the right support and training so that there isn’t a repeat of that. I think that’s probably the difference that we just see the locums as a service and if they’re not providing that service then we just dump it, really. (Interview 22, Medical Staffing, Secondary Care) | |
| It’s very variable. And some hospitals, some trusts, some ROs in the NHS are excellent at handing back to us the reason why they’ve let a doctor go. And others, no, the doctor is just asked to leave, and just some vague term of incompatibility is reported back through the recruitment officers, and the HR or doctors’ management team at the hospital, and we get nothing that we can, not use to criticise the doctor, but to begin to understand why the doctor failed at that particular trust. My duty is to make sure patients are safe. But my duty is also to help doctors understand where things are going wrong … but if the hospital doesn’t tell me what the concern is about, what the complaint is about, the reason, and they don’t have to provide a reason, then I’m stuck. And all we do is mark the file and know not to try to place that doctor at that trust anymore. (Interview, 47, Locum Agency RO) | |
| I remember being in a pub once at one of these locum group meetings and there was a new GP there. And I introduced myself and we got chatting. He said, oh, yeah, you’re that locum who missed that annular rectal carcinoma, aren’t you? I said, what, what surgery are you at? He said, oh, yeah, no, I was a trainee in one of your surgeries, yeah, you saw this patient and you did a rectal examination. And I remembered the guy completely. And you found an abnormal prostate, so you sent him to urology and the urologist saw him and diagnosed an annular rectal carcinoma. So yeah, that was you. And no one had ever told me and I’ve never worked at that practice again. I had no idea [why I hadn’t been asked back] … I just thought I wasn’t working at that place because they just didn’t need locums. But no, it was because I’d missed something. And obviously since then, every time I do a rectal examination, I think I mustn’t miss that. It’s a fantastic way to learn, it’s the best way, it’s a gift you’re given, you know, to learn from your mistakes. But you’re denied that because it’s much easier to say … oh, don’t worry, we just won’t use that locum again. And, you know, that gets the patient off their back. It’s so wrong. (Interview 63, Locum GP, Primary Care) |
Appendix 6 Additional material for Chapter 8: patient perceptions and experiences of locum doctor care
Additional participant quotations
| Theme | Example quotes |
|---|---|
| Patient perceptions | I think it comes down to personalities. You’ve got good doctors who are thorough and then you’ve got other doctors. So it doesn’t really matter whether they’re a locum or not, it’s their ability to read notes, to understand the notes and then to know … have the power to action the correct treatment, without being worrying about the cost of sending someone for tests and things … And we need locums. The days of the one GP forever has gone. So that’s my take-away is that we need to be aware that the doctors that we’re seeing want to do it and that they’ve got the right tools to do it. (Focus Group B, R1) |
|
For me it’s to be told that he’s a locum, and maybe even reiterate his – not his training and history, but he’s fully qualified, because some people might think, oh, locum is junior or something like that as well. (Interview 75, Patient)
I feel from their point of view that they are GPs in waiting, obviously waiting for a position somewhere. (Focus Group D, R3) |
|
|
That I think locums are no different than regular doctors and they find themselves sometimes in a difficult position because they are thrown into unknown place and they have to figure it out quickly. And as I said, they sometimes lack this confidence that a regular doctor has, just from being in single place for a number of years … locums shouldn’t be treated any differently than regular doctors, they’ve completed their education, their training, they want to help, they want to be professional, et cetera. Just perhaps the patients should be more tolerant. (Patient Interview, 09_85)
I don’t think of locums, or not locums, I just think of going to see the doctor … because these days you can’t even get to see the same doctor twice … So going to see a locum is just like going to see a doctor you haven’t seen before. (Patient Interview, 09_61) |
|
|
It seems to be the issue isn’t really whether you’re a locum or not, it’s to do with the supporting infrastructure and the person themselves. (Focus Group B, R2)
I think it comes down to personalities. You’ve got good doctors who are thorough and then you’ve got other doctors. So it doesn’t really matter whether they’re a locum or not, it’s their ability to read notes, to understand the notes and then to know … have the power to action the correct treatment, without being worrying about the cost of sending someone for tests and things … And we need locums. The days of the one GP forever has gone. So that’s my take-away is that we need to be aware that the doctors that we’re seeing want to do it and that they’ve got the right tools to do it. (Focus Group B, R1) |
|
|
I find some locums are very, very good and some are not as good, but I also find some consultants who are very good … I think from what I’m hearing along with my own opinion is that with locums, with GPs, with senior registrars, with consultants we’ve got good ones, medium ones and not all that good. Occasionally we’ve got some who are fantastically excellent. It’s just like the rest of the world, it’s mixed. (Focus Group C, R4)
I think it just depends on not necessarily whether they’re locum or whether they’re a permanent doctor but I suppose what the personality is like, how much they’re enjoying the job, what their interests are. Whether they’re willing to listen, how much experience they’ve had, whether they’re tired of the job and they’re not really interested in it as much anymore, whether they’re stressed … So I think it kind of depends more on the person and I suppose the environment that they’re working in and the systems that they’re maybe using. (Focus Group B, R3) |
|
| Fortunately for the first time I had a guy there who actually explained what my problem was and why they couldn’t do any surgery on it. I said to him, oh how come that I’ve been waiting three years being messed about. And in three minutes you showed me what was wrong with me, you explained why it can’t be done, why the dangers are higher than the benefits. He looked at me and smiled like Mona Lisa and said, well some of us are better than others. And the moral of that to me is actually that’s exactly the same as locums, some are better than others. If you get a good one, they can be very, very good, because they’re really, really going to be careful. And if you get a bad one I think this is the thing, they’ve not got the confidence or the experience to say, yeah, we’re going to do this. And have they got the confidence or the clout to say straight up I’m going to refer you to such and such consultant? … But as far as locums are concerned, as I say, I treat them as being as good as anybody else until I find out that they’re not. (Focus Group C, R4) | |
| I think the issues with your medical history and with follow-up is with locum doctors, but I think in terms of the response to what you’re actually presenting with I don’t think, my opinion is it’s not a specific thing to being a locum doctor; I think that just can be the individual doctor and consultants themselves … I’ve been in that situation where I have been seeing my regular GP and not been satisfied … I’d be happy to see a locum, because that fresh set of eyes made a massive difference to me because it meant that at an early age my endometriosis wasw dealt with, I had surgery, I’ve been able to have two children. (Focus Group E, R1) | |
|
Somebody who can’t find full time employment … To me, if they wanted to be doctors, they would be looking for a permanent position either as a GP or in a hospital situation. I’m never happy with them, but that’s my view. It’s they’re not unemployable in that respect, but they don’t seem to fit into one category? (Focus Group C, R1)
I don’t have a particularly positive impression of speaking with them. I found them … lazy. (Patient Interview, 09_116) My mother has seen locums in A&E; she was a frequent flyer, my mum. She had pneumonia five times in one year, the fifth time took her, but that’s how often we were in hospital. We did see locums then, I confess to speaking to them like they were children, because I’d been through it that many times, I was saying, no, I’m not doing this again. (Patient Interview 05_41) |
|
| Patient awareness | The receptionist told me when I was booking the appointment, it was along the lines of, will you be happy to see a locum, or, it’s Dr X, it’s a locum, or I would have said, is that the new doctor, but again, I don’t think a lot of people would [know]. (Interview 21, Patient) |
|
Why would a locum doctor feel the need to say to a patient, I’m the locum, when actually that patient is probably used to the registrar changing every six months anyway on rotation? Invariably, they’ll see someone different, why would you not just say I’m Miss Smith’s registrar, she’s in the next room. Why would you badge it with locum because I think if the reality is if you do use the word locum, I think most patients are familiar with the word locum and they’ll see it in a negative way as this is somebody that’s not going to know me, this is somebody that’s not going to be as close to my history and it’ll put those barriers up almost immediately … If you don’t say you’re the locum at the start of the clinic and then it becomes really apparent that you can’t find the records on the electronic system ’cause you’re not familiar with it, would that be worse in terms of the doctor/patient dynamic if you hadn’t signalled that that might be an issue than if it just becomes apparent? Is it something that locum doctors will say explicitly ’cause they’re aware of that vulnerability and the fact that they’re likely to be more scrutinised and therefore they almost use it as a defence, I don’t know. (Interview 27, Medical Director)
I’ve seen various locums at the surgery now. And prior to COVID-19 you would go to the surgery, not be offered, most of the time, a choice of who you see. So often you’d seen a locum and not even know that. And there’d also be like trainee GPs, so it’s hard to distinguish who’s who. (Focus Group A, R2) |
|
|
Typically patients don’t know that they’ve been seen by a locum. Patients have conveyed to me in my experience that they feel locums aren’t committed to the organisation, so can come in, do slapdash and leave if it gets hot, if it gets too complicated. They don’t have any emotional investment that this is their organisation, this is what they’re going to help control and take pride in that, because they’re only there for a period of time and can leave. (Interview 20, Director of Patient Experience, Secondary Care)
When you see somebody, do you even know if you’re seeing a locum? I mean, yes, if you go on your computer and you look up your practice, and you look at the list of doctors there and so on, you can do it. But quite often, if you ring up the doctor because you’re ill and they say, well, I’ll give you an appointment with Dr Whatsit. And you haven’t a clue who Dr Whatsit is and you’ve never seen Dr Whatsit before, Dr Whatsit apparently has never seen your notes either, it’s quite muddling. So I think there are things one could do to make it a bit less muddling if one puts one’s mind to it. (Focus Group A, R3) |
|
|
When you’re in hospital you might see lots of different doctors and some of the situations where I work it probably wouldn’t be a good idea to say doctors here to see you now, by the way he’s a locum, he doesn’t know anything about the hospital, the area, the district. All he knows … no. So I don’t know is my answer. In a lot of cases I wouldn’t say that. I wouldn’t. (Focus Group D, R1)
Sometimes at my surgery I don’t know about anybody’s else’s but I don’t know if I’m seeing a locum or not … I don’t know who’s a locum, who’s doing what and who’s the nurse? I think it runs quite smoothly but sometimes … it is a bit scary not knowing who you’re going to see. But thinking back over the last 18 months, 13 months, whatever it is, that I’d sooner have a little bit of something than nothing at all. (Focus Group D, R5) I’d say in the past … you’d ring the doctors and they would say to you. But I find in more recent years at my GP practice that there’s not even that really. My GP practice is also a training practice, so we have lots of different doctors coming and going. (Focus Group E, R1) |
|
|
If you’re ill enough to be in hospital, you’re glad to see anybody, is my bottom line. I’m not aware I’ve ever seen a locum. (Patient Interview, 05_41)
My own GP … when I say my own GP, it’s so difficult, in fact, it’s impossible at my practice to say which GP you want to see anyway. So every time you go, there’s a different GP. And as it happens, I think probably because of pension ages and pensions or something, and they’re all about my age which is, you know, retirement age, they’ve been leaving anyway and new ones have been coming. So it made absolutely no difference whether I saw a locum or a GP because it was a new person. (Focus Group B, R4) None of the receptionists or anything mentioned anything, because, like you say, probably they would have some members of the public, going back to the example I gave about everybody demanding to see the consultant at the hospital, well they’d be the … no, no, I want to see doctor suchabody, he’s been here ten years, I want to see doctor suchabody, she’s been here 15 years. Whereas, to me, you know, I just see whoever is available, I’m just glad to live in a country where somebody is available that will see me. (Interview 77, Patient) |
|
|
I: Do you think you should be told when the doctor is a locum?
R: Yeah, absolutely. But as a patient, I’ve never been told, or it’s only when I’ve questioned, why has the doctor disappeared as a result, and they’ve said that the doctor is a locum. And not unless when I did some research to find out, what is a locum, then I found out what a locum is. (Interview 95, Patient) I think when it’s long term patients, as it mostly is with mental health, I think they do need to know that it’s a locum, because it will be a long term relationship usually … So, where I think sometimes they’re passive, patients wouldn’t say the same, and they dread it, particularly that woman’s ward, they used to have new consultants every six months. And it’s just horrendous for them. (Interview 86, Clinical Lead Secondary Care) |
|
| Why would a locum doctor feel the need to say to a patient, I’m the locum, when actually that patient is probably used to the registrar changing every six months anyway on rotation? Invariably, they’ll see someone different, why would you not just say I’m Miss Smith’s registrar, she’s in the next room. Why would you badge it with locum because I think if the reality is if you do use the word locum, I think most patients are familiar with the word locum and they’ll see it in a negative way as this is somebody that’s not going to know me, this is somebody that’s not going to be as close to my history and it’ll put those barriers up almost immediately. I was really struck by why would you say that and I was thinking about it, if we had an agency nurse coming in covering a shift on our ward, would they tell all the patients that they were the agency nurse, I’m not sure that they would, they’d say, I’m the nurse looking after you. I was struck by why doctors might feel obliged to tell patients that they were the locum. And I think one of the reasons that they will do that is to … I nearly used the word inadequacies which is not the word I was looking for at all, but I was going to say to almost excuse some of the frustrations that might play out subsequently. If you don’t say you’re the locum at the start of the clinic and then it becomes really apparent that you can’t find the records on the electronic system ’cause you’re not familiar with it, would that be worse in terms of the doctor/patient dynamic if you hadn’t signalled that that might be an issue than if it just becomes apparent? Is it something that locum doctors will say explicitly ’cause they’re aware of that vulnerability and the fact that they’re likely to be more scrutinised and therefore they almost use it as a defence, I don’t know. (Interview 27, Medical Director) | |
| I: Do patients in your practice know when they’re seeing a locum? R: Yes, so at the point of booking, you know, reception staff, by nature, will say who they are seeing, what their job role is. I: Okay. And do you think that that’s important for patients to know? R: I think it’s essential, it’s patient choice, a patient needs to know who they’re seeing and they can choose to see them or not. (Interview 1, GP and CCG Medical Director) |
|
| Yes, they do care on the whole because sometimes they say are you a locum, and that gives me two ideas, first of all, they know the system a bit better than the average patient, and secondly, or they might be approaching it from a different angle which is are you one of the regular doctors or are you a fly by night locum who’s just going to fob me off and I’ll be palmed off again? So it works both ways. But it’s usually the case that they’ve already come with a predetermined idea given to them by the staff, unconsciously or otherwise that he’s just a stopgap, he’s filling in and we’ve got nobody else except him today so you’re going to have to lump him. But it goes both ways, I suppose, and there’s a large chunk in the middle who don’t really care and if they’ve seen somebody and most locums do keep coming back unless they really don’t get on, then they will just take it at face value and take it in their stride. Once you become part of the practice, you become part of the furniture then they don’t usually bat an eye-lid, like I’ve been in this practice now as a regular for the past year and more, so they don’t bat an eye-lid after that. (Interview 58, Locum GP) | |
|
Do you think patients should know whether a doctor is a locum or not?
R: My instinct is no. I mean, we use, and especially now with PCNs, the clinician a patient sees now could be one of a number of people. You know, we’ve got five pharmacists and two PAs working in our PCN and they’re contacting our patients, the PAs are there, they’re not on our website as full time members of staff. But, no, I don’t think so. A patient is coming to [PRACTICE NAME], we’ll put them with the best person that we can in that moment for whatever it is that they need. Who that person is is our choice and if they don’t like that variety of choice, they have a choice themselves. A lot of them will specify a particular clinician but we don’t always enable that. We will where we can where it’s appropriate but where we can’t we’ll say, we can’t do that for you this time, what do you want to do, do you want to wait or see someone else. But who that other person is, no I don’t think we should be labelling people as not officially part of the team. |
|
|
R: I mean it’s certainly not going to do anything to help the locum feel like they are part of the team is it. (Interview 73, Practice Manager)
I: Yeah, yeah. How do patients generally respond to locums? Do they know that they’re seeing a locum at your practices, are they told by the receptionist or is it something that comes up ad-hoc? R: We try and use the same ones as much as we can so there’s that regular contact for the patient, they are aware who’s locum and who’s not locum. But it gets to the extreme whereby some of our employed staff are deemed to be locum staff because they only work two days a week. |
|
| And you try and tell patients, that’s the modern way of working, unfortunately, we’ve gone past the days where your GP would work 24/7, five days a week and so on, some people now only work two days a week, three days a week. There’s an education to be had within our patient group ’cause now they just think everyone’s a locum because they only work one day or two days. (Interview 84, GP Lead) Some, obviously, patients just don’t care, and a doctor’s a doctor, they don’t really care about whether you’re locum, salaried, partner or … they don’t really know the difference and they’re not bothered. So yeah, but you can get some negative views, I think. |
|
|
Do you think patients should know or need to know that they’re seeing a locum?
R: No, I don’t really think they do need to know. Because theoretically, we’re all doing the same thing, we’re all treating the patients’ clinically, and the best way that we think they need to be treated. So, in that respect, no, particularly at our practice, we don’t have that much continuity, because, as I say, the partners work half weeks, and then me as a salaried as well, I do Wednesday to Friday, there’s no one who’s there Monday–Friday and has that sort of constant presence at the practice. So, most of the time, a patient rings and they just get booked in with whoever’s available. So, it’s not, where I know other practices, they can have systems where doctors have their own specific lists and the same patients ring up and they have to be booked in with a particular doctor. It doesn’t work like that at our practice, so I think, particularly our practice, I don’t think there’s any reason why they need to know really. (Interview 97, Salaried GP) |
|
|
Well we … when we give them a badge it has locum written on it, we know that. So, that is policy here. But obviously the badge can be on the belt on the waist, you know, and … you know, whether they introduce themselves to patients as a locum consultant or as a consultant I honestly don’t know actually, or whether they even show them the badge, or if the patients can read it of course, you know? So, there’re all sorts of issues, but, yeah, we do insist the badge has the word ‘locum’ on it. (Interview 10, Consultant Secondary Care)
Personal view is that I don’t think they need to know, particularly. If they’ve got a problem for whatever reason with a doctor, then we need to know that regardless if they’re a locum or substantive appointment or whatever their contractual status is. It’s still an issue that we need to sort out and address. So I’m not sure there’s any benefit from that, no. (Interview 26, Assistant Medical Director) |
|
| Continuity of care | Is it the individual and the continuity, or is it, you know, something else? And I think at the back of my mind … well, at the forefront of my mind, I desperately want it to all be about seeing the GP and having continuity, and them knowing me and my family inside out. But I do think we’re at the stage where that’s kind of like a media construct of a GP, it’s like a country practice version of a GP. And it hasn’t existed for like five decades. And we moved to this system where you see whoever you see, whether they’re just another GP in the practice or a locum or whatever. And the theory was that it shouldn’t matter who you see because what matters is the recording and the system and the process. But as I think we’ve all vividly described, we’re all on the same page really that the systems behind what we have now aren’t good enough. And that’s what the issue is rather than anything else. (Focus Group B, R2) |
| The opening gambit, when you do actually go and see the locum is, what can I do for you today? So he’s obviously never read your notes. I’m sure they’re like an A&E doctor, they haven’t got a clue what’s going to walk through that door … It must be really difficult for them to make that decision based on a few minutes’ conversation. (Focus Group C, R1) | |
| And we moved to this system where you see whoever you see, whether they’re just another GP in the practice or a locum or whatever. And the theory was that it shouldn’t matter who you see because what matters is the recording and the system and the process. But as I think we’ve all vividly described, we’re all on the same page really that the systems behind what we have now aren’t good enough. And that’s what the issue is rather than anything else. (Focus Group B, R2) So I’m very much pro locum, providing that the infrastructure, the service that they’re working with is … and I did mention the word continuity earlier on, is able to cope. It appears to me that everybody’s experience comes down to the administrative aspects with things letting people down, that one system doesn’t connect with another. The network of how it works isn’t connected … I visited the locum and gone back and seen another doctor, then I’ve mentioned what was said and done and what have you, and they have no record of it. And that concerns me. There’s no accountability. (Focus Group B, R5) |
|
| One thing that occurred to me is that the whole business of continuity of care seems to be focused on continuity of doctors’ notes. In the old days you’d have a wodge of them about that thick wouldn’t you or that thin depending on how often you’ve been, and now it’s on a computer screen. They look at the screen rather than you when they’re talking to you. I suppose they can’t avoid that. But that’s okay as long as that works. But my experience of the few as time goes on, you get more hospital visits for various reasons, is that people don’t always know about you when you go to hospital. So you go to see one consultant about something, that might be related to something else you’re seeing another consultant about, they’re connected in some way, but they don’t know … they don’t communicate with each other about what’s going on. And then eventually you get your notes back to your GP. I think one thing I would say is that if I want continuity of care, I want continuity of information passing and consultants prepared to be open to let other people see their notes, for goodness sake. Rather than hoarding them away which I feel sometimes is the case because they don’t want them misinterpreted in some way by someone who is seen not to be competent. (Focus Group D, R4) That binary choice of seeing a doctor or not seeing a doctor … we see a locum doctor or you see nobody. (Focus Group A, R5) |
|
| You can never book an appointment with your doctor at our surgery. It’s as simple as that. So you’ve got a choice, you have a locum or you don’t see a doctor. (Focus Group B, R2) My general experience with the GP practice is that I mostly see locums and I mostly choose to see locums over the permanent doctor. (Focus Group B, R2) In our surgery, it’s just the fact we’ve got a lack of doctors. We’ve got 25 doctors’ rooms and we’ve got two or three doctors and the rest are locums. But they’re not even … you know, we haven’t got 18 locums, we’ve got three or four a day. So to get an appointment is a nightmare and if you do get an appointment, you see a locum, which nine out of 10 times is better than seeing a doctor. (Focus Group B, R8) |
|
|
I would much rather see a locum than not be able to see anybody at all. (Focus Group C, R2)
And I have an occasion I’ve been and my regular doctor hasn’t been available and then they’ve said, oh, I’m sorry, the locum’s going to see you today. (Focus Group B, R1) I got told that a doctor wasn’t available but the locum was. Therefore, I went with the locum because you never know when you’re going to get a doctor’s appointment. (Focus Group A, R2) So to get an appointment is a nightmare and if you do get an appointment, you see a locum, which nine out of 10 times is better than seeing a doctor. (Focus Group B, R8) |
|
| So my surgery, whenever I try and make an appointment, they do say that you can be seen by a different GP, but I insist I’d rather be seen by my regular GP, who’s aware of my treatment, who’s aware of my plans. So I insist and I request that, otherwise I don’t want to be making an appointment, because on occasions, I’ve seen other GPs in the surgery. It’s like we’re starting from fresh again, and you’re trying to explain everything, and it’s just not helpful … I don’t seem to see any point of seeing another doctor. Because my GP should be the point of call. I shouldn’t be having to, as a patient, try to change from one GP to another GP, as a result, because the level of care would be affected. I don’t feel comfortable, or there’s trust issues, or, you know, there’s misuse of management, do you know. It’s like you’re going round and round in circles, but you’re not stopping. Because it’s happened before, where I’ve been seen by another GP, they’ve put me onto this service, that service. (Interview 95, Patient) | |
| The opening gambit, when you do actually go and see the locum is, what can I do for you today? So he’s obviously never read your notes. I’m sure they’re like an A&E doctor, they haven’t got a clue what’s going to walk through that door. What are they going to be presented with? It must be really hard for them that people like us that have got long term illnesses, who know how the illness develops, how our bodies work when it’s telling us it’s something wrong. And we tell him what’s going on and he only has a snippet so he must feel really uncomfortable, do I err on the side of caution or do I go with my gut instinct? It must be really difficult for them to make that decision based on a few minutes’ conversation. (Focus Group C, R1) | |
| Communication and practice | How they differ from the permanent staff is very much that they are very cautious in their approach as to … I think what I said before about them going out to check with, you know, another GP who might know you, is that it’s almost like they don’t want to take too much of what you’re saying on board without having it verified … they have access to electronic notes. But that’s another issue, sometimes they don’t … I’ve seen a locum GP who doesn’t have access to your notes. So really, they’re very cautious on what they can prescribe because they can’t see your notes and, you know, they don’t want to rely on you as an historian as to what kind of medication you’re on. So yeah, it can affect your care in that way as well if they haven’t got access to the notes. But even when they do have access, my experience is that they are, you know, cautious. And it feels very much that you’re seeing somebody on kind of like an interim basic sort of … it feels like an emergency type of … not emergency but it feels like they’re going to do the bare minimum and fill in. And I’ve found that they’re telling me to come back again … So when you get offered something, you take it. Even though it might mean it’s a complete waste of time, you see somebody who really doesn’t feel able or willing to treat you and advises you to come back and see a regular doctor, you’d do anything because you’re not being offered a choice even to have an appointment. (Focus Group A, R2) |
| I saw a locum, or in fact first of all I had a telephone conversation and she said, I think need to see you. I went to the surgery, which was quite an experience in itself because this was, I think, two weeks into lockdown. I don’t think she’d had time to read my extensive notes, but she certainly didn’t listen to my explanation which would have saved her doing 18 different blood tests and sending me for … or trying to send me for all sorts of different scans. It was like she starting again from day one. I’ve got a history going back 13 years and if she’d have just listened, I could have explained it in ten minutes and saved an awful lot of toing and froing. (Focus Group C, R2) | |
| I often wonder with particularly with junior locums whether they’ve got the confidence to make a decision or whether they just go out the room and have a word with the senior GP or what have you. (Focus Group C, R4) So that doctor, through that line of questioning and not having any sort of prior history … may have, you know, had a chance to look at my notes beforehand, ordered the right tests and didn’t feel constrained in that practice about what tests that they could order. And someone subsequently … because when you get referred to hospital, the consultant said that that doctor was very much on the ball. And, of course, that’s a change to lifelong medication. And literally within a month of the medication kicking in, it transformed my life. (Focus Group A, R1) |
|
| I was in A&E for a good six hours and they said right, we’re going to send you home in care of the GP. Which is a fair comment but I still couldn’t see, my blood sugar was still raising in the thirties. And lo and behold who walks in but this locum who introduces himself to me that I’ve spoken to on the phone. And said, what they doing? I said, well nothing, they’re going to send me home and refer me to you. He said, well we’re going nowhere. Either they give you a dose of insulin or they give you a litre of fluids to try and flush out your sugar. Now that … I was just blown out of this world, that one the guy had turned up and number two he was going to over-rule the A&E. So, yes, that is a positive side to it. (Focus Group C, R1) | |
| So to get an appointment is a nightmare and if you do get an appointment, you see a locum, which nine out of 10 times is better than seeing a doctor because, you know, he hasn’t got the time for you. If it’s one of our regular doctors, they haven’t got the time, they want you in and out. A locum will spend, you know, five or 10 minutes longer to try and figure out what’s wrong and get something done about it. (Focus Group A, R8) I have actually had a positive experience with a locum … she was a breath of fresh air. What I didn’t know was, she was a locum. I didn’t know she was only there for 12 months. She was absolutely fabulous and she gave me much more time than the general GP would. And she actually dealt with about two or three different issues in the one meeting. And then she asked me to arrange for a blood test in six months’ time. (Focus Group A, R5) |
|
| I’d seen a locum once regarding my migraines, and they prescribed me this medication that really helped me, and then when I’d gone back to get it again I was being refused the medication. Almost being told, when I was giving the name of it the GP was like, I don’t even know what that is. And I’m like, but this locum gave it to me and this is the name. And they just wouldn’t give it to me … So, I think that can be a benefit of a locum because they won’t necessarily be aware of the ins and outs of which medications practices are trying to reduce. (Focus Group E, R1) When I last spoke to a locum in my … because I’ve had a kidney transplant, I have regular … about every three-month appointments with the hospital, the renal team. And that was where I saw a locum. And I have ongoing issues with my regular doctor. I tell them things, it’s the same issues that’s come up and then they just don’t do anything. So this locum, in one appointment with the locum, they changed my blood pressure tablets, which I’d been advocating for; they’d increased my anaemia medication, which I had been asking about; and they got me in to see a nutritionist. (Focus Group A, R4) |
|
|
So each doctor had some sort of specialism within the practice. If a locum goes into a practice like that, then a) I think that they do often ask for more tests than your doctor would because the familiarity breeds contempt thing that we were talking about earlier, you get overconfident. They’re more likely to ask you … get the blood tests, do the tests and they’re probably not worried about how that affects the budget as much as a partner in the practice is going to be. That might be a thing. (Focus Group B, R4)
But the locum who did come, who had the experience, was very good. Took lots of tests. Instead of taking things for granted and just a quick in and out, he seemed to take the time to find the history, which the first one didn’t have time for or wouldn’t have done. So it’s about looking back at who the patient is in front of you. A lot might be to do with maturity, time, stress, things like that. (Focus Group B, R4) |
|
|
I went back and on this occasion it was a locum I saw and immediately this person before I even mentioned the background to that, I said what I was concerned about, this person immediately took it on-board. And in fact, examined me and I got an immediate referral to the hospital and got treatment. This was just pre COVID actually, so I was I guess fortunate with timing and that and had the treatment I needed. So my experience of seeing a locum was incredibly positive, if I hadn’t seen that person on that day, I may not have got treated and that would have had very significant negative outcomes for me personally. (Focus Group D, R4)
And I recognise that GPs have to have a huge amount of experience but even so, you know, with an individual patient you perhaps can make assumptions about their condition until someone comes in and starts asking what appear to be the same questions again and you feel you’re repeating yourself. But something different occurs to them. And that can actually be life-changing. (Focus Group A, R1) |
|
| A locum actually worked in my favour … I had a chest infection. And I tend to have them at least once a year, so it’s not something my GP’s not aware of. But on this occasion when I went in, it was a locum doctor … And she said, oh, let me just examine your chest … She goes, I think you’ve got a heart murmur. And I didn’t ever know what heart murmur meant, never mind what it is … And she said … I’m going to send you for a re-examination with a heart specialist. And she worked in my favour, I mean it was a blessing in disguise for me because if she didn’t do that, I would have probably carried on and my heart would have got weaker. Because I put my shortness of breath and my palpitations down to anxiety and depression and mental health, and nothing to do with physical health. So I had a very positive experience with a locum. (Focus Group A, R6) | |
| I’d gone to the GP surgery just for a review of the contraceptive pill actually. And at the time, my dad was dealing with cancer so I was a little bit stressed. Took my blood pressure and it was a little bit raised. And that just kind of escalated, getting like loads of blood tests done. And there were some abnormalities in that … I eventually got diagnosed with a genetic condition from that point but I actually hadn’t gone to the GP surgery with any kind of complaints. So I suppose on reflection, it was quite a positive experience because had I had not seen that locum, that may not have happened because she might not have triggered those blood tests or I might have been diagnosed later than I was. So my experience I suppose is quite positive. (Focus Group B, R3) | |
| In my practice, there must be about five doctors which are permanent. And they do have locums that come in and out. You never see the same locum again … sometimes they can give you a fresh view on things … The condition that I’ve got now was discovered late in life … he identified something in me that I had neurologically, which is a rare genetic problem, and which was the answer to everything, it just sort of all fell into place. All my worries, all my concerns seemed to melt when this guy identified what it was. I said this fellow knows what he’s talking about … And he explained the situation but he wanted me to see a colleague within hospital and he referred me to [hospital] I’ve never looked back since. I probably owe … I reckon my health would have deteriorated far more quickly … I’ve got a lot to say positively. (Focus Group B, R5) | |
| I’ve got quite a few different medical conditions, one of them being fibromyalgia and arthritis. I’ve had it a long time and I manage it quite well. But I injured my knee. And I saw a first locum who sort of said, well, it’ll be your fibromyalgia, it’ll be okay, blah, blah, blah. Time went on again and I went back to my practice and saw another locum. And she was absolutely amazing and examined me and I’d actually torn my meniscus in my knee. So I’d been hobbling around for six weeks, knowing it wasn’t my arthritis or the fibromyalgia and I had actually injured myself. And she arranged for me to go to be checked out at hospital, which was when then they picked up that I’d torn my meniscus. But had the first doctor not looked at my notes and just thought, oh, she’s got fibromyalgia and arthritis, it’s that, it needed investigating. And I knew … I know what different pain levels are and what they are and I knew something wasn’t right. I was having to lift my knee up to actually move my leg, so I knew that wasn’t part and parcel. So in that respect, the locum … the first locum who sort of dismissed it, I think sometimes they can get scared that you see someone with a lot of different medical conditions that are all intertwined with each other and it can be easy to dismiss someone as overweight and it’s down to weight and different things, without realising there’s lots of other factors that go with it. But the second locum, I’ll always be thankful for her because, you know, I could have ended up having a lot longer without treatment. And subsequently, I had an operation on my knee. (Focus Group B, R1) | |
| The whole system of the surgery … of our surgery anyway, is just nothing ever gets done. So much as I’ve had to get all my records from the doctor’s surgery because they keep telling me that there’s nothing wrong. And they’ve been telling me there’s nothing wrong for 11 years, right up to the point I had my heart attack and then the point when I kept on getting pancreatitis. And this has gone on and on and on and on. And eventually, a locum said, I think you may have a gluten problem. It turns out I’m a celiac. But our doctor’s surgery couldn’t manage to pick up on that because you see one doctor, then you don’t see the doctor. Then you see another doctor who knows nothing about the appointment you had a month ago. And it goes on and on and on and on. (Focus Group B, R8) | |
| I wanted to pick up on was something that’s been said a few times now. Just it is interesting isn’t it that a locum can pick something up new … (Focus Group B, R6) I have benefited from some locum doctors in the past because they’ve brought a fresh pair of eyes and perspective on it … So, it’s not always a bad thing having a different person in front of you….there has been that element of they brought something fresh to the table to look at or they’ve been aware of a different way of treating something to what your GP previously said. But then there’s the follow-up session again because then you’re back to that, you’re not going to see them again. It’s mainly the inconsistency that gives you the uncertainty. (Focus Group E, R1) |
|
| The positive: a fresh pair of eyes. So, my experience was really exceptional. It was a German locum doctor, very young, but I soon did build a rapport with her and I was reassured that they were taking her to the team meetings, so the senior doctors in the practice were involved. It was very unusual, I presented with a cough and had an x-ray quick and there were abnormalities. So, she put me through the cancer 14-day appointment with the hospital, so it all happened very quickly. And I do wonder if because she was so vigilant that it kind of saved my life. And if it had been my own GP he may well have looked at me and thought, well she’s always been healthy up until now; he might have come with a different perspective and had a slower response than what the German locum doctor had. She was just very thorough. (Focus Group E, R3) |
Appendix 7 Additional material for Chapter 9: consultation patterns and differences in the clinical practice and performance of locum and permanent doctors in primary care in the United Kingdom
A retrospective cohort analysis of consultation events from CPRD GOLD, 2010–21.
Sensitivity analyses using only practices participating CPRD GOLD in all years, n = 381.
| Year | Locum consultations (%) – AURUM | Locum F2F consultations (%) – AURUM | Locum telephone consultations (%) – AURUM | Locum consultations (%) – GOLD | Locum F2F consultations (%) – GOLD | Locum telephone consultations (%) – GOLD |
|---|---|---|---|---|---|---|
| 2010 | 0.65 | 0.54 | 1.35 | 9.08 | 10.76 | 6.83 |
| 2011 | 0.58 | 0.49 | 1.04 | 9.40 | 11.34 | 6.52 |
| 2012 | 0.47 | 0.38 | 0.68 | 9.50 | 11.53 | 6.43 |
| 2013 | 0.48 | 0.40 | 1.06 | 9.18 | 11.20 | 5.56 |
| 2014 | 0.60 | 0.52 | 1.20 | 9.47 | 11.62 | 5.07 |
| 2015 | 0.53 | 0.46 | 0.79 | 9.70 | 11.96 | 6.32 |
| 2016 | 0.50 | 0.53 | 0.38 | 9.52 | 12.09 | 8.21 |
| 2017 | 0.60 | 0.71 | 0.78 | 9.49 | 12.07 | 8.71 |
| 2018 | 0.80 | 1.10 | 0.81 | 9.64 | 12.34 | 9.31 |
| 2019 | 0.65 | 1.11 | 0.92 | 9.44 | 12.52 | 11.13 |
| 2020 | 0.64 | 0.64 | 1.18 | 8.73 | 11.53 | 12.12 |
| Code | Description |
|---|---|
| 1 | Senior partner 1,271,021 |
| 2 | Partner 8,033,530 |
| 3 | Assistant 129,795 |
| 4 | Associate 112,496 |
| 5 | Non-commercial local rota of ˂ 10 GPs 294 |
| 6 | Commercial Deputising service 3822 |
| 7 | Locum 1,367,260 |
| 8 | GP Registrar 1,082,008 |
| 9 | Consultant 4003 |
| 10 | Sole Practitioner 12,989 |
| 47 | Salaried partner 1,538,224 |
| 50 | GP retainer 141,013 |
| Code | Description |
|---|---|
| 1 | Clinic |
| 2 | Night visit, Deputising service |
| 3 | Follow-up/routine visit |
| 4 | Night visit, local rota |
| 5 | Mail from patient |
| 6 | Night visit, practice |
| 7 | Out of hours, practice |
| 8 | Out of hours, non-practice |
| 9 | Surgery consultation |
| 10 | Telephone call from a patient |
| 11 | Acute visit |
| 17 | Mail to patient |
| 18 | Emergency consultation |
| 21 | Telephone call to a patient |
| 24 | Children’s home visit |
| 27 | Home visit |
| 28 | Hotel visit |
| 30 | Nursing Home visit |
| 31 | Residential Home visit |
| 32 | Twilight visit |
| 33 | Triage |
| 34 | Walk-in Centre |
| 35 | Co-op telephone advice |
| 36 | Co-op surgery consultation |
| 37 | Co-op Home visit |
| 38 | Minor Injury Service |
| 50 | Night visit |
| 55 | Telephone consultation |
| 61 | Extended hours |
| Types of consultation | Codes used to classify type of consultation (from Table 30) |
|---|---|
| All consultations | 1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 17, 18, 21, 24, 27, 28, 30, 31, 32, 33, 34, 35, 36, 37, 38, 50, 55, 61 |
| F2F consultations | 1, 2, 3, 4, 6, 7, 8, 9, 11, 18, 24, 27, 28, 30, 31, 32, 33, 34, 36, 37, 38, 50, 61 |
| Telephone consultations and online consultations | 10, 21, 35, 55, 5, 17 |
| Percentiles (%) | Yearly consultation volume all GPs, N (%) | Yearly consultation volume locums, N (%) | Number of days worked all GPs, N (%) | Number of days worked, locums, N | Number of weeks worked, all GPs, N | Number of weeks worked locums, N | Average interval between consultations, in days, all GPs, N | Average interval between consultations, in days, locums, N |
|---|---|---|---|---|---|---|---|---|
| 5 | 2 | 6 | 1 | 1 | 1 | 1 | 1 | 1 |
| 25 | 1395 | 30 | 79 | 2 | 22 | 2 | 1.2 | 3 |
| 50 | 5306 | 122 | 238 | 7 | 52 | 5 | 1.5 | 7 |
| 75 | 9413 | 595 | 286 | 33 | 52 | 18 | 1.8 | 17 |
| 95 | 15,853 | 3837 | 329 | 175 | 52 | 50 | 8 | 63 |
| Mean (SD) | 6096 (5400) | 803 (2036) | 189 (114) | 34 (62) | 38 (19) | 12.5 (15) | 4 (14.5) | 16 (28) |
| Years | Number of practices by years of contribution to GOLD, all countries | Number of practices by years of contribution to GOLD, England only | Region | Number of practices by region, all years |
|---|---|---|---|---|
| > 1 | 889 | 487 | North East and Yorkshire | 26 |
| > 2 | 866 | 465 | North West | 82 |
| > 3 | 839 | 439 | Midlands | 75 |
| > 4 | 788 | 391 | East of England | 44 |
| > 5 | 716 | 319 | South West | 96 |
| > 6 | 621 | 228 | London | 131 |
| > 7 | 559 | 171 | South East | 58 |
| > 8 | 521 | 139 | England | 511 |
| > 9 | 489 | 117 | Wales | 127 |
| > 10 | 446 | 80 | Scotland | 234 |
| > 11 | 381 | 42 | N. Ireland | 42 |
| Total | 914 |
| Outcome | |
|---|---|
| Opioids | Opioid analgesics included oral and transdermal formulations of codeine, dihydrocodeine, dextropropoxyphene, meptazinol, fentanyl, morphine, oxycodone, buprenorphine, hydromorphone, pethidine, tramadol and tapentadol. |
| Hypnotics prescriptions | Benzodiazepines including: alprazolam, amitriptyline hydrochloride/chlordiazepoxide, bromazepam, chlordiazepoxide hydrochloride, chlordiazepoxide hydrochloride, chlordiazepoxide/clidinium bromide, clobazam, diazepam, dipotassium clorazepate, flunitrazepam, flurazepam hydrochloride, loprazolam mesilate, lorazepam, lormetazepam, nitrazepam, oxazepam, temazepam, triazolam. Z-drugs including: zaleplon, zolpidem tartrate, zopiclone. |
| Emergency admissions | Each admission has the method of admission field which we used to derive information on emergency admissions. We defined an emergency admission as one where the method of admissions was A&E; GP direct to hospital; GP via a bed bureau; consultant clinic; mental health crisis resolution team; or other means. Emergency admissions were only included if both the admission and discharge dates were recorded and if the admission date was on or before the discharge date. |
| Year | All GP consultations | All locum consultations | F2F GP consultations | F2F locum consultations | Telephone and online GP consultations | Telephone and online locum consultations | Total patient count | N of practices |
|---|---|---|---|---|---|---|---|---|
| 2010 | 8,139,545 | 1,080,393 | 7,429,761 | 1,011,445 | 710,960 | 69,019 | 1,628,346 | 381 |
| 2011 | 8,283,676 | 1,127,899 | 7,466,835 | 1,047,058 | 818,296 | 80,967 | 1,699,898 | 381 |
| 2012 | 8,596,087 | 1,196,195 | 7,691,333 | 1,096,835 | 905,991 | 99,451 | 1,733,287 | 381 |
| 2013 | 8,836,801 | 1,171,809 | 7,873,772 | 1,069,011 | 964,150 | 102,875 | 1,759,436 | 381 |
| 2014 | 8,986,653 | 1,170,294 | 7,981,755 | 1,069,009 | 1,006,136 | 101,381 | 1,762,497 | 381 |
| 2015 | 9,071,875 | 1,178,916 | 8,040,283 | 1,081,957 | 1,033,064 | 97,042 | 1,770,446 | 381 |
| 2016 | 9,064,695 | 1,142,534 | 8,022,558 | 1,060,237 | 1,043,226 | 82,385 | 1,766,414 | 381 |
| 2017 | 8,864,930 | 1,054,047 | 7,821,261 | 975,615 | 1,044,336 | 78,473 | 1,755,180 | 381 |
| 2018 | 8,694,995 | 1,006,019 | 7,724,033 | 929,490 | 971,493 | 76,588 | 1,744,502 | 381 |
| 2019 | 8,606,593 | 988,021 | 7,577,949 | 911,996 | 1,029,214 | 76,117 | 1,739,155 | 381 |
| 2020 | 7,690,481 | 870,956 | 5,024,764 | 582,833 | 2,669,733 | 289,134 | 1,509,056 | 381 |
| 2021 | 5,869,358 | 703,540 | 3,968,290 | 489,157 | 1,902,107 | 214,771 | 1,404,621 | 381 |
| Description of indicator | Group at risk (denominator) | Group exposed to hazardous prescribing (numerator) | Operationalisation of hazardous prescribing indicators for locum and permanent GPs |
|---|---|---|---|
| Outcome: GI bleed | |||
| Prescription of an oral NSAID, without co-prescription of an ulcer healing drug, to a patient aged ≥ 65 years | Patients aged ≥ 65 years without co-prescription of an ulcer-healing drug (PPI or H2 antagonist) in the 3 months leading up to the index date | Patients prescribed an oral NSAID in the 3 months leading up to the index date |
|
| Prescription of an oral NSAID, without co-prescription of an ulcer healing drug, to a patient with a history of peptic ulceration | Patients aged ≥ 18 years with a Read code for peptic ulcer or upper GI bleed at least 3 months before index date and not prescribed an ulcer healing drug (PPI or H2 antagonist) within the 3 months leading up to the index date | Patients prescribed an oral NSAID within the 3 months leading up to the index date |
|
| Prescription of an antiplatelet drug without co-prescription of an ulcer-healing drug, to a patient with a history of peptic ulceration | Patients aged ≥ 18 years with a Read code for peptic ulcer or GI bleed at least 3 months before index date and not prescribed an ulcer healing drug (PPI or H2 antagonist) within the 3 months leading up to the index date | Patients prescribed an antiplatelet drug (aspirin or clopidogrel or prasugrel or ticagrelor) within the 3 months leading up to the index date |
|
| Prescription of warfarin or DOAC in combination with an oral NSAID | Patients aged ≥ 18 years prescribed warfarin or a DOAC (apixaban or dabigatran or rivaroxaban) within the 3 months leading up to the index date | Patients prescribed an oral NSAID within the 3 months leading up to the index date |
|
| Prescription of warfarin or DOAC and an antiplatelet drug in combination without co-prescription of an ulcer-healing drug | Patients aged ≥ 18 years prescribed warfarin or DOAC without co-prescription of ulcer-healing drug (PPI or H2 antagonist) within the 3 months leading up to the index date | Patients prescribed an antiplatelet drug (aspirin or clopidogrel or prasugrel or ticagrelor) within the 3 months leading up to the index date and within 28 days of the warfarin/DOAC prescription |
|
| Prescription of aspirin in combination with another antiplatelet drug (without co-prescription of an ulcer-healing drug) | Patients aged ≥ 18 years prescribed aspirin without co-prescription of ulcer-healing drug (PPI or H2 antagonist) within the 3 months leading up to the index date | Patients prescribed another antiplatelet drug (clopidogrel or prasugrel or ticagrelor) within the 3 months leading up to the index date and within 28 days of the aspirin prescription |
|
| Outcome: exacerbation of asthma | |||
| Prescription of a non-selective beta-blocker to a patient with asthma | Patients aged ≥ 18 years with a Read code for asthma at least 3 months before index date and no subsequent asthma resolved code during that time period | Patients prescribed a non-selective beta-blocker within the 3 months leading up to the index date |
|
| Prescription of a long-acting beta-2 agonist inhaler (excluding combination products with inhaled corticosteroid) to a patient with asthma who is not also prescribed an inhaled corticosteroid | Patients aged ≥ 18 years with a Read code for asthma at least 3 months before index date (and no subsequent asthma resolved code during that time period) who have been prescribed a long-acting beta-2 agonist inhaler (excluding combination products with inhaled corticosteroid) within the last 3 months | Patients not prescribed an inhaled corticosteroid within the 3 months leading up to the index date |
|
| Outcome: heart failure | |||
| Prescription of an oral NSAID to a patient with heart failure | Patients aged ≥ 18 years who have a diagnosis of heart failure at least 3 months before the index date | Patients prescribed an oral NSAID within the 3 months leading up to the index date |
|
| Outcome: cardiovascular events, including stroke | |||
| Prescription of antipsychotics for > 6 weeks in a patient aged ≥ 65 years with dementia but not psychosis | Patients aged ≥ 65 years with a Read code for dementia at least 3 months before the index date and no Read code for psychosis (or have a psychosis Read code and a subsequent psychosis resolved Read code) at least 3 months before the index date | Patients prescribed antipsychotic drugs at least once within the 3 months leading up to the index date |
|
| Practice revisits | Antibiotic prescriptions | Opioid prescriptions | Hypnotic prescriptions | |
|---|---|---|---|---|
| Locum consultations | 0.877 (0.871 to 0.884), < 0.001 (0.003) | 1.215 (1.207 to 1.222), < 0.001 (0.004) | 1.078 (1.065 to 1.093), < 0.001 (0.007) | 0.962 (0.942 to 0.984), < 0.001 (0.010) |
| Gender (reference = male) | 1.177 (1.172 to 1.181), < 0.001 (0.002) | 1.107 (1.103 to 1.112), < 0.001 (0.002) | 1.044 (1.037 to 1.052), < 0.001 (0.003) | 1.179 (1.166 to 1.194), < 0.001 (0.007) |
| Age | 1.005 (1.004 to 1.005), < 0.001 (0.001) | 0.988 (0.988 to 0.989), < 0.001 (0.001) | 1.018 (1.018 to 1.018), < 0.001 (0.001) | 1.012 (1.012 to 1.013), < 0.001 (0.001) |
| Comorbidity score | 1.197 (1.194 to 1.199), < 0.001 (0.001) | 1.016 (1.013 to 1.019), < 0.001 (0.001) | 1.033 (1.029 to 1.037), < 0.001 (0.001) | 0.998 (0.991 to 1.004), < 0.535 (0.003) |
| Years registered with practice | 0.998 (0.997 to 0.998), < 0.001 (0.001) | 1.001 (1.001 to 1.002), < 0.001 (0.001) | 0.998 (0.998 to 0.999), < 0.001 (0.001) | 0.994 (0.994 to 0.995), < 0.001 (0.001) |
| Patient list size | 1.001 (1.000 to 1.001), < 0.001 (0.001) | 1.000 (1.000 to 1.001), < 0.001 (0.001) | 0.999 (0.999 to 1.000), < 0.218 (0.001) | 0.999 (0.999 to 0.999), < 0.001 (0.001) |
| IMD quintile (1 = most deprived) | ||||
| Quintile 2 | 1.016 (1.009 to 1.022), < 0.001 (0.003) | 1.009 (1.003 to 1.015), < 0.005 (0.003) | 1.161 (1.146 to 1.176), < 0.001 (0.007) | 1.028 (1.008 to 1.048), < 0.004 (0.009) |
| Quintile 3 | 1.027 (1.020 to 1.034), < 0.001 (0.003) | 1.000 (0.994 to 1.006), < 0.880 (0.003) | 1.286 (1.270 to 1.303), < 0.001 (0.008) | 1.086 (1.065 to 1.107), < 0.001 (0.010) |
| Quintile 4 | 1.049 (1.041 to 1.057), < 0.001 (0.004) | 0.992 (0.985 to 0.999), < 0.028 (0.003) | 1.451 (1.431 to 1.470), < 0.001 (0.010) | 1.193 (1.168 to 1.219), < 0.001 (0.012) |
| Quintile 5 | 1.057 (1.049 to 1.066), < 0.001 (0.004) | 0.977 (0.970 to 0.984), < 0.001 (0.003) | 1.702 (1.678 to 1.727), < 0.001 (0.011) | 1.336 (1.305 to 1.368), < 0.001 (0.016) |
| Rurality | 1.002 (0.994 to 1.011), < 0.677 (0.004) | 1.000 (0.992 to 1.008), < 0.988 (0.004) | 0.925 (0.910 to 0.941), < 0.001 (0.007) | 0.972 (0.948 to 0.997), < 0.047 (0.012) |
| Region (reference = North East) | ||||
| North West | 0.854 (0.697 to 1.049), < 0.133 (0.090) | 1.216 (1.001 to 1.476), < 0.048 (0.120) | 0.983 (0.823 to 1.174), < 0.852 (0.090) | 1.208 (0.925 to 1.580), < 0.164 (0.165) |
| Yorkshire and Humber | 0.933 (0.724 to 1.202), < 0.593 (0.120) | 1.110 (0.875 to 1.407), < 0.390 (0.134) | 0.961 (0.773 to 1.195), < 0.719 (0.108) | 1.019 (0.734 to 1.414), < 0.909 (0.170) |
| Midlands | 0.866 (0.703 to 1.169), < 0.179 (0.088) | 1.110 (0.910 to 1.350), < 0.303 (0.111) | 0.941 (0.786 to 1.127), < 0.509 (0.087) | 1.320 (1.007 to 1.731), < 0.044 (0.182) |
| East of England | 0.942 (0.758 to 1.170), < 0.588 (0.104) | 1.078 (0.881 to 1.321), < 0.468 (0.111) | 0.857 (0.711 to 1.032), < 0.107 (0.082) | 1.560 (1.180 to 2.062), < 0.002 (0.222) |
| London | 0.851 (0.696 to 1.044), < 0.121 (0.090) | 1.104 (0.909 to 1.340), < 0.298 (0.109) | 0.694 (0.581 to 0.829), < 0.001 (0.063) | 1.221 (0.935 to 1.593), < 0.141 (0.165) |
| South East | 0.943 (0.770 to 1.155), < 0.572 (0.099) | 1.164 (0.965 to 1.410), < 0.118 (0.113) | 0.841 (0.706 to 1.001), < 0.052 (0.076) | 1.429 (1.098 to 1.857), < 0.008 (0.191) |
| South West | 1.102 (0.893 to 1.361), < 0.365 (0.119) | 1.044 (0.856 to 1.273), < 0.669 (0.105) | 0.869 (0.725 to 1.043), < 0.132 (0.082) | 1.512 (1.151 to 1.986), < 0.003 (0.211) |
| Year (reference year = 2010) | ||||
| 2011 | 1.040 (1.034 to 1.049), < 0.001 (0.003) | 0.947 (0.941 to 0.953), < 0.001 (0.003) | 1.004 (0.992 to 1.018), < 0.478 (0.006) | 0.974 (0.954 to 0.994), < 0.010 (0.010) |
| 2012 | 1.079 (1.071 to 1.087), < 0.001 (0.004) | 0.974 (0.968 to 0.981), < 0.001 (0.003) | 0.964 (0.952 to 0.977), < 0.001 (0.006) | 0.910 (0.891 to 0.929), < 0.001 (0.009) |
| 2013 | 1.096 (1.088 to 1.124), < 0.001 (0.004) | 0.865 (0.859 to 0.871), < 0.001 (0.003) | 0.962 (0.950 to 0.976), < 0.001 (0.007) | 0.913 (0.893 to 0.932), < 0.001 (0.010) |
| 2014 | 1.110 (1.099 to 1.116), < 0.001 (0.004) | 0.860 (0.854 to 0.867), < 0.001 (0.003) | 0.944 (0.930 to 0.958), < 0.001 (0.007) | 0.886 (0.866 to 0.906), < 0.001 (0.010) |
| 2015 | 1.114 (1.105 to 1.127), < 0.001 (0.005) | 0.759 (0.752 to 0.765), < 0.001 (0.003) | 0.941 (0.926 to 0.956), < 0.001 (0.008) | 0.866 (0.845 to 0.889, < 0.001 (0.011) |
| 2016 | 1.136 (1.125 to 1.146), < 0.001 (0.005) | 0.732 (0.724 to 0.739), < 0.001 (0.003) | 0.907 (0.890 to 0.923), < 0.001 (0.008) | 0.848 (0.823 to 0.872), < 0.001 (0.012) |
| 2017 | 1.139 (1.126 to 1.150), < 0.001 (0.006) | 0.724 (0.717 to 0.732), < 0.001 (0.004) | 0.858 (0.841 to 0.876), < 0.001 (0.009) | 0.835 (0.809 to 0.863), < 0.001 (0.013) |
| 2018 | 1.116 (1.102 to 1.129), < 0.001 (0.006) | 0.673 (0.665 to 0.680), < 0.001 (0.004) | 0.806 (0.788 to 0.824), < 0.001 (0.009) | 0.795 (0.768 to 0.824), < 0.001 (0.013) |
| 2019 | 1.118 (1.104 to 1.132), < 0.001 (0.007) | 0.662 (0.654 to 0.671), < 0.001 (0.004) | 0.760 (0.742 to 0.780), < 0.001 (0.009) | 0.740 (0.711 to 0.770), < 0.001 (0.013) |
| 2020 | 1.470 (1.449 to 1.492), < 0.001 (0.010) | 0.632 (0.621 to 0.644), < 0.001 (0.005) | 0.774 (0.750 to 0.798), < 0.001 (0.011) | 0.731 (0.694 to 0.770), < 0.001 (0.017) |
| 2021 | 1.468 (1.441 to 1.497), < 0.001 (0.014) | 0.644 (0.630 to 0.660), < 0.001 (0.007) | 0.749 (0.718 to 0.782), < 0.001 (0.015) | 0.656 (0.607 to 0.710), < 0.001 (0.023) |
| Constant | 0.051 (0.042 to 0.063), < 0.001 (0.005) | 0.149 (0.124 to 0.179), < 0.001 (0.014) | 0.009 (0.007 to 0.010), < 0.001 (0.001) | 0.004 (0.002 to 0.005), < 0.001 (0.001) |
| Emergency admissions – same day | Emergency admissions – within 1–7 days | A&E attendances – same day | A&E attendances – within 1–7 days | |
|---|---|---|---|---|
| Locum consultations | 0.976 (0.930 to 1.025), < 0.344 (0.025) | 0.999 (0.948 to 1.052), < 0.972 (0.026) | 1.043 (1.008 to 1.078), < 0.014 (0.017) | 1.052 (1.022 to 1.084), < 0.001 (0.015) |
| Gender (reference = male) | 0.810 (0.790 to 0.832), < 0.001 (0.011) | 0.911 (0.887 to 0.937), < 0.001 (0.012) | 0.768 (0.753 to 0.782), < 0.001 (0.007) | 0.870 (0.856 to 0.885), < 0.001 (0.007) |
| Age | 0.998 (0.998 to 0.999), < 0.001 (0.001) | 1.008 (1.007 to 1.009), < 0.001 (0.001) | 0.988 (0.988 to 0.989), < 0.001 (0.001) | 0.987 (0.986 to 0.987), < 0.001 (0.001) |
| Comorbidity score | 1.352 (1.336 to 1.369), < 0.001 (0.001) | 1.370 (1.354 to 1.386), < 0.001 (0.001) | 1.185 (1.172 to 1.199), < 0.001 (0.007) | 1.190 (1.178 to 1.203), < 0.001 (0.006) |
| Years registered with practice | 1.001 (1.000 to 1.002), < 0.013 (0.001) | 0.998 (0.997 to 0.999), < 0.001 (0.001) | 1.002 (1.002 to 1.003), < 0.001 (0.001) | 0.999 (0.997 to 0.999), < 0.001 (0.001) |
| Patient list size | 0.999 (0.999 to 1.001), < 0.824 (0.001) | 0.999 (0.998 to 0.999), < 0.001 (0.001) | 1.000 (0.999 to 1.000), < 0.688 (0.001) | 0.999 (0.998 to 0.999), < 0.001 (0.001) |
| IMD quintile (1 = most deprived) | ||||
| Quintile 2 | 1.060 (1.014 to 1.107), < 0.009 (0.024) | 1.098 (1.049 to 1.150), < 0.001 (0.025) | 1.087 (1.053 to 1.121), < 0.001 (0.017) | 1.096 (1.064 to 1.127), < 0.001 (0.016) |
| Quintile 3 | 1.118 (1.068 to 1.169), < 0.001 (0.026) | 1.192 (1.137 to 1.249), < 0.001 (0.028) | 1.139 (1.102 to 1.177), < 0.001 (0.019) | 1.123 (1.091 to 1.157), < 0.001 (0.017) |
| Quintile 4 | 1.166 (1.111 to 1.224), < 0.001 (0.029) | 1.257 (1.196 to 1.321), < 0.001 (0.030) | 1.179 (1.138 to 1.221), < 0.001 (0.021) | 1.211 (1.174 to 1.250), < 0.001 (0.019) |
| Quintile 5 | 1.218 (1.157 to 1.283), < 0.001 (0.032) | 1.336 (1.266 to 1.409), < 0.001 (0.035) | 1.209 (1.162 to 1.256), < 0.001 (0.024) | 1.268 (1.223 to 1.311), < 0.001 (0.022) |
| Rurality | 0.995 (0.944 to 1.049), < 0.866 (0.027) | 0.927 (0.877 to 0.979), < 0.005 (0.025) | 0.966 (0.926 to 1.007), < 0.001 (0.021) | 0.945 (0.910 to 0.981), < 0.003 (0.018) |
| Region (reference = North East) | ||||
| North West | 0.786 (0.610 to 1.011), < 0.061 (0.101) | 0.992 (0.802 to 1.226), < 0.940 (0.107) | 0.971 (0.732 to 1.290), < 0.843 (0.141) | 1.355 (1.103 to 1.664), < 0.004 (0.142) |
| Yorkshire and Humber | 0.682 (0.496 to 0.939), < 0.019 (0.111) | 0.985 (0.756 to 1.284), < 0.913 (0.133) | 0.707 (0.496 to 1.008), < 0.056 (0.128) | 1.104 (0.856 to 1.424), < 0.444 (0.143) |
| Midlands | 0.858 (0.664 to 1.110), < 0.244 (0.113) | 1.141 (0.920 to 1.414), < 0.229 (0.125) | 1.068 (0.801 to 1.425), < 0.653 (0.157) | 1.358 (1.101 to 1.674), < 0.004 (0.145) |
| East of England | 0.783 (0.600 to 1.022), < 0.072 (0.106) | 1.009 (0.808 to 1.260), < 0.937 (0.114) | 1.022 (0.759 to 1.375), < 0.887 (0.155) | 1.218 (0.981 to 2.511), < 0.072 (0.134) |
| London | 0.496 (0.385 to 0.641), < 0.001 (0.064) | 0.927 (0.750 to 1.146), < 0.483 (0.099) | 1.253 (0.944 to 1.662), < 0.117 (0.181) | 1.576 (1.284 to 1.934), < 0.001 (0.165) |
| South East | 0.669 (0.522 to 0.858), < 0.002 (0.085) | 0.922 (0.749 to 1.136), < 0.447 (0.098) | 1.019 (0.771 to 1.347), < 0.894 (0.145) | 1.249 (1.020 to 1.530), < 0.031 (0.129) |
| South West | 0.738 (0.570 to 0.958), < 0.022 (0.098) | 0.851 (0.684 to 1.058), < 0.147 (0.094) | 1.071 (0.801 to 1.432), < 0.645 (0.159) | 1.169 (0.946 to 1.444), < 0.145 (0.126) |
| Year (reference year = 2010) | ||||
| 2011 | 1.000 (0.953 to 1.048), < 0.992 (0.024) | 1.075 (1.022 to 1.131), < 0.005 (0.028) | 1.087 (1.049 to 1.128), < 0.001 (0.020) | 1.142 (1.106 to 1.179), < 0.001 (0.019) |
| 2012 | 0.966 (1.038 to 1.014), < 0.160 (0.024) | 1.083 (1.028 to 1.141), < 0.001 (0.029) | 1.087 (1.048 to 1.128), < 0.001 (0.020) | 1.187 (1.150 to 1.225), < 0.001 (0.019) |
| 2013 | 0.987 (1.013 to 1.037), < 0.603 (0.025) | 1.057 (1.001 to 1.114), < 0.014 (0.029) | 1.147 (1.105 to 1.190), < 0.014 (0.022) | 1.191 (1.154 to 1.231), < 0.014 (0.020) |
| 2014 | 0.988 (1.024 to 1.041), < 0.654 (0.027) | 1.089 (1.030 to 1.152), < 0.005 (0.031) | 1.144 (1.100 to 1.190), < 0.005 (0.023) | 1.222 (1.182 to 1.265), < 0.005 (0.021) |
| 2015 | 1.016 (1.019 to 1.076), < 0.583 (0.030) | 1.090 (1.027 to 1.158), < 0.009 (0.033) | 1.198 (1.149 to 1.249), < 0.009 (0.026) | 1.240 (1.195 to 1.285), < 0.009 (0.023) |
| 2016 | 0.985 (1.054 to 1.052), < 0.650 (0.033) | 1.117 (1.044 to 1.196), < 0.001 (0.039) | 1.208 (1.152 to 1.266), < 0.001 (0.029) | 1.211 (1.162 to 1.262), < 0.001 (0.026) |
| 2017 | 1.100 (1.072 to 1.182), < 0.001 (0.040) | 1.168 (1.084 to 1.258), < 0.001 (0.044) | 1.287 (1.224 to 1.353), < 0.001 (0.033) | 1.250 (1.195 to 1.308), < 0.001 (0.029) |
| 2018 | 1.179 (1.177 to 1.270), < 0.001 (0.045) | 1.174 (1.177 to 1.371), < 0.001 (0.050) | 1.636 (1.557 to 1.719), < 0.001 (0.041) | 1.327 (1.265 to 1.390), < 0.001 (0.032) |
| 2019 | 1.216 (1.225 to 1.319), < 0.001 (0.050) | 1.225 (1.225 to 1.448), < 0.001 (0.057) | 1.591 (1.507 to 1.681), < 0.001 (0.044) | 1.261 (1.197 to 1.330), < 0.001 (0.034) |
| 2020 | 1.175 (1.157 to 1.304), < 0.001 (0.062) | 1.196 (1.157 to 1.476), < 0.001 (0.071) | – | – |
| 2021 | – | – | – | – |
| Constant | 0.002 (0.001 to 0.002), < 0.001 (0.001) | 0.001 (0.001 to 0.001), < 0.001 (0.001) | 0.004 (0.002 to 0.005), < 0.001 (0.001) | 0.004 (0.004 to 0.006), < 0.001 (0.001) |
| ACSC admissions – same day | ACSC admissions – within 1–7 days | Referrals | Tests | |
|---|---|---|---|---|
| Locum consultations | 0.977 (0.929 to 1.027), < 0.362 (0.025) | 0.981 (0.932 to 1.032), < 0.729 (0.025) | 0.850 (0.842 to 0.858), < 0.001 (0.004) | 0.805 (0.796 to 0.814), < 0.001 (0.005) |
| Gender (reference = male) | 0.786 (0.766 to 0.808), < 0.001 (0.011) | 0.906 (0.881 to 0.931), < 0.001 (0.013) | 0.927 (0.922 to 0.932), < 0.001 (0.003) | 0.995 (0.989 to 1.001), < 0.120 (0.003) |
| Age | 0.999 (0.998 to 0.999), < 0.005 (0.001) | 1.008 (1.007 to 1.009), < 0.001 (0.001) | 1.008 (1.008 to 1.009), < 0.001 (0.001) | 0.997 (0.997 to 0.998), < 0.001 (0.009) |
| Comorbidity score | 1.339 (1.322 to 1.356), < 0.001 (0.008) | 1.376 (1.361 to 1.391), < 0.001 (0.007) | 0.877 (0.874 to 0.881), < 0.001 (0.001) | 1.090 (1.086 to 1.094), < 0.001 (0.002) |
| Years registered with practice | 1.002 (1.001 to 1.003), < 0.001 (0.001) | 0.997 (0.996 to 0.998), < 0.001 (0.001) | 0.999 (0.998 to 0.999), < 0.001 (0.001) | 1.000 (0.998 to 1.001), < 0.103 (0.001) |
| Patient list size | 0.999 (0.999 to 1.000), < 0.223 (0.001) | 0.999 (0.998 to 0.999), < 0.001 (0.001) | 1.000 (0.999 to 1.001), < 0.458 (0.002) | 1.000 (1.000 to 1.001), < 0.001 (0.002) |
| IMD quintile (1 = most deprived) | ||||
| Quintile 2 | 1.056 (1.010 to 1.104), < 0.016 (0.024) | 1.103 (1.054 to 1.153), < 0.001 (0.025) | 0.984 (0.977 to 0.993), < 0.001 (0.004) | 1.009 (0.999 to 1.019), < 0.094 (0.005) |
| Quintile 3 | 1.121 (1.070 to 1.173), < 0.001 (0.026) | 1.154 (1.102 to 1.209), < 0.001 (0.027) | 0.963 (0.954 to 0.972), < 0.001 (0.004) | 1.006 (0.995 to 1.016), < 0.300 (0.005) |
| Quintile 4 | 1.132 (1.078 to 1.189), < 0.001 (0.028) | 1.264 (1.204 to 1.327), < 0.001 (0.031) | 0.939 (0.929 to 0.948), < 0.001 (0.005) | 1.017 (1.006 to 1.029), < 0.003 (0.006) |
| Quintile 5 | 1.132 (1.073 to 1.194), < 0.001 (0.031) | 1.287 (1.220 to 1.356), < 0.001 (0.035) | 0.976 (0.899 to 0.921), < 0.001 (0.005) | 0.999 (0.986 to 1.012), < 0.848 (0.006) |
| Rurality | 0.939 (0.890 to 0.991), < 0.005 (0.026) | 0.893 (0.845 to 0.943), < 0.005 (0.025) | 1.028 (1.014 to 1.040), < 0.001 (0.007) | 0.977 (0.963 to 0.990), < 0.001 (0.007) |
| Region (reference = North East) | ||||
| North West | 0.828 (0.644 to 1.064), < 0.140 (0.105) | 0.943 (0.767 to 1.159), < 0.576 (0.099) | 0.942 (0.366 to 2.425), < 0.901 (0.454) | 1.190 (0.661 to 2.142), < 0.562 (0.357) |
| Yorkshire and Humber | 0.727 (0.530 to 0.998), < 0.048 (0.117) | 0.885 (0.682 to 1.149), < 0.358 (0.117) | 0.262 (0.080 to 0.860), < 0.027 (0.159) | 1.342 (0.653 to 2.758), < 0.423 (0.493) |
| Midlands | 0.884 (0.685 to 1.140), < 0.341 (0.115) | 1.077 (0.873 to 1.329), < 0.487 (0.115) | 0.829 (0.317 to 2.169), < 0.702 (0.407) | 1.187 (0.653 to 2.157), < 0.574 (0.362) |
| East of England | 0.808 (0.621 to 1.052), < 0.114 (0.109) | 0.966 (0.777 to 1.201), < 0.759 (0.107) | 0.715 (0.264 to 1.935), < 0.509 (0.363) | 1.498 (0.809 to 2.772), < 0.198 (0.470) |
| London | 0.506 (0.393 to 0.651), < 0.001 (0.065) | 0.880 (0.716 to 1.082), < 0.227 (0.093) | 1.137 (0.443 to 2.919), < 0.789 (0.547) | 1.733 (0.964 to 3.114), < 0.066 (0.519) |
| South East | 0.710 (0.555 to 0.909), < 0.007 (0.089) | 0.889 (0.726 to 1.089), < 0.257 (0.092) | 0.690 (0.274 to 1.739), < 0.432 (0.325) | 1.078 (0.604 to 1.923), < 0.799 (0.318) |
| South West | 0.821 (0.635 to 1.063), < 0.135 (0.108) | 0.812 (0.655 to 1.004), < 0.055 (0.088) | 0.513 (0.195 to 1.353), < 0.177 (0.254) | 0.903 (0.495 to 1.648), < 0.740 (0.277) |
| Year (reference year = 2010) | ||||
| 2011 | 1.009 (0.961 to 1.059), < 0.723 (0.025) | 1.060 (1.007 to 1.115), < 0.024 (0.027) | 0.925 (0.916 to 0.934), < 0.319 (0.005) | 0.939 (0.929 to 0.949), < 0.001 (0.005) |
| 2012 | 1.003 (0.954 to 1.054), < 0.904 (0.025) | 1.095 (1.041 to 1.152), < 0.001 (0.028) | 0.869 (0.860 to 0.878), < 0.001 (0.004) | 0.905 (0.895 to 0.915), < 0.001 (0.005) |
| 2013 | 0.982 (0.932 to 1.033), < 0.480 (0.026) | 1.048 (0.994 to 1.106), < 0.079 (0.028) | 0.882 (0.873 to 0.891), < 0.001 (0.005) | 0.839 (0.830 to 0.849), < 0.001 (0.005) |
| 2014 | 1.028 (0.974 to 1.084), < 0.319 (0.028) | 1.114 (1.055 to 1.177), < 0.001 (0.030) | 0.914 (0.904 to 0.923), < 0.001 (0.005) | 0.830 (0.820 to 0.840), < 0.001 (0.005) |
| 2015 | 0.982 (0.926 to 1.042), < 0.549 (0.030) | 1.098 (1.035 to 1.165), < 0.002 (0.032) | 0.944 (0.934 to 0.955), < 0.001 (0.006) | 0.817 (0.806 to 0.827), < 0.001 (0.005) |
| 2016 | 1.035 (0.968 to 1.107), < 0.317 (0.035) | 1.114 (1.042 to 1.191), < 0.002 (0.037) | 0.977 (0.965 to 0.989), < 0.001 (0.007) | 0.839 (0.826 to 0.851), < 0.001 (0.006) |
| 2017 | 1.086 (1.009 to 1.169), < 0.028 (0.041) | 1.145 (1.065 to 1.233), < 0.001 (0.043) | 0.971 (0.957 to 0.985), < 0.001 (0.007) | 0.887 (0.873 to 0.902), < 0.001 (0.007) |
| 2018 | 1.228 (1.139 to 1.325), < 0.001 (0.047) | 1.275 (1.182 to 1.376), < 0.001 (0.049) | 1.039 (1.022 to 1.052), < 0.001 (0.008) | 0.926 (0.910 to 0.942), < 0.001 (0.008) |
| 2019 | 1.204 (1.108 to 1.309), < 0.001 (0.051) | 1.356 (1.250 to 1.471), < 0.001 (0.057) | 1.015 (0.999 to 1.032), < 0.072 (0.008) | 0.955 (0.937 to 0.973), < 0.001 (0.009) |
| 2020 | 1.229 (1.107 to 1.364), < 0.001 (0.065) | 1.347 (1.213 to 1.492), < 0.001 (0.071) | 0.656 (0.640 to 0.673), < 0.001 (0.008) | 0.322 (0.310 to 0.334), < 0.001 (0.006) |
| 2021 | – | – | 0.757 (0.734 to 0.781), < 0.001 (0.011) | 0.437 (0.418 to 0.458), < 0.001 (0.010) |
| Constant | 0.001 (0.001 to 0.002), < 0.001 (0.001) | 0.001 (0.001 to 0.001), < 0.001 (0.001) | 0.026 (0.011 to 0.063), < 0.001 (0.001) | 0.020 (0.011 to 0.035), < 0.001 (0.006) |
| Indicator A | Indicator B | Indicator C | Indicator D | Indicator E | |
|---|---|---|---|---|---|
| Locum consultations | 1.116 (1.077 to 1.157), < 0.001 (0.020) | 1.442 (0.939 to 2.217), < 0.095 (0.316) | 1.351 (0.720 to 2.535), < 0.349 (0.434) | 0.772 (0.641 to 0.931), < 0.007 (0.074) | 1.066 (0.790 to 1.438), < 0.675 (0.163) |
| Gender (reference = male) | 0.756 (0.736 to 0.777), < 0.001 (0.010) | 0.948 (0.696 to 1.291), < 0.735 (0.149) | 0.821 (0.538 to 1.252), < 0.360 (0.177) | 1.029 (0.902 to 1.175), < 0.665 (0.070) | 1.255 (0.869 to 1.811), < 0.226 (0.235) |
| Age | 0.983 (0.981 to 0.985), < 0.001 (0.001) | 0.995 (0.985 to 1.005), < 0.354 (0.005) | 1.019 (1.001 to 1.039), < 0.044 (0.010) | 0.953 (0.948 to 0.959), < 0.001 (0.003) | 1.001 (0.984 to 1.018), < 0.918 (0.008) |
| Comorbidity score | 0.992 (0.980 to 1.004), < 0.193 (0.006) | 0.975 (0.843 to 1.127), < 0.731 (0.072) | 0.959 (0.827 to 1.112), < 0.579 (0.073) | 0.874 (0.831 to 0.918), < 0.001 (0.022) | 0.593 (0.496 to 0.710), < 0.001 (0.054) |
| Years registered with practice | 0.999 (0.998 to 1.000), < 0.001 (0.001) | 1.001 (0.992 to 1.016), < 0.502 (0.006) | 0.998 (0.984 to 1.011), < 0.721 (0.007) | 1.004 (0.996 to 1.004), < 0.838 (0.002) | 1.013 (1.001 to 1.025), < 0.026 (0.005) |
| Patient list size | 1.000 (1.000 to 1.001), < 0.001 (0.001) | 1.000 (1.000 to 1.001), < 0.093 (0.001) | 1.000 (0.999 to 1.000), < 0.475 (0.001) | 1.000 (1.000 to 1.000), < 0.001 (0.001) | 0.999 (0.999 to 1.000), < 0.219 (0.001) |
| IMD quintile (1 = most deprived) | |||||
| Quintile 2 | 1.059 (1.020 to 1.100), < 0.003 (0.020) | 1.183 (0.685 to 2.046), < 0.547 (0.331) | 1.923 (0.980 to 3.770), < 0.057 (0.661) | 0.947 (0.780 to 1.149), < 0.582 (0.094) | 1.690 (1.014 to 2.818), < 0.044 (0.441) |
| Quintile 3 | 1.137 (1.093 to 1.182), < 0.001 (0.023) | 1.130 (0.664 to 1.192), < 0.653 (0.307) | 1.326 (0.695 to 2.533), < 0.392 (0.438) | 0.867 (0.711 to 1.058), < 0.159 (0.088) | 0.990 (0.612 to 1.599), < 0.966 (0.243) |
| Quintile 4 | 1.171 (1.122 to 1.222), < 0.001 (0.025) | 0.938 (0.557 to 1.580), < 0.810 (0.249) | 1.160 (0.583 to 2.306), < 0.673 (0.407) | 1.055 (0.857 to 1.300), < 0.611 (0.112) | 0.741 (0.400 to 1.371), < 0.339 (0.233) |
| Quintile 5 | 1.338 (1.275 to 1.404), < 0.001 (0.033) | 1.119 (0.661 to 1.894), < 0.675 (0.301) | 2.007 (0.984 to 4.095), < 0.055 (0.730) | 0.945 (0.753 to 1.186), < 0.627 (0.110) | 0.529 (0.287 to 0.975), < 0.041 (0.165) |
| Rurality | 0.787 (0.760 to 0.814), < 0.001 (0.014) | 1.126 (0.699 to 1.814), < 0.625 (0.274) | 1.066 (0.564 to 2.015), < 0.843 (0.346) | 1.261 (1.057 to 1.506), < 0.010 (0.113) | 2.055 (1.253 to 3.370), < 0.004 (0.519) |
| Region (reference = North East) | |||||
| North West | 0.842 (0.753 to 0.943), < 0.003 (0.048) | 1.411 (0.584 to 3.407), < 0.444 (0.635) | 1.166 (0.277 to 4.912), < 0.834 (0.856) | 3.666 (1.773 to 7.580), < 0.001 (1.358) | 0.164 (0.047 to 0.566), < 0.004 (0.104) |
| Yorkshire and Humber | 2.057 (1.793 to 2.361), < 0.001 (0.144) | 1.483 (0.432 to 5.091), < 0.531 (0.933) | 4.520 (0.691 to 29.585), < 0.116 (4.333) | 3.697 (1.600 to 8.544), < 0.002 (1.580) | 2.975 (0.606 to 14.607), < 0.179 (2.416) |
| Midlands | 0.828 (0.739 to 0.928), < 0.001 (0.048) | 1.773 (0.705 to 4.461), < 0.224 (0.835) | 1.301 (0.302 to 5.604, < 0.724 (0.969) | 3.020 (1.452 to 6.281), < 0.003 (1.128) | 1.142 (0.313 to 4.168), < 0.841 (0.754) |
| East of England | 1.067 (0.948 to 1.200), < 0.281 (0.064) | 2.441 (0.880 to 6.769), < 0.086 (1.270) | 2.317 (0.500 to 10.724), < 0.282 (1.811) | 2.424 (1.149 to 5.116), < 0.020 (0.924) | 1.755 (0.470 to 6.552), < 0.403 (1.180) |
| London | 0.990 (0.882 to 1.111), < 0.866 (0.058) | 0.904 (0.359 to 2.276), < 0.830 (0.426) | 1.507 (0.347 to 6.538), < 0.584 (1.128) | 2.472 (1.184 to 5.162), < 0.016 (0.929) | 0.214 (0.058 to 0.789), < 0.021 (0.142) |
| South East | 0.912 (0.816 to 1.019), < 0.104 (0.052) | 1.946 (0.801 to 4.727), < 0.141 (0.881) | 1.607 (0.377 to 6.849), < 0.522 (1.188) | 3.388 (1.644 to 6.982), < 0.001 (1.250) | 0.670 (0.190 to 2.360), < 0.532 (0.430) |
| South West | 0.939 (0.837 to 1.052), < 0.277 (0.055) | 1.881 (0.739 to 4.786), < 0.185 (0.896) | 1.706 (0.375 to 7.766), < 0.490 (1.319) | 4.018 (1.933 to 8.353), < 0.001 (1.500) | 1.684 (0.466 to 6.085), < 0.426 (1.104) |
| Year (reference year = 2010) | |||||
| 2011 | 0.800 (0.776 to 0.826), < 0.001 (0.012) | 0.846 (0.562 to 1.272), < 0.422 (0.176) | 0.991 (0.609 to 1.614), < 0.973 (0.246) | 1.120 (0.955 to 1.315), < 0.164 (0.091) | 0.506 (0.374 to 0.683), < 0.001 (0.078) |
| 2012 | 0.676 (0.654 to 0.698), < 0.001 (0.011) | 1.166 (0.749 to 1.815), < 0.496 (0.263) | 1.732 (0.996 to 3.013), < 0.052 (0.489) | 1.005 (0.852 to 1.186), < 0.953 (0.085) | 0.464 (0.336 to 0.639), < 0.001 (0.076) |
| 2013 | 0.609 (0.589 to 0.630), < 0.001 (0.010) | 1.013 (0.627 to 1.637), < 0.959 (0.248) | 2.071 (1.157 to 3.707), < 0.014 (0.615) | 0.886 (0.746 to 1.051), < 0.165 (0.077) | 0.491 (0.359 to 0.671), < 0.001 (0.078) |
| 2014 | 0.577 (0.556 to 0.598), < 0.001 (0.011) | 1.134 (0.668 to 1.925), < 0.642 (0.306) | 1.802 (0.943 to 3.442), < 0.075 (0.595) | 0.960 (0.805 to 1.145), < 0.651 (0.086) | 0.523 (0.373 to 0.733), < 0.001 (0.090) |
| 2015 | 0.484 (0.464 to 0.504), <0.001 (0.010) | 0.882 (0.493 to 1.578), < 0.673 (0.262) | 2.867 (1.371 to 5.992), < 0.005 (1.078) | 0.857 (0.711 to 1.032, < 0.104 (0.082) | 0.468 (0.322 to 0.680), < 0.001 (0.089) |
| 2016 | 0.422 (0.402 to 0.442), < 0.001 (0.011) | 1.181 (0.578 to 2.416), < 0.648 (0.431) | 3.066 (1.298 to 6.993), < 0.011 (1.295) | 0.793 (0.646 to 0.973), < 0.026 (0.083) | 0.172 (0.109 to 0.271), < 0.001 (0.040) |
| 2017 | 0.391 (0.370 to 0.414), < 0.001 (0.011) | 0.835 (0.352 to 1.987), < 0.683 (0.369) | 1.009 (0.363 to 2.805), < 0.986 (0.526) | 0.623 (0.496 to 0.782), < 0.001 (0.072) | 0.139 (0.087 to 0.220), < 0.001 (0.033) |
| 2018 | 0.351 (0.330 to 0.373), < 0.001 (0.011) | 0.940 (0.332 to 2.661), < 0.907 (0.499) | 1.704 (0.473 to 6.132), < 0.415 (1.113) | 0.383 (0.294 to 0.501), < 0.001 (0.052) | 0.063 (0.036 to 0.111),< 0.001 (0.018) |
| 2019 | 0.289 (0.269 to 0.311), < 0.001 (0.011) | 1.021 (0.330 to 3.162), < 0.971 (0.589) | 0.266 (0.051 to 1.374), < 0.114 (0.223) | 0.319 (0.234 to 0.433), < 0.001 (0.050) | 0.120 (0.065 to 0.221), < 0.001 (0.037) |
| 2020 | 0.316 (0.287 to 0.349), < 0.001 (0.016) | 1.713 (0.418 to 7.028), < 0.455 (1.234) | 9.810 (0.772 to 124.623), < 0.078 (12.722) | 0.223 (0.143 to 0.347), < 0.001 (0.050) | 0.020 (0.009 to 0.045), < 0.001 (0.008) |
| 2021 | 0.382 (0.331 to 0.441), < 0.001 (0.028) | 22.005 (0.923 to 524.69), < 0.056 (35.607) | – | 0.285 (0.148 to 0.545), < 0.001 (0.094) | 0.010 (0.001 to 0.068), < 0.001 (0.010) |
| Constant | 13.369 (11.145 to 16.036), < 0.001 (0.005) | 1.402 (0.436 to 4.515), < 0.571 (0.836) | 0.011 (0.013 to 0.080), < 0.001 (0.010) | 0.003 (0.001 to 0.007), < 0.001 (0.013) | 180.80 (29.810 to 1096.55), < 0.001 (166.27) |
| Indicator F | Indicator G | Indicator H | Indicator I | Indicator J | |
|---|---|---|---|---|---|
| Locum consultations | 0.992 (0.915 to 1.076), < 0.852 (0.041) | 0.994 (0.906 to 1.090), < 0.894 (0.047) | 0.888 (0.848 to 0.929), < 0.001 (0.021) | 0.958 (0.812 to 1.130), < 0.613 (0.010) | 0.487 (0.193 to 1.229), < 0.128 (0.230) |
| Gender (reference = male) | 0.668 (0.555 to 0.806), < 0.001 (0.063) | 1.565 (1.416 to 1.728), < 0.001 (0.080) | 1.070 (1.007 to 1.136), < 0.001 (0.032) | 0.962 (0.850 to 1.087), < 0.534 (0.007) | 0.568 (0.279 to 1.156), < 0.119 (0.206) |
| Age | 0.965 (0.958 to 0.972), < 0.001 (0.004) | 0.933 (0.930 to 0.936), < 0.001 (0.002) | 1.008 (1.006 to 1.009), < 0.001 (0.001) | 0.966 (0.961 to 0.970), < 0.001 (0.001) | 1.097 (1.034 to 1.164), < 0.002 (0.033) |
| Comorbidity score | 0.556 (0.506 to 0.611), < 0.001 (0.026) | 0.665 (0.637 to 0.693), < 0.001 (0.014) | 1.106 (1.077 to 1.134), < 0.001 (0.014) | 0.891 (0.854 to 0.930), < 0.001 (0.003) | 0.889 (0.698 to 1.130), < 0.337 (0.109) |
| Years registered with practice | 1.008 (1.002 to 1.014), < 0.006 (0.003) | 0.997 (0.994 to 1.002), < 0.151 (0.001) | 1.005 (0.998 to 1.003), < 0.655 (0.001) | 1.001 (0.998 to 1.004), < 0.509 (0.001) | 1.021 (0.999 to 1.042), < 0.052 (0.011) |
| Patient list size | 1.000 (1.000 to 1.001), < 0.002 (0.001) | 1.000 (1.000 to 1.001), < 0.818 (0.001) | 0.999 (0.999 to 1.000), < 0.001 (0.001) | 0.999 (0.999 to 1.000), < 0.656 (0.001) | 1.000 (0.998 to 1.001), < 0.667 (0.001) |
| IMD quintile (1 = most deprived) | |||||
| Quintile 2 | 0.964 (0.738 to 1.260), < 0.791 (0.132) | 1.035 (0.893 to 1.200), < 0.647 (0.078) | 0.861 (0.788 to 0.941), < 0.001 (0.039) | 1.093 (0.906 to 1.318), < 0.353 (0.009) | 0.806 (0.296 to 2.190), < 0.672 (0.411) |
| Quintile 3 | 0.836 (0.638 to 1.095), < 0.195 (0.115) | 0.932 (0.803 to 1.083), < 0.351 (0.071) | 0.748 (0.684 to 0.819), < 0.001 (0.034) | 0.962 (0.794 to 1.166), < 0.695 (0.010) | 0.441 (0.174 to 1.120), < 0.085 (0.210) |
| Quintile 4 | 0.798 (0.599 to 1.064), < 0.124 (0.117) | 0.934 (0.804 to 1.085), < 0.375 (0.071) | 0.736 (0.675 to 0.804), < 0.001 (0.033) | 1.057 (0.867 to 1.288), < 0.582 (0.012) | 0.816 (0.304 to 2.190), < 0.686 (0.411) |
| Quintile 5 | 0.400 (0.285 to 0.560), < 0.001 (0.069) | 0.892 (0.763 to 1.043), < 0.151 (0.071) | 0.763 (0.695 to 0.837), < 0.001 (0.036) | 1.178 (0.958 to 1.448), < 0.120 (0.015) | 1.724 (0.517 to 5.751), < 0.375 (1.059) |
| Rurality | 1.264 (1.005 to 1.591, < 0.045 (0.148) | 0.975 (0.846 to 1.122), < 0.721 (0.070) | 0.824 (0.752 to 0.902), < 0.001 (0.038) | 0.959 (0.809 to 1.137), < 0.631 (0.012) | 1.288 (0.481 to 3.448), < 0.615 (0.647) |
| Region (reference = North East) | |||||
| North West | 0.149 (0.086 to 0.259), < 0.001 (0.042) | 1.085 (0.761 to 1.548), < 0.651 (0.196) | 0.392 (0.325 to 0.472), < 0.001 (0.037) | 2.269 (1.277 to 4.031), < 0.165 (0.168) | 0.042 (0.007 to 2.375), < 0.124 (0.086) |
| Yorkshire and Humber | 0.753 (0.397 to 1.428), < 0.385 (0.246) | 1.027 (0.626 to 1.684), < 0.916 (0.259) | 0.877 (0.668 to 1.151), < 0.001 (0.122) | 2.231 (1.126 to 4.423), < 0.021 (0.177) | 0.023 (0.002 to 1.892), < 0.094 (0.052) |
| Midlands | 0.263 (0.151 to 0.457), < 0.001 (0.074) | 0.894 (0.620 to 1.289), < 0.547 (0.167) | 0.410 (0.339 to 0.496), < 0.001 (0.040) | 3.084 (1.725 to 5.514), < 0.001 (0.190) | 0.029 (0.001 to 1.677), < 0.087 (0.059) |
| East of England | 0.229 (0.128 to 0.411), < 0.001 (0.068) | 0.787 (0.537 to 1.155), < 0.222 (0.154) | 0.497 (0.406 to 0.609), < 0.001 (0.052) | 1.824 (0.991 to 3.357), < 0.053 (0.230) | 0.111 (0.015 to 7.694), < 0.309 (0.240) |
| London | 0.055 (0.029 to 0.103), < 0.001 (0.018) | 0.899 (0.623 to 1.297), < 0.569 (0.168) | 0.827 (0.684 to 0.999), < 0.049 (0.080) | 2.273 (1.262 to 4.094), < 0.006 (0.171) | 0.019 (0.001 to 1.115), < 0.056 (0.039) |
| South East | 0.209 (0.123 to 0.357), < 0.001 (0.057) | 0.861 (0.603 to 1.228), < 0.409 (0.156) | 0.347 (0.288 to 0.418), < 0.059 (0.033) | 2.466 (1.388 to 4.382), < 0.002 (0.199) | 0.050 (0.008 to 2.898), < 0.148 (0.103) |
| South West | 0.681 (0.399 to 1.164), < 0.161 (0.186) | 0.907 (0.622 to 1.321), < 0.609 (0.174) | 0.368 (0.302 to 0.448), < 0.145 (0.037) | 2.737 (1.526 to 4.910), < 0.001 (0.218) | 0.026 (0.001 to 1.550), < 0.080 (0.054) |
| Year (reference year = 2010) | |||||
| 2011 | 0.815 (0.748 to 0.888), < 0.001 (0.036) | 0.876 (0.778 to 0.986), < 0.028 (0.053) | 0.760 (0.732 to 0.790), < 0.001 (0.015) | 0.902 (0.779 to 1.043), < 0.163 (0.010) | 0.826 (0.340 to 2.006), < 0.673 (0.374) |
| 2012 | 0.687 (0.627 to 0.753), < 0.001 (0.032) | 0.805 (0.713 to 0.908), < 0.001 (0.050) | 0.648 (0.623 to 0.674), < 0.001 (0.013) | 0.653 (0.554 to 0.770), < 0.001 (0.009) | 0.911 (0.366 to 2.269), < 0.842 (0.424) |
| 2013 | 0.595 (0.541 to 0.654), < 0.001 (0.029) | 0.785 (0.696 to 0.887), < 0.001 (0.049) | 0.478 (0.459 to 0.498), < 0.001 (0.010) | 0.669 (0.565 to 0.792), < 0.001 (0.010) | 1.423 (0.528 to 3.835), < 0.485 (0.720) |
| 2014 | 0.594 (0.537 to 0.658), < 0.001 (0.031) | 0.753 (0.664 to 0.853), < 0.001 (0.048) | 0.387 (0.370 to 0.404), < 0.001 (0.009) | 0.686 (0.575 to 0.820), < 0.001 (0.010) | 0.857 (0.320 to 2.292), < 0.758 (0.430) |
| 2015 | 0.474 (0.424 to 0.529), < 0.001 (0.027) | 0.758 (0.664 to 0.865), < 0.001 (0.051) | 0.274 (0.260 to 0.288), < 0.001 (0.007) | 0.510 (0.416 to 0.625, < 0.001 (0.011) | 1.361 (0.422 to 4.394), < 0.606 (0.814) |
| 2016 | 0.359 (0.318 to 0.406), < 0.001 (0.022) | 0.726 (0.630 to 0.837), < 0.001 (0.053) | 0.228 (0.214 to 0.241), < 0.001 (0.007) | 0.499 (0.399 to 0.624), < 0.001 (0.012) | 2.422 (0.615 to 9.541), < 0.206 (1.694) |
| 2017 | 0.326 (0.286 to 0.373), < 0.001 (0.022) | 0.703 (0.604 to 0.819), < 0.001 (0.055) | 0.171 (0.160 to 0.184), < 0.001 (0.006) | 0.402 (0.309 to 0.523), < 0.001 (0.013) | 3.228 (0.522 to 19.954), < 0.207 (3.000) |
| 2018 | 0.332 (0.287 to 0.384), < 0.001 (0.025) | 0.721 (0.612 to 0.849), < 0.001 (0.060) | 0.121 (0.111 to 0.132), < 0.001 (0.005) | 0.233 (0.168 to 0.324), < 0.001 (0.013) | 2.495 (0.329 to 18.935), < 0.377 (2.580) |
| 2019 | 0.265 (0.225 to 0.312), < 0.001 (0.022) | 0.784 (0.658 to 0.934), < 0.006 (0.070) | 0.085 (0.077 to 0.095), < 0.001 (0.005) | 0.323 (0.234 to 0.446), < 0.001 (0.013) | 0.978 (0.179 to 5.353), < 0.979(0.848) |
| 2020 | 0.346 (0.281 to 0.427), < 0.001 (0.037) | 0.616 (0.486 to 0.781), < 0.001 (0.075) | 0.049 (0.041 to 0.057), < 0.001 (0.004) | 0.262 (0.171 to 0.403), < 0.001 (0.017) | 4.105 (0.273 to 61.700), < 0.307 (5.676) |
| 2021 | 0.497 (0.380 to 0.650), < 0.001 (0.068) | 0.539 (0.373 to 0.779), < 0.001 (0.101) | 0.023 (0.017 to 0.031), < 0.001 (0.003) | 0.378 (0.214 to 0.668), < 0.001 (0.023) | 2.247 (0.040 to 126.372), < 0.694 (4.619) |
| Constant | 2,624.92(1,285.25 to 5361.01), < 0.001 (956.37) | 3.632 (2.393 to 5.514), < 0.001 (0.773) | 0.001 (0.001 to 0.001), < 0.001 (0.001) | 0.010 (0.005 to 0.020), < 0.001 (0.004) | 48.753 (0.111 to 21,361.8), < 0.210 (151.30) |
FIGURE 44.
All locum consultations as a proportion of all GP consultations.
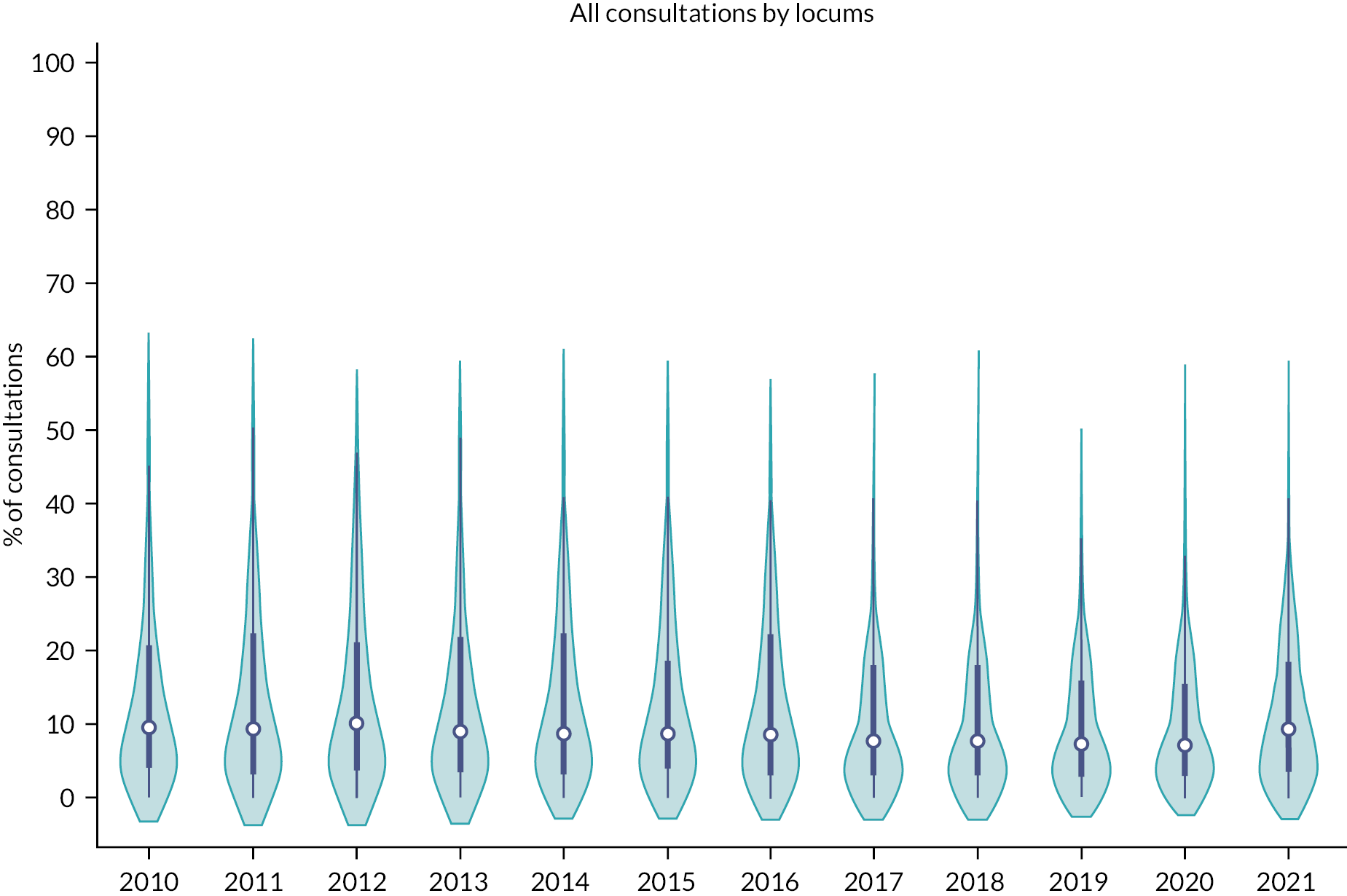
FIGURE 45.
All locum F2F consultations as a proportion of all GP F2F consultations.

FIGURE 46.
All locum telephone and online consultations as a proportion of all GP telephone and online consultations.

FIGURE 47.
Regional variation in the proportion of locum consultations in 2010–21.

FIGURE 48.
Regional variation in the proportion of F2F locum consultations in 2010–21.
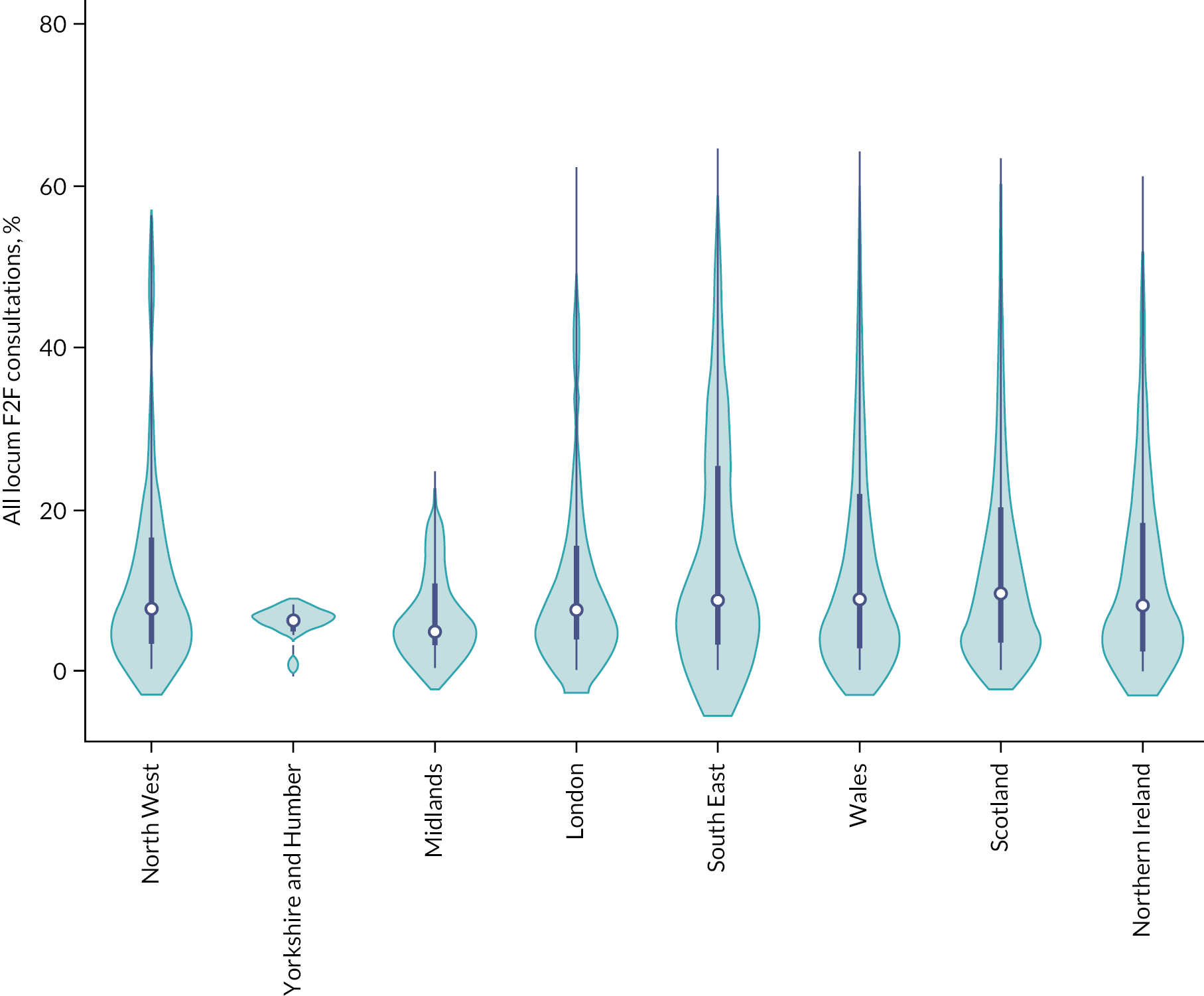
FIGURE 49.
Regional variation in the proportion of telephone and online locum consultations in 2010–21.
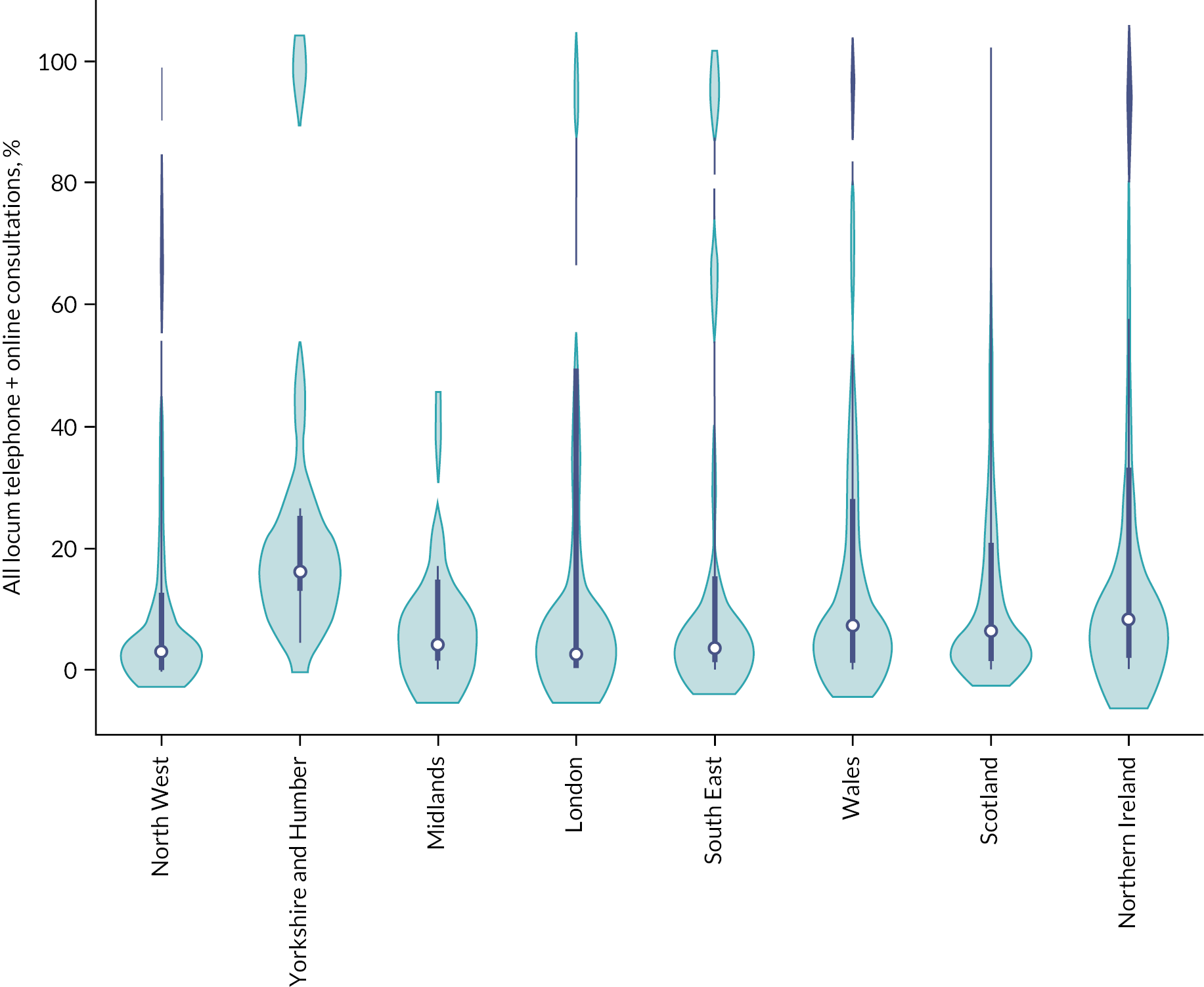
FIGURE 50.
Total consultation by GP type and day of week, aggregated over 2010–21.
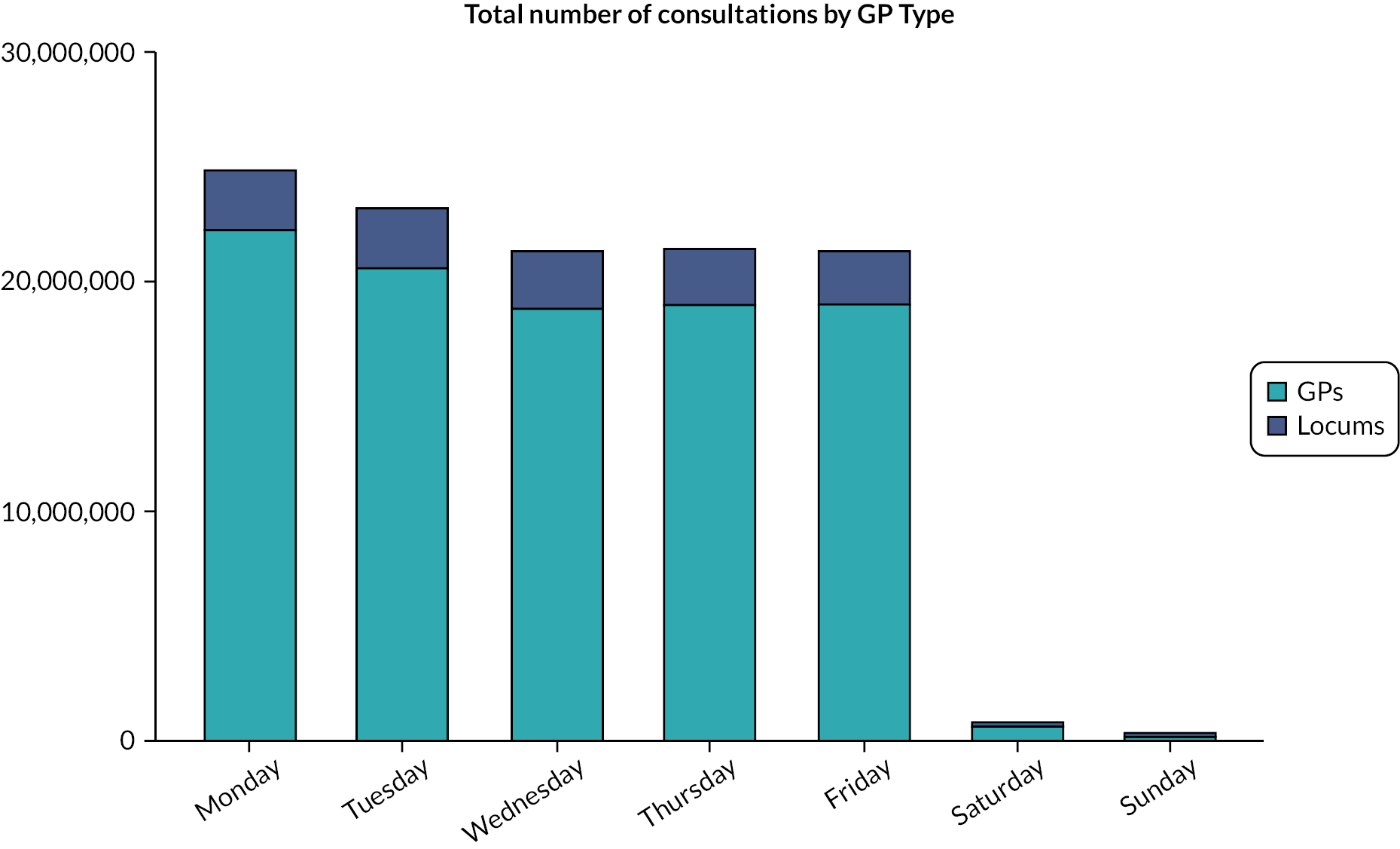
FIGURE 51.
Mean proportion of GP locum consultation by day of week, over 2010–21. Bar labels show the average number of GP consultations done in each day across 381 practices in England.
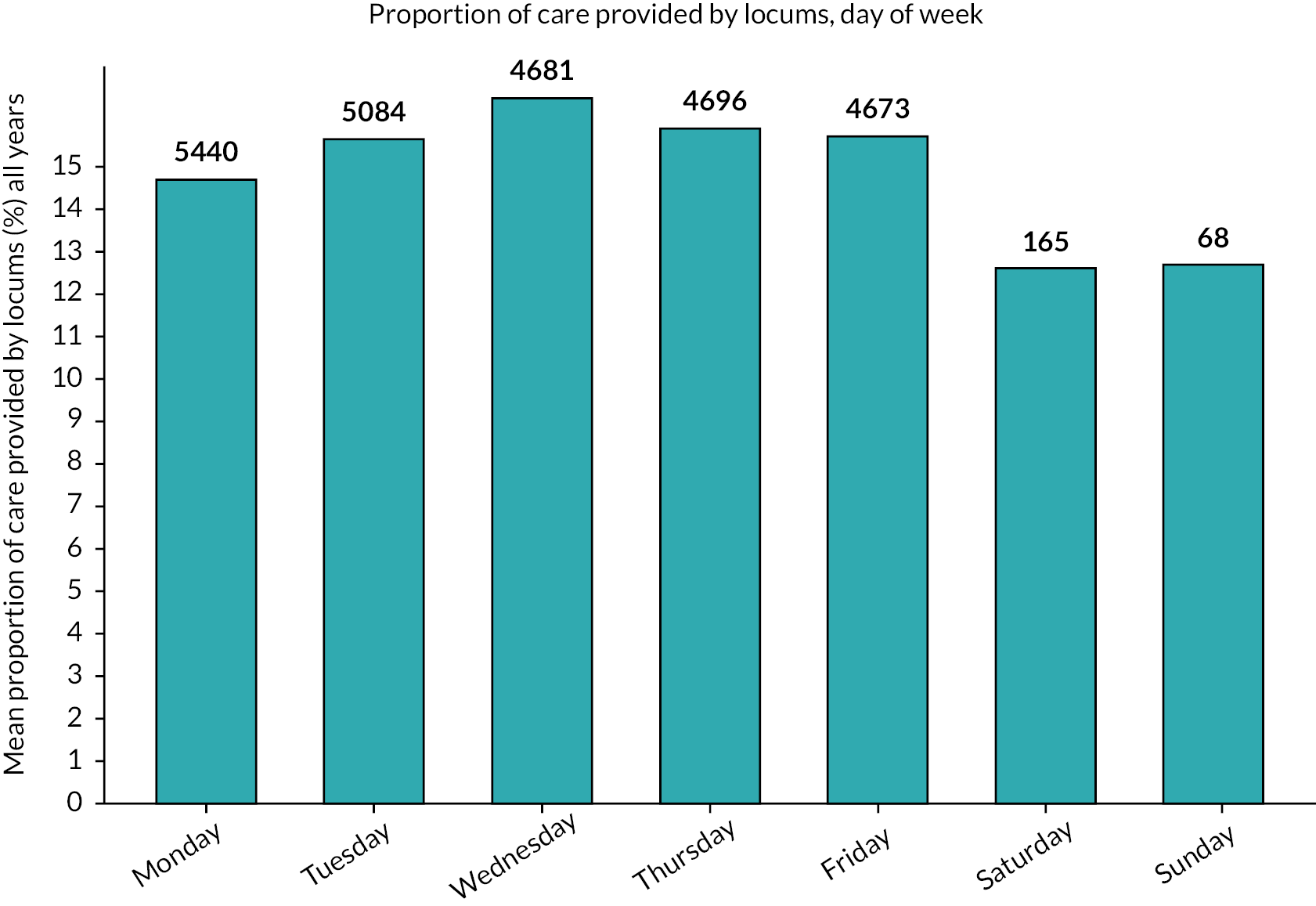
FIGURE 52.
Mean values with CIs for non-hospital outcomes by GP type, over time (2010–21).
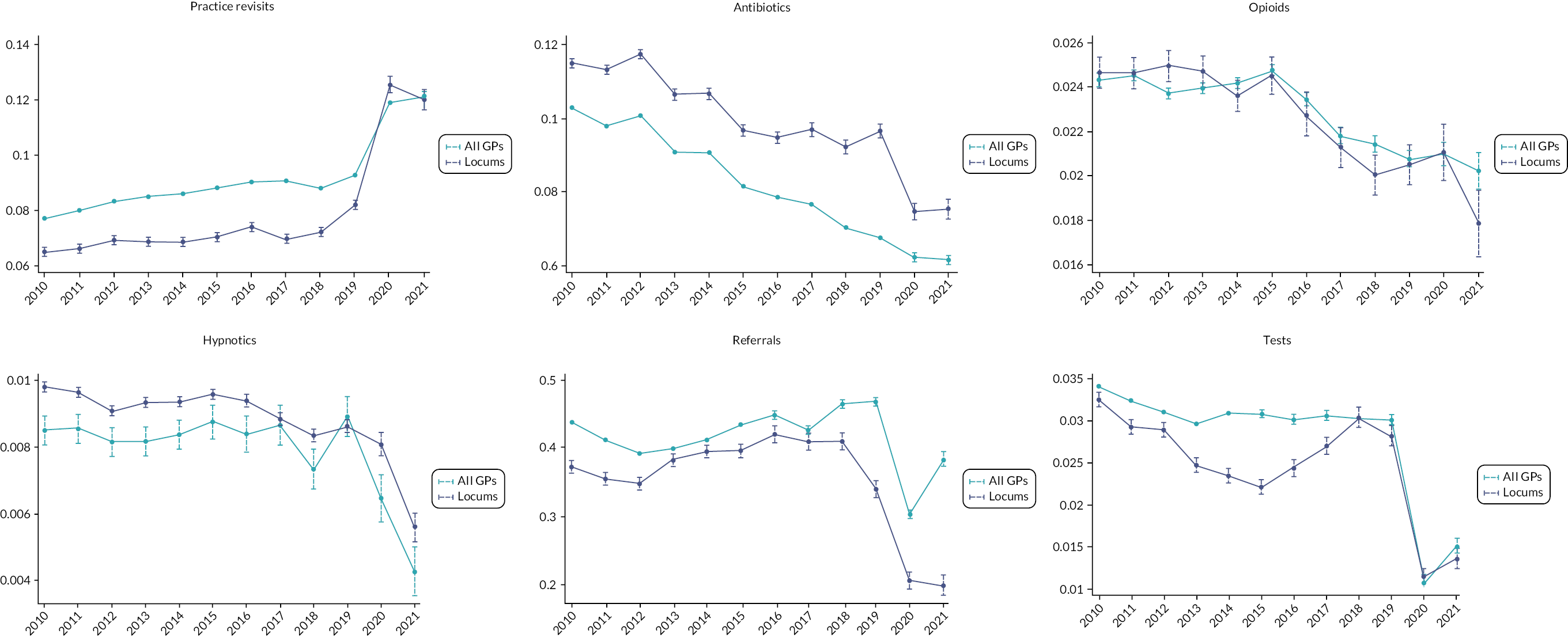
FIGURE 53.
Mean values with CIs for hospital outcomes by GP type, over time (2010–20).
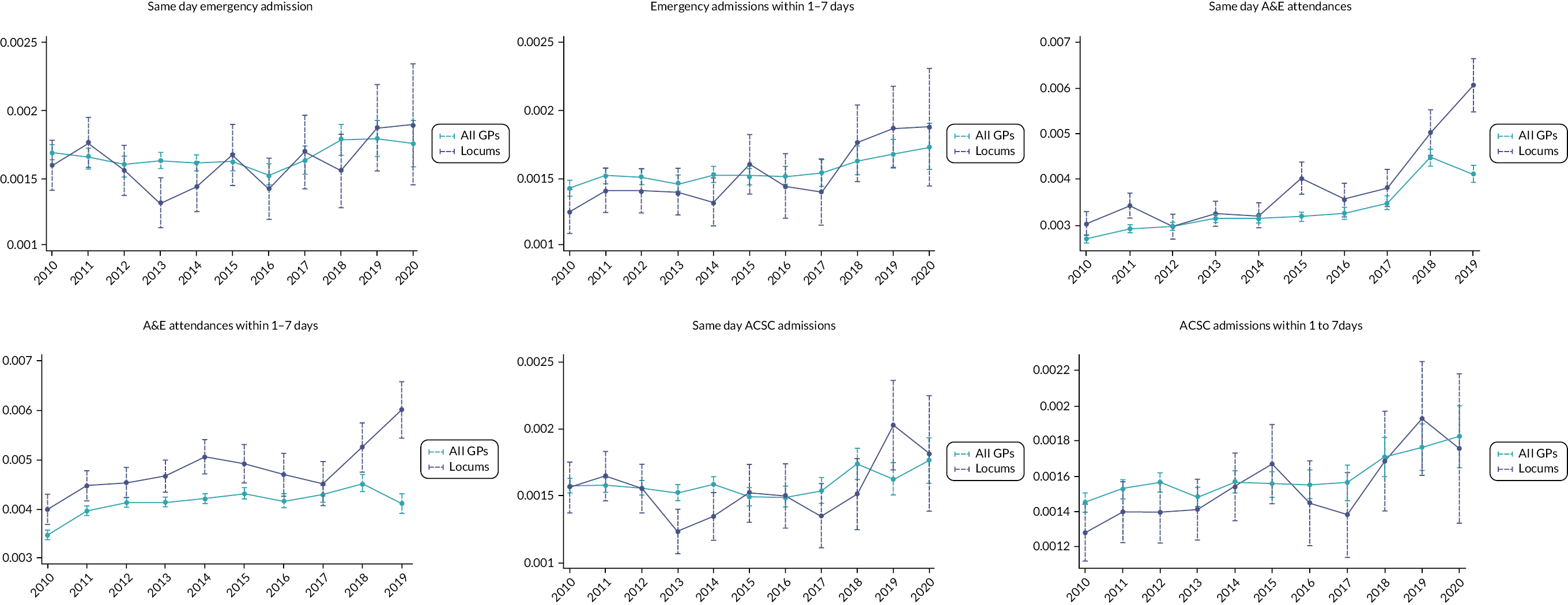
Appendix 8 Additional material for Chapter 10: the use of locum doctors in National Health Service trusts in England: analysis of electronic patient records
FIGURE 54.
Bradford EPR data for total patients and orders per week September 2017–November 2021.
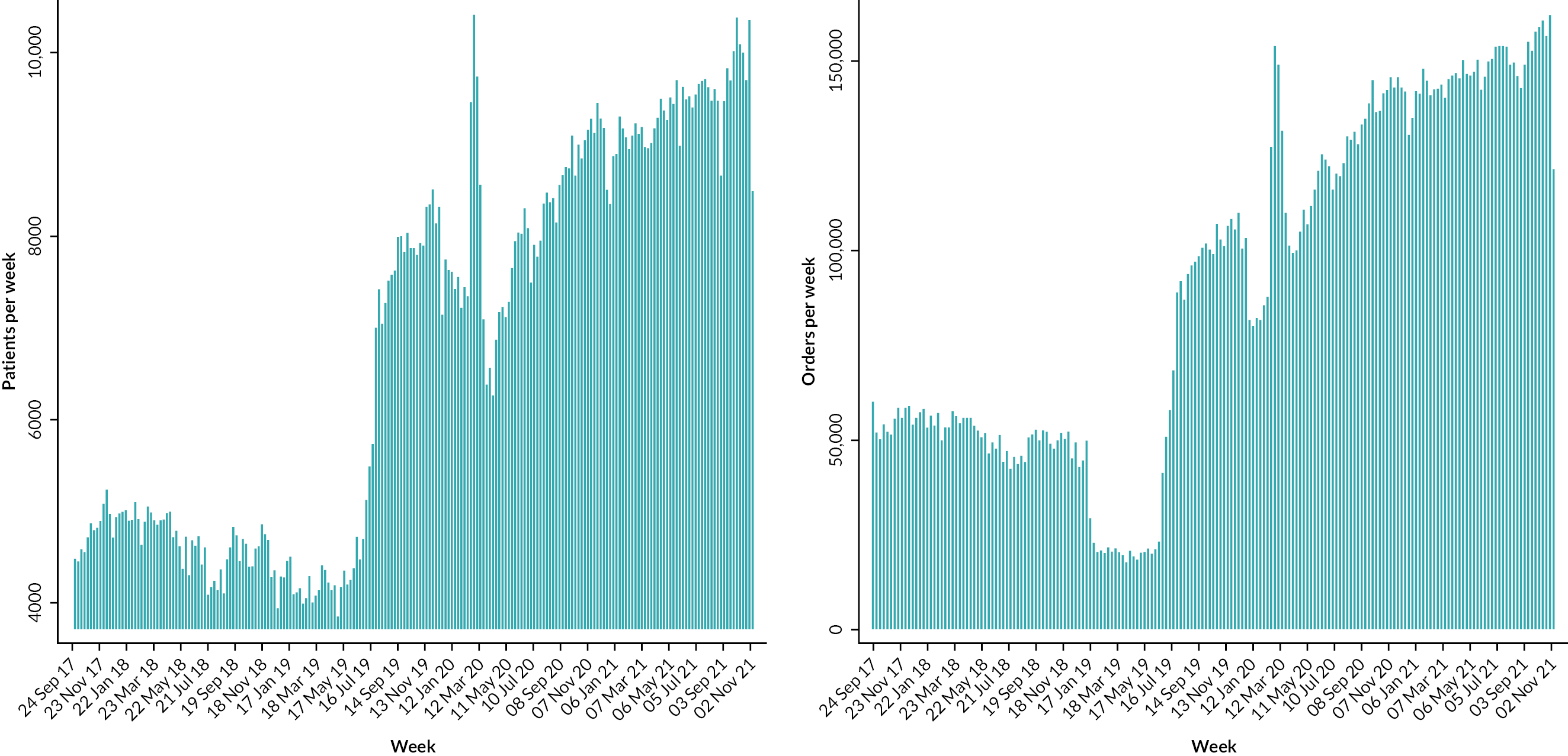
Appendix 9 Locum doctors in the NHS: Understanding and improving the quality and safety of healthcare (policy report)




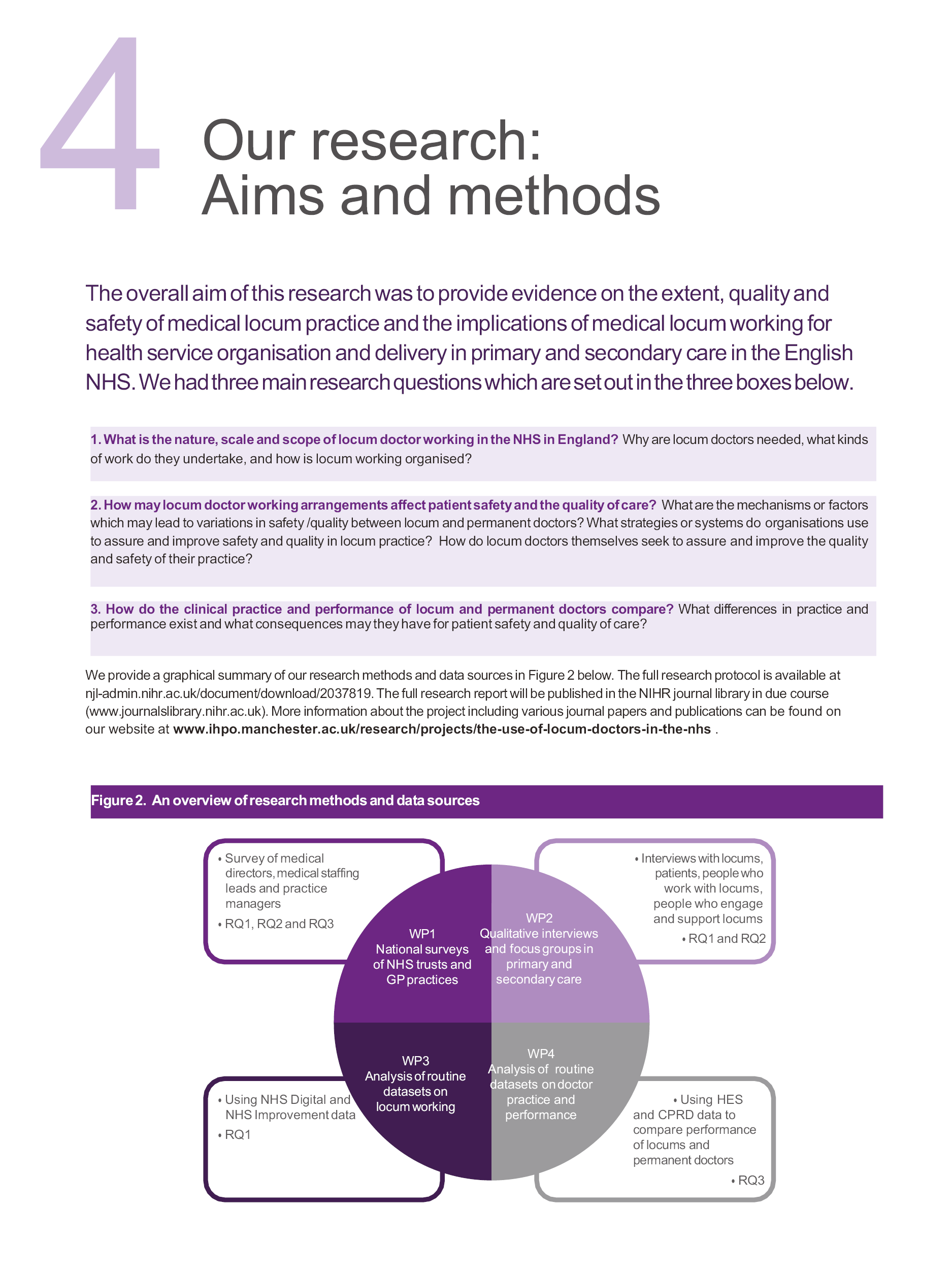






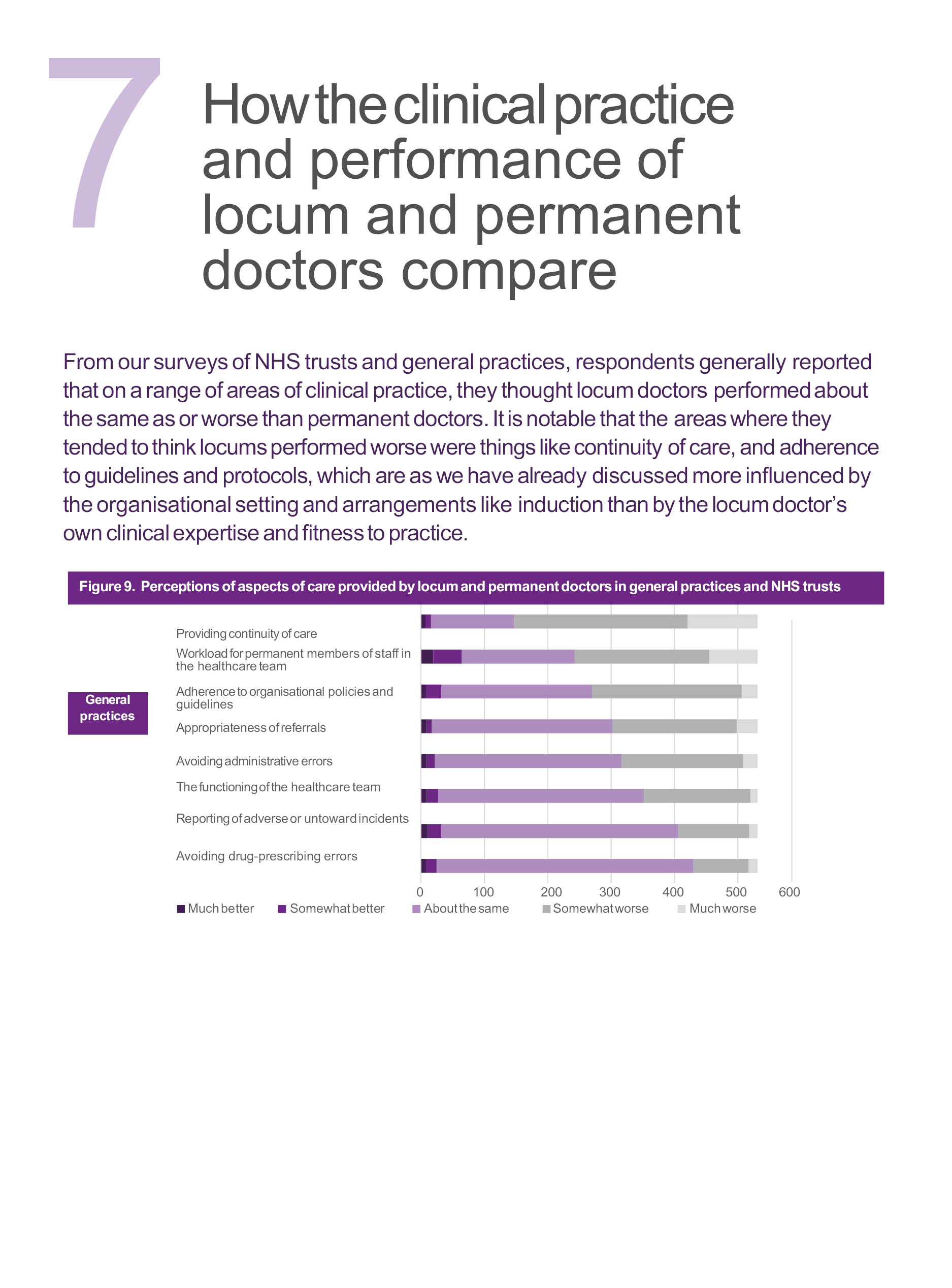
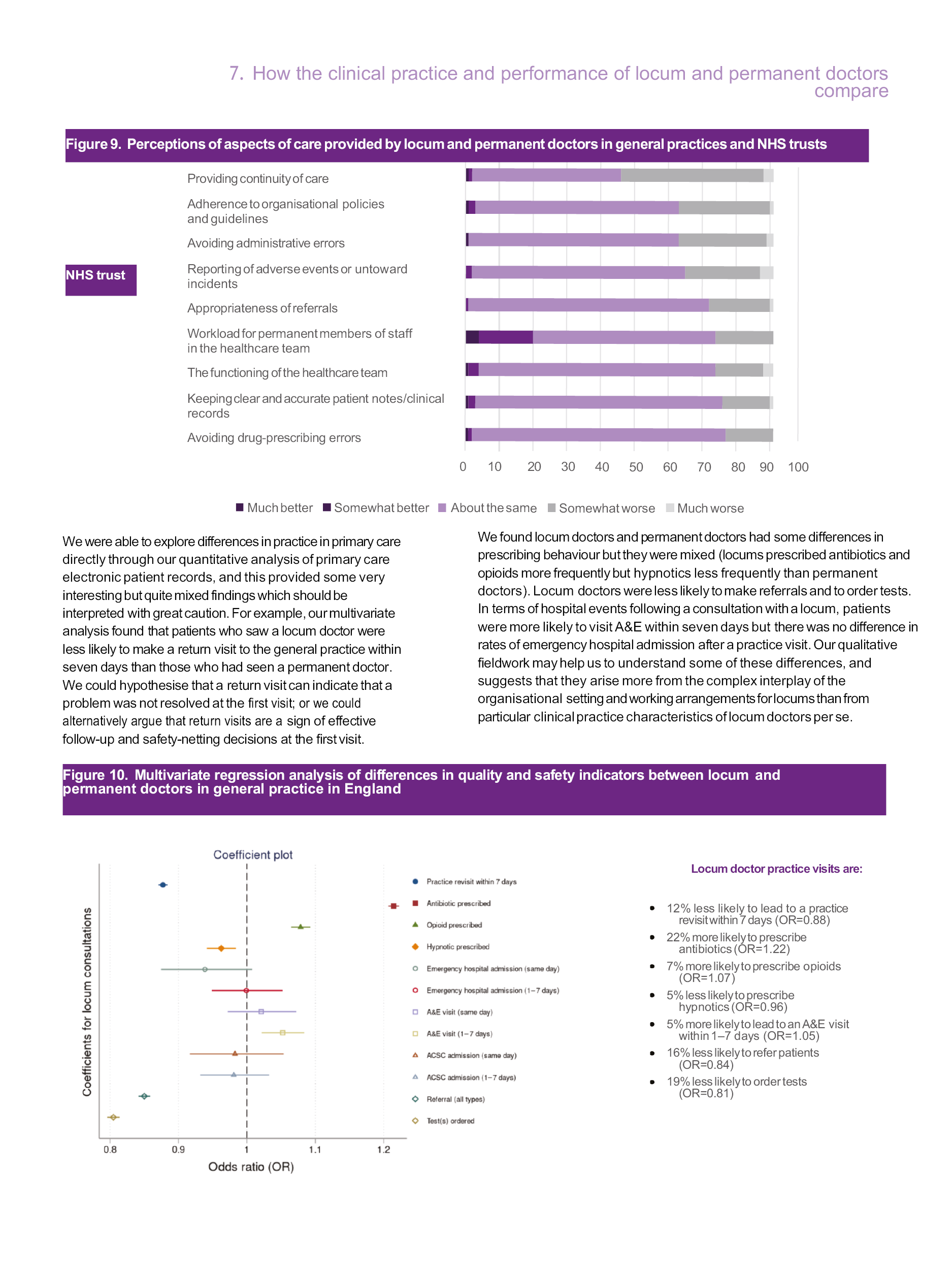


List of abbreviations
- ACSC
- ambulatory care sensitive condition
- CCG
- Clinical Commissioning Group
- CPD
- continuing professional development
- CPRD
- Clinical Practice Research Databank
- CQC
- Care Quality Commission
- EPR
- electronic patient record
- ESR
- electronic staff record
- F2F
- face to face
- FTE
- full-time equivalent
- GMC
- General Medical Council
- GP
- general practitioner
- HES
- Hospital Episode Statistics
- IMD
- Index of Multiple Deprivation
- IMG
- international medical graduate
- IRAS
- Integrated Research Application System
- LSOA
- lower-layer super output area
- MDT
- multidisciplinary team
- MPIT
- medical practice information transfer
- NIHR
- National Institute for Health and Care Research
- ODS
- organisation data service
- PPI
- patient and public involvement
- QOF
- Quality and Outcomes Framework
- REC
- Research Ethics Committee
- RO
- responsible officer
- RTA
- reflexive thematic analysis
- STP
- Sustainability and Transformation Partnership
