Notes
Article history
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as award number 17/09/08. The contractual start date was in October 2018. The draft manuscript began editorial review in May 2022 and was accepted for publication in April 2023. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ manuscript and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this article.
Permissions
Copyright statement
Copyright © 2024 Pryjmachuk et al. This work was produced by Pryjmachuk et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2024 Pryjmachuk et al.
Chapter 1 Introduction and background
This study arose from a successful application to a 2017 National Institute for Health and Care Research (NIHR) commissioning call on research to improve services for children and young people (CYP) with common mental health problems (CMHPs). 1 Originally scheduled for 3 years beginning late 2018, it was extended for 7 months because of unanticipated delays caused by the coronavirus disease 2019 (COVID-19) pandemic.
The study is linked to another study funded from the same call, ‘Queer Futures 2’ (QF2),2 which focuses on mental health services for lesbian, gay, bisexual, trans, queer (LGBTQ) young people. The NIHR asked the two studies to collaborate. This was facilitated through: our research associates (Fraser, Lane) having regular contact with QF2’s three research associates; this study’s chief investigator (Pryjmachuk) being a QF2 coinvestigator; representatives from the two studies sitting on each other’s study advisory group (SAG); and ensuring there was as little duplication as possible regarding the populations and services relevant to each study.
Background
Children and young people’s mental health
Over the last decade or so, CYP’s mental health has been a growing public health concern both nationally3–6 and internationally. 7 In 2004, around 1 in 10 CYP in England were estimated to have a mental disorder, that is, a mental health problem sufficient to warrant professional intervention. 8 In 2017, the time of the commissioning call, these estimates rose to one in eight CYP in England. 9 The most recent estimates, published in 2021 and covering the height of the COVID-19 pandemic, suggest around one in six CYP in England may have a mental disorder. 10 Moreover, data from NHS Digital11 indicate a near doubling (92%) in referrals to children’s mental health services in England from December 2017 to December 2021 and a 62% increase in contacts with children’s mental health services during the same period.
Within adult mental health, CMHPs are defined as a range of emotional disorders – notably depression, anxiety and anxiety-related disorders like panic, obsessive–compulsive disorder (OCD) and post-traumatic stress disorder (PTSD) – affecting a significant proportion of the population, hence the label ‘common’. 12 In adult mental health, CMHPs can be contrasted with ‘serious mental illness’ (SMI). SMI covers more disabling disorders affecting fewer people, for example, schizophrenia. This is not to say CMHPs cannot lead to serious difficulties but, where this is the case, a qualifying label is often added to the disorder’s name to indicate it may be more an SMI than a CMHP. Compare, for example, mild-to-moderate depression (CMHP) with severe depression (SMI).
Regarding CYP’s mental health, the commissioning brief largely reflected the demarcation between CMHPs and SMI seen in adult mental health with emotional disorders (depression and anxiety-related disorders) being included and psychoses excluded. However, the brief outlined a somewhat extended view of CMHPs including behavioural disorders, substance misuse, self-harm, gender identity disorders and emerging personality disorders. It also excluded learning disability, autism and eating disorders from its definition of CMHPs. This stance on CMHPs is in line with the latest English prevalence data:9,10 emotional disorders (anxiety and depression) remain the most prevalent (common) disorders among CYP; self-harm and suicide attempts among those with a mental disorder are relatively common, affecting 25% of such CYP; and gender identity problems increase the risk of developing a mental disorder. Though excluded from the brief, it seems eating disorders are becoming more common with prevalence rates in England in 11- to 16-year-olds doubling from 2017 to 2021. 10
Importantly, this study focuses on services for CYP experiencing, rather than diagnosed with, CMHPs; this allowed for greater inclusivity because not every CYP exhibiting signs and symptoms of a CMHP necessarily has a diagnosed mental health problem.
Mental health services
The seminal 1995 report Together We Stand13 led to the establishment of the de facto model for UK children’s mental health services, the so-called ‘tiers’ model. This model specifies four tiers of service provision according to clinician-perceived needs of CYP and their families. Tier 1, reflecting non-specialist, universal services, is concerned largely with mental health promotion and mental ill-health prevention. Tiers 2–4 reflect formal mental health services [i.e. ‘Child and Adolescent Mental Health Services (CAMHS)’], with Tiers 2–3 mostly equating to outpatient services. Tier 4 (very specialised services) mostly equates to inpatient services.
The tiers model has dominated UK service provision for at least two decades. However, for more than a decade, it has become increasingly clear that it has not met the needs of most CYP experiencing mental health problems. Numerous reports and reviews, including a 1999 Audit Commission report,14 the independent CAMHS review of 2008,15 the 2013 Chief Medical Officer’s report,3 the English Children’s Commissioner’s 2016 ‘lightning’ review6 and reports from the Welsh National Assembly in 20144 and 201816 have consistently described UK children’s mental health services as fragmented, unco-ordinated, variable, inaccessible and lacking an evidence base. Moreover, providing more money for existing services has not necessarily solved these concerns given that the financial responses to crises in children’s mental health identified in 1999 and 2008 did not result in any wholesale improvements in the quality of, or access to, services in subsequent reports or reviews. More recently, there have been attempts to transform services using initiatives such as the ‘Choice and Partnership Approach’ (CAPA),17 a CYP’s version of the adult Improving Access to Psychological Therapies’ programme (CYP-IAPT)18 and ‘THRIVE’,19 a putative alternative to the four-tier model. However, little is known about the effectiveness of these initiatives nor the effectiveness of service models in CYP’s mental health in general. Our previous NIHR work on self-care support in CYP’s mental health20 found factors like choice, child-centredness and staff flexibility to be more important than a service’s theoretical stance or a particular service model. Moreover, we found a service predicated on seemingly effective, evidence-based interventions may not necessarily be effective in itself, that is, specific interventions are often emphasised in services at the expense of important secondary service characteristics like accessibility, child-centredness and the ‘fit’ with individual CYP.
Study rationale
Given that little is known about the effectiveness of, and implementation complexities associated with, service models for CYP experiencing CMHPs is in itself a justification for the study. That services for CYP experiencing CMHPs are often early intervention services additionally strengthens this study’s value, as does exploring how services might be accessed and navigated.
Intervening early with CYP experiencing CMHPs helps prevent milder mental health problems becoming more severe during childhood, an important consideration, given the link between CYP’s health and well-being and educational attainment. 21 More significantly, intervening early can help prevent the continuation of problems into adulthood and the associated costs and burdens of treating adult mental health problems. Half of all adult mental health problems begin before age 14 and 75% before age 18,22 so there are clear benefits in identifying what constitutes an effective children’s mental health service.
The disparate factors associated with accessing and navigating services for CYP experiencing CMHPs have not been synthesised into a coherent model of effective and acceptable service provision. In reviewing the international literature and exploring specific services in England and Wales, we have been able to examine the accessibility of services for CYP experiencing CMHPs and how they are navigated and so identify what it is about services that seems to work and what CYP and their families think about services.
Study overview
Aim and objectives
The study’s overarching aim was to develop a model of effective, high-quality service design for CYP experiencing CMHPs by identifying services available to this population group, the barriers and enablers to access, and the effectiveness (including cost effectiveness) and acceptability of those services.
This aim was operationalised via several study objectives:
-
to systematically search, appraise and synthesise the international literature on services for this population group in order to (1) build evidence of the effectiveness and acceptability of current service provision and (2) assist with objective 2
-
to develop a descriptive typology of services for this population group using the literature referred to in objective 1 and a survey of service provision in England and Wales
-
through primary research, to explore the barriers and enablers that CYP and their families experience in accessing and navigating services
-
to identify the key factors influencing effectiveness and acceptability in order to build an evidence-based model of high-quality service provision for this population group
-
to estimate provider and user costs/benefits associated with different service models
-
to make evidence-based recommendations to the NHS about future service provision.
Design
The study combines evidence syntheses with primary research, using a sequential, mixed-methods design we have used in previous NIHR studies. 20,23 This design is useful for contrasting systematic syntheses of secondary research/policy data with primary data from service users and service providers. Such primary data can offer insights into help-seeking behaviour, access barriers and facilitators and why services underpinned by notionally effective interventions do not always have their intended outcomes.
Table 1 outlines how the study’s four work streams map onto the study’s objectives as well as listing specific research questions underpinning each work stream. The flow chart in Figure 1 illustrates how the four work streams interconnect.
| Work stream | Objectives | Research questions |
|---|---|---|
| 1: Literature reviews | 1, 2, 4, 5, 6 | What does the international literature say about the types of services available for CYP experiencing CMHPs? What is the international evidence for the effectiveness, cost effectiveness and acceptability of these services? |
| 2: Service map | 2, 4, 6 | What out-of-hospital services are available in England and Wales for CYP experiencing CMHPs? What are the characteristics of these services? |
| 3: Case study | 3, 4, 5, 6 | What are the barriers and enablers that CYP and their families and carers experience in accessing and navigating services for CYP experiencing CMHPs in England and Wales? What factors determine whether a service is perceived as viable, accessible, appropriate and cost-effective? |
| 4: Model development | 4, 6 | In what ways might the key factors associated with access to, navigating, and receiving help from these services be synthesised into a model (or models) of effective and acceptable, high-quality service design for CYP experiencing CMHPs? |
FIGURE 1.
Study flow chart. PPI, patient and public involvement.
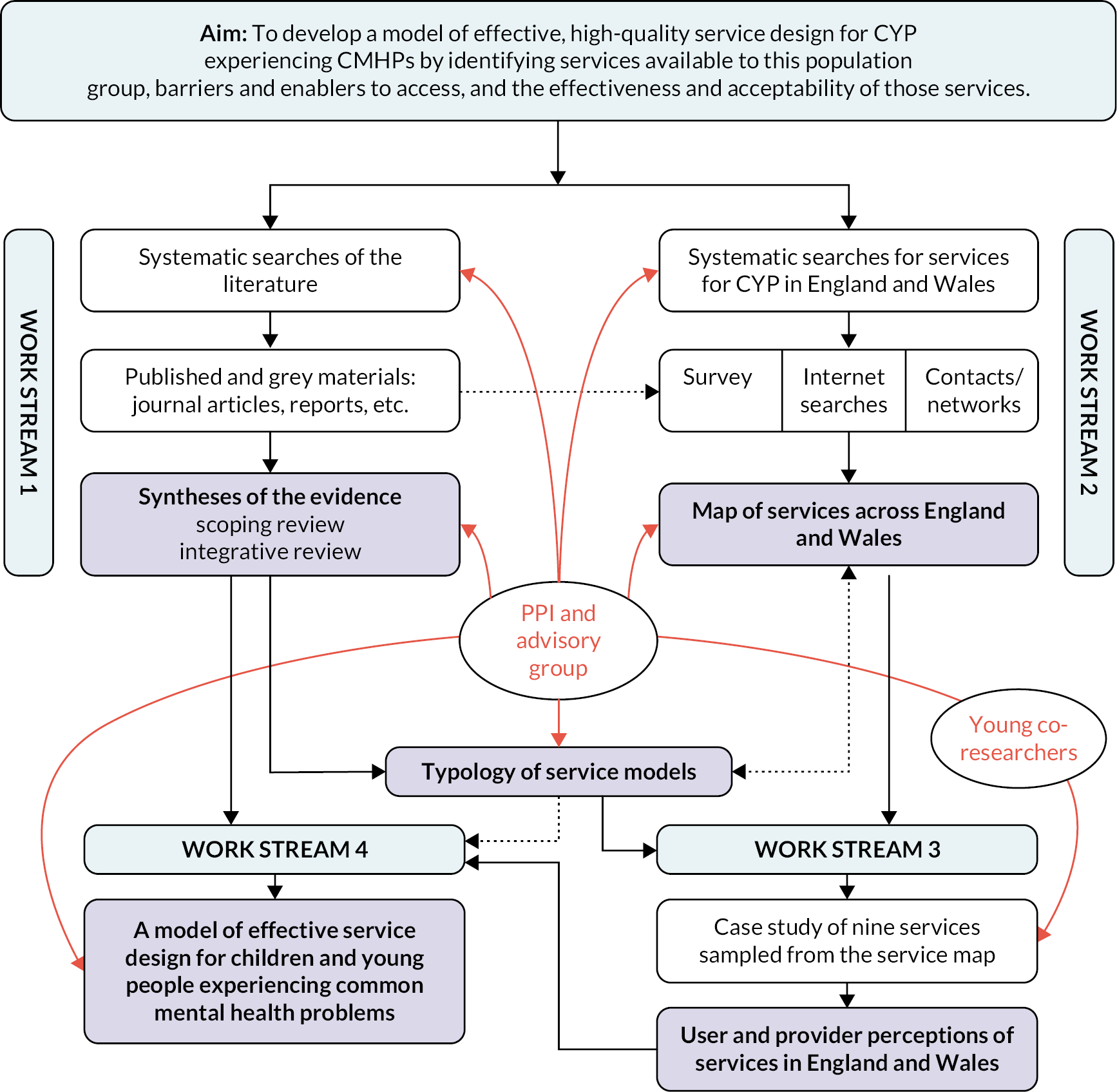
In Work Stream 1, we conducted two literature reviews: a scoping review and an integrative review. To make sense of the fragmented, variable and often unco-ordinated services described in the literature, a typology of service models for CYP experiencing CMHPs was derived from the scoping review data.
In Work Stream 2, we mapped service provision for CYP experiencing CMHPs in England and Wales using an online survey together with desk research that involved internet searches and following up leads provided by relevant networks we knew of. In using our typology to categorise services identified in Work Stream 2, we were able to both validate the typology and establish a sampling frame for Work Stream 3.
In Work Stream 3, we paid several ‘young co-researchers’ (see Chapter 2) to assist the study’s substantive researchers in data collection and analysis. We collected data from nine case study sites reflecting the various service models in our typology. We collected quantitative and qualitative data from key stakeholders in each site to further explore issues such as accessibility, acceptability and (perceptions of) effectiveness. We also collected, where possible, data on resource use and associated costs.
In Work Stream 4, the research team, young co-researchers and SAG collaboratively synthesised the data from the other work streams into a model illustrating the key factors associated with, and which underpin, high-quality service provision for CYP experiencing CMHPs.
Report organisation
Chapter 2 describes the study’s patient and public involvement (PPI). Chapter 3 outlines the methods underpinning Work Stream 1, the literature reviews. Scoping review findings are reported in Chapter 4, alongside our definitive service model typology. So that the service provision profile reported in the literature could be contrasted with service provision in England and Wales, the service mapping (Work Stream 2) methods and findings are reported next in Chapter 5. In Chapter 6 (integrative review findings), evidence for the various service models within our typology is outlined. Chapter 7 provides an overview of the methods for, and findings from, Work Stream 3, the collective case study. Chapter 8, focusing on Work Stream 4, outlines how data from the other work streams were synthesised into a model of high-quality service design for CYP experiencing CMHPs. Chapter 9 discusses the implications of our model for service design and delivery in CYP’s mental health. It also outlines the study’s strengths and limitations, concluding with some recommendations for commissioning, practice and research colleagues.
Chapter 2 Patient and public involvement
This chapter outlines how PPI permeated the study. To ensure the study remained relevant to those accessing and providing services, we involved young people and parents/carers, as well as those who commission and provide mental health services throughout the study, from its inception through to dissemination.
Patient and public involvement also led to the study receiving an informal, short title of ‘Blueprint’. In conducting the study, we tended to use Blueprint to refer to the study rather than using its formal, long title.
Involvement during study development
Patient and public involvement influenced the study’s development in several ways. A director of Common Room (Neill), a young people’s consultancy led by lived experience, was a study co-applicant. Through Common Room, young people with lived experience of mental health issues provided constructive advice on initial study design, further fine-tuned the study proposal and helped co-write the study protocol.
In disseminating findings from our previous NIHR study on self-care support in CYP’s mental health,20 we held a priority-setting stakeholder event using James Lind Alliance principles24 in early 2015. At this event, CYP, parents/carers, service user groups and researchers identified several research questions that influenced the study’s development, including ‘what characteristics facilitate engagement in mental health services?’ and ‘how can the NHS develop and commission accessible, flexible and child-centred services?’ Around the same time, at a research planning meeting held in Manchester, young service users and parents provided critical comments about, and endorsed, the mixed-methods design we subsequently employed in this study.
Research team members felt the study findings would have more validity and credibility if young people were actively involved in the research – that is, data collection and analysis – rather than merely providing advice and guidance. Consequently, for the study’s fieldwork (primary research) aspects, six ‘young co-researchers’ were employed to work alongside the study’s two research associates.
Involvement during study delivery
Study advisory group
The study was guided by a SAG (see additional files www.fundingawards.nihr.ac.uk/award/17/09/08; accessed 26 March 2024), which included young service users and parents/carers of CYP who had accessed services. Its membership, drawn from across England and Wales, additionally included representatives from children’s mental health services, social care, education, the third sector, academia and NHS service commissioning. We appointed two co-chairs to oversee planned six-monthly meetings: a mental health nursing academic with significant research and clinical experience in CYP’s mental health; and a young person with experience of both mental health services and PPI activities.
Prior to our first SAG meeting, we held a separate induction and training session for the PPI SAG members, delivered by the Manchester research associate (Fraser) who had extensive experience of PPI work in a previous NIHR programme grant. 25 This session included an introduction to the study and its research methods as well as a general introduction to PPI. We provided all PPI members with a copy of a research methods handbook designed specifically for PPI contributors. 26
At the SAG’s successful inaugural meeting in March 2019, we generated a list of potential short names for the study since the SAG considered the study’s formal, long title unwieldy. Shortly after this meeting we were saddened to hear of the unexpected death of our young person co-chair (see Dedication). A few months later, we organised a celebration of her life which was well attended by friends, family and former colleagues. Moreover, in recognition of her PPI contributions, we nominated her for a (posthumous) University of Manchester PPI award, which we – and her family – were delighted to hear she won. At our second six-monthly SAG meeting, we discussed whether we should appoint another young person co-chair: the SAG unanimously agreed we should. We subsequently appointed a new young co-chair who saw the study through to its completion.
The COVID-19 pandemic meant we had to modify our originally planned PPI engagement strategies. We had planned to hold all six SAG meetings in Manchester. We met in person for the second meeting in September 2019 but our third scheduled meeting, due March 2020, coincided with the initial pandemic lockdown period and had to be cancelled. Subsequent SAG meetings during 2020–1 were held remotely via videoconferencing which impacted on attendance and engagement. Our final SAG meeting (April 2022) was held as a hybrid in-person/remote meeting to accommodate requests for both options and, though overall attendance was reasonable, in-person attendance was low.
Throughout the pandemic, we maintained regular contact with our SAG via videoconferencing, e-mail and newsletters. While SAG engagement drop-off was observed among both PPI and service provider representatives, continued engagement with young person members was particularly difficult. We tried on several occasions to invite additional young people to the SAG with limited success since only one new young person was appointed. To address this gap, and to ensure we got substantial young person feedback on our final Work Stream 4 model (see below), our Common Room coinvestigator (Neill) facilitated access to another group of young people.
Despite the challenges above, we held six SAG meetings as planned and there has been SAG input into every stage of the study. Our SAG helped us define ‘common mental health problems’ for the purposes of the research and advised on inclusion/exclusion criteria for the literature search (see Chapter 3). In Work Stream 2 (see Chapter 5), the SAG used their networks to help publicise the mapping survey across England and Wales. SAG members also publicised our study website and Twitter feed and helped us refine the draft model typology emerging from Work Stream 1. Prior to submitting documentation for Work Stream 3’s ethical review, young person, parent and professional SAG members helped us refine the style and language of our participant information sheets, consent forms and topic guides. In Work Stream 4, SAG members provided feedback on our final model. We will continue to draw on SAG members’ expertise as we disseminate our findings.
Common Room
Following involvement in the study’s design and application stages, Common Room engaged with young people within its network to provide us with guidance on information and publicity about the study. Common Room facilitated a young person discussion group to determine an informal, short study title/name. As outlined earlier, suggestions were made at our inaugural SAG meeting, but we felt young people should have the final say. We made it clear that titles on the SAG shortlist should not constrain them; they could choose their own if preferred. In the end, the young people settled on a SAG shortlist option: ‘Blueprint’.
Common Room’s young people also provided feedback on initial designs for the study website. We had also planned to work with Common Room to recruit and employ Work Stream 3’s young co-researchers, but an organisational change within Common Room prevented us from pursuing this. However, we had contacts at a mental health research charity, the McPin Foundation (‘McPin’), that had substantial experience of supporting lived experience co-researchers and they agreed to facilitate our young co-researchers into post. McPin also provided a PPI representative for the study steering committee (see additional files www.fundingawards.nihr.ac.uk/award/17/09/08; accessed 26 March 2024) required under NIHR governance regulations.
Common Room also facilitated a group of six young people, aged 13–23 years and all with lived experience of mental health services, to provide feedback on our preliminary Work Stream 4 model (see Chapter 8).
In addition, two young people provided feedback on draft versions of this report’s Plain language summary.
Young co-researchers and McPin
As noted earlier, we wanted young people with lived experience to work collaboratively with us as co-researchers during Work Stream 3’s data collection and analysis phases. We chose to work with young adults (aged 18–25 years) because there were fewer bureaucratic challenges in employing those over 18 years; their lived experiences would, nonetheless, still be relatively recent.
In recognising there could be inherent power issues in working with young co-researchers, we specified that our young co-researchers would have equal status as research team members and that renumeration would match typical pay for junior university research assistants. However, we were also cognisant that the young co-researchers would need supporting, both pastorally and in terms of research training. Given McPin’s extensive experience in supporting and training young people in advocacy, co-production and consultation, McPin were ideally placed to help us ensure the co-researchers’ expertise by experience was recognised and valued in a supportive and nurturing environment.
Due to their expertise in working with young people in similar roles, McPin provided mentorship in addition to being the formal employer. This helped us overcome bureaucratic challenges in trying to recruit and employ co-researchers via the host universities or contracting NHS trust. Using their extensive experience of training and working collaboratively with service user researchers, research team members Fraser, Neill and Bee designed a bespoke 2-day co-researcher induction and research methods training package. Our decision to train and work collaboratively with young co-researchers was commended by the NHS Research Ethics Committee that reviewed our application for the Work Stream 3 fieldwork.
We worked with McPin to advertise the co-researcher roles having agreed a cohort of up to six young people would best suit the study’s timeline. Six co-researchers would also prevent the role being burdensome for one or two researchers since the roles were expected to involve travel to several case study sites across England and Wales. We were also keen to provide opportunities for involvement in real-world research to as many young people as possible, within the funding available. A cohort approach would also accommodate any holiday, sickness or study periods.
We received 27 applications for the roles and were due to interview shortlisted candidates in March 2020, but these plans (and our April 2020 training plans) had to be cancelled due to the COVID-19 pandemic. When it became clear that travel restrictions would not be lifted for some time, we sought ethical approval to adapt the study to accommodate remote data collection procedures. Consequently, we revised the co-researcher job description to emphasise remote data collection and asked previous applicants to indicate if they still wished to be considered. Twenty-two applications went forward for review and eight were shortlisted for (online) interview. Six candidates were offered a position and all accepted. We assigned three co-researchers to the University of Manchester and three to Cardiff University.
We adapted our bespoke induction and research methods training for online delivery and delivered the training over five sessions during autumn 2020. Contractual delays (between the universities, the contracting NHS trust and McPin) and governance delays (regarding NHS research passports) – also partly down to the pandemic – prevented the cohort from being involved in data collection until early 2021. The co-researchers subsequently worked with the study’s two research associates (Fraser, Lane) to co-interview CYP, parents/carers and service providers during remote video calls. We also delivered a remote qualitative analysis training session to support their involvement in data interpretation during Work Stream 3’s analysis phase. During this phase, the co-researchers helped us contextualise the data by assisting with the development of frameworks and the identification of themes.
The co-researchers co-designed and recorded a video version of the CYP participant information sheet to support recruitment of CYP participants to the case study interviews. This was used by case study sites to introduce the study to potential participants, and we received positive feedback on the accessibility of this medium compared to written document alternatives.
The co-researchers helped coproduce Work Stream 3’s findings, provided useful feedback on Work Stream 4’s final model and they will be involved in dissemination. We have received considerable interest from the wider research community about our collaborative approach to co-researching. As part of our dissemination plan, a co-authored paper capturing this journey and reflecting on the successes and challenges of this approach has been published. 27
Reflections on the study’s patient and public involvement
We set out to achieve meaningful PPI and to ensure the views of our PPI partners permeated each stage of the study. We met several challenges along the way, not least the impact of a global pandemic, but we also achieved successes and believe we have met the PPI goals specified in the original funding application.
Successfully collaborating with experts by experience takes time and resources and should be viewed as a journey throughout a study’s lifetime. Put simply, to do PPI well takes time and money and we are grateful to the NIHR for enabling us to provide the dedicated resources and financial support to cover our PPI partners’ time and expertise.
Working with McPin has been extremely valuable. Importantly, McPin helped provide a supportive and nurturing environment for the young co-researchers. Our decision to employ a cohort of six co-researchers proved sensible as all were able to set their own pace while gaining valuable real-world research experience. Taking a cohort approach allowed us a more flexible and nuanced approach to co-researcher involvement. For example, some were more comfortable with co-interviewing and wanted a lot of opportunities to be involved in data collection. Others were happier with a more reflective and analytical approach, focusing more on data analysis. All six co-researchers have used their experiences to move into new roles or further study. Four are pursuing research careers, two of which are health focused; the other two are studying to become healthcare practitioners.
In hindsight, although PPI costs would have increased, it might have been better to have had the co-researchers in post from the study’s inception rather than a year or so into the study. This would have enabled involvement in pre-fieldwork activities such as devising topic guides or applying for ethical review.
We finish this chapter with some co-researcher reflections:
I have learnt so much whilst working on Blueprint. This was my first experience of interviewing people and conducting qualitative research. I have since been able to take on many other mental health related roles that I do not think I would have been able to do had it not have been for the Blueprint Project. It improved my confidence tenfold.
[Blueprint] didn’t ask for any formal qualifications, instead focussing on experiences and qualities of candidates. Furthermore, one essential criterion was ‘personal experience of living with a mental health problem’. I personally found this hugely refreshing and welcoming. In the past, I have always felt the need to hide my mental health difficulties, particularly regarding employment for fear of being seen as unreliable or less able to work. The fact that the Blueprint project recognised that people with mental health difficulties have a lot to give in terms of lived experience, and provide an important perspective was extremely inclusive … it made me feel welcome, included, and valid.
My experience … has been overwhelmingly positive. The researchers at Cardiff and Manchester universities as well as McPin have helped to make the experience rewarding (in terms of knowledge gained for myself), productive (in terms of knowledge shared with the research team) and enjoyable (with little of the ‘burden’ people with lived experience typically feel in the world of work).
Chapter 3 Literature reviews methods
This chapter focuses on the methods underpinning the scoping and integrative reviews conducted in Work Stream 1. Since a single search underpinned both reviews, the methods for both are reported here. The scoping review findings are reported in Chapter 4 and the integrative review findings in Chapter 6.
In the agreed protocol (see additional files www.fundingawards.nihr.ac.uk/award/17/09/08; accessed 26 March 2024), we stated that we would conduct four interconnected literature reviews on services for CYP experiencing CMHPs: (1) a descriptive review of service models; (2) a review of the effectiveness of these service models; (3) a review of their acceptability; and (4) a cost-effectiveness review. A protocol for these reviews was published in PROSPERO in August 2018, reference CRD42018106219. 28 However, in implementing the study, we amended our Work Stream 1 plans slightly: the descriptive review was refashioned as a scoping review, and we combined the effectiveness, cost effectiveness and acceptability reviews into a single integrative review.
Scoping and integrative reviews
A descriptive review is fundamentally the same as a scoping review. We shifted to the latter term because of calls for consistency in the health research field. 29 Scoping reviews are similar to systematic reviews: both are conducted using transparent and systematic processes. However, while the main purpose of a systematic review is to summarise the available literature in order to answer a focused question, a scoping review is useful where there is a need to clarify a concept (in our case, ‘service models for CYP experiencing CMHPs’) and/or identify key characteristics or factors relating to that concept. 30 Since scoping reviews focus on the literature’s breadth (scope) rather than depth, there are fewer restrictions on the types of literature than can be included compared to systematic reviews: documents do not have to be peer-reviewed, the literature can be ‘grey’ and document quality may be less important. Thus, scoping reviews often include a larger volume of literature than systematic reviews and, unlike systematic reviews, formal quality assessment of included documents is generally not required. 29–31
A principal outcome of a scoping review is a map of the available literature;30,31 indeed, where that map is presented visually, scoping reviews have been called ‘evidence maps’ or ‘evidence and gap maps’. 29,32–34 Since a typology is a form of map, a scoping review is an ideal vehicle for achieving one of the study’s principal outcomes: a descriptive typology of services for CYP experiencing CMHPs.
The integrative review was originally planned as discrete effectiveness, cost effectiveness and acceptability reviews. However, given the heterogeneity of research designs employed in the included studies, the variability in the outcomes of the effectiveness studies (such that meta-analysis was unfeasible), the overlap between the types of evidence available in each included paper and the very limited cost-effectiveness data, we made a pragmatic decision to combine the effectiveness, cost effectiveness and acceptability reviews into a single integrative review. An integrative review still meets the study aims and objectives outlined in Chapter 1.
Integrative reviews allow for the simultaneous inclusion of experimental and non-experimental (or quantitative and qualitative) research so that a particular phenomenon can be understood more fully. 35 They also provide opportunities for insight on a particular topic (in our case, services for CYP experiencing CMHPs) by synthesising knowledge across different ‘communities of practice’,36 whether these communities reflect different disciplines or different research traditions. Our integrative review is essentially a mixed-methods systematic review designed to answer specific questions about which services for CYP experiencing CMHPs work and what those delivering and receiving services think of them.
Methods
Review questions
The literature reviews address research objectives 1 and 2 and these research questions:
-
What does the international literature say about the types of services available for CYP experiencing CMHPs?
-
What is the international evidence for the effectiveness, cost effectiveness and acceptability of these services?
The first research question underpinned the scoping review; the second, the integrative review. The scoping review was also used to finalise a definitive typology of services for CYP experiencing CMHPs (see later in this chapter). Together with the service map (Work Stream 2; see Chapter 5), this definitive typology also provided the sampling frame for our subsequent case study research (Work Steam 3; see Chapter 7).
Search strategy
A Population, Intervention, Comparator, Outcomes and Study Design (PICOS) formulation37 was used to frame the inclusion/exclusion criteria for the reviews (see Appendix 1). To identify and classify service models and find empirical evidence supporting different models, and because little was known about the breadth of service models for CYP experiencing CMHPs, we needed to conduct as broad a search of services for this population group as possible. Consequently, only the population (P) and intervention (I) elements of PICOS were used to devise the search strategy (see Appendix 2).
Since both reviews were focused on the same population (CYP experiencing CMHPs) and same ‘intervention’ (services for this population group), a single search was conducted. Search terms were established from combinations of the research team’s knowledge of, and expertise in, children’s mental health services, specific models and/or services mentioned in the commissioning brief and SAG contributions. The research team and SAG were aware of some literature that had attempted to categorise services, both in CYP’s mental health and in broader healthcare provision. This literature influenced both the ‘intervention’ search terms and a preliminary typology. Detail about the literature influencing this preliminary typology is provided later in this chapter.
Full searches were conducted using a variety of search platforms to access relevant bibliographic databases (see Appendix 2). Searches were limited to documents published from 1 January 1995 onwards as 1995 can be considered a watershed in UK children’s mental health service delivery, being the year in which the seminal report Together We Stand13 was published. No other limiters were applied.
The searches were conducted in May 2019. Additional documents (obtained from screening the reference lists of relevant literature reviews, citations in included documents and the research team’s networks) continued to be added to the literature pool until the end of 2020. The searches were not updated at a later point because the scoping review’s primary objective was the development of a typology (which was subsequently endorsed by the research team and SAG). Moreover, according to a recent consensus paper on updating systematic reviews,38 searches do not need updating if the findings or credibility of a review are unlikely to change, which was the case for both the scoping and integrative reviews.
Inclusion and exclusion criteria
A single set of PICOS inclusion/exclusion criteria was used for both reviews (see Appendix 1), although some PICOS elements were irrelevant for the scoping review and for the acceptability data within the integrative review. The criteria were developed with SAG advice and fine-tuned after some preliminary engagement with the literature.
Several exclusions merit further brief discussion. Firstly, gender identity issues were excluded because they were a focus of the parallel QF2 study. Documents relating to services for gender identity issues were, however, passed onto the QF2 team. Secondly, during screening it became clear that many potentially relevant US documents were focused on CYP with ‘serious emotional disturbance’ (SED; sometimes ‘severe emotional disorder’), a concept which does not map well onto CMHPs. Serious emotional disturbance is not a formal diagnosis but rather a legal administrative term used by US state and federal agencies to identify CYP with high needs. 39 Sometimes documents describing SED populations clearly mapped onto our inclusion/exclusion criteria, for example, by further defining SED as including those with depression or anxiety (included) or those with complex needs at risk of an out-of-home placement (excluded). However, many documents did not delineate SED further. Consequently, following discussions with our SAG, we agreed to exclude SED unless there was further explicit reference to an included condition. Thirdly, relevant literature reviews were not included unless they described service models in sufficient detail, in which case they were included in the scoping review. Reference lists of reviews were, however, screened for potentially relevant documents. Any such documents not already identified by the search were added to the pool of literature for eligibility assessment. A final issue related to the study’s focus which was services for CYP experiencing CMHPs and not interventions or treatments for this group. As outlined earlier, a principal objective of the study was to produce a service model typology using information gleaned primarily from the scoping review. During initial screening we realised that to do this, we would need to distinguish between documents describing services (included) and documents merely describing treatments or interventions, for example, cognitive–behaviour therapy or parenting programmes (excluded). We scoured the generic healthcare management literature and asked colleagues in one of our affiliated business schools if they knew of any clear criteria for defining ‘service model’, but both our search of the generic healthcare management literature and responses from our business school colleagues only reinforced our views that the concept was somewhat ‘fuzzy’. We had further discussions at one of our SAG meetings and agreed some criteria that might define a service model for the purposes of this study (Box 1).
-
Purpose: to improve access or quality of care, provide discrete pathways through services and/or reduce costs
-
Target: to meet the needs of a population or population subgroup (e.g. CYP with mental health problems or CYP with depression)
-
Structure: requires defined standards, a framework, a standard operating procedure or guiding principles against which performance can be audited
-
Processes: complex system where the sum of the parts (e.g. staff, culture, interventions, funding) is greater than the whole
-
Outcomes: are system-wide or population level as well as individual level
Service model, intervention or feature?
In determining whether a document described, or provided evidence for, a particular service model, we met several challenges during screening. One significant challenge, mentioned above, concerned discriminating between interventions and services/service models. The English IAPT40 initiative illustrates how interventions and service models might overlap. In its original iteration, IAPT was predicated on cognitive–behavioural therapy (CBT) (an intervention), but IAPT is more than an intervention: it has specific operating procedures covering staff training, levels of intervention (stepped-care), outcome measures and quality assurance and thus we would categorise IAPT as a service model. However, many of the documents we examined were not as straightforward as the IAPT example and, while the criteria outlined in Box 1 helped, reviewers had to make independent judgements as to whether a service model or an intervention was being described, with disagreements being resolved by discussion or referral to a third reviewer. The second significant challenge with some service descriptions was whether what was being described in the document was, indeed, a service model or something more akin to a characteristic or feature of the service. Some examples we had to work through which ended up as ‘features’ of a model were telepsychiatry, open access, case management, integrated care and consultation-liaison. As with the service model/intervention dilemma we encountered, judgements within the research team mostly resolved any model/feature dilemmas that arose. The features we ultimately identified (see Chapter 4) were thus determined through extensive discussion among the research team with additional SAG feedback.
In hindsight, the challenges we encountered here are unsurprising. Most service models we identified had several interacting components, required those delivering or receiving the services to change their behaviour and were often designed to elicit a range of outcomes – traits that are typical of complex interventions. 41,42
Search results, screening and document selection
The aggregate results from the databases and resources searched totalled 87,928 records which were exported into Endnote X9 (Clarivate Analytics, Philadelphia, PA, USA). After automatic and further manual deduplication in Endnote, 39,396 records remained. Given screening this many records manually would be unwieldy, research team members Pryjmachuk and Fraser used a two-stage, semi-automatic rapid title/abstract screen (using Endnote’s search function) to both screen in relevant, and screen out irrelevant, records (see Appendix 3). Stage 1 screening-in, determined largely by using terms from the original search strategy, resulted in 6412 of the 39,396 records being retained. Stage 2 screening-out involved rapidly reviewing record titles in Endnote for irrelevant terms (some, like eating disorders and psychosis, were predetermined by the commissioning brief) and then using those terms to find further irrelevant records. For Stage 2 screening-out (but not Stage 2 screening-in), individual record titles were manually inspected prior to exclusion to reduce the risk of missing potentially relevant records. Of the 6412 records retained, screening-out led to a further 1691 removals, leaving 4271 records. These records were exported to Covidence (Veritas Health Innovation Ltd, Melbourne, Australia), an online review management tool, for title and abstract screening against the inclusion/exclusion criteria.
Screening was conducted independently by two reviewers. For consistency (particularly regarding service/intervention discrimination), research team member Pryjmachuk screened all Covidence records with Evans, Fraser, Kirk or Lane as a second reviewer. Disputes were settled by a third reviewer. Following screening, 839 of the 4271 records were identified as potentially relevant and flagged for full-text retrieval. A further 220 unique documents were identified as potentially relevant from other sources (relevant literature reviews, citations in included documents and the research team’s networks), of which 191 were retrieved for full-text review. In total, 1030 full-text documents were assessed for eligibility against the inclusion/exclusion for each of the two reviews, and 310 documents in total were included in one or both reviews. Many documents met the eligibility criteria for both the scoping and integrative reviews (Figure 2).
FIGURE 2.
Venn diagram of documents included in each review. SCO, scoping review; EFF, ACC, ECO, respectively, effectiveness, acceptability and economic elements of integrative review. Total included documents = 310; SCO included = 296. EFF + ACC + ECO (integrative) included = 98 (EFF included = 56; ACC included = 62; ECO included = 3). Diagram produced using the tool available at http://bioinformatics.psb.ugent.be/webtools/Venn/.
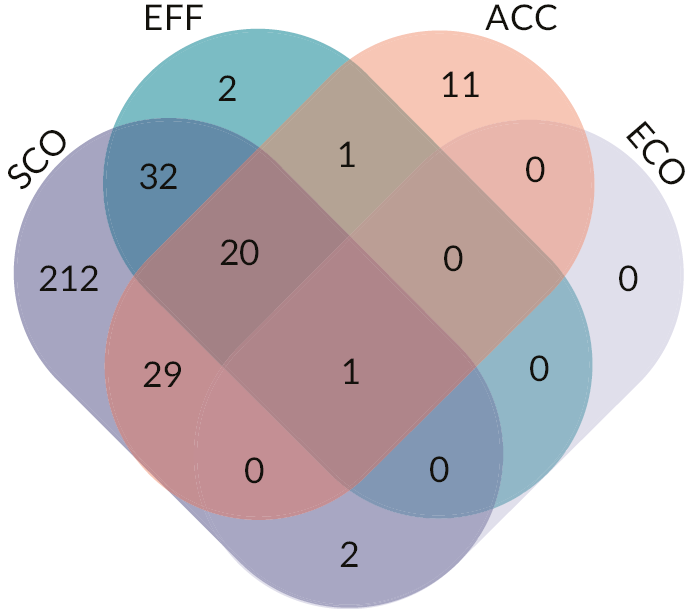
Two hundred and ninety-six documents were included in the scoping review, 84 of which contained empirical evidence and were thus also included in the integrative review. An additional 14 documents containing empirical evidence but an insufficient service description to be included in the scoping review meant 98 documents were included in the integrative review. Of these 98 documents, 56 provided effectiveness data, 62 acceptability data and 3 economic (cost-effectiveness) data.
Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) 202043 diagrams for the scoping and integrative reviews are presented, respectively, in Figures 3 and 4.
FIGURE 3.
PRISMA 2020 for the scoping review. (a) Eighteen of the 103 included other sources reports were picked up via the databases but incorrectly screened out during the semi-automated rapid title screen.
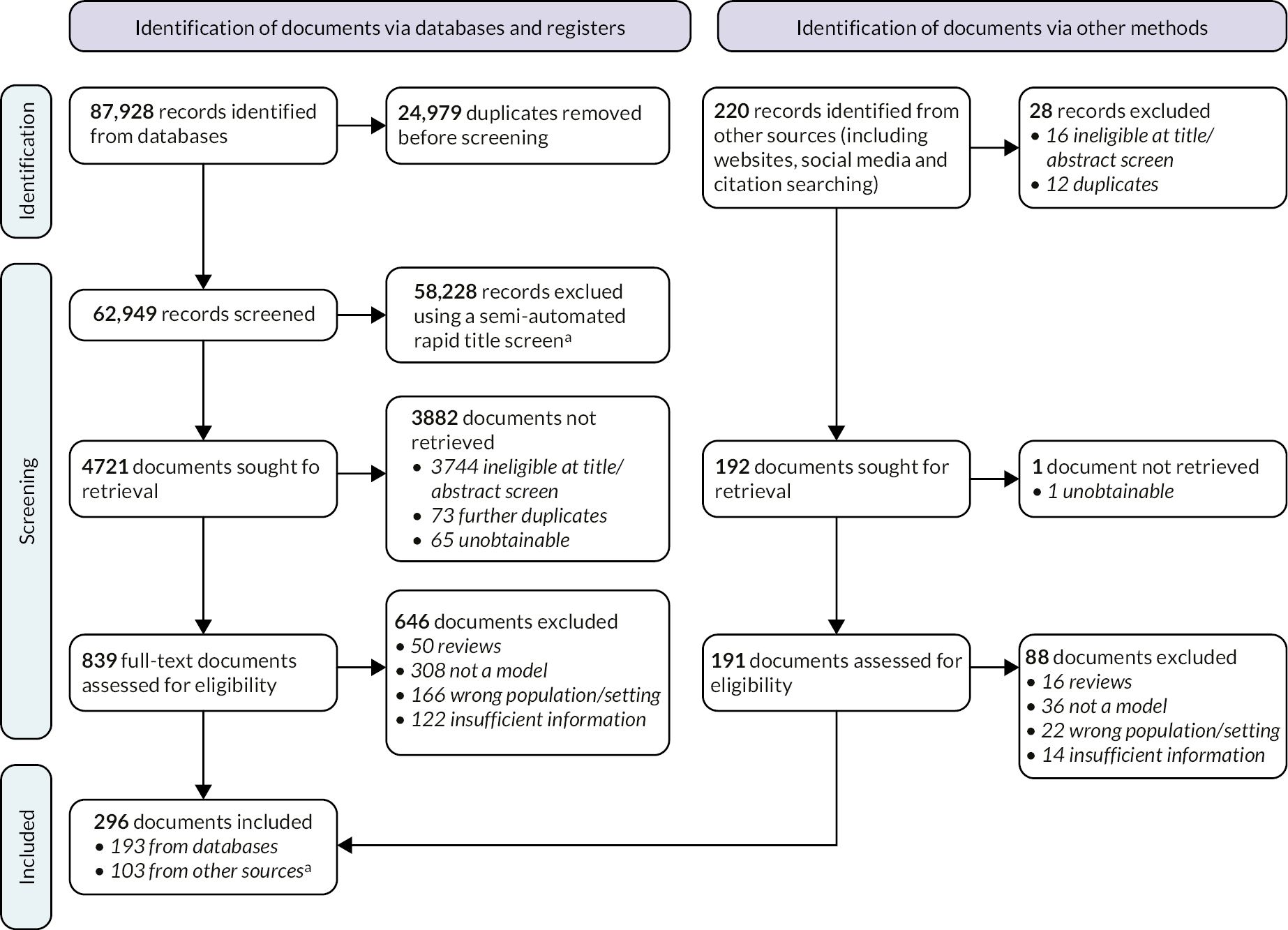
FIGURE 4.
PRISMA 2020 for the integrative review. (a) Eight of the 35 included other sources documents were picked up via the databases but incorrectly screened out during the semi-automated rapid title screen. (b) Total papers exceeds 98 as some papers provided a combination of effectiveness, acceptability and economic (cost-effectiveness) data.
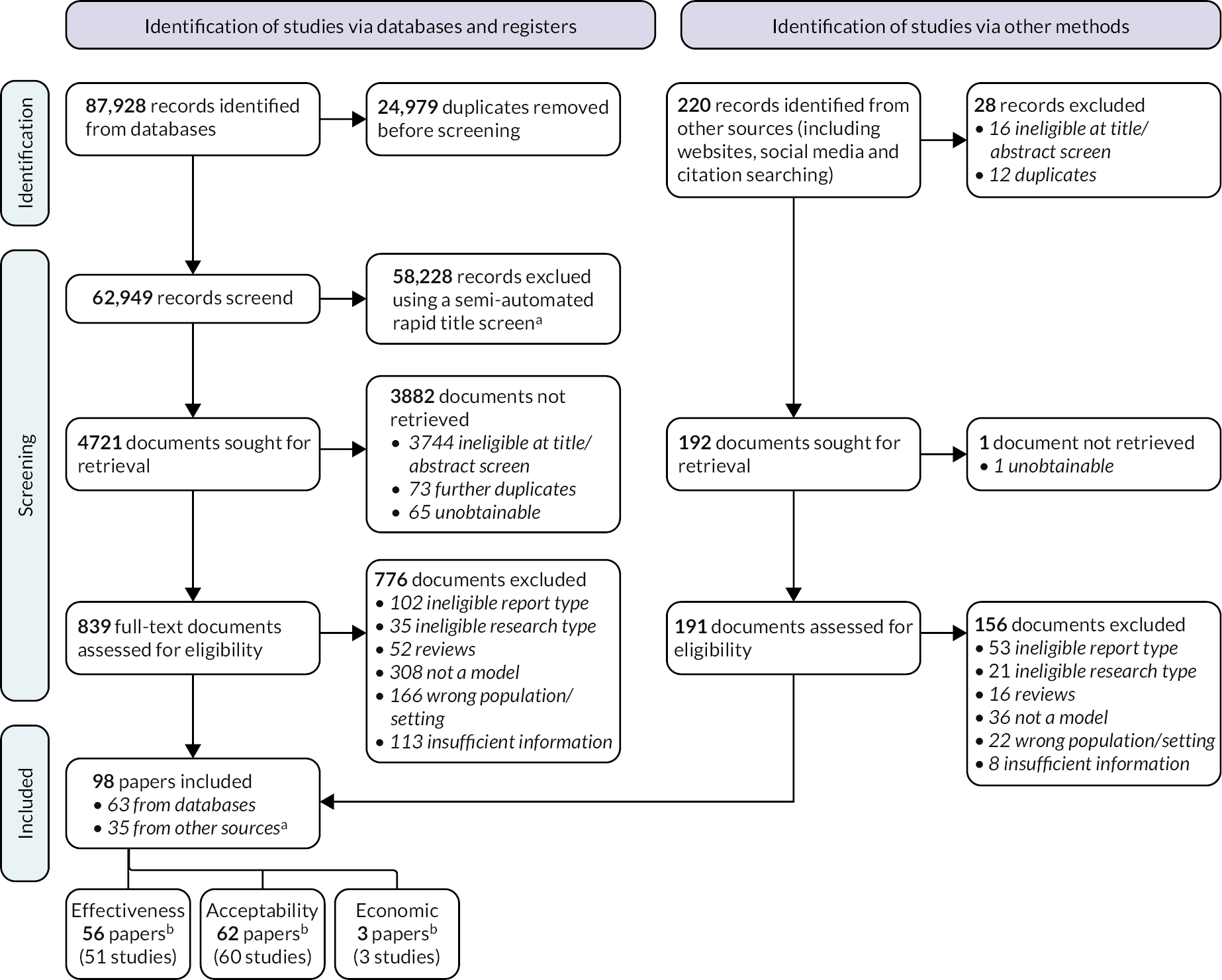
For both reviews, documents were excluded because they: (1) were literature reviews (though reference lists were screened); (2) did not describe or evaluate a service model or the document contained insufficient information for reviewers to be sure a service model was being discussed; or (3) were targeted at the wrong population. For the integrative review, additional reasons for exclusion included ineligible document type (e.g. thesis, conference abstract or book chapter) and ineligible research type.
Several documents identified via other methods and subsequently included (18 out of 103 for the scoping review; 8 out of 35 for the integrative review) were picked up by the original database searches yet missed by the semi-automated rapid title screen. Some potentially relevant documents (66 in total) were unobtainable because document supply services could not access physical library resources at the time because of COVID-19 restrictions.
A note on document and report identification labels
For the reviews, we have used the syntax (first listed author) (publication year) to identify a specific document or report, for example, ‘Asarnow 2005’ or ‘Lim 2017’. Studies reported in more than one paper are identified by a combination of their component papers, for example, ‘Asarnow 2005/Asarnow 2009’. Despite a similar appearance, these IDs are not in-text citations like those used in Harvard-style referencing systems; they are thus not listed in this report’s reference list. Instead, the full references of documents and reports included in the reviews are listed in Appendix 4. Where an included document or report is cited in this report, the standard Vancouver-style convention of superscript numbers has been used and that document/report does, indeed, appear in the reference list.
Data extraction
Non-English documents were translated prior to extraction. The 310 documents eligible for either of the reviews were extracted using a data extraction sheet devised in Microsoft Excel (see additional files www.fundingawards.nihr.ac.uk/award/17/09/08; accessed 26 March 2024). This data extraction sheet was used for both reviews. For the scoping review, data extraction of all 296 included documents was completed only by Pryjmachuk, though Evans and Fraser checked a 10% sample of extractions for accuracy with both demonstrating high levels of agreement. For the integrative review, Pryjmachuk again extracted all 98 papers, but this time each paper was also extracted independently by either Evans, Fraser, Kirk or Lane (plus Camacho for any economic papers). For each paper, the two data extractions were compared by Pryjmachuk and any discrepancies resolved by discussion or (rarely) referral to a third reviewer.
Quality assessment
As mentioned earlier, scoping reviews typically do not include a quality assessment and so no scoping review documents were quality assessed. For the integrative review, we anticipated included studies would incorporate a wide variety of research methods, so we employed the Mixed-Methods Appraisal Tool (MMAT; version 2018)44 as our single quality appraisal tool. MMAT was embedded into our data extraction sheet (see additional files www.fundingawards.nihr.ac.uk/award/17/09/08; accessed 26 March 2024). MMAT has five categories of study design: (1) qualitative; (2) quantitative randomised controlled trial (RCT); (3) quantitative non-randomised; (4) quantitative descriptive; and (5) mixed methods. For each study design category, appraisers consider a set of five specific questions, answering ‘yes’, ‘no’ or ‘can’t tell’ to each. To be considered a mixed-methods study (MMAT category 5), the data from the different research elements needed to be integrated. Where it was not, we used the approach of Scott et al. ,45 assessing each element individually and choosing the lowest quality rating to represent the study.
Mixed-Methods Appraisal Tool discourages calculation of an overall quality score; so, we have presented MMAT results for the included studies in ‘raw’ format, colour-coding appraisers’ agreed judgements as green for ‘yes’, orange for ‘can’t tell’ and red for ‘no’. We also provide information about the MMAT study design category and the study type or methods used (see Report Supplementary Materials 1–3). When presented in tabular format (see Appendix 5; discussed further in Chapter 6, integrative review findings), the reader can get a visual representation of the included literature’s overall quality and so draw their own conclusions.
Scoping review mapping: service model typology
As mentioned earlier, literature in a scoping review tends to be mapped rather than synthesised. The resultant map from our scoping review is essentially our typology of service models for CYP experiencing CMHPs. We used an iterative process to develop our service model typology starting with existing (pre-search) knowledge of relevant literature we and our SAG were aware of (Table 2). These sources gave us a preliminary (version 1) typology – an initial list of service model types – which in turn informed the search strategy outlined earlier.
| Source | Context | Notes |
|---|---|---|
| Jensen 199646 | Mental health care for CYP | Identifies several different services: clinic-based outpatient services; family preservation; therapeutic foster care;a day treatment; intensive case management; family support; inpatient hospitalisation;a systems of care |
| Bower and Gilbody 200547 | CMHPs in adults in primary care | Identifies four models of quality improvement in primary care: (1) training primary care staff; (2) consultation-liaison; (3) collaborative care; (4) replacement/referral |
| Schmied et al. 200648 | CYP with ‘high needs’ | Identifies four broad approaches: (1) therapeutic foster care;a (2) residential care;a (3) Multisystematic Therapy (MST); (4) service co-ordination and integration (includes case management, wraparound and systems of care) |
| Biggins 201449 | Home-based treatment in CYP’s mental health | Identifies four types of home-based treatment: (1) preservation; (2) treatment foster care;a (3) intensive case management and wraparound; (4) adult mobile crisis teams applied to CYP |
| McDougall 200850 | Tier 4 CAMHS in England | Identifies alternatives to inpatient care: day patient care; home-based treatment; case management; multisystemic treatment; multidimensional treatment foster carea |
| Kurtz 200951 | Tier 4 CAMHS in England | Similar categorisation to McDougall 2008 but with family preservation added |
| Shepperd et al. 200952 Lamb 200953 |
Alternatives to inpatient care in CYP’s mental health | Eight approaches identified: (1) MST; (2) intensive home-based crisis intervention (homebuilders); (3) intensive home treatment; (4) intensive specialist outpatient treatment; (5) day hospital; (6) case management; (7) therapeutic foster care;a (8) short-term residential carea |
| Shailer et al. 201354 | Young people with serious mental health problems in New Zealand | Identifies several community-based approaches: standard CAMHS; treatment foster care;a MST; strengthening families; auxiliary supports; out-of-home placements |
| Kwok et al. 201655 | Alternatives to inpatient care in CYP’s mental health | Five alternatives identified: (1) MST; (2) day patient; (3) specialist outpatient; (4) intensive home treatment; (5) supported dischargea |
| Social Services Improvement Agency 201556 | CYP with mental health/substance misuse/behavioural issues | Potential service models identified included: multidimensional treatment foster care;a strengthening families; MST; homebuilders |
| Houses of Parliament POST 201757 | CYP’s mental health | Classified services into four broad groups: (1) whole system models; (2) school-based models; (3) community-based models; (4) other models |
During the screening process (reading titles/abstracts and reading full-text articles for inclusion), we had periodic research team discussions about the classification of emerging model types, which led to further refinements and a more developed typology (version 2) once screening was complete. We used version 2 of the typology to initially code services in our service map (see Chapter 5). Once coded, the service map provided the sampling frame for Work Stream 3’s case study sites. The data extraction process for the scoping review led to some further (relatively minor) modifications to the typology. This modified typology (version 3) was endorsed by the SAG and is our final typology, described in detail in Chapter 4.
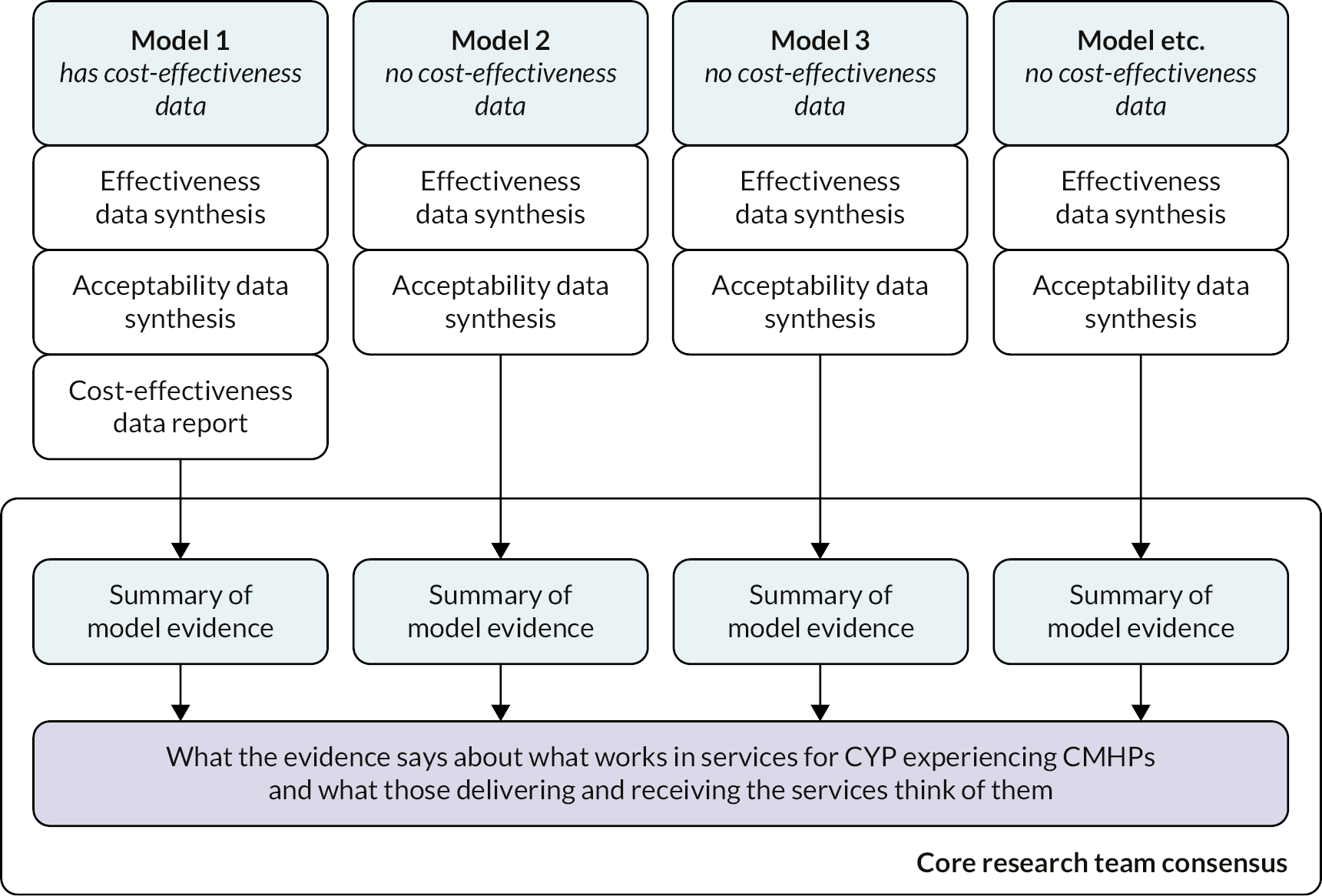
Integrative review synthesis
The integrative review’s synthesis method is based on the Evidence for Policy and Practice Information and Co-ordinating (EPPI)-Centre’s mixed-methods approach,58 whereby the different data sources (effectiveness, cost effectiveness and acceptability) are first analysed separately but subsequently compared and contrasted. Driving this approach was an intention to identify whether any of the specific models in the typology were more effective and acceptable than others, primarily to inform funders, commissioners and providers of services.
Following independent extraction by two reviewers, there was a comprehensive set of 98 combined data extraction sheets, each containing data relevant to effectiveness, cost effectiveness, acceptability or any combination of these. Key information from the data extraction sheets was then collated into separate summary tables for each of the three data sources (see Report Supplementary Materials 1–3).
The heterogeneity of the research designs and outcomes in the effectiveness studies meant that meta-analysis was unfeasible and so a narrative approach to synthesis was taken. The key effectiveness findings within each typology model group were synthesised by Pryjmachuk to provide an effectiveness evidence overview for each model group. A similar approach was taken for the acceptability studies. Quantitative synthesis for the cost-effectiveness studies was unfeasible since only three studies were included. Instead, cost-effectiveness data for the three studies were reported within the respective typology model group, after any aggregate effectiveness or acceptability data had been discussed.
For each model group, once the three data sources had been independently considered, the data were combined to summarise the effectiveness, acceptability and cost effectiveness of each model.
As a final stage in the integrative review synthesis, all of the data from across the various models were discussed among the core research team (Evans, Fraser, Kirk, Lane, Pryjmachuk) for a consensus on what the evidence says about what ‘works’ in services for CYP experiencing CMHPs and what those delivering and receiving such services like or dislike about them. The integrative review synthesis process is schematically outlined in Figure 5. The integrative review findings are reported in Chapter 6.
FIGURE 5.
Integrative review synthesis process.
Chapter 4 Scoping review findings and service model typology
This chapter presents the scoping review findings, starting with a descriptive overview of the body of included literature, after which we introduce our definitive typology of service models for CYP experiencing CMHPs. We also discuss some ‘features’ of services described in the included literature; in particular, we explore whether specific features are associated with specific service models.
Descriptive overview of included literature
The main inclusion criterion for the scoping review was a sufficiently detailed service description that enabled categorisation into one (or more) of the model types in our preliminary typology or into some new model type. Using this criterion, we identified 296 documents and extracted 342 service descriptions from those documents. Some documents described multiple services and some services were described in multiple documents.
Publication trends
Figure 6 outlines publication trends across time for the included documents. Data for 2019 and 2020 are incomplete because of the search date and cut-off date for inclusion. Since the search was conducted in May 2019, there are only partial data for 2019. The search was not repeated (for reasons outlined in Chapter 3) though additional documents were included up until the end of 2020 which explains the small number of 2020 documents. The trendline indicates a general increase in publications with notable peaks around 2003, 2009 and 2016–7.
FIGURE 6.
Included documents by publication year. (a) No date available for two documents.

There is no clear explanation for the peaks in Figure 6, though one explanation may be that (academic) interest in health topics wax and wane according to political priorities and/or public concerns and the availability of any associated funding, either for service development or research.
Country
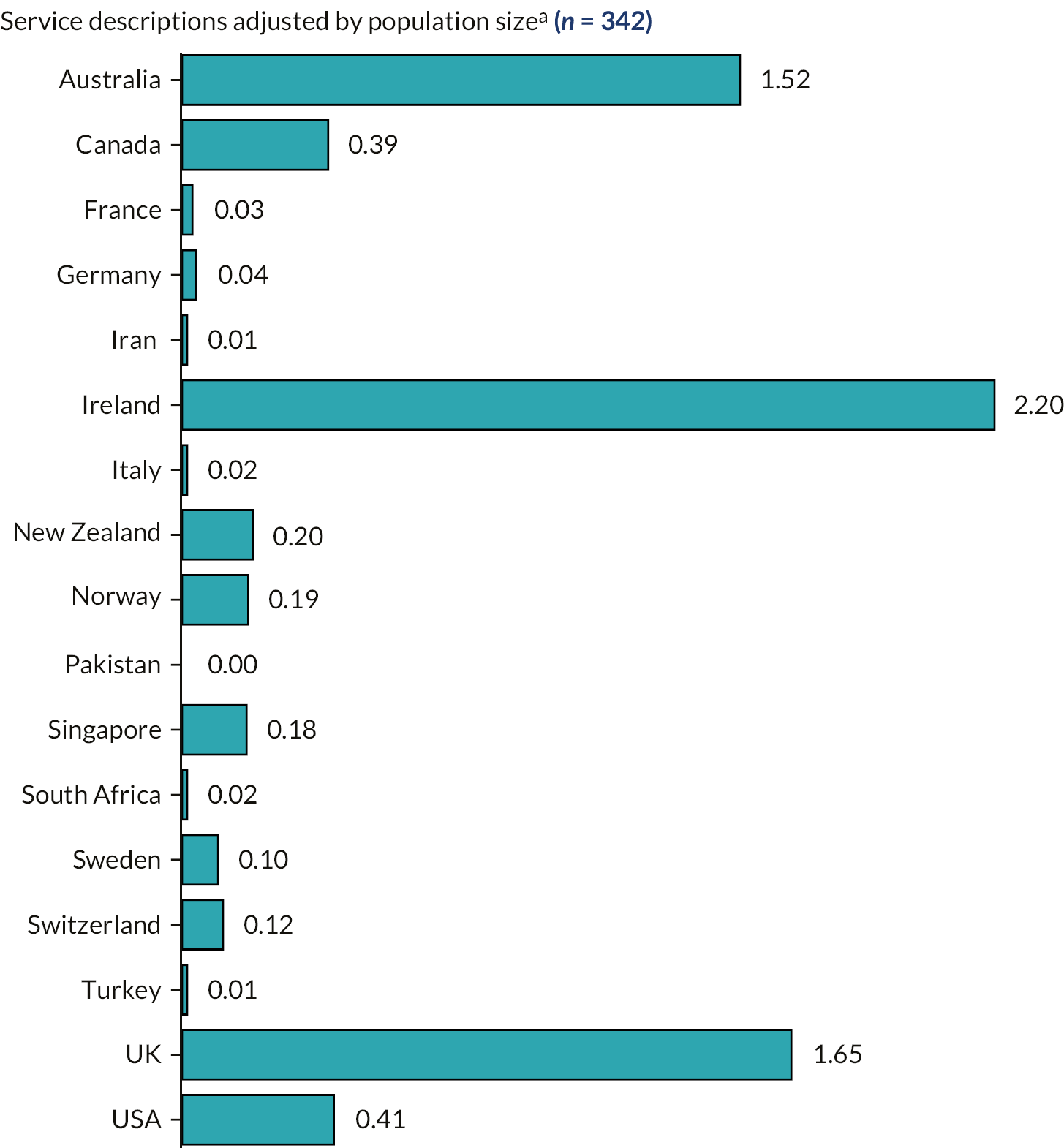
Figure 7 illustrates that more than 90% of services originated from the ‘Anglosphere’ (USA, UK, Australia, Canada and Ireland). Interestingly, if the numbers of service descriptions are adjusted for population size (using 2020 World Bank data59), Ireland punches above its weight in terms of population size while the USA punches below it (Figure 8).
FIGURE 7.
Service descriptions by country.
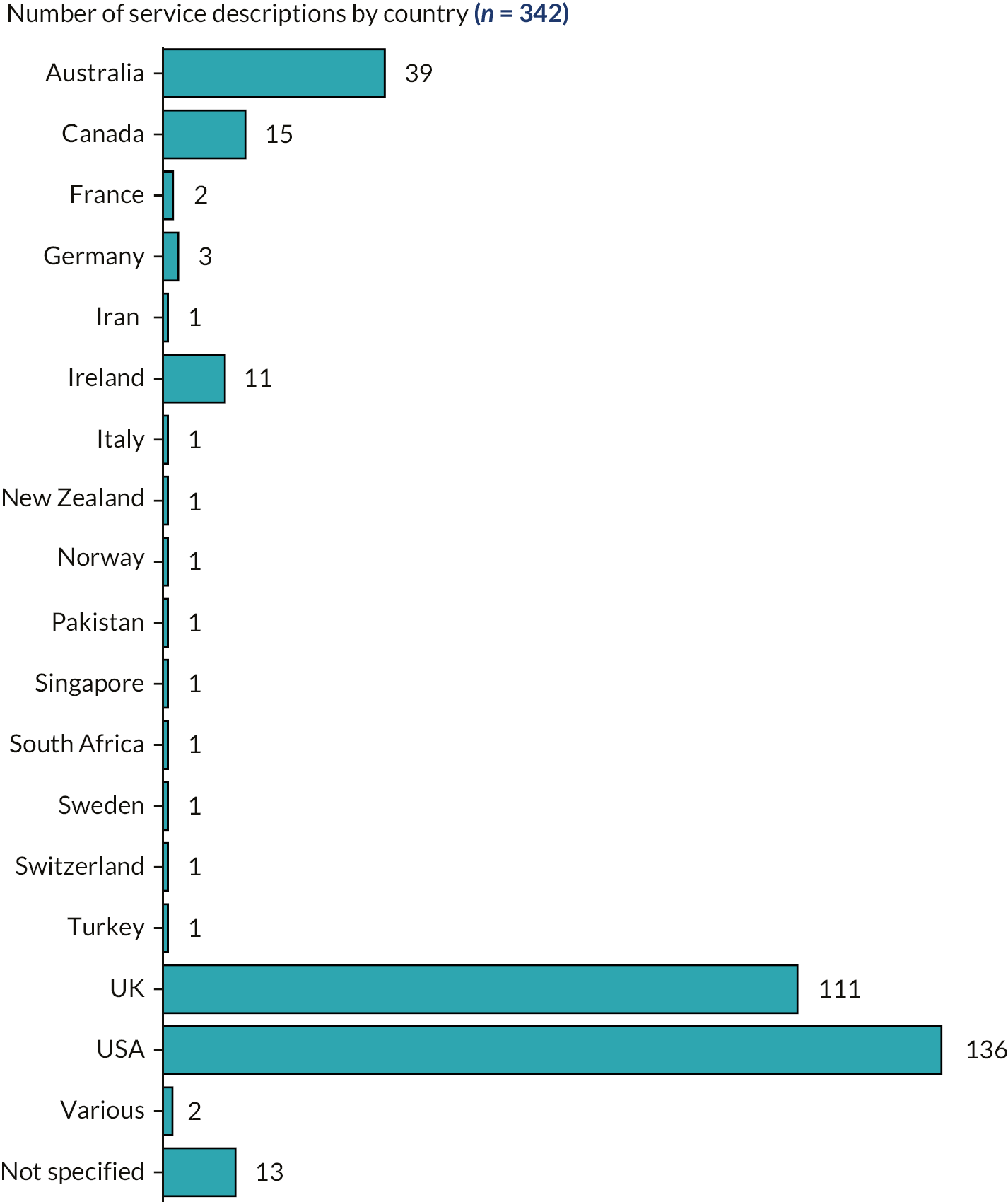
FIGURE 8.
Service descriptions by country adjusted by population. (a) Equal to number of services described/population size in millions.
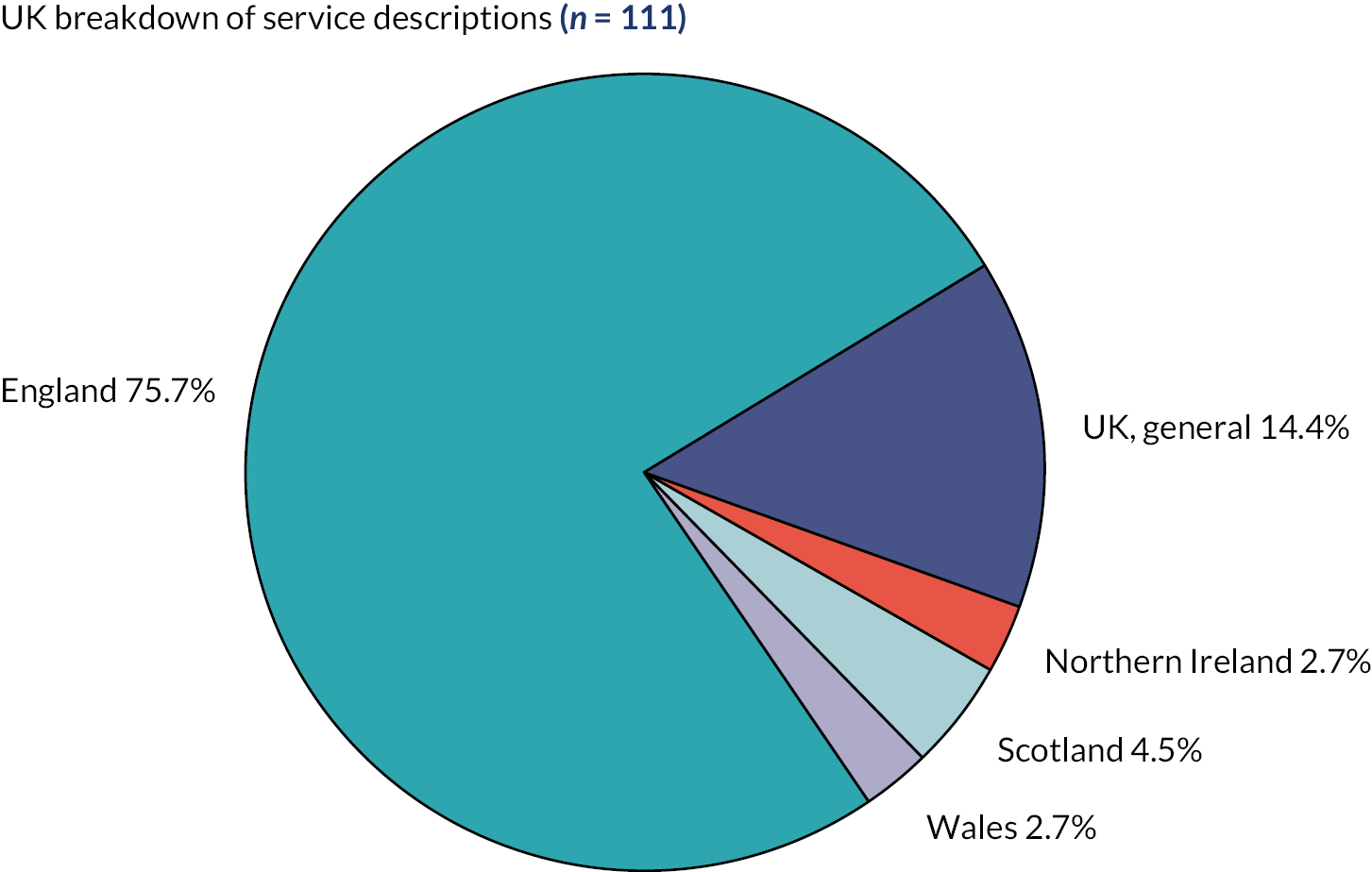
UK services
Regarding the UK services described, most emanated from England with a sizeable minority (14%) having a presence across the whole UK. Relatively few services were unique to Scotland, Wales or Northern Ireland (Figure 9).
FIGURE 9.
Service descriptions by UK constituent nation.
Document types
Most (80%) of the 296 documents were journal articles (Figure 10).
FIGURE 10.
Included document types.
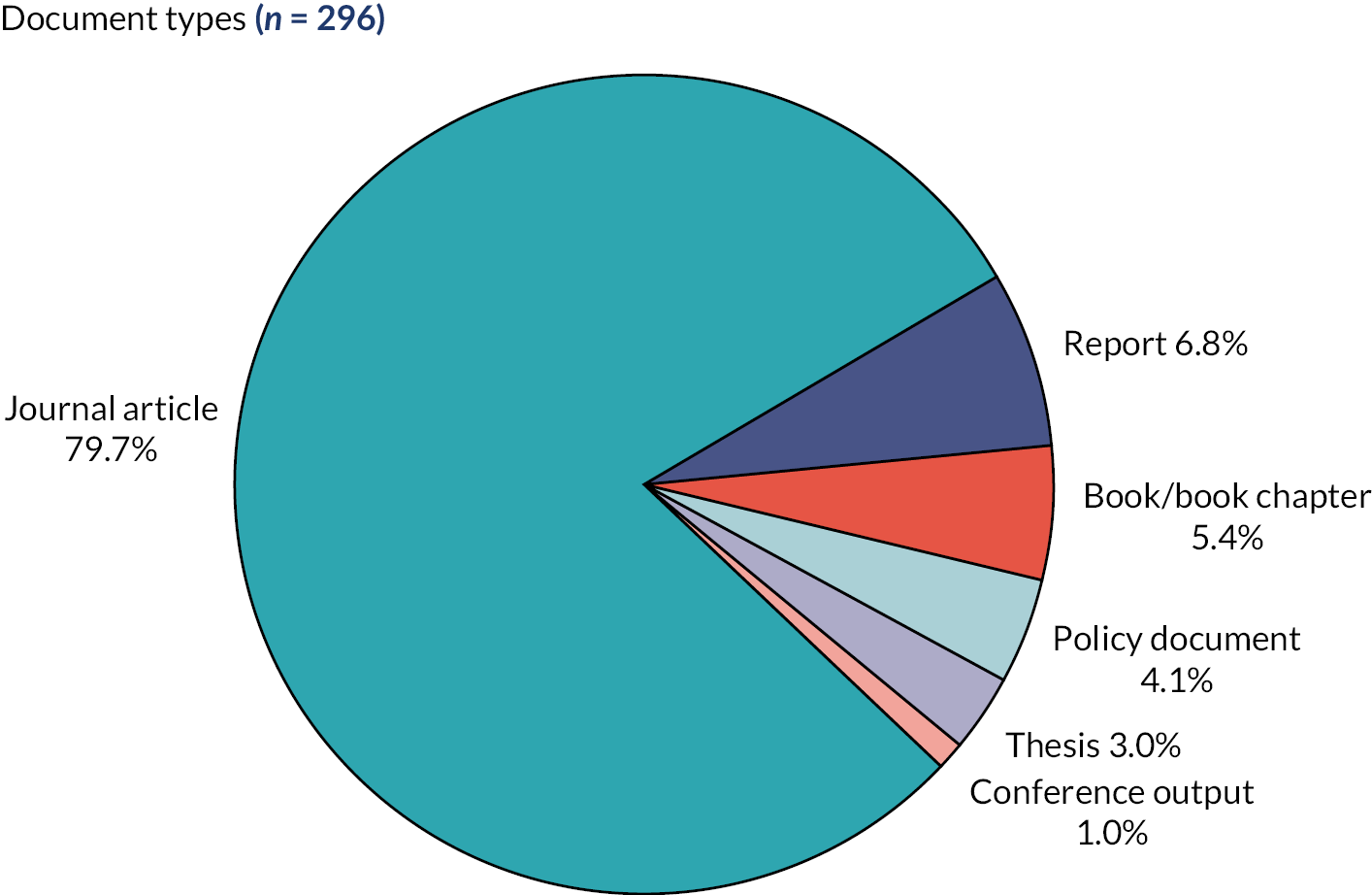
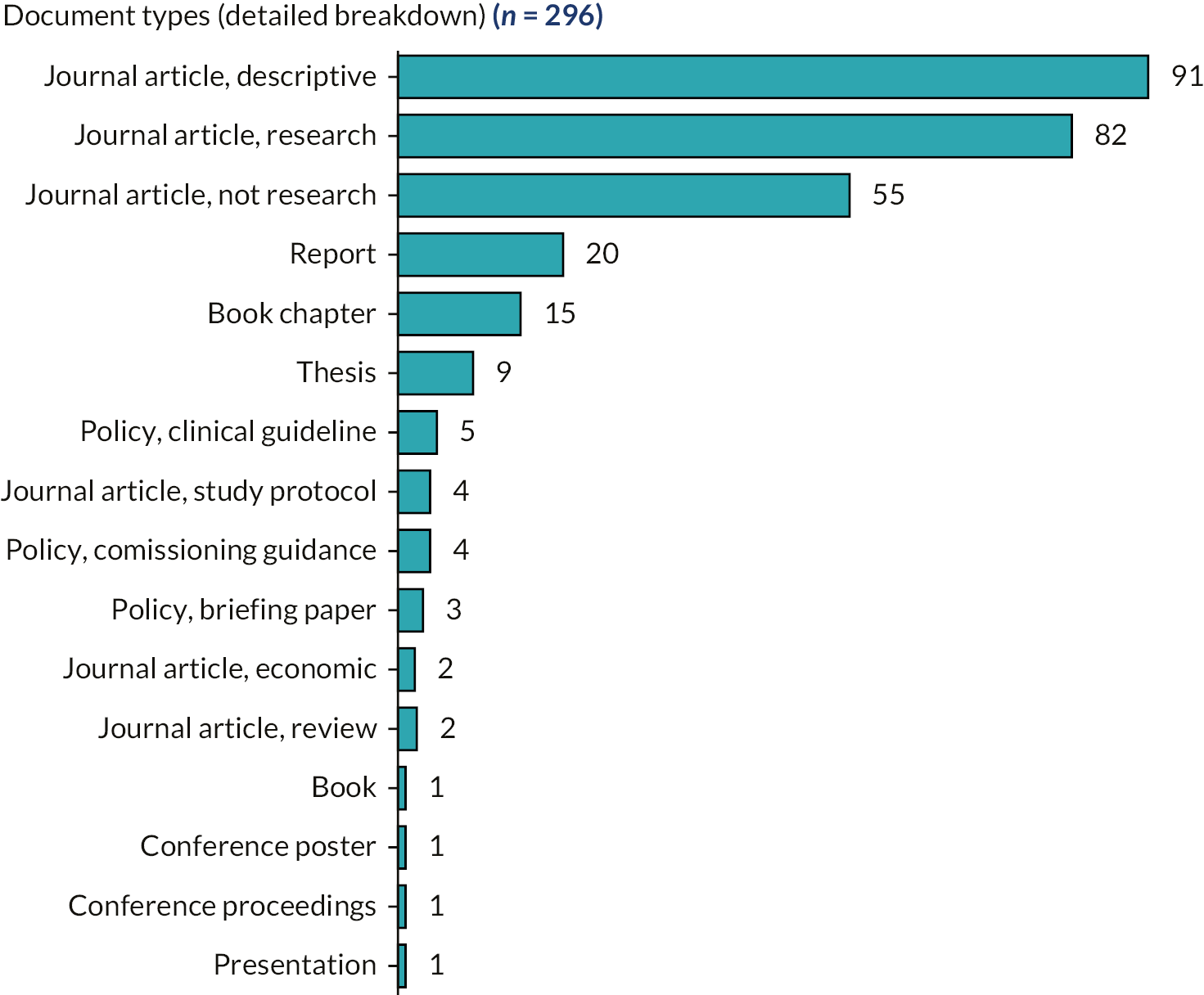
A significant proportion of journal articles were descriptive or they reported research that was ineligible for the integrative review (Figure 11).
FIGURE 11.
Detailed breakdown of document types.
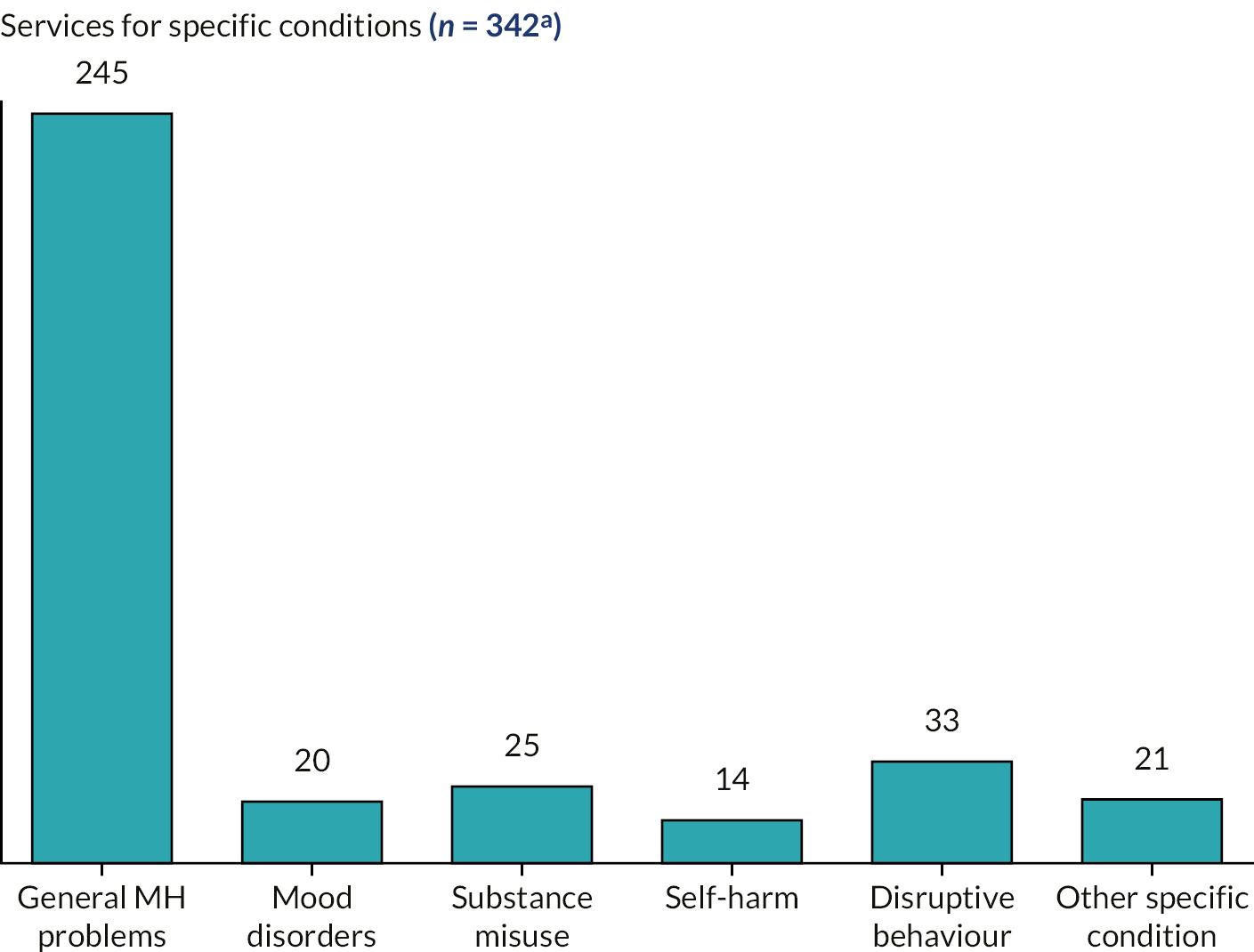
Services for specific conditions
Most identified services were targeted at CYP with general mental health problems (Figure 12). A minority targeted specific conditions such as anxiety and depression (mood disorders), substance misuse, self-harm and disruptive behaviour disorders.
FIGURE 12.
Services for specific conditions. (a) Total > 342 as some services cover multiple conditions.
Service model typology
Our final service model typology, derived from the scoping review and the knowledge and expertise of the research team and SAG, is presented diagrammatically in Figure 13. We identified 17 model types in six principal model groups (A–F). In addition, seven potential models seemed less rigid and more flexible than models in groups A–F, in that they tended to provided ‘scaffolding’ to services through a structured framework and often coexisted with models in groups A–F. Hence, our seventh group (G) is a group of (service transformation) frameworks rather than models.
FIGURE 13.
Typology of service models. NGO, non-governmental organisation.

Although the typology presents six discrete model groupings and a group of service transformation frameworks that cut across the six model groupings, real-life service provision often operates within a mixture of models and frameworks. Thus, the boundaries between models can overlap or be somewhat fuzzy (we revisit this point in Chapter 5). The arrowed lines in Figure 13 demonstrate some of the major relationships between the models. For example, there are links between in/outreach models (D), specialist CAMHS (A and B) and non-specialist CAMHS (C) – those providing in/outreach services are often experts drawn from specialist or non-specialist CAMHS and those providing in/outreach usually need to liaise with CAMHS. Another example relates to ecological models (E): ecological models assume any formal or informal mental health services a CYP receives are also part of their ecology.
Within each main model grouping are several submodels. Again, these are represented as discrete models, but in reality, they often overlap and/or are closely connected to one another. For example, the difference between school-embedded (B2) and schools outreach services (D2) is down to whether the staff providing the service are permanently located in the school (perhaps employed by the school) or whether the service is peripatetic, being provided by ‘visiting’ experts.
A detailed description of the typology models follows shortly; before this, it is worth exploring some additional characteristics of the services described in the included documents and how these services map onto our typology.
Distribution of services across models
The 342 service descriptions extracted from the 296 documents were subsequently categorised into one or more of the 24 different service models/frameworks within the seven broad groupings A–G. For reasons outlined earlier, many services could be categorised across multiple models/frameworks; however, to simplify analyses, a primary category was agreed for each service description during data extraction (Figure 14).
FIGURE 14.
Model distribution by primary category. ARC, availability, responsiveness and continuity.

The model grouping with the largest number of included documents (113) was in/outreach (D), followed by community-embedded specialist CAMHS (B; 89 documents) and service transformation frameworks (G; 54 documents), although a significant number of these (20) focused on a single framework, systems of care (G1). There were relatively few included documents for specialist CAMHS (A), community-embedded non-specialist CAMHS (C), ecological models (E) and demand management models (F).
Features associated with models
In Chapter 3, we mentioned the challenges we had in determining whether what was being described was a service, an intervention or a feature. Documents describing what we agreed to be interventions were excluded because of our focus on services. We did, however, record information about the features of a service when extracting data as we thought such information might be useful for model building in Work Stream 4. Features we extracted data about are listed in Table 3.
| Feature | Brief description |
|---|---|
| The service … | |
| X1 transitions | refers to the transition between childhood and adulthood; is often accessible between ages 18 and 25 years |
| X2 trauma informed | focuses on trauma and/or employs trauma-informed approaches |
| X3 family work | emphasises the importance of working with the family and not just the CYP |
| X4 intervention protocol | uses specific interventions (e.g. CBT, parenting), delivered according to a strict protocol |
| X5 interagency working | emphasises the importance of interagency or interdisciplinary working |
| X6 transdiagnostic | does not use clinical diagnosis, providing instead support focusing on (self-reported) problems or symptoms |
| X7 digital/remote | is delivered wholly or partially via digital (e.g. online) or remote (e.g. telepsychiatry) means |
| X8 task-shifting | has elements normally delivered by highly trained specialists delivered instead by associate specialists, parents or peers |
| X9 self-management | is predicated on the CYP/family learning how to self-manage problems |
| X10 shared decision-making | explicitly mentions shared decision-making or co-production |
| X11 care pathway | is explicitly underpinned by a care pathway |
| X12 early intervention | explicitly identifies as an early intervention service |
| X13 triage | has triage as a critical component |
| X14 integrated care | explicitly identifies as integrated care |
| X15 information and advice | has the provision of information and advice as an explicit function |
| X16 crisis care | provides care for CYP in crisis |
| X17 consultation-liaison | offers consultation with service users and/or liaison with other professionals |
| X18 peer work | uses parents and/or CYP with lived experience (paid or volunteer) to provide aspects of the service |
| X19 case management | uses a case manager (or similar) to manage/co-ordinate care |
| X20 open access | has few, if any, barriers to access (e.g. drop-in services, self-referral) |
We mapped the features reviewers identified during data extraction across the various models to see if specific features were associated with specific models. To do this, we used a crude methodology of scoring 1 if a feature was evident in the data extraction for the service, 0 if it was not and 0.5 if, after discussion, the reviewers thought it ambiguous. The 342 extraction records from the 296 documents were grouped by primary model type and for each model type we counted the number of references to each feature (by totalling the 1, 0 and 0.5 scores), dividing the total by the number of extractions to produce a percentage of extractions mentioning that feature.
We have presented ‘percentage mentioning feature’ information as ‘heatmaps’ in Figure 15 (submodels) and Figure 16 (overall model groupings). By looking at higher percentages (greener cells), it is possible to get a sense of which features are associated with which models.
FIGURE 15.
Heatmap of features by model subgroupings. Numbers in coloured boxes indicate percentage of service descriptions mentioning feature.
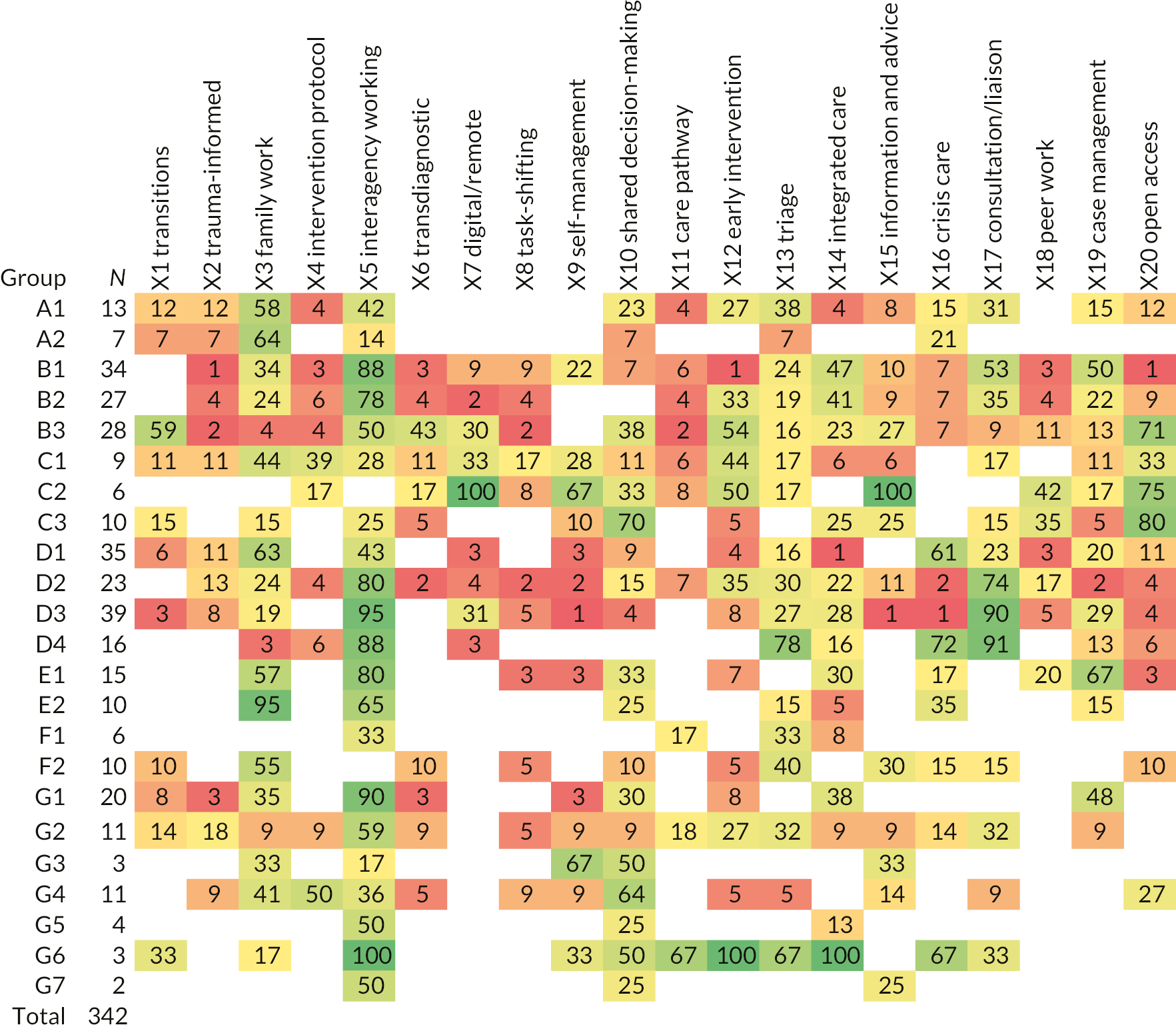
FIGURE 16.
Heatmap of features by major model groups. Numbers in coloured boxes indicate percentage of service descriptions mentioning feature.
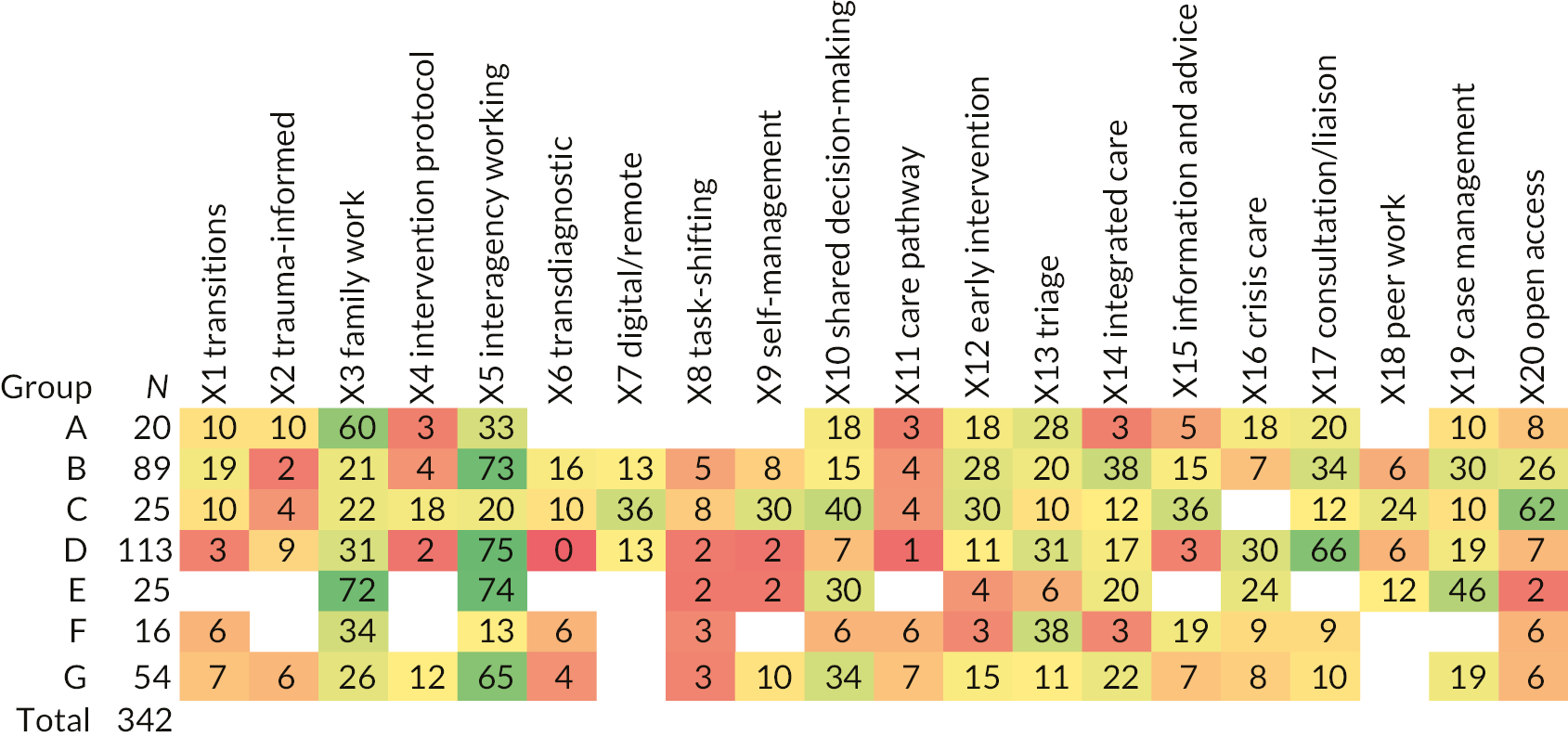
In the submodel analysis (see Figure 15), there were relatively few extractions for some model groups. There were no more than seven extractions for specialist CAMHS day care (A2), digital service (C2) and organisation-level demand management (F1), so any claims regarding features for these models should be treated with caution. In addition, since there were no more than four extractions for (i)THRIVE (G3), availability, responsiveness and continuity (ARC) (G5), formal partnerships (G6) and Evergreen Canada (G7), we have not speculated on features for these frameworks.
If an arbitrary rate of 50% or more of extractions mentioning a feature is used to signify a moderate association and an arbitrary rate of 75% or more a strong association, it is reasonable to argue that certain features seem to be associated with certain models. These associations are discussed shortly when we describe the models in detail but, before this, it is worth discussing several features rarely mentioned in the extracted service descriptions: trauma-informed (X2), transdiagnostic (X6), task-shifting (X8), care pathway (X11), integrated care (X14) and peer work (X18). Since a decision on identifying these as features was taken early in the screening process, it may be no services with these features subsequently appeared as we progressed through screening and data extraction. The absence of some, however, is surprising, notably integrated care and peer work.
Integrated care is important because it has been, for several decades, a central policy objective of many healthcare systems worldwide. 60 Though there is confusion in the literature,60,61 integrated care generally refers to attempts to provide holistic services to populations by asking providers to work together and collaborate or through creating single organisations to deliver integrated services. The literature is unclear as to which disparate entities require integration:61 there could be ‘vertical’ integration, such as the integration of primary, secondary and tertiary care or the integration of mental and physical health care, or there could be ‘horizontal’ integration such as the integration of health and social care (and perhaps even education where CYP are concerned). Two other features are closely aligned with integrated care – interagency working (X5) and case management (X19) – and it might be the confusion around what integrated care is means it is represented in these two features rather than as a specific, unique feature.
Peer work (X18), often seen as powerful adjunct to mental health service provision,62 featured in relatively few documents. We are unsure why but perhaps what seems a good idea is blocked by bureaucratic and organisational barriers in (often state-controlled) public health systems. Peer work was most frequently mentioned (though it did not meet the 50% threshold) in digital/remote (C2) and non-governmental organisation (NGO)-derived community hub (C3) services, services having more operational flexibility because they tend to be provided by the non-statutory sector.
Theoretical underpinnings
Only around one-third of services (29%) specified they were underpinned by theory. The most common theories cited were socioecological theory (27 services) and CBT (16 services). Services citing socioecological theory were largely ecological (E) services, while services citing CBT were mostly collaborative care (B1) or primary care mental health (C1) services. These observations are relatively unsurprising and will be discussed further as we consider each model in turn.
Model descriptions
Each model type is described in detail in this section, together with some examples of services categorised within that model type. For a full list of services identified in the scoping review, grouped by model type (see Appendix 6).
Group A: specialist Child and Adolescent Mental Health Services
Specialist CAMHS is the incumbent service model in many countries. It encompasses ‘standard’, institutionally based, medically (psychiatry) oriented CAMHS. In the UK, it is sometimes referred to as ‘statutory CAMHS’. It is a baseline against which other models can be compared and is frequently used as ‘usual care’ in effectiveness studies. Importantly, ‘specialist’ in this context is used to distinguish between mental health care delivered by mental health specialists and mental health care delivered by generalists like school nurses or general practitioners (GPs).
Specialist CAMHS comprises three components: outpatient services; day patient services; and inpatient services. While these can be considered models in their own right, the literature sometimes considers specialist CAMHS as an integrated whole. This may reflect variability in service delivery and organisation since the three components are sometimes provided by the same organisation and sometimes by separate organisations. Outpatient CAMHS (A1), often referred to as ‘clinics’ in the literature, may be based in hospital or community settings. In community settings, outpatient CAMHS may morph into a group B (community-embedded specialist CAMHS) model, for example, when an outpatient service moves out of a hospital setting into a setting such as a health centre or school. While many outpatient CAMHS are generic (A1a), clinics targeted at specific conditions (A1b) such as attention deficit hyperactivity disorder (ADHD) (included in the study’s remit) or eating disorders (excluded) are fairly common. Specialist CAMHS day care (A2) is also known as day hospital or partial hospitalisation. Inpatient care (A3) was outside of our remit.
Heatmap analyses found family work (feature X3) was moderately associated with all aspects of specialist CAMHS, suggesting most group A services target families rather than just CYP.
There were 20 service descriptions in total for group A, 13 for outpatient CAMHS (A1) and 7 for CAMHS day care (A2). Group A services were found in many countries. Examples of generic A1 services include Child Mental Health Clinic (Syed 2007, Pakistan), Innovative Tier 2 Service (Worral-Davies 2004, UK) and Norwegian Outpatient CAMHS (Bjørngaard 2008). Examples of specialist A1 services include ADHD Specialty Clinic (Campbell 2014, USA; McGonnell 2009, Canada), AtR!sk for emerging personality disorder (Kaess 2017, Germany) and Transcultural Child Psychiatry Team (Measham 2005, Canada).
Day services (A2) identified all included ‘day’ in their names, for example, a Turkish Day Clinic (Çakin Memik 2010), Day Service for Adolescents (Gatta 2009, Italy) and Extended Day Treatment (Vanderploeg 2009, USA).
Group B: community-embedded specialist Child and Adolescent Mental Health Services
B and C models are community-based, rather than hospital-based or institutionally based, services in which key mental health staff are embedded (‘co-located’) within, rather than being ‘visitors’ to, the service. Where key mental health staff visit a service, we classified it as an in/outreach (D) service. What distinguishes B from C models is the key mental health staff in B models are those drawn from traditional specialist CAMHS (e.g. psychiatrists, psychologists and mental health nurses), whereas C models tend to draw staff from less medically orientated professions like counselling and youth work.
We identified 89 group B service descriptions in total: 34 for collaborative care (B1), 27 for school-embedded mental health services (B2) and 28 for psychiatry-derived community hubs (B3).
B1 collaborative care
There is uncertainty over what collaborative care is. The Centre for Mental Health63 sees collaborative care as systematic, multidisciplinary, team-based care involving a case manager, co-produced care plans and patient management protocols. In our typology, we see collaborative care as the co-location of specialist CAMHS staff within primary care in order to effect closer and more collaborative working. Consistent with the Centre for Mental Health’s perspective, our heatmap analyses did however identify interagency working (feature X5) as strongly associated with collaborative care and case management (X19) as moderately associated.
Unlike most models, a theoretical basis – usually CBT – was often specified for B1 models. This is relatively unsurprising given collaborative care mainly focuses on mood disorders (anxiety and depression) for which CBT is seen as an effective treatment. 64
In the 34 collaborative care service descriptions, US services dominated. Examples include Child and Adolescent Psychiatry for Primary Care (CAP PC) (Kaye 2017), Reaching Out to Adolescents in Distress (ROAD) (Richardson 2014, Wright 2016) and Youth Partners in Care (Asarnow 2005, Asarnow 2009, Rapp 2017). A few services were identified in other countries including Primary Care CAMH Outreach Clinic (Day 2006, UK), Shifted Outpatient Clinics (Bower 2003, UK) and the Hamilton Family Health Team Mental Health Program (Kates 2011, Canada). Across the world, many services were explicitly referred to as Collaborative Care (Clarke 2005, Coffey 2017, Myers 2010, Richardson 2009, Silverstein 2015, all USA; Nadeau 2017, Canada; Sharifi 2019, Iran) or a derivative such as Colocated Collaborative Care (Keller 2013, USA; Moore 2018, USA) or Integrated Collaborative Care (Henderson 2017, Canada; Moore 2018, USA).
B2 school-embedded mental health service
These services differ from schools outreach (C3) in that the school employs mental health staff directly or they are embedded into the school for a significant amount of time. Staff may work solely for a particular school, or they may work across several. While the staff involved might provide liaison services (to teachers and parents, for example), they generally offer more than outreach.
Unsurprisingly, interagency working (feature X5) was strongly associated with school-embedded mental health services in our heatmap analyses.
The 27 service descriptions for B2 were largely US services and included Recovery High Schools (Finch 2014, Finch 2018), School-based Health Centres (Colon 2005, Larson 2016, Liu 2010, Mitchell 2007) and School Health Clinic (Armbruster 2002). A few services were also identified other countries: CAMHS Counsellor in Schools (McKenzie 2011, UK), Doc On Campus (DOC) (Doley 2008, Australia) and the Canadian School-based Pathway to Care (Kutcher 2013b, Wei 2011).
B3 psychiatry-derived community hubs
These services have their roots in the work of Australian psychiatrist Patrick McGorry. 65,66 Although McGorry’s work originally focused on centres for early intervention in psychosis, they have subsequently grown, alongside a ‘transdiagnostic’ perspective, to cover young people experiencing any mental health issue. Psychiatry-derived community hubs are one-stop (integrated) primary care centres for those aged 12–25 years needing help with anything troubling them: mental, physical or sexual health issues; alcohol and drugs; or work and study support. They have a specific focus on early intervention. Indeed, in our heatmap analyses, early intervention (feature X12) was moderately associated with B3 services as was transitions (X1) and interagency working (X5). There was a strong association with open access (X20).
Of the 28 B3 service descriptions, almost all concerned McGorry’s Headspace Centres in Australia (e.g. Abidi 2017, Howe 2014, Malla 2016, McGorry 2018, Rickwood 2019) or an Irish offshoot, Jigsaw Centres (e.g. Abidi 2017, Malla 2016, O’Keeffe 2015, Peiper 2017).
Group C: community-embedded non-specialist Child and Adolescent Mental Health Services
As noted earlier, C models are similar to B models since they are community-embedded, but they differ in that C models tend to have key mental health staff drawn from less psychiatry-orientated professions. C models also tend to have more open approaches to access.
We identified 25 group C service descriptions in total: 9 for primary care mental health service (C1), 6 for digital service (C2) and 10 for NGO-derived community hubs (C3).
C1 primary care mental health service
These services are delivered in primary care settings (e.g. GP clinics), but, unlike B1 services, they are not delivered by staff from specialist CAMHS nor are the staff necessarily co-located. No specific features were associated with C1 services in our heatmap analyses.
Of the nine C1 service descriptions, most focused on stepped-care models in primary care. In the UK, for example, there is Stepped Care Model for Depression [National Institute for Health and Care Excellence (NICE) 2019] and England’s adult IAPT programme applied to those aged 14–19 years, 1419 IAPT Pilot (Humphrey 2016). In Australia, there is Stepped Care for Anxious Youth (Chatterton 2019, Rapee 2017) and the Child Mental Health Service within Australia’s Access to Allied Psychological Services (ATAPS) programme (Bassilios 2016a, Bassilios 2016b, Bassilios 2017). There was also an Australian service predicated on the Transdiagnostic Staging Model (Cross 2017). In stepped-care models, those receiving treatment usually start with a low-level (often CBT-based) treatment and either exit the service if treatment is successful or step-up to a higher-level treatment if it is not. In staging models, however, treatment stratification is based on disease severity rather than treatment response.
Like B1, C1 was a model group for which a theoretical basis – almost always CBT – was often specified. Again, this is unsurprising given most stepped-care treatments are based on CBT principles.
C2 digital services
These are services where the ‘community’ is the internet. Unlike services which offer telephone or video alternatives to face-to-face contact, C2 services operate solely as digital or remote services and they normally operate as open access or self-referral services.
Six C2 service descriptions were identified: four described Kooth in the UK (Frith 2017, Houses of Parliament POST 2017, Hanley 2019, Prescott 2017), one described eheadspace in Australia (Cotton 2019) and one ProHEAD online in Germany (Kaess 2019).
Predictably, digital/remote (feature X7) was strongly associated with C2 services in our heatmap analyses, as were information and advice (X15) and open access (X20). Self-management (X9) and early intervention (X12) were also moderately associated with C2 services.
The small number of C2 services identified in the review is surprising given advances in technology and the ‘digital immersion’ of CYP in recent years. Although the COVID-19 pandemic provided an external stimulus for the expansion of C2 services,67 our search would not have picked up reports of these services since it was conducted before the height of the pandemic. It is not unreasonable to assume, however, literature on C2 services will increase over the next few years.
C3 NGO-derived community hubs
Group C3 is analogous to B3 (psychiatry-derived community hubs) though C3 services have a clear non-medical/non-psychiatry ethos and are usually provided by a NGO like a charity or social enterprise. On top of providing services directly to CYP, these organisations often offer outreach (D) services.
All 10 C3 service descriptions were from the UK, except for the US Family Empowerment Program (Cleek 2012). Most UK services identified were Youth Information, Advice and Counselling Services (YIACS) (Houses of Parliament POST 2017, NIHR ARC NWC n.d., Nolan n.d., Rayment 2014). YIACS offer a one-stop, integrated health and well-being approach for CYP aged 13–25 years. Other UK C3 services identified include The Junction (Walker 2010) and The Wish Centre (Durcan 2018).
Like B3 services, C3 services cover mental, physical and sexual health, substance misuse and work/study support; in addition, YIACS deal with safeguarding, homelessness, money and benefits, and they often provide peer support opportunities. In our heatmap analyses, shared decision-making (feature X10) and open access (X20) were strongly associated with C3 services. Interestingly, and unlike B3 services, transitions (X1) were not explicitly associated with C3 services.
Group D: in/outreach
Inreach and outreach are often conflated in the literature but generally ‘outreach’ means mental health experts delivering services in the general community, whereas ‘inreach’ means they deliver services in specific (community) settings like schools, prisons or even the family home. For simplicity, we have used ‘outreach’ to cover both inreach and outreach activities. Outreach services tend to have an early intervention focus and the bulk of outreach work is either consultation (offering triage, assessment and low-level intervention work to CYP/families) or liaison (offering training, advice and support to non-mental health staff). 68 Consultation-liaison is thus a key feature of D models and it is no surprise we found associations between consultation-liaison (X17) and D models in our heatmap analyses.
Group D provided the most service descriptions: 113 in total, with 35 for outreach to home (D1), 23 for schools outreach (D2), 39 for community outreach and liaison (D3) and 16 for paediatric liaison (D4).
D1 outreach to home
These services include assertive outreach, mobile crisis teams and home treatment. While these services are usually provided for more serious mental health problems such as psychosis (outside our remit), some D1 services are available for CYP at the more complex end of the CMHPs spectrum. Unsurprisingly, for at-home, often crisis-based, services our heatmap analyses found (moderate) associations between D1 services and both family work (feature X3) and crisis care (X16).
The 35 D1 service descriptions mainly emanated from the USA with 1 UK and 1 Canadian service. D1 services had various names though most included words expressing an urgency of some sort for example, ‘intensive’, ‘crisis’ and ‘emergency’. US examples include Ventura County Children’s Crisis Continuum (Sowar 2018), Intensive Home-based Services (Daleiden 2010) and KidCare Emergency Mobile Psychiatric Service (Guerra 2006). The UK service was Lothian CAMHS Intensive Treatment Service (Duffy 2014) and the Canadian one, Family Preservation (Wilmshurst 2002).
D2 schools outreach
D2 services involve mental health experts going into schools to work directly with CYP/families, train and support school staff, and/or carry out preventative and low-level intervention work. Schools outreach differs from school-embedded (B2) services in that the mental health staff are ‘visitors’ rather than permanent members of staff. Unsurprisingly, our heatmap analyses identified interagency working (X5) and consultation-liaison (X17) as features strongly associated with D2 services.
A significant proportion of the 23 D2 service descriptions were UK services and included School nurse drop-in clinics (Clarke 2003), Mental Health Services and Schools Link Pilots (Day 2017, Houses of Parliament POST 2007), Mental Health Link Worker (Hunter 2009) and, most recently, Mental Health Support Teams in Schools (BPS 2019). Several US services were also identified including Early Childhood Consultation Partnership (ECCP) (Gilliam 2006, Gilliam 2007), C3: Classroom-Community Consultation (Lee 2017) and Links to Learning (L2L) (Atkins 2015). Services identified in other countries included Fil Harmonie (Oppetit 2018, France) and Response, Early Assessment and Intervention in Community Mental Health (REACH) (Cai 2016, Lim 2017, Singapore).
D3 community outreach and liaison
In D3 services, mental health experts consult-liaise in the wider community – schools and colleges, youth centres, primary care centres and religious buildings, for example. Staff in D3 services have a wider remit than those working solely in outreach to home (D1) or schools outreach (D2); some D3 services also overlap with those in paediatric liaison (D4). As with schools outreach, it was unsurprising to find D3 services strongly associated with interagency working (feature X5) and consultation-liaison (X17).
Around half of the 39 D3 service descriptions described UK services. Many of these focused on the Primary Mental Health Worker (PMHW) (e.g. Callaghan 2003a, Callaghan 2003b, Callaghan 2004, Conlon 2009, MacDonald 2004, Walker 2005), a key role requirement of the original 1995 ‘four-tier’ framework. 13 Other UK services included Newham Child and Family Consultation Service (Aggett 2006) and Primary Mental Health Team (Gale 2003, England; Whitworth 2004, Wales). Some UK services were targeted at specific populations, for example, Direct Access Mental Health Service for Looked-after Young People (Arcelus 1999). Several service descriptions considered state-wide US initiatives, for example Massachusetts Child Psychiatry Access Project (MCPAP) (e.g. Aupont 2013, Coffey 2017, Sarvet 2011, Straus 2014) and Washington’s Partnership Access Line (e.g. Barclay 2016, Gabel 2012).
D4 paediatric liaison
These are hospital-based services aimed at improving care through the integration of physical and mental health care. Consultation-liaison underpins these services with mental health staff supporting paediatric (children’s physical health) services. Paediatric liaison’s core business covers two main areas: psychiatric emergencies and supporting the mental health of CYP with (usually long-term) physical health conditions. Services delivered in a community rather than hospital setting are better classified as D1, D2 or D3. Unremarkably, our heatmap analyses found D4 services to be strongly associated with interagency working (feature X5), triage (X13) and consultation-liaison (X17) and moderately associated with crisis care (X16).
The 16 D4 service descriptions came from many countries and many explicitly referred to ‘liaison’ in their name, for example, Paediatric Liaison Psychiatry (McNicholas 2018, Ireland), Paediatric Liaison Child and Adolescent Mental Health Services (PL-CAMHS) (Garralda 2016, UK), Paediatric Liaison (Woodgate 2006, UK), Liaison Psychiatry Service (Lenoir 2009, France) and Child and Adolescent Psychiatry Consultation-Liaison Service (Sheridan 2017, USA). D4 services with more esoteric names included Onsite Child Guidance Model (Mahajan 2007, USA), Emergency Room Follow-up Team (ERFUT) (Greenfield 1995, Canada) and Kids’Link Hotline (Roman 2018, USA).
Group E: ecological models
These are models that take all aspects of CYP’s lives into consideration – school, peers, friends, housing, income, health, well-being, criminality and so on. Bronfenbrenner’s socioecological systems theory69 usually underpins these models. Most E models have their roots in social work or youth offending; we have included them only when the service has specifically focused on mental health problems rather than disruptive behaviours (e.g. aggression) or youth offending.
Most documents describing ecological models we screened focused on populations with severe or complex problems rather than CMHPs, hence most were ineligible for the study. Nonetheless, 25 group E service descriptions were eligible, 15 focusing on wraparound approaches (E1) and 10 on multisystemic therapy (MST; E2).
E1 wraparound approaches
Wraparound is a collaborative, team-based approach to service and support planning for CYP with complex needs and their families. This includes, but is not restricted to, CYP with mental health problems. Much of the wraparound literature, however, focuses on youth offending. The core components of formal wraparound, agreed by consensus in 1998, underpin what the National Wraparound Initiative70 calls ‘high-quality wraparound’. High-quality wraparound requires youth participation, collaborative working, community- and strength-based approaches, cultural competence, ‘natural supports’ (relatives, friends, neighbours, etc.) and flexibility. Regardless of whether a service met the criteria for high-quality wraparound or not, we coded into E1 any service making explicit reference to support being ‘wrapped around’ the CYP/family.
Wraparound and systems of care (G1; see later) are closely related, in that the principles of systems of care are implemented through wraparound. 71 Case management (feature X19) was associated (moderately) with E1 services in our heatmap analyses. Additionally, and unsurprisingly, E1 services were moderately associated with family work (X3) and strongly associated with interagency working (X5).
Of the 15 service descriptions categorised as wraparound, almost all were from the USA and most explicitly named the service Wraparound (e.g. Barrow 2017, Bonham 2010, Durbin 2012, Karpman 2013, Painter 2012), though a few used more esoteric names such as Full Service Partnership (Chambers 2008, Cordell 2017a, Cordell 2017b) or In2School (McKay-Brown 2019). In2School, an Australian service, was unusual because a school, rather than a health, social care or youth justice agency, co-ordinated wraparound.
E2 multisystemic therapy
Multisystemic therapy is a ‘family-ecological’, community-based model targeting young people aged 11–17 years at risk of placement in care or custody. Its principal proponent is psychologist Scott W Henggeler. 72 It is most often used in youth offending though some MST services exist for CYP experiencing CMHPs. While most E2 services are USA-based, there is a UK and Ireland MST network. 73
Despite being a ‘therapy’, MST does fulfil the criteria for a service model. It has a rigid set of nine principles covering assessment, strength-based approaches, multiple systems collaboration and continuous evaluation. 72 Multisystemic therapy can be seen as an individual level analogue to system level wraparound. 74 Again, heatmap analyses provided unremarkable findings: E2 services were associated strongly with family work (feature X3) and moderately associated with interagency work (X5).
All 10 service descriptions incorporated MST into their names, most simply calling the service MST (e.g. Barrow 2017, Löfholm 2009, Sheidow 2013, Shepperd 2009, Wells 2010), though a few added a qualifier, for example, MST-Psychiatric (McDougall 2014) and Adapted MST (Rowland 2005). Almost all E2 service descriptions were from the USA, though Swedish (Löfholm 2009, Sundell 2008) and UK (McDougall 2008, McDougall 2014, Wells 2010) services were also described.
Group F: demand management models
As the name implies, F models are characterised by a need to manage service demand, flow and capacity, often in the face of long waiting lists. Demand can be managed at organisation level or at patient level. We identified 16 group F service descriptions, 6 focusing on organisation-level (F1) demand management and 10 on patient-level (F2) demand management.
F1 organisation-level demand management
In F1 models, an entire service is subject to new ways of working to manage demand, flow and/or capacity.
Five of the six F1 service descriptions were from the UK, with the other from Australia. Of the six F1 service descriptions, four focused on Choice and Partnership Approach (Fuggle 2016, Robotham 2009/Robotham 2010, Wilson 2015 in the UK; Naughton 2015 in Australia). Devised by UK psychiatrists Anne York and Steve Kingsbury, the ‘choice’ element in CAPA refers to giving CYP/families a choice: in appointments, treatment options or whether or not they engage further, for example. 75 The ‘partnership’ element is what CAPA calls the treatments/interventions available, ostensibly because CAPA claims to be predicated on shared decision-making. 75 Our heatmap analyses, however, did not identify shared decision-making – nor any other features for that matter – as being associated with F1 services.
F2 patient-level demand management
In F2 services, attempts are made to manage demand by training staff in brief assessment and intervention approaches. A limited number of appointments (often between one and three) are made available for both assessment and any subsequent work the CYP/family are expected to engage in. Our heatmap analyses found family work (feature X3) was moderately associated with F2 services which suggests many of these services expect family, rather than just CYP, involvement.
F2 services were identified in the UK, Ireland, Canada and Australia but not in the USA. Of the 10 F2 service descriptions, only a few mentioned brevity in their names, for example Brief Consultation and Advice (Heywood 2003, UK; McGarry 2008, Ireland), Brief Intervention Service (Gallagher 2015, UK; Wagner 2017, Australia) and Opt-in Appointment and Brief Therapy (Stallard 1998, UK). Other services had names masking the service’s underlying focus, for example, Janeway Family Centre Change Clinic (Hair 2013, Canada), See To Assess, Review, Treat, Evaluate, Review (STARTER) (York 2004, UK) and Young People’s Consultation Service (Young 2012, UK).
Group G: service transformation frameworks
Group G frameworks are designed to transform whole systems, often coexisting with A–F group models. Underpinning these service transformation frameworks is an attempt to tackle service fragmentation in mental health systems by encouraging disparate providers to collaborate. Unsurprisingly, our heatmap analyses identified interagency working (feature X5) as moderately associated with these services.
One or more of the G frameworks were evident in 54 service descriptions. The majority (20) were coded as systems of care (G1). Eleven were coded as UK psychological frameworks (G4) and 11 as various tiers approaches (G2). Four were coded as ARC (G5) and three each as (i)THRIVE (G3) or formal partnerships (G6). The remaining two were coded as Evergreen Canada (G7).
G1 systems of care
Systems of care is a US approach to the delivery of children’s mental health services, first conceptualised in the mid-1980s and later refined and implemented in the mid-1990s with the release of federal funds. It is a philosophy of how care should be delivered76 with 13 guiding principles focusing on availability and access, strengths-based individualised services, wraparound (see above), evidence-informed practice, partnerships with CYP/families, integrated services, care (case) management, transitions support and continuous accountability and quality improvement mechanisms. One of the first systems of care was the Fort Bragg initiative. 77–79
Stroul et al. 80 define a ‘system of care’ as:
A spectrum of effective, community-based services and supports for children and youth with or at risk for mental health … that is organized into a co-ordinated network, builds meaningful partnerships with families and youth, and addresses their cultural and linguistic needs, in order to help them to function better at home, in school, in the community, and throughout life.
p. 6
Given this definition is unremarkable that our heatmap analyses found strong associations between systems of care and interagency work (feature X5) though no associations were found with other features (including family work, shared decision-making and case management).
As a USA-specific approach, all 20 G1 service descriptions were from the USA. Many services were explicitly named as a system of care either alone (e.g. Barrow 2017, Bartlett 2006, Biebel 2007, Evans 2006, Miller 2012, SAMHSA 2016, Stroul 2010) or with a qualifier such as Early Childhood Systems of Care (Champine 2018), Systems of Care in Schools (Powers 2011) and California Children’s System of Care (Zanglis 2002). Others such as Family Mosaic Project (Measelle 1998) and Urban Trails (Desmond 2011) were more obscure, referring only to a system of care in the service description.
G2 tiers approaches
These are frameworks for organising services according to a hierarchy based on, for example, clinician-assessed need or case complexity. These frameworks also require some degree of collaboration – or even integration – between service providers. Despite this, integrated care (feature X14) was not associated with G2 services in our heatmap analyses, though interagency working (X5) was moderately associated.
Of the 11 G2 service descriptions, 6 referred to UK tiers frameworks (G2a) and 5 to tiers approaches in other countries (G2b). Four UK G2a descriptions (Atkinson 2015, Houses of Parliament 2017, JCPfMH 2013, Wolpert 2016) referred to the 1995 four-tier framework of English CAMHS;13 the other two (HSCBNI 2018; NICCY 2018) referred to Northern Ireland’s Integrated Care Pathway,81 which also uses tiers.
The English four-tier framework has significant overlap with specialist CAMHS (A) and, to some extent, community-embedded specialist CAMHS services (B) in that, for many years, it has been the organising framework for those services in England. Of the four tiers, Tier 1 (universal) was excluded from the study since its focus is mental health literacy and CYP’s general emotional well-being. Tier 4 refers to very specialised services (usually inpatient) for those with more serious mental health problems like psychosis and eating disorders and so was also excluded. Thus, Tier 2 and Tier 3 services were most relevant to us. These services offer assessment and treatment for those with mild-to-moderate mental health problems, though service entry thresholds have increased in recent years because of rising demands for services. 82 Tier 2 services usually consist of outpatient or community-based appointments with a single professional; Tier 3 services involve multidisciplinary team contact and may also include day patient (A2) services. Tier 2 services were originally expected to employ ‘PMHWs’ to perform extensive outreach and liaison. While we categorised service descriptions focusing on PMHWs as community outreach and liaison (D3) services, most can also be categorised as G2 services.
Tiers approaches in countries other than the UK (G2b) include Multi-tier Systems of Support (MTSS) (Bruns 2016, Lyon 2016; both USA), Life-course Model of Care (Evans 2014, USA) and Multi-layered Care System (Jordans 2010, several low-income countries).
G3 (i)THRIVE
THRIVE is a set of principles for creating coherent and resource-efficient communities of mental health devised by the Anna Freud Centre and the Tavistock in London. 19,83 The psychologist Miranda Wolpert has been key to its development. iTHRIVE is the name for the roll-out (implementation) of THRIVE.
Since only three service descriptions covering THRIVE (Houses of Parliament POST 2017, Wolpert 2016, Wolpert 2019) were identified, we have disregarded the heatmap analyses for THRIVE.
THRIVE is not incompatible with CYP-IAPT (see G4 below) or CAPA (F1 above) and has been mooted as an alternative to the four-tier (G2a) approach discussed above. 19 Its principal focus is the needs of CYP rather than the structures or interventions supposedly meeting those needs. THRIVE identifies five categories of need: ‘THRIVING’ is a general community need, resolved through preventative and mental health promotion work (thus irrelevant to this study); ‘Getting Advice’ is a need resolved through signposting, self-management and one-off contact; ‘Getting Help’ is a need resolved by the provision of evidence-informed and outcome-focused interventions; ‘Getting Risk Support’ is a need resolved through risk management and crisis response; and ‘Getting More Help’ is a need resolved through extensive treatment.
G4 UK psychological therapies frameworks
Two UK psychological therapies frameworks were described in 11 service descriptions. Ten focused on England’s CYP-IAPT (e.g. Edbrooke-Childs 2015, Fonagy 2017, Kingsbury 2014, Ludlow 2020) and one on Matrics Plant in Wales (Improvement Cymru 2020).
Children and young people-improving access to psychological therapy aims to improve the availability of, and access to, evidence-based psychological therapies such as CBT, parenting and interpersonal therapy. However, unlike adult IAPT (see C1 above), CYP-IAPT is not a stepped-care approach. Training existing specialist CAMHS (group A) staff in these evidence-based psychological therapies is a key aspect of CYP-IAPT. In addition to training and outcome measurement, shared decision-making is also a feature. Given the key roles parenting programmes and shared decision-making play in CYP-IAPT, it was unremarkable to find G4 services moderately associated with family work (feature X3) and shared decision-making (X10) in our heatmap analyses.
Matrics Plant (literally ‘Children’s Matrix’) is an all-Wales framework for the development, planning and delivery of ‘psychologically minded’ services to CYP/families which has similarities to (and notable differences from) both adult IAPT and CYP-IAPT in England.
G5 availability, responsiveness and continuity
Availability, responsiveness and continuity is a focused organisational intervention designed to help community-based mental health services improve their social context and thus address barriers impeding service and treatment outcomes. It draws influence from several organisational psychology theories, notably general systems theory and diffusion of innovation theory. Its principal proponent is social worker Charles Glisson. 84 Availability, responsiveness and continuity has three core assumptions: (1) the implementation of ‘technology’ (in its truest sense, meaning the application of theories or ideas) is a social as well as technical process; (2) mental health services exist in a social context encompassing the service, service provider, service organisation and wider community; and (3) service effectiveness is a function of the ‘fit’ between social context and technology. Change agents (drawn from social work, counselling, clinical and occupational psychology) are trained to work at community, organisational and individual levels to bridge these social and technological gaps. At community level, change agents work with stakeholder groups; at organisational level, they facilitate the delivery of mental health services; at an individual level, they work with relevant community opinion leaders such as judges, mayors and religious leaders.
We identified four ARC service descriptions, all from Glisson’s team in the USA (Glisson 2002, Glisson 2012, Glisson 2013, Glisson 2016). Given the small number of service descriptions, we have disregarded the heatmap analyses for ARC.
G6 formal partnerships
There were three disparate service descriptions – all local and all from England – we were unable to categorise elsewhere, but which nevertheless appeared to be examples of formal (legal) partnerships between various organisations. These were Community Children’s Health Partnership (Hewitt 2011), REACH-IN (Ivings 2018) and Solar (Vusio 2020).
The Community Children’s Health Partnership, located in Bristol, is a formal partnership between an NHS Trust and a children’s charity providing a full range of children’s mental health services. REACH-IN, a collaboration between statutory and non-statutory services, is Greater Manchester’s integrated crisis care pathway for CYP aged up to 18 years. It is underpinned by (i)THRIVE (see G3 above). Only outreach (D) services of REACH-IN were within the study’s scope. Solar is a community mental health partnership for CYP aged 0–19 years in the Solihull area of Birmingham. It is a partnership between an NHS trust, a children’s charity and an autism charity with single governance arrangements including single patient records and single care plans. Solar also uses CAPA (see F1 above).
Since we identified only three service descriptions for G6, we have disregarded its heatmap analyses.
G7 Evergreen Canada
Another service description which we were unable to categorise elsewhere was Evergreen, a Canadian national framework for youth mental health care led by psychiatrist Stan Kutcher. 85 It is a framework for Canadian local and federal governments to consider when developing policies, plans and services in CYP’s mental health. It is premised on six values: human rights; dignity, respect and diversity; best available evidence; choice; collaboration; and access to information and services. Two Evergreen service descriptions were identified (Kutcher 2013a, Mulvale 2015).
Most other group G frameworks are either prescriptive or require some degree of framework fidelity; Evergreen, however, is explicitly non-prescriptive. This could explain why, unlike the other frameworks, we did not find any documents outlining how Evergreen had been implemented.
Summary
In completing this scoping review, we have inductively developed a typology of service models for CYP experiencing CMHPs. Across the international literature, the most commonly described models were in/outreach models (D), followed by community-embedded specialist CAMHS models (B). Service transformation frameworks (G) were also relatively common.
Our typology is an attempt to simplify the complexities associated with fragmented, variable and often unco-ordinated services for CYP experiencing CMHPs. Complexities remain, however: some models in our typology overlap with others and actual service delivery is frequently guided by multiple, connected models rather than a single, discrete model. Comparing services described in the literature with actual service delivery across England and Wales is the next chapter’s focus.
Chapter 5 Mapping services in England and Wales
This chapter focuses on Work Stream 2, in which services for CYP experiencing CMHPs were mapped across England and Wales. While the primary purpose of mapping was to provide a sampling frame for Work Stream 3 (see Chapter 7), mapping also provides a snapshot of the variety of services available across England and Wales. Moreover, through understanding how services are actually delivered, the service map also helped shape our service model typology. Attempts to code services in the map against early iterations of the typology enabled us to test and refine the typology to produce the definitive typology presented earlier in Chapter 4.
Methods
Research questions
The mapping stage addressed study objective 2 and these research questions:
-
What out-of-hospital services are available in England and Wales for CYP experiencing CMHPs?
-
What are the characteristics of these services?
Identifying services
The service map was derived from established mapping procedures we have used previously,20,86 namely a survey and systematic desk-based searches.
The survey
The primary tool for capturing data on the range of services operating across England and Wales was an online survey via SelectSurvey (v.4; ClassApps, Apollo Beach FL). Our SAG assisted in survey development and piloting and in devising accompanying ‘frequently asked questions’ (FAQs).
The survey was distributed during May and June 2019 and remained open until the end of January 2020. Research team members and the SAG identified both potential respondents and networks that might facilitate access to the survey. E-mails with a survey weblink were sent to relevant e-mail distribution lists, organisations and individuals across the statutory and non-statutory sectors, including all English and Welsh NHS CAMHS. The survey was also publicised through the study’s website87 and Twitter feed (@BlueprintMH). Hard-copy English and Welsh versions of the survey were available for completion by e-mail or post if respondents preferred, or where e-mail addresses were unavailable or no longer in use. See additional files www.fundingawards.nihr.ac.uk/award/17/09/08 (accessed 26 March 2024), for the survey, covering letter and FAQs.
Desk-based searching
Searches of online service directories (e.g. those on the Anna Freud Centre88 and Youth Access89 websites) and general Google searches were employed to supplement the survey information. We used the same principles as for the literature reviews, using combinations of the population (‘P’) and intervention (‘I’) search terms (see Appendix 2). Because Google is not generally geared towards complex searches, these combinations were simpler than they were for the literature reviews.
In addition, all English ‘local transformation plans’ for CYP’s mental health available online were checked for relevant information. The literature search also identified some relevant English and Welsh services which were included in the map if still operational.
Inclusion and exclusion criteria
For consistency, we used the same inclusion and exclusion criteria as for the scoping review (see Appendix 1) with two additions: the service had to operate in England or Wales (or, for digital services, be accessible by CYP living in these areas) and be operational during the 9-month data collection period, May 2019 to January 2020.
Search results
The survey and desk-based searches identified 212 separate services, of which 154 met the inclusion criteria (Figure 17). One hundred and twenty-three different service providers provided these 154 services.
FIGURE 17.
Flow diagram for included services.
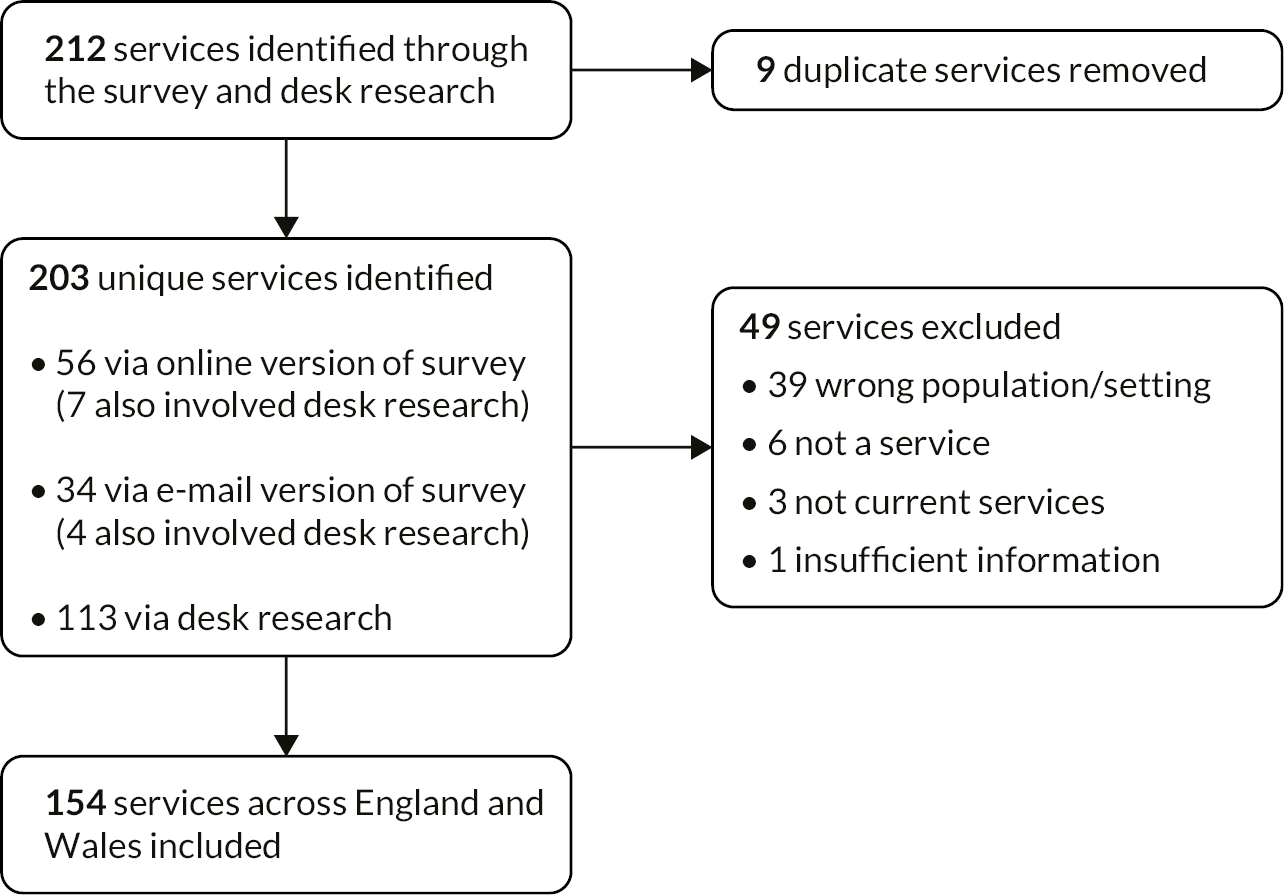
Data extraction and analysis
On closing the survey, data were downloaded from SelectSurvey in Microsoft Excel format. For e-mail submissions and desk-derived information, data were inputted into the same Excel spreadsheet by either Fraser or Lane. A final Excel spreadsheet containing both survey and desk data was subsequently imported into IBM SPSS Statistics (v.25; IBM Corp., Armonk, NY) so that service characteristics could be analysed. Variable names were created within SPSS to reflect the various survey questions (see additional files www.fundingawards.nihr.ac.uk/award/17/09/08; accessed 26 March 2024), with two sets of post hoc variables being added: ‘service models’, coded against the models in typology version 2 (see Chapter 4); and ‘service features’, coded against the features of services (also Chapter 4). Service model codes were also used to determine potential eligibility for the case study (see Chapter 7).
Missing data
Since there was a significant number of missing data in the final Excel spreadsheet, particularly from the desk-based searches, many mapping findings relate only to a proportion of the 154 included services. Where this is the case, the number of services providing data is specified.
A few variables (e.g. service funder and service interaction) were not analysed because the data collected were limited or difficult to code into discrete categories. Because economic data might be confidential or commercially sensitive, the economic data questions were optional; consequently, few services chose to provide these data.
Service map findings
Service location
Service location can be thought of in several ways: in terms of the country in which the service operates; whether it serves urban or rural areas; and in terms of the sector and/or setting in which it is located.
Country
Of the 154 services, 114 (74.0%) operated in England, 30 (19.5%) in Wales and 10 (6.5%) across several, or all 4, of the UK’s constituent nations. Predictably, given the populations of England and Wales in mid-2020 were, respectively, 56.6 and 3.2 million,90 more services were identified in England than Wales. However, proportionally more services against population size were found in Wales (around nine per million) compared to England (around two per million), possibly because Wales (like Scotland and Northern Ireland) spends more per person on health than England. 91
Urban versus rural
Of services providing data, most operated within urban areas (city/metropolitan areas or towns), with fewer operating in rural areas and fewer still operating online (Figure 18). Through additional free-text responses, six services defined themselves by geography or setting rather than population density stating, for example, they provided services across a number of schools or they operated at county- or country-wide level. Although services were identified in all English and Welsh NHS health regions, most mapped sites were in the main metropolitan areas of England and Wales.
FIGURE 18.
Proportion of services operating in urban vs. rural locations.
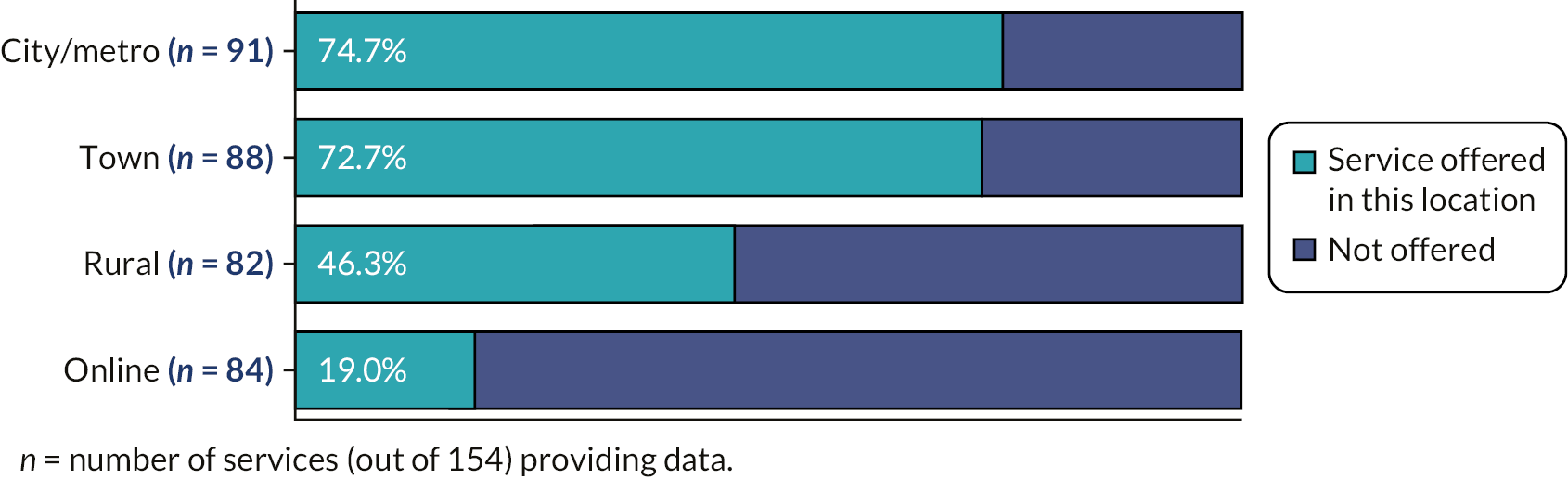
Sector and setting
Service provision was distributed almost equally across the statutory and third sectors (Figure 19). Services provided by the statutory sector, either as a single agency (NHS or local authority) or collaboratively, accounted for 45% of services, while the third sector accounted for 44%. A small proportion of services were provided by the private sector and a similarly small proportion provided collaboratively across all sectors (statutory, private, third). The ‘other’ provider was a university licensing a service to schools.
FIGURE 19.
Proportion of services offered by sector.

The most common settings for services were non-health community settings (Figure 20), which included schools as well as settings such as youth or community centres. Fewer services were located within health settings with only a minority operating in hospitals. Around a quarter of services reported delivering services in the CYP’s home or online.
FIGURE 20.
Proportion of services operating in specific settings.
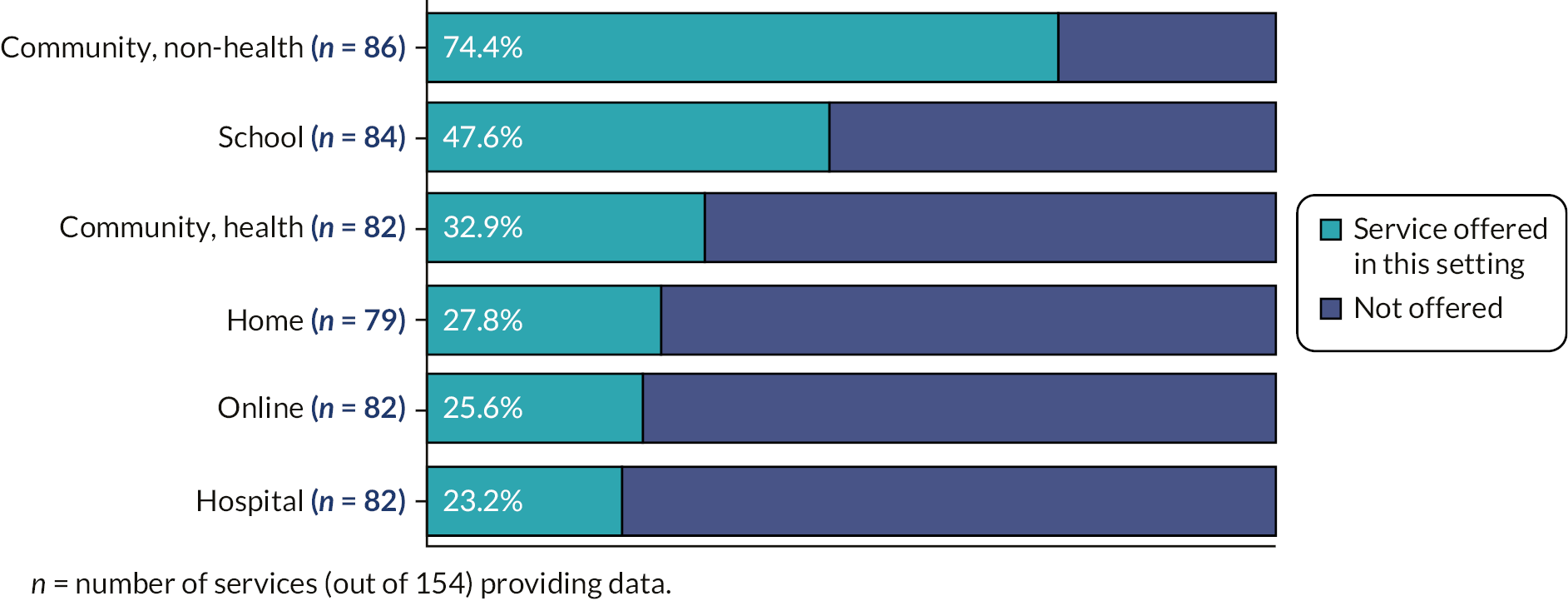
Cross-tabulating service settings with sector (see Table 4, reading by row), we found, unsurprisingly, that most hospital and health-based community services were delivered by NHS providers and that services in non-health settings were mostly delivered by the third sector. The third sector was also the largest provider of online services. The NHS and the third sector were both significant providers of home-based services.
| Setting | Sector | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Local authority | NHS | Third | Cross-statutory | Cross all sectors | Private | Other | Total | ||
| Hospital | n | 0 | 15 | 1 | 2 | 1 | 0 | 0 | 19 |
| %a | 0.0 | 78.9 | 5.3 | 10.5 | 5.3 | 0.0 | 0.0 | 100 | |
| Community, health | n | 0 | 15 | 8 | 2 | 2 | 0 | 0 | 27 |
| % | 0.0 | 55.6 | 29.6 | 7.4 | 7.4 | 0.0 | 0.0 | 100 | |
| Community, non-health | n | 3 | 9 | 40 | 4 | 4 | 4 | 0 | 64 |
| % | 4.7 | 14.1 | 62.5 | 6.3 | 6.3 | 6.3 | 0.0 | 100 | |
| School | n | 2 | 7 | 24 | 3 | 2 | 1 | 1 | 40 |
| % | 5.0 | 17.5 | 60.0 | 7.5 | 5.0 | 2.5 | 2.5 | 100 | |
| Online | n | 1 | 4 | 10 | 2 | 2 | 2 | 0 | 21 |
| % | 4.8 | 19.0 | 47.6 | 9.5 | 9.5 | 9.5 | 0.0 | 100 | |
| Home | n | 4 | 8 | 8 | 1 | 1 | 0 | 0 | 21 |
| % | 18.2 | 36.4 | 36.4 | 4.5 | 4.5 | 0.0 | 0.0 | 100 | |
Support offered
Figure 21 outlines the proportion of services offering specific types of support. Many services provided a range of different types of support, the most common being advice, self-management facilitation, assessment, early intervention and counselling. While many services reported facilitating CYP and families to self-manage (through skills training, for example), an additional number also provided direct self-help (i.e. by supplying self-help materials). Fewer services reported using triage and fewer still waiting-list management.
FIGURE 21.
Types of support offered by services.
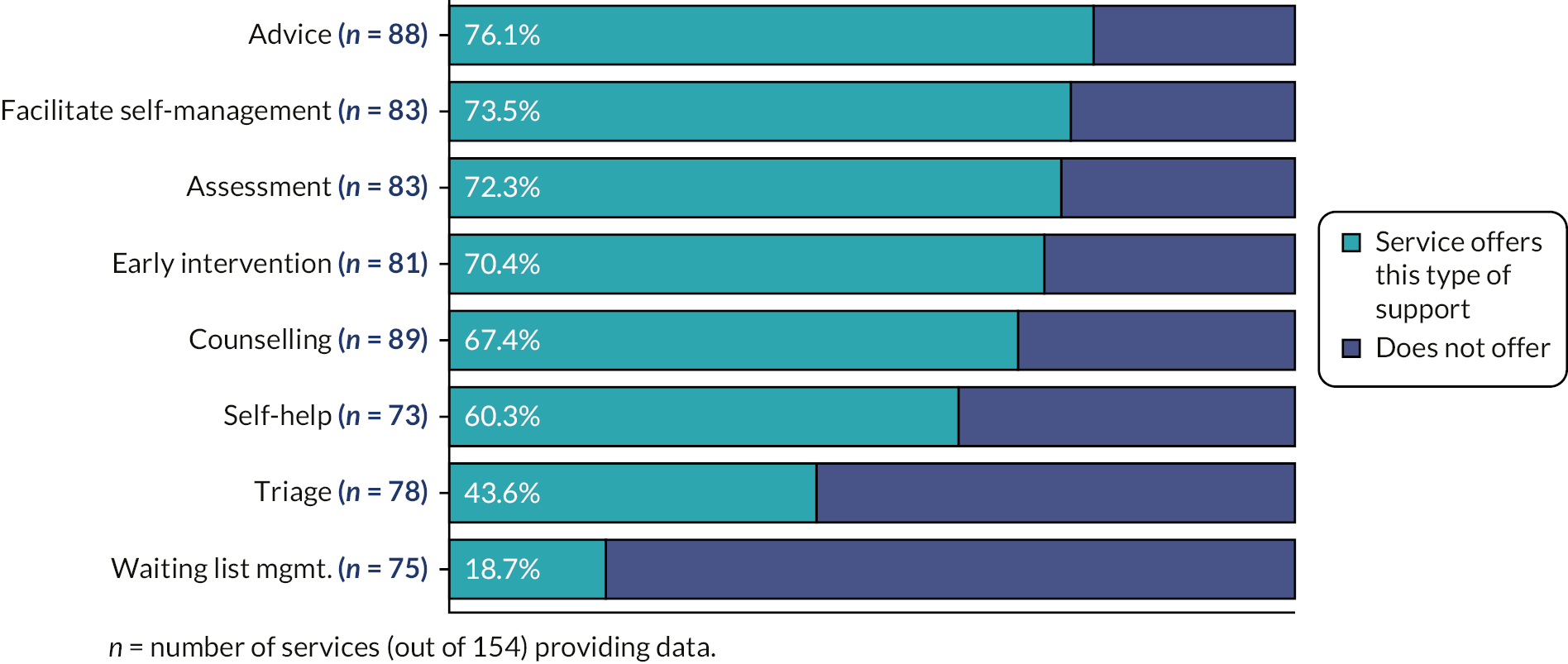
Support offered versus features
As outlined in Chapter 3, we coded services in the literature reviews against a list of service features as well as against the service models in our typology. Since most support functions listed in Figure 21 ultimately turned out to be features, responses to survey questions about these functions were used to code the post hoc ‘features’ variables. Analyses of these variables appear later in this chapter.
Target groups and conditions
Mental health conditions
Services offered support for a range of CMHPs (Figure 22). More than 90% of services offered support for general anxiety issues and depression and almost 90% offered support for self-harm. These findings are unsurprising given anxiety, depression and self-harm are some of the UK’s most prevalent disorders (see Chapter 1). Less than 50% offered support for adjustment disorder and prodromal psychosis. A significant number of services reported (in additional free-text responses) offering services for a range of mental health difficulties rather than specific conditions, for example, ‘we see anyone for anything’, ‘no diagnoses specified’ and ‘a range of mental health difficulties’. Other free-text responses identified support for sleep problems, stress, isolation, attachment concerns, bullying and exam pressure.
FIGURE 22.
Conditions supported by services.
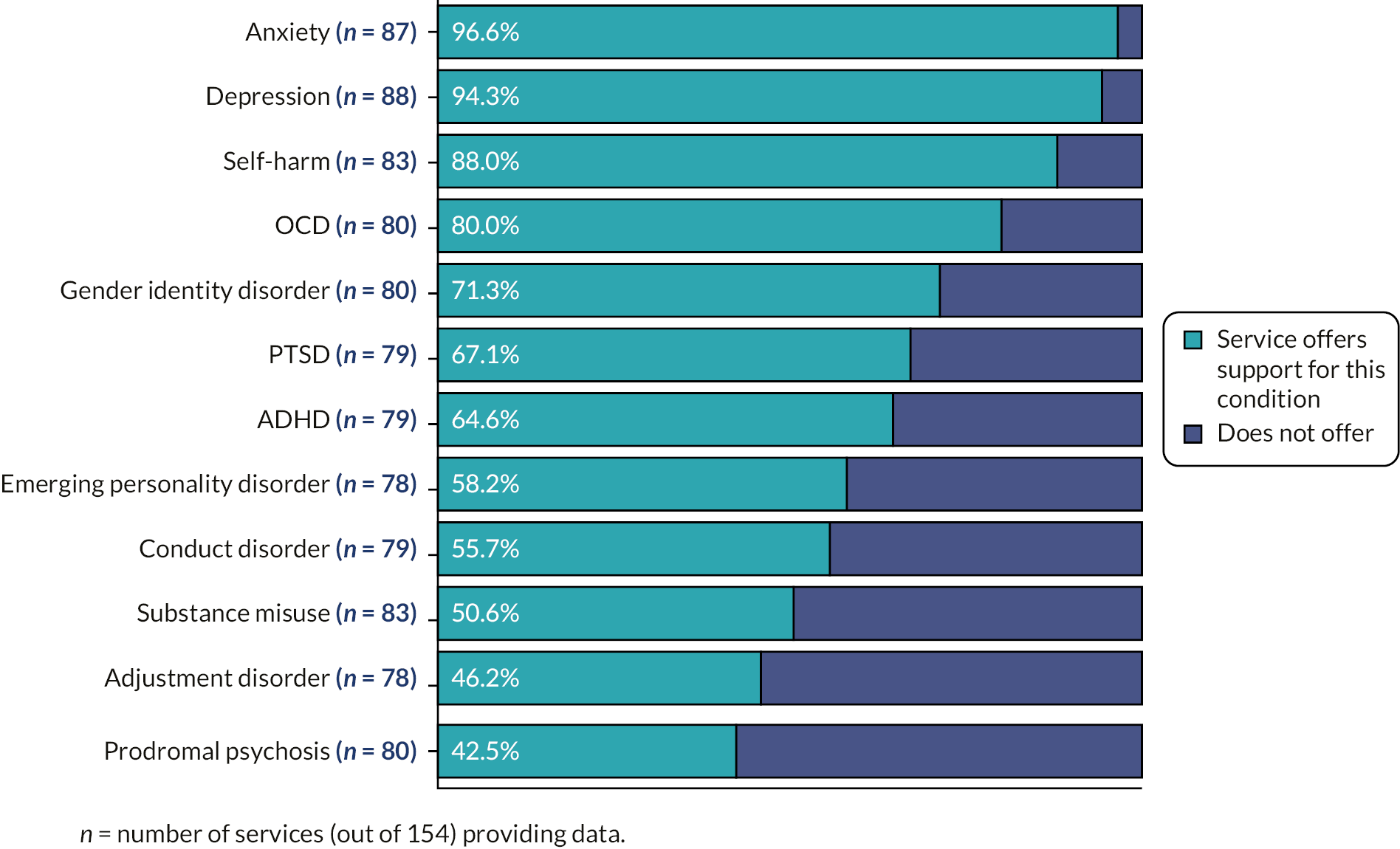
Some services also reported specifically targeting groups of CYP at greater risk of developing mental health problems, including looked-after children and care leavers, unaccompanied asylum-seeking children, LGBTQ+ youth, young carers and ‘NEETs’ (those aged 15–29 years not in education, employment or training).
Age groups
Services tended to focus mainly on secondary school children, with more than 90% offering support to those aged 12–16 years and/or 17–18 years (Figure 23). Around three-quarters of services offered support to those aged 5–11 years and over 60% offered support to young adults (those over 18 years), perhaps reflecting concerns around transitions between child and adult mental health services. Less than half offered services to the under-fives.
FIGURE 23.
Age groups services support.
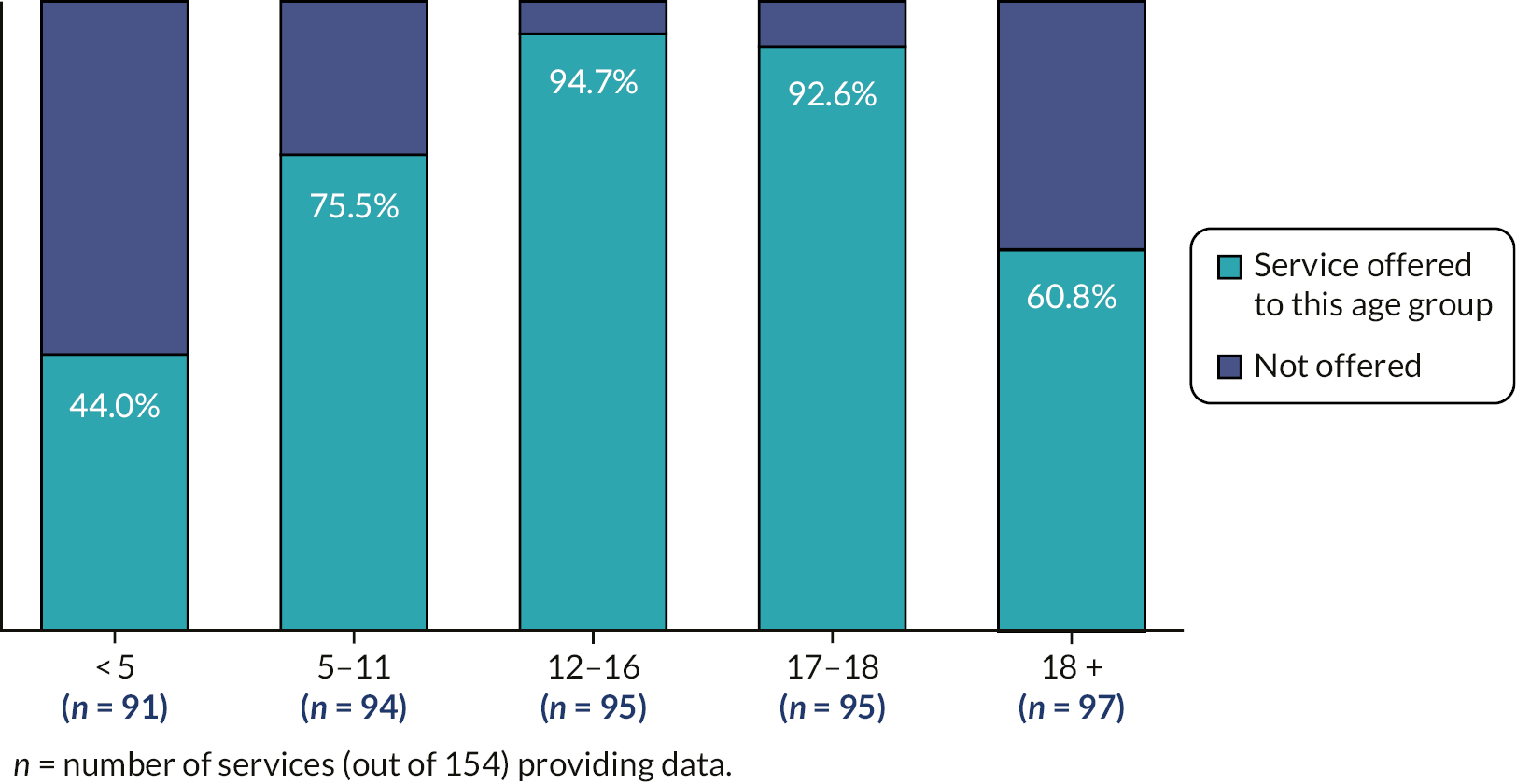
Cross-tabulating age groups with service sector (see Table 5, reading by row), the third sector provided more post-16 services but fewer services for under-fives than the NHS.
| Age group | Sector | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Local authority | NHS | Third | Cross-statutory | Cross all sectors | Private | Other | Total | ||
| Under 5 years | n | 2 | 24 | 6 | 1 | 4 | 3 | 0 | 40 |
| %a | 5.0 | 60.0 | 15.0 | 2.5 | 10.0 | 7.5 | 0.0 | 100 | |
| 5–11 years | n | 5 | 26 | 28 | 2 | 5 | 4 | 1 | 71 |
| % | 7.0 | 36.6 | 39.4 | 2.8 | 7.0 | 5.6 | 1.4 | 100 | |
| 11–16 years | n | 4 | 29 | 42 | 4 | 5 | 5 | 1 | 90 |
| % | 4.4 | 32.2 | 46.7 | 4.4 | 5.6 | 5.6 | 1.1 | 100 | |
| 17–18 years | n | 4 | 26 | 44 | 3 | 6 | 5 | 0 | 88 |
| % | 4.5 | 29.5 | 50.0 | 3.4 | 6.8 | 5.7 | 0.0 | 100 | |
| 18 + years | n | 2 | 7 | 40 | 2 | 5 | 3 | 0 | 59 |
| % | 3.4 | 11.9 | 67.8 | 3.4 | 8.5 | 5.1 | 0.0 | 100 | |
Service delivery
Type of contact
Almost all services (96 of 97 services providing data) offered face-to-face support, and over 50% (46 of 85 services) offered remote support either online, by telephone or through some other means such as an app or e-mail. Importantly, the mapping data were collected before the COVID-19 pandemic; had it been collected later, the proportion of services offering remote support would likely have been higher.
Most services providing data offered individual one-to-one support (Figure 24), with around two-thirds offering group support and around 60% mixed individual/group support. Around 45% of services offered telephone support and around 30% online support. A smaller proportion offered ‘proxy’ support, that is, consultation with someone acting on the CYP’s behalf.
FIGURE 24.
Type of contact provided by services.

Service target
Predictably, all services offered support to CYP (Figure 25), with around 70% offering support to parents and 35% to siblings. Almost a third reported they would also support peers, for example by allowing friends to attend with the CYP.
FIGURE 25.
Target of services.

Service availability and contact time
Services reported they operated mostly during the working week (Monday–Friday), either during standard office hours (‘nine-to-five’) or through extended hours such as into the evening (Figure 26). Relatively few services operated at weekends.
FIGURE 26.
Service availability.
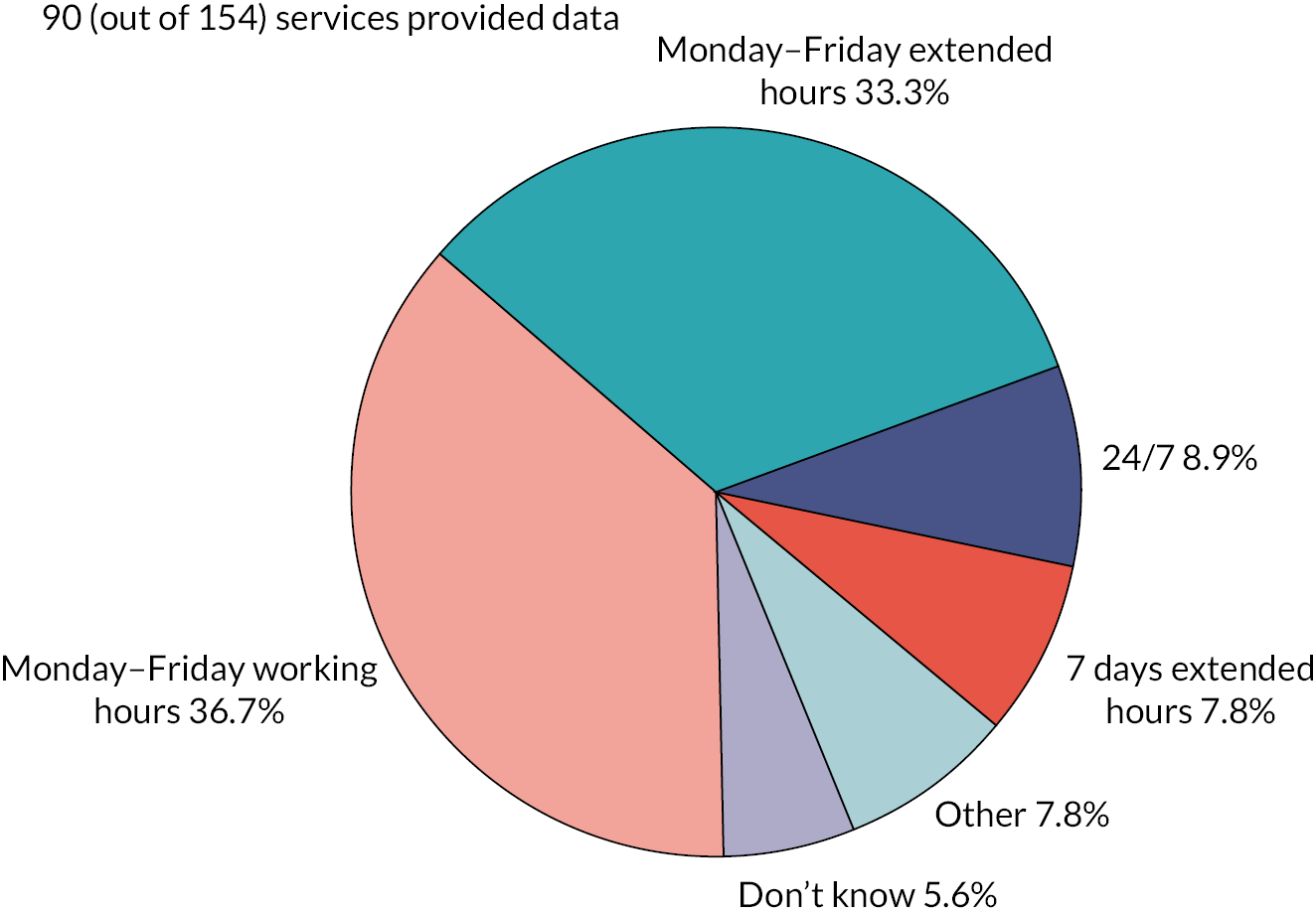
Of services providing data, around 60% (47 of 82 services) provided time-limited support compared to around 40% (35 of 82 services) providing unlimited access. Those providing time-limited support usually offered a maximum of six to eight sessions, although in some services it was based purely on the CYP’s level of need.
Most services (around 57%) saw CYP on a weekly basis (Figure 27). Few services offered daily or twice-weekly contact. A significant number of services (around a quarter) provided additional free-text responses stating contact was variable depending on individual needs or the treatment modality.
FIGURE 27.
Contact time.
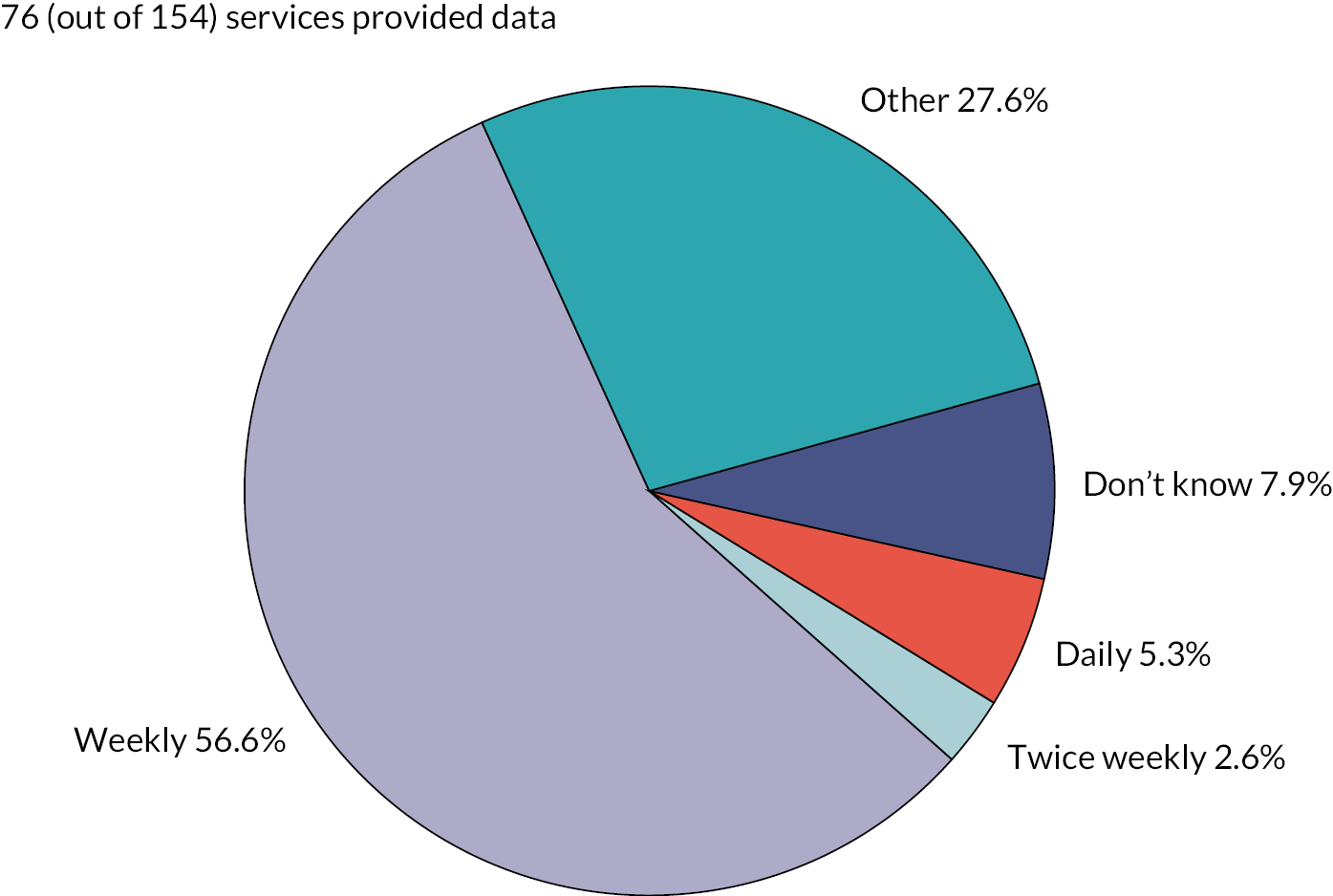
Service staffing
Only 68 services provided staffing profile data (Figure 28). The data, however, illustrate a wide variety of professional and lay staff working in services across England and Wales. Unremarkably, the most frequently reported staff members were mental health professionals such as psychologists, counsellors, mental health nurses and psychiatrists. Around a quarter of services (16 out of 68) added free-text responses to the ‘other staff’ category; other staff identified included emotional well-being practitioners, administrative staff, dieticians, paediatricians, behaviour support staff and student professionals on placement.
FIGURE 28.
Number of services employing specific staff types. AHP, allied health professional; PWP, psychological well-being practitioner.
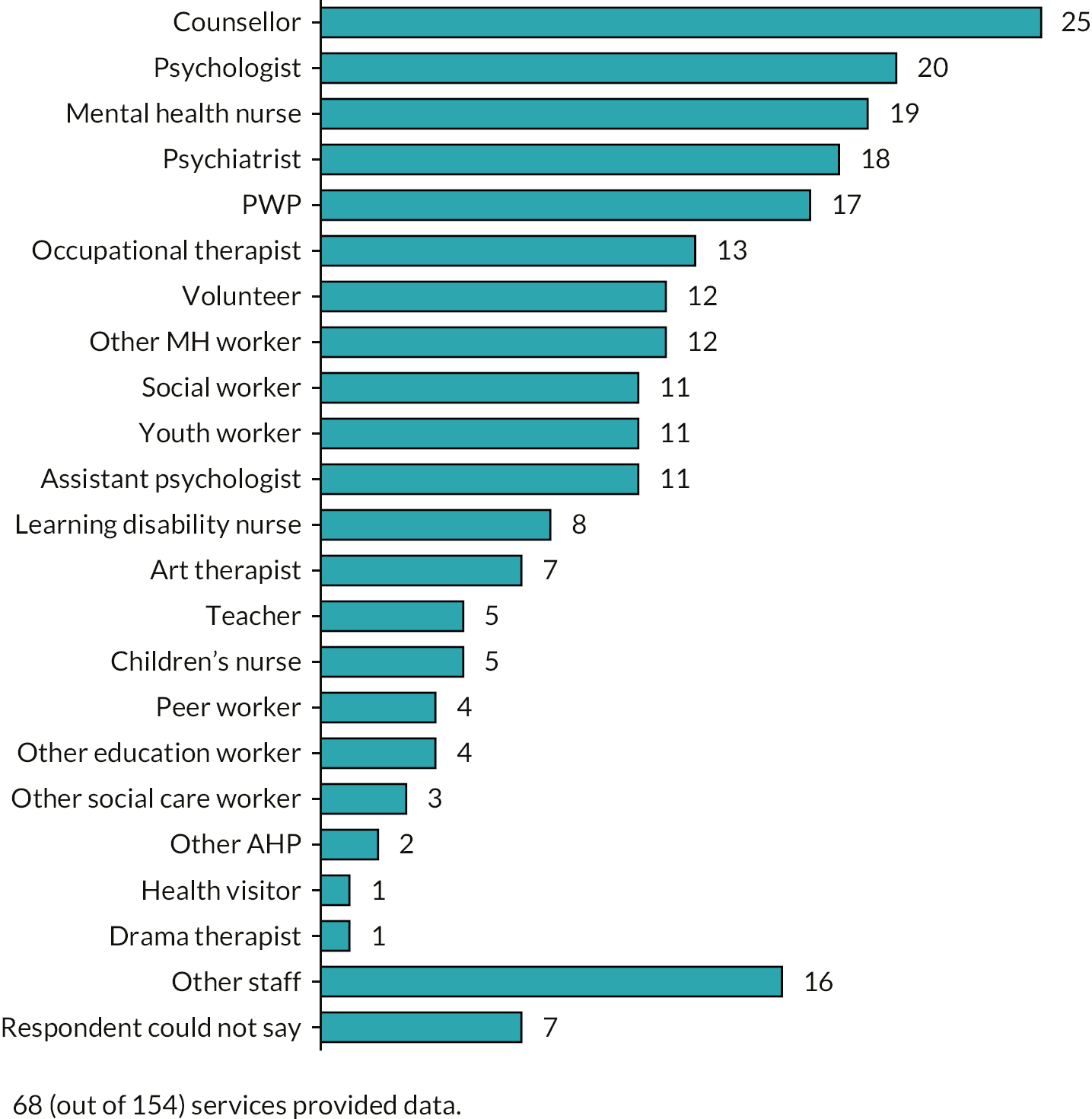
Service access
Various referral routes into services were reported (Figure 29). Over 80% of services accepted self-referrals from CYP and over 70% referrals from parents or carers. Almost 80% accepted referrals from schools. The least-reported referral routes were paediatrics and accident and emergency (A&E), possibly because these services cater more for CYP with severe mental health problems.
FIGURE 29.
Referral routes.

Table 6 shows the cross-tabulation of referral routes by sector. The percentages shown are the proportion of services within each sector offering a specific referral route.
| Referral route | Offering | Sector | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Local authority | NHS | Third | Cross-statutory | Cross all sectors | Private | Other | Total | ||
| Self | n | 3/5 | 15/28 | 46/50 | 3/3 | 5/5 | 4/4 | 1/1 | 77/96 |
| % | 60.0 | 53.6 | 92.0 | 100.0 | 100.0 | 100.0 | 100.0 | 80.2 | |
| GP | n | 2/5 | 22/28 | 30/45 | 2/2 | 3/4 | 2/5 | 0/1 | 61/90 |
| % | 40.0 | 78.6 | 66.7 | 100.0 | 75.0 | 40.0 | 0.0 | 67.8 | |
| School | n | 5/5 | 23/28 | 37/46 | 2/2 | 4/4 | 0/5 | 1/1 | 72/91 |
| % | 100.0 | 82.1 | 80.4 | 100.0 | 100.0 | 0.0 | 100.0 | 79.1 | |
| Parents | n | 4/5 | 15/28 | 34/46 | 3/3 | 4/4 | 4/5 | 1/1 | 65/92 |
| % | 80.0 | 53.6 | 73.9 | 100.0 | 100.0 | 80.0 | 100.0 | 70.7 | |
| Social care | n | 4/5 | 23/28 | 24/45 | 2/2 | 3/4 | 0/5 | 0/1 | 56/90 |
| % | 80.0 | 82.1 | 53.3 | 100.0 | 75.0 | 0.0 | 0.0 | 62.2 | |
| A&E | n | 1/5 | 20/26 | 9/43 | 2/2 | 2/4 | 0/5 | 0/1 | 34/86 |
| % | 20.0 | 76.9 | 20.9 | 100.0 | 50.0 | 0.0 | 0.0 | 39.5 | |
| Paediatrics | n | 2/5 | 27/28 | 15/45 | 3/3 | 2/4 | 0/5 | 0/1 | 49/91 |
| % | 40.0 | 96.4 | 33.3 | 100.0 | 50.0 | 0.0 | 0.0 | 53.8 | |
More non-statutory sector services offered self-referral routes than statutory sector services, although more than half of NHS services reported a self-referral route. There was a similar profile for parental referral, though the lower number of third-sector services offering parental referral could be because some services offered confidential support to CYP without parental knowledge or involvement. Most services in the statutory and third sectors offered referral routes for school staff, though the private sector did not. GP referrals were most prominent in NHS services, though two-thirds of third-sector services accepted them. Few third-sector services received referrals via paediatrics or A&E.
Service features
All 154 services were coded post hoc by Fraser, Lane and Pryjmachuk against the 20 features described in Chapter 4. Many services received multiple codes. Figure 30 summarises the number of services reporting a specific feature. The number of services with specific features may be much higher than reported since a feature was coded only if explicit in the data. Features were coded from answers to certain questions in the survey (see additional files www.fundingawards.nihr.ac.uk/award/17/09/08; accessed 26 March 2024), which not every respondent completed, and from additional, desk-based information which was often difficult to obtain. Nonetheless, the available data provide some insight into the features of English and Welsh services for CYP experiencing CMHPs.
FIGURE 30.
Number of services reporting specific features.
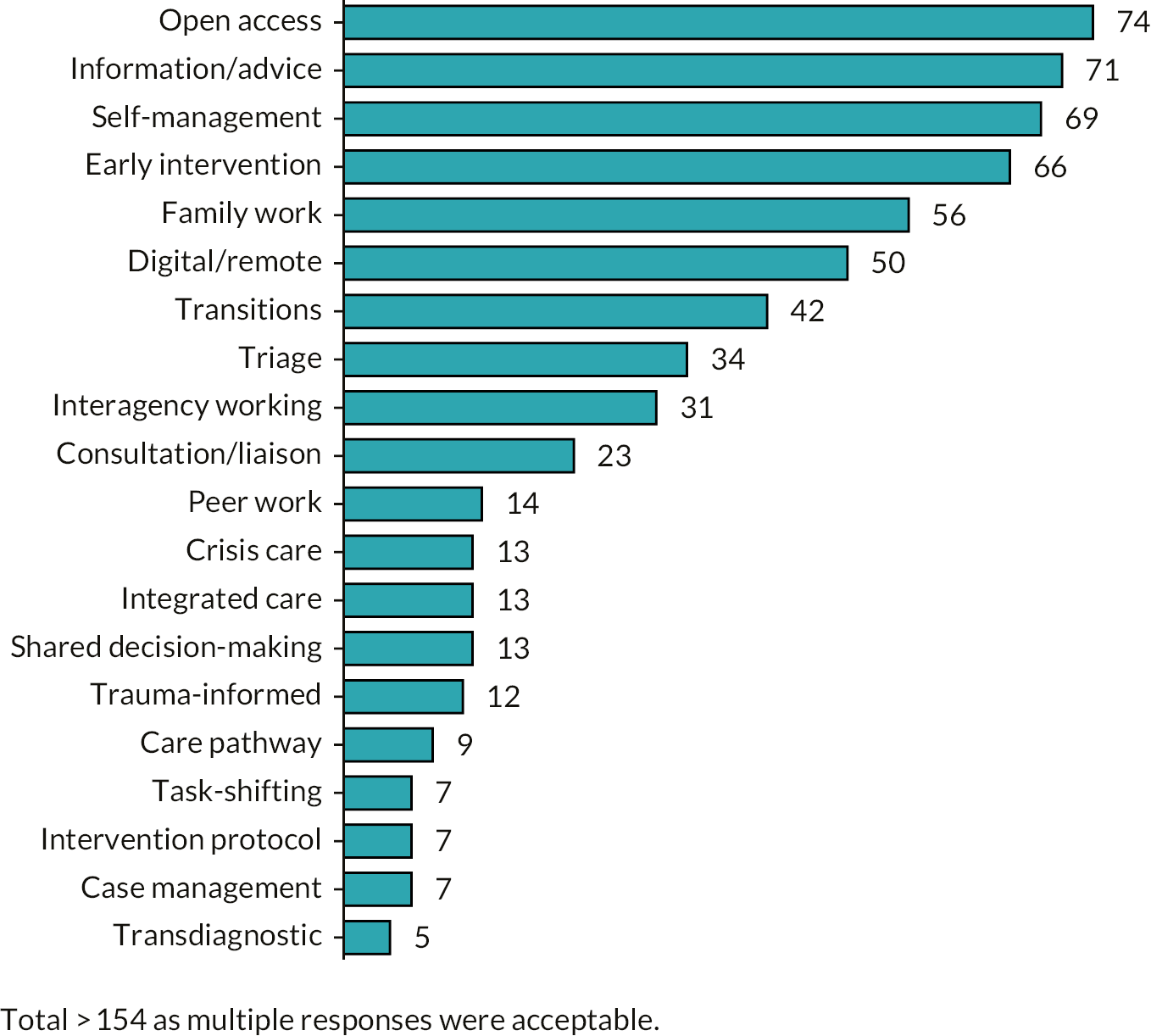
The features coded most frequently were open access (74 services), information and advice (71), self-management (69), early intervention (66), family work (56), digital/remote (50) and transitions (42). These features paint a picture of generally open and flexible services, providing information and advice, self-management support and support for transitions to adult mental services, and which are family-focused and primed for early intervention.
The features for which there was little explicit mention may be down to an artefact of the limited data collected (as mentioned above) or because the feature is associated with models or services relatively uncommon in the UK. For example, the transdiagnostic approach – in which services focus on presenting problems rather than diagnoses – is mostly associated with psychiatry-derived community hubs (B3), which are common in Australia (Headspace Centres) and Ireland (Jigsaw Centres) but less so in the UK. Case management, as another example, is often associated with collaborative care (B1) and systems of care (G1), both of which are commonplace in the USA but less so in the UK. Trauma-informed approaches tend to be linked to specialist services dealing with PTSD or adverse childhood events and we identified few such services in our service map. Crisis care is more likely a feature of services for CYP experiencing more severe mental health problems, two of which – psychosis and eating disorders – were specifically excluded from the study.
The relatively low profile of peer work and shared decision-making is surprising since these two features reflect current aspirations within CYP’s mental health. 62,92 Again, this could be an artefact of the limited data collected, or it may be peer work and shared decision-making are implicit features of services so were consequently not mentioned or reported.
Service models
As with features, all 154 services were coded post hoc by Fraser, Lane and Pryjmachuk, firstly against typology version 2 (see Chapter 3) so we could sample for Work Stream 3’s case study work, and later against the final typology presented in Chapter 4. As with features, many services received multiple model codes. However, unlike the literature reviews, we did not assign a primary code to each service for two reasons: because real-world service delivery is often ‘fuzzier’ than that described in research or professional literature; and because multiple coding aided our sampling for the case study work because it increased the chances our sample would capture all seven main typology model groups, A–G.
Figure 31 compares the number of services coded against the models in our final typology for the service map and for the scoping review. It illustrates differences between what is reported in the international literature and the landscape of service provision in England and Wales.
FIGURE 31.
Typology model frequency in the scoping review and service map.
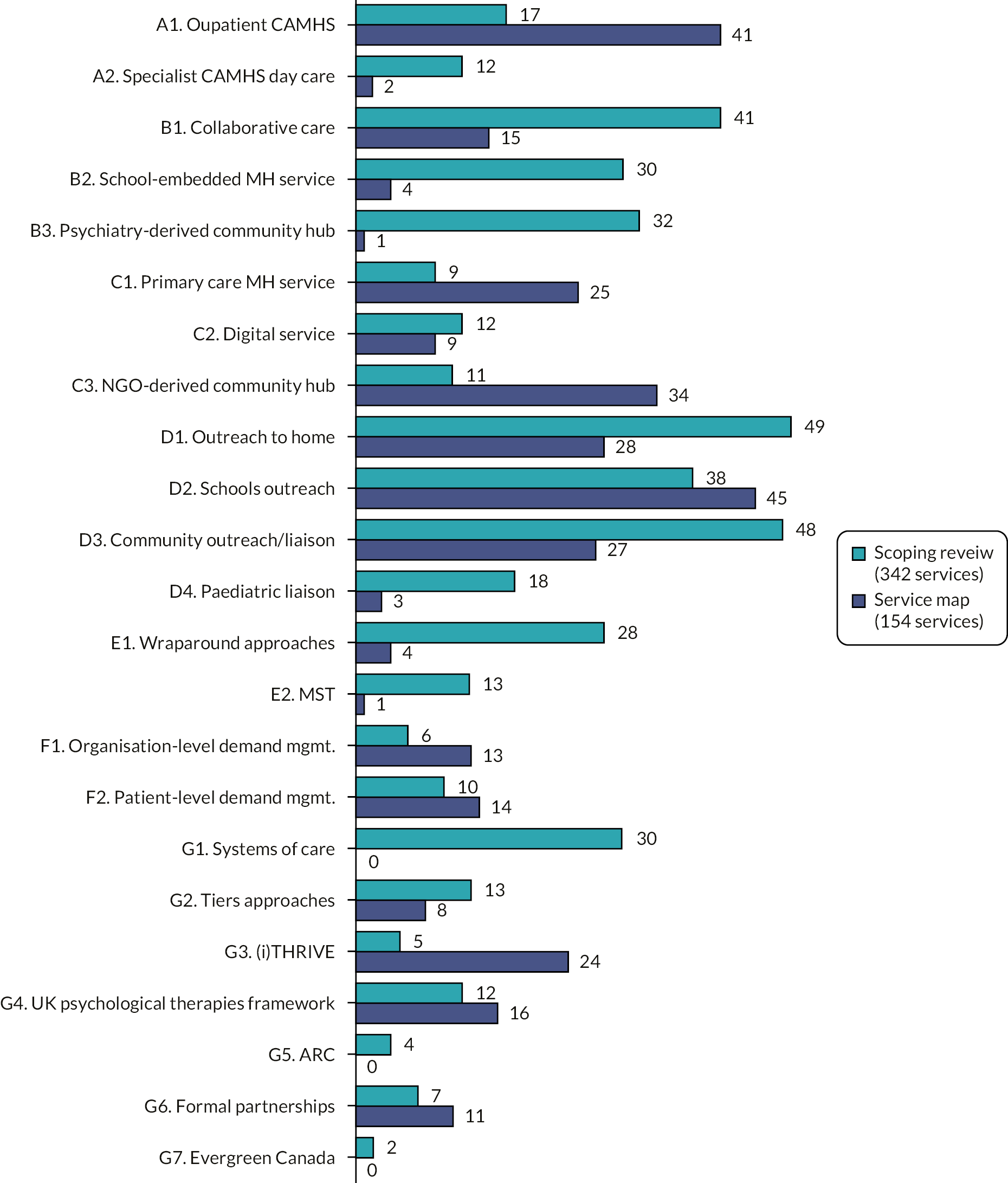
The most common service models employed in England and Wales are community outreach models: schools outreach (D2, 45 services); outreach to home (D1, 28 services); and community outreach and liaison services (D3, 27 services). The next most common models were outpatient CAMHS (A1, 41 services), NGO-derived community hubs (C3, 34 services), primary care mental health services (C1, 25 services) and the (i)THRIVE (G3) and UK psychological therapies (G4, mainly CYP-IAPT) frameworks, employed in 24 and 16 services, respectively. The latter two frameworks are UK-specific, so their presence is unsurprising, as is the absence in the service map of non-UK frameworks like systems of care (G1), ARC (G5) and Evergreen (G7). Few services were explicitly coded as a tiers approach (G2) despite the UK four-tier framework still having influence in England and Wales. This could be an artefact of coding since services had to explicitly refer to ‘tiers’ to be coded as such and, while we suspected many (particularly NHS) services still operated within the four-tiers framework, few explicitly stated this. Then again, a few services, especially those using (i)THRIVE (G3), explicitly stated they had moved on from a tiers approach.
While significantly reported in the international literature, relatively few English and Welsh services employed specialist CAMHS day patient models (A2), collaborative care approaches (B1), school-embedded mental health services (B2), psychiatry-derived community hubs (B3), paediatric liaison services (D4), wraparound approaches (E1) and MST (E2).
Day patient models may be more common in countries (especially the USA) with insurance-based health systems since they are cheaper alternatives to inpatient care. Collaborative care is common in US child health provision because there is a tradition of separating paediatric and adult general practice which makes it easier for children’s mental health and children’s primary care specialists to work collaboratively. This may also explain why paediatric liaison is more common in the literature since many of the paediatric liaison papers were from the USA. Unlike the USA, there is no UK tradition of providing formal health (primary care) clinics within schools which could explain the differences in school-embedded mental health service provision. As outlined earlier, psychiatry-derived community hubs are common in Australia and Ireland but less so in the UK. They also have their roots in early intervention for psychosis and psychosis was specifically excluded from the study. The ecological models (wraparound approaches and MST) are USA-derived models which are also relatively expensive to deliver; a low UK profile is thus unsurprising. Moreover, both were developed for CYP with more serious (rather than common) mental health problems, often in the context of youth offending, so finding few such services is unremarkable. The difference between the service map and scoping review profiles for organisation-level demand management could be a result of demand being managed in the UK through initiatives like CAPA rather than through insurance-imposed restrictions.
Summary
Our service map reveals service provision across England and Wales for CYP experiencing CMHPs is diverse, with various statutory, private and third-sector providers operating in a range of settings and supporting CYP with a wide range of CMHPs. No single model from our typology is particularly dominant, though some medically driven services (day care, psychiatry-derived hubs, paediatric liaison) have limited profiles, as do wraparound approaches and MST. Most services were provided in community, non-health settings, most focused on secondary school children and most offered support for the ‘most common’ of the CMHPs, namely general mood disorders and self-harm. Open access via self- or parent referral was relatively widespread, particularly in the third and private sectors.
While diversity in service provision can be beneficial (particularly if CYP and families have a choice), it also raises concerns about consistency and equity of access. The diversity we found in our service map may, in part, explain past and ongoing concerns regarding service variability discussed in Chapter 1. Moreover, while open access and delivery largely in community settings is to be welcomed, we have identified some shortcomings in English and Welsh service provision: urban areas appear to be better provided for than rural areas (though this may simply reflect different population densities), there appear to be fewer services for the under-12s, open access is less common in the statutory sector (especially the NHS) than the third and private sectors and few services exist outside of standard office hours.
Chapter 6 Integrative review findings
This chapter presents findings from the 98 empirical papers reporting effectiveness, acceptability (‘views’) and/or cost-effectiveness data. As outlined in Chapter 3, we used the EPPI-Centre approach to evidence synthesis,58 analysing the individual data sets separately before synthesising them. It makes sense to structure our integrative review around the typology described in Chapter 4, that is, analyse the evidence separately for each main model group (A–G) before drawing general conclusions about the effectiveness and acceptability of services for CYP experiencing CMHPs.
General observations on the included papers
Fifty-six of the 98 empirical papers provided effectiveness data, 62 acceptability data and just 3 cost-effectiveness data about the various service models. These numbers total more than 98 because 22 papers provided data from more than one perspective (see Figure 2, Chapter 3). Summary tables for the extracted effectiveness, acceptability and cost-effectiveness data can be found in Report Supplementary Materials 1–3.
Regarding effectiveness, 56 papers provided data from 51 studies. Five studies were reported in paired papers: Asarnow 2005/Asarnow 2009; Evans 1997/Evans 2003; Cai 2016/Lim 2017; Window 2004/Vostanis 2006; and Sundell 2008/Löfholm 2009. Three studies compared more than one relevant model: Zima 2010 compared two models across different typology categories – outpatient CAMHS (A1) versus collaborative care (B1) – while Silverstein 2015 compared two different forms of collaborative care (B1) and Evans 1997/Evans 2003 three different forms of outreach to home (D1).
Regarding acceptability, 62 papers provided data from 60 studies, with 2 studies being reported in paired papers (Asarnow 2005/Asarnow 2009; Callaghan 2003b/Callaghan 2004). The Zima 2010 study comparing two models across different typology categories provided acceptability as well as effectiveness data. Bower 2003 also explored two models across two different typology categories: collaborative care (B1) and community outreach and liaison (D3).
Regarding cost effectiveness, three papers provided data from three studies: Cai 2016 (Cai2016/Lim2017 study); Wright 2016 (Richardson 2014/Wright 2016 study) and Chatterton 2019 (Rapee 2017/Chatterton 2019 study). Cai 2016 reported cost-effectiveness data alongside effectiveness data, while Wright 2016 and Chatterton 2019 reported only cost-effectiveness data.
Study types
Figure 32 outlines the types of study providing effectiveness, acceptability and economic (cost-effectiveness) data, according to the MMAT study type categories described in Chapter 3.
FIGURE 32.
Data sources by MMAT study type. ACC, acceptability; ECO, economic; EFF, effectiveness.
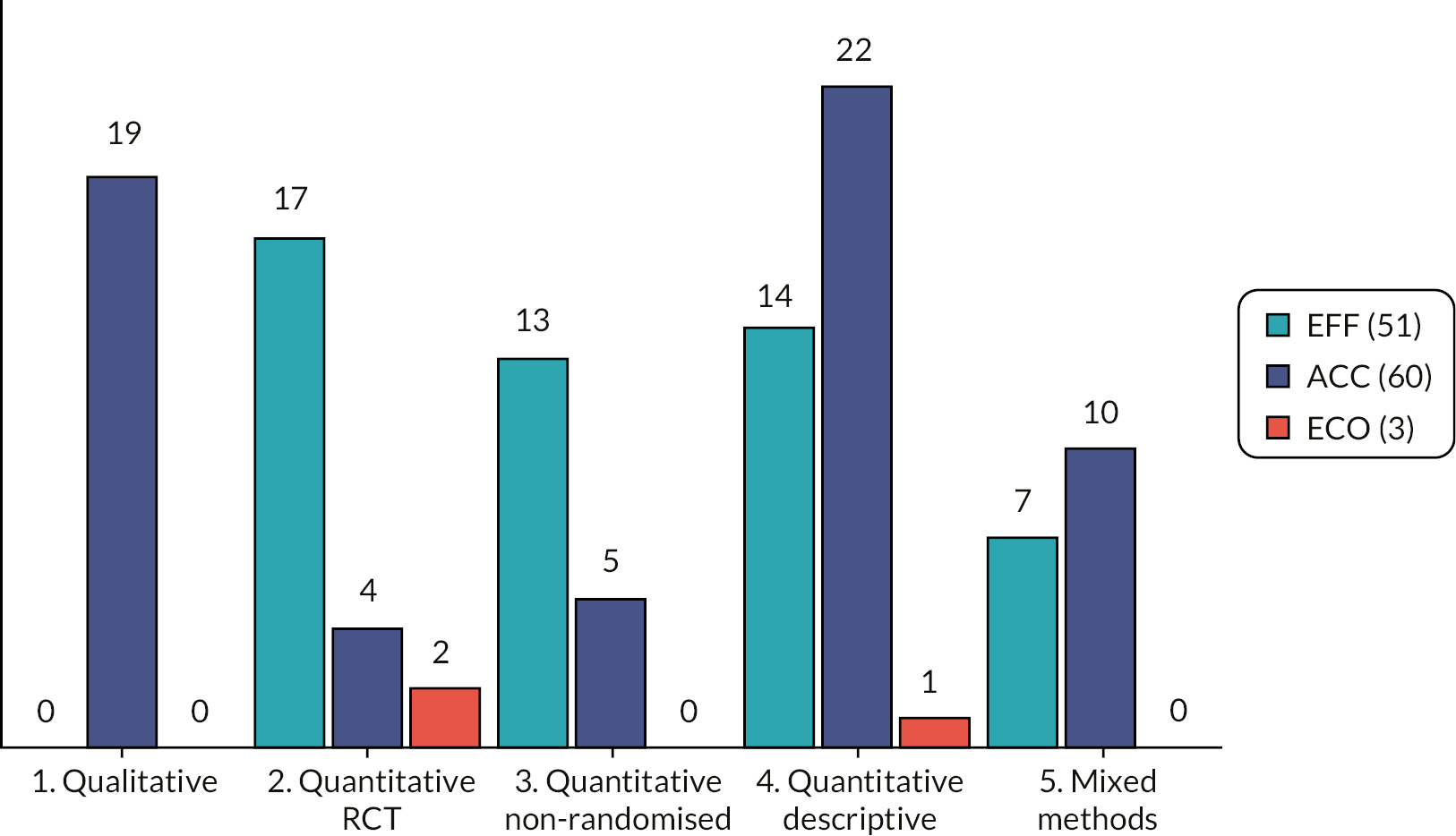
Effectiveness data were obtained in roughly equal amounts from all three MMAT quantitative study types (RCTs, non-RCTs and descriptive quantitative studies) as well as from a smaller number of mixed-methods studies.
Acceptability data were obtained mostly from qualitative and descriptive quantitative studies, with some data from randomised and non-RCTs and mixed-methods studies. That qualitative studies provided most of the acceptability data is unremarkable. The quantitative descriptive studies providing acceptability data tended to be surveys or studies in which satisfaction measures were taken pre/post intervention or post only. Similarly, the acceptability data in the small number of trials (MMAT groups 2–3) were mostly from satisfaction measures employed in those trials.
Cost-effectiveness data were obtained from two RCTs and an uncontrolled retrospective cohort study.
In the ensuing sections, we discuss, in turn, the findings for each typology model group. Where there is sufficient effectiveness and acceptability data for a specific submodel within a model group (e.g. B1 in group B), we have considered those submodels separately as well as within the whole model group; where there are insufficient data, we have merely discussed the overall model group.
Further detail about the study types and research designs employed in the included studies, along with details of MMAT appraisals for each study, can be found in Appendix 5. As outlined in Chapter 3, MMAT discourages the calculation of an overall score from ratings on each of the five criteria. Instead, we present MMAT appraisal data in a colour-coded format so that readers can get a sense of the quality of each typology group’s studies by simply eyeballing the tables in Appendix 5.
No included papers provided effectiveness data for digital services (C2), NGO-derived community hubs (C3), organisation-level demand management (F1), tiers approach (G2), (i)THRIVE (G3), UK psychological therapy frameworks (G4), formal partnerships (G6) and Evergreen Canada (G7). No acceptability data were available for psychiatry-derived community hubs (B3), digital services (C2), MST (E2) or for any group G framework except systems of care (G1). There were scant cost-effectiveness data, available only for collaborative care (B1), primary care mental health service (C1) and schools outreach (D2).
Group A: specialist Child and Adolescent Mental Health Services
As a reminder, this is the model group encompassing ‘standard’ institutionally based children’s mental health services. Group A encompasses outpatient (A1), day patient (A2) and inpatient (A3) services. The latter were outside of the study’s remit.
Fifteen studies provided group A data (see Appendix 5), with four providing effectiveness and 14 providing acceptability data. Quality appraisals of group A studies suggest the acceptability data are generally of higher quality (more green colouring) than the effectiveness data.
Effectiveness
There were four group A effectiveness studies, one each from England (Worral-Davies 2004), the USA (Zima 2010), Turkey (Çakin Memik 2010) and Australia (Ray 1998). There were no RCTs; two (Rey 1998, Zima 2010) were controlled studies without randomisation and two (Worral-Davies 2004, Çakin Memik 2010) were uncontrolled studies measuring pre/post outcomes in a single cohort. No studies were published within the last 10 years and two (Rey 1998, Worral-Davies 2004) are more than 15 years old.
Regarding outpatient CAMHS (A1), Worral-Davies 2004 explored a generic ‘Innovative Tier 2’ service in which CAMHS staff acted as a first point of contact for anyone concerned about emotional-behavioural problems in CYP. They found that median Health of the Nation Outcome Scales for Children and Adolescents (HoNOSCA) scores fell significantly from assessment to post intervention. Zima 2010 compared a specialist ADHD clinic with the management of ADHD in primary care (a collaborative care model, see later); finding outcomes did not vary between the two groups of CYP.
Regarding day care (A2), Çakin Memik 2010 found young people completing a day programme combining activities and psychotherapies appeared to function better globally at discharge. Families also perceived the programme as helpful. Rey 1998 examined a day programme providing a range of psychotherapies, finding young people attending the programme functioned better overall and used fewer services than matched non-day patients.
Acceptability
Fourteen studies provided group A acceptability data. Four included acceptability studies (Bone 2015, Crouch 2019, Hinrichs 2012, Teggart 2006) – all UK studies – did not specify whether the services they described were outpatient, day patient or inpatient services, or indeed a combination of all three. These studies may reflect UK mental health service configuration such that ‘CAMHS’ can mean a service with one component (usually outpatients) or with two or three. Eight acceptability studies explored either generic outpatient CAMHS (Bjørngaard 2008, Coyne 2015, Kapp 2017, Mitchell-Lowe 2009, Persson 2017, Solberg 2015) or condition-specific outpatient CAMHS (McGonnell 2009, Zima 2010). The two A2 effectiveness studies (Çakin Memik 2010, Rey 1998) also provided acceptability data.
Acceptability data for group A models came from various European, North American and Australasian countries and largely from interviews, focus groups and surveys. The A2 data came from satisfaction measures employed in quantitative studies. Of the 14 acceptability studies, roughly half are from the last decade and half are more than 10 years old. All but one (Hinrichs 2012) obtained data from service users, that is, CYP and/or their parents or caregivers.
Overall, the group A acceptability studies suggest there is uncertainty and apprehension around the processes for accessing specialist CAMHS, both from service users (Bone 2015, Crouch 2019, Coyne 2015, Mitchell-Lowe 2009) and referrers (Hinrichs 2012), and that lengthy waiting times are an issue (Crouch 2019, Teggart 2006, Bjørngaard 2008, Coyne 2015, Kapp 2017, Persson 2017, McGonnell 2009). However, once families had overcome any access barriers, specialist CAMHS was generally viewed positively (Teggart 2006, Solberg 2015, McGonnell 2009, Zima 2010). Interestingly, both Solberg 2015 and Zima 2010 reported no difference in satisfaction levels between those who improved after treatment and those who did not, suggesting merely gaining access to services can influence satisfaction.
The group A acceptability studies also identify user involvement in delivering services as important (Bone 2015, Coyne 2015, Kapp 2017, Persson 2017), as are positive relationships between service users and professionals (Bjørngaard 2008, Coyne 2015, Mitchell-Lowe 2009) and positive interprofessional relationships (Hinrichs 2012).
Cost effectiveness
No cost-effectiveness data were available for any group A model.
Group A evidence summary
The two included A1 studies provided little effectiveness evidence for specialist CAMHS outpatient services; in contrast, the two A2 studies provided some limited evidence that day hospital may improve functioning. Accessing specialist CAMHS can cause apprehension for service users and uncertainty for both service users and referrers. User involvement in CAMHS is important to CYP and parents as is the quality of relationships with specialist CAMHS staff. Inter- and intraprofessional relationships between specialist CAMHS and other staff are important. Specialist CAMHS was generally viewed positively by families once access was gained.
Group B: community-embedded specialist Child and Adolescent Mental Health Services
In this model group, key staff from specialist CAMHS (group A) physically move to become embedded (‘co-located’) within community settings like primary care clinics or schools. As a reminder, collaborative care (B1) is the co-location of specialist CAMHS staff in primary care, school-embedded mental health service (B2) is where mental health staff are either employed directly by a school or embedded into a school for significant time periods, and psychiatry-derived community hubs (B3) are one-stop primary care centres for those aged 12–25 years who need help with anything troubling them.
Twenty-six studies provided group B data. Seventeen studies provided effectiveness data, 19 acceptability data and 1 cost-effectiveness data (see Appendix 5). Ten studies provided more than one data type. Eighteen studies considered collaborative care models, six considered school-embedded mental health services and two considered psychiatry-derived community hubs.
Effectiveness
Eleven studies provided effectiveness data for collaborative care, four for school-embedded mental health services and two for psychiatry-derived community hubs.
B1 collaborative care
Ten of the 11 collaborative care studies were conducted in the USA, with 1 UK study (Day 2006). Ten studies were controlled trials with six being RCTs, mostly of reasonably good quality according to our MMAT appraisals. Seven studies were reported in the last 10 years. Most B1 studies focused on depression (Asarnow 2005, Asarnow 2009, Clarke 2005, Richardson 2019, Richardson 2014, Shippee 2018) or ADHD (Kolko 2012, Kolko 2014, Power 2014, Silverstein 2015, Zima 2010). The roles mental health professionals take in collaborative care varies with some jointly delivering care to CYP and families (Clarke 2005), some providing care in liaison with primary care colleagues (Day 2006, Shippee 2018) but most providing support and co-ordination (in the form of case management) to primary care colleagues (Asarnow 2005/Asarnow 2009, Kolko 2012, Richardson 2009, Richardson 2014, Silverstein 2015).
Most B1 studies suggest that, compared to usual care, collaborative care is effective in improving depressive symptoms or behaviour in ADHD. Nonetheless, Clarke 2015 found collaborative care was not much more effective than well-delivered provision of selective serotonin reuptake inhibitor (SSRI) antidepressants by primary care practitioners. Power 2014 found that collaborative care offered no benefits over the addition of brief education and support to usual ADHD care and, as reported earlier, Zima 2010 found outcomes generally did not vary between children receiving ADHD care in specialist outpatient clinics and those receiving (collaborative) care in primary care settings.
B2 school-embedded mental health services
For school-embedded mental health services, two of the four included studies were UK studies (McKenzie 2011, Scotland; Wolpert 2013, England) and two from the USA (Beehler 2012, Finch 2018). Only one RCT, part of a mixed-methods study (Wolpert 2013), was included; one study (Finch 2018) was a non-randomised controlled study and the remaining two (Beehler 2012, McKenzie 2011) were uncontrolled studies. All four studies were conducted within the last 10 years. Although the services considered were all school-embedded, they are somewhat dissimilar. Cultural Adjustment and Trauma Services (CATS) (Beehler 2012) is a US school-based model focusing on immigrant children exposed to trauma. Recovery high schools (Finch 2018) are US specialist schools targeting young people misusing substances. The McKenzie 2011 study describes embedding a specialist CAMHS counsellor into schools in Scotland, and the English Targeted Mental Health in Schools (TaMHS) initiative (Wolpert 2013) facilitated schools to deliver mental health services however they wanted.
Despite their dissimilarities, all four studies hinted at improvements in emotional and behavioural outcomes. Beehler 2012 reported that CATS was effective, especially when its various service components (e.g. relationship building, outreach and case management) are used in combination. Finch 2018 reported that, compared to ‘usual’ schools, recovery high schools improved overall abstinence, lowered marijuana use and improved absenteeism. McKenzie 2011 reported positive changes in student functioning, problems and well-being following the introduction of a specialist CAMHS counsellor. In the Wolpert 2013 mixed-methods study, both the RCT and longitudinal components indicated TaMHS provision benefitted children in primary schools but not necessarily those in secondary schools.
B3 psychiatry-derived community hubs
Given there were 28 scoping review documents describing B3 models, it was surprising only two B3 effectiveness studies met the integrative review criteria. Both are relatively recent: Rickwood 2015a explored Headspace Centres in Australia, while O’Keefe 2015 explored an Irish analogue, Jigsaw Centres. Both studies hinted at improvements in both psychological distress and psychosocial functioning. Both, however, were uncontrolled studies. Importantly, Rickwood 2015a noted not all young people benefit from Headspace Centres; around a fifth ended up worse after using them.
Acceptability
Fifteen studies provided acceptability data for collaborative care and four studies provided data for school-embedded mental health services. Again, given the 28 B3 scoping review documents, it is notable that there were no B3 acceptability data for the integrative review. The MMAT quality profile of the group B acceptability studies is somewhat mixed.
B1 collaborative care
For collaborative care, most of the acceptability studies (11) were, again, conducted in the USA, with two UK studies (Bower 2003, Day 2006), one Australian study (Bor 2013) and one Canadian study (Nadeau 2017). Most were < 10 years old. Given the number of controlled studies providing B1 effectiveness data, it is unsurprising to find quantitative satisfaction measures providing much of the acceptability data. Generally, satisfaction data from the controlled and descriptive B1 studies suggest parents (Adams 2016, Bor 2013, Day 2016, Kolko 2012, Kolko 2014, Power 2014) and staff (Adams 2016, Bor 2013, Fallucco 2017, Kaye 2017) are satisfied with collaborative care services. Only two studies (Asarnow 2005/Asarnow 2009, Richardson 2014) – both RCTs – obtained satisfaction ratings from CYP. Both reported an intervention effect on satisfaction at 6-month follow-up but not at later points.
There were some common themes within the B1 acceptability studies, notably – but not exclusively – in the four studies with major qualitative components (Kolko 2012, Nadeau 2017, Richardson 2009, Rodriguez 2019). Issues around access and waiting times were reported, including the value parents (Day 2006), CYP (Richardson 2009) and primary care clinicians (Bower 2003, Fallucco 2017, Rodriguez 2019) placed on the swift access to mental health specialists that collaborative care seemed to bring about. Kolko 2012 emphasised the importance of on-site (co-located) mental health support. Four studies (Adams 2016, Bower 2003, Faullco 2016, Rodriguez 2019) reported on incidental opportunities for the education, training and professional development of non-mental health primary care staff. Several studies emphasised specific qualities of services and/or the staff delivering services, including care continuity (Day 2006, Nadeau 2017), welcoming and easily accessible environments (Richardson 2009, Nadeau 2017), and person-centred approaches underpinned by shared decision-making (Nadeau 2017, Richardson 2019, Rodriguez 2019).
B2 school-embedded mental health services
Of the four B2 acceptability studies, two were UK studies (McKenzie 2011, Scotland; Wolpert 2013, England) and two were US studies (Nabors 1999, Powers 2013). Nabors 1999 is over 20 years old. Acceptability data for two studies (McKenzie 2011, Nabors 1999) were derived from descriptive quantitative studies; the other two (Powers 2013, Wolpert 2013) from substantive qualitative designs. Data were obtained from CYP in three studies (McKenzie 2011, Nabors 1999, Wolpert 2013) and from staff in three studies (McKenzie 2011, Powers 2013, Wolpert 2013).
As with the B2 effectiveness studies, B2 services in the acceptability studies are somewhat dissimilar. Services in two of the studies (McKenzie 2011, Wolpert 2013) have already been described as these studies also provided effectiveness data. The other two studies describe similar approaches: in Nabors 1999, mental health professionals (psychologists) delivered services in a school-based health centre and in Powers 2013, mental health professionals are embedded in schools to both deliver clinical care and work with school staff.
Informants were generally positive about the B2 services. However, access and waiting times were again an issue. Nabors 1999 reported students wanted rapid access to the embedded mental health professional and session lengths and frequencies that suited them. Powers 2013 argues locating mental health professionals in schools enabled vulnerable students to access care they might not have otherwise accessed. Good relationships with mental health professionals were important to both CYP (Nabors 1999) and staff (Powers 2013). Nabors 1999 and Wolpert 2013 additionally emphasised the importance of mental health professionals supporting the development of CYP’s coping and self-management skills.
Cost effectiveness
In a robust and well-conducted analysis, Wright 2016 compared collaborative care for depression (B1) with usual care. Net benefits of 0.04 quality-adjusted life-years (QALYs) [95% confidence interval (CI) 0.02 to 0.09], net cost of US$ 883 (95% CI −US$ 920 to US$ 3759) and incremental cost-effectiveness ratio of US$ 18,239/QALY (95% CI dominant to 24,408) were identified, implying collaborative care was likely to be cost-effective.
Group B evidence summary
Overall, the strongest evidence of effectiveness is for collaborative care (B1). Most of this evidence is relatively recent and derived from controlled studies; there is also cost-effectiveness evidence. In addition, parents and staff seem generally satisfied with collaborative care. However, most of the evidence is from the USA so its applicability to UK health systems is debatable. Despite their dissimilarities, improvements in emotional and behavioural outcomes were evident in all four school-embedded mental health service (B2) studies. Informants were also generally positive about these services. This is important given the recent introduction, in England, of school-based mental health support teams. 93 (These teams were introduced during the lifetime of this study, but not bedded in, so no evidence for them was available.) There is little effectiveness evidence for psychiatry-derived community hubs (B3): the most notable observation here is that some young people might end up worse from using Headspace Centres. There were no B3 acceptability data.
Access and waiting times, co-locating mental health professionals and positive relationships between service users and staff and between multidisciplinary team members were themes common to both collaborative care (B1) and school-embedded mental health services (B2). The qualities of both services and the staff delivering them and incidental opportunities for the professional development of primary care staff were themes within the B1 acceptability data. The importance of developing CYP’s coping and self-management skills was a theme within the B2 acceptability data.
Group C: community-embedded non-specialist Child and Adolescent Mental Health Services
Of the group C models, effectiveness evidence was available for primary care mental health services (C1) and acceptability evidence for primary care mental health services and NGO-derived community hubs (C3). There was no evidence for digital services (C2). As a reminder, C1 services are analogous to collaborative care (B1) services in that they sit in primary care settings. However, C1 services’ mental health staff tend to come from less medically orientated professions like counselling or youth work and they are not always co-located. Similarly, NGO-derived community hubs (C3) are analogous to psychiatry-derived community hubs (B3) except staff come from, and services tend to be embedded within, the non-governmental/third sector rather than the statutory sector.
Four studies provided group C data (see Appendix 5), with two providing effectiveness data, three acceptability data and one cost-effectiveness data.
Effectiveness
The two C1 effectiveness studies are from Australasia, and both are relatively recent. Clark 2014 studied Your Choice in New Zealand, a service facilitating the collaborative, multidisciplinary triage of CMHPs. In an Australian RCT, Rapee 2017 compared a three-step approach for anxious youth (low-intensity self-help → the Cool Kids programme → individual CBT) with just its intermediate level, Cool Kids. The Clark 2014 study provides some effectiveness evidence: those completing Your Choice reported significant improvements from intake to completion in psychosocial functioning, reduced risk of mental health concerns and reductions in substance misuse. Rapee 2017 reported that, in terms of symptom reduction, stepped care was not superior to Cool Kids alone but may require less therapist time for equivalent outcomes.
Acceptability
The two C1 acceptability studies are also from Australasia and, again, both are relatively recent. In the Your Choice study (Clark 2014; described above), CYP anonymously completed a bespoke feedback form. In Bassilios 2017, the Child Mental Health Service of Australia’s ATAPS initiative was investigated via telephone interviews with staff. In the single C3 acceptability study, Walker 2010 employed focus group and one–one interviews with CYP and staff to explore The Junction, a mental health service embedded into an existing English third-sector youth service.
Although there were only three acceptability studies, informants were generally satisfied with the services provided. Access issues were also evident: there was satisfaction with the speed at which appointments were made (Clark 2014) and with venue accessibility (Walker 2010). Other important factors emerging from the group C acceptability data were the number of sessions available (Clark 2004), flexible services (Bassilios 2017, Walker 2010), user involvement (Walker 2013), linkages and relationships with stakeholders such as schools and GPs (Bassilios 2017) and support for the development of CYP’s coping and self-management skills (Clark 2004). Interestingly, staff informants in Walker 2010 felt their non-statutory role gave them freedom and flexibility in their working processes that a statutory CAMHS role could not.
Cost effectiveness
Chatterton 2019 is a companion paper to Rapee 2017 described above. In a robust and well-conducted analysis, a three-step approach for anxious youth was compared with just the intermediate step, Cool Kids. Rapee 2017 found that young people randomised to the full three-step approach had a net QALY loss of 0.011 (95% CI 0.037 loss to 0.015 gain) compared to those receiving just the intermediate step, and their parents a net QALY loss of 0.002 (95% CI 0.014 loss to 0.010 gain). However, neither difference was statistically significant and, especially for parents, the QALY loss was small. The three-step approach was associated with a net cost saving from both a health sector (AU$ −563; 95% CI −AU$ 1353 to AU$ 643) and a societal perspective (AU$ −1334; 95% CI −AU$ 2386 to AU$ 510). No incremental cost-effectiveness ratio (ICER) was reported. The largest grouping of points on the cost-effective plane were in the southwest quadrant indicating the three-step approach was less costly but also less effective than Cool Kids alone. The lower cost of parental time required to deliver stepped care was a key driver of cost savings from the societal perspective. While there was no significant difference in the benefit of either approach, there were potentially lower costs associated with stepped care. Differences in costs were not statistically significant, however.
Group C evidence summary
Regarding effectiveness and cost effectiveness, only two C1 studies met the inclusion criteria. It is thus difficult to draw firm conclusions about the effectiveness or cost effectiveness of group C services. Despite the limited number of group C acceptability studies, there were some common themes relating to access, linkages and relationships with stakeholders, the number of sessions available to CYP, service flexibilities, user involvement and support for the development of coping and self-management skills.
That no evidence for digital services (C2) met our inclusion criteria is noteworthy especially since, as noted in Chapter 4, the COVID-19 pandemic provided an external stimulus for the expansion of such services. We suspect there will be increased interest – and research outputs – associated with C2 services over the next few years.
Group D: in/outreach
As a reminder, the service is taken directly to the user in group D models. Where the user is a CYP or their caregivers, the service is one of consultation; where the user is another (non-mental health) professional, the service is one of liaison. 68 Hence, consultation-liaison is a key component (indeed, as reported in Chapter 4, a key feature) of all group D services. Models within this group are distinguished largely by the setting in which consultation-liaison takes place: the home (D1), schools (D2), the community at large (D3) and hospitals (D4).
Twenty-four studies provided group D data (see Appendix 5) with 13 studies providing effectiveness data, 15 acceptability data and 1 cost-effectiveness data. Four studies provided more than one data type. Four studies considered outreach to home (D1), 10 schools outreach (D2), 7 community outreach and liaison (D3) and 3 paediatric liaison (D4).
Effectiveness
Four studies provided effectiveness data for outreach to home, five for schools outreach, and two each for community outreach and liaison and paediatric liaison.
D1 outreach to home
These are services delivered in the CYP’s own home or alternative to home. While crisis care approaches fit here, only studies with populations falling within our definition of CMHPs were included. A recent, complementary NIHR study (led by research team member Evans) considers crisis care in CYP in more detail. 94
Three of the four D1 studies (Duffy 2014, Evans 1997/Evans 2003, Wilmshurst 2002) focus on home-based crisis care; the other (Tischler 2002) focuses on an outreach service for homeless families. Two are UK studies (Duffy 2014, Tischler 2002) and two from North America (Evans 1997/Evans 2003, USA; Wilmshurst 2002, Canada). Two are RCTs (Evans 1997/2003, Wilmshurst 2002), one is a controlled study within a mixed-methods design (Tischler 2002) and one is an uncontrolled study (Duffy 2014). All except Duffy 2014 are more than 15 years old.
The D1 effectiveness studies hint that home-based outreach may be effective for CYP experiencing various CMHPs, though our MMAT appraisals suggest not especially robust studies. In a RCT, Evans 1997/Evans 2003 compared three different approaches to home outreach finding all three equally successful in preventing hospitalisations and keeping young people in the community. In another RCT, Wilmshurst 2002 compared a family preservation programme having intensive home support workers available 24/7 with a 5-day residential programme. At 1-year follow-up, significantly higher percentages of family preservation children showed reductions in ADHD, anxiety and depression symptoms, whereas a significant proportion of residential children showed clinical deterioration.
Of the UK studies, Tischler 2002 compared homeless families in England receiving a specialised outreach service with a control group of homeless families not receiving the service. Tischler 2002 found that while parental well-being decreased in both groups, outreach children had a significantly higher reduction in Strengths and Difficulties Questionnaire (SDQ) scores than control group children. In an uncontrolled Scottish study, Duffy 2014 reported on the effectiveness of the Lothian CAMHS intensive treatment service, finding positive changes on a range of child-focused outcomes including functioning, symptomatology, self-concept and quality of life.
D2 schools outreach
Schools outreach differs from school-embedded services (B2) in that mental health staff are ‘visitors’ rather than permanent staff members. Four of the five included D2 studies were US studies (Atkins 2006, Atkins 2015, Gilliam 2016, Holmes 2015), with the other from Singapore (Cai 2016/Lim 2017). Apart from Atkins 2006, most studies are relatively recent. Three studies were RCTs (Atkins 2006, Atkins 2015, Gilliam 2016); the other two (Cai 2016/Lim 2017, Holmes 2015) were uncontrolled descriptive studies.
Most studies focused on behavioural disorders like ADHD, oppositional defiant disorder (ODD) and conduct disorder. Most targeted primary school children, with two (Gilliam 2016, Holmes 2015) focusing on early childhood. All involved mental health professionals working with teachers and other education staff. In addition, Atkins 2006 and Atkins 2015 involved parent advocates and ‘key opinion leader’ teachers – teachers other staff used informally for advice about students.
Generally, included D2 studies suggest schools outreach approaches are effective, especially for externalising behaviour. However, according to our MMAT appraisals, most had significant quality limitations.
D3 community outreach and liaison
In these models, mental health experts consult/liaise with non-mental health specialists in the wider community, for example, those working in schools and colleges, primary care, youth services and religious organisations. Staff in D3 services tend to have a wider remit than the other forms of outreach.
Two D3 effectiveness studies were included (Callaghan 2004, Window 2004/Vostanis 2006), both English and both exploring the ‘PMHW’ role. Primary mental health workers were designated workers acting as a bridge between non-mental health specialists and formal CAMHS. Both studies hinted PMHWs might be effective, though both are over 15 years old. Callaghan 2004 focused on looked-after CYP in an uncontrolled study, finding at 5-month follow-up significant improvements in adult-rated child emotional problems and child-rated peer relationship problems. Window 2004/Vostanis 2006 compared PMHWs in two ‘family support’ services against usual services. Referral to one family support service was open, while referral to the other was facilitated via social services. The study found both family support models provided earlier responses and both resulted in reductions in HoNOSCA and SDQ scores. Of the two models, the open referral model was more accessible; the social services facilitated model, however, was associated with significantly more positive child behaviour and family life outcomes.
D4 paediatric liaison
D4 services are hospital-based services – such as A&E liaison and joint clinics – that aim to improve care through the integration of physical and mental health care. Two D4 effectiveness studies were included, both North American.
A relatively recent, uncontrolled retrospective study (Holder 2017; USA) found using mental health social workers alongside paediatric emergency physicians significantly reduced length of emergency department stay. In a much older ‘natural’ experiment (Parker 2003; Canada), a psychiatrist introduced urgent phone consultations with non-mental health staff or emergency appointments with CYP and families in a ‘rapid response’ model. The psychiatrist’s availability varied over time; consequently, so did the service. Admissions from the emergency department to adolescent inpatients dropped when the rapid response service was available and rose when it was suspended.
Both D4 studies suggest having mental health experts working with emergency departments can reduce the length of emergency department stay and the likelihood of inpatient admission.
Acceptability
Only one study provided acceptability data for outreach to home, six studies provided acceptability data for schools outreach, six for community outreach and liaison and two for paediatric liaison. The MMAT quality profile for these acceptability studies is perhaps the best of all the model groups.
D1 outreach to home
The single included study (Tischler 2002), concerning an outreach service for homeless families, has already been described above. Informants (staff and parents) had generally favourable opinions about the service, especially regarding its accessibility.
D2 schools outreach
Three of the six included D2 acceptability studies were conducted in England (Gowers 2003, Hunter 2009, Rothi 2006) with one each being conducted, respectively, in Australia (Corboy 2007), the USA (Lee 2017) and Singapore (Lim 2017). Most of these studies are more than 10 years old. Most D2 acceptability data came from staff informants and most described services whereby mental health professionals provided in-school consultation to CYP and/or their families and liaison to other professionals. The exception was Rothi 2006 who described a liaison-only service in which teachers were trained by mental health professionals to deliver basic mental health consultations.
While staff seemed largely satisfied with D2 services (Corboy 2014, Hunter 2009, Lim 2017), getting access to their mental health counterparts was sometimes a source of dissatisfaction (Gowers 2004, Rothi 2009), though having a link person with whom to liaise could resolve this (Gowers 2004, Hunter 2009). Liaison, whether formal or informal, was especially valued by staff (Gowers 2004, Hunter 2009) and often helped school staff’s professional development (Lee 2017); Rothi 2006 noted, however, that teachers felt their expertise with CYP was often undervalued by mental health liaison staff.
D3 community outreach and liaison
Of the six included D3 acceptability studies, four (Bower 2003, Callaghan 2003a, Callaghan 2003b/Callaghan 2004, McDonald 2004) are from England. Of these, three (Callaghan 2003a, Callaghan 2003b/Callaghan 2004, McDonald 2004) concern the PMHW discussed above; the fourth (Bower 2003) was discussed earlier as it also considered collaborative care (B1). The remaining two studies (Sarvet 2010b, Sheldrick 2012) focused on the Massachusetts Child Psychiatry Access Project, a liaison service to paediatricians, family practice physicians and nurse practitioners in community settings. All D3 acceptability studies had professionals as informants; only Callaghan 2003b/Callaghan 2004 included caregivers and CYP as additional informants. Acceptability data were obtained from surveys in four studies (Bower 2003, Callaghan 2003a, Sarvet 2010b, Sheldrick 2012) and qualitative methods in the remaining two (McDonald 2004, Callaghan 2003b/Callaghan 2004).
The D3 acceptability data identified access and waiting times as an issue, either as a source of dissatisfaction (Bower 2003, Callaghan 2003b/Callaghan 2004) or as a valued service aspect in that users tended to be satisfied when they could obtain access (Callaghan 2003a, Sarvet 2010b, Sheldrick 2012). In addition, organisational barriers such as unclear role expectations (McDonald 2004), lack of user involvement (Callaghan 2003b/Callaghan 2004) and lack of information (Bower 2003) were seen as threats to the successful implementation of these consultation-liaison services.
D4 paediatric liaison
Two studies provided D4 acceptability data, both from Canada and both quantitative descriptive designs. Lee 2014 described an alternative to the use of on-call psychiatry in emergency departments by employing a social worker directly in the emergency department. The rapid response study described above (Parker 2003) also provided effectiveness data. Given the limited D4 acceptability data, no clear themes emerged though Lee 2014 noted that parental satisfaction was associated with waiting time and appointment length as well as the degree to which parents felt listened to by consultants and Parker 2003 reported staff were positive about the rapid response model which implies quick access to mental health expertise may be important in improving services.
Cost effectiveness
Cai 2016/Lim 2017 explored ‘REACH’, a Singaporean schools outreach (D2) service, conducting a cost-effectiveness analysis by comparing some of those with ADHD who entered REACH and who were subsequently referred to hospital-based outpatient care with those who remained within community-based care. Because of poor reporting in the two papers, it is hard to tell whether ‘community-based care’ meant simply continuing to receive the service in school as a consultation-liaison service or whether additional options were available. A negative ICER of SG$ 18,303/QALY was reported suggesting that the community service was likely to be cost-effective (i.e. lower net costs and greater net health benefits than hospital-based care). However, the study has vital information missing (e.g. perspective, time horizon, what costs were included, allocation to hospital vs. community care) and only a very small number of participants (18) contributed data. Although the study met the review’s inclusion criteria, its methodological issues are so great no robust conclusions can be drawn.
Group D evidence summary
Although the MMAT appraisals for the group D effectiveness studies indicate that most have significant limitations, there are consistent suggestions outreach approaches are effective. Access was a common theme across the group D acceptability data, as was the value of liaison provided by mental health staff. It was difficult to determine the value of consultation (i.e. services provided to CYP and/or parents) because there were few CYP or parent informants. The single cost-effectiveness study was disregarded because of poor reporting.
Group E: ecological models
As a reminder, these are models stressing the importance of the CYP’s ecosystem when delivering services. While the literature on ecological models is relatively widespread, most of it was ineligible because it focused on populations with severe and complex mental health problems (often regarding youth offending) rather than CMHPs. Wraparound approaches (E1) are collaborative, team-based approaches to service and support planning for CYP with complex needs and their families; MST (E2) is a ‘family-ecological’, community-based model targeting young people aged 11–17 years at risk of placement in care or custody.
Seven studies provided group E data: six provided effectiveness data, and one acceptability, data (see Appendix 5). Four studies focused on wraparound approaches and three on MST. Since wraparound may simply be a system-level analogue of MST (which operates at individual level),74 we discuss the two approaches together.
Effectiveness
Three of the group E effectiveness studies considered wraparound approaches (Cordell 2017a, McKay-Brown 2019, Painter 2012), and three MST (Painter 2009, Rowland 2005, Sundell 2008/Löfholm 2009). Four are US studies (Cordell 2017a, Painter 2009, Painter 2012, Rowland 2005), the other two from Australia (McKay-Brown 2019) and Sweden (Sundell 2008/Löfholm 2009). The wraparound studies are relatively more recent than the MST ones.
Cordell 2017a reported reductions in crisis service use; Painter 2012 found that wraparound can improve functioning, strengths and mental health symptoms in CYP. Both studies, however, note that it is difficult to identify which of the many wraparound components might be responsible for any effects. McKay-Bown 2019 investigated wraparound for school-refusing CYP, finding that it may help the return to mainstream school. The wraparound studies thus suggest that wraparound is effective, though all three studies were uncontrolled. The two US MST studies (Painter 2009, Rowland 2005) suggest that MST is effective, but the Swedish study (Sundell 2008/Löfholm 2009) found MST to be no more effective than usual care.
Acceptability
Only a single group E acceptability study was included, a relatively recent Canadian study (Bartlett 2018) looking at school-based wraparound. Data were collected from parents as well as a range of staff. While it is difficult to draw conclusions from a single study, the study does suggest that schools are ideal wraparound environments because they are accessible, non-stigmatising, closely connected to the community and because staff have daily contact with CYP.
Cost effectiveness
No cost-effectiveness data were available for any group E model.
Group E evidence summary
There are hints that ecological models may be effective especially for wraparound approaches. The wraparound data are reasonably recent, though derived from uncontrolled studies. The data for MST are old and more equivocal. The single acceptability study means it is hard to draw conclusions about wraparound’s value, especially since no perspectives from CYP were obtained.
Group F: demand management models
Group F services focus on managing demand, flow and capacity in children’s mental health services, often in the face of long waiting lists. Demand can be managed at organisation level (F1) or at patient level (F2).
Seven studies provided group F data (see Appendix 5), four provided effectiveness data and six acceptability data. Three studies provided both effectiveness and acceptability data. There were six F2 studies and only one F1 study. All F2 studies described a ‘brief intervention and action’ approach. The single F1 study (Robotham 2010) focused on the CAPA.
Effectiveness
No effectiveness evidence was available for organisational-level demand management (F1). The four patient-level demand management (F2) effectiveness studies were conducted in four different countries. Barwick 2013 explored a Canadian walk-in centre offering brief therapy, finding an effect on total mental health problems and internalising behaviours. Heywood 2003 explored an English ‘2 + 1’ service offering two initial sessions and a single follow-up session, finding a decrease in symptoms and increase in functioning between the first and final sessions. McGarry 2008 report on an Irish service offering a single session with an option for a follow-up session finding that, compared to usual care, it was effective at 3-month and 6-month follow-ups on a range of mental health and other outcomes. Wagner 2017 explored an Australian service offering a maximum of six sessions over a 3-month period and, while usual care was found to be equally effective in terms of symptomatology, their brief intervention service needed fewer paid resources and was accessed faster. Three studies (Barwick 2013, McGarry 2008, Wagner 2017) were controlled studies and two (Barwick 2013, Wagner 2017) are < 10 years old.
Thus, there is consistent evidence from several countries that brief interventions may be effective, be less resource intensive and serve as intended in reducing demand on specialist CAMHS. Two of the studies (Barwick 2013, Heywood 2003), however, were of questionable quality according to our MMAT appraisals.
Acceptability
The single F1 acceptability study (Robotham 2010) provided staff perspectives on CAPA. Staff reported CAPA reduced waiting lists for families coming into the service, but once in the service (i.e. after an initial ‘choice’ meeting), they experienced bottlenecks in accessing follow-up ‘partnership’ (treatment) sessions. This suggests CAPA may merely shift a lengthy wait from an earlier to a later part of the patient journey.
There were five F2 acceptability studies. On top of the three F2 effectiveness studies which also had acceptability data (Barwick 2013, Heywood 2003, McGarry 2008), a further two studies, both English, provided acceptability data. In a relatively recent study, Gallagher 2015 explored a service offering a maximum of six sessions. Stallard 1998 explored a brief therapy approach requiring families to positively confirm their wish for an appointment and/or attendance at it.
Barwick 2013 and McGarry 2008 both reported no statistically significant differences in satisfaction between the services studied and usual care. Both had data from CYP: Barwick 2013 emphasising the importance of immediate access and McGarry 2008 of not having lengthy waiting times. In the other three F2 acceptability studies, there was a consistent theme of CYP/parents generally being satisfied with services but also having reservations about access and waiting times. For example, Heywood 2003 reported parents were glad they did not have to wait, Gallagher 2015 identified difficulties accessing the service as a barrier and Stallard 1998 found parents were dissatisfied with the wait for a first appointment. Gallagher 2015 also reported that families want more information before sessions and that more sessions would be useful, although the latter is contrary to a supposedly brief interventions approach.
Cost effectiveness
No cost-effectiveness data were available for any group F model.
Group F evidence summary
There is consistent evidence from several countries that patient-level demand management – specifically, brief intervention approaches – may be effective, less resource intensive and serve as intended in reducing demand on specialist services. Waiting times were seen as a barrier to services and seem to be connected to whether a demand management service is seen favourably or not.
Group G: service transformation frameworks
As a reminder, group G service transformation frameworks are less rigid and more flexible than the models in groups A–F, tending to provide ‘scaffolding’ to services.
Only two of the seven service transformation frameworks identified in our typology had any effectiveness or acceptability data: systems of care (G1) and ARC (G5), both US models (see Appendix 5). Nine studies provided data for these two models, six studies providing effectiveness, and four acceptability, data. Only systems of care had acceptability data.
Effectiveness
Six studies provided effectiveness data, three each for systems of care and ARC.
G1 systems of care
Systems of care is an approach to the delivery of children’s mental health services based on 13 guiding principles. While wraparound (E1) is a means through which systems of care operates, wraparound services can exist independently of a system of care.
One of the first systems of care was the Fort Bragg initiative (Lambert 1996). Lambert 1996 compared a children’s mental health service for military families operating under a system of care (Fort Bragg) with services for military families (at Forts Stewart and Campbell) operating without any formal framework, finding neither approach provided superior results. The two more recent systems of care studies (Champine 2008, Manteuffel 2002) both report significant improvements in CYP’s general behaviour and functioning, from intake to follow-up, but since both are uncontrolled studies, the effect cannot be confidently attributed to systems of care.
G5 availability, responsiveness and continuity
Availability, responsiveness and continuity is a framework in which change agents are trained to work at community, organisational and individual levels in order to bridge gaps between social context and technology. All three ARC studies are reasonably robust RCTs (see our MMAT appraisals) and all are < 10 years old. Findings from these RCTs consistently support the notion that organisational factors can not only improve youth mental health and functioning outcomes (Glisson 2013, Glisson 2016) but also organisational outcomes like staff morale and job satisfaction (Glisson 2012).
Acceptability
The only group G acceptability data were for systems of care. Three studies obtained information from parents (Champine 2018, Heflinger 1996, Measelle 1998), another information from staff (Powers 2011). Champine 2018 investigated an early childhood system of care finding there was no universal agreement on the most helpful aspect of services, but many parents found family support and parenting skills education to be the most helpful. Heflinger 1996 provided acceptability data from the Fort Bragg initiative noting parents were significantly more satisfied with Fort Bragg services on access and convenience, explanation and process, waiting times, involvement and relationships with staff. Measelle 1998 explored satisfaction with case managers in systems of care, finding greater monthly contact with case managers predicted satisfaction. Powers 2011, a ‘microethnography’ study involving just two staff informants, found many challenges to systems of care because of their ‘multilayeredness’: challenges included role conflicts between staff from the various organisations in a system of care, governance overlaps, leadership stability and the system of care’s sustainability.
Cost effectiveness
No cost-effectiveness data were available for any group G framework.
Group G evidence summary
Of the two frameworks for which we had evidence, there was only robust effectiveness evidence for ARC (G5). The acceptability data, available only for systems of care (G1), are difficult to interpret, perhaps because as the architects of systems of care point out,80 systems of care are different in every community so it is difficult to evaluate them in the same way. Nonetheless, data around access and waiting times, contact time with services and improving the self-management skills of parents were evident in the G1 acceptability data. Interestingly, no evidence met our inclusion criteria for any other G framework including the two mentioned in the commissioning call, (i) THRIVE (G3) and CYP-IAPT (categorised within G4).
Overall evidence for the typology models
Overall, there was effectiveness evidence only for collaborative care (B1), outreach approaches in general (D), brief intervention services in patient-level demand management (F2) and the ARC (G5) service transformation framework. The strongest effectiveness evidence was for collaborative care, particularly for CYP with depression or ADHD. Collaborative care also appears to be cost-effective. However, since most collaborative care evidence was from the USA, applicability to UK health systems is debateable.
No model was more acceptable than others. Nonetheless, there were some cross-cutting themes highlighting what CYP, parents and mental health professionals expected from services. These themes are: (1) access, particularly regarding waiting times and service location; (2) professional development of staff, in that several models (mostly in groups B and D) provided staff with incidental opportunities for gaining knowledge about, or developing professional skills in, CYP’s mental health; (3) the qualities of services and the staff delivering those services, a theme covering factors such as physical environment, availability of information about a service and its processes, staff child-centredness, degree of CYP/parental involvement and care continuity (e.g. seeing the same staff); (4) positive relationships, in that good services appeared to be predicated on good relationships, both between staff and service users and between the different professionals involved; and (5) the facilitation of self-management skills, in that CYP and parents wanted services to provide them with skills to help themselves.
Our integrative review findings suggest that effective and acceptable services for CYP experiencing CMHPs are often underpinned by: few barriers to access; some degree of interagency working (interagency working is central to both collaborative care and outreach approaches and is reflected in the ‘positive relationships’ theme above); the use of consultation-liaison (a key aspect of group D models, and which often contributes to staff professional development); and a consideration of a service’s wider culture (reflected in the ‘qualities of services’ theme). Brief intervention approaches may be especially good at managing waiting lists (and so improving accessibility); given their brief nature, they may also facilitate the acquisition of self-management skills.
Chapter 7 Collective case study of services
This chapter focuses on Work Stream 3, in which we conducted a collective case study of services for CYP experiencing CMHPs in England and Wales. The chapter starts with an outline of the research methods used in Work Stream 3. A brief overview of the individual case study sites then follows, after which we present our findings, organised around three cross-cutting themes.
Methods
Research questions
The case study addressed research objectives 3, 4 and 5 and these research questions:
-
What are the barriers and enablers that CYP and their families and carers experience in accessing and navigating services for CYP experiencing CMHPs in England and Wales?
-
What factors determine whether a service is perceived as viable, accessible, appropriate and effective?
Design
The design was a collective case study. In case study research, a phenomenon is examined in its real-life context with the goal of describing that phenomenon in depth or explaining it. 95 Collective case studies are those in which multiple cases are studied, either simultaneously or sequentially, to illuminate contextual issues relating to the phenomenon. 95 ‘Case’ is a broad concept and may be an individual, an event, an organisation or a policy, the case in this study being ‘a service for CYP experiencing CMHPs’. Case study research typically involves studying the phenomenon from different perspectives via multiple methods. In line with this, we planned for data to be collected through individual interviews, focus groups, observation and documentary analysis. The COVID-19 pandemic, however, resulted in some necessary modifications to these plans (see Data collection).
Sampling and recruitment
Case study sites
A sampling frame of current services across England and Wales was derived from the service map outlined in Chapter 5. From this sampling frame, we purposively sampled 38 services (26 in England; 12 in Wales) to ensure variability in characteristics such as sector (NHS, non-statutory), locality/setting (urban, rural; home, clinic, school), target age group, mode of delivery (face-to-face, online, telephone) as well as ensuring we captured the spread of models in version 2 of our typology (see Chapter 3). For maximum variation, we also included innovative services (e.g. digital services), services targeting specific specialist groups (e.g. looked-after children), as well as services using models specified in the commissioning brief (CAPA, CYP-IAPT and THRIVE). From this purposive sample of 38 services and in consultation with our SAG, we identified and invited 19 potential sites to participate in the study. Seventeen sites responded within the recruitment time frame, of which three were outside the scope of the study aims. Of the 14 remaining, 9 (5 in England; 3 in Wales; 1 UK-wide) agreed to take part. Online meetings were subsequently held with these sites to negotiate access.
Participants
At each case study site, we aimed to recruit a purposive sample reflecting the characteristics of that specific service. We wanted to include younger and older children, parents/carers, CYP and parents who had declined or disengaged from services, staff that reflected the service’s skill mix and those commissioning services. At each site, we aimed to recruit six to eight CYP, two to three parents/carers and two to three staff members or commissioners. The sample inclusion/exclusion criteria are presented in Box 2.
Current or previous service users
CYP (aged 8–18 years)
Young adults (18 + years)
Parents/carers of CYP using services
StaffFront-line staff delivering the service to CYP/families at the case study sites
Service managers at the sites
Those commissioning services at the sites
Exclusion criteriaChildren aged under 8 years
Service users or parents/carers unable to fully understand the study and provide informed consent
At each site, a key contact was identified who could approach potential research participants and provide them with information about the study, which was supplied via letter, e-mail or, in the case of CYP and parents, directly when attending the service. For CYP under 16 years, information about the study (including a CYP information leaflet) was first sent or given to parents; only with parental permission were CYP contacted to discuss participation in the study. At some sites, we placed advertisements on the service’s website to alert potential participants to the study.
A range of information sheets for different participant groups were developed with our SAG and some additional young people and parents. All written recruitment materials were available in both English and Welsh. To increase the accessibility of information and allow potential participants to ‘see’ the researchers and young co-researchers prior to taking part (since COVID-19 restrictions prevented the research team physically visiting sites), we created, with the young co-researchers, a video to supplement the written information sheets. This video was hosted on the study website along with the relevant participant information sheets. Site key contacts were asked to direct potential participants to this website.
After receiving information about the study, potential participants were asked to contact the research team directly to indicate their interest in taking part. The research team then further discussed the study with them and, if they wished to take part, arranged a convenient interview time. Attempts were made to recruit CYP who had declined or disengaged from services, but this was unsuccessful.
Data collection
We planned to use several methods to collect data at our case study sites: individual interviews (in person, by telephone or through videoconferencing); focus groups; documentary review (of operational manuals, for example) and, where possible, observation (of, e.g. referral meetings, initial assessment reviews, team meetings and interventions with CYP).
Because of the COVID-19 pandemic, all primary data collection (apart from one interview) was collected remotely. Participants agreeing to an individual interview could choose between a telephone interview or a Zoom or Microsoft Teams videoconferencing interview. We did manage to conduct one group interview with CYP. Semistructured interviews were conducted with CYP, parents and service providers/managers. Topic guides (see additional files www.fundingawards.nihr.ac.uk/award/17/09/08; accessed 26 March 2024) were developed using the study’s aims and objectives and in consultation with our SAG. The broad purpose of the interviews was to capture participants’ experiences of the service and their perceptions of its appropriateness, accessibility and effectiveness. Interviews with service providers and commissioners also explored areas relating to service development and delivery.
In total, 96 interviews involving 108 participants were conducted. Eighty-three were conducted via Zoom/Microsoft Teams, 12 by telephone and 1 face to face after the COVID-19 restrictions were relaxed. With participant assent/consent, 90 interviews were recorded using encrypted digital audio recorders. Six participants (five CYP, one parent) did not consent for audio-recording and notes were taken instead. For participating, CYP and parents were offered a £10 gift voucher as a token of appreciation. Of the 96 interviews, 87 were individual, 8 were dyadic CYP–parent interviews and 1 was a group interview with 4 CYP. Twenty-two interviews were conducted jointly by the young co-researchers. Mean interview length was 56 minutes (range 31–84 minutes).
COVID-19 restrictions meant we could not conduct observations of any activities at the sites, and it proved difficult to negotiate observing meetings held via videoconferencing. However, relevant, freely available documents about the service were collected from each site to provide contextual and background information.
We collected data about annual service delivery budgets and funding source. We also requested information about key areas of spending and resource use including staffing and the number of CYP using the service. We had planned to collect data on user costs (travel costs to services and out-of-pocket expenses); however, given CYP and parents were not visiting services in person because of COVID-19 restrictions, these cost data were not collected.
Data analysis
Interview audio-recordings were transcribed and imported into NVivo 11 (QSR International, Victoria, Australia). Data analysis occurred in parallel to data collection and was informed by framework,96,97 a matrix-based analytic method widely used in qualitative health services research. Framework has five stages: familiarisation; identification of a thematic framework; indexing; charting; and interpretation. The core qualitative research team (Evans, Fraser, Kirk, Lane) and the young co-researchers read and discussed the transcripts in detail to familiarise themselves with the data and identify any areas requiring further exploration in future interviews. The data were then coded deductively (‘indexed’) in NVivo using a thematic framework based on the study’s aims and objectives, after which the data were ‘charted’ by the core qualitative research team and young co-researchers. Team members charted the data independently before meeting to agree the final charts. Charting enabled the deductive coding for each theme to be examined within each case study site and comparatively across sites (see Appendix 7 for an example chart). The data were then analysed inductively and iteratively by the team to identify, and agree on, a set of cross-cutting themes. Examining the dimensions of these themes, exploring relationships between them and searching for explanations allowed us to interpret them.
Site cost data were summarised into a table (see Service costs). For NHS sites, staff costs were estimated by multiplying the number of working hours by the NHS unit cost per hour98 for the respective pay band. Staff costs for non-NHS sites could not be calculated because equivalent cost data were not available.
Research ethics and governance
Ethical and other approvals for Work Stream 3 were granted by the NHS Health Research Authority (reference: 20/SC/0174) and by the organisations operating the services at the case study sites. Four substantial and two minor amendments were subsequently approved, all relating to the COVID-19 pandemic.
A range of information sheets and assent/consent forms were developed for different participant groups, co-designed with young advisors and SAG members. Written or verbal informed consent (or assent for children under 16 years) was obtained from all participants. For children under 16 years, parental consent was obtained as well as the CYP’s assent. However, the final decision on participating rested with the CYP. Consent/assent was regarded as a continual process with attention paid to any nonverbal signs suggesting participants no longer wished to take part.
Given there was a risk some participants might become distressed when describing difficult personal experiences and that safeguarding disclosures might occur during an interview, distress and debrief procedures were developed (see additional files www.fundingawards.nihr.ac.uk/award/17/09/08; accessed 26 March 2024) to ensure that participants were supported both during and after participation in the study.
Information and data were handled in line with UK General Data Protection Regulations and the Data Protection Act 2018. All data from, and about, services and participants were anonymised. Transcripts were password-protected and securely stored. Case study sites are referred to by a number rather than name. Participant quotes are attributed using a code reflecting the site, participant type and individual participant, for example, CYP04-34 = a CYP participant at Site 4, SP09-46 = a staff (service provider) participant at Site 9 and P05-35 = a parent participant at Site 5.
The case study sites
For brief descriptions of the case study sites, see Box 3; for a summary of their characteristics, see Table 7. Detailed case study site descriptions can be found in Appendix 8.
| Site | Model(s) | Sector location | Setting | Target group(s) | Referral route | Mode of delivery Times of operation |
|---|---|---|---|---|---|---|
| 1 | C3, D3 | Third Wales; urban/rural |
Community (non-health); schools | CYP aged 10–18 years experiencing mental health difficulties; families; LGBTQ+ and ethnic minorityCYP with trauma aged 10–25 years | Self/family; professionals | Face to face; remote Monday–Friday, working hours |
| 2 | D2 | Third UK-wide; urban/rural |
Schools (outreach) | CYP aged 13–19 years scoring 20 + on CES-D scale | CES-D scale (in school) score of 20 + | Face to face (when schools open); remote during the pandemic Monday–Friday, working hours |
| 3 | C1, D3, G6 | Third England; urban/rural |
Community (non-health); schools | CYP aged 5–21 years experiencing mental health difficulties | Self/family; professionals | Face to face; remote Sunday–Friday, extended hours |
| 4 | C2, G3 | Private (plc) UK-wide; urban/rural |
Online | CYP aged 10–25 years with mental health problems | Self-referral in commissioned areas | Remote 24/7 web resources; live chat 8 a.m.–10 p.m. |
| 5 | A1a, A1b, B1, D3, E1, G3, G4 | Statutory England; urban/rural |
Community health-based site; some outreach to other community settings | CYP aged 0–19 years (up to 25 years for care leavers) with CMHPs; + specialist ADHD service | Professionals | Some face to face (high risk; ADHD assessments) plus remote Monday–Friday, working hours (7 p.m. Weds) |
| 6 | D1, E1, G2a, G3, G6 | Statutory England; urban |
Home (outreach) | Children in crisis aged up to 18 years | Professionals | Face to face (including during the pandemic) 7 days, 8 a.m.–10 p.m. |
| 7 | A1a, A1b, D1, D2, F1 | Statutory Wales; urban/rural |
Community health-based site; some outreach to other community settings | CYP with mental health problems aged up to 18 years; substance abuse; young offenders | Professionals | Face to face; remote Monday–Friday, 9 a.m.–5 p.m.; crisis team to 9.30 p.m. |
| 8 | D3, E1 | Statutory Wales; urban |
Community (non-health) | Looked-after CYP aged up to 18 with developmental trauma (and carers) | Self/family; professionals | Face to face; remote Monday–Friday, working hours |
| 9 | C3, D3, F2, G2a, G3, G4, G6 | Third/statutory sector partnership England; urban/rural |
‘One-stop shop’ centre and community-based hubs (pre-pandemic) | CYP with mental health problems aged up to 25 years | Self/family; professionals | Mostly remote due to the pandemic but face-to-face returning |
Site 1: Branch of a UK-wide, third-sector mental health organisation providing several different services including school-based outreach, family support, a peer support group and a service supporting ethnic minority or LGBTQ+ CYP with recent trauma.
Site 2: Third sector-led, targeted school-based well-being programme teaching CYP emotional resilience to reduce low mood and anxious thoughts.
Site 3: Third-sector organisation providing peripatetic, open access, one-to-one counselling support to CYP.
Site 4: Private sector online counselling service targeting CYP.
Site 5: Specialist NHS CAMHS providing an emotional well-being and mental health service. Serves a large, mainly rural geographical area.
Site 6: NHS crisis response service providing home- and community-based rapid assessment and brief intensive support to CYP.
Site 7: Specialist CAMHS providing several different services including ‘core’ CAMHS, substance misuse, home treatment and youth offending services.
Site 8: NHS service within a child psychology team focusing on looked-after CYP.
Site 9: Third-sector, Tier 2 service in formal partnership with a local NHS trust acting as a hub for all CYP mental health referrals via joint triage.
Service costs
Resource/cost data reported by the sites are summarised in Table 8. However, these need to be interpreted with caution as there is no comparable measure of benefit or efficiency. Training costs could not be summarised in any meaningful way since they were reported variably by the sites.
| Service model(s) | Total annual cost (£) | No. of CYP using service per year | NHS main funder | Clinical staff description | Staff costsb (NHS/clinical) (£) | |
|---|---|---|---|---|---|---|
| Site 1 | C3, D3 | 250,000 (average) |
Not reported | No | Not available | Not available |
| Site 2 | D2 | 100,000 | 400 | No | Not available | Not available |
| Site 3 | C1, D3, G6 | 1,600,000 | 3300 | No | Counsellor led | Not available |
| Site 4 | C2, G3 | 140,000 | 2160 | ?? | Peer and counsellor led | Not available |
| Site 5 | A1a, A1b, B1, D3, E1, G3, G4 | 2,200,000 | 1551 referrals 1440 discharges |
Yes, direct | Mixed: social worker, clinical psychologist, nurse | 1,711,300 |
| Site 6 | D1, E1, G2a, G3, G6 | 2,827,065 | 1130 referrals | Yes, direct | Nurse led | 1,428,304 |
| Site 7 | A1a, A1b, D1, D2, F1 | Not available | Not available | Not available | Not available | Not available |
| Site 8 | D3, E1 | Not reported | 600 (based on 50 per month) | Yes, direct | Clinical psychology led | 627,372 |
| Site 9 | C3, D3, F2, G2a, G3, G4, G6 | 700,338 | 1999 | Yes, indirect | Therapist led | 535,447c |
For services providing an annual budget or estimated running costs, these ranged from £100,000 to over £2,000,000. Predominantly NHS-funded services typically had larger annual budgets and were larger services. For NHS-funded services, clinical staff costs ranged from £535,447 to £1,711,300. As expected, the main driver of service costs is staff. Of the services who provided staff breakdowns, most were led by a particular group of clinical staff which is reflected in the costs (see Table 8 and Figure 33), although Site 5 had a mixed staffing profile reflecting its multidisciplinary nature (see Figure 33).
FIGURE 33.
Breakdown of clinical staff roles at the NHS-funded sites.

Participant characteristics
Table 9 presents the participant composition at each site. Services at Site 8 focused on parents and hence no CYP participants; similarly, Site 4 focused only on supporting CYP. Difficulties were experienced in recruiting CYP at Site 5. Sites 1 and 9 focused mainly on supporting CYP.
| CYP | Parent/carer | Service provider | Total | |
|---|---|---|---|---|
| Site 1 | 7 | 1 | 4 | 12 |
| Site 2 | 5 | 2 | 9 | 16 |
| Site 3 | 5 | 3 | 3 | 11 |
| Site 4 | 6 | 0 | 2 | 8 |
| Site 5 | 2 | 5 | 5 | 12 |
| Site 6 | 6 | 4 | 5 | 15 |
| Site 7 | 6 | 3 | 5 | 14 |
| Site 8 | 0 | 7 | 2 | 9 |
| Site 9 | 4 | 1 | 6 | 11 |
| Total | 41 | 26 | 41 | 108 |
In total, 41 CYP, 26 parents and 41 service providers participated in the study. Their characteristics are presented in Table 10. The mean CYP age was 17 years (range 9–22 years); almost three-quarters identified as female and 90% were White British. Almost 90% of parent/carer participants were female and most (almost 90%) were White British. Over 90% of service provider staff were practitioners or managers at the service; over 70% were female and 100% were White British.
| Characteristic | CYP (n = 41) | Parents/carers (n = 26) | Service providers (n = 41) |
|---|---|---|---|
| Gender (%) | Female: 30 (73.2) Male: 10 (24.4) Gender fluid: 1 (2.4) |
Female: 23 (88.5) Male: 3 (11.5) |
Female: 29 (70.7) Male: 12 (29.3) |
| Age | Range: 9–22 years Mean: 17 years |
Not collected | Not collected |
| Ethnicity (%) | White British: 37 (90.2) Asian British: 1 (2.4) British Indian: 1 (2.4) Black African: 1 (2.4) White and Black Caribbean: 1 (2.4) |
White British: 23 (88.5) White other: 1 (3.8) Black African: 1 (3.8) Declined: 1 (3.8) |
White British: 41 (100) |
| Role (%) | Not applicable | Not applicable | Practitioner: 24 (58.5) Manager: 11 (26.8) Manager/practitioner: 2 (4.9) School staff: 2 (4.9) Peer support worker: 1 (2.4) Commissioner: 1 (2.4) |
Cross-case analysis findings
From the cross-case analysis, three themes explained participants’ perceptions of the factors influencing the accessibility, acceptability and effectiveness of services. These were: pathways to support; service engagement; and learning and understanding.
Pathways to support: service access and exit
This theme describes referral and assessment processes, the availability of support, the key barriers and enablers influencing access and ‘exits’ from services.
Being referred
Children and young people and parents accessed services via self-referral, professional referral or a mixture of the two. At Site 2, CYP were selected and offered the service based on a screening test (CES-D) result. The three sites not offering self-referral were all NHS services.
For services requiring a professional referral (usually from a GP or school), CYP and parents described the need to present a case that would trigger a referral to CAMHS rather than be normalised or disbelieved:
I phoned up my GP, I said my daughter is attempting to kill herself and wants to kill herself and my GP turned around to me and said children that age don’t kill themselves … [he] said you need to be stronger and you need to have stronger parenting skills.
P05-35
Parents described how it was important to use the ‘right’ language to get a successful referral and explained how they needed to be advocates for their child. As one mother recalled:
You have to really push hard to be able to get the support you actually really need. I’m quite pushy as a person so I do get there eventually … I said she will be a statistic if you don’t help now.
P06-47
Two mothers described being ‘coached’ in how to present their case:
He [nurse] was, like, coaching us what to say. He goes, unless you say this, they are not going to do this for you … say this, this will be the outcome. And that’s why we’ve had the success with getting [daughter] into CAMHS.
P06-47
They were adamant that … her current level of anxiety was not suitable for their service … the school nurse then did say, well, they’ll only really take the referral if they think they’re actually taking it because there’s an issue with her weight not because of the anxiety.
P05-39
At five sites, CYP could self-refer via an online form or by telephone. CYP valued self-referral because they did not have to discuss their feelings with their GP or school to access support and so there was less risk of them being ‘judged’. It also avoided the need for a professional referral which could involve disclosing their difficulties to their parents or discussing them in their presence. While the NHS sites recognised the value of self-referral in improving access, they were concerned that it might also increase demand for their services. Site 5 provides an example:
Are young people taken seriously when they go to try and get a referral? … to have a professional referral, they have to tell school or they have to tell a GP … the referral process I think is definitely a barrier for some. And for families as well … when people go to the GP … and then you get this referral, when you read it back to mum and she’s saying, ‘I didn’t ask for that’.
SP05-10
Do we go to a self-referral system? But then that’s taking people away from actually delivering therapy to young people. So, that means our waiting list is going to go up. So, what do you prioritise, really? It’s difficult, isn’t it? A difficult decision.
SP05-07
Another site had implemented procedures to prevent their service being ‘inundated’ via the online self-referral system:
A young person or a parent has to ring head office … we just check the age of the young person and whether they live in [local area] and then they’re given a password. We can’t not password our online referral form because young people just having a bad day [would] just fill it in and actually never come for counselling, so it kind of prevents us from being overwhelmed … So they’re given a password to access the online referral form and then they have until Sunday evening after … to fill in that online referral form and, if they haven’t filled it in by then, they’d have to ring again to get a new password … We couldn’t just have an open referral form because we’d just be inundated …
SP03-18
Self-referral was predicated on CYP and parents being aware of the service and this referral route. As one young person noted, greater publicity directed at CYP was important because of their perceived reluctance to seek support from GPs:
More publicity about the service because, yeah, I’m pretty sure the only way I found out was through the doctors, and I know there’s a lot of people that don’t like going to the doctors about mental health … So, I don’t know, if it was published in more places or more detail about it, I think that would be better.
CYP09-48
Some sites described how they promoted their service directly to CYP via schools (e.g. in assemblies) and social media. Promoting services via schools was seen as having a greater reach than social media which relied on CYP and families following the relevant channels:
I suppose we try and do as much as we can on social media but … we only have about three or four hundred followers on Instagram … so a lot of [school] students won’t be seeing that, or aren’t following us, so don’t see what we’ve got.
SP01-01
I first found about [Site 4] in college where someone from [Site 4] came and they were talking about how [Site 4] … helped young people and I was feeling very like stressed in terms of college.
CYP04-44
A Site 2 teacher highlighted the importance of providers ‘selling’ services to CYP during school assemblies:
They were very good at delivering their assemblies, the content was really pitch perfect and, you know, I remember the assemblies that ran, you could hear a pin drop around the room. They [students] were listening, they really enjoyed it and that was a really, really positive experience … from the get go it was sold to them because of the way the workers delivered that, that was really positive … they hear the worker and they want to be part of that.
SP02-23
Working with other organisations to raise awareness of a service was also important since CYP could be signposted to the service by colleges, schools, GPs and specialist CAMHS. To support this, one site employed specific engagement leads who planned promotional activities with other services. At Site 1 and Site 7, the presence of an integrated, multiagency referral panel across a geographical district raised awareness of the services available for CYP and helped reduce inappropriate referrals:
Having the [Wellbeing] Panel has meant that we’re actually aware of a lot of the services that we wouldn’t … they’re all on the Panel, we kind of know what they’re doing … it’s good to be able to keep up-to-date of what they’re able to offer … we have noticed since the Wellbeing Panel’s been in place that … we were getting more appropriate referrals.
SP07-31
Sites 2 and 5 described how they had changed the name of their service to better reflect the service provided. For one site, this had involved changing their name from ‘CAMHS’ to a name reflecting a more multidisciplinary approach and one with fewer negative connotations.
Being assessed
Services assessed referrals against eligibility criteria based largely on the nature of the CYP’s mental health problems and, for most services, the locality in which the CYP lived. Sometimes it was unclear whether CYP aged 16 years and above were eligible for the service.
Service providers highlighted the difficulties posed by poor-quality referrals that lacked information, demonstrated poor understanding of the service’s remit or did not have the CYP’s agreement. Poor-quality referrals could lead to delays in accessing appropriate support or the CYP being assessed as not meeting eligibility criteria:
Some of the quality of referrals that we’re getting from the professionals haven’t been particularly great … from some GPs, we’ll just get the real bare bones and it’s hard to identify what the mental health issue is from the information they’ve given us … But actually when you speak to the parents and you get that little bit more information, you see there is [something] but from the information the professionals have given us there’s no evidence of anything going on really.
SP05-15
One parent described how she was unaware of which service the GP was referring her child to and was confused to find they had been referred to several services including CAMHS:
The doctor referred her, but I didn’t know who she was being referred to. She just said she would refer her for counselling and support, so it was very confusing because I had no idea where she was being referred to … I started getting various letters from different services. It was really confusing … they didn’t tell me that she’d been referred to CAMHS; I didn’t know what CAMHS was.
P07-34
Self-referral and involving families during the assessment process facilitated service entry by enhancing the quality of information available to providers. This information enabled providers to understand the contextual issues surrounding the CYP’s problems when assessing service eligibility:
We like self-referrals because there’s more information and it’s bulky, there’s a bigger narrative around what might be going on. And if I’m truthful, I find the referrals that sometimes come from professionals, there’s not the information that we need.
SP09-21
We actually call them, we call the parent, the young person … with this additional information from the young person’s voice or the parent’s voice, they are suitable for our service.
SP05-10
At multiservice sites, service providers described how having a single point of access (SPoA), where referrals were assessed by a multidisciplinary/multiagency team, helped ensure CYP received the most appropriate service for their needs and in a timelier way. A SPoA also reduced duplication and referral rejection:
I think that [the Wellbeing Panel] works really well in getting families the right support in the first instance rather than them traditionally going to the GP, being referred somewhere, being rejected, go back to the GP, being referred again.
SP01-02
This approach to interagency working and shared professional expertise was also important in managing the flow of referrals into CAMHS by identifying those CYP who might not meet the CAMHS threshold and thus needed support from elsewhere:
It might not be that a young person coming through [the Panel] has moderate to severe mental health problems, which is normally what CAMHS would look at, but they would receive a service, whether it’s a community service, whether it’s a primary mental health team, whether it’s one of the charity organisations. So children are assessed and are given the right service for the mental health need that they present with.
SP07-22
If we are running effectively then we ought to be taking the pressure off CAMHS by seeing those young people who are not serious enough to get referred to CAMHS, but actually if you leave them for another year without support then they will be serious enough to get to CAMHS.
SP01-02
However, for CYP and parents, the processes they encountered and navigated via a SPoA could feel complex and confusing if it resulted in multiple assessments and waiting lists. One young person described how destabilising and depersonalising it was being moved between the third sector and CAMHS parts of a joint service as their level of risk was assessed:
I applied to [service name] and then I got an e-mail saying that I had been put on CAMHS … and then I got moved back to [service name] which was annoying … they told me that because I hadn’t self-harmed in three weeks … I wasn’t doing it enough to access CAMHS … obviously if you’re trying to not do that, that’s the last thing you want to hear … you kind of need a bit of stability and not being moved between the services … you kind of just feel like a number, just being like moved around.
CYP09-45
Participants sometimes experienced a lack of information about the service prior to commencing the therapy or programme provide by the service which may be another barrier to accessing and engaging with services. CYP described not knowing what to expect from sessions or not understanding the nature of the service.
Waiting for support
Sites varied in how timely they were in responding to CYP’s needs. At some sites, an assessment led to immediate or rapid access to therapy and support, mainly because of the assessed level of risk or because it was an intrinsic characteristic of the service:
It [an online service] helps because if you have a meeting with the community mental health team at some point later in the week or month or whatever it is but you’re not having a bad day [then] … it’s just not useful. The point of talking to someone is when you’re struggling in the moment, and I think you can get the best help [then] … And that’s what’s so good about these online services is that if I’m struggling now, I can literally just get on now and talk to someone.
CYP04-56
For many, however, an assessment led to a waiting list for support. As noted earlier, some CYP (e.g. those on ADHD pathways) could be on several waiting lists if they were assessed as needing several services or therapies. Waiting lists were seen as problematic by CYP, parents and service providers for the delays they imposed on receiving support. Children and young people described how they felt their mental health had worsened while waiting to be assessed and then waiting to be allocated a therapist. For one young person, the wait led to feelings her mental health difficulties were not valid:
I saw about three different GPs before they actually referred me as urgent. Like, it was urgent but they kept saying oh, well, the waiting list is pretty long so you might be there for a while. So then when I did get on the waiting list I had to wait for an initial assessment and then I had to wait again, months, for an actual worker to be allocated to me, even though it was urgent … that’s really bad because I was waiting months and months on the wrong medication before I could get help … It kind of made me feel invalid …
CYP06-040
The time between seeking and receiving help was also difficult for parents to contend with. Parents described how communication could be poor while on a waiting list which led to uncertainty over when their child would finally access support, a situation that could lead to parents ‘chasing’ and ‘pushing’ for appointments:
I got really concerned about it, and so I contacted CAMHS. I tried calling, I tried e-mailing, but I wasn’t getting anywhere. Nobody was calling me back … there was such a gap between the initial assessment and getting that follow up, and I did chase it … we didn’t see anyone till the middle of April, and that was because I pushed and pushed.
P07-34
One service provider recognised that for parents on a waiting list, services could be seen as not acknowledging their child’s difficulties:
If you’re a parent who’s gone to the GP because you’ve found out your [child] is self-harming, and you’ve got to sit there and wait for a month before anyone even acknowledges, it’s not that we don’t acknowledge it, but it can be really distressing [for them].
SP01-03
Site 3 had introduced a system of contacting CYP on their waiting list to reassure them they had not been forgotten though there was uncertainty about the frequency of contact:
We’d send them a text after four weeks to say, oh, you’re still on our list. But then we got feedback from some of our young people on our advisory group to say that they didn’t feel cared for because it was such a long time since. So we started to send them a text after every two weeks.
SP03-17
Notably, most sites appeared to have a role in managing demand for specialist CAMHS. For some services, the focus was on preventing referral to CAMHS in the first place (e.g. those unlikely to meet entry thresholds); for others, it related to managing and supporting CYP on CAMHS waiting lists or preventing hospital admission. Some service providers noted, however, higher CAMHS access thresholds had resulted in their services increasingly supporting CYP with greater needs.
Availability of support
Children and young people and parents valued services that were available evenings and weekends. Indeed, many felt services should be accessible 24/7. The ability to make direct contact with practitioners when needed rather than waiting for the next scheduled appointment was also important:
They give you a number and you can just ring them whenever you need them and there’ll always be someone there to speak to you.
CYP06-036
I literally had [practitioner] on speed dial at certain times and she’d call me back. Because I just needed that lifeline.
P08-44
The service location’s convenience could also influence access and perceived service availability. Services not requiring travel due to being delivered at home or in schools or which were provided digitally were seen by CYP and parents as more physically accessible. Indeed, during the data collection period, online services expanded significantly at most sites because of the pandemic (except for Site 6 and for Site 4 which was already a wholly digital service). Adding digital provision appeared to promote access to support by removing travel time and costs and boosting appointment time flexibility. However, there were also drawbacks. Home, digital and school-based services could present privacy and confidentiality issues for CYP (see also Privacy and confidentiality) and accessing digital services had financial implications in terms of the costs of equipment (e.g. mobile phones) and internet access. Digital provision could also challenge engagement as some CYP found it difficult to express their feelings via video or in writing. Moreover, text-based counselling could be problematic for CYP with learning disabilities, literacy difficulties or where English was not their first language. Because video appointments can create additional communication barriers for CYP on neurodevelopmental pathways, some parents felt it inappropriate to use video appointments to assess or provide therapy for these CYP.
Exiting services and continuity of support
Sites varied in relation to whether support was offered for a fixed period or for a more individually determined period according to the CYP’s needs. Once support had ended, most services provided families with information about additional local and national support services. Some sites allowed self-referral back into the service rather than expecting families to restart the referral process from the beginning. One parent described how the service had kept the ‘door open’ and another described self-rereferral as ‘a safety net’:
We went back via that route because that door was already open to us. So, you know, at that point, I was like, look, you know, we are struggling … they are like actively keeping the door open to their service for me.
P08-41
That reassurance again that they were there, we could always go back to them if we were really struggling … For me, it was that bit of a safety net, that comfort that, yes, we’re not struggling with this on our own, they are there.
P06-32
Receiving follow-up contact from services after exiting a service was valued by CYP and parents. One CYP felt reassured the service was planning to ‘check-in’ with her 3 months after discharge to see if she wished to resume therapy; another stated follow-up contact would have made her feel cared for and valued:
In about three months’ time … they’re going to do like a check-in meeting. Me and the therapist that I had are going to be like, hey, how are you doing? Do you want to go back to therapy now or are you feeling a lot better or worse? … It doesn’t feel like they’re just sending me off on an adventure … it feels like they’re actually there, in case I need it.
CYP09-53
She [CYP02-52] said that after the last session, she had been sent a certificate and a stress ball but that there was no further follow-up or contact [with the service]. What she would have really liked … is for the practitioner to follow-up with her after a short period, to check in and see how she was doing … she said if the programme incorporated a follow-up element, it would ‘make me feel I’m important in their eyes and that they care about me’.
CYP02-52; researcher notes
Another CYP would have liked to have remained in contact with the service after being formally discharged rather than being handed over ‘like a basketball’ to another service:
It would be nice if [service] would directly call me, maybe at, like, two weeks later and then a month later, or, you know, come back to the house and see me again. Because it’s almost like they’ve just dropped me off and handed me over to somewhere else now; it’s like I’m a basketball being thrown around. And, like, maybe I’ll stay at one basketball post for longer than the other, but, you know, still slowly deflating.
CYP06-29
Some CYP moved from the service to their local specialist CAMHS due to worsening mental health. However, this service transfer could lead to duplication and delays in receiving appropriate support:
I waited about 11 months [for CAMHS] … it was a very long time. Considering that, I mean, I was quite ill then … I had a choice appointment, and the lady in that basically said to me like, yeah, like … we’ll get you in the system and we’ll get you on some medication. I then waited another, like, six months and had my first appointment through. And they were like oh, we can offer you eight weeks of CBT. And no mention of medication. And I was like well, I’ve just done like 18 months of that already.
CYP03-12
In Site 6, aftercare was planned via a post-discharge support pathway. However, difficulties could still be experienced in transferring CYP to specialist CAMHS, especially in terms of waiting lists and meeting eligibility criteria. Non-NHS sites continued to support young people after they reached 18 years, whereas there was a perceived service gap for those aged 16 and 17 years in some NHS services. Most NHS sites stopped supporting young people once they reached 18 years and some would not accept new referrals from those aged 16 years and above:
The 16- to 18-year-olds, that’s a challenge in some [areas] … where they don’t have a fully comprehensive CAMHS … so we’ve identified that this young person’s got a mental health need but … they might not typically meet the criteria for an adult service and there’s no CAMHS … in that 16 to 18 gap.
SP06-19
Interestingly at Site 9, a multiagency site, services provided by the third-sector partner continued to support young people up to 25 years, while NHS services stopped at 18 years. Extending services beyond 18 years can still create difficulties, however, if the eligibility criteria differ between child and adult mental health services.
Service engagement
This theme describes CYP, parent and service provider perceptions of the acceptability and effectiveness of support provided by the services and how service engagement is influenced by the personalisation of support, choice and involvement in decision-making, practitioner qualities, positive relationships and respect for confidentiality.
Personalisation of support
Participants highlighted the importance of services which offered personalised support or person-centred engagement and which were not constrained by organisational processes, time or risk management concerns. Participants stressed the importance of services being tailored to individual needs and preferences:
Everybody’s experience differs … I wouldn’t want what some of my friends would want and I think that’s the main thing … the type of therapy that I did that, like, helped me probably the most out of everything that I’ve done, that’s got me to the point where I could say that I’m much better, I was talking to my friend about it, she said I couldn’t think of anything worse than doing that … an ideal mental health service would be that everybody recognised that everybody is different, so not everybody’s going to respond from the same things.
CYP03-12
The sites approached personalisation of services in different ways. Some service providers described adopting a person-centred, solution-focused approach to support based on the CYP’s current needs or personal interests:
The fact that we tailor the therapy we give to each child as well. So it’s not like they’re coming to the service and then they get, right, this is week one, we’re going to do this and that’s that. If we started the therapy sessions and we can tell that something is really bothering that child that week, then our plans kind of go out the window and we focus on the child and what they need that week …
SP05-15
Site 2, a school-based service, used scenarios during group exercises that were tailored to the local geographical area or socioeconomic context:
When you’re in a grammar school, you’ll use a different example than you would use necessarily in a school where the education side is not as important … One of the examples … is around ‘you failed on a test’ and in one of our schools they’d be, like, ‘I don’t care’, that’s not an issue for them.
SP02-01
Across third-sector sites, in particular, there was a focus on providing session content that was CYP-centred, that is, age-appropriate, enjoyable and accessible. CYP described how they became more engaged when sessions were fun and when they adopted an informal, creative or interactive approach. For example, one young person – a self-described ‘not a talker’ – enjoyed the opportunity to write blog content, stories and poetry, describing the impact of this as ‘calming and comforting’ (CYP04-34). In addition to being fun, sessions needed to focus on strengths rather than deficits:
What you’re learning was helpful, but then at the same time it was fun. It wasn’t boring, it wasn’t like a class or something … I had [practitioners] who were both like just really fun and really nice and the way they spoke and stuff like that, they were welcoming and nice … And it was the way that they started the sessions as well … everyone would say something that they’d done that week that they were proud of or they’d enjoyed that week, so we all realised that we had something to be grateful for and something to look forward to.
CYP02-26
Not operating under a ‘medical model’ or diagnosis-led approach gave some non-statutory providers the freedom and ability to be more CYP-centred:
We’re not a medical model really … it’s more relaxed and less formal. It’s kind of, how are things going? What do you want to talk about today? Any ‘wow’ moments? I like talking to the kids about any wow moments and any less wow moments. I think it’s the lack of formality that helps and going with their [CYP] agenda.
SP09-21
We’re not a diagnostically led service … there’s no, sort of, protocols and pathways based on that so you’re, kind of, just interacting as a human. And, I think, seeing you as a whole and working with you in your situation I think, for some people, has been really helpful.
SP04-31
Using co-production and feedback from CYP accessing the services to design CYP-centred session content was well established at some sites. Services providing a non-judgemental space for parents and carers, where they did not feel blamed for their child’s difficulties and where the approach was parent-centred rather than deficit-focused seemed to promote meaningful service engagement:
It’s really great for parents not to have another setting in which the child has to comply or behave … it can be very shaming for parents who have children with challenging behaviours to come to many settings that feel very public. And I think something that is a positive experience for parents is that kind of safe experience that they [get here].
SP09-46
However, for some parents of CYP on neurodevelopmental pathways, services were often perceived as overly structured with a ‘tick-box’, deficit-focused approach which could be distressing for both parent and child:
It’s really hard when your child is sat next to you, to talk about their problems. It’s a bit brutal for the child … they never ask about his good points, or what we love about him. [Son asked] ‘why am I different mum?’, it’s rough on the kids … you feel quite bad when you come out of these meetings … I like to call the service the ‘shit parenting course’ … I understand they have a job to do but sometimes it is just like bullet points.
P05-16
Some sites – Site 6 in particular – adopted a holistic, ecological approach to support, working with the wider family as well as the CYP. Service providers thought this important in ensuring services could understand the wider context of family life and tailor support accordingly:
Because it might not be just one person working on a case, we can, sort of, all do different things. So, we have that bit of a luxury where we can, sort of, plough a bit more of our time in … You know, you can really, sort of, get to know these young people and their families, as well … [they] trust us because, you know, we’re always just on the end of the phone; if they want us to come out, we’ll come out.
SP06-17
Parents welcomed holistic family support and felt it promoted their child’s engagement with the service:
Whilst they were there for [child], they were there for us … And I know fundamentally, it was around [daughter] and what she needed, but actually that support was there for us … really friendly, really approachable … [daughter] doesn’t really say anything to anyone, but she was talking to them … [daughter] took to [practitioner] straightaway and would chat with her. And I don’t see that very often.
P06-32
The ability of Site 6 (an NHS service) to provide a personalised approach may relate to the intensive and short-term nature of the support provided and that the setting was the family home. There were, however, concerns from staff about the impact increased workloads might have on this valuable aspect of service delivery:
At times quality may have been compromised slightly just because workload did increase. So rather than seeing maybe one or two people a day and being able to spend three days with them and doing all that liaison work, it might be that you had to see two or three people each day, so you just did not have time to do all of that liaison work in detail as you would have done previously … you just don’t feel like you’ve done as good a job, if that makes any sense.
SP06-09
Choice and involvement in decision-making
Children and young people and parents valued services which involved them in decision-making and which offered them choice: choice in how to access services (including self-referral), in the mode of delivery and service setting, choice of practitioner and in the type of support/therapy provided. Some service providers saw involvement in decision-making as an ongoing process:
It’s about, you know, asking what they want as they go along … You know, the young person says, ‘I’ve changed my mind, I don’t want to try and get this’, then we’ll say ‘okay, what is it you want to do?’ … a central part is that their voice is really important.
SP01-04
Some sites were able to offer CYP a choice of delivery mode (e.g. online vs. in-person, group vs. individual) and some provided options for the location of in-person delivery. However, other services were unable to offer CYP a choice because their programmes were designed to be delivered in a specific way, for example, peer support through group approaches. Group approaches were also deemed necessary to manage service demand or reduce treatment waiting times. Lack of choice was not always problematic, however:
Generally the response was I don’t want to do group work but I’ll do it. And then, by the end of the group, they’ve gone I don’t want to leave, I really enjoyed it … So, it was both good for the young people and it was also good for the service … previously of those eight people, maybe four or five of them would have ended up on a one-to-one waiting list, now they’ve done the group maybe only two or three will.
SP05-07
While some CYP valued the opportunity of accessing a supportive peer group where shared experiences could be discussed, there were caveats to this approach. Not all CYP felt confident about discussing their feelings in a group setting. For instance, there were issues about confidentiality in school settings:
I’d say the best thing is that it’s, like, the groups weren’t in, like, your classes, so it wasn’t, like, people you were used to talking to and I think that made it a bit better, because you could be more open about things, because you wouldn’t be worried that, like, you’d be talking to your friends about it, and things, because they were just other people in the year who you hadn’t really spoken to. But you get to know them more at the same time and you can become, like, friends with them, without having that fear that they might, like, talk to other people about what you’ve said.
CYP02-54
Site 4 (a wholly digital service) was predicated on having a self-directed process in which CYP made their own decisions about what elements of support they wanted to access, for example, engage in live chat with a practitioner versus access website resources only. Having this choice was valued by CYP:
The nice thing is it is a not a counselling service unless you want it to be. It can be as formal or as informal as you want it to be … it is nice that you don’t have to talk, that is optional.
CYP04-43
Children and young people could also select a preferred practitioner at Site 4, based on information provided on their website:
A good option is where it says ‘meet the team’ and you can see who each person is, they usually have a background of themselves and what they do … I can see who they are … Sometimes you can even ask for a preference to speak to someone …
CYP04-56
At some sites, the potential for choice was more limited, as therapeutic interventions were based on practitioner assessment of clinical need, demand management or diagnosis-led pathways. One service provider talked about CYP’s ‘best interests’, though not necessarily from the CYP’s perspective:
We are focused on what’s right for that young person, whether they agree or not sometimes. Most of the time they do, but whether they agree or not, we will tell them that this is in your best interests, this is why we’re doing this … I do think it’s important that we have that best interest right at the forefront of everything we do.
SP05-07
Another service provider acknowledged that the presumption of choice based on, for example, information provided on a service’s website might be misleading for CYP and families as practitioners had to balance CYP/family preferences with their own clinical assessments of ‘best interests’:
I think the other challenge is clearly defining each service offer, while saying these are our service offers but you might not necessarily get to where you want to go, which is a tricky thing in terms of triage and assessment and what comes out of that assessment. Should they really go to canine therapy, should they really go to CBT? … that is a continuous challenge to weigh up … the choice of the child or the young person with what is clinically best for them in terms of treatment.
SP09-14
Practitioner qualities
Across all sites it was staff attributes – notably, staff expertise, personal qualities and interpersonal skills – that appeared to influence which services were perceived as acceptable and effective by CYP and parents.
Children and young people and parents valued being supported by staff perceived to be experienced and knowledgeable, including in some cases by virtue of the staff member’s lived experience of mental health difficulties. Lived experience alone, however, was insufficient. CYP and parents wanted staff recognised as skilled or specialists in mental health, staff who were well trained or ‘accredited’ in some way:
It was also the fact that it wasn’t just any old person. It was someone that knew what they were doing and had dealt with this type of thing before and had, like, ideas of how to fix that already … That [it was] backed up in more than just feelings.
CYP01-28
This was particularly so for parents accessing support for CYP on neurodevelopmental pathways and for digital service providers who wanted to demonstrate ‘authenticity’ to remote service users. Particularly within NHS services, being seen by an accredited, trained mental health professional (rather than a support worker) indicated that the severity of their mental health difficulties had been recognised:
I’ve not really met any bad mental health nurses. I’ve met bad support workers … they’ve just not had any training, I think, with mental health issues. They get surprised by everything they see … and they don’t really know what to do. And they have to get the nurses to take over most of the time. Because when I was at [Site 5], I never had a support worker, it was always a nurse … Yeah, it was crucial that it was a nurse.
CYP05-08
Service providers highlighted the importance of interagency, multidisciplinary teams in providing the range of expertise necessary to effectively support and signpost CYP and families:
I think the fact that we are one service and we’re not split into the different teams does work very, very well. So, you can move almost internally within the service, you’re not having to be referred onto other people. You can go into Crisis, and that’s not a different team, and young people are not having to be referred back …
SP05-07
In addition to expertise, the personal qualities and interpersonal skills of practitioners were important. Staff considered to be non-judgemental, genuine and empathic were able to build trust with CYP which, in turn, helped to normalise and de-stigmatise their experiences. These skills, along with a passion for their role, appeared to support engagement with services and the development of positive therapeutic relationships:
It was almost like talking to a friend … she made me feel as though she’d known me for a very long time, and I felt like she really understood, like, the things that I was like battling with … Sometimes, with some of the people that I’ve seen for my mental health, it … literally just feels like I’m sat talking to this person and they’re literally sat listening to me because that’s what they’re paid to do. And I didn’t get that feeling at all with her. It felt like she wanted to be there and help me … It felt like, you know, she actually like cared about me.
CYP03-12
She’s amazing, [practitioner]. She’s so passionate … and I think that’s the thing, you know? I don’t know if everybody that works for [Site 8] is as passionate … I don’t know whether that’s their own life experiences but yeah, they really, really care, they don’t just go through the motions of the job and that really hits home, so it does pull you, it really does pull you in.
P08-44
Children and young people valued practitioners who remembered details of their lives and used this to engage and build trust with them in subsequent sessions. Older children valued services which were able to communicate in an age-appropriate way and which recognised their developing independence and maturity:
I’ve been in and out of counselling and stuff since I was little … with [counsellor], I didn’t really want the sessions to actually end because it was very helpful for me … the best I had throughout life really … it’s the way she would speak to me, she wouldn’t talk down to me, because that’s something that happens quite a lot … It’s a little bit condescending or, I don’t know, or they go like the other way, it’s too pampered and I’m like babied too much whereas [counsellor] would do it like perfectly when she’d speak to me like an adult but wouldn’t make me feel like I have loads of responsibilities …
CYP09-48
Positive relationships
Positive relationships between professionals and CYP and their parents appeared to be underpinned by good communication and ‘relational’ continuity of care (i.e. seeing the same practitioner). Communication and regular contact with CYP and parents, both prior to service access and between sessions, were important in developing therapeutic relationships, building trust and maintaining engagement. CYP valued seeing the same practitioner each time (or having a named worker) as this provided consistency and so facilitated the development of trusting, positive therapeutic relationships. In some services, however, the consistency of a named worker needed to be balanced against the convenience of drop-in support:
I think it [having a named worker] is good, like you have someone who understands you. But it depends because … they have a special time when they can be available and you might not be able to be available then because you might be going out … whilst the other one [live chat drop-in support] it’s like you can easily come on whenever you want to.
CYP04-44
Some services placed a particular emphasis on the continuity of the therapeutic relationship. In Site 2 (a school-based service), continuity of staff from the programme was seen to promote positive relationships and good communication with the school (both staff and students), which in turn facilitated the programme’s delivery and the mobilisation of support resources:
The [service] staff who do the assembly [to introduce the programme] are the ones who are going to be there on the day, so they’ll say, hi I’m [name], it’ll be us you’re coming to see … any anxiety they [students] might have about coming to a group, we kind of break down those barriers …
SP02-01
Some services promoted continuity by giving CYP the option of working with the same practitioner when reaccessing a service, although this could lead to a wait for appointments. Where relational continuity was disrupted by maternity leave, staff sickness or practitioners leaving the service, continuity could be facilitated by staff sharing information and offering gradual transitions to any new practitioners:
My key workers came to see me, and it was like this is who you’re going to have when you come out [of inpatient care], they’re going to come and see you, we’re going to make sure that we have a good relationship before you come out … [later] it changed because, well she had a baby, so she left … I got passed on, but we built up to it, so it was a steady process … I met my new therapist a few weeks before she left, and she came in and sat with us.
CYP05-08
However, such continuity could be undermined by poor interagency communication and a lack of shared systems resulting in CYP having to repeatedly share information, often when transitioning to adult services:
It’s a nightmare. The thought of that [transition] is just terrifying because I’ve obviously built a good relationship with my current worker so then for them to say right let’s start again … I’m hoping that the child services and the adult services work together more so I don’t have to keep repeating stuff over and over again … like, just give them my file, let them read it for five minutes and then … It would save so much time and resources and everything …
CYP06-40
Positive relationships between staff within service provider teams were also important. Service providers described how teamwork was an important support mechanism in coping with emotionally charged work:
It’s important that we feel cohesive and have that support from each other. It’s not really work you can do in isolation. We often pair up, which is probably a difference between us and other services.
SP08-29
Good teamwork appeared to be important for staff coping with increasing service demands and workload. Service providers associated service effectiveness with having manageable caseloads and appropriate administrative support. Liaison work facilitated through good interagency relationships, whether formal or informal, appeared to be another factor associated with service acceptability and effectiveness:
[Site 1] have a good relationship with like high schools and stuff like that … so I did get her [practitioner from Site 1] to message the head of inclusion … So I even went in for a chat with her [head of inclusion] … and she was like … what can we do as a school to help you? And I just said, you know, tell the teachers to chill out a bit. Like to do with schoolwork and like maybe a bit more accepting … she kind of resolved them for me, if you get what I mean.
CYP01-15
Privacy and confidentiality
How privacy and confidentiality were managed was an important factor in service engagement. Three areas seemed to impact on service acceptability and effectiveness: safeguarding and managing risk; tensions and challenges arising within families; and service settings.
Regarding safeguarding and managing risk, CYP were sometimes unclear about limits to confidentiality which challenged their engagement with services and their trust in practitioners:
Them telling my parents about [safeguarding matter]. Because I was 16, they were like we need to tell them ’cause you’re not an adult. Yeah, that was a really hard thing to go through. My first CAMHS nurse sat my parents down and literally told them everything, and I was like are you for real? … she was like, right, I need to talk to your parents, so they’re coming in. She went out of the room and rang them, and I didn’t know. She was like, oh, I’ll be back in a minute … And then she brought them in, and told them everything that I had told her … I didn’t tell her everything … I just told her a smaller thing, to see if I could trust her … I didn’t really trust her again.
CYP05-08
Thus, a failure to fully inform and involve CYP in decisions affecting them and a failure to manage risks around confidentiality and the disclosure of information could undermine trust in services:
When I was at college, I was seeing a counsellor and I had told them some information about stuff that was going on at home … It was nothing to do with safeguarding, it was generally nothing that would have been worrying, and obviously I was told that was confidential. But then that got passed on to my head at the college and then that somehow got back to my mum, which obviously caused issues at home. So from that, I lost all trust in counselling and I refused to see the counsellor at college … So yeah, stuff like that, trust, my trust is very easy to go, especially with adults, so I’ve had a history of bad experiences with adults and teachers and people who betray my trust.
CYP09-48
Regarding tensions and challenges within families, some CYP felt empowered and ‘in control’ when they accessed services without parental involvement:
It was completely up to me and there was no, like, parental involvement [at Site 3, a third sector organisation] … I decided I didn’t want my parents involved with it. I wanted it to be something that I did by myself. And so she was like, yeah, that’s fine … It was nice to be in control when everything else that I’d done was sort of dictated to me …
CYP03-12
However, respecting CYP’s right to confidentiality and privacy could also present challenges for parents who sometimes felt excluded when they just wanted to support their child as best they could:
Sometimes I feel like they don’t tell us everything … I think whatever conversation they had they should tell us as a parent for us to know how to deal with [daughter]. Because sometimes, like [daughter] sometimes, say, she’s not open … I think if they give us a summary about the conversation or something like that I think it will help … she [daughter] might say one thing which might help us to change or to do something differently.
P06-33
One parent, in recognising the competing priorities of a CYP’s right to confidentiality and a parent’s desire to help, suggested services could engage with CYP and parents through ‘bookending’, that is, facilitating CYP and parents to discuss access to future support both prior to, and at the end of, (individual) support:
It is just that if I’d had had perhaps more feedback, I know they’re confidential sessions … I completely understand that, but maybe if I’d had a kind of the session’s bookend: ‘We’ve spoken with [son]. We can’t talk about what we spoke about. However, we feel that maybe he may benefit from moving on to this or moving on to that.’ Yeah, I think the only thing I would suggest would be about bookending the start and the end of the session …
P01-21
Regarding service settings, while particular service settings or locations might facilitate service access, some could also present privacy and confidentiality challenges if other people could be aware of the CYP accessing mental health services or if the setting did not afford sufficient privacy.
Locating a mental health service within a school could positively influence a school’s culture, through increasing mental health awareness within the school, increasing the frequency of conversations about mental health and through challenging stigma:
The good thing about doing it [mental health work] with the year group is that if you work with a third of the year, the culture of the year changes … feedback has been great and we’ve had some of ours [students] who have gone on to be wellbeing officers for the school … others who have, yeah, kind of, ran the mental health days as part of mental health awareness week … it’s opened conversations and, if anything, our aim as well, we take away the stigma of mental health in a school … Being able to say, actually, I don’t feel this way and it being okay, that changes the culture of a school.
SP02-01
However, services located in schools and colleges could challenge confidentiality. Names could be read out in class, for example, revealing mental health difficulties to peers and potentially increasing stigma:
They read it out, in the lesson, who was in what group. I didn’t really mind, but I know other people were a bit annoyed that they read it out. Because if you get put in there [the programme] they were a bit like ‘you’re dead sad’ …
CYP02-26
I remember being knocked by, like, sort of being singled out … the teacher would come and collect me, and there’d be like a laugh or something like that.
CYP02-06
Indeed, service providers acknowledged potential peer group stigma may prevent some CYP accessing services:
There probably is a bit of a stigma in the schools as well where young people don’t want to admit that they are going to a mental health support session and they have got to do that [for] six weeks or whatever. So, you will probably get some who will just disregard that and say, ‘I don’t want to do it’ or ‘I’ll give it a go, but I’m not coming back’ … because they are a bit worried about what other people think of them.
SP02-06
I do think sometimes they are a bit embarrassed and that’s why I don’t burst into a tutor group and say, you, you, you, you have been selected [for the programme] … It’s why I pull them out of the classroom and try to do it sensitively …
SP02-55
While accessing services within schools could appeal to CYP who did not want their parents involved, there were nonetheless concerns that information would be shared with teaching staff:
A lot of young people were saying to us that they were not quite as honest on [the screening questionnaire] as what they wanted to be because they were worried about who in school was going to see that questionnaire … Schools work differently … so in some schools, our teams were going in and doing the questionnaires and in others, the teachers were doing them. And we always gave them a big brown envelope for the kids just to put them all in and seal it … children were telling us that they knew that teachers were looking at them and they have a real issue around sharing of information with teachers; they don’t feel like their information is safe.
SP02-03
At Site 5, a young person described not being given any choice about being seen by her CAMHS worker in college despite privacy concerns:
When they [CAMHS worker] first started coming into college, I was a bit like I don’t really want it to be at college … I think they wanted to see me in an educational background, how I was, because my mood sort of like went up when I was at college … It’s a big thing when you’re like 16 and they see an NHS worker walk into a room with you, and all your friends are like, what is she doing? … and even when she took her lanyard off, they get visitor badges and everyone’s like who are you seeing on a weekly basis? And I’m like … I don’t want to say, because it’s a bit personal …
CYP05-08
Home visits or accessing services digitally from home sometimes impacted on CYP’s privacy given parents and siblings could be present or in the vicinity:
To have it over video chat is not brilliant. Because I live in a house, my mum works in a school, so like breaks like Easter and things like that, you know, she’s home. And to have the privacy is actually really hard like because a lot of my issues are around her. So I can’t sort of be, you know, honest if you like … I have my sessions then in my bedroom rather than downstairs but, you know … my brother’s next door and he can hear me.
CYP03-14
For one young person, this was their ‘worst nightmare’:
It felt quite uncomfortable, them coming to my house … I didn’t like that at all … That was like my worst nightmare because I feel like I can’t open up … like I can’t really express how I’m feeling.
CYP06-40
Site 4, a wholly digital service, was predicated on being anonymous and offering confidential access:
Everything about [Site 4] is completely anonymous. We are quite unique in that aspect of having no identifiable markers at all when a young person signs up … The feedback we’ve had from young people is they found that quite safe, so they can kind of let go of some things and not have to worry about consequences … The anonymity, I think, speaks for itself; it’s such an empowering tool that young people can use, where they can just come, and they can feel heard and seen and valued and not have to worry about the consequence of what they say in that moment, which is just something that they might not experience in any other place in their life at this moment …
SP04-42
I do think there’s something about, what’s the word? Like, I guess, decrease in shame and, kind of, stigma … you don’t have to go and sit in a waiting room, you’re not at CAMHS or you’re not going to that one room in the school that everybody knows is where you go to see the counsellor, psychologist, therapist …
SP04-31
This was important for some CYP because without the assurance of anonymity they did not feel able to talk openly when accessing the service:
It’s because it’s an online platform, so no one knows that you’re going on it, so your parents don’t need to know … It’s like it’s confidential and the person you’re talking to, a named worker, so it’s like it’s a bit different to school in terms of safeguarding – they [school] tell everything … like once I was on about self-harm and stuff and … I said that to my teacher and she goes ‘I’m going to have to report this to safeguarding’ … but on [Site 4] it’s like none of that, so like they were able to give me techniques like why don’t you just like use ice or something but in school it’s ‘we’ll phone your mum and dad’ …
CYP04-44
However, there was scepticism about claims made by sites regarding anonymity:
If something like was to happen and they needed your details, they would then ask for them but instead of like getting rid of them after that incident, they then keep them [on file] … so like now when they ask me, I’m like ‘I’m not giving it to you’ and they’re like ‘well, we already have it’.
CYP04-49
Children and young people could feel a lack of control and ownership over content they shared online which raised digital privacy concerns for some:
I can’t control a lot of things on here, like I can’t delete an entry or I can’t delete a goal. I can’t delete messages … sometimes it feels like they’re controlling a lot of it. I think it would have been better if we could have equal control over this whole site or personal accounts. You can’t even delete your account apparently … you have to message the team and talk to them, and then they have to refer this to some IT staff and the IT people delete it … I just really don’t like that because what if you don’t want to use it and it’s just still there?
CYP04-56
Learning and understanding
Within this theme, three levels of learning and understanding appeared to influence service acceptability and effectiveness: practitioners learning new skills or developing their practice through a culture of ongoing learning; CYP acquiring skills and increasing self-awareness of their mental health; and the acquisition of relevant skills by parents/carers.
Practitioner learning
A culture in which learning was fundamental to the organisation was valued by service providers and seen as vital in providing effective support for CYP and families since it increased practitioner competence and openness to new ways of working:
Constant learning, innovation and improvement mentality at service level … There’s quite regular continuous professional development (CPD) as well … I like the fact that we have regular training as well and there are always opportunities to do things, to learn more. I’m on a course tomorrow …
SP03-19
One service described how they learnt from one another using formal mechanisms like clinical supervision to develop their practice, as well as more informal mechanisms like team meetings:
We have clinical supervision once a month, which we’re really pushed on, and rightly so, but we also have, once a month we’ll have a group case formulation, where somebody will bring a complex case. But you’re not expected to know everything’, cause it is complicated, and there can be a lot of stuff going on. So, the fact that there’s a culture of being able to say, you know what, I don’t know what to do here, is really positive.
SP05-07
Reflexive practice contributed to a culture of ongoing learning with staff sharing expertise and skills and learning from one another while being supported by their peers. This helped to improve team cohesion and staff retention:
We have a team reflective session with one of the psychotherapists which I think is really helpful … there’s quite a good sense of team camaraderie … the idea of it is to have an opportunity just to reflect and say, ‘God, it’s really hard’.
SP03-37
At one site, practitioners were encouraged to test out new approaches to improving service delivery:
The team are really passionate about pushing boundaries … so if anybody has a new idea or has a thought of something that can work better or that we’re not providing and lacking in … they’re encouraged to put that into place and give it a try. And I think that is really good from the top-down, so [manager] and everybody below really supports that. Plus if you have an idea that you think would be beneficial, that they are more than happy to support you in any training that you need … to be an independent practitioner and know exactly that you’re going to get the support to kind of push those boundaries is amazing.
SP05-15
Such teams appeared to be resourceful and flexible, adapting the way they delivered services to meet the needs of CYP and parents, while being supported by colleagues and managers. Site 5’s focus on innovation was felt to have enhanced their reputation which also facilitated staff recruitment:
We never have problems recruiting to our service … They want to come and have the experience. And I think it’s because of reputation …
SP05-04
In services where a more formulaic approach to mental health work was used, practitioners engaged in ongoing training, reflection and peer review to ensure fidelity to the therapy model (which was seen as ensuring effectiveness) and to improve their knowledge and skills:
The staff are required … to record three sessions, which goes back to people who are higher up, who’ve been signed off to check, and then they listen through them and mark them. There’s two elements, so it’ll be like kind of, the fidelity of it and sticking to the content and then also just generally how the session goes …
SP02-01
Service providers described using feedback from CYP – through a young person’s advisory group or the routine use of service satisfaction questionnaires, for example – to improve their own practice and inform service development or redesign.
Acquiring self-care skills and self-awareness
A common feature across all sites that CYP, parents and professionals associated with service acceptability and effectiveness was that CYP learnt new skills, while also acquiring knowledge and expertise around mental health and mental health issues in general. These skills and knowledge enabled CYP to cope better with their own mental health difficulties. CYP consequently developed self-awareness which helped prepare them for self-management of their mental health issues. One CYP explained:
I just think I know more about myself than I did before. I know how to calm myself down; I know how to process things and now I can do that without even thinking about it. And I’m just a lot more open now than I ever have been, about my past, and my mental health and stuff.
CYP05-08
Skills, strategies and techniques learnt typically centred on emotional regulation or the management of anxiety through relaxation or breathing techniques, ‘self-soothing boxes’ or challenging unhelpful ways of thinking. Some had names like ‘CBT toolkit’ or ‘surfing the wave’ (a mindfulness technique to manage self-harm urges). CYP associated acquiring these skills, strategies and techniques with improvements in their mental health:
I can remember last year, I was feeling like really stressed and stuff, and then afterwards I went on [Site 4] and then there was a lady called [practitioner name] and then she like taught me this technique and I always use it now, like whenever I’m stressed. Like breathe in, like calm and then breathe out, stop, and it just helped me, that really helped me, and I always use that technique.
CYP04-44
I think, they call it ‘where’s the evidence?’ So … if you ever have that feeling of your friends no longer want to be friends with you or something along those lines, it was ‘where’s the evidence to back that up?’ So when you come up with that in your mind, but then you can’t actually justify it, it’s able to reduce that anxiety or reduce that panic because until you speak to them [your friends], or until you actually do find the evidence, that’s just a negative thought …
CYP02-11
And a service provider reported:
I had a little girl who said, ‘my counsellor listened to me and taught me how to surf the edge [of a wave] when I wanted to self-harm’ … she didn’t stop self-harming, but she managed it. So we talked about this wave of feeling an emotion that triggered the self-harm and whether she could surf that wave for a little while. And the time that she could surf it increased and she developed more strategies, and so her self-harm was reduced significantly.
SP09-21
Participants said it was important these skills, strategies and techniques were taught at the right level and so CYP could successfully develop their own coping techniques and achieve a level of independence. This helped CYP identify their own trigger points, recognise how to access appropriate resources when they felt in crisis and understand their own emotional states. For some CYP, having the opportunity to talk about their feelings was a learning activity in itself:
When I was accessing [Site 9] for the first time, I really, really couldn’t talk about anything, and I think, just generally practising talking about what’s going on, it helped me … I’m a much more open person now, I’m very open, and I think practising opening up and being able to put your emotions into words, that practice was really good, ’cause I can now do that with my friends.
CYP09-45
I think [Site 4 has] helped me to talk instead of internalising things … I guess it helps. I don’t speak to Samaritans as much anymore because I’ve got [Site 4].
CYP04-056
Participants described how the use of tools and techniques could result in longer-term benefits for CYP in that they developed coping skills that helped prevent deteriorations in their mental health:
And then there was a mood diary … And me and my other mate from the session have carried that on where you say what you did in the day and then you rate your day and triggers and stuff like that, we learnt all that as well. So, say me and my mum have an argument in the day then that’s going to trigger a bad day, so then I can think about what I can do to stop an argument or prevent one.
CYP02-26
It was a lot of learning how to deal with anxiety, or how to deal with mental health when it does arise … if you do ever start to experience it again, then you’ve always got those techniques that you’ve learned in the past that you can use again, and you can use them over and over again to help you.
CYP02-11
Parents learning new skills
Some services offered parents opportunities to learn skills to support their children. These included skills to help their child with anxiety, low mood and anger, either through peer-supported approaches or through more formalised (face to face or online) teaching:
We’re running some parent support face-to-face groups as well, which are really popular … It’s multi-functional, so, you know, we’re looking at some key things like anxiety, how to help your child with anxiety … some very basic techniques and stuff, low mood, anger, emotional intelligence … looking at recognising a child’s emotions, and how to listen … it’s semi-structured … part psycho-ed [psychoeducation], but part just sharing and support.
SP03-17
A lot of parents do appreciate the fact that we also train the parents if they need it … so the training courses we have on our website we make freely available to all the parents … if the child is a lot younger, we’ll teach the parents all the skills so that they can then support the child …
SP05-15
Another parent described how they had successfully implemented a strategy they had learnt to improve communication with their child:
We recognised that obviously she needs to manage her emotions, but also she didn’t communicate with us effectively how she was feeling. So, we looked at communication strategies so she could really try and tell us how she’s feeling about having to tell us so much. So, we used the traffic light system … although, when I tried it with [child’s name] later, she was a little bit like [pulls face], do we have to? Yes, we do, come on, let’s get it done … Whilst she weren’t back to being the [child’s name] we knew, we noticed a change in her which was massive for us … she’s spending more time with us downstairs.
P06-32
Site 8 provided a service supporting the carers of looked-after children. Carers received specific training on trauma-informed care, which increased their understanding and awareness of the issues facing looked-after children, and helped them acquire skills in how to engage with CYP in trauma-informed way:
It had a really nice flow to it. Obviously, been very well thought out, but it was a mix of kind of the psychology … a mix of kind of stress response systems, and, you know, this is how a brain works, without getting too kind of neurological. A mix of really good case studies. Kind of one of the core elements was pace as a sort of therapeutic style, playfulness, acceptance, curiosity and empathy … I think it was great that they were a week apart because … I would kind of go to the first session, learn about 15 things, and immediately be thinking, oh that could help …
P08-41
Summary
Work Stream 3 aimed to identify the enablers of, and barriers to, access to mental health support and the factors influencing whether a service is perceived as accessible, acceptable and effective by those who commission and provide services and, more importantly, by CYP and parents attempting to access and navigate such services. Box 4 summarises the main findings from this work stream.
Self-referral: avoids the need to navigate gatekeepers and improves the quality of information available at assessment. However, to self-refer, CYP/families need to be aware of (need information about) the service.
Availability of services, in terms of the timeliness of receiving support, extended contact hours and CYP/families being able to contact staff directly.
A SPoA may help direct CYP/families to an appropriate service (but it may also be a barrier to receiving support if it leads to further assessments and waiting lists).
Physically accessible service locations.
Discharge pathways facilitating continuity of support.
BarriersProfessional referrals may require CYP/parents to present mental health problems in a way practitioners will validate; they also raise concerns for CYP about disclosure, for example, that parents might find out about a CYP’s difficulties.
Poor-quality referrals may result in delays to CYP/families accessing appropriate support or the CYP/family being judged as not meeting service eligibility criteria.
Waiting lists delay access to support.
Lack of information about services.
Lack of clear pathways for those aged 16 years and over who need ongoing support from NHS mental health services.
Service engagementPerson-centredness and tailoring to individual needs lead to more personalised and meaningful engagement.
CYP can be engaged through less formal, age-appropriate session content which is also fun and creative.
A focus on strengths rather than deficits.
The involvement of CYP/families in decision-making and co-production helps inform service design and development.
Choice and flexibility in relation to service access and service delivery are important.
Ecological or holistic approaches which work with the wider family as well as the CYP.
Staff who are motivated, experienced and expert; staff who are non-judgemental, empathic and compassionate. Relational continuity between staff and CYP supports engagement, trust and the development of therapeutic relationships.
Good interagency liaison work and care co-ordination.
Respect for CYP’s confidentiality balanced against parents’ desires to support their child.
Learning and understandingHelping CYP acquire knowledge, skills, strategies and techniques to understand and (self-)manage their mental health.
Providing parents with opportunities to learn new skills to support their child in managing symptoms and facilitate effective communication within families.
An organisational culture which: supports practitioners in ongoing learning and reflective practice; is open to innovative practice to improve service delivery; and which values coproduction and learning from CYP and parents/carers, from others within their own disciplines, and from other disciplines.
Regarding the enablers of, and barriers to, access, it is self-referral, timeliness and availability of support, physical accessibility, and discharge support planning that are important; in other words, these are the factors that appear to influence whether a service is seen as accessible or not by CYP and families. A SPoA to multiagency services may also be beneficial if it does not result in multiple assessments and multiple waiting lists.
Acceptability and effectiveness are also considered across two dimensions: service engagement and learning and understanding. These two dimensions highlight the importance of personalised, holistic and flexible services that involve CYP and families, respect confidentiality, ensure relational continuity, focus on strengths and engage CYP in creative ways. Staff qualities are important not only regarding expertise and professional competency but also in relation to empathy and compassion. A learning culture was perceived as being fundamental to service acceptability and effectiveness: it was important for staff to work in environments emphasising staff learning and development, supporting reflective practice and which valued service improvement especially when CYP/families could contribute to (co-design) services. Service effectiveness was linked to CYP developing the knowledge and skills to both understand and manage their own mental health. Children and young people, parents and services providers associated this learning with improvements in CYP’s mental health, self-confidence, social relationships and school engagement. Providing CYP with opportunities to express their feelings was associated with improving CYP’s confidence and their ability to articulate their emotions to others, including those working in services they might access in the future.
Chapter 8 Model building
This chapter focuses on Work Stream 4. In this final work stream, we synthesised data from the integrative review (Work Stream 1) and the case study (Work Stream 3) to produce an evidence-based model of high-quality service provision for CYP experiencing CMHPs. We firstly describe the data synthesis method used (integration through narrative), after which we discuss the mixed-methods matrices that aided our data synthesis. We end by presenting the coproduced model of high-quality service provision for CYP experiencing CMHPs that emerged from our synthesis.
Methods
Research question
Work Stream 4 addressed study objectives 4 and 6 and the following research question:
-
In what ways might the key factors associated with access to, navigating and receiving help from, services be synthesised into a model (or models) of effective and acceptable, high-quality service design for CYP experiencing CMHPs?
Data synthesis process
Our synthesis method was ‘integration through narrative’. 99 During a series of online and face-to-face meetings, core research team members Evans, Fraser, Kirk and Pryjmachuk firstly compared and contrasted the Work Stream 3 case study data with the Work Stream 1 integrative review data using the ‘weaving’ approach to integration through narrative. In the weaving approach, different data sets are analysed, interpreted and reported together on a theme-by-theme or concept-by-concept basis. 99 To do this, we used the three themes from the case study analysis (see Chapter 7) to create three mixed-methods matrices. In these matrices (see Appendix 9), the case study data were presented transparently alongside the review data so we could look for similarities and differences and see how the case study data might provide an extended understanding of the review data (and vice versa).
Meta-model
Next, from the matrices, we devised a preliminary model of high-quality services for CYP experiencing CMHPs that attempted to integrate all of the factors associated with access to, navigating, and receiving help from, such services. We used the principle of ‘scientific parsimony’100 to produce this preliminary model, that is, we aimed for an explanatory model of service provision that was comprehensive yet understandable. Importantly, this explanatory model is different to the models categorised into our typology and discussed in Chapter 4. Technically, it is a ‘meta-model’ or ‘model of models’; pragmatically, however, we shall continue to refer to it as a ‘model’.
The preliminary (meta-)model was presented for feedback at a meeting (March 2022) that included research team members and the young co-researchers and at the final SAG meeting (April 2022). Research team and SAG members unable to attend the respective meetings were e-mailed details of the preliminary model and invited to provide feedback through e-mail or a videoconference call. Common Room also facilitated an additional group of young people with lived experience to provide feedback on the model. In all, we obtained feedback on the preliminary model from CYP, a parent, commissioners and academics, researchers and clinicians in psychiatry, general practice, nursing and social work. Both the statutory and non-statutory sector sectors were represented in our feedback. Following this feedback, core research team members Evans, Fraser, Kirk and Pryjmachuk met several times to revise the preliminary model into the final model presented at the end of this chapter.
Integration through narrative
A narrative for each of the three themes in the mixed-methods matrices (see Appendix 9) is presented below. Within each theme, we analysed and interpreted the case study and integrative review data across several key concepts, which we identify using quotation marks in each narrative below.
Pathways to support
‘Referral routes’ contrasted the advantages of self-referral against those of professional referral. Only case study data were available here; there was no evidence for specific referral routes in the review data. Self-referral was generally seen to promote service access, while professional referral was seen as problematic; poor-quality professional referrals in particular seemed to increase the risk of rejection by a service. In both data sets, there was a consistent perspective on ‘availability of information’ in that a lack of information about services made CYP and parents apprehensive about services and was seen as a barrier to access. Both data sets were also consistent regarding ‘speed of access’ and ‘waiting lists’: families generally wanted rapid access to services without lengthy waiting times for both assessment and therapy. The case study data also indicated some services had a role in supporting CYP while they waited for access to more specialist services. ‘Accessibility at all stages of the CYP’s journey’, picked up in both data sets, reflects frustrations with approaches that nominally improve access but which often move bottlenecks further along the CYP’s journey. For example, services with a SPoA may provide more rapid access to assessment but might still have lengthy therapy waits. ‘Physical accessibility and convenience of the service’ was noted in both data sets though in more detail in the case study data. While the review data simply specified that venues need to be accessible, the case study data expand on this by identifying service hours, ability to contact service providers directly and physical convenience (including mode of delivery) as characteristics of an accessible service. ‘Post-service support’ was reported in the case study data only and refers to signposting to further support, self-referral back into services, post-discharge follow-up and planning for transition to adult mental health services.
Service engagement
There were significant and consistent data supporting the concept of ‘personalised services’ in both data sets, with ‘involvement’ (including service co-design) being central to a personalised approach. CYP and parents want services to be person-centred, age-appropriate, focused on strengths rather than deficits, tailored to individual needs and interests and flexible enough to meet changing needs. In addition, service co-design should be ongoing process rather than one-off. Furthermore, CYP want services which are engaging, fun and creative. Both the review and case study data also suggested the non-statutory sector may have more freedom and flexibility to offer personalisation than the statutory sector, possibly because these services are rarely diagnosis-led. ‘Choice’ was a key concept in both data sets, though there was more detail in the case study data which reported that CYP and parents want choice in how to access services, the mode of delivery, service setting and the type of support or therapy provided. Moreover, the case study data suggest, where choice is necessarily restricted, it should be clearly communicated to the CYP/family. A significant concept arising in the case study, but not the review, data was ‘confidentiality’. The way confidentiality was managed was an important issue for CYP and parents and there were sometimes tensions between confidentiality and safeguarding. Confidentiality can influence decisions about which services CYP will access or the extent to which they will share information with practitioners. For example, CYP may worry about peers finding out about them accessing help in school settings and there was doubt as to whether at-home, remote services (telephone or online) could provide the same levels of privacy as office-based appointments. Though identified in both data sets, the case study data provide significantly more detail about ‘practitioner qualities’, best summarised in the phrase ‘compassionate and competent staff’. Regarding compassion, staff need to be approachable, non-judgemental, empathic, genuine and passionate about their work with CYP. Regarding competence, CYP and parents want staff to be experienced, knowledgeable and therapeutically skilled; this could mean being seen by an accredited mental health professional rather than a support worker. ‘Positive relationships’ covered therapeutic relationships between practitioners and CYP/families as well as effective team working. Both data sets provided strong evidence for this concept and both included ‘continuity of care’ as important in establishing positive relationships. The case study data identify good communication and practitioner skills as underpinning therapeutic relationships, demonstrating some overlap with ‘practitioner qualities’.
Learning and understanding
The key concept ‘practitioner learning’ was identified in both data sets and refers to staff learning reflectively from other disciplines, from others within their own discipline or, indeed, from the CYP in their care. An example from the integrative review is non-mental health specialists gaining knowledge and skills from mental health specialists, particularly in services featuring consultation-liaison. ‘Acquiring skills for self-care’ was also identified in both data sets. The review data outline CYP and parents often wanted services to provide them with skills to help themselves. The case study data further expand on this by identifying the nature of the self-care skills required: skills to regulate emotions, challenge ways of thinking, manage anxiety and self-soothe, for example. ‘Personalised approaches to learning’ overlaps with ‘personalised services’ discussed in Service engagement, with ‘involvement’ being a common characteristic of both. The review data refer to staff who were CYP-centred and the degree to which CYP and parents are involved, while the case study data refer to sessions being pitched at a level that works for individual CYP. ‘Impact of learning skills for self-care’ was substantially more evident in the case study data. Reported impacts in the case study data include reduced anxiety and stress, being better able to cope at school and during lockdown, preventing deterioration in mental health, promoting independence, improved resilience and better problem solving. The review data focused mainly on the impact of brief intervention approaches which are often underpinned by training in self-care skills.
Final model of high-quality effective and acceptable services
Integrating the three narratives above, together with feedback from various stakeholders, led to our final model of high-quality effective and acceptable services for CYP with CMHPs. The model is represented visually in Figure 34.
FIGURE 34.
An evidence-based model of high-quality services for CYP experiencing CMHPs.

Elements in cyan on the left-hand side of Figure 34 are the core characteristics a service needs to possess to be considered high-quality; the blue elements on the right are the necessary underpinning characteristics than cut across these core characteristics.
Table 11 further explains the individual model components and outlines how each component was derived from the integration through narrative synthesis.
| Model component | Explanation | Derived from theme (and key concepts) |
|---|---|---|
| Rapid access and short waiting times | CYP can access services quickly and once accessed, therapies and support are provided in a timely manner | Pathways to support (referral routes; speed of access; waiting lists; accessibility at all stages of the CYP’s journey) Service engagement (confidentiality) |
| Opportunities to learn practical skills and strategies for self-care | The key to providing effective and acceptable support for CYP experiencing CMHPs is the provision of skills to enable CYP and families to help themselves | Learning and understanding (acquiring skills for self-care; impact of learning skills for self-care) |
| Individualised support | Services offer choice and flexibility to CYP/families, considering the needs, views interests and hobbies of CYP (personalisation) | Service engagement (personalised services; involvement; choice) Learning and understanding (acquiring skills for self-care; personalised approaches to learning; involvement) |
| Clear and accessible information | Clear information about services is provided to CYP, parents and professionals using a variety of media, (not all families have private access to the internet); information is available to help CYP and families navigate the most appropriate services when given a choice | Pathways to support (referral routes; availability of information) |
| Compassionate and competent staff | Staff are approachable, caring, empathic and person-centred; staff are appropriately qualified and experienced | Service engagement (practitioner qualities; positive relationships; continuity of care) Learning and understanding (practitioner learning) |
| Aftercare planning | Processes and systems for navigating out of services as well as into services are available; covers transitions to adult services, ongoing support, potential for rereferrals and continuity of care | Pathways to support (post-service support) Service engagement (positive relationships; continuity of care) |
| Values that respect confidentiality | CYP’s autonomy and perspectives on confidentiality are prioritised and balanced against any safeguarding concerns | Service engagement (confidentiality) |
| Engagement and involvement of CYP at the core | Activities and therapies provided are accessible engaging, developmentally appropriate, creative and fun; CYP are involved in shared decision-making for their own care as well as for service design and delivery | Pathways to support (physical accessibility and convenience of service) Service engagement (personalised services; involvement) Learning and understanding (personalised approaches to learning; involvement) |
| Collaborative relationships: with CYP, families and other disciplines and agencies | Trust is predicated on good interagency/interprofessional relationships and good therapeutic (practitioner-CYP/family) relationships | Pathways to support (referral routes; post-service support) Service engagement (positive relationships) Learning and understanding (practitioner learning) |
| A learning culture | A learning culture is demonstrated through good team relationships and a reflective learning environment that includes learning from each other as well as from those using services | Service engagement (choice; practitioner qualities; positive relationships) Learning and understanding (practitioner learning) |
How our evidence-based model might be contextualised within past and current policy and practice in CYP’s mental health and how it might be used to influence future service provision are discussed in the next, and final, chapter.
Chapter 9 Discussion and conclusions
The commissioning call behind this study was released in 2017 when the main policy driver in CYP’s mental health in England and Wales was the 2015 report, Future in Mind. 5 Future in Mind outlined a set of key proposals for transforming the design and delivery of children’s mental health services. A green paper22 steered a consultation on these proposals during late 2017 and early 2018, after which proposals for transforming children’s mental health services were embedded into the 5-year NHS Mental Health Implementation Plan (MHIP),101 published in 2019 as part of the NHS Long Term Plan.
The commissioning call specifically asked for research proposals exploring models and frameworks that might facilitate the transformational changes in services called for in Future in Mind and the MHIP. This study has identified models/frameworks for improving children’s mental health services in the international literature, classifying these model/frameworks into a typology and seeking evidence of their effectiveness, cost effectiveness and acceptability. Our service map and case study work subsequently explored the implementation of these models/frameworks in the local context of England and Wales.
In synthesising the review and case study data (see Chapter 8), we argue that, while there is some limited evidence of effectiveness for specific models/frameworks in our typology, focusing on specific models and frameworks is not particularly important when designing and delivering children’s mental health services. This includes those UK models/frameworks the commissioning call cited, namely CAPA, CYP-IAPT and THRIVE. Instead, it is certain fundamental components – those outlined in our (meta-)model (see Figure 34 and Chapter 8) – that are important in the commissioning, design and delivery of services.
Comparing our model with previous research and policy
The components in our model reflect observations in Future in Mind and the MHIP, namely that services should offer prompt entry, individualised care, a workforce with the right skills, welcoming environments, the facilitation of self-care skills and managed transitions to adult services.
Our findings also reflect findings and recommendations from previous research and reports. In 2006, a report on young people-friendly general health services102 identified accessibility, publicity (information), confidentiality, environment, staff attributes (e.g. skills, attitudes and values), joined-up working and CYP’s involvement as markers of quality services. The 2008 CAMHS Review15 noted parents and professionals need information about services, that there should be swifter access to services and that CYP should be able to develop trusting relationships with staff for the length of time they need. Our NIHR work on self-care support in CYP’s mental health, published in 2014,20 found choice, child-centeredness and staff flexibility to be more important than a service’s theoretical stance or a particular service model. A 2016 report from an independent commission on CYP’s mental health103 identified co-production with young people, system (multiagency) working, easily accessible services, workforce development and support for transitions as important factors in children’s mental health services. In 2021, the National Children’s Bureau104 stressed the importance of personalising services and therapies for CYP with poor mental health. Finally, a 2022 paper on YIACS105 (published after our review searches had been completed) identified opportunities to self-refer, timely provision of support, non-clinical environments, age-appropriate services (personalisation), a non-hierarchical workforce (learning culture) and interagency collaboration as key facilitators of access to, and engagement with, YIACS. These factors are strikingly similar to those in our model.
Though we have discounted specific models/frameworks in favour of a more generic model, it is worth discussing CAPA, CYP-IAPT and THRIVE as they were cited in the commissioning call. We found little research-based evidence about these approaches in the literature and, although several case study sites used one or more of them, the service providers interviewed did not mention them when asked about access, effectiveness and acceptability. Nonetheless, a scoping review of CAPA,106 published after our reviews had been completed, found that CAPA may reduce waiting times without compromising quality of care, but none of the studies in the review were particularly robust. A qualitative study on CYP-IAPT in Cambridge,107 again published after our reviews were completed, found staff with little understanding of the programme, variable levels of stakeholder investment and difficulties with collaborative working. As with all our typology models/frameworks, we are not discounting their value; rather, we argue their use should be secondary to a consideration of the fundamental components in our final model.
Novel findings
Given our findings are consistent with previous research and aligned with current policy, readers may question what contribution this study makes to the evidence base and policy development. Firstly, we provide confirmatory evidence about the organisation and delivery of children’s mental health services from more than 300 documents and more than 90 interviews with over 100 stakeholders that is consistent with previous research, and which supports the current policy direction. In short, a consistent organisational evidence base spanning more than 15 years appears to have had little impact on service delivery.
Secondly, there are novel aspects to our findings. While support for transitions to adult services is often identified as a service gap, we think aftercare is a more comprehensive concept than transitions since it considers ongoing support following discharge, the potential for rereferrals and continuity of care – that is, ‘what happens next?’ – for all CYP and not just those approaching 18 years.
Our model also emphasises the importance of balancing confidentiality against issues like safeguarding and CYP’s autonomy. Confidentiality may be a particular issue in services provided in schools. Schools are often seen as ideal places for mental health services because they are accessible, non-stigmatising, closely connected to the community and relevant staff have daily contact with CYP. 15,108,109 Yet, confidentiality can easily be breached in school settings, for example, by reading out lists of students ‘selected’ for a mental health intervention or having counselling/therapy offices located where others might see students attend. In terms of balancing confidentiality against safeguarding, Jenkins110 notes confidentiality in therapeutic work with CYP, which is often framed in terms of assumed legal obligations (e.g. to report abuse or underage sexual activity), may be more nuanced and negotiable than practitioners realise.
Another novel finding is how those using services perceive staff competence and compassion. Competence is not just ticking every box in a competency framework: it covers staff expertise and experience and their capacity to operate within, and recognise the limits of, their own knowledge and abilities. Recognising your own limitations fits in with our notion of a learning culture, one embracing reflective practice and reflexive learning and coproduction with CYP and parents. Competence also has implications for peer and associate worker roles since these workers may be best employed to augment, rather than substitute, trained and experienced mental health professionals. In any case, peer and associate workers are likely to benefit from support, supervision and/or mentoring from experienced mental health professionals. 62 There are economic implications too. Attempting to drive down service costs through staff costs (through, e.g. using self-help apps, associate professionals or peer workers) is a false economy if supervision and support costs are ignored or if these approaches are assumed to have no impact on service efficacy. Moreover, compassionate care generally requires staff time (or ‘presence’) which is at loggerheads with the targets and cost savings of market-driven health services,111 particularly when, as now, services have significant staff vacancy rates. 112
The importance of a learning culture is also a novel finding. While many of the reports cited earlier stress the importance of environment and workforce development, a learning culture also encompasses good team relationships, training opportunities (at the organisation’s expense) and a reflective learning milieu in which practitioners learn from each other and, indeed, from service users. Interestingly, some of the most robust effectiveness evidence in the integrative review came from the ARC (G5) studies. 113–115 A learning culture is implicit in ARC since ARC requires effective organisations to demonstrate participation, ‘psychological safety’ (speaking freely without fear of punishment or humiliation), openness to change, responsive rather than reactive services and a commitment to continuous development. 113
Inconsistencies with previous research and policy
Some notionally good practice outlined in Future in Mind and the MHIP was not particularly evident in our data and is thus not explicit in our final model. One example is single points of access (SPoA). In our data, speed of access and not having long waits for therapeutic support was more important than SPoA. A recent (2020) study116 found SPoA can improve access to children’s mental health services through addressing access barriers, simplifying where to get help and making it easier to contact services. Single points of access are, however, not necessarily accompanied by increased capacity and thus do not resolve long waiting times. This reflects the case study data: while a SPoA could facilitate initial access, it could also be confusing to navigate and lead to further assessments and waiting lists for support.
Another example of notionally good practice is dedicated (named) staff responsible for mental health in schools. Nothing in our data confirmed this, though this may be an artefact of our sampling. We did, however, identify collaborative interagency relationships as important. While there is ample evidence in the literature that good collaborative relationships between schools and mental health services are important,109,117,118 imposed relationships may not work as well as more ‘organic’ relationships. Moreover, an evaluation of the recent English ‘mental health services and schools link’ pilots found services may not have the resources to implement named contacts. 118
Given our previous NIHR study on self-care support in CYP’s mental health,20 we are not surprised at the inclusion of ‘opportunities to learn practical skills and strategies for self-care’ in our model. In Future in Mind, self-care is equated with apps and digital tools, a rather narrow view; the Anna Freud Centre,119 conversely, outlines an expansive list of activities (e.g. listening to music, watching television or going outside) that CYP could engage in to help themselves without mental health professionals being involved. CYP and parents in our case study sites provided a more nuanced perspective: they certainly wanted the ability to help themselves but preferred services to facilitate this through supported self-care (through staff providing them with tangible skills, e.g. to help regulate emotions or manage anxiety), often for the period while waiting for more specialist services.
There was also an expectation in Future in Mind and the MHIP that digital services would play a significant role in future service provision. These expectations were set, however, before the COVID-19 pandemic which, as mentioned in Chapter 4, provided an external stimulus for the expansion of digital services. That no evidence for digital services met our integrative review’s inclusion criteria is noteworthy, though we should add one of our sites was a wholly digital service. The general literature on digital approaches is more tempered than the hyperbole seen in some quarters and backs up the notion of digital being an option for those who prefer it. 120,121 A recent review of digital services engagement in CYP’s mental health122 found generally good retention rates for digital services though service design and modality were important here. Risks exist with digital services that are not present in traditional office-based services (and vice versa). In a recent provider review involving feedback from over 1700 CYP, the Care Quality Commission67 concluded that pandemic-driven digital services both highlighted and exacerbated health inequalities, and that digital services might miss cues in-person services would not. This latter point was also reported by some of our case study service provider participants. Confidentiality and safety may also be issues. At home, a CYP may be overheard by siblings or parents while using a service, or the CYP may not want parents to know they are accessing services. Moreover, it may be more difficult to offer emergency help remotely. A recent rapid review of digital services in CYP’s mental health120 found digital services were often much briefer than traditional office-based services, leaving no time for identifying action plans or goals.
Study strengths and limitations
Overall strengths and contribution of the study
This study’s main strength – and its principal contribution – is the robust and transparent development of a comprehensible, evidence-based model of high-quality service design for CYP experiencing CMHPs that is transferable across services, sectors and geography. In doing this, we have achieved the study’s overarching aim. Our high degree of PPI (see Chapter 2), especially the involvement of young co-researchers, is another strength. Despite conducting the bulk of our empirical research during the COVID-19 pandemic, we nonetheless recruited to target; moreover, we learnt much about the advantages and disadvantages of using remote research methods. That the study builds upon our previous (mostly NIHR-funded) work and its potential to influence future research in CYP’s mental health – a generally under-researched area – are additional strengths.
General limitations
As discussed in Chapter 3 (see Service model, intervention or feature?), conceptual difficulties surrounding defining, and distinguishing between, interventions and service models were, if not a limitation, a challenge. Additionally, we could have had a more definitive view on ‘counselling’ since counselling was central to some services but could also be considered an intervention. Conceptual difficulties surrounding ‘common’ mental health problems were resolved largely by discussions with our SAG though, as outlined in Chapter 3, it was not always easy to make an inclusion/exclusion decision for US papers using the quasi-legal term ‘serious emotional disturbance’.
Some service initiatives we were aware of were too new to have filtered through into the literature or service map in any meaningful way, for example, the introduction in England of schools mental health support teams, alongside a new role of educational mental health worker. 22,93,101 While a limited number of ‘trailblazer’ teams were established in December 2018, logistical and training requirements meant it would be several years before they became embedded. 93 School closures during the pandemic further complicated their establishment. Thus, we have no data on these teams, which we would classify as schools outreach (D2) services. While we did find some evidence of effectiveness for outreach services in general, our findings suggest that these teams will be successful only if strong collaborative school-mental health service relationships exist, staff have the right attitudes and skills, confidentiality and safeguarding are balanced and any support offered is personalised. The pandemic also brought about a surge in remote/digital (C2) services and while we explored some of these services in our case study sites, these services would have been under-represented in the literature when our searches were conducted. We suspect there will be significant future increases in literature regarding these services as researchers and practitioners find time, post pandemic, to evaluate and reflect on them.
Limitations with the literature reviews
The main limitations with the literature reviews arose from conceptual difficulties in identifying what a ‘service model’ was and from having to handle an unexpectedly large number of documents. The former we discussed above. The latter was not necessarily an issue with the scoping review because scoping reviews seek to include all relevant material and do not require deep data extraction. 29–31 However, it took longer than expected to screen the 800-odd documents flagged for full-text review. The semiautomated rapid title screen technique used initially may have resulted in us overlooking some relevant documents manual inspection might have picked up. Indeed, as reported in Chapter 3, some documents missed were identified later through other sources. Additionally, 66 potentially relevant documents (around 1.5% of documents sought for retrieval) were unobtainable because pandemic restrictions prevented document supply services accessing physical library resources.
Service map limitations
While the service map provided a robust sampling frame for Work Stream 3, we doubt we have a comprehensive picture of the range of English and Welsh services available since it is unlikely we identified all relevant services. Some services, particularly those identified via desk research, had significant quantities of missing data. Follow-up telephone or e-mail contacts occasionally provided additional information but, generally, there was no response to requests for further information.
Case study limitations
We had planned to use observation as a data collection method; however, COVID-19 restrictions meant we could not directly observe activities at the case study sites and it proved difficult to negotiate observing activities remotely. Thus, our findings lack the additional insights that observing actions and interactions in a natural setting might generate.
While we met our overall participant target, we recruited fewer CYP than our sampling goal. However, this should be considered within the context of the pandemic, consequent lockdowns and school closures. Collecting data remotely may have both encouraged and discouraged study participation and may have influenced the data generated in interviews. The service provider participant profile was not especially diverse being all White British and 70% female, though this may be a systemic, rather than sampling, issue given 78% of NHS CAMHS staff are White British and 85% female. 112
In the study protocol, we said we would try to recruit participants who refused or disengaged from services. However, despite asking our case study site contacts to facilitate this, we could not recruit these participants.
Economic aspects limitations
There were few relevant economic data available in the literature – three papers in all, with one being so poorly reported it was of little use. That economic evaluations generally focus on specific interventions rather than overall services is the most likely explanation for the dearth of literature. We did find studies reporting only costs but, lacking incremental analyses, these did not meet our inclusion criteria.
At the case study sites, there was wide variability in the amount of data available, or which sites were willing to provide, on service, training and staff costs. One site provided no data at all. Service costs should be considered with caution as no comparable measures of health benefit (e.g. QALYs, or impact on use of other healthcare services) were available. Training costs, which could be one-off or recurring, could not be summarised in any meaningful way but are likely to reflect staffing profiles. For example, nurse- or clinical psychology-led services likely draw on training already completed as part of clinical qualifications whereas lay- or peer-led services may have higher in-house training costs. Staff costs were estimated for NHS-funded services (using standard NHS costs) and appear to be a key driver of service costs. We could not estimate costs for non-NHS services. As outlined in Chapter 7, we had planned to collect user cost data (e.g. travel costs to services or out-of-pocket expenses) but since CYP and parents were not attending in-person services because of COVID-19 restrictions, we did not collect these data.
Commissioners deciding which services to fund might find it helpful to compare the relative cost effectiveness of various services models as well as their effectiveness. A standardised ‘reference case’ for economic evaluations in CYP’s mental health with agreed measure(s) of health benefit would allow meaningful comparisons to be made between service models.
Equality, diversity and inclusion
Strengths in terms of equality, diversion and inclusion include employing young people with lived experience of mental health problems as co-researchers. To avoid tokenism, we paid an hourly rate equivalent to a junior university researcher. We also worked with young people with lived experience to help us produce CYP-friendly participant information sheets and a video version of the same. Young people also provided feedback on our final model. There was substantial service user representation (CYP/parents) on our SAG, including a young person co-chair. Two of our case study sites delivered services targeting specific minority groups (ethnic minorities and looked-after children). Finally, Welsh translations of study materials were available for Welsh sites.
If conducting similar studies in the future, there are several things we (and other researchers) could do to improve research inclusivity, for example, we could look to recruit a more diverse pool of young co-researchers. While bureaucratic barriers prevented us from employing under 18s, we need to think about ways of encouraging young people from more disadvantaged backgrounds to apply for such roles. We should try to recruit research participants from seldom heard groups and try to obtain a more diverse or representative set of provider participants, perhaps by checking staff profiles before recruiting at sites or targeting culturally adapted services. The impact of remote data collection can be double-edged: it can be more inclusive (e.g. no need for travel and CYP already technology immersed may prefer such approaches), but it also potentially excludes others, for example, those who do not have internet access or fast connections (or even a mobile phone signal, as in parts of rural Wales), or those who cannot afford a smartphone or the costs associated with using one.
Conclusions
In conducting this study, we have addressed both the demands of the original commissioning call and the aims and objectives set out in the protocol. We have explored different service models for CYP experiencing CMHPs, preferring not to recommend any one model over others because the review data were equivocal and there was no strong support for any particular model in the case study data. Instead, we have developed an alternative, evidence-based model that outlines the fundamental components necessary for high-quality services for CPY experiencing CMHPs. Our model has utility for policy, practice and research, supports previous research and reports in this area and adds significant depth around core issues like confidentiality, aftercare, personalised approaches, engagement and organisational culture.
Implications for health care
In the face of wide service variability, many of the models/frameworks identified in our typology were devised, understandably, to provide some consistency across services. However, consistency can lead to a ‘one size fits all’ approach which can be inappropriate in local contexts: rural areas require different service configurations to urban areas, CYP out of education have different needs to school attenders, as may those who have access to technology and those who do not. This study’s main implication is therefore:
-
Using our model components to support the design and delivery of services – rather than the ‘top–down’ imposition of specific local or national models – could improve the consistency of services for CYP experiencing CMHPs. Our model still permits tailoring to the local context, as envisaged by Future in Mind and the MHIP. Moreover, such tailoring requires building on local relationships and local capacity,123 which can only come about through good collaborative relationships.
The following also have implications for policy, practice and education in CYP’s mental health:
-
We found aftercare arrangements are often neglected, not just in terms of transitions to adult services but also regarding exiting and re-entering services, longer-term ad hoc support and continuity of care. Those aged 16 or 17 years are particularly disadvantaged, often caught between CYP’s services refusing new post-16 referrals and adult services unable to accept under-18s. This is rarely a problem in services catering for those up to age 25 years like the UK YIACS and Australian Headspace Centres.
-
The learning culture component of our model strongly implies that services need more than mere staff training and development. While workforce development is rarely excluded from CYP’s mental health policy, a learning culture requires leadership and workforce development strategies that incorporate learning opportunities, clinical supervision, reflexive learning, reflective practice and the freedom to innovate in practice. In educating the children’s mental health workforce – both at pre-qualifying and post-qualifying levels – it goes without saying that practitioners need to be compassionate and competent. However, judgements on these qualities are often made by the workers and professions involved without consultation with service users; CYP and families should be the main arbiters of what compassion and competence mean.
-
Lived experience in service provision is valuable but may work better when delivered alongside professional support rather than as a substitute.
-
Stakeholders in children’s mental health services want more information about services, specifically what services are available locally, how services might be accessed, the support offered and what happens once the CYP leaves the service. More publicity about the services available, both locally and nationally, should be provided in schools.
-
Ideally, a range of services, whether provided by one provider or competing providers, should be on offer to CYP and families so they are able to choose services best tailored to their individual needs. In (mainly urban) areas where a range of service options is available, CYP and parents want sufficient information to enable them to choose the most appropriate service.
-
The private and third sectors appear more agile when it comes to offering choice, personalisation and flexibility. Exploring the reasons behind this may help develop future statutory (NHS) services.
Recommendations for research
We make the following recommendations for further research:
-
That our model is consistent with what has been reported in the literature for many years suggests there is little value in conducting further exploratory work in this area; instead, research should focus on how to implement the components in our model into practice.
-
Though our model is evidence-based, research should be conducted into whether using our model to design, deliver or audit services has any impact on outcomes (both CYP/family-focused and organisational).
-
Given the limited evidence found for digital services and the surge in their use during the pandemic, more research exploring the advantages and disadvantages of digital/remote platforms in delivering children’s mental health services is required.
-
Research exploring what the statutory sector could learn from the private and third sectors in terms of choice, personalisation and flexibility.
-
We know little about those who chose not to engage with children’s mental health services, so there is potential for research with those who refuse and/or disengage from services and others whose voices are seldom heard. Often these are CYP with co-occurring issues such as offending behaviour, neurodiversity or substance misuse, which this study did not explore in depth.
-
When researching services, a diverse profile of service providers/staff should be included; if there is a lack of diversity due to systemic issues, research should be conducted into how the staff delivering services might be more representative of those using them.
-
Further work on the cost effectiveness of different approaches in CYP’s mental health should be conducted, taking account of both costs and benefits especially where digital self-help strategies, peer workers or associate professionals might substitute or augment highly trained and experienced mental health professionals.
-
To understand more about the comparative cost effectiveness of different approaches, one or more standardised measures of health benefit should be established and used in all economic evaluations of children’s mental health services.
Additional information
Acknowledgements
We are grateful to our case study participants and the organisations who permitted us to use their services as case study sites. We are also grateful to individuals and organisations that helped facilitate this study including Sue Pargeter at the NIHR, our study advisory and independent steering group members (see additional files www.fundingawards.nihr.ac.uk/award/17/09/08; accessed 26 March 2024), Rachel Temple and Thomas Kabir at McPin, the young people from Common Room who provided feedback on the study’s various aspects, the NIHR Clinical Research Networks (health services research, mental health and children specialties) and the peer reviewers who provided constructive feedback on the original funding application and this report.
We are especially grateful to our six young co-researchers – Bekah Carrington, Jodie Crooks, James Diffey, Rose McGowan, Georgia Naughton and Keeya. As outlined in Chapter 2, their participation has been mutually beneficial in that not only have they brought valuable user perspectives to the study, working on the study has provided them with opportunities for personal and career development.
Contributions of authors
Steven Pryjmachuk (https://orcid.org/0000-0002-6976-1727) (Professor, Mental Health Nursing) led on study design and conceptualisation; supervised the literature review and service map work streams; conducted the literature searches; led on screening, data extraction and analysis for the literature reviews; contributed to the model building synthesis; wrote the scoping and integrative review chapters; led on writing and editing this report.
Susan Kirk (https://orcid.org/0000-0002-1485-8804) (Professor, Child and Family Health) helped design and conceptualise the study; assisted with screening, data extraction and analysis for the literature reviews; co-supervised the case study work stream; contributed to case study data analysis and model building synthesis; co-wrote the case study chapter; reviewed and approved this report.
Claire Fraser (https://orcid.org/0000-0003-3684-3168) (Research Associate, Health Services Research) assisted with the literature searches; assisted with screening, data extraction and analysis for the literature reviews; co-led the service map data collection and analysis; co-wrote the service map chapter; obtained the necessary ethical permissions; provided research training support for the young co-researchers; conducted case study interviews; contributed to case study data analysis and model building synthesis; co-wrote the case study chapter; reviewed and approved this report.
Nicola Evans (https://orcid.org/0000-0001-5154-0478) (Reader, Health Services Research) helped design and conceptualise the study; assisted with screening, data extraction and analysis for the literature reviews; co-supervised the case study work stream; contributed to case study data analysis and model building synthesis; co-wrote the case study chapter; reviewed and approved this report.
Rhiannon Lane (https://orcid.org/0000-0002-4964-2472) (Research Associate, Health Services Research) assisted with screening, data extraction and analysis for the literature reviews; co-led the service map data collection and analysis; co-wrote the service map chapter; provided research training support for the young co-researchers; conducted interviews for the case study; contributed to case study data analysis; reviewed and approved this report.
Liz Neill (Director, Common Room North) supported the study’s PPI elements; provided training support for the young co-researchers; provided expert opinion on the model typology and final model; reviewed and approved this report.
Elizabeth Camacho (https://orcid.org/0000-0001-9574-7710) (Senior Research Fellow, Health Economics) helped design and conceptualise the study; led on the study’s health economics aspects; provided expert opinion on the model typology and final model; reviewed and approved this report.
Peter Bower (https://orcid.org/0000-0001-9558-3349) (Professor, Heath Services Research) helped design and conceptualise the study; offered advice and guidance regarding the literature reviews; provided expert opinion on the model typology and final model; reviewed and approved this report.
Penny Bee (https://orcid.org/0000-0002-5600-0400) (Professor, Health Service Research) helped design and conceptualise the study; provided research training support for the young co-researchers; provided expert opinion on the model typology and final model; reviewed and approved this report.
Tim McDougall (https://orcid.org/0000-0002-9843-9315) (NHS Director of Nursing and Quality) helped design and conceptualise the study; provided expert opinion the model typology and final model; reviewed and approved this report.
Disclosure of interests
Full disclosure of interests: Completed ICMJE forms for all authors, including all related interests, are available in the toolkit on the NIHR Journals Library report publication page at https://doi.org/10.3310/DKRT6293.
Primary conflicts of interest: Steven Pryjmachuk is an unpaid non-executive director of Six Degrees CIC, a mental health social enterprise, holds a strategic honorary contract with Greater Manchester Mental Health NHS Foundation Trust and was a member of the 2021 NIHR i4i Digital Health Technologies for Children and Young People’s Mental Health funding panel. Susan Kirk is a member of the NIHR Research for Patient Benefit funding panel. Nicola Evans was Chief Investigator on an NIHR-funded study on crisis care in children and young people’s mental health (NIHR128359). Liz Neill is Director of Common Room North, a consultancy organisation led by lived experience in mental health, a member of the programme board for Future in Mind: Leeds and a trustee of The Market Place, a youth service provider. Elizabeth Camacho was a member of the 2019–21 NIHR Research for Patient Benefit funding panel and is a member of the NIHR Health Technology Assessment funding panel. Peter Bower is an NIHR Senior Investigator and a member of the NIHR Programme Grants for Applied Research funding panel. Penny Bee is a member of the NIHR Programme Grants for Applied Research funding panel. Tim McDougall is Director of Nursing and Quality (Specialist Services) at Lancashire and South Cumbria NHS Foundation Trust.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review.
Ethics statement
The Work Stream 3 case study component received a favourable ethical opinion from South Central-Berkshire Research Ethics Committee on 28 April 2020 (reference 20/SC/0174). Health Research Authority (HRA) and Health and Care Research Wales (HCRW) approvals were granted 4 August 2020. Four substantial amendments received favourable ethical opinions in July, October and November 2020 and in February 2021, as did two minor amendments in March and June 2021.
Information governance statement
The University of Manchester and Cardiff University are committed to handling all personal information in line with the UK Data Protection Act (2018) and the General Data Protection Regulation (EU GDPR) 2016/679. Under Data Protection legislation, The University of Manchester and Cardiff University are Data Controllers for their respective contributions to the data collected for this project and we process personal data in accordance with their instructions. You can find out more about how we handle personal data, including how to exercise your individual rights and the contact details for the respective Data Protection Officers here www.manchester.ac.uk/discover/privacy-information/data-protection/ (The University of Manchester) and here www.cardiff.ac.uk/public-information/policies-and-procedures/data-protection (Cardiff University).
Department of Health and Social Care disclaimer
This publication presents independent research commissioned by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by the interviewees in this publication are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, MRC, NIHR Coordinating Centre, the Health and Social Care Delivery Research programme or the Department of Health and Social Care.
This monograph was published based on current knowledge at the time and date of publication. NIHR is committed to being inclusive and will continually monitor best practice and guidance in relation to terminology and language to ensure that we remain relevant to our stakeholders.
Publication
Pryjmachuk S, Kirk S, Fraser C, Evans N, Lane R, Crooks J et al. A collaboratively produced model of service design for children and young people with common mental health problems. BMC Health Serv Res 2024;24:133. https://doi.org/10.1186/s12913-024-10562-7
Disclaimers
This article presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care.
References
- National Institute for Health Research Health Services and Delivery Research . Commissioning Brief 17 09 – Services to Support Early Intervention and Self-Care for Children and Young People Referred to Children and Young People’s Mental Health Services CAMHS With Common Emotional and Behavioural Problems 2017.
- National Institute for Health and Care Research (NIHR) . Research Award: Identifying and Evaluating Mental Health Early Intervention Services and Self-Care Support for Lesbian, Gay, Bisexual and Transgender Young People: A Mixed Methods Study, 17 09 04 2017. https://fundingawards.nihr.ac.uk/award/17/09/04 (accessed 13 April 2022).
- Murphy M, Fonagy P. Our Children Deserve Better: Prevention Pays, Annual Report of the Chief Medical Officer 2012. London: Department of Health; 2013.
- National Assembly for Wales Children, Young People and Education Committee . Inquiry into Specialist Child and Adolescent Mental Health Services 2014.
- NHS England . Future in Mind: Promoting, Protecting and Improving Our Children and Young People’s Mental Health and Wellbeing 2015.
- Children’s Commissioner for England . Lightning Review: Access to Child and Adolescent Mental Health Services, May 2016 2016.
- World Health Organization . Mental Health Action Plan 2013–2020 2013.
- Green H, McGinnity A, Meltzer H, Ford T, Goodman R. Mental Health of Children and Adolescents in Great Britain, 2004. Basingstoke: Palgrave MacMillan; 2005.
- Sadler K, Vizard T, Ford T, Marcheselli F, Pearce N, Mandalia D, et al. Mental Health of Children and Young People in England, 2017: Summary of Key Findings. Leeds: NHS Digital; 2018.
- Newlove-Delgado T, Williams T, Robertson K, McManus S, Sadler K, Vizard T, et al. Mental Health of Children and Young People in England, 2021. Leeds: NHS Digital; 2021.
- NHS Digital . Mental Health Services Referrals and Care Contacts for Children and Young People Aged 0 to 18 2021. https://digital.nhs.uk/data-and-information/data-tools-and-services/data-services/mental-health-data-hub/mental-health-services-monthly-statistics (accessed 13 April 2022).
- National Institute for Health and Care Excellence (NICE) . Common Mental Health Problems: Identification and Pathways to Care Clinical Guideline [CG123] 2011.
- NHS Health Advisory Service . Child and Adolescent Mental Health Services: Together We Stand 1995.
- Audit Commission . Children in Mind: Child and Adolescent Mental Health Services 1999.
- CAMHS Review . Children and Young People in Mind: The Final Report of the National CAMHS Review 2008.
- National Assembly for Wales Children, Young People and Education Committee . Mind Over Matter: A Report on the Step Change Needed in Emotional and Mental Health Support for Children and Young People in Wales 2018.
- Robotham D, James K, Cyhlarova E. Managing demand and capacity within child and adolescent mental health services: an evaluation of the Choice and Partnership Approach. Mental Health Rev J 2010;15:22-30. https://doi.org/10.5042/mhrj.2010.0656.
- Kingsbury S, Rayment B, Fleming I, Thompson P, York A, Hemsley M, et al. CYP IAPT Principles in Child & Adolescent Mental Health Services: Values and Standards: ‘Delivering with and Delivering Well’. London: CAMHS Press; 2014.
- Wolpert M, Harris R, Hodges S, Fuggle P, James R, Weiner A, et al. THRIVE Framework for System Change. London: Anna Freud National Centre for Children and Families/Tavistock and Portman NHS Foundation Trust; 2019.
- Pryjmachuk S, Elvey R, Kirk S, Kendal S, Bower P, Catchpole R. Developing a model of mental health self-care support for children and young people through an integrated evaluation of available types of provision involving systematic review, meta-analysis and case study. Health Serv Deliv Res 2014;2:1-212.
- Public Health England . The Link Between Pupil Health and Wellbeing and Attainment: A Briefing for Head Teachers, Governors and Staff in Education Settings 2014.
- Department of Health/Department for Education . Transforming Children and Young People’s Mental Health Provision: A Green Paper 2017.
- Hannigan B, Edwards D, Evans N, Gillen E, Longo M, Pryjmachuk S, et al. An evidence synthesis of risk identification, assessment and management for young people using tier 4 inpatient child and adolescent mental health services. Heath Serv Deliv Res 2015;3:1-228.
- Cowan K, Oliver S. The James Lind Alliance Guidebook, Version 5. Southampton: James Lind Alliance; 2013.
- Lovell K, Bee P, Bower P, Brooks H, Cahoon P, Callaghan P, et al. Training to enhance user and carer involvement in mental health-care planning: the EQUIP research programme including a cluster RCT. Programme Grants Appl Res 2019;7:1-140. https://doi.org/10.3310/pgfar07090.
- A Research Handbook for Patient and Public Involvement Researchers. Manchester: Manchester University Press; 2018.
- Fraser C, Carrington B, Crooks J, Diffey J, Evans N, . The Blueprint Writing Collective . A blueprint for involvement: reflections of lived experience co-researchers and academic researchers on working collaboratively. Res Involv Engagem 2022;8. https://doi.org/10.1186/s40900-022-00404-3.
- Pryjmachuk S, Kirk S, Fraser C, Evans N, Lane R, Bee P, et al. A Systematic Review of the Effectiveness, Acceptability and Cost-Effectiveness of Services for Children and Young People With Common Mental Health Problems 2018. www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42018106219 (accessed 13 April 2022).
- Colquhoun HL, Levac D, O’Brien KK, Straus S, Tricco AC, Perrier L, et al. Scoping reviews: time for clarity in definition, methods, and reporting. J Clin Epidemiol 2014;67:1291-4. https://doi.org/10.1016/j.jclinepi.2014.03.013.
- Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol 2018;18. https://doi.org/10.1186/s12874-018-0611-x.
- Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol 2005;8:19-32. https://doi.org/10.1080/1364557032000119616.
- Hetrick SE, Parker AG, Callahan P, Purcell R. Evidence mapping: illustrating an emerging methodology to improve evidence-based practice in youth mental health. J Eval Clin Pract 2010;16:1025-30. https://doi.org/10.1111/j.1365-2753.2008.01112.x.
- Pham MT, Rajić A, Greig JD, Sargeant JM, Papadopoulos A, McEwen SA. A scoping review of scoping reviews: advancing the approach and enhancing the consistency. Res Syn Meth 2014;5:371-85. https://doi.org/10.1002/jrsm.1123.
- Sargeant JM, O’Connor AM. Scoping reviews, systematic reviews, and meta-analysis: applications in veterinary medicine. Front Vet Sci 2020;7. https://doi.org/10.3389/fvets.2020.00011.
- Whittemore R, Knafl K. The integrative review: updated methodology. J Adv Nurs 2005;52:546-53. https://doi.org/10.1111/j.1365-2648.2005.03621.x.
- Cronin MA, George E. The why and how of the integrative review. Organ Res Methods 2020;26:168-92. https://doi.org/10.1177/1094428120935507.
- Centre for Reviews and Dissemination . Systematic Reviews: CRD’s Guidance for Undertaking Reviews in Health Care 2008.
- Garner P, Hopewell S, Chandler J, MacLehose H, Schünemann HJ, Akl EA, et al. Panel for Updating Guidance for Systematic Reviews (PUGs) . When and how to update systematic reviews: consensus and checklist. BMJ 2016;354. https://doi.org/10.1136/bmj.i3507.
- Brauner CB, Stephens CB. Estimating the prevalence of early childhood serious emotional/behavioral disorders: challenges and recommendations. Public Health Rep 2006;121:303-10. https://doi.org/10.1177/003335490612100314.
- NHS England . Adult Improving Access to Psychological Therapies Programme n.d. www.england.nhs.uk/mental-health/adults/iapt/ (accessed 13 April 2022).
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Medical Research Council Guidance . Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 2008;337. https://doi.org/10.1136/bmj.a1655.
- O’Cathain A, Croot L, Duncan E, Rousseau N, Sworn K, Turner KM, et al. Guidance on how to develop complex interventions to improve health and healthcare. BMJ Open 2019;9. https://doi.org/10.1136/bmjopen-2019-029954.
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372. https://doi.org/10.1136/bmj.n71.
- Hong Q, Pluye P, Fàbregues S, Bartlett G, Boardman F, Cargo M, et al. Mixed Methods Appraisal Tool (MMAT) Version 2018 User Guide. Gatineau, QC: Canadian Intellectual Property Office, Industry Canada; 2018.
- Scott SD, Rotter T, Flynn R, Brooks HM, Plesuk T, Bannar-Martin KH, et al. Systematic review of the use of process evaluations in knowledge translation research. Syst Rev 2019;8. https://doi.org/10.1186/s13643-019-1161-y.
- Jensen PS, Hoagwood K, Petti T. Outcomes of mental health care for children and adolescents: II. Literature. J Am Acad Child Adolesc Psychiatry 1996;35:1064-77. https://doi.org/10.1097/00004583-199608000-00018.
- Bower P, Gilbody S. Stepped care in psychological therapies: access, effectiveness and efficiency: narrative literature review. Br J Psychiatry 2005;186:11-7.
- Schmied DV, Brownhill DS, Walsh P. Models of Service Delivery and Interventions for Children and Young People with High Needs. Ashfield, NSW: NSW Department of Community Services; 2006.
- Biggins T. Specialist Mental Healthcare for Children and Adolescents: Hospital, Intensive Community and Home-based Services. Abingdon: Routledge; 2014.
- McDougall T, Worrall-Davies A, Hewson L, Richardson G, Cotgrove A. Tier 4 Child and Adolescent Mental Health Services (CAMHS) – inpatient care, day services and alternatives: an overview of Tier 4 CAMHS provision in the UK. Child Adolesc Ment Health 2008;13:173-80. https://doi.org/10.1111/j.1475-3588.2007.00481.x.
- Kurtz Z. The Evidence Base to Guide Development of Tier 4 CAMHS. London: Department of Health; 2009.
- Shepperd S, Doll H, Gowers S, James A, Fazel M, Fitzpatrick R, et al. Alternatives to inpatient mental health care for children and young people. Cochr Datab Syst Rev 2009;2. https://doi.org/10.1002/14651858.CD006410.pub2.
- Lamb CE. Alternatives to admission for children and adolescents: providing intensive mental healthcare services at home and in communities: what works?. Curr Opin Psychiatry 2009;22:345-50. https://doi.org/10.1097/YCO.0b013e32832c9082.
- Shailer JL, Gammon RA, de Terte I. Youth with serious mental health disorders: wraparound as a promising intervention in New Zealand. Aust N Z J Fam Ther 2013;34:186-213. https://doi.org/10.1002/anzf.1028.
- Kwok KHR, Yuan SNV, Ougrin DR. Alternatives to inpatient care for children and adolescents with mental health disorders. Child Adolesc Ment Health 2016;21:3-10. https://doi.org/10.1111/camh.12123.
- Social Services Improvement Agency . Known Effectiveness of Models and Frameworks for Interventions With Children and Families: Phase 1 2015.
- Houses of Parliament Parliamentary Office of Science & Technology . POSTNote 563: Mental Health Service Models for Young People 2017.
- Harden A, Thomas J. Methodological issues in combining diverse study types in systematic reviews. Int J Soc Res Methodol 2005;8:257-71. https://doi.org/10.1080/13645570500155078.
- The World Bank . Population, Total 2020. https://data.worldbank.org/indicator/SP.POP.TOTL (accessed 13 April 2022).
- Gröne O, Garcia-Barbero M. WHO European Office for Integrated Health Care Services . Integrated care: a position paper of the WHO European Office for Integrated Health Care Services. Int J Integr Care 2001;1.
- Goodwin N. Understanding integrated care. Int J Integr Care 2016;16. https://doi.org/10.5334/ijic.2530.
- Theodosiou L, Glick O. Peer Support Models for Children and Young People with Mental Health Problems. London: Centre for Mental Health/Children & Young People’s Mental Health Coalition; 2020.
- Shah S. Collaborative Care: An Exploration into Core Tenets, Fidelity, and Policy. London: Centre for Mental Health; 2018.
- Wergeland GJH, Riise EN, Öst L-G. Cognitive behavior therapy for internalizing disorders in children and adolescents in routine clinical care: a systematic review and meta-analysis. Clin Psychol Rev 2021;83. https://doi.org/10.1016/j.cpr.2020.101918.
- McGorry PD, Mei C. Early intervention in youth mental health: progress and future directions. Evid Based Mental Health 2018;21:182-4. https://doi.org/10.1136/ebmental-2018-300060.
- McGorry P, Trethowan J, Rickwood D. Creating headspace for integrated youth mental health care. World Psychiatry 2019;18:140-1. https://doi.org/10.1002/wps.20619.
- Care Quality Commission . Provider Collaboration Review: Mental Health Care of Children and Young People During the COVID-19 Pandemic 2021. www.cqc.org.uk/publications/themes-care/provider-collaboration-review-mental-health-care-children-young-people (accessed 13 April 2022).
- Academy of Consultation-Liaison Psychiatry . What Is Consultation-Liaison Psychiatry? n.d. www.clpsychiatry.org/about-aclp/whatis-clp/ (accessed 13 April 2022).
- Bronfenbrenner U. Making Human Beings Human: Bioecological Perspectives on Human Development. Thousand Oaks, CA: Sage; 2005.
- Bruns EJ, Walker J, Adams J, Miles P, Osher T, Rast J, et al. Ten Principles of the Wraparound Process. Portland, OR: National Wraparound Initiative, Research and Training Center on Family Support and Children’s Mental Health, Portland State University; 2014.
- Tolan PH, Dodge KA. Children’s mental health as a primary care and concern: a system for comprehensive support and service. Am Psychol 2005;60:601-14. https://doi.org/10.1037/0003-066X.60.6.601.
- Henggeler SW. Multisystemic therapy: an overview of clinical procedures, outcomes, and policy implications. Child Psychol Psychiatr Rev 1999;4:2-10. https://doi.org/10.1017/S1360641798001786.
- MST UK & Ireland . MST Teams in the UK & Ireland. MST UK &Amp; Ireland n.d. www.mstuk.org/mst-uk/mst-uk-teams (accessed 13 April 2022).
- Faw Stambaugh L, Mustillo SA, Burns BJ, Stephens RL, Baxter B, Edwards D, et al. Outcomes from wraparound and multisystemic therapy in a center for mental health services system-of-care demonstration site. J Emot Behav Disord 2007;15:143-55. https://doi.org/10.1177/10634266070150030201.
- York A, Kingsbury S. The Choice and Partnership Approach: A Guide to CAPA. Bournemouth: Caric Press; 2009.
- Powers J, Webber K, Bower H. Promoting school mental health with a systems of care approach: perspectives from community partners. Soc Work Ment Health 2011;9:147-62. https://doi.org/10.1080/15332985.2010.534363.
- Burchard JD. Evaluation of the Fort Bragg managed care experiment. J Child Fam Stud 1996;5:173-6. https://doi.org/10.1007/BF02237939.
- Friedman RM. The Fort Bragg study: what can we conclude?. J Child Fam Stud 1996;5:161-8. https://doi.org/10.1007/BF02237937.
- Bickman L. The evaluation of a children’s mental health managed care demonstration. J Ment Health Adm 1996;23:7-15. https://doi.org/10.1007/BF02518639.
- Stroul BA, Ed M, Blau GM, Friedman RM. Updating the System of Care Concept and Philosophy. Washington, DC: Georgetown University Center for Child and Human Development, National Technical Assistance Center for Children’s Mental Health; 2010.
- Northern Ireland Commissioner for Children and Young People . ‘Still Waiting’: A Rights Based Review of Mental Health Services and Support for Children and Young People in Northern Ireland 2018.
- Crenna-Jennings W, Hutchinson J. Access to Children and Young People’s Mental Health Services: 2018. London: Education Policy Institute; 2018.
- Wolpert M, Harris R, Hodges S, Fuggle P, James R, Weiner A, et al. THRIVE Elaborated. London: CAMHS Press; 2016.
- Glisson C. The organizational context of children’s mental health services. Clin Child Fam Psychol Rev 2002;5:233-53.
- Kutcher S, McLuckie A. creating a child and youth mental health framework for Canada. Psychiatr Serv 2013;64:479-82. https://doi.org/10.1176/appi.ps.201100269.
- Kirk S, Beatty S, Callery P, Milnes L, Pryjmachuk S. Evaluating Self-Care Support for Children and Young People With Long-Term Conditions 2010.
- Blueprint . Blueprint: Service Design for Children and Young People’s Mental Health n.d. https://sites.manchester.ac.uk/blueprint/ (accessed 13 April 2022).
- Anna Freud National Centre for Children and Families . Youth Wellbeing Directory n.d. www.annafreud.org/on-my-mind/youth-wellbeing/ (accessed 13 April 2022).
- Youth Access . Find Your Local Service n.d. www.youthaccess.org.uk/services/find-your-local-service (accessed 13 April 2022).
- Office for National Statistics . Census 2021: Population Estimates 2021. www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates (accessed 13 April 2022).
- Paun A, Cheung A, Nicholson E. Funding Devolution: The Barnett Formula in Theory and Practice. London: Institute for Government; 2021.
- Hayes D, Edbrooke-Childs J, Town R, Wolpert M, Midgley N. Barriers and facilitators to shared decision making in child and youth mental health: clinician perspectives using the Theoretical Domains Framework. Eur Child Adolesc Psychiatry 2019;28:655-66. https://doi.org/10.1007/s00787-018-1230-0.
- British Psychological Society . Mental Health Support Teams: How to Maximise the Impact of the New Workforce for Children and Young People 2019.
- National Institute for Health and Care Research (NIHR) . Research Award: Crisis Responses for Children and Young People: An Evidence Synthesis of Service Organisation, Effectiveness and Experiences (CAMH Crisis), NIHR128359 2019. https://fundingawards.nihr.ac.uk/award/NIHR128359 (accessed 13 April 2022).
- Yin R. Applications of Case Study Research. London: Sage; 2012.
- Ritchie J, Spencer L. Analysing Qualitative Data. London: Routledge; 1994.
- Ritchie J, Spencer L. Qualitative Research Practice: A Guide for Social Science Students and Researchers. London: Sage; 2003.
- Curtis LA, Burns A. Unit Costs of Health & Social Care 2020. Kent: PSSRU, University of Kent; 2020.
- Fetters MD, Curry LA, Creswell JW. Achieving integration in mixed methods designs: principles and practices. Health Serv Res 2013;48:2134-56. https://doi.org/10.1111/1475-6773.12117.
- Gaugh HG. Scientific Method in Practice. Cambridge: Cambridge University Press; 2003.
- NHS England . NHS Mental Health Implementation Plan 2019 20–2023 24 2019.
- Department of Health . You’re Welcome Quality Criteria: Making Health Services Young People Friendly 2006.
- Frith E. Children and Young People’s Mental Health: Time to Deliver (the Report of the Commission on Children and Young People’s Mental Health). London: Education Policy Institute; 2016.
- National Children’s Bureau . Making a Difference to Young People’s Lives Through Personalised Care: Mental Health Inequalities and Social Deprivation 2021.
- Hassan SM, Worsley J, Nolan L, Fearon N, Ring A, Shelton J, et al. An exploration of young people’s, parent/carers’, and professionals’ experiences of a voluntary sector organisation operating a Youth Information, Advice, and Counselling (YIAC) model in a disadvantaged area. BMC Health Serv Res 2022;22. https://doi.org/10.1186/s12913-022-07800-1.
- Pajer K, Pastrana C, Gardner W, Sivakumar A, York A. A scoping review of the Choice and Partnership Approach in child and adolescent mental health services. J Child Health Care 2022. https://doi.org/10.1177/13674935221076215.
- Burn A-M, Vainre M, Humphrey A, Howarth E. Evaluating the CYP-IAPT transformation of child and adolescent mental health services in Cambridgeshire, UK: a qualitative implementation study. Implement Sci Commun 2020;1. https://doi.org/10.1186/s43058-020-00078-6.
- Bartlett NA, Freeze TB. Community schools: new perspectives on the wraparound approach. Exceptionality Educ Int 2018;28:55-81. https://doi.org/10.5206/eei.v28i2.7765.
- Pryjmachuk S, Graham T, Haddad M, Tylee A. School nurses’ perspectives on managing mental health problems in children and young people: school nurses and mental health. J Clin Nurs 2012;21:850-9. https://doi.org/10.1111/j.1365-2702.2011.03838.x.
- Jenkins P. Having confidence in therapeutic work with young people: constraints and challenges to confidentiality. Br J Guid Couns 2010;38:263-74. https://doi.org/10.1080/03069885.2010.483128.
- Tierney S, Bivins R, Seers K. Compassion in nursing: solution or stereotype?. Nurs Inq 2018;26. https://doi.org/10.1111/nin.12271.
- NHS Benchmarking Network . Children and Young People’s Mental Health Services Workforce: Report for Health Education England 2021.
- Glisson C, Hemmelgarn A, Green P, Dukes D, Atkinson S, Williams NJ. Randomized trial of the availability, responsiveness, and continuity (ARC) organizational intervention with community-based mental health programs and clinicians serving youth. J Am Acad Child Adolesc Psychiatry 2012;51:780-7. https://doi.org/10.1016/j.jaac.2012.05.010.
- Glisson C, Hemmelgarn A, Green P, Williams NJ. Randomized trial of the availability, responsiveness and continuity (ARC) organizational intervention for improving youth outcomes in community mental health programs. J Am Acad Child Adolesc Psychiatry 2013;52:493-500. https://doi.org/10.1016/j.jaac.2013.02.005.
- Glisson C, Williams NJ, Hemmelgarn A, Proctor E, Green P. Aligning organizational priorities with ARC to improve youth mental health service outcomes. J Consult Clin Psychol 2016;84:713-25. https://doi.org/10.1037/ccp0000107.
- Rocks S, Glogowska M, Stepney M, Tsiachristas A, Fazel M. Introducing a single point of access (SPA) to child and adolescent mental health services in England: a mixed-methods observational study. BMC Health Serv Res 2020;20. https://doi.org/10.1186/s12913-020-05463-4.
- Pettitt B. Effective Joint Working Between Child and Adolescent Mental Health Services and Schools. Nottingham: Department for Education and Skills; 2003.
- Day L, Blades R, Spence C, Ronicle J. Mental Health Services and Schools Link Pilots: Evaluation Report. London: Department for Education; 2017.
- Garland L, Dalzell K, Wolpert M. What Works for Me: The Self-care Approaches of Children and Young People. London: CAMHS Press; 2019.
- James K. Remote Mental Health Interventions for Young People: A Rapid Review of the Evidence. London: Youth Access; 2020.
- Hollis C, Falconer CJ, Martin JL, Whittington C, Stockton S, Glazebrook C, et al. Digital health interventions for children and young people with mental health problems – a systematic and meta-review. J Child Psychol Psychiatr 2017;58:474-503. https://doi.org/10.1111/jcpp.12663.
- Liverpool S, Mota CP, Sales CMD, Čuš A, Carletto S, Hancheva C, et al. Engaging children and young people in digital mental health interventions: systematic review of modes of delivery, facilitators, and barriers. J Med Internet Res 2020;22. https://doi.org/10.2196/16317.
- Nolte E. How Do We Ensure That Innovation in Health Service Delivery and Organization is Implemented, Sustained and Spread? Policy Brief. Copenhagen: World Health Organization Regional Office for Europe; 2018.
Appendix 1 Inclusion/exclusion criteria
Population: CYP experiencing CMHPs
Included:
-
< 18 years; up to 25 if core provision is for under 18s.
-
CMHPs were agreed by the research team and advisory group to be: anxiety and related disorders (OCD, phobias, school refusal); depression; self-harm; PTSD; ‘emerging personality disorder’; adjustment disorder; ADHD or attention deficit disorder; conduct disorder; ODD; substance misuse disorders; ‘at risk of psychosis’.
Excluded:
-
Adults.
-
Excluded by the commissioning brief: eating disorders; psychosis; autism/autism spectrum disorder.
-
Excluded because of the parallel QF2 study: gender identity issues.
-
Agreed by the research team and advisory group: ‘ultra-high risk of psychosis’; enuresis; encopresis; ‘behaviour problems’ not identified as ADHD, ODD or conduct disorder; primary focus on juvenile offending or learning disability; serious antisocial behaviour or complex needs where main risk is removal from home.
-
‘Emotional disturbance’ or ‘SED’ without explicit reference to any of the included conditions above.
Intervention: services for CYP experiencing CMHPs
Included:
-
Current and historical services; pilot or experimental services.
-
Settings: day hospital; outpatients; community; CYP’s home or home alternative; educational institutions.
-
Scoping review: service is described in sufficient detail to enable its categorisation into a typology.
Excluded:
-
Treatments/interventions rather than services; services for preventing mental ill-health or for promoting mental well-being.
-
Services provided in institutional settings (inpatient services, residential services, youth offending institutions); treatment foster care.
-
Scoping review: insufficient detail about the service.
Comparators:
-
Scoping review: not applicable.
-
Integrative review: effectiveness data – other service models, standard care/treatment as usual, inpatient/residential care; acceptability data – not applicable; economic data – as effectiveness data.
Outcomes:
-
Scoping review: not applicable.
-
Integrative review: effectiveness data – relevant measures of CYP’s mental health, family functioning, educational attainment or quality of life; acceptability data – qualitative and quantitative data capturing stakeholder views; economic data – incremental cost effectiveness of service model versus comparator.
Study (document) type:
Included:
-
Scoping review: any document (journal papers, books, book chapters, reports, theses, policy documents, opinion papers, editorials, commentaries, protocols) with a sufficiently detailed description of a service.
-
Integrative review: effectiveness data – peer-reviewed quantitative studies with at least one pre/post outcome measure; acceptability data – peer-reviewed qualitative or quantitative studies in which either participants’ views are expressed or in which participation data are available; economic data – peer-reviewed studies reporting costs, health outcomes, and incremental cost-effectiveness analyses.
Excluded:
-
Both reviews: conference abstracts/posters (but checked for any relevant full-study papers); reviews (reference lists checked for any relevant documents).
-
Integrative review: books, book chapters, reports, theses, policy documents, opinion papers, editorials, commentaries, protocols.
Appendix 2 Search strategy
Search terms used:
-
Population: CYP experiencing CMHPs:
-
[CYP] – child* OR p?ediatric* OR teen* OR adolescen* OR young person OR young people OR young adult OR youth OR student OR pupil OR juvenile
-
[CMHPs] – anxiet* OR anxious OR worr* OR depress* OR obsessive compulsive OR OCD OR traumatic stress OR PTSD OR suicid* OR parasuicd* OR self harm* OR self injur* OR phobi* OR school refusal OR panic OR gender identity OR mental disorder* OR psychiatr* OR mental* ill* OR mental* distress* OR mental health problem* OR mental health difficult* OR mood disorder* OR affective disorder* OR emotional problem* OR emotional difficult* OR emotional* distress* OR ADHD OR attention deficit OR conduct disorder* OR behavio?r* problem* OR oppositional defian* OR adjustment disorder* OR substance misuse OR substance abuse OR ‘substance use’
-
-
Intervention: service models for CYP experiencing mental health problems:
-
[generic terms] – service* ADJ2 organi?ation* OR service* ADJ2 model* OR service* ADJ2 delivery OR service* ADJ2 (framework* OR frame work*) OR service* ADJ2 system* OR service ADJ2 (pathway* OR path way*) OR service ADJ2 program* OR care ADJ2 organi?ation* OR care ADJ2 model* OR care ADJ2 delivery OR care ADJ2 (framework* OR frame work*) OR care ADJ2 system* OR care ADJ2 (pathway* OR path way*) OR care ADJ2 program* OR digital ADJ2 model* OR digital* ADJ2 deliver* OR digital ADJ2 service* OR digital ADJ2 system* OR digital ADJ2 care OR digital ADJ2 program* OR e health OR ehealth OR m health OR mhealth OR tele health OR tele care OR tele psychiatr*
-
[proprietary terms] – KOOTH OR Thrive OR iThrive OR ‘i Thrive’ OR IAPT OR ‘improving access to psychological therap*’ OR CAPA OR ‘choice and partnership approach’ OR ‘brief consultation’ OR brief assessment OR therapeutic assessment OR tier OR early intervention OR wrap around OR wraparound OR MST OR multi systemic OR multisystemic OR rapid assessment OR ARC OR ‘Availability Responsiveness and Continuity’ OR stepped care OR multi modal OR multimodal OR CAMH* OR liaison psychiatry OR A&E liaison OR crisis care
-
[additional terms] – triage OR self?manage* OR self?care OR self?help OR peer support OR peer mentor* OR recovery
-
Aggregate search = (1a OR 1b) AND (2a OR 2b OR 2c).
Notes: OVID syntax displayed; equivalents used in other databases. ADJ2 = within two words proximity of each other; * = truncation; ? = wildcard.
Databases/resources searched
Accessed via Ovid (Ovid Technologies Inc., New York, NY):
-
PsycINFO
-
MEDLINE
-
Cochrane EBM Reviews
-
Heath Management Information Consortium (HMIC)
-
Social Policy and Practice
-
EMBASE
-
Allied and Complementary Medicine Database (AMED)
Accessed via EBSCO (EBSCO Industries Inc., Birmingham, AL):
-
CINAHL Plus
-
Social Sciences Full Text
-
British Education Index
Accessed via ProQuest (ProQuest LLC, Ann Arbor, MI):
-
British Nursing Index
-
Sociological Abstracts
-
Applied Social Sciences Index and Abstracts (ASSIA)
-
Social Services Abstracts
-
Education Resources Information Center (ERIC)
Simpler searches were conducted in the following resources with less sophisticated database querying:
-
SCOPUS
-
Cochrane Library
-
Community Care Inform (Children)
-
Social Care Online
-
Campbell Collaboration
-
OpenGrey
-
North Grey Literature Collection
-
NHS Evidence
-
NIHR Journals Library
Appendix 3 Screen in/out terms
Stage 1 screen in terms:
-
[services terms] – service; model; framework; frame work; system; pathway; deliver; program; manage; collab; approach; digital; electronic; technolog; e-health; ehealth; m-health; mhealth; mobile health; tele; KOOTH; thrive; IAPT; improving access to psychological; CAPA; choice and partnership; brief consult; brief assess; therapeutic assess; mental health assess; psychiatric assess; tier; early intervention; wraparound; wrap around; MST; multi systemic; multi-systemic; multisystemic; rapid assess; availability and responsiveness; stepped; multi modal; multi-modal; multimodal; liaison; crisis; triage; self manage; self-manage; self care; self-care; self help; self-help; peer; mentor; peer; support; recovery; alternative; CAMH
-
[CYP terms] – child; adolesc; youth; young; teen; paediatr; pediatr; juven
-
[mental health terms] – mental; psychiatr
Six thousand four hundred and twelve of 39,396 records were screened in as they contained a AND b AND c terms in their title or abstract.
Stage 2 screen out terms
-
[population terms] – adult; old; elder; dement; veteran; men; women; mother; father; parent
-
[conditions terms] – eating disorder; anorex; bulmi; HIV; AIDS; asthma; diabet; cancer; brain; TBI; enceph; neuro; autis; ASD; disab; pain; cyst; CF; arth; spina; heart; cardio; cardia; psychosis; psychot; schiz; disease; fail to thrive; obes; weight; lupus; physical; bully
-
[settings or context terms] – partum; pregnan; birth; matern; natal; inpatient; in-patient; hospital; violen; aggress; resident; foster; prison; detention; institute; sex; gender
-
[psychometrics terms] – psychom; scale; measure; instrument; valid; reliab; tool
Of the 6412 screened in records, a further 1691 were screened out because of these terms; 4721 records thus remained.
Appendix 4 List of included documents in the literature reviews
| No. | Document ID | Document full reference | SCO | Integrative | ||
|---|---|---|---|---|---|---|
| EFF | ACC | ECO | ||||
| 1 | Abidi 2017 | Abidi S. Paving the way to change for youth at the gap between child and adolescent and adult mental health services. Can J Psychiatry 2017;62:388–92. | ✓ | |||
| 2 | Acri 2016 | Acri MC, Bornheimer LA, O’Brien K, Sezer S, Little V, Cleek AF, et al. A model of integrated health care in a poverty-impacted community in New York City: importance of early detection and addressing potential barriers to intervention implementation. Soc Work Health Care 2016;55:314–27. | ✓ | |||
| 3 | Adams 2016 | Adams CD, Hinojosa S, Armstrong K, Takagishi J, Dabrow S. An innovative model of integrated behavioral health: school psychologists in pediatric primary care settings. Adv Sch Ment Health Promot 2016;9:188–200. | ✓ | ✓ | ||
| 4 | Aggett 2006 | Aggett P, Boyd E, Fletcher J. Developing a Tier 1 CAMHS foundation course: report on a 4-year Initiative. Clin Child Psychol Psychiatry 2006;11:319–33. | ✓ | |||
| 5 | Allison 2007 | Allison S, Gilliland D, Mayhew K, Wilson R. Personal reflections on the development of an integrated service delivery for child and adolescent mental health services. Child Care Pract 2007;13:67–74. | ✓ | |||
| 6 | Appleton 2000 | Appleton PL, Hammond-Rowley S. Addressing the population burden of child and adolescent mental health problems: a primary care model. Child Adolesc Ment Health 2000;5:9–16. | ✓ | |||
| 7 | Arcelus 1999 | Arcelus J, Bellerby T, Vostanis P. A mental-health service for young people in the care of the local authority. Clin Child Psychol Psychiatry 1999;4:233–45. | ✓ | |||
| 8 | Armbruster 1997 | Armbruster P, Gerstein SH, Fallon T. Bridging the gap between service need and service utilization: a school-based mental health program. Community Ment Health J 1997;33:199–211. | ✓ | |||
| 9 | Armbruster 2002 | Armbruster P. The administration of school-based mental health services. Child Adolesc Psychiatr Clin N Am 2002;11:23–41. | ✓ | |||
| 10 | Asarnow 2005 | Asarnow JR, Jaycox LH, Duan N, LaBorde AP, Rea MM, Murray P, et al. Effectiveness of a quality improvement intervention for adolescent depression in primary care clinics: a randomized controlled trial. JAMA 2005;293:311–9. | ✓ | ✓ | ✓ | |
| 11 | Asarnow 2009 | Asarnow JR, Jaycox LH, Tang L, Duan N, LaBorde AP, Zeledon LR, et al. Long-term benefits of short-term quality improvement interventions for depressed youths in primary care. Am J Psychiatry 2009;166:1002–10. | ✓ | ✓ | ✓ | |
| 12 | Atkins 2003 | Atkins MS, Graczyk PA, Frazier SL, Abdul-Adil J. Toward a new model for promoting urban children’s mental health: accessible, effective, and sustainable school-based mental health services. School Psych Rev 2003;32:503–14. | ✓ | |||
| 13 | Atkins 2006 | Atkins MS, Frazier SL, Birman D, Adil JA, Jackson M, Graczyk PA, et al. School-based mental health services for children living in high poverty urban communities. Adm Policy Ment Health 2006;33:146–59. | ✓ | ✓ | ||
| 14 | Atkins 2015 | Atkins MS, Shernoff ES, Frazier SL, Schoenwald SK, Cappella E, Marinez-Lora A, et al. Redesigning community mental health services for urban children: supporting schooling to promote mental health. J Consult Clin Psychol 2015;83:839–52. | ✓ | ✓ | ||
| 15 | Atkinson 2015 | Atkinson M, Owen D. CAMHS: A Time to Transform. London: iMPOWER Consulting; 2015. | ✓ | |||
| 16 | Aupont 2013 | Aupont O, Doerfler L, Connor DF, Stille C, Tisminetzky M, McLaughlin TJ. A collaborative care model to improve access to pediatric mental health services. Adm Policy Ment Health 2013;40:264–73. | ✓ | |||
| 17 | Barclay 2016 | Barclay RP, Hilt RJ, Garrison M. A statewide pediatric psychiatry consultation to primary care program and the care of children with trauma-related concerns. J Behav Health Serv Res 2016;43:691–9. | ✓ | |||
| 18 | Barrow 2017 | Barrow RN. Addressing Barriers to Mental Health Treatment: Why Not Wraparound? Doctor of Psychology thesis. Los Angeles, CA: Alliant International University; 2017. | ✓ | |||
| 19 | Bartlett 2006 | Bartlett R, Herrick CA, Greninger L. Using a system of care framework for the mental health treatment of children and adolescents. J Nurse Pract 2006;2:593–8. | ✓ | |||
| 20 | Bartlett 2018 | Bartlett NA, Freeze TB. Community schools: new perspectives on the wraparound approach. Except Educ Int 2018;28:55–81. | ✓ | |||
| 21 | Barwick 2013 | Barwick M, Urajnik D, Sumner L, Cohen S, Reid G, Engel K, et al. Profiles and service utilization for children accessing a mental health walk-in clinic versus usual care. J Evid Based Soc Work 2013;10:338–52. | ✓ | ✓ | ✓ | |
| 22 | Bassilios 2016a | Bassilios B, Nicholas A, Reifels L, King K, Spittal MJ, Fletcher J, et al. Improving access to primary mental health care for Australian children. Aust N Z J Psychiatry 2016;50:1074–84. | ✓ | |||
| 23 | Bassilios 2016b | Bassilios B, Nicholas A, Reifels L, King K, Fletcher J, Machlin A, et al. Achievements of the Australian Access to Allied Psychological Services (ATAPS) program: summarising (almost) a decade of key evaluation data. Int J Ment Health Syst 2016;10:61. | ✓ | |||
| 24 | Bassilios 2017 | Bassilios B, Nicholas A, Ftanou M, Fletcher J, Reifels L, King K, et al. Implementing a primary mental health service for children: administrator and provider perspectives. J Child Fam Stud 2017;26:497–510. | ✓ | ✓ | ||
| 25 | Beehler 2012 | Beehler S, Birman D, Campbell R. The effectiveness of Cultural Adjustment and Trauma Services (CATS): generating practice-based evidence on a comprehensive, school-based mental health intervention for immigrant youth. Am J Community Psychol 2012;50:155–68. | ✓ | ✓ | ||
| 26 | Bickman 1996a | Bickman L. The evaluation of a children’s mental health managed care demonstration. J Ment Health Adm 1996;23:7–15. | ✓ | |||
| 27 | Bickman 1996b | Bickman L. The application of program theory to the evaluation of a managed mental health care system. Eval Program Plann 1996;19:111–9. | ✓ | |||
| 28 | Biebel 2007 | Biebel K, Geller JL. Challenges for a system of care. In Fisher W, editor. Research on Community-based Mental Health Services for Children and Adolescents (Research in Community and Mental Health, Vol. 14). Bingley: Emerald Group Publishing Ltd; 2007. pp. 179–99. | ✓ | |||
| 29 | Biggins 2014 | Biggins T. Home-based treatment. In McDougall T, Cotgrove A, editors. Specialist Mental Healthcare for Children and Adolescents: Hospital, Intensive Community and Home-based Services. Abingdon: Routledge; 2014. | ✓ | |||
| 30 | Bjørngaard 2008 | Bjørngaard JH, Wessel Andersson H, Osborg Ose S, Hanssen-Bauer K. User satisfaction with child and adolescent mental health services: impact of the service unit level. Soc Psychiat Epidemiol 2008;43:635–41. | ✓ | ✓ | ||
| 31 | Bloom 2005 | Bloom S. Mental health services. In Dryfoos JG, Quinn J, Barkin C, editors. Community Schools in Action: Lessons from a Decade of Practice. Oxford: OUP; 2005. pp. 98–113. | ✓ | |||
| 32 | Böge 2019 | Böge K, Karnouk C, Hahn E, Schneider F, Habel U, Banaschewski T, et al. Mental health in refugees and asylum seekers (MEHIRA): study design and methodology of a prospective multicentre randomized controlled trail [sic] investigating the effects of a stepped and collaborative care model. Eur Arch Psychiatry Clin Neurosci 2019;270:95–106. | ✓ | |||
| 33 | Bone 2015 | Bone C, O’Reilly M, Karim K, Vostanis P. ‘They’re not witches. …’ Young children and their parents’ perceptions and experiences of child and adolescent mental health services. Child Care Health Dev 2015;41:450–8. | ✓ | |||
| 34 | Bonham 2010 | Bonham E ‘Beth’. Approaches for mental health well-being in children and adolescents: ACAPN news. J Child Adolesc Psychiatr Nurs 2010;23:242–3. | ✓ | |||
| 35 | Bor 2013 | Bor W, Heath F, Heussler H, Reuter R, Perrett C, Lee E. Can a multi-disciplinary assessment approach improve outcomes for children with attention deficit hyperactivity disorder? Australas Psychiatry 2013;21:499–503. | ✓ | ✓ | ||
| 36 | Bower 2003 | Bower P, Macdonald W, Sibbald B, Garralda E, Kramer T, Bradley S, et al. Postal survey of services for child and adolescent mental health problems in general practice in England. Prim Care Ment Health 2003;1:17–26. | ✓ | ✓ | ||
| 37 | Breda 1996 | Breda CS. Methodological issues in evaluating mental health outcomes of a children’s mental health managed care demonstration. J Ment Health Adm 1996;23:40–50. | ✓ | |||
| 38 | BPS 2019 | British Psychological Society. Mental Health Support Teams: How to Maximise the Impact of the New Workforce for Children and Young People. Leicester: British Psychological Society; 2019. | ✓ | |||
| 39 | Brockie-Trombley 2005 | Brockie-Trombley MJ. The Effects of Intensive Mental Health Services on Child and Parent Emotional Functioning and Family Stress. PhD thesis. Washington, DC: Howard University; 2003. | ✓ | |||
| 40 | Bruns 2016 | Bruns EJ, Duong MT, Lyon AR, Pullmann MD, Cook CR, Cheney D, et al. Fostering SMART partnerships to develop an effective continuum of behavioral health services and supports in schools. Am J Orthopsychiatry 2016;86:156–70. | ✓ | |||
| 41 | Burchard 1996 | Burchard JD. Evaluation of the Fort Bragg managed care experiment. J Child Fam Stud 1996;5:173–6. | ✓ | |||
| 42 | Burns 2014 | Burns J, Birrell E. Enhancing early engagement with mental health services by young people. Psychol Res Behav Manag 2014;4:303–12. | ✓ | |||
| 43 | Byrne 2011 | Byrne P, Power L, Boylan C, Iqbal M, Anglim M, Fitzpatrick C. Providing 24-hour child and adolescent mental health services: demand and outcomes. Psychiatrist 2011;35:374–9. | ✓ | |||
| 44 | Cai 2016 | Cai SY, Fung DSS. Community mental health as a population-based mental health approach. Isr J Psychiatry Relat Sci 2016;53:33–9. | ✓ | ✓ | ✓ | |
| 45 | Çakin Memik 2010 | Çakin Memik N, Yildiz Öç Ö, Karakaya I, Gülen ŞiŞmanlar Ş, Ağaoğlu B. Çocuk ve ergen psikiyatrisinde bir gündüz kliniği deneyimi [An experience of a child and adolescent psychiatry day clinic treatment program]. Turkiye Klinikleri J Pediatr 2010;19:103–12. | ✓ | ✓ | ✓ | |
| 46 | Callaghan 2003a | Callaghan J, Pace F, Young B, Vostanis P. Primary mental health workers within youth offending teams: a new service model. J Adolesc 2003;26:185–99. | ✓ | ✓ | ||
| 47 | Callaghan 2003b | Callaghan J, Young B, Richards M, Vostanis P. Developing new mental health services for looked after children: a focus group study. Adopt Foster 2003;27:51–63. | ✓ | ✓ | ||
| 48 | Callaghan 2004 | Callaghan J, Young B, Pace F, Vostanis P. Evaluation of a new mental health service for looked after children. Clin Child Psychol Psychiatry 2004;9:130–48. | ✓ | ✓ | ✓ | |
| 49 | Callaly 2010 | Callaly T, Von Treuer K, Dodd S, Berk M. Mental health services for young people – the challenge of integrating services. Acta Neuropsychiatr 2010;22:158–60. | ✓ | |||
| 50 | Callaly 2014 | Callaly T. Early intervention for young people with mental illness. In Byrne P, Rosen A, editors. Early Intervention in Psychiatry. Chichester, UK: John Wiley & Sons, Ltd; 2014. pp. 68–78. | ✓ | |||
| 51 | Campbell 2014 | Campbell L, Allan C. The ADHD clinic: a collaborative model of care. Mo Med 2014;111:199–201. | ✓ | |||
| 52 | Campo 2005 | Campo JV, Shafer S, Strohm J, Lucas A, Cassesse CG, Shaeffer D, et al. Pediatric behavioral health in primary care: a collaborative approach. J Am Psychiatr Nurses Assoc 2005;11:276–82. | ✓ | |||
| 53 | Casat 1999 | Casat CD, Sobolewski J, Gordon J. School-based mental health services (SBS): a pragmatic view of a program. Psychol Sch 1999;36:403–13. | ✓ | |||
| 54 | Chambers 2008 | Chambers R, Tullys T, Mayer K, Wigand D. Regional collaborative practice in psychiatric rehabilitation and recovery: a best practice model. J Soc Work Disabil Rehabil 2008;7:187–231. | ✓ | |||
| 55 | Champine 2018 | Champine RB, Whitson ML, Kaufman JS. Service characteristics and family involvement in an early childhood system of care. J Child Fam Stud 2018;27:324–38. | ✓ | ✓ | ✓ | |
| 56 | Chanen 2009 | Chanen AM, Jackson HJ, McCutcheon LK, Jovev M, Dudgeon P, Yuen HP, et al. Early intervention for adolescents with borderline personality disorder: quasi-experimental comparison with treatment as usual. Aust N Z J Psychiatry 2009;43:397–408. | ✓ | |||
| 57 | Chatterton 2019 | Chatterton ML, Rapee RM, Catchpool M, Lyneham HJ, Wuthrich V, Hudson JL, et al. Economic evaluation of stepped care for the management of childhood anxiety disorders: results from a randomised trial. Aust N Z J Psychiatry 2019;53:673–82. | ✓ | ✓ | ||
| 58 | Chiumento 2011 | Chiumento A, Nelki J, Dutton C, Hughes G. School-based mental health service for refugee and asylum seeking children: multi‐agency working, lessons for good practice. J Public Ment Health 2011;10:164–77. | ✓ | |||
| 59 | Clark 2014 | Clark TC, Johnson EA, Kekus M, Newman J, Patel PS, Fleming T, et al. Facilitating access to effective and appropriate care for youth with mild to moderate mental health concerns in New Zealand. J Child Adolesc Psychiatr Nurs 2014;27:190–200. | ✓ | ✓ | ✓ | |
| 60 | Clarke 2003 | Clarke M, Coombs C, Walton L. School based early identification and intervention service for adolescents: a psychology and school nurse partnership model. Child Adolesc Ment Health 2003;8:34–9. | ✓ | |||
| 61 | Clarke 2005 | Clarke G, Debar L, Lynch F, Powell J, Gale J, O’Connor E, et al. A randomized effectiveness trial of brief cognitive-behavioral therapy for depressed adolescents receiving antidepressant medication. J Am Acad Child Adolesc Psychiatry 2005;44:888–98. | ✓ | ✓ | ||
| 62 | Cleek 2012 | Cleek EN, Wofsy M, Boyd-Franklin N, Mundy B, Howell TJ. The Family Empowerment Program: an interdisciplinary approach to working with multi-stressed urban families. Fam Process 2012;51:207–17. | ✓ | |||
| 63 | Coffey 2017 | Coffey S, Vanderlip E, Sarvet B. The use of health information technology within collaborative and integrated models of child psychiatry practice. Child Adolesc Psychiatr Clin N Am 2017;26:105–15. | ✓ | |||
| 64 | Colon 2005 | Colon BA. School-based health services. In Dryfoos J, Quinn J, Barkin C, editors. Community Schools in Action: Lessons from a Decade of Practice. Oxford: OUP; 2005. pp. 84–97. | ✓ | |||
| 65 | Conlon 2009 | Conlon M. The role of primary mental health workers in child and adolescent mental health services in Scotland. J Ment Health Train Educ Pract 2009;4:21–5. | ✓ | |||
| 66 | Connor 2006 | Connor DF, McLaughlin TJ, Jeffers-Terry M, O’Brien WH, Stille CJ, Young LM, et al. Targeted child psychiatric services: a new model of pediatric primary clinician-child psychiatry collaborative care. Clin Pediatr (Phila) 2006;45:423–34. | ✓ | |||
| 67 | Corboy 2007 | Corboy D, McDonald J. An evaluation of the CAST program using a conceptual model of school-based implementation. AeJAMH 2007;6:63–77. | ✓ | ✓ | ||
| 68 | Cordell 2017a | Cordell KD, Snowden LR. Reducing mental health emergency services for children served through California’s Full Service Partnerships. Med Care 2017;55:299–305. | ✓ | ✓ | ||
| 69 | Cordell 2017b | Cordell KD, Snowden LR. Embracing comprehensive mental health and social services programs to serve children under California’s Mental Health Services Act. Adm Policy Ment Health 2017;44:233–42. | ✓ | |||
| 70 | Cotton 2019 | Cotton R. Using Digital Technology to Design and Deliver Better Mental Health Services: Perspectives from Australia and the USA. London: Winston Churchill Memorial Trust; 2019. | ✓ | |||
| 71 | Coyne 2015 | Coyne I, McNamara N, Healy M, Gower C, Sarkar M, McNicholas F. Adolescents’ and parents’ views of child and adolescent mental health services (CAMHS) in Ireland. J Psychiatr Ment Health Nurs 2015;22:561–9. | ✓ | ✓ | ||
| 72 | Cross 2014 | Cross SPM, Hermens DF, Scott EM, Ottavio A, McGorry PD, Hickie IB. A clinical staging model for early intervention youth mental health services. Psychiatr Serv 2014;65:939–43. | ✓ | |||
| 73 | Cross 2017 | Cross S, Hickie I. Transdiagnostic stepped care in mental health. Public Health Res Pr 2017;27:e2721712. | ✓ | |||
| 74 | Crouch 2019 | Crouch L, Reardon T, Farrington A, Glover F, Creswell C. ‘Just keep pushing’: parents’ experiences of accessing child and adolescent mental health services for child anxiety problems. Child Care Health Dev 2019;45:491–9 | ✓ | |||
| 75 | Daleiden 2010 | Daleiden EL, Pang D, Roberts D, Slavin LA, Pestle SL. Intensive home based services within a comprehensive system of care for youth. J Child Fam Stud 2010;19:318–25. | ✓ | |||
| 76 | Day 2006 | Day C, Davis H. The effectiveness and quality of routine child and adolescent mental health care outreach clinics. Br J Clin Psychol 2006;45:439–52. | ✓ | ✓ | ✓ | |
| 77 | Day 2017 | Day L, Blades R, Spence C, Ronicle J. Mental Health Services and Schools Link Pilots: Evaluation Report. London: Department for Education; 2017. | ✓ | |||
| 78 | Desmond 2011 | Desmond B. Evolution of San Francisco Bay Area Urban Trails. J Psychoact Drugs 2011;43:331–6. | ✓ | |||
| 79 | DfCSF 2008 | Department for Children, Schools and Families. Targeted Mental Health in Schools Project. Using the Evidence to Inform Your Approach: A Practical Guide for Headteachers and Commissioners. London: HMSO; 2008. | ✓ | |||
| 80 | Doley 2008 | Doley A, Sibly C, Wigg C, Crawford P, Cowper L, Barker C, et al. Doctor on campus: a general practice initiative for detection and early intervention of mental health problems in a rural Australian secondary school. Health Sociol Rev 2008;17:53–63. | ✓ | |||
| 81 | Dryfoos 1995 | Dryfoos JG. Full service schools: revolution or fad? J Res Adolesc 1995;5:147–72. | ✓ | |||
| 82 | Dryfoos 2002 | Dryfoos J. Partnering full-service community schools: creating new institutions. Phi Delta Kappan 2002;83:393–9. | ✓ | |||
| 83 | Duffy 2014 | Duffy F, Skeldon J. A CAMHS intensive treatment service: clinical outcomes in the first year. Clin Child Psychol Psychiatry 2014;19:90–9. | ✓ | ✓ | ||
| 84 | Durbin 2012 | Durbin CJ. Conflict and Collaboration in a Wraparound Project: Taking Action Through Research. PhD thesis. Minneapolis, MN: Capella University; 2012. | ✓ | |||
| 85 | Durcan 2018 | Durcan G, Snell J. A Space to Talk: An Evaluation of the Wish Centre’s Services with Young People Who Self-harm. London: Centre for Mental Health; 2018. | ✓ | |||
| 86 | Eapen 2012 | Eapen V, Lee L, Austin C. Health and education: service providers in partnership to improve mental health. Int J Ment Health Syst 2012;6:19. | ✓ | |||
| 87 | Edbrooke-Childs 2015 | Edbrooke-Childs J, Calderon A, Wolpert M, Fonagy P. Children and Young People’s Improving Access to Psychological Therapies. Rapid Internal Audit: National Report. London: Anna Freud Centre/UCL; 2015. | ✓ | |||
| 88 | Evans 1997 | Evans ME, Boothroyd RA, Armstrong MI. Development and implementation of an experimental study of the effectiveness of intensive in-home crisis services for children and their families. J Emot Behav Disord 1997;5:93–105. | ✓ | ✓ | ||
| 89 | Evans 2003 | Evans ME, Boothroyd RA, Armstrong MI, Greenbaum PE, Brown EC, Kuppinger AD. An experimental study of the effectiveness of intensive in-home crisis services for children and their families: program outcomes. J Emot Behav Disord 2003;11:92–102. | ✓ | ✓ | ||
| 90 | Evans 2006 | Evans ME. Integrating nursing care into systems of care for children with emotional and behavioral disorders. J Child Adolesc Psychiatr Nurs 2006;19:62–8. | ✓ | |||
| 91 | Evans 2014 | Evans SW, Owens JS, Mautone JA, DuPaul GJ, Power TJ. Toward a comprehensive life-course model of care for youth with attention-deficit/hyperactivity disorder. In Weist MD, Lever NA, Bradshaw CP, Owens JS, editors. Handbook of School Mental Health. Boston, MA: Springer US; 2014. pp. 413–26. | ✓ | |||
| 92 | Fallucco 2017 | Fallucco EM, Blackmore ER, Bejarano CM, Kozikowksi CB, Cuffe S, Landy R, et al. Collaborative care: a pilot study of a child psychiatry outpatient consultation model for primary care providers. J Behav Health Serv Res 2017;44:386–98. | ✓ | ✓ | ||
| 93 | Fealy 2006 | Fealy S, Story I. The mental health risk assessment and management process (RAMP) for schools: I. The model. AeJAMH 2006;5:284–94. | ✓ | |||
| 94 | Finch 2014 | Finch AJ, Frieden G. The ecological and developmental role of recovery high schools. Peabody J Educ 2014;89:271–87. | ✓ | |||
| 95 | Finch 2018 | Finch AJ, Tanner-Smith E, Hennessy E, Moberg DP. Recovery high schools: effect of schools supporting recovery from substance use disorders. Am J Drug Alcohol Abuse 2018;44:175–84. | ✓ | ✓ | ||
| 96 | Fonagy 2015 | Fonagy P, Clark DM. Update on the improving access to psychological therapies programme in England. BJPsych Bull 2015;39:248–51. | ✓ | |||
| 97 | Fonagy 2017 | Fonagy P, Pugh K, O’Herlihy A. The Children and Young People’s Improving Access to Psychological Therapies (CYP IAPT) programme in England. In Skuse D, Bruce H, Dowdney L, editors. Child Psychology and Psychiatry. Chichester: John Wiley & Sons, Ltd; 2017. pp. 429–35. | ✓ | |||
| 98 | Friedman 1996 | Friedman RM. The Fort Bragg study: what can we conclude? J Child Fam Stud 1996;5:161–8. | ✓ | |||
| 99 | Friedman 2000 | Friedman K, Damare MM, Leone P. Relationship of school-based mental health services to assessment of student behavior. 13th Annual Conference Proceedings – A System of Care for Children’s Mental Health: Expanding the Research Base 2000:138–40. | ✓ | |||
| 100 | Frith 2016 | Frith E. Children and Young People’s Mental Health: Time to Deliver (the Report of the Commission on Children and Young People’s Mental Health). London: Education Policy Institute; 2016. | ✓ | |||
| 101 | Frith 2017 | Frith E. Online Mental Health Support for Young People. London: Education Policy Institute; 2017. | ✓ | |||
| 102 | Fuggle 2015 | Fuggle P, McHugh A, Gore L, Dixon E, Curran D, Cutinha D. Can we improve service efficiency in CAMHS using the CAPA approach without reducing treatment effectiveness? J Child Health Care 2016;20:195–204. | ✓ | |||
| 103 | Furman 2002 | Furman R, Jackson R. Wrap-around services: an analysis of community-based mental health services for children. J Child Adolesc Psychiatr Nurs 2002;15:124–31. | ✓ | |||
| 104 | Gabel 2010 | Gabel S. The integration of mental health into pediatric practice: pediatricians and child and adolescent psychiatrists working together in new models of care. J Pediatr 2010;157:848–51. | ✓ | |||
| 105 | Gabel 2012 | Gabel S. Innovations in practice: child and adolescent psychiatrists and primary care – innovative models of consultation in the United States. Child Adolesc Ment Health 2012;17:252–5. | ✓ | |||
| 106 | Gale 2003 | Gale F, Vostanis P. The primary mental health worker within child and adolescent mental health services. Clin Child Psychol Psychiatry 2003;8:227–40. | ✓ | |||
| 107 | Gallagher 2015 | Gallagher J, Schlösser A. Service users’ experiences of a brief intervention service for children and adolescents: a service evaluation. Child Care Pract 2015;21:374–91. | ✓ | ✓ | ||
| 108 | Garralda 2016 | Garralda ME, Slaveska-Hollis K. What is special about a paediatric liaison child and adolescent mental health service? Child Adolesc Ment Health 2016;21:96–101. | ✓ | |||
| 109 | Gatta 2009 | Gatta M, Bertossi L, Dal Zotto L, Del Col L, Testa P, Battistella P. Approccio psicoeducativo all’adolescente psichiatrico: l’esperienza di un servizio semiresidenziale [Psycho-educational intervention for psychiatric adolescents: the experience of a daily service]. Gior Neuropsich Età Evol 2009;29:132–44. | ✓ | |||
| 110 | Gilliam 2007 | Gilliam WS. Early Childhood Consultation Partnership: Results of a Random-Controlled Evaluation. New Haven, CT: Yale School of Medicine; 2007. | ✓ | |||
| 111 | Gilliam 2016 | Gilliam WS, Maupin AN, Reyes CR. Early childhood mental health consultation: results of a statewide random-controlled evaluation. J Am Acad Child Adolesc Psychiatry 2016;55:754–61. | ✓ | ✓ | ||
| 112 | Glisson 2002 | Glisson C. The organizational context of children’s mental health services. Clin Child Fam Psychol Rev 2002;5:233–53. | ✓ | |||
| 113 | Glisson 2012 | Glisson C, Hemmelgarn A, Green P, Dukes D, Atkinson S, Williams NJ. Randomized trial of the availability, responsiveness, and continuity (ARC) organizational intervention with community-based mental health programs and clinicians serving youth. J Am Acad Child Adolesc Psychiatry 2012;51:780–7. | ✓ | ✓ | ||
| 114 | Glisson 2013 | Glisson C, Hemmelgarn A, Green P, Williams NJ. Randomized trial of the availability, responsiveness and continuity (ARC) organizational intervention for improving youth outcomes in community mental health programs. J Am Acad Child Adolesc Psychiatry 2013;52:493–500. | ✓ | ✓ | ||
| 115 | Glisson 2016 | Glisson C, Williams NJ, Hemmelgarn A, Proctor E, Green P. Aligning organizational priorities with ARC to improve youth mental health service outcomes. J Consult Clin Psychol 2016;84:713–25. | ✓ | ✓ | ||
| 116 | Godoy 2017 | Godoy L, Long M, Marschall D, Hodgkinson S, Bokor B, Rhodes H, et al. Behavioral health integration in health care settings: lessons learned from a pediatric hospital primary care system. J Clin Psychol Med Settings 2017;24:245–58. | ✓ | |||
| 117 | Gowers 2004 | Gowers S, Thomas S, Deeley S. Can primary schools contribute effectively to tier I child mental health services? Clin Child Psychol Psychiatry 2004;9:419–25. | ✓ | ✓ | ||
| 118 | Greenfield 1995 | Greenfield B, Hechtman L, Tremblay C. Short-term efficacy of interventions by a youth crisis team. Can J Psychiatry 1995;40:320–4. | ✓ | |||
| 119 | Grimes 2006 | Grimes KE, Kapunan PE, Mullin B. Children’s health services in a ‘system of care’: patterns of mental health, primary and specialty use. Public Health Rep 2006;121:311–23. | ✓ | |||
| 120 | Guerra 2006 | Guerra PA. Variables Associated with Completion and Non Completion of an in-Home Crisis Intervention Service for Children and Adolescents. PhD thesis. West Hartford, CT: University of Hartford; 2006. | ✓ | |||
| 121 | Hagell 2016 | Hagell A, Lamb S. Developing an integrated primary health care and youth work service for young people in Lambeth: learning from the Well Centre. J Child Serv 2016;11:233–43. | ✓ | |||
| 122 | Hair 2013 | Hair HJ, Shortall R, Oldford J. Where’s help when we need it? Developing responsive and effective brief counseling services for children, adolescents, and their families. Soc Work Ment Health 2013;11:16–33. | ✓ | |||
| 123 | Hanley 2019 | Hanley T, Sefi A, Grauberg J, Green L, Prescott J. A Positive Virtual Ecosystem: The Theory of Change for Kooth: Comprehensive Report. Manchester: XenZone/The University of Manchester; 2019. | ✓ | |||
| 124 | Heflinger 1996 | Heflinger CA, Sonnichsen SE, Brannan AM. Parent satisfaction with children’s mental health services in a children’s mental health managed care demonstration. J Ment Health Adm 1996;23:69–80. | ✓ | |||
| 125 | Henderson 2017 | Henderson JL, Cheung A, Cleverley K, Chaim G, Moretti ME, de Oliveira C, et al. Integrated collaborative care teams to enhance service delivery to youth with mental health and substance use challenges: protocol for a pragmatic randomised controlled trial. BMJ Open 2017;7:e014080. | ✓ | |||
| 126 | Hewitt 2011 | Hewitt K. Developing community children’s health services. Health Serv J 2011. URL: www.hsj.co.uk/interactive/developing-community-childrens-health-services/5026093. | ✓ | |||
| 127 | Heywood 2003 | Heywood S, Stancombe J, Street E, Mittler H, Dunn C, Kroll L. A brief consultation and advisory approach for use in child and adolescent mental health services: a pilot study. Clin Child Psychol Psychiatry 2003;8:503–12. | ✓ | ✓ | ✓ | |
| 128 | Hinrichs 2012 | Hinrichs S, Owens M, Dunn V, Goodyer I. General practitioner experience and perception of child and adolescent mental health services (CAMHS) care pathways: a multimethod research study. BMJ Open 2012;2:e001573. | ✓ | |||
| 129 | Holder 2017 | Holder SM, Rogers K, Peterson E, Shoenleben R, Blackhurst D. The impact of mental health services in a pediatric emergency department: the implications of having trained psychiatric professionals. Pediatr Emerg Care 2017;33:311–4. | ✓ | ✓ | ||
| 130 | Holmes 2015 | Holmes C, Levy M, Smith A, Pinne S, Neese P. A model for creating a supportive trauma-informed culture for children in preschool settings. J Child Fam Stud 2015;24:1650–9. | ✓ | ✓ | ||
| 131 | Houses of Parliament POST 2017 | Houses of Parliament Parliamentary Office of Science & Technology. POSTNote 563: Mental Health Service Models for Young People. London: The Parliamentary Office of Science and Technology; 2017. | ✓ | |||
| 132 | Howe 2014 | Howe D, Coates D, Batchelor S. Headspace Gosford data: the local application of a national model. Australas Psychiatry 2014;22:374–7. | ✓ | |||
| 133 | HSCBNI 2018 | Health and Social Care Board (Northern Ireland). Working Together: A Pathway for Children and Young People through CAMHS . Belfast: Health and Social Care Board; 2018. | ✓ | |||
| 134 | Humphrey 2016 | Humphrey A, Eastwood L, Atkins H, Vainre M, Lea-Cox C. An exemplar of GP commissioning and child and adolescent mental health service partnership: Cambridge 1419 young people’s service. J Integr Care (Brighton) 2016;24:26–37. | ✓ | |||
| 135 | Hunter 2009 | Hunter A, Playle J, Sanchez P, Cahill J, McGowan L. Introduction of a child and adolescent mental health link worker: education and health staff focus group findings. J Psychiatr Ment Health Nurs 2008;15:670–7. | ✓ | ✓ | ||
| 136 | Illback 2010 | Illback RJ, Bates T, Hodges C, Galligan K, Smith P, Sanders D, et al. Jigsaw: engaging communities in the development and implementation of youth mental health services and supports in the Republic of Ireland. J Ment Health 2010;19:422–35. | ✓ | |||
| 137 | Improvement Cymru 2020 | Improvement Cymru. Matrics Plant: Guidance on the Delivery of Psychological Interventions for Children and Young People in Wales. Cardiff: Improvement Cymru; 2020. | ✓ | |||
| 138 | Ivings 2018 | Ivings K, Barnes S. Integrated Crisis Care for Children and Young People up to Age 18 Across Greater Manchester: The REACH-IN Model. Manchester: Greater Manchester and Eastern Cheshire Strategic Clinical Networks; 2018. | ✓ | |||
| 139 | JCPfMH 2013 | Joint Commissioning Panel for Mental Health. Guidance for Commissioners of Child and Adolescent Mental Health Services. Joint Commissioning Panel for Mental Health; 2013. | ✓ | |||
| 140 | Jordans 2010 | Jordans MJ, Tol WA, Komproe IH, Susanty D, Vallipuram A, Ntamatumba P, et al. Research development of a multi-layered psychosocial care system for children in areas of political violence. Int J Ment Health Syst 2010;4:1–12. | ✓ | |||
| 141 | Kaess 2017 | Kaess M, Ghinea D, Fischer-Waldschmidt G, Resch F. Die ambulanz für risikoverhalten und selbstschädigung (AtR!Sk) – ein pionierkonzept der ambulanten früherkennung und frühintervention von borderline-persönlichkeitsstörungen [The outpatient clinic for adolescent risk-taking and self-harm behaviors (AtR!Sk) – a pioneering approach of outpatient early detection and intervention of borderline personality disorder]. Prax Kinderpsychol Kinderpsychiatr 2017;66:404–22. | ✓ | |||
| 142 | Kaess 2019 | Kaess M, Ritter S, Lustig S, Bauer S, Becker K, et al. Promoting Help-seeking using E-technology for ADolescents with mental health problems: study protocol for a randomized controlled trial within the ProHEAD consortium. Trials 2019;20:94. | ✓ | |||
| 143 | Kapp 2017 | Kapp C, Perlini T, Jeanneret T, Stéphan P, Rojas-Urrego A, Macias M, et al. Identifying the determinants of perceived quality in outpatient child and adolescent mental health services from the perspectives of parents and patients. Eur Child Adolesc Psychiatry 2017;26:1269–77. | ✓ | ✓ | ||
| 144 | Karpman 2013 | Karpman H. Is Everything Coming up Rosie? What is the Impact of a Redesigned Medicaid Funded Mental Health System on Child Mental Health, Caregiver Needs and Strengths, and Youth Risk Factors for Substance Abuse? PhD thesis. Waltham, MA: Brandeis University; 2013. | ✓ | |||
| 145 | Kataoka 2018 | Kataoka SH, Vona P, Acuna A, Jaycox L, Escudero P, Rojas C, et al. Applying a trauma informed school systems approach: examples from school community-academic partnerships. Ethn Dis 2018;28:417–26. | ✓ | |||
| 146 | Kates 2011 | Kates N, McPherson-Doe C, George L. Integrating mental health services within primary care settings: the Hamilton family health team. J Ambul Care Manage 2011;34:174–82. | ✓ | |||
| 147 | Kaye 2017 | Kaye DL, Fornari V, Scharf M, Fremont W, Zuckerbrot R, Foley C, et al. Description of a multi-university education and collaborative care child psychiatry access program: New York State’s CAP PC. Gen Hosp Psychiatry 2017;48:32–6. | ✓ | ✓ | ||
| 148 | Keller 2013 | Keller D, Sarvet B. Is there a psychiatrist in the house? Integrating child psychiatry into the pediatric medical home. J Am Acad Child Adolesc Psychiatry 2013;52:3–5. | ✓ | |||
| 149 | Kingsbury 2014 | Kingsbury S, Rayment B, Fleming I, Thompson P, York A, Hemsley M, et al. CYP IAPT Principles in Child & Adolescent Mental Health Services: Values and Standards: ‘Delivering with and Delivering Well’. London: CAMHS Press; 2014. | ✓ | |||
| 150 | Knapp 2016 | Knapp M, Ardino V, Brimblecombe N, Evans-Lacko S, Iemmi V, King D, et al. Youth Mental Health: New Economic Evidence. London: Personal Social Services Research Unit, London School of Economics and Political Science; 2016. | ✓ | |||
| 151 | Kolko 2012 | Kolko DJ. Doctor-office collaborative care for pediatric behavioral problems: a preliminary clinical trial. Arch Pediatr Adolesc Med 2012;166:224. | ✓ | ✓ | ✓ | |
| 152 | Kolko 2014 | Kolko DJ, Campo J, Kilbourne AM, Hart J, Sakolsky D, Wisniewski S. Collaborative care outcomes for pediatric behavioral health problems: a cluster randomized trial. Pediatrics 2014;133:e981–92. | ✓ | ✓ | ✓ | |
| 153 | Kraemer 2008 | Kraemer S. Paediatric liaison. Psychiatry 2008;7:371–4. | ✓ | |||
| 154 | Kutcher 2013a | Kutcher S, McLuckie A. Evergreen: creating a child and youth mental health framework for Canada. Psychiatr Serv 2013;64:479–82. | ✓ | |||
| 155 | Kutcher 2013b | Kutcher S, Wei Y. Challenges and solutions in the implementation of the school-based pathway to care model: the lessons from Nova Scotia and beyond. Can J Sch Psychol 2013;28:90–102. | ✓ | |||
| 156 | Lamb 2009 | Lamb CE. Alternatives to admission for children and adolescents: providing intensive mental healthcare services at home and in communities: what works? Curr Opin Psychiatry 2009;22:345–50. | ✓ | |||
| 157 | Lambert 1996 | Lambert EW, Guthrie PR. Clinical outcomes of a children’s mental health managed care demonstration. J Ment Health Adm 1996;23:51–68. | ✓ | |||
| 158 | Larson 2016 | Larson S. School-based Health Centers: A Model of Care to Meet the Behavioral and Mental Health Needs of Children and Adolescents. PhD thesis. San Francisco, CA: University of California, San Francisco; 2016. | ✓ | |||
| 159 | Law 2016 | Law D, Goforth A. CYPIAPT and Children & Young Peoples Mental Health Service Transformation: An Essential Guide for Commissioners (v1.3). London: London and South East CYP-IAPT Learning Collaborative; 2016. | ✓ | |||
| 160 | Lee 2009 | Lee RC, Tiley CE, White JE. The Place2Be: measuring the effectiveness of a primary school-based therapeutic intervention in England and Scotland. Couns Psychother Res 2009;9:151–9. | ✓ | |||
| 161 | Lee 2013 | Lee VWW, Murphy BP. Broadening the early intervention paradigm: a one stop shop for youth: one stop shop for youth. Early Interv Psychiatry 2013;7:437–41. | ✓ | |||
| 162 | Lee 2014 | Lee J, Korczak D. Factors Associated with Parental Satisfaction with a Pediatric Crisis Clinic (PCC). J Can Acad Child Adolesc Psychiatry 2014;23:118–27. | ✓ | ✓ | ||
| 163 | Lee 2017 | Lee MY, Danna L, Walker DW. Classroom–Community Consultation (C3) 10 years after Hurricane Katrina: a retrospective look at a collaborative, school-based referral model. Child Sch 2017;39:119–27. | ✓ | ✓ | ||
| 164 | Lenoir 2009 | Lenoir P, Maloy J, Desombre H, Abert B, Taleb MO, Sauvage D. La psychiatrie de liaison en pédiatrie: ressources et contraintes d’une collaboration interdisciplinaire [Consultation-liaison psychiatry in pediatrics: resources and constraints of an interdisciplinary collaboration]. Neuropsychiatr Enfance Adolesc 2009;57:75–84. | ✓ | |||
| 165 | Lim 2017 | Lim C, Loh H, Renjan V, Tan J, Fung D. Child community mental health services in Asia Pacific and Singapore’s REACH model. Brain Sci 2017;7:126. | ✓ | ✓ | ✓ | |
| 166 | Liu 2010 | Liu RY, Ramowski SK, Nystrom RJ. Health service integration in Oregon school-based health centers: meeting the mental health needs of young people. Adv Sch Ment Health Promot 2010;3:26–36. | ✓ | |||
| 167 | Löfholm 2009 | Löfholm CA, Olsson T, Sundell K, Hansson K. Multisystemic therapy with conduct-disordered young people: stability of treatment outcomes two years after intake. Evid Policy 2009;5:373–97. | ✓ | ✓ | ||
| 168 | Ludlow 2020 | Ludlow C, Hurn R, Lansdell S. A current review of the children and young people’s improving access to psychological therapies (CYP IAPT) program: perspectives on developing an accessible workforce. Adolesc Health Med Ther 2020;11:21–8. | ✓ | |||
| 169 | Lynch 2017 | Lynch F, Kehoe C, MacMahon S, McCarra E, McKenna R, D’Alton A, et al. Paediatric consultation liaison psychiatry services (PCLPS) – what are they actually doing? Ir Med J 2017;110:652. | ✓ | |||
| 170 | Lyon 2016 | Lyon AR, Whitaker K, French WP, Richardson LP, Wasse JK, McCauley E. Collaborative care in schools: enhancing integration and impact in youth mental health. Adv Sch Ment Health Promot 2016;9:148–68. | ✓ | |||
| 171 | Macdonald 2004 | Macdonald W, Bradley S, Bower P, Kramer T, Sibbald B, Garralda E, et al. Primary mental health workers in child and adolescent mental health services. J Adv Nurs 2004;46:78–87. | ✓ | ✓ | ||
| 172 | Mahajan 2007 | Mahajan P, Thomas R, Rosenberg DR, Leleszi JP, Leleszi E, Mathur A, et al. Evaluation of a child guidance model for visits for mental disorders to an inner-city pediatric emergency department. Pediatr Emerg Care 2007;23:212–7. | ✓ | |||
| 173 | Malla 2016 | Malla A, Iyer S, McGorry P, Cannon M, Coughlan H, Singh S, et al. From early intervention in psychosis to youth mental health reform: a review of the evolution and transformation of mental health services for young people. Soc Psychiatry Psychiatr Epidemiol 2016;51:319–26. | ✓ | |||
| 174 | Manteuffel 2002 | Manteuffel B, Stephens RL, Santiago R. Overview of the national evaluation of the comprehensive community mental health services for children and their families program and summary of current findings. Child Serv 2002;5:3–20. | ✓ | ✓ | ||
| 175 | McDougall 2008 | McDougall T, Worrall-Davies A, Hewson L, Richardson G, Cotgrove A. Tier 4 child and adolescent mental health services (CAMHS) – inpatient care, day services and alternatives: an overview of Tier 4 CAMHS provision in the UK. Child Adolesc Ment Health 2008;13:173–80. | ✓ | |||
| 176 | McDougall 2014 | McDougall T. Multisystemic therapy. In McDougall T, Cotgrove A, editors. Specialist Mental Healthcare for Children and Adolescents: Hospital, Intensive Community and Home-based Services. Abingdon: Routledge; 2014. | ✓ | |||
| 177 | McDougall 2016 | McDougall T. CAMHS transformation: CAMHS transformation: modernising therapeutic interventions and outcomes. In McDougall T, editor. Children and Young People’s Mental Health: Essentials for Nurses and Other Professionals. Abingdon: Routledge; 2016. pp. 36–43. | ✓ | |||
| 178 | McGarry 2008 | McGarry J, McNicholas F, Buckley H, Kelly BD, Atkin L, Ross N. The clinical effectiveness of a brief consultation and advisory approach compared to treatment as usual in child and adolescent mental health services. Clin Child Psychol Psychiatry 2008;13:365–75. | ✓ | ✓ | ✓ | |
| 179 | McGonnell 2009 | McGonnell M, Corkum P, McKinnon M, MacPherson M, Williams T, Davidson C, et al. Doing it right: an interdisciplinary model for the diagnosis of ADHD. J Can Acad Child Adolesc Psychiatry 2009;18:283–6. | ✓ | ✓ | ||
| 180 | McGorry 2013 | McGorry P, Bates T, Birchwood M. Designing youth mental health services for the 21st century: examples from Australia, Ireland and the UK. Br J Psychiatry 2013;202:s30–5. | ✓ | |||
| 181 | McGorry 2016 | McGorry P, Goldstone S. Transforming cultures for the mental health care of young people. In Hordes M, Gau S, editors. Positive Mental Health, Fighting Stigma and Promoting Resiliency for Children and Adolescents. London: Academic Press; 2016. pp. 173–84. | ✓ | |||
| 182 | McGorry 2018 | McGorry PD, Mei C. Early intervention in youth mental health: progress and future directions. Evid Based Mental Health 2018;21:182–4. | ✓ | |||
| 183 | McGuinness 2009 | McGuinness TM. Youth in the mental health void: wraparound is one solution. J Psychosoc Nurs Ment Health Serv 2009;47:23–6. | ✓ | |||
| 184 | McKay-Brown 2019 | McKay-Brown L, McGrath R, Dalton L, Graham L, Smith A, Ring J, et al. Reengagement with education: a multidisciplinary home-school-clinic approach developed in Australia for school-refusing youth. Cogn Behav Pract 2019;26:92–106. | ✓ | ✓ | ||
| 185 | McKenzie 2011 | McKenzie K, Murray GC, Prior S, Stark L. An evaluation of a school counselling service with direct links to child and adolescent mental health (CAMH) services. Br J Guid Couns 2011;39:67–82. | ✓ | ✓ | ✓ | |
| 186 | McNicholas 2018 | McNicholas F. Child & adolescent emergency mental health crisis: a neglected cohort. Ir Med J 2018;111:841. | ✓ | |||
| 187 | Measelle 1998 | Measelle JR, Weinstein RS, Martinez M. Parent satisfaction with case managed systems of care for children and youth with severe emotional disturbance. J Child Fam Stud 1998;7:451–67. | ✓ | ✓ | ||
| 188 | Measham 2005 | Measham T, Rousseau C, Nadeau L. The development and therapeutic modalities of a transcultural child psychiatry service. Can Child Adolesc Psychiatr Rev 2005;14:68–72. | ✓ | |||
| 189 | Mendenhall 2019 | Mendenhall AN, Grube W, Jung E. Implementing strengths model for youth in community mental health: impact on case managers’ professional quality of life. Child Youth Serv Rev 2019;102:1–6. | ✓ | |||
| 190 | Miller 2012 | Miller BD, Blau GM, Christopher OT, Jordan PE. Sustaining and expanding systems of care to provide mental health services for children, youth and families across America. Am J Community Psychol 2012;49:566–79. | ✓ | |||
| 191 | Mitchell 2007 | Mitchell SA. Examining the Effectiveness of a School-based Mental Health Center’s Service. PhD thesis. Kingston, RI: University of Rhode Island/Rhode Island College; 2007. | ✓ | |||
| 192 | Mitchell-Lowe 2009 | Mitchell-Lowe M, Eggleston M. Children as consumer participants of child and adolescent mental health services. Australas Psychiatry 2009;17:287–90. | ✓ | |||
| 193 | Moore 2018 | Moore JA, Karch K, Sherina V, Guiffre A, Jee S, Garfunkel LC. Practice procedures in models of primary care collaboration for children with ADHD. Fam Syst Health 2018;36:73–86. | ✓ | |||
| 194 | Motes 2014 | Motes PS, Smith CO. Systems of caregiving: the promotion of positive mental health outcomes in children and adolescents. In Talley RC, Fricchione GL, Druss BG, editors. The Challenges of Mental Health Caregiving. New York, NY: Springer; 2014. pp. 103–21. | ✓ | |||
| 195 | Muir 2009 | Muir K, Powell A, Patulny R, Flaxman S, McDermott S, Oprea I, et al. Headspace Evaluation Report: Independent Evaluation of Headspace: The National Youth Mental Health Foundation. Sydney: Social Policy Research Centre; 2009. | ✓ | |||
| 196 | Mulvale 2015 | Mulvale G, Kutcher S, Randall G, Wakefield P, Longo C, Abelson J, et al. Do national frameworks help in local policy development? Lessons from Yukon about the Evergreen child and youth mental health framework. Can J Commun Ment Health 2015;34:111–28. | ✓ | |||
| 197 | Myers 2010 | Myers K, Stoep AV, Thompson K, Zhou C, Unützer J. Collaborative care for the treatment of Hispanic children diagnosed with attention-deficit hyperactivity disorder. Gen Hosp Psychiatry 2010;32:612–4. | ✓ | |||
| 198 | Nabors 1999 | Nabors LA, Weist MD, Reynolds MW, Tashman NA, Jackson CY. Adolescent satisfaction with school-based mental health services. J Child Fam Stud 1999;8:229–36. | ✓ | |||
| 199 | Nadeau 2017 | Nadeau L, Jaimes A, Johnson-Lafleur J, Rousseau C. Perspectives of migrant youth, parents and clinicians on community-based mental health services: negotiating safe pathways. J Child Fam Stud 2017;26:1936–48. | ✓ | ✓ | ||
| 200 | Nash 2016 | Nash A, Collier C. The alternative peer group: a developmentally appropriate recovery support model for adolescents. J Addict Nurs 2016;27:109–19. | ✓ | |||
| 201 | Nash 2019 | Nash AJ, Hennessy EA, Collier C. Exploring recovery capital among adolescents in an alternative peer group. Drug Alcohol Depend 2019;199:136–43. | ✓ | |||
| 202 | NICE 2019 | National Institute for Health and Care Excellence (NICE). Depression in Children and Young People: Identification and Management. London: NICE; 2019. | ✓ | |||
| 203 | Naughton 2015 | Naughton J, Basu S, O’Dowd F, Carroll M, Maybery D. Improving quality of a rural CAMHS service using the Choice and Partnership Approach. Australas Psychiatry 2015;23:561–5. | ✓ | |||
| 204 | Neira-Munoz 1998 | Neira-Munoz E, Ward D. Side by side. Health Serv J 1998. URL: www.hsj.co.uk/home/side-by-side/33995.article | ✓ | |||
| 205 | NICCY 2018 | Northern Ireland Commissioner for Children and Young People. ‘Still Waiting’: A Rights Based Review of Mental Health Services and Support for Children and Young People in Northern Ireland. Belfast: Northern Ireland Commissioner for Children and Young People; 2018. | ✓ | |||
| 206 | NIHR ARC NWC n.d. | NIHR Applied Research Collaboration North West Coast. Understanding the Impact of the YIAC (Youth Information, Advice and Counselling) Model on Access, Engagement and Mental Health for Young People Aged 14–25 Years. Liverpool: ARC NWC; n.d. | ✓ | |||
| 207 | Nissen 2004 | Nissen LB, Hunt SR, Bullman S, Marmo J, Smith D. Systems of care for treatment of adolescent substance use disorders: background, principles and opportunities. J Psychoactive Drugs 2004;36:429–38. | ✓ | |||
| 208 | No author 2001 | No author. Significant achievement awards: a unique approach to mental health care for young children – the Multnomah County, Oregon, Early Childhood Mental Health Program. Psychiatr Serv 2001;52:1389–90. | ✓ | |||
| 209 | Nolan n.d. | Nolan L. Evaluation for understanding the impact of the YIAC (Youth Information Advice and Counselling) model on access, engagement and mental health. Poster presentation; n.d. | ✓ | |||
| 210 | NTA 2008 | National Treatment Agency for Substance Misuse. The Role of CAMHS and Addiction Psychiatry in Adolescent Substance Misuse Services. London: National Treatment Agency; 2008. | ✓ | |||
| 211 | O’Herlihy 2016 | O’Herlihy A, Fonagy P, Pugh K. Future in Mind – CYP IAPT and ED. PowerPoint presentation; 2016. | ✓ | |||
| 212 | O’Keeffe 2015 | O’Keeffe L, O’Reilly A, O’Brien G, Buckley R, Illback R. Description and outcome evaluation of Jigsaw: an emergent Irish mental health early intervention programme for young people. Ir J Psychol Med 2015;32:71–7. | ✓ | ✓ | ||
| 213 | O’Reilly 2015 | O’Reilly A, Illback R, Peiper N, O’Keeffe L, Clayton R. Youth engagement with an emerging Irish mental health early intervention programme (Jigsaw): participant characteristics and implications for service delivery. J Ment Health 2015;24:283–8. | ✓ | |||
| 214 | Oppetit 2018 | Oppetit A, Brébant C, Monchablon D, Bourgin J, Gaillard R, Olié J-P, et al. Détection précoce des troubles psychiques en milieu scolaire: le dispositif Fil Harmonie [Early detection of mental health disorders at school: The Fil Harmonie pilot program]. L’Encéphale 2018;44:232–8. | ✓ | |||
| 215 | Painter 2009 | Painter K. Multisystemic therapy as community-based treatment for youth with severe emotional disturbance. Res Soc Work Pract 2009;19:314–24. | ✓ | |||
| 216 | Painter 2012 | Painter K. Outcomes for youth with severe emotional disturbance: a repeated measures longitudinal study of a wraparound approach of service delivery in systems of care. Child Youth Care Forum 2012;41:407–25. | ✓ | ✓ | ||
| 217 | Parker 2003 | Parker KCH, Roberts N, Williams C, Benjamin M, Cripps L, Woogh C. Urgent adolescent psychiatric consultation: from the accident and emergency department to inpatient adolescent psychiatry. J Adolesc 2003;26:283–93. | ✓ | ✓ | ✓ | |
| 218 | Pearlman 2018 | Pearlman DN, Vendetti T, Hill J. Linking public schools and community mental health services: a model for youth suicide prevention. R I Med J 2018;101:36–8. | ✓ | |||
| 219 | Pearson 1998 | Pearson G, Jennings J, Norcross J. A program of comprehensive school-based mental health services in a large urban public school district: The Dallas model. In Esmann A, editor. Adolescent Psychiatry: The Annals of the American Society for Adolescent Psychiatry, vol. 23. Hillsdale, NJ: Analytic Press; 1998. pp. 207–31. | ✓ | |||
| 220 | Peiper 2017 | Peiper N, Illback RJ, O’Reilly A, Clayton R. Latent class analysis of need descriptors within an Irish youth mental health early intervention program toward a typology of need: Irish youth mental health. Early Interv Psychiatry 2017;11:37–46. | ✓ | |||
| 221 | Persson 2017 | Persson S, Hagquist C, Michelson D. Young voices in mental health care: exploring children’s and adolescents’ service experiences and preferences. Clin Child Psychol Psychiatry 2017;22:140–51. | ✓ | |||
| 222 | Pettitt 2003 | Pettitt B. Effective Joint Working Between Child and Adolescent Mental Health Services and Schools. Nottingham: Department for Education and Skills; 2003. | ✓ | |||
| 223 | Pillay 1997 | Pillay AL, Lockhat MR. Developing community mental health services for children in South Africa. Soc Sci Med 1997;45:1493–501. | ✓ | |||
| 224 | Power 2014 | Power TJ, Mautone JA, Marshall SA, Jones HA, Cacia J, Tresco K, et al. Feasibility and potential effectiveness of integrated services for children with ADHD in urban primary care practices. Clin Pract Pediatr Psychol 2014;2:412–26. | ✓ | ✓ | ✓ | |
| 225 | Powers 2011 | Powers J, Webber K, Bower H. Promoting school mental health with a systems of care approach: perspectives from community partners. Social Work Mental Health 2011;9:147–62. | ✓ | ✓ | ||
| 226 | Powers 2013 | Powers JD, Edwards JD, Blackman KF, Wegmann KM. Key elements of a successful multi-system collaboration for school-based mental health: in-depth interviews with district and agency administrators. Urban Rev 2013;45:651–70. | ✓ | ✓ | ||
| 227 | Prescott 2017 | Prescott J, Hanley T, Ujhelyi K. Peer communication in online mental health forums for young people: directional and nondirectional support. JMIR Ment Health 2017;4:e29. | ✓ | |||
| 228 | Radford 2011 | Radford S, van Driel ML, Swanton K. Improving health outcomes in young people: a holistic, team based approach. Aust Fam Physician 2011;40:153–6. | ✓ | |||
| 229 | Rapee 2017 | Rapee RM, Lyneham HJ, Wuthrich V, Chatterton ML, Hudson JL, Kangas M, et al. Comparison of stepped care delivery against a single, empirically validated cognitive-behavioral therapy program for youth with anxiety: a randomized clinical trial. J Am Acad Child Adolesc Psychiatry 2017;56:841–8. | ✓ | ✓ | ||
| 230 | Rapp 2017 | Rapp AM, Chavira DA, Sugar CA, Asarnow JR. Integrated primary medical-behavioral health care for adolescent and young adult depression: predictors of service use in the youth partners in care trial. J Pediatr Psychol 2017;42:1051–64. | ✓ | |||
| 231 | Rayment 2014 | Rayment B. On the Right Tracks: A Guide to Commissioning Counselling Services for Young People 13–25 Years. London: Youth Access; 2014. | ✓ | |||
| 232 | Rey 1998 | Rey JM, Enshire E, Wever C, Apollonov I. Three-year outcome of disruptive adolescents treated in a day program. Eur Child Adolesc Psychiatry 1998;7:42–8. | ✓ | ✓ | ✓ | |
| 233 | Rice 2017 | Rice SM, Halperin S, Cahill S, Cranston I, Phelan M, Hetrick SE, et al. The Youth Mood Clinic: an innovative service for the treatment of severe and complex depression. Australas Psychiatry 2017;25:112–6. | ✓ | |||
| 234 | Richardson 2009 | Richardson L, McCauley E, Katon W. Collaborative care for adolescent depression: a pilot study. Gen Hosp Psychiatry 2009;31:36–45. | ✓ | ✓ | ✓ | |
| 235 | Richardson 2014 | Richardson LP, Ludman E, McCauley E, Lindenbaum J, Larison C, Zhou C, et al. Collaborative care for adolescents with depression in primary care: a randomized clinical trial. JAMA 2014;312:809. | ✓ | ✓ | ✓ | |
| 236 | Rickwood 2015a | Rickwood DJ, Mazzer KR, Telford NR, Parker AG, Tanti CJ, McGorry PD. Changes in psychological distress and psychosocial functioning in young people visiting headspace centres for mental health problems. Med J Aust 2015;202:537–42. | ✓ | ✓ | ||
| 237 | Rickwood 2015b | Rickwood DJ, Telford NR, Mazzer KR, Parker AG, Tanti CJ, McGorry PD. The services provided to young people by headspace centres in Australia. Med J Aust 2015;202:533–7. | ✓ | |||
| 238 | Rickwood 2019 | Rickwood D, Paraskakis M, Quin D, Hobbs N, Ryall V, Trethowan J, et al. Australia’s innovation in youth mental health care: the headspace centre model. Early Interv Psychiatry 2019;13:159–66. | ✓ | |||
| 239 | Robinson 2000 | Robinson KE. Outcomes of a school-based mental health program for referred youth. 13th Annual Conference Proceedings – A System of Care for Children’s Mental Health: Expanding the Research Base 2000:141–4. | ✓ | |||
| 240 | Robotham 2009 | Robotham D, James D. Evaluation of the Choice and Partnership Approach in Child and Adolescent Mental Health Services in England. London: The Mental Health Foundation; 2009. | ✓ | |||
| 241 | Robotham 2010 | Robotham D, James K, Cyhlarova E. Managing demand and capacity within child and adolescent mental health services: an evaluation of the Choice and Partnership Approach. Ment Health Rev J 2010;15:22–30. | ✓ | ✓ | ||
| 242 | Rodriguez 2019 | Rodríguez EM, Gulbas LE, George-Jones J, Leija A, Burrows D, Neavel C. Interdisciplinary perspectives on an integrated behavioral health model of psychiatry in pediatric primary care: a community-based participatory research study. Community Ment Health J 2019;55:569–77. | ✓ | ✓ | ||
| 243 | Roman 2018 | Roman SB, Matthews-Wilson A, Dickinson P, Chenard D, Rogers SC. Current pediatric emergency department innovative programs to improve the care of psychiatric patients. Child Adolesc Psychiatr Clin N Am 2018;27:441–54. | ✓ | |||
| 244 | Rothi 2006 | Rothi D, Leavey G. Child and adolescent mental health services (CAMHS) and schools: inter-agency collaboration and communication. J Ment Health Train Educ Pract 2006;1:32–40. | ✓ | |||
| 245 | Rowland 2005 | Rowland MD, Halliday-Boykins CA, Henggeler SW, Cunningham PB, Lee TG, Kruesi MJP, et al. A randomized trial of multisystemic therapy with Hawaii’s Felix Class youths. J Emot Behav Disord 2005;13:13–23. | ✓ | ✓ | ||
| 246 | Rowlandson 2009 | Rowlandson PH, Smith C. An interagency service delivery model for autistic spectrum disorders and attention deficit hyperactivity disorder. Child Care Health Dev 2009;35:681–90. | ✓ | |||
| 247 | Salloum 2014 | Salloum A, Scheeringa MS, Cohen JA, Storch EA. Development of stepped care trauma-focused cognitive-behavioral therapy for young children. Cogn Behav Pract 2014;21:97–108. | ✓ | |||
| 248 | SAMHSA 2016 | U.S. Department of Health and Human Services Substance Abuse and Mental Health Services Administration (SAMHSA). The Comprehensive Community Mental Health Services for Children with Serious Emotional Disturbances Program: Report to Congress 2016. Rockville, MD: SAMHSA; 2016. | ✓ | |||
| 249 | Sarvet 2010a | Sarvet BD, Wegner L. Developing effective child psychiatry collaboration with primary care: leadership and management strategies. Child Adolesc Psychiatr Clin N Am 2010;19:139–48. | ✓ | |||
| 250 | Sarvet 2010b | Sarvet B, Gold J, Bostic JQ, Masek BJ, Prince JB, Jeffers-Terry M, et al. Improving access to mental health care for children: the Massachusetts Child Psychiatry Access Project. Pediatrics 2010;126:1191–200. | ✓ | ✓ | ||
| 251 | Sarvet 2011 | Sarvet B, Gold J, Straus JH. Bridging the divide between child psychiatry and primary care: the use of telephone consultation within a population-based collaborative system. Child Adolesc Psychiatr Clin N Am 2011;20:41–53. | ✓ | |||
| 252 | Schley 2008 | Schley C, Ryall V, Crothers L, Radovini S, Fletcher K, Marriage K, et al. Early intervention with difficult to engage, ‘high-risk’ youth: evaluating an intensive outreach approach in youth mental health. Early Interv Psychiatry 2008;2:195–200. | ✓ | |||
| 253 | Schley 2011 | Schley C, Radovini A, Halperin S, Fletcher K. Intensive outreach in youth mental health: description of a service model for young people who are difficult-to-engage and ‘high-risk’. Child Youth Serv Rev 2011;33:1506–14. | ✓ | |||
| 254 | Schley 2012 | Schley C, Yuen K, Fletcher K, Radovini A. Does engagement with an intensive outreach service predict better treatment outcomes in ‘high-risk’ youth? Engagement as outcome predictor. Early Interv Psychiatry 2012;6:176–84. | ✓ | |||
| 255 | Schmied 2006 | Schmied DV, Brownhill DS, Walsh P. Models of Service Delivery and Interventions for Children and Young People with High Needs. Ashfield, NSW: NSW Department of Community Services; 2006. | ✓ | |||
| 256 | Scott 2009 | Scott E, Naismith S, Whitwell B, Hamilton B, Chudleigh C, Hickie I. Delivering youth-specific mental health services: the advantages of a collaborative, multi-disciplinary system. Australas Psychiatry 2009;17:189–94. | ✓ | |||
| 257 | Shannahan 2016 | Shannahan R, Fields S. Services in Support of Community Living for Youth with Serious Behavioral Health Challenges: Mobile Crisis Response and Stabilization Services. Baltimore, MD: The National Technical Assistance Network for Children’s Behavioral Health, School of Social Work, University of Maryland; 2016. | ✓ | |||
| 258 | Sharifi 2019 | Sharifi V, Shahrivar Z, Zarafshan H, Ashkezary SB, Stuart E, Mojtabai R, et al. Collaborative care for child and youth mental health problems in a middle-income country: study protocol for a randomized controlled trial training general practitioners. Trials 2019;20:405. | ✓ | |||
| 259 | Sheidow 2013 | Sheidow AJ, Houston JL. Multisystemic therapy for adolescent substance use. In Miller P, editor. Interventions for Addiction (Comprehensive Addictive Behaviors and Disorders, Volume 3). San Diego, CA: Academic Press; 2013. pp. 77–86. | ✓ | |||
| 260 | Sheldrick 2012 | Sheldrick RC, Mattern K, Perrin EC. Pediatricians’ perceptions of an off-site collaboration with child psychiatry. Clin Pediatr (Phila) 2012;51:546–50. | ✓ | ✓ | ||
| 261 | Shepperd 2009 | Shepperd S, Doll H, Gowers S, James A, Fazel M, Fitzpatrick R, et al. Alternatives to inpatient mental health care for children and young people. Cochrane Database Syst Rev 2009;2:CD006410. | ✓ | |||
| 262 | Sheridan 2017 | Sheridan JS, Sheridan DC, Johnson KP, Marshall RD. Can’t we just get some help? Providing innovative care to children in acute psychiatric crisis. Health Soc Work 2017;42:177–82. | ✓ | |||
| 263 | Shippee 2018 | Shippee ND, Mattson A, Brennan R, Huxsahl J, Billings ML, Williams MD. Effectiveness in regular practice of collaborative care for depression among adolescents: a retrospective cohort study. Psychiatr Serv 2018;69:536–41. | ✓ | ✓ | ||
| 264 | Shortt 2006 | Shortt AL, Fealy S, Toumbourou JW. The mental health risk assessment and management process (RAMP) for schools: II. Process evaluation. AeJAMH 2006;5:295–306. | ✓ | |||
| 265 | Silverstein 2015 | Silverstein M, Hironaka LK, Walter HJ, Feinberg E, Sandler J, Pellicer M, et al. Collaborative care for children with ADHD symptoms: a randomized comparative effectiveness trial. Pediatrics 2015;135:e858–67. | ✓ | ✓ | ||
| 266 | Simmons 2018 | Simmons MB, Coates D, Batchelor S, Dimopoulos-Bick T, Howe D. The CHOICE pilot project: challenges of implementing a combined peer work and shared decision-making programme in an early intervention service. Early Interv Psychiatry 2018;12:964–71. | ✓ | |||
| 267 | Solberg 2015 | Solberg C, Larsson B, Jozefiak T. Consumer satisfaction with the child and adolescent mental health service and its association with treatment outcome: a 3–4-year follow-up study. Nord J Psychiatry 2015;69:224–32. | ✓ | |||
| 268 | Sowar 2018 | Sowar K, Thurber D, Vanderploeg JJ, Haldane EC. Psychiatric community crisis services for youth. Child Adolesc Psychiatr Clin N Am 2018;27:479–90. | ✓ | |||
| 269 | Stallard 1998 | Stallard P, Sayers J. An opt-in appointment system and brief therapy: perspectives on a waiting list initiative. Clin Child Psychol Psychiatry 1998;3:199–212. | ✓ | ✓ | ||
| 270 | Straus 2014 | Straus JH, Sarvet B. Behavioral health care for children: the Massachusetts Child Psychiatry Access Project. Health Aff (Millwood) 2014;33:2153–61. | ✓ | |||
| 271 | Stroul 2010 | Stroul BA, Ed M, Blau GM, Friedman RM. Updating the System of Care Concept and Philosophy. Washington, DC: Georgetown University Center for Child and Human Development, National Technical Assistance Center for Children’s Mental Health; 2010. | ✓ | |||
| 272 | Sundell 2008 | Sundell K, Hansson K, Löfholm CA, Olsson T, Gustle L-H, Kadesjö C. The transportability of multisystemic therapy to Sweden: short-term results from a randomized trial of conduct-disordered youths. J Fam Psychol 2008;22:550–60. | ✓ | ✓ | ||
| 273 | Syed 2007 | Syed EU, Hussein SA, Yousafzai AW. Developing services with limited resources: establishing a CAMHS in Pakistan. Child Adolesc Ment Health 2007;12:121–4. | ✓ | |||
| 274 | Taylor 2010 | Taylor E, Duffy F. Service-user evaluation in two outpatient CAMHS teams. DCP Scotland Newsletter 2010:62–7. | ✓ | |||
| 275 | Teggart 2006 | Teggart T, Linden M. Investigating service users’ and carers’ views of child and adolescent mental health services in Northern Ireland. Child Care Pract 2006;12:27–41. | ✓ | |||
| 276 | Timimi 2013 | Timimi S, Tetley D, Burgoine W, Walker G. Outcome orientated child and adolescent mental health services (OO-CAMHS): a whole service model. Clin Child Psychol Psychiatry 2013;18:169–84. | ✓ | |||
| 277 | Timimi 2015 | Timimi S. Children and young people’s improving access to psychological therapies: inspiring innovation or more of the same? BJPsych Bull 2015;39:57–60. | ✓ | |||
| 278 | Tischler 2002 | Tischler V. Evaluation of a mental health outreach service for homeless families. Arch Dis Child 2002;86:158–63. | ✓ | ✓ | ✓ | |
| 279 | Trainer 2015 | Trainer M, Smith S, Reid A. County Durham CAMHS Crisis and Liaison Service: Service Evaluation Report. Darlington: Tees, Esk and Wear Valleys NHS Foundation Trust; 2015. | ✓ | |||
| 280 | van Roosmalen 2013 | van Roosmalen M, Gardner-Elahi C, Day C. A systems relations model for Tier 2 early intervention child mental health services with schools: an exploratory study. Clin Child Psychol Psychiatry 2013;18:25–43. | ✓ | |||
| 281 | Vanderploeg 2009 | Vanderploeg JJ, Franks RP, Plant R, Cloud M, Tebes JK. Extended day treatment: a comprehensive model of after school behavioral health services for youth. Child Youth Care Forum 2009;38:5–18. | ✓ | |||
| 282 | Vanderploeg 2016 | Vanderploeg JJ, Lu JJ, Marshall TM, Stevens K. Mobile crisis services for children and families: advancing a community-based model in Connecticut. Child Youth Serv Rev 2016;71:103–9. | ✓ | |||
| 283 | Vostanis 2006 | Vostanis P, Anderson L, Window S. Evaluation of a family support service: short-term outcome. Clin Child Psychol Psychiatry 2006;11:513–28. | ✓ | ✓ | ||
| 284 | Vusio 2020 | Vusio F, Thompson A, Laughton L, Birchwood M. After the storm, Solar comes out: a new service model for children and adolescent mental health. Early Interv Psychiatry 2020;15:731–8. | ✓ | |||
| 285 | Wagner 2017 | Wagner GA, Mildred H, Gee D, Black EB, Brann P. Effectiveness of brief intervention and case management for children and adolescents with mental health difficulties. Child Youth Serv Rev 2017;79:362–7. | ✓ | ✓ | ||
| 286 | Walker 2003 | Walker S. Multidisciplinary family support in child and adolescent mental health services. Clin Child Psychol Psychiatry 2003;8:215–26. | ✓ | |||
| 287 | Walker 2005 | Walker S. Releasing potential – the future of social work and CAMHS. J Soc Work Pract 2005;19:235–50. | ✓ | |||
| 288 | Walker 2010 | Walker S. A description of the establishment of a new child and adolescent mental health service in the United Kingdom. J Child Adolesc Ment Health 2010;22:35–9. | ✓ | ✓ | ||
| 289 | Wei 2011 | Wei Y, Kutcher S, Szumilas M. Comprehensive school mental health: an integrated ‘school-based pathway to care’ model for Canadian secondary schools. McGill J Educ 2011;46:213–29. | ✓ | |||
| 290 | Wells 2010 | Wells C, Adhyaru J, Cannon J, Lamond M, Baruch G. Multisystemic therapy (MST) for youth offending, psychiatric disorder and substance abuse: case examples from a UK MST team: case examples of multisystemic therapy. Child Adolesc Ment Health 2010;15:142–9. | ✓ | |||
| 291 | Whitworth 2004 | Whitworth D, Ball C. The impact of primary mental health workers on referrals to CAMHS. Child Adolesc Ment Health 2004;9:177–9. | ✓ | |||
| 292 | Wilmshurst 2002 | Wilmshurst LA. Treatment programs for youth with emotional and behavioral disorders: an outcome study of two alternate approaches. Ment Health Serv Res 2002;2:85–96. | ✓ | ✓ | ||
| 293 | Wilson 2015 | Wilson S, Metcalfe J, McLeod S. Comparing Choice and Partnership Approach assumptions to child and adolescent mental health services in NHS Greater Glasgow and Clyde. Int J Health Care Qual Assur 2015;28:812–25. | ✓ | |||
| 294 | Window 2004 | Window S, Anderson L, Vostanis P. A multi-agency service for child behavioural problems. Community Pract 2004;77:180–4. | ✓ | ✓ | ||
| 295 | Wolpert 2011 | Wolpert M, Deighton J, Patalay P, Martin A, Fitzgerald-Yau N, Demir E, et al. Me and My School: Findings from the National Evaluation of Targeted Mental Health in Schools 2008–2011. London: Anna Freud Centre/UCL; 2011. | ✓ | |||
| 296 | Wolpert 2012 | Wolpert M, Fugard AJB, Deighton J, Görzig A. Routine outcomes monitoring as part of children and young people’s improving access to psychological therapies (CYP IAPT) – improving care or unhelpful burden? Child Adolesc Ment Health 2012;17:129–30. | ✓ | |||
| 297 | Wolpert 2013 | Wolpert M, Humphrey N, Belsky J, Deighton J. Embedding mental health support in schools: learning from the Targeted Mental Health in Schools (TaMHS) national evaluation. Emot Behav Diffic 2013;18:270–83. | ✓ | ✓ | ✓ | |
| 298 | Wolpert 2016 | Wolpert M, Harris R, Hodges S, Fuggle P, James R, Weiner A, et al. THRIVE Elaborated. 2nd edn. London: CAMHS Press; 2016. | ✓ | |||
| 299 | Wolpert 2019 | Wolpert M, Harris R, Hodges S, Fuggle P, James R, Weiner A, et al. THRIVE Framework for System Change. London: Anna Freud National Centre for Children and Families/Tavistock and Portman NHS Foundation Trust; 2019. | ✓ | |||
| 300 | Woodgate 2006 | Woodgate M, Garralda ME. Paediatric liaison work by child and adolescent mental health services. Child Adolesc Ment Health 2006;11:19–24. | ✓ | |||
| 301 | Woodward 2003 | Woodward RM. The Interrelationship Between Children’s School-based and Outpatient Specialty Mental Health Service Use: A Consumer Demand Analysis. PhD thesis. Baltimore, MD: Johns Hopkins University; 2003. | ✓ | |||
| 302 | Worral-Davies 2004 | Worrall-Davies A, Cottrell D, Benson E. Evaluation of an early intervention Tier 2 child and adolescent mental health service. Health Soc Care Community 2004;12:119–25. | ✓ | ✓ | ||
| 303 | Worral-Davies 2013 | Worrall-Davies A. Day services. In McDougall T, Cotgrove A, editors. Specialist Mental Healthcare for Children and Adolescents: Hospital, Intensive Community and Home-based Services. Abingdon: Routledge; 2014. | ✓ | |||
| 304 | Wright 2015 | Wright E, Ord J. Youth work and the power of ‘giving voice’: a reframing of mental health services for young people. Youth Policy 2015;115:63–84. | ✓ | |||
| 305 | Wright 2016 | Wright DR, Haaland WL, Ludman E, McCauley E, Lindenbaum J, Richardson LP. The costs and cost-effectiveness of collaborative care for adolescents with depression in primary care settings: a randomized clinical trial. JAMA Pediatr 2016;170:1048. | ✓ | ✓ | ||
| 306 | York 2004 | York A, Anderson Y, Zwi M. Eight months to eight weeks: reducing waiting times in a child and adolescent mental health service. Ment Health Rev (Brighton) 2004;9:15–9. | ✓ | |||
| 307 | York 2009 | York W. Developing a school team to improve links between education and mental health services. Nurs Times 2009;105:25–7. | ✓ | |||
| 308 | Young 2012 | Young L, Lowe F. The young people’s consultation services: a model of engagement. In Lemma A, editor. Contemporary Developments in Adult and Young Adult Therapy. Abingdon: Routledge; 2012. pp. 89–110. | ✓ | |||
| 309 | Zanglis 2002 | Zanglis I. Mental Health and Schools: Nobody Ever Said Interagency Collaboration was Easy. PhD thesis. Santa Barbara, CA: University of California, Santa Barbara; 2002. | ✓ | |||
| 310 | Zima 2010 | Zima BT, Bussing R, Tang L, Zhang L, Ettner S, Belin TR, et al. Quality of care for childhood attention deficit/hyperactivity disorder in a managed care Medicaid program. J Am Acad Child Adolesc Psychiatry 2011;49:1225–37.e11. | ✓ | ✓ | ||
| TOTALS | 296 | 56 | 62 | 3 | ||
Appendix 5 Included studies’ key characteristics and Mixed-Methods Appraisal Tool appraisal by model group
Note: MMAT appraisal numbers refer to the question numbers for the respective MMAT group. Appraisers’ agreed responses were coded green for ‘yes’, orange for ‘can’t tell’ and red for ‘no’.
Group A studies (specialist Child and Adolescent Mental Health Services)
| Grp | Report ID | Locale | MMAT group/study type | MMAT appraisal |
|---|---|---|---|---|
| Effectiveness | ||||
| A1a. | Worral-Davies 2004 | UK, England | 4. uncontrolled retrospective cohort study | ①②③④⑤ |
| A1b. | Zima 2010a (see also B1) | USA | 3. controlled retrospective cohort study | ①②③④⑤ |
| A2. | Çakin Memik 2010a | Turkey | 4. uncontrolled pre/post study | ①②③④⑤ |
| A2. | Rey 1998a | Australia | 3. matched controls study | ①②③④⑤ |
| Acceptability | ||||
| A. | Bone 2015 | UK, England | 1. interviews with CYP/parents | ①②③④⑤ |
| A. | Crouch 2019 | UK, England | 1. telephone interviews with parents | ①②③④⑤ |
| A. | Hinrichs 2012 | UK, England | 1. face-to-face interviews with staff | ①②③④⑤ |
| A. | Teggart 2006 | UK, Northern Ireland | 5. survey of families + focus groups with CYP | ①②③④⑤ |
| A1a. | Bjørngaard 2008 | Norway | 4. parent satisfaction survey | ①②③④⑤ |
| A1a. | Coyne 2015 | Ireland | 1. interviews with CYP/parents | ①②③④⑤ |
| A1a. | Kapp 2017 | Switzerland | 4. survey of CYP/parents | ①②③④⑤ |
| A1a. | Mitchell-Lowe 2009 | New Zealand | 1. interviews with CYP/parents | ①②③④⑤ |
| A1a. | Persson 2017 | Sweden | 1. focus groups with CYP | ①②③④⑤ |
| A1a. | Solberg 2015 | Norway | 4. longitudinal survey of CYP inc. satisfaction | ①②③④⑤ |
| A1b. | McGonnell 2009 | Canada | 5. survey of parents/staff + staff interviews | ①②③④⑤ |
| A1b. | Zima 2010a (see also B1) | USA | 3. parent-rated satisfaction in controlled cohort study | ①②③④⑤ |
| A2. | Çakin Memik 2010a | Turkey | 4. parent-rated satisfaction in uncontrolled pre/post study | ①②③④⑤ |
| A2. | Rey 1998a | Australia | 3. CYP-/parent-rated satisfaction in matched controls study | ①②③④⑤ |
Group B studies (community-embedded specialist CAMHS)
| Grp | Report ID | Locale | MMAT group/study type | MMAT appraisal |
|---|---|---|---|---|
| Effectiveness | ||||
| B1. | Asarnow 2005a
Asarnow 2009a |
USA | 2. RCT | ①②③④⑤ |
| B1. | Clarke 2005 | USA | 2. RCT | ①②③④⑤ |
| B1. | Day 2006a | UK, England | 3. controlled study | ①②③④⑤ |
| B1. | Kolko 2012a | USA | 5. RCT (within a mixed-methods study) | ①②③④⑤ |
| B1. | Kolko 2014a | USA | 2. cluster RCT | ①②③④⑤ |
| B1. | Power 2014a | USA | 3. controlled study | ①②③④⑤ |
| B1. | Richardson 2009a | USA | 5. uncontrolled pre/post (within a mixed-methods study) | ①②③④⑤ |
| B1. | Richardson 2014a (same study as Wright 2016) | USA | 2. RCT | ①②③④⑤ |
| B1. | Shippee 2018 | USA | 3. controlled retrospective cohort study | ①②③④⑤ |
| B1. | Silverstein 2015 | USA | 2. RCT | ①②③④⑤ |
| B1. | Zima 2010a (see also A1b) | USA | 3. controlled retrospective cohort study | ①②③④⑤ |
| B2. | Beehler 2012 | USA | 4. uncontrolled longitudinal study | ①②③④⑤ |
| B2. | Finch 2018 | USA | 3. controlled study | ①②③④⑤ |
| B2. | McKenzie 2011a | UK, Scotland | 4. uncontrolled pre/post study | ①②③④⑤ |
| B2. | Wolpert 2013a | UK, England | 5. RCT + observational longitudinal study | ①②③④⑤ |
| B3. | O’Keefe 2015 | Ireland | 4. uncontrolled retrospective cohort study | ①②③④⑤ |
| B3. | Rickwood 2015a | Australia | 4. uncontrolled retrospective cohort study | ①②③④⑤ |
| Acceptability | ||||
| B1. | Adams 2016 | USA | 4. survey of parents/staff | ①②③④⑤ |
| B1. | Asarnow 2005a
Asarnow 2009a |
USA | 2. CYP-rated satisfaction in RCT | ①②③④⑤ |
| B1. | Bor 2013 | Australia | 4. mail/phone survey of parents/staff | ①②③④⑤ |
| B1. | Bower 2003 (see also D3) | UK, England | 4. postal survey of staff | ①②③④⑤ |
| B1. | Day 2006a | UK, England | 3. parent-rated satisfaction in controlled study | ①②③④⑤ |
| B1. | Fallucco 2017 | USA | 4. satisfaction survey of staff | ①②③④⑤ |
| B1. | Kaye 2017 | USA | 4. satisfaction survey of staff | ①②③④⑤ |
| B1. | Kolko 2012a | USA | 5. focus groups with/survey of staff + parent-rated satisfaction in RCT | ①②③④⑤ |
| B1. | Kolko 2014a | USA | 2. parent-rated satisfaction in RCT | ①②③④⑤ |
| B1. | Nadeau 2017 | Canada | 1. case study interviews with families/staff | ①②③④⑤ |
| B1. | Power 2014a | USA | 3. parent-rated acceptability in controlled study | ①②③④⑤ |
| B1. | Richardson 2009a | USA | 5. interviews with CYP/parents + CYP-/parent-rated satisfaction from an uncontrolled pre/post study | ①②③④⑤ |
| B1. | Richardson 2014a (same study as Wright 2016) | USA | 2. CYP-rated satisfaction in RCT | ①②③④⑤ |
| B1. | Rodriguez 2019 | USA | 1. interviews with staff | ①②③④⑤ |
| B1. | Zima 2010a (see also A1b) | USA | 3. parent-rated satisfaction in controlled cohort study | ①②③④⑤ |
| B2. | McKenzie 2011a | UK, Scotland | 4. CYP-/referrer-/counsellor-rated helpfulness in uncontrolled pre/post study | ①②③④⑤ |
| B2. | Nabors 1999 | USA | 4. survey of YP | ①②③④⑤ |
| B2. | Powers 2013 | USA | 1. interviews with staff | ①②③④⑤ |
| B2. | Wolpert 2013a | UK, England | 5. qualitative interviews with CYP/parents/staff | ①②③④⑤ |
| Cost-effectiveness | ||||
| B1. | Wright 2016 (same study as Richardson 2014a) | USA | 2. cost–utility analysis within RCT | ①②③④⑤ |
Group C studies (community-embedded non-specialist CAMHS)
| Grp | Report ID | Locale | MMAT group/study type | MMAT appraisal |
|---|---|---|---|---|
| Effectiveness | ||||
| C1. | Clark 2014a | New Zealand | 5. uncontrolled pre/post study | ①②③④⑤ |
| C1. | Rapee 2017 (same study as Chatterton 2019) | Australia | 2. RCT | ①②③④⑤ |
| Acceptability | ||||
| C1. | Bassilios 2017 | Australia | 1. telephone interviews with staff | ①②③④⑤ |
| C1. | Clark 2014a | New Zealand | 5. CYP completed narrative feedback form | ①②③④⑤ |
| C3. | Walker 2010 | UK, England | 1. focus groups and interviews with CYP/staff | ①②③④⑤ |
| Cost-effectiveness | ||||
| C1. | Chatterton 2019 (same study as Rapee 2017) | Australia | 2. cost–utility analysis within a RCT | ①②③④⑤ |
Group D studies (in/outreach)
| Grp | Report ID | Locale | MMAT group/study type | MMAT appraisal |
|---|---|---|---|---|
| Effectiveness | ||||
| D1. | Duffy 2014 | UK, Scotland | 4. uncontrolled pre/post study | ①②③④⑤ |
| D1. | Evans 1997 Evans 2003 |
USA | 2. RCT | ①②③④⑤ |
| D1. | Tischler 2002a | UK, England | 5. controlled study | ①②③④⑤ |
| D1. | Wilmshurst 2002 | Canada | 2. RCT | ①②③④⑤ |
| D2. | Atkins 2006 | USA | 2. cluster RCT | ①②③④⑤ |
| D2. | Atkins 2015 | USA | 2. cluster RCT | ①②③④⑤ |
| D2. | Cai 2016a
Lim 2017a |
Singapore | 4. uncontrolled retrospective cohort study | ①②③④⑤ |
| D2. | Gilliam 2016 | USA | 2. cluster RCT | ①②③④⑤ |
| D2. | Holmes 2015 | USA | 4. uncontrolled pre/post study | ①②③④⑤ |
| D3. | Callaghan 2004a (same study as Callaghan 2003b) | UK, England | 5. uncontrolled pre/post study | ①②③④⑤ |
| D3. | Window 2004 Vostanis 2006 |
UK, England | 3. matched controlled study | ①②③④⑤ |
| D4. | Holder 2017 | USA | 4. uncontrolled retrospective cohort study | ①②③④⑤ |
| D4. | Parker 2003a | Canada | 4. uncontrolled ‘natural experiment’ | ①②③④⑤ |
| Acceptability | ||||
| D1. | Tischler 2002a | UK, England | 5. focus groups with staff/interviews with parents | ①②③④⑤ |
| D2. | Corboy 2007 | Australia | 1. individual and group face-to-face and telephone interviews with staff | ①②③④⑤ |
| D2. | Gowers 2004 | UK, England | 4. survey of staff | ①②③④⑤ |
| D2. | Hunter 2009 | UK, England | 1. focus group interviews with staff | ①②③④⑤ |
| D2. | Lee 2017 | USA | 1. case study: individual interviews with staff | ①②③④⑤ |
| D2. | Lim 2017a (same study as Cai 2016a) | Singapore | 4. satisfaction ratings (informants unclear) in uncontrolled retrospective cohort study | ①②③④⑤ |
| D2. | Rothi 2006 | UK, England | 1. interview with staff | ①②③④⑤ |
| D3. | Bower 2003 (see also B1) | UK, England | 4. postal survey of staff | ①②③④⑤ |
| D3. | Callaghan 2003a | UK, England | 4. staff service satisfaction questionnaire | ①②③④⑤ |
| D3. | Callaghan 2003b Callaghan 2004a |
UK, England | 5. grounded theory study using focus groups (2003b) and post-service satisfaction questionnaire (2004) with CYP/carers/staff | ①②③④⑤ |
| D3. | McDonald 2004 | UK, England | 1. case study involving interviews with staff | ①②③④⑤ |
| D3. | Sarvet 2010b | USA | 4. survey of staff | ①②③④⑤ |
| D3. | Sheldrick 2012 | USA | 4. online survey of staff | ①②③④⑤ |
| D4. | Lee 2014 | Canada | 4. telephone survey of parental satisfaction | ①②③④⑤ |
| D4. | Parker 2003a | Canada | 4. survey of A&E staff within an uncontrolled ‘natural’ experiment | ①②③④⑤ |
| Cost-effectiveness | ||||
| D2 | Cai 2016a (same study as Lim 2017a) | Singapore | 4. cost–utility analysis within an uncontrolled retrospective cohort study | ①②③④⑤ |
Group E studies (ecological models)
| Grp | Report ID | Locale | MMAT group/study type | MMAT appraisal |
|---|---|---|---|---|
| Effectiveness | ||||
| E1. | Cordell 2017a | USA | 3. retrospective interrupted time series | ①②③④⑤ |
| E1. | McKay-Brown 2019 | Australia | 4. uncontrolled pre/post study within action research project | ①②③④⑤ |
| E1. | Painter 2012 | USA | 4. uncontrolled longitudinal study | ①②③④⑤ |
| E2. | Painter 2009 | USA | 3. controlled study | ①②③④⑤ |
| E2. | Rowland 2005 | USA | 2. RCT | ①②③④⑤ |
| E2. | Sundell 2008 Löfholm 2009 |
Sweden | 2. RCT | ①②③④⑤ |
| Acceptability | ||||
| E1. | Bartlett 2018 | Canada | 1. case study with parent/staff interviews | ①②③④⑤ |
Group F studies (demand management models)
| Grp | Report ID | Locale | MMAT group/study type | MMAT appraisal |
|---|---|---|---|---|
| Effectiveness | ||||
| F2. | Barwick 2013a | Canada | 3. controlled study | ①②③④⑤ |
| F2. | Heywood 2003a | UK, England | 5. uncontrolled pre/post study | ①②③④⑤ |
| F2. | McGarry 2008a | Ireland | 2. RCT | ①②③④⑤ |
| F2. | Wagner 2017 | Australia | 3. controlled retrospective cohort study | ①②③④⑤ |
| Acceptability | ||||
| F1. | Robotham 2010 | UK, England | 5. interviews and focus groups with staff | ①②③④⑤ |
| F2. | Barwick 2013a | Canada | 3. CYP-rated satisfaction in controlled study | ①②③④⑤ |
| F2. | Gallagher 2015 | UK, England | 1. interviews with YP/family members | ①②③④⑤ |
| F2. | Heywood 2003a | UK, England | 5. interviews with CYP/parents + completion of an engagement questionnaire | ①②③④⑤ |
| F2. | McGarry 2008a | Ireland | 2. parent-rated satisfaction in RCT | ①②③④⑤ |
| F2. | Stallard 1998 | UK, England | 4. satisfaction survey of parents/staff | ①②③④⑤ |
Group G studies (service transformation frameworks)
| Grp | Report ID | Locale | MMAT group/study type | MMAT appraisal |
|---|---|---|---|---|
| Effectiveness | ||||
| G1. | Champine 2018a | USA | 4. uncontrolled pre/post study | ①②③④⑤ |
| G1. | Lambert 1996 | USA | 3. controlled study | ①②③④⑤ |
| G1. | Manteuffel 2002 | USA | 4. uncontrolled longitudinal study | ①②③④⑤ |
| G5. | Glisson 2012 | USA | 2. RCT | ①②③④⑤ |
| G5. | Glisson 2013 | USA | 2. RCT | ①②③④⑤ |
| G5. | Glisson 2016 | USA | 2. RCT | ①②③④⑤ |
| Acceptability | ||||
| G1. | Champine 2018a | USA | 4. parent-rated satisfaction in uncontrolled pre/post study | ①②③④⑤ |
| G1. | Heflinger 1996 | USA | 4. repeated parent satisfaction survey | ①②③④⑤ |
| G1. | Measelle 1998 | USA | 4. survey with parental satisfaction measure | ①②③④⑤ |
| G1. | Powers 2011 | USA | 1. staff interviews in a microethnography study | ①②③④⑤ |
Appendix 6 Services described in the scoping review by model group
| Primary service model group | Service model subgroup | Service name (document ID, country) |
|---|---|---|
|
A. Specialist CAMHS
Encompasses ‘standard’ institutionally based, medically (psychiatry) driven child and adolescent mental health services in the country of origin |
A1a. Outpatient CAMHS, generic service | CAMHS (Coyne 2015, Ireland); CAMHS Outpatients (Kapp 2017, Switzerland); Child Mental Health Clinic (Syed 2007, Pakistan); Innovative Tier 2 Service (Worral-Davies 2004, UK); Norwegian Outpatient CAMHS (Bjørngaard 2008, Norway); Outcome-Oriented CAMHS (Timimi 2013, UK) |
| A1b. Outpatient CAMHS, condition-specific service | ADHD Specialty Clinic (Campbell 2014, USA; McGonnell 2009, Canada); AtR!sk (emerging personality disorder) (Kaess 2017, Germany); HYPE: Helping Young People Early (emerging personality disorder) (Chanen 2009, Australia); Transcultural Child Psychiatry Team (ethnic minorities) (Measham 2005, Canada); Youth Mood Clinic (mood disorders) (Rice 2017 Australia); Young People’s Drug and Alcohol Service (NTA 2008, UK) | |
| A2. Specialist CAMHS Day Care | Day Clinic (Çakin Memik 2010, Turkey); Day Service for Adolescents (Gatta 2009, Italy); Day Services (all UK: McDougall 2008; Worral-Davies 2013); Day Treatment (Rey, 1998 Australia); Extended Day Treatment (Vanderploeg 2009, USA); Intensive Day Treatment (Lamb 2009, no country specified) | |
| A3. Inpatient care | Not in scope | |
|
B. Community-embedded specialist CAMHS
Community-based, rather than institutional, services in which key mental health workers from Specialist CAMHS (A group) are embedded (colocated) within the service rather than being ‘visitors’ to that service |
B1. Collaborative Care
Embedding Specialist CAMHS (A Group) workers into primary care settings so they can work closely and collaboratively |
Behavioural Health Clinician Integration in Primary Care (all USA: Coffey 2017;a Godoy 2017); CAP PC: Child and Adolescent Psychiatry for Primary Care (Kaye 2017, USA); Child Psychiatry Consultation Model (Fallucco 2017, USA); Collaborative Care (Clarke 2005, USA; Coffey 2017,a USA; Myers 2010, USA; Nadeau 2017, Canada; Richardson 2009, USA; Sharifi 2019, Iran; Silverstein 2015,a USA); Colocated Collaborative Care (all USA: Keller 2013; Moore 2018);a Community Care of North Carolina (Gabel 2010, USA); Co-ordinated System of Assessment and Diagnosis for ADHD (Rowlandson 2009, UK); DOCC: Doctor-Office Collaborative Care (all USA: Kolko 2012, Kolko 2014; EMERALD: Early Management and Evidence-based Recognition of Adolescents Living with Depression (Shippee 2018, USA); Enhanced Collaborative Care (Silverstein 2015,a USA); Hamilton Family Health Team Mental Health Program (Kates 2011, Canada); Integrated Behavioural Health (all USA: Adams 2016; Rodriguez 2019); Integrated Collaborative Care (Henderson 2017, Canada; Moore 2018,a USA); Integrated Healthcare Service Delivery System (Acri 2016, USA); Multidisciplinary Partnership for Children with Attention Problems (Bor 2013, Australia); PASS: Partnering to Achieve School Success (Power 2014, USA); Primary Care CAMH Outreach Clinic (Day 2006, UK); Primary Care Collaborative Mental Health Team (Campo 2005, USA); ROAD: Reaching Out to Adolescents in Distress (all USA: Richardson 2014; Wright 2016); Shifted Outpatient Clinics (Bower 2003, UK); Stepped Care Collaborative Care for Refugees and Asylum Seekers (Böge 2019, Germany); Youth Partners in Care (all USA: Asarnow 2005; Asarnow 2009; Rapp 2017) |
|
B2. School-embedded Mental Health service
Embedding Specialist CAMHS (A Group) workers into schools |
ACCESS: Accessible, Collaborative Care for Effective School-based Services (Lyon 2016, USA); CAMHS Counsellor in Schools (McKenzie 2011, UK); CATS: Cultural Adjustment and Trauma Services (Beehler 2012, USA); The Children’s Behaviour Therapy Unit (Robinson 2000, USA); Clinics within Full Service Schools (Dryfoos 1995, USA); Dallas Youth and Family Centres (Pearson 1998, USA);DOC: Doc On Campus (Doley, 2008, Australia); Full-service Community Schools (Dryfoos 2002, USA); Linkages to Learning (Friedman 2000, USA); Mental Health Service in Community Schools (Bloom 2005, USA); Multi-System Partnership for School-based Mental Health (Powers 2013, USA); The Place2Be (all UK: Houses of Parliament POST 2017; Lee 2009); RAMP: Risk Assessment and Management Process (all Australia: Fealy 2006; Shortt 2006); Recovery High Schools (all USA: Finch 2014; Finch 2018); School-based Health Centres (all USA: Colon 2005; Larson 2016; Liu 2010; Mitchell 2007); School-based Mental Health Care (Woodward 2003, USA); School Mental Health Team (York 2009, UK); School-based Pathway to Care (all Canada: Kutcher 2013b; Wei 2011); School Health Clinic (Armbruster 2002, USA); TaMHS: Targeted Mental Health in Schools (all UK: DfCSF 2008; Wolpert 2011; Wolpert 2013) | |
|
B3. Psychiatry-derived community hub
One-stop (integrated) primary care centres for those aged 12–25 needing help with mental health, physical health (including sexual health), alcohol and other drugs, or work and study support; has roots in psychiatry, particularly early intervention in psychosis work |
ACCESS: Adolescent Connections to Community-driven Early Strengths-based and Stigma-free Services (Malla 2016,b Australia); CHOICE (Simmons 2018, Australia); Clinical Staging within Headspace Centres (Cross 2014, Australia); Headspace Centres (all Australia: Abidi 2017b Burns 2014; Callaly 2010; Callaly 2014; Cotton 2019; Howe 2014; Malla 2016;b McGorry 2013;b McGorry 2016; McGorry 2018; Muir 2009; Radford 2011; Rickwood 2015a; Rickwood 2015b; Rickwood 2019; Scott 2009b); Headstrong/Jigsaw (all Ireland: Abidi 2017;b Illback 2010; Malla 2016;b McGorry 2013;b O’Keeffe 2015; O’Reilly 2015; Peiper 2017); Norfolk and Suffolk Specialist Youth Mental Health Service (Knapp 2016, UK); Youth Mental Health Clinic (Scott 2009,b Australia); YStop: Psychiatry Clinic in Youth Stop (Lee 2013, Australia) |
|
|
C. Community-embedded non-specialist CAMHS
Community-based, rather than institutional, services in which key mental health workers from ‘less medical’ professions (e.g. counselling or youth work) are embedded (colocated) within the service rather than being ‘visitors’ to that service |
C1. Primary care mental health service
Services delivered in primary care settings but which are not delivered by staff from Specialist CAMHS (A Group) nor are the staff necessarily colocated |
1419 IAPT Pilot (Humphrey 2016, UK); ATAPS: Access to Allied Psychological Services, Child Mental Health Service (all Australia: Bassilios 2016a; Bassilios 2016b; Bassilios 2017); Stepped Care for Anxious Youth (all Australia: Chatterton 2019; Rapee 2017); Stepped Care Model for Depression (NICE 2019, UK); Stepped Care Trauma-focused CBT (Salloum 2014, USA); Strengths Model for Youth (Mendenhall 2019, USA); Transdiagnostic Staging Model (Cross 2017, Australia); Your Choice (Clark 2014, New Zealand) |
|
C2. Digital Service
Services that operate solely as digital/remote services |
eHeadspace (Cotton 2019, Australia); Kooth (all UK: Frith 2017; Houses of Parliament POST 2017; Hanley 2019; Prescott 2017); ProHEAD Online (Kaess 2019, Germany) | |
|
C3. NGO-derived community hub
One-stop, integrated health and well-being services for young people aged 13–25; analogue of model B3 but with a clear non-medical/psychiatry ethos, often provided by third-sector organisations |
Family Empowerment Program (Cleek 2012, USA); The Junction (Walker 2010, UK); Pause, Forward Thinking Birmingham (Frith 2016, UK); Rural Youth Work Project (Wright 2015, UK); The Well Centre (Hagell 2016, UK); The Wish Centre (Durcan 2018, UK); YIACS: Youth Information, Advice and Counselling Services (all UK: Houses of Parliament POST, 2017; NIHR ARC NWC n.d.; Nolan n.d.; Rayment 2014) | |
|
D. In/outreach
In/outreach services tend to have an early intervention focus and the bulk of the work is either consultation (offering triage, assessments and low-level intervention work to CYP and their families) or liaison (offering training, advice and support to non-mental health staff). |
D1. Outreach to home
While these services are most often provided for more serious mental health problems such as psychosis (which is out of scope), some are available for those at the more complex end of the CMHPs spectrum |
(Assertive) Outreach Services (Lamb 2009,c no country specified; McDougall 2008,c UK);
CAMHS Specialist Substance Misuse Service (NTA 2008,c UK); Children’s Crisis Outreach Response System (Shannahan 2016,c USA); Community Intensive Therapy Team (Biggins 2014,c UK); Connecticut Mobile Crisis Intervention Service (all USA: Sowar 2018;c Vanderploeg 2016); Crisis Case Management (all USA: Evans 1997;c Evans 2003c); Enhanced Home-based Crisis Intervention (all USA: Evans 1997;c Evans 2003c); Family Preservation (Lamb 2009,c no country specified; Wilmshurst 2002, Canada); Flux: Wiltshire Young People’s Substance Misuse Service (NTA 2008,c UK); Home-based Crisis Intervention (all USA: Evans 1997;c Evans 2003c); Home-based Treatment (McDougall 2008,c UK); Homebuilders (Shepperd 2009,c no country specified); IICAPS: Intensive In-Home Child and Adolescent Psychiatric Service (Biggins 2014,c UK); IMYOS: Intensive Mobile Youth Outreach Service (all Australia: Schley 2008; Schley 2011; Schley 2012); Intensive Home-based Services (Daleiden 2010, USA; Lamb 2009,c no country specified; Shepperd 2009,c no country specified); Intensive Mental Health Services (Brockie-Trombley 2005, USA); KidCare Emergency Mobile Psychiatric Service (Guerra 2007, USA); Lambeth’s Virtual Integrated Team (NTA 2008,c UK); The Lock Young People’s Substance Misuse Service (NTA 2008,c UK); Lothian CAMHS Intensive Treatment Service (Duffy 2014, UK); Massachusetts Mobile Crisis Intervention (Shannahan 2016,c USA); Mental Health Outreach Service for Homeless Families (Tischler 2002, UK); Milwaukee Mobile Urgent Treatment Team (Shannahan 2016,c USA); Mobile Response and Stabilisation Services (Shannahan 2016,c USA); Orygen Youth Access Team (McGorry 2013, Australia); No. 29: Bradford Young People’s Service (NTA 2008,c UK); Ventura County Children’s Crisis Continuum (Sowar 2018,c USA); WAARM: Washburn Allina Acute Response Model (Roman 2018, USA);The Young People’s Drug Treatment Service Bristol (NTA 2008,c UK) |
|
D2. Schools outreach
Mental health experts go into schools to work directly with families, train and support school staff, and do mental health promotion/preventative work and low-level interventions van Roosmalen 2013 |
C3: Classroom-Community Consultation (Lee 2017, USA); CAMHS delivering services to schools (Armbruster 1997, USA); CAMHS Liaison with Schools (Gowers 2004, UK); CAMHS-Schools Joint Working (Pettitt 2003, UK); CAST: CAMHS and Schools Together (Corboy 2007, Australia); ECCP: Early Childhood Consultation Partnership (all USA: Gilliam 2006; Gilliam 2007); Fil Harmonie (Oppetit 2018, France); The Haven Project (Chiumento 2011, UK); Head Start Trauma Smart (Holmes 2015, USA); Hill Top Project (Eapen 2012, Australia); Independent School-based Mental Health Program (Armbruster 2002, USA); L2L: Links to Learning (Atkins 2015, USA); Luton Community CAMH Early Intervention and Prevention Service (van Roosmalen 2013, UK); Mental Health Link Worker (Hunter 2009, UK); Mental Health Services and Schools Link Pilots (all UK: Day 2017; Houses of Parliament POST 2007); Mental Health Support Teams in Schools (BPS 2019, UK); PALS: Positive Attitudes Toward Learning in Schools (all USA: Atkins 2003; Atkins 2006); REACH: Response, Early Assessment and Intervention in Community Mental Health (all Singapore: Cai 2016; Lim 2017); Rhode Island Suicide Prevention Initiative (Pearlman 2018, USA); School-based Mental Health Service (Casat 1999, USA); School nurse drop-in clinics (Clarke 2003, UK) | |
|
D3. Community outreach and liaison
Mental health workers consult/liaise with non-mental health specialists in the wider community, which may include, for example, schools and colleges, primary care services, youth workers and religious organisations; remit is wider than for models D1 and D2 |
A-DASH: Adolescent Drug and Alcohol Service (NTA 2008,d UK); Alternative Peer Group (all USA: Nash 2016; Nash 2019); Birmingham Young People’s Substance Misuse Service (NTA 2008,d UK); CAMHS/GP Consultation-Liaison Model (Bower 2003, UK); Community Intervention Model (Pillay 1997, South Africa); Direct Access Mental Health Service for Looked After Young People (Arcelus 1999, UK); Early Childhood Mental Health Programme (No Author 2001, USA); Enhanced Care Co-ordination (Roman 2018, USA); Family Centres (Allison 2007, UK); Family Support Service (all UK: Vostanis 2006; Walker 2003; Window 2004); Flintshire Primary Care Service for Children (Appleton 2000, UK); MCPAP: Massachusetts Child Psychiatry Access Project (all USA: Aupont 2013; Coffey 2017; Connor 2006; Gabel 2010;d Gabel 2012;d Sarvet 2010a; Sarvet 2010b; Sarvet 2011; Sheldrick 2012; Straus 2014); Newham Child and Family Consultation Service (Aggett 2006, UK); Offsite Collaborative Care (Keller 2013, USA); PAL: Partnership Access Line (all USA: Barclay 2016; Gabel 2010;d Gabel 2012d); Primary Mental Health Team (all UK: Gale 2003; Whitworth 2004); Primary Mental Health Worker (all UK: Callaghan 2003a; Callaghan 2003b; Callaghan 2004; Conlon 2009; MacDonald 2004; Neira-Munoz 1998; Walker 2005); Project TEACH (all USA: Gabel 2010;d Gabel 2012d); Youthspace (McGorry 2013, UK) |
|
|
D4. Paediatric liaison
Services aimed at improving care through the integration of physical and mental health care; includes A&E liaison services and joint clinics |
CAMHS Crisis and Liaison Service (Trainer 2015, UK); Child and Adolescent Psychiatry Consultation-Liaison Service (Sheridan 2017, USA); ERFUT: Emergency Room Follow-up Team (Greenfield 1995, Canada); Kids’Link Hotline (Roman 2018,e USA); Liaison Psychiatry Service (Lenoir 2009, France); Mental Health Liaison Team (Byrne 2011, Ireland; Kraemer 2008, UK); Onsite Child Guidance Model (Mahajan 2007, USA); Outpatient Crisis Model (Roman 2018,e USA); Paediatric Emergency Department Programme (Holder 2017, USA); PL-CAMHS: Paediatric Consultation-Liaison Psychiatry Service (Lynch 2017, Ireland); Paediatric Liaison (Woodgate 2006, UK); Paediatric Liaison CAMHS
(Garralda 2016, UK); Paediatric Liaison Psychiatry (McNicholas 2018, Ireland); Rapid Response Model (Parker 2003, Canada); Urgent Referral Model (Lee 2014, Canada) |
|
|
E. Ecological models
Models where all aspects of the CYP’s life are taken into consideration (school, peers, friends, housing, income, health, well-being, criminality, etc.); often explicitly underpinned by Bronfenbrenner’s ecological systems theory |
E1. Wraparound approaches
Collaborative, team-based approaches for CYP with complex needs in which services are ‘wrapped around’ the family |
Early and Periodic Screening, Diagnosis and Treatment (Furman 2002, USA); Full Service Partnership (all USA: Chambers 2008; Cordell 2017a; Cordell 2017b); In2School (McKay-Brown 2019, Australia); Wraparound (Barrow 2017, USA; Biggins 2014, USA/UK; Bonham 2010, USA, Durbin 2012, USA; Karpman 2013, USA; Lamb 2009, no country specified; McDougall 2008, UK; McGuiness 2009, USA; Painter 2012, USA; Schmied 2006, no country specified) |
|
E2. Multi-systemic therapy
A ‘family-ecological’, community-based model targeting CYP aged 11–17 who are at risk of placement in care or custody |
Adapted MST (Rowland 2005, USA); MST: Multi-systemic Therapy (Barrow 2017, USA; Lamb 2009, no country specified; Löfholm 2009, Sweden; McDougall 2008, UK; Schmied 2006, no country specified; Sheidow 2013, USA; Shepperd 2009, no country specified; Sundell 2008, Sweden; Wells 2010, UK); MST-Psychiatric (McDougall 2014, UK) | |
|
F. Demand management models
Characterised primarily by a need to manage flow, demand and capacity in CYP’s mental health services, often in the face of long waiting lists. |
F1. Organisation-level demand management
The whole organisation is subject to new ways of working in order to manage flow/demand |
CAPA: Choice and Partnership Approach (Fuggle 2016, UK; Naughton 2015, Australia; Robotham 2009, UK; Robotham 2010, UK; Wilson 2015, UK); Liverpool Integrated Comprehensive CAMHS Pathway (Houses of Parliament POST 2017, UK); Outpatient CAMHS Team (Taylor 2010, UK) |
|
F2. Patient-level demand management
Demand is managed by introducing and training staff in brief assessment and intervention approaches |
Black Young People’s Consultation Service (Young 2012,e UK); Brief Consultation and Advice (Heywood 2003, UK; McGarry 2008, Ireland); Brief Intervention Service (Gallagher 2015, UK; Wagner 2017, Australia); Janeway Family Centre Change Clinic (Hair 2013, Canada); Opt-in Appointment and Brief Therapy (Stallard 1998, UK); STARTER: See To Assess, Review, Treat, Evaluate, Review (York 2004, UK); Walk-in Counselling Centre (Barwick 2013, Canada); Young People’s Consultation Service (Young 2012,e UK) |
|
|
G. Service transformation frameworks
Designed to transform whole systems. Less rigid and more flexible than the models above, providing ‘scaffolding’ to services through a structured framework. Often coexist with specific models in groups A–F. A common feature is an attempt to get disparate providers to collaborate and work together |
G1. US Systems of Care
A spectrum of effective, community-based services and supports for children and youth with or at risk for mental health or other challenges and their families, that is organised into a co-ordinated network |
All USA: California Children’s System of Care (Zanglis 2002); CASSP: Child and Adolescent Service System Programme (Motes 2014); Early Childhood Systems of Care (Champine 2018); Family Mosaic Project (Measelle 1998); Fort Bragg Demonstration (Bickman 1996a; Bickman 1996b; Breda 1996; Burchard 1996; Friedman 1996); Mental Health Services Program for Youth (Grimes 2006); Strengthening Communities – Youth (Nissen 2004); Systems of Care (Atkins 2003; Barrow 2017; Bartlett 2006; Biebel 2007; Bonham 2010; Evans 2006; Manteuffel 2002; Miller 2012; SAMHSA 2016; Schmied 2006; Stroul 2010); Systems of Care in Schools (Powers 2011); Urban Trails (Desmond 2011) |
|
G2a. Tiers Approach, UK
Services operating under the ‘four-tier’ framework established by the NHS Health Advisory Service in 1995 |
All UK: CAMHS Tiers (Atkinson 2015; Houses of Parliament 2017; JCPfMH 2013; Wolpert 2016); Northern Ireland Integrated Care Pathway (HSCBNI 2018; NICCY 2018) | |
|
G2b. Tiers Approach, non-UK
Service provision predicated on organisational steps (tiers) |
Life-course Model of Care (Evans 2014, USA); MTSS: Multi-tier Systems of Support (all USA: Bruns 2016; Lyon 2016); Multi-layered Care System (Jordans 2010, various low-income countries); Trauma-informed School Systems (Kataoka 2018, USA) | |
|
G3. (i)THRIVE
A set of principles for creating coherent and resource-efficient communities of mental health |
THRIVE (all UK: Houses of Parliament POST 2017; Wolpert 2016; Wolpert 2019) | |
|
G4. UK Psychological Therapies Framework
Frameworks devised to improve access to psychological therapies |
All UK: CYP-IAPT: Children and Young People’s Improving Access to Psychological Therapies (Edbrooke-Childs 2015; Fonagy 2015; Fonagy 2017; Kingsbury 2014; Law 2016; Ludlow 2020; McDougall 2016; O’Herlihy 2016; Timimi 2015; Wolpert 2012); Matrics Plant (Matrix Children) (Improvement Cymru 2020) | |
|
G5. ARC
US-focused organisational intervention designed to help mental health services improve their social context and thus address barriers that impede service and treatment outcomes |
All USA: ARC: Availability Responsiveness and Continuity (Glisson 2002; Glisson 2012; Glisson 2013; Glisson 2016) | |
|
G6. Formal Partnerships
Service provision is underpinned by frameworks that establish formal partnerships between organisations |
All UK: Community Children’s Health Partnership (Hewitt 2011); REACH-IN (Ivings 2018); Solar (Vusio 2020) | |
|
G7. Evergreen Canada
A national framework for CYP’s mental health services in Canada |
All Canada: Evergreen (Kutcher 2013a; Mulvale 2015) |
Appendix 7 Example of a cross-case analysis framework: effectiveness (of services)
| Theme | Case Study 2 – school based | Case Study 4 – digital | Case Study 5 – NHS CAMHS | Case Study 6 – NHS crisis service | Case Study 9 – combined NHS/third-sector service |
|---|---|---|---|---|---|
| Practical strategies/techniques | YP learn techniques in the sessions which help them to manage feelings and thoughts. Sessions include the practical application of the techniques as the theory behind them. Techniques taught include: where is the evidence? Mood diaries and journaling. Skills learnt help YP to counteract negative thoughts (using positive counter-thoughts) and give them the tools to manage situations and relationships. YP felt they had ‘helped quite drastically’, reduced anxiety/panic and stress and helped them cope better at school and with school work. Learning practical techniques provides YP with a toolkit that they can use in their own time, so provides longer-term support beyond the session. YP talked about using the techniques to cope during lockdown. One YP described feeling guilty if don’t complete mood diaries. |
YP learn practical techniques, e.g. relaxation and breathing techniques to reduce stress and anxiety; how to create a safety box (‘self-soothe boxes’) to help manage feelings; using journaling for offloading/venting and self-reflection/checking in on yourself. YP welcome these techniques, find them helpful – they act as a distraction tool. |
YP describe learning skills and strategies which help them cope with feelings, manage emotions and prevent self-harm. Improvements linked to DBT, CBT, skills training and medication. YP report feeling happier and more equipped to deal with anxiety. One parent noted that their child had found an intervention for OCD helpful as it was less structured/more flexible in approach. Impact relies on parents implementing skills learnt (in parenting groups) at home. Staff note Managing strong emotions group is less effective with older children/not well attended. Outcomes reported by YP include reduced panic attacks, improvements in mood, anxiety and weight. |
YP describe being given resources to use when in crisis including detailed care plan, distraction technique sheets, and booklets. YP use these to manage negative thoughts and develop positive thinking. A range of outcomes were reported by YP: Reduced suicidal thoughts; improved sleeping routine and motivated to get out of bed; feeling safe and supported as feelings/thoughts normalised. Parents – improved parent–child relationships and mental health of CYP. Staff reported increased parent and CYP self-confidence to cope; Improvements in sleep; YP returning to school; reduced A&E attendances; reduced Tier 4 admissions; reduced demand on core CAMHS. |
The more practical-focused CBT sessions seen as most helpful in reducing anxiety. Learning strategies to use when feeling sad such as breathing techniques, counting exercise, using positive thoughts to change mindset/listing the positives about yourself. This has led to feeling less sad. Service approach incorporates a number of practical approaches: Drama therapy interventions are practically focused on expression of feelings and techniques that reduce anxiety (e.g. relaxation). Other practical strategies taught – example of managing self-harm urges (‘surfing the wave’ – mindfulness technique) that reduces self-harm. YP reported outcomes include being more open about feelings; decreased anxiety/sadness. Parent described how child has learnt strategies to use when sad has improved their mental health. |
| Staff-reported outcomes for YP include improved self-confidence, mood and self-esteem. YP reported outcomes include feeling more positive, positive impact on stress and anxiety and coping better in school, being better able to concentrate and focus in class. May prevent need for CAMHS for some YP and therefore reduce referrals to CAMHS. Service gives YP an understanding of their MH which then improves engagement with CAMHS. |
|||||
| Learning and understanding | Learning about how thoughts affect feelings and actions (cognitive triangle) was helpful and helped YP to better understand triggers of low mood and anxiety. It increases understanding of their feelings/mood, well-being and helps them learn about what helps/actions to take, e.g. going outside, being active. Provides a new perspective. Learning these CBT techniques helps YP with learning a sense of self, understanding what’s going on for them. Helps them develop autonomy – understand that they have control over feelings – service view. The content is pitched at a level that works for all YP – it is basic and not too complex or confusing. |
Supports YP to develop confidence/literacy to access other services. | One YP described increased understanding of feelings/thoughts/self as a result of support received. However, two parents of YP on the Access Pathway noted that lack of understanding and memory problems were barriers to impact of therapy and a CBT intervention. The service assessment tools were also considered to be inappropriate for children on the Access Pathway due to lack of understanding of the questions. |
HCPs have an improved holistic understanding of family needs from crisis team intervention. | YP report greater understanding about anxiety and pinpointing the triggers. |
| Communication | Staff believe YP are more able to talk about their feelings as a result of sessions due to increased MH literacy but also feeling more open about talking about MH. YP feel listened to and valued during sessions. Teaching staff feel that the sessions can increase communication about MH in the school. Some schools report reduced use of pastoral services = ↑ resilience and/or ↑MH literacy. One YP and parent talked about how techniques learnt in the session had been shared at home with mum (who also has MH difficulties). They also felt they don’t argue as much now (due to using techniques learnt). The sessions teach it is ok to talk and ask for support and may facilitate YP reaching out to other services. |
YP find the site helpful for offloading – putting down your feelings, getting them off your chest/out there – in a safe way. Being able to do this helps YP to ask for help. Similarly, staff note that YP sometimes try out talking about things in the sessions and if that goes ok, will then be prepared to go on to discuss in their CAMHS sessions. The service may therefore play a role in empowering YP to engage more with other services, to gain confidence to open up about things. YP note that it helps to talk instead of internalising things and accessing the site helps YP to communicate and express their feelings which in turn helps their MH. |
YP described feeling more open about their feelings after accessing support. | Session helped YP to be able to talk about emotions. Felt listened to by service. Parents described receiving support around communication strategies to help the child and parent communicate. Parent feels support from service helped YP open up a bit. Staff note the importance of talking to and listening to parents – important for them to feel heard. Shared system with Core CAMHS teams (within same Trust only though?) means they have access to contextual information on YP/family and can reassure them they don’t need to re-tell story – can just focus on here and now. Lack of access to systems/lack of shared IT in other Trust CAMHS teams = barrier to above approach, communication is difficult, a massive barrier. Some teams still using paper records = challenge. Good working systems, communication and info sharing – conference call each evening. Case notes are shared with service Y to facilitate continuation of support for YP. |
YP describe impact of support on being more able to talk about and communicate their feelings. Sessions help YP to be more open, to practice putting emotions into words and reflect on their feelings. As a result, some YP feel more able to talk to their friends about how they are feeling. Talking about feelings helps YP to realise they are not to blame. YP feels able to communicate and disclose feelings to worker due to development of trust and confidentiality. Service has good working relationships with schools – particularly in areas where high need/deprivation or where there is no school counsellor. Good relationships with service A and B and tier 3 CAMHS – holistic approach to support – which service is best for this person – done via triage process which facilitates communication across different services. |
| Social connection and relationships | Sessions provide an opportunity to meet others, to know that you are not alone/that others struggle too, to make new friends. Sessions may improve relationships with others and also provide access to positive adult role models. Teaching staff note improved relationships between students in school. |
Provides peer support via discussion boards – opportunity to connect with other YP with shared experience. | DBT group work – developed friendships with other attendees. | No data | No data |
| Organisation culture/ethos | Sessions focus on the positive not the negative – YP are helped to recognise the positives in their life. Sessions impact positively on school culture – increases communication about MH in the school, ↑ MH literacy and reduces stigma. Anecdotal evidence from parents and teachers about ‘seeing a difference’ in YP after attendance. Good partnership between school and service. Service works well with teachers and recognise that they are very busy – delivery organisation understands the school culture/structure. |
No data | No data | Team works collectively and has a good working relationship; cross cover in place for short staffing. | No data |
| Continuity | Lack of continuity once the programme is completed there is no follow-up. As a result, YP (who had attended 1-2-1 support) reported it can be difficult to be motivated to continue using strategies and no longer feel cared for once complete programme due to lack of follow-up. | Named worker is available over the weekend – knowing she is there is helpful. | YP found it helpful to see the MH nurse weekly as it was helpful to focus on 1 week at a time to get through the week. Lack of continuity – DBT sessions not completed due to YP’s transition to adult services. |
One of key aims of service is to liaise with other services to ensure support is in place for YP for after discharge after 72 hours. Having youth support workers in team has been key to developing relationships with third sector and social care to support this liaison. | No data |
Appendix 8 Case study site characteristics
The following descriptive summaries of the case study sites are based on information gathered from service documentation, the Work Stream 2 map and data generated from interviews with service providers during Work Stream 3.
Site 1
Model categories: C3 (NGO-derived community hub); D3 (community outreach and liaison).
Site 1 was a branch of a UK-wide third-sector mental health organisation that supported CYP aged up to 25. Site 1 provided several different services for CYP, including a school-based outreach service providing one-to-one support in local secondary schools, a family support service, a peer support group and a new service supporting ethnic minority or LGBTQ+ young people and their families who had experienced recent trauma. The one-to-one support used solution-focused approaches tailored to the needs of the young person. The peer support service was provided by ‘Wellbeing Ambassadors’, volunteer young people aged 14–25. These ambassadors had multiple roles including helping to train professionals on mental health topics, contributing to staff recruitment, informing the organisation’s social media presence and fundraising. The family support service provided support, aimed at building resilience, to CYP aged up to 18 and their families for a fixed period of 10–12 weeks.
Access was via a single point of access, operated by multiagency panel consisting of representatives from the third-sector, health and education. Both self-referral (e.g. completing a website referral form) and professional referral were accepted. This panel also processed referrals from Site 7. Service access was only available to families living within the local authority boundary.
Coronavirus disease 2019 impact on service delivery
Consultations with CYP were largely offered by phone. Groups for CYP and parents/carers were delivered (separately) online. Some online work is likely to continue in the future alongside a return to in-person sessions.
Funding and sustainability
This service was dependent on temporary funding streams with the service having to apply for specific funding to carry out projects with a specific remit.
Site 2
Model categories: D2 (schools outreach)
Site 2 was a targeted, third sector-led, school-based well-being programme for young people aged 13–19 which aims to teach CYP emotional resilience and reduce low mood and anxious thoughts. The service is exclusively delivered by trained staff from a charity. The 6-week programme is delivered in several UK regions and is based on an evidence-based intervention developed in the USA. Eligibility for the programme was assessed by asking groups of students (e.g. in a given year group) to complete the CES-D depression scale (the CES-D). 98 Those scoring 20 and above were considered likely to benefit from the programme. Following screening, schools informed eligible students and classroom-based sessions were delivered to groups of 8–10 students during the school day. Sessions lasted for an hour and were timed to avoid timetable clashes with core subjects. Session content was based on CBT principles of challenging negative thoughts and included home tasks between sessions to embed coping skills. At programme completion all students were given information about sources of ongoing support which they could self-refer to. If further need was identified, the charity’s practitioners worked with school staff to signpost to school pastoral support and/or local CAMHS. The programme has engaged with more than 7000 young people to date.
Coronavirus disease 2019 impact on service delivery
The programme was adapted for virtual delivery during lockdown-induced school closures. When schools re-opened, in-person sessions were re-established with reduced group sizes. Catch-up sessions were provided for CYP who had missed sessions due to COVID-19 isolation. One-to-one virtual sessions were also made available in some areas to young people struggling with their mental health as part of a government initiative to support vulnerable children struggling because of COVID-19. Additionally, in some areas, the service supported young people on waiting lists for specialist CAMHS.
Funding and sustainability
Time-limited philanthropic funding has allowed the programme to be provided at no cost to schools.
Site 3
Model categories: C1 (primary care mental health service); D3 (community outreach and liaison); G6 (formal partnerships)
Site 3 was a third-sector organisation providing open access one-to-one counselling support to young people aged 9–21. The counselling was peripatetic with practitioners travelling to a location suitable to the young person, for example schools or community settings. Access was also available via remote methods. Counselling was time-limited but could be extended if needed. The counselling could be face to face (in-person or virtual) or through text messaging. In addition to pre-booked appointments, there was also a live service which could be accessed online or via the telephone without an appointment. A telephone advice and support line for parents was also available as were parent support groups. Practitioners drew upon a range of therapeutic styles including CBT, play therapy and brief solution-focused therapy, although most delivered humanistic/integrative style counselling. Young people could self-refer to the service by self-completing a referral form. The service also received referrals from other third-sector organisations and from the statutory sector, and it had a formal mutual referral pathway with local CAMHS. Although Site 3 was a faith-based service, the service was open to CYP of any or no faith and faith did not influence the work carried out with young people.
Coronavirus disease 2019 impact on service delivery
Online (video) and telephone counselling provision was developed in response to COVID-19 and will be retained alongside in-person provision. Parent support groups moved online to Zoom and were well attended but are scheduled to return to in-person delivery.
Funding and sustainability
The charity behind Site 3 is funded by donations, legacies, fundraising and a contract with a local NHS clinical commissioning group (CCG).
Site 4
Model categories: C2 (digital service); G3 (THRIVE)
Site 4 was a private sector online counselling service targeting CYP aged 10–25. The web-based platform provided anonymous access to text-based, one-to-one live and asynchronous chat, online forums, advice and information and journaling. Self-referral was the only access method. The service was sometimes used as a ‘stepping-stone’ to support from other services. It could also be used by statutory CAMHS to manage demand (e.g. for those not meeting the entry threshold or for waiting list management). Self-help resources on the platform were accessible 24/7 while access to live chat with trained emotional well-being practitioners and counsellors was provided from 12 to 10 p.m. weekdays and 6 to 10 p.m. weekends. The service aimed to increase the accessibility of support by providing rapid access at any time to anyone with an internet connection and by providing a choice of self-directed support options through a single platform. Access to online forums and discussion boards aimed to empower young people by providing peer support and shared experiences. Registration was required to use the service though a non-identifying username could be used to maintain anonymity. When additional needs and/or risks were identified, the service could signpost to other services but only if the CYP was prepared to give up their anonymity.
Coronavirus disease 2019 impact on service delivery
As an already established digital service, service provision was largely unaffected. However, an increase in service demand was observed which had to be managed by prioritising need and risk.
Funding and sustainability
The service was funded locally by various CCGs across England and Wales and was provided free at the point of access to CYP. Service eligibility was determined by the CYP’s home postcode at self-referral. CYP who attempted self-referral but lived outside a commissioned area were signposted to other services.
Site 5
Model categories: A1a, A1b (outpatient child and adolescent mental health services); B1 (collaborative care); D3 (community outreach and liaison); E1 (wraparound approaches); G3 (THRIVE); G4 (UK psychological therapies framework)
Site 5 was specialist NHS CAMHS providing an emotional well-being and mental health service for CYP aged up to 18 (up to 19 if already in treatment; up to 25 for care leavers or those with special educational needs). It served a large, mainly rural geographical area. Service access was via professional referral only, although a parental advice line was established in response to the COVID-19 pandemic (see below). The service aimed to prevent mental health crises escalating by responding quickly and to help young people manage their emotional well-being within the community. The service operated from a single base and provided a range of services from preventative and early help to complex crisis support and intensive home treatment. The service comprised a multidisciplinary team of nurses, social care practitioners and clinical psychologists with additional input from occupational therapy, psychiatry, psychology assistants, and support and peer workers. The service was based on the THRIVE framework and provided a full range of evidence-based interventions including brief advice and information, CYP-IAPT-recognised therapies, complex emergency mental health treatment, intensive home treatment and parent/carer workshops. The appropriateness of referrals was assessed at daily multidisciplinary team meetings. The service contributed to the assessment of CYP on a neurodevelopment pathway for ADHD and provided a service for looked-after CYP. Schools outreach via a ‘school links’ team provided dedicated support to students from pupil referral units. Service development was proactively informed through CYP and parent participation groups. These groups also helped devise an age-appropriate care plan for CYP known as a ‘well-being passport’.
Coronavirus disease 2019 impact on service delivery
Most assessment and therapeutic interventions became phone-based rather than face to face. A parental advice line was established to enable parents to speak to a duty worker. Online psychoeducational resources were also developed to support parents as were e-resources (e.g. animations and teachers’ notes) for schools to support the roll-out of ‘well-being assemblies’.
Funding and sustainability
The service was funded via statutory NHS funding.
Site 6
Model categories: D1 (outreach to home); E1 (wraparound approaches); G2a (tiers approach, UK); G3 (THRIVE); G6 (formal partnerships)
Site 6 was an NHS crisis response service providing community-based rapid assessment and brief intensive support to CYP (aged 5–18) in their own homes. Referrals were via mental health professionals only and through telephone only. This ensured immediate and consistent responses and enabled inappropriate referrals to be quickly identified via robust triage. An assertive outreach approach was used: young people were seen rapidly to try and prevent escalation and unnecessary A&E attendances, Tier 4 referrals and admissions to general paediatric beds. The service forms part of an integrated, district-wide crisis care pathway within the ‘getting more help’ and ‘getting risk support’ aspects of the THRIVE. CYP were seen within 4 hours of referral and received intensive support over a 72-hour period from a multidisciplinary team. The service operated from 8 a.m. to 10 p.m., 7 days a week. It was designed to address the resilience of support systems as well as the distress of CYP in crisis. Thus, the service had an ‘ecological’ dimension, working with the wider family as well as the young person in crisis using a home-based treatment approach alongside intensive family interventions. Support was predicated on dialectical behaviour therapy (DBT) principles, alongside brief intervention and family therapy approaches. Staff engaged with partner agencies to ensure support mechanisms were in place beyond the 72-hour period to reduce the likelihood of future crisis episodes. The service’s discharge pathway included partnerships with third-sector agencies. However, young people were not discharged until the service was confident that their needs could be met and thus support could be extended in some cases beyond 72 hours. Restricted staff caseloads supported this approach. Young people and families accessing the service were able to self-refer for 6 months if another crisis arose.
Coronavirus disease 2019 impact on service delivery
Service provision was largely unaffected by the pandemic.
Funding and sustainability
The service was developed with additional local funding and as an adjunct to existing mental health services for CYP; it did not therefore commandeer resources/practitioners from elsewhere (e.g. local specialist CAMHS provision).
Site 7
Model categories: A1a, A1b (outpatient child and adolescent mental health services); D1 (outreach to home); D2 (schools outreach); F1 (organisational-level demand management)
The service at Site 7 was embedded in specialist CAMHS and was composed of several different services: ‘core CAMHS’ providing clinic-based appointments and community services; a substance abuse service; a home treatment service; and a youth offending service. The multidisciplinary teams in the service included mental health nurses, family therapists, physiotherapists, psychotherapists, dieticians, psychiatrists and occupational therapists. The service remit was around CYP with moderate to severe mental health difficulties. The service used CAPA, with a ‘choice’ appointment offered initially for assessment, followed by a ‘partnership’ appointment to establish treatment plans. The same multidisciplinary panel as for Site 1 was used to assess initial referrals within the locality.
Coronavirus disease 2019 impact on service delivery
Home visits and all in-person consultations were halted as services were moved online. Virtual appointments will be retained post pandemic.
Funding and sustainability
The service is funded via statutory NHS funding.
Site 8
Model categories: D3 (community outreach and liaison); E1 (wraparound approaches)
Site 8 was an NHS service within a child psychology team, based within community child health, alongside specialist CAMHS. The team comprised of clinical psychologists, graduate mental health workers, trainee clinical psychologists and an occupational therapist who provided therapeutic and consultation support for looked after CYP (aged 0–18). This service was geographically restricted to CYP living within a defined area and currently on the looked-after children pathway. The service’s focus was supporting carers of CYP that have experienced developmental trauma. The service was ‘diagnosis-blind’, but the young people usually presented with behavioural or mental health problems. Self-referrals from carers were accepted. Different forms of support were available depending on level and type of need, forming a stepped approach to care. For example, the service provided courses for young people, carers and relevant professionals (e.g. social workers and teachers) on therapeutic parenting and developmental trauma with the aim of increasing awareness around these issues, and it also offered consultation, advice and support to foster carers, social workers and schools around supporting CYP in their care. CYP who had a high level of need were offered one-to-one therapeutic support directly. Foster carers were sometimes involved in these therapy sessions.
Coronavirus disease 2019 impact on service delivery
Services were delivered online to families, but the staff team continued to meet in person to manage, and respond to, the substantial increase in referrals observed during the pandemic. A rise in urgent referrals also led to stronger interagency working with a local crisis team.
Funding and sustainability
The service is funded via statutory NHS funding.
Site 9
Model categories: C3 (NGO-derived community hub); D3 (community outreach and liaison); F2 (patient-level demand management); G2a (tiers approach, UK); G3 (THRIVE); G4 (UK psychological therapies framework); G6 (formal partnerships)
Site 9, a third-sector Tier 2 emotional well-being service, is underpinned by a formal partnership between a third-sector organisation and an NHS Trust. The service acted as a hub for all mental health referrals for CYP in the local area including, via a joint triage process, referrals to specialist CAMHS. The service offered short-term mental health interventions to CYP aged 4–25 with mild-to-moderate mental health presentations. Referrals to the service were from a range of other agencies (health, education, social care) as well as self-referrals from parents and older children. The service aimed to improve the well-being of CYP and families and to ensure young people had access to timely and appropriate support wherever possible. The service model was ‘THRIVE-informed’ and was blended with the YIACS integrated health and well-being approach. It offered various support options including one-to-one counselling and CBT (via the NHS Trust partner), low-intensity psychological interventions, digital support via an ‘e-well-being’ service and group work, as well as alternative approaches like drama, play and canine-assisted therapy. Services were provided in community locations as well as the main service hub. A brief intervention over four sessions was available for CYP who were subthreshold for CAMHS. This service provided quick access to support (within 6 weeks) via a ‘see and treat’ model. A family therapist was employed to provide specialist one-to-one support to parents/carers of younger children and to develop dyadic group work between parents and CYP.
Coronavirus disease 2019 impact on service delivery
Service provision was adapted to offer a range of support and therapies via telephone and video consultation in lieu of face-to-face services.
Funding and sustainability
Funding is provided via the local CCG.
Appendix 9 Mixed-methods matrices
| Theme (matrix no.) | Key concept(s) | Case study data (Work Stream 3) | Integrative review data (Work Stream 1) |
|---|---|---|---|
| Pathways to support (1) | Referral routes | Self-referral is perceived to promote access to mental health services (based on families having information about services) Professional referrals seen as problematic because of presentation and disclosure issues for families and poor-quality professional referrals to service providers which can lead to delay and/or denied access |
No evidence for specific referral routes in the review |
| Availability of information |
CYP may lack of information about the nature of the service prior to entering services which increases anxiety Parents may lack information while on waiting lists which creates uncertainty |
Families experience uncertainty and apprehension about the processes associated with accessing mental health services Families want information before sessions |
|
| Speed of access; waiting lists | Timely access to support is important Some services have a role in providing support while CYP wait to access specialist services Waiting lists are problematic for families and can be a consequence of poor referral information |
Families want rapid access to the service without lengthy waiting times | |
| Accessibility at all stages of the CYP’s journey | Single point of access may mean that CYP access more appropriate support and reduces duplication; however, for families it can just be the first stage in accessing support and may lead to further waiting lists for therapy | Some approaches appear to reduce waiting lists for families entering a service, but once in the service there are bottlenecks in accessing therapy sessions, i.e. lengthy wait is shifted from an earlier part of the patient journey to a later part | |
| Physical accessibility and convenience of service | The service needs to be ‘open’ to families in terms of hours of service, ability to contact service providers directly and physical convenience though physical convenience may have to be balanced with ‘negatives’ associated with mode of service | The venue needs to be accessible | |
| Post-service support | Continuity of support after leaving service is important and involves: signposting to further support; self-referral back into service; post-discharge follow-up; and planning for transfer to adult mental health services | No findings from the review on post-service support | |
| Service engagement (2) | Personalised services; involvement |
CYP and parents want services to be person-centred, tailored to individual needs and interests, age-appropriate and flexible to meet changing needs; CYP want services which are engaging, fun and creative and to focus on strengths rather than deficits; parents want non-judgemental services which are parent-centred rather than CYP deficit-focused, not tick-box or overly structured Services should adopt a less formal or clinical approach (perhaps not diagnosis-led) to increase engagement and accessibility for CYP; may be easier to achieve outside of NHS Working holistically with CYP and the wider family can help services to understand the wider context and (in conjunction with other services) tailor support accordingly Co-production is important to ensure that services are designed by and for CYP and co-production should be ongoing rather than one-off |
Person-centred approaches important especially in terms of shared decision-making Services could have flexibilities, e.g. more sessions would be useful for some families In some models, staff felt that their non-statutory role gave them freedom and flexibility in their working processes that a statutory CAMHS role would not Service user involvement in CAMHS is important to CYP and parents; lack of user involvement could thwart the successful implementation of consultation-liaison services |
| Choice | One size does not fit all: CYP and parents should have choice in how to access services, mode of delivery, service setting and type of support/therapy provided; choice and involvement in decision-making should be an ongoing process Lack of involvement in decision-making was observed in relation to safeguarding and medication decisions; lack of involvement can undermine trust in services Choice may be restricted by demand management and resource availability; where choice is restricted by clinical assessment of need this should be clearly communicated to the CYP/family |
Students wanted choice over session lengths and frequencies that suited them Locating MH professionals in school enabled vulnerable students to access quality care they might not have otherwise been able |
|
| Confidentiality | Confidentiality is a key area for CYP and can determine decisions about which service they will access or the extent to which they share information with a practitioner Service procedures regarding safeguarding, confidentiality and ownership of data/content shared are not always clear to CYP accessing digital services Respect for confidentiality can create tensions within families when older children are accessing services Confidentiality can be undermined by the service setting, e.g. school-based services; support in the family home/digital access from home |
No mention of confidentiality as relevant issue in the review data | |
| Practitioner qualities (compassionate and competent staff) | Service acceptability can be determined by practitioner attributes CYP and parents want staff to be experienced and knowledgeable; lived experience can be important but is not sufficient alone and needs to be accompanied by training and accreditation; being seen by an accredited mental health professional (rather than a ‘support worker’) can be validating for CYP, in that it recognises their need Practitioner qualities and interpersonal skills are as important as knowledge and expertise; staff need to be non-judgemental, empathic, genuine and passionate about their work with CYP Staff need to be approachable and to be able to relate to CYP, using humour and informal approaches where appropriate to build trust and ameliorate power imbalances |
The qualities of services and the staff delivering those services; this includes issues such as the quality of the physical environment; the availability of information about the service and its processes; the person-centredness of the staff, the degree to which CYP/parents are involved and continuity within the service (e.g. seeing the same staff) | |
| Positive relationships; continuity of care | Good communication and practitioner skills underpin therapeutic relationships Continuity of care is important in establishing and maintaining therapeutic relationships; CYP benefit from access to a named/key worker as it provides consistency and enables trust to be built, thus supporting the therapeutic relationships Access to the same worker on re-referral to a service is welcomed but the benefits of access to a named worker has to be balanced against the convenience of drop-in ‘live chat’ services Effective team working is important where professionals gained a sense of enjoyment from doing their work, mutual support, positive team relationships, manageable caseloads, well-organised/administered services; high caseloads affected practitioners’ ability to maintain enthusiasm and invest in CYP. |
Good services appeared to be predicated on good relationships both between staff and patients/service users and between the different professionals involved The qualities of services and the staff delivering those services; this includes issues such as the quality of the physical environment; the availability of information about the service and its processes; the person-centredness of the staff, the degree to which CYP/parents are involved and continuity within the service (e.g. seeing the same staff). Good services appeared to be predicated on good relationships both between staff and patients/service users and between the different professionals involved. Glisson’s ARC work clearly identifies that organisational factors can improve outcomes such as staff morale and job satisfaction |
|
| Learning and understanding (3) | Practitioner learning | The creation of a learning culture where learning was fundamental to service provision – staff could learn from one another through positive team relationships. Staff incorporate reflective learning and learning from CYP to improve practice and service design | In several of the typology models (especially those featuring consultation-liaison), staff got incidental opportunities for gaining knowledge about, or developing their professional skills in, CYP’s mental health |
| Acquiring skills for self-care | CYP learn skills and techniques or use toolkits (for emotional regulation, goal setting, challenging ways of thinking, anxiety management, relaxation, self-soothing) which leads to better understanding of self and development of coping techniques and independence | Facilitation of self-care skills is important, in that CYP/parents wanted services to provide them with skills to help themselves | |
| Personalised approaches to learning; involvement | Sessions are pitched at a level that works for all CYP; not basic or convoluted; use of scenarios to think about how techniques might be used | The qualities of services and the staff delivering those services, the person-centredness of the staff and the degree to which CYP/parents were involved are all markers of a good service | |
| Impact of learning skills for self-care | Reported impact of learning skills: reduced anxiety and stress; better able to cope at school/with school work; techniques helpful with coping during lockdown Providing tools and techniques helps provide (informal) longer-term support and so prevents mental health deteriorating and promotes independence and resilience, and helps CYP to find solutions Parents learn skills to use at home with younger children |
Brief intervention approaches may be especially good at managing waiting lists (and so improving accessibility); given their brief nature, these approaches may also facilitate self-management skills There is consistent evidence from several countries (though from somewhat weakly reported and/conducted studies) that brief interventions may be effective, may be less resource intensive and may serve as intended as amodel for reducing demand on specialist CAMH services |
List of abbreviations
- A&E
- accident and emergency
- ADHD
- attention deficit hyperactivity disorder
- ARC
- availability, responsiveness and continuity (framework)
- ATAPS
- Access to Allied Psychological Services
- CAMHS
- Child and Adolescent Mental Health Services
- CAPA
- Choice and Partnership Approach
- CBT
- cognitive–behavioural therapy
- CCG
- clinical commissioning group
- CMHPs
- common mental health problems
- COVID-19
- coronavirus disease 2019
- CYP
- children and young people or child/young person
- DBT
- dialectical behaviour therapy
- GP
- general practitioner
- HCRW
- Health and Care Research Wales
- HoNOSCA
- Health of the Nation Outcome Scales for Children and Adolescents
- HRA
- Health Research Authority
- IAPT
- Improving Access to Psychological Therapies (programme)
- LGBTQ+
- lesbian, gay, bisexual, trans, queer and other (+) ‘non-binary’ people
- MHIP
- mental health implementation plan
- MMAT
- Mixed-Methods Appraisal Tool
- MST
- multisystemic therapy
- NGO
- non-governmental organisation
- NIHR
- National Institute for Health Research (now National Institute for Health and Care Research)
- OCD
- obsessive–compulsive disorder
- ODD
- oppositional defiant disorder
- PMHW
- primary mental health worker
- PPI
- patient and public involvement
- PRISMA
- Preferred Reporting Items for Systematic reviews and Meta-Analyses
- PTSD
- post-traumatic stress disorder
- QALY
- quality-adjusted life-year
- QF2
- ‘Queer Futures 2’ NIHR study
- RCT
- randomised controlled trial
- SAG
- study advisory group
- SDQ
- Strengths and Difficulties Questionnaire
- SED
- serious emotional disturbance or severe emotional disorder
- SMI
- serious mental illness
- SPoA
- single point(s) of access
- YIACS
- Youth Information, Advice and Counselling Services
Notes
-
Data extraction summary tables by principal model type for the effectiveness studies
-
Data extraction summary tables by principal model type for the acceptability studies
-
Data extraction summary tables by principal model type for the cost-effectiveness studies
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/DKRT6293).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
