Notes
Article history
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as award number 17/51/08. The contractual start date was in February 2019. The draft manuscript began editorial review in July 2022 and was accepted for publication in October 2023. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ manuscript and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this article.
Permissions
Copyright statement
Copyright © 2024 Holti et al. This work was produced by Holti et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2024 Holti et al.
Chapter 1 Overview of the improving care for trans adults project
Context
The adult trans population has significant and distinctive health and well-being needs, which the NHS currently struggles to meet. Throughout this report we use the term trans to refer to the diverse people whose gender identities do not correspond to how they were assigned at birth or in early life. The term includes non-binary people.
This research concerns improving the range of NHS health services that trans adults need. These include services intended to support people who are making a medical transition, and many other services relevant to wider aspects of physical and mental health and well-being. Not all trans people need to make a medical transition, and transition can take many different forms. However, issues of co-ordination arise between different aspects of transition-related care, and between transition-related care and general health care.
Currently, trans people over 17 who need to make a medical transition can seek care at one of the UK’s 10 specialist NHS Gender Identity Clinics (GICs), sometimes also known as Gender Identity Services (GISs). As we shall see, people experience very long waits to be seen. Since 2020, NHS England (NHSE) has also funded three pilot primary care gender clinics, providing most of the same transition care options.
Transition-related care is also likely to involve other NHS services. These may include a trans person’s own general practitioner (GP), practice nurse and local pharmacies, in prescribing, dispensing, administering, monitoring and managing long-term hormone replacement therapy (HRT). Various surgical specialists may be involved, with the NHS offering ‘top surgery’ for trans people who were assigned female at birth (AFAB), and genital reconstruction surgery for AFAB people and people assigned male at birth (AMAB). The NHS also offers some voice coaching and hair removal services.
Many trans people require the support of NHS mental health services, because of the prevalence of poor mental health, attributable to the minority stigma trans people face.
In the 2021 UK Census, 262,000 people (0.5% of returns) indicated that their gender was ‘different from their sex registered at birth’. 1 Waiting lists for the GICs in England have grown significantly in recent years, apparently due to a combination of significant increases in demand and relatively static capacity. Waiting lists totalled over 2300 in 2015, with a total clinic population at that point of 6000 (which can be estimated as ˂ 5% of the trans population). Waiting times for first appointments at that point varied between 9 and 64 weeks. 2 Following temporary reductions in their capacity during the coronavirus disease discovered in 2019 (COVID-19) pandemic, the majority of GICs are at the time of writing reporting 4- to 5-year waits, with the largest GIC alone reporting over 11,000 people waiting. 3
Because of barriers to accessing NHS care they need within an acceptable timescale, many trans people in the UK, who can afford to, turn to private providers of hormone therapy and gender-related surgery, within the UK and abroad. Many also access private provision of procedures important to their transition which are not offered by the NHS, such as facial feminisation surgery.
The need for better co-ordinated care across services and specialisms and over time was recognised by the House of Commons Women and Equalities Select Committee Report on Transgender Equalities. 4 This concluded that ‘The NHS is letting down trans people’,4 referring to overly complex referral pathways and lack of joint working between primary care and specialist services, particularly over long-term hormone therapy. The Medical Director for Specialist Services in NHSE raised explicit concerns about long waiting times at GICs, systemic failings in the care that trans people receive, and a pervasive lack of cultural awareness among NHS staff. 5 Whether their healthcare needs were associated with a medical transition or not, it was apparent that trans people typically experience serious barriers to receiving appropriate and well-integrated care. 6
This research has sought to build on initiatives to improve care and its integration, including those involving third-sector lesbian, gay, bisexual, transgender, queer and intersex, plus (LGBTQI+) organisations working in partnership with primary care organisations or with GICs. It has also sought to explore how lessons about effective integration of trans health care can best be implemented in the context of an NHS still coping with the consequences of the COVID-19 pandemic.
In the remainder of this chapter, we set out the research aims and objectives and review the main guidelines that shape the current provisions, as well as the relevant existing literature on experiences of trans health care and related topics. The following chapter then summarises the research design and methodology.
Research aims and objectives
The aims of this collaborative research were:
-
To analyse empirically the current realities and derive conceptually informed future possibilities as to how various NHS services and third-sector organisations can work together effectively to address the needs of trans adults at different stages of their lives.
-
To disseminate this analysis and its implications for wider learning, improving the effectiveness of specialist and non-specialist services in meeting the needs of trans adults.
The overall objective was to produce guidance material and online educational materials for trans people who use services, commissioners and staff in specialist and generalist services, so that they can better understand and shape cost-efficient and integrated provision.
The research questions (RQs) were:
-
What is the range of models recently used in the UK for providing integrated care for meeting the specific health and well-being needs of trans people?
-
Which factors make services more or less accessible and acceptable to the variety of trans adults who need them?
-
In the different integrated service models, how effective are the different aspects of services and their interaction in meeting the needs of people at different stages of their gender transition and at different ages?
-
What lessons emerge as to how models for providing integrated care can be successfully implemented and further improved in meeting the needs of trans people, within limited resources and continuing constraints resulting from the COVID-19 pandemic?
Guidelines shaping the current system of care
As institutions, GICs serve multiple functions – medical and legal – in terms of regulating trans identities and access to health care. They provide a key route to accessing a diagnosis of ‘gender dysphoria’ through the NHS, which leads to various gender-affirming treatments. The same diagnostic criteria, applied within a GIC by a certified member of the Ministry of Justice’s panel of gender specialists, provide the basis for subsequent signing off for gender-affirming surgery as well as the application for a Gender Reassignment Certificate (GRC).
The criteria for and approach to diagnosing and creating treatment plans are set out in four main places.
-
The Diagnostic and Statistical Manual (DSM) of the American Psychiatric Association (APA). This is widely influential internationally in terms of providing lists of symptoms to be used in mental health diagnoses. The latest version of this DSM-57 espouses the aim of moving away from the pathologising category of ‘gender identity disorder’ present in DSM-4. 8 It offers a set of criteria for the diagnosis of ‘gender dysphoria’, which is seen as the distress that can result from having a gender identity different from the sex assigned at birth. DSM-5 lists symptoms such as ‘a strong desire to be of the other gender’ [sic] alongside ‘clinically significant impairment in social, occupational, or other important areas of functioning’. 8 It also requires these symptoms to be present on a stable basis, for at least 6 months.
-
The International Classification of Diseases, ICD-11. 9 This is generally understood within psychiatry as closely related to the DSM. The latter is seen as providing more detailed guidance on diagnostic criteria for conditions identified in the former. ICD-11 replaces the term ‘transsexualism’ used in ICD-1010 with ‘gender incongruence’, and situates this as a condition relevant to sexual health, rather than mental health. The criteria for applying it to a person are cast in terms of ‘a marked and persistent incongruence between an individual’s experienced gender and the assigned sex, which often leads to a desire to “transition”, in order to live and be accepted as a person of the experienced gender’. There is no requirement to identify a state of distress as in DSM-5. This is based on a body of evidence that distress in trans people is related to minority stress, rather than to being trans in itself. 11
-
The Royal College of Psychiatrists’ Good Practice Guidelines for the Assessment and Treatment of Adults with Gender Dysphoria. 12 These guidelines briefly introduce the concept of gender dysphoria in terms of a state of ‘distress associated with the experience of one’s personal gender identity being inconsistent with the phenotype or the gender role typically associated with that phenotype’ (p. 12),12 but also acknowledge that the terminology and criteria are under review by the ICD. The guidelines stress the need for respect for patient autonomy in decision-making on treatment, based on informed consent (p. 28). 12 They also emphasise that clinicians should adopt a patient-centred approach and customise treatment plans around individual circumstances and needs, specifically mentioning non-binary people (p. 19). 12 The guidelines refer to being informed by the World Professional Association for Transgender Health (WPATH) Standards of Care,13 which advocate patient-centred assessment and treatment. Alongside these collaborative features, the guidelines recommend that assessment conversations should explore whether there is history of ‘mental disorder’, childhood or adolescent cross-dressing with ‘possible erotic accompaniment’, and current relationship status. The latter appears to be a reference to the theory of ‘autogynephilia’, whereby trans women’s identities can be a by-product of sexual orientation. This theory has been severely critiqued as stemming more from anti-trans ideology than any evidence. 14 The guidelines fail to clarify how any of these lines of inquiry might affect the assessment of gender dysphoria, other than a statement that suspension of gender treatment ‘can only occur where there is evidence that a mental health condition is giving rise to a misdiagnosis of gender dysphoria or renders the patient untreatable until their condition is reasonably well controlled’ (p. 23). The guidelines further clarify that mental health conditions can ‘more usually’ be treated in parallel with ‘the gender treatment process’ (p. 23).
-
The Service Specifications for GICs for Adults (Non-surgical Interventions). 15 These specify that entering the NHS treatment pathway is dependent on an assessment that results in a diagnosis of gender dysphoria, while grounding this in the definition of transsexualism in ICD-10 as ‘a disorder characterized by a strong and persistent cross-gender identification’. The specification states that this assessment will normally take the form of two clinician sessions, conducted several months apart, with the second carried out by a doctor or clinical psychologist (p. 24). 15 It also refers to assessments and interventions being ‘personalised and based on shared decision-making, with service flexibility and reasonable adjustments to the delivery of care to match the individual’s needs and circumstances’ (p. 3). 15 It further stresses the importance of informed consent, including provision of full information about the possible risks of treatment (p. 7),15 but such considerations are clearly meant to apply after the diagnostic decision has been made.
Literature review
Experiences of trans health care
There is a limited body of existing literature that directly concerns the organisation and delivery of trans health care, with some UK-based studies. Some strands within this are relevant to the research reported here. These concern the dynamics underlying inadequate and poorly integrated care for trans people, which need to be overcome.
A first strand of literature concerns trans people’s experiences of health care in general, and the common negative experiences that lead people to delay or avoid accessing health care when they need to. A large-scale five-country survey of healthcare experiences revealed that more than half of the trans people surveyed delayed accessing health care in general, because of previous experiences of being misgendered or treated disrespectfully by clinicians, administrative staff or receptionists. 16 A qualitative study of trans individuals in Canada brings out some of the dynamics behind and consequences of such patterns. It concluded that trans adults often feel either explicitly or subtly discriminated against by health services, yet are expected to educate clinicians about transition-related matters and remain positive despite lack of recognition of their needs and everyday experiences of exclusion. 17 This was seen as linked to poorer overall health outcomes for trans people.
A second strand concerns experiences of transition-related health care. In the UK, as in many countries, trans people must go through a process of psychological evaluation, leading to a diagnosis of gender dysphoria or gender incongruence, before they can access gender-affirming treatment, such as hormone therapy or surgeries. One relatively small study of patient satisfaction ratings within an English GIC indicated high rates of satisfaction. 18 This satisfaction rating was, however, focused on the experience of the GIC itself, rather than the overall experience of transition-related care from different sources over time. A rather different picture emerges from a range of qualitative studies which bring out the difficulties and stresses that trans people face in their healthcare encounters.
In an analysis of qualitative survey data of trans users of mental health services and GICs, Ellis et al. 19 concluded that practitioners tend to be poorly informed about trans issues and the realities of trans people’s lives and that intrusive questioning and restrictive treatment pathways all contributed to actually having a negative impact on mental health and well-being, particularly in the context of the minority stress trans people experience in everyday life. A focus-group-based study of the experiences and transition-related needs of non-binary people attending a GIC concluded it was necessary to adapt GIC clinical assessment approaches to affirm rather than question a person’s gender identity and provide space for a non-binary person to explore and articulate their goals for treatment, taking account of the person’s likely pervasive experiences of transphobia and social isolation. 20
An in-depth study of the experiences of 14 trans people in Sweden concluded that they found the process of clinical evaluation needed to access gender-affirming medical treatment problematic. This was because of the length of time they had to wait and the lack of support while doing so, and clinicians appearing not to be familiar with important aspects of trans experience. Some trans people experienced themselves as paradoxically expected to take some elements of initiative with their medical transition – for example, through ordering hormones from abroad, in order to be judged by clinicians as sufficiently committed to transitioning to receive medical support. 21
A third important strand of literature concerns trans people’s experience of mental health care. A review of evidence suggests that the trans population carries a higher than average prevalence of common mental health conditions as well as suicidality. 22 Other studies indicate that the experience of receiving mainstream psychological therapies can be a difficult, unsatisfactory and even a fearful one for many trans people, often because clinicians can appear reluctant to engage with, or even recognise, a trans identity. 23,24 Therapists may imply that a trans identity is problematic, rather than focusing on the mental health difficulties that result from the transphobia to which trans people are subjected. In reaction to this, some clinicians in the UK and USA have advanced models for meeting the needs of trans clients more effectively,25–27 within a framework of affirming trans identities, while recognising the impact of minority stigma.
A further strand of literature relevant to this study critiques established models for accessing gender-affirming treatment through a process of psychological diagnosis. Several authors describe the emergence of clinical practice based on an informed consent model (ICM). 28,29 Ashley et al. 28 identify a variety of ICMs. The common element is that the focus of assessment shifts from diagnosis of gender dysphoria to that of clarifying treatment goals and ensuring the trans person concerned has a full understanding of the likely benefits and the medical risks, as well as the capacity to give their informed consent.
We did not study an example of an ICM in the research reported here. However, as reported in Chapter 4, the future desirability of ICMs emerged frequently during the interviews with trans people. In later chapters, we will explore the relevance of literature on ICMs to our findings on improving the integration of care for trans adults.
Wider literature on person-centred, co-ordinated care
The research reported here also builds on wider health policy and organisational studies literature to enable critical evaluation and learning from attempts to improve the integration of care for trans adults.
A first area concerns co-ordinated or integrated care. These closely related concepts have many different definitions referring to a wide variety of initiatives in designing and delivering health and social care (HSC) services. 30 However, most commentators agree on some core principles, which reflect the different perspectives of policy-makers, commissioners, service managers, clinicians and service users or patients. In any particular initiative to provide integrated care, based on the work of Lloyd and Wait,31 the following concerns are reflected to a greater or lesser extent:
-
Service users requiring several distinct branches of medical or social care benefit from experiencing seamless or ‘person-centred’ care, rather than a fragmented experience of separate attendances at different services, each lacking a full understanding of what others are doing.
-
Clinicians and other service professionals often want to improve their interdisciplinary co-ordination around cases, improving outcomes and preventing errors.
-
Managers want to improve the efficiency of services, removing duplication – for example, in the form of similar clinical or administrative work being carried out with the same person in different places.
-
Commissioners or policy-makers aspire to align the incentives of different services focusing on the needs of the same group of people, provide a more holistic system of care and improve clarity as to who is accountable for achieving health outcomes.
What these principles mean in practice, however, and the processes, methods and tools suitable for achieving them, depend greatly on context. 30,32
Second, there are strong connections between co-ordinated or integrated care and innovations in ‘person-centred’ approaches to health care, as well as user involvement in the shaping and delivery of care. 33 A large body of evidence indicates that improved patient satisfaction and clinical outcomes are strongly related to a person-centred and co-ordinated approach to health care. 34 Clear and full communication of clinical options to service users or patients, their involvement in decisions about their care and continuity in the clinical and support personnel working with them all have positive effects. A related body of work elaborates the social, clinical and resource effectiveness of users being involved, either as individuals or collectively, in the design and delivery of the services they need. 35 Ideas of user-led approaches to service design are relevant to understanding innovations in health services for trans people, given the role of third-sector organisations in advocating for and involving members of trans communities in shaping services.
Overall, we take from the literature on healthcare innovation the notion of person-centred, co-ordinated care as a useful conceptual guide for assessing the acceptability of current services for trans adults. These ideas are equally relevant for assessing progress resulting from initiatives to improve integration of care.
Chapter 2 Research design, data collection and analysis
The overall research design was a multicomponent and mixed-methods study of current realities and initiatives to improve health care for trans people, leading to the identification of areas for improvement and production of educational materials. The empirical research took place over a period of two and a half years, from March 2019 to September 2021, with a 6-month pause during the initial phases of the COVID-19 pandemic, from March to October 2020.
The research followed the plan and detailed procedures set out in the study protocol, revised in the light of the pandemic during 2020, with all subsequent interviewing – the vast majority of the data gathering in the project – carried out remotely. 36 Changes to the plan are noted below. Data collection plans obtained research governance approval from the Health Research Authority (IRAS 262467).
We describe below the methodological approach for each of the four main research work packages (WPs), to demonstrate the rigour of this qualitative research against the ‘Standards for Reporting Qualitative Research’ in the healthcare sector published by O’Brien et al. 37 In keeping with these, we first summarise the composition and stance of the research team on key issues in researching trans health care, to make transparent the perspectives brought to interpreting research data.
Research team and project community
The core Improving Care for Trans Adults (ICTA) research team comprised nine white people:
-
four investigators, three cis men and one cis woman, all with established academic posts, and part-time on the project, all over 50;
-
two full-time research fellows, both trans and non-binary, employed on fixed-term contracts at the Open University, in their late 20s and early 30s;
-
three part-time co-researchers, all trans, one woman, one man and one non-binary person, employed by third-sector LGBTQI+ project partners, all aged between 25 and 40.
As described under WP 2 below, the core team was supplemented between June 2021 and January 2022 by two part-time trans researchers, who were Black, non-binary and in their 20s. An external organisation was engaged to provide an online platform for the national survey of trans healthcare experiences also described below.
The research benefited from extensive involvement of the ICTA patient and public involvement (PPI) group, all trans people, led by a non-binary person in the role of PPI lead, who met regularly with the research team. The PPI lead and group commented on the content of research instruments and participant information sheets, as well as on sampling priorities, interim analyses and report drafts. The whole project had a focus on health inequalities and equality, diversity and inclusion (EDI). The PPI group played a vital role in keeping such concerns foregrounded, repeatedly advocating steps to increase participation from marginalised groups of trans people. This report includes a statement from the PPI group (see Patient and public involvement group statement: patient and public involvement on improving care for trans adults project), which identifies the challenges the group experienced in taking up its role in relation to the research team as a result of how the project was organised. These included difficulties in influencing the research team to give enough attention to trans participation in general and to the involvement of the most marginalised trans voices of Black people and people of colour. In the final stages of the project, with permission from the funder, the PPI lead was also engaged for some additional hours as a researcher to assist with analysis of data as a part-time member of the research team because of their knowledge of the mental health provision for trans people.
Research team assumptions and standpoints
Team members shared a recognition that the most important interests to be served by the project were those of trans people and trans communities. They also held a commitment to advancing the rights of trans people in society and within healthcare systems, given that most health care internationally has historically failed to see trans identities as part of normal human diversity. For most of the last century trans identities were either ignored, regarded as deviant or treated as a form of mental illness. 38 In the current century, medical frameworks no longer classify being trans as a mental health condition,9 but most institutions in society enact cisnormativity in terms of expecting people to be cisgender, and are often harmfully transphobic as a result. 39 This may take a less overt form, such as treating trans people as outside of social norms and not deserving of recognition or welcome. Frequently, however, transphobia takes the form of overt and harmful aggression, including outright denial that a trans person’s gender identity is different to that assigned at birth.
A related shared perspective was that trans people carry unique experience and knowledge of how they are marginalised in a variety of ways within current UK society, and how this affects their lives, including their encounters with health services. The accounts of trans people are thus a vital source of insight and analysis into how health services function and affect them, rather than mere sources of data. Hence our approach to interviewing trans people sought to bring out not only their experiences of health care, but also their views on what had given rise to these experiences and how care could be improved in the future.
The active and effective involvement of trans people in roles other than informants was also a central element in seeking integrity in the research process. Early meetings of the research team acknowledged that its senior positions were all filled by cis academics with permanent university posts, with trans researchers and PPI group members on various kinds of fixed-term contract. The involvement of trans people in the PPI group, Steering group and Advisory Group in the analysis and interpretation of data was intended to give voice to a variety of trans perspectives on the interpretation of research data, while keeping in sight the overall goal of understanding how to improve health services for trans people and communities. We attempted to address the structural imbalance in terms of the roles of cis and trans team members by maintaining a culture of circulating drafts of outputs and responding to all comments made. In the final chapter of this report, we reflect on the difficulties that emerged, however, in achieving meaningful trans participation – trans colleagues were often placed in the position of commenting on work done rather than collaboratively shaping it from an earlier stage.
A final perspective central to the research process concerned researchers being reflexively aware of their assumptions and experiences of trans health care so that they were both open to and critically aware of what was emerging from data being collected or analysed. While the harmful impact of cisnormativity and transphobia is likely to be found in trans people’s accounts of their experience of health services, researchers needed to be open to identifying care practices that break with previous norms and understand how these have improved service-user experience. At the same time, researchers considered critically ways in which cisnormative assumptions remained present and could still have harmful consequences. They considered how far trans people’s more positive accounts of services may have been shaped by their awareness and stoical acceptance of poor care provided by many NHS services, as concluded by the House of Commons report already referred to. Trans people may be understood as sometimes ‘settling’ for questionable aspects of care.
While it is possible to set out perspectives shared across the team, there were also recurrent interpretative tensions. These arose in particular from gaps in the understanding of cis members of the team as to the wider history and context of trans health care. Such tensions were often about the extent to which a new service model should be seen as beneficial, because alongside a helpful aspect it preserved practices that compromised the dignity or rights of trans people. To an extent, such tensions were resolved through productive debate. While we have taken a clear stance on many conclusions and recommendations in this report, our interpretations of data in some areas remain unresolved, as is apparent from the PPI lead statement included in this report. We do not seek to gloss over such unresolved issues and also do not see them as undermining the scientific quality of our work. They are an inevitable aspect of researching a contested and politicised field such as trans health care.
Work Package 1: desk research on current arrangements across the United Kingdom
This addressed RQ1, broken down into two related RQs:
-
What range of models/approaches exists for the provision of health and well-being services to trans adults?
-
What examples are there of initiatives to improve the integration of healthcare services oriented to trans adult care?
Researchers adapted a process for qualitative document analysis (QDA), as detailed by Altheide and Schneider,40 to review available documents across the UK concerning the current range of policies and services relevant to trans health care. This involved developing a strategy for sampling relevant documents, and developing a protocol for reviewing their content, which provided a basis for thematic analysis.
Appendix 1 summarises the QDA process and the protocol used to review documents. This WP was completed during the first year of the project and led to an interim project output. 41 It also informed the selection of initiatives to improve care researched empirically in WP 3.
Beginning with the English context, relevant policy documents were obtained from the websites of one NHS Clinical Commissioning Group (CCG) from each of the 44 Sustainability and Transformation Partnerships (STPs) across England. Six STPs were then selected for more detailed consideration, with their constituent CCGs and provider organisations searched for documentation on trans healthcare policies and relevant services:
-
Birmingham and Solihull STP
-
Kent and Medway STP
-
Northumberland, Tyne and Wear, and North Durham STP
-
Somerset STP
-
Greater Manchester HSC Partnership
-
Sussex and East Surrey STP
The first four were chosen to represent different kinds of region. The last two were chosen because the cities of Manchester and Brighton (which respectively sit within these STPs) are known to contain services which may offer positive examples of integration and awareness of trans health care. In addition, researchers collated documents related to the gender dysphoria pathways as they exist in each of the four nations, and good practice guidance specifically related to trans health.
Following a review of the information available from NHS organisations in the selected areas, it was decided that further investigation into services provided by third-sector organisations was required due to the role which they may play in the integration of care. Materials from the websites of third-sector organisations within these areas were selected according to the criterion that they exemplified instances of collaborative working or service provision around health care. Social spaces for trans people were excluded as they are typically not a direct collaboration between third sector and local authorities. The benefits they can have to a trans individual’s well-being are significant, but these groups generally tend to affect this through personal advocacy and community building, rather than working with structures of health care.
Work Package 2: an investigation of factors associated with service use and non-use
This addressed RQ2, concerning what makes services more or less accessible or acceptable for trans adults. An initial online and paper screening survey was used to gather data on demographics and service use across the UK, and received over 2055 responses, compared to a target of 500. The paper version of the survey appears in Appendix 2, as does a summary of the response data. The survey was promoted widely by project partners and through LGBTQI+ networks and organisations. Response options included offering to be interviewed, with over 800 people putting themselves forward. Researchers used data on demographics and service use to construct five purposive subsamples, to be invited for individual qualitative interviews. The underlying rationale was to identify groups more likely to experience social exclusion or stigma in everyday life, and who were also more likely to experience difficulties in accessing and receiving health care. The experience of these groups would be an indication of the priorities for improving services to make them more inclusive and more effective in addressing health inequalities.
In discussion with the PPI group, the following groups were identified as priorities for subsamples of trans service users:
-
older people and trans ‘elders’ (e.g. historic transitioners)
-
disabled or chronically ill people
-
people with low income or educational qualification
-
people living in rural areas
-
Black people and people of colour
The individuals invited within each subsample were selected to give diversity in factors such as gender, location (according to the Office of National Statistics postcode classification of rurality) and age. When the last two were being sampled for, diversity was sought in other respects. The list of survey respondents to be contacted for each subsample was identified by researchers prior to accessing their names or personal details. Researchers then invited respondents for interview. This gave rise to a total of 65 interviews, lasting between 1 and 3 hours. Most were carried out by trans researchers. The first 10 were conducted face-to-face, immediately before the onset of pandemic restrictions, in early 2020. All the remainder were carried out online from September 2020 to mid-2021. The interviewer guide appears in Appendix 3.
The interview offers from trans adults resulting from the survey included relatively few Black people and people of colour. The survey was kept open for several months and additional targeted recruitment attempted, but with the continuing pandemic, recruitment of these groups remained low. The research team engaged two trans Black researchers, who recommended recruiting people to focus groups rather than individual interviews, because this would be perceived as a more supportive environment within which people could talk about their experiences. These researchers recruited focus groups and worked with the research team to adapt the interview protocol to a group context. A further amendment to the favourable research ethics opinion was obtained. Twenty-three people attended across eight online focus groups for trans Black people and people of colour (TBPoC), each lasting between 1 and 3 hours. Each group was audio-recorded, transcribed and the transcriptions anonymised. The total national sample of service users participating in this WP was thus 88 trans people, of which 65 were interviewed and 23 attended focus groups.
Across all the subsamples, individuals were invited for interviews because their survey response indicated relevance to a particular subsample. However, most interviewees had social characteristics or experiences that were relevant to more than one subsample. Many were treated during data analysis as belonging to more than one subsample. In analysing each subsample, the experiences of each interviewee were analysed primarily in terms of aspects relevant to that subsample – for example, that they were disabled, but also bearing in mind that they were a Black person or living on a low income. These intersectional aspects of their experience then featured in the analysis of other subsamples where they were also included.
Table 1 summarises the numbers of service users from the national sample who provided data within each subsample, indicating how many in each were also included in other subsamples.
| Subsample | No. of interviews | No. also in other subsamples |
|---|---|---|
| Older trans people and trans ‘elders’ | 28 | 24 |
| Trans people with low income and/or low educational qualifications | 16 | 13 |
| Trans people with chronic illness or disabled | 27 | 23 |
| Trans people living in rural areas | 17 | 17 |
| Trans Black people and people of colour | 16 (plus 23 focus-group participants) | 11 |
Table 1 indicates the substantial overlap in membership across subsamples. It shows that interviewees were in fact considered and incorporated within the analysis of all subsamples for which they had relevant characteristics. Of the total of 65 people in the national sample of individual interviews, 23 were included in 2 subsamples, 11 in 3, and 1 in 4. Just under one-third of those interviewed, 22 participants, featured in a single subsample. The transcriptions of the focus groups with the 23 Black people and people of colour were also not included in any of the analysis under other subsamples. This was because the focus groups took place at the very end of data collection and the analysis of other subsamples was largely complete.
The use of subsamples thus allowed firstly an analytical focus across a group of individuals on common characteristics that potentially made accessing or using health care challenging. Second, through interpreting data from individuals within two or more subsamples, researchers sought to capture the intersectional implications of combinations of social positions or perspectives.
In terms of data analysis procedures, interview and focus-group audio-recordings were transcribed, checked for fidelity and anonymised. The transcripts relevant to each subsample were then analysed thematically,42 as distinct groups of transcripts. A subteam of at least two researchers analysed each subsample, one of these a co-researcher from a third-sector partner organisation. At least one member of each subteam was trans.
For each subsample, each researcher on the subteam first of all read all of the transcripts and then coded each one independently, corresponding to Phases 1 and 2 of thematic analysis as described by Braun and Clarke. 42 Codes were entered using NVivo (QSR International, Warrington, UK) qualitative analysis software. A coding frame, adapted for each subsample, prompted identification of text relevant to RQ2 (factors affecting the accessibility or acceptability of services), using a set of codes corresponding to different categories of service-user experience. These descriptive codes were generated by the whole research team and then refined within each subteam, based on everyone reading an initial set of transcripts and sharing views on the aspects of service-user experience that were relevant to the RQ. The codes were thus inductively generated while also informed by the experience and perspectives in particular of the trans members of the research team. Appendix 3 shows the codes generated across the NVivo database of interviews, encompassing the five subsamples. It shows codes that were applicable to all subsamples, as well as those that were used to identify aspects of experience distinctively relevant to each subsample.
Codes were discussed and reviewed at regular subteam meetings. Researchers coded independently, using local copies of the database of interview transcripts for the subsample. Coding from the different researchers working on the subsample was then amalgamated by uploading and merging these local copies. Since the purpose of this stage of the analysis was to identify text relevant to different and well-specified aspects of service-user experience, there was little contention over differences in how text was coded. Some differing perceptions about the relevance of a portion of text to a code were discussed and resolved at subteam meetings, but quantitative measures or calculations of inter-coder reliability were not seen as necessary or meaningful, given the clarity with which codes could be formulated. Such measures and calculations can also be seen as at odds with the nature of an interpretative methodology. 43
One of the subteam members then led on further interpretation of the data as categorised under the codes for each subsample. This corresponded to Braun and Clarke’s Phases 3, 4 and 5 of thematic analysis (‘Searching for themes’, ‘Reviewing themes’ and ‘Defining and naming themes’). 42 The researcher refined and combined codes to produce a set of themes that captured the range of user experiences and topics revealed within the subsample, and produced a draft report on these themes. Particular attention was paid to interpreting data from individuals on positive or negative aspects of their care in the context of wider experiences they reported of coming out and living as a trans person, taking account also of the range of social positions or identities they held and social context. The researcher producing the initial draft was trans for four of the five subsamples. A Black researcher produced the draft of the report on the experiences of trans Black people and people of colour (TBPoC).
Draft subsample reports were then discussed and refined collaboratively by the wider team, resulting in each subteam producing a revised subsample report. Summaries of the refined subsample reports appear in Chapter 3, with the resulting themes appearing as the subheadings in the sections devoted to each subsample. In this phase of analysis, researchers compared the experiences described under each theme with those found in related research within the literature, sometimes drawing on concepts from other research to illuminate or explain the data. This stage of analysis thus combined inductive refinement of themes with use of relevant concepts or theories, such as theories of minority stress and microagressions,22,44 ideas of transnormativity38 concerning how trans identities have been regulated and controlled by cis-dominated medical professions, and analyses of how health inequalities are produced within LGBTQI+ populations through mechanisms that make services difficult or unattractive to access. 45 The idea of intersectionality46 also played a role in bringing out how trans people’s experiences of health care need to be differentiated depending on which other marginalising social categorisations, such as non-white ethnicity, they are subject to. Such concepts set the analysis of data in the context of wider social processes reported elsewhere. Combining inductive refinement with the application of concepts and comparison with findings from other research is recognised as a rigorous methodology for qualitative data analysis. 37,43
Work Package 3: case studies of initiatives to improve integration of care
This was initially planned to comprise six case studies of initiatives to improve aspects of the integration of care for trans adults, based on qualitative interviewing of service users and staff involved. This was to address RQ3, concerning the effectiveness of different aspects or features of services in improving care, and contribute to answering RQ4, concerning the lessons learnt for improving care.
Four such case studies of service improvement or innovation were completed. In collaboration with the study steering group, two case studies of initiatives to improve care were replaced with two case studies of a different kind. One focused on the experiences of trans service users with mental conditions in using health care, as well as the views of third-sector mental health professionals on the current state of mental health services in supporting trans adults. The second focused on service-user and third-sector experiences of trans health care in Northern Ireland, where the low level of resourcing of a single specialist gender service has meant that it has not seen any new patients for several years.
The reasons for these changes were partly difficulties in gaining research access and local ethics and governance approvals to study NHS services during the pandemic, beyond the four case studies already approved. However, the significance of the topics studied in the new cases was also a major factor. The propensity of stigma-related mental health concerns in the trans population means that it is important to study how people experience relevant services and how they might be improved. The effective absence of an NHS specialist gender service in Northern Ireland means that it is important to understand how trans people needing care and third-sector organisations that support them are coping and what can be learnt from this in terms of making future care more acceptable and integrated.
In the four case studies of service improvement, the research team worked with a key staff contact within each service provider to agree the scope of the case study and identify which staff had been involved in the initial conceptualisation, design and implementation of the initiative to improve the integration of care for trans adults. The cohort of service users with experience of the innovation was also identified. Participant information sheets were then created and submitted for local ethical and governance approval. Staff were then invited to participate in interviews because of their role and experience relevant to the initiative being studied. Service users were invited to participate based on their having completed the national screening survey of trans adults’ healthcare experiences (see Work Package 2: an investigation of factors associated with service use and non-use), and indicated that they had used the services being studied and were willing to be interviewed. A service provider involved in one of the case studies mailed out details of the study to service users, indicating they could participate in the national survey if they were interested in being interviewed.
In Case Studies 5 and 6, staff interviewees were all third-sector professionals, recruited through an initial collaboration between the research team and an agency active in promoting services for trans people. In Case Study 5, this was a LGBTQI+ organisation active in promoting health care for trans people in Northern Ireland. In Case Study 6, this was an agency that provided mental health support for trans people. In both cases, the research team did not attempt to recruit NHS organisations or staff as research participants. This was partly because the need for these two cases emerged at a late stage of the overall project and there was insufficient time to secure NHS ethical and governance approvals. However, it was also because the scope of these particular case studies was to understand the experience of service users rather than that of NHS staff.
Table 2 shows the numbers interviewed in each case. The majority were carried out by video conference, apart from 15 staff interviews on Case Study 1 and 2 on Case Study 2 carried out face-to-face, all before the onset of the pandemic in March 2020. In each case, in the context of the pandemic there were limited numbers of service users offering to be interviewed so there was no scope for selection – the research team accepted the offers made and interviewed as many people as possible. The samples for each case were not held to be representative of the total population of service users for a particular service, rather to illustrate a variety of experiences.
| Case study | Staff | Service users |
|---|---|---|
| Case 1: Third-sector gender-outreach workers attached to a GIC | 16 | 15 |
| Case 2: Primary care liaison and psychology services within a GIC | 9 | 7 |
| Case 3: Primary care training and accreditation for trans health care | 9 | 7 |
| Case 4: The Welsh Gender Service | 8 | 10 |
| Case 5: Experiences of trans health care in Northern Ireland | 6 | 4 |
| Case 6: Healthcare experiences of trans adults with mental health conditions | 7 | 2 (plus 72 recruited elsewhere) |
| Totals | 55 | 45 |
The additional 72 service users whose interviews were analysed for Case Study 6 were recruited either in one of the other case studies or as part of the national sample of service users in WP 2. For both categories of research participant, their consent to participate included the provision that their data could be used for multiple kinds of analysis within the project. All service users included in the Case Study 6 analysis indicated the presence of a mental health condition in their survey response or during their interview. Of these 72, 56 came from those recruited for interviews in WP 2 (the vast majority of the 65 interviews already described), and the remaining 16 from those interviewed within other case studies. Two interviewees were recruited from the responses to the screening survey specifically for the mental health case study, because they had indicated extensive experience of psychiatric services.
Table 3 shows the numbers of interviewees among the total of 46 recruited across the case studies who met the criteria for being included within the analysis of one or more of the subsamples already described under WP 2, as well as the figure already given for those included in the mental health case study. Data on their experiences of health care were analysed within the context of these subsamples, as well as from the perspective of revealing the impact of innovations or circumstances that were the focus of the case study through which they had been recruited. As in WP 2, this approach to analysing experiences from more than one perspective was intended to recognise and reveal the intersectional nature of trans lives. Table 3 also indicates again the numbers already given in Table 2 for the national sample participants within each subsample. The final column then shows the resulting total number of participating service users within each subsample. The make-up of the participating service users in Case Study 6, Trans people living with mental health conditions, appears as an additional sixth row in the table, because in many respects this case study was more akin in its purpose to the subsamples recruited under WP 2. The emphasis was on understanding user experiences in relation to the accessibility and acceptability of services (RQ2), rather than studying the results of attempts to innovate (RQ3).
| Subsample | Interviews included from across case studies | Interviews included from the national sample | Focus-group participants | Total participants providing data |
|---|---|---|---|---|
| Older trans people and trans ‘elders’ | 5 | 28 | 0 | 33 |
| Trans people with low income and/or low educational qualifications | 7 | 16 | 0 | 23 |
| Trans people with chronic illness or disabled | 16 | 27 | 0 | 43 |
| Trans people living in rural areas | 5 | 17 | 0 | 22 |
| TBPoC | 0 | 16 | 23 | 39 |
| Case Study 6: Trans people living with mental health conditions | 18 | 56 | 0 | 74 |
Within the population of 46 service users recruited across the case studies, just under half, 22 people, were not included in any of the other subsamples or Case Study 6 for analysis. Twelve people featured in one of the groups listed in Table 3, as well as in one of Case Studies 1–5. Four people featured in two groups, five people in three groups, and two people in four groups. One person fitted criteria for inclusion in five groups, that is four subsamples as well as Case Study 6, in addition to the case study where they were recruited.
Distinct, but overlapping, research subteams took responsibility for the interviews in each of Case Studies 1–5. Each subteam contained trans and cis researchers, with the trans researchers carrying out most of the interviews with service users, as well as carrying out some staff interviews. Appendix 4 contains typical topic guides for staff and service-user interviews. As described in the study protocol, interviews were audio-recorded, transcribed, and transcriptions then anonymised. Interviews with staff typically lasted between 1 hour and 90 minutes. Interviews with service users were between 1 and 3 hours long.
Case study data analysis was primarily based on these interviews, but also involved some analysis of service documents, such as policies and progress reports. As in WP 2, thematic analysis42 was used to summarise and interpret staff and service users accounts of changes to care practices, the extent to which achievements and benefits resulted, and the issues or challenges encountered. As in WP 2, there were two overall stages of the analysis carried out within each case. In the first phase, each staff and service-user transcript was coded independently by two different researchers on the case study subteam, at least one of whom was trans. The descriptive codes used allowed identification of text relevant to different aspects of RQ3, for example the motivations for the new care practices being studied, the practices themselves, the benefits, issues or difficulties encountered, as well as views on their overall effectiveness and the implications for future service development.
Appendix 5 shows the descriptive codes used in NVivo for staff and services user transcripts in one of the case studies. The coding frames were different because staff and service-user interviews contained data relevant to different as well as overlapping aspects of the overall case. For example, staff could be expected to provide most of the data on the reasons behind an initiative to improve care. When analysing service-user transcripts, researchers were careful to code accounts of benefits or shortcomings of care experienced only after absorbing the totality of a transcript and the wider personal history it contained. Researchers saw it as important to interpret an individual’s experiences of benefits, issues and difficulties with a current service in the context of their wider experiences of life or health care over time.
Descriptive codes were then merged and compared by a research team member responsible for producing a second-order analysis of each case in the form of a draft case study report. As in WP 2, differences between coders concerning the initial descriptive coding were noted and discussed where necessary, but mostly seen as helpful indications that additional text could be seen as relevant to understanding the impact of attempts to improve care (i.e. RQ3). Second-order analysis mainly took the form of inductively refining and combining descriptive codes to identify themes that adequately summarised the range of views across informants on the rationale for the innovation being studied, the practices that emerged, and the achievements, shortcomings and challenges encountered, as well as the implications for further service development. In the study of services in Northern Ireland and the mental health case study, the themes identified focused on the range of service-user experiences, rather than the course of an innovation. In three cases, the author of the draft was the PI, a cis man, and in one other case authorship was shared between a cis woman Co-I and a non-binary researcher. In the other two cases, the author was a trans researcher, in one case a woman and in the other a non-binary person.
As in WP 2, second-order analysis authors drew to some extent on concepts from existing related research in arriving at a set of themes to summarise the data, alongside inductive development. In the mental health case study, frameworks for understanding the relationship between mental health, microagressions and marginalisation22,44 were brought to bear. For Cases 1–4, concepts from institutional theory47 proved useful in structuring the analysis. These concepts concerned the process by which new service logics come into being, as clinicians and service designers seek to break with some aspects of existing services and perpetuate others. Existing literature has drawn attention to the role of interdisciplinary networks of health professionals joining with user communities to share a moral ethos about service priorities that challenges existing services. Such networks can then advocate and develop innovative practices. 48
For Cases 1 and 2, draft reports were fed back for validation to the interviewees, as a presentation, for discussion, in online workshops. Separate workshops for staff and service users were held for each case. Points of accuracy and interpretation were incorporated into subsequent drafts. Reports were fed back to key participants in Cases 3–5, with a request to correct issues of accuracy.
The analyses of all the cases in this report present anonymised data, including direct quotations from participants, preserving participant confidentiality. Most of the case analyses do not identify the services involved or their geographical setting, other than in very general terms. However, following discussions with key participants in Cases 4 and 5 (concerning services in Wales and Northern Ireland respectively), we did not attempt ‘geographical anonymisation’ for these cases. The configuration of social context and healthcare delivery issues in these cases would have made anonymisation of the setting involved difficult and arguably impossible. As in the other cases, anonymised quotations from participants are attributed only in terms of the speaker’s generic role and have been scrutinised so that they do not contain any clue as to the speaker’s identity.
Across WP 2 and WP 3, an important methodological element was the interviewing of trans service users by trans researchers, although cis researchers also undertook such interviews. Trans researchers were often able to identify where follow-up questioning could lead to fuller data. This, however, put trans researchers in the position of hearing accounts of care that placed them at risk of vicarious trauma or retraumatisation due to their own experiences. The trans researchers requested and were provided with a trans-led supervision forum, where they could process this impact on them.
Work Package 4: synthesis of findings and implications for improving practice
This addressed RQ4, concerning the lessons learnt for improving health care for trans adults. This included the development and comparison of analyses of the five purposive subsamples and the six case studies.
The drafts of case reports were first discussed and further developed within the research team. Authors worked to an extent inductively, refining and combining themes to represent the data succinctly but comprehensively, while also drawing on concepts from existing literature identified above under WP 2 and WP 3. In addition, ideas of integrated or co-ordinated care30,32 and person-centred care33,49 played a key role in conceptualising deficiencies in care reported and in analysing attempts to improve it.
During this stage, the project team discussed and agreed the structure of this final report, with the findings in two parts. Chapter 3 combines the analyses of the five subsamples within the national sample in WP 2 and Case Study 6 from WP 3, concerning experiences of trans people with mental health conditions, to reveal the dynamics of problematic and often poor care received by the majority of people in our sample. Chapter 4 then presents the remaining five case studies from WP 3 to analyse the extent to which attempts to improve and better integrate care have addressed the deficiencies described.
Chapters 5 and 6 then draw out the implications. In particular, two trans researchers within the team led on conceptualising a possible trajectory for the future of trans health care, based on three distinct underlying paradigms or models. The first paradigm involved improving the established model based on formal diagnosis of gender dysphoria as the gateway to gender-affirming treatment being available only through specialist gender services. The second and third paradigms involved progressively more integration of gender-affirming care within primary care and a diminishing role for specialist diagnosis. Developed versions of the paradigms appear in Chapter 6 and Appendix 9.
A day-long online workshop of the ICTA project community, comprising the research team, the study steering group, the advisory group and the PPI group played a key role in debating the emerging analysis. A total of 32 people, 21 of whom were trans, took part.
Leading up to it, trans members of the project team aired concerns that their perspectives and, in particular, conclusions that were critical of current services would be diluted in the final drafting of project outputs by their senior colleagues, to avoid alienating NHS project partners. A key purpose of the workshop was to ensure that a wide variety of trans voices were present among the stakeholders contributing to analysis. In structuring the workshop, the research team sought to balance presentations of draft findings, including the idea of the three paradigms, with focused small group discussions. The design intent was that there should be ample space for trans people to formulate and express views and statements about project outputs in groups that did not include representatives of NHS services.
The workshop design appears in Appendix 6. Participants were each pre-allocated to two different small groups of four or five people that met at different points during the day to discuss various presentations or topics. One set of groups was based on role: service users, primary care staff, mental health staff, GIC staff and third-sector staff. So trans people were either in a service-user group, or another grouping based on their professional role. The other set of groups comprised mixed ‘home groups’, which first met at the beginning of the day and were intended for participants to work together with others in different roles. Small group and plenary discussions were recorded, either through the online meeting software, or by note-takers. Anonymised examples of small group outputs are included in Appendix 6. The discussions and outputs from the workshop indicated broad agreement with the idea of representing possible futures of trans health care in terms of the three paradigms, and contributed to clarifying their content.
Following the workshop, the PI made arrangements to extend the duration of funding of the PPI group until the end of the writing-up period after the conclusion of the research contract, so that drafts of Chapters 5 and 6 were reviewed by this group of trans people. The two trans research fellows had both moved on to new posts by the time of final drafting and submission of this report but contributed their time to review drafts out of goodwill.
Such inputs were important in identifying possible gaps or negative impacts on equality issues in rationales for service improvement within case studies. For example, PPI group members foregrounded the data on the mental health burden on trans people of extended assessments, and the dangers of additional assessment being seen as necessary for people who already experience multiple forms of marginalisation, such as neurodivergent people or people with mental health conditions.
Clinical leads were also asked to comment on drafts of the case studies they were involved in. In response to feedback, the research team refined some case reports to focus more precisely on the learning from the intended service innovation, rather than the entire service. Revised case reports also differentiated the accounts of experiences of the relatively small number of service users interviewed, bringing out their range and relating them to personal histories and contexts. Service-user accounts thus served to illustrate different ways that individuals responded to the innovation studied, rather than claiming to represent user satisfaction or dissatisfaction with the service in general. NHS project partners were not involved in the shaping of the analysis in Chapters 5 and 6 of this report, although they, together with the study steering group, were given the opportunity to comment on Chapter 6.
Project outputs
All of this work provided the basis for project outputs and their dissemination. In addition to this report, the project has produced online educational materials for GPs, psychological therapists and members of the public, in particular trans people and their supporters. The materials concern rationales and practical issues involved in achieving improved integration of care for trans people. They are available free of charge from late 2024.
Chapter 3 Healthcare experiences of trans people
Introduction
This chapter focuses on the healthcare experiences of trans (including non-binary) people. It presents data relevant to RQ 2, namely:
Which factors make services more or less accessible and acceptable to the variety of trans adults who need them?
Additionally, the analytic focus is on exploring the extent to which participants experienced care as (1) person-centred and (2) co-ordinated.
The chapter reports on the experiences of six (overlapping) subsamples within the ICTA national sample of interviewees: people with mental health concerns or conditions, older trans people and trans ‘elders’ (those who transitioned years or decades ago); disabled or chronically ill people; people with low income or low educational qualifications; people living in rural areas; and TBPoC. The six subsamples were drawn from the 65 interviews and 8 focus groups (with 23 people) conducted for the national sample; the analytic group also included 24 of the 46 service-user participants interviewed for the case studies, giving a total sample of 111 people included across the 6 subsamples. The first subsample was the largest, in fact including all but 9 of the 65 interviewees, as shown in Table 3 in the previous chapter. It revealed themes that are fundamental to understanding the experience of the other groups, given this extensive overlap in membership. We therefore begin with the findings from this subsample, to set the context for the others that follow. Table 6 in Appendix 7 shows the demographic breakdown of each subsample, including by gender. The chapter concludes with a summary of the findings regarding the healthcare experiences across the subsamples.
People with mental health concerns or conditions
Prevalence of mental health difficulties
The original ICTA research plan did not call for a case study focused on mental health. The decision to conduct one came about as a result of the researchers noticing the high levels of mental health disclosures among the participants. This suggested the value of a focus on trans adults’ experiences of mental health and mental health treatment.
The responses to the survey used to recruit interviewees showed that, from a total sample of 2055:
-
23% (481) had accessed/were currently accessing transition-related psychotherapeutic support, of which:
-
262 or 54% accessed private psychotherapy
-
158 or 33% accessed NHS psychological therapies
-
61 or 13% accessed both NHS and private psychotherapy
-
-
11% (232) reported being on a waiting list for such support
-
21% (431) would have liked to be able to access such support.
In other words, half the survey respondents had accessed or wanted to access psychotherapy support for their transition journey.
From the same sample, in the 2 years prior to completing the survey:
-
26% (535) had accessed/were currently accessing NHS psychotherapeutic services for non-transition-related reasons.
-
28% (585) had accessed/were currently accessing third-sector/private psychotherapy for non-transition-related reasons.
-
18% (376) have been under the care of Community Mental Health Teams in the previous 2 years.
These data suggest a high level of felt need for psychotherapeutic support in this population (over one in four participants) but also a high level of engagement with community mental health services, given estimates of population average caseloads for adult community care of 100,000 people of 1632 (1.6%) according to an NHS report for 2019–20. 50 The finding of high levels of mental health felt need and service usage in this population corresponds with prior research. 19,51
The interview data analysed below resulted from 74 interviews with trans people, all included because they talked about experiencing mental health difficulties which included commonly reported experiences of anxiety and/or depression as well as reports of having been suicidal in the past. Additionally, participants reported mental health difficulties including personality disorders, obsessive compulsive disorder, bipolar depression, and trauma-related mental health concerns. A number of participants reported neurodiversity (e.g. autism, dyslexia and dyspraxia).
Non-healthcare-related contributors to mental health
An initial analysis was conducted to examine what the interview data suggest participants understand or perceive as non-healthcare-related contributors (positive or negative) to their mental health. The key finding was that a variety of contextual factors create significant mental health burden for trans people, including loss of relationships and negative work experiences as a result of transitioning, threat of anti-trans violence and experience of microaggressions, and the inter/intrapersonal impacts of living in a trans-hostile society. One participant commented, ‘I mean like in the 80s your white hetero males used to throw stones at me, threw bottles at me, call me a poof all that sort of thing. I got beaten up a couple of times.’ There were also accounts of violence that were more recent, such as an experience of being physically attacked in a workspace. One participant talked about experiencing ‘stones (thrown) through the window’ of their house and being harassed by a group of teenagers on the street outside it.
This analysis also explored how participants attributed their mental health difficulties. Some attributed these to gender incongruence, but it was more common that they talked about mental health difficulties as linked to not transitioning and mental health improvements to transitioning:
My mental health is the bit that I’ve struggled with, and it’s been a definite benefit to that … for me transition has been only beneficial from a health perspective. Because if we’re talking about it, is ill health limiting then the thing that was limiting me was my mental health, which has improved.
Overall, the findings accord with a contextual or social understanding of the higher rates of mental health difficulties within trans populations. This understanding aligns with the ‘minority stress model’,52 a theoretical and explanatory framework that suggests that mental health disparities for trans people are largely explained by the stressors caused by living in a transphobic social context, such as harassment, discrimination and targeted violence. 11
Experiences of general health care
A second analysis focused on how participants understood relationships between their mental health and their experiences of general (neither transition-related nor mental health-related) health care. ICTA participants’ accounts suggested that positive experiences of health care were associated with encounters that were free of transphobic microaggressions, and supportive of trans patients’ medical transition. Conversely, negative experiences of health care were associated with experience of transphobic microaggressions, which are known to damage well-being. 44,53,54 Examples of microaggressions included being misgendered, deadnamed, subject to cisnormative or transphobic assumptions (e.g. about sexual history), health professionals being overly curious/questioning about trans status/experience when transness is not medically relevant, and medical staff making presumptions about trans health/identity that effectively dismiss a trans person’s knowledge of themselves. To exemplify this, one participant talked about their distress at being deadnamed:
I know walking into A&E that they’ve looked at my name, they’ve looked at my records, they’ve got me down as male and Mr [name] on the system and yet the staff have turned around and said to a nurse, oh this lady over here. And I’m like you have Mr [name] in front of you on the screen, you literally have it in front of you on the screen with a male marker, I’d already confirmed that that’s me, and yet you’ve still misgendered me and that’s [sigh] – I find those sort of situations difficult.
Participants also talked about their experiences of not receiving appropriate or (in the patient’s view) satisfactory health care, which contributed to stress and hence negative mental health. Often this was due to healthcare professionals’ lack of understanding of trans healthcare needs – for example, in one account a GP making a medically inappropriate and (for the patient) very damaging decision to stop a participant’s HRT. There were also accounts of non-transition specialist health services simply not providing health care to trans patients on the basis that they did not have a protocol for them. One participant described having urgent surgery cancelled because:
The surgeon said that they had no policy on how to treat transgender patients and then after time I was then informed that he would no longer be dealing with me and he would be passing me on to another hospital.
This person was subsequently treated without issue by another service.
The impact of repeated negative experiences of health care was a wary or anxious attitude towards seeking medical care, which is likely to contribute to health inequalities for this population, and might lead to self-exclusion from healthcare settings. Overall, there was evidence of iatrogenic harm in general healthcare settings that was trans-specific, that is beyond the level of iatrogenic harm experienced in the general population. Prominent issues concerned healthcare professionals’ apparent lack of training or cultural competence in working with trans patients, and transphobia in the form of doubting and undermining trans identity.
Experiences of transition-related health care
The third analysis examined how participants understood relationships between their mental health and their experiences of transition-related (GIC) health care. The accounts of waiting to access medical transition health care clearly suggest that a multiyear waiting list has a significant and detrimental impact on trans people’s mental health. As one participant said: ‘Waiting with gender dysphoria that long can be crippling. As I’m sure you’ve heard from others, it’s crippling.’ Another participant stated:
[The waiting list]’s so absolutely soul destroying for everybody going through it. It takes so long and everyone is so emotionally fed up of it and exhausted by the whole thing. That even if you consider yourself to be pretty resilient and if you think of yourself as a resilient person and that your mental health is strong it still gets exhausting and the wait is just interminable.
This finding is in line with other research on the negative impact of waiting to access health care. 55,56
Participants’ accounts of the experience of diagnosis within GICs suggest that for some the experience is positive and validating. For others, however, the experience is intrusive, uncomfortable/distressing and potentially destabilising or even re-traumatising, where patients were made to go over historic trauma without a trauma-informed support structure in place to manage potential risk. To exemplify, one participant described the questions they were asked as invasive and the experience as ‘deeply humiliating’:
At the beginning, they want to know everything. They want to know all about your masturbatory history and all that kind of stuff. That was deeply humiliating. That happened in the first two sessions that I had there before they put me onto the doctor to start me on hormones and stuff. I mean I don’t have a problem talking about this kind of stuff now, but it felt very invasive at the time.
Another participant talked about the impact of questions that were experienced as transphobic:
The psychiatrist just bluntly asked something like, ‘do you think you’re trans because you were abused as a child?’ I was just looking at him like completely baffled. You’re supposed to be a doctor and you’re saying those words? You’re just repeating what the TERFs are saying? I just couldn’t grasp it.
The data also at times point to the possibility of intersectional issues such as age, race, class, weight, mental health, disability, neurodiversity and gender factors (for trans women and non-binary people) within the diagnostic process being implicated in worse patient outcomes/satisfaction with treatment (c.f. Riggs et al. ). 38
The accounts also suggest that the rationale for diagnosis of gender dysphoria or the diagnostic processes involved in sign-off for surgery is rejected by many trans people and that GIC appointments are experienced as contexts in which trans patients have to ‘prove’ trans identity, and in which there is inconsistency from clinician to clinician. Exemplar quotes include:
If I was being less kind I’d say [the screening appointment is about] making sure you were trans enough to be on the waiting list … They just want to make sure that you’re – in heavy air quotes – ‘really trans’.
I’m having to prove this [gender identity] to higher-grade people and continually do that where the one thing that has been firm and fixed in my life has been my gender identity.
The accounts suggest that trans people who feel like they have to ‘prove’ their trans identity experience GIC health care as subjecting them to a stream of microaggressions since these assessment processes are intrinsically questioning/doubting of trans people’s knowledge of themselves and undermining of their identities. In this way, the diagnostic assessment processes that are central to GIC pathways are, as evidenced by the accounts of ICTA participants, clearly contributing to the mental health burden of some trans people. This is iatrogenic harm, and ties into the broader transphobic context of a climate of doubt over the validity of trans identities, Bettcher’s ‘denial of authenticity’ and undermining of ‘first-person authority’. 53 From the accounts, it appears there is a lack of understanding and acknowledgement of the harm caused to trans people by waiting for and being denied trans-related health care. The accounts also suggest a lack of awareness of the power imbalance of predominantly cis clinicians gatekeeping access to trans health care.
It should be noted that the accounts of negative experience of diagnosis prototypically involved depiction of an assessment process that is adversarial, aggressive or hostile, involving a sharp power differential between patient and doctor and an understanding of the trans patient as untrustworthy and/or lacking in credibility. Conversely, positive experiences of diagnosis involve encounters described as caring, nurturing, collaborative and affirming, where the power differential is not remarked on and where the trans patient experiences themself as respected and listened to. The contrast appears to be of a climate of power-with, seeing the trans patient as the expert on themself to be collaborated with, and power-over, with the trans person seen in an infantalising way, to be treated adversarially, doubted and caught out.
Many participants expressed doubt about the legitimacy of the gender dysphoria diagnosis; this is important given the core finding that a diagnostic stance that involves doubting that trans people are the experts on their own gender identity is detrimental to the mental health of trans people.
Experiences of mental health services
The fourth analysis examined how participants understood relationships between their mental health and their experiences of mental health services including counselling. Many of the participants talked about how access to counselling/mental health support during transition was or would be very helpful; participants also talked about how hard it was to access transition-related counselling support.
The data on participants’ experiences of mental health systems and professionals (such as psychiatrists and psychiatric nurses) included accounts of positive experiences. However, there were also some notable accounts of transphobic treatment. The transphobia was sometimes systemic – for example, gendered wards created significant issues in some accounts – but the accounts also contained quite shocking examples of transphobia that were expressed interpersonally by mental health professionals. For example:
When I was showering or using the bathroom, because I was on constant observations when I first got there, they would watch me shower and they didn’t close the door. And because I was listed as male, I had male nurses watching me. They did not know that I was trans, and this was before I had my top surgery. So they were basically just watching me shower and looking me up and down, really confused, giving me dirty looks while I was showering, whilst I was being through it. I remember one time I had a shower and sat on the floor of my room. I had a pair of nurses outside my room arguing over whether I was a boy or a girl. And then eventually they were just, ‘What is it? What?’
These experiences of having trans identity dismissed, challenged and not believed, and having the views and preferences of trans patients ignored or dismissed, are echoed in other accounts. Yet the starkness of the accounts perhaps illustrates the intersectional impact of being a person who is both trans and understood within a system as having mental illness – being seen as even less credible or trustworthy than a person who is either trans or mentally ill.
In terms of accounts of therapeutic treatment, there were both positive and negative experiences. As illustrated in Table 4, these were broadly complementary:
| Positive experiences of therapy involve | Negative experiences of therapy involve |
|---|---|
| Being asked for pronouns/preferred name | Being persistently misgendered |
| Accepting of trans identities, trans-affirmative stance, actively rejecting conversion therapy | Counsellor evidences transphobic sympathies or expresses transphobic assumptions about trans people/identities |
| Facilitates exploration of gender identity including any doubts, does not dismiss/deny trans identity | Expression of gender questioning is glossed over, not explored (avoided) or shut down |
| Good therapy relationship | Sense of lack of interpersonal connection and lack of safety |
| Avoiding inappropriate focus on transness and ‘trans broken arm syndrome’ | Over-focus on transness and instances of ‘trans broken arm syndrome’ |
| Trans aware/trans knowledgeable, insider understandings (trans therapists) – by implication, not having/expressing transphobic/heteronormative assumptions | Lack of knowledge (being ‘clueless’) but also lack of knowledge being associated with therapist expressing transphobic and heteronormative assumptions |
System/service issues:
|
Summary of mental health experiences
The analysis of ICTA survey responses from participants who reported experience of mental health difficulties echoes prior research. This is a population that experiences a high mental health burden. Further, the analysis of the interviews indicates that this burden is directly related to trans people’s experiences of trans-related stigma and microaggressions. Participants’ reports of experiences of health care shows that trans people are quite regularly experiencing in healthcare settings the same transphobia and microaggressions as in other social contexts, and that when this happens the outcome is poorer experience of health care and consequent mistrust of healthcare providers. Both of these contribute to poorer mental health, and, probably, health inequalities for this population. Research attributing poorer maternal and infant health outcomes for non-white patient groups to racism within maternity services57–60 provides a related example of the significant negative health outcomes of societal prejudice enacted systemically or interpersonally in healthcare settings.
Analysis of participant reports of GIC healthcare experiences strongly suggests that prejudice against trans people is also experienced by some participants in the very healthcare setting dedicated to providing specialised health care for this population, with reported negative impacts on the mental health of patients. By participant accounts, when undergoing a gender dysphoria diagnosis is experienced as a process of having to prove trans identity, diagnosis is experienced as enacting trans microaggressions, something which, in participant accounts, creates negative mental health impact. The multiyear waiting times to access GIC services was experienced as another systemic expression of transphobia which participants reported as creating significant mental health burden.
Analysis of experiences of mental health treatment by participants suggest that trans people are also experiencing significant transphobia in mental health settings (e.g. psychiatric hospitals and community mental health clinics) and within counselling/psychological services, those in the NHS, in third-sector (charity) and educational settings, and within paid/private counselling and psychotherapy. The accounts of good experiences of mental health and counselling treatment indicate that service satisfaction is linked with services being (broadly) trans accepting, trans knowledgeable and avoiding enacting transphobia and microaggressions.
Across all services, but in particular GIC services, participant accounts suggest that for a significant number of trans people NHS health care is creating iatrogenic harm – by exposing them to trans prejudice and trans microaggressions and consequently further increasing the mental health burden of this population.
Older trans people and trans ‘elders’
This analysis focuses on the healthcare needs and experiences of older trans people in the UK. Ageing is associated with increasing healthcare needs as well as emergence of comorbid conditions that need to be concurrently managed. Co-ordination of health care (a focus for the ICTA project) is thus particularly relevant for older adults and, research suggests, often problematic. 61 Access to health care for older adults may be impacted by locality62 as well as socioeconomic factors63 and ageism. 64 Further, a recent study in Wales of people seeking to transition later in life indicated that such older trans adults have to carry a dual burden of educating GPs about their healthcare needs while experiencing cisnormative assumptions, which impede their access to transition-related care. 65 All of this indicates the importance of examining the healthcare experiences of older trans people, who face unique health challenges, both with transition-related care and non-transition-related care.
We use ‘older’ as a very broad term, referring to research participants aged between 51 and 82. The data reported here include semistructured interviews with 33 trans people living in the UK; 9 in their 50s, 15 in their 60s, 8 in their 70s and 1 in their 80s at the time of the interview. The overall ‘younger’ age of this sample means that there is less information about the experiences of health care in older age, and about issues such as increasing physical frailty, dementia and needing social care. These findings are further limited by it being a majority white sample.
Accessing services
Waiting
While the long waiting times for transition-related health care have impacted most participants, older trans people provide a unique perspective. As one participant succinctly put it, ‘I’m well past the halfway point in my estimated life. I need to get on with it’ (Woman, aged 71). These participants are experiencing waiting at a stage of their life where time feels particularly precious. For many this delay in care comes after years of waiting to make the decision to transition, which makes accessing transition-related care feel particularly urgent for them. Many older participants described a wish for a more accelerated timeline for transition. This was in relation to many factors, in particular a sense of ‘not having much time left’ as well as having a good understanding of oneself in older age and feeling capable of making transition-related decisions. (It is important to note that people of all ages in our sample expressed similar sentiments, and be aware of the ageism implicit in the idea it takes age to achieve this self-understanding.) As one participant described, however, this experience of not transitioning until later in life but once having made that decision moving along quite quickly, can be fraught:
My third assessment at [GIC E] or whatever they call it was a third doctor, by the fourth I was back to the first one. He, in his report he reckoned that I was too slow deciding to transition because of my age. Then in another report he reckoned I was too fast deciding to transition because it only took a year from deciding to going full-time.
This 71-year-old participant received pushback from the GIC for transitioning at her own pace, first that she had waited too long to start transitioning and later that she was going too quickly. Across the ICTA sample participants talked about having little control over the pace of their transitions, being subject to arbitrary waits, but also to potentially infantilising notions of what is ‘good for them’ in terms of timescales. This issue of not being able to transition at a pace that was right for them was particularly present for older people.
Hormone replacement therapy
Older people accessing HRT will have additional health considerations. For people taking oestrogen, the risk of heart disease or stroke is low but there is an increased risk after the age of 60. As one 72-year-old participant explained,
After my heart attack my GP said, ‘You do realise that the hormone treatment is contraindicated in this case, don’t you?’ ‘Yes.’ He said, ‘But you’re not going to stop it are you?’ ‘No.’ ‘OK, fine.’
In this case, the doctor was concerned about an increased risk but was still prescribed her oestrogen on the basis of her informed consent. Several older participants talked about having been put on oestrogen patches or gel instead of pills due to the decreased risk of heart disease, stroke and blood clots. One older woman who did not respond well to the patches described struggling to, but ultimately succeeding in, having her informed consent accepted and acquiring oestrogen pills. Other ICTA participants reported similar experiences feeling that they needed to fight to access care. The mental health impact of experiencing barriers in health care has already been discussed.
Another concern for older people is osteoporosis, which is directly linked to hormone levels. Not having enough oestrogen or testosterone can lead to bone density loss. For people who no longer produce enough oestrogen or testosterone for whatever reason, correct hormone maintenance is crucial. Older AFAB participants reported navigating HRT for menopause, and in some cases requiring testosterone rather than (or in addition to) oestrogen HRT. Such accounts illustrate the complexity of hormone management in older trans people, and suggest the need for a patient-centred approach to HRT prescribing.
Social care
While no one in this subsample had first-hand experiences of social care, several participants discussed end of life planning in relation to gender. One concern was getting a GRC so that their death certificate would have the correct gender. Some people were also concerned that unsupportive family members might not respect their name or gender after death. Appropriate future social care was a concern. It should be noted here that obtaining a GRC is contingent on a diagnosis of gender dysphoria and medical evidence.
Outpatient services
Screenings
The NHS offers a range of screening programmes, many of which are primarily offered to older people. Difficulties can arise when people are invited for screenings based on the gender marker in their medical records, which may or may not be accurate or accurately reflect a person’s screening needs. Because the ‘m’ or ‘f’ is currently used as a stand-in for the presence or absence of certain body parts and risk factors, anyone who does not fit into those boxes, for example a man with a cervix or a woman without one, may be disadvantaged. This can happen to someone at any age but was particularly prominent with the older participants as they qualify for more screenings.
Many older ICTA participants reported getting invited for only the screenings associated with the gender marker on their NHS records. For people with an ‘m’ marker, this means being invited for abdominal aortic aneurysm (AAA) screenings but not being invited for breast cancer screenings even if that would be medically indicated. For those with an ‘f’ marker this means receiving breast and cervical cancer screening invitations but having to chase down other screenings if they are required. Several participants reported being erroneously invited for cervical cancer screenings once they had changed their gender marker to ‘f’, but most were able to consent to being removed from that list when they explained to their GP that they did not require that screening. Similarly, other participants removed themselves from the breast cancer screening list after having top surgery while remaining on the cervical cancer screening list if relevant. In addition to removing themselves from certain screening lists, participants have also had to initiate putting themselves back on other lists, particularly for AAA and breast cancer screenings. This requires, however, that an individual is aware of what screenings they need, which not all of our participants were. While prostate cancer does not have a national screening programme, some participants with an ‘f’ marker have tried to access prostate cancer screenings with mixed success. Furthermore, some participants reported avoiding screenings altogether due to gender dysphoria. Bowel cancer screenings, however, remained uninterrupted for participants, as that is not a gendered programme.
Breast cancer screenings were the most commonly cited and highlight the array of experiences trans people have with this type of health care. While some participants reported positive experiences, significant lapses in care were reported as well. For example, the following 54-year-old participant experienced a complete absence of care:
I’d been putting off having a mammogram because I knew I was going for top surgery anyway. But then I developed this breast abscess and the GP’s advice was go and get yourself a mammogram. So I rang Breast Test Wales to get a mammogram and was told that we don’t see trans people in this service … so even if you’re a man with breast cancer or if you’re male identifying you have to book a mammogram through your local hospital rather than through the Breast Test people. And it usually takes longer because you’re accessing a specialised service because they don’t run male clinics very often.
This is a clear example of healthcare discrimination – he was not able to access the same care provision that cis women are able to access despite having the same need.
Our findings highlight the ineffectiveness of screening programmes run on the basis of a gender marker rather than on the basis of medical need. As several participants have echoed, a better system would be to track an individual’s need for various screenings, such as ticking a box that this patient has a cervix or not. This would ensure that all people receive the proper invitations for the body they have at that point in time. The findings also evidence barriers to accessing screening for trans people, which could potentially lead to higher incidence rates of cancer in trans communities. Further research may be required to understand how best to overcome these. In Case Study 3 in Chapter 4, we report on some initiatives in primary care to ensure that trans people are called for screenings appropriate to them, and also to mitigate the distress caused by screenings likely to trigger experiences of gender dysphoria.
Hair removal
Hair removal as part of transition-related health care can involve general facial and body hair removal as well as targeted hair removal on a part of the body to prepare for surgery, for example hair removal on the skin graft donor site in advance of phalloplasty. The specific services provided are laser/intense pulsed light (IPL) or electrolysis. Many participants (this was true across the ICTA sample) reported that the existing NHS provision for hair removal is too minimal to be helpful, driving many to pay for treatment out of pocket, where they have the means.
While some noted white hair being less visible for lighter skinned people, several participants also pointed out that laser and IPL are not effective on light hair. This highlights the way certain groups face extra disadvantages in trans healthcare costs – more pricey electrolysis is the only effective option with grey or fair hair, and for people with darker skin. Participants in this group in particular reported having to pay for extra hair removal. This presents an often unaffordable financial burden. Not being able to access sufficient hair removal presents a threat to well-being and safety for trans women, particularly older, poorer and darker skinned trans women. Without it, they may be unable to navigate the world safely and without dysphoria. Lack of access to hair removal can amount to an additional inequality trans women face in getting the transition care they require.
Surgery later in life
As with HRT, there are additional risks for older people undergoing surgery, risks which factored into participant’s decision-making processes. In addition to surgical risks, some participants discussed not wanting to bother with certain surgeries, such as lower surgery, because of their age (rationales included both worry about medical complications related to age and, for some, a sense that their age meant that more medically complex forms of lower surgery were not ‘worth it’). While surgery is not right for all older people, it is important that older trans people have access to good information in order to make decisions about their care and that they are able to access the care options that are best for them as individuals.
Historic transition
Historic transitioners, people who accessed medical transition many years ago, will have faced an additional barrier to accessing transition-related health care. The previous model for GIC referrals was for a GP to refer an individual to a psychologist who would complete an assessment and then decide whether or not to refer the person to the GIC. Participants reported that this added an additional delay as well as a possible roadblock if the psychologist decided not to refer.
Some such ICTA participants highlighted the issues having been discharged from their GIC created in accessing ongoing hormone prescriptions. Barriers to ongoing health care and the risks attached to its removal – for example, of osteoporosis – point to the lack of integration of trans health care in mainstream medicine and the health inequalities this creates.
Transitioning later in life
Transitioning later in life has its own unique set of challenges. Older trans people face difficulties accessing transition-related health care, as discussed above, but participants who transitioned later in life described additional social barriers. Many of these participants did not know about transness earlier in their life and by the time they did typically had family and work pressures which kept them in the closet. Several participants described having some understanding of their gender at a younger age but not feeling able to come out due to prevailing societal stigma, lack of information and family and career pressures, among other reasons.
While not everyone did express regret or negative feelings about transitioning later, some wished they had been younger and therefore at lower risk for various medical interventions. Some also felt that the changes they experienced on hormones had been limited by their age, such as the 68-year-old participant who stated, ‘If I’d done this when I was a lot younger then my facial features would have changed, they would have softened more. Given my age, the hormones they’ve got an uphill task.’ Other participants expressed concern that not transitioning earlier meant they were not ‘really trans’ or were not ‘trans enough’; as one 51-year-old explained:
I felt, one of the things I was worried about is transitioning being old. I got all tied up in this ‘am I trans enough, if I’d have been really bothered, I should have done this when I was 18’, but when I was 18 trans men didn’t exist.
Of course, it was possible to transition in the early to mid-twentieth century and indeed people did, but many participants lacked access to critical information and the safety and support to do so until later in life, which may relate to prevailing attitudes at the time.
Participants sometimes cited upsides or silver linings to later transitions. Even those who had some regret around not transitioning earlier discussed feeling better prepared and more sure of themselves during the process as a result of their age. Having support systems in place and knowing where to get information helped many older participants in their transition. Those older participants who were retired when they transitioned explained how that was beneficial; they talked about how they did not have to worry about coming out at work or taking time off for medical appointments or surgical recovery (although that needs to be understood in the context of participants’ perception that coming out at work and taking time off would have been treated as a problem). Having children grown up and out of the house and other similar family pressures being removed were also cited as catalysts for transitioning later in life. While it is impossible to know what different choices participants might have made were there no transphobia in society or barriers to coming out as trans, the importance of people being able to transition at any age and at their own pace is a key finding from this subsample analysis.
Disability/chronic illness
Research has documented that, while disabled people may have greater healthcare needs, they also experience significant barriers to accessing health care. These include both issues related to physical access (transportation to appointments, access into and within buildings, accessibility of medical equipment), financial barriers (e.g. affordability of medications) and issues around cultural competence of medical providers and the rigidity of healthcare practices. 66,67 These barriers create reduced access to health care for disabled patients,68–70 with consequent impacts on health outcomes for this population. This existing research thus suggested that it would be important to focus on the healthcare experiences of disabled trans people.
This analysis examined the healthcare experiences of 43 people who self-identified as disabled and/or chronically ill. The specific conditions included a wide variety of physical and mental health conditions as well as neurodivergence. The participants in this sample ranged in age from 20 to 82 years old.
Frequency of healthcare experiences
In general, disabled and chronically ill participants had frequent interactions with medical professionals for transition-related care, care related to their condition(s), and general health care. While there were certainly positive experiences, this report will largely discuss the challenges as that is what most participants focused on in describing their experiences. Frequent encounters with medical professionals, common for disabled and chronically ill people, put them in more situations where they might experience poor health care as a result of medical transphobia (and its intersection with other forms of discrimination including ableism, racism and fatphobia).
Experiences of general health care
Accessing health care that is gendered in any way is one of the challenges of this group. Many hospitals have gender-segregated wards so being put on the appropriate ward or there not being any appropriate ward were concerns for participants. For example, one woman described being put in a side room instead of on the women’s ward, where she felt ‘like a naughty child being put out of the way’. Even though this individual was eventually moved to the women’s ward, she continued to be misgendered by hospital staff.
The disabled and chronically ill participants’ experiences of general health care were further shaped, in many cases, by medical trauma. Participants typically reported a history of numerous and sometimes traumatic encounters with medical professionals which in some cases, they said, left them reluctant to seek care. When encountering poor care, many participants discussed filing complaints. However, it is important to note that going through complaints procedures is time- and energy-intensive and can be emotionally challenging for what participants said often amounted to little or no results.
Trans broken arm syndrome
‘Trans broken arm syndrome’ is the phenomenon where a trans person seeks out medical care for something unrelated to their trans status and yet their transness is focused on by medical professionals, sometimes to the point where the real cause of the issue is not investigated. This syndrome is not only experienced by disabled/chronically ill trans people, but we discuss it here because of how prevalent it was in this sample. While some participants highlighted that transness can be relevant to various health concerns, good medical practice dictates it should not be seen as the only possible cause. In addition to over-focus on transness being frustrating for patients and potentially stalling or blocking their health care, there are also legal implications if someone’s trans status is shared when it is not medically relevant. ‘Gender reassignment’ is a protected characteristic and therefore it should only be shared with the patient’s consent and where it is necessary for care. For many medical encounters, it is up to the patient to disclose their trans status or not. One participant described this decision-making process:
I’m actually quite protective of my trans status in general around medics, they generally don’t need to know … and let’s be honest there is a chance that I will get this wrong and I will withhold it the one time in a thousand that it was relevant and suffer some harm from that, OK. But when I go up against some unknown doctor it’s 50/50 that they’ll trans broken arm me and **** me off, I play the odds. And in how many years now? In 18 years of playing the odds on that one I’ve always won.
While some trans people may always choose not to disclose their trans status, it is concerning when people feel they cannot disclose something that might be relevant for fear of health care being delayed or withheld. We return in later chapters, particularly in Chapter 4, Case Studies 3 and 4, to the issues of the kind of education needed for healthcare providers, above all in primary care, to ensure that clinicians take appropriate account of trans status on the one hand, and do not use it inappropriately as a pretext for delaying care or referring elsewhere.
Experiences of trans-specific health care
Hormone regimes can be impacted by various physical health conditions. Different hormone levels may be required depending on individual need; however, knowing what those needs are depends upon the patient’s GP or GIC having an understanding of their condition(s) and/or their specialist doctors having an understanding of HRT. Different types of hormones may also be indicated – for example, some participants in this group discussed going on oestrogen patches instead of pills, or testosterone gel instead of injections, due to their medical conditions. Hormone regimes can also have a positive impact on a person’s general health, such as one participant who experienced relief from their chronic migraines after starting oestrogen.
While across the ICTA sample people talked about difficulties with their GPs refusing or being reluctant to refer to a GIC, this seemed to be a particular issue for this group, with participants describing being referred to other services instead. One participant, who had their GIC referral initially refused because their doctor was insistent that they only needed trauma therapy, had another roadblock put up when they sought out another doctor, this time with the doctor only referring them to the GIC on the condition that they also attend the weight clinic. The poor treatment from the doctor in this case was offset by the positive experience this participant had at the weight clinic, but the example still illustrates the additional healthcare barriers experienced by some trans patients as a result of weight stigma. Consultations with trans service users involved in the ICTA project revealed further experiences of facing extra barriers to a necessary healthcare referral due to weight, and of persistent fatphobia that trans (and particularly disabled/chronically ill) people face.
Another source of delays for this group happened once people reached the GIC. There are typically long waits between the two or more appointments involved in a GIC assessment process. For this group, often seen as more medically complex, clinicians can decide that additional appointments are required before an individual can access hormones or surgical referrals. Once those referrals are given, they are only valid for 1 year, even though many surgeons have a waiting list that is more than 1 year. One participant, who had his lower surgery delayed due to a chronic medical condition, described his experience of trying to get his referral renewed on a phone appointment. The clinician made him revisit old trauma that was not relevant to renewing his referral, sent the details of these disclosures to clinicians in other organisations who did not need this information (including some who were no longer providing this individual with care), and after all of that failed to renew the surgical referral. Not only was this ICTA participant not able to access the care he required in this instance, but he was retraumatised and there was an unethical breach of patient privacy.
Service-user agency in management of care
While not exclusive to this group, disabled and chronically ill participants commonly showed a high level of (necessary) agency in the management of their health care as well as a great deal of expertise and medical literacy. As one participant said:
So I literally went to my GP with a list of information for them, so I actually did their job for them, slammed it on their desk and said ‘Right refer me now unless you want a dead body in 48 hours.’ So I was really, so yeah at this point I then got referred, it took me about I think eight months to get that referral through. I then got, I did a few trips up to the joyous [city] and got sat in front of stuffy, uptight, inappropriate men asking me stupid questions that weren’t really relevant about how do I masturbate for example.
Another participant, who was seeing an endocrinologist to investigate the basis of her intersex traits, had a different and more problematic experience of agency. She recounted how her doctor warned her that pursuing an investigation into her intersex traits would delay her access to transition-related health care. While this participant was given choices around managing her own care, she had to sacrifice accessing one type of care for another. Yet another participant took control of her care by ensuring she was not discharged from the gender clinic after she had finished accessing interventions from them. Her diabetes means that her hormone monitoring is slightly more complex, which is one reason she was more comfortable staying under the care of the GIC.
While this was (again) not exclusive to disabled and/or chronically ill participants, the high number of medical interactions experienced by this group highlights the common experience of lack of communication between various medical services. Primary care, specialist care and gender care are all interacting for many of these participants, and it was clear from participant reports that the lack of integration between them acts to exacerbate their health issues. Even when service users are able to take up agency and influence their own care, addressing some of the fragmented decision-making they encountered, this is not always an empowering experience. Some participants expressed that they wished they had more support while navigating health care, particularly with exploring their gender and what, if any, transition steps they may wish to take before entering gender services.
Absence of care
As we have indicated, there were instances of complete failure to provide care. For many disabled and/or chronically ill participants, this was directly linked to their condition(s). For example, one participant described her decision-making process around vaginoplasty as someone with inflammatory bowel disease. There is a type of procedure that does not use a colon graft which would be ideal for her; however, that procedure is not currently available on the NHS. This greatly limits her access to health care, due to the inflexibility of what is available. Other participants failed to even get referred to the GIC, as one person said, ‘Well, if I hadn’t have backed down, if I hadn’t have got ill, then maybe I would have pushed further about GIC.’ This participant was denied care but was too ill to pursue it further.
Another barrier for disabled/chronically ill trans people was navigating multiple doctors and specialist services. In addition to not being able to access a GIC and avoiding the GIC because of the admin burden, others, like this participant, avoided the GIC out of fear: ‘Yeah I would say I’ve probably avoided the gender clinics. Like because I don’t want to deal with it. Not because I think it’ll be bad necessarily but just out of fear.’
Another participant described his experience of a failure of care in great detail. He was under the care of an anal surgery team for complications from an assault and at the same time also seeking out lower surgery. However, the anal surgeon’s lack of knowledge of transition-related health care had become a barrier in accessing both surgeries. A complete lack of communication between the GIC, the lower surgery team, and this patient’s other surgical team meant his care had ground to a halt. This participant told his medical teams he was ready to go ahead with the lower surgery and accept the possible health ramifications, but he still ran into delays, including several referrals expiring and having to be renewed with further invasive appointments at the GIC. At the time of his interview this participant was still stuck in the cycle of managing the stringent requirements of various services and had not yet been able to access any of the required care. His experience appears to have shown him that he can be only one thing to the NHS, either trans or chronically ill, and that he certainly cannot be trans and chronically ill in more than one way.
This patient’s experience of a healthcare system that has an apparent inability to treat him as a whole person with various complex healthcare needs exemplifies the lack of person-centred and co-ordinated care predominantly experienced within this subsample. This patient’s experience also speaks to the ways in which being trans can be a barrier to receiving other necessary care, and being disabled and/or chronically ill can be a barrier to receiving trans health care, in this case leaving the patient with no care at all, with all the potential consequences to his physical and mental well-being. Finally, this example also points to a lack of cultural competence around trans people, a theme that particularly impacts this subsample, although reiterated many times elsewhere in this research, speaking to a structural problem of transphobia within healthcare systems.
Low income/low educational qualifications
Background and sample
Studies have shown enduring links between education level, socioeconomic status and health,45,71–73 with adults with higher educational attainment and higher socioeconomic status having better health and longevity. 74 A number of explanatory theories have been investigated to explain this. First, such health inequalities have been attributed to lack of social and financial capital. 75,76 Second, areas of deprivation may have lower coverage of clinical health services and less availability of health-promoting/supporting services. 77–79 Third, forms of social and cultural support associated with working-class sociality and community are rarely promoted or utilised at an institutional level. 80 Thus, health inequality associated with education and socioeconomic status are supposed to emanate from lack of social cohesion and ingrained intergenerational deprivation. Although these are complex and intersectional relationships, there is no reason to suppose that education and socioeconomic status do not similarly influence the health of sexual and gender minorities. 81,82
Accordingly, for this subsample, we set out to recruit interview respondents who reported low educational qualifications, low income and/or the experience of struggling significantly on their income. This section is based on an analysis of interviews with 23 people who reported education that stopped after the age of 16 (15 participants) and/or reported that they were ‘really struggling on present income’ (9 people). A further six people in this group reported that they were ‘struggling on their present income’ (e.g. experiencing difficulty but not ‘really struggling’).
Barriers to accessing general identity clinic care
Income, employment and housing precarity and benefit dependency interacted with people’s domestic and intimate contexts to present barriers to accessing gender-related care. For many, limited employment opportunities, lifelong income precarity or being employed in gendered occupations meant that the life changes associated with transitioning (such as dissolution of relationships or changes in job) were not as feasible as they may have been for others. The following respondent reported how a work context that she experienced as sexist and assumed would be transphobic coincided with a lack of employment opportunities elsewhere to inhibit her in exploring her gender experience.
I worked for the Navy and I worked on submarines and I was in an environment that needed, well it was a very macho environment, but there were women there and things. Because we had a couple of women that were the first apprentices, that were the first female apprentices that were in our area as well, so they were, it was starting to change, the environment; however, the work that I was doing needed security clearance and bits and pieces. And effectively I started getting involved into a bubble that there was no way that I could afford, if I wanted to keep my career, to be found out. So things had to be pushed and kept really secret.
Precarity also made it difficult to leave relationships that inhibited the pursual of gender-related care, even when those relationships were characterised by anti-trans violence. The following respondent had to move in with their biological family after leaving their spouse.
… a huge stressor was being left economically completely vulnerable. Going from having good regular income from [former partner] to having nothing and then being dependent on my parents. I didn’t have the wherewithal to access the benefit system, which I’m finally accessing now. But yeah, I was dependent on my parents for money and they used that as a quid pro quo to basically endure a weekly transphobic rant that looked like the comment section on Mumsnet […] And so I then went through all the hoops and got on T with [clinical provider] but unfortunately, there’s been a lot of stuff going on in my life outside health care. […] In the end I sought out the help from a domestic violence charity and they said look, you know, we’ve done this assessment, the statistics say that if you stay there you’ll be dead in six months, so you’ll have to go. […] and so I was put into homeless hostels and this was week one or week two on T because the abuse at home got worse when I started T.
In the context of financial precarity, the need to combine paid work with care of others is common. The following respondent described how they could not attend to their gender-transition needs until the person they cared for had died.
I had to work night shifts and then I had to care for [mother] during the day and so that’s why I was in that position. Now, eventually of course I lost my mum and that was the only thing, because I’d retired from work […] so in the end I decided, ‘well, I’ve done everything for everybody else, I think it’s time I did something for me now’ …
Paying for care
This study collected many instances of people accessing aspects of care privately (private hormone prescriptions, mental health treatments, hair removal, etc.). However, the widespread experience that clinical gender transition will inevitably entail personal financial expenditure makes what should be standard care, free at the point of need, more aspiration than reality for those on the lowest incomes.
[Any form of self-funded care] is completely out of the question for me unfortunately. I’ve been, I’ve never had a real job […] so, I wouldn’t be able to get loans and stuff. I wouldn’t be able to, I’m on PIP, I’m on Personal Independence Payments and on ESA. And I’ve always been on one form or another. Before I was on my own DLA and stuff.
Moreover, the experience of care is profoundly affected by income precarity and low income. After waiting several years for their initial appointment, the following respondent found they could not afford to travel.
… but I couldn’t get [to my first appointment] because while they do give you fuel money for your visits if you live out of a certain amount of area, I had to have fuel in the first place to get there, to then get a refund and I didn’t have it. So I wrote to them by e-mail and said, look I’m really sorry but I just don’t have the fuel to get there and while I appreciate you do give me fuel money I still have to have fuel in the first place, so can I rearrange the appointment? I didn’t even get a reply …
Others, particularly disabled participants, described having to depend on friends or charity for transport to their appointments. The geographic distance between gender clinics is relevant to this discussion, illustrating one consequence of trans health care being centralised into specialist services rather than integrated into local healthcare services.
Where standard NHS provision is absent or inadequate to meet an individual’s health needs or where waiting lists means that needs go unmet, those on low incomes simply cannot afford to make up even modest shortfalls.
… you can’t get NHS funding to get facial hair removal until you’ve got a diagnosis. Now if you’re looking at the gender clinics at the moment with the waiting list and then the wait to see the doctor, to get a diagnosis […] It’s only at that point when the NHS may give you a limited budget to do facial hair removal. You’ve had to struggle for five years walking around with a beard – I’ve still got a beard, mine’s never going to go because I’m a pensioner and I cannot afford to get rid of it […] The electrolysis for example, I’ve got £1,500 at about £60 an hour [provided by the NHS]. So what’s that work out? … About 25 hours’ worth of treatment. I was quoted by a friend who was an electrologist that it was 300 to 400 hours I would need to do my face […] And the fact is, I’d have to pay for it. I can’t afford as a pensioner to pay for more than that.
For those who could periodically afford private care, loss of care associated with income precarity could have serious consequences to health and care.
And [private provider] got really nasty with me and they were like ‘well if you don’t pay we’re going to kick you out of the clinic’, and I was like well ‘OK like I guess that’s that then’. So yeah they kicked me out the clinic. They knew I was homeless as well, they didn’t give a crap.
This was also the case with accessing hormones. For many people, starting hormone therapy had an immensely helpful impact on their mental health, often relieving serious symptoms of dysphoria related to gender incongruence (as already noted earlier in this chapter under People with mental health concerns or conditions). Within this context the need to commence hormone treatments becomes urgent, not only because it often commences a clinical transition journey, but as a mental health intervention in its own right. The following respondent was buying their hormones, but had to discontinue this due to money issues:
… the way that the gender identity services decide whether or not you should have hormones is so very long and so very protracted that I was forced to buy [hormones] because they made me feel both physically and mentally better. So my mental health is also deteriorating because I haven’t had any oestrogen or antiandrogens or anything since about March. I’m holding on literally by the skin of my fingernails to my sanity. My skin and my features are returning back to how they were pre-hormones.
Finally, people on low income were disproportionately affected when NHS Trusts made changes to what they would pay for or when coverage differed from each other. Thus, some respondents reported going without care that others in nearby areas were receiving while others reported that cutbacks meant that treatments they relied on to alleviate the side effects of their gender-transition treatments were no longer available.
Gender identity clinics’ processes
Although strong concerns were expressed across the entire sample around inflexible bureaucratic procedures in many GIC clinics, respondents in this group reported particular concerns. We have seen already how financial precarity can place significant barriers to being able to attend GIC appointments promptly. Moreover, those on low income or in precarious employment do not have the same capacity as others to take time off work to attend appointments or to be flexible when appointments are rescheduled. A particular fear among many in this group was that of missing appointments. This fear was based on a well-founded assumption that a missed appointment might put treatment back significantly.
If you miss an appointment for whatever reason, there could be a million reasons why you miss an appointment. Your bus might be late, your taxi might not turn up, or you might physically not be able to get out because you’re poorly that day, whatever, etc. If you miss an appointment, it’s considered to be some kind of a black stain against your name […] that could potentially send you right back for years on the merry-go-round all again. Now to a trans woman or trans person that’s like, it’s the most horrific thing that can happen to them, apart from being refused treatment. It is the second most horrific thing that a trans person can go through, to be put back on the wait list again as a form of punishment. And I do think, I suspect as well that it is used as a form of, not only punishment but a form of culling of the wait list.
Many respondents reported experiencing a particular burden of responsibility to spot and act on potential administrative errors by GICs that could have a catastrophic impact on their care and health.
So they sent me a letter welcoming me to the waiting list of [GIC]. And they said your referral date was October 2019. What? Well I was on the phone. I’m having none of that. I said no, I was, my referral date is when I was referred to GIC and that was October 2018. […] and the current waiting time is something like 24 months. I’m thinking you’re not putting me back another bloody two years. Sod that for a game of monkeys. And when I rang up and voiced my opinion, the very nice lady at the other end of the phone said, ‘oh I’m ever so sorry about that’ she says, ‘we don’t know when anyone was done so we’ve just had to do it from when we opened the clinic and hopefully people like yourself will get in touch and tell us.’ And I had another letter back saying they’d amended it and I was, my referral’s now 2018 not ’19 … If I wasn’t savvy enough to pick up the phone and sort it, it wouldn’t have got done. There you go.
People in rural areas
Rural populations are theorised to experience potentially reduced access to health care due to the need to travel further to healthcare appointments. 83 A systematic review examining healthcare outcomes and healthcare experiences for rural lesbian, gay, bisexual and transgender (LGBT) people suggests that they experience both poorer health outcomes and worse healthcare experiences that urban LGBT people. 84 This analysis examines the healthcare experiences of rural-dwelling participants and was based on 22 interviews with people aged between 23 and 82.
Travelling for care
Travelling for gender identity-related medical services is different from travel for many other types of health care because GIC clinics typically operate under a national (vs. regional) referral system which means that patients may end up travelling a significant distance. For those in more rural locations, or in lower population areas, accessing other types of specialist healthcare services may also involve significant travel – for example, one participant talked about travelling ‘100 miles each way’ for electrolysis and over 60 miles to access a sexual health screening. Participants talked about travelling for health care involving crossing locality and funding boundaries (e.g. clinical commission group, local authority) as well as national borders (e.g. Wales to England), and in some cases international borders (e.g. a patient who accessed medication from Thailand). For example, as reported in the case study in Chapter 4, in Northern Ireland, all services providing gender-affirming care are located within the Belfast area, creating significant disparities in accessibility of care between those close to the capital and trans people at the furthest edges of the region.
Rural participants talked about how travel to access health care was associated with difficulties relating to financial cost and in terms of time and stress. For example, this participant talked about how stressful, difficult and expensive it was for them to get to their GIC appointment:
So, for me to be able to get to [City 1] with all my accessibility stuff that I need and everything. The easiest way is train. Train from here to [City 1] with needing first class and a seat for my carer and everything is easily 50 quid one way. So then that’s 100 quid both ways, plus taxi from the train station to the thing. And the thing is my wheelchair’s bigger than the average wheelchair because I’m fat. So it’s wider. So, I need a van or accessible thing to be able to fit it in the boot. Even though it folds down and everything I need a bigger, like 16-seater or 12-seater or one of the bigger ones which they price gouge you for. So typically, a taxi in [City 1] from town centre to anywhere is at least 20 quid. We’ll conservatively say 30. One way. So that’s 60 quid for taxis, 100 quid for train and that’s just the bare essentials. That’s not including, because it’ll be an all-day trip, food or what have you.
This quotation provides an example of how ICTA participant accounts evidenced the way in which different marginalisations have a cumulative effect on increasing barriers to health care, evidencing how intersectionality works in creating extra barriers (see next section).
Other participants talked about the stress of travel, having to negotiate how to take a bus in a strange city and ‘find accommodation and stay overnight and that sort of thing – which was stressful enough on its own let alone the fact that I was going into this [GIC] appointment not entirely sure how it was going to work’.
Rural participants talked about how their access to health care was shaped by the distance to healthcare services. For example, one person recounted how losing access to their car led to them having to rely on a third-sector organisation to pick up their prescriptions and to think twice about whether they needed to go to the doctor: ‘I can only afford a limited number of taxis, like one a month. I had two last month, because I had to go and have my [COVID] vaccination.’ Other participants talked about choosing GICs on the basis of distance from home, rather than other factors that might be more important: ‘Afterwards I did think that maybe I should have done some more research and found out where the shortest waiting list was and just got the train or whatever when an appointment came up.’ Other participants talked about how the difficulties of travel to appointments led to them avoiding health care.
Participants also talked about how being in a rural area meant reduced choice of healthcare services, leaving them stuck even if they felt their local services were unhelpful. One talked about how their GP would not give them a bridging prescription:
You have no choice on GP practices here. It isn’t the case that, I can’t just move. If I live within a 20-mile radius of that clinic that is the clinic I have to go to. I knew of other people who are trans who were going to another clinic, another GP practitioner say and they were getting support and they were getting bridging prescriptions. And it was only what, 12 miles away.
Another participant talked about how they felt that being rural meant that they were stuck with a local NHS Trust which is ‘not as forward thinking’ as urban trusts. These accounts evidence how transphobia and lack of cultural competence from healthcare providers represent an extra risk for rural patients who lack patient choice. This may lead people to be denied or delayed in accessing health care. The possible profound impacts on their physical and mental well-being have already been referred to.
Being rural for some participants meant being in a healthcare context where they feared the potential for gossip or felt that local healthcare providers were not trustworthy, leading them to avoid local services. One participant talked about seeking sexual health screening outside of their area:
I decided that I needed to do an HIV test and I decided to do the full HIV STI one. And I looked, because I didn’t want to go, because we’re such a small practice, if I’d gone into the practice and asked for, a screen for this you can never guarantee, although they’re meant to be discrete you can never guarantee that somebody’s not going to say something and that’s going to be, you know. And of course then that sort of tars you with a brush doesn’t it because you’re going in for that sort of screening. And I went to [organisation 2]. The online one and I did […] I think they’re called third generation tests.
The logistical difficulties associated with travelling to clinic for appointments meant that some people welcomed virtual (online) appointments as providing a better way to access services. The lack of availability of this approach prior to the pandemic is noteworthy, because clearly for many the access issue was already present. For example, one participant mentioned how happy they were when they were able to get a virtual GIC assessment after years of difficulty in getting access:
I had an online assessment, surgical assessment in the autumn and then in December I had my second referral appointment. Again that was an online appointment, both of these with medical specialists by the way at the clinic and I was very happy.
Social repression of trans identity and isolation from trans communities
Rural participants talked about experiencing isolation related to their trans identity, and how the sense that everyone knows everyone in smaller rural communities can make the process of coming out as trans more challenging or sometimes impossible, due to transphobia. One participant had a prominent position within their community, having been the headteacher of the small village primary school for over two decades. This position of trust and care within the community meant that they were ‘terrified’ to come out because they feared how the village would react.
Not because it’s illegal as well you know but in a situation like that you just need a few people in a community go against you and life becomes intolerable. I’ve seen it happen to other people.
Another participant recalled how before they came out, they would be themself only when away from the rural community they lived in – for example, when they went on holiday or to cities far from home.
And on all those occasions when we were away from home I was [respondent’s name]. But back to who I used to be when we got home again … I was [respondent’s name] and we were about to go shopping and I live at the end of a cul-de-sac, a long cul-de-sac and I was looking to see if anyone would see me before I scuttled into the car to [City 1] or [City 2] or wherever it was we were going to go shopping. And I thought this is ridiculous, why am I still hiding? By this time I was working at the university and I was beyond teacher retirement age of 62, 63 I suppose, and I thought well, what’s the worst that could happen?
Coming out as trans only on retirement was something that other rural-living participants reported.
Socially ingrained transphobia was perceived by participants as being more prevalent in rural areas compared to towns and cities, with one participant describing how their community was ‘pretty much still stuck in the 80s, probably 90s, but they’re so far behind with everything, socially, medically …’. This participant compared their rural community with one of their nearest cities which has its own LGBTQI+ café and a much more visible trans and LGBTQI+ community. This individual felt geographically isolated from the local trans community to the extent that they felt they were effectively living in a different time:
Sociologically we’re sort of, compared to [city 1] or [city 3], we’re sort of, well Neanderthal really … When I’ve visited [city 2] I’ve seen trans women and trans men wandering around the streets and living their lives. So I know that there is a community for want of a better word in [city 2], but it’s not, I can’t just jump on a bus or drive up there because it’s 20-odd miles.
For rural participants who feel unable to present as trans due to the way that trans identities are stigmatised in their local community, there are health consequences. One participant explained that the reason they used illegal drugs and abused alcohol was because where they lived they didn’t feel that they could be themself.
When I get depressed I treat myself badly, I start drinking a lot of wine, I start smoking more cigarettes, I might have a joint, I might even contemplate the idea of having a line or two of something stronger because I feel bad and the reason I feel bad is because I can’t present myself to the world as I feel I am.
Social isolation from trans communities is thus associated with negative mental health impacts for rural-dwelling trans people. Negative impacts of social isolation are also relational. For example, being isolated from other trans people impacted participants’ sex life, one reporting that they had not had an intimate or sexual experience since 1995: ‘I don’t really miss it so much as I miss being in a relationship.’ Other rural trans participants talked about finding it difficult to even open up to friends for hugs and tactile comfort; while they attributed this in part to sexual abuse they experienced as a child, they also related this to their trans identity and being historically fearful of developing connections with people.
Social isolation is additionally a health risk for trans people in rural communities, in the sense that, if someone becomes unwell and they are cut off from their local community because they are trans, they have fewer people to rely on for help.
… living alone, when I have felt unwell, and it’s only, it can get scary, let’s put it that way. I can get scared when I’m, if I’m unwell feeling very vulnerable I can get, I can get scared.
Another participant similarly talked about their fear of becoming ill, because they live on their own and have little to no help available if they were to become bed/house bound. This would make them extremely vulnerable, which might have worrying implications for people considering trans-related surgeries.
Living in a small rural setting also makes healthcare encounters potentially more difficult. For example, one participant spoke about how the rural setting they live in has a very strong religious community where most of the village – including one of the GPs – is part of the church. This made them very anxious about going to the doctor:
So you don’t know who you’re going to get if you go to the doctor, unless you know them already … I don’t think it holds me back from seeking help when I need it. But it maybe delays me seeking help because I have to go through that process of thinking or mentally preparing myself of what’s going to happen here and just preparing myself for the possibilities.
While some participants reported very supportive GPs/healthcare providers in their rural context, other participants talked about how they left their location due to very poor experiences with health services: ‘So I move here and I’m so absolutely, I’m so panicked by the idea of talking to medical services again, making contact with a GP. And then I did, and they were wonderful. They set my mind at rest.’
Trans Black people and trans people of colour
This section of the report focuses on the healthcare experiences faced by TBPoC. The analysis is based on interviews (16) and focus groups (8 with 23 people) with 39 people; the youngest participant was 19 and the oldest 57. Previous literature and reports on the experiences of trans people in the UK have not always included data or experiences from trans people who are marginalised due to ethnicity, and inclusion of the experiences of this group was thus very important.
Focusing on the healthcare experiences of TBPoC is also important because of the empirical evidence that experience of racism is associated with poorer health outcomes. 85,86 This analysis thus used an intersectional lens, which acknowledged that trans Black people and trans PoC are not just facing transphobia in medical settings, they are also dealing with the impacts of medical racism and other types of oppression. ‘Intersectionality’ is a term coined and developed by Kimberlé Crenshaw46 in 1989 to address this phenomenon. It can be defined as an analytical framework that describes how a person can experience discrimination that is specifically produced by a combination of two or more social categorisations such as class, race, sexuality, gender identity and disability.
Multiple themes raised by participants applied across different racial and ethnic backgrounds. There were also multiple instances where participants of a similar background, and different genders, made reference to the same factors that would encourage a lack of distrust in medical professionals. This section summarises these themes. We make a clear distinction between trans Black people and trans PoC as the Black voice was less represented in the ICTA interview data and we wished to redress this imbalance in the focus groups. While communities do have many commonalities in the way they are treated, each group also respectively faces a unique set of barriers to navigate and comprises many unique and distinct cultures.
Accessing mental health services
Many of the TBPoC group findings echo the general findings set out earlier in this chapter, of how trans health care and being trans impact mental health. However, some findings are specific to this group.
Participants reported discrimination on multiple fronts in terms of the mental health support that they had either accessed or attempted to access. Discrimination based on being trans was discussed as a common occurrence, something which seemed to be a product both of transphobia and of a lack of substantial training to provide adequate support to trans people. One participant expressed their difficulty in accessing a counselling service that was safe for all aspects of their marginalised identity:
I wasn’t given the correct support for what I needed … it was counselling through local services but I wasn’t allowed to speak about my transness or any other issues, so I just had to talk about the surface anxiety and depression and not go into anything deeper …
This participant described how they had already struggled with the emotional labour required to seek help for their deteriorating mental health; they were hoping that their efforts would result in transformative support, but described how they were instead met with discrimination on the basis that they were trans. This meant that they were not afforded the safety and care that is expected in all therapeutic settings and instead were further traumatised.
The knowledge that reaching out for support did not guarantee a positive outcome was prominent among the participants in this group and several said that this had deterred them from seeking out further help, instead turning to their communities for support. Many of the participants said that they did not feel safe enough to disclose that they were trans in mental health/counselling spaces, for fear of being refused help or pathologised.
Another issue shared by the majority of participants was the lack of cultural competence within counselling and therapy services. It was quite rare for participants to be able to speak to therapists and counsellors who shared their whole lived experience. Participants said that if they were able to access a therapist who was Black or a PoC, it was not guaranteed that they were not transphobic. Similarly, if they were able to access a LGBTQI+ or trans therapist, or one that was supposedly knowledgeable about trans issues, racism and cultural insensitivity were often prevalent. People in this group also commonly experienced therapists as lacking knowledge about trans experiences.
These participants’ experiences of racism and transphobia result directly from the fact that they live at an intersection of identity that has been continuously overlooked by the decision-makers who provide these services. When asked about any alternatives, participants noted that very few mental health services exist that acknowledge and tailor to the intersections of their identities and those that do often lack the resources needed to support their service users. Many were aware of community organisations such as the Black Trans Foundation and the Black LGBTQIA+ Therapy Fund. However, these organisations are oversubscribed and underfunded to manage the demand for tailored mental health support. One participant remarked that the lack of appropriate provision left them feeling hopeless about getting help with their mental health. While counselling can be accessed privately, the significant costs of this mean that many TBPoC were unable to access support with the cultural competence to understand their struggles and effectively support improved mental health outcomes.
Cultural transphobia and cultural insensitivity
Family relations in some Black and PoC communities can differ from those of white communities. One reason for this is the higher presence of strong faith backgrounds in some communities. 87 Faith is often not separate from culture and instead intricately linked with how people from certain communities form their identities. Religiously based bias in multiple cultural contexts has resulted in trans and queer identities being ostracised and invalidated. 88 Many of the participants of this TBPoC group talked about the struggle to come out to family because of the risk of being cut off entirely due to the homophobia and transphobia that they would face. Participants talked about how the risk does not just include immediate family but extended family too. Not only does coming out thus jeopardise their safety and stability, but it can also sever their ties with their heritage and therefore potentially destabilise their sense of self. Participants talked about how, in certain cultural contexts, it is often a choice between maintaining their safety and stability by hiding their identity from their family or choosing to be themselves and facing family rejection. It is important to note that family rejection in this case is not just judgement and disapproval; participants talked about instances of coming out that resulted in houselessness, disownment and, in extreme cases, violence. The high potential risks of coming out to family are at odds with some GIC clinicians’ insistence that individuals must come out to their family before being given access to care; this GIC stance evidences a potentially dangerous failure of cultural understanding. It is also noted that this issue is neither exclusive to nor ubiquitous in BPoC communities and suggests the need for clinicians to be able to apply a person-centred, culturally aware approach, understanding diverse ideas of family and community beyond the idea of nuclear family.
Familial or community understandings may also shape the experiences of TBPoC with mental health difficulties. Participants talked about how the attitudes towards mental health in some Black and PoC communities can differ greatly depending on generation, with older generations tending to see discussion of mental health issues as taboo and something negative. Participants noted that emergence of mental health difficulties can be interpreted as evidence that a parent/carer or family has failed their child in some way. Opinions of the extended family and community can also influence how a parent/carer or family reacts to mental health issues displayed by their child. Participants talked about how the dismissal of mental health discussions in the homes of TBPoC suppresses the possibility of mental health solutions. This, said participants, can lead to TBPoC feeling the need to become hyper-independent, especially when it comes to their mental health care, as a result of not having safe and protective channels to express these health concerns in the home. In turn, this hyper-independence can take a toll on their mental health as it precludes building a robust support system.
Race, citizenship and class
Some participants talked about how citizenship status had had an effect on their access to trans-related health care. GICs expect trans people to change their names, a straightforward process in the UK. However, people not born in the UK may face significant barriers to changing their name, and it may even be impossible if their country of origin does not recognise trans people. Another issue discussed by participants was the expectation that patients seeking trans-related health care would want or need to change their name, a finding explored in-depth in Treatment of non-binary identities in trans-related care. For some TBPoC, their name holds cultural meaning and heritage rather than being gendered. Some participants did not see name change as an essential part of their transition and so this expectation from GICs was a barrier to them accessing care.
Participants also talked about feeling that racism in healthcare services provided a further barrier to accessing health care. Many participants believed they were not taken seriously at their GP practices due to the way they spoke and the way they looked. Participants talked about their experiences of linguistic profiling (racist discrimination based on language use),89 one participant noting how they seemed to be treated differently due to their accent and their ethnicity: ‘I would sometimes [pre-COVID] take my white friends to my doctor’s appointments, so they can call out when the doctor isn’t taking me seriously.’ Due to the 4-year-plus waiting lists for GICs, many trans people resort to going private for their medical transition health care. Black people and some PoC communities, however, fall into the lowest income bands in the UK and have less access to generational wealth and savings. 90,91 Thus, for TBPoC it is often impossible to afford the considerable costs of private health care, which leaves them disproportionally impacted by the multiyear waiting lists for transition-related health care.
Black participants of different genders made reference to misogynoir, the term for misogyny that is specifically levelled at Black women, femmes and those perceived as women. 92 Within the healthcare setting, misogynoir generally presents as assuming that patients can handle more pain than their white counterparts, as reports of pain not being listened to (often until it’s too late and sometimes irreversible damage has taken place), and as when a patient’s well-being is placed below that of patients of other racial groups. 19 The severity of misogynoir is often linked with the shade of the Black person – darker people are treated worse than those with lighter skin.
One trans Black person when asked if they thought healthcare professionals did not take them seriously because of their trans status, their race or their disabilities said: ‘It’s definitely all three, they seem to hate it when I know a lot about my own conditions because it suggests that I’m completely fine, if I’m able to speak about it in detail.’
One trans Black person cited issues with the limited pool of gender surgeons on offer for trans people in the UK, saying that people of colour or Black people specifically have to weigh up their willingness to receive care from those who have inflicted harm on themselves or others due to their race, or explore costly private health care (in the UK or abroad) to limit racist interactions that occur when seeking to access trans-affirming surgery.
Another trans Black person also referred to the public humiliation they experienced from GP reception staff and GP managers after they handed in their deed poll for a name change on NHS systems, and to how their deadname was continuously used subsequently:
And he came out and he called me this name that was all jumbled up and I just broke down in tears in the surgery and started crying. And the man literally said to me, ‘You need to calm down, you’re causing a scene. We have an anti-abuse policy’ and all of this. And I was thinking, you wouldn’t say this if I was a cis white female crying about my health and stuff like that. You’re saying I’m causing a scene, is that because I’m a PoC?
This quote exemplifies the kinds of racism that trans Black people may experience at the hands of healthcare professionals, and how Black patients, particularly those subject to misogynoir, are often mislabelled as angry or aggressive. 93 Mismanagement of care by staff (here deadnaming) translates to poor outcomes for patients. This participant reported significant distress and a long-term distrust of healthcare services.
Treatment of non-binary identities in trans-related care
Non-binary identities are still a point of contention in many trans-related healthcare settings. In the accounts of TBPoC people in this study, non-binary identities within GIC settings are still not seen as valid by clinicians, with many participants reporting being refused care on the basis that they did not seem ‘binary’ enough.
If anyone mentions a GIC I immediately roll my eyes … the way the NHS GICs are completely backward, completely outdated. If you don’t fit this binary version of what you think trans is, we’re not going to give you care.
One participant remarked that their Black non-binary friend wanted to use a name that was meaningful to them and their heritage but was refused by the GIC on the grounds that it was insufficiently gendered. This highly problematic resistance to non-binary identities, reported by many non-binary ICTA participants, can also be understood in the context of Eurocentrism and colonisation; historical scholarship documents that many pre-colonial cultures did not have a binary approach to gender. 94–96 In this way, bias against non-binary genders intersects with a lack of cultural awareness and racism to create additional marginalisation.
While a recent legal ruling suggests that, in the UK, non-binary people are now legally recognised under equality legislation,97 TBPoC who are non-binary remain in a vulnerable position when their identity is not recognised or is challenged in trans-related healthcare settings.
Weight bias
The relationship between racism and both weight stigma and body mass index (BMI) as a measure of ‘healthy’ weight is increasingly acknowledged, as is the role of racism in assumptions that for some populations fatness is a cause of health problems, compared to a broader understanding of health determinants. 98,99 Many ICTA participants talked about how their body weight became implicated in healthcare encounters. However, this was particularly expressed by this subsample, with many TBPoC participants reporting being refused health care on the sole basis of their weight. One participant was told that in order to access health care they would need to be within a ‘healthy’ weight as defined by BMI scale, something which they said frightened them as they had not been that weight since puberty.
Other participants were told to lose weight to access health care despite having a history with anorexia which made dieting a potential trigger for relapse. Research on weight bias (discrimination against higher-weight individuals) evidences both the negative impact on experiences and outcomes of health care100 as well as the relationships between body weight and socioeconomic status and ethnicity, with poverty and being a non-majority ethnicity both associated with higher rates of obesity. 101,102 This research literature suggests that TBPoC people may be particularly vulnerable to experiencing weight bias in their medical encounters as well as experiencing the negative impacts of internalisation of weight bias. Indeed, participants noted how constant images and centralisation of thin white bodies in movies, TV shows and other consumable media had impacted their mental health. 103 Relatedly, participants talked about the negative impacts of not seeing representations of Black and Brown trans people in images of transition-related post-surgery results, another example of the absence of representation or inclusion of TBPoC bodies in trans health care.
Reception staff
Almost all of the focus-group participants explicitly mentioned the role that reception staff play in allowing transphobia to take place within the healthcare service. As one participant said, ‘The true gatekeepers are the admin people.’ When there were positive experiences with reception staff, they made the participant’s whole experience with health care more positive. When looking to how health care can be improved for trans users in the UK, training of reception staff needs to be included as a point of urgency to ensure that a trans person’s first human touchpoint with health care is positive.
Integrated and disintegrated care
Participants who noted smooth communication between different healthcare departments, both related to their trans health care and general care, were the exceptions. Most participants noted problems with referrals being bounced between departments, leaving them unaware of when their necessary specialised care would begin. For non-trans related health care, the accounts of lack of communication between GPs and referral services were sometimes shocking, with participants talking about how the lack of communication forced them to have to advocate for themselves, often without warning. Participants in this subsample wondered if the patient labour forced on them (to bridge lack of communication between services) was related to their ethnicity and while this issue (lack of co-ordinated health care) was widely reported by ICTA participants in general, the accounts of TBPoC participants suggest that this issue may be particularly stark for this population. The accounts already discussed have shown that TBPoC have to deal with healthcare professionals who enact racist microaggressions, which act to dissuade people from accessing health care. The impact of the lack of co-ordinated health care compounds this.
Chapter summary
This chapter summarises the findings of the ICTA project about the experiences of health care of 111 trans people, selectively recruited for interview from a pool of over 2000 survey respondents to maximise the diversity of the sample. The recruitment strategy allowed the healthcare experiences of trans people in the following groups to be considered: older trans people and historic transitioners; disabled and chronically ill people; trans people with low educational attainment or low income; trans people living in rural areas; TBPoC; and trans people with mental health difficulties.
In line with the RQ driving this part of the ICTA study, the focus for the analyses summarised here was the accessibility and acceptability of health care for participants. The findings across the subsamples in this chapter strongly suggest that NHS healthcare services, including general, specialist and medical-transition (GIC) services, are, for far too many of the trans participants, not acceptable. This is a very regrettable finding but perhaps not surprising given the conclusion of the Select Committee Report on Transgender Equalities in 2016, that ‘The NHS is letting down trans people.’4 To unpack this conclusion further, it is important to note that the interview data suggest that experiences of health care were often highly variable, with participants concurrently reporting experiencing excellent care for some health needs and unsatisfactory/unacceptable care for other healthcare needs. A common reported experience was that moving from one service, GP practice, hospital, healthcare trust or region to another could result in a significant change in the quality of health care, such that those experiencing poor health care often looked to move services/practices.
It is also important to note that across the sample it was very clear that the most expressed dissatisfaction was with gender specialist services. This related to both the accessibility of care (multiyear waiting lists) and to the types of care received; in particular there was widespread dissatisfaction with the current care pathway in terms of its rigidity, perceived bureaucracy and requirements for receipt of a gender dysphoria diagnosis in order to access gender-affirming care. The analyses suggest that, while participants expressed both positive (minority) and negative (majority) views about the need for a formal diagnosis, the lack of acceptability of GIC services was for many participants linked to diagnostic practices experienced as the patient having to ‘prove’ their trans identity, as well as diagnostic interactions experienced as hostile, dismissive and authoritarian, as opposed to person-centred and collaborative.
In terms of accessibility of services, the multiyear (and growing) waiting list to access GIC services is a major concern and will be discussed further in Chapter 4. The data from across the subsamples clearly show the damage (in terms of mental health impacts) caused to trans people by the extraordinary waits that they endure to access (and during) medical transition health care. Beyond the waiting list, the data on participants’ experiences of other types of healthcare evidence other kinds of barriers to accessing services. Participants’ accounts suggest that lack of understanding of the healthcare needs of trans people, including the relevance or not of trans status for specific health issues, and a general lack of trans cultural competence and prevalent transphobia, act as barriers for trans people seeking to access healthcare services. Sometimes these barriers, as per the accounts, lead to trans people being denied health care or being abruptly transferred to another service, as well as health care being delayed. The analysis also suggests that repeated negative experiences of health care can further reduce the accessibility of services because trans people may develop considerable reluctance to access healthcare services due to fear about how they may be treated.
The subsample analyses provide a compelling explanation for the poor healthcare experiences reported by participants – namely, discrimination towards trans people that is enacted both systemically (e.g. waiting list to access GICs, or healthcare services and systems that are rigidly gendered) and interpersonally (by healthcare providers to trans patients). Poor healthcare experiences were associated with participants’ trans status not being seen (or alternatively over-focused on), experiences of being trans/associated healthcare needs not being understood, and trans status being stigmatised. The (in)visibility, misunderstanding and stigmatising of trans patients was, as described by participants, expressed through microaggressions as well as experience of explicit anti-trans discrimination. It was also associated with a lack of trans cultural competence as well as lack of knowledge of the healthcare needs of trans people on the part of healthcare providers. Conversely, good health care was associated in participant accounts with respectful, person-centred care that was free of trans microaggressions, evidenced trans cultural awareness (e.g. respecting patient pronouns) and a knowledge of the healthcare needs of trans people including when a patient’s trans status is relevant for particular types of health care.
The subsample analyses also point to the impact of intersecting discrimination, such as that described by ICTA participants who are TBPoC, or experience mental health difficulties, or who are disabled, older or lower-incomed. Participants’ accounts strongly suggest that being doubly (or more) marginalised is associated with a particularly strong likelihood of negative experience of health care which is neither person-centred nor co-ordinated. The analyses also point to the high levels of patient labour needed both to access health care and to achieve co-ordinated care.
These negative experiences of health care are concerning because they are likely to be associated with poorer healthcare outcomes for trans people. The section in this chapter summarising the healthcare experiences of trans people with mental health difficulties made the argument that negative healthcare experiences exacerbate minority stress, resulting for this population in trans-specific iatrogenic harm. A broader argument about iatrogenic harm may be warranted. While this project did not systematically assess health outcomes of participants, extensive prior research suggests worse physical and mental health outcomes for trans people. 104–107 These are most typically explained in terms of the impact of anti-trans stigma that includes ‘systematic social and economic marginalisation, pathologisation, stigma, discrimination, and violence’. 108,109 Crucially, prior research suggests that negative health outcomes also result from the fact that anti-trans stigma is experienced within healthcare systems and settings. 108,110,111 While many ICTA participants did report some good experiences of health care and a minority reported overall good experiences of NHS health care, in general participants’ reports of their experiences of health care were more negative than positive. Since negative healthcare experiences for trans people are likely to be associated with poorer health outcomes for this population, it seems that the main finding of this chapter is that the NHS is (still) letting down trans people.
Chapter 4 Case studies
Introduction
This chapter presents findings from the various ICTA case studies. It provides the material to inform a more evaluative discussion, in the following chapter, about what has been learnt concerning how to improve the integration of trans health care, and the implications for the future.
There are six sections. The first four contain summaries of findings from case studies of initiatives to improve the integration of care. Fuller versions of each case, with more extensive quotations for interviews, appear in Appendix 8. The cases are:
-
gender-outreach workers attached to a GIC
-
primary care liaison and psychology services within a GIC
-
training and accreditation in trans health care for GPs within a locality
-
the Welsh Gender Service (WGS): a new specialist gender service linked to primary care local gender teams (LGTs) and third-sector support
The summaries of each case convey the rationale and objectives behind the initiative, what has been implemented in practice, the impact on service-user experiences, and the issues encountered. The fuller reports of each case in the appendices contain more extensive quotations from interviews and also an analysis of interview data, indicating likely future developments.
A fifth section summarises a report on the experiences of service users and third-sector organisations that support trans people with getting access to health care in Northern Ireland. There has been extremely limited access to any NHS specialist gender service in Northern Ireland for some years. The case concerns how service users and third-sector organisations have faced this situation, their struggles to make the case for adequate services, and their views as to what kinds of services are needed. A fuller report on this case appears alongside that of the other four case studies in Appendix 8.
The sixth and final section summarises views from across all the case studies, from both the service users and the various professionals interviewed, as to how trans health care could be improved or reorganised in the future.
Case Study 1: third-sector gender-outreach workers attached to a gender identity clinic
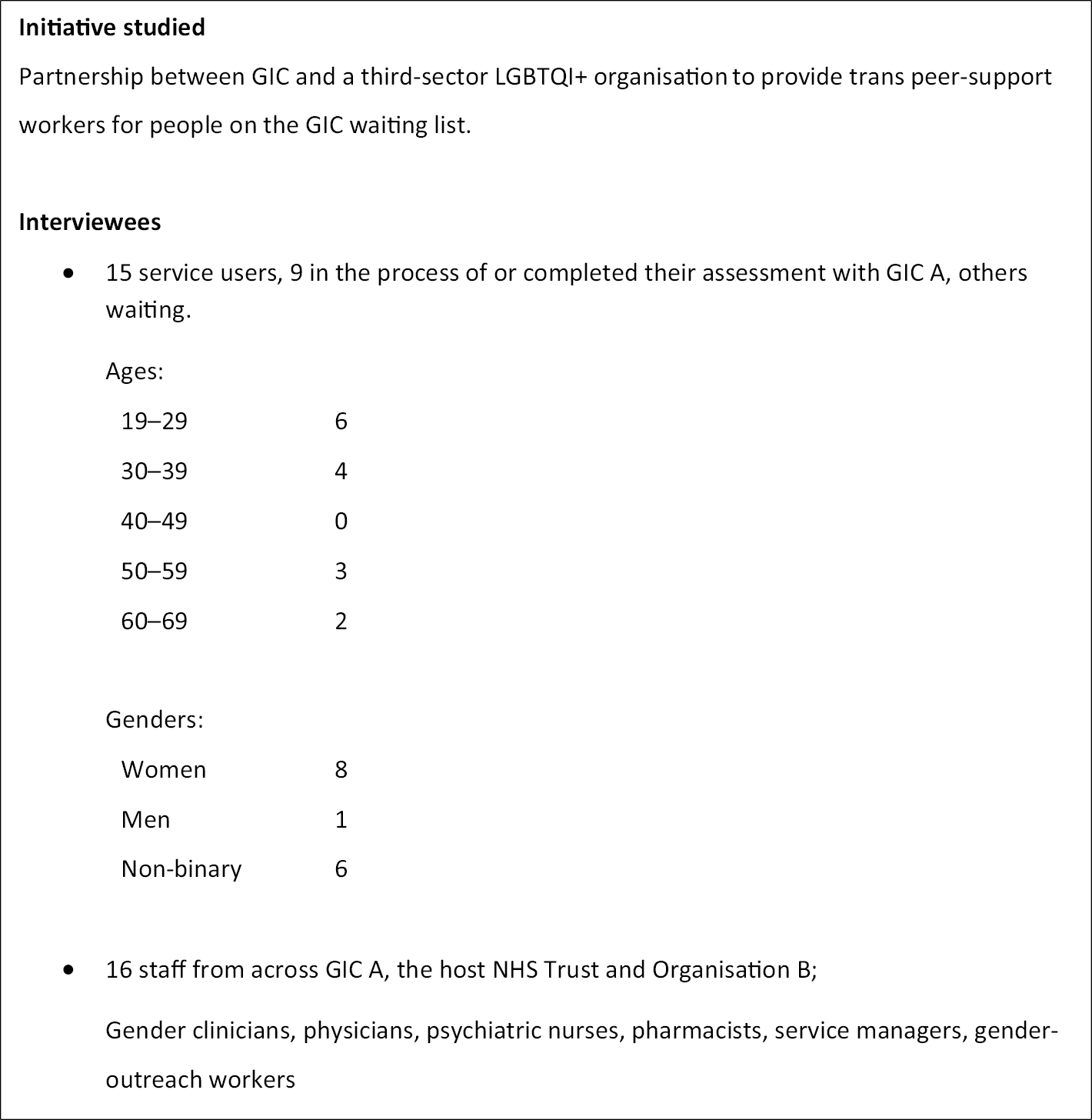
Rationale and implementation
Discussions took place between Trust A hosting the GIC and NHSE about ‘how to manage waiting’. There was a shared concern about the number of people now on the GIC waiting list, due to increasing demand, and the length of waiting for first clinical appointments. Discussions also took place with third-sector Organisation B, about a new gender-outreach worker role, with lived experience of being trans. Funding was agreed for this new role, employed by the GIC, and offering information, advice and peer support, targeted at people on the waiting list. Two part-time trans outreach workers were recruited by the GIC, working with staff from Organisation B. Outreach workers were based primarily on Organisation B premises, but had the opportunity to be involved in meetings and aspects of care provision at the main GIC site.
At the time of interviewing, from late 2019 through 2020, GIC A had over 1000 people on its waiting list. Its mode of operating followed the NHSE Service Specification for Gender Identity Services for Adults (Non-surgical Interventions). 15 Waiting times were typically 2 years for the first clinical appointment, and a further 2 years for the second. Following diagnosis, some service users who needed hormone therapy waited further, for around 12 months, for an appointment with an endocrinology team, typically 5 years after referral.
Achievements of gender outreach
-
Service users valued a variety of support groups set up by the outreach workers and how they were run.
I also started going to … plus 25 group. She always redirected towards positivity and she was good at setting boundaries in a way that made the environment feel very safe. And yeah, I would talk about things that were very difficult and then she would reframe it … that’s a huge positive.
Service user C1
-
In particular, a trans swimming group was widely appreciated, providing access to activity that otherwise poses significant barriers.
… we’ve got people who’ve not been swimming since they were a kid because of the fears that they have around changing facilities or doing swimming, because it’s a vulnerable activity putting on a swimming costume and doing these things …
GIC staff 1
-
Outreach workers provided emotional and practical support one-to-one for people on the waiting list.
… sat down for an hour and just had a chat … that’s one of the biggest things that I discovered was when you speak to other trans people, there are a lot of things that happened in your life which they recognise … that’s where you’re thinking, oh well, it’s not just me. Everyone’s gone through this.
Service user C2
GIC clinicians also began to refer people for support at a later stage in their journey, including on diagnosis.
-
Outreach workers were seen by GIC staff as deeply committed to their clients and ‘always fighting somebody’s corner’ across a range of arenas concerning health care and other aspects of their life.
-
Outreach workers improved clinic–community communications in both directions. They drew on personal and third-sector digital and other communication skills to reach members of the trans communities.
… they’re more expert than us at posters. It’s something simple but it’s something that will bring in 100 people. If we did one it would look, we’d only bring in 10.
GIC staff 2
-
They arranged meetings where trans community members could meet and talk with GIC clinicians and arranged for the GIC to be represented at trans community events.
-
Outreach workers were seen by GIC staff as not only representing the concerns of service users and potential service users, but also stimulating a constructive GIC response. Outreach workers instigated direct dialogue with non-binary people over their concerns about how they were received by GIC clinicians.
-
An outreach worker led on establishing a monthly trans sexual and reproductive health clinic, based in third-sector premises, through developing a working relationship with another NHS Trust.
-
Gender-outreach workers referred people from out of the area they covered to trans support groups in their area.
-
Outreach workers established collaboration with the local police in reporting hate crime.
Issues and challenges experienced
-
There was widespread and often painful awareness that the length of the waiting list was the most pressing concern for service users. Both staff and service users saw the gender-outreach workers themselves as unable to address this issue.
We had great discussions but again she couldn’t really do anything. For me it just felt that you could go there and vent your frustrations a little bit and then that was it. But it has absolutely no influence by the sounds of things.
Service user C3
-
Many saw outreach workers as uncomfortably ‘caught in the middle’ of allegiances to the trans community and the NHS GIC. Gender-outreach workers were seen in a compromised position, representing the requirements of the established NHS GIC system, and its long waits, to trans communities. Working with the tensions inherent in their ‘dual belonging’ was often stressful and involved considerable skill in relating.
-
Outreach workers felt they were left supporting service users with the high levels of distress. GIC staff also appreciated that outreach workers shouldered the responsibility of responding to service-user distress at anti-trans media coverage.
-
Some service users were of the view that the association of the gender-outreach workers with the GIC was problematic because things said to the outreach workers might reach clinicians involved in their assessment.
-
Some users felt that gender-outreach workers should be more explicit in advocating ways of moving forward with transition through routes for obtaining hormone prescriptions other than through GICs:
They should get a list together of endocrinologists who are willing to take responsibility for trans patients and prescribing them hormones … they should give you that list on the helpful resources while you wait, not things that I knew already.
Service user C4
-
Staff from both the GIC and Organisation B felt that the gender-outreach workers were overstretched relative to the demands on them, and this was borne out by the experience of some service users, much as they appreciated the support offered.
-
Several staff spoke of the challenge of reaching people on the GIC waiting list who lacked the confidence to participate in trans events and networks, or who perhaps lived in a rural area without nearby trans contacts.
-
A related challenge concerned the management of group events so that they provided an opportunity for interaction and mutual support, without pressuring those attending to interact or participate more than they wanted to.
-
The gender-outreach workers and staff involved in their supervision were clear about the difference between providing emotional and practical support to service users and providing mental health support. There was confidence that the supervision of the gender-outreach workers meant that they knew when to refer people on to other services, usually provided by third-sector organisations. There remained, however, the issue of the capacity of such services to meet the demand placed on them.
Case Study 2: primary care liaison and psychology services within a gender identity clinic
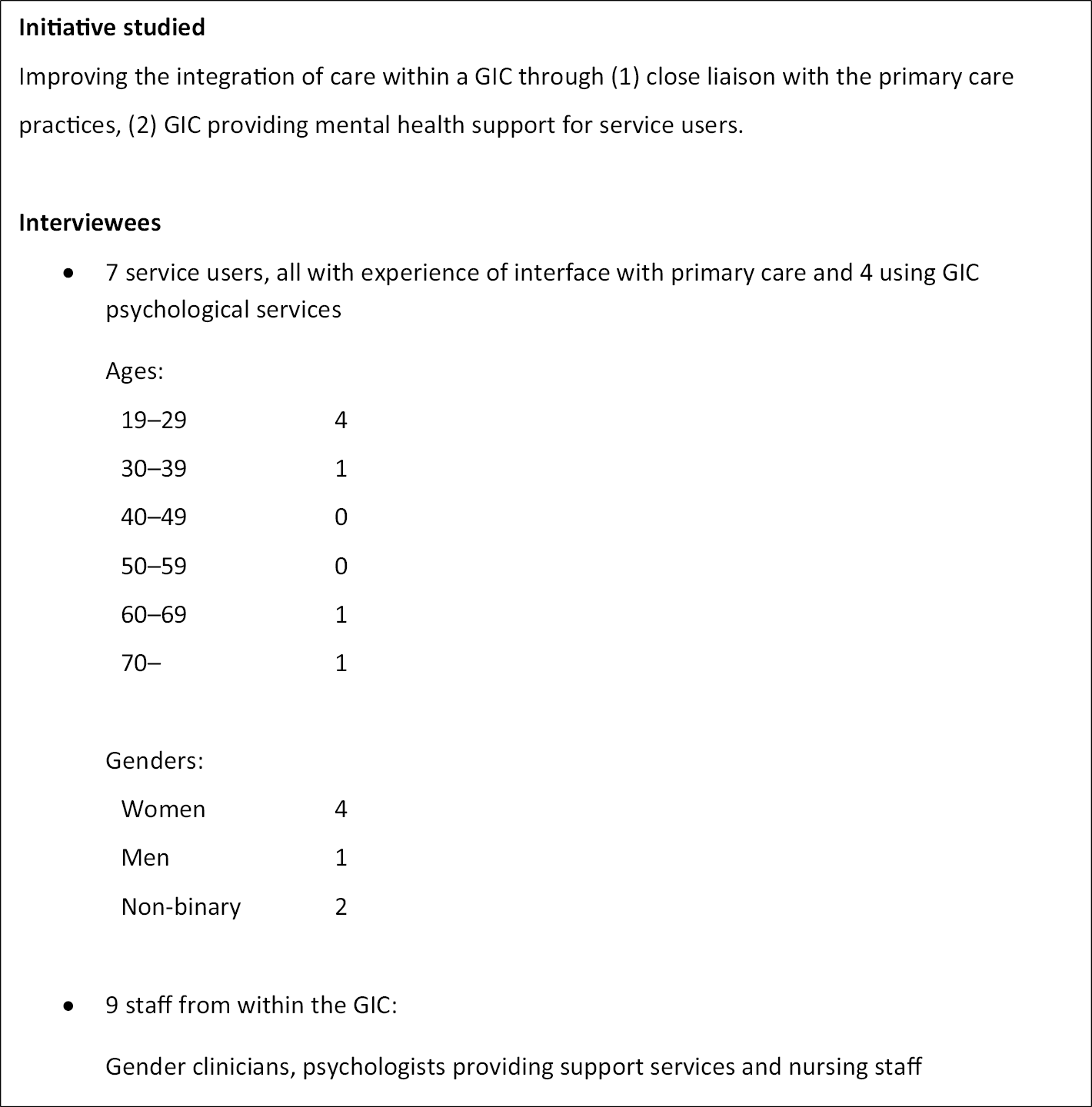
Background
For the GIC studied, the length of time from referral to first assessment appointment was around 2.5 years and grew significantly over the course of the COVID-19 pandemic. Service users interviewed reported waits of between one and nearly 3 years, depending on when they had been referred. All found the wait very stressful, with some deciding to ‘go private’ for assessment and access to hormone therapy before being seen by the GIC.
Consistent with the NHSE Gender Identity Services (Adults) specification,15 there were two clinical assessment appointments by a senior gender clinician for each person, with additional ones in between if clinicians considered this necessary. There was also a physical examination for detecting issues that might complicate hormone therapy.
Gender identity clinics’ interfaces with primary care
Service users reported widely divergent experiences of being referred to the GIC by their GP. For some, their GP referred them quickly and competently. For others, their GP appeared both reluctant to refer and lacked knowledge about how to do so.
They genuinely made me feel like I was being an annoyance to them by asking to be looked after, for them to a do a thing that only they can.
Service user C5
On receipt, referrals are processed by the GIC nurses, who request any missing information from the GP. Acceptance of the referral involves the GP signing a memorandum of understanding (MoU) which sets out the detailed arrangements for shared care between the GIC and a GP practice, above all with respect to hormone therapy. The GP is expected to prescribe, following GIC advice, and arrange regular blood tests, which the GIC interprets and discusses with the person concerned, leading to revised prescribing advice as necessary. The GIC introduced the MoU at the referral acceptance stage in response to uneven responses from referring GPs across the country to shared care.
GIC staff have developed template letters to make sure that GPs are fully informed about service users’ progress, and the implications for prescribing. Liaison between GPs and the GIC over blood tests and prescription change issues is well established, using a shared digital patient record system. Service users and GIC clinicians, however, reported persistent problems with blood test information not being provided in time to be of use at scheduled GIC review sessions. Service users found they had to intervene frequently.
Both gamete storage and hysterectomy commonly require a person’s GP to complete an individual funding request (IFR) to the local CCG. The GIC has developed ways of supporting GPs with this, making them aware of recent NHSE guidance which indicates that gamete storage should not be withheld.
Psychology services within the gender identity clinic
Staff were aware of people entering the service with a mental health burden from the stress of daily experiences of transphobic interactions, as well as the impact of the extended waiting period and experiences of having little control over their access to gender-affirming care through the GIC system.
… causing a weight or a drain on my mental health.
Service user
The GIC provides psychological support separately from the main assessment pathway, through a small psychology team. Group-based models introduce an element of peer support as well as being cost-effective in utilising staff, including clinical psychology trainees. A mix of groups, workshops, individual sessions and some family and couples work has evolved to meet perceived needs. These can be accessed ‘at any point’ once service users are being seen by the GIC. Staff estimated that around 20% of the people seen by the GIC are seen by the psychology team in one of these ways.
Pre-pandemic, there were face-to-face weekly groups and longer workshops for those not able to travel to weekly groups. More recently, the service has developed online groups for trans-affirmative CBT and compassion-based therapy.
The clinic nurses were seen by staff and service users as the key link by which people could access the psychology services, as well as providing informal counselling to people on the pathway.
Experiences of benefits and achievements
Several service users reported that group work provided experiences of both receiving help from peers and of helping others. For example, one user felt that the ‘improving confidence group’ provided a structure for effective peer support:
So, I came away from that group with some sheets that I still keep around to this day, because I got a lot of help from the other people in that group, saying, these are our experiences … It was that sort of thing, where it allowed for much more freedom of conversation, rather than a minute-by-minute, this is our topic …
Service user C6
Another experienced an online compassion therapy group as similarly providing ‘space for us to bounce ideas and talk about experiences’ while also providing a helpful framework:
… the general attitude of, stop being so hard on yourself. Again, it’s one thing to have a drive and a motivation. It’s another thing to be lashing the whip at yourself, to be like, no, go faster, go faster, you’re a failure for not having done more …
Service user C7
Staff reported that online delivery of the various groups has been successful, with therapeutic work happening in a slightly different way from a face-to-face model, but equally effectively. Online models made weekly attendance and a more intensive way of working more viable, and supported peer engagement, particularly for geographically dispersed participants.
In an experience of individual counselling, a trans person felt the psychologist had helped them focus appropriately on the difficulties of navigating various aspects of their transition, while affirming their underlying identity.
Experiences of issues and challenges
-
GIC psychologists recognised that they had limited capacity to address the considerable mental health burden of many trans people entering the service, with the group provisions addressing the milder end of the spectrum of severity. GIC psychologists were aware that many service users had mental health conditions, such as anxiety, depression, or obsessive compulsive disorder, which in their view were not directly related to their gender and which therefore should be treated by mainstream local NHS mental health services. Local mental health services, however, often refused to treat such cases, referring them back to the GIC.
If I detailed every single instance of when basic mental health support was, not necessarily denied, but refused to me, because I’ve got gender issues and they’re not trained to deal with that …
Service user C8
-
GIC staff saw their role in addressing this serious gap in access to provision, arguably affecting those with the highest need, in terms of acting as explicit advocates for people to get treatment. Some GIC staff expressed concern that the local services taking on these clients might not take a sufficiently holistic approach to mental health, applying only a limited range of techniques for addressing specific common mental health conditions, and lack skills in helping people affected by minority stigma.
-
Some staff were concerned at the contradictions between taking up a therapist role and working within a setting that assesses people as to whether they are appropriate for trans health care. The same GIC clinic both sets out to provide an open and exploratory space for people to consider what they want from treatment, and determines within an assessment process whether they fulfil diagnostic criteria. Staff also acknowledged that pressure to reduce the waiting list and maximise utilisation of diagnostic capacity can lead to issues of ‘sidelining’ people who are perceived to be ‘unsure’ about their treatment goals.
-
Further evidence of tension between receiving psychological help and GIC assessment came from staff perceptions that some service users learnt not to disclose mental health difficulties to gender clinicians. This could lead to mental health conditions going unsupported, and only emerging when people came for psychological assessment separate from the gender assessment.
-
Overall, the psychology team had limited capacity to offer psychological interventions, particularly individual counselling. This meant that programmes of treatment were more limited in length than was desirable for some individuals, to keep waiting times down. It was also difficult for staff to keep in mind all the individuals on their caseloads, which were considerably larger than in most psychology services, with more people seen less often, sometimes with several months between sessions. The groups or workshops meant, however, that it was possible to offer follow-on interventions after seeing someone individually.
Case Study 3: primary care training and accreditation
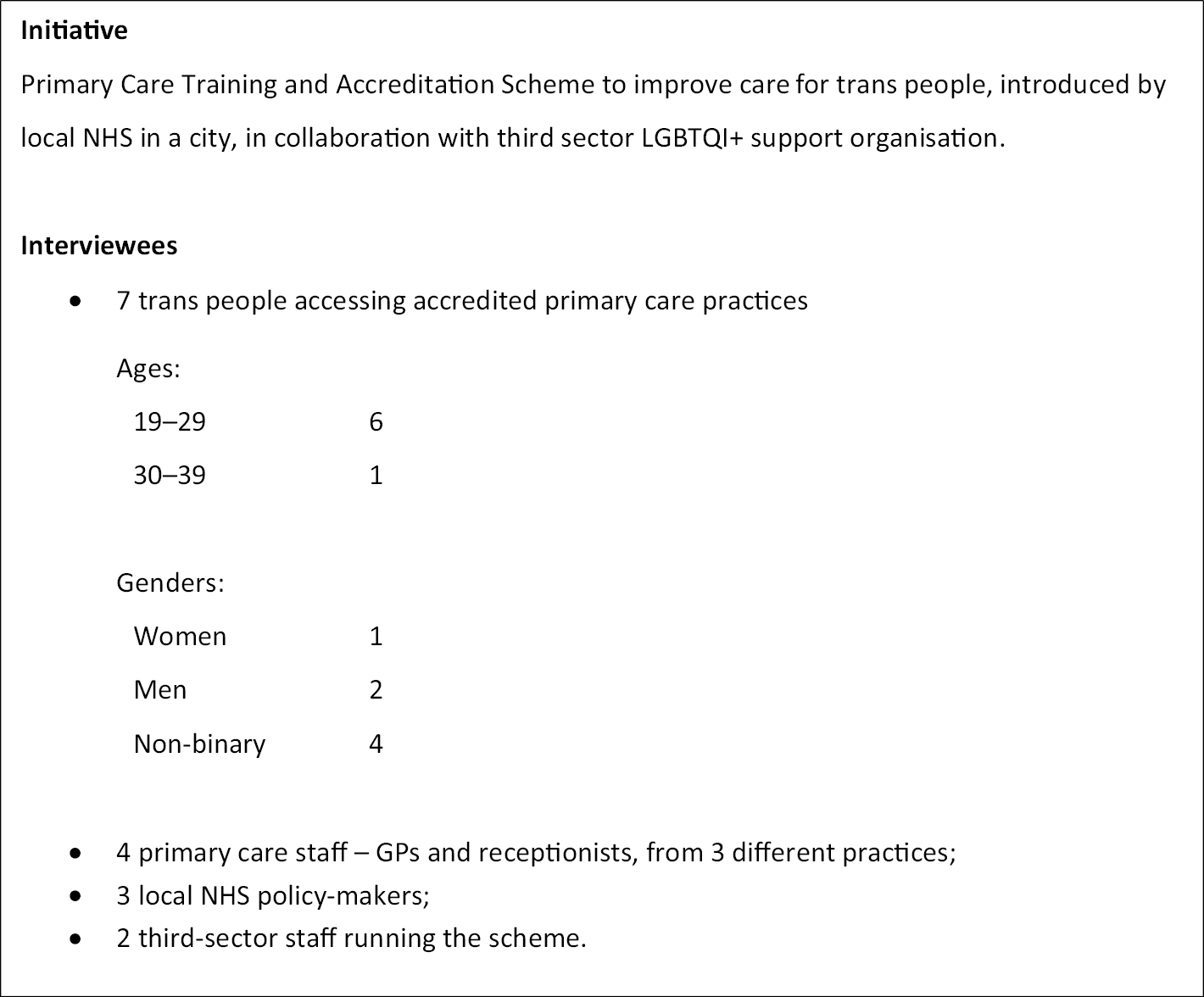
Rationale and implementation
This case study concerns an NHS primary care training and accreditation scheme (TAS) focusing on meeting the healthcare needs of LGBTQIA+ communities. It focuses on the ‘trans-inclusive’ elements of TAS intended to improve the health care received by trans people, introduced in 2016 within MetroCity by the local NHS in collaboration with Alpha, a third-sector organisation providing support and advocacy for LGBTQIA+ populations.
TAS was launched, initially for GP practices, in MetroCity in 2013. In 2016, TAS was relaunched and rebranded as a trans-inclusive scheme. The motivation to make the scheme trans-inclusive appears to have been strongly shared between Alpha and MetroCity Commissioning (MC). Prior to 2016, they became aware that primary care and other branches of health care in MetroCity were often not meeting the needs of trans people. The new version of TAS is funded so that Alpha provides training and accreditation services to primary care practices without charging them a fee.
On the basis of local research into the barriers faced by trans people in accessing services, TAS staff at Alpha developed standards for primary care of trans people, as well as a framework for accrediting competence at the level of a GP practice.
General practitioner motivation to work with trans-inclusion aspects followed from their commitment to the earlier versions of TAS that focused on improving the experience of lesbian, gay and bisexual (LGB) patients. One GP cited the strong motivating effect of TAS staff with lived experience of trans health care coming to their practice to explain the barriers that trans people face.
The TAS philosophy is that trans community membership and needs are fluid and changing, and that training and accreditation need to be co-produced to reflect this. The TAS steering group includes people with lived experience of receiving trans health care, as well as GPs, dentists, pharmacists, optometrists and commissioners.
How training and accreditation work
Training sessions for GP practices typically last 1 hour, intended to involve all practice staff. These sessions may be several months or even 1 or 2 years apart, depending on how rapidly the practice is able to progress with its development in the trans healthcare standards.
Training covers: LGBT basics, including the differences between concepts of sex, gender identity and sexuality; ideas of cis and trans, including non-binary, people; health inequalities experienced by LGBT people, the additional inequalities faced by trans people; the importance of recognising protected characteristics and addressing inequalities; and best practice in terms of inclusive primary health care. Clinical and non-clinical staff alike commented on the importance of having the training delivered by a trans person.
Assessment for accreditation typically takes place on the same day as training, in a separate session with a smaller group of practice staff. This includes discussion of policies and questioning of staff about how they have dealt with or would deal with various scenarios involving trans patients.
Assessments also explore the questions typically asked by clinicians in their consultations with patients, whether patients are given the opportunity to give information appropriately about trans identities and whether there is exploration of related health issues such as relevant screenings.
The assessment result is fed back in terms of a bronze, silver or gold TAS award, with recommendations for areas of improvement. Typical feedback at bronze level might concern ensuring a well-intentioned policy is better understood and acted on by practice staff.
Features of trans-inclusive healthcare resulting
The picture emerging from the perceptions of service users and TAS staff is that some accredited practices have developed competence in many aspects of trans health care and have acquired a substantial trans clientele. However, the experiences of service users suggest that trans healthcare expertise was not consistently held by all staff in a practice, or consistently supported by administrative systems. Commissioners were also concerned that trans healthcare understanding and competence was limited to a relatively few more advanced practices. In these:
-
Patient registration forms allow people to indicate their gender in an inclusive way, as well as trans status, pronouns and anatomical details relevant to screenings. Practices have also developed expertise in how to change gender markers on medical records and how to transfer appropriate information from an old record to a new one.
… their registration form was really good, I think it had multiple gender options. It asked a question about whether or not you have a cervix rather than just assuming that women have a cervix and men don’t.
Service user C9
-
Practice receptionists showed awareness of some key aspects of trans inclusion.
I went in to book an appointment and that stresses the hell out of me, and I went in in person, because I thought they were less likely to think I was joking. Because I don’t look like the kind of thing they would be expecting … And the receptionist was just, yes, how about Tuesday? She didn’t even blink …
Service user C10
-
Two trans men commented on the respectful and sensitive way that cervical smear testing was carried out.
Some service users, however, reported significant problems, indicating inconsistencies within practices:
-
One person had difficulty achieving a change in their name and gender marker on the patient record. The surgery staff consistently referred to the participant by their correct name, but documents printed out from the record contained their deadname.
-
Another participant attended for a minor procedure. They were deadnamed in the waiting room, and then found the treating clinicians were surprised by their gender. They experienced having to deal with the clinicians’ embarrassment, rather than receiving support for their own reactions.
-
Another participant pointed out that even seemingly minor failings in respectful behaviour towards them were all the more painful because of their past experiences of healthcare settings.
… it’s the fact that I have repeatedly had bad experiences. I’ve had more negative experiences than positive experiences. So, even though I have a relative assumption that my GP practice probably is fairly culturally competent as far as a bunch of cis people go, that past experience isn’t going to magically disappear either […].
Service user C11
Developments in transition-related care
Training and accreditation scheme staff reported that it was increasingly rare for a practice not to know how to refer someone to a GIC, or to avoid doing so when asked to. Following repeated difficulties in getting a referral to a GIC from their GP in a different part of England, one service user reported that their new TAS-accredited GP proactively asked if they had as yet been referred. The GP then completed the referral within a week.
Higher levels of TAS award are tied to practices demonstrating competence in prescribing hormone therapy for trans people, and TAS staff described how they could connect less capable practices with other GPs already skilled in this. Some GPs indicated that they were already experienced and confident in prescribing and monitoring hormones under shared care with a GIC, as well as prescribing hormones for harm reduction to people on a GIC waiting list.
However:
-
Some service users reported that their TAS GPs lacked knowledge about how to work with the GIC system. In one case, at a gold-accredited practice, a service user had to overcome several barriers to receiving care via a GIC.
-
Someone who had already transitioned when registering with their practice was referred by their TAS-accredited GP to a local endocrinologist for hormone prescriptions. This person questioned why this was necessary:
… I’m just on hormones for the rest of my life, why on earth can a GP not manage that?
Service user C12
Case Study 4: the Welsh Gender Service

Rationale
This case study concerns delivery of the WGS since 2019. Prior to this, access to specialist gender services was via funded access to a specified GIC in England. Welsh patients, however, first had to be screened by local mental health services. This created significant inequities to accessing gender-affirming care for Welsh patients. The entire trans population of Wales was placed on to the waiting list of a single English clinic.
The instigators of the WGS were a small network of people from different settings, who shared a moral commitment to establishing a new kind of service for trans communities. The network included a GP who had established a working relationship with Welsh government health policy-makers in another clinical area. Others involved in the design included individuals from trans communities and a third-sector LGBTQI+ leader with a history of working with communities to deliver innovative services. Staff and community representatives consulted widely within local trans communities, gathering views as to how the new services should run.
The Welsh Gender Service in practice
Specialist clinic
The WGS specialist clinic assesses people for gender-affirming care. While working within a formal framework of diagnosing gender incongruence, clinicians saw the assessment process as fundamentally a collaborative one:
[W]e are affirmative practitioners and we work with patients, with their consent, and inform them around their combined joint decision-making.
Gender clinician
They prioritised giving people access to care, while recognising that it was vital to ensure the person was fully aware of what treatment would involve, including medical risks, and that they had mental capacity to consent. Clinicians reported that it was extremely rare for them to have concerns about a person’s capacity to consent. They did not follow the practice of exploring a person’s trauma history as part of assessment, a practice critiqued in Chapter 3.
The WGS pathway requires an opinion from only one gender clinician for a diagnosis to be confirmed. WGS gender clinicians can also approve people for top surgery and provide a first signature for lower surgery.
Local gender teams
Local gender teams are small teams of practitioners based in each of the local health boards (LHBs) across Wales, who provide and manage care after people have been assessed by the specialist clinic. Care typically includes hormone prescriptions but can also include speech and language therapy and fertility preservation. LGTs also take responsibility for ‘harm reduction’ hormone prescribing for people who present at GP surgeries as self-medicating with hormones. LGT prescribers have regular videoconferences with clinicians from the WGS specialists to discuss cases where blood results show problematic hormone levels or other kinds of abnormalities.
Support service
This is a third-sector organisation that provides a Gender Information and Support Team. It is funded to provide a full-time service manager – a social worker – and a full-time equivalent peer-support post. They provide advocacy for individuals wanting help getting their GP to refer them to the WGS or else with getting a bridging prescription. They also help people with waiting list issues, above all making sure that people with referrals had been transferred from the English GIC waiting list, and also making sure that their referral date was correct.
Peer support is provided through telephone sessions, usually four sessions over as many months. This can also involve liaison with the specialist clinic on behalf of a service user.
Benefits experienced
-
Service users had positive experiences of the integrated service provision:
… my three years with the [WGS] and with the local gender teams has just been so relaxed. It basically comes down to what do you want from your transition? What effects do you want, what is bothering you?
Service user C13
-
Gender clinicians experienced the fact that initiation and management of hormone prescribing was taken over by LGTs as a welcome release of their time from the kind of follow-up appointments that occur in other GICs.
-
LGT prescribers welcomed their integrated responsibility for carrying out blood tests, monitoring and optimising hormone therapy, as well as taking overall charge of the relationship with the patient. They emphasised the benefits of integrating hormone therapy with other aspects of primary care, also appreciated by service users:
The doctor that I see for trans healthcare stuff […] I go in about one thing, she asks about my history and sorts me out for 10 things I didn’t even know I was able to get help with, I love her.
Service user C14
-
Both service users and WGS staff value the social and emotional support offered by the support service:
… They didn’t seem to be trans people, but they just didn’t put a foot wrong. They were so open and empathetic and would never accidentally misgender anyone […] I haven’t really had that experience in any medical setting before.
Service user C15
Challenges experienced
-
There were widespread concerns at the level of resourcing of the system as a whole, given the size of the waiting list, even though the situation for all other GICs was recognised as being considerably worse. While service users were appreciative of the support service, some spoke of long delays in getting a response.
-
Some staff raised concerns that, even within the gender-affirming values of the WGS, there could be unwarranted additional assessment appointments for some groups, because clinicians ‘maybe sometimes still having a slightly narrower view of transness than they should or they could to support those people’. The danger was that certain groups of people might be seen as ‘unsure’ when in their own minds this was not the case. This was a concern particularly for autistic people and also for non-binary people.
-
Several service users and clinicians were very concerned that there is no funding for hair removal under the WGS, seeing this as an integral part of providing psychological well-being for transfeminine people, as well as essential in preparation for any lower surgery, and an unreasonable financial burden to place on service users.
… we don’t get the advantages of English patients … We don’t get electrolysis.
Service user C16
-
While the WGS has taken steps to streamline the process for surgical referrals, several service users pointed out the impact of being dependent on providers elsewhere in the UK, the lack of capacity and waiting times involved, and the need to travel a considerable distance and usually recover away from home.
-
There were also some operational issues. Prescribing clinicians within LGTs reported having to take on the somewhat improvised creation of patient record systems for their WGS work, because there were no existing systems that linked effectively between the assessment clinic, the LGTs and GP practices that they might subsequently discharge people to.
-
LGT clinicians indicated that they were either near their planned capacity or else would be at it within a few months. At that point, unless sufficient service users had been discharged on to other GPs, bottlenecks would appear at the LGTs.
-
Creation of a direct enhanced service (DES) agreement, by which GP practices could have additional payments for managing HRT for trans patients, was widely welcomed by clinicians as a mechanism for overcoming GP resistance to taking on seemingly unfamiliar work. However, progress has been slow in persuading practices throughout Wales to engage. Possible reasons for reluctance included the general pressure on GP workloads and many GPs being wary of engaging with HRT for cis women following concerns with risks of cancer and thromboembolism with earlier generations of treatments in the 1990s.
-
Data protection rules have so far prevented a service-user data-sharing agreement being put in place between Umbrella Cymru and WGS. WGS has to send people information about the support service with a consent form for Umbrella Cymru to be able to contact them. It could be problematic to send out a letter from the gender service, using an appropriate current name and title, to people referred prior to the new service opening in 2019. There was a danger that the person concerned had changed their name since the referral and that the name on the letter might ‘out’ them to people they were living with.
Case Study 5: trans healthcare experiences in Northern Ireland
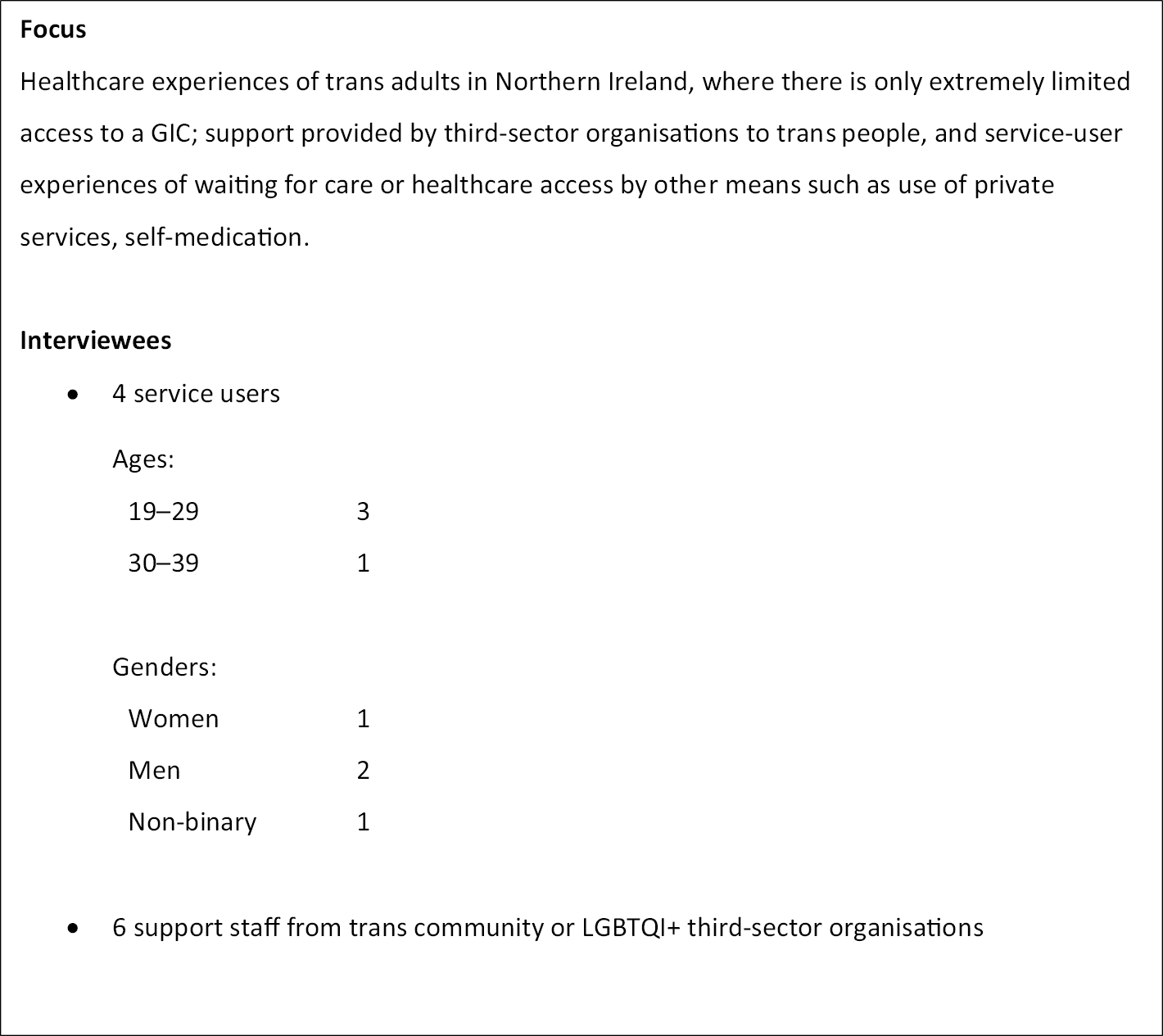
Background: ‘a case study of nothing’
This case study looks at existing services available for the assessment and provision of care for trans adults in Northern Ireland, where there are widespread perceptions of a ‘trans healthcare crisis’. A specialist gender clinic in Belfast has seen patients 18 and older for assessment and provision of care related to gender incongruence. The clinic is not a GIC in the same sense as GICs in England; it primarily functions as a psychosexual service. Crucially, it has a very small clinical staff and did not see any new trans patients between January 2018 and June 2020. New patients are now being seen from existing referrals. New referrals are still not being accepted.
In 2019, the NI HSC Board was tasked by the Department of Health with reviewing GISs in Northern Ireland. A review group, with some trans community participation, was established with ‘listening events’ taking place in November and December 2019.
Third-sector support for trans people
Third-sector organisations are not involved in the delivery of commissioned healthcare services but attempt to manage the high demand for support from trans people who have no NHS gender service available to them. In late 2018, a number of trans people set up a trans-led campaigning and human rights organisation to improve health care. This led to a position paper on ‘what we want to see from gender-affirming healthcare in the region’. They also pushed for progress with the review of the specialist clinic, securing limited trans representation.
Alongside its policy and training work, this trans-led organisation provides healthcare support and advocacy for individuals. Other third-sector LGBTQ+ organisations also provide counselling and advocacy for trans individuals engaging with health care.
Several service users reported receiving counselling or informal advice from LGBT+ or trans community organisations, as well as from trans friends. This had helped them decide how to move forward with private care or self-medication. One interviewee reported that they had benefited hugely from attending a week-long ‘trans training’ residential. This had included a variety of workshops, including on how to manage a name change.
One third-sector interviewee called Northern Ireland an ‘ethno-nationalist state’ where society is heavily divided into two groups with antagonistic views of national identity. This is linked to rigid gender roles, which has implications for making transition experiences ‘extremely difficult’, even compared to those in other parts of the UK.
Experiences of the gender identity clinic
Of the three interviewees who had been seen by the GIC, one found the overall experience acceptable. Another described the initial appointment with two clinicians feeling like ‘interrogation to see if I was trans’, and experienced questioning concerning their sexuality as ‘weird and not really related’.
Another found the GIC process adversarial and unsupportive:
… the service right now is designed so that a cisgender person doesn’t accidentally transition … It’s not made for trans people or to support trans people […] And I think overall it’s so infantalising …
Service user C17
Third-sector interviewees also recounted reports from trans people of a stringent policy regarding mental health within the GIC. People who disclosed any mental health condition were likely to have their assessment suspended.
There was a variety of experiences of care following assessment at the GIC. Some reported that the system for regular prescribing of hormones through their GP, with periodic blood tests and reviews by the endocrinologist, had worked well. Others felt there appeared to be ‘no formal strategy, care package, intention for looking after trans people long term’.
Experiences of private gender services and self-medication
In response to long or indefinite GIC waiting times, both third-sector workers and service users interviewed indicated widespread use of private services for accessing assessment, hormones, hair removal, voice coaching and gender-related surgery. Many people resorted to crowd funding. GPs were widely cited as refusing to enter into shared care arrangements with private gender services, for prescribing hormones or carrying out blood tests for monitoring, leading to people having to pay additional fees to the private gender service.
Several interviewees referred to an emerging pattern where trans men with sufficient funds obtained a referral from a private gender service and then paid for private top surgery in Poland.
Several interviewees described their experiences of private gender services as accepting of their own views on being trans and taking a pragmatic approach to finding out what they needed:
[an] informed consent approach … Trusting the patient I think was the biggest thing for me. The fact that they trusted what I said. And trusted that this is what I needed, rather than being interrogated for it all.
Service user C18
Other interviewees recounted how they had decided to self-medicate with hormones because they could not afford a private gender service. GPs were widely experienced as refusing to provide blood tests or monitoring in such cases, or to prescribe as a harm-reduction measure, usually giving as a reason that they could not ‘take on liability’ for a person’s health if they were self-medicating. The choice to self-medicate meant bearing the associated health risks oneself:
… it was very much I balanced the risk and the reward and on the whole, it has been a positive thing for me.
Service user C19
Experiences of general health care within general practitioner practices
One interviewee reported positive experiences of staying with a small-town GP practice they had grown up with, where the GP was willing to engage positively when they came out as trans. This person had worked with the staff to improve their understanding of trans health care, and the use of appropriate pronouns.
Many more of the experiences were negative: name changes and requests to change pronouns were not being followed through on medical records, and in one example, reception staff apparently deliberately and repeatedly misgendered someone so they felt compelled to move to a different practice.
A number of interviewees relayed accounts that GPs had attempted to refer trans people to the GIC for health issues that were not connected with a medical transition; with the GIC not functioning, some GPs had taken to referring people to third-sector LGBTQI+ or trans organisations, sometimes with physical health problems. Third-sector staff felt placed in an impossible position by such referrals.
Several interviewees reported that GPs did not know about the health conditions different trans people might be at risk of:
… what are things you can watch out for for a trans person? What are they more at risk for? Because the onus is very much on the trans person to know that … Because they absolutely know less than I know.
Service user C20
Interviewees reported there were a small number of trans-affirming and trans-inclusive practices in Belfast. However, trans people experienced huge variability between different practice staff. This created stress and disparities in the health care available to different trans individuals.
Experiences of other health services
Two interviewees reported distressing experiences of NHS sexual health clinics, contrasting this with the respect shown when they attended sexual health screening clinics run by a LGBTQI+ organisation. They were, for example, asked for their pronouns as they registered at the latter.
Others reported avoiding NHS health care in general, because they expected to encounter either or both of an insensitive and inappropriate curiosity about their history as a trans person, or else a lack of cultural understanding of:
what trans means, knowing what kind of people and bodies and physiology is covered by the term woman and man … constantly using terms like male and female and referring to body parts.
Service user C21
Some of our interviewees had found NHS counselling for anxiety or depression helpful, although limited in what it could achieve given the short programmes on offer.
Community action to improve services
Many interviewees shared a view that ‘the mainstream doesn’t want to know’, meaning that addressing the deficiencies in trans health care appeared not to be a consistent priority for the devolved administration or for the HSC service, in spite of the costs of not providing adequate care. These included above all the mental health burden carried by those unable to access any treatment, often leading to chronic suicidality as well as actual instances of suicide. There was also the increased burden placed on other NHS and third-sector services:
… it actually costs more to not fund the service because we’re seeing the impact on voluntary community sectors like ourselves or other healthcare providers or back into the NHS in primary mental health teams where people are self-harming …
Third-sector worker
Views on future health care for trans adults
Data from services users and staff across the case studies included a wide range of suggestions, requests and recommendations concerning how to improve health care for trans adults, including how to improve integration between services. Many of these ideas were in tension with each other, as they appeared to be based within different views of what scope of change is possible.
Here we summarise these ideas. We outline three broad views or paradigms for consideration. These differ in key assumptions, such as where different aspects of care are best provided, by whom, and whether a formal process for diagnosing gender incongruence is necessary. Table 5 summarises the three paradigms.
| Paradigm 1: Improving provision based on the current specialist service model Underlying assumptions Care based on the current NHSE specialist service specification, with gender-affirming treatment requiring prior in-depth diagnosis by GIC clinicians, who are members of the Ministry of Justice gender specialists list, according to the ICD-11 definition of gender incongruence. |
| Paradigm 2: Provision of most transition-related health care within primary care settings Underlying assumptions Most people who seek gender-related care have their needs met within a primary care setting, from an appropriately skilled GP-led local gender service. Diagnosis and treatment planning for hormone therapy and other gender-affirming treatments normally carried out within a primary care-based service. The role of specialist gender services needs to be reconfigured. |
| Paradigm 3: Removal of gender incongruence diagnostic requirement and further rethinking the role of specialist services Underlying assumptions Access to hormone therapy, and other gender-affirming care, including surgical procedures, based on informed consent. Specialist gender services support service users who choose to be referred because they feel the need for more exploration, or those that primary care services consider requiring specialist endocrinologist input. |
An earlier version of these paradigms was presented and discussed at an ICTA workshop in summer 2021, including researchers, the advisory and steering groups, as well as lead clinicians involved in the case studies. The understanding emerging was that they are a convenient way of organising elements of trans health care for discussion, rather than fully coherent and distinct models. The paradigms indicate the range of future possibilities in terms of how far they diverge from the current model, so facilitate exploration and discussion of a direction of travel for future years. None of the paradigms should be taken as representing straightforwardly the views of particular interviewees or groups. Many people advocated developments relevant to more than one paradigm. For example, some had strong views on the longer-term desirability of Paradigm 2 or Paradigm 3, but also wanted to make immediate improvements within Paradigm 1.
Appendix 9 contains four tables which summarise the suggestions and proposals made by service users and staff across the case studies as to how each paradigm could be taken forward. Under Paradigm 1, Table 8 is an additional table, labelled Paradigm 1b. This captures suggestions made as to additional elements that should be added to the current specialist service specification, within its underlying assumptions. These additional elements are also relevant to Paradigms 2 and 3.
The views and suggestions summarised under Paradigms 1 and 2 came from across the 48 staff and 42 service users interviewed for the five case studies that appear in this chapter. The pattern for Paradigm 3 was markedly different, with the suggestions coming overwhelmingly from trans service users, as well as the small number of third-sector staff we interviewed, most of whom were themselves trans. The suggestions and views summarised under Paradigm 3 are consistent with a significant body of opinion within trans communities that access to gender-affirming care should be solely based on informed consent, rather than clinical diagnosis of gender dysphoria, on the basis that diagnosis is inherently dehumanising. 112 The kinds of service-user experience reported in Chapter 3, where people found the extended process of diagnosis harmful, lend support to this position.
The case for informed consent has been articulated for trans communities – for example, by activist platforms such as Informed Consent for Access to Trans Healthcare in the USA113 as well as within academic publishing (e.g. Schulz). 114 Clinics operating an ICM have been studied in both the USA and Australia. 115,116 Ashley et al. 28 distinguish a number of variants of ICMs, along a continuum between ‘strong’ and ‘weak’. In strong ICMs, the clinician ensures that people fully understand the benefits and risks of treatment options and undertakes a formal assessment of mental capacity to consent, but the decision to proceed with treatment lies solely with the service user:
… the aim is to elucidate and best meet the patient’s embodiment goals rather than establish eligibility for hormones. Strong ICMs recognize that using independent assessments of gender identity and/or gender dysphoria to establish eligibility may be distressing and contribute to the pathologization of trans communities. 28
Under weak ICMs, there is collaborative assessment by the clinician and service user of readiness for hormone therapy and joint decision-making, which may include a formal diagnosis of gender incongruence. However, the assessment foregrounds ‘the patient’s decision to initiate hormone therapy’28 and joint clarification of treatment goals.
In the next chapter, we will discuss further the implications of the findings from the ICTA project for developing ICMs. For the moment, we note that almost all the views and suggestions from trans people summarised under Paradigm 3 were consistent with the strong version of informed consent. These views were generally linked with a stance that access to transition-related care through informed consent should not be through GICs as currently constituted, but through primary care clinics, local sexual health clinics or else clinics based on LGBTQI+ or trans third-sector settings. Many trans advocates of a strong ICM did not see GICs as culturally able to deliver this kind of care, given their history of responsibility for an extended diagnostic process. One person argued in effect that cis clinicians who have positioned themselves as experts in diagnosing trans identities cannot be seen as trusted collaborators by trans people:
I think even a few years ago, if you’d asked me that question, I would say, ‘they need to lower the wait times’ … Now having gone through the system myself and seeing it first-hand, you got to get rid of that system. It’s broken. It’s beyond repair. […] The wait times are but a symptom of everything that’s wrong with the GIC. These people who have been positioned as experts don’t have the first clue what they’re talking about, and they have been given far too much power …
Service user C22
Another person similarly held that GICs need to be replaced by other kinds of care provider, because of the combined legacy of the diagnostic model and waiting times associated with it:
My honest answer is I think they should be gone. I don’t think they should exist anymore. I don’t think that can happen until we’ve made a move into primary health care or there’s an alternative solution. But I don’t think they’re fit for purpose anymore. We know how much the demand has increased but the actual supply of services hasn’t. Or it’s not been able to meet that demand. When there’s a target waiting time of 16 weeks on the NHS and people are waiting years and years and years for their treatment that’s a sign that you can put as much Sellotape on the hull of a boat as you want but sometimes you just need a new boat.
Service user C23
We need to be cautious in using our qualitative interviews as an indication of the degree to which different paradigms were supported by different constituencies – the samples of service users and staff were not selected to be representative of a wider population. However, across the 42 trans service users interviewed, just under half said that in various ways the role of specialist GICs needed to be reworked, with far more assessment carried out in primary care or other community clinics. Further, just under one-third said that trans adults should have access to hormone therapy through some version of informed consent.
Third-sector trans support workers also tended to advocate a future based on informed consent, often with a caveat that service users need to have full information and understanding about treatments:
… open, honest explanation of if you’re going to be accessing hormones this is what happens, this is what could happen. Having people making the decisions that affect their bodies with that 100% clarity is very, very important I think.
Third-sector trans support worker
The distribution of views relevant to Paradigms 2 and 3 across the 21 GIC staff interviewed suggests the presence there too of a significant body of opinion that the current model needs to change. Just over one-fifth of (mainly cis) GIC staff interviewed indicated they supported moving towards a version of an ICM. And just over half said that the role of tertiary GICs needed to become more circumscribed, with much more routine assessment done in suitably staffed primary care clinics.
A final significant theme across our interviews on the future of trans health care concerned the need to improve how all branches of health care respond to the non-transition-related needs of trans people. Fundamental points were that services need to demonstrate that they are aware that trans people exist, and find ways of ensuring that people are referred to by their correct pronouns.
There are 100,000 different reasons why trans people would go to a healthcare service, that have nothing to do with being trans, and I think that tends to get forgotten by the health service in general. They seem to think that trans people will only ever come to the healthcare service if it’s about being trans and nothing else.
Service user C24
And a trans person that walks into a clinic where they say to everybody, regardless of if you pass, regardless of if you don’t, if you’re cis, if you’re trans, whatever, that every single person that they talk to, the first thing they do is they ask for a name and pronouns, perfect. You’re going to feel so much better. And it’s just really little things like that.
Service user C25
Chapter conclusion
In this chapter, we have summarised the experiences of a range of initiatives to improve the integration of care for trans adults, as well as the experiences of service users and trans advocacy organisations in Northern Ireland. We have also summarised views on the future of trans health care across the service users and staff we interviewed for these case studies. In the next chapter, we explore what can be learnt from all of this, together with the experiences of care reported in Chapter 3, in terms of the general implications for improving the integration of trans health care.
Chapter 5 Discussion
Introduction
At the end of Chapter 3, we referred back to the findings of the House of Commons Women and Equalities Committee report. 4 We concluded that, on the evidence summarised in that chapter, it is still true that in many ways ‘The NHS is letting trans people down’ (p. 82). 4 Our aim in this chapter is to summarise and distil what has been learnt, from studying the initiatives reported on in Chapter 4, to improve care and its integration, and how far this addresses the deficiencies identified in Chapter 3.
We begin by summarising what we have learnt about the overall terrain of trans health care that needs to be better integrated and improved. Figure 1 presents a provisional map of this, based on the experiences of receiving and providing health care heard during in-depth interviews and focus groups, involving over 180 people throughout the UK, over the course of the project.
FIGURE 1.
Arenas of care for trans adults: improving care and its integration.
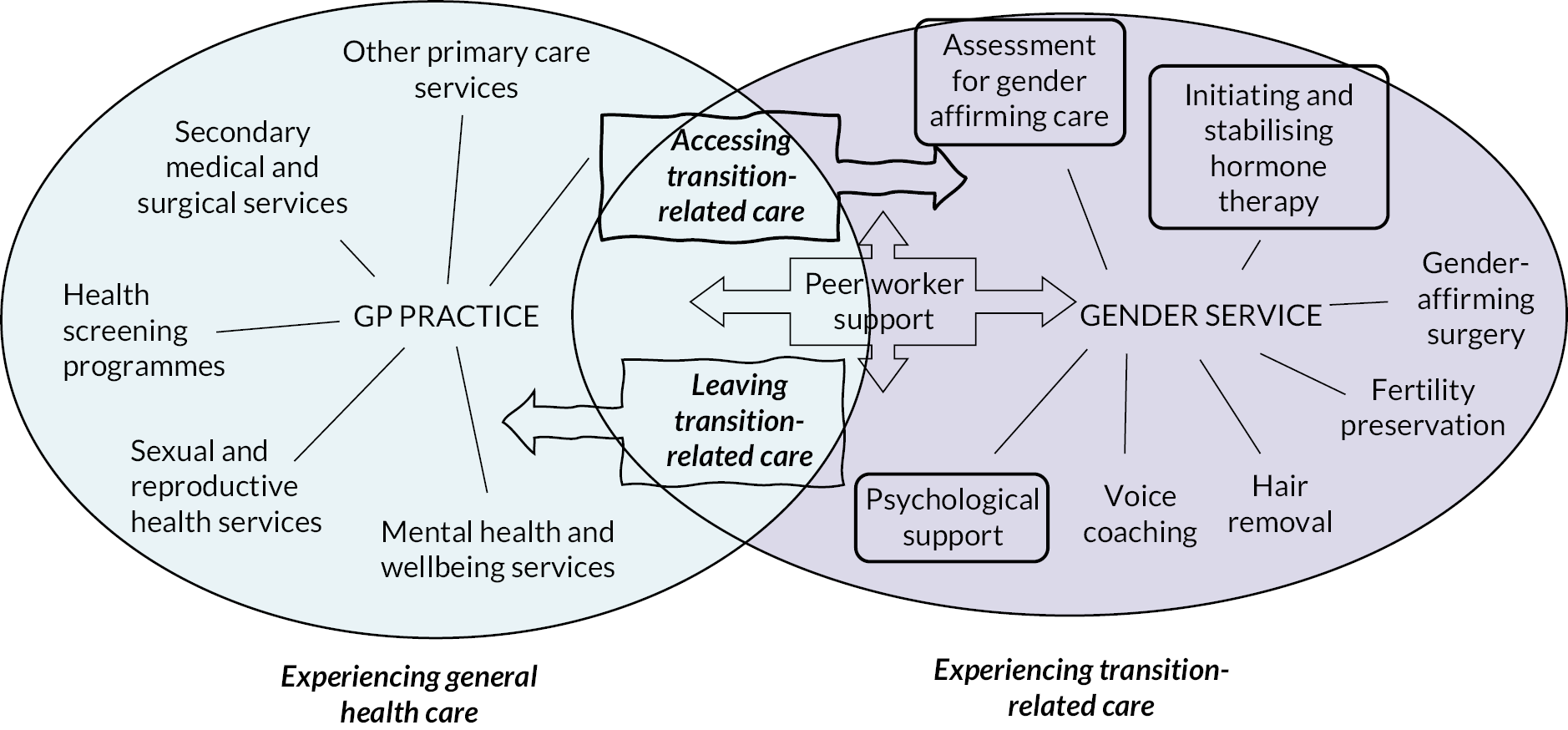
Figure 1 shows two overlapping ovals: one on the left, depicting what is involved in trans people receiving general health care; and one on the right depicting transition-related care. The two ovals are shown overlapping only slightly, reflecting how people currently have to find a way of navigating out of a general healthcare space into a specialist gender-service space. Showing the two ovals in this way is not intended to indicate how things should be, but rather how they currently are, in terms of how trans people access and use general and transition-related health care from NHS providers. Later in this chapter and in the final chapter of this report we will return to arguments about how transition health care should be far more integrated with the rest of health care, with greater overlap between these two ovals.
Figure 1 shows GPs as the co-ordinating agents for general health care, in the centre of the left-hand oval. This reflects NHS policy. It is the GP who has ultimate responsibility for referring someone to the services they need, authorising access and co-ordinating different strands of care. In the right-hand oval, we have shown a ‘gender service’ as having a similar role in co-ordinating different aspects of transition-related care, according to individual need. These aspects are the assessment for care, hormone therapy, gender-affirming surgery, voice coaching, hair removal and psychological support.
Again, the positioning of a ‘gender service’ in Figure 1 reflects what currently happens, rather than being a recommendation of what should happen. Up to around 2020, it was GICs alone among NHS organisations that fulfilled this role. Since then, pilot primary care services have been commissioned and have taken on providing or co-ordinating almost all of the aspects of care shown in the right-hand oval. It should be further noted, of course, that it is also possible for a private gender service to act as the hub of the right-hand oval – many of our interviewees felt they had no option but to engage with this non-NHS option. Further, many people access non-NHS services for general health care, such as therapy or counselling, or for transition-related care such as hair removal, while also accessing NHS services. The diagram also does not attempt to show aspects of statutory care or support outside of health care that may be very important to the overall experience of trans people, such as housing or benefits.
The terrain depicted in these two ovals is vast. The initiatives reported in Chapter 4 provide learning relevant to some key elements and their integration, but do not encompass the whole picture. In what follows, we summarise the learning with respect to four key areas, shown in boxes with bold surrounds in the diagram. These concern: how people gain access to transition-related care; how processes of assessment for care can be improved; how hormone therapy can be initiated and stabilised over an initial period of months; and how people can be supported psychologically. In this chapter, for each of these areas, we first summarise the dynamics of poor and unco-ordinated care emerging across the interviews. We then distil what has been learnt about how to improve and better co-ordinate care, drawing on the notion of person-centred co-ordinated care as the touchstone. Under each heading we also identify the issues and contradictions that have emerged and remain to be addressed.
A further section of the chapter summarises some limited learning from our case studies as to directions for improving other aspects of gender-affirming care, such as surgery, hair removal and fertility preservation. A final section then summarises what has been learnt about improving experiences of general health care, including the long-term management of hormone therapy and other longer-term aspects of trans health, both transition-related and non-transition-related.
Accessing and waiting for transition-related care
Dynamics underlying poor experiences
While we heard about some GP practices that were knowledgeable, supportive, sensitive and effective in referring people to a specialist gender service, the following deficiencies were repeatedly reported by service users, in both Chapters 3 and 4.
We heard about GPs who admitted to their patients that they did not know how to refer them to a GIC, or claimed erroneously that the person needed first to have a psychological or psychiatric assessment. This process has long been superseded in England, Scotland and Northern Ireland, more recently in Wales.
A related dynamic occurs where a GP simply refuses to refer someone, sometimes explaining this in terms of the trans person not knowing their own mind, appearing to believe that referral to the GIC commits the person concerned to a medical transition. In a few cases, GPs appear to have taken their authority to base a refusal to refer on their own anti-trans beliefs. We also found cases where trans people were told they could not be referred immediately because their BMI was too high, because they had a history of mental health concerns, or because the GP saw both of these as linked. Some TBPoC we spoke to experienced their ethnicity as making it more difficult to get a GP referral, within a general picture of having to persuade their GP to take their requests and experiences seriously. They were also likely to have been told that their BMI was a barrier to accessing health care, sometimes because clinicians seemed additionally concerned about a Black person’s BMI, or because clinicians were apparently unaware of how erroneous assumptions about the universal applicability of BMI can exclude Black people.
Another pattern we heard about frequently is where a GP apparently agrees to make a referral, but repeated follow-up by the person concerned reveals that the GP has not in fact made the referral or waited weeks or even months before doing so. Still another way in which trans people have experienced their GP as departing from putting the patient’s needs first is in writing a referral statement that undermines the integrity or identity of the person concerned. An example of this was a referral letter depicting someone ‘thinking about becoming a different gender’, when the person concerned was quite clear about their gender identity.
The idea of person-centredness is often used to consider the experiences of an individual passing through a health clinic or service. Our findings show that the experience of waiting between referral to a GIC and the beginning of an assessment process has possibly the most profound negative impact on the extent to which trans people perceive themselves as recognised and considered by the NHS.
We noted in Chapter 3 that the length of waiting as experienced by service users is not merely the time elapsed since a referral is acknowledged by a GIC, or even the time elapsed since a referral was made by the GP. Many people delay asking for referral via their GP for a significant amount of time, often years, for a variety of reasons. They may have in their own minds already been in a state of waiting long beforehand. For example, an individual may wait until they are certain which medical interventions they require before seeking a referral, meaning that for them they may have been waiting many years outside of the medical system. A feeling of being in suspense can be deepened by uncertainties already referred to as to whether the referral has actually been made by the GP or received by the GIC. We heard of several cases where, after an extended period of silence from the GIC, sometimes over a year, a waiting person has managed to contact the GIC and found out that the GP did not actually make the referral, or did so months later than originally indicated.
We saw in Chapter 3 that people on GIC waiting lists experienced anxious uncertainty, often severely. Waiting was deeply difficult due to living with untreated gender incongruence, the many ways in which this put life ‘on hold’, and awareness that the outcome of their GIC assessment was not ultimately under their control. This was all the more difficult for people living in family or community contexts which were unaccepting of or hostile towards their trans identities. Many trans people found that GICs, until quite recently, failed to provide updates on the likely waiting times, and are difficult to contact to get current information about when one is likely to be seen. This uncertainty leads to fears of losing one’s place in the waiting list, through missing a letter or an e-mail, or through the clinic making a mistake and not sending a communication, resulting in a missed appointment. Many of our respondents reported feeling unable to bear the continued wait, and so taking a decision to self-medicate with hormones or go to a private gender service if they could afford that. This option was, of course, more open to those in employment with reasonable incomes, and less open to the economically marginalised, above all TBPoC.
A further, often distressing, aspect of waiting was that associated with the minimum of two or more assessment appointments required in most GIC assessment processes. While diagnostic guidelines (e.g. DSM-5)7 refer to the need for stability of gender identity over a 6-month period, the capacity issues faced by GICs and the approach adopted to managing queues has led in some GICs to much larger gaps between diagnostic appointments, with still further extended waits for subsequent surgical assessments and other treatments. We therefore heard from people who had prepared in great anticipation for an initial assessment, received a positive signal about the likelihood of a diagnosis, and then realised there was yet further waiting before they could receive treatment. The experience of many was that they had already been waiting months or years prior to their first appointment, in a state of clarity and stability about their gender identity. The additional wait seemed to be ‘for the doctors’.
Many clinicians we spoke to were deeply concerned about the waits experienced by their clients. They were, however, relatively shielded from direct encounters with the anxiety and distress of those waiting. Some distanced themselves from feeling responsible, because there was apparently little they could do to improve the situation. Others were outspoken in their criticism of the NHS commissioners of their service, for completely failing to acknowledge that demand for services – in terms of numbers of referrals received – has grown by several hundred per cent in recent years. Commissioners were seen as expecting increased demand to be met within existing levels of resources or marginal increases.
This raises troubling questions about how the NHS and those who control its funding can tolerate waits of several years for trans people to receive treatment. Following the COVID-19 pandemic, there are widespread concerns when some physical health outpatient services have perhaps 8% of people on their waiting lists waiting a year or more for consultant-led treatment. 117 In mental health services, the proportion of people in 2020 waiting more than 6 months for assessment and treatment was 11%. 118 The only waits that approximate those for gender-affirming treatment were those for treatment for severe mental illness, commonly up to 4 years. All trans adults currently being referred for GIC appointments can expect to wait at least 4 years. We return in the final chapter to the societal dynamics that may underlie this.
The severity of the extent of waiting for GIC care is borne out by some ICTA modelling (reported separately) on a number of realistic GIC staffing models, based on typical current rates of referrals and referral backlogs. With some loosening of current assumptions that all people require two assessments before they can be prescribed hormones or receive other gender-affirming treatments, it appears that even with staffing at around 1.5 times that needed to meet current demand, the queues of people waiting will not be drained for between 3 and 4 years. The acceptability of such waits is widely challenged within trans and LGBTQI+ communities. This has also been taken up in a legal case by social justice campaigners,119 arguing that NHSE should honour the 18-week target time from referral to treatment for trans health care. The basis of the case is that failure to do so stems from an ideology that trans needs for health care are less urgent than others, linked to a belief that trans people should have plenty of time to achieve certainty. Our data from service users do not bear this belief out. Across our sample of over 100 service users from the various subpopulations reported in Chapter 3 and the case studies in Chapter 4, few appeared to arrive at their GIC assessments without a clear sense of their direction. Our interviews and consultations with trans people involved in the project also strongly suggest that those who do wish to take some time to explore their gender identity want to do so on a timescale much shorter than the waiting times currently typical of GIC pathways. Service-user interviews and focus groups provide ample evidence of the distress and indeed harm caused by waiting.
Learning from initiatives to improve access to more integrated transition-related care
Case Studies 3 and 4 in Chapter 4 both indicate that trans-informed training can result in GPs understanding how to respond helpfully and straightforwardly to requests from trans adults to be referred to a specialist gender service. However, even when some GPs in a practice have received training and shown they are able to make referrals, some of our service-user interviewees encountered other GPs in the same practice who were not well informed and made the process of referral unnecessarily difficult and stressful. The implication is that training needs to be readily available to all practice staff, both clinical and administrative, with an expectation that everyone will undertake training at least in the essentials of trans health care and referral pathways. Case Study 3 provides some evidence of the benefits of an accreditation system for badging competence in trans health care. It also suggests that periodic reviews of consistency in competence and knowledge across staff in a primary care practice are needed to ensure that trans people get the specialist referrals they are entitled to according to General Medical Council (GMC) ethical guidance. 120
Case Study 4 illustrates the value of having a framework for working relationships between a regional GIC and primary care practices, based on a network of practices that act as local centres of expertise. This network can be used to deliver advice to primary care practices experiencing uncertainty as to how to refer. In other contexts, we heard of primary care practices experiencing English GICs as unresponsive to requests for advice concerning referrals or the management of people waiting for GIC assessment. This was probably in part because English GICs all take referrals from any GP practice across the country, and, at least at the time of fieldwork, only a few areas had developed local networks of primary care expertise in trans health care for GPs to draw on.
The widespread experiences of people having difficulty gaining access to transition-related care reported in both Chapters 3 and 4 highlight the importance of third-sector services, employing mainly trans staff to provide support and advocacy for gaining access to care. Case Studies 3 and 4 in Chapter 4 illustrate the role of such services for people who simply want information on how to get a referral to a gender service, or who are experiencing barriers in getting access to care they have a right to, in particular bridging prescriptions. 121
In Case Study 4, third-sector workers brokered arrangements by which NHS LGTs prescribed hormone therapy for people who had been assessed by a private gender service, and provided blood tests to be monitored by the private service, under a shared care arrangement. This was crucial when the person’s usual GP had refused to participate in shared care. Similarly, in this same case, third-sector workers put people in touch with their LGT to provide a bridging prescription when they were self-medicating. There is a strong indication that the integrated way of working of the WGS, with regular meetings between staff from the specialist gender clinic, the LGTs and the third-sector support organisation, plays a key role in maintaining the standing and influence of the support staff within the system. It also allows the system to bring expertise to bear rapidly in assessing whether medical issues might complicate giving an individual a bridging prescription. This allows third-sector staff to be effective advocates in helping people access care. An implication is that support service staff, and in particular trans peer-support staff, need to be fully included as fellow professionals in the operational decision-making and development of a gender service.
A further useful mechanism at the point of referral to a GIC, emerging from Case Study 2, is a detailed MoU, issued by the receiving GIC, setting out GP and GIC responsibilities in the initiation and management of HRT. This is thus a tool for integrating care across the primary care–GIC boundary. Case Study 2 suggests this can be effective in dealing with GP resistance to hormone prescribing, through GIC staff intervening with the GP at a relatively early stage. However, in at least one case it led to the service user concerned being held in suspense while their GP practice took several weeks to agree to sign the MoU. This suggests the MoU on its own may have limited effectiveness and could create additional barriers to care, if not reinforced by education of GP practices on their responsibilities for supporting trans patients.
The challenges of being referred to a GIC and having the framework for shared care agreed between a GP and a GIC are, of course, only part of the picture emerging from our research about the difficulties trans people face in accessing care. It is important to note that the GMC ethical guidance for GPs in trans health care120 indicates that it’s a GP’s responsibility to support people while waiting for GIC assessment, referring them to a mental health service if they have concerns on that front. Our research did not uncover any examples of GP practices able to put such supports in place. And across our interviews there is strong evidence that many local mental health services are not well equipped to support trans people in general, including when experiencing distress during the extraordinary wait involved.
Our case studies indicate some learning about how third-sector trans peer-support workers can deliver support during waits. However, support appears more difficult to deliver with integrity when all concerned are aware that it does not deal with service users’ main concern, the months and years they have to wait.
Case Studies 2 and 4 show how peer-support workers have delivered a number of forms of support: practical support, with issues such as using a deed poll to change one’s name; emotional support for people experiencing isolation, distress, or having difficulties with family relationships or housing; social support, for people who want access to trans-led events, activities or groups; and information about the GIC assessment process, including where people are in the waiting list and what to expect in clinical assessment appointments. Peer workers have achieved this through one-on-one support meetings, often by phone, and through facilitating trans groups and activities. The positive experiences of the trans swimming group described in Case Study 2 suggest that such trans-led group activities can deliver important contributions to well-being. Funded trans peer workers have a vital role in understanding community needs and then brokering the funding and delivery of activities that meet them. This, however, needs to be set in the context of the need for much better access to both transition-related medical care and adequate mental health services. Peer support is not a substitute for either, and needs to avoid transferring unreasonable responsibility for providing care to lower-paid trans community members.
The case studies also indicate issues involved in providing peer support to people waiting for assessment. First, staffing needs to be adequate. The level of demand for this kind of support is indicated in Case Study 4, where we heard that around 700 out of 1000 people on the waiting list indicated that they wanted to talk to a support worker, whereas a single full-time-equivalent peer-worker post was actually able to engage with around 300 people over roughly a 12-month period. The consequence, seen in both cases of peer-support services, was that response times were considerably longer than the workers considered desirable.
Second, we saw that it may be difficult for peer workers to contact people on waiting lists, particularly if people have been waiting for months or years and their contact details are held by the NHS GIC. Data protection requirements mean that an NHS organisation has to seek consent before passing any details to a third-sector support organisation. Third-sector LGBTQI+ organisations may have highly developed skills in soliciting contact through social media and attending existing trans events and forums. However, there remains the challenge of contacting more isolated trans people who do not attend events or use social media. These may be the people who are most in need of support.
Third, we saw evidence that the role of peer workers involves considerable social skill in navigating a kind of ‘dual belonging’, to trans communities and to an NHS-based system of care. Peer workers may be called on both to explain what is involved in an NHS assessment, and to hear the distress of people who have been waiting an unreasonable amount of time and do not feel their ‘transness’ requires extended assessment. Peer workers can experience themselves as deeply compromised in their ability to advocate for people, when employed by a GIC with power over the timescales by which people can be recognised as trans, and ultimately over whether this recognition is bestowed. This situation is made less stressful when peer workers have some agency and influence within the GIC system. This may take the form of having ready access to information on how to access bridging prescriptions and to the clinicians involved, or access to the NHS administration of waiting lists. The latter allows them to respond with clarity to someone anxious about their position on the waiting list.
A final area of challenge that remains to be addressed concerns the common lack of local mental health services adequate to support a trans person on a GIC waiting list who is experiencing mental health difficulties. Peer workers may be trained in how to identify someone who needs more than the kind of emotional or social support they themselves can provide. However, the lack of effective mental health services that someone can be referred to places peer workers – and their clients – in a very difficult position. We return shortly to the implications for how mental health services need to develop.
Assessment for gender-affirming care
Dynamics underlying negative experiences of assessment
In Chapter 3, we summarised the characteristics of trans people’s negative experiences of GIC diagnostic assessments. A significant number of service-user interviewees found that their experience of GIC diagnostic sessions strayed, to varying degrees, beyond the bounds of what could be interpreted as ‘person-centred’, becoming adversarial and even hostile. A common aspect was being asked the same questions on multiple occasions about childhood, family background and a person’s sense of their gender at different points in their life. Some experienced this as being under suspicion, that clinicians were trying to catch them ‘in a lie’ or find a flaw in their ‘story’ of being trans. This kind of repeated questioning can amount to a microaggression44 because it belittles a trans person’s account of themselves through asking for it repeatedly, rather than joining with their first-person authority. 53 It also serves to undermine the development of a collaborative relationship between trans person and clinician, rather leading to one where the trans person chooses to offer or withhold information strategically, based on what they believe the clinician will respond positively to, leading to a desired result.
A more serious failure of person-centredness occurs in some of the accounts we heard. In these, people experienced themselves as questioned in-depth about a history of childhood sexual abuse, and then confronted directly with the proposition that their trans identity is the result of this. In Chapter 3, we discussed the lack of evidence to support the link between childhood abuse and trans identity, and the danger of further stigmatising trans people through implying it. Interviewees experienced this as unrelated to the issues they were currently facing in moving forward as a trans person, and distressing and destabilising in restimulating earlier traumas, often without appropriate support. Similarly, intense questioning about their difficulties in being accepted in family, school or other social contexts could leave people feeling vulnerable and unsupported.
It is possible to relate the potential for harmful interactions of this nature to the frameworks of guidance and institutional frameworks within which GICs are expected to operate. These were summarised in Chapter 1.
These can be seen as placing contradictory pulls on clinicians’ roles and accountabilities.
First, clinicians are charged within the NHS service specification with diagnosing whether someone has gender dysphoria, in the face of evolving guidance and standards that have moved away from the idea that being trans is a mental health condition or any kind of disorder. Davy and Toze122 point out that the diagnostic criteria for gender dysphoria set out in DSM-5 do not clearly separate out the diagnosis of distress from the identification of a trans identity when distress is not present. They further argue that the evidence for the reliability of the symptoms listed as indicating gender dysphoria is at best weak. Since no underlying research evidence has ever been made available by the APA working group responsible for DSM-5, the published criteria are ‘primarily reliant upon clinical consensus’, which is considered by the APA as a relatively weak form of scientific evidence. 122
Second, clinicians are expected to challenge a person’s sense of their gender identity. They should consider whether there are ‘alternative mental health diagnoses’ that might apply. The Royal College of Psychiatry Good Practice Guidelines12 seem to recommend lines of investigation that suggest looking for the cause of a trans identity in childhood trauma or some form of sexual repression. We have already referred to scholarly critique of the latter idea and in Chapter 3 to critique of there being a link from childhood trauma to a trans identity. Further, we note the lack of reference to evidence of mental health conditions that might explain a trans identity in any of the four guidance documents summarised in Chapter 1. Clinicians we spoke to were all clear that when people decide to detransition, not only is this extremely rare, but in most cases this is because of family or community hostility to their trans identity.
Some clinicians we spoke to were very aware of possible legal challenges to their diagnostic decision-making. Such concerns may be reinforced by NHS Trust management anxious to avoid future litigation when someone may claim they should not have been deemed by an adult GIC as able to give informed consent to gender-affirming treatment. While this led some clinicians to emphasise their responsibility as diagnosticians, it did not appear to alter their view that misdiagnosis was very unlikely.
A further layer of explanation of the distressing nature of many of the assessment experiences we heard from trans people may lie in clashes of understanding about what it is to know that one is trans. Riggs et al. 38 analyse the history of the development of gender services and the very limited role of trans people in the shaping of frameworks, standards and services. They argue that trans people have gained access to gender-affirming treatment through a shifting series of compliances with norms of what it means to be trans, referred to as transnormativity. For example, the notion of the ‘transsexual’ and the transition from a ‘male sexed body’ and gender role to a ‘female sexed body’ and gender role, underpinned the services offered by the early GICs in the USA and UK from the 1960s onwards. Riggs et al. trace this to the influential work of Harry Benjamin,123 a white, male and cis psychiatrist. While the role of trans people as activists in creating the social environment needed to recognise these services was significant, and there were a few prominent trans supporters, including funders, there was little or no trans professional input. The understandings of trans identities in the diagnostic guides described in Chapter 1 are arguably mainly those of cis professionals. Riggs et al. identify as central the underlying assumption that trans identities needed to be diagnosed by a professional from the ‘psy establishment’. 123 They further argue, drawing on Pearce,124 that ‘to obtain the treatment they sought, patients needed to first articulate their experiences in a manner that would be taken seriously by the predominantly middle-class, White, cisgender male psychiatrists and clinical psychologists who oversaw these institutions’. 123 We found very similar perceptions among many of our interviewees.
As we discussed in Chapter 3, Bettcher53 argues for a more radical break with the idea that professionals have the authority to pronounce on whether someone is trans. She proposes that trans identities should move beyond transnormative ideas rooted in the societal norm or ‘natural attitude’, where one’s male or female gender identity and role signify which kind of genitalia one possesses. Rather, identities stem from the first-person authority of a trans person’s account of their gender identity and the bodily, social and medical actions they want to take to express it.
This perspective suggests how we can understand the distressing experiences of GIC assessments within our sample. Trans people may encounter clinicians who, in pursuing a line of inquiry that seeks to find an ‘alternative diagnosis’, seem unable to take in what the trans person is saying about themselves. Further, clinicians may ask questions that trans people experience as an unwarranted invasion of confidential matters concerning their sexuality. Such assessment experiences stifle rather than enhance exploration and development of trans identities, sometimes becoming mired in an enactment of transnormativity, as service users try and second guess what clinicians are looking for, to enable their treatment. There seems to be a fundamental clash between some forms of psychiatric or psychological practice, based on the idea of expert diagnosis of a disorder, and the kinds of knowledge about self and its expression through the body that trans people develop. This can be seen as underlying the distress that many of our interviewees expressed at having to account for themselves to cis clinicians who have the right to pronounce on whether they are actually trans. Where this clash comes to the fore, any notion of ‘person-centredness’ goes by the board. As Bettcher53 puts it, the trans person experiences a denial of authenticity, of their own account of themselves as trans.
Learning from an initiative with collaborative assessment
A central aspect of Case Study 4 in Chapter 4 concerns the approach to assessing people for access to gender-affirming care, including hormone therapy, which differs significantly from the negative elements of psychiatric diagnostic assessment described above. It has clear advantages in setting a person-centred approach, and is also consistent with the more positive and collaborative experiences of assessment summarised at the end of Chapter 3. We return shortly to the links between this approach to assessment and a more person-centred and co-ordinated way of managing the initiation and stabilisation of HRT in primary care.
There are three main respects in which this approach to assessment emerges as beneficially patient-centred. The first is that, for many people, the assessment can be considerably shorter than we heard was common experience with other GICs. In the GIC in Case Study 4, assessments can be based on a single assessment appointment with a single gender clinician. We heard that around half of the people entering assessment had a treatment plan after a single assessment, because their treatment goals were clarified, and there were no complicating medical issues. The fact that blood tests were easily arranged through local primary care practices integrated with the gender service made it straightforward to clarify if there were endocrinal issues. We return shortly to the issues raised by clinical decisions to extend an assessment with one or more further appointments.
The second and perhaps most important aspect concerns the collaborative and gender-affirming approach used by clinicians in interacting with the person being assessed. Clinicians emphasised their respect for trans identities, their focus on jointly clarifying treatment goals based on sharing information about options, potential benefits and medical risks. They recognised they needed to screen people for mental capacity to understand treatment options and consent to them, but did not, for example, foreground exploration of past trauma as a possible ‘alternative explanation’ of a trans identity. They also recognised and sought to minimise the inherently traumatic nature of any kind of medical assessment for a trans person, who will almost certainly have suffered repeated microaggressions in past healthcare encounters.
Clinicians also sought to relate to service users in ways that de-emphasised differences in power, rather than directly asserting their medical authority and knowledge. Shuster (p. 195)125 draws attention to the importance of clinicians working collaboratively with trans people’s own knowledge and experience on issues such as the effects of hormone therapies, avoiding claiming spurious authority and maintaining humility about the extent or reliability of medical knowledge on many aspects of trans health care, including, for example, the long-term effects of HRT.
The third beneficial aspect of the assessment process concerns the use of videoconferencing for the assessment appointments themselves, combined with basic physical data and blood work collected from the person during a separate trip either to their own GP or gender-specialised primary care clinic within their locality. This way of working emerged in part in response to the restrictions of the COVID-19 pandemic, but places much less of a time and travel burden on the person being assessed. This contrasts with some of the experiences reported in Chapter 3, of people having to travel long distances at considerable expense to attend a GIC assessment, often worrying that transport difficulties will result in missing their appointment and losing their place on the waiting list.
Overall, this assessment approach appears to have been experienced as low in stress for the limited number of service users experiencing it we were able to interview. The emphasis on collaborative decision-making, fostering of mutual trust and exchange of knowledge in the clinician–service user encounter, and joint exploration of desired effects and risks of treatment, are markedly similar to the assessment approaches documented by clinics in the USA126 and Australia127 which espouse an ICM. As we saw in Paradigm 3 for the future of trans health care in the last chapter, under an ICM no formal diagnosis of gender dysphoria is required in order to access gender-affirming treatment. In these examples of ICMs, assessment by a clinician still takes place but its focus is on sharing relevant information and establishing that the person concerned has mental capacity to consent. 28
Clinicians in Case Study 4 recognised that they were practising a gender-affirming approach to assessment within a formal NHS context that required them to give a diagnosis of gender dysphoria. They were not working formally within an ICM. Yet, in a variety of ways, they distanced themselves from the idea that they were working according to a psychiatric diagnostic model. They variously described the diagnosis itself as ‘tokenistic’, ‘something that surgeons like to see’, or an indication of ‘governance for the decisions we make with patients’. They can be seen as conforming with ambivalence, even reluctance, to some of the requirements of the institutional field they were operating within. 47 At the same time they can be seen as holding themselves accountable to other emerging institutional pressures, in the sense of socially held bodies of knowledge as to what are acceptable ways of practising. 128 While we did not collect data directly on the content of the regular consultations between the gender service in this case and representatives of trans communities, these can be seen as a way of institutionalising how trans voices and trans community knowledge can be involved in the articulation of a respectful and productive approach to assessment. And the collaborative approach to assessment can also be seen as drawing on parts of institutional guidelines such as the ‘Good practice guidelines for the assessment and treatment of adults with gender dysphoria’12 and the international WPATH Standards of Care Version 7. 13 This selective use of existing institutional supports and engagement with new networks and norms can be understood as part of a process of innovation and moving towards new norms of trans health care, as has often happened in other areas of health care. 48 We may speculate that future institutional guidance for trans health care will continue to move to a much clearer espousal of collaborative and non-pathologising processes of assessment, that recognise the authenticity of trans identities and experience. The emerging evidence of the benefits of the assessment approach in Case Study 4 supports such developments.
This case study also revealed learning as to substantial issues that need to be addressed in developing this kind of model. Above all, it raises ethical concerns about how to avoid collaboration being on offer to the more privileged and medically articulate, but overridden by medical authority for trans people who are seen as in some way less trustworthy or less able to explain themselves.
One set of issues concerns the basis upon which decisions are made that someone will need a more extended assessment, including at least one further appointment with a gender clinician. It was not possible in our interviews with clinicians to explore in-depth how far such decisions to extend assessment could always be collaborative, as opposed to in effect required by the clinician. The prerogative of an assessing clinician to require a second appointment raises concerns in the light of experiences reported in Chapter 3 of extended assessments over which trans people felt they had little control, and for which there did not seem to be valid reasons. Some older trans people reported how they were required to attend a series of assessment appointments, apparently because they had not transitioned at an earlier age; some chronically ill people were also given additional GIC assessment appointments. TBPoC reported their assessments at GICs becoming complicated over issues because their chosen, culturally meaningful, name apparently did not convey a sufficiently binary gender identity. In Chapter 4, the NI case study also reported how some people avoided disclosing mental health concerns because they judged it would lead to a more extended assessment. There was also evidence of this in Case Study 2.
In discussing and interpreting findings from across the ICTA project, members of the PPI group and other trans people involved in the research or as advisers have raised strong concerns, based on trans community experiences, about the way clinician prerogative to extend assessments can be used. The concerns are twofold: first, distorted clinician perceptions of the risk involved in gender-affirming treatment; and second, a tendency for some clinicians to fall into a kind of ableism that sees certain groups of trans people, regrettably often those most stigmatised, as not able to know their own minds or best interests. We briefly explore both these areas of concern below.
In terms of perceptions of risk, some cis clinicians emphasise the need to take time over an assessment to be sure that a person will not regret their transition, or to establish whether there could be an ‘alternative explanation’ of gender incongruence stemming from a mental health condition. The rationale is that it is necessary to protect an individual against the risk of undergoing gender-affirming treatment that they might later regret. However, medical practice takes a more accommodating stance on the risks of possible regret taken by cis people who are keen to undergo plastic surgery or fertility enhancement, for example. Psychological evaluation is not required for either treatment. Further, many cisgender clinicians do not appear to take similar account of the risks of delaying gender-affirming treatment in terms of mental health deterioration. These risks are apparent in some of the service-user experiences reported in Chapter 3.
Possible explanations of this particular way of evaluating the risks associated with hormone therapy lie with the social stigma still widely attached to being trans, the lack of value attached to trans identities in a cis-normed society28 and indeed the possibility of clinicians being subject to hostility in the media or in a legal context, from anti-trans individuals or groups. However well-intended, cis clinicians can experience themselves as held accountable for validating someone’s trans identity in the face of anti-trans currents in society, which view being trans as something best avoided and likely to carry a risk of regret in the future. This view is not supported by reviews of outcomes of gender-affirming treatment. These have repeatedly demonstrated the widespread benefits to mental health, the very low incidence of regret, and that this is most often linked to poor surgical outcomes or experiences of social stigma or rejection. 129
Second, there is concern that cis clinicians can make decisions about delaying or even denying access to gender-affirming care based on what has been called ‘subtle ableism’. Shuster125 found that even within US clinics that espoused informed consent for accessing trans health care, clinicians could fall into reasserting their medical authority because they distrusted the rationality of their trans clients:
Justifying their rationale was the subtle ableism that providers brought into the clinical encounter with trans people. In asking their patients to resolve mental health issues first, or referring to mental health issues as a ‘co-occurring’ conditions, [they] revert back to paternalistic medicine where ‘doctor knows best’. 125
Related concerns have been expressed by trans people within our extensive sample of interviews and reinforced in consultations with members of trans communities. These include that clinicians can misinterpret someone’s uncertainty about treatment goals, or uncertainty as to whether they have a binary or non-binary identity while still being sure that they want hormone therapy, as an indication that a diagnosis should be delayed. Further, such situations may arise for autistic people, people with learning difficulties, people with mental health conditions or who use substances, and people who live in trans-hostile family settings or communities. This can lead to these most vulnerable groups being subject to additional scrutiny or even denied transition-related care.
Further research is urgently needed to clarify what forms of assessment are appropriate for these groups of trans people who clinicians may see as having an impaired ability to understand and consent to specific treatments. These are groups who typically experience multiple forms of stigma across many settings, including health care. Addressing these inequalities requires developing forms of assessment which do not discriminate unfairly against them in accessing gender-affirming treatment. Such forms of assessment need to balance giving access to treatment with thorough and collaborative exploration of intended goals, likelihood of benefits as well as the medical and social risks. Assessments also need to identify needs for additional social and psychological support to accompany gender-affirming medical care. The integrity of such forms of assessment will depend on the availability of these additional forms of support, in contrast to the stories of limited support reported in Chapter 3.
It is worth noting that these issues in assessment for trans people in groups subject to multiple forms of stigma may be just as pressing for gender clinics working explicitly within some versions of an ICM. 28 Such clinics have been functioning in the USA for many years29,115 and more recently in Australia, and operate within published protocols, which are compatible with the WPATH Version 7 Standards of Care. 13 While emphasising collaborative and patient-centred decision-making, these protocols also require the assessing clinician (usually a GP) to screen for mental health conditions and recommend referral as needed to a psychologist before prescribing hormones. 126,127 In recent research in an Australian clinic working within this framework, levels of user satisfaction with care were high, but slightly lower among the 8% of service users asked to undergo assessment with a psychologist before receiving gender treatment. 116 The grounds given for most of these extended assessments concerned a recent history of post-traumatic stress disorder or schizophrenia. The Callen-Lorde protocol126 similarly allows for extended assessment in cases where the clinician judges that the person is not yet able to give informed consent.
Initiating and stabilising hormone therapy
Dynamics underlying poor experiences
Across our case studies and interviews with the national sample of service users, we heard many examples of GPs who refused to prescribe hormones recommended by private gender services, or to prescribe bridging hormones for people waiting for assessments, on a harm-reduction basis, despite guidance on how to do so from GIC websites and national bodies. 12 This refusal affected people who were self-medicating and others who had been receiving hormones via a private gender service that proved no longer viable.
We also heard some examples of people whose GPs refused to sign a shared care arrangement with a GIC, with GIC clinicians monitoring blood hormone levels and recommending what should actually be prescribed. Sometimes initial refusal to be involved in shared care led to delays in hormone prescribing. All of these can be seen as GPs refusing to take up a role in a nationally specified model of co-ordinated care for trans people, leaving the person concerned anxious and unsure how their care is to be carried forward. The cause in all of these circumstances appears to be GPs feeling that any involvement in prescribing hormones for trans adults is beyond their competence and an unreasonable responsibility for them to shoulder – even if specialists are also involved. This is borne out by several of our interviews with more enlightened GPs, who expressed frustration that many of their colleagues appear swayed by spurious fears about links between hormones and cancer or thromboembolism, based on problems with earlier forms of HRT prescribed to cis women.
More generally, both service users and GIC clinicians reported breakdowns in the process of administration of hormones. GPs or practice nurses might fail to recognise specific hormones being prescribed or to understand their role in administration or monitoring. Even going to the retail pharmacy to pick up what had been prescribed could be a fraught experience for a trans person. There was the possibility – and in some cases the actuality – that the pharmacist would require an explanation, in earshot of whoever was listening, as to why a hormone was being prescribed to someone who did not appear to fit with the licensed use.
A separate but related issue occurs where someone who has been discharged from GIC care and has been receiving prescription hormones for an extended period, then relocates and signs up with a new GP practice. They may encounter a GP who simply refuses to continue a long-established repeat prescription.
A related breakdown in care co-ordination concerns flows of information needed to review and manage hormone therapy under a shared care arrangement between a GP and a GIC. We heard both from service users and GIC clinicians about repeated difficulties in GIC clinicians obtaining in good time the results from blood tests carried out within a GP surgery, prior to consultations intended to review dosages. Service users reported that changes to dosages that were important to their continued transition and well-being were being postponed until the next scheduled appointment usually months ahead. GIC clinicians felt that a significant amount of their time was spent chasing blood test results to get them in time for an appointment.
We also heard about a reciprocal dynamic, with problems about information flows from GICs to GP practices. Service users were also often uncertain and anxious about when or indeed if their GP practice would hear about a recommendation from the GIC to change a hormone prescription or dose. Several reported resorting to carrying documented details of the change physically into their surgery and making sure they were passed to their GP.
Learning from initiatives to improve hormone therapy initiation and management
Case Study 4 in Chapter 4 reports on the establishment and initial development of regional primary care clinics, spread across Wales, which take responsibility for prescribing and monitoring HRT for trans adults following assessment at the specialist gender clinic. This is the most significant initiative we studied to address lack of integration between an assessing gender service and arrangements for prescribing and monitoring HRT. The key features are as follows. Their effectiveness and efficiency would appear to be of wider relevance to other gender services and NHS primary care commissioners.
The regional clinics were largely staffed by GPs, located within established GP practices and funded by the local NHS. They took responsibility for prescribing hormones, monitoring blood tests and titrating doses immediately following assessment, aiming to pass service users on to their usual practice after around 12 months, on the basis that their doses and prescriptions would by then be stable. This arrangement avoids the costly and damaging difficulties in communication between GICs and primary care practices over blood tests and dosage changes, experienced by many people attending other GICs. It also frees up gender specialists to devote more time to assessments, rather than review appointments for people already on hormones. Local clinicians, however, worked in an integrated way with their specialist colleagues, attending joint training on trans health care, and holding regular joint clinical consultations.
Further advantages emerging from this arrangement include the regional clinics rapidly becoming established as having GPs confident in prescribing under shared care with a GIC, whether based on a full GIC assessment or on the basis of a ‘harm reduction’ bridging prescription. These more knowledgeable GPs can then advise and educate colleagues in their own and neighbouring practices. Above all, both service users and GPs involved in these regional clinics were enthusiastic about how they brought HRT for trans people into the mainstream of primary care. Doctors in the regional clinics helped service users deal with a range of health issues, and hormone therapy came to be experienced as part of primary care, rather than something specialised, difficult, or in any way stigmatised.
The development of these regional clinics at the time of fieldwork raised some issues that remain to be resolved. Significantly, a DES arrangement was created, to provide a contractual basis for local GP practices to take on service users with stable hormone prescriptions once they were discharged from the regional clinic. However, there appeared to be low take-up of the DES in some regions, possibly because GP practices experienced a combination of the national staff shortages and increasing workload as other clinical areas have responded to NHS-wide policies of transferring more care for chronic conditions from secondary services to primary care. Lack of widespread primary care education about the relatively straightforward realities of much trans health care also appears to have played a role. While the arrangements in Case Study 4 were not at the stage where there were many service users as yet ready for transfer from the regional hormone management clinics, the need to increase the capability of the wider GP system to manage hormone prescribing remains a pressing issue for the near future. The idea of GP practices nominated to provide trans healthcare expertise for a locality, acting as a kind of hub for a cluster of other practices, emerged in both Case Studies 4 and 5 as an interim step. This would ensure that, if a trans person found their existing GP practice unable to support them, they would not have to travel far to find one that could. The increased use of videoconferencing and telephone appointments in health care generally during the pandemic can also be a means for increasing the accessibility of trans-inclusive health care across localities.
The trans-led primary care TAS reported in Chapter 4, Case Study 3, indicates how wider GP capability in trans health care can be strengthened. In particular, the linking of higher levels of accreditation to competence in hormone prescribing for trans people, including bridging prescriptions, appears to have been effective in motivating GP practices to increase their capability. Case Studies 3 and 4 both suggest that GP motivation to engage with trans health care is often linked to a general commitment to be inclusive and overcome health inequalities. This suggests directions for promoting trans healthcare training and competence development. A further enabling factor appears to be the ready availability of backup expertise in areas such as HRT. While the conurbation GP practices in Case Study 3 were frustrated at their difficulties in communicating with GICs, they were able to tap into local networks of GPs who had taken a lead in trans health care, as well as an emerging regional primary care-based specialist gender service. This suggests that primary care TASs need to be linked to local sources of specialist expertise.
Finally, a consistent theme of difficulty across a range of attempts to improve the integration of hormone therapy with GIC assessment concerns lack of integration of electronic patient records. In Case Study 2 in Chapter 4, a GIC achieved limited success by adopting one of the most-used digital systems that allows primary care practices to share patient records and notes with a secondary or specialist clinic. This facilitated ready communication of test results, revised prescribing recommendations and the answering of queries between GPs and gender specialists. The coverage of primary care practices using this ‘shareable’ system nationally was not, however, extensive enough to avoid common situations where test results had to be chased by clinicians, or service users had to lean on their GPs to catch up with changed prescribing recommendations. Even in Case Study 4, where there was some organisational integration between the regional prescribers and the central specialist service, the primary care patient record system could not fully support the level of clinical collaboration taking place. Much of this had to be carried out and documented by e-mail. Problems of lack of digital support for integrated working are not peculiar to transition-related care for trans people. It will be important for gender services and their primary care collaborators to learn from solutions emerging in other branches of health care.
Mental health and psychological support
Trans healthcare dynamics with negative impacts on mental health
In Chapter 3, we reported data from the ICTA national survey of over 2000 trans adults as to the disproportionate mental health burden commonly experienced by trans people. We saw, for example, that the occurrence of people within the sample who had received treatment for severe mental health conditions from community mental health teams was over ten times the prevalence in the general population.
We also presented evidence from our data as to the causes of this amount of mental illness. Interviews and focus groups with trans people revealed the impact of pervasive transphobic interactions in society and the unfortunate role of health services in adding to this to the extent of causing harm, sometimes manifestly damaging mental health and sense of well-being. Interviewees described experiencing in healthcare settings the same transphobia and microaggressions as in other social contexts, and how this led them to mistrust healthcare providers, leading in some cases to a spiral of deteriorating mental and physical health. Microaggressions included being misgendered, deadnamed or subjected to transphobic assumptions (e.g. about sexual history). More subtle undermining could take the form of health professionals being overly curious or questioning about trans status when transness was not medically relevant, or making presumptions about trans health or identity that effectively dismissed a trans person’s knowledge of themself.
We have already in this chapter reviewed the mental health burden placed on trans people by their multiyear wait for specialist care, and by further waits during the process of assessment. We have also discussed how the process of making a gender dysphoria diagnosis, carried out in non-collaborative mode, can itself be a microaggression, because people experience having to prove their trans identity. In Chapter 3, we argued that this creates negative mental health impacts.
Chapter 3 further brought out the kinds of affective and interpretative labour that trans people commonly have to engage in, in order to get the care they need from both transition-related and other branches of health care. The demanding nature of this labour places people under further stress, particularly for the most marginalised who may find the barriers to accessing care are more pronounced and the dangers of not getting the care they need more distressing.
Across the service-user interviews and focus groups reported on in Chapters 3 and 4, we found a significant number of trans people articulating a further unmet need in terms of the kind of mental health support available to them from health services. This concerned the need for ‘gender counselling’, a place to explore their gender identity and/or feelings about how to express it more fully, bodily and socially. This crucial unmet need stemmed from widespread assumptions that this kind of open, person-centred exploration would not be possible with a professional who was also carrying out a diagnostic assessment, or even with one who was not actually responsible for diagnosis but still worked for a gender assessment organisation, such as a GIC. Some people were aware that they might receive some helpful independent counselling from a third-sector LGBTQI+ or trans organisation, but that they would otherwise struggle to find or afford the kind of counselling help they sought.
Learning from initiatives to improve and integrate mental health support
One of our ICTA case studies concerned the provision of psychological support within a GIC. It reveals learning as to what is possible in terms of improving mental health and well-being support during the process of assessment and beginning gender-affirming treatment. It also indicates unresolved issues and unfilled gaps in mental health support.
In Chapter 4, Case Study 2, we saw that groups, both face-to-face and online, can be devised using trans-affirmative enhancements to established group therapy techniques such as CBT. Such groups can help emphasise a sense of connectedness between participants, who are likely to be experiencing a degree of social isolation in their day-to-day lives. They can also facilitate the sharing of knowledge and expertise about how to tackle everyday challenges of trans lives, and encourage people to experience compassion for themselves and others about progress with such struggles. Groups of this kind have been designed and delivered by cis clinicians, but informed by consultations with a panel of trans service users.
The achievements of such groups, however, need to be set in the context of the breadth and depth of mental health need within the trans population. Groups of this kind are targeted at trans people experiencing relatively mild forms of anxiety and depression. The extent of more severe mental ill health within the trans population indicated by our survey indicates significant need that this kind of group work does not claim to address.
Psychologists working with the GIC concerned were clear that more severe mental health conditions needed to be met by other, general NHS mental health services, such as Increasing Access to Psychological Therapies and Community Mental Health Teams. There were, however, significant problems of co-ordination of care. We saw that people often came to the GIC having had very negative experiences of general mental health and psychotherapy services – for example, being told that their trans identity meant they could not be treated by a mainstream mental health service. In response, GIC psychologists formulated referrals for trans people to their local mental health services, asserting their needs and that the local mental health service was the appropriate place to address these needs. GIC psychologists claimed to have been successful with this approach. However, they also expressed concern that many clinicians in mental health services lacked understanding of how to work with people who experienced minority stress and transphobia in particular. This suggests that lack of availability of NHS mental health services appropriate for trans people who most need them continues to be a major concern.
We also heard about the availability of individual counselling within a GIC, to help people explore unresolved issues concerning their transition – for example, how to work with difficult family or other relationships. Based on the limited number of service users we interviewed who had experienced this, this kind of support helped trans people address the social and psychological aspects of their transition. As with the psychology groups, people who participated in receiving support after receiving diagnosis were able to do so with little apparent anxiety that whatever they disclosed to staff would affect their continued access to gender-affirming care. However, there was evidence across our service-user interviewees, and also from some clinicians, that service users do not feel safe disclosing or discussing complex facets of their identity to anyone involved in their diagnostic assessment, or to anyone who might be involved in team discussions about them. Further, some clinicians are painfully aware of the difference between being in an assessor role and in a therapist role. The implication is that effective psychological support for trans people needs to be clearly separated from the system for accessing gender-affirming care.
Experiences of other gender-affirming procedures
None of our case studies focused primarily on attempts to improve the integration of other aspects of gender-affirming care, such as surgeries, hair removal, voice coaching or fertility preservation. These all consistently emerged as highly problematic areas across our sample of service users and need to be addressed by further initiatives and research.
For both upper and lower surgery, the very small number of NHS surgeons able and available to carry out either transmasculine or transfeminine procedures added further extended waits, and often meant that people had to travel long distances from their homes for surgery. This added to their financial burden, particularly if they needed to arrange accommodation for an initial recovery period. Undergoing surgery away from home also meant being away from established networks of people who might help them during recovery. We further noted in Chapter 3 the impact on TBPoC of the lack of inclusion of Black and Brown people in indicative images of post-surgery results.
In Chapter 3 and in Case Studies 4 and 5 in Chapter 4, we also noted how insufficient funding of hair removal undermines the whole system of care for transfeminine people. The need for hair removal is experienced as fundamental to a sense of well-being and being safe in transphobic society where there are constant threats of violence. Most trans people end up funding their own hair removal with significant financial impact. In Wales, there was at the time of writing no funding for any hair removal, and elsewhere people estimated that the amount of funding available for the NHS covers only a small proportion of what people actually need. Older trans women with grey hair, those with light hair, and those with darker skins need considerably more sessions, and often laser treatments are not effective, with more expensive electrolysis required. It is the people more likely to be poorer who face the greatest financial burden if they are to achieve the hair removal they need. These are also the people most likely to be exposed to harassment and violence in their daily lives.
Across the sample of service users, we heard of several examples where GPs appeared to interpret a recommendation from a GIC, that a trans person attend a fertility preservation clinic before beginning hormone therapy, as over-riding the person’s wish to begin taking hormones as soon as possible. The GIC in Case Study 2 in Chapter 4 undertook an initiative to improve the integration of care in this respect by encouraging service users to make an informed decision about fertility preservation well in advance of their second assessment appointment. This GIC also worked with service users’ GPs to advise them on local policies for funding gamete storage and drafting IFRs if needed.
Experiencing general health care
Experiences of general practitioner practices
Throughout our service-user data, as reported in Chapters 3 and 4, while we heard some examples of highly effective care received from GP practices, we heard many more examples of trans people experiencing various ordeals. This could lead them then to avoid health services in general, with potentially highly damaging impacts. We have already discussed the common difficulties in obtaining a referral to a GIC. Beyond this, many people experienced being misgendered by receptionists and clinicians, having difficulties in changing their name and pronouns in their patient record, and not being referred for cancer screenings that were appropriate for them because the practice had not taken account of their trans status. Above all, in Chapter 3, we noted the cumulative impact of repeated microaggressions of this nature on trans people’s mental health. These microaggressions are likely to be compounded and particularly severe for TBPoC and also particularly significant for trans people living in rural contexts, who may effectively have no choice about the GP practice to attend.
Case Study 3 in Chapter 4 described a trans-led approach to training and accrediting GP practices to address these deficiencies. We interviewed some clinicians and receptionists who had begun to work with a new understanding of health inequalities faced by trans people and the pressing need to ensure that trans people are welcomed and included by their primary care practice. This led to administrative systems that readily reflect trans identities and clinical practices that ensure that people are asked appropriate and respectful questions about their general health concerns, without making assumptions about links between gender identity and anatomy. We also heard examples of the benefits of this kind of intervention for trans people, who experienced inclusive patient registration systems, the use of a trans status marker on their record to make sure that they were invited to appropriate screenings, practice staff using correct pronouns at all times, and respectful conduct of screenings that might otherwise lead to dysphoric experiences.
In both this case study and in the experiences of local primary care practices specialising in trans health care in Case Study 4, some service users have also begun to experience trans health care as appropriately integrated into the everyday life of a GP practice. Some clinicians saw this as reflecting what is possible when delivering trans health care in a primary care setting, as one aspect of person-centred care. This contrasts strongly with the idea that trans health care is something that is specialised and particularly difficult, to be separated out from the mainstream of health care within a GIC.
While Case Studies 3 and 4 illustrate the potential for improving how GP practices support trans people, they also indicate how much remains to be done. Within the small sample of service users we interviewed in each case, we heard experiences of inconsistent practices and standards of care. Some people experienced difficulties in getting their names changed on patient records, or were deadnamed or misgendered, depending on which members of the practice they were dealing with. We also heard about the damaging impact of these inconsistent experiences given the history of microaggressions that trans people typically experience – emerging trust in a GP practice can be easily undermined.
Experiencing secondary services
In our service-user interviews, we heard some examples of trans people experiencing respectful care from a specialist medical or surgical discipline, on a matter not directly related to their transition. We also heard examples of an apparent complete breakdown in communication between a specialist medical or surgical team and surgical team responsible for lower surgery, with issues unresolved or both transition-related and non-transition-related surgeries held up seemingly indefinitely because neither team was willing to take any initiative. None of our case studies, however, addressed initiatives to improve the experiences of trans people with secondary medical and surgical services. This area too requires further research.
Chapter conclusion
This chapter began by mapping the terrain of trans health care, in terms of how people move between general health care and transition-related health care. It then summarised the dynamics underlying experiences of poor care and the learning that has emerged from our case studies as to how to improve care and its integration within four areas: accessing transition-related care; undergoing assessment for gender-affirming care; initiating and stabilising hormone therapy; and mental health support. We also summarised what our data have revealed about how to improve general health care from GP practices for trans people, and its integration with transition-related care.
The final chapter of this report summarises the conclusions of the ICTA project against the RQs set out in the first chapter. It draws out the implications of the learning described in this chapter for improving the integration of health care for trans adults in the future.
Chapter 6 Conclusions and implications
Introduction
As set out in Chapter 1, the ICTA RQs are addressed as follows.
RQ1. What is the range of models recently used in the UK for providing integrated care for meeting the specific health and well-being needs of trans people?
This was addressed in the Report on WP 141 and paved the way for identifying the initiatives to improve care studied in this project. Figure 1 in Chapter 5 summarises the current picture in terms of how elements of transition-related and non-transition-related care are typically organised.
RQ2. Which factors make services more or less accessible and acceptable to the variety of trans adults who need them?
In Chapter 3, we summarised findings from interviews with trans people, purposively sampled to include older people, people with chronic health conditions and disabled people, people living in rural areas, people with a low income or a low educational attainment, and Black people and people of colour. We identified key factors that make health services difficult to access or which lead to problematic, unacceptable and even harmful experiences of care. These included GP practices failing to treat trans people respectfully or understand their identities, health concerns and referral routes for transition-related care; the extraordinarily lengthy waiting times for GIC appointments once referrals have been made; the extended nature of GIC diagnostic assessments, which can seem to doubt that trans people know their own minds; the difficulties of receiving psychological support within a GIC system experienced as seeing a mental health condition as a reason for delaying gender-affirming treatment; and mental health services that appear unwilling to treat trans people simply because they are trans.
Overall, trans people can experience themselves as being regarded in one part of the health service as highly responsible for their own health, as active participants in health care expected to educate their GP about their health concerns or how to make a referral to a GIC. Yet elsewhere, at a GIC they can experience themselves as denied their own voice as to their needs, until these have been corroborated by a clinician. This places contradictory burdens on trans people already managing the effects of stigma in many social settings. In Chapter 3, we reported ways in which these dynamics can be compounded for the groups of trans people who are the most stigmatised in society. In Chapters 3 and 4, we further saw ways in which hormone therapy can be seriously affected by breakdowns in collaboration between GICs and GP practices.
RQ3. In the different integrated service models, how effective are the different aspects of services and their interaction in meeting the needs of people at different stages of their gender transition and at different ages?
The benefits and unresolved issues stemming from the initiatives to improve aspects of health care for trans adults and their integration are set out in Chapter 4. In Chapter 5, we presented these initiatives as aspects of a system of trans health care, while also identifying other important aspects which we were unable to study within the current project.
RQ4. What lessons emerge as to how models for providing integrated care can be successfully implemented and further improved in meeting the needs of trans people, within limited resources and continuing constraints resulting from the COVID-19 pandemic?
The remainder of this final chapter focuses on answering this RQ.
Table 11 in Appendix 10 summarises the learning from six kinds of initiatives for improving aspects of trans health care, emerging from the cases discussed in Chapters 4 and 5. It summarises the potential benefits, the unresolved issues arising in practice, and possible future developments.
In what follows, we consider the implications for the three paradigms for the future of trans health care identified in Chapter 4 (Table 5). We first explore how the benefits summarised in Appendix 10, Table 11 could be further realised by extending these initiatives within the current model (Paradigm 1 from Chapter 4), where most transition-related care is delivered through accessing a tertiary gender service, a GIC. We also summarise the issues that remain unaddressed by the initiatives we studied, above all the need to address the huge challenge of waiting times and the backlog of people waiting. We further set out the learning from our research about how to implement service improvements effectively through the participation of trans staff and trans communities.
We then explore the implications of the initiatives in Appendix 10, Table 11 for improving trans health care delivered through primary care-based gender services (Paradigm 2 from Chapter 4) and through services that move beyond a diagnostic model to one based on informed consent (Paradigm 3 from Chapter 4).
We conclude by setting out the limitations of the ICTA project, outlining its implications for future research, and identifying some of the key challenges in moving trans health care forward. This includes further reflection on the partial extent to which the project addressed EDI issues.
Implications for improving current arrangements (Paradigm 1)
The wider take-up of each initiative shown in Appendix 10, Table 11 will improve the degree to which trans people experience person-centred care within the current model of needing to be referred to a GIC. Widespread training of GPs in trans health care and the referral pathway, the establishment of local lead practices as centres of expertise, and the establishment of regional trans-led support services delivered by third-sector organisations would considerably improve the experiences of trans people approaching the NHS.
Moves toward a collaborative approach to assessment appear to be possible within the existing, albeit contested, requirement for a diagnosis of gender dysphoria. Case Study 4 in Chapter 4 suggests that a collaborative assessment can for many people be completed within a single appointment with a clinician. Further, if the relevant routine health checks, including blood tests, needed to screen for complications with hormone therapy, are carried out by a local GP and data passed to the gender clinician, it is possible to conduct assessments virtually, using videoconferencing. This can be of considerable benefit to service users, in terms of saving travel time and expense, and may also allow clinicians to work more effectively.
Indications from our interviewees, consistent with many other studies,129 suggest that the risks of regret of people who undertake gender-affirming procedures are very small, and there is nothing to indicate that an affirmative approach to assessment adds to them. Rather, a quicker and more collaborative approach is likely to have benefits in terms of lessening and shortening the distress trans people often experience before and during assessment, improving their mental health, as well as alleviating the mental health burden caused by long waits. It is also likely to reduce the extent to which trans people feel they need to present themselves as free from mental health concerns such as anxiety or depression, meaning they can feel freer to seek timely mental health support. Trans people may also feel more able to express their identity congruently, rather than experiencing pressure to conform to transnormative or binary stereotypes.
Closer links between GICs and GP practices serving a locality will provide a more integrated system for initiating and monitoring hormone therapy and other gender-affirming treatments. Further, across localities widespread training of GP practices in trans health care, in particular the use of hormone therapy, will make it easier for trans people to receive continuing therapy from their GP throughout their lives, once discharged from an initial period with a ‘locality lead’ practice.
Widespread training of local NHS mental health professionals in carrying out psychological therapies in a trans-affirmative manner will greatly improve the ability of trans people to access existing, albeit severely stretched, NHS mental health support. This would ensure trans people have equal access to services that may be more appropriate than GIC psychology teams.
The combination of these initiatives for improvement will have an even greater impact in making care consistent and co-ordinated. The intricacies involved make carrying out a detailed cost benefit analysis for any of these initiatives, or comparing them with a null state, very difficult. However, none of these initiatives are inherently costly, compared to currently commissioned services, and all could be included within existing commissioning frameworks and plans. The issues and possible future directions identified in Appendix 10, Table 11 are also tractable – services and commissioners should be able to find ways to make progress with them, taking account of the analysis set out in Chapters 4 and 5. The future possibilities emerging from the case studies, as listed in Appendix 10, Table 11, in fact cover most of the suggestions from interviewees for improving the current GIC system reported in the final section of Chapter 4 and in Tables 7 and 8 in Appendix 9. Additional ideas for service improvements from the latter list concern: the wider availability of hair removal treatments, which are needed for any lower surgery, as well as for the removal of facial hair; and surgical procedures that protect the everyday safety of trans women or transfeminine people, such as facial feminisation surgery.
The unaddressed issues: waiting times and access to surgery
Such developments and their incremental contribution to delivering person-centred co-ordinated care, however, need to be set in the context of the enormous waits for treatment trans people have experienced. We have seen repeatedly in our data the distress and often deep despair this causes. Many trans people feel compelled to ‘go private’ for assessment and prescription of hormone therapy, and/or upper and lower surgery, often when they can scarcely afford to. Others have resorted to self-medicating with hormones bought from internet pharmacies or shared with them through trans communities. Our interviews with service users, even in the initiatives to improve care, indicated how common it was for people to feel they had no option but to find a way of accessing hormones privately before they even got to their first GIC assessment. As one put it, it was apparent at their welcome workshop at the GIC that:
… half the people here are already three-quarters of the way down the line […] already transitioned and living full-time and probably on HRT … and you’re saying that you do this assessment … and it’s like ‘the horse has bolted’.
Many professionals working with trans people have told us they feel profoundly compromised by this state of affairs.
Based on the experience of the WGS reported in Chapter 4, an approach to assessment for hormone therapy based on the possibility of a single clinical opinion and assessment appointment would help clear waiting lists and reduce waiting times. However, the thousands of people already waiting in the system across the UK mean that, even if this practice were adopted widely, it would still take several years for waiting times to reduce.
Our research suggests that the dynamics giving rise to such waiting times are complex. The rising numbers of referrals and a relatively static level of resourcing for specialist services play a role, but need to be looked at in the context of a wider debate as to what exactly should be invested in. Many of the initiatives summarised in Appendix 10, Table 11 have implications for making assessment and treatment less costly to deliver, as well as more person-centred to receive. And the frameworks for delivering transition-related care described below, under Paradigms 2 and 3, also have significant potential for simpler, more flexible assessment processes with less reliance on particular groups of senior staff. Increasing the financial resourcing of trans health care cannot therefore be separated from consideration of the models that would allow people quicker access to care.
Above all, there is an underlying question of the relative priority of trans health care within NHS budgets, set against many other pressures, in the post-pandemic context. There are growing backlogs of elective care in many areas and huge demand pressures on acute services. Even in this context, as we noted in the previous chapter, the duration of waiting experienced by trans people is extraordinary. In Chapter 4, we saw that in Northern Ireland a complete absence of referral opportunities has been regarded as tolerable by the NHS for several years. As one service user put it, with heavy irony, there is a common misperception that being trans is a choice, and therefore not a priority: ‘… it’s not just a delay because there don’t happen to be enough surgeons. It’s a delay because it’s us, and we’re no one’s priority because we’ve chosen to be in this situation’. Some clinicians too suggested that current anti-trans currents in society were affecting NHS priority-setting, leading to reluctance to increase funding for GICs.
All of this suggests the need for commissioners and health service policy-makers to reflect on the value – or lack of it – that is being placed on meeting healthcare needs of trans people when allocating resources. The current backlogs imply a perspective that trans identities are in some way undesirable, marginal or optional for the people involved – society should not place meeting the needs of trans people at the same level as other mental or physical needs. Ashley et al. 28 contrast this with a perspective that sees trans identities as part of normal human diversity, to be supported out of commitment to social justice for a stigmatised minority, and indeed to be treasured. Such a perspective prompts re-evaluating how healthcare resources are allocated, however strong the competing pressures.
An area for further exploration in justifying greater expenditure on gender services is that of the costs to other services – particularly mental health services – of having thousands of people waiting several years for treatment. Exploring these costs and the potential for reducing them was beyond the scope of this project. However, as reported in Chapter 3, a high proportion of the 2000 trans people who participated in the ICTA survey were using, or wanting to use, mental health services. In Chapter 3, we argued that the experience of waiting has in many cases intensified this mental health burden. The costs of investing more in trans health care should therefore be set against the benefits of freeing up the capacity of overstretched mental health services, with potential impact on reducing waiting for these services, leading both to human and economic benefits as more people receive treatment more quickly. There are additional considerations of the costs of waiting emerging from our interviews in terms of the likelihood of GIC administrative errors and rework needed when people on the waiting list change their address, or when their medical records are misplaced as time passes.
The initiatives we studied did not include making inroads into the additional long waits most trans people experience for upper and lower surgery. These were, however, mentioned frequently by service users, many of whom paid large amounts of money for private surgery, often overseas. For many trans people, surgery is an essential healthcare need, and part of the picture of co-ordinated care that needs to be addressed. While the ICTA project can claim to have contributed to distilling knowledge about how to improve access to assessment and the initial stages of hormone therapy, it can only claim to have revealed the need for further initiatives in the provision of upper and lower surgery. The planning and development of the clinical workforce needed appears to be one important element, given the shortage of providers. A better regional distribution of the surgical facilities appears to be another, reducing the distance that many people currently travel for major surgery.
Trans participation in shaping and providing services
In Chapter 4, we reported widespread views from interviewees that there should be more trans people working in GIC staff roles, whether as gender clinicians, nurses or support workers. Most of the service users we interviewed perceived that the great majority of GIC staff they met were cis. Many indicated that they did not trust cis GIC clinicians to understand the experiences, perceptions and needs of trans people. A stronger trans staff profile, still more evidence of trans people in senior clinical positions, would be an effective intervention in this dynamic.
The GICs participating in Case Studies 1, 2 and 4 in Chapter 4, and the primary care training and accreditation initiative in Case Study 3, have all in different ways sought to involve people from trans communities in shaping their provision. These provide indications for others to build on as to how to make sure trans perspectives are reflected in clinical and administrative practices. In Case Study 3, a coproduction group of GIC staff and service users examined proposals for new service offerings. In Case Studies 3 and 4, trans communities were represented on overall steering boards, to which staff involved in taking initiatives forward reported progress and were held accountable. In Case Study 4, attempts at community accountability were made by having a trans community member on all staff appointment boards, and also present at all training sessions for GPs. These were seen as steps toward staff operating within a framework of supporting trans rights and understanding trans perspectives and cultures.
In Case Study 4, we saw how the new gender service in Wales has been developed by an expanding and innovating network, which brings together representatives of trans communities, clinical and third-sector leaders and health service policy-makers. This network shares a moral commitment to trans rights and overcoming health inequalities experienced by trans people, as the basis for improving trans health care. Its members also appear to hold in common some central cognitive frameworks and operational concepts. These include the ideas of affirmative practice, and of a network of regional primary care clinics and third-sector support agencies working together with a hub specialist gender clinic. The well-articulated moral justification and trans participation in creating it are arguably key features that other services can learn from. This may well provide the basis for progressive recruitment of a higher proportion of trans staff.
Implications for primary care gender services (Paradigm 2)
Three gender services based in primary care clinics have been piloted in England since 2020. The pilot schemes are open to people who are already on GIC waiting lists, and attend a GP practice within a catchment area defined for each scheme. These services intend to offer trans health care that is ‘local, timely and easier to access’. 130 They initially offered diagnosis of gender incongruence and access to hormone therapy. They work within the NHSE Gender Identity Service Specification and so require people to have at least two assessment appointments with a gender clinician, usually a GP who has undertaken additional training. Some services have rapidly moved on to offering referrals for top surgery and one of the two sign-offs required for lower surgery. People still need to go through a GIC for the required second gender specialist sign-off for lower surgery. Like the gender service in Case Study 4, and the primary care training scheme in Case Study 3, all three pilot services emphasise the extent to which there has been trans community participation in their design and implementation, and the degree to which trans people are involved in professional roles and in oversight or governance bodies.
While these services are still at the stage of trial and evaluation, some important aspects of their future potential as well as issues they may need to address emerge from our analysis of the initiatives studied within the ICTA project.
First, these primary care gender services appear to reflect the thinking summarised in Chapter 4 and in Appendix 9, Table 9 under Paradigm 2 for the future of trans health care. Many people will have been aware of these services being designed or even initially implemented when, during their ICTA interviews, they offered their thoughts about desirable future arrangements. These pilot schemes appear to offer a closer integration between everyday health care and transition-related care, with a prominent role for GPs in carrying out assessments. We have seen in Case Studies 3 and 4 the advantages of this, with symbolic benefits to affirming trans people, as well as medical benefits in terms of co-ordinating transition-related care with other aspects of health care. Above all, this marks a kind of institutional shift in trans health care away from being the specialist domain of psychiatrists and clinical psychologists.
Primary care gender services, coupled with strong trans participation in design and delivery also appear to offer an environment conducive to the practice and further development of the kind of collaborative approach to assessment reported in Case Study 4, and identified in Chapter 3 as more acceptable to service users. Currently the NHSE specification still requires a minimum of two assessment appointments. The evidence of Case Study 4 is that this aspect of the specification could fruitfully be revisited, in that for many people one such appointment allows all aspects of an assessment to be covered, particularly for people who have in fact been living with full expression of their trans identity for several years, waiting for an assessment. This would increase service capacity.
The new primary care-based gender services have also already incorporated trans peer-support roles, including the role of care navigator. 130 This is consistent with the finding from our case studies that peer-support workers are most effective when clearly integrated into the administrative structure of a gender service, and so able to mediate effectively in getting information on waiting times and giving support in making and rearranging appointments. The new services also offer professional psychological counselling, often delivered by trans staff. This appears to be kept separate from the process of assessing people for access to gender-affirming treatment,130 consistent with the learning from the initiatives we have studied. This kind of arrangement appears to have great potential for meeting the need for ‘gender counselling’, for people who feel they need professional support in thinking through their gender identity or goals for gender-affirming treatment, independent from their assessment for access to gender-affirming medical treatment. As reported in Chapter 4, this was identified by several interviewees as a largely unmet need within the current GIC system. The implication is, however, that primary care services will need to continue to make it very clear that psychological support is independent of the assessment process and confidential.
The development of a cadre of therapists and counsellors able to support trans people, with trans-affirmative therapeutic approaches, also raises the possibility of developing this kind of capability within local NHS mental health services more generally. This will be an important avenue for future exploration, to address the difficulties reported in Chapter 3 that trans people commonly experienced in accessing effective mental health support.
Figure 2 summarises these possibilities for improving the integration of care through local primary care gender services.
FIGURE 2.
Possibilities for experiencing integrated trans-affirming health care.
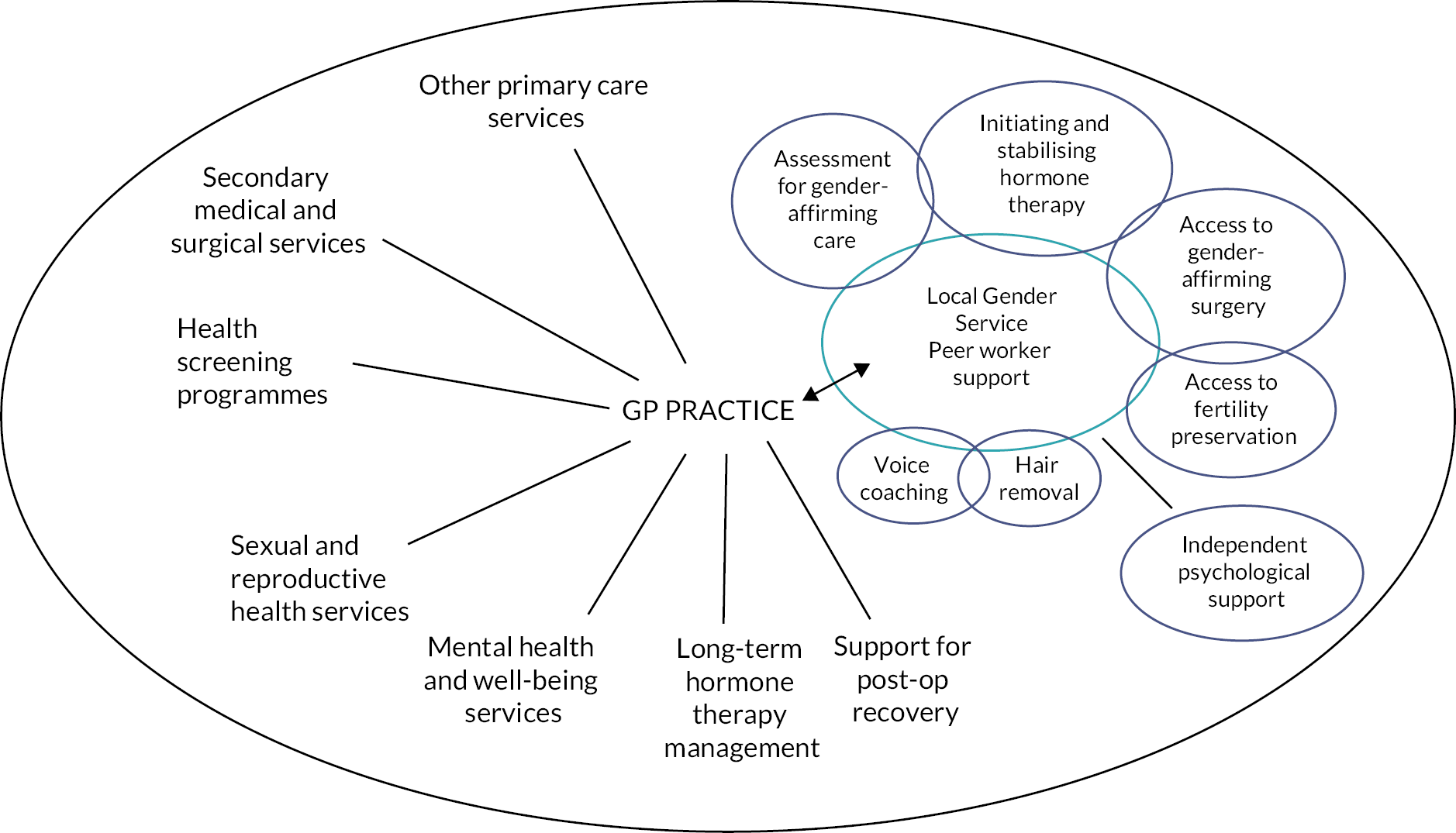
Our findings illuminate issues to be resolved in the development of this model. Currently, at least one of the pilot schemes is connected with an established GIC,130 with GIC clinicians acting in an advisory and supervisory capacity to GPs. This raises the question of what the continuing role of GICs would be if primary care gender services expand. A possible answer suggested by several of the GIC clinicians we interviewed is that GICs would in time shift to primarily a supportive role, with most people seen by primary care gender services. From our interviews, some trans people felt it was important that the option should remain to request a more extended assessment by a tertiary service. However, many others were very clear that this was not an option they would value.
As we saw in Case Study 4, primary care services are also likely to need to resolve how to achieve transparency in clinical decision-making as to when it is appropriate to extend an assessment and to find ways of doing this in a way that respects person-centredness. It will be important to avoid the impact of ableist assumptions that, for example, neurodivergent people, those with pre-existing mental health conditions or trauma history and people with learning difficulties are less able to know their own minds, and so require further assessment. This model could give rise to a two-tier trans healthcare system with more marginalised people facing increased delays that could impact their mental health.
A further important area of challenge concerns how to support service users, typically from multiple stigmatised groups, who face adversity in their family or community context in moving forward with expression of their gender identity. If regret following transition is often linked to hostility experienced or breakdown in relationships, how can it be made possible for them to transition according to a timescale that they themselves choose? What kinds of support or connection to trans community activities can be facilitated to help someone facing this extremely difficult situation? It is likely to be trans support staff who are called upon to engage with such complex, fraught circumstances, and it is important that they have resources available for doing so, including training in the cultural competences required to work with marginalised groups.
The key role of GPs in primary care gender services places trans health care in the midst of a highly problematic aspect of NHS staffing, the national shortage of GPs. Throughout this research, we heard of GPs keen to take on responsibility for trans health care, but also wary of widespread concerns among their colleagues that many practices are short of staff and at the same time being expected to take on additional clinical procedures that many hospital-based specialisms have identified as best carried out in primary care. Gender services are not alone in appreciating how population health and well-being can be more effectively delivered through earlier intervention in primary care, moving more assessment, monitoring and control of long-term conditions into the realm of GPs and their immediate colleagues.
One response to this situation is to argue that the development of primary care gender services adds further weight to the case for investing more in the training of GPs and in campaigns that emphasise the value and intrinsic rewards of general practice as a career choice for medical trainees. Another, however, is to explore the viability of alternative primary care staffing models. Many clinicians we interviewed were clear that people with either a general nursing or psychiatric nursing background would be well equipped to carry out gender assessments, with appropriate training and supervision. This would reflect the increasing role of nurses and nurse practitioners in primary care in general. Further, there is a strong case for developing forms of medical supervision for non-prescribing nurses working in assessment so that they are readily connected to prescribing expertise.
Another promising possibility is the involvement of primary care nurses or clinical pharmacists in prescribing and monitoring HRT for trans people. Across our case studies, we saw that hormone prescribing and management for trans people is performed by clinicians with diverse specialisms. Endocrinologists, psychiatrists and GPs operate in this area with confidence, on the basis of endocrinological knowledge common to most areas of medical practice. They coupled this with their experience of understanding of what works for most people who want to undertake various kinds of transitions. We found GPs who had developed trans healthcare expertise, having previously worked with hormone prescribing for cis people with various medical conditions. We also found psychiatrists or GPs with trans prescribing expertise who described how even endocrinology specialists working in general hospital trusts often lacked an understanding of the needs and experiences of trans people concerning hormone therapy, and so did not, for example, have in-depth knowledge of the implications for effective titration of doses. This prominent role for experience-based knowledge suggests that non-medical prescribers could readily take up a role within a supervised framework of HRT prescribing, once they had gained practical experience.
Several clinicians questioned the appropriateness of nurses becoming prescribers for hormone therapy. Some felt that, given the ‘off label’ nature of such prescribing, this was ‘a specialism too far’ for nurse prescribers. An implication is that further integrating trans health care within primary care requires revisiting of the contexts in which hormone therapy is seen as normal and safe, and further clinical research and guideline development if necessary. The ‘off label’ nature of HRT for trans people would then no longer be necessary.
Implications for moving beyond the diagnostic model (Paradigm 3)
The issue of whether the future of trans health care should be based around a diagnosis of gender incongruence (or gender dysphoria, according to which guideline is invoked) is one of the major controversies emerging from our research. We saw at the end of Chapter 4 that there is a substantial body of opinion within trans communities that the requirement of a diagnosis for access to hormone therapy or other kinds of gender-affirming procedures is a denial of trans people’s right to assert their own identity. Ashley112 argues that it is simply dehumanising:
Referral requirements for HRT treat self-reports of gender dysphoria not as one would treat reports of normal mental experiences, but as one would treat reports of mental illnesses […] treating gender dysphoria in this way is pathologising and, because it pathologises normal human variance, dehumanising. 112
In Chapter 3, we argued that both the impact of years of waiting for diagnosis and negative experience of diagnosis itself can cause iatrogenic harm, that is harm from the healthcare system itself. Some trans people expressed a positive experience of GICs, particularly in cases where their trans identities were affirmed and transitions supported. In other cases, trans people experienced clinicians as asking potentially intrusive questions but believed this was a necessary part of the process and done respectfully. Some found clinicians receptive to what they were saying, without imposing categories or norms. While we do not know if our sample was proportionately representative of the relative frequency of these different experiences in the wider population of trans people passing through GICs, it was clear that the negative experiences were in the majority in our sample.
In Chapter 5, we attempted to make sense of these patterns by identifying the characteristics of the system of assessment and diagnosis itself which can undermine trans adults’ self-authority and inhibit their authenticity, through raising questions about whether their experience of gender might stem from some form of pathology. One implication is that more positive experiences of collaborative assessment, where trans people feel their perceptions are being validated, may occur because the clinicians involved have adopted a stance and method of working that allows affirmation of trans experiences, and enacts that they are valued. This can be seen as occurring despite, rather than because of, some aspects of the lines of questioning or topic guides for assessments set out in various guidelines. It may also be that some groups are treated more affirmatively than others, with data from Chapter 3 suggesting that trans people who are Black, people of colour, non-binary, neurodivergent or trauma survivors may experience more antagonistic, less affirmative care.
The case for an ICM for accessing gender-affirming medical treatments is that it shifts medical assessment still further away from considerations of pathology, and does so at the level of the system of care rather than relying on the discretion and commitment of clinicians. We have not studied an ICM of care within the ICTA project – we were not aware of one operating within the UK. However, based on related initiatives that we have been able to study, and limited literature available on experiences with ICMs elsewhere in the world,115,116 we can see a case for arguing that this approach offers benefits in facilitating person-centred, co-ordinated care.
First, ICMs appear to have the potential to combine a person-centred focus on the goals of care with medical diligence and authorisation of treatment. As Ashley et al. 28 point out, even the strong form of an ICM does not amount to ‘hormones on demand’. While ICMs can take many forms, and there is a need for further research,28 it appears that in many forms there is still a clinical assessment involved, but not one that involves a diagnosis related to a trans identity. Clinicians must ensure they have fully disclosed all information relevant to treatment goals being discussed, that their client has understood this and that they have the capacity to consent to chosen options. Examples of clinic protocols126,127 were referred to in Chapter 5.
Second, effective co-ordination of care could be achieved by locating an ICM within the kind of primary care gender service described in the preceding section. A primary care gender clinic working according to an ICM would be highly consistent with the ethos, described under the previous heading, of normalising trans health care as part of primary care, rather than constructing it as a specialised tertiary service. Such primary care clinics could affirm trans identities as part of normal human diversity.
Third, ICMs are highly relevant to political debates within the UK (and elsewhere) about changing the legal basis for gender reassignment to one of self-identification. If this were to become law, gender reassignment would no longer require, as under the current Gender Recognition Act (GRA),131 that two members of the MoJ list of gender specialists have diagnosed the person with gender dysphoria. This would greatly reduce the legal role and significance of gender dysphoria diagnosis. Further, its role in providing a basis for access to NHS resources, and using NHS resources in the lengthy process of assessment, might then be questioned on two additional grounds. An ICM is compatible with the WPATH Standards of Care, particularly in its most recent revision, Version 8. 132 And GPs or other doctors in community settings prescribe NHS treatments in other clinical areas, such as antidepressants, abortion, or indeed HRT for cis women experiencing the menopause, because there is evidence, following a process of exploration of the likely benefits and risks, that these are helpful to well-being. There does not need to be a specialised diagnosis of pathology.
These potential benefits and associated issues require further exploration by policy-makers and clinicians, working together with trans communities. An important focus for future research will be to study the experiences of trans people going through such clinics, with qualitative richness similar to that achieved in our ICTA interviews.
In this spirit, it is worth reflecting on a further likely advantage of moving beyond the diagnostic model. Many of the experiences of service users we heard about were dominated by their sense that they had to present at assessment appointments in a strongly binary-gendered way, and talk about their history in a way that would allow a clinician to ‘tick the diagnostic boxes’. Many trans people are keenly aware of a collective narrative that GIC clinicians are unlikely to understand their needs and perceptions as trans people. Whether grounded in the realities of current GIC practice or not, there is a legacy of distrust, coupled with many trans people experiencing a pronounced power imbalance in the clinical encounter – clinicians control the authorising of their diagnosis and access to the care they need. This, at best, inhibits free discussion and person-centred care. At worst, it leaves people in despair and traumatised.
An additional potential benefit of moving beyond the accumulated distrust associated with the current system of assessment is that there could be a rather freer exchange of information between clinicians and service users as to what the latter are learning about different ways of delivering hormones and dosages. Our interviews and consultations suggested that trans individuals and communities have developed a considerable body of informal practice-based knowledge about the impact of different dosing and delivery methods in hormone therapy. Yet some people are reluctant to share what they are discovering because it might be seen as acting irresponsibly and affect their continued access.
Our research findings also suggest some issues that will need to be addressed in the development of ICMs.
The first is that clinics and clinicians able to operate within an ICM will still need to respond to people who want professional support in clarifying their gender identity and treatment goals. As with the primary care clinics described under Paradigm 2, they will need to offer appropriate counselling. The issue of separating this from diagnostic assessment would become much less of an issue. It is also likely that some people will want to go to someone perceived as having clinical expertise and have a form of diagnostic assessment. This, however, would be at the request of the service user, not a requirement.
Second, in Chapter 4, we alluded to the issues that may arise when, even under an ICM, a clinician forms a view that someone lacks capacity to give informed consent, or where a medical practitioner is of the view that treatment is actually dangerous for purely endocrinal reasons, and the person concerned is both aware of this and still wants to proceed. Tensions between person-centred control of care and medical responsibility and norms of decision-making may remain. Such tensions are, however, present in other domains of medical care.
Limitations and implications for further research
This research involved collecting in-depth qualitative data from over 180 trans users of health care and over 50 healthcare professionals, and interrogated a substantial and purposively sampled body of data to understand the dynamics underlying experiences of poor and better care. The data collected was sufficient and appropriate to achieve the research objectives, despite difficulties during the COVID-19 pandemic in recruiting participants and gaining access to some intended case studies. These findings are of broader relevance to helping a wide range of health services improve the care they provide for trans people. Above all they are vital for avoiding the kinds of iatrogenic harm to trans people, revealed in our interviews, that can unfortunately occur across a range of NHS contexts.
That said, the research does not claim to represent the full variety of experiences of receiving or providing trans health care across the UK. The case studies did not, for example, include any of the NHSE pilot primary care gender services, which were established after this research was designed. While our findings have a considerable amount to offer in understanding the issues likely to be encountered by gender services operating according to some version of an ICM, we were unable to study such a service – there were none operating within the UK during the period of the research. We have already indicated the need for further research into the benefits and issues emerging with such services.
A further set of limitations and implications for future research concern the extent to which we succeeded in engaging with the profound EDI involved in trans health care. The following section addresses these.
Implications of equality, diversity and inclusion issues in this research
We noted in Chapter 2 that this research is fundamentally about EDI in health care. It concerns how the NHS can provide care that better includes trans people and addresses their diverse needs. Across the strands of our research design, we made efforts to recruit service users subject to multiple forms of social stigma, including being disabled, Black or a person of colour, or having low educational attainment. It is through these experiences that the majority of EDI issues in service provision are revealed. Reflecting on the research, however, reveals limitations in how far we included diverse trans voices and perspectives. For example, we made no attempt specifically to recruit neurodivergent people, although several participants identified themselves as neurodivergent.
Three particular EDI-related limitations of the data collected, and of the analysis and interpretation we achieved, have additional implications for the focus and conduct of future research.
First, as the PPI group statement indicates, our focus on understanding the dynamics of poor and better care meant that we carried out no systematic analysis of differences in the experiences of trans people of different genders. This should be a priority for future research.
Our service-user participants numbered 133 in all, with many giving a complex, sometimes multipart answer to the interview question about how they described their gender. However, 50 said they were a woman or female as the main part of their answer, 23 said they were a man or male, while the remaining 60 said they were either non-binary or described a non-binary identity using a different term, such as genderqueer, agender, or gender-fluid. A closer look at the make-up of the participant group, however, illustrates the complexity of capturing how far different identities and transition needs have been included in a study of trans health care. Of the 60 people giving their gender as non-binary or using a related term, around half had undertaken, were in the process of undertaking, or were contemplating a transmasculine medical transition. So, across the sample, transfeminine and transmasculine experiences were both well represented. For future research, it will be important to bear in mind that identity demographics do not correlate to healthcare need in a simple way. For example, transmasculine non-binary people and trans men have considerable overlap in the gender-affirming treatment they need.
That said, some important differences between genders do emerge across the ICTA accounts, which can inform further research. These concern in particular the nature of negative experiences of diagnostic processes. Trans women and transfeminine non-binary people commonly experienced as humiliating and irrelevant questions stemming from discredited ideas that clinicians should investigate the possibility of ‘autogynephilia’. 14 Trans men and transmasculine non-binary people experienced as humiliating, and often traumatising, questions that implied that their experience of their gender identity might be a consequence of childhood sexual abuse, an equally contestable notion. 25 Non-binary people frequently reported a lack of cultural understanding of their identity by GIC and general healthcare professionals, leading them to present their gender tactically in a more binary way, in order to access treatment. Across the genders, there was also a variety of experiences in terms of the details of accessing different forms of HRT and monitoring their effectiveness. All of these issues merit further research focusing on experiences of different social and medical transition pathways, and the specific cultural and medical issues that people with different identities and transition needs encounter.
Some specific gender-related disparities emerge from the ICTA data that should be explored in future research. These include the implications of the availability of chest reconstruction only for transmasculine people, and the safety differences and other disparities between trans women and trans men inherent in expecting someone to present in gender-congruent ways prior to treatment. For example, trans women dressing in overtly feminine ways may for some present a safety concern, and require additional labour and cost (e.g. make-up/hair removal) compared to the requirements experienced by trans men. It would also be worthwhile to research how far transmasculine and transfeminine non-binary people feel able or safe to access health care openly as non-binary. In the current context of hostile media rhetoric particularly against trans women, there may well be differences.
A second limitation with significant implications for future research concerns the limited participation in our research of Black people and people of colour. This is also taken up in the PPI group statement. In hindsight, the research team went about recruiting Black people and people of colour as if there were no structural issues to be addressed in doing so. Particularly the senior members of the research team did not adequately see how their ‘unmarked’133 white and cis identities failed to indicate that the ICTA research project was working with, and could be trusted by, global majority trans communities. Reaching out to these communities was left to the project’s third-sector partners, and this proved to have limited success. It was only after repeated discussions with the PPI lead and PPI group that senior researchers agreed to allocate funds to two part-time trans Black researchers, embedded in community networks, and substantial participation was achieved. This was, however, at a late stage in the fieldwork, which meant that Black people and people of colour were largely absent from the purposive subsamples of elders, chronically ill people, people in rural areas and people on low incomes or with low educational qualifications. This compromised intersectional analysis within these subsamples. The implication is that future fuller participation by Black people and people of colour requires their representation on the research team from the outset.
Finally, while the research was greatly enhanced and strengthened in the extent to which it addressed EDI issues by the committed work of an energetic PPI lead and PPI group, this was also limited by the established structural arrangements for PPI participation in a research project of this nature. The PPI group were essential to bringing insights from diverse trans communities into the interpretation of data, and in many respects worked alongside the research team, integral to developing interpretations. We have already referred to the need to extend PPI contracts through the writing-up period. Some members of the group have continued on a goodwill basis to comment on revisions to this report made in response to peer and editorial review. In future there is a strong case that members of marginalised communities should be funded to contribute to research on health care they are involved in for the full cycle of research, including final revisions. These can be just as crucial as any other stage in a research project in their impact on the validity of the research and its relevance to communities.
A further dynamic that deserves reflecting upon is that the research team took time and care to summarise large amounts of qualitative data, but in so doing left little time at the end of the project for PPI input. This is to some extent the result of the established distinction, enshrined in research ethics procedures, between research team members, who have direct access to research data, and PPI members, who do not. The PPI group had to wait for the data to be analysed and summarised before commenting. Research teams on future projects need to find ways of feeding back intermediate analyses earlier to a PPI group, to elicit reactions and achieve a more extended dialogue in developing interpretations.
Some overall challenges
We conclude by briefly noting three overall challenges, which emerge from our research and which will need to be addressed by trans communities, health policy-makers, practitioners and researchers.
The first challenge concerns the overall implications of the discussion here of the three paradigms for trans health care and their ability to deliver person-centred and integrated health care for trans people.
The House of Commons Women and Equalities Committee report which prompted the commissioning of this research expressed ‘concern that Gender Identity Services continue to be provided as part of mental health services, giving the impression that trans identity is a disease or disorder of the mind’. 4 It also stated that ‘The evidence is overwhelming that there are serious deficiencies in the quality and capacity of NHS Gender Identity Services’ (para 229). 4
Our discussion of Paradigm 1 above summarises the severe challenges the existing system, based on specialist GICs, faces. It indicates what has been learnt through some initiatives to improve care, and the issues that remain unresolved. The discussion of Paradigms 2 and 3 indicates the possibilities for integrating trans health care with primary care. These are in keeping with the direction set by the Women and Equalities Committee in 2016 and also with the expressed needs of the majority of trans people who participated in this research, as we saw in Chapter 4. There is a strong case that over time the system of care should move from one based on GICs to one based on primary care gender clinics, with appropriate specialist services able to support primary care clinicians carrying out assessments and managing gender-affirming treatments. This offers the opportunity to deliver transition-related care that is better co-ordinated, as well as integrated with the rest of the health care a person needs. We have suggested that the primary care pilot schemes in England can benefit from the learning within the initiatives we have studied. We have also strongly suggested the need to explore how a system based on some version of an ICM might operate, with potentially considerable benefits both in terms of social justice for trans people and the effective use of NHS resources.
Unsurprisingly, our findings focus attention on the need for significantly increased funding of trans health care. In a situation of severe lack of NHS capacity overall, the problem remains of how to balance investment in new and emerging models with addressing the problems in existing services. Our findings have implications for low-cost interventions in how care is currently provided – for example, revisiting of diagnostic guidelines and strengthening the involvement of trans people in the governance and delivery of services, and the widespread training of NHS staff in the values and competencies of trans health care. Alongside this, the primary care pilot schemes appear to offer an important focus for evaluation, leading to the development and funding of models for the future.
The second and related challenge concerns issues of achieving equity of access to transition-related care across different localities within the UK, in the context of a mix of established and developing services. Waiting times for GICs are extremely long everywhere, but some localities now have a primary care pilot gender service. Elsewhere, there is wide variation in the degree to which GPs are willing to give bridging prescriptions for hormone therapy to people on GIC waiting lists. In some localities, secondary care endocrinology clinics will similarly provide bridging hormones. However, both kinds of arrangements are relatively rare, so that many trans people may have no such possibility. Considerations of overcoming health inequalities require that this postcode lottery needs to be further investigated and addressed.
The final challenge is best summarised in the words of one of the trans people we interviewed. It concerns confronting the assumption common in many parts of society that it is somehow optional to consider whether to prioritise meeting the healthcare needs of trans people.
… you’ve got to realise that we’re … most people, years ago either just lived and died not being themselves. But now we’re seeing the ability, we’re seeing an opportunity, a possibility to be accepted … And within the younger generation of course it’s going to happen. They’ve got people out there, they’ve got their role models out there. And I said it is going to happen, so it’s only going to get, not worse, but it’s only going to get better and brighter, whatever. All we need is the services to follow suit.
Service user
Patient and public involvement group statement: patient and public involvement on improving care for trans adults project
The ICTA project, though brave in scope and accomplishments, has nevertheless reflected existing societal dynamics in the processes connected to its design, execution and outputs. This does not render any of the findings invalid, but it may at times have excluded or watered down certain voices.
Trans people are marginalised within their own healthcare system, and the research has clearly demonstrated this. Much of the existing research has been by cis practitioners, and the health care is performed almost entirely by cis clinicians to standards set by cis decision-makers and norms and biases of a cis-dominated society.
The ICTA project itself was conceived by cis people, and more junior trans researchers were only brought in after its inception, although trans people and organisations were consulted in the earlier stages. The research appeared to have been designed, at least in some ways, around the concerns of existing service providers rather than patients. Given that the findings of the research, as described in Chapter 3 of this report, pointed to iatrogenic harm by service providers, and service providers were also project partners, this ultimately constituted a conflict of interest, and limited the ability of this research and the PPI group themselves to address power and unequal structures.
This for me was a critical point of failure and it was predictable before the research began … it’s far from best practice for qualitative research about a marginalised group to be designed and coded by anyone without that lived experience. How can a person without the lived experience possibly know what they’re looking for? Even with the best of intention, they simply lack the direct experience.
PPI Group Member Feedback*
Formation of the patient and public involvement group
The PPI lead, a white, disabled, neurodivergent, non-binary person, from a non-academic, EDI training and therapy background, was recruited after the original PPI lead, recruited in 2018, became an ICTA researcher. This created an extra delay in the PPI group becoming meaningfully involved in the project. The process of recruiting the seven group members did not begin until July 2019. Members were intentionally recruited to reflect a wide diversity of marginalised voices from within the trans community, including members representing Wales, Northern Ireland and Scotland as well as marginalised demographics. An introductory workshop was run to select participants.
The PPI lead was contracted to work 17 hours per month; members were paid to attend four meetings a year.
The PPI lead now reflects that their role would more usefully have been given to a trans person who also experienced racism. They believed at the time that the recruitment of more than one PPI group member from marginalised ethnicities would be sufficient; however, they now reflect that, despite giving this issue considerable attention, multiple systemic factors led to the marginalisation of the voices of trans people impacted by racism within this project, and this mirrors the way that, despite the best efforts of cis researchers, trans voices have also been marginalised.
… this comes back to the question around race and other forms of marginalisation – the design was such that they would be add-ons rather than integral to how transphobia manifests. This seems particularly true of class (as intersecting with race) and how the entire landscape of care is very much shaped by material inequalities and access to intergenerational resources.
PPI Group Member Feedback*
It is not necessarily through a lack of awareness or deliberate overlooking that this happened. It is simply that there is no substitute for marginalised voices being given the opportunity to speak for themselves, and there are many systemic barriers to marginalised voices coming through authentically when a space is conceived, designed and ordered by the dominant group, however mindful they are of inequality.
Concerns about minimising the severity of the trans healthcare crisis
More trans oversight and influence at the very beginning of ICTA might have impacted how the research was conceived and implemented. Decisions made at the start of the project have created a structure we continued to need to abide by, despite much growth and learning from cis team members and increasing trans involvement.
An example of this is the involvement of GICs as project partners. At times through the project, the PPI group were concerned about cis clinician voices being weighed as equal to trans voices, and issues around this were picked up by the PPI group in the writing of the final report. For example, writers using terms that suggested equivalency between the distress of clinicians and patients regarding long waiting lists. Given the severe risks to trans people associated with delays and denial of health care, including long-term mental health impacts and suicide, many of the PPI group were troubled to see clinician stresses apparently treated as equivalent.
At times the PPI group also felt that, given the severity of experiences trans participants were relating with respect to GICs, the reporting of this was ‘toned down’ in order to be more palatable, and the GICs being project partners may have been an influencing factor in this.
The mental health report of this project makes clear the concerning levels of iatrogenic harm from GICs in terms of both the waits for treatment and the manner of assessment. Gatekeeping and systemic barriers are particularly experienced by marginalised groups – non-binary people from colonised cultures, autistic people, those with mental health conditions or past trauma, for example, are named in the report as facing additional obstacles on top of the already considerable barriers.
The pervasive lack of concern for what happens to a trans person when their treatment is delayed or blocked was highlighted in the mental health section, but overall, language has been diluted to an extent that the scale of this crisis appears to have been obscured.
PPI members were also at pains to highlight the way the research shows that iatrogenic harm related to transphobia extends to medical neglect and structural violence throughout health care, and to elderly and end of life care. Particularly the negligent journey patients experience after discharge from GISs, a direct result of the way trans health care has been siloed into GICs, while training, addressing transphobia and embedding trans needs systemically throughout health and social care have been entirely overlooked.
We were left with concerns that the outputs would be cis-voiced and that without meaning to, cis biases and interpretations would overlay the words of members of our community. It is not that the cis researchers were not aware of or mindful of this risk, it is simply that trans voices are more authentically heard when presented, collated and interpreted by other trans people. Equally so with the voices of trans people impacted by racism, trans people impacted by transmisogyny, disabled and neurodivergent trans people, etc. From the group’s perspective the considerable structural inequalities built into the trans healthcare system did not fully come through in the reporting, although they were clear to see in the data; ‘the framing does not even correspond to the severity apparent in the data’ (PPI Group Member Feedback*).
Impact of coronavirus disease and the research climate
Coronavirus disease impacted the project in multiple ways. Some of these perpetuated marginalisation already in place. For example, the PPI group planned for ways to recruit survey participants offline through trans groups and other spaces. Older trans people who might be less involved in online spaces and other more marginalised trans people who do not go online were left out of the data when COVID made alternative data collecting impossible.
Coronavirus disease disproportionately impacted many more marginalised groups. It is reasonable to speculate that the people who had the time and mental energy to think about filling an online survey and considering being interviewed in the middle of a global pandemic were more likely to be among socially secure groups and were not, for example, key workers. Certainly, the PPI group had more problems retaining members from more marginalised groups during the pandemic as a direct result of the extra pressures they were under.
These inequalities came through in the case studies of specific populations – the most marginalised of those groups seemed not to be present. The low SES group did not speak of the extreme deprivation PPI members see for some in trans communities; the older trans people group was skewed towards the lower end of the age range it covered; the TBPoC group appeared to be somewhat missing the voices of trans women, to give some examples.
The impact of the pandemic and staffing issues on ICTA meant that at the end of the project, the trans researchers had left before final reports or outputs had been created or viewed by the PPI group. Indeed, the PPI group found that, as deadlines kept shifting, it was hard to arrange a meeting and know that they would have sight of information to be able to usefully comment on.
Some of this is recognised as a feature of the climate in academia currently. Over-promising on research grants has become so commonplace that projects impose unreasonable expectations. All concerned with ICTA have been very committed to deliver what they promised; however, this took a toll disproportionately on trans employees of ICTA, including the PPI group, who felt the weight of community obligations to commit to at times working unreasonable hours to ensure the research met its potential.
The workload associated with reviewing outputs by the PPI group was substantially greater than budgeted for, and it was goodwill and investment in ensuring the trans voice was safeguarded that led the PPI lead and group to devote considerable unpaid time to the task, amid the commitments of their other work, study and life challenges. Participation was intensely stressful and burdensome beyond what it should have been precisely because trans voices were not properly embedded in the project.
The PPI lead acknowledges the enormous commitment, dedication and wisdom shown by the group, and the robustness of the cis researchers in receiving at times very strong feedback. However, concern remains that there was insufficient time and space to ensure each analysis had been given due attention and time for a thorough, reflective feedback process.
In effect it has reduced the voice and ability to comment when every deadline is so short. This reduces our impact.
PPI Group Member Feedback*
Intersectional issues
The PPI group very much wanted researchers to hold in mind the diversity of the trans community as they wrote their outputs. A checklist for researchers to refer to as they wrote was created to assist this purpose of holding intersectional issues in mind. For this document to have been useful, it needed to be constantly reviewed during writing, and there was sadly little evidence of this happening. This is likely to be simply the overwhelm of deadlines and the size of the administrative task of pulling such a complex project together, but it points to the way intersectional issues, seen as an add-on rather than fully embedded, can get left out.
The recruitment of specific researchers to look into trans health care for people affected by racism was important but also very much an afterthought, and only after poorly funded attempts to engage those voices via the PPI group had failed in their reach. Originally, the PPI group made attempts to do further engagement work when it was identified that Black voices specifically were missing from the research. These failed due to a number of complicating factors, including COVID, but largely because they were under-resourced and not tapped into the right networks, which relates back to the PPI lead being white. Finally, specific focus groups, under the banner of ‘Black trans people and trans people of colour (TBPoC)’ were run towards the end of the project. The PPI group welcomed this, although the decision to separate out Black voices but amalgamate others was questioned:
Why is there an assumption that racialisation is somehow uniform except in relation to blackness?
PPI Group Member Feedback*
The PPI group had in fact previously cautioned the researchers against using the term ‘People of Colour’ as well as the term BAME and to think more carefully about who is actually being spoken of and included in any given instance. It should also be noted that ‘PoC’ is a US-centric term that can be seen to exclude marginalised ethnicities that in certain contexts may be perceived as white – for example Ashkenazi Jewish and Roma people. With the extreme marginalisation of Roma people in the UK currently, and in particular stark health inequalities and low life expectancy (Matthews and Gavin, 2017), further unpacking of which racially marginalised voices were being heard/not heard could have been fruitful.
Another concern raised early in the process of framing the research outputs and repeatedly recurring was about the unquestioning acceptance of the validity of the notion of ‘more complex’ cases that should face extra barriers, even though the mental health report demonstrated the harm of this assumption. This extra burden falls precisely on the shoulders of those who can least afford it, those already experiencing a greater mental health burden, such as those with a trauma history or neurodiversity, and would put them at undue risk, given the mental health benefits of transitioning and the harm of waiting and gatekeeping described in Chapter 3 of this report. These concerns appear to be addressed in the final report; however, the number of times similar issues needed to be raised underlines the entrenched nature of the ableist assumptions often being made regarding access to trans health care.
Despite gender being a substantial aspect of the subject of being trans, the group observed that gender disparities were little acknowledged in the outputs – the trans healthcare experience is very different for trans women, trans men and non-binary people, and there are fundamental inequalities between the pathways. This was mostly overlooked.
It’s quite startling how little gender is actually taken into account in what we read.
PPI Group Member Feedback*
Issues of power replicated
An overall concern was the way in which issues of power and inequality were not made sufficiently explicit in the research outputs, a reluctance to name transphobia, for example, where it was clearly being demonstrated.
There’s also a further risk with that approach of placing the issue with the individual or with particular identities rather than with interlocking structures of oppression – and tying in with some of our concerns earlier about GIC defensiveness etc., I think there is maybe an issue with this report in terms of being scared of actually addressing issues of power.
PPI Group Member Feedback*
The power issues in this research process mirrored power dynamics of trans health care – trans voices ending up in a place of criticising from an outsider position rather than fully shaping or indeed leading the process. And as trans voices were marginalised so the less heard trans voices were doubly so, including within the PPI group, and despite the best of intentions.
Towards the end of the project, the PPI group were in the stressful predicament of needing to give tough feedback while remaining concerned about being unable to endorse the final report. There was never a question of the good intention or allyship on the part of the remaining cis researchers, but nevertheless the systems and processes that created this research served to unintentionally marginalise trans voices.
Writing wasn’t a collaborative process – I think in some ways part of it was that this project took on too much data so writing had to be very rushed and then our thoughts were kind of tacked on at the end. Whereas to do engaged research you need to involve communities at every stage of analysis and writing.
PPI Group Member Feedback*
The value of extending PPI contracts until the report submission must be recognised. This ensured a critical, independent set of trans voices had an overview. The final stages of the writing required extensive and strong feedback, and largely this feedback was taken on board and concerns listened to and reflected on. However, the concerns expressed in this section still stand. The group requests that readers of the report tune into just how much systemic injustice and inequality is shown in the ICTA findings, and at times inadvertently replicated or unconsciously minimised.
Conclusion
In conclusion, the learning this group has taken from the process has been:
-
It is not enough to involve marginalised people in matters related to their needs. Those groups need to lead research in this area.
-
Awareness of diversity and intersectional issues needs to be built-in from the start. Holding in mind class, race, gender and other intersections at all times and not siloing them into separate issues.
-
We learn most about a group from the experiences of those most marginalised within it.
-
Oppression is often unintentional, produced unconsciously, replicated through mundane systems – it can occur even with the best intentions through pressure of deadlines and the imposition of existing structures.
-
Cultural competence on trans issues is in severe deficit. Within health care, but also within academia. A lack of established pathways to developing knowledge means a cis person may enter the field and find themself in a position of power over trans lives with no relevant trans-related qualification or particular trans-specific expertise.
There needs to be full acknowledgement of the enormous labour that has gone into the ICTA project by all concerned, including participants. This report of the ICTA findings begins to honour that work and is a valid and useful, if overly tentative, piece of work. It is the hope of the PPI group that exploration of the data will not stop here but will deepen. The opportunity for it to save trans lives by lessening the transphobia-specific iatrogenic harm currently being caused by healthcare systems needs to be fully realised.
*Quotes are taken from comments on NIHR report and the process of writing this summary.
References: Matthews Z, Gavin M. Health and Social Care Briefing: Gypsy, Roma and Traveller Equality and Inclusion. Friends, Families and Travellers. 2017. URL: www.gypsy-traveller.org/wp-content/uploads/2017/12/Health-and-Social-Care-Briefing-Master-Copy.pdf (accessed 16 February 2024).
Additional information
Acknowledgements
The authors are extremely grateful to the members of trans communities who gave so much time and commitment to being interviewed for this research. The authors wish also to thank all the staff from NHS and third sector organisations who were interviewed or helped with arranging the case studies reported on. The research benefited immensely from a wide range of inputs throughout its course from its Patient and Public Involvement Group, a Project Steering Group and an Advisory Group, as well as from collaboration with Gendered Intelligence, the Gender Identity Research and Education Society (GIRES), and the British Association for Counselling and Psychotherapy (BACP). The authors are profoundly grateful for all of this.
The following people also contributed to this report:
Azekel Axelle (independent researcher, trans health) conducted focus groups for TBPoC and produced draft material from them.
Tajah Hamilton (independent researcher, trans health) conducted focus groups for TBPoC and produced draft material from them.
Peter Keogh (Professor, public health) led on the design of some research instruments, the training of interviewers and the approach to analysis of interview data.
Michael Petch (researcher, trans health) participated in the design of the study, carried out interviews of service users, contributed to analysis of interviews in the national subsamples of service users.
Benji Talbot (researcher, trans health) managed fieldwork, contributed to analysis of data from interviews in the national subsamples and in the case studies of initiatives to improve care.
Contributions of authors
Richard Holti (https://orcid.org/0000-0003-4769-8621) Professor, Health Innovation. Led design of the study, carried out fieldwork, led data analysis for the case studies, and led writing of the report.
Evelyn Callahan (https://orcid.org/0000-0002-0360-4657) Research Fellow, Trans Health. Participated in the design of the study, managed and carried out fieldwork interviews, led on analysis and writing up of qualitative interviews in the national samples.
Jamie Fletcher (https://orcid.org/0000-0003-2929-7613) Researcher, Trans Health. Participated in the design of the study, carried out interviews of service users, contributed to analysis of and writing up of case studies.
Sam Hope (https://orcid.org/0000-0001-8160-4620) Independent Researcher, Trans Mental Health. Co-led in the analysis and writing up of the mental health case study, and reviewed drafts of other sections of the report.
Naomi Moller (https://orcid.org/0000-0002-9756-0367) Professor, Psychology and Psychotherapy. Participated in the design of the study, carried out interviews of service users and staff, co-led on analysis of and writing up of the mental health case study.
Ben Vincent (https://orcid.org/0000-0002-3110-3008) Research Fellow, Trans Health. Participated in the design of the study, managed fieldwork and carried out interviews of service users and staff, contributed to the overall analysis framework and led on analysis of and writing up of one case study of innovation.
Paul Walley (https://orcid.org/0000-0002-1877-013X) Senior Lecturer, Health Operations Management. Participated in the design of the study, carried out interviews of service staff, led on modelling of the impact of different staffing models on GIC waiting lists, contributed to analysis and reviewed drafts of the report.
Disclosure of interests
Full disclosure of interests: Completed ICMJE forms for all authors, including all related interests, are available in the toolkit on the NIHR Journals Library report publication page at https://doi.org/10.3310/EWTA4502.
Primary conflicts of interest: Naomi Moller: British Association for Counselling and Psychotherapy Research Committee Member; Chair of Training, Research Counselling Centre Consortium (TRACCs); UK Chapter President Society for Psychotherapy Research.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review and appropriate agreements. Please note that electronic files containing anonymised research data will be held securely on the OU’s Open Research Data Online system. According to OU research data management policy, after 10 years there will be a review of whether the data should be retained for further research use. If there is no case for its further use, it will be destroyed.
Ethics statement
Detailed data collection plans for this research led to favourable opinions on research ethics from the NHS East Midlands-Leicester Central Research Ethics Committee (Ref. 19/EM/0289) on 17 July 2020 (amendment ref. 661833/02) and the Open University Human Research Ethics Committee (Ref. HREC/3141/Holti). These plans included measures to protect participant confidentiality and take account of the distress that might be involved in being interviewed about potentially sensitive and difficult experiences.
Information governance statement
The Open University is committed to handling all personal information in line with the UK Data Protection Act (2018) and the General Data Protection Regulation (EU GDPR) 2016/679. Under the Data Protection legislation, the Open University is the Data Controller, and you can find out more about how we handle personal data, including how to exercise your individual rights and the contact details for our Data Protection Office here: www5.open.ac.uk/foi/main/sites/www.open.ac.uk.foi.main/files/files/ecms/web-content/Data_protection_policy_May_2018_pdf.pdf.
Department of Health and Social Care disclaimer
This publication presents independent research commissioned by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by the interviewees in this publication are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, MRC, NIHR Coordinating Centre, the HSDR programme or the Department of Health and Social Care.
This monograph was published based on current knowledge at the time and date of publication. NIHR is committed to being inclusive and will continually monitor best practice and guidance in relation to terminology and language to ensure that we remain relevant to our stakeholders.
Disclaimers
This article presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care.
References
- Office for National Statistics . Gender Identity, England and Wales: Census 2021 2023.
- AIR Unit . Operational Research Report Following Visits and Analysis of Gender Identity Clinics in England 2015.
- GIC n.d. https://tavistockandportman.nhs.uk/services/gender-identity-clinic-gic/#waiting-times (accessed 8 February 2024).
- House of Commons . Report of the Women and Equalities Committee on Transgender Equality 2016.
- Palmer J. We Are Meeting Concerns on Gender Services 2017. www.england.nhs.uk/blog/we-are-meeting-concerns-on-gender-services/ (accessed 6 February 2018).
- LGBT Foundation . Transforming Outcomes: A Review of the Needs and Assets of the Trans Community 2017.
- American Psychiatric Association (APA) . American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders 2013.
- Bell CC. DSM-IV: Diagnostic and Statistical Manual of Mental Disorders. JAMA 1994;272:828-9.
- World Health Organization (WHO) . International Classification of Diseases (ICD-11) 2021.
- World Health Organization (WHO) . International Classification of Diseases (ICD-10) 2016.
- Robles R, Fresán A, Vega-Ramírez H, Cruz-Islas J, Rodríguez-Pérez V, Domínguez-Martínez T, et al. Removing transgender identity from the classification of mental disorders: a Mexican field study for ICD-11. Lancet Psychiat 2016;3:850-9.
- Royal College of Psychiatrists . Good Practice Guidelines for the Assessment and Treatment of Adults With Gender Dysphoria: College Report CR181 2013.
- Coleman E, Bockting W, Botzer M, Cohen-Kettenis P, DeCuypere G, Feldman J, et al. Standards of care for the health of transsexual, transgender, and gender-nonconforming people, Version 7. Int J Transgend 2012;13:165-232.
- Serano J. Autogynephilia: a scientific review, feminist analysis, and alternative ‘embodiment fantasies’ model. Sociol Rev 2020;68:763-78.
- NHS England . Service Specification – Gender Identity Services for Adults (Non-Surgical Interventions) 2019.
- Burgwal A, Motmans J. Trans and gender diverse people’s experiences and evaluations with general and trans-specific healthcare services: a cross-sectional survey. Int J Impot Res 2021;33:679-86.
- Vermeir E, Jackson LA, Marshall EG. Barriers to primary and emergency healthcare for trans adults. Cult Health Sex 2018;20:232-46.
- Davies A, Bouman WP, Richards C, Barrett J, Ahmad S, Baker K, et al. Patient satisfaction with gender identity clinic services in the United Kingdom. Sex Relatsh Ther 2013;28:400-18.
- Ellis SJ, Bailey L, McNeil J. Trans people’s experiences of mental health and Gender Identity Services: a UK study. J Gay Lesbian Ment Health 2015;19:4-20.
- Taylor J, Zalewska A, Gates JJ, Millon G. An exploration of the lived experiences of non-binary individuals who have presented at a gender identity clinic in the United Kingdom. Int J Transgend 2019;20:195-204.
- Linander I, Alm E, Hammarström A, Harryson L. Negotiating the (bio)medical gaze – experiences of trans-specific healthcare in Sweden. Soc Sci Med 2017;174:9-16.
- Millet N, Longworth J, Arcelus J. Prevalence of anxiety symptoms and disorders in the transgender population: a systematic review of the literature. Int J Transgend 2017;18:27-38.
- Applegarth G, Nuttall J. The lived experience of transgender people of talking therapies. Int J Transgend 2016;17:66-72.
- McCann E, Sharek D. Survey of lesbian, gay, bisexual, and transgender people’s experiences of mental health services in Ireland. Int J Ment Health Nurs 2014;23:118-27.
- Hope S. Person-centred Counselling for Trans and Gender Diverse People: A Practical Guide. London: Jessica Kingsley Publishers; 2019.
- Hendricks ML, Testa RJ. A conceptual framework for clinical work with transgender and gender nonconforming clients: an adaptation of the Minority Stress Model. Prof Psychol Res Pr 2012;43:460-7.
- Austin A, Craig SL. Transgender affirmative cognitive behavioral therapy: clinical considerations and applications. Prof Psychol Res Pr 2015;46:21-9.
- Ashley F, Amand CM, Rider GN. The continuum of informed consent models in transgender health. Fam Pract 2021;543.
- Schulz SL. The informed consent model of transgender care: an alternative to the diagnosis of gender dysphoria. J Humanist Psychol 2018;58:72-9.
- Kodner DL. All together now: a conceptual exploration of integrated care. Healthc Q 2009;13:6-15.
- Lloyd J, Wait S. Integrated Care: A Guide for Policymakers. London: Alliance for Health and the Future; 2005.
- Goodwin N. Understanding integrated care. Int J Integ Care 2016;16.
- Coulter A. Engaging Patients in Healthcare. London: McGraw-Hill Education (UK); 2011.
- Voices N. Prioritising Person-centered Care – The Evidence. London: National Voices; 2014.
- Greenhalgh T, Humphrey C, Woodard F. User Involvement in Health Care. Oxford: Blackwell; 2010.
- Holti R. Improving the Integration of Care for Trans Adults: Study Protocol Version 2.0. Milton Keynes: Open University; 2020.
- O’Brien BC, Harris IB, Beckman TJ, Reed DA, Cook DA. Standards for reporting qualitative research: a synthesis of recommendations. Acad Med 2014;89:1245-51.
- Riggs DW, Pearce R, Pfeffer CA, Hines S, White F, Ruspini E. Transnormativity in the psy disciplines: constructing pathology in the Diagnostic and Statistical Manual of Mental Disorders and Standards of Care. Am Psychol 2019;74:912-24.
- Berger I, Ansara YG. The SAGE Encyclopedia of Trans Studies. Thousand Oaks, CA: SAGE Publications Ltd; 2021.
- Altheide DL, Schneider CJ. Qualitative Media Analysis. Thousand Oaks, CA: SAGE Publications Ltd; 2012.
- Vincent B, Petch M, Holti R. Review of the Integration of Trans Health. Milton Keynes: Open University; 2020.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77-101.
- Gioia DA, Corley KG, Hamilton AL. Seeking qualitative rigor in inductive research: notes on the Gioia methodology. Organ Res Methods 2013;16:15-31.
- Nadal KL, Whitman CN, Davis LS, Erazo T, Davidoff KC. Microaggressions toward lesbian, gay, bisexual, transgender, queer, and genderqueer people: a review of the literature. J Sex Res 2016;53:488-50.
- Zajacova A, Lawrence EM. The relationship between education and health: reducing disparities through a contextual approach. Annu Rev Public Health 2018;39:273-89.
- Crenshaw K. Demarginalizing the intersection of race and sex: a Black feminist critique of antidiscrimination doctrine, feminist theory and antiracist politics. U Chi Legal F. 1989:139-67.
- Jepperson RL. The New Institutionalism in Organizational Analysis. Chicago, IL: University of Chicago Press; 1991.
- Storey J, Holti R. Abingdon: Routledge; 2019.
- Håkansson Eklund J, Holmström IK, Kumlin T, Kaminsky E, Skoglund K, Höglander J, et al. ‘Same same or different?’ A review of reviews of person-centered and patient-centered care. Patient Educ Couns 2019;102:3-11.
- NHS Benchmarking Network . Mental Health Sector, Adult and Older Persons Mental Health 2020 Key Findings 2021. www.nhsbenchmarking.nhs.uk/mental-health-sector#londonmental (accessed 8 February 2024).
- Tan KK, Schmidt JM, Ellis SJ, Veale JF, Byrne JL. ‘It’s how the world around you treats you for being trans’: mental health and wellbeing of transgender people in Aotearoa New Zealand. Psychol Sex 2021:1-13.
- Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol Bull 2003;129:674-97.
- Bettcher TM. You’ve Changed: Sex Reassignment and Personal Identity. Oxford: Oxford University Press; 2009.
- Freeman L, Stewart H. Microaggressions in clinical medicine. Kennedy Inst Ethics J 2018;28:411-49.
- Gagliardi AR, Yip CYY, Irish J, Wright FC, Rubin B, Ross H, et al. The psychological burden of waiting for procedures and patient-centred strategies that could support the mental health of wait-listed patients and caregivers during the COVID-19 pandemic: a scoping review. Health Expect 2021;24:978-90.
- Nikolova S, Harrison M, Sutton M. The impact of waiting time on health gains from surgery: evidence from a national patient‐reported outcome dataset. Health Econ 2016;25:955-68.
- Khan Z. Ethnic health inequalities in the UK’s maternity services: a systematic literature review. Br J Midwifery 2021;29:100-7.
- Limb M. Disparity in maternal deaths because of ethnicity is ‘unacceptable’. BMJ 2021;372.
- Summers H. Black women in the UK four times more likely to die in pregnancy or childbirth. Guardian 2021. www.theguardian.com/global-development/2021/jan/15/black-women-in-the-uk-four-times-more-likely-to-die-in-pregnancy-or-childbirth (accessed 8 February 2024).
- Wallace S, Nazroo J, Bécares L. Cumulative effect of racial discrimination on the mental health of ethnic minorities in the United Kingdom. Am J Public Health 2016;106:1294-300.
- Osborn R, Moulds D, Squires D, Doty MM, Anderson C. International survey of older adults finds shortcomings in access, coordination, and patient-centered care. Health Aff (Hope) 2014;33:2247-55.
- Jo O, Kruger E, Tennant M. GIS mapping of healthcare practices: do older adults have equitable access to dental and medical care in the UK?. Br Dent J 2021;1.
- Almeida APSC, Nunes BP, Duro SMS, Facchini LA. Socioeconomic determinants of access to health services among older adults: a systematic review. Rev Saude Publica 2017;51. www.ncbi.nlm.nih.gov/pmc/articles/PMC5779074/ (accessed 8 February 2024).
- Chang ES, Kannoth S, Levy S, Wang S-Y, Lee JE, Levy BR. Global reach of ageism on older persons’ health: a systematic review. PLOS ONE 2020;15.
- Willis P, Dobbs C, Evans E, Raithby M, Bishop J-A. Reluctant educators and self-advocates: older trans adults’ experiences of health-care services and practitioners in seeking gender-affirming services. Health Expect 2020;23:1231-40.
- Sakellariou D, Rotarou ES. Access to healthcare for men and women with disabilities in the UK: secondary analysis of cross-sectional data. BMJ Open 2017;7.
- Williams V, Read S, Mason-Angelow V, Heslop P, Miles C. Being a disabled patient: negotiating the social practices of hospitals in England. Soc Incl 2018;6:74-82.
- Sakellariou D, Anstey S, Gaze S, Girt E, Kelly D, Moore B, et al. Barriers to accessing cancer services for adults with physical disabilities in England and Wales: an interview-based study. BMJ Open 2019;9.
- Gibson J, O’Connor R. Access to health care for disabled people: a systematic review. Soc Care Neurodisability 2010;1:21-3.
- Matin BK, Williamson HJ, Karyani AK, Rezaei S, Soofi M, Soltani S. Barriers in access to healthcare for women with disabilities: a systematic review in qualitative studies. BMC Women’s Health 2021;21:1-23.
- Freedman VA, Martin LG. The role of education in explaining and forecasting trends in functional limitations among older Americans. Demography 1999;36:461-73.
- Mackenbach JP, Kunst AE. Measuring the magnitude of socio-economic inequalities in health: an overview of available measures illustrated with two examples from Europe. Soc Sci Med 1997;44:757-71.
- Pamuk ER. Social-class inequality in infant mortality in England and Wales from 1921 to 1980. Eur J Popul 1988;4:1-21.
- Raghupathi V, Raghupathi W. The influence of education on health: an empirical assessment of OECD countries for the period 1995–2015. Arch Public Health 2020;78:1-18.
- Wilkinson RG. Class and Health. Abingdon: Routledge; 1986.
- Coburn D. Income inequality, social cohesion and the health status of populations: the role of neo-liberalism. Soc Sci Med 2000;51:135-46.
- Acheson SD. Independent Inquiry into Inequalities in Health. London: The Stationery Office; 1998.
- Muntaner C, Lynch J, Oates GL. The social class determinants of income inequality and social cohesion. Int J Health Serv 1999;29:699-732.
- Scambler G, Higgs P. ‘The dog that didn’t bark’: taking class seriously in the health inequalities debate. Soc Sci Med 2001;52:157-9.
- Cattell V. Poor people, poor places, and poor health: the mediating role of social networks and social capital. Soc Sci Med 2001;52:1501-16.
- Weatherburn P, Davies P, Hickson F, Hartley M. A Class Apart. The Social Stratification of HIV Infection among Homosexually Active Men. London: Sigma Research; 1999.
- Hope V, MacArthur C. Safer sex and social class: findings from a study of men using the ‘gay scene’ in the West Midlands Region of the United Kingdom. AIDS Care 1998;10:81-8.
- Kelly C, Hulme C, Farragher T, Clarke G. Are differences in travel time or distance to healthcare for adults in global north countries associated with an impact on health outcomes? A systematic review. BMJ Open 2016;6.
- Rosenkrantz DE, Black WW, Abreu RL, Aleshire ME, Fallin-Bennett K. Health and health care of rural sexual and gender minorities: a systematic review. Stigma Health 2017;2:229-43.
- Ben J, Cormack D, Harris R, Paradies Y. Racism and health service utilisation: a systematic review and meta-analysis. PLOS ONE 2017;12.
- Paradies Y, Ben J, Denson N, Elias A, Priest N, Pieterse A, et al. Racism as a determinant of health: a systematic review and meta-analysis. PLOS ONE 2015;10.
- Bullivant S. The ‘No Religion’ Population of Britain: Recent Data from the British Social Attitudes Survey (2015) and the European Social Survey (2014). Catholic Research Forum; 2017.
- Strassfield M, Henderson-Espinoza R. Introduction: mapping trans studies in religion. Transgender Stud Q 2019;6.
- Baugh J. Black Linguistics. Abingdon: Routledge; 2005.
- Office for National Statistics . People Living in Deprived Neighbourhoods 2020. www.ethnicity-facts-figures.service.gov.uk/uk-population-by-ethnicity/demographics/people-living-in-deprived-neighbourhoods/latest/ (accessed 8 February 2024).
- Office for National Statistics . Household Wealth by Ethnicity in Great Britain (April 2016 to March 2018) 2020. www.ons.gov.uk/peoplepopulationandcommunity/personalandhouseholdfinances/incomeandwealth/articles/householdwealthbyethnicitygreatbritain/april2016tomarch2018 (accessed 8 February 2024).
- Bailey M. Misogynoir in medical media: on Caster Semenya and R Kelly. Catal Feminism Theor Technoscience 2016;2:1-31.
- Walley-Jean JC. Debunking the myth of the ‘angry Black woman’: an exploration of anger in young African American women. Black Women Gender Families 2009;3:68-86.
- Hunt S. An Introduction to the Health of Two-spirit People: Historical, Contemporary and Emergent Issues. Prince George, BC: National Collaborating Centre for Aboriginal Health; 2016.
- Käng DB. Kathoey ‘In trend’: emergent genderscapes, national anxieties and the re-signification of male-bodied effeminacy in Thailand. Asian Stud Rev 2012;36:475-94.
- Singh H, Kumar P. Hijra: an understanding. J Psychosoc Res 2020;15:79-8.
- Taylor v. Jaguar Land Rover. London: HM Employment Tribunals; 2020.
- Da’Shaun LH. Belly of the Beast: The Politics of Anti-fatness as Anti-blackness. Berkeley, CA: North Atlantic Books; 2021.
- Strings S. Fearing the Black Body. New York: New York University Press; 2019.
- Phelan SM, Burgess DJ, Yeazel MW, Hellerstedt WL, Griffin JM, van Ryn M. Impact of weight bias and stigma on quality of care and outcomes for patients with obesity. Obes Rev 2015;16:319-26.
- Krieger N, Kosheleva A, Waterman PD, Chen JT, Beckfield J, Kiang MV. 50-year trends in US socioeconomic inequalities in health: US-born Black and White Americans, 1959–2008. Int J Epidemiol 2014;43:1294-313.
- Himmelstein MS, Puhl RM, Quinn DM. Intersectionality: an understudied framework for addressing weight stigma. Am J Prev Med 2017;53:421-31.
- Pearl RL, Puhl RM. Weight bias internalization and health: a systematic review. Obes Rev 2018;19:1141-63.
- Castro VA, King WM, Augustaitis L, Saylor K, Gamarel KE. A Scoping review of health outcomes among transgender migrants. Transgender Health 2021;7:385-96.
- Goodman M, Nash R. Examining Health Outcomes for People Who Are Transgender. Washington, DC: Patient-Centered Outcomes Research Institute; 2019.
- Kattari SK, Walls NE, Speer SR, Kattari L. Exploring the relationship between transgender-inclusive providers and mental health outcomes among transgender/gender variant people. Soc Work Health Care 2016;55:635-50.
- Lefevor GT, Janis RA, Franklin A, Stone W-M. Distress and therapeutic outcomes among transgender and gender nonconforming people of color. Couns Psychol 2019;47:34-58.
- Reisner SL, Poteat T, Keatley J, Cabral M, Mothopeng T, Dunham E, et al. Global health burden and needs of transgender populations: a review. Lancet 2016;388:412-36.
- Winter S, Diamond M, Green J, Karasic D, Reed T, Whittle S, et al. Transgender people: health at the margins of society. Lancet 2016;388:390-40.
- Hibbert M, Wolton A, Crenna-Jennings W, Benton L, Kirwan P, Lut I, et al. Experiences of stigma and discrimination in social and healthcare settings among trans people living with HIV in the UK. AIDS Care 2018;30:836-43.
- Reisner SL, Pardo ST, Gamarel KE, Hughto JMW, Pardee DJ, Keo-Meier CL. Substance use to cope with stigma in healthcare among US female-to-male trans masculine adults. LGBT Health 2015;2:324-32.
- Ashley F. Gatekeeping hormone replacement therapy for transgender patients is dehumanising. J Med Ethics 2019;45:480-2.
- ICATH . Informed Consent for Access to Trans Health n.d. https://icathorg.wordpress.com (accessed 8 February 2024).
- Schulz SL. The informed consent model of transgender care: an alternative to the diagnosis of gender dysphoria. J Human Psychol 2017;58:72-9.
- Deutsch MB. Use of the informed consent model in the provision of cross-sex hormone therapy: a survey of the practices of selected clinics. Int J Transgend 2012;13:140-6.
- Spanos C, Grace JA, Leemaqz SY, Brownhill A, Cundill P, Locke P, et al. The informed consent model of care for accessing gender-affirming hormone therapy is associated with high patient satisfaction. J Sex Med 2021;18:201-8.
- The King’s Fund Institute . Waiting Times for Elective (Non-Urgent) Treatment: Referral to Treatment 2021. www.kingsfund.org.uk/insight-and-analysis/data-and-charts/waiting-times-non-urgent-treatment#the-number-of-long-waits (accessed 8 February 2024).
- Royal College of Psychiatrists . Two Fifths of Patients Waiting for Mental Health Treatment Forced to Resort to Emergency or Crisis Services 2020. www.rcpsych.ac.uk/news-and-features/latest-news/detail/2020/10/06/two-fifths-of-patients-waiting-for-mental-health-treatment-forced-to-resort-to-emergency-or-crisis-services?searchTerms=waiting%20for%20treatment (accessed 8 February 2024).
- Good Law Project . Good Law Project Will Appeal High Court Decision on Trans Waiting Times 2023. https://goodlawproject.org/update/good-law-project-will-appeal-high-court-decision-on-trans-waiting-times/ (accessed 9 February 2024).
- General Medical Council Ethical Hub . Trans Healthcare: How to Make Your Practice More Inclusive n.d. www.gmc-uk.org/professional-standards/ethical-hub/trans-healthcare#Trans%20healthcare (accessed 10 February 2024).
- General Medical Council Ethical Hub . Trans Healthcare: How to Make Your Practice More Inclusive n.d. www.gmc-uk.org/professional-standards/ethical-hub/trans-healthcare#Prescribing (accessed 10 February 2024).
- Davy Z, Toze M. What is gender dysphoria? A critical systematic narrative review. Transgend Health 2018;3:159-69.
- Benjamin H. The transsexual phenomenon. Trans N Y Acad Sci 1967;29:428-30.
- Pearce R. Understanding Trans Health: Discourse, Power and Possibility. Bristol: Policy Press; 2018.
- Shuster SM. Performing informed consent in transgender medicine. Soc Sci Med 2019;226:190-7.
- Callen-Lorde . Protocols for the Provision of Hormone Therapy n.d. https://ceitraining.org/documents/Callen-Lorde-TGNC-Hormone-Therapy-Protocols.pdf (accessed 1 February 2024).
- AusPATH . Australian Informed Consent Standards of Care for Gender Affirming Hormone Therapy n.d. https://ceitraining.org/documents/Callen-Lorde-TGNC-Hormone-Therapy-Protocols.pdf (accessed 10 February 2024).
- Kraatz MS. Institutional Work: Actors and Agency in Institutional Studies of Organizations. Cambridge: Cambridge University Press; 2009.
- What We Know project . What Does the Scholarly Research Say about the Effect of Gender Transition on Transgender Well-Being 2018. https://whatweknow.inequality.cornell.edu/topics/lgbt-equality/%20what-does-the-scholarly-research-say-about-the-well-being-of-transgender-people%20/ (accessed 11 February 2024).
- Indigo Gender Service . Indigo Gender Service n.d. https://indigogenderservice.uk/ (accessed 10 February 2024).
- Gender Recognition Act 2004. www.legislation.gov.uk/ukpga/2004/7/contents (accessed 10 February 2024).
- Coleman E, Radix AE, Bouman WP, Brown GR, de Vries ALC, Deutsch MB, et al. Standards of care for the health of transgender and gender diverse people, version 8. Int J Transgend Health 2022;23:S1-S259.
- De Vries KM. Transgender people of color at the center: conceptualizing a new intersectional model. Ethnicities 2015;15:3-27.
- Fennell MJV. Low self-esteem: a cognitive perspective. Behav Cogn Psychother 1997;25:1-26.
- Pepping CA, Lyons A, McNair R, Kirby JN, Petrocchi N, Gilbert P. A tailored compassion-focused therapy program for sexual minority young adults with depressive symotomatology: study protocol for a randomized controlled trial. BMC Psychol 2017;5.
Appendix 1 Methodology for Work Package 1
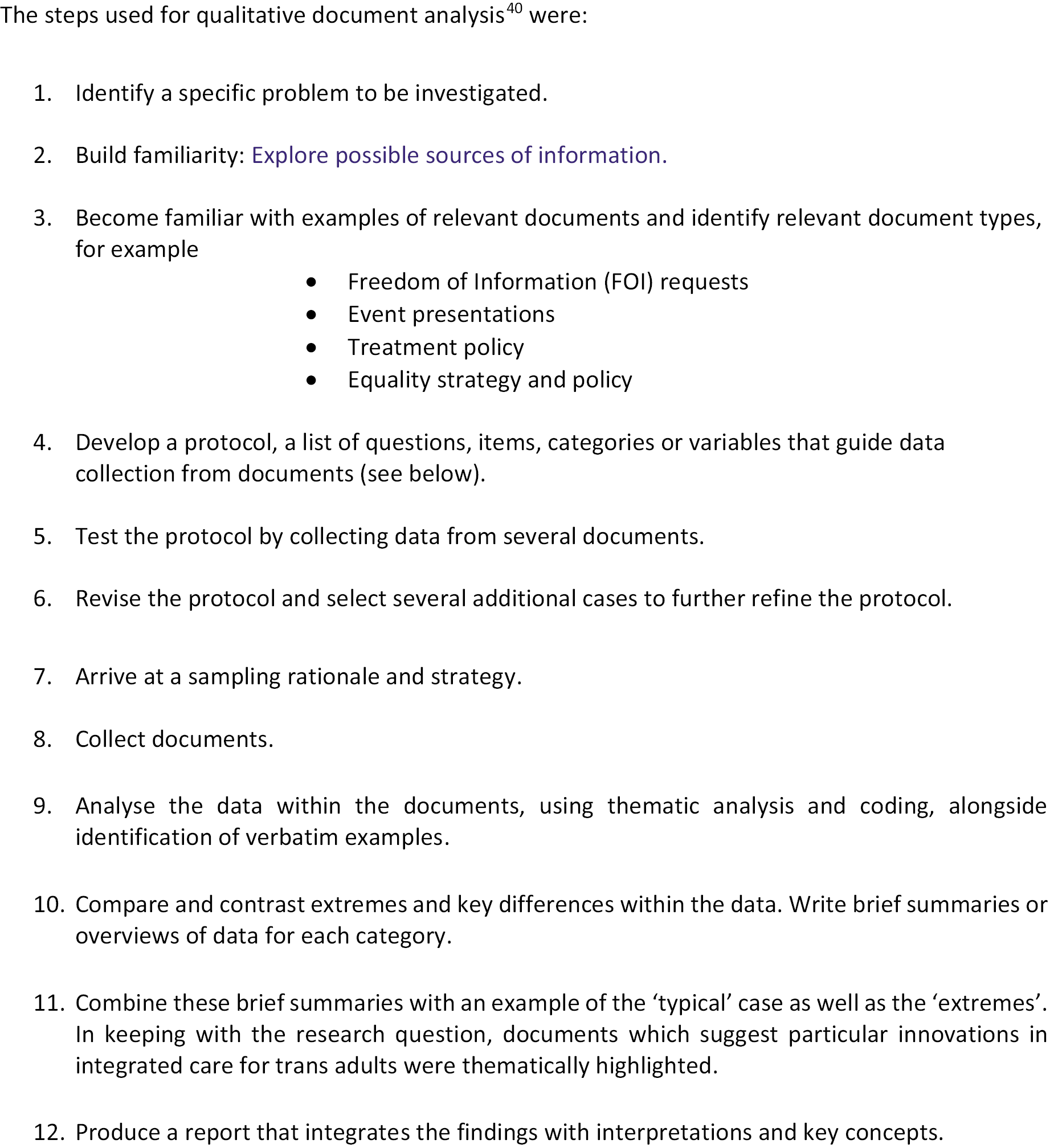
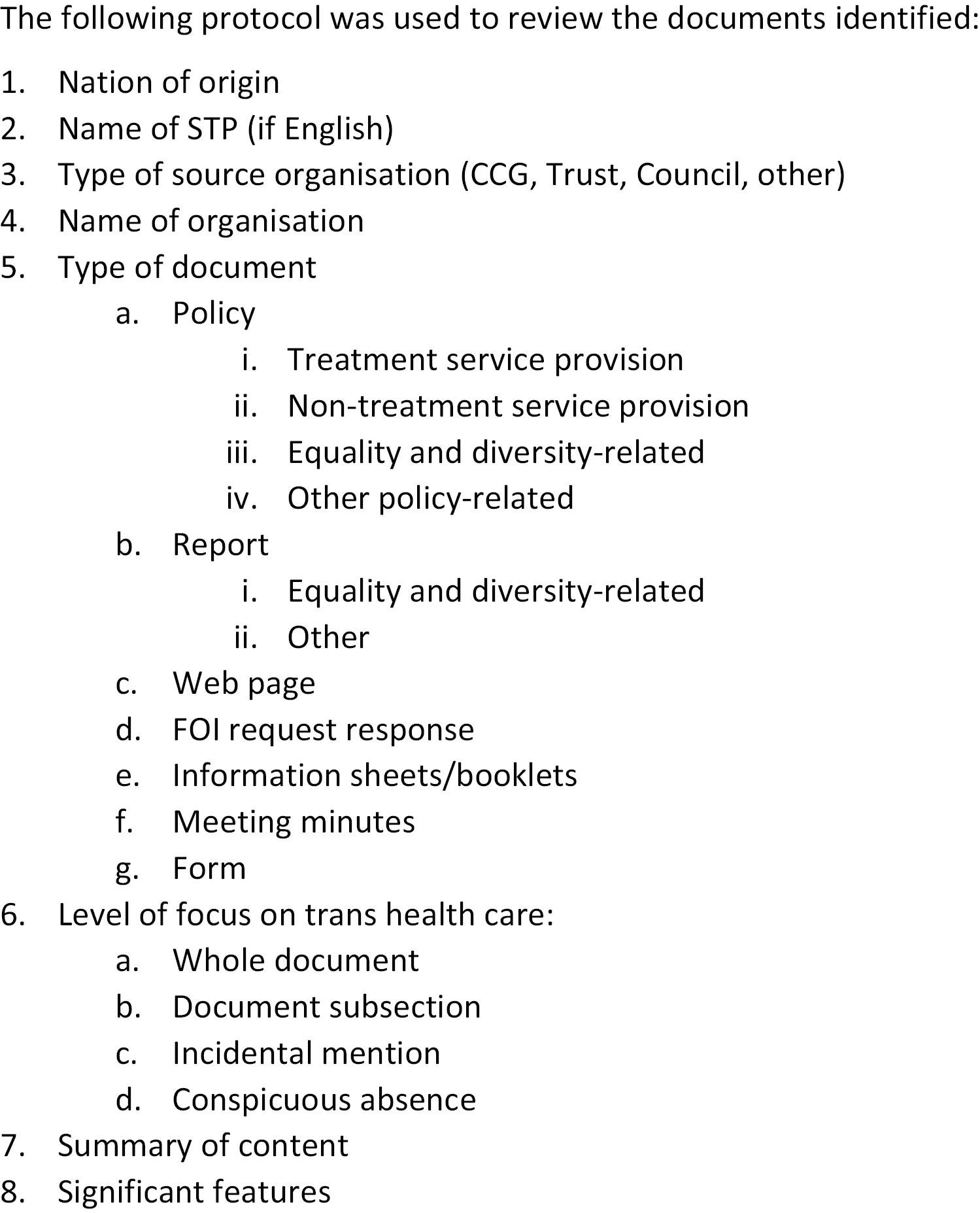
Appendix 2 The screening survey
The survey instrument
The paper version of the screening survey instrument appears on the pages that follow. This replicates the questions in the online version completed by all but a handful of the 2055 respondents.
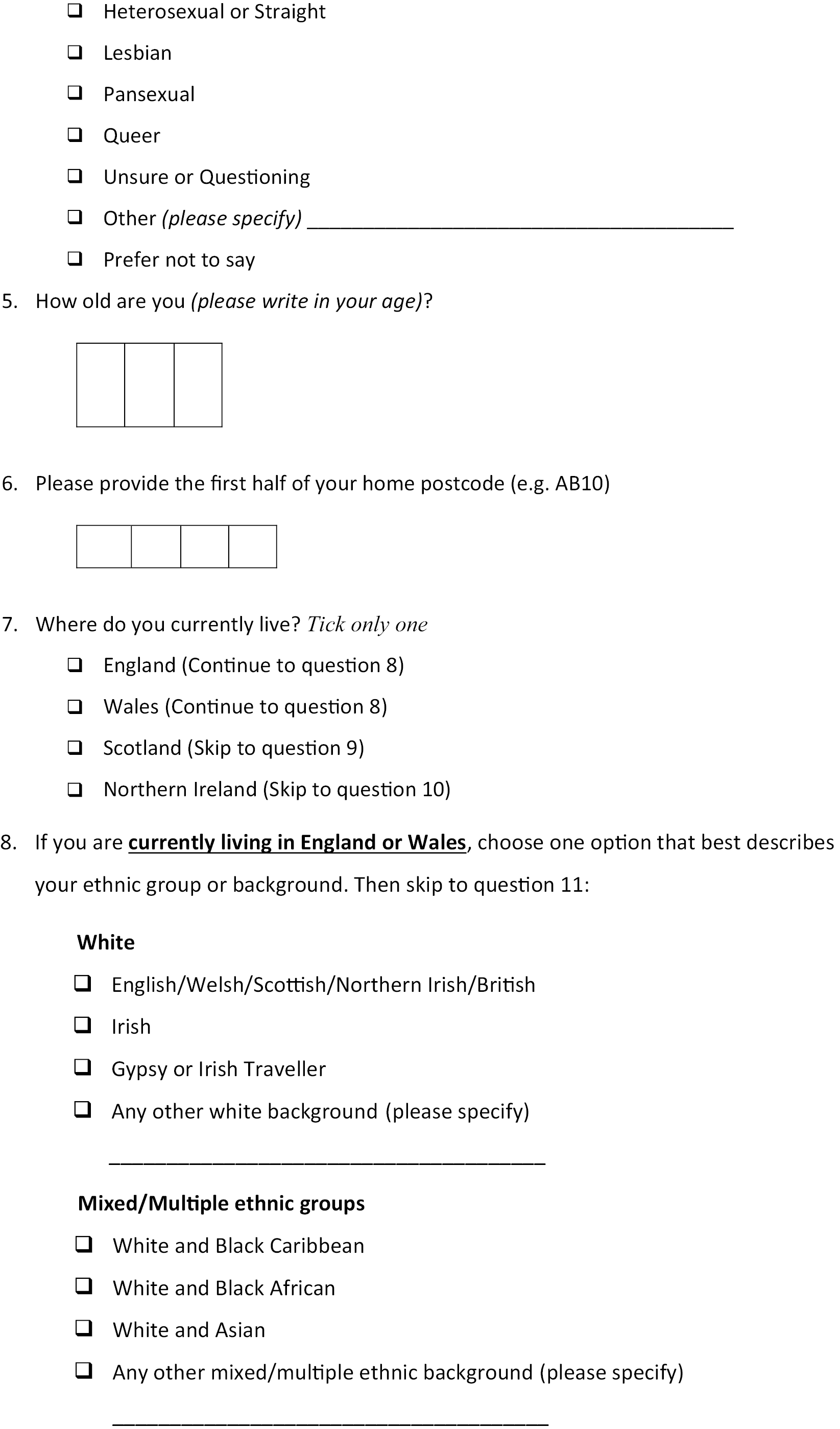

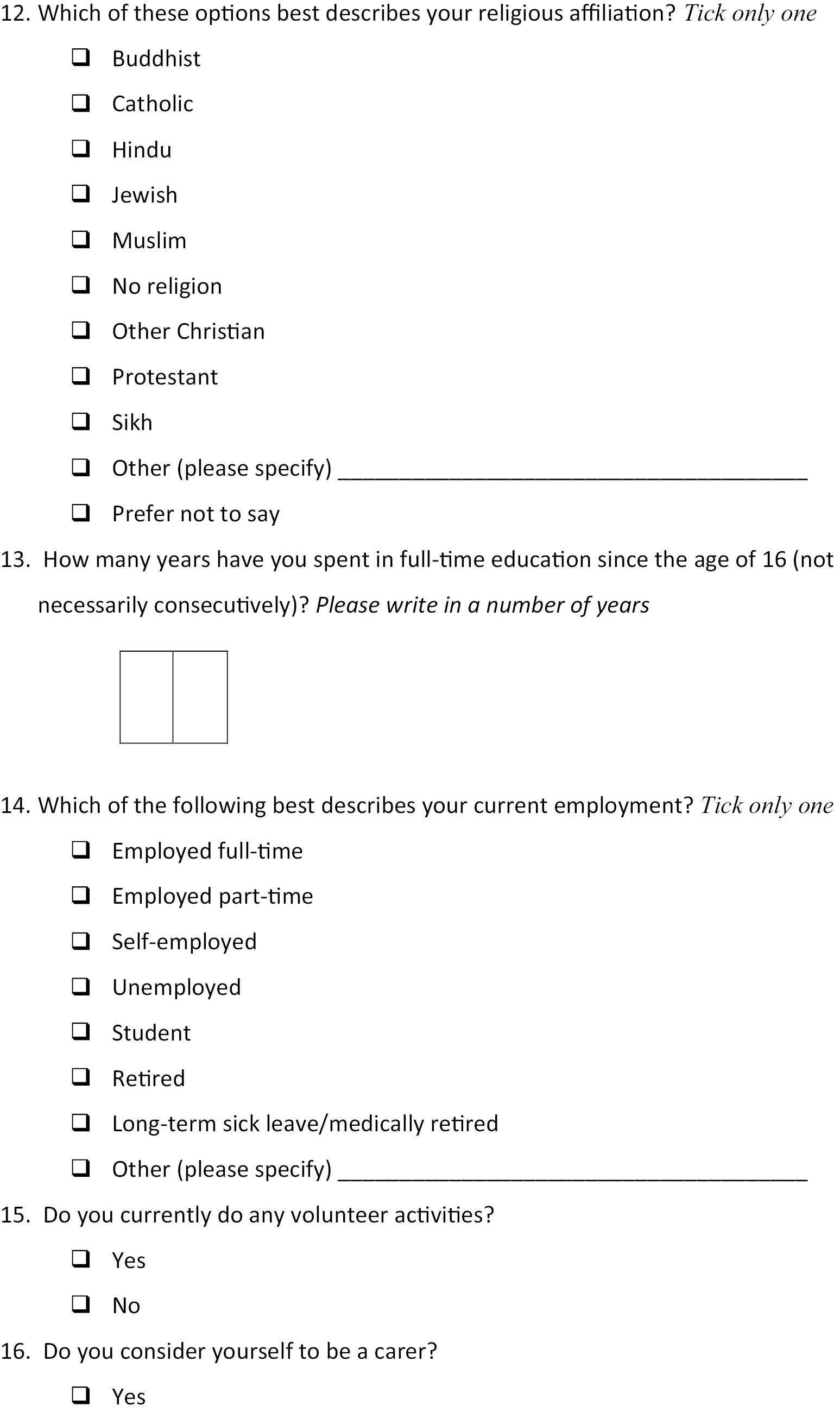
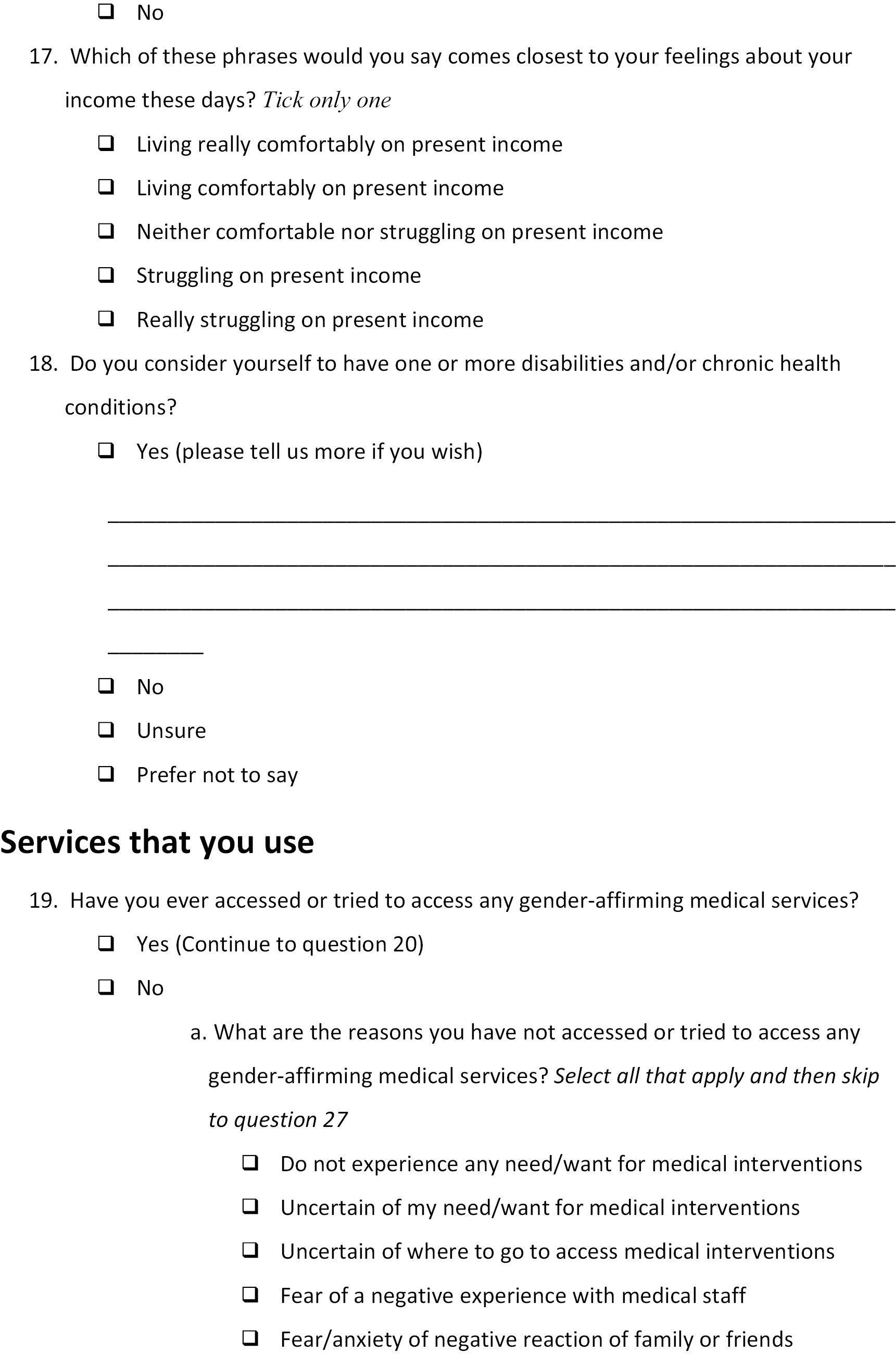

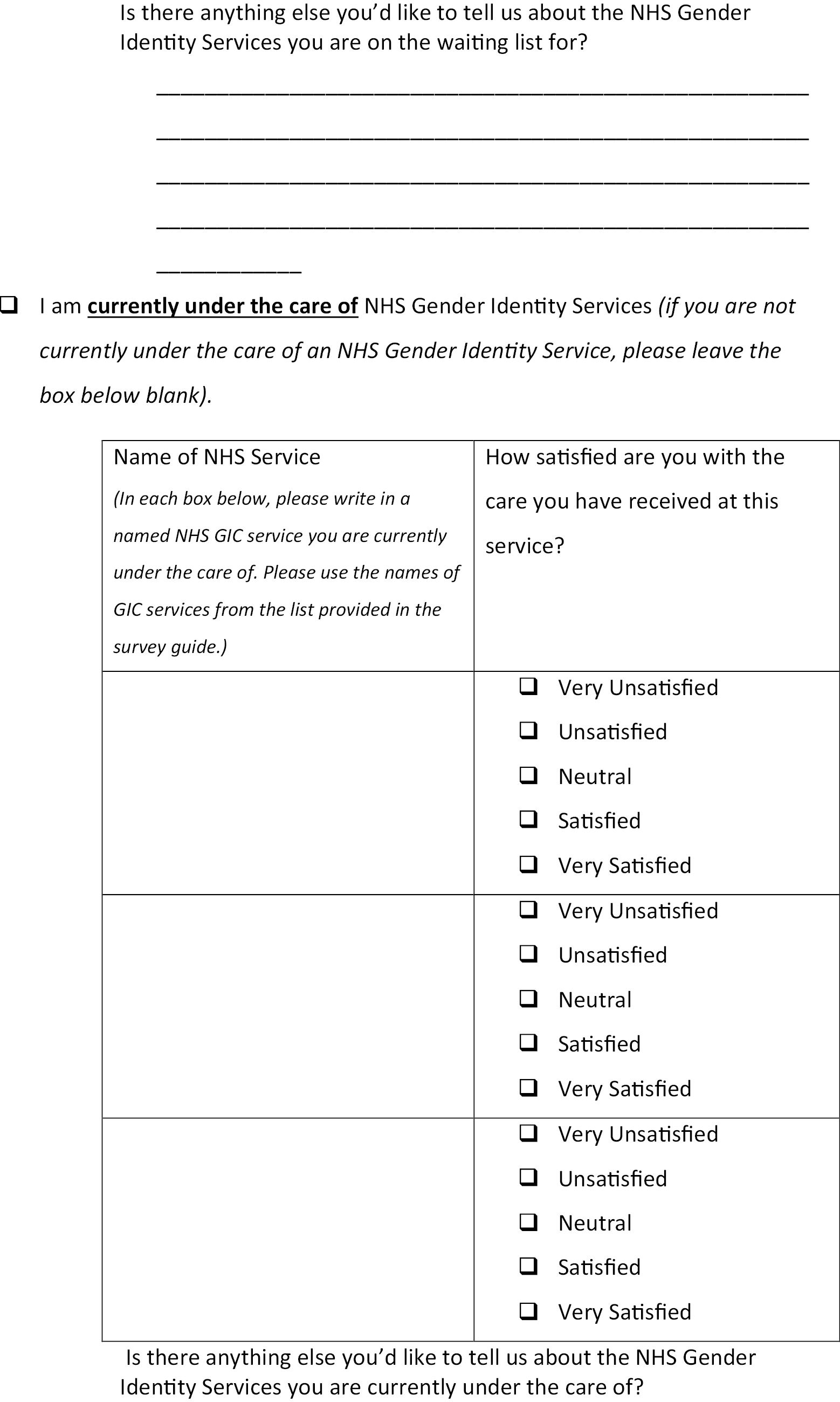
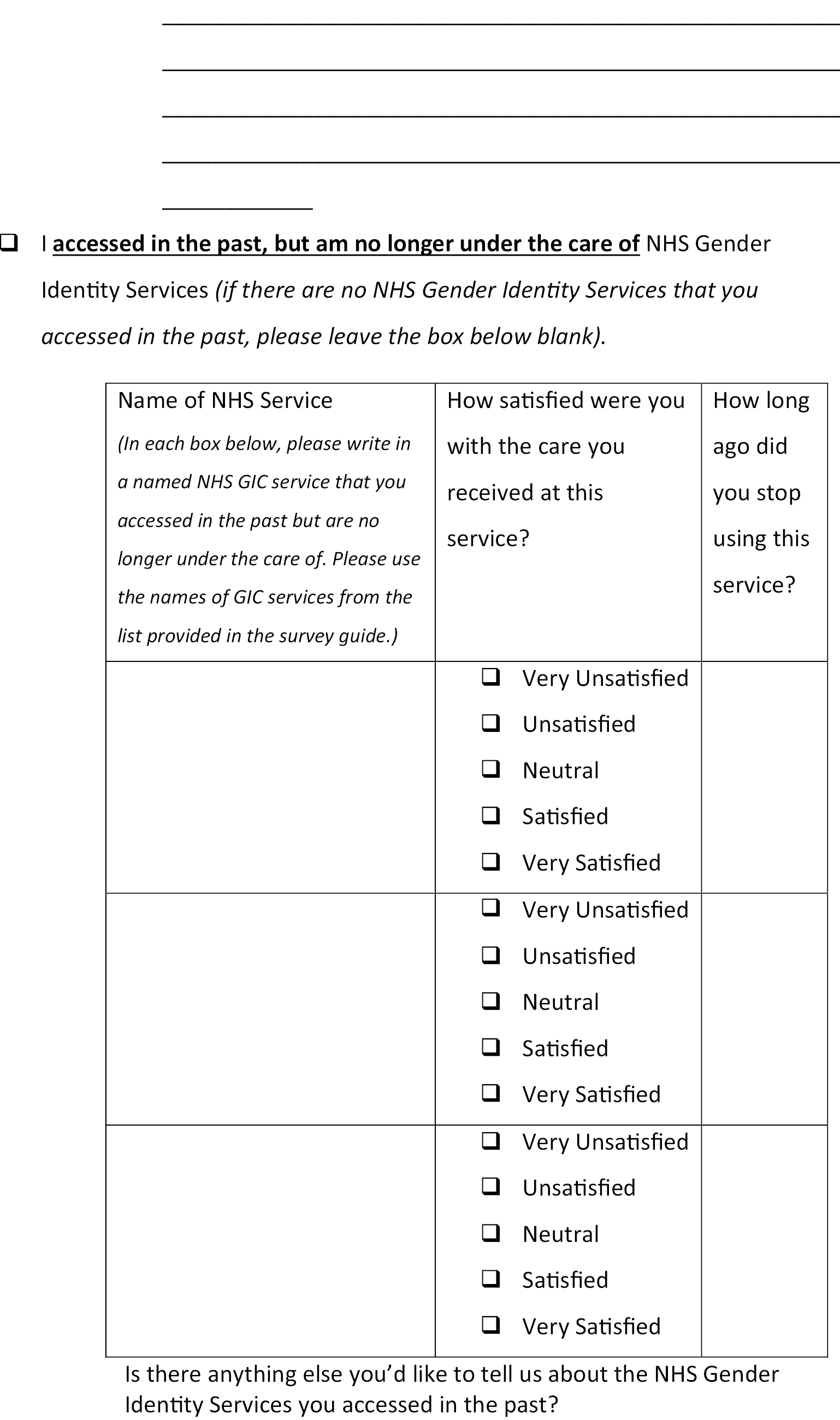
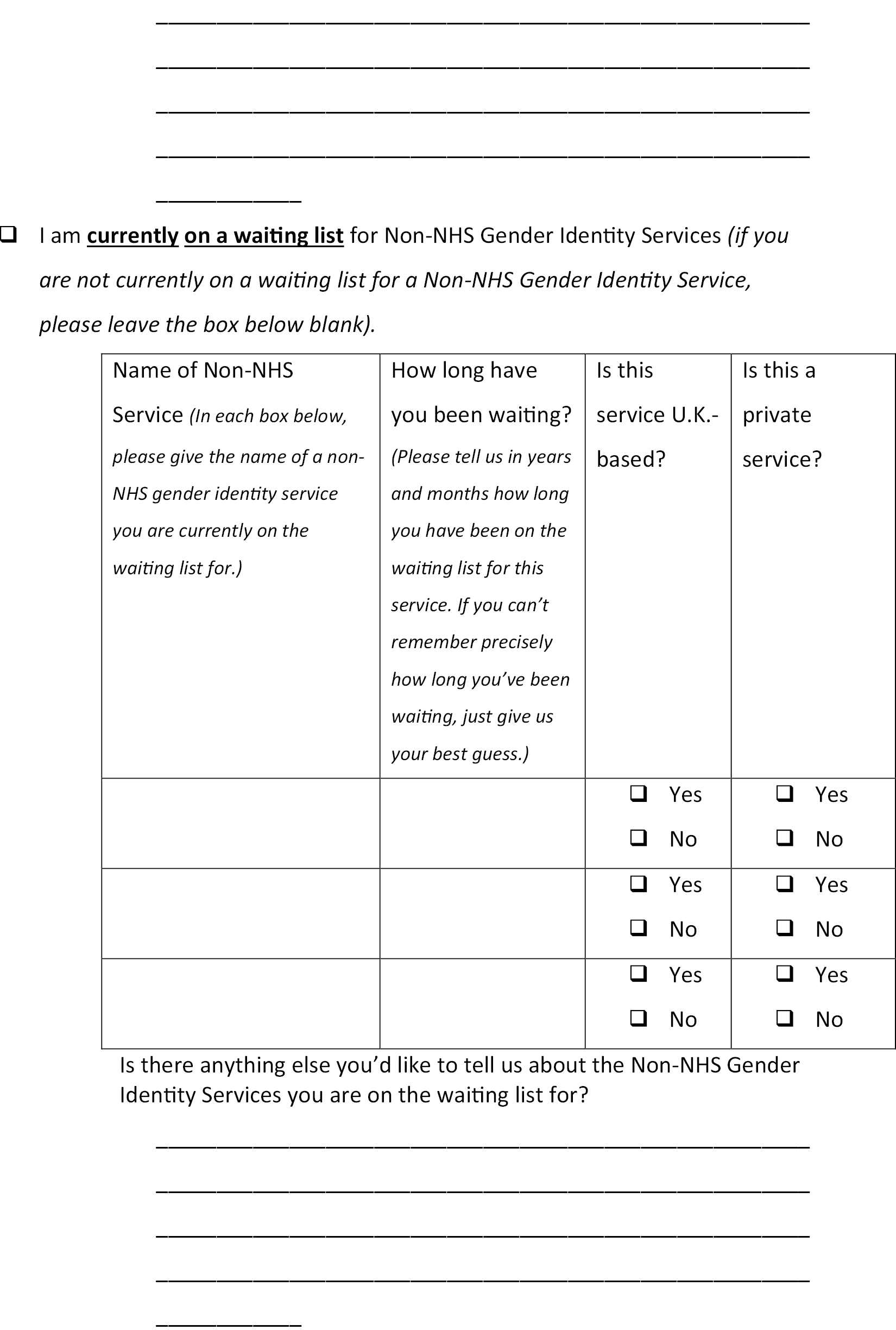
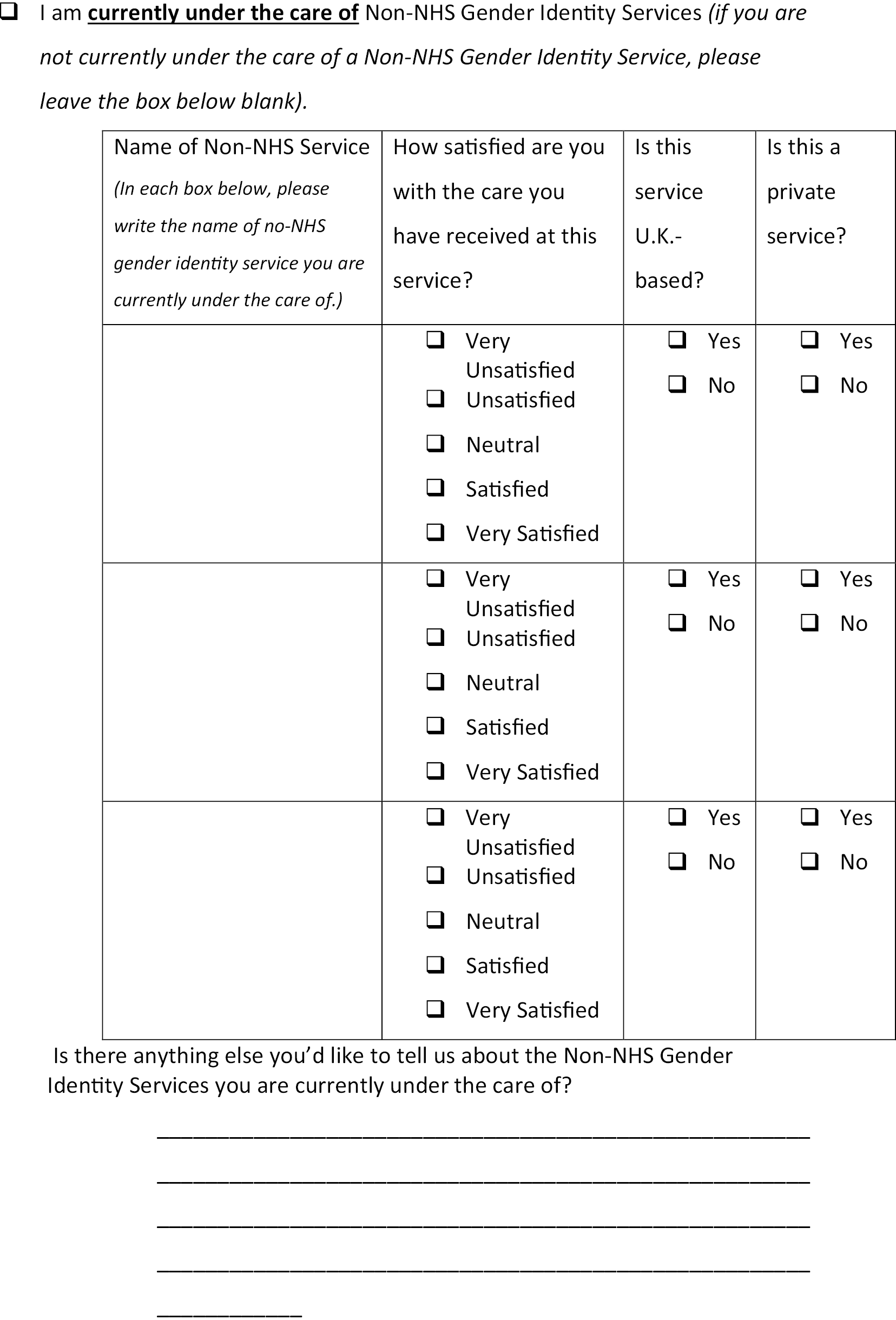
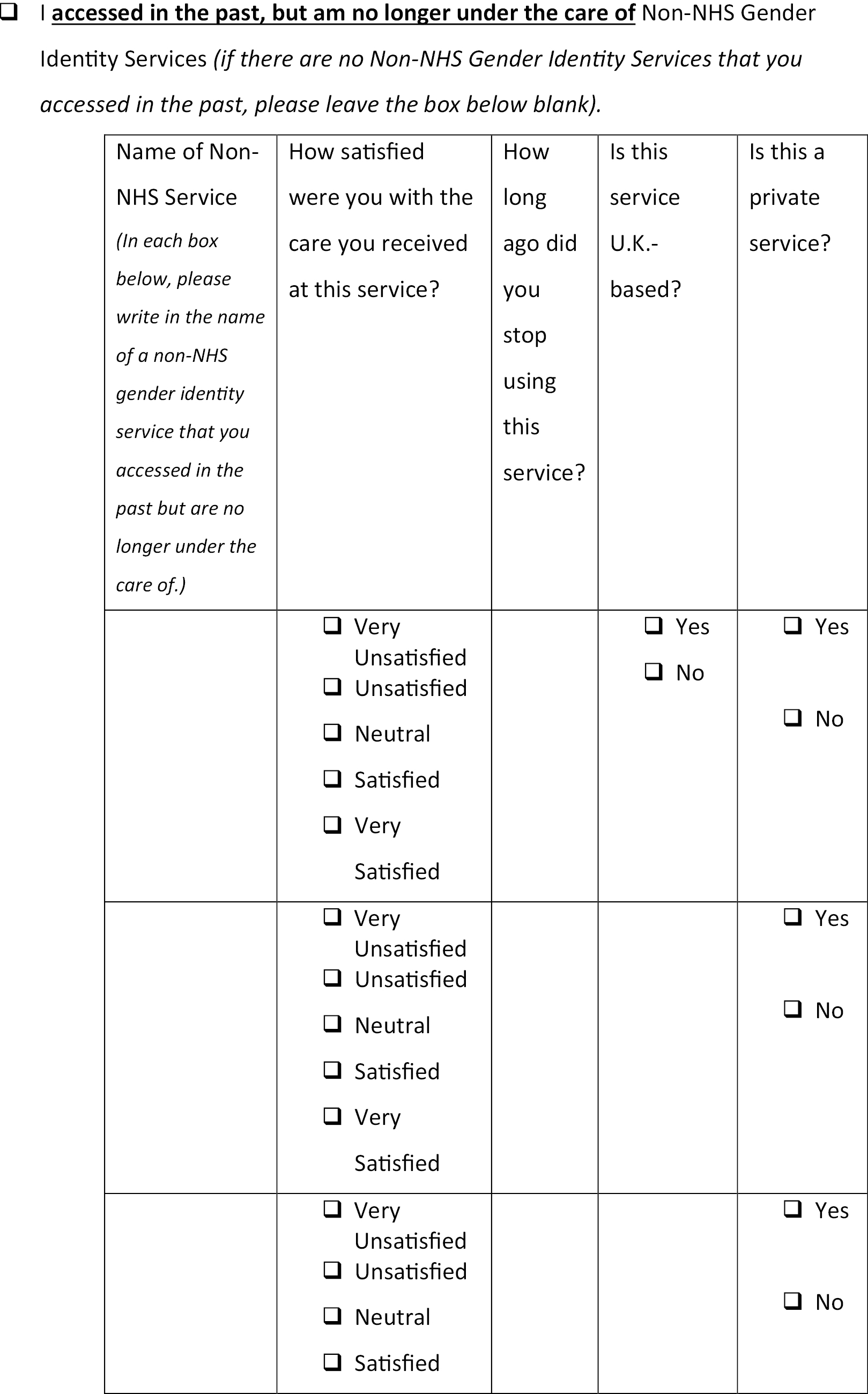
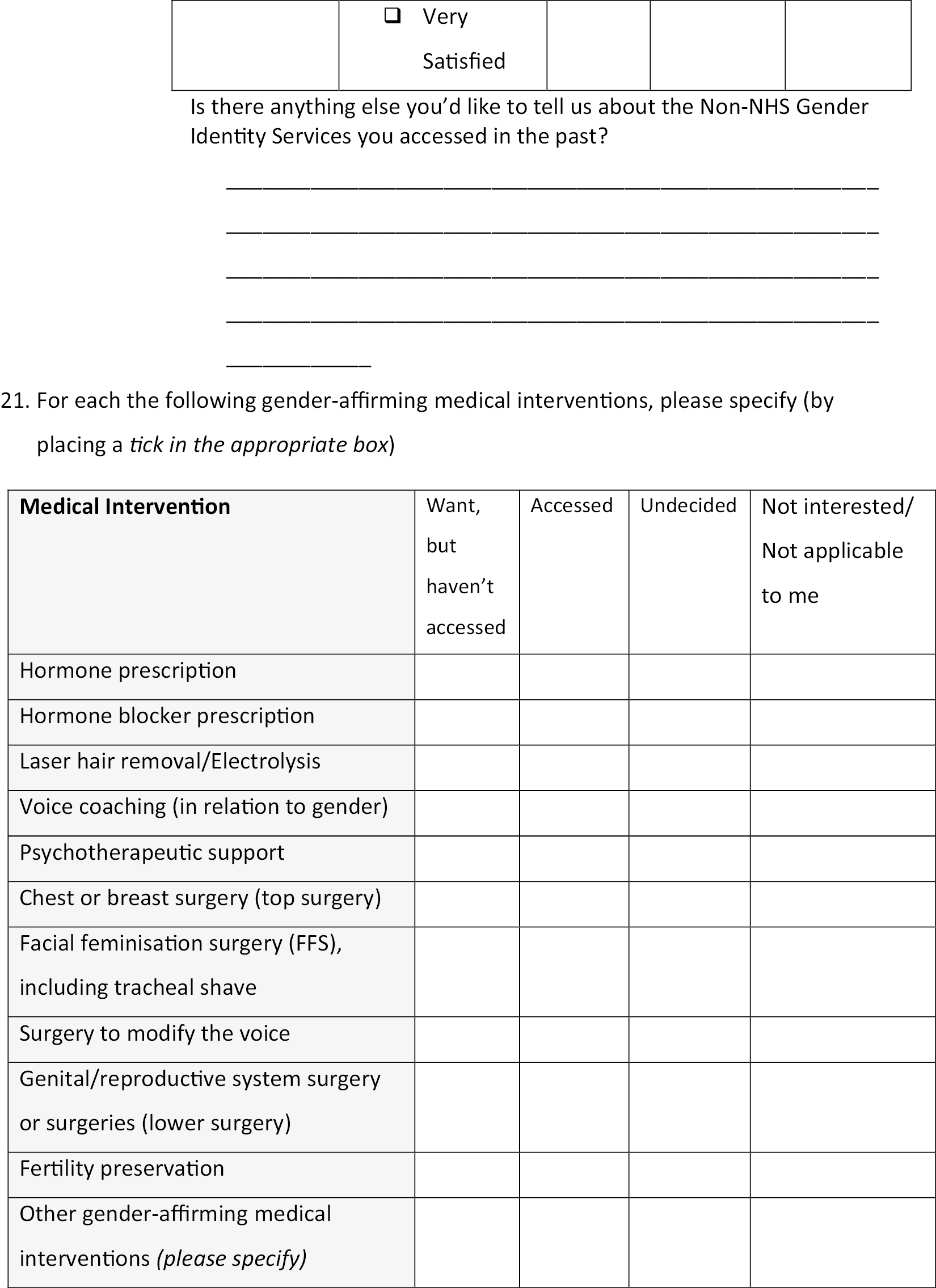
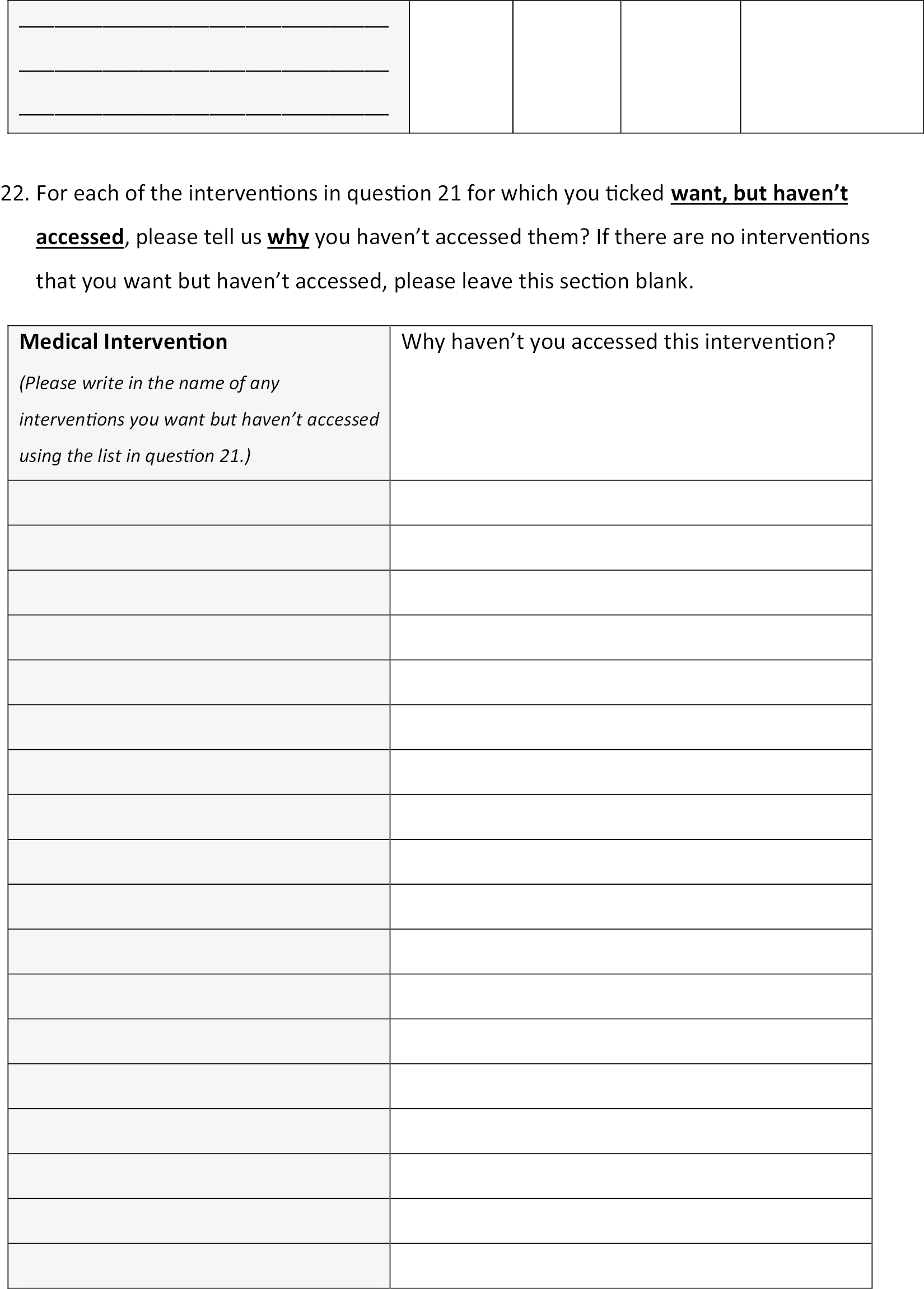
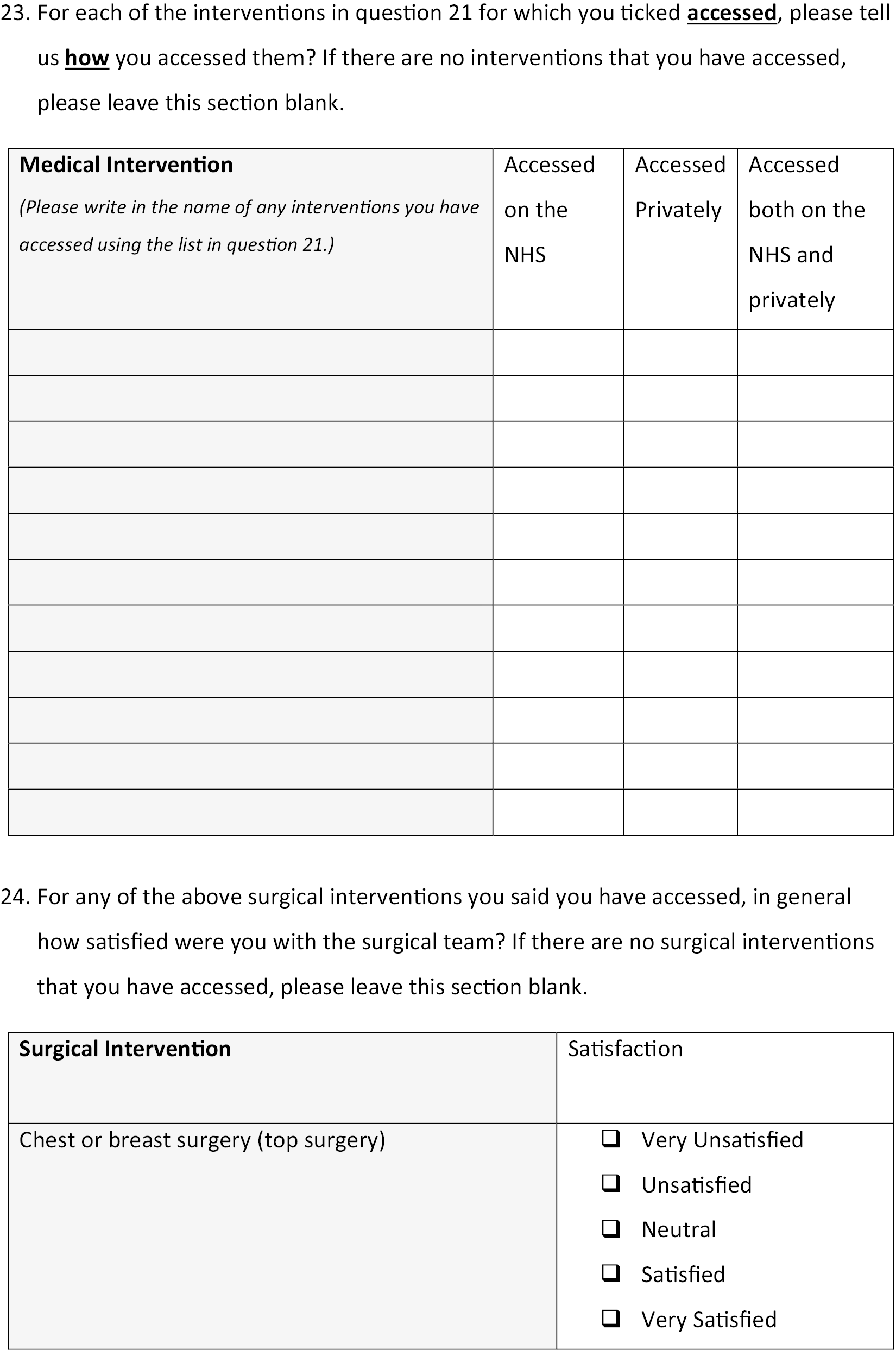

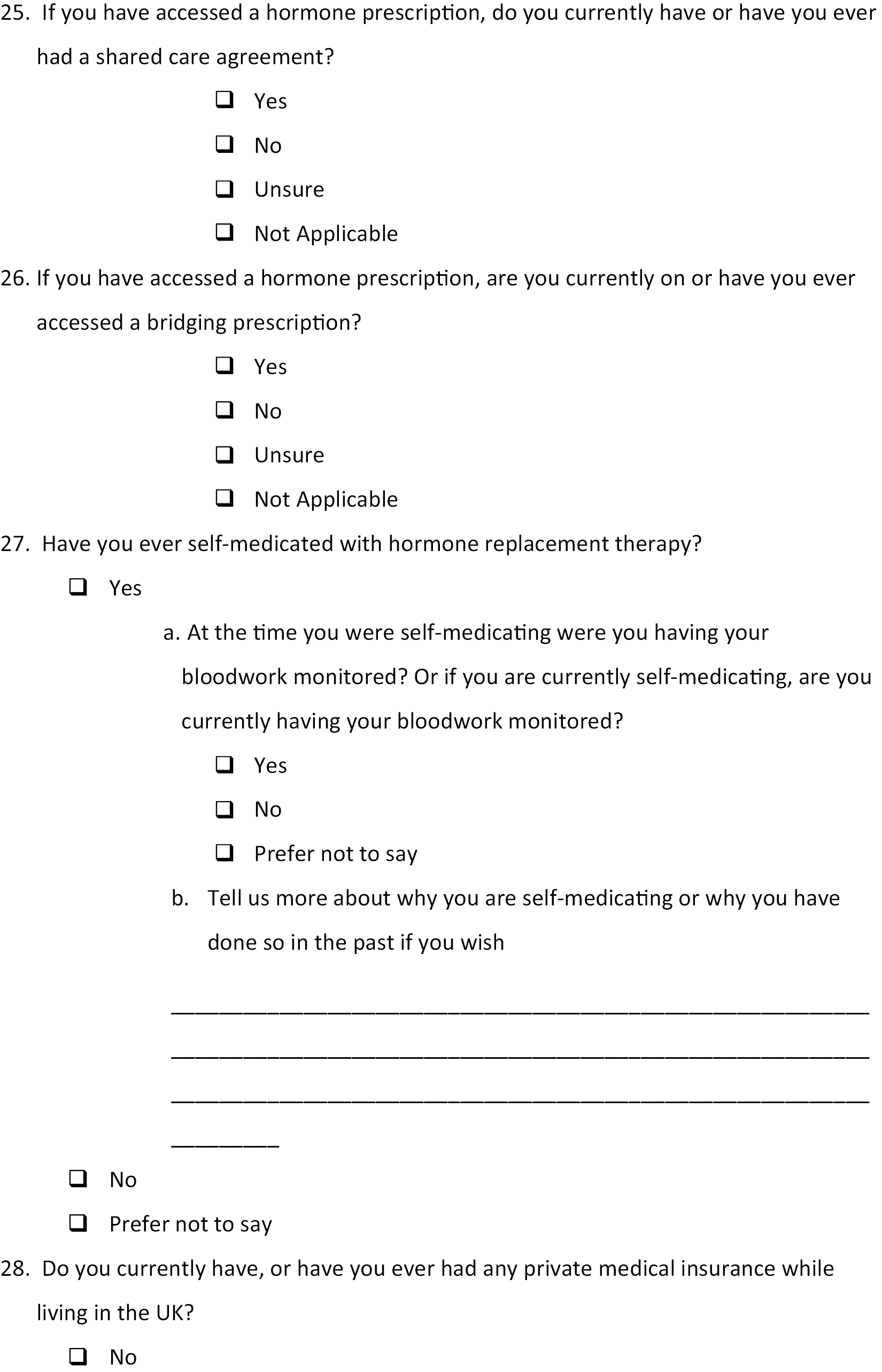
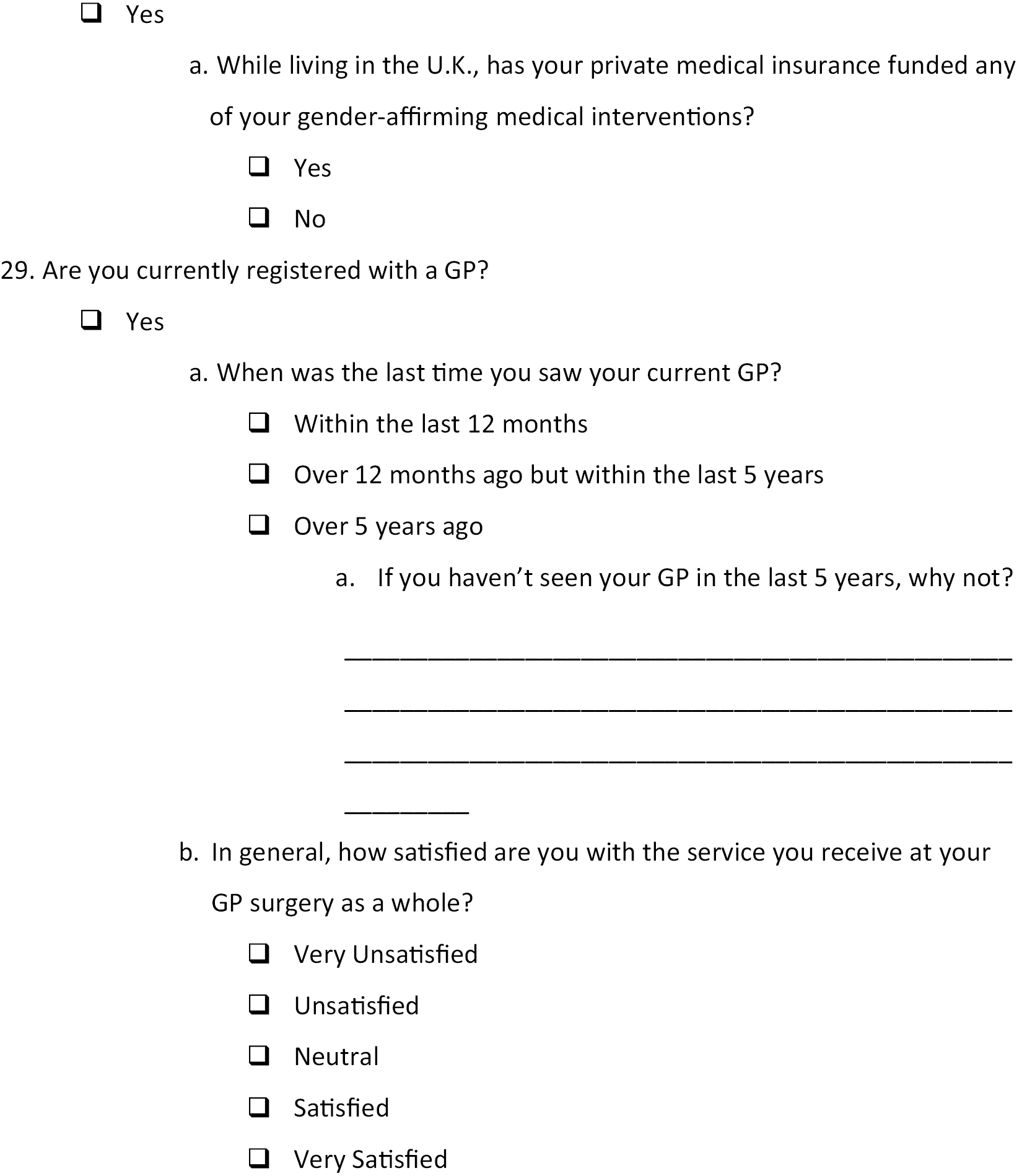
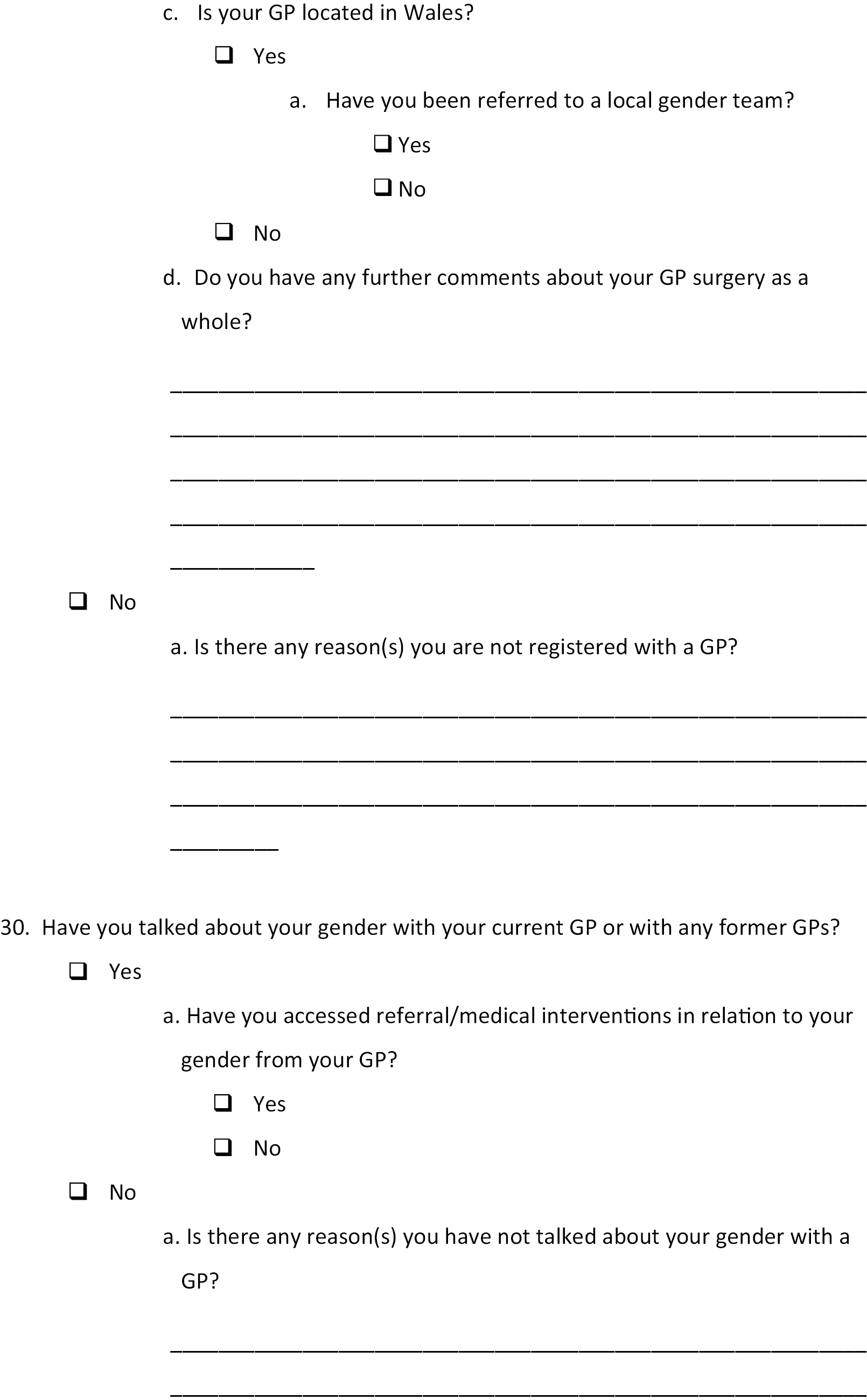
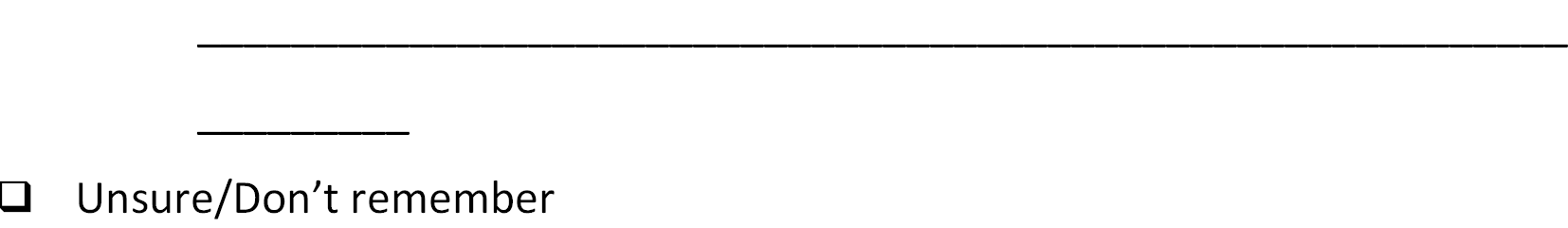
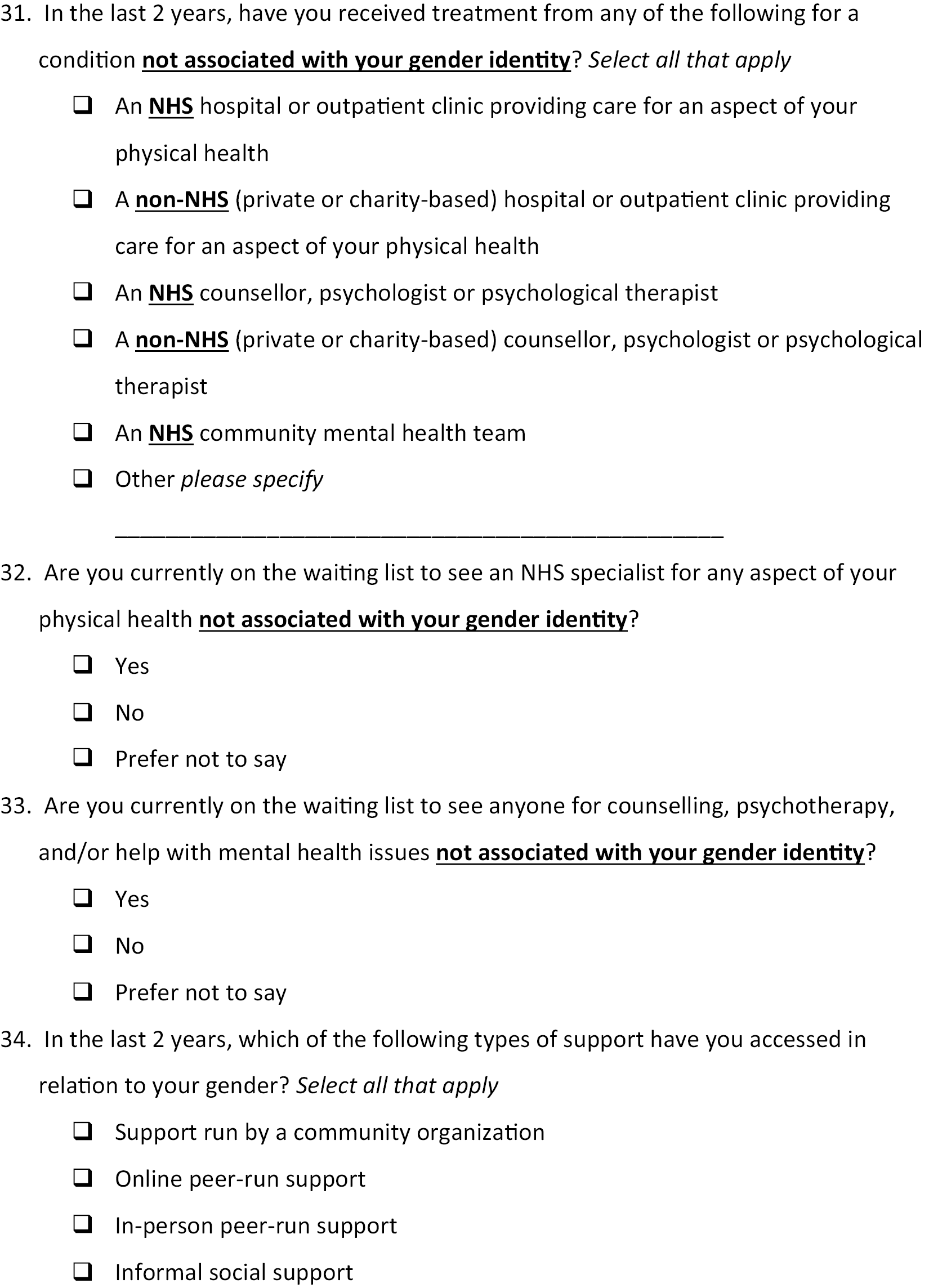
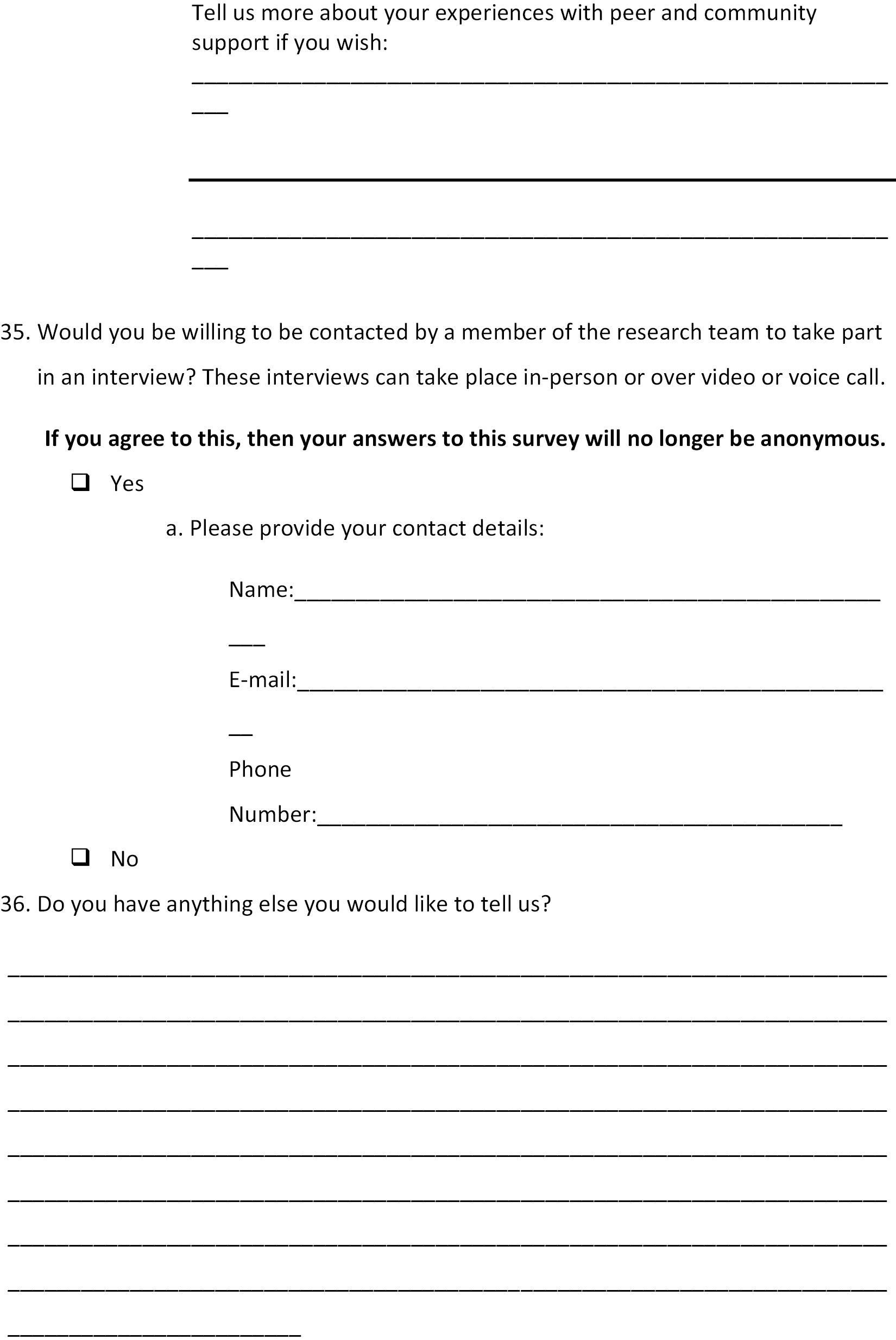
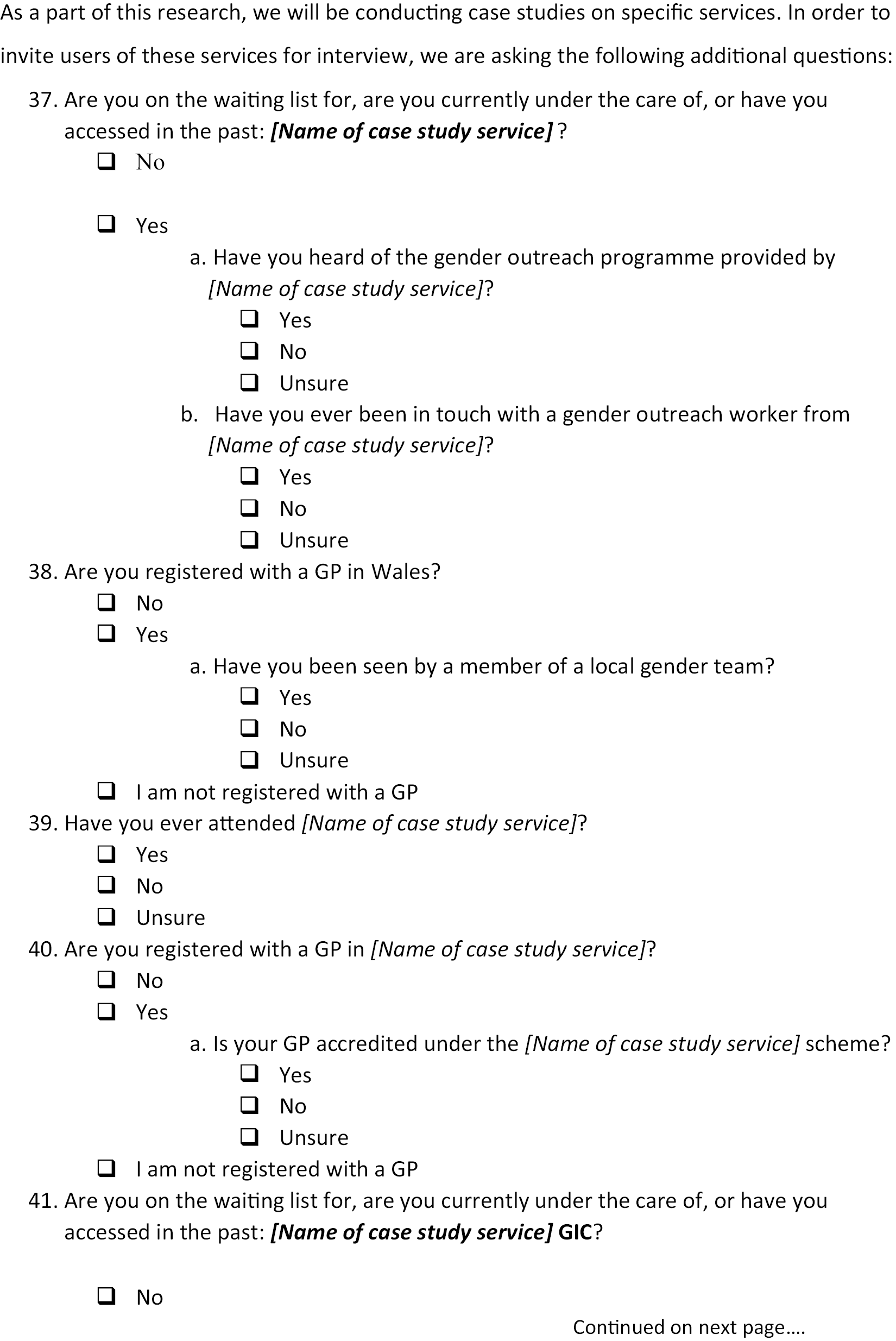
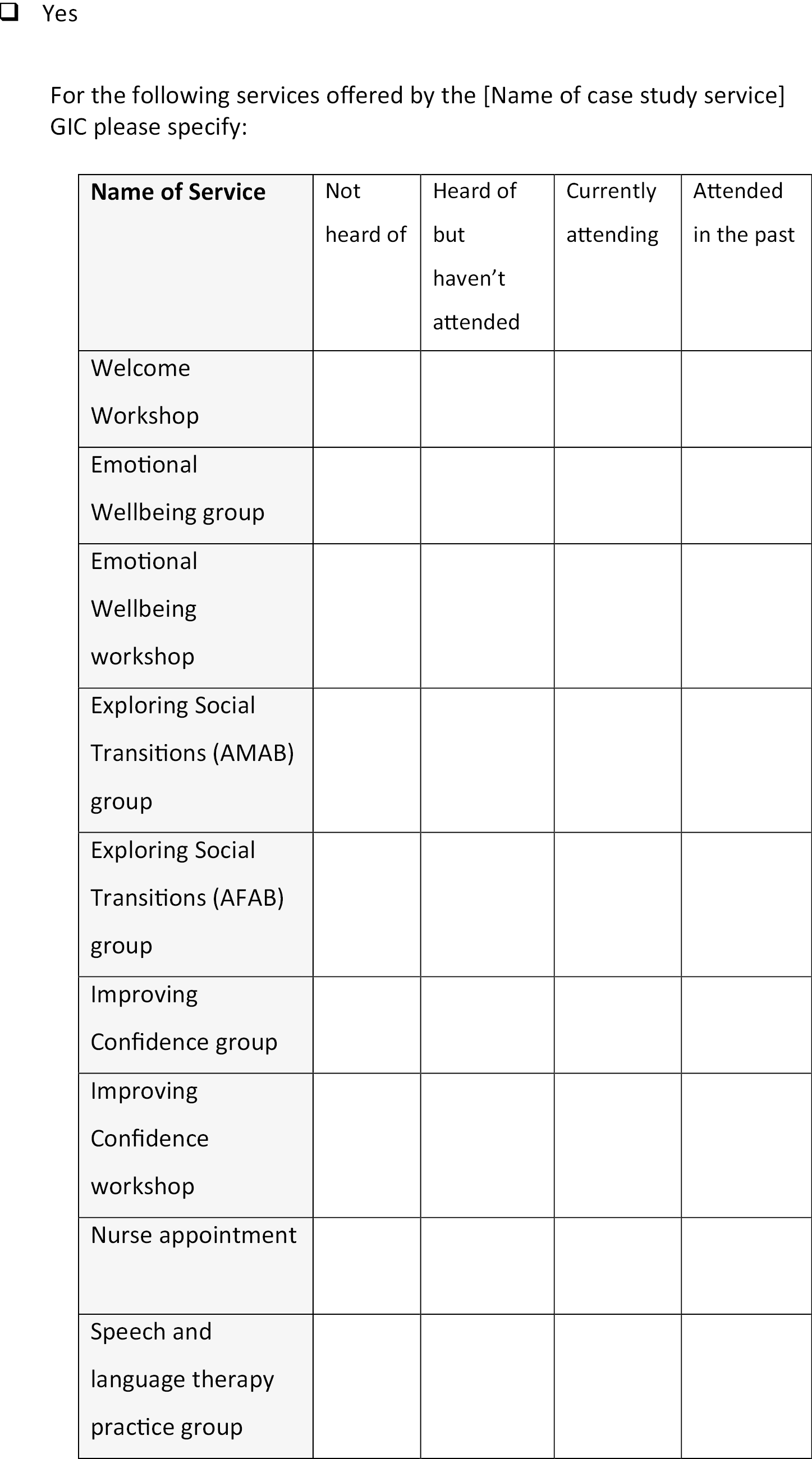
THANK YOU FOR TAKING THE TIME TO COMPLETE THIS SURVEY
Summary of survey respondent demographics
Introduction
We summarise here the demographic and healthcare characteristics of the population of 2055 survey respondents. These were all drawn on in various ways in selecting people for the various purposive subsamples of interviewees, described in Chapters 2 and 3.
Data on which services had been accessed by people were also drawn on to identify which people to invite for interview within the case studies of particular services, described in Chapter 4. Some data on service satisfaction were also collected in the survey. The intention behind this was to allow identification of people with higher or lower levels of satisfaction with particular services, so that these could be represented in a balanced way within subsamples and case studies. In fact, the numbers of people offering to be interviewed relevant to each subsample and case study did not provide any scope for further structuring of subsamples according to level of service satisfaction. Service satisfaction data were not drawn upon when inviting people for interview.
Demographic characteristics
Across the 2055 respondents, many people selected more than one option offered as a description of their gender. There were 3293 options selected in all, by 2055 people, summarised in Figure 3. Responses indicating a non-binary gender identity were more common overall, although in many cases people indicated both a binary and a non-binary identity.
FIGURE 3.
Gender reported by survey respondents.

Similarly, many respondents selected more than one of the options offered as a description of their sexuality. A total of 3297 terms were selected across the 2055 respondents, summarised in Figure 4. Being lesbian, gay or heterosexual accounted for only 24% of responses.
FIGURE 4.
Sexual orientation reported by survey respondents.

Figure 5 shows that the age distribution of participants was significantly skewed towards the younger adult range, with 56% of respondents under 30. Attempts were made in all the subsamples of interviewees to make sure that the fuller range of ages were more equally represented. The only exception was the subsample of older trans people. Given the relative lack of survey respondents and interview offers from people over 70, this subsample was made up of people aged 50 upwards.
FIGURE 5.
Age distribution of survey respondents.
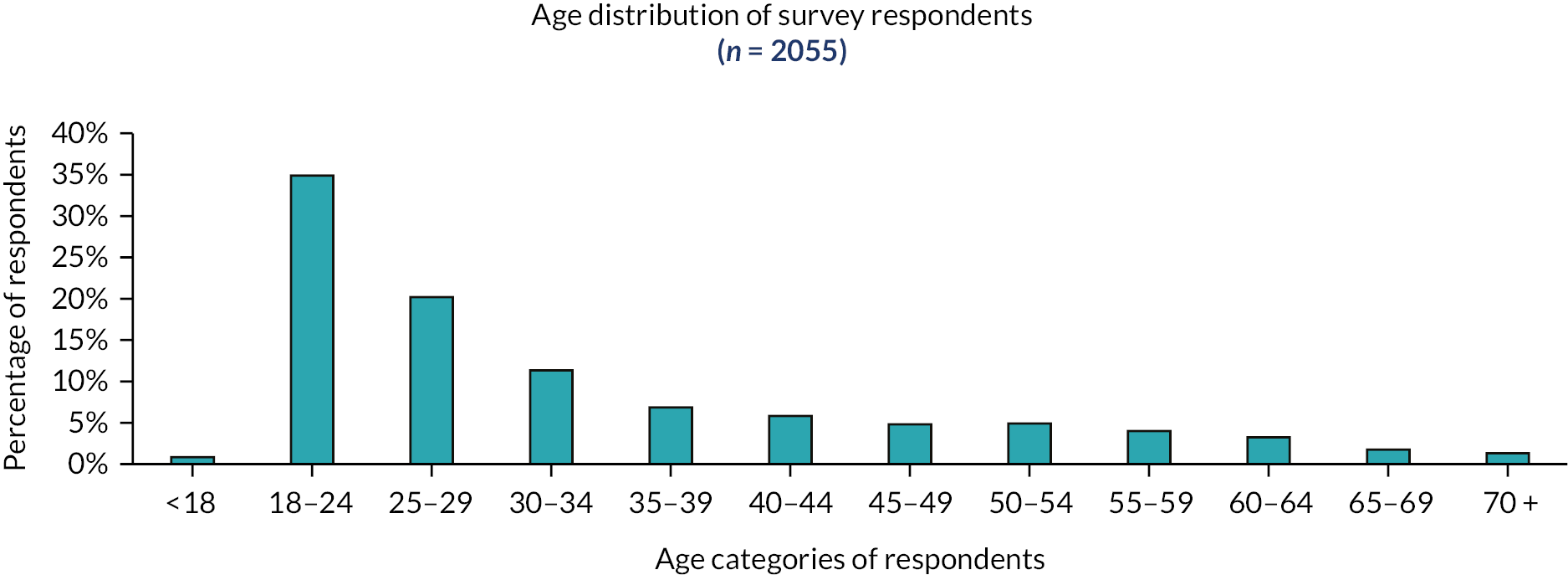
Eighty-nine per cent of respondents entered that they were born in the UK, rather than elsewhere. Figure 6 shows the distribution of responses on ethnicity, grouping responses into four main categories. Respondents were predominantly white (93%). Efforts were made to recruit global majority interviewees to all subsamples – place of birth was not a criterion for selection.
FIGURE 6.
Ethnicity of survey respondents.

Figure 7 shows that survey respondents included a wide range of religions. However, 67% selected the ‘no religion’ response option.
FIGURE 7.
Religion of survey respondents.
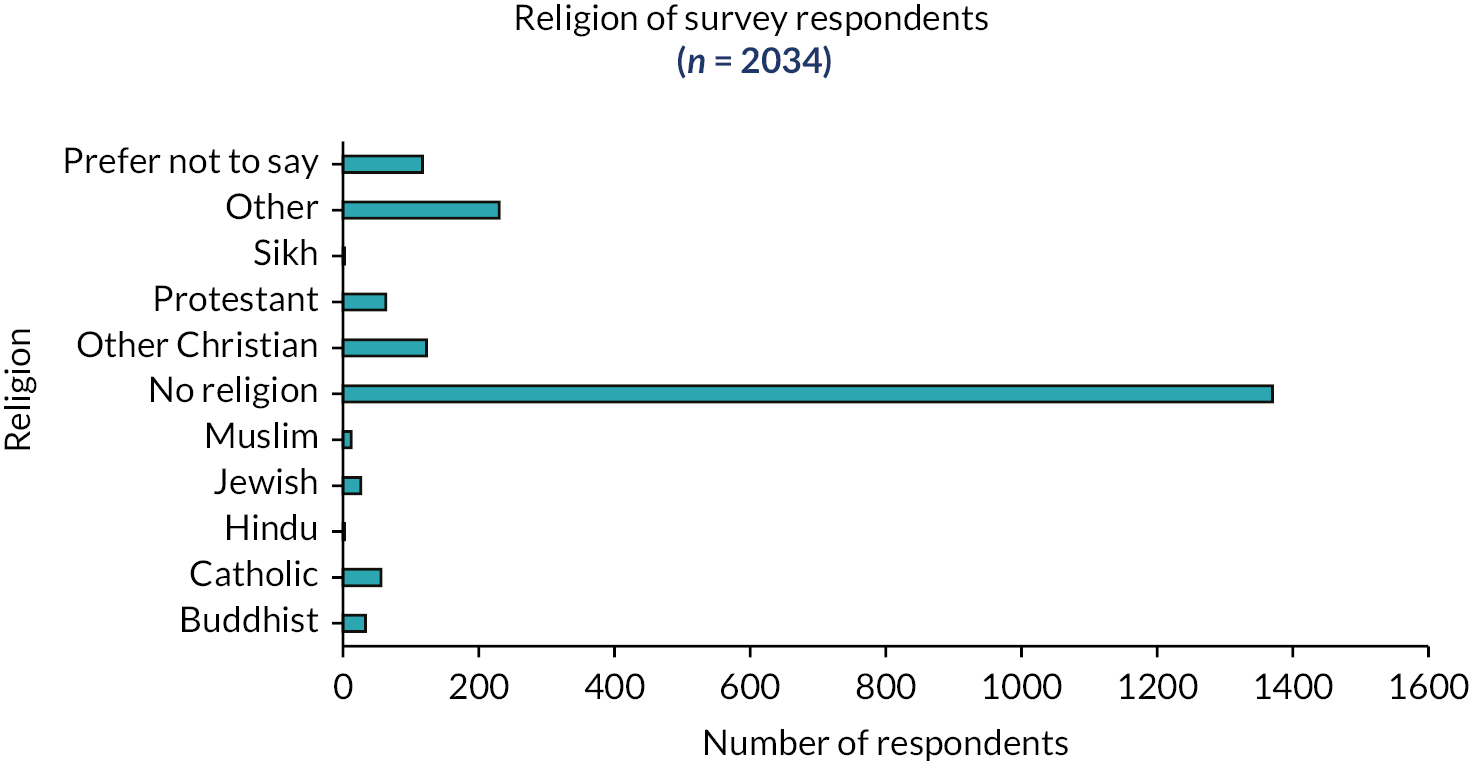
Figure 8 shows that the majority of participants had received post-18 education, with 40% leaving after 3 years of higher or further education, and a further 39% studying longer. Only 6% had left education at 16, and a further 15% at 18. Again, wherever possible, subsamples were constructed to represent a variety of educational attainment.
FIGURE 8.
Education since age 16.

Figure 9 summarises responses on employment status. Full-time employment and student status were the commonest responses, with just over half of respondents (53%) overall indicating that they were either employed or self-employed. Thirty-five per cent of respondents said that they undertook volunteer activities, and 11% considered themselves to be carers.
FIGURE 9.
Employment status of survey respondents.

Figure 10 summarises respondents’ perceptions as to the adequacy of their income. This shows fairly balanced distribution around a median response of ‘neither comfortable nor struggling’, with 28% saying they were either ‘struggling’ or ‘really struggling’.
FIGURE 10.
Income adequacy of survey respondents.
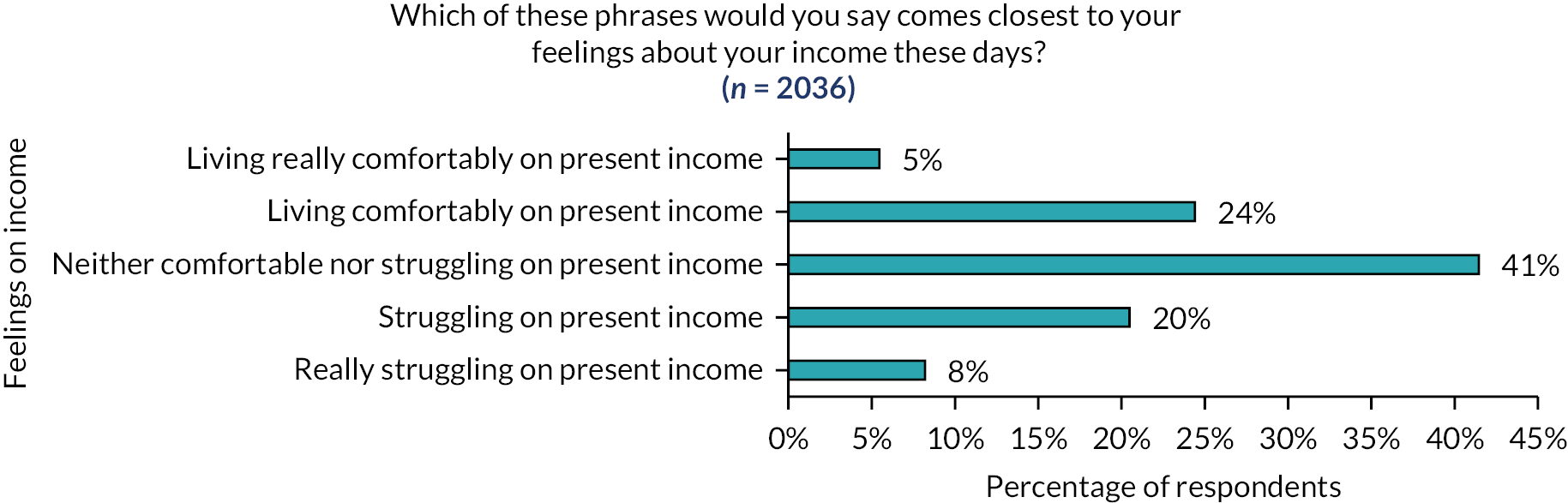
Figure 11 shows that the majority of people in the population of respondents considered themselves to be disabled in one or many ways, or to have a chronic health condition. This preponderance may of course reflect selection bias, in that people were responding to a survey about health care. Whether or not this is the case does not of course compromise the validity of the criteria used to select people for the purposive subsamples.
FIGURE 11.
Health conditions of survey respondents.

Appendix 3 The national sample qualitative data
This appendix contains the interview protocol for the qualitative interviews carried out across the subsamples. It also contains an illustration of the descriptive codes used in the first stage of data analysis described in Chapter 2, in the form of a screenshot from NVivo data analysis software.
Interview protocol
The guide for service-user interviews within the national sample appears over the following pages.
Interviewer guide for ‘service-user’ interviews
Prior to interview:
-
Introduce yourself.
-
Describe the overall project.
-
Describe the purpose of this interview.
-
Check that they have consented.
-
State that the interview will be recorded, what will happen to this recording, how it will be stored, transcribed, anonymised and when/how it will be destroyed.
-
Check that they are OK for you to turn the recorder on.
Before we start, I just want to walk you through the interview so you know what to expect. The interview will be in four parts. We will start with some general information about you. I’ll just ask you a few questions about who you are, and about your health in general. We are interested in all health experiences, not just transition-related health care. In the second part, I’ll be asking you about your experience of using GIC services and hopefully we will be able to talk in more detail about some of those experiences. In the third part, I’d like to broaden this out to think about the different general health services you might have used in the past or are using now. This could include your GP, hospital services or even social support or social care services. Finally, we’ll spend a little time talking about your views on Trans, including GNB, health generally and how health services could be improved.
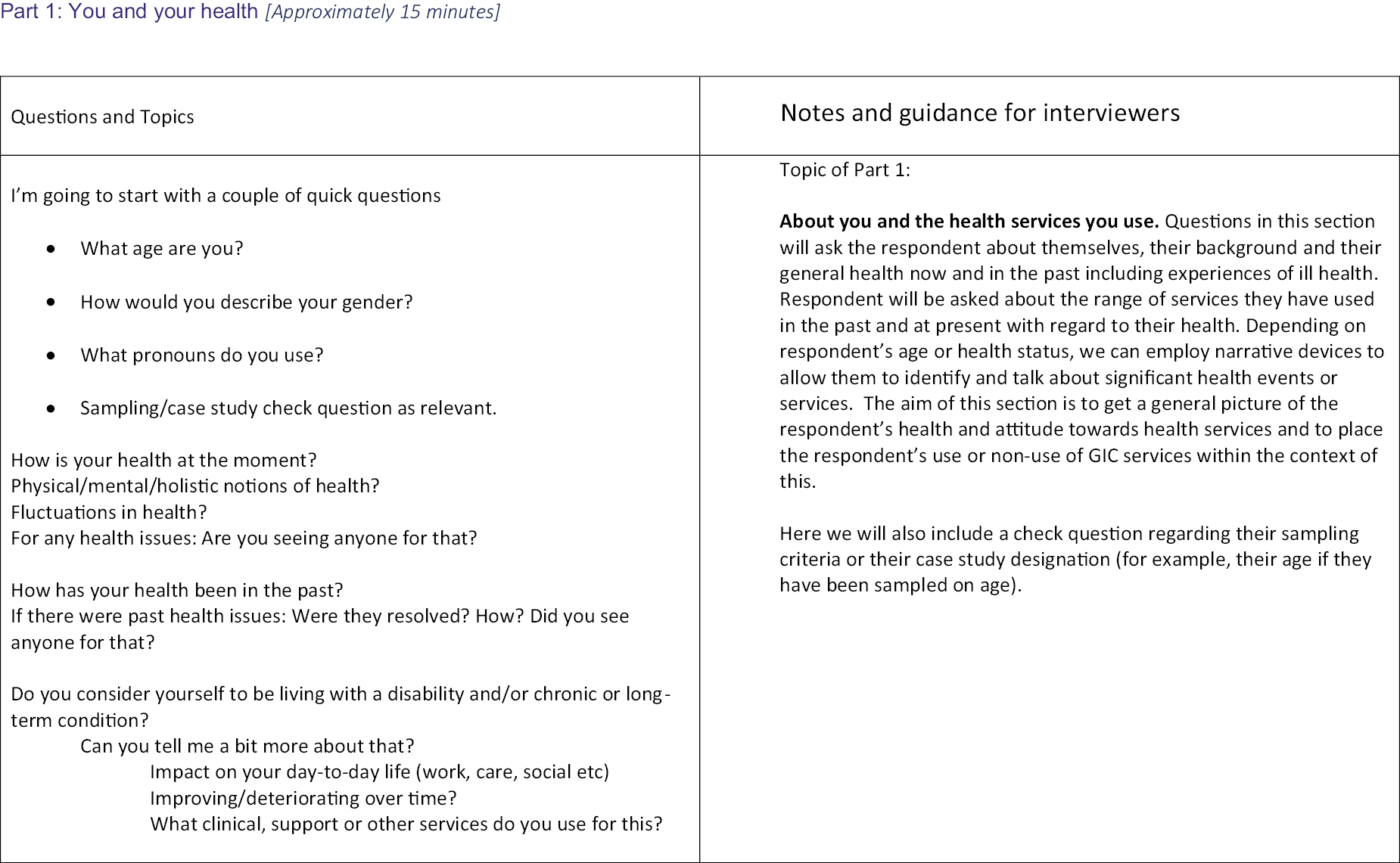
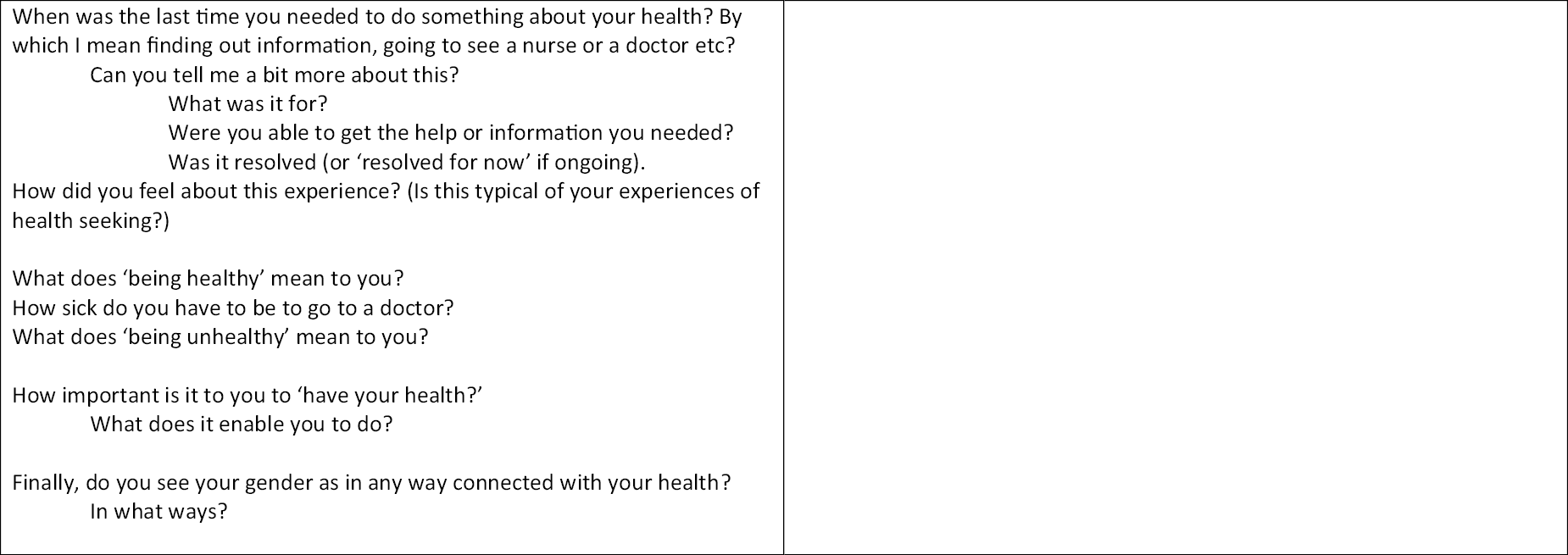
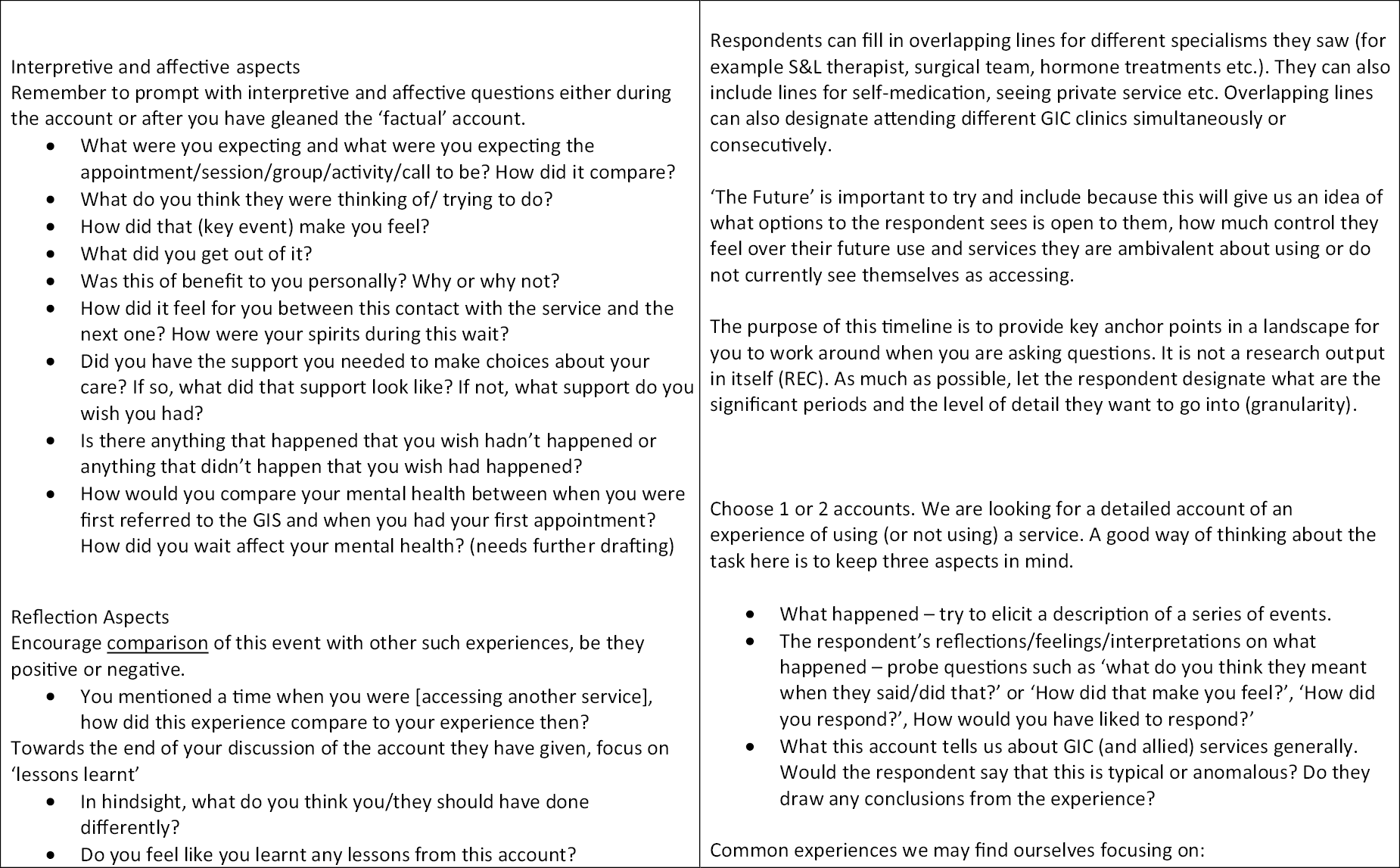
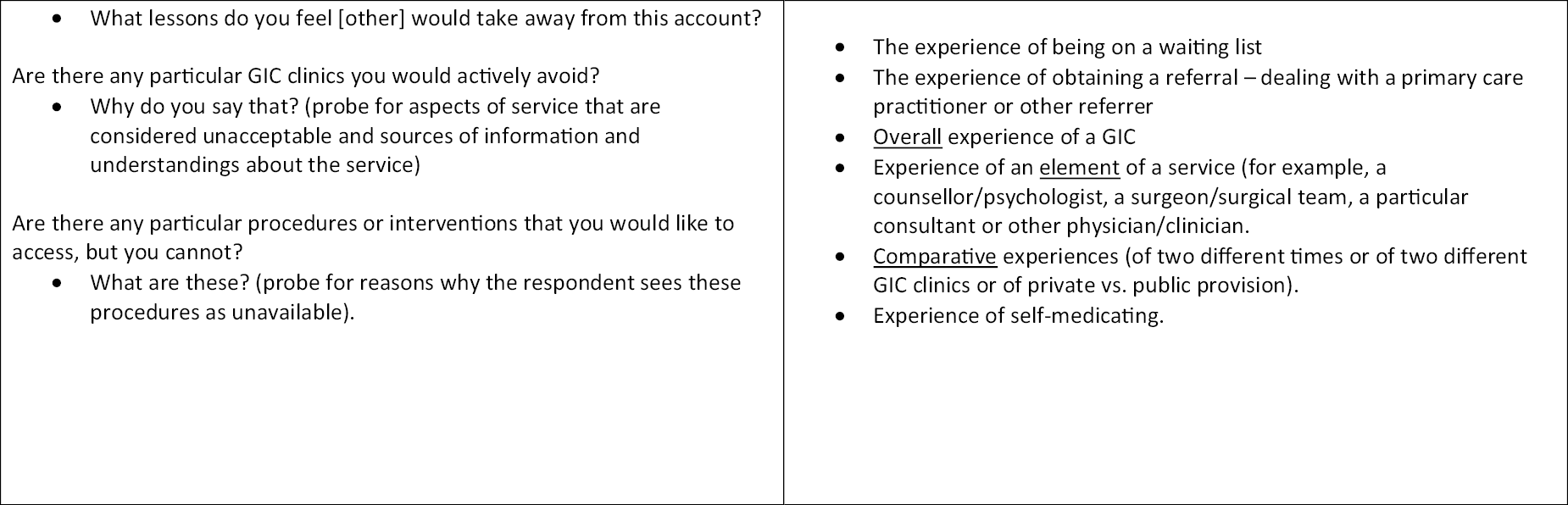
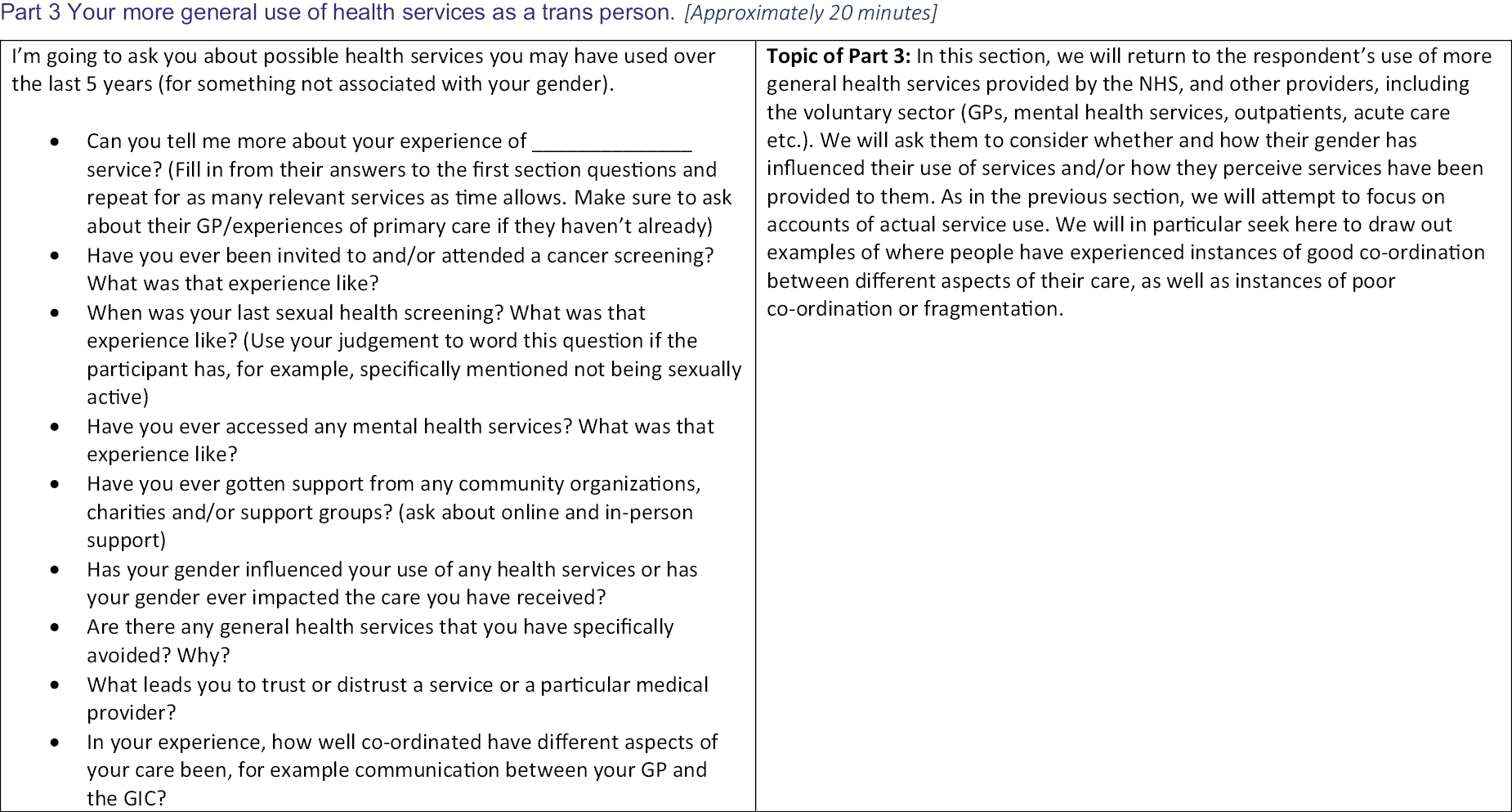

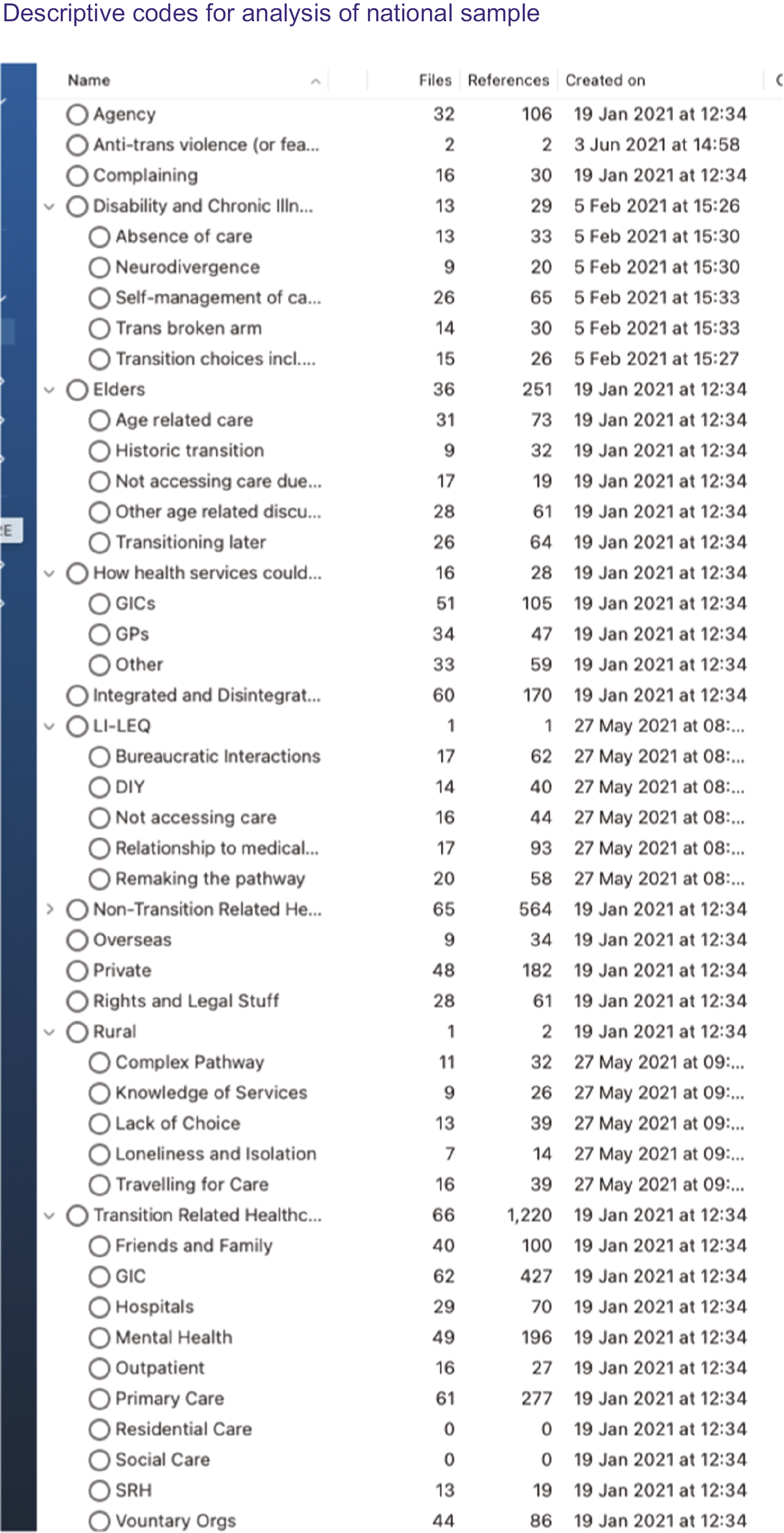
Appendix 4 Case study interview guides
Example of interviewer questions for staff interviews
-
What is your role in the GIC? What does this involve?
-
What has been your involvement to date in designing or implementing elements of care for trans adults that improve the integration of care (e.g. case study specifics)?
-
As you see it, why were these additional service elements put in place? Who were key people involved and what benefits they were looking for, and for whom?
-
What has now happened in terms of implementing these ideas? How do they affect what you do in your own role?
-
What has been achieved through this, or is currently working well?
-
In your own experience, what issues or challenges have been encountered?
-
What further plans are you aware of for further developing or improving these initiatives and the integration of care for users of the GIC more generally?
-
In your view, what else needs to happen to improve the service, and why, and what would help or hinder this happening, particularly during and following the COVID-19 pandemic?
-
Is there anything else you want to add?
Service-user interview guide
The same interview guide was used for service-user interviews in the case studies as in the national sample. This appears above in Appendix 3. In Part 2 of the interview, the guide indicates that the interviewer should add additional questions exploring the interviewee’s experience of using the service that is the subject of the case study.
Appendix 5 Descriptive codes for initial analysis of case studies
This appendix contains screenshots from NVivo illustrating the descriptive codes used in the first stage of analysis of interview data from staff and service-user interviews, as described in Chapter 2.
Figure 12 shows an example of the descriptive codes used to analyse staff interviews within one of the case studies.
FIGURE 12.
Example of descriptive codes for case study staff interviews.

Figure 13 shows a corresponding example of descriptive codes used to analyse case study service-user interviews.
FIGURE 13.
Example of descriptive codes for case study service-user interviews.
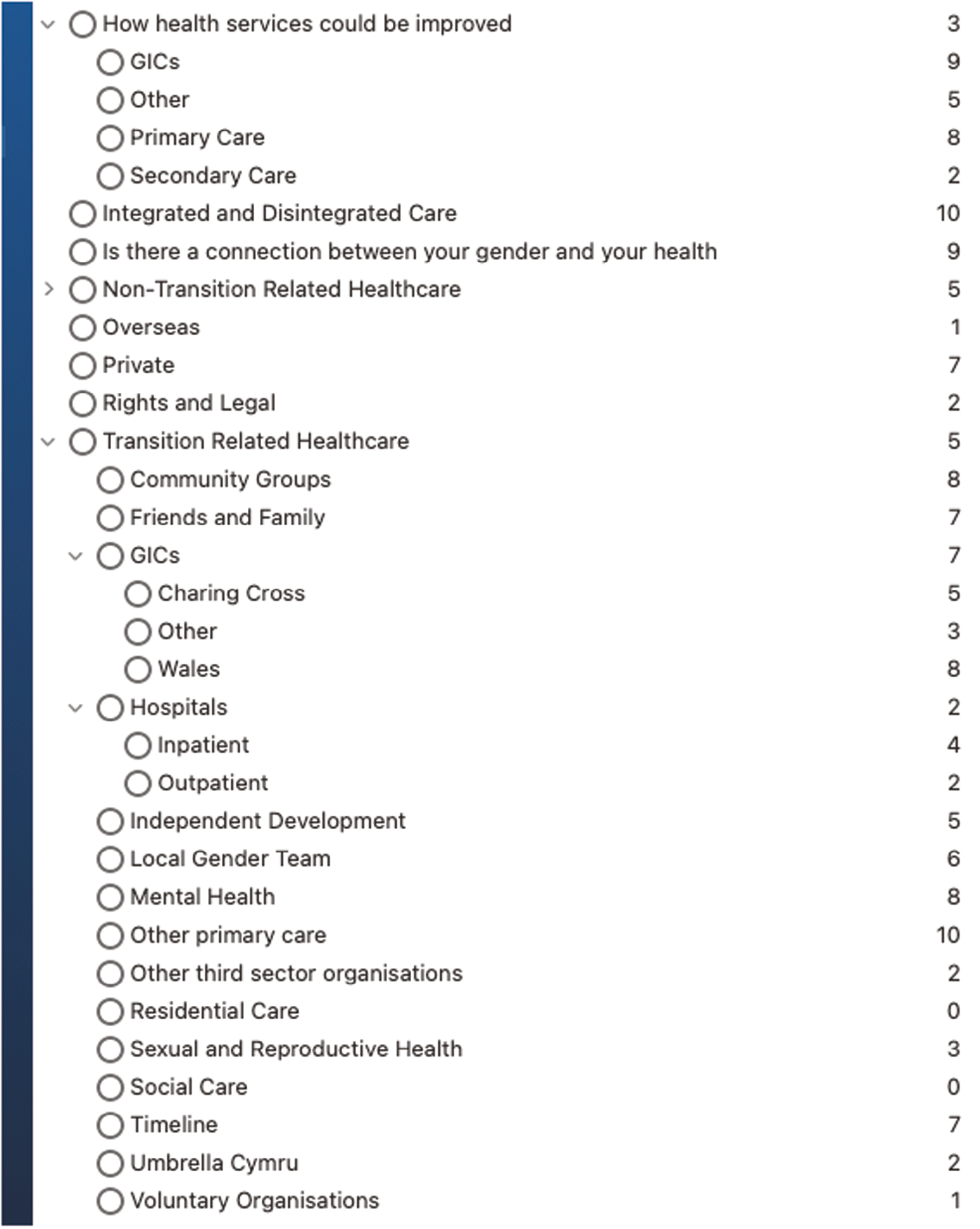
Appendix 6 The project partners workshop
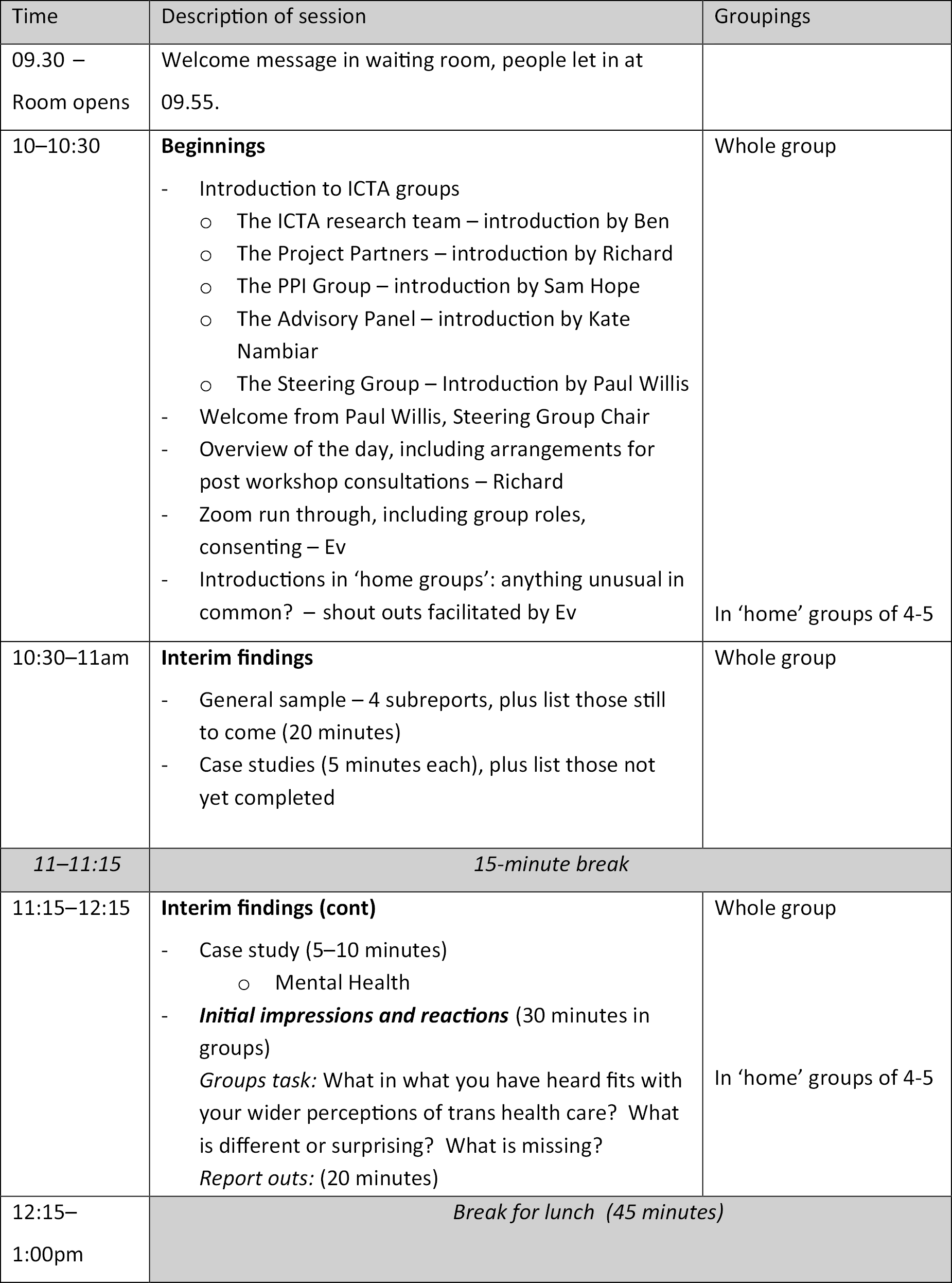
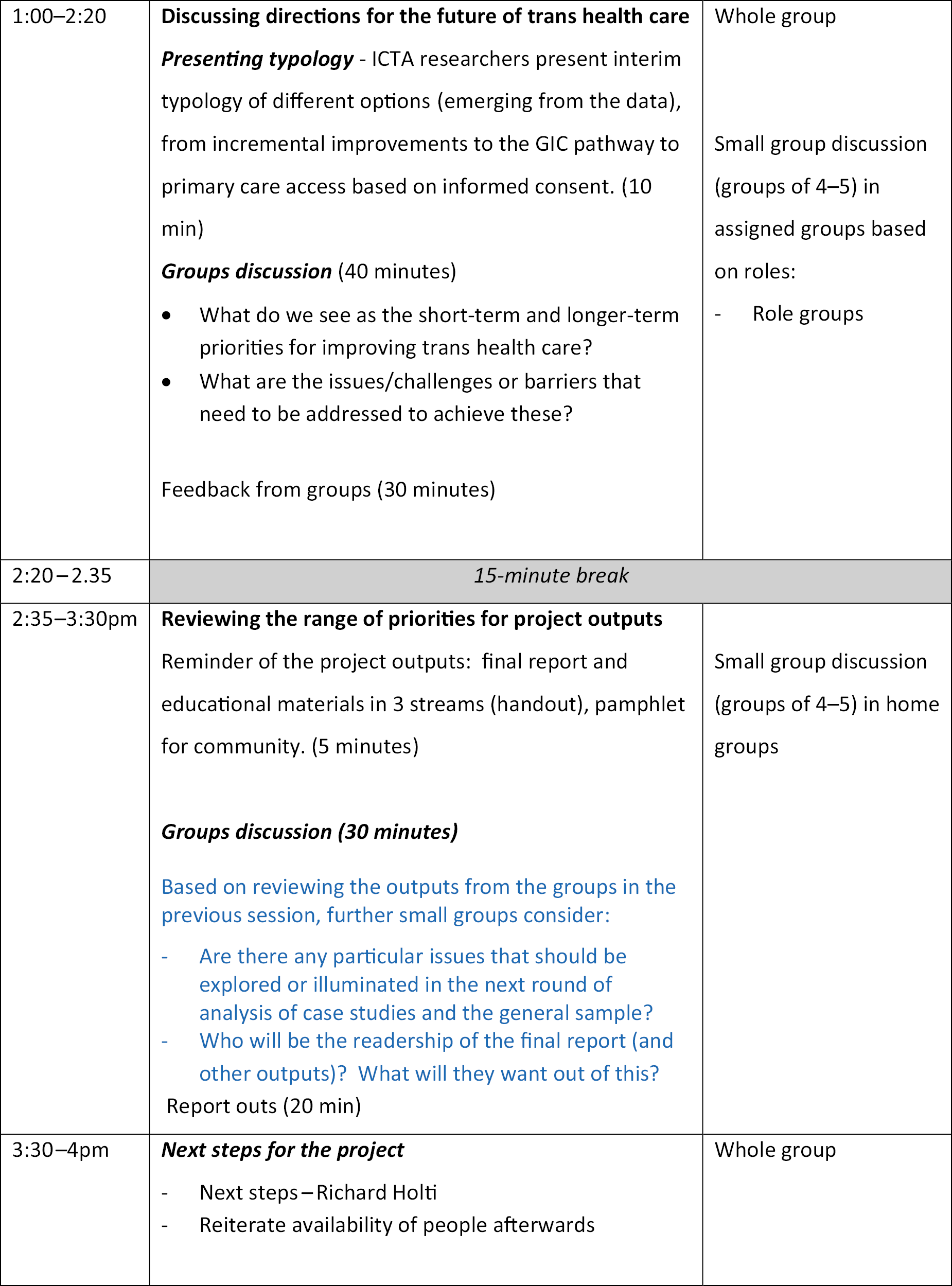
ICTA Workshop 20 Jul 2021: Examples of feedback from three ‘Home Groups’.
Feedback from Group A
What are implications for issues to focus in further analysis of ICTA data?
Who is the final report for and what will they need to get from it?
The final report needs to recognise that some trans healthcare issues are NHS-wide issues; for example, trans health care will be much improved if different systems can talk to one another. Digitisation of the NHS has been under way for over a decade now but hasn’t actually moved on very far. It is a further example of a broken system that holds back trans health care.
At the same time, it is important to recognise that overly free flow of patient records without authorisation can cause a lot of distress. Every last detail of what is in GIC records does not need to go to GPs or be read by the NHS in general. It certainly shouldn’t become central to the patient record, which has on occasion happened, with the record in effect giving a headline, ‘This person is trans’.
In the report, it will be useful to articulate the different kinds of gender services operating in different regions. For example, how the Welsh model actually functions, in terms of the process and the kinds of practices involved at each stage.
Recommendations in general need to be realistic and take account of the need to recruit and retain staff in GICs. People are put off working in them. It is difficult to get people in post and then difficult to keep them. It is important to engage healthcare workers more generally in trans health care, make the system more inclusive and so more effective in how care flows between primary care and specialist services.
Recommendations also need to take account of the fact that there is such a large backlog of people already in the system, waiting for care. We are not starting from a blank slate. The 18 months of backlog that the Welsh service started from is relatively modest compared to most other areas.
The tone of the final report will be vital. Recommendations should be constructed in a way that is reasoned, applying criteria of effectiveness and efficiency, and informed by what is happening in other countries. The logic should carry the reader along, in a way that is factual and unbiased. The report should also take the reader through the subject ‘like it is’ – for example, explaining that most trans people are actually not that complex in terms of the care they need, although some are; and also that clinicians are working very hard within a system that isn’t properly funded. The ICM needs to be explained very clearly.
Feedback from Group B
The report should also take account of ‘the critical moment’. There are currently significant forces organising against GISs. There needs to be an acknowledgement that there are some detransitioners and that this is a risk to be borne in mind in decision-making. However, this needs to be balanced by the (much larger?) risks represented by delaying decision-making in care or making it more complicated than it needs to be.
-
‘No-brainer’ to change the current model.
-
Training is needed across the board.
-
Service specification needs to be actually used (self-referral).
-
Not getting value for money, using alternative sources of funding through primary care.
-
Patient Knows Best records system.
-
Cultural change is needed in NHS organisations.
-
The situation is so bad, is it too far gone to enact meaningful change?
Feedback from Group C
-
Group acknowledged the level of trauma and distress associated with interactions with healthcare systems for trans patients as suggested by the ICTA data and also by some workshop participant experiences – for example, community work as well as personal experiences. That correspondingly means there could potentially be difficult emotions being experienced by workshop participants.
-
Suggestion that in order to effect change the outputs need to speak to distinct but equally important groups:
-
healthcare providers of all kinds
-
trans communities
-
service commissioners
-
-
Very important the outputs are written in a way that is accessible to all these groups – for example, ‘plain English’ versions of outputs. Also, important (for credibility for trans communities) that trans participants in the ICTA project and trans communities more broadly see themselves/recognise themselves in the outputs.
-
Important the reports reflect on who is/is not in the ICTA sample and thus what stories and understandings are excluded from the project reports/outputs.
-
Important that the reports/outputs are not read as wholly negative about current provision (in particular GICs) given the project aim to effect positive change in healthcare systems (risk of project outputs being rejected). Need for there to be tangible options for services to take up to improve care provision/solve identified issues.
-
Need to clearly (upfront) recognise systemic factors – for example, around how healthcare pathways are commissioned and to avoid blaming services for issues that are outside their control.
-
Importance of presenting change models that build on current provision and allow evolution of services towards paradigm change; changes to current provision are critical because it is the current system and so important to have good suggestions for this.
-
Importance of both suggesting practical/concrete changes in current practice and naming/identifying structural conditions that negatively impact the healthcare experiences of trans people (e.g. report must span current treatment context/practical/concrete/solution-focused to future-focused/conceptual/paradigm shift plus forensic identification of systemic factors that create healthcare inequalities for this population).
-
Value of developing service delivery models that involve coproduction between clinicians, commissioners, and representatives of trans communities where each are equal contributors – benefits in terms of models that work for all parties.
-
Important to consider outputs in terms of the GP pathways for Paradigm 2/3 – what would that look like, for example, in England (much larger population)?
-
Important to consider as an adaptation (in the paradigms) a return to more localised/regional services as integration is much more possible if strong relationships can be built with local services (e.g. GPs).
-
Important to understand the impact, on all involved in trans health care (e.g. patients and healthcare professionals), of a broader societal context that is hostile to trans people.
-
Really important to consider how project outputs will be disseminated to the trans communities so that they can draw benefit from the ICTA project findings/conclusions.
-
Important that overall outputs provide strong evidence for the health inequalities of trans people and how they are underserved in healthcare systems; also impacts of intersectionality – for example, for trans people who are also disabled, older, people of colour, etc.
-
Outputs should highlight how the pandemic has hit trans communities and whether shifts in care (e.g. move towards more online working) have/have not been experienced as beneficial.
Appendix 7 Gender breakdown of interview samples
Table 6 shows the gender breakdown of the subsamples of interviews analysed in Chapter 3.
| Subsample | Non-binary | Women | Men | Total |
|---|---|---|---|---|
| People living with mental health conditions | 29 | 35 | 10 | 74 |
| Trans elders | 5 | 22 | 6 | 33 |
| Low income or low educational quals. | 5 | 15 | 3 | 23 |
| Disabled/chronic illness | 22 | 15 | 6 | 43 |
| People living in rural locations | 3 | 14 | 5 | 22 |
| Black people and people of colour | 26 | 8 | 5 | 39 |
Appendix 8 Fuller case study reports
Case Study 1: third-sector gender-outreach workers attached to a gender identity clinic
Introduction
Case Study 1 examines a partnership between GIC A and a third-sector LGBTQI+ organisation, Organisation B, to provide trans peer-support workers for people on the GIC waiting list. Sixteen staff involved in this initiative were interviewed from across GIC A, the NHS Trust that hosted it and Organisation B. Fifteen service users were interviewed, recruited from those who had responded to the ICTA national screening survey, and indicated they had engaged with the gender-outreach workers. Of these, nine were in the process of or had completed their assessment with GIC A. Others were either waiting for assessment or had been assessed elsewhere. Some proved to have only passing experience of the gender-outreach workers. In what follows, as a consequence, there is a rather fuller depiction of staff views on gender outreach, with service-user views included when available.
The gender identity clinic context
At the time of interviewing, from late 2019 through 2020, GIC A had over 1000 people on its waiting list. Its mode of operating followed the NHSE Service Specification for Gender Identity Services for Adults (Non-Surgical Interventions). 15 As people entered the service from the waiting list, they had two assessment appointments, with additional ones in between if clinicians considered them necessary. The first appointment was typically with a gender clinician with a nursing background. The second was with the same person, together with a consultant psychiatrist or psychologist who was also a member of the MoJ list of gender specialists. At the time of interviewing, waiting times were typically 2 years for the first clinical appointment, and a further 2 years for the second. Following diagnosis, service users waited further, for around 12 months, for an appointment with an endocrinology team to prescribe hormones, typically 5 years after referral.
Objectives and nature of the gender-outreach initiative
In late 2014 and early 2015, discussions took place between Trust A, hosting GIC A, and NHSE about ‘how to manage waiting’. There was a shared concern about increasing demand, and the length of waiting for first appointments. Discussions took place with Organisation B about a new gender-outreach worker role, with lived experience of being trans. Funding was agreed for this new role as a member of GIC staff, offering information, advice and peer support, for people waiting. Two part-time outreach workers, both trans, were recruited by the Trust, in collaboration with Organisation B. They were based primarily on Organisation B premises but were involved in meetings and aspects of care provision at the main GIC site.
Gender-outreach practices and achievements
Building awareness of gender outreach
The gender-outreach workers were jointly supervised and supported by a senior nurse within the GIC staff and a manager within Organisation B. There were initial difficulties in publicising their existence to people on the GIC waiting list. The GIC lacked administrative capacity to send out letters, and data protection rules prevented the passing of contact details to Organisation B to make contact. The gender-outreach workers, supported by Organisation B, therefore went about contacting people on the waiting list through engaging with local trans communities, including through social media.
… right we’re just going social media … we’re going venues, we’re going communities and what we’re going to have to do is work with when people turn up to these events, say manage to discuss, are you on the waiting list for [GIC A]? Great, we’ll continue to be able to provide you with both group support and one-to-one support …
Gender-outreach worker
After some months, GIC resources allowed letters and additional information about groups and activities to be sent out. The GIC and Organisation B further established a system by which people were informed about what the gender-outreach workers offered, when their referral to the GIC was accepted. GIC clinicians reported that they too brought outreach to the attention of clients at each stage of the assessment process. They encouraged people to contact gender-outreach workers for help with overcoming isolation, with social aspects of transitioning, such as coming out to family, friends or their workplace, or with practical or legal aspects such as changing their name on their medical record at their GP surgery. They were offered the options of contacting outreach workers directly by phone or social media, or just turning up to a group-support session.
Service users we interviewed found out about the gender-outreach workers through a variety of routes, with informal contacts within friendship and trans community networks, including social media, at least as significant as information provided through the GIC.
Gender-outreach activities
Staff and service users had consistent views that the various support groups run by the gender-outreach workers were valued by participants. The groups or sessions were places where people could share experiences, ask for and receive advice, often concerning practical challenges and ‘trans admin’ tasks (such as completing a deed poll as part of a name change), within a supportive and safe environment.
I also started going to [gender-outreach worker’s] Plus 25 group. She always redirected towards positivity and she was good at setting boundaries in a way that made the environment feel very safe. And yeah, I would talk about things that were very difficult and then she would reframe it – that’s a huge positive.
Service user
Several people spoke about the value and pleasure simply of being with other trans people.
A regular weekly trans swimming group in particular was widely seen as both innovative and beneficial. This was established at the suggestion of one of the gender-outreach workers, and involved the GIC successfully making a case to NHS Trust senior management that additional resources should be used, because of the benefits to well-being. Again, on the advice of the gender-outreach worker, the NHS sponsorship of these sessions was not included in the promotional material, so that service users would see them as independent of the GIC. An outreach worker hosted the sessions in collaboration with staff from the swimming pool, which was closed to the general public. As well as a trans environment, the sessions provided physical exercise and mental health benefits. Above all, they provided access to an activity that typically poses significant barriers for trans people:
… but it was nice to actually be doing something which was not, which was open to trans people, because that’s what it was there for, but it was actually doing something, not just sitting around […] it was purely rock up to the swimming pool, get changed and go swimming. But it was also because there was safety from, you could be like, if there was something, I felt like I could talk to them about it.
Service user
Outreach workers also provided emotional and practical support one-to-one for people on the waiting list.
… sat down for an hour and just had a chat … that’s one of the biggest things that I discovered was when you speak to other trans people, there are a lot of things that happened in your life which they recognise … that’s where you’re thinking, oh well, it’s not just me. Everyone’s gone through this.
Service user
Outreach workers were seen by GIC staff as deeply committed to their clients and ‘always fighting somebody’s corner’ across a range of arenas concerning health care and other aspects of their life. In some cases, gender-outreach workers accompanied a client to their first assessment appointment at the GIC.
GIC clinicians also began to refer people for outreach support after diagnosis, recognising that the trans outreach staff could provide information and support in ways not possible for the mainly cis GIC clinical staff.
So someone might want to progress to surgery … so it could be helpful for them to speak to an outreach worker about how to go about that, the things that they need to consider, again someone that’s been through that process …
GIC staff
Outreach workers and GIC staff encouraged wider engagement of service users with the various outreach groups, beyond a narrow definition of use by people on the waiting list. People living within the locality and attending other GICs were welcomed.
Drawing on dual belonging
Outreach workers were seen by colleagues from both sides of the partnership as skilfully drawing on a kind of dual belonging – to the GIC staff and to the local trans community.
A significant arena concerned how the outreach workers communicated with potential users of the service. They drew on their own experience and capabilities with communications within trans communities.
… they’re more expert than us at posters. It’s something simple but it’s something that will bring in a 100 people. If we did one it would look … we’d only bring in 10. Because of the approach, because of the language, because of the styling we are bound by.
GIC staff member
They were also seen as highly responsive to NHS clinical and administrative colleagues in providing advice on how to respond to service users on a range of issues where lived experience was vital. This included how to find material with which to persuade an obstructive GP to give a referral to the GIC, how to get a GP practice to change the title on a medical record to reflect a new name and gender, and how to approach using gendered public toilets as a trans person.
The outreach workers were seen as crucial to bringing GIC staff out of traditional clinical settings so that people had the opportunity to ask them questions. This happened at LGBTQI+ and trans events, as well as at events for trans people convened by the gender-outreach workers themselves.
So, there was a big [name of location] trans memorial event recently, and actually we were really involved in that, and that’s only because she’d challenged and had said we really want to support the trans community, why are we not visible in this? And that was great.
GIC staff member
Outreach workers were seen by GIC staff as not only representing the concerns of service users and potential service users, but also stimulating a constructive GIC response. Outreach workers instigated direct dialogue with non-binary people over their concerns about how they were received by GIC clinicians. The workers also explained service users’ concerns about lack of understanding of trans health care within local primary care, and the need for GIC staff to educate primary care colleagues.
Expanding the scope of service integration
We heard of four examples where gender-outreach workers were instrumental in expanding the range of services offered to GIC service users.
The first concerns the establishment of a monthly sexual and reproductive health clinic, specifically targeted at trans adults. Gender-outreach workers developed a working relationship with the reproductive and sexual health department of a local NHS hospital Trust. A sexual health doctor contacted Organisation B because she was interested in developing services for trans sex workers, and this led to identification of a need for sexual and reproductive health screening for trans people more generally. Trans needs were often not understood and ignored by GPs and other providers. The outcome was a successful proposal to the host Trust to run a sexual health session for trans people at Organisation B. This clinic was publicised by the GIC, broadening the range of services offered in an integrated way.
In a second example, an outreach worker initiated a workshop for trans women on the waiting list, run by the GIC Speech and Language Therapist. Third, gender-outreach workers collaborated with the local police, to develop a system for reporting hate crime. The final example was where gender-outreach workers helped identify other trans-led forms of support for people who were not within the area covered by the Organisation B outreach or who were under 17, drawing on their knowledge of trans organisations across the region.
Support and supervision of gender-outreach workers
Staff from both the GIC and Organisation B were clear that a key element in achieving the effectiveness of the gender-outreach workers was the attention given to their professional supervision and support. In addition to their line management within the GIC, they attended multidisciplinary team (MDT) meetings within the GIC and also had supervision meetings within Organisation B. The latter provided opportunities to discuss activities they were engaged in and issues arising. They were also supported in activities such as attending community events by well-established Organisation B protocols for ensuring staff safety, which had evolved over time within a workforce well used to going out to meet clients and potential clients of sexual health services, in community rather than clinic contexts. This combination of NHS and voluntary-sector supervision meant that the outreach workers felt well supported.
Challenges of gender outreach
Long waits remained
While both the service users and staff we spoke to recognised the value of the support offered by the gender-outreach workers and the groups they ran, there was widespread and often painful awareness that the length of the waiting list was the most pressing concern for service users. Both staff and service users saw the gender-outreach workers themselves as unable to address this issue.
For service users who felt they did not need practical or social support with transition, usually because they already had a lot of contact with other trans people, this led to anger and frustration.
We had great discussions but again she couldn’t really do anything. For me it just felt that you could go there and vent your frustrations a little bit and then that was it. But it has absolutely no influence by the sounds of things.
Service user
Staff from both the GIC and Organisation B were also aware that the initiative was leaving unaddressed the underlying problem of the long waiting times between referral and first appointment. At the same time, some staff emphasised the benefits brought by the outreach workers as something that was valuable and needed regardless of the highly unsatisfactory waiting times:
We’re not trying to placate people by saying oh here’s a swimming club, keep yourself quiet … if we didn’t have a waiting list we would have still embarked on this project.
GIC staff member
Outreach workers as caught ‘in the middle’
Many staff saw outreach workers as uncomfortably ‘caught in the middle’ of allegiances to trans community and the NHS GIC. Gender-outreach workers were seen in a compromised position, representing the requirements of the established NHS GIC system, and its long waits, to trans communities. Working with the tensions inherent in their dual belonging was often stressful and involved considerable skill in relating.
The outreach workers were often called upon to provide information about the GIC treatment pathway, what it required of people at the various stages and the length of waiting involved. They had to respond both with accurate information and sympathy at the implications.
Outreach workers felt they were left supporting service users with the high levels of distress. GIC admin staff were also pulled into the role of consoling distressed callers while also managing their expectations by emphasising the length of the waiting list. Some staff considered whether it might be possible for greater collaboration between admin staff and the gender-outreach workers, in determining how best to deal with such calls. While several interviewees implied that individual staff members should not feel responsible for the length of the waiting list, it was apparent that admin and outreach staff had a key role in actually facing the deep distress of those waiting for a desperately needed service, on a timescale that was often unbearable.
Gender identity clinic staff also appreciated that outreach workers shouldered the responsibility of responding to service-user distress at anti-trans media coverage.
Some service users were of the view that the association of the gender-outreach workers with the GIC was problematic because things said to the outreach workers might reach clinicians involved in their assessment:
I didn’t necessarily feel I could confide in them massively or talk to them at length about my treatment because I knew they had the connection to the GIC. My fear was that they would feed that back then to my practitioners and almost tell tales on me for being a bad trans.
Service user
Some users felt that gender-outreach workers should be more explicit in advocating ways of moving forward with transition through routes for obtaining hormone prescriptions other than through GICs:
They should get a list together of endocrinologists who are willing to take responsibility for trans patients and prescribing them hormones … they should give you that list on the helpful resources while you wait, not things that I knew already.
Service user
Some staff raised the issue as to whether there could be clearer prioritisation of gender-outreach work, given the extent and range of needs to be met. One suggestion was that gender-outreach workers might seek to work more with people as they came off the waiting list and prepared to attend their first assessment appointment. This would be to help people deal with the weight of expectation, and possibly also fear and distress, that had built up over the years of waiting.
… you’ve got people on websites saying a lot of negatives, and that’s why some people come to our service and they’re very apprehensive.
Staff member
Limited resourcing of gender outreach
A further challenge widely identified concerned the level of staffing for gender outreach. Staff from both the GIC and Organisation B felt that the gender-outreach workers were overstretched relative to the demands on them, and this was borne out by the experience of some service users, much as they appreciated the support offered:
I just get this very strong feeling that [Gender-Outreach Worker 2] is extremely overworked and she’s not able to respond to messages, because there’s just too many … there just needs to be more …!
Service user
Supporting people not already connected to trans communities
Several staff spoke of the challenge of reaching and then working with people on the waiting list who lacked the confidence to participate in trans events and networks, or who perhaps lived in a rural area without nearby trans contacts.
A related challenge concerned the management of group events so that they provided an opportunity for interaction and mutual support, without pressuring those attending to interact or participate more than they wanted to.
Managing the boundary between peer support and psychological intervention
The gender-outreach workers and staff involved in their supervision were aware of the need to clarify the difference between providing emotional and practical support to service users and providing mental health support. The time of most staff was taken up with conducting assessments, although some staff reported that they were able to provide ‘low level CBT’ interventions to deal with anxiety or depression. However, there was confidence that the supervision of the gender-outreach workers meant that they knew when to refer people on to other services, usually provided by third-sector organisations.
Further development of gender outreach
At the time of interviewing, the provision of gender outreach was already being expanded to other geographical areas. Some of these were being covered by an additional worker employed by Organisation B. Others were being covered or planned to be covered through new collaborations between the GIC and other third-sector organisations in different localities. There was a related initiative for GIC nurses to run first assessment sessions at one of the new regional locations.
Several staff felt that the amount of outreach worker time needed to be increased to deal with the demand and also that more time for discussion between outreach workers and GIC nurses would improve understanding of what outreach workers could offer. Even before the COVID-19 pandemic, thought was being given to how remote video calling could be used to extend the ability of outreach workers to support people at a distance.
A further initiative concerned outreach workers raising awareness at GP practices as to how they could support people on the GIC waiting list. Beyond this, the outreach workers were influential in supporting the development of policies for treating trans patients appropriately elsewhere in the mental health Trust hosting the GIC, including making sure that inpatients were allocated and welcomed within wards according to their correct gender.
Case Study 2: primary care liaison and psychological services within a GIC
Introduction
This case concerns attempts to improve the integration of care within a GIC on two fronts: liaison with the primary care practices and mental health support for service users. Between mid-2020 and mid-2021, we interviewed nine members of GIC staff, including gender clinicians, psychologists providing support services and nursing staff. We interviewed seven service users, recruited through the national screening survey on the basis that they had engaged to some extent with the psychological support at this GIC. Their ages ranged from 22 to 70, and they included one man, four women and two non-binary people. All reported on experiences of the interface between GIC and primary care, while four had experiences of receiving GIC psychological services. Of these, one was offered psychological support but didn’t feel the need to accept. Three attended group programmes over several weeks, with two of these also receiving individual counselling at some point.
In describing the services below, we bring out the service-user experience where we have data on it, alongside views of clinicians. We first summarise the main features of the GIC assessment and treatment pathway, as context.
The gender identity clinic context
At the time of interviewing, the GIC had around 1000 service users at various points of assessment or treatment, with around 1200 people on its waiting list. The length of time from referral to first assessment appointment was around 2.5 years and grew significantly over the course of the COVID-19 pandemic. Service users interviewed reported waits of between 1 and nearly 3 years, depending on when they had been referred. All found the wait very stressful, with three of the seven deciding to ‘go private’ for assessment and access to hormone therapy before being seen by the GIC.
… the wait became harder than I had expected, or the mental reserves I’d had, that I thought would be able to get me through the wait, ran out, and I was like, I need to starting doing something now …
Service user
Consistent with the NHSE Gender Identity Services (Adults) specification,15 there were two clinical assessment appointments by a senior gender clinician for each person, with additional ones in between if clinicians considered this necessary. The service users we interviewed in fact all received a diagnosis after two appointments. There was also a physical examination, covering height, weight and blood pressure, combined with an endocrinal consultation, for detecting issues that might complicate hormone therapy.
At the time of interviewing, the second appointment usually followed the first within 6 months. Service users reported waiting between 4 and 6 months, apart from one who had waited 10. With the pandemic, most first assessment appointments were held via video. Given the need for the physical examination, many second appointments have continued to be face-to-face, with the two sessions on the same day or sometimes combined.
According to clinicians, diagnoses were formalised in a MDT meeting shortly after the second assessment. The service users we spoke to all reported that they were actually told of their diagnosis during their second appointment. This included explanation of the nature and impacts of gender-affirming treatments – including some or all of hormone therapy, voice coaching, hair removal, fertility preservation and gender surgery. Service users reported that hormone treatment, if desired, was also initiated at the second appointment, with a recommendation to their GP to prescribe under shared care.
Service users’ commentaries on their experiences of the assessment appointments varied. Of the six who had first assessments, three found the clinician supportive and well informed. One of these found the approach to questioning ‘a little invasive […] not in a negative or particularly uncomfortable way’. The other three had problematic experiences, finding the clinician unsympathetic either because they asked intrusive questions without making it clear why, appeared oppositional or challenging, or failed to convey recognition of ways of thinking about gender that were important to the person:
Why are you asking me about my childhood? What relevance does that have? I don’t think it’s relevant at all … I’m bending, twisting the narrative to be the right narrative … It was like they were trying to catch me out …
Service user
Experiences of second appointments, with completion of assessment and treatment planning, were more positive. Clinicians were experienced as ‘positive and optimistic’ or:
… generally putting me at ease about pretty much everything. Answering all the questions I had, relating them to me as a person, rather than just a checklist to tick off […] listening to what was bothering me and giving actual examples, from his experience …
Service user
One person drew attention to the impact on them of having two independent assessments – they were asked the same set of questions at each, which felt like going over what the service already knew about them:
… it was just a rehashing of the first, totally identical to the first appointment. But it got me my second signature and then I’m officially diagnosed.
Service user
Two further clinician signatures are required to refer someone for top and/or lower surgery, as per the service specification. One user was disturbed and baffled by being further probed for a consistent story about their gender identity, as if their trans status was still in doubt, as well as by what seemed irrelevant questioning about their relationship status. Another person was appreciative of a flexible approach by clinicians, leaving them to decide about surgery in their own time:
The gender clinic’s pretty much the one thing that I haven’t had trust destroyed in, at this point, that I trust them to ask, when it comes, okay, time for referral for surgery, let’s go over some points again.
Service user
Gender identity clinic interfaces with primary care
Service users reported widely divergent experiences of being referred to the GIC by their GP. For some, their GP referred them quickly and competently. For others, their GP appeared both reluctant to refer and lacked knowledge about how to do so. In one case, a GP incorrectly referred them to a mental health service rather than the GIC – the referral was refused with a request to redirect. In another case, a GP said they first required a letter from a counsellor the person had been seeing.
On receipt, referrals are processed by the GIC nurses, who request any missing information from the GP. Acceptance of the referral involves the GP signing a MoU which sets out the detailed arrangements for shared care between the GIC and a GP practice, above all with respect to hormone therapy. The GP is expected to prescribe, following GIC advice, and arrange regular blood tests, which the GIC interprets and discusses with the person concerned, leading to revised prescribing advice as necessary.
The GIC introduced the MoU at the referral acceptance stage in response to uneven responses from referring GPs across the country to shared care. While GMC guidelines emphasise the risks to patients of not prescribing cross-gender hormones important to their well-being, GPs in different commissioning areas encounter different policies as to whether HRT prescriptions for trans people are funded or require an IFR. GIC staff reported that some Local Medical Committees were also taking a stance that GPs should not prescribe or administer hormones for trans people unless their practice received an enhanced payment from the CCG for handling this.
The GIC experience was that some practices refused to take part in shared care even when commissioned to do so, usually claiming that they were not competent to provide hormone therapy for a trans person. This could emerge even after a service user has received a diagnosis and recommendation for hormone prescribing from the GIC, with ‘devastating impact’ on the person concerned. The MoU attempts to address funding issues and any other source of GP resistance early, well before it has such consequences. However, one service user reported that their referral had been delayed because their GP practice took several weeks to consider signing the MoU:
They genuinely made me feel like I was being an annoyance to them by asking to be looked after, for them to a do a thing that only they can.
Service user
In such cases, the GIC nurses follow up with a GP practice in the first instance. If necessary, GIC gender clinicians speak directly to the GP to help them understand that HRT for trans people is usually straightforward medically, emphasising that most GPs already have experience of prescribing testosterone and oestrogens to cis people, and that the GIC will take responsibility for monitoring blood work.
Another service user found their GP was initially resistant to shared care. Once an appointment was made with the nurse, however, things went much better:
… then they said, well, it’s just an intramuscular injection, so that’s easy.
Service user
The GIC has attempted to address further difficulties that typically arise in liaising with GPs once someone has begun their GIC assessment. Staff have developed template letters to keep GPs informed following each assessment appointment. These cover whether there is a provisional or final diagnosis, implications for prescribing and other treatments, and any further aspects of medical transition currently being considered. Once a treatment plan is agreed, usually at the second appointment, the letter contains full information on the possible risks of treatment, short-term and long-term, so that these are clear to the GP as well as to the service user.
Following initiation of hormone therapy, the GIC uses SystmOne, a leading shared online patient record system, but still only used in around 25% of UK GP practices, as a platform for communicating over blood tests and dosages. Clinic nurses mediate the interchange of queries and answers within the system. This allows GPs and GIC clinicians to resolve issues without having to arrange phone calls – for example, over a request from a service user for a change in dosage, or a GP enquiry about GIC perceptions of the general well-being of a service user.
Given the limited use of SystmOne in primary care, service users and GIC clinicians reported persistent problems with blood test information not being provided in time to be of use at scheduled GIC review sessions. Service users found they had to intervene frequently:
… sometimes if they send information from one to the other, it will get a bit lost. Like something on my GIC system, wouldn’t work on the GP system. And he wouldn’t realise for a while until I say, hey why hasn’t this happened?
Service user
One gender clinician gave their e-mail address and mobile number to service users so that problems with getting tests done could be sorted out prior to review appointments.
A further area of liaison with primary care likely to arise on or before the initiation of hormone therapy was arranging for fertility preservation or hysterectomy, if desired by an individual. Both gamete storage and hysterectomy commonly require a person’s GP to complete an IFR to the local CCG. The GIC has developed ways of supporting GPs with this, making them aware of recent NHSE guidance which indicates that gamete storage should not be withheld. The GIC also advises on which CCGs now have a policy of funding gamete storage for trans people, making an IFR unnecessary.
Psychological support
In 2017, the GIC reviewed the need to provide psychological support for service users. Staff were aware of people entering the service with a mental health burden from the stress of daily experiences of transphobic interactions:
… issues about social anxiety and the knock-on effect of depression and self-esteem disturbance … of course the difference for trans people is actually they’ve got good reason to feel anxious and afraid and socially isolated.
GIC staff
There was also awareness of the impact of the extended waiting period and experiences of having little control over their access to gender-affirming care through the GIC system. As one service user put it, this was:
… causing a weight or a drain on my mental health.
Service user
The direction the GIC set was to provide psychological support separately from the main assessment pathway, through a small psychology team, consisting of a principal clinical psychologist, one other clinical psychologist and an assistant psychologist. There are also usually two clinical psychology trainees assigned to the service each year, working with service users under supervision.
The psychology team has run group-based therapy programmes, and also provided some individual and family or couples counselling. The last-mentioned were typically one-off consultations to help a service user and others close to them work through issues related to their transition. All of these interventions are in principle available to service users ‘at any point in the pathway’, once someone has had their first assessment. With the pandemic, staff reported increasing referrals to the psychology team on first assessment due to people experiencing social isolation. Sometimes people were also signposted to local trans groups.
The psychology team has led on establishing a coproduction group for the GIC. The latter consists of four or five members of staff, from nursing and psychology, and an equal number of service users and has been considering how to improve services. Its initiatives have included improving information and support for those on the waiting list. A trans ‘expert by experience’ has been recruited to the GIC staff team, to offer support to people on the waiting list as well as take part in the delivery of workshops and coproduction activities.
Staff estimated that around 20% of the people seen by the GIC are seen by the psychology team in one of the above ways. There are typically 100 people receiving psychological intervention at any one time. The clinic nurses were seen by both staff and service users as central in making sure that service users are aware of what the psychology team offers:
As I approached every appointment I think, it was, oh and if you ever need, if you need to reach out to things like workshops and groups, we can, they always made sure that I knew there was an option on the table for me.
Service user
One service user also experienced the nurses as offering a kind of informal counselling at regular check-in sessions:
I guess, the therapy-esque sessions, they were just short little half an hour, an hour-sessions, where you can just talk about whatever.
Service user
Psychology groups
Groups are intended to facilitate peer support as well as helping people work with therapeutic ideas and are seen as a cost-effective way of providing support, drawing on assistant psychologist and psychology trainee staff alongside senior psychologists. Clinicians emphasised that in all groups they aimed to facilitate a sense of connectedness between participants, because many came with ‘… a sense of anxiety about coming to groups and a sense of isolation from other people’.
Prior to the pandemic restrictions of 2020, the following were run as face-to-face groups of six to eight sessions, on a weekly or fortnightly basis:
-
Exploring social transitions, for those who have had difficulty in achieving a social transition in the expression of their gender.
-
Emotional well-being, for people experiencing ‘mild levels of anxiety and depression’, based on trans-affirmative approaches to cognitive–behavioural therapy (CBT) (e.g. Austin and Craig27).
-
Improving confidence, run by psychology staff jointly with a speech and language therapist, specifically for trans women post affirmative treatment, based on well-established CBT resources for helping with low self-esteem (e.g. Fennell134), ‘adapted to be trans affirmative’.
Staff emphasised the importance of these groups for people to gain support in a context that was not about assessment. Three of the service users we interviewed attended the face-to-face weekly groups, in each case after they had received their diagnosis and had begun hormone therapy. One person in their early 20s experienced themself as ‘helping the older patients’ in the Emotional Well-being group and valued this. Another service user, however, experienced the Emotional Well-being group as not able to help the severity of their anxiety:
… It was designed around being practical for day-to-day issues, rather than, shall we say, intense mental health issues.
Service user
We return shortly to the issue of how far the targeting of the group interventions can be seen as addressing the range of more severe mental health concerns that may affect trans people entering a GIC service, as indicated by the findings of the ICTA survey reported in Chapter 3.
A third person found that the Improving Confidence group provided an effective structure for learning from others about how to deal with practical aspects of living with a changed expression of their gender, such as using a different public toilet:
So, I came away from that group with some sheets that I still keep around to this day, because I got a lot of help from the other people in that group, saying, these are our experiences … It was that sort of thing, where it allowed for much more freedom of conversation, rather than a minute-by-minute, ‘this is our topic’ …
Service user
Realising that service users living at greater distances found it difficult to attend regular sessions, staff subsequently adapted each of these programmes to take the form of two day-long workshops, 1 month apart, as an alternative mode of delivery. Around 2 weeks after each workshop, staff followed attendees up individually by telephone.
Face-to-face groups and workshops were suspended during the pandemic, with some relaunched in virtual mode. At the same time, psychology staff explored setting up new online groups and drew on recent evidence of the effectiveness of compassion-focused therapy with young LGB adults,135 adapting this approach to recognise the impact of transphobic microaggressions that participants repeatedly experience. The concept was to give participants an opportunity to work with ideas of increasing their self-compassion, affirming a positive view of how they are living their lives and disrupting learnt negative feelings. This concept was discussed at an early stage with the coproduction group.
The resulting design involved a range of experiential exercises such as giving and receiving compassionate comments with trans peers. At the time of fieldwork, several groups of 11 participants had attended 8 weekly online sessions. The group was found to be relevant and helpful by one interviewee who participated after they had begun hormone therapy:
… the general attitude of, stop being so hard on yourself … Again, it’s one thing to have a drive and a motivation. It’s another thing to be lashing the whip at yourself, to be like, no, go faster, go faster, you’re a failure for not having done more.
Service user
Staff reported that online delivery of the various groups has been successful, with therapeutic work happening in a slightly different way to a face-to-face model, but equally effectively. Online models made weekly attendance and a more intensive way of working more viable, and supported peer engagement, particularly for geographically dispersed participants. More generally, staff reported that self-assessment scores for anxiety, depression, well-being, or self-esteem generally improved following groups, and that qualitative feedback was positive, with service users mostly asking to have more of the kind of sessions they had received, rather than something different.
Individual counselling
The psychology team offer programmes of individual counselling on issues related to a person’s gender or transition. This happens in blocks of six fortnightly sessions, extendable following reviews. Staff reported that those who were considered not to be clear about their treatment goals could be told they were being taken out of the assessment process while they were receiving psychological therapy. The implication was that this could sometimes be a joint decision between clinician and service user, but that the decision ultimately lay with the clinician. According to staff, such people could then resume their assessment once they had clarified treatment goals. In Chapter 5, we discuss the problematic issues that may arise in a clinician deciding that someone’s treatment goals are not clear enough to proceed with a diagnostic assessment.
Alternatively, for those whose treatment goals were perceived to be clear, but who were:
[…] quite distressed or […] having difficulties with the family in relation to gender, then the psychological work and the medical treatment pathway would run in parallel.
Staff member
Following a set of sessions, people are often put on a ‘follow-up’ list, seeing a psychologist after several months, in effect for repeated stand-alone consultations, usually when also attending the GIC for a follow-up hormone therapy or surgery consultation.
Individual therapy is generally based on ‘acceptance and commitment’ therapy models, adapted to take account of the minority stress that trans people experience as they encounter transphobic microaggressions. Clinicians espoused an approach of supporting clients in articulating what is important to them in how they live and helping them develop strategies for managing negative feelings. Therapeutic work could also, for example, help someone process their reactions to gender-affirming treatments, including surgery, or consider how to approach problematic close relationships.
Two of the service users we interviewed received individual counselling, again after receiving a diagnosis. One felt the psychologist had helped them focus appropriately on the difficulties of navigating various aspects of their transition, while affirming their underlying identity:
… by the time I got to this counselling, I’d been sitting on 18 months of waitlist, so I’d done a lot of thinking and working things out beforehand … So, I didn’t learn things about myself from it, but I was able to feel better about things that were distressing me, like things like dealing with wait times, with the admin process […] the uncertainty with social reception, with going through the process of changing my gender marker […] in terms of my emotional feelings about my identity in and of itself, those were pretty much always positive … I absolutely trust the gender clinic, because my experience with them has been 99% positive and beneficial.
Service user
The other person was referred for counselling after repeated setbacks in getting medical help following undiagnosed severe pain after lower surgery. They appreciated being referred by the GIC and getting help with the psychological aspects of pain management but felt that other NHS services were failing to take seriously the need to diagnose the pain being experienced. They eventually got the NHS medical help they needed.
Issues with psychological support
Gender identity clinic psychologists recognised that they had limited capacity to address the considerable mental health burden of many trans people entering the service. As already indicated, the group provisions can be seen as only addressing the milder end of the spectrum of severity. GIC psychologists were aware that many service users had mental health conditions, such as anxiety, depression or obsessive–compulsive disorder, which in their view were not directly related to their gender and which therefore should be treated by mainstream local NHS mental health services. Local mental health services, however, often refused to treat such cases, referring them back to the GIC. GIC staff saw their role in addressing this serious gap in access to provision, arguably affecting those with the highest need, in terms of acting as explicit advocates for people to get treatment:
I can assess and formulate people and write a really thorough letter based on their needs and what they’re presenting with. I’ve had a fairly good success rate, touch wood, with GPs and services who’ve refused people because they’re trans essentially. Not for any rhyme or reason.
GIC staff member
Some GIC staff expressed concern that the local services taking on these clients might not take a sufficiently holistic approach to mental health, applying only a limited range of techniques for addressing specific common mental health conditions. They were also concerned that clinicians in local NHS services lacked understanding of how to work with people experiencing transphobia in their everyday lives and the interaction this has with mental health conditions. The implication was that local mental health services need to gain competence to provide appropriate therapy for trans people with mental health needs, rather than exclude trans people by referring them back to the GIC.
We were unable to explore with any service users who received counselling prior to diagnosis whether they felt inhibited about exploring psychological material in counselling because they were also still under assessment. Experiences reported with other GICs in Chapter 3 indicate this has been an issue elsewhere. We were also unable to explore the kinds of circumstances under which people might be asked to suspend their assessment while they received counselling, and how people experienced this. As already mentioned, in Chapters 5 and 6, we raise more generally the difficulties and ethical issues associated with a clinical judgement that a person is ‘unsure’ and so should have their assessment delayed.
The importance of such issues is borne out by the concerns expressed by some staff at the contradictions between taking up a therapist role and working within a setting that assesses people as to whether or not they are trans and can therefore receive treatment. As they put it, the same GIC clinic both sets out to provide an open and exploratory space for people to consider what they want from treatment and determines within an assessment process whether they fulfil diagnostic criteria for gender dysphoria. They also acknowledged that pressure to reduce the waiting list and maximise utilisation of diagnostic capacity can lead to considerations of ‘sidelining’ people who are perceived to be unsure about their treatment goals. Even though different clinicians are involved in the two different kinds of clinical encounter, the tensions between them can emerge in team discussions, and can have profound implications for service users. One staff member described these dynamics:
… a couple of times where the team might have been pushing back if somebody has been unsure what they want with regards to medical treatment for a while, and I’m just doing open-ended kind of exploration and hand-holding […] But the team might be saying ‘Discharge them. They can come back whenever, without waiting. But if they don’t want treatment, then we should close them. And they can just let us know when they’re ready’ … And then that being understandably very frustrating, confusing, and difficult for people.
GIC staff member
Further evidence of tension between receiving psychological help and GIC assessment came from staff perceptions that some service users learnt not to disclose mental health difficulties to gender clinicians, instead telling them:
… what they think you need to hear … having a sense of the boxes that need to be ticked […] I guess that mirrors the minority stress thing of feeling they need to hide part of themselves in order to get by in the world.
GIC staff member
This could lead to mental health conditions remaining hidden, and only emerging when people came for psychological assessment separate from the gender assessment.
Staff reported that an overall major issue the GIC faced was lack of capacity to offer psychological interventions, particularly individual counselling. Programmes of treatment had to be more limited in length than was desirable for some individuals, to keep waiting times down. It was also difficult for staff to keep in mind all the individuals on their caseloads, which were considerably larger than in most psychology services, with more people seen less often, sometimes with several months between sessions. The groups or workshops meant, however, that it was possible to offer follow-on interventions after seeing someone individually.
Developments under consideration
Staff and service users held a variety of views as to how transition-related care in general should develop in the future. The final section of Chapter 4 summarises this range of views, along with those of interviewees in the other case studies. Here we present the views relevant to the further development of primary care liaison and psychological support within this GIC.
Many staff and service users emphasised the importance of improving training for GP practices in trans health care, in particular in their responsibilities for prescribing hormone therapy. Some staff members felt that the GIC itself should also develop the capacity to prescribe, take bloods, dispense and administer hormones and hormone blockers, for service users who do not have a GP willing to enter into shared care.
A related suggestion was the development of a comprehensive coding system for patient records, that could be shared with primary care, which would reflect what it is medically important for services to know about trans service users – for example, which organs they have that require cancer screenings.
In terms of psychology provision, staff were of the view that online groups will continue to be an important mode of delivery for the foreseeable future, in combination with face-to-face. Staff saw continued development of compassion-focused and trans-affirmative approaches within individual and group therapies. Staff wanted to explore development of more inclusive group-support models that recognise the variety of medical and social transition that people engage with. The need for this is suggested by the experience of a non-binary service user we interviewed. They wondered why they had not been offered any groups, and whether this might be because the groups were designed for people with binary identities.
This would require the adoption of instruments for measuring the extent (and intended reduction) of minority stress in a more inclusive way than is possible using existing measurement instruments, which tend to assume a binary gender identity.
Staff were strongly aware of the need for psychological support among the 1200 people on the waiting list. They explored a partial but low-resource solution, using the Recovery College model to develop peer-led well-being workshops. Although this proved not to attract take-up, a range of shorter peer-led courses and online resources, on topics such as physical health and harm prevention when self-medicating, were being developed.
Case Study 3: primary care training and accreditation
Introduction
This case study concerns an NHS primary care TAS focusing on meeting the healthcare needs of LGBTQIA+ communities. This study focuses on the ‘trans-inclusive’ elements of TAS intended to improve the health care received by trans people, introduced in 2016 within MetroCity by the local NHS in collaboration with Alpha, a third-sector organisation providing support and advocacy for LGBTQI+ populations.
It is based on interviews with four primary care staff – GPs and receptionists – drawn from three different GP practices. These practices were selected because of the length of time they had been involved with the scheme and were drawn from urban areas with a range of social and economic characteristics. Seven trans service users were interviewed, on the basis they had completed the ICTA national screening survey on healthcare experiences of trans adults and indicated that they had used a TAS-accredited GP practice within MetroCity. One was a woman, two were men and four non-binary. All were aged between 20 and 30.
Three senior staff working for the NHS in MetroCity and involved in the commissioning of the scheme were also interviewed, as were two Alpha staff running the scheme. The study also draws on published TAS documents.
Below, we summarise what prompted the trans-inclusive elements of TAS, and how GP practices were engaged. We summarise the nature of the training and accreditation, how trans-inclusive health care has been stimulated by it, and how staff and service users experienced this. We were able to gather experiences from services users relevant to some, but not all, aspects of trans health care which TAS was attempting to influence. We summarise what has been achieved by the scheme, the concerns and issues that have arisen, and plans for developing the scheme.
Why were the trans-inclusion elements of training and accreditation scheme put in place?
Training and accreditation scheme was launched, initially for GP practices, in MetroCity in 2013, with the intention of improving care for LGB people. The scheme was run by Alpha and commissioned by MetroCity NHS. In 2016, TAS was relaunched and rebranded as a trans-inclusive scheme. The motivation to make the scheme trans-inclusive appears to have been strongly shared between Alpha and MetroCity Commissioning (MC). MC has two senior officers responsible for inclusion and equality, as well as a Head of Engagement, with a remit of establishing relationships with marginalised communities. Prior to 2016, they became aware that primary care and other branches of health care in MetroCity were often not meeting the needs of trans people. This contributed to the disadvantage trans populations face in terms of physical and mental health outcomes, and the barriers that many trans people face in accessing health services. At the same time, Alpha strengthened its focus on improving trans health care, increasing its recruitment of trans staff, including a new TAS co-ordinator:
… among LGBT community members, the greatest need, the poorest outcomes, the most difficult barriers to overcome, are experienced by trans and non-binary people, so let’s focus on that.
TAS staff member
The new version of TAS was commissioned by the MetroCity region administration, with additional financial backing from NHSE. From 2017, there has been a trans member of the TAS team employed by Alpha with specific responsibility for trans inclusion, as well as three staff roles working with primary care practices on training and accreditation, each focusing on a different section of the city. The funding allows Alpha to provide training and accreditation services to primary care practices without charging them a fee. The scheme was also expanded to cover a wider range of primary care practices beyond GP surgeries.
Engaging general practitioners
On the basis of local research into the barriers faced by trans people in accessing services, TAS staff at Alpha developed standards for primary care of trans people, as well as a framework for accrediting competence at the level of a GP practice. MC and Alpha have promoted the new TAS within primary care meetings and forums since 2017.
TAS staff realised that there was within GP practices a combination of demand for knowledge about how to meet the needs of trans patients, coupled with a fear of being exposed as ill-equipped to do so. The solution was to seed information about the scheme wherever possible within the primary care system.
… to just go somewhere and be a friendly face, and do a five-minute little pitch … don’t worry, you don’t need to be scared of us. Actually, our job is to help you …
TAS staff member
General practitioner motivation to work with trans-inclusion aspects also followed from their positive experience and commitment to the earlier versions of TAS that focused on improving the experience of LGB patients. Awareness of the need for trans health care among student populations also seems to have been significant. One GP interviewed cited the strong motivating effect of TAS staff with lived experience of trans health care coming to the practice to explain the barriers that trans people face, and what can be done to improve their health care.
… it was to a large extent someone coming into the practice and encouraging me to think more deeply about my work.
GP
How training and accreditation work
At the time of fieldwork, 49 GP practices in MetroCity, around 75% of the total, had signed up for TAS training and achieved at least bronze accreditation.
Training sessions for GP practices typically last 1 hour, intended to involve all practice staff. These sessions may be several months or even 1 or 2 years apart, depending on how rapidly the practice is able to progress with its development in the trans healthcare standards. This reflects the limited time that practice staff can set aside for in-service training.
Training covers: LGBT basics, including the differences between concepts of sex, gender identity and sexuality; ideas of cis and trans, including non-binary, people; health inequalities experienced by LGBT people, the additional inequalities faced by trans people; the importance of recognising protected characteristics and addressing inequalities; and best practice in terms of inclusive primary health care.
Training sessions are designed so that there is space for practice staff to raise questions or talk about encounters with trans patients which they experienced as not going well, so that there can then be discussion of what can be learnt.
… they just really embraced that as a learning opportunity rather than being scared of it as a mistake […] I think people carry a lot of shame around the topics of discrimination and marginalisation. And wanting to be an ally but not necessarily being in a marginalised group … they know that things are kind of bad for trans people, and they know that they haven’t personally really done anything to make it better …
TAS staff member
The volume of training has increased markedly during recent years. At the time of interviewing, virtual sessions were being delivered in several different practices each day.
Clinical and non-clinical staff alike commented on the importance of having the training delivered by a trans person. GPs indicated the value they attached to having clear information about the health inequalities and problems accessing services typically experienced by trans people, and that this freed them up from hesitancy about admitting what they didn’t know.
Assessment for accreditation typically takes place on the same day as training, in a separate session with a smaller group of practice staff. This includes discussion of policies and questioning of staff about how they have dealt with or would deal with various scenarios involving trans patients. One example is what the response would be if a receptionist overheard a patient in the waiting room making a transphobic joke about another patient. According to TAS staff, the aim is to ‘create the conditions for services to tell us things’, rather than a more formal process of assessment.
… do they feel confident to intervene if they witness transphobia, and is there a general culture that … is their manager going to back them up on intervening?
TAS staff member
Assessments also explore the questions typically asked by clinicians in their consultations with patients, whether patients are given the opportunity to give information appropriately about trans identities and whether there is exploration of related health issues such as relevant screenings.
TAS staff subsequently review practice documentation and policies on topics such as equality and inclusion, and the extent to which the handling of patient records conforms with privacy and confidentiality rights for trans people enshrined in the GRA. They also form a view on the extent to which understanding of these issues is shared across practice staff.
The assessment result is fed back in terms of a bronze, silver or gold TAS award, with recommendations for areas of improvement. TAS staff felt that the different levels of award were effective in recognising progressive achievement in delivery of care. Typical feedback at bronze level might concern the need to ensure that a well-intentioned policy is better understood and acted on by practice staff. Another example of a developmental direction could be that of learning about the particular issues faced by LGBT and trans people from a particular ethnic or religious group prominent in a practice’s catchment area.
TAS staff each act as account managers for practices in particular areas of the city. The intention is that this continuing relationship provides the basis for learning within an atmosphere of openness. Training and accreditation materials are reviewed and updated annually, in consultation with focus groups of trans community members, as well as a TAS Steering Group, overseen by the TAS trans co-ordinator at Alpha. The TAS philosophy is that trans community membership and needs are fluid and changing, and that training and accreditation need to be co-produced to reflect this. The TAS Steering group includes people with lived experience of receiving trans health care, as well as GPs, dentists, pharmacists, optometrists and commissioners.
Features of trans-inclusive care resulting
Trans-inclusive administration
Practices have developed new patient registration forms that allow people to indicate their gender in an inclusive way, as well as trans status, pronouns and anatomical details relevant to screenings. This allows the creation of a trans status marker on the system, which allows clinicians to review which screenings are appropriate.
At the instigation of commissioners, practices also now collect anonymised demographic monitoring information from patients relevant to improving social inclusion. Trans status is included in this monitoring.
Practice receptionists showed awareness of some key aspects of trans inclusion:
We have to identify ourselves, what pronoun we want for ourselves … we have to identify that with the patients as well …
Receptionist
Practices have developed expertise in how to change gender markers on medical records and how to transfer appropriate information from an old record to a new one.
General practitioners showed awareness that they should not depend exclusively on administrative systems for ensuring they address people appropriately:
… if I’m not sure, I always ask a patient. I don’t know if that’s the right thing to do or not, but I think it’s better to ask than to assume and offend.
GP
Practice staff interviewed expressed confidence in the accuracy of names on the records of trans patients, and that their practices were responsive to trans needs, including on occasion the need to set up an urgent appointment with someone who has forgotten to book a hormone injection sufficiently in advance. A phlebotomist reported being able to use the patient record to identify when someone had transitioned and made sure that they were addressed appropriately when setting up an appointment.
One practice indicated that they had been able to carry out an audit of the care that their trans patients were receiving – for example, whether they were receiving regular blood tests to support hormone therapy and whether appropriate screenings had been carried out. Commissioners reported that they were aware of a handful of more advanced GP practices that had developed this capability but were unsure of how far this had been achieved by others.
These perceptions were borne out by a number of the service users we interviewed, who variously noted that registration processes were respectful and gathered appropriate information, that changing their gender marker on their practice health record had been a smooth process, that check-in procedures no longer involved giving a gender or a title, that they were always addressed on the phone with the correct name, and that arranging appointments appropriate for their anatomy had been straightforward.
… their registration form was really good, I think it had multiple gender options. It asked a question about whether or not you have a cervix rather than just assuming that women have a cervix and men don’t.
Service user
I went in to book an appointment and that stresses the hell out of me, and I went in in person, because I thought they were less likely to think I was joking. Because I don’t look like the kind of thing they would be expecting … And the receptionist was just, yes, how about Tuesday? She didn’t even blink …
Service user
Other service users, however, reported significant problems, indicating inconsistencies in how these administrative systems functioned. One person had difficulty achieving a change in their name and gender marker on the patient record. The surgery staff consistently referred to the participant by their correct name, but documents printed out from the record contained their deadname. When they asked for this to be corrected, the practice, apparently incorrectly, told them they ‘would have to go through the GIC first’.
Another participant, whose record had not been changed, attended for a minor procedure. They were deadnamed in the waiting room, and then found the treating clinicians were surprised by their gender. They experienced having to deal with the clinicians’ embarrassment, rather than receiving support for their own reactions.
In another case, a less informed member of practice staff initially refused to respond to a request to change a person’s name on the record:
[W]hen I went to change my name, I ended up with a bit of adversity from one of the reception staff and I ended up having to just get the reception manager. And as soon as she came out, she was like, yes, this is the process. It’s absolutely fine. […] but it was that initial barrier.
Service user
Cultural competence
TAS staff perceived growing awareness of trans healthcare needs in GP practices:
Nowadays, it’s very rare that I go to a practice where either they say they don’t know if they’ve got trans patients […] So, that awareness from healthcare professionals about trans people existing has really changed in the last four years.
TAS staff member
General practitioners and TAS staff alike emphasised the importance of developing an overall approach within the practice that was welcoming to trans people, underpinned by awareness of the fears they may carry into healthcare settings. GPs emphasised that this cultural understanding was best demonstrated by not making unnecessary assumptions about many aspects of a person’s life or health, and also being willing to apologise when making a mistake in an interaction, asking to be put right.
So, it’s finding that balance … not wanting someone to think you are probing when you don’t need to, but also feeling, okay, I need to ask for this reason, I need to know about your anatomy, for example for this physical health reason …
GP
Competence in working with trans people was seen by some as needing to be developed over time:
I think key in terms of trans inclusion is the opportunity to create an education or thinking space for the practice staff in the broadest sense … because I don’t think that people can change overnight, assumptions about gender identity that they’ve grown up with, that their parents have grown up with, their communities have grown up with …
GP
One service user, however, felt that even seemingly minor failings in respectful behaviour towards them were all the more painful because of their past experiences of healthcare settings. While a well-intended practice offered them benefits, they realised that they often remained hypersensitised to staff using inappropriate language or making erroneous assumptions, and often they had to ‘settle’ for a limited standard of care.
… it’s the fact that I have repeatedly had bad experiences. I’ve had more negative experiences than positive experiences. So, even though I have a relative assumption that my GP practice probably is fairly culturally competent as far as a bunch of cis people go, that past experience isn’t going to magically disappear either […] it’s not always the case that the staff you end up seeing are the most knowledgeable.
Service user
Another person explained that a good experience with a practice could have the paradoxical effect of making them feel more dependent on the particular staff involved and anxious about what would happen if they were no longer available:
I wish that the whole process hadn’t felt like overlaying with this ever-present fear of refusal or withdrawal, or things being suddenly withdrawn … Like I’ve never left that GP, I have done all kinds of gymnastics to stay there because when it comes down to it, I’m still scared of something happening to cut me off.
Service user
Referring to GICs
TAS staff reported that it was increasingly rare for a practice not to know how to refer someone to a GIC, or to avoid doing so when asked to. Following repeated difficulties in getting a referral to a GIC from their GP in a different part of England, one service user reported that their new TAS-accredited GP proactively asked if they had been as yet referred. The GP then completed the referral within a week.
However, other service users reported that their TAS GPs lacked knowledge about how to work with the GIC system. In one case, at a gold-accredited practice, a service user had to overcome several barriers to receiving care via a GIC:
First of all, [the GP] wanted to refer me to a mental health unit […] went away, did their research … and got on top of it, and got me my referral to the GIC….And then […] when I first got prescribed hormones, my GP was very reluctant to give them to me just because I think they didn’t want the liability. And they were very adamant that it was the case that the GIC gives that to me, gives me that prescription, and I had to explain and point out a letter where it’s actually, no, they give their recommendation and then you prescribe it …
Service user
General practitioners were also critical of some GIC referral processes, which seemed to make referral more complicated than necessary. One example given was of a referral form that required a BMI to be entered, and a letter received in response to a failure to do so that threatened to remove the patient from the waiting list. The GP pointed out that giving a BMI at this point was of little use, given that the person would not be seen by the GIC for at least 2 years.
General practitioners expressed frustration with the length of the waiting lists for patients referred to GICs. They found it additionally difficult that GIC policies meant it was impossible to discuss or receive advice on cases on the waiting list, or discharged on long-term hormone therapy, since GICs will only discuss with GPs patients who have been seen but not yet discharged. GPs contrasted this situation with many hospital specialisms, who, particularly during the pandemic, have been increasingly open to e-mail and phone exchanges about how best to manage patients waiting to be seen by a specialist service, or who have been seen and then discharged from the specialist service.
Hormone therapy
Some GPs indicated that they were already experienced and confident in prescribing and monitoring hormones under shared care with a GIC, as well as prescribing hormones for harm reduction to people on a GIC waiting list. These GPs indicated that they were supporting colleagues within their own practices, and also more widely across the city, in developing skills in this area.
Two service users commented on how safe they felt that the same nurse was always the one to give them their hormone injection – this removed anxiety about having to explain anything to a previously unknown staff member. One service user, however, reported repeated failure from their accredited GP practice to send blood test results to the GIC in time for their consultations to review hormone dosages. This prevented a timely discussion of their need for an increase in dosage.
In another instance, someone who had already transitioned when registering with their practice was referred by their accredited GP to a local endocrinologist for hormone prescriptions. This person questioned why this was necessary:
… I’m just on hormones for the rest of my life, why on earth can a GP not manage that?
Service user
One GP felt less experienced but was committed to finding colleagues who could provide advice:
If a patient’s come in, needing something and you, as their doctor don’t try your best to help them, it doesn’t sit right with me. I think you’re constantly trying to find the balance between, are you going to cause more harm doing the thing, or by not doing anything, you know?
GP
Higher levels of TAS award are tied to practices demonstrating competence in prescribing hormone therapy for trans people, and TAS staff described how they could connect less capable practices with other GPs already skilled in this.
Other aspects of health care
Two trans men commented on the respectful and sensitive way that cervical smear testing was carried out. One had been encouraged to stay with their current practice when moving out of its normal catchment area, in order to provide continuity of this kind of supportive care.
… they understood that it would be a really distressing thing for me to go through […] They asked for my pronouns […] they gave me the option of not looking at the screen when it was happening.
Service user
Some clinicians referred to having become more sensitised to the potential mental health needs of their trans patients. However, one service user had not experienced their TAS GP as being open to hearing about both their mental health concerns and their trans identity.
TAS staff also provide workshops for trans people, to improve people’s knowledge of and ability to get the best use out of health services. They further provide advice to individuals on where to find an inclusive primary care practice.
Several users and GPs reported frustration that it was difficult to communicate to hospital labs that specific blood hormone levels appropriate to a trans person should be monitored, with norms different from those for a cis person. Information about the trans status and gender of a service user did not always transfer into other NHS organisations.
Overall achievements and issues
The picture emerging from the perceptions of service users and TAS staff is that some accredited practices have developed competence in many aspects of trans health care and have acquired a substantial trans clientele. However, the experiences of service users suggest that trans healthcare expertise was not consistently held by all staff or consistently supported by administrative systems.
These kinds of failings were also reported by TAS staff, who have been contacted by trans people following negative experiences with an accredited practice. TAS staff follow up these reports with the practice identified, as an opportunity to bring about improvement.
Commissioners and GPs we spoke to also expressed concerns about continuing resistance to TAS from a minority of GP practices within the city.
… we do still have a few transphobe comments and feedback come through from our GPs who don’t understand why we should be focusing our services or any support around specific groups, especially trans people. […] And it’s a constant reminder to practices around what their duty of care is that we share […] get our medical director to step in …
Commissioner
Future developments
Commissioners and TAS staff described a number of fronts for expanding TAS. These included a further level of award for practices demonstrating consistent achievement in trans health care beyond the gold award level. TAS and its trans-inclusive requirements were also being expanded to other kinds of primary care, such as retail pharmacy, optometry and dentistry. TAS has been expanded to other areas within England.
Several members of staff interviewed were involved in designing and winning funding for a new pilot primary care-based gender service in the same city. They held that the experience of trans community stakeholders and GPs working together to create TAS had provided the basis for further conversations and joint shaping of the new service:
… we wouldn’t have been able to have a collaborative conversation with trans communities and GPs if there hadn’t have been [TAS] … What it would mean to think about trans health as a normal part of normal everyday life. Because that’s what general practice is.
TAS staff member
A number of staff described the new service as intended to provide holistic care for trans people, including mental health support. They emphasised the importance of understanding the intersectional nature of needs, that people can be disabled, non-white and/or refugees as well as trans, indicating how TAS has promoted ideas of person-centred or patient-centred care:
… the principles we’re talking about are about patient-centred care. They’re about not making assumptions. […] They’re about recognising multiple marginalised communities and the barriers people have.
TAS staff member
Case Study 4: the Welsh Gender Service
Introduction
This case study looks at the setup and delivery of the WGS. This comprises:
-
a specialist Gender Identity Clinic (GIC) based at a hospital site in Cardiff
-
local gender teams (LGTs), practitioners based in each of the local health boards (LHBs) across Wales, who provide and manage care after people have been assessed by the GIC
-
Umbrella Cymru, a third-sector organisation that provides a Gender Information and Support Team.
This case study is based on semistructured interviews conducted with 8 staff and 10 service users of the WGS.
NHS Wales is comprised of seven LHBs, each of which has its own LGT, shown in Figure 14.
FIGURE 14.
Map of Welsh LHBs. Source: www.rcgp.org.uk/getmedia/8de53cd2-93b5-4d5e-88eb-5d1700aacbef/RCGP-NHS-in-wales-oct-2017.pdf

Pathway
The WGS is commissioned by the Welsh Health Specialised Services Committee (WHSSC). Prior to its commissioning in 2019, access to specialist gender services was via funded access to a specified GIC in England. Welsh patients, however, first had to be screened by local mental health services. Figure 15 summarises the differences between the new and old pathways.
FIGURE 15.
Map of former and current pathways for gender-affirming care for Welsh patients. Original figure, derived from data collected for this case study.
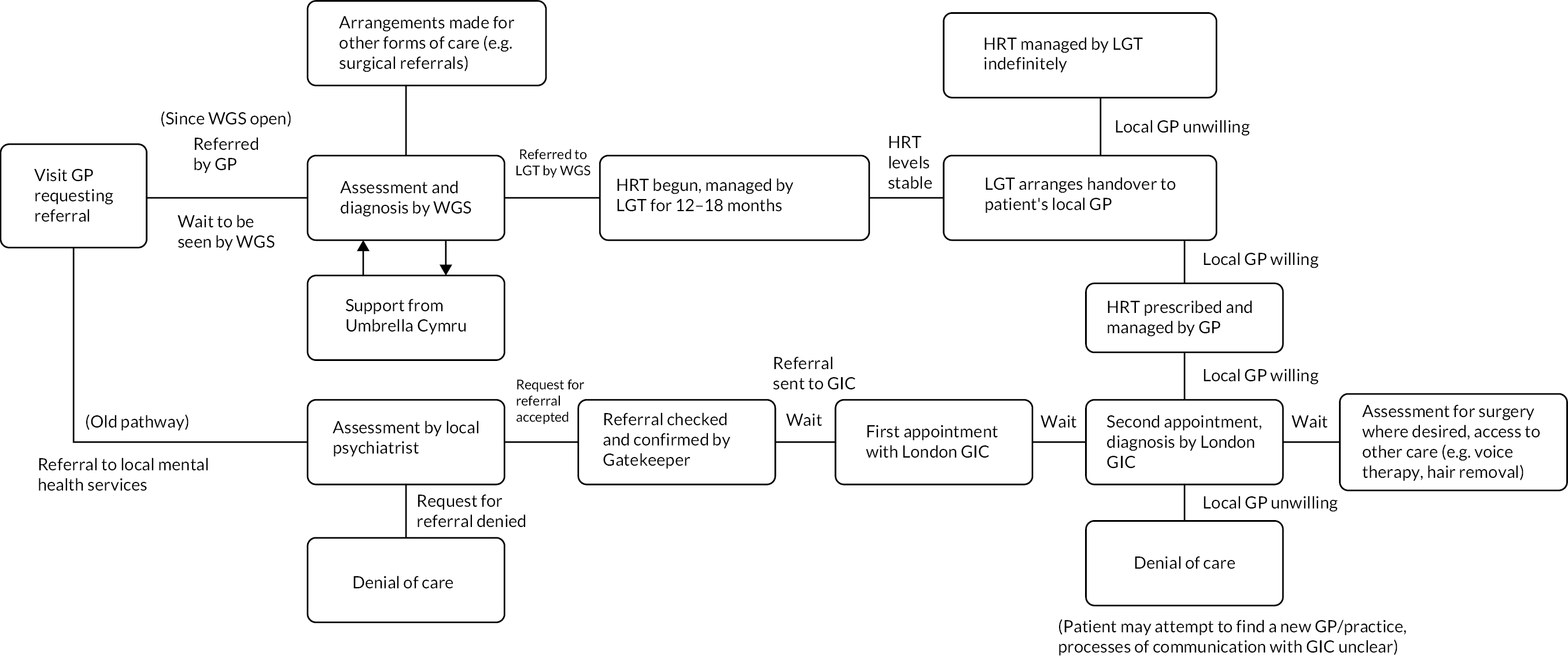
Rationale and implementation
Staff explained how, historically, the earlier pathway created significant inequities to accessing gender-affirming care for Welsh patients. Some local psychiatrists would believe they had found ‘some psychological issues’ that they ‘needed to explore’ and would correspondingly not refer those patients on to the English GIC. The staff member highlighted that ‘obviously’ gender dysphoria was the source of mental distress being experienced by these patients. Others highlighted that there ‘wasn’t a great deal of clinical use’ to the local psychiatric appointments.
A related point was that ‘our patients were not getting a Welsh service in the slightest’, highlighting that the entire trans population of Wales was placed on to the waiting list of a single English clinic, ‘without extra provision for that, really’. Service users needed to travel for multiple assessment meetings – a significant burden of cost and time.
A key factor identified by staff as contributing to the rationale for the implementation of LGTs as part of the service model was that, even when assessment was successfully accessed via the English GIC, patients were dependent on their local GP being willing to enter a shared care arrangement. In rural areas with very limited GP provision, should the only available practitioner(s) refuse, patients could be left without care. Access to care was therefore a ‘postcode lottery’.
The creation of the WGS/LGT system ‘was remodelling the whole service to focus on local care’. This was rendered possible by political support. Interviewees explained how in 2017 the devolved Welsh government was aware of service inequalities, and recognised political as well as practical benefits to reform:
It was at the behest of the Health Minister, Cabinet Secretary who wanted to see this work and had an eye for it being successful in order that he could make an announcement ahead of one of the Pride events.
WGS staff member
The instigators were a small network of people from different settings, who shared a moral commitment to establishing a new kind of service. The network included a GP who had established a working relationship with Welsh government health policy-makers in another clinical area and had also become concerned about the difficulties experienced by their own trans patients. This GP engaged with the WHSSC priority of establishing a WGS and was funded to gain experience of gender assessments and prescribing elsewhere in the UK, alongside being appointed as adviser to WHSSC on gender services. They worked with a WHSSC project manager to design the new service.
Others involved in the design included individuals from trans communities and a third-sector LGBTQIA+ leader with a history of working with communities to deliver innovative services. People involved in service design and implementation expressed personal connections with trans communities through being part of the wider LGBTQIA+ umbrella, which functioned not only to motivate but also informed network integration:
And so, from the very beginning I have felt really connected to the community and I belong to the LGBT community as an out lesbian. So, for me these were my siblings, there is a personal sense of connection as well as a duty of care as a clinician.
WGS staff member
The design of the new service was overseen by a wider group of senior health board representatives and trans community stakeholders. Staff and community representatives consulted widely within local trans communities, gathering views as to how services should run, while also recognising that for many:
The relationship between themselves and general practice was completely broken.
WGS staff member
The instigators accepted that the existing waiting lists would immediately place significant pressure on the new service in Wales. Referrals were backdated in accordance with the original GP referral on the old pathway. Support for people while they waited was identified as vital because of distress and harm that long waits had caused, including concerns that there had been a number of suicides as a result. The service designers considered an existing model of trans peer-support workers attached to an English GIC, and also drew on the support for gender and sexual diversity that Umbrella Cymru had been delivering since 2015. The group establishing the WGS successfully put a support service specification to WHSSC and Umbrella Cymru bid successfully to deliver this.
Alongside establishing the new specialist clinic, the instigating group developed the concept of LGTs – identified primary care practices managing care for people for an initial period of around 12 months after assessment. About a year in advance of the formal launch of the WGS, with funding from WHSSC, the GP leading on gender services began to run a primary care prescribing clinic a day a week, initiating hormone therapy for trans people living within the LHB area who had been assessed by the English GIC, but then found their local Welsh GP or endocrinologist unwilling to prescribe. This provided the model for a LGT. The instigating GP welcomed a number of colleagues from other parts of Wales to sit in on clinics as a means for them to develop the skills needed to run a similar service.
The setup of the WGS with LGTs was formally implemented between the planning function within each LHB and WHSSC. Each LHB appointed a senior gender lead, responsible for funding and appointing LGT clinicians to deliver hormone prescribing and monitoring, and speech and language therapy. The gender lead also oversaw funding for hormone prescriptions.
Local gender team prescribers across the health boards had a range of medical backgrounds. Most were GPs, but some were medical specialists – for example, in sexual and reproductive health. Taking up the role did not depend on having any prior experience with trans patients, but most had prior experience with hormone management in some clinical context. Some staff or practices came to be involved because of educational work being done by staff working to create the WGS, which stimulated commitment to address the health inequalities faced by trans people. Decisions on where to site LGTs sometimes took into account the strategic benefit of specific (accessible) locations, and the level of support that interested clinicians had from practice partners.
A further element in the initial design of the system was negotiation, between NHS Wales and the General Practitioners Committee Wales of the BMA, of a DES for providing HRT. The DES provides GP practices with additional payment for taking over prescribing and monitoring of hormones for people who are endocrinologically stable after around 12 months with a LGT, thus freeing up LGT capacity. Members of the WGS instigating network made the case to commissioners as to how important the DES was to the functioning of the new WGS system, as well as specifying the clinical content. The funding for the LGTs and the DES payments to GPs was ring-fenced legislatively.
The Welsh Gender Service in practice
Here we summarise the data reported as to what happens within the WGS specialist clinic, the LGTs and the peer support. Several interviewees highlight the close collaboration between organisations, disciplines and perspectives that shaped practices across the different areas. Umbrella Cymru staff saw acting as a ‘critical friend’, challenging established NHS practices, as an important part of their role.
Umbrella Cymru leads on engaging the trans community and other stakeholders with the development of the WGS. In addition to 6-monthly stakeholder meetings involving NHS managers and clinicians from across the service, there are monthly online meetings open to trans groups to review the service and disseminate information. Engagement is further sustained through having a trans community member on all staff appointment panels, including for clinical posts, and a community observer at GP training sessions.
All staff across the specialist clinic, Umbrella Cymru, and the LGTs are invited to monthly online professional development sessions, with inputs by external experts on different aspects of trans experience. These are seen as reinforcing staff cohesion across the system.
Specialist clinic
The central activity associated with the WGS specialist clinic is assessment of people for gender-affirming care. With the COVID-19 pandemic, assessment appointments were rapidly moved in mid-2020 to videoconferencing. Blood tests needed to initiate hormone prescribing are carried out separately at the relevant LGT, usually after the person has had their initial virtual session at the specialist clinic. During 2020 and 2021, there has been a steady increase in clinical capacity as gender specialists, including an endocrinologist, have been recruited. The move to virtual working has enabled the recruitment of a number of experienced gender clinicians based in England, alongside others based in Wales.
Since its opening in September 2019, approximately 1000 service users who had previously been referred to the English GIC but not yet seen were transferred to the new Welsh clinic. At the time of interviewing, the backlog, as well as new referrals, meant that there was a waiting time of around 30 months for an assessment appointment.
While working within a formal framework of diagnosing gender incongruence, clinicians saw the assessment process as fundamentally a collaborative one:
We are affirmative practitioners and we work with patients, with their consent, and inform them around their combined joint decision-making.
Gender clinician
They prioritised giving people access to care, while recognising that it was vital to ensure the person was fully aware of what treatment would involve, including medical risks, and that they had mental capacity to consent. Clinicians reported that it was extremely rare for them to have concerns about a person’s capacity to consent. They did not follow the practice of exploring a person’s trauma history as part of assessment, in contrast to the experiences reported in Chapter 3 by many people assessed in other GICs. The problems associated with this practice, including lack of evidence for it, were discussed in the section of Chapter 3 covering experiences of trans people with mental health conditions.
The WGS pathway requires an opinion from only one gender clinician for a diagnosis to be confirmed. The specialist clinic also operates on the basis that many people can be diagnosed and passed on to their LGT for initiation of hormone therapy after a single assessment appointment. Roughly half of those seen are asked to attend a follow-up appointment, usually a few months later, to complete assessment for hormone therapy. A common reason for the second appointment was that the person concerned needed some more time to explore their treatment goals. Staff, including those providing support independent of the assessing clinicians, indicated that both they and the people being assessed generally understood why a second appointment was beneficial, although clinicians had ultimate authority over whether a second appointment was needed. In Chapter 5, we discuss the ethical issues that may be raised by decisions to prolong assessments.
One clinician described their approach to assessment as follows:
With me that’s an interview that’s approximately an hour long […] Firstly, I am making a diagnosis that feels a little bit tokenistic, or perhaps ritualistic these days, but I have to go through a diagnostic process and make an actual ICD-11 diagnosis based on their criteria. […] The second thing I have to do is to gauge capacity of the individual to be making adult treatment decisions in sound mind. And the third thing is treatment delivery, so I have to inform and put together a treatment plan in the way that’s least traumatising to my actual patient, and also, I suppose holding the hand of other medical professionals involved, especially the GP.
WGS staff member
The choice of language – ‘least traumatising’ – suggests that, despite the intentions of clinicians and the improvements the service has made relative to the former pathway, the requirement for formal psychiatric diagnosis prior to access to gender-affirming interventions, and the requirements for medical evidence as part of a gender recognition process, can potentially be traumatising in and of itself.
Staff may also discuss clinical cases within a weekly MDT meeting, but this was relatively infrequent: ‘Usually I don’t need to, actually.’
Subsequent to appointments, WGS clinical staff use letters to communicate a care plan with relevant services, above all the LGT and the patient’s GP, but perhaps also fertility preservation and speech and language therapy.
Clinicians were critically aware that the diagnostic criteria for gender incongruence in ICD-11 amounted to making a general judgement that someone was trans – there are no specific or objective indicators. They tended to see the practice of diagnosis rather as a means to access care:
If you’re asking me ‘do I put a diagnosis of gender incongruence on my letters’, then, yes, I do. Some people want to have that. Why do I put it on? I could see it just as a coding thing as you’ve got a diagnostic code and that means you get treatment. If you’re asking me on a personal level, ‘do I think making a diagnosis is what I do and is this something that I spend an hour making a diagnosis’, then absolutely not. I see it as potentially a tool. I think surgeons like to see it on their letters, for example, that they’ve had a diagnosis. So, I’m pragmatic about it. I will use it but, if you read what is the criteria of a diagnosis of gender incongruence, you could answer that in two seconds, couldn’t you?
WGS staff member
Welsh Gender Service staff with psychiatric backgrounds did not view this as essential, clarifying that colleagues with clinical psychology or general practice backgrounds conducted assessments in the same way.
Welsh Gender Service gender clinicians can also approve people for top surgery and provide a first signature for lower surgery. The option of surgery is usually raised at the first clinical appointment. From late 2020, the WGS commissioned a clinician in a nearby part of England to provide the required second assessment for surgery.
Local gender teams
A key function of the LGT within each LHB was the delivery of gender-affirming care under the treatment plans resulting from assessments. Care typically included hormone prescriptions but could also include speech and language therapy and fertility preservation. While LGTs were established to initiate and stabilise hormone therapy for people assessed through the WGS, three of the people we spoke to who were being prescribed by a LGT had in fact been assessed by a private gender service. A further person had been assessed by the English GIC previously responsible for assessments, and another by a different English GIC, prior to moving to Wales. LGTs appeared to be willing to prescribe regardless of where assessments had been done.
Each LGT typically included one or two identified prescribers, usually GPs, each commissioned to deliver typically one or two half-day clinic sessions per week specifically for the WGS. Some LGT clinicians indicated, however, that they saw WGS patients during the course of their general sessions. This was either because the specific clinic sessions had not yet been organised or because of general disruption to primary care clinics due to COVID-19.
Local gender team prescribers were equipped for their role by a combination of sitting in on other WGS clinics and using comprehensive guidelines on hormone therapy produced by clinicians at the specialist service. They expressed confidence in their ability to manage hormone prescribing, pointing out that much hormone management was routine in comparison to other clinical areas. This was borne out by the experiences of users. One said of their LGT:
There’s a GP who works from a different surgery to my own, but still local, so I go there and see them every now and then, every few months. Yes, really good. They’re obviously well trained in what they do and are really comfortable with working with trans people or with me, at least.
Service user
Local gender teams also took responsibility for ‘harm reduction’ hormone prescribing for people who had presented at GP surgeries as self-medicating with hormones, while waiting to be referred to the WGS. The GP would then consult the WGS specialists as to the medical viability of a hormone prescription, which would then be managed through the health board’s LGT. One of the service users we interviewed had approached their GP for support after beginning to self-medicate and was then rapidly supported with a prescribing arrangement through their LGT.
Local gender teams have a remit for providing advice on trans health care to GP practices across their health board. One of our service-user interviewees described a kind of shared care arrangement between their own GP practice and a GP from the LGT. This may have been partially the result of pandemic restrictions during 2020. Their hormones were prescribed by the LGT, but all blood tests and face-to-face consultations were with their GP, who was ‘good friends’ with the LGT clinician based some miles away. The service user could, with some difficulty, arrange to speak on the phone to the LGT clinician, but otherwise relied on GP-to-GP collaboration. Over a year they had never met the LGT GP. They had heard from a friend that a LGT clinician in another health board was more readily available via instant messaging:
The person I believe is on Messenger and will answer questions as in yes I will phone you, that sort of thing, on Messenger.
Service user
Another user noted that there was ‘really good’ communication between their prescribing GP and the WGS, in contrast to difficulties in GP communications with a GIC they had previously experienced while living in England.
Local gender teams have regular fortnightly videoconferences with clinicians from the WGS specialist clinic. These calls are an opportunity to discuss the management of any more complex cases – for example, where blood results show problematic hormone levels or other kinds of abnormalities.
Support service
At the time of interviewing, Umbrella Cymru was funded to provide a full-time service manager – a social worker by background – and a full-time equivalent peer-support post. The latter had been split between three part-time people, all of them trans. Part of the work of the service manager comprised advocacy for individuals who contacted the support service directly, wanting help getting their GP to refer them to the WGS or else with getting a bridging prescription, particularly in cases when the GP did not appear to know how the new pathway worked. One of the service users we interviewed was helped by the support service to obtain a bridging prescription through the WGS after their relationship with a private gender service broke down. In another case, the support service negotiated a shared care arrangement for hormone management through a LGT when someone with a diagnosis from a private gender service found their own GP practice unwilling to enter into a shared care arrangement.
Another substantial element was dealing with waiting list issues, above all making sure that people with referrals had been transferred from the English GIC waiting list, and also making sure that their referral date was correct, particularly if a GP had delayed in actually making the referral. There were, in some cases, considerable difficulties in getting GPs to provide evidence of having made a referral, when one had not apparently been received by the WGS. However, staff highlighted the benefits of administrative tenacity in the backdating of referrals made via the former pathway:
… so, somebody recently said to me the road to [name of English GIC] was so – what did they say? The road to [name of English GIC] was so cold and lonely, thank you for scooping me up.
WGS staff member
In terms of physical space, Umbrella Cymru has a base office as well as an office within the WGS that allows for the service manager to attend the weekly MDT meetings. Having in-person working practices in the same place prior to remote working (during the COVID-19 pandemic in 2020) was experienced as significantly beneficial in developing working relationships among staff from different backgrounds:
… any third-sector organisation being attached to an NHS organisation can have its bumps in the road. So having that physical space was really useful at that time to make sure that it was a seamless integration […] it worked really well to have all staff popping in and out of the clinic as and when on different days …
WGS staff member
Staff reported that, of the approximately 1000 patients whose referrals had been received by WGS (as of late 2020), around 70% had expressed interest in accessing support, with around 300 of those contacted. The purpose of an initial support assessment by the service manager was to understand a person’s overall history, their family and/or home life, their wider social supports, any financial issues they were facing, or any issues with drugs or alcohol. This would then lead to the person either receiving one-on-one peer support, or else ‘enhanced support’ from the service manager or a trainee social worker also attached to the service.
Peer support was provided through telephone sessions, usually four sessions over as many months. Peer-support workers were also available to interact on instant messaging. Support was in principle available not only to people waiting for WGS assessment, but also to people who needed support to approach their GP to get themselves referred, or those who wanted peer support after being seen by a GIC. It could involve:
emotional support, practical support, advocacy with other services… or providing support with building a trans person’s confidence in their identity or in their gender presentation.
WGS staff member
It could also involve liaison with the specialist clinic, through application of trans-specific sensitivity and cultural competency, as well as competency in accessing NHS systems and records.
… calling up and saying either, is this person on the waiting list? Where are they on the waiting list? When can they expect their next appointment? … Or they’ve got an appointment coming up but they can’t remember what date and what time, who it’s with, what it’s about, etc. […] It’s checking things on behalf of a client … maybe they’re not confident to call up or they don’t have the time to call up or maybe they have voice dysphoria …
WGS staff member
One service user was deeply appreciative of the support service for working with the specialist clinic to track down a letter from a private gender clinic to their previous GP, which confirmed their diagnosis.
Enhanced support addressed in more depth challenges some trans people might be facing and worked on how they might be addressed. The service manager and the social work trainees attached to the service drew on social work techniques to deliver this, identifying ‘personal outcomes’. The manager ensured that trainees attached to the service were working from within a commitment to trans rights. Examples of the focus for enhanced support given by staff members included ‘building confidence with gender expression’ as part of social transition, coming out to a partner or other family members, or simply supporting people experiencing ‘low mood and then dysphoria’ after finding a generalist NHS mental health clinician unwilling to engage with issues of gender identity. Enhanced support usually involved 8–12 telephone sessions.
Umbrella Cymru staff also saw their support work as helping prepare people for their assessment session at the specialist clinic. This might involve reassuring them that certain things they feared would not be problematic – for example, that clinicians would not expect them to ‘prove they are trans’, present themselves as a man or a woman if they were non-binary, or avoid disclosing mental health struggles. It might also involve explaining that clinicians were likely to raise topics such as progress with coming out in different contexts and fertility preservation options. Peer-support workers reported that they generally encouraged service users to think about aspects of their transition in addition to the medical ones if they were not already doing so.
Benefits experienced
Welsh Gender Service staff saw the simpler assessment process, usually based on a single opinion, as an important achievement in terms of service-user experience and allowing more rapid progress through the inherited waiting list. One view was that most people who have been waiting for 2–3 years have already sufficiently demonstrated their determination to medically transition. Another was:
I think it’s well-received. I think people obviously understand having to see one clinician, they don’t understand having to see two, for two opinions. So yes, I think it’s made it more streamlined, and it’s also made it more palatable.
WGS staff member
Service users also had positive experiences of the integrated service provision:
… my three years with the [WGS] and with the local gender teams has just been so relaxed. It basically comes down to what do you want from your transition? What effects do you want, what is bothering you? […] And then sorting out a way to do it, it has just been so easy and so laid back in the best way… they know what they’re doing, and you feel very safe in their hands.
Service user
I think honestly the local gender teams service needs to just be adopted everywhere because it’s so much more efficient in every way. Because you get to know the local gender team which are local to you, it’s less pressure on the gender clinic itself. It encourages more GPs to know more about hormones so then maybe even further down the line, if someone only wants hormones and not surgery they could just be with their GP and not go to the Gender Service.
Service user
Gender clinicians experienced the fact that initiation and management of hormone prescribing was taken over by LGTs as a welcome release of their time from the kind of follow-up appointments that occur in other GICs. Some, who had worked or continued to work part-time in other GICs, contrasted the integrated way that LGTs took responsibility for blood testing and hormone management with the difficulties involved in typical GIC shared care arrangements. A great deal of time and effort in the latter typically went into getting hold of blood results from dispersed GP practices.
Within LGTs, prescribers welcomed their integrated responsibility for carrying out blood tests, monitoring and optimising hormone therapy, as well as taking overall charge of the relationship with the patient, including consent forms, and making sure that all contact details were up to date and included the correct name and title. Some emphasised the benefits of integrating hormone therapy with other aspects of primary care:
This is everyday life, this is everyday patients … one of my patients, not my gender clinic, came to an appointment with myself I believe for a bad toe or something like that, but it was on the day that my gender clinic was running. And then a week later she rung and said that she had feelings that, she was trans, she was a trans lady, and the following week, the first time ever, she had dressed more feminine and came to surgery to talk about her gender … There’s an element of the more you single out and create a specific route, we’re reinforcing prejudices without realising it. There’s no reason why someone should be going to a hospital for this treatment. That’s not right.
LGT prescriber
The benefits of this integration were reflected in the experiences of some of the service users. One described their relationship with their LGT doctor, who was also their long-term GP:
… she’s brilliant. So, I see obviously her every nine weeks for my testosterone injection. So generally we catch up then and if there’s been anything I bring it to her then.
Service user
Another spoke about how their LGT clinician was able to integrate hormone prescribing with the treatment of a chronic condition, within a collaborative way of working:
The doctor that I see for trans healthcare stuff, it’s phenomenal and she’s actually the one that has been helping me to get stuff seen for [chronic condition] and also, I go in about one thing, she asks about my history and sorts me out for 10 things I didn’t even know I was able to get help with, I love her … she showed me the results. Like she doesn’t just sit as this omniscient doctor, so she showed me what was going on, talked me through everything.
Service user
The use of telemedicine and digital messaging by clinicians, particularly within the specialist clinic, has improved the accessibility of services, regarded favourably in terms of both provision and information access:
And some of them I spoke to on Facebook, which is very cool … a lot of them are on Facebook and in the group on Facebook, so if I have a problem I can just post, and within a few hours, [doctor 1] and [doctor 5] are replying on the post, which is hugely helpful … if you just have a quick two-minute question, you can go directly to [doctor 5] and ask her. She was having an MDT meeting about me about my bottom surgery and she was asking me questions over Facebook about it. And she told me then and there what happened in the meeting where she was – it was a very weird experience.
Service user
Both service users and the range of WGS staff placed high value on the social and emotional support offered by the support service – several staff emphasised that this support was not simply needed because of the length of waiting times. A service user described the ethos of the support service:
… They didn’t seem to be trans people, but they just didn’t put a foot wrong. They were so open and empathetic and would never accidentally misgender anyone. They’re just really, really great, but they’re all quite Mumsie in a way, so you feel like they really care about you, which is really nice. I haven’t really had that experience in any medical setting before.
Service user
Challenges experienced
A number of system-level challenges were raised by both service users and clinicians. There were widespread concerns at the level of resourcing of the system as whole, given the size of the waiting list, even though the situation for all other GICs was recognised as being considerably worse. While service users were appreciative of the work done with them by the support service, some spoke of long delays in getting a response:
I still don’t know how they exist … Anyway, they were really brilliant and really, really nice to me, but their response times, it took an incredibly long time for me to get to speak to someone.
Service user
Some service users experienced their GPs as lacking understanding about current referral pathways – one was told by their GP practice that there were no gender identity referrals possible during the pandemic. On the other hand, some staff argued that there was a vanguard of younger GPs, often women, who were leading engagement with HRT for trans people. Once they demonstrated how straightforward hormone therapy management was for most patients, others in their practices would follow.
Some staff raised concerns that, even within the gender-affirming values of the WGS, there could be unwarranted additional assessment for some groups, because of clinicians ‘maybe sometimes still having a slightly narrower view of transness than they should, or they could, to support those people’. The danger was that certain groups of people might be seen as ‘unsure’ when, in their own minds, this was not the case. This was seen as a concern particularly for autistic people and also to an extent for non-binary people. As already mentioned, in Chapter 5, we discuss more generally the need for further consideration of how to avoid a two-tier system of assessment, with additional barriers or delays in obtaining care arising for some groups, such as autistic people, people with mental health conditions and those with learning difficulties. Such groups carry stigma and clinicians may be less experienced and skilled in understanding and working with them. We also discuss how similar dynamics may affect TBPoC, as well as non-binary people.
Several service users and clinicians were very concerned that there is no funding for hair removal under the WGS, seeing this as an integral part of providing psychological well-being for transfeminine people, as well as essential in preparation for any lower surgery, and an unreasonable financial burden to place on service users.
… we don’t get the advantages of English patients … We don’t get electrolysis.
Service user
While the WGS has taken steps to streamline the process for surgical referrals, several service users pointed out the impact of being dependent on providers elsewhere in the UK, the lack of capacity and waiting times involved, and the need to travel a considerable distance and usually recover away from home. Some were also concerned that the relatively new NHS hub system for surgical referrals was opaque in the way it worked and difficult to get information on progress from. Many of our interviewees had decided to raise money to pay for private surgery in the UK or in Poland.
A number of service users and staff also drew attention to the perceived inequities of waiting times for people still on the old pathway, working through a set of appointments with the English GIC, compared to those on the new Welsh pathway. Some had been denied requests to transfer, even when they required a sign-off for surgery rather than an initial assessment, and it was not clear what arrangements were in place for someone who had been through most of the pathway on the old system. There appeared to be unresolved issues of continuity of care for people who had first accessed transition-related care under the old pathway.
There were also some operational issues. Prescribing clinicians within LGTs reported having to take on the somewhat improvised creation of patient record systems for their WGS work, because there were no existing systems that linked effectively between the assessment clinic, the LGTs and GP practices that they might subsequently discharge people to under the DES. One LGT, for example, registers its service users as ‘temporary residents’ at the GP practice hosting the LGT, and then uses the practice’s electronic patient record system. This is, however, not accessible by the assessment clinic, which communicates patient details and treatment plans via e-mail. Any further communication about a particular case between the LGT and the specialist clinic tends also to be via e-mail. Consequently, the LGT prescribers have created a parallel paper file for each WGS service user, containing print-outs of e-mail exchanges with the specialist service and also with the service user themself. At the point of discharge to the person’s GP, a LGT clinician needs to craft a further letter, summarising the care plan, again sent by e-mail. As one LGT GP pointed out, there is no online NHS system for one GP practice to refer a patient to another GP.
At the time of interviewing, LGT clinicians indicated that they were either near their planned capacity or else would be at it within a few months. At that point, unless sufficient service users had been discharged on to other GPs under the DES, bottlenecks would appear at the LGTs. One LGT prescriber reported that they had just reached capacity and so were now starting a waiting list of people passed to them by the specialist service. The as yet handful of service users who could readily be passed on by the LGT included those who had previously been diagnosed and prescribed hormones by a private gender service, and so were already stable:
There was nothing to titrate […] There was nothing really to do for them. But at the minute I’m sort of a babysitter for want of a better term … it’s just how to get that next step up and running.
LGT prescriber
The DES was widely welcomed by clinicians as a mechanism for overcoming GP resistance to taking on seemingly unfamiliar work. However, interviewees indicated that progress has been slow in persuading practices throughout Wales to engage. A figure for one LHB was that just over 10% of practices, or 15 in total, had signed up.
Possible reasons for reluctance to engage with supporting trans patients on hormone therapy included the general pressure on GP workloads, given the tendency for many secondary clinical areas to identify aspects of care that can be managed in primary care. However, a more specific reason was also offered. Many GPs in Wales have been wary of engaging with HRT with cis women following concerns with risks of cancer and thromboembolism with earlier generations of treatments in the 1990s. Particularly in the context of the pressures on primary care during the pandemic, it has been difficult to engage GPs with more recent education about the comparative safety and simplicity of hormone therapy for trans people:
I think that’s the deep-seated, you know, the bad way that HRT was publicised in the 90s. I truly think that’s the actual block is people think hormones cause cancer … if we could get a room full of people I think you would get that out of them.
LGT prescriber
A further operational challenge stems from the fact that data protection rules have so far prevented a service-user data-sharing agreement being put in place between Umbrella Cymru and WGS. WGS has to send people information about the support service with a consent form for Umbrella Cymru to be able to contact them. While this was cumbersome but relatively straightforward for new referrals, it could be problematic to send out a letter from the gender service, using an appropriate current name and title, to people referred prior to the new service opening in 2019. For example, there was a danger that the person concerned had changed their name since the referral and that the name on the letter might ‘out’ them to the people they were living with.
Future developments
Of the service users interviewed, only one had experienced assessment within the WGS clinic – the others had been taken on by a LGT or were receiving HRT at their own GP practice after assessment elsewhere. Several users had strong views that the diagnostic approach in other GICs and private gender services was unnecessary.
Clinicians offered suggestions for the future development of the specialist clinic. This included the idea of a gender nurse specialist taking over many first appointments, for ‘review and endorsement’, with support from the endocrinologist. There was also a view that trans representation within the staff group should be increased, in combination with more consistent trans community representation at internal meetings as well as continuing the regular stakeholder meetings.
At the time of interviewing, some LGTs were planning an arrangement to have common hormone medications available onsite, to avoid the delays involved in first issuing a prescription that the service user needs to take to a pharmacy, and then in some cases make a further appointment for an injection. A further development under consideration in the way of working is that the current widespread use of telephone consultations within LGTs, backed up by e-mail exchanges, will be expanded further, to become the norm, with blood pressure and weight monitoring carried out at the service user’s local GP. This has benefits in terms of reducing travel time and increasing accessibility for service users. Some also anticipated LGTs introducing video consultations.
Several interviewees emphasised the importance of increasing the take-up of the DES among GP surgeries throughout all LHBs. A key mechanism for this would be widespread education on trans health care for practices, emphasising the simplicity of the new referral process to the specialist gender clinic, the straightforward nature of much HRT management, the guidance available and the ease of accessing support from LGTs. One model being considered by one health board was that practices could be put in small clusters, of perhaps seven. A lead practice for each cluster could then take responsibility for HRT patients under the DES, if not all practices signed up. GP education should also cover general health care and topics such as asking about contraception needs in an open way without making assumptions about patients’ relationships or sexuality. Clinicians should also be trained as to how to avoid referring to body parts in a gendered way.
At the time of interviewing, there were plans for making a business case for expanding the capacity for peer support. A related plan concerned facilitating the formation of local mutual support groups for people waiting for one-to-one support while on the WGS waiting list. We have already referred to the likelihood of the need to consider expansion of the capacity of LGTs.
Some LGT clinicians indicated they had been encouraged to train further in trans health care through a Royal College of Physicians postgraduate diploma. They anticipated that this would increase their expertise and standing, particularly with respect to being able to provide signatures for surgery. Some anticipated that this expanding pool of expertise could provide the basis for establishing a North Wales specialist clinic, thus improving accessibility. Related to this were ideas of increasing the visibility of gender services and care options on health board websites throughout Wales, rather than leaving this awareness-raising to local trans community networks and third-sector organisations. Leaflets or website downloads should be available much more widely across primary care and other NHS services. A video could be used to explain to people what to expect at their assessment appointment.
Case Study 5: trans healthcare experiences in Northern Ireland
Introduction: ‘a case study of nothing’
This case study looks at existing services available for the assessment and provision of care related to gender incongruence for adults in Northern Ireland. Since there is currently very limited access to a specialist gender service within Northern Ireland, the case focuses on support provided by third-sector organisations to trans (including non-binary) people, and service-user experiences of waiting for care or healthcare access by other means such as use of private services, or self-medication [do it yourself (DIY)].
Contextualising existing services
Healthcare services in Northern Ireland are free at the point of delivery and provided by HSC, analogous to NHS England. The HSC Board (HSCB) commissions services, with Northern Ireland divided into five HSC Trusts which deliver them (Figure 16).
FIGURE 16.
Map of Northern Irish HSC Trust areas. Based on information from: http://online.hscni.net/hospitals/health-and-social-care-trusts/
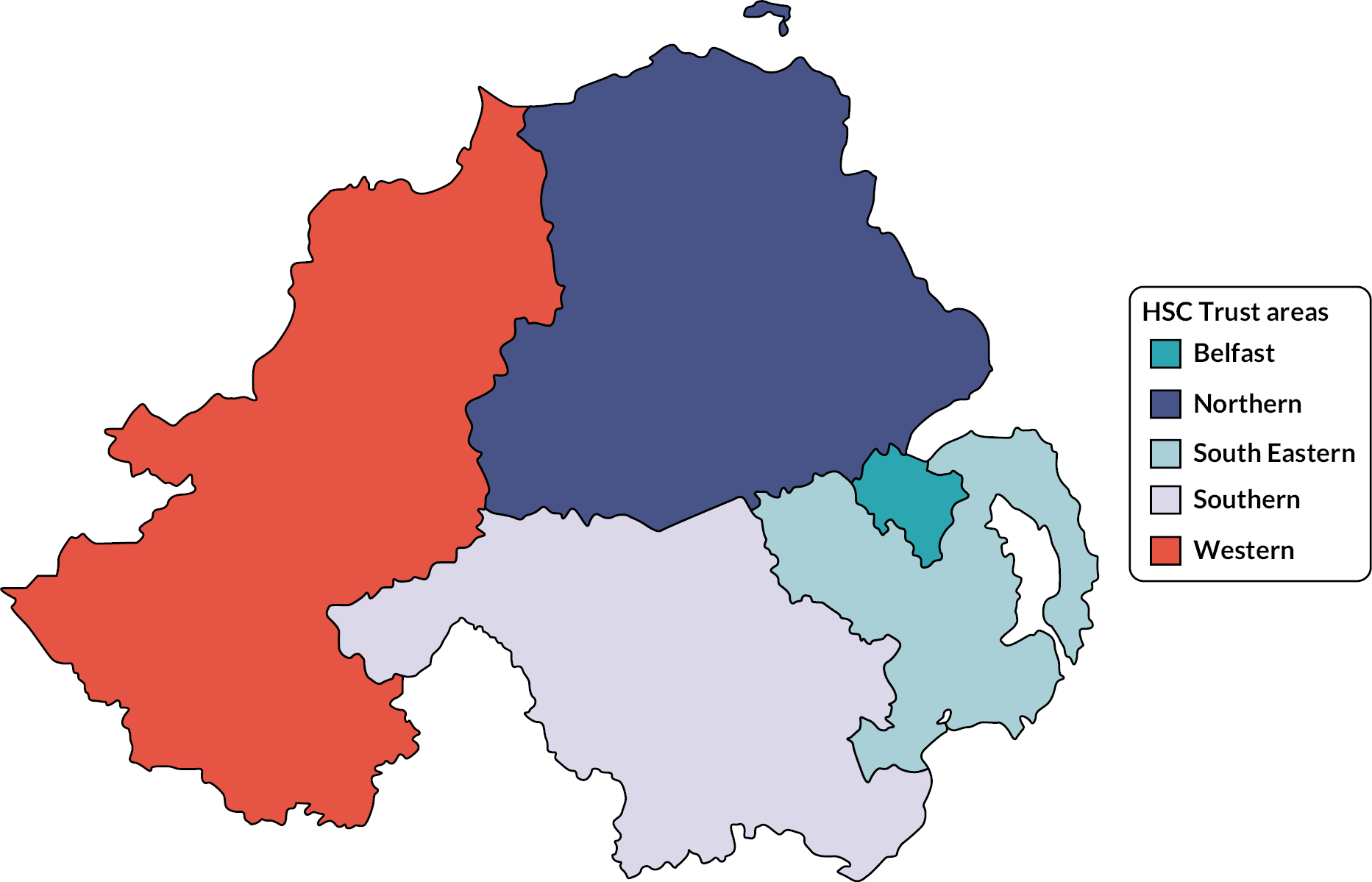
The specialist gender clinic
A specialist gender clinic in Northern Ireland has seen patients 18 and older for assessment and provision of care related to gender incongruence. This is based within Belfast HSC Trust. The clinic is not a GIC in the same sense as GICs in England; it primarily functions as a psychosexual service. Historically, it was not formally commissioned to provide GISs, though did offer appointments for assessment and care related to gender dysphoria.
While there is a lack of information available, the specialist clinic did not see any new patients between January 2018 and June 2020. New patients are now being seen from existing referrals, but new referrals are still not being accepted due to the extensive backlog. In January 2021, a FOI request established that the clinic waiting list was comprised of 493 patients. Funding dropped from £224,181 in 2015–6 to £147,700 in 2019–20.
As of October 2020, the clinic had an available staffing of a 0.4 WTE (whole time equivalent) consultant psychiatrist, and a 0.4 WTE therapist. To address the patient backlog, a new clinician was recruited from elsewhere in the UK, who travels to Northern Ireland once per month to provide a clinic. A letter from the Northern Irish Health Minister specified that this additional staff resource was ‘to support the ongoing management of people who have started their gender journey’ under the Northern Irish gender service for people under 18.
Previously, the adult specialist clinic accepted referrals from GPs, NHS consultants, mental health practitioners, or specialist nurses. Self-referral, or referral from third-sector organisations, is not possible in Northern Ireland.
Service review
In 2019, the HSCB was tasked by the Department of Health with reviewing GISs in Northern Ireland. A review group was established with ‘listening events’ taking place in November and December 2019. The group’s activities were paused during the COVID-19 pandemic but resumed mid-2020. As of November 2021, the HSCB website had not been updated, and indicated the review was originally intended to be completed by Spring 2021. Our understanding is the report was completed and submitted for review by the NI Department for Health during 2022.
Third-sector organisational support
Third-sector organisations are not involved in the delivery of commissioned healthcare services but attempt to manage the high demand for support trans people need due to the context outlined above.
In late 2018, some trans people who had been working with a family support organisation set up a separate trans-led campaigning and human rights organisation to improve health care. This is funded via revenue raised by providing trans-awareness training to GP practices, medical students, other healthcare staff, and through donations. Volunteers also contribute their time to support and advocate for trans people. During 2019, both organisations consulted with over 100 trans people, gathering views of current services and what should be in place, as well as reviewing service models internationally. This led to a position paper on ‘what we want to see from gender-affirming healthcare in the region’. They also pushed for progress with the review of the specialist clinic, securing limited trans representation on this, as well as on a government-led co-design group developing a LGBTQI+ strategy for Northern Ireland.
Alongside its policy and training work, the trans-led organisation provides healthcare support and advocacy for individuals. Other third-sector LGBTQI+ organisations also provide counselling and advocacy for trans individuals engaging with health care.
In this case study, six support organisation workers (some of whom were also trans and had accessed services) and four trans people who had accessed, were waiting to access, or wished to access gender-affirming medical interventions were interviewed. Interviewees were aged between 21 and 41, and included one trans woman, five trans men, one non-binary and one agender person, and one person who gave their gender as trans.
Several interviewees referred to a ‘trans healthcare crisis’ in Northern Ireland. They referred to the effective closure of the specialist clinic and the size of its official waiting list, as well as the number of people who have since been unable to gain a referral or simply not seen the point in trying to get one.
Views of the cultural context of trans identities in Northern Ireland
One third-sector participant called Northern Ireland an ‘ethno-nationalist state’ where society is heavily divided into two groups with antagonistic views of national identity. The history of the Troubles has led to emphasis on:
… traditionally masculine behaviours, ideologies, roles … the gender roles have hardened and almost crystalised in these very, very strict almost again soldier roles. You have a purpose in society and that’s really obvious in gender roles.
Third-sector worker
This has implications for the making of transition experiences ‘extremely difficult’, even compared to those in other parts of the UK. Interviewees further pointed out that many within the population remain ‘traumatised by civil war’. Mental health services are severely overstretched as a consequence.
Experiences of the gender identity clinic
Several of our interviewees had found their GP receptive to referring them to the GIC, when it was still taking referrals. Two participants, however, experienced considerable difficulties. When one person went to their GP practice saying they wanted to transition, a GP first of all directed them to an out-of-date list of trans community groups. When this person made an appointment with a different GP in the practice, this GP referred them directly to an endocrinologist. After 2 months waiting for the appointment, the endocrinologist told them that he could not treat them but would have to refer them to the GIC. At that point, the GIC waiting time was 6 months, but this still felt like ‘being left in limbo’. Another (non-binary) person experienced their GP as dissuading them from a referral to the GIC apparently because this GP saw the GIC as only for people who wanted to go through a binary transition.
Of our interviewees, only three had direct experience of assessment and treatment through the GIC – the others had either decided against being referred or were still waiting to be seen, in one case still waiting for a first appointment after 6 years. One person on the waiting list was invited to an information session with a group of others, to hear about the process ahead. They reported that some of the named information sheets given out deadnamed participants. GIC staff were apologetic, citing a systems error, but this still created an impression of lack of caring and was seen as reducing service-user trust in the cultural competence of the service.
Of the three interviewees who had been seen by the GIC, one found the overall experience acceptable. Another described the initial appointment with two clinicians feeling like ‘interrogation to see if I was trans’, and experienced questioning concerning their sexuality as ‘weird and not really related’:
… it was kind of to see like, oh, do you have sex as a man or as a woman? I wasn’t really very clear on what the motive of that was.
Service user
This led to over a year of monthly meetings with a GIC ‘therapist person’, where future treatments were discussed repeatedly, as was the timetable for this service user to come out socially as their gender. They felt that the GIC was waiting for them to transition socially before prescribing hormones, whereas they themselves felt that hormones would make their social transition much easier. After ‘a year of battling’ they were referred back to the same endocrinologist they had seen previously and were prescribed hormones. They told the GIC they were unsure about whether they wanted lower surgery and were told they could ‘come back’ when they were ready to talk further.
A third interviewee reflected that the GIC process had felt adversarial and unsupportive:
The service right now is designed so that a cisgender person doesn’t accidentally transition … It’s not made for trans people or to support trans people […] And I think overall it’s so infantilising … And I really take issue with having to convince a cisgender person that I’m trans when their understanding of what trans is really hasn’t progressed past the 90s. I just feel like their psychiatric assessment is there to trip you up rather than actually encourage you into what you think and what you feel. It’s not a safe space. It’s not therapy by any mention.
Service user
A number of third-sector workers interviewed reported that people who had been through the GIC assessment had told them of experiences of pressure to conform to binary stereotypes. Their gender identity became ‘unexplored and solidified’.
People still have the GIC suit, the GIC dress that they wear to their appointments.
Third-sector worker
Third-sector interviewees also recounted reports from trans people of a stringent policy regarding mental health within the GIC. People who disclosed any mental health condition were likely to have their assessment suspended, apparently without recognition that living in a transphobic culture as a trans person, whether openly or not, is damaging to mental health.
They make mental health care and hormone care inaccessible at the same time […] There are still people who are still patients who were seen way before, who are scared to talk about their mental ill health. Because they’re worried about their hormone treatment is going to be taken away from them …
Third-sector worker
There was a variety of experiences of care following assessment at the GIC. Some reported that the system for regular prescribing of hormones through their GP, with periodic blood tests and reviews by the endocrinologist, had worked well. Others had less consistent experiences. Participants stated that their endocrinology reviews had become up to 2 years apart, apparently because of the demand for the endocrinologist, and questioned whether there were any succession plans for the single endocrinologist who supports the GIC. There appeared to be ‘no formal strategy, care package, intention for looking after trans people long term’. One person was left reflecting on the degree to which they had persistently to advocate for their own care as a trans person.
And it is truly exhausting to try and advocate for yourself, and also to have so many doors closed in your face.
Service user
Experiences of private gender services and self-medication
In response to long or indefinite GIC waiting times, or a perceived lack of a possibility of referral, both the third-sector workers and service users interviewed indicated widespread use of private services for accessing assessment, hormones, hair removal, voice coaching and gender-related surgery.
The cheapest private provider commonly used charged £30–£40 per month for hormone prescribing, in addition to the costs of initial assessment. Some people were able to fund this, but those with insecure or no employment found this ‘a huge burden’. Many resorted to crowd funding.
General practitioners were widely cited as refusing to enter into shared care arrangements with private gender services, for prescribing hormones or carrying out blood tests for monitoring. There were a few exceptions reported. Three participants had found their GPs were willing to work with a private service to monitor and prescribe hormones, as well as administer injections when needed. One person, however, chose to continue paying their private provider to monitor and prescribe on the basis of blood tests carried out at the GP surgery, ‘because they’re just a lot more reliable’.
Several interviewees referred to an emerging pattern where trans men with sufficient funds obtained a referral from a private gender service and then paid for private top surgery in Poland. We were told that there were no surgeons performing top surgery in Northern Ireland at the time of interviewing, and that, in any case, the only way to access this through the NHS would have been through the blocked GIC route.
Several interviewees described their experiences of private gender services as accepting of their own views on being trans and taking a pragmatic approach to finding out what they needed. One service user likened this to:
[an] informed consent approach … Trusting the patient I think was the biggest thing for me. The fact that they trusted what I said. And trusted that this is what I needed, rather than being interrogated for it all.
Service user
Another felt that private clinicians made it clear that intrusive questions needed to be asked to cover diagnostic guidelines, and that this contextualisation of the questioning had reduced the distress of answering. Private gender services were also experienced as prompt and reliable in correspondence.
Other interviewees recounted how they had decided to self-medicate with hormones, or relayed the experiences of others. The reasons in all cases were lack of access to the GIC and not being able to afford a private gender service. The remaining option for affirming their gender was buying hormones from internet pharmacies, or else receiving them through friends or networks who had found ways of accessing or sharing supplies.
General practitioners were widely experienced as refusing to provide blood tests or monitoring in such cases, or to prescribe as a harm-reduction measure, usually giving as a reason that they could not ‘take on liability’ for a person’s health if they were self-medicating. The choice to self-medicate meant bearing the associated health risks oneself. One person was told by a GP who they felt was ‘on side’ that the practice policy would only allow a one-off blood test. This person then felt in a state of constant anxiety about their health. However:
… it was very much I balanced the risk and the reward and on the whole, it has been a positive thing for me.
Service user
While wanting professional monitoring of hormone treatment, this person was also wary of giving up control of their dose to a cis doctor. They feared that a doctor would rigidly follow hormone ranges specified as normal for male and female bodies, rather than a trans person’s perceptions of what felt right to their own sense of their body and their gender.
Others expressed anger with GP refusals to prescribe as a harm-reduction measure, aware there is provision for this in medical guidelines:
… there are times when you need to stick your neck out for your patients. If there is harm coming to your patients, you need to implement supports for them, and inaction is harm.
Third-sector worker
Experiences of general health care within general practitioner practices
One interviewee reported positive experiences of staying with a small-town GP practice they had grown up with, where the GP was willing to engage positively when they came out as trans. Arguably the distance from an urban centre and a wider choice of GP practice made this the most viable option. This person had worked with the staff to improve their understanding of trans health care, and the use of appropriate pronouns. They felt that their continuing good relationship with their GP also meant that they continued to use health services in general with confidence.
Many more of the experiences of primary care were negative, however. We heard further accounts of trans people being treated dismissively by practice staff. There were examples of name changes and requests to change pronouns not being followed through on medical records and one example of reception staff apparently deliberately and repeatedly misgendering someone who felt that they had a good relationship with the GP themself. This person felt compelled to move to a different practice.
A number of interviewees reported accounts from other trans people that GPs had attempted to refer them to the GIC for health issues that were not connected with a medical transition, simply because they felt something like a skin condition might be hormone-related. A related development was that, with the GIC not functioning, some GPs had taken to referring people to third-sector LGBTQI+ or trans organisations, sometimes with physical health problems, sometimes because people wanted to transition and there was nowhere else to refer them. Third-sector staff felt placed in an impossible position by such referrals – they were unable to provide the help being sought.
Several interviewees reported that they lacked trust in GPs and other medical professionals, because of their health concerns as trans people not being taken seriously. In particular, there were concerns that most GPs did not know about the health conditions that trans people with different histories might be at risk of:
… what are things you can watch out for as a trans person? What are they more at risk for? Because the onus is very much on the trans person to know that … Because they absolutely know less than I know.
Service user
Several people reported there were a small number of trans-affirming and trans-inclusive practices in Belfast. However, even with these, third-sector workers reported that trans people had experienced huge variability between different practice staff – for example, in how much attention they paid to which health screenings are relevant to trans people with different anatomies. This added to the stress of navigating health care as a trans person and also in effect created disparities in the health care available to different trans individuals depending on which staff they saw.
Experiences of third-sector support
Several service users reported how they had received formal counselling or informal advice from LGBTQI+ or trans community organisations, as well as from trans friends. This had helped them decide how to move forward with private care or self-medication. One person, however, felt that there needed to be more options in terms of trans community support, recounting an experience of not fitting in with the views of others in a particular context.
One interviewee reported that they had benefited hugely from attending a week-long ‘trans training’ residential. This had included a variety of workshops, including on how to manage a name change. Above all, it had been valuable and also fun to meet and spend time with trans people.
Experiences of other health services
Two interviewees reported distressing experiences of NHS sexual health clinics. One received normative comments about the possibilities of becoming pregnant in the future, which they felt were irrelevant and impertinent. Another found that the rigid separation of binary male and female services led to them having to explain that their anatomy, identity and needs did not conform to either template. They experienced the clinical staff as not listening to or taking in important information, with one member of staff ignoring complaints about pain involved in a procedure, and another spending time asking ‘nosey’ questions about their history as a trans person. This led the person concerned to avoid NHS sexual health clinics, and also fed into a pattern of avoiding disclosing their trans status in other clinical settings, to avoid curious questioning.
Both these individuals contrasted their experience of NHS sexual health services with the respect shown when they attended sexual health screening clinics run by a LGBTQI+ organisation. They were, for example, asked for their pronouns as they registered with the latter.
Others reported avoiding NHS health care in general, because they expected to encounter either or both of an insensitive and inappropriate curiosity about their history as a trans person, or else a lack of cultural understanding of:
What trans means, knowing what kind of people and bodies and physiology is covered by the term woman and man … constantly using terms like male and female and referring to body parts.
Service user
Some of our interviewees had found NHS counselling for anxiety or depression helpful, although limited in what it could achieve given the short programmes on offer. A third-sector worker reported very negative experiences of trans people who had been referred to their local NHS mental health services – for example, being asked questions about how they have sex as part of a mental health assessment. Others considered that there was no effective mental health support for trans people.
Views on overall co-ordination of services
Several interviewees conveyed the view that the various services involved in trans health care work in a disconnected way, with separate appointment systems and lack of awareness of what is happening for a person elsewhere in the system. This applied to the GIC, the fertility clinic, the endocrinology clinic and the speech and language clinic, with the surgeons all being based in England. Service users living in other parts of Northern Ireland also pointed out that all of the transition-related services were concentrated in Belfast. They had to travel an hour or more to access each service.
Interviewees cited instances of young people discharged from the youth gender service, being told that they would have to wait 5 years before being seen by the adult service. Typically, they would be on a prescription for hormone blockers from the youth service, and their only option for continued treatment was to pay for care through a private adult gender service.
The experience of one interviewee illustrated a lack of co-ordination between GICs across the UK. This person, in their 20s, found unco-ordinated GICs unable to respond to their pattern of periodic relocations, which would be a normal expectation for many people at this stage of life:
Every time I move, I go to the back of the surgery list.
Service user
Community action to improve services
One third-sector interviewee felt that NHS services lack the capacity and funding to engage with trans communities and find out about their needs. Increasing awareness of trans health care seemed to be down to the initiative of individual members of staff. Many interviewees shared a view, often expressed angrily, that ‘the mainstream doesn’t want to know’, meaning that addressing the deficiencies in trans health care appeared not to be a consistent priority for the devolved administration or for the HSC service, in spite of the costs of not providing adequate care. These included, above all, the mental health burden carried by those unable to access any treatment, often leading to chronic suicidality as well as actual instances of suicide. There was also the increased burden placed on other NHS and third-sector services:
… it actually costs more to not fund the service because we’re seeing the impact on voluntary community sectors like ourselves or other healthcare providers or back into the NHS in primary mental health teams where people are self-harming …
Third-sector worker
Some pointed out the difficulties of gaining widespread public support for adequate services, in contrast to the recent successful campaigns for abortion rights and for equal marriage. Misleading coverage in the media implying that it is too easy for young people to transition was also damaging.
I’m constantly talking about the waiting list, the denial of service, the impact that that has on trans people’s mental health. So, we are trying to put that message out there you know with stakeholders … whether it be the police, whether it’s housing associations.
Third-sector worker
Summary and implications
The key features of this case are: a trans healthcare crisis with hundreds of people denied access to gender-affirming care on the NHS; for individuals, consequent use of private services and self-medication; and for the trans community the development of campaigning and support forums and services. Some trans individuals and LGBTQI+ organisations are involved in reviewing the current GIC and in planning future services, albeit within a context of needing to campaign for adequate funding, as well as for a greater degree of involvement of trans organisations. The context of the GIC not functioning has sharpened perceptions that trans healthcare needs to be accepted by government, and indeed the population, as a much greater priority, and that trans people need to be involved in the design and delivery of services.
All of our interviewees held the view that much transition-related care could in principle be delivered through primary care, with suitably trained GPs. Many also expressed a strong view that trans people need to be able to access suitably skilled counselling, but that this needs to be entirely separate from the system for accessing gender-affirming care. People need a space to explore feelings, including doubts and confusions about their gender identity, but this requires a removal of the fear that what they say will affect their access to hormones or other treatment. Chapters 5 and 6 of this report include a wider discussion of the issues raised by such views.
In the shorter term, priorities also emerged for improving the competency of GPs with the monitoring and prescribing of hormones, as well as improving the willingness of GPs to recognise their responsibilities for effective care of trans people. This would reduce the financial and mental health burden on trans people unable to access a GIC.
Appendix 9 Views on three paradigms for the future of trans health care
This appendix contains four tables which summarise the suggestions and proposals made by service users and staff across the case studies as to how each paradigm could be taken forward. Under Paradigm 1, there are two tables, Tables 7 and 8. Table 8, also labelled Paradigm 1b, captures suggestions made as to additional elements that should be added to the current specialist service specification, within its underlying assumptions. These additional elements are also relevant to Paradigms 2 and 3. Table 9 refers to suggestions made under Paradigm 2 and Table 10 refers to suggestions made under Paradigm 3.
| Underlying assumptions: the current NHS England specialist service specification, with in-depth diagnosis by GIC clinicians, members of the MoJ gender-specialists list, according to ICD-11 definition of gender incongruence, prior to gender-affirming treatment | ||
|---|---|---|
| Domain | Specific suggestions | Illustrative quotes |
| Improving GIC communication with service users |
|
‘When you get put on the waiting list for a gender clinic, they could say to you […], here are the things you could be doing now that will aid your process once you get here, that will provide evidence and make the process quicker for you.’ (Service user) ‘ … a lot of people find out stuff about gender identity services through anecdotal information either through Facebook groups, through Reddit, things like that […] if there were more actual resources on [GIC] website …’ (Service user) |
| Reducing delay between referral and hormone prescribing |
|
‘If there is sufficient expertise let’s say from a nursing professional or an occupational therapy professional, why not? You know, what stops such professionals from being able to make a diagnosis?’ (GIC staff member) ‘They should get a list together of endocrinologists who are willing to take responsibility for trans patients and prescribing them hormones …’ (Service user) |
| Improving GIC collaboration with primary care |
|
‘GPs need […] better training around hormones, monitoring and prescribing. A lot of them need training just on simple things like how to do a GIC referral …’ (GIC staff member) ‘I feel that they don’t even have access to your NHS records, and I thought the NHS record is the thing that’s meant to follow you around […] Why are people not accessing it?’ (Service user) |
| Expanding capacity of GICs and related gender-affirming treatment services |
|
‘… if there’s some standardisation of care, I think there can be a bit more effort as well as pressure on commissioners […]. Because if you don’t speak from one voice, I think you find that commissioners will act differently to different GICs.’ (GIC staff member) ‘… The last time I checked there were like, three surgeons and that’s just a ridiculous number, right?’ (Service user) |
| Introduce explicit standards for trans health care |
|
‘I think that if they’re asking questions it should be sort of upfront about why they’re asking them. Because a lot of the questions they asked me it felt like I wasn’t really getting any idea of why they’re asking, of what their motives were. And then, beyond that I feel like, sort of trusting the people there to know what they want.’ (Service user) |
| Increasing trans representation and voice within GICs |
|
‘They’re not trans, they don’t understand trans and their attitudes to trans people are 20 years out of date. It’s as simple as that.’ (Service user) ‘I would love there to be knowledge in the profession about the barriers that trans people face accessing health care or accessing society in general, about how that can impact on my mental health’ (Service user) |
| Expanding trans peer support within the GIC system |
|
‘I think finding ways to fund those community groups […] and to help put structures around them so that people don’t burn out or have boundary issues when working with people […].’ (GIC staff member) |
| Underlying assumptions: in-depth diagnosis by GIC clinicians, members of the MoJ gender-specialists list, according to ICD-11 definition of gender incongruence, prior to gender-affirming treatment, but with additional service elements not included in current service specification | ||
|---|---|---|
| Domain | Specific suggestions | Illustrative quotes |
| Improving support for gender recognition certification |
|
‘… if I wanted to go and apply for my gender recognition certificate now, I can’t because I still haven’t accessed [Name of GIC] … There are a lot of things that I cannot do because I haven’t yet received the medical diagnosis. And that system is broken because it’s taking so long. So, again it’s another one of those things that puts your life on hold.’ (Service user) |
| Availability of a wider range of surgical and medical gender-affirming procedures |
|
‘… people are going to want and need access to different surgery or different medical procedures that are going to improve their life […] making them safer in an environment that might be more hostile or in particular communities that are less welcoming …’ (Service user) ‘And for those who can’t afford private treatment for hair removal […] the number of sessions the NHS will pay for is ridiculously inadequate. Eight. […] I’ve had hundreds, literally hundreds […] to ask them to do a social transition in that role without providing those services first, I think it’s cruel and immoral.’ (Service user) |
| Improved support and provision for mental health and well-being |
|
‘… when I was feeling really down, and I was thinking I don’t want to go on anymore, one of the things that was going through my head was I can’t reach out for help to my GP or the GIC on this, because they will bin me off their waiting list […] we need to […] explain that a lot better, so […] it is OK to reach out for help …’ (Service user) |
| Making patient records trans-inclusive |
|
‘It’ll be a more accurate system and it’ll give people better health care to, for example, simply record what body parts somebody has in the records, rather than an M or an F and using that as a stand-in. It’s important for a doctor to know if someone has a cervix, regardless of the gender of that person …’ (Service user) ‘… Asking people’s pronouns. Having that be on their medical records and then actually using them …’ (Service user) |
| Underlying assumptions: most people who seek gender-related care have their needs met within a primary care setting, from a GP-led local gender service. Role of specialist gender services reconfigured. | ||
|---|---|---|
| Domain | Specific suggestions | Illustrative quotes |
| Primary care assessment for hormone therapy |
|
‘… the integration of trans health care into primary health care is a big one for me. About moving trans health care away from that idea of being incredibly specialised and segmented away from the rest of health care […] into the open where I can go to my GP and have these blood tests done and then have them look at my results, you know, I need that greater integration.’ (Service user) ‘I think primary care will be able to co-ordinate care better than us … for me there is required to be the robustness in the diagnosis and the robustness in the process […] who does that I don’t mind, as long as it’s robust.’ (GIC staff member) |
| Revised role for specialist gender clinics |
|
‘ … The GP can only do so much, if you pile it all at the GP, then they will be even more stretched. And they’ve got a ton of different, other areas, they can have a trans specific unit at the GIC, it does help a lot because they are professionals at transitioning.’ (Service user) ‘ … develop GP skills to the point where they are registered specialists. In which its then about supporting them with complex cases and they become a truly autonomous, independent diagnostic and treatment partner.’ (GIC staff member) |
| Funding and managing the shift to a new system of care |
|
‘The capacity is just not there. And so anything that just tries to evolve it is going to fail ultimately […] the NHS is never going to fund the current model with sufficient people in it to have a sensible service. So you’ve just got to go back to the drawing board and think how you’d deliver it.’ (GIC staff member) ‘I’d be very much for GPs not only being trained on it, so anyone we speak to would be knowledgeable about trans issues, be able to prescribe hormones, talk to them about mental health, and talk to them about surgeries, talk to them about particular medical complications …’ (Service user) ‘Integrating primary care diagnosis and hormone treatments […] can obviously have an impact but it is going to take some time I think before such services, competent services can be set up.’ (GIC staff member) |
| Underlying assumptions: access to hormone therapy, and related treatments, including surgical procedures, based on informed consent; specialist gender services support service users who chose to be referred because they feel the need for more exploration, or those requiring specialist endocrinology | ||
|---|---|---|
| Specific suggestions | Illustrative quotes | |
| Access to gender-affirming medical care |
|
‘I think far too often GICs will see neurodivergence or anything along those lines, being non-binary as being complex and therefore needing all of these additional things when actually it’s all about the ability to give informed consent. […] If an adult is capable of giving informed consent to a treatment then I don’t see why that treatment should be withheld from them …’ (Service user) ‘The simple questions as a medical professional, is this safe? Is this a good idea? Is there anything glaring that would make us think that you might regret this? That you might need some time and space to think about? … you’re put in the position of holding all this power and responsibility […] But then what happens if they let that go and let people make their own decisions.’ (GIC staff member) ‘… Just listening to me as the expert, the pre-eminent expert in my body, as the person who has lived in it the longest and can tell you what’s going on […] I think that’s what we tend to call a person-centred care approach would really be beneficial.’ (Service user) |
| Specialist gender support services |
|
‘… staffed by trans people. Some kind of service that allows people to safely and nonjudgmentally and nondirectively explore their gender identity, and that shouldn’t take the form of an assessment. It should be nondirective support. I don’t think that you should have to access that in order to access gender-affirming health care … maybe that should be delivered in collaboration with community organisations because that’s where the expertise lies …’ (Third-sector trans support worker) |
Appendix 10 Summary of learning from case study initiatives to improve care
| Aspect of care | Initiatives | Benefits | Key issues | Future possibilities |
|---|---|---|---|---|
| Improving access to transition-related care | Training for GPs on how to refer to GICs and offer bridging hormone prescriptions for people waiting for a GIC appointment. Local lead trans healthcare GPs provide advice to other GPs. Third-sector trans support workers provide individuals with referral advice and advocacy. |
Trans adults able to obtain GIC referral without stress and labour of convincing GP this is their right, and straightforward. Trans adults waiting for a GIC appointment more likely to receive a ‘harm reduction’ bridging prescription. |
Even where training available for GP practices, levels of competence and commitment to trans perspectives and rights may be variable across practice staff. GP advice networks only emerging in some areas, otherwise absent in many. Deficiencies in local mental health support for trans people enduring years of waiting for a GIC appointment. |
Mandatory trans healthcare training and standards for primary care, antidiscrimination initiatives. |
| Practical, social and emotional support while waiting for assessment and afterwards | Third-sector peer workers attached to a gender service provide individual advice and support and facilitate support groups. | Trans adults receive practical and emotional support on challenges of social transition, including ‘trans admin’, and social support through trans-led activities and events. Trans peer-support workers understand needs for support within communities and devise ways for meeting them with NHS resources. |
Difficulties in contacting people on waiting lists because of data protection. Peer-support workers need to be fully included within the GIC professional team – for example, able to deal with queries about position on the waiting list. Peer workers navigate stressful ‘dual belonging’ to trans communities and to a gender service, unable to influence length of waiting or nature of assessments. |
Regional third-sector support hubs for trans people, independent of agencies delivering gender-affirming medical care – utilisation of existing trans-led organisations and networks. |
| Assessment for gender-affirming care | Gender service clinicians provide collaborative and gender-affirming approach to assessment, focusing on clarifying treatment options, potential benefits and risks. Use of videoconferencing for assessment sessions, with physical data, including blood tests, carried out by a GP local to service user. |
The majority of trans people experience a quicker and less stressful assessment. Trans people do not have to travel long distances to participate in assessment or worry about missing appointments because of travel difficulties. |
Clinician decisions to extend assessment process may stem from ‘subtle ableism’ of clinicians and lack of understanding of trans people. Neurodivergent people, those with mental health conditions or learning difficulties, and Black people or people of colour may be subject to unwarranted delay in progressing to treatment. |
Approaches that recognise diversity in ways of talking about gender and treatment goals. Greater involvement of trans staff in assessments. Revisit assessment guidelines to support an affirmative approach. |
| Initiating and stabilising hormone therapy | Regional GP-led hormone therapy clinics, working in collaboration with endocrine specialists in a gender service, handle prescribing for approximately 12 months after an individual completes their assessment. | Trans adults receive hormones rapidly, prescribing and monitoring integrated. GP prescribers co-ordinate individuals’ other transition-related and general healthcare needs. GP prescribers disseminate trans healthcare expertise to primary care colleagues. |
Encouraging a person’s own GP practice to take over prescribing after approx. 12 months, in order to free up capacity of the regional clinic. Lack of integrated electronic patient records able to support collaboration between specialist gender service, regional clinics and local GPs. |
Denser network of local GP practices able to lead on hormone prescribing and other aspects of trans health care. Wider availability of bridging prescriptions within local primary care. |
| Mental health and well-being support | Psychology team attached to a gender service provides individual counselling and facilitated group programmes. | Trans people receive help with working through problematic aspects of their social transition and/or their emotional reactions to medical transition. Groups help people to overcome sense of isolation, to give and receive practical and emotional support. |
Tensions between therapy and the assessment function of a GIC – challenges to ethics of confidentiality if therapists expected to disclose client material, beyond just safeguarding concerns, that impacts diagnosis. People may withhold exploring mental health difficulties or avoid seeking support from any GIC staff, to avoid extending assessment. |
Clearer separation between mental health support and diagnostic assessment, ensuring confidentiality and independence of therapeutic support. Education in trans-affirmative therapeutic approaches for mental health services in general. |
| General primary health care | Training for GP practices in social and medical aspects of primary health care for trans people. Assessment and accreditation for standards of trans health care within GP practices. |
Trans people experience administrative systems that welcome trans identities, and clinical practices that avoid assumptions about links between gender identity and anatomy. Trans people are offered appropriate cancer screenings. Trans people and clinicians begin to experience trans health care as a routine part of everyday primary care, with GP practices competently providing hormone therapy and routine post-op care. |
Following a positive experience with a particular member of practice staff, trans people may not be able to rely on a consistent standard of care within the same practice. Different members of staff may not share the same awareness or competence. Wider NHS systems mean that problems with changing names, pronouns and gender markers on patient records persist when people are referred to secondary care. |
Trans healthcare standards become integrated with wider notions of patient-centred care, focusing on individual need, and avoiding making assumptions about identities, anatomies or priorities. Trans-inclusive patient records, breaking with binary gender markers and anatomical assumptions. |
Glossary
Cis person A person whose gender is the same as that assigned at birth or in early life.
Cisnormativity Social expectations and practices that privilege cis people, often by assuming that people are cis and identify with a binary gender.
Disabled people People disabled by barriers in society, as defined by the social model of disability.
Gender-affirming care Medical treatment, including but not limited to hormone therapy and/or surgical procedures, that supports and affirms an individual’s gender identity.
Non-binary A gender identity that is neither man nor woman and therefore not binary.
Trans person A person whose gender differs from that assigned at birth or in early life.
Transfeminine Trans and aligned with social or physical aspects of femininity.
Transmasculine Trans and aligned with social or physical aspects of masculinity.
Transnormativity The social expectation that a trans person should present as if they are cis, conforming to gender norms commonly applied to cis people.
List of abbreviations
- AAA
- abdominal aortic aneurysm
- AFAB
- assigned female at birth
- AMAB
- assigned male at birth
- APA
- American Psychiatric Association
- BMI
- body mass index
- CCG
- Clinical Commissioning Group
- COVID-19
- coronavirus disease discovered in 2019
- DES
- direct enhanced service
- DLA
- disability living allowance
- DSM
- Diagnostic and Statistical Manual
- EDI
- equality, diversity and inclusion
- ESA
- employment and support allowance
- FOI
- freedom of information
- GIC
- Gender Identity Clinic
- GIS
- Gender Identity Service
- GMC
- General Medical Council
- GP
- general practitioner
- GRA
- Gender Recognition Act
- GRC
- Gender Recognition Certificate
- HRT
- hormone replacement therapy
- HSC
- health and social care
- ICD
- International Classification of Diseases
- ICM
- informed consent model
- ICTA
- Improving Care for Trans Adults
- IFR
- individual funding request
- IPL
- intense pulsed light
- LGB
- lesbian, gay and bisexual
- LGBT
- lesbian, gay, bisexual and transgender
- LGBTQI+
- lesbian, gay, bisexual, transgender, queer and intersex, plus
- LGBTQIA+
- lesbian, gay, bisexual, transgender, queer, intersex and asexual, plus
- LGT
- local gender team
- MDT
- multidisciplinary team
- MoU
- memorandum of understanding
- NHSE
- NHS England
- PIP
- Personal Independence Payment
- PPI
- patient and public involvement
- QDA
- qualitative document analysis
- RQ
- research question
- STP
- Sustainability and Transformation Partnership
- TAS
- training and accreditation scheme
- TBPoC
- trans Black people and people of colour
- WGS
- Welsh Gender Service
- WHSSC
- Welsh Health Specialised Services Committee
- WP
- work package
- WPATH
- World Professional Association for Transgender Health
