Notes
Article history
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as project number 14/70/73. The contractual start date was in March 2017. The final report began editorial review in April 2021 and was accepted for publication in January 2022. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
Copyright © 2022 Annandale et al. This work was produced by Annandale et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaption in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2022 Annandale et al.
Chapter 1 Introduction and background
This report presents findings from a study funded by the UK’s National Institute for Health and Care Research (NIHR) Health and Social Care Delivery Research programme. The study’s broad aim was to identify and describe key situated interactional practices of decision-making that take place during labour in midwife-led units (MLUs). Understanding how decisions are made in clinical practice is important because women’s retrospective accounts of birth show that greater involvement in decision-making is associated with greater postnatal satisfaction and well-being, and decreased anxiety. 1–5 Drawing evidence together, Hodnett5 showed, almost 20 years ago, that when women evaluate their childbirth experience the ‘influences of pain, pain relief, and intrapartum medical interventions on subsequent satisfaction are neither as obvious, as direct, nor as powerful as the influences of the attitudes and behaviours of the caregivers’. 5
This basic finding has been replicated over time,6–9 and the need for effective, sensitive and inclusive communication is enshrined in policy guidelines. For example, National Institute for Health and Care Excellence (NICE) guidelines10 recommend the following:
Treat all women in labour with respect. Ensure that the woman is in control of and involved in what is happening to her . . . establish a rapport . . . ask her about her wants and expectations for labour, and be aware of tone and demeanour, and of the actual words used . . .
However, despite the evidential and policy drivers, there are challenges to implementation in practice. 11 A critical issue in addressing these challenges is the dearth of evidence concerning how interactions actually happen during labour. 12 As Pilnick13 observes, ‘The potential implications of these interactional processes [. . .] are immense, since . . . “good” practice is ultimately achieved through interaction rather than through policy or regulation’. 13
Accordingly, at the core of this study is fine-grained analysis [using conversation analysis (CA)] of the interactions that took place between women, health-care practitioners (HCPs) and birth partners (BPs) during 37 video-recorded or audio-recorded labours. Recordings took place in two MLUs in the UK, where midwives are the lead HCPs caring for pregnant people who are (1) defined as low risk for pregnancy or birth complications and (2) have opted for midwife-led care.
Midwife-led care refers to the autonomous care by midwives of pregnant persons who present to maternity services as low risk for complications. 14 During the intrapartum period, midwife-led care takes place in units staffed and managed by midwives, although referrals to obstetric-led care occur should complications arise. Notions of normality and risk, therefore, underpin the distinction between midwife- and obstetric-led care. 15 Midwife-led care is associated with facilitating, when appropriate, the normality of birth as a spontaneous physiological process and, therefore, less intervention. 16,17 Emphasis is placed on midwives’ professional expertise and women’s embodied and agentic capacities to manage labour. This does not mean, however, that risk surveillance is absent from midwife-led care,15 nor that pregnant people and midwives are not engaged in decision-making. Those people with low-risk pregnancies have many options for their care during labour and birth, including (but not limited to) choices around pain relief, vaginal examinations (VEs) and management of the third stage. These are routine (likely not medically urgent) decisions of the kind that might be relevant to any labouring person in any context. The routine and widespread nature of these decisions during labour and birth make it particularly important to understand how they are managed in practice. Accordingly, decision-making in MLUs forms the focus of our research.
The two key research questions were:
-
What communication strategies (e.g. open questions, option listing, requests) are used by HCPs, women and their BPs to initiate decision-making?
-
What responses are made relevant by these strategies (e.g. an open question makes relevant a narrative response and a request makes relevant a granting/declination; see Chapter 2, Conversation analysis)?
Addressing these questions provides an understanding of interactional practices for managing decision-making and how far it is shared between HCPs and labouring people. In keeping with CA, which is the leading methodology for analysing talk-in-interaction, decision-making is treated here as a visible and practical set of interactional activities (as opposed to internal cognitive processes).
The study had four objectives:
-
To create a rich data set based on recordings of people giving birth in MLUs. We collected data via (1) antenatal questionnaires (ANQs) surveying women’s expectations and preferences for birth, (2) intrapartum video-/audio-recordings of labour and births, and (3) postnatal questionnaires (PNQs) about women’s experiences of, and satisfaction with, decision-making during labour.
-
To contribute to the evidence base for shared decision-making through a fine-grained analysis of the verbal and non-verbal details of interactions that take place in real time during birth, specifically how decisions are initiated, who initiates them and how different ways of initiating decisions are responded to. Using CA, the primary analytic focus was on how talk is used (by all parties) to encourage or discourage involvement in decision-making over the course and events of a birth.
-
To assess whether or not women’s actual experiences reflect their antenatal expectations and whether or not there is an association between interactional strategies used (by all parties) during labour (particularly the extent to which decisions are shared) and women’s later reported level of satisfaction. In this way, we could assess whether or not satisfaction is related to definable aspects of care in MLUs.
-
To disseminate findings to health-care providers and service users to contribute to translating existing Department of Health and Social Care and NHS policy directives on sharing decision-making into clinical practice.
Our study primarily focuses on decisions made during the intrapartum period. However, we recognise the importance of decision-making during the antenatal period and have included antenatal surveys of women’s expectations and wants. We know that women do not, on the whole, enter MLUs without having given some thought to their preferences around key aspects of their care during labour and women may also develop written birth plans. Birth plans are an important method for inviting participation in decision-making and for personalising care. 18,19 However, the effectiveness of birth plans at translating antenatal preferences into intrapartum practice is variable19 and relies on the contingencies of actual intrapartum events,20 as well as the flexibility of HCPs (who might also be subject to clinical contingencies). 21 Once in labour, a woman may face numerous decisional moments that might or might not have been foreseen and that have to be acted on in the moment. 11,22 For these reasons, it is vital to understand how decision-making occurs in real time during labour and birth.
A note on the terminology of birthing persons
All of the people in labour who participated in our recordings appeared to identify as women (as evidenced by the uncontested gendered pronouns by which others referred to them). Accordingly, when referring to our data set, we use the term ‘women’ to refer to people in labour. In common with broader maternity-related literature and policy documents, we also often use the term ‘women’ to refer to persons who labour when discussing labour and birth more generally. However, we recognise that this language does not include those who experience pregnancy and labour without identifying as women (e.g. trans-men and gender non-binary persons). Therefore, when discussing labour and birth beyond the context of our specific data set, we also use more gender-neutral terms, such as ‘labouring person’ or ‘service user’. Our use of this dual language aims to acknowledge the complexities involved in gendering people who give birth.
Choice and participation in decision-making in the NHS
The NHS firmly advocates service user choice. 23 Nevertheless, choice is a disputed concept, particularly in its application to health-care services. 24–26 Successive policies characterise service users as self-determining consumers,27,28 but both service users and HCPs are constrained in a range of ways relative to commercial encounters. For instance, although service users have the right to refuse care, they do not have the right to demand particular treatments and/or investigations. 29 HCPs have a duty to act in the best interests of service users and cannot simply agree to their choice if doing so would cause harm. In this sense (as well as others), the consumer choice model works imperfectly in health care. Nevertheless, respect for service user autonomy can act as a corrective to the long-standing perception of paternalism within medical encounters,30–32 in which HCPs might assume authority and afford service users little or no say in what happens to them. However, there remains a possibly inescapable (although perhaps narrowing) asymmetry between HCPs and service users in terms of medical and institutional knowledge, expertise and skill. 33 Where there is low health literacy or self-efficacy, the choice agenda risks placing an onerous burden on service users. 34,35
Shared decision-making is an approach to health care that attempts to occupy the middle ground between consumerism and paternalism by recognising, respecting and incorporating both HCPs’ and patients’ domains of expertise in medical encounters. 36,37 Therefore, shared decision-making is designed to counteract potentials for both consumerist patient abandonment and paternalist coercive action, and is seen as, ‘the pinnacle of patient-centred care’. 38 However, a range of conceptual39–42 and practical barriers43–45 have resulted in a limited and inconsistent implementation of shared decision-making in practice. 46–48 Barriers include (variable) patient ambivalence about their role as decision-makers45,49 and HCP concerns about, or experience of, time and resource constraints (including human resources). 44,50
A focus on involving women in decisions relating to intrapartum care has been a long-standing principle of UK maternity policy (and elsewhere). 10,51,52 These policies are clear that service users benefit from active engagement in decision-making. However, as noted above, fine-grained analyses of how decisions are initiated and managed in interactions between HCPs, labouring people and BPs is under-researched. Maternity care provides an ideal context to study the implementation of participatory approaches to decision-making because, relative to other aspects of health-service delivery, service users are, for the most part, healthy and able to function without complication. 53 In this sense, pregnancy and birth ought not to routinely provide agentic barriers to enacting informed choice in care decisions.
Decision-making during labour and birth
Although its history overlaps with the development of the choice/shared decision-making agenda in the NHS, policy emphasis on involving women in decision-making during labour has also been shaped by a distinct and long-standing critique of the medicalisation of childbirth.
Medicalisation of birth and its critique
The medicalisation of birthing practices over the nineteenth and particularly twentieth centuries is well documented. 54–56 Childbirth practices transformed from a ‘natural’ physiological, domestically located event, accompanied by an often lay female attendant, to a mainly ‘medical’ event, taking place in an institution, accompanied by a hierarchy of trained professionals and potentially involving multiple medical and technological procedures. In the UK, for example, homebirth was reasonably standard until the 1920s, when a shift towards hospital birth began, rising to around 65% by the 1950s. 57 In the 1970s, the Peel Report58 recommended that, on the grounds of safety, all births should take place in a hospital. By the 1980s, less than 1% of births took place at home and, since then, homebirth rates have remained consistently low (the figure for 2018 was 2.1%). 59
The factors that contributed towards and maintain medicalisation are complex and multifaceted,60 but include (1) the emergence and proliferation of biomedicine in general and in obstetrics in particular;61 (2) a focus on maternal and fetal risk;15,62–64 and, relatedly, (3) the development of technologies that enable a preventative approach by permitting a range of measurements and an assessment of body functions and processes. 65–67 Taken together, these factors of medicalisation are often associated, although in variously contested ways,68 with achieving safer childbirth. 69
For some women, having access to a medicalised setting offers reassurance and might be a key component for their satisfaction levels and feeling in control. 70–73 However, medicalisation has also occasioned resistance from feminists, midwives and childbirth activist groups [e.g. the National Childbirth Trust (London, UK), the Association for the Improvement of Maternity Services (Surrey, UK) and the Association of Radical Midwives (Northumberland, UK)]. The advancement of (male) biomedical authority is historically gendered and arguably disempowers women both as birthing subjects74,75 and as midwives61 by pathologising childbirth (and the pregnant body more broadly), bringing it under medical surveillance and intervention. 76,77 Although birth is generally safe in the UK, the focus on risk has intensified64,78 and has become normative so that most people give birth not only in hospital but also under obstetric-led care. 79,80 This can be explained in multiple ways, but might relate to the perceived risks of birth. 2,81–83
In the latter part of the twentieth century, mounting resistance to medicalisation went some way to reopening discussions about the normal physiology of birth, women’s bodily capabilities and midwives’ essential skills. 62 One response to the medicalisation of birth – variously called ‘humanist’60 or ‘feminist’,20 or identified by its features (e.g. woman-centred84–86) or by its central (but contested)87 association with midwife-led care88–90 – is more akin to ideas about shared decision-making adopted in the NHS more broadly. In this multifaceted approach, which, for the sake of consistency, we will call midwife led, the potential for normality (variously conceptualised)91 is promoted in an attempt to rebalance medical authority over women and midwives. Women are viewed more holistically, as more than birthing bodies, and there is recognition of the inter-relationships between psychological, emotional, social, cultural and physiological aspects of birth. 70,75,92,93 In this approach, midwives are the lead professionals and work in partnership with women to establish and support their needs and preferences, ‘being ‘with women’ as opposed to being ‘with institution’94 (see also Fottler et al. 95). There is also recognition that the process and experience of birth matters, not just the outcome. 96,97 Being involved in decision-making, having choice and feeling in control are positively associated with women’s reporting of high levels of satisfaction and positive birth experience,18,98–100 which has implications for postnatal well-being of mother and baby. 101,102
In the UK, critique of the medicalisation of childbirth culminated in the publication of the ground-breaking Changing Childbirth report,103 which reversed the Peel Report’s58 recommendation for 100% hospital births, acknowledged the psychosocial aspects of birth and promoted woman-centred care through supporting choice, control and continuity of carer (i.e. the so-called ‘three Cs’). 51 These ideas continue to resonate and are visible in subsequent maternity care policies. 52,104 However, realising the ideals of the ‘three Cs’ has been challenging. 87,105
Challenges of involving women in decision-making
Despite persuasive evidence that the choice and control that accompany engagement in decision-making are beneficial, women’s accounts suggest that there is considerable variation in the extent to which they report being included in decision-making during birth. 106–112 Indeed, the most recent Care Quality Commission report113 shows that 22% of women surveyed in 2019 said that they were only sometimes (18%) or never (4%) involved in decisions. Other studies report highly variable optionality around different types of clinically routine decisions,112 especially where this concerns personally sensitive/invasive procedures, such as VEs and fetal monitoring. 114
Villarmea and Kelly11 ask why involving women in decisions during labour is ‘so good in theory yet seemingly so difficult in practice’. 11 They11 suggest that there is a tension between individualising decisions and the broader organisational context of decision-making, and argue that it is possible that what sounds theoretically possible at the level of individual women might not be deliverable in the reality of a busy, under-resourced unit/ward. For example, the Royal College of Midwives (RCM) (London, UK)115 reports that, in 2019, the NHS was short of the equivalent of almost 2500 full-time midwives. However, Villarmea and Kelly11 suggest that these organisational issues might be inappropriately augmented by a stereotype that women in labour lack full capacity because of the deleterious effects of pain and tiredness. 116,117
Whatever the reasons for the inconsistent implementation of policies that promote the inclusion of labouring women in decisions, most existing studies have relied on women’s (and HCPs’) retrospective accounts that are variously removed from the actual experience and may, therefore, be subject to a range of biases. 118–120 Ethnographic observations121–124 have provided valuable insights into more situated practice, but tend to gloss the details of interaction (for exceptions see Jordan93,125 and Korstjens et al. 126). Moreover, one scoping study on collaboration and communication in maternity care found that few studies have researched both women/partners and HCPs. 12 To investigate the subtleties of discussions among women, partners and HCPs, a fine-grained analytic approach is needed. This approach will enable the examination of the specific context in which decision-making is ultimately accomplished. As a consequence of the reliance on retrospective data and the lack of specific focus on actual instances of interaction, only general recommendations for effective practice are usually offered. For example, Better Births52 requires that:
Women should be able to make decisions about their care during pregnancy, during birth and after their baby’s birth, through an ongoing dialogue with professionals that empowers them. They should feel supported to make well informed decisions through a relationship of mutual trust and respect with health professionals, and their choices should be acted upon.
However, there is little specific guidance on exactly how HCPs can facilitate this involvement in decision-making.
Conversation analysis: real-time decision-making in health-care interaction
Conversation analysis is a theoretically and methodologically distinctive approach to studying precisely how talk-in-interaction works on the micro level in everyday practice. CA uses audio-recordings and video-recordings of authentic interactions in real time (and associated transcripts) to enable direct observation and fine-grained analysis of not only what is said but also how it is said (e.g. emphasis, breathiness and evidence of hesitation), when and by whom. The key methodological advantages of CA are that it does not rely on recall and that it investigates interactional conduct at a fine level of detail that people cannot easily articulate (e.g. in a research interview) and, indeed, of which they are largely unaware.
A focus on the detail of communication matters because, as noted above, talk-in-interaction is central to the activity of medical health care. 127 By focusing on the details of authentic interactions, CA can expose and interrogate the micro-level realisation of interactional challenges faced by HCPs and patients. Examining the precise wording that HCPs use reveals features that can affect interaction in ways that might not be open to speakers’ intuitions. For example, a small change in question format from ‘is there anything else you want to address today’ to ‘is there something else you want to address today’ elicits significantly more reported concerns from patients. 128
A small number of CA studies have explicitly addressed shared decision-making. 129 However, conversation analysts do not begin with a particular model of decision-making, but rather try to inductively understand how agency in decision-making gets differentially distributed through the process of interaction. By examining health-care interactions, conversation analysts have identified a continuum of HCP approaches to opening decision-making that are more or less authoritative, ranging from those that are more ‘unilateral’ or ‘presumptive’ to those that are more ‘bilateral’ or ‘participatory’. 130–132 Collins et al. 130 define these dimensions in the following terms:
In ‘bilateral’ approaches, the practitioner talks in a way which actively pursues patient’s [sic] contributions, providing places for the patient to join in, and building on any contributions the patient makes . . . In ‘unilateral’ approaches the practitioner talks in formats less conducive to patient’s [sic] participation: e.g., the scene for the decision is already set; the decision is presented as ‘made’. 130
That is, turns are designed to convey levels of authority and involvement in decision-making. A presumptive or unilateral format (e.g. ‘I am going to . . .’) informs a recipient that something has already been decided and does not actively invite an interactional response and, therefore, makes resistance or negation more difficult. This format conveys (claims) a speaker’s authority over the decision. In contrast, a participatory or bilateral format (e.g. ‘what are your thoughts about . . .’) actively encourages recipient involvement in the decision. Of course, recipients may avoid the constraints of a turn, and other CA studies have shown the ways that patients can influence decision-making by, for example, resisting recommendations133–135 or by introducing their own agendas. 136–139 Taken together, these findings highlight the ways that health-care decisions are negotiated as joint social activities between service users and HCPs,140 as well as the subtle ways that agency may be enacted or constrained in interactions.
Conversation analytic studies in the context of labour and birth
In the main, CA studies of decision-making have focused on consultations between HCPs and patients in a range of primary and secondary care settings, that is, contexts in which decision-making is chiefly concerned with events or procedures that will likely be enacted outside the consultation (e.g. treatment, testing or referral decisions). Exceptions include analyses of surgical practice141 and physiotherapy sessions,142 and performing obstetric ultrasound scans. 143 In the context of maternity care, CA studies have examined antenatal appointments144–147 and genetic counselling,13,148,149 as well as calls to a homebirth helpline. 150,151 Very few studies have examined interactional practices of situated decision-making in the fast-moving, time-limited context of childbirth. There are three exceptions (all based in obstetric-led care): Jordan125,152 and Bergstrom et al. ,153,154 which both focus on the (transition to) second stage of labour, and our own pilot study155 conducted on analyses of extracts from the British television show One Born Every Minute (OBEM) (Dragonfly, London, UK). 155
Jordan152 (recorded in the USA in the mid to late 1980s) focuses on the ways that a labouring woman’s embodied knowledge and expertise is subjugated to the doctor’s technical expertise, such that she has to wait for his assessment of her cervix before being permitted to push. For example, as she waits for the doctor to come, a nurse instructs the woman to resist what her body is telling her to do, saying, for example, ‘It won’t be long. It’ll feel better for you to push. But in the meantime, I don’t want you to, okay?’. 152 When the doctor does the examination, he announces his verdict to the nurse (‘she can push’152) and the nurse speaks to the labouring woman (‘you can push’152). Bergstrom et al. 154 extended findings about the interactional realisation of an apparent ‘don’t push’ rule that applies until there has been some objective assessment of the readiness of the cervix. This study was based on analyses of three (of 23) video-recordings of the second stage of labour (including the one analysed by Jordan) in which the camera just happened to be switched on before second stage had been officially declared. In a different report on the whole data set of 23 recordings, Bergstrom et al. 153 describe the sequential structure of conducting VEs and suggest that these are accomplished as a ‘ritual’ that transforms an intimate act into a socially acceptable act.
More recently, in preparation for the current project, we conducted a pilot study of decision-making in labour based on data from the television programme OBEM (an observational documentary series shown in the UK on Channel 4). We transcribed, in detail, the interactions between HCPs, women and BPs for 26 births taken from the first three series (broadcast between 2010 and 2012). We considered a spectrum of decisions, including investigative/monitoring activities (e.g. VEs and fetal monitoring), pain management decisions and decisions for assisted or surgical deliveries. HCPs used a range of interactional practices that varied the ‘optionality’ afforded to the participant in the responding turn. For example, there were omissions (e.g. implementing a decision without discussion), directive pronouncements (e.g. ‘you need to . . .’ and ‘we are going to . . .’), propositional constructions (e.g. ‘do you want to do . . . ?’ and ‘why don’t you . . . ?’) and open questions (e.g. ‘what is your plan for pain relief?’). Two phrases were routinely deployed: ‘we need to . . . ’ and ‘we’re going to . . . ’. These assertive formulations were used in both situations of risk [e.g. ‘Uhm. We will need to take you (down) to theatre to deliver the baby. Baby doesn’t like this after you’ve pushed’] and in routine activities [e.g. ‘Now what I need to do uhm (2.5) find out how dilated you are’]. Overwhelmingly, women agreed to these decisions; however, when they did not, it was interactionally effortful for them to decline.
The OBEM data afforded fascinating insight into interactional practices for managing and negotiating decision-making during birth and provided good grounds for conducting this type of research. However, these data were not ideal for conversation analytic purposes because they are heavily edited to be produced as a 1-hour television programme. Therefore, our findings were based on a less than optimum data set for these purposes and could not represent the range of decision-making practices used either across the specific births shown or across the labour wards that were filmed. Therefore, we needed to produce a bespoke data set based on unedited recordings of the birthing event as it happens to more completely track nuanced interactions as they occur across the (perhaps many) hours of labour. It is this novel data set that forms the basis of the current report.
Inductive coding of interactional data based on conversation analysis
As outlined above, qualitative analysis, using CA, is at the heart of our analyses and enables us to explore how talk is used (by all parties) to encourage or discourage involvement in decision-making over the course and events of a birth (study objective 2). However, as interactional practices are definable and can be categorised in clear ways,156,157 it is also possible to design and apply a coding frame to quantify the interactional practices that take place during labour and birth. Nonetheless, extensive inductive conversation analytic work is first necessary to ensure that quantitative coding is thoroughly underpinned by observed nuanced interactional realities. This means that influential and effective coding systems, such as the Roter Interaction Analysis System,158 are not suitable for our purposes because, although they can be used flexibly, they ultimately rely on application of pre-established categories.
The reward of combining conversation analytic work with quantitative coding is that it permits exploration of distributional159 and comparative156 research questions (for illustrative studies, see Robinson and Heritage160). Examples of both distributive and comparative research of this kind are illustrated in a recent NIHR-funded study of decision-making in neurology consultations reported by Reuber et al. 161 Using CA, the authors had previously identified HCP practices for constructing a decision as a choice (or not) for patients. 162 In their follow-up study, Reuber et al. 161 developed a novel coding scheme (on which ours is modelled; see Chapter 2, Quantitative coding and analysis of interactional data) to facilitate extensive and nuanced coding of instances of HCPs’ use of recommendations, option lists (i.e. when HCPs provide a menu of options from which patients might select) and what they called ‘patient-view elicitors’ (PVEs) (i.e. a range of HCP turn designs that invite patients to express a preference). The coding scheme captured the qualitative data relating to how turns were initiated and responded to, as well as any follow-up discussions in pursuit of a decision. These internal-to-consultations data were next combined with data collected external to the consultation (via questionnaire), such as patient satisfaction and perception of whether or not choice had been offered. The final combined data set facilitated both distributional and comparative analyses. For example, the three focal practices (recommendations, option lists and PVEs) were not evenly distributed, with recommendations being the most common approach to decision-making overall. Furthermore, the frequency with which each practice was employed depended on the type of decision being made. Decisions relating to investigations and tests tended to involve recommendations, whereas treatment and referral decisions were relatively more likely to include option lists and PVEs. In comparing the consequences of the three practices, one striking finding was that recommendations consistently led to agreement with a proposed course of action, whereas PVEs were more likely to lead to rejection and option lists to postponement of a decision.
An important implication of Reuber et al. ’s161 findings (discoverable primarily from the distinctive methodological approach) is that the guidelines concerning patient choice are not routinely being enacted (at least in the context of neurology). Moreover, the tendency to accept recommended courses of action (as opposed to those offered as optional or as dependent on patient preference) sets up a possible conflict between what might be seen as a duty of care and a responsibility to provide patient choice. When the HCP has compelling clinical grounds for favouring a particular course of action, a recommendation is more likely than either of the choice-implicative formats to achieve acceptance. Therefore, previous work suggests that patient choice tends to be reserved for decisions for which clinical outcomes may be less contingent on patient preference.
In the present study, the quantitative coding of interactions enabled us to explore (1) the extent and distribution of different practices (objective 2) and (2) relationships between these practices and women’s postnatally reported levels of satisfaction with their experiences (objective 3). This analysis builds on Reuber et al. ’s projects,161,162 but with important adaptations to include decisions initiated by women and their BPs. In the context of labour and birth, with long-standing debate about the empowerment of maternity service users, we did not think it was appropriate to exclude analyses of the decisions that they might initiate.
Much existing research about decision-making in the intrapartum period excludes BPs (for related exceptions, see Hildingsson163 and Thies-Lagergren and Johansson164). There are understandable reasons for this, given that people in labour and their HCPs are the ratified decisional parties (except in certain critical situations in which the person is unable to consent for themselves and their BP is also their next of kin). However, as we showed in our analysis of data from OBEM,155 BPs do participate in decisional discussions and their role should not be neglected. 165
As a consequence of including analyses of decisions initiated by HCPs, labouring people and their BPs, in comparison with Reuber et al. ,161 we identified a broader range of initiating formats in relation to a broader range of decision types. This is not surprising given the very different context for the research. The extensive nature of our data and findings (which also includes data from interviews and surveys) cannot be easily summarised in a single report. We have necessarily had to compromise on the depth and breadth of what it is possible to include and have chosen to focus on key areas of decision-making during labour and birth. Through our analysis of these key areas, we illustrate the full range of interactions that were observed.
Unpacking ‘satisfaction’
As already highlighted at various points, previous studies have indicated that women’s perceptions of their involvement in decision-making are associated with postnatal satisfaction. A key objective of this study is to understand this relationship more precisely by exploring whether or not there are associations between women’s reported levels of postnatal satisfaction and the ways that decision-making actually unfolds through interaction (as explored by our inductive coding of the interactional data). In this way, we aim to determine whether or not satisfaction is related to definable aspects of practice in the MLU.
Conceptualising satisfaction
Satisfaction is a deceptively simple concept, but attempts to measure it are complex, multidimensional and often poorly defined. 1,119,166 In discussion of how satisfaction should be conceptualised, two approaches dominate:166–168 (1) the fulfilment approach, which sees satisfaction as determined by the outcome of the experience (e.g. a healthy baby), and (2) the discrepancy approach, which treats satisfaction as arising from (in)congruity between what was expected and what actually happened. 1,169 The latter approach was used by Christiaens and Bracke1 and is summarised as follows:
Satisfaction is a state of mind reflecting the evaluation of the birth experience as a whole compared to several antenatal values and expectations. If expectations are met, the corresponding values and beliefs are affirmed. If not, conflicts arise, which may bring about distress.
Christiaens and Bracke1
In the present study, we also take the discrepancy approach, collecting data about our participants’ expectations antenatally (at 35 weeks) and asking them whether or not they were met postnatally (at 6 weeks). These data will be related to measures of satisfaction related to aspects of their care (i.e. being listened to by staff, views taken into account and the decisions made). Uniquely, we are also able to relate satisfaction to what happens in decision-making during labour.
Structure of the rest of the report
Chapter 2 describes our methods and analytic approaches. Chapter 3 presents key findings from the questionnaires and the coded interactional data to address research objective 3. Thereafter, analytic chapters address research objectives 1 and 2 by exploring decision-making in four common specific contexts: fetal monitoring (see Chapter 4), progress (see Chapter 5), pain relief (see Chapter 6) and third-stage decisions (see Chapter 7). Finally, Chapter 8 presents our conclusions, discusses the implications of our findings and suggests avenues of future research.
Chapter 2 Methodology
Introduction
The principal focus of the study was CA and subsequent coding of recordings of labour and birth, with additional methods (i.e. questionnaires and interviews) being used to supplement this analysis and address our research objectives. Through these mixed methods, we explored decision-making during labour and birth in MLUs at two English NHS trusts.
Recordings of labour and birth
Recordings of labour and birth were analysed using two approaches. First we adopted a qualitative approach, using CA to explore how decision-making takes place. The focus of the CA was on how talk was used (by all parties) to encourage or discourage women’s involvement in decision-making over the course and events of labour and birth. Second, quantitative codings of the recordings of labour and birth were analysed. Each recording was coded to quantify the number of types of interaction that took place during decision-making (i.e. how decisions were initiated, who initiated them and how different ways of initiating decisions were responded to). The coding frame was derived inductively from the qualitative CA.
Antenatal and postnatal questionnaires
Antenatal questionnaires and PNQs surveyed women’s expectations, experiences and satisfaction with labour and birth. These questionnaires made it possible to compare women’s antenatal expectations with what actually happened during labour, as captured by the recordings and as reported by women. In combination with the quantitative coding of the recordings of labour and birth, the PNQ was also used to determine whether or not there is an association between interactional strategies used during labour and women’s postnatally reported level of satisfaction.
Semistructured interviews with midwives and obstetricians
Semistructured interviews with midwives and obstetricians were conducted at each research site and analysed using thematic analysis. These interviews (1) supported local study implementation (by exploring perceptions of recording feasibility) and (2) explored HCPs’ perceptions of factors that facilitate, or constrain, women’s involvement in decision-making during labour.
Owing to the innovative nature of the study, concerns were expressed by colleagues, reviewers and service user groups (SUGs) about its feasibility. These concerns included whether or not women and HCPs would agree to the recording of labours and births and whether or not it would be possible to generate high-quality recordings suitable for CA. Key to addressing and overcoming these concerns was an extensive period of planning and service user consultation (see Patient and public involvement). Critical ethics issues resolved through this planning process included:
-
concerns about the intimate nature of the recordings and ensuring that those in labour had control over, and felt comfortable with, this process
-
managing the sensitivities of initial approach and follow-up during the period of participation (i.e. from 20-week scan to 6 weeks post partum) because of the potential for miscarriage, stillbirth or neonatal death to occur within this time frame
-
managing consent for recordings involving multiple participants
-
navigating HCPs’ concerns about the potential use of recordings in litigation.
These issues were addressed through our recruitment and consent procedures, which we outline in this chapter. Given the sensitive nature of the data, participant anonymity is paramount. Accordingly, all participants and study sites have been given pseudonyms throughout this report.
Ethics approval was granted by the National Research Ethics Service Committee for Yorkshire and the Humber (South Yorkshire) following a meeting on 23 March 2017. Approval was confirmed by the University of York Economics, Law, Management, Politics and Sociology Research Ethics Committee. The protocol underwent Health Research Authority-approved substantial and non-substantial amendments (see Pregnant people) to produce the final methodology reported in this chapter. The study was accepted as part of the NIHR’s Clinical Research Network Portfolio of studies (and received a ‘green’ red-amber-green rating for recruitment).
Given concerns about feasibility, the study was designed with a 12-month pilot phase, with review points at 4 and 12 months. Owing to a delay in the start of recruitment (waiting for all research and development approvals to be in place at trust level), the final review point for the pilot was moved from 12 months (February 2018) to 16 months (June 2018). At the end of this 16-month period, feasibility had been established and the study was approved by NIHR to progress to the main phase.
In what follows, we provide an overview of our two study sites, moving on to describe the data collection and analytic procedures for each of the three forms of data source (i.e. recordings of labour, questionnaires and interviews) described above. We conclude the chapter by reflecting on the role of patient and public involvement (PPI) in the study, and how this positively shaped the design and conduct of our research.
The study sites
There are four settings for labour and birth in the English NHS: (1) home, (2) freestanding midwifery units, (3) alongside midwifery units and (4) obstetric units (OUs). ‘Freestanding midwifery units’ are at a geographical distance from an OU and, therefore, vehicle transfer is required if complications arise during labour. The more common ‘alongside midwifery units’ provide midwife-led care in a setting adjacent to, or in the same building as, an OU. 52
We collected data in alongside MLUs at two NHS trusts in England between April 2018 and October 2019. Sites were selected to enable access to a population of participants diverse in ethnicity and socioeconomic status (SES). Site A is a very large, purpose-built unit that includes an OU and an alongside MLU. This MLU is adjacent to the OU and, therefore, depending on the clinical scenario, doctors may attend the unit when called on. In 2020, approximately 6200 babies were born at site A (OU and MLU figures combined). Site B contains a medium-sized alongside MLU, which is located on a separate floor to the OU. Doctors do not attend to women on this unit (except in certain emergency situations) and, instead, women who develop complications are transferred to the OU. In 2020, approximately 4500 babies were born at site B (OU and MLU figures combined).
Rather than conducting a comparative analysis of practice, our aim in selecting MLUs A and B was to include examples of midwife-led care from two units considered sufficiently similar that major differences in interactional practices of decision–making would not be expected. These similarities were confirmed through the HCP interviews and recordings of labour. Semistructured interviews explored HCPs’ perceptions of the factors that shape decision-making, enabling us to consider the impact of potential organisational differences between MLUs A and B (e.g. site-specific practices; see Semistructured interviews with health-care practitioners). These interviews revealed no differences in accounts of the factors that shape decision-making and, indeed, pointed to the shared set of professional resources (national clinical guidelines) that govern practice in this context. Similarities were further verified through our CA and coding of interactional practices during labour and birth, and the analytic patterns identified were observed at both sites. On this basis, the data gathered at both sites were pooled for the purpose of analysis and analytic generalisation. 170
Recordings of labour and birth
The recordings of labour and birth enabled us to study real-time interactions. Recordings took place in the MLUs only and were stopped if women were transferred to another location for obstetric-led care (women were informed of this possibility on the information sheet).
Data collection
There were three groups of participants for each recording: (1) individuals (aged ≥ 16 years) with a healthy singleton pregnancy expected to labour spontaneously and give birth vaginally at term, (2) their BPs and (3) HCPs (i.e. clinical staff at each site). Although we did not ask participants about their gender identity, those recorded all had names conventionally assigned to females and were gendered as women (and accepted this gendering) during interactions with BPs and midwives. Accordingly, each woman was given a ‘female name’ pseudonym (see Appendix 1). These pseudonyms were selected on the basis that no other consented participant shared this name and that it had the same number of syllables as the original name (which is important to retain for CA purposes). Birth partners are referred to as ‘BP’ plus numbers (e.g. BP1) in the order of their appearance in the recordings. HCPs who were recorded were given pseudonyms based on their professional role and order of appearance in recordings (e.g. M1, M2, Doc1 and Doc2). As the number of male midwives at each site is very small, we refer interchangeably to all midwives in our analysis as female or using the gender-neutral ‘they/them’ to preserve anonymity.
All participants were informed that only the research team would see the un-anonymised footage, and each participant was given the option of choosing in what form the anonymised data could be shared publicly (i.e. as an anonymous transcript, as anonymised video clips, as anonymised audio clips and/or as anonymised photographs). When participants in the same recording selected conflicting ‘levels’ of consent, anonymity was prioritised and the option providing the highest level of anonymity was adhered to. For example, if one participant agreed that anonymised transcripts, photographs and video clips could be shared, but another only agreed to transcripts, then only the anonymised transcripts would be shown publicly. Below we describe the data collection procedures for each group of participants involved in the recordings and provide an overview of the recordings collected.
Pregnant people
Recruitment
Research midwives screened and approached eligible pregnant people to provide details of the study at the 20-week scan appointment (after the scan had been completed, at which point it was felt that they would be less anxious) or at antenatal appointments thereafter. Pregnant people also had the option of self-referring into the study at any point after their 20-week scan appointment, for example by responding to study information on posters (see Appendix 2). The information provided addressed all three aspects of the study in which people were being invited to participate, namely the recording of labour and the two questionnaires (i.e. the ANQ and the PNQ). It made clear that whether or not recording ultimately took place was dependent on a number of contingent circumstances (e.g. availability of equipment and staff agreement).
Those people who were certain that they wanted to participate following the research midwife’s initial approach had the option of providing consent then and there. Alternatively, the research midwife followed up those people who expressed interest in the study with a telephone call and arranged to take consent face to face in their home (or other location of their choosing), remotely via Skype™ (Microsoft Corporation, Redmond, WA, USA) or telephone, or at another antenatal appointment. Consent was reconfirmed verbally on arrival in labour. Women in labour were instructed to identify themselves as a study participant when they contacted the MLU and both MLUs also used systems to flag up study participation on patient records.
There were no existing data available from the trusts on which to base estimates of recruitment figures (i.e. how many women would have to be recruited into the study to achieve the original study target of 50 recordings of labour and birth). The rationale for a sample size of 50 women, as specified in the study protocol, was to allow for a diverse range of participants to take part while producing data that would be manageable for the conversation analytic work. Assuming a 60% conversion rate from consented women into recorded labours, we had anticipated that we would need to recruit 85 women to the study. However, in the initial months of the pilot phase, it became clear that we would have to revise these targets because the conversion rate proved much lower than anticipated (closer to 20%). Therefore, we gained NIHR and Health Research Authority approval for the following:
-
To lower the target number of recordings to a target number of 20–30 on the basis of advice from experts in CA who confirmed that this would remain a powerful qualitative sample for the purpose of our research objectives. This change was approved by our Study Steering Committee.
-
To recruit a larger number of participants than originally anticipated (estimated n = 150) to achieve this target.
-
To extend the study recruitment period.
-
To increase the points of potential recruitment into the study by enabling pregnant people to be recruited at any antenatal care appointment after the 20-week scan appointment and/or to self-refer into the study. The original protocol described recruitment only at the 20-week scan appointment and up to 35 weeks of pregnancy.
Characteristics of the recorded sample of women
The study successfully recruited and consented 154 women (site A, n = 111; site B, n = 43), producing 37 recordings for analysis. From the outset, given their different patient populations, it was not anticipated that the two sites would recruit equal numbers.
Table 1 shows that only 24% of the consented women went on to be recorded. This figure includes women who were admitted to the MLU but who were later transferred to the OU (in which case only the MLU part of their labour was recorded). A further 18% of consented women laboured/gave birth in the MLU but were not recorded. This occurred for a number of reasons, including insufficient time to set up the camera before starting care because women were in advanced labour on admission (n = 8), the fact that no midwife who had consented to the study was on duty (n = 8), user error in setting up the camera (n = 7) and other reasons that could not be determined (n = 5). Nearly half (49%) of the sample of consented women (all of whom were anticipating labouring and giving birth in the MLU) were not admitted to the MLU at any point and, therefore, were not recorded. This is higher than reported in the NHS Patient Survey Programme’s 2019 Survey of Women’s Experience of Maternity Care,113 which found that 22% of those planning to labour and birth in a MLU, instead, entered an OU. In the present study, this occurred for a range of clinical reasons during pregnancy or at the point of admission, which made women ineligible for midwife-led care. Finally, there was a small group (13%) of women who did not enter the MLU for other reasons, for example because no birthing room was available on the MLU or because they had moved to another area or had withdrawn from the study after initially consenting (applying to only five women). Notably, all withdrawals of consent occurred prior to labour commencing and there were no instances where a woman withdrew her consent following recording.
| Site | Labour/birth in MLU, n (%) | Labour/birth took place in OU: not recorded, n (%) | Other: not recorded, n (%) | Total, n (%) | |
|---|---|---|---|---|---|
| Recorded | Not recorded | ||||
| A | 30 (27) | 19 (17) | 52 (47) | 10 (9) | 111 (100) |
| B | 7 (16) | 9 (21) | 24 (56) | 3 (7) | 43 (100) |
| Total | 37 (24) | 28 (18) | 76 (49) | 13 (9) | 154 (100) |
In summary, contrary to concerns expressed by reviewers and commentators that people would not want to have their labours recorded, people were willing to take part. The key challenge concerned the high proportion of people who, although intending to give birth in the MLU, became ineligible to do so because they developed complications in pregnancy or on admission that meant that it was recommended that they give birth on the OU.
We aimed to recruit as diverse as possible a sample of women by SES and ethnicity. SES was measured using the Index of Multiple Deprivation (IMD),171 an area-based measure of relative deprivation based on household postcode (see Appendix 3 for details of the IMD). The IMD ranks areas in deciles from 1 (most deprived) to 10 (least deprived). Our respondents fell in all deprivation deciles, indicating some level of diversity, but a mean score of 6.30 and skewness of –0.89 indicates that there was a larger percentage of participants from least deprived areas. The sample was overwhelmingly white, with 97% of participants identifying as such. The proportions of women of different ethnicities who were approached by the research midwives were broadly similar to the proportions of women of different ethnicities who gave birth at each trust during the study recruitment period (see Appendix 4 for ethnicity figures, although note that these figures cannot be directly compared, as the numbers are calculated at trust level only and incorporate women who birthed in OUs as well as MLUs). The predominantly white make-up of the recorded sample (see Chapter 3) seems primarily explained by the comparatively smaller potential recruitment pool of ethnic minority women and that, in general, members of these groups who were approached were less likely to give their consent to participate in the study. We reflect on the implications of this as a study limitation in the discussion (see Chapter 8, Limitations).
Comparison of recorded and non-recorded samples
As explained, all of the women who consented to the study were intending to give birth in MLUs. Likelihood ratio chi-squared and Mann–Whitney U-tests were conducted, as appropriate, to explore if there were significant differences between the recorded (n = 37) and non-recorded samples (n = 87 or fewer). The demographic and satisfaction information are derived from ANQ and PNQ responses and, therefore, total numbers do not always add up to 154 due to full or partial missing data in participants’ ANQ and/or PNQ responses (see Questionnaires for more information on ANQ and PNQ data collection and the satisfaction variables).
Tables 2–5 show that there were no significant differences between the recorded and non-recorded samples in terms of ethnicity, parity, SES or any of the aspects of satisfaction. This provides evidence that the two samples are, to a large extent, equivalent. It should be remembered that, although the recorded sample of women all laboured for a period of time in the MLU, they did not necessarily give birth there (i.e. they may have been transferred to an OU). Therefore, these data should not be taken to represent relative satisfaction between women who received care in the MLU and those who received care elsewhere. Rather, theses data are presented here only to assess the characteristics of the recorded sample compared with the consented sample.
| Sample | Ethnicity, n (%) | Total, n (%) | ||||
|---|---|---|---|---|---|---|
| White | Mixed/multiple ethnic group | Asian/Asian British | Black/African/Caribbean/black British | Other | ||
| Recorded | 36 (29.3) | 1 (0.8) | 37 (100.0) | |||
| Non-recorded | 80 (65.0) | 1 (0.8) | 2 (1.6) | 2 (1.6) | 1 (0.8) | 86 (100.0) |
| Total | 116 (94.3) | 1 (0.8) | 3 (2.4) | 2 (1.6) | 1 (0.8) | 123 (100.0) |
| Sample | Parity, n (%) | Total, n (%) | |
|---|---|---|---|
| First baby | Subsequent baby | ||
| Recorded | 22 (19.0) | 12 (10.3) | 34 (100.0) |
| Non-recorded | 55 (47.4) | 27 (23.3) | 82 (100.0) |
| Total | 77 (100.0) | 39 (100.0) | 116 (100.0) |
| Sample | n | Mean rank |
|---|---|---|
| Recorded | 37 | 60.19 |
| Non-recorded | 87 | 67.93 |
| Total | 124 |
| Question | n | Mean rank |
|---|---|---|
| How satisfied were you that you were listened to by staff?a | ||
| Recorded | 32 | 45.77 |
| Non-recorded | 62 | 50.84 |
| Total | 94 | |
| How satisfied were you that your views were taken into account by staff?b | ||
| Recorded | 32 | 49.59 |
| Non-recorded | 62 | 46.42 |
| Total | 94 | |
| How satisfied were you with the decisions that were made?c | ||
| Recorded | 31 | 52.61 |
| Non-recorded | 61 | 43.39 |
| Overall satisfactiond | ||
| Recorded | 31 | 50.81 |
| Non-recorded | 61 | 44.31 |
Birth partners
Birth partners received information at 20 weeks or thereafter (via women, who were asked to pass study information sheets to anyone likely to attend the birth). In instances in which it was not possible to obtain consent from a BP prior to labour (e.g. because a different person attended the birth than originally planned), MLU staff verbally confirmed consent for recording. MLU staff noted when a recording took place in a logbook and indicated if there was a need for research midwives to obtain retrospective written consent from the BP. If written consent was not given, or could not be determined (i.e. because of a lack of response), BP footage was edited out of the recording, and this was necessary in three recordings. A total of 158 BPs consented, of whom 43 featured in recordings.
Health-care practitioners
Health-care practitioners at both sites were briefed in writing and at meetings, and were given opportunities to provide written consent to opt in to the study. Anticipating that HCPs were likely to be concerned about the potential use of recordings in litigation (owing to high rates of litigation in this field of health care, leading to the UK’s most expensive clinical negligence claims172), we sought advice from the sponsor’s contracts manager and made clear the status of these data in our information sheets. Specifically, we informed participants that all research material, irrespective of its nature, could potentially be used if requested to corroborate a complaint and that, in these circumstances, it would not be possible to maintain confidentiality. In addition, participants were informed that in the highly unlikely event that poor practice was observed on the recordings, the research team would have an ethical and legal obligation to follow institutional procedures for reporting this. However, if care was given according to usual best practice standards, then accurate recording would be an advantage if care was to be questioned subsequently.
Project information posters were placed around both study locations to ensure that non-clinical staff (e.g. cleaners and administrators) were aware of the study. Recording signs were used to indicate if recording was in progress inside a room and these highlighted that no footage of staff would be used in the study unless written consent was given. Where staff who had not previously consented entered to provide care during labour, we contacted them subsequently to ask for their retrospective written consent. If consent was not given, then their footage was edited out of the recording. A total of 121 HCPs consented (site A, n = 104; site B, n = 17), of whom 74 were recorded.
Procedure for recording labour and birth
Each participating unit was provided with a mobile Smots™ camera (Scotia UK plc, Edinburgh, UK), a stand-alone recording device (independent of the research or health-care team once set up) that provides high-quality video-/audio-recordings in clinical settings. Data were recorded to a securely located bespoke encrypted laptop via a secure intranet connection, which was separate from the hospital intranet [and later uploaded to a military-grade password-protected hard drive, returned to the University of York (York, UK) and uploaded to its secure server].
Women and their BPs were advised in the consenting process that they could position the camera and could switch it on/off (or to request that others do so) at any point. In switching the camera off, our procedures prioritised the woman’s consent. Therefore, HCPs could not switch the camera off without the woman’s consent (unless there was a medical emergency) and BPs were encouraged to switch the camera off only with the woman’s consent whenever possible. Our preference was to capture video data to be able to observe non-verbal interactions; however, women had the option of choosing audio-only recording. Of the 37 recordings, 24 (65%) were video-recordings and 13 (35%) were audio-only recordings. Women were recorded ideally as soon as the first stage of labour was established until the end of the third stage of labour (i.e. after delivery of the placenta). In practice, some recordings began during the latent stage of labour and in several recordings the camera was switched off immediately after the baby was born, meaning that the third stage was not recorded. The total recorded time was 166 hours and 56 minutes (for further detail of recording parameters, see Appendix 5).
Data analysis of recordings
Recordings of labour and birth were analysed through two approaches. CA was used to develop an in-depth qualitative understanding of how decision-making is carried out during labour and birth. The insights developed from this analysis informed the development of a standardised coding scheme through which a quantitative coding of the interactional data was conducted.
Conversation analysis
In intrapartum care, midwives and women are engaged in a range of context-specific activities, such as discussing options for care and investigations. It is the analysis of how these activities are accomplished that formed the basis of our analyses. Therefore, we adopted an ‘action-based’ approach to understanding communication in care, derived from the micro-analytic tradition of CA. A fundamental CA insight is that talk is highly organised and that there is, as the founder of the approach Sacks173 suggests, ‘order at all points’. Therefore, talk is suitable for systematic analysis. CA focuses on participants’ objectively observable conduct, based on detailed analysis of actual interactions, and avoids claims about interactants’ internal (and unobservable) intentions, cognitions or desires.
Conversation analysis is predicated on the understanding that talk is used to perform social actions (i.e. to ‘do’ things). Of relevance here, actions might include offering (e.g. ‘would you like X’), requesting (e.g. ‘please can I have X’) and recommending (e.g. ‘I think we should give you some X’). However, a long-standing CA finding is that first actions (like those just illustrated) set up a relevant next action for recipients to respond,174–176 that is, actions are packaged in pair-related sequences, comprising a first pair part (from speaker A) and a second pair part (from speaker B), known as adjacency pairs. A request, for example, sets up a conditional responsive slot for a recipient to grant or decline. If the request is not followed by a relevant next turn, then the second pair part is relevantly missing and the adjacency pair is incomplete. 176
Therefore, the provision of a type-related second pair part is normative in that if it is missing then the speaker of the first pair part regularly pursues a relevant response. 176 Therefore, the basic two-part sequence might be expanded in various ways, as illustrated in Figure 1. In Figure 1 (which is just one way in which a request sequence might be expanded), we see that the recipient of the request remains silent after the first request and the first speaker then pursues a response by reissuing the request, which is again met with silence, prompting a second pursuit, to which the recipient does respond (here, declining the request).
FIGURE 1.
Schematic illustration of expanding a request sequence in talk.

Accordingly, turns at talk do not occur merely serially, but are structured by reference to one another, ‘in some before and after relationship’. 177 The organisation of adjacency pairs, however, does not imply that speakers have little option in selecting responses, as a range of relevant next actions is possible. 178,179 A request might, for instance, be relevantly followed by acceptance, declination or some form of hedge that defers the granting. Therefore, the production of any particular relevant response is always a selection by the respondent from alternatives. However, these alternatives are not equivalent, as some responses are ‘preferred’ over others. 178 Preference refers not to ‘personal, subjective, or “psychological” desires or dispositions’,178 but, instead, to a distinction between preferred responses that ‘forward’ the action of the initiating turn (e.g. granting a request) and dispreferred responses that ‘block’ it (e.g. declining a request), regardless of what the individual responding personally wants. 180 Put more simply, it is interactionally more straightforward to provide a preferred response.
Preference is oriented to in the grammatical and lexical design of turns and in their timing. Therefore, relative to preferred responses, which tend to be immediately and straightforwardly delivered by the respondent, dispreferred responses tend to be delayed, and contain markers of hesitation, as well as accounts for why the preferred response cannot be provided179 (e.g. in turning down a request, speakers do not ‘just say no’). 181 Speakers of initiating actions (i.e. talk) might also encode something of their expectation relating to the ease with which action might be progressed. For example, in making a request, a speaker might convey something about both their entitlement to ask and the burden that fulfilling the request might have for the recipient. 182 Therefore, modal requests (e.g. ‘can you . . . ’) display an entitlement to ask and an expectation of ease of granting, whereas ‘I wonder if . . . ’ displays low entitlement and some expectation that granting the request might be burdensome for the recipient. Recipients (and speakers generally) have agency in talk, but they are constrained by the way the initiating actions are formulated.
Therefore, doing CA requires paying systematic attention to the organisation of turns at talk, the relationship between turns, the ways that turns are designed to build the action they are producing, and how dimensions, such as entitlement and other contingencies, are conveyed and managed. As outlined in Chapter 1, CA in the context of health care has illustrated how talk can be organised in ways that either invite or discourage patient participation in decision-making. Our analysis focuses on illuminating these aspects of interaction in MLUs to facilitate an understanding of the extent to which decisions become jointly negotiated (or ‘shared’) and whether or nor they are initiated by particular participants in the interaction.
Given the breadth and depth of data and the intensive nature of conversation analytic work, we were necessarily selective in the topics we focused on for the purposes of this report. A key finding of our preliminary analysis (subsequently verified by the quantitative coding of the data) was that the way decisions are initiated appears to be contingent on what kind of decision is being made (e.g. monitoring and pain relief). To elucidate these differences, we elected to explore decisions about monitoring, VEs, artificial rupture of membranes and pain relief, and ‘third-stage’ decisions relating to delivery of the placenta and cord clamping/cutting. These were decisions that we asked about in the questionnaires and were initiated in ways that were either relatively constraining (e.g. monitoring and VEs) or more participatory (e.g. pain relief and third-stage decisions) with respect to women’s agency. These topics form the basis of Chapters 4–7 of this report.
The interactions between HCPs, women and BPs were identified and edited for verbatim transcription (i.e. for budgeting purposes, we did not generally send whole recordings to the transcriber). Data concerning the decision types outlined above were selected from the professionally transcribed verbatim transcripts and re-transcribed using the conventions of CA (known as Jeffersonian transcription;183 see Appendix 6 for CA transcription conventions).
The data, plus the associated transcripts, were then examined in detail for how decisions were initiated and responded to so to establish how far decision-making was shared (research objective 2). Where possible (i.e. where we had video), our qualitative CA included embodied actions (e.g. gaze and head movements). Given the mix of audio-only recordings and video-recordings, a focus on these non-verbal features has not been possible across the data set. However, in the title of each of the data extracts presented in the CA chapters (see Chapters 4–7), we include information about whether the extract is based on audio or video, and, if the latter, whether or not the participants were on camera.
Quantitative coding and analysis of interactional data
Development and application of the coding scheme
In creating the coding scheme to generate quantitative data, we were committed to carrying out the necessary act of data reduction (for quantitative analysis) without sacrificing CA’s sensitivity to interaction. 156 Although informed by existing formal coding frameworks (see Stivers et al. 132 and Reuber et al. 161), the coding scheme was primarily developed through an iterative bottom-up process in which we drew on the CA from the study to adequately capture what was going on in the interactions.
Inspired by Reuber et al. ’s161 use of an online questionnaire to ‘extract’ quantitative data, the coding scheme comprised a codebook (see Appendix 7) and an online data extraction form constructed using Qualtrics® software (Qualtrics, Provo, UT, USA). The coding scheme was developed and refined through an iterative process. The first step was an extensive data familiarisation process that involved three members of the team (LB-J, CJ and VL) watching and listening to an opportunity sample of recordings (i.e. as recordings were completed, transcribed and subject to preliminary CA). Following this, the coding scheme was developed through a process of trial and error, whereby definitions of interactional practices (derived from the CA) were produced, and where we considered the different ways in which participants could immediately respond to the different decisional practices and how best to capture the often extensive decision-making sequences that occurred. Multiple versions of the coding scheme were developed and the coding team met frequently to discuss the coding process, the success of the coding scheme in providing valid descriptions of real interactional practice and any disagreements. After each meeting, a new version of the codebook and data extraction form was constructed, taking into account discussions and any agreed changes before the independent coding process started again. Through the application of this iterative process, a final coding scheme was developed that would allow for the identification of interactional phenomena identified in the CA, while allowing the classifications to be reliably applied between coders.
The coding scheme was designed so that, when applied, the following could be coded for each recording:
-
The stages in labour when the recording started and ended, together with length and format (i.e. audio-only, video or mixed) of recording.
-
All decisions about the key aspects of care asked about in the ANQs and PNQs (described in Data analysis of recordings). There were 12 categories of decision, including, for example, pain relief, fetal monitoring, manual (not visual) VEs, position for first stage, position for birth and active/physiological third stage.
-
For each decision identified, we recorded who it was initiated by (i.e. midwife, doctor, labouring woman or BP).
-
Decisions were commonly made through extended sequences and, therefore, to track decision-making across time we followed Reuber et al. ’s161 methodology, and made a distinction between a decision and the decision points that constituted it. Each decision could have any number of decision points that represented the chain of decision-making relating to that decision. This was carried out so that our coding retained the sequential order of decision points and so that it was possible to compare first decision points with later ones within a single decision. Each decision point was classified as one of 11 types, including pronouncements, recommendations, requests, offers, open questions and indecipherable. Note that, following our pilot work and that of Reuber et al. ,161 we maintained a distinction between the strongly directive recommendations (pronouncements) and those that contained a proposal.
-
We coded the immediate recipient response to each decision point. Coders selected one of 11 response types, including ‘no audible response’, ‘acknowledges’, ‘agrees/accepts/aligns/selects option’ and ‘disagrees/rejects/denies/misaligns’ (misalignment refers to not going along with a proposed course of action).
-
For each decision point, we also recorded the specific section of transcribed text that constituted the decision point.
-
When all decision points for a single decision had been coded (i.e. the decision was complete and there were no further initiating turns for that decision), we coded whether or not the possible course of action was pursued, agreed and acted on, agreed but not acted on, or abandoned.
-
For each decision, we assessed the level of ‘sharedness’ and ‘balance’ in decision-making by selecting one of seven categories on an ordinal scale. Researcher-based judgements were made for each separate decision according to who led the decision-making process and to what extent the other party had some say in the decision-making. For these purposes, we combined midwives and doctors into the category ‘HCP’ and women and BPs into the category ‘birth party’. Decisions were coded as (1) unilateral HCP, (2) HCP led but birth party had some say, (3) HCP led but birth party had most say, (4) equal balance between HCP and birth party, (5) birth party led but HCP had most say, (6) birth party led but HCP had some say or (7) unilateral birth party.
However, some exceptions applied (see Appendix 7). For example, we coded only those decisions that were asked about in the questionnaires, and only on occasions when decisions were discussed between HCPs and women and/or BPs (i.e. not decisions that were discussed only between HCPs or between women and BPs).
Table 6 provides our codebook definitions for each interactional practice that could constitute a decision point, with examples. For ease of reading, full Jeffersonian transcription notation is not used here, but was used to conduct the CA work. As can be seen from the definitions, our codebook was heavily influenced by the CA work in that it captures the ways in which initiating turns can vary the dimensions of entitlement and decisional domain. 132
| Format | What is conveyed | Example |
|---|---|---|
| No verbal initiation (just do it) | Conveys entitlement, but there are always embodied actions that women might notice and resist | Monitoring without asking/informing |
| Pronouncements | Something is going to, needs to or will happen. High entitlement/ownership, expects agreement | [Midwife] said she examined you about 8:40? So I’ll examine you about 12:40 |
| Instruction/command/demand | A decision is initiated as a directive to the other party to do something, high entitlement and expectation of agreement | Get up and walk about. You will have your baby |
| Recommendation/suggestion/proposal | Endorses a course of action, expects agreement, but leaves some room for the other to decide | I’m just wondering about examining you really, to be honest. I’m just, I’m not getting a clear picture really. So I just think it might just be helpful |
| Request | A decision is initiated in a way that asks the other to grant something. Might convey entitlement to ask, but decisional domain is with the other | Please can I have some pethidine? |
| Offer | A decision is initiated in a way that self has the right/possibility to enact on behalf of the other but is seeking the other’s view/permission | I could offer you some codeine as well if you wanted that |
| Option list | Decision initiated that includes a menu of options from which the other should select, conveys entitlement to construct option, but places decision with other | So you can either have a good few pushes (.) on the bed, or we can get you up on the stool to push, or push on the toilet, or you can have the injection and the placenta just comes out |
| Open question | Wh- questions,a allow other to narrate their own decision | Wo, how do you feel about getting back in the pool? |
| Decision-implicative statement | A declarative statement that may have decision-implicative relevance, but does not place pressure on the other to respond | I don’t feel like I’m in a comfortable position |
Figure 2 shows an example of how the rules laid out in the codebook were applied to code for interactional practice for one woman (Judy; VIP04) and demonstrates the hierarchical nature of the data, as each decision can be made up of a chain of decision points. In decision 1, regarding whether or not an injection for the placenta should be administered, the decision is coded as concerning active or physiological third stage initiated by the midwife through the use of an option list. This is clearly an example of an option list because the midwife gives two different options and then places the decision in the decisional domain of the labouring woman. Judy responds by saying ‘I don’t know what I want’, which is coded as the response option ‘doesn’t know’, again according to the rules in the codebook. After the birth, the same placenta issue arises three more times, each time initiated again by a midwife. The three further decision points and the responses are classified, that is, as a request that is deferred by another midwife and as an option list that is agreed by Judy (although Judy does not explicitly select an option, in context she is heard to be agreeing to the injection). The slight ambiguity of Judy’s response is checked in a further decision point as a request that is accepted by Judy, according to the codebook rules. The overall decision is coded as having been acted on and classified as being HCP led, but the birth party had most say. Decision 2 is a simpler and more directive decision regarding fetal monitoring in that it involves a single decision point classified as a midwife-initiated pronouncement, and responded to with no audible response. Given the directive nature of the decision-making, the decision was classified as being unilateral HCP led.
FIGURE 2.
Example of how a recording might be coded for more than one decision and one or more decision points per decision. DP, decision point.

Intercoder reliability testing
Intercoder reliability was tested using cross-tabulation and Cohen’s kappa. Three coders (LB-J, CJ and VL) independently produced coding for two randomly selected recordings to ensure that coders reliably identified the same forms of interactional practice, through the application of the coding scheme. The three coders agreed the identification of 16 decisions in common across the two recordings and reliability figures were calculated for four variables in each of these decisions (n = 64). These variables were the initiating format used in the first decision point, the responsive format that followed, whether or not the decision was pursued and the sharedness of the decision (overall). In accordance with Landis and Koch’s184 guidelines, there was substantial agreement for response format and sharedness (with κ between 0.50 and 0.81 and between 0.54 and 0.91, respectively), outstanding agreement for initiating format (with κ between 0.84 and 0.92) and moderate agreement for whether or not the course of action was pursued (with κ between 0.26 and 0.69). However, these figures can be partially explained by the variation between coding pairs, where a higher level of reliability was achieved between Clare Jackson and Victoria Land (i.e. the two project conversation analysts). Experience of CA was, therefore, an advantage. Given the time-consuming nature of continuing efforts to achieve reliability across all three coding pairs, it was agreed that Clare Jackson would code all of the data with Victoria Land’s oversight.
Interactional measures
The end result of the data extraction process was a multilevel hierarchical data set in which each labour was classified as consisting of a number of decisions and each decision classified as consisting of a number of decision points. Data from some decision point- and decision-level variables were aggregated to create higher-level variables. Therefore, the 37 recordings were the starting point for generating the overall quantitative figures used for statistical analyses (i.e. for analytical purposes, n may be the number of decision points, the number of decisions or the number of recordings). These variables are explained below.
Decision point-level variables used in the analysis were as follows:
-
Who initiated the decision-making.
-
Who responded.
-
What initiating format was used.
-
What response was given.
Decision-level variables used in the analysis were as follows:
-
What type of decision was being made.
-
How many decision points made up the decision.
-
Whether or not the proposed action was acted on.
-
An ordinal variable was derived from the researcher-coded level of sharedness question to measure the ‘balance’ in decision-making between HCPs and the birth party. The seven-point scale (see Development and application of the coding scheme) was used in its original form, with a low score on the scale indicating that decision-making was led more by the HCP and a high score indicating that decision-making was led more by the birth party.
-
Who initiated the decision-making in the first decision point.
-
Who responded to the first decision point.
-
What initiating format was used in the first decision point.
-
What response was given in the first decision point.
Labour-level variables used in the analysis were as follows:
-
Frequency of decision points in the labour.
-
Frequency of decisions in the labour.
-
Frequency of midwife-initiated decision points, midwife-initiated pain relief decision points and midwife-initiated fetal monitoring decision points that included each of the forms of decisional practice and equivalent variables showing the proportion of all decisions points that were initiated using each of the forms of decisional practice (e.g. the frequency of all midwife-initiated decision points in a single birth that were pronouncements and the proportion of all midwife-initiated pain relief decision points in a single birth that were option lists). Frequency variables were employed only if there were > 10 of the relevant decision points in the whole data set and proportion variables were used only for labours with > 10 of the relevant decision points. These variables measured the extent of the use of different forms of decisional practice by midwives.
-
Frequency of all woman-initiated decision points, all woman-initiated fetal monitoring decisions points and all women-initiated pain relief decision points that included each of the forms of decisional practice. Frequency of women-initiated decision points were employed only if there were > 10 of the relevant decision points in the whole data set. No proportion variables were used for women-initiated decision points, as most births had very few instances of each type. These variables measured the extent of the use of different forms of decisional practice by women.
-
Mean balance and sharedness scores across all midwife-initiated, pain relief and fetal monitoring decisions.
Quantitative analysis
Quantitative data analysis was conducted using IBM SPSS 25 (IBM SPSS Statistics, Armonk, NY, USA). Univariate analyses (e.g. frequencies, descriptive statistics, normality diagnostics) were conducted to summarise the data and explore the typical decision-making characteristics of the labours, including the average number of decisions per recording and the average number of decision points per decision, the types of decisions being made and the forms of decision-making most commonly used. Descriptive and inferential bivariate analyses (e.g. cross-tabulation with likelihood ratio chi-squared tests or comparisons of central tendency with Mann–Whitney U-tests, as appropriate) were used to investigate the associations between variables, including, for example, if certain types of decisions had more decision points, if certain responses were more commonly used in response to certain initiating formats and if different people were more likely to use certain forms of initiating format. There were relatively small numbers of missing values, but pairwise deletion was employed to deal with missing values to maximise sample size without the use of imputation methods.
The interactional data were also merged with, and used in combination with, the questionnaire data, and these analyses are discussed in Analysis of questionnaires.
Questionnaires
With permission from the authors (research team members JG and HB) and the University of Leeds, two self-completion questionnaires were adapted (with oversight from our lay collaborator and SUGs) from the ANQs and PNQs that had been validated and used to study decision-making in childbirth in the Great Expectations2 and Greater Expectations185 studies. Women chose to complete the surveys electronically (via Qualtrics) or by post.
The ANQ used a series of closed questions to survey key demographic information (e.g. age, ethnicity) and to establish women’s expectations of labour and birth. The ANQ covered aspects such as interactions with HCPs, birth planning, wants and expectations about labour and birth, dealing with pain, preferences about procedures during labour and birth, and experiences during the third stage. In addition, the ANQ included two questions about completing the questionnaire itself.
The PNQ sought to discover the extent of women’s satisfaction with labour and birth, and the degree to which they had wanted to be and actually were involved in decision-making. In this respect, the PNQ paralleled the ANQ topically, but contained a total of 71 questions and these, again, were divided into six sections: (1) medical staff, (2) what happened during labour (e.g. pain, BPs, complications/interventions, birth position, pushing and mode of delivery), (3) third stage, (4) labour as a whole, (5) being part of the study and (6) satisfaction (detail on response rates, which were high, can be found in Chapter 3).
Data collection
Consented women were invited to complete the ANQ at around 35 weeks of pregnancy and the PNQ at around 6 weeks after birth. Some women completed and returned the questionnaires after these times, often after a reminder text from the research midwives and/or from the researcher via Qualtrics. Confirmation was sought from the research midwives before sending out questionnaires in case women’s circumstances had changed (e.g. because of stillbirth). PNQs were sent to all women, whether or not they had been recorded, as we were interested in analysing the reported experiences of all women who gave birth in the MLU (i.e. recorded and non-recorded, and including those who moved to an OU, although the postnatal data from the latter are not included in this report).
Analysis of questionnaires
Antenatal questionnaire and PNQ data were captured via Qualtrics. Questionnaires completed in hard copy and returned by post were inputted into Qualtrics manually by the study intern (VÁT) and the questionnaire data exported to SPSS. This questionnaire data set, ethnicity (census categories) and SES (based on postcode, coded to IMD 2015) obtained from information at consent and the birth-level interactional data set were merged in SPSS and analysed using pairwise deletion to deal with missing values. The majority of the variables were employed with minimal recoding required beyond a reordering of a minority of response categories for analysis (e.g. in the PNQ, the questions on satisfaction were ordered on a five-point scale from very satisfied to very dissatisfied and these were reversed so that a value of 1 represents the most dissatisfied option and 5 the most satisfied) and setting some values as missing (e.g. ‘other’, ‘not applicable’). Some of the ordinal variables covering wants, expectations and experiences were recoded to combine adjacent categories with small numbers together. Satisfaction was measured (on a five-point scale, from very dissatisfied to very satisfied) through three separate questions:
-
How satisfied were you that you were listened to by staff?
-
How satisfied were you that your views were taken into account by staff?
-
How satisfied were you with the decisions that were made?
A single score conceptualised as ‘overall satisfaction’ was created by taking the mean of the three variables. Cronbach’s alpha indicates that the overall satisfaction measure is internally consistent (α = 0.827).
Descriptive univariate analyses were conducted to explore the characteristics of the sample, as well as women’s wants, expectations, experiences and satisfaction levels. Descriptive and non-parametric inferential bivariate analyses (i.e. cross-tabulations with likelihood ratio chi-squared tests, Kruskal–Wallis tests and Spearman’s correlations, as appropriate) were employed to explore associations between variables (e.g. the links between women’s expectations of involvement in decision-making and accounts of what actually happened and how they felt about it, and between questionnaire satisfaction data and what they reported actually happened in the labour and birth). In this analysis, which was focused solely on ANQ and PNQ data (see Chapter 3, Antenatal wants and expectations, and Chapter 3, The realities of choice: were wants and expectations met?), the full available sample was employed (rather than just the data from recorded births) because, as shown in Characteristics of the recorded sample of women, the reduced sample had similar demographic and satisfaction characteristics to the extended sample. This allowed us to fully exploit the data available to us.
For analyses involving both questionnaire data and interactional data (see Chapter 3, Interactional strategies of decision-making used during labour and birth, and Chapter 3, Decision-making practices and satisfaction with labour and birth), the same statistical methods were employed, but with the reduced sample. This analysis allowed us to investigate issues such as whether women’s levels of postnatal satisfaction were associated with researcher-coded measures of ‘sharedness’ and ‘balance’ or with the use of particular interactional formats during labour (described in Chapter 3, Decision-making practice and satisfaction).
Semistructured interviews with health-care practitioners
Data collection
In addition to their role in study set-up (see Introduction), interviews were used to understand HCPs’ perceptions of factors that facilitate or constrain women’s involvement in decision-making. The interviewees were a purposive sample of seven midwives and three obstetricians at each site (i.e. 14 midwives and six obstetricians in total), covering a range of grades and experience (for further details see Appendix 8). Obstetricians were included because, in one of the study sites (as already noted in The study sites), obstetricians may attend the MLU if called on and because, more generally, obstetricians have a role in maternity guidelines that affect midwives’ practice. HCPs were invited to take part by the principal investigators at each site and were provided with an information sheet. Written consent was obtained from HCPs prior to interviews and reconfirmed by the interviewers (EA, LB-J, SB-J and VL). All HCPs agreed to their interview being audio-recorded. Interviews lasted approximately 45 minutes and took place in a pre-booked room at each site. The interviews were professionally transcribed verbatim by a third party and transcripts anonymised (i.e. HCPs were given a pseudonym based on their site location, professional role and participation number). The interviewees and video-/audio-recorded HCPs were not purposively sampled to overlap because we did not seek to link interview accounts and interactional practices, but rather to use them to obtain a broad understanding of the practice context from a wide sample of HCPs. None of the obstetricians and only three of the midwives interviewed took part in the recordings of labour.
Thematic analysis of interviews
The interview transcripts were subjected to thematic analysis in their entirety by two of the researchers (EA and SB-J). This analysis started with a process of familiarisation via multiple readings of transcripts before developing a coding frame (which was discussed with the wider team). Both researchers coded the same two interviews (one obstetrician and one midwife) against the pilot coding frame, revised the coding frame and subsequently coded all interviews using NVivo 12 (QSR International, Warrington, UK).
Twelve principal themes were identified (see Appendix 9). Collectively, the themes revealed that staff perceived women’s involvement in decision-making as crucial yet constrained by a number of factors, such as unpredictable clinical contingencies during labour, guidelines concerning the management of risk and the varying extents to which women wanted to be involved. Although space precludes detailed engagement with interview data, these overarching findings provided vital insights into staff perspectives, helping us to contextualise and understand practices observed in the video-recordings/audio-recordings of labour, which are the primary focus of this report. When interviews provided specific insights, these are referenced in the analytic chapters (see Chapters 3–7).
Project documents
Project documents not included in the appendices of this report, including copies of the antenatal and postnatal questionnaires, consent forms, participant information sheets, HCP interview topic guide, and the conversation analysis data extraction form, can be found on the study Project page on the NIHR Journals Library website https://www.journalslibrary.nihr.ac.uk/programmes/hsdr/147073/#/).
Patient and public involvement
Patient and public involvement was central to the study design from the outset. Our research team originally included a lay member (Laura Cook), who was involved in the design of the research pre funding and also in PPI-related activities for the period post funding. In addition, we set up two SUGs comprising 22 users of maternity services (but not all members attended all SUG meetings). One group was in the vicinity of each study site for reasons of convenience to the membership (e.g. travel) and to advise on local aspects. One of the groups met before recruitment for the study commenced (chaired by Laura Cook) and both groups met three times (chaired by LB-J) during data collection and analysis periods to facilitate engagement with key stages of the research process (note that SUG members were paid for their time at INVOLVE rates and had expenses returned to them). Meetings were minuted to ensure that discussion accurately fed into the project. In addition, two service user representatives were recruited to the Study Steering Committee to ensure that PPI informs the development of dissemination activities from the study. Service users were involved with the study in the following ways.
Advising on type, and use, of camera
We presented various options for recording equipment and procedures. Following PPI, we selected Smots cameras because, despite their expense, they were viewed as the least intrusive and most secure option.
Advising on ethical challenges
Patient and public involvement generated crucial insights into how to deal with the ethics complexities of this project. The SUGs were asked to consider a series of key ‘ethical dilemmas’ and their answers informed the development of our recruitment and consent procedures (see Recordings of labour and birth). The SUGs also informed our protocol for camera operation and the prioritisation of the labouring person’s control over this (see Procedure for recording labour and birth). The NHS Research Ethics Committee opinion was that good PPI had been sought.
Revising participant-facing materials
Following PPI, we made major amendments to participant-facing materials, making them more accessible. This included the development of a lay summary that was subsequently used by NIHR as an example of good practice. PPI also raised issues that the research team had not previously considered. For example, a woman might think she could not take part in the study if she wanted a water birth and, therefore, the information sheet was revised to make it clear that water births were not an obstacle to participation.
Feeding into the analytic process by commenting on transcripts and work in progress by the study team
The SUGs were given anonymised transcripts of some early findings and asked to comment on what they thought was going on in the transcript. These discussions contributed to our understanding of service user perspectives on decision-making in maternity care.
Dissemination of findings
Service user group members were asked how best to disseminate the project findings and valuable information was received from both groups. In addition, some SUG members volunteered to assist with the delivery of dissemination workshops (currently postponed because of COVID-19).
Overall, although PPI was valuable throughout the study, its most significant contribution was to the development of an ethically robust research protocol. It is likely that the study design and recruitment materials would have been less effective without the modifications made in response to service user feedback.
Conclusion
This chapter has detailed the data collection and analysis procedures used in this mixed-methods study, including recordings of labour and birth analysed by CA and quantitative coding, ANQs and PNQs concerning women’s expectations about and experiences of decision-making, and background interviews with HCPs. In the chapter that follows (see Chapter 3), we illustrate how the two principal methods (i.e. questionnaires and quantitative coding of recordings of birth) were brought together to address the relationship between the interactional strategies used during labour and women’s later reported levels of satisfaction (study objective 3). In the remaining data analysis chapters (see Chapters 4–7), we focus primarily on the qualitative CA analysis of recordings to provide a fine-grained analysis of the verbal and non-verbal detail of interactions that take place in real time during birth (study objective 2). As noted in Chapter 1, the detailed CA of these interactions represents the core of this study.
Chapter 3 Expectations, experiences and satisfaction with care
Introduction
This chapter addresses the third study aim:
-
To assess whether or not women’s actual experiences reflect their antenatal expectations and whether or not there is an association between interactional strategies during labour (particularly the extent to which decisions are shared) and women’s later reported levels of satisfaction.
The first part of this chapter draws on ANQs to examine women’s ‘wants and expectations’ for how decision-making should take place during labour and birth. We then use PNQs to explore how far these wants and expectations were met. The second part of this chapter reports the range of interactional strategies used during labour and birth using data from the video-/audio-recordings and explores associations between women’s reports of how decision-making took place, researcher-coded interactional strategies of decision-making and postnatally reported satisfaction.
Sample and data: questionnaire analysis
As detailed in Chapter 2, the objective was to study women who laboured and gave birth in the two MLUs. Table 7 shows that almost 51% of the total questionnaire data set (comprising women who completed an ANQ and/or PNQ) spent at least some time in a MLU (some were transferred to an OU) and that just under 30% (n = 37) of these women were recorded and, therefore, subject to coding for the analysis of decision points and decision content (described later in this chapter). Although anticipating labouring and giving birth in a MLU, 46% (n = 57) of women became clinically ineligible and entered OUs rather than MLUs. This is higher than the 22% reported by the NHS Patient Survey Programme’s 2019 Survey of Women’s Experience of Maternity Care. 113 The remainder (n = 4, 3.2%) comprises women who, for example, moved to a new geographic area or chose to withdraw from the study in pregnancy.
| Care received | Recorded, n (%) | Non-recorded, n (%) | Total, n (%) |
|---|---|---|---|
| Midwife led | 37 (29.8) | 26 (21.0) | 63 (50.8) |
| OU | 0 | 57 (46.0) | 57 (46.0) |
| Other | 0 | 4 (3.2) | 4 (2.3) |
| Total | 37 (29.8) | 87 (70.2) | 124 (100) |
As Table 8 shows, the questionnaire response rates were very high, especially for the recorded sample: almost 92% (n = 34) of women completed an ANQ and just over 86% (n = 32) of women completed a PNQ. Around 78% (n = 29) of the recorded and almost 67% (n = 58) of the non-recorded samples completed both questionnaires. There was no overlap between the three recorded women who did not complete the ANQ and the five recorded women who did not complete the PNQ. We are unable to determine why these women (and others) did not respond. (As explained in Chapter 2, Data collection, reminders were sent.)
| Questionnaire | Questionnaire completed | Recorded: midwife led, n (%) | Non-recorded, n (%) | Total, n (%) | ||
|---|---|---|---|---|---|---|
| Midwife led | OU | Other | ||||
| ANQ | Yes | 34 (91.9) | 26 (100.0) | 53 (93.0) | 4 (100) | 117 (94.4) |
| No | 3 (8.1) | 0 | 4 (7.0) | 0 | 7 (5.6) | |
| Total | 37 (100) | 26 (100.0) | 57 (100.0) | 4 (100.0) | 124 (100.0) | |
| PNQ | Yes | 32 (86.5) | 21 (80.8) | 40 (70.2) | 1 (25.0) | 94 (75.8) |
| No | 5 (13.5) | 5 (19.2) | 17 (29.8) | 3 (75.0) | 30 (24.2) | |
| Total | 37 (100) | 26 (100.0) | 57 (100.0) | 4 (100.0) | 124 (100.0) | |
| Both | Yes | 29 (78.3) | 21 (80.8) | 36 (63.2) | 1 (25.0) | 87 (70.2) |
| = 58 (66.6) | ||||||
| No | 8 (21.6) | 5 (19.2) | 21 (36.8) | 3 (75.0) | 37 (29.8) | |
| Total | 37 (100) | 26 (100.0) | 57 (100.0) | 4 (100.0) | 124 (100.0) | |
Sample description
Table 9 describes key sample characteristics (recorded and non-recorded women) that, with the exception of SES (which was derived from residential postcodes), are based on ANQ responses. Here, and elsewhere, where samples do not comprise the total number eligible, then this reflects missing data. The sample is predominantly white. Almost two-thirds of the sample were expecting a first baby and one-third of the sample a subsequent baby. SES is widely distributed, although is slightly skewed towards residence in least deprived areas (for methodological detail, see Chapter 2). We are unable to account empirically for the slight skewness of the sample towards residence in higher SES areas. It is possible that respondents in least deprived areas feel more comfortable in engaging in research and are more able to devote the time to completing study questionnaires. As discussed in Chapter 2, there are no statistically significant differences in these key characteristics between recorded and non-recorded women.
| Characteristic | Sample result |
|---|---|
| Ethnicity, n (%) | |
| White | 116 (94.3) |
| Mixed/multiple ethnic group | 1 (0.8) |
| Asian/Asian British | 3 (2.4) |
| Black/African/Caribbean/black British | 2 (1.6) |
| Other | 1 (0.8) |
| Total | 123 (99.9) |
| Parity, n (%) | |
| First labour/birth | 77 (66.4) |
| Subsequent labour/birth | 39 (33.6) |
| Total | 116 (100.0) |
| SES | |
| Mean | 5.89 |
| Median | 6.0 |
| Mode | 4 |
| SD | 2.841 |
| Skewness | –0.029 |
| n | 124 |
Antenatal wants and expectations
As all women who completed ANQs were expecting to give birth in MLUs, the analysis of wants and expectations is based on the total sample (n = 117) (i.e. irrespective of whether or not they actually laboured/birthed there and whether or not they were recorded or not). Here, and elsewhere, the wording of question response options is abbreviated for ease of presentation.
As Chapters 4–7 use video and/or audio data to explore how decision-making takes place, we describe women’s orientation to communication and feelings about common procedures and pain relief. Most (90%) women reported being fully able to discuss what they wanted during pregnancy either ‘always’ or ‘most of the time’ (and the remainder said this happened ‘only occasionally’ or ‘hardly ever’). Most women were ‘always’ (46%) or ‘sometimes, but sometimes not’ (49%) as assertive as they want to be in communication with HCPs (and for 5% of women this was ‘hardly ever’ the case). Moreover, the large majority (73%) of women wanted to know as much as possible about what might happen during labour. At the time of completing their ANQ, slightly less than half (47%) of women had made a birth plan, although 23% of women were ‘intending’ to and 11% were ‘considering’ it. Postnatally, 68.5% of women reported having done so (including the majority of those who were ‘intending’ to antenatally), whereas 31.5% of women had not.
Women’s feelings about common procedures are shown in Figure 3. Most women were positively disposed towards or ‘don’t mind’ fetal monitoring at intervals and primarily ‘don’t mind’ VEs. As these procedures are part of the NICE intrapartum care pathway,10 they are probably part of women’s routine expectations. The other five procedures, however, show a different pattern. Women generally preferred not to have or ‘don’t mind’ continuous fetal monitoring, drugs to speed labour, induction and episiotomy, bearing out previous research that women tend to choose MLUs because they prefer physiological over managed birth. 20,186,187 Although around half of women ‘don’t mind’ having their waters broken, most of the rest preferred not to have or definitely did not want this to happen.
FIGURE 3.
What happens in labour: feelings about procedures that may be proposed.
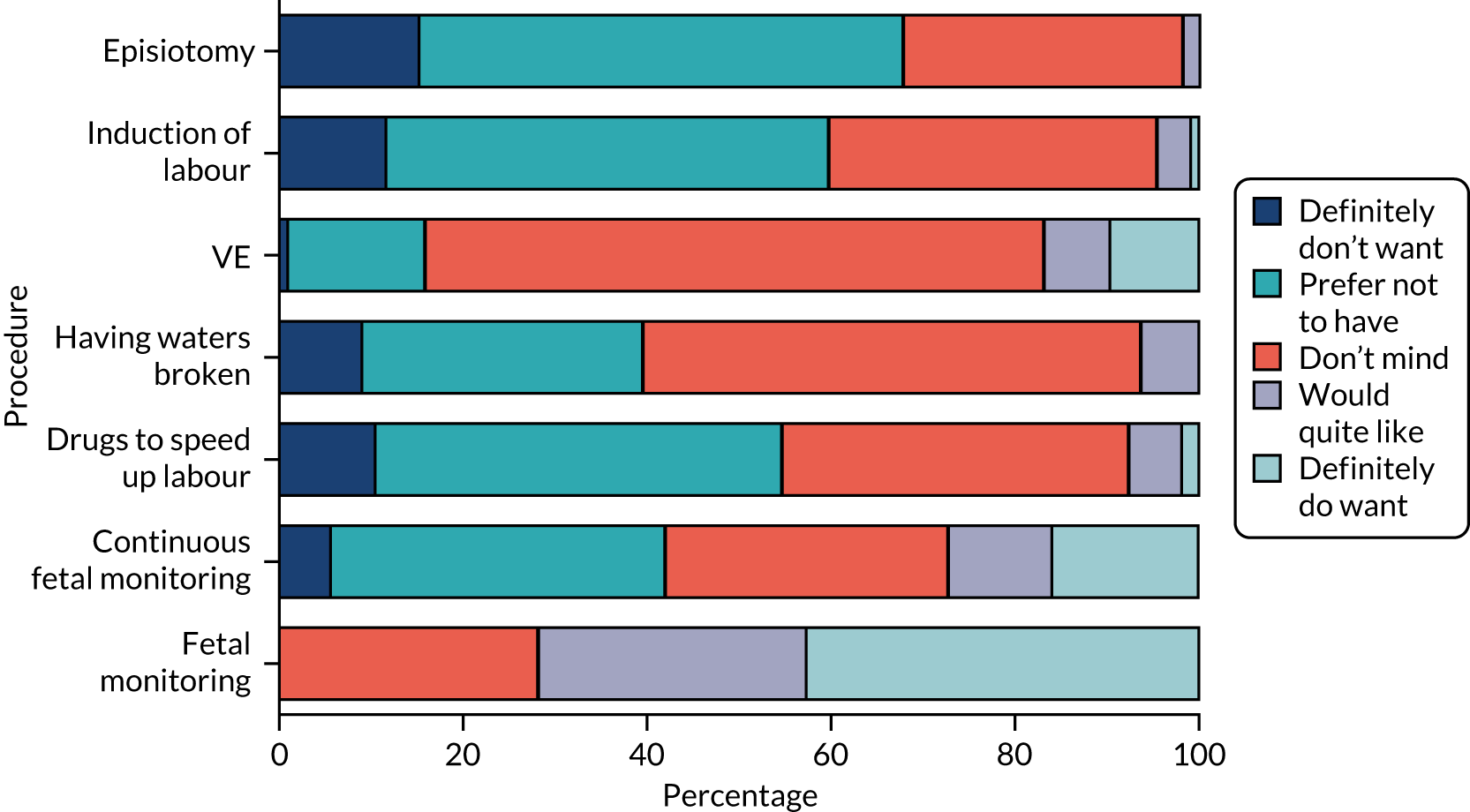
Figure 4 shows that sizeable majorities of women would ‘quite’ or ‘definitely’ like to use breathing and relaxation, and gas and air. Although many women ‘preferred not to use’ or ‘definitely did not want’ an epidural and an injection of opiate, it is notable that 23.0% and 26.4%, respectively, said that they would ‘not mind’ these.
FIGURE 4.
Methods of pain relief.
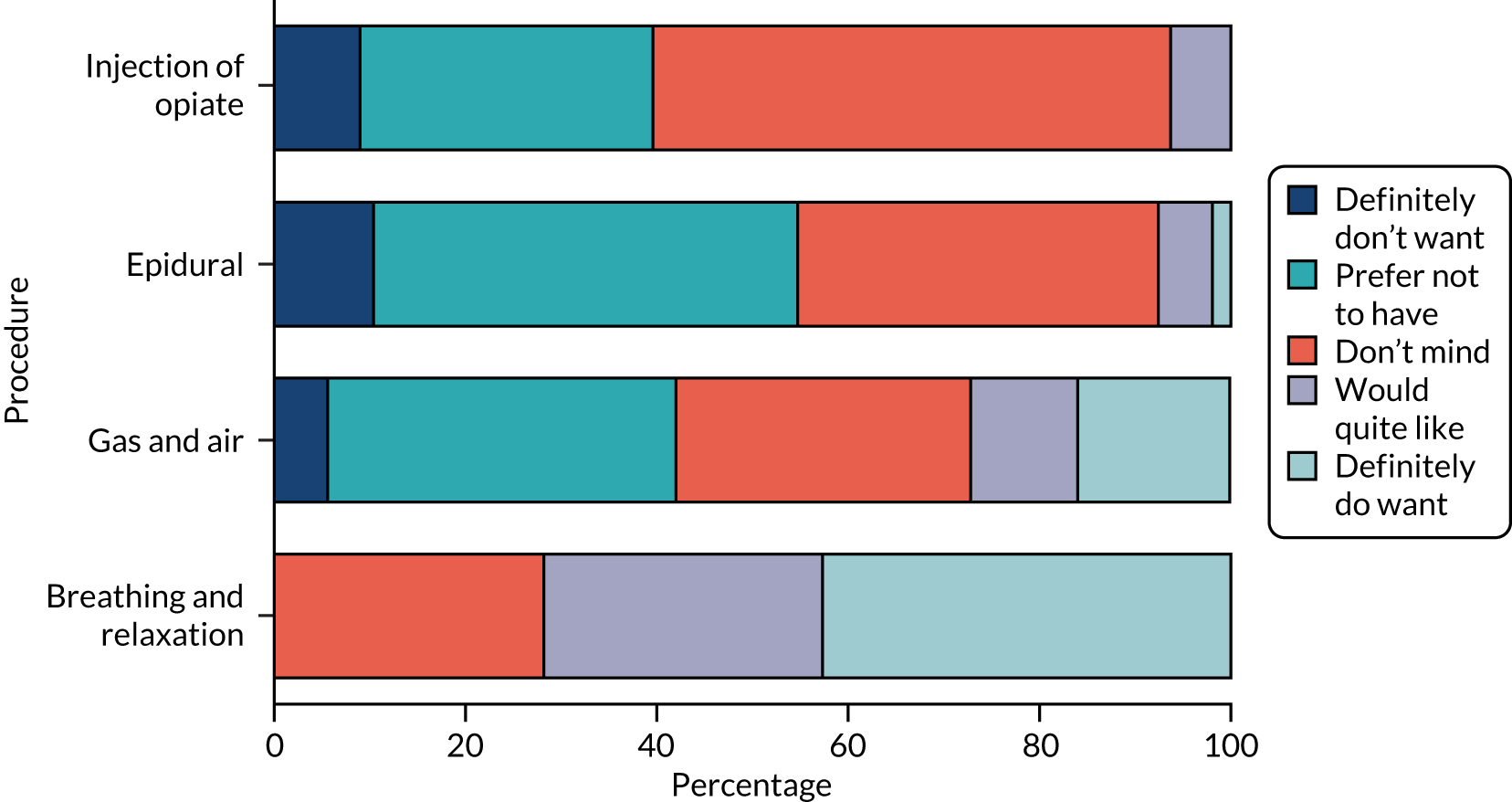
Although women articulated clear preferences for pain relief and for many procedures, sizeable numbers ‘didn’t mind’, suggesting a neutral or open-minded position. Given that making a choice may be seen as a gamble and planning can lead to disappointment,99,188–190 this may be a way of managing the unpredictability of labour and birth. Consequently, some women may have felt that they wanted to ‘go with the flow’,186,191 a corollary of open-mindedness, rather than to formulate preferences (something also conveyed by midwives in interviews). Moreover, women may have wished to retain an element of potential control through articulated preferences while simultaneously entrusting those providing care. 192
Our analysis of reported wants and expectations of ‘being in control of what is done to you’ during labour revealed that most women either wanted ‘very much’ (51%) or would ‘quite like’ (34%) to be in control, whereas the rest ‘didn’t mind’ (12%) or ‘preferred not to be’ (3%) (none ‘definitely didn’t want to be’). Most women expected that they ‘probably’ would (54%), or were ‘sure’ (14%) they would, be in control. However, a notable 26% of women ‘didn’t have any expectations’ (only 6% expected that they ‘probably wouldn’t be’ and only one was ‘sure’ she would not be in control). To explore statistical associations between wants and expectations, we recoded variables to reflect what we conceptualised as either ‘woman oriented’ or ‘staff oriented’. Women-oriented wants included ‘want very much’, ‘quite like’ and ‘don’t mind’ and woman-oriented expectations included ‘sure will be’, ‘probably will be’ and ‘don’t have any expectations’. Staff-oriented wants included ‘prefer not to be’ and ‘definitely don’t want to be’ and staff-oriented expectations included ‘probably won’t be’ and ‘sure won’t be’. Table 10 shows a statistically significant association (p < 0.001) between wants and expectations. The majority of women both wanted and expected control to be woman oriented. Even so, almost 20% of women wanted control to be ‘women oriented’, but expected that it would actually be ‘staff oriented’.
| Expectations | Orientations | Want to be in control, n (%) | ||
|---|---|---|---|---|
| Staff oriented | Woman oriented | Total | ||
| Expect to be in control | Staff oriented | 15 (12.9) | 23 (19.8) | 38 (32.7) |
| Woman oriented | 2 (1.7) | 76 (65.5) | 78 (67.2) | |
| Total | 17 (14.6) | 99 (85.3) | 116 (99.9) | |
As pain relief features strongly in communication during labour193 (see Chapter 6), we considered how involved women wanted and expected staff to be in decision-making generally. In terms of ‘wants’, most women rejected the extremes of ‘leaving it totally up to the staff to make the right decision’ and not wanting ‘any staff involvement’, opting for the middle categories of ‘I would like staff to advise me and I will probably take their advice’ (just over 37%) and ‘I would like to staff to advise me, but I will still make my own mind up even if my decision is different to their advice’ (59%). This broadly supports research by O’Cathain et al. ,112 who found that 54% of women preferred ‘to make the final choice after seriously considering the midwives’ and doctors’ opinion’. Expectations about pain relief decision-making in our study also fell primarily into the middle two categories, with slightly more women expecting staff to advise them but to still make up their own mind even if their decision may be different (53%) than to be advised by staff and probably to take that advice (45%).
To analyse relationships between wants and expectations about pain relief decision-making, we similarly recoded variables into ‘staff oriented’ (combining ‘I will leave it totally up to the staff to make the right decision’ and ‘I would like the staff to advise me, but I will still make up my own mind even if my decision is different to their advice’) and ‘woman oriented’ (combining ‘I would like staff to advise me, but will still make up own mind even if my decision is different to their advice’ and ‘I don’t want any staff involvement’). Table 11 shows a highly significant association (p < 0.001) between wants and expectations, with just over half (51.7%) of the sample both wanting and expecting pain relief decision-making to be ‘woman oriented’. Women held these wants and expectations even though most were expecting labour (‘without drugs’) to be ‘very’ (61.7%) or ‘unbearably’ (19.1%) painful.
| Expectations | Orientations | Want to be in control, n (%) | ||
|---|---|---|---|---|
| Staff oriented | Women oriented | Total | ||
| Expect to be in control | Staff oriented | 41 (35.3) | 12 (10.3) | 53 (45.7) |
| Women oriented | 3 (2.6) | 60 (51.7) | 63 (54.3) | |
| Total | 44 (37.9) | 72 (62.0) | 116 (100.0) | |
In summary, women generally felt assured in their interactions with practitioners, wanted to know about what would happen in labour and, with the important exceptions of VEs and intermittent fetal monitoring, in the main ‘didn’t mind’ or preferred not to have the range of procedures that often accompany hospital birth. The large majority of women wanted to use breathing/relaxation and gas and air for pain, but most preferred not/definitely did not want to have an epidural or opiate injection (although a substantial minority of women ‘didn’t mind’ these). Most women expressed an overall desire for control over what doctors and midwives would do to them during labour and aspired to be engaged with decision-making (although to varying degrees). Moreover, most women expected a match between what they wanted to happen/what should happen and what actually would happen during labour and birth, be this wanting and expecting control and decision-making to be women oriented (generally preferred) or to be staff oriented (much less preferred).
The realities of choice: were wants and expectations met?
The analysis of how far wants and expectations were met includes only women who laboured in the MLUs for at least a period of time because it is their experiences that primarily concern us. This analysis comprises a maximum of 53 women (recorded, n = 32; non-recorded, n = 21) who completed a PNQ or a maximum of 50 women (recorded, n = 29; non-recorded, n = 21) for combined ANQ and PNQ data (see Table 8).
The significant majority (98%) of women had not met any of the midwives who looked after them during labour. However, 79% of women had at least one midwife who was with them throughout and all had a BP. As already noted, just over 68% of women had prepared a birth plan. Rather than being ‘exactly followed’ (8%), plans mostly ‘guided what happened’ (50%), although 19% of women indicated that staff ‘did not use’ the plan. Of the remainder, a few (8%) reported changing their mind about the plan or that it changed because of an emergency (11%) (one woman was not sure how the plan was used).
Over half (60%) of the women were as assertive as they wanted to be when talking to staff during labour and birth, 34% ‘sometimes were and sometimes weren’t’ as assertive as they wanted to be and just 6% reported that that they were ‘hardly ever’ as assertive as they wanted to be. No relationship was found between antenatal reports of assertiveness when talking to health professions generally and women’s postnatal accounts of whether or not they were as assertive as they wanted to be (ρ = 0.156; p = 0.278). Moreover, the majority of women were ‘sure’ (26%) that they were, or ‘probably’ (49%) were, in control of what midwives did to them in labour (with 23% ‘sometimes’ sure they were and 2% ‘sure they were not’).
Research points to what Lally et al. 194 characterise as the ‘expectation–experience gap’, in which antenatal expectations and postnatal reports of personal control and procedures/interventions either fail to match up (i.e. expecting fewer, but having more)195,196 or are lowly correlated. 197 Furthermore, the greater the incongruence between planned and actual experience, the lower levels of satisfaction with labour and birth have been found to be. 70,195,196,198,199 Therefore, we analysed how far women’s postnatal accounts of what they had wanted reflected their antenatal expressions. We asked three antenatally/postnatally matched questions to measure the extent to which women wanted to be in control of decision-making, each on an ordinal scale ranging from ‘no, I would prefer/preferred not to be’ to ‘yes, I want/wanted this very much’. Table 12 shows the cross-tabulation of ‘wants’ for being in control expressed antenatally and postnatally regarding control over what staff do during labour. We observe a significant moderate correlation between the two ordinal variables (ρ = 0.335; p = 0.018) (i.e. women who indicated they wanted to be in control antenatally were more likely to specify postnatally that they had wanted to be in control during labour/birth). Further analyses indicate a similar correspondence between antenatal expectations of wants and postnatal reporting of wants during labour in the extent to which women wanted to be in control of decisions about labour (ρ = 0.337; p = 0.017; n = 50) and the extent to which they thought decisions about labour should be made by staff or by themselves, assuming no complications (ρ = 0.342; p = 0.016; n = 49) (cross-tabulations not shown).
| Wants | Wanted during birth (reported postnatally), n (%) | |||||
|---|---|---|---|---|---|---|
| No, I preferred not to be | I didn’t mind | Yes, I quite wanted this | Yes, I wanted this very much | Total | ||
| Wanted antenatally | No, I would prefer not to be | 0 (0.0) | 0 (0.0) | 0 (0) | 1 (100.0) | 3 (100.0) |
| I don’t mind | 0 (0.0) | 4 (44.4) | 5 (55.6) | 0 (0) | 9 (100.0) | |
| Yes, I would quite like this | 0 (0.0) | 9 (45.0) | 6 (30.0) | 5 (25.0) | 20 (100.0) | |
| Yes, I want this very much | 0 (0.0) | 3 (15.8) | 6 (31.6) | 10 (52.6) | 19 (100.0) | |
| Total | 0 (0.0) | 16 (32.7) | 17 (34.7) | 16 (32.7) | 49 (100.0) | |
As shown in Table 13, when asked about common procedures and pain relief, women tended to report postnatally that they had wanted ‘staff to advise them and expected to take staff advice’. Even so, almost 43% of women reported that they had wanted to leave decisions about fetal monitoring ‘totally’ up to midwives, and just over 64% ultimately wanted to ‘make up their own mind’ about pain relief. Therefore, it is unsurprising that their postnatal accounts of what actually happened (Table 14) show how uncommon it was to go against staff advice. More frequently, decisions were either made entirely by staff or women reported taking the advice staff gave them (which mostly was what they said they had wanted). However, a comparison of the data in Tables 13 and 14 shows that differences between what women said they had wanted and their reports of what actually happened (both reported postnatally) were primarily between wanting ‘staff to advise me but still make up my own mind (even if my decision different from staff)’ to reporting that actually ‘staff advised me and I took the advice’ (see Appendix 10 for cross-tabulations confirming this). Although, ostensibly, this shows that decisions turned out to be more ‘staff oriented’ (or midwife initiated) than women had wanted, it is perhaps more likely to suggest that although women may have been reserving the option to go against staff advice, the need do so did not arise and/or that what they personally wanted coincided with what staff advised.
| Procedure | Decision wanted, n (%) | ||||
|---|---|---|---|---|---|
| Leave totally to staff | Staff advise and expected to take advice | Staff advise me, make up own mind | No staff involvement | Total | |
| Fetal monitoring | 21 (42.9) | 22 (44.9) | 6 (12.2) | 0 (0.0) | 49 (100.0) |
| VE | 9 (17.9) | 29 (56.6) | 13 (25.5) | 0 (0.0) | 51 (100.0) |
| Pain relief | 2 (3.5) | 17 (32.1) | 34 (64.2) | 0 (0.0) | 53 (100.1) |
| Placenta | 6 (12.0) | 18 (36.0) | 21 (42.0) | 5 (10.0) | 50 (100.0) |
| Cord clamping | 11 (23.9) | 18 (39.1) | 12 (26.1) | 5 (10.9) | 46 (100.0) |
| Skin to skin | 5 (10.2) | 21 (42.9) | 12 (24.9) | 11 (22.4) | 49 (100.0) |
| Vitamin K injection | 1 (2.0) | 36 (72.0) | 6 (12.0) | 7 (14.0) | 50 (100.0) |
| Procedure | Decision made, n (%) | ||||
|---|---|---|---|---|---|
| Entirely by staff | Staff advised me, I took the advice | Staff advised me, I decided not to take the advice | No staff involvement | Total | |
| Fetal monitoring | 24 (50.0) | 20 (41.7) | 3 (6.3) | 1 (2.1) | 48 (100.1) |
| VE | 7 (14.3) | 40 (81.6) | 1 (2.0) | 1 (2.0) | 49 (99.9) |
| Pain relief | 3 (5.9) | 44 (86.3) | 2 (3.9) | 2 (3.9) | 51 (100.0) |
| Placenta | 6 (12.5) | 28 (58.3) | 4 (8.3) | 10 (20.8) | 48 (99.9) |
| Stitches | 24 (58.5) | 17 (41.5) | 0 (0.0) | 0 (0.0) | 41 (100.0) |
| Cord clamping | 22 (45.8) | 22 (45.8) | 4 (8.3) | 0 (0.0) | 48 (99.9) |
| Skin to skin | 7 (14.9) | 26 (55.3) | 1 (2.1) | 13 (27.7) | 47 (100.0) |
| Vitamin K injection | 1 (1.9) | 44 (84.6) | 0 (0.0) | 7 (13.5) | 52 (100.0) |
Table 15 reports correlations between postnatal reports of how women wanted decision-making to take place and what actually happened for the majority of the common procedures. The strength of the effect sizes varies, being strong for decisions about skin to skin (ρ = 0.769) and fetal monitoring (ρ = 0.513), but only moderate for VEs (ρ = 0.320), placenta (ρ = 0.301), cord clamping (ρ = 0.364) and vitamin K injection (ρ = 0.452). There was no significant relationship between what women reported postnatally that they had wanted to happen and what actually happened for pain relief (ρ = 0.219; p = 0.136). It is worth noting that when this same analysis was undertaken with the subsample (n = 37) of women whose births were recorded (results not shown here), the findings were very similar, although the positive pain relief correlation increased in magnitude and became significant (Spearman’s r = 0.364; p ≤ 0.046; n = 31). In combination, these findings on the links between antenatal wants and postnatally reported wants and actual experiences during labour/birth suggest that the ‘expectation–experience gap’ was less apparent in our sample than in previous research,194,195 but that it varied greatly according to the type of decision concerned.
| Procedure | Spearman’s r | Significance | n |
|---|---|---|---|
| Pain relief | 0.146 | Non-significant | 50 |
| Fetal monitoring | 0.513 | p < 0.01 | 47 |
| VE | 0.320 | p < 0.05 | 49 |
| Placenta | 0.301 | p < 0.05 | 48 |
| Skin to skin | 0.769 | p < 0.01 | 45 |
| Cord clamping | 0.364 | p < 0.05 | 45 |
| Vitamin K injection | 0.452 | p < 0.01 | 50 |
To summarise, the majority of women antenatally reported a wish to be involved in decision-making during labour and birth. Most women also expected there to be a match between what they wanted to happen/what should happen and what would happen, whether this was for more ‘woman-oriented’ (the majority) or more ‘staff-oriented’ (the minority) decision-making. However, postnatal responses tend to show that women wanted decision-making either to be led by staff or to be advised by staff and to take that advice, and, broadly, this is what actually happened (based on their reports). Instances of women being advised by staff but not taking the advice, or of there being no staff involvement in decisions, were relatively rare. However, shifts between what women said they had wanted and what actually happened (both reported postnatally) were primarily between wanting ‘staff to advise me but still make up my own mind (even if my decision different from staff)’ and ‘staff advised me and I took the advice’, which probably reflects that the need to go against staff advice did not arise. In the next part of the chapter, we analyse how decision-making actually took place during the 37 labours and births that were video-/audio-recorded.
Interactional strategies of decision-making used during labour and birth
All 37 recordings included at least one codeable decision, and the total number of decisions coded was 858. The number of decisions coded per recording ranged from 1 to 67, with a median number of 22 coded decisions. There were 1574 decision points, and the number of decision points per decision ranged from 1 to 18, with a median of 1. A large majority (96.8%) of coded decisions were completed within five or fewer decision points.
Almost half (n = 403, 47.0%) of coded decisions concerned fetal monitoring. This is not surprising given NICE guideline recommendations for monitoring every 15 minutes during first stage of labour and every 5 minutes during second stage of labour. 10 The next largest category was of decisions related to pain relief (n = 119, 13.8%). A further 8.2% (n = 70) and 10.4% (n = 89) were related to position during first and second stage, respectively, with 8.5% (n = 73) related to VEs. Because there are more of these kinds of decisions than we have recordings, the implication is that these decisions occur recurrently in any labour. We captured relatively few decisions about other aspects of care, including artificial rupture of membranes and ‘third-stage’ decisions (e.g. placental delivery, cord clamping, skin to skin and vitamin K injections). These decisions are typically discussed and/or carried out only once during the intrapartum period and so small numbers are to be expected.
There is statistically significant variation in the number of decision points needed to complete a decision by decisional content [H(11) = 251.0; p < 0.001; ε2 = 0.293]. Figure 5 illustrates this by showing the percentage of decisions that took only a single decision point to complete for each type of decision coded. For example, the majority of skin-to-skin (93.8%) and fetal monitoring decisions (86.6%) were initiated and agreed within a single decision point, whereas this is true for only 33.1% of pain relief decisions. In fact, the only decisions that took more than eight decision points to complete were related to pain relief (data not shown). As elaborated in Chapter 5, only 23% of VE and artificial rupture of membranes decisions were completed within a single decision point.
FIGURE 5.
Percentage of decision types completed at first decision point by decisional content. ARM, artificial rupture of membranes.
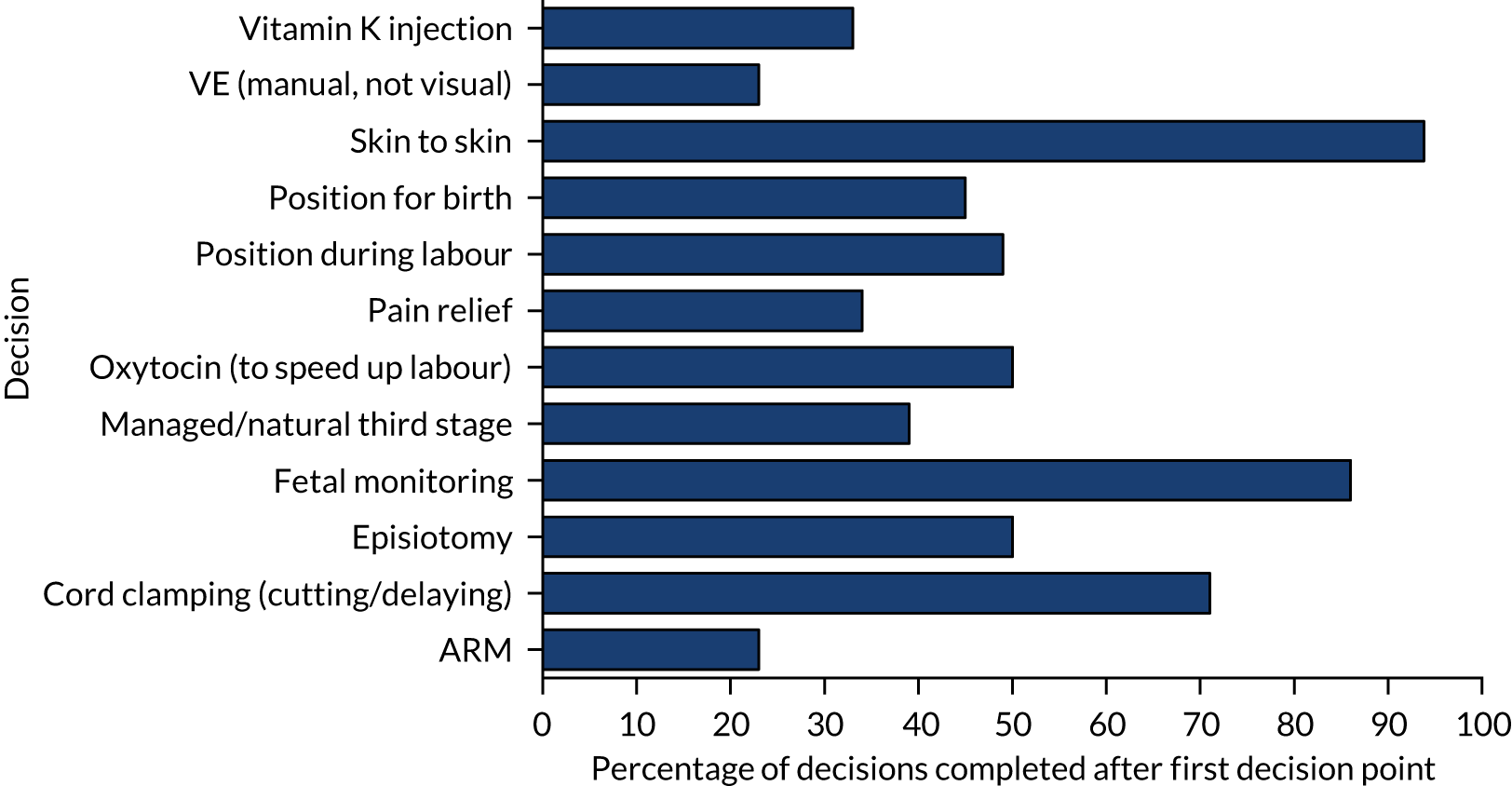
Who initiates decisions and how?
A majority of decisions (88.5%) were initiated by midwives at the first decision point, and midwives initiated the majority (85.3%) of decision points overall. Labouring women initiated only 7.6% of decisions at the first decision point and only 9.7% of all decision points. Taken together, this suggests that decision-making tends to be midwife initiated, which is supported by women’s PNQ responses (see Tables 13 and 14). However, this does not take into account the format of initiating turns, which might variably invite women’s participation (e.g. by option listing or offering).
Table 16 shows the frequency of initiating formats used across all decision points by midwives and women. There is a highly significant difference (p < 0.001) between midwives and women in terms of the initiating formats they employ. Pronouncements and recommendations/suggestions/proposals make up the largest proportion of midwife-initiated decision points (together appearing in 47.0% of all midwife-initiated decision points). Midwives do use the more participatory formats of offers and option lists, but more rarely than the ‘unilateral’ formats.
| Format used | Midwives, n (%) | Women, n (%) |
|---|---|---|
| Just do it (no audible initiating turn) | 107 (8.0) | 0 (0.0) |
| Pronouncement with/without tag | 341 (25.4) | 5 (3.3) |
| Instruction/command/demand | 46 (3.4) | 9 (6.0) |
| Recommendation/suggestion/proposal | 290 (21.6) | 8 (5.3) |
| Request | 128 (9.5) | 41 (40.4) |
| Offer | 181 (13.5) | 1 (0.7) |
| Open question | 42 (3.1) | 18 (11.9) |
| Option list | 83 (6.2) | 0 (0.0) |
| Closed yes/no question | 94 (7.0) | 15 (9.9) |
| Decision-implicative statement | 26 (1.9) | 32 (21.2) |
| Indecipherable | 3 (0.2) | 2 (1.3) |
| Total | 1341 (100.0) | 151 (100.0) |
In addition, we see that, although midwives use all the formats on which we coded, women do not. This reflects the institutionalised statuses and associated rights that each group embodies. Women, for example, are not really in a position to generate option lists (although they may request options). The highest proportion of women-initiated decision points are in the format of requests (just over 40% of total initiating decision points), which, in general, passes the decision to the HCPs. The nil return on women’s ‘just do it’ is a factor of the coding scheme. This category was introduced to capture fetal monitoring decisions, which we could hear as happening even when we had access to audio-only recordings. Women do ‘just’ change position, for example, but we could not include this in the coding scheme to manage audio and visual data equitably.
In general, on the question of who initiates decisions, it is clear that it is midwives and, with the exception of pain relief, this broadly matches women’s postnatal reports. In answer to how decisions are made, it is equally clear that, overall, decisions are initiated more frequently in what might be characterised as unilateral, rather than in participatory, formats. The relatively low frequency of women-initiated decisions (and decision points) suggests that women generally have a more responsive than initiating role in decision-making (at least as coded). However, the format used by midwives varies significantly [χ2(12) = 164.789; p < 0.001, Cramer’s V = 0.392] according to the type of decision being made (here, and in the analyses in the remainder of Interactional strategies of decision-making used during labour and birth, only categories with total frequencies > 20 are included in the analysis for chi-squared tests to minimise empty and low n cells in the cross-tabulation). Figure 6 shows the percentage of formats midwives used to initiate different types of decisions. It is clear that fetal monitoring (the only decision type that occurs with no verbal initiator) is generally pronounced or requested (see Chapter 4). Offers occur in pain relief decisions, as do open questions, recommendations and option lists. Instructions/demands/commands do not occur frequently; however, when they do, a large proportion is in relation to position during the second stage. The ways that women are interactionally invited to participate in decision-making, then, depends on the type of decision being made. Interestingly, although there are few decisions about managed or physiological third stage and cord clamping, these do tend to be participatory (i.e. initiated by midwives’ option lists or offers, respectively; see Chapter 7). There is, perhaps surprisingly, a high proportion of VEs initiated via pronouncements (see Chapter 5).
FIGURE 6.
Stacked bar chart of initiating format used by midwives (at first decision points) by decision type. ARM, artificial rupture of membranes.

Figure 7 shows the percentage formats used by women to initiate different types of decisions. Women initiate a smaller range of decisions (never, for example, initiating decisions about fetal monitoring or vitamin K injection) and use a smaller number of formats than midwives. Embodying their institutional position vis-à-vis midwives, women tend to use requests, especially in relation to pain relief. Decision-implicative statements and open/closed questions are used across a variety of decision types (significance testing was not conducted for this comparison because of small numbers in many groups).
FIGURE 7.
Stacked bar chart of initiating formats used by women (across first decision points) by decision type. ARM, artificial rupture of membranes.
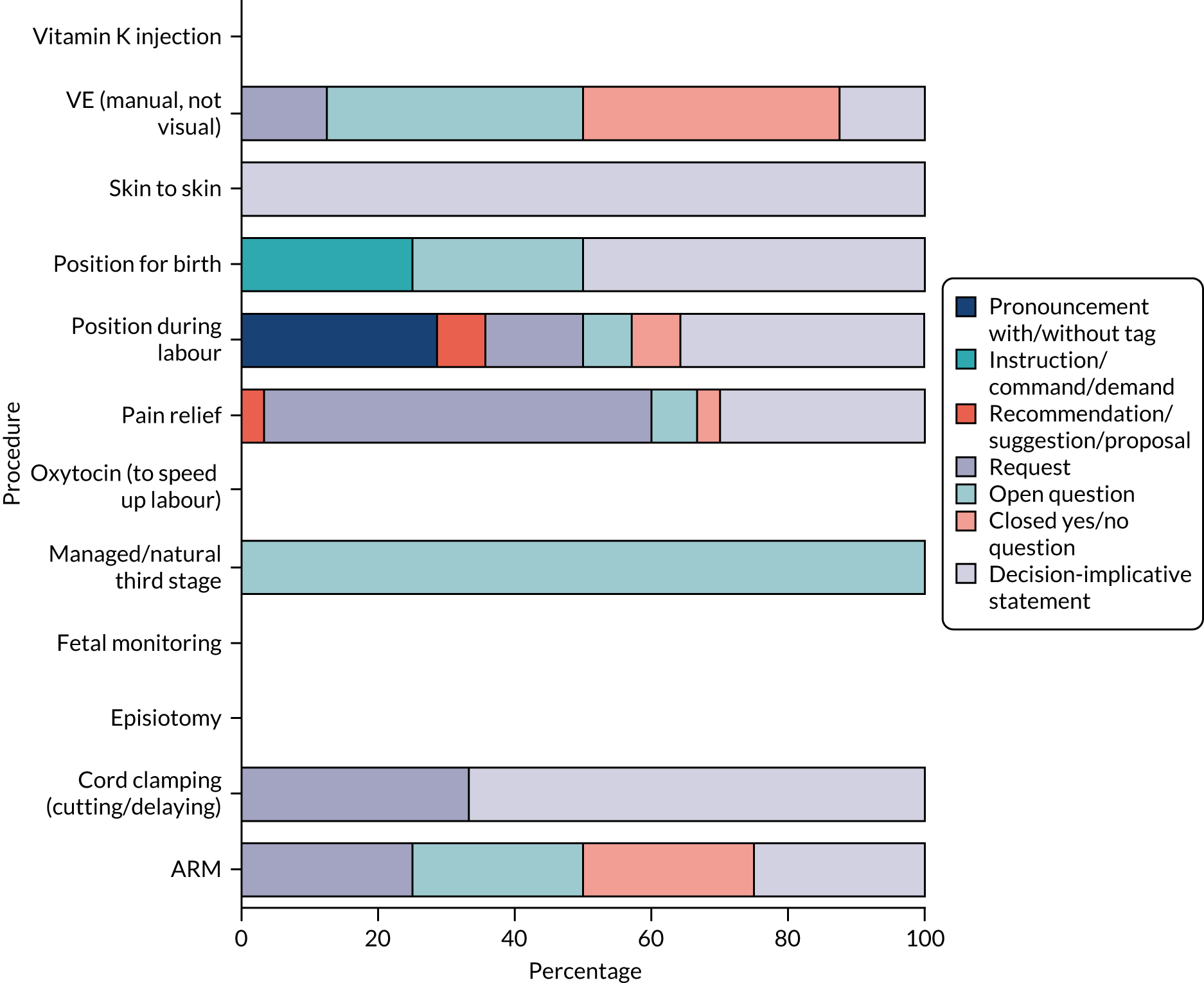
Who responds and how?
When midwives initiate decisions, around half (46.6% at the first decision point and 53.4% across all decision points) of the decisions are responded to by the woman. In contrast, a large majority (90.8% of first decision points and 88.1% across all decision points) of women-initiated decisions are responded to by midwives. As these figures represent the largest proportion of decisions and responses, it is clear that BPs do not play a major interactional role in decision-making.
When midwives initiated decisions, almost half (49.1% at the first decision point and 41.0% across all decision points) of the decisions received no verbal response from anyone (as noted, we did not code for non-verbal responses because of the matter of handling both audio- and video-recordings). Across all decision points, < 5% of midwife-initiated decision points are verbally rejected/declined and 35.4% are agreed/accepted/option selected (with 40.6% getting no verbal response). In contrast, when women initiate decisions, 23.8% are rejected/declined and 24.5% are agreed/accepted. Around 10% of women-initiated decisions are deferred and another 11.9% occasion information provision from midwives.
These overall figures obscure the fact that there are significant differences in response based on initiating form [χ2(6) = 49.816, p < 0.001; Cramer’s V = 0.325] and also in outcome based on initiating form [χ2(9) = 242.2; p < 0.001; Cramer’s V = 0.417]. The ‘just do it’ initiating format, for example, nearly always (96.3%) occasions no verbal response and the suggested action also ends up happening 96.3% of the time. In contrast, only 38.3% of actions initiated as offers are agreed and 35.7% are carried through. As requests are used by both midwives and women (although generally in relation to different decisions, i.e. fetal monitoring and pain relief, respectively), it is interesting to see how these are responded to. Midwife-initiated requests are agreed to on 49.6% occasions, but rejected on only 1.6% of occasions. In contrast, women’s requests are agreed to on 30% of occasions and rejected 30% of the time. The context of what the decision is about is important here because fetal monitoring appears to be treated by all parties as routine and pain relief as negotiable.
In summary, the analysis shows that decision-making was primarily midwife initiated. Pronouncements and recommendations predominate in midwife-initiated decision points. However, for women, requests (especially in relation to pain relief) and, to a lesser extent, decision-implicative statements, prevail.
Decision-making practices and satisfaction with labour and birth
Women’s perception of decision-making and satisfaction
Part of our third study aim involved the exploration of associations between interactional strategies used during labour and the measures of women’s satisfaction, as described in Chapter 2. Table 17 shows that satisfaction was very high. The distributions are highly skewed (Shapiro–Wilks p < 0.001), showing that there is only limited discrimination among respondents.
| Satisfaction measure | n | Minimum | Maximum | Median | Mean | SD | Shapiro–Wilks p-value |
|---|---|---|---|---|---|---|---|
| Listened to | 32 | 1 | 5 | 5 | 4.38 | 1.1 | < 0.001 |
| My views taken into account | 32 | 2 | 5 | 5 | 4.44 | 0.914 | < 0.001 |
| How decisions made | 31 | 2 | 5 | 5 | 4.74 | 0.682 | < 0.001 |
| Mean (overall) satisfaction | 31 | 2 | 5 | 5 | 4.548 | 0.777 | < 0.001 |
Analyses examining associations between satisfaction measures and women’s postnatal reports of decision-making showed strong (ρ > 0.05) significant correlations (p < 0.01) between ‘feeling of being in control’ and two of the three dimensions of satisfaction [i.e. ‘listened to by staff’ (ρ = 0.543), ‘my views were taken into account’ (ρ = 0.569) and overall satisfaction (ρ = 0.523)] and there was a moderate-strength correlation (ρ = 0.300) with ‘satisfied with decisions made’ (ρ = 0.380). The more in control women felt, the more satisfied they were. However, none of the correlations between satisfaction and ‘who made the decisions’ was significant. There were some interesting patterns in the seven decision-specific variables, including the fact that women who were more involved in the decision about how the placenta came away reported a higher satisfaction in terms of being ‘listened to’ by staff (ρ = 0.384; p < 0.05). However, we also found some negative correlations with satisfaction. There were moderate-strength negative correlations between women’s involvement in decisions about VEs and satisfaction with ‘decisions made’ (ρ = –0.468; p < 0.01) and with ‘overall’ satisfaction (ρ = –0.430; p < 0.05), as well as between involvement in pain relief and satisfaction with ‘decisions made’ (ρ = –0.376; p < 0.05). This means that participants with greater involvement in decision-making around these procedures actually reported lower satisfaction (see Appendix 11 for the correlation matrix).
Decision-making practice and satisfaction
To explore decision-making and satisfaction further, we examined the links between researcher-coded decision-making variables and satisfaction. These variables were derived from the decisional coding (see Interactional strategies of decision-making used during labour and birth) and based on (1) the researcher-coded ‘subjective’ measure of ‘balance’ and (2) the different initiating formats used across all midwife-initiated decisions or for certain types of midwife-initiated decisions (see Chapter 2, Interactional measures, for methodological details).
Table 18 shows descriptive statistics for mean ‘balance’. We see more responses towards the lower end of the overall ‘balance’ scale (rounded mean 2.23), indicating that decision-making was more midwife initiated. The decision-specific balance variables show somewhat similar mean scores to these overall measures, although it is worth noting that the pain relief decision-specific balance score is notably higher (mean = 3.3), indicating that it tended to be more birth party initiated than other decisions.
| Statistic | n | Minimum | Maximum | Median | Mean | SD | Shapiro–Wilks p-value |
|---|---|---|---|---|---|---|---|
| Mean balance | 37 | 1 | 3.3 | 2.3 | 2.2297 | 0.477 | 0.294 |
| Pain relief mean balance | 34 | 1 | 6 | 3.083 | 3.262 | 0.990 | 0.584 |
| Monitoring mean balance | 37 | 1 | 2 | 1.5 | 1.488 | 0.260 | 0.695 |
The associations between birth party–HCP ‘balance’ in decision-making and satisfaction can be seen in Table 19. We see significant moderate-strength negative correlations between mean ‘balance’ and two components of satisfaction, that is, the extent to which women felt that they had been ‘listened to’ (ρ = –0.453; p < 0.009) and their ‘views were taken into account’ (ρ = –0.367; p < 0.039), showing that births that were more HCP initiated tend to have higher scores on these aspects of satisfaction. There were similar strength significant negative correlations between ‘balance’ in pain relief decisions and all aspects of satisfaction.
| Listened to by staff | Views taken into account by staff | Satisfaction with decisions made | Satisfaction combined | Mean balance | Pain relief mean balance | Monitoring mean balance | |
|---|---|---|---|---|---|---|---|
| Listened to by staff | 0.791*** | 0.512** | 0.906*** | –0.453** | –0.452** | 0.086 | |
| Views taken into account | 0.677*** | 0.920*** | –0.367* | –0.424* | 0.145 | ||
| Satisfaction with decisions made | 0.674*** | –0.242 | –0.399* | 0.329 | |||
| Satisfaction combined | –0.353 ∼ | –0.420* | 0.235 | ||||
| Mean ‘balance’ | 0.612*** | 0.432** | |||||
| Pain relief mean balance | 0.052 | ||||||
| Monitoring mean balance | |||||||
| n | 32 | 32 | 31 | 31 | 37 | 34 | 37 |
We explored possible associations between the forms of decision-making practice used and satisfaction, considering midwife- and women-initiated decisions.
For midwife-initiated decisions, we analysed Spearman’s correlations between the 10 initiating formats of pronouncements, closed questions, decision-implicative statements, instructions/demands/commands, ‘just do it’, offers, open questions, option lists, recommendations and requests, and women’s satisfaction levels. This was undertaken for both frequencies of decision points used and for proportions of decision points that are of each type of decision (note that, for the latter, only births with ≥ 10 decision points were included, reducing the sample size to a maximum of 28). We found no statistically significant correlations between the total number of midwife-initiated decision points and satisfaction, or between the use of any of the different forms of midwife-initiated decision-making practice and any of the measures of satisfaction (for data, see Appendix 12). Further analyses focusing only on pain relief or fetal monitoring decisions also showed no significant correlations between different forms of midwife-initiated decisional practice and satisfaction (analyses not shown).
For women-initiated decision-making and satisfaction, only four initiating formats (i.e. closed questions, decision-implicative statements, open questions and requests) were included in the analysis. Table 20 shows the frequency of decision points used and Table 21 shows the frequency of decision points specifically for pain relief decisions. There was a significant moderate negative correlation between the number of decision points used and satisfaction with being ‘listened to’ by staff (ρ = –0.363; p = 0.041), meaning that births with more woman-initiated decision-making overall tended to have lower levels of satisfaction on this dimension. However, it is decision-implicative statements that are particularly of note, with women’s use of this initiating format showing a significant strong negative correlation with ‘listened to’ by staff (ρ = –0.515; p = 0.003), and significant moderate negative correlations with ‘decisions made’ (ρ = –0.401; p = 0.023) and with ‘overall satisfaction’ (ρ = –0.404; p = 0.024). There was also a moderate negative correlation between women’s use of requests and their satisfaction that their ‘views were taken into account’ (ρ = –0.389; p = 0.028).
| Listened to by staff | Views taken into account by staff | Satisfaction with decisions made | Satisfaction combined | Number of decision points | Closed yes/no | Decision-implicative statements | Open questions | Requests | |
|---|---|---|---|---|---|---|---|---|---|
| Listened to by staff | 0.791*** | 0.512** | 0.919*** | –0.363* | –0.009 | –0.515** | –0.220 | –0.312 ∼ | |
| My views were taken into account by staff | 0.677*** | 0.920*** | –0.329 ∼ | 0.000 | –0.401* | –0.217 | –0.389* | ||
| Satisfied with decisions made | 0.674*** | –0.198 | –0.026 | –0.314 ∼ | –0.214 | –0.278 | |||
| Satisfaction combined | –0.249 | 0.010 | –0.404* | –0.129 | –0.261 | ||||
| Number of decision points | 0.608** | 0.686** | 0.491** | 0.804** | |||||
| Closed yes/no | 0.392* | 0.220 | 0.409* | ||||||
| Decision-implicative statements | 0.309 ∼ | 0.440** | |||||||
| Open questions | 0.267 | ||||||||
| Requests | |||||||||
| n | 32 | 32 | 31 | 31 | 37 | 37 | 37 | 37 | 37 |
| Listened to by staff | Views taken into account by staff | Satisfaction with decisions made | Satisfaction combined | Number decision points | Closed yes/no | Decision-implicative statements | Open questions | Requests | |
|---|---|---|---|---|---|---|---|---|---|
| Listened to by staff | 0.791*** | 0.512** | 0.919*** | –0.431* | –0.036 | –0.493** | –0.251 | –0.315 ∼ | |
| My views were taken into account by staff | 0.677** | 0.920** | –0.394* | –0.036 | –0.329 ∼ | –0.257 | –0.400* | ||
| Satisfied with decisions made | 0.674** | –0.235 | –0.151 | –0.363* | –0.099 | –0.260 | |||
| Satisfaction combined | –0.348 ∼ | –0.030 | –0.472** | –0.123 | –0.277 ∼ | ||||
| Number of decision points | 0.499** | 0.533** | 0.378 * | 0.880*** | |||||
| Closed yes/no | 0.248 | 0.167 | 0.460** | ||||||
| Decision-implicative statements | 0.187 | 0.315 ∼ | |||||||
| Open questions | 0.164 | ||||||||
| Requests | |||||||||
| n | 32 | 32 | 31 | 31 | 37 | 37 | 37 | 37 | 37 |
We see very similar findings for pain relief decision points in that there are negative correlations between satisfaction and larger numbers of woman-initiated decision points, as well as between the use of requests and, in particular, decision-implicative statements and satisfaction. The similarity between the pain relief-specific and all decisions findings indicates that it is pain relief decisions that are driving the negative correlations seen in Table 20 (i.e. women who initiate multiple pain relief decisions report lower satisfaction). This could help to explain the earlier (see Table 19) counterintuitive finding that birth party-initiated births tend to be rated lower in terms of women’s satisfaction. It may be that labouring women who are in excessive pain tend to (1) take control of decision-making and (2) rate their satisfaction with decision-making lower postnatally.
To explore this possibility, correlations between the researcher-coded ‘balance’ variable and interactional practice variables were conducted. Table 22 shows moderate-strength (bordering on strong strength) statistically significant positive correlations between the frequency of women-initiated decision-implicative statements and balance (ρ = 0.485; p = 0.02), as well as between women-initiated requests and balance (ρ = 0.497; p = 0.02). This indicates that births with these interactional formats were more likely to be researcher rated as more birth party led. We do not have the necessary sample size to run multivariate analyses to explore these issues further and cannot say with any certainty why any labouring woman may be less satisfied with the decision-making in their labour. However, taken together, and alongside the earlier finding from the PNQ analysis that self-reported involvement in pain relief is negatively correlated with satisfaction with decisions made, these correlations suggest that if women are expressing a lot of pain, then they are likely to take the lead and proactively ask for pain relief and are also more likely to rate their overall satisfaction with decision-making less positively.
| Decision point | Practice and balance | |
|---|---|---|
| Midwife initiated | Woman initiated | |
| Total decision points | 0.107 | 0.603*** |
| Pronouncements | –0.082 | N/A |
| Closed yes/no | 0.395* | 0.082 |
| Decision-implicative statements | 0.174 | 0.485** |
| Instructions/commands/demands | 0.180 | N/A |
| ‘Just do it’ | –0.003 | N/A |
| Offers | 0.347* | N/A |
| Open questions | 0.000 | 0.295 |
| Option lists | 0.269 | N/A |
| Recommendations | –0.073 | N/A |
| Requests | 0.127 | 0.497** |
| n | 37 | 37 |
Conclusion
In this chapter, we have found that, antenatally, most women expressed a desire for involvement in decision-making and to be in control of what happens in labour and birth. In addition, women expected a match between how they felt decision-making should and would happen, which was mostly in the direction of being woman led rather than midwife led. However, women’s postnatal reports indicated that they had wanted decision-making to be more staff led or to be advised by staff and to take that advice, and this was broadly what they reported did happen. However, the seeming incongruity may, at least, in part, be explained by the likelihood that women had reserved the option to go against staff advice (to varying degrees), but the occasion did not arise, as what they wanted at the time (as reported postnatally) coincided with what midwives advised.
Analyses of the interactional data broadly bore out women’s accounts of decision-making as midwife initiated. Pronouncements and recommendations predominated midwives’ initiating formats (although this varied by type of decision), whereas requests (notably with regard to pain relief) and, to a lesser extent, decision-implicative formats mostly prevailed for women.
Postnatal reports show high satisfaction for all three domains (i.e. being listened to, views taken into account and with decisions made) and thereby for overall satisfaction. The more women reported that they were ‘listened to’ and that their ‘views were taken into account’, the more in control they felt. However, women whose labour and births were more ‘balanced’ towards midwife-initiated decision-making tended to be more satisfied that they had been ‘listened to’ and that their ‘views had been taken into account’, which was also found when satisfaction with pain relief was specifically analysed (applying to all three satisfaction dimensions). There were no significant associations between any of the different forms of midwife-initiated decision-making practice and measures of satisfaction. However, women who initiated decision-making through the decision-implicative format were statistically more likely to have lower satisfaction for being ‘listened to’, for ‘decisions made’ and for overall satisfaction. In addition, women’s use of requests was associated with lower satisfaction in ‘views being taken into account’. The similarity between pain relief-specific findings and all decisions tells us that it is pain relief decisions that are driving these associations (i.e. women who initiate more pain relief decision points report lower satisfaction). Therefore, women who pursue decision-making tend to rate their satisfaction with decision-making lower postnatally. We explore this qualitatively in Chapter 6.
Chapter 4 Fetal monitoring
Introduction
In this chapter, we focus on the most common decisions enacted in the data set, which are those relating to fetal monitoring during labour. Fetal heart rate (FHR) has been recognised as an indicator of fetal well-being for over two centuries,200 and auscultation (i.e. listening to the sounds) of the fetal heart is now routine in antenatal and intrapartum care. 201 The main purpose of monitoring FHR during the intrapartum period is to detect signs of fetal distress to facilitate early intervention and, therefore, prevention of fetal morbidities. 201 There are two main types of FHR monitoring in current use: (1) intermittent auscultation (IA) using either a Pinard or, more commonly, a handheld Doppler; and (2) continuous monitoring using an electronic fetal monitor (EFM), which is a form of cardiotocography. All 37 recordings, including the shortest (8-minute) recording, contained instances of IA monitoring (overwhelmingly using a Doppler, with only a single use of a Pinard) and eight recordings included decision-making about EFM.
The literature pertaining to fetal monitoring focuses on the contested bioethics and efficacy of continuous EFM,75,202–204 and has led to re-examination of, and advocacy for, the use of IA in low-risk labours. 75,201,202,205–207 These studies repeatedly show that IA is a safe option for most women and babies, and this message has been taken up in practice guidelines. 208–210 For example, the 2017 amendment to the NICE guidelines (section 1.10.1)208 explicitly states that EFM should not be offered to women who are at a low risk of complications. This amendment was endorsed in a RCM and Royal College of Obstetrician and Gynaecologists (London, UK) 2017 consensus statement. 211 EFM is not, therefore, in routine use in MLUs (and, therefore, there are fewer instances in our data set), but it remains an important tool if complications arise.
The wording of NICE guidelines10 appears to position women as decision-makers vis-à-vis monitoring by including the direction to HCPs to ‘offer IA’ (section 1.10.2 © NICE 2014 Intrapartum Care for Health Healthy Women and Babies. Available from www.nice.org.uk/guidance/cg190. 10 All rights reserved. Subject to Notice of rights NICE guidance is prepared for the National Health Service in England. All NICE guidance is subject to regular review and may be updated or withdrawn. NICE accepts no responsibility for the use of its content in this product/publication). However, such ‘offering’ happens rarely in practice. Instead, as we will show, both midwives and women orient to IA as something that will inevitably happen.
Despite the availability of, and debates about, different technologies, surprisingly few studies have assessed women’s antenatal preferences around monitoring (for exceptions see Hindley et al. 212 and Mangesi et al. 213). As we report in Chapter 3 (see Figure 3), no women in this study (full sample) indicated that they ‘definitely did not want’ or ‘preferred not to have’ IA, whereas over 40% of women either ‘definitely did not want’ or ‘preferred not to have’ EFM. In terms of decision-making, half of the full sample reported postnatally (see Chapter 3 and Table 14) that decisions about monitoring were taken entirely by staff. The finding that women report generally low involvement in monitoring decisions is supported by the coding of the interactional data from the recordings. We see this primarily in two ways. First, echoing NICE guidelines10 (sections 1.10.2 and 1.13.2) relating to frequency of monitoring, it is common for midwives to inform women (in ways that presume acceptance) about the planned incidences of monitoring both in early labour [example shown in extract 1 (Figure 8)] and at the beginning of second stage [example shown in extract 2 (Figure 9)]. Second, thereafter, midwives’ initiating formats also tend to be presumptive. (Note that for all data extracts please see Appendix 6 for CA transcription conventions.)
FIGURE 8.
Extract 1 (VIP36:Pheobe:Video): presumptive scheduling of monitoring during first stage.
FIGURE 9.
Extract 2 (VIP22:Claudia:Video): presumptive scheduling of monitoring during second stage.

Monitoring decisions are overwhelmingly initiated by midwives. There is only a single instance of a woman-initiated monitoring decision [following a midwife’s earlier abandoned attempt to monitor, the labouring woman offers ‘Want to do that again. Do you want to listen’ (VIP03)]. Chapter 3, Figure 6, shows that the most common formats for midwife-initiated decisions are those that narrow recipients’ participatory opportunities, that is, pronouncements (46% of monitoring decisions) and ‘just do it’ (25%). There is, however, a reasonable proportion of requests (20%) that do invite recipient responses (even if it is only ‘yes/no’). A smaller proportion of requests are recommendations/suggestions/proposals (5%), but these tend to be used in relation to EFM decisions (although not all EFM decisions are recommendations). The remaining 4% of midwife-initiated monitoring decisions comprise single instances of other formats. Crucially, there is no instance of an option list used for monitoring decisions. We turn now to examine the interactional data in more detail to illustrate how the key formats used affected opportunities for women’s involvement in decision-making.
When monitoring is ‘just done’
In some ways, ‘just done’ is a misnomer because what we mean by this is that there is no verbal initiating turn. Monitoring, however, is quite a physical activity and involves some preparation on the part of midwives. For example, midwives might wheel a Doppler trolley to wherever the woman is located in a room, detach the monitor and add gel to the sensor before accessing the woman’s abdomen. There are also auditory cues, for example, by the wheeling trolley or the ‘crackle’ of the monitor as it is switched on. Finally, midwives often wait for an opportunity to monitor between contractions, which means that they might be standing with a prepared monitor for some time before they actually begin auscultation (this is shown in Figure 10, in which a student midwife waits for almost 4 minutes with monitor in hand, at all times observing when might be an opportune moment to begin monitoring). These preparatory actions are all likely to be noticeable by women.
FIGURE 10.
Student midwife waiting watchfully with monitor in hand (VIP12).

Figure 11 shows a series of images of non-verbalised monitoring when the midwife is behind a woman (Lydia) who is kneeling over the bed. Lydia is in second stage and is close to giving birth. In the first image, the midwife returns to kneeling after she has been bent down to observe the woman’s vagina as Lydia is pushing. When the midwife kneels up again, she has the monitor in her right hand. In image 2, the midwife reaches to the left for the gel, applies the gel in image 3 and then returns the gel to the shelf in image 4. Lydia remains kneeling, with her head down, throughout these activities. The only sign she gives to demonstrate possible awareness of an upcoming monitoring is that she raises her left elbow, placing her hand on the bed (image 4), which might more easily accommodate a move away from the bed. In image 5, the midwife reorients to Lydia and, just following this, bends down at Lydia’s left-hand side. In image 6, as the midwife begins monitoring, Lydia lifts her head and, therefore, becomes more upright and twists slightly to give the midwife more space. All of this is unspoken. Lydia is deeply focused on her labour and is not engaging in interaction throughout the period represented by the images. However, not only does Lydia accept the monitoring, but she also actively co-operates with the midwife.
FIGURE 11.
Non-verbalised monitoring from behind woman (VIP08).
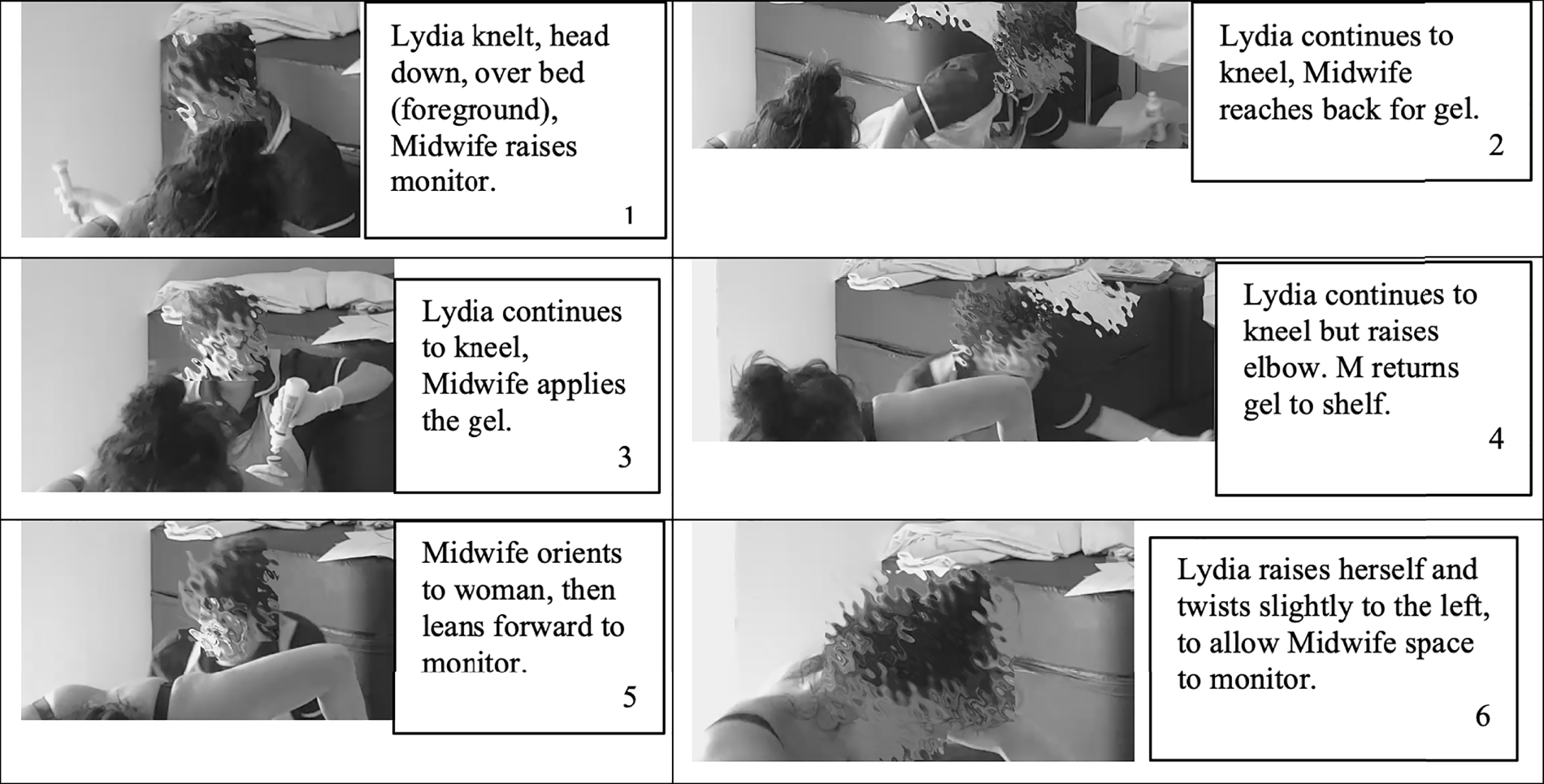
It is rare for a woman to resist monitoring in whatever way it is initiated, but we do have one example of a woman, Harmony, who defers a non-verbalised move to monitor [see extract 3 (Figure 12)]. This occurs at a moment just following a VE that has shown that there has been no cervical dilatation since the previous examination. This occasions a negatively formulated request (i.e. ‘can’t you . . . ’) from one of the BPs present to ‘help her along a bit’. In the silence that follows (L2) the midwife can be seen looking for and picking up the monitor. The machine crackles as she moves back towards Harmony and deals with the BP’s request (L3–4). Unfortunately, after seeing the midwife pick up the monitor, all parties are off camera and so we cannot see the exact moment that the midwife moves the monitor towards Harmony’s abdomen. However, there is no verbal initiating turn. Nevertheless, Harmony cries out (L5) and instructs the midwife to wait. The midwife agrees to wait (L6) before continuing the conversation about progress.
FIGURE 12.
Extract 3 (VIP30: Harmony:Video-but-mostly-off-camera): woman defers a non-verbalised initiation of monitoring.
In a physiological approach to birth, there is a common understanding that women are doing the work and are best left undisturbed to facilitate an inner focus,214–216 and, at this time, midwives attempt to minimise interaction when women display that they are ‘in the zone’. However, as Reed et al. 216 point out, midwives are often caught between what they call ‘rights of passage’, which are women’s rights to labour without disturbance and women’s ‘rights to protection’, which is clinical risk management. Fetal heart monitoring is a case in point because midwives reportedly acknowledge its potential for disturbance and disruption of women’s focus, but nevertheless carry it out as it is required both to manage risk and to adhere to policy guidelines. It is possible that non-verbalised initiations are one way that midwives can minimise the disruption caused by monitoring by not pressing for verbal interaction.
Verbal initiations in monitoring decisions
Pronouncements
Pronouncements, the most common format midwives use to initiate monitoring decisions, are declarative statements of intent and so also place little pressure on women to respond. Elsewhere, Stivers et al. 132 researched doctors’ use of pronouncements in treatment recommendations in primary care. In that context, Stivers et al. 132 show that pronouncements present a treatment decision as already determined, that is, the doctor was both instigator and decision-maker. We cannot assume that pronouncements in the context of midwife-led care decisions work in exactly the same way as doctors’ treatment decisions. However, there is some evidence that pronouncements are used in relation to investigations in secondary care (see Reuber et al. 161), and there is clear overlap in the ways that midwives use pronouncements to encode their authority to decide unilaterally to monitor the FHR.
The two most common turn designs, which are variations of ‘I will . . . ’ (n = 66, 35%) and ‘I am going to . . . ’ (n = 60, 32%), account for 67% of pronouncements. These formats are illustrated in Table 23. Another 25% (n = 48) of pronouncements are truncated versions of these two designs [e.g. ‘Just quickly listen’ (VIP36) and ‘Just have a little listen’ (VIP14)]. The remaining pronounced formats include ‘need to’ formulations (n = 6, 3%) [e.g. ‘We need to just have a quick listen in to baby again, OK’ (VIP01)] and a small number of infrequently used formats [e.g. ‘Sorry, Gracie, it’s that time again, OK’ (VIP37)].
| ‘I will’ (elided to ‘I’ll’) | ‘I am going to’ (elided to ‘I’m’, but also includes turns that omit the self-reference) |
|---|---|
| I’ll just listen inVIP29 | I’m gonna listen to babyVIP35 |
| I’ll just have a quick listenVIP07 | Just going to listen to baby, MarthaVIP24 |
| I’ll have a little listen in now while I’m hereVIP10 | Just going to listen to baby, lovelyVIP08 |
| I’ll just have another quick little listen inVIP14 | I’m just going to have a listen after the next oneVIP23 |
Both ‘I’ll’ and ‘going to’ formats have the action of informing women that monitoring is imminent. These formats do not invite deliberation from recipients and present the decision to monitor as inevitable. The grammatical and lexical design of these turns index high entitlement217 to conduct the activity of auscultation, place little pressure on the woman to respond and convey, via minimisers (e.g. ‘just’, ‘little’ or ‘quick’), that the activity will not be onerous. In doing so, these formats modulate the potential for disruption of labour by conveying a non-negotiable commitment to imminent monitoring that does not require verbal interaction from recipients.
It is perhaps not surprising, then, that the majority (n = 130, 68%) of the full collection of pronounced decisions to monitor receive no verbal response from recipients (although they maybe consented to non-verbally through embodied co-operation or nods). When there is a verbal response (n = 61, 32%), the majority are agreements (n = 47, 77% of verbal responses), most commonly, ‘Yeah’. Only one participant (VIP16; Addison) declines to be monitored following an asserted decision. Addison declines twice, saying ‘no, no’ on the first occasion and ‘no’ on the subsequent occasion. On both occasions, Addison apologises therefore, orienting to her transgression of the expectation for agreement. These declinations do lead to deferral of monitoring but only temporarily.
Requests
The request format provides more leeway for women’s involvement and can be categorised broadly in two ways: (1) ‘Can I . . . ’ (n = 41, 50%) and (2) ‘alright/OK to . . . ’ (n = 25, 31%) (both ways are illustrated in Table 24). The remaining types of requests include ‘do you mind’ formats (n = 6, 7%) [e.g. ‘Nina do you mind if I have a quick listen to baby’ (VIP17)], more complicated formats where the request to monitor is rolled up with another request (n = 5, 6%) [e.g. ‘Am I OK just to lift this up and have a listen?’ (VIP22)] and a small number of other formats seldom used (n = 4, 5%) [e.g. ‘. . . let me just have a listen in then’ (VIP28), which we coded as a request but note that its declarative format could make this more presumptive218].
| Can I . . . | Alright/OK to . . . |
|---|---|
| Can I just listen inVIP11 | Alright just to have a listen againVIP29 |
| Can I just have a quick listenVIP22 | Am I alright just to listen in to baby?VIP02 |
| Nina, can I have a listenVIP17 | Is it OK to have another listen to the babyVIP14 |
| Can I just have a listen in to baby, BryonyVIP05 | Is it alright if I just have another little listen?VIP12 |
We have called these turns ‘requests’, but this perhaps is another misnomer (see Kendrick and Drew219 on the wider notion of recruitment). Couper-Kuhlen,220 for example, differentiates social actions, such as offers, requests, proposals and suggestions, in terms of who is understood to be the agent of an act and who is understood to be its beneficiary. According to Couper-Kuhlen,220 a request can be said to be such because the speaker intends the recipient to be the agent of an act that benefits themselves (i.e. as a speaker). For example, in the hypothetical request ‘Can I have a lift?’, the speaker is asking the other to do something for them. Although the grammatical formulation of something like ‘Can I have a lift?’ bears a strong resemblance to ‘Can I have a listen?’, and both share the quality of asking a question as opposed to asserting an action (e.g. compare with ‘I am going to need a lift’ or ‘I’ll just listen in’), there are important differences in terms of agents and beneficiaries. The turns that we have identified as requests do not fall neatly into Couper-Kuhlen’s220 category of ‘other doing something on behalf of self’. Rather, the speakers (i.e. the midwives) are the intended agents of the act of auscultation, albeit they may need women’s assistance in accessing the necessary part of the body. The question of who benefits is also somewhat unclear because although labouring women, or, more directly, their fetuses, potentially benefit from monitoring, it is also an activity that is required of midwives (and obstetricians). Failing to monitor could have consequences for all parties. Although not commenting specifically on IA, midwives interviewed for this study did regularly discuss the necessity of documenting events during labour in line with clinical guidelines, as well as their concerns about the personal consequences of not doing so, for example if care was subsequently to be questioned. Concerns about blame and its shaping of midwives’ perceptions of, and actions concerning, the management of risk through monitoring activities, such as IA and VEs, is also well documented in existing research. 124,221
It may be that what we mean by a ‘request’ in our data is something more akin to permission-seeking, that is, midwives are using a ‘request’ format to seek permission to conduct an action involving the woman. These permissional ‘requests’ were also seen in Harwood et al. ’s222 study of clinical encounters between HCPs and dementia patients, particularly during a physical examination, when, for example, a doctor might seek to listen to a patient’s chest. It remains to future analyses as to whether or not there is overlap between these formats and other form of request analysed in the CA literature; a caveat to be kept in mind below.
Conversation analysis studies on requests have shown the significance of ‘entitlement’ and ‘contingency’. 182,223,224 Entitlement refers to the rights a speaker has/takes to make a request and contingency orients to the ease or difficulties of it being granted. These exigencies are consequential for the grammatical and syntactical construction of a turn. At one end, imperatives (e.g. ‘put that down’)223 convey high entitlement to ask and an expectation of ease of granting (low contingency). At the other end, ‘I wonder if’ formats convey low entitlement or an expectation of difficulty in or obstacles to granting. 182 Modal verb interrogative formats (e.g. ‘can/could’, ‘will/would’), although not as strong as imperatives (because of the interrogative that more easily allows for a declination/refusal), nevertheless index high levels of entitlement and grantability. To the (uncertain) extent that our permission-seeking formats resemble requests, the ‘can I . . . ’ format in our data exhibits high entitlement and low contingency. The ‘alright/OK . . . ’ format appears to allow more syntactical flexibility so that midwives using this format might select from personalised and depersonalised formats [e.g. ‘Am I alright to (personalised) . . .’ vs. ‘Is it OK to’ (depersonalised)], and are able to increase the degree of conditionality via the use of ‘if’222 (e.g. compare ‘Is it OK to . . .’ with ‘is it alright if I . . . ’). The flexibility of the ‘alright/OK’ format means that it might appear as part of a high entitlement/low contingency turn (e.g. ‘Alright just to have a listen again?’) or a low-entitlement/high-contingency turn (e.g. ‘Is it alright if I just have another little listen?’). If entitlement and contingency are conceptualised as continua rather than binaries (i.e. from high to low rather than high vs. low) then we can see that tweaks in turn design may shift the ‘force’ of a turn further along continua in one direction or another.
A distinction between ‘can I’ and ‘alright to’ along the dimensions of contingency and entitlement bears further research, especially in the context of permission-seeking requests. Nevertheless, if we explore the way in which recipients respond then it is apparent that the ‘alright/OK to’ format occasions more verbal responses than the ‘can I’ format (49% vs. 24%, respectively). This suggests that the ‘alright to’ format places slightly higher pressure on women to respond verbally to make a decision. In contrast, the ‘can I’ formats act more like pronouncements in conveying high entitlement/low contingency to proceed to monitoring without explicit (verbal) agreement.
Once again, whatever format is used by midwives to enact a permission-seeking request, recipients overwhelmingly agree to be monitored. We have no examples of an outright declination and there are just two participants who defer. In the first of these, the woman (Claudia; VIP22), responds ‘sorry’ to a midwife’s request (‘Am I OK to have a listen in’) just as a contraction begins. The apology in the context of a contraction acts as an account for delaying the monitoring. We know that the midwife treats the apology this way because she/he does not withdraw from her/his position and, instead, waits kneeling, with monitor in hand, until Claudia says ‘Go for it’ and the monitoring proceeds.
The second participant to defer following a request (Gracie; VIP37) does so in the context of a prior orientation to the disturbance of monitoring, in which Gracie had accepted a request, but with a request of her own for the midwife to be ‘quite quick’. On the next occasion, Gracie moves to defer the monitoring, saying ‘better if you just leave it a minute’. In response, the senior midwife in the room utters a turn designed to persuade Gracie that monitoring every 15 minutes is not only routine, but also recommended by NICE guidelines10 (i.e. ‘Every 15 minutes we listen in. That’s recommended by NICE guidelines’). This reference to guidelines resonates with Drew’s225 finding that citing documents in interaction occurs systematically in problematic or defensive environments. Drew225 suggests that the document invokes a depersonalised objective account that warrants a particular agenda or action. Here, the senior midwife is warranting fetal monitoring as something that is subject to external guidelines rather than being at the discretion of midwives (or, by implication, women). This is accepted by Gracie, but she indicates the reason for her deferral is the imminence of a contraction. Following the contraction, Gracie gives the go-ahead to monitor but again requests the midwife to ‘be quick’.
In the prior sections, we have explored the ways that monitoring decisions are initiated, showing that these decisions are generally treated as being in midwives’ domain. In our observations, women never initiate these decisions and have generally low involvement in them. This said, we can also see that midwives orient to and attempt to minimise the potential for disturbance of labouring women. There is a strong expectation of agreement, and women’s resistance is highly unusual, but does occur. It is worth remembering that most women in the full sample reported antenatally that they wanted or did not mind IA and so low resistance is unsurprising.
‘Routine’ versus ‘non-routine’ monitoring
The handheld Doppler is used with every woman in our data set. The guidelines are omnipresent both in the practice of 5- or 15-minute schedules (depending on stage of labour) and in the announcements about this practice (see extracts 1 and 2 in Figures 8 and 9). These implicit orientations to the guidelines mark IA as a routine activity, but rarely expand on either the reasons for conducting the activity or how it will be carried out. However, we also have occasional uses of EFM and, unusually for midwife-led care, a single use of a fetal scalp electrode to monitor the fetal heart. Decisions to use these monitoring technologies tend to involve more explanation and are carried out as recommendations rather than pronouncements, marking their non-routine status in this context. In using a recommendation, despite making clear that the midwife is endorsing a course of action, there is less presumption than pronouncements [extracts 4 and 5 are illustrative (Figures 13 and 14)].
FIGURE 13.
Extract 4 (VIP07:Martha:Audio): example 1 of midwife recommending EFM.
FIGURE 14.
Extract 5 (VIP36:Phoebe:Video-but-off-camera): example 2 of a midwife recommending EFM.
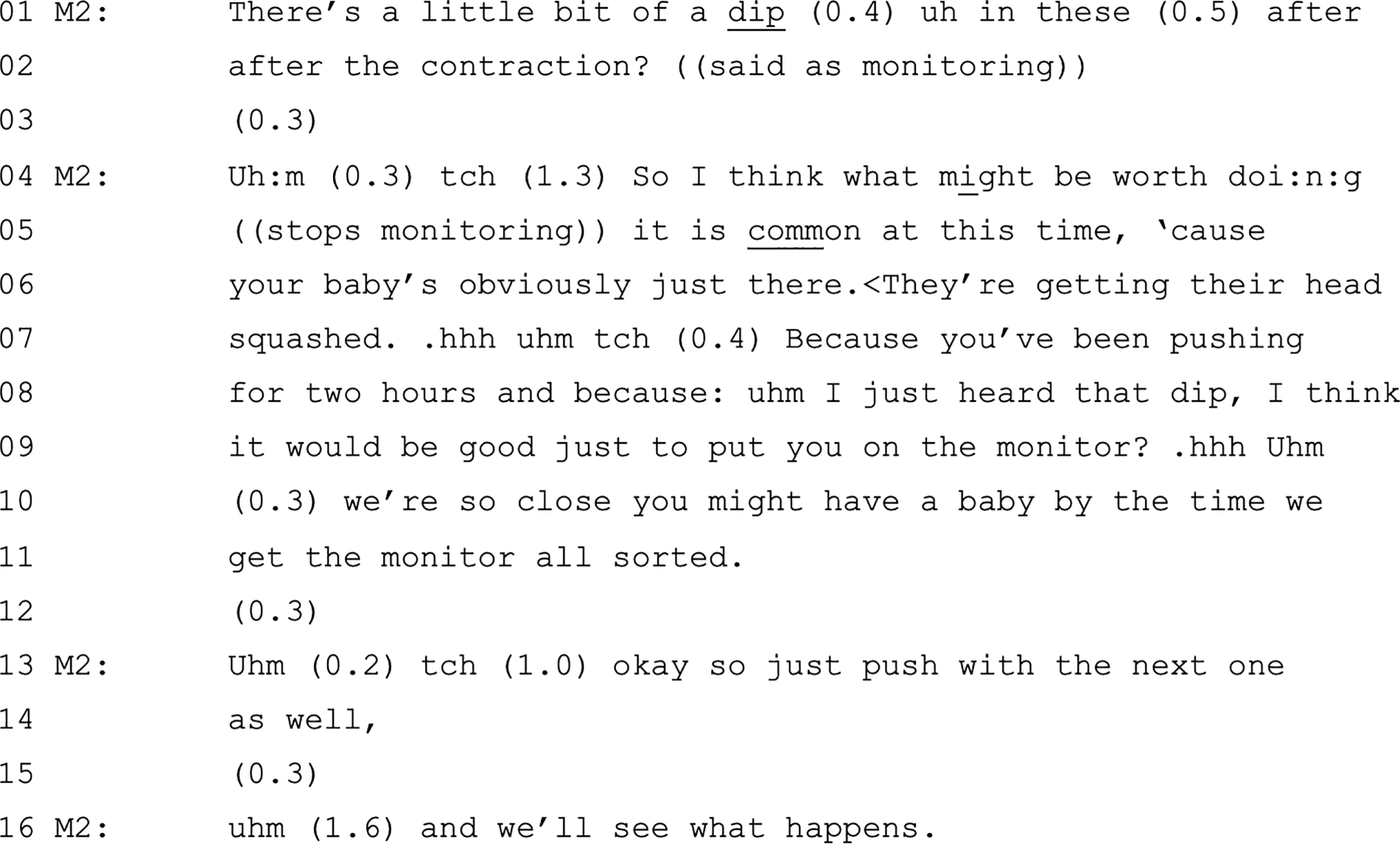
The recommendation for EFM in both extracts is built off a description of a problem with the FHR and, in fact, is presented as a consequence of this problem (with the ‘so’ prefacing). 226 The problem itself is described with some delicacy and qualification as ‘a little lower’ than a previous monitoring (see extract 4 in Figure 13) and as a ‘little dip’ (see extract 5 in Figure 14). In both cases, the midwife is describing the problem as they are monitoring the FHR using a handheld Doppler and, therefore, these turns are a form of online commentary227 that foreshadows a recommendation. In neither case is the recommending turn pronounced, as neither midwife says that they ‘will’ or are ‘going to’ use EFM. Instead, each midwife describes what they ‘would like to do’ (see extract 4 in Figure 13) or something they think might be ‘worth doing’ (see extract 5 in Figure 14, although note that this is abandoned and comes back as a slightly stronger ‘I think it would be good . . .’). Both midwives provide (with some delicacy) a rationale for using the EFM. In extract 4 (see Figure 13), the midwife says that the baby’s heart rate is under the lower acceptable limit. In extract 5 (see Figure 14), the midwife breaks off from her first attempt at the recommendation to insert a rationale (framed as ‘common’), that is, the baby’s head is being squashed as Phoebe has already been pushing for the maximum ‘normal’ period (i.e. 2 hours for nulliparous women10) and a dip in the heart rate has been detected.
In extract 5 (see Figure 14), there are no verbal responses to the midwife’s recommendation and, unfortunately, as Phoebe was off camera at this point, we were unable to observe non-verbal responses. It is possible that there might have been agreement by the time the midwife suggests that Phoebe might have her baby before they get her on to a monitor. In fact, EFM is used on Phoebe and her baby is born with the assistance of ventouse. In extract 4 (see Figure 13), Martha does respond verbally to accept EFM (L10), but it is notable that the midwife pursues confirmation of agreement (L15; after asserting authority over the conditions under which the EFM would stop, L11). Martha subsequently has a second period of continuous EFM, and eventually her baby is monitored by use of a fetal scalp electrode and Martha is later transferred to the OU. These recommending sequences invoke quite a different scenario to that in which Doppler monitoring is typically performed. The contrast between non-routine and routine is instantiated in the details of interaction. We do, however, have one example of an EFM decision that is pronounced. In this case (Diana; VIP21), use of EFM is not related to detection of a problem with the FHR, but rather follows a decision to use an oxytocin drip to speed up contractions in the second stage. The use of EFM is routine with oxytocin drip,10 but this is not explained to Diana. Having secured Diana’s agreement to the drip, the midwife says simply ‘So I’ll bring on a:: monitor as well as and pop you on the monitor as well. Yeah?’. The tag at the end of the pronouncement does some work to invite Diana’s agreement (which is given as ‘OK’), but clearly the turn was designed to convey the midwife’s commitment to using EFM and, having agreed to the oxytocin drip, it would be quite difficult for Diana to refuse continuous monitoring.
Conclusions
Guidelines10 position women as potential decision-makers in IA through the notion that it should be ‘offered’. However, we have shown that, in practice, IA is a decision made by HCPs and, indeed, that the guidelines are drawn on to reinforce HCPs’ authority to make this decision.
Midwives face the difficulty of conducting the regular monitoring specified in guidelines10 in a way that does not disrupt the flow of labour. Just doings and pronouncements (which do not require responses from women) are a possible solution, but this also means low involvement in decision-making.
We have shown that IA decisions are consequential, as illustrated by the occasions on which they lead to further interventions (e.g. EFM). These interventions are treated as non-routine and as requiring some participation from women in decision-making. However, these interventions are still initiated in ways (e.g. recommendations) that create little space for women’s involvement.
Women themselves report a preference for IA in questionnaires, and very few women attempt to defer or decline monitoring in recordings. However, women do occasionally attempt to defer or decline monitoring in the moment. When they do so, midwives respect the woman’s agency, but only temporarily, that is, following declinations, the decision to monitor is renewed and/or pursued.
Chapter 5 Vaginal examinations to assess progress
Introduction
Assessing progress is central to intrapartum care and is predicated on detecting and preventing morbidities for both the labouring woman and her baby. 228 Following Freidman’s229,230 influential work in the 1950s, describing temporally normative progress through distinct stages and phases of labour, clinicians routinely plot cervical dilatation against time to detect and take action on any deviations from the expected rate. After full dilatation has been achieved, the monitoring of progress against time continues, but attention switches from the cervix to the birth of the baby.
There are empirically grounded reservations about the appropriateness of an idealised model of progress, as well as doubts about the accuracy and effectiveness of VEs. 231–234 Nevertheless, norms and practices for assessing progress are instantiated in NICE guidelines10 so that VEs (i.e. the mainstay of procedures for monitoring progress234,235) are recommended every 4 hours during the active first stage of labour (section 1.12.7) and dilatation of at least 2 cm per 4-hour period is expected (section 1.12.14). NICE guidelines10 do, however, acknowledge that VEs might be distressing for women and that the need for a VE should be explained and consent must be given (section 1.4.5). There is also a suggestion that women might request a VE (section 1.12.710). However, the frequency and necessity of VEs are positioned as decisions that lie in the HCPs’ domain. It could be argued, then, that the guidelines themselves do not present decision-making about VEs as a joint accomplishment, but as a HCP-led intervention that requires the woman’s consent.
In this chapter, we focus on decision-making pertaining to VEs conducted to assess progress. We show that, although these decisions tend to be midwife initiated in ways that construct VEs as routine, decision-making takes place over time and involves regular phases of activities (see Overview of data set relating to vaginal examinations) that afford women opportunities for consent, which is pursued if not forthcoming (see Responses to midwife-initiated decisions about scheduled vaginal examinations). The 4-hourly schedule (hence, guidelines) forms the backdrop of decision-making about VEs, even during the latent phase, when this schedule does not apply (see Vaginal examinations during the latent phase: an opportunity for ‘choice’). Decision-making about ‘off-schedule’ VEs (e.g. during the second stage) have a distinctive quality that constructs these VEs as non-routine and more accountable (i.e. requiring greater acknowledgement of women’s potential role in decision-making) (see Decisions to conduct vaginal examinations to establish full dilation before/during second stage). Finally, we demonstrate that, like IA, VE decisions are consequential and have implications for subsequent actions, such as amniotomy (i.e. breaking waters) (see Vaginal examination outcomes are consequential).
Overview of data set relating to vaginal examinations
Our ANQ data (see Chapter 3 and Figure 3) shows that the large majority of respondents ‘didn’t mind’ VEs (although one woman indicated that she definitely did not want VEs during labour). Overall, this suggests that women generally expect VEs as a routine part of labour. The fact that ‘didn’t mind’ was selected over the more favourable ‘quite like’ or ‘definitely want’ perhaps suggests, however, a level of resignation.
In our data set of 37 recordings, there are 73 decisions relating to VEs. This figure does not represent the total number for these women because they may have had VEs on an assessment unit before admission and/or otherwise before/after the camera was switched on/off. Nor does the figure include the times when midwives inserted fingers into the vagina to conduct directed pushing, to catheterise or to conduct an amniotomy. Of the VE-relevant decisions recorded, a majority (n = 45, 62%) related to assessing progress. The remainder of VE-relevant decisions were associated with managing maternal requests for pain relief (the granting of which depends on progress; see Chapter 6) and checking for tears postnatally.
In our data set, VE decisions relating to assessing progress (in the absence of pain relief requests) fall broadly into two types: (1) those that are scheduled (4-hourly) and (2) those used to assess whether or not the cervix is fully dilated when pushing. Almost all of these decisions are initiated by midwives (n = 39, 87%). Pronouncements [e.g. ‘((Midwife)) said she examined you about 8.40? So I’ll examine you about 12.40’ (VIP22)] and recommendations [e.g. ‘Josie, I’m just wondering about examining you really, to be honest. I’m just, I’m not getting a clear picture really, so I just think it might just be helpful’ (VIP35); see extract 9 in Figure 18] make up the largest category (74%) of initiating formats (pronouncements, n = 15; recommendations, n = 14) overall. Notably, pronouncements generally pertain to scheduled VEs and not to those used for checking readiness to push. The remaining 26% of initiating formats comprise the more participatory formats of offers [e.g. ‘So in about half an hour it’ll have been 4 hours since we last examined you, so we can offer another examination if you wanted one’ (VIP32)] and option lists [e.g. ‘If we can’t see anything externally, like the baby’s head coming down, my suggestion would be to either get up and have a wee or I can do another examination down below’ (VIP20); see extract 11 in Figure 20]. There is also an example of a doctor requesting permission to do a VE [i.e. ‘Can I examine you to see where we are’ (VIP21)]. These figures, which are showing that decisions relating to VEs tend to be presented as lying in the midwives’ domain, do not fully represent the multiple opportunities afforded to women to consent to VEs. Interestingly, despite the prevalence of pronouncements, small numbers of women in the full sample report experiencing decision-making pertaining to VEs as entirely staff led (14.3%) (see Chapter 3 and Table 14). This might be explained by the contrasting ways that monitoring and VE decisions are initiated and enacted. Monitoring decisions tend to occur after a single initiation. Similar to monitoring, VEs are an expected and predictable part of labour. VEs are also, however, intimately intrusive. This expected-but-intrusive character of VEs is handled in quite regular ways across our data set and so it is possible to discern an overarching interactional structure to their use in practice (see Appendix 13 for a table showing the overall architecture of VE decisions), affording women multiple opportunities to participate in decision-making (e.g. forewarning about when a VE is next due, pronouncing a VE is imminent and getting consent before initiating the examination).
There is some overlap between our findings and those presented by Bergstrom et al. 153 (although note that Bergstrom et al. 153 analysed only second-stage VEs), especially in the verbal pronouncement that a VE is forthcoming. As in Bergstrom et al. ’s153 study, the need for a scheduled VE is rarely explained in our data set (although VEs conducted ‘off schedule’ are accompanied by explanations). As in Bergstrom et al. ’s153 study, the word vagina is rarely used, but euphemistic terms [e.g. ‘down below’ (VIP20)] are also rare (‘cervix’ is commonly used). Just as the activity of monitoring is described as ‘listening in’, the activity of conducting a VE is almost always referred to as ‘examine you’. However, in contrast to Bergstrom et al. ’s153 findings, the midwives in our data set always inform women of the outcome.
It is important to note that women do request VEs, but they tend to do so in the context of asking about pain relief. In terms of progress, women seem more generally to ask how much longer they are likely to be in labour, but this tends not to lead to a discussion about a VE unless one is due. Occasionally, although rarely (and we have only three cases), BPs might ask about the timing of VEs. However, midwives treat these queries as inapposite. In the remainder of this chapter we focus, therefore, on decisions about VEs to assess progress that are initiated by midwives.
Responses to midwife-initiated decisions about scheduled vaginal examinations
When midwives initiate decisions about scheduled VEs, women overwhelmingly agree to them. No women in our data set refused a scheduled VE. Nonetheless, it is clear that midwives orient to issues of consent and explicitly require some form of response from labouring women, particularly about when and how the VE is conducted. Therefore, agreement is overwhelmingly pursued when it is not immediately forthcoming. This is illustrated in extract 6 (Figure 15), where the midwife forewarns the labouring woman (Elise) sometime ahead of an upcoming VE, taking for granted that a VE will happen (L1), but also checks and pursues Elise’s agreement (L6).
FIGURE 15.
Extract 6 (VIP02:Elise:Video): midwife pursues agreement to conduct VE.
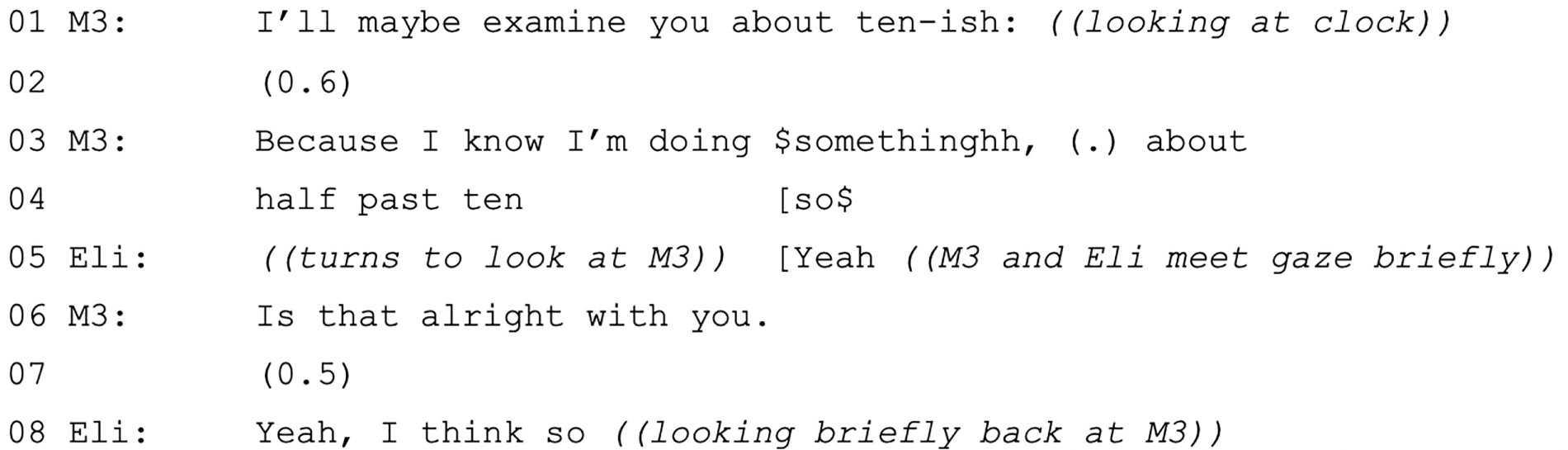
Respectfully conducted VEs require bodily co-ordination and co-operation between labouring women and HCPs. Therefore, although initiating turns might not construct optionality for recipients, there are ways that women are afforded and can express co-operation. For example, having agreed to a VE, women tend to be guided through positioning their body to allow the examination. This might be carried out fairly elaborately, especially on first examination [e.g. ‘And (0.2) what I’d like you to do is.hh bring your feet up. And like you know like in meditation position when you’re gonna just sort of relax your knees and like (0.4) meditate’ (VIP31)] or more straightforwardly [e.g. ‘so frog legs’ (VIP30)]. These positionings tend to be followed by a verbal query about readiness and when this is not forthcoming, HCPs hold off beginning the examination. Consent is, therefore, conveyed through embodied actions, as well as verbally.
Although clearly an activity that requires co-operation and co-ordination, the design of the initiating turns tends to expect agreement. There are, however, just a few instances in which midwives do explicitly provide optionality. In relation to scheduled VEs, optionality tends to occur during the latent phase.
Vaginal examinations during the latent phase: an opportunity for ‘choice’
The latent phase of labour is variously described in the literature,236 but NICE10 defines it as a period of painful contractions, cervical effacement and dilatation up to 4 cm. Following (contested) evidence-based guidelines,237 women in the latent phase are discouraged from attending or remaining in hospital to manage increased risk of intervention associated with early attendance. 238,239 This expectation also facilitates midwives’ primary workload focus on women in active labour. 240 This approach to care during early labour, however, is also associated with women’s confusion and dissatisfaction,241 especially if they experience themselves as being in labour despite not cohering with formal clinical definitions. 242 Women report feeling anxious about when to attend hospital243 and, following admission, fear of being sent home again. 244,245 Women who are sent home again report feeling unsupported, anxious, disappointed and exhausted244,246 (i.e. feeling states with possible implications for progress of labour).
In our data set, women display apprehension concerning progress and it is also clear that ‘slow’ progress can be anticipated by midwives. The 4-hourly scheduling of VEs does not apply until a woman is considered to be in established labour. However, the general 4-hourly scheduling does seem to be oriented to as normative, even during the latent phase. For example, women might notice/comment on the absence of VEs [see extract 7 (Figure 16)] and midwives orient to timing when they are deciding not to conduct a VE [see extract 8 (Figure 17)].
FIGURE 16.
Extract 7 (VIP06:Kay:Video): explicit choice relating to VE.
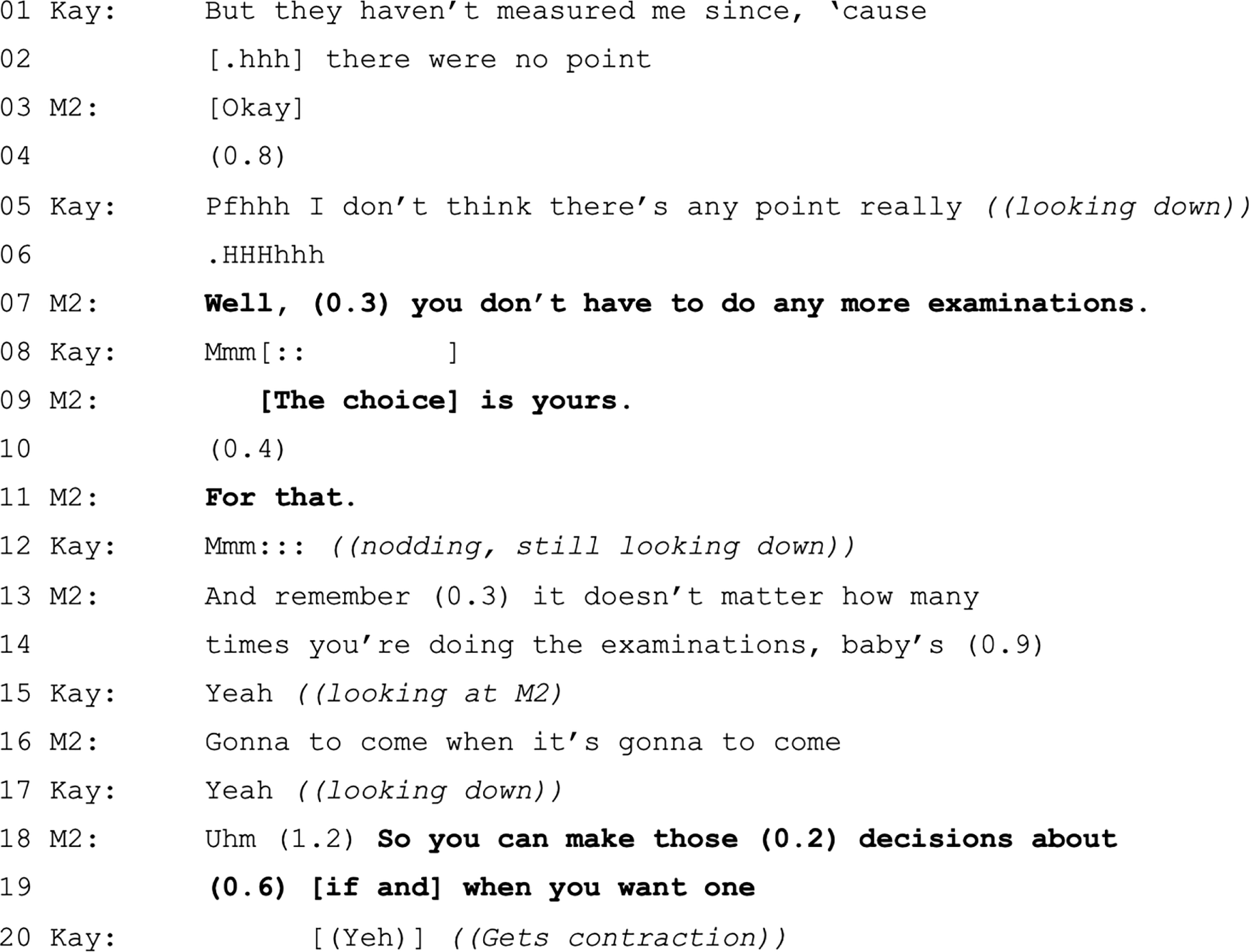
FIGURE 17.
Extract 8 (VIP10:Gabi:Video): explicit choice relating to VE.

In extract 7 (see Figure 16), a woman (Kay), who has already been sent home once and is resisting being sent home again, mentions during the history taking that she has not been ‘measured’ since yesterday, adding that there was ‘no point’ (L1–2 and L5). This mention of not having been recently examined is a negative observation247 that points to some relevant absence of expected activity. In adding ‘there were no point’ and reiterating this futility in the present tense at L5, Kay orients to the lack of progress and provides her own account of why the expected activity (i.e. a VE) has not occurred. Faced with Kay’s assessment that further examinations are probably futile, the midwife states (resonating with NICE guidelines10 for care during early labour) that further VEs are not compulsory (L7) and are a matter of maternal choice (L9). In explicitly making the VE a choice, the midwife arguably downplays its clinical significance (at this stage). Following Kay’s non-committal response (and perhaps withholding of eye gaze; L12) the midwife invokes known-in-common knowledge (‘remember . . .’) that having further VEs does nothing to bring the baby sooner (L13–14 and L16). This seems to be an orientation to and warding-off of the possible implication that Kay’s negative observation acts to ‘fish’ for a VE. Therefore, despite the apparent autonomy afforded to Kay, the midwife is deterring a decision to conduct a VE. This warding-off is elaborated in later lines (data not shown) by pointing out the likely disappointment of a no-change outcome and the consequent impact on labour.
In extract 8 (see Figure 17), an explicit offer of choice is similarly used to deter a decision to conduct a VE. The midwife first offers to do a VE at a specific time point in accordance with the 4-hourly convention (L1–2) by expressing willingness – ‘I could’ – predicated on whether or not this is what Gabi wants (and, therefore, downplaying clinical grounds). Gabi appears to accept the offer (L5), but, notably, the midwife does not engage with this response and instead continues the prior turn by stating overtly that the timing of the next VE is a choice for the woman (L6). Despite the apparent autonomy afforded to Gabi at this point, the midwife pursues an agenda to defer the VE by voicing a conditional criterion from Gabi’s perspective (i.e. ‘if you think the contractions have gone off and it would be better to wait then . . . ’; L7–8 and L10; meeting Gabi’s gaze only for ‘better to wait’). The inference that it would be better to delay is not lost on Gabi and, despite having agreed to have a VE, she now agrees to delay (L9; notably before the completion of the midwife’s turn). As in extract 12 (see Figure 21), the midwife next provides psychophysiological advantages of avoiding disappointment (data not shown).
These instances show ‘choice’ being used in rather a specific way to permit and encourage declination of an otherwise expected VE in circumstances in which the outcome of that activity might disappoint the woman and impede labour. In this sense, although these decisions are apparently being placed with the women, the fact that they are placed with women downplays the clinical ‘necessity’ of the activity. Therefore, when midwives suspect that labour is not yet established, then one way to manage anticipation of VEs is to initiate the decision as optional, predicated on what the woman wants rather than on clinical grounds (see also Reuber et al. 161). It is notable that midwives in our data set do not negatively pronounce about VEs, that is, they do not say ‘I am not going to examine you’.
Occasionally, midwives might initiate a decision about conducting a VE outside the 4-hourly schedule, particularly during or just before the second stage, when they want to be certain that a woman is fully dilated. Similar to decisions about VEs during the latent phase, these ‘off-schedule’ VEs appear not to be pronounced, and we consider them further below.
Decisions to conduct vaginal examinations to establish full dilatation before/during second stage
Earlier conversation analytic studies, conducted by Jordan152 and Bergstrom et al. 154 in the USA on data collected in the mid to late 1980s, established that the interactional operation of a ‘no push’ rule until second stage had been authoritatively established via a VE. This ‘rule’ is not routinely applied in our data set. Instead, midwives encourage women to ‘go with’ their bodies and leave labour to progress into second stage without the intervention of a VE. For example, women often report feeling a ‘pushy’ pressure and when this happens midwives tend to say things like ‘Well if you need to push, push’ (VIP17). However, on occasion, based on the midwives’ reading of bodily signs, midwives do recommend holding off pushing, saying, for example, ‘I wouldn’t push at the moment, it might be just the head’s low enough down so you can feel like that . . . I can’t see any sign’ (VIP07). Nevertheless, in these circumstances, a VE is not routinely immediately suggested and, instead, midwives work with women to help them cope with these ‘early’ urges to push.
When ‘off-schedule’ decisions about VEs do arise because of uncertainty about the cervix’s ‘readiness’, they do so in relation to contingent bodily events that are not necessarily anticipated or expected. This might explain why these VEs are not pronounced and/or appear to involve relatively elaborate explanations. Extracts 9–11 in Figures 18–20 show three examples: the first example is a recommendation (i.e. suggestion) (see extract 9 in Figure 18), the second example is an offer (see extract 10 in Figure 19) and the third example is an option list (see extract 11 in Figure 20).
FIGURE 18.
Extract 9 (VIP35:Josie:Video): midwife recommends a VE after period of pushing.

FIGURE 19.
Extract 10 (VIP37:Gracie:Audio): midwife offers VE after an hour of pushing.
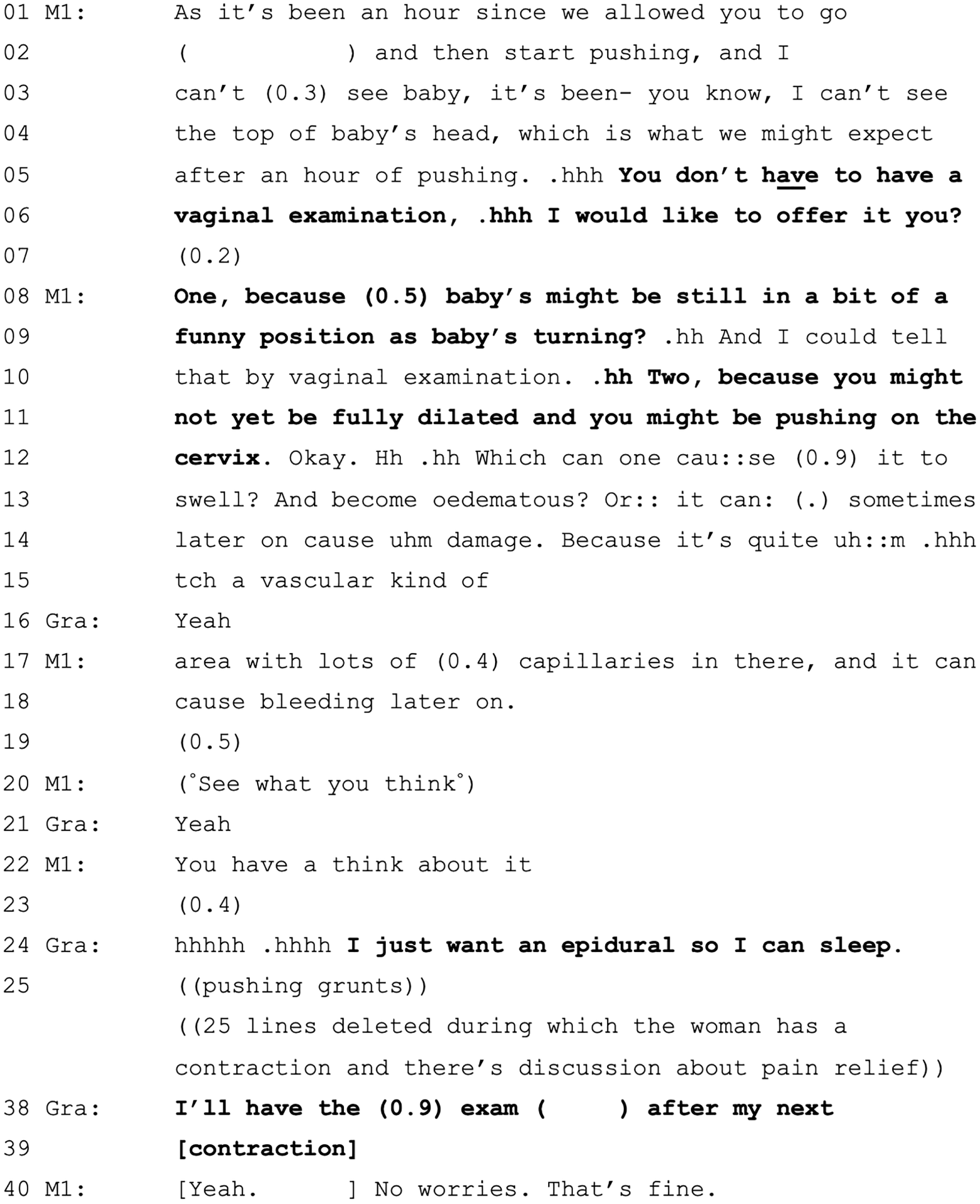
FIGURE 20.
Extract 11 (VIP20:Abigail:Video): following a period of pushing, midwife uses option listing that includes VE.

In all three extracts (see Figures 18–20), the women have been experiencing pushing for a period of time but without external signs of fetal descent. None were ‘due’ a VE in the sense of the 4-hourly schedule. Although each midwife uses a different initiating format, it is clear these decisions have quite a different character to those about scheduled VEs. In extract 9 (see Figure 18), the midwife recommends a VE, but as something that she is ‘wondering about’ (L1) rather than something she is going to do. In extract 10 (see Figure 19), the midwife offers a VE, although the unusual formulation – ‘I would like to offer it you’ (L6) – has something of the quality of a recommendation because it is a ‘myside’ offer, said because the midwife ‘would like to’). Extract 11 (in Figure 20) contains a full-form option list,248 which sets up a menu of two options, that is, having a wee (L8) or a VE (L10), from which Abigail can select. All three extracts (see Figures 18–20) contain explanations for why a VE might be conducted. In extract 11 (see Figure 20), the explanation is not very specific, with ‘I’m not getting a clear picture really’ (L3–4) and that a VE might be ‘helpful’ (L6) and ‘useful’ (L14). The explanations in extracts 10 and 11 (see Figures 19 and 20) are more specific, and both involve describing the possibility that the babies are in a ‘funny position’ (see L9 in Figure 19 and L16–17 in Figure 20), the effects of which are described in unusually medicalised terms in extract 10 (see L10–18 in Figure 19). The explanations in all three extracts work to account for the decision, but also do some persuasive work [it is notable, for example, that while extract 11 (see Figure 20) contains an option list, only the VE option, not the alternative of having a wee, is explained]. In all three cases, the women (eventually) agree to the VE, but it takes some time for Gracie (see extract 10 in Figure 19) to do so. Following the VEs, all three women are found to be fully dilated. Gracie and Abigail go on to give birth soon afterwards. Josie, however, following another period of pushing, is later transferred to the OU for an instrumental delivery.
Vaginal examination outcomes are consequential
The outcomes of VEs are consequential and tend to be followed by some form of decision-making. There is a clear expectation of and preference for progress of cervical dilatation, and this is not lost on women who might utter such things as ‘fingers crossed’ (VIP22) and ‘If I’m not more than three centimetres just knock me out’ (VIP36). The potential for women’s disappointment is generally treated as something to be managed (e.g. see extracts 8 and 9 in Figures 17 and 18 where midwives steer decisions towards postponing VE precisely to avoid disappointment). Extract 12 (Figure 21) is illustrative of interactional work to manage perception of low dilatation.
FIGURE 21.
Extract 12 (VIP07:Martha:Audio): midwife’s management of woman’s perception of low dilatation.
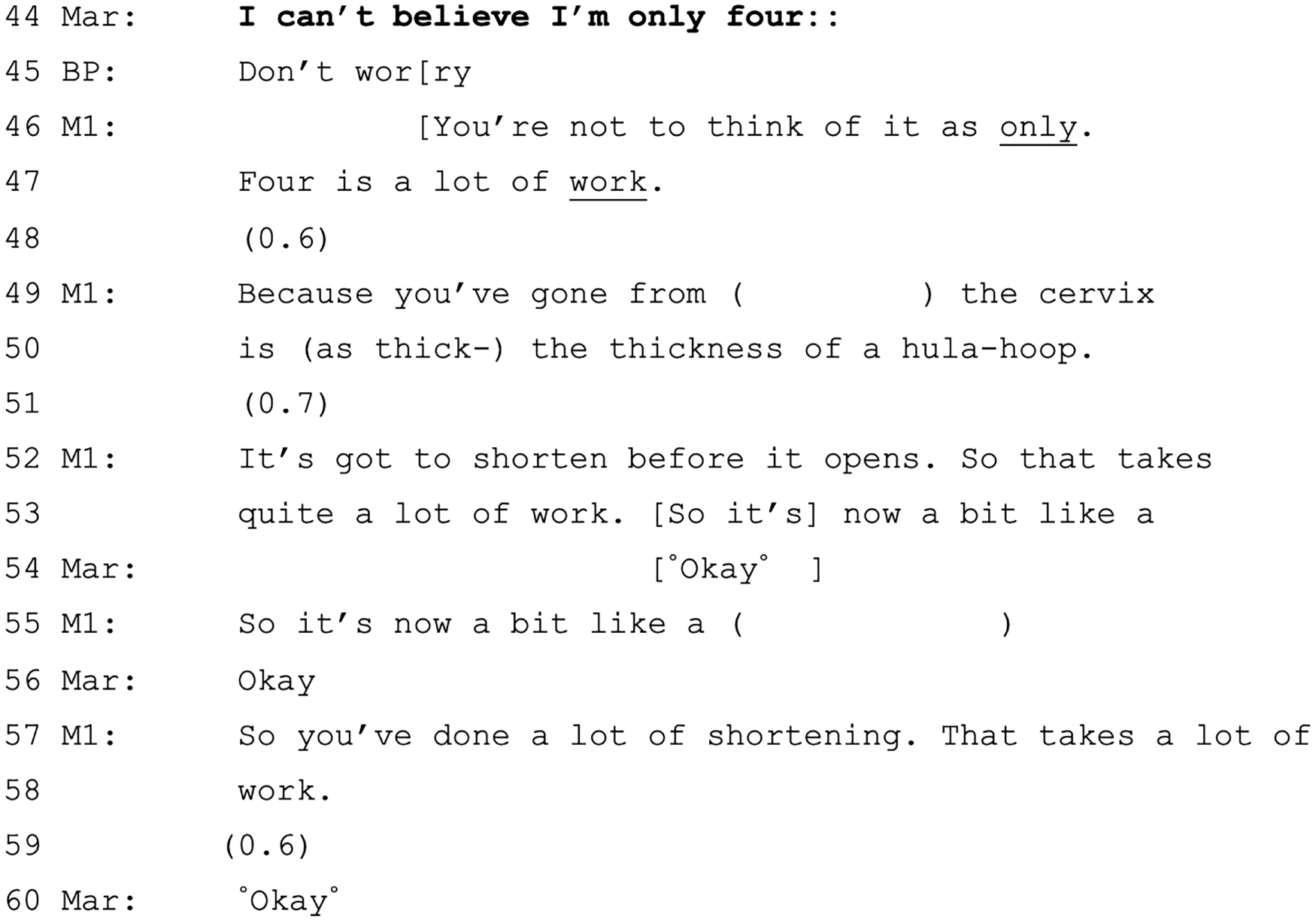
Martha’s statement of disbelief occasions slightly different responses from the others in the room. The BP provides a sympathetic ‘directive’ ‘don’t worry’ (L45), but the midwife reproves Martha’s use of ‘only’ and stresses again the amount of work that it has taken to get to this point (L46–7). The midwife follows this with a contrastive description of the starting thickness and current thickness of the cervix (L49–55), therefore, providing evidence of effective progress.
On some occasions, the outcome of the VE is not normalised this way and further action is specified. If labour is not yet established, then this may be a general recommendation about hydrating [e.g. ‘So you need to make sure you’re drinking plenty’ (VIP02)], encouraging mobilisation [e.g. ‘I’d walk around a little bit more’ (VIP10)] or the midwife might carry out a sweep of the membranes [e.g. ‘I’m just going to do a really good sweep and see if I can get these contractions coming a bit more’ (VIP14)]. If the woman is considered to be in established labour but found not to have progressed at the expected rate, then a decision about amniotomy is considered.
Amniotomy
In our data set, there are seven midwife-initiated decisions about amniotomy (i.e. breaking of waters) and one of these is a recommendation against doing so [‘I think I would like to just leave it a little while before I do anything,.hh just let your body do its own thing I think rather than breaking your waters at the moment’ (VIP14)]. Of those decisions remaining, five were initiated in ways that place the decision with the midwife (using pronouncement/recommendation). Four of these five pronouncements/recommendations led to amniotomy, but we cannot be certain about the fifth because the woman was transferred to the OU. The sixth example more explicitly, and unusually, left the decision to the woman (using an offer). We conclude this section by considering these contrasting forms of decision-making about amniotomy as a decision in the context of slower than expected progress.
Extract 13 (Figure 22) is an illustration of a decision about amniotomy that is pronounced. The woman (Philippa) has had an unscheduled VE to manage a maternal request for opiate pain relief and was found to be 6-cm dilated. As the interactants are engaged in decision-making about opiates, there is no immediate mention of a problem with progress. However, following a shift change shortly afterwards, the new midwife asserts that they are going to conduct an amniotomy via an explanation for conducting another VE, that is, first there is a pronouncement to re-examine (L8) (albeit with an inflection of inviting involvement via the tag question; L9) and then a plan to (try to) conduct an amniotomy is stated as reason for doing so (L9–10). The addition of ‘for you’ (L10) conveys that the intervention is being carried out on Philippa’s behalf, but does not quite transform the turn into an offer. As a whole, the decision is not designed to provide an opportunity for Philippa to participate in decision-making regarding the amniotomy. Philippa does, however, immediately agree (L11) and the amniotomy is conducted soon afterwards without further discussion.
FIGURE 22.
Extract 13 (VIP11:Philippa:Video): pronouncing plan to conduct amniotomy.

There is a notable lack of explanation in extract 13 (see Figure 22). It is only after the procedure has been conducted and the woman is experiencing painful contractions and demanding more pain relief that its side effects (‘It feels worse . . . because there’s nothing protecting him’), advantages (‘he’s pushing down and stretching everything inside’) and clinical reasoning (‘there were a bit of slow progress and we’ve done this to help you’) are described.
The next example (extract 14 in Figure 23) begins in a way that also places the decision to conduct an amniotomy in the midwife’s domain, but the decision subsequently becomes optional for the woman (Claudia). This example also involves a shift change. It becomes clear that Claudia had been showing signs of slow progress at the previous VE, but that this had not been acted on. Therefore, the new midwife begins a decision about amniotomy by referring to the fact (attributed to a ‘consultant’) that it ‘should’ have already happened (L3–4 and L6). The midwife then go on to explain the reasons by referring to clinical expectations, which were not met at the time of the previous VE, of 2 cm dilatation in a 4-hour period (L8–9, L11–12, L14–15, L17 and L20).
FIGURE 23.
Extract 14 (VIP22:Claudia:Video): decision to conduct amniotomy midwife-led, contingent on dilatation.
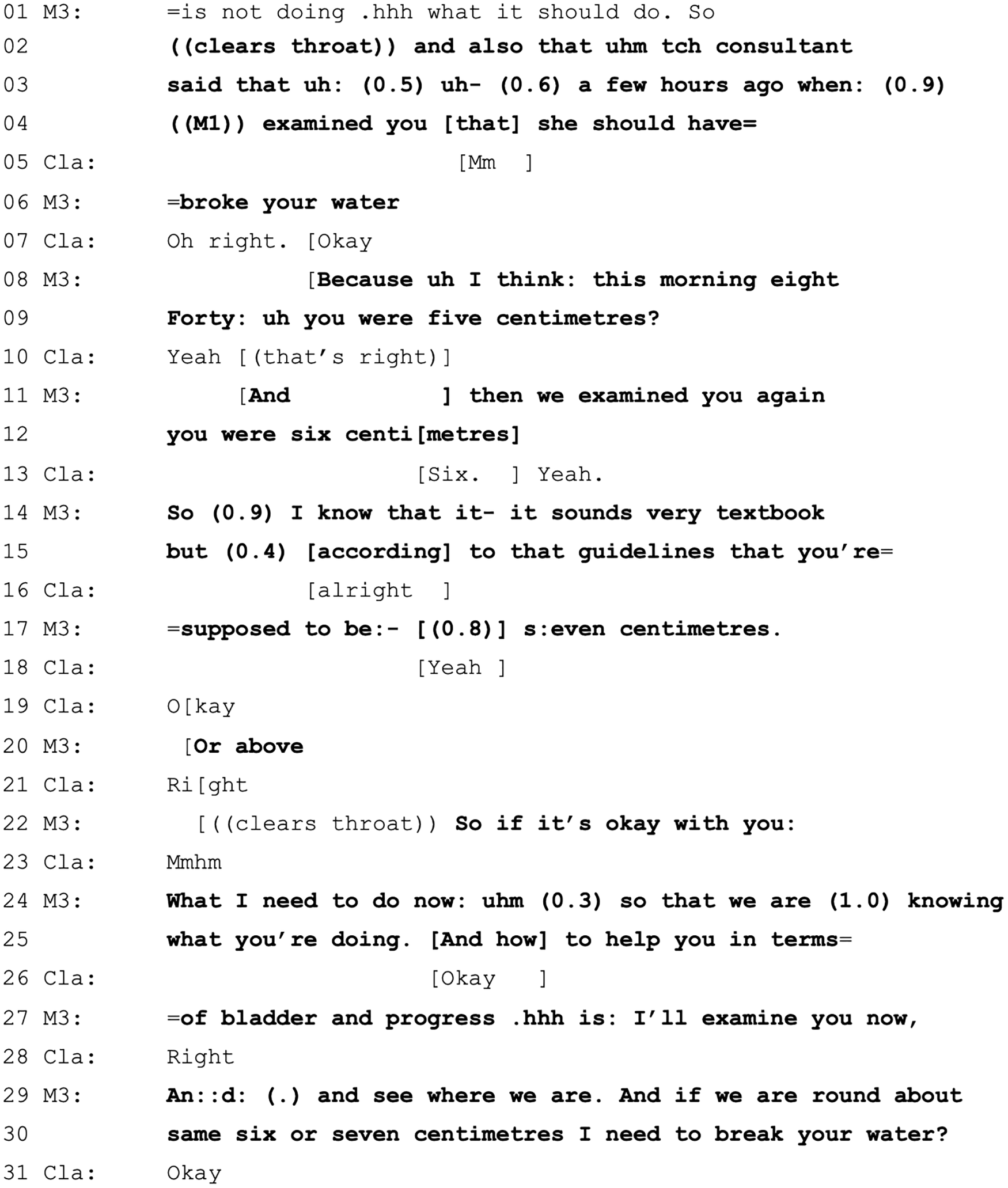
The midwife sets up the decision about amniotomy as being contingent on the outcome of the current VE (L29–30). The whole decision is framed in terms of what the midwife ‘needs’ to do (L24), but is prefaced with ‘if it’s OK with you’ (L22), therefore, affording Claudia some opportunity to decline. In fact, Claudia does agree to the terms set out by the midwife (L31).
However, the contingencies set up for conducting the amniotomy are not in fact met because the VE reveals that Claudia’s cervix is now 8 cm dilated. On discovering this, the midwife does not withdraw the decision but, instead, offers to conduct an amniotomy (‘Uh Claudia do you want me to break your waters to help speed up the situation’). The offer is ‘weighted’ in favour of acceptance by the addition of a named benefit. However, Claudia seeks further information, asking what the benefits and, particularly, the negatives are of amniotomy. The midwife’s response to this query continues to favour breaking the waters by saying that there ‘isn’t much negative’ beyond the fact that it will be considered an intervention. There follows a long question and answer sequence in which Claudia pursues and receives more information, including the fact that it is likely to be more painful, and eventually asks her partner what he thinks. He encourages her to go for it, saying ‘I think you should just do it’. After some further discussion, Claudia agrees to the amniotomy.
In contrast to the case shown in extract 13 (see Figure 22), there is more interactionally grounded provision for informed decision-making in extract 14 (see Figure 23). This is largely attributable to two factors not present in the earlier case. First, the midwife explains the clinical rationale for the amniotomy and, therefore, when these considerations are found not to be relevant, the medical grounds are no longer pressing. Hence, the decision becomes less about what is needed than what the woman wants. Second, when faced with a choice, Claudia is able to seek and respond to further information as the basis for her decision. Notably, for both women, the starting point for the decision about amniotomy allows little opportunity for choice because they have fallen outside the guidelines for expected progress. Arguably, optionality emerges in Claudia’s case only because of the extent of the dilatation of her cervix.
Conclusion
Vaginal examinations and IA are both technologies of monitoring (of progress or FHR). Our analysis shows how scheduled VEs, such as scheduled IA, are oriented to as ‘routine’, that is, a form of care that is necessary during labour. Decisions about the frequency and necessity of VEs (in the absence of pain relief requests) are treated as lying in the midwives’ domain. Permission about whether or not a VE can proceed at any particular moment lies with the woman, and no intervention takes place without consent, but women are generally not involved in the decision about whether or not the VE should happen. This maps onto NICE guidelines,10 which specify that VEs should take place at regular intervals, with women’s consent.
The process of establishing consent for VEs is elaborate, requiring participation from the woman at multiple points. This may explain why women report feeling more involved in these decisions in spite of them being HCP led, in comparison with monitoring.
There are occasions where HCPs treat VEs as more optional decisions, in which women should be involved, for example during the latent phase of labour. Interestingly, however, the CA of these interactions demonstrates that optionality enables particular outcomes (e.g. the avoidance of VE to prevent disappointment). This demonstrates the value of a detailed analysis of interaction, that is, optionality does not automatically lead to equal weighting of options/opportunities to participate.
The outcomes of VEs are consequential. Evidence that labour is not progressing at the rate expected leads to decisions about further intervention (e.g. amniotomy). As with decision-making about scheduled VEs during established labour, decision-making about amniotomy is HCP led and involves orientation to clinical guidelines about the measurement of progress in ways that narrow the scope for women’s involvement.
Chapter 6 Pain relief
Introduction
In this chapter, we focus on decisions pertaining to pain relief. Labour pain can be one of the most challenging and intense pain experiences, but it is also highly subjective and variable. 249,250 Women variously, and even concurrently, report welcoming the pain, despite its challenges, because it heralds the arrival of their baby,249,251 but also report that it is the aspect of birth they most fear. 252 Women’s experience of pain is affected by a range of psychosocial factors, including anxiety/control,253 and the quality of support from caregivers. 5,90,185 How to deal with pain is a key aspect of antenatal and intrapartum decision-making.
A range of non-pharmacological and pharmacological pain relief is available;254 however, given the subjectivity of pain, and people’s personal preferences for managing it, there is no ideal type. For some labouring persons, pharmacological methods, although associated with potential side effects255,256 and increased risk of intervention (with epidurals),257 offer a positive birth experience by (variably) reducing pain. 258 For others, a positive experience relies on working ‘with’ the pain259 (e.g. by using relaxation techniques) rather than by trying to alleviate it. NICE guidelines (section 1.8.1),10 therefore, instruct HCPs to be mindful about their own attitudes and preferences about forms of pain relief so as to impartially inform and support women’s choices. Similarly, the RCM260 suggests maintaining awareness of personal bias, such as underestimating the intensity of pain women experience in labour and/or overestimating the effectiveness of analgesic drugs. The Care Quality Commission261 suggests that women report negative birth experiences when they encounter some form of coercion around pain relief techniques or when their decisions are not supported, as well as when chosen methods do not meet their expectations. Discussions pertaining to pain, then, can be complex and consequential for labouring persons’ experiences.
In our data set, decisions relating to pain relief are certainly among the most complex. Although midwives initiate more of these decisions than women, much more optionality is afforded to women than we have seen in relation to decisions about fetal monitoring (see Chapter 4) or VEs (see Chapter 5). As we saw in Chapter 3, women initiate decisions about pain relief more than any other type of decision, thereby positioning themselves as active in this domain of decision-making. However, pain relief includes the longest chains of decision-making (ranging from 1 to 18 decision points), suggesting that there is also substantial pursuit and negotiation.
Overview of coding of interactional data about pain relief decisions: initiations and responses
Pain relief decisions are launched using a variety of formats; however, as seen in Figure 6 (see Chapter 3), just over half of midwife-initiated decisions place decisions with women (i.e. via offers, option lists and open-questions). Pronouncements [e.g. ‘I’m just gonna put my hand on your back and I’ll just push a little, yeah’ (VIP11)] are rare, but one-quarter of midwife-initiated pain relief decisions are recommendations/suggestions/proposals. However, on closer analysis of these recommendations, almost half (45%) are suggestions to stop using the Entonox [e.g. ‘Might be worth trying without the gas. A, it can make you dizzy, and B, it might distract you from the business of pushing’ (VIP09)]. The other initiations are mainly recommendations about non-pharmacological methods or oral analgesics. Taken together with the relatively frequent use of offers, it appears that, even when midwives initiate pain relief decisions, there is a marked tendency to hand over the decision to women (see also Cole et al. 146).
In contradistinction to midwives, who most commonly used offers, when women initiated pain relief decisions they most commonly used requests (17/30, 56.7%) (see Chapter 3 and Figure 7). Such requests tended to be formatted as either ‘can I . . . ’ interrogatives [e.g. ‘Can I have the gas’ (VIP08)] or ‘I need . . . ’ statements {e.g. ‘I need something. I need I need I need [opiate]’ (VIP17)}. Decision-implicative statements [e.g. ‘I was hoping to have a water birth when I have it, but I don’t know whether I’d like it or not’ (VIP06)] accounted for 30% of women-initiated decisions. The remaining initiations were (request-like) queries about what was available [e.g. ‘is there any pain relief you can have’ (VIP24)].
Looking closely at what midwives offered and what women requested, it is clear that midwives generally used offers to initiate decisions about non-pharmacological pain relief [e.g. ‘Do you want me to give you a bit of a massage’ (VIP13)] and Entonox [e.g. ‘Do you want to try some gas and air now’ (VIP28)]. In contrast, women tended to use (declarative) requests in relation to pharmacological methods, specified [e.g. ‘I need an epidural’ (VIP28)] or unspecified [e.g. ‘Oh I need more drugs’ (VIP17)].
When midwives offered pain relief, 45% of offers were accepted and 17% were rejected [e.g. ‘No, it’s not desperately painful’ (VIP03)]. Remaining responses included raising a concern {e.g. ‘I thought you was only allowed [opiate] once’ (VIP30)}. In contrast, 23% of the women’s requests were immediately agreed to [e.g. ‘yeah yeah, you can have [codeine] any time you need it’ (VIP31)] and 29% were immediately declined [e.g. ‘No. You’re doing fine, you don’t need that epidural, honestly’(VIP37)]. A further 17% of requests were deferred [e.g. ‘Well we’ll see after this. Let’s have a listen first. And then see what’s happening with the next one’ (VIP07)] and a further 17% are met with questions [e.g. ‘what time did you have the last’ (VIP02)]. The remaining women’s requests do not get any verbal response from the midwife. The requests that are immediately granted mostly relate either to non-pharmacological pain relief or oral analgesics (e.g. codeine). The requests that are immediately rejected, are immediately deferred or occasion a follow-up question generally relate to pharmacological pain relief, particularly opiates and epidurals.
In Chapter 3, we showed that women’s decision-implicative statements are negatively associated with satisfaction for ‘listened to’ by staff, ‘decisions made’ and for ‘combined’ (overall) satisfaction. In some ways, this is not surprising because, by nature, decision-implicative statements do not place interactional pressure on recipients to respond. 262 Compare, for example, Imogen’s (VIP24) ‘maybe gas and air’s not strong enough’ with her later request of ‘is there any more pain relief I can have?’. The former occasions no discussion relating to pain relief (the midwife, instead, suggests cleaning the water in the pool because Imogen has vomited), whereas the latter occasions decision-making about conducting a VE to ‘see what’s happening’ and, therefore, decide ‘what will be the best course of action’ (on examination, the cervix is 6 cm, the waters are broken and then the midwife reopens discussion of pain relief with an option list, from which Imogen selects an opiate injection). Therefore, decision-implicative statements on their own tend not to lead to a decision being made and, instead, appear as part of longer chains of decisions that women pursue through the use of more direct requests.
It generally appears, however, that women are not immediately granted pharmacological pain relief, even when they directly request it. Nonetheless, this does not mean that this is accepted by women, nor that women do not eventually get the pain relief that they request. As revealed below, decision-making about the use of drugs that might have clinical implications for women and babies is highly complex and is contingent on a number of uncertain parameters. This means that it is not always possible for a midwife to immediately fulfil a woman’s request for pain relief. Through CA, we demonstrate how midwives and women negotiate these complex interactions.
Limiting optionality: laddering of options and invoking stage of labour
Progress underlies and even constrains much of the decision-making about pain relief during labour, particularly that pertaining to pharmacological methods. We see this in two ways: (1) via the interactional ‘laddering’ of pain relief so that options are presented by the midwife as ordered from non-pharmacological through to strong analgesics, and (2) the invoking by the midwife of stage of labour in decision-making. Below, we illustrate this through pain relief decisions taken during early labour, decisions taken during transition from first to second stage and decisions concerning the timing of opiate injections in relation to birth. In all cases, echoing findings reported in Chapter 5 concerning amniotomy, optionality concerning methods of pain relief is treated as contingent on the (perceived) progress of labour.
Early labour
Pain relief is commonly discussed with women during the early part of their admission, when midwives seek women’s views [e.g. ‘Have you thought about what you want to do for pain relief?’ (VIP14)]. Descriptions of alternatives tend to follow these opening questions, in which opiates and epidurals (the latter are not available in MLUs and so require transfer to OUs) are presented later in a hierarchy of options. As one midwife puts it, ‘ideally we’d like to start off with things small’ (VIP02). Extract 15 (Figure 24) is illustrative. The extract begins just after an initial VE has revealed that the woman’s (Kailani’s) cervix is ‘3 to 4’ centimetres (and, therefore, the woman is not yet in established labour). The midwife tells Kailani not to ‘be disheartened’ and encourages her to be ‘a bit more patient’ before initiating a discussion about pain relief.
FIGURE 24.
Extract 15 (VIP28:Kailani:Audio): laddering of pain relief.

The above discussion sets up a future decision about pain relief rather than a here and now (e.g. ‘have a think about . . .’; L1). The midwife then lists broadly four options: (1) aromatherapy massage, (2) birthing ball, (3) Entonox and (4) opiates/epidurals. However, the options are ordered so that the non-pharmacological options are available presently (or when the midwife has time; e.g. ‘can do . . . ’ and ‘can get’) and the Entonox is an option for when Kailani feels she needs it (L20–22). The stronger methods are conveyed as not yet being available to her and are explicitly treated as for ‘further down the line’ (L26). This ordering of options from non-pharmacological to mild analgesics to strong analgesics is typical across the data set.
Women are generally aware that there is an expected ordering of pain relief options. For example, one woman (Martha; VIP07), following a VE showing her cervix to be 4 cm, is invited to say what pain relief she would like to try from a list of ‘simple things’ like positioning, birthing ball or mat. Martha’s response, orienting to the lack of mention of pharmacological methods, is that ‘it’s too early for proper pain relief, isn’t it . . . ’.
Early labour seems especially to be a phase of limited optionality around pain relief. For example, Kailani, who features in extract 15 (see Figure 24), is later encouraged by a second midwife to stop using Entonox until she is ‘a bit more established’. Later, a third midwife rejects Kailani’s request for an epidural, saying ‘Not until you’re in established labour’ (although this midwife suggests codeine and a ‘nice warm bath’ to make her ‘more comfortable’). Subsequently, Kailani is transferred to an antenatal ward and there is no further recording of her labour after that.
Transition from first to second stage
Early labour, however, is not the only time that strong analgesia, particularly epidural, is discouraged. In transition (i.e. a period of intense and frequent contractions during which labouring women might become distressed and panicky), women’s requests for epidurals might be seen as symptomatic of nearing second stage. 263 This means that a request made at this time is likely to be resisted by midwives because it is treated as characteristic of a particular stage of labour, nearing second stage, and not as an expression of pain that requires ‘treatment’. As one midwife puts it in conversation with a woman in our recordings:
I’ll just kind of warn you now. There’s a bit before you get to fully dilated, which we call transition, when you will become a bit agitated and and a bit grrr, and it will all feel too much and you’ll change your mind, you don’t want one, and you’ll change your mind you’re going home, it’ll be like grrr. But what that means – we need to look out for it – is that you’re nearly there. So, if you decided that you’re probably not wanting an epidural, that isn’t the point at which to go oh, alright then, because you’re nearly there . . . It’s a shame to go for it at that point when you’re about to start pushing.
VIP10; simplified transcript
The above quotation was designed to be informative about a future point in labour, as the woman to whom it is directed (Gabi) was 5 cm dilated at the point of discussion. It is worth noting, however, that as soon as the midwife leaves the room Gabi whispers to her partner ‘sounds like she doesn’t want me to have the epidural though, doesn’t it?’ and so the ‘informing’ has been heard as a deterrent.
In practice, we do see midwives and BPs orienting to increased pain and distress as a sign of progress. For example, in response to a woman’s (Madeline; VIP 22) statement that she does not ‘want to do this any more’, her BP declares ‘that’s a good sign’. Similarly, there are occasions when a request for something like an epidural is treated as being characteristic of transition. For example, Gracie (VIP37) responds to a midwife’s recommendation for a VE that she, instead, ‘just want[s] an epidural so [she] can sleep’. The midwife first acknowledges and then declines this request on the grounds that the woman was ‘doing fine’ and does not ‘need that epidural’, and summarises with ‘everybody wants an epidural at this stage’.
So far, we have presented evidence that strong analgesia is treated as lying at the top of a hierarchy of pain relief that begins with non-pharmacological methods. Epidurals, in particular, are discouraged in the latent phase and in transition, although for slightly different reasons (however, three women in our data set do opt for and receive epidurals during active first stage). It is worth noting that almost 70% of women in our larger sample reported antenatally that they would either definitely not want or prefer to avoid an epidural, and all had opted for midwife-led care, in which epidurals are not available without transfer to the OU. Midwives might, therefore, be working to uphold that earlier choice (which may be reflected in the midwife’s characterisation of having an epidural ‘close to pushing’ as a ‘shame’ in the above quotation). This possibility is supported by our interview data, in which several HCPs highlighted the complexities involved when women request pain relief that they had previously stated they categorically did not want. For example:
And you don’t want women to have regrets, because, you know, they might not be in the right frame of mind [when requesting, for example, an epidural]. But then you don’t want to deny women anything that they could be really angry about.
Midwife A4
Timing opiates in relation to birth
Unlike epidurals, opiates are available as an option in midwife-led care. In line with NICE guidelines (section 1.8.12),10 midwives describe the impact of opiates as uncertain and variable, as well as potentially causing (temporary) drowsiness and respiratory depression in the mother and baby. 264 Opiates quickly cross the placenta and enter the fetal bloodstream, peaking at 1–5 hours following the injection. 265 Therefore, there is a preference to give opiates well before the second stage to allow the concentration to reduce in maternal and fetal bodies prior to birth. As a consequence, decision-making about opiate use typically hinges on assessments of progress (see extract 16 in Figure 25).
FIGURE 25.
Extract 16 (VIP02:Elise:Video): invoking stage of labour in opiate decision.
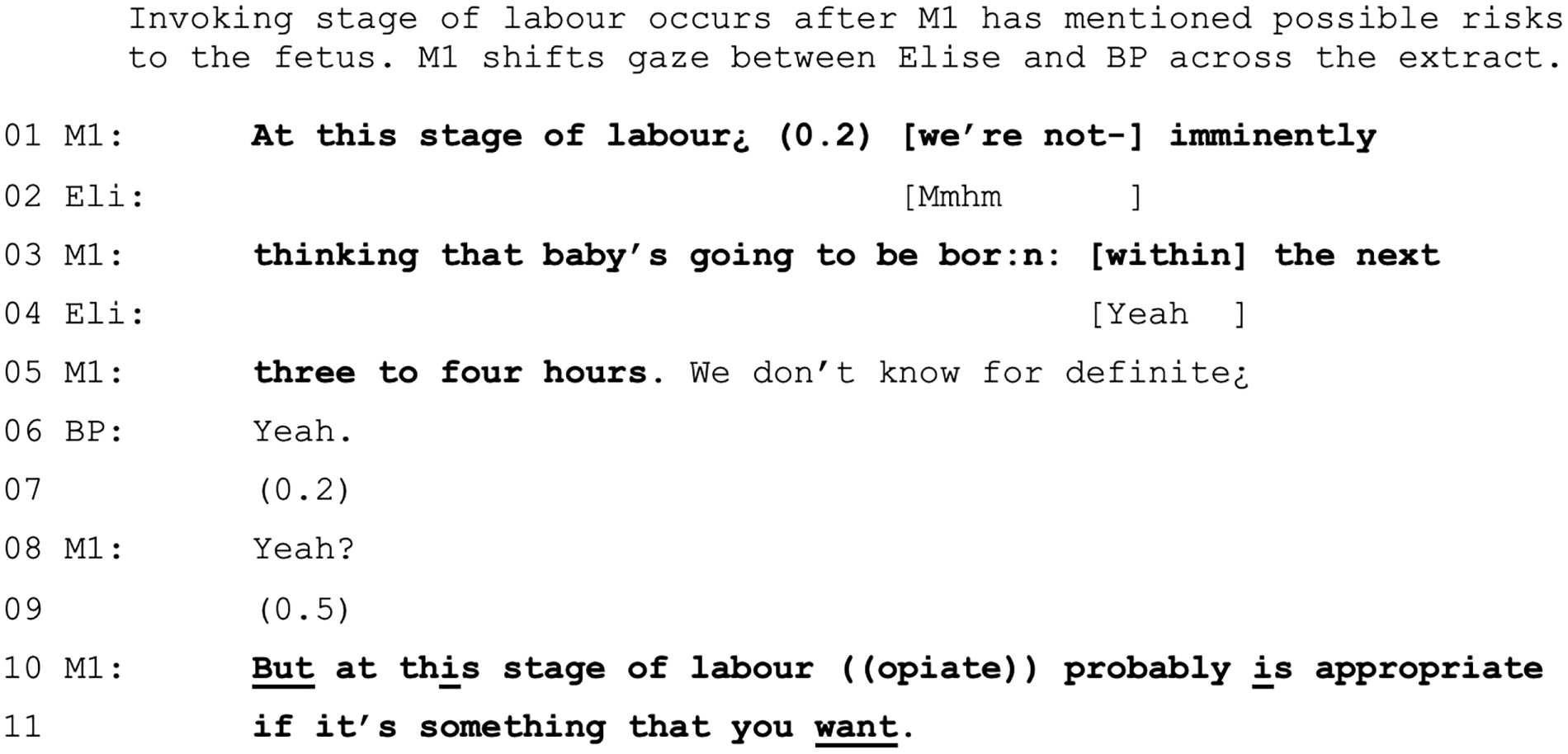
That decision-making about opiates as contingent on stage of labour is also evident when opiates are offered following a VE that has shown progress that falls short of transition (which, as noted above, is a point at which midwives seek to deter requests for pain relief). For example, after discovering that a woman is 6 cm, dilated a midwife says, ‘options for pain relief, you could carry on with the gas, you could get a bath, could try aromatherapy or ((opiate))’ (VIP24) (note that the woman selects the opiate). Alternatively, a VE might be proposed so that a woman can make an informed decision about opiates, that is, if labour is ‘still sort of at the earlier part’ (VIP36).
Progress (or at least perceived estimated time left until birth) is also a feature of women’s decision-making about opiates. For example, later on in the recording shown in extract 16 (see Figure 25), and with a different midwife, Claudia agrees to a VE to see if she needs to have an amniotomy, but also to inform her decision about opiates, saying ‘I think I want to see how close I was. Because if I’d only gone up to like seven or something then obviously there’s a long time left to go. And I was thinking I’d like ((opiate))’ (VIP22).
In keeping with the contingency of opiate use on stage of labour, and the laddering of pain relief, midwives use various strategies to defer or deter opiates. These are illustrated in extracts 17–20 (Figures 26–29), which are from one recording (Nina; VIP17) but are evident more broadly across the data set. To provide some context, Nina received an opiate earlier in labour, some time before the recording starts. Early in the recording, the midwife mentions that Nina can now get in the pool because it has been 2 hours since the injection. Nina begins asking for ‘more drugs’ before the permitted time has elapsed for a second dose and just after she has reported needing to push. Therefore, there are two factors at play that inform the midwife’s deferrals: (1) the time interval between doses and (2) the possibility that Nina is in transition. As time passes, the latter becomes the most significant. Strategies of deferral that the midwife uses include contradiction and encouragement (see extract 17 in Figure 26), an explanation of transition (see extract 18 in Figure 27), tying in the decision to a VE (see extract 19 in Figure 28) and pointing to the risks of opiates and proffering alternatives (see extract 20 in Figure 29).
FIGURE 26.
Extract 17 (VIP17:Nina:Audio): contradiction and encouragement.
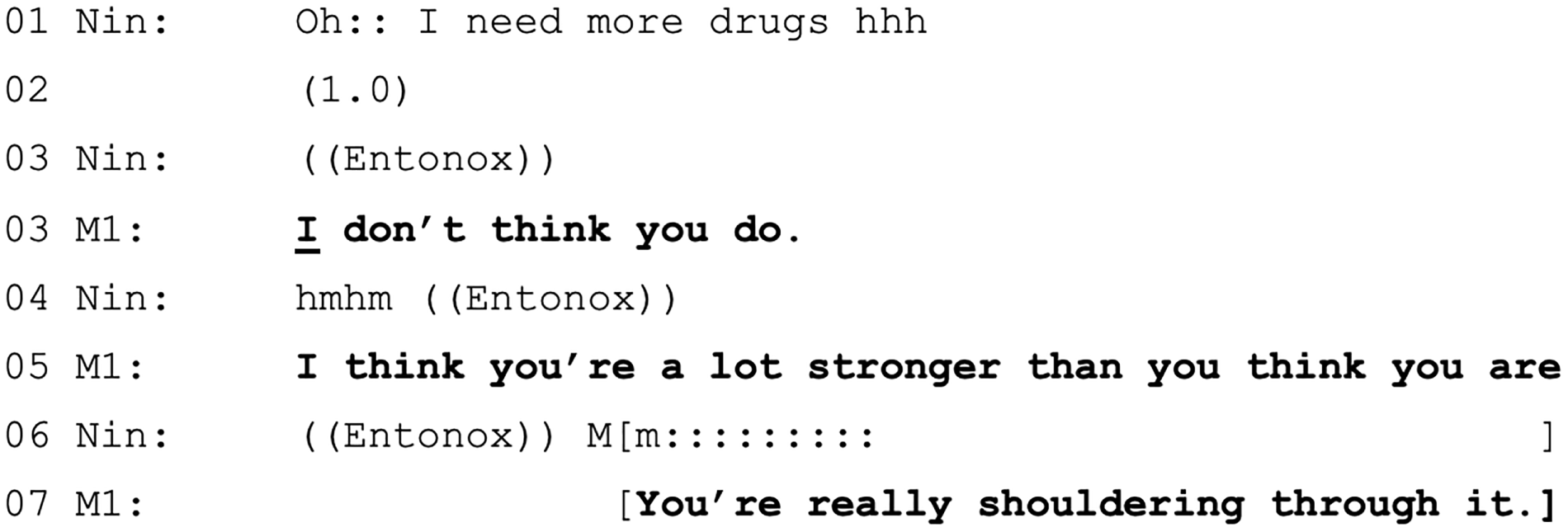
FIGURE 27.
Extract 18 (VIP17:Nina:Audio): explanation of transition.

FIGURE 28.
Extract 19 (VIP17:Nina:Audio): tying in decision to a VE.

FIGURE 29.
Extract 20 (VIP17:Nina:Audio): pointing to risks of opiates and proffering alternatives.
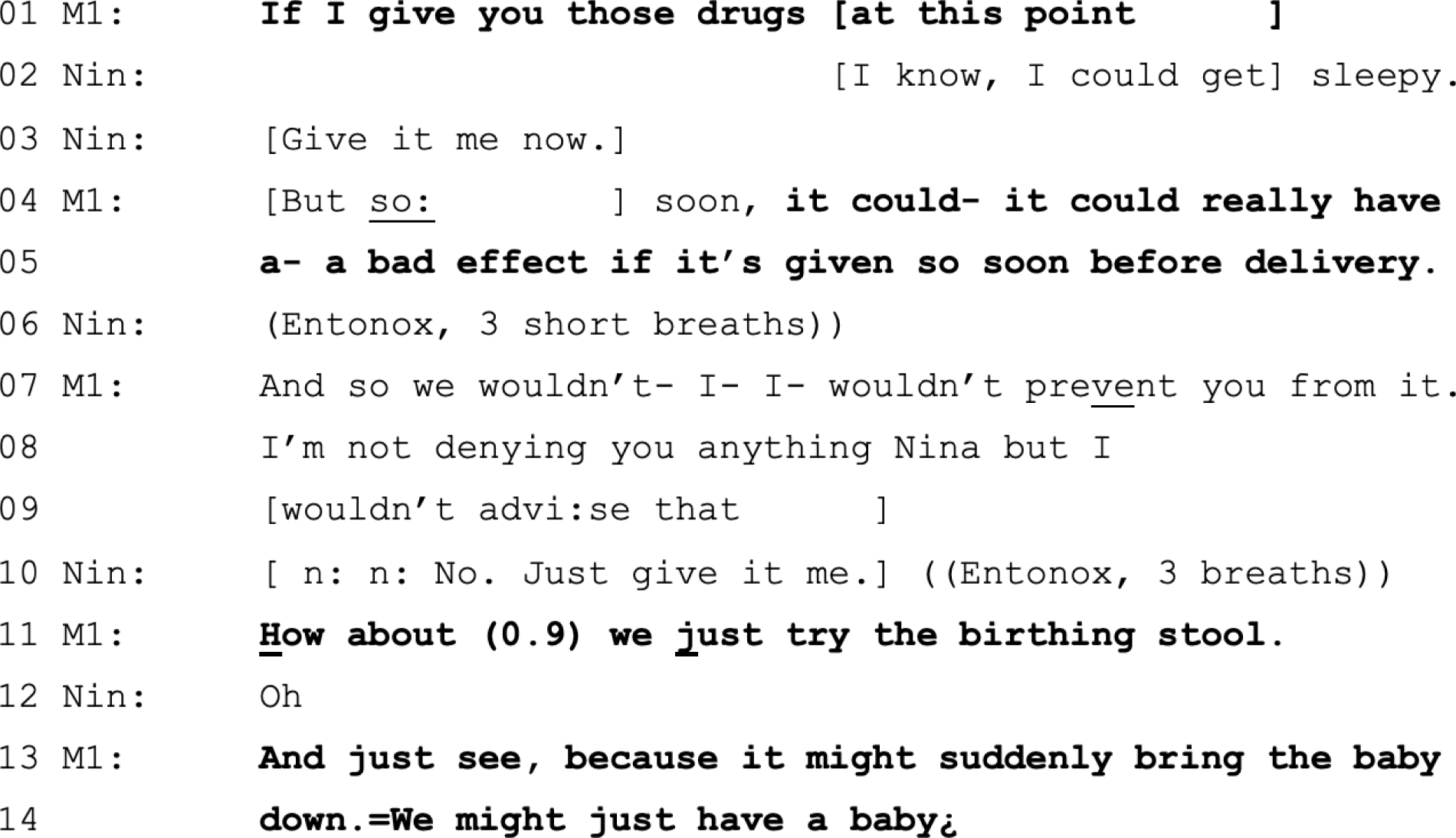
A notable feature of all these strategies is that, although they involve deterring opiates, they also offer women support through other means (i.e. encouragement, explanation or trying alternative birthing positions). Ultimately, Nina does, in fact, get an opiate (some 4 hours into the recording) as an alternative to having an epidural, which she requests when she is fully dilated (bar a ‘rim’ of cervix) and beginning to push (although irregularly). Having spoken to a senior colleague, the midwife negotiates, saying ‘we can give you ((opiate)) if you want, rather than an epidural’, which Nina accepts on the basis that she can have the epidural after she has the opiate (and, therefore, the option of an epidural is kept open). (Note that the immediacy of pain relief is Nina’s primary concern and she does not want to wait for transfer to OU.) The midwife also gives Nina an aromatherapy massage to help manage the pain. The baby is born 3 hours after the injection, with Nina having experienced a long and difficult second stage.
Pursuing opiates
We have demonstrated above that, although women actively lead pain relief decision-making, midwives are not generally immediately acquiescent, hence the interactional ‘need’ for women’s pursuit. As we have seen in Chapter 3, there is a negative statistical association between the number of times a woman pursues a request in a decision about pain relief and postnatally reported levels of satisfaction. The longest chains of decisions in our data set relate to decisions about the use of opiates. In the final section of the chapter, we use CA to qualitatively explore what takes place during two examples of particularly lengthy chains of decision-making concerning the use of opiates. In doing this, we illuminate aspects of the interactional contexts in which repeated requests for pain relief were generated in our data set.
Progress in labour, as midwives acknowledge to women, is uncertain and unpredictable. Midwives are generally cautious about offering precise timings of birth and, instead, constantly observe for signs of progress (e.g. women’s behaviour and their reported sensations). Given the uncertainty of progress, the signs may occasionally leave midwives to conclude that a woman is further on in labour than she actually is, with implications for decisions about opiates. For example, one (VIP11) of the two recordings that each contain the longest chains of decision points involves a multiparous woman (Philippa) who is seeking opiates at the same time as reporting pressure to push. As is fairly common across the data set, Philippa attempts to initiate a decision for stronger pain relief in various ways, including decision-implicative statements (e.g. ‘I don’t think I’m going to do it on gas and air’) and requests [e.g. ‘I need something stronger’ and ‘please can I have some ((opiate))’]. Concurrently, her spontaneous verbal reports (e.g. ‘That felt like a lot of pressure then’), the frequency and length of contractions (e.g. the midwife comments ‘These are whopping great contractions’), and multiple attempts to obtain stronger pain relief give a possible impression of approaching transition. The midwife regularly checks this by asking Philippa to report her sensations (e.g. ‘Have you been pushing at all?’, ‘Is it feeling any different?’ and ‘Where is the pain now. Is it at the back or the front?’) and, via their assessments (e.g. ‘This is the really tough part’ and ‘Nearly there. Whopping great contractions and you’re coping’), conveys the possibility that Philippa is closing in on second stage. The possible signs of transition are used by the midwife to deter a decision about opiates. For example, responding to pressure for opiates, the midwife says ‘Might be a little late for something . . . might have a baby first’ and later says ‘I think things are happening quite quickly’. At the same time, the midwife coaches Philippa through contractions, helping her to slow her breathing, inspires her to move and try different positions, regularly praises her for her ‘courage’ and for how ‘amazing’ she is, and encourages her to stay ‘in the moment’ and to take contractions ‘one at a time’. This amounts to enormous emotional labour on the midwife’s part to support the woman through physical labour (and, again, is a regular feature of work carried out by midwives across the data set).
Approximately 1 hour after Philippa first mentions needing something more than Entonox, she requests opiates again, using a negative formulation of ‘Can I not have any ((opiate))?’. There is some evidence that negatively formulated requests display greater entitlement to make the request – and, therefore, greater expectation of grantability – than the same request formulated positively [e.g. ‘can I not have . . . ’ vs. ‘can I have . . . ’, and see also the BP’s request of ‘can’t you help her along a bit’ in extract 3 (L1 in Figure 12)]. 224 The exchange that immediately follows is shown in extract 21 (Figure 30).
FIGURE 30.
Extract 21 (VIP11:Philippa:Video): VE offered in face of 11th decision point relating to woman’s request for opiate.
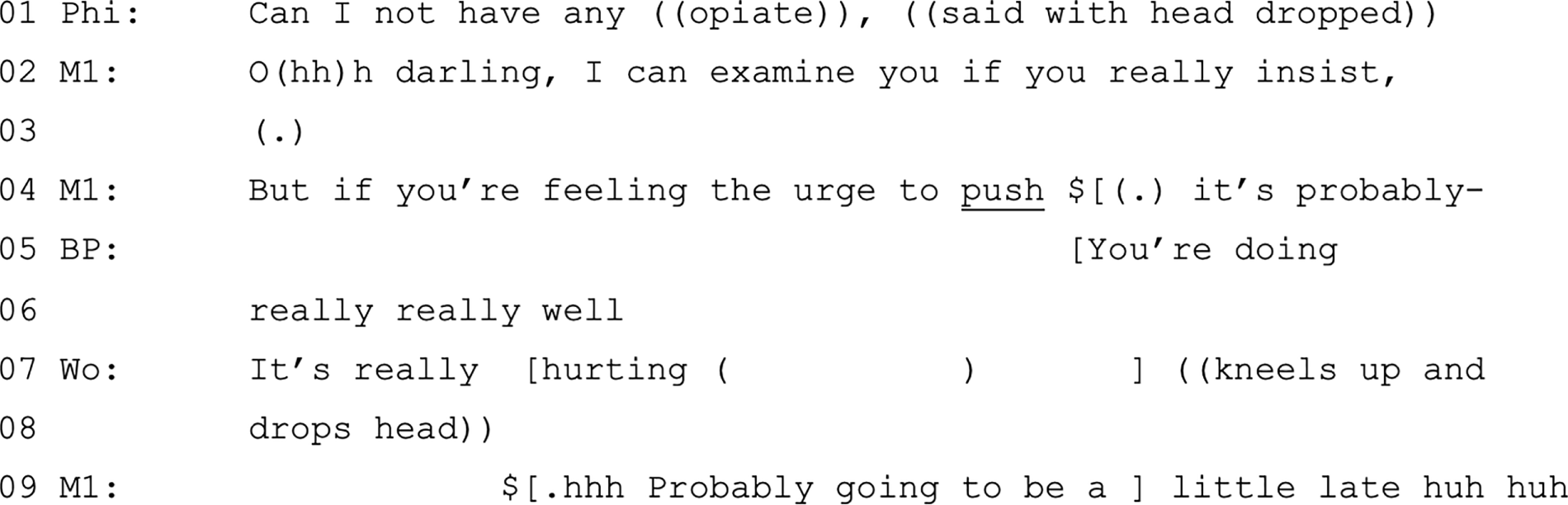
Faced with what is now the 11th decision point relating to the decision about opiates, the midwife offers a VE (L2). The offer is predicated on what the midwife characterises is Philippa’s insistence. Out of context, invoking Philippa’s insistence appears misplaced because Philippa has not been pursuing a VE. However, the need for the VE is entwined with a decision about opiates, which she has been pursuing. This relationship between opiates and progress is made explicit in the midwife’s following turns, that is, if the woman is ‘feeling the urge to push’ (L4) it is probably going to be a ‘little late’ for opiates (L9). The midwife then encourages Philippa to continue, talking her through contractions for another half an hour, after which Philippa issues another request (for an unspecified ‘something else’), followed quite quickly by yet another request of ‘is there nowt else I can have’. The midwife then, again, offers a VE in similar terms to the previous offer [i.e. ‘I can examine you (.) if you really want me to’]. Following a question-and-answer sequence, Philippa issues a conditional request that implicitly accepts the VE by enquiring whether or not she can have an opiate if she is ‘only 7 centimetres’. The midwife unequivocally agrees. When she had the VE, Philippa’s cervix is 6 cm dilated and the opiate is given. Not long after, Philippa also has an amniotomy (see Chapter 5 and extract 13 in Figure 22) and the baby is born within 90 minutes of the opiate injection and, therefore, the midwife warns her that he may be drowsier than usual. In her PNQ, Philippa is one of the outliers relative to the majority of the CA data set in having a neutral (as opposed to positive) satisfaction score.
Long decision-making chains, such as the one outlined above, are a common feature of decision-making about opiates. In all cases, the women are highly engaged in extending the sequences. These decisions take place over time, sometimes hours, with plenty of other activities (especially monitoring) happening between relevant turns. In this sense, the CA notion of ‘sequence’ has to be extended to include revisiting the same decision, even if the utterances are separated in time or by the discussion of other topics. For example, we would not want to see Philippa’s negatively formulated request (see extract 21 in Figure 30) without the broader context of all the prior occasions she forwarded her agenda to seek opiates.
As reflected in our survey findings, having to repeatedly pursue requests for opiates can lead to women feeling unheard. Fiona, who was involved in the longest chain of decisions in our data set (n = 18), writes in her PNQ:
I don’t feel that the midwife in the later stages of my labour listened to what I was saying. All in all the experience was positive. However, I asked for increased pain relief around 6.30 a.m. and repeatedly after that, and the midwife did not have a discussion with me about why it would be advisable not to have the pain relief until around 8.20 a.m. In the meantime I was very frustrated that no one was listening.
VIP12
Looking at the details of this opiate decision, a likely key issue for Fiona arises because of a shift change, as a consequence of which a previously agreed decision about pain relief has to be renegotiated. The first midwife, to whom the initial request for an opiate is posed, appears to agree to it (i.e. ‘That’s fine. Whatever you want’), but then offers a VE ‘just to check that you’ve not progressed and sort of got to a point where you’re ready to push baby out’. Fiona eventually accepts the offer of a VE, but the midwife goes off shift before it is conducted, explaining that she has been on duty for 12.5 hours and the new shift has started and, therefore, ‘There’s no point me examining you, because then they can carry on’. Fiona reissues her request for opiates as part of her response to the incoming midwife’s open query (i.e. ‘how are you doing’) by saying that she is ‘struggling now’ and wishes to ‘get out [of the pool]’ because she ‘want[s] some ((opiate))’. The midwife defers responding to the request, first by asking what form of pain relief Fiona had in her previous labour, second by enquiring about the nature of her current pains and third by asserting an imminent need to conduct observations (e.g. blood pressure). Nevertheless, the midwife keeps open the matter of opiates by then saying ‘Bear with me and then we’ll keep having a bit more of a chat about your options’. It is, however, another 30 minutes before opiates are mentioned again [see L8 in extract 22 (Figure 31)].
FIGURE 31.
Extract 22 (VIP12:Fiona:Video).
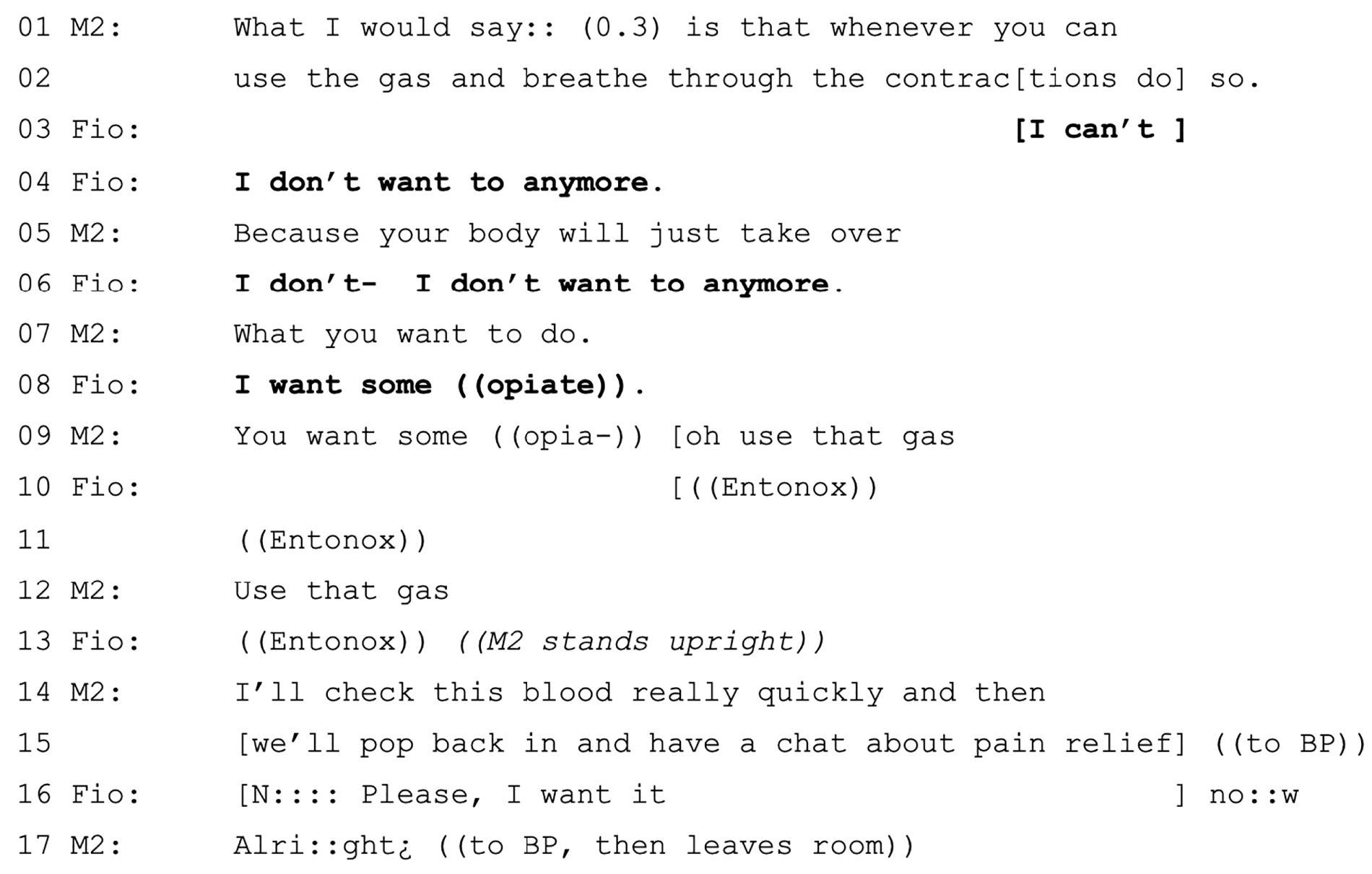
The midwife’s response, which starts with a repeat of Fiona’s request (L9), is halted, as Fiona has another contraction. The midwife instructs her to use the Entonox and then asserts that they are leaving to check bloods ‘really quickly’ (L14) and will ‘have a chat’ on her return (L15). Fiona, treating the midwife’s plans as delaying her own, pleads for opiates (L16) in overlap with the midwife’s turn at L15. Both speakers persist simultaneously to complete their turns, suggesting a competitive element. 266 In fact, the midwife does not respond to Fiona and, instead, completes the turn at L15 with a tag ‘all right’ (L17) directed to the BP. The midwife is out of the room for about 10 minutes, during which time Fiona complains to her BP, saying, for example, ‘I want to get out and have some ((opiate)) but they’re not bringing it’ and, later, that she has been asking ‘forever’. The BP, aligning with the (absent) midwife, entreats Fiona to ‘trust them’. On returning, the midwife once again defers discussion about pain relief, saying that they will discuss it after monitoring the baby [Figure 32]. On completion of monitoring, the midwife returns to the topic (L1, see extract 24 in Figure 33) and essentially recommends a VE (L7–8). The midwife makes the granting of opiates conditional on the outcome of the VE (L10–11 and L13–16). Optionality (using an option list) is afforded to Fiona in terms of timing for the VE (L20–22).
FIGURE 32.
Extract 23 (VIP12:Fiona:Video).
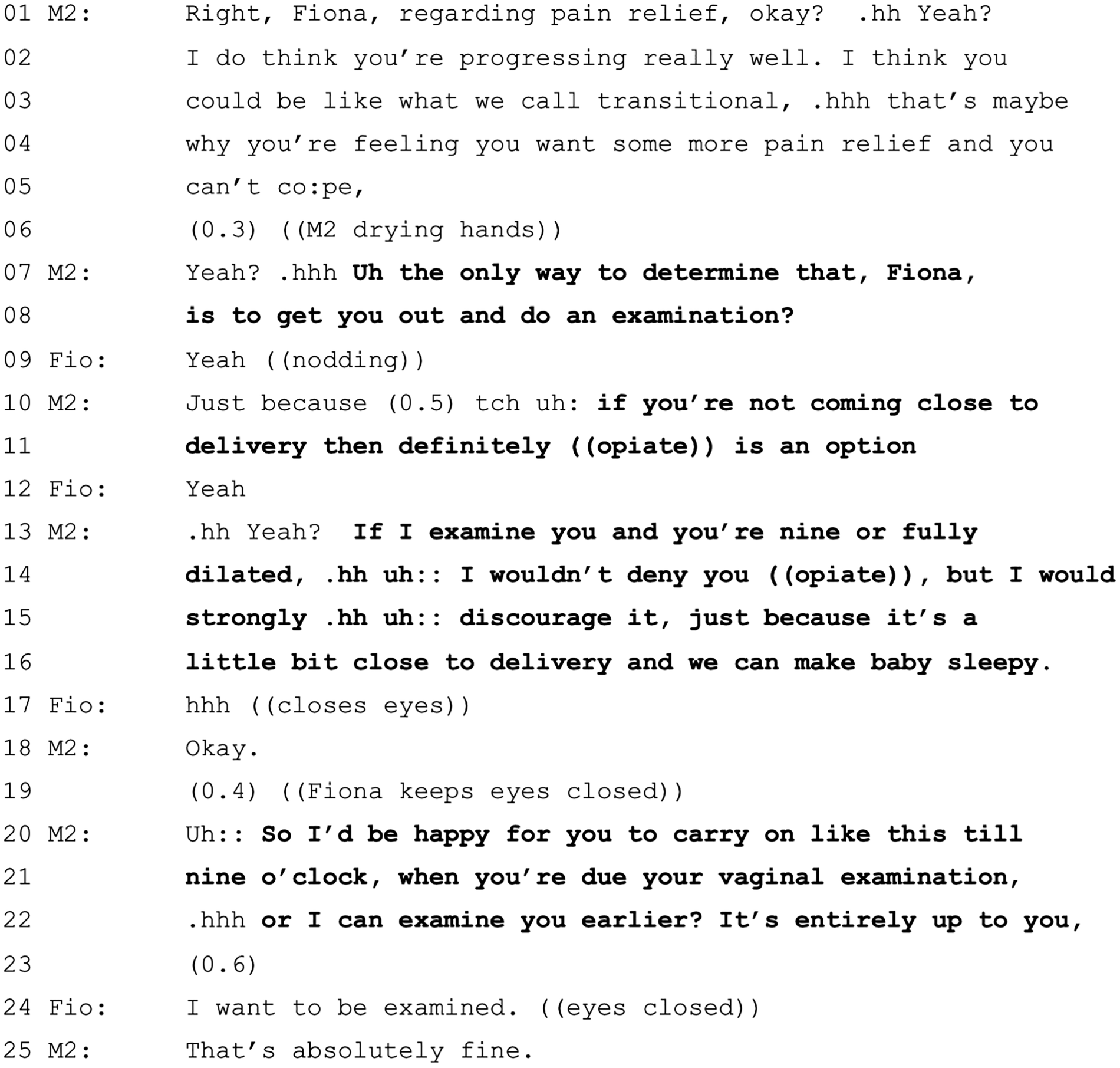
FIGURE 33.
Extract 24 (VIP12:Fiona:Video-but-off-camera).

The examination is conducted about 20 minutes later (the delay being accounted for by getting Fiona out of the pool, drying off, going to the toilet and experiencing a number of contractions). On completion of the VE, the midwife monitors the baby before announcing dilatation, therefore, delaying the news that she is 8 cm. On hearing the news, Fiona immediately requests opiate again and the midwife responds by pointing to the risks of opiates given at this stage of labour. It is at this point that Fiona displays most frustration, saying ‘But I can’t I can’t do this. I’ve been wanting it for like an hour and a half. I real- I really just need it’. Fiona is accurate in her estimation of the time since she first asked for opiates. The turning point comes some moments later with an option list [see extract 24 (Figure 33)], providing choice between two options of carry on with support or an opiate.
The options are not equally weighted, partly because of where this option list happens in the chain of decision points (i.e. coming after recommendations against opiate based on risk) and partly from the way in which the option list itself is built. The first option of support, Entonox and pool (L10–11 and L13–14) is built around minimising the time left (‘last little bit of cervix’). The support worker’s positive assessments (L5–6 and L9) also lend support to this option. The alternative option is opiate (L16) and an uncertain outcome (‘we’ll just see what happens’; L18). Faced with this, Fiona equivocates, saying that she does not know which one to take (L19), although she does reject the pool (L12). This is the first time Fiona displays hesitation about wanting opiates. In response, the midwife hands the decision back to Fiona (L20). There follows (data not shown) some discussion and reassurance about possible time left to delivery before Fiona accepts the first option (i.e. Entonox plus support). She is then encouraged onto a birthing stool and the baby is born 12 minutes later. In the PNQ, Fiona reports being satisfied with the decisions that were made and so she was presumably content that she did not have opiates. However, as noted in her qualitative comments, the way in which the decision was experienced interactionally (rather than the outcome) – feeling that she was not listened to – was a source of dissatisfaction.
Conclusion
Interactional decision-making about pain management is highly complex. In this chapter, our focus has been necessarily narrow, and this means that we have not been able to explore some of the fundamental practices that shape a woman’s experience of pain. For example, we have not discussed the clearly important role BPs and midwives have in supporting and coaching women through contractions. Nor have we discussed the more subtle ways that pain is oriented to (e.g. pain displays and responses to them). We have, instead, focused primarily on decisions about methods of pain relief, noting that there is a clear laddering of options that are tied to matters of progress. As we have demonstrated, progress has its own epistemological challenges.
Decision-making about opiates is particularly complex because their timing is potentially consequential for women and babies. Matters of timing in labour are imprecise and can be unpredictable. The impression, based on a range of data, that a woman is nearing second stage may or may not be accurate. Although opiates may be deterred in the context of (suspected) advanced progress, midwives do not abandon women to their pain. Rather, they are attentive and encouraging, and provide support for women to ‘work with’ their pain. 259 However, for some women, not getting access to the opiate they want can leave them feeling unheard.
The more a woman is involved in pursuing pain relief decisions, the less satisfied she is. If we simply counted the number of times women spoke during decisions relating to pain management, then they would appear to be highly active and the relationship to satisfaction would seem paradoxical. However, through CA of these interactions, we can see that what is occurring here is that pain relief decisions are sometimes being kept ‘open’ by midwives, necessitating women’s further pursuits of requests. In some cases, these decisions take place over very extended time periods. Our analysis has pointed to two interactional contexts in which these lengthy chains of decision-making may arise: (1) uncertainty about progress and (2) shift changes. However, further research (with our data set) is needed to systematically understand the ways in which women escalate their requests for pain relief and the ways in which midwives respond to them.
Chapter 7 Third-stage decisions
Introduction
The third stage of labour is defined as the period between the birth of the baby and the expulsion of the placenta. There is a range of interventions and procedures that occur during it and immediately beyond (e.g. cord clamping and cutting, placental expulsion, skin to skin, breastfeeding, catheterisation, suturing, positioning and pain relief). NICE guidelines10 include reference to respecting this time for getting to know the baby and, therefore, ensuring that care is handled sensitively with separation and disruption minimised (point 1.14.1, updated 201710). Our rationale for addressing ‘the third stage’ is that, although it encompasses a range of decisions, these tend, on the whole, to be ones in which women’s (or their BPs’) participation is invited to greater extents than observed elsewhere in our data set. We focus on two key decisions: (1) whether to use oxytocic drugs to induce separation and expulsion of the placenta (i.e. active management) or for the placenta to be expelled in its own time (i.e. physiological management) and (2) clamping and cutting of the umbilical cord.
Of the 37 recordings, 20 include at least some of the third stage. Of the 17 cases in which the recording ends before the baby is born, seven recordings include some discussion of third stage (and immediately beyond) decisions. Therefore, the analysis in this chapter is based on a subset of 27 of the 37 recordings of the complete data set.
Active or physiological third stage
NICE guidelines10 suggest that the decision about active or physiological third stage should be discussed in advance and that statistical information regarding the likelihood of haemorrhage, nausea/vomiting and blood transfusion should be given (points 1.14.7–8, updated 201710). NICE guidelines10 recommend that women are advised to have an actively managed third stage; however, if women are considered low risk, then HCPs should ‘support her in her choice’ (point 1.14.11, updated 201710) for a physiological third stage. If a situation of a retained placenta arises, then the guidelines are much more directive (points 1.14.21–8, updated 201710). The RCM267 recommends that women should be informed that there is a reduced risk of haemorrhage if active management is chosen. This advice is rooted in evidence,268 but the quality of research is often low and there are potential negative effects of the drugs, such as increase in maternal blood pressure, afterpains and vomiting, that should be communicated in advance of the decision. 269
Options chosen across the data
In the ANQs, a large proportion (48%) of participants in the larger sample indicated that they wanted an oxytocin injection to speed up delivery of the placenta and 20% selected a preference for allowing the placenta to come away in its own time. The remainder of participants selected either not knowing enough to make a decision (11%) or having no preference (15%) (missing data account for the residual 6%). As mentioned in Chapter 3, Table 14, decisions pertaining to the placenta were one of the few types that some (20.8%) participants postnatally reported having experienced no staff involvement, suggesting (cautiously) that a relatively higher level of ‘control’ may have been given to women.
Decision-making about whether or not to have an actively managed third stage is present in all the recordings that include post-birth footage (i.e. 20 recordings) and all seven of the recordings that end before the moment of birth but that also contain discussion of third-stage decisions. Consistent with the NICE guidelines,10 overwhelmingly, the decision made was to take the drug-managed option (i.e. ‘active’). The decision not to have the oxytocin injection was chosen in only 2 of these 27 recordings. In one of these two recordings, the decision was made after the baby had been born. Although this choice was accepted, the midwife, nonetheless, presented the option of the injection if the physiological third stage was unsuccessful. In the second instance, there is a provisional decision, but the footage ends before the birth of the baby and so there is no evidence of how this decision was actually enacted. The statistical information that NICE recommends10 is shared with women regarding the numbers of women affected by risks of both options (e.g. nausea and vomiting are associated with haemorrhage of more than 1 litre in 13/1000 vs. 29/1000 women with active vs. physiological management, respectively) was not present in any of the decisions captured in the data.
Timing of decision-making
Usually, decision-making about management of the third stage was initiated in these 27 births during the first stage of labour or prior to labour. There are six cases in which third-stage options are not discussed until after the baby has been born; however, in all but one of these cases, there is evidence to indicate that previous discussions had taken place (i.e. before the recording began or in a birth plan). Moreover, in one case (VIP04), a discussion of active or physiological options occurs during the first stage of labour, but no decision is reached, and then, after the birth of the baby, a different midwife moves toward administering the injection, presuming that the decision had already been made (giving evidence for administration of the oxytocin injection as the normative option). This assumption shows the routine expectation that the decision will have already been made prior to the time of its implementation.
Initiation of the decision
Option lists are the most common way (8/27) in which this decision is initiated (note that there is an additional option list when an offer is converted to an option list after a silence; see extract 30 in Figure 39). Option listing is likely to be heard by the recipient as offering opportunity for choice. 162 Extracts 25–27 (Figures 34–36) show three different ways in which option listing is accomplished.
FIGURE 34.
Extract 25 (VIP04:Judy:Audio).

FIGURE 35.
Extract 26 (VIP06:Kay:Video).
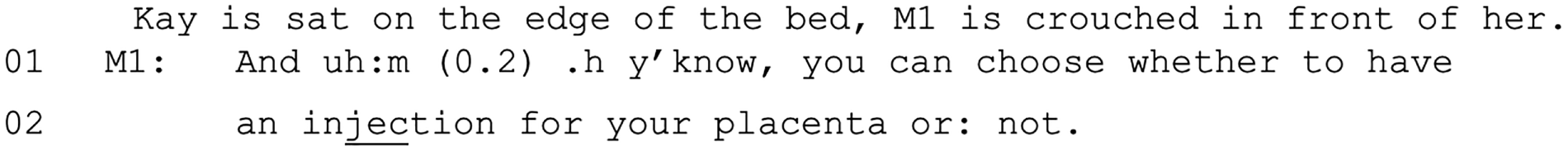
FIGURE 36.
Extract 27 (VIP20:Abigail:Video-but-off-camera).
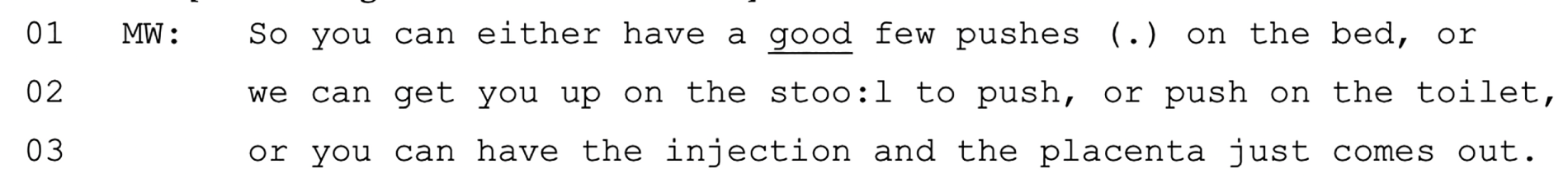
In extract 25 (see Figure 34), both options are articulated fully. In extract 26 (see Figure 35), one option is explicated fully (i.e. ‘to have an injection for your placenta’) and the other option is indicated by contrast (i.e. ‘or not’). Finally, in extract 27 (see Figure 36), four options are presented. Three options relate to different ways to have a physiological third stage (i.e. pushing on the bed, getting on the birth stool to push and pushing on the toilet) and one option is to have oxytocic drugs.
Offers are the second most common way (6/27) in which these decisions are initiated, although one of these offers is subsequently revised as an open question. In extract 28 (Figure 37), the midwife offers active management through reference to ‘the injection’.
FIGURE 37.
Extract 28 (VIP09:Freya:Audio).

Although offers ostensibly position the recipient of the offer as the decision-maker, they do not necessarily give an unbiased opportunity to accept or reject the action put forward. Extract 29 (Figure 38), for instance, shows a midwife preceding the offer with an informing that they have the injection already prepared (L1). Furthermore, the injection is minimised (‘little’) and described as being ‘to help’ (L1).
FIGURE 38.
Extract 29 (VIP08:Lydia:Video).
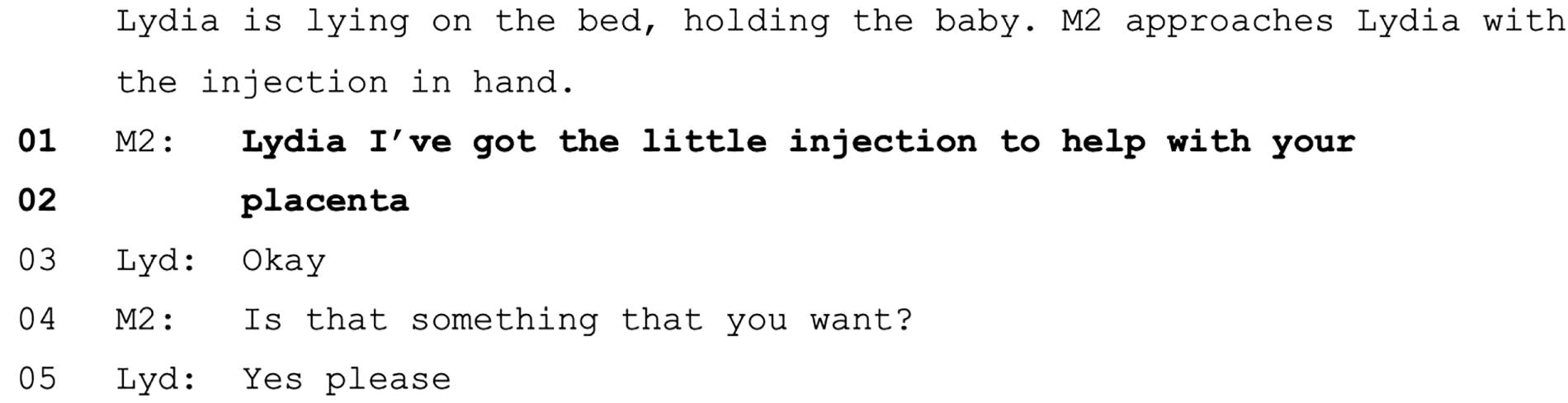
However, outright rejection is usually not required for recognition of approaching non-acceptance and midwives often adapt their turns to head-off possible rejection. In the extracts 30 and 31 (Figures 39 and 40) an offer, which presupposes acceptance, is revised.
FIGURE 39.
Extract 30 (VIP19:Leigh:Audio).
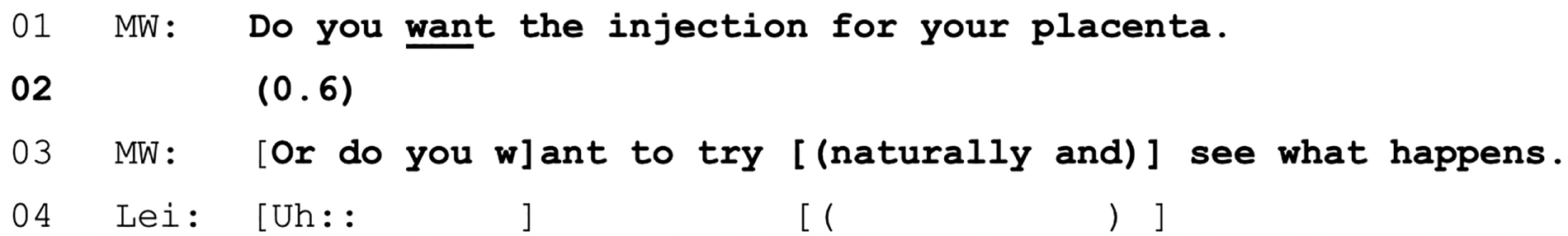
FIGURE 40.
Extract 31 (VIP37:Gracie:Audio).
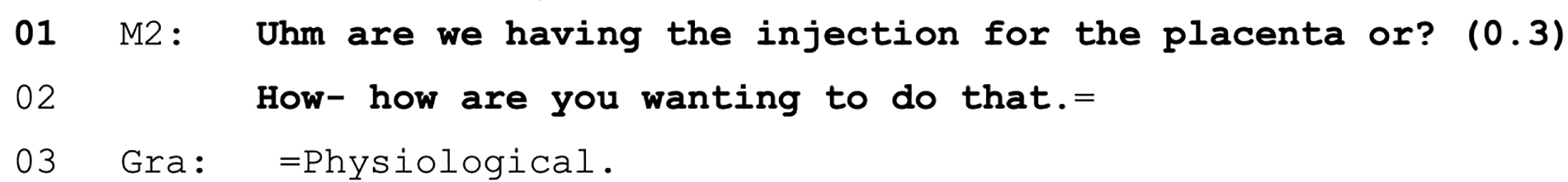
After the initial decision initiations in extracts 30 and 31 (see Figures 39 and 40), there is silence (represented in seconds in brackets on L2 and L1, respectively). Silence after an offer is indicative of a possible upcoming rejection of that offer. 270 In both examples, midwives display an orientation to that by adapting the initiating format to one that is more inclusive of both options. In extract 30 (see Figure 39), an incremental addition (L3) changes the offer to an option list and in extract 31 (see Figure 40) the offer is rephrased as an open question. Open questions are a way in which midwives can elicit views about preferences for placenta management without presupposing which option is likely to be selected [see extract 32 (Figure 41)].
FIGURE 41.
Extract 32 (VIP05:Bryony:Audio).
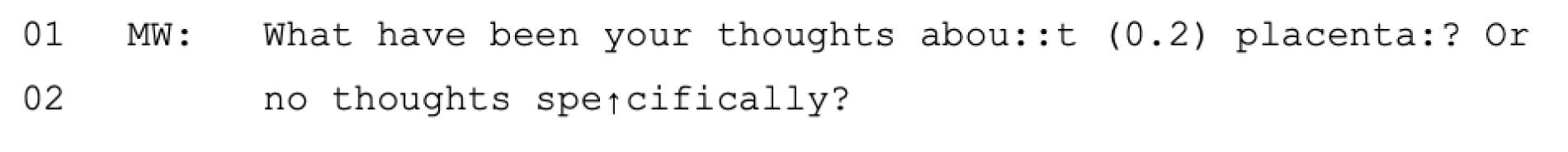
This interaction occurs early in the labour and, therefore, this stage might be more fitted to this format of initiation, as it does not require a definite answer immediately. In this instance, the woman does not answer as a contraction begins. Instead, the BP refers to the birth plan in response to the midwife. There are two other instances in which reference to the birth plan is used as a way of initiating discussion of this decision (one in which the midwife raises it and another in which the woman does).
Reference to birth plans (2/27), open questions (2/27), options lists (8/27) and, perhaps to a slightly lesser extent, offers (6/27) are ways in which the decision is placed with the person giving birth. There was one other instance in which a woman anticipated an offer after the midwife sought to establish the woman’s understanding of the decision by accepting the injection before it had been offered (see extract 37 in Figure 46). Therefore, in 19 instances, decision-making about third-stage management is initiated in a way that treats the decision as being in the woman’s domain.
Health-care practitioners’ input in these decisions
That the initiations treat the decision as being in the woman’s domain does not preclude input from HCPs, as the options in the lists may be weighted or the offer might come as the midwife is assembling the equipment for the injection.
In extract 33 (VIP06) (Figure 42), the midwife provides an options list (L1–2). The woman (Kay), who is chewing toast, begins to respond with ‘I’ll see how’ (L3) and the midwife provides the full turn (‘just see how it goes’; L4), which defers the decision-making. Nevertheless, the midwife then provides a rationale for physiological delivery of the placenta and, therefore, weight for that option, with ‘if you’ve birthed a baby then chances are you’ll probably manage to have your placenta as well’ (L6–7), which Kay resists by suggesting she is unlikely to care what happens at that stage (L9). In extract 34 (VIP24) (Figure 43), after the initial option list (L4–5) is receipted, but no option selected (L6), the midwife provides a general recommendation (L7) that weights the decision towards having the injection. Unlike extracts 33 and 34, in which the decision is weighted after choice has been presented, in other cases HCPs initiated this decision with recommendations/suggestions. For example, in extract 35 (Figure 44) the woman has just given birth and the midwife recommends an actively managed third stage (L4–5), having noticed some bleeding (L3).
FIGURE 42.
Extract 33 (VIP06:Kay:Video).
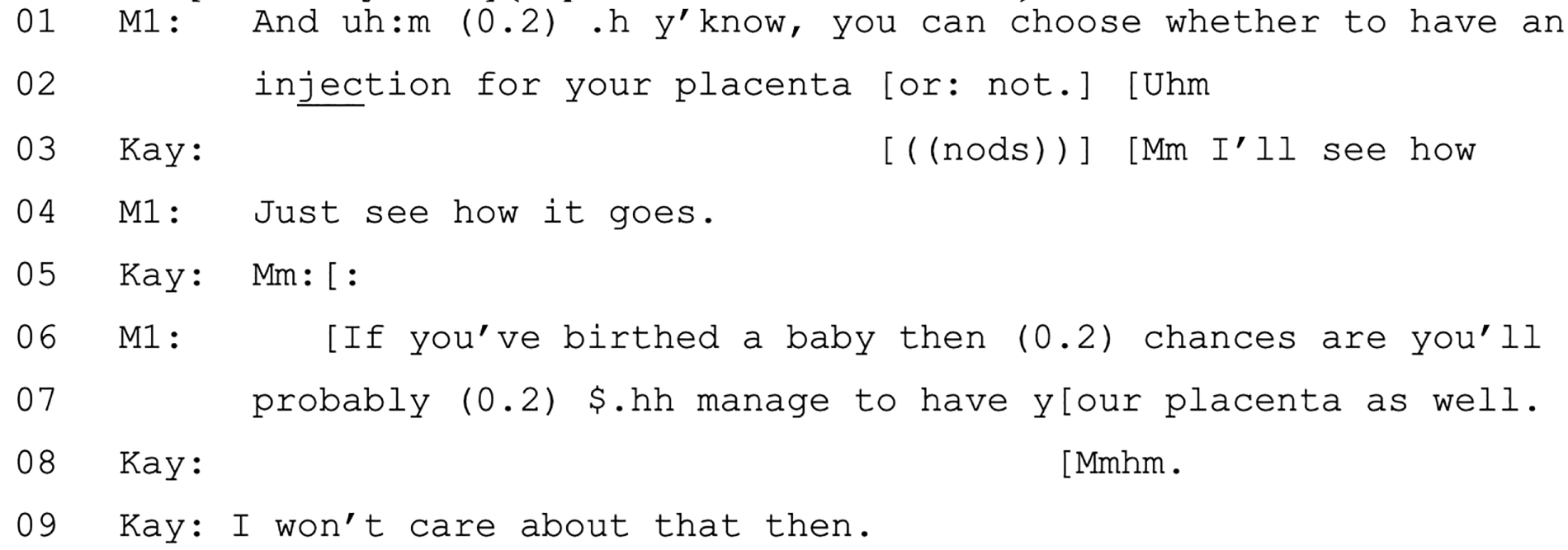
FIGURE 43.
Extract 34 (VIP24:Imogen:Video-but-off-camera).

FIGURE 44.
Extract 35 (VIP26:Bella:Video).
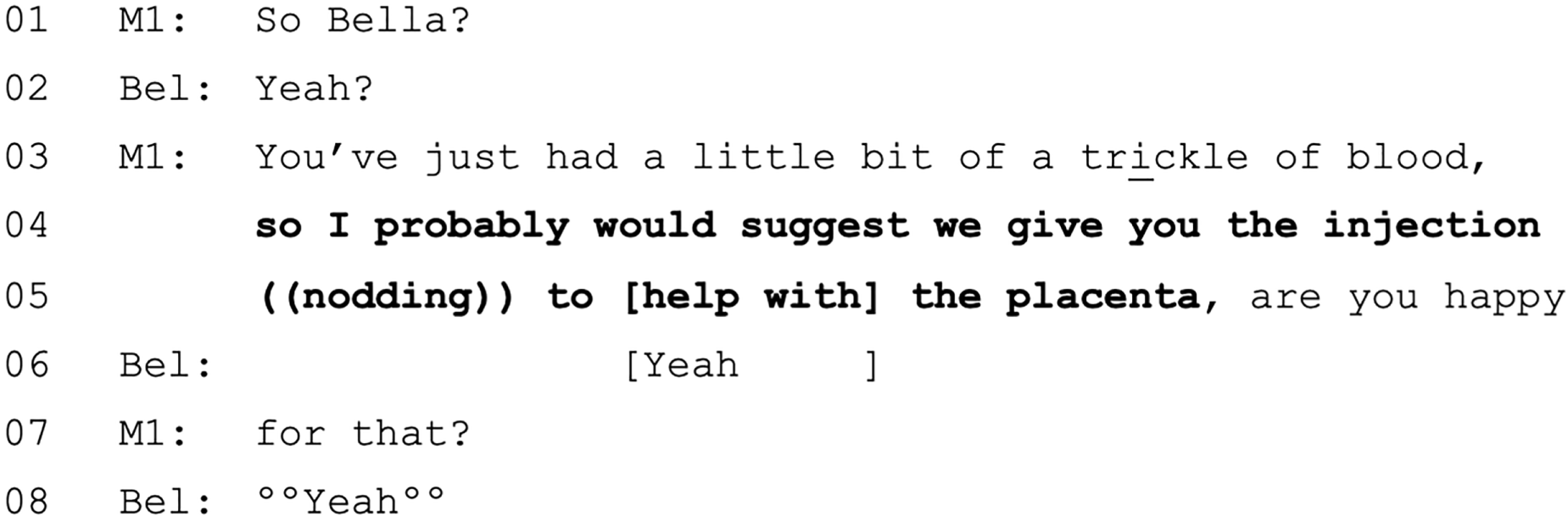
There are three instances (3/27) of the active or physiological decision being initiated by a recommendation and in each one the recommendation is grounded in specific details of the woman’s case.
In the remaining cases (5/27), reference to this decision is made with pronouncements [e.g. extract 36, L1 (Figure 45)].
FIGURE 45.
Extract 36 (VIP21:Diana:Video).
As we have noted in Chapter 4, this format provides for minimal recipient input (beyond, in this case, the confirmation-seeking tag question – ‘OK?’; L2). That is not to say that a person giving birth could not contest it, but that there is little interactional space provided for them to do so. However, the use of the indexical ‘that’ (L1) indicates that the injection has been discussed previously (as opposed to ‘a’, for example). In four of the five instances there is this interactional evidence that an already agreed decision is being indexed. In addition, four of these instances occur at the point at which the injection is about to be administered. Throughout the data set, when a decision about placenta management is made prior to the birth of the baby, then there is often a consent check or pronouncement at the time of execution of the decision (akin to the consent checks made before conducting VEs discussed in Chapter 5). Therefore, for these five cases of pronouncements, the evidence suggests that earlier discussions are likely to have occurred before the onset of the recording.
Sharing information
Health-care practitioners do not always assume that the woman will know about the options available with regard to delivery of the placenta. RCM267 and NICE guidelines,10 particularly the latter, recommend that midwives should provide detailed information about each option. In our data, midwives may launch into information-giving with reference to this decision, but that is rare. Usually, a midwife produces an understanding check prior to an action that will bring the woman to a decision point (e.g. option list, offer).
In extract 37 (Figure 46), the midwife begins what is likely to have been ‘were you wanting’ (L1) and then cuts off to do the understanding check (L1–3). Phoebe responds to both the understanding check (‘yeah’; L4) and the not articulated but implicit offer with ‘I think I would’ (L6). In extract 38 (Figure 47), Yvonne’s confirmation (L3) in response to the midwife’s understanding check (L1–2) claims (but does not demonstrate) knowledge of the choice available. The midwife treats this as a go ahead and so moves to enquire about the decision reached (L4). However, in this case, Yvonne seeks further information before reaching a decision (L5). These understanding checks are positioned prior to movement towards a decision initiation point and are used to ensure that utterances are recipient designed, based on the constraint that ‘speakers should not tell recipients what they suppose . . . the recipient already knows’176 (i.e. in first asking if they have had previous discussions, midwives are establishing current levels of understanding/knowledge women may have to make an informed decision, hence providing the grounds for either launching information provision or moving directly to decision-making). Extract 37 (see Figure 46) demonstrates the recipient’s recognition of the understanding check as being in service of an offer (rather than a stand-alone action) by the provision of a response to an offer that has not actually been articulated. By providing information in this way, midwives are attentive to the varying levels of knowledge that people giving birth may have and are able to tailor the information given to match this.
FIGURE 46.
Extract 37 (VIP36:Phoebe:Video-but-off-camera).

FIGURE 47.
Extract 38 (VIP13:Yvonne:Audio).
Decision-making in the event of delayed placenta expulsion
Once the decision has been made and the injection administered, in most cases, the delivery of the placenta is usually fairly straightforward. Of the 20 births that include recording after the birth of the baby, 13 involve unproblematic delivery of the placenta and in four the recording ends before the placenta is delivered (this includes the one case in which a physiological third stage was chosen). However, the remaining three cases involve some problem with the delivery of the placenta. In all three instances the midwives offer multiple suggestions to encourage the placenta (e.g. breastfeeding, urinating/catheterisation, bearing down, birthing stool, smelling clary sage and blowing into a glove) and in one case these are successful. In the other two instances, the options available to the women become limited, as is spelled out clearly in extract 39 (Figure 48).
FIGURE 48.
Extract 39 (VIP22:Claudia:Video).

In extract 39 (see Figure 48), we see that surgical removal is presented as something to be avoided (L8), but may become necessary and, therefore, by implication, it is not a decision that is subject to negotiation. Similarly, in the other case of delayed placenta expulsion (VIP08; not shown here) the midwife posits the option of going to theatre as inevitable if the measures to encourage placenta delivery are unsuccessful. In particular, in relation to the use of a catheter, the midwife states ‘we’re doing all this with the idea of saving you from going to theatre to have your placenta taken out’. In the first of these two cases (see extract 39 in Figure 48), Claudia does go to theatre for placenta removal and in the second the recording ends while they are waiting for the doctor to arrive.
Summary
In summary, active management of third stage is more frequent than physiological delivery of the placenta. There is evidence that this decision is discussed prior to birth and, therefore, some time ahead of its implementation. In these data, the way in which the decision regarding active or physiological management of the placenta is initiated usually provides for input from the women. Of the 27 cases, 16 cases are initiated using these high-involvement methods (e.g. option lists, offers, open questions), two cases are referred to by indexing birth plans in which the decision has already been made and in one case the decision is made in response to an understanding check (which typically precedes one of these actions). This provision for choice is associated with shared decision-making. Nevertheless, the options may be weighted towards having an actively managed third stage, even when midwives provide choice. This may contribute to the extent to which active management is selected, although it should be remembered that almost 50% of participants did indicate antenatally that they wanted the oxytocin injection.
Before initiating decisions, midwives sometimes check whether or not the women have the information necessary to make the decision (unlike other decisions during birth, it is not assumed that women will have the knowledge necessary to make these decisions). Information-sharing is integral to shared decision-making. Nevertheless, we did not find examples of the kind encouraged in NICE guidelines10 regarding the statistical outcomes of one choice versus the other.
Cord clamping and cord cutting
To permit placental blood to flow to the infant, there has been a move towards consensus that delayed cord clamping should occur in all births unless there is a threat to the baby’s life,271 and this is now widely recommended in maternity guidelines (e.g. NICE section 1.14.14, updated 201710). In addition, there is evidence to suggest that fathers who cut the cord benefit in terms of their emotional bond with the baby and feeling of empowerment, and this, therefore, should be encouraged. 272 [No equivalent research exists concerning cutting the cord/bonding when the co-parent is also a mother, necessitating further research concerning this issue with LGBT+ (lesbian, gay, bisexual, trans plus) people.]
Delayed cord clamping as the norm
In ANQs, 60% of participants in the larger sample selected a preference to delay clamping until after the cord has stopped pulsating and only 3% of participants indicated that they would want immediate clamping. However, a large proportion of participants indicated that they did not know enough to make a decision (19%). The remainder of participants (12%) reported that they did not have a preference (with another 6% missing values). Delayed cord clamping is referenced explicitly in 12 of the recordings. Discussion of delayed cord clamping may occur before the baby is born (7/12) or after (5/12). Usually the HCPs initiate cord clamping (9/12), but it may also be women (1/12) or BPs (2/12). Where it is referenced, there is always a consensus towards delayed or deferred cord clamping. When midwives are referring to delayed cord clamping it is rarely treated as a decision but, rather it is taken as a given [see extracts 40 and 41 (Figures 49 and 50)].
FIGURE 49.
Extract 40 (VIP04:Judy:Audio).

FIGURE 50.
Extract 41 (VIP11:Philippa:Video).
In extracts 42 and 43 (Figures 51 and 52), there is discussion of the birth plan. In extract 42 (see Figure 51), the BP voluntarily refers to their plan for delayed cord clamping (L1) and in extract 43 (see Figure 52) Lexi requests delayed cord clamping (L4) after the midwife has raised it as a topic (L3).
FIGURE 51.
Extract 42 (VIP05:Bryony:Audio).
FIGURE 52.
Extract 43 (VIP3:Lexi:Audio).
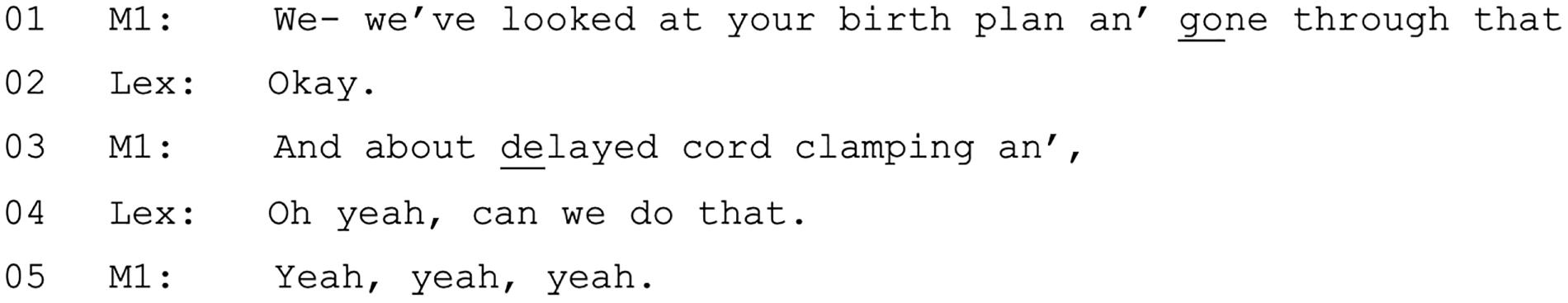
This latter case (see extract 43 in Box 43) is the only instance across the 12 recordings in which a midwife orients to delaying of cord clamping as an issue requiring decision-making. The upgraded response from the midwife in each case [i.e. ‘Absolutely’ in extract 43 (see Figure 52) and multiple repeats of ‘yeah’ in extract 44 (in Figure 53)] endorses the decision.
There was just a single episode in which delayed cord clamping was treated as something that may not be known about. It is worth noting that the midwife is here interacting with the BPs. In extract 44 (VIP18), the midwife is explaining to the BPs what will happen after the baby is born [L1–2 in extract 44 (Figure 53)]. As part of this, delayed cord clamping is assumed, and the midwife seeks to establish the BPs’ understanding (L6–7) as a prelude to providing that information (L9–12). Subsequently, the midwife refers to delayed cord clamping as ‘kind of standard procedure’ (L15). This is echoed in another case, in which the midwife states ‘it’s standard practice in this hospital anyway’ (VIP33; data not shown).
FIGURE 53.
Extract 44 (VIP18:Zoe:Audio).
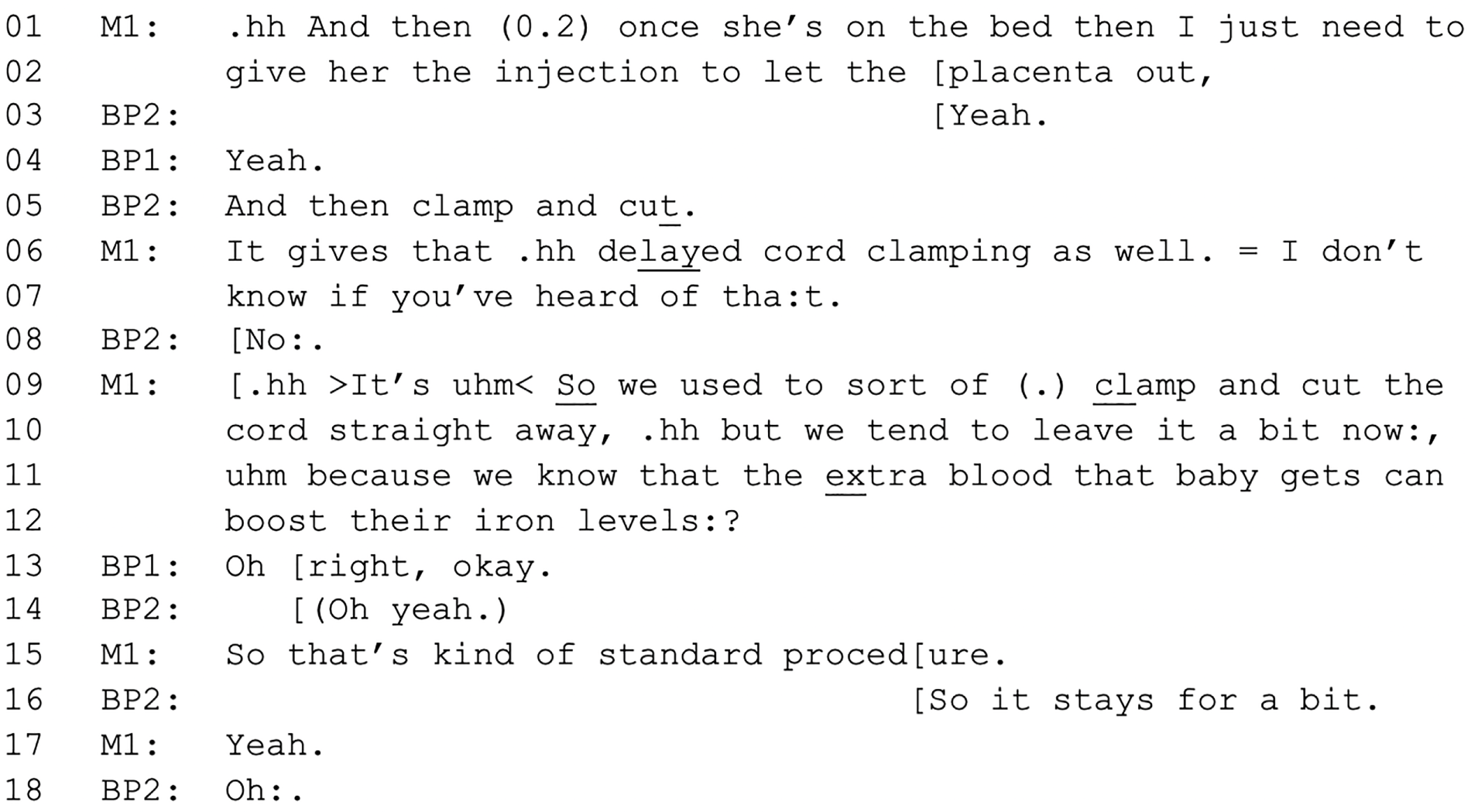
Initiating the decision to cut the cord
Decision-making occurs around the cutting of the cord. It is assumed that the cord will be cut (‘lotus birth’273 is never considered) and so the decision-making focuses on who will cut it. Talk about cutting the cord occurs in 23 of the recordings, including all 20 recordings for which there are video-recording/audio-recordings after the birth of the baby. Overwhelmingly, the most frequent way in which this is carried out is through offers, which occur in 18 instances [the remaining five cases involve the midwife assuming that the BP is cutting the cord (n = 1), midwife pronouncement (n = 1), the midwife announcing that it will be carried out but not stating by whom (n = 2) and the birth party initiates by requesting to do it in advance of the birth (n = 1)].
Offers in the CA literature involve one party offering help to the other party. Therefore, research has often explored how a need or problem is built in an interaction and how offers are produced as a possible remedy to this need/problem (e.g. see Curl274). The context of ‘offering’ cord cutting is different because it is one party offering an opportunity to the other party, rather than in response to a problem/need. Moreover, the offers in the current data set are different, as traditionally an offer embodies some object (e.g. either action or thing) that the speaker is proposing to do/give that will be for the benefit of the recipient (e.g. problem: ‘I’m going to be late to collect my daughter’; offer: ‘I’ll collect her’). In our current corpus, the action will be for the benefit of the recipient, but the action will be carried out by the recipient too, albeit with a midwife’s guidance. Therefore, what we have glossed as ‘offers’ may not overlap with offers as defined in the wider CA literature.
There are 18 cases in which cutting the cord is offered. These offers are almost exclusively directed towards BPs [e.g. ‘Now do you want to cut the cord, Daddy’ (VIP11) and ‘Do you want tuh cut the cor:d, ((BP name))?’ (VIP18)]. The exceptions occur when there are multiple BPs present, for example ‘Who wants to cut the cor:d.’ (VIP04).
When the offer is accepted, the response is accepted and the interaction moves on. However, when the offer is turned down, the offer is pursued, suggesting that there is a strong expectation that BPs enact the cord cutting [see extracts 45 and 46 (Figures 54 and 55)].
FIGURE 54.
Extract 45 (VIP01:Jacqueline:Audio).
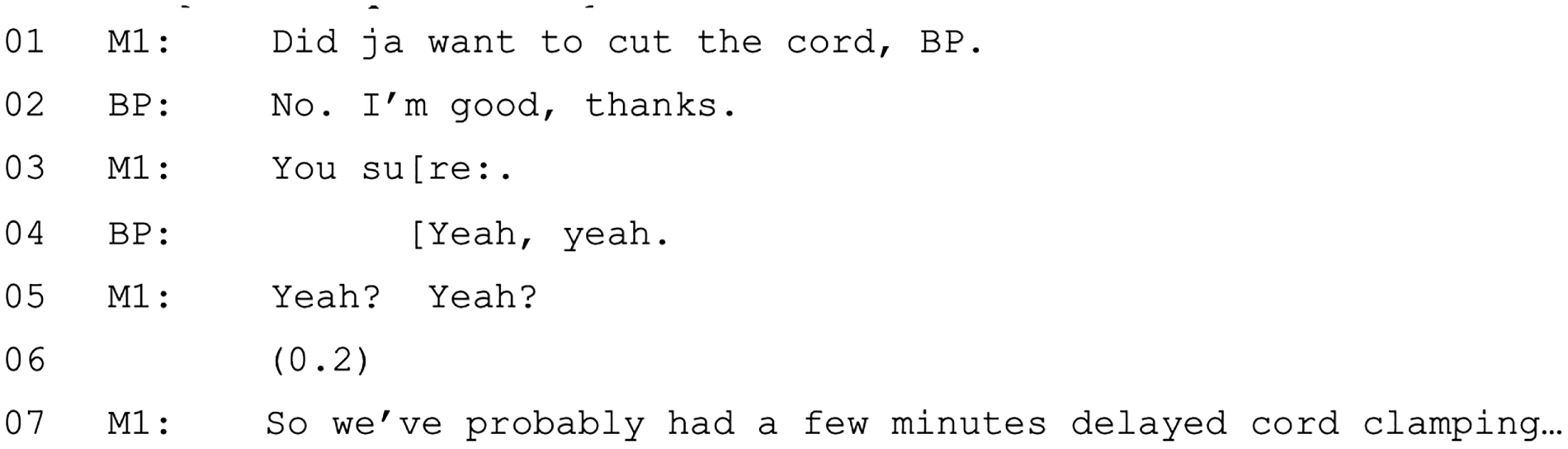
FIGURE 55.
Extract 46 (VIP03:Willow:Video).
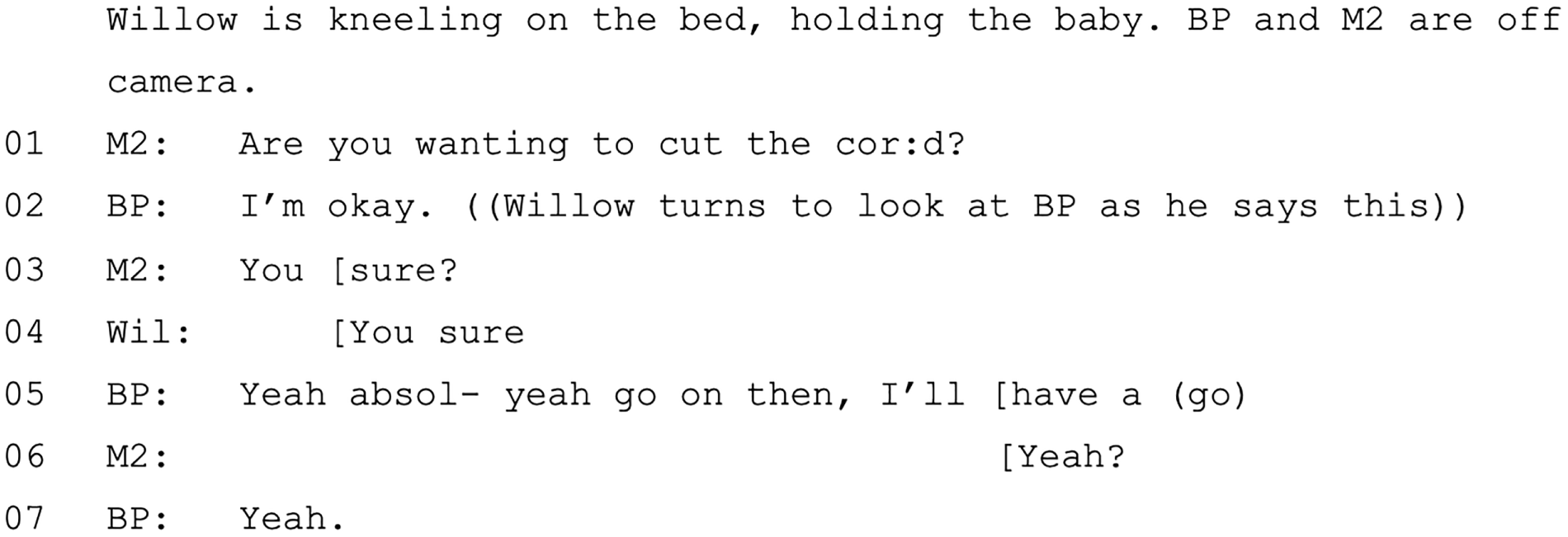
In both extracts 45 and 46 (see Figures 54 and 55), the midwives pursue acceptance of the offer with elliptical interrogatives [e.g. ‘you sure’, L3 in extracts 45 and 46 (see Figures 54 and 55)]. In extract 45 (VIP01), there is another declination (L4) followed by a second, more tentative, pursuit (L5) before the midwife accepts the BP’s answer and moves on to cutting the cord (L7) (see extract 45 in Figure 54). In extract 46 (VIP03), the pursuits – notably uttered by both the midwife (L3) and the woman (L4) – result in a revised response from the BP [i.e. the beginning of the second declination is cut off and, instead, he accepts the offer to cut the cord (see L5 in extract 46 in Figure 55)].
In a single case (VIP32), when the BP declines the offer, the midwife does not immediately pursue, but rather offers the woman the opportunity to cut the cord herself [see extract 47 (Figure 56)].
FIGURE 56.
Extract 47 (VIP32:Natalie:Video).
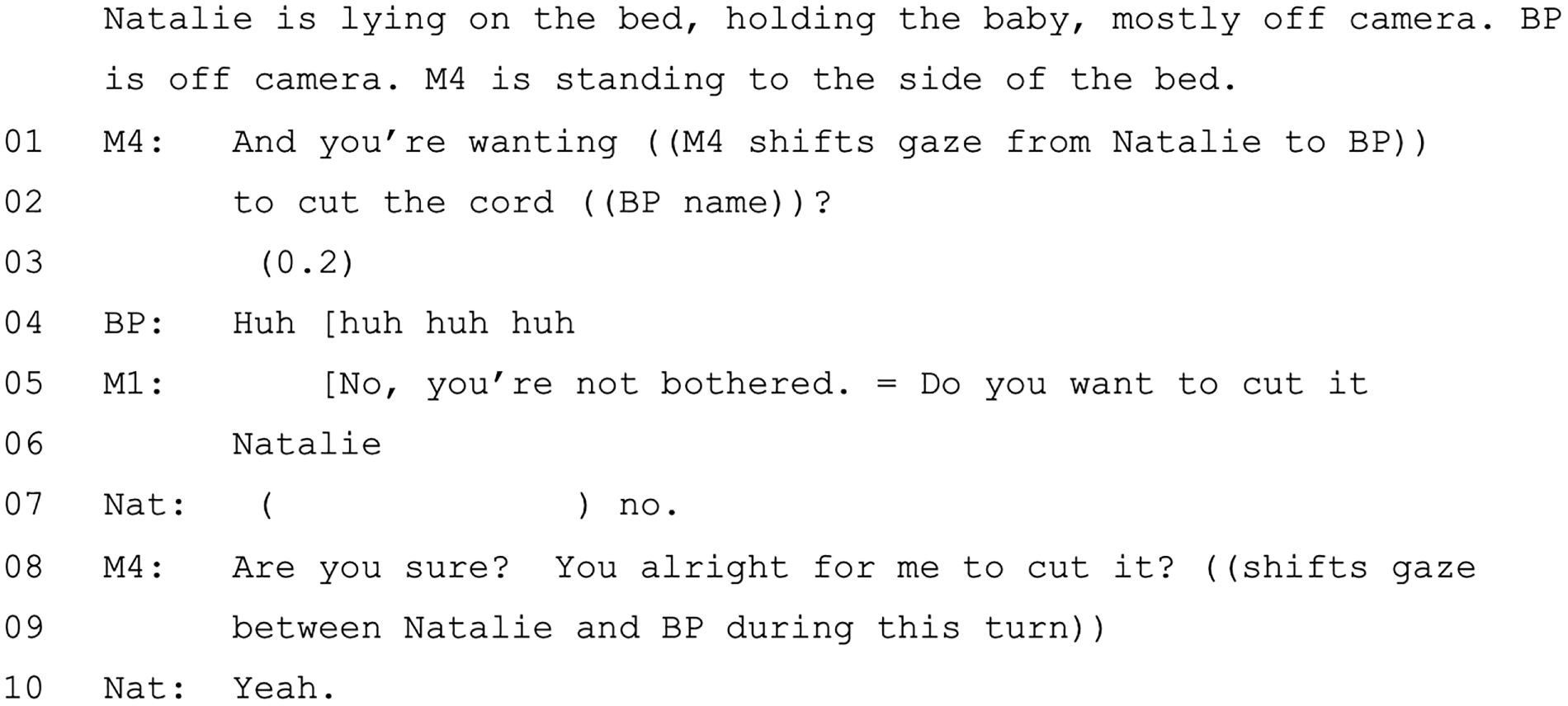
Extract 47 is the only example in the study of a mother being invited to cut her own cord. The mother also declines and, subsequently, the midwife does pursue the BP, but ultimately the midwife cuts the cord. Overall, then, cutting the cord is a decision (perhaps the only decision during labour and birth) that is treated as within the BP’s domain (but with a strong expectation of agreement). There are two instances across the collection in which people in early labour informs midwives that their partner would like to cut the cord, but generally the person giving birth is not treated as involved in this decision. Extract 48 (VIP12) is the only case in which the midwife seeks confirmation that the woman also agrees to the BP cutting the cord [see extract 48 (Figure 57)].
FIGURE 57.
Extract 48 (VIP12:Fiona:Video).
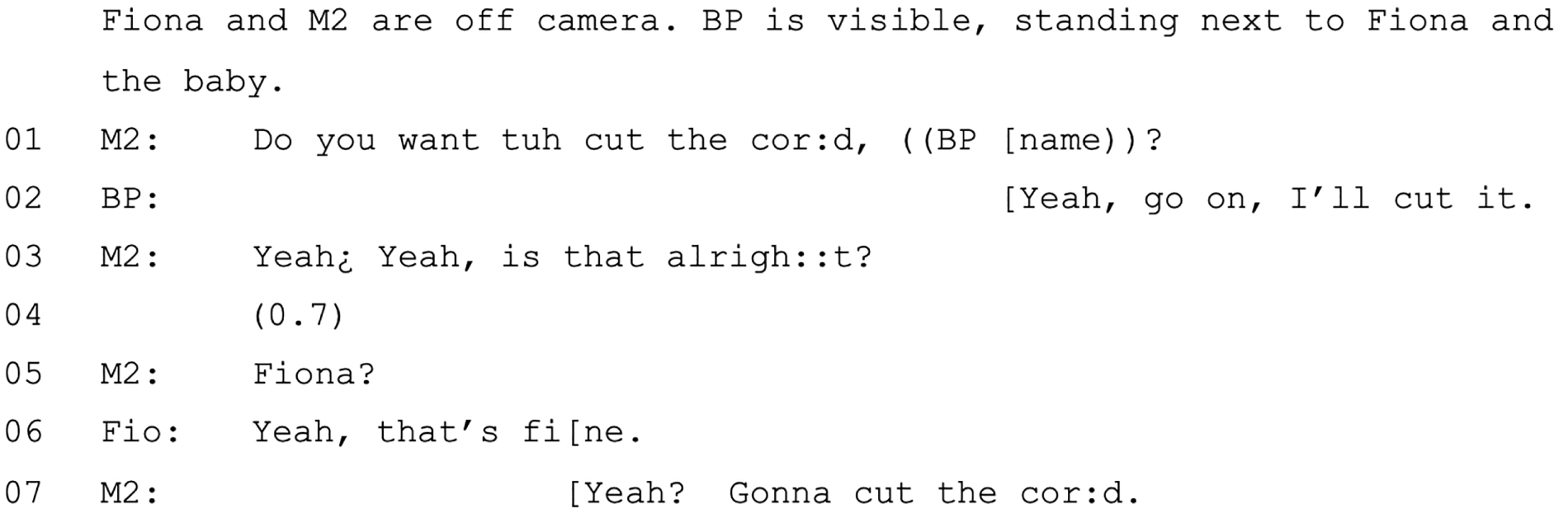
Summary
In summary, cutting the cord is assumed by all parties. There is some orientation to when it is cut, with delayed cord clamping being oriented to as preferred by midwives and the birth party alike (providing that they are aware of this option). However, delayed cord clamping is often not treated as a decision by the midwives. Offers are the most common way in which cord cutting decisions are initiated. There is an expectation that the BP will cut the cord. Furthermore, the decision about who is going to cut the cord is the only decision that is treated as positioned in the BP’s domain.
Discussion and conclusion
Two key decisions that are made after the baby is born are (1) cord cutting and (2) physiological/active third stage. These decisions are present in every recording in which we have post-birth footage (and are, in any case, likely to apply universally to all births).
Third stage is a place for high involvement in decisions overall (although this is less so when the placenta is not coming out as fast as the midwives would expect). These decisions are usually initiated in ways that provide for input (e.g. offers, option lists), which gives evidence for that claim. Many of the decisions that occur in this third phase are distinct from others during labour in that the baby is now a separate entity and so decisions are not affecting multiple parties in the same way.
Even though these decisions may technically be optional, our analysis demonstrates that there are normative choices (i.e. an actively managed third stage, delayed/deferred cord clamping and BP to cut the cord), and little choice to delay placenta expulsion. Dispreferred choices may be challenged by midwives, whereas preferred choices are not (e.g. a BP cutting the cord).
NICE guidelines10 indicate lots of information that should be given to people concerning the third stage; however, in reality, practice is nuanced to accommodate the variable prior knowledge of women and their BPs. Across the decisions pertaining to management of the placenta, there is careful navigation of assessing the birth party’s understanding and providing information that is tailored to their needs.
Overall, the third stage, and the period immediately following, is a time in which decision-making is predominantly in the woman’s domain (with the exception of delayed delivery of placenta). There are elements of shared decision-making evident during this phase. However, women seem not to convey having strong preferences (at least interactionally) suggesting, somewhat paradoxically, that the place they have the most optionality is the place they appear to have least concern about their involvement.
Chapter 8 Discussion and conclusion
Introduction
The study had four objectives:
-
To create a rich data set based on recordings of giving birth in MLUs. We collected data via (1) ANQs surveying women’s expectations and preferences for birth, (2) intrapartum video-/audio-recordings of labour and births and (3) PNQs about women’s experiences of, and satisfaction with, decision-making during labour.
-
To contribute to the evidence base for shared decision-making through fine-grained analysis of the verbal and non-verbal details of interactions that take place in real time during birth, specifically how decisions are initiated, who initiates them and how different ways of initiating decisions are responded to. Using CA (and CA-derived coding), the analytic focus was on how talk is used (by all parties) to encourage or discourage involvement in decision-making over the course and events of a birth.
-
To assess whether or not women’s actual experiences reflect their antenatal expectations and whether or not there is an association between interactional strategies used (by all parties) during labour (particularly the extent to which decisions are shared) and women’s later reported satisfaction. In this way, we could assess whether or not satisfaction is related to definable aspects of care in MLUs.
-
To disseminate findings to health-care providers and service users to contribute to translating existing Department of Health and Social Care and NHS policy directives on sharing decision-making into clinical practice.
In this chapter, we outline how objectives 1–3 were met and summarise the main findings. Objective 4 is not addressed in this report because our bespoke dissemination activities (i.e. two national-level workshops working with the RCM’s Progress Theatre, planned for Autumn 2020) have been postponed because of the COVID-19 pandemic. We continue to disseminate our findings at national and international academic and practitioner conferences.
This study is grounded in the fine-grained analysis of a data set of 37 recordings (totalling more than 166 hours) of women in labour in MLUs, which was the basis for both CA and the inductive quantitative coding of the interactional accomplishment of decision-making. Together with ANQs and PNQs, we have, therefore, met our first research objective to generate a rich set of data pertaining to women’s observable (and self-perceived) experiences of midwife-led childbirth.
Meeting this objective was a significant achievement in its own right. We have demonstrated the feasibility of this type of study not only in practical terms (i.e. the ethical collection of analysable recordings), but also in terms of establishing the willingness of pregnant people, BPs and HCPs to participate. We had little difficulty in recruiting to our project. Instead, our unanticipated challenge was in maintaining women’s eligibility for the study because it quickly became evident that the majority of women who consented were transferred to obstetric care before labour (i.e. they were never admitted to the MLUs) (see Chapter 2). The number of people who transferred from one service to another before labour began was significant and did not reflect national statistics (e.g. in 2019, the Care Quality Commission113 reported that 77% of women gave birth in the place they had planned to antenatally).
The recordings are the central data set in our mixed-methods study. The recordings will undoubtedly have analytic utility in numerous future studies (and we have sought participants’ consent in this regard275). Here, however, we have used the recordings as a specific basis for conducting CA of decision-making. Our use of CA to analyse interactions between midwives, labouring persons and BPs addresses a significant gap in existing knowledge about decision-making and, to our knowledge, is unique in the UK. This also represents a distinctive context for CA more broadly because CA studies of health-care interactions generally focus on primary and secondary care consultations. Relative to labour, these consultations are (much) shorter and involve fewer participants and, although decision-making clearly occurs, we rarely get to see the decisions as they are enacted. In contrast, decision-making during labour often takes place over hours and may involve numerous participants (e.g. multiple midwives and/or BPs), and the decisions made are enacted within the intrapartum period. In this sense, our recordings may provide the full ‘life’ of a decision, from initiation, through negotiation, to enactment and outcome. The inclusion of decisions initiated by recipients of health care (in this case, labouring persons), as well as third parties (e.g. BPs), is also relatively unusual in projects of this kind, as the HCP has been the typical focus of research (for notable exceptions see Elsey,276 Ekberg et al. 277 and Pino et al. ,278 and articles in Beach279).
The present study incorporates novel findings of likely interest to conversation analysts (e.g. the ‘permissional’ requests evident in the fetal monitoring decisions) and suggests further lines of conversation analytic inquiry (e.g. contrasting turn designs of pronouncements, including ‘I will . . . ’ vs. ‘I’m going to . . . ’). We will follow up these analyses in specialist CA publications. However, we have not foregrounded a conversation analytic audience in this report. Instead, we have written primarily for a health-care audience and, for this reason, have focused on addressing the study objectives.
We next discuss the main findings in relation to objectives 2 and 3. Objective 2: how is talk used (by all parties) to encourage or discourage involvement in decision-making over the course and events of a birth? addresses objective 2 and deals with the ways talk is used to encourage/discourage involvement in decision-making. Objective 3, part 1: assessing whether or not women’s actual experiences reflect their antenatal expectations deals with whether or not women’s antenatal expectations were reflected in their experience of labour, and part 2 [see Objective 3, part 2: is there is an association between interactional strategies used (by all parties) during labour (particularly the extent to which decisions are shared) and women’s later reported level of satisfaction?] pertains to the association between interactional practices and satisfaction. We highlight the methodological innovations achieved (see Innovative methods) and consider the research limitations (see Limitations). We then make suggestions for further research (see Further research) before drawing some final conclusions (see Conclusions).
Objective 2: how is talk used (by all parties) to encourage or discourage involvement in decision-making over the course and events of a birth?
Midwives initiate the majority of decision-making during labour and birth in MLUs. Both women and midwives orient to decisions as lying within the midwives’ domain. We see this in both the ways in which midwives initiate decisions (e.g. by pronouncements and recommendations) and in women’s ready agreement to proposed courses of action. This tells us that labouring persons rarely challenge the ‘direction’ of decisions, although in and of itself this does not tell us how they felt about decisions. Lack of challenge may indicate agreement with the decision or it may reflect a felt inability to challenge for various reasons. Our finding that decision-making is practitioner led accords with previous CA work,161 maternity research53 and health-care research more broadly46 regarding the discrepancy between policy that emphasises participatory decision-making and practice at the level of health-care interactions.
In this regard, our findings support what is evident in existing maternity research regarding the tendency towards guideline-driven care,87,280,281 predicated on an increased concern with risk management,62,221 at the same time, somewhat paradoxically,282 that policies require midwives to respect labouring people’s agency. Therefore, our findings demonstrate the interactional realisation of the tension between enacting shared decision-making and meeting clinical guidelines.
The potential for women’s involvement in decision-making varies according to the decision being made. When clinical guidelines (e.g. concerning frequency of fetal and cervical observations, or the expected progress of labour) and clinical knowledge (e.g. concerning the impacts of pharmacological methods of pain relief at various stages of labour) make a particular course of action normative, midwives tend not to use interactional formats that invite women to participate in decision-making. Our data illustrate the impact of these formats in the sense that the decisional outcomes tend to match the goal being pursued by the midwives. It is important to highlight that, although women’s participation in decisions is not consistently invited, their consent to procedures is sought and is pursued if not forthcoming. Although the non-verbal initiations of fetal monitoring might be considered an exception to this, we have shown that women may have considerable access to a forthcoming monitoring via the noises that accompany retrieval and preparation of the Sonicaid and that they can (although rarely do) resist decisions of this kind. Women’s consent to procedures may be given verbally (most frequently as ‘yeah’), but also may be indicated through embodied actions (e.g. turning their bodies to permit monitoring).
Our findings resonate with previous work161 that suggests that patient choice tends to be reserved for decisions in which clinical outcomes may be less contingent on patient preference. As indicated throughout the report (see, particularly, Chapters 5–7), option listing might be considered the most participatory or ‘shared’ form in clinical interaction. In our study, women are explicitly presented with option lists during decision-making in quite specific circumstances only. These circumstances include (1) options around the frequency of VEs in early labour and (2) options concerning the use of methods to deliver the placenta.
In these cases, optionality exists in clinical guidelines (i.e. VEs do not have to be conducted every 4 hours in early labour and women should be offered a choice about the mode of placental delivery). Nonetheless, use of CA demonstrates that, even in these circumstances, optionality may be interactionally constructed in ways that emphasise outcomes that are preferred by midwives and/or guidelines (e.g. weighted against use of VEs in early labour because of the risk of disappointment/slowing progress and towards administering oxytocic drugs to facilitate placental delivery without risk of bleeding).
Another situation in which decision-making is treated as potentially lying more in the woman’s domain is the use of pain relief. Both midwives and (unusually, in comparison with other decisions) women orient to pain relief as a decision that ‘belongs’ to the person in labour. However, as is the case with other decisions, our analysis has demonstrated that the optionality that women are afforded in decision-making about pain relief is heavily contingent on clinical parameters and expertise. When requests for pharmacological pain relief are in tension with normative decisional outcomes (i.e. that opiates should not be given too early in labour or too close to birth), midwives use various strategies to deter/defer their use. By this, they offer women multiple alternative means of support; however, our data also illustrate that having to continue to pursue requests for pain relief can leave women feeling less satisfied with their experiences of decision-making [see Objective 3, part 2: is there is an association between interactional strategies used (by all parties) during labour (particularly the extent to which decisions are shared) and women’s later reported level of satisfaction?].
A final example of optionality concerns cutting of the cord. Our recordings reveal the key supportive and encouraging role played by BPs (e.g. supporting women through contractions, ensuring hydration and through both physical and verbal affective displays). However, the data indicate that BPs do not play a major role overall in decision-making (as they rarely initiate decisions and, when they do, midwives treat the initiations as inapposite). The one exception is the cutting of the cord, in which not only are BPs involved in decision-making, but the decision is also treated as belonging exclusively to them (the cord is not considered to belong to the woman). Moreover, there is a normative expectation that the BP should cut the cord, which is constructed in the ways in which midwives formulate their interactions regarding these decisions.
Objective 3, part 1: assessing whether or not women’s actual experiences reflect their antenatal expectations
Antenatal questionnaire data revealed that the majority of women (in the larger sample) intending to labour and birth in the MLUs both wanted to be involved in decision-making and expected there to be a correspondence between what they wanted to happen/what should happen and what would actually happen, be this for more ‘woman-oriented’ (the majority) or more ‘staff-oriented’ (the minority) decision-making. As explained in Objective 2: how is talk used (by all parties) to encourage or discourage involvement in decision-making over the course and events of a birth?, our CA of recordings found that decision-making was primarily midwife initiated and led, and women oriented to most decisions as lying within the midwives’ domain. This was underscored by the analysis of the quantitatively coded data on decision types and formats for the recorded sample, which showed that most decisions were midwife initiated both at the first decision point and for decision points as a whole. Midwives were more likely to use unilateral formats (e.g. pronouncements, recommendations) than they were more participatory formats (e.g. offers, option lists), although, as previously illustrated in Chapters 4–7, there was variation according to what the decision concerned. When women sought to initiate decisions, this was primarily via requests and this especially concerned pain relief. The qualitative CA and the quantitative coding of decision-making help us to interpret the PNQ responses (from recorded and unrecorded women who laboured in the MLUs) about their expectations and experiences. The questionnaire responses were principally in the direction of women having wanted decision-making either to be led by staff or to be advised by staff and to take that advice. Reports of being advised by staff but not taking the advice, or of no staff involvement in decisions, were relatively rare. When there were differences between what women said they had wanted and what they said actually happened (both self-reported postnatally), these differences were primarily between having wanted ‘staff to advise me but still make up my own mind (even if my decision is different from staff)’ and reporting that ‘staff advised me and I took the advice’. From this, we can infer that women probably did not feel the need to go against, and therefore largely acceded to, the decisions initiated by midwives.
Objective 3, part 2: is there an association between interactional strategies used (by all parties) during labour (particularly the extent to which decisions are shared) and women’s later reported level of satisfaction?
Postnatal questionnaire responses showed that the majority of the women were very satisfied on all dimensions (i.e. with being listened to, with their views taken into account, with how decisions were made and overall satisfaction score). We derived measures based on the quantitative coding of decision types and decision formats (for each separate decision), which enabled us to determine how far the ‘balance’ of decisions was midwife initiated or birth party initiated for the recorded sample. Supporting the analysis of the wider sample, the ‘balance’ of decision-making was more towards midwives, although the balance of pain relief decision-making was more birth party initiated than other typical decisions.
Based on mean balance scores of all decisions for each birth, statistically significant moderate-strength negative correlations were found between mean ‘balance’ and two components of satisfaction: (1) the extent to which women felt that they had been ‘listened to’ and (2) the extent to which their ‘views were taken into account’, showing that births that were more midwife initiated tended to have higher scores on these aspects of satisfaction. There were similar-strength significant negative correlations between ‘balance’ in pain relief decisions and all aspects of satisfaction. No significant relationships were found between fetal monitoring decision-specific measures of balance and satisfaction.
To investigate this further, we explored relationships between midwives’ and women’s initiating formats and satisfaction levels. No associations were found between midwives’ initiating formats and satisfaction. However, for women’s initiating formats, there were significant negative associations between some dimensions of satisfaction, particularly in relation to pain relief decisions. Notably, women who initiated decision-making by decision-implicative statements were more likely to have lower satisfaction for being ‘listened to’, ‘decisions made’ and overall satisfaction. There were also moderate negative correlations between women’s use of requests and satisfaction with their ‘views being taken into account’. As there were very similar findings for pain relief decision points and satisfaction, this suggests that pain relief decisions were likely to be driving the negative correlations (i.e. women who were taking the lead in pain relief decisions reported lower satisfaction).
This apparently paradoxical association can be explained using the CA (underscoring the importance of underpinning quantitative coding with qualitative analysis). Specifically, we have shown that, owing to normative clinical/practice orientations regarding pharmacological pain relief, midwives often deter/defer the use of opiates in ways that necessitate women’s pursuit of these decisions. Our analysis is suggestive of some contexts in which lengthy decision-making chains may arise, in particular when there is clinical uncertainty about progression and/or when decisions are interrupted during changes of staff. However, further research is needed to systematically explore the interactional contexts in which women pursue pain relief requests and the ways in which midwives respond to them.
Innovative methods
As noted, there are very few CA studies of labour and birth. Rather than start from a model of what decision-making should look like, CA allows us to understand how agency/involvement is distributed in practice through the actions of participants (e.g. midwives, people in labour and their BPs). CA also helps us to see the consequences of the ways in which decisions are formulated through the responses they make possible. This provides an actual basis for understanding what decision-making looks like and, therefore, some awareness of the challenges to implementing policy recommendations.
The present research coheres methodologically with the growing body of research that integrates CA with formal coding. 157 CA’s commitment to describing clearly defined interactional practices makes it well suited to coding while maintaining the sequential temporality that is important in CA. That is, we were able to identify, with a high degree of intercoder reliability, where and how initial decision points were produced and how these were responded to and/or extended across subsequent decision points. Inevitably, as we address in Limitations, tensions arose between the relative crudeness of the coding and the richness of the qualitative CA.
Limitations
There are a range of limitations. Despite our committed attempts to recruit an ethnically diverse sample (including, for example, provision of translated recruitment information and targeted selection procedures) the sample is overwhelmingly white. We acknowledge the importance of understanding the experiences of ethnic minority people in labour and of including analysis of interactions in labours involving ethnic minority people. This is particularly important in the light of higher rates of stillbirth/maternal mortality in ethnic minority women,283,284 and that women of colour often cite poor communication as a significant factor in suboptimal care. 285,286 The under-representation of ethnic minority people in medical research remains a concern in the UK,287 and there are efforts to understand and improve the situation. 288–290 As a priority, researchers need to become informed about the outcomes of these efforts and to incorporate any recommended practices.
An allied point is that our study was not designed to collect information about the gender or sexual orientations of participants. However, on reflection, this is a limitation of the study that could be easily addressed in future research by ensuring that participants are given the opportunity to define these aspects of their identity in questionnaires. This would enable assessment of whether research concerning decision-making in labour is inclusive of LGBT+ people.
As noted above, despite a thorough grounding in interactional data and the retention of sequences of action, the reduction of complex interaction to codable categories inevitably resulted in a blunt instrument with which to measure decision-making. For example, by combining all requests, the coding could not account for important distinctions in their turn design that invoke differential contingencies and beneficiaries. Arguably, by maintaining a coding distinction between strongly directive recommendations (e.g. pronouncements) and other forms of recommending, we were able to at least incorporate this variation of turn design in our analysis (and to good effect because to describe what midwives do when initiating, say monitoring, as recommending would be to understate their action). However, in general, coding is inevitably reductive. Therefore, we have tried to show the more nuanced fine-grained analysis in our qualitative chapters (see Chapters 4–7).
Our narrow focus on decision initiation and responses on aspects of care that we asked about in the questionnaires (necessary for comparative analyses to address study research objectives) has meant there are multiple aspects that are unexplored in the CA that would benefit from further in-depth analyses. For example, we noticed decisions that were not asked about in the questionnaires but that we found to be reasonably routine, such as decisions about catheterisation and, during the latent phase, being sent home or to an antenatal ward. Women’s experience of bladder care during labour is under-researched291 and, although more is known about their experiences of the latent phase, our data suggest that these ‘gatekeeping’ decisions about remaining in the MLU before active labour are sensitive and consequential. 292
Our focus directly on the initiation of, and responses to, decision initiations also meant that we excluded aspects of care that might frame decision-making,129 for example discussions about birth plans that may (or may not) frame recommendations in ways that align with women’s preferences (see Barnes293 for relevant CA work in general practitioner consultations). It would also be helpful to more systematically examine the role of information provision in decision-making. For example, in Chapters 4 and 5, we noted that recommendations for less anticipated decisions relating, respectively, to continuous fetal heart monitoring and ‘off-schedule’ VEs included explanations. It is not clear if this accounting for the decision is intended to be persuasive and, therefore, encouraging acceptance or if it creates the conditions for more informed decision-making (see Parry294 for related research in physiotherapy). Another important element of involving persons in labour that we have not been able to explore is midwives’ regular invitations to ask questions.
Relatedly, a primary focus on decision-making meant that we excluded analysis of the interactional techniques for managing/working with pain, which are central to midwives’ work. Our findings suggest that decisions related to pain are a key site of women’s agency and satisfaction. The apparently paradoxical suggestion that greater ‘involvement’ in these decisions leads to lower satisfaction is a product of the coding system that quantified women’s pursuits (using decision implicative statements and requests) as a measure of involvement. This is an accurate description because it indicates women’s persistence in seeking their preferred option. Nevertheless, the notion of women’s ‘involvement’ in these long chains of decision-making does not properly capture what is happening for the participants. These interactions are difficult for all participants and are consequential for women’s experience. Therefore, there is clearly a need for more systematic analysis of the ways pain relief is pursued and decided on. This may involve, for example, an analytic focus on the interactional ‘markers’ of what we might characterise as emotional labour295–297 enacted by midwives and BPs to facilitate women’s working with pain. 259
As BPs are not generally ratified by midwives and labouring persons as participants in decision-making, our focus on decision-making necessarily excludes BPs’ other significant roles, particularly in the management of pain. A broader focus on the interactional techniques of supporting and encouraging labouring persons (loosely characterised as emotional labour) would address this gap. This might involve more systematic and fine-grained analysis of ‘coaching’ through contractions, including, crucially, the embodied features of interaction (e.g. the role of touch). In common with many CA studies, we have privileged the spoken interaction over the embodied. 298 Thorough multimodal analysis is enormously time-consuming and would have been impossible in the life of the current project. We acknowledge, however, the importance of more systematic analyses of the embodied and non-linguistic features of interaction. A promising avenue of research is recent studies of pain expression in primary care299 and oncology. 300
Our focus on only midwife-led care was important to reflect the context of low-risk birth, in which participatory decision-making is most likely to be found and in which many of the routine forms of care provided (e.g. VEs, pain relief, placental delivery) are likely to be relevant to all persons in labour. However, it is possible that the ‘routine’ nature of many decisions that take place in MLUs means that their midwife-led nature is uncontroversial (e.g. frequent monitoring/VEs). Antenatally, the larger sample of women generally either wanted or did not mind the interventions that midwives sought to pursue in HCP-led ways as part of routine care, such as fetal monitoring at intervals and VEs. In this sense, there may have been no tension between the outcomes sought by midwives and those desired by women, perhaps reflected in the high levels of satisfaction. However, because there is little optionality/choice in MLUs, and because options become further reduced through any clinical complication in this context, there is an indication of the importance of conducting similar research in obstetric-led care, where labours are, by definition, high risk and more clinically complex, with decisions being less expectable and predictable.
There is the potential for a methodological problem in the way we have associated interactional data (i.e. decision points) and satisfaction scores. In designing the PNQ, we perhaps needed to be more careful to delineate satisfaction with care given in MLUs and that in OUs to account for when women transferred from the former to the latter during labour. Inspection of the PNQs (particularly the qualitative open comments) suggests that our participants were responding holistically to the satisfaction questions. This means that we cannot always be certain that satisfaction scores can be related to the aspects of the labour/birth that were recorded. This could be addressed more broadly in future studies if labouring persons could be recorded across the full experience in all birth contexts. Comments from non-recorded participants suggest disappointment at exclusion from being recorded at all or having to stop recording following transfer during labour.
Although a strength of this data set, vis-a-vis more traditional CA studies, is the potential to explore decisions ‘end to end’, as enacted in real time, its limitation is that the ‘real-time’ contingencies of labour and birth (e.g. responses to pain or to clinical need) mean that recordings do not ‘start’ and ‘stop’ at the same points for each participant during the interaction. Nonetheless, our data set includes a large amount of analytically comparable material concerning decision-making.
The number of recordings (n = 37) may be viewed as a limitation, despite the number of hours (over 166 hours) of material. Certainly, our original aim to collect 50 recordings had to be revised (to a minimum target of 30) in the light of the unanticipated attrition of consented participants to obstetric care. Nevertheless, this ambitious project has generated a large number of complex and rich data that we have not been able to do justice to in the confines of this report. For example, the HCP interview data, which was analysed thematically (using NVivo), informed the analysis as intended, but has been underutilised in the report. It is clear from these data that the midwives (who were not necessarily those who appear in recordings) are keenly aware that women’s choices and wishes may be marginalised to avoid professional challenge and to align care with clinical guidelines. The interactional analyses, based on CA and CA-informed coding, could easily each have been the basis of full-length reports in their own right and there was far more potential for analysis of questionnaire data. The attempt to combine both forms of analysis into a single report has meant that we have been necessarily selective in our presentation of findings.
Nevertheless, we have produced, to our knowledge, the first UK and only conversation analytic study of real-time interactional practices of decision-making in midwife-led care. Overall, the project has combined self-report, interview and interactional data, allowing for mixed-methods quantitative and qualitative analyses. We suggest that, although the specifics of decisions vary widely, the practices that HCPs and service users use to initiate and negotiate decision-making will be applicable beyond MLUs, especially to other time-sensitive contexts in which decisions are discussed and enacted in situ contingent on emerging clinical factors (e.g. emergency care). We agree with Heritage301 regarding:
. . . the compelling educational value of real data, in which real clinicians deal with the real dilemmas of real patients in real time. Recordings have the power to evoke analysis and reflection that is wide and deep and that is, on occasion, an important stimulus to changes in practice.
Heritage301
Further research
On the basis of this study, we suggest the following six directions of research (note that recommendation 1 should underpin all new research and recommendations 3, 4 and 5 could be conducted with our existing data set):
-
Research is needed to explore more effective ways of including ethnic minority people at all stages (i.e. from initial approach to recording) and what barriers exist to this inclusion (e.g. whether or not this population of women are more likely than white women to enter OUs rather than MLUs).
-
An extension of our methodology should be used to study decision-making in obstetric-led care. We have demonstrated the willingness of participants to consent to recording and the practicalities of collecting data of this nature. Given that, by definition, obstetric care involves high-risk labours and our finding that optionality is contingent on clinical factors, it is important to systematically analyse decision-making in this context. The very different and, potentially, more consequential (in terms of women’s experiences) nature of decision-making in obstetric care was strongly emphasised by our SUGs.
-
Further systematic understanding of how pain relief is pursued/resolved is required, given that this is the area in which we found some significant associations between decision-making practice and satisfaction.
-
Research should consider broadening the study of interactional practices of participatory decision-making to include practices that occur outside the (necessarily) narrow confines of initiation, pursuit and response adopted in this study. These practices might include, for example, information provision and the opportunity to ask questions. Other factors, such as continuity of a midwife and the number of midwives involved in the intrapartum period, might also be consequential for decision-making.
-
Relatedly, there is a need to understand the interactional markers of the emotional labour enacted by both midwives and BPs. Further analysis of the role played by both midwives and BPs, for example by ‘coaching’ women through contractions, words of encouragement and use of touch, might provide broader context for understanding the ways in which decision-making occurs in practice.
-
Although ambitious, it would be helpful to be able to follow pregnant persons across their antenatal encounters into the intrapartum period. This would allow us to examine not just women’s perceptions of their antenatal wants and expectations, but their actual decision-relevant interactions with HCPs throughout pregnancy (including childbirth), therefore, facilitating further empirically grounded analysis of the relationship between future-oriented decision-making and the decisions that are made during labour.
Conclusions
As reviewed in Chapter 1, existing research has illustrated that women’s involvement in decision-making during labour is important for their well-being and that, in spite of evidential and policy drivers, such involvement is challenging to realise in practice. A key issue in addressing these challenges is that there is limited research knowledge concerning the fine-grained detail of the interactions that take place between women, HCPs and BPs during labour. This study has demonstrated the feasibility of using CA of recordings of labour to understand these interactions. In doing so, it has highlighted the barriers that may exist to women’s involvement in decision-making.
In line with other CA studies of health care,161,248 we have demonstrated that policy initiatives that emphasise patient involvement in decision-making are challenging to enact in practice. Our CA of the recordings illustrates that midwives’ interactions are oriented to a particular set of guidelines/clinical norms. When guidelines/clinical practice indicate a normative outcome, midwives appear to avoid the use of interactional formats that offer women choice.
Therefore, to require midwives to share decision-making with people in labour by giving optionality in all circumstances is, simultaneously, to require midwives to, potentially, contradict another set of imperatives. We suggest that the significance of this challenge for midwives needs to be acknowledged in policy initiatives regarding decision-making, and that such initiatives should reflect on these challenges at the level of communication between midwives and women. For example, what might an interaction look like that takes account of a midwife’s accountability to document 4-hourly VEs and to give a labouring person optionality about whether or not a VE should take place? If this is very difficult to achieve (as our data suggest may be the case), then institutional reflection is needed about the reconciliation of these goals in ways that can enable people’s involvement in decision-making during labour.
We have found that, despite reporting a desire for significant participation in decision-making, women in this study postnatally reported that decisions were more staff led and, moreover, that this was broadly (again reflecting postnatally) what they had preferred to happen. This suggests that women were generally accepting of midwife-led decision-making and satisfied with this. It is notable that over half of women reported being as assertive as they wanted to be and most others that they sometimes were as assertive as they wanted to be when talking to staff in labour and, in addition, the majority of women were either ‘sure’ they were or ‘probably’ were in control of what midwives did to them. This underscores that most women may have felt that they had no reason to disagree with the staff advice (i.e. women may have been satisfied with staff-led decision-making because they agreed with the decisions being made). As outlined previously, this may have been a product of some of the relatively routine and uncontroversial decisions that typify labour in MLUs, which was the focus of our study.
One area in which the goals of midwives and women in labour did sometimes observably diverge in the interactional data was during decision-making about pain relief. CA demonstrates that such ‘women-led’ decision-making is necessitated by midwives’ clinical preference to avoid the use of pharmacological methods of pain relief at particular stages of labour. In other words, pain relief decision-making is sometimes necessarily women led because of midwives’ deferrals or deterring of pain relief decisions, meaning that the interactional formats employed by midwives still shape decision-making in this context. The negative association between this form of decision-making and women’s satisfaction suggests that it can, in some cases, leave women feeling unheard by staff. This demonstrates the consequential nature of the decision-making that takes place during even low-risk birth.
Acknowledgements
We are enormously grateful to all the people and organisations who helped us to produce this research. In particular, we would like to thank the following.
Members of the Study Steering Committee for their valuable contributions and guidance: Margaret Jackson (chairperson), Maria Booker, Jeremy Dearling, Paul Drew (until January 2020), Kim Hinshaw, Josephine Green, Marion Laemle, Joyce Marshall and Patrick Titley.
Members of the SUGs for their significant insight and support: Laura Cook (also co-applicant until 2017), Wiebke Acton, Lauren Brooks, Agnieszka Burke, Marie Canning, Jorandi Daneel, Amina Day, Rachel Elwell, Sally Fisher, Samina Furniss, Rebecca Goodheart, Jessica Harris, Alexandra Haworth, Heather Hughes, Rehana Jomeen, Nikki Leigh, Rebecca Lomax, Pauline May, Daisy Minton, Ceira Pabla, Rosie Scott, Sophie Simpson, Laura Smyth, Lauren Smyth, Rachel Summers and Vicky Tallon.
The administrative and support staff at both research sites who made sure the project ran smoothly, especially Hilary Rosser for her excellent recruitment and diligent following-up with consents; Clare Pye and members of the PPI group in obstetrics, gynaecology and neonatology research at one of our study sites; and Susan Townend, who was one of our original co-applicants and local principal investigators and who made an invaluable contribution to the study design and data collection.
Members of the Department of Television, Film and Theatre, University of York, especially Patrick Titley, for their invaluable guidance about filming and editing. In addition, Andrew Middleton and colleagues at Scotia UK, for great customer service before and after our purchase of the Smots™ cameras.
Our transcriber, James Gunn, for his accurate and timely verbatim transcription of recordings.
Our two study interns (funded with additional support from the Department of Sociology, University of York): Víctor Ávila Torres, for his meticulous work on data entry, the transfer and cleaning of questionnaire data from Qualtrics to SPSS and his guidance concerning quantitative analyses, and for questionnaire distribution and follow-up of non-responders; and Mary Potts, for her sterling assistance in literature searching.
Members of the RCM’s Progress Theatre Group, with whom we were planning our dissemination events when the pandemic struck. We very much look forward to our future work together.
Sophie Bramley (Sociology Department, then Research Facilitator, University of York) and Lisa Lack (Research Grant Co-ordinator, University of York), for their research support.
Christine Morton and Brigitt Jordan, who believed in our project from its very beginnings and provided invaluable support in helping us to get started.
Our conversation analytic reviewers, Danielle Jones and Merran Toerien, for their careful and constructive feedback on an earlier version of the project report.
Our NIHR project manager, Martin Simpson-Scott, for his speedy and clear responses to our many queries along the way, and NIHR Assistant Research Manager Alexis Palmer for assistance at the editorial stage. In addition, Catriona McDaid and colleagues at the NIHR Research Design Team Yorkshire and Humber for their insightful assistance at the application stage of the research.
The anonymous NIHR reviewers for their very supportive feedback on the first draft of this report and their suggestions for revision.
Finally, and most of all, our very special and humbled thanks to all the women, BPs, midwives, doctors and support workers who so generously participated in this research.
Contributions of authors
Ellen Annandale (https://orcid.org/0000-0002-0607-0435) (Professor, Sociology) was chief investigator and was responsible for management of the project, and contributed to the study design, data collection (majority of interviews), setting up and cleaning of SPSS questionnaire databases, data analysis (interviews, questionnaires), and drafting and editing of chapters of the report.
Helen Baston (https://orcid.org/0000-0002-8527-3061) (Consultant Midwife) was a local principal investigator and was responsible for site induction and management, was originator of the study concept and provided subsequent contributions to the design and its implementation [including consenting staff (interviews and recording), supervising related research midwife activities, preparing staff for their role in data collection and day-to-day monitoring of study progress], and provided critical academic and clinical reviews of the draft report and dissemination strategy.
Siân Beynon-Jones (https://orcid.org/0000-0002-6795-7101) (Senior Lecturer, Sociology) contributed to the study design, was lead on the ethics approval process and was involved in data collection (interviews), data analysis (interviews), and drafting and editing of chapters of the report.
Lyn Brierley-Jones (https://orcid.org/0000-0003-0395-9447) (now Research Fellow, University of Leeds) was a full-time research associate on the project and contributed to ethics applications, project design (particularly the inductive coding frame), convening SUG meetings, data collection (questionnaires and interviews), CA, and drafting and editing of chapters of the report.
Alison Brodrick (https://orcid.org/0000-0003-1905-7704) (Consultant Midwife) contributed to the study design and implementation, including consenting staff for video-recordings, day-to-day monitoring of study progress at a local research site, editing, and clinical review of draft chapters and final report.
Paul Chappell (https://orcid.org/0000-0002-3587-570X) (Honorary Research Fellow, Sociology; Research Consultant) contributed to the design of the quantitative coding scheme, construction of quantitative interactional data sets, data cleaning and management, quantitative data analysis, and drafting and editing of Chapters 2 and 3 of the report.
Josephine Green (https://orcid.org/0000-0002-7688-9534) (Professor Emeritus, Health Sciences, previously Professor of Psychosocial Reproductive Health) provided substantial contributions to the conception and design of the work and, as a member of both the project team and the Project Steering Committee, made contributions to the interpretation of data and critical revision of draft chapters.
Clare Jackson (https://orcid.org/0000-0002-1269-1836) (Senior Lecturer, Sociology) is a conversation analyst and contributed to the study design, design and implementation of interactional coding, conversation analytic transcription and analysis, and drafting and editing of chapters of the report.
Victoria Land (https://orcid.org/0000-0003-4542-6163) (Research Fellow, Sociology) is a conversation analyst specialising in health-care interactions and contributed to the study design, design of the PNQ, carrying out interviews with HCPs, design and testing reliability of the interactional coding, conversation analytic transcription and analysis, and drafting and editing of chapters of the report.
Tomasina Stacey (https://orcid.org/0000-0003-2002-6200) (Associate Professor in Midwifery Practice) was a local principal investigator and study site co-ordinator, and contributed to recruitment, data collection, data analysis and editing of chapters of the report.
Data-sharing statement
The removal of all potential identifying information from this large and complex data set will involve a significant time investment. Accordingly, if accepted, all available data will be deposited in the UK Data Archive, managed by the UK Data Service (URL: https://ukdataservice.ac.uk/) within 12 months of the publication of this report. ‘Available data’ refers to data for which participants have given specific consent for this use. Participants were asked whether or not they consented to the depositing of the anonymised verbatim transcripts of recordings of labour and birth, anonymised verbatim interview transcripts and anonymised survey responses. It should be noted that, as some recordings of labour and birth were of significant length, verbatim transcripts were produced for only the sections that were analytically significant for the aims of the study detailed in this final report.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care.
References
- Christiaens W, Bracke P. Assessment of social psychological determinants of satisfaction with childbirth in a cross-national perspective. BMC Pregnancy Childbirth 2007;7. https://doi.org/10.1186/1471-2393-7-26.
- Green JM, Coupland VA, Kitzinger J. Great Expectations: A Prospective Study of Women’s Expectations and Experiences of Childbirth. Hale: Books for Midwives Press; 1998.
- Karlström A, Nystedt A, Hildingsson I. The meaning of a very positive birth experience: focus groups discussions with women. BMC Pregnancy Childbirth 2015;15. https://doi.org/10.1186/s12884-015-0683-0.
- Bell AF, Rubin LH, Davis JM, Golding J, Adejumo OA, Carter CS. The birth experience and subsequent maternal caregiving attitudes and behavior: a birth cohort study. Arch Womens Ment Health 2019;22:613-20. https://doi.org/10.1007/s00737-018-0921-3.
- Hodnett ED. Pain and women’s satisfaction with the experience of childbirth: a systematic review. Am J Obstet Gynecol 2002;186:160-72. https://doi.org/10.1016/S0002-9378(02)70189-0.
- Lundgren I, Berg M. Central concepts in the midwife–woman relationship. Scand J Caring Sci 2007;21:220-8. https://doi.org/10.1111/j.1471-6712.2007.00460.x.
- Nilsson L, Thorsell T, Hertfelt Wahn E, Ekström A. Factors influencing positive birth experiences of first-time mothers. Nurs Res Pract 2013. https://doi.org/10.1155/2013/349124.
- Macpherson I, Roqué-Sánchez MV, Legget Bn FO, Fuertes F, Segarra I. A systematic review of the relationship factor between women and health professionals within the multivariant analysis of maternal satisfaction. Midwifery 2016;41:68-7. https://doi.org/10.1016/j.midw.2016.08.003.
- Perriman N, Davis DL, Ferguson S. What women value in the midwifery continuity of care model: a systematic review with meta-synthesis. Midwifery 2018;62:220-9. https://doi.org/10.1016/j.midw.2018.04.011.
- National Institute for Health and Care Excellence (NICE) . Intrapartum Care for Health Healthy Women and Babies 2014.
- Villarmea S, Kelly B. Barriers to establishing shared decision-making in childbirth: unveiling epistemic stereotypes about women in labour. J Eval Clin Pract 2020;26:515-19. https://doi.org/10.1111/jep.13375.
- van Helmond I, Korstjens I, Mesman J, Nieuwenhuijze M, Horstman K, Scheepers H, et al. What makes for good collaboration and communication in maternity care? A scoping study. Int J Childbirth 2015;5:210-23. https://doi.org/10.1891/2156-5287.5.4.210.
- Pilnick A. ‘It’s something for you both to think about’: choice and decision making in nuchal translucency screening for Down’s syndrome. Sociol Health Illn 2008;30:511-30. https://doi.org/10.1111/j.1467-9566.2007.01071.x.
- Walsh D, Devane D. A metasynthesis of midwife-led care. Qual Health Res 2012;22:897-910. https://doi.org/10.1177/1049732312440330.
- Scamell M, Alaszewski A. Fateful moments and the categorisation of risk: midwifery practice and the ever-narrowing window of normality during childbirth. Heal Risk Soc 2012;14:207-21. https://doi.org/10.1080/13698575.2012.661041.
- Sandall J, Devane D, Soltani H, Hatem M, Gates S. Improving quality and safety in maternity care: the contribution of midwife-led care. J Midwifery Womens Health 2010;55:255-61. https://doi.org/10.1016/j.jmwh.2010.02.002.
- Sutcliffe K, Caird J, Kavanagh J, Rees R, Oliver K, Dickson K, et al. Comparing midwife-led and doctor-led maternity care: a systematic review of reviews. J Adv Nurs 2012;68:2376-86. https://doi.org/10.1111/j.1365-2648.2012.05998.x.
- Green JM, Baston HA. Feeling in control during labor: concepts, correlates, and consequences. Birth 2003;30:235-47. https://doi.org/10.1046/j.1523-536x.2003.00253.x.
- Mirghafourvand M, Mohammad Alizadeh Charandabi S, Ghanbari-Homayi S, Jahangiry L, Nahaee J, Hadian T. Effect of birth plans on childbirth experience: a systematic review. Int J Nurs Pract 2019;25. https://doi.org/10.1111/ijn.12722.
- Malacrida C, Boulton T. The best laid plans? Women’s choices, expectations and experiences in childbirth. Health 2014;18:41-59. https://doi.org/10.1177/1363459313476964.
- Whitford HM, Entwistle VA, van Teijlingen E, Aitchison PE, Davidson T, Humphrey T, et al. Use of a birth plan within woman-held maternity records: a qualitative study with women and staff in northeast Scotland. Birth 2014;41:283-9. https://doi.org/10.1111/birt.12109.
- Nieuwenhuijze M, Low LK. Facilitating women’s choice in maternity care. J Clin Ethics 2013;24:276-82.
- Department of Health and Social Care . NHS Choices 2017. www.nhs.uk/ (accessed 7 March 2022).
- Downie R. Education patients and consumers. J R Coll Physicians Edinb 2017;47:261-6. https://doi.org/10.4997/JRCPE.2017.311.
- Fotaki M. What Market-Based Patient Choice Can’t Do for the NHS: The Theory and Evidence of How Choice Works in Health Care. London: Centre for Health and the Public Interest; 2014.
- Whiteman I. The fallacy of choice in the common law and NHS policy. Health Care Anal 2013;21:146-70. https://doi.org/10.1007/s10728-011-0198-4.
- Lindberg J, Lundgren AS. Positioning the ageing subject: articulations of choice in Swedish and UK health and social care. Policy Stud 2021;42:289-307. https://doi.org/10.1080/01442872.2019.1599839.
- McDonald R, Mead N, Cheraghi-Sohi S, Bower P, Whalley D, Roland M. Governing the ethical consumer: identity, choice and the primary care medical encounter. Sociol Health Illn 2007;29:430-56. https://doi.org/10.1111/j.1467-9566.2007.00493.x.
- Department of Health and Social Care (DHSC) . Reference Guide to Consent for Examination or Treatment 2009.
- Parsons T. The Social System. New York, NY: Free Press; 1951.
- Mishler EG. The Discourse of Medicine: Dialectics of Medical Interviews. Westport, CT: Greenwood Publishing Group; 1984.
- Starr P. The Social Transformation of American Medicine. New York, NY: Basic Books; 1982.
- Pilnick A, Dingwall R. On the remarkable persistence of asymmetry in doctor/patient interaction: a critical review. Soc Sci Med 2011;72:1374-82. https://doi.org/10.1016/j.socscimed.2011.02.033.
- Joseph-Williams N, Edwards A, Elwyn G. Power imbalance prevents shared decision making. BMJ 2014;348. https://doi.org/10.1136/bmj.g3178.
- Price S, Noseworthy J, Thornton J. Women’s experience with social presence during childbirth. MCN Am J Matern Child Nurs 2007;32:184-91. https://doi.org/10.1097/01.NMC.0000269569.94561.7c.
- Charles C, Gafni A, Whelan T. Shared decision-making in the medical encounter: what does it mean? (or it takes at least two to tango). Soc Sci Med 1997;44:681-92. https://doi.org/10.1016/S0277-9536(96)00221-3.
- Charles C, Gafni A, Whelan T. Decision-making in the physician–patient encounter: revisiting the shared treatment decision-making model. Soc Sci Med 1999;49:651-61. https://doi.org/10.1016/S0277-9536(99)00145-8.
- Barry MJ, Edgman-Levitan S, Billingham V. Shared decision making – the pinnacle of patient-centered care. N Engl J Med 2012;366:780-1. https://doi.org/10.1056/NEJMp1109283.
- Entwistle VA, Watt IS. Patient involvement in treatment decision-making: the case for a broader conceptual framework. Patient Educ Couns 2006;63:268-78. https://doi.org/10.1016/j.pec.2006.05.002.
- Makoul G, Clayman ML. An integrative model of shared decision making in medical encounters. Patient Educ Couns 2006;60:301-12. https://doi.org/10.1016/j.pec.2005.06.010.
- Griffey RT, Shah MN. What we talk about when we talk about SDM. Acad Emerg Med 2016;23:493-4. https://doi.org/10.1111/acem.12907.
- Siyam T, Shahid A, Perram M, Zuna I, Haque F, Archundia-Herrera MC, et al. A scoping review of interventions to promote the adoption of shared decision-making (SDM) among health care professionals in clinical practice. Patient Educ Couns 2019;102:1057-66. https://doi.org/10.1016/j.pec.2019.01.001.
- Gravel K, Légaré F, Graham ID. Barriers and facilitators to implementing shared decision-making in clinical practice: a systematic review of health professionals’ perceptions. Implement Sci 2006;1. https://doi.org/10.1186/1748-5908-1-16.
- Légaré F, Ratté S, Gravel K, Graham ID. Barriers and facilitators to implementing shared decision-making in clinical practice: update of a systematic review of health professionals’ perceptions. Patient Educ Couns 2008;73:526-35. https://doi.org/10.1016/j.pec.2008.07.018.
- Joseph-Williams N, Elwyn G, Edwards A. Knowledge is not power for patients: a systematic review and thematic synthesis of patient-reported barriers and facilitators to shared decision making. Patient Educ Couns 2014;94:291-309. https://doi.org/10.1016/j.pec.2013.10.031.
- Elwyn G, Scholl I, Tietbohl C, Mann M, Edwards AG, Clay C, et al. ‘Many miles to go . . . ’: a systematic review of the implementation of patient decision support interventions into routine clinical practice. BMC Med Inform Decis Mak 2013;13. https://doi.org/10.1186/1472-6947-13-S2-S14.
- Blair L, Légaré F. Is shared decision making a utopian dream or an achievable goal?. Patient 2015;8:471-6. https://doi.org/10.1007/s40271-015-0117-0.
- Roy NT, Ulrich EE. Quantifying the relationship between patient characteristics and involvement in developing and implementing a treatment plan. Drug Healthc Patient Saf 2017;9:1-8. https://doi.org/10.2147/DHPS.S107065.
- Frosch DL, May SG, Rendle KA, Tietbohl C, Elwyn G. Authoritarian physicians and patients’ fear of being labeled ‘difficult’ among key obstacles to shared decision making. Health Aff 2012;31:1030-8. https://doi.org/10.1377/hlthaff.2011.0576.
- Dimopoulos-Bick T, Osten R, Shipway C, Trevena L, Hoffmann T. Shared decision making implementation: a case study analysis to increase uptake in New South Wales. Aust Health Rev 2019;43:492-9. https://doi.org/10.1071/AH18138.
- McIntosh T, Hunter B. ‘Unfinished business’? Reflections on changing childbirth 20 years on. Midwifery 2014;30:279-81. https://doi.org/10.1016/j.midw.2013.12.006.
- NHS England . National Maternity Review: Better Births: Improving Outcomes of Maternity Services in England. A Five Year Forward View for Maternity Care 2016. www.england.nhs.uk/wp-content/uploads/2016/02/national-maternity-review-report.pdf (accessed 3 March 2022).
- Begley K, Daly D, Panda S, Begley C. Shared decision-making in maternity care: acknowledging and overcoming epistemic defeaters. J Eval Clin Pract 2019;25:1113-20. https://doi.org/10.1111/jep.13243.
- van Teijlingen E. A critical analysis of the medical model as used in the study of pregnancy and childbirth. Sociol Res Online 2005;10:63-77. https://doi.org/10.5153/sro.1034.
- Johanson R, Newburn M, Macfarlane A. Has the medicalisation of childbirth gone too far?. Br Med J 2002;324:892-5. https://doi.org/10.1136/bmj.325.7355.103.
- Henley-Einion A. The Social Context of Birth. Abingdon: Radcliffe Medical Press; 2003.
- Warriner S. Looking at midwifery over the last 100 years. Br J Midwifery 2002;10:520-1. https://doi.org/10.12968/bjom.2002.10.8.10603.
- Department of Health and Social Security . Peel Report: Domiciliary Midwifery and Maternity Bed Needs 1970.
- Office for National Statistics . Birth Characteristics 2018 2019. www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/livebirths/datasets/birthcharacteristicsinenglandandwales (accessed 12 May 2020).
- Clesse C, Lighezzolo-Alnot J, de Lavergne S, Hamlin S, Scheffler M. The evolution of birth medicalisation: a systematic review. Midwifery 2018;66:161-7. https://doi.org/10.1016/j.midw.2018.08.003.
- Cahill HA. Male appropriation and medicalization of childbirth: an historical analysis. J Adv Nurs 2001;33:334-42. https://doi.org/10.1046/j.1365-2648.2001.01669.x.
- Scamell M. Childbirth within the risk society. Sociol Compass 2014;8:917-28. https://doi.org/10.1111/soc4.12077.
- Smith V, Devane D, Murphy-Lawless J. Risk in maternity care: a concept analysis. Int J Childbirth 2012;2. https://doi.org/10.1891/2156-5287.2.2.126.
- Chadwick RJ, Foster D. Negotiating risky bodies: childbirth and constructions of risk. Heal Risk Soc 2014;16:68-83. https://doi.org/10.1080/13698575.2013.863852.
- Davis-Floyd RE. The technological model of birth. J Am Folk 1987;100. https://doi.org/10.2307/540907.
- Davis-Floyd RE. The technocratic body: American childbirth as cultural expression. Soc Sci Med 1994;38:1125-40. https://doi.org/10.1016/0277-9536(94)90228-3.
- Kornelsen J. Essences and imperatives: an investigation of technology in childbirth. Soc Sci Med 2005;61:1495-504. https://doi.org/10.1016/j.socscimed.2005.03.007.
- Tew M. Safer Childbirth? A Critical History of Maternity Care. Berlin: Springer; 1990.
- Stoll K, Edmonds J, Sadler M, Thomson G, McAra-Couper J, Swift EM, et al. A cross-country survey of attitudes toward childbirth technologies and interventions among university students. Women Birth 2019;32:231-9. https://doi.org/10.1016/j.wombi.2018.07.025.
- Lazarus ES. What do women want – issues of choice, control and class in pregnancy and childbirth I. Med Anthropol Q 1994;8:25-46. https://doi.org/10.1525/maq.1994.8.1.02a00030.
- Christiaens W, Bracke P. Place of birth and satisfaction with childbirth in Belgium and the Netherlands. Midwifery 2009;25:e11-19. https://doi.org/10.1016/j.midw.2007.02.001.
- Miller AC, Shriver TE. Women’s childbirth preferences and practices in the United States. Soc Sci Med 2012;75:709-16. https://doi.org/10.1016/j.socscimed.2012.03.051.
- Greer J, Lazenbatt A, Dunne L. ‘Fear of childbirth’ and ways of coping for pregnant women and their partners during the birthing process: a salutogenic analysis. Evid Based Midwifery 2014;12:95-100.
- Rothman BK. In Labor: Women and the Power in the Birthplace. New York, NY: W.W. Norton and Company; 1982.
- Martin E. The Woman in the Body: A Cultural Analysis of Reproduction. Milton Keynes: Open University Press; 1989.
- Riessman CK. Women and medicalization: a new perspective. Soc Policy 1983;14:3-18.
- Brubaker SJ, Dillaway HE. Medicalization, natural childbirth and birthing experiences. Sociol Compass 2009;3:31-48. https://doi.org/10.1111/j.1751-9020.2008.00183.x.
- MacKenzie Bryers H, van Teijlingen E. Risk, theory, social and medical models: a critical analysis of the concept of risk in maternity care. Midwifery 2010;26:488-96. https://doi.org/10.1016/j.midw.2010.07.003.
- Hollowell J, Li Y, Malouf R, Buchanan J. Women’s birth place preferences in the United Kingdom: a systematic review and narrative synthesis of the quantitative literature. BMC Pregnancy Childbirth 2016;16. https://doi.org/10.1186/s12884-016-0998-5.
- Scarf VL, Rossiter C, Vedam S, Dahlen HG, Ellwood D, Forster D, et al. Maternal and perinatal outcomes by planned place of birth among women with low-risk pregnancies in high-income countries: a systematic review and meta-analysis. Midwifery 2018;62:240-55. https://doi.org/10.1016/j.midw.2018.03.024.
- Oakley A, Rajan L. Obstetric technology and maternal emotional well-being: a further research note. J Reprod Infant Psychol 1990;8:45-5. https://doi.org/10.1080/02646839008403607.
- Possamai-Inesedy A. Confining risk: choice and responsibility in childbirth in a risk society. Heal Sociol Rev 2006;15:406-14. https://doi.org/10.5172/hesr.2006.15.4.406.
- Coxon K, Sandall J, Fulop NJ. To what extent are women free to choose where to give birth? How discourses of risk, blame and responsibility influence birth place decisions. Health Risk Soc 2014;16:51-67. https://doi.org/10.1080/13698575.2013.859231.
- Fontein-Kuipers Y, de Groot R, van Staa A. Woman-centered care 2.0: bringing the concept into focus. Eur J Midwifery 2018;2. https://doi.org/10.18332/ejm/91492.
- Leap N. Woman-centred or women-centred care: does it matter?. Br J Midwifery 2009;17:12-6. https://doi.org/10.12968/bjom.2009.17.1.37646.
- Brady S, Lee N, Gibbons K, Bogossian F. Woman-centred care: an integrative review of the empirical literature. Int J Nurs Stud 2019;94:107-19. https://doi.org/10.1016/j.ijnurstu.2019.01.001.
- Newnham E, Kirkham M. Beyond autonomy: care ethics for midwifery and the humanization of birth. Nurs Ethics 2019;26:2147-57. https://doi.org/10.1177/0969733018819119.
- Lundgren I, Berg M, Nilsson C, Olafsdottir OA. Health professionals’ perceptions of a midwifery model of woman-centred care implemented on a hospital labour ward. Women Birth 2020;33:60-9. https://doi.org/10.1016/j.wombi.2019.01.004.
- Gibson E. Women’s expectations and experiences with labour pain in medical and midwifery models of birth in the United States. Women Birth 2014;27:185-9. https://doi.org/10.1016/j.wombi.2014.05.002.
- Sandall J, Soltani H, Gates S, Shennan A, Devane D. Midwife-led continuity models versus other models of care for childbearing women. Cochrane Database Syst Rev 2016;4. https://doi.org/10.1002/14651858.CD004667.pub5.
- Young D. What is normal childbirth and do we need more statements about it?. Birth 2009;36:1-3. https://doi.org/10.1111/j.1523-536X.2008.00306.x.
- Wagner M. Fish can’t see water: the need to humanize birth. Int J Gynaecol Obstet 2001;75:25-37. https://doi.org/10.1016/S0020-7292(01)00519-7.
- Jordan B. Birth in Four Cultures: A Cross Cultural Investigation of Childbirth in Yucatan, Holland, Sweden, and the United States. Montreal, QC: Eden Press; 1978.
- Leap N, Hunter B. Supporting Women for Labour and Birth: A Thoughtful Guide. Abingdon: Routledge; 2016.
- Bradfield Z, Duggan R, Hauck Y, Kelly M. Midwives being ‘with woman’: an integrative review. Women Birth 2018;31:143-52. https://doi.org/10.1016/j.wombi.2017.07.011.
- Hodnett ED, Gates S, Hofmeyr GJ, Sakala C. Continuous support for women during childbirth. Cochrane Database Syst Rev 2003;3. https://doi.org/10.1002/14651858.CD003766.
- Oakley A. Essays on Women, Medicine and Health. Edinburgh: Edinburgh University Press; 1993.
- Cook K, Loomis C. The impact of choice and control on women’s childbirth experiences. J Perinat Educ 2012;21:158-68. https://doi.org/10.1891/1058-1243.21.3.158.
- Fair CD, Morrison TE. The relationship between prenatal control, expectations, experienced control, and birth satisfaction among primiparous women. Midwifery 2012;28:39-44. https://doi.org/10.1016/j.midw.2010.10.013.
- Conesa Ferrer MB, Canteras Jordana M, Ballesteros Meseguer C, Carrillo García C, Martínez Roche ME. Comparative study analysing women’s childbirth satisfaction and obstetric outcomes across two different models of maternity care. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2016-011362.
- Taheri M, Takian A, Taghizadeh Z, Jafari N, Sarafraz N. Creating a positive perception of childbirth experience: systematic review and meta-analysis of prenatal and intrapartum interventions. Reprod Health 2018;15. https://doi.org/10.1186/s12978-018-0511-x.
- Michels A, Kruske S, Thompson R. Women’s postnatal psychological functioning: the role of satisfaction with intrapartum care and the birth experience. J Reprod Infant Psychol 2013;31:172-82. https://doi.org/10.1080/02646838.2013.791921.
- Department of Health and Social Care (DHSC) . Changing Childbirth: Report of the Expert Maternity Group 1993.
- Department of Health and Social Care (DHSC) . Maternity Matters: Choice, Access and Continuity of Care in a Safe Service 2007.
- Hill M. Give Birth Like a Feminist: Your Body. Your Baby. Your Choices. London: Harper Collins; 2019.
- Boyle S, Thomas H, Brooks F. Women’s views on partnership working with midwives during pregnancy and childbirth. Midwifery 2016;32:21-9. https://doi.org/10.1016/j.midw.2015.09.001.
- Bylund CL. Mothers’ involvement in decision making during the birthing process: a quantitative analysis of women’s online birth stories. Health Commun 2005;18:23-39. https://doi.org/10.1207/s15327027hc1801_2.
- Cole L, LeCouteur A, Feo R, Dahlen H. ‘Trying to give birth naturally was out of the question’: accounting for intervention in childbirth. Women Birth 2019;32:e95-101.
- Attanasio LB, Kozhimannil KB, Kjerulff KH. Factors influencing women’s perceptions of shared decision making during labor and delivery: results from a large-scale cohort study of first childbirth. Patient Educ Couns 2018;101:1130-6. https://doi.org/10.1016/j.pec.2018.01.002.
- De Freitas C, Massag J, Amorim M, Fraga S. Involvement in maternal care by migrants and ethnic minorities: a narrative review. Public Health Rev 2020;41. https://doi.org/10.1186/s40985-020-00121-w.
- Koster D, Romijn C, Sakko E, Stam C, Steenhuis N, de Vries D, et al. Traumatic childbirth experiences: practice-based implications for maternity care professionals from the woman’s perspective. Scand J Caring Sci 2020;34:792-9. https://doi.org/10.1111/scs.12786.
- O’Cathain A, Thomas K, Walters SJ, Nicholl J, Kirkham M. Women’s perceptions of informed choice in maternity care. Midwifery 2002;18:136-44. https://doi.org/10.1054/midw.2002.0301.
- Care Quality Commission . 2019 Survey of Women’s Experiences of Maternity Care: Statistical Release 2020.
- Thompson R, Miller YD. Birth control: to what extent do women report being informed and involved in decisions about pregnancy and birth procedures?. BMC Pregnancy Childbirth 2014;14. https://doi.org/10.1186/1471-2393-14-62.
- Royal College of Midwives . England Short of Almost 2500 Midwives, New Birth Figures Confirm 2019. www.rcm.org.uk/news-views/rcm-opinion/2019/england-short-of-almost-2-500-midwives-new-birth-figures-confirm/ (accessed 17 March 2021).
- Ladd RE. Women in labor: some issues about informed consent. Hypatia 1989;4:37-45. https://doi.org/10.1111/j.1527-2001.1989.tb00590.x.
- Wolf AB, Charles S. Childbirth is not an emergency: informed consent in labor and delivery. IJFAB Int J Fem Approaches to Bioeth 2018;11:23-4. https://doi.org/10.3138/ijfab.11.1.23.
- Salovey P, Sieber W, Smith A, Turk D, Jobe J, Willis GB. Reporting Chronic Pain Episodes on Health Surveys 1992.
- van Teijlingen ER, Hundley V, Rennie AM, Graham W, Fitzmaurice A. Maternity satisfaction studies and their limitations: ‘what is, must still be best’. Birth 2003;30:75-82. https://doi.org/10.1046/j.1523-536X.2003.00224.x.
- Beecher C, Greene R, O’Dwyer L, Ryan E, White M, Beattie M, et al. Measuring women’s experiences of maternity care: protocol for a systematic review of self-report survey instruments. Syst Rev 2020;9. https://doi.org/10.1186/s13643-019-1261-8.
- Annandale EC. How midwives accomplish natural birth: managing risk and balancing expectations. Soc Probl 1988;35:95-110. https://doi.org/10.2307/800734.
- Hunt SC, Symonds A. The Social Meaning of Midwifery. Basingstoke: McMillan Press; 1995.
- Walsh D. Subverting the assembly-line: childbirth in a free-standing birth centre. Soc Sci Med 2006;62:1330-40. https://doi.org/10.1016/j.socscimed.2005.08.013.
- Scamell M. The swan effect in midwifery talk and practice: a tension between normality and the language of risk. Sociol Health Illn 2011;33:987-1001. https://doi.org/10.1111/j.1467-9566.2011.01366.x.
- Jordan B, Davis-Floyd RE, Sargent C. Childbirth and Authoritative Knowledge: Cross-Cultural Perspectives. Los Angeles, CA: University of California Press; 1997.
- Korstjens I, Mesman J, van Helmond I, de Vries R, Nieuwenhuijze M. The paradoxes of communication and collaboration in maternity care: a video-reflexivity study with professionals and parents. Women Birth 2021;34:145-53. https://doi.org/10.1016/j.wombi.2020.01.014.
- Heritage J, Maynard DW. Communication in Medical Care. Cambridge: Cambridge University Press; 2006.
- Heritage J, Robinson JD, Elliott MN, Beckett M, Wilkes M. Reducing patients’ unmet concerns in primary care: the difference one word can make. J Gen Intern Med 2007;22:1429-33. https://doi.org/10.1007/s11606-007-0279-0.
- Land V, Parry R, Seymour J. Communication practices that encourage and constrain shared decision making in health-care encounters: systematic review of conversation analytic research. Health Expect 2017;20:1228-47. https://doi.org/10.1111/hex.12557.
- Collins S, Drew P, Watt I, Entwistle V. ‘Unilateral’ and ‘bilateral’ practitioner approaches in decision-making about treatment. Soc Sci Med 2005;61:2611-27. https://doi.org/10.1016/j.socscimed.2005.04.047.
- Opel DJ, Heritage J, Taylor JA, Mangione-Smith R, Salas HS, Devere V, et al. The architecture of provider-parent vaccine discussions at health supervision visits. Pediatrics 2013;132:1037-46. https://doi.org/10.1542/peds.2013-2037.
- Stivers T, Heritage J, Barnes RK, McCabe R, Thompson L, Toerien M. Treatment recommendations as actions. Health Commun 2018;33:1335-44. https://doi.org/10.1080/10410236.2017.1350913.
- Koenig CJ. Patient resistance as agency in treatment decisions. Soc Sci Med 2011;72:1105-14. https://doi.org/10.1016/j.socscimed.2011.02.010.
- Stivers T. Parent resistance to physicians’ treatment recommendations: one resource for initiating a negotiation of the treatment decision. Health Commun 2005;18:41-74. https://doi.org/10.1207/s15327027hc1801_3.
- Ekberg K, LeCouteur A. Clients’ resistance to therapists’ proposals: managing epistemic and deontic status. J Pragmat 2015;90:12-25. https://doi.org/10.1016/j.pragma.2015.10.004.
- Gill VT. Doing attributions in medical interaction: patients’ explanations for illness and doctors’ responses. Soc Psychol Q 1998;61:342-60. https://doi.org/10.2307/2787034.
- Gill VT, Pomerantz A, Denvir P. Pre-emptive resistance: patients’ participation in diagnostic sense-making activities. Sociol Health Illn 2010;32:1-20. https://doi.org/10.1111/j.1467-9566.2009.01208.x.
- Stivers T, Heritage J. Breaking the sequential mold: answering ‘more than the question’ during comprehensive history taking. Text 2001;21:151-85. https://doi.org/10.1515/text.1.21.1-2.151.
- Toerien M, Jackson C, Murray AJ, Durrheim K. Qualitative Studies of Silence: The Unsaid as Social Action. Cambridge: Cambridge University Press; 2019.
- Costello BA, Roberts F. Medical recommendations as joint social practice. Health Commun 2001;13:241-60. https://doi.org/10.1207/S15327027HC1303_2.
- Mondada L. Instructions in the operating room: how the surgeon directs their assistant’s hands. Discourse Stud 2014;16:131-61. https://doi.org/10.1177/1461445613515325.
- Parry RH. The interactional management of patients’ physical incompetence: a conversation analytic study of physiotherapy interactions. Sociol Health Illn 2004;26:976-1007. https://doi.org/10.1111/j.0141-9889.2004.00425.x.
- Ostermann A, Frezza M. Ephemeral Visual Referents and Their Consequences to Intersubjectivity in Fetal Ultrasound Scans. Lyon: Interactions Multimodales par ECran; 2008.
- Petraki E, Clark S. Affiliating through agreements: the context of antenatal consultations. Aust J Linguist 2016;36:273-89. https://doi.org/10.1080/07268602.2015.1121535.
- Petraki E, Clark S. Escalating the positive in antenatal consultations: midwife support in (inter)action. Commun Med 2018;14:241-55. https://doi.org/10.1558/cam.36356.
- Cole L, Turnbull D, Dahlen H. How are decisions made to access a planned epidural in labour? Midwife-woman interactions in antenatal consultations. Midwifery 2020;82. https://doi.org/10.1016/j.midw.2019.102618.
- Cole L, LeCouteur A, Feo R, Dahlen H. ‘Cos you’re quite normal, aren’t you?’: epistemic and deontic orientations in the presentation of model of care talk in antenatal consultations. Health Commun 2021;36:381-91. https://doi.org/10.1080/10410236.2019.1692492.
- Pilnick A. ‘It’s just one of the best tests that we’ve got at the moment’: the presentation of nuchal translucency screening for fetal abnormality in pregnancy. Discourse Soc 2004;15:451-65. https://doi.org/10.1177/0957926504043710.
- Pilnick A, Zayts O. Advice, authority and autonomy in shared decision-making in antenatal screening: the importance of context. Sociol Health Illn 2016;38:343-59. https://doi.org/10.1111/1467-9566.12346.
- Shaw R, Kitzinger C. Calls to a home birth helpline: empowerment in childbirth. Soc Sci Med 2005;61:2374-83. https://doi.org/10.1016/j.socscimed.2005.04.029.
- Shaw R, Kitzinger C. Managing distress, effecting empowerment: a conversation analytic case study of a call to the Home Birth Helpline. Int Rev Soc Res 2013;3:7-28. https://doi.org/10.1515/irsr-2013-0008.
- Jordan B. Technology and social interaction: notes on the achievement of authoritative knowledge in complex settings. Talent Dev Excell 2014;6:95-132.
- Bergstrom L, Roberts J, Skillman L, Seidel J. ‘You’ll feel me touching you, sweetie’: vaginal examinations during the second stage of labor. Birth 1992;19:10-8. https://doi.org/10.1111/j.1523-536x.1992.tb00365.x.
- Bergstrom L, Seidel J, Skillman-Hull L, Roberts J. ‘I gotta push. Please let me push!’ Social interactions during the change from first to second stage labor. Birth 1997;24:173-80. https://doi.org/10.1111/j.1523-536x.1997.tb00582.x.
- Jackson C, Land V, Holmes EJ. Healthcare professionals’ assertions and women’s responses during labour: a conversation analytic study of data from One Born Every Minute. Patient Educ Couns 2017;100:465-72. https://doi.org/10.1016/j.pec.2016.10.004.
- Robinson JD. The role of numbers and statistics within conversation analysis. Commun Methods Meas 2007;1:65-7. https://doi.org/10.1080/19312450709336663.
- Stivers T. Coding social interaction: a heretical approach in conversation analysis?. Res Lang Soc Interact 2015;48:1-19. https://doi.org/10.1080/08351813.2015.993837.
- Roter D, Larson S. The Roter Interaction Analysis System (RIAS): utility and flexibility for analysis of medical interactions. Patient Educ Couns 2002;46:243-51. https://doi.org/10.1016/S0738-3991(02)00012-5.
- Heritage J. Conversation analysis at century’s end: practices of talk-in-interaction, their distributions, and their outcomes. Res Lang Soc Interact 1999;32:69-76. https://doi.org/10.1080/08351813.1999.9683609.
- Robinson JD, Heritage J. Physicians’ opening questions and patients’ satisfaction. Patient Educ Couns 2006;60:279-85. https://doi.org/10.1016/j.pec.2005.11.009.
- Reuber M, Chappell P, Jackson C, Toerien M. Evaluating nuanced practices for initiating decision-making in neurology clinics: a mixed-methods study. Heal Serv Deliv Res 2018;6. https://doi.org/10.3310/hsdr06340.
- Reuber M, Toerien M, Shaw R, Duncan R. Delivering patient choice in clinical practice: a conversation analytic study of communication practices used in neurology clinics to involve patients in decision-making. Heal Serv Deliv Res 2015;3. https://doi.org/10.3310/hsdr03070.
- Hildingsson I. Swedish couples’ attitudes towards birth, childbirth fear and birth preferences and relation to mode of birth – a longitudinal cohort study. Sex Reprod Healthc 2014;5:75-80. https://doi.org/10.1016/j.srhc.2014.02.002.
- Thies-Lagergren L, Johansson M. Intrapartum midwifery care impact Swedish couple’s birth experiences – a cross-sectional study. Women Birth 2019;32:213-20. https://doi.org/10.1016/j.wombi.2018.08.163.
- Fontein-Kuipers Y, van Duijvenbode J, Pluymaekers M. Portrayal of shared decision-making in lifetime documentary series ‘One Born Every Minute’. SM J Nurs 2019;5:1-7. https://doi.org/10.36876/smjn.1021.
- Sawyer A, Ayers S, Abbott J, Gyte G, Rabe H, Duley L. Measures of satisfaction with care during labour and birth: a comparative review. BMC Pregnancy Childbirth 2013;13. https://doi.org/10.1186/1471-2393-13-108.
- Bramadat IJ, Driedger M. Satisfaction with childbirth: theories and methods of measurement. Birth 1993;20:22-9. https://doi.org/10.1111/j.1523-536x.1993.tb00175.x.
- Sitzia J, Wood N. Patient satisfaction: a review of issues and concepts. Soc Sci Med 1997;45:1829-43. https://doi.org/10.1016/S0277-9536(97)00128-7.
- Preis H, Lobel M, Benyamini Y. Between expectancy and experience: testing a model of childbirth satisfaction. Psychol Women 2019;43:105-17. https://doi.org/10.1177/0361684318779537.
- Carminati L. Generalizability in qualitative research: a tale of two traditions. Qual Health Res 2018;28:2094-101. https://doi.org/10.1177/1049732318788379.
- UK Government . English Indices of Deprivation 2015 2015. www.gov.uk/government/statistics/english-indices-of-deprivation-2015 (accessed 30 June 2020).
- Anderson A. Ten years of maternity claims: an analysis of the NHS Litigation Authority data – key findings. Clin Risk 2013;19:24-31. https://doi.org/10.1177/1356262213486434.
- Sacks H. Lectures on Conversation. Volumes I and II. Oxford: Blackwell; 1992.
- Schegloff EA. Sequencing in conversational openings. Am Anthropol 1968;70:1075-95. https://doi.org/10.1525/aa.1968.70.6.02a00030.
- Sacks H, Schegloff EA, Psathas G. Everyday Language: Studies in Ethnomethodology. New York, NY: Irvington; 1979.
- Schegloff EA. Sequence Organization in Interaction. Vol. 1. Cambridge: Cambridge University Press; 2007.
- Sacks H, Button G, Lee JR. In Talk and Social Organisation. Clevedon: Multilingual Matters; 1987.
- Pomerantz A, Atkinson M, Heritage J. Structures of Social Action: Studies in Conversation Analysis. Cambridge: Cambridge University Press; 1984.
- Pomerantz A, Heritage J, Sidnell J, Stivers T. The Handbook of Conversation Analysis. Chichester: John Wiley & Sons, Ltd; 2012.
- Heritage J. Garfinkel and Ethnomethodology. Cambridge: Polity Press; 1984.
- Kitzinger C, Frith H. Just say no? The use of conversation analysis in developing a feminist perspective on sexual refusal. Discourse Soc 1999;10. https://doi.org/10.1177/0957926599010003002.
- Curl TS, Drew P. Contingency and action: a comparison of two forms of requesting. Res Lang Soc Interact 2008;41:129-53. https://doi.org/10.1080/08351810802028613.
- Jefferson G, Lerner G. Conversation Analysis: Studies from the First Generation. Amsterdam: John Benjamins; 2004.
- Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics 1977;33:159-74. https://doi.org/10.2307/2529310.
- Green J, Baston H, Easton S, Mccormick F. Greater Expectations? Interrelationships Between Women’s Expectations and Experiences of Decision Making, Continuity, Choice and Control in Labour, and Psychological Outcomes. Leeds: Mother and Infant Research Unit, University of Leeds; 2003.
- Downe S, Finlayson K, Oladapo OT, Bonet M, Gülmezoglu AM. What matters to women during childbirth: a systematic qualitative review. PLOS One 2018;13. https://doi.org/10.1371/journal.pone.0194906.
- Armstrong N, Kenyon S. When choice becomes limited: women’s experiences of delay in labour. Health 2017;21:223-38. https://doi.org/10.1177/1363459315617311.
- Borrelli SE, Walsh D, Spiby H. First-time mothers’ expectations of the unknown territory of childbirth: uncertainties, coping strategies and ‘going with the flow’. Midwifery 2018;63:39-45. https://doi.org/10.1016/j.midw.2018.04.022.
- Snowden A, Martin C, Jomeen J, Hollins Martin C. Concurrent analysis of choice and control in childbirth. BMC Pregnancy Childbirth 2011;11. https://doi.org/10.1186/1471-2393-11-40.
- Divall B, Spiby H, Nolan M, Slade P. Plans, preferences or going with the flow: an online exploration of women’s views and experiences of birth plans. Midwifery 2017;54:29-34. https://doi.org/10.1016/j.midw.2017.07.020.
- Lundgren I. Swedish women’s experience of childbirth 2 years after birth. Midwifery 2005;21:346-54. https://doi.org/10.1016/j.midw.2005.01.001.
- Westergren A, Edin K, Walsh D, Christianson M. Autonomous and dependent – the dichotomy of birth: a feminist analysis of birth plans in Sweden. Midwifery 2019;68:56-64. https://doi.org/10.1016/j.midw.2018.10.008.
- Lally JE, Thomson RG, MacPhail S, Exley C. Pain relief in labour: a qualitative study to determine how to support women to make decisions about pain relief in labour. BMC Pregnancy Childbirth 2014;14. https://doi.org/10.1186/1471-2393-14-6.
- Lally JE, Murtagh MJ, Macphail S, Thomson R. More in hope than expectation: a systematic review of women’s expectations and experience of pain relief in labour. BMC Med 2008;6. https://doi.org/10.1186/1741-7015-6-7.
- Gibbins J, Thomson AM. Women’s expectations and experiences of childbirth. Midwifery 2001;17:302-13. https://doi.org/10.1054/midw.2001.0263.
- Slade P, Macpherson SA, Hume A, Maresh M. Expectations, experiences and satisfaction with labor. Br J Clin Psychol 1993;32:469-83. https://doi.org/10.1111/j.2044-8260.1993.tb01083.x.
- Ayers S, Pickering AD. Women’s expectations and experience of birth. Psychol Heal 2005;20:79-92. https://doi.org/10.1080/0887044042000272912.
- Lindholm A, Hildingsson I. Women’s preferences and received pain relief in childbirth – a prospective longitudinal study in a northern region of Sweden. Sex Reprod Healthc 2015;6:74-81. https://doi.org/10.1016/j.srhc.2014.10.001.
- Goodman P, Mackey MC, Tavakoli AS. Factors related to childbirth satisfaction. J Adv Nurs 2004;46:212-19. https://doi.org/10.1111/j.1365-2648.2003.02981.x.
- Chez BF, Harvey MG, Harvey CJ. Intrapartum fetal monitoring: past, present, and future. J Perinat Neonatal Nurs 2000;14:1-18. https://doi.org/10.1097/00005237-200012000-00002.
- Patey AM, Curran JA, Sprague AE, Francis JJ, Driedger SM, Légaré F, et al. Intermittent auscultation versus continuous fetal monitoring: exploring factors that influence birthing unit nurses’ fetal surveillance practice using theoretical domains framework. BMC Pregnancy Childbirth 2017;17. https://doi.org/10.1186/s12884-017-1517-z.
- Alfirevic Z, Devane D, Gyte GM, Cuthbert A. Continuous cardiotocography (CTG) as a form of electronic fetal monitoring (EFM) for fetal assessment during labour. Cochrane Database Syst Rev 2017;2. https://doi.org/10.1002/14651858.CD006066.pub3.
- Sartwelle TP, Johnston JC, Arda B. Perpetuating myths, fables, and fairy tales: a half century of electronic fetal monitoring. Surg J 2015;1:e28-e34. https://doi.org/10.1055/s-0035-1567880.
- Sartwelle TP, Johnston JC, Arda B. A half century of electronic fetal monitoring and bioethics: silence speaks louder than words. Matern Health Neonatol Perinatol 2017;3. https://doi.org/10.1186/s40748-017-0060-2.
- Devane D, Lalor JG, Daly S, McGuire W, Cuthbert A, Smith V. Cardiotocography versus intermittent auscultation of fetal heart on admission to labour ward for assessment of fetal wellbeing. Cochrane Database Syst Rev 2017;1. https://doi.org/10.1002/14651858.CD005122.pub5.
- Hersh S, Megregian M, Emeis C. Intermittent auscultation of the fetal heart rate during labor: an opportunity for shared decision making. J Midwifery Womens Health 2014;59:344-9. https://doi.org/10.1111/jmwh.12178.
- Bloom SL, Belfort M, Saade G. Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network . What we have learned about intrapartum fetal monitoring trials in the MFMU Network. Semin Perinatol 2016;40:307-17. https://doi.org/10.1053/j.semperi.2016.03.008.
- National Institute for Health and Care Excellence (NICE) . Intrapartum Care for Healthy Women and Babies. Clinical Guideline [CG190] 2014.
- World Health Organization (WHO) . WHO Recommendations: Intrapartum Care for a Positive Childbirth Experience 2018.
- Lewis D, Downe S. FIGO Intrapartum Fetal Monitoring Expert Consensus Panel . FIGO consensus guidelines on intrapartum fetal monitoring: Intermittent auscultation. Int J Gynaecol Obstet 2015;131:9-12. https://doi.org/10.1016/j.ijgo.2015.06.019.
- Royal College of Midwives, Royal College of Obstetricians and Gynaecologists . RCM/RCOG/Consensus/Statement/on/Electronic/Fetal/Monitoring/(EFM) 2017. www.rcm.org.uk/media/5602/rcm-rcog-consensus-statement-on-efm.pdf (accessed 13 July 2020).
- Hindley C, Hinsliff SW, Thomson AM. Pregnant womens’ views about choice of intrapartum monitoring of the fetal heart rate: a questionnaire survey. Int J Nurs Stud 2008;45:224-31. https://doi.org/10.1016/J.IJNURSTU.2006.08.019.
- Mangesi L, Hofmeyr G, Woods D. Assessing the preference of women for different methods of monitoring the fetal heart in labour. S Afr J Obstet Gynaecol 2009;15:58-9.
- Davis-Floyd R. Birth as an American Rite of Passage. Los Angeles, CA: University of California Press; 1992.
- Blix E. Avoiding disturbance: midwifery practice in home birth settings in Norway. Midwifery 2011;27:687-92. https://doi.org/10.1016/j.midw.2009.09.008.
- Reed R, Rowe J, Barnes M. Midwifery practice during birth: ritual companionship. Women Birth 2016;29:269-78. https://doi.org/10.1016/j.wombi.2015.12.003.
- Stevanovic M, Peräkylä A. Deontic authority in interaction: the right to announce, propose, and decide. Res Lang Soc Interact 2012;45:297-321. https://doi.org/10.1080/08351813.2012.699260.
- Kent A, Kendrick KH. Imperative directives: orientations to accountability. Res Lang Soc Interact 2016;49:272-88. https://doi.org/10.1080/08351813.2016.1201737.
- Kendrick KH, Drew P. Recruitment: offers, requests, and the organization of assistance in interaction. Res Lang Soc Interact 2016;49:1-19. https://doi.org/10.1080/08351813.2016.1126436.
- Couper-Kuhlen E. What does grammar tell us about action?. Pragmatics 2014;24:623-47. https://doi.org/10.1075/prag.24.3.08cou.
- Scamell M. The fear factor of risk – clinical governance and midwifery talk and practice in the UK. Midwifery 2016;38:14-20. https://doi.org/10.1016/j.midw.2016.02.010.
- Harwood RH, O’Brien R, Goldberg SE, Allwood R, Pilnick A, Beeke S, et al. A staff training intervention to improve communication between people living with dementia and health-care professionals in hospital: the VOICE mixed-methods development and evaluation study. Heal Serv Deliv Res 2018;6. https://doi.org/10.3310/hsdr06410.
- Craven A, Potter J. Directives: entitlement and contingency in action. Discourse Stud 2010;12:419-42. https://doi.org/10.1177/1461445610370126.
- Heinemann T. ‘Will you or can’t you?’: displaying entitlement in interrogative requests. J Pragmat 2006;38:1081-104. https://doi.org/10.1016/j.pragma.2005.09.013.
- Drew P, Drew P, Raymond G, Weinber D. Talk and Interaction in Social Research Methods. London: SAGE Publications Ltd; 2006.
- Raymond G. Prompting action: the stand-alone ‘so’ in ordinary conversation. Res Lang Soc Interact 2004;37:185-218. https://doi.org/10.1207/s15327973rlsi3702_4.
- Heritage J, Stivers T. Online commentary in acute medical visits: a method of shaping patient expectations. Soc Sci Med 1999;49:1501-17. https://doi.org/10.1016/S0277-9536(99)00219-1.
- Gharaibeh A, Mahmood T. Abnormal labour. Obstet Gynaecol Reprod Med 2019;29:129-35. https://doi.org/10.1016/J.OGRM.2019.02.006.
- Friedman E. Graphic analysis of labour. Am J Obstet Gynecol 1954;68:1568-75. https://doi.org/10.1016/0002-9378(54)90311-7.
- Friedman EA. Primigravid labor; a graphicostatistical analysis. Obstet Gynecol 1955;6:567-89. https://doi.org/10.1097/00006250-195512000-00001.
- Oladapo OT, Diaz V, Bonet M, Abalos E, Thwin SS, Souza H, et al. Cervical dilatation patterns of ‘low-risk’ women with spontaneous labour and normal perinatal outcomes: a systematic review. BJOG 2018;125:944-54. https://doi.org/10.1111/1471-0528.14930.
- Lavender T, Hart A, Smyth RM. Effect of partogram use on outcomes for women in spontaneous labour at term. Cochrane Database Syst Rev 2013;7. https://doi.org/10.1002/14651858.CD005461.pub4.
- Lavender T, Cuthbert A, Smyth RM. Effect of partograph use on outcomes for women in spontaneous labour at term and their babies. Cochrane Database Syst Rev 2018;8. https://doi.org/10.1002/14651858.CD005461.pub5.
- Downe S, Gyte GM, Dahlen HG, Singata M. Routine vaginal examinations for assessing progress of labour to improve outcomes for women and babies at term. Cochrane Database Syst Rev 2013;7. https://doi.org/10.1002/14651858.CD010088.pub2.
- Shepherd A, Cheyne H. The frequency and reasons for vaginal examinations in labour. Women Birth 2013;26:49-54. https://doi.org/10.1016/j.wombi.2012.02.001.
- Hanley GE, Munro S, Greyson D, Gross MM, Hundley V, Spiby H, et al. Diagnosing onset of labor: a systematic review of definitions in the research literature. BMC Pregnancy Childbirth 2016;16. https://doi.org/10.1186/s12884-016-0857-4.
- Kobayashi S, Hanada N, Matsuzaki M, Takehara K, Ota E, Sasaki H, et al. Assessment and support during early labour for improving birth outcomes. Cochrane Database Syst Rev 2017;4. https://doi.org/10.1002/14651858.CD011516.pub2.
- Holmes P, Oppenheimer LW, Wen SW. The relationship between cervical dilatation at initial presentation in labour and subsequent intervention. BJOG 2001;108:1120-4. https://doi.org/10.1111/j.1471-0528.2003.00265.x.
- Rota A, Antolini L, Colciago E, Nespoli A, Borrelli SE, Fumagalli S. Timing of hospital admission in labour: latent versus active phase, mode of birth and intrapartum interventions. A correlational study. Women Birth 2018;31:313-18. https://doi.org/10.1016/j.wombi.2017.10.001.
- Spiby H, Walsh D, Green J, Crompton A, Bugg G. Midwives’ beliefs and concerns about telephone conversations with women in early labour. Midwifery 2014;30:1036-42. https://doi.org/10.1016/j.midw.2013.10.025.
- Green JM, Spiby H, Hucknall C, Richardson Foster H. Converting policy into care: women’s satisfaction with the early labour telephone component of the All Wales Clinical Pathway for Normal Labour. J Adv Nurs 2012;68:2218-28. https://doi.org/10.1111/j.1365-2648.2011.05906.x.
- Dixon L, Skinner J, Foureur M. The emotional journey of labour-women’s perspectives of the experience of labour moving towards birth. Midwifery 2014;30:371-7. https://doi.org/10.1016/j.midw.2013.03.009.
- Barnett C, Hundley V, Cheyne H. ‘Not in labour’: impact of sending women home in the latent phase. Br J Midwifery 2008;16:144-53. https://doi.org/10.12968/bjom.2008.16.3.28692.
- Spiby H, Green J, Hucknall C, Richardson-Foster H, Andrews A. Labouring to Better Effect: Studies of Services for Women in Early Labour. The OPAL Study (OPtions for Assessment in Early Labour). Report for the National Co-Ordinating Centre for NHS Service Delivery and Organisation R&Amp;D 2007. https://njl-admin.nihr.ac.uk/document/download/2027469 (accessed 8 March 2022).
- Beake S, Chang YS, Cheyne H, Spiby H, Sandall J, Bick D. Experiences of early labour management from perspectives of women, labour companions and health professionals: a systematic review of qualitative evidence. Midwifery 2018;57:69-84. https://doi.org/10.1016/j.midw.2017.11.002.
- Bick DE, Rycroft-Malone J, Fontenla M. A case study evaluation of implementation of a care pathway to support normal birth in one English birth centre: anticipated benefits and unintended consequences. BMC Pregnancy Childbirth 2009;9. https://doi.org/10.1186/1471-2393-9-47.
- Schegloff EA, Drew P, Wootton AJ. Erving Goffman: Exploring the Interaction Order. Cambridge: Polity Press; 1988.
- Toerien M, Reuber M, Shaw R, Duncan R. Generating the perception of choice: the remarkable malleability of option-listing. Sociol Health Illn 2018;40:1250-67. https://doi.org/10.1111/1467-9566.12766.
- Lowe NK. The nature of labor pain. Am J Obstet Gynecol 2002;186:S16-24. https://doi.org/10.1016/s0002-9378(02)70179-8.
- Whitburn LY, Jones LE, Davey MA, Small R. The meaning of labour pain: how the social environment and other contextual factors shape women’s experiences. BMC Pregnancy Childbirth 2017;17. https://doi.org/10.1186/s12884-017-1343-3.
- Whitburn LY, Jones LE, Davey M-A, Small R. Women’s experiences of labour pain and the role of the mind: an exploratory study. Midwifery 2014;30:1029-35. https://doi.org/10.1016/j.midw.2014.04.005.
- Haines HM, Rubertsson C, Pallant JF, Hildingsson I. The influence of women’s fear, attitudes and beliefs of childbirth on mode and experience of birth. BMC Pregnancy Childbirth 2012;12. https://doi.org/10.1186/1471-2393-12-55.
- Lundgren I, Dahlberg K. Women’s experience of pain during childbirth. Midwifery 1998;14:105-10. https://doi.org/10.1016/s0266-6138(98)90007-9.
- Thomson G, Feeley C, Moran VH, Downe S, Oladapo OT. Women’s experiences of pharmacological and non-pharmacological pain relief methods for labour and childbirth: a qualitative systematic review. Reprod Health 2019;16. https://doi.org/10.1186/s12978-019-0735-4.
- Smith LA, Burns E, Cuthbert A. Parenteral opioids for maternal pain management in labour. Cochrane Database Syst Rev 2018;6. https://doi.org/10.1002/14651858.CD007396.pub3.
- Anim-Somuah M, Smyth RM, Cyna AM, Cuthbert A. Epidural versus non-epidural or no analgesia for pain management in labour. Cochrane Database Syst Rev 2018;5. https://doi.org/10.1002/14651858.CD000331.pub4.
- Cambic CR, Wong CA. Labour analgesia and obstetric outcomes. Br J Anaesth 2010;105:i50-60. https://doi.org/10.1093/bja/aeq311.
- Jones L, Othman M, Dowswell T, Alfirevic Z, Gates S, Newburn M, et al. Pain management for women in labour: an overview of systematic reviews. Cochrane Database Syst Rev 2012;3. https://doi.org/10.1002/14651858.CD009234.pub2.
- Leap N, Dodwell M, Newburn M. Working with pain in labour: an overview of evidence. New Dig 2010;49:22-6. https://doi.org/10.1002/14651858.CD004667.pub2.
- Royal College of Midwives (RCM) . Understanding Pharmacological Pain Relief 2012.
- Care Quality Commission . 2017 Survey of Women’s Experiences of Maternity Care 2018.
- Stivers T, Rossano F. Mobilizing response. Res Lang Soc Interact 2010;43:3-31. https://doi.org/10.1080/08351810903471258.
- Charles C, Chapman V, Charles C. The Midwife’s Labour and Birth Handbook. Oxford: Wiley-Blackwell; 2018.
- Reynolds F. The effects of maternal labour analgesia on the fetus. Best Pract Res Clin Obstet Gynaecol 2010;24:289-302. https://doi.org/10.1016/j.bpobgyn.2009.11.003.
- Tuckey JP, Prout RE, Wee MY. Prescribing intramuscular opioids for labour analgesia in consultant-led maternity units: a survey of UK practice. Int J Obstet Anesth 2008;17:3-8. https://doi.org/10.1016/j.ijoa.2007.05.014.
- Schegloff EA. Overlapping talk and the organization of turn-taking for conversation. Lang Soc 2000;29:1-63. https://doi.org/10.1017/S0047404500001019.
- Royal College of Midwives (RCM) . Midwifery Care in Labour Guidance for All Women in All Settings 2018.
- Leduc D, Senikas V, Lalonde AB. Clinical Practice Obstetrics Committee . Active management of the third stage of labour: prevention and treatment of postpartum hemorrhage. J Obstet Gynaecol Can 2009;31:980-93. https://doi.org/10.1016/S1701-2163(16)34329-8.
- Begley CM, Gyte GM, Devane D, McGuire W, Weeks A, Biesty LM. Active versus expectant management for women in the third stage of labour. Cochrane Database Syst Rev 2019;2. https://doi.org/10.1002/14651858.CD007412.pub5.
- Davidson J, Maxwell J, Heritage J. Structures of Social Action: Studies in Conversation Analysis. Cambridge: Cambridge University Press; 1984.
- Burleigh A. Delaying the clampers. AIMS 2012;2.
- Brandão S, Figueiredo B. Fathers’ emotional involvement with the neonate: impact of the umbilical cord cutting experience. J Adv Nurs 2012;68:2730-9. https://doi.org/10.1111/j.1365-2648.2012.05978.x.
- Zinsser LA. Lotus birth, a holistic approach on physiological cord clamping. Women Birth 2018;31:e73-76. https://doi.org/10.1016/j.wombi.2017.08.127.
- Curl TS. Offers of assistance: constraints on syntactic design. J Pragmat 2006;38:1257-80. https://doi.org/10.1016/j.pragma.2005.09.004.
- Parry R, Pino M, Faull C, Feathers L. Acceptability and design of video-based research on healthcare communication: evidence and recommendations. Patient Educ Couns 2016;99:1271-84. https://doi.org/10.1016/j.pec.2016.03.013.
- Elsey C, Wilkinson R, Rae J, Rasmussen G. Atypical Interaction. Basingstoke: Palgrave Macmillan; 2020.
- Ekberg K, Meyer C, Scarinci N, Grenness C, Hickson L. Family member involvement in audiology appointments with older people with hearing impairment. Int J Audiol 2015;54:70-6. https://doi.org/10.3109/14992027.2014.948218.
- Pino M, Doehring A, Parry R. Practitioners’ dilemmas and strategies in decision-making conversations where patients and companions take divergent positions on a healthcare measure: an observational study using conversation analysis. Health Commun 2021;36:2010-21. https://doi.org/10.1080/10410236.2020.1813952.
- Beach WA. Lay diagnosis [special issue]. Text 2001;21:13-268. https://doi.org/10.1515/text.1.21.1-2.13.
- Kirkham M, Kirkham M. Informed Choice in Maternity Care. Basingstoke: Palgrave Macmillan; 2004.
- Kotaska A. Guideline-centered care: a two-edged sword. Birth 2011;38:97-8. https://doi.org/10.1111/j.1523-536X.2011.00469.x.
- Symon A. Risk and Choice in Maternity Care: An International Perspective. London: Churchill Livingstone; 2006.
- Knight M, Bunch K, Tuffnell D, Shakespeare J, Kotnis R, Kenyon S, et al. Saving Lives, Improving Mothers’ Care: Lessons Learned to Inform Maternity Care from the UK and Ireland Confidential Enquiries into Maternal Deaths and Morbidity 2015–17 2019. www.npeu.ox.ac.uk/assets/downloads/mbrrace-uk/reports/MBRRACE-UK%20Maternal%20Report%202019%20-%20WEB%20VERSION.pdf (accessed 8 March 2022).
- Esegbona-Adeigbe S, Olayiwola W. Reducing the incidence of stillbirth in black women. Br J Midwifery 2020;28:297-305. https://doi.org/10.12968/bjom.2020.28.5.297.
- Khan Z. Ethnic health inequalities in the UK’s maternity services: a systematic literature review. Br J Midwifery 2021;29:100-7. https://doi.org/10.12968/bjom.2021.29.2.100.
- Altman MR, Oseguera T, McLemore MR, Kantrowitz-Gordon I, Franck LS, Lyndon A. Information and power: women of color’s experiences interacting with health care providers in pregnancy and birth. Soc Sci Med 2019;238. https://doi.org/10.1016/j.socscimed.2019.112491.
- Smart A, Harrison E. The under-representation of minority ethnic groups in UK medical research. Ethn Health 2017;22:65-82. https://doi.org/10.1080/13557858.2016.1182126.
- Fry G, Gilgallon K, Khan W, Reynolds D, Spencer G, Wright A, et al. Recruitment of south Asian carers into a survey-based research study (innovative practice). Dementia 2020. https://doi.org/10.1177/1471301220909246.
- Jomeen J, Redshaw M. Ethnic minority women’s experience of maternity services in England. Ethn Health 2013;18:280-96. https://doi.org/10.1080/13557858.2012.730608.
- Jutlla K, Raghavan R. Improving the Recruitment of Black, Asian and Minority Ethnic (BAME) Communities in Health and Social Care Research: A Review of Literature 2017. https://dora.dmu.ac.uk/handle/2086/13221 (accessed 17 March 2021).
- Gutiérrez VB, Fader M, Monga A, Kitson-Reynolds E. Lack of care? Women’s experiences of maternity bladder management. Br J Midwifery 2019;27:15-2. https://doi.org/10.12968/bjom.2019.27.1.15.
- Rayment J, Rance S, McCourt C, Sandall Cbe Rm J. Barriers to women’s access to alongside midwifery units in England. Midwifery 2019;77:78-85. https://doi.org/10.1016/j.midw.2019.06.010.
- Barnes RK. Preliminaries to treatment recommendations in UK primary care: a vehicle for shared decision making?. Health Commun 2018;33:1366-76. https://doi.org/10.1080/10410236.2017.1350915.
- Parry R. Practitioners’ accounts for treatment actions and recommendations in physiotherapy: when do they occur, how are they structured, what do they do?. Sociol Health Illn 2009;31:835-53. https://doi.org/10.1111/j.1467-9566.2009.01187.x.
- Hunter B. Emotion work in midwifery: a review of current knowledge. J Adv Nurs 2001;34:436-44. https://doi.org/10.1046/j.1365-2648.2001.01772.x.
- Riley R, Weiss MC. A qualitative thematic review: emotional labour in healthcare settings. J Adv Nurs 2016;72:6-17. https://doi.org/10.1111/jan.12738.
- Toerien M, Kitzinger C. Emotional labour in action: navigating multiple involvements in the beauty salon. Sociology 2007;41:645-62. https://doi.org/10.1177/0038038507078918.
- Barnes RK. Conversation analysis of communication in medical care: description and beyond. Res Lang Soc Interact 2019;52:300-15. https://doi.org/10.1080/08351813.2019.1631056.
- McArthur A. Getting pain on the table in primary care physical exams. Soc Sci Med 2018;200:190-8. https://doi.org/10.1016/j.socscimed.2018.01.012.
- Chapman CR, Beach WA. Patient-initiated pain expressions: interactional asymmetries and consequences for cancer care. Health Commun 2020;35:1643-55. https://doi.org/10.1080/10410236.2019.1654178.
- Heritage J, Beach WA. Handbook of Patient–Provider Interactions Raising and Responding to Concerns About Life, Illness & Disease. New York, NY: Hampton Press Inc.; 2013.
- Ministry of Housing Communities & Local Government . English Indices of Deprivation 2015. Postcode Lookup n.d. https://imd-by-postcode.opendatacommunities.org/imd/2015 (accessed 11 March 2022).
- Stivers T, Sidnell J. Proposals for activity collaboration. Res Lang Soc Intertact 2016;49:148-66. https://doi.org/10.1080/08351813.2016.1164409.
Appendix 1 Pseudonyms for recordings and labouring women
| Recording number (randomised) | Woman’s pseudonym |
|---|---|
| VIP01 | Jacqueline |
| VIP02 | Elise |
| VIP03 | Willow |
| VIP04 | Judy |
| VIP05 | Bryony |
| VIP06 | Kay |
| VIP07 | Martha |
| VIP08 | Lydia |
| VIP09 | Freya |
| VIP10 | Gabi |
| VIP11 | Philippa |
| VIP12 | Fiona |
| VIP13 | Yvonne |
| VIP14 | Brenna |
| VIP15 | Faith |
| VIP16 | Addison |
| VIP17 | Nina |
| VIP18 | Zoe |
| VIP19 | Leigh |
| VIP20 | Abigail |
| VIP21 | Diana |
| VIP22 | Claudia |
| VIP23 | Gina |
| VIP24 | Imogen |
| VIP25 | Kyla |
| VIP26 | Bella |
| VIP27 | Jasmine |
| VIP28 | Kailani |
| VIP29 | Madeline |
| VIP30 | Harmony |
| VIP31 | Lexi |
| VIP32 | Natalie |
| VIP33 | Ruth |
| VIP34 | Daisy |
| VIP35 | Josie |
| VIP36 | Phoebe |
| VIP37 | Gracie |
Appendix 2 Study poster
Appendix 3 Index of Multiple Deprivation 2015
The IMD is the official government measure of relative deprivation based on small areas (i.e. lower-layer super output areas) or neighbourhoods. In total, there are 32,844 areas in England, which are designed to be of a similar population size, with an average of 1500 residents and 650 households in each.
The Index comprises seven domains, each with different weightings: (1) income deprivation (22.5%); (2) employment deprivation (22.5%); (3) education, skills and training deprivation (13.5%); (4) health deprivation and disability (13.5%); (5) crime (9.3%); (6) barriers to housing services (9.3%); and (7) living environment deprivation (9.3%).
It is important to bear in mind that the IMD is a measure of relative deprivation that compares each neighbourhood with all the others in England. Neighbourhoods are ranked against one another from 1 (the most deprived area) to 32,844 (the least deprived area). Data are grouped into deciles from 1 (most deprived) to 10 (least deprived). The numeric value attached to an area does not indicate how deprived that area is in itself, only how it compares to other areas. The IMD is not a measure of an individuals’ deprivation level, as, for example, there can be variation within an area.
The IMD 2015 Postcode Lookup302 facility was used to determine the decile within which each respondents’ household fell. Postcode was provided by respondents during the consenting process. The 2015 IMD was used because when recruitment commenced this was the most recent data set.
For further details see URL: www.gov.uk/government/statistics/english-indices-of-deprivation-2015 (accessed 11 March 2022).
Appendix 4 Ethnicity figures for each study site
| Trust | Percentage (n/N) of women who gave birth during the recruitment period:a April 2018 to October 2019 (all birth settings) | Percentage (n/N) of women approached | Percentage (n/N) of women approached who consented |
|---|---|---|---|
| A | |||
| White | 50 (7790/15,570) | 80 (675/846) | 15 (102/675) |
| Asian/Asian British | 12 (1925/15,570) | 10 (86/846) | 5 (4/86) |
| Black/African/Caribbean/black British | 7 (1025/15,570) | 4 (30/846) | 7 (2/30) |
| Mixed/multiple ethnic group | 4 (590/15,570) | 2 (20/846) | 0 (0/20) |
| Other | 26 (4040/15,570) | 4 (35/846) | 6 (2/35) |
| B | |||
| White | 75 (5849/7842) | 85 (194/227) | 21 (40/194) |
| Asian/Asian British | 17 (1294/7842) | 12 (28/227) | 11 (3/28) |
| Black/African/Caribbean/black British | 2 (174/7842) | < 1 (1/227) | 0 (0/1) |
| Mixed/multiple ethnic group | 4 (284/7842) | < 1 (2/227) | 0 (0/2) |
| Other | 3 (241/7842) | < 1 (2/227) | 0 (0/2) |
Appendix 5 Recording parameters
| Recording information | Parameter |
|---|---|
| Total hours | 166.56.00 |
| Format | 23 video-recordings, 14 audio-recordings |
| Mean hours | 04.30.42 |
| Median hours | 03.28.00 |
| Maximum hours | 15.20.00 |
| Minimum hours | 00.08.00 |
| SD | 0.141 |
| Moment of birth recorded | 21/37 (of these, 19 are unassisted and two are ventouse deliveries on the MLU) |
| When moment of birth is not recorded | |
| Transferred to obstetric care | 7/16 (e.g. meconium in waters, low FHR, ketones) |
| Transferred for epidural | 3/16 |
| Latent phase of labour | 3/16 (i.e. women go home or transferred to an antenatal ward) |
| Camera stops for no apparent reason | 3/16 (these require further investigation) |
| Recording starts |
Latent stage: 9 First stage: 21 Second stage: 7 |
| Recording ends |
Latent stage: 6 First stage: 6 Second stage: 3 Third stage: 7 Post third stage: 15 |
Appendix 6 Conversation analytic transcription conventions
Following Jefferson;183 symbols reproduced with permission from John Benjamins Publishing Company, Amsterdam, the Netherlands.
| [] square brackets | Overlapping talk |
| = equals sign | Latched speech (no silence between turns at talk) |
| (0.4) time in parentheses | Intervals of silence within or between talk (measured in tenths of a second) |
| (.) period in parentheses | A silence in talk but too short to measure (less than 2 tenths of a second) |
| < | ‘Jump’ started talk |
| Features of speech delivery – punctuation symbols are not used grammatically | |
| . period | Closing (downward) intonation |
| , comma | Continuing or slightly rising intonation |
| ? question mark | Rising intonation |
| - dash | Cut off |
| : colon | Sound stretch – the more colons the greater the stretch |
| word underlining | Emphasis |
| .tch | Tongue click |
| hhh | Audible outbreath (number of h’s indicates length) |
| .hhh | Audible in breath (number of h’s indicates length) |
| TALK (capital letters) | Loud |
| °Talk° (degree signs) | Quiet (more degree signs, quieter the talk) |
| >Talk< | Speeded up talk |
| <Talk> | Slowed down talk |
| # | Creaky voice |
| £ | Smiley voice |
| ↑↓ | Change in pitch |
| Hah hah or huh huh | Laughter |
| () empty single brackets or words enclosed in single brackets | Transcriber uncertainty |
| ((word)) words enclosed in double brackets | Transcribers’ comments |
Appendix 7 Codebook for use with data extraction form
The base-level unit of analysis we are working with are decisions and decision points.
Decisions
A decision is one of the actions covered in the ANQ and PNQ. The following a priori categories were derived from the Great/Greater Expectations studies:2,185
-
pain relief
-
fetal monitoring
-
VE (manual, not visual)
-
artificial rupture of membranes
-
position during labour (verbalised/topicalised)
-
oxytocin (to speed up labour)
-
position for birth (verbalised/topicalised)
-
episiotomy
-
managed/natural third stage
-
cord clamping (cutting/delaying)
-
skin to skin
-
vitamin K injection.
The list excludes ‘pushing decisions’ because we found our coding of these to be unreliable in early versions of the data extraction form.
Do not code on decisions that are not in this list.
Decision points
A decision point is an interactional turn started by a HCP (i.e. midwife or doctor) or a member of the birth party (i.e. woman or BP) that initiates discussion about one of the decision types (i.e. actions covered in the ANQs and PNQs). You are asked to copy and paste the turn into the form. The initiating turn is coded on the basis of its grammatical formulation. These formats were generated inductively from multiple inspections of the interactional data (SB-J, LB-J, CJ and VL) and deductively from the literature (e.g. Stivers et al. 132). Examples follow.
Just do it (no initiating turn)
There is no audible initiation, but some key decision is acted on in first position. In practice, these relate only to monitoring because we can hear the monitor (whereas, we cannot, for example, reliably hear women change position when there is no video).
Example
Uses fetal monitor with no verbal initiator.
Pronouncement (with or without tag)
A decision is asserted as going/needing to happen or that it will happen (something that the self is going to do, despite occasional use of institutional ‘we’).
Examples
I’m just going to listen to baby.
And then what we’ll do is uhm: (0.5).hh re-examine you if that’s OK.
Instruction/command/demand
A decision is initiated as a directive to the other party to do something.
Example
Pop her waters (BP).
Recommendation/suggestion/proposal
A decision is initiated in a way that clearly endorses a proposed course of action but leaves some room for the other to decide.
Examples
I think I would like to just leave it a little while before I do anything,.hh just . . . Rather than breaking your waters at the moment.
And I- I think probably we ought to just check after 2 hours rather than 4.
With your next pu:sh let’s just drop the gas::. And let’s just go for it.
Sometimes (0.2) if on your side, you don’t- you’re not keen on all fours can take the pressure off your back, (.) can help sometimes?
Shall we see if there’s any change? (VE decision)
Note that ‘Shall we X’ is treated as a proposal rather than an yes/no interrogative because it is not seeking information per se and is, in essence, a suggestion to do something together (see Stivers and Sidnell303).
Request
A decision is initiated in a way that asks the other to grant something.
Examples
Please can I have some pethidine?
Can I just have a listen?
Do you mind if she has a little listen?
Offer
A decision is initiated in a way that self has the right/possibility to enact on behalf of the other, but is seeking the other’s view/permission.
Examples
I could offer you some codeine as well if you wanted that.
Uh ((Wo)) do you want me to break your waters to help speed up the situation?
Option list
Decision initiated that includes a menu of options from which the other should select.
Examples
but it’s a (.) choice there’s a- huh huh the(h)re’s a choi(h)ce no(h)w. Whether you want the catheter to stay in, Or you want me to (0.9) uh do uhm do an in and out one.
Are you happy in that position or do you want to switch around a bit?
Yes/no interrogative (closed question)
Question designed for yes or no that seeks information regarding a key decision.
Example
Is it too late for pethidine?
Open question
‘Wh-‘ questions that are not otherwise covered elsewhere by the coding scheme.
Example
What other pain relief can I have?
Decision-implicative statement
A declarative statement that has decision-implicative relevance
Examples
I think she needs a bit of help (BP).
I don’t know if I need something stronger.
I don’t feel like I’m in a comfortable position.
Indecipherable
Use if it is possible to hear that a turn at talk has occurred, but we are unable to decipher its content.
Exceptions
Not every decision point will end up being coded. The following exceptions apply:
-
All courses of action not included in the ANQ and/or PNQ.
-
For decisions about position during labour/for birth, subtle movements like ‘keep your belly in the water’.
-
Decisions discussed between HCPs that do not include the woman, and those discussed between woman and BP(s) that do not include HCPs.
-
Decisions about readiness once a decision has been agreed (e.g. readiness for a VE that has already been agreed).
-
Decisions where the initiating turn at the first decision point is indecipherable in the recording.
Other notes
Note that in the ANQs/PNQs, decisions about using the pool are treated as pain relief and this is how we should treat them in coding (i.e. do not treat pool as a matter of position).
Fetal monitoring can stop during a contraction and start again once the contraction has completed. If this happens, do not code the decision to restart monitoring in this context as a new decision. Code as a pursuit only if the restart is verbalised.
The distinction between position for labour and position for birth is that position for labour refers to first stage and position for birth refers to second stage.
It is not practicable to code every ‘decision implicative statement’ and so code only those that are oriented to by the recipient (if the recipient is a member of the ‘opposite’ party, i.e. where a midwife/doctor is recipient of a woman/BP’s decision implicative statement, and vice versa).
Where the options in a list are separated by silence, we need to treat them on a case-by-case basis for whether we hear the first option as an offer followed by pursuit or as a through-produced option list. Seek consensus where not sure.
The form provides an opportunity to characterise the action of a turn if the grammatical format does not capture action. For example, the following is carried out as an offer, but the action is recommending:
You don’t have to have a vaginal examination, I would like to offer it you, one, because babies might be still in a bit of a funny position as baby’s turning, and I could tell that by vaginal examination. Two, because you might not yet be fully dilated and you might be pushing on the cervix, OK? Which can then cause () it to swell and become oedematous, or it can () sometimes later on cause damage, because it’s quite a tch a vascular kind of area with lots of capillaries in there, can cause bleeding later on.
Responses
The data extraction form asks who responds – no audible response, midwife, doctor, labouring woman, BP, or more than one person – and then asks for a classification of the response, as follows:
-
no audible response
-
acknowledges
-
agrees/accepts/aligns/selects option
-
agrees/accepts/aligns with caveat
-
offers
-
provides information
-
seeks more information/raises concern
-
defers
-
disagrees/rejects/denies/misaligns
-
says does not know
-
speakers differ in response (add details)
-
indecipherable.
The classifications that include multiple descriptions (e.g. agrees/accepts/aligns/selects option) are an attempt to capture cognate responses to different initiating formats. It is important to remember to discount non-verbal responses (e.g. nodding) because we need to maintain parity across video-recordings and audio-only recordings. The form allows coders to include additional description where the format and action of a responsive turn differ.
More on decision points
Some decision points will be the first decision point (and known as first decision points) in a particular decision-making sequence. Decision points that follow (i.e. pursuits in interactional terms) will be recorded as related to the initiating sequence. This is achieved automatically by a prompt that asks ‘Is the decision pursued again in one of the ways we’re coding?’. There are five possible responses: (1) yes; (2) no, decision that was initiated is acted on; (3) no, decision that was initiated is agreed but not acted on; (4) no, decision that was initiated is not agreed nor acted on/is abandoned; and (5) not known (use where there is no access to the end of the decision because the recording ends).
Some decision contents are initiated, agreed (or not) and acted on (or not) fairly adjacently (e.g. monitoring), but others might be initiated and pursued across minutes or hours (e.g. pain relief). The aim is to track a decision until the point where it is agreed (even if the agreement is to abandon the decision), but always check whether or not the decision resurfaces at a later point. If it does resurface, include it in the original chain of decision points for this decision content. If the same decision content re-occurs after a previous one has been enacted, then code it as a new decision. For example, if a woman requests and receives an opiate but then asks for more, code the second round as a new decision.
‘Sharedness’
At the end of each decision-making sequence, the form asks the coder to estimate the sharedness of the decision they have just coded. There are seven options:
-
unilateral HCP
-
HCP led but birth party had some say
-
HCP led but birth party had most say
-
equal balance between HCP and birth party
-
birth party led but HCP had most say
-
birth party led but HCP had some say
-
unilateral birth party.
Recording-level questions
There are also recording-level questions that must be filled in at the end of the coding of each recording. These questions relate to the format of the recording (video/audio), the stage in labour the camera is switched on and off and the length of the recording.
Appendix 8 Health-care practitioner interviews, grades and experience of sample
| HCP | Hospital (n) | |
|---|---|---|
| A | B | |
| Midwife | ||
| Grade 5 | 2 | 1 |
| Grade 6 | 4 | 3 |
| Grade 7 | 1 | 2 |
| Matron | 0 | 1 |
| Registrar | 1 | 1 |
| Consultant obstetrician | 2 | 2 |
Appendix 9 Health-care practitioner interview NVivo codes (high order)
Main themes
-
Normality.
-
Unpredictability of birth.
-
Women’s involvement in decision-making.
-
Involving women in decisions, supporting their decisions.
-
Tension between women having choice/providing choice and knowing what is best.
-
Capacity to involve women influenced by policies/procedures/fear of complaints litigation.
-
BPs.
-
HCPs’ level of experience (mainly in reference to midwives).
-
Role of context.
-
Relationships with colleagues.
-
Why things have to/need to happen.
-
Pain relief.
Appendix 10 Decision-making: what women wanted and what happened (reported postnatally)
| What women wanted | What actually happened, n (%) | ||||
|---|---|---|---|---|---|
| Decision entirely by staff | Staff advised me, I took their advice | Staff advised me, I chose not to take their advice | No staff involvement | Total | |
| Pain relief | |||||
| Leave decision totally to staff | 0 (0.0) | 2 (3.9) | 0 (0.0) | 0 (0.0) | 2 |
| Staff to advise me, expected to take the advice | 1 (2.0) | 14 (27.5) | 0 (0.0) | 0 (0.0) | 15 |
| Staff to advise me, but make up own mind (even if different to advice) | 2 (3.9) | 28 (27.5) | 2 (3.9) | 2 (3.9) | 34 |
| No staff involvement | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Total | 3 | 44 | 2 | 2 | 51 |
| Fetal monitoring | |||||
| Leave decision totally to staff | 16 (76.2) | 4 (19.0) | 1 (4.8) | 0 (0.0) | 21 |
| Staff to advise me, expected to take the advice | 6 (28.6) | 15 (71.4) | 0 (0.0) | 0 (0.0) | 21 |
| Staff to advise me, but make up own mind (even if different to advice) | 1 (20.0) | 1 (20.0) | 2 (40.0) | 1 (20.0) | 5 |
| No staff involvement | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Total | 23 | 20 | 3 | 1 | 47 |
| VEs | |||||
| Leave decision totally to staff | 4 (44.4) | 5 (55.6) | 0 (0.0) | 0 (0.0) | 9 |
| Staff to advise me, expected to take the advice | 2 (7.1) | 25 (89.3) | 1 (3.6) | 0 (0.0) | 28 |
| Staff to advise me, but make up own mind (even if different to advice) | 1 (8.3) | 10 (8.3) | 0 (0.0) | 1 (8.3) | 12 |
| No staff involvement | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Total | 7 | 40 | 1 | 1 | 49 |
| Placenta | |||||
| Leave decision totally to staff | 1 (16.7) | 4 (66.7) | 0 (0.0) | 1 (16.3) | 6 |
| Staff to advise me, expected to take the advice | 2 (11.8) | 12 (70.6) | 2 (11.8) | 1 (5.9) | 17 |
| Staff to advise me, but make up own mind (even if different to advice) | 3 (15.0) | 11 (55.0) | 2 (10.0) | 4 (20.0) | 20 |
| No staff involvement | 0 (0.0) | 1 (20.0) | 0 (0.0) | 4 (80.0) | 5 |
| Total | 6 | 28 | 8 | 16 | 45 |
| Skin to skin | |||||
| Leave decision totally to staff | 4 (80.0) | 1 (20.0) | 0 (0.0) | 0 (0.0) | 5 |
| Staff to advise me, expected to take the advice | 1 (5.0) | 18 (90.0) | 0 (0.0) | 1 (5.0) | 20 |
| Staff to advise me, but make up own mind (even if different to advice) | 1 (10.0) | 7 (70.0) | 1 (10.0) | 1 (10.0) | 10 |
| No staff involvement | 0 (0.0) | 0 (0.0) | 0 (0.0) | 10 (100.0) | 10 |
| Total | 6 | 26 | 1 | 12 | 45 |
| Cord clamping | |||||
| Leave decision totally to staff | 9 (81.8) | 0 (0.0) | 2 (18.2) | 0 (0.0) | 11 |
| Staff to advise me, expected to take the advice | 7 (38.9) | 0 (0.0) | 10 (55.6) | 1 (5.6) | 18 |
| Staff to advise me, but make up own mind (even if different to advice) | 2 (18.2) | 0 (0.0) | 8 (72.7) | 1 (9.1) | 11 |
| No staff involvement | 3 (60.0) | 0 (0.0) | 0 (0.0) | 2 (40.0) | 5 |
| Total | 21 | 0 (0.0) | 20 | 4 | 45 |
| Vitamin K injection | |||||
| Leave decision totally to staff | 0 (0.0) | 1 (100.0) | 0 (0.0) | 0 (0.0) | 1 |
| Staff to advise me, expected to take the advice | 1 (2.8) | 34 (94.4) | 0 (0.0) | 1 (2.8) | 36 |
| Staff to advise me, but make up own mind (even if different to advice) | 0 (0.0) | 6 (100.0) | 0 (0.0) | 0 (0.0) | 6 |
| No staff involvement | 0 (0.0) | 3 (42.9) | 0 (0.0) | 4 (57.1) | 7 |
| Total | 1 | 44 | 0 (0.0) | 5 | 50 |
Appendix 11 Correlation matrix: Spearman’s correlations between perception of decision-making and satisfaction
| Listened to by staff | My views were taken into account by staff | Satisfied with decisions made | Mean satisfaction | Who made decisions | Feeling in control | Pain relief | Fetal monitoring | VE | Placenta coming away | Stitches | Cord clamped | Skin to skin | Vitamin K injection | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Listened to by staff | 1 | 0.791*** | 0.512** | 0.919*** | 0.245 | 0.543** | –0.127 | 0.103 | –0.16 | 0.384* | 0.331 ∼ | –0.169 | –0.009 | 0.017 |
| My views were taken into account by staff | 1 | 0.677*** | 0.920*** | 0.153 | 0.569** | –0.281 | –0.134 | –0.275 | 0.146 | 0.091 | 0.032 | –0.124 | 0.039 | |
| Satisfied with decisions made | 1 | 0.674*** | –0.028 | 0.380* | –0.376* | –0.350 | –0.468** | 0.133 | –0.071 | 0.108 | –0.228 | 0.142 | ||
| Mean satisfaction | 1 | 0.277 | 0.523** | –0.196 | –0.041 | –0.430* | 0.195 | 0.116 | –0.118 | 0.03 | 0.026 | |||
| Who made decisions | 1 | 0.372 ∼ | 0.335 ∼ | 0.328 ∼ | –0.018 | 0.222 | 0.021 | 0.148 | 0.539** | 0.207 | ||||
| Feeling in control | 1 | 0.131 | 0.164 | –0.002 | 0.269 | 0.420* | 0.173 | 0.108 | 0.128 | |||||
| Pain relief | 1 | 0.517** | 0.058 | –0.077 | 0.389∼ | 0.134 | 0.430* | 0.078 | ||||||
| Fetal monitoring | 1 | 0.381* | 0.004 | 0.406* | 0.28 | 0.311 | 0.064 | |||||||
| VE | 1 | 0.031 | 0.294 | 0.21 | 0.126 | –0.077 | ||||||||
| Placenta coming away | 1 | 0.356 ∼ | 0.279 | 0.426* | 0.467* | |||||||||
| Stitches | 1 | 0.271 | 0.146 | 0.154 | ||||||||||
| Cord clamped | 1 | 0.382* | 0.461* | |||||||||||
| Skin to skin | 1 | 0.520** | ||||||||||||
| Vitamin K injection | 1 |
Appendix 12 Non-significant correlations between total number of midwife-initiated decision-making practices and satisfaction
| Spearman’s rho | Satisfaction_listened_to_by_staff | Satisfaction_views_were_taken_into_account_by_staff | Satisfaction_with_decisions_made | Satisfaction_combined_mean | DP: Assertions. Proportion |
|---|---|---|---|---|---|
| Satisfaction_listened_to_by_staff | |||||
| Correlation coefficient | 1.000 | 0.791** | 0.512** | 0.919** | –0.071 |
| Significance (two-tailed) | . | 0.000 | 0.003 | 0.000 | 0.698 |
| n | 32 | 32 | 31 | 31 | 32 |
| Satisfaction_views_were_taken_into_account_by_staff | |||||
| Correlation coefficient | 0.791** | 1.000 | 0.677** | 0.920** | –0.136 |
| Significance (two-tailed) | 0.000 | . | 0.000 | 0.000 | 0.459 |
| n | 32 | 32 | 31 | 31 | 32 |
| Satisfaction_with_decisions_made | |||||
| Correlation coefficient | 0.512** | 0.677** | 1.000 | 0.674** | –0.064 |
| Significance (two-tailed) | 0.003 | 0.000 | . | 0.000 | 0.730 |
| n | 31 | 31 | 31 | 31 | 31 |
| Satisfaction_combined_mean | |||||
| Correlation coefficient | 0.919** | 0.920** | 0.674** | 1.000 | –0.164 |
| Significance (two-tailed) | 0.000 | 0.000 | 0.000 | . | 0.379 |
| n | 31 | 31 | 31 | 31 | 31 |
| DP: Assertions. Proportion | |||||
| Correlation coefficient | –0.071 | –0.136 | –0.064 | –0.164 | 1.000 |
| Significance (two-tailed) | 0.698 | 0.459 | 0.730 | 0.379 | . |
| n | 32 | 32 | 31 | 31 | 37 |
| DP: Closed_yn_n. Proportions | |||||
| Correlation coefficient | –0.347 | –0.335 | –0.088 | –0.213 | –0.024 |
| Significance (two-tailed) | 0.052 | 0.061 | 0.636 | 0.249 | 0.887 |
| n | 32 | 32 | 31 | 31 | 37 |
| DP: Decision_implicative_statement. Proportion | |||||
| Correlation coefficient | 0.133 | 0.156 | 0.314 | 0.299 | –0.183 |
| Significance (two-tailed) | 0.469 | 0.395 | 0.085 | 0.103 | 0.279 |
| n | 32 | 32 | 31 | 31 | 37 |
| DP: Indecipherable. Proportion | |||||
| Correlation coefficient | –0.058 | –0.048 | –0.229 | –0.086 | 0.043 |
| Significance (two-tailed) | 0.752 | 0.792 | 0.216 | 0.646 | 0.799 |
| n | 32 | 32 | 31 | 31 | 37 |
| DP: Instruction_command_demand. Proportion | |||||
| Correlation coefficient | –0.047 | –0.030 | –0.197 | 0.008 | –0.129 |
| Significance (two-tailed) | 0.800 | 0.870 | 0.288 | 0.965 | 0.448 |
| n | 32 | 32 | 31 | 31 | 37 |
| DP: Just_do_it. Proportion | |||||
| Correlation coefficient | –0.025 | –0.021 | 0.056 | –0.008 | –0.431** |
| Significance (two-tailed) | 0.894 | 0.910 | 0.764 | 0.965 | 0.008 |
| n | 32 | 32 | 31 | 31 | 37 |
| DP: Offer. Proportion | |||||
| Correlation coefficient | –0.122 | 0.006 | –0.225 | –0.037 | –0.322 |
| Significance (two-tailed) | 0.506 | 0.976 | 0.224 | 0.844 | 0.052 |
| n | 32 | 32 | 31 | 31 | 37 |
| DP: Open_question. Proportion | |||||
| Correlation coefficient | 0.069 | 0.088 | 0.062 | 0.203 | –0.204 |
| Significance (two-tailed) | 0.708 | 0.632 | 0.740 | 0.273 | 0.226 |
| n | 32 | 32 | 31 | 31 | 37 |
| DP: Option_list. Proportion | |||||
| Correlation coefficient | –0.136 | 0.099 | 0.155 | 0.012 | –0.176 |
| Significance (two-tailed) | 0.457 | 0.591 | 0.404 | 0.948 | 0.298 |
| n | 32 | 32 | 31 | 31 | 37 |
| DP: Recommendation_suggestion_proposal. Proportion | |||||
| Correlation coefficient | 0.104 | 0.203 | 0.219 | 0.142 | –0.252 |
| Significance (two-tailed) | 0.573 | 0.265 | 0.236 | 0.447 | 0.132 |
| n | 32 | 32 | 31 | 31 | 37 |
| DP: Request. Proportion | |||||
| Correlation coefficient | –0.021 | –0.096 | 0.063 | 0.051 | –0.174 |
| Significance (two-tailed) | 0.911 | 0.603 | 0.735 | 0.785 | 0.304 |
| n | 32 | 32 | 31 | 31 | 37 |
Appendix 13 Overall architecture of vaginal examination decisions
| Interactional activity | Example (simplified transcription) |
|---|---|
| On admission, general informing that VEs will be conducted 4-hourly | So we examine you every 4 hours, see what’s happeningVIP22 |
| Forewarning of upcoming VE | And I examined you about 10.30, and I would normally look at doing another one 4 hours from there, . . . So 10, 11, 12, 1, 2. So in an hourVIP31 |
| Check agreement to conduct VE imminently | So would that be OK to examine you like we planned?VIP14 |
| Ensure/check comfort (other activities are also conducted here, including monitoring and feeling abdomen for position of the baby) | You think you can try and have a wee for me? You’ll be more comfortable for the vaginal examination having had a weeVIP37So it’s just going to be a bit of cold gel at first. If you want me to stop, or if you’re getting a contraction, just say and we’ll stopVIP22 |
| Check consent/readiness before starting VE | Are you ready for me to (0.5) for me to go aheadVIP30 |
| Online commentary15 | So baby’s head is very low, I can feel that. The waters are still there . . . Cervix is really thinVIP14 |
| Announcement of cervical dilatation | So it’s about 3 to 4 centimetres, it’s really stretchy, it’s at the frontVIP28 |
| Decision-making/reassurance | ((Following the VE)) Alright, go with it, push if you need toVIP37Three to four’s good, it’s stretchy, waters are still there. Don’t be disheartened. Try not to be sad. It’s just like this one’s taking a bit longer, but you’ll still get a baby at the end of it, you’ll just have to be a bit more patientVIP28 |
List of abbreviations
- ANQ
- antenatal questionnaire
- BP
- birth partner
- CA
- conversation analysis
- EFM
- electronic fetal monitor
- FHR
- fetal heart rate
- HCP
- health-care practitioner
- IA
- intermittent auscultation
- IMD
- Index of Multiple Deprivation
- LGBT+
- lesbian, gay, bisexual, trans plus
- MLU
- midwife-led unit
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health and Care Research
- OBEM
- One Born Every Minute
- OU
- obstetric unit
- PNQ
- postnatal questionnaire
- PPI
- patient and public involvement
- PVE
- patient-view elicitor
- RCM
- Royal College of Midwives
- SES
- socioeconomic status
- SUG
- service user group
- VE
- vaginal examination
