Notes
Article history
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as award number NIHR131800. The contractual start date was in September 2021. The draft manuscript began editorial review in June 2023 and was accepted for publication in March 2024. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ manuscript and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this article.
Permissions
Copyright statement
Copyright © 2024 McConnell et al. This work was produced by McConnell et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2024 McConnell et al.
Chapter 1 Background
Sections of this chapter have been reproduced with permission from McConnell et al. 1 This is an Open Access article distributed under the terms of the Creative Commons Attribution Licence, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. The text below includes minor additions and formatting changes to the original text.
Cardiovascular disease is the most common cause of death worldwide. 2 Heart failure (HF) characterises the final phenotype of many cardiovascular diseases3 estimated affect 64.3 million people worldwide in 2017. 4 Its prevalence is expected to rise due to the improved survival following an acute myocardial infarction associated with the availability of life-saving evidence-based treatments and due to ageing populations. 5,6 Patients with HF experiencing New York Heart Association (NYHA) Class III or Class IV symptoms account for over 1 million hospitalisations per year in the USA and Europe. 7 Additionally, HF is the most frequent cause of hospitalisation among individuals aged > 65 years. 8 In 2012, HF was estimated to account for £22.5B of health expenditure globally; between 2012 and 2030, it is estimated that total costs will increase by 127%. 9 Integrating palliative care (PC) with routine management of HF has been shown to significantly reduce healthcare costs overall compared to usual care (without PC)10 and significantly reduce the number of hospital visits and duration of inpatient stays. 11,12 The National Audit Office review of end-of-life (EoL) care recommended PC for patients with HF, due to a potential cost savings by reducing utilisation of acute services. 13 An example of potential savings from integrating care is found in the work by Atkinson et al. 14 in Wales who set up a co-specialty PC and HF hospital-community service with a catchment population of approximately 445,000 people, with 350 to 400 HF admissions each year. Over the 5-year study period, the introduction of the integrated service resulted in an estimated average saving of at least £10,218.36 per referral; as year-on-year savings have increased, in 2020 this figure rose to £14,109.36 per referral. 14 Overall, it is estimated that the integrated service has saved approximately £2.4M over 5 years, with almost £1.3M saved in 2020 alone for that catchment area. 14
There is evidence of improved patient and informal caregiver outcomes when PC is integrated in HF management. A review of carers’ needs identified that integrated PC in HF management led to an improvement in satisfaction with care from both the patient and their informal caregiver. 15 Informal caregivers are typically defined as those who provide unpaid care to individuals with whom they have a relationship, that is family members or spouses. 16 Informal carers are crucial to facilitating independent living and supporting quality of life (QoL) for patients with HF, and therefore PC can address caregivers’ needs and help them care for their loved one. 17 Integrated PC in HF management can benefit QoL, symptom burden and levels of depression in patients with the condition. 18
Integrated palliative and HF care aims to achieve continuity of care by integrating administrative, organisational and clinical services that make up the patients care network. 19 Examples of integrated PC and HF interventions include collaborations and shared goal-setting between PC and clinical cardiology teams to ameliorate symptoms with PC goals, alongside HF management. 20 The addition of social-worker-led PC services alongside HF management21 improved the physical, psychological, social, spiritual and EoL outcomes of patients. In 2020, the European Association for Palliative Care Task Force22 concluded that the inclusion of PC within the regular clinical framework for people with HF provides improvement in QoL as well as comfort and dignity. This was echoed in a position paper by the European Society of Cardiology (ESC)23 Heart Failure Association (HFA), which stated that many patients with HF would benefit from earlier integration of a palliative approach into the care provided by the multidisciplinary team (MDT) involved.
However, although two decades have passed since the first publication on the benefits of PC for patients with HF,24 the HFA Atlas identified only 10 out of 42 European countries with designated PC units for patients with HF. 23 The poor integration of PC into HF management can be explained by a number of factors, including uncertainty around the HF disease trajectory and complexities of communicating this uncertainty to patients and informal caregivers. 25–27 HF is an unpredictable illness, with periods of stability of symptoms, interjected with numerous exacerbations, and a gradual progression of the disease towards death. Many patients with HF overestimate survival,28 further adding to cardiology providers’ reluctance to initiate difficult conversations around prognosis. 27 This difficulty is further compounded by lack of patient and practitioner knowledge around what PC is and a general misunderstanding that PC is applicable only at EoL. 26,27,29,30 The fragmentation of inpatient and outpatient services also creates a barrier to the holistic need’s assessment required for an integrated PC approach. 31
Overview of existing evidence
Until recently, the lack of evidence from clinical trials demonstrating benefits of PC for people with HF posed an additional barrier. However, there has been an exponential increase in published literature since the turn of the century, increasing from 10 publications on average in 2000 to over 100 publications per year in 2017. 32 McIlvennan and Allen31 published a review summarising the evolving role of PC for patients with HF, along with the barriers and opportunities for its integration into routine practice. Findings from the review highlighted the need for evidence on how best to integrate PC and HF given the cultural and environmental differences in how PC services are delivered. 31 Three systematic reviews of PC interventions for patients with HF by Diop et al. ,33 Datla et al. 18 and Sahlollbey et al. 32 all highlighted the benefits of PC in HF management for patient-centred outcomes and reducing hospital utilisation. A recent scoping review examining elements of integrated PC in HF management34 identified the need for a multidisciplinary approach to integration, and for cardiology staff to champion the benefits of PC. This review also highlighted the need for research with robust theoretical underpinnings given the complex behaviour changes required for sustaining integrated care in practice. 34
A recent editorial35 exploring the phenomenon of inconsistent implementation of integrated PC and HF interventions proposed a realist approach could provide a sound theoretical understanding of the barriers and facilitators to routine implementation. Research to date has focused on trying to evidence effectiveness through a linear cause and effect approach, which fails to ignore the messy, non-linear world of real-life practice. 35 Datla et al. 18 also identified a lack of clear consensus around: (1) the core components of integrated PC and HF interventions; (2) the ideal configuration for the MDT; and (3) the most effective service provision model to ensure that generalist and/or specialist PC is tailored to patient needs. The issue of heterogeneity was further highlighted in a narrative literature review aimed at identifying the key characteristics of integrated PC and HF interventions. 36 Of the nine studies included, all integrated PC and HF interventions were implemented in different countries with different models of health service provision for citizens (USA, Sweden, Hong Kong), different settings (inpatient, outpatient and home-based), delivered by a heterogeneous mix of MDTs [HF physicians, HF nurses, general practitioners (GPs), community nurses, occupational therapists], using different modes of delivery (face to face, telemedicine), and involving different intervention components (symptom management, advance care planning). Therefore, we still do not know:
-
which intervention produces the best outcomes for patients and their informal carers (what works: specialist vs. primary care etc.)
-
when best to initiate PC (for whom; at what stage in the disease trajectory), or
-
the optimal delivery method (in what circumstances; required infrastructure, staff competencies etc.).
Rationale explaining why this research is important now
Globally the population is living longer than ever before. In 2022, there were 771 million people aged 65 years or over globally, three times more than in 1980 (258 million). 37 Globally, the older population is projected to reach 994 million by 2030 and 1.6 billion by 2050 ‒ a rise of 10% in 2022 to 16% in 2050. 37 Although we can celebrate this achievement in life expectancy, it comes with significant challenges for an already struggling healthcare service now and in the future. Older people have complex health needs, with on average 4.5 comorbidities. HF often dominates their physical and psychological needs,24 along with being the costliest aspect of their care due to high rates of hospitalisation and pharmaceutical, device, and surgical interventions as their HF progresses. 38–40 Older people with HF have undeniably had their needs overlooked, with calls for more attention to, and research for, this vulnerable group to ensure they receive appropriate, effective treatment and care. 31,41,42 The 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic HF highlighted the need for studies to determine specific options for PC within the treatment of HF. 43
Although we have some promising examples of integrated PC and HF interventions,20,21 there is heterogeneity in terms of countries, healthcare settings, delivery by mix of MDTs, modes of delivery and different intervention components. 44 Hence, this review is vital for identifying which model works best, for whom, or in what circumstances.
Aims and objectives
Aim
To understand how integrated PC and HF interventions may work in different healthcare settings for example inpatient/outpatient, and for which groups of people, so we can recommend strategies to maximise the potential for widespread implementation, reduce healthcare costs, and improve QoL for patients and informal carers.
Objectives
-
To conduct a realist synthesis (RS) to build an understanding of which integrated PC and HF interventions work best together, in which contexts and for which patients who have HF and informal carers
-
To co-produce implications with an expert stakeholder group, to maximise potential for widespread implementation through a user guide for healthcare providers and user-friendly summaries for patients and the public
Review questions
-
What are the mechanisms by which integrated PC and HF interventions work to produce their intended outcomes?
-
What are the contexts which determine whether integrated PC and HF interventions produce their intended or unintended outcomes?
-
In what settings are integrated PC and HF interventions likely to be effective?
Chapter 2 Review methods
This methods chapter is based on previously published work45,46 by our methodological expert, Geoff Wong (GW), the lead researcher on the Realist And Meta-narrative Evidence Syntheses: Evolving Standards (RAMESES) project (www.ramesesproject.org/) which developed realist review quality and publication standards and training materials (see Report Supplementary Material 1).We used a realist approach to understand and make sense of the complexity of integrating PC in HF management and to examine what works for whom, in what circumstances, how and why. Realist synthesis is a theory-driven approach for understanding existing diverse multiple sources of evidence relating to complex interventions. It is theory driven because it uses evidence to iteratively develop and test structurally coherent explanations (i.e. theories) of complex interventions. The review methodology followed Pawson’s47 five iterative stages for RS: (1) locating existing theories; (2) searching for evidence; (3) selecting documents; (4) extracting and organising data; and (5) synthesising the evidence and drawing conclusions (Figure 1). The review project ran for 22 months, from September 2021 to June 2023. The RS protocol was published in BMJ Open1 and the review was registered on PROSPERO (number CRD42021240185).
FIGURE 1.
Project flow diagram using Pawson’s five iterative steps.

Stakeholder group
An international stakeholder group was recruited during the planning stages of this project to provide clinical management, clinical practice, academic, policy and service user expertise to guide programme theory refinement and development, and our comprehensive dissemination strategy. Our stakeholder group comprised 32 individuals, including medics, nurses and policy staff representing healthcare professionals involved in the delivery of PC and HF management; research clinicians in PC and HF at national/international level; policy and community groups; and patient and public involvement (PPI) partners. Stakeholder meetings (n = 5) lasted 2 hours (with the exception of the fourth meeting which lasted 3 hours to present and discuss implications) and took place at regular quarterly intervals throughout the project (Table 1). Meetings took place on the teleconferencing application Zoom (Zoom Video Communications, San Jose, CA, USA) to facilitate engagement from all stakeholder members, and also due to the COVID-19 pandemic restrictions. All participants provided verbal consent for the recording prior to each meeting. Recordings were not used as a form of data, but to ensure accurate notetaking of stakeholders’ expert feedback and advice. Stakeholder meetings began with a short presentation to introduce and reacquaint stakeholders with the topic, review methods and issues for discussion. Discussions at the early stages were open-ended; however, the project team encouraged discussion around the ‘preliminary’ initial programme theory and key ideas from the initial literature searching to draw out our initial programme theory. Stakeholders also kept in regular communication with the project team through e-mail, adding any further comments or thoughts from the meetings, which were added to the initial programme theory. Stakeholders also provided relevant documents included within this review (n = 11). Later stakeholder meetings focused on actionable findings and the dissemination strategy.
| Date | Stakeholder attendees | Topics discussed | Examples of stakeholders’ contributions |
|---|---|---|---|
| 3 November 2021 | 14 stakeholder participants including nursing staff, consultants, PPI members and GPs | Stakeholders reminded about research topic and realist methods. Open discussion around preliminary initial programme theory, integrated PC in HF, contexts that work, outcomes and what matters for healthcare professionals (HCPs) and patients |
|
| 30 March 2022 | 12 stakeholder participants including cardiology and PC consultants, GPs, PPI members and researchers | Stakeholders were presented with the initial programme theory and the initial findings. Open discussion around what a clear pathway for integrated PC in HF would look like, the issues around terminology for PC, the culture within cardiology and education |
|
| 6 July 2022 | 14 stakeholder participants including specialist HF nurses, cardiology and PC consultants, PPI members and researchers | Stakeholders were presented with our emerging findings focused around three key areas: need for a clear pathway; the role of education; and the impact of wider and organisational issues |
|
| 12 October 2022 | 20 stakeholder participants including specialist HF nurses, cardiology and PC consultants, PPI members and researchers. This meeting also incorporated additional HF nursing specific feedback that was gained through an interactive question and answer session at the Irish Nurses Cardiovascular Association event. This event was attended by over 100 HF nurses, from undergraduate to clinical nurse specialists | Stakeholders were presented with key findings and associated implications based around education; buy-in; resourcing; and guidelines. In addition, identifying a future programme of work was discussed |
|
| 8 March 2023 | 12 stakeholder participants including specialist HF nurses, cardiology and PC consultants, PPI members and researchers | Stakeholders were presented with the final animation, followed by a detailed discission on the implications and dissemination plan. Additionally, the refined future plan of work was presented |
|
Patient and public involvement
Our PPI group were involved throughout the planning and execution of this project. The PPI group was recruited by TM during April 2020 from members of two established public involvement and engagement groups (Marie Curie PPI Research Voices Group London and British Heart Foundation PPI Network members). We received eight responses from PPI members, three of whom agreed to membership of our stakeholder group. At this initial stage their input was sought in relation to the importance of our proposed study, how we should focus on our review and our plain language summary.
During the review, we asked PPI stakeholder group members:
-
to help us to develop our initial programme theory
-
for their advice and feedback on our programme theory as it evolved
-
to consider our findings and implications from their varied perspectives
-
to provide input and support into our dissemination strategy and
-
to review and contribute to our materials, to ensure they met the needs of patients and the wider public.
Informal meetings were arranged with our PPI members prior to main stakeholder meetings (Table 1) to provide any support that was needed. For example, before the first stakeholder meeting, our PPI meeting focused on realist terminology, emphasising the importance of ensuring PPI voices were heard at meetings. This meeting also provided an opportunity for any other questions or concerns that our PPI members had about their role. We witnessed the value of having these informal meetings with our PPI members in the stakeholder group meetings. For example, in the first stakeholder meeting, PPI members made significant contributions to developing the programme theory. Their perspectives and opinions were welcomed by all stakeholders and illuminated real-world implications for service users in terms of what works, and what does not work when integrating PC with HF management. The strength of PPI involvement in this project is evident in the considered pieces provided for the website (https://palliatheartsynthesis.co.uk/blog/) and reflective pieces (see Appendix 4). The review methods adopted within this RS are outlined in the following section.
Step 1: locate existing theories
Within the first stage of the review, we conducted exploratory searches to locate key literature sources and to identify any existing theories that may be relevant. Exploratory searches were carried out on MEDLINE using key terms for PC and HF. The informal searches conducted within step 1 differed from the more formal searching that was carried out in step 2, as their purpose was to identify quickly a set of highly relevant documents. Thus, exploratory and informal search methods including citation tracking and snowballing based on known existing documents were also used. Drawing on the literature identified in the informal searches and the project team’s experiential and content knowledge, we developed a ‘preliminary’ initial programme theory to explain how integrated PC in HF management may work, and the core mechanisms which generate its outcomes (Figure 2). This preliminary initial programme theory was presented to our stakeholder group to facilitate discussion for the further development of our initial programme theory.
FIGURE 2.
Preliminary initial programme theory.
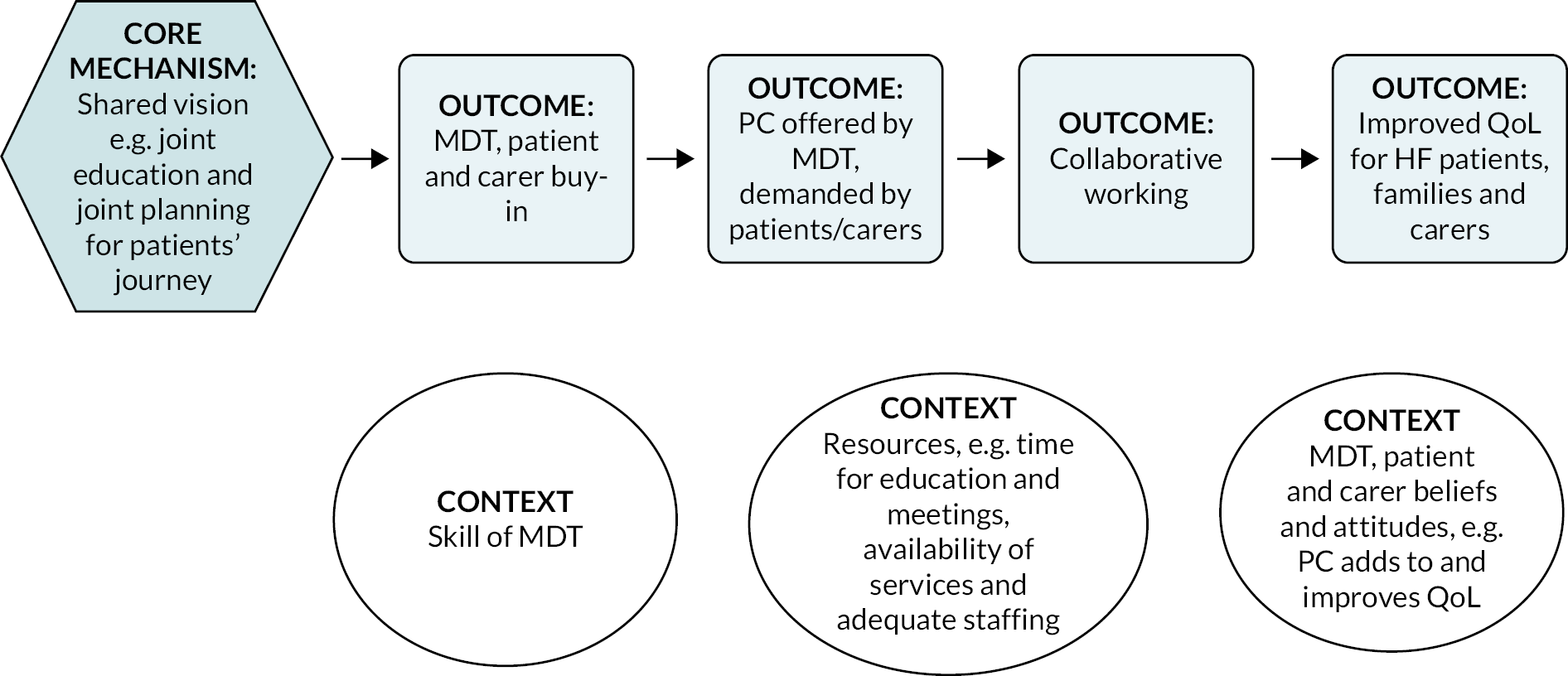
Refinement of the preliminary initial programme theory
Following the presentation of the preliminary initial programme theory at our first stakeholder group, we found that stakeholders focused on HCPs’ perspectives as providing key explanations for challenges around implementation of integrated PC in HF management. This indicated that we should narrow the scope of the synthesis to focus on HCPs’ perspectives on integrated PC. We still considered the importance of patient and informal caregiver perspectives; however, stakeholders emphasised the gatekeeping nature of HCPs to access integrated PC in HF.
Step 2: search strategy
Formal search
Our search strategies were designed, piloted and implemented by an information specialist with experience of carrying out iterative searches for RS ‒ Claire Duddy (CD), in collaboration with Clare Howie (CH) and TM.
For the main search, CH identified potential search terms using published search strategies from existing systematic reviews18,19,31–34 and by reading other relevant published research documents22–24,36,48–50 that were identified via earlier scoping searches and during protocol development. Other search terms were chosen based on suggestions of key documents and language used by our stakeholder group.
Claire Duddy used MEDLINE (via Ovid) to iteratively develop a search strategy, identifying a core set of free text and subject heading (MeSH) terms and then testing the effect of adding, removing and refining terms. We used existing sets of known relevant documents to benchmark the search strategy and assess the impact of making changes. These were documents that were cited in the protocol, and documents included in two recent systematic reviews. 18,34 Our overall aim was to reach an appropriate balance of sensitivity and specificity, such that the search strategy retrieved a range of relevant literature that was likely to contain data that could be used to refine and develop our initial programme theory, while minimising the retrieval of irrelevant literature. The final agreed strategy for the main search combined terms for HF with terms for PC and is outlined in full in Appendix 1.
In November 2021, CD conducted searches in the following databases: MEDLINE (via Ovid), EMBASE (via Ovid), PsycINFO (via Ovid), AMED (The Allied and Complementary Medicine Database via Ovid), HMIC (The Healthcare Management Information Consortium via Ovid) and CINAHL (Cumulative Index to Nursing and Allied Health Literature via EBSCOhost) (see Appendix 1). We adapted the search strategy developed for MEDLINE for use in each database, adjusting the search syntax and subject heading terms as appropriate. All search results were exported to EndNote X9 (Clarivate Analytics, Philadelphia, PA, USA) reference management software and duplicates were removed using the ‘Find Duplicates’ function and additional manual checks by CD.
In addition to the database searches, we sought to identify additional academic and grey literature via several supplementary searching methods. We ran simplified versions of our search strategy in Google, OpenGrey and the NICE Evidence search website with the aim of identifying relevant grey literature. Results (up to the first 500 for Google and NICE Evidence) from these resources were screened ‘on screen’ to identify material that described PC for patients who have HF and new material was added to the EndNote library.
Although our protocol documented we may undertake forward citation searching, we judged the large volume of documents retrieved did not necessitate additional searching. We asked our stakeholder group and wider networks to suggest additional relevant literature that we should consider for inclusion.
Following the main search in November 2021, we set up an alert using Google Scholar to help us to identify any newly published relevant material. The alert used the terms ‘heart failure’, ‘palliative care’ and ‘end of life’. New results were collated by CD on a monthly basis until August 2022 and shared with CH, TM and Carolyn Blair (CB) who considered them for inclusion throughout the project.
Step 3: document selection
Inclusion criteria
We kept the initial inclusion and exclusion criteria for the review deliberately broad as we aimed to identify all relevant quantitative, qualitative, mixed-methods and non-empirical documents relating to HF and PC.
The following inclusion criteria was applied:
The screening process was piloted by CH with a sample of 50 titles and abstracts to ensure the application of the inclusion criteria was suitable. Consistency checks were carried out by a second reviewer (TM) on a 10% random sample of the screening (title, abstract and full text) and the coding process for the main search. Very few inconsistencies were identified and, when identified, these were resolved through discussion.
We also included all documents from the stakeholders and the alerts that contributed to the evolving programme theory. Documents were screened initially by title and abstract, using the inclusion criteria detailed in Table 2. Following this process, 1066 documents met the initial inclusion criteria (January 2022). Selection was predominantly focused on whether documents were likely to contain data that would contribute to the refinement of the initial programme theory. Documents were organised according to perspective reported, that is whether they included data speaking to patient, informal caregiver, HCP perspectives related to PC in HF management (or no particular perspective). Discussions were held with Joanne Reid (JR), TM, CH, CD, Loreena Hill (LH) and GW to refine the inclusion criteria (25 January 2022). At this point, based on the initial programme theory and stakeholder discussions, it was decided to refine the inclusion criteria further to align with the focus of the review (see Chapter 2, Refinement of the preliminary initial programme theory).
| Categories | Inclusion criteria |
|---|---|
| Document types | All documents focused on PC for patients with HF |
| Study design | All study designs. Non-empirical data (e.g. from opinion/commentary pieces) which help direct/shape theory development |
| Types of settings | All documents about inpatient or outpatient or home-based care settings |
| Types of participants | All adult patients (18 years and over) with HF |
| Types of intervention | Any combination of PC strategies for the management of patients with HF |
| Outcome measures | All integrated PC- and HF-related outcome measures |
Documents that described HCPs’ perspectives on PC in HF were included for full-text screening. With the refinement of the inclusion criteria, 140 documents from the main search were found to provide data relating to HCPs’ experiences of PC in HF. All documents containing data thought to contribute to programme theory refinement were included.
Step 4: extracting and organising data
When document selection was completed, CH and CB uploaded the full texts of included documents into NVivo (Version 12, 2018) (QSR International, Warrington, UK) qualitative data analysis software, to assist with data management. Data extraction involved coding data within NVivo. Initial coding of the documents retrieved by the main search was undertaken by CH and 10% was independently checked by TM. Coding was both inductive (codes emerging through data analysis) and deductive methods (codes determined prior to analysis through initial programme theory and stakeholder discussions). The coding framework resulted from the analysis of the richest documents, which were documents that we judged had the most potential to inform the programme theory; within this review, these were mostly qualitative research documents. Examples of initial codes identified were ‘biomedical culture within cardiology’ and ‘terminology – understanding what PC is and is not’. We concurrently worked to identify ‘guiding principles’ and features underpinning the interventions, and relevant implications discussed mostly in policy documents, reviews and commentaries. The framework generated was applied to the rest of the documents and refined as the analysis progressed. For example, we identified relevant contexts when these mechanisms were likely to be ‘triggered’, such as a shared understanding (across patient, informal caregiver and HCPs) that PC in HF management positively contributes to optimised QoL. Such contexts and mechanism became ‘codes’.
The coding frame was based on the richest documents and then was conducted chronologically (CH), starting with the most current documents to identify any improvements in relation to implementation of integrated PC and HF overtime that could help direct/shape our programme theory. Alerts and stakeholder documents were then imported into NVivo, coded by CB and checked by JR. Regular team meetings throughout this phase focused on analysing the codes and their relationship to the developing programme theory. These regular team discussions and engagement with the data enabled and facilitated understanding of how emerging data may influence the refinement of our programme theory. Based on these discussions, additional coding was undertaken by CB and checked by JR. This then in turn led onto the realist analysis (step 5) to help explain and develop the final programme theory and context–mechanism–outcome configurations (CMOcs).
Data extraction was conducted on included documents from the main search (CH, 10% checked by TM), alerts (CB and JR) and stakeholder documents (JR) to capture descriptive categories captured within an Excel spreadsheet. These descriptive categories included participant characteristics (i.e. which type of healthcare professionals), study characteristics and implications provided. While we included an international evidence base within this review, we were mindful of the medico-legal context within the NHS and details on the county of origin of each included document are captured in the data extraction tables. The characteristics of the included documents are summarised in Appendix 2, Tables 37–40.
Step 5: synthesising and drawing conclusions
The analysis was driven by a realist logic. We sought to interpret and explain mechanisms, such as shared vision and provision of joint PC and HF education, in which integrated PC in HF management would occur (or not). We used the coding of the included documents within NVivo to draw relationships between contexts, mechanisms and outcomes, and to further develop our initial programme theory. To develop and refine the CMOcs, and the programme theory, we made judgements about the relevance and rigour of data extracted from the included documents following a series of questions that are commonly used in realist reviews. 46 Our data synthesis process was informed by the following questions (Box 1).
Are the contents of a section of text within an included document referring to data that might be relevant to programme theory development?
Judgements about trustworthiness and rigourAre the data sufficiently trustworthy to warrant making changes (if needed) to the programme theory?
Interpretation of meaningIf the section of text is relevant and trustworthy enough, does its contents provide data that may be interpreted as functioning as context, mechanism or outcome?
Interpretations and judgements about CMOcsWhat is the CMOc (partial or complete) for the data?
Are there data to inform CMOcs contained within this document or other included documents? If so, which other documents?
How does this CMOc relate to CMOcs that have already been developed?
Interpretations and judgements about programme theoryHow does this (full or partial) CMOc relate to the programme theory?
Within this same document are there data which inform how the CMOc relates to the programme theory? If not, are there data in other documents? Which ones?
In light of this CMOc and any supporting data, does the programme theory need to be changed?
Reproduced with permission from Papoutsi et al. 46 This is an Open Access article distributed under the terms of the Creative Commons Attribution Licence (https://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution and reproduction in any medium, provided the original work is properly cited. The text above includes minor additions and formatting changes to the original text.
We followed a process of constantly moving from data to theory as we refined explanations for patterns of particular behaviours or outcomes. We attempted to frame these explanations at a level of abstraction that could encompass a variety of phenomena or behaviour patterns. We worked on identifying relationships between contexts, mechanisms and outcomes within and across different documents (e.g. mechanisms inferred from one document could help explain how contexts influenced outcomes reported in a different document). We regularly synthesised data from different documents to build CMOcs, as complete CMOcs could not always be found in the one document.
As described above, we identified ‘guiding principles’ and implications that underpin existing interventions. The juxtaposition of these ‘guiding principles’ (underpinning interventions and implications) with the ‘possible mechanisms’ identified allowed us to identify particular configurations of mechanisms and contexts that were more likely to be conducive, or hinder implementation of integrated PC in HF management. Additionally, this work helped to identify barriers to the effectiveness of implementing integrated PC into HF management. Within this review, the most self-explanatory example of this may be PC and HF specialisms working within silos and a consequential lack of shared learning and reciprocal partnership working to facilitate integrated PC within HF management.
Direct quotations from included documents coded within NVivo were collated and presented to help demonstrate/explain emerging CMOs and contribute towards the synthesis. These CMOcs were compared to and contrasted with our evolving programme theory to understand relationships between each CMOc and their place within the programme theory. As the review progressed, we iteratively refined the programme theory driven by interpretations of the data included in the literature, and by feedback received by our stakeholders.
In summarising, the evidence synthesis process was achieved using the below analytic processes:51
-
Juxtaposition of data sources: data reported in different documents were compared and contrasted.
-
Reconciling ‘contradictory’ or disconfirming data: when outcomes differed in seemingly comparable circumstances, further investigation was undertaken to find explanations for why different outcomes happened. This involved looking closer at what made up the context for different kinds of ‘problems’, to understand how the mechanisms triggered could explain different outcomes.
-
Consolidation of sources of evidence: when the findings from different documents had similarities, a judgement was made as to whether these similarities could adequately form patterns to inform the development of CMOcs and programme theory, or whether there were nuances that needed to be highlighted, and for what purpose.
The aim of the analysis was to reach theoretical saturation, that sufficient information had been captured to portray and explain the processes leading to the implementation of integrated PC in HF management and the mechanisms that can aid this implementation.
Use of substantive theory
As realist syntheses are a form of theory-driven review, they commonly use existing theoretical frameworks (or substantive theories) to either provide analogy or as ‘lenses’ to help explain, for example, the underlying mechanisms behind our findings. Taking this into account, the use of substantive theory was discussed within our regular team meetings throughout this project. Based on the content expertise within the project team, a key theoretical framework that was considered at these meetings was the capability, opportunity, motivation, behaviour (COM-B) model. The COM-B model of behaviour presents three components required for any behaviour (B). These factors are capability, opportunity, and motivation,52 visually detailed in Figure 3.
FIGURE 3.
The COM-B model of behaviour.

Capability refers to having the knowledge, skills and abilities to engage in a behaviour, and is comprised of two areas: psychological capability and physical capability. Opportunity, within the context of the COM-B model, refers to the external factors needed to engage in a particular behaviour and describes two components: physical opportunity and social opportunity. Motivation refers to internal processes that influence behaviour and has two components: reflective and automatic motivation. This theoretical model was deemed particularly relevant to help frame our findings, as the successful implementation of integrated PC and HF can be largely explained by healthcare professional capabilities, opportunities and their motivation (or lack of) to integrate care.
Chapter 3 Results
Sections of this report have been reproduced with permission from McConnell et al. 53 This is an open access article distributed under the terms of the Creative Commons Attribution Licence, which permits unrestricted use, distribution, and reproduction in any medium, providing the original author and source are credited. The text within this report includes minor additions and formatting changes to the original text.
Results of the review
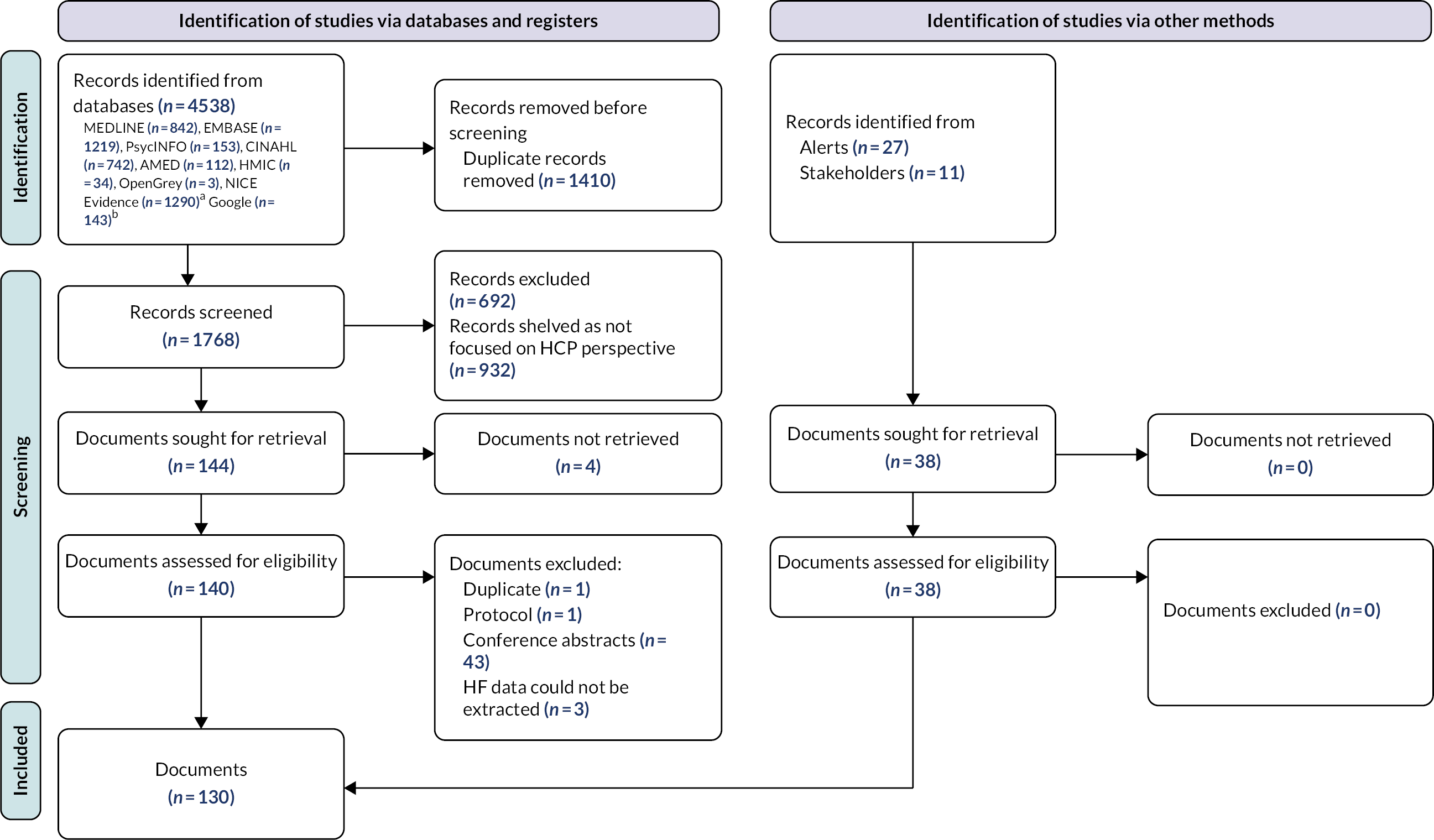
The Preferred Reporting of Items for Systematic Review and Meta-Analyses (PRISMA) flow diagram54 reports the number of documents that were identified, included and excluded in the review (Figure 4). In total, 1768 records were identified through database searching and screened, with 1076 documents meeting the initial inclusion criteria. Given the large number of eligible documents, we consulted with our stakeholders during our first meeting held on 3 November 2021 (see Chapter 2, Stakeholder group) to agree on the most pertinent aspects of our preliminary programme theory to focus on so we could make the most substantial contribution to our programme theory. The background literature and our stakeholder group collectively emphasised the key role that HCP perspectives play in influencing whether or not PC is integrated within HF management. Therefore, we narrowed our inclusion criteria to documents focused more specifically on HCPs’ perspectives on PC in HF management. The number that met these narrowed criteria was 140, of which 48 were removed based on exclusion criteria. A further 38 documents were returned from alerts (n = 27) and stakeholder documents (n = 11). In total, 130 documents were included in the review (see Appendix 2, Tables 37–40). No discrepancies were identified during the 10% check of coding and data extraction from the main search.
FIGURE 4.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses 2020 flow diagram for new systematic reviews. a NICE Evidence search (evidence.nhs.uk) is now retired. A total of 1290 hits were ranked by relevancy and the first 500 hits were screened ‘on screen’. b Google search (google.com) estimated 20,200,000 hits but only the first 143 were available and were screened ‘on screen’. Reproduced with permission from Page et al. 54 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) licence, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The text above includes minor additions and formatting changes to the original text.
Study characteristics
The majority of documents ‒ 36% (n = 46/130) ‒ were conducted in the USA and a smaller number ‒ 26% (n = 34/130) ‒ conducted in the UK. The majority of documents ‒ 37% (n = 48/130) ‒ focused on a combination of HCPs, patients and informal caregivers. A total of 6% (n = 8/130) of documents focused on physicians (of different specialties), 6% (n = 8/130) focused specifically on nursing staff, and a minority 1% (n = 1/130) focused on GPs. The date of publication ranged from 2000 to 2022, with the majority 69% (n = 90/130) of documents published between 2011 and 2021. The majority 66% (n = 86/130) of documents were research, including 29% (n = 37/130) qualitative work, 15% (n = 19/130) survey designs, with a small number (4%) of trials (n = 5/130) and 17% (n = 22/130) literature reviews. The majority 72% (n = 94/130) of documents focused on barriers and facilitators to PC in HF management. A small number of documents, 10% (n = 13/130), focused on aspects of integrated service design or tools to assist needs assessment. Appendix 2 provides a detailed overview of the characteristics of all included documents.
Summary of context–mechanism–outcome configurations
Table 3 contains a summary of the 6 CMOcs and 30 sub CMOcs uncovered from our review of the literature, in three main clusters.
| Cluster/CMOc | Summary | ||
|---|---|---|---|
| Main CMOc | Sub CMOc | ||
| Cluster 1: culture change Understanding the impact of a biomedical culture |
|||
| CMOc 1 | When HF physicians and HF nurses work within a biomedical culture that equates PC with EoL care only (C), they are less likely to integrate PC early (O) because they do not think it is appropriate (M) | ||
| CMOc 1.1 | When HF physicians’ and HF nurses’ training focuses predominantly on biomedical interventions to prolong life (C), they can be reluctant to consider PC (O), because they perceive they have failed in their care of the patient by doing so (M) | ||
| CMOc 1.2a | When HF physicians and HF nurses experience discomfort with poor prognosis (C), they may use language to soften a diagnosis/prognosis (O) because they do not want to erode the patient’s hope for more curative treatments (M) | ||
| CMOc 1.2b | When HF physicians and HF nurses use language that they feel may soften a diagnosis/prognosis (C), patients may be less upset but also less aware of the seriousness of their illness (O) because they do not fully understand (M) | ||
| CMOc 1.3 | When HF physicians and HF nurses synonymise PC with EoL care (C), they are reluctant to discuss this with patients who have HF receiving active treatments (O), because they do not think the patient is at the end of their life yet (M) | ||
| CMOc 1.4 | When the health and QoL of a patient with HF is deteriorating (C), HF physicians and HF nurses are still reluctant to integrate PC (O), because they are concerned this will signal to the patient that they are giving up on them (M) | ||
| CMOc 1.5 | When HF physicians and HF nurses believe that PC is suitable only for people with cancer who have a more predictable prognosis (C), they are unlikely to discuss PC with patients (O), because they believe it will not be helpful (M) | ||
| CMOc 1.6 | When HF physicians are focused on exhausting treatment options to prevent patients from dying (C), they are less likely to accept the need for PC (O) or want to discuss it with patients (O) because they do not believe the two approaches (biomedical and PC) can be provided in parallel to alleviate patient suffering (M) | ||
| CMOc 1.7a | When life-prolonging devices are futile (C), HF physicians infrequently discuss deactivation (O) because they lack confidence discussing this with the patient and their informal caregivers (M) | ||
| CMOc 1.7b | When life-prolonging devices are no longer appropriate for patients who have HF (C), PC physicians and PC nurses are uncertain about how to discuss this with patients (O) because they lack the specialist knowledge to do so (M) | ||
| Cluster 1: culture change Achieving culture change, using educational opportunities to change the culture for PC in HF |
|||
| CMOc 2 | When HF physicians and HF nurses have exposure to educational strategies that teach and prioritise PC (C), they are more willing to provide generalist PC and know when to refer to or seek input from specialist PC (O) because they have greater knowledge and confidence in their abilities to do so (M) | ||
| CMOc 2.1 | When HF and PC physicians and nurses take part in joint education that focuses on effective partnership working and patient care-co-ordination across different care settings (C), they are better able to identify and address the PC needs of patients with HF earlier (O) because they can learn how to share and mobilise their different knowledge and skills (M) | ||
| CMOc 2.2a | When PC physicians and PC nurses assess suitability for PC and provide care based on prognosis (i.e. in a similar way to cancer patients) (C), patients with HF are less likely to receive timely needs-based PC (O) because their condition is so variable and unpredictable (M) | ||
| CMOc 2.2b | When those involved in the care of patients with HF across settings have access to and seek advice, support and education for any challenges they face in managing patients who have HF (C), patients with HF are more likely to get better care (O) because HCPs are more able to identify their PC needs (M) | ||
| CMOc 2.3 | When those working in HF have access to and attend education for any challenges they face in managing patients who have HF with PC needs (C), patients with HF are more likely to get timely PC (O) because HF physicians and HF nurses have better knowledge of when PC may be needed (M) | ||
| CMOc 2.4 | When HF physicians and HF nurses have access to, and attend UG, PG or ongoing PC education that focuses on the purpose and role PC can play in HF clinical practice (C), they are likely to better appreciate when PC is needed for patients (O) because of their increased understanding (M) | ||
| CMOc 2.5a | When HF and PC physicians and nurses take part in experiential learning with peer support and reflection (C), they develop better mutual understanding and relationship building between disciplines (O) because they come to appreciate their respective strengths and skills (M) | ||
| CMOc 2.5b | When physicians and nurses in HF and PC are given protected time and choice of educational settings (e.g. online, face to face or hybrid) (C), they are more likely to attend (O) because they are empowered to do so (M) | ||
| CMOc 2.6 | When HF physicians and HF nurses who find it challenging to discuss PC with patients who have HF are offered and attend suitable education in communication skills (C), they are more likely to raise this issue with patients and their informal caregivers (O) because they have the confidence and knowledge needed (M) | ||
| CMOc 2.7 | When patients with HF, who think that PC lacks relevance for them, are provided early on with individually appropriate information about the purpose and role of PC in HF (C), they are more likely to have a better understanding of when they might benefit from PC (O) because they have a better appreciation of it (M) | ||
| Cluster 1: culture change Winning hearts and minds, using leadership and examples of benefit to change the culture for PC in HF |
|||
| CMOc 3 | When service providers and users have sufficient appreciation about the benefits of PC (C), they are more motivated to advocate for integrated PC in HF management (O), because they understand its role in improving patient outcomes (M). | ||
| CMOc 3.1 | When a respected and influential HF clinician in an organisation consistently advocates for the benefits of integrating PC into HF (C), they are more likely to be able to overcome indifference and resistance to integration (O) because they are perceived to have authority and credibility (M) | ||
| CMOc 3.2a | When patients who have HF and their informal caregivers are able to directly experience the benefits of early integrated HF and PC (C), they are more likely to ask for it (O) because they have an appreciation of its value (M) | ||
| CMOc 3.2b | When HF physicians and HF nurses are able to directly see the benefits for their patients of early integrated HF and PC (C), they are more likely to implement it (O) because they have an appreciation of its value (M) | ||
| Cluster 2: practice change Facilitating practice change for example considering the impact of wider context and organisational issues on PC integration |
|||
| CMOc 4 | When HF and PC physicians and nurses have opportunities to work collaboratively with relevant professionals to provide integrated PC and HF management (C), they are better able to assess and address their patients’ PC needs (O) because they learn when and how to draw on each other’s skills and knowledge (M) | ||
| CMOc 4.1 | When well-functioning MDTs consist of a wider range of relevant professionals (C), the team has access to a wider range of expertise (O) because each brings unique perspectives and experiences (M) | ||
| CMOc 4.2 | When MDTs are well organised with clearly defined roles and responsibilities (C), it enables high-quality parallel planning and more effective decision-making across care settings (O) because members know what is expected of them (M) | ||
| CMOc 4.3 | When HF physicians and HF nurses caring for a patient with HF are able to identify the relevant staff member(s) who has the most frequent contact with the patient with HF (C), patients are more likely to be receptive to advice delivered by them (O) because they trust them (M) | ||
| CMOc 4.4 | When HF physicians and HF nurses work in a clinical hierarchy where important decisions around key aspects of patient care are made by those higher up the hierarchy (C), those further down the hierarchy (usually HF nurses) feel unable to discuss PC with patients (O) because they do not believe they have the permission to do so (M) | ||
| Cluster 2: practice change Facilitating improved practice by overcoming the organisational barriers to integration |
|||
| CMOc 5 | When organisations help staff to overcome the barriers to integration of HF with PC (C), staff are more likely to focus on its delivery (O) because they are enabled to do so (M) | ||
| CMOc 5.1 | When organisations help staff to overcome barriers to the integration of PC in HF management that are beyond their individual control (C), staff are more likely to focus on timely integration (O) because they are enabled to do so (M) | ||
| CMOc 5.2 | When HF physicians and HF nurses take the time early in the HF disease trajectory to learn from patients and their informal caregivers about their goals of care (C), they can provide them with more tailored care and make decisions together (O) because they have a better understanding of their needs (M) | ||
| CMOc 5.3 | When HCPs co-operatively and collaboratively utilise each other’s areas of expertise and information for the management of patients throughout their illness trajectory (C), the patient experiences greater continuity of care (O) because the information and care they receive is not fragmented or inconsistent (M) | ||
| Cluster 3: organisational change The need to embed clear, visible guidelines to integrate PC into HF management |
|||
| CMOc 6 | When guidelines outlining who should be doing what and when are clear, visible and implemented (C), then patients with HF have their PC needs assessed and addressed at the right time, by the right people (O), because staff have clarity over expectations and roles (M) | ||
| CMOc 6.1 | When HF physicians and HF nurses perceive that guidelines for the integration of HF and PC do not provide adequate clarity over roles and responsibilities (C), they are not likely to be guided by them (O) because they lack clinical relevance or ease of implementation (M) | ||
| CMOc 6.2 | When organisations have provided both guidelines and the time and resources needed to implement them (C), HCPs are more likely to follow them (O), because they have clarity of what their organisation expects of them (M) | ||
Overview of context–mechanism–outcome configuration synthesis
The following sections present the programme theory and its underpinning CMOcs and sub CMOcs in such a way as to be transparent as well as accessible. The CMOc synthesis is further illustrated in Appendix 3, Table 41. Each section starts with an overarching CMOc, or series of CMOcs (Tables 4–34) supplemented by an explanation of the evidence base which underpins the CMOcs – that is what works/or what does not work, for whom, and in what circumstances. Illustrative data (e.g. extracts from included documents) are included in boxes under the narrative for each subsection (Boxes 2–26) as a way of showing how we made our interpretations and inferences for each of the CMOcs. Although documents included within the review refer to various terms for stages of HF (e.g. chronic HF, advanced HF, congestive HF), for inclusivity we use the term HF throughout.
| CMOc | Description |
|---|---|
| CMOc 1 | When HF physicians and HF nurses work within a biomedical culture that equates PC with EoL care only (C), they are less likely to integrate PC early (O) because they do not think it is appropriate (M) |
Cluster 1: culture change
CMOc 1: understanding the impact of a biomedical culture
Overarching CMOc 1 highlights the ‘biomedical culture’ within cardiology, and the need and potential for this culture to be challenged before PC can be successfully integrated into HF management. 48,55–58 We deem this overarching CMOc to be one of the most important explanations of why certain HF physicians and HF nurses are less likely to work to support integration of PC. 48,55–58 The narrative below describes and explains the nuances of how this biomedical culture prevents timely access to PC. This includes the difficulties with terminology in HF and PC, covering common misunderstandings which impact perceptions of PC and hence when it is most appropriately integrated. 56,59–63 Due to the complexity of the HF, illness trajectory prognostication is evidently challenging, which can cause delays in timely PC integration. 29,61,63–66 Finally, we consider specific issues relating to life-prolonging devices, and the challenges these pose for HF physicians and HF nurses conducting PC conversations with patients and their caregivers. 62,67–70 The perspectives of key HCPs have been cited in the narrative that follows. It is however important to note that, despite differences in perspectives that are likely to occur within practice across the subspecialties in cardiology (i.e. electrophysiologists), the majority of sources do not necessarily distinguish between these different subspecialties, and therefore an accurate comparison of perspectives is not possible. Furthermore, given that international literature has been included in this synthesis, we are aware that the differences in medico-legal systems within countries may result in differing perspectives on care delivery.
CMOc 1.1: biomedical culture and fears of clinical failure
Cardiology is described as active and interventional,71 and as such, HF physicians are trained to treat patients’ cardiac conditions with urgent effect which has been very successful in terms of the marked reduction in deaths now following myocardial infarction (MI). However, the intense, fast-paced environment and expectations of cardiology do not naturally permit HF physicians time to reflect on palliative and/or EoL needs. 65,72 Rather the literature illustrates that HF physicians’ clinical focus is firmly set on the need for immediate medical action to prevent patients with HF illness progression or death. 57,67,73,74 Interpretation of the data shows that HF physicians are reluctant to engage with PC, as moving from a biomedical to more holistic PC focus is seen as medical failure. 48,55–58 The fear of medical failure is not restricted to physicians, it is also evident in a proportion of nurses (24%) when they are not able to change the natural progression of HF. 58 These feelings may be embedded with a reported discomfort with death, which is often incorrectly seen as synonymous with PC. 75 PC discussions are viewed as ‘taboo’ and perpetuated by moral discomfort and a biomedical approach. 56,59,60 Within the literature reviewed PC was predominantly aligned with EoL care29,76 and a determination to prolong life is perpetuated by the mindset that anything other than biomedical treatment means clinical failure. 55–57 Therefore, hospitalisation or aggressive treatment73 is considered less of a ‘defeat’ than ensuring PC is integrated earlier in the illness trajectory to improve QoL and relieve distressing symptoms. 77 There is a clear necessity to create more willingness and ease in discussing PC needs alongside medical care directed specifically at treating HF. Building skills which will help identify PC needs in patients with HF is also key, and this is addressed under CMOc 2.
| Sub CMOc | Description |
|---|---|
| CMOc 1.1 | When HF physicians’ and HF nurses’ training focuses predominantly on biomedical interventions to prolong life (C), they can be reluctant to consider PC (O), because they perceive they have failed in their care of the patient by doing so (M) |
-
Wotton et al. :78
Transition to palliative care was made difficult when physicians viewed this as having failed the patient.
-
Borbasi et al. :73
Medicine’s fixation with cure-at-all-costs might well be the reason why patients with ESHF (early-stage heart failure) are treated aggressively until the very end.
-
Green et al. :55
Some doctors suggested that cardiologists could be reluctant to take responsibility for a patient’s transition to a palliative approach because it could give rise to a sense of failure.
-
Green et al. :55
It’s a sort of mental barrier to some cardiologists … palliative care is a sort of admission of defeat that you can’t do anything more.
-
Ziehm et al. :48
Generally, physicians of all subgroups (cardiologists and general practitioners) described cardiology as a discipline which is not able to accept medical limits. This means that cardiology is perceived as prolonging non-palliative treatment because palliative care is seen as defeat.
-
Ziehm et al. :48
As a cardiologist you are taught very early that there is always a way and that everything can be done.
-
Ziehm et al. :48
Healthcare providers, especially physicians express also their feelings about PC in terms of losing the patients or experiencing a defeat when the patients die … based on ‘an inappropriate notion of ideal medicine’.
-
Ecarnot et al. :71
In cardiology, the end of life is generally quite sudden, and when it’s sudden and unexpected, we are very physically active and interventional, and we don’t really have the time to be asking ourselves all these questions.
-
Higginbotham et al. :57
There was a belief held amongst some of the doctors that recognizing dying was equivalent to failure and so they felt morally justified in continuing to provide medical intervention.
-
Singh et al. :58
35% (n = 11) of physicians … and 24% (n = 18) of nurses … agreed that they experienced a sense of failure when they were not able to change the natural progression of heart failure or slow clinical worsening.
CMOc 1.2a and 1.2b: terminology and misunderstandings of palliative care
Another barrier to integrating PC identified in the literature is around terminology. In the context of a biomedical culture where the focus is on saving lives, hearing the words ‘heart failure’ is described by HF physicians and HF nurses as a shock to most patients and informal caregivers. As a result, physicians and HF nurses sometimes adapt their terminology to, for example, a pumping problem to soften the diagnosis. 61–63 The justification for this approach is rooted in the physicians’ desire to prevent upset and discomfort with the emotional responses evoked by the word ‘failure’ (interpreted by patients as meaning their heart would stop abruptly). 61–63,79 As a result, the term ‘heart failure’ is avoided by some physicians, who feel it is too emotive or inappropriate for the patient to hear. 61–63,79 The issue with semantics is also present when discussing PC. 80 Findings consistently point towards the discomfort among HF physicians about discussing a term associated with EoL care with their patients. 64,80 The consequence is a lack of information being given to patients regarding HF severity and prognosis,81 hindering patient-centred, holistic care and hindering patient and family opportunities to make advance preparations, which impacts on the patient’s QoL. 62,80,82 As with the stigma around PC terminology, the diagnostic term ‘heart failure’ evidently incites difficulties in communication for HF physicians and HF nurses. Therefore, training in communication skills with patients and informal caregivers could help to more easily facilitate confident conversations which ensure that patients and informal caregivers are fully aware of the diagnosis and holistic care options.
| Sub CMOc | Description |
|---|---|
| CMOc 1.2a | When HF physicians and HF nurses experience discomfort with poor prognosis (C), they may use language to soften a diagnosis/prognosis (O) because they do not want to erode the patient’s hope for more curative treatments (M) |
| CMOc 1.2b | When HF physicians and HF nurses use language that they feel may soften a diagnosis/prognosis (C), patients may be less upset but also less aware of the seriousness of their illness (O) because they do not fully understand (M) |
-
Harding et al. :61
(Heart failure is) chronic and intractable … This long-term chronic deterioration is probably something we’re not terribly good at, particularly the psychosocial aspect.
-
Chattoo and Atkin:62
… it was interesting to note how one of the patients (in his late sixties), who had been treated by a cardiologist for a year, seemed shocked when the HFN (heart failure nurse) mentioned the term ‘heart failure’.
-
Chattoo and Atkin:62
The HFN remarked that cardiologists often introduced her as ‘the nurse who takes care of pumping problems’ or ‘nurse who will take care of your tablets’, without engaging with the diagnosis or her role.
-
Chattoo and Atkin:62
Healthcare professionals are often reluctant to talk about heart failure because of the implications of the words ‘heart failure’, and if they don’t have time to sit down with somebody and explain then it can be quite a frightening term to hear.
-
Stocker et al. :63
I mean, how would you … explain heart failure to someone? I don’t like the term heart failure because failure just sounds like you’re about to pop it which generally speaking they’re not.
-
Stocker et al. :63
It doesn’t always work that way in practice. If that patient is in shock or in denial or very upset still about the fact that they’ve got heart failure, because the term (palliative care) itself is a scary term.
-
Ament et al. :82
You have to help the patient to get the right information. Otherwise, you don’t know if the information they’re getting is giving them realistic expectations, because that’s where it starts. You have to know what they understand and what they can expect.
CMOc 1.3: the problems associated with terminology and misunderstandings of palliative care
| Sub CMOc | Description |
|---|---|
| CMOc 1.3 | When HF physicians and HF nurses synonymise PC with EoL care (C), they are reluctant to discuss this with patients who have HF receiving active treatments (O), because they do not think the patient is at the end of their life yet (M) |
As alluded to earlier in CMOc 1, integration of PC for patients with HF may be suboptimal due to limited knowledge and misperceptions of PC as a service reserved for those near death and not suitable for patients with chronic conditions like HF. 58,74,75,83 The evidence suggests PC is being inaccurately synonymised with EoL care and this attitude evidently informs whether and how early HF physicians integrate PC into HF management. 58,74–76,83 Given HF physicians’ self-perceived identity as life-savers84 and considering that PC is synonymised with EoL care, this paradigm does not naturally nor easily merge with the role of conducting PC conversations. PC is described as a ‘grey area’ which evidently incites a fear for HF physicians and HF nurses that post-conversation patients will have the perception that they going to die imminently. 82,85–87 Although time issues to initiate PC conversations is often blamed on inadequate staffing67,85 (expanded on in CMOC 4), the widespread reference to lack of time may actually hide a lack of confidence in HF physicians and HF nurses to conduct PC conversations, as has been suggested in the literature – respondents working in the hospital mentioned that they do not feel comfortable to make time for conversations with patients about PC needs. 88 HF physicians report not having adequate knowledge and feeling under-skilled, thus lacking in confidence in a palliative approach, which then makes them reticent to discuss PC. 63,82,85–88 The term ‘supportive care’ as a service name was viewed by HF physicians and HF nurses to be less synonymous with EoL and hospice; less prognosis dependent compared to the term ‘palliative care’; and is deemed more suitable to adopt in HF care. 64 The issue of rebranding is part of a current, larger debate among PC specialists, which has not been studied among HF physicians and patients with HF. 64 However, changing the name to ‘supportive care’ without adequate education around what this type of care involves may raise the same problems as those found for the term ‘palliative care’. What is necessary is to ensure that there is adequate PC education to improve knowledge in the underlying ethos and components of PC and how this can be integrated at all stages of HF illness trajectory. 58,64,74,75,83 The literature also highlights communication difficulties between the clinician and the patient in relation to the core aspects of PC,58,74,75,83 so whether or not PC is rebranded64 HF physicians and HF nurses require training to improve communication skills in order to accurately convey what PC means.
-
Kavalieratos et al. :83
When asked to describe eligibility and appropriateness criteria for palliative care (for which there are none, aside from patient need), cardiology and primary care providers used the terms ‘hospice’ and ‘palliative care’ interchangeably unless prompted for clarification.
-
Kavalieratos et al. :83
Interviewer: And, so in your mind, is there a distinction between palliative care and hospice care? Cardiologist: No. Not in my mind. Is there?
-
Schallmo et al. :75
The term ‘palliative care’ was often used interchangeably with end-of-life care and sometimes interchangeably in the same article. This led to confusion because the reader was unsure whether the author was referring to communication barriers of PC or hospice, or both.
-
Janssen et al. :74
… and at a certain moment you get to using the words ‘PC’. But it is so loaded because palliative is confused with terminal.
-
Singh et al. :58
… most healthcare professionals providing care to individuals with heart failure regard palliative care as an end-of-life approach.
-
Singh et al. :58
A high proportion of participants believed the service name ‘palliative care’ was a barrier to referral, synonymous with hospice, decreases hope and was viewed to be prognosis dependent, in comparison to the service name ‘supportive care’.
-
Bonares et al. :64
57.4% believed that their patients have negative perceptions of the term ‘Palliative Care’, and 44.1% (243 of 551) stated that they would be more likely to refer to SPC (specialised palliative care) earlier if it was renamed ‘Supportive Care’.
-
Bonares et al. :64
There is evidence that, among medical oncologists and patients with cancer, the term supportive care is received more favourably than palliative care. This has not been studied among cardiologists and patients with heart failure.
-
Bonares et al. :64
Referral frequency was associated with … less equation of palliative care with end-of-life care (P < 0.001).
-
Graham et al. :85
I need to be able to take the time to introduce it in a way that I don’t walk out of the room and they actually think ‘what the hell is he talking about – I’m gonna die so I need palliative care?’
CMOc 1.4: heart failure physicians and heart failure nurses’ fears in relation to giving up on patients
The presence of a biomedical culture within cardiology, combined with the stigma around the term PC as synonymous with EoL, also generates moral tension, as HF physicians feel that they have given up on patients with HF and their informal caregivers when they introduce PC. 57,88–90 As a primary care physician in an American qualitative study explains: ‘It’s that dance around giving up, the perception of giving up on them when you start talking about end‐of‐life in hospice and that sort of thing’. 67 The distress caused through fears of diminishing hope for patients when introducing PC is evidently closely linked to HF physicians’ misperception of PC and concerns of ‘walking away from’ or giving up on patients. 57,67,78,89 There is also dual pressure from HF physicians’ clinical perception of their role as ‘life-savers’84 and their possible (inadvertent) misconstruction of what patients and informal caregivers need and want that is holistic individualised care. 60,67 However, this attachment to their professional identity is in part understandable as evidence suggests that HF physicians are not the only group who view themselves as life savers. 90 Patients with HF and informal caregivers have an understandable confidence in cardiology teams’ competency to prolong life and many may have a resistance to PC through lack of understanding and misconceptions that it is EoL care only. Therefore, public health campaigns to help communicate a wider knowledge of the benefits of PC and regarding the integration of PC into HF management early in the illness trajectory may help provide more familiarisation and realistic expectations. Knowledge of PC and adequate time to provide continuity of care could also help to relieve undue pressure relating to HF physicians’ concerns about ‘walking away’ from patients and informal caregivers.
| Sub CMOc | Description |
|---|---|
| CMOc 1.4 | When the health and QoL of a patient with HF is deteriorating (C), HF physicians and HF nurses are still reluctant to integrate PC (O), because they are concerned this will signal to the patient that they are giving up on them (M) |
-
Kavalieratos et al. :83
… cardiology providers frequently discussed the ‘point at which you are unable to do more’ … the trigger to get (the palliative care service) involved was knowing that my patient was dying and that I didn’t have other medical options for them.
-
Ismail et al. :84
Important and underemphasised aspect of cardiology. We like to think of ourselves as life savers, is that possibly why we don’t address the end-stage heart failure issues so well.
-
Glogowska et al. :90
This curative culture is not exclusive to cardiologists. Patients … may have received many successful treatments over the span of their heart failure trajectory, so may also believe that the cardiologist will always be able to find a new treatment.
-
Shinall:56
The culture of medicine, designed to prolong life at all costs, had trouble accounting for the need to stop at some point, and providers acutely felt the clash between honoring a patient’s wishes and their own discomfort in stopping life support, which at times felt like murder.
-
Singh et al. :91
Yeah I think there’s probably a perception, a real perception of you know … we haven’t done our job.
-
Hutchinson et al. :67
[Patients] want to know that everything possible is being done. And they feel as if going home is like people giving up. (CARD6U)
-
Hutchinson et al. :67
… no one likes to get angry phone calls or be sort of accused of not taking the best care of their loved one, or giving up on them … when you start talking about end-of-life in hospice and that sort of thing.
-
Higginbotham et al. :57
Several doctors recognized that prolongation of life was not right but at times felt obliged to meet the treatment expectations of both the patient and their families.
CMOc 1.5: the complexity of the illness trajectory: delays to palliative care
A further barrier to integrated PC for patients with HF relates to complexity of the illness trajectory, which can follow an extremely variable clinical course with periods of stability interrupted by exacerbations that may rapidly lead to instability and ultimately death. 61,62,76,92 HF physicians and HF nurses point towards the various barriers that delays a PC conversation with patients with HF. Firstly, given the alternating phases of acute HF and phases of prolonged relative stability, HF physicians and HF nurses emphasise that it is very difficult to make a definitive prognosis. 61,66,86 The complexity in formulating a short- to medium-term prognosis is further compounded by HF physicians’ and HF nurses’ perception of patients’ readiness, or lack of readiness for PC conversations. 65,66,85 When twinned with the biomedical culture, and misunderstandings of PC this creates barriers to shared decision-making93 (expanded in CMOc 4) and ultimately a delay in timely PC conversations. Some HF physicians and HF nurses acknowledged that this delay in having PC conversations was suboptimal, and primary care physicians in particular highlighted how this can lead to the inequity of PC provision for patients with HF compared to those with a cancer diagnosis, where they would routinely discuss ‘prognosis’ and PC needs at the same time. 61 The evidence suggests that HF physicians and HF nurses mistakenly intertwine PC needs with an EoL prognosis29 and therefore opportunities to have PC conversations based on a patient needs, rather than on solid evidence that nothing more can be done from a life-prolonging treatment-only perspective, are missed. 61,63–66 Some HF physicians and HF nurses highlighted an awareness that they should discuss prognosis early (which in the literature also generally means discuss PC), ideally at the point of diagnosis. 56,67,71 However, they rarely did, as this was perceived as inappropriate (or ‘cruel’) and generated fears around causing excessive distress for patients; or perhaps, as previously noted in the literature, this masked their lack of confidence in having PC conversations. 63 This feeling of being under-skilled in discussing prognosis and PC issues led to a ‘trickling down’ of prognostic information and indirect and abstract communication about the progressive and terminal nature of HF. 63 While it is evident that HF physicians and HF nurses want to ensure patients have the best care possible, they are constrained by underpinning barriers including a lack of PC knowledge and confidence in communication skills. 25,66,82,85,86 There is clearly a need for education and training for HF physicians and HF nurses so they understand that PC for patients with non-malignant chronic illness such as HF should be based on patient need and not on their prognosis, and that PC can be integrated into any point of their HF management plan when symptoms are more problematic, and stopped when patients are feeling better. 29,61,63–66
| Sub CMOc | Description |
|---|---|
| CMOc 1.5 | When HF physicians and HF nurses believe that PC is suitable only for people with cancer who have a more predictable prognosis (C), they are unlikely to discuss PC with patients (O), because they believe it will not be helpful (M) |
-
Brännström et al. :86
As chronic heart failure (CHF) is an unpredictable disease it is more difficult to talk about existential issues with these persons than with those with cancer.
-
Harding et al. :61
Cardiac staff identified the unpredictable disease trajectory as a reason why future care options are not discussed.
-
Harding et al. :61
They can be really, really poorly, and then suddenly their heart seems to gain a bit more strength and they’re up and pottering about, so it’s very difficult to prognosticate, and I think that’s what’s often so uncertain and difficult.
-
Chattoo and Atkin:62
We propose that issues of meaning of illness and pain that seem so closely embedded within popular and professional understandings of cancer … are muted within the mechanical, clinical representations of heart failure as a ‘pumping problem’.
-
Green et al. :55
I think it may be a lot easier for people to approach talking about palliative care with patients in cancer, because they’re already straight away, ‘Cancer – I’m going to die’, and with heart failure: ‘What does that mean?’
-
Lum et al. :92
The cancer patient has a downward slope and it’s pretty predictable … The HF patient crashes and gets better … So their acceptance of the dying process is different.
-
Stocker et al. :63
This (difficulties in prognosis) led most clinicians, regardless of specialty, to delay conversations about prognosis and palliative care until often very late in the disease trajectory, or at all.
-
Romanò:93
The problem seems to be more of a cultural one, linked to the belief that PC is destined exclusively for patients [with] … cancer, or to fears that initiating PC means all attempts to actively treat the HF will be discontinued.
-
Bonares et al. :64
Of the respondents, 29% delayed SPC referral because of prognostic uncertainty … In actual practice, nearly three-fourths of cardiologists referred late.
-
Higginbotham et al. :57
… the disabling of the shared decision-making process between healthcare professionals and the patient … [results] in a consistent failure to transition patients to a palliative care approach as might more often happen in cancer care.
CMOc 1.6: the reluctance to accept the need for palliative care and distress in decision-making
| Sub CMOc | Description |
|---|---|
| CMOc 1.6 | When HF physicians are focused on exhausting treatment options to prevent patients from dying (C), they are less likely to accept the need for PC (O) or want to discuss it with patients (O) because they do not believe the two approaches (biomedical and PC) can be provided in parallel to alleviate patient suffering (M) |
Underlying the biomedical culture in cardiology are a wide range of therapeutic options which are used to ‘fix the problem’ including numerous interventional procedures and devices. 65,67,93 Cardiology is described as a discipline which is known to prolong treatment for as long as possible, referred to as ‘cracking on until the end’57 as the limits of modern medicine are difficult to accept. 57,67,73,74 The evidence suggests that this culture causes notable difficulties in merging with the principles and needs-based holistic approach of PC that focuses on relieving psychological, social, spiritual and physical suffering48,56,60,71,90,93,94 which leads to a certain cognitive dissonance. 71,77,86 Most patients who have HF reach an advanced stage in their illness without an advance care plan in place, which is recognised as important for all chronic, life-limiting conditions, to ensure patient-centred treatment goals, along with ensuring that EoL care needs and preferences are met. 72,95,96 When the disease has reached an advanced stage, HF physicians and HF nurses are evidently subject to distress when deciding whether to permit the continuation of unnecessary treatments to prolong life, or discuss EoL options with patients. 55–57,72 As one source suggests, incremental increases in PC as the HF progresses until life-prolonging care is discontinued causes incoherence and can be challenging for HF teams to navigate. 86 Therefore, the timing of PC conversations, which should include advance care plans, is often deferred to the point when all medical options are exhausted; it is only when HF physicians perceive themselves as no longer useful that PC is perceived as patients’ ‘only option’. 72,83,97 Clinical guidelines acknowledge that integrating PC into HF management is a complex task; however, they clearly state that initiating PC early is advised to relieve patient suffering and improve QoL from the point of a HF diagnosis if needed. 43,93 Despite high adherence to clinical practice guidelines on optimising active treatments, guidelines in relation to early integration of PC remain largely unpractised72,93,98 (expanded in CMOc 5). HF physicians and HF nurses’ reflections largely illustrate difficulties in acceptance that PC needs to be implemented. 48,57,67,74,93 Overall, both disciplines (PC and cardiology) report that HF physicians tend to focus on treatment and neglect the more holistic palliative approach until all medical options have been exhausted which evidently delays a timely integration of PC. 63,82,85–88 Further training on how PC can be, and why PC should be incrementally increased based on patients’ needs while active treatments are ongoing would aid in reducing distress in decision-making for HF physicians and HF nurses (see CMOc 2).
-
Brännström et al. :86
Being on unstable ground about the unpredictable process of dying means: being uncertain about anticipating the course of dying; being concerned about not preparing the patient and next of kin for death; and being uncertain about integrating curative treatment and palliative care.
-
Selman et al. :65
… you can get a whole load of consultants, dare I say it, who are interested in all the ritzy things of putting stents in arteries and myocardial infarction, and that’s saving lives, so actually when you’re at the termination of life they’re not so interested. …
-
Matlock et al. :98
Over half of the cardiologists sampled for this study recommended care that was discordant from these guidelines (ACC/AHA guidelines) and this discordance was worse in the regions performing more intense medical care in the last 6 months of life.
-
Ziehm et al. :48
In the group of cardiologists, palliative care for CHF patients was partly seen as unnecessary because of the medical progress in the improvement and development of new therapies.
-
Romanò:93
The knowledge and attitudes of cardiologists in this field (PC) is quite low, and this also arises from the assumption that the frequent use of high-tech treatments, even in late HF stages, is beneficial.
-
Hutchinson et al. :67
… part of that I think is the idea that we can fix everything. There’s always a new procedure that can be done as opposed to oncology where you actually run out of things you can do. In cardiology, there’s always this perception that there’s one more thing you can try.
-
Hutchinson et al. :67
But I don’t feel like … I was trained well to have (conversations) because we were sort of trained well to … try to fix the problem and (move) on, you know?
-
Janssen et al. :74
We have to search for something, not static, but dynamic. There is so much technology available.
-
Higginbotham et al. :57
This type of medical model of managing heart failure patients was considered by doctors to be ‘sticky plaster medicine’ (Geoff, Consultant) and that often it was just a case of ‘cracking on until the end’.
| Sub CMOc | Description |
|---|---|
| CMOc 1.7a | When life-prolonging devices are futile (C), HF physicians infrequently discuss deactivation (O) because they lack confidence discussing this with the patient and their informal caregivers (M) |
| CMOc 1.7b | When life-prolonging devices are no longer appropriate for a HF patient with them (C), PC physicians and PC nurses are uncertain about how to discuss this with patients (O) because they lack the specialist knowledge to do so (M) |
CMOc 1.7a and CMOc 1.7b: the complexity of life-prolonging devices and the associated palliative care-related issues
As already noted in previous sections, the continuous rapid advancements in life-prolonging treatments in cardiology generates a belief that technology will always continue to prolong patients’ lives, adding to the tension of integrating PC into active HF management. 62,68,99 Rapid developments and advancements in pharmaceutical management and devices such as mechanical circulatory support (MCS) devices, implantable cardioverter defibrillators (ICDs) and cardiac resynchronisation therapies (CRT) can improve symptoms and prevent sudden cardiac death. 62,67–70 However, the use of advanced HF therapies such as MCS should not mean that PC is not discussed or integrated. 67,100 Recent randomised controlled trials (RCTs) have demonstrated that patients awaiting implantation of MCS, or cardiac transplantation should be offered the opportunity to have a PC consultation. 21,101 Indeed, this is recommended within the ESC HF position paper and is now mandatory in the USA. HF physicians openly admit their bias toward interventions, and when combined with communication issues, this helps explain why some patients with HF receive overly aggressive, non-beneficial care. 67 An important part of PC input would take into account the patient’s expectation of treatment and their preference regarding deactivation of their implantable device, when appropriate. 67 In regard to ICD insertion, a survey of HF physicians and trainees indicated that only 9.4% of respondents involved in the insertion of ICDs always explained the possibility of future deactivation of the device, with a significant proportion of trainees never raising this issue before implantation. 84 Many HF physicians and trainees reported a lack of knowledge and thus a need for education on how to discuss and include the patient and their informal caregivers in deactivation decisions. 62,77,87,99 Although HF physicians may realise that they should engage in these types of conversations with patients, they rarely do. This again illustrates the significant communication challenges which are evidently underpinned by a lack of confidence in how to respond to patients’ questions relating to PC needs62,70,77,100 and fear of ‘information overload’ for the patient and their informal caregivers prior to implantation. 26 HF physicians require knowledge and communication skills to discuss PC issues with patients who have HF referred not only for an implantable device or transplantation as well as during the course of the patient’s illness. 84 Given that this literature spans over a decade with the same questions occurring again and again, there is still a need to bridge the cultural divide between PC and cardiology as opportunities for PC conversations are still consistently missed. 62,77
Palliative care physicians and PC nurses working in hospice also note the clinical complexity and the need for expertise related to care of patients with HF with cardiac devices (i.e. ICDs) or advanced HF therapies (i.e. MCS). 69,70,102,103 The literature indicates that there is significant moral complexity surrounding the withdrawal of life-prolonging devices such as MCS, raising the question as to whether death would be deemed a natural outcome of HF or an act of assisted suicide for patients for whom a device was deactivated at the EoL (although this is more of an issue in the USA than in Europe). 102–104 Just over a quarter of HF physicians felt comfortable personally switching off the MCS,102,103 although this number was higher in PC physicians. 103 This points towards a difference in culture between consultants specialising in PC compared to cardiology around the acceptance of death and ease with being actively involved in the cessation of life-prolonging treatments. Bridging the gaps and engaging in dialogue and shared education between these two specialties is a critical first step in creating a more cohesive approach to care for patients with HF. 103 It is evident that PC physicians and PC nurses would benefit from HF-specific PC education which highlights the importance of joint education/working to harness shared learning between PC and HF disciplines (expanded in CMOc 2). There are also unique communication needs when considering relevant patients with HF PC needs including expectations of a cardiac device and how the technology impacts QoL and the dying process, which point towards the need for a joint education and shared decision-making approach. 77
-
Chattoo and Atkin:62
I think the tension seems to arise at the moment in use of implantable devices for defibrillating and decision-making as to whether that’s a useful aid anymore. So I think that’s where the, sort of, microcosm of it (philosophical difference) is.
-
Bouamrane et al. :87
Crucial [PC] conversations about important subjects such as implantable cardioverter defibrillator deactivation are simply not happening as a matter of routine.
-
Ismail et al. :84
Of those trainees involved in the insertion of implantable cardiac defibrillators (ICDs), only 9.4% always explained the possibility of future deactivation of the device, with a significant proportion of trainees never raising this issue before implantation.
-
Lum et al. :92
Our organization just developed a new LVAD clinic. (LVADs are) used as a destination therapy for people and it has some symptom benefits. So we are asking, ‘Can people be in hospice with an LVAD? Is that a quality of life intervention?’
-
McIlvennan et al. :103
When asked how comfortable the clinician would be personally turning off the LVAD, few cardiology clinicians (26%) but most HPM (hospice/palliative medicine) clinicians (59%) responded that they would be comfortable (P < 0.001).
-
McIlvennan et al. :103
… the majority of HPM clinicians (88%) responded that requests for turning off an LVAD in a patient who is not nearing death should be honored. Fewer cardiology clinicians (57%) agreed with this statement (P < 0.001).
-
McIlvennan et al. :103
87% of cardiology vs. 100% of HPM clinicians believed the cause of death following LVAD deactivation was from underlying disease (P < 0.001), with 13% of cardiology clinicians considering it to be a form of euthanasia or physician-assisted suicide.
-
Hutchinson et al. :67
One physician described this predisposition using LVADs as an example: ‘and we’re offering these advanced platforms like they’re magic. And they’re incredibly over-marketed by hospitals that want to put them in’.
-
Hjelmfors et al. :77
Many professionals reported a lack of knowledge of how to discuss questions about devices, which made it hard to discuss these issues.
-
Tomasoni et al. :81
Patients with advanced HF might overestimate their life expectancy. It is important that advanced care planning is engaged at an early phase of the disease, before heart transplantation or LVAD implantation. Such process aims to enhance patients’ autonomy in decision-making.
CMOc 2: achieving culture change, using educational opportunities to change the culture for palliative care in heart failure
The overarching CMOc 2 highlights that educational strategies which teach and prioritise PC are essential to integrating PC into HF management. These are explained in more detail in sub CMOcs 2.1–2.7. In this section, we focus on the evidence which points towards the importance of shared learning across PC and HF and developing a learning collaborative across relevant settings. This includes formal training and education but also informal knowledge transfer between the various professional groups. 34,48,55,61,87,88,105–110 In CMOc 2.2, we report on the lack of confidence PC physicians and PC nurses have in their understanding of HF management, which highlights a need for experiential learning through informal and formal training. 62,65,85,107 CMOc 2.3 covers HF physicians and HF nurses, where we report on why more confidence and supportive communication skills in PC is needed through specialised training in PC. 87,108,109,111–114 In CMOc 2.4 we report why formal ongoing education is necessary for all professionals caring for patients with HF. Two aspects are discussed: integrating PC modules into the undergraduate (UG) and post graduate (PG) curriculum;23,75,83,88,115–117 and continuing professional development (CPD) for the wider care team. 85,87,112,117 CMOc 2.5 illustrates how the evidence suggests that it is clearly not enough to suggest formalised education as a solution to integrating PC into HF management; rather it is important to consider the specific techniques and strategies needed to best educate HF and PC physicians and nurses. 58,75,85,86,112,118 CMOc 2.6 report on why specific techniques and strategies that enhance supportive communication skills in PC can help HF physicians and HF nurses to increase their confidence and put learning into practice. 58,75,85,86,112,118 Finally, in CMOc 2.7 we report on why education for patients and their informal caregivers is important. Three aspects are discussed in this section: the importance of direct conversations, techniques which may make conversations easier and the need to prioritise a public health approach to education in relation to PC. 55,77,87,119,120
| Cluster/CMOc | Summary |
|---|---|
| CMOc 2 | When HF physicians and HF nurses have exposure to educational strategies that teach and prioritise PC (C), they are more willing to provide generalist PC and know when to refer to or seek input from specialist PC (O) because they have greater knowledge and confidence in their abilities to do so (M) |
CMOc 2.1: the importance of shared education
The evidence suggests that shared education, that is learning from and with each other, between PC and HF health and social care (HSC) professionals, is an essential component towards the integration of PC into HF management. 34,48,55,61,87,88,105–110,121–123 The Caring Together (CT) programme is a useful example of a partnership developed to pioneer integrated models of HF and PC that was implemented across different care settings in Glasgow. 87,124 A core component of this model of care includes the provision of shared HF and PC training,87,124 with success of the programme hinging on both formal training and education, but also importantly through informal knowledge transfer and shared learning between the various specialist groups. 87,124 It should be noted, however, that this programme was supported by funding from two charitable organisations and local government. However, additional evidence suggests that a collaborative approach to educating HF and PC HF physicians and HF nurses would improve the competence of these specialists in providing patient information and facilitate agreement about care pathways and issues such as referral criteria to SPC. 55,87,124,125 Data highlight that through shared learning and knowledge transfer, a learning collaborative could develop which could take place during both formal events (i.e. dedicated study days), as well as through informal discussions on an opportunistic or ‘needs based’ approach. 87,88 Importantly, sources report that this flow of knowledge transfer must operate in multiple directions, from cardiology to PC, community/hospice to acute care and vice versa (see CMOc 4). 59,87,126 In particular, shared education is central to influence HF physicians’ and HF nurses’ perceptions of PC’s role and similarly to help PC physicians and PC nurses understand the uncertain disease trajectory of patients with HF (see CMOc 1).
Being mindful that PC and cardiology are two distinctly different specialties, as Graham et al. report ‘this mutual understanding allows the specialty-specific skills to be leveraged more effectively as they are grounded in the same core philosophy of care’. 85 The evidence suggests that shared education can also help to establish processes for joint working between PC and cardiology (see CMOc 4). Multidisciplinary working and improved team working are considered essential to ensure patients receive more joined up and consistent care (see CMOc 4). 61,87,110,121,127 Overall, shared education creates the opportunity for improved patient and informal caregiver care through a mutual understanding and increase in provider knowledge of PC for HF physicians and HF nurses (see CMOc 6) and of HF management for PC physicians, PC nurses and the wider MDT121,128 (see CMOc 4). 34,48,55,61,87,88,106–110,122,123
| Sub CMOc | Description |
|---|---|
| CMOc 2.1 | When HF and PC physicians and nurses take part in joint education that focuses on effective partnership working and patient care-co-ordination across different care settings (C), they are better able to identify and address the PC needs of patients with HF earlier (O) because they can learn how to share and mobilise their different knowledge and skills (M) |
-
Hanratty et al. :107
I think one needs to meet with the two specialties (cardiology and palliative medicine) to work the thought and processes through a bit … there’s too much of a gap between.
-
Harding et al. :61
… clinical staff recommended mutual education and joint working between cardiology and palliative care.
-
Green et al. :55
An inter-professional approach to the education of palliative medicine specialists and cardiologists could help to eliminate this perceived uncertainty by increasing the confidence of each HCP in his or her capacity to make decisions.
-
Cheang et al. :106
A need and desire by PC professionals to improve training in relevant PC skills for cardiology and vice versa for PC.
-
Ziehm et al. :48
It is suggested to educate HCPs about PC services and aims and that HCPs caring for patients with CHF should collaborate with those experienced in PC.
-
Singh et al. :34
A joint educational program should encompass heart failure and palliative symptom management, including opioids and diuretics goals of care discussions and understanding of palliative approaches.
-
Tilley et al. :108
Educating providers on the utilization of PC for heart failure patients need to be prioritized … In doing so, providers and PC can work together … and decrease the uncertainty, thus enhancing patient quality of life.
-
Ament et al. :88
Organizing educational meetings, educational outreach visits by an expert, training sessions, creating a learning collaborative and developing educational materials are strategies that could be used to improve the knowledge among HCPs.
-
Graham et al. :85
Our study demonstrates that integration of an educational framework that focused specifically on … a collaborative model of care, and improved communication between specialty services fosters mutual understanding of the overall direction for the provision of care.
| Sub CMOc | Description |
|---|---|
| CMOc 2.2a | When PC physicians and PC nurses assess suitability for PC and provide care based on prognosis (i.e. in a similar way to cancer patients) (C), patients with HF are less likely to receive timely needs-based PC (O) because their condition is so variable and unpredictable (M) |
| CMOc 2.2b | When those involved in the care of patients with HF across settings have access to and seek advice, support and education for any challenges they face in managing patients who have HF (C), patients with HF are more likely to get better care (O) because they are more able to identify their PC needs (M) |
CMOc 2.2a and 2.2b: palliative care training is needed for all involved in the care of patients with heart failure across settings
The evidence points to three specific areas of importance in relation to training: (1) the need for PC physicians and PC nurses to understand that PC for patients with HF must be needs based due to the uncertainty of the HF illness trajectory;112 (2) similarly HF physicians and HF nurses also need to understand that PC must be needs-based; and (3) the importance of PC training for all those involved in the care of patients with HF across settings. Firstly, PC physicians and PC nurses may lack confidence in their understanding of HF management,62,65,85,107,123 with the literature indicating that experiential learning through informal and formal training is essential. 85,129 Secondly, the literature also indicated that training in HF is also needed across settings to include community PC nurses, GPs, unscheduled care staff, social workers, care home staff and care assistants involved in PC. 21,112,122 The quote which follows, from the CT programme, illustrates the importance of good communication and relationships between PC and HF physicians and nurses and the necessity for PC physicians to be open to guidance and advice from HF physicians and HF nurses when integrating PC into HF management:
P13: … (talking about key cardiologist & HF nurse) they are very good to go to for advice and they can bounce ideas off of us so that’s very important time, when they manage to come up (i.e. to MDTs) […] if there is anything outstanding about any medication or anything that we maybe need to go back to the GP about, or we need to go back to the heart failure specialist, then we would do that as well but it would be outlined. 87
It is evident that HF physicians and HF nurses also encounter covert and overt difficulties integrating PC into HF management when PC physicians incorrectly translate the guidelines for a malignant PC model with a predictable prognosis to patients with HF who have an unpredictable disease trajectory. 25,62,129 An example is given of a HF nurse who was unable to refer a patient to the local hospice: ‘ … they were actually reluctant to take him until the consultant had given us a prognosis, a predicted time of life’. 62 Further areas where PC physicians and PC nurses require training include HF specific medications,85 symptom management62,65,85 and interventions including medical devices. 106
-
Addington-Hall and Gibbs:129
In any case, palliative care services need experience in heart failure if they are to be able to educate others in the use of the palliative care approach with these patients.
-
Hanratty et al. :107
I mean I haven’t come across a palliative care physician yet who’s comfortable in treating heart failure.
-
Selman et al. :65
Palliative care staff suggested that they would benefit from training in CHF symptom management.
-
Chattoo and Atkin:62
… the heart failure drugs are quite different to the symptom control medication that we would normally use … But I might not know how to regulate the heart failure drugs we can use (PCN). I don’t think I could do that on my own.
-
Millerick et al. :112
… community nurses and care home staff regard themselves as competent and confident in their palliative care role, but much less so in relation to heart failure knowledge and competency. This clearly highlights an area of priority learning and training need.
-
Cheang et al. :106
Two of the greatest barriers to good care by palliative services for patients with heart failure is … the limited knowledge that palliative specialist doctors and nurses have into the current best management of heart failure (esp. cardiac drugs and interventions).
-
Graham et al. :85
I (Palliative care HCP) feel better equipped to manage patients with heart failure at home … largely because of the conversations that I’ve had with colleagues … and … partly related to the communications and the training and teaching that we’ve received.
-
Graham et al. :85
My learning came partly through self-directed learning … sort of foundational ideas around heart failure and then reading a bit about symptom control, often that was more palliative oriented.
-
Graham et al. :85
… (A cardiologist and a palliative care doctor) gave a few presentations that were very helpful, where they reviewed, first of all, that it was quite possible for us to manage heart symptoms, and second of all an outline of how to do that.
CMOc 2.3: training for heart failure physicians and heart failure nurses in palliative care
The American Heart Association has endorsed integration of PC into the early care of all patients with HF,50 yet no explicit recommendations exist to guide the content and quality of PC education for cardiology trainees. The evidence suggests that more specialised education in the principles of PC is needed for trainees and continuing education is essential for HF physicians and HF nurses. 87,94,108,109,111–114,130 Millerick et al. 112 conducted a PC- and HF-specific training needs assessment in Scotland in 2015 involving GPs, community nurses, HF and PC nurses, care home staff, out-of-hours nursing staff, hospital-based nursing staff, care home liaison nurses, HF physicians, care-of-the-elderly physicians, care assistants and other professionals involved in care of patients with HF, such as pharmacists, allied health professionals, social care staff and chaplains working across all settings (acute and community care). This training needs assessment (which received 470 responses) highlights the in-depth knowledge and skill set of HF specialist nurses. 112 It also reveals that over 60% of HF-professional-specific respondents had not received any specific training in relation to PC in HF. 112 A later review of the international literature by Singh et al. 113 conducted in 2017, and published in 2019, which includes studies of HF providers, reports that 53% had received no formal education in PC. Furthermore, HF nurses directly reported needing further PC training to enable them to become more confident and skilled in communication, and in the integration of PC into patient management. 109 This indicates a major training and knowledge gap that is essential to the early identification, comprehensive assessment and anticipatory care management of PC needs in patients with HF. 94,109,112,113,130 As covered in CMOc 1, evidence suggests that the lack of integration of PC into HF management relates to a misconception that PC is synonymous with patients facing imminent death or close to EoL. 108,114 It is also important to note that this is not solely relating to HF physicians and HF nurses but rather many primary PC providers, including nurses, also have misconceptions of PC, which again points towards the need for education across settings and disciplines. 131 The sources reviewed identify specific training needs for HF physicians and HF nurses such as symptom identification/management and supportive communication skills. 65,117,130 The evidence suggests that it is imperative that HF physicians and HF nurses have access to, and allocated time to avail of, PC learning opportunities to raise awareness of PC benefits and how PC can be integrated alongside life-prolonging treatment. 87,108,109,111–114,130
| Sub CMOc | Description |
|---|---|
| CMOc 2.3 | When those working in HF have access to and attend education for any challenges they face in managing patients who have HF with PC needs (C), patients with HF are more likely to get timely PC (O) because HF physicians and HF nurses have better knowledge of when PC may be needed (M) |
-
Addington-Hall and Gibbs:129
Better education in the principles of palliative care is indeed needed for all health professionals, especially the growing number of heart failure nurses.
-
Selman et al. :65
Breaking bad news and discussing end-of-life issues in a supportive way were specific suggested training needs for cardiac staff.
-
Kavalieratos et al. :117
Participants from all specialties perceived the need to develop ‘palliative care basics’ (e.g. symptom identification/management in serious illness, communication skills regarding goals of care).
-
Ziehm et al. :119
In particular education of professionals regarding possibilities for palliative care of CHF patients should be intensified as patients could benefit from (early) admission to palliative care.
-
Ziehm et al. :119
Cardiologists’ training programmes should try to convey a more realistic picture about medical limits especially when it comes to non-communicable diseases, and palliative care should be covered in more depth.
-
Barrett and Connaire:111
With appropriate training and education, it is possible that cardiac nurses could meet many of the palliative care needs of the patients and families within their care.
-
Barrett and Connaire:111
… an appropriate starting point for any further education for cardiac nurses is on the core philosophy and principles of palliative care, with an emphasis … [that it] is indeed appropriate and compatible with active HF management.
-
Constantine et al. :132
Palliative care should be part of the training of all PAH-CHD providers, who should address the palliative care needs of their patients in close collaboration with palliative care specialists.
PAH-CHD, pulmonary arterial hypertension associated with congenital heart disease.
CMOc 2.4: continuing professional development
Evidence suggests that increasing knowledge of PC requires integration of PC education into the existing curriculum for all prospective providers during UG and/or PG training23,75,83,88,115–117 as well as ongoing education for those in practice. 85,87,112,117 Shared education needs to be available for the broader care team across settings to help guard against siloed working and successfully integrate PC into HF management. 34,131 Therefore, evidence-based inter- and multidisciplinary education is advocated to improve PC knowledge while also increasing understanding of clinical roles for all who currently provide PC and will provide PC to patients with HF in the future. 34,131 Although the educational experiences proposed by the literature vary between medical specialties, the commonalities were clear and centre on clarifying misconceptions about PC and hospice, identifying PC needs, effective working with respective disciplines (HF or PC) and when to refer to SPC. 85,117 It is evident that training and education have resource implications and need to be ongoing rather than seen as a one-off expense. 87
| Sub CMOc | Description |
|---|---|
| CMOc 2.4 | When HF physicians and HF nurses have access to, and attend UG, PG or ongoing PC education that focuses on the purpose and role PC can play in HF clinical practice (C), they are likely to better appreciate when PC is needed for patients (O) because of their increased understanding (M) |
-
Buck and Zambroski:116
… offering palliative care electives provides education to those already interested in palliative care, integration into the existing curriculum would provide the principles of palliative care to all who will care for patients in the future.
-
Kavalieratos et al. :83
… clinical education must be improved to expose all learners to palliative care topics … [to] correct misconceptions [on] … how to identify palliative needs in their patients; how to provide primary palliative care themselves … and, how to effectively work with palliative care specialists.
-
Kavalieratos et al. :83
… educating HF physicians on the value and availability and the utilization of palliative care services is key. I don’t think we get a good job of learning about that during our medical school or residency or fellowship training.
-
Bouamrane et al. :87
Thus education, training and shared learning of the broader care team are crucial … continued effort is needed in this arena and investments in training and shared learning need to be ongoing and cannot be considered a ‘one off expense’.
-
Millerick et al. :112
Formal or informal heart failure and palliative care education strategies should be considered as an integral component to the ongoing professional development of healthcare professionals involved in the care management of persons living with and dying from advanced heart failure.
-
Schallmo et al. :75
Palliative care and end-of-life care are not universally taught in the university or residency setting. Research authors support that inadequate education or inexperience in PC led to HCP resistance or decreased use of PC.
-
Hill et al. :23
Healthcare providers need to appreciate the importance of palliative care, and this should be highlighted and incorporated more definitively in the specialist HFA training curricula for both cardiologists and nurses.
-
Singh et al. :34
A method for improving the education and training … is integrating … an evidence-based inter- and multidisciplinary education module involving nurses, physicians, social workers, occupational therapists, dieticians, speech therapists, pharmacists, chaplains and physical therapists with specialist palliative care providing support.
-
Kim et al. :131
… it is necessary to develop interprofessional education curricula for primary PC providers, who need to provide adequate PC intervention for patients with HF, even without professional qualifications.
-
Graham et al. :85
HCPs identified participation in continuing medical education that focused specifically on the delivery of palliative care for patients with advanced heart failure as a key facilitator to the delivery of home-based palliative care for patients with AHF.
CMOc 2.5a and 2.5b: educational techniques and strategies
Identifying the optimal techniques and strategies is important when considering how to best educate HF and PC physicians and nurses. This review identified some promising educational techniques for improving their understanding of PC for HF management, such as experiential learning and peer support. 58,75,85,86,112,118 It is evident that experiential learning opportunities present in everyday clinical practice, which can complement more formal knowledge, skills and expertise, and occurs naturally on a patient-by-patient basis during times of real clinical need. 75,85–87 As Millerick and Armstrong112 report, this ‘… encourages cross-fertilization of knowledge and skills that deepens our understanding of needs and the challenges that can often inhibit effective care across care settings’. This type of ‘on-the-job’ learning is reported to encourage mutual understanding and the recognition of the unique contribution of each individual’s clinical role, thus building relationships and care co-ordination. 75,85,112 Evidence suggests that experiential learning such as this helps to identify and manage comorbidities and patient needs collaboratively between HF and PC, guarding against siloed working. 75,85,112 HF physicians and HF nurses may also benefit from peer support, mentoring and supervision from PC physicians and PC nurses, and vice versa, to enhance experiential learning and provide a supportive culture which is receptive to learning. 58,75,85,86,118 In particular, HF physicians and HF nurses experiencing feelings of failure (see CMOc 1) may need peer support from other HF physicians and HF nurses combined with training in reflective practice which may also serve to improve the quality of PC delivered to patients. 58
| Sub CMOc | Description |
|---|---|
| CMOc 2.5a | When HF and PC physicians and nurses take part in experiential learning with peer support and reflection (C), they develop better mutual understanding and relationship building between disciplines (O) because they come to appreciate their respective strengths and skills (M) |
| CMOc 2.5b | When physicians and nurses in HF and PC are given protected time and choice of educational settings (e.g. online, face to face or hybrid) (C), they are more likely to attend (O) because they are empowered to do so (M) |
The evidence overwhelmingly suggests that the preferred learning method was formal face-to-face activities, including conferences, seminars and discussions, with alternative modes of delivery, such as multimedia and full online platforms less favoured. 59,112 However, it must be noted that these findings are based on pre-COVID-19 data, so we cannot be sure that face-to-face learning is still the preferred learning mode post-COVID-19.
Regardless of the mode of delivery, in the context of increasing time constraints on busy HF and PC physicians and nurses, educational and learning opportunities must be accessible to encourage attendance. 59,87,112 Fitting educational programmes within existing programmes of work is deemed essential for sustainability, accessibility and attendance. As Schichtel et al. report, ‘Ideally, the training should take place at their local surgery. In this way, learning activities would also reach those professionals, who normally would not attend a palliative care event’. 59 Allocated time to participate in these activities is deemed an essential prerequisite to success in educating HF and PC HF physicians and nurses in how to best integrate PC into HF management (see CMOc 4). 87
-
Brännström et al. :86
… having support and togetherness with the team members [is important] … to try out ideas, to receive some understanding for your shortcomings, to be listened to, validated and questioned as to whether you have done what is required.
-
Bouamrane et al. :87
… problems with staff being released to attend events and back fill to allow this training must also be in place to allow the ongoing training.
-
Millerick et al. :112
Formal face-to-face learning methods … were highlighted by over 50% of respondents as their preferred method of learning. Just over 20% of recipients preferred online learning and only 17% identified peer shadowing as their preferred learning mode.
-
Ziehm et al. :119
… a huge need for further professional education in palliative care was expressed by all interviewed professional groups … a palliative care unit introducing their opportunities to the care staff or multidisciplinary educational programmes in which every discipline/profession profits from each other.
-
Schallmo et al. :75
Communication and skills training are necessary to assist the HCP to transfer knowledge into practice. Practice change can be supported through mentoring from experienced PC specialists.
-
Schichtel et al. :59
In order for training to be effective and sustainable, it needed to fit into existing educational programmes of GPs and nurses. Ideally, the training should take place at their local surgery.
-
Singh et al. :58
A proportion of cardiologists and HF nurses providing care for individuals with chronic heart failure may require peer support and supervision from other cardiovascular nurses and physicians … this may improve the quality of end-of-life care delivered to patients.
-
Bierle et al. :118
Careful self-examination as well as participation in palliative care education may alleviate moral distress for critical care nurses.
-
Graham et al. :85
Learning was largely centered around having effective advance care planning and/or goals of care conversations, and recognition of the value of a holistic approach to care brought by the palliative care team.
-
Graham et al. :85
These included self-directed reading, formal and informal peer-to-peer support from palliative care colleagues, formal and informal education from cardiology colleagues, and on-the-job experience.
CMOc 2.6: communication skills
It is clearly not enough to suggest formalised education as a solution to integrating PC into HF management, rather the evidence suggests that it is important to consider what specifically any education should focus on. 75 The evidence strongly suggests that HCPs across care settings would benefit from training in communication skills. 30,55,73,116,127,133 Improved communication skills are linked to increased competence and confidence, which in turn is likely to have an impact on earlier integration of PC into HF management. 55,58,84,134–136 Evidence suggests that training in how to conduct direct PC conversations with patients and their informal caregivers may help increase HF physicians and HF nurses’ competency in sensitive communication. 67,77,87,91,108,126,137 Furthermore, it is evident that inter-professional and interprovider education focused on communication for HF and PC physicians and nurses may also aid in building relationships, improve the flow of communication between disciplines and result in improved care co-ordination. 34,87,138 The CT programme is a useful example of co-ordination of care which ensured ease of communication between disciplines. As Bouamrane et al. state, ‘[with the CT programme] it was seen as easier and more straightforward making it more likely for individuals to be willing to just pick up the phone and contact others as required’. 87 It is also important to note that, the introduction of CT was particularly successful where it served to build on pre-existing good links or relationships. 87
| Sub CMOc | Description |
|---|---|
| CMOc 2.6 | When HF physicians and HF nurses who find it challenging to discuss PC with patients who have HF are offered and attend suitable education in communication skills (C), they are more likely to raise this issue with patients and their informal caregivers (O) because they have the confidence and knowledge needed (M) |
-
Selman et al. :65
Both specialties recognised that cardiac staff often lack the communication skills necessary to handle sensitive issues such as prognosis and end-of-life preferences.
-
O’Hanlon and Harding:109
Nurses felt they needed training in many aspects of communication, the most common being counselling courses, training in spirituality, and bereavement care training.
-
O’Hanlon and Harding:109
Nurses felt that improving their communication skills was very important and that they would benefit greatly from attending advanced communication skills training.
-
Hjelmfors et al. :30
In total, 18% of the nurses agreed that a lack of communication skills is a barrier and 30% agreed that they did not know how to discuss prognosis or end-of life care with the patient.
-
Schallmo et al. :75
Communication and skills training are necessary to assist the HCP to transfer knowledge into practice.
-
Schallmo et al. :75
Many HCPs cited inexperience in communication skills, a lack of confidence, or lack of education as a barrier to initiating the conversation with patients and their family.
-
Schallmo et al. :75
Education regarding PC should involve both a basic understanding of key principles and communication techniques to increase the HCPs’ knowledge, attitude, and preparedness to practice PC.
-
Abedini et al. :138
Additionally, interventions specifically aiming to enhance interprofessional and interprovider communication could help clarify roles and expectations around when and how to introduce PC to patients who traverse many care settings and providers.
-
Singh et al. :34
Knowing how to engage CHF clinicians to partake in primary palliative care education, such as communication, is important for integrated palliative care as well as structured educational-behavioural interventions on primary palliative care in the context of CHF.
-
Waller et al. :105
Generalist and specialist providers should receive targeted education and training to ensure they are equipped with the skills to: recognize palliative care needs; appropriately communicate this with patients; and provide appropriate care.
CMOc 2.7: educating patients with heart failure and their informal caregivers
As discussed earlier, a significant barrier to a needs-based approach to PC is that many patients with HF and their informal caregivers have misconceptions of what PC is and when it is appropriate to avail of these services (see CMOc 1). Therefore, educating patients with HF and their informal caregivers early in the disease trajectory about the life-limiting nature of HF and PC options is essential. 77,87,119,120,139 Two key educational opportunities were identified: the importance of HF physicians and HF nurses having direct conversations with patients, and a more generic and wider public information campaign relating to PC in HF management. 55,77,87,119,120,137 Bouamrane et al. 87 suggest that patient-centred education should include discussions about prognosis, and education regarding the clinical progression of HF including associated symptoms and functional decline. Direct conversation with the HF clinician initially is crucial to ensure the patient fully understands their condition, how PC can benefit them and the options available. 55 However, some HF physicians and HF nurses have concerns about the appropriate timing to open this conversation, which can impede opportunities for patient education early in the illness trajectory. For example, a patient’s condition and related psychological state may hinder a discussion, as Stocker et al. 63 suggest: ‘Sensitive discussions of palliative issues are complicated by the fact that many patients experience symptoms which confound their ability to think clearly’. As Dionne-Odom et al. 140 report, ‘Cardiologists commented that it was important to offer PC “early, but not too early”’. Finally, as a participant in Bouamrane et al. ’s87 study explains: ‘… there is also some patients who if you told them at an earlier stage they wouldn’t do well, you know, psychologically that would impact on them … ’ It is likely that training in PC would reduce some of the uncertainties in opening conversations about PC; however, HF physicians and HF nurses may also find it helpful to have structured education at clinical appointments132 whereby they can signpost to PC public health initiatives as a positive second step in educating patients with HF and their informal caregivers. 77 It must also be noted that there are patients with HF who may not want to know more about their condition. Therefore, it is necessary to ensure that all initiatives are non-obligatory as the decisions of these individuals must be respected. As Hjelmfors et al. 77 suggest, HF-specific patient education materials on PC can be used. Another option may include using a patient needs assessment as an educational opportunity and signposting to HF support groups who are knowledgeable about the benefits of PC. 87,139 Although HF physicians and HF nurses concerns regarding timing of PC discussions are important considerations, it is evident that raising awareness of PC earlier rather than later in the disease trajectory, through the most appropriate means for the individual patient, is important for ensuring needs-oriented care is delivered to patients with HF and their informal caregivers alike. 34,55,61,73,93,127 It is also important to note that patient education is likely to be a useful tool to encourage patient empowerment which could further help in patients championing for their PC needs. 88
| Sub CMOc | Description |
|---|---|
| CMOc 2.7 | When patients with HF, who think that PC lacks relevance for them, are provided early on with individually appropriate information about the purpose and role of PC in HF (C), they are more likely to have a better understanding of when they might benefit from PC (O) because they have a better appreciation of it (M) |
-
Bouamrane et al. :87
The comprehensive assessment of patients is also taken as an opportunity for patient education about symptoms, self-management and disease trajectory. Cardiological review and holistic assessment is therefore an essential component of most models of care.
-
Bouamrane et al. :87
… shared care and care coordination was best implemented within a programme of shared-learning and knowledge-transfer, both for patients … and care providers. Feedback about this aspect of Caring Together was positive.
-
Ziehm et al. :119
Information about content and structure of palliative care could be given to patients at an early stage as this might facilitate care at a time when patients might benefit from it.
-
Ziehm et al. :48
… heart failure patients should be educated about the course and the consequences of their disease as early as possible (e.g. at the time of diagnosis) in order to enable them to communicate their wishes and treatment preferences with HCPs.
-
Namukwaya et al. :120
Patient education, I think we are not doing enough.
-
Constantine et al. :132
The process of educating ourselves and our patients cannot be purely opportunistic … Rather, structured education at clinic appointments designed for this purpose, through patient groups and using digital platforms and new technologies is necessary.
-
Hjelmfors et al. :77
On a professional level, knowledge, confidence, and skills are needed. On an organization level, it is necessary to provide professionals with time, room, and information material for patients and families … HF-specific patient education materials can be used.
CMOc 3: winning hearts and minds, using leadership and examples of benefit to change the culture for palliative care in heart failure
The overarching CMOc 3 highlights how winning hearts and minds is an important consideration when integrating PC into HF management. These are explained in detail in sub CMOcs 3.1–3.3. Two aspects of this are clearly illustrated through the literature: (1) the importance of champions; and (2) the importance of knowledge translation of benefits to service providers and service users. Champions are important across all levels. The included literature clearly illustrated how HF and PC physicians and nurses can win the hearts of those responsible for integrating PC and HF. 34,83,87,117,119,141 Winning hearts is demonstrated primarily through their everyday practice, communicating the benefits of integrating PC and HF, and advocacy for more multidisciplinary teamwork across settings. 34,83,87,117,119,141 The literature reports the multiple benefits of integrating PC into HF management including improved patient, informal caregivers and healthcare system outcomes,14,34,81,85,87,131,132,142 and how important it is that service providers and service users are made aware of these benefits so they understand the role of the benefits in improving patient outcomes.
CMOc 3.1: the importance of champions to advocate for integrating palliative care into heart failure management
Championing the benefits of PC to patients and colleagues involves multiple activities, including garnering organisational support and required resources, dissolving boundaries in communication with colleagues, modelling practice which demonstrates the benefits of PC, raising awareness, and taking time to develop interdisciplinary liaisons. 34,83,87,117,119,141,143,144 Multiple clinical roles including HF physicians, HF nurses, PC physicians, PC nurses and GPs are reported as being well placed to champion for the early integration of PC into HF management. 34,83,87,117,119,141 The evidence suggests that PC champions can help to influence their colleagues through their practice and also through communicating the benefits of early intervention to meet the holistic needs of patients and informal caregivers living with HF. 34,87,117,119,141,143 In multidisciplinary HF teams, the literature reports that an interdisciplinary approach must be championed by a respected and influential leader. It is also important that they advocate for the need for respectful understanding of the value of each other’s clinical roles and patient-centred care. 34,87,144 Authenticity is essential for champions: it is necessary that they can communicate the benefits of PC in HF management but also are genuinely passionate about the benefits for patients. As Bouamrane et al. 87 explain:
… we’ve got two individuals that are in the programme who are such passionate speakers and also passionate in how they actually manage this group of patients, although we suspected there were people out there to begin with. I think having them both join the programme, and work so well with the programme, has exceeded our expectations as well …
| Cluster/CMOc | Summary |
|---|---|
| CMOc 3 | When service providers and users have sufficient appreciation about the benefits of PC (C), they are more motivated to advocate for integrated PC in HF management (O), because they understand its role in improving patient outcomes (M) |
| Sub CMOc | Description |
|---|---|
| CMOc 3.1 | When a respected and influential HF clinician in an organisation consistently advocates for the benefits of integrating PC into HF (C), they are more likely to be able to overcome indifference and resistance to integration (O) because they are perceived to have authority and credibility (M) |
With appropriate education and support, all members of the MDT can become champions for PC needs. This can help to attain engagement and overcome resistance from more indifferent colleagues to identify and manage patient needs in collaboration with PC, hence guarding against a siloed approach. 34,83,87,88,111,117,119,141,143,144
-
Kavalieratos et al. :117
Palliative care providers were viewed as experts in ‘difficult communication’, and were therefore seen as the ideal agents to promote and market the role of palliative care amongst their primary care and cardiology colleagues.
-
Kavalieratos:117
… in a good-natured way, [I] really try to do a little education with folks, and I think they really appreciate it … I think once he realized that we’re not the grim reaper service and that we’re really about what does the patient want, they sort of lay down their baggage.
-
Kavalieratos et al. :83
Additionally, identifying and supporting ‘internal champions’ within primary care or cardiology to serve as interdisciplinary liaisons with palliative care may be another mechanism by which to enhance meaningful collaboration between specialties.
-
Gelfman et al. :141
The key to establishing a collaborative relationship is to identify a palliative care champion within the cardiology group at one’s own institution … This collaboration can serve to help ‘translate’ the palliative care paradigm to HF clinicians and vice versa.
-
Bouamrane et al. :87
‘Because we had champions on each site – who were keen to take things forward in the majority of sites – that kind of … required the least effort to actually get everybody together to start thinking about this’.
-
Westlake et al. :127
By championing patients’ needs, clinicians can ensure that there is clear communication and improve the multidisciplinary team’s collaboration to provide well coordinated, patient-focused care.
-
Barrett et al. :111
Nurses are highly motivated to provide the best care possible for their patients and should, with appropriate education and support, be able to champion a palliative care approach in caring for their HF patients.
-
Ziehm, Farin, Seibel, et al. ,119
A wish is to get the foot in the door earlier to raise awareness: ‘Ok, the basic situation cannot be changed but one can do a lot regarding quality of life or life expectancy’– without maintaining any empty promises.
-
Singh et al. :34
A key strategic element at the professional level is cardiologists as palliative care champions for integrated palliative care, in order to facilitate change efforts through developing organisational support and obtaining required resources.
-
Ament et al. :88
Interdisciplinary champions working with a virtual collaborative structure need to be identified, who dedicate themselves to supporting, marketing, and driving through an implementation process, overcoming indifference or resistance in the current context of advanced CHF and palliative care.
| Sub CMOc | Description |
|---|---|
| CMOc 3.2a | When patients who have HF and their informal caregivers are able to directly experience the benefits of early integrated HF and PC (C), they are more likely to ask for it (O) because they have an appreciation of its value (M) |
| CMOc 3.2b | When HF physicians and HF nurses are able to directly see the benefits for their patients of early integrated HF and PC (C), they are more likely to implement it (O) because they have an appreciation of its value (M) |
CMOc 3.2a and 3.2b: evidencing benefits
A key historical barrier to integration of PC into HF management cited in the literature was the relatively weak evidence base for the benefits of integrating PC into HF management. 141 More recent literature demonstrates a growing evidence base showing the benefits of integrated PC for patients with HF, from relieving symptoms, providing psycho-social support, reducing hospital visits, admissions and time spent in hospital, and meeting the priorities of care that matter most to patients. 14,34,81,85,87,131,132,142,145 However, this significant increase in the evidence base has not resulted in higher levels of integrated care; rather, more subtle barriers have emerged, such as the lack of service provider and service user knowledge and appreciation of the diversity of PC interventions and their benefits. 138 CMOc 2, which highlights the importance of education, and has implications for this section. When service providers receive education showing tangible benefits for their patients, they can come to appreciate its value for improving patient outcomes. 88,110 The literature also supports the age-old adage that ‘seeing is believing’, as was the case for service users. When patients with HF had positive experiences of PC integrated into their HF management, they were much more likely to be advocates for integrated PC. 14
-
Gelfman et al. :141
Improving collaboration can be a challenge because the research base demonstrating the benefits of palliative care on outcomes and quality of care for patients with HF is still in its early development.
-
Gasper et al. :110
Following the implementation of the education program, 100% (n = 21) of the clinicians who completed the survey strongly agreed that palliative care can enhance the quality of life for patients with heart failure.
-
Abedini et al. :138
… low knowledge of the benefits of PC in advanced patients with HF throughout the disease continuum (has frequently been cited as a barrier to timely PC and hospice referral).
-
Atkinson et al. :14
This model of care (HFSCSa) was designed to better address patient needs and the high proportion of service users reporting a willingness to recommend the service to others (85%) and rating the service favourably suggest this is being achieved.
-
Ament et al. :88
Organizing educational meetings, educational outreach visits by an expert, training sessions, creating a learning collaborative and developing educational materials are strategies that could be used to improve the knowledge among HCPs (working in Chronic HF).
a HFSCS – co-specialty hospital-community service, Heart Failure Supportive Care Service.
Cluster 2: practice change
CMOc 4: facilitating practice change considering the impact of wider context and organisational issues on palliative care integration
| Cluster/CMOc | Summary |
|---|---|
| CMOc 4 | When HF and PC physicians and nurses have opportunities to work collaboratively with relevant professionals to provide integrated PC and HF management (C), they are better able to assess and address their patients’ PC needs (O) because they learn when and how to draw on each other’s skills and knowledge (M) |
The overarching CMOc 4 highlights the importance of collaboration between specialties (i.e. PC and HF) in MDT working, which was widely cited throughout the literature. 14,22,23,34,85,87,88,124,128,131,142,146–148 There are important nuances and detail that underlie CMOc 4 regarding what factors facilitate and impede practice change in relation to integrated PC in HF management. First, the evidence suggests it is important to consider the composition of the MDT across care settings, to ensure that all relevant specialties are included, providing access to a breadth of clinical expertise. It is evident from the literature that positive working relationships can be enhanced through education and training to learn about each other’s strengths and skills. 22,87,148 Furthermore, clearly defined roles and responsibilities in collaborative models encourages needs and value-based care provision and communication between services. 14,85,88,142,146 Second, the importance of making use of discipline-specific strengths across settings to encourage timely recognition of PC needs was emphasised. 55,59,87,88,146,149 The literature also emphasises the importance of trusting relationships between the MDT members and the problems created by established clinical hierarchies within clinical teams in integrating PC into HF management. 30,55,71,78,149,150 Finally, enhancing and consolidating approachable working relationships between HCPs from differing specialties with the central focus on patient-centred care was key to diminishing fragmentation and increasing individually tailored, co-ordinated care. 23,87,124,148
CMOc 4.1: composition of multidisciplinary teams
It is evident that many patients with HF would derive benefit from the early integration of needs-based PC provided by a suitably skilled MDT to initiate discussions, alleviate burdensome symptoms and signpost to supportive resources. 22,23,34,87,131,147,148 Across a wide range of national healthcare structures and local service configurations, sources suggest that a broad range of disciplines should be included in the MDT; however, input is identified as resource dependent. 23,87 Disciplines include PC specialists, geriatricians, nurses, social workers, chaplains, pharmacists allied health professionals and care workers. 22,23,34,87,122,131 The CT programme report87 emphasises the importance (and success) of adapting existing resources and service redesign as opposed to recruiting additional staff. However, we need to be mindful that this publication is dated 2014, and while service redesign drawing on existing resources would remain the ideal, given current resource issues within the health service, more research is required to ascertain if service redesign would work in the current understaffing climate.
The importance of collaborating through multidisciplinary work is deemed critical to success, and should involve efficient regular team meetings, an individual appointed to co-ordinate care, communication and information sharing to ensure optimum needs-based care for patients and informal caregivers. 22,23,34,87,131,132,137 One commonly undernvolved discipline highlighted by Stevenson et al. 147 is clinical pharmacists. These authors argue that pharmacists should be an integral part of the MDT to provide the required expertise to optimise medication regimens, and avoid potential adverse outcomes from polypharmacy (taking multiple medications). 25,147,151,152 Overall, it is important that decisions are synchronised through the MDT process, providing access to a breadth of clinical expertise. 23,87,147,148 Having the perspective of medication experts is seen as an invaluable asset to MDTs, not only for medication regimen review but also for pain and non-pain symptom management. 147 Furthermore, as Hill et al. 23 suggest, it is important to ensure the availability of HF medication. One approach to promote this lies in ‘anticipatory prescribing’, namely writing prescriptions for medications that might be needed as a matter of urgency in the near/intermediate future in accordance with local governance arrangements. 23
| Sub CMOc | Description |
|---|---|
| CMOc 4.1 | When well-functioning MDTs consist of a wider range of relevant professionals (C), the team has access to a wider range of expertise (O) because they can each bring their perspectives and experiences to bear (M) |
-
Bouamrane et al. :87
… the allocation of a care manager – usually a nurse with specialised training in HF – tasked with coordinating the care management plan of the patient, training and education for patients, family and carers … have all been identified as essential elements of successful integrated palliative care models for HF.
-
Bouamrane et al. :87
The CT programme was much more about service redesign and adapting existing structures rather than parachuting in more staff.
-
Bouamrane et al. :87
… HF palliative care programs should include a nurse and social worker or psychologist. The nurse is also likely to be best placed to act as the HF care manager, particularly if trained and committed to both palliative and disease management goals.
-
Sobanski et al. :22
Most PC concerns should be within the skills of the usual care teams (cardiology, primary care, care of older adults), supported by a specialist PC for education, training, and clinical care if needed.
-
Hill et al. :23
Current models have a ‘shared care’ or collaborative approach … These are centred on MDT involvement with input from allied professionals, depending on individual patients’ needs.
-
Singh et al. :34
It is recommended the team consist of primary care, advanced CHF clinicians, palliative care specialists, geriatricians, nurses, social workers, chaplains, pharmacists and allied health, through team meetings and collaboration, partnering healthcare professionals with patients and carers.
-
Singh et al. :34
A favourable model of care involves primary palliative care delivered in routine heart failure care by cardiology, primary care physicians and nurses with support from specialist palliative care for education and support between the teams.
-
Roikjær et al. :148
Our analysis shows a need to form an interdisciplinary team around the patient to better understand, assess and relieve symptoms of a psychosocial and existential nature … [to] ensure a bridge between perspectives, which will eventually strengthen the quality of treatment.
-
Stevenson et al. :147
It is crucial to recognize palliative care-trained clinical pharmacists as an integral part of the palliative care team and their role as medication experts who can identify problematic polypharmacy.
-
Kim et al. :131
In the case of outpatient settings, including home and outpatient clinics, most studies emphasized the comprehensive approach between the cardiology team (cardiologist, HF nurse) and PC specialists (PC physician and nurse).
CMOc 4.2: co-ordination of multidisciplinary teams
The evidence suggests that to integrate PC into HF teams there is a need for interdisciplinarity across care settings which requires better treatment co-ordination and direction of resources. 14,22,23,34,85,87,88,131,132,142,145–148 There is a strong body of evidence emphasising the importance of consultation between practitioners in community-based care and HF physicians. 55,59,87,88,146,149 As explained in CMOc 3, communication between the different HCPs working in different settings is deemed essential to the co-ordination of MDTs. 48,88 For example, sources highlighted that it is important to strengthen communication between these HCPs to ensure that important information on PC needs is passed across from the HF physician to the GP. 55,59,87,88,146,149 Sources also indicated that this should include a prompt from the HF physician to have a PC conversation to help increase GPs’ confidence in opening conversations with patients and informal caregivers. 55,59,87,88,146,149 Evidence also suggests that effective working across care settings allows expertise to be taken from secondary care back to community, enhancing support of primary care teams caring for patients with HF at home. 14,131,145 There is evidently a need to understand each of these roles and their importance in the MDT, which should be integral to education on integrating PC into HF management (see CMOc 4). 85,88,128 In particular Graham et al. 85 indicated that there needs to be better clarification of who is primarily responsible for the patient’s medical care in the community, suggesting that it would be beneficial to appoint a point of contact to aid patients in navigating the medical system, overseeing the variety of care tasks and delineating which providers are responsible for which tasks at which time. Similarly, other sources suggest that MDT working can be enhanced by identifying a lead co-ordinator of care to integrate inputs from different disciplines. 23,34,87,131 As Hill et al. 23 suggest, the responsibilities of the team members within such MDTs should be defined, and it may be helpful to nominate a HCP to act as interlocutor between the patient/informal caregiver and service provider. A multidisciplinary co-ordinated approach to PC for patients with HF has multiple benefits; it challenges the misconception that PC is only for EoL interventions while enabling high-quality parallel planning during the HF illness journey. 14,132,145
| Sub CMOc | Description |
|---|---|
| CMOc 4.2 | When MDTs are well organised with clearly defined roles and responsibilities (C), it enables high-quality parallel planning and more effective decision-making across care settings (O) because members know what is expected of them (M) |
-
Bouamrane et al. :87
… there does need to be this collaborative approach to provide the best possible end of life care and will need a member of the team to take on responsibility for care coordination and liaison.
-
Ziehm et al. :48
They wrote that ‘all physicians should work together and should exchange information about the patient in order to provide the best care in all stages of life and death’ and that ‘therapy should be in consensus among all disciplines involved’.
-
Hill et al. :23
Specialist palliative care and a palliative care approach by all professionals. Both should be considered within HF management, the latter predominately addressing symptom alleviation, ensuring treatment modalities are aligned with preferences for care, offering psychosocial support, and fostering care coordination.
-
Singh et al. :34
A multidisciplinary approach involves an identified leader integrating inputs from different disciplines, highlighted by the support of a palliative care champion in this review.
-
Constantine et al. :132
A multidisciplinary approach to palliative care for PAH-CHD patients can target intractable symptoms and address complex issues, discordant patient–family goals, and unrealistic expectations of prognosis or treatment effects.
-
Ament et al. :88
Specification of responsibilities and roles on all levels of the interdisciplinary organization and having a professional responsible increase the chance for sustainable integration of timely recognition of palliative care needs.
-
Graham et al. :85
With the development of the collaborative model of care, both cardiology and palliative care providers indicated that there was an increased awareness of the role of the other specialty, including services and limitations of the care each specialty provides.
-
Atkinson et al. :14
Overlapping care between specialties is especially important … consistent cardiology input helps support palliative care providers who may be daunted by managing patients with HF alone.
-
Graham et al. :85
I think it would be great if there were kind of point people in the community that would be helpful as liaisons between the community, the hospital, and the clinic.
CMOc 4.3: trusting relationships
While the literature often frames HF physicians as having an active, biomedical frame of mind, HF nurses generally are portrayed as more inclined to a holistic approach, and more apt to acknowledge that patients require PC at an earlier stage. 30,58,71,78,119,150 A 2021 survey of cardiovascular nurses and physicians in Australia and New Zealand found that 94% of HF physicians have a distinct reluctance to refer to PC when patients are classified as stable and NYHA Class II‒III compared with 65% of nurses. 58 The literature signifies that there is a difference between nurses’ and HF physicians’ perception of the appropriate timing for PC. 30,58,71,78,150 Sources identify that there is not only a difference in perception, but also a difference in the dynamic of relationships that HF physicians and HF nurses form with patients and informal caregivers. A trusting relationship with the patient and informal caregiver is deemed an important aspect when initiating a conversation about PC needs. 55,71,78,149 HF nurses would appear to be better placed to discuss palliative issues, as the evidence clearly shows they see the patient and their informal caregivers more frequently, develop a trusting bond, and can make time to discuss these issues at length if needs be. 55,59,71,78,88,149 The resource of time is a significant issue which requires more in-depth exploration and will be discussed more fully in CMOc 5. Some HF physicians and primary care physicians mentioned that the HF nurses should be given the most prominent role in these PC discussions given their insight into the patient and informal caregivers’ needs. 71,90,149 However, two sources55,92 suggested that due to the chronic nature of their condition, patients with HF may have a closer relationship with cardiology specialists (comparing to other disciplines); therefore, the HF physician may be best placed to discuss PC needs. Overall, more sources suggested that patients would confide in HF nurses and would honestly convey their needs,71,90,149 with one source suggesting that some HF physicians may be seen as unapproachable. 55 The overriding consensus was that the quality of the relationship with the patient was more important than the grade or discipline of the HCP in guiding who should be responsible for having PC conversations. 55,71,77,78,149 A trusting relationship is evidently key to assessing patient needs and conducting PC conversations with patients with HF and their informal caregivers alongside the evident importance of continuation of care (see CMOc 5). 55,71,78,149 With the current developments of the nursing profession adopting more autonomous roles in the UK, nurses will have the advanced knowledge and skills to champion PC integration as they often have a key position within the HF team. 30,150 Therefore, it may be helpful when integrating PC into HF management for HF nurses to take a stronger leadership role in the assessment and management of the needs and preferences of patients with HF. 30,150
| Sub CMOc | Description |
|---|---|
| CMOc 4.3 | When HF physicians and HF nurses caring for a patient with HF are able to identify the relevant staff member(s) who has the most frequent contact with the patient with HF (C), patients are more likely to be receptive to advice delivered by them (O) because they trust them (M) |
-
Wotton et al. :78
… knowing the patient was seen as essential in developing an understanding of the patient’s current physical and psychological status, knowledge of patient and family routines, coping resources and physical capacities, and a patient-nurse relationship based on confidence and trust.
-
Green et al. :55
Participants said that nurses can be more approachable than doctors, at times … [they] are often in the best position to discuss sensitive issues with patients due to the amount of daily contact they have with patients.
-
Green et al. :55
You don’t want the first time you hear that your prognosis is awful and that you should be palliative to come from the new doctor … that needs to be … the people that the patient trusts the most (HF physician and HF nurse).
-
Green et al. :55
I think that patients talk more to nurses than they do to doctors, for two reasons … mainly contact time, because doctors … aren’t there as much as nurses, and secondly, a readiness to talk to someone who’s not a doctor.
-
Waterworth and Gott:149
[Patients] tell things to the nurse that they won’t necessarily tell to the doctor, so you sort of get a fuller picture of what is happening.
-
Glogowska et al. :90
The participants expressed views on which professionals were best placed to have ‘the conversation’ with patients. One GP valued the input of specialist heart failure nurses in this regard.
-
Ecarnot et al. :71
Families and patients often confide things in nurses that they won’t say to the physician. The role of the nurses in communicating the wishes and values of the patients and their families when discussing individual cases is thus vital.
-
Singh et al. :91
Whether health professionals asked the right questions and patients were comfortable discussing their issues was based on the strength of the patient–provider relationship.
-
Hjelmfors et al. :77
It was suggested that the nurse functions as a ‘spider in the web’, recognizing needs and wishes of the patient and family, as the nurse often spends more time with them than the physician.
-
Singh et al. :58
The majority of physicians (n = 29; 91%) agreed they would not refer a patient who is stable on current therapy and is classified as New York Heart Association Class (NYHA) II‒III.
-
Singh et al. :58
In comparison, only 65% of nurses (n = 48) agreed they would not refer a patient who is stable on current therapy and classified as NYHA II‒III and this difference between physicians and nurses was statistically significant (p = 0.032).
CMOc 4.4: clinical hierarchy
Heart failure nurses are the HCPs who have the most regular contact with the patient and their informal caregivers throughout the HF journey. This can result in them having the most comprehensive appreciation of the patients’ holistic PC needs. Nonetheless, the clinical hierarchy in which they work appears to stifle their willingness (or ability in medico-legal systems where they have less autonomy) to initiate PC conversations. 30,78,150 The role of the HF nurse varies across geographical location, for example in Poland and Lithuania HF nurses are an important part of the MDT; however, they have less autonomy due to medico-legal considerations within such countries. 23,33 In other European countries (e.g. Russia and Serbia), nurses working in HF do not have a recognised specialist role. 23,33 Sources identify this difference in geographical location as being an important point to remember when considering the roles and responsibilities of HF nurses. For example, Hjelmfors et al. 77 explain that within their Swedish study, roles and expectations might be different than other countries. Generally, the literature suggests that HF nurses are more aware of the need for and value of PC,58 but in many countries the HF physician must be in agreement, otherwise PC will not be smoothly integrated into HF management. 71,150 Although both HF physicians and HF nurses report that discussing prognosis and EoL care is an important part of their work, they have different responsibilities in these conversations. 74,77 The HF nurses take a supportive role,30,77,150,153 while the HF physicians often initiate the discussion. In one study, a HF nurse described instances where they were left to deal with the patient and informal caregivers’ distress post-PC conversations. 74 One source suggested that HF nurses may feel disempowered by the lack of regard for their input and opinion by those further up in the clinical hierarchy. 71 Although the literature suggests that HF nurses are most suitably placed to discuss PC with patients with HF, if the HF physician has not started these conversations, some HF nurses within certain countries are reluctant to initiate. 30,71 Although the literature suggests that HF nurses are an essential part of the HF MDT43,154 and are suitable placed to discuss PC with patients with HF, if the HF physician has not started these conversations some HF nurses within certain countries are reluctant to initiate. HF nurses’ discourse suggests that they try to convince doctors to transition from a purely biomedical to a more palliative-oriented approach (i.e. informally discuss holistic needs and advance care planning issues), especially when the HF physician’s instructions are not aligned to patients and informal caregivers’ wishes. 30,71 There is clearly a clinical hierarchy in cardiology which can create barriers to integrating PC and HF management and, in some cases, may cause disharmony in cardiology teams. 30,71,74 Communication issues are alluded to in the literature as a possible barrier to HF nurses’ decision-making around timely integration of PC with HF management. Therefore, adequate training on respectful communication within the clinical hierarchy may be required (see CMOc 2). HF nurses have the most regular contact with patients and informal caregivers throughout the HF journey and this combined with their eagerness to provide early intervention for PC needs may indicate that the responsibilities of HF nurses could be increased in alignment with the medico-legal context of where they are geographically located. 30,71,74,153
| Sub CMOc | Description |
|---|---|
| CMOc 4.4 | When HF physicians and HF nurses work in a clinical hierarchy where important decisions around key aspects of patient care are made by those higher up the hierarchy (C), those further down the hierarchy (usually HF nurses) feel unable to discuss PC with patients (O) because they do not believe they have the permission to do so (M) |
-
Wotton et al. :78
Nurses indicated their desire for more timely palliative care but felt cardiologists were intent on life sustaining treatment.
-
Wotton et al. :78
By the same token, nurses’ ability to address and implement orders for end-of-life care was influenced by a reluctance of physicians to issue ‘not for resuscitation’ orders.
-
Hjelmfors et al. :30
‘If the physician has not talked about it [end-of-life care] with the patient, I hesitate to discuss it myself’
-
Hjelmfors et al. :150
… they perceive these discussions (PC) to be beyond their responsibility and authority. ‘It’s not my place as a nurse’.
-
Ecarnot et al. :71
We find ourselves blocked by physicians who want to continue curative care, but without doing too much either … We put a bit of pressure on the doctors, but we don’t really know where to position ourselves.
-
Ecarnot et al. :71
It’s difficult when you’re not being heard or respected as a nurse, when you’re sounding alarm bells and they (the physicians) just respond ‘no, no, that’s not how it is … ’.
-
Ecarnot et al. :71
… the nurses’ actions are basically motivated by the fundamental desire to maximize the patient’s comfort, even if this involves coaxing the physician towards a palliative approach so as to relieve the suffering they perceive the patient to be experiencing.
-
Janssen et al. :74
You don’t know how a patient will react. He can show almost no response, until you (nurse points at cardiologist) leave and then we have a patient who is completely in distress.
-
Hjelmfors et al. :77
The nurse sits along as an extra ear and sounding board in that situation, both for the patient’s sake and for our own, for feedback and for questions about care.
-
Hjelmfors et al. :77
Our study took place in a Swedish context where roles and expectations might be different than other countries. Nurses and doctors were described as having different responsibilities in conversations about prognosis and end-of-life care; however, they should work closely together.
CMOc 5: achieving culture change, using educational opportunities to change the culture for palliative care in heart failure
The overarching CMOc 5 highlights the barriers and facilitators which impact prioritising integrated PC in HF management. There are important issues raised in CMOc 5 concerning the nuances that facilitate and impede practice change and these are explained in CMOc 5.1–5.3 below. First, the literature emphasised that time pressures often caused by inadequate staffing was a barrier to integrating PC into HF management. 59,61,63,67,71,75,84,89,155 The evidence indicates that the reorganisation of existing services is urgently required to provide a more equitable healthcare system for patients with HF. 84,85,87,105,113,129 Equity in PC provision should be regardless of geographical region, regardless of whether patients want to remain at home and should be based on need rather than disease (i.e. PC in HF management should be prioritised in a similar way to PC in cancer). 84,85,87,105,113,129,145 For example, Graham et al. 85 state that it is necessary to re-examine the way in which resources are distributed in the community considering that patients with HF have a variable disease trajectory and require different levels of support over that trajectory. Considering that this does not align with the way that PC resources (e.g. nursing hours, PC unit beds, personal support worker hours, etc.) are currently distributed in the community patients with HF typically have less resources, resulting in suboptimal PC. 85 Second, sources suggest that involvement of and partnership with the patient and their informal caregivers at an early stage using shared decision-making must be prioritised to create goals of care early in the HF disease trajectory. 23,57,95,114,118,132 Finally, continuity in care is highlighted as a priority as stated in CMOc 4 given that co-operation and collaboration between disciplines improves when HCPs utilise each other’s areas of expertise throughout the patient’s illness trajectory. This results in multidisciplinary HCPs and patients feeling more connected and maintaining trusting relationships with their care providers. 55,61,86,107,114,119,156
| Cluster/CMOc | Summary |
|---|---|
| CMOc 5 | When organisations help staff to overcome the barriers to integration of HF with PC (C), staff are more likely to focus on its delivery (O) because they are enabled to do so (M) |
CMOc 5.1: organisational issues impeding practice change
From a cardiology perspective, time constraints often limit HCPs’ ability to have a conversation with patients and their informal caregivers about PC needs. 71,85,134 The literature emphasises that given the pressures on the cardiology team, mainly due to staffing constraints, there is limited time to communicate complex issues which causes aversion to initiating PC conversations. 59,61,63,67,71,75,84,89,155 Potential barriers to the integration of PC into HF management include the lack of organisational resources, staff training and available time. 23,73,78,90,113,126,149 These organisational barriers evidently have an impact on limited communication, co-ordination and collaboration between HCPs which are described as barriers for timely recognition of PC needs in HF management. 88,126,132,156 The evidence emphasises that a lack of funding and services adds to difficulties in addressing patients with HF’s needs, and urgent investment in PC and HF management is required. 78,87,106,113,129 Despite evidence from the CT programme suggesting that integrating PC into HF management does not impinge on time as significantly as was feared,87 a number of more recent sources suggest system-level improvements, such as adequate PC beds85 and community resources21,146 are required to provide optimum PC for patients with HF. 84,85,87,105,113,129
| Sub CMOc | Description |
|---|---|
| CMOc 5.1 | When organisations help staff to overcome barriers to the integration of PC in HF management that are beyond their individual control (C), staff are more likely to focus on timely integration (O) because they are enabled to do so (M) |
-
Borbasi et al. :73
Structural and organisational changes would be essential to provide the necessary skills, time, resources, collaboration and support for effective palliative care.
-
Waterworth et al. :149
… GPs identified that the actual involvement of the practice nurse (PN) in the management of older people with HF was minimal and reasons reported for this … included lack of organization, the practice being too busy [and] associated financial incentives.
-
Bouamrane et al. :87
Expected negative impacts on workload did not necessarily materialise across all sectors contributing to the CT. … some heart failure specialist nurses also felt that the introduction of CT had not been as burdensome an experience as they had anticipated.
-
Bouamrane et al. :87
The facilitation groups allowed for the service to be implemented in a way that considered the local needs and priorities and allowed implementation of the Caring Together programme into the existing structure and services.
-
Ecarnot et al. :71
By the time you talk to the patient, the family, the team […] it can take all afternoon. But at least, everyone benefits. And then it’s so much easier after that in the unit, the family isn’t aggressive, nor is the patient.
-
McCambridge et al. :146
GPs highlighted a wider issue within health care of inadequate social resources in the community to support such patients in their homes.
-
Ament et al. :88
Collaboration and sharing information is needed to make timely recognition of palliative care needs more efficient and compatible. Research revealed that team work regarding advanced CHF and palliative care is the most promising strategy to improve patient-centered outcomes.
-
Graham et al. :85
Accessing palliative care beds is a huge challenge, particularly since over the years, certain palliative care units have actually created more limited guidelines … getting palliative care service like (palliative care unit) admission for heart failure is very difficult.
-
Graham et al. :85
Additionally, this work highlights the need for system level change to address limited access of homecare services and equipment for this patient population to help improve care delivery.
-
Tilley et al. :108
Patients reported social isolation, decreased independence, and increased caregiver burden caused by their deteriorating health status. Additionally, patients reported a lack of resources and availability of community services to address these needs.
CMOc 5.2: shared decision-making
Preferences for treatment and care of patients and their informal caregivers need to be taken into account and addressed more systematically throughout all stages of HF. 55,67,76,83,86,153,157 Involvement of, and partnership with, the patient and their informal caregivers at an early stage of their HF journey using shared decision-making is essential to enhance the likelihood of meeting goals of care. 23,57,95,114,118,132 Emphasising and respecting QoL, autonomy and preferences of the patients and their informal caregivers are essential in the shared decision-making process. 55,67,83,86,153 As Hill et al. 23 and Waller158 explain, tools and programmes that assist patients and informal caregivers undertaking difficult discussions and supporting shared decision-making on treatment options, should be developed and implemented. Similarly, Schichtel et al. 59 emphasise the value of shared decision-making tools to facilitate the conversations to give patients a sense of control over what they do or do not want to discuss and similarly help HF physicians and HF nurses to understand patient’s preferences. The evidence confirms that an individualised assessment of patients’ needs and preferences is essential and will be aided by HCPs’ skills in communication. 55,86,96,116,131,157–159 The organisational aspect of integrating PC across structures and settings requires prioritised time to invest in shared decision-making between HCPs and patients’ with an understanding of the changing responsibilities and roles relevant to the patient’s healthcare trajectory. 23,34,55,57,76,86,114,116,118,131,159
| Sub CMOc | Description |
|---|---|
| CMOc 5.2 | When HF physicians and HF nurses take the time early in the HF disease trajectory to learn from patients and their informal caregivers about their goals of care (C), they can provide them with more tailored care and make decisions together (O) because they have a better understanding of their needs (M) |
-
Brännström et al. :86
Being a palliative nurse for persons with severe congestive heart failure in advanced homecare means being adaptable to the patient’s way of life, that is striving to make the patient’s goal one’s own. …
-
Green et al. :55
Even at the risk of increasing a patient’s psychological morbidity, each patient’s individual health beliefs, coping strategies, and receptiveness to information should be evaluated.
-
Buck et al. :116
Earlier access to palliative care can be advocated for by supporting the importance of the patient’s goals in the care process … to assess long-term goals including use of advanced directions and potential hospice utilization when appropriate.
-
Hill et al. :23
Families and informal caregivers are crucial partners in the HF care team, their support influencing patients’ self-care and mental well-being, as well as prognosis, their involvement often changing and intensifying during clinical crises and the terminal phase.
-
Singh et al. :114
It is also important to consider how healthcare professionals are working as a multidisciplinary team to enable shared decision-making … the patient and the physician taking steps to partake in the process of decision-making regarding treatment.
-
Higginbotham et al. :57
The absence of a structured management plan and a fragmented care system leads to the disabling of the shared decision-making process between healthcare professionals and the patient, resulting in a consistent failure to transition patients to a palliative care approach.
-
Bierle et al. :118
To ease the burden of caregiving, the critical care nurse and the palliative care team should offer family caregivers support and straightforward information in an unhurried and caring manner.
-
Constantine et al. :132
The privileged position of PAH-CHD specialists, providing long-term, often lifelong, care for their patients, allows a strong rapport and a sense of collaborative decision making to be formed over time.
-
Singh et al. :34
Involvement of and partnership with the patient and their carers using shared decision making is essential to create goals of care early in the heart failure disease trajectory.
CMOc 5.3: continuity in care
| Sub CMOc | Description |
|---|---|
| CMOc 5.3 | When HCPs cooperatively and collaboratively utilise each other’s areas of expertise and information for the management of patients throughout their illness trajectory (C), the patient experiences greater continuity of care (O) because the information and care they get is not fragmented or inconsistent (M) |
The evidence suggests that HCPs see a need for closer cooperation between the disciplines (cardiology, general medicine, PC) to ensure continuity at an early stage (see CMOc 4). 55,61,86,107,114,119,156 The evidence reports that continuity of care (especially of their treatment) improves when HCPs collaborate closely with colleagues from different disciplines across care settings when they have a shared understanding that they are all working towards the same patient-centred goal. 85,88,136 HCPs in cardiology reported a greater sense of satisfaction when working in partnership with PC physicians and PC nurses, knowing that they could accompany patients on their entire journey and therefore do not feel disassociated at a certain point in the relationship. 85,88,136 The literature strongly stated the importance of continuity of care to safeguard patients against feelings of abandonment; therefore, maintaining a role for HF physicians and HF nurses is paramount as patients often have strong bonds and trust in their long-standing HF physicians and HF nurses. 85,88,136 HF physicians’ expert opinion on clinical complexities of cardiac medications and devices is also essential at all stages of the patient’s journey to benefit patients, their informal caregivers, and physicians and nurses in PC. 85,89 With strong lines of communication and willing collaboration between PC and HF specialists across care settings, the complex symptoms in HF can be managed, providing optimum holistic care to improve the patient’s QoL and improve continuity in care. 55,61,62,71,86,90,107,113,119,156,160 A further point is reducing patient burden when PC is integrated into HF management, as this comanagement of care helps to guard against fragmentation of care allowing for a more seamless transition at different stages of their illness trajectory. 67,85,89,155 Comanagement of care, sharing information and sharing expertise through patient-centred meetings and interdisciplinary case reviews are deemed essential. 55,61,86,107,114,119,156 It is evident that the interface between PC and cardiac teams needs to be negotiated to ensure continuing links and clear lines of communication to improve management and support available to patients with HF. 55,61,62,71,73,86,87,90,107,113,119,155,156,160
-
Hanratty et al. :107
I think it’s something that’s been lost in modern medicine, the continuity of care and not just in heart failure, across the board.
-
Brännström et al. :89
… better structured follow-ups and continuity of care is emphasised … the importance of being involved throughout the disease trajectory and there also needs to be more cooperation with palliative care services.
-
Kaasalainen et al. :136
All participant groups expressed concern about the perceived lack of continuity in care when patients were transitioning from the cardiac ‘community’ to a palliative care service.
-
Brännström et al. :89
On the other hand what emerges is uncertainty about whether the patient will, in the future, receive optimal heart failure treatment when responsibility has been handed over.
-
Bouamrane et al. :87
Equally, a lack of continuity in the care provided to those with AHF remains evident and there remains inconsistency regarding when to change the emphasis of care from life prolonging to supportive.
-
Hutchinson et al. :67
Many participants felt involving palliative care teams is beneficial, some felt that additional providers increase fragmentation of care and may be burdensome for patients, who already see many specialists.
-
Kogan et al. :155
In addition, patients experience multiple care transitions and see various providers over the course of a progressive illness, making it difficult to have regular ACP discussions that foster a shared understanding of a patient’s goals.
-
Graham et al. :85
… this degree of collaboration provided improved continuity of care from all HCPs, creating a model for patients that is flexible, decreases the risk of patient perceptions of abandonment by the cardiologist, and allows more seamless transition between different care settings.
-
Ament et al. :88
What’s also important to us is to have those patients come back regularly to someone they know and not to different people, because that happens regularly as well for scheduling reasons. Trust is important in the relationship too.
-
Graham et al. :85
Overall, HCPs felt that care transitions were facilitated (between outpatient/inpatient/home) by having team members positioned in each of these settings to take on primary responsibility for patient care.
Cluster 3: organisational change
CMOc 6: the need to embed clear, visible guidelines to integrate palliative care into heart failure management
The overarching CMOc 6 highlights the final points for consideration when embedding PC into HF management. Additional factors which underpin CMOc 6 are explained in CMOc 6.1–6.2. The narrative below describes and explains why visible guidelines are essential to bridge the gap between clinical practice and guidelines. First, the evidence suggests that guidelines need to clarify roles, responsibilities and decision-making to ensure that HCPs can provide expert care despite the uncertainty of the HF illness trajectory. 26,34,85,88,91,125,161 Second, to make guidelines relevant, integrated care pathways must be supported at policy level to facilitate stronger collaborative relationships between cardiology, primary care and specialist PC (see CMOc 4 and 5). 34,85,87,91,125,162
| Cluster/CMOc | Summary |
|---|---|
| Facilitating practice change considering the impact of wider context and organisational issues on PC integration | |
| CMOc 6 | When guidelines outlining who should be doing what and when are clear, visible and implemented (C), then patients with HF have their PC needs assessed and addressed at the right time, by the right people (O), because staff have clarity over expectations and roles (M) |
CMOc 6.1: guidelines for integrating palliative care into heart failure management
Guidelines for integrating PC into HF management exist. For example, the World Health Organization (WHO) and the ESC suggest PC should be available and integrated at an early stage into the routine care for patients with HF alongside disease modifying treatment and PC in HF management. This is supported by a growing body of research. 26,34,79,85,88,91,125,145,161,163 However, the evidence suggests that there is a gap between the evidence and translation into everyday clinical practice, with guidelines on integration of PC into HF management being not being embedded into practice. 26,34,79,85,88,91,125,161 Although international experts have recently reached consensus on a large number of criteria for referral to SPC,164 currently HF physicians and HF nurses operate from ‘broad guidance’ rather than integrated PC and HF specific guidance125 when considering PC access. The lack of visibility and implementation of integrated PC and HF specific guidelines are presented as a barrier to decision-making, defining roles and responsibility and care pathways reducing the potential for optimal care for patients with HF who have PC needs. 34,57,71,85,91,125,163 Although HF guidance [e.g. The Canadian Cardiovascular Society, HFA of the ESC, Heart Failure Society of America (HFSA)] do not give details of specific integrated models, there is consensus that care should be co-ordinated. However, there is disagreement over at what point PC should be considered for patients with HF and when it is appropriate to initiate PC. 87,163 Although guidelines discuss the ‘team’ involved in the palliative management of patients with HF, there needs to be clarity over involvement across care settings, defining roles and responsibilities of HCPs from a broad range of social and health service sectors. 85,87,91,125,163 Evidence strongly suggests that guidelines for PC in HF management and implications for their implementation need to be more specifically tailored for patients who have HF, recognising the distinctive challenges faced by this population, including the uncertain illness trajectory and the various procedures and devices which may be used in their HF management. 150,165,166 Alongside ensuring the visibility and implementation of current guidelines as part of routine practice, specific guidelines need to be formulated on how to proceed with appropriate protocols for various circumstances, for example, the role of palliative sedation for terminal-stage patients who have HF,166 potential difficulties with polypharmacy147,151,152 and how ICDs are managed when the patient is approaching EoL. 26,69,70,100
| Sub CMOc | Description |
|---|---|
| CMOc 6.1 | When HF physicians and HF nurses perceive that guidelines for the integration of HF and PC do not provide adequate clarity over roles and responsibilities (C), they are not likely to be guided by them (O) because they lack clinical relevance or ease of implementation (M) |
-
Selman et al. :125
Eight services had no criteria and reported operating instead with broad guidance. In these services the confidence of the cardiac team in meeting the needs of the patient was the deciding factor in whether to refer.
-
Kim and Hwang:165
Our palliative care guidelines are governed by oncology healthcare systems, making it difficult to develop palliative care guidelines or regulations for those with cardiac disease.
-
Ecarnot et al. :71
The nurses seem eager for there to be some guidance, or official consensus about when a patient should be considered to be in palliative care, and how this decision should be materialized.
-
Singh et al. :91
… we have some guidelines around when is the right time to refer to palliative care in our heart failure bundle of care … I have no doubt that they are ignored by most people but the fact is that they exist.
-
Singh et al. :91
Certain hospitals had guidelines to help clinicians decide whether a patient would benefit from palliative care, although the utilisation of the guideline was questioned.
-
Higginbotham et al. :57
The barrier to expert end of life care was perceived by some doctors involved to be the lack of clear guidance … having defined guidance provided the necessary support and assurance to know when to refer onto the palliative care team.
-
de Sousa et al. :161
Despite consensus about the need for integration of palliative care in the management of HF, there are still no clear indications on how to implement the guidelines and early select patients who benefit from a specialised approach.
-
Graham et al. :85
Despite expert guidelines emphasizing the importance of non- abandonment of patients as they transition to a more comfort- focused approach to care, a number of studies have shown that patients and caregivers still experience abandonment.
-
Ament et al. :88
More attention to palliative care in heart failure-specific clinical practice guidelines is needed to implement palliative care in current CHF care and to remind HCPs of palliative care.
-
Hill et al. :26
There is a gap between guideline recommendations and everyday clinical practice concerning implantable cardioverter defibrillator (ICD) deactivation.
CMOc 6.2: policy and integrated care pathways
Integrated care pathways are needed to provide a structured collaborative approach towards the provision or models of PC. 34,85,87,91,125,167 The literature suggests that consistent guidance, policy changes, and a shared vision of how to implement an integrated PC and HF care pathway across all care settings (primary, secondary and tertiary) is necessary to counteract the ongoing deficiencies in management of this patient population. 57,65,87,162 As Higginbotham et al. 57 state, this pathway needs to include a clearly defined decision-making algorithm in order to optimise the patients’ and informal caregivers’ experience both when identifying needs and providing palliation. As noted in CMOc 4 and 6.1, clarifying staff roles and responsibilities and provision of routine assessment of the need for PC is essential as part of this pathway to facilitate clear communication and early access to PC services when appropriate. 57,65,114,167 Despite agencies (e.g. WHO) making progress to ensure that PC is equitable across all chronic conditions, it is essential that everyday clinical practice reflects policy stipulations and access to PC is based on need, not prognosis. 34,116,117,158,167 Policy-makers must consider the need for organisational restructuring to help provide the infrastructure necessary for the provision of equitable care. This infrastructure should equip HCPs to deliver generalist PC as part of routine HF management and access to SPC when required irrespective of geographical location or prognosis. 57,117,167 Clarity is also needed in policy documentation as to who leads PC for patients with HF. Despite statements by NICE and the British Heart Foundation that this is a cardiology role, there is still a lack of clarity among providers. Given this ongoing uncertainty around roles, guidelines must be used and prioritised. 34,109,117 Other recommendations emerging from the literature support pre-existing policy statements. 50 As stated in CMOc 5, goals of care and treatment decisions must be facilitated through a shared decision-making process early in the illness trajectory, with due consideration of the needs of patients and their informal caregivers. 23,25,57,114,118,132 Shared education (see CMOc 2) in PC is essential to equip HF and PC physicians and nurses to integrate PC into HF management. 34,48,55,61,87,88,105–110,121 It is evident through the literature that policy changes and organisational restructuring are essential to facilitate stronger collaborative relationships between specialists (e.g. HF and PC) and across care settings (e.g. primary, secondary and tertiary settings) to ensure that patients with HF and their informal caregivers receive optimum care at the earliest opportunity. 34,85,87,91,113,125
| Sub CMOc | Description |
|---|---|
| CMOc 6.2 | When organisations have provided both guidelines and the time and resources needed to implement them (C), HCPs are more likely to follow them (O), because they have clarity of what their organisation expects of them (M) |
-
Selman et al. :65
Referral criteria and care pathways would clarify staff roles, provide routine assessment of the need for palliative care, facilitate referral to palliative care services when necessary and enable flexible care, including preferred place of death.
-
Buck and Zambroski:116
The World Health Organization has identified pressing policy issues such as integrating palliative care across current health services, making palliative care access needs based rather than diagnosis based, and developing palliative care programs for all with life-threatening illnesses.
-
Kavalieratos et al. :117
Additionally, given that palliative care utilization may be a function of local availability, policymakers should also facilitate the development of palliative care services in currently underserved geographic regions.
-
Swetz et al. :102
… ESC-HFA,a ISHLT,b and HFSAc should develop a detailed consensus statement on the management of these patients that encompasses ethical, legal, and religious principles, advance care planning, logistics of withdrawal of LVAD support, and the role of palliative care consultants.
-
Hjelmfors et al. :150
Community based programmes for long-term conditions, including heart failure, need to include a framework that ensures regular review along with a shift in care goals and the services provided as the patient moves from chronic disease management to a supportive and palliative care phase, then to terminal care.
-
Singh et al. :113
Most CHF nurses contacted specialist PC for referral or educational activities. These nurses believed care pathways between cardiology, primary care and specialist PC facilitated access to specialist care.
-
Singh et al. :114
The analytical systems of thinking in providing palliative care to patients with chronic heart failure involved the professional role and experience influencing palliative care referral, pre-existing decision pathways including care strategies facilitating referral.
-
Singh et al. :34
A strong and effective national palliative care policy framework, subsidised fees and a renumeration model for palliative care are crucial system level palliative care strategies to integrate palliative care for individuals with CHF.
-
Singh et al. :34
… integrated palliative care in CHF can be utilised in future research to determine key priorities from a patient, provider and policy perspective to integrate palliative care in CHF care across the care continuum and improve the quality of life in individuals and their families, while optimising the delivery of care.
-
Singh et al. :34
Professional and policy organisations and societies have a role in continuing to highlight the importance and incentivise palliative care.
a ESC‒HFA – European Society of Cardiology Heart Failure Association.
b ISHLT – International Society for Heart and Lung Transplantation.
c HFSA – Heart Failure Society of America.
Chapter 4 Discussion
We know that HF has become a modern-day epidemic across the world, with prevalence rates similar to the leading forms of cancer. 2,4 We anticipate the numbers of people living with HF will rise with an ageing population,5,6 and that both patients and their informal carers have high burden of physical, psychological and social symptoms. 24,26,27,30 Costs to healthcare services are also substantial. 8,9
We know that integrating PC with HF management can offer a feasible solution to many of these issues, from providing holistic care aimed at relieving suffering and improving the QoL for patients and their informal carers,15,17 to reducing healthcare costs through reduced hospital visits and inpatient time. 10–12,14 However, over two decades worth of research, policy and clinical guidelines later, integrated PC in HF management is still not part of routine practice. 26,27,30
The RS approach employed for this review of the literature provided a way for us to understand and offer implications to tackle this evidence to practice gap. Although narrative and descriptive reviews have added to the evidence base, in this review the goal was to explicitly and specifically provide an understanding of what works, for whom and in what circumstances when integrating PC into HF management. 44 The value of the realist approach has been in allowing us to include a diverse range of literature and valuable contributions from an expert stakeholder group, whose insights were interwoven throughout the discussion of findings from the literature. This expert stakeholder input helped us to draw out implications which are actionable for key audiences, including: policy; service providers; and the public, including those impacted by HF and their informal carers.
Summary of key findings
In summary, our key findings identified several challenges, but also multiple opportunities to support the early integration of PC into HF management. Challenges include a pervading biomedical culture that tends to focus predominantly on the medical needs of patients with HF and on life-prolonging treatments. There is also a misunderstanding among clinicians, patients and their informal caregivers alike that PC is solely for patients with cancer, or for EoL care. PC provision for patients with HF should be based on need, and not prognosis, and the importance of this is underscored by the unpredictable disease trajectory within HF. This is further compounded by PC clinicians’ training in the traditional PC cancer disease model, which does not sufficiently translate to those with non-malignant disease with an unpredictable prognosis, such as HF.
Additional key challenges to integrating PC and HF management included the ever-increasing time pressure on clinicians and lack of confidence to initiate PC conversations with patients. Inadequate SPC services also caused difficulties when referring patients with more complex needs, which presented challenges to integrated MDT working. Investment in adequate infrastructure and resourcing to support integrated PC services is imperative to prevent bottlenecks. Finally, lack of knowledge among clinicians in relation to who is responsible for making decisions around integrating PC and HF, along with when and how key decisions should be implemented, prevented integration of PC into HF management.
Opportunities to change culture and address misconceptions included PC education for all HSC staff. Education should focus on helping clinicians to understand that PC for non-cancer illnesses should be based on need and not prognosis. Learning should be embedded throughout UG, PG and CPD. Educational strategies that are likely to be effective include experiential learning among both disciplines of PC and cardiology. Communication skills training is important and needed so that all clinicians have the core skills and confidence to have meaningful PC conversations from the point of a HF diagnosis, if appropriate, or soon after a diagnosis. Such conversations would ensure that PC runs in parallel with HF management and is introduced in a sensitive way as early as is appropriate. Setting up and running MDT meetings for those involved in PC and HF is also key for the development of trusting relationships, collaborative working and creating opportunities for clinicians to learn from each other. Wider public messaging can also help dispel myths and misunderstanding around PC so that patients and their informal caregivers can become their own champions and advocate for a more holistic PC approach to HF management.
Finally, champions are important across all levels, from patients and informal carers to clinicians, right up to senior decision-makers in the HSC system, in order to win the hearts and minds of those responsible for integrating PC and HF. Winning both is also a key opportunity to support integration and can be achieved through showing examples of good practice and improved patient, informal caregiver, and healthcare system outcomes.
Using a behaviour change framework to leverage desired behaviour
Reflecting on our preliminary programme theory and during ongoing refinement, it was apparent that certain behaviours largely explained both ‘blockages’ and ‘flows’ to integration of PC into HF management. Based on the content expertise within the project team, a key theoretical framework that was considered most appropriate to help us make sense of how to address these behavioural challenges was the COM-B model. The COM-B model of behaviour presents three components required for any behaviour (B). These components, or determinants of behaviour, are capability, opportunity and motivation. 52 This model proposes that for behaviour change to occur, an individual must believe they have the physical strength, skill or stamina, and the psychological ability (knowledge, resilience, skills and stamina) to undertake that behaviour. Individuals must also have the required social (cultural norms and social cues) and physical (time and resource) opportunity. Furthermore, the behaviour must be more desirable and important than other competing priorities. The motivation component refers to the internal processes which affect decision-making and resulting behaviour. These internal processes include reflective motivation (reflecting on past experiences and making plans), and automatic motivation (impulses, desires and reservations). Each component can influence the other, and each component can be further influenced by the behaviour change itself. Therefore, this model is useful for helping us explain why integrating PC into HF management has been so difficult, and systematically working out what interventional strategies might be needed for targeting long-term behaviour change. The components within this model interact; as a positive change in behaviour can strengthen capabilities, opportunities, or motivation, therefore behaviour change is more likely to be sustained over time.
The following section is focused on the three components of the COM-B model – capability, motivation and opportunity. We chose to discuss our findings this way as both the literature and stakeholder feedback indicated that the key barriers to integrating care largely involve human behaviour in response to underlying processes (motivation, etc.) shaped by the contexts in which key players operate. Our discussions made us consider how we could draw on our findings to produce implications that are useful for policy, practice and research (Table 35). To produce our review implications, we focused on identifying which interventional strategies were likely to be effective in changing contexts that were linked to desired outcomes. The COM-B model helped us in two ways. First, we used it to identify potentially useful intervention strategies that might change context. Second, we used it to categorise intervention strategies according to which component of COM-B they addressed. In Figure 5, we provide an overview which lists our intervention strategies by COM-B component and for each strategy we indicate which CMOc(s) the strategy addresses.
| Implications | Targeted at/actionable by |
|---|---|
| Integrated PC and HF services must be prioritised by senior decision-makers in the health and care system |
|
| Services must be adequately funded to ensure that staff are able to develop and run fully integrated PC and HF services | As above |
| Service design should start with an assessment of the availability of PC and HF services in their locality (e.g. ‘postcode lottery’ issues) and find solutions | As above |
| Services integrating PC into HF management must be provided which are reflective of the diversity of the whole population within the local healthcare context | This is everyone’s business across all levels of care and decision-making |
Develop service delivery models that provide continuity of care for patients with HF including:
|
|
| Develop resources for all settings (e.g. primary and secondary care) and all audiences involved (e.g. patients, carers, and clinicians) with clear and consistent messages about PC and HF. For example, develop a patient information leaflet, co-designed by PPIE, to highlight what integrated PC in HF management is and when this might be suitable | As above |
Develop guidelines for MDT meetings to identify who, when and how each of the below key decisions and action will be completed for each patient with HF:
|
As above |
| Evaluate current PC education in undergraduate and post-registration medical, nursing, allied HSC professional curriculum to identify deficits in the PC curriculum around caring for those with HF |
|
| Effective communications skills training is required across all levels of the curriculum in nursing, medicine and allied HSC professional education to ensure all have the means to communicate the value of PC and HF and provide ongoing care | As above |
| Facilitate joint decision-making: Set up and run MDT meetings for those involved in PC and HF that enable members to develop trusting relationships, work collaboratively and learn from each other | Commissioners and providers at national/place level |
| Create active engagement by demonstrating the value of integrated PC in HF, for example, through the sharing of examples of good practice, for example through visits and placements | Governments HSC professionals |
| Develop effective patient PC education for individuals diagnosed with HF | Governments/commissioners |
| Equip and enable all people involved with PC and HF (e.g. patients, consultants, nurses, informal carers) to champion the value and need for integrated PC and HF | Communities |
| Address any public (mis)understanding of PC and HF through public health campaigns focused on raising awareness of PC as a holistic, wrap around care plan for improving QoL for those with HF | Governments in partnership with communities |
FIGURE 5.
An overview of intervention strategies likely to produce desired behaviours and avoid undesired behaviours to facilitate the integration of PC into HF management structured around the COM-B model.
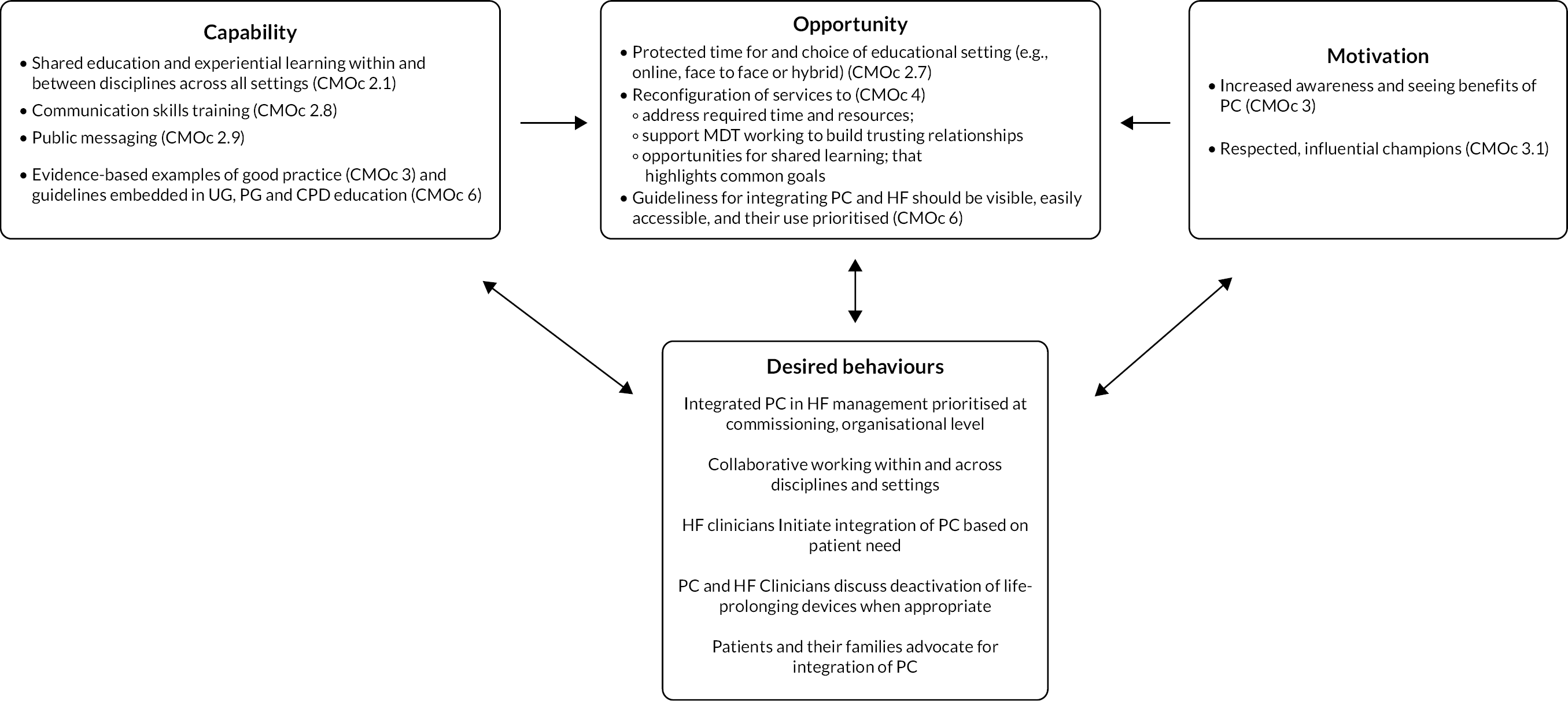
Capacity
According to the ‘capacity’ component of the COM-B model, individuals must believe they have the required knowledge and skills to carry out a behaviour. Unsurprisingly, education was a key intervention strategy for providing HCPs with the required knowledge and skills to overcome many of the blockages identified in the literature. This is evident in a biomedical culture (CMOc 1–1.1), misunderstandings around terminology which equate PC with EoL care only (CMOc 1.2–1.5), complexities of the HF illness trajectory (CMOc 1.6–1.7) and the challenges of integrating PC in the context of patients with HF who have life-prolonging devices (CMOc 1.8a–1.8b). However, the realist analysis and synthesis of the literature helped uncover what ‘types’ of educational strategies are required to achieve integration of PC into HF management, and these are outlined in the following sections.
Shared education and experiential learning within and between disciplines across all settings (CMOc 2.1)
Shared learning is an essential intervention strategy to bridge the cultural divide between HF and PC by highlighting the common goals of both PC and HF specialties (to improve patient outcomes), and to increase understanding of what PC is (holistic care that can be delivered alongside active HF management based on patient need, not prognosis) and what it is not (for patients with cancer and EoL care only). Stakeholders further supported findings on the importance of informal education, through experiential learning, which can include PC staff attending cardiology MDT meetings. During the MDT meetings, mutual team education and support can help HCPs get to know each other, understand each other’s roles, and build and reinforce team ethos and common goals. Stakeholders fully agreed with findings that knowledge of PC and HF is important, but also skills and how HCPs discuss/talk about PC with patients is vital. In their experience, and as supported in the literature, clinical exposure through watching/observing/shadowing can have the greatest impact on learning. There is also an important role for simulation training in exposing HCPs and trainees to clinical scenarios to provide experiential learning in a safe space, to allow learning from mistakes. International stakeholders shared useful learning from exchange programmes for HF professionals and PC professionals to experience each other’s roles, for example HF nurses’ placement in PC and vice versa.
These intervention strategies are crucial for overcoming key blockages to integrated PC uncovered in the literature, such as the pervading biomedical culture that tends to focus predominantly on the medical needs of patients with HF and on life-prolonging treatments. The biomedical culture within which cardiology teams receive their education, train and work helps explain why early integration of PC in HF management has been so problematic and slow to become part of routine practice. According to the ‘opportunity’ component of the COM-B model, cultural norms and social cues are a key determinant of behaviour. Culture refers to the shared and fundamental beliefs, normative values and related social practices of a group that are so widely accepted that they are implicit and no longer scrutinised. 168 Because individual, organisational and social culture is implicit, it is an unseen but very powerful force driving behaviour.
Stakeholders acknowledged the life-sustaining culture among cardiology healthcare professionals, driven by training in a medical model and continuous improvements in therapies. Cardiology as a specialty has been at the forefront of successes in modern medicine, with people with HF living longer in response to evidence-based advances in mechanical circulatory support devices, coronary revascularisation, cardiac resynchronisation and medication management (e.g. beta-blockers and angiotensin-converting enzyme inhibitors). 169 This modern-day success still operates in the context of medicine’s historical focus on molecular biology and technology, dating as far back as the 1800s, which tended to overlook the more holistic dimensions of ill health. 170 Changes in the nineteenth century combined medicine with physical and life science, which resulted in the well-known ‘biomedical model’. This refers to a collection of views resulting in set beliefs about disease and its treatment, focusing medicine towards a predominately technical and scientific discipline170 which is at odds with a holistic PC approach.
Stakeholders re-emphasised the importance of cardiology and PC teams understanding each other’s roles, with joint education needed to bring specialties together. PC is a relatively new specialty which has taken years to build up expertise in cancer care. Some PC clinicians fear taking on patients who have HF as it is out of their comfort zone. No one specialty needs to do it all, so a key aspect of PC education for all HCPs is to provide a good understanding of generalist PC and also how to recognise when specialist PC is appropriate. Those working in PC need to receive education and training, working with HF colleagues, to understand the specific PC needs of patients with HF. For those working with patients living with HF, training in PC should also be mandatory.
Communication skills training (CMOc 2.8)
Effective communication is a core PC skill and essential for the successful integration of PC into HF management. This core intervention strategy should therefore be embedded in UG, PG and CPD education for all HCPs caring for patients with non-malignant illness such as HF. The literature strongly supported this strategy, showing that the HCPs (most prominently physicians in HF) required to initiate integrated PC into patients’ HF management did not believe they had adequate communication skills and as a result lacked confidence to have meaningful PC conversations from the point of a HF diagnosis, if appropriate, or soon after a diagnosis (CMOc 2.8). The ‘if appropriate’ caveat is important as not all patients are ready or want to discuss the life-limiting nature of HF, and that must be respected. Communication skills training should therefore also cover how to assess the communication and information needs of individual patients to ensure their perspective on what they want is heard and addressed. 61
Public health approach/messaging (CMOc 2.9)
A public health approach/positive messaging around PC was identified as a core intervention strategy to help dispel myths and public misunderstanding around PC. For example, both PC and HF were referred to as ‘loaded terms’ in the literature and by stakeholders, which, if misunderstood by patients and their informal carers, can generate strong emotional responses which made clinicians less motivated to talk about them. This overlaps with the reflective motivation component within the COM-B model, which proposes that reflecting on previous negative experiences can be a demotivator and prevent a behaviour from occurring (in this case integration of PC). In support of this theory, the literature showed that when clinicians experience discomfort with the terms PC and/or HF they may use language to soften a diagnosis/prognosis of HF, and avoid PC conversations because, like their patient, they do not fully understand that PC does not mean EoL care only, and do not want to erode the patient’s hope. However, the unintended consequence is that patients may be less aware of the seriousness of their illness or that they could be benefiting from a more holistic approach to their HF care that could help manage physical symptoms and improve their psychological, social and spiritual well-being. Stakeholders also raised similar issues around terminology throughout the stakeholder meetings. They discussed the confusion around the term ‘palliative care’, agreeing that PC is still largely associated with cancer and EoL care. To add to that, a diagnosis of HF can also sometimes be interpreted by patients as meaning impending death, with their heart about to fail at any moment. Although there was much debate among stakeholders, with patient partners strongly advocating for a change in the terminology of ‘palliative care’ to ‘supportive’ or ‘comfort care’ and a change in terminology from heart ‘failure’ to heart ‘function’ (see https://palliatheartsynthesis.co.uk/some-thoughts-on-terminology-a-patients-view/), there was consensus that the most important thing is for the meaning behind the terms to be understood by service providers and service users. That is: that PC is a beneficial component of care to help patients live well, and that it can be introduced if/when needed from the point of HF diagnosis to more advanced stages of the illness.
Evidence-based examples of good practice (CMOc 3) and guidelines embedded in undergraduate and postgradudate education (CMOc 6)
The final educational intervention strategies under the capacity component of the COM-B model included PC education that includes evidence-based examples of good practice and guidelines on who should be doing what, when and how in relation to integrating PC and HF for all HCPs involved in HF management. The reasons why both educational components are required for integrating PC into HF management are expanded on further under Opportunity and Motivation.
Opportunity
Protected time for and choice of educational setting (for example online, face to face, or hybrid) (CMOC 2.7)
As a recap, the opportunity component of the COM-B model proposes that individuals must have the required physical (time and resources) opportunities for behaviour change to occur. Therefore, providing evidence-based educational strategies is not enough to create behaviour change without due attention to the required opportunities. The literature and stakeholders both stressed the importance of having protected time for registered staff to attend training, and also highlighted the importance of ensuring that opportunities are maximised, such as holding training at the workplace and in the preferred format (which was face to face preCOVID-19 – this would need to be re-evaluated in a post-COVID-19 context).
Reconfiguration of services (CMOc 4) to:
-
address required time and resources
-
support MDTs working to build trusting relationships
-
provide opportunities for shared learning that highlights common goals.
The literature and stakeholder discussions were also awash with references to lack of physical opportunity (lack of time and resources) to integrate PC into HF management. Stakeholders acknowledged that HF nurse specialists do consider holistic care including PC as key parts of their role; however, adequate staffing is necessary to provide time, and manage patient caseloads. Service developers and planners need to be cognisant of the importance of having adequate time throughout the patient’s journey and not just see PC discussions as a one-off conversation. There are issues around regional provision and integration of PC in HF as this varies across regions. In some areas, stakeholders referred to it as ‘fitting a square peg in a round hole’ when they were describing patients who have HF trying to access into local PC services. When considering resourcing across staff, provision is required and time needed for all relevant HCPs, including physiotherapy, occupational therapy, etc. as MDTs are crucial for building trusting relationships/highlighting common goals for improved patient outcomes and creating opportunities for shared learning within and across disciplines and settings. Planners and commissioners may express concern at the extra funding required but need to be made aware of longer-term savings from early integration of PC, as evidenced in the research literature. Stakeholders also highlighted the importance of learning from existing integrated PC and HF services which have successfully reconfigured their services without additional funding.
Guidelines for integrating palliative care and heart failure should be visible, easily accessible and their use prioritised, so that staff have clarity over expectations and roles, and patients receive the right care, from the right people, at the right time (CMOc 6)
Guidelines evaluate and summarise existing evidence in order to assist HCPs make evidence-based decisions around management of specific conditions for specific patient groups, and in consultation with patients and their informal caregivers. Guidelines can also be used for benchmarking against best practice, and as an educational tool to improve care quality and patient outcomes. 43 The importance of having guidelines was highlighted by our review findings, which identified the lack of clarity among HF nurses, HF physicians and GPs around who is responsible for initiating PC conversations, when this should happen and how often, as a key barrier to integrating PC and HF.
However, as with education, it is not enough to simply propose an intervention strategy without a full understanding of how it works, and in what circumstances. For example, the first position paper presenting guidelines for integrated PC for HF dates back to 2009,171 followed over a decade later by the most recent guidelines in 2020,23 yet little has changed in terms of their implementation26,27,30 and such implementation is noted to be inconsistent. 172
The realist analysis and synthesis of the literature helped uncover what strategies are required to optimise ‘use’ of integrated PC and HF guidelines. Unless these guidelines are visible, easily accessible and prioritised in routine clinical practice, they will not create behaviour change. As covered under the capacity component, embedding guidelines in UG, PG and CPD education is a key strategy to heighten their visibility and accessibility. Prioritising guidelines in clinical practice via policy support is also crucial to ensure their use in routine practice. These findings are supported by the wider literature on optimising implementation of guidelines, which include strategies such as strengthening awareness of specific guidelines with key stakeholders; supporting organisational changes to facilitate practitioners use of guidelines’ implementation; and motivating key stakeholders to use the guidelines173 This leads us into the motivation component of the COM-B model.
Motivation
Increased awareness and seeing benefits of palliative care (CMOc 3)
According to the COM-B model, motivation is a core component necessary for behaviour change, meaning that the behaviour must be more desirable and important than other competing priorities. CMOc 3 identified the importance of increased awareness and seeing the benefits of PC for HF as key intervention strategies. However, stakeholders acknowledged cardiology as an evidence-driven discipline, and as such HF physicians may need to know what ‘dose’ of PC is required and have compelling evidence of why they need to integrate PC. However, what counts as evidence matters, and it can be challenging to generate evidence on effect sizes with complex phenomena – such as the integration of PC with HF.
Respected, influential champions (CMOc 3.1)
Stakeholders noted that evidence may win minds, but we also need to convince hearts, and so emphasised the importance of winning both hearts and minds. This is a term that can be understood in a number of ways, but essentially conveys an attempt to achieve a desired goal using emotive and intellectual appeals. The synthesis of the international evidence also supported the importance of conveying the emotive and intellectual need for integrating PC and HF via credible champions, seeing direct patient benefit, and evidence-based education. As already mentioned above, stakeholders emphasised the importance of sharing examples of good practice through visits and placements as this provides an excellent opportunity for clinicians to ‘see’ evidence of patient and health service benefit. Equipping and enabling all key players involved with PC and HF (e.g. patients, consultants, nurses and carers) to champion the value and need for integrated PC and HF can also help win over those who may not have considered PC as an important component of HF management. The role of patient champions can promote attitude change in cardiology HCPs and can help to break down barriers – as was the experience of some stakeholders from their own services.
Stakeholders recommended ensuring that evidence of benefit is relatable to key audiences, and this is reflected through their active involvement in refining implications (see Appendix 4). For example, in their experience, the cardiology community is data driven and value evidence of benefit from RCTs. Those in policy and commissioning value health economic data most, with patients valuing more patient specific outcome data.
Equality, diversity and inclusion
Both the literature and expert stakeholder group highlighted inequity of PC access for patients with HF across care settings, compared to other patient populations (e.g. those with cancer diagnoses). Our UK wide PPI partners (both male and female) in particular felt very strongly that there are ongoing inequalities depending on diagnosis:
I also cared for my father who received palliative care for lung cancer. He received really great support from the McMillan nurses and was taken into hospice care before he died. The difference between the two types of care, [heart failure and cancer] even with both being terminal, was quite profound. (See Appendix 4)
Specific studies looking at the equality, diversity and inclusion in relation to access to PC for patients with HF would be beneficial in the future, in order to recognise and respond to the inequities that are present.
Chapter 5 Conclusions and implications
PalliatHeartSynthesis review implications
In concluding, we draw out the implications for policy and practice from our data (Table 4), and recommendations for future research (Table 5). Service commissioners or providers will all likely have different starting points in their journey in integrating HF and PC. As such not all the implications we provide will be relevant and need to be acted on for all services. We see our implications as providing decision support to services. In other words, the implications help services to identify the areas that they may wish to focus on when trying to further integrate HF and PC.
Following ongoing refinement of our programme theory at each stakeholder meeting, we co-produced implications with our expert stakeholder group. These implications outline the required steps to take to ensure the core components and determinants of behaviour are in place so that all key players have the capacity, opportunity and motivation to integrate PC into HF management. Previous research evidence shows a reduction in healthcare costs and improved QoL for patients and informal carers when PC is introduced into HF management. Therefore, maximising implementation of the implications to support integration is key to achieving these aims.
Strengths and limitations
The key strengths of this report include the completion of a robust and comprehensive realist analysis, following Realist And Meta-narrative Evidence Syntheses: Evolving Standards (RAMESES) quality standards for RS. 44 This has enabled us to go beyond the evidence for effectiveness provided in the existing research base to build theories of how integration of PC and HF is more likely to be implemented, and in what circumstances. Although previous reviews have focused on outcomes related to barriers and facilitators, and quantifiable measures, such as reduced hospital visits, time in hospital and QoL, we have been able to uncover a range of intermediate, essential resources, behaviours and actions that are required at key points along the integrated PC and HF journey. This has allowed us to uncover why it has been so hard to integrate PC into HF management and produce review implications based on that understanding.
Another key strength has been our highly engaged, enthusiastic stakeholder group, made up of a diverse range of local, national and international expertise in PC and HF, including our PPI partners who often took the lead in stakeholder meetings and ensured our findings included what is most important to service users as well as service providers. Our PPI partners went above and beyond for this project, writing engaging blog posts, and a special issue for our project website, inspired by theory building during stakeholder discussions. Stakeholders have been instrumental throughout all stages of the review, drawing on their real-world experience to inform the ongoing refinement of our programme theory, co-producing implications and the project animation, informing our dissemination plan, and identifying key areas for future research (Table 36). As such all of our project outputs are grounded in real-world practice, policy and service user experience.
| Recommendation | Area |
|---|---|
| 1 | Identify more cost-effectiveness data, particularly for the UK context as most data originates from the USA |
| 2 | Review of the literature to examine what is a good outcome(s) to demonstrate patient benefit |
| 3 | How do we implement meaningful outcome measures for integrated PC and HF? |
| 4 | Map inequity of PC and HF provision – for example who does not get access to a HF nurse? |
| 5 | What is the minimum PC input that needs implemented into HF to see a positive outcome(s)? |
| 6 | Education:
|
| 7 | Further research is required to evaluate existing integrated PC and HF services to identify what works/does not work, for whom, and in what circumstances. This would provide an opportunity to test (i.e. confirm, refute, or refine) the programme theory from this RS of the literature and develop detailed ‘how to’ guidance for setting up integrated PC and HF services |
| 8 | Research on assisted dying for patients with multiple long-term conditions including heart failure is an area that requires further research to guide integrated palliative care services internationally, and for the NHS in the future should this become part of legislation |
A real strength of the RS approach employed for this project rests in the potential transferability of our findings. As this approach to reviewing the evidence is theory driven and focuses on understanding commonly occurring mechanisms that cause outcomes our findings are likely to be useful wherever these same mechanisms can be reasonably inferred to be in operation. Based on our understanding of these mechanisms, we were able to develop review implications for implementation strategies that are likely to work across a range of different settings, wherever people are trying to integrate PC into HF management. Therefore, our findings are versatile, and their relevance is maximised for use across the NHS.
In the case of this review, limitations included lack of clarity over cardiac subspecialties (e.g. interventional cardiology, electrophysiology and advanced HF and transplant cardiology), where these may have been reported within the subcategories of participants, these were rarely reported within the presentations of the findings. The vast majority of the studies were focused on HF physicians and HF nurses and did not reflect the multidisciplinarity of the HF team that would provide PC, for example limited perspectives from pharmacists, community nurses and GPs.
A further limitation of this review may have been the low number of RCTs included (Table 9). Inclusion of RCTs in systematic reviews is important for the collation of robust trial outcome data to provide evidence for guiding clinical decisions. 174 However, when the focus of a review is on understanding what works, for whom and in what circumstances to provide evidence for guiding ‘how to’ implement a complex intervention, RCTs have limited data on context, and mechanisms to help answer these questions. 175
Including a greater diversity in perspectives would have strengthened this project, in particular, bringing in the expertise of Dutch, Belgian and Spanish colleagues with experience in assisted dying, as this was an important aspect of context that was not found in the literature reviewed, and an area requiring further research. This may have limited some of the CMOcs.
Finally, we acknowledge that the realist approach to analysis means that our findings are based on our interpretation of the data. A different team of researchers could have reached different interpretations. However, the close involvement of our key stakeholders makes us confident that our findings are credible and have been strengthened through a robust, iterative RS process.
Recommendations for future research
Our findings and stakeholder discussions identified seven key areas for future research.
Additional information
Acknowledgements
We thank the members of our key stakeholder group, who actively contributed through individual and group meetings to offer their valuable and diverse perspectives. Key stakeholders significantly contributed to the evolved programme theory and actionable findings and outputs, including blogs on the study website (https://palliatheartsynthesis.co.uk). Key stakeholders included Phillipa Ashcroft (UK), Clea Atkinson (UK), John Burden (UK), Ronnie Burns (UK), Rachel Campbell (UK), Linda Cooper (UK), Alice Crabtree (UK), Akshay Desai (USA), Lana Dixon (UK), Edith Donnelly (UK), Grainne Doran (UK), Ruth Driscoll (UK), Karen Hogg (UK), Gillian Hutchinson (UK), Miriam Johnson (UK), Robert Jones (UK), Mary Kennedy (Ireland), Donna-Louise Laird (UK), Denise McAnena (UK), Karen McCammon (UK), Mary McGeough (UK), Emma McMullan (UK), Yvonne Millerick (UK), Teresa O’Nwere-Tan (UK), Austin Orr (UK), Joseph Rogers (USA), Bob Ruane (UK), Gursharan Singh (Australia), Carol Stone (UK), Grainne Toal (UK), Ellie Wagstaff (UK), and Marni Willens (UK). We also thank the NIHR reviewers for their helpful comments which have helped to strengthen this report.
CRediT statement
Tracey McConnell (https://orcid.org/0000-0003-1292-8597): Conceptualisation (lead), Data curation (equal), Formal analysis (equal), Funding acquisition (equal), Investigation (equal), Methodology (equal), Project administration (equal), Writing – original draft (equal), Writing – editing and reviewing (lead).
Carolyn Blair (https://orcid.org/0000-0001-5454-5813): Data curation (equal), Formal analysis (equal), Investigation (supporting), Project administration (supporting), Writing – original draft (equal), Writing – editing and reviewing (Equal)
Geoff Wong (https://orcid.org/0000-0002-5384-4157): Conceptualisation (equal), Funding acquisition (equal), Methodology (equal), Writing – editing and reviewing (equal).
Claire Duddy (https://orcid.org/0000-0002-7083-6589): Conceptualisation (equal), Data curation (equal), Funding acquisition (equal), Methodology (equal), Writing – editing and reviewing (equal).
Clare Howie (https://orcid.org/0000-0002-4359-6831): Data curation (supporting), Formal analysis (equal), Investigation (equal), Project administration (supporting), Writing – original draft (equal), Writing – editing and reviewing (equal).
Loreena Hill (https://orcid.org/0000-0001-5232-0936): Conceptualisation (equal), Writing – editing and reviewing (equal).
Joanne Reid (https://orcid.org/0000-0001-5820-862X): Conceptualisation (lead), Data curation (equal), Formal analysis (equal), Funding acquisition (equal), Investigation (equal), Methodology (equal), Project administration (equal), Writing – original draft (equal), Writing – editing and reviewing (lead).
Disclosure of interests
Full disclosure of interests: Completed ICMJE forms for all authors, including all related interests, are available in the toolkit on the NIHR Journals Library report publication page at https://doi.org/10.3310/FTRG5628.
Primary conflicts of interest: Geoff Wong reports membership of HTA Prioritisation Committee 2015–22, HTA Remit and Competitiveness Committee 2015–21, HTA Post-Funding Committee 2018–21. Loreena Hill reports honoraria payment from Vifor, and Chair of Digital Health and Patient care committee of the Heart Failure Association of the European Society of Cardiology.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to full text documents may be granted following review.
Ethics statement
This was not necessary as this was a realist synthesis of the literature.
Information governance statement
As this was a systematic review, the project did not handle any personal information. Therefore, an information governance statement is not required.
Department of Health and Social Care disclaimer
This publication presents independent research commissioned by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, MRC, NIHR Coordinating Centre, the Health and Social Care Delivery Research programme or the Department of Health and Social Care.
This monograph was published based on current knowledge at the time and date of publication. NIHR is committed to being inclusive and will continually monitor best practice and guidance in relation to terminology and language to ensure that we remain relevant to our stakeholders.
Publication
McConnell T, Burden J, Duddy C, Hill L, Howie C, Jones B, et al. Integrating palliative care and heart failure: a protocol for a realist synthesis (PalliatHeartSynthesis). BMJ Open 2022;12:e058848. https://doi.org/10.1136/bmjopen-2021-058848
Disclaimers
This article presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care.
References
- McConnell T, Burden J, Duddy C, Hill L, Howie C, Jones B, et al. Integrating palliative care and heart failure: a protocol for a realist synthesis (PalliatHeartSynthesis). BMJ Open 2022;12. https://doi.org/10.1136/bmjopen-2021-058848.
- World Health Organization (WHO) . Global Status Report on Noncommunicable Diseases 2014. www.who.int/publications/i/item/9789241564854 (accessed 20 October 2022).
- Ponikowski P, Anker SD, AlHabib KF, Cowie MR, Force TL, Hu S, et al. Heart failure: preventing disease and death worldwide. ESC Heart Fail 2014;1:4-25. https://doi.org/10.1002/ehf2.12005.
- GBD 2017 Disease and Injury Incidence and Prevalence Collaborators . Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018;392:1789-858. https://doi.org/10.1016/S0140-6736(18)32279-7.
- Savarese G, Lund LH. Global public health burden of heart failure. Card Fail Rev 2017;3:7-11. https://doi.org/10.15420/cfr.2016:25:2.
- Savarese G, Becher PM, Lund LH, Seferovic P, Rosano GMC, Coats AJS. Global burden of heart failure: a comprehensive and updated review of epidemiology. Cardiovasc Res 2022;118:3272-87. https://doi.org/10.1093/cvr/cvac013.
- Ambrosy AP, Fonarow GC, Butler J, Chioncel O, Greene SJ, Vaduganathan M, et al. The global health and economic burden of hospitalizations for heart failure: lessons learned from hospitalized heart failure registries. J Am Coll Cardiol 2014;63:1123-33. https://doi.org/10.1016/j.jacc.2013.11.053.
- Blecker S, Paul M, Taksler G, Ogedegbe G, Katz S. Heart failure-associated hospitalizations in the United States. J Am Coll Cardiol 2013;61:1259-67. https://doi.org/10.1016/j.jacc.2012.12.038.
- Gomez-Soto FM, Andrey JL, Garcia-Egido AA, Escobar MA, Romero SP, Garcia-Arjona R, et al. Incidence and mortality of heart failure: a community-based study. Int J Cardiol 2011;151:40-5. https://doi.org/10.1016/j.ijcard.2010.04.055.
- Morrison RS, Dietrich J, Ladwig S, Quill T, Sacco J, Tangeman J, et al. Palliative care consultation teams cut hospital costs for Medicaid beneficiaries. Health Aff (Millwood) 2011;30:454-63. https://doi.org/10.1377/hlthaff.2010.0929.
- Gonzalez-Jaramillo V, Fuhrer V, Gonzalez-Jaramillo N, Kopp-Heim D, Eychmuller S, Maessen M. Impact of home-based palliative care on health care costs and hospital use: a systematic review. Palliat Support Care 2021;19:474-87. https://doi.org/10.1017/S1478951520001315.
- Sahlen KG, Boman K, Brannstrom M. A cost-effectiveness study of person-centered integrated heart failure and palliative home care: based on a randomized controlled trial. Palliat Med 2016;30:296-302. https://doi.org/10.1177/0269216315618544.
- Report by the Comptroller and Auditor General [HC 1043 Session 2007–2008]. London: National Audit Office; 2008.
- Atkinson C, Hughes S, Richards L, Sim VMF, Phillips J, John IJ, et al. Palliation of heart failure: value-based supportive care. BMJ Supportive &Amp; Palliative Care 2024;14:e1225-33. https://doi.org/10.1136/bmjspcare-2021-003378.
- Doherty LC, Fitzsimons D, McIlfatrick SJ. Carers’ needs in advanced heart failure: a systematic narrative review. Eur J Cardiovasc Nurs 2016;15:203-12. https://doi.org/10.1177/1474515115585237.
- Broese van Groenou MI, De Boer A. Providing informal care in a changing society. Eur J Ageing 2016;13:271-9. https://doi.org/10.1007/s10433-016-0370-7.
- Fitzsimons D, Doherty LC, Murphy M, Dixon L, Donnelly P, McDonald K, et al. Inadequate communication exacerbates the support needs of current and bereaved caregivers in advanced heart failure and impedes shared decision-making. J Cardiovasc Nurs 2019;34:11-9. https://doi.org/10.1097/JCN.0000000000000516.
- Datla S, Verberkt CA, Hoye A, Janssen DJ, Johnson MJ. Multi-disciplinary palliative care is effective in people with symptomatic heart failure: a systematic review and narrative synthesis. Palliat Med 2019;33:1003-16. https://doi.org/10.1177/0269216319859148.
- Siouta N, van Beek K, Preston N, Hasselaar J, Hughes S, Payne S, et al. Towards integration of palliative care in patients with chronic heart failure and chronic obstructive pulmonary disease: a systematic literature review of European guidelines and pathways. BMC Palliat Care 2016;15:1-12. https://doi.org/10.1186/s12904-016-0089-4.
- Rogers JG, Patel CB, Mentz RJ, Granger BB, Steinhauser KE, Fiuzat M, et al. Palliative care in heart failure: the PAL-HF randomized, controlled clinical trial. J Am Coll Cardiol 2017;70:331-41. https://doi.org/10.1016/j.jacc.2017.05.030.
- O’Donnell AE, Schaefer KG, Stevenson LW, DeVoe K, Walsh K, Mehra MR, et al. Social worker-aided palliative care intervention in high-risk patients with heart failure (SWAP-HF): a pilot randomized clinical trial. JAMA Cardiol 2018;3:516-9. https://doi.org/10.1001/jamacardio.2018.0589.
- Sobanski PZ, Alt-Epping B, Currow DC, Goodlin SJ, Grodzicki T, Hogg K, et al. Palliative care for people living with heart failure: European Association for Palliative Care Task Force expert position statement. Cardiovasc Res 2020;116:12-27. https://doi.org/10.1093/cvr/cvz200.
- Hill L, Prager Geller T, Baruah R, Beattie JM, Boyne J, de Stoutz N, et al. Integration of a palliative approach into heart failure care: a European Society of Cardiology Heart Failure Association position paper. Eur J Heart Fail 2020;22:2327-39. https://doi.org/10.1002/ejhf.1994.
- Anderson H, Ward C, Eardley A, Gomm SA, Connolly M, Coppinger T, et al. The concerns of patients under palliative care and a heart failure clinic are not being met. Palliat Med 2001;15:279-86. https://doi.org/10.1191/026921601678320269.
- Browne S, Macdonald S, May CR, Macleod U, Mair FS. Patient, carer and professional perspectives on barriers and facilitators to quality care in advanced heart failure. PLOS ONE 2014;9. https://doi.org/10.1371/journal.pone.0093288.
- Hill L, McIlfatrick S, Taylor BJ, Jaarsma T, Moser D, Slater P, et al. Patient and professional factors that impact the perceived likelihood and confidence of healthcare professionals to discuss implantable cardioverter defibrillator deactivation in advanced heart failure: results from an international factorial survey. J Cardiovasc Nurs 2018;33:527-35. https://doi.org/10.1097/JCN.0000000000000500.
- Barclay S, Momen N, Case-Upton S, Kuhn I, Smith E. End-of-life care conversations with heart failure patients: a systematic literature review and narrative synthesis. Br J Gen Pract 2011;61:e49-62. https://doi.org/10.3399/bjgp11X549018.
- Allen LA, Yager JE, Funk MJ, Levy WC, Tulsky JA, Bowers MT, et al. Discordance between patient-predicted and model-predicted life expectancy among ambulatory patients with heart failure. JAMA 2008;299:2533-42. https://doi.org/10.1001/jama.299.21.2533.
- Lowey S. Factors affecting post-acute referrals for palliative home health care among patients with end-stage heart failure. J Pain Symptom Manage 2016;51:426-7. https://doi.org/10.1016/j.jpainsymman.2015.12.039.
- Hjelmfors L, Stromberg A, Friedrichsen M, Martensson J, Jaarsma T. Communicating prognosis and end-of-life care to heart failure patients: a survey of heart failure nurses’ perspectives. Eur J Cardiovasc Nurs 2014;13:152-61. https://doi.org/10.1177/1474515114521746.
- McIlvennan CK, Allen LA. Palliative care in patients with heart failure. Br Med J 2016;353. https://doi.org/10.1136/bmj.i1010.
- Sahlollbey N, Lee CKS, Shirin A, Joseph P. The impact of palliative care on clinical and patient-centred outcomes in patients with advanced heart failure: a systematic review of randomized controlled trials. Eur J Heart Fail 2020;22:2340-6. https://doi.org/10.1002/ejhf.1783.
- Diop MS, Rudolph JL, Zimmerman KM, Richter MA, Skarf LM. Palliative care interventions for patients with heart failure: a systematic review and meta-analysis. J Palliat Med 2017;20:84-92. https://doi.org/10.1089/jpm.2016.0330.
- Singh GK, Ivynian SE, Davidson PM, Ferguson C, Hickman LD. Elements of integrated palliative care in chronic heart failure across the care continuum: a scoping review. Heart Lung Circ 2022;31:32-41. https://doi.org/10.1016/j.hlc.2021.08.012.
- McConnell T, Diffin J, Fitzsimons D, Harrison C, Stone C, Reid J. Palliative care and heart failure: can implementation science help where the evidence alone has failed?. Eur J Cardiovasc Nurs 2020;19:190-1. https://doi.org/10.1177/1474515119894215.
- Lewin WH, Schaefer KG. Integrating palliative care into routine care of patients with heart failure: models for clinical collaboration. Heart Fail Rev 2017;22:517-24. https://doi.org/10.1007/s10741-017-9599-2.
- United Nations, Department of Economic and Social Affairs, Population Division (2022) . World Population Prospects 2022, Data Sources. UN DESA POP 2022 DC NO. 9 n.d. https://www.un.org/development/desa/pd/content/World-Population-Prospects-2022 (accessed 10 March 2023).
- Braunschweig F, Cowie MR, Auricchio A. What are the costs of heart failure?. Europace 2011;13:ii13-7. https://doi.org/10.1093/europace/eur081.
- Bews HJ, Pilkey JL, Malik AA, Tam JW. Alternatives to hospitalization: adding the patient voice to advanced heart failure management. CJC Open 2023;5:454-62. https://doi.org/10.1016/ j.cjco.2023.03.014.
- Bharani A, Mehta A, Hiensch K, Zeng L, Lala A, Goldstein NE, et al. Referral-based versus embedded-based palliative care consultation models among people hospitalized with heart failure: improving the flow (Sch457). J Pain Symptom Manage 2023;65:e609-10. https://doi.org/10.1016/j.jpainsymman.2023.02.194.
- Hill L, Carson MA, Vitale C. Care plans for the older heart failure patient. Eur Heart J Suppl 2019;21:L32-5. https://doi.org/10.1093/eurheartj/suz243.
- DeGroot L, Pavlovic N, Perrin N, Long Z, Gilotra N, Szanton S, et al. Unmet palliative care needs and quality of life of physically frail adults with heart failure. J Card Fail 2023;29. https://doi.org/10.1016/j.cardfail.2022.10.008.
- McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Bohm M, et al. Corrigendum to: 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: developed by the task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) With the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J 2021;42. https://doi.org/10.1093/eurheartj/ehab670.
- Wong G, Greenhalgh T, Westhorp G, Buckingham J, Pawson R. RAMESES publication standards: realist syntheses. BMC Med 2013;11:1-14. https://doi.org/10.1186/1741-7015-11-21.
- Price T, Wong G, Brennan N, Withers L, Cleland J, Wanner A, et al. Remediation programmes for practising doctors to restore patient safety: the RESTORE realist review. Health Serv Deliv Res 2021;9:995-1010. https://doi.org/10.3310/hsdr09110.
- Papoutsi C, Mattick K, Pearson M, Brennan N, Briscoe S, Wong G. Interventions to improve antimicrobial prescribing of doctors in training (IMPACT): a realist review. Health Serv Deliv Res 2021;6:1-136. https://doi.org/10.3310/hsdr06100.
- Pawson R. Realist Synthesis: New Protocols for Systematic Review. London: SAGE Publications. Ltd; 2006.
- Ziehm J, Farin E, Schäfer J, Woitha K, Becker G, Köberich S. Palliative care for patients with heart failure: facilitators and barriers-a cross sectional survey of German health care professionals. BMC Health Serv Res 2016;16:1-10. https://doi.org/10.1186/s12913-016-1609-x.
- Hill L, Beattie JM, Geller TP, Baruah R, Boyne J, Stolfo GD, et al. Palliative care: essential support for patients with heart failure in the COVID-19 pandemic. Eur J Cardiovasc Nurs 2020;19:469-72. https://doi.org/10.1177/1474515120932814.
- Braun LT, Grady KL, Kutner JS, Adler E, Berlinger N, Boss R, et al. American Heart Association Advocacy Coordinating Committee . Palliative care and cardiovascular disease and stroke: a policy statement from the American Heart Association/American Stroke Association. Circulation 2016;134:e198-225. https://doi.org/10.1161/CIR.0000000000000438.
- Pawson R. The Science of Evaluation: A Realist Manifesto. London: SAGE Publications Ltd; 2013.
- Michie S, Richardson M, Johnston M, Abraham C, Francis J, Hardeman W, et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med 2013;46:81-95. https://doi.org/10.1007/s12160-013-9486-6.
- McConnell T, Blair C, Burden J, Duddy C, Hill L, Howie C, et al. Integrating palliative care and heart failure: a systematic realist synthesis (PalliatHeartSynthesis). Open Heart 2023;10. https://doi.org/10.1136/openhrt-2023-002438.
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Br Med J 2021;10:n71-11. https://doi.org/10.1136/bmj.n71.
- Green E, Gardiner C, Gott M, Ingleton C. Exploring the extent of communication surrounding transitions to palliative care in heart failure: the perspectives of health care professionals. J Palliat Care 2011;27:107-16. https://doi.org/10.1177/082585971102700.
- Shinall MC. The evolving moral landscape of palliative care. Health Aff (Millwood) 2018;37:670-3. https://doi.org/10.1377/hlthaff.2017.1121.
- Higginbotham K, Jones I, Johnson M. A grounded theory study: exploring health care professionals decision making when managing end stage heart failure care. J Adv Nurs 2021;77:3142-55. https://doi.org/10.1111/jan.14852.
- Singh GK, Ferguson C, Davidson PM, Newton PJ. Attitudes and practices towards palliative care in chronic heart failure: a survey of cardiovascular nurses and physicians. Contemp Nurse 2021;57:113-27. https://doi.org/10.1080/10376178.2021.1928522.
- Schichtel M, MacArtney JI, Wee B, Boylan AM. Implementing advance care planning in heart failure: a qualitative study of primary healthcare professionals. Br J Gen Pract 2021;71:e550-60. https://doi.org/10.3399/BJGP.2020.0973.
- Schichtel M, Wee B, Perera R, Onakpoya I, Albury C. Effect of behavior change techniques targeting clinicians to improve advance care planning in heart failure: a systematic review and meta-analysis. Ann Behav Med 2021;55:383-98. https://doi.org/10.1093/abm/kaaa075.
- Harding R, Selman L, Beynon T, Hodson F, Coady E, Read C, et al. Meeting the communication and information needs of chronic heart failure patients. J Pain Symptom Manage 2008;36:149-56. https://doi.org/10.1016/j.jpainsymman.2007.09.012.
- Chattoo S, Atkin KM. Extending specialist palliative care to people with heart failure: semantic, historical and practical limitations to policy guidelines. Soc Sci Med 2009;69:147-53. https://doi.org/10.1016/j.socscimed.2009.02.025.
- Stocker R, Close H, Hancock H, Hungin APS. Should heart failure be regarded as a terminal illness requiring palliative care? A study of heart failure patients’, carers’ and clinicians’ understanding of heart failure prognosis and its management. BMJ Support Palliat Care 2017;7:464-9. https://doi.org/10.1136/bmjspcare-2016-001286.
- Bonares MJ, Mah K, MacIver J, Hurlburt L, Kaya E, Rodin G, et al. Referral practices of cardiologists to specialist palliative care in Canada. CJC Open 2021;3:460-9. https://doi.org/10.1016/j.cjco.2020.12.002.
- Selman L, Harding R, Beynon T, Hodson F, Coady E, Hazeldine C, et al. Improving end-of-life care for patients with chronic heart failure: ‘let’s hope it’ll get better, when I know in my heart of hearts it won’t’. Heart 2007;93:963-7. https://doi.org/10.1136/hrt.2006.106518.
- Chandar M, Brockstein B, Zunamon A, Silverman I, Dlouhy S, Ashlevitz K, et al. Perspectives of health-care providers toward advance care planning in patients with advanced cancer and congestive heart failure. Am J Hosp Palliat Care 2017;34:423-9. https://doi.org/10.1177/1049909116636614.
- Hutchinson RN, Gutheil C, Wessler BS, Prevatt H, Sawyer DB, Han PKJ. What is quality end-of-life care for patients with heart failure? A qualitative study with physicians. J Am Heart Assoc 2020;9. https://doi.org/10.1161/JAHA.120.016505.
- Steitieh D, Sharma N, Singh HS. How technology is changing interventional cardiology. Curr Cardiovasc Risk Rep 2022;16:1-10. https://doi.org/10.1007/s12170-021-00686-4.
- Knoepke CE, Mandrola JM. Don’t be afraid: using an ICD means having difficult conversations. Circ Heart Fail 2019;12. https://doi.org/10.1161/CIRCHEARTFAILURE.119.006289.
- Tokunaga-Nakawatase Y, Ochiai R, Sanjo M, Watabe S, Tsuchihashi-Makaya M, Miyashita M, et al. Perceptions of physicians and nurses concerning advanced care planning for patients with heart failure in Japan. Ann Palliat Med 2020;9:1718-31. https://doi.org/10.21037/apm-19-685.
- Ecarnot F, Meunier-Beillard N, Seronde MF, Chopard R, Schiele F, Quenot JP, et al. End-of-life situations in cardiology: a qualitative study of physicians’ and nurses’ experience in a large university hospital. BMC Palliat Care 2018;17. https://doi.org/10.1186/s12904-018-0366-5.
- Ahluwalia SC, Levin JR, Lorenz KA, Gordon HS. ‘There’s no cure for this condition’: how physicians discuss advance care planning in heart failure. Patient Educ Couns 2013;91:200-5. https://doi.org/10.1016/j.pec.2012.12.016.
- Borbasi S, Wotton K, Redden M, Chapman Y. Letting go: a qualitative study of acute care and community nurses’ perceptions of a ‘good’ versus a ‘bad’ death. Aust Crit Care 2005;18:104-13. https://doi.org/10.1016/S1036-7314(05)80011-6.
- Janssen DJ, Ament SM, Boyne J, Schols JM, Rocca HB, Maessen JM, et al. Characteristics for a tool for timely identification of palliative needs in heart failure: the views of Dutch patients, their families and healthcare professionals. Eur J Cardiovasc Nurs 2020;19:711-20. https://doi.org/10.1177/1474515120918962.
- Schallmo MK, Dudley-Brown S, Davidson PM. Healthcare providers’ perceived communication barriers to offering palliative care to patients with heart failure: an integrative review. J Cardiovasc Nurs 2019;34:E9-E18. https://doi.org/10.1097/JCN.0000000000000556.
- Singh GK, Ferguson C, Hickman LD. Integrating heart failure palliative care delivery in an uncertain disease trajectory. Heart Lung Circ 2022;31:755-6. https://doi.org/10.1016/j.hlc.2022.04.001.
- Hjelmfors L, Mårtensson J, Strömberg A, Sandgren A, Friedrichsen M, Jaarsma T. Communication about prognosis and end-of-life in heart failure care and experiences using a heart failure question prompt list. Int J Environ Res Public Health 2022;19. https://doi.org/10.3390/ijerph19084841.
- Wotton K, Borbasi S, Redden M. When all else has failed: nurses’ perception of factors influencing palliative care for patients with end-stage heart failure. J Cardiovasc Nurs 2005;20:18-25. https://doi.org/10.1097/00005082-200501000-00006.
- Beattie JM, McGregor D, Connolly M. Plus ca change, plus c’est la meme chose? Musings from Montreal. Curr Opin Support Palliat Care 2013;7:1-2. https://doi.org/10.1097/SPC.0b013e32835dbfd5.
- Hupcey JE, Penrod J, Fogg J. Heart failure and palliative care: implications in practice. J Palliat Med 2009;12:531-6. https://doi.org/10.1089/jpm.2009.0010.
- Tomasoni D, Vishram‐Nielsen JK, Pagnesi M, Adamo M, Lombardi CM, Gustafsson F, et al. Advanced heart failure: guideline‐directed medical therapy, diuretics, inotropes, and palliative care. ESC Heart Failure 2022;9:1507-23. https://doi.org/10.1002/ehf2.13859.
- Ament SMC, van den Beuken-Everdingen M, Maessen JMC, Boyne J, Schols JMGA, Stoffers HEJH, et al. Professionals guidance about palliative medicine in chronic heart failure: a mixed-method study. BMJ Support Palliat Care 2020:1-8. https://doi.org/10.1136/bmjspcare-2020-002580.
- Kavalieratos D, Mitchell EM, Carey TS, Dev S, Biddle AK, Reeve BB, et al. ‘Not the “grim reaper service”’: an assessment of provider knowledge, attitudes, and perceptions regarding palliative care referral barriers in heart failure. J Am Heart Assoc 2014;3. https://doi.org/10.1161/JAHA.113.000544.
- Ismail Y, Nightingale AK, Shorthose K. Trainee experiences of delivering end-of-life care in heart failure: key findings of a national survey. Br J Cardiol 2015;22. https://doi.org/10.5837/bjc.2015.008.
- Graham C, Schonnop R, Killackey T, Kavalieratos D, Bush SH, Steinberg L, et al. Exploring health care providers’ experiences of providing collaborative palliative care for patients with advanced heart failure at home: a qualitative study. J Am Heart Assoc 2022;11. https://doi.org/10.1161/JAHA.121.024628.
- Brännström M, Brulin C, Norberg A, Boman K, Strandberg G. Being a palliative nurse for persons with severe congestive heart failure in advanced homecare. Eur J Cardiovasc Nurs 2005;4:314-23. https://doi.org/10.1016/j.ejcnurse.2005.04.007.
- Bouamrane MM, Saunderson KM, Mair F. Manualisation of Models of Caring Together in NHS Greater Glasgow and Clyde FINAL REPORT. British Heart Foundation/Marie Curie Cancer Care; 2014.
- Ament SMC, van den Broek LM, van den Beuken-van Everdingen MHJ, Boyne JJJ, Maessen JMC, Bekkers SCAM, et al. What to consider when implementing a tool for timely recognition of palliative care needs in heart failure: a context-based qualitative study. BMC Palliat Care 2022;21:1-9. https://doi.org/10.1186/s12904-021-00896-y.
- Brännström M, Forssell A, Pettersson B. Physicians’ experiences of palliative care for heart failure patients. Eur J Cardiovasc Nurs 2011;10:64-9. https://doi.org/10.1016/j.ejcnurse.2010.04.005.
- Glogowska M, Simmonds R, McLachlan S, Cramer H, Sanders T, Johnson R, et al. ‘Sometimes we can’t fix things’: a qualitative study of health care professionals’ perceptions of end of life care for patients with heart failure. BMC Palliat Care 2016;15:1-10. https://doi.org/10.1186/s12904-016-0074-y.
- Singh GK, Ramjan L, Ferguson C, Davidson PM, Newton PJ. Access and referral to palliative care for patients with chronic heart failure: a qualitative study of healthcare professionals. J Clin Nurs 2020;29:1576-89. https://doi.org/10.1111/jocn.15222.
- Lum HD, Jones J, Lahoff D, Allen LA, Bekelman DB, Kutner JS, et al. Unique challenges of hospice for patients with heart failure: a qualitative study of hospice clinicians. Am Heart J 2015;170:524-30.e3. https://doi.org/10.1016/j.ahj.2015.06.019.
- Romanò M. Barriers to early utilization of palliative care in heart failure: a narrative review. Healthcare (Basel) 2020;8. https://doi.org/10.3390/healthcare8010036.
- Matsui M. Nurses’ symptom management and views on death and caring for heart failure and chronic obstructive pulmonary disease. Int J Palliat Nurs 2022;28:214-21. https://doi.org/10.12968/ijpn.2022.28.5.214.
- Lewis EF. End of life care in advanced heart failure. Curr Treat Options Cardiovasc Med 2011;13:79-8. https://doi.org/10.1007/s11936-010-0100-y.
- Formiga F, Chivite D, Pujol R. Improving the management of terminal heart failure patients. Am J Med 2005;118:1446-7. https://doi.org/10.1016/j.amjmed.2005.06.031.
- Matsunuma R, Matsumoto K, Yamaguchi T, Sakashita A, Kizawa Y. Comprehensive palliative care needs in outpatients with chronic heart failure: a Japanese cross-sectional study. Palliat Med Rep 2022;3:65-74. https://doi.org/10.1089/pmr.2021.0063.
- Matlock DD, Peterson PN, Sirovich BE, Wennberg DE, Gallagher PM, Lucas FL. Regional variations in palliative care: do cardiologists follow guidelines?. J Palliat Med 2010;13:1315-9. https://doi.org/10.1089/jpm.2010.0163.
- Brännström M, Jaarsma T. Struggling with issues about cardiopulmonary resuscitation (CPR) for end-stage heart failure patients. Scand J Caring Sci 2015;29:379-85. https://doi.org/10.1111/scs.12174.
- Standing H, Exley C, Flynn D, Hughes J, Joyce K, Lobban T, et al. A qualitative study of decision-making about the implantation of cardioverter defibrillators and deactivation during end-of-life care. Health Serv Deliv Res 2016;4:1-150. https://doi.org/10.3310/hsdr04320.
- Crespo‐Leiro MG, Metra M, Lund LH, Milicic D, Costanzo MR, Filippatos G, et al. Advanced heart failure: a position statement of the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail 2018;20:1505-35. https://doi.org/10.1002/ejhf.1236.
- Swetz KM, Cook KE, Ottenberg AL, Chang N, Mueller PS. Clinicians’ attitudes regarding withdrawal of left ventricular assist devices in patients approaching the end of life. Eur J Heart Fail 2013;15:1262-6. https://doi.org/10.1093/eurjhf/hft094.
- McIlvennan CK, Wordingham SE, Allen LA, Matlock DD, Jones J, Dunlay SM, et al. Deactivation of left ventricular assist devices: differing perspectives of cardiology and hospice/palliative medicine clinicians. J Card Fail 2017;23:708-12. https://doi.org/10.1016/j.cardfail.2016.12.001.
- Beattie JM. Withdrawal of life-sustaining medical devices at the end of life. BMJ Support Palliat Care 2013;3:9-10. https://doi.org/10.1136/bmjspcare-2012-000428.
- Waller A, Hobden B, Fakes K, Clark K. A systematic review of the development and implementation of needs-based palliative care tools in heart failure and chronic respiratory disease. Front Cardiovasc Med 2022;9. https://doi.org/10.3389/fcvm.2022.878428.
- Cheang MH, Rose G, Cheung CC, Thomas M. Current challenges in palliative care provision for heart failure in the UK: a survey on the perspectives of palliative care professionals. Open Heart 2015;2. https://doi.org/10.1136/openhrt-2014-000188.
- Hanratty B, Hibbert D, Mair F, May C, Ward C, Capewell S, et al. Doctors’ perceptions of palliative care for heart failure: focus group study. Br Med J 2002;325:581-5. https://doi.org/10.1136/bmj.325.7364.581.
- Tilley D. Improving Utilization of Palliative Care for Heart Failure Patients. Gardner-Webb University; 2022.
- O’Hanlon D, Harding R. Are specialist heart failure nurses currently able to provide palliative care to their patients?. Prog Palliat Care 2011;19:165-71. https://doi.org/10.1179/1743291X11Y.0000000010.
- Gasper AM, Magdic K, Ren D, Fennimore L. Development of a home health-based palliative care program for patients with heart failure. Home Healthc Now 2018;36:84-92. https://doi.org/10.1097/NHH.0000000000000634.
- Barrett M, Connaire K. A palliative care approach in heart failure: knowledge and attitudes of cardiac nurses. Br J Card Nurs 2016;11:136-42. https://doi.org/10.12968/bjca.2016.11.3.136.
- Millerick Y, Armstrong I. Heart failure and palliative care: training needs assessment to guide priority learning of multiprofessionals working across different care settings. Curr Opin Support Palliat Care 2015;9:31-7. https://doi.org/10.1097/SPC.0000000000000113.
- Singh GK, Davidson PM, Macdonald PS, Newton PJ. The perspectives of health care professionals on providing end of life care and palliative care for patients with chronic heart failure: an integrative review. Heart Lung Circ 2019;28:539-52. https://doi.org/10.1016/j.hlc.2018.10.009.
- Singh GK, Ivynian SE, Ferguson C, Davidson PM, Newton PJ. Palliative care in chronic heart failure: a theoretically guided, qualitative meta-synthesis of decision-making. Heart Fail Rev 2020;25:457-67. https://doi.org/10.1007/s10741-019-09910-1.
- Howlett J, Morin L, Fortin M, Heckman G, Strachan PH, Suskin N, et al. End-of-life planning in heart failure: it should be the end of the beginning. Can J Cardiol 2010;26:135-41. https://doi.org/10.1016/s0828-282x(10)70351-2.
- Buck HG, Zambroski CH. Upstreaming palliative care for patients with heart failure. J Cardiovasc Nurs 2012;27:147-53. https://doi.org/10.1097/JCN.0b013e318239f629.
- Kavalieratos D. Exploring the Role of Palliative Care in Heart Failure: Referral Barriers, Care Gaps, and Quality of Care. Department of Health Policy and Management, University of North Carolina at Chapel Hill; 2012.
- Bierle RS, Vuckovic KM, Ryan CJ. Integrating palliative care into heart failure management. Crit Care Nurse 2021;41:e9-e18. https://doi.org/10.4037/ccn2021877.
- Ziehm J, Farin E, Seibel K, Becker G, Köberich S. Health care professionals’ attitudes regarding palliative care for patients with chronic heart failure: an interview study. BMC Palliat Care 2016;15:1-8. https://doi.org/10.1186/s12904-016-0149-9.
- Namukwaya E, Grant L, Downing J, Leng M, Murray SA. Improving care for people with heart failure in Uganda: serial in-depth interviews with patients’ and their health care professionals. BMC Res Notes 2017;10. https://doi.org/10.1186/s13104-017-2505-0.
- Brännström M, Fischer Gronlund C, Zingmark K, Soderberg A. Meeting in a ‘free-zone’: clinical ethical support in integrated heart-failure and palliative care. Eur J Cardiovasc Nurs 2019;18:577-83. https://doi.org/10.1177/1474515119851621.
- Baik D, Leung PB, Sterling MR, Russell D, Jordan L, Silva AF, et al. Eliciting the educational needs and priorities of home care workers on end-of-life care for patients with heart failure using nominal group technique. Palliat Med 2021;35:977-82. https://doi.org/10.1177/0269216321999963.
- Zapka JG, Hennessy W, Carter RE, Amella EJ. End-of-life communication and hospital nurses: an educational pilot. J Cardiovasc Nurs 2006;21:223-31. https://doi.org/10.1097/00005082-200605000-00011.
- Johnson MJ, McSkimming P, McConnachie A, Geue C, Millerick Y, Briggs A, et al. The feasibility of a randomised controlled trial to compare the cost-effectiveness of palliative cardiology or usual care in people with advanced heart failure: two exploratory prospective cohorts. Palliat Med 2018;32:1133-41. https://doi.org/10.1177/0269216318763225.
- Selman L, Harding R, Beynon T, Hodson F, Hazeldine C, Coady E, et al. Modelling services to meet the palliative care needs of chronic heart failure patients and their families: current practice in the UK. Palliat Med 2007;21:385-90. https://doi.org/10.1177/0269216307077698.
- Boyd KJ, Worth A, Kendall M, Pratt R, Hockley J, Denvir M, et al. Making sure services deliver for people with advanced heart failure: a longitudinal qualitative study of patients, family carers, and health professionals. Palliat Med 2009;23:767-76. https://doi.org/10.1177/0269216309346541.
- Westlake C, Smith VJ. Nursing concerns with palliative care and at the end-of-life in patients with heart failure. Dove Press 2015;5:33-47. https://doi.org/10.2147/NRR.S45298.
- Ryder M, Beattie JM, O’Hanlon R, McDonald K. Multidsciplinary heart failure management and end of life care. Curr Opin Support Palliat Care 2011;5:317-21. https://doi.org/10.1097/SPC.0b013e32834d749e.
- Addington-Hall JM, Gibbs JSR. Heart Failure Now on the Palliative Care Agenda. Thousand Oaks, CA: SAGE Publications Ltd; 2000.
- Crousillat DR, Keeley BR, Buss MK, Zheng H, Polk DM, Schaefer KG. Palliative care education in cardiology. J Am Coll Cardiol 2018;71:1391-4. https://doi.org/10.1016/j.jacc.2018.02.019.
- Kim C, Kim S, Lee K, Choi J, Kim S. Palliative care for patients with heart failure: an integrative review. J Hosp Palliat Nurs 2022;24:E151-8. https://doi.org/10.1097/NJH.0000000000000869.
- Constantine A, Condliffe R, Clift P, Tulloh R, Dimopoulos K, Committee CS. Palliative care in pulmonary hypertension associated with congenital heart disease: systematic review and expert opinion. ESC Heart Fail 2021;8:1901-14. https://doi.org/10.1002/ehf2.13263.
- Sebern MD, Sulemanjee N, Sebern MJ, Garnier-Villarreal M, Whitlatch CJ. Does an intervention designed to improve self-management, social support and awareness of palliative-care address needs of persons with heart failure, family caregivers and clinicians?. J Clin Nurs 2018;27:e643-57. https://doi.org/10.1111/jocn.14115.
- Dunlay SM, Foxen JL, Cole T, Feely MA, Loth AR, Strand JJ, et al. A survey of clinician attitudes and self-reported practices regarding end-of-life care in heart failure. Palliat Med 2015;29:260-7. https://doi.org/10.1177/0269216314556565.
- LeMond L, Goodlin SJ. Management of heart failure in patients nearing the end of life-there is so much more to do. Card Fail Rev 2015;1:31-4. https://doi.org/10.15420/cfr.2015.01.01.31.
- Kaasalainen S, Strachan PH, Brazil K, Marshall D, Willison K, Dolovich L, et al. Managing palliative care for adults with advanced heart failure. Can J Nurs Res 2011;43:38-57.
- Russell D, Luth EA, Baik D, Jordan L, Creber RM. On board: interdisciplinary team member perspectives of how patients with heart failure and their families navigate hospice care. J Hosp Palliat Nurs 2020;22:351-8. https://doi.org/10.1097/NJH.0000000000000673.
- Abedini NC, Guo G, Hummel SL, Bozaan D, Beasley M, Cowger J, et al. Factors influencing palliative care referral for hospitalised patients with heart failure: an exploratory, randomised, multi-institutional survey of hospitalists and cardiologists. BMJ Open 2020;10. https://doi.org/10.1136/bmjopen-2020-040857.
- Ivany E, While A. Understanding the palliative care needs of heart failure patients. Br J Community Nurs 2013;18:441-5. https://doi.org/10.12968/bjcn.2013.18.9.441.
- Dionne-Odom JN, Kono A, Frost J, Jackson L, Ellis D, Ahmed A, et al. Translating and testing the ENABLE: CHF-PC concurrent palliative care model for older adults with heart failure and their family caregivers. J Palliat Med 2014;17:995-1004. https://doi.org/10.1089/jpm.2013.0680.
- Gelfman LP, Kalman J, Goldstein NE. Engaging heart failure clinicians to increase palliative care referrals: overcoming barriers, improving techniques. J Palliat Med 2014;17:753-60. https://doi.org/10.1089/jpm.2013.0675.
- Quinn KL, Stukel TA, Campos E, Graham C, Kavalieratos D, Mak S, et al. Regional collaborative home-based palliative care and health care outcomes among adults with heart failure. Can Med Assoc J 2022;194:E1274-82. https://doi.org/10.1503/cmaj.220784.
- George S, Leasure AR. Application of transformational leadership principles in the development and integration of palliative care within an advanced heart failure program. Dimens Crit Care Nurs 2016;35:59-65. https://doi.org/10.1097/DCC.0000000000000166.
- Hendricks-Ferguson VL, Stallings DT. Case study of an African American woman with heart failure: ethical and palliative care considerations. J Hosp Palliat Nurs 2022;24:225-31. https://doi.org/10.1097/NJH.0000000000000865.
- Davidson PM, Paull G, Introna K, Cockburn J, Davis JM, Rees D, et al. Integrated, collaborative palliative care in heart failure: the St. George Heart Failure Service experience 1999–2002. J Cardiovasc Nurs 2004;19:68-75. https://doi.org/10.1097/00005082-200401000-00011.
- McCambridge J, Keane C, Walshe M, Campbell P, Heyes J, Kalra PR, et al. The prehospital patient pathway and experience of care with acute heart failure: a comparison of two health care systems. ESC Heart Fail 2021;8:1076-84. https://doi.org/10.1002/ehf2.13089.
- Stevenson MH, McPherson A, Tavares C, Groninger HR. Polypharmacy in palliative care for advanced heart failure: the PAL-HF experience. J Card Fail 2022;28:1382-3. https://doi.org/10.1016/j.cardfail.2022.04.010.
- Roikjaer SG, Timm H, Simonÿ C. First steps to integrate general palliative care into a cardiac hospital setting–using dialogue‐based workshops. Scand J Caring Sci 2022;36:203-14. https://doi.org/10.1111/scs.12978.
- Waterworth S, Gott M. Involvement of the practice nurse in supporting older people with heart failure: GP perspectives. Prog Palliat 2012;20:12-7. https://doi.org/10.1179/1743291X11Y.0000000019.
- Hjelmfors L, van der Wal MHL, Friedrichsen MJ, Martensson J, Stromberg A, Jaarsma T. Patient-nurse communication about prognosis and end-of-life care. J Palliat Med 2015;18:865-71. https://doi.org/10.1089/jpm.2015.0037.
- Granger BB, Tulsky JA, Kaufman BG, Clare RM, Anstrom K, Mark DB, et al. Polypharmacy in palliative care for advanced heart failure: the PAL-HF experience. J Card Fail 2022;28:334-8. https://doi.org/10.1016/j.cardfail.2021.08.021.
- McPherson A, Nguyen C, Groninger H, Anderson KM, Henderson P, Rao A. Continuous intravenous inotropic support for advanced heart failure: palliative considerations. J Pain Palliat Care Pharmacother 2022;36:59-67. https://doi.org/10.1080/15360288.2022.2050456.
- Clarke LM. A Qualitative Analysis of the Experiences of Heart Failure Specialist Nurses Working with Patients with End Stage Heart Failure. University of Leicester; 2009.
- McDonagh TA, Blue L, Clark AL, Dahlstrom U, Ekman I, Lainscak M, et al. European Society of Cardiology Heart Failure Association Committee on Patient Care . European Society of Cardiology Heart Failure Association Standards for delivering heart failure care. Eur J Heart Fail 2011;13:235-41. https://doi.org/10.1093/eurjhf/hfq221.
- Kogan AC, Kraus K, Olsen B, Bandini JI, Ahluwalia SC. Clinician perspectives on group visits for advance care planning among caregivers and older adult patients with heart failure. J Am Board Fam Med 2021;34:375-86. https://doi.org/10.3122/jabfm.2021.02.200270.
- Low J, Pattenden J, Candy B, Beattie JM, Jones L. Palliative care in advanced heart failure: an international review of the perspectives of recipients and health professionals on care provision. J Card Fail 2011;17:231-52. https://doi.org/10.1016/j.cardfail.2010.10.003.
- Blum M, Gelfman LP, McKendrick K, Pinney SP, Goldstein NE. Enhancing palliative care for patients with advanced heart failure through simple prognostication tools: a comparison of the surprise question, the number of previous heart failure hospitalizations, and the Seattle heart failure model for predicting 1-year survival. Front Cardiovasc Med 2022;9. https://doi.org/10.3389/fcvm.2022.836237.
- Waller A, Girgis A, Davidson PM, Newton PJ, Lecathelinais C, Macdonald PS, et al. Facilitating needs-based support and palliative care for people with chronic heart failure: preliminary evidence for the acceptability, inter-rater reliability, and validity of a needs assessment tool. J Pain Symptom Manage 2013;45:912-25. https://doi.org/10.1016/j.jpainsymman.2012.05.009.
- Kane PM, Ellis-Smith CI, Daveson BA, Ryan K, Mahon NG, McAdam B, et al. BuildCARE . Understanding how a palliative-specific patient-reported outcome intervention works to facilitate patient-centred care in advanced heart failure: a qualitative study. Palliat Med 2018;32:143-55. https://doi.org/10.1177/0269216317738161.
- Anscombe R, Middlemiss T. Palliative care in end-stage heart failure: experience of a collaborative approach in a secondary care setting. Intern Med J 2019;49:404-7. https://doi.org/10.1111/imj.14218.
- Egídio de Sousa I, Pedroso A, Chambino B, Roldão M, Pinto F, Guerreiro R, et al. Palliative care in heart failure: challenging prognostication. Cureus 2021;13. https://doi.org/10.7759/cureus.18301.
- Gelfman LP, Kavalieratos D, Teuteberg WG, Lala A, Goldstein NE. Primary palliative care for heart failure: what is it? How do we implement it?. Heart Fail Rev 2017;22:611-20. https://doi.org/10.1007/s10741-017-9604-9.
- Brennan EJ. Chronic heart failure nursing: integrated multidisciplinary care. Br J Nurs 2018;27:681-8. https://doi.org/10.12968/bjon.2018.27.12.681.
- Chang YK, Allen LA, McClung JA, Denvir MA, Philip J, Mori M, et al. Criteria for referral of patients with advanced heart failure for specialized palliative care. J Am Coll Cardiol 2022;80:332-44. https://doi.org/10.1016/j.jacc.2022.04.057.
- Kim S, Hwang WJ. Palliative care for those with heart failure: nurses’ knowledge, attitude, and preparedness to practice. Eur J Cardiovasc Nurs 2014;13:124-33. https://doi.org/10.1177/1474515113519521.
- Kuragaichi T, Kurozumi Y, Ohishi S, Sugano Y, Sakashita A, Kotooka N, et al. Nationwide survey of palliative care for patients with heart failure in Japan. Circ J 2018;82:1336-43. https://doi.org/10.1253/circj.CJ-17-1305.
- DeGroot L, Koirala B, Pavlovic N, Nelson K, Allen J, Davidson P, et al. Outpatient palliative care in heart failure: an integrative review. J Palliat Med 2020;23:1257-69. https://doi.org/10.1089/jpm.2020.0031.
- Shanafelt TD, Schein E, Minor LB, Trockel M, Schein P, Kirch D. Healing the professional culture of medicine. Mayo Clin Proc 2019;94:1556-66. https://doi.org/10.1016/j.mayocp.2019.03.026.
- Steitieh D, Zaidi A, Xu S, Cheung JW, Feldman DN, Reisman M, et al. Racial disparities in access to high-volume mitral valve transcatheter edge-to-edge repair centers. J Soc Cardiovasc Angiography Interv 2022;1. https://doi.org/10.1016/j.jscai.2022.100398.
- Davis JE. Biomedicine and Its Cultural Authority 2016. https://thenewatlantis.com/wp-content/uploads/legacy-pdfs/201606101_TNA48Davis.pdf (accessed 4 May 2023).
- Jaarsma T, Beattie JM, Ryder M, Rutten FH, McDonagh T, Mohacsi P, et al. Advanced Heart Failure Study Group of the HFA of the ESC . Palliative care in heart failure: a position statement from the palliative care workshop of the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail 2009;11:433-43. https://doi.org/10.1093/eurjhf/hfp041.
- Steiner B, Neumann A, Pelz Y, Ski CF, Hill L, Thompson DR, et al. Challenges in heart failure care in four European countries: a comparative study. Eur J Public Health 2023;33:448-54. https://doi.org/10.1093/eurpub/ckad059.
- Uchmanowicz I, Hoes A, Perk J, McKee G, Svavarsdóttir MH, Czerwińska-Jelonkiewicz K, et al. Optimising implementation of European guidelines on cardiovascular disease prevention in clinical practice: what is needed?. Eur J Prev Cardiol 2021;28:426-31. https://doi.org/10.1177/2047487320926776.
- Young AE, Davies A, Bland S, Brookes S, Blazeby JM. Systematic review of clinical outcome reporting in randomised controlled trials of burn care. BMJ Open 2019;9. https://doi.org/10.1136/bmjopen-2018-025135.
- Kane SS, Gerretsen B, Scherpbier R, Dal Poz M, Dieleman M. A realist synthesis of randomised control trials involving use of community health workers for delivering child health interventions in low and middle income countries. BMC Health Serv Res 2010;10:1-7. https://doi.org/10.1186/1472-6963-10-286.
- Bekelman DB, Rabin BA, Nowels CT, Sahay A, Heidenreich PA, Fischer SM, et al. Barriers and facilitators to scaling up outpatient palliative care. J Palliat Med 2016;19:456-9. https://doi.org/10.1089/jpm.2015.0280.
- Schichtel M, Wee B, MacArtney JI, Collins S. Clinician barriers and facilitators to heart failure advance care plans: a systematic literature review and qualitative evidence synthesis. BMJ Support Palliat Care 2019;12:e1-9. https://doi.org/10.1136/bmjspcare-2018-001747.
- Schallmo M, Dudley-Brown S, Davidson P. Nurses’ knowledge, attitude, and confidence in delivering palliative care for hospitalized patients with heart failure: an integrative review. J Pain Symptom Manage 2019;55:659-60. https://doi.org/10.1016/j.jpainsymman.2017.12.361.
- Kavalieratos D, Gelfman LP, Tycon LE, Riegel B, Bekelman DB, Ikejiani DZ, et al. Palliative care in heart failure: rationale, evidence, and future priorities. J Am Coll Cardiol 2017;70:1919-30. https://doi.org/10.1016/j.jacc.2017.08.036.
- Curtis BR, Rollman BL, Belnap BH, Jeong K, Yu L, Harinstein ME, et al. Perceptions of need for palliative care in recently hospitalized patients with systolic heart failure. J Pain Symptom Manage 2021;62:1252-61. https://doi.org/10.1016/j.jpainsymman.2021.06.001.
- Villalobos JP, Bull SS, Portz JD. Usability and acceptability of a palliative care mobile intervention for older adults with heart failure and caregivers: observational study. JMIR Aging 2022;5. https://doi.org/10.2196/35592.
- Graven LJ, Abbott L, Schluck G. The coping in heart failure (COPE-HF) partnership intervention for heart failure symptoms: implications for palliative care. Prog Palliat Care 2022;31:169-78. https://doi.org/10.1080/09699260.2022.2124144.
Appendix 1 Search strategies
Main searches
MEDLINE
Host: Ovid
Data parameters: MEDLINE Epub Ahead of Print, In-Process & Other Non-Indexed Citations, Ovid MEDLINE Daily and Ovid MEDLINE
Date range searched: 1946 to present (Daily update)
Date searched: 11 November 2021
Searcher: CD
Hits: n = 842
| 1 | exp *Heart Failure/ | 104,436 |
|---|---|---|
| 2 | heart failure.ti | 77,005 |
| 3 | cardiac failure.ti | 2226 |
| 4 | or/1-3 | 117,436 |
| 5 | *Palliative Care/ | 33,835 |
| 6 | *Palliative Medicine/ | 352 |
| 7 | *‘Hospice and Palliative Care Nursing’/ | 1313 |
| 8 | *Hospices/ | 3946 |
| 9 | *terminal care/or hospice care/ | 27,184 |
| 10 | *Terminally Ill/ | 3921 |
| 11 | palliat*.ti | 30,880 |
| 12 | end of life.ti | 12,006 |
| 13 | terminal care.ti | 771 |
| 14 | hospice*.ti | 6860 |
| 15 | supportive care.ti | 2043 |
| 16 | or/5-15 | 73,905 |
| 17 | 4 and 16 | 842 |
EMBASE
Host: Ovid
Date range searched: 1974 to present (Daily update)
Date searched: 11 November 2021
Searcher: CD
Hits: n = 1219
| 1 | exp *heart failure/ | 232,486 |
|---|---|---|
| 2 | heart failure.ti | 121,813 |
| 3 | cardiac failure.ti | 2552 |
| 4 | or/1-3 | 239,376 |
| 5 | *palliative therapy/ | 37,650 |
| 6 | *hospice/ | 6293 |
| 7 | exp *terminal care/ | 39,032 |
| 8 | exp *terminally ill patient/ | 3118 |
| 9 | palliat*.ti | 44,147 |
| 10 | end of life.ti | 15,823 |
| 11 | terminal care.ti | 817 |
| 12 | hospice*.ti | 8308 |
| 13 | supportive care.ti | 3716 |
| 14 | or/5-13 | 101,105 |
| 15 | 4 and 14 | 1219 |
PsycInfo
Host: Ovid
Date range searched: 1806 to present (weekly update)
Date searched: 11 November 2021
Searcher: CD
Hits: n = 153
| 1 | *heart disorders/ | 8637 |
|---|---|---|
| 2 | heart failure.ti | 1906 |
| 3 | cardiac failure.ti | 12 |
| 4 | or/1-3 | 8847 |
| 5 | exp *palliative care/ | 13,835 |
| 6 | exp *hospice/ | 2954 |
| 7 | *terminally ill patients/ | 3587 |
| 8 | palliat*.ti | 6070 |
| 9 | end of life.ti | 4141 |
| 10 | terminal care.ti | 92 |
| 11 | hospice*.ti | 2227 |
| 12 | supportive care*.ti | 306 |
| 13 | or/5-12 | 19,250 |
| 14 | 4 and 13 | 153 |
AMED (Allied and Complementary Medicine)
Host: Ovid
Date range searched: 1985 to November 2021 (Monthly update)
Date searched: 11 November 2021
Searcher: CD
Hits: n = 112
| 1 | heart failure congestive/ | 479 |
|---|---|---|
| 2 | heart failure.ti | 553 |
| 3 | cardiac failure.ti | 6 |
| 4 | or/1-3 | 613 |
| 5 | palliative care/ | 6653 |
| 6 | hospices/ | 394 |
| 7 | exp terminal care/ | 5589 |
| 8 | terminal illness/ | 2961 |
| 9 | palliat*.ti | 7421 |
| 10 | end of life.ti | 2470 |
| 11 | terminal care.ti | 138 |
| 12 | hospice*.ti | 1995 |
| 13 | supportive care.ti | 131 |
| 14 | or/5-13 | 16,334 |
| 15 | 4 and 14 | 112 |
CINAHL
Host: EBSCOhost
Date range searched: Unknown (from database inception to present)
Date searched: 11 November 2021
Searcher: CD
Hits: n = 742
| S1 | MM ‘Heart Failure’ | 34,996 |
|---|---|---|
| S2 | TI ‘heart failure’ | 32,976 |
| S3 | TI ‘“cardiac failure’ | 254 |
| S4 | S1 OR S2 OR S3 | 44,106 |
| S5 | MM ‘Palliative Medicine’ | 29 |
| S6 | MM ‘Hospice and Palliative Nursing’ | 3665 |
| S7 | MM ‘Hospices’ | 1686 |
| S8 | MM ‘Terminal Care+’ | 50,499 |
| S9 | MM ‘Terminally Ill Patients+’ | 7832 |
| S10 | TI palliat* | 24,439 |
| S11 | TI ‘end of life” OR “end-of-life’ | 12,284 |
| S12 | TI ‘terminal care’ | 223 |
| S13 | TI hospice* | 7785 |
| S14 | TI ‘supportive care’ | 1464 |
| S15 | S5 OR S6 OR S7 OR S8 OR S9 OR S10 OR S11 OR S12 OR S13 OR S14 | 68,172 |
| S16 | S4 AND S15 | 742 |
HMIC (Health Management Information Consortium)
Host: Ovid
Date range searched: 1979 to September 2021 (Bimonthly update)
Date searched: 11 November 2021
Searcher: CD
Hits: n = 34
| 1 | heart failure.ti | 376 |
|---|---|---|
| 2 | cardiac failure.ti | 10 |
| 3 | 1 or 2 | 386 |
| 4 | palliative care/ | 2436 |
| 5 | exp ‘End of life care’/ | 1000 |
| 6 | hospices/ | 541 |
| 7 | hospice care/ | 163 |
| 8 | exp terminal care/ | 994 |
| 9 | terminal care hospitals/ | 29 |
| 10 | terminal illness/ | 716 |
| 11 | palliat*.ti | 1239 |
| 12 | end of life.ti | 912 |
| 13 | terminal care.ti | 76 |
| 14 | hospice*.ti | 424 |
| 15 | supportive care.ti | 23 |
| 16 | or/4-15 | 4111 |
| 17 | 3 and 16 | 34 |
OpenGrey
Host: www.opengrey.eu (now archived)
Date range searched: Unknown (from database inception to present)
Date searched: 12 November 2021
Searcher: CD
Hits: n = 3
‘heart failure’ AND (palliat* OR hospice* OR ‘end of life’ OR ‘terminal care’ OR ‘supportive care’)
NICE Evidence search
Host: www.evidence.nhs.uk (now closed)
Date range searched: Unknown (from database inception to present)
Date searched: 12 November 2021
Searcher: CD
Hits: n = 1290 (Screened first 500 ‘on screen’, ranked by relevance)
‘heart failure’ AND (palliat* OR hospice* OR ‘end of life’ OR ‘terminal care’ OR ‘supportive care’)
Host: www.google.com (Incognito window)
Date range searched: Unknown (from database inception to present)
Date searched: 12 November 2021
Searcher: CD
Hits: n = 143 (20,200,00 estimated; viewing 100 per page and screening ‘on screen’ only 143 were available to review)
‘heart failure’ AND (palliative OR hospice OR ‘end of life’ OR ‘terminal care’ OR ‘supportive care’)
Appendix 2 Characteristics of all included studies
| Authors | Year of publication | Country | Type of paper | Aim(s) | Study design/methods | Sample/setting |
|---|---|---|---|---|---|---|
| Anscombe and Middlemiss160 | 2019 | New Zealand | Personal Viewpoint | To discuss the authors experiences of working in a collaborative approach to PC in HF in their hospital’s cardiology supportive care clinic | N/A | Hospital cardiology secondary care setting |
| Shinall56 | 2018 | USA | Case study | To discuss a case around EoL care with an individual with HF and ventricular assist device, and associated ethical issues | Case study | Hospital setting |
| Clarke153 | 2009 | UK | Thesis | To identify and explore the experiences of HF specialist nurses who work with patients with end stage HF, to understand how such experiences affected nurses, how they approached their work, and how they were supported | Qualitative design | Community-based HF specialist nurses |
| Knoepke and Mandrola69 | 2019 | USA | Editorial | To discuss issues around conversations that should be conducted relating to ICDs and physicians’ responsibilities with this | Editorial paper | N/A |
| Tokunaga-Nakawatase et al.70 | 2020 | Japan | Research | To investigate the perceptions of physicians and nurses concerning ACP for patients with HF | Surveys via self-report questionnaire | Physicians and nurses who belonged to certified institutions for ICD and/or CRT |
| Swetz et al.102 | 2013 | International | Research | To study the attitudes and practices of HF clinicians regarding withdrawal of LVAD support in patients approaching death | Web-based surveys using self-report questionnaire | Members of the European Society of Cardiology-HF Association (ESC-HFA), International Society for Heart and Lung Transplantation (ISHLT) and the HFSA |
| Dunlay et al.134 | 2015 | USA | Research | To examine clinicians’ practices, expectations, and personal level of confidence in discussing goals of care and providing EoL care to their patients | Surveys via self-report questionnaire | Physicians, nurse practitioners/physician assistant from tertiary care, and community cardiology and primary care settings |
| Barrett and Connaire111 | 2016 | Ireland | Research | Examined the knowledge and attitudes of cardiac nurses of a PC approach when caring for patients who have HF | Surveys via self-report questionnaire | Cardiac nurses from three large university hospitals |
| Abedini et al.138 | 2020 | USA | Research | To identify factors influencing cardiologists’ and hospitalists’ decisions regarding PC referral among hospitalised patients with advanced HF | Vignette- based survey | Hospitalists and cardiologists, including fellows, attendings, nurse practitioners, and physicians’ assistants from academic, veteran’s affairs, community, and other settings |
| Green et al.55 | 2011 | UK | Research | To assess, from the HCPs’ perspective, the extent of communication between patients who have HF and HCPs regarding transitions to a PC approach | Qualitative design | PC/cardiology/care-of-the-elderly consultants, cardiology/PC registrars, general hospital nurses, PC clinical nurse specialists, and HF clinical nurse specialists from a range of care settings |
| Ziehm et al.119 | 2016 | Germany | Research | To evaluate healthcare providers´ (nurses and physicians) attitudes towards and experiences with PC for patients with CHF in order to identify barriers and facilitators and hence develop recommendations for improvement of those patients’ access to PC | Qualitative design | Healthcare professionals including hospital/outpatient/HF/PC/palliative nurses and cardiologists resident/hospital and GPs from hospital and community settings |
| Cheang et al.106 | 2015 | UK | Research | To investigate the reasons for the perceived underutilisation of PC services throughout the UK and identify if there are significant problems with current provision of PC for HF | Prospective online survey study | Healthcare professionals including consultants, clinical nurse specialists, other PC nurses, and non-consultant doctors from hospital, community, and hospice settings |
| Kim and Hwang165 | 2014 | South Korea | Research | To describe nurses’ knowledge and attitude regarding clinical PC, and to evaluate how knowledge of, and attitude towards, PC in nurses influence their clinical practice of PC | Cross-sectional descriptive design | Nursing staff based in cardiovascular inpatient/intensive care/outpatient units from two tertiary university hospitals |
| Schichtel et al.59 | 2021 | England | Research | To explore the views of primary care HCPs on how to improve their engagement with ACP in HF | Qualitative design | Healthcare professionals including GPs and general practice/HF specialist/district nurses from primary care settings in one region of England |
| Baik et al.122 | 2021 | USA | Research | To elicit the educational needs and priorities of home care workers caring for community dwelling adults with HF at the EoL | Nominal group technique involving a semi-quantitative structured group process and point rating system | Home care workers from a non-profit training and education organisation within one city |
| Higginbotham et al.57 | 2021 | England | Research | To explore how healthcare professionals in an acute medical setting make decisions when managing the care of patients diagnosed with NYHA III and NYHA IV HF, and how these decisions impact directly on the patient’s EoL experience | Qualitative design | Healthcare professionals including staff nurses from acute medicine/respiratory acute medicine/cardiology/medical assessment, and doctors including foundation year/specialty trainee/specialist registrar years 1 and 2/consultants from a range of clinical specialisms including cardiology/care of elderly/emergency department/PC. Patients with NYHA III and IV. Setting – acute medicine department in a district hospital |
| Singh et al.58 | 2021 | Australia and New Zealand | Research | To determine the attitudes of cardiovascular HCPs towards EoL care and its impact on specialist PC referral and to determine the association between EoL attitudes and the cardiovascular healthcare professionals’ self-reported delivery of supportive care and the HCPs’ characteristics | Online self-report questionnaires | Cardiovascular HCPs including physicians, nurses, and allied healthcare professionals from both metropolitan and rural locations of work |
| Bonares et al.64 | 2021 | Canada | Research | To determine the referral practices of cardiologists to SPC | Self-report survey | Cardiologists from general cardiology, critical care, transplant medicine, congenital heart disease, HF, electrophysiology, mechanical assistive devices and paediatric cardiology working within academic centres, community hospitals and private practice |
| Hutchinson et al.67 | 2020 | USA | Research | To explore how physicians (cardiologists and primary care physicians) define high-quality EOL care for patients with AHF, and what barriers they encounter in delivering such care | Qualitative design | Physicians including general cardiologists, electrophysiology, and HF specialists from rural, semirural and urban practice settings |
| Brännström and Jaarsma99 | 2015 | Sweden | Research | To describe the experiences and thoughts of members of an integrated HF and PC team concerning talking about cardiopulmonary resuscitation with patients who have end-stage HF | Qualitative design | HCPs including cardiologists, general practitioner specialised in palliative medicine, district nurses, HF nurse specialised in PC, occupational therapist physiotherapist from one community hospital |
| Stocker et al.63 | 2017 | England | Research | To explore experiences of giving or receiving a prognosis and advanced PC planning (ACP) for those with HF | Qualitative design | Patients, carers and healthcare professionals including specialists, GPs and specialist HF nurses from domiciliary and secondary care settings |
| Bekelman et al.176 | 2016 | USA | Research article | To understand organisational factors that could influence the adoption and scale-up of outpatient PC in chronic advanced illness, using the example of HF | Qualitative design | Healthcare professionals including primary care staff, primary care providers, cariology clinicians (physicians, advanced practice nurses), chiefs of service, regional and national leadership from the local, regional and national health system |
| Zapka et al.123 | 2006 | USA | Research article | To describe a pilot educational seminar and participants’ ratings of (a) their skills related to EoL care, (b) their attitudes about EoL care and (c) the participants’ most recent experience with a patient’s death | Pretest and post-test design | HCPs including nursing and other staff from cardiology and general medicine within the hospital setting |
| Borbasi et al.73 | 2005 | Australia | Research | To explore the views of nurses on EoL care for patients with ESHF | Qualitative design | Registered nurses, clinical nurse consultants, clinical nurses and nurse managers from three acute care sites and palliative community/hospice settings |
| Kaasalainen et al.136 | 2011 | Canada | Research | To explore the care processes experienced by community-dwelling adults dying from advanced HF, their family caregivers, and their health-care providers | Qualitative design | Patients with advanced HF, informal caregivers, nurses, physicians and pharmacists from a community setting |
| Harding et al.61 | 2008 | UK | Research | To generate recommendations for the appropriate provision of feasible and acceptable information to patients who have CHF and their family carers, in line with UK and international policy guidelines | Qualitative design | Cardiology staff, PC staff, patients and families at one tertiary hospital |
| Glogowska et al.90 | 2016 | England | Research | To explore the perceptions and experiences of HCPs working with patients with HF around EoL care | Qualitative design | HCPs including GPs, cardiologists, care of the elderly physicians, psychiatrists, specialist HF nurses, cardiac rehabilitation manager/practitioner and community matron from primary, secondary and community care settings |
| Brännström et al.86 | 2005 | Sweden | Research | To illuminate the meaning of being a palliative nurse for persons with CHF in advanced homecare as disclosed through nurses’ narratives | Qualitative design | All registered nurses within one unit for advanced palliative homecare based at a county hospital |
| Ismail et al.84 | 2015 | UK | Research | To evaluate the confidence of trainee doctors in managing EoL issues in HF | Online survey | Cardiologists in training across the range of different specialties, including interventional cardiology, electrophysiology, cardiac imaging, adult congenital heart disease, HF and device implantation, as well as academic trainees |
| Hjelmfors et al.150 | 2015 | Sweden and Netherlands | Research | To explore how often and why HF nurses in outpatient clinics discuss prognosis and EoL care in the context of patient education | Descriptive and comparative study | HF registered nurse–patient conversations from hospital-based HF clinics, public healthcare centres with an HF service, hospital-based HF clinics |
| Wotton et al.78 | 2005 | Australia | Research | To describe registered nurses’ perceptions of factors influencing care for patients in the palliative phase of end-stage HF | Qualitative design | HCPs’ experience in cardiac and PC including registered nurses, clinical nurse consultants, clinical nurses and nurse managers from hospital and community settings |
| Lum et al.92 | 2015 | USA | Research | To enhance understanding of the perspectives of hospice clinicians regarding the unique needs of patients with HF related to transitioning from life-prolonging to comfort-focused care, the role and availability of cardiac therapies in the hospice setting, and opportunities to improve care for hospice patients with HF | Qualitative design | Hospice HCPs, including physicians, advanced practice nurses and nurses |
| Ecarnot et al.71 | 2018 | France | Research | To describe the perceptions and attitudes of physicians, nurses and nurses’ aides in cardiology regarding EoL situations | Qualitative design | HCPs including physicians, nurses and nurses’ aides from one cardiology department in teaching hospital |
| Matlock et al.98 | 2010 | USA | Research | To examine whether an association existed between cardiologists’ tendencies to discuss PC for patients with advanced HF and the regional use of health care in the last 6 months of life | Postal survey | Cardiology physicians from specialties including general cardiology, invasive, interventional and electrophysiology |
| Ament et al.82 | 2020 | Netherlands | Research | To develop a comprehensive tool to enable HCPs in timely recognising and directing PC needs in CHF | A four-stage mixed- method study | Patients, family members and HCPs including cardiologists, HF nurse specialists, registered nurses, cardiologist in training, general practice-based nurse specialists, general practitioners, elderly care physicians, PC specialists/consultants, cardiology physician researchers cardiology, medical doctor (nursing home), certified nurse assistant and teams leaders from hospital, general practice and long-term care facilities |
| Ahluwalia et al.72 | 2013 | USA | Research | To evaluate the extent to which physicians engage in recommended elements of ACP communication during outpatient clinic visits with patients who have HF | Qualitative design | Audio-recorded outpatient visits with patients and physicians |
| Waterworth and Gott149 | 2012 | New Zealand | Research | To explore the views of general practitioners regarding the involvement of the practice nurse in supporting older people with HF throughout the disease trajectory and identify specific implications for initiating advance care planning and improving EoL care | Qualitative design | GPs recruited from a range of GP practices |
| Ziehm et al.49 | 2016 | Germany | Research | This study aims to identify German HCP perception of barriers and facilitators to PC of patients with CHF | Online cross-sectional survey | HCPs including physicians, GPs, resident/hospital cardiologists and hospital/community nurses |
| Selman et al.65 | 2007 | UK | Research | (1) To formulate guidance and recommendations for improving EoL care in CHF; and (2) to generate data on patients’ and carers’ preferences regarding future treatment modalities, and to investigate communication between staff, patients and carers on EoL issues | Qualitative design | Patients, carers and clinicians including specialist registrar, consultant, specialist inpatient nurses, specialist community nurses from PC, specialist nurses, cardiology consultants, specialist registrar from one teaching hospital |
| Kuragaichi et al.166 | 2018 | Japan | Research | To clarify the current status of PC for patients who have HF in Japan | Cross-sectional survey design | Circulation Society-authorised cardiology training hospitals |
| Selman et al.125 | 2007 | UK | Research | To describe current provision of specialist PC for patients who have HF, and explore challenges, referral criteria and recommendations to inform service development | Qualitative design | HCPs including PC physicians/consultants, medical directors, chief executives, outpatient service co-ordinators, consultant cardiologists, PC/HF/community HF nurse specialists, and a director, service improvement facilitator and network manager from hospital, community and hospice settings |
| Gasper et al.110 | 2018 | USA | Research | To implement a PC programme for patients with HF who were admitted to home healthcare services | Quality improvement project | HCPs who were home healthcare clinicians within a not-for-profit home healthcare organisation |
| Lowey29 | 2016 | USA | Research | To examine factors that influence the transition of patients with end-stage HF to palliative home care | Prospective mixed- method study | Nurses who were currently working as home care co-ordinators/discharge nurses (phase 1) and nurses who were employed (phase 2) from care home agencies across one state |
| O’Hanlon and Harding109 | 2011 | UK | Research | To describe the current PC skills and knowledge of specialist HF nurses | Cross-sectional survey design | British HF nurses |
| Janssen et al.74 | 2020 | Netherlands | Research | To identify characteristics of a tool to assess PC needs in chronic HF that are needed for successful implementation, according to patients, their family and healthcare professionals | Qualitative design | Patients, family members and HCPs including registered nurses, certifies nurse assistants, HF nurse specialists, general-practice-based nurse specialists, family physicians, cardiologists, PC specialists/consultants, elderly care physicians, medical doctorand team leader from general practice, academic hospitals and nursing homes |
| Schichtel et al.177 | 2019 | UK | Review | To identify the barriers and facilitators to the implementation of ACP by healthcare professionals in HF and to synthesise the evidence on recommendations on how to engage clinicians with ACP in HF | Systematic review | N/A |
| Kogan et al.155 | 2021 | USA | Research | To understand clinician perspectives on group visits for ACP among older adult patients with HF and caregivers | Qualitative study | Healthcare professionals including physicians and advanced practice providers from family/internal medicine, cardiology, or PC from one clinical site |
| McIlvennan et al.103 | 2017 | USA | Research | To explore the differences between cardiology and HPM clinician perspectives on deactivation of LVAD therapy and, for the first time, report the qualitative data gathered from these surveys | Convergent parallel mixed-methods survey design | Cardiology and HPM clinicians |
| Sebern et al.133 | 2018 | USA | Research | To conduct a formative evaluation of the iPad‐Enhanced Shared Care Intervention for Partners among persons with HF, family caregivers and clinicians | Qualitative design | Patient/informal caregiver dyads and healthcare professionals including advanced practice nurses, nurse clinicians, pharmacist, and dietitian from one healthcare institution |
| Waller et al.158 | 2013 | International panel of experts | Research | To adapt the Needs Assessment Tool: Progressive Disease-Heart Failure (NAT: PD-HF) to a HF population based on comments from a multidisciplinary expert panel, and to test the psychometric properties of the newly developed tool with patients in an HF service | Acceptability and reliability study | Healthcare professionals including cardiologists, doctors, PC physicians, cardiovascular nurses, nursing staff research fellows in nursing, and a nurse practitioner |
| Formiga et al.96 | 2005 | Spain | Letter | Letter to the editor | N/A | N/A |
| Beattie104 | 2013 | UK | Letter | Letter to the editor | N/A | N/A |
| Ryder et al.128 | 2011 | UK and Ireland | Review | To discuss MDT HF management with EoL | Literature review | N/A |
| Bierle et al.118 | 2021 | USA | Review | To review the models of PC and the role that the critical care nurse plays in symptom palliation and preparation of the patient and their family for transition to other levels and settings of care | Literature review | N/A |
| Ivany and White139 | 2013 | UK | Review | This review shows that individuals living with HF have a number of PC needs, including education, communication, symptom management and psychosocial needs | Literature review | N/A |
| Singh et al.114 | 2020 | UK, Sweden, USA and Netherlands | Research | To examine healthcare professionals’ decision-making processes and explore factors impacting decisions to refer or deliver PC in CHF | Qualitative meta-synthesis | N/A |
| Standing et al.100 | 2016 | UK | Research | To explore patients’/relatives’ and clinicians’ views/experiences of decision-making about ICD and CRTD implantation and deactivation, to establish how and when ICD risks, benefits and consequences are communicated to patients, to identify individual and organisational facilitators and barriers to discussions about implantation and deactivation and to determine information and decision-support needs for shared decision-making | Qualitative design | Patients/carers and healthcare professionals including implanting cardiologists, cardiologists, arrythmia nurses, secondary care and community HF nurses, cardiac physiologists, health psychologists and PC clinicians from tertiary-care centres and district general hospitals |
| Lewis95 | 2011 | USA | Review | Review focusing on the optimal care for complex decision-making in patients who have advanced HF facing EoL | Review | N/A |
| Beattie et al.79 | 2013 | UK and Canada | Editorial | To present views of attendees at a workshop of the 18th International Congress on PC on their perception of evolving HF PC services | Discussion piece | N/A |
| Westlake and Smith127 | 2015 | USA | Review | To address the PC through HC continuum and for whom, when, and where PC and HC is appropriate; describe critical components of PC and HC; and discuss the communication and decision-making needs of patients and their families during PC and HC | Review | N/A |
| Millerick and Armstrong112 | 2015 | UK | Research | A training needs assessment was undertaken as part of a programme to inform the development of training specific to HF and PC – Caring Together programme | Electronic questionnaire | Healthcare professionals including GPs, community nurses, HF nurses, care home staff, out-of-hours nursing staff, hospital-based nursing staff, PC nurses, care home liaison nurses, cardiologists, PC/care-of-the-elderly physicians and care assistants from different care setting across three sites |
| Romanò93 | 2020 | N/A | Review | To review the barriers to early utilisation of PC in HF management | Narrative review | N/A |
| Singh et al.34 | 2022 | N/A | Review | To examine the key elements of integrated PC recommended for individuals living with chronic HF across the care continuum | Scoping review methods | N/A |
| Gelfman et al.141 | 2014 | N/A | Review | To discuss a road map for collaborating with HF clinicians by reviewing the needs of patients with HF | Review | N/A |
| Howlett et al.115 | 2010 | N/A | Special article | Overview of the literature on relation to EoL planning in HF | N/A | N/A |
| Low et al.156 | 2011 | N/A | Review | To collate qualitative and quantitative evidence on: (1) patients’ perceived needs and experiences of care provision; and (2) the perspectives and understanding of health professionals on care delivery | Systematic literature review | N/A |
| Crousillat et al.130 | 2018 | USA | Research | To identify essential PC competencies for cardiology trainees | Electronic survey | Fellows and faculty from academic cardiology fellowship programmes |
| Schallmo et al.178 | 2019 | USA | Review | To conduct an integrative review on how nurses perceived communication barriers to delivering information to individuals in the palliative phase of HF | Integrative review | N/A |
| Russell et al.137 | 2020 | USA | Research | To explore sociocultural components that influence how patients with HF and their families navigate hospice care | Qualitative design | Interdisciplinary team members including nurses, social workers, physicians, and bereavement/spiritual counsellors at a large, not-for-profit hospice agency |
| Namukwaya et al.120 | 2017 | Uganda | Research | To elicit patients’ and HPs’ views of patients who have HF’ needs over the course of their illness to enable generalists, cardiologists, and PC clinicians to develop guidelines to provide patient-centred realistic care | Qualitative design | Patients, carers and healthcare professionals including doctors, nurses, and social workers from a general cardiology ward within a national hospital |
| LeMond et al.135 | 2015 | USA | Review | To provide clinicians with a basic framework for administration of EoL care in patients with HF, specifically focusing on decision-making, symptom management, and functional management | Review | N/A |
| Kavalieratos et al.83 | 2014 | USA | Research | To uncover potential barriers to PC referral for patients who have HF | Qualitative design | HCPs from cardiology, primary care, and PC, including nurse practitioners, physicians and physician assistants working in academic and non-academic practice settings |
| Kane et al.159 | 2018 | Ireland | Research | To explore whether and how a PC-specific patient-reported outcome intervention involving the Integrated Palliative care Outcome Scale influences patients’ experience of patient-centred care in nurse-led CHF disease management clinics | Qualitative design | Patients and nurses involved in nurse-led CHF disease management clinics in two tertiary referral centres |
| Hupcey et al.80 | 2009 | USA | Research | To uncover whether the conceptualisation of PC for HF as EoL care may inhibit the provision of PC for HF services | Mixed methods | Family caregivers and HF healthcare professionals, including HF physicians and advanced practice/research nurses from one HF team |
| Dionne-Odom et al.140 | 2014 | USA | Research | To translate a cancer-focused concurrent PC intervention into one that would be appropriate for rural-dwelling adults with NYHA Class III–IV HF and their primary caregivers. | Two-stage formative evaluation study | Patient/informal caregiver dyads and HCPs from specialties including primary care, internal medicine, cardiology, hospitalist and family practice from primary care and hospital |
| DeGroot et al.167 | 2020 | USA | Review | To synthesise the literature of outpatient PC in HF to identify the current landscape, the impact on patient health outcomes, key stakeholders’ perspectives, and future implications for research and practice | Integrative literature review | N/A |
| Chattoo and Atkin62 | 2009 | UK | Personal Viewpoint | To explore the continuities and discontinuities in recent policy initiatives on the extension of specialist PC to people with HF | N/A | N/A |
| Chandar et al.66 | 2017 | USA | Research article | To clarify attitudes of oncologists, cardiologists and primary care physicians towards ACP and to identify persistent barriers to timely ACP discussion following a quality improvement initiative at our health system geared at improvement in ACP implementation | Cross-sectional online survey | HCPs from primary care, cardiology and oncology including attending physicians, nurse practitioner, nurse, or administrative staff from an integrated, community-based health system |
| Brännström et al.89 | 2011 | Sweden | Research | To describe physicians’ experiences of PC for patients who have HF | Qualitative design | Physicians from a medical geriatrics clinic based in one county hospital with a specialised palliative advanced home care team |
| Brännström et al.121 | 2019 | Sweden | Research | To describe the experiences of clinical ethical support among professionals in a MDT in integrated HF care and palliative homecare after a period of 3 years | Qualitative design | Healthcare professionals including cardiologists, GPs specialising in PC, registered nurses (district/HF nurses specialised in PC), occupational therapists and physiotherapists from one integrated HF and specialist palliative in-home programme |
| Boyd et al.126 | 2009 | UK | Research | To evaluate the key components of services for people with advanced HF from multiple perspectives and recommend how care might be delivered in line with UK policies on long-term conditions, palliative and EoL care | Qualitative design | Patients, carers, and HCPs from a breadth of clinical and service management perspectives of regional HF services |
| Davidson et al.145 | 2004 | Australia | Research | To describe the development of a model of an integrated, consultative, PC approach within a comprehensive HF community-focused disease management programme | Development and evaluation | Teaching hospital |
| George and Leasure143 | 2016 | USA | Review | To examining the use of transformational leadership principles for integrated PC in HF service. | Review | N/A |
| Hjelmfors et al.30 | 2014 | Sweden | Research | To describe HF nurses’ perspectives on, and daily practice regarding, discussing prognosis and EoL care with patients who have HF in outpatient care. It further aims to explore barriers, facilitators and related factors | Survey study | HF nurses who had dedicated time for patients who have HF from outpatient clinics and primary healthcare centres |
| Singh et al.91 | 2020 | N/A | Research | To explore healthcare professionals’ perspectives on access to PC for patients with chronic HF, focusing on patient, provider and system factors | Qualitative design | Cardiologists, PC specialists, HF nurses, and PC nurses in acute and community care settings were interviewed using semistructured interviews |
| Hanratty et al.107 | 2002 | UK | Research | To identify doctors’ perceptions of the need for PC for HF and barriers to change | Qualitative design | GPs and consultants in cardiology, geriatrics, PC and general medicine |
| Buck et al.116 | 2012 | USA | Research | To explore the meaning of PC for HF and then discuss its relationships with both chronic care and EoL care | Case study | N/A |
| Singh et al.113 | 2019 | N/A | Research | To examine the knowledge, attitudes, and perspectives of healthcare professionals towards EoL care and PC for patients with chronic HF | Integrative review | Cardiologists, PC specialists, HF nurses and PC nurses in acute and community care settings were interviewed using semistructured interviews |
| Addington-Hall and Gibbs129 | 2000 | UK | Editorial | To highlight the emergence of coronary heart disease on the PC agenda and to emphasise that this is an important opportunity to ensure that PC is provided on the basis of need, not diagnosis | Editorial paper | N/A |
| Kavalieratos et al.179 | 2017 | USA | Review | To describe the potential role of PC in improving outcomes in patients with HF, characterise typical PC delivery models and each model’s existing evidence, and describe future priorities for PC research and clinical practice models in HF | Review | N/A |
| Selman et al.65 | 2007 | UK | Research | To describe current provision of specialist PC for patients who have CHF, and explore challenges, referral criteria and recommendations to inform service development | Qualitative design | Key professionals involved in CHF PC representing 17 services comprising three main types: hospital-based, community-based, and hospice-based |
| Kavalieratos117 | 2012 | USA | Thesis | To explore (1) palliative care referral barriers in HF; (2) the unresolved symptoms and treatment gaps of HF patients prior to palliative care consultation; and (3) the link between palliative processes and patient outcomes in a cohort of HF patients receiving community-based palliative care | Mixed methods | Physician and non-physician providers (i.e. nurse practitioners and physician assistants) involved in both cardiac and PC service provision |
| Documents from stakeholders | ||||||
|---|---|---|---|---|---|---|
| Authors | Year of publication | Country of study | Type of publication | Aim | Study design | Sample/setting |
| Atkinson et al.14 | 2022 | UK | Research | To create and evaluate a co-specialty cross-boundary service model for patients with HF that better provides for their PC needs in the latter stages of life, while delivering a more cost-effective patient journey | Questionnaire using patient-reported experience measure-based questions and electronic medical records | Patients with HF from a co-specialty hospital-community service, the HF supportive care service in an NHS hospital |
| Bouamrane et al.87 | 2014 | UK | Report | To define and manualise the models developed in the three areas; to identify components that could be transferred to other areas of the UK and other disease groups; and to undertake a scoping review comparing the components with those of other initiatives in the UK and internationally | Scoping review and qualitative interviews | Stakeholders from community, out-of-hours care and acute care from sites across the UK |
| Johnson et al.124 | 2018 | UK | Research | To assess the feasibility (recruitment/retention, data quality, variability/sample size estimation, safety) of a clinical trial of palliative cardiology effectiveness | Non-randomised feasibility | Adults with symptomatic HF and family carers recruited from a single UK site |
| Browne et al.25 | 2014 | UK | Research | To examine patient, informal caregiver and professional perceptions of advanced HF, and barriers and facilitators to improved models of care, with a particular focus on issues relating to the management of crises or unexpected events as this is a particularly challenging issue for patients, carers and professionals | Qualitative design | Patients with advanced HF and their carers from a HF liaison service; primary care; PC clinic for advanced HF; and local hospital admission units from one region in the UK. Healthcare professionals from a range of disciplines including cardiology, medicine for the elderly, district nursing, general practice, pharmacy, the ambulance service, and a HF liaison nurse service |
| Hill et al.23 | 2020 | UK | Position paper | To synthesise the available evidence and provide clinical guidance on integrating palliative and HF care and highlight gaps in knowledge, and signpost areas for future research | Review of existing research informed by ESC Patient Forum representatives | N/A |
| Brennan163 | 2018 | UK | Summary paper | To discuss the evidence and guidelines supporting an integrated multidisciplinary approach to CHF nursing care | N/A | N/A |
| Hill et al.26 | 2018 | International | Research | To explore patient and professional factors that impact perceived likelihood and confidence of healthcare professionals to discuss ICD deactivation | Online cross-sectional factorial survey, encompassing a demographic questionnaire and clinical vignettes | Healthcare professionals involved in the daily management of patients with an ICD, including specialist nurses, cardiologists, cardiac physiologists, general nurses, physicians, physiotherapists and electrophysiologists |
| Steitieh et al.68 | 2022 | USA | Review | To highlight recent essential advances in recent years as well as the technological advances on the horizon; and to delve into the advances in percutaneous coronary intervention and structural heart disease, the use of imaging for complex cases, and the anticipated changes that this new technology will bring with it | N/A | N/A |
| McDonagh et al.154 | 2011 | International | Position statement | To summarise the key elements which should be involved in, as well as some more desirable features which can improve, the delivery of care in a HF management programme | N/A | N/A |
| McDonagh et al.43 | 2021 | International | Guidelines | To present ESC guidelines for the diagnosis and treatment of acute and chronic HF | N/A | N/A |
| Braun et al.50 | 2016 | USA | Policy statement | To present a policy statement from the American Heart Association/American Stroke Association in relation to PC and cardiovascular disease and stroke | N/A | N/A |
| Documents from alerts | ||||||
|---|---|---|---|---|---|---|
| Authors | Year of publication | Country of study | Type of publication | Aim | Study design | Sample and setting |
| Graham et al.85 | 2022 | Canada | Research | To understand HCPs’ experiences with the collaborative delivery of a palliative approach to care to patients with AHF at home | Qualitative design | Cardiology and palliative care healthcare professionals whose location was practice was hospital/home/combination involved in collaborative care for patients with AHF from a heart centre and PC centre |
| Hendricks-Ferguson and Stallings144 | 2022 | USA | Feature article | To highlight ethical principles of concern, the role of an interdisciplinary team approach for patients with heart failure, and the advocacy role of nurses | Case study | N/A |
| Tilley108 | 2022 | USA | PhD thesis | To educate providers regarding PC care for HF patients | Brief educational course with pre and post survey | Cardiology and PC care healthcare professionals from one acute care setting |
| Matsunuma et al.97 | 2022 | Japan | Research | To comprehensively assess the prevalence and characteristics of PC needs of CHF outpatients | Cross-sectional study | Patients with CHF from one hospital HF outpatient clinic |
| Singh et al.76 | 2022 | Australia | Editorial | To highlight the clinical variation in PC provision in the context of HF | Opinion piece | N/A |
| Gelfman et al.162 | 2017 | USA | Article | Overview of primary PC for patients with HF | Article | N/A |
| Sobanski et al.22 | 2020 | European | Expert position statement | European Association for Palliative Care Task Force expert position statement | Expert position statement | N/A |
| Stevenson et al.147 | 2022 | USA | Letter to editor | To highlight concerns related to the brief report entitled ‘Polypharmacy in palliative care for advanced heart failure: the PAL-HF experience’ | Opinion piece | N/A |
| Constantine et al.132 | 2021 | UK | Review | To provide an expert statement on the role of palliative care in PAH-CHD patients, based on the results of a systematic review of available evidence | Systematic review and expert opinion | N/A |
| Curtis et al.180 | 2021 | USA | Research | To identify characteristics of patients who have HF associated with perceived need for PC | Data from the Hopeful Heart Trial analysed, focusing on the efficacy of a collaborative care intervention for treating both systolic HF and depression | Patients with either HF or HF plus depression were recruitment from eight hospitals in one region of the USA |
| de Sousa et al.161 | 2021 | Portugal | Research | To assess the accuracy of the Meta-Analysis Global Group in Chronic Heart Failure score in predicting the 3-year mortality of hospitalised patients with acute HF | Retrospective study | All patients consecutively discharged from one acute HF unit of a tertiary hospital |
| McCambridge et al.146 | 2021 | Ireland and UK | Research | To analyse community management of patients during the symptomatic period prior to admission with acute decompensated heart failure | Mixed- methods observational study | Patients admitted to hospital with acute decompensation HF two-centre (hospitals), two-country (Ireland and UK) |
| Ament et al.88 | 2022 | Netherlands | Research | To explore factors that contribute positively and negatively to timely screening of PC needs in advanced CHF | Qualitative study | Healthcare professionals including cardiologists, HF nurse specialists, GPs, general-practice-based nurses, PC specialists/consultants, registered nurses, certifies nurse assistants, team leaders, HCPs specialised in palliative care working in HF recruited from six general practices and two hospitals |
| Hjelmfors et al.77 | 2022 | Sweden | Research | To describe HCPs’ perceptions of communication about prognosis and EoL in HF care, and to describe their experiences of using a heart-failure-specific question prompt list (HF-QPL) | Qualitative design | Nurses and physicians working in both hospital and primary care who were using a HF-QPL and participating in a communication course |
| Chang et al.164 | 2022 | USA | Research | To identify consensus referral criteria for specialist PC for patients with advanced HF | Delphi study | International clinical (physician, advanced practice provider, nurse practitioner, or consultant) experts from cardiology/palliative care/cardiology and palliative care/critical care from five continents with extensive knowledge of cardiology and/or palliative care through their training, clinical practice, and/or research |
| Kim et al.131 | 2022 | Republic of Korea | Review | To identify the features of RCTs for adult patients with HF and to provide basic references for the development of future trials | Integrative review | N/A |
| Matsui94 | 2022 | Japan | Research | To investigate nurses’ symptom management and their views on death and caring for HF and chronic obstructive pulmonary disease | Cross-sectional survey | Nurses working in cardiology or respiratory wards at 11 hospitals, which were community support hospitals and university hospitals with specialised departments in one metropolitan area |
| McPherson et al.152 | 2022 | USA | Review | To address pharmacology, guideline recommendations, benefits and burdens, considerations related to hospice and EoL care, and future directions of continuous intravenous inotropic support in advanced HF care | Literature review | N/A |
| Quinn et al.142 | 2022 | Canada | Research | To determine whether regionally organised, collaborative, home-based palliative care – involving cardiology, primary care and PC – was associated with increased rates of out-of-hospital death among adults who died with HF | Cohort study | Patients with CHF across two large health regions |
| Roikjaer et al.148 | 2022 | The Nordic region | Research | To produce new insight for developing and integrating general PC care in HF treatment | Qualitative research | Healthcare professionals including nurses, physicians, physiotherapists and a hospital chaplain involved in the standard care of patients with HF from one local or adjoining hospital setting |
| Tomasoni et al.81 | 2022 | Italy | Review | To summarise medical management of patients with advanced HF | Literature review | N/A |
| Villalobos et al.181 | 2022 | USA | Research | To test the acceptability and usability of Convoy-Pal among older adults with advanced heart failure and their social convoys | Observational study | Domiciliary dwelling patients (and caregivers) receiving follow-up HF care from one hospital |
| Waller et al.105 | 2022 | Poland | Review | To examine PC needs tools for people diagnosed with advanced HF or chronic respiratory diseases, to determine their: (1) psychometric quality; and (2) acceptability, feasibility and clinical utility when implemented in clinical practice | Systematic review | N/A |
| RCTS from alert | ||||||
|---|---|---|---|---|---|---|
| Authors | Year of publication | Country of study | Type of publication | Aim | Study design | Sample and setting |
| Blum et al.157 | 2022 | USA | Research | To compare the prognostic utility of the Seattle HF model, the surprise question, and the number of hospitalisations within the last 12 months for predicting 1-year survival in patients with advanced HF | Multisite cluster randomised controlled trial | Patients with advanced HF and HF physicians who were board certified in advanced HF and transplant cardiology within primary care |
| Graven et al.182 | 2022 | USA | Research | To examine the preliminary effectiveness of the Coping in Heart Failure Partnership telehealth intervention on HF symptom frequency, severity, and symptom-related degree of interference with physical activity and enjoyment of life | Three-group randomised controlled pilot study | Patients admitted with HF from two hospitals |
| Granger et al.151 | 2022 | USA | Brief report | To describe the patterns of medication use and to evaluate the effects of the Palliative Care in HF (PAL-HF) intervention on the amount of polypharmacy present | Randomised controlled trial | Patients with advanced HF from a single centre |
| O’Donnell et al.21 | 2018 | USA | Research | To determine if early initiation of goals of care conversations by a PC–trained social worker would improve prognostic understanding, elicit advanced care preferences, and influence care plans for high-risk patients discharged after HF hospitalisation | Pilot randomised clinical trial | Hospitalised or recently hospitalised patients with HF from one hospital |
Appendix 3 Mapping of overarching context–mechanism–outcome configurations to included papers
| Authors | CMOc 1 | CMOc 2 | CMOc 3 | CMOc 4 | CMOc 5 | CMOc 6 | |
|---|---|---|---|---|---|---|---|
| Original search | |||||||
| 1. | Anscombe and Middlemiss160 | ✓ | ✓ | ||||
| 2. | Shinall56 | ✓ | |||||
| 3. | Clarke153 | ✓ | ✓ | ||||
| 4. | Knoepke and Mandrola69 | ✓ | ✓ | ||||
| 5. | Tokunaga-Nakawatase et al.70 | ✓ | ✓ | ||||
| 6. | Swetz et al.102 | ✓ | |||||
| 7. | Dunlay et al.134 | ✓ | ✓ | ✓ | |||
| 8. | Barrett and Connaire111 | ✓ | ✓ | ✓ | |||
| 9. | Abedini et al.138 | ✓ | ✓ | ||||
| 10. | Green et al.55 | ✓ | ✓ | ✓ | ✓ | ✓ | |
| 11. | Ziehm et al.119 | ✓ | ✓ | ✓ | ✓ | ✓ | |
| 12. | Cheang et al.106 | ✓ | ✓ | ✓ | ✓ | ||
| 13. | Kim and Hwang165 | ✓ | |||||
| 14. | Schichtel et al.59 | ✓ | ✓ | ✓ | ✓ | ||
| 15. | Baik et al.122 | ✓ | ✓ | ||||
| 16. | Higginbotham et al.57 | ✓ | ✓ | ||||
| 17. | Singh et al.58 | ✓ | ✓ | ||||
| 18. | Bonares et al.64 | ✓ | |||||
| 19. | Hutchinson et al.67 | ✓ | ✓ | ✓ | |||
| 20. | Brännström and Jaarsma99 | ✓ | |||||
| 21. | Stocker et al.63 | ✓ | ✓ | ✓ | |||
| 22. | Bekelman et al.176 | ✓ | |||||
| 23. | Zapka et al.123 | ✓ | |||||
| 24. | Borbasi et al.73 | ✓ | ✓ | ✓ | |||
| 25. | Kaasalainen et al.136 | ✓ | ✓ | ✓ | |||
| 26. | Harding et al.61 | ✓ | ✓ | ✓ | ✓ | ||
| 27. | Glogowska et al.90 | ✓ | ✓ | ||||
| 28. | Brännström et al.86 | ✓ | ✓ | ✓ | ✓ | ||
| 29. | Ismail et al.84 | ✓ | ✓ | ✓ | |||
| 30. | Hjelmfors et al.150 | ✓ | ✓ | ||||
| 31. | Wotton et al.78 | ✓ | ✓ | ||||
| 32. | Lum et al.92 | ✓ | |||||
| 33. | Ecarnot et al.71 | ✓ | ✓ | ✓ | |||
| 34. | Matlock et al.98 | ✓ | |||||
| 35. | Ament et al.82 | ✓ | |||||
| 36. | Ahluwalia et al.72 | ✓ | |||||
| 37. | Waterworth and Gott149 | ✓ | ✓ | ✓ | |||
| 38. | Ziehm et al.49 | ✓ | ✓ | ||||
| 39. | Selman et al.65 | ✓ | ✓ | ✓ | |||
| 40. | Kuragaichi et al.166 | ✓ | |||||
| 41. | Gasper et al.110 | ✓ | ✓ | ✓ | ✓ | ||
| 42. | Lowey29 | ✓ | |||||
| 43. | O’Hanlon and Harding109 | ✓ | ✓ | ✓ | |||
| 44. | Janssen et al.74 | ✓ | ✓ | ||||
| 45. | Schichtel et al.177 | ✓ | |||||
| 46. | Kogan et al.155 | ✓ | ✓ | ||||
| 47. | McIlvennan et al.103 | ✓ | |||||
| 48. | Sebern et al.133 | ✓ | ✓ | ||||
| 49. | Waller et al.158 | ✓ | ✓ | ||||
| 50. | Formiga et al.96 | ✓ | ✓ | ||||
| 51. | Beattie104 | ✓ | |||||
| 52. | Ryder et al.128 | ✓ | ✓ | ||||
| 53. | Bierle et al.118 | ✓ | ✓ | ✓ | |||
| 54. | Ivany and White139 | ✓ | |||||
| 55. | Singh et al.114 | ✓ | ✓ | ✓ | ✓ | ✓ | |
| 56. | Standing et al.100 | ✓ | ✓ | ||||
| 57. | Lewis95 | ✓ | ✓ | ✓ | |||
| 58. | Beattie et al.79 | ✓ | ✓ | ||||
| 59. | Westlake and Smith127 | ✓ | ✓ | ✓ | |||
| 60. | Millerick and Armstrong112 | ✓ | ✓ | ||||
| 61. | Romanò93 | ✓ | ✓ | ||||
| 62. | Singh et al.34 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| 63. | Gelfman et al.141 | ✓ | ✓ | ||||
| 64. | Howlett et al.115 | ✓ | ✓ | ||||
| 65. | Low et al.156 | ✓ | ✓ | ✓ | |||
| 66. | Crousillat et al.130 | ✓ | |||||
| 67. | Schallmo et al.178 | ✓ | ✓ | ✓ | |||
| 68. | Russell et al.137 | ✓ | ✓ | ||||
| 69. | Namukwaya et al.120 | ✓ | ✓ | ||||
| 70. | LeMond et al.135 | ✓ | ✓ | ||||
| 71. | Kavalieratos et al.83 | ✓ | ✓ | ✓ | ✓ | ✓ | |
| 72. | Kane et al.159 | ✓ | ✓ | ||||
| 73. | Hupcey et al.80 | ✓ | |||||
| 74. | Dionne-Odom et al.140 | ✓ | ✓ | ||||
| 75. | DeGroot et al.167 | ✓ | |||||
| 76. | Chattoo and Atkin62 | ✓ | ✓ | ✓ | |||
| 77. | Chandar et al.66 | ✓ | |||||
| 78. | Brännström et al.89 | ✓ | |||||
| 79. | Brännström et al.121 | ✓ | ✓ | ||||
| 80. | Boyd et al.126 | ✓ | ✓ | ✓ | |||
| 81. | Davidson et al.145 | ✓ | ✓ | ✓ | ✓ | ||
| 82. | George and Leasure143 | ✓ | |||||
| 83. | Hjelmfors et al.30 | ✓ | ✓ | ||||
| 84. | Singh et al.91 | ✓ | ✓ | ✓ | |||
| 85. | Diop et al.33 | ✓ | |||||
| 86. | Hanratty et al.107 | ✓ | ✓ | ✓ | ✓ | ||
| 87. | Buck et al.116 | ✓ | ✓ | ✓ | ✓ | ||
| 88. | Singh et al.113 | ✓ | ✓ | ||||
| 89. | Kavalieratos117 | ✓ | ✓ | ✓ | |||
| 90. | Addington-Hall and Gibbs129 | ✓ | ✓ | ||||
| 91. | Kavalieratos et al.179 | ✓ | |||||
| 92. | Selman et al.125 | ✓ | |||||
| Stakeholder paper s | |||||||
| 1. | Atkinson et al.14 | ✓ | ✓ | ✓ | |||
| 2. | Bouamrane et al.87 | ✓ | ✓ | ✓ | ✓ | ✓ | |
| 3. | Johnson et al.124 | ✓ | ✓ | ✓ | |||
| 4. | Browne et al.25 | ✓ | ✓ | ✓ | ✓ | ||
| 5. | Hill et al.23 | ✓ | ✓ | ✓ | ✓ | ||
| 6. | Brennan163 | ✓ | |||||
| 7. | Hill et al.26 | ✓ | |||||
| 8. | McDonagh et al.154 | ✓ | |||||
| 9. | McDonagh et al.43 | ✓ | |||||
| 10. | Steitieh68 | ✓ | |||||
| 11. | Braun et al.50 | ✓ | ✓ | ||||
| Alerts | |||||||
| 1. | O’Donnell et al.21 | ✓ | ✓ | ||||
| 2. | Graham et al.85 | ✓ | ✓ | ✓ | ✓ | ✓ | |
| 3. | Granger et al.151 | ✓ | ✓ | ||||
| 4. | Hendricks-Ferguson and Stallings144 | ✓ | |||||
| 5. | Tilley108 | ✓ | ✓ | ✓ | ✓ | ||
| 6. | Matsunuma et al.97 | ✓ | |||||
| 7. | Singh et al.76 | ✓ | ✓ | ||||
| 8. | Gelfman et al.162 | ✓ | |||||
| 9. | Sobanski et al.22 | ✓ | ✓ | ||||
| 10. | Stevenson et al.147 | ✓ | ✓ | ✓ | |||
| 11. | Constantine et al.132 | ✓ | ✓ | ✓ | ✓ | ✓ | |
| 12. | Curtis et al.180 | ✓ | |||||
| 13. | de Sousa et al.161 | ✓ | ✓ | ||||
| 14. | McCambridge et al.146 | ✓ | ✓ | ✓ | |||
| 15. | Ament et al.88 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| 16. | Blum et al.157 | ✓ | |||||
| 17. | Graven et al.182 | ✓ | |||||
| 18. | Hjelmfors et al.77 | ✓ | ✓ | ✓ | |||
| 19. | Chang et al.164 | ✓ | |||||
| 20. | Kim et al.131 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| 21. | Matsui94 | ✓ | ✓ | ||||
| 22. | McPherson et al.152 | ✓ | ✓ | ||||
| 23. | Quinn et al.142 | ✓ | ✓ | ✓ | |||
| 24. | Roikjaer et al.148 | ✓ | ✓ | ||||
| 25. | Tomasoni et al.81 | ✓ | ✓ | ||||
| 26. | Villalobos et al.181 | ✓ | |||||
| 27. | Waller et al.105 | ✓ | ✓ | ✓ | |||
Appendix 4 Reflective pieces from British Heart Foundation patient and public involvement network members
Reflective piece on patient’s involvement and contribution to PalliatHeartSynthesis: palliative care in heart failure project
Why it was important to me as a patient to be involved in this project
Yes, I had experienced serious illness with dilated cardiomyopathy. At one stage I was given only weeks to live by the cardiac consultant unless I received a heart transplant. Fortunately, I was lucky.
I also cared for my father who received palliative care for lung cancer. He received really great support from the McMillan nurses and was taken into hospice care before he died. The difference between the two types of care, [heart failure and cancer] even with both being terminal, was quite profound.
I therefore wanted to help this project accordingly.
Robert Ruane
As a patient who has survived the initial journey along the Heart Failure pathway, I felt that the opportunity to become a part of this research should not be missed. Having been retired for twenty years and certainly not up to speed on the branch of Research Methods called Realist Synthesis, only added to that feeling. I was immediately impressed by the whole research team and their emphasis on recruiting equality and diversity within the Stakeholders.
Robert Jones
It was important to me to be involved in this project. I was diagnosed with heart failure ten years ago after three hearts attacks and ongoing persistent Atrial fibrillation (AF). I have been fortunate that I have not experienced serious symptoms as the condition has, so far, been successfully controlled by medication. I also try to keep myself reasonably fit through regular exercise which has helped enormously.
So, it was the Heart Failure element which first attracted me to the project which I saw as another way of ‘giving back’ to the NHS, having dodged the grim reaper several times thanks to the dedicated staff of the NHS. But I wondered whether I was a suitable person for this project as I had no direct experience of palliative care, at least as I understood the term.
What I did know from friends and my wife, a retired OT, was that, unlike its popular image, palliative care was usually a positive experience for all involved.
John Burden
How I felt about my involvement and contribution
Despite the odd personal health hiatus (usually sorted by medication changes, or in one case by an ICD Generator change) I have attended all the on-line Stakeholder events since they started in November 2021. From my point of view as a heart failure patient I have always felt welcomed and valued; my views positively received, listened to and respected. I am sure my fellow patient Stakeholder members feel the same. Each meeting was professionally organised via Zoom group connectivity, a fitting use of this technology. Each session had a pre-circulated agenda and was conducted in a user-friendly manner.
The inclusion of the animation in cartoon format as part of the project website is a masterstroke.
Robert Jones
We were consulted several times for comments on documentation and the animation and while I cannot quote chapter and verse, I feel that my comments were appreciated and taken onboard where appropriate or relevant.
Our meetings were run inclusively with many opportunities to contribute to discussions by all stakeholders. I wonder if I said too much in fact!
But the good thing was that I felt I could say what I wanted even if it didn’t necessarily agree with the professional members of the stakeholders group.
Though there were many technical terms bandied about, I didn’t feel excluded and could ask for clarification in layman’s terms if I felt the need. I feel the professional members of the stakeholder group were very tolerant and open to the views of the PPI members. Moreover, the project team held pre-meetings for our PPI group before the main stakeholders meeting to keep us briefed which was very good.
The atmosphere in all the Zoom meetings was always warm and friendly, largely due to the approach and values of the project team which set the tone. The meetings were very stimulating, and this led me, on my own initiative, to do some mostly linguistic research around the term ‘palliative care’ and to a lesser extent, ‘heart failure’ as they are both increasingly controversial terms amongst health professionals let alone patients and carers, the health system’s clients or customers. To my surprise this short paper was taken in by the project team, tidied up and put on the project blog where it has been read and appreciated. I have never experienced this before on any of my PPI involvements these past several years.
John Burden
Final reflections
I really enjoyed working with Tracey and the team. I am more than happy to help wherever I can. I realise my experience is now somewhat outdated [prior to having a heart transplant], but I believe I can still offer plenty of insight into many aspects in managing heart failure.
Robert Ruane (14 March 2023)
At the outset of this project, the end-of-project date seemed a long and distant time away. I confess to some doubts concerning my own appropriate longevity to be ‘around’ at this time. Advances in successful Ablation technology have added to the Surgical, Medical and Pharmacological successes of earlier years. Realist Synthesis was a challenge initially: however reading some of University College London Kate Hind’s output made me make the connection to Operations Research which I had used formerly in my earlier professional choice of Mechanical Engineering.
I have thoroughly enjoyed this phase of the project and am more than willing to help in any way I can in the subsequent phases.
Robert Jones (9 March 2023)
The experience has been personally rewarding, that trite and over-used expression. But it has. By rubbing shoulders with medics, albeit via Zoom, I’ve come to learn more about how the health system works (and not just in the UK or England) from the grass roots to academia and the constraints imposed on it by resource limitations and the perceptions of the various stakeholders: patients, carers and professionals. From my fellow PPI contributors, I’ve appreciated the range of cardiovascular conditions and the surprising, remarkable and sometimes unbelievable health journeys they have made and how the health service has benefitted them.
The involvement has been rewarding in another sense, that of the very generous recompense for our time. I suspect we would all have done it for nothing, and there are no travel expenses involved either, thanks to Zoom.
I suppose it is only fair to PPI members to acknowledge materially the contribution PPI makes ultimately to health provision. After all, PPI is a form of employment, a kind of consultancy in a way, and generous material reward can make you feel valued.
Which sums up my whole experience really, I feel my contribution has been valued.
Many thanks to Tracey, Joanne and colleagues and good luck with the next stage of the project.
John Burden (15 March 2023)
Reflective piece on a carer’s involvement and contribution to PalliatHeartSynthesis: palliative care in heart failure project
Why I think this project is important, and why I, as a carer, wanted to be involved
My father had chronic heart failure (CHF) and died in June 2022 after many years of poorly controlled symptoms. When he died, we, as a family, wanted to be involved in palliative care in some way to make a difference and help someone or their families have a more positive palliative and end-of-life experience.
When Tracey approached me about the ongoing project and that it was looking at CHF and palliative care, I knew right away that it was the perfect opportunity to be involved and influence change.
Key barriers to integrating palliative care and heart failure, and key solutions
In hindsight, I can now see how Dad may have benefited from palliative care at an earlier stage of his illness. I suppose this didn’t happen for several reasons. The main one I see is that firstly we were never given a diagnosis of CHF although it is now obvious that was what his diagnosis was.
There is certainly a lack of understanding from both the public and medical community about what palliative care is and what it isn’t. The perception is that palliative care is an end-of-life process and until that changes then the benefits of it won’t be seen or offered to those who can benefit from it.
Dad would have benefited from palliative care support certainly in his last year and it would have prevented unnecessary hospital admissions that were so distressing to my Dad and our whole family.
Dad always felt that his medication would eventually be balanced, and his symptoms would ease. If he and we had been better informed that his condition was palliative, then we would have had a better understanding of his prognosis and we would have had more realistic expectations. Dad wouldn’t have been waiting to ‘get better’ and could have lived his life with a different mental attitude and accepted his condition and symptoms more readily and looked for other ways to relieve his symptoms or to come to terms with their limitations.
Solutions for integrating palliative care and heart failure
Awareness for both the general public and healthcare professionals is the first and most important step on this journey. This project has made great advances and has the all-important data to back up its recommendations, but next step is how to implement it in a practical manner.
Building networks between services like physiotherapy, pharmacy, dietetics and GPs to co-ordinate their services to offer a package of care tailored to the patients’ needs is key.
Patient and public involvement and involvement of those people living positively palliative lives is also key to changing public attitudes and perceptions.
As heart disease is one of the most prevalent health conditions in UK/Ireland then integrated care pathways are essential to ensure improved quality of life for its sufferers and to reduce unnecessary hospital admissions in the currently overworked emergency care, wards & departments.
As a family we had no awareness of palliative care prior to Dad’s last week of life. We assumed that palliative care and end-of-life care were one and the same. Looking back now I believe that the ward staff were unsure of the differences either. Dad wasn’t actually palliative, I believe, but end-of-life and even then, this service was lacking in what it could provide.
There is a need to demystify palliative care and to reinforce the positive benefits.
Clear, simple and honest definitions of palliative care and CHF directly related to real life situations will help to educate everyone.
If we think of other situations/conditions that were once taboo subjects that are now integrated into everyday life and mirror them. Also, look at other cultures that have a more positive outlook on palliative and end-of-life care and see how that was achieved.
Final reflections
My son looked up the definition of palliative care and it said it was: ‘Treating the symptoms but not the underlying disease’. He said, ‘If you had the flu and took paracetamol that is technically a palliative treatment’.
I thought that was quite a good way to look at it.
Glossary
This glossary is based on previously published work by our methodological expert Geoff Wong (GW), the lead researcher on the RAMESES project (www.ramesesproject.org) which developed realist review quality and publication standards and training materials.
Context–mechanism–outcome configurations Relationships between the building blocks of realist analysis (i.e. how mechanisms are triggered under specific contexts to cause particular outcomes).
Contexts Settings, structures, environments, conditions or circumstances that trigger behavioural and emotional responses (i.e. mechanisms) in those affected.
Mechanisms The way in which individuals and groups respond to, and reason about, the resources, opportunities or challenges offered by a particular programme, intervention or process. Mechanisms are triggered in specific contexts and lead to changes in behaviour.
Outcomes Impacts or behaviours resulting from the interaction between mechanisms and contexts.
Programme theory A set of theoretical explanations or assumptions about how a particular programme, process or intervention is expected to work.
Rayyan QCRI A web application used to facilitate the screening process for a literature review.
For a more comprehensive glossary, see the RAMESES project (www.ramesesproject.org).
List of abbreviations
- AHF
- advanced heart failure
- AMED
- The Allied and Complementary Medicine Database
- CHF
- chronic heart failure
- CINAHL
- Cumulative Index to Nursing and Allied Health Literature
- CMOc
- context–mechanism–outcome configuration
- COM-B
- capability, opportunity, motivation, behaviour
- CPD
- continuing professional development
- CRT
- cardiac resynchronisation therapy
- CT
- Caring Together
- EoL
- end of life
- ESC
- European Society of Cardiology
- ESHF
- early-stage heart failure
- GP
- general practitioner
- HCP
- healthcare professionals
- HF
- heart failure
- HFA
- Heart Failure Association
- HFN
- heart failure nurse
- HMIC
- The Healthcare Management Information Consortium
- HSC
- health and social care
- ICD
- implantable cardioverter defibrillator
- MCS
- mechanical circulatory support devices
- MDT
- multidisciplinary team
- MI
- myocardial infarction
- NYHA
- New York Heart Association
- PAH-CHD
- pulmonary arterial hypertension associated with congenital heart disease
- PC
- palliative care
- PG
- postgraduate
- PN
- practice nurse
- PPI
- patient and public involvement
- PPIE
- patient and public involvement engagement
- PRISMA
- Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- QoL
- quality of life
- RAMESES
- Realist and Meta-narrative Evidence Synthesis: Evolving Standards
- RCT
- randomised controlled trials
- RS
- realist synthesis
- SPC
- specialist palliative care
- UG
- undergraduate
- WHO
- World Health Organization
Notes
-
RAMESES checklist
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/FTRG5628).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
