Notes
Article history
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as award number NIHR130588. The contractual start date was in July 2022. The draft manuscript began editorial review in January 2023 and was accepted for publication in September 2023. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ manuscript and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this article.
Permissions
Copyright statement
Copyright © 2024 Cantrell et al. This work was produced by Cantrell et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2024 Cantrell et al.
Background and structure of the report
In general terms, signposting means pointing people to sources of information, help or advice that they should find useful. The UK health and social care system is complex and many people are unaware of the diverse services available. This gives rise to a need for signposting from their first point of contact with the service (often a general practice) to other sources of information and support where appropriate. The resources signposted could be information about a specific condition, information about an online support group or details of support or activities offered by health and social care organisation and the voluntary and community sectors (VCSs). Many members of health and social care staff carry out signposting as part of their role and its importance has increased in recent years in conjunction with the development of social prescribing as an alternative or add-on to conventional medical treatment. The need for signposting also reflects how demand for many services exceeds the available supply, potentially leading to long waiting lists and frustration on the part of patients.
Against this background, it is important to consider how the concept of signposting has developed; it was defined in 2013 as ‘new roles and support for navigators, health trainers and advisers who help patients and service users understand, access and navigate community-based services that will improve their health’. 1
The diversity of approaches to signposting is illustrated by a survey of Clinical Commissioning Groups (CCGs) in England conducted in 2018–9. 2 Of the 195 CCGs approached for the survey, 162 provided usable data and 147 provided some form of ‘care navigation’ service in primary care. Services were delivered by existing practice staff, dedicated paid employees and volunteers in various combinations. Seventy-five different titles were used to describe the role, with ‘care navigator’ and ‘link worker’ being most common. Care navigators (CNs) are people who help patients to navigate the healthcare system from screening, diagnosis, treatment and follow-up for a specific medical condition. Link workers (LWs) can be based in primary care practices or community or voluntary organisation and help support people to access resources from their local community to address and support their health and social care needs. The majority of services were available to all adult patients (‘generic’ services), particularly when delivered by receptionists or other members of practice staff, but some were only available to those meeting particular criteria such as older people or those with a long-term health condition.
Another variable was the method of referral into, or contact, with the service, the most common being referral by a primary care or community health professional, followed by self-referral and at contact with a general practitioner (GP) surgery. 2 Signposting or care navigation can also be delivered through diverse channels: face to face, by phone or virtually or by technology assisted by humans or by technology that has been developed to undertake signposting.
Signposting can be one element within social prescribing. Social prescribing interventions with a clear signposting element will be included in the review, extracted data will focus on the signposting element.
This diversity of approaches suggests a need to investigate what is known about which works best and why. The topic was identified as an evidence gap by Health and Care Research Wales following a prioritisation exercise in 2020. The original research question was: ‘What approaches improve signposting to services for people with health and social care needs? What works best, for whom, in what circumstances and why? Are there any benefits from implementing options in combination’? A realist review approach3 was thus specified from the outset. Programme theories identified from a review of theoretical and empirical literature led us to develop questions and then synthesise the evidence from the distinct perspectives of the service user, the provider of signposting services and the commissioner or funder.
Experimental report format
This report uses an experimental format to optimise its usefulness to its target audiences. This audience-centric method of presentation seeks to minimise ‘academic formatting’ as requested by policy/decision-makers. 4,5 It starts by introducing the problems and then covers the findings from each of the three questions that the report is addressing. Each of the questions is introduced together with any subquestions. Information is then provided about the perspective the questions is being answered for, for example service user, provider of a signposting service and commissioner/funded of a signposting service. Findings from the literature are then presented together with the initial conclusions specific to that perspective supported by data extraction tables. The report then finishes with an overall conclusion and references.
The report appendix provides supporting detail for the methodology. This experimental format thus seeks to optimise usefulness to the intended audience by providing the findings much earlier in the report. It recognises that a detailed research methodology is of comparatively less interest to primary audiences. Nevertheless, full methods are still provided for researchers with the time or methodological interest to require more from the report. Further details of the methodology can be found in Appendices. Appendix 1 covers the report methodology, the MEDLINE search strategy is reported in Appendix 2 and the document flow diagram for the review is detailed in Appendix 3, Figure 1. Appendix 4.The full date extraction of context-mechanism-ouctome (CMO) configurations in the programme theory signposting table, Report Supplementary Material 1.
Appendix 4, Table 12 provides details of the consolidated programme theory, and the data extraction tables are in Appendix 5, Tables 13–15. Full details of the realist review questions can be found in Appendix 6, and public and patient involvement in Appendix 7.
Statement of problem
Signposting is an informal process that involves giving information to patients to enable them to access external, usually non-clinical, services and support. 6 Signposting also includes self-referral, which often requires patients to contact health and support services by telephone or the internet. Signposting may also take place within clinical interactions or within more extensive social prescribing.
Typically, signposting is conceived as a brief activity – one of the ways it is distinguished from social prescribing or care navigation – perhaps comparable in duration to the GP consultation. Concern has been expressed that this may represent an inappropriate response for those with complex health and social care needs. Accompanying and competing narratives focus on diversion away from inappropriate utilisation of primary care or health service resources or on an improved joined-up service for service users, thereby improving the overall quality of care. The team at the National Institute for Health and Care Research (NIHR) Evidence Synthesis Centre at the University of Sheffield was therefore asked to conduct a focused realist synthesis to explore how signposting services work, for whom and under what circumstances. In answering these questions, the research team concentrated on three complementary perspectives (service user, service provider and commissioner). Full details of the realist reviews questions are provided in Appendix 6. These three perspectives are captured in three complementary questions and considered in turn before integrating the three sets of findings below.
Research question 1 (service user perspective)
Question 1: What do people with health and social care needs require from a signposting service to believe it is a valuable and useful service?
Subquestions
To address this overarching question, the following subquestions were formulated:
-
What do people with health and social care needs require from a signposting service to believe it is a valuable and useful service?
-
What do people with health and social care needs require to be confident in accessing a signposting service?
-
Which aspects of signposting services help people with health and social care needs to engage with signposting services?
-
Which aspects of signposting services enable people with health and social care needs to be satisfied with the service provided?
Perspective
This question and subquestions take the perspective of the individual using signposting services. Service users may use a generic service designed to handle people with different conditions or circumstances or may use a service designed for people with a specific condition or situation (or their carers, families, etc.).
Findings for Question 1 (value and usefulness): service user perspective
Findings for Question 1 are organised under the four identified subquestions. A total of 19 items of evidence were reviewed including 4 reviews and 15 individual items reporting UK studies or service evaluations. Few items featured ‘signposting’ as the focus of the study or research question. Relevant literature included studies of navigator roles and social prescribing and qualitative studies of patient and receptionist interactions in primary care. The focus of the questions means that included items are mainly qualitative or mixed-methods studies. However, one quantitative study reported a correlation between patient satisfaction and ‘patient burden’ – the extent to which the patient had to ‘push’ themselves through their interactions to achieve appropriate options and choices. For data extraction table for Question 1, see Tables 1–4.
| Author (year) | Review year | Included country/countries | Type of review | Number of included studies | Review findings | Review implications |
|---|---|---|---|---|---|---|
| Bickerdike et al. (2017)7 | 2017 | UK | Systematic review | 15 evaluations | Mostly small-scale evaluations, limited by poor design and reporting and rated with a high risk of bias. Common design issues included lack of comparative controls, short follow-up durations, a lack of standardised and validated measuring tools, missing data and failure to consider potential confounding factors. Most evaluations presented positive conclusions | Current evidence fails to provide sufficient detail to judge either the success or value for money of social prescribing. If social prescribing is to realise its potential, future evaluations of social prescribing must use comparative designs and consider when, by whom, for whom, how well and at what cost |
| Chatterjee et al. (2017)8 | 2017 | Evaluation of UK social prescribing schemes | Systematised review | 86 schemes located including pilots, 40 evaluated primary research materials: 17 used quantitative methods (6 RCTs); 16 qualitative methods, and 7 mixed methods; 9 exclusively involved arts on prescription | Outcomes included increase in self-esteem and confidence; improvement in mental well-being and positive mood; and reduction in anxiety, depression and negative mood | Despite positive findings, the review identifies gaps in the evidence base and makes recommendations for future evaluation and implementation of referral pathways |
| Liebmann et al. (2022)9 | 2022 | Canada, Sweden, UK, USA | Qualitative meta-synthesis | 18 (19 papers) | Analysis identified three themes: increased sense of well-being, factors that engendered an ongoing desire to connect with others and perceived drawbacks of social prescribing. Themes illustrate benefits and difficulties people perceive in social prescribing programmes addressing loneliness and social isolation, with overall balance of more benefits than drawbacks | Given some unhelpful aspects of social prescribing, greater thought should be given to potential harms. Further qualitative and quantitative research is needed to better understand mechanisms and effectiveness and how different components of social prescribing might be best matched to individual participants |
| Mossabir et al. (2015)10 | 2015 | Sweden, UK | Scoping review | 7 | Mental health conditions and social isolation were most common reasons for referral to interventions. Referrals were usually made through general practices. Studies reported improvement to participants’ psychological and social well-being as well as decreased use of health services. Limited measures of participant physical health outcomes | Interventions linking patients from healthcare setting to community-based resources target and address participant psychosocial needs |
| Author (year) | Study year | Study country/countries | Study design | Study sample | Sample size | Population age | Population gender | Health condition |
|---|---|---|---|---|---|---|---|---|
| Bertotti et al. (2018)11 | 2018 | Hackney UK | Realist evaluation – focus groups and individual interviews | Two quantitative GP online surveys with GP surgeries, qualitative interviews with stakeholders, two learning events involving SPCs, commissioners, community organisation representatives and service users, and observations of sessions between SPCs and individuals | Seventeen patients using social prescribing services, three community organisations, three SPCs, commissioners and GPs | Not stated | Not stated | Social isolation, mild–moderate mental health problems, presenting with a social problem, or frequent attenders to GP/A&E |
| Brunton et al. (2022)12 | 2022 | England | Qualitative | Stakeholder staff | Thirty-four respondents in 17 semistructured interviews 1 focus group of 14 practice managers | Not stated | Not stated | N/A |
| Burroughs et al. (2019)13 | 2019 | Staffordshire, England | Feasibility study | Phase 1 older people and third-sector providers Phase 2 support workers Phase 3 study participants, support workers and GPs |
Six support workers – four actually worked with older people in intervention arm Intervention arm – 19 Usual care – 20 Overall randomised – 38 participants |
Participants (older people) – median age: Intervention arm – 73 years Usual care – 70 years Total – 71 years |
Participants (older people) – female sex, n: Intervention arm – 10 Usual care – 12 Total – 22 |
Older people with anxiety or depression |
| Carduff et al. (2016)14 | 2016 | South East Scotland, UK | Semistructured qualitative interviews | Carers, carer liaison and GP from each practice (total = 19) | Eleven carers who had received intervention from their practice and with the carer liaison and one GP in each practice (total = 19) | Mean age of 74 years (range 58–86 years), interviewed across participating practices | Of 83 carers, 55 (66%) female and 28 (34%) male | Carers for persons with dementia (40%), 16% carers for person with cancer and 16% for lung disease |
| Carstairs et al. (2020)15 | December 2018–January 2019 | Scotland | Exploratory study utilising semistructured interviews | Primary care patients and HPs from one UK NHS board | Patients (n = 14) and HPs (n = 14) from one UK NHS board | Health professionals aged 25–64 years Patients aged 25 to ≥ 65 years |
Health professionals seven female and seven male Patients eight female and six male |
Primary care patients referred for physical activity opportunities |
| Foster et al. (2021)16 | 2020 | UK | Included: (a) analysis of routine quantitative data (May 2017 – December 2019) (b) semistructured interviews and (c) SROI analysis | Interviews with 60 service users, LWs and volunteers | All service users n = 10,643 Subsample of service users with pre and post scores on the UCLA loneliness scale n = 2250 Subsample of service users with follow-up UCLA n = 101 |
Mean age = 65.5 years (SD: 19.3) | Female 5388 (65.8) Male 2802 (34.2) |
18 years or older referred from any source. No specific eligibility criteria for loneliness but service targeted at young parents, individuals with health and/or mobility issues, recently bereaved, retired or with children leaving home |
| Gauthier et al. (2022)17 | 2022 | Canada | Case study | ARC navigators | Sixty-six journal entries from 2 ARC navigators (NB and NN) | Not stated | Not stated | Navigators worked with vulnerable populations, for example those with frailty, chronic illness and mental health problems |
| Hammond et al. (2013)18 | 2009–11 | North West England | Ethnographic observation in North West England. Seven researchers conducted 200 hours of ethnographic observation, predominantly in reception of each practice | Seven urban general practices. Forty-five receptionists asked about their work as they carried out their activities. | Observational notes taken. Analysis involved ascribing codes to incidents considered relevant to role and organising these into clusters | Not stated | Not stated | General practice patients |
| Harris et al. (2020)6 | 2020 | Yorkshire and Humber region of Northern England | Qualitative – Semistructured interviews | Primary care team – GPs, nurses and health and social care workers (healthcare assistants and social prescribers) | Twenty-one members of primary care team | Not stated | Not stated | Three exemplars of common health problems: physical LTCs; common mental health problems; and medically unexplained symptoms |
| Hibberd and Vougioukalou (2012)19 | 2012 | UK | Three-phase evaluation (May–August 2010; September–December 2010 and January–March 2011). Questionnaires and focus groups | People with dementia and their carers who had contacted an adviser | Not stated. Total users 392 | Mainly in 70s and 80s | Not stated | People with confirmed diagnosis of dementia and their carers |
| Papachristou Nadal et al. (2022)20 | 2022 | South London UK | Qualitative one-to-one semistructured interviews within wider pilot intervention study | In-depth interviews conducted directly after end of the intervention | Sixteen participants were interviewed: 10 healthcare professionals 6 (of the 19 intervention group participants) participants with severe mental illness and diabetes | Age of the 19 participants in the intervention group Mean (SD) 45.8 (9.7) Median (minimum, maximum) 46.0 (25.0, 64.0) IQR (lower quartile, upper quartile)17.00 (35.00, 52.00) |
Gender of the 19 participants in the intervention group (%) Male 8 (42.1) Female 11 (57.9) |
People with type 2 diabetes and severe mental illness |
| Stokoe et al. (2016)21 | 2016 | UK | Qualitative conversation analysis of incoming patient telephone calls, recorded ‘for training purposes’ | Total number of receptionists 9(9) 9(8) 10(10) (number of receptionists audiotaped in brackets) | Three English GP surgeries | Not stated | Data from GP1, GP2, GP3 Total patients 5987, 7691, 10,943 Proportion appointments booked by phone 96%, 92%, 91%. Number of calls collected for study 613, 582, 1585 Number of calls selected for analysis [final number 150 (149) 150 (148) 150 (150)] |
Not stated |
| White and Kinsella (2010)22 | 2010 | UK | Evaluation | GPs, practice staff and patients | Twenty-two (including 12 patients) | Under 35 years 33% 36–65 years 48% Over 65 years 15% Not recorded/declined 4% |
Female 66% Male 34% |
Not stated (patients with mental health and social issues) |
| White et al. (2022)23 | 2022 | UK | Evaluation of social prescribing service (January 2019–December 2020) | Interviews and focus groups | Total participants: 57 key stakeholders; social prescribing managers, LWs, referrers (GPs and social work practitioners), clients, VCS agencies and groups |
Those aged 16 years and over | Not stated | Loneliness and isolation; anxiety; becoming healthy and active |
| Wildman et al. (2019)24 | 2019 | UK inner-city area in west Newcastle upon Tyne (population n = 132,000) ranked among 40 most socioeconomically deprived areas in England | Qualitative methods using semistructured follow-up interviews | Users of LW social prescribing service who had participated in earlier study | Twenty-four service users | Participants aged between 40 and 74 years | Eleven women and 13 men | People with LTCs living in socioeconomically disadvantaged region. Two-thirds of participants experiencing mental health and social isolation issues |
| Author (year) | Signposting context | Setting | Generic or specialist | Signposting features | By whom | Type of resources required | Length of interaction |
|---|---|---|---|---|---|---|---|
| Bertotti et al. (2018)11 | Primary care | Twenty-three GP surgeries located in the London Borough of Hackney and the City of London | Generic | GP referral process; interaction with SPC; interaction with community/statutory organisations. To co-produce a well-being plan resulting from discussions about needs and aspirations of each patient and availability of local support services |
SPC | Eighty-five community organisations in borough which delivered physical activity classes, health advice, networking activities (e.g. lunch clubs), psychological support, art and other services | Up to six, 40 minutes long, sessions |
| Brunton et al. (2022)12 | Challenges of integrating signposting into general practice | Primary care | Generic | Integrating signposting into general practice | Reception staff as CNs Social prescribing LWs |
Not reported | Not reported |
| Burrough et al. (2019)13 | Primary care | General practice | Specialist | Older people received support for anxiety and depression and to attend a community group or usual care | Support worker employed by Age UK North Staffordshire | Training, support materials and manual | Three to six sessions, lasting 15 minutes to 4 hours Supervision time varied between 60 and 280 minutes per support worker |
| Carduff et al. (2016)14 | Primary care | General practices | Specific | Carers identified opportunistically, from register and through self-identification (poster) | Carer liaison | Carer toolkit including assessment form, fridge magnet with contact numbers etc. | Not stated |
| Carstairs et al. (2020)15 | Primary care | General practice | Specialist | Jog leaders and group members hosting ‘meet and greet’ sessions at practice could allow HPs to gain knowledge about this option. Provide opportunity to signpost patients to group members for more information, support and reassurance and to establish ‘buddy’ to start activity journey with | LWs | Access to resources advising on available option, and time to seek out this information is a critical barrier for HPs. To help overcome these barriers, HPs need up-to-date resources, and alternative connecting solutions that rely on an intermediary or resource including practice champions, LWs within practices, and community hubs | Not stated |
| Foster et al. (2021)16 | Social prescribing service across 37 different sites throughout the UK | Varies | Generic | Developing supportive relationship with service users, assessing their needs and providing person-tailored care | Paid LWs alongside volunteers | Access to appropriate community activities and services (signposting) such as craft groups, adult learning and leisure facilities | Support provided for up to 12 weeks |
| Gauthier et al. (2022)17 | Primary care | Generic | ARC navigators | Not reported | Navigator 1 logged 433 encounters [mean total duration per patient = 126 minutes (range: 6–466 minutes)] with 66% of encounters occurring via telephone (n = 284) Navigator 2 logged 1025 encounters (mean total duration/patient = 91 minutes) | ||
| Hammond et al. (2013)18 | Primary care | GP surgery | Generic | Face-to-face interactions | Receptionists | Knowledge of practice | Brief contact |
| Harris et al. (2020)6 | Primary care | Thirteen general practices | Generic |
|
GP: 12 (57%) Nurse: 7 (33%) Health and social care worker: 2 (10%) |
Information and self-help resources and peer and community support groups. Practical support – tangible services and aids; equipment provision, vouchers, books, self-monitoring diaries, completing forms and teaching practical skills to help patients use specific health-related equipment |
Brief consultations (< 15 minutes) |
| Hibberd and Vougioukalou (2012)19 | Community | Commissioned by Council’s Adult Social Care Services in partnership with NHS | Specialist | Face to face at home, telephone or e-mail. Referral to or contacting health or social services. Filling in forms. Practical support and advice. Information about clubs/activities | Dementia advisers | Detailed information about practical help (phone numbers etc.) and understanding of who and what to contact. Details of benefits and information about local services | Up to 2 hours mentioned |
| Papachristou Nadal et al. (2022)20 | Community | Community Mental Health Unit | Specialist | Referral to social and leisure resources and help with navigating health system | CN | Swimming, living well programmes, leisure centres or food clubs | Not stated but CN not only booked appointments but attended with service user |
| Stokoe et al. (2016)21 | Primary care | GP surgery | Generic | Telephone interactions | Receptionists | Help with appointments | Not stated but within usual primary care reception interactions |
| White and Kinsella (2010)22 | Primary care | GP surgery | Generic | Not described | Social prescribing health trainers | Signposting to other agencies and working with service users to find ways of coping with issues they are facing | Initially 1 hour |
| White et al. (2022)23 | Primary care | Based within GP practices and other locations including community centres | Generic | Separate social prescribing services available to support housing, debt and welfare benefits; such issues directed to separate in-house welfare service, and not dealt with directly by LWs, so excluded from data analysis | Social prescribing service co-delivered by two VCS organisations with support provided by LWs (four or five variously during evaluation) | Buddying to support clients on initial agency visits | Service offered short-term support but with need for flexibility to tailor duration of support to meet individual needs |
| Wildman et al. (2019)24 | Primary care | GP surgery | Generic | Highly personalised service to reflect individual goal-setting priorities and a focus on gradual and holistic change dealing with issues beyond health | LWs | Emotional support and ‘everyday reassurance’ for service users lacking self-esteem and experiencing anxiety; ‘instrumental support’ (e.g. filling out welfare benefit application forms); ‘informational’ support in identifying sources of help within wider community; and ‘appraisal’ support with decision-making and problem solving | Service users remain for up to 2 years or longer if required. During patient’s engagement, face-to-face contact is supplemented by telephone, e-mail or text contact. Meeting duration frequency increases or decreases according to need |
| Author (year) | Outcomes measured | Main findings | Key messages including limitations |
|---|---|---|---|
| Bertotti et al. (2018)11 | Referral to SPC (stage one)
|
Data collection shows that beneficial outcomes for patients result from combination of multiple stages working together effectively. Realist evaluation approach enabled identification of three stages of interaction between the patient and three other stakeholders: the GP (stage one), the SPC (stage two) and community organisations (stage three) | SPCs pivotal to effective functioning of social prescribing service and responsible for activation and initial beneficial impact on users. There are significant potential benefits from social prescribing but also several challenges. ‘Buy-in’ from some GPs, branding and funding for third sector in context of social care cuts are some of the challenges that need to be thought about and overcome. The SPC is central to social prescribing and their role needs to be understood more clearly practically and conceptually |
|
|||
| Brunton et al. (2022)12 | Stakeholder views on challenges of integrating signposting into general practice | Three themes that highlight the challenges of integrating signposting into general particle were role perceptions, role preparedness and integration and co-ordination of roles | Key factors that affect signposting in practice are: clarity of role purpose and remit, appropriate training and skill development for role holders and adequate communication and engagement between stakeholders/partnership working Limitations: views of CNs from only 1/5 areas where they were working and their experience could be different to CNs working in different areas of Greater Manchester |
| Burroughs et al. (2019)13 | Participation in study did not impact on routine care, other than response to calls from study team about risk of self-harm. GPs not aware of work done by support workers (SWs) with patients |
Older people found sessions with SWs acceptable, although signposting to, and attending, groups not valued by all participants. GPs recognised need for additional care for older people with anxiety and depression, which they could not provide |
SWs recruited from Age UK employees can be trained to deliver an intervention, based on principles of BA, to older people with anxiety and/or depression. Training and supervision model acceptable to SWs, and intervention acceptable to older people |
| Carduff et al. (2016)14 | Development of an intervention model to identify, assess, support and refer carers. To evaluate if the intervention is feasible and acceptable | Eighty-three carers identified from four practices: 36 from practice registers, 28 by practice staff and 7 self-identified. Eighty-one carers received the pack and 25 returned the CSNAT form. Follow-up calls to discuss support were received by 11 carers and an additional 12 carers were referred/signposted for support. The qualitative interviews suggest carers valued the connection with their practices but found the paperwork in the toolkit burdensome | Carers did not describe need for intensive support, preferring smaller interventions. Feeling ‘connected’ was very important to the well-being of carers. They endorsed the provision of carer support being available in their community through their local GP practice. The approach this study used to identify and support carers was acceptable. The success of the intervention was dependent on engagement within the whole practice. Carers needed to be proactively identified by practices as they did not tend to self-identify or ask for help. Practices need to adopt a public health approach to raise carer awareness about support within their communities |
| Carstairs et al. (2020)15 | Barriers and facilitators for patient connection | Three methods of connecting patients to community-based groups identified: informal passive signposting, informal active signposting and formal referral or prescribing. Barriers and facilitators fell into five theoretical framework domains for HPs and two COM-B model components for patients. Patients liked their HP to connect them to resources on specific PA opportunities to consider and potentially follow up on. Patients described that connecting to tangible PA options is favourable instead of just being told ‘you should get more active’ given as they think it helps them towards implementing the changes |
HPs raising the topic of PA can help patients to justify, facilitate and motivate action to change. The workload for HPs associated with the different methods of connecting patients with community-based opportunities varied, and is central to implementation by HPs. Combining resource solutions and social support for patients can provide them with a larger range of PA options along with the information and support they require to connect with local opportunities |
| Foster et al. (2021)16 | Loneliness scores Return on investment |
The majority of service users (72.6%) felt less lonely after receiving support. The mean decrease in UCLA score −1.84 (95% CI −1.91 to −1.77) indicates an improvement. Improved well-being, increased confidence and life having more purpose were some of the additional benefits. Base-case analysis estimated a SROI of £3.42 per £1 invested in the service. Key aspects for the service were having skilled LWs and support tailored to individual needs. There were challenges though included utilising volunteers, meeting some service users’ needs in relation to signposting and sustaining improvements in loneliness. Nevertheless, the service appeared to be successful at supporting service users experiencing loneliness | This national social prescribing programme was found to help reduce people’s loneliness as well as improving their well-being and increasing their sense of purpose. The model achieves a positive net social value for money invested (£3.42 return per £1 invested). Key to the service success is having skilled LWs who deliver personalised support. Challenges to service delivery include using volunteers, signposting and sustaining improvements in loneliness |
| Gauthier et al. (2022)17 | Navigators learning experience | Reflective journal entries analysed using five framework categories
|
Experiences suggests that navigator education programmes should include learning opportunities from experiences of primary care, which could be testimonials from patients during training or initial supervised patient interactions. Supervision could help navigators with managing expectation, confidence building and help them start developing skills to apply person-centred care Limitations: limited generalisability firstly due to journal entries from only two navigators. Additionally, the navigators knew that the journals would be read by others which may introduce social desirability bias |
|
|||
| Hammond et al. (2013)18 | Receptionist attitudes and behaviours | Receptionists face difficult task of prioritising patients, despite having little time, information and training. They felt responsible for protecting patients who were most vulnerable; however, this was sometimes made difficult by protocols set by the GPs and by patients trying to ‘play’ the system | Framing receptionist–patient encounter as between the ‘powerful’ and the ‘vulnerable’ impairs a full understanding of the complex tasks receptionists perform and contradictions inherent in their role. Calls for more training, without reflective attention to practice dynamics, risk failing to address systemic problems, portraying them instead as individual failings |
| Harris et al. (2020)6 | Participants’ accounts showed that referral and signposting to external services and resources was most common SMS activity used across all three exemplar common health problems | From the interview analysis three categories and six subcategories, illustrating different self-management support activities across common health problems, were identified. Referral and signposting were frequently used to facilitate patient engagement with services and resources. Challenges were experienced by practitioners in balancing medical management and psychosocial support and motivating patients to engage with self-management | Digital repository of available community services and additional training in motivational interviewing would support practitioners and enable them to increase their confidence and skills in SMS across common health problems. Limited consultation time was a common obstacle but unclear exactly what the optimum duration and pattern of consultations should be. Recommendation from this research includes increasing awareness of practical support initiatives for people with common mental health problems and mediclally unexplained symptoms (MUS) and for healthcare commissioners the setting targets for management of physical LTCs |
| Hibberd and Vougioukalou (2012)19 | Service user perceptions Service provider perceptions |
Immediacy is very important. Service users feel able to recontact service at any time without restrictions. The service did not use answerphones which are off-putting for those with hearing or cognitive problems. Service users appreciated being listened to by someone who knew what they were talking about. Adviser independence from health and social services was appreciated making it easier to talk about problems and issues with services |
Can ‘oil the wheels’ within a longer pathway (often seen as disconnected). Some overlap, for example, with post-diagnostic counselling but not seen as an issue because of special need for reinforcement among this cognitively impaired population |
| Advisers particularly appreciated when service users feel frustrated, upset or vulnerable. Service users value (1) repeated back information and (2) review of action points at end of call. Written reminders sent as follow-up. Need for emotional support not just practical support. Relaxed environment also appreciated |
|||
| Papachristou Nadal et al. (2022)20 | Thematic analysis | From analysis of 19 participants, five main themes emerged regarding the care-navigator role: administrative service; signposting to local services; adhering to lifestyle changes and medication; engaging in social activities; further skills and training needed | Key findings emphasise benefits of care-navigator role in helping people with severe mental illness to better manage their diabetes, that is, through diet, exercise medication and attending essential health check-ups |
| Stokoe et al. (2016)21 | Published satisfaction survey scores | Analysis identified ‘burden’ on patients to drive calls forward and achieve service. ‘Patient burden’ occurred when receptionists unable to meet patients’ initial request did not offer alternatives to or did not summarise relevant next actions at the end of calls. ‘Patient burden’ frequency differed across the three GP services. Increased ‘patient burden’ was associated with decreased satisfaction scores on satisfaction survey |
Patients in some practices have to push for effective service when calling GP surgeries. Conversation analysis specifies what constitutes (in)effective communication. Findings can then underpin receptionist training to improve patient experience and satisfaction |
| White and Kinsella (2010)22 | Six of 12 patients signposted to another service or activity. Some patients primarily need space to discuss their troubles. Some are signposted to another agency after only one or two sessions with the SPHT; patients seen for three or more sessions are encouraged to develop a personal health action plan | In only 9 months, 484 patients were supported to cope better and improve their health. 51% of patients seen were referred to community-based service for support. 48% made personal action plan. 87% of those signed off had made changes that enabled them to cope better and improve their health |
Benefits for practices of the health trainer and social prescribing service:
|
| Patients seen were among the most vulnerable and disadvantaged they had mild mental health problems, relationship difficulties or were socially isolated. The service was valued very highly be patients – they really liked the friendly, informal approach, someone with time to listen and the support to develop with their own solutions to their difficulties |
|
||
| GPs and other practice staff liked having a service to refer patients with primarily social problems. There was some evidence that patients, who had seen a health trainer, visited their GP less with social problems |
|
||
| White et al. (2022)23 | Number of users referred to social prescribing service. Sources of referral to service. Thematic analysis of interview data |
Two thousand one hundred and ninety-nine users referred to social prescribing service (September 2017–August 2020). Sources of referral included self-referral (28%); social workers (20%); HPs (12.5%). Despite emphasis on social prescribing as a resource to help primary care manage demand, only 4.2% referrals were from GPs, a significant proportion (41.5%) were from two practices. The five themes identified from the qualitative data were: Theme One, Accessing Link Worker Support; Theme Two, How Link Workers Support Clients; Theme Three, Getting on: Accessing Support in the Community; Theme Four, Perceived Benefits of Social Prescribing; Theme Five, Working to Deliver Social Prescribing |
Key support included referral into and onwards from social prescribing services (in addition to signposting), longer-term LW support and buddying. Practitioner responses highlighted the balance between empowerment and dependency featured in practitioner responses. There is a need for good support and supervision for LWs to enable them to provide support while minimising client dependency. Further exploration is needed of why GP referrals were lower than expected and how referrals could be increased. Social workers were key referrers to social prescribing services suggesting a potential need to investigate in greater depth the role of social prescribing in UK social work practice |
| Wildman et al. (2019)24 | Service users’ perspective on social prescribing service | Participants reported reduced social isolation and improvements in their condition management and health-related behaviours. Findings indicated that, in this sample of people facing complex health and socioeconomic issues, longer-term intervention and support were required. | Highlights issues of interest to commissioners and providers of social prescribing:
|
Positive features of LW social prescribing for service users included:
|
From research perspective, diversity of improvements and their episodic nature suggest that evaluation of social prescribing interventions requires longitudinal quantitative and qualitative data | ||
| Requires strong, supportive relationship with an easily accessible LW in promoting sustained behaviour change. Highlights importance of LW continuity. A barrier for some participants was a lack of suitable and accessible voluntary and community services for onward referral |
What do people with health and social care needs require from a signposting service to believe it is a valuable and useful service?
People with health and social care needs in the UK carry a strong expectation that they will be seen by health professional staff, particularly by their GP. 12 Any attempt to direct them to non-clinical staff carries the risk that they will see themselves as being ‘fobbed off’. 12,25,26
Practice manager 2: So, the patient loses faith in the call handler because they think that [they’ve] just been fobbed off. ‘You can’t even get through to that doctor’s, and then when you do, she’s telling me that I need to go there, and then I’m phoning there again and then to be told that they’re fully booked up’. And then it gives us a bit of a bad…it’s not fair really. 12[6]
This phenomenon has been reported for patients who are directed towards self-care options,27 as well as for patients with psychosis being handled within primary care. 28 This means it is likely that the threat of being ‘fobbed off’ may exist for both users of generic signposting services and users of specialist signposting services. A patient who feels ‘fobbed off’ is more likely to re-present to the surgery within a short period of time27 in search of a response that they view as appropriate. Staff members involved in signposting have a small window of opportunity within which to counter this potential negative attitude. This contrasts with extensive social prescribing or social navigation options which report the build-up of trust over a sustained period of time.
It is significant, from the literature relating to LWs, that patients may be prepared to ‘trade’ the extra time, used to develop a full and accurate picture of their individual need taken by a LW against the clinical interaction with a GP or practice nurse. 24
There’s a huge difference [between a link worker and a nurse or doctor]. The practice nurse just wants to stick the jab in your arm, and let them get on with it, and that’s it. Doesn’t ever really have time to do the in-depth analysis of where you’re at and what you’re doing. The Ways to Wellness person has that concern. 24[6]
The implication of this statement is that signposting services, as individually configured for brief contact, cannot satisfy the need for ‘in-depth analysis’ as articulated here. Potentially, an alternative source of ‘capital’ that can be traded against clinical knowledge and expertise is the detailed knowledge of community resources which can be acquired through training, experience and a suitable directory or resource of activities and opportunities:
…it’s important to have someone there, who has a finger on the pulse, knows all these different things. Doctors can’t know everything and I mean, what they know obviously helps improve your health, but things like support in the community and things, I don’t think enough of them know about it. I don’t even know that the practice nurses know enough about it. 24[6]
A less tangible benefit but, nevertheless one valued by the service user, is the ability to link together an otherwise disjointed health and social care response; someone who “puts all the links together, which is a link worker in an intervention where ‘everything was involved’.”24
Although this benefit was described in the context of a LW, who fulfils many diverse roles, it can be transparently attributed to the signposting component with its focus on both ‘navigation’ and ‘joining up’.
An adequate response requires multiple expectations to be satisfied sequentially – that the one signposting will identify options efficiently, that these options will be available, that they will be feasible and that they will be appropriate to the needs of the individual. 12 These demanding requirements correspond to provision identified for Question 2, namely well-trained staff, supported by information resources, directories or lists of contacts, underpinned by an appropriately resourced community infrastructure and informed by a knowledge of the needs of the individual. A qualitative meta-synthesis9 highlights the matching of response to need as one of the persistent challenges of linking schemes, requiring further research and this appears to be equally true of a briefer signposting intervention where time to establish a full and accurate picture of complex need may be even more limited.
Within the limited contact time implied by active signposting, it is likely to prove challenging to build up the confidence of the user in the signposting service and trust of the service user in the service provider with whom they are in contact. One GP reports how trust between a GP and their patient is fundamental to them subsequently listening to their advice and trusting the recommended destination for the referral. 6 The relationship between GP and patient is at best an ambivalent one – trust can be built up over many years or lost speedily by a negative episode of care. While recognisable reception staff may have built up a comparable relationship with service users in their community, they represent only a small proportion of potential signposting contacts and so, in many cases, the relationship may equate to ‘cold calling’ requiring the build-up of trust from ground zero.
Trust can be built up within a signposting service through the quality of the initial response (achieved by staff training and experience), the quality of the advice and its appropriateness to the individual service user and the quality of the resources as subsequently accessed. 12 A paradox exists that repeat use may be a sign that the original need remains unfulfilled given that repeated contact works contrary to a programme theory of subsequent self-management. The value of the service is seen not when a user returns to the service for the same need, but when they have the confidence to return to the service for a different but related need, when they recommend the service to others in a similar situation or, in some cases, where they themselves volunteer to become part of the pathway either within the initial signposting service or in contributing to the community back-up response.
Signposting services are intended to build up service user self-esteem and confidence, thereby improving their self-direction and, in the case of chronic conditions, their resourcefulness and self-management. While this is undoubtedly evidenced in sustained social prescribing services,7,8,16,29 it is difficult to attribute this to a brief variant of the intervention, as in signposting. Intermediaries, whether those signposting or those in social prescribing roles, describe how building up of service user self-esteem and confidence may require extended time, multiple contacts or, commonly, both.
As identified elsewhere in this review, the quality of the community response may be determined by the level of resourcing received by the organisations to which the service user is referred. One way in which a signposting service may mitigate their dependence on community resource levels is through access to a wide range of service providers. For example, one evaluation describes how it referred just over half of its service users to other organisations, including literacy courses at colleges, volunteering and community allotments, line dancing and the local Citizen Advice Bureau. 22
What do people with health and social care needs require to be confident in accessing a signposting service?
Users of signposting services have varying levels of need. Two particular factors were identified as shaping the signposting response to users with different needs. First, those delivering the service may attempt to accommodate the needs of vulnerable service users. 18 This may be done by providing extra help – such as filling out forms – or by moving from being a service interface to becoming a patient champion. In some cases, this may involve actually making the decision for the service user when their capacity or confidence to make their own decision is thrown into question. Signposting services are particularly valued by those who are frustrated, upset or vulnerable. One evaluation report highlights how those being targeted by signposting services were those seen as being among the most vulnerable and disadvantaged, those with mild mental health problems and those with relationship difficulties or who were socially isolated. 23 Paradoxically, however, the extent and nature of these types of challenge may require more intensive involvement than just signposting, moving much more towards social prescribing. 23 As a general finding, those who superficially most likely to benefit from the extra support in navigation offered by signposting are also those who might benefit from more intensive forms of support. This not only makes it challenging to demark where signposting ends and social prescribing begins, but also means that the more time that is spent in establishing the service user’s needs, the more extensive the awareness of the full scale and complexity of their needs and thus the more intensive a response is required. A corollary may be resistance to pressures from those seeing themselves as entitled; assuming a gatekeeper role against those who might seek access to opportunities or resources at the expense of those who are more in need.
Second, signposting services may serve different functions for different age groups, even if they share the same apparent symptoms such as social isolation, depression or anxiety – younger service users may value initiation of opportunities, and therefore be more amenable to signposted activities, whereas older people’s loneliness is often entrenched, arising from diminishing social networks, attributed to the deaths of family/friends and a loss of functional ability to engage in activities. 16
Which aspects of signposting services help people with health and social care needs to engage with signposting services?
The evidence identifies three critical points in the signposting process with a bearing on engagement with signposting. First, the one signposting should be able to offer options. 21 Second, the ‘patient burden’ in seeking to progress, for the one using the service, should be kept to a minimum. 21 Third, the one signposting should summarise the suggested actions to confirm resolution and closure. 21 This feature is considered particularly important where the service user experiences cognitive difficulties as with those with memory problems or dementia. A written summary may be used to reinforce the agreed action. Significantly, offering options and summarising what has been agreed feature as important characteristics of medical receptionist interactions and communications generally, aside from a signposting role. However, fulfilment of these requirements has been found to be variable. An additional contingent requirement is a further loop whereby unsatisfactory or unacceptable options are rechannelled to acceptable alternatives. 21 Again, this is described as reducing ‘patient burden’. 21
Signposting services are primarily transactional, rather than relational, and, particularly if delivered by those identifiable from former or split receptionist roles, may create an expectation in speedy and brief resolution to avoid tying up the service for other users. In contrast, navigators document the importance of gaining and building service user trust. 17 Question 2 documents how this requires that navigators develop relationships with patients ‘actively listening and digging deeper’17 in order to tailor their response to patient needs and individual preferences. 10 It further notes how four included studies in a scoping review of linking schemes10 found that relationships with facilitators that were described as ‘being flexible, trustworthy, empathetic and accessible (Andersson 1985, Woodall and South 2005, Brandling and House 2007, White et al. 2010)’10(:480) encouraged service user engagement. Evidence is equivocal on the optimal balance between transactional and relational roles for a service as a whole and available data suggest that service users hold different individual preferences for these roles and these, in turn, may fluctuate according to the situation being encountered and the urgency of the response being required. Evidence suggests that access to requisite skills in questioning are needed for both services that aim to provide signposting or extensive social prescribing.
Signposting services may provide a misleading picture of their success when a service user, either intentionally or unintentionally, gives the impression that they plan to follow up on the suggestion but does not actually follow through. Service users describe how the ‘right’ advice may not have been timely for them, particularly, when they have multiple issues of competing priority with which to contend. In these cases, the otherwise apposite action may be deferred or even ignored all together. Evidence captures from signposting staff, specifically navigators, a note of hopefulness, that service users will respond positively to the direction being offered and will subsequently benefit, rather than secure expectation that they will do so. 17
Which aspects of signposting services enable people with health and social care needs to be satisfied with the service provided?
Service users may feel that a signposting service is merely a way to steer ‘them away from GP appointments, rather than steering them towards the most appropriate care’. 12 Service users may feel dissatisfied that they are being ‘managed’ by non-clinical staff who are not equipped to handle their situation. This very much depends upon the nature of the advice, for example, whether the referral is to community groups and activities or to other ‘more appropriate’ health services. This concern ties in to the reciprocal concern (Question 2) of staff involved in signposting being drawn into a clinical role. While the concerns of clinical staff may centre on safety,12 those of service users may focus on the perceived quality of the response.
Evidence suggests that service users may not initially identify what intervention they require. They may not be aware that a signposting service exists or that it can help them in relation to the specific issues that they face (the issue of ‘who will signpost to the signposters?’). Knowledge of available services and their roles is variable among potential referrers such as primary healthcare staff. Even if they access a signposting service, it may take time in order to elicit what they actually require, as well as to establish realistic expectations, both what can be achieved and what cannot be achieved by the service. One qualitative study evaluating a social prescribing service23 reports that ‘sometimes they just don’t know what they need and they need to talk, so it’s important to just listen … the questions that you ask them are important for getting out information’23(:6, e5110).
Mismatched expectations are potentially a source of dissatisfaction with a signposting service even when it closely fulfils its intended remit. A further issue relates to follow-up – expectations from the service can be shaped by previous experiences with the service so that repeat service users may feel more comfortable in accessing the service when they require ‘more of the same’ that they are in accessing a wider diversity of services that may or may not be offered by the signposting service.
Summary for value and usefulness of signposting: service user perspectives
Interpretation of the review brief became more challenging as our review team became sensitised to the nuances of signposting provision. Should we literally focus only on the signposting component in isolation? In which case, we could reasonably conclude that beneficiaries from signposting in isolation are likely to represent only a small proportion of service users, for whom the referral target is simply the missing piece in their route to self-management and resolution. In such a situation, a 2- to 5-minute intervention may be viewed as sufficient. Or is signposting to be considered as an adjunct that must always be backed up with more extensive social prescribing that provides for those for whom signposting will not be enough?
Two further complexities were identified. First, where signposting is prolonged beyond its brief 2- to 5-minute ‘dosage’, it may offer an opportunity to elicit more information on user need; therefore, increasing the likelihood that referral to more intensive services is required – effective, rather than efficient, signposting thereby potentially subverts its own programme theory of brief contact and referral onwards. This tension plays out against the two driving and competing narratives for signposting, namely the driver to deflect inappropriate non-health-related demands away from the health service, particularly primary care (‘to free up GPs’ time by directing patients to other sources of help’), and the driver to use signposting as a way to improve the quality of care through better integration and linking of services (‘to enable patients to be signposted at the first point of contact, to the “right” professional or service’). 12
Second, where signposting cannot be extended beyond its 2- to 5-minute duration, it may represent an inappropriate response to more profound needs, thereby functioning to cloak levels of actual need. This links to the need identified in a qualitative metasynthesis9 to evaluate potential harms of social prescribing which can be extrapolated to encompass equally the briefer interventions delivered by signposting.
Conceptually, the challenges presented by signposting services mirror, albeit on a wider scale, those posed by the creation of the NHS111 service as an alternative to urgent primary and secondary care. Service users require reassurance that the response that they are receiving is not of inferior quality, that the operatives with whom they are dealing are proficient, that the response is appropriate and that the eventual outcome that they receive is the best possible for their current situation. Similarly, signposting services may be seen to be equally vulnerable to high-profile accounts of occasional inappropriate response, evidenced in concerns from signposting staff about ‘stepping into clinical areas’ and patient safety. Such concerns may require that specialist signposting for high-risk groups, for example, for patients with psychosis, receive additional safeguards (whether this be training, expertise or procedures) for both signposting staff and their service users.
Initial conclusions for value and usefulness of signposting (service user perspective)
-
Although a distinction between brief signposting services and intensive extended social prescribing services is meaningful from the perspective of service funding and training and expectations on staff, this distinction is less useful from the perspective of service user need.
-
A small proportion of potential service users have their needs satisfied by the largely navigational brief intervention offered by signposting. A much larger proportion of service users will require extensive support, perhaps requiring an extended duration of contact or multiple episodes of contact or both.
-
A key issue is whether signposting and social prescribing, as two distinct levels of service provision, are delivered within a fully integrated service, whether they represent separate services with a fluid interface or whether they are loosely linked and largely dysfunctional.
-
A related key issue concerns the potentially diverse relationships between the signposting service and the opportunities or activities to which they direct the service users; these could be formally integrated within a common ‘scheme’, loosely confederated with minimal governance and quality control or opportunistically aggregated with little commonality of candidacy or expectation.
-
The signposting service operates as a ‘shop window’ for services, statutory or voluntary, on offer. Deficiencies in the signposting service may impact negatively on take-up of the available opportunities. Conversely, poor access to, resourcing of and delivery by, supporting services may reflect negatively on the credibility of the signposting service influencing numbers of repeat users or testimonials to the signposting service.
Research question 2 (service provider perspective)
What resources (training, directories/databases, credible and high-quality services for referral) do providers of front-line signposting services require to confidently provide an effective signposting service?
Perspective
Question 2 is from the perspective of the individual providing a signposting service. Many different people provide these services including volunteers, lay people, receptionists and various health professionals including GPs, physiotherapists, nurses and pharmacists.
Findings for Question 2 (required resources): service provider perspective
For Question 2, a total of 14 items of evidence were reviewed, 1 review and 13 individual items reporting UK, USA or Canadian studies or service evaluations. The findings from the included studies are discussed within themes. The data extraction tables follow the findings; see Tables 5–8.
| Author (year) | Review year | Included country/countries | Type of review | Number of included studies | Review findings | Review implications |
|---|---|---|---|---|---|---|
| Mossabir et al. (2015)10 | 2015 | Sweden, UK | Scoping review | Seven studies | Almost all interventions were facilitator-led, whereby the facilitator works to identify and link participants to appropriate community-based resources. Studies reported improvement to participants’ psychological and social well-being as well as decreased use of health services. Limited measures of participant physical health outcomes | Interventions linking patients from healthcare setting to community-based resources target and address participant psychosocial needs. Health professionals aid the referral of patients to the intervention and role of intervention facilitators is key to the interventions |
| Author (year) | Study year | Study country/countries | Study design | Study sample | Sample size | Population age | Population gender | Health condition |
|---|---|---|---|---|---|---|---|---|
| Bertotti et al. (2018)11 | 2018 | Hackney UK | Realist evaluation – focus groups and individual interviews | GPs, stakeholders, SPCs, commissioners, community organisation representatives and service users | Seventeen patients using social prescribing services, three community organisations, three SPCs, commissioners, and GPs | Not stated | Not stated | Social isolation, mild–moderate mental health problems, presenting with a social problem, or frequent attenders to GP/A&E |
| Brunton et al. (2022)12 | 2022 | England | Qualitative | Stakeholder staff | Thirty-four respondents in 17 semistructured interviews, 1 focus group of 14 practice managers | Not stated | Not stated | N/A |
| Burroughs et al. (2019)13 | 2019 | Staffordshire, England | Feasibility study | Phase 1 older people and third-sector providers Phase 2 support workers Phase 3 study participants, support workers and GPs |
Six support workers – four actually worked with older people in intervention arm Intervention arm – 19 Usual care – 20 Overall randomised – 38 participants |
Participants (older people) – median age: Intervention arm – 73 years Usual care – 70 years Total – 71 years |
Participants (older people) – female sex, n: Intervention arm – 10 Usual care – 12 Total – 22 |
Older people with anxiety and depression |
| Carstairs et al. (2020)15 | December 2018–January 2019 | Scotland | Exploratory study utilising semistructured interviews | Primary care patients and HPs from one UK NHS board | Patients (n = 14) and HPs (n = 14) from one UK NHS board | Health professionals aged 25–64 years Patients aged 25 to ≥ 65 years |
Health professionals seven female and seven male Patients eight female and six male |
Primary care patients referred for physical activity opportunities |
| Donovan and Paudyal (2016)30 | Northumberland Region, England | Qualitative | Pharmacy support staff from 12 HLP initiatives | Twenty-one pharmacy support staff | Age range < 30–69 years < 30 years: 4 40–49 years: 6 50–59 years: 8 60–69 years: 3 |
Female: 21 | Pharmacy customers | |
| Farr et al. (2021)31 | 2020 | England | Qualitative | Professionals and service users involved with implementing the THRIVE framework for CYP’s mental health | Eighty (CAMHS clinicians, commissioners, service leads, service users and their parents or carers. Participants from the wider referral pathway and implementation team were also included) | Not stated | Not stated | Mental health conditions referred to CAMHS |
| Gauthier et al. (2022)17 | 2022 | Canada | Case study | ARC navigators | Sixty-six journal entries from two ARC navigators (NB and NN) | Not stated | Not stated | Navigators worked with vulnerable populations, for example, those with frailty, chronic illness and mental health problems |
| Hammond et al. (2013)18 | 2009–11 | North West England | Ethnographic observation in North West England. Seven researchers conducted 200 hours of ethnographic observation, predominantly in reception of each practice | Seven urban general practices. Forty-five receptionists asked about their work as they carried out their activities | Observational notes taken. Analysis involved ascribing codes to incidents considered relevant to role and organising these into clusters | Not stated | Not stated | General practice patients |
| Harris et al. (2020)6 | 2020 | Yorkshire and Humber region of Northern England | Qualitative – semi-structured interviews | Primary care team – GPs, nurses and health and social care workers (healthcare assistants and social prescribers) | Twenty-one members of primary care team | Not stated | Not stated | Three exemplar types of common health problems: physical LTCs; common mental health problems; and medically unexplained Symptoms |
| Kennedy et al. (2016)32 | England | Qualitative | Community | Fifteen case studies of observations facilitator–participant interactions at intervention delivery and interviews with participants | Adults over 18 years, range from 43 to 76 years | Six female, nine male | Type 2 diabetes | |
| Komaromy et al. (2018)33 | 2011 (training CHWs for CARS program) 2015 (training CHWs for ‘Let’s move New Mexico’ family obesity prevention training programme) | USA | Training programme evaluation | CHWs attending CARS program CHWs attending ‘Let’s move New Mexico’ family obesity prevention training programme |
CARS training programme – 139 individuals have completed training programme ‘Let’s move New Mexico’ family obesity prevention training programme – 25 CHWs |
Not stated | Not stated | Patients with substance use disorders Families at risk of obesity |
| Toal-Sullivan et al. (2021)34 | 2017–8 | Canada | Evaluation (training programme) | Navigators attending ARC training programme | Programme piloted May 2017 – 13 participants: five experienced multicultural health navigators, four members of ARC research team, three university students and one ARC patient navigator Second implementation training programme with 11 participants comprising 5 multicultural health navigators, 4 members of research team and 2 ARC patient navigators | Not reported | Not reported | Navigators worked with vulnerable populations such as those with frailty, chronic illness and mental health problems |
| White et al. (2022)23 | 2022 | UK | Evaluation of social prescribing service (January 2019–December 2020) | Interviews and focus groups | Total participants: 57 key stakeholders; social prescribing managers, LWs, referrers (GPs and social work practitioners), clients, VCS agencies and groups |
Those aged 16 years and over | Not stated | Loneliness and isolation; anxiety; becoming healthy and active |
| Author (year) | Signposting context | Setting | Generic or specialist | Signposting features | By whom | Type of resources required | Length of interaction |
|---|---|---|---|---|---|---|---|
| Bertotti et al. (2018)11 | Primary care | Twenty-three GP surgeries located in the London Borough of Hackney and the City of London | Generic | GP referral process; Interaction with SPC; Interaction with community/statutory organisations. To co-produce a well-being plan resulting from discussions about needs and aspirations of each patient and availability of local support services |
SPC | Eighty-five community organisations in borough which delivered physical activity classes, health advice, networking activities (e.g. lunch clubs), psychological support, art and other services | Up to six, 40-minute-long sessions |
| Brunton et al. (2022)12 | Challenges of integrating signposting into general practice | Primary care | Generic | GP referral process; Interaction with SPC; Interaction with community/statutory organisations. To co-produce a well-being plan resulting from discussions about needs and aspirations of each patient and availability of local support services |
Reception staff as CNs Social prescribing LWs |
Not reported | Not reported |
| Burroughs et al. (2019)13 | Feasibility of support workers employed by Age UK | Community | Specialist | Older people received support for anxiety and depression and to attend a community group or usual care | Support workers employed by Age UK North Staffordshire | Training Manual Support material Supervision |
Three to six sessions, lasting 15 minutes to 4 hours Supervision time varied between 60 and 280 minutes per support worker |
| Carstairs et al. (2020)15 | Primary care – GPs identifying patients who could benefit from jogScoltland | General practice | Specialist | Informal, active or referral to JogScotland. Jog leaders and group members hosting ‘meet and greet’ sessions at practice could allow HPs to gain knowledge about this option. Provide opportunity to signpost patients to group members for more information, support and reassurance and to establish ‘buddy’ to start activity journey with | GPs | Videos, leaflets | Standard GP appointment |
| Donovan and Paudyal (2016)30 | Pharmacy support staff views and attitudes on the HLP initiative | Primary care | Generic | Developing supportive relationship with service users, assessing their needs and providing person-tailored care | Pharmacy support staff | Knowledge of services, resources, community support | Brief consultation |
| Farr et al. (2021)31 | Improving access to mental health services against background of long waiting times and strict referral criteria | Four London boroughs | Specialist | Discussion with families and referrers of those not meeting CAMHS criteria | CAMHS staff, including STAR workers focusing on school outreach and signposting | Support from schools, local authorities and third sector/CVS | Variable |
| Gauthier et al. (2022)17 | Navigators’ experiences of assisting patients’ access to health and social resources in the community | Primary care | Generic | Navigators’ document their experience as a navigator through reflective journaling | ARC navigators | Not reported | Navigator NB logged a total of 433 encounters [mean total duration per patient was 126 minutes (range: 6–466 minutes)] with 66% of encounters occurring via telephone (n = 284) Navigator NN logged a total of 1025 encounters (mean total duration per patient was 91 minutes) |
| Hammond et al. (2013)18 | Primary care | Seven general practices | Generic | Face-to-face interactions | Receptionists | Knowledge of practice | Brief consultations – phone or in-person |
| Harris et al. (2020)6 | Primary care | Thirteen general practices | Generic |
|
GP: 12 (57 %) Nurse: 7 (33 %) Health and social care worker: 2 (10%) |
Information and self-help resources and peer and community support groups. Practical support – tangible services and aids; equipment provision, vouchers, books, self-monitoring diaries, completing forms and teaching practical skills to help patients use specific health-related equipment |
Brief consultations (< 15 minutes) |
| Kennedy et al. (2016)32 | Initial evaluation of a web-based tool GENIE consisting of network mapping, user-centred preference elicitation and needs assessment and facilitated engagement with resources | Community | Specialist | Facilitators guided participants through the GENIE process, an online tool to map social networks, and help participants to find and access relevant resources | Facilitators were local health trainers and CNs | Database of relevant resources and activities | GENIE process designed to take 30–40 minutes |
| Komaromy et al. (2018)33 | Evaluation of using Extension for Community Healthcare Outcomes (ECHO) model for CHW training | Community | Specialist | Training and ongoing support | CHS training using ECHO model | Not stated | Not stated |
| Toal-Sullivan et al. (2021)34 | Evaluation of training programme for lay navigators | Primary care | Generic | Training for lay navigators in primary care | Lay navigators | Not stated | Twelve-module blended approach |
| White et al. (2022)23 | Primary care | Based within GP practices and other locations including community centres | Generic | Separate social prescribing services available to support housing, debt and welfare benefits; such issues directed to a separate in-house welfare service, and not dealt with directly by LWs, so excluded from data analysis | Social prescribing service co-delivered by two VCS organisations with support provided by LWs (four or five variously during evaluation) | Not stated | Service Offered short-term support but with need for flexibility to tailor the duration of support to meet individual needs |
| Author (year) | Outcomes measured | Main findings | Key messages including limitations |
|---|---|---|---|
| Bertotti et al. (2018)11 | Referral to SPC (stage one)
|
Beneficial outcomes for patients result from combination of multiple stages working together effectively. Realist evaluation approach enabled identification of three stages of interaction between the patient and three other stakeholders: the GP (stage one), the SPC (stage two) and community organisations (stage three) | SPCs’ pivotal effective functioning of social prescribing service and responsible activation and initial beneficial impact on users. Social prescribing shows significant potential for benefit, but several challenges must be considered and overcome, including ‘buy-in’ from some GPs, branding and funding for third sector in context of social care cuts |
|
|||
| Brunton et al. (2022)12 | Stakeholder views on challenges of integrating signposting into general practice | Three themes that highlight the challenges of integrating signposting into general particle were role perceptions, role preparedness and integration and co-ordination of roles | Key factors that affect the success of signposting in practice are: clarity of role purpose and remit, appropriate training and skill development for role holders and adequate communication and engagement between stakeholders/partnership working. Limitations: views of CNs from only 1/5 areas where they were working and their experience could be different to CNs working in different areas of Greater Manchester |
| Burroughs et al. (2019)13 | Feasibility of non-traditional support workers delivering psychosocial intervention to older people with anxiety and depression and encouraging to attend a group | Recruiting and retaining the support workers was possible. They found the training support materials and manual acceptable and delivered the intervention as intended. Signposting to group activities was not acceptable to all older adults | This feasibility study found that support workers recruited from Age UK employees can be trained to deliver a psychosocial intervention. The support workers found the training and supervision model acceptable. Limitations: target recruitment was not achieved |
| Carstairs et al. (2020)15 | Health professionals and patients views of connecting patients to jogScotland including barriers and facilitators | Patients referred to community-based groups through informal passive signposting, informal active signposting and formal referral/prescribing Patients often presumed that active signposting was referral by HPs Barriers for HPs included need for current knowledge of options Patient barriers included need for social support to attend for first time |
HPs promoting PA could benefit from:
|
| Limitation: HPs interviewed had interest in promotion of PA and patients could have similar response bias mean that generalisation of the findings is not possible and any findings should be implemented with caution | |||
| Donovan and Paudyal (2016)30 | Pharmacy support staff views and experiences of HLP initiative | Facilitators/barriers included training, access to information | To promote the engagement of pharmacy staff with HLP initiative, need to involve them at the beginning. Training for staff on certain public health areas would be beneficial Limitations: All participants were female and white British, meaning any generalisation of findings should be cautious |
| Farr et al. (2021)31 | Qualitative data on the implementation of the THRIVE model of care, including collaboration and inter-agency working | Outreach into schools helped to promote the appropriate use of CAMHS and, consistent with other studies, to strengthen schools’ knowledge of suitable referrals and help them to signpost. A constraint on the use of signposting was insufficient third-sector resources |
Major challenge to system change was shortage of resources within the community to facilitate signposting. Insufficient capacity within CAMHS is a barrier to implementation, scalability and sustainability of programme change, particularly because signposting, outreach and mapping require focused resources Limitations: project still at an early stage of implementation; unequal representation of different stakeholder groups |
| Gauthier et al. (2022)17 | Navigators’ learning experience | Reflective journal entries analysed using five framework categories:
|
Experiences suggest that navigator education programmes should include learning opportunities from experiences of primary care, which could be testimonials from patients during training or initial supervised patient interactions. Supervision could help navigators with managing expectation, confidence building and help them start developing skills to apply person-centred care Limitations: limited generalisability journal entries from only two navigators. Also, navigators were aware that journals would be read by others so possibility of social desirability bias |
|
|||
| The journal entries demonstrated that navigators were applying skills learnt in training as well as learning from their patients. An awareness of what each patient can teach their navigator should be a key part of future training courses. Peer learning from other navigators also helped navigator’s personal growth. Potential to have community of navigators to learn from each other. When navigators were challenged with difficult situations, they asked for help from primary care team. Their position in the team helped them provide a bridge between health and social care providers in primary care and community |
|||
| Hammond et al. (2013)18 | Complexity of general practice receptionists’ role | Receptionists had the hard job of prioritising patients with limited time, information and training. Receptionists felt responsible for protecting patients they considered most vulnerable but protocols and patients trying to ‘play’ the system make this difficult | While more training is often suggested for receptionists, the difficulties that they face are helped or hindered by other members of staff at the practice and the organisation, structure and context of the practice which need addressing instead of present the problems as the receptionists |
| Harris et al. (2020)6 | Participants’ accounts showed that referral and signposting to external services and resources was the most common SMS activity used across all three exemplar common health problems | From the interview analysis, three categories and six subcategories, illustrating different self-management support activities across common health problems, were identified. Referral and signposting were frequently used to facilitate patient engagement with services and resources. Challenges were experienced by practitioners in balancing medical management and psychosocial support and motivating patients to engage with self-management | Digital repository of available community services and additional training in motivational interviewing would support practitioners and enable them to increase their confidence and skills in SMS across common health problems. Limited consultation time was a common obstacle but unclear exactly what the optimum duration and pattern of consultations should be |
| Kennedy et al. (2016)32 | Intervention acceptability, possible to implement and whether participants took up new activities | Most participants identified and started new activities following use of the tool | Key aspects of successful implementation including background work (reliable database, tailored preferences option reduction) for facilitator Limitation: results not generalisable on basis of health condition or location |
| Komaromy et al. (2018)33 | Participants’ self-reported abilities and attitudes evaluated using pre/post-program surveys and open-ended case scenarios | Obesity prevention CHWs reported increased skills and knowledge on post-training programme surveys. CARS CHWs motivational interview skills improved after training |
ECHO model shows promise to provide distance training and mentoring for CHWs. The needs of local communities and CHS will need to be understood to tailor programmes to the local communities |
| Toal-Sullivan et al. (2021)34 | Navigators’ learning experience | Participants found teaching material engaging and appropriate; sessions were relevant to their role; and content of face-to-face training met intended learning objectives | ARC navigator training programme shows promise, but effectiveness must be demonstrated with implementation and evaluation data. Learning from developing the programme, the pilot and implementation will be used to revise the curriculum for education of new navigators involved in a planned RCT of ARC. Potential to adapt programme for different setting, populations of patients and navigator qualifications (lay, clinical). The programme described develops our understanding of a theoretically grounded and competency-based curriculum designed to get lay navigators ready to support patients’ in accessing community resources for health and well-being Limitations: small sample of learners in pilot training and second implementation |
| White et al. (2022)23 | Number of users referred to social prescribing service Sources of referral to service Thematic analysis of interview data |
2199 users referred to social prescribing service (September 2017–August 2020) Sources of referral included self-referral (28%); social workers (20%); HPs (12.5%) Despite emphasis on social prescribing as a resource to help primary care manage demand, only 4.2% referrals were from GPs, a significant proportion (41.5%) were from two practices. The five themes identified from the qualitative data were: Theme One, Accessing Link Worker Support; Theme Two, How Link Workers Support Clients; Theme Three Getting on: Accessing Support in the Community, Theme Four, Perceived Benefits of Social Prescribing; Theme Five, Working to Deliver Social Prescribing |
Key support included referral into and onwards from social prescribing services (in addition to signposting), longer-term LW support, and buddying. Practitioner responses highlighted the balance between empowerment and dependency featured in practitioner responses. There is a need for good support and supervision for LWs to enable them to provide support while minimising client dependency. Further exploration is needed of why GP referrals were lower than expected and how referrals could be increased. Social workers were key referrers to social prescribing services suggesting a potential need to investigate in greater depth the role of social prescribing in UK social work practice |
Front-line providers of signposting services require training
Training is important to help front-line providers offer an effective signposting service. Numerous training courses, either generic or tailored to support particular populations, are currently available. One recent qualitative study12 found that some reception staff felt insufficiently trained to take on a role of active signposting as a CN. Receptionists may either lack formal training or have to wait for care navigation training, making them feel even less prepared for their role:
Receptionist 4 (CN): Well, whenever we started the care navigating, me and my colleague didn’t go on the course till a long time after, like months after…12(p5).
There were some receptionists who were excited to develop their role. Receptionists can potentially have a key role in signposting, but there is a need for adequate training and support from the practice team. Receptionists already have an important role within their practice; a high workload and their location in the waiting area are all issues that could make it difficult to fulfil a signposting role. An observational study in seven urban general practices in the north-west of England involving 45 receptionists explored the complexity of the receptionist role. 18 The study found that receptionists had the difficult role of prioritising patients for which they had limited time, training and information. Receptionists felt it was important for them to protect the patients who were most vulnerable, but that was not always possible due to the procedures they had to follow and also some patients knowing how to ‘play the system’. The knowledge that receptionists have of patients from living in the community could be helpful but could also mean that receptionists could get asked about work by patients they meet when not at work. To help GP practices to manage workload, receptionists ask each patient their problem to record on the booking system. From the information added, the GPs can then determine each patient’s level of need for an appointment. One practice in the study required the receptionists to ask each patient why they wanted to see a doctor. The receptionists’ response in the study indicated that they found it difficult. The study concluded that while more training is often suggested for receptionists, the challenges they encounter cannot always be addressed by training. These challenges may be exacerbated or improved by the actions of other staff in the practice and the organisation, structure and context of the individual practice. The situation can be improved by providing receptionists with the opportunity to give feedback on how policies can impact on their job and getting the wider practice team to consider the full role of the receptionist and the challenges that they are facing. The study was published in 2013 and the observations were conducted in 2009–11 and may be out of date, but the pandemic has potentially intensified some of these issues.
In addition, some reception staff felt that active signposting was a form of clinical triage leading to their concerns about patient safety when they as non-clinicians were undertaking the role. 12
Pharmacists can also be involved in signposting and are well placed in the community for this role. A qualitative study explored the view and attitudes of pharmacy support staff on the Healthy Living Pharmacy (HLP) initiative. 30 Pharmacy counter-based roles were found to be more suited to this public health role than dispensing roles. Initial training on the Royal Society of Public Health training programme was needed to become a Level 1 HLP; some described the training as useful, but many did not feel that the training had helped them to develop the skills that they required to work with clients. Offering advice or signposting about smoking was seen as easier than proactively delivering public health advice on topics they found difficult to bring up, for example, obesity, alcohol consumption or sexual behaviour, indicating the need for training on delivering advice in these areas. Nineteen facilitators and barriers became apparent from the interview data which included training as discussed above. Another barrier or facilitator was access to information, whether they knew of services they could refer patients to and how much information to give to clients. Additionally, confidential conversations could be difficult due to the availability of space and facilities. Pharmacies are often busy and there might not be a consultation room or quiet area available for confidential conversation. Time and competing priorities was another barrier, for example, pressure to focus on other services for which the pharmacy received financial rewards. Increased engagement with HLP required other staff to be involved from the introduction of the HLP initiative.
Training for community health workers (CHWs) working with patients with addiction and obesity prevention was developed using the Extension for Community Healthcare Outcomes (ECHO) model33 and included initial face-to-face skills training followed by weekly teleECHO sessions providing mentorship and community of practice. The training programme was tailored to the needs of the community and the CHWs but could be adapted to other settings. Two linked studies investigated the development and evaluation of a training programme for navigators34 and then a case study used reflective journals to document the navigator’s journey. 17 The researchers developed the Access to Resources in the Community (ARC) patient navigator training programme. The ARC training programme34 was structured around key competencies determined by undertaking an initial educational need assessment. The training course consisted of 12 learning modules and used a blended learning approach. Additionally, navigators had access to discussion forums and a navigator journal as part of the training course. Each navigator had weekly meetings with an experienced multicultural health navigator and support and mentorship from the research team; this continued for the 2 years of the evaluation study to support the navigators’ practice. 34 The training was generally well received. Experience suggested that navigator education programmes should include learning opportunities from experiences of primary care, which could be testimonials from patients during training or initial supervised patient interactions. 17 Qualitative data from mentorship meetings and journals revealed that the training programme was effective in preparing them for practice.
Front-line providers of signposting services require ongoing support and supervision
Ongoing support and supervision is important to enable front-line providers to provide successful signposting services The NOTEPAD trial13 offered two ways of supervision for the support workers, group meeting with two members of the research team and other support workers to discuss practicalities and share experiences and local resource knowledge or individual supervisory support for support workers with one of the research team. This model of supervision was acceptable to the support workers. Usual and ongoing support was also received from support workers’ nominated manager at Age UK. Support workers highlighted how important the supervision was at the final group meeting for reflection on their sessions with the older people and to help them decide how to support them. Training developed using the ECHO model included weekly teleECHO sessions,33 whereby CHWs could discuss their work and receive support and advice from ECHO specialists and other CHWs providing mentorship and a community of practice which were found to be important for CHWs development. The teleECHO session did not include CHWs’ supervisors as when used previously their presence could make CHWs feel less comfortable in discussions. However, including supervisors could help with team integration and teaching CHWs about the resources within their own community. To help community addiction recovery specialist (CARS) CHWs learn about resources within their own community, part of their training was to create a resource directory for their community. A training programme evaluation highlighted that mentorship and additional professional development were needed to support learning in the field. 34 The case study17 using reflective journals of patient navigators that had attended the ARC training programme found the need for ongoing support from peers and supervision. The case study also found that navigators were learning from their peers, the other navigators, suggesting the potential to have community of navigators to learn from each other. Supervision or support from their line managers could help navigators with managing expectation, confidence building and help them start developing skills to apply person-centred care.
Front-line providers of signposting services need to be flexible to meet individual needs
A qualitative study,15 considering patient and health professionals’ views on connecting primary care patients to community resources, found that some patients would have liked a buddy to attend with or someone to meet and greet them to help them attend for the first time. This indicates again that different patients need different things from a signposting service but also that health professionals could be spending time referring patients who feel unable to attend without the extra support in place. A scoping review10 investigated the relationship that LWs developed with participants. The following characteristics of facilitators that were identified in the included studies were ‘skills in tailoring activities to the needs and preferences of participants and the ability to encourage attendance and flexibility in their approach’. 10 Four of the included studies found that the relationship that facilitators developed with participants encouraged their engagement due to the facilitators ‘being flexible, trustworthy, empathetic and accessible’. 10 In the NOTEPAD trial,13 it was intended that support workers would tailor the intervention to the specific participant by being flexible with the number of sessions, if delivered face to face or by phone, and at the initial interview, patient preference was explored. Support workers need skills to do this properly.
Two navigators who had attended the ARC programme documented their experiences as navigators using reflective journals. 17 The journals demonstrated the importance for navigators of gaining and building their patients’ trust. Navigators needed to develop relationships with patients by actively listening and digging deeper to understand what patients needed and their individual preferences. Before a patient shares their health and social care needs, they might want to build up trust with, be listened to by their navigator or LW. 6,17
In the case study,17 the navigators worked with the patients for 3 months and some patients indicated that they needed support for longer. This suggested a variability of support that different patients need and the need for navigators to be flexible in their interactions with individual patients determining the level of support they need (some might need a navigator to attend a service with them initially) and the length of time that patients might require support for. Patients requiring support over different periods of time were also identified in another qualitative study23 where LWs were meant to be providing short-term support. Ideally, clients would have an initial appointment where they describe their problems and what they need help with, the LW would then refer and signpost them and then there would be a follow-up call. However, many clients required more and LWs needed to have skills to realise when this was the case. With complex cases, workers needed to build relationships, find services that meet their needs and then help them with accessing the appropriate service. Sometimes, clients needed help with contacting the service or perhaps attending initially, although this did not necessarily mean that they engaged long term with the service.
Front-line providers of signposting services need knowledge of good-quality available services for referrals
The quality of the resources and services to which patients are referred is clearly important. This was reflected by a Child and Adolescent Mental Health Services (CAMHS) Support Time and Resilience (STAR) worker whose service would only signpost young people to services that they had visited so they know that the services actually exist, are financially viable and able to support the needs of their young people. 31 This qualitative study also found a lack of community resources to refer patients to. People signposting need resources to meet the needs of referrals. A GP interviewed in a qualitative study6 on supporting self-management for patients with different health conditions said that he did not feel confident referring patients as he was unsure of resources or services available as they change over time. To help primary care staff feel confident referring or signpost patients to community services, they need greater and current knowledge of these services. To provide more effective self-management support to patients, many of the participants, from primary care, thought that they needed ‘a “signposting directory” of information resources and local clinical and non-clinical support services’. 6 The qualitative study found that, in the area of mental health, GPs had more knowledge of online services or self-referral services and so would feel more confident referring patients to these services.
A realist evaluation of social prescribing highlighted an important point about voluntary and community services. 11 Representatives from the third sector involved in the evaluation felt that there was an expectation that their services had spare capacity to accommodate extra referrals from social prescribing. However, their services had actually experienced extensive funding cuts, which was a major problem for continuing to deliver social prescribing services. Receptionists acting as CNs found it dissatisfying when they referred patients to services that did not have the capacity to accept them. 12 Another qualitative study15 found that health professionals were reticent to refer patients to physical activity opportunities as they were unsure if the opportunities were current. The study suggested that health professionals could benefit from resources such as a community resource with current community opportunities or an intermediary person to refer patients to. Navigators could experience feelings of helplessness when signposting patients to services due to challenges of barriers to access, cost and waiting times and lack of response from patients;17 navigators, therefore, need available services to refer their patients to and skills in encouraging patients to access services.
Online signposting
Recent years have witnessed increased interest in online or hybrid signposting services. 35 An initial evaluation of GENIE, an online social network intervention for people with type 2 diabetes, was positive. 32 Facilitators, who were local health trainers and CNs, worked through the process with participants. Facilitators received two training sessions on how to use the tools needed to deliver GENIE. A database of community resources was created for GENIE which links to the preference questions and selects potentially appropriate resources for participants. Facilitators worked through GENIE once with participants to create their social network map and prioritise three activities or forms of support. Facilitators understood GENIE and what their role was in delivering the intervention. The facilitators had an important role in the process: they were recruited from local populations, and this meant they could work together and collaborate at each stage of the process which might not have happened if there had been a sense of difference in status. Facilitators often took the lead but encouraged participants to play an active role. Training and skills are needed to enable a facilitator to help the participant play this active role. The study found that having the facilitator’s human presence helped participants to focus, stay motivated and persevere with the process. This indicates how important the facilitator’s role was and how even if a web tool has great promise, a facilitator can help participants to fully engage and complete the process. Facilitators did have ongoing working relationships with some of the participants, but the idea was that GENIE was completed just once with a facilitator. Facilitators spent much time on network mapping, and future training could place emphasis on discussing preferences and options. This would ensure that adequate attention is given to establishing that activities and resources are appropriate for service users. GENIE is a promising intervention that could be adapted for other conditions and is useful for lay health trainers or CNs to use with new or existing service users or to for use by service users who are health literate to help them identify activities.
Initial conclusions for required resources (service provider perspective)
-
Providers of front-line signposting services require appropriate training, ongoing support and supervision.
-
Providers of front-line signposting services require good knowledge of services to which they can refer.
-
Providers of front-line signposting services need to be flexible in order to meet individual needs.
-
Providers of front-line signposting services need competencies in matching appropriate services or resources to the needs of service users.
-
Signposting services need to be underpinned by well-resourced, good-quality accessible services to which providers are able to refer.
Research question 3 (commissioner perspective)
Question 3: How can commissioners/funders specify, monitor and evaluate signposting services (generic or specific) to optimise value for money and outcomes for service users? Specifically, do factors favour funding of generic versus specialist services or vice versa?
Perspective
The perspective is that of commissioners/funders responsible for providing signposting services. This could be CCGs (replaced by Integrated Care Boards in 2022), local authorities or national/regional bodies. The evidence is taken from studies conducted in England; Wales, Scotland and Northern Ireland have separate organisational arrangements, but similar principles apply. For the data extraction table for Question 3, see Tables 9–11.
| Author (year) | Study year | Study country/countries | Study design | Study sample | Sample size | Population age | Population gender | Health condition |
|---|---|---|---|---|---|---|---|---|
| Allen and Drabble (2017)36 | 2015–7 | England | Evaluation of Primary Care Navigator (PCN) service | Patients and key stakeholders | Unclear | N/R | N/R | Diabetes |
| Dayson et al. (2016)37 | 2012–5 | England | Evaluation of social prescribing service | Client management and monitoring data, hospital episode statistics and case studies involving service users | Unclear | Predominantly older people | 62% female | Long-term conditions |
| Farr et al. (2021)31 | 2020 | England | Qualitative | Professionals and service users involved with implementing the THRIVE framework for CYP’s mental health | 80 (CAMHS clinicians, commissioners, service leads, service users and their parents or carers. Participants from the wider referral pathway and implementation team were also included) | N/R | N/R | Mental health conditions referred to CAMHS |
| Tierney et al. (2019)2 | 2018–9 | England | Survey of CCGs | All CCGs in England (195) | 162 provided usable data | N/A | N/A | N/A |
| Author (year) | Signposting context | Setting | Generic or specialist | Signposting features | By whom | Type of resources required | Length of interaction |
|---|---|---|---|---|---|---|---|
| Allen and Drabble (2017)36 | Support for people with diabetes and related conditions provided through pharmacies and GP surgeries | Lambeth (inner London) | Specialist | Work with patients who have difficulty accessing services or who have specific needs | Primary CNs | Space for consultations; training and support | Variable |
| Dayson et al. (2016)37 | People with long-term conditions referred to social prescribing service | Rotherham CCG area | Generic for people with long-term conditions | Wide range of activities available | GP practices | Funded activities and other VCS activities | Variable but multiple referrals from SP service to funded activities not uncommon |
| Farr et al. (2021)31 | Improving access to mental health services against background of long waiting times and strict referral criteria | Four London boroughs | Specialist | Discussion with families and referrers of those not meeting CAMHS criteria | CAMHS staff, including STAR workers focusing on school outreach and signposting | Support from schools, local authorities and third sector/CVS | Variable |
| Tierney et al. (2019)2 | Specification and funding of relevant services | Local CCG areas | Both (but predominantly generic, i.e. open to all adults) | Range of care navigation services provided | Range of people including receptionists, practice managers, paid workers and volunteers | Variable | Variable |
| Author (year) | Outcomes measured | Main findings | Key messages including limitations |
|---|---|---|---|
| Allan and Drabble (2017)36 | Range of qualitative and quantitative outcomes from patient, staff and organisational perspectives | Recommendations relevant to commissioners were provided and furthermore a detailed evaluation was recommended to address identified limitations | Recommendations: Clearly establish what service users can expect from PCN services Develop a database of PCN episodes to understand outcomes and resource use Consider how access and referral might be affected by the employment and support model available for PCNs Review the impact of PCN availability on patient awareness of, and access to, the service and consider ways of providing greater flexibility of access Explore digital methods of compiling and disseminating the navigation prescription Collect patient data to monitor impact on health inequalities Develop succession planning for PCNs and continuous recruitment to ensure maintenance of the service. |
| Limitations: the scope and scale of the evaluation were limited and the quality of the data was generally not robust in the absence of a longitudinal element. Future evaluations would benefit from further in-depth access, particularly before and after surveys to measure patient outcomes and measures of primary care usage by the target group at the beginning and end of the intervention | |||
| Dayson et al. (2016)37 | Activities and referrals; impact on demand for hospital services; social impact; economic and social cost/benefit | The Rotherham Social Prescribing Service is one of the largest in the UK. During 2012–5 it engaged with over 3000 people with long-term conditions. Evaluation found evidence of reduced use of urgent care and improved well-being in service users. Economic benefits to commissioners were estimated based on NHS costs avoided through reduced demand for urgent hospital care. Authors reported that between 2012 and 2015, the estimated total NHS costs avoided exceeded £500,000 representing an initial return on investment of 43 pence per pound invested. |
Key messages: ‘NHS Rotherham CCG and its statutory partners have made a large and long-term financial and strategic commitment to Social Prescribing as a mainstream component of health provision’. This ensures that diverse activities are funded or available elsewhere in the VCS. Cost benefits to social prescribing need to be understood on a long-term time frame. Service users who engage fully with the programme appear to benefit most. Evaluation highlights importance of Case Management Teams in ensuring that those most likely to benefit are referred. |
| The costs of delivering the service would be regained after about 2 and 1/2 years if the benefits identified are fully sustained over a longer period. Costs avoided after 5 years could approach £1.1 million: return on investment of £1.98 for each pound (£1) invested. If the benefits are sustained but drop off at a rate of 33% each year, they could lead to total cost reductions of £0.46 million: return on investment of £0.83 for every £1 invested. Value of service user well-being outcomes (from financial proxies and techniques associated with SROI analysis) estimated as between £0.57 and £0.62 million in first year following engagement with social prescribing: greater than costs of delivering the service |
Future evaluation could follow service users for longer and seek to develop a matched control group. ‘Other areas future evaluation might consider include the impact on GP time and the introduction of a standardised measure of health-related quality of life’. Limitations: relatively short-term and uncontrolled evaluation |
||
| Farr et al. (2021)31 | Qualitative data on the implementation of the THRIVE model of care, including collaboration and interagency working | Service accessibility ‘was seen to be promoted through integration of a needs-based approach, flexible re-referral, signposting and information sharing, the use of goal-orientated interventions and collaboration over risk and treatment endings’. ‘The use of signposting to redirect CYP referred into CAMHS to services that would better meet their needs was seen by participants as more equitable, and increased CYP and family awareness of other sources of support. Outreach into schools was seen to promote appropriate use of CAMHS and, consistent with other studies, to foster schools’ knowledge of suitable referrals and enable them to signpost’. ‘Insufficient third sector resources were seen to constrain the use of signposting and timely discharge, the impact of which relied on adequate support in the community to promote accessibility’ |
‘A major challenge to system change was a shortage of resources in the community to facilitate signposting. Three of six commissioners recognized the priority to build support in the system’. Insufficient capacity within CAMHS ‘was seen as a barrier to implementation, scalability and sustainability of programme change, particularly because signposting, outreach and mapping required focused resources’. Limitations: project still at an early stage of implementation; unequal representation of different stakeholder groups |
| Tierney et al. (2019)2 | Type of people providing care navigation; type of people to whom the service is available; methods of referral; whether service has been evaluated | Over 90% of CCGs providing usable data (147/162) had some form of care navigation service. Seventy-five different titles were used to describe the role. Most services were open to all adults, but some targeted particular groups, for example, older people and those with long-term conditions. Referrals tended to be made by a professional, or people were identified by a receptionist when presenting to a surgery. Only 22% of CCGs reported that at least one service in their area had been evaluated. Services that had been evaluated tended to be dedicated schemes, involving staff employed to undertake care navigation type work. Services delivered in-house by existing primary care staff were least likely to have been evaluated | Implementation of care navigation by CCGs was highly heterogeneous. Generic services provided by trained surgery staff were most common. Variation could hamper comparison between areas and be confusing for patients. Few services had been evaluated. Results reflect CCG perceptions only and represent the situation in late 2018 |
Findings for Question 3 – specification, monitoring and evaluation: service commissioner/funder perspective
For Question 3, a total of four items of evidence were reviewed; data were extracted from a survey of CCGs in England; evaluations of a social prescribing service and a primary care diabetes care navigation service; and a qualitative study of a new care model in CAMHS.
Commissioned care navigation services in England are highly diverse in terms of client groups, staff delivering the service, referral routes and how the role is described. Evaluation of services is uncommon, and this could be a barrier to effective commissioning.
Evaluations in primary and secondary care have identified key recommendations for commissioners. Lack of availability of services in the VCS may limit the effectiveness of signposting/care navigation in both primary and secondary care. A successful social prescribing programme has made a long-term commitment to social prescribing as a key component of health provision. This involves working closely with the VCS to ensure that diverse activities are funded, including direct funding by the CCG. The evaluation found evidence of reduced urgent care use and improved well-being in those who engaged with the service. Methods are available to estimate economic benefits of social prescribing and similar services to commissioners based on reduced use of other services.
Brief signposting interventions may be sufficient for some service users. Others require intensive support to overcome barriers to engaging with either the care signposting/care navigation process or subsequently to engaging with services to which they are referred. From the commissioner perspective, it is important that referral processes provide intensive support to those most likely to benefit in the longer term.
Tierney et al. 2 surveyed English CCGs to understand how ‘care navigation’ is understood and implemented. Of the 195 CCGs in existence at the time, 162 provided usable data. Over 90% of these CCGs (147/162) had some form of care navigation service. A total of 75 different titles were used to describe the role. Most services were open to all adults, but some targeted particular groups, for example, older people and those with long-term conditions. Some areas had both universal and more targeted services but the rationale for this was not reported in the paper. Referrals tended to be made by a professional, or people were identified by a receptionist when they presented to a surgery. Only 22% of CCGs reported that at least one service in their area had been evaluated. Services that had been evaluated tended to be dedicated schemes, involving staff employed to undertake care navigation type work. Services delivered in-house by existing primary care staff were least likely to have been evaluated.
Wide variation in service provision and nomenclature can make it challenging to compare performance between areas. Service users could also find this variation confusing. 2 Although not explicitly discussed by the authors, the low level of evaluation of services noted in the study should be of concern to commissioners because they fund training for staff providing brief signposting as well as intensive care navigation support. One limitation of this study was that it reflects the situation in late 2018 and therefore before the COVID-19 pandemic.
Evaluations of a primary care diabetes care navigator (PCN) programme36 and a large social prescribing programme37 took different approaches to data collection. The former involved interviews with a range of key stakeholders, while the latter combined quantitative data with case studies involving service users.
The PCN programme evaluation produced several recommendations relevant to commissioners:
-
Clearly establish what service users can expect from PCN services.
-
Develop a database of PCN episodes to understand outcomes and resource use.
-
Consider how access and referral might be affected by the employment and support model available for PCNs.
-
Review the impact of PCN availability on patient awareness of, and access to, the service and consider ways of providing greater flexibility of access.
-
Explore digital methods of compiling and disseminating the navigation prescription.
-
Collect patient data to monitor impact on health inequalities.
-
Develop succession planning for PCNs and continuous recruitment to ensure maintenance of the service.
Limitations of this evaluation include its cross-sectional design. Further in-depth evaluation, including a before-and-after evaluation of primary care resource use by the target population, was recommended. 36
Commissioners need to evaluate the value for money of their services, and this was addressed in an evaluation of the Rotherham social prescribing service. 37 The service is one of the largest in the UK. During 2012–5, it engaged with over 3000 people with long-term conditions. The evaluation found evidence of reduced use of urgent care and improved well-being in service users.
The economic benefits to commissioners were estimated based on the NHS costs avoided through reductions in the demand for urgent hospital care. The authors reported that ‘the estimated total NHS costs avoided between 2012 and 2015 were more than half a million pounds: an initial return on investment of 43 pence for each pound invested’. 37 Examples were provided on possible return on investment over 5 years based on different assumptions about sustainability of the initial benefits. The value of service users’ well-being outcomes was estimated using financial proxies and techniques associated with social return on investment (SROI) analysis. The estimated value of these benefits was between £0.57 and £0.62 million in the first year after engagement with social prescribing, which exceeded the costs of delivering the service.
The evaluation also highlighted the importance of Case Management Teams in ensuring that those most likely to benefit were referred. The authors noted that future evaluations could follow service users for longer and seek to develop a matched control group. They could also consider the impact of the service on GP time and take a standardised approach to measuring health-related quality of life. 37
A qualitative study of the implementation of the THRIVE model of care, including collaboration and inter-agency working, in CAMHS in London31 identified a role for signposting in a specialist setting where demand exceeds supply and strict referral criteria are applied by commissioners. Service accessibility ‘was seen to be promoted through the integration of a needs-based approach, flexible re-referral, signposting and information sharing, the use of goal-orientated interventions and collaboration over risk and treatment endings’. 31 Signposting was used to redirect children and young people (CYP) referred into CAMHS to services that better meet their needs. Participants considered this to be more equitable, and to increase the awareness of CYP and their families in connection with other sources of support. Appropriate use of CAMHS services was promoted through outreach into schools, thereby increasing knowledge of suitable referrals within schools and enabling signposting.
Insufficient resources for signposting within CAMHS and alternative sources of support within the CVS were recognised by commissioners as barriers that needed to be tackled,31 supporting the findings of the Rotherham social prescribing service evaluation37 and reflecting the fact that this service was at a relatively early stage of implementation.
Initial conclusions for Question 3 – specification, monitoring and evaluation: the service commissioner/funder perspective
-
A small purposive sample of studies illustrates the diversity of commissioned signposting services in the UK (England) and provides exemplars of service specification, monitoring/data collection and evaluation (including a possible approach to economic evaluation).
-
Evaluation of services is uncommon, and this absence presents a potential barrier to effective commissioning.
-
Lack of availability of services in the VCS may limit the effectiveness of signposting/care navigation in both primary and secondary care and their potential to reduce urgent care use and improve well-being in service users.
-
Brief signposting interventions may be sufficient for some service users. Others require intensive support to overcome barriers to engagement with either the care signposting/care navigation process or, subsequently, services to which they are referred.
-
If commissioners are to avoid demands on long-term resource use, it is essential that referral processes provide intensive support to those most likely to benefit from navigation services in the longer term.
Overall conclusions
Across the three perspectives (service user, service provider and commissioner of services), certain common findings could be observed.
First, the variation of terminology and intensity of service provision is unhelpful. Service users find it difficult to understand what services are being offered. Service commissioners may find it challenging to specify services and to identify an appropriate evaluation frame. Conversely, it is important for a clear distinction to be made between service provider responses that focus on signposting and those that require intensive and sustained support.
Second, it is unhelpful to consider signposting services in isolation. While a small proportion of service users may benefit from brief signposting interventions, the complex health and social needs of many service users, especially given how non-generic services are targeted specifically at users because of their intensive needs, require an extended response. Furthermore, the risk that commissioners and service providers might believe that signposting in itself is sufficient could lead to needs being hidden.
Third, the satisfaction of service users, their perception of the value of service providers and the service providers’ own confidence in their role rely on a knowledge of accessible and available resources. At times of economic constraints, pressures are placed not only on health services but also on informal social provision. Service users lose confidence in signposting services if they are not supported by adequate opportunities and activities.
Fourth, the drivers for signposting services are equivocal. The efficiency argument – relieving pressure on primary care and other front-line services – figures prominently in many of the reviewed studies. At the same time, the improved quality of care argument – services being joined up and enabling service user progress across organisations and sectors – is also invoked. While these two narratives may be seen as inter-related in terms of appropriate service utilisation, they start to diverge when considerations of whether the service should involve brief interactions with large numbers of generic users or sustained, and even prolonged, support to a targeted user group with complex health and social needs.
Finally, evaluation of signposting services is challenging. Claimed benefits for services that include signposting often derive from more sustained and intensive interactions: for example, improvements in self-confidence or gains in health literacy. Brief interventions of any type find it difficult to demonstrate either immediate or sustained benefit and this is particularly likely to be the case when the intervention involves referral to other agencies where the quality of response may be uncontrolled and, therefore, variable.
Equality, diversity and inclusion
As a secondary data study, coverage of populations within the review is determined by the samples of included studies. Study authors did not focus on population variables such as ethnicity or religious belief. Indeed, coverage of any protected characteristics was very limited. The review team has identified a need to explore in a structured and systematic way aspects of diversity already shown to be important when accessing health and care services, particularly information-based services comparable to signposting. For example, a systematic review of social prescribing services found little emphasis on cultural appropriateness. 7
Of particular importance might be cultural differences in question asking behaviour and the practical need for translation or interpretation services, both in promoting and in delivering services. Although we found that personal characteristics were critical in the delivery of signposting services, issues such as matching service providers and service user groups by ethnicity or other similarities remain to be explored. It is not known whether particular ethnic minorities, gender or other protected characteristics are more or less likely to use signposting services; evidence from other health services such as ambulance services suggests a need for caution in assuming underutilisation. Recruitment processes for service providers may offer structural barriers to delivery of an ethnically and language-diverse service.
The literature did not highlight issues of diversity as they relate to setting up a service; theoretically, we might hypothesise that it is easier for a service commissioner to profile population needs for a specific service rather than provide a culturally appropriate generic service. For the latter, training may be targeted more at delivering a culturally appropriate service rather than on the cultural content of the signposting services required by the former.
Methodological limitations/lessons from experimental format
As previously mentioned, the review authors have intentionally re-engineered an experimental report format in an attempt to avoid the academic AMRAD (Abstract Methods Results and Discussion format) and to acknowledge current understanding of policy-maker report preference. However, acknowledging that this format may carry certain limitations in addition to providing an opportunity for lessons learnt, the review authors observe that:
-
Researchers might not understand the methodology used and any assumptions on which the findings are based.
-
Readers may not be able to navigate the report format.
-
The review team have identified a need for feedback and evaluation for the report once published to determine the extent to which it meets the requirements of different target audiences.
-
In future, earlier discussions on experimental formats with the NIHR Health and Social Care Delivery Research Programme staff and the editorial team could facilitate timely publication of report findings.
Research priorities/gaps
-
There is a need to evaluate different levels of intensity of service provision and their differential benefits and value for money.
-
Productive comparison and evaluation (through benchmarking and audit) of similar services is required (i.e. signposting services to be compared with similar brief services and services providing more intensive and sustained to be compared with similar).
-
Further comparison and evaluation of signposting services could explore levels of service provided by different staff roles.
-
Specialist services may particularly benefit from evaluation tailored to the needs and objectives of each specific service.
-
Issues of diversity are particularly absent from the literature particularly as they relate to setting up a service; thus, we have identified a need for research around setting up and providing services for diverse populations.
-
Research examining the impact of economic constraints on informal social provision would be potentially informative.
-
Further consideration of the extent to which each service developed should prioritise and manage brief interactions with large numbers of generic users or sustained, and even prolonged, support to a targeted user group with complex health and social needs.
Additional information
Contributions of authors
Anna Cantrell (https://orcid.org/0000-0003-0040-9853) (Research Fellow) was the lead reviewer and carried out proposal development, information retrieval, study selection, data extraction, and report writing.
Andrew Booth (https://orcid.org/0000-0003-4808-3880) (Professor in Evidence Synthesis) was the methodological adviser and lead proposal developer, conducted study selection, data extraction, taxonomy development, and report writing, and was the guarantor of the review.
Duncan Chambers (https://orcid.org/0000-0002-0154-0469) (Research Fellow) carried out study selection, data extraction, and report writing.
All authors commented on drafts of the proposal and report.
Disclosure of interests
Full disclosure of interests: Completed ICMJE forms for all authors, including all related interests, are available in the toolkit on the NIHR Journals Library report publication page at https://doi.org/10.3310/GART5103.
Primary conflicts of interest: Andrew Booth is a member of the NIHR Health Services and Delivery Research (HS&DR) Funding Committee and the NIHR Systematic Reviews Advisory Group, and Convenor of the Cochrane Qualitative and Implementation Methods Group.
Data-sharing statement
Any additional data not included in this report and its appendices are available on request. All queries should be submitted to the corresponding author.
Ethics statement
This review did not involve the collection or analysis of any data that were not included in previously published research in the public domain. Therefore, it was exempt from formal ethical review by the University of Sheffield Ethics Committee.
Information governance statement
National Institute for Health and Care Research is committed to handling all personal information in line with the UK Data Protection Act (2018) and the General Data Protection Regulation (EU GDPR) 2016/679. Under Data Protection legislation, NIHR is the Data Processor; the Department for Health and Social Care (DHSC) is the Data Controller, and we process personal data in accordance with their instructions. You can find out more about how we handle personal data, including how to exercise your individual rights and the contact details for DHSC’s Data Protection Officer here www.nihr.ac.uk/documents/nihr-privacy-policy/12242#how-we-protect-your-personal-data.
Department of Health and Social Care disclaimer
This publication presents independent research commissioned by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, MRC, NIHR Coordinating Centre, the HSDR programme or the Department of Health and Social Care.
This monograph was published based on current knowledge at the time and date of publication. NIHR is committed to being inclusive and will continually monitor best practice and guidance in relation to terminology and language to ensure that we remain relevant to our stakeholders.
Disclaimers
This article presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care.
References
- Nesta . More Than Medicine, New Services for People Powered Health 2013.
- Tierney S, Wong G, Mahtani KR. Current understanding and implementation of ‘care navigation’ across England: a cross-sectional study of NHS clinical commissioning groups. Br J Gen Pract 2019;69:e675-81.
- Pawson R, Greenhalgh T, Harvey G, Walshe K. Realist review – a new method of systematic review designed for complex policy interventions. J Health Serv Res Policy 2005;10:21-34. https://doi.org/10.1258/1355819054308530.
- Petkovic J, Welch V, Jacob MH, Yoganathan M, Ayala AP, Cunningham H, et al. Do evidence summaries increase health policy-makers’ use of evidence from systematic reviews? A systematic review. Campbell Syst Rev 2018;14:1-52.
- Sharp MK, Baki DABA, Quigley J, Tyner B, Devane D, Mahtani KR, et al. The effectiveness and acceptability of evidence synthesis summary formats for clinical guideline development groups: a mixed-methods systematic review. Implement Sci 2022;17:1-20.
- Harris E, Barker C, Burton K, Lucock M, Astin F. Self-management support activities in primary care: a qualitative study to compare provision across common health problems. Patient Educ Couns 2020;103:2532-9. https://doi.org/10.1016/j.pec.2020.07.003.
- Bickerdike L, Booth A, Wilson PM, Farley K, Wright K. Social prescribing: less rhetoric and more reality. A systematic review of the evidence. BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2016-013384.
- Chatterjee HJ, Camic PM, Lockyer B, Thomson LJM. Non-clinical community interventions: a systematised review of social prescribing schemes. Arts Health 2017;10:97-123. https://doi.org/10.1080/17533015.2017.1334002.
- Liebmann M, Pitman A, Hsueh Y-C, Bertotti M, Pearce E. Research Square Platform LLC. 2022.
- Mossabir R, Morris R, Kennedy A, Blickem C, Rogers A. A scoping review to understand the effectiveness of linking schemes from healthcare providers to community resources to improve the health and well-being of people with long-term conditions. Health Soc Care Community 2015;23:467-84. https://doi.org/10.1111/hsc.12176.
- Bertotti M, Frostick C, Hutt P, Sohanpal R, Carnes D. A realist evaluation of social prescribing: an exploration into the context and mechanisms underpinning a pathway linking primary care with the voluntary sector. Prim Health Care Res Dev 2018;19:232-45. https://doi.org/10.1017/s1463423617000706.
- Brunton L, Tazzyman A, Ferguson J, Hodgson D, Nelson P. The challenges of integrating signposting into general practice: qualitative stakeholder perspectives on care navigation and social prescribing in primary care. BMC Primary Care 2022;23. https://doi.org/10.1186/s12875-022-01669-z.
- Burroughs H, Bartlam B, Bullock P, Lovell K, Ogollah R, Ray M, et al. Non-traditional support workers delivering a brief psychosocial intervention for older people with anxiety and depression: the NOTEPAD feasibility study. Health Serv Deliv Res 2019;7:1-120. https://doi.org/10.3310/hsdr07250.
- Carduff E, Jarvis A, Highet G, Finucane A, Kendall M, Harrison N, et al. Piloting a new approach in primary care to identify, assess and support carers of people with terminal illnesses: a feasibility study. BMC Fam Pract 2016;17. https://doi.org/10.1186/s12875-016-0414-2.
- Carstairs SA, Rogowsky RH, Cunningham KB, Sullivan F, Ozakinci G. Connecting primary care patients to community-based physical activity: a qualitative study of health professional and patient views. BJGP Open 2020;4. https://doi.org/10.3399/bjgpopen20X101100.
- Foster A, Thompson J, Holding E, Ariss S, Mukuria C, Jacques R, et al. Impact of social prescribing to address loneliness: a mixed methods evaluation of a national social prescribing programme. Health Soc Care Community 2021;29:1439-49. https://doi.org/10.1111/hsc.13200.
- Gauthier AP, Bourgoin N, Ndihokubwayo N, Lemonde M, Toal-Sullivan D, Timony PE, et al. Learning from reflective journaling; the experience of navigators in assisting patients access to health and social resources in the community. Int J Health Promot Educ 2022;60:354-64. https://doi.org/10.1080/14635240.2022.2073900.
- Hammond J, Gravenhorst K, Funnell E, Beatty S, Hibbert D, Lamb J, et al. Slaying the dragon myth: an ethnographic study of receptionists in UK general practice. Br J Gen Pract 2013;63:e177-84. https://doi.org/10.3399/bjgp13X664225.
- Hibberd P, Vougioukalou S. Flexible, immediate support and signposting. J Dementia Care 2012;20:12-3.
- Papachristou Nadal I, Cliffton C, Tolani E, Achilleos S, Winkley K, Chamley M, et al. Eliciting the mechanisms of action of care navigators in the management of type 2 diabetes in people with severe mental illness: a qualitative study. Diabet Med 2022;39. https://doi.org/10.1111/dme.14894:e14894.
- Stokoe E, Sikveland RO, Symonds J. Calling the GP surgery: patient burden, patient satisfaction, and implications for training. Br J Gen Pract 2016;66:e779-85. https://doi.org/10.3399/bjgp16X686653.
- White J, Kinsella K. An Evaluation of Social Prescribing Health Trainers in South and West Bradford. Leeds: Leeds Metropolitan University; 2010.
- White C, Bell J, Reid M, Dyson J. More than signposting: findings from an evaluation of a social prescribing service. Health Soc Care Community 2022;30:e5105-14. https://doi.org/10.1111/hsc.13925.
- Wildman JM, Moffatt S, Steer M, Laing K, Penn L, O’Brien N. Service-users’ perspectives of link worker social prescribing: a qualitative follow-up study. BMC Public Health 2019;19. https://doi.org/10.1186/s12889-018-6349-x.
- Baddeley B, Sornalingam S, Cooper M. Social prescribing in general practice. InnovAiT 2016;11:119-21. https://doi.org/10.1177/1755738016667967.
- O’Callaghan D. Understanding the Social Prescribing Approach: Insights from the Health and Well-Being Community Referral Service in Cork. Ireland: Community-Academic Research Links/University College Cork; 2020.
- Richards S. Putting self-care into practice. Practice Nurse 2012;42:26-30.
- Ryan S, Rogers A, Lester H. GPs’ and patients’ views on recovery from psychosis. Ment Health Rev J 2014;19:99-109. https://doi.org/10.1108/mhrj-11-2013-0035.
- Kilgarriff-Foster A, O’Cathain A. Exploring the components and impact of social prescribing. J Public Ment Health 2015;14:127-34. https://doi.org/10.1108/jpmh-06-2014-0027.
- Donovan GR, Paudyal V. England’s Healthy Living Pharmacy (HLP) initiative: facilitating the engagement of pharmacy support staff in public health. Res Social Adm Pharm 2016;12:281-92. https://doi.org/10.1016/j.sapharm.2015.05.010.
- Farr J, Moore A, Bruffell H, Hayes J, Rae JP, Cooper M. The impact of a needs-based model of care on accessibility and quality of care within children’s mental health services: a qualitative investigation of the UK i-THRIVE Programme. Child Care Health Dev 2021;47:442-50. https://doi.org/10.1111/cch.12855.
- Kennedy A, Vassilev I, James E, Rogers A. Implementing a social network intervention designed to enhance and diversify support for people with long-term conditions. A qualitative study. Implement Sci 2016;11. https://doi.org/10.1186/s13012-016-0384-8.
- Komaromy M, Ceballos V, Zurawski A, Bodenheimer T, Thom DH, Arora S. Extension for Community Healthcare Outcomes (ECHO): a new model for community health worker training and support. J Public Health Policy 2018;39:203-16. https://doi.org/10.1057/s41271-017-0114-8.
- Toal-Sullivan D, Lemonde M, Gauthier AP, Dahrouge S. Adopting a lay navigator training programme in primary care. Health Edu J 2021;80:210-24. https://doi.org/10.1177/0017896920959364.
- Kiely B, Croke A, O’Shea E, Connolly D, Smith SM. Effectiveness of link workers providing social prescribing on health outcomes and costs for adult patients in primary care and community settings. A protocol for a systematic review of the literature. HRB Open Res 2019;2. https://doi.org/10.12688/hrbopenres.12936.2.
- Allen R, Drabble D. South Lambeth Primary Care Navigation for Diabetes: Final Evaluation Report. London: The Tavistock Institute; 2017.
- Dayson C, Bashir N, Bennett E, Sanderson E. The Rotherham Social Prescribing Service for People With Long-Term Health Conditions: Annual Report 2016.
- Southby K, Robinson O. Information, advocacy and signposting as a low-level support for adults with high-functioning autism spectrum disorder: an example from the UK. J Autism Dev Disord 2018;48:511-9. https://doi.org/10.1007/s10803-017-3331-x.
- MacInnes J. Care navigators decision-making in prescribing Telecare for older people. Health Soc Care Community 2020;28:2431-40. https://doi.org/10.1111/hsc.13066.
- Hagan RJ. What next? Experiences of social support and signposting after a diagnosis of dementia. Health Soc Care Community 2020;28:1170-9. https://doi.org/10.1111/hsc.12949.
- Saunders B, Foster NE, Hill JC, Sowden G, Evans N, Bishop A, et al. First contact practitioners’ (FCPs) and general practitioners’ perceptions towards FCPs delivering vocational advice to patients with musculoskeletal conditions: a qualitative investigation of the implementation potential of the I-SWAP initiative. J Occup Rehabil 2022;32:147-55. https://doi.org/10.1007/s10926-021-09992-5.
- Brandborg CE, Skjerning HT, Nielsen RO. Physical activity through social prescribing: an interview-based study of Danish general practitioners’ opinions. Health Soc Care Community 2021;30:1969-78. https://doi.org/10.1111/hsc.13577.
- Holding E, Thompson J, Foster A, Haywood A. Connecting communities: a qualitative investigation of the challenges in delivering a national social prescribing service to reduce loneliness. Health Soc Care Community 2020;28:1535-43. https://doi.org/10.1111/hsc.12976.
- Tod AM, Kennedy F, Stocks AJ, McDonnell A, Ramaswamy B, Wood B, et al. Good-quality social care for people with Parkinson’s disease: a qualitative study. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2014-006813.
- Kokorelias KM, Shiers-Hanley JE, Rios J, Knoepfli A, Hitzig SL. Factors influencing the implementation of patient navigation programs for adults with complex needs: a scoping review of the literature. Health Serv Insights 2021;14. https://doi.org/10.1177/11786329211033267.
- Valaitis RK, Carter N, Lam A, Nicholl J, Feather J, Cleghorn L. Implementation and maintenance of patient navigation programs linking primary care with community-based health and social services: a scoping literature review. BMC Health Serv Res 2017;17. https://doi.org/10.1186/s12913-017-2046-1.
- Tierney S, Wong G, Roberts N, Boylan AM, Park S, Abrams R, et al. Supporting social prescribing in primary care by linking people to local assets: a realist review. BMC Med 2020;18. https://doi.org/10.1186/s12916-020-1510-7.
- McMurray A, Ward L, Johnston K, Yang L, Connor M. The primary health care nurse of the future: preliminary evaluation of the Nurse Navigator role in integrated care. Collegian 2018;25:517-24. https://doi.org/10.1016/j.colegn.2017.12.003.
- Dominguez A. Decreasing Primary-Care-Related Emergency Department Visits in the Hispanic Population Using Patient Navigators n.d. https://scholarworks.waldenu.edu/dissertations/4616.
- Cooper SL, Pelly FE, Lowe JB. Assessment of the construct validity of the Australian Health Star Rating: a nutrient profiling diagnostic accuracy study. Eur J Clin Nutr 2017;71:1353-9. https://doi.org/10.1038/ejcn.2017.23.
- Bauer A, McDaid D, Tinelli M, Guy D. Signposting and Navigation Services for Older People: Economic Evidence. London: London School of Economics and Political Science Care Policy and Evaluation Centre; 2019.
- May M, Brousseau DC, Nelson DA, Flynn KE, Wolf MS, Lepley B, et al. Why parents seek care for acute illness in the clinic or the ED: the role of health literacy. Acad Pediatr 2018;18:289-96. https://doi.org/10.1016/j.acap.2017.06.010.
- Wade M, Brown N, Steele J, Mann S, Dancy B, Winter S, et al. The impact of signposting and group support pathways on a community-based physical activity intervention grounded in motivational interviewing. J Public Health (Oxf) 2021;44:851-62. https://doi.org/10.1093/pubmed/fdab198.
- Green E, Shaw SE, Harris T. ‘They shouldn’t be coming to the ED, should they?’ A qualitative study of why patients with palliative care needs present to the emergency department. BMJ Support 2019;9. https://doi.org/10.1136/bmjspcare-2015-000999.
Appendix 1 Methodology
Rationale for using realist synthesis
Several considerations determined the choice of realist synthesis as the preferred review method. The original request from the commissioner of the review had suggested, based on initial scoping, that a realist synthesis would be justified by the type of question and characteristics of the data. This was confirmed by the review team following their own review of the commissioning documents based on their experience of multiple realist reviews. The commissioner of the review suggested a broad line of inquiry, and this was then explored through multiple candidate programme theories which were then prioritised to represent one for each of the patient/carer, service provider and commissioner of services perspective.
Although some researchers prefer to use the label of ‘rapid realist review’, the review team privileges the label ‘focused realist review’ together with its implication that the number of programme theories to be explored would be limited by time and resource constraints. The scattered, elusive and fragmented nature of the evidence meant that the ‘bricolage’ required to explore and test programme theories would be appropriate in piecing together an evidence trail.
Scoping the literature
An exploratory search was conducted to find terms and related concepts for signposting in early June 2022. The initial searches guided the development of the searches to identify programme theory(ies). The search for theories was developed on MEDLINE and adapted for the other databases. The search included synonyms and related terms for signposting combined with terms for programme theory and relevant study types. The searches were conducted in June 2022.
Sources searched:
-
MEDLINE via OvidSP.
-
Cumulative Index to Nursing and Allied Health Literature (CINAHL) via EBSCOhost.
-
Social Sciences Citation Index (SSCI) via Web of Science.
Searches were limited to research published in English from 2016 to current. In 2016 signposting was discussed in NHS England 2016. General Practice Forward View. www.england.nhs.uk/wp-content/uploads/2016/04/gpfv.pdf
The MEDLINE search is provided in Appendix 2. Search steps 1–2 and 4–6 are the terms and concepts associated with signposting. Search steps 8–11 are broad terms around theory and then search step 15 relates to focused theory terms.
The broad search retrieved 716 unique references and the focused search retrieved 31 references. Both searches were used to explore the programme theories. However, the broad search was used to privilege an understanding of the contexts for signposting services, whereas the focused terms prioritised the identification of mechanisms.
One reviewer (AB) reviewed the results of the focused and then the broader search and selected 22 core studies to use for theory identification. The three reviewers divided these studies between them and extracted initial programme theories in the form of IF (context) – THEN (mechanism) – LEADING TO (outcome) statements (CMO configurations). Extracted data related to IF (WHO? DO WHAT? FOR WHOM?) THEN (THE RESPONSE IS) LEADING TO (WHAT OUTCOMES? FOR WHOM?) followed by the reference source.
Complete configurations were prioritised, whenever possible, although a limited number of two element configurations were included when they provided unique insights, for completeness. Appendix 4, Table 12 shows the signposting programme theories identified.
All CMO configurations were checked by a single reviewer experienced in realist synthesis to ensure that they were complete, in a common format and that agency (i.e. who was the agent for action) could be identified. The review team then met to discuss the initial programme theories and identified a need to address three complementary perspectives: those of the service user, service provider and commissioner. Identification of programme theory led to the development of a priority question constructed to match each perspective.
Searching processes
Exploratory scoping of the literature was accompanied by creation of a reference management (EndNote) database across multiple databases. In August 2022, the team’s information specialist revisited the EndNote database to run targeted searches in order to identify key items relating to the service user, service provider and service funder or commissioner perspectives from their titles and abstracts. Simultaneously another information professional conducted ‘context sensitive’ searches of article full text using the scite tool and Google Scholar (via Publish or Perish), as is evidenced from the tables of included studies papers could relate to more than one of the prioritised questions, thereby covering multiple perspectives. Each question lead researcher would cross-refer studies to other lead researchers where it was apparent that multiple perspectives had been addressed within an individual study,
Selection and appraisal of documents
Selection of documents for full analysis was prioritised to optimise richness, rigour and relevance. Formal quality appraisal was not undertaken. All documents that made specific reference to ‘signposting’ in their title were included as a core set of data sources. In addition, evaluations or qualitative research studies on social prescribing and care navigation were included where ‘signposting’ featured multiple times in the full text. Documents with only an isolated mention of signposting were not included unless supported by a substantive data extract. A purposive sample of documents describing specialist services that include a substantive signposting function was created to reflect condition-specific variations (e.g. people with dementia, those with autism, frail elderly etcetera). The concentration of signposting functions within the receptionist function in primary care required inclusion of documents describing qualitative studies of receptionist–patient interactions, particularly where signposting was either explicitly mentioned or where the functions of signposting (e.g. referral to other health, social or community resources was clearly identifiable).
Inclusion criteria
We based eligibility on the following [Patient/Problem–Intervention–Comparison–Outcome(s), i.e. PICO] aspects:
-
adults and children with health and social care needs (Patient/Problem)
-
signposting (Intervention)
-
none (Comparison)
-
patient outcomes; health services outcomes; patient and carer satisfaction; resource use (Outcomes).
Study designs – Systematic reviews, randomised controlled trial (RCTs), qualitative, economic evaluations and UK initiatives.
Unpublished reports evaluating signposting services will be included.
Context – UK studies were predominantly included to optimise the usefulness of the synthesis findings with a UK context. Studies from the USA or other comparable countries will be included if referred to within relevant studies.
Only UK initiatives will be included.
A document flow diagram (see Appendix 3, Figure 1) was produced to record the number of documents assessed for eligibility and included in the review, together with an indication of their source of origin (e.g. from searching databases, reference lists). The number of documents across the three review questions was less than the aggregate figure for all three reviews to reflect that several studies supplied data for multiple questions.
Data extraction
Data for supporting or refuting the prioritised programme theories were extracted from papers prioritised for relevance, rigour and richness. Due to the interpretative nature of the review question and the time constraints under which the review was performed, no attempt was made to assess the methodological limitations of each study. Instead, studies were considered to be less susceptible to methodological limitations if they employed recognisable research methods of data collection and data analysis, whether quantitative or qualitative. Similarly, richness was judged according to the pragmatic nature of the extent of data relevant to the phenomenon of interest (signposting services) rather than through application of an arbitrary and unvalidated richness scale. Relevance was achieved by ensuring an exclusive focus on the UK, except in the case of more generalisable systematic reviews, and by considering whether findings related to a signposting service or to signposting within a larger service and by considering whether findings related to signposting for a specific population or a generic service open to all who are entitled to health and/or social care services.
Analysis and synthesis processes
Extracted data were tabulated against relevant headings for both review level evidence (Review ID; Author; Review year; Included country/countries; Type of review; Number of included studies; Review findings; Review implications) and for primary studies (Study ID; Author; Study year; Study country/countries; Study design; Study sample; Sample size; Population age; Population gender; Health condition; Signposting context; Setting; Generic or specialist; Signposting features; By whom; Type of resources required; Length of interaction; Outcomes measured; Main findings; Key messages including limitations); see Appendix 5, Tables 13–15.
The data extraction table is provided in Appendix 5.
In addition, qualitative findings were extracted and mapped against the most relevant question or subquestion. A narrative summary was then produced that summarised data from the data table and additional qualitative data where available.
Data synthesis was undertaken either by AC, DC or AB and synthesis results were regularly shared and discussed within the team as a way to ensure validity and consistency in the underlying inferences. The review team sought to identify prominent recurrent patterns of contexts and outcomes (demi-regularities) in the data. We then sought to explain these through the means (mechanisms) by which they occurred. For example, we noted that included articles often characterised the information-seeking behaviours of those who required only ‘light-touch’ navigation to appropriate services and those who required more intensive support. Data synthesis enabled us to explain differential reporting of processes and outcomes through the identification of contrasting mechanism(s) that presuppose instant fulfilment of information needs or more sustained relationship building and trust. Further examination of included articles, and expanding these to other contexts and services through purposive searching, allowed us to understand that while the case for signposting was often articulated around assumptions of minimal necessary contact those requiring signposting often presented with complex needs that could not be addressed speedily. We interpreted these within two contrasting rationales for service provision; first, in a context of service substitution where a signposting service seeks to divert or deflect patient and carer needs from established medical or care services and, second, within a context of service enhancement whereby services of which patients or carers were initially unaware or unlikely to use where presented within an integrated coherent response. When additional studies were sought to enable programme theory testing, such as in relation to social prescribing, which more closely resembled the more intensive form of signposting, data handling processes, synthesis and analysis were repeated.
Document characteristics
Details of the characteristics of documents included in the review are given for each review question.
Appendix 2 MEDLINE search strategy
Database: Ovid MEDLINE(R) and Epub Ahead of Print, In-Process, In-Data-Review and Other Non-Indexed Citations and Daily <1946 to 21 June 2022>
Search strategy:
------------- ------------------ ----------------------- --------------------------
-
signposting.kw. (8)
-
signpost*.tw. (1065)
-
1 or 2 (1067)
-
care navigat*.tw. (193)
-
health trainer*.tw. (80)
-
health adviser*.tw. (137)
-
or/1–2,4–6 (1466)
-
concept*.tw. (545,373)
-
framework*.tw. (351,979)
-
model*.tw. (3,417,968)
-
theor*.tw. (745,466)
-
8 or 9 or 10 or 11 (4,511,751)
-
7 and 12 (404)
-
limit 13 to (english language and yr=‘2016 –Current’) (267)
-
(‘logic model’ or ‘theory of change’ or ‘theory of action’ or ‘outcomes chain’ or ‘program* theory’ or ‘program* logic’ or ‘logical framework*’).tw. (2934)
-
7 and 15 (3)
***************************
Appendix 3 Document flow diagram
A document flow diagram was produced to record the number of documents assessed for eligibility and included in the review, together with an indication of their source of origin (e.g. from searching databases, reference lists). The number of documents across the three review questions was less than the aggregate figure for all three reviews to reflect that several studies supplied data for multiple questions.
FIGURE 1.
Document flow diagram.
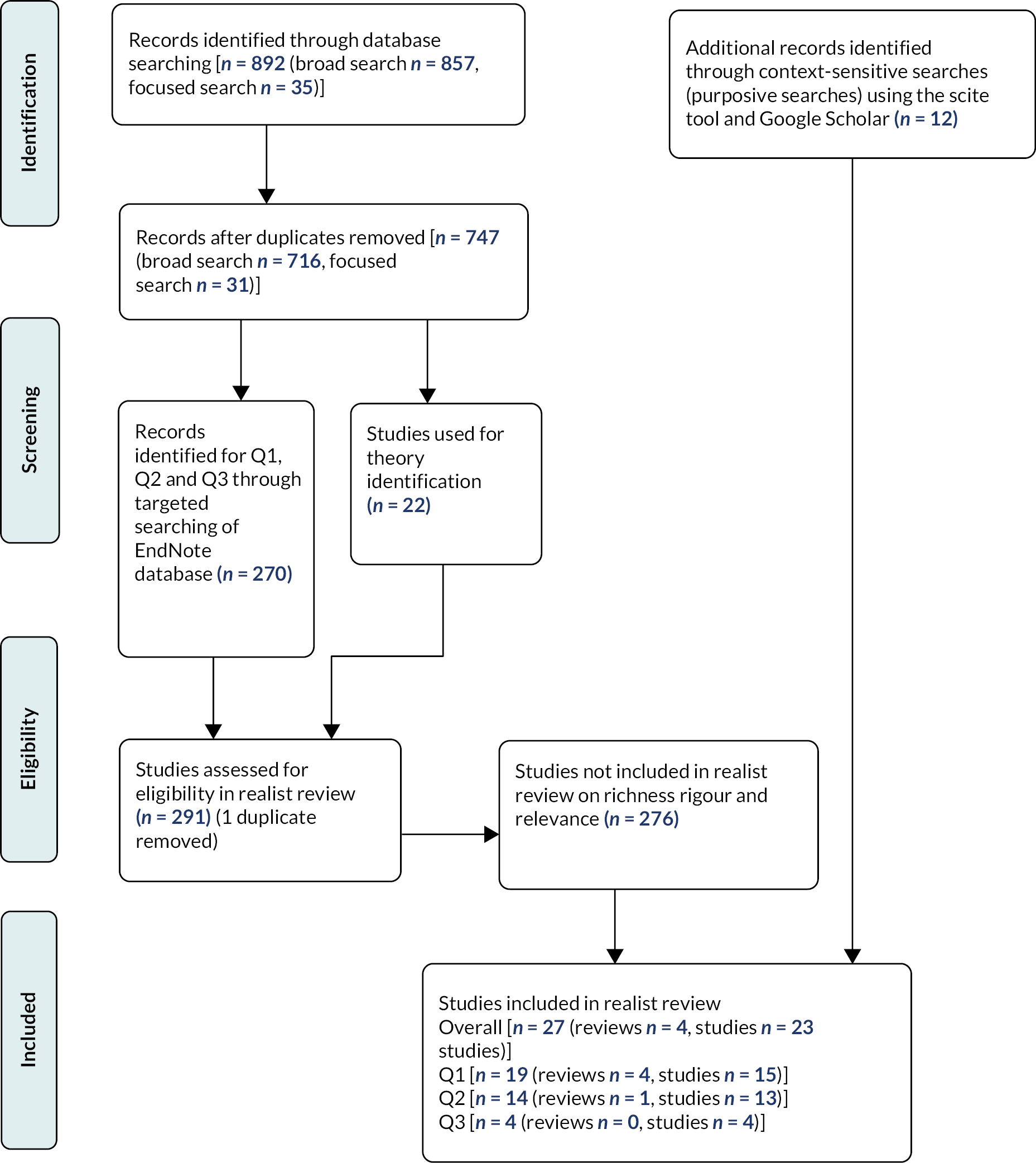
Appendix 4 Consolidated programme theory
| Who | What | Impacted by | With what outcomes | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Who | For whom | Commissioned/organised by whom | Signposting activity | Subsequent activity | Enabling activity | Barriers | Enablers | Individual | Health | Health service | Society |
| Autism support service staff | Adults with high- functioning autistic spectrum disorder | Listen | Peer mentors | Provide low stress environment | Poor resource provision (austerity climate) | Mutual trust and respect | Tolerance of self | Prevention of infections, symptom deterioration and mental health deterioration | Appropriate service use | ||
| CNs | Employers of first contact practitioners | Make recommendations | Provide telecare equipment | Public and community transport | Poor transport infrastructure | Tolerance of others | Improved health, quality of life and well-being | Support at home | Recognition of social support needs | ||
| Dementia advisers/dementia navigators | Carers of people with dementia | Equipment manufacturers | Encourage service users to develop relationships and interactions with family and friends | Befriending services | Training (staff) | Relationships with family and friends (as alternative) | Access to services | Reduced anxiety, depression or socially isolation | Reduced dependence | Improved access to community resources | |
| Diagnosing medical professionals | Female breast cancer patients | Health planners | Provide written information on condition | Ongoing support | Skilled LWs and volunteers | Patient expectations of treatment | Know they have been listened to | Increase in appropriate use | Appropriate use of community resources | ||
| First-time parents of young children | Vocational advice | Non-medical activities | Non-medical activities | Poor motivation for participation and engagement | Confident to reuse service | Alternative use to health services | Increased use of voluntary/third sector services | ||||
| First contact practitioners | Immigrants with health conditions | Healthcare organisations | Social prescribing | Social support services | Social support services | Inappropriate signposting | Confidence in navigating service | Tailored care plans | Utilisation of craft groups, adult learning and leisure facilities | ||
| GPs | Non-indigenous healthcare users | Health services | Support and encourage patient to develop social connections/activities | Community physiotherapy | Community engagement initiative to understand gaps in accessing care | Possible need for referral back to GP when sessions end | Enhanced community well-being and social inclusion | Adherence to treatment | Increased numbers of volunteers | ||
| GP surgery staff | Local authorities | Physical activities | High-quality safe physical activities | Dependence on seeing LW | Improved self-efficacy, self-management or empowerment | Patient satisfaction with services for themselves or their children | |||||
| Health professionals | Refer to under-used programmes | Social care assessment | Good-quality social care | Inappropriate LWs (e.g. gender) | Financial, employment and health claims addressed | Follow-up and uptake of screening | |||||
| Lay navigators | Older people | Bridge to wider health services | Training (users) | Appropriate funding | Conflict and loss of trust from health professionals | Improved problem solving | Prevention of premature institutionalisations | ||||
| LWs | Older people needing support at home | Provide written information on how to navigate the health system | Conduct holistic risk assessment | Leadership | Delayed/prevented access to services | Health literacy | Improved communication among primary care providers and community services or providers | ||||
| Local communities | Older adults with anxiety and depression | Develop supportive relationship | Review care plan | Supervision | Older men do not want to be passive recipients of services | Increased engagement in physical activity | Improved care co-ordination | ||||
| Memory clinics | Emotional support | Training manual | Volunteers not able to fulfil role | Reduced use of GPs | |||||||
| Nurse navigators | Palliative Care patients | Assess user needs | Creative activities, lifelong learning, befriending, volunteering and peer support | Role definition | Non-utilisation of emergency care services | ||||||
| Paediatricians | Isolated older individuals | Service commissioners | Refer to groups | Computer classes, art groups, ‘Men in Sheds’, walking groups | Navigation programme | Timely referrals | |||||
| Patient navigation programme teams | Provide person-tailored care | Swimming, walking, bowls | Longer-term support | Increased utilisation of signposting services | |||||||
| Patient navigators | Patients offered physical activities | Appropriate communication with patients | Motivational interviewing | Directory or list of resources | Improved retention in physical activity programmes | ||||||
| Patients with chronic conditions | Instant phone advice | Develop health literacy | Health professional understanding of role | Continuity of care | |||||||
| Receptionists | Patients with complex health needs | Health professional understanding of eligibility | |||||||||
| Signposting services | People with dementia | Develop relationships with statutory and third sector partners | |||||||||
| Patients with musculoskeletal pain | Remove stigma around psychological and social health | ||||||||||
| Social prescribing LW | Patients who are inactive | Social services | |||||||||
| Staff in libraries | People suffering from or at risk of loneliness | ||||||||||
| Staff in shopping centres | People with frailty, chronic illness and mental health problems | ||||||||||
| People with ‘non-medical’ needs | |||||||||||
| People with Parkinson’s | |||||||||||
| Patients with significant physical and/or psychosocial difficulties | |||||||||||
| Support workers | Service users | ||||||||||
| Trained volunteers | Statutory agencies | ||||||||||
| Volunteers | |||||||||||
Appendix 5 Data extraction tables
| Author (year) | Study year | Study country/countries | Study design | Study sample | Sample size | Population age | Population gender | Health condition |
|---|---|---|---|---|---|---|---|---|
| Author (year) | Signposting context | Setting | Generic or specialist | Signposting features | By whom | Type of resources required | Length of interaction |
|---|---|---|---|---|---|---|---|
| Author (year) | Outcomes measured | Main findings | Key messages including limitations |
|---|---|---|---|
Appendix 6 Realist review questions
Question 1 (value and usefulness of signposting) considers the service user perspective
What do people with health and social care needs require from a signposting service to believe it is a valuable and useful service?
To address this question the team formulated the following subquestions:
-
What do people with health and social care needs require from a signposting service to believe it is a valuable and useful service?
-
What do people with health and social care needs require to be confident in accessing a signposting service?
-
Which aspects of signposting services help people with health and social care needs to engage with signposting services?
-
Which aspects of signposting services enable people with health and social care needs to be satisfied with the service provided?
Question 2 (required resources) considers the perspective of the front-line provider of the signposting service
What resources (training, directories/databases, credible and high-quality services for referral) do providers of front-line signposting services require to confidently deliver an effective signposting service?
Question 3 (specification, monitoring and evaluation) considers the viewpoint of the commissioner/funder
Under what circumstances should commissioners commission generic or specialist signposting services?
Purposive searching was undertaken for each of the three questions to find a sample of rich relevant studies to answer each of the questions. The searching included forward and backward citation searching of relevant studies from the theories searches, focused searches and searching for UK initiatives.
Where possible we predominantly included UK studies to optimise the usefulness of the synthesis findings with a UK context. Studies from other comparable countries were included where relevant.
Several studies supplied data to address more than one question and were therefore included in multiple sections.
Appendix 7 Public and patient involvement
On 22nd August at 1 p.m. we conducted an online meeting of the Health Service and Delivery Research Sheffield Evidence Synthesis Centre Public Advisory Group. Three members attended plus Anna Cantrell, review lead and Sue Baxter, patient and public involvement (PPI) lead for Sheffield Evidence Synthesis Centre.
The group were asked about their understanding of the term signposting and their experiences of accessing signposting services, a summary of the discussion and issues raised is provided.
All of the members had heard of the term signposting, different people had different perceptions of what it means. Some of the members thought signposting could be part of social prescribing.
What helps/hinders signposting?
-
Speed of ability to digest information
-
May need help from carer
-
Speed of giving information is important
-
Can people use the information given
-
Levels of health literacy
-
Self-confidence to navigate the systems.
Quality of signposting information is important:
-
depends who is providing information
-
need to avoid too much information
-
needs to be relevant
-
needs to link to patient priorities
-
needs to be timely (ongoing).
Patient needs to feel valued that
-
they are not being fobbed off
-
signposting is not for purpose of ticking a box
-
someone checks if signposting is effective
-
someone will come back and ask if any of services were taken up or not.
Would they follow up resources or service signposted to?
-
Some yes, and some no.
-
Would depend on confidence to contact and motivation.
-
Often people do not like to contradict a professional, so will just nod and say yes.
-
Need to follow up with people afterwards.
-
After resources or services suggested give people a chance to say what do you think and their thoughts on what has been suggested.
Additional comments:
Knowing an individual’s circumstances is really important to determine what might work for them.
Urgency of need might affect follow-up, geographical restrictions, access city/rural areas, resources for travel.
General comments: people with low status often given the job of signposting but it should be perceived as of great importance and role not de-valued, everybody could benefit from signposting, should be a key part of patient management, need to better understand the holistic nature of living with a condition – MH or physical, need training to be able to navigate, need to understand personal circumstances.
Felt that a receptionist would not be ideal – open reception area, have busy role already, suggestion of a bespoke health educator or navigator role as it should be valued/important need to do it properly.
The PPI meeting was useful and it was interesting to get group members’ responses to how they understood the term ‘signposting’ and their experiences of accessing signposting services. The information from the PPI group supported issues highlighted in the literature and was useful in developing the overall conclusions of the realist review. The rapid nature of the project meant that consultation took place at a single PPI meeting. It would have been useful to have PPI input throughout the review life cycle including for the scope of the review, particularly in developing the questions, and to discuss our findings. Three members of the PPI group advised on the plain language summary.
List of abbreviations
- ARC
- Access to Resources in the Community
- CAMHS
- Child and Adolescent Mental Health Services
- CCG
- Clinical Commissioning Group
- CHW
- community health worker
- CMO
- context–mechanism–outcome
- CN
- care navigator
- CYP
- children and young people
- ECHO
- Extension for Community Healthcare Outcomes
- GP
- general practitioner
- HLP
- Healthy Living Pharmacy
- LW
- link worker
- NIHR
- National Institute for Health and Care Research
- PCN
- primary care diabetes care navigator
- PPI
- patient and public involvement
- STAR
- Support Time and Resilience
- VCS
- voluntary and community sector
Notes
-
Programme theory for signposting table, full data extraction of context-mechanism-outcome (CMO) configurations
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/GART5103).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
