Notes
Article history
The research reported here is the product of an HSDR Rapid Service Evaluation Team, contracted to undertake real time evaluations of innovations and development in health and care services, which will generate evidence of national relevance. Other evaluations by the HSDR Rapid Service Evaluation Teams are available in the HSDR journal.
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as project number 16/138/31. The contractual start date was in October 2018. The final report began editorial review in July 2020 and was accepted for publication in September 2020. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
Copyright © 2022 Smith et al. This work was produced by Smith et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaption in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2022 Smith et al.
Chapter 1 Context
Primary care networks are groups of general practices that were brought together across England in 2019 to hold shared budgets and develop new services in response to national policy that was intended to bring about better integration of health care within local communities.
Primary care networks were to build on the many pilots of new ‘vanguard’ models of integrated health care that had been developed as a result of the NHS Five Year Forward View. 2
Primary care networks offer the possibility of significant levels of additional funding for general practice through a compulsory, formal and incentivised model that differs from many predecessor schemes of collective primary care.
There were (as at May 2020) 1259 PCNs in England, serving populations ranging from 20,000 to well above the 50,000 suggested in policy. 3
Primary care networks sometimes build on prior general practice collaborations and are often supported by the organisational infrastructure of the extant collaborations. Other networks are brand new entities in the process of becoming established and working out how best to source their management support.
The research took place in a rapidly changing policy and service context: initially as a result of the implementation of The NHS Long Term Plan4 and subsequent professional challenge to the PCN policy and contractual proposals, and thereafter as a result of the global COVID-19 pandemic emerging in early 2020.
PCN, primary care network.
Parts of this report have been reproduced from Parkinson et al. 1 This is an open access article distributed in accordance with the Creative Commons Attribution 4.0 Unported (CC BY 4.0) license, which permits others to copy, redistribute, remix, transform and build upon this work for any purpose, provided the original work is properly cited, a link to the licence is given, and indication of whether changes were made. See: https://creativecommons.org/licenses/by/4.0/.
Introduction
The aim of this rapid evaluation study was to provide early evidence about the implementation of primary care networks (PCNs) in the NHS across England, with a particular focus on understanding what has helped or hindered their progress, how they operate in relation to pre-existing collaborations in general practice (GP), and exploring issues for rural as compared with urban PCNs. The detailed research questions (RQs) for the study are set out in Chapter 2.
Primary care networks are groups of GPs that were brought together in 2019 to hold shared budgets and develop new services in response to national policy intended to bring about better integration of health care within local communities. The study entailed a review of existing international research evidence about collaborations within GP and then, based on identified knowledge gaps, case study research to examine the nature, functioning, potential and shortcomings of PCNs. The research took place in a rapidly changing policy and service context – initially as a result of the implementation of The NHS Long Term Plan4 and subsequent professional challenge to the PCN policy and contractual proposals, and thereafter as the global COVID-19 pandemic emerged.
The findings from this rapid evaluation study are intended to inform NHS England and Improvement’s (NHSE&I’s) and the primary care community’s future planning and guidance for PCNs. Our analysis of these findings forms the basis of recommendations for how the sustainability of PCNs can be assured and how they might develop in the future, including in the context of the significant changes taking place in primary health care and GP as a result of the COVID-19 global pandemic.
Policy context
General practice is one of the main first points of contact that patients have with the NHS and acts as a gateway that connects people to specialist care at treatment centres, hospitals, mental health services and community health-care services. NHS GP has until recently had high approval ratings among patients and the public,5 and is considered important and cost-effective in that it enables health outcomes to be improved and health inequalities to be addressed while helping to contain costs in the wider health system. 6,7
In its Five Year Forward View strategic plan,2 published in 2014, NHS England (now NHSE&I) identified the need for new models of care that increasingly require collaboration across a range of health and social care services and providers. Related to this, it was asserted that GPs needed to work together (and with other primary care practitioners and services) in a more systematic, sustained and organised manner. 2 The 2016 General Practice Forward View8 built on the NHS Five Year Forward View,2 describing how the NHS needed to change to make sure that sufficient and sustainable primary health care could be provided. The NHS Five Year Forward2 view also noted that GPs needed to be flexible and ready to change, including by adapting to evolving health needs (in particular, those of an ageing population living with multiple complex conditions) and the opportunities presented by new technology. The context for these plans was one of GP in the UK being under considerable strain, as evidenced by the Commonwealth Fund’s 2019 survey9 of primary care physicians, in which just 6% of UK general practitioners reported feeling ‘extremely’ or ‘very satisfied’ with their workload (the lowest of all countries surveyed), and 49% reported wanting to reduce their clinical hours in the next 3 years.
The NHS Long Term Plan,4 published in January 2019, confirmed that spending on primary and community health services was to be at least £4.5B higher in 5 years’ time to ‘fund expanded community multidisciplinary teams aligned with new primary care networks based on neighbouring GP [general practitioner] practices’ (contains public sector information licensed under the Open Government Licence v3.0). Subsequent guidance10 published by NHS England and the British Medical Association (BMA) later in January 2019 confirmed the requirement for all GPs in England to form local ‘primary care networks’ (PCNs) covering patient populations of 30,000–50,000 by July 2019, ‘so that no patients or practices are disadvantaged’ (contains public sector information licensed under the Open Government License v3.0).
Primary care networks were to build on the many pilots of new ‘vanguard’ models of integrated health care that had been developed as a result of the Five Year Forward View,2 and these new networks were advocated by NHS England to be ‘an essential building block of every Integrated Care System’ (contains public sector information licensed under the Open Government License v3.0). Those vanguard models of care entailed pilots of significant integration of GP and community health services; hospital, mental health, community and primary care; GP and social care (particularly in providing support to residential care homes); and services focused on particular clinical conditions such as cancer. The funding for these vanguard schemes ended in March 2018, and early and interim assessment of their progress concluded that their long-term impact and sustainability was unproven. 11,12 Our evaluation of the early implementation and progress of PCNs took place in the context of these prior vanguard schemes; in some sites the work of the networks was building on aspects of those schemes and the joint working in health and social care that had underpinned the vanguard projects.
General practice collaborations in the NHS in England
Collaborations in GP, also sometimes known in international health policy as ‘organised general practice’ or ‘managed primary care’, have emerged in many health systems over the past three decades. 13 PCNs represent the latest incarnation of such collaborations in the NHS in England.
In 2017, the Nuffield Trust and the Royal College of General Practitioners (RCGP) undertook a survey of all GPs across England, to establish the pattern and frequency of collaborative working across practices. 14 Eighty-one per cent of respondents reported that their practice was already working in collaboration with other local GPs, this having been at 73% in the prior iteration of the survey in 2015. 15 The primary reasons given for working collaboratively were to improve access for patients to GP; to transfer more health services into the community; to strengthen financial and organisational sustainability of GP; and to improve staff experience, training and education. The survey results also emphasised that:
-
Working at scale in collaborative arrangements was broadly accepted as the future for GP in England.
-
There were many forms of GP collaboration across the NHS, with GP federations being the most commonly reported (see Table 1 for an explanation of GP federations).
-
In almost all cases these collaborations had emerged from within GPs rather than being mandated in national policy.
-
GPs were often part of more than one collaboration.
-
These collaborations varied in size, with > 50% having > 100,000 registered patients.
-
Networks varied in focus and motivation for collective working, with smaller groups tending to prioritise practice sustainability, staff experience and patient access. Larger groups tended to prioritise patient access and transferring services to the community.
-
Time and work pressures were considered the main barrier to collaborations achieving their aims. 14
Table 1, drawing on the work of Rosen et al. ,16 sets out the main GP collaboration models in England in place in 2019, and thus provides important contextual details about the pre-existing GP collaborations from (or alongside which) new PCNs have formed. The interplay of pre-existing GP collaborations and PCNs formed a core aspect of this evaluation study (see Chapter 2, Methods). The collaboration models in Table 1 vary considerably. For example, super-partnerships represent a formal merger of practices and have a board of directors to oversee the collaboration, together with a shared contract that binds all practices together. GP federations can be either informal or formal in the way they are set up and members work together, and they can take a variety of legal and contractual forms. Networks are typically informal in nature, coming together around a set of specific issues, such as enabling extending the opening hours of GP or a 24 hours per day, 7 days per week, out-of-hours service, or to inform the planning of local services. 16
| Collaboration model | Key characteristics |
|---|---|
| Informal network | Networks (described as ‘informal networks’ here to distinguish between them and ‘primary care networks’ as set out in The NHS Long Term Plan4) are one way in which GPs can collaborate. There are no formal ties between the practices; instead, they rely on informal discussions, meetings and co-operation. All practices in such a network keep their own contracts and funding sources, and no particularly tangible objectives are typically set |
| Multisite practice organisation | These organisations are very formal in nature and there is one core company or group of directors holding one GP contract for all practices within that management framework. The goals of each practice, therefore, should be in alignment with those of the organisation as a whole. Funds are held in the central hub of the organisation and disseminated to practices for specific purposes |
| Super-partnership | Similar to multisite practice organisations, super-partnerships represent mergers of previously independent GPs into a single new organisation. The governance for super-partnerships is complex. Practices may choose either to manage each of their contracts separately, although activities and goals are shared and aligned across all participating practices, or to draw up a new GMS contract and appoint an executive board to oversee the work of all participating practices. In the latter case, funds will be redistributed in accordance with any new processes in place |
| Federation | Federations are more formal than networks but less formal than multisite practice organisations and super-partnerships. In federations, participating GPs maintain responsibility for their own contracts. However, some additional legal agreements might be pursued and put into place to carry out joint activities. An executive board function typically exists to oversee the federation; however, each practice may set its own goals and objectives and these may not necessarily align with those of the organisation as a whole |
| PCH | The PCH model was created by the NAPC building on the Health Care Home from the USA.17 An integrated care model, it has four key characteristics that need to be met for a collaboration to be categorised as a PCH: (1) the partnership must span across primary, secondary and social care; (2) there is a strong element of personalised care with the aim of improving the health of the population as a whole; (3) all funding is channelled through one central budgetary system between all stakeholders in the collaboration; and (4) it covers a population of 30,000–50,000 registered patients across collaborators |
| Hubs | Hubs often emerge as part of existing collaborative relationships among different GPs that are already in place and are usually focused on delivering extended access to GP care. Their aims and objectives can differ depending on local population needs; however, a core feature is that they provide same-day urgent appointments to registered patients. For example, this can been done by having a shared triage system to point patients to the most appropriate route of care. In addition, they may offer out-of-hours care. More recently, COVID-19 primary care hubs have been formed18 |
Along with different models of collaborative working, GP collaborations also vary in terms of how they are set up geographically. Although GPs can group together based on geographical proximity (as is the case for PCNs), some collaborations are not geographically contiguous; rather, they are regional or national multipractice organisations that are geographically dispersed. 19 Notably, some types of collaborations may go by more than one name (federation, super-partnership, primary care group, etc.) but may share common characteristics in terms of the functions performed. 20
The nature and extent of these prior GP collaborations is important context to the implementation and development of PCNs, as many collaborations have continued to operate alongside new networks, often providing management and infrastructure support. It has been noted in prior analysis21 that GP collaborations can bring opportunities for smaller practices that have struggled to tailor services for patients living with complex needs in both rural and urban areas. It is of note that the prior collaborations in place as PCNs were established are largely ones that evolved from within general practice and primary care (as opposed to being mandated in national policy), and are typically considered to be ‘owned’ by local practices and practitioners (or may indeed be formally owned by them). By contrast, PCNs have been mandated in national policy, and the issue of general practitioners’ sense of ownership of and belonging to the new networks is explored in the research reported here.
Primary care networks
Primary care networks are the latest attempt on the part of the NHS in England to engage GP (and other primary care practitioners and teams) in bringing about a range of service changes intended to support local populations living with ever more complex long-term conditions, and reduce the reliance of such people on inpatient hospital care. Previous similar policy initiatives have included GP fundholding, total purchasing pilots (TPPs), personal medical services (PMS) schemes and primary care groups. 22 Furthermore, with PCNs there is a desire to use this more collaborative approach as a means to strengthen the sustainability of GP, including in respect of its workforce and financial health.
Primary care networks are distinct from previous collaborations in terms of the context in which they are being implemented. Almost half of general practitioners in the NHS in England are employed on a salaried or sessional basis (as opposed to having equity ownership of the practice), and a majority are women (many of whom work part-time and/or wish to have portfolio careers, as do some of their male colleagues). 23 Even before the COVID-19 pandemic, a significant shortfall had been seen in the availability of general practitioners and other health professionals (including community and practice nurses) at a time of rising demand for services. Furthermore, the sustainability of GP is a key current concern, in respect both of securing sufficient workforce and of matching supply of services to growing patient demand. 9
Primary care networks are particularly noteworthy in that they offer GPs the possibility of significant levels of additional funding, and in that there is a contractual basis to this. Hence, PCN working has a formal, incentivised and compulsory feel to it in comparison with many predecessor schemes of collective primary care. Unsurprisingly, given the PCN approach outlined above, with additional funding on offer from NHSE&I to develop new services for local patients, almost all GPs have joined a PCN,24 although the extent to which this is an enthusiastic and committed move is explored within this evaluation. In late 2019, NHSE&I ran a consultation about the service specifications to underpin the PCN contract, which resulted in major concerns on the part of GP about the pace, scope and scale of what was expected. 25 Subsequent revisions to the PCN service specifications in early 2020 extended the timescale for networks to take on responsibility for some services, such as early cancer diagnosis. Once the COVID-19 pandemic emerged in the UK in March 2020, a decision was taken to defer the implementation of some PCN services set out in national specifications, although the Enhanced Healthcare in Care Homes scheme26 was brought forward to start in May 2020, causing further consternation in the primary care community. 27
Primary care networks commenced on 1 July 2019 as required by NHS England and Improvement and in 2020 there were around 1250 networks across England covering populations of approximately 30,000–50,000 patients,28 a size that is consistent with the primary care home model (National Association of Primary Care). Each PCN holds a Directed Enhanced Services (DES) contract as a formal agreement across the constituent practices, with one practice typically holding this on behalf of those within the network. The DES contract provides funds for the network to operate new services that are specified by NHSE&I as noted in the previous paragraph.
These services provided by a PCN are being phased in over a period of 3 years with social prescribing and practice-based pharmacy being the first to be implemented, followed by enhanced health services for care homes. The intention was to provide a total of £1.8billion in funding through PCNs by 2023–24, including resource to operate the networks and help pay for additional primary care staff. For this latter aspect – paying for additional staff – the Additional Roles Reimbursement Scheme was introduced by NHS England and Improvement in 2019 and its early progress has been evaluated for the Department of Health and Social Care by the King’s Fund. 29
These PCNs sometimes build on prior GP collaborations and are often supported by the organisational infrastructure of the extant collaborations. Other networks are brand-new entities in the process of becoming established and working out how best to source their management support. For this latest iteration of GP collaborations in the English NHS, there is much to be learnt from examining research evidence on the nature and speed of implementation and the development and impact of previous primary care organisations dating back to the early 1990s, in particular those that were brought together to hold shared contracts to deliver health services for a local population.
In the next chapter, we describe the methods used for this rapid evaluation of the implementation and early development of PCNs, what helped and hindered their progress, how they worked with the GP collaborations that were already in place as the new networks were formed and what this means for future development of PCNs. Following this, we set out the findings of our rapid evidence assessment (REA) of GP collaborations, using this to frame questions for exploration in the case study research that is presented and discussed in subsequent chapters.
Chapter 2 Methods
The overarching purpose of this evaluation was to produce early evidence of the development and implementation of PCNs introduced into the NHS in England in July 2019. The evaluation had a particular focus on seeking to understand how practices entered into collaborations, why some collaborations stall or fail, and if and how the experience of rural collaborations may differ from that of urban examples.
We completed a qualitative cross-comparative case study evaluation comprising four work packages:
-
a REA
-
a stakeholder workshop with leading academics, policy experts, and patient/public representatives to share findings from the REA and shape REAs for case study work
-
interviews with key stakeholders across case study sites alongside observations of strategic meetings, online surveys and analysis of key documents
-
analysis of findings from work packages 1–3 to develop a set of lessons for the next stage of development of PCNs in the NHS in England, for dissemination to policy-makers, practitioners and representatives of patients, carers and the public.
We undertook a multifaceted sampling process to select four case study sites, based on identifying appropriate primary care collaborations through clinical commissioning groups that had not been previously evaluated.
A content analysis approach to documentary reviews and observations was undertaken. Data analysis for interviews was informed by a framework method for the analysis of qualitative data in multidisciplinary health research. Our analysis was guided by theoretical and policy literature on collaborations of GPs.
Aims and research questions
The overarching purpose of this evaluation was to produce early evidence of the development and implementation of PCNs introduced into the NHS in England in July 2019, to inform subsequent policies and support that was to be provided for these new collaborations. The evaluation therefore sought to identify the forms of GP collaboration previously used in primary care in England, the reasons for GPs to enter (or not) into collaborations, and evidence about the impact of PCNs and prior GP collaborations, along with any barriers to or facilitators of progress.
The evaluation had a particular focus on seeking to understand the rationale behind why and how practices entered into collaborations, the potential influence of prior collaborative working on PCNs, and if and how the experience of rural collaborations may differ from that of urban examples. The findings from the evaluation are intended to feed into NHSE&I’s planning and implementation guidance for PCNs and inform proposals for longer-term study of PCNs.
To address our aims, we sought to answer the following evaluation questions:
-
What was the contextual and policy background within which PCNs were introduced?
-
What were the pre-existing forms of GP collaborative working across primary care in England?
-
How have new PCNs been implemented in a sample of urban and rural settings?
-
How do new PCNs relate to pre-existing GP collaborations?
-
-
What are the rationales and motivations for GPs to enter into GP collaborations, including new PCNs? In particular, what role do financial incentives play in facilitating or inhibiting collaboration? What are the expected outcomes for PCNs?
-
What evidence exists about the positive or negative impacts associated with different experiences of establishing GP collaborations, and how do these relate to newly formed PCNs?
-
What appear to be the barriers to and facilitators of effective collaboration across GPs, with respect to both to whether or not collaborations were successful and to whether or not collaborations achieved an impact?
-
What does the analysis of prior experience of GP collaborations, and the early implementation of PCNs, suggest in terms of the likely progress of PCNs in the NHS in England, including in the light of the COVID-19 pandemic and associated challenges?
General approach
We completed a mixed-methods cross-comparative case study evaluation30–32 comprising four work packages [(WPs) Table 2]:
-
a REA
-
a stakeholder workshop with leading academics, policy experts and patient/public representatives, to share findings from the REA and shape REAs for case study work
-
interviews with key stakeholders across case study sites alongside observations of strategic meetings, online surveys and analysis of key documents
-
analysis of findings from WPs 1–3 to develop a set of recommendations for the next stage of development of PCNs in the NHS in England, for dissemination to policy-makers, practitioners and representatives of patients, carers and the public.
| WP | Description | Research questions |
|---|---|---|
| 1: a REA | An overview of published evidence to distil prior learning and inform the development of propositions to be tested through comparative case studies of new primary care collaborations/networks | 1.1, 3 |
| 2: stakeholder workshop |
A workshop led by members of the study team for relevant stakeholders (e.g. academic and policy experts in the field, PPI representatives), in which initial findings from the REA were shared and discussed The aim of this workshop was to clarify evidence gaps and evaluate questions of particular relevance to emerging policies on PCNs and thus inform the next steps for WP3 |
1.1, 2, 3 |
| 3: comparative case studies of four PCNs (minimum of two in rural settings) | Interviews with those involved in the conceptual design and implementation of PCNs in their sites and exploration of relationships with any prior GP collaboration in the case study site; analysis of key documentation (both internal and publicly shared); non-participant observation of strategic meetings; and an online survey to collate information on challenges associated with collaborative working and to measure early impacts | 1.2, 1.3, 3, 4 |
| 4: analysis of findings from WPs 1–3 to develop a set of recommendations for the next stage of development of PCNs in the NHS in England | Share and discuss findings generated from data collection from WP3 | 1, 3, 4, 5 |
| 4: dissemination to policy-makers, practitioners and representatives of patients, carers and the public | Develop recommendations for commissioners, providers and policy-makers through academic outputs, virtual meetings with policy-makers, blogs, podcasts and online media | 1, 3, 4, 5 |
Work package 4 was originally designed to be a number of face-to-face case study-specific workshops, as well as round table discussion with key experts. As a result of the COVID-19 pandemic (March 2020 onwards), the study team, following guidance from the National Institute for Health and Care Research (NIHR) Health and Social Care Delivery Research (HSDR) programme, suspended data collection and focused on the analysis and writing-up of findings. NHS colleagues at case study sites were made aware that they were no longer expected to comment on or respond to our communication (May 2020). We were, however, able to use digital slide decks to share and discuss with policy experts, academics and staff at our case study sites in autumn 2020/winter 2021 (n = 3) to share and discuss emerging findings (academic outputs available online and possibly in the form of blogs and executive summaries), and to ensure their applicability to the next stage of development of PCNs.
Protocol sign-off
The study topic was identified and prioritised for rapid evaluation by NIHR HSDR after receiving a request from NHS England (in 2018) in respect of PCN planning and implementation. This varies from the approach to the identification of innovation usually adopted by the Birmingham, RAND and Cambridge Evaluation (BRACE) Centre, which involves horizon scanning.
An initial topic specification (first stage protocol) was prepared (September 2018) and, once approved, was used as the basis for writing the full research protocol (March 2019), which drew on the findings of the initial REA (WP1) and workshop (WP2). The full research protocol was revised further (October 2019) as PCN implementation shifted with regard to policy changes.
Ethics approval
An application for an ethics review to the University of Birmingham’s Research Ethics Committee was made by the project team and approval was gained in May 2019 (ERN_13-1085AP34). The project team received confirmation from the Health Research Authority (HRA) that this study was to be categorised as a service evaluation and therefore approval by the HRA or a NHS Research Ethics Committee was not required. At each case study site, we approached relevant local research and development offices to register our service evaluation, and received confirmation that all were content for the evaluation to proceed in their local area.
Work package 1: rapid evidence assessment
A REA followed a systematic approach, in line with guidance on literature reviews in health care,33 but the scope of the search was restricted to key search terms and review criteria to allow for a focused review of the literature within a limited time frame. 34 The REA aimed to synthesise the body of evidence on GP collaborations across primary care drawing on UK and international literature.
Searches were undertaken in two stages on 21 September 2018. First, the study team completed a search for reviews and evidence summaries published during the period 1998–2012, inclusive, to account for the breadth of published literature. Second, a search was then undertaken of all published literature (including primary research studies and reviews) from the year 2013 until September 2018 using key search terms in titles and abstracts. Searches were undertaken in PubMed® (National Library of Medicine, Bethesda, MD, USA), Ovid® (Wolters Kluwer, Alphen aan den Rijn, the Netherlands) MEDLINE® (National Library of Medicine), Web of Sciences™ (Clarivate™, Philadelphia, PA, USA) [Social Sciences Citation Index™ (Clarivate) only] and Scopus® (Elsevier, Amsterdam, the Netherlands) (restricted to the following subject areas: medicine, social sciences, nursing, multidisciplinary and health professions) for literature published in the English language and containing selected search terms (Box 3), which were then adapted to other publication databases. Forward and backward citation searching of relevant articles were undertaken to ensure that key articles had been identified through our search strategy. Search terms were developed in collaboration with an experienced health services research librarian (Rachel Posaner of the University of Birmingham).
((“Primary care*” OR “primary health care*” OR “general practice” OR “GP*” OR “family physician*” OR “family doctor*” OR “primary care*” OR “family health team*”) AND (“collaborat*” OR alliance OR “primary care network*” OR network* OR “super-partnership*” OR “super partnership*” OR “superpartnership*” OR “federation*” OR “multi-site practice organi*” OR “ multi site practice organi*” OR “multisite practice organi*” OR “cooperat*” OR “co-operat*” OR “cluster*”) AND (“effective*” OR “efficien*” OR “success*” OR “valu*” OR “impact*” OR “cost*” OR “econom*”) AND (“review*”))
OR
((“collaborat*” OR “alliance” OR “primary care network*” OR “network” OR “super-partnership*” OR “super partnership*” OR “superpartnership*” OR “federation*” OR “multi-site practice organi*” OR “multi site practice organi*” OR “multisite practice organi*” OR “cooperat*” OR “co-operat*” OR “cluster*”) AND (“primary care*” OR “primary health care*” OR “general practice” OR “GP*” OR family physician*” OR “family doctor*” OR “primary care*” OR “family health team*”) AND (“economies of scope” OR “at scale” OR “scope” OR “cost*” OR “economies at scale*”) AND (“review*”))
OR
((“primary commissioning” OR “independent practice assessment” OR “community health organi*” OR “independent practice organi*” OR “independent practitioner organi*” OR “health care home” OR “community-oriented primary care” OR “community-owned primary care” OR “community health trust”) AND (“review*”))
These are the search terms for 1998–2012, inclusive, for the BRACE primary care collaborations REA (restricted to review only); 2013 onwards includes all the same terms but drops the term “review*”.
The year 2013 was considered of particular importance to GP collaborations in the NHS in England given the introduction of clinical commissioning groups (CCGs) in April of that year, replacing primary care trusts (PCTs) as the bodies responsible for commissioning most NHS services for their local populations. CCGs have all the GPs in a geographic area as members and are governed by boards comprising general practitioners, other clinicians (including a nurse and a secondary care consultant) and lay members. Thus, since April 2013, GPs in England have been required to collaborate for purposes of commissioning secondary and tertiary care services for their registered populations, but have not been required to collaborate to provide health-care services. Our REA and evaluation were, therefore, restricted to collaborations for service provision rather than collaborations for commissioning. The evidence review was registered with PROSPERO before screening began (PROSPERO protocol registration number CRD42018110790).
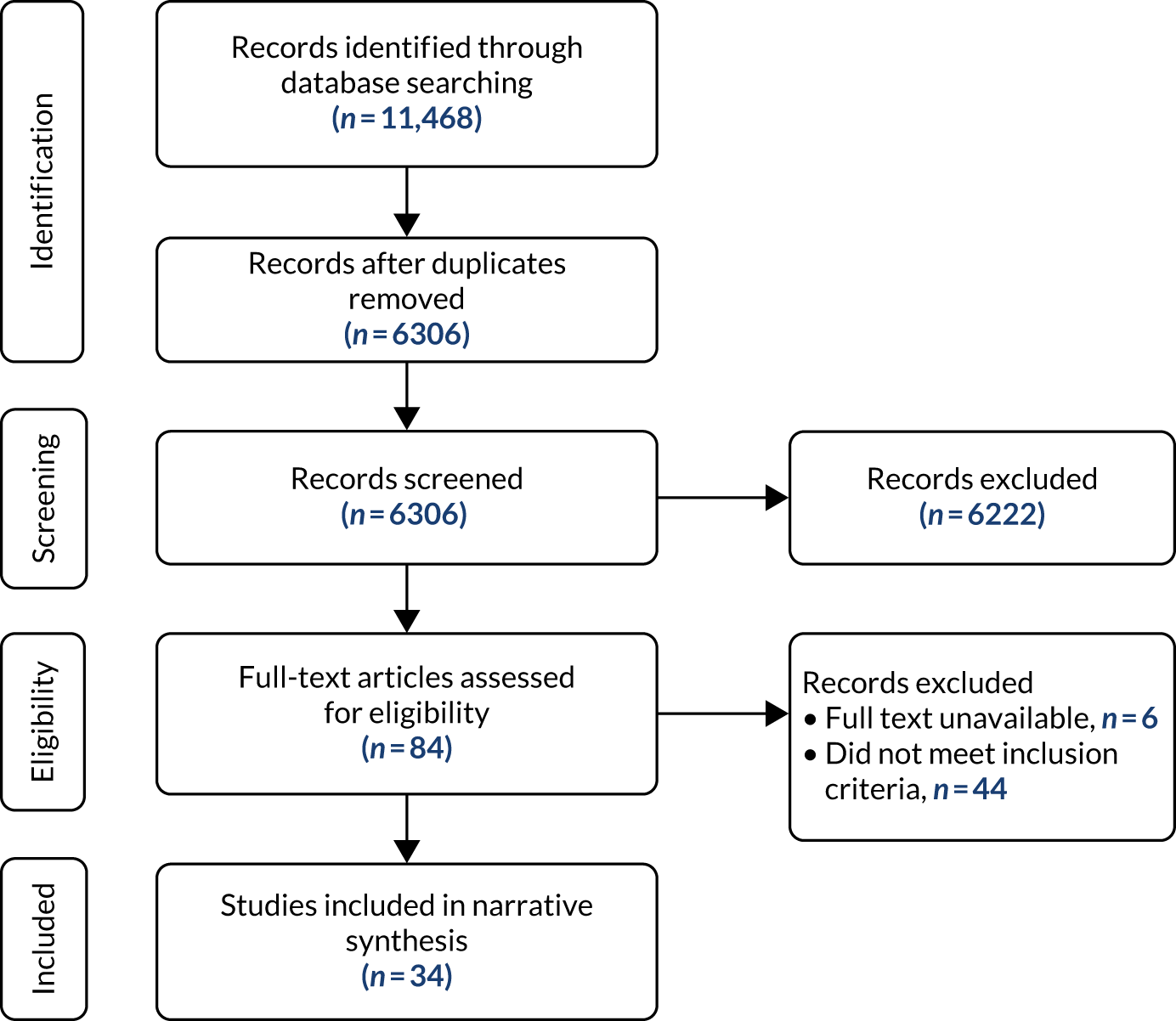
Five review articles and 34 peer-reviewed primary research studies were eligible for inclusion. In addition, we identified 16 grey literature publications, bringing the total number of included publications in this REA to 55. We present these numbers using an adapted version of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram35 in Figures 1 and 2.
FIGURE 1.
A PRISMA flow diagram of screening decisions: 1998–2012, inclusive (reviews only).
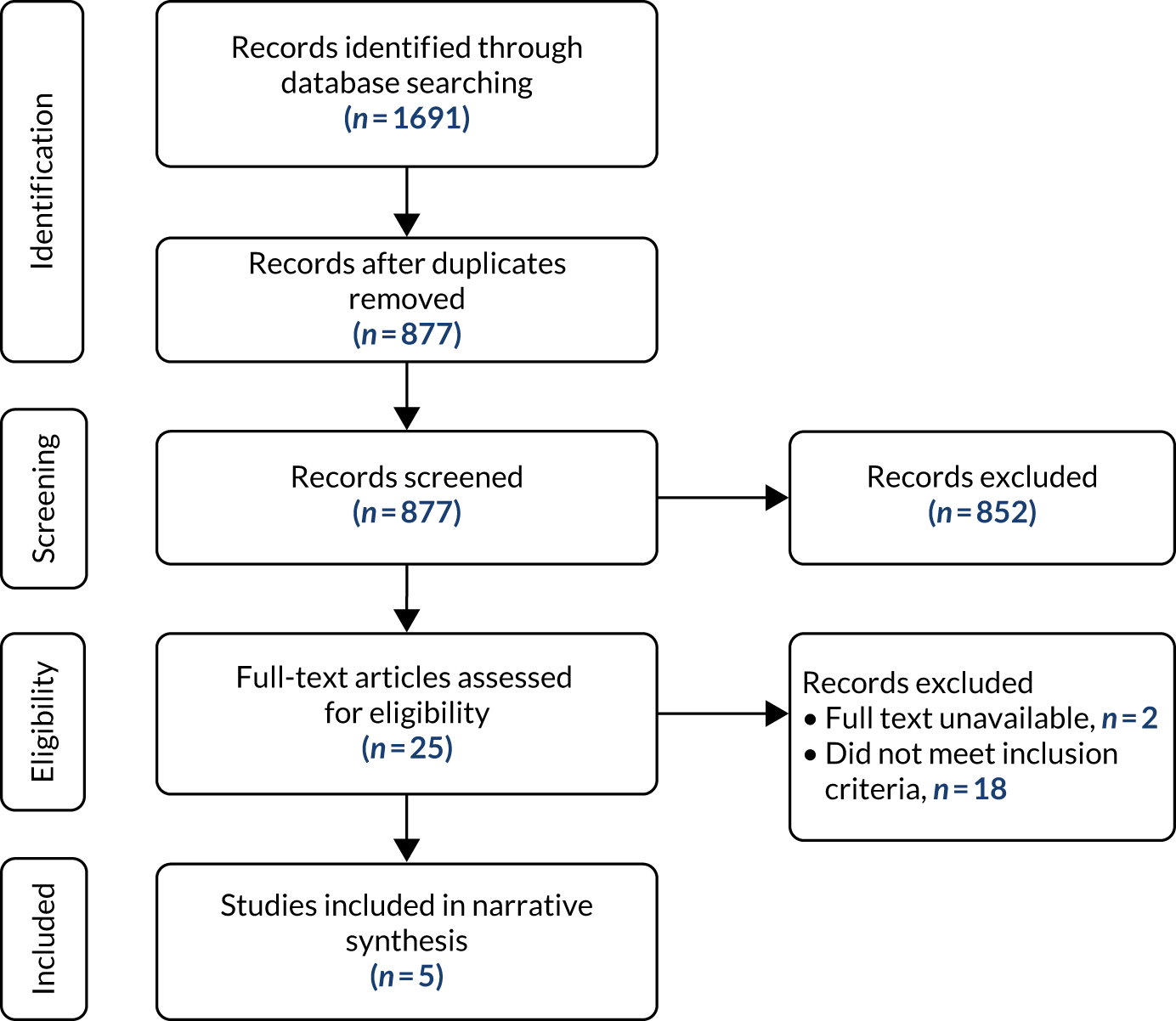
FIGURE 2.
A PRISMA flow diagram of screening decisions: 2013–18, inclusive (all methodologies).
In summary, the REA included both scholarly (academic) literature and grey literature (i.e. reports and articles not submitted to a peer-reviewed journal) that described and evaluated models of GP collaboration in the UK and internationally, including demographics of GP collaborations, impacts of primary care collaborative working, and any reported barriers to and facilitators of implementing these arrangements.
Although we aimed to be inclusive in our approach to the REA and capture an accurate representation of the body of literature published on collaborations, there were some limitations of the review:
-
Defining ‘collaboration’ was challenging given the numerous ways that it was described in the literature and the associated terms attached to it. Despite this, we believe that we captured relevant publications to provide a sufficient overview of evidence relevant to the objectives of this study, as the reviewers erred on the side of inclusion when screening the titles, abstracts and full texts when there was doubt about the relevance of a publication after discussion.
-
We found that in several cases a particular collaborative model, in particular the GP federation in the London Borough of Tower Hamlets, was discussed in more than one paper. 36,37 Consequently, there is a risk of over emphasising that model.
-
We found little evidence of measured outcomes and costs to back up the expected impacts of collaborations. Examples of such outcomes that may be desirable to measure include the incremental costs/savings associated with collaboration, measures of staff satisfaction and changes in patient health outcomes.
Work package 2: project design stakeholder workshop
A half-day project design workshop38 was held in November 2018 and involved, in addition to the research team, primary care policy officials from NHSE&I, a patient representative (from the BRACE Health and Care panel, a source of advice from the health and care sector that acts as a sounding board in relation to the choice, design, delivery and dissemination of rapid evaluations conducted at BRACE) and academics with experience of researching primary care organisations and policy experts in the field (n = 12). The aim of the workshop was to discuss the findings of the REA (WP1), to help identify gaps in the literature, and thereby identify and agree the appropriate focus of evaluation questions for the case studies in WP3. Furthermore, the results of the REA were consolidated into a slide set and working paper at this stage, providing vital resources for the evaluation team to shape the data collection strategy for case study sites.
A structured agenda was prepared in advance of the workshop and included time for plenary discussions, presentations of findings from the REA (also shared with participants in advance) and smaller group discussions. Members of the study team took detailed notes during the workshop, which were used to further develop and refine the case study design (WP3). Notes from the workshop, including proposed detailed evaluation questions and confirmed evidence gaps, were shared with all participants following the workshop. For more information on this, see Report Supplementary Material 1.
Results from the workshop highlighted a number of evidence gaps that could be addressed throughout the evaluation. Participants felt that it was important to understand how ‘participation’ in a collaboration is understood and how ‘success’ within a primary care collaboration would be defined.
Participants at the workshop also felt that a key unexplored area was experiences of primary care collaborations in rural, as opposed to urban, areas to better understand regionally specific challenges in primary care. First, questions were raised with regard to how PCNs can cater for different types of rural and coastal populations, where the population is older than the national average, with subsequent implications for demand on health and care services as well as for the workforce. Second, good innovation and practice were felt to be too often based on urban examples of primary care delivery, with relatively little being known about whether or how easily such learning is transferable to rural settings.
Notably, the study team was encouraged to steer away from case study sites that had already been well evaluated. Finally, attendees were keen for the evaluation to include an exploration of what management and organisational development skills/capacity are needed to make a collaboration work and from where collaborations are drawing these skills and capacity.
Following the project design workshop, the study team continued to communicate and share preliminary learning from the evaluation with key stakeholders and policy experts in attendance to acknowledge and incorporate learning from other national evaluations/research happening in parallel, and ensure that data collection remained responsive to emerging insights captured by policy experts. Thus, the study team, throughout the duration of the rapid evaluation, held regular teleconference meetings with policy experts from NHSE&I, the Department of Health and Social Care (DHSC), The Health Foundation (London, UK) and senior academics in primary care policy research at the University of Manchester (Manchester, UK).
Work package 3: comparative case studies of four primary care collaborations
We conducted comparative case studies of four primary care collaborations in England (three PCNs and one GP super-partnership comprising several PCNs). This work package involved three phases:
-
case study selection and site recruitment
-
data collection at four case study sites
-
analysis and reporting.
These phases were undertaken between April 2019 and April 2020. Given that our evaluation began in September 2018, our initial search for case study sites was focused on primary care collaborations [e.g. GP federation, primary care home (PCH), 24-hour access hub or GP super-partnership] rather than having a sole focus on PCNs. However, after the implementation of NHSE&I’s PCNs model in July 2019, and discussion with the NIHR HSDR secretariat, the research team’s focus turned to recruiting PCNs as case study sites (unless the team was already in the process of recruiting another form of primary care collaboration).
Phase 1: case study selection and site recruitment
Sampling strategy
We undertook a multifaceted sampling process to select four case study sites, based on identifying appropriate primary care collaborations through CCGs that had not been previously evaluated and varied with respect to:
-
rural or urban setting [based on the 2011 rural–urban classification (RUC) of CCGs in England39]
-
collaborations facing significant challenges compared with those that were operating without significant operational complications.
With the support of the University of Birmingham Health Services Management Centre’s Knowledge and Evidence Service team, two members of the research team (AH and MS) carried out a search of three online non-academic databases – GPOnline, Pulse and the Health Service Journal (January 2018 to April 2019) – to identify well- and poor-performing primary care collaborations using the following terms: “collaboration” OR “alliance” OR “primary care network*” or “network*” OR “super-partnership*” OR “super partnership*” OR “superpartnership*” OR “federation*” OR “multi-site practice organisation*”.
However, from the search results, it remained difficult to identify primary care collaborations but easier to ascertain CCGs encountering challenges with the delivery of primary care. In addition, at the time of identifying potential case study sites (May 2019), there was no definitive database/source detailing the existence of primary care collaborations in England. Therefore, the research team obtained an anonymised list of all responses from the Nuffield Trust and RCGP’s Collaboration in General Practice survey14 to identify CCGs to approach, and contacted a number of experts in the field to support the identification of collaborations that may be interested in taking part in our evaluation (May 2019). From July 2019, the study team primarily focused on recruiting PCNs for its case study sites. Our inclusion/exclusion criteria are detailed in Table 3.
| Inclusion criteria | Exclusion criteria |
|---|---|
|
Rural or urban setting (based on the 2011 RUC of CCGs in England) Collaborations facing significant challenges compared with those who were operating without significant operational complications Informal networks, multisite practice organisations, super-partnerships, federations, PCH (pre July 2019) or a PCN (post July 2020) Collaborations either active or that have ceased to be operational in the past 12 months Collaborations consisting of any number of collaborators/GPs (pre July 2019) or that meet PCN model specifications (post July 2019) |
Collaborations that have already been the focus of research or evaluation within the previous 2 years |
Case selection and site recruitment
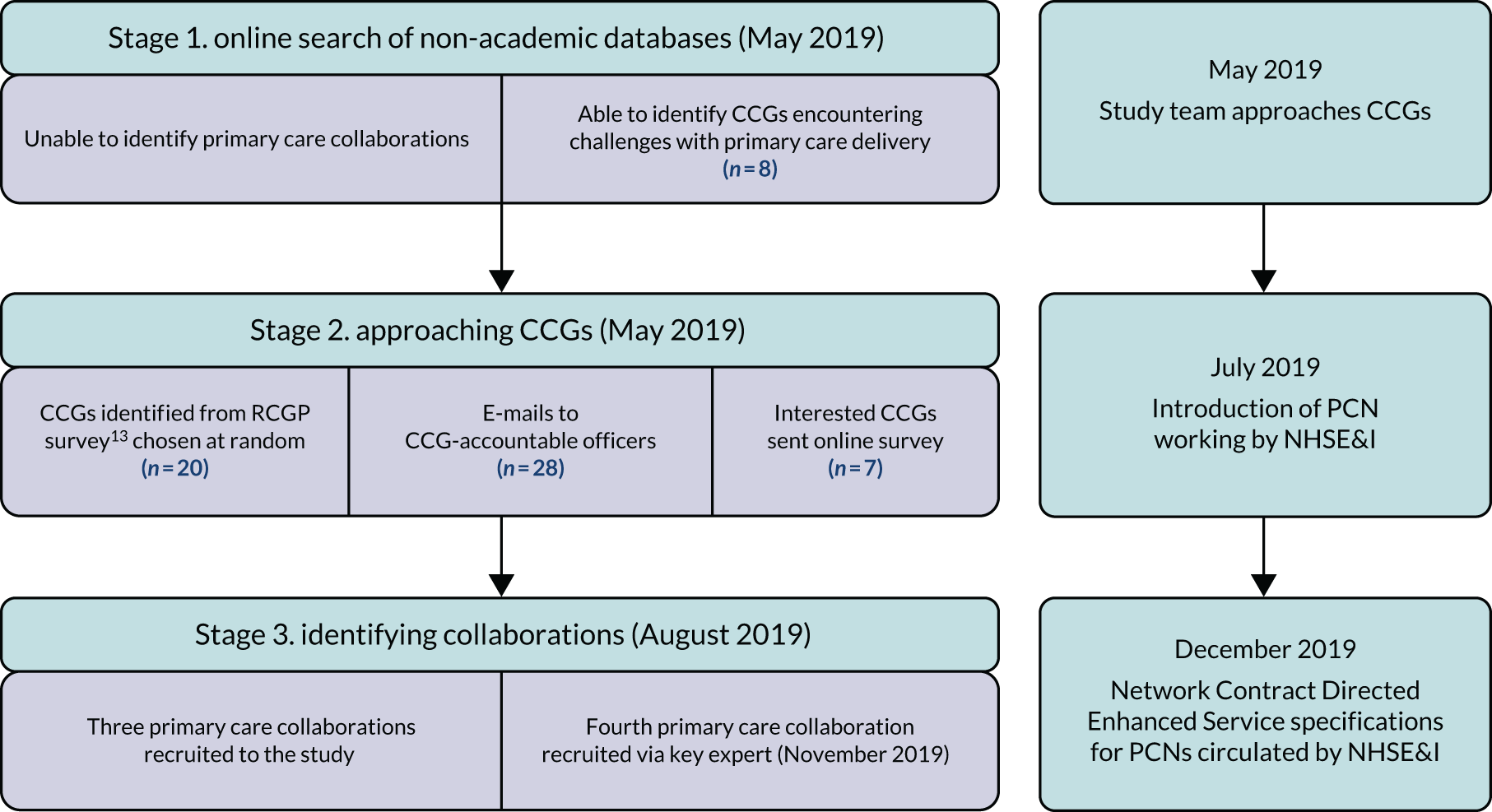
Amelia Harshfield and Manbinder Sidhu identified eight potential CCGs (seven of which were urban and one of which was rural) from online searches. Of the CCGs that responded to the 2017 RCGP survey,14 the total number classified as rural was 28, whereas the total number classified as urban was 133 (based on the 2011 RUC of CCGs in England). The study team took an executive decision to approach 28 rural and urban CCGs in England in May 2019 [comprising eight collaborations identified from online searches (rural, n = 1; urban, n = 7) and 20 CCGs identified from the 2017 RCGP survey14 chosen at random (rural, n = 10; urban, n = 10) based on resources and to begin data collection in a timely fashion].
The study team sent e-mail correspondence directed to CCG accountable officers (or their equivalent) on behalf of the principal investigator (JS) (with a follow-up e-mail sent 4 weeks after the initial invitation). The e-mail was accompanied by an information sheet and a reply form asking the CCG to name all operational/non-operational primary care collaborations (from the previous 12 months) in their area, and was followed up with a telephone conversation between Amelia Harshfield or Manbinder Sidhu and the primary care lead at the CCG. Seven of the 28 CCGs invited responded expressing a willingness to know more about the evaluation with the possibility of taking part.
To support the identification of primary care collaborations via CCGs, the study team disseminated a short online survey (see Appendix 1) to those groups that had responded to our initial approach, asking them to provide details about their primary care collaborations and whether pre-existing collaborations were now PCNs or how they were part of the local emerging network configuration. The survey was pilot tested with two policy experts prior to circulation.
By August 2019, only three primary care collaborations that met our inclusion criteria, from three different CCGs, were committed to taking part in our evaluation (two PCNs and one GP super-partnership). All three primary care collaborations were recruited as our case study sites. Our fourth case study site (a PCN), which met our inclusion criteria, was recruited directly via a key expert employed by a GP super-partnership in England (November 2019). Figure 3 summarises our sampling process.
FIGURE 3.
Summary of case study site sampling.
Phase 2: data collection at four case study sites
The study team followed Johl and Renganathan’s40 phased framework for responsible engagement with organisations and gatekeepers, which includes ‘pre-entry’, ‘during fieldwork’, ‘after fieldwork’ and ‘getting back’ phases. The use of this framework helped the study team to establish a communication plan to build gatekeeper trust and support for the project. A gatekeeper was defined as a person based at our case study sites who could act as an intermediary between a researcher and potential participants with the authority to deny or grant permission for access to potential research participants. 41
Potential participants for interviews were identified, when possible, via a stakeholder mapping exercise with a gatekeeper at each site. Individuals were purposively sampled for maximum variation42 with regard to knowledge of impacts and enablers of, and barriers to, GP collaboration in their area. When stakeholder mapping was not possible, the team incorporated both snowballing and convenience sampling methods to identify interviewees. 43
The gatekeeper helped the team by forwarding documents for analysis and arranging interviews with participants. Communication with gatekeepers across case study sites was often challenging given the changing policy landscape of primary care during late 2019 (such as Brexit planning, NHS financial and workforce challenges, and the scope and pace of PCN policy implementation, as discussed in Chapter 1). Although the research team established significant rapport with gatekeepers, it was difficult to engage clinical and non-clinical staff responsible for delivering front-line primary care health services during a period of policy turbulence, which was made more difficult with the rise of the COVID-19 pandemic.
Our data collection involved four components: stakeholder interviews, non-participant observation of meetings at PCN or GP collaboration executive board level, document review and an online survey.
Stakeholder interviews
Interviewees included CCG staff (related to the set-up and implementation of PCNs), GPs in collaboration lead roles, practice managers (PMs), pharmacists, and those in roles focused on the financial and operational management of collaborations/PCNs. Depending on the size of the primary care collaboration/PCN, the evaluation team planned to complete 10–15 interviews across each case study site or until data saturation had been reached. 44
All interviewees received an information sheet (by e-mail or in person) and were given time to make a decision with regard to participation and to ask questions about the process. Participants signed a consent form prior to participating in the interview, including whether or not they consented to the recording of the interview. Participants were allowed to withdraw from the study at any time (without giving a reason) and were given information about how to find out more about the study or raise any concerns about its conduct.
Individuals participated in a semistructured interview with either one or two members of the study team, either in person or via telephone, and interviews lasted between 30 and 60 minutes. A topic guide was developed and used during interviews (see Appendix 2), although the semistructured nature of the interviews allowed interviewers to deviate from the topic guide based on the interviewee’s knowledge, experience and previous responses. The topic guide contained questions relevant to understanding barriers to and facilitators of PCNs (and/or larger collaborative working within which PCNs exist), operational challenges associated with establishing and running the PCN/collaboration, and the early successes/impacts achieved at each case study site.
Interviews were audio-recorded (all participants gave consent) and transcribed verbatim by a professional transcription service. These transcriptions were anonymised and kept in compliance with the General Data Protection Regulation (GDPR) in the Data Protection Act 2018. 45
In total, we interviewed 25 participants across four case study sites. Table 4 provides a description of those we interviewed.
| Site | Description of staff | Number of staff (interview numbers) |
|---|---|---|
| A | Primary care clinical | 4 (1–4) |
| Primary care non-clinical | 5 (5–9) | |
| B | Primary care clinical | 3 (10–12) |
| Primary care non-clinical | 3 (13–15) | |
| CCG | 2 (16 or 17) | |
| C | Primary care clinical | 4 (18, 20–22) |
| Primary care non-clinical | 2 (23 or 24) | |
| CCG | 1 (19) | |
| D | Primary care non-clinical | 1 (25) |
| Total | 25 |
Non-participant observation of meetings
We observed meetings (at an executive and managerial level where operational and clinical deliveries were discussed) between key stakeholders at case study sites to gain a deeper understanding of how the collaboration was operating and what priorities and challenges it was addressing. These interactions were recorded on an observation template based on the agenda for the meeting, as well as using sociograms (i.e. visual representations of relationships between individuals in a given setting) when possible (at meetings with fewer attendees) to map the nature of interactions within the meeting. 46 This observation template can be found in Report Supplementary Material 2.
Participant information sheets and written consent forms were circulated in advance or on the day of the meeting to all attendees. Prior to each observation, a member of the study team provided a verbal explanation of the project and its aims and gave attendees an opportunity to ask questions. Individuals who did not consent were omitted from recorded observation notes. Two participants from different case study sites requested that their comments be omitted from observation notes. During meetings, team members were seated appropriately to record observations but remain unobtrusive to the discussion.
Throughout the evaluation, being able to attend meetings proved to be challenging for staff in three of the four case study sites; for example, meetings were regularly rescheduled at short notice and the study team often had limited access to high-level strategic meetings. Thus, collaborations were selective with regard to the nature of meetings they allowed the evaluation team to attend. In addition, it was sometimes difficult to gain access to meetings at which staff from individual practices expected that they might divulge information that may represent their primary care collaboration in a negative manner. Therefore, such concerns had a significant impact on the number of observations that were completed (n = 9), despite extensive efforts on the part of the evaluation team working with case study gatekeepers.
Document review
Members of the study team gathered documents describing and containing data on the nature of primary care collaborations, and the priorities and aims, challenges and objectives, activities, set-up, operation, staff involvement, and costs and outcomes of collaboration. These were used to contextualise the development and functioning of the collaboration/PCN and to provide a historical perspective. Documents were sourced through case study gatekeepers and included:
-
material related to the structure of the collaboration/PCN
-
infrastructure and governance arrangements and charts
-
agendas and minutes of collaboration/PCN board and other meetings
-
local communications materials.
Data were extracted from source documents using a structured Microsoft Excel® Version 2108 (Microsoft Corporation, Redmond, WA, USA) template, which is available in Report Supplementary Material 3. The research team summarised information from documents that informed the writing of our context (see Chapter 1) and case study summaries (see Chapter 4).
Online smart survey
Throughout data collection, members of the evaluation team across all four case study sites struggled to arrange and complete interviews with clinical staff working in primary care (who were time limited), although other non-clinical staff were more available for interviewing. Therefore, in January 2020, the research team designed a short online survey (taking no more than 10 minutes to complete; see Appendix 3) to supplement data collected from interviews and observations, as well as to gather further data from general practitioners, nurses, PMs and newly introduced staff members recruited via the implementation of NHSE&I’s PCN model (i.e. social prescribers, pharmacists). Prior to circulation, a draft version of the survey was piloted with two senior and experienced general practitioners who were external to the case study sites to ensure that questions were appropriate to our evaluation questions, and to check for ease of comprehension and completion. Once redrafted following their comments, the survey was distributed across case study sites via gatekeepers (February–March 2020). A breakdown of survey responses from each site and characteristics of participants is provided in Tables 5 and 6. The results are discussed in Chapter 5, and additional information on survey responses is available in Appendix 5, Tables 8 and 9.
| Site | Number of responses |
|---|---|
| A | 2 |
| B | 14 |
| C | 4 |
| D | 8 |
| Total | 28 |
| Role | Number of respondents |
|---|---|
| Primary care clinical staff | 17 |
| Primary care non-clinical staff | 4 |
| Primary care organisational management-related staff | 3 |
| Other (community-based health-care providers/leaders) | 4 |
| Total | 28 |
Phase 3: analysis and write-up
Between January and April 2020, the insights gained through interviews, documents, non-participant observations and the online survey were analysed for each case study site.
We took a content analysis approach to documentary reviews and observations, hence, an iterative process of reading appropriate primary care literature and engaging in interpretation. To aid in the process of analysing and interpreting the data, the core evaluation team (MS, SP and JS) undertook an online data analysis half-day workshop in March 2020 followed by regular weekly online video calls (March–April 2020). These meetings had to take place online, as the COVID-19 pandemic was under way during the majority of phase 3, and the evaluation team was working from home as per government guidance.
Our analysis was guided by theoretical and policy literature on collaborations of GPs and in particular the framework developed by Smith and Mays,22 seeking to identify and understand the following:
-
objectives underpinning a collaboration
-
measures (or proxy measures) of the impact of a collaboration
-
degree of success in ‘tipping the balance’, that is shifting policy attention away from more traditionally powerful elements of health systems, such as acute hospitals, towards primary health care (in this case the local PCN area and overarching CCG)
-
the role played by primary care collaborations in strengthening primary care services and influence. 13
Data analysis for interviews was informed by the Gale et al. 47 framework method for the analysis of qualitative data in multidisciplinary health research. This method of analysis is a highly systematic method of categorising and organising data while continuing to make analytical and interpretive choices transparent and auditable. Hence, the aim for the project team was to facilitate comparison across the case studies.
There are seven stages to analysis within the framework approach:47
-
transcription
-
familiarisation with the interview
-
coding
-
developing a working analytical framework
-
applying the analytical framework
-
charting data in a framework matrix
-
interpreting the data.
Data analysis and early interpretation of emerging findings was led by Amelia Harshfield (November 2019 to February 2020). However, Amelia Harshfield was on maternity leave from March 2020 onwards and Sarah Parkinson led data analysis and writing up of the findings, with input from Judith Smith and Manbinder Sidhu throughout.
Stage 1: transcription
All interviews across the four case study sites were transcribed verbatim through a professional outsourced transcribing company; a single organisation, specialising in transcribing health-related qualitative interviews, was used for all interviews.
Stage 2: familiarisation with the interview
Members of the project team (AH and MS) established familiarity with the data by reading two transcripts (or one-page summaries of transcripts) from each case study site and discussing emerging findings and areas of interest (which warranted further probing in subsequent interviews) and was discussed during telephone weekly meetings (November 2019 to February 2020). During meetings, team members were able to reflect on, discuss and share preliminary thoughts and impressions of early findings. This in turn led the evaluation team to construct detailed case descriptions for each of the four sites (see Chapter 4).
Stage 3: coding
Stages 3 and 4 (coding and developing a working analytical framework) of analysis occurred in tandem. The study team applied a deductive approach, having first developed an initial coding framework focusing on specific areas of interest identified from our REA and primary care policy literature, as well as interview guides and an initial reading of interview transcripts and field notes. Second, two researchers (SP and MS) independently coded the one interview transcript to ensure that no important aspects of the data were missed. The qualitative data analysis software package NVivo 12 (QSR International, Warrington, UK) was used to undertake coding.
Stage 4: developing a working analytical framework
After piloting the initial coding framework and revising it based on the coding of an initial transcript, an analytical coding framework was agreed by all project team members (see Appendix 4). The analytical coding framework differed from the initial framework in that it had fewer codes, and these were more grounded in relation to the study REAs. Once agreed, all remaining interview transcripts were coded (n = 24). The codes in the final analytical framework were categorised under the following broad themes, namely general information (including the nature of primary care collaboration, governance and pragmatic information with regard to implementation, e.g. stakeholder involvement); description of, and reasons for, developing a collaboration/PCN; understanding and measuring impact (e.g. service delivery, financial and organisational); goals/metrics; what had gone well and poorly since the introduction of PCNs; and future steps.
Stage 5: applying the analytical framework
The working analytical framework was then applied by indexing (the systematic application of codes from the agreed analytical framework to the whole interview data set) by two project team members (SP and MS). Manbinder Sidhu coded data from two sites where he had collected data to build on existing levels of immersion. However, Sarah Parkinson coded data across all four sites to build a wider encompassing understanding of the data. Each code (n = 140) was shortened in name (if possible) for easier application. Data from observations and document analysis were discussed in data analysis meetings (March and April 2020) with regard to supporting emerging findings from interview data.
Stage 6: charting codes
As opposed to traditional methods of charting data (summarising data from each transcript by category of code), the project team took a novel rapid approach of a single researcher reading all content (from interviews across each site) under each code. The summary of codes was discussed at a second data analysis online video half-day workshop attended by team members (April 2020). Divergent interpretations with the coded data were resolved, and theoretical engagement with the coded data was undertaken, through discussions during the workshop among study team members. As a result, the evaluation principal investigator (JS) wrote a critical summative narrative paper of our findings and their relevance to policy literature, which was checked by Sarah Parkinson and Manbinder Sidhu. This overarching narrative paper helped team members to understand the scope and relevance of their findings, and supported the team in working out how best to write up themes in a coherent and integrated manner. No data were recoded following the second data analysis workshop.
Stage 7: interpreting the data
The critical summative narrative paper was circulated to wider team members (SP and MS) for comments (April 2020). The narrative was further refined with some outstanding queries remaining, with the intention that these would be resolved during the writing of Chapter 6. In addition, refinements to the narrative summary paper supported the interpretation of data across the four case study sites, interrogating theoretical concepts relational to our evaluation questions and mapping connections across our themes. Once all members of the project team agreed on the summative narrative, writing up of findings commenced. The project team circulated a summary of findings (digital slide deck) to each case study site providing an opportunity to give comments [i.e. member validation48 (June 2020)]. These comments were acknowledged and incorporated into findings.
Summary of analysis
We have provided a transparent account of our adapted framework analysis model suitable for rapid evaluation in which we detail significant discussion and contributions of project team members. Our approach supported engagement with the data in a timely fashion while iteratively returning to the literature to create a summative narrative paper. In the following chapter, we present a summary of our findings from the REA. A summary of Chapter 2 is given in Box 3.
Follow-up interviews on the COVID-19 response
Owing to the COVID-19 pandemic, data collection for this evaluation concluded in March 2020, at which point only limited information about the response of each case study site to the pandemic was available. To help fill some of these gaps, the research team contacted the gatekeepers at each site in June 2020 for a short 30-minute semistructured telephone interview on collaborative responses to COVID-19 through PCNs. Gatekeepers were contacted by e-mail, at which point the study team also sent preliminary findings and the case study site description (see Chapter 4) to check the text for accuracy. This member validation process allowed the study team to check the factual accuracy of information about each case study site.
Three follow-up interviews were conducted with representatives from sites B, C and D. The interviews addressed the following questions:
-
What changes to service delivery have been made across your PCN since the beginning of the pandemic? Has any support or guidance been received from NHSE&I, CCG, local foundation/acute trusts? Success stories?
-
How has PCN policy helped/hindered primary care delivery during this period? (Organisational/managerial/leadership/governance issues.)
-
What has been the impact on staff? (Clinical and non-clinical.)
-
What changes do you think will continue beyond the pandemic and why?
The information from these interviews is summarised at the end of Chapter 5.
Chapter 3 Lessons from the evidence
The REA sought to answer the following questions:
-
What are the forms of organisational collaboration used in GP?
-
What are the reasons for GPs to enter into collaboration, or not?
-
What are the perceived facilitators of, or barriers to, effective GP collaborations?
-
What evidence is there of positive or negative impacts (both intended and unintended) brought about by collaborations in GP?
There are many diverse models that GPs adopt to collaborate with one another and different approaches taken to developing services. Forty-seven different ways of describing a GP collaboration were identified and the population covered by a GP collaboration ranges from < 1000 people to > 500,000 people.
In an English context, reasons to collaborate in various types of arrangements have included to hold budgets and bid together for contracts; to commission services for a local population as part of national policy on primary care-led commissioning; to deliver a wider range of services for patients; to strengthen practices’ resilience by providing better primary care management and better staffing resources; and to enable better access to care for patients by extending opening hours of GPs.
The main factors reported in the literature to have an impact on the progress of GP collaborations, and of particular relevance to the development of PCNs, can be summarised within four themes: management and leadership, engagement of general practitioners and the wider primary care team, strategic direction and objectives, and relationship of the GP collaboration with the wider health and care system.
Impacts claimed for GP collaborations included enabling the delivery of high-quality health care; introducing new specialist services in primary care settings; providing direct access to diagnostic facilities for general practitioners, hence avoiding unnecessary outpatient referral; pooling resources to avoid duplication of effort; and a sense of overwhelming workload in respect of understanding what is required to participate in the collaboration.
Rapid evidence assessment
Given the > 30-year history of development of GP collaborations in the UK and internationally, and the existence of a significant body of research and evaluation, it was considered important to undertake a rapid assessment of this evidence to inform this evaluation of the early implementation of PCNs. A major review of the evidence relating to large-scale GP was undertaken by Pettigrew et al. 21 at the London School of Hygiene & Tropical Medicine in 2016. Therefore, the evidence assessment for this evaluation of PCNs focused primarily on more recent literature (2013–18), using 55 publications from the UK context and from all high-income countries (as defined by the Organisation for Economic Co-operation and Development49), as well as examining reviews and syntheses of prior research (1998–2018). Full details of the methods for the REA are given in Chapter 2.
The REA sought to answer the following questions:
-
What are the forms of organisational collaboration used in GP?
-
What are the reasons for GPs to enter into collaboration, or not?
-
What are the perceived facilitators of, or barriers to, effective GP collaborations?
-
What evidence is there of positive or negative impacts (both intended and unintended) brought about by collaborations in GP?
Forms of organisational collaboration in general practice
The traditional model of GP in the UK, in common with many other developed countries, is of small, privately owned partnerships operating under a contract with the publicly funded national health system. Over the past three decades, there has been an international move towards more organised and collective GP, largely based on horizontal integration across practices, and typically involving practices working in networks, federations or more formal mergers in super-partnerships. 19,20,50 In some of these arrangements, dedicated management and organisational support are put in place centrally, and formal entities that are owned and operated by groups of practices are established.
The REA offered insights into the diverse models that GPs adopt to collaborate with one another and the different approaches taken by GP collaborations when developing services. Forty-seven different ways of describing a GP collaboration were identified in this evidence assessment, including those summarised in Table 1 in Chapter 1 that reflect the policy context of GP collaborations in the UK.
The evidence review revealed that, in the international context, the population covered by a GP collaboration ranges from < 1000 people through to > 500,000 people. In 2017, 28% of GP collaborations in England covered a population of < 50,000 people and 31% covered a population of > 200,000. 15 In the research literature, there is frequent analysis of the size of GP collaborations and discussion about the advantages and disadvantages of different scales. Many of these discussions conclude that, rather than be overly prescriptive about a particular size or structure for GP collaborations, policy-makers should seek, where possible, to allow organisational form to follow function21,51,52 and that there are perils in a national policy or funding body mandating a specific size or form. 13,53 In the case of PCNs, size and form have been mandated (albeit implementation has in practice allowed more flexibility), with the justification being that this builds on the National Association of Primary Care’s suggestion of a population of 30,000–50,000 people being appropriate for the PCH model of care. 17
Reasons for general practice collaboration
Collaborative GP is most frequently associated with a desire to strengthen and extend the provision of primary care and community-based health and care services, along with enabling financial, workforce and organisational efficiencies. 20,24,50 In some countries, and particularly in England, networked and collaborative primary care has tended to be focused on engaging GP in the purchasing or commissioning of wider health services (as in GP fundholding, TPPs, PCTs and, more recently, CCGs). Research into different iterations of primary care commissioning has, however, shown that they tend to focus mainly on developing local primary care service provision and networking, rather than planning and purchasing a wider range of community and secondary care services. 22 PCNs have been established primarily to focus on extending the provision of local health and care services, and are commissioned and funded to do this by NHSE&I. There is an aspect to the work of PCNs that is arguably about commissioning (the assessment of local health needs, and then developing services to meet those needs) but this is within a context of service specifications set out by NHSE&I.
In the international context, primary care physician-led and -owned groups have typically emerged as a means to hold contracts with funders or insurers, or to deliver a range of health-care services that seek to keep quality high while containing costs. 13,53,54 Although examples of GP collaborations in countries such as New Zealand, Canada and the USA have often been able to demonstrate some success in meeting these goals, evaluation studies have found that primary care organisations often underestimate the complexity and scale of the management capacity required, and pay insufficient attention to the time and support needed to engage local health-care professionals in the new service delivery arrangements. 54–56 The vital importance of infrastructure and management support to primary care-led organisations is also reported in studies of community-owned and -led services, including in New Zealand57 and the UK. 58
General practitioner collaborations have often focused on working together to provide a range of new health services. Some GPs may start collaborating to bid for contracts to offer these services, or assume budgets to provide them, whereas others may start collaborating for different reasons (e.g. to have greater influence in the local or regional health system, to fend off a perceived threat to GP independence or provide training and development support for primary care teams) and find that as part of their collaborative process they then start introducing new services. The latter happened with primary care groups in the NHS,50 physician groups in California54,55 and independent practitioner associations in New Zealand. 13,53
In the English context, GPs have entered into various collaborative arrangements over the past 30 years, citing different reasons for doing so. These reasons include to hold budgets and bid together for contracts,19,59 to commission services for a local population as part of national policy on primary care led commissioning,20,51,60 to deliver a wider range of services for patients,16,36 to strengthen practices’ resilience by providing better primary care management and better staffing resources,61 and to enable better access to care for patients by increasing opening hours,3,62 among others. 21 Unsurprisingly, these collaborations vary in form, functions, staffing arrangements and culture. It is often difficult to divorce the commissioning aspect of a GP collaboration from its role in developing service provision (and, as noted above, there are elements of this overlap within PCN policy), given that many commissioning collaborations moved to focus on the provision of care within primary and community services. 20,51,63 A summary of reasons for forming a GP collaboration is set out in Box 5.
To improve and extend service provision for patients in primary care including, for example, practice-based physiotherapy, specialist asthma and diabetic care, pharmacy-led medication reviews in GP or care homes, dementia cafés and carer support, and intensive home support for people living with multiple complex conditions. 14,19,21,36,61,64–74
To engage general practitioners and their teams in local care planning and purchasing. 21,50,51,60
To encourage greater integration of local health services, including through the development of effective multidisciplinary teamworking. 3,19,20,61
A response to governmental mandate or recommendation, including to take on responsibility for commissioning or purchasing certain local health services. 3,13,15,36,61,62,66,70,75–78
To enable GP to gain greater influence in the local or regional health system. 21,50,51,53,60
To improve the sustainability and resilience of GP. 19,61,79–82
To reduce costs and become more cost-effective. 65,68,83–86
To increase, recruitment, retention, job satisfaction or staff experience within primary care. 14,68
Nevertheless, it is clear from literature from different countries that, even where GP collaboration is considered a key feature of the policy and organisational landscape, some GPs have historically chosen not to enter into any collaborative model, presumably for various reasons including fear of loss of professional status or autonomy. 21,87 Little research appears to have been undertaken to understand the nature of, and reasons for, non-collaborative working across GPs in the NHS or internationally.
Enablers of and barriers to general practice collaboration
The REA explored those factors perceived to enable or hinder GP collaborations. These factors varied in focus, ranging from leadership and organisational skills, through governance arrangements, to having appropriate technology. Often, an absence of the perceived facilitators was the main barrier to collaboration. The main factors reported in the literature to have an impact on the progress of GP collaborations, and of particular relevance to the development of PCNs, can be summarised within four themes:
-
management and leadership
-
engagement of general practitioners and the wider primary care team
-
strategic direction and objectives
-
relationship with the wider health and care system.
Management and leadership
A theme that recurs across forms of GP collaborations in the UK and overseas, and across three decades, is the need for sufficient management and leadership capacity. 3,50,60,84,88,89 This expresses itself in relation to the need for clear roles for those leading the collaboration to enable primary care colleagues within and across practices to work together effectively. 70,79,80,83,90,91 This can include very practical matters such as obtaining physical premises for the GP collaboration core team and shared service delivery. 70,78,92 Undertaking the necessary organisational development work early in the development of a GP collaboration is critical to ensuring that roles are clearly defined, understood and enacted. Likewise, there is a need for time and resources,15,36,59,62,79,89,93,94 ensuring that those running a GP collaboration have the necessary clinical and non-clinical skills59,64,72,79,88,94 and development support to achieve the aims and objectives of the collaboration. 59,62
Organisational and managerial support is not just about the capacity that is available within the GP collaboration itself: it is also vital that there is adequate health system and management support available from the wider local and national health system, for example in relation to training resources, information technology (IT) systems, policy advice, governance and regulatory matters. 62,66,85,86,93,95 Clear and agreed governance and regulations for the establishment and maintenance of the GP collaboration are important and are often underestimated by GP groups at the outset. 15,59,75,88,94
Funding for management support and leadership capacity is reported as critical50,63,73,85 (yet often insufficient) for the development and operation of GP collaborations, and is typically underestimated at the outset. 61,67,85 Related to this issue of resources, access to integrated patient records and other IT systems across practices in the collaboration is considered vital to the functioning of GP collaborations, but is often difficult to put in place and hence becomes a barrier to progress. 3,21,59,66,70,85,88,90,93,94
Engagement of general practitioners and the wider primary care team
Studies of GP collaborations in the UK and overseas repeatedly emphasise the vital importance of ensuring that there is sufficient trust between members of the GP collaboration21,36,50,59 and also that there are effective working relationships within and across the practices that make up the organisation. 21,37,59,68,79,80,88,96 Without these, the collaboration will struggle to secure support for its objectives or to enact its plans. This can be summed up as the need for a strong sense of active participation in the GP collaboration, rather than general practitioners and their teams being passive members. 21,59,69,79,88,91,93,97 It can, however, be harder for some (often smaller, or single-handed) practices to feel that their voice is heard within a GP collaboration, particularly in its early stages of development. Some studies have shown that practices that have traditionally been vocal about local service delivery often take on the leading role in new collaborations. 21,60
There is also evidence emphasising the importance of close geographic proximity of practices within a collaboration, together with the possibility of using shared infrastructure such as back office administrative support, out-of-hours shared cover arrangements, or joint appointments of specialist nursing, pharmacy and other staff. 3,19,68,72,84
Strategic direction and objectives
Many evaluation studies – including TPPs and PMS pilots (see Boxes 5 and 6) – have highlighted the need for a GP collaboration to have clear aims and objectives, and to ensure that these have been developed with the active engagement of constituent GPs and their teams. This is linked to the need for clarity about the outcomes a GP collaboration wants to achieve50,63,75,76 and its ability to achieve these outcomes. A regional or national top-down approach to developing a particular form of GP collaboration may introduce priorities and policies that are not fully aligned with local needs,21,50,92,98 as collaborations initiated and driven by GPs and primary care teams themselves may be able to respond better to assessments of local needs. There will, however, be trade-offs in respect to achieving national and local priorities, and a key task for a GP collaboration is to undertake this planning and priority-setting work. 89
Relationships with the wider health and care system
A frequently reported tension or barrier to the development and longer-term success of GP collaborations has been for policy-makers and funders to adopt what is perceived by GP to be a top-down approach, whether expressed through excessive governmental legislation or regulations, too much prescription of governance arrangements and service priorities, and overbearing performance management approach. 53,54,68 This can lead to general practitioners feeling that their autonomy and core purpose are being challenged or that they are under threat. 16,75,76,79,89
Short-term political cycles have been reported in some studies13,21,50,79,88 to introduce uncertainty about what GP collaborations are required to do, leading to cynicism and lack of engagement on the part of general practitioners and their teams. Furthermore, leaders of some collaborations can find it time-consuming and distracting to navigate a complex wider health system infrastructure,21,50,61,79,84 which points to the importance of policy-makers and funders being thoughtful and proportionate in how far they expect GP collaborations to be integrated with overall health system management infrastructure. Finally, a frequent barrier to the sustained progress of GP collaborations is the disillusionment they and their teams encounter following initial over-optimism (often on the part of policy-makers and funders who are impatient for ‘results’) about what is achievable in a limited time frame,15,50,59,99 or feeling that the contributions of the collaboration are not being acknowledged. 70 This in many ways reflects a cultural clash between large-scale health policy organisations and newer, smaller and more fragile GP collaborations.
The reported impact of general practice collaborations
The evidence review identified a number of areas of impact associated with GP collaborations. There was, however, a relative lack of quantitative evidence to support these claims, and many evaluation studies3,56,57,59 had focused more on the initial implementation of GP collaborations rather than on the sustained tracking of progress in achieving service or health outcomes. Nevertheless, impacts claimed for GP collaborations included enabling the delivery of high-quality health care (e.g. practice-based physiotherapy, specialist asthma and diabetic care, pharmacy-led medication reviews in GP or care homes, dementia cafés and carer support, and intensive home support for people living with multiple complex conditions19,36,50,61,63,68,69,71,72,77,85,90); introducing new specialist services in primary care settings;50,63,66 providing direct access for GPs to diagnostic facilities and hence avoiding unnecessary outpatient referrals;3,100 and pooling resources (e.g. electronic health records) to avoid duplication of effort. 59,66,79,83,84 Other areas of impact associated with GP collaborations were focused on organisational or infrastructure matters, including improved employee satisfaction62,68,69,83,90 and strengthened working relationships between staff. 68,79,84 There have also been negative unintended impacts from GP collaborations that were identified in the literature, including challenging the role and sense of autonomy of general practitioners68,75 and a sense of overwhelming workload in respect of understanding what is required to participate in the collaboration, to set it up and make it succeed. 50,75
Lessons from two particular prior forms of general practice collaboration
There is particular learning to be gained for PCNs from an examination of the experience of two particular UK experiments with GP collaborative working, both of which were subject to 3-year national evaluation studies. These are the TPP schemes that were established in 1995 as extensions to the Conservative Government policy of GP fundholding, and the PMS scheme of local contracts for primary care, brought in as part of the implementation of the National Health Service (Primary Care) Act 1997. 101 Our REA and the key policy components of the PCN approach in 2019 has led us to consider that these two prior forms of GP collaboration have particularly relevant insights for current developments, given that they also took the opportunity to have additional funding, through a contract held collectively across practitioners or practices, to purchase or deliver a wider range of local health services. The summary of learning from TPPs and PMS schemes is set out in Boxes 6 and 7 below.
There were 53 TPPs in the first wave of these schemes introduced in 1995 and they remained in place until 1999. The TPPs comprised GPs in a local area that came together to hold a budget with which to purchase the majority of hospital and community health services, building on the GP fundholding scheme that had commenced in 1991. They varied in size from populations of 7000 people to those of 80,000 people and adopted a range of organisational forms. TPPs were evaluated by a national team of researchers led by Nicholas Mays of The King’s Fund. Some of the key lessons from the evaluation were as follows.
Enablers of and barriers to progressClarity of objectives and planning for the TPP was seen to be a key enabler of progress.
Progress was enabled significantly where there were higher levels of management capacity and expertise.
Smaller TPPs appeared to have more success in engaging their clinical community in their work than larger TPPs.
Effective GP leadership of a TPP was considered critical; however, some struggled to engage the wider GP and practice membership of the TPP, citing a lack of direct incentives for GPs.
Data and IT were barriers to progress, including problems in securing utilisation and financial data.
They struggled to engage social care and local authorities in their work, and likewise local communities and service users.
ImpactTheir achievements were typically modest in scale, local and incremental, and tended to focus on improving and extending primary and community health service provision.
They were able to make some changes to patients’ use of emergency secondary care services by providing alternative forms of community health care.
They were found to have increased the cost of running the local health system, given the additional transaction costs of smaller health purchasers.
Adapted with permission from the Open University Press, from The Purchasing of Health Care by Primary Care Organisations: An Evaluation and Guide to Future Policy, Mays N, Wyke S, Evans D, editors, 2001.
Personal medical services pilots were established in ‘waves’ following implementation of the National Health Service (Primary Care) Act 1997,101 which was passed with cross-party support just prior to the Labour general election victory of 1997. PMS was a voluntary scheme that allowed a GP (or group of practices) to take on a local contract to deliver an extended range of primary care services to meet local population needs in a flexible and multidisciplinary manner, working to quality and service standards negotiated with the local health authority and, subsequently, the PCT. PMS contracts proved popular (22% of general practitioners were working to them in 2002) and continued beyond the initial pilot phase. In 2002, a national contractual framework was introduced for PMS schemes, alongside wider reform of primary care contracts. It is notable that PMS has remained an attractive approach for general practitioners across the years. PMS contract pilots were evaluated by a number of academic teams funded through a national DHSC programme of research. Key findings included the following:
Enablers of and barriers to progressEnablers of progress cited by evaluators were clear objectives for the local scheme, effective management support and expertise, commitment and support from clinicians in the scheme, and strong teamwork and shared culture within practices/practice groups. 102,103
The contractual freedoms on offer were considered to enable practices/practice groups to develop innovative services.
A small number of PMS schemes were led by nurses, who held the contract for the organisation and provided overall leadership to the practice team.
ImpactPersonal medical services schemes led to modest and steady improvements in the quality of primary care. 103
Personal medical services schemes led to innovation in the form of use of a greater mix of skills in primary care, including the employment of salaried general practitioners, practice-based pharmacists and nurse practitioners.
Personal medical services schemes were able to develop services that went some way to addressing long-standing inequities in primary care, for example in establishing services for homeless people, refugees and those with severe mental ill health. 104
Patients’ experience of primary care did not change as much as had been hoped for in PMS schemes, and innovations in care provision were not as significant as vaunted in the initial policy.
Gaps in existing evidence on general practice collaborations
In preparation for our stakeholder workshop at which we shared the findings of our REA, we distilled what we considered to be the main gaps in the evidence on GP collaborations, framing these as questions that needed to be answered by future research and, where possible, our own rapid evaluation of the implementation and early development of PCNs. These questions were as follows:
-
What are the benefits of collaboration for (1) patients, (2) staff and (3) the local health system?
-
What are the costs of collaboration (financial costs, opportunity costs and other kinds of cost)?
-
To what extent are the enablers/facilitators for successful collaboration in place within local systems of care?
-
What further kinds of support and/or investment are most needed to create an environment for effective collaboration?
-
Why do some practices choose not to collaborate? What happens in areas where practices choose not to collaborate? Does this affect care outcomes in any way and if so, how?
-
Do GPs need to collaborate to achieve key outcomes (e.g. improving access, achieving sustainability)?
These questions informed our methods and approach for the case study element of our evaluation, and are examined as part of the discussion chapter (see Chapter 6) when reflecting on what this study has revealed in respect of collaboration within GP, and in particular for the future monitoring and development of PCNs in the NHS in England.
Summary of the rapid evidence assessment
The REA underlined many of the factors considered essential to the operation of effective GP collaborations that have been identified in prior reviews, which provide important lessons for new PCNs to consider, as we have reported elsewhere. 99 Some important lessons for PCNs to consider include the time it is likely to take for them to become established as well-functioning organisations in a wider health system, and the level of high-quality management and leadership capacity required to ensure their success.
Lessons from previous GP collaborations suggest that PCNs will need an appropriate balance of autonomy and control in relation to health funders and planners, along with clarity of remit and objectives that enables them to develop plans and work programmes aligned with the expectations of both policy-makers and local primary care stakeholders. PCNs will also require sufficient time and capacity to develop trusting and supportive relationships within the GP collaboration and with other partner organisations, especially early in their implementation. Finally, from the literature on previous forms of GP collaboration it is clear that PCNs have the potential to use the funding allocated to them to enable new and extended forms of primary care service provision, but that expectations should be managed to ensure that they can make progress in a measured manner that is proportionate to the challenges that evidence suggests they will face.
Our rapid review enabled us to identify important gaps in the research evidence, which we explored in a workshop of key stakeholders (see Chapter 2, Methods), then using these insights to frame questions for the case study research set out in Chapters 4 and 5 of this report. In the next chapter, we describe the four case study PCNs and their extant GP collaborations, and then set out the findings of our research in these sites.
Chapter 4 Description of case study sites
This chapter provides a brief overview and context to each of the four case study sites, along with their core characteristics.
Site A is a PCN of eight GPs serving a population of 75,000 patients in a rural setting in England dispersed over a large geographical area. The stated overall aim of the PCN is to improve access for local people to the resources they need to lead healthier lives.
Site B is a super-partnership containing 13 practices serving over 130,000 patients, which was formed in 2017 in response to a workforce crisis. Site B is located in a largely rural area of England characterised by a largely ageing white British population. The super-partnership aims to create efficiencies from working at scale, including by providing some centralised back office functions for constituent practices.
Site C is a PCN of eight practices serving a population of 60,000–70,000 patients in a largely urban setting in England dispersed over a town-based geographical area. The area is socioeconomically disadvantaged with a large elderly population, many of whom live with long-term health conditions. The current PCN mirrors the previous collaborative model, the site C neighbourhood, with the aim of providing better integrated care for the local community.
Site D is a PCN of four practices, serving a population of > 30,000 patients. It is located in a rural area in England, characterised by an ageing and dispersed population with complex health and social care needs. Prior to becoming a PCN, there was a strong sense of collaborative working between all the practices currently in the PCN.
In this chapter, a brief overview is given of the background and context to each of the four case study sites, along with their core characteristics. Particular attention has been paid to previous and existing forms of GP collaboration within each case study site, illustrating the complex and varying context within which PCNs have been introduced. The way in which these sites were selected for study is set out in Chapter 2.
Site A
Site A is a PCN of eight GPs serving a population of 75,000 patients in a rural setting in England dispersed over a large geographical area.
The area is characterised by an ageing, white British population, with many living with a range of long-term health conditions. The patient population has good access to primary care services (the majority will be seen by their general practitioner within 48 hours) compared with the general English population. The stated aim of the PCN is to improve access for local people to the resources they need to lead healthier lives.
There was an established history of these eight practices working collaboratively prior to the creation of the PCN, in an informal model of locality working, as well as engaging in partnership working with practices that are part of neighbouring PCNs. The locality model focused on developing an integrated multiprofessional workforce to enable primary care, community health and social care professionals to work in partnership with acute and community care providers. Hence, locality working was based on:
-
delivering a more community-focused service
-
multidisciplinary clinical and social care team service delivery
-
making the most of existing relationships between practices and those delivering community services
-
reducing organisational boundaries and increasing collective working through networked arrangements.
The PCN is supported by a large GP super-partnership established across two counties in England serving over 350,000 patients; some, but not all, of the practices within the PCN are members of the super-partnership. The GP super-partnership offers practices administrative and management support, which frees up time for clinical work, enables economies of scale and builds on established relationships with acute and community providers of care. As a result, the eight practices decided collectively to use PCN funding to pay the GP super-partnership to provide certain services for the PCN, including legal advice, setting up contracts, financial management, monitoring support and procurement. As part of this GP super-partnership structure, the PCN continues to have strong relationships with a neighbouring network that also has constituent practices from within the GP super-partnership.
The PCN holds 6-weekly governance meetings with one lead general practitioner and one PM from each practice in attendance. The PCN also has a core management structure made up of the clinical director (CD), two general practitioners and a PM informally acting as a PCN manager, who provide oversight to the network’s operational and service development decision-making and day-to-day management. At the time of data collection, there was a newly appointed CD.
A diagram of site A’s organisational structure is in Figure 4. The orange represents the unit of analysis for this evaluation (i.e. case study site collaboration), and the purple represents parts of the organisational structure within each site that were outside the focus of this evaluation.
FIGURE 4.
Site A organogram.

Site B
Site B is a super-partnership containing 13 practices serving > 130,000 patients, which was formed in 2017. The practices within the super-partnership are part of four PCNs. Some of these networks have a majority of practices from the super-partnership, although in some PCNs super-partnership practices are in the minority. Site B practices had previously collaborated through an integrated neighbourhood team, a GP hub and a GP federation, which is still in place and whose membership overlaps with that of the super-partnership. Although PCNs and the GP federation continue to exist in parallel, the collaboration that seems to hold the most influence over collaborative working within site B is the super-partnership.
Site B is located in a largely rural area of England characterised by an ageing, white British population.
The super-partnership was created in part to respond to a workforce crisis, to help address general practitioner recruitment issues, to meet service pressures caused by changes in patient demand and to attract more investment into primary care. The super-partnership aims to create efficiencies from working at scale, including by providing some centralised back office functions for constituent practices.
A central tenet of the super-partnership is to create parity between partners and safety in numbers, seeking to reduce the risk borne by any one partner. One way that the super-partnership accomplishes this is through a ‘property solution’ in which property in the super-partnership is held jointly by all partners, which has been highlighted as a key success. Within the super-partnership, each practice retains clinical autonomy and is its own profit/loss centre, although the super-partnership carries the overall risk for any financial losses. The super-partnership has a set of clear due diligence procedures for new practices wishing to become part of the organisation, and they pay a joining fee based on their number of registered patients.
The super-partnership has a two-tier system of governance in which some decisions are made by the full partnership: a managing board with GP partners who represent different localities from across the super-partnership, and a team of executive directors. The full super-partnership meets on a quarterly basis, with the management board meetings held monthly and the executive team meeting weekly.
A diagram of site B’s organisational structure is provided in Figure 5.
FIGURE 5.
Site B organogram.
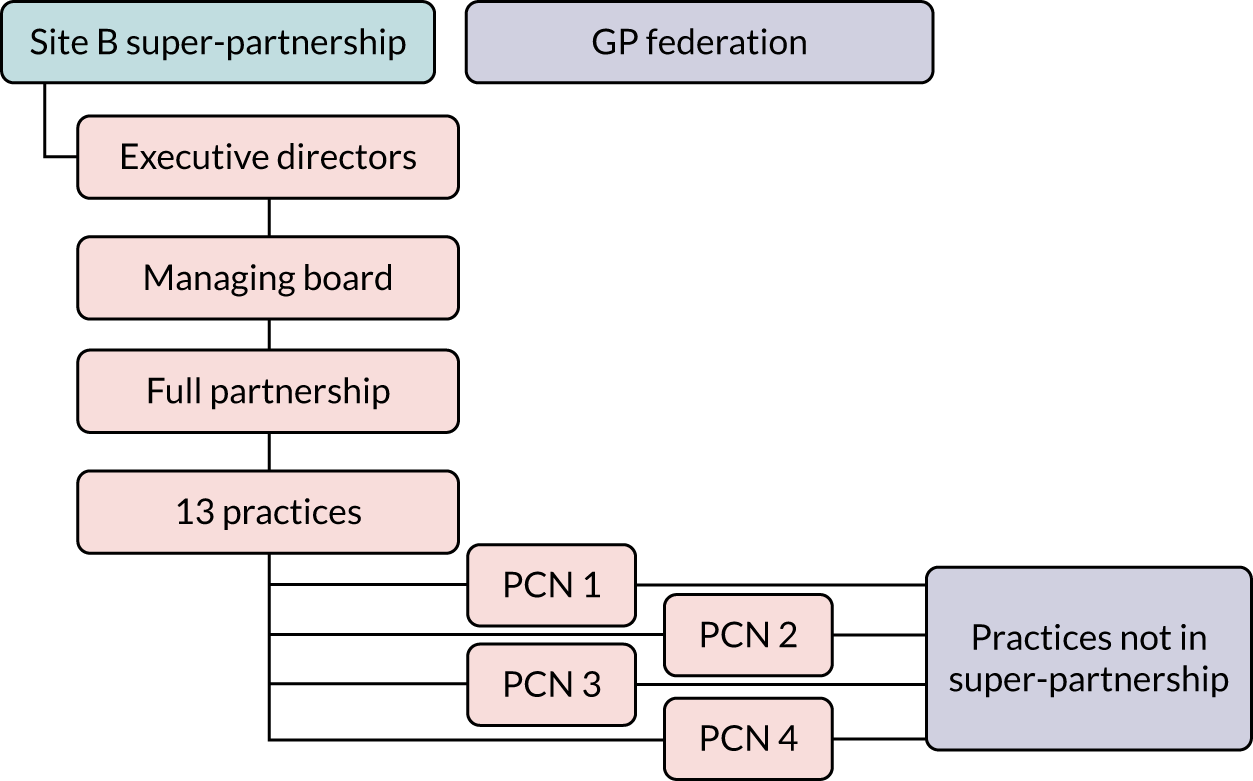
Site C
Site C is a PCN of eight practices serving a population of 60,000–70,000 patients in a largely urban setting in England dispersed over a town-based geographical area.
The area is socioeconomically disadvantaged with a large elderly population, many of whom live with long-term health conditions. There is also a significant minority-ethnic South Asian community representing a mainly younger cohort.
The current PCN mirrors the previous collaborative model, the site C neighbourhood, which comprised the same eight practices. The purpose of the neighbourhood, integrated with the local NHS foundation trust, was to promote greater patient self-management by enabling care nearer to home through closer working across primary care and health and social care services, in addition to voluntary, community and faith sector service provision. Hence, the neighbourhood promoted multidisciplinary working across a range of services including GP teams. The neighbourhood model was implemented in 2017 and was expected to end in 2020 (based on pre-COVID-19 pandemic information). At the time of data collection, the PCN and the neighbourhood were working in parallel. The governance and management structure of the neighbourhood and of the PCN had both similarities and differences: both models were led by two CDs (one neighbourhood lead was also a joint PCN lead). Neighbourhood working was led via monthly meetings attended by both clinical and managerial staff, as well as by patient participation group leads, with collective input with regard to decision-making and strategic direction. In comparison, monthly PCN meetings were attended by lead general practitioners from each of the eight practices, with discussions fed back once meetings had concluded. Nevertheless, the PCN was established to build on the aims and objectives of the neighbourhood, as detailed below:
-
to address health inequalities in the area and improve access for patients at a reduced cost
-
to support patients living with long-term conditions to support self-management
-
to have better integrated care in the community with the development of mental health teams, increased social prescribing and training receptionists as care navigators
-
to develop and support the workforce to deliver a range of extended health services.
To help achieve these aims, the PCN has appointed a manager to oversee governance and manage a shared budget across the eight practices, whereas the CD’s focus is on improving service-level provision aligned with quality improvement monitoring.
A diagram of site C’s organisational structure is provided in Figure 6.
FIGURE 6.
Site C organogram.
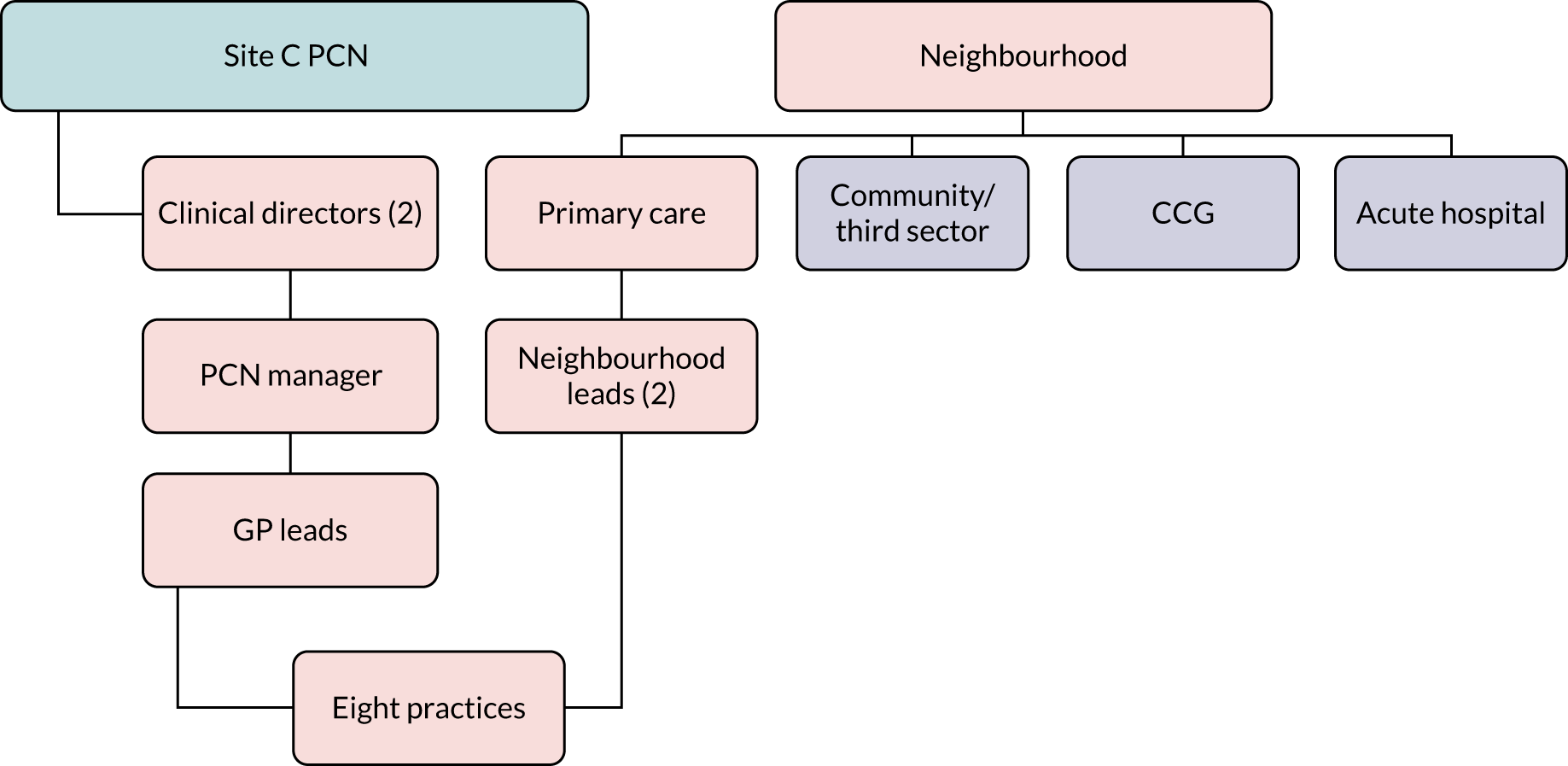
Site D
Site D is a PCN of four practices, serving a population of around 30,000 patients. It is located in a rural area in England, characterised by an ageing, dispersed population with complex health and social care needs. The population is mostly white British, and faces issues such as frailty, isolation and living with long-term health conditions.
Prior to becoming a PCN, there was a strong sense of collaborative working between all the practices currently in the network. This informal collaboration had grown to meet the needs of practices working to support the local rural population, and to encourage effective links with community providers, the voluntary sector, social care and others in the health and social care system.
The PCN board is made up of one general practitioner and one PM from each practice, with an overall PCN manager on the board working alongside the CD. There is also a working group with representatives from across the PCN, which implements network-level decisions, comprising general practitioners, PMs, IT staff and others. The PCN board meets monthly, whereas the working group meets fortnightly.
A diagram of site D’s organisational structure is provided in Figure 7.
FIGURE 7.
Site D organogram.

In the next chapter, we set out the findings of the research undertaken in these four case study sites, using the themes from the rapid review of evidence about GP collaborations to organise and contextualise the results, and explore the early experience of PCNs, including their implementation and what enabled or hindered progress.
Chapter 5 Findings from case study research
General practices across England have seized the opportunity to access new funding to form PCNs. General practitioners and their teams place particular priority on enhancing the sustainability of primary care. However, there are mixed views about the purpose of PCNs, with some people supportive of the national policy and approach, and others frustrated at having to adhere to a government line to receive new funding.
In all four case study sites, the new PCN was established in the context of a prior general practitioner collaboration. Previous collaborations helped the PCN to build on previous successes such as the strong existing relationships between practices and integrated service delivery. However, it was often a source of tension in sites where the PCN was perceived to be undoing aspects of the work of the previous collaboration.
This evaluation has revealed a tension between the desire by general practitioners and their teams for local autonomy and influence over PCNs and the perceived top-down nature of PCN policy. Developing shared goals and objectives emerged as an enabler of progress, and of positive working relationships within and beyond the PCN.
The need for effective leadership of the PCN, together with sufficient high-quality management support, was a strong theme in the evaluation fieldwork.
It was clear that, although they are small organisations, PCNs need a significant range of administrative and management capacity and skills, including finance and accounting, human resources, IT, staff engagement and governance support, which were not present in all case study sites in this evaluation. In addition, the evaluation revealed significant challenges faced by CDs in terms of workload, and pointed to the need to improve non-clinical management skills in this role.
The allocation of a new source of funding that is channelled directly into GP rather than through an intermediary organisation such as the CCG or sustainability and transformation partnership, is clearly welcomed in principle by most practices.
In some instances, CCGs have enabled and supported PCNs, providing resource and expertise to help establish inter-practice working, hire new staff and operate contracts. In other areas, however, there is evidence of the CCG attempting to hold on to resources or control that have been delegated to PCNs and are therefore not perceived to be operating within the spirit and expectation of PCN policy.
Rural collaborations feel that PCN policy has been developed with urban practices and collaborations in mind, and are concerned the policy does not adequately account for the distinctive experience of delivering primary care in rural areas.
With regard to COVID-19, PCNs were part of an integrated response alongside the CCGs, the extended-hours access providers, and local community, foundation and acute trusts. In response to patient demand and access to primary care, PCNs experienced a significant drop in patients requesting appointments with general practitioners, with the majority of consultations carried out by video or telephone, a transition that the majority of patients were pleased with as they received a quicker than usual response from their practice. However, requests for general practitioner appointments are gradually increasing. Throughout the pandemic, all four PCNs continued to deliver the Network Contract Direct Enhanced Service specification.
The findings from the case study research are presented below, examining reasons to work as part of PCNs and other forms of GP collaboration, the early impact of network implementation and other forms of collaborative working, and facilitators and barriers that PCNs have faced within their first 9 months of operation. Barriers faced by rural PCNs and small practices are also highlighted. When possible, this chapter includes consideration of how PCNs and other collaborative working arrangements have responded to the COVID-19 pandemic, which first started to affect the UK health services in the final stages of this evaluation (March 2020).
These findings draw together the primary data collected for this evaluation through interviews and non-participant observations, as well as evidence from documentary analysis (see Chapter 2). Where relevant, evidence is contextualised through learning from the background review of research literature (see Chapter 3).
Reasons to collaborate in primary care
In Chapter 3 we examined the rationale and incentives for GP to enter into different forms of collaboration, as noted over several decades in the UK and overseas, including the role of financial incentives, the desire of general practitioners to have greater influence in the local health system, the aim of improving and extending primary care service delivery, and a need to secure the sustainability of GP for the longer term. Throughout this evaluation, it has become clear that the rationale and incentives associated with PCNs are in some ways distinct from those associated with GP collaborations more broadly, and, therefore, these have been treated separately in the sections below.
Reasons to enter into a collaboration within primary care
Over the past decade, primary care in the UK has faced challenges in terms of workforce, efficiency and resilience, which cause serious issues in terms of the sustainability of primary care. 9 These issues of sustainability, in terms of both finances and the primary care workforce, emerged as significant across the case study sites in this evaluation, and were identified as key reasons to enter into collaborations in primary care [Interview (Int)1, Int3, Int10, Int13, Int14, Int15, Int20].
Collaborations can help address issues of GP sustainability in a number of ways. First, practices collaborating with one another can help to distribute workload and pressures between them, and can enable some tasks and procedures to be shared between practices to reduce the burden on any one practice team (Int6, Int7, Int10, Int15, Int20). Collaboration between practices can also help recruit and retain staff within primary care, including by enabling the organisation to offer better training resources, flexible work arrangements and better benefits to staff (Int10, Int14, Int15):
It’s very difficult for small, singlehanded GP practices to survive with the workloads that are on them in terms of the pressures. And only by working together and collaborating can we sort of be strong enough to face the issues that we face on a daily basis in general practice. So those were the sort of ideas around making it sustainable and future proof.
Int15
There was a recognition some time ago . . . that nine practices are essentially from an administration point in very many cases doing the same thing nine times over, which is a fundamental waste of time and money. There was an argument that things such as practice policies, methods of using clinical systems, scanning and coding could all be, if not the same, similar, so that when we did make changes we could try and use one person to make the bulk of the changes, and then the other nine, well the other eight would just be tinkering around the edges.
Int7
Collaborations can also help address issues with the financial sustainability of primary care. For example, before PCNs, some discretionary funding was available through the CCG to improve collaboration between GPs at many of the case study sites, increasing the budget for primary care (Int17, Int21, Int22, Int25). Economies of scope and scale, creating financial efficiencies, and implementing better financial and organisational management were also mentioned as reasons to form collaborative organisations in GP (Int13, Int16, Int17):
If you look at [redacted] . . . there was a lot more clarity about what they wanted to do, so they wanted to actually see primary care at scale in a structured way where they could get the economies of scale from a bigger organisation, get rid of that kind of corner shop mentality that a lot of practices have got, inject some professional management into general practice.
Int17
Improvements to patient care and service provision were also mentioned as reasons to form collaborations in primary care. Collaborating between practices can help fill gaps in service provision when single practices are not able to provide all services (Int3, Int15, Int17, Int20), and help provide patients with better co-ordinated care, particularly for patients with complex health and social care needs (Int3, Int24). Collective working in primary care also helps with planning and providing services at a population level, and the evaluation heard about some pre-PCN collaborations having started as a result of undertaking population-level service planning for a locality (Int6) and devising ways to improve care for older people (Int22, Int24, Int25). However, some interviewees thought that providing care at a larger scale would result in poorer patient experience and outcomes, which is explored in Impact of primary care networks:
We’re only a small network, 35,000 patients in the network . . . I sort of see the 35,000 rather than the 3000 we’ve got on our list. So I’m really enthusiastic, and I want to make sure that the 35,000 are looked after, as much as my 3000.
Int6
Reasons to enter into a primary care network
Although the reasons for entering into GP collaborations are diverse, as noted in Chapter 3, the reasons for entering into PCNs appear to be more tightly focused on policy and financial incentives, which is unsurprising given the nature of the policy with its national approach to contracts and service specifications. Many interviewees said that practices were effectively obligated to form PCNs, and that practices had no choice but to accept the financial incentives associated with networks for fear that they would be ‘left behind’ (Int1, Int2, Int4, Int5, Int8, Int12, Int17, Int23). Some of these interviewees negatively framed the PCN policy, stating that practices were coerced into entering into collaborative arrangements despite having some concerns. However, others expressed ambivalence about PCN requirements, describing them as an external policy development to which practices needed to adapt (Int1, Int17):
With the PCNs we’ve been told we have to, and if we don’t we’re being told that our patients will go into a PCN . . . and it will be out of our hands. So we’re being bullied into something that the doctors don’t have time for.
Int8
If we’re going to talk about the PCNs, the rationale for getting involved is it’s a national policy and there’s a lot of cash on the back of it, and their motivation has been OK, because general practice is very good at adapting to contractual context and particularly when there’s a set of incentives which is what primary care networks are partially about.
Int17
Although the majority of reasons that were identified by interviewees for joining or forming a PCN focused on policy and funding, survey responses revealed more varied reasons, albeit the survey was completed by only 28 respondents across the four case study sites at a time when data collection was stalling because of the COVID-19 pandemic. When asked to rate reasons why they had formed a PCN, over half of respondents rated, ‘To help sustain the viability/sustainability of general practice’ and ‘Improving co-ordination and delivery of primary care services for patients’ as very important. Figure 8 shows the mixed response to this survey item.
FIGURE 8.
Reasons to form or join a PCN from survey (n = 28). NA, not applicable.
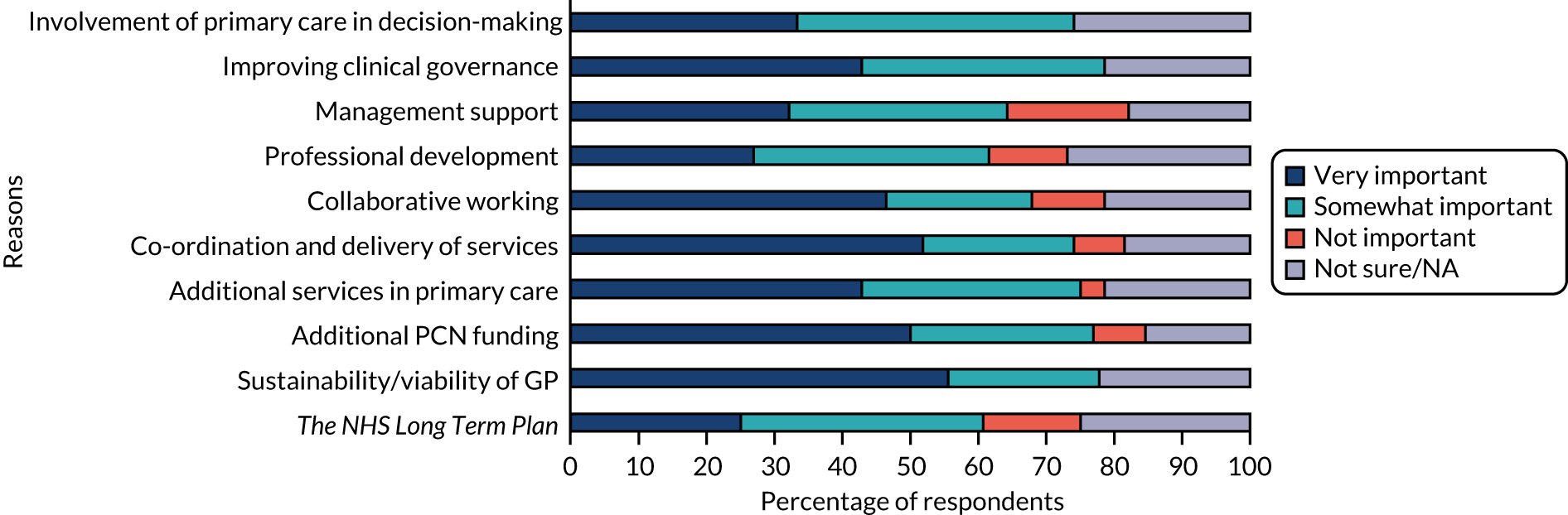
Fundamental question around the purpose of primary care networks
A central tension about the purpose of PCNs arose again and again throughout this evaluation. Some respondents had a view that PCN funding should be spent to help improve the financial sustainability of primary care and reduce general practitioner workload, whereas others thought that the new resource should be allocated to developing new primary care services (Int3, Int18, Int21, Int22 Int24). This tension about the purpose of PCNs has revealed itself in disagreements among those active in management of the networks, and also raises questions about whether or not the new organisations have effectively accomplished their goals.
Some mentioned that they felt that PCNs were being ‘sold’ as a cure-all within primary care, and that there should be a more realistic assessment of what they could reasonably expect to achieve (Int17, Int19, Int24), something that will probably be all the more acute in the context of the COVID-19 pandemic and its aftermath. This underlined the need to identify clear goals for PCNs to help solve some of these tensions about their direction:
There’s other areas and snippets of conversation where you can imagine that PCNs are seen to be the cure of the world’s woes really, or diabetes care or care home care or keeping people out of hospital. And I think, again that is another tension because really they’re trying to make up for there being 6000 GPs short. They’re not saying we can do any more of these, we’re just saying we need this to do what we can do . . . the enthusiasm is great but undoubtedly some of the clinical leads . . . see the potential as being wider than it actually is. I mean I have said myself, I think actually being called a primary care network is a bit egging the pudding that isn’t it? We’re not really are we? We’re a GP network. We’re not going to devolve control of optometry or pharmacy or anything else, but hey, wasn’t me that picked the name.
Int19
Impact of primary care networks
This evaluation sought to examine the early impact of PCNs, and identified positive and negative consequences that have stemmed from these networks in their first 9 months of operation. The evidence for this impact is largely qualitative, drawn from interviews and non-participant observations. Unsurprisingly, at this early stage of network development, very little quantitative evidence was found in respect of their impact. Survey respondents were asked about the advantages and disadvantages of PCNs, and these are set out in Figures 9 and 10.
FIGURE 9.
Primary care network advantages from survey (n = 28).
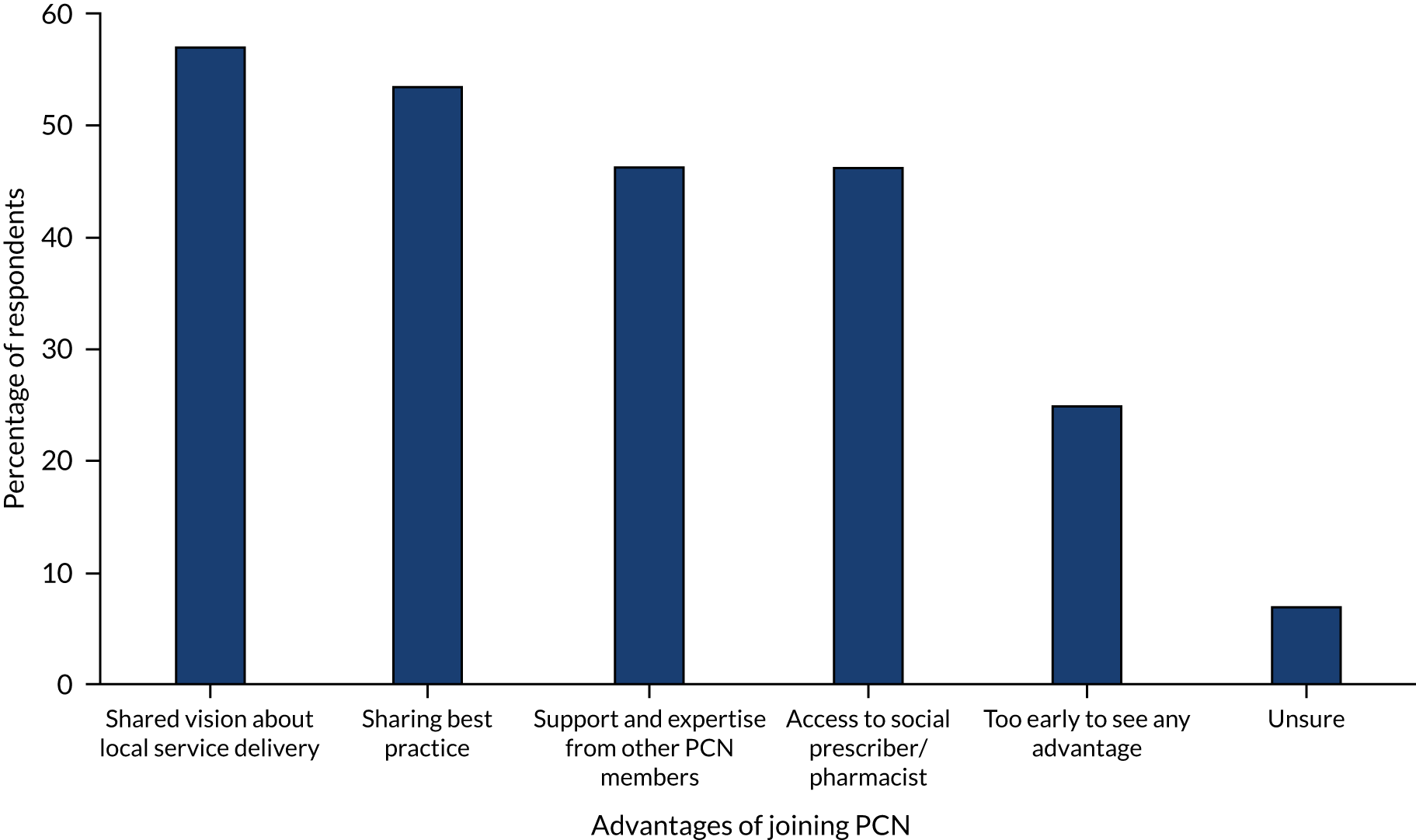
FIGURE 10.
Primary care network disadvantages from survey (n = 28).
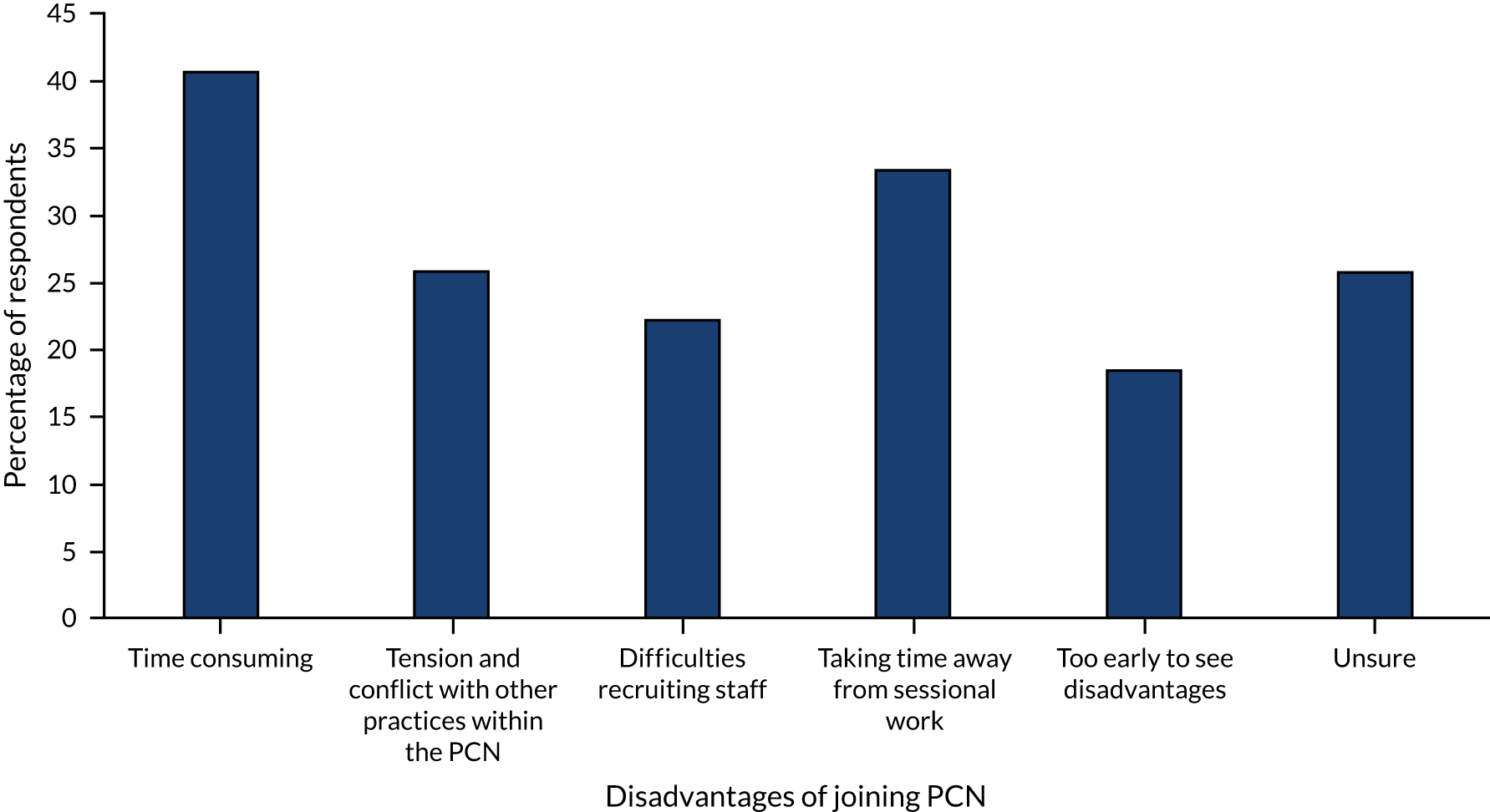
It is important to note that some respondents in this evaluation study reported that it was too early to see the impact of PCNs, particularly as many areas were still working to address operational, back office and regulatory issues before shifting their attention to health service redesign (Int14, Int15, Int17, Int21, Int23). This also aligned with survey evidence, as 26% of survey respondents reported that it was too early to see any advantages of working as part of a PCN.
A large proportion of interviewees emphasised that, although PCNs had changed the policy landscape in terms of some of the requirements made of primary care, they had not yet led to any substantial changes to modes of working within practices, services offered to most patients or ways of collaborating between practices (Int2, Int4, Int6, Int7, Int8, Int9, Int12, Int19, Int23, Int25, site A observation). When exploring the impacts described below, it is important to note that many of those interviewed reported that PCNs had had no or very little impact thus far:
As far as I’m aware we haven’t made any changes to service delivery . . . I think we’ve all carried on doing what we’ve always done, the same way we’ve always done it.
Int7
From somebody who comes into the PCN meetings and just responds to the information and isn’t involved in attending meetings for the leads or the finance and things – there doesn’t seem to be an awful lot done . . . Occasionally I sit there and am thinking why on earth are we here? Because we’re not actually achieving anything.
Int9
Some respondents reported that the implementation of PCNs had been a negative change when compared with how things had been before. For example, during an observation of a network meeting at site A, those present were asked by a facilitator (funded through NHSE&I’s Time for Change programme105) to report how they viewed changes resulting from the PCN. Ten network members rated the PCN as ‘negative’ or ‘very negative’, whereas only three rated it as ‘positive’ or ‘very positive’. Reasons cited for negative views of the PCN included a lack of long-term vision, an excessive burden for practices (and lead general practitioners in particular) in terms of workload, failure to move quickly to implement the PCN, perceived irrelevance of national PCN policy in rural contexts and a perceived lack of leadership from NHSE&I. Some of the reasons for positive views of the PCN included the additional funding coming into GP and support given by the super-partnership (site A observation). These themes were common across the sites and are explored below in more detail.
Service delivery and patient-level impact
Extended-hours GP services had been put into place by PCNs as per the NHSE&I specification (Int2, Int5, Int7, Int9, Int5, Int20, Int21), along with some PCN-determined services such as group counselling services (Int6), older people’s community care (Int3), integrated care for those with hypertension (Int24) and diabetes (site D observation), a rapid diagnostic pathway for patients with a suspected cancer diagnosis (site D observation), video consultation services (site C observation) and multidisciplinary teams to discuss and plan care for patients with complex needs (Int18). Site D was also in the process of planning the building of a central hub for integrated working with other areas of the health and social care system, to be led by primary care and have its own dedicated facilities (site D observation). Several interviewees also commented that PCNs had the potential to increase the influence of primary care in the local health system (Int17), and act as a mechanism to build relationships with community providers and the voluntary sector (Int16), which was supported by the number of integrated services described above.
Some interviewees reported that practices in their area were already meeting PCN service specifications prior to their introduction in January 2020 (Int21, Int24). For example, practices at sites A, B and C were already collaborating to work to provide primary care support to local care homes (Int8, Int13, Int14, Int15, Int17, Int21, Int22, Int24). Sites B and C had also already been working on drug monitoring with high-risk medications, resulting in safer prescribing of opiates and other medications (Int11, Int20, Int22, Int23, site C observation):
When the PCN was first published, and we first heard about this, I looked at it and thought well this is everything that I’m doing with the network, surely it’s the same thing.
Int21
Prior to PCNs, many practices already worked collaboratively to improve care for their patients. For example, the site B super-partnership had already hired mental health nurses, developed services to improve mental health in primary care and created new standardised protocols for managing long-term conditions (Int13, Int14, Int15). Likewise, the neighbourhood at site C had already been working with district nurses, the voluntary sector, the mental health sector and local schools on asthma care (Int21, Int22, Int23, Int24). In addition, practices in site D had worked collaboratively to audit those in the local population who used services the most, as a basis to plan the optimum provision of social care for this population, as well as putting in place a paramedic visiting service and introducing enhanced dementia care services for older people (Int25). Sites A and B had also worked jointly across constituent practices to improve safety measures through training and developing and implementing standard operating procedures, together with internal audit controls and peer-based benchmarking across practices (Int2, Int11, Int13). In providing these services, many collaborations and practices had also previously engaged with community health-care teams, mental health services, local councils, care homes and social services through relationships that had grown organically through years of joint working (Int8, Int16, Int17, Int18, Int21, Int24):
We also developed a healthy memory café which has been much more of a success than we expected it to be, and that’s held once a month . . . We have a GP there . . . nurses . . . Alzheimer’s nurse . . . a dementia practitioner . . . the fire service . . . occupational health, social worker and it is just an opportunity for anybody that’s got a diagnosis of dementia or may just be worried about their memory to pop in and have some advice and help and guidance should they need it. So, I think we’ve been running 4 months and we’ve had about 95 patients attend so far all of which have gone away really grateful for the input. Quite a few are returning on a monthly basis because actually it’s a really nice place to just sit and socialise and specifically for carers.
Int24
As many PCNs had already been working collaboratively to deliver services and improve patient care prior to becoming a network, some felt that the PCN was a step backwards and that these new networks had started to undo the work of previous GP collaborations. Some reported that the PCNs were smaller in scope in terms of what services would be delivered through the network (Int18, Int24) and that the parties involved in the collaboration (Int2, Int6) were more limited in number and type of profession, particularly as the early focus of PCNs has been on sorting out the managerial and administrative aspects of setting them up (Int2, Int24). A few interviewees reflected that because PCNs were more focused on GP than some other prior forms of collaboration that include different parts of the health and social care system (such as multispecialty community provider vanguard schemes2 or integrated care and support pioneers106) PCNs offered fewer options in terms of referring patients to alternative services (Int9). Several respondents also reported that they felt that the NHS direction of travel in terms of consolidation of independent practices into larger entities would negatively affect the continuity of care that patients experienced in smaller practices (Int19), and the ability for services to be planned on a smaller scale in a way that aligns with local population needs (Int4):
The PCN is so far behind, or the new model of the PCN is so far behind where we already are, that I feel we’re thwarted. And in fact since it was launched I feel as though lots of things have kind of been in abeyance, lots of kind of projects and things that were moving forward sort of seem to be on hold because we’re waiting for the PCNs to evolve.
Int18
I just can’t see how on earth the PCN is going to be even remotely in a position to take on that kind of level of work. I just can’t. And I think we would be setting ourselves up to fail massively if we even tried . . . I think because you’ve already got a neighbourhood set up, and its actually worked very well, to have then a PCN is all . . . it’s duplication.
Int24
NHS England has really bought into this . . . making things bigger, bigger providers, bigger scale. It seems to be ignoring much stronger evidence for the advantages of continuity of care . . . There is a tension between access and continuity of care, and at the moment we’re following the one that isn’t evidence based.
Int19
New roles and staff
Primary care networks have provided funding explicitly to hire additional roles in primary care, which has been one of the most substantial changes described by those consulted in this evaluation. The case study sites had all recruited (or were in the process of hiring):
-
pharmacists
-
social prescribers
-
complex care nurses, community matrons and dementia nurses
-
community paramedics
-
physiotherapists
-
administrators
-
care co-ordinators
-
dementia specialist practitioners and advanced practitioners to help take some of this workload from general practitioners.
Because PCNs are not independent legal entities, hiring arrangements for staff varied between the case study sites, with some sites having a lead practice to recruit staff on behalf of the others, and some sites having the CCG, super-partnership or a local NHS trust hire staff. Sometimes the recruitment of staff by entities other than primary care groups had been viewed positively, although it had also caused difficulties, which are described in Facilitators of and barriers to the early implementation of primary care networks. Although the PCNs had progressed in terms of getting people hired for these roles, some respondents reported difficulty in terms of the time it had taken to put together job descriptions (Int8, Int24) and sort out details such as who would induct PCN staff (Int7). There were also reports of challenges in terms of high staff turnover, particularly for PCN nurses, which was observed at site C (site C observation).
Other forms of GP collaboration had enabled the creation of additional roles for primary care prior to PCNs being introduced in our case study sites. Several sites had introduced sharing staff between practices, including mental health professionals (Int13), community matrons (Int22, Int24), community paramedics (Int15, Int25), social prescribers (Int10) and community pharmacists (Int19). Some individual practices had also hired staff for roles that were later funded by PCNs (Int1, Int5, Int8). For collaborations and practices that had already been working with the network-funded roles, there was a view that hiring roles through the PCN could cause a disruption where previous ways of working were already functioning well (Int7, Int8, Int24).
Some respondents commented on the positive impact that these new roles were expected to have on PCNs, on GP and on wider community health provision. For example, it was noted that social prescribers would be able to look at lifestyle factors and could potentially bring about improvements in patients’ health (Int2, Int5, Int6, Int8), and that roles such as social prescribers, pharmacists and physiotherapists would be able to provide more community services to support primary care (Int17, Int21). Others commented that new roles would help to reduce general practitioner workload by creating efficiencies (e.g. by having a single pharmacist to work across all care homes in an area) and by taking away work from general practitioners (Int6, Int9, Int20, Int22, Int24).
Many were, however, more conservative in their assessment of the difference that these new roles would be likely to make in primary care. Some commented that, although new roles might help a small number of patients, the roles would not make a difference for most patients who may not need or have contact with the new PCN-funded roles (Int5, Int21), and would not reduce workload for most staff (Int5, Int17). In addition, even with new network-funded roles, some had reflected that there might not be the workforce available to make primary care sustainable to the extent needed (Int7, Int9), particularly in rural areas (Int9, Int12, Int17, Int24). Although new funding is provided for additional roles through PCNs, some interviewees said that the additional requirements and targets set out in the national PCN specification were such that the additional roles might not reduce general practitioner workloads, and that a moratorium on new targets was needed to reduce workload (Int1, Int17):
At the moment, it’s an extra person, but here’s the work for an extra two people is what it feels like for your average GP. So they don’t feel the benefit, that’s been the problem.
Int17
You know, one new worker over eight practices ain’t doing much for anybody really. But we’re not going to say no, obviously, but they’re not going to change the world are they?
Int21
Impact on practice staff
In some instances, PCNs appeared to be starting to have a positive impact on staff in GPs. One interviewee commented that, in practices with a small number of partners, PCNs were providing security to partners and had given them the confidence that, if the other general practitioners pulled out of the partnership, they would not be left isolated (Int9). It was also reported that PCNs had generated enthusiasm in terms of general practitioners becoming involved in local strategic planning for health services (Int19) and resulted in new training and shared resources (Int5, Int18):
We’ve got a couple of practices within our PCN that are only two-partner practices – and I think that it’s knowing that they have got the support of a larger organisation and that they can share resources and that it doesn’t have to all fall down on them I think would be encouraging for somebody coming in, knowing that they have that wider support and networking . . .
Int9
The main thing that has come in – and this isn’t just here – is the enthusiasm with which mostly a new set of GP [general practitioner] faces have really taken on a new role and are invigorated and believe they’re a bit empowered, and they’re doing something at a bigger, more strategic level than out of practice.
Int19
Much of the positive impact on staff described by interviewees was attributed to other prior models of collaboration, rather than the PCN. For example, the super-partnership at one site had been able to offer improved support and resources to staff, including additional training, flexible working arrangements and more generous benefits (Int11, Int14, Int16). Collaboration also enabled it to offer more opportunities for specialisation within the field of primary care, which was described as having the potential to enhance career options (Int10, Int11, Int14):
The fact that you’ve got the support of peers has helped to retain GPs [general practitioners] who would have otherwise retired, and has been an attraction for people to move from not wanting to contemplate partnerships to being partners, because actually we’re demonstrating that there’s so much support around the things that put people off, whether it’s the property management, HR [human resources] or whatever, actually you don’t need to worry about that. So I think that’s in part one of the attractions.
Int11
Although some have reported a positive impact on staff from the introduction of PCNs, the evidence collected through this early evaluation suggests that networks have to date tended to be experienced in a rather negative light by some primary care staff. Workload for existing clinical and non-clinical staff was a significant cause of tension given the time required to set up and establish PCNs across practices. For example, being part of a PCN often entailed multiple weekly and monthly meetings, in which many of the same staff were involved, on top of their clinical duties and other responsibilities (Int4, Int13, Int14). The administrative and managerial aspect of PCNs was also time-consuming, particularly for PMs and CDs, despite funding being made available for managerial aspects of networks (Int1, Int3, Int4, Int5, Int7, Int8), and many mentioned that PCN-related tasks felt too much on top of the regular day job (Int1, Int5, Int7, Int8, Int9, Int12, Int14). This was also supported by survey evidence. When asked about the disadvantages of PCNs, 41% of survey respondents selected that a disadvantage was that networks were time-consuming, making it the disadvantage most frequently selected by survey respondents:
It can’t be a bolt on to the day job, and that’s what it is at the moment. I have been averaging . . . 55–60 hours over the last couple or 3 months and that in itself wouldn’t be a problem . . . what is a problem is that for all of that we’re no further forward than when I started 3 months ago. That is fundamentally a problem, and when I listen to all the other PCNs I get the impression that there’s a lot that are in the same boat.
Int7
Primary care networks not only add to workload in terms of managerial and administrative duties, but also shift a proportion of the responsibility for funding and implementing local primary care service development from the CCG and community health trust to PCNs. Some respondents commented that this shift, while providing more funding to primary care, had caused issues in terms of increased workload, as GPs found it difficult to meet the additional services in the national PCN specifications even with the additional new staff that had been funded (Int1, Int6, Int8, Int9, Int19, Int24):
We want to make our working lives better rather than just having more money, and we couldn’t really see the PCNs initially were going to make our working lives better. But we had a hope . . . that we would have more clinical support and that would make us be able to deliver more sustainable general practice. Of course that’s been turned on its head completely by the targets that have been set up and in the specifications, which are completely unachievable.
Int1
Organisational impact
Primary care networks had, however, led to perceptions on the part of some respondents of more efficient working and the introduction of more robust managerial and administrative structures. At site C, the PCN had implemented centralised human resource management support, governance structures and training resources (Int20, Int21), along with a shared process and support for the Quality and Outcomes Framework primary care contract monitoring requirements107 (Int21). Practice managers at this site had worked together to align back office procedures, helping to ensure that administrative tasks could be completed centrally by appropriately skilled staff (Int20, Int23, Int24), and that staff such as nurses and receptionists could move around practices as needed (Int18). Site D had set up a PCN triaging process using a commercially available online symptom assessment system to help refer patients to allied health professionals in a standardised way across the network. This was reported to create efficiencies in terms of triaging processes, and had helped the PCN collect data on the use of allied health professionals to aid its resource planning (Int25). Across PCNs in which centralised and standardised processes had been implemented, some respondents commented on what they considered to be the increased stability of their organisations (Int4, Int6):
We do know that in each practice you’ll say, ‘oh yeah such a body brilliant at admin’ or ‘great at coding’, ‘brilliant on scripts’, so why not take them and have them taken out of the practice and just working centrally, because we’re electronic nowadays.
Int23
Some of the organisational impact from collaborating across practices was attributed to other forms of collaboration that preceded, and were continuing alongside, PCNs. For example, the super-partnerships at sites A and B had both provided practices with centralised support for Care Quality Commission inspections, including a joint Care Quality Commission registration at site A (Int2, Int6, Int16, site B observation). The super-partnership at site B had also set up standardised processes for GP reception and patient triaging, and for back office functions including accounting and financial reporting, and a standardised way to respond to GDPR policy, and the logging and handling of complaints and incidents. These processes had created efficiencies and increased stability across the super-partnership and its practices, and allowed staff to move across practices as required (Int11, Int15):
We now have one way of doing the books across all of the practices, with one accountancy firm that has driven down cost. And there’s been bumps in the road on that one, trying to get everyone aligned to a single year end and trying to align all of the different financial reporting mechanisms that we all have into one way of doing it, which was never going to be simple. We’ve now got to the position – it has taken 3 years but we have now got to a position where it feels a lot more stable.
Int11
Although PCNs could be a vehicle to introduce more effective and efficient processes across primary care, this evaluation pointed to potential organisational challenges. By obliging practices to form collaborations, the implementation of PCN policy had in effect forced some practices to work together that had fundamental and sometimes long-standing differences in terms of their operational environment, ways of working and values (Int1, Int2, Int4, Int9, Int17). Although practices within a PCN were required to be geographically contiguous, there have been instances when the border of a network appears geographically contiguous on a map, but has failed to encapsulate areas with similar demographic factors or what are locally considered to be ‘natural communities’ for local people or health professionals (Int12, Int19). Bringing together practices in this top-down fashion had caused tensions within some PCNs, which are explored further in Facilitators of and barriers to the early implementation of primary care networks:
The challenges really were that PCN were something that were . . . an arbitrary formation . . . The idea of collaborative working sounds great, but, you know, when you are forced into a relationship rather than a relationship happening organically, it is very challenging . . . Some of the practices in our PCN area footprint . . . always had different viewpoints of how a PCN should be run.
Int1
Sometimes the reason you’ve got two practices in a particular area is a practice split 10 years ago and now one or two of the GPs left the other two or three GPs and started another practice inside a town. And you still get some of that hangover even now.
Int17
Financial impact
The evidence from this evaluation about the financial impact of PCNs is mixed. On the one hand, these new networks provide a mechanism through which more funding has come into primary care, which has been seen by some as a very important early impact (Int1, Int4, Int14, Int17, Int20, Int21, Int25), and has encouraged practices to work together that would not otherwise have done so (Int17):
Obviously in some respects this exercise is just a rechurning of cash inflow into practices and rebadging it under a different name.
Int4
So the average PCN in our patch in the year that we’re about to go into is going to have just under half a million pound each . . . if you can access that resource, that is a big incentive to put up with Dr X and Dr Y who you find quite irritating. If there wasn’t a lot of resource being invested, I suspect they’d go ‘I really can’t stand him or her, I’m not getting involved’.
Int17
The funding coming directly into primary care had given more financial freedom and security to primary care. Some interviewees commented that there were fewer ‘strings’, or caveats, associated with funding for PCNs, as the CCG or local trust does not have the power to dictate precisely how it is spent (Int19, Int20), and that there was a more steady flow of funding than with previous arrangements (Int23). However, there had also been tensions with CCGs and trusts attempting to maintain oversight of PCN budgets, which are discussed in Facilitators of and barriers to the early implementation of primary care networks below:
When this DES [Directed Enhanced Services] PCN came along, it was a voluntary contract but it was quite [an] autonomous independent contract, there were no strings attached to it, so the CCG could not dictate, you know, what we do and how we do it. Our . . . local trust, could not dictate how we set the whole thing up and what thing we should do or we shouldn’t do . . . So it’s us, we’re deciding what is best for general practice and what is best for our patients.
Int20
Some evidence pointed to more efficient spending and achieving economies of scale (Int14, Int15), for example through better financial management centrally within PCNs or the prior collaboration (Int2, Int16), or the ability to purchase medications at wholesale prices (Int11). However, some of these positive impacts in terms of financial efficiency may have been attributable to other forms of GP collaboration rather than the introduction of PCNs:
There is a contribution that is made by the practices to run the organisation, but through collaborative working, through better use of staff and resources, effectively that money comes back . . . the idea obviously if we are delivering high-performance and high-quality care, that our performance targets will be higher, that will achieve more, which will generate additional income, but income that we can then not just think of it as profit but a way to sort of develop the organisation even further. So there is initially obviously a financial implication in joining [redacted] but we feel that the practices get that back, get that benefit back in higher values than what they contributed.
Int15
Despite some examples of success, there was evidence that PCNs could have a negative financial impact on practices. Some people expressed a view that, although new funding was coming into primary care, this money had had to be spent on the up-front additional management and administrative costs associated with the new networks owing to an underestimation of the time and resources needed (Int3, Int7). There had also been reports that funding from NHSE&I had not been sufficient to cover expenses, leading to financial disbenefit for some practices as a result of joining PCNs (Int5, Int13). Similarly, some commented that the new funding would be spent on the additional services required through the national PCN specification (Int7) or on topping up where the full cost of these new roles was not covered by new resources for networks [although the funding for these roles has since been increased by NHSE&I to cover 100% of the costs108 (Int1, Int13)]:
I think one of the dangers is underestimating the amount of time and commitment people would put into it so it then makes it a negative impact on the finances of practices for time put in.
Int3
The £1.50 per patient is fixed as well that’s going to be used up very quickly by . . . employing additional roles. And actually, we were always worried even when we started that . . . this was going to end up making more work for GPs and it will cost us more in the long run because of all this overlay . . . And certainly, that’s the way it’s looking at the moment and I can’t really see that there is much in it for us at the moment.
Int1
Some asserted that, although CDs were being paid for their role, the remuneration was not enough to cover the number of clinical sessions they needed to drop to attend to PCN-related tasks (Int2, Int3, Int20). The loss of clinical sessions for CDs also had the potential to affect practices: at least one practice was reported in our fieldwork as not having allowed one of their general practitioners to stand for election for the CD role because GP shifts would be left uncovered (Int2, Int5, Int7, Int8, site A observation):
It’s not that any GP didn’t want to take the clinical directorship from a prospective of finances. We actually had two GPs that were very interested in doing it. The problem was that practices stopped them because they could not afford the lack of capacity.
Int7
It was suggested that the existence of a ‘dual system’, in which practices contribute to the financial costs of the collaboration for centralised functions such as management and administration while also continuing to operate these same activities on a practice-by-practice basis, had been detrimental to PCNs trying to realise their full potential in terms of financial savings (Int10, Int12, Int13). The practices risked bearing the up-front costs required to implement collaborations without realising the potential financial benefits from moving towards shared back office functions, economies of scale and improved financial management, among other mechanisms for potential cost savings.
Facilitators of and barriers to the early implementation of primary care networks
This evaluation has explored facilitators that have contributed to the early progress of PCNs along with their pre-existing GP collaborations, and the barriers that they have faced to date. In many cases, facilitators and barriers are closely linked and, therefore, they are discussed in parallel below. The barriers and facilitators are also very resonant with those identified in Chapter 3, suggesting that PCNs are in many ways closely related to their antecedent forms of GP collaboration. Although most of evidence around the facilitators and barriers reported below stems from interviews and observations, survey respondents were also asked about the challenges that PCNs had faced in their early months, which are summarised in Figure 11, although responses to the survey were limited.
FIGURE 11.
Primary care network challenges from survey (n = 28). NA, not applicable.
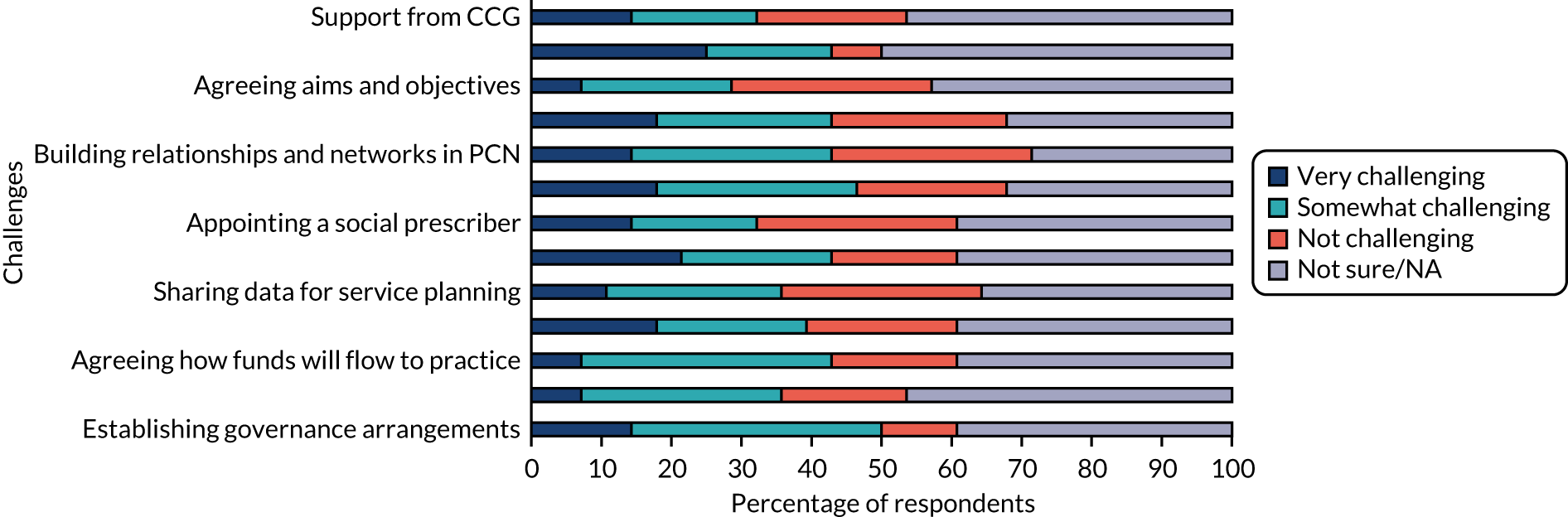
Management and leadership
Many of the facilitators of collaborative working focused on strong leadership and management of the PCN and other forms of pre-existing collaboration. A few interviewees reported that their network had effective meetings and that learning was shared at a managerial level across the organisation (Int18, Int20). Characteristics of good leadership encompassed strong consensus around decisions made at a board and managerial level (Int14, Int20), as well as having people in leadership roles who listened to the concerns of staff (Int14):
Everyone knows that you’re voting as a partnership. Everyone knows that we go by the majority so . . . you can’t bring that many partners together and everyone be 100% happy with the outcome. Believe it or not, the majority of stuff that we’ve done and delivered we have had 100% of those there because they’ve bought into the ethos of what we’re trying to do . . . If someone is unhappy, we always look at what they’re unhappy about and we try and address that, which we have done on many occasion. And 9 times out of 10 obviously we find a solution.
Int14
Some interviewees commented on the importance of the CD role in terms of ensuring the success of PCNs. They noted that having a single person responsible for resolving issues, facilitating collaboration and building relationships between members was an important aspect of networks (Int10, Int17), which might help facilitate their development and ensure that they succeed. Some also commented on qualities that a CD should have, which go beyond clinical skills to encompass good leadership, communication, being personable and approachable, drive, enthusiasm and being politically ‘savvy’ (Int1, Int2, Int3, Int5, Int6, Int9, Int23), along with a genuine desire to get involved with management functions (Int1, Int5):
That higher-level management work, with all the management speak and the politics and that kind of thing, is not really my cup of tea at all, and I think to be a good clinical director it has to be your cup of tea. It’s got to be the kind of thing you actually enjoy doing and the challenge . . . that you actually want to take on . . . I think that’s probably one of the most important skills to have is an enthusiasm for that kind of work.
Int1
We’ve got three groups [of CDs]. We’ve got those who’ve been around, quite experienced, been involved with local medical committee and the local federation or CCG. They know how the system works, they’re quite experienced and so on. There’s another group that are younger generally, quite enthusiastic, also quite idealistic sometimes, but they’re not sure how to make it work yet, which levers to pull or necessarily how to work things, but they are really relatively quite motivated. And then there’s a third group who look a bit bewildered and they’ve got into it because nobody else wanted to do it and they were probably the least unwilling . . . and there’s a few of those who are doing it but they’re not sure why they’re doing it or how they got to be doing it. And their motivation and experience is different so (a) they’re not quite as motivated to develop themselves or their PCN, and also they’ve probably got fewer tools to enable them to do it as well. . . . I call the final group the permanently bewildered – they’re not quite sure what they’re doing or why they’re there or how they got there!
Int17
Although strong leadership and management can act as facilitators, these were not yet reported as being present in the PCNs in our case study sites. Many interviewees commented on the lack of strong leadership within their network, resulting in frustrating meetings and an inability to achieve progress (Int3, Int8, Int9, Int21, Int24). In some cases, this resulted from the CD role being taken on reluctantly after difficulties in filling the role, which was felt to have inhibited the appointment of a CD with the necessary mix of skills, communication abilities, experience, and time and energy (Int2, Int3, Int4, Int5, Int6, Int7, Int8). Difficulty in filling the CD role was reported by some respondents, and in one case this had resulted in less than ideal arrangements, such as the rotation of the CD role on a yearly basis (Int2, Int4, Int6, Int7):
We have tended to just go round in circles on discussions on how we do things . . . everybody will be in agreement and then somebody else will bring it back round to the start again and say, ‘but what about this’.
Int9
I don’t think we think things are progressing very quickly and not quickly enough. We’ve had a clinical director who isn’t very communicative I’m not saying [redacted] is not doing his job because I understand he has been going to lots of meetings and everything and when he comes to talk to us he’s, he does give feedback but in between we’ve no idea what’s going on so I just think he’s finding it difficult to do his day job go to all the meetings and make sure we’re all kept up to speed with things.
Int5
Some interviewees suggested that PCNs were relying too heavily on the CD, who may not have all the managerial and financial skills, or time, to successfully manage the network (Int2, Int4, Int7, Int23). This issue was observed at a PCN board meeting in one site, at which the CD and other clinicians discussed the technical details of building maintenance and legal details about holding property as a PCN, yet the CD admitted to having little experience of such matters. To make up for this lack of managerial capacity, several interviewees suggested that a professional, non-clinical management role should be implemented to support the effective management of PCNs (Int4, Int7), signalling the importance of role allocation within these new organisations. One site was already considering splitting the CD post into two roles, one focused on clinical leadership and the other on operational management, and had discussed increasing administrative support as the PCN grows (site A observation):
I think [what] NHS England did get completely wrong is that they should have funded immediately a management position for a professional manager to come in and actually get the structure sorted, I think to ask a clinician to also be an expert when we are talking about management set-up, about roles, about job descriptions, [is] fundamentally wrong it should have been somebody brought in to concentrate on those tasks.
Int7
At one site, there were tensions with regard to leadership and the purpose of the PCN. There was a divide between network staff who wished to continue and build on the achievements of the neighbourhood collaboration and its integrated working in wider health economy (Int 20, Int22, Int24) and those who wanted to use newly acquired PCN resources specifically to decrease general practitioner workload and improve the financial situation of practices (Int21, Int22, Int23). The division, with regard to the purpose of the PCN, manifested itself during early board meetings (Int20, Int21, Int22, Int23, Int24) at which even democratically decided decisions about care delivery were challenged (Int22):
It had quite a negative effect because they’re coming from two completely different ends of the spectrum, so [redacted] was wanting the PCN to actually work for the GPs, clinicians, so he wanted a system that meant the pressure was taken off the clinicians, whereas [redacted]’s always been for what’s best for the patient and patient care. And really there should have been something in the middle but they are at extremes. So initially it’s caused quite a lot of conflict and board meetings have been a bit – I’ve not been, this is hearsay, so I can’t confirm – a bit fraught at times.
Int23
The way that they work is they do a vote on a decision and they go with the majority, and that was agreed when the PCN was set up that that would be the way forward . . . That isn’t happening – if the CD doesn’t agree with the unanimous decision that was made, he seems to be going off and doing his thing.
Int22
Relationships with clinical commissioning groups
Some interviewees reported that the local CCG was supportive of PCN development (Int1, Int11, Int13, Int16, Int25), and had been helpful in tasks such as the recruitment and hiring of new staff (Int15, Int16), fostering relationships between practices and providing practices with dedicated time for network meetings (Int11). It was noted that it was important for CCGs to be supportive of PCNs and other forms of pre-existing GP collaboration, while also providing them with room to innovate and make autonomous decisions (Int16, Int25). This echoed the messages in Chapter 3 about the importance of effective relationships between a GP collaboration and its funding or authorising body.
Although positive relationships with CCGs were viewed as facilitators of collaborative working, they was not present across all the case study sites. Some respondents reported that support for the PCN from the CCG was weak, something that seemed to be a particular issue in one site (Int4, Int5, Int7). This poor relationship with the CCG was also observed during a PCN meeting at this site, at which some felt that the commissioning group was meddling with the PCN’s jurisdiction in terms of recruiting staff for new roles (site A observation). Some reported a concern about how their CCG was distributing funds to the PCN, including instances in which the CCG had allegedly not distributed funds as was agreed (Int1, Int4, Int7, Int20, Int22, Int24). There were also reported instances when it had been unclear under what conditions funding would be distributed by the CCG to the PCN, and how much scrutiny would be made of network expenditure (Int17, Int23, Int24).
The issues apparently causing poor relationships between some networks and their local CCG brought to the surface a more fundamental tension about the role of PCNs in commissioning care. PCNs represent a shift of some commissioning power away from the CCG into primary care. Some respondents reported that the local commissioning group had attempted to exert control of budgets allocated directly to PCNs (Int1, Int4, Int18, Int19, Int21, Int22, Int24). It was also reported that the agenda of PCNs and that of CCGs did not necessarily align, as some general practitioners were more likely to want to spend network budgets on supporting practices and decreasing general practitioner workload than the commissioning group, which would probably want something different to be done with the money (Int2, Int19, Int21), such as an increased community-focused approach to population health:
They’ve kind of held back on some of the funds that probably should have come directly to us, I don’t think they were doing anything with that, I think that they just sort of felt they had some role in kind of redirecting it really, but I think that’s probably misguided.
Int4
I have not found it a positive experience there’s the PCN view that the Clinical Commissioning Group should not dictate then how the money that has been given to the PCN is spent.
Int22
Ways of working and relationships across practices
Many respondents noted that clear communication across the network and a good relationship between practices, and particularly between PMs, was important in facilitating effective PCN development (Int2, Int7, Int9, Int23, Int24). Establishing shared goals and aims (Int7) was also cited as important, particularly in moving towards a more meaningful sharing of resources to cover the whole population of the network, rather than each practice focusing exclusively on its own patients (Int3). Staff away days and other forums for staff from across the collaboration to talk to one another were reported to create a sense that staff are working as part of a unified team rather than a collection of practices (Int14, Int15, Int16):
I think as a group of people all the doctors in the primary care network group and all the practice managers work very well together, we have very open discussions and we have a common wish and a common aim to create a better service.
Int7
I think the biggest challenge was getting 12 practices together who have worked differently to suddenly think about working as one organisation, and there’s still ongoing work with that around the culture of being part of one organisation, being part of [redacted] rather than just the individual practice that you were part of previously. I think there’s always going to be a struggle with that and things we can learn and how we can do that better or improve how we integrate staff and practices. But certainly I think we’ve come a long way from where we were sort of 2 years ago and you can already see the difference with people.
Int15
Despite strong relationships and shared ways of working acting as a facilitator of collaboration, there had also been challenges associated with joint working in the early development of PCNs. Interviewees reported that differences in ethos, operational environments, organisational culture and operating procedures had made it difficult at times to get activities or services under way across practices in the PCN (Int1, Int10, Int11, Int13, Int14, Int15, Int24). This had even led some practices in one site to leave the PCN, and in another site to leave the super-partnership. (Int13, Int15, Int16, Int25). As one general practitioner commented regarding the differences in priorities and attitudes between different partners:
When I was in my 30s, I was quite ambitious and I wanted, you know, if you set up some goal I would try and get the right end of it. As I’ve got older, I’ve probably done what most people do which is I want to just sit somewhere around the mean so that people just leave me alone. And I don’t want to be a trailblazer, I don’t want to be a laggard, I just want to sit in the middle. That I think that what we’ve done with [redacted] is we are right outside of the normal general practice and I think that exposes us to the potentially benefits, I mean, that’s why we’re doing it, but it exposes to the risk that actually policy just doesn’t fit.
Int10
Some people were happy to work in low-cost, low-value environments and some of us wanted higher-value environments that came at a higher cost, and therefore a profit would be lower. And trying to move towards a parity of drawing drove out one partnership . . . Another partnership left because it felt that it wasn’t getting change that was creating value quick enough . . . they didn’t feel they were getting enough really.
Int11
I know what they say about groups that they need to form, storm and norm, but we’re definitely in the storm version at the moment and there’s a lot of clashing of heads from my point of view. It seems a bit of a shame really.
Int24
As PCNs have brought together practices that often did not organically form a partnership, there have been challenges that have arisen because of the sometimes ‘imposed’ nature of PCN collaborations. Many expressed an anxiety that general practitioners may have about the loss of independence caused by PCNs and other forms of collaboration (Int6, Int7, Int9, Int13, Int14, Int18, Int23, Int24), particularly compared with more bottom-up forms of collaboration that were perceived to better retain the autonomy of GPs (Int2, Int23):
Joining six practices was challenging enough – I hate to think about bigger practices, bigger networks – because I think by the nature of GPs, they can be quite strong-willed. They have their ideas. It’s their own business. And now we’re saying in a way, forget being your own business, we’ll join up with another five, and work together for the greater good.
Int6
Technical issues have also stood as a barrier to shared ways of working, such as a lack of shared IT systems and record-keeping systems (Int4, Int7, Int9, Int11, Int13, Int14, Int24).
Many sites had struggled so far to promote staff engagement below the PCN governance level, which threatened to hinder the formation of a shared sense of identity and working across the network (Int6, Int10, Int15, Int24, site C observation). Lack of engagement within constituent practices of a PCN was also reported to be a challenge, something that is consistent with the historical experience of GP collaborations reported in Chapter 3. It was observed that practices with poorer engagement with the PCN were less likely to utilise network resources such as social prescribers, hence undermining the overall mission of the new organisation (site C observation). However, several interviewees noted that this was not necessarily a bad thing, as it allowed staff who did not wish to be engaged in the PCN to continue with their regular way of working and get involved at their own pace (Int15, Int20):
It’s not easy, because every staff member is different. We’ve done staff newsletters and things like that to communicate. Our chief officer does a weekly update that goes to all staff, so update on what we’re doing, and some staff will find that really interesting, and some staff will say ‘Why am I reading this? I don’t care. I just want to do my job and go home and get paid’. So it’s trying to understand what your staff want to hear.
Int15
Some of the staff wouldn’t know that we were in a network, even though we’ve told them about it. If you then said about the PCN, they’d say well what’s that? Because there’s no – there isn’t any sort of joined up working at the moment.
Int6
The relationship between a primary care network and previous general practice collaborations
Where the establishment and implementation of PCNs had built on the strengths of previous GP collaborative working arrangements, this was almost always reported to have been a facilitator of network development. For example, at site A it was reported that the super-partnership (of which some PCN members were a part) had been able to help share learning across the network about how to manage collaborations (Int2, Int8), and provided support for legal matters, governance, finances and data management (Int7, Int9). Some also commented that, at site B, the goals of PCNs were largely aligned with the goals of the super-partnership (Int15), and that the super-partnership had helped foster a maturity of collaborative working that put them ahead of other networks (Int17) including in terms of what the PCN had been able to accomplish in just a few months (Int18, Int19, Int23, Int25, site D observation).
All four sites had been able to build on the success of previous GP collaborations in some way, although each had faced tensions and challenges associated with the interplay of the former and newer organisational arrangements. Many interviewees expressed a concern that PCNs had affected previous ways of collaborative working in a negative way (Int2, Int6, Int17, Int18, Int21, Int22, Int24), and some respondents continued to view the pre-existing forms of collaboration as more relevant and helpful than the PCN, albeit the new networks were only a few months ‘old’ (Int9, Int19, Int23). At one site’s super-partnership board meeting, one of the operational priorities for the year ahead was to address the mismatch between the priorities of the super-partnership and the PCN, pointing to the issues caused when these do not align:
When PCNs were being set up, there was an awful lot of discussion about what about the existing collaboratives and the relationships that had been developed and formed were really helpful . . . But in most cases . . . it’s caused the end of the existing collaborative arrangements. They’re still there but . . . they’re a shadow of their former selves.
Int17
Previous GP collaborations were reported by some to be a source of tension in instances when some practices within a PCN belonged to a pre-existing GP organisation and others did not. For instance, at two sites, only some of the practices in PCNs were part of a wider super-partnership, and these differing allegiances had caused tension and distrust among the PCN members about whether the super-partnership was exerting control over the network, or even if the partnership was positioning itself to take over the practices outside the super-partnership. In at least one PCN, professional mediation had helped them to devise a voting solution to address this, so that the practices that were a part of the super-partnership could not secure a majority just by voting as a block (Int1, Int6, Int15, Int16):
It was a bit like getting peace in the Middle East you know, we had to reach a compromise where . . . all the parties felt that it was – specifically these two non [redacted] practices – felt that we had to rig the voting so that we didn’t have a simple majority . . . When decisions are being made that we had to have sort of a fail-safe put in there that they, we as collective four [redacted] practices, we couldn’t overrule the two other practices if they dissented with us . . . so we eventually reached a compromise after much horse trading . . . quite a lot of emotional sort of anger and people being suspicious and that sort of thing, and we eventually reached a PCN agreement.
Int1
There have also been practical issues that have arisen out of pre-existing collaborative arrangements across GPs, most notably through confusion related to the hiring of new staff. In cases when a PCN was not established as a legal entity able to hire staff, it was unclear which party should recruit the new roles funded through networks (Int2, Int4, Int23, site B observation), particularly with respect to the overhead costs and the risk to hiring practices if other practices were to leave the PCN, or if it were to be discontinued (Int2, Int6, Int7). When shared staff had already been hired by collaborations that existed prior to the implementation of PCNs, this had often caused confusion about how these human resources (HR) arrangements should adapt, particularly when the interests of the hiring body (e.g. the CCG, trust or super-partnership) did not align with those of the PCN (Int7, Int10, Int16, Int19, Int20, Int23, Int24). However, several interviewees reported that they were happy for the trust or super-partnership to hire staff and deal with the administrative details, overheads and risks (Int2, Int6, Int7, Int20).
Challenges in fulfilling the national primary care network specifications and expectations
This evaluation has identified some policy-related challenges faced by PCNs. Some of these relate to the national PCN service specifications (as explored in Chapter 1), which, although considered by case study sites to have improved from their first version (Int1, Int2, Int17, Int20), were sometimes still considered too demanding and overly prescriptive considering the (pre-COVID-19 pandemic) financial and workforce challenges in primary care (Int1, Int6, Int8).
Although PCNs were viewed positively by some respondents in terms of the increased power of primary care to negotiate contracts when they worked in collaboration (Int2), there was a countervailing view that the national nature of the specification risked lumping together requirements that would have traditionally been negotiated separately and/or locally (Int1). This was particularly an issue in cases in which the services described in the PCN specification were not considered to align with the needs of local populations (Int1, Int5, Int12, Int19, Int21, Int23, Int24):
Each time, the contract is being renegotiated it’s for 12 months, it’s got lots of promises about what’s going to happen in the future, but the first contract that they brought out was rejected by everybody this time. So, in a way, we might have more strength now we are in networks to actually say no, than we did have as individual GPs so that could be good.
Int2
Similarly, some interviewees expressed a view that too much was being expected too soon from PCNs (Int4, Int5, Int24), particularly as they were still working out how to function operationally before they could accomplish goals such as decreasing workload and improving care to align with The NHS Long Term Plan4 ambitions (Int1, Int6, Int19). There was a view among some interviewees that PCNs had been rushed in their implementation, and had not been given sufficient time to find a model that worked across primary care (Int7, Int14, Int24):
NHS England . . . they have ideas, they seem to have ideas and then these ideas get filtered through with not a lot of meat on the bones. And I find – and this is nationally – everyone then has their own interpretation of what they’re trying to achieve and what they’re trying to deliver . . . if you’re all going off on a tangent what you’re going to end up with isn’t going to work.
Int14
The PCN is in its infancy, and they seem to be desperately trying to run before they can walk which I can’t quite understand.
Int24
In one site, which had a more formalised and permanent structure in place for its pre-existing collaboration, the PCN policy was seen as a ‘curve ball’ (Int10, Int13, Int15):
Everything takes a lot longer than everyone envisages. And the NHS has a habit of changing just at the point when you’re mastering something . . . consistency should not be underestimated.
Int13
Most of us I think felt quite annoyed when PCNs came along because actually we were trying to do something similar but then all of a sudden the ground changed underneath us.
Int10
Some PCNs seemed to have responded to the new policy context by taking (at least for the initial few months) a ‘box ticking’ approach to fulfilling the national specification (Int1, Int24, site B observation, site D observation). Although not uncommon, this approach had the potential to undermine some of the broader goals and priorities of PCNs:
We just thought, well we’ve been there before. We deal with the box ticking. Get the box ticking done and then deliver what . . . might improve care for our patients, but this is on a completely different level to anything we’ve found we’ve done before.
Int1
Some interviewees also commented on what they considered to be a lack of clarity about how PCNs should be set up and what their longer-term vision was to be (Int8, Int20, Int23). This was supported by our survey evidence, for when asked what challenges PCNs have faced, ‘Support and guidance provided by NHS England’ was ranked as ‘Very challenging’ by 25% of survey respondents, the highest proportion among the challenges listed in the survey, although only 28 respondents completed the survey.
Barriers for rural areas and small practices
Barriers for rural primary care networks
Rural areas face particular challenges in establishing and operating PCNs. Some interviewees in this evaluation felt that the overall PCN policy had been designed more for urban areas, and had not been sufficiently well thought out in terms of implications for rural practices (Int2, Int4, Int7):
I think they are the right way forward, I don’t have any problem with the concept of a primary care network as such. Where I think there are issues is that at very short notice we were asked to create a primary care network based on a model that had been tested in an urban environment . . . While I agree there are a lot of things that we could do to generate additional time and capacity in the practices, what I don’t think works is the urban model in the rural location. So we are at short notice being pushed into accepting a method of working that in our, certainly my, heart of hearts, I don’t think is fit for this county.
Int7
Some of these challenges were related to distance and the time taken to drive across the geographical boundary of a rural PCN, which could make it difficult for shared staff such as district nurses, as well as unpaid volunteers, to be able to attend to many patients within a single working day. Distance and a lack of reliable public transport could also make it undesirable or challenging for both patients and staff to travel to health centres other than their home practice, making some of the PCN specifications and sharing of primary care roles seem less relevant than in a setting where practices and their patients were in a small geographical area (Int2, Int3, Int4, Int5, Int7, Int8, Int9, Int12, Int20, site C observation).
Some interviewees mentioned extended-hours GP as a service that was rarely accessed in rural areas, as patients were considered less likely to be willing to travel long distances between practices to be seen more quickly (Int2, Int4, Int5, Int8, Int9). Digital or telephone solutions were mentioned as a potential way to address issues in terms of distance and travel (before the COVID-19 pandemic suddenly increased the use of such approaches across UK primary care), although it was noted that rural areas face unique challenges in terms of digital access and broadband speeds (Int2, Int3):
The first one that is critical across everything we do is drive time . . . the reality is patients can get everywhere, albeit in a rural location that is much more difficult because of course there are very often no buses and no transport methods. But it’s not can a patient get there, it’s how long will it take them. For us in a rural location very often if a patient can’t come to the local surgery . . . they have to be taken by volunteers so drive time becomes key because you’re actually asking people to give up their own time to take somebody to somewhere else and bring them back that cannot take hours because you’re not going to get volunteers to do that.
Int7
Rural areas face particular workforce challenges that have an impact on their ability to hire shared staff across a PCN and deliver on requirements within the national service specification. For example, rural areas may be less attractive to locums, who get paid on a fee-for-service basis, as they will necessarily cover fewer patients in a less populated area than in a busy urban setting (Int4, Int7, Int9, site C observation):
There are locums in the area. There aren’t many – they’re not easy to get hold of . . . the difficulties with [being a] locum over here is that if you’re working one practice in the morning, you could actually find yourself too far away from any other practice for the afternoon. So of course they by nature tend to congregate around the urban areas where they know they can earn a greater income.
Int7
Finally, PCNs were said to present an issue in rural areas in that country localities typically have fewer options in terms of practices that are geographically contiguous to form a PCN. It is likewise potentially more challenging in rural areas to find geographically contiguous practices that share common outlooks and ways of working than in urban areas (Int1, Int2, Int9):
Some of the practices in our PCN area footprint . . . had different viewpoints of how a PCN should be run, and then because we are a very rural PCN . . . we had to form a PCN with the practices that were geographically continuous, whereas for example in a big city or a big town in theory you would be those things would be diluted or you could pick and choose.
Int1
Barriers for smaller practices
Primary care networks also pose a particular challenge for smaller practices, some of which may be situated in rural areas. Smaller practices may be less able to adapt to meet PCN specifications (e.g. extended-hours access to GP), because of limitations of staff and resources. In fact, some interviewees commented that networks risked pushing out smaller practices rather than supporting them to meet PCN requirements (Int2, Int19). Smaller practices were also reported by some to be potentially less able to allocate staff time to set up, operate or engage with the PCN, and that there would be a disproportionate effect on a small practice if a partner wished to be the CD of the network (Int2, Int6):
There’s as much chance that a primary care network is hostile and says to a smaller practice, ‘cause it is usually the smaller ones that can’t stretch to meet those hours, ‘You’re not part of the team’ as opposed to ‘Well we’ll help you and support you’.
Int19
There was likewise a view among respondents that PCNs might prove less beneficial to smaller practices, as, in the case of practices that are paid through PCN funding on a per-patient basis, the remuneration may not prove to be enough to cover the costs associated with being part of the network (Int2, Int24):
The PCN funding I think it depends who you asked isn’t it? . . . Your £1.76 that the individual practices have got it’s great if you’re a large practice. You are absolutely stuffed if you’re a small practice because actually your level of commitment and work is exactly the same, but the funding is considerably less.
Int24
Along with these challenges, it was asserted by some respondents that there might also be increased sensitivity among smaller practices in terms of being susceptible to a takeover, as several interviewees recounted a history of smaller practices being taken over by larger practices in terms of the context surrounding PCNs (Int1, Int3, Int19), together with a perceived government agenda of wanting more consolidation of practices into larger groups (Int9). This issue also came up in the context of voting arrangements within PCNs, as one site struggled about whether votes should be distributed equally across practices or by patient population (Int19, Int20):
I’m a smaller practice and the two practice one is a huge practice. Their history is that they’ve taken over five smaller practices. If history were to repeat itself they would take over another . . . A bigger practice will see it as an opportunity to just firm up and make life really quite hard until a smaller practice gives up and goes away . . . I think for me the biggie is whether PCNs are going to be supportive of all practices or are they not.
Int19
Primary care network-level responses to COVID-19
The timescale of this study was such that fieldwork concluded just as the COVID-19 pandemic was gaining hold across the UK. Although the evaluation did not set out to examine collaborative responses to public health emergencies, the study team attempted to conduct short interviews with the gatekeepers at each case study site to gather information about each collaboration’s response to COVID-19. In the discussion (see Chapter 6) and conclusion (see Chapter 7), we suggest tracking how the role of PCNs changes in the longer term as a result of COVID-19, its further progression and the changes to primary care service provision made rapidly in early 2020.
Site A
A follow-up interview with the site A gatekeeper informed the study team that the COVID-19 response had been ‘pretty good’, with an integrated response involving the CCG, the extended-hours access provider and the local community trust. GPs were heavily involved in strategically planning a countywide response, and the majority of practices were on board; however, some practices from neighbouring PCNs developed their own localised approach. GPs from the PCN and the CCG were part of a virtual group to co-ordinate the response to the pandemic. These meetings were initially held thrice weekly and then once per week. At the time of the interview, the virtual group was in preparation for a second wave of rising infections. The recent appointment of a CD had significantly improved leadership and decision-making within the PCN, which was pivotal in enabling the PCN to move at speed and with decisiveness during the pandemic response.
Throughout the pandemic, the PCN continued to deliver the Network Contract Directed Enhanced Service specification. 25 Owing to the PCN’s county-wide approach, two ‘hot’ sites were set up across the local area to treat suspected COVID-19 patients, which prevented PCNs from having to set up individual ‘hot’ and ‘cold’ sites. In addition, more clinical and non-clinical staff were volunteering to give their time to support PCN initiatives such as supporting patients with suspected COVID-19 in nursing homes, people with learning difficulties and people receiving cancer care.
The study team collected a number of documents generated by the PCN to communicate operational- and service-level changes related to the pandemic. These documents were a mixture of standard operating procedures, guidance and information, and updates covering the following: changes to outpatient services at the local acute trust, impact on patients receiving palliative care treatment, how to address safeguarding issues and how best to support people experiencing domestic abuse, and continued treatment for long-term health conditions (particularly those being ‘shielded’), as well as those living with mental illnesses. Finally, specific guidance was developed to help GPs acquire personal protective equipment (PPE).
In response to patient demand and access to primary care, the PCN experienced a significant drop in patients requesting appointments with general practitioners, and those who did were happy with video or telephone consultations and pleased with quicker than usual responses from their practice. Some general practitioners were reluctant to familiarise themselves with video consultations, largely because they were inexperienced in holding these, required further skills training and/or felt potentially out of their ‘technological comfort zone’. Unsurprisingly, as the pandemic lockdown restrictions eased, patients started to return and ask for face-to-face appointments, these patients being those considered to be ‘frequent users’ of primary care. Finally, communication between the PCN and the wider local health economy had improved, along with a sense of togetherness. This had compelled the CCG to complete its own evaluation of the primary care pandemic response, to explore what changes to primary care should remain beyond the COVID-19 pandemic.
Site B
The follow-up interview with the site B gatekeeper revealed that since the evaluation study team had ceased data collection in March 2020, the super-partnership had expanded considerably, assuming a greater degree of control of the PCNs within the super-partnership. This had led it to create one large PCN covering a population of > 150,000 patients. Several practices that were not part of the site B super-partnership were now members of the expanded PCN, although these practices had not been part of the collaborative responses to COVID-19 that are described below. As the super-partnership was now running a single large PCN, primary care pandemic responses had been co-ordinated by the super-partnership.
In response to COVID-19, several site B practices had been designated as ‘hot’ and ‘cold’ practices (with respect to suspected COVID-19 patients), and staff redistributed between practices as appropriate. The super-partnership had also conducted a PPE audit of all practices and had conducted weekly staff absence and sickness audits to respond rapidly to early warning signs of practice closure. A shared telephone messaging system, virtual teleconference system and e-consultation service had been implemented across all practices, along with a shared communications system and a COVID-19 planning communications channel to share learning across practices (although it was noted that fewer than half of partners and < 10% of staff had to date used the COVID-19 planning channel). The super-partnership had also provided guidance for GPs on routine services that could safely be suspended or altered during the pandemic, as well as those that could be provided appropriately in the patient’s home (by either a practitioner or the patient themselves). It had, however, been at the clinicians’ and practices’ discretion to implement these changes to clinical practice.
It was reported that some of the positive changes that had been implemented at site B would be continued after the pandemic, such as offering telephone and video consultations for patients.
Site C
At site C, the PCN had continued to deliver as much of the national PCN service specification as possible, including social prescribing, medicines optimisation, extended-hours access, newly appointed musculoskeletal practitioners and practice receptionists trained as care co-ordinators. In response to tackling the spread of COVID-19, a newly established pandemic response team with representatives from the PCN (eight lead GPs), the CCG and the local trust had been set up with the aim of delivering a co-ordinated response with regard to diagnosis/treatment of suspected COVID-19 patients.
More specifically, all eight practices within the PCN had agreed to share staff to address the geographical challenges of treating patients during the pandemic and established two ‘hot hubs’. At these two locations, patients with suspected COVID-19 were able to undergo tests for temperature, blood pressure and oxygen saturation through their car window before completing a face-to-face consultation. It was reported that the PCN had helped with the co-ordination of the local response to the pandemic but that the most significant facilitator of collaborative working had been the pre-existing collaborative working in the area (familiarity with other staff across the network, understanding GP working in the area, and having knowledge of local population health needs and challenges).
Finally, despite the PCN having introduced telephone consultation in the past 6 years, the pandemic had created a shift in patient opinion, with patients now more inclined to request digital consultations because of an unwillingness to come into practice. Increased availability of telephone (and video) consultations, coupled with a decrease in a patient demand for general practitioner appointments, had improved access to primary care services. Hence, almost three-quarters of patients were now able to have some form of initial primary care contact within 24–48 hours (compared with 1–2 weeks prior to the pandemic).
Site D
At site D, a slightly slower response to COVID-19 was observed in a non-participant observation in early March 2020 in which a PCN board member commented that there had been no discussion at a board level regarding COVID-19 and that there seemed to be undue hesitancy in talking about it. Despite this initially hesitant response, the later follow-up interview with the site D gatekeeper revealed that the PCN had enacted a number of network-wide changes because of the COVID-19 pandemic, after a meeting with all GPs within the network later in March 2020 to remodel service delivery.
The PCN had established one practice within the network as its ‘hot hub’ to lead COVID-19-related work and see patients who had potentially contracted the virus, whereas the other three practices remained open for routine GP. The PCN had purchased additional PPE, respiratory kit and individual cleanable consultation cabins to be used outdoors at the ‘hot’ practice. The network had also conducted a risk assessment exercise within the overall primary care clinical team to identify staff at an increased risk of COVID-19-related harms, and these staff had been prioritised to work in the ‘cold’ practices where possible.
The PCN had increased its capacity to conduct video and telephone consultations for both routine and COVID-19 patients, and had implemented a network-wide communications strategy informing patients of services within each practice. A GP co-ordinator had been appointed to help share learning and knowledge across the PCN, and to help form links with acute care teams for patients requiring hospital admission or respiratory support. The site D PCN was asked by its local CCG to provide ‘hot hub’ services for a number of surrounding practices outside the network, and saw COVID-19 patients from external practices during the pandemic.
Although the practices would in any case have probably implemented some forms of collaborative working during the pandemic, it was reported that without the formal PCN they would not have been able to accomplish the same level of impact.
It was reported that the pandemic had meant that fewer patients had contacted their general practitioner, giving clinical staff time for critical reflection and an opportunity to provide better personalised care to complex patients by reducing the number of patients presenting with less acute issues. Clinical staff were also reported to have benefited from the technological resources and telephone triaging systems that were now available as a result of the pandemic, as well as rapid support from NHS Digital. It was noted, however, that non-clinical staff in the PCN might have faced more significant challenges with changed ways of working and rotation between practices. The gatekeeper from site D reported that the PCN was likely to retain some of the positive COVID-19-related changes, such as the telephone triaging system and video consultations.
Summary
In the next chapter, we reflect on the findings of this evaluation of the implementation and early development of PCNs, doing so in the context of our review of research evidence from > 30 years of GP collaborations, and examining the extent to which PCNs are similar to, or distinctive from, their predecessor primary care organisations. This analysis is then used as the basis for drawing conclusions and making recommendations about the future direction of PCNs (see Chapter 7).
Chapter 6 Discussion
Primary care networks are exhorted in policy to be central to NHSE&I plans to enable better integrated health and care services, more community-based provision of care, less reliance on hospital services and a more population-focused approach to determining local health needs.
There is a paradox for PCNs in that on the one hand they are expected to meet local population health needs, yet on the other hand they face nationally specified requirements to employ certain professionals and introduce defined services, irrespective of whether or not these are considered most pressing in terms of local need.
Prior collaborations in some instances provided significant management and infrastructure support to the new PCN, and organisational capacity to implement and run new networks required by NHSE&I. How far prior collaborations prove able to provide ongoing support to PCNs, and together become a force for change and influence in primary care, remains to be seen.
This evaluation has revealed this tension between the desire for local professional autonomy and influence over the PCN and the top-down nature of PCN policy. However, the variation in experiences reported across just four PCNs indicates that there is, in practice, flexibility in how the new organisations have been implemented and the degree of freedom they have been afforded by their CCG, and also by their constituent practices.
The CD role is emphasised strongly in PCN policy and this was similarly evident in our evaluation case study work. The varying nature of leadership and management able to be provided by PCN CDs raises a concern about the sustainability of these roles in the longer term, and the time commitment required risks those who take on such roles experiencing burnout and deciding to step down.
The allocation of a new source of funding that is channelled directly to GP is viewed as offering greater security to local practices previously very worried about long-term sustainability, and in some cases as liberating, giving an opportunity to plan new services without some of the perceived constraints of waiting for the local CCG to offer (or withhold) support.
A key aspect of rural primary care and GP is that PCNs in these areas may comprise a greater number of smaller practices and arguably be accustomed to being more independent in how they work than those in urban areas. Our rural case studies wished to pursue the PCN policy, but appeared to be finding it more challenging to coalesce as PCNs and develop a clear rationale and plan for new services
The aim of this rapid evaluation study was to provide early evidence about the implementation of PCNs in the NHS across England, with a particular focus on understanding what has helped or hindered their progress, how they operate in relation to pre-existing collaborations in GP and exploring issues for rural as compared with urban PCNs. In this chapter we set out an overview of our evaluation findings, reflect on the robustness of our results and distil lessons for the conduct of rapid evaluation studies.
Overview of case study findings
Purpose of primary care networks
Primary care networks are exhorted in policy to be central to NHSE&I plans to enable better integrated health and care services, more community-based provision of care, less reliance on hospital services and a more population-focused approach to determining local health needs. In this, PCNs are very similar to many prior iterations of GP collaborations in the UK and overseas.
This evaluation has revealed that those working to implement and run PCNs largely support the overarching policy aims set for them, and GP across England have seized the opportunity to access new funding to form networks. However, many general practitioners and their teams may place a higher priority on matters of particular pressing concern to those working in GP and primary care, namely those related to enhancing the sustainability of primary care itself and improving the availability and co-ordination of local primary care services than PCNs. The challenges facing GP, in terms of workforce scarcity, rising demand for services and falling job satisfaction on the part of general practitioners and their teams, were acknowledged in The NHS Long Term Plan,4 and seem to underpin the formation of PCNs, alongside other motivations such as increasing integration of health and social care. At times, these potentially conflicting aims of PCNs were a source of frustration among those charged with their implementation, as it was not always possible to work towards increased integration of the health and social care system while also working towards addressing sustainability and workload-related concerns for general practitioners.
There is a paradox for PCNs in that on the one hand they are expected to meet local population health needs, yet on the other hand they face nationally specified requirements to employ certain professionals (e.g. pharmacists, social prescribers) and introduce defined services (e.g. enhanced health care in care homes) irrespective of whether or not these are considered by PCN leadership teams to be the most pressing in terms of local need. This paradox was a significant source of tension within our evaluation findings, with a rich and varied mix of views about the purpose of PCNs, with some positive and supportive of the national approach, and others frustrated at having to toe a government line to receive new funding, reportedly feeling that the ‘PCN policy’ had been imposed on GP in a rather rushed manner.
There was, however, evidence of PCNs enabling GPs to come together to share services and create collective solutions to long-standing problems related to the sustainability of primary care. This included new practice-based pharmacy support and reviews for people using multiple medications, the opportunity to work together to provide extended-hours access to GP, and sharing ‘back office’ administrative and management support, including for HR and training purposes. However, as with the paradox referred to above, networks often reported that they felt that new services were likely to benefit only a relatively small number of patients and, as nationally specified, were sometimes considered ‘must do’s’ from on high, rather than a reflection of the main priorities for the local population and primary care teams, something that was a particular concern for rural PCNs.
In addition, there was evidence of ‘soft’ benefits such as getting to know other practices, finding support at a time of policy turbulence (Brexit, The NHS Long Term Plan4 and then the COVID-19 pandemic), new general practitioner leaders emerging from within the clinical community, and feeling the value of long-awaited investment in primary care and its services. These positive aspects very much echo the wider international experience of GP collaborations, where ‘strength in numbers’ becomes a key feature of primary care organisations, along with mutual support, shared expertise and opportunities for new clinical leaders and PMs taking on wider responsibilities.
Prior general practitioner collaborations
In all four case study sites, the new PCN was established in the context of a prior GP collaboration. This is unsurprising, given that the Nuffield Trust and RCGP established in 2017 that > 80% of GPs in England were part of one or more collaborations, including GP federations, super-partnerships, locality groups or community health organisations. 14 This complex organisational landscape was reflected in our evaluation fieldwork. For example, when respondents described a particular service innovation or other success, it was often attributed to previous forms of local GP collaboration, with the PCN seen as a way of sustaining or extending such development, especially when practices were collaborating for the first time (in the PCN).
Prior collaborations in some instances provided significant management and infrastructure support to the new PCN, as well as organisational capacity to implement and run new networks as required by NHSE&I. This echoes the experience of independent practice associations (IPAs) in New Zealand providing management support for nationally mandated primary health organisations in the early 2000s. 56 IPAs represented a pragmatism on the part of the primary care community and also an attempt to ‘survive and thrive’, which they did, as well as provide important capacity, leadership and support for New Zealand primary care more generally. 56
Although in the English NHS some PCNs have been able to utilise the management support and organisational capacity from prior collaborations, the mapping of prior collaborations to new PCNs has not been straightforward. For example, PCNs are expected to be geographically contiguous, whereas federations, super-partnerships and other such organisations are typically ‘coalitions of the willing’ based on a shared vision or set of goals, and draw from an often wide and dispersed area. Indeed, in our case study sites, the PCN was sometimes regarded as an additional bureaucratic burden, including in respect of meetings, hiring staff, and handling budgets and contracts. Where the boundaries of prior collaborations and PCNs did not align, the support provided by prior collaborations was at times contentious, particularly for PCN members who were not part of prior collaborative working arrangements. How far prior collaborations prove able to provide ongoing support to PCNs, and together become a force for change and influence in primary care (as in New Zealand56), remains to be seen.
What is clear is that three decades of increasingly frequent and intense collective working in GP have made collaboration (for a majority of practices) the usual way of operating. Our evaluation revealed hardly any fundamental protest or disagreement about the value of working, and need to work, in collaboration with other practices, whether for service planning and development or to share administrative and management support. What was notable, however, was the extent and depth of involvement of prior collaborations in PCNs. In two case study sites (sites A and B), the prior collaboration (a super-partnership) was in effect running the PCN with some resistance from practices not in the super-partnership. In another case (site C), the prior collaboration (a neighbourhood focused on integrated care) clashed with the new PCN (focused more on the sustainability of GP), and in the fourth case (site D) the prior ways of collaborative working simply morphed into a more formal collaboration through the establishment of the network.
In a similar vein, the capacity, expertise and experience of prior collaborations was often highly valued by those in new PCNs, saving time and offering useful learning for the new organisation. There were, however, some reservations (particularly in practices that had not been part of the prior collaboration) of being ‘taken over’ or subsumed into something they had not previously wished to join, thus reflecting the well-documented culture of autonomous GP. Furthermore, the existence of parallel primary care collaborations does entail some overlap of functions and management support, and this evaluation revealed some early concerns about the transaction costs of this ‘dual operation’.
In most cases, however, it was clear that PCNs were working out with prior collaborations how best to clarify roles, responsibilities and sources of organisational support. This is something that has been experienced by many collaborations cited in the research literature, for GP-developed and GP-owned collaborations often sustain and thrive alongside new government-instigated primary care organisations, which our evaluation suggests is likely to be the case with PCNs. Evidence from prior GP collaborations, including TPPs63 and primary care groups and trusts,50 underlines the importance of having such clarity of roles and functions, and the challenge of attempting to determine the precise nature of transaction costs and hence any duplication. PCNs, as with their antecedents, build on and learn from previous primary care collaborations, and need to be attentive to roles, functions and governance (and the cost of these) as they work alongside one another. In particular, they have to determine their own distinctive role in funding, planning and running primary care services, and how this fits with the functions and remit of the CCG, and (where relevant) the activity of the pre-existing GP collaboration(s) in their area.
Ownership of and engagement with primary care networks
Primary care networks are fundamentally about the bringing together of GPs into wider networks, albeit they are quite small in scale compared with many prior GP collaborations. The smaller scale of the PCN, comprising sometimes just a few practices, means that the potential for close engagement of general practitioners and their teams with the network is significant. Evidence on GP collaborations points to the importance of the scale of the collaboration for the ‘ownership’ and engagement of professionals with the network, federation or super-partnership. 20 The other key factor in the research literature in respect of practice and GP engagement with collaborations is the need for general practitioners to consider the cross-practice organisation as ‘theirs’ and ideally to have an active role in creating these organisations, as opposed to being required to form them by a funder or planning body. 13,20
This evaluation has revealed this tension between the desire for local professional autonomy and influence over the PCN and the top-down nature of national PCN policy. This is clearly something that is built into the policy design, given that it is a nationally mandated scheme intended to accomplish national health priorities as part of a significant investment in primary care and GP. However, the variation in experiences reported across just four PCNs indicates that there is in practice flexibility in how the new organisations have been implemented and the degree of freedom they have been afforded by their CCG and also by their constituent practices. In this way, despite some frustration about having to focus on national priorities, PCNs are proving fleet of foot in developing something of a mosaic of organisational forms – echoing the metaphor used in work on primary care-led commissioning nearly 25 years ago. 109
Taking time to clarify roles within the PCN, and to develop shared goals and objectives for the work of the collaboration, emerged from this evaluation as an enabler of progress and of positive working relationships within and beyond the network. For some respondents to our evaluation, time and resources for organisational development across practices and with other primary care services were important, including through staff away days, joint training events and forums for PMs and/or nurses from across the PCN. This comment echoes the sentiment expressed in this study, yet could come from any one of countless prior evaluations of collaborations in GP and primary care: ‘I think the biggest challenge was getting 12 practices together who have worked differently to suddenly think about working as one organisation, and there’s still ongoing work with that around the culture of being part of one organisation’ (Int15). The fact that this remains an issue after 30 years bears witness to its profoundly important nature – cultural change within primary care is complex and often fragile, reflective of the typically small and independent nature of the constituent practices.
Leadership and management
The need for effective leadership of the PCN, together with sufficient high-quality management support, was a strong theme in the evaluation fieldwork, and one prefigured in the prior research evidence about enablers of successful GP collaborations. In the case study PCNs, it was clear that, although small organisations, they need a significant range of administrative and management capacity and skills, including finance and accounting, HR, IT, staff engagement and governance support. Resourcing such capacity and skills for a collective of a few practices is a considerable challenge, and hence it is not surprising to find a diversity of approaches, sometimes involving prior collaborations, as described above. Other PCNs seek to find shared roles for administration and management or to access additional expertise from the local CCG or NHS trust.
In terms of management challenges for PCNs, the time required for meetings, recruiting staff, implementing new roles and services alongside core services, and administration and management of the network was of particular note. The time pressure for those involved in PCN development was reported as an acute concern, especially for CDs and PMs, who have to do this on top of their usual ‘day jobs’. The CD role is emphasised strongly in PCN policy and this was similarly evident in our evaluation case study work. The varied quality of leadership and management from PCN CDs that was reported by respondents to our evaluation raises a concern about the sustainability of these roles in the longer term, and the time commitment required of them presents a risk of burnout and deciding to step down, something that had already happened in one of our case study sites and was reported as a worry in another. As PCNs move forward and take responsibility for running a wider range of integrated health and care services, they will probably need to have a more distributed approach to leadership and management, perhaps sharing the CD role (or elements of it) with other clinicians in the network, and/or also employing a non-clinical general manager to provide professional management support. This general management may come from one or more local PMs, or from a CCG or trust.
The management challenge for PCNs is complex and sophisticated, especially for new and small network-based organisations, and research evidence consistently points to the difficulty of bringing about new forms of integrated care,110 something that is a key ambition within national PCN policy. It was striking in this evaluation to find that, just a few months into their operation, PCNs had undertaken collective management work, including implementing innovative ways of increasing extended access to primary care; hiring a range of new professionals to deliver services such as pharmacy and social prescribing; sharing back office functions such as accounting, Quality and Outcomes Framework data reporting, and Care Quality Commission registration; setting up shared triage for access to allied health professional services; and organising away days, training and other engagement activities. There was a range of concerns and frustrations about management and leadership, and it seemed that the quality of management available to PCNs was varied, albeit they were often able to draw on the capacity and expertise of prior collaborations. They were, however, largely accustomed to some form of cross-practice working and had clear ideas about what was needed for the next phase of development.
The role of funding and incentives
A strong and consistent message across our evaluation fieldwork was that PCNs have been established in a near universal manner as a result of NHSE&I using them as the mechanism through which to offer new funding to GP. Although NHS GP has had prior experience of new forms of contract being offered for collective service commissioning and provision – most notably TPPs in the 1990s and PMS schemes in the 2000s (see Chapter 3) – this is the first time that there has been what is effectively a national mandate for practices to hold a joint cross-practice contract to receive new funding. This use of funding to incentivise different forms of organisation, planning and service delivery is, in cultural and organisational development terms, radical for GP, and has the potential to revolutionise or destabilise the way in which practices operate.
The allocation of a new source of funding that is channelled directly to GP, rather than through an intermediary organisation such as a CCG or sustainability and transformation partnership, is clearly welcomed in principle by most practices, fulfilling the promise in The NHS Long Term Plan4 to invest in primary care. Our evaluation revealed that, for some, this investment is viewed as offering greater security to local practices previously very worried about long-term sustainability, and in some cases as liberating, giving an opportunity to plan new services without some of the perceived constraints of waiting for the local CCG to offer (or withhold) support. This was encapsulated in the reflection ‘so it’s us, we’re deciding what is best for GP and what is best for our patients’ (Int20).
Others, however, reported that the experience of setting up the PCN, establishing cross-practice working and having largely to use the new resource to deliver services required by NHSE&I, have led to frustration, disappointment and even talk of leaving the network. This view was typically based on an assessment of the amount of work (and hence resource) entailed in setting up and running a PCN and its shared services, and the burden experienced by practices ‘losing’ general practitioner and management time to support the network. This was reflected in the comment ‘I can’t really see that there is much in it for us at the moment’ (Int1). In this way, the allocation of new resources reflects the paradox and tension evident in the purpose of PCNs, one that can be conceptualised as liberating or constraining, bottom up or top down, an issue to which we return in the discussion below about PCNs’ relationship with the wider health system.
Money, as a metaphor for wider dynamics within GP organisation, is something that has been explored in the international research literature, including in relation to the charging and subsidising of user fees for GP consultations in New Zealand111 and the allocation of budgets to physician groups in the USA and UK. 54 Our early evaluation of PCNs indicates the need to further explore the tension between budget holding as a freedom or as a constraint as these new organisations take on a wider range of responsibilities over the coming years, together with larger budgets.
Relationship with the wider NHS system
The development of PCNs represents a shift of responsibility for the allocation of part of the funding for primary care service development away from the CCG to a collective of practices, something that will be important to track as time goes on and PCNs assume increasing levels of funding to provide a wider range of additional services. Although this accords with the policy narrative of empowering and strengthening primary care to deliver a wider range of integrated health and care services, it will change and challenge elements of how CCGs work with their local GPs. Our evaluation reveals how much the relationship between a CCG and a PCN can vary. In some instances, respondents reported that CCGs have clearly enabled and supported PCNs, providing resources and expertise to help the establishment of inter-practice working, the hiring of new staff and the operation of contracts. In other areas, however, it was reported that the CCG was attempting to hold onto control, exerting close monitoring of budgets and spending decisions, and not operating within the spirit and expectation of the overall PCN policy.
This tension between a budget-holding primary care organisation and its funding or authorising body is widely reported in the research literature from the UK and internationally, as noted in Chapter 3. This issue appears as a particular fault-line in those countries with a nationally funded health system, yet with more independent GP in the business or partnership model, namely New Zealand, Australia, Canada, the Netherlands and the UK. This is likely to be a result of an inherent clash of organisational cultures within the health system, the one national, collective and tending to bureaucratic roles and control, and the other more small scale, responsive and prone to locally determined decisions among a small group of business partners. 13 This appears to play out again with PCNs, with comments in our evaluation such as ‘they [general practitioners] appear to be distrustful of everybody and they want to be independent,’ (Int18) and others alleging that the local CCG had withheld development funding for PCNs that had been allocated by NHSE&I. The perhaps inevitably awkward position of a regional or district funding body in a health system with regard to how to relate to GP collaborations was evident from the comment in this study: ‘Everybody has frustrations, don’t they, with the CCGs on the whole’ (Int24).
It is important to note that this evaluation took place during the first 9 months of operation of PCNs, and hence they were still very much in their formative phase and were learning not only how to work as a collective of practices, but also with their CCG(s), local NHS trusts and other partners such as community pharmacies, third-sector organisations and social services providers. The varying nature of the relationship between a PCN and the local CCG(s) was not, therefore, surprising, and has been reported in other studies such as those of GP fundholding,112 TPPs63 or primary care groups and trusts. 50,113 This may reflect the increasingly common presence of collaborative working in English GP20,69 and an associated increase in trust between GP and local commissioning or funding bodies.
The experience of rural primary care networks
Two of our case study PCNs were in rural areas, one was semirural, and another was on the edge of a conurbation and abutting rural communities. The study set out to examine the experience of rural PCNs to fill this gap in the literature, given that prior evidence suggested that case studies of GP collaboration are more frequently drawn from urban settings.
There was a theme in our fieldwork of PCN policy being considered by those in more rural areas to be one developed with urban practices and collaborations in mind. For example, national policy dictated the expectation of recruiting new professional staff for a PCN on the basis that they would deliver services for patients across the network, but the challenges of geography, travel time (for staff, patients and carers) and public transport made this much more difficult in rural areas. Also, although people in rural areas are used to having to travel a distance to access health and other public services, they are typically less keen to travel to primary care hubs or specialist services to be seen by providers other than their own general practitioner. Our study took place prior to the emergence of the COVID-19 pandemic, but it will be interesting for further evaluations of PCNs to explore how far innovations with telephone, digital and video consultation – as described in Chapter 5 – will have taken root in rural areas, what appetite there is among rural and/or elderly populations for these approaches and what role PCNs will play in the longer term in sustaining and developing such services.
A key aspect of rural primary care and GP is that PCNs in these areas may comprise a greater number of smaller practices, and arguably be accustomed to being more independent in how they work than urban practices, because of being ‘on their own’ and having to serve a wider range of health and care needs, with less easy access to specialist and other support. 114 Furthermore, some aspects of the PCN national specification may already be taking place in rural areas, causing confusion about how services may need to adapt to fit with PCN policy. For example, practices in rural areas often have dispensing rights, and in effect work as integrated GP and pharmacy services, and may be more likely to already have been providing support to care homes. Our rural case studies wished to pursue the PCN policy, but appeared to be finding it hard to coalesce as networks and develop a clear rationale and plan for new services. Rurality is an aspect of PCN development that we suggest should be examined in more depth in future evaluations of these networks and other primary care innovations, as with the BRACE Centre study of hospitals managing GP115 for which a follow-up phase of research is planned.
Maturity of development of primary care networks
Primary care networks had been established for just a few months when fieldwork for this rapid evaluation study was undertaken. Despite this, it was of note that all the case study sites had established governance arrangements, developed plans for local service development and recruited (or taken steps about how to recruit) new professional staff to deliver PCN services as required by NHSE&I service specifications. There were inevitable frustrations as practices within PCNs ‘formed, stormed and normed’116 but there were clear signs of them starting to achieve operational success as new organisations.
The reason for this relatively swift organisational progress appears to be in part the existence of prior GP collaborations that have been able to support the establishment of PCNs. Furthermore, for some, the local CCG or a NHS trust have been able to offer management advice and support. More generally, it would seem that GP in the NHS in England is demonstrating the way in which it has moved, over the past 30 years, to a much more collective and collegial way of working, whereby the forming of new networks is not as troublesome and challenging as with, say, GP fundholding in the 1990s or primary care groups and trusts in the early 2000s.
Perhaps the main challenge facing PCNs in terms of their ability to deliver on the many policy expectations placed on them will be the way in which they are able to respond to the complex and uncertain context of the COVID-19 pandemic in 2020 and after. We know from follow-up fieldwork with case study gatekeepers that PCNs have provided vital support for practices, and a basis for planning rapid service innovations such as online and telephone access to primary care, enhanced health service support to care homes and ‘hot hub’ centres for patients suspected of having COVID-19 symptoms. How far these developments are sustained in the longer term, and the role of PCNs in enabling or inhibiting this, remains to be seen, and will be an important matter for further studies in this area.
Primary care networks in a time of COVID-19
Fieldwork for this evaluation concluded just as the COVID-19 pandemic was emerging in the UK. As a result, we have limited evidence (gathered via follow-up interviews in July 2020 with our gatekeeper contact in each case study PCN) about how the four case study sites reacted to the pandemic and the extent to which the PCN proved helpful or otherwise as changes to GP service provision were made in response to COVID-19. Given the reported rapid and extensive changes to the mode of delivery of many GP services (typically moving from face to face to telephone or online117), it will be interesting in the longer term for researchers to examine the role of PCNs in supporting and enabling such change, and reviewing whether or not it should be sustained following the pandemic. Likewise, it will be useful to explore how far practices might have retreated into their own teams in a time of emergency, when it was necessary to make rapid changes to workforce and other service delivery issues. Another area of interest might be the ways in which PCNs and practices have worked with other NHS organisations, social care and the voluntary sector as part of wider community support efforts intended to support people during the pandemic lockdown. Finally, in relation to the focus on this evaluation on GP collaborations, the extent to which a pre-existing GP collaboration was instrumental in providing support to primary care as it faced the need for urgent change, or if this was more focused on the new PCN collective, is worthy of further research.
Reflection on robustness of results
The study team completed this mixed-methods comparative evaluation following established methodology and guided by previous evidence of implementation studies while engaging iteratively with published literature. The robustness of our findings has been shown in a number of ways throughout our evaluation. We used a rapid assessment of the evidence on GP collaborations to establish the key elements of such organisational arrangements, and specifically to identify where there remain gaps in the research evidence. These evidence gaps (see Chapter 3) informed our scoping of case study research and, in particular, the precise nature of questions posed. The use of triangulation118 (collecting data through interviews, non-participant observation, online surveys and documentary analysis) enabled the team to develop a comprehensive understanding of the barriers and facilitators associated with the implementation and early development of PCNs.
First, we interviewed a range of stakeholders across primary care, but more specifically those involved with establishing a strategic direction and providing leadership with regard to PCNs, seeking to fill gaps identified from our rapid evidence review. Second, we were able to capture rich, detailed accounts, being privy to a number of discussions and decision-making processes in our non-participant observations. These varied data sources permitted the evaluation team to reach what we considered to be adequate saturation. 119
Throughout the evaluation, the team made use of member validation120 with regard to data collection, analysis, write-up and checking of REAs and emerging findings. The team held a number of meetings with NHSE&I, and DHSC primary care policy leads, to share early learning and seek insights into evolving policy about the implementation of PCNs. A summary of project findings was circulated to case study sites during the drafting of this report, allowing site staff an opportunity to reflect and comment on the findings and add insights about the work of PCNs in a time of pandemic.
The evaluators sought to establish good rapport with gatekeeper managers in the case study sites, which assisted with data collection. However, data collection proved challenging at times given the pressures faced by primary care in a changing policy context, and there was a need for adaptability within the evaluation team and approach, as described in Chapter 2, including greater use of observation of meetings, to compensate for some interviews that could not be secured. During analysis, we adopted novel approaches to expedite the interpretation and synthesis of findings, for example by discussing case study summaries during online digital team workshops, allowing open discussion and cross-analysis.
Overall, there was a need for the evaluation team to be responsive to the changing policy context, most specifically in shifting the focus of the research away from all GP collaborations towards the implementation of PCNs in particular, albeit the relationship of prior collaborations with new networks formed an important theme in the evaluation.
Limitations of our findings
There were a number of limitations to this rapid evaluation. As noted above, gaining access and arranging and carrying out interviews proved difficult in all four case study sites. This delayed data collection considerably, and we carried out more interviews and observations in some sites than in others. In particular, the team were able to carry out only one interview at site D. However, a number of meeting observations were recorded and a large number of participants from site D responded to the online survey, which strengthened our findings. On reflection, rather than pursuing data collection using interviews, it would have been preferable to distribute the online survey earlier, despite a low response rate.
There are a number of reasons that might explain why we encountered such difficulties with data collection and access. First, the study team intentionally approached cases study sites without a prior history of taking part in research/evaluation and those with well-documented challenges in delivering primary care services. Therefore, staff at our sites may have underestimated the time involved in taking part in a formal research study. Second, data collection commenced when PCNs were first registered, which was a difficult time for the set-up and implementation of network-based collaborative working and, therefore, many case study sites deprioritised the need for interviews in the short term. Third, towards the conclusion of fieldwork in early 2020, a number of scheduled observations were cancelled at short notice and others were postponed because of the onset of the COVID-19 pandemic. Nevertheless, one case study site continued to give study team access to documentation relevant to service-level changes that arose as a result of the pandemic (which has been presented in Chapter 5).
The evaluation took 9 months longer than originally anticipated in the original study protocol. The delay was, in part, due to the study team shifting focus. The initial premise for the evaluation was to explore primary care collaborations, and the study team (with input from the BRACE Centre steering group) shifted focus to evaluate PCNs, to be responsive to emerging NHS policy. This shift had a considerable impact on the sampling and recruitment of case study sites, as the initial aim had been to ascertain a maximum variation sample of case study sites by type of GP collaboration. Ultimately, this resulted in super-partnerships and PCNs with a prior history of collaborative working forming our final sample, which might not be as representative of current GP, as some PCNs are formed of practices with no experience of collaboration.
Despite these challenges, there is strong substantive learning from our evaluation in relation to the early implementation of PCNs, particularly given the research team’s responsiveness to changing primary care policy and ability to complete data collection during the COVID-19 pandemic.
This evaluation project had relatively limited patient and public involvement (PPI), notwithstanding input from BRACE Health and Care Panel patient/public members to our project design workshop in November 2018, and one of these colleagues undertaking peer review of the full study proposal. The study team kept BRACE Health and Care Panel members updated about project progress through quarterly e-bulletins, and we presented a full update of the study and its emerging themes at a Health and Care Panel workshop in Birmingham in September 2019, seeking advice and challenges about the focus of the project, and its likely dissemination.
In addition, project updates were shared on a 4-monthly basis with members of the BRACE Steering Group, which includes Charlotte Augst (Chief Executive of National Voices, the network that represents health and social care user organisations in the UK), who, in May 2020, advised the study team to undertake further interviews about the impact of COVID-19 on PCNs. The study team recognises the drawback of not involving GP patient participation groups in our case study data collection. However, understanding the patient experience of GP since the introduction of PCNs and the subsequent changes introduced because of COVID-19 may be explored in forthcoming BRACE Centre evaluations.
In conclusion, despite using multiple methods for data collection, additional interviews and observations would have strengthened the robustness of our findings. Finally, owing to the onset of the COVID-19 pandemic occurring during project write-up, the team were unable to undertake planned site-specific and overall face-to-face workshops with policy experts. The team did, however, share a concise slide deck of the project findings with each site in June 2020 without the obligation of providing comments, and completed virtual seminars with three out of four sites in late 2020 and early 2021.
Lessons about the conduct of rapid evaluations
We have summarised some of the main lessons learned from our experiences of conducting a NIHR-funded rapid evaluation below:
-
Responsiveness.
At the request of our funders (NIHR HSDR programme) the team was responsive to immediate national policy changes to support learning in relation to the implementation of PCNs in England. The team completed a REA as opposed to a formal systematic literature review, which saved time and resources, but the quality and breadth of relevant evidence was limited. The evaluation took longer to complete (9 months longer than stated in the original protocol) because of challenges with recruiting suitable case study sites (at a time of national policy changes) and arranging data collection. The onset of the COVID-19 pandemic has been detrimental to sharing real-time feedback to case study sites, especially with those sites seeking to learn from our findings to inform their PCN implementation strategy. There was also difficultly in determining whether our study should be categorised as research or a service evaluation using the HRA online algorithm.
-
Relevance.
There has been continued and close collaboration with the BRACE Health and Care panel (which includes members of the BRACE PPI group) to discuss the priority of our evaluation, comment on our participant-facing material (e.g. information sheets) and listen to our emerging findings. The involvement of key stakeholders and policy experts in the project design ensured that the team answered the most appropriate REAs with regard to current health policy changes. However, collaboration from stakeholders has been largely consultation rather than co-production.
-
Rigour.
Throughout the evaluation the study team shared early insights with regard to the conduct and learning of their rapid evaluation with colleagues from NHSE&I, the DHSC, researchers at the University of Manchester and policy experts. The team engaged iteratively with theoretical and policy-relevant literature throughout the design, data collection and analysis/interpretation stages of the evaluation. Online surveys, designed for primary care colleagues, were member checked by two general practitioners before dissemination. During data analysis, there was appropriate use of online workshops to add rigour to analysis and interpretation.
Chapter 7 Conclusion and implications
This evaluation of the early implementation of PCNs provides a rich source of learning about the implementation and early development of PCNs in four case study sites in England. The data collected through this evaluation provide policy-relevant insights for each of the REAs that formed the basis of the evaluation. The evaluation REAs are set out in Box 11, followed by a short explanation of how each question has been addressed.
-
What was the contextual and policy background within which PCNs were introduced?
-
What were the pre-existing forms of GP collaborative working across primary care in England?
-
How have new PCNs been implemented in a sample of urban and rural settings?
-
How do new PCNs relate to pre-existing GP collaborations?
-
-
What are the rationales and motives for GPs to enter into GP collaborations, including new PCNs? In particular, what role do financial incentives play in facilitating or inhibiting collaboration? What are the expected outcomes for PCNs?
-
What evidence exists about the positive or negative impacts associated with different experiences of establishing GP collaborations and how do these relate to newly formed PCNs?
-
What appear to be the barriers to and facilitators of effective collaboration across GPs, with respect to both successful and unsuccessful collaboration, and achieving impact or not?
-
What does the analysis of prior experience of GP collaborations, and the early implementation of PCNs, suggest in terms of the likely progress of these networks in the NHS in England, including in the light of the COVID-19 pandemic and associated challenges?
Evaluation findings
We found that PCNs had been implemented in the context of many well-established ways of formal and informal collaborative working in GP across rural and urban settings. In some cases, these previous collaborations provided much-needed support in terms of management, leadership and infrastructure, although they could also be a source of tension within PCNs, as interests, goals and ways of working of the prior collaboration and new network did not necessarily align (RQs 1.1–1.3). Reasons for collaborative working in GP typically focused on the desire to enhance the sustainability of primary care and offer better integrated care for patients, although the reasons cited for joining or forming a PCN were often more narrowly focused on policy and financial incentives, indicating the top-down nature of network formation (RQ2).
At the time of writing this report (June 2020), it was too early to determine the impact of PCNs, but early evidence pointed to operational success in networks in terms of setting up managerial structures, hiring for new roles and providing integrated services, as set out in the national PCN specification. There was also evidence that PCNs could address sustainability issues in primary care by bringing in new funds, creating efficiencies such as shared back-office support functions, and increasing managerial and leadership capacity. Furthermore, it was striking that all of this had been achieved in just 9 months, with almost all practices remaining in their PCN, suggesting that networks had been able to form, plan and mobilise more swiftly than most of their predecessor primary care organisations, and we posit that this was due in part to the experience and support of prior GP collaborations.
Primary care networks have, however, caused some negative impacts, such as increased workload and organisational tensions, particularly in the initial set-up phase as they worked out managerial and decision-making processes, and practices negotiated the role of networks in a landscape of previous collaborative working arrangements (RQ3). In terms of facilitators of and barriers to the operation of PCNs, we found that effective management and leadership, particularly with respect to having a committed CD who was able to take on the role for the medium to longer term, and constructive relationships with CCGs and trusts, were important in ensuring the success of PCNs.
It is essential for PCNs to build on the learning of previous collaborations in GP rather than undoing their work, and to explore and build a new shared understanding of the goals of networks in the context of prior collaborations. For example, there seemed to be some tension among respondents to this evaluation as to whether the central purpose of PCNs is to reduce general practitioner workload and improve sustainability of primary care or to improve integrated care for patients. In rural areas, there was evidence of particular barriers to the establishment and operation of PCNs, such as a perceived lack of fit with aspects of the national PCN specification and local capabilities and needs, alongside existing challenges of providing primary care to rural populations (RQ4). What is clear is that PCNs will need to be able to handle multiple and at times competing priorities set by NHSE&I, together with seeking to meet the needs of local practices and patient populations. Critical to this will be having sufficient policy and organisational headroom to make choices about service priorities, and adequate management support to get the work done.
Weighing the evidence from this evaluation and from previous experiences of GP collaboration within the English NHS, it seems that PCNs have significant potential in terms of increasing sustainability in primary care and delivering integrated health and care services to local populations. The case study sites examined in this evaluation have mobilised quickly, focused on seeking to achieve the expectations set out in national PCN policy, and all at a time of a complex and shifting political and societal backdrop (i.e. Brexit, The NHS Long Term Plan,4 COVID-19). To realise the full potential of PCNs, it will be important to increase commitment on the part of local GPs and wider community health and care teams to their local network, build managerial and leadership capacity, and clarify the role of previous GP collaborations within the PCN landscape, which is explored in more detail in the recommendations below. PCNs provide a potentially powerful and effective mechanism to co-ordinate primary care responses to the COVID-19 pandemic in England, including new forms of service delivery that are resilient to heath emergencies, playing a role in public health testing and tracking, and supporting vulnerable patients and families needing to be ‘shielded’. Follow-up research is needed to understand better how PCNs have responded to the pandemic so far, and their role in enabling new forms of primary care service provision in a post-COVID-19 England (RQ5).
Implications for decision-makers
The implications of our evaluation for those making decisions about PCN policy and development at a national and a local level are summarised in Box 12, organised into three categories, and are explained in more detail below. These implications are directed mainly at national decision-makers and, in particular, those related to the engagement and the role of PCNs in the wider health and social care system. Those relating to leadership and management capacity are directed primarily at local decision-makers, albeit they will probably require resources and expertise from a national level to support PCN development activity.
-
There is a need for consistent long-term national policy about PCNs and other forms of GP collaboration that allows for local diversity of size and form of network, while also avoiding the temptation to merge or reorganise PCNs.
-
It is important that realistic and clear goals are set for PCNs against which the performance and progress of the networks can be measured.
-
Efforts should be made to ensure that PCN policy is compatible with both rural and urban area primary care delivery.
-
It is important to build on the experience and expertise of pre-existing GP collaborations.
-
There is a need to ensure sufficient and distributed management and organisational support for the PCN CD role.
-
Ensure that the wider primary care team is able to be part of PCN leadership.
-
It would be helpful to revisit the role of the PCN in the context of the health and social care system as it emerges from the COVID-19 pandemic.
-
Ensure that PCNs are monitored and performance managed in a way that enables them space and permission to develop and pursue local priorities within the context of a national framework.
-
There is a need to clarify the role of CCGs in relation to PCNs.
Increasing the engagement of general practices and wider primary care teams with primary care networks
Increasing the commitment to PCNs by GPs and others in primary care will be important in ensuring that the full benefits of networks can be realised. Some practices are inevitably (at this set-up stage) still running a dual system, spending up front on the implementation and management of PCNs without realising the full benefits of communal working. Increased engagement in PCNs will also help address tensions around the autonomy of GP alongside a desire to collaborate with other practices, which were found in this evaluation, and which have been a historical tension within the experience of GP collaborations in the UK and internationally. Based on our evaluation findings, we propose the following, which may help increase engagement in PCNs among practices and others involved in the delivery of primary care services:
-
There is a need for national decision-makers to ensure consistent long-term policy about PCNs and other forms of GP collaboration, allowing for local diversity of size and form of network, and avoiding the temptation to merge or reorganise PCNs. Primary care planning and commissioning is often subject to policy reform, which has caused some lack of trust among primary care practitioners consulted in this evaluation about whether or not PCNs will be an enduring policy and one in which it is worth investing significant time, commitment and engagement.
-
It is important that national decision-makers and local CCGs set realistic and clear goals for PCNs. There is currently some tension within the PCNs included in this study as to whether they should be mostly focused on addressing general practitioner workload and the sustainability of primary care or on providing a wider range of integrated services to local populations. Helping PCNs to develop an appropriate balance in terms of how they focus on multiple (and at times competing) local and national goals is an important challenge for NHSE&I, and for PCNs as they gain organisational confidence and maturity. Setting clear and realistic goals will also help to monitor the performance and progress of PCNs, providing a framework against which to measure the networks.
-
Efforts should be made to ensure that PCN policy is compatible with both rural and urban area primary care delivery. PCNs are a central government initiative based on the major The NHS Long Term Plan4 and an investment in primary care, with nationally defined service specifications. This appears from our evaluation to present a particular potential challenge in rural areas, where it is sometimes perceived that PCN policy does not align easily with local capabilities and needs. By working closely with rural as well as urban PCNs (and some who are struggling, as well as those making quick progress) in creating future iterations of the PCN specification, and avoiding the understandable temptation to work with the ‘leading light’ networks, which are often in urban settings, national policy-makers can ensure that the evolution of NHS guidance and service specifications for PCNs achieves an appropriate balance of national direction and space for local delivery.
Building leadership and management capacity
Our evaluation has the following implications for local decision-makers who are seeking to build further capacity within PCNs to help address the varied quality of leadership and management within networks as revealed in this evaluation:
-
It is important to build on the experience and expertise of pre-existing GP collaborations. In some of our case study sites, the PCN was able to draw on important managerial capacities and infrastructure from previous (and current) GP collaborations, which helped the network achieve operational success. Where managerial and leadership capacities have been enhanced by previous collaborations, PCNs should be encouraged by NHSE&I and local CCGs to draw on this resource. Local ways of working will determine the exact nature of how PCNs can best work with pre-existing GP collaborations, and may range from informal advice and support to using paid logistical support from previous collaborations.
-
There is a need for CCGs and PCN governing bodies to ensure sufficient and distributed management and organisational support for the PCN CD role. From this evaluation, it has become clear that PCN CDs, at least in our case study sites, are often overextended and they do not always have the appropriate mix of non-clinical skills and capacity needed to successfully lead a network. A greater degree of professional managerial roles and support within PCNs may help address this shortcoming, and sharing of good practice at a local and national level is also likely to be helpful.
-
Local PCN governing bodies should ensure that the wider primary care team is able to be part of PCN leadership. There may be local staff within practices and the broader primary care and community health sector (e.g. PMs, nurses, pharmacists, voluntary sector managers) who would want to further their career and would welcome the opportunity to become more involved in managing PCN activity.
Clarifying how primary care networks fit into the wider health and social care system
Nationally, there may be a need for further guidance on the scope and boundaries of PCNs, as they evolve and take on more significant leadership roles within their sustainability and transformation partnership and/or local authority area. As the NHS and local government adapt to a post-COVID-19 way of organising public health and primary care work (including testing, tracing and isolating people found to have or be at risk of COVID-19) and ensuring the sustainability of all other local health services that may have been paused during the pandemic, the role of the PCN will probably be important, and needs to be clarified, supported and resourced by both national and local decision-makers. Specific implications from our evaluation about clarification of the PCN role include the following:
-
It would be helpful for NHSE&I to revisit the role of the PCN in the context of the health and care system as it emerges from the COVID-19 pandemic. There is likely to be a need for further flexing of the PCN service specifications as the NHS, social care and the voluntary sector grapple with the consequences of the pandemic, and work out (and continually adapt) local service development priorities. NHSE&I has already shown its readiness to do this (e.g. in raising the priority of care home support) and it will be important that this flexibility continues, and also that it is developed and agreed in collaboration with networks, and those from a range of urban and rural settings.
-
National decision-makers need to ensure that PCNs are monitored and their performance managed in a way that enables them space and permission to develop and pursue local priorities within the context of a national framework. Achieving a balance of local goals within a national framework will require sophisticated and flexible performance management and guidance, but will increase the likelihood of sustainable success for PCNs.
-
There is a need to clarify the role of CCGs in relation to PCNs. Where CCGs have been perceived as exerting undue influence over PCNs and associated funding, tensions have arisen between networks and commissioning bodies. As PCNs are a departure from previous commissioning arrangements, and put more planning and purchasing power in the hands of GP, further guidance by NHSE&I is likely to be needed, not least in the context of COVID-19 and the associated temporary suspension of some commissioning activity (and reverting to national block allocations of resource to NHS trusts and foundation trusts, and temporary suspension of some targets). As the NHS emerges from the pandemic and takes stock of service changes (including the significant innovations in the ways in which GP and primary care services are delivered), there will be a need to clarify the role of PCNs (alongside CCGs) in funding and supporting such developments for the longer term.
Conclusions and suggestions for further research and evaluation
This evaluation has demonstrated the considerable potential for PCNs to improve sustainability within primary care and provide integrated services to patients, and the early operational success that PCNs in four case study sites across England have been able to achieve. As PCNs move forward, it will be important to ensure that they reach their full potential, particularly in the light of the resources, time and energy that have been put into this new form of collaboration in the English NHS. We have identified several priority areas above with respect to implications from our evaluation for the future direction and support of PCNs, which will require engagement and close working between NHSE&I, CCGs and local PCNs across a variety of rural and urban settings.
As PCNs become more deeply embedded in local care landscapes, it will be important to monitor their development, including measurement of their impact, and understand better the facilitators of and barriers to them achieving their goals. In monitoring their progress and impact, a blend of qualitative and quantitative measures will be needed, for it was clear from our REA that GP collaborations have typically been subject to extensive qualitative evaluation, and have much less sustained quantitative analysis of their progress.
Areas in which evidence could helpfully be gathered about PCN progress therefore include:
-
achievement of targets set out in the national PCN specification
-
based on this monitoring, a clear articulation of the benefits of PCN activity for patients, staff and the local health and care system
-
careful monitoring of the management and transaction costs of PCNs, to enable cost–benefit analyses of their operation
-
comparative analysis of such measures across PCNs in a region and nationally, to provide the basis for in-depth exploration of what enables or inhibits progress.
This quantitative tracking of PCNs can then form the basis for a qualitative study of what has enabled or hindered progress, and an exploration of what additional support and investment may be needed to enable effective collaboration and achievement of goals. It will be important not only to study those PCNs that appear to be making effective progress, but also to explore and understand why some networks struggle and find it hard to collaborate, and in turn whether or not this affects health and care goals set for networks. Ultimately, research into the longer-term operation of PCNs needs to be able to answer this question raised by our REA for this study: do GPs need to collaborate to achieve key outcomes (e.g. improving access, achieving sustainability)?
Limited information about PCNs’ response to the COVID-19 pandemic was collected through this evaluation, although additional data gathering on how networks formed part of the primary care response to COVID-19 would be useful in understanding this more fully. Along with providing information on the COVID-19 primary care response itself and the role of PCNs within this, additional information gathering would contribute to an understanding of whether practices revert to prior and individual ways of working or draw more on shared resources within collaborations during moments of stress.
In further research, it will also be important to evaluate how PCNs move from an initial stage characterised by relatively high up-front costs to a more established stage in which the resources put into networks might contribute more meaningfully to sustainability and efficiency in primary care. In addition, the ongoing relationship between PCNs and prior GP collaborations will be important to track, for this evaluation has revealed just how established the concept of collegial or collective working now is across English GP.
Acknowledgements
We are extremely grateful to all the participants who took part in this study and to our contacts at each case study site who helped to co-ordinate our interactions with interviewees and provided documents to, and answered queries from, the research team.
We would also like to thank members of the BRACE Centre Executive, Health and Care Panel, PPI Group, and Core Team for their input and constructive comments throughout the study, and colleagues from NHSE&I, DHSC, The King’s Fund, the Nuffield Trust, and the University of Manchester for their contributions at our half-day project design workshop.
Specifically, we would like to thank Natasha Elmore, Dr Sarah Ball and Jon Sussex (all from RAND Europe) for their contribution to data collection, gaining ethics approval and providing project advice; Dr Rebecca Fisher (Senior Policy Fellow, Health Foundation) and Dr Mina Gupta (general practitioner, Modality) for peer review of our online surveys; Samantha Hinks (NHSE&I) and Professor Katherine Checkland (University of Manchester) for their ongoing advice and sharing learning from their own evaluations and research throughout; Professor Russell Mannion (University of Birmingham), Dr Katie Colman and Mark Platt (BRACE Health and Care Panel) who reviewed our study protocol from a theoretical, policy and PPI perspective; Cathy Dakin (BRACE Administrator, University of Birmingham) who reviewed our Plain English summary and provided excellent support throughout; and Professor Justin Waring (University of Birmingham) and Dr Anna Dixon [Chief Executive, Centre for Ageing Better (London, UK)] for undertaking critical reviews of the draft report.
Contributions of authors
Judith Smith (https://orcid.org/0000-0003-4036-4063) (Professor of Health Policy and Management, and Director of the BRACE Centre) was the principal investigator and led the study. She contributed to the conception and design of the study, the theoretical framework, data collection at one study site, and overall data analysis and interpretation, and is corresponding author of the final report. She led the writing on Chapters 1, 3 (co-led) and 6 while contributing to Chapters 2, 5 and 7. Professor Smith took responsibility for overall editing of the final report and is the guarantor.
Sarah Parkinson (https://orcid.org/0000-0002-2858-1842) (Analyst, RAND Europe) was the project manager for the study (January–June 2020). She contributed to data collection at two study sites, led overall data analysis and interpretation, and is a co-author of the final report. She led the writing on Chapters 4 (co-led), 5 and 7 while contributing to Chapter 6.
Amelia Harshfield (https://orcid.org/0000-0001-5549-6451) (Analyst, RAND Europe) was the project manager for the study (July 2018–December 2019). She contributed to the conception and design of the study, the theoretical framework and data collection at two study sites, and is a co-author of the final report. She co-led the writing on Chapter 3.
Manbinder Sidhu (https://orcid.org/0000-0001-5663-107X) (Research Fellow, University of Birmingham) was a researcher for the study. He contributed to the design of the study, the theoretical framework, data collection at two study sites, and overall data analysis and interpretation, and is a co-author of the final report. He led the writing on Chapters 2 and 4 (co-led) while contributing to Chapters 5–7.
All authors contributed to integrating the findings of the study. Judith Smith, Sarah Parkinson and Manbinder Sidhu made critical revisions to the report for important intellectual content and approved the final manuscript. All authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the article are appropriately investigated and resolved.
Patient and public involvement
A member of the BRACE Health and Care Panel attended the project design workshop and a PPI member of the panel reviewed and helped shape the proposal for the evaluation. The ‘plain English’ summary of the report has been reviewed by another PPI adviser. Project updates were shared on a 4-monthly basis for the duration of the project with members of the BRACE Steering Group, which includes our BRACE Centre co-investigator Charlotte Augst (Chief Executive of National Voices), who advised the study team in May 2020 to complete further interviews with regard to the impact of COVID-19 on PCNs. Updates on the project were given to our BRACE Health and Care Panel in regular e-bulletins, and a presentation of emerging themes from the study was given at a panel workshop in Birmingham in September 2019, when challenges and advice were given to the evaluation team. Project findings were shared and discussed at a further meeting of the full BRACE Health and Care Panel in early 2021 – the panel includes eight patient and public members. We will seek further advice from these members concerning how best to communicate the evaluation’s findings to patient and public audiences, building on the steer they gave to us in discussion at the September 2019 workshop.
Publications
Parkinson S, Smith J, Sidhu M. Early development of primary care networks in the NHS in England: a qualitative mixed-methods evaluation. BMJ Open 2021;11:e055199.
Smith J, Parkinson S, Harshfield A, Sidhu MS. Primary Care Networks in the English NHS: (Another) Triumph of Hope Over Experience? Health Services Research UK Annual Conference, July 2020.
Smith J and Harshfield A. Primary Care Networks: A Marathon Not a Sprint. 2019. URL: https://www.hsj.co.uk/primary-care/primary-care-networks-a-marathon-not-a-sprint/7025889.article (accessed 28 August 2020).
Data-sharing statement
Owing to the consent process for data collection at case study sites within this evaluation, there are no data that can be shared.
Disclaimers
This report presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care.
References
- Parkinson S, Smith J, Sidhu M. Early development of primary care networks in the NHS in England: a qualitative mixed-methods evaluation. BMJ Open 2021;11. https://doi.org/10.1136/bmjopen-2021-055199.
- NHS England and Improvement . Five Year Forward View 2014.
- Baird B, Ross S, Honeyman M, Sahib B, Reeve H, Nosa-Ehima M, et al. Innovative Models of General Practice. London: The King’s Fund; 2018.
- NHS England and Improvement . The NHS Long Term Plan 2019.
- Robertson R. Public Satisfaction with GP Services Drops to Lowest Level in 35 Years. London: The King’s Fund; 2018.
- Kringos D, Boerma W, Bourgueil Y, Cartier T, Dedeu T, Hasvold T, et al. The strength of primary care in Europe: an international comparative study. Br J Gen Pract 2013;63:e742-50. https://doi.org/10.3399/bjgp13X674422.
- Starfield B. Primary Care: Balancing Health Needs, Services, and Technology. New York, NY: Oxford University Press; 1998.
- NHS England and Improvement . General Practice Forward View 2016.
- Fisher R, Turton C, Gershlick B, Alderwick H, Thorlby R. Feeling the Strain: What the Commonwealth Fund’s 2019 International Survey of General Practitioners Means for the UK. London: The Health Foundation; 2020.
- NHS England and Improvement and the British Medical Association General Practitioners Association . Investment and Evolution: A Five-Year Framework for GP Contract Reform to Implement 2019.
- National Audit Office . Developing New Care Models through NHS Vanguards 2018.
- Tallack C, Hinks S. Lessons from the English National Health Service new care models programme. Int J Integrat Care 2019;19:1-8. https://doi.org/10.5334/ijic.s3405.
- Smith J, Mays N. Primary care organizations in New Zealand and England: tipping the balance of the health system in favour of primary care?. Int J Health Plann Manage 2007;22:3-19. https://doi.org/10.1002/hpm.866.
- Kumpunen S, Curry N, Farnworth M, Rosen R. Collaboration in General Practice: Surveys of GP Practices and Clinical Commissioning Groups. London: The Nuffield Trust, Royal College of General Practitioners; 2017.
- Kumpunen S, Curry N, Ballard T, Price H, Holmes M, Edwards N. Collaboration in General Practice: Surveys of GPs and CCGs. London: The Nuffield Trust, Royal College of General Practitioners; 2015.
- Rosen R, Kumpunen S, Curry N, Davies A, Pettigrew L, Kossarva L. Is Bigger Better? Lessons for Large-scale General Practice. London: The Nuffield Trust; 2016.
- National Association of Primary Care . National Association of Primary Care n.d. https://napc.co.uk/primary-care-home/ (accessed 29 May 2020).
- Fisher R. General practice in the time of covid-19 2020. https://blogs.bmj.com/bmj/2020/05/05/rebecca-fisher-general-practice-in-the-time-of-covid-19/ (accessed 25 May 2020).
- Smith J, Holder H, Edwards N, Maybin J, Parker H, Rosen R, et al. Securing the Future of General Practice: New Models of Primary Care. London: The Nuffield Trust, The King’s Fund; 2013.
- Pettigrew LM, Kumpunen S, Rosen R, Posaner R, Mays N. Lessons for ‘large-scale’ general practice provider organisations in England from other inter-organisational healthcare collaborations. Health Policy 2019;123:51-6. https://doi.org/10.1016/j.healthpol.2018.10.017.
- Pettigrew L, Mays N, Kumpunen S, Rosen R. Large-scale General Practice in England: What Can We Learn from the Literature. London: The Nuffield Trust; 2016.
- Smith JA, Mays N. GP led commissioning: time for a cool appraisal. BMJ 2012;344. https://doi.org/10.1136/bmj.e980.
- Salisbury H. Oh, those lazy, part time GPs!. BMJ 2019;367. https://doi.org/10.1136/bmj.l6813.
- Baird B, Beech J. Primary Care Networks Explained. London: The King’s Fund; 2019.
- NHS England and Improvement . Network Contract DES – Engagement on Draft Outline Service Specifications Summary Report 2020.
- NHS England and Improvement . The Framework for Enhanced Health in Care Homes 2020 21 – Version 2 2020. www.england.nhs.uk/wp-content/uploads/2020/03/theframework-for-enhanced-health-in-care-homes-v2-0.pdf (accessed 29 April 2022).
- Serle J. Contentious NHS Scheme to Bolster Care Homes Brought Forward 2020. www.hsj.co.uk/contentious-nhs-scheme-to-bolster-carehomes-brought-forward/7027530.article (accessed 27 August 2020).
- Baird B, Beech J. Primary Care Networks Explained 2020. www.kingsfund.org.uk/publications/primary-care-networks-explained (accessed 28 July 2022).
- Baird B, Lamming L, Bhatt RT, Beech J, Dale V. Integrating Additional Roles Into Primary Care Networks. London: The King’s Fund; 2022.
- Stake RE. Multiple Case Study Analysis. New York, NY: Guilford Press; 2005.
- Yin RK. Case Study Research: Design and Methods. Thousand Oaks, CA: SAGE Publications Ltd; 2009.
- De Silva MJ, Breuer E, Lee L, Asher L, Chowdhary N, Lund C, et al. Theory of Change: a theory-driven approach to enhance the Medical Research Council’s framework for complex interventions. Trials 2014;15. https://doi.org/10.1186/1745-6215-15-267.
- Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. Cochrane Handbook for Systematic Reviews of Interventions. Chichester; 2019.
- Barends E, Rousseau DM, Briner RB. CEBMa Guideline for Rapid Evidence Assessments in Management and Organizations. Amsterdam: Center for Evidence Based Management; 2017.
- Moher D, Liberati A, Tetzlaff J, Altman DG. PRISMA Group . Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLOS Med 2009;6. https://doi.org/10.1371/journal.pmed.1000097.
- Pawa J, Robson J, Hull S. Building managed primary care practice networks to deliver better clinical care: a qualitative semi-structured interview study. Br J Gen Pract 2017;67:e764-e774. https://doi.org/10.3399/bjgp17X692597.
- Robson J, Hull S, Mathur R, Boomla K. Improving cardiovascular disease using managed networks in general practice: an observational study in inner London. Br J Gen Pract 2014;64:e268-74. https://doi.org/10.3399/bjgp14X679697.
- Ørngreen R, Levinsen K. Workshops as a research methodology. Electron J E-Learn 2017;15:70-81.
- Bibby P, Brindley P. Urban and Rural Definitions for Policy Purposes in England and Wales: Methodology (v1.0) 2013. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/239477/RUC11methodologypaperaug_28_Aug.pdf (accessed 28 August 2020).
- Johl SK, Ranganathan S. Strategies for gaining access in doing fieldwork: reflection of two researchers. Electron J Bus Res Methods 2010;8.
- Andoh-Arthur J, Atkinson P, Delamont S, Cernat A, Sakshaug JW, Williams RA. SAGE Research Methods Foundations. London: SAGE Publications Ltd; 2020.
- Ritchie J, Lewis J, Nicholls CM, Ormston R. Qualitative Research Practice: A Guide for Social Science Students and Researchers. London: SAGE Publications Ltd; 2014.
- Patton MQ. Qualitative Research & Evaluation Methods: Integrating Theory and Practice. London: SAGE Publications Ltd; 2014.
- Baker SE, Edwards R. How Many Qualitative Interviews is Enough? Expert Voices and Early Career Reflections on Sampling and Cases in Qualitative Research. Swindon: National Centre for Research Methods Review Paper and Economic and Social Research Council; 2012.
- Great Britain . Data Protection Act 2018 2018.
- Tubaro P, Ryan L, D’angelo A. The visual sociogram in qualitative and mixed-methods research. Sociologic Res Online 2016;21:180-97. https://doi.org/10.5153/sro.3864.
- Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol 2013;13. https://doi.org/10.1186/1471-2288-13-117.
- Miles MB, Huberman AM. Qualitative Data Analysis: An Expanded Sourcebook. London: SAGE Publications Ltd; 1994.
- Organisation for Economic Co-operation and Development . List of OECD Member Countries – Ratification of the Convention of the OECD n.d. www.oecd.org/about/document/ratification-oecd-convention.htm (accessed 28 August 2020).
- Smith J, Goodwin N. Towards Managed Primary Care: The Role and Experience of Primary Care Organizations. Farham: Ashgate Publishing, Ltd; 2006.
- Smith J, Mays N, Dixon J, Goodwin N, Lewis R, McClelland S, et al. A Review of the Effectiveness of Primary Care-led Commissioning and its Place in the NHS. London: The Health Foundation; 2004.
- Bojke C, Gravelle H, Wilkin D. Is bigger better for primary care groups and trusts?. BMJ 2001;322:599-602. https://doi.org/10.1136/bmj.322.7286.599.
- Thorlby R, Smith J, Barnett P, Mays N. Primary Care for the 21st Century: Learning from New Zealand’s Independent Practitioner Associations. London: The Nuffield Trust; 2012.
- Casalino L. GP Commissioning in the NHS in England: Ten Suggestions from the United States. London: The Nuffield Trust; 2011.
- Ham CJ. GP Budget Holding: Lessons from Across the Pond and from the NHS. Birmingham: Health Services Management Centre, University of Birmingham; 2010.
- Thorlby R, Rosen R, Smith J. GP Commissioning: Insights from Medical Groups in the United States. London: The Nuffield Trust; 2011.
- Crampton P, Starfield B. A case for government ownership of primary care services in New Zealand: weighing the arguments. Int J Health Serv 2004;34:709-27. https://doi.org/10.2190/FMJW-R4R9-C4R1-W8RJ.
- Imison C, Williams S, Smith J, Dingwall C. Toolkit to Support the Development of Primary Care Federations. London: Royal College of General Practitioners, The King’s Fund, The Nuffield Trust, Hempsons; 2010.
- Elvey R, Bailey S, Checkland K, McBride A, Parkin S, Rothwell K, et al. Implementing new care models: learning from the Greater Manchester demonstrator pilot experience. BMC Fam Pract 2018;19. https://doi.org/10.1186/s12875-018-0773-y.
- Checkland K, Coleman A, McDermott I, Segar J, Miller R, Petsoulas C, et al. Primary care-led commissioning: applying lessons from the past to the early development of clinical commissioning groups in England. Br J Gen Pract 2013;63:e611-9. https://doi.org/10.3399/bjgp13X671597.
- Erler A, Bodenheimer T, Baker R, Goodwin N, Spreeuwenberg C, Vrijhoef HJ, et al. Preparing primary care for the future – perspectives from the Netherlands, England, and USA. Z Evid Fortbild Qual Gesundhwes 2011;105:571-80. https://doi.org/10.1016/j.zefq.2011.09.029.
- Rosen R, Kumpunen S, Smith J. Developing Care for a Changing Population: Learning from GP-led Organisations. London: The Nuffield Trust; 2016.
- Mays N, Wyke S, Evans D. The Purchasing of Health Care by Primary Care Organisations: An Evaluation and Guide to Future Policy. Maidenhead: Open University Press; 2001.
- Angstman KB, Horn JL, Bernard ME, Kresin MM, Klavetter EW, Maxson J, et al. Family medicine panel size with care teams: impact on quality. J Am Board Fam Med 2016;29:444-51. https://doi.org/10.3122/jabfm.2016.04.150364.
- Beehler GP, Funderburk JS, King PR, Wade M, Possemato K. Using the Primary Care Behavioral Health Provider Adherence Questionnaire (PPAQ) to identify practice patterns. Transl Behav Med 2015;5:384-92. https://doi.org/10.1007/s13142-015-0325-0.
- Breton M, Maillet L, Haggerty J, Vedel I. Mandated Local Health Networks across the province of Québec: a better collaboration with primary care working in the communities?. London J Prim Care 2014;6:71-8. https://doi.org/10.1080/17571472.2014.11493420.
- Ham C. GPs Must Adapt to a New Model of Care. London: Pulse; 2012.
- Harris MF, Advocat J, Crabtree BF, Levesque JF, Miller WL, Gunn JM, et al. Interprofessional teamwork innovations for primary health care practices and practitioners: evidence from a comparison of reform in three countries. J Multidiscip Healthc 2016;9:35-46. https://doi.org/10.2147/JMDH.S97371.
- Kumpunen S, Rosen R, Kossarova L, Sherlaw-Johnson C. Primary Care Home: Evaluating a New Model of Primary Care. London: The Nuffield Trust; 2017.
- Lane R, Russell G, Bardoel EA, Advocat J, Zwar N, Davies PGP, et al. When colocation is not enough: a case study of General Practitioner Super Clinics in Australia. Aust J Prim Health 2017;23:107-13. https://doi.org/10.1071/PY16039.
- Oelke ND, Milkovich L, Whitmore B. Using the awareness, motivation, skills, and opportunity framework for health promotion in a primary care network. Health Promot Pract 2018;21:457-63. https://doi.org/10.1177/1524839918801912.
- Richters A, Nieuwboer MS, Olde Rikkert MGM, Melis RJF, Perry M, van der Marck MA. Longitudinal multiple case study on effectiveness of network-based dementia care towards more integration, quality of care, and collaboration in primary care. PLOS ONE 2018;13. https://doi.org/10.1371/journal.pone.0198811.
- Valentijn PP, Vrijhoef HJ, Ruwaard D, de Bont A, Arends RY, Bruijnzeels MA. Exploring the success of an integrated primary care partnership: a longitudinal study of collaboration processes. BMC Health Serv Res 2015;15. https://doi.org/10.1186/s12913-014-0634-x.
- Henderson J, Javanparast S, MacKean T, Freeman T, Baum F, Ziersch A. Commissioning and equity in primary care in Australia: views from primary health networks. Health Soc Care Community 2018;26:80-9. https://doi.org/10.1111/hsc.12464.
- Dowswell G, Harrison S, Wright J. The early days of primary care groups: general practitioners’ perceptions. Health Soc Care Community 2002;10:46-54. https://doi.org/10.1046/j.0966-0410.2001.00332.x.
- Rodríguez C, Bélanger E. Stories and metaphors in the sensemaking of multiple primary health care organizational identities. BMC Fam Pract 2014;15. https://doi.org/10.1186/1471-2296-15-41.
- Rousseau C, Pontbriand A, Nadeau L, Johnson-Lafleur J. Perception of interprofessional collaboration and co-location of specialists and primary care teams in youth mental health. J Can Acad Child Adolesc Psychiatry 2017;26:198-204.
- Thomas P. Achieving community oriented integrated care through the 2014 England GP contract. London J Prim Care 2014;6:55-64. https://doi.org/10.1080/17571472.2014.11493416.
- Anaf J, Baum F, Freeman T, Labonte R, Javanparast S, Jolley G, et al. Factors shaping intersectoral action in primary health care services. Aust N Z J Public Health 2014;38:553-9. https://doi.org/10.1111/1753-6405.12284.
- Bailie R, Matthews V, Brands J, Schierhout G. A systems-based partnership learning model for strengthening primary healthcare. Implement Sci 2013;8. https://doi.org/10.1186/1748-5908-8-143.
- Rosen R. Transforming General Practice: What are the Levels for Change?. London: The Nuffield Trust; 2015.
- Toop L. Steps towards more integrated care in New Zealand: a general practice perspective. BJGP Open 2017;1. https://doi.org/10.3399/bjgpopen17X100845.
- Jaruseviciene L, Liseckiene I, Valius L, Kontrimiene A, Jarusevicius G, Lapão LV. Teamwork in primary care: perspectives of general practitioners and community nurses in Lithuania. BMC Fam Pract 2013;14. https://doi.org/10.1186/1471-2296-14-118.
- Addicott R, Ham C. Commissioning and Funding General Practice: Making the Case for Family Care Networks. London; 2014.
- Bienkowska-Gibbs T, King S, Saunders CL, Henham ML. New Organisational Models of Primary Care to Meet the Future Needs of the NHS: A Brief Overview of Recent Reports 2015.
- Miller R, Weir C, Gulati S. Transforming primary care: scoping review of research and practice. J Integr Care 2018;26:176-88. https://doi.org/10.1108/JICA-03-2018-0023.
- Baird B, Charles A, Honeyman M, Maguire D, Das P. Understanding Pressures in General Practice. London: The King’s Fund; 2016.
- Brown LJ, Oliver-Baxter J. Six elements of integrated primary healthcare. Aust Fam Physician 2016;45:149-52.
- Sangaleti C, Schveitzer MC, Peduzzi M, Zoboli ELCP, Soares CB. Experiences and shared meaning of teamwork and interprofessional collaboration among health care professionals in primary health care settings: a systematic review. JBI Database System Rev Implement Rep 2017;15:2723-88. https://doi.org/10.11124/JBISRIR-2016-003016.
- Barnett S, Jones SC, Bennett S, Iverson D, Bonney A. General practice training and virtual communities of practice – a review of the literature. BMC Fam Pract 2012;13. https://doi.org/10.1186/1471-2296-13-87.
- Yates R, Wells L, Carnell K. General practice based multidisciplinary care teams in Australia: still some unanswered questions. A discussion paper from the Australian General Practice Network. Aust J Prim Health 2007;13:10-7. https://doi.org/10.1071/PY07018.
- Suter E, Mallinson S, Misfeldt R, Boakye O, Nasmith L, Wong ST. Advancing team-based primary health care: a comparative analysis of policies in western Canada. BMC Health Serv Res 2017;17. https://doi.org/10.1186/s12913-017-2439-1.
- Morgan S, Pullon S, McKinlay E. Observation of interprofessional collaborative practice in primary care teams: an integrative literature review. Int J Nurs Stud 2015;52:1217-30. https://doi.org/10.1016/j.ijnurstu.2015.03.008.
- Rosen R, Parker H. New Models of Primary Care: Practical Lessons. London: The Nuffield Trust; 2013.
- Hespe C, Rychetnik L, Peiris D, Harris M. Informing implementation of quality improvement in Australian primary care. BMC Health Serv Res 2018;18. https://doi.org/10.1186/s12913-018-3099-5.
- Mannion R. General practitioner-led commissioning in the NHS: progress, prospects and pitfalls. Br Med Bull 2011;97:7-15. https://doi.org/10.1093/bmb/ldq042.
- Jolanki O, Tynkkynen LK, Sinervo T. Professionals’ views on integrated care. J Integr Care 2017;25:247-55. https://doi.org/10.1108/JICA-06-2017-0018.
- Stukel TA, Glazier RH, Schultz SE, Guan J, Zagorski BM, Gozdyra P, et al. Multispecialty physician networks in Ontario. Open Med 2013;7:e40-55.
- Smith J, Harshfield A. Primary Care Networks: A Marathon Not a Sprint 2019. www.hsj.co.uk/primary-care/primary-care-networks-a-marathon-not-a-sprint/7025889.article (accessed 28 August 2020).
- Smits M, Rutten M, Keizer E, Wensing M, Westert G, Giesen P. The development and performance of after-hours primary care in the Netherlands: a narrative review. Ann Intern Med 2017;166:737-42. https://doi.org/10.7326/M16-2776.
- Great Britain . National Health Service (Primary Care) Act 1997 1997.
- Leese B, Petchey R. Achievements of the first wave personal medical services (PMS) pilots in England. A health authority perspective. J Health Organ Manag 2003;17:181-93. https://doi.org/10.1108/14777260310480730.
- Campbell S, Steiner A, Robison J, Webb D, Raven A, Richards S, et al. Do Personal Medical Services contracts improve quality of care? A multi-method evaluation. J Health Serv Res Policy 2005;10:31-9. https://doi.org/10.1177/135581960501000108.
- Lewis R, Gillam S. Personal medical services. BMJ 2002;325:1126-7. https://doi.org/10.1136/bmj.325.7373.1126.
- NHS England & Improvement . Working With Time To Change to Build on Positive Practice in Mental Health Services 2016. www.england.nhs.uk/2016/02/ttc/#:~:text=NHS%20England%20has%20worked%20with,use%20services%20and%20NHS%20professionals.
- NHS England and Improvement . Integrated Care Pioneers n.d. www.england.nhs.uk/integrated-care-pioneers/ (accessed 28 August 2020).
- NHS England and Improvement . 2020/21/General/Medical/Services/(GMS)/Contract/Quality/and/Outcomes/Framework./Guidance/for/GMS/Contract/2020/21/in/England n.d. www.england.nhs.uk/wp-content/uploads/2020/09/C0713-202021-General-Medical-Services-GMS-contract-Quality-and-Outcomes-Framework-QOF-Guidance.pdf (accessed 28 August 2020).
- Primary Care Strategy, NHS Contracts Group and Systems Transformation Group . Network Contract Directed Enhanced Service: Additional Roles Reimbursement Scheme Guidance 2019.
- Smith J, Bamford M, Ham C, Scrivens E, Shapiro J. Beyond Fundholding: A Mosaic of Primary Care Led Commissioning and Provision in the West Midlands. Birmingham: Health Services Management Centre, University of Birmingham; 1997.
- Curry N, Ham C. Clinical and Service Integration: The Route to Improved Outcomes. London: The King’s Fund; 2010.
- Croxson B, Smith J, Cumming J. Patient Fees as a Metaphor for So Much More in New Zealand’s Primary Health Care System. Wellington: Health Services Research Centre; 2009.
- Glennerster H, Cohen A, Bovell V. Alternatives to fundholding. Int J Health Serv 1998;28:47-66. https://doi.org/10.2190/E5MT-HHGH-5AAA-RC1X.
- Dowling B, Glendinning C. The New Primary Care: Modern, Dependable, Successful?. Maidenhead: Open University Press; 2003.
- Palmer B, Appleby J, Spencer J. Rural Health Care: A Rapid Review of the Impact of Rurality on the Costs of Delivering Health Care. London: The Nuffield Trust; 2019.
- Sidhu M, Pollard J, Sussex J. Vertical integration of GP practices with acute hospitals in England and Wales: why, how and so what? Findings from a qualitative, rapid evaluation study. BMJ Open 2022;12. https://doi.org/10.1136/bmjopen-2021-053222.
- Tuckman BW. Developmental sequence in small groups. Psychol Bull 1965;63:384-99. https://doi.org/10.1037/h0022100.
- Baird B. How has General Practice Responded to the Covid-19 (Coronavirus) Outbreak?. London: The King’s Fund; 2020.
- Flick U, Flick U, von Kardorff E, Steinke I. A Companion to Qualitative Research. Thousand Oaks, CA: SAGE Publications Ltd; 2004.
- Fusch PI, Ness LR. Are we there yet? Data saturation in qualitative research. The Qual Rep 2015;20:1408-16. https://doi.org/10.46743/2160-3715/2015.2281.
- Pope C, Ziebland S, Mays N. Qualitative research in health care. Analysing qualitative data. BMJ 2000;320:114-16. https://doi.org/10.1136/bmj.320.7227.114.
Appendix 1 Primary care collaborations survey as part of sampling strategy
Appendix 2 Topic guide for interviews
Evaluation questions
-
What are the different forms of GP collaboration in primary care in England and how have they been implemented in a sample of urban and rural settings?
-
What are the rationales and incentives for general practices to enter into different forms of collaboration, and what are the reasons for and consequences of not doing so? In particular, what role do financial incentives play in facilitating or inhibiting collaboration? What are the expected outcomes of GP collaborations?
-
What evidence exists about the positive or negative impacts associated with different experiences of establishing (or not) GP collaborations?
-
What are the barriers to and facilitators of effective collaboration across GPs, with respect to both successful and unsuccessful collaboration, and achieving impact or not?
Before the interview begins
-
Ensure that the participant has read the information leaflet.
-
Ensure that the participant feels able to ask any questions about the evaluation including issues about confidentiality, the findings and/or dissemination before being asked to sign a consent form.
-
Explain that they do not have to answer all the questions just because they have consented to the interview, and that they can take a break or stop the interview at any time.
-
Check that they are happy to be audio-recorded and have signed for this on the consent form.
-
Start audio-recording and begin the interview.
Themes to be covered in the interview
-
Describe your current model of collaboration in your area at present:
-
current stakeholders
-
number of practices
-
length of time since collaboration commenced
-
the population being covered by the network (has there been any learning from the ‘primary care home model’?).
-
-
Describe any specific challenges the network has faced for being located in an urban/rural setting.
-
Describe how current collaborative working model has evolved since commencement/past 12 months:
-
Have the numbers of collaborators increased/decreased? Why?
-
What have been the issues of tension? How have they been resolved?
-
Describe improvements (if any) to GP working in your area since the formation of the network (i.e. increasing access and extending services).
-
Integration across secondary, community and third-sector organisations?
-
-
Discussion on the nature of relationships that exist within the network (perhaps use the stakeholder mapping document):
-
Across the different layers of stakeholders.
-
Among GPs.
-
How is the collaboration being led and by whom.
-
Is there greater/lesser interdependency?
-
-
What have been some of the reasons for choosing this particular model of collaboration over others?
-
Describe the financial incentives involved as part of this model of collaboration.
-
Describe the financial drawbacks involved as part of this model of collaboration.
-
What are the risks associated with maintaining and supporting this collaboration?
-
-
What are some of the key goals/outcomes you would like to achieve, both in the immediate and the medium/long term?
-
What processes/changes in practice have taken place in order to achieve said goals/outcomes?
-
How is ‘success’ being determined and/or measured?
-
-
What benefits have you seen since the development/commence of this collaboration?
-
indemnity
-
governance
-
data sharing
-
improved organisational development
-
workforce satisfaction.
-
-
Have there ever been occasions when practices have an expressed a desire to leave the collaboration and/or left? If yes, could you please describe what happened?
Appendix 3 Survey
Appendix 4 Code book for interview analysis
The code book presented in Table 7 was exported from NVivo12. The number of files represents the number of unique interviews within that code, and the number of references refers to the number of text sections within that code.
| Name | Files (n) | References (n) |
|---|---|---|
| 01 General information | 0 | 0 |
| 01.01 Models | 0 | 0 |
| 01.01.01 Primary care networks | 22 | 109 |
| 01.01.02 Super partnerships | 8 | 25 |
| 01.01.03 Other collaboration models | 13 | 46 |
| 01.02 Governance | 0 | 0 |
| 01.02.01 Management, leadership and decision-making | 20 | 132 |
| 01.02.02 Regulation | 3 | 6 |
| 01.02.03 Meetings | 21 | 53 |
| 01.02.04 Commissioning | 14 | 34 |
| 01.02.05 Important documents or policies | 2 | 2 |
| 01.02.06 Other governance topics | 3 | 3 |
| 01.03 Stakeholder involvement | 0 | 0 |
| 01.03.01 Internal stakeholders | 0 | 0 |
| 01.03.01.01 Management staff | 9 | 29 |
| 01.03.01.02 GPs | 8 | 12 |
| 01.03.01.03 Nurses | 5 | 13 |
| 01.03.01.04 Mental health | 2 | 3 |
| 01.03.01.05 Social care | 2 | 2 |
| 01.03.01.06 Social prescribers | 13 | 30 |
| 01.03.01.07 Pharmacists | 14 | 36 |
| 01.03.01.08 Practice managers | 10 | 18 |
| 01.03.01.09 Other clinical staff | 3 | 5 |
| 01.03.01.10 Other non-clinical staff | 4 | 6 |
| 01.03.01.11 Other community-based staff | 6 | 9 |
| 01.03.01.12 Other staffing comments | 13 | 28 |
| 01.03.02 External stakeholders | 20 | 49 |
| 01.03.03 Relationships between stakeholders | 7 | 11 |
| 01.03.04 Other stakeholder information | 0 | 0 |
| 01.04 Demographic information | 0 | 0 |
| 01.04.01 Patient population | 4 | 16 |
| 01.04.01.01 Patient demographics | 4 | 4 |
| 01.04.01.02 Health issues | 0 | 0 |
| 01.04.01.03 Number of patients | 9 | 10 |
| 01.04.02 Geography | 0 | 0 |
| 01.04.02.01 Rural | 12 | 39 |
| 01.04.02.02 Urban | 0 | 0 |
| 01.04.02.03 Other | 2 | 4 |
| 01.04.03 Other demographic information | 2 | 2 |
| 01.05 GP practices in collaboration | 0 | 0 |
| 01.05.01 Number of practices | 17 | 40 |
| 01.05.02 Information on specific practice in collaboration | 9 | 10 |
| 01.05.03 Other information on GP practices | 5 | 5 |
| 01.06 Implementation of collaboration | 0 | 0 |
| 01.06.01 Timeline | 4 | 5 |
| 01.06.02 Prior to becoming collaboration | 14 | 49 |
| 01.06.03 Process of implementation and rationale | 13 | 43 |
| 01.06.04 Other information on implementation | 0 | 0 |
| 01.07 Other general information | 0 | 0 |
| 02 Reason for becoming GP collaboration | 1 | 1 |
| 02.01 Policy and regulation-related reasons | 0 | 0 |
| 02.01.01 NHS Long Term Plan | 1 | 1 |
| 02.01.02 GP contract | 0 | 0 |
| 02.01.03 Other policy and regulation reason | 3 | 3 |
| 02.02 Care-related reasons | 0 | 0 |
| 02.02.01 More or improved services | 8 | 16 |
| 02.02.02 Patient outcomes | 2 | 3 |
| 02.02.03 Other care-related reasons | 3 | 4 |
| 02.03 Organisational reasons | 0 | 0 |
| 02.03.01 Financial reasons | 1 | 1 |
| 02.03.01.01 Money received by collaboration | 8 | 28 |
| 02.03.01.02 Money spent or used by collaboration | 4 | 4 |
| 02.03.01.03 Other financial reasons | 7 | 9 |
| 02.03.02 Non-financial organisational efficiency | 8 | 10 |
| 02.03.03 Other organisational reasons | 4 | 4 |
| 02.04 Other reasons to become collaboration | 4 | 4 |
| 03 Collaboration services | 0 | 0 |
| 03.01 Patient services | 0 | 0 |
| 03.01.01 Community-based services | 13 | 27 |
| 03.01.02 Digital services | 2 | 2 |
| 03.01.03 Extended hours | 9 | 14 |
| 03.01.04 Personalised or specialised services | 2 | 2 |
| 03.01.05 Population-level services | 6 | 9 |
| 03.01.06 Other additional services | 7 | 12 |
| 03.02 Organisational resources | 0 | 0 |
| 03.02.01 Shared administration and back office support | 10 | 21 |
| 03.02.02 Pooled resources | 8 | 13 |
| 03.02.03 Data sharing | 8 | 13 |
| 03.02.04 Other organisational resources | 8 | 10 |
| 03.03 Other collaboration services | 0 | 0 |
| 04 Impacts | 0 | 0 |
| 04.01 Services delivery impacts | 0 | 0 |
| 04.01.01 Positive | 12 | 34 |
| 04.01.02 Negative | 7 | 19 |
| 04.01.03 No or neutral impact | 13 | 14 |
| 04.02 Patient outcome impacts | 0 | 0 |
| 04.02.01 Positive | 9 | 14 |
| 04.02.02 Negative | 2 | 2 |
| 04.02.03 No or neutral impact | 4 | 5 |
| 04.03 Staff impacts | 0 | 0 |
| 04.03.01 Positive | 14 | 32 |
| 04.03.02 Negative | 10 | 25 |
| 04.03.03 No or neutral impact | 5 | 5 |
| 04.04 Organisational impacts | 0 | 0 |
| 04.04.01 Positive | 13 | 25 |
| 04.04.02 Negative | 8 | 20 |
| 04.04.03 No or neutral impact | 9 | 10 |
| 04.05 Financial impacts | 0 | 0 |
| 04.05.01 Positive | 12 | 20 |
| 04.05.02 Negative | 6 | 14 |
| 04.05.03 No or neutral impact | 11 | 19 |
| 04.06 Other impacts | 0 | 0 |
| 04.06.01 Positive | 2 | 3 |
| 04.06.02 Negative | 3 | 4 |
| 04.06.03 No or neutral impact | 3 | 3 |
| 05 Goals and metrics | 0 | 0 |
| 05.01 Stated goals of collaboration | 14 | 41 |
| 05.02 Metrics used to measure success | 10 | 15 |
| 05.03 Other information on goals and metrics | 4 | 5 |
| 06 What is going well | 0 | 0 |
| 06.01 Types of successes | 0 | 0 |
| 06.01.01 Ways of working and collaborating between staff | 15 | 39 |
| 06.01.02 Management and governance | 12 | 22 |
| 06.01.03 Services provision improvements | 13 | 37 |
| 06.01.04 Policy and regulation successes | 2 | 2 |
| 06.01.05 Resources | 7 | 9 |
| 06.01.06 Other types of successes | 6 | 7 |
| 06.02 Facilitators of success | 2 | 2 |
| 06.03 Other information on successes | 2 | 2 |
| 07 What is not going well | 0 | 0 |
| 07.01 Types of challenges or failures | 0 | 0 |
| 07.01.01 Ways of working and collaborating with staff | 20 | 39 |
| 07.01.02 Management and governance | 18 | 87 |
| 07.01.03 Services provision challenges | 11 | 27 |
| 07.01.04 Patient-level challenges | 3 | 5 |
| 07.01.05 Policy and regulation challenges | 17 | 63 |
| 07.01.06 Resources | 15 | 49 |
| 07.01.07 Other types of challenges or failures | 14 | 36 |
| 07.02 Tensions | 17 | 58 |
| 07.03 Overcoming challenges or failures | 12 | 21 |
| 07.04 Other information on challenges or failures | 2 | 3 |
| 08 Future of collaboration | 0 | 0 |
| 08.01 Future priorities | 22 | 74 |
| 08.02 Future challenges | 17 | 34 |
| 08.03 Other information on future of collaboration | 1 | 1 |
| 09 Other topics | 1 | 1 |
| 10 Interviewee information | 0 | 0 |
| 10.01 Role | 24 | 35 |
| 10.02 Other information about interviewee | 5 | 6 |
| 11 Quotes | 24 | 122 |
Appendix 5 Additional survey tables
Tables 8 and 9 provide additional information on survey responses for this evaluation.
| Reasons | Response, n (%) | |||
|---|---|---|---|---|
| Very important | Somewhat important | Not important | Not sure or N/A | |
| To help us meet the objectives of The NHS Long Term Plan4 | 7 (25) | 10 (36) | 4 (14) | 7 (25) |
| To help sustain the viability/sustainability of general practice | 15 (56) | 6 (22) | 0 (0) | 6 (22) |
| Access additional funding available to our practice via the PCN contract | 13 (46) | 7 (25) | 2 (7) | 6 (21) |
| Secure additional primary care services (practice-based pharmacy, social prescribing, etc.) | 12 (43) | 9 (32) | 1 (4) | 6 (21) |
| Improving co-ordination and delivery of primary care services for patients | 14 (52) | 6 (22) | 2 (7) | 5 (19) |
| Increasing collaborative working with other practices and primary care providers | 13 (46) | 6 (21) | 3 (11) | 6 (21) |
| Increasing opportunities for professional development for general practitioners and other members of staff | 7 (27) | 9 (35) | 3 (12) | 7 (27) |
| Enabling us to strengthen the management support available to our practice and local primary care services | 9 (32) | 9 (32) | 5 (18) | 5 (18) |
| Improving clinical governance arrangements across local practices and services (i.e. having a systematic approach to maintaining and improving the quality of patient care and service delivery) | 12 (43) | 10 (36) | 0 (0) | 6 (21) |
| Increasing involvement of primary care and general practice in decision-making about the commissioning of local health services | 9 (33) | 11 (41) | 0 (0) | 7 (26) |
| Challenges | Response, n (%) | Response total | |||
|---|---|---|---|---|---|
| Very challenging | Somewhat challenging | Not challenging | Not sure or N/A | ||
| Establishing governance arrangements for the PCN | 4 (14) | 10 (36) | 3 (11) | 11 (39) | 28 |
| Accessing funds specific to supporting collaborative/PCN working | 2 (7) | 8 (29) | 5 (18) | 13 (46) | 28 |
| Agreeing how funds will flow from the PCN to practice | 2 (7) | 10 (36) | 5 (18) | 11 (39) | 28 |
| Sharing data across practices with regard to clinical governance | 5 (18) | 6 (21) | 6 (21) | 11 (39) | 28 |
| Sharing data across practices with regard to service planning | 3 (11) | 7 (25) | 8 (29) | 10 (36) | 28 |
| Appointing a pharmacist | 6 (21) | 6 (21) | 5 (18) | 11 (39) | 28 |
| Appointing a social prescriber | 4 (14) | 5 (18) | 8 (29) | 11 (39) | 28 |
| Securing enough management and administration support | 5 (18) | 8 (29) | 6 (21) | 9 (32) | 28 |
| Building relationships and networks between those involved in the PCN | 4 (14) | 8 (29) | 8 (29) | 8 (29) | 28 |
| Securing sufficient leadership by senior members of collaboration | 5 (18) | 7 (25) | 7 (25) | 9 (32) | 28 |
| Agreeing aims and objectives for the PCN | 2 (7) | 6 (21) | 8 (29) | 12 (43) | 28 |
| Support and guidance provided by NHSE&I | 7 (25) | 5 (18) | 2 (7) | 14 (50) | 28 |
| Support provided by CCG | 4 (14) | 5 (18) | 6 (21) | 13 (46) | 28 (bottom of form) |
List of abbreviations
- BRACE
- Birmingham, RAND and Cambridge Evaluation
- CCG
- Clinical Commissioning Group
- CD
- clinical director
- DHSC
- Department of Health and Social Care
- GDPR
- General Data Protection Regulation
- GP
- general practice
- HR
- human resources
- HRA
- Health Research Authority
- HSDR
- Health and Social Care Delivery Research
- Int
- interview
- IT
- information technology
- NHSE&I
- NHS England and Improvement
- NIHR
- National Institute for Health and Care Research
- PCH
- primary care home
- PCN
- primary care network
- PCT
- primary care trust
- PM
- practice manager
- PMS
- personal medical services
- PPE
- personal protective equipment
- PPI
- patient and public involvement
- PRISMA
- Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- RCGP
- Royal College of General Practitioners
- REA
- rapid evidence assessment
- RQ
- research question
- RUC
- rural–urban classification
- TPP
- total purchasing pilot
- WP
- work package
Notes
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/GBUO3259).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
