Notes
Article history
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as project number 15/144/29. The contractual start date was in July 2017. The final report began editorial review in April 2022 and was accepted for publication in November 2022. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ manuscript and would like to thank the reviewers for their constructive comments on the final manuscript document. However, they do not accept liability for damages or losses arising from material published in this manuscript.
Permissions
Copyright statement
Copyright © 2024 Spilsbury et al. This work was produced by Spilsbury et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2024 Spilsbury et al.
Chapter 1 Introduction
Background and rationale
In England and Wales, an estimated 425,000 older people live in circa 18,000 care homes. 1 The care home population represents the oldest and most vulnerable groups in society. Older people are entering care homes later, approximately 70% are living with cognitive impairment2 and 76% requiring assistance with mobility. 3 People now living in residential homes (care homes without nursing) would likely have been in nursing homes (care homes with nursing) 5–10 years ago. Nursing homes today provide care once delivered in acute hospitals. 4–7 This is due to increase in chronic progressive conditions that require more intensive care and resources, changes in the role of care homes to manage acute patients following a hospital admission (step-down care) and to prevent an admission to hospital (step-up care). 8 Care homes deliver end-of-life care for many. 9,10 This complex mix of residents shapes the type and level of care and services required. Change will continue as the social care system responds to financial constraints and reduced healthcare support to care homes.
Staffing is the largest operating cost for care homes11 and the quality of care provided within care homes is contingent on the nursing and direct care support workforce – a resource that homes struggle to recruit and retain. 12,13 The coronavirus disease 2019 (COVID-19) pandemic has exacerbated the pre-existing effects of the variation in staffing between and within homes. 14 This study was commissioned in part due to the lack of understanding about factors influencing variations in direct care staffing and turnover, and the impact on residents and relatives, staff and healthcare resources. Previous studies commissioned by the National Institute for Health and Care Research (NIHR) focused on the interface between care homes and the healthcare inputs needed for equitable and optimum care. 15 Our study is unique in that its focus is on direct care staff employed within the care home and the ways in which deploying this workforce and its skill mix impact on quality. This study was commissioned at the same time as a study on the relationship between workforce employment conditions and training, Care Quality Commission (CQC) quality ratings and the health- and care-related quality of life of care home residents. 16
At the time of reporting – 2 years after the first cases of COVID-19 were detected in the UK – there is increasing recognition of the pivotal role of care homes in supporting older people and meeting their long-term needs in ways that reflect their preferences for care and support. 17 Understanding how best to provide care and support for residents through effective use of human resources in homes is societally and politically important. Ensuring quality for care home residents is the subject of ongoing international debate involving the public, policy-makers, commissioners, providers, clinicians and researchers. 4,18 The government recognises the role of social care staff and the need to recognise, reward and invest in development of this workforce. 19
We consider below the care home context and its workforce, the concept of quality for this setting and previous studies of the staffing–quality relationship.
Care homes and the direct care workforce
Care homes are not part of the NHS; they are independent organisations, including for-profit chains, not-for-profit third-sector organisations and privately owned homes or companies with only a small number of homes. 20 Care in this sector is funded through a mix of self-funding, means-tested support from local authorities and continuous healthcare funding from the NHS. Over one-third of people living in care homes pay (in full or in part) for their own care; others are supported by public funding (local authority, NHS continuing care or through some combination of local authority, charity and NHS support). 21 Self-funding residents are reported to pay higher fees compared to those funded by local authorities and this price differential is perceived by many as unfair and predicted as unsustainable for future care provision. 20,22
Care homes in England (the context for this study) include homes with nursing (or nursing homes), without nursing (or residential homes), or both (dual registered homes). There is considerable overlap in dependency levels and care needs among residents in care homes with and without nursing. 5 However, important differences exist in the workforce in different types of care homes.
In homes with nursing care, registered nurses (RNs) are employed around the clock to supervise care delivery which is mainly provided by a large workforce of non-registered care staff, also known as care support staff or care assistants (CAs). RNs in these homes will provide clinical care and support and liaise with other healthcare professionals on behalf of residents. In care homes without nursing, the workforce comprises only social care staff. The NHS provides healthcare input (including nursing care) on an ‘as required’ basis. Registered NHS nurses may be involved in supporting specialist care for residents in both types of care homes (e.g. palliative care). Care staff in either of these settings (with and without nursing or dual registered) are employed at different levels (e.g. as CA, senior CA or nursing assistant). While not registered with any professional body (e.g. the Nursing and Midwifery Council), many of these social care staff possess vocational qualifications or have completed the Care Certificate. 14 In recent years (from 2019), the nursing associate role has been introduced into the sector. 23 Nursing Associates work alongside RNs, taking on some clinical skills previously undertaken solely by RNs.
The most recent Skills for Care report provides a detailed profile of the care home workforce (2020/21):14
-
there are 470,000 direct care staff in care homes with and without nursing;
-
there are 31,000 RNs in care homes with nursing;
-
there has been a significant decrease (33%) in number of RNs in the sector since 2012–3;
-
there are high turnover rates of RNs and care support workers;
-
vacancy rates are high in the sector with the highest vacancy rates for registered managers;
-
the majority of the workforce identify as female (82%) and were more likely to work in direct care roles (83%) than in managerial roles (79%);
-
over one-quarter (27%) of workers are aged 55 years and over;
-
the social care workforce is more diverse (21% ethnic minorities) than the general population (14%).
Staffing profiles and establishments vary across provider organisations due to funding arrangements and geographical location. This variation means studying care homes and those who work in them is complex.
Quality in care homes
Quality – as a concept – is similarly complex: it is contested and dynamic. Several formulations are both possible and legitimate and individual stakeholder perspectives shape its definition. In the care home context, these perspectives include residents, relatives, care home staff, NHS staff, provider or commissioning organisation, regulatory bodies and policy-makers. The ways in which quality is measured, monitored and reported in care homes is a topic debated internationally and difficulties arise because of the diverse range of views, values, expectations and preferences held by these different key stakeholders.
In England, care home quality is regulated by the CQC. CQC conduct inspections and award publicly available ratings of care homes. Quality ratings are based on inspectors’ assessment of evidence gathered using five key lines of enquiry (KLOEs): ‘safe’, ‘effective’, ‘caring’, ‘responsive’ and ‘well led’ (see Appendix 1). Inspectors use four sources of information: (1) CQC’s ongoing relationship with the provider; (2) ongoing local feedback and concerns; (3) pre-inspection planning and evidence-gathering; and (4) the inspection visit. An overall rating is aggregated from ratings for each of the KLOEs, with ratings awarded on a four-point scale: ‘outstanding’, ‘good’, ‘requires improvement’ or ‘inadequate’. 24 In 2021, 85% of residential homes and 78% of nursing homes were rated as good or outstanding. 22 The frequency of CQC inspection visits varies depending on a care home’s rating, but care homes may be inspected at any time. 24 Local authorities and commissioners ensure that care homes they work with are fulfilling their statutory and contractual responsibilities, but this information is not publicly available.
Understanding the staffing–quality relationship in care homes
Two dimensions of quality need to be considered in this context: quality of care and quality of life. While the nature and characteristics of the care home workforce, and their approaches to care, are likely major determinants of quality, research into the staffing–quality relationship is comparatively scarce – when compared to acute health care. There is some evidence that care home staff have an impact on satisfaction. 25,26 The measurement of quality in homes (with an emphasis on staffing) has predominantly focused on clinical outcomes: pressure ulcer prevalence, falls or medication errors. Evidence, mainly from North America, suggests ‘inadequate’ staffing levels in care homes reduce quality and that the numbers – rather than skills – of workers improve quality. 17,27 These findings must be treated cautiously as they are drawn mainly from cross-sectional studies, are inconsistent, involve non-contemporaneous data sets and assume staffing and quality are linearly related. Most extant longitudinal studies which have attempted to address these limitations have been conducted in North America. 27,28 There are no previous studies on the relationship between nurse staffing and quality in English care homes. Previous analyses of care homes in England found quality was positively correlated with staff retention and a significant negative relationship with job vacancies;29 and that a deficiency in staffing could lead to care home closure. 30 More recently, Towers et al. 16 identified that improving working conditions (such as wages and training) and reducing staff turnover are associated with increased quality and outcomes for care home residents.
Our mixed-method (QUAL-QUANT) parallel design study builds on existing work and addresses some of the methodological challenges associated with understanding the staffing–quality relationship, using a theoretical framework31 to understand quality through structures, processes and outcomes.
Chapter 2 Study aim and objectives
The aim of the Staffing Relationship to Quality in care homes (StaRQ) mixed-methods study was to investigate the most effective workforce models of nursing and care support in care homes for the sustained benefit of residents, relatives and staff.
Study objectives were to:
-
describe variations in the characteristics of the care home nursing and support workforce [work package (WP) 1];
-
identify the dependency and needs of residents and relatives in care homes and their association with care home staffing (WP2, WP3);
-
examine how different care home staffing models (including new roles) impact on quality of care, resident outcomes and NHS resources (WP1, WP2, WP3);
-
explain how care home workforce (numbers, skill mix and stability) might meet the dependency and needs of residents (WP1, WP2, WP3, WP4);
-
explore and understand the contributions of the nursing and support workforce (including innovations in nursing and support roles) in care homes to enhance quality of care (WP1, WP4);
-
translate methods used for modelling the relationships between staffing and quality to provide a platform for sector-wide implementation (WP5).
Chapter 3 Methodology and methods
Donabedian’s theoretical framework31 of quality (focusing on structures, processes and outcomes) framed our understanding of the relationship between care homes’ workforce and quality for residents. Structure is the (relatively) stable features of the organisation that affect its ability to deliver care and services. Process is the interactions between provider and consumer; what is done for and with residents by the provider. Outcomes are those end results attributable to antecedent care.
Quality is complex, contested and dynamic; several definitions are possible and legitimate. Individual perceptions, values, expectations and preferences in the care system all shape the concept. The care home system includes residents, relatives and care home staff, as well as external health and social care providers: NHS staff, commissioning organisations, regulatory bodies and policy-makers. Quality is further complicated as homes must address both quality of care and quality of life. Our mixed-method (QUAL-QUANT) parallel design study was designed to address the complex nature of quality; it was viewed broadly, and our five interlinked WPs – involving literature reviews, quantitative analysis, documentary analysis and qualitative fieldwork – sought to unpick structures, processes and outcomes from a variety of perspectives.
Work package 1 highlights the care home workforce context for quality by (1) reviewing descriptive research into the roles and responsibilities of RNs and CAs and (2) a realist review generating and outlining theories of how and why workforce is related to quality in care homes. In WP2 and WP3 we used routinely collected measures of staffing and examined (longitudinally) the relationship of these to measure of quality (outcomes). WP3 also examines the costs of quality – to care home providers the wider impacts of variable quality on the health and social care system. In WP4 we analysed CQC inspection reports of homes rated outstanding or inadequate, to develop understanding of how (1) care homes ensure a workforce to support people living in care homes and (2) the workforce enhances quality for residents. WP5 constitutes an important translational phase; we explore the advice and influence networks between home staff and ‘readiness’ for implementing innovations.
Our study was impacted by the COVID-19 pandemic. Accordingly, deviations from our original protocol were necessary (see Appendix 2). We used alternative methods wherever possible to address our original study objectives.
Work package 1: determining the characteristics of the care home workforce and understanding quality
Two literature reviews were conducted.
Work package 1i: roles and responsibilities of the care home workforce linked to quality
A systematic review synthesised studies of care home staff (RNs and CAs) perceptions of their role. The protocol was registered with PROSPERO. 32
Data sources
Search strategy and information sources
A search strategy was developed with an information specialist in February 2021 (see Appendix 3). Text words and subject headings (where available) were used. Limits applied to the search included a date limit (2010 onwards) and English language. This date restriction was applied to ensure the evidence reflected the current practice of staff in care homes. The following databases were searched: MEDLINE I ALL (Ovid), EMBASE (Ovid), APA PsycINFO® (Ovid), CINAHL (EBSCO), Web of Science (all databases, Clarivate) and Applied Social Science Index and Abstracts (ProQuest). The database search identified 3871 records.
Study selection
Search results were imported into Rayyan (https://rayyan.qcri.org/). Two reviewers (RD, KH) independently screened all titles and abstracts, assessing against the inclusion/exclusion criteria (Box 1). This process ensured the criteria were consistently applied. Discrepancies were resolved through discussion (RD, KH) or by including a third reviewer (KS). The full articles of included papers (n = 109) were retrieved, and two reviewers (RD, KH) confirmed study eligibility (n = 25). The reference lists of included studies were also screened: 11 additional studies were included. The review includes a total of 36 studies (see Appendix 4).
Inclusion criteria – studies needed to meet all of these criteria to be eligible:
-
staff employed by the care home (RNs and care staff)
-
staff describing their roles and responsibilities related to general day-to-day care and life for residents to live well
-
links established between roles and responsibilities and residents’ quality of care or quality of life
-
reporting original research
-
published in full, and in English between 2010 and 2021
Exclusion criteria – the study focus was on:
-
the care home manager, who has a broader role than direct care for residents
-
staff employed in care homes but who do not provide direct care for residents (e.g. housekeeping or catering staff)
-
healthcare professionals who are not employed by a care home but who may visit the care home to provide care for residents (e.g. RNs working for community nursing teams)
-
temporary staff employed by agencies who intermittently work in a care home
-
staff experiences and attitudes towards their work
-
end-of-life care
-
non-empirical (such as opinion or discussion articles) published prior to 2010
Data extraction
Data on author, year, study location, study aim, study rationale, theoretical framework, research question, participant characteristics, study setting and data collection and analysis methods were extracted. The review question guided extracting data from the results and discussion sections of included studies. Results of interest were staff perceptions of their roles and responsibilities that contributed to quality: we were interested in both quality of care and quality of life because of the care context. Links between roles and responsibilities and qualities could be explicit or related to concepts indicating quality. For example, relationships or dignity were considered indicators of quality of life and identifying and recognising deterioration in residents were indicators of quality of care. Data were extracted and organised for results using three worksheets in Microsoft Excel to extract data for studies focused on (1) CAs, (2) RNs and (3) both CAs and RNs. Data were extracted by one reviewer (RD or KH) and checked by the other (RD, KH). Discrepancies were discussed with a third reviewer (KS). Included studies were those where authors made explicit links between staff responsibilities and quality of care and life, or made links to a concept or concepts.
Quality assessment of studies
Studies were quality assessed using the Mixed Methods Appraisal Tool (MMAT). 33 Two reviewers (RD and KH) independently screened and assessed methodological quality. Disagreements were resolved through discussion with a third reviewer (KS). We did not exclude studies based on quality assessment, but we were able to appraise the quality of evidence available to address our question. See Appendix 5.
Data analysis
We used content analysis:34 this approach supports analysis of large amounts of text data. There were four stages to our analysis: (1) familiarisation with the data; (2) organising data into meaning units; (3) coding data to higher level themes; and (4) refining higher level themes. One researcher (RD) iteratively coded data relating to roles and responsibilities and quality of care and life. Coding was developed for different roles: RNs and CAs. Organising data in this way supported comparative analysis so that we could identify similarities, differences and patterns in roles and responsibilities. We ensured an audit trail of the review process to enhance transparency. A team of three researchers was used for analysis and interpretation.
A narrative synthesis of our analysis is presented in Chapter 4.
Work package 1ii: care home staff behaviours for promoting quality of resident experience
Our realist review developed evidence and theory-based explanations of how care home staff promote resident quality of care and quality of life, why and in what circumstances. 35,36 Theories were developed in three stages: (1) elicitation, (2) development and testing and (3) refinement. Consultation with residents, relatives, staff, providers, commissioners, regulators and policy-makers ensured sense-checking of our theories and improved our explanation and analysis. 37,38 See Appendix 6 for review process.
The review protocol was registered with the Research Registry (registration number 1062: https://tinyurl.com/mxt8s2h6). RAMESES reporting standards guided our review processes. 36 Our methods have been published by Elsevier Ltd, Crown Copyright © 2021;39 permission is granted by Elsevier for use in this report.
Stage 1: theory elicitation
Defining the scope of the review: concept mining and initial theory development
This stage provided the structure and framework for exploring and synthesising diverse research. 40 First, the most recent systematic review of the relationship between staffing and quality27 was used to develop preliminary explanations by identifying key concepts and theories. Six ‘If–Then’ statements41 derived from the included studies, were further mined to develop ideas and assumptions about how and why staffing influences quality (see Appendix 7). We used these statements to articulate programme theories containing possible social rules, values or sets of interrelationships38 that might limit or trigger programme mechanisms and their linked outcomes.
In line with Pawson et al. ,40 our programme theories were iteratively scrutinised and agreed with stakeholders to refine review scope. We had two stakeholder groups: (1) care home residents and relatives (n = 5) and (2) care home managers (n = 7). Each group met three times during the review period. In the first meeting, residents and relatives directed us towards one area: how everyday human interactions that occur between staff and residents shape residents’ experiences of care. In the words of stakeholders, ‘how staff made residents feel’. Care home managers confirmed the importance of this link. Staff behaviours became a key concept (theory area) linked to ‘quality’.
Mapping staff behaviours against research-reported staffing model characteristics and quality outcomes42–44 confirmed the working hypothesis. By way of illustration, in one qualitative study, behaviours such as ‘getting to know the resident’ and ‘treating residents like their mum or dad’, generated resident ‘joy’ and ‘satisfaction’. 45 These behaviours became the focus for our review and theory development.
To frame our review and help isolate key behaviours and associated triggers, we used Michie et al. ’s COM-B theory. 46 COM-B suggests behaviour results from three interacting components in people or teams: capabilities (the psychological or physical abilities of people to enact behaviours); opportunities (the physical or social environment that enables behaviours); and motivations (reflective and automatic mechanisms that activate or inhibit behaviour). Using COM-B and bespoke data extraction forms we coded data from studies on staffing and quality as capabilities, opportunities, motivations or behaviours. Demi-regularities, or patterns, then provided the basis for context–mechanism–outcome configuration development. 35 By the end of stage 1, our review questions had evolved to become:
-
What staff behaviours influence care home residents’ experience of quality?
-
What influences the behaviour of care home staff?
-
What impact does the interaction between staff behaviours and context have on care home residents’ experience of quality?
We sense checked our review questions in stakeholder meetings where the importance of the multilayered relationships staff had with those they care for and work with and how these relationships influence staff behaviours and quality as experienced by residents was highlighted.
Stage 2: theory development and testing
Search, appraisal, extraction and synthesis of evidence
This stage involved systematically searching, appraising, extracting and narratively synthesising evidence to test and develop emergent programme theory from stage 1. 40
Search strategy
With an information scientist, we designed an inclusive search strategy to maximise data for extraction around three central concepts – long-term care facilities, staffing and quality – and searched a range of databases from inception to November 2019 (see Appendix 8). To minimise the risk of missing eligible studies we additionally: (1) consulted experts from the research team members’ networks; (2) forward citation matched; and (3) scanned reference lists of identified papers.
Selection and appraisal of documents
Search results were saved, managed and duplicates removed using EndNote. Titles and abstracts of the retrieved papers were screened for inclusion by the study team (KH, KS, CT, BH, AA, DV).
Studies were included if they:
-
addressed the relationship between staffing models and quality (quality of life and/or quality of care);
-
took place in a care home context;
-
explicitly focused on quality or, implicitly, accounts of quality similar to our working model of quality based on ‘how staff make people feel’;
-
addressed capabilities, opportunities, motivations and/or behaviours.
Studies were excluded if they:
-
did not focus on staffing AND quality;
-
were not research, that is unsystematic approach to inquiry;
-
were not conducted in care homes;
-
if they focused on external providers – this work has already been done. 47
Study quality was assessed qualitatively for:
-
relevance – degree of contribution to theory building and/or testing; and
-
rigor – whether the method used to generate the data was credible and trustworthy. 36
Studies were included if they contributed to the initial programme theory of stage 1. Full-text papers marked for inclusion were retrieved and read in full by (KH and KS). Any disagreements were resolved through discussion with members of the wider research team (CT, BH, AA, DV) and with reference to the review framework and emergent programme theory. 40 Sixty-six studies were included in this review.
Data extraction
Data on staff behaviours and triggers (capability, opportunity, motivation) and their interaction in care home settings were extracted. KH and KS double-extracted data from over a third of the included papers (n = 25; 38%). This was done in three stages: KH and KS both extracting from five papers then discussing, followed by two further rounds (with 10 papers in each round) with discussion. Piloting and double extraction from a sample of papers were used to promote consistent and comprehensive data extraction. KH extracted data for all included papers. Data from author explanations and discussions can help make explicit in what context, which mechanisms lead to which outcomes48 and so were included.
Stage 3: theory refinement
In this final stage, we refined context–mechanism–outcome configurations and examined supporting evidence in three researcher-led discussions during November to December 2019 with our stakeholder groups which included: residents and relatives (group 1) and care home managers (group 2), and our Study Steering Committee (SSC) members (including representatives from provider organisations, policy-makers, regulators, methodologists and members of the public). Stakeholders were invited to comment critically on the resonance, relevance and gaps in our theories. Revision of context–mechanism–outcome configurations after each discussion led to the final set of refined context–mechanism–outcome configurations (presented in Chapter 4).
Work package 2: modelling relationships between staffing and quality at a national level
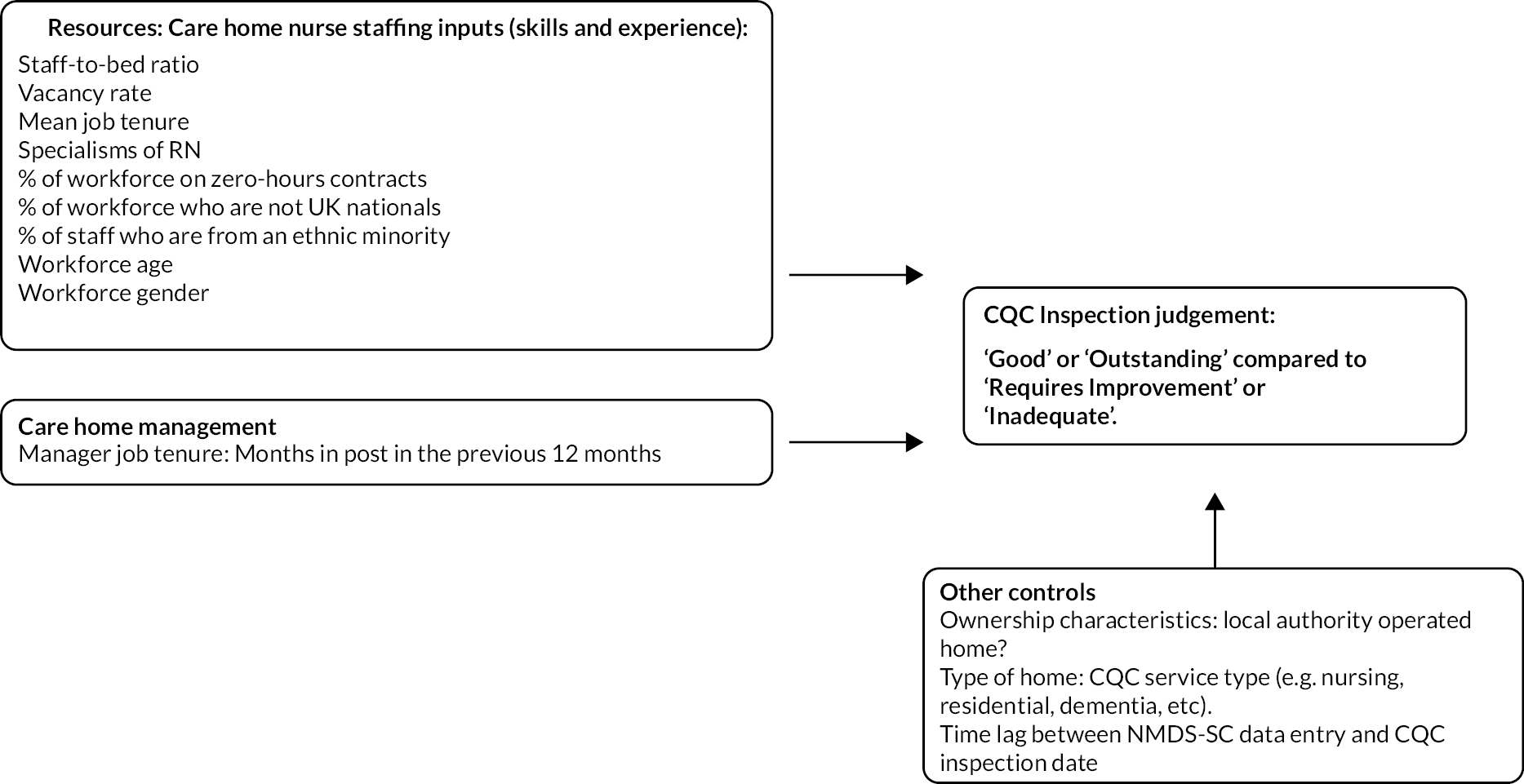
This was a cross-sectional observational study of a subpopulation of English care homes providing workforce data to Skills for Care for the National Minimum Data Set for Social Care (NMDS-SC) in the period September 2014–July 2017: the NMDS-SC was replaced by the Adult Social Care Workforce Data Set (ASC-WDS) in August 2019. CQC inspection judgements about care quality (see below) were modelled as functions of the staffing resources of the homes while accounting for organisational characteristics of the home operator (Figure 1).
FIGURE 1.
The relationship between workforce characteristics and care quality outcomes in the NMDS-SC.
Measuring care quality
All care homes in England are subject to regular inspection by the CQC, with the precise timings of inspections dependent on a risk-based model developed by the CQC using data regularly reported to it by care homes. CQC inspectors make judgements about whether care homes (with and without nursing) are (1) safe, (2) effective, (3) caring, (4) responsive and (5) well-led (see Appendix 1). The results of their judgements are reported as being inadequate, requiring improvement, good or outstanding, with a judgement using this scale for each of the five categories and an overall judgement. 49 In practice, over 75% of inspection judgements are ‘good’, with around a fifth requiring improvement and much smaller numbers in the ‘outstanding’ and ‘inadequate’ categories. 22
This inspection method assesses care quality through expert professional judgements informed by data analysis and relatively short audit visits to care homes. Whether this approach accurately conceptualises and measures care quality is debatable, but we took a pragmatic view that CQC inspection judgements tell us something useful and interesting about the care quality that homes provide. In particular, we are interested in relationships between the CQC measure of care quality and care homes’ staffing establishments. Is there evidence of different approaches to staffing establishments and do different approaches lead to different outcomes? Our approach was novel because existing studies of relationships between staffing and care quality focus on clinical indicators. These may be sensitive to the quality of nursing care50,51 but miss broader conceptions of care(r) quality.
Data sources
The study draws on NMDS-SC data from September 2014 to July 2017. It includes records from 5028 individual care homes in England, in the CQC-regulated activities category of ‘accommodation for persons requiring nursing or personal care’ which reported that they provided services to older people. This is approximately 50% of care homes for older people regulated by the CQC: 36% of homes (n = 1785) in the data set were care homes with nursing, the remainder (n = 3243) without nursing (residential care). Data are collected through care home operators making voluntary returns, detailing aspects of their workforce and home characteristics, to Skills for Care. Substantially incomplete records, and/or records that contained obvious data entry errors, were excluded from our analysis.
Participation in the NMDS-SC is voluntary. While the data set covers a high proportion of English care homes, it may not be representative of the whole sector. Internal analysis from Skills for Care52 suggests independent care home operators are less likely to participate than local authority-run homes (24% of homes in our data set are operated by local authorities). Homes in London and the South East are less likely to participate, while homes in the North East are more likely to participate. Larger multihome operators are more likely to participate than smaller operators. Care home operators who do not participate, or who participate but provide incorrect or substantially incomplete data may also differ from those included in our analysis in important but unobservable ways. However, it is worth highlighting that CQC inspection scores did not differ substantially between care homes that submitted data to the NMDS-SC and those that did not.
The data should be thought of as a population data set (where the population is all care homes that participate in NMDC-SC without significant amounts of missing data and date-entry errors) rather than a sample. Results will not necessarily generalise to care homes that do not participate in the study, but the analysis is still of value because of the large proportion of English care homes that participate. Skills for Care extracted data from the NMDS-SC data set that included measures of care home and workforce characteristics (Box 2).
Workforce measures
-
Total staff (including non-care staff)
-
Percentage of staff who are on permanent contracts (as opposed to staff provided by an employment agency or on temporary contracts)
-
Percentage of staff on zero-hours contracts (i.e. where staff are not contracted to work a specific number of hours a week but are called into work when they are needed)
-
Percentage of posts that are unfilled (vacancy rate)
-
Average staff job tenure
-
Percentage of staff who are full-time
-
If a care home with nursing, the specialism of the RN working in the home (four categories: community nursing, older people, adults, mental health)
-
Number of months that the registered manager had been in post in the year prior to the most recent inspection
Care home characteristics measures
-
Number of resident beds (including occupied and unoccupied beds)
-
Staff-to-bed ratio was computed from data on staff and bed numbers
-
Whether the home was operated by a local authority or independent operator
-
Whether the home provides specialist dementia care
-
Whether the home provides nursing care
-
Dates on which care homes provided data to the NMDS-SC
Data on each home’s latest CQC inspection scores along with the date of the inspection were added to this data set. CQC scores are reported in Table 1. The time between data entry into the NMDS-SC and the date of the CQC inspection was calculated and included in the analysis to control for measurement error arising from changes to staffing between data entry and inspection (the median gap between data entry and inspection was 2 months with half of all inspections within 7 months of data entry). Table 1 reports the distribution of CQC scores among homes in the sample.
| All (%) | Care homes without nursing (%) | Care homes with nursing (%) | |
|---|---|---|---|
| Outstanding | 1.9 | 2.0 | 1.8 |
| Good | 72.8 | 67.8 | 74.8 |
| Requires improvement | 23.5 | 27.6 | 21.9 |
| Inadequate | 1.8 | 2.6 | 1.5 |
| Number of observations | 5028 | 1785 | 3243 |
Note that 72.8% of homes were judged to be good, with just 1.9% judged outstanding, 23.5% requiring improvement and 1.8% inadequate. Residential care homes without nursing care were slightly more likely to be in both the outstanding and require improvement category than homes with nursing care. This lack of variation in our key outcome measure has implications for our analytical approach which we explain below. Descriptive statistics for all these measures are reported in Table 2. The data set also contain data on CQC service type (e.g. dementia, learning difficulties, mental health) as some homes reported providing care to residents in more than one CQC category (i.e. not just to older people). These variables were not used in the analysis reported below (because preliminary analysis found no relationship between them and CQC scores) but they are reported for information.
| Variable | Nursing and residential homes | Care homes with nursing | Residential homes | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Median | IQR | Mean | SD | Median | IQR | Mean | SD | Median | IQR | |
| CQC rating (good + outstanding) | 0.747 | 0.435 | – | 0.698 | 0.459 | – | 0.766 | 0.423 | – | |||
| Number of beds | 37.331 | 20.684 | 48.194 | 23.457 | 33.067 | 18.164 | ||||||
| Total number of staff (headcount) | – | 36.000 | 31.000 | – | 52.000 | 34.000 | – | 24.000 | 24. | |||
| Staff-to-bed ratio | 1.230 | 0.554 | – | 1.310 | 0.546 | – | 1.183 | 0.537 | – | |||
| Proportion of staff who are on permanent contracts | 0.918 | 0.098 | 0.906 | 0.095 | 0.924 | 0.099 | ||||||
| Vacancy rate | 0.021 | 0.085 | 0.021 | 0.08 | 0.021 | 0.086 | ||||||
| Staff tenure (years) | 4.451 | 2.605 | 4.010 | 2.185 | 4.624 | 2.763 | ||||||
| Proportion of workforce who are employed full time | 0.528 | 0.240 | 0.583 | 0.21 | 0.507 | 0.248 | ||||||
| Proportion of workforce on zero-hours contracts | – | 0.00 | 0.078 | – | 0.023 | 0.1 | – | 0.00 | 0.067 | |||
| Specialism of RN – older people (yes, proportion) | – | – | 0.331 | 0.406 | – | – | – | |||||
| Specialism of RN – adults | 0.232 | 0.349 | ||||||||||
| Specialism of RN – learning difficulties | 0.026 | 0.127 | ||||||||||
| Specialism of RN – mental health | 0.060 | 0.171 | ||||||||||
| Specialism of RN – community care | 0.003 | 0.028 | ||||||||||
| Specialism of RN – other | 0.005 | 0.039 | ||||||||||
| Workforce age | 43.643 | 4.544 | 43.339 | 3.998 | 43.747 | 4.757 | ||||||
| Proportion of workforce who are female | 0.866 | 0.102 | 0.847 | 0.087 | 0.875 | 0.107 | ||||||
| Proportion of workforce with a disability | – | 0.00 | 0.018 | – | 0.00 | 0.017 | – | 0.00 | 0.02 | |||
| Proportion of workforce who are not UK nationals | 0.026 | 0.088 | 0.045 | 0.11 | 0.016 | 0.073 | ||||||
| Proportion of workforce who are ethnically white | 0.925 | 0.21 | 0.629 | 0.135 | 0.944 | 0.174 | ||||||
| Number of months that a manager was in post in the 12 months prior to inspection | 12.000 | 0.00 | 12.000 | 1.0 | 12.000 | 0.0 | ||||||
| Months between NMDS-SC data entry and CQC inspection | 2.000 | 7.0 | 2.000 | 8.0 | 2.0 | 6.0 | ||||||
| Proportion of homes operated by local authorities | 0.235 | 0.403 | – | 0.221 | 0.347 | – | 0.254 | 0.413 | – | |||
| NMDS service flag (care homes with nursing, proportion) | 0.355 | 0.478 | 1.000 | 0.000 | – | |||||||
| CQC service type: dementia (proportion) | 0.653 | 0.476 | 0.674 | 0.469 | 0.648 | 0.477 | ||||||
| CQC service type: children 0–18 years of age | 0.002 | 0.047 | 0.003 | 0.053 | 0.001 | 0.044 | ||||||
| CQC service type: learning disabilities | 0.111 | 0.314 | 0.074 | 0.262 | 0.124 | 0.329 | ||||||
| CQC service type: mental health | 0.175 | 0.38 | 0.183 | 0.387 | 0.170 | 0.376 | ||||||
| CQC service type: people who misuse drugs and alcohol | 0.012 | 0.11 | 0.013 | 0.115 | 0.012 | 0.111 | ||||||
| CQC service type: people detained under MHA | 0.01 | 0.101 | 0.016 | 0.115 | 0.009 | 0.097 | ||||||
| CQC service type: people with an eating disorder | 0.009 | 0.095 | 0.011 | 0.105 | 0.009 | 0.096 | ||||||
| CQC service type: physical disabilities | 0.362 | 0.481 | 0.481 | 0.5 | 0.313 | 0.464 | ||||||
| CQC service type: sensory impairment | 0.184 | 0.388 | 0.192 | 0.394 | 0.180 | 0.384 | ||||||
| CQC service type: whole population | 0.002 | 0.042 | 0.002 | 0.047 | 0.002 | 0.044 | ||||||
| CQC service type: younger adults | 0.216 | 0.412 | 0.295 | 0.456 | 0.181 | 0.384 | ||||||
| CQC-regulated activities: accommodation for persons requiring nursing or personal care | 1.0 | 0.017 | 1.000 | 0.0 | 1.000 | 0.019 | ||||||
| CQC-regulated activities: nursing care | 0.001 | 0.034 | 0.003 | 0.058 | – | |||||||
| CQC-regulated activities: personal care | 0.026 | 0.158 | 0.016 | 0.126 | 0.028 | 0.167 | ||||||
| CQC-regulated activities: assessment or medical treatments | 0.349 | 0.476 | 0.898 | 0.302 | 0.116 | 0.321 | ||||||
| N observations (locations) | 5028 | 1785 | 3243 | |||||||||
Table 2 provides some insight into between home variations in care home workforce. The average number of beds per home was 37, with homes that provided nursing care typically larger (mean beds = 48) than residential homes (mean beds = 33). The median number of staff employed was 36 (52 in homes with nursing; 33 in homes without nursing. Note that we focus on total staff employed as our main measure of staffing because in preliminary analysis including more detailed measures of staffing by job grade prevented our multilevel models from converging; in our judgement the total staff measure was the best way of balancing parsimony with model performance). The interquartile ranges for this measure were quite large: 34 for homes with nursing and 18 for homes without nursing, suggesting significant variation in numbers of staff employed in different homes. The mean staff-to-bed ratio was 1.23 (1.31 in homes with nursing and 1.18 in homes without nursing). On average, 2% of posts were vacant, but with a relatively high standard deviation suggesting a significant proportion of homes with large numbers of vacancies. Mean staff tenure was 4.5 years. On average, 53% of staff were employed in full-time posts. Mean staff age was 44 years. Over 85% of the workforce were female. Around 8% were from ethnic minorities and 2.5% were not UK nationals.
The NMDS-SC has a number of strengths and weaknesses compared to the extant literature. The data cover a high proportion of care homes in England (although as discussed above, results cannot necessarily be generalised to the total population of care homes). It includes measures of aspects of staffing likely to be important for care quality that have not been present in many previous studies, specifically the extent to which a home uses temporary staff, the role-related experience of staff and the proportion of jobs unfilled and detailed measures of staffing by job grade. Key factors likely to have a causal impact on care quality, specifically the acuity of resident care needs and occupancy levels, and many characteristics of the home (e.g. whether it is run for profit, whether it is a purpose-built facility) are not captured by the data set. These limitations need to be kept in mind when considering the results of our analysis below.
Data analysis
Latent profile analysis
To examine whether it was possible to discern any patterns in variations in staffing between homes and whether different care home staffing models might be associated with care quality we first examined whether it was possible to detect distinct home/staffing models. Specifically, we attempted to see if it was possible to identify homes with similar workforce characteristics (e.g. similarities/differences in staff-to-bed ratios, patterns of staff experience or temporary staffing use). To do this, we used latent profile analysis (LPA) using the R package tidyLPA. 53,54 LPA is a type of modelling that uses Expected Maximisation algorithms to find maximum likelihood parameters of the statistical model, assuming that it is derived from unobserved latent variables. 55 LPA is a data-driven approach pertinent to a research design in which a number of clusters is not assumed in advance. However, this analysis did not provide any evidence of distinct care home staffing models.
Next, we used multilevel logistic regression to test for relationships between the workforce characteristics described in Table 2 and CQC scores to examine whether differences in workforce characteristics were associated with differences in CQC assessments of quality.
Multilevel logistic regression
We originally planned to treat CQC inspection scores as an ordinal measure of quality. However, 75% of CQC ratings were reported as ‘good’ (see Table 1). However, preliminary analyses suggested that ordered logit analysis was technically inappropriate because the proportional odds assumption was violated. Further confusion matrices derived from ordered logit models found that these models failed to correctly predict both inadequate and outstanding homes. Therefore, we split the CQC score variable into homes rated ‘inadequate’ or ‘requires improvement’ in one category and ‘good’ or ‘outstanding’ in the other and proceeded with logit analysis on this binary outcome.
Local authorities in England act as commissioners and funders of social care for residents and have statutory responsibilities to promote the efficient and effective operation of a market for care services in their locality and must foster workforce development and continuous improvements in service quality. 56 Further, around a fifth of homes in the data set were directly operated by local authorities. Therefore, to account for variations in approach taken by local authorities in managing these homes and in fulfilling their statutory duties, we took a multilevel approach. Where homes are clustered within local authorities, we fitted multilevel logistic regression models using R software environment for statistical programming and data visualisation. The main effects were estimated by multilevel (hierarchical) logistic regression. This is a nested model: care homes represent level one and local authorities with social care responsibilities level two.
Multilevel (hierarchical) regression was appropriate because CQC inspection ratings varied significantly by local authority – as evidenced by the intraclass correlation (ICC) score in regression outputs (ICC score captures the proportion of variation in CQC scores that is due to differences between local authorities). Conditional and marginal R-squared show the proportion of variance explained by fixed effects only and the entire model, respectively. We fitted three separate models. The first is for all homes for older people (nursing and residential), the second is for homes that provide residential care only, and the third is for homes that provide nursing care. This is because relationships between workforce characteristics and quality may differ in these different contexts.
Cost–benefit analysis
Our initial study protocol outlined a planned cost analysis to estimate the additional staffing costs needed to bring about improvements in inspection scores. However, because the size of the relationship between additional staffing resources and increased chances to a good or outstanding inspection score were so small, the results of such an analysis would not be meaningful in any practical sense, as the additional staffing costs needed to bring about small improvements in quality evaluations would be so large that it would not represent a realistic or feasible intervention. We have therefore not included a cost–benefit analysis in WP2.
Work package 3: modelling relationships between staffing, quality, outcomes and resource use at an organisational level
This study sought to answer two questions: Are adverse events for residents more likely when a lower proportion of care is provided by nurses; and is the lower level of nursing input the likely cause of greater risk of these adverse events for residents? To answer these questions, we need to understand why skill mix changes over time. We analysed routinely collected longitudinal data from a single care home provider over 42 months. The data were more fine-grained: staffing, planned and actual hours worked by CAs and RNs, and data on resident and home characteristics. We utilised nurse-sensitive indicators of care quality as our outcome measures (see Data sources).
Study setting
The setting was a care home owner operator with 134 homes with and without nursing in England, a total of 7,624 resident beds, and an average occupancy rate of 86.5% (interquartile range = 13.75). The average share of residents with nursing needs was 66.1% (interquartile range = 42.4). Around 20% of residents were in dedicated dementia care units. Around a fifth of residents paid for their care, with funding from local authorities or the NHS via clinical commissioning groups constituting the remainder.
The study period was December 2014–May 2018 (42 months). The unit of analysis of the study is the care home month, so there were 5628 (134 × 42) care home month observations in the study. Because we used routinely collected administrative data, essential for business, there were no missing values.
Care home staffing arrangements and skill mix: implications for our study
This care home provider’s target nurse staffing levels were (relatively) fixed: one or two nurses per shift depending on the number of available nursing beds in the home. Home occupancy rarely drops to radically reduced nurse staffing levels. However, carer shifts may reduce as occupancy rates decline – lower occupancy rates increase skill mix. As occupancy rates, particularly low occupancy, may be the result of confounders (including care quality) that impact risk of adverse events. To counter this, we controlled statistically for occupancy.
Skill mix falls if there are shortages of nurses and rises when shortages of carers occur because of staff illness or unfilled vacancies. The provider tried to avoid being short of nurses by using (temporary) agency staff – but this was not always possible. We included measures of nurse and carer shortages in the analysis to identify any increased risk to residents that results from short-term staffing shortages as opposed to increased risk due to inadequate staffing establishments.
For a given level of skill mix, processes of care may change if demands on staff time increase or staff must adjust to a shift in care context. For example, in care homes with nursing, new resident admissions increase demands on nurses because they require nurses to assess residents’ needs, then develop and monitor the effectiveness of care plans until residents become settled into the home. The use of agency nurses as a result of unfilled vacancies or staff illness will substitute nursing staff who know residents and their care needs with nurses without home-specific experience, risking a change in care quality. To test whether these factors affected our measures of care quality, we included a measure of the proportion of care hours provided by agency nurses in a given home/month and the average number of weekly admissions as a proportion of the total beds in the home.
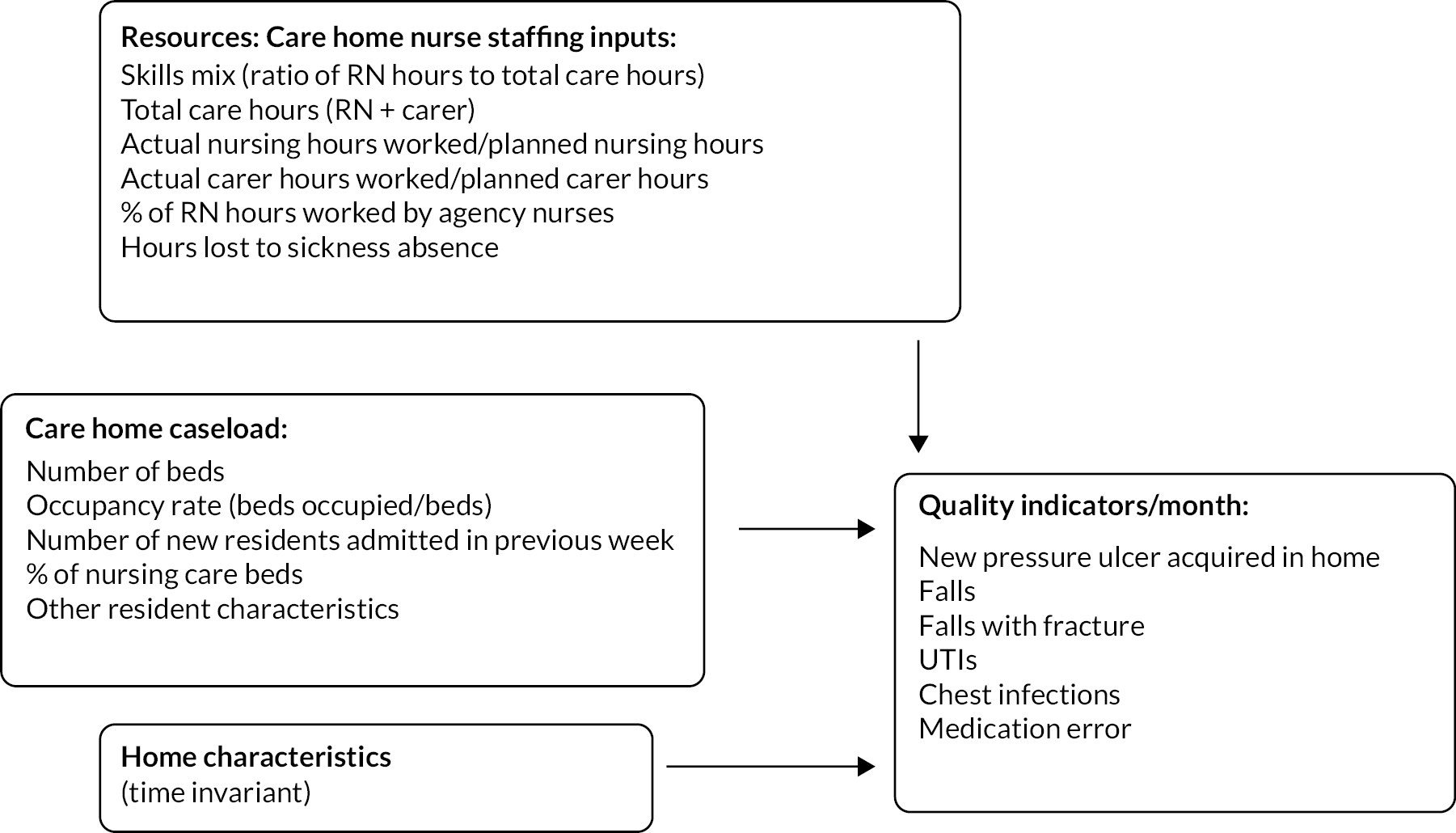
Finally, skill mix will change as resident care needs change. Skill mix falls as resident care needs increase – residents need more personal care and carer hours increase but nursing hours remain constant. Increased resident care needs may increase the risk of resident adverse events because greater care needs are likely associated with poorer health and more frailty. In interpreting our analysis, a lower skill mix and greater risk of adverse events could be caused by inadequate nurse staffing but could also be caused by unobserved changes to resident-specific risks influencing skill mix. We used the econometric method of growth mixture modelling (explained below) to control for medium-term unobserved changes to resident care needs influencing trajectories of nurse-sensitive indicators of care quality over time and skill mix. We could not control for short-run changes in resident care needs resulting in month-to-month fluctuations in care workers’ hours and therefore skill mix. See Figure 2 for our theoretical reasoning.
FIGURE 2.
The relationship between staffing and care quality outcomes at the care home/month level.
Data sources
Measures of quality
Quality outcomes were operationalised using nurse-sensitive indicators of care quality. Nurse-sensitive indicators of care quality investigated were: pressure ulcers developed in the care home; falls; falls that result in a fracture; urinary tract infections (UTIs); and chest infections. We also examined reported medication error rates as a broad measure of care quality. These measures all represent adverse incidents within the care home. All outcome measures were transformed to a ‘rate per occupied bed per care-home month’. See Table 3 for statistical description of measures. All these indicators constituted relatively rare events. The most common falls occurred at a rate of ~one per five occupied beds a month. Falls resulting in a fracture were much less common: ~1 per 335 occupied beds per month. Chest infections occurred at rate of ~1 per 20 occupied beds per month, UTIs 1 per 14 occupied beds per month, pressure ulcers 1 per 100 occupied beds per month and medication errors 1 per 62 occupied beds per month. We discuss the limitations of these data sets in Chapter 5.
| Mean | SD | Median | IQR | |
|---|---|---|---|---|
| Outcomes (rate per occupied bed per month) | ||||
| Pressure ulcers | 0.01 | 0.021 | 0 | 0.009 |
| Falls | 0.197 | 0.181 | 0.151 | 0.201 |
| Falls with fracture | 0.003 | 0.009 | 0 | 0 |
| UTIs | 0.069 | 0.082 | 0.044 | 0.103 |
| CI | 0.051 | 0.07 | 0.029 | 0.072 |
| Medication errors | 0.016 | 0.05 | 0 | 0.018 |
| Staffing characteristics | ||||
| Total monthly care hours per occupied bed per month (RN + carer) | 124.52 | 31.10 | 122.482 | 35.481 |
| Skill mix: proportion of monthly care hours provided by RNs | 0.203 | 0.093 | 0.225 | 0.101 |
| Agency nurses (proportion of monthly care hours provided by agency nurses) | 0.047 | 0.07 | 0.019 | 0.067 |
| Proportion of planned RN hours per month actually worked | 0.982 | 0.116 | 0.973 | 0.123 |
| Proportion of planned carer hours per month actually worked | 1.001 | 0.134 | 0.99 | 0.136 |
| Total care hours (RN + carer) lost to sickness absence per month | 0.051 | 0.036 | 0.043 | 0.046 |
| Control variables | ||||
| Total number of beds | 56.611 | 25.838 | 52 | 29 |
| Occupied beds (average per week) | 48.377 | 22.137 | 44.25 | 25.275 |
| Occupancy rate (average per week) | 0.865 | 0.122 | 0.9 | 0.138 |
| Admissions as a proportion of total beds (average per week) | 0.024 | 0.024 | 0.02 | 0.022 |
| Resident characteristics (measures at a single point in time, April 2018, only) | ||||
| Proportion of residents with nursing needs | 0.661 | 0.323 | 0.714 | 0.424 |
| Proportion of residents in dedicated dementia units | 0.198 | 0.254 | 0.053 | 0.344 |
| Proportion of residents in dedicated dementia units who also exhibited challenging behaviour | 0.005 | 0.014 | 0 | 0 |
| Proportion of young disabled residents | 0.049 | 0.147 | 0 | 0.022 |
| Proportion of residents with learning difficulties | 0.002 | 0.007 | 0 | 0 |
| Proportion of residents with Parkinson’s disease | 0.007 | 0.017 | 0 | 0 |
| Proportion of residents with Huntington’s disease | 0.002 | 0.018 | 0 | 0 |
| Proportion of residents receiving end-of-life care | 0.055 | 0.076 | 0.031 | 0.076 |
| Proportion of residents with other specific care needs | 0.045 | 0.088 | 0.013 | 0.048 |
Measures of workforce
We calculated total care hours (nurses and carers), carer hours and nurse hours per occupied bed per month and a skill mix variable – the proportion of care hours provided by RNs per occupied bed/month. The median number of total care hours per occupied bed per month was 122.5 (interquartile range = 35.5). The median percentage of these hours provided by RNs (skill mix) is 22.5% (interquartile range = 10%). If nurses are off sick or there are unfilled RN vacancies, the care home provider would seek to cover shifts using RN provided by agencies. The median percentage of care hours provided by agency nurses per month was 1.9% (interquartile range = 6.7%). We also have measures of whether nurse and carer hours were at or below their planned levels. We used this to calculate the proportion of planned hours worked each month, providing a combined measure of staff absence due to uncovered shifts arising from sickness and absence. The median percentage of planned hours worked for RN hours worked is 97.3%, although an interquartile range for this variable of 12.3% indicates that shifts where nurse staffing was below target were not uncommon. For carer hours worked as a proportion of planned carer hours worked, the median is higher, 99%, although the interquartile range is slightly larger at 13.4%. See Table 3.
Control variables
Other variables included in the analysis measure aspects of time-varying, home case load, that is changes to demand for care that could therefore affect the processes of care, specifically (see Table 3): (1) ratio of average weekly new residents admitted to available beds (median = 0.02, interquartile range = 0.022); (2) number of occupied beds (median = 44.3, interquartile range = 25.3) and the total number of beds (occupied and unoccupied, median = 52, interquartile range = 29).
We computed the proportion of beds occupied per month (median = 0.9, interquartile range = 0.138) and included this in the regression modelling instead of separate measures of number of beds occupied and total beds. The care home provider shared data constituting proxy measures of potential need: the proportion of residents who were elderly, receiving specialist dementia care and exhibiting challenging behaviours, younger residents with disabilities, receiving specialist care for Parkinson’s or Huntington’s disease and residents receiving specialist end-of-life care. The data were from a single time point (April 2018) and included to examine whether their inclusion affected results.
Data analysis
We estimated a number of different regression models with the indicators of care quality as dependent variables. First, we used simple pooled, cross-sectional ordinary least squares (OLS) models as a more easily interpretable benchmark to assess the results of more complex models against. Next, we fitted models with care home fixed effects to control for time-invariant omitted variables (i.e. home specific structures of care). These models also included time effects to control for variables that are constant across care homes but tend to vary over time, for example gradual changes to home caseload.
Finally, we specified multilevel growth models (growth mixture modelling with a random intercept) that account for different trajectories of outcomes between care homes. For example, unobserved processes of care changed over time due to (unobserved) changes in home caseload. The ICC was used to illustrate the proportion of total variation in nurse-sensitive outcomes of care quality due to differences in home-specific trajectories over time (except the models with falls with fracture where the ICC score was low). The difference between conditional (variance explained by fixed effects only) and marginal (variance explained by the entire model) R2 shows – our preferred – mixed effects models outperform models with separate fixed and time effects. Marginal effects were calculated from the results of the growth mixture models to use as an input into our cost–benefit analysis of changing skill mix.
We used models with lagged and lead measures of key variables to test whether staffing in previous months might explain nurse-sensitive indicators of care quality in future months – a form of sensitivity analysis. Results were not statistically significant. Exploration of non-linear relationships between the outcome variables, total staffing and skill mix using squared terms for skill mix and other workforce measures, also yielded small and statistically non-significant results and these analyses are not reported. Although note that regression analysis is typically only able to detect non-linear relationships if the non-linear relationship follows a very specific functional form, there may therefore be non-linear relationships we are unable to detect with these methods. 57
We shared results of our preliminary analyses with quality and operational managers from the care home provider who provided the data in order to sense check our results against their experiences. This did not result in any significant changes to the analysis.
Cost–benefit analysis
The cost perspective taken in the analysis was, as far as possible, that of the NHS (with costs presented in 2019–20 prices). This is where most notable healthcare services for outcomes associated with staffing are likely to take place, although not exclusively. The NHS will also bear costs of nursing time, although these costs are shared by multiple stakeholders. The financing of nursing hours in care homes is complex including NHS, local authority and private funding, as is the provision of healthcare services to this population. 58–61 Regardless of this, the aim was to present indicative estimates of NHS cost savings that would arise from positive changes to workforce attributes. Unit costs are summarised in Table 4.
| Cost variable | Unit cost (£) | Unit | Source |
|---|---|---|---|
| Nursing time (skill mix) | 39.23 | Per hour | Curtis and Amanda62 |
| Medication errors | 3.07 | Per error | Elliott et al.70 |
| Falls with fractures | 4247.00 | Per event | Franklin and Hunter71 inflated using indices provided by Curtis and Amanda62 |
| UTI | 337.00 | Per event | Derived from NHS Reference Costs, Hospital Episodes Statistics and ONS population estimates85–87 |
In the absence of any care home-specific nursing unit costs, data from Personal Social Services Research Unit (PSSRU) Unit Costs of Health and Social Care were used to determine costs of nursing hours. 62 These estimates were derived from Agenda for Change pay scales and other indirect costs, including overheads and were assumed to be broadly indicative of appropriate unit costs. This gave an hourly cost for a Band 5 community-based nurse of £39.23, equating to a cost of £23,460 per month or £281,520 per year for an average home.
We next needed to estimate treatment cost savings for falls with fractures, UTIs and medication errors. To do this, a series of pragmatic literature reviews were conducted to identify unit costs. Literature was consulted rather than immediately piecing together assumed resource use and nationally available unit cost sources for two reasons: either they were not directly measurable healthcare costs, but rather an impact of some causative events (medication errors, fall with fractures), or to attempt to gather costs that reflected the average severity and resource use of these events over an appropriate time horizon (ideally to resolution) in an appropriate population (UK care home residents).
Data sources and analysis
Searches were performed in December 2020 using PubMed, supplemented by Google Scholar and citation snowballing, date restricted to 10 years or 2010 to present (as of December 2020), with search terms: Cost of medication errors in care home UK and Cost of medication errors in the UK. For other searches, ‘medication errors’ was replaced with the appropriate outcome of interest: ‘falls’ and ‘UTIs’.
Sources were chosen to inform the cost calculations on the basis of a series of suitability criteria. Data were preferred if they were UK specific, relevant to a care home population, in appropriate units to match the outcomes as defined in the analysis, and contemporaneous. In the event that competing sources were identified, consideration was given to factors such as the nature of the evidence, including sample size and study design. Only sources that were considered as potentially suitable are referred to in the summary provided here. While it is recognised that these methods do not guarantee that all the potentially relevant literature will have been identified, it is expected that sources of most relevant cost data will have been encountered.
Cost of medication errors
The search identified a relatively small literature relating to the costs of medication errors. 63–70 Of these, only one estimated the prevalence and burden (in terms of healthcare resource use and deaths) in care home settings. 70 This study utilised several other studies to produce aggregate-level estimates of the Cost of medication errors to the NHS. In the base case, the authors estimated that 237,287,788 ‘definitely avoidable’ adverse drug events occurred annually, at a cost of £98,462,582 (mean of £0.41 per error). Including ‘probably avoidable’ adverse drug events increased this to £728,462,837 (£3.07 per error). While these estimates were not without limitations, they came close to fitting the requirements of this study (UK, contemporary, most comparable population, able to derive a ‘per error’ cost). The price year for which costs were presented was not clear in the publication and so no inflation indices were applied.
Cost of falls resulting in fractures
Six studies of interventions or trials designed to reduce falls in older people that included cost–benefit analysis were identified. 71–76 Only one of these studies, which was in non-care home setting, included UK-specific cost estimates of a fall74 while another presented costs in British Pound (GBP) but was based on Australian resource use estimates. 71 Franklin and Hunter71 presented age-group specific cost estimates for minor (£427.84 for 75- to 89-year-olds) and major falls (£4014.52) in the UK (2016–17 GBP), the major distinction being the requirement for hospital admission. While it might be assumed that this correlates with fractures, the study did not specifically distinguish between falls resulting in fracture. Two other studies also considered a UK setting but presented mean costs of fractures for each arm or associated costs, but not mean cost per fall resulting in a fracture. 75,76 Two further studies77,78 estimated the costs of managing falls in older adults living in the community but it was difficult to ascertain how costs cited related to falls specifically. Guidelines produced by the National and Institute for Health and Care Excellence in the UK were identified which costed falls based on PSSRU unit cost data. 79,80 However, the care home data did not distinguish between underlying cause of fracture, or site of fracture, so it is unclear how suitable these data were.
Therefore, none of the sources offered costs that were both reflective of the institutional setting or country (UK specific). The study by Franklin and Hunter71 did (at least) present estimates that were broadly consistent with the characterisation required (fall with fractures vs. major falls) and stratified for an older population (75–89 years old). It was assumed that a fall resulting in a fracture would likely lead to a hospital admission in an older frail population. These costs were inflated to 2019–20 prices (£4247) using NHS cost of inflation estimates. 62
Costs of urinary tract infections
Searches for sources of costs of UTIs did not yield many publications. Of studies identified three referenced costs, however it was not possible to isolate the cost per UTI from them. 81–83 A study by Pickard and colleagues82 suggested an increased cost of £547.63 for patients undergoing catheterisation who experienced a UTI. One study considered an economic perspective of UTIs and measured direct costs to the Italian health service in women with cystitis and a history of UTIs (mean annual cost of €229 per woman). A quality improvement project aimed at reducing UTI related to dehydration in care homes was identified. 84 The authors suggest that the project was effective and state that every avoided hospital admission would lead to a cost saving of £1300, but the study did not directly collect resource use/cost data.
In the absence of a suitable source, a cost was estimated based on the proportion of clinically significant UTIs that lead to hospitalisation. Secondary care costs are likely to significantly outweigh any costs associated with antibiotic treatment. Further pragmatic searches were performed but did not yield usable data. An estimate was computed (Table 5) based on UK population estimates (2020) and estimates of the incidence of clinically significant UTI in adults aged 70 years and over in the UK to derive a denominator and hospital episode statistics (2019–20) to derive a numerator. 85–87 It was estimated that in 2019–20, approximately 21% of clinically significant UTIs led to hospitalisation in those aged 70 years and above. A unit cost derived from NHS Reference Costs (2018–9) was weighted using 21% to derive a mean cost per UTI (Table 6),88 equating to an average treatment cost of £337.
| Population | UTI rate/100 person years | UTI (men) |
UTI (women) |
Admission (men) |
Admission (women) |
% UTI w/admission | ||
|---|---|---|---|---|---|---|---|---|
| Men | Women | |||||||
| 70–74 | 3,363,906 | 3.05 | 10.96 | 50,696 | 186,512 | 10,632 | 15,337 | 11 |
| 75–79 | 2,403,759 | 6.13 | 14.34 | 72,808 | 174,379 | 13,947 | 20,117 | 14 |
| 80–84 | 1,726,223 | 6.13 | 14.34 | 52,286 | 125,227 | 18,755 | 27,053 | 26 |
| 85–89 | 1,049,866 | 10.54 | 19.8 | 54,677 | 105,160 | 19,005 | 27,414 | 29 |
| 90 and over | 609,503 | 10.54 | 19.8 | 31,743 | 61,051 | 16,331 | 23,558 | 43 |
| 262,208 | 652,330 | 78,670 | 113,479 | 21 | ||||
| HRG code | Description | Activity | Unit cost (£) | Weighted cost (£) |
|---|---|---|---|---|
| LA04H | Kidney or UTI, with Interventions, with CC Score 12+ | 2145 | 6014 | 49 |
| LA04J | Kidney or UTI, with Interventions, with CC Score 9–11 | 3042 | 4668 | 54 |
| LA04K | Kidney or UTI, with Interventions, with CC Score 6–8 | 4411 | 3836 | 65 |
| LA04L | Kidney or UTI, with Interventions, with CC Score 3–5 | 4105 | 3000 | 47 |
| LA04M | Kidney or UTI, with Interventions, with CC Score 0–2 | 2261 | 2475 | 21 |
| LA04N | Kidney or UTI, without Interventions, with CC Score 13+ | 8560 | 3051 | 100 |
| LA04P | Kidney or UTI, without Interventions, with CC Score 8–12 | 45,706 | 2210 | 386 |
| LA04Q | Kidney or UTI, without Interventions, with CC Score 4–7 | 89,469 | 1536 | 526 |
| LA04R | Kidney or UTI, without Interventions, with CC Score 2–3 | 51,153 | 1078 | 211 |
| LA04S | Kidney or UTI, without Interventions, with CC Score 0–1 | 50,630 | 738 | 143 |
| Total activity | 261,482 | – | – | |
| Weighted unit cost | 1602 a | |||
| Cost per UTI | 337 b |
Work package 4: understanding the contributions of the care home workforce to enhance quality
This was a documentary analysis of CQC inspection reports – one mechanism used in the sector to assess quality. We aimed to explore:
-
how staffing structures and/or workforce models (numbers, skill mix and stability) influenced quality; and
-
care processes involving care home staff associated with quality and explain the relationship between staffing and quality.
We used document analysis89 to elicit meaning, gain understanding and develop empirical knowledge. 90 This is the first published systematic analysis and synthesis of regulatory reports to explore the relationship between staffing and quality. It represents a novel approach for understanding and explaining quality in this context by synthesising data usually viewed and reported for single homes in isolation.
Data sources
Publicly available CQC inspection reports91 were the data. Our two-stage sampling approach started with CQC reports (n = 125) for our care provider partner from WP3. We included reports from homes rated outstanding (n = 8) or inadequate (n = 2) (Table 7). We piloted our data extraction methods on these 10 care home reports and then (in stage 2) extended the sample to homes from other providers rated as outstanding or inadequate.
| Care home ID | Type | Location | Size | Resident mix | CQC rating |
|---|---|---|---|---|---|
| Care Home 1 | Dual registered | London | 42 beds | Treatment of disease, disorder or injury, caring for adults over 65 years | Outstanding |
| Care Home 2 | Dual registered | East Midlands | 55 beds | Accommodation for persons who require nursing or personal care, physical disabilities, treatment of disease, disorder or injury, caring for adults over 65 years | Outstanding |
| Care Home 3 | Dual registered | South East | 49 beds | Accommodation for persons who require nursing or personal care, dementia, treatment of disease, disorder or injury, caring for adults over 65 years | Outstanding |
| Care Home 4 | Dual registered | South West | 56 beds | Accommodation for persons who require nursing or personal care, dementia, treatment of disease, disorder or injury, caring for adults over 65 years | Outstanding |
| Care Home 5 | Dual registered | South West | 49 beds | Accommodation for persons who require nursing or personal care, treatment of disease, disorder or injury, caring for adults over 65 years | Outstanding |
| Care Home 6 | Dual registered | North East | 59 beds | Accommodation for persons who require nursing or personal care, dementia, physical disabilities, treatment of disease, disorder or injury, caring for adults over 65 years | Outstanding |
| Care Home 7 | Dual registered | East of England | 40 beds | Accommodation for persons who require nursing or personal care, physical disabilities, treatment of disease, disorder or injury, caring for adults over 65 years | Outstanding |
| Care Home 8 | Dual registered | London | 52 beds | Accommodation for persons who require nursing or personal care, treatment of disease, disorder or injury, caring for adults over 65 years | Outstanding |
| Care Home 9 | Residential care | East | 35 beds | Dementia, caring for adults over 65 years | Inadequate |
| Care Home 10 | Dual registered | North West | 78 beds | Accommodation for persons who require nursing or personal care, dementia, treatment of disease, disorder or injury, caring for adults over 65 years | Inadequate |
Of the 1066 care homes in England rated as outstanding and 277 rated as inadequate on the CQC website in January 2021 (www.cqc.org.uk/search/services/care-homes), we purposively (Box 3) sampled 20 CQC reports (10 rated as outstanding and 10 as inadequate). Purposive sampling criteria were chosen as ownership, care home size, geographical location influence home structures (numbers/mix of staff, pay, occupancy, resident mix) and organisational processes – impacting on quality and resident experience. Table 8 describes our final 20 care homes in stage 2 and Appendix 9 details our criteria for purposive sampling.
-
Care home ownership: Care home services are mostly supplied by independent care providers, made up of a mix of both for-profit and not-for-profit businesses, but with some local authority provision.
-
Size of the provider organisation: Care home provider organisations vary in size. The vast majority are small providers with around 4000 owning just one home. There are six large care organisations each owning over 100 homes in their portfolio. On a national basis, these six providers have a combined share of 11% of all care homes.
-
Geographical location: There are regional, as well as urban and rural, variations in the CQC reports of quality in care homes. 22
-
Individual care home size: Small care homes (1–10) beds are more often rated as ‘good’ or ‘outstanding’ than larger care homes (50+ beds). 22
| Care home ID | Type | Size of provider organisation | Ownership | Location | No of beds | Resident mix | CQC rating |
|---|---|---|---|---|---|---|---|
| Care Home 11 | Dual registered |
Large | For-profit | Northeast | 43 | Accommodation for persons who require nursing or personal care, dementia, treatment of disease, disorder or injury, caring for adults over 65 years | Outstanding |
| Care Home 12 | Dual registered |
Large | For-profit | Northeast | 29 | Accommodation for persons who require nursing or personal care, dementia, caring for adults over 65 years | Outstanding |
| Care Home 13 | Residential care |
Large | Not-for-profit | Hull, Yorkshire and Humber | 87 | Accommodation for persons who require personal care, dementia, caring for adults over 65 years | Outstanding |
| Care Home 14 | Dual registered | Large | Not-for-profit | Southwest | 71 | Accommodation for persons who require nursing or personal care, dementia, caring for adults over 65 years | Outstanding |
| Care Home 15 | Dual registered | Large | Not-for-profit | Hull, Yorkshire and Humber | 34 | Accommodation for persons who require nursing or personal care, caring for adults over 65 years | Outstanding |
| Care Home 16 | Residential care | Medium | Not-for-profit | Southeast | 22 | Accommodation for persons who require personal care, dementia, caring for adults over 65 years | Outstanding |
| Care Home 17 | Dual registered | Medium | For-profit | Southeast | 71 | Accommodation for persons who require nursing or personal care, dementia, physical disabilities, treatment of disease, disorder or injury, caring for adults over 65 years | Outstanding |
| Care Home 18 | Dual registered | Small | For-profit | Northwest | 64 | Accommodation for persons who require nursing or personal care, physical disabilities, treatment of disease, disorder or injury, caring for adults over 65 years | Outstanding |
| Care Home 19 | Residential care | Small | For-profit | West Midlands | 24 | Accommodation for persons who require personal care, dementia, caring for adults over 65 years | Outstanding |
| Care Home 20 | Residential care | Local authority | Local authority | Northwest | 40 | Accommodation for persons who require personal care, dementia, caring for adults over 65 years | Outstanding |
| Care Home 21 | Residential care | Local authority | Local authority | East | 32 | Accommodation for persons who require personal care, dementia, physical disabilities, caring for adults over 65 years | Outstanding |
| Care Home 22 | Dual registered | Large | For-profit | East | 55 | Accommodation for persons who require nursing or personal care, caring for adults over 65 years | Inadequate |
| Care Home 23 | Dual registered | Large | For-profit | London | 146 | Accommodation for persons who require nursing or personal care, people living with dementia | Inadequate |
| Care Home 24 | Dual registered | Medium | For-profit | East Midlands | 50 | Accommodation for persons who require nursing or personal care, dementia | Inadequate |
| Care Home 25 | Residential care | Medium | For-profit | East Midlands | 33 | Accommodation for persons who require personal care, dementia | Inadequate |
| Care Home 26 | Residential care | Medium | Not-for-profit | Southeast | 25 | Accommodation for persons who require personal care, people, dementia | Inadequate |
| Care Home 27 | Residential care | Medium | Not-for-profit | Southeast | 50 | Accommodation for persons who require personal care, dementia | Inadequate |
| Care Home 28 | Residential care | Small | Not-for-profit | Northwest | 39 | Accommodation for persons who require personal care, dementia | Inadequate |
| Care Home 29 | Residential care | Small | For-profit | Hull, Yorkshire and Humber | 15 | Accommodation for persons who require personal care, caring for adults over 65 years | Inadequate |
| Care Home 30 | Residential care | Small | For-profit |
Southwest | 13 | Accommodation for persons who require personal care, caring for adults over 65 years | Inadequate |
Data extraction and analysis
Data on home characteristics and the five key CQC domains of quality (safe, effective, caring, responsive and well-led) were extracted from the CQC reports by a single researcher (KH). A second team member (KS, RD) checked the data extraction. Data were organised into matrices using spreadsheets with each home on a row and characteristics in columns.
Using content analysis34 we focused on three units of analysis: organisational structures, unit-level processes and individual staff actions. There were four stages to our analysis: (1) familiarisation with the data; (2) organising data into meaning units; (3) coding data to higher-level themes; and (4) refining higher-level themes. We used findings from the realist review to guide our analysis in six areas: resident-focused care, information sharing, teamworking, organisation of care, leadership and composition of staff.
To enhance trustworthiness,92 we recorded the process and decision made during the study as an audit trail. Three researchers (KH, RD, KS) undertook coding, analysis and interpretation with iterative questioning (of data and each other) and probing for detail and debriefing after each coding stage and keeping a reflective commentary.
A narrative synthesis of our analysis is presented in Chapter 4.
Work package 5: a platform for sector-wide implementation
This was a mixed-methods parallel case study:93 with each care home constituting a case. Methods used involved social network analysis (SNA) based on self-report questionnaires, and manager-completed (on behalf of the home) questionnaire-based survey using an adapted version of the NoMAD tool. 94
Due to homes’ varied characteristics (differing ownership, organisational and home size and geographical locations), we purposively sampled for diversity. Eleven care homes were recruited through contact with Leeds Care Association, the care provider in WP3 and support from NIHR EnRICH Yorkshire and Humber and West Midlands. Recruitment was in two stages. First, letters were sent to the care home managers or senior executive team to establish potential interest in participating. After home-level consent, staff were provided with information about the study and made an individual decision to participate.
Data sources
Social network analysis
The SNA was focused on the advice and influence relationships within the care homes. A roster name generation method95 was used with the care home staff (including managers) in each case site. A blank name slot was added to allow respondents to mention people not included in the roster. The care home managers from the corporate provider were also asked to consider other managers from within the wider corporate network in their responses. All employees were listed, and respondents chose staff in response to three questions asked: (1) Who do you seek advice from on quality of care? (2) Who do you influence on quality of care? (3) Who influences you on quality of care?
This method has the benefit of being efficient; essential in a time-poor environment with competing demands for staff attention. On average, it took staff approximately 10 minutes to answer the survey. Managers took longer (average 39 minutes) to complete the survey as they also completed the NoMaD survey tool (see below).
Staff completed the questionnaire at the care home with the researcher or online. In two homes surveys were left for staff to self-complete and returned to the research team. Most homes had unreliable internet access and so paper-based questionnaires were provided with an optional link to the online questionnaire.
NoMAD
We used the NoMAD survey tool created by Finch et al. ;94 this is based on normalisation process theory (NPT). 96 NoMAD is a 23-item instrument for measuring implementation processes from the perspective of social actors directly involved in the work of implementing an innovation. 97 The manager in each home (n = 11) completed the NoMAD survey. They were asked to imagine (their) ‘ideal’ website bringing together staffing and quality. Care home managers were asked to complete the survey because they would most likely instigate and lead the management of the implementation of any translational technology arising from our study.
Pilot study
The pilot study site was a medium-sized care home from a six-home group. It was chosen because no other homes in this group were used in the main study. Two key points arose from the pilot. First, the effectiveness of the three questions was confirmed. Second, multiple visits would be needed to try to get a sufficient response from the staff. The visit to the pilot care home lasted several hours as care duties significantly reduced the number of staff members available to participate.
Data analysis
Social network analysis
The SNA was used to determine the central players for the flow of advice and influence in home networks. We focused on incoming influence: these responses were more trustworthy than the outgoing influence responses due to the weakness Rogers98 identified in the self-designation method of identifying opinion leaders. We focused on Roger’s sociometric measure of identifying opinion leaders. 98 First, on individuals who have the most connections in the advice network and the influence network: degree centrality. Second, on individuals who serve most often as a bridge in the network: betweenness centrality in SNA. This identifies who serves as connectors between different parts of the network. All respondents were asked about length of service they had in the care home and in the sector, as well as their gender, race, shifts worked and home role.
The responses were processed using UCINET, a SNA software package. 99 The software was used to generate network diagrams and network statistics.
NoMAD
The NoMAD tool has 23 questions to determine readiness for innovation based on four constructs: coherence (the sense-making work that people do individually and collectively when faced with operationalising a set of practices); cognitive participation (the relational work that people do to build and sustain a community of practice around an innovation); collective action (the operational work that people do to enact a set of practices associated with the innovation); and reflexive monitoring (the appraisal work that people do to assess and understand the ways that an innovation and set of practices affect them and others around them). 96
After three general questions on readiness with responses ranging from 1 to 10, 20 Likert scale questions measure the four constructs. Data were analysed descriptively.
Public and stakeholder involvement and engagement
We have worked closely with the public and stakeholders throughout the research, from question formulation through to synthesis, and we consider this a strength of our research to conduct research with and for the sector. We formed two advisory groups: (1) a resident and relative group and (2) a care home manager group. The SSC also had representation of key stakeholders including relatives to guide our work. These mechanisms ensured that alternative perspectives (beyond the research team) fed into and improved the design and implementation, as well as promoted conversations and learning to benefit the research.
Ethics approval
Ethics approval was required for the empirical studies undertaken in WP2, WP3 and WP5: WP1 and WP4 comprised evidence reviews and documentary analysis. WP2 and WP3 were reviewed and approved (2 August 2017) by the Social Care Research Ethics Committee (17/WM/0232). WP5 was reviewed and approved (21 June 2019) by the University of Leeds, Faculty of Medicine and Health, Ethics and Governance Committee (HREC 18-028). Data-sharing agreements were established between the University of Leeds and Skills for Care (WP2) and the care provider organisation (WP3).
Chapter 4 Findings
Work package 1: determining the characteristics of the care home workforce and understanding quality
Work package 1i: roles and responsibilities of the care home workforce linked to quality
Thirty-six studies were included in the review. Representing international studies: North America (n = 13);100–112 Europe (n = 12),113–124 Asia (n = 6),125–130 Australia (n = 4)131–134 and one comparative (Canada and Sweden) study (n = 1)135 (Table 9). Most studies used qualitative methods (n = 32); three studies used survey methods and one used mixed methods (Table 9).
| Author, year and country136 | Study aim | Study design, data collection method and analysis | Number of care homes represented (terminology used in paper to refer to care homes) | Number of participants (terminology used in paper to refer to staff group) | Participant characteristics |
|---|---|---|---|---|---|
| Abrahamson, 2020, USA100 | To examine nursing assistant perspective of their role in the nursing home resident experience | Qualitative, semistructured interviews. Interpretive approach to identify codes and themes |
17 organisations (including assisted-living clinics, skilled nursing facilities and community colleges) | 25 nursing assistants | Gender: 100% female Age: not reported Years in position: average 2.6 years (SD = 3.58) |
| Andersen, 2016, Canada108 | To explore the complexities of care; working environments; and knowledge, skills and efforts of care aides who work in nursing homes | Qualitative, interviews Inductive interpretive analysis |
5 nursing homes | 22 care aides | Gender: 91% female Age: 20–30 – 14% 31–50 – 72% 51–60 – 14% Years of experience: 1 – 9% 2–5 – 14% 6–10 – 5% 11–15 – 18% 16–20 – 9% 21–25 – 36% 26–30 – 4% > 30 – 4% |
| Backhaus, 2018, the Netherlands117 | To understand how nursing homes employ BRNs and how they view the unique contributions of baccalaureate-educated RNs to staff and residents in their organisations | Qualitative, semistructured individual and group interviews. Content analysis |
6 nursing home organisations | Board members and directors (n = 8), ward/nursing home manager (n = 12), vocationally trained RNs (n = 3), certified nurse assistants (n = 6), nurse assistants (n = 5), baccalaureate-educated RNs (n = 6) | Description for vocationally trained RNs, CNAs and nurse assistants (n = 14): Gender: 100% female Age (mean/range): 41 (25–62) years Years in position (mean/range): 13 (0–31) years Description for baccalaureate-educated RNs (n = 6): Gender: 100% female Age (mean/range): 39 (30–49) years. Years in position (mean/range): 3 (2–7) years |
| Banerjee, 2015, Canada109 | To explore the experience of care workers, who we understand as labouring on the ‘fault line’ between the human needs of the residents they care for and institutional processes | Qualitative. Open-ended survey questions and focus groups Inductive approach |
Open-ended survey: 71 residential care facilities Focus groups: number of care homes represented not reported |
Survey participants included 415 care workers, 139 licenced practical nurses and 141 RNs Focus groups (n = 9) comprised between 3 and 8 frontline care workers |
Open-ended survey questions: Gender: 95% Age: not reported Years of experience: almost two-thirds worked in residential care for a decade or longer Focus group: Gender: primarily female (number not reported) Age: not reported Years of experience: not reported |
| Bedin, 2013, Switzerland122 | To explore the daily experience of RNs in nursing homes and the way this role is implemented through the interactions with all the other professional caregivers of the institution | Qualitative Observations and focus groups Content analysis |
9 nursing homes | 16 RNs and other participants included community health assistants, auxiliary nurses, as well as community social workers, members of administrative services, technical/logistical staff members and food service employees | Description of RNs Gender: not reported Age: not reported Years of experience in gerontological care: ranged from 3 to 27 years |
| Cho, 2020, Korea125 | To describe RNs’ perceptions of nursing services as important and necessary for nursing home residents, facilitators and challenges in taking care of these residents, and their needs to improve the quality of care in the nursing home setting | Qualitative Semistructured interviews Thematic analysis |
6 nursing homes | 19 RNs (7 of which were department directors or unit managers, and 12 were staff RNs) | Gender: 100% female Age (average and range): 48.5 (32–59) Employment duration: 9 months – 18 years (including former working experience) |
| Chung 2010, USA101 |
To examine beliefs and assumptions held by nursing assistants working in nursing homes about their roles in caring for residents | Qualitative Semistructured interviews | Study participants were recruited through a long-term care workers’ union affiliated with 24 skilled nursing facilities | 21 nursing assistants | Gender: 71% female Age: average age 42 years (range 22–58 years) Average time working as a nursing assistant: 11 years (range 1–30 years) |
| Craftman, 2016, Sweden113 | To describe RNs’ experience in the context of delegating the administration of medication to unlicenced personnel in residential care homes | Qualitative Semistructured interviews Manifest content analysis |
11 residential care homes | 18 RNs | Gender: 94% female Age: range 38–66 years Average number of years of work experience as RN: 15 years (range 2–25) |
| Daly, 2012, Canada and Sweden135 | To analyse the everyday work life of long-term care facility workers in Canada and Sweden | Qualitative Open-ended survey questions Thematic content analysis |
Residential care (number of homes not reported) | 345 assistant nurses (licenced or registered practical nurses) 504 care aides (personal support workers) |
Gender: not reported Age: not reported Experience: two-thirds of the workers in Canada and slightly more of them in Sweden have worked in this capacity for a decade or more |
| Ellis, 2012, Canada110 | To explore medication management as described by licenced nurses working in long-term care | Qualitative Focus groups Thematic analysis |
2 long-term care facilities | 10 RNs and 12 registered practical nurses | RNs: Gender: 100% female Average age: 42.5 years Years of work experience: 8.5 years Registered practical nurses: Gender: 100% female Average age: 39 years Years of work experience: 6.9 years |
| Ellis, 2015, Australia131 | To explore nurses’ and personal CAs’ role in improving the relocation of older people into a nursing home | Qualitative Interviews Thematic analysis |
4 nursing homes | 7 RNs, 5 enrolled nurses and 8 personal CAs | Gender: majority female (figure not provided) Average age: 47 years Average length of employment: 4 years Average length of care experience: 17 years |
| Forss, 2018, Sweden114 | To illuminate the experience of participating in nutritional care from the perspectives of older people and RNs | Qualitative Semistructured interviews Content analysis |
6 nursing homes | 8 RNs and 4 older people | Characteristics of RNs Gender: 75% female Average age: 44.1 (range 28–67) years Years of work experience ranged from 2 to 43 years |
| Halifax, 2018, USA102 | To describe how certified nursing assistants understood, recognised, interpreted and responded to residents’ pain | Qualitative Semistructured interviews Constant comparative analysis |
2 care home sites (nursing home and a memory care clinic) | 16 certified nursing assistants | Gender: 81% female Average age: average 45.6 years (range 27–62, SD 9.47) Average length of time working as a certified nursing assistant – 15.4 years (range 4–33 years, SD 10.83) Average length of time working at current location – 11.8 years (range 1–31 years, SD 9.33) |
| Heath, 2010, UK119 | To illuminate the distinct contributions made by RNs to outcomes for older people in UK (nursing) care homes and to identify the outcomes of their work | Qualitative Participants provided written feedback describing ‘significant’ work (phase 1), observations, semistructured interviews and relevant documentation (phase 2) Thematic analysis |
Participants taking part in phase 1 were recruited from care homes around the UK (number not provided), and phase 2 conducted in 3 care homes | Phase 1: 16 RNs and 18 CAs Phase 2: 73 observations, interviews with 25 RNs (including care home managers), 24 CAs, 3 physiotherapists, 1 general practitioner, 1 clinical psychologist, 1 head of residential care, 4 relatives and 18 residents. Documents reviewed included care plans, medication charts, medical and therapy notes, tools used to measure pressure risk or resident dependency and audits |
Gender: not reported Age: not reported Years in position: not reported |
| Hunter, 2010, Australia132 | To provide a contemporary description of the practice of nurses caring for older people in long-term care | Mixed methods Questionnaire, reviewing relevant documentation and semistructured interviews Descriptive statistics, Wilcoxon t-test and content analysis |
6 long-term aged care facilities | RNs working in a clinical capacity (n = 48) and nurse managers whose role was administrative (n = 16) | Characteristics of RNs Gender: 100% female Age: 0–35 years – 11% 36–40 years – 7% 41–45 years – 31% 46–50 years – 16% > 51 years – 35% Years working as a RN: 0–4 – 17% 5–10 – 23% 11–15 – 26% > 16 years– 34% |
| Johansson-Pajala, 2016, Sweden115 | To explore RNs’ experience of medication management in municipal care of the elderly in Sweden | Qualitative Focus groups Content analysis |
5 long-term care organisations | 21 RNs | Gender: 81% female Age: median age of 50 years (range 27–65) Years of nursing experience: 19 years (median), range 4–34 |
| Kusmaul, 2017, USA103 | To capture the certified nursing assistants’ perspectives on what direct care behaviours make up quality care | Qualitative Semistructured interviews Content analysis |
8 nursing homes | 23 certified nursing assistants | Gender: 91% female Age: not reported Years of experience: < 5 years – 30% 5–10 years – 17% 11–15 years – 9% 16–20 years – 17% > 20 years – 26% |
| Knopp-Sihota, 2015, Canada111 | To describe the nature and frequency of rushed or missed care by healthcare aides in western Canadian nursing homes | Quantitative Questionnaire Descriptive statistics |
36 nursing homes | 583 healthcare aides | Gender: 94% female Age: < 30 years – 13% 30–39 years – 22% 40–49 years – 32% 50–59 years – 24% > 60 years – 9% Years worked as a care aide: Average (SD): 11 (8.7) years ≤ 10 years: 58% > 10 years: 42% |
| Kuk, 2017, the Netherlands118 | To examine the extent to which nursing staff in the Netherlands perceive that they encourage functional activity in nursing home residents | Quantitative Questionnaire Descriptive statistics |
41 nursing homes | 275 certified nurse assistants and 93 RNs | Gender: 94% female Age: ≤ 35 years – 33% > 35–≤ 50 years – 40% > 50 years – 27% Years of professional experience: ≤ 10 years – 38% > 10 years ≤ 20–30% > 20 years – 32% |
| Laging, 2018, Australia133 | To explore the recognition and assessment of resident deterioration in the nursing home setting | Qualitative Observations and semistructured interviews Constant comparative analysis |
2 nursing homes | Observation component involved 184 hours of observations of 66 participants (3 GPs, 10 RNs, 10 enrolled nurses, 8 personal CAs, 20 residents and 15 family members) took part in the observational component of the study 40 participants completed semistructured interviews (3 GPs; 10 RNs; 9 enrolled nurses; 8 personal CAs; 5 residents and 5 family members) |
Gender: not reported Age: not reported Years in position: not reported |
| Liu, 2014; Hong Kong128 | To explore nursing assistant’s roles during the actual process of pain management for residents | Qualitative, semistructured interviews and focus groups Content analysis |
12 nursing homes | 49 nursing assistants | Gender: 96% female Age: < 18: 2.04% 18–25: 16.33% 26–35: 24.49% 36–45: 44.9% 46–55: 12.24% Years’ experience working with cognitively impaired home residents: 6 months – 1 year: 2% 1–3 years: 14% 3–5 years: 29% 5–10 years: 24% > 10 years: 31% |
| Lung, 2016; Hong Kong129 | To explore the perspectives of nursing home residents and nursing assistants on their daily interactions | Qualitative Unstructured interviews Content analysis |
6 nursing homes | 18 nursing assistants and 15 residents | Characteristics of nursing assistants: Gender: 100% female Average age (SD): 51 years (6.7) (range 37–62) Average length of employment: 7.4 years |
| Marshall, 2020, Canada112 | To describe the perceptions of the roles and work of nurses and CAs in long-term care from interprofessional perspectives | Qualitative Focus groups, interviews Framework analysis |
10 long-term care facilities | Focus group participants (n = 75) comprised physicians, administrators, extended care paramedics, RNs, licenced practical nurses, continuing CAs, personal care workers and residents and/or family members (number of specific professional roles participating in focus groups not provided) Interview participants: regulated nurses (n = 18); continuing CAs and personal care workers (n = 8); nurse practitioner (n = 1). Participants also included physicians (n = 1), administrators (n = 3), residents and/or family members (n = 10) |
Gender: not reported Age: not reported Years in position: not reported |
| Mueller, 2012, USA105 | To examine Licenced Practical Nurse perceptions about their role and responsibilities in nursing homes | Quantitative Questionnaire Descriptive statistics |
Participants recruited via boards of nursing, (number of nursing homes represented not reported) | 142 licenced practical nurses | Gender: 98.4% female Age: 47.8 (SD 12.5). Average number of years as a licenced practical nurse: 18.6 (SD – 12.2). Average number of years in current position: 7.5 (SD – 7.4) |
| Medvene, 2010, USA104 | To identify the communication behaviours and strategies used by socially skilled geriatric nurse aides working with residents in long-term care facilities | Qualitative Semistructured interviews Structured content analysis |
9 long-term care facilities (mix of nursing homes and assisted living facilities) | 16 geriatric nurse aides | Gender: 94% female Average age: 42.2 (SD 12.23) years (range 22–63 years) Average number of years worked at the facility: 7 years (SD 6.71) (range 1–20 years) |
| Odberg, 2018, Norway123 | To expand the knowledge of the nurses’ role during medication administration in the context of nursing homes | Qualitative Observations, semistructured interviews Inductive content analysis |
Two nursing homes | Interview participants – staff nurses (n = 8), nurse assistants (n = 3), nurse managers (n = 2) and doctors (n = 2) | Gender: 80% female Age: not reported Years in position: not reported |
| O’Doherty, 2013, Ireland124 | To explore nurses’ perceptions of their role in the rehabilitation of older people in long-term care residences | Qualitative Semistructured interviews Framework analysis |
2 long-term care residences | 10 nurses | Gender: 100% female Age: 26–60 years Experience in care of older people ranged from 1 to 30 years |
| Olsson, 2014, Sweden116 | To describe RNs’ perceptions of their profession concerning medication management in elderly care in nursing homes | Qualitative Interviews Content analysis |
8 nursing homes | 16 RNs | Gender: 94% female Age: not reported Years of working as RN: 20 years (median), 1–39 years (range) Duration working in current workplace: 5 years (median), few months – 18 years (range) |
| Ostaszkiewicz 2016, Australia134 | To examine, describe and explain how continence care was determined, delivered and communicated in Australian long-aged care facilities | Qualitative Interviews and observations Open coding, theoretical coding and selective coding |
Interviews carried out in long-term aged care facilities across Australia (number not reported), and observations in 2 care homes | The interview sample included RNs (n = 6), enrolled nurses (n = 6), and personal care workers (n = 6) | Gender: not reported Age: range 18–69 years Years in current long-term care facility: range 1–15 years Years working in long-term care: range 1–20 years |
| Park, 2018, Korea126 | To search for ways to invigorate and foster the remaining functions of this complex-disability group, based on practical nursing strategies in nursing homes | Qualitative Interviews Thematic analysis |
11 nursing homes | 29 nurses | Gender: 100% female Average age: 41.6 years (range 26–57 years) Average length of experience in nursing homes: 4 years and 3 months |
| Sun-Young, 2020, Korea127 | To clarify and conceptualise the ways in which nurses manage the ego integrity of residents of nursing homes in their daily practice | Qualitative Interviews Specific analysis approach not reported |
6 nursing homes | 8 nursing home nurses | Gender: not reported Age: not reported Years in position: not reported |
| Talbot (2016), UK120 | To provide an in-depth phenomenological understanding of the experience of staff caring for service users with dementia in long-term residential and nursing care environments | Qualitative Semistructured interviews Interpretive phenomenological analysis |
Residential and nursing care homes (number of homes not reported) | 8 CAs | Gender: 88% female Age range: 21–42 years Length of current employment: 18 months – 5 years (range) |
| Vandrevala (2017), UK121 | To explore nursing staff roles adopted while responding and managing sexual needs and expression of/for nursing home residents with dementia | Qualitative Semistructured interviews Interpretative phenomenological analysis |
2 nursing homes | 8 nursing staff (7 health CAs, and 1 unit manager) | Gender: 75% female Age: 20–30 – 37.5% 31–40 – 37.5% 41–50 – 25% Length of time working as a care worker: under 1 year – 25% 1–5 years – 62.5% 11–15 years – 12.5 % |
| Vogelmeirer, 2011, USA107 | To describe medication reconciliation practices in nursing homes with a specific focus on nursing staff involvement in the process | Qualitative Interviews and observations Content analysis |
8 nursing homes | Number of RN staff observed: 18 Number of RN observations: 27 Number of licenced practical nurse staff observed: 15 Number of licenced practical nurse observations: 19 |
Participant characteristics not reported |
| Vogelmeirer, 2014, USA107 | To explore nursing home leader and staff nurse perceptions about the process of medication reconciliation, with a specific focus on identifying medication order discrepancies | Qualitative Interviews and focus groups Thematic analysis |
8 nursing homes | 13 RNs, 28 licenced practical nurses and 18 nursing home leaders (of which 15 were RNs) | Gender: not reported Age: not reported Years’ experience at current nursing home: Staff nurses: 75% had less than 5 years of experience in their nursing home Leaders: 50% had 6 or more years of experience in their current nursing home |
| Yektatalab, 2012, Iran130 | Explore Iranian caregiver’s perceptions in elderly care homes which can improve the care and quality of the patient’s life | Qualitative Focus groups and interviews Inductive content analysis |
2 care homes | 10 caregivers, and 4 head nurses and supervisors | Gender: 71% female Age: 25–35 years Average number of years working in care home: 30 years (range 1–11 years) |
Most studies (n = 31) were assessed as good quality against the MMAT. 100–102,104–110,112–121,123,125–131,133–135 Five studies were of lower quality, due to difficulty in assessing some MMAT criteria103,111,122,124,132 (see Appendix 5).
Five themes represent the literature: (1) ensuring personalisation of care; (2) assessing, supporting and monitoring resident health and well-being; (3) promoting safety; (4) leading and co-ordinating care; and (5) supporting residents to live with purpose. Cross-cutting themes included leadership, relationships and quality assurance (Figure 3).
FIGURE 3.
Roles and responsibilities of care home staff Based on NHS England House of Care – a framework for long-term condition care. 137
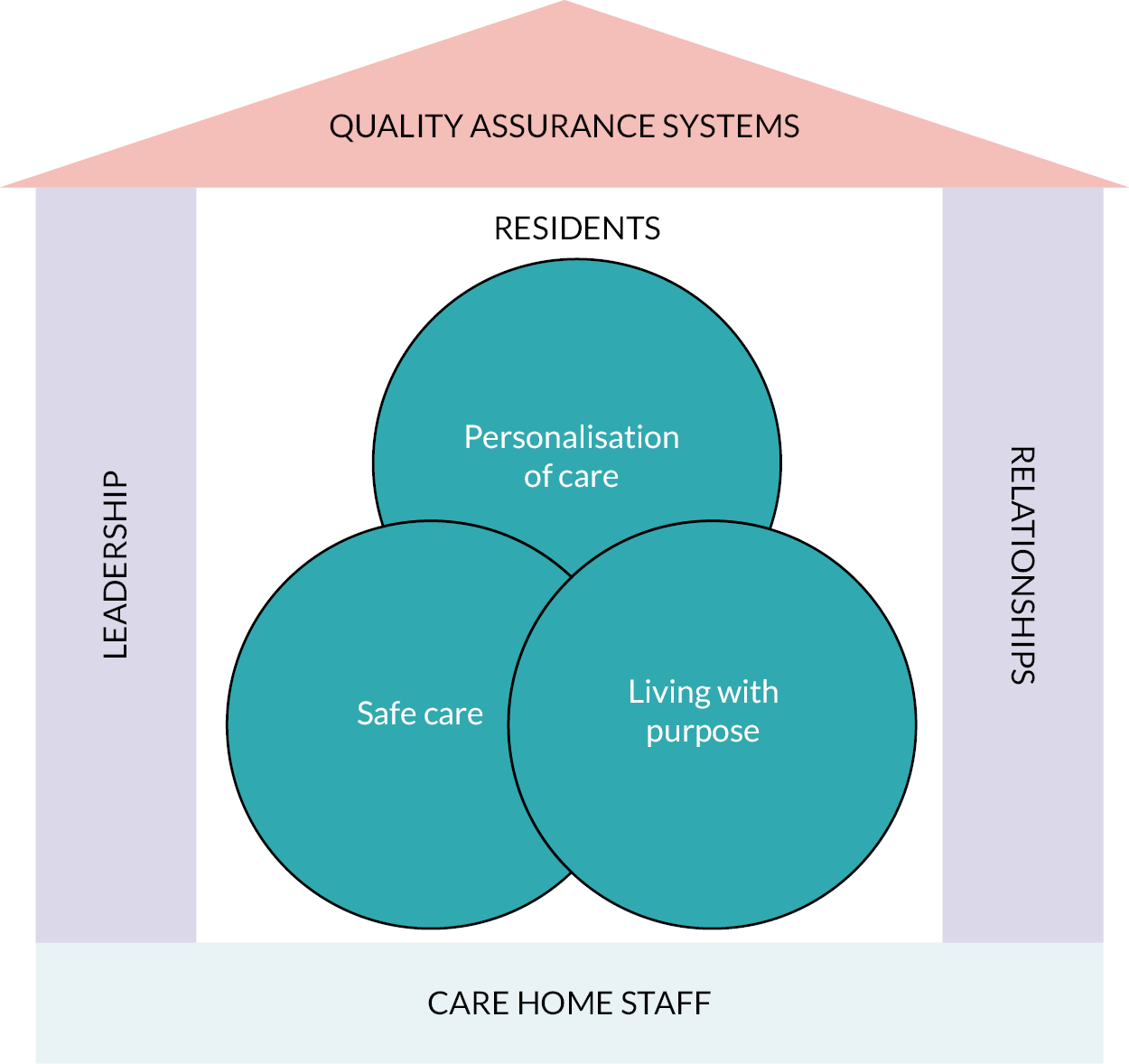
Ensuring personalisation of care
Personalisation refers to the focus on the older person’s specific needs, wishes and preferences by care home staff (including RNs and CAs) and using this knowledge and understanding for planning and providing individualised, personally appropriate and respectful care.
Registered nurses and CAs described the importance of establishing close, ‘family-like’ relationships with residents to enhance their knowledge and understanding of the individual. 101,112,125,128,131,135 ‘Getting to know’ the resident required investment of time by RNs and CAs. 104,108,112,122 Work undertaken during and outside of contracted hours; for example, spending time with residents after a shift or on days off. 109,112 Not all CAs prioritised relationship building, focusing instead on task-orientated care. 120,138 Relationships, and ‘knowing’ an individual, were perceived to help staff be responsive in the support and care provided for residents. 101,104,112,122,126,133 RNs reported it supported efficient decision-making to address health and social care needs of residents, whereas infrequent interactions or lack of familiarity with residents negatively impacted on care. 133 CAs perceived personal relationships ensured a ‘human touch’101 and helped them carry out their work,104 for example, recognising signs of pain for a resident and then ensuring adequate pain relief. 128 It also provided strong motivation to provide a level of care that they would for their own family members. 101,103
Staff described using a range of communication methods to build trusting relationships with residents and enhance quality of care and quality of life: greeting a person by name, complimenting a resident, engaging in conversation on topics of resident interest, accepting how a resident is feeling, using humour, or sharing information about hobbies or family as appropriate with residents. 101,104,108,129 While humour was considered an important strategy for building relationships, care home staff emphasised the importance of determining a resident’s reaction or response to humour and adjusting the content and/or tone of this form of communication. 129 Similarly, staff disclosure of information about themselves to a resident needed to be appropriate and acceptable for the resident. 129 Non-verbal communication strategies used included displaying affection, gentle touch or hugging, smiling, being present, not rushing and small gestures aimed at demonstrating understanding of what matters for the resident. 100,101,104,135
Care staff perceived relationship building as important for residents as part of a comfortable and supportive living environment,104,112 and ensuring resident perspectives and experiences were respected. 103,104,129 Building trust was important if residents were able to communicate their needs, such as their physical status or pain or discomfort experienced. 126 CAs described the importance of ‘family-like’ relationships for residents who did not have regular visits from family and friends: CAs described that they fulfilled this role for these residents. 108 RNs had an important role in supporting residents to establish and maintain meaningful relationships with staff, other residents, visiting family and friends. 127 This included assessing any communication difficulties that the resident may be experiencing, for example any difficulties with hearing which could be addressed to support relationship building. 119
Care home staff reported their important role in preserving and promoting personal dignity for residents and involving them in care. RNs played key roles in assessing and planning care,119,122 including finding solutions for, or new ways of addressing, care issues. For example, when a resident refused or resisted assistance with personal care then it was important to find respectful ways to support the resident. 122 RNs also had to clearly communicate any plans for care with CAs. 100 CAs had an important role in supporting residents with personal care to meet personal preferences for maintaining their physical appearance or to ensure their living space was maintained;103,134 this included activities such as timely care to assist someone to maintain their hygiene when incontinent, minimising unpleasant odours by removing wet or soiled linen or clothes, or tidying personal belongings. CAs also perceived it important to provide this personal care with empathy103 and to control non-verbal responses when providing intimate care to not offend an individual resident. 100
Care home staff considered it important to maintain residents’ rights to make choices and decisions about their care, alongside assessing individual capacity to consent:100,104,121 this was promoted by listening to residents, gaining permission from residents, involving residents in decisions and offering information and choices. 114 CAs described that they had an important role in translating complex medical information into lay language for residents,100 and advocating for residents. 100,103,135 RNs described that involving residents in their care required knowledge, competence and effective communication skills, as well as time and opportunities to interact with residents. 114
Assessing, supporting and monitoring resident health and well-being
Care home staff (RNs and CAs) described the importance of their interactions with residents for timely assessment, support and monitoring of residents’ health and well-being. Relationships and ‘knowing’ the resident have been described above. This section provides more depth of how care home staff gather intelligence through these relationships for the purpose of enhancing quality of care and quality of life for residents.
Staff recognised that residents were not always able to articulate when they felt unwell, or when their symptoms were worsening. Therefore, knowing a person helped staff to recognise subtle changes in a resident that may indicate a change in their health status or deterioration and that could promote timely care or interventions;126,128 for example, identifying new or worsening pain for a resident. 102 Examples of observations used by staff for this purpose included changes in resident daily behaviour patterns (e.g. sleep or appetite patterns), body movements or non-verbal gestures (e.g. pointing at or rubbing an affected area), interpersonal interactions (e.g. agitated or not talking) and external appearance (e.g. a bed sore or rash). 102,104,126,128 CAs also described assessing verbal tone or expression of emotions104 as indicators of potential change when a resident could not verbalise their health status. Daily assessment for all residents, and in particular for residents living with cognitive impairment, was considered an important role for all staff to enhance quality of care and quality of life. 126,128
Being able to competently undertake these observations required consistent assignment of staff to build understanding of the person and recognise changes. 133 This could be particularly challenging for RNs who often delegated caring responsibilities to other staff and so had to rely on these staff to report resident changes back to them. 133 RNs perceived it important to direct the care team to ensure these observations were undertaken when providing day-to-day care for, and interacting with, residents. 126 RNs also recognised that particular resident groups (e.g. those being cared for in bed) required careful observation and monitoring. 126 CAs described themselves as ‘proxy reporters’, ‘middle person’, ‘gate-keeper’ and ‘bridging the gap between nurses and residents’. 128 However, some studies reported that some CAs did not consider resident assessment as part of their role, nor their responsibility. 128,133 CAs were cautious and wanted to avoid being responsible for errors so focused on fundamental aspects of care rather than engaging in assessment activities. 128 A task-focused approach, for example CAs focusing on helping a resident to wash and dress but not looking at the condition of their skin, meant that health problems could go unnoticed and untreated, and negatively impact on a resident’s quality of life. 133 Conversely, some CAs reported that when they recognised changes in a resident’s health, for example level of pain being experienced by them, this assessment was not always acknowledged by RNs. 119,128,133 RNs have an important role in supervising and supporting CAs to monitor and report changes in resident status through constant dialogue and engaged teamworking. 113 CAs have not always been adequately trained to assess residents and so without this level of support and supervision by RNs, residents are at increased risk of deteriorating133 or not having their condition or state (such as pain and whether medicines are relieving their pain) reassessed. 128 RNs also have a key responsibility to assess and liaise with other healthcare professionals to ensure the health and care needs of residents are appropriately reported, addressed and managed. 122,133 The importance of team relationships is considered further below (See Leading and co-ordinating care).
Registered nurses described taking actions to ‘nip things in the bud’ and prevent further worsening of a health condition or to minimise deterioration of the resident’s overall health and well-being. 110,115,119,123 RNs described their responsibility to use their knowledge and assessment skills to ensure appropriate care and support for residents, which included for example requesting review and reductions in medicines being administered or obtaining appropriate equipment for assisting residents to move and to prevent pressure area damage. 119 The physical presence of a RN ensured early identification, or anticipation, of problems for residents and so had potential to prevent deterioration of resident health or well-being and also promptly manage acute situations. 119,125
Promoting safety
Registered nurses have an essential role in promoting safety for care home residents, including the delegation and supervision of care provided by CAs. Leading and co-ordinating care is an important aspect of safety and is also considered as a separate theme below (See Leading and co-ordinating care). RNs also interface with external healthcare professionals. Studies highlighted the ways in which RNs work with the range of internal and external staff to ensure appropriate and timely interventions and care by staff to promote quality and safety for residents, as well as to create safe environments.
Registered nurses coach the direct care team and their physical presence is reported to improve care delivery and support teams to reflect on what works well or may need to be improved. 117 The RN has an important role in co-ordinating care and role modelling best practice and professional standards of care. 132 Studies revealed that RNs adapted their ways of working to accommodate best use of the skills set of colleagues for the benefit of residents’ care and to compensate for any perceived deficiencies in staff knowledge, skills and competence, or to accommodate organisational challenges such as staff shortages in the care home or access to other healthcare professionals. 115,123
The RN anticipates care demands, planning work and being responsive and flexible in care delivery and their work to ensure resident safety. Studies highlighted how RNs filled gaps in care while fulfilling their own roles and responsibilities through ‘workarounds’ or adaptations. 115,123 Unintended consequences were identified when RNs were filling gaps in care over extended periods while fulfilling their own role and responsibilities: higher workloads for RNs were perceived to increase errors in care delivery. 123
Record keeping was considered an important source of information about care ‘done’ or ‘not done’ by the care team; CAs recognised their role in supporting the maintenance of accurate care records. 100 RNs audit these care records and following up on any missed care or ensuring accurate records to reflect the care provided. 116 Deficiencies in care records were perceived by all staff (RNs and CAs) as neglectful and opening opportunities for criticism or blame cultures. 100 Learning from adverse incidents (such as medicine administration errors) was also used by RNs to support the care team and to develop a more open culture and climate that would benefit residents’ care and promote safety. 113
Knowledge of, and adherence to, policies and protocols were considered a prerequisite for achieving safety for residents, but RNs acknowledged that these did not always accommodate the challenges and realities of working in a care home environment. 113 This led staff to find workarounds to ensure safe care delivery, for example to ensure the administration of medicines when short-staffed. 110,123
Registered nurses were considered essential for creating safe environments for resident care. 119 Examples of ways in which nurses contributed to safe environments included carrying out risk assessments, documenting and recording care, minimising potential harms/hazards, using protocols to help prevent falls, obtaining appropriate equipment for moving and handling of residents, and preventing pressure area damage,119 and preventing medication errors. 110,116,125 Decisions related to creating safe environments had to be balanced with the RN’s ambition to promote resident choice and freedom within the context of a shared residential environment meeting the needs of a varied resident population. 122
Leading and co-ordinating care
The importance of RNs leading and co-ordinating care has already been raised in the themes above. We develop understanding specific to leadership and co-ordination in this section. In particular, we consider the ways that RNs work collaboratively to promote good quality care, support planning activities and ensure safe delegation of care.
Studies described RNs working collaboratively with members of the care home team, relatives and external healthcare professionals. This collaboration was perceived to improve resident’s health status and quality of life. 119,125,132 Collaboration required RNs to effectively listen to others and gather information about the resident and their needs and preferences from residents themselves, their relatives and the care team. 107,110,114,115,125 RNs translated this intelligence into a care plan that promoted personalisation of care (discussed above), and then played an important role in ensuring the right people were involved at the right time to support the resident.
A significant proportion of personal care and support is provided by CAs in care home settings. CAs had a pivotal role in monitoring residents and reporting changes in residents’ health and well-being to RNs125 and to initiate additional care or services, for example from the medical team. 100 RNs reinforced this perception: CAs were described as their ‘eyes and ears’115 but it was the RN who led and co-ordinated care.
Registered nurses were described as having a key role in liaising with medical and allied health professionals. These services – medical care, physiotherapy, occupational therapy and dietetics – are often provided for care home residents by external services. RNs liaised with relevant professionals to ensure timely inputs to meet residents’ health, care and support needs. This requires RNs knowledge of the resident and a comprehensive assessment to help inform decision-making about care and to guide these inputs. 110,114,133 Involving the resident and family with these services and care was also deemed the role of the RN. 125 Despite being pivotal for collaboration and co-ordination, it is important to highlight that RNs reported that they often worked alone in the care home setting:106,107,115,116 they described themselves as a ‘solitary worker’. 116 This highlights a distinction between RNs working in this context to, for example, in an acute care environment where there are often more RNs working at one time and access to medical staff.
The RN had a role in planning activities, which was closely linked with ensuring leadership and co-ordination of care for residents’ benefit. Planning activities occurred at a number of levels; for example, to ensure adequate resourcing and staff rostering (facility level), to prioritise, plan and delegate daily work and activities for the team (team level) and to respond to residents changing needs (individual level). 122,123,132 Delegation of care activities by RNs to CAs required:105,113,115,116,119,125,132
-
The RN to clearly communicate with CAs and to have understanding of the knowledge and skills of the care team for appropriate delegation.
-
RN and CA relationships based on trust so that the RN had confidence that delegated care would be carried out appropriately and the CA would report if they did not feel capable to perform, or did not understand, the delegated care.
-
The CA to report any concerns about the resident to the RN and the RN to follow up on delegated tasks with the CA, monitor residents and outcomes and any unintended consequences of delegation for residents or the care team.
As leaders and co-ordinators of care, the RNs required an understanding of the care team for safe delegation. When delegating, RNs had to ensure they maintained a level of engagement with residents and their care so that they could review and respond to any changes in care needs for the resident. 133 RNs also had to minimise task-based approaches to care when delegating: while carrying out delegated care tasks (e.g. bathing), CAs needed flexibility in their work (and the organisation of this work) to be able to respond to immediate needs of residents. 109 Task-based approaches or routines were perceived by care home staff to have a negative impact on residents and their experiences of care. 109
Supporting residents to live with purpose
In this final theme, we acknowledge that the roles and responsibilities of care home staff are carried out in the residents’ home. Therefore, in addition to meeting the personal and healthcare needs of residents, staff have an important role in supporting residents to live with purpose and to promote their quality of life and well-being. In many ways, this theme overlaps with our consideration of the ways in which care home staff ensure personalisation of care. However, we considered it important to also consider how care home staff support residents to ‘live with purpose’, alongside the tensions in their work that may inhibit this ambition.
Registered nurses described their role in helping residents with their personal well-being and quality of life. 119,127 This was perceived by care home staff as ensuring residents: felt safe and secure; established and maintained meaningful relationships (including intimate relationships); fulfilled their spiritual needs; had time to reminisce; had physical or emotional needs addressed; and maintained their functional and/or cognitive abilities for as long as possible. 100–102,104,108,112,118–121,124,125,127,130,131,138
Importantly, care home staff helped create a ‘home’ environment. Recognising individual residents within a communal living arrangement was a key concern for care home staff. 131 Care home staff liaised with residents and their families and friends to promote a sense of home for the residents. This included surrounding the resident with familiar possessions,127 or encouraging residents to maintain routines or do tasks they may have previously done. 124 Promoting residents’ choice and control about how they spent their time was also highlighted by care home staff as important. 119 RNs identified their role in maintaining balance and harmony within the communal living environment: this included supporting residents in distress or behaving in ways that may upset or disrupt other residents. 119,122 A range of strategies and approaches used by care home staff to promote resident well-being were identified in the literature, and included: providing one-to-one company; engaging in activities of the resident’s choice and promoting diverse activities, both social and recreational; and promoting a home-like environment with opportunities to engage in household tasks. 103,104,112,118–120,122,124,125,130,131,135,138 However, studies revealed the challenges for care home staff when supporting residents in the care home environment.
Staff shortages, alongside workload demands and pressures which included the administrative burden of care, limited available time for care home staff in these more supportive activities. 111,120,131,135 Physical care was often prioritised over psychosocial care130,134 and the organisation of care, particularly task-based approaches, could limit the engagement of CAs with residents’ social, spiritual and emotional care needs. 109,120,135 Cultural differences also impacted on whether CAs considered psychosocial care as within their roles and responsibilities. 129 Leadership played an important role in creating cultures that balanced the range of residents’ needs to support both quality of care and quality of life.
-
Promoting personalisation of care and establishing ‘family-like’ relationships between residents and staff (RN and CA) enables staff to tailor care to residents’ needs and preferences, to be responsive and to support efficient decision-making, as well as promoting feelings of comfort and safety for residents and maintaining their rights to make choices and decisions about their own care.
-
Knowing a person helped staff to recognise subtle changes in a resident that may indicate a change in their health status or deterioration and that could promote timely care or interventions.
-
Assessing, supporting and monitoring resident health and well-being was the responsibility of the RN – supported by the care team. RNs have an important role in supervising and supporting CAs and promoting teamwork.
-
RNs have an essential role in promoting safety, including mechanisms for quality assurance, in homes. RNs work with a range of internal and external staff to ensure appropriate and timely interventions and care by staff to promote quality and safety for residents and in care environments.
-
RNs have an important role in anticipating care demands, planning work and being responsive and flexible in care delivery and work designed to ensure resident safety.
-
RNs collaborative work with members of the home team, relatives and external healthcare professionals to create intelligence-informed care plans, promoting personalisation of care for residents, followed by co-ordinating the right people to be involved at the right time to support residents.
-
Staff have a key role in supporting residents to live with purpose and promote residents’ quality of life and well-being.
Work package 1ii: care home staff behaviours for promoting quality of resident experience
The realist review offered six theoretical propositions (context–mechanism–outcome configurations) as necessary conditions to create systems for staff behaviour that influence quality as experienced by long-term care facility residents (Figure 4). Evidence informing the development of these theoretical propositions is presented below. These results have been published. 39
FIGURE 4.
Six theoretical propositions
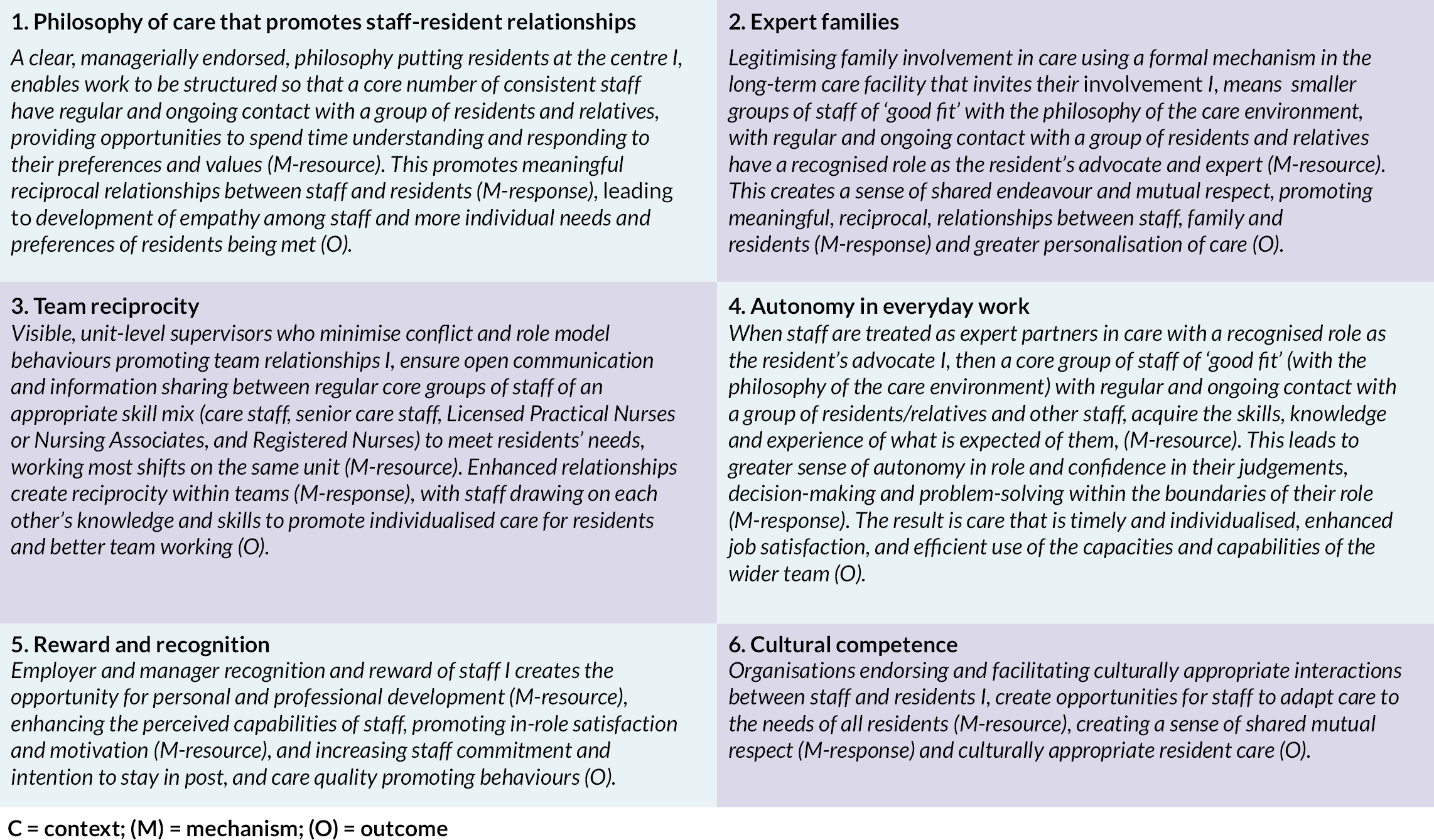
As Figure 5 illustrates, these propositions connect and impact on each other. One thread ran through all of them: effective leadership behaviours (at all levels) were necessary to trigger the effective use of resources (mechanism), that cultivated the relationships (mechanism response) required for staff to behave in ways that promoted quality (outcome).
FIGURE 5.
Summary of context–mechanism–outcome configurations.
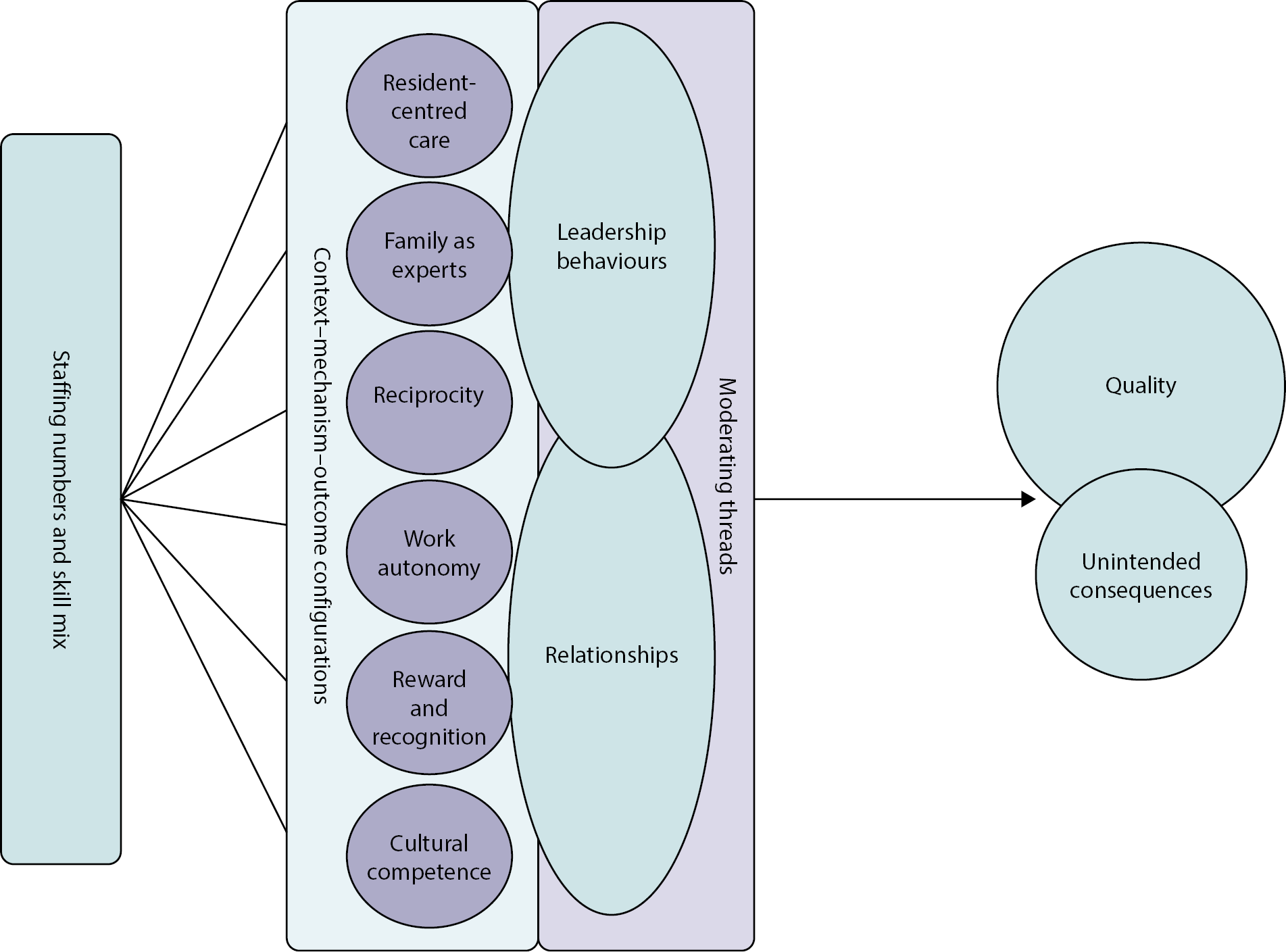
Philosophy of care that promotes staff–resident relationships
Philosophies of care promoting relationships between staff and residents support staff behaviours that foster individualised resident care. 139–145 Philosophies should include an explicit care-focused mission statement,139,142,146 clearly articulated and enacted through the everyday behaviours of managers/supervisors. 139,140,142,143,147 Philosophies should go beyond assisting residents with physical tasks, and address residents’ social and emotional needs through relationships. 143,144 To be effective, work needs to be organised around such philosophies. 144,145,147 For example, a core number of staff who are a ‘good fit’ with the philosophy of the care environment, who engage consistently with the same group of residents and with sufficient resources will better meet residents’ needs and preferences. 148–153 Staff who are a ‘good fit’ with the philosophy of the care environment, were those that actively valued older people:45,144,154–161 displaying or willing to learn empathy, compassion and kindness45,144,153,155,156,162–167 and enacting these attributes through behaviours; performing duties beyond the bare minimum specified in contracts, helping others45,144,155,156 and working well with coworkers. 153 Sufficient staff subscribing and enacting the philosophy meant it was reinforced, sustained and relationships developed. 153,154,159
Cross-sectional50 and longitudinal studies27,167 were inconsistent and contradictory, but revealed no critical number of staff. Numbers varied from 5 to 15 residents per staff member. 148,150–152 Relative criteria were more useful: sufficient staff for timely care, such as, avoiding residents crying out for help with no care workers around to notice,140 and consistent staff with regular contact with a group of residents and families. 168 Small groups of linked residents and staff promoted familiarity, communication and a familial environment for cultivating relationships111,150,152 with more time for residents, families168 and coworkers. 111,149,152
Managerial behaviours encouraged relationship building:139,140,146 clearly communicating role expectations and responsibilities;140,146,153,169,170 reinforcing individual staff contribution to collective care;144,146,163 physically helping out with resident needs and supporting staff;139,146,171–173 actively listening to staff, resident and families’ concerns;139,141,146 and openly discussing challenges faced. 139,141,143,147,171–174 Staff that feel supported, valued and with (managerial) ‘permission’ to prioritise residents’ needs adapt and adopt behaviours that foster expression of residents’ preferences while providing care144,147,157 and experimentation of novel ways of engaging residents. 136,153,175 A relationships-focus enables greater appropriateness in behaviours given resident preferences. 45,136,139,144,155,176,177 Strategies employed included associating residents’ stories to their own experiences, stimulating empathy and taking more responsibility for putting ‘learning’ (about individual residents) into practice. 45,156,177 Unsupported staff provided less support to colleagues,147 weakening the generative mechanisms behind quality.
Developing close bonds with residents is not without risks: relationships developed over time can increase the emotional burden of care,156,176,178 feelings of helplessness and distress when unable to reduce suffering;144 not always mitigated by caring experience. 178 Accordingly, some workplaces discouraged relationship-building with residents157,178 to reduce the emotional burden for staff. 147,176,178
Expert families
Family members are an important and valuable source of information and understanding for residents’ needs and preferences. 140,153,164,166,173,179–181 Staff engagement with family members – if desired – leads to family acting as experts in their relative’s care. 166,172,179,180 In a philosophically and behaviourally supportive context, these roles positively influence staff behaviours and create opportunities for relationship-centred care140,164,182,183 – especially for residents living with de5mentia. 179
Family involvement is legitimised via formal mechanisms for involvement. This also encourages relationship building168,179,182,184 built around ‘informing staff’ and ‘consulting with staff’ through to ‘co-deciding with staff’. 179 Mechanisms for meaningful participation include: invitations to care planning meetings,166,179,182,185 support groups for family members,184 formal introductions to staff members at the facility,179,182 and regular family information meetings. 182,185
Relationships between staff and family members should be reciprocal and act as a vehicle for sharing information about residents,144,164,168,172,179,181,182 their preferences and other personal information for informed care164,179–181 and care planning. 179 Practical manifestations can be seen in staff avoiding foods that a resident dislikes and using personal belongings to create homely environments. 164,172 Family may demonstrate successful behavioural strategies and interpretation with residents. 144,179,184 In turn, staff feel rewarded from positive relationships with families. 144 Establishing relationships with family members takes time. 140,144,153,164,181,182 Once established, communicating care plan changes,182 health,144 and participation in activities can be sustained,164 generating a greater sense of shared caring responsibilities and mutual respect. 144,164,172,173
Risks for staff associated with greater familial involvement include feelings of stress and anxiety arising from unrealistic demands and expectations on care provided140,144,178,179,183 or an unwillingness from family to accept a resident’s deterioration178 or challenging behaviours. 144 One consequence is negative feedback loops of poor staff experience and negative attitudes towards families, diminishing recognition of continued importance of staff–family relationships,140,179,183 and subsequent relationship breakdown. 140,144,178,183
Team reciprocity
Companionship is important in care work; being seen, needed and supported by reciprocating colleagues provides satisfaction and meaning in work. 157,158 Expressions of reciprocity included, ‘we depend on each other’,157,172 ‘show respect for one another’,146,173 ‘we take turns’,186 and ‘we are a part of each other’s decision-making’. 146 Sometimes reciprocity was implicit in teamwork,143 meaningful relationships with colleagues,144,171 shared values,141,143,158,170,172 mutual respect,141 a mutual understanding of each other’s work,144,171 strong group relations142 and unified commitment. 142,157,187 Whether explicit or implicit, reciprocity was linked with information exchange and the ability to draw on each other’s knowledge and skills to promote individualised care and enhance quality. 139,141–144,146,153,157,170–173,188,189 Teams with high degrees of reciprocity were more open to advice seeking and collaborating. 158,189
Leaders – at unit level – exhibited various behaviours designed to foster reciprocity:
-
Clearly communicating expectations of staff, ways of working and their behaviours. 139,146,153,170
-
Holding regular meetings inclusive of all staff. 139,146,170
-
Openly discussing and resolving problems as a team. 139,141,146
-
Flexible working structures for staff. 143,145,147,153,171,173
-
Bringing staff together as a close-knit group bound together by common interests and experiences. 141,170,172
Role experience was a modifier of reciprocity-reinforcing behaviours. Experienced staff often used reciprocal behaviours to build confidence with less experienced/confident staff. 147,153,155,158,159,190–194 Such behaviours were nested in relationships built on open communication and respect for the less experienced. 193,195 Managerial support meant experienced staff shared greater knowledge and experiences;147,155,157,192,196 especially among staff caring for people living with dementia. 157,165,180,197 Units that discouraged coworker relationships often lacked team reciprocity,178 and were of poorer quality. Unit-level supervisors that minimise conflict and role model relationship-building behaviours provide the context in this context–mechanism–outcome configuration.
Role modelling and reciprocity do not always coexist. Negative outcomes include complacent staff generating and sustaining power imbalances or bullying – particularly in chronically short-staffed homes. Examples included ignoring or excluding team members or withholding information about resident care. 198 Understaffed care teams have higher workloads, less time available for interpersonal discussions and less time for defusing frustrations, leading to conflict. 198 Effective leadership and management are crucial for minimising such unintended outcomes. 149,178,194,198
Autonomy in everyday work
Greater perceived autonomy means greater staff engagement with work140,144,169,199 or role empowerment. 140,189,194,200 Autonomy is a positive and necessary feature of delivering individualised resident care. 140,144,166,199,200 Flexibility in staff responses to needs is highly valued, leading to higher perceived quality among family and residents. 142,180,199 Increasing autonomy is easier in smaller teams of staff, working consistently with the same group of residents and colleagues. 152
Autonomy, behavioural enactment and leadership coexist in a positive feedback loop. Collective agreement resulting from reciprocity strengthens collective knowledge and shared values/mission, which in turn gives staff greater confidence to act independently. 158 Shared values are vital to developing professional values and integrity, refining staff skills, supporting further learning and development of skills and satisfaction with work. 158 These leadership elements constitute the context in this context–mechanism–outcome configuration. In such long-term care facilities, management practices foster staff with the skills, knowledge,140 opportunity139 and confidence to become autonomous workers. 197
Staff exhibit active autonomy in resident care in various ways that promote quality of care: reporting they are involved in care planning,45,140,199,200 asking for advice,45,140 being encouraged to innovate with different ways of providing care or undertaking work,140,144,169,171 meeting residents’ needs flexibly157,171 and being consulted for their views, ideas and opinions,140,150,156,189,200,201 and feeling valued for such input. 45,140,159,189
Staff who see themselves as equal partners in care experienced a sense of shared responsibility45 and mutual respect. 140 Staff capacities and capabilities when recognised and used efficiently result in work geared to meeting individual resident needs, rather than institutional routines. 45,140,156,159,171,199,200 Autonomy allowed staff time to ‘do the little extra’s’. 158 As a result, staff were more likely to be independent in their work,169 considered themselves able to make decisions,189,200,201 and shared work. 140,159,169 A high degree of flexibility in their work plans makes it easier for staff to collaborate and consult with each other in short informal meetings and, further, to support and help each other during the shift. 158
Reward and recognition
Rewarding and recognising staff influenced how staff felt about their work and shaped behaviours. Reward and recognition happen formally and informally. Formal endorsement arises from:
-
the senior executive team (organisational level) and/or care home leaders;200
-
the organisational mission statement (placing as much value on staff as residents);45,139,156
-
training and education;45,140,142,145,160,169,196,200,202,203
-
involvement in decision-making about resident care for the resident’s they knew well. 45,156,202
Surprisingly, little evidence exists regarding the influence of pay on perceptions of work and staff behaviours.
Informally, recognition can be:
-
Managers addressing staff by first or preferred name and praising staff for their contribution. 139,140,146,163,200
-
Utilising the unique knowledge staff have about individual residents by asking them for their opinions on how best to support the resident population. 140,146
-
Managers ‘pitching in’ with the day-to-day work, such as making beds and assisting at mealtimes, to support staff;139,146 and
-
Providing emotional support for any anxieties staff experience as a result of providing care. 147,148
Rewards are wide-ranging but included offering small gifts or arranging social gatherings to demonstrate appreciation for a job well done. 139,170 The investment in staff through rewards and recognition had a positive impact on how staff felt about their work, enhanced staff–manager relationships and led to behaviours that promoted quality in the long-term care facility and for the benefit of residents. 45,139,142,148,156,159,163,200
Cultural competence
Cultural competence, the ability to understand, communicate and effectively interact with people of different cultures, helps staff meet residents’ needs and promote quality of care and life. 140,147,184,204 Manifestations of cultural competence included:
-
Employing staff from different backgrounds, which was identified as valuable for promoting cross-cultural relationships with residents, family and coworkers. 140,147,162,177,184,193
-
Respecting religious beliefs,147,177,193 cultural norms,140,154,162,193,205 and sexual orientation,204,206 made a positive difference to daily lives of residents. 140,147,154,162,193
-
Knowing how to provide culturally appropriate personal care – such as meal preparation,162,205 honouring rituals,140,147,162,169 greeting residents using their first language,193 being in tune with local dialects,207 touching a resident in a culturally appropriate manner,140,193 and/or using appropriate non-verbal communication. 147,162,184,193
These factors all helped develop and maintain (cross-cultural) relationships between staff and residents. 140,162,193
Quality-promoting relationships are hindered184,193 when staff experience discriminatory behaviour from residents, for example, verbal abuse on the basis of skin colour,162 accent,162 sexual orientation204,206 and language difficulties. 162,180,184,189,193,206 Management intervention is essential to repair relationships. 147
Cultural competence is developed on the job147,180,193,204 and reinforced through team reciprocity,162,193 exhibited as respect and tolerance of each other’s cultures, effective cross-cultural communication and learning,193,206 and promotion of relationships between coworkers. 162,180
The theoretical propositions capture the key findings of this review (see Figure 4).
Work package 2: modelling relationships between staffing and quality at a national level
The overall aim of this WP was to understand whether and how variations in staffing between home explains variations in care quality as evaluated by the CQC. The dependent variable in our analysis is CQC inspection score (dichotomised into inadequate/requires improvement and good/outstanding) with independent variables measure of home characteristics that homes report to Skills for Care for inclusion in the NMDS-SC. To investigate the relationships, we estimated multilevel logistic regression models.
A note on interpretation
Results are reported in Table 10 as odds ratios – interpreted as the likelihood of a change in CQC inspection report score (from ‘inadequate’ or ‘requires improvement’ to ‘good’ or ‘outstanding’) associated with a one-unit change in each independent variable. An odds ratio below one indicates a home is less likely to be good or outstanding. For example, the odds ratio for total number of beds (0.994) suggests an increase in the number of beds is associated with a reduction in the likelihood of a home being rated good or outstanding. Conversely, an odds ratio above one signals an increased likelihood of being rated good or outstanding. If the odds ratio for total number of beds were 2 instead of 0.99, it would indicate that one extra bed would double a home’s likelihood of being rated good or outstanding. Because odds ratios are not always straightforward to interpret, we discuss the percentage changes in probability of a home being rated good or outstanding (often described as marginal effects) for some of our key results below. We also report 95% confidence intervals (CIs) for each odds ratio. These indicate the range of odds ratios likely to be observed 95% of the time if different samples of homes were drawn at random from the same population.
| Outcome: CQC good or outstanding rating | Nursing and residential homes | Nursing homes | Residential homes | |||
|---|---|---|---|---|---|---|
| Predictors | Odds ratios | CI | Odds ratios | CI | Odds ratios | CI |
| (Intercept) | 2.772 | 0.146 to 52.689 | 0.942 | 0.001 to 1014.368 | 5.580 | 0.210 to 147.928 |
| Number of beds | 0.994 | 0.988 to 1.000 | 0.993 | 0.982 to 1.005 | 0.991* | 0.983 to 1.000 |
| Total number of staff | 0.855 | 0.696 to 1.051 | 0.860 | 0.505 to 1.464 | 0.859 | 0.672 to 1.097 |
| Staff-to-bed ratio | 1.233** | 1.080 to 1.409 | 1.898** | 1.274 to 2.826 | 1.125 | 0.970 to 1.305 |
| % of staff on permanent contracts | 1.109 | 0.515 to 2.389 | 1.748 | 0.366 to 8.342 | 1.020 | 0.418 to 2.488 |
| Vacancy rate | 0.530 | 0.255 to 1.103 | 2.934 | 0.547 to 15.734 | 0.418* | 0.182 to 0.956 |
| Staff tenure (years) | 1.040* | 1.008 to 1.074 | 1.007 | 0.934 to 1.086 | 1.048* | 1.011 to 1.086 |
| % full-time employees | 1.254 | 0.894 to 1.760 | 2.171* | 1.024 to 4.604 | 1.012 | 0.694 to 1.477 |
| % of workforce on zero hours | 1.708* | 1.046 to 2.789 | 1.261 | 0.610 to 2.606 | 1.710 | 0.966 to 3.027 |
| Specialism of RN – older people | 0.954 | 0.682 to 1.336 | ||||
| Specialism of RN – adults | 0.877 | 0.599 to 1.282 | ||||
| Specialism of RN – mental health | 0.665 | 0.346 to 1.280 | ||||
| Specialism of RN – community care | 0.716 | 0.011 to 47.216 | ||||
| Specialism of RN – other | 0.181 | 0.018 to 1.816 | ||||
| Workforce age | 0.936 | 0.448 to 1.955 | 0.902 | 0.161 to 5.059 | 0.866 | 0.383 to 1.959 |
| % women in total workforce | 1.239 | 0.425 to 3.615 | 0.527 | 0.029 to 9.415 | 1.073 | 0.336 to 3.427 |
| % non-UK workers | 1.222 | 0.516 to 2.892 | 1.975 | 0.403 to 9.685 | 0.863 | 0.322 to 2.315 |
| % minority ethnic workers | 0.939 | 0.487 to 1.812 | 0.856 | 0.284 to 2.580 | 1.225 | 0.573 to 2.622 |
| Number of months that a manager was in post in the 12 months before inspection | 1.104*** | 1.082 to 1.126 | 1.116*** | 1.075 to 1.158 | 1.099*** | 1.072 to 1.125 |
| Months between NMDS-SC data entry and CQC inspection | 0.973*** | 0.966 to 0.980 | 0.974** | 0.959 to 0.990 | 0.971*** | 0.963 to 0.979 |
| Home operated by local authority | 1.148 | 0.944 to 1.397 | 1.021 | 0.679 to 1.536 | 1.231 | 0.982 to 1.543 |
| CQC service type: dementia | 0.801** | 0.680 to 0.943 | 0.912 | 0.693 to 1.202 | 0.804* | 0.659 to 0.981 |
| CQC service type: elderly | 0.805 | 0.632 to 1.025 | 0.885 | 0.512 to 1.530 | 0.734* | 0.557 to 0.967 |
| Random effects | ||||||
| σ 2 | 3.29 | 3.29 | 3.29 | |||
| τ00 councils with social care responsibilities | 0.34 | 0.20 | 0.36 | |||
| ICC | 0.09 | 0.06 | 0.10 | |||
| N councils with social care responsibilities | 151 | 141 | 151 | |||
| Observations | 5028 | 1785 | 3243 | |||
| Marginal R2/conditional R2 | 0.127/0.209 | 0.120/0.171 | 0.115/0.203 | |||
Results
Higher staff-to-bed ratio is associated with a greater chance of a good or outstanding CQC inspection score (odds ratio 1.233, 95% CI 1.080 to 1.409). This effect was greater in nursing homes (odds ratio 1.898, 95% CI 1.274 to 2.826), implying that increasing staff per bed from an average of 1.3 to 2.3 would almost double the likelihood that a home would be rated good or outstanding.
Having more experienced staff (i.e. with higher mean job tenure at the home) was associated with a slight increase in chance of a good or outstanding inspection rating (odds ratio 1.04, 95% CI 1.008 to 1.074): a result mainly driven by nursing homes. Each month that a manager was in post in the 12 months prior to the inspection increased the likelihood of a good or outstanding inspection rating (odds ratio 1.104, 95% CI 1.082 to 1.126). This implies homes without managers in post in the 12 months prior to the inspection were less likely to be rated as good or outstanding, with the chances of being rated good or outstanding lower the longer the period without a manager.
Homes that had a greater proportion of their staff on zero-hours contracts were more likely to be rated positively (odds ratio 1.708, 95% CI 1.046 to 2.789), with the odds ratio higher in residential care homes compared to nursing homes. Although there is no obvious causal mechanism to explain this result, it is conceivable that more flexible staffing arrangements may allow homes to better ensure adequate staffing that meets residents’ needs in the context of resource constraints. Residential homes with more unfilled vacancies were less likely to be rated good or outstanding (odds ratio 0.418, 95% CI 0.182 to 0.956). Residential homes were more likely to be rated positively when they had more full-time (as opposed to part-time) staff, although the mechanism through which this might cause a better inspection score is not clear. Larger residential homes were less likely to be rated positively (although there was no clear relationship between home size and quality ratings in nursing homes).
In interpreting these results, it is important to keep in mind that we are observing associations between measures of quality and staffing at a single point in time. These associations do not necessarily represent causal relationships. For example, higher-quality homes may find it easier to retain staff and managers so part of the association may be explained by quality causing more experienced staff and managers rather than more experienced staff and managers causing higher quality.
Sensitivity analyses
To test whether results were sensitive to choices made when organising and preparing data for analysis, we carried out sensitivity analyses. We used raw, numeric CQC scores as outcome variables and applied a linear random intercept model. Sensitivity analysis results were similar to the main results in terms of statistical significance and effect size (Table 11). We examined how sensitive main results were to the addition and withdrawal of individual variables from the models. Results were broadly stable. We performed cross-validation to ensure our models retained accuracy in out-of-sample predictions, with no material consequences for their predictive accuracy. We manipulated some of our independent variables to check whether results are sensitive to measurement scales. Specifically, we dichotomised the ‘manager in post’ variable; results did not alter.
| Model 1: NMDS-SC nursing and residential homes with controls hierarchical logit model | Model 2: Care home provider: bivariate logit model | Model 3: Care home provider: logit model with controls | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Odds ratio | 95% CI | p-value | Odds ratio | CI | p-value | Odds ratio | 95% CI | p-value | |
| Staff-to-bed ratio | 1.23 | 1.082 to 1.41 | < 0.05 | 1.04 | 1.01 to 1.07 | < 0.001 | 1.173 | 1.06 to 1.29 | < 0.001 |
| Pseudo R-squared | – | 0.01 | 0.01 | ||||||
Cross-sectional analyses of relationships between care quality and care home staffing are likely to be biased because of omitted variables and measurement error. 50 To estimate omitted variable bias in this study, we estimated comparable models looking at relationships between jobs-to-beds ratios and CQC judgements in the NMDS-SC and separately for homes operated by the care home operator who provided us with additional, non-NMDS-SC data, for WP3. Therefore, we were interested in whether the key relationships between the staff-to-bed measures and CQC inspection score were broadly similar in both studies. If the relationship in NMDS-SC was greater than the relationship in the care home provider data, this would imply omitted variable bias. (See Chapter 5.)
Summary
In summary, our results suggest that having more staff with greater experience in role is associated with more positive evaluations of quality in care homes by the CQC. However, effect sizes are small with only a small proportion of the variance in outcomes explained by our model.
Marginal effects more clearly quantify the size of key relationships. Taking the baseline probability of being rated as good or outstanding for an average home as 74.7%, increasing average staff experience in role by 5 years or doubling the number of staff would both improve the home’s chances of being rated positively by nearly three percentage points (i.e. from 74.7% to 77.2%). Numerical staffing measures have only a limited impact on CQC inspectors’ evaluations of care quality.
We originally planned to make estimates of the costs (in terms of higher costs) and benefits (in terms of fewer homes rated negatively by the CQC) of different staffing models. We explained in Chapter 3 why this analysis was not undertaken.
-
Having more experienced staff is likely to improve care quality for residents.
-
Care homes with a manager in post in the 12 months prior to the inspection were more likely to be rated as good or outstanding.
-
Very large staffing increases would be needed to create small improvements in quality. However, imprecise measurements of staffing and quality may cause the size of the staffing–quality relationship to be underestimated.
-
Our analysis of NMDS-SC has not identified distinct patterns or models of home staffing characteristics so there is no evidence that different models may result in different quality outcomes. Whether this is because there is limited variation in care home staffing models (e.g. because funding and resource constraints mean that most homes operate with similar staffing models) or our data were too limited is uncertain.
Work package 3: modelling relationships between staffing, quality, outcomes and resource use at an organisational level
The overall aim of this WP was to explain how the care home workforce (numbers, skill mix and stability) might meet the dependency and needs of residents through analysing routinely collected longitudinal data from a single care home provider organisation. In WP3, we sought to overcome some of the shortcomings of the previous study (WP2) and to develop estimates of care quality–staffing relationships, using nurse-sensitive indicators of care quality (including falls, falls with fracture, UTIs, chest infections and pressure ulcers) and a broader measure of quality, medication errors.
Results
Falls
The pooled OLS model suggests a higher skill mix is associated with a reduced rate of falls. However, this result was not statistically significant in fixed effects and our preferred multilevel growth model. The results of this model also suggested that falls were higher in homes with more residents in specialist dementia units, although none of the workforce measures were associated with statistically significant changes in the rate of falls (Table 12).
| Predictors | Pooled OLS | Fixed effects | Mixture (multilevel growth) model | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Regression coefficient | 95% CI | p-value | Regression coefficient | 95% CI | p-value | Regression coefficient | 95% CI | p-value | |
| Skill mix (proportion of total care hours provided by RNs) | −0.262 | −0.373 to −0.151 | < 0.001 | −0.103 | −0.340 to 0.133 | 0.39 | −0.178 | −0.380 to 0.024 | 0.084 |
| Proportion of care provided by agency nurses | 0.07 | −0.020 to 0.160 | 0.127 | −0.006 | −0.100 to 0.088 | 0.897 | 0.002 | −0.090 to 0.094 | 0.961 |
| Total care hours (RN + carer) | −0.001 | −0.025 to 0.023 | 0.926 | −0.013 | −0.035 to 0.010 | 0.269 | −0.014 | −0.036 to 0.009 | 0.234 |
| Proportion of planned nursing hours actually worked | 0.211 | 0.075 to 0.348 | 0.002 | 0.058 | −0.109 to 0.225 | 0.495 | 0.11 | −0.046 to 0.265 | 0.166 |
| Proportion of planned carer hours actually worked | −0.177 | −0.289 to −0.066 | 0.002 | −0.069 | −0.216 to 0.077 | 0.353 | −0.103 | −0.238 to 0.032 | 0.135 |
| Admissions as a proportion of total beds (average per week) | 0.268 | 0.036 to 0.500 | 0.024 | 0.143 | −0.149 to 0.435 | 0.338 | −0.041 | −0.284 to 0.203 | 0.744 |
| Occupancy rate (average per week) | 0.158 | 0.107 to 0.208 | < 0.001 | −0.124 | −0.226 to −0.023 | 0.016 | 0 | −0.070 to 0.069 | 0.99 |
| Proportion of residents with nursing needs | −0.035 | −0.068 to −0.002 | 0.038 | −0.049 | −0.127 to 0.029 | 0.219 | −0.049 | −0.127 to 0.029 | 0.219 |
| Proportion of residents in dedicated dementia units | 0.209 | 0.186 to 0.232 | < 0.001 | −0.155 | −0.310 to −0.000 | 0.05 | 0.147 | 0.081 to 0.213 | < 0.001 |
| Proportion of residents in dementia units who exhibit challenging behaviour | −0.54 | −0.946 to −0.133 | 0.009 | −0.706 | −4.460 to 3.049 | 0.713 | −0.725 | −2.007 to 0.557 | 0.268 |
| Proportion of young disabled residents | −0.151 | −0.190 to −0.111 | < 0.001 | −0.366 | −1.088 to 0.356 | 0.321 | −0.161 | −0.287 to −0.036 | 0.012 |
| Proportion of residents with learning disabilities | −3.47 | −4.247 to −2.694 | < 0.001 | 6.181 | −1.897 to 14.259 | 0.134 | −2.499 | −4.990 to −0.008 | 0.049 |
| Proportion of residents with Parkinson’s disease | 0.962 | 0.633 to 1.291 | < 0.001 | −0.35 | −2.361 to 1.661 | 0.733 | 0.471 | −0.464 to 1.405 | 0.324 |
| Proportion of residents with Huntington’s disease | −0.232 | −0.534 to 0.071 | 0.134 | 0.967 | −4.721 to 6.655 | 0.739 | −0.129 | −1.144 to 0.886 | 0.803 |
| Proportion of residents receiving end-of-life care | 0.008 | −0.070 to 0.086 | 0.834 | −0.581 | −1.242 to 0.080 | 0.085 | −0.062 | −0.302 to 0.179 | 0.615 |
| Proportion of residents with other specific care needs | −0.088 | −0.149 to −0.026 | 0.005 | 0.327 | −0.366 to 1.021 | 0.355 | −0.043 | −0.241 to 0.155 | 0.67 |
| R2 adjusted | 0.217 | 0.004 | – | ||||||
| Marginal/conditional R-squared | – | 0.161/0.466 | |||||||
| ICC 1 | 0.36 | ||||||||
Falls with fractures
A higher skill mix was associated with a lower risk of falls with fractures, with the size of the relationship stable across different model specifications (a coefficient of −0.008). However, the effect size itself was small and the models were only able to explain a very small proportion of the variation in the incidence of falls. No other workforce characteristics were associated with rates of falls with fractures, although once again there was an association between more residents in dementia units and a higher rate of falls (Table 13).
| Predictors | Pooled OLS | Fixed effects | Mixture (multilevel growth) model | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Regression coefficient | 95% CI | p-value | Regression coefficient | 95% CI | p-value | Regression coefficient | 95% CI | p-value | |
| Skill mix (proportion of total care hours provided by RNs) | −0.008 | −0.012 to −0.004 | < 0.001 | −0.008 | −0.012 to −0.004 | < 0.001 | −0.008 | −0.012 to −0.004 | < 0.001 |
| Proportion of care provided by agency nurses | −0.002 | −0.007 to 0.003 | 0.418 | −0.003 | −0.010 to 0.003 | 0.305 | −0.002 | −0.007 to 0.003 | 0.377 |
| Total care hours (RN + carer) | 0 | −0.001 to 0.002 | 0.678 | 0.001 | −0.001 to 0.002 | 0.435 | 0 | −0.001 to 0.002 | 0.656 |
| Proportion of planned nursing hours actually worked | −0.005 | −0.013 to 0.002 | 0.162 | 0.002 | −0.009 to 0.013 | 0.679 | −0.005 | −0.013 to 0.003 | 0.215 |
| Proportion of planned carer hours actually worked | 0.003 | −0.003 to 0.009 | 0.339 | −0.002 | −0.012 to 0.008 | 0.678 | 0.003 | −0.004 to 0.009 | 0.391 |
| Admissions as a proportion of total beds (average per week) | 0.001 | −0.012 to 0.014 | 0.877 | −0.009 | −0.028 to 0.011 | 0.384 | 0 | −0.013 to 0.013 | 0.996 |
| Occupancy rate (average per week) | −0.003 | −0.006 to −0.000 | 0.04 | 0.002 | −0.004 to 0.009 | 0.478 | −0.003 | −0.006 to 0.000 | 0.056 |
| Proportion of residents with nursing needs | −0.001 | −0.003 to 0.001 | 0.174 | −0.001 | −0.003 to 0.001 | 0.222 | −0.001 | −0.003 to 0.001 | 0.222 |
| Proportion of residents in dedicated dementia units | 0.002 | 0.000 to 0.003 | 0.008 | −0.005 | −0.016 to 0.005 | 0.312 | 0.002 | 0.000 to 0.003 | 0.017 |
| Proportion of residents in dementia units who exhibit challenging behaviour | 0 | −0.022 to 0.022 | 0.982 | −0.294 | −0.544 to −0.044 | 0.021 | −0.002 | −0.026 to 0.023 | 0.904 |
| Proportion of young disable`d residents | −0.003 | −0.005 to −0.000 | 0.019 | −0.008 | −0.056 to 0.040 | 0.732 | −0.003 | −0.005 to −0.000 | 0.034 |
| Proportion of residents with learning disabilities | −0.028 | −0.070 to 0.015 | 0.201 | 0.534 | −0.004 to 1.071 | 0.052 | −0.027 | −0.075 to 0.021 | 0.267 |
| Proportion of residents with Parkinson’s disease | 0.005 | −0.013 to 0.023 | 0.615 | 0.024 | −0.110 to 0.158 | 0.725 | 0.005 | −0.015 to 0.025 | 0.654 |
| Proportion of residents with Huntington’s disease | 0.002 | −0.015 to 0.018 | 0.824 | 0.115 | −0.263 to 0.494 | 0.55 | 0.002 | −0.017 to 0.020 | 0.842 |
| Proportion of residents receiving end-of-life care | 0.005 | 0.000 to 0.009 | 0.031 | 0.054 | 0.010 to 0.098 | 0.016 | 0.005 | −0.000 to 0.010 | 0.051 |
| Proportion of residents with other specific care needs | 0 | −0.003 to 0.004 | 0.863 | 0.035 | −0.011 to 0.081 | 0.134 | 0 | −0.003 to 0.004 | 0.853 |
| R2 adjusted | 0.012 | 0.007 | – | ||||||
| Marginal/conditional R-squared | – | 0.017/0.026 | |||||||
| ICC 1 | 0.01 | ||||||||
Marginal effects analysis suggests that for an average care home with 48 occupied beds, if the proportion of care provided by RNs increased from a mean of 0.2 to 0.3 (one standard deviation above the mean) – equivalent to an increase in full-time nursing posts of around 3.5, from 7 to 10.5 – the increase might lead to a reduction in the number of 0.5 falls per year for that home 1.7 (95% CI 1.54 to 1.87) to 1.2 (95% CI 0.89 to 1.5).
Urinary tract infections
A higher skill mix was associated with lower rates of UTIs in all three models, although the size of the association was smaller in the fixed effects and multilevel growth models. Marginal effects suggest that a one standard deviation increase in skill mix equivalent to 3.5 extra full-time equivalent nursing posts in an average home with 48 occupied beds, would be associated with a fall in UTIs from 41 a year (95% CI 35.3 to 46.7) to 32.1 a year (95% CI 24 to 40.3). The rate of UTIs was higher when the proportion of planned nursing hours worked was higher and lower when the proportion of planned carer hours worked was higher (Table 14).
| Predictors | Pooled OLS | Fixed effects | Mixture (multilevel growth) model | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Regression coefficient | 95% CI | p-value | Regression coefficient | 95% CI | p-value | Regression coefficient | 95% CI | p-value | |
| Skill mix (proportion of total care hours provided by RNs) | −0.233 | −0.288 to −0.177 | < 0.001 | −0.142 | −0.262 to −0.022 | 0.02 | −0.153 | −0.259 to −0.048 | 0.004 |
| Proportion of care provided by agency nurses | 0.047 | 0.002 to 0.092 | 0.04 | 0.029 | −0.019 to 0.077 | 0.233 | 0.027 | −0.020 to 0.074 | 0.257 |
| Total care hours (RN + carer) | 0.01 | −0.002 to 0.022 | 0.117 | −0.004 | −0.015 to 0.008 | 0.544 | 0 | −0.011 to 0.012 | 0.981 |
| Proportion of planned nursing hours actually worked | 0.156 | 0.088 to 0.224 | < 0.001 | 0.13 | 0.045 to 0.214 | 0.003 | 0.144 | 0.064 to 0.224 | < 0.001 |
| Proportion of planned carer hours actually worked | −0.106 | −0.162 to −0.050 | < 0.001 | −0.072 | −0.146 to 0.002 | 0.057 | −0.088 | −0.158 to −0.018 | 0.013 |
| Admissions as a proportion of total beds (average per week) | 0.092 | −0.024 to 0.208 | 0.119 | −0.13 | −0.278 to 0.018 | 0.086 | −0.006 | −0.132 to 0.120 | 0.926 |
| Occupancy rate (average per week) | −0.029 | −0.054 to −0.004 | 0.024 | 0.009 | −0.042 to 0.060 | 0.733 | −0.02 | −0.057 to 0.016 | 0.279 |
| Proportion of residents with nursing needs | 0.019 | 0.002 to 0.035 | 0.024 | 0.03 | −0.013 to 0.072 | 0.175 | 0.03 | −0.013 to 0.072 | 0.175 |
| Proportion of residents in dedicated dementia units | −0.04 | −0.051 to −0.028 | < 0.001 | 0.074 | −0.004 to 0.153 | 0.064 | 0.007 | −0.030 to 0.043 | 0.717 |
| Proportion of residents in dementia units who exhibit challenging behaviour | −0.197 | −0.400 to 0.005 | 0.056 | −0.656 | −2.561 to 1.249 | 0.5 | −0.392 | −1.108 to 0.324 | 0.283 |
| Proportion of young disabled residents | −0.022 | −0.042 to −0.002 | 0.028 | −0.12 | −0.486 to 0.247 | 0.522 | −0.029 | −0.099 to 0.042 | 0.43 |
| Proportion of residents with learning disabilities | −0.187 | −0.573 to 0.200 | 0.344 | 2.091 | −2.007 to 6.190 | 0.317 | −0.165 | −1.560 to 1.230 | 0.817 |
| Proportion of residents with Parkinson’s disease | 0.851 | 0.687 to 1.015 | < 0.001 | 1.433 | 0.413 to 2.453 | 0.006 | 0.913 | 0.397 to 1.428 | 0.001 |
| Proportion of residents with Huntington’s disease | 0.106 | −0.044 to 0.257 | 0.166 | −2.319 | −5.205 to 0.567 | 0.115 | 0.032 | −0.541 to 0.605 | 0.913 |
| Proportion of residents receiving end-of-life care | 0.029 | −0.010 to 0.068 | 0.145 | 0.143 | −0.192 to 0.479 | 0.402 | −0.009 | −0.143 to 0.125 | 0.898 |
| Proportion of residents with other specific care needs | −0.015 | −0.046 to 0.016 | 0.343 | −0.411 | −0.763 to −0.059 | 0.022 | −0.063 | −0.174 to 0.048 | 0.266 |
| R2 adjusted | 0.065 | 0.013 | – | ||||||
| Marginal/conditional R-squared | – | 0.044/0.442 | |||||||
| ICC 1 | 0.42 | ||||||||
Chest infections
There was no statistically significant relationship between skill mix and the rate of chest infections in our preferred multilevel growth model. Once again, the rate of chest infections was higher the greater the proportion of planned nursing hours worked and lower the greater the proportion of carer hours worked (Table 15).
| Predictors | Pooled OLS | Fixed effects | Mixture (multilevel growth) model | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Regression coefficient | 95% CI | p-value | Regression coefficient | 95% CI | p-value | Regression coefficient | 95% CI | p-value | |
| Skill mix (proportion of total care hours provided by RNs) | −0.174 | −0.221 to −0.126 | < 0.001 | −0.05 | −0.153 to 0.052 | 0.338 | −0.058 | −0.154 to 0.039 | 0.241 |
| Proportion of care provided by agency nurses | 0.037 | −0.002 to 0.075 | 0.06 | 0.02 | −0.021 to 0.061 | 0.344 | 0.019 | −0.022 to 0.060 | 0.362 |
| Total care hours (RN + carer) | 0.007 | −0.003 to 0.018 | 0.158 | 0.001 | −0.009 to 0.010 | 0.92 | 0.003 | −0.007 to 0.013 | 0.553 |
| Proportion of planned nursing hours actually worked | 0.143 | 0.085 to 0.202 | < 0.001 | 0.099 | 0.027 to 0.172 | 0.007 | 0.112 | 0.041 to 0.182 | 0.002 |
| Proportion of planned carer hours actually worked | −0.095 | −0.143 to −0.048 | < 0.001 | −0.061 | −0.125 to 0.002 | 0.058 | −0.071 | −0.133 to −0.010 | 0.023 |
| Admissions as a proportion of total beds (average per week) | 0.195 | 0.096 to 0.294 | < 0.001 | −0.089 | −0.216 to 0.038 | 0.169 | 0.01 | −0.105 to 0.124 | 0.869 |
| Occupancy rate (average per week) | −0.001 | −0.023 to 0.020 | 0.91 | 0.008 | −0.036 to 0.052 | 0.71 | −0.024 | −0.059 to 0.010 | 0.164 |
| Proportion of residents with nursing needs | 0.013 | −0.001 to 0.027 | 0.075 | 0.021 | −0.028 to 0.070 | 0.395 | 0.021 | −0.028 to 0.070 | 0.395 |
| Proportion of residents in dedicated dementia units | −0.03 | −0.040 to −0.021 | < 0.001 | 0.031 | −0.036 to 0.098 | 0.367 | 0.025 | −0.016 to 0.066 | 0.224 |
| Proportion of residents in dementia units who exhibit challenging behaviour | −0.307 | −0.480 to −0.133 | 0.001 | −1.174 | −2.803 to 0.455 | 0.158 | −0.679 | −1.519 to 0.162 | 0.113 |
| Proportion of young disabled residents | −0.023 | −0.040 to −0.006 | 0.007 | −0.137 | −0.450 to 0.177 | 0.393 | −0.036 | −0.124 to 0.053 | 0.427 |
| Proportion of residents with learning disabilities | −0.18 | −0.511 to 0.152 | 0.289 | 2.878 | −0.626 to 6.383 | 0.108 | 0.035 | −1.628 to 1.699 | 0.967 |
| Proportion of residents with Parkinson’s disease | 0.537 | 0.397 to 0.678 |
< 0.001 | 1.044 | 0.171 to 1.916 | 0.019 | 0.484 | −0.088 to 1.056 | 0.097 |
| Proportion of residents with Huntington’s disease | 0.083 | −0.046 to 0.212 | 0.208 | −1.296 | −3.764 to 1.172 | 0.303 | −0.016 | −0.732 to 0.700 | 0.965 |
| Proportion of residents receiving end-of-life care | −0.001 | −0.035 to 0.032 | 0.935 | 0.38 | 0.093 to 0.667 | 0.009 | 0.045 | −0.109 to 0.200 | 0.565 |
| Proportion of residents with other specific care needs | −0.002 | −0.028 to 0.024 | 0.88 | −0.223 | −0.524 to 0.078 | 0.147 | −0.062 | −0.196 to 0.073 | 0.369 |
| R2 adjusted | 0.054 | 0.011 | – | ||||||
| Marginal/conditional R-squared | – | 0.031/0.635 | |||||||
| ICC 1 | 0.62 | ||||||||
Pressure ulcers
The only relationship between staffing measures and pressure ulcers in our (preferred) multilevel growth model was that more hours worked (RN plus carer) was associated with a greater risk of pressure ulcers. However, the size of this relationship was small, and only a low proportion of the variance in incidence of pressure ulcers was explained. Which is not surprising given the rare occurence of pressure ulcers in our data. Risk of pressure ulcers increases as the number of care hours provided increases. This could reflect more care hours being provided in homes where residents have more acute care needs which reflect frailty, ill-health and co-morbidities that put residents at increased risk of developing pressure ulcers. (Table 16).
| Predictors | Pooled OLS | Fixed effects | Mixture (multilevel growth) model | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Regression coefficient | 95% CI | p-value | Regression coefficient | 95% CI | p-value | Regression coefficient | 95% CI | p-value | |
| Skill mix (proportion of total care hours provided by RNs) | 0 | −0.015 to 0.015 | 0.973 | −0.006 | −0.021 to 0.009 | 0.405 | 0.001 | −0.023 to 0.025 | 0.959 |
| Proportion of care provided by agency nurses | 0.016 | 0.004 to 0.028 | 0.011 | 0.020 | 0.008 to 0.032 | 0.001 | 0.005 | −0.008 to 0.019 | 0.451 |
| Total care hours (RN + carer) | 0.001 | −0.003 to 0.004 | 0.698 | 0.018 | 0.011 to 0.024 | < 0.001 | −0.003 | −0.007 to 0.000 | 0.055 |
| Proportion of planned nursing hours actually worked | −0.006 | −0.024 to 0.012 | 0.5 | −0.017 | −0.036 to 0.001 | 0.071 | −0.007 | −0.028 to 0.015 | 0.536 |
| Proportion of planned carer hours actually worked | 0.002 | −0.013 to 0.017 | 0.758 | 0.003 | −0.012 to 0.018 | 0.698 | 0.007 | −0.011 to 0.026 | 0.448 |
| Admissions as a proportion of total beds (average per week) | 0.037 | 0.006 to 0.068 | 0.02 | 0.027 | −0.004 to 0.058 | 0.091 | 0.005 | −0.029 to 0.039 | 0.772 |
| Occupancy rate (average per week) | −0.004 | −0.011 to 0.003 | 0.26 | 0.003 | −0.004 to 0.011 | 0.35 | −0.008 | −0.017 to 0.001 | 0.07 |
| Proportion of residents with nursing needs | 0.005 | 0.000 to 0.009 | 0.037 | 0.001 | −0.003 to 0.006 | 0.572 | 0.006 | −0.002 to 0.013 | 0.139 |
| Proportion of residents in dedicated dementia units | −0.002 | −0.005 to 0.001 | 0.242 | −0.004 | −0.007 to −0.001 | 0.02 | −0.004 | −0.007 to −0.001 | 0.02 |
| Proportion of residents in dementia units who exhibit challenging behaviour | 0 | −0.054 to 0.054 | 0.996 | −0.001 | −0.055 to 0.053 | 0.968 | 0.003 | −0.105 to 0.110 | 0.962 |
| Proportion of young disabled residents | −0.007 | −0.013 to −0.002 | 0.005 | −0.014 | −0.020 to −0.009 | < 0.001 | −0.006 | −0.016 to 0.004 | 0.235 |
| Proportion of residents with learning disabilities | −0.06 | −0.164 to 0.043 | 0.253 | −0.057 | −0.160 to 0.046 | 0.278 | −0.08 | −0.286 to 0.126 | 0.446 |
| Proportion of residents with Parkinson’s disease | −0.007 | −0.051 to 0.037 | 0.765 | −0.005 | −0.048 to 0.039 | 0.831 | 0.02 | −0.063 to 0.102 | 0.644 |
| Proportion of residents with Huntington’s disease | −0.025 | −0.065 to 0.015 | 0.225 | −0.037 | −0.077 to 0.003 | 0.072 | −0.025 | −0.107 to 0.056 | 0.543 |
| Proportion of residents receiving end-of-life care | 0.003 | −0.007 to 0.014 | 0.542 | 0.004 | −0.006 to 0.015 | 0.405 | 0.002 | −0.019 to 0.022 | 0.866 |
| Proportion of residents with other specific care needs | 0.007 | −0.001 to 0.015 | 0.091 | 0.004 | −0.005 to 0.012 | 0.397 | 0.008 | −0.008 to 0.024 | 0.343 |
| R2 adjusted | 0.015 | 0.016 | – | ||||||
| Marginal/conditional R-squared | – | 0.016/0.123 | |||||||
| ICC 1 | 0.11 | ||||||||
Medication errors
We observe a number of statistically significant relationships between medication errors and staffing measures. A higher skill mix was associated with a lower rate of medication errors, with the coefficients stable across all three models. Medication errors were also more likely when a greater proportion of care hours were provided by agency nurses. We also see the same pattern of results that we observed with UTIs and chest infections; medication errors are higher where a higher proportion of planned nursing hours are worked and lower where a higher proportion of carer hours are worked. The consistency of this result across all three measures lends credence to the idea that this may reflect how staffing affects the accuracy of record keeping (Table 17).
| Predictors | Pooled OLS | Fixed effects | Mixture (multilevel growth) model | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Regression coefficient | 95% CI | p-value | Regression coefficient | 95% CI | p-value | Regression coefficient | 95% CI | p-value | |
| Skill mix (proportion of total care hours provided by RNs) | −0.085 | −0.150 to −0.020 | 0.01 | −0.085 | −0.150 to −0.020 | 0.01 | −0.086 | −0.149 to −0.022 | 0.008 |
| Proportion of care provided by agency nurses | 0.059 | 0.033 to 0.086 | < 0.001 | 0.033 | 0.007 to 0.059 | 0.013 | 0.032 | 0.006 to 0.058 | 0.015 |
| Total care hours (RN + carer) | 0.009 | 0.002 to 0.017 | 0.011 | −0.002 | −0.008 to 0.004 | 0.582 | −0.001 | −0.007 to 0.005 | 0.727 |
| Proportion of planned nursing hours actually worked | 0.04 | −0.000 to 0.081 | 0.05 | 0.078 | 0.032 to 0.124 | 0.001 | 0.077 | 0.031 to 0.122 | 0.001 |
| Proportion of planned carer hours actually worked | −0.029 | −0.062 to 0.004 | 0.085 | −0.058 | −0.099 to −0.018 | 0.004 | −0.059 | −0.099 to −0.019 | 0.004 |
| Admissions as a proportion of total beds (average per week) | 0.518 | 0.449 to 0.587 | < 0.001 | 0.049 | −0.032 to 0.129 | 0.236 | 0.108 | 0.031 to 0.185 | 0.006 |
| Occupancy rate (average per week) | −0.04 | −0.055 to −0.025 | < 0.001 | 0.043 | 0.015 to 0.071 | 0.002 | 0.017 | −0.009 to 0.042 | 0.196 |
| Proportion of residents with nursing needs | −0.001 | −0.011 to 0.008 | 0.771 | −0.004 | −0.060 to 0.052 | 0.887 | −0.004 | −0.060 to 0.052 | 0.887 |
| Proportion of residents in dedicated dementia units | −0.011 | −0.018 to −0.005 | 0.001 | 0.183 | 0.141 to 0.226 | < 0.001 | 0.117 | 0.081 to 0.152 | < 0.001 |
| Proportion of residents in dementia units who exhibit challenging behaviour | 0.031 | −0.089 to 0.152 | 0.61 | 0.287 | −0.744 to 1.317 | 0.585 | 0.014 | −0.782 to 0.811 | 0.972 |
| Proportion of young disabled residents | 0.001 | −0.010 to 0.013 | 0.809 | 0.269 | 0.071 to 0.467 | 0.008 | 0.077 | −0.025 to 0.180 | 0.139 |
| Proportion of residents with learning disabilities | 0.032 | −0.198 to 0.262 | 0.784 | −1.32 | −3.538 to 0.897 | 0.243 | −0.429 | −2.068 to 1.209 | 0.608 |
| Proportion of residents with Parkinson’s disease | −0.009 | −0.107 to 0.088 | 0.853 | 0.414 | −0.138 to 0.966 | 0.142 | 0.327 | −0.152 to 0.807 | 0.181 |
| Proportion of residents with Huntington’s disease | −0.071 | −0.161 to 0.019 | 0.12 | −0.25 | −1.812 to 1.311 | 0.753 | −0.171 | −0.997 to 0.655 | 0.685 |
| Proportion of residents receiving end-of-life care | −0.023 | −0.046 to 0.001 | 0.056 | −0.191 | −0.372 to −0.009 | 0.04 | −0.121 | −0.264 to 0.022 | 0.096 |
| Proportion of residents with other specific care needs | −0.022 | −0.040 to −0.004 | 0.019 | 0.055 | −0.135 to 0.245 | 0.571 | 0.009 | −0.128 to 0.145 | 0.9 |
| R2 adjusted | 0.088 | 0.034 | – | ||||||
| Marginal/conditional R-squared | – | 0.114/0.893 | |||||||
| ICC 1 | 0.88 | ||||||||
Examining marginal effects, an average home of 48 occupied beds, a one standard deviation increase in skill mix – equivalent to around 3.5 additional full-time equivalent nursing posts – would be associated with that home having an annual fall in medication errors of around 5, from 12.5 per year (95% CI 3 to 22) to 7.6 (95% CI −2.6 to 17.1).
Cost–benefit analysis
We first estimated the additional nursing costs. We estimated treatment cost savings for falls with fractures, UTIs and medication errors. This was informed by a series of pragmatic literature reviews conducted to identify unit costs (presented in Methods).
Additional nursing costs
We reported above, that a one standard deviation increase in skill mix would result in the percentage of care being provided by RNs increasing from 20% to 30%. In an average care home with 48 occupied beds, this would equate to an increase in nursing hours of 598 hours per month. In the absence of any care home specific nursing unit costs, data from PSSRU Unit Costs of Health and Social Care were used to determine costs of nursing hours. 208 These estimates are derived from Agenda for Change pay scales and other indirect costs, including overheads and are assumed to be broadly indicative of appropriate unit costs. This gives an hourly cost for a Band 5 community-based nurse of £39.23, equating to a cost of £23,460 per month or £281,520 per year for an average home.
Cost of falls resulting in fractures
A one standard deviation increase in nursing hours would be associated with a reduction in falls with fractures of 0.5 per year in an average home. This suggested an annual treatment cost saving of £2123.50.
Costs of urinary tract infections
The results reported above suggested that a one standard deviation in skill mix would be associated with a reduction in UTIs of 41 per year in an average home, suggesting a treatment cost saving of £13,817.
Cost of medication errors
Our results suggested that increasing skill mix by one standard deviation would be associated with a reduction of five medication errors per year in an average care home. This equates to an annual saving of £15.35.
Our cost–benefit analysis reveals that an expensive increase in nursing care (a total cost of £281,520 per year for an average-sized home of 48 beds) would be associated with total treatment cost savings of around £35,058 that is a net additional cost of £246,462. There is of course a degree of uncertainty around both the costs of treatment and the estimates of reductions in falls with fractures, medication errors and UTIs. It would be possible to compute upper and lower bound estimates of the net additional cost but given the small size of the marginal effects of skill mix increases on the incidence of nurse-sensitive indicators of care quality, more nuanced estimates would not change the big picture: additional staff costs are likely to substantially outweigh reduced treatment costs.
Summary of cost–benefit analysis
The costs of adverse outcomes are not purely financial: one in five UTIs is likely to require treatment in hospital. In an average home, this would mean around ten residents hospitalised with UTIs per year. These are experiences that are painful, uncomfortable and distressing for the residents and their families. Hospitals also come with a risk of iatrogenic harm themselves – and older people are overrepresented in the population affected. Similarly, a rare fall with a fracture is likely to have significant negative consequences for the resident. These then are not events that should be reduced to treatment costs. However, and overall, our results indicate that simply increasing nursing inputs in this setting – and in the absence of other interventions – is unlikely to be a cost-effective way of reducing adverse incidents for care home residents.
-
Statistically significant but small relationships suggest a higher proportion of care being provided by RNs may result in lower incidence of falls with fractures, UTIs and medication errors. There were no such relationships for all other falls, chest infections or pressure ulcers.
-
There was no evidence found for non-linear relationships between staffing and outcomes although this may be an artefact of methods used. 57
-
Using agency nurses to cover for nurse sickness or unfilled vacancies was not associated with increased risk of falls, infections, or pressure ulcers, but was associated with increased risk of medication errors.
-
An expensive increase in nursing care would be associated with minimal total treatment cost savings and, therefore, an increased net additional cost for care home providers. Simply increasing nursing inputs in this setting is unlikely to be a cost-effective way of reducing adverse incidents for care home residents.
Work package 4: understanding the contributions of the care home workforce to enhance quality
Our findings are presented in two sections: (1) ensuring a care home workforce to support people living in care homes and (2) understanding of the contributions of the care home workforce to enhance quality for care home residents. Key structural, process and outcome components of the relationship between care home staffing and quality as derived from regulatory reports are presented in Figure 6.
FIGURE 6.
Key structural, process and outcome components of the relationship between care home staffing and quality as derived from regulatory reports.

Ensuring a care home workforce to support people living in care homes
‘Enough’ staff
Care Quality Commission reports did not provide details of staff numbers, skill mix or deployment within the care home. This omission applied to all care homes in our sample (which included care homes of differing size and ownership). However, our analyses offered qualitative insights into how staff numbers may influence ‘quality’ in the care home. All care homes rated outstanding were considered to have ‘enough staff’ or ‘sufficient staff’ with the skills, knowledge and experience to ‘meet residents’ needs’, or ‘keep people safe’:
All of the residents said there were enough staff available to them and they never had to wait for support.
Care Home 18
Residents were supported by enough staff with the skills, experience and knowledge to meet their needs.
Care Home 14
Perceived adequate numbers of staff were positively appraised by residents and their relatives for providing individualised care in a timely manner, and by staff to feel supported and to be able to spend time with residents:
A person we spoke with told us there were enough staff to support them if needed, they said, ‘There is always someone151 here. If I use the call bell they come quickly’.
Care Home 19
We saw staff had enough time to sit and talk to people and ensure their emotional and social needs were also being met.
Care Home 21
Staff felt there were enough staff to meet people’s needs. One explained, ‘If we have a resident who needs more care, [registered manager] will make sure there’s enough staff to meet their needs’.
Care Home 2
For care homes rated inadequate, staff numbers were often considered to be below the number required to meet residents’ needs and to ensure care was safe and this had an impact on workload for staff, their ability to meet demands and staff well-being:
Relatives we spoke with told us there were rarely enough staff. One relative said, ‘There just never seemed to be enough staff there.’ Staff we spoke with told us there weren’t enough staff. One staff member said, ‘Staffing is a bit dodgy, it’s hit and miss if there are enough staff or not.’ A different staff member said, ‘There is a lot of staff sickness, it’s because staff are so overworked.’ Another staff member said, ‘We are short staffed and it’s a safety issue.’
Care Home 24
Lower staffing levels were of particular concern at the weekend and at night. Staff sickness was higher in those care homes with lower staffing levels. The reports of care homes rated inadequate highlighted system deficiencies related to (1) calculating staffing levels and (2) effectively managing staffing in these care homes:
Systems were either not in place or robust enough to demonstrate staffing levels were effectively managed. This placed people at risk of harm.
Care Home 25
In care homes rated as outstanding, registered managers were reported to have the authority to secure the workforce that they judged necessary to meet demand and to ensure safety for residents.
Care home manager: judgement and authority for staffing levels
When the care home was rated as outstanding, there were examples that highlighted the pivotal role of the care home manager for judging staffing requirements to meet residents’ needs and promote safe care, coupled with the authority to enact these decisions within the care home. This was highlighted across the sample rated as outstanding and not specific to characteristics, such as ownership or size. These reports indicated that a degree of flexibility and judgement by the manager about staffing in these care homes was considered essential for promoting quality. Good working relationships between the care home manager and the provider senior management team in care homes rated as outstanding were reported to support the care home manager when determining staffing levels and structures:
The registered manager told us that although the provider was a ‘corporate brand’, the provider worked with them and gave them flexibility to manage and run the home. For example, to vary staffing levels and arrange specific activities.
Care Home 11
The manager was therefore afforded authority based on confidence and trust in their abilities to manage their care home. Some managers were given authority by the provider organisation or owner to consistently staff the service slightly above the ‘required’ levels to ensure that staff had more time to spend with residents. Staffing above required levels had additional benefits:
We were advised the service was staffed 10% over the estimated required levels, in order to allow for annual leave, training and unplanned absence.
Care Home 15
There was minimal detail in the reports as to how care home managers made judgements about staffing levels. In some homes rated as outstanding, it was reported that the manager used a dependency tool to calculate staffing levels based on resident need, while others were considering the utility of a dependency tool for better predicting staffing levels. For many of these managers, they used professional judgement and understanding about the needs of residents.
The reports of care homes rated as inadequate did not refer to the use of any tools for calculating staffing levels, nor how managers determined these levels using their judgement:
There was no evidence to demonstrate how staffing levels were calculated.
Care Home 28
In addition, our analyses revealed that senior management teams in large and medium provider organisations were reported as largely ‘absent’ from the care home or involved with care home managers when deficiencies in care were identified. In some cases, provider senior management teams were ineffective: this created a ripple effect where inadequacies of senior teams were associated with poorer quality:
We had concerns about the quality of the provider’s response when issues were raised with them … we found the response of the services senior management team was not robust.
Care Home 23
‘At our last inspection the provider had failed to ensure there were sufficient numbers of care staff deployed to meet peoples assessed care and support need’ … ‘At this inspection the provider had not made enough improvement and was still in breach of regulations’
Care Home 25
Proactive and cohesive relationships between the manager of the care home and the provider senior management team (or owner) therefore appeared important to support the manager with making decisions about staffing and to empower them to staff as they determined most suitable for the people living in the care home and to ensure quality of service. For independently owned single-care home operators, where there was no access to a provider senior management team, then managers (and owners) sought external support from larger organisations (such as the local authority) or healthcare professionals.
Transparency, oversight and monitoring of decisions about staffing levels were identified as important for assessing, planning and maintaining the contribution of care home staff to quality. However, our analyses revealed that staffing numbers only partially explained the relationship between staffing and quality.
Quality is more than staff numbers
We identified other factors related to care home staffing that had an influence on quality. Stability of staffing and low levels of use of agency or temporary staff, coupled with a skilled and competent care workforce, were clearly necessary for promoting quality:
There was a stable staff team and people and relatives told us they knew staff well. The service had low levels of use of agency staff and had high levels of staff retention due to the positive and supportive culture. The registered manager told us they and the head of care would work a care shift rather than use agency staff. The service had the lowest staff turnover of the eight homes in the provider’s local region.
Care Home 5
Stability of the care home workforce was linked to appropriate induction for all staff, and enabled opportunities to address training to support staff and promote skill and competence. Stability of the workforce ensured that residents were supported by a consistent team of staff and staff were able to develop understanding of the needs and preferences of the people living in the care home to provide personalised care. Stability was also reported to promote teamworking which had benefits for staff and their day-to-day work:
The registered manager had a strong focus on developing a permanent staff group and teamwork. They valued their staff team and provided opportunities for continuous learning and development for staff. The registered manager told us how they had worked hard to employ permanent staff and reduce the number of hours that agency staff were used to cover shifts.
Care Home 4
Staff working in care homes where there was stability within the team reported their job satisfaction and well-being at work. Staff at a care home rated as outstanding provided the following comments: ‘It’s a really nice place to work’, ‘I love my job’ and ‘I’ve worked here for 20 years, I must be happy’ (Care Home 15). Care home managers had a key role in providing environments for these important factors associated with staffing and quality to flourish. However, the presence of the provider senior management team (or owner) was also important and to reinforce staff were valued for their role and contribution. Examples of how this was achieved were offered. Some organisations offered induction days for new staff to learn about the organisation and its values, as well as providing opportunity for staff to meet the senior executive team (such as the Director and Chairman) and the senior management team. A staff member reported:
This really makes you feel you are part of [organisation name].
Care Home 17
Another example was provider senior managers spending time at the care home so that they got to know staff, could offer opportunities for staff to promote quality in the care home, or to address barriers for promoting quality:
The provider tried to engage with members of staff through planned ‘surgeries’ by the human resources department. This was so staff could talk through any concerns they had to drive progress. It was also so the provider could share any benefits staff got working for the company. This was to promote staff retention and provide consistency for the people living at the home.
Care Home 16
Provider senior management involvement in care homes rated as inadequate was often lacking or, if present, ineffectual for creating staff stability, minimising use of agency staff, or ensuring the skills and competence of the care home workforce.
Realising and supporting the potential of the staffing resource
Opportunities for the continuing professional development and training of staff were extensive in care homes rated as outstanding. This was linked to developing skilled and competent staff which impacted positively on quality for care home residents. The care home manager had a key role in supporting staff to develop and to help realise their potential to benefit residents. New staff were supported through induction and mandatory training that supported staff to obtain the nationally recognised Care Certificate, and some care homes offered a period of shadowing of a more experienced member of staff:
In addition to completing the induction training, staff were provided with opportunities to shadow more experienced staff. This enabled them to get to know people and learn how they liked to be cared for as well as developing their knowledge and skills.
Care Home 17
In care homes rated outstanding development opportunities included skills development to support role extension, bespoke training through an extensive library of courses, targeted development to accelerate staff development for more senior roles, experiential learning to enhance understanding for delivering compassionate care, formal health and social care qualifications, and support for RNs for revalidation. In addition, there were opportunities for staff to become a champion for a particular aspect of care and enhance service delivery or to change roles within the care home to make better use of an individual staff member’s skill set. In these care homes, mandatory training for staff was maintained and regularly updated. The records of staff in these care homes were up to date, with plans for their training and development identified. In addition, there was evidence of supervision and appraisals for staff:
Supervision sessions enabled staff to discuss their personal development objectives and goals. We also saw records confirming that staff had received annual appraisals of their individual performance and had an opportunity to review their personal development and progress. A member of staff told us, ‘I am always more confident after supervision’.
Care Home 17
Encouragement by the manager for development and training was valued by staff and a motivating force for quality and excellence in the service:
Staff told us, ‘The manager has continued to encourage us to [strive for excellence] and is so enthusiastic. I think we are doing even more things with the residents than we did in the past. We haven’t stopped. We want this place to be as good as it can be’.
Care Home 20
While the importance of continuing professional development was recognised and actively promoted by managers of small independent care homes, there were less structured opportunities for staff and on occasion staff had to leave to pursue development opportunities:
We always encourage staff to achieve their own potential. If that means they leave us to move forward, that’s fine. We’re happy that social care in general is benefitting from their development.
(Care Home 19)
In care homes rated inadequate, opportunities for staff training and continuing professional development were limited (regardless of size or ownership), as well as limited supervision arrangements to ensure staff were supported in their roles:
The management team were not routinely assessing the competency of all staff and responding to shortfalls in their knowledge in an effective and proactive way.
Care Home 23
Staff told us they had received training although the amount of training varied and we could not establish from the records we reviewed that staff had received training that would equip them with the skills and knowledge to carry out their role and responsibilities.
Care Home 29
In these organisations, specific concerns were raised across the CQC reports about limited knowledge, skills and competence for staff in the following areas: safeguarding; infection prevention and control; falls prevention; oral health; end-of-life care; fire safety; management and administration of medicines; and moving and handling.
In addition to continuing professional development, training and supervision, other mechanisms to reward and recognise staff were considered important to ensure staff felt valued by the management team. Feeling valued was linked with enhancing staff commitment and supporting their potential contribution to quality:
Staff felt constantly supported, valued and praised. They told us, ‘There is no shortage of praise, and we get thanked for all we do’, ‘I feel valued by everyone I work with’ and ‘Teamwork is essential and we have no problems there’.
Care Home 14
Reward and recognition varied in care homes of different sizes and ownership and relied on the available resources for the care home manager. Examples of the ways in which staff were rewarded and recognised are provided in Box 4. Reward and recognition by smaller providers were often less structured and involved smaller gestures, such as thanking staff or listening to staff. For example, one care home invested in refurbishing a staff room based on staff input and feedback. This highlights that reward and recognition were not always financial, in terms of monetary rewards for staff, but involved other approaches to promote staff satisfaction and well-being, and to realise and support the potential of the staffing resource.
-
Annual care awards.
-
Staff loyalty schemes, including long service awards.
-
Employee of the month award.
-
‘Kindness in care’ awards.
-
Regular recognition of colleagues who ‘go the extra mile’ or ‘above and beyond the call of duty’ with a reward from the care home manager or provider organisation.
-
Sharing positive feedback from people living in, or visiting, the care home.
-
Inviting external speaker to cover a subject identified as important by care staff.
-
Team building days.
-
Financial rewards and providing a ‘living wage’ (not a minimum wage).
-
Personal letters or cards to thank staff for their contribution to the work of the care home.
-
Celebrating and supporting the social and cultural diversity, values and beliefs of staff.
Understanding of the contributions of the care home workforce to enhance quality for care home residents
Person (not system) focused
In care homes rated as outstanding, the focus on the person living in the care home was evident. Our analyses highlighted the ways in which staff engaged positively with residents, offered choice, attended to diverse personal, social or cultural needs, promoted dignity, focused on abilities of the individual and promoted independence. By working in these ways, staff were described as being ‘present’ or ‘visible’ for residents, were able to develop relationships with residents, gained in-depth understanding of individual residents and their needs and preferences, and as a result were able to recognise and respond to changes in their presentation or condition. This had a positive impact on residents because it enabled tailored care and interventions, promoted individual purpose and well-being, ensured residents were involved in daily decisions, created a sense of personal security and safety and promoted resident and relative satisfaction:
People told us they thought the staff were ‘excellent’. Relatives told us how they thought the care and the management were ‘excellent’. One relative told us, ‘It [the care home], is fantastic.’ They went on to say, ‘It is not a home, it is my family member’s home.’ One relative had written a compliment thanking staff for the ‘Love and passion they provided.’ They went on to say, ‘The work staff did was amazing’.
Care Home 21
Developing relationships to support the person living in the care home was an important aspect of ways of working in care homes rated as outstanding. Residents and families were consulted to ensure that their views on personal support needed, as well as their preferences, were included in plans for care and ongoing reviews of care. Some care homes had a rolling programme of ‘resident of the day’ where the resident and their family met with a range of staff from the care home to provide feedback on the service they received and to review their care plan to make sure it fully reflected their current needs and preferences:
One person described their ‘resident of the day’ experience as ‘An extra special day’.
Care Home 18
Care home staff in these homes consulted with relevant health and social care professionals to ensure support for residents was sought in an appropriate and timely manner. Advice offered by external health and social care professionals was incorporated into care plans:
‘We do have people with some complex needs here so want to ensure all carers have knowledge of the issues and needs that people have, especially new care staff.’ Relatives agreed, ‘[The family member] has better access here to health services than she did at home in the community’.
Care Home 1
Care homes rated as inadequate reported staff working in ways which displayed some of these person-focused aspects. However, the reports also highlighted when these aspects were not fulfilled and where care was systems-focused:
We found examples of institutionalised practices where staff had not considered people’s feelings or if they were promoting their dignity. These practices were neglectful and could cause emotional harm.
Care Home 23
We found pre-admission assessments to make sure the service could meet people’s care and support needs, lacked detail about people’s physical, mental, social needs and preferences, with no information about identified risks.
Care Home 26
A person-focused approach required effective mechanisms for staff to work together and share information for resident care and quality assurance.
Working together
The combined action of staff to effectively and efficiently support and care for people living in a care home constituted teamwork. CQC inspectors described teamwork in care homes as outstanding when staff: ‘worked together’, ‘were on the same page’, ‘had shared values’ and ‘valued each other’.
In care homes rated outstanding, working together and supporting each other in the collective endeavour of care was highlighted: ‘It’s really good. Everyone is supportive, friendly and professional.’ (Care Home 13). In addition, there was acknowledgement that within the team there were individuals with different skills and that each team member should be able to make a contribution and flourish in their role:
A staff member said: ‘We all have different skills and can offer something different’.
Care Home 11
Working together was often underpinned by a clear philosophy of care that staff were keen to deliver:
Staff were driven by the philosophy that ‘every individual at the care home should receive an outstanding service’.
Care Home 2
Staff in care homes rated as outstanding displayed compassion, kindness and empathy towards each other. Teams were described as motivated, passionate and committed to improving residents’ lives. A shared philosophy of care and values led staff to share information with one another, ask their colleagues for advice and support, and to learn from each other. Leadership was key for promoting teamwork and staff reported that they valued teamworking, and enjoyed working in these environments and with their colleagues:
A staff member said: ‘The manager works with us as a team, that’s how it works, there is no them and us’.
Care Home 15
One staff member said, ‘I absolutely love it here, I like working with older people and all the staff are very nice. It is like one big family’.
Care Home 21
The care homes rated outstanding were also characterised by open and honest cultures that also supported learning from incidents and reflective practice:
The manager said: ‘getting things wrong makes us learn and get better as a team. We should never be afraid to fail, it is what we learn from it that is so important’.
Care Home 3
There was evidence of staff working as a team in some reports of care homes rated as inadequate: ‘We have a good staff team and create a nice working and living environment for everyone. It really is a home’ (Care Home 29). However, staff at these care homes described their day-to-day work as disorganised, that there was poor communication between staff, that their workloads were burdensome and they did not feel supported by colleagues or the manager. Therefore, despite acknowledging being part of a team, teamworking (as described above) was not apparent.
Structure in teams was also an important feature of care homes rated as outstanding. The registered manager was responsible for the overall service but was supported by leaders working in clinical areas and support services (such as laundry, kitchen and maintenance). These ‘unit level’ leaders were essential for cascading information to staff, delegating work and supervising staff, and monitoring service delivery. In a number of care homes rated outstanding in our sample, unit leaders did regular checks to ensure quality practices were thoroughly embedded in the service, for example medicines management procedures, confidentiality processes, responding promptly to call bells and treating residents with care with dignity.
Information sharing to benefit residents
Information sharing involved but was not limited to: giving and receiving details about the physical and psychosocial needs and preferences of individual residents; acting on information received; and sharing experiences, expertise and insights to benefit resident care. This required systems for comprehensive recording of individual residents and their circumstances and included written and verbal communication with the purpose of enhancing quality of service received by residents and their families.
Information sharing in care homes rated outstanding included staff in close consultation with residents, families and health and social care professionals. Systems for information sharing in these homes were reported as comprehensive and robust, and staff engaged in both written and verbal forms of communication. Written forms of communication provided staff with the knowledge, instruction and awareness to meet resident’s needs safely and effectively. These also provided a formal record of care for people living in or visiting the care home, and for internal and external reviews and audits of care within the home. Verbal communication supplemented written forms of communication and had the potential to promote effective discussions between staff, or between staff and residents and relatives, or other professionals involved with care. Conversely, information sharing in care homes rated inadequate was described as ineffective, lacked managerial oversight and there was an over reliance by care staff on verbal handover or informal communication rather than a mix of verbal and written communication. This resulted in missed opportunities to mitigate risks and promote safety.
While systems for written communication varied between care homes, there were some that were common to all outstanding homes including: policies and procedures; and care plans and risk assessments. Verbal communication included (but was not limited to) staff handover between shifts, team meetings and informal conversations.
Policies and procedures
In care homes rated as outstanding, there were detailed policies and procedures in place that were evidence-informed and reflected current legislation to guide staff with best practice. Documents identified in our analyses included policies on safeguarding, the Mental Capacity Act (2005), health and safety, infection prevention and control and medicines management. Staff were reported to be engaged with these policies and procedures and this was linked to promoting safer care for residents. Examples in these outstanding reports included accurate medicines administration records and evidence of adherence to infection prevention policies:
Protocols were in place that clearly described when medicines prescribed for use ‘as required’ should be administered. Staff had excellent knowledge of people’s medicines and the signs or indicators of when medication would be required.
Care Home 15
In inadequate care homes, while the provider had policies and procedures in place, many did not reflect current legislation or best practice. These policies and procedures were therefore not fit for purpose and created potential risks to safety and quality of care within the care home:
We concluded the provider was not evaluating and improving their practice sufficiently to meet regulation. They did not operate effective systems and processes, and the systems and processes did not enable the provider to assess, monitor and improve the service or assess, monitor and mitigate risk.
Care Home 29
Care plans and risk assessments
In care homes rated as outstanding, care plans were reported as comprehensive and person-focused and included a resident’s preferences: ‘I prefer a small snack before bed like a yoghurt or a banana and to watch some television. I like to have my bedroom light off with the door half open’ (Care Home 14). Staff engaged with these plans, which were also regularly reviewed and updated to reflect changing needs of residents. Whereas in care homes rated as inadequate, care plans were reported as often not reflective of current care needs of residents, lacked specific detail, were not well presented or organised and were often not used by care staff:
Although we found no impact on people’s care, not all staff spoken with had read people’s care plans. Staff referred to not having the time to do this and stated they were solely reliant on senior members of staff providing key information at handover meetings.
Care Home 22
Some care plans lacked detail instructing staff how to meet people’s needs. One person’s care plan referred to ‘regular repositioning’ to reduce the risk of developing pressure sores but did not specify how often the person required this.
Care Home 30
Some care homes in our sample had transitioned to electronic care planning to enhance quality. Electronic care planning supported ‘real time’ information recording by staff about the care and support of residents. Electronic systems were considered to raise staff awareness of residents’ needs and any changes to prompt timely interventions. Finally, these systems enabled efficient audits to improve resident care. Staff perceived that electronic care plans freed up time for them to spend with residents.
Risk assessments were completed by care home staff to help identify potential risks specific to an individual, for example mobility and risk of falls, continence, nutrition and hydration, or skin integrity, or as a result of the environment, such as fire and safety, infection prevention and control. The care plan addressed how these personal risks should be mitigated for an individual. Plans to manage environmental risks, for example how to evacuate residents in the event of an emergency, were also documented. In outstanding care homes, effective risk assessments supported staff to balance potential risks and resident’s choice, and to support and maintain residents’ safety or report concerns or incidents through appropriate routes. Risk assessments were regularly reviewed, and care plans were updated in these homes:
We saw that all potential risks were recorded and used to inform changes to people’s care plans.
Care Home 19
In care homes rated as inadequate, there was a lack of engagement with risk assessments by both management and staff. Validated risk assessment tools were not always used in these environments. Where risk assessments had been completed, some were generic and not always reflective of the needs and preferences of the resident. Planned care did not always reflect identified risk for an individual and not all risks to people’s safety and well-being were recorded or monitored:
Risks associated with the stoma had not been considered or recorded, for example, the risk of skin irritation, leakage, retraction or prolapse and dehydration.
Care Home 22
Verbal communication
Verbal communication – such as handover, team meetings and informal conversations – complemented written communication that guided or recorded care delivery. In care homes rated as outstanding, handovers were considered effective for catching up about resident care, listening to the views and concerns of care colleagues and promoting the involvement of all staff in supporting resident care decisions:
Staff worked well as a team to provide effective care to people. There was a handover every morning with nurses and care staff. Staff ensured that any changes to people’s needs were mentioned and known about. One member of staff said, ‘When I’m not here for a few days I get a handover from a nurse. I catch up with the care staff and talk to people too.’ Another member of staff said, ‘We have good relationships, we all work together.’ A third said, ‘We support each other. It’s a positive team and one thing I like about working here is that they are all people orientated’.
Care Home 1
However, in care homes rated as inadequate there was often an over-reliance on verbal reports about care during handover and neglect of the written documents detailed above which had an important role in promoting quality and safety within the care home environment.
Team meetings were reported to have a range of important functions associated with resident care (such as reinforcing the home’s philosophy of care, reviewing care plans and/or risk assessments, or revising work organisation to benefit residents) and staff development and recognition (e.g. learning from incidents, taking time to recognise and value staff contributions and achievements). The extent to which these functions were achieved varied depending on whether the care home was rated outstanding or inadequate, and whether there was strong relational leadership of the care home.
In addition to handovers and team meetings, managers of care homes rated outstanding engaged in informal conversations on a regular basis with staff. Many had ‘open door’ policies and did regular ‘walk around’ the care home. Other homes used afternoon ‘huddles’ so staff could meet and discuss events of the day. These strategies were considered to support and encourage staff to informally discuss their work and encouraged recognition of staff, as well as opportunities for ongoing problem solving:
Staff felt listened to and clear about their roles and responsibilities towards people living at the home. Staff felt confident to raise issues, concerns and ideas with the registered manager and were given regular opportunities to do so.
Care Home 19
The combined use of both written and verbal communication using the systems described above contributed to effective information sharing that benefited resident care. These systems were observed more frequently in care homes rated as outstanding. In addition, these homes had effective leaders that led the care teams. Working together and information sharing enhanced team cohesiveness and were important foundations for staff to ensure quality of support and care for residents.
-
Managers of care homes rated outstanding had the authority and flexibility to secure the workforce they judged necessary to meet residents’ needs and keep people safe.
-
Cohesive working relationships between the care home manager and provider senior management teams or owners ensured managers were supported and empowered to enact staffing decisions.
-
Low levels of staffing negatively impacted residents’ care and support, increased workload for staff, and decreased staff well-being and job satisfaction, which led to higher levels of staff sickness.
-
There was minimal detail in the CQC reports of how staffing levels were determined by care home managers and no consistent use of tools to support professional judgement about staffing.
-
Staffing numbers only partially explained the relationship between staffing and quality. Stability of staffing and low levels of use of agency or temporary staff, coupled with a skilled and competent care workforce, were necessary conditions for quality.
-
Opportunities for continuing professional development and training of staff, alongside staff supervision, were extensive in care homes rated as outstanding.
-
Mechanisms to reward and recognise staff were considered important to ensure staff felt valued by the management team. Feeling valued was linked with enhancing staff commitment and supporting the contribution of staff to quality.
-
Developing relationships to support the person living in the care home was an important aspect of ways of working in care homes rated as outstanding and included consultation between care home staff with residents, families and health and social care professionals.
-
In care homes rated outstanding, staff worked together and supported each other in the collective endeavour of care and support for residents.
-
A shared philosophy of care and values led staff to share information with one another, ask their colleagues for advice and support, and to learn from each other.
-
In care home rated as outstanding, there was clarity of leadership, team structure and roles and responsibilities of staff.
-
The combined use of both written (policies and procedures, care plans and risk assessments) and verbal communication (staff handover between shifts, team meetings and informal conversations) contributed to effective information sharing that benefited resident care. These systems were observed more frequently in care homes rated as outstanding.
Work package 5: a platform for sector-wide implementation
The structure of a social network determines how it functions,209–211 such network structures are thus pivotal for the diffusion of innovations. 212 Knowing a network structure can help in knowing who is in the network and where to target to help the spread and adoption of innovations. Even the absence of relationships within the network can present an opportunity for interventions to shape the network itself.
Appendix 10 explains the key SNA concepts used in the findings.
The innovation context
As part of the SNA, we wanted to introduce the idea of innovation (Table 18) and to standardise the innovation across the homes. We asked people to imagine an (their) ideal website bringing together staffing and quality. All of the participating homes were familiar with website resources, such as Capacity Tracker (https://capacitytracker.com/) and Skills for Care (www.skillsforcare.org.uk/adult-social-care-workforce-data/adult-social-care-workforce-data.aspx). We adapted the NoMAD survey94 for managers in the homes, to capture a sense of ‘newness’ (of their ‘ideal’ website), the chance of such a site being a ‘normal’ part of current or future work, and the four NPT core concepts representing work needed to introduce and sustain use of an innovation such as a staffing and quality website. The survey was in effect a heuristic device to help guide our interpretation of the observed social networks in the homes pertaining to advice and influence. There were no obvious points of difference regarding the four core concepts of NPT between the homes – all homes centred around ‘neither agreeing or disagreeing’ or ‘moderate agreement’.
| Home | Familiar?a | Part of current work?b | Part of future work?c | Coherenced | Cognitive participatione | Collective actionf | Reflexive monitoringg |
|---|---|---|---|---|---|---|---|
| 1 | 8 | 5 | 6 | 2.25 | 2.25 | 2 | 2 |
| 2 | 5 | 5 | 7 | 2.25 | 1.25 | 2 | 2.6 |
| 3 | 3 | 7 | 8 | 2 | 2 | 2.29 | 3.4 |
| 4 | 9 | 8 | 8 | 3 | 2.25 | 2.57 | 2.4 |
| 5 | 3 | 7 | 8 | 2 | 2 | 2.4 | 3 |
| 6 | 1 | 4 | 4 | 3 | 3 | 3 | 3 |
| 7 | 4 | 4 | 4 | 3 | 2.75 | 2.57 | 2.6 |
| 8 | 3 | 7 | 8 | 2 | 2.2 | 2 | 3 |
| 9 | 10 | 10 | 10 | 2 | 2 | 2 | 2.2 |
| 10 | 8 | 5 | 6 | 2.25 | 2.25 | 2 | 2 |
| 11 | 1 | 8 | 8 | 2 | 2 | 2.29 | 2 |
Care home networks of influence and advice
Care homes comprise people connected via active networks of relationships. Advice, influence and social capital (such as trust) flow through these networks. Some networks have key individuals at their heart – others are more diffuse, with wider groups of connections. Networks and their characteristics (such as the degree of reciprocity between social actors) can promote or hinder the mechanisms behind behaviours that influence quality – an important finding from our realist review.
We describe below – and in Table 19 – the characteristics and potential mechanisms for promoting innovation uptake and spread in the ‘advice’ (who do you influence?) and ‘influence’ (who influences you?) networks in the 11 study care homes.
| Care Home #1 | Care Home #2 | Care Home #3 | Care Home #4 | Care Home #5 | Care Home #6 | Care Home #7 | Care Home #8 | Care Home #9 | Care Home #10 | Care Home #11 | Overall mean | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| #Bedsa | 74 | 57 | 28 | 174 | 62 | 20 | 32 | 20 | 69 | 84 | 84 | 64.00 |
| #Employeesb | 99 | 57 | 35 | 121 | 84 | 34 | 43 | 14 | 72 | 94 | 75 | 66.18 |
| #Respondentsc | 18 | 37 | 17 | 24 | 14 | 14 | 8 | 11 | 10 | 39 | 27 | 19.91 |
| %Responsed | 18 | 65 | 49 | 20 | 17 | 41 | 19 | 79 | 14 | 41 | 36 | 36.17 |
| #Advice Relationshipse | 222 | 590 | 109 | 78 | 74 | 123 | 72 | 26 | 68 | 254 | 500 | 192.36 |
| %Reciprocal Advice Relationshipse | 8 | 24.7 | 11 | 4 | 2.7 | 13 | 16 | 0 | 0 | 12.6 | 14 | 9.64 |
| #Influence Relationshipse | 331 | 722 | 168 | 80 | 87 | 98 | 24 | 31 | 75 | 375 | 548 | 230.82 |
| %Reciprocal Influence Relationshipse | 8.5 | 29.4 | 22.6 | 0 | 2.3 | 6.1 | 8.3 | 6.5 | 2.7 | 16 | 15.3 | 10.70 |
| #Advice Cliquese | 70 | 70 | 34 | 11 | 16 | 32 | 17 | 7 | 25 | 106 | 162 | 50.00 |
| #Influence Cliquese | 131 | 66 | 32 | 9 | 30 | 32 | 5 | 7 | 20 | 145 | 168 | 58.64 |
| Overall Advice Clustering Coeff% (×100)e | 45.7 | 60.1 | 66.3 | 21.1 | 16.1 | 67.2 | 60.5 | 35.3 | 14.7 | 27.6 | 60.6 | 43.20 |
| Overall Influence Clustering Coeff% (×100)e | 73 | 63.4 | 76.9 | 14.5 | 15.3 | 60.5 | 15.4 | 43.2 | 29.1 | 40.4 | 64.5 | 45.11 |
| Advice Densitye | 0.023 | 0.161 | 0.08 | 0.005 | 0.011 | 0.079 | 0.04 | 0.143 | 0.021 | 0.028 | 0.075 | 0.06 |
| Influence Densitye | 0.034 | 0.197 | 0.126 | 0.006 | 0.012 | 0.057 | 0.013 | 0.17 | 0.015 | 0.039 | 0.084 | 0.07 |
| Highest Advice Betweennesse | Care Asst (676) | Home Mgr (954) | Maintenance (111) | Manager (7) | Snr Care Asst (41) | Nurse (182) | Dep Mgr (245) | Care Mgr (5) | 2 Care Asst (22) | Nurse (668) | Home Mgr (1026) | |
| Highest Influence Betweennesse | Dep Mgr (1279) | Home Mgr (710) | Unit Mgr (231) | Carer (4) | Care Asst (49) | Domestic (71) | Dep Mgr (14) | Support Worker (5) | Care Asst (58.5) | Nurse (1139) | Home Mgr (962) | |
| Highest Advice Out Degree Centralitye | Mgr and Dep Mgr (12) | 2 Mgrs (29, 28) | Unit Mgr (14) | CLM (8) | Dep Gen Mgr (6) | Home Mgr (14) | Dep Mgr (6) | Care and Dep Care Mgr (7) | Home Mgr (6) | Home Mgr (29) | Home and Dep Home Mgr (19) | |
| Highest Influence Out Degree Centralitye | Mgr and Dep Mgr (11) | Home Mgr (31) | Unit Mgr (13) | Carer (8) | Dep Gen Mgr (6) | Home Mgr (11) | Mgr and Dep Mgr (4) | Care Mgr (7) | Care Asst (5) | Nurse (21) and Home Mgr (21) | Home Mgr (20) | |
| CQC Ratingf | Requires Imp | Outstanding | Good | Requires Imp | Outstanding | Good | Good | Good | Good | Good | Good |
Care Home 1
Network characteristics
Advice and influence networks can be described as radial (Figure 7: Care Home 1 a and b). At the centre were a single respondent who felt they influenced, and were influenced by, everyone and a second respondent who was influenced by everyone. The relatively low reciprocity in the home suggests that while these two individuals may feel as if they are influential, it may not be reciprocated: advice and influence flowed to these two individuals, but they may not provide good targets for messaging around innovation.
FIGURE 7.
Advice network and influence network across 11 care homes.
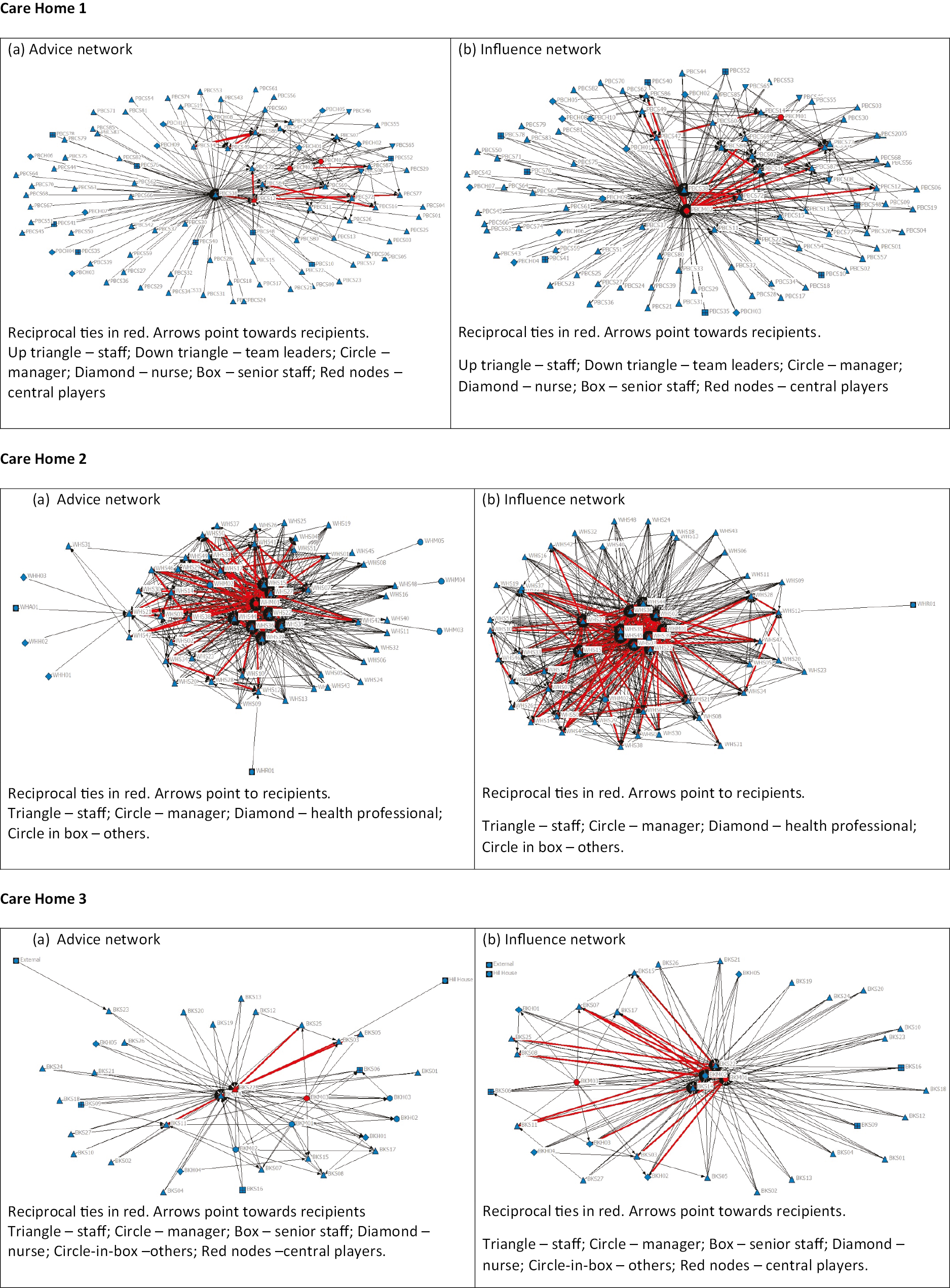
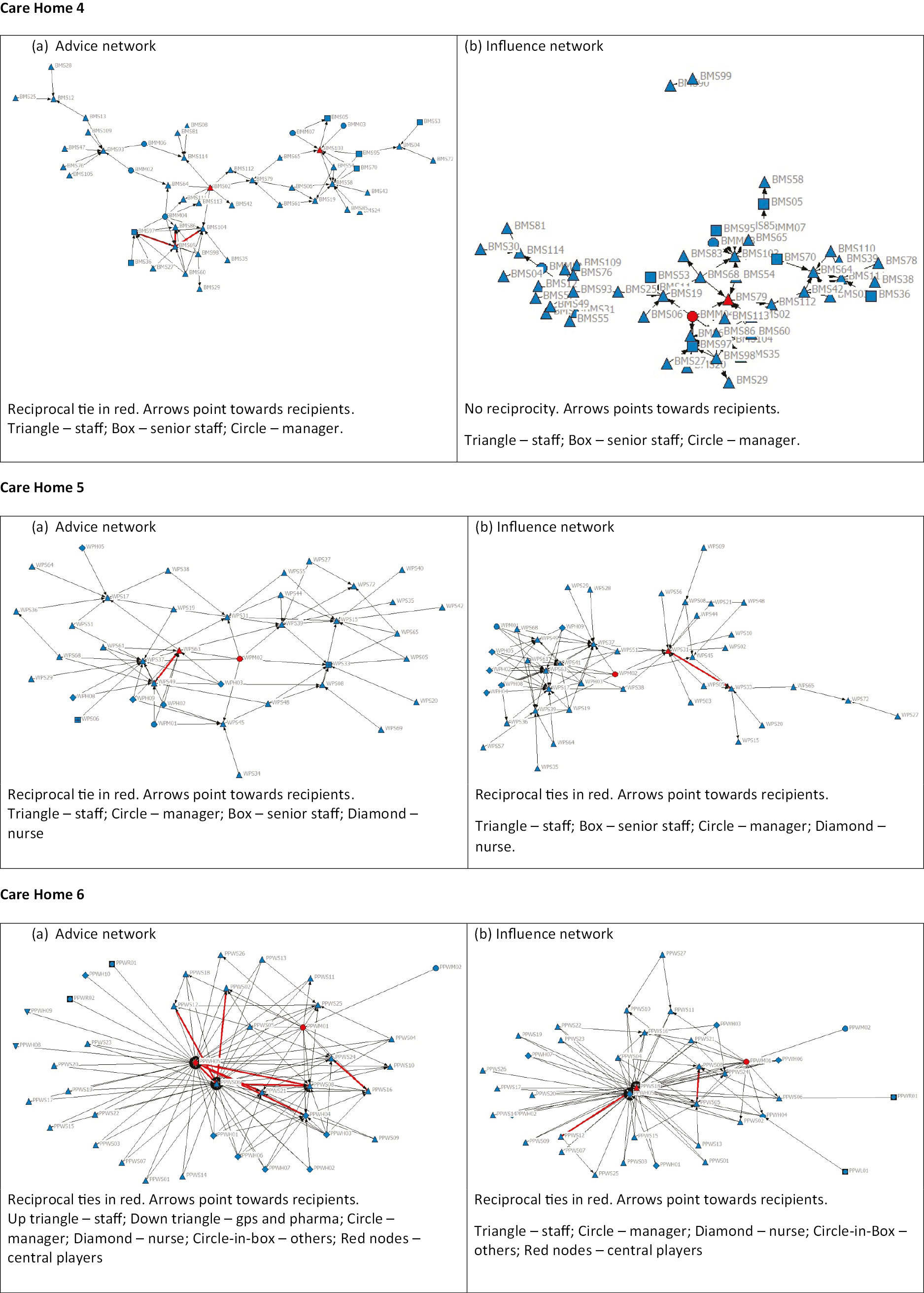
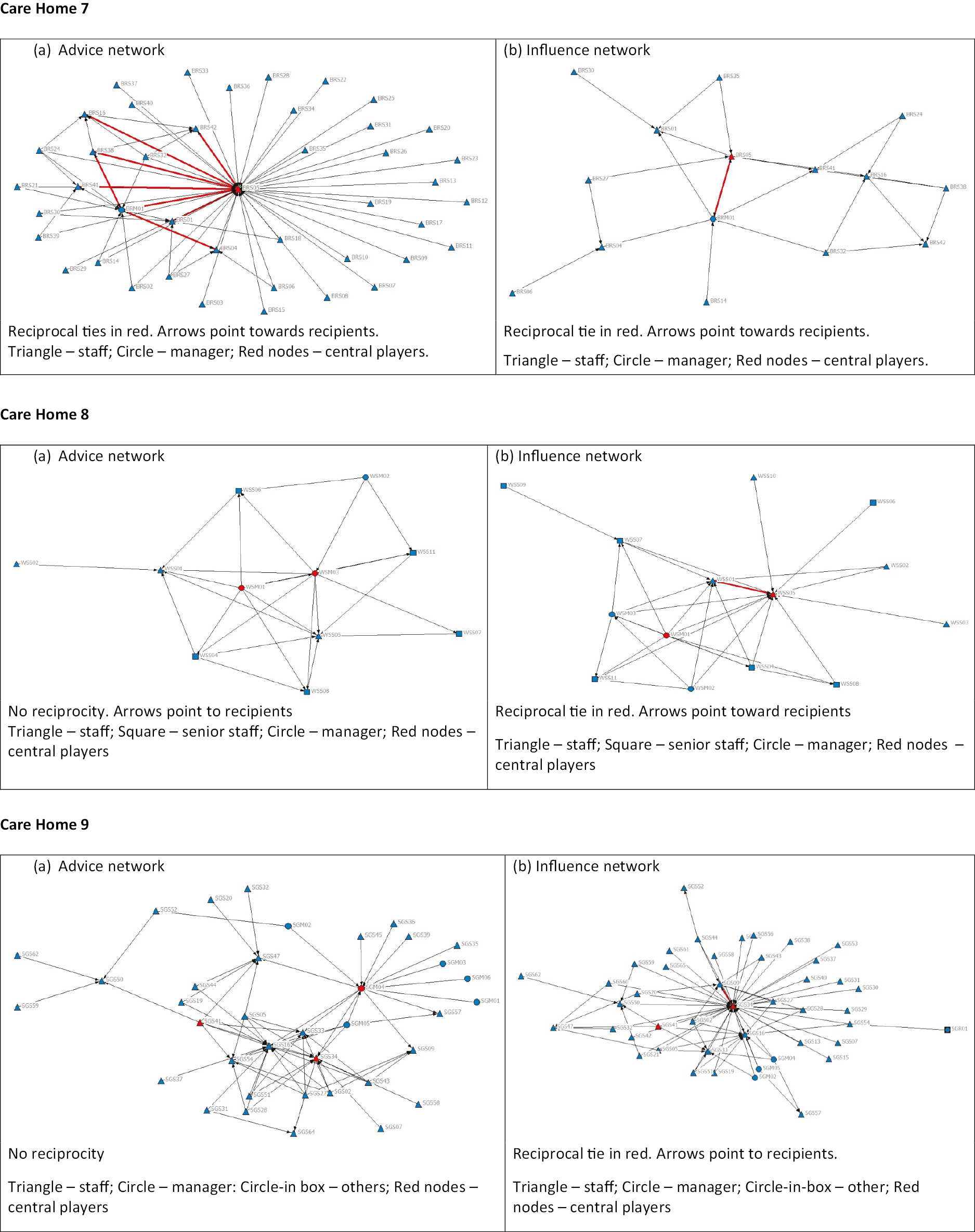
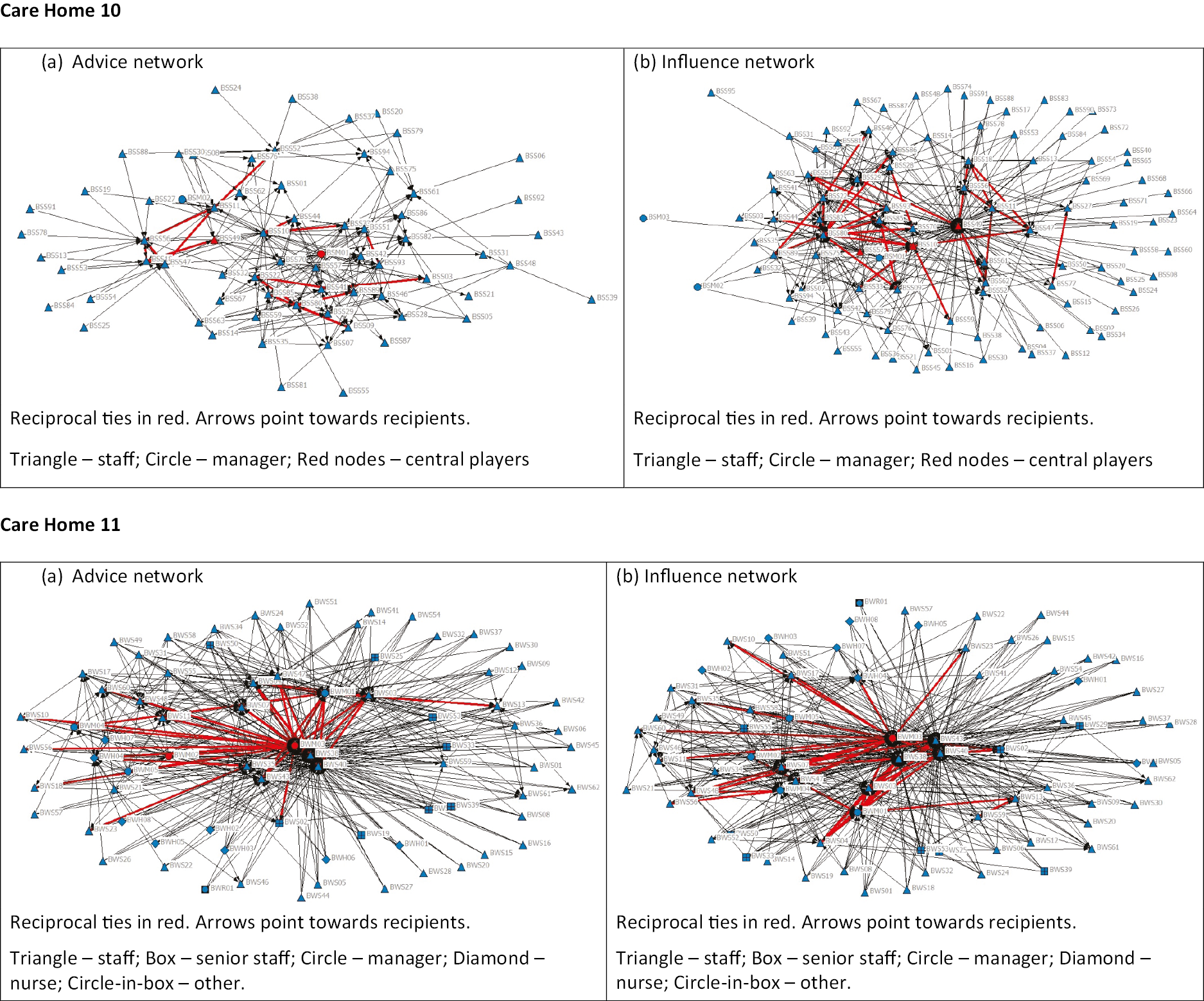
Staff were mainly drawn from the local area, with multiple families providing care home employees. Social relationships – formed in the local community – existed between staff and were maintained in the home. These mutual connections may provide some network cohesion, which in turn may help with sustaining adopted innovations. The advice and influence networks reflect relationships formed in the outside community being present in the care home: both networks have a large number of relationships and cliques. The relatively high clustering coefficient suggests tendencies for network clusters to form. However, network densities are low – possibly because the more people in the network the lower the density.
The low-density and low-reciprocity nature of the networks mean fewer connections and a barrier to spreading innovation.
Implementation of innovation
The manager felt a website on staffing and quality would feel somewhat familiar and largely ambivalent regarding the chances of such a resource becoming a normal component of current or future work (Table 18). Implementing innovations is helped by harnessing the power of the most central players in the network: those providing the most advice and influence. The manager (PBCM01) and deputy manager (PBCM02) were the ones providing advice and influence. The deputy manager was the most used bridge in the influence network. Perhaps surprisingly, a CA was the most used bridge in the advice network (receiving advice and passing it on) (Table 19).
It was very possible that a considerable degree of homophily had developed in Care Home 1 due to (1) staff mainly living in the area local to the care home and (2) multiple families who had multiple members employed by the care home. Homophily is the tendency to form strong social connections among those who share something in common – including living in the same area or being from the same family. 213 This should lead to more cohesion in the network due to increased number of connections, but also creates more cliques and clusters in the care home network. Care Home 1 had higher than average cliques and clustering, especially in the influence network. Staff relationships outside the care home influenced the networks within it. Any weak bridging ties between the network clusters and cliques would provide routes for moving innovation-related knowledge (and behaviours) from one group to another.
Care Home 2
Network characteristics
The home has core–periphery structure advice and influences social networks (see Figure 7: Care Home 2 a and b). Most of the relationships are either within the core, or between the core and the periphery.
This care home had the highest number of advice and incoming influence relationships and the most reciprocity between staff. It was also the densest, with above-average numbers of cliques. The networks’ tendency to form clusters was also higher than average (Table 19). The overall picture is one of heavily interconnected care home staff with strong reciprocal advice and influence relationships. These characteristics suggest innovation is more likely to spread – relative to homes such as #1 or #3 – widely and quickly.
Implementation of innovation
The manager was ambivalent towards a website on staffing and quality in terms of familiarity and chances of incorporation into normal work (Table 18). The care home manager was the key central player in both networks serving both as a bridge and providing the most advice and influence. The care home manager was the key opinion leader: they also received influence and advice, making them a significant bridge in these networks. Their support for any implementation of an innovation would be crucial.
Care Home 2 (and see also Care Home 10) had low numbers of staff living near the care home, but both homes had a high number of cliques and clustering. The networks were denser, making them more cohesive and with weak bridging ties connecting the clusters and cliques. The cohesion of these networks was most likely due to management efforts at increasing the sense of belonging (to the home and subteams) among staff. Dense and cohesive networks should encourage the transfer of innovations within these networks.
Care Home 3
Network characteristics
Like Care Home 2, both networks in this care home had star-shaped core–periphery structures (see Figure 7: Care Home 3 a and b), with just a handful of relationships not involving the core. One manager (BKM01) in the influence network was the biggest receiver of influence but also provided the most influence. This individual was a natural bridge between influence-based cliques.
While the number of relationships based on advice and influence was relatively small, there was a fair degree of reciprocity (advice network was slightly above average and for influence, double the average). The ability to cluster in both networks was above average, but the number of cliques formed was well below average. Both advice network and influence network densities were above average but limited connectivity in these networks may inhibit the spread of new ideas.
Implementation of innovation
The manager felt a website on staffing and quality would likely feel new and were moderately positive regarding the chances of such a resource becoming a normal component of current or future work (see Table 18). The care home manager (BKM01) was most sought after for advice and the strongest influencer. The unit manager (BKM03) held a clear bridge role in the influence network – bringing less connected groups together through influence. Surprisingly, one of the most connected staff was an estate maintenance employee who sought advice from almost everyone in the home (reflected in their betweenness centrality score). The extent to which this individual would be a good opinion leader is unknown.
Care Home 3 provided the perfect example of a network bridge. The unit manager received the most influence in the influence network and was also the person who influenced the most staff members. This individual would therefore be the most logical choice for an opinion leader given their influence in the care home.
Care Home 4
Network characteristics
Care Home 4 differed from the previously described networks as there were no obvious focal points (see Figure 7: Care Home 4 a and b) for advice and influence. Spreading innovation-related messages/information from one side of the network to the other would need several intermediate members to co-operate. There were no ‘bridges’ to enable the efficient spread of information (using people) from one side to the other in a couple of steps.
The number of advice and influence relationships were below average. And reciprocity, the number of cliques within the networks and potential for clustering were also low. The densities of both networks were about average (Table 19). Relative to other care homes’ network structures these networks would not represent a supportive context for the diffusion of innovation.
Implementation of innovation
The manager felt a website on staffing and quality would feel very familiar and was strongly positive regarding the chances of such a resource becoming a normal component of current or future work (Table 18). The care home manager had the highest betweenness centrality in the advice network. A carer – with 3–5 years of care sector experience – was highest in the influence network. Both roles would be potential knowledge brokers. The highest out-degree centrality in the advice network was the care home manager, while in the influence network it was another carer who had been employed in the care home industry for over 15 years. All the centrality scores were similar – representing no clear advantages in trying to identify potential brokers/influencers for innovation (Table 19).
There was no obvious central point in the network structure of Care Home 4. It did not have either a core–periphery or radial structure. This meant there was danger of blockages of best practice intervention or innovations within this network (see also Care Home 5 for another example of network structure impacting on function). For this network, the ties were not evenly distributed. Because the relationships are clustered on the left-hand side of the network, the benefits of these relationships (including social capital, influence and innovations) will go to the left-hand side first.
Care Home 5
Network characteristics
The influence network had a clear bifurcation (see Figure 7: Care Home 5 b). The network component to the left of node WPS31 is focused on six caregivers who receive a lot of influence from managers, nurses and other CAs. The component on the right had no influence from nurses or managers – with just two exceptions: CAs WPS31 and WPS45 influenced by the deputy general manager (WPM02). The deputy general was a bridge in the influence network. These structures suggest that the spread and adoption of an innovation is more likely in the left-hand part of the network because influential people and those they influence are more closely connected. In the right-hand component, CA WPS45 (influenced by the deputy general manager) influenced only one other person. Unlike the influence network, the advice network was less divided. Most of those receiving advice had a manager or a nurse involved.
Reciprocity in both networks was low. The number of cliques formed, the ability to cluster, and the density of each network was below average-reflecting fragmentation.
Implementation of innovation
The manager felt a website on staffing and quality would feel somewhat new and was largely positive regarding the chances of such a resource becoming a normal component of current or future work (see Table 18). The deputy manager (WPM02) was the most influential and the most sought-after person for advice. But the difference between them and others was not large. A senior CA had the highest betweenness centrality in the advice network, and a CA had the highest betweenness centrality in the influence network. See Table 19. Given that lack of a single clear source of advice in the care home, the safest strategy would be channel innovation messages to the home via the nurses and managers.
Care Home 6
Network characteristics
Of the nine largest recipients of advice, seven had reciprocal ties with each other (see Figure 7: Care Home 6 a). The care home manager advised eight (of the nine) biggest recipients. Like the advice network, the influence network structure is focused on those most influenced (see Figure 7: Care Home 6 b). However, unlike the advice network, there were fewer reciprocal ties and thus fewer interconnections among members.
Reciprocity and numbers of cliques in both networks were below average. The clustering coefficient was well above average, suggesting strong potential for clusters to form – especially the case in the advice network. The network densities were higher than average probably because these were relatively small networks (see Table 19).
Implementation of innovation
The manager felt a website on staffing and quality would feel new and were ‘cautious’ regarding the chances of such a resource becoming a normal component of current or future work (see Table 18). The most central players in a network are an obvious target for implementation efforts. If the home manager targeted the nine most likely recipients of advice (who then advised a handful of others), then the chances of spread and adoption of something new may be improved. Perhaps unsurprisingly, the manager providing the most advice was also influential. While the nurse serving as the most used bridge in the advice network had only been employed by this particular care home for less than a year, they had more than 15 years of care home sector experience. Of note, was the housekeeping assistant acting as the most used bridge in the influence network. While she said everyone influenced her on quality of care, she in turn only influenced two other people – suggesting her usefulness as a bridge in knowledge translational terms was limited. The structure of the two networks suggests that diffusion of an innovation will be more successful if focused on providing and encouraging the use of advice.
The advice and influence network structures of Care Home 6 (and also 11) have a small number of central players with reciprocal ties with each other. This structure facilitated an easier flow from one side of the network to the other than those networks that did not have this feature.
Care Home 7
Network characteristics
The advice network resembled spokes on a wheel. The hub was the deputy manager who received advice from everyone (see Figure 7: Care Home 7 a) and yet was at the heart of the reciprocal ties in this network. Outside of the reciprocal ties, there were very few interconnections in this network. The influence network was much smaller and unlike the advice network, lacked an obvious individual as focal point (see Figure 7: Care Home 7 b).
Both the advice and influence networks were small in terms of connections, with clear reciprocity in the advice network (above average) but not in the influence network. There were relatively few cliques in both networks. The reciprocal ties with the deputy manager meant clear potential for clustering in the advice network. However, in the absence of such reciprocity in the influence network, there was little potential for clustering. The density of the advice network was about average, while the density of the (small) influence network was well above average (see Table 19).
Implementation of innovation
The manager felt a website on staffing and quality would feel somewhat familiar and largely ambivalent regarding the chances of such a resource becoming a normal component of current or future work (see Table 18). The potential opinion leader in the advice and influence networks was the deputy manager (BRS05). This individual had the highest betweenness and degree of centrality in both networks. She was at the centre of a cluster of reciprocal relationships through which advice flowed. The manager influenced the same number of people as the deputy manager giving her the same level of degree centrality (see Table 19).
Care Home 8
Network characteristics
In the advice network, the focus was on the care home manager and deputy managers who tied together the network while in the influence network, the focus was on two individuals who received the most influence (see Figure 7: Care Home 8 a and b). The small number of employees at this care home had an impact on the characteristics of these two networks: not surprisingly, the number of relationships in both networks was below average. The level of reciprocity and cliques was well below average in both networks. But having the fewest possible connections – because it was a small home with few staff – meant clustering was just below average, and density well above average (see Table 19). This was due to the small number of people in the networks which means fewer possible connections.
Implementation of innovation
Despite the manager feeling a website on staffing and quality would be reasonably new, the manager was positive regarding the chances of a web resource becoming a normal component of current or future work (see Table 18). The care home manager was an obvious choice as a potential opinion leader. She had the highest betweenness centrality in the advice network – providing the most advice and was a clearly influential figure. One of the support workers (WSS05) had the highest betweenness centrality in the influence network. However, with 12 people influencing her and her only influencing one other person, she was unlikely to succeed as a key bridge in the influence network.
Care Home 9
This care home served as our pilot site where we were concerned with testing the feasibility of our methods rather than the response rate. The response rate was low in this care home.
Network characteristics
Despite some overlaps, there was segmentation among the advice givers in this network. Some of those receiving advice get it from those where it was not shared with others (see Figure 7: Care Home 9 a). On the other hand, the influence network had a generally radial structure focused on the carer receiving the most advice (SGS34). The radial nature comes from the fact that the carer in the centre was influenced by almost everyone (see Figure 7: Care Home 9 b).
Numbers of relationships and cliques, reciprocity, clustering and density were all lower than average (see Table 19).
Implementation of innovation
The manager felt a website on staffing and quality would feel completely familiar and were extremely positive regarding the chances of such a resource becoming a normal component of current or future work (see Table 18: note they were a pilot site and had lots of experience working with Skills for Care infrastructure). Two CAs with almost 30 years’ experience had the highest betweenness centrality in the advice network and one of those also had the highest betweenness centrality in the influence network. However, while they received the most advice and influence, they connected outwardly to only a couple of others who were not well connected. These two CAs would not make great candidates for roles as opinion leaders. The care home manager was the most sought-after for advice and a CA was seen as the biggest influencer. The number of people advised and influenced by the manager was small, suggesting more people may be needed for a sense of critical mass in influence and spread of behaviours. See Table 19. In the advice network, those targeted for innovation diffusion would need to be selected carefully – based on their cliques – because of the segmentation of advice givers.
Care Home 10
Network characteristics
This was a strongly interconnected home with equally strong levels of reciprocity. This drives the increased number of cliques and makes it possible for this network to form more clusters. This was another broadly radial structure with one staff member being influenced by everyone. But the relationships and interconnections in the influence network meant that cliques and reciprocal ties were dispersed. (see Figure 7: Care Home 10 a and b). Both advice and influence networks were conducive to diffusing innovations.
Relationship numbers were above average in both networks while clustering coefficients and the densities of both networks were below average. This was likely due to the size of the network as a whole – and therefore a higher denominator for the measures (see Table 19).
Implementation of innovation
The manager felt a website on staffing and quality would feel familiar but were ambivalent regarding the chances of such a resource becoming a normal component of current or future work (see Table 18). Top providers of advice and influence were a nurse and the care home manager, suggesting suitability as opinion leaders. The best bridges in this advice network were a team leader and a staff member who was both a nurse and the unit manager. Both these bridges provided as much advice as they received – confirming their value as bridging connections. The two staff with the highest betweenness centrality as influencers network were influenced by many more people than they influenced, limiting their roles as bridges for implementation or brokers for knowledge/messaging in the network (see Table 19).
Care Home 11
Network characteristics
This well-connected home’s advice network was radial in nature and driven by the three staff who took advice from almost everyone. The reciprocal relationships in the advice network of these three people formed a clique. It was similar structure for the influence network: four people were influenced by everyone (see Figure 7: Care Home 11 a and b). There were multiple cliques of reciprocal relationships between people. With some overlap in their connections, each member is also connected to unique people. This makes these cliques a solid target for diffusing innovations.
This care home had network characteristics that were well above average for both networks, indicative of its well-connected nature (see Table 19).
Implementation of innovation
The manager felt a website on staffing and quality would be very new. However, they were also positive regarding the chances of a web resource becoming a normal component of current or future work (see Table 18). Advice network reflected hierarchy and roles in the home: top advice providers included 4 (of 5) managers, 2 (of 8) senior CAs and 1 nurse (of 8). The staff member connecting the most people in this advice network was the care home manager (see Figure 7: Care Home 11 a). The top influencers at this care home were the care home manager and three of the other four remaining managers: a senior CA and a single assistant (see Figure 7: Care Home 11 b).
The care home manager was connected to the most influencers and so served as the biggest connector in this network of influence. The managers were prime candidates for opinion leadership roles (see Table 19). In both the advice and influence networks, the cliques identified above would be a good entry point for innovations, due to the breadth of their reach.
-
For the first time in the UK, we have described advice and influence networks within a sample of UK care homes.
-
These network structures serve as key for understanding who (and where) in the network should be targeted to implement changes associated with innovation.
-
Networks and their characteristics (such as the degree of reciprocity between social actors) can promote or hinder the mechanisms behind behaviours that influence quality – an important finding from the realist. 39
-
Some people within a home may feel they are influential, but it may not be reciprocated: advice and influence may flow to them, but they may not be connected to others in the network for wider influence.
-
Networks that are interconnected, dense or cohesive, with strong advice and influence relationships have higher chances of implementing change associated with innovation.
-
The care home manager – as opinion leader (i.e. providing most advice and influence and receiving most advice and influence) – is often pivotal for implementing innovation-related change.
Chapter 5 Discussion
Our mixed-methods study explored the relationship between staffing and quality in care homes using six interlinked WPs. We used Donabedian’s framework31 to examine the connections between structures, processes and outcomes that promote quality for people living in care homes. This chapter uses a synthesis of our findings to present a logic model explaining this relationship.
The context in which our findings were produced and will be received is significantly different to the pre-pandemic context at the time the study was commissioned and started. The impact of COVID-19 for residents arising from changes to everyday care and practices, infection prevention and control – including isolation of residents from family and friends – is not yet fully understood. The impact on staff is also being realised: staff shortages in the sector as a direct result of the pandemic are of real concern as we report. 214,215
We consider our findings will have international relevance for rebuilding care home communities and realising the importance of the relationship that exists between the staffing resource and quality in this sector as experienced by the people living or working in care homes, their family and friends, and staff who support residents and the sector (including NHS staff, commissioners, regulators and policy-makers). In addition, we acknowledge that care homes are located within a broader socio-political context and that there are enduring challenges for the sector associated with economic, regulatory, political and legislative pressures, societal and political debates about ageing and the value and contribution of care homes, as well as operating within fragmented health and care systems. Although not the focus of our research, our work and findings need to be understood within these debates and context.
We have addressed our original research objectives. We have developed a logic model to synthesise findings from our research.
Developing our logic model of the relationship between staffing and quality
The logic model (Figure 8) captures structures, processes and outcomes identified through our WPs. It helps explain empirically and theoretically what works, why and how, as well as the interactions between the constituent parts (structure, processes and outcomes) that we consider important for the staffing–quality relationship. This is the novel contribution of our study: we bring together constituent parts of the care home staffing–quality relationship.
FIGURE 8.
Logic model of staffing–quality relationship.

As well as identifying components of the staffing–quality relationship, the logic model provides a useful visual aid for the sector. ‘Sense-checking’ of the logic model with care home management teams revealed that the logic model had resonance, was considered relevant and all teams identified ‘gaps’ in their own staffing–quality relationship. The logic model therefore offers opportunities for individual care home management teams to review and appraise what works well, and target areas that require improvements and/or innovation. Links between structures, processes and outcomes are not unidirectional; this is captured in our logic model. For example, when staff are satisfied in their role then they are more likely to remain in their post, which creates stability in the team.
First, we synthesise findings related to important structural components related to the staffing quality relationship. The care home manager has a pivotal role in the care home216,217 and their responsibilities are detailed in the Health and Social Care Act 2008 (Regulated Activities) Regulations 2010. 218 Stability of the manager is important for quality: our findings reveal that care homes with a manager in post in the 12 months prior to a CQC inspection were more likely to be rated as good or outstanding (WP2). The manager makes decisions about the workforce they consider necessary to meet residents’ needs and to keep people safe. Managers of care homes rated good or outstanding had authority and flexibility to secure the workforce they judged necessary (WP4). Cohesive working relationships between managers and the provider senior management team or owner supported and empowered managers to enact their staffing decisions (WP4).
Higher staff-to-bed ratios are associated with a greater chance of a good or outstanding CQC inspection score (WP2). We found a statistically significant, but small, relationship between a higher proportion of care being provided by RNs and a lower incidence of falls with fractures, UTIs and medication errors (WP3): a novel finding in the UK context but that resonates with other international longitudinal studies. 27 Use of agency nurses to cover for nurse sickness or unfilled vacancies is not associated with increased risk of falls, infections, or pressure ulcers, but is associated with increased risk of medication errors (WP3). However, simply increasing nursing inputs in this setting is unlikely to be a cost-effective way of reducing adverse incidents for care home residents (WP3). Based on our modelling work we cannot confidently quantify ‘sufficient’ staff: linear regression methods are not particularly good at identifying non-linear relationships. 219 While agency nurses are often perceived as negative for quality in the sector,220 our study suggests that more RNs improve quality (or reduce adverse clinical incidents), regardless of whether they are permanent or agency staff. However, use of agency staff is perceived to impact on the organisation of care work and residents’ experiences of care when care is provided by unfamiliar staff (WP4). Having ‘enough’ or ‘sufficient’ staff is a feature of findings in other WPs: ensuring timely care for residents (WP1ii); and recognising that low levels of staffing negatively impact on residents’ care and support, workload for staff, and staff well-being and job satisfaction, leading to higher levels of staff sickness (WP4). However, there is a lack of detail on how staffing levels are determined by managers and there is no consistent use of tools to support professional judgement about staffing (WP4).
Our work also highlights the importance of workforce stability: the manager and the care workforce (RNs and CAs). Stability of the care workforce, which results in lower levels of use of agency or temporary staff, was necessary condition for quality (WP4). We also found that having more experienced care staff, that is staff in post for 5 years, is likely to improve the quality rating for the care home (WP2), and therefore quality for residents. Importantly, a stable workforce was associated with skills and competence, which includes clinical, care, social and cultural skills and competence (WP1i, WP1ii, WP4). Cultural competence refers to an individual’s ability to understand, communicate and effectively interact with people of different cultures, and therefore to meet residents’ needs and promote quality of care and life (WP1ii). Cultural competence is an important consideration for workforce planning and subsequent recruitment and retention of the care team. Opportunities for staff induction, training and continuing professional development, alongside staff supervision, were extensive in care homes rated as outstanding (WP4). High staff turnover minimised opportunities for developing staff skills and competence: the focus for care homes with high turnover being staff induction and mandatory training (WP4).
Numbers of staff are an important but not sufficient condition for care home quality. Our work offers insights into processes that support quality. Importantly, ‘sufficient’ staff and staff ‘stability’ are important conditions for two key harmonious components for quality: person-focused care and teamworking.
Staffing consistency – ‘sufficient’ staff and stability – is important for the organisation of care and work. Larger homes were less likely to be rated positively (WP2), but other WPs highlighted the importance of size of the team (rather than the home) and the resultant impact on care organisation to promote quality (WP1i, WP1ii, WP4). Our work reveals that small groups of linked residents and staff (5–15 residents per staff member based on level of resident dependency) promoted familiarity, communication and a familial environment for cultivating relationships (WP1ii). Establishing ‘family-like’ relationships between residents and staff and ‘knowing’ a person was perceived by staff to promote personalisation of resident care (WP1i) and to support staff to go beyond assisting residents with physical tasks, to address their social and emotional needs through relationships (WP1ii).
Developing relationships to support the person living in the care home is a feature of care homes rated as outstanding and includes care home staff consulting with residents and their families, health and social care professionals (WP1i, WP1ii, WP4). These relationships inform care planning and personalisation of resident care (WP1i). Relationships between care home staff and families also legitimise family involvement in care to support quality (WP1i). Unit-level supervisors that role model relationship-building behaviours are important for this to be realised and enacted by care teams (WP4).
Staffing consistency (numbers and stability as described above) is also important for teamworking. In care homes rated outstanding, staff were reported to work together and supported each other in the collective endeavour of care and support for residents (WP4). The relationship between how staff feel in their day-to-day work and quality of health care is well recognised,221 and a finding of our work. Staff that feel supported, valued and with (managerial) ‘permission’ to prioritise residents’ needs adapt and adopt behaviours that foster expression of residents’ preferences while providing care (WP1ii, WP4). Greater perceived autonomy in day-to-day work, with associated accountability, led to greater staff engagement and satisfaction with work (WP1ii, WP4).
Team reciprocity was linked with open communication and information exchange (WP1ii). Reciprocity also supported teams to draw on each other’s knowledge and skills to promote individualised care and enhance quality (WP1i, WP1ii, WP4). The combined use of both written (policies and procedures, care plans and risk assessments) and verbal communication (staff handover between shifts, team meetings and informal conversations) contributed to effective information sharing that benefited resident care: these systems were observed more frequently in care homes rated as outstanding (WP4). Visible unit-level supervisors (not necessarily the manager) that foster teamworking and minimise conflict provide the contexts in which team reciprocity and relationships flourish (WP1ii). Networks and their characteristics (such as the degree of reciprocity) can promote or hinder the mechanisms behind behaviours that influence quality. Networks that are interconnected, dense or cohesive, with strong advice and influence relationships have higher chances of implementing change associated with innovation to promote quality (WP5). The care home manager – as opinion leader (i.e. providing most advice and influence and receiving most advice and influence) – is often pivotal for implementing innovation-related change (WP5).
We recognise not all care homes in England employ RNs. In care homes without nursing, senior care staff, with community-based RNs, will ensure resident needs are met. Our review work offered insights into the roles and responsibilities of the care team. Where RNs are employed by a care home, they are responsible for assessing, supporting and monitoring resident health and well-being, with support of the care team (WP1i). RNs have an important role in supervising and supporting CAs, and to promote teamworking for residents’ benefit (WP1i). In addition, RNs have an important role in anticipating care demands, planning work and being responsive and flexible in care delivery and their work to ensure resident safety (WP1i). Promoting resident safety, alongside quality assurance, and working with (and co-ordinating) a range of staff (internal and external) to ensure appropriate and timely interventions and care is also perceived as the role of the RN (WP1i). When enacted this promotes quality and safety for residents, creates comfortable and safe environments, as well as supporting efficient decision-making (WP1i). The end result is tailored and responsive care and ensuring timely (and appropriate) interventions by the right person (employed by the care home or employed by an external organisation but with a responsibility for residents) which impact on outcomes and quality. There is a gap in understanding the roles and responsibilities of staff in care homes without nursing and the impacts when these are undertaken by a workforce comprised of CAs, that is social care staff.
There are leadership and management behaviours that are important for the realisation of the key processes described above. Our realist review (WP1ii) considered leadership behaviours that lead to quality, including promoting a resident-centred approach, ensuring effective communication, promoting staff confidence, offering practical support to staff, providing emotional support, recognising staff contribution and encouraging diversity. 39 Managerial behaviours encourage relationship building (WP1ii). Staff feeling valued is linked with enhancing staff commitment and supporting their contribution to quality (WP4). A managerially endorsed philosophy of care (valuing residents and staff) also supports staff behaviours that foster individualised resident care (WP1ii, WP4). We acknowledge that all these components are located within mechanisms for regulatory compliance.
We consider these structural and process components as essential characteristics to support the staffing–quality relationship. We have considered the concept of quality (and outcomes) broadly in this mixed-methods study. This is an important and novel contribution of our work. Previous studies to understand this relationship have focused on modelling structural characteristics and clinical outcomes. Our work has empirically and theoretically progressed this understanding and the links between structure, processes and outcomes (beyond clinical indicators). Quality in our work includes resident needs and preferences being met (and culturally appropriate) (WP1i, WP1ii, WP4), resident and family satisfaction (WP1i, WP1ii, WP4), residents living with purpose to promote their quality of life and well-being (WP1i, WP1ii, WP4), and safe care for residents (which includes clinical outcomes) (WP1i, WP1ii, WP2, WP3, WP4). We have also considered staff well-being and job satisfaction as we consider this influences quality as experienced by residents.
Strengths and limitations
Strengths of this study are our mixed-methods approach, our broad conceptualisation of quality and theoretical framework to understand and explain the staffing–quality relationship. These factors supported our synthesis and informed the development of a logic model. Our work was significantly impacted by the COVID-19 pandemic (see Appendix 2), but our revised methods enabled us to address our original objectives.
We have worked closely with the public and stakeholders throughout the research, from question formulation to synthesis. Our intention was to ensure that the research was carried out ‘with’ and ‘for’ the public and stakeholders, rather than it being ‘about’ them. 222 We formed two advisory groups for the study that met regularly (pre-pandemic): (1) a resident and relative group and (2) a care home manager group. The SSC also had representation of key stakeholders (see Acknowledgements) to guide our work and met throughout the study period. These mechanisms ensured that alternative perspectives (beyond the research team) fed into and improved the design, implementation and quality of the research, and promoted conversations and learning to benefit the research. 223
Our reviews include international literature. Much of the evidence base informing our reviews is descriptive, lacks comparison or controls and is small scale. Nonetheless, these studies have contributed to understanding the roles and responsibilities of the care home workforce for promoting quality (WP1i) and to offer theory-based explanations of how, why and in what circumstances staff behaviours promote quality for older people living in care homes (WP1ii). When considering the staffing–quality relationship, both reviews have moved evidence-based discussion beyond numbers of staff and their relationship to quality, to a focus on the importance of what they do and how they do it. These findings are important for people and organisations making policy and delivering services on the best ways to deploy and support quality in care homes through the most valuable resource for any care home: its staff. However, we acknowledge that this understanding is developed through international studies, where the long-term care context may be different. In particular, these studies predominantly focused on the role and responsibilities of the RN. In the UK, most care homes do not employ RNs, with nursing care being provided by nurses employed by primary and community care services. The roles and responsibilities of CAs are considered in our analyses for these reviews, but there is no consideration of the varied levels of workers in this support category in our analyses. This constitutes an important gap for consideration in future studies. Primary data collection, as we originally proposed, would have provided this more nuanced understanding and knowledge.
We worked closely with a national organisation (Skills for Care) for WP2. This constitutes a cross-sectional observational study of a subpopulation of care homes in England that supplied their workforce data to Skills for Care for inclusion in the NMDS-SC and CQC inspection ratings. There are debates of how well this approach accurately conceptualises and measures care quality. 224,225 We adopt the pragmatic view that CQC inspection judgements are one measure of care home quality, and we focused on relationships between the CQC measure of quality and care homes’ staffing establishments. This approach is novel: existing studies of the staffing–quality relationship tend to focus on clinical indicators that are sensitive to staffing inputs. 17,27 This work therefore contributes evidence based on broader conceptions of quality. However, we acknowledge some limitations of this approach.
In our methods we acknowledge the potential for bias in cross-sectional analyses of relationships between quality and staffing because of omitted variables and measurement error. 17 Following sensitivity analyses, we are confident that the omission of home caseload measures in the NMDS-SC may not be a significant source of bias in our WP2 analysis. However, small effect sizes may be a consequence of the limitations of the data: particularly imprecise measurement of staffing and quality which mean measurement error is likely to bias estimates downwards. Given our data source, the extent to which the results generalise to homes that do not contribute data to NMDS-SC is not clear. We had originally proposed to estimate the costs (in terms of higher costs) and benefits (in terms of fewer homes rated negatively by the CQC) of different staffing models. However, we did not pursue this analysis: it was not possible to discern clearly different staffing models in the data and effect sizes were relatively small. Any cost–benefit analysis results would therefore not be meaningful.
We worked with a large care home provider organisation for WP3. This is the first study in the UK to work with a large care organisation for this purpose and so a key contribution of our work is to provide novel evidence on relationships between nurse staffing and care quality in English care homes drawing on longitudinal data that allow many of the limitations of previous studies to be addressed. 17,27,28 Most longitudinal studies in this field have been conducted in North America; findings from other countries may not generalise to the English context because of differences in the fundings and organisation of care between countries. Against these strengths, it is important to consider limitations of our modelling work.
Nurse-sensitive indicators of care quality do not address residents’ quality of life. However, there is a link between health status and impact on quality of life. Therefore, these indicators are one aspect of quality, and have implications for potentially preventable treatment costs that fall on the wider healthcare system. Our findings are based on data from a single care home operator and so may not be generalised to the wider population of care homes. The care home provider has developed management systems and processes for determining and ensuring what it considers to be appropriate staffing levels, so this places limits on the amount of variation in staffing arrangements we observed, and this limited variation may mute results that would be apparent if there was more variation in staffing. Our study was designed to minimise measurement error by using large administrative data sets. However, we noted that error rates recorded in the data set underestimate true rates; for example, medication errors. 226 This is likely to be because these errors are being self-reported (and may be influenced by staffing levels) and may only record the most obvious and possibly serious errors. This influenced the data and impacted on our modelling and cost analysis. This study lacks measures of resident characteristics and resident-specific risk, the omission of which may bias results: an issue debated. 28 It also does not take into account work variations of RNs and CAs employed by different homes. However, we have controlled for time invariant and time-varying home-specific characteristics and our focus on a single care home provider may mitigate this: staff are employed on common job descriptions and similar policies and processes will exist across care homes in the organisation. One key thing to keep in mind when interpreting our results is that the accuracy of measurements may be affected both by staffing levels and by (unobserved) determinants of care quality like the competence and ‘quality’ of managers and/or staff. For example, well-managed homes may be more likely to record quality-related incidents more accurately than poorly managed homes’ where staffing and the organisation of care may make adverse events more likely.
Our documentary analysis of CQC inspection reports offered novel insights into the structural, process and outcome components of the staffing–quality relationship and complemented the findings of other linked studies in terms of explanation and theorising. This qualitative analysis focuses on associations rather than causal relationships. Our analysis is limited to the text available and any inherent reporting biases of the inspectors who authored the reports. It is also limited to the purposive sample of care homes rated as outstanding or inadequate. Transparency of our approach and methods promotes transferability.
The NoMAD survey enabled us to describe care home managers’ views about how a staffing and quality online resource might impact their work and their expectations of whether it could become a routine part of their current or future work. SNA identified opinion leaders in care homes by either their number of connections or how often they served as a bridge in the network. There are implications of SNA relevant for managers: to identify the most connected people and the possibility of recruiting them to be innovation champions; to reveal bottlenecks in the flow of information and advice; to identify gaps (or structural holes) in networks that need to be brokered; to highlight that proximity matters in networks and that it can be used to assemble teams; and to remind managers that central players in one network are not necessarily central players in other networks and that they may need to manage multiple networks. 227,228 These findings are novel but limited by cross-sectional nature and response rates. Seven managers from eight care homes completed the NoMAD survey. For some of the case sites (n = 11) the response rate was low. Revisiting the care homes with low response rates was limited by the pandemic. We acknowledge the low response rate at some of the care homes may affect the representativeness of the networks we describe.
Finally, we acknowledge the limitations imposed on this study due to COVID-19 (see Appendix 2). In particular, not being able to undertake the in-depth case study data collection activities which would have gathered primary data from people living and working in, or visiting, care homes.
Equality, diversity and inclusion
Our approach and methods optimised participation of the diverse care home population: people living and working in care homes. Using national and organisational data sets ensured equality and inclusivity, as well as ensuring diversity on characteristics such as age, sex, disability, race, religious beliefs, marital status and sexual orientation. Diversity of care home residents, particularly those lacking capacity, and staff are often under-represented in research. The use of anonymised data sets for these populations enabled their representation and inclusion in our study.
We have worked closely with the public and stakeholders throughout the research, from question formulation through to synthesis (described in Chapter 3, and above under section Strengths and limitations). Involvement and engagement included residents, relatives, care home staff, NHS staff, providers, provider representative bodies, commissioners, regulators and policy-makers. Our SSC had representatives from these stakeholder groups and we were also guided by our two advisory groups – (1) residents and relatives and (2) care home managers and RNs – to ensure we promoted inclusive, accessible and active engagement in our study. This is reflected in blogs that we wrote with our residents and relatives’ advisory group (see e.g. https://bit.ly/3E8yf0V) and SSC members (see, e.g. https://bit.ly/3uBdQhJ).
Our approach to involvement and engagement ensured that alternative perspectives (beyond the research team) fed into and improved the design, implementation and quality of the research, and promoted conversations and learning to benefit the research. The research team was comprised of individuals with methodological, subject and sector expertise; appointed research fellows had health and social care research experience.
Chapter 6 Conclusions
Quality is complex, contested and dynamic. The perspective of those living in care homes, their families, or those who work in or with homes (care home staff, NHS staff, providers or commissioners, regulators and policy-makers) will influence individual perspectives. Care homes represent a range of service types and structures that influence staffing arrangements. Studying the staffing–quality relationship then is not straightforward. This complexity merited a mixed-methods research design. In this final chapter, we revisit the research objectives set out at the start of the study (see Chapter 2). We summarise the extent to which we met these and highlight implications for social care and future research of the staffing–quality relationship in care homes.
Study objectives revisited
Objective 1: describe variations in the characteristics of the care home nursing and support workforce
The two evidence reviews in WP1 provide evidence and theory-based explanations of variations in care home workforce characteristics associated with higher quality care. We explored staff roles and responsibilities (WP1i) and the conditions necessary for staff to behave in ways that promote quality (WP1ii). The review findings focus on different staff within care homes: leaders and managers, unit supervisors, RNs, CAs and staff with ‘informal’ influence within the care team. The reviews add depth to understanding of variations in care home workforce characteristics and how they shape quality. Specifically, they paint a picture of who staff are, what they do (and why) and how they act for the benefit of residents and their families.
We did not survey managers and staff to describe recruitment and retention challenges and staff roles as originally planned (due to the pandemic). Since our study was commissioned descriptions of the care home workforce and the challenges of securing the workforce have been forthcoming in national reports from Skills for Care (as presented in Chapter 1).
Objective 2: identify the dependency and needs of residents and relatives in care homes and their association with care home staffing
This objective was partially met. Data were limited as the NMDS-SC lacked a measure of resident characteristics and resident-specific risk (WP2). Care home provider cross-sectional organisational data were based on their own internal classification scheme indicating, for example, the proportion of residents with nursing needs or those receiving specialist dementia care (WP3). Some of the NMDS-SC data and variables were fit for inclusion in our models – meaning we could address information deficits that affect workforce planning, quality improvement and commissioning by incorporating measures of dependency and functional needs of care home residents. WP4 revealed decisions about staffing needed for resident needs and preferences are often based on (largely intuitive) managerial judgements as opposed to systematic use of validated tools. Our findings reveal the impact on residents when actual staffing levels fall below the planned level (WP3, WP4), and the consequences for staff well-being and job satisfaction when there are insufficient staff to meet residents’ needs (WP1ii, WP4).
Objective 3: examine how different care home staffing models (including new roles) impact on quality of care, resident outcomes and National Health Service resources
The relative absence of clearly discernible and distinct staffing models in homes meant our analysis did not identify how distinct patterns or models of care home staffing impact on quality and outcomes (WP2). In WP2, care home staffing models exhibited limited variation (funding and resource constraints meant most homes operate with similar staffing models). The possibility that data were too limited for analysis cannot be excluded. The care provider organisation (WP3) developed management systems and processes for determining and ensuring its ‘appropriate’ staffing levels. Where RNs were employed, there was little variation in numbers between homes. Consequently, variation in staffing was less than expected. WP2 findings made cost–benefit analysis nonsensical: it was not possible to apply meaningful cost estimates to data. Our cost–benefit analysis in WP3 suggests additional staffing costs are likely to substantially outweigh reduced treatment costs – recognising that the true costs of adverse outcomes often extend beyond the financial. It is possible that our estimates of benefits are inaccurate: the linear regression models used in this study may have missed important non-linear relationships between staffing and quality. 57 Machine learning methods are better able to detect non-linear relationships so they could usefully be employed in future studies to investigate if there are inflection points beyond which additional staffing does not improve quality outcomes.
Objective 4: explain how care home workforce (numbers, skill mix and stability) might meet the dependency and needs of residents
Our findings indicate – albeit cautiously – that having more staff is likely to improve care quality for residents (WP2) and more care by RNs may lead to fewer adverse events for falls with fractures, UTIs and medication errors (WP3). Expensive increases in nursing care would be associated with minimal total treatment cost savings and, therefore, an increased net additional cost for care home providers: simply increasing nursing inputs is unlikely to be a cost-effective way of reducing adverse incidents for care home residents (WP3). We acknowledge the limitations of data sets included in our research (see Chapter 5).
Having ‘sufficient’ staff is important for quality: ensuring timely care for residents (WP1ii); and recognising that low levels of staffing negatively impact on residents’ care and support, workload for staff and staff well-being and job satisfaction, leading to higher levels of staff sickness (WP4). However, there is a lack of detail of how staffing levels are determined by managers and there is no consistent use of tools to support professional judgement about staffing (WP4).
Based on our modelling work we cannot confidently quantify ‘sufficient’ staff because results suggest linear relationships between staffing measures and quality outcomes where incremental increases in staffing numbers, skill and experience are associated with small incremental increases in quality measures. It is therefore not clear from the data whether there are minimum thresholds below which these staffing measures should not fall without increasing risks for residents. Methods better able to identify non-linear relationships between staffing and quality (i.e. machine learning) could help to quantify what sufficient staffing means. Stability of the care home manager and the care workforce was important to meet the dependency and needs of residents and to enhance quality (WP1i, WP1ii, WP2, WP3, WP4). Stability of the workforce results in lower levels of use of agency or temporary staff. Agency or temporary staff were perceived to compromise quality (WP4); however, we found that use of agency nurses to cover for sickness or unfilled vacancies was not associated with increased risk of adverse events other than an increased risk of medication errors (WP3). A stable workforce was aligned with a skilled and competent workforce (WP1i, WP1ii, WP4) and to benefit the organisation of care to better meet residents’ needs.
Objective 5: explore and understand the contributions of the nursing and support workforce (including innovations in nursing and support roles) in care homes to enhance quality of care
Our research suggests the nursing and support workforce are well placed to enact the behaviours that ensure personalised care, tailored to resident needs and preferences, with interventions that are appropriate and timely (WP1i, WP1ii, WP4). We have highlighted specific workforce-related factors that support teamworking and relationships that benefit residents (WP1i, WP1ii, WP4). Leadership and managerial behaviours which reward and recognise staff contribution are key to realising these components of care and teamworking (WP1ii, WP4).
Care staff with more (contextualised) experience – that is, care staff in post for 5 years, care home managers for more than 12 months – are likely to improve quality, at least as judged by the regulator (WP2). A stable workforce equated to better skills and competence in clinical, caring, social and cultural areas of work (WP1i, WP1ii, WP4). High staff turnover minimised opportunities for developing staff skills and competence – reducing quality, as experienced by residents (WP4).
The pandemic meant we were limited in our study of innovations in nursing and support roles. We were unable to administer surveys or undertake the planned in-depth case studies. Exploration and understanding of contributions of the workforce is derived from evidence reviews and documentary analysis. While relevant, they may reduce internal validity or be more prone to reporting and other biases. Relying on these data sources means we may have missed roles and responsibilities in environments that do not employ RNs: care homes without nursing or residential homes.
Objective 6: translate methods used for modelling the relationships between staffing and quality to provide a platform for sector-wide implementation
Work packages 1–4 findings were brought together in a logic model. We demonstrated the feasibility of SNA for unpacking the relationships, ties and flow of social capital in homes. Knowledge of this picture creates potential for planning implementation efforts required to enhance quality via staffing judgements and staff-focused interventions (WP5). Ultimately, securing high quality, complete, samples of staff required face-to-face intensive researcher involvement in homes; many were not used to participating in research. COVID-19 restrictions further limited this work. Despite the restrictions and varied effects, we have shown that potential opinion leaders for quality improvement can be identified (based on their network position) and that metrics such as reciprocity, betweenness and centrality could be produced and – at least at the researcher level – help steer potential strategies and interventions to increase the adoption and spread of innovation. Delays with WPs 2 and 3 limited our translational activities for modelling. We were able to adapt the NoMAD survey tool to capture a sense of the work potentially required to introduce and sustain the use of an innovation – such as a staffing and quality online resource aimed at home managers.
Concluding remarks
The logic model explains empirically and theoretically what works, why and how, as well as the interactions between the constituent parts (structure, processes and outcomes) that we consider important for the staffing–quality relationship. Understanding how to meet the needs and preferences of residents in care homes efficiently (given rising costs and demand) and how to use the workforce resources in care homes to promote quality and effective working is a societal priority. Our study makes a novel and important contribution to understanding the relationship between staffing and quality in the UK (and international) care home context.
Implications for social care
-
Understanding that numbers of staff alone are a necessary but not sufficient condition for care home quality.
-
Quality improves in homes when more care is provided by RNs.
-
Simply introducing ‘more’ staff (particularly RNs) is unlikely to be a cost-effective way of reducing adverse incidents in care homes.
-
Quality relies on the who, what and how of staffing arrangements and organisation of work.
-
Leadership is key, influencing how organisational resources are used to promote the environments and cultures needed for quality promoting relationships to flourish.
-
Realising and supporting the potential of the staffing resource (clinical, care, social and cultural skills and competence) is essential for quality. Opportunities for learning and development demonstrate an organisation values staff and may support staff retention.
-
A focus on the structures that support staffing consistency (stability, skill and competence) is important for influencing processes (the organisation of care and teamworking) and outcomes for residents and staff.
-
Developing transparent approaches that enable care home managers to effectively judge and make decisions about staffing levels is crucial for safe and appropriate care for residents.
-
Reciprocal relationships beyond the immediate care team, and including residents, their families and health and social care professionals, promote quality.
-
Leadership and management behaviours influence staff commitment and thus their contribution to quality.
-
A ‘visible’ unit supervisor and staff who ‘connect’ and influence the team are essential for quality and innovation in care homes.
Implications for research
Future research should:
-
Unpack the contribution of direct care support workforce (including CAs, senior CAs and nursing associates) working at different levels of skills and competence to care home quality.
-
Explore how training for CAs, senior CAs and nursing associates contributes to improving quality.
-
Consider differences for temporary (i.e. step-up or step-down care) versus permanent (i.e. long-term placement) care home residents.
-
Explore how resident population levels of dependency are related to quality.
-
Use innovative methods to capture quality in ways that recognise individual stakeholder views, values, expectations and preferences and address both quality of care and quality of life.
-
Develop robust social network interventions to change network structures to enhance reciprocity and advice and influence relationships to embed innovations for enhancing quality.
-
Consider machine learning methods for analysis of routine data because these methods are better able to identify non-linear relationships between staffing and care quality indicators than traditional regression analysis in order to better identify minimum adequate staffing levels.
-
Use methods to promote more accurate modelling of the staffing–quality relationship through data linkage.
-
Further test and develop our logic model.
Additional information
Acknowledgements
We acknowledge and thank members of our Study Steering Committee (SSC) for their guidance and wisdom throughout the study. Chaired by Professor Peter Griffiths, our SSC members included: Sharon Blackburn, Professor Kevin Brazil, Jean Christensen, Annie Dransfield, Professor Claire Goodman, Sally Gordon, Professor Martin Green, Ruth Holt, Cherelle Lyons, Trevor Murrells, Denise Nightingale, Michelle Platton, Professor Matt Sutton and Ian Turner.
We particularly thank residents, relatives and care home managers and RNs who willingly gave their time to our study advisory groups, providing critical comment and keeping the research team grounded in the everyday life for people living and working in care homes. We also thank the care home managers and teams who assisted in setting up the fieldwork sites originally planned for WP4 but abandoned due to COVID-19.
We thank many senior care home colleagues for discussions that informed our work but in particular the thoughtfulness and critique of Richard Adams, Liz Jones, Peter Hodkinson, Graeme Lee, Angela Randle, Anita Astle, Ros Heath, Margot Whitaker and Geoffrey Cox.
Finally, we acknowledge, with thanks, the contributions of the following colleagues and research staff: Suzanne Banks, Lyn Bulmer, Janet Dixson, Dorota Karasek, Michelle Ridge, Rosemary Roberts and Gabriela Seed for assistance with the finances and administration; support from colleagues at the Leeds Institute for Data Analytics; Kate Farley for supporting the application process; Claire Skinner, Rachel D’Souza, Jean Uniake and Ruchi Higham for assistance with ethics and governance approvals; and Anna Cronin de Chavez contributing to some data collection activities.
Contributions of authors
Karen Spilsbury (https://orcid.org/0000-0002-6908-0032) contributed to the design of the study and led WPs 1i, 1ii and 4. She authored Chapters 1, 2, 3 and 4 (reporting WP1i, 1ii and 4), 5 and 6, and prepared the Scientific summary. She coauthored methods and findings for other WPs in Chapters 3 and 4.
Andy Charlwood (https://orcid.org/0000-0002-5444-194X) contributed to the design of the study and led WPs2 and 3. He authored Chapters 3 and 4 (reporting WP2 and 3). He assisted with preparation of the final report, edited and reviewed other sections of the report for clarity and content.
Carl Thompson (https://orcid.org/0000-0002-9369-1204) contributed to the design of the study and led WP5. He authored Chapters 3 and 4 (reporting WP5) and prepared the Abstract and Plain English summary. He assisted with preparation of the final report, edited and reviewed the report for clarity and content.
Kirsty Haunch (https://orcid.org/0000-0002-5013-1258) was lead research fellow for WP1ii and WP4 and assisted with WP1i. She co-ordinated and facilitated the advisory groups, comprised of residents, relatives and care home managers and staff. She coauthored Chapters 3 and 4 (reporting WP1i, 1ii and 4). She reviewed other sections of the report for clarity and content.
Danat Valizade (https://orcid.org/0000-0003-3005-2277) contributed to the design of the study and was lead research fellow for WPs2 and 3. He coauthored Chapters 3 and 4 (reporting WP2 and 3). He reviewed other sections of the report for clarity and content.
Reena Devi (https://orcid.org/0000-0003-2834-8597) was lead research fellow for WP1i and assisted with WP4. She coauthored Chapters 3 and 4 (reporting WP1i, 1ii and 4). She assisted with preparation of the final report and reviewed other sections of the report for clarity and content.
Cornell Jackson (https://orcid.org/0000-0001-6185-7997) was lead research fellow for WP5. He coauthored Chapters 3 and 4 (reporting WP5). He reviewed other sections of the report for clarity and content.
David Phillip Alldred (https://orcid.org/0000-0002-2525-4854) contributed to the design of the study and edited and reviewed the final report for clarity and content.
Antony Arthur (https://orcid.org/0000-0001-8617-5714) contributed to the design of the study and edited and reviewed the final report for clarity and content.
Lucy Brown (https://orcid.org/0000-0002-3179-1293) contributed to the design of the study, facilitated WP3 and reviewed the final report for clarity and content.
Paul Edwards (https://orcid.org/0000-0002-4015-9943) contributed to the design of the study, facilitated WP3 and reviewed the final report for clarity and content.
Will Fenton (https://orcid.org/0000-0002-4852-6453) contributed to the design of the study, facilitated and contributed to WP2 and reviewed the final report for clarity and content.
Heather Gage (https://orcid.org/0000-0002-2049-9406) contributed to the design of the study, supervised cost–benefit analysis for WP2 and WP3 and reviewed the final report for clarity and content.
Matthew Glover (https://orcid.org/0000-0001-9454-2668) led the cost–benefit analysis for WP3 and reviewed the final report for clarity and content.
Barbara Hanratty (https://orcid.org/0000-0002-3122-7190) contributed to the design of the study and reviewed sections of the final report for clarity and content.
Julienne Meyer (https://orcid.org/0000-0001-5378-2761) contributed to the design of the study and edited and reviewed the final report for clarity and content.
Aileen Waton (https://orcid.org/0000-0002-6148-9802) facilitated WP3 and reviewed the final report for clarity and content.
Disclosure of interests
Full disclosure of interests: Completed ICMJE forms for all authors, including all related interests, are available in the toolkit on the NIHR Journals Library report publication page at https://doi.org/10.3310/GWTT8143.
Primary conflicts of interest: Karen Spilsbury is part funded by the National Institute for Health and Care Research (NIHR) Applied Research Collaboration Yorkshire and Humber. She was a member of the NIHR Health and Social Care Delivery Research (HSDR) Funding Committee (2014–8). Carl Thompson was a member of the NIHR HSDR Funding Committee (2019–22). David Phillip Alldred is part funded by the NIHR Yorkshire and Humber Patient Safety Translational Research Centre. Antony Arthur was a member of the NIHR Health and Social Care Delivery Research (HSDR) Funding Committee (2014–6). Heather Gage is part funded by the National Institute for Health and Care Research Applied Research Collaboration Kent, Surrey and Sussex. Barbara Hanratty is part funded by the National Institute for Health and Care Research Applied Research Collaboration North East and North Cumbria and is Deputy Director of the National Institute for Health and Care Research Older People and Frailty Policy Research Unit. Kirsty Haunch is a current member of the NIHR Health Technology Assessment Prioritisation Committee A (Out of hospital) March 2022–3. Aileen Waton is Company Director with Bupa UK and Executive Director with Scottish Care. All data requests should be submitted to the corresponding author for consideration. Commercially sensitive data provided for the study by the care home organisation cannot be shared.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Commercially sensitive data provided for the study by the care home organisation cannot be shared.
Ethics statement
WP2 and WP3 were approved (2 August 2017) by the Social Care Research Ethics Committee (17/WM/0232). WP5 was approved (21 June 2019) by the University of Leeds, Faculty of Medicine and Health, Ethics and Governance Committee (HREC 18-028).
Department of Health and Social Care disclaimer
This publication presents independent research commissioned by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by the interviewees in this publication are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, MRC, NIHR Coordinating Centre, the HSDR programme or the Department of Health and Social Care.
This monograph was published based on current knowledge at the time and date of publication. NIHR is committed to being inclusive and will continually monitor best practice and guidance in relation to terminology and language to ensure that we remain relevant to our stakeholders.
Disclaimers
This manuscript presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care.
References
- Buisson LW. Care of Older People: UK Market Report 26th Edition 2013 2014 2014.
- Alzheimer’s Society . Facts for the Media n.d. www.alzheimers.org.uk/about-us/news-and-media/facts-media (accessed 14 April 2022).
- Gordon AL, Franklin M, Bradshaw L, Logan P, Elliott R, Gladman JR. Health status of UK care home residents: a cohort study. Age Ageing 2014;43:97-103.
- British Geriatrics Society . Quest for Quality: British Geriatrics Society Joint Working Party Inquiry into the Quality of Healthcare Support for Older People in Care Homes: A Call for Leadership, Partnership and Quality Improvement 2011.
- Lievesley N, Crosby G, Bowman C. The Changing Role of Care Homes. London: BUPA and Centre for Policy on Ageing; 2011.
- British Geriatrics Society . BGS Commissioning Guidance – High Quality Healthcare for Older Care Home Residents n.d. www.bapen.org.uk/images/pdfs/news/bgs-commissioning-guidance.pdf (accessed 14 April 2022).
- Office for National Statistics . Changes in the Older Resident Care Home Population Between 2001 and 2011 2014.
- Moore A. The care homes with the full care spectrum. Health Serv J 2013. www.hsj.co.uk/supplement-archive/the-care-homes-with-the-full-care-spectrum/5059974.article (accessed 16 January 2024).
- Hanratty B, Lowson E, Grande G, Payne S, Addington-Hall J, Valtorta N, et al. Transitions at the end of life for older adults – patient, carer and professional perspectives: a mixed-methods study. Health Serv Deliv Res 2014;2:1-102.
- Goodman C, Froggatt K, Amador S, Mathie E, Mayrhofer A. End of life care interventions for people with dementia in care homes: addressing uncertainty within a framework for service delivery and evaluation. BMC Palliat Care 2015;14:1-9.
- Laing W. Calculating a Fair Market Price for Care. A Toolkit for Residential and Nursing Homes. London: Laing & Buisson; 2008.
- Care Quality Commission . The State of Health Care and Adult Social Care in England 2013 14 2014. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/364440/CQC_StateOfSocial_2014.pdf (accessed 14 April 2022).
- Skills for Care . The State of the Adult Social Care Sector and Workforce in England 2015.
- Skills for Care . The State of the Adult Social Care Sector and Workforce in England 2021 2021. www.skillsforcare.org.uk/adult-social-care-workforce-data-old/Workforce-intelligence/documents/State-of-the-adult-social-care-sector/The-State-of-the-Adult-Social-Care-Sector-and-Workforce-2021.pdf (accessed 14 April 2022).
- Goodman C, Davies SL, Gordon AL, Dening T, Gage H, Meyer J, et al. Optimal NHS service delivery to care homes: a realist evaluation of the features and mechanisms that support effective working for the continuing care of older people in residential settings. Health Serv Deliv Res 2017;5:1-204.
- Towers AM, Smith N, Allan S, Vadean F, Collins G, Rand S, et al. Care home residents’ quality of life and its association with CQC ratings and workforce issues: the MiCareHQ mixed-methods study. Health Serv Deliv Res 2021;9:1-188.
- Spilsbury K, Hewitt C, Stirk L, Bowman C. The relationship between nurse staffing and quality of care in nursing homes: a systematic review. Int J Nurs Stud 2011;48:732-50.
- Rochira S. A Place to Call Home?: A Review Into the Quality of Life and Care of Older People Living in Care Homes in Wales: Older People’s Commissioner for Wales 2014. www.olderpeoplewales.com/Libraries/Uploads/A_Place_to_Call_Home_-_A_Review_into_the_Quality_of_Life_and_Care_of_Older_People_living_in_Care_Homes_in_Wales.sflb.ashx (accessed 14 April 2022).
- Department of Health and Social Care . People at the Heart of Care: Adult Social Care Reform 2022. www.gov.uk/government/publications/people-at-the-heart-of-care-adult-social-care-reform-white-paper/people-at-the-heart-of-care-adult-social-care-reform (accessed 14 April 2022).
- Competition and Markets Authority . Care Homes Market Study: Summary of Final Report 2017. www.gov.uk/government/publications/care-homes-market-study-summary-of-final-report/care-homes-market-study-summary-of-final-report (accessed 14 April 2022).
- Care Quality Commission . The State of Health Care and Adult Social Care in England 2018 19 2019. www.cqc.org.uk/sites/default/files/20191015b_stateofcare1819_fullreport.pdf (accessed 14 April 2022).
- Care Quality Commission . The State of Health Care and Adult Social Care in England 2020 21 2021. www.cqc.org.uk/sites/default/files/20211021_stateofcare2021_print.pdf (accessed 14 April 2022).
- Care Quality Commission . Briefing for Providers: Nursing Associates 2019. www.cqc.org.uk/sites/default/files/20190123_briefing_for_providers_nursing_associates_0.pdf (accessed 14 April 2022).
- Care Quality Commission . How CQC Monitors, Inspects and Regulates Adult Social Care Services 2021. www.cqc.org.uk/sites/default/files/How_CQC_regulates_adult_social_care_November_2021.pdf (accessed 14 April 2022).
- Chou SC, Boldy DP, Lee AH. Factors influencing residents’ satisfaction in residential aged care. Gerontologist 2003;43:459-72.
- Lucas JA, Levin CA, Lowe TJ, Robertson B, Akincigil A, Sambamoorthi U, et al. The relationship between organizational factors and resident satisfaction with nursing home care and life. J Aging Soci Policy 2007;19:125-51.
- Backhaus R, Verbeek H, van Rossum E, Capezuti E, Hamers JPH. Nurse staffing impact on quality of care in nursing homes: a systematic review of longitudinal studies. J Am Med Dir Assoc 2014;15:383-93.
- Clemens S, Wodchis W, McGilton K, McGrail K, McMahon M. The relationship between quality and staffing in long-term care: a systematic review of the literature 2008–2020. Int J Nurs Stud 2021;122.
- Allan S, Vadean F. The association between staff retention and English care home quality. J Aging Soci Policy 2021;33:708-24.
- Netten A, Williams J, Darton R. Care-home closures in England: causes and implications. Ageing Soc 2005;25:319-38.
- Donabedian A. Evaluating the quality of medical care. Milbank Q 2005;83:691-729.
- Spilsbury K, Devi R, Haunch K, Dalton S, Thompson C, Alldred D, et al. A Systematic Review of Care Home Staff Perceptions of Their Roles and Responsibilities to Enhance Quality in Care Homes for Older People 2021. www.crd.york.ac.uk/prospero/display_record.php?RecordID=241066 (accessed 14 April 2022).
- Hong QN, Fàbregues S, Bartlett G, Boardman F, Cargo M, Dagenais P, et al. The Mixed Methods Appraisal Tool (MMAT) version 2018 for information professionals and researchers. Educ Inf 2018;34:285-91.
- Erlingsson C, Brysiewicz P. A hands-on guide to doing content analysis. Afr J Emerg Med 2017;7:93-9.
- Pawson R, Greenhalgh T, Harvey G, Walshe K. Realist review – a new method of systematic review designed for complex policy interventions. J Health Serv Res Policy 2005;10:21-34. https://doi.org/10.1258/1355819054308530.
- Wong G, Westhorp G, Manzano A, Greenhalgh J, Jagosh J, Greenhalgh T. RAMESES II reporting standards for realist evaluations. BMC Med 2016;14. https://doi.org/10.1186/s12916-016-0643-1.
- Davidoff F, Dixon-Woods M, Leviton L, Michie S. Demystifying theory and its use in improvement. BMJ Qual Saf 2015;24:228-38.
- Pawson R, Tilley N. Realistic Evaluation. London: SAGE Publications Ltd; 1997.
- Haunch K, Thompson C, Arthur A, Edwards P, Goodman C, Hanratty B, et al. Understanding the staff behaviours that promote quality for older people living in long term care facilities: a realist review. Int J Nurs Stud 2021;117.
- Pawson R, Greenhalgh T, Harvey G, Walshe K. Realist Synthesis: An Introduction. Manchester: University of Manchester; 2004.
- Pearson M, Brand SL, Quinn C, Shaw J, Maguire M, Michie S. Using realist review to inform intervention development: methodological illustration and conceptual platform for collaborative care in offender mental health. Implement Sci 2015;10:134-34. https://doi.org/10.1186/s13012-015-0321-2.
- Madden C, Clayton M, Canary HE, Towsley G, Cloyes K, Lund D. Rules of performance in the nursing home: a grounded theory of nurse–CNA communication. Geriatr Nurs 2017;38:378-84. https://doi.org/10.1016/j.gerinurse.2016.12.013.
- Bishop CE, Weinberg DB, Leutz W, Dossa A, Pfefferle SG, Zincavage RM. Nursing assistants’ job commitment: effect of nursing home organizational factors and impact on resident well-being. Gerontologist 2008;48:36-45.
- Ericson-Lidman E, Larsson LL, Norberg A. Caring for people with dementia disease (DD) and working in a private not-for-profit residential care facility for people with DD. Scand J Caring Sci 2014;28:337-46. https://doi.org/10.1111/scs.12063.
- Eldh AC, van der Zijpp T, McMullan C, McCormack B, Seers K, Rycroft-Malone J. ‘I have the world’s best job’ – staff experience of the advantages of caring for older people. Scand J Caring Sci 2016;30:365-73. https://doi.org/10.1111/scs.12256.
- Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci 2011;6:42-. https://doi.org/10.1186/1748-5908-6-42.
- Goodman C, Dening T, Gordon AL, Davies SL, Meyer J, Martin FC, et al. Effective health care for older people living and dying in care homes: a realist review. BMC Health Serv Res 2016;16. https://doi.org/10.1186/s12913-016-1493-4.
- Wong G, Pawson R, Owen L. Policy guidance on threats to legislative interventions in public health: a realist synthesis. BMC Public Health 2011;11:222-22. https://doi.org/10.1186/1471-2458-11-222.
- Care Quality Commission . Key Lines of Enquiry, Prompts and Ratings Characteristics for Healthcare Services 2018. www.cqc.org.uk/sites/default/files/20180628%20Healthcare%20services%20KLOEs%20prompts%20and%20characteristics%20FINAL.pdf (accessed 14 April 2022).
- Spilsbury K, Hewitt C, Stirk L, Bowman C. The relationship between nurse staffing and quality of care in nursing homes: a systematic review. Int J Nurs Stud 2011;48:732-50. https://doi.org/10.1016/j.ijnurstu.2011.02.014.
- Backhaus R, van Rossum E, Capezuti E, Hamers JP. Nurse staffing impact on quality of care in nursing homes: a systematic review of longitudinal studies. J Am Med Dir Assoc 2014;15.
- Skills for Care . Drawing Conclusions about All CQC Regulated Providers Based on a Sample from the NMDS-SC. Strategic Workforce Intelligence Group Methodology Discussion Paper. Personal Correspondence Skills for Care 2014.
- Rosenberg JM, Beymer PN, Anderson DJ, van Lissa CJ, Schmidt JA. tidyLPA: an R package to easily carry out Latent Profile Analysis (LPA) using open-source or commercial software. J Open Source Softw 2019;3.
- De Boeck P, Bakker M, Zwitser R, . The estimation of item response models with the lmer function from the lme4 package in R. J Stat Softw 2011;39:1-28.
- Cloitre M, Garvert DW, Weiss B, Carlson EB, Bryant RA. Distinguishing PTSD, complex PTSD, and borderline personality disorder: a latent class analysis. Eur J Psychotraumatol 2014;5.
- Legislation Gov UK . Care Act 2014 2014. www.legislation.gov.uk/ukpga/2014/23/contents/enacted (accessed 14 April 2022).
- Breiman L. Statistical modeling: the two cultures (with comments and a rejoinder by the author). Stat Sci 2001;16:199-231, 33.
- Davies SL, Goodman C, Bunn F, Victor C, Dickinson A, Iliffe S, et al. A systematic review of integrated working between care homes and health care services. BMC Health Serv Res 2011;11:1-21.
- Forder JE, Allan S. Competition in the Care Homes Market. A Report for the OHE Commission. Kent: University of Kent; 2011.
- Iliffe S, Davies SL, Gordon AL, Schneider J, Dening T, Bowman C, et al. Provision of NHS generalist and specialist services to care homes in England: review of surveys. Primary Health Care Res Dev 2016;17:122-37.
- Steventon A, Roberts A. Estimating length of stay in publicly-funded residential and nursing care homes: a retrospective analysis using linked administrative data sets. BMC Health Serv Res 2012;12:1-8.
- Curtis LA, Amanda B. Unit Costs of Health & Social Care 2020 2020. https://doi.org/10.22024/UniKent%2F01.02.84818.
- Patel K, Jay R, Shahzad MW, Green W, Patel R. A systematic review of approaches for calculating the cost of medication errors. Eur J Hosp Pharm 2016;23:294-301.
- Walsh EK, Hansen CR, Sahm LJ, Kearney PM, Doherty E, Bradley CP. Economic impact of medication error: a systematic review. Pharmacoepidemiol Drug Saf 2017;26:481-97.
- Dreischulte T, Grant A, Donnan P, McCowan C, Davey P, Petrie D, et al. A cluster randomised stepped wedge trial to evaluate the effectiveness of a multifaceted information technology-based intervention in reducing high-risk prescribing of non-steroidal anti-inflammatory drugs and antiplatelets in primary medical care: the DQIP study protocol. Implement Sci 2012;7:1-13.
- Avery AJ, Rodgers S, Cantrill JA, Armstrong S, Cresswell K, Eden M, et al. A pharmacist-led information technology intervention for medication errors (PINCER): a multicentre, cluster randomised, controlled trial and cost-effectiveness analysis. Lancet 2012;379:1310-9.
- Elliott RA, Putman KD, Franklin M, Annemans L, Verhaeghe N, Eden M, et al. Cost effectiveness of a pharmacist-led information technology intervention for reducing rates of clinically important errors in medicines management in general practices (PINCER). PharmacoEconomics 2014;32:573-90.
- Parekh N, Ali K, Stevenson JM, Davies JG, Schiff R, Van der Cammen T, et al. PRIME study group . Incidence and cost of medication harm in older adults following hospital discharge: a multicentre prospective study in the UK. Br J Clin Pharmacol 2018;84:1789-97.
- Bradley MC, Fahey T, Cahir C, Bennett K, O’Reilly D, Parsons C, et al. Potentially inappropriate prescribing and cost outcomes for older people: a cross-sectional study using the Northern Ireland Enhanced Prescribing Database. Eur J Clin Pharmacol 2012;68:1425-33.
- Elliott RA, Camacho E, Jankovic D, Sculpher MJ, Faria R. Economic analysis of the prevalence and clinical and economic burden of medication error in England. BMJ Qual Saf 2021;30:96-105.
- Franklin M, Hunter RM. A modelling-based economic evaluation of primary-care-based fall-risk screening followed by fall-prevention intervention: a cohort-based Markov model stratified by older age groups. Age Ageing 2020;49:57-66.
- Jenkyn KB, Hoch JS, Speechley M. How much are we willing to pay to prevent a fall? Cost-effectiveness of a multifactorial falls prevention program for community-dwelling older adults. Can J Aging 2012;31:121-37.
- Kunigkeit C, Stock S, Müller D. Cost-effectiveness of a home safety intervention to prevent falls in impaired elderly people living in the community. Arch Osteoporos 2018;13:1-10.
- McLean K, Day L, Dalton A. Economic evaluation of a group-based exercise program for falls prevention among the older community-dwelling population. BMC Geriatr 2015;15:1-11.
- Sach TH, Logan PA, Coupland CA, Gladman JRF, Sahota O, Stoner-Hobbs V, et al. Community falls prevention for people who call an emergency ambulance after a fall: an economic evaluation alongside a randomised controlled trial. Age Ageing 2012;41:635-41.
- Snooks HA, Anthony R, Chatters R, Dale J, Fothergill R, Gaze S, et al. Support and Assessment for Fall Emergency Referrals (SAFER) 2: a cluster randomised trial and systematic review of clinical effectiveness and cost-effectiveness of new protocols for emergency ambulance paramedics to assess older people following a fall with referral to community-based care when appropriate. Health Technol Assess 2017;21:1-218.
- Craig J, Murray A, Mitchell S, Clark S, Saunders L, Burleigh L. The high cost to health and social care of managing falls in older adults living in the community in Scotland. Scott Med J 2013;58:198-203.
- Tian Y, Thompson J, Buck D. The cost of falls: exploring the cost of the whole system pathway for older people in a rural community in England. J Integr Care 2014;22:165-73.
- National Institute for Health and Care Excellence (NICE) . Falls Assessment and Prevention of Falls in Older People 2013. www.nice.org.uk/guidance/cg161/evidence/falls-full-guidance-190033741 (accessed 14 April 2022).
- Compston J, Cooper A, Cooper C, Cooper C, Edwards J, Gittoes NJL. UK clinical guideline for the prevention and treatment of osteoporosis. Arch Osteoporos 2017;12:1-24.
- Kilonzo M, Vale L, Pickard R, Lam T, N’Dow J. Catheter Trial Group . Cost effectiveness of antimicrobial catheters for adults requiring short-term catheterisation in hospital. Eur Urol 2014;66:615-8.
- Pickard R, Lam T, Maclennan G, . Types of urethral catheter for reducing symptomatic urinary tract infections in hospitalised adults requiring short-term catheterisation: multicentre randomised controlled trial and economic evaluation of antimicrobial-and antiseptic-impregnated urethral catheters (the CATHETER trial). Health Technol Assess 2012;16. https://doi.org/10.3310/hta16470.
- Smith DR, Pouwels KB, Hopkins S, Naylor NR, Smieszek T, Robotham JV. Epidemiology and health-economic burden of urinary-catheter-associated infection in English NHS hospitals: a probabilistic modelling study. J Hosp Infect 2019;103:44-5.
- Lean K, Nawaz RF, Jawad S, Vincent C. Reducing urinary tract infections in care homes by improving hydration. BMJ Open Qual 2019;8.
- Ahmed H, Farewell D, Jones HM, Francis NA, Paranjothy S, Butler CC. Incidence and antibiotic prescribing for clinically diagnosed urinary tract infection in older adults in UK primary care, 2004–2014. PLOS ONE 2018;13.
- NHS Digital . Hospital Admitted Patient Care Activity 2019–20 2020.
- Office for National Statistics . Population Estimates for the UK, England and Wales, Scotland and Northern Ireland: Mid-2020 2021. www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/bulletins/annualmidyearpopulationestimates/mid2020/previous/v1/pdf (accessed 14 April 2022).
- NHS England . 2018/19/National/Cost/Collection/Data/Publication 2019. www.england.nhs.uk/publication/2018-19-national-cost-collection-data-publication/ (accessed 14 April 2022).
- Bowen GA. Document analysis as a qualitative research method. Qual Res J 2009;9:27-40.
- Rapley T. Doing Conversation, Discourse and Document Analysis. Thousand Oaks, CA: SAGE Publications Ltd; 2007.
- Care Quality Commission . Inspection Reports n.d. www.cqc.org.uk/what-we-do/how-we-do-our-job/inspection-reports (accessed 14 April 2022).
- Bryman A. Social Research Methods. Oxford: Oxford University Press; 2016.
- Teddlie C, Tashakkori A. Mixed Methods Research. The Sage Handbook of Qualitative Research 2011;4:285-300.
- Finch T, Girling M, May C, . NoMAD: implementation measure based on normalization process theory. [Measurment instrument] 2015. http://www.normalizationprocess.org (accessed 16 January 2024).
- Lazega E. The Collegial Phenomenon: The Social Mechanisms of Cooperation Among Peers in a Corporate Law Partnership. Oxford: Oxford University Press; 2001.
- May C, Finch T, Mair F, Ballini L, Dowrick C, Eccles M, et al. Understanding the implementation of complex interventions in health care: the normalization process model. BMC Health Serv Res 2007;7:1-7.
- Toolkit N. NPT Toolkit Website 2020. www.normalizationprocess.org/nomad-study/ (accessed 14 April 2022).
- Rogers E. Diffusion of Innovations. New York: Free Press; 2003.
- Borgatti SP, Everett MG, Freeman LC. UCINET 6 for Windows: Software for Social Network Analysis. Harvard, MA: Analytic Technologies; 2002.
- Abrahamson K, Fox R, Roundtree A, Farris K. Nursing assistants’ perceptions of their role in the resident experience. Nurs Health Sci 2020;22:72-81.
- Chung G. Nursing assistant beliefs about their roles and nursing home residents: implications for nursing home social work practice. Soc Work Health Care 2010;49:718-33.
- Halifax E, Miaskowski C, Wallhagen M. Certified nursing assistants’ understanding of nursing home residents’ pain. J Gerontol Nurs 2018;44:29-36.
- Kusmaul N, Bunting M. Perspectives on caregiving: a qualitative evaluation of certified nursing assistants. Geriatr Nurs 2017;38:146-51.
- Medvene LJ, Lann-Wolcott H. An exploratory study of nurse aides’ communication behaviours: giving ‘positive regard’ as a strategy’. Int J Older People Nurs 2010;5:41-50.
- Mueller C, Anderson RA, McConnell ES, Corazzini K. Licensed nurse responsibilities in nursing homes: a scope-of-practice issue. J Nurs Regul 2012;3:13-20.
- Vogelsmeier AA, Scott-Cawiezell JR, Pepper GA. Medication reconciliation in nursing homes: thematic differences between RN and LPN staff. J Gerontol Nurs 2011;37:56-63.
- Vogelsmeier A. Identifying medication order discrepancies during medication reconciliation: perceptions of nursing home leaders and staff. J Nurs Manag 2014;22:362-72.
- Andersen EA, Spiers J. Care aides’ relational practices and caring contributions. J Gerontol Nurs 2016;42:24-30.
- Banerjee A, Armstrong P, Daly T, Armstrong H, Braedley S. ‘Careworkers don’t have a voice:’ epistemological violence in residential care for older people. J Aging Stud 2015;33:28-36. https://doi.org/10.1016/j.jaging.2015.02.005.
- Ellis W, Kaasalainen S, Baxter P, . Discourse/discours-medication management for nurses working in long-term care. Can J Nurs Res Arch 2012;44:128-49.
- Knopp‐Sihota JA, Niehaus L, Squires JE, Norton PG, Estabrooks CA. Factors associated with rushed and missed resident care in western Canadian nursing homes: a cross-sectional survey of health care aides. J Clin Nurs 2015;24:2815-25.
- Marshall EG, Power M, Edgecombe N, Andrew MK. Above and beyond: a qualitative study of the work of nurses and care assistants in long term care. Work 2020;65:509-16.
- Gransjön Craftman A, Grape C, Ringnell K, Westerbotn M. Registered nurses’ experience of delegating the administration of medicine to unlicensed personnel in residential care homes. J Clin Nurs 2016;25:3189-98.
- Forss KS, Nilsson J, Borglin G. Registered nurses’ and older people’s experiences of participation in nutritional care in nursing homes: a descriptive qualitative study. BMC Nurs 2018;17:1-13.
- Johansson-Pajala RM, Jorsäter Blomgren K, Bastholm-Rahmner P, Fastbom J, Martin L. Nurses in municipal care of the elderly act as pharmacovigilant intermediaries: a qualitative study of medication management. Scand J Prim Health Care 2016;34:37-45.
- Olsson IN, Wätterbjörk I, Blomberg K. Registered nurses’ perception of their professional role regarding medication management in nursing care of the elderly. J Nurs Educ Pract 2014;4.
- Backhaus R, Verbeek H, van Rossum E, Capezuti E, Hamers JPH. Baccalaureate-educated registered nurses in nursing homes: experiences and opinions of administrators and nursing staff. J Adv Nurs 2018;74:75-88.
- Kuk NO, den Ouden M, Zijlstra GA, Hamers JPH, Kempen GIJM, Bours GJJW. Do nursing staff encourage functional activity among nursing home residents? A cross-sectional study of nursing staff perceived behaviors and associated factors. BMC Geriatr 2017;17:1-10.
- Heath H. Outcomes from the work of registered nurses working with older people in UK care homes. Int J Older People Nurs 2010;5:116-27.
- Talbot R, Brewer G. Care assistant experiences of dementia care in long-term nursing and residential care environments. Dementia 2016;15:1737-54.
- Vandrevala T, Chrysanthaki T, Ogundipe E. ‘Behind closed doors with open minds?’: a qualitative study exploring nursing home staff’s narratives towards their roles and duties within the context of sexuality in dementia. Int J Nurs Stud 2017;74:112-9.
- Bedin MG, Droz-Mendelzweig M, Chappuis M. Caring for elders: the role of registered nurses in nursing homes. Nurs Inq 2013;20:111-20.
- Odberg KR, Hansen BS, Wangensteen S. Medication administration in nursing homes: a qualitative study of the nurse role. Nurs Open 2019;6:384-92.
- O’Doherty E. Nurses’ role in care home rehabilitation. Nurs Times 2013;109:18-21.
- Cho E, Kim HJ, Chang SJ, Kim H, Kim J. Exploring nurses’ perceptions of nursing home care in South Korea: a qualitative study. J Korean Gerontol Nurs 2020;22:85-94.
- Park MS, Lim SY, Kim EY, Lee SJ, Chang SO. Examining practical nursing experiences to discover ways in which to retain and invigorate the remaining functions of the elderly with a demented and complex disability in nursing homes. Jpn J Nurs Sci 2018;15:77-90.
- Sun-Young L, Chang SO. The conceptual structure of the management by nurses of the ego integrity of residents of nursing homes. J Nurs Res 2020;28.
- Liu JY. Exploring nursing assistants’ roles in the process of pain management for cognitively impaired nursing home residents: a qualitative study. J Adv Nurs 2014;70:1065-77.
- Lung CC, Liu JYW. How the perspectives of nursing assistants and frail elderly residents on their daily interaction in nursing homes affect their interaction: a qualitative study. BMC Geriatr 2016;16. https://doi.org/10.1186/s12877-016-0186-5.
- Yektatalab S, Kaveh M, Sharif F, Khoshknab MF, Petramfar P. Characteristics of care and caregivers of Alzheimer’s patients in elderly care homes: a qualitative research. Iran Red Crescent Med J 2012;14.
- Ellis JM, Rawson H. Nurses’ and personal care assistants’ role in improving the relocation of older people into nursing homes. J Clin Nurs 2015;24:2005-13.
- Hunter S, Levett-Jones T. The practice of nurses working with older people in long term care: an Australian perspective. J Clin Nurs 2010;19:527-36.
- Laging B, Kenny A, Bauer M, Nay R. Recognition and assessment of resident’ deterioration in the nursing home setting: a critical ethnography. J Clin Nurs 2018;27:1452-63.
- Ostaszkiewicz J, O’Connell B, Dunning T. ‘We just do the dirty work’: dealing with incontinence, courtesy stigma and the low occupational status of carework in long-term aged care facilities. J Clin Nurs 2016;25:2528-41.
- Daly T, Szebehely M. Unheard voices, unmapped terrain: care work in long-term residential care for older people in Canada and Sweden. Int J Soc Welf 2012;21:139-48.
- Abbott KM, Heid AR, Van Haitsma K. ‘We can’t provide season tickets to the opera’: Staff perceptions of providing preference-based person centered care. Clin Gerontol 2016;39:190-209.
- NHS England . House of Care – A Framework for Long Term Condition Care 2019. tinyurl.com/NHSE-houseofcare (accessed 30 March 2020).
- Lung CC, Liu JYW. How the perspectives of nursing assistants and frail elderly residents on their daily interaction in nursing homes affect their interaction: a qualitative study. BMC Geriatr 2016;16:1-14.
- Forbes-Thompson S, Leiker T, Bleich MR. High-performing and low-performing nursing homes: a view from complexity science. Health Care Manage Rev 2007;32:341-51.
- Cohen-Mansfield J, Parpura-Gill A. Practice style in the nursing home: dimensions for assessment and quality improvement. Int J Geriatr Psychiatry 2008;23:376-86.
- Gittell JH, Weinberg D, Pfefferle S, Bishop C. Impact of relational coordination on job satisfaction and quality outcomes: a study of nursing homes. Hum Resour Manag J 2008;18:154-70.
- Andre B, Sjovold E, Rannestad T, Ringdal GI. The impact of work culture on quality of care in nursing homes – a review study. Scand J Caring Sci 2014;28:449-57. https://doi.org/10.1111/scs.12086.
- Lyons SS. How do people make continence care happen? An analysis of organizational culture in two nursing homes. Gerontologist 2010;50:327-39. https://doi.org/10.1093/geront/gnp157.
- Bennett MK, Ward EC, Scarinci NA, Waite MC. Service providers’ perceptions of working in residential aged care: a qualitative cross-sectional analysis. Ageing Soc 2015;35:1989-2010.
- Edvardsson D, Fetherstonhaugh D, McAuliffe L, Nay R, Chenco C. Job satisfaction amongst aged care staff: exploring the influence of person-centered care provision. Int Psychogeriatr 2011;23:1205-12. https://doi.org/10.1017/S1041610211000159.
- Anderson RA, Toles MP, Corazzini K, McDaniel RR, Colón-Emeric C. Local interaction strategies and capacity for better care in nursing homes: a multiple case study. BMC Health Serv Res 2014;14. https://doi.org/10.1186/1472-6963-14-244.
- Casey D, Murphy K, Ni Leime A, Larkin P, Payne S, Froggatt KA, et al. Dying well: factors that influence the provision of good end-of-life care for older people in acute and long-stay care settings in Ireland. J Clin Nurs 2011;20:1824-33. https://doi.org/10.1111/j.1365-2702.2010.03628.x.
- Verbeek H, van Rossum E, Zwakhalen SM, Kempen GIJ, Hamers JP. Small, homelike care environments for older people with dementia: a literature review. Int Psychogeriatr 2009;21:252-64.
- Eika M, Dale B, Espnes GA, Hvalvik S. Nursing staff interactions during the older residents’ transition into long-term care facility in a nursing home in rural Norway: an ethnographic study. BMC Health Serv Res 2015;15. https://doi.org/10.1186/s12913-015-0818-z.
- Nakrem S. Understanding organizational and cultural premises for quality of care in nursing homes: an ethnographic study. BMC Health Serv Res 2015;15. https://doi.org/10.1186/s12913-015-1171-y.
- Rantz MJ, Hicks L, Grando V, Petroski GF, Madsen RW, Mehr DR, et al. Nursing home quality, cost, staffing, and staff mix. Gerontologist 2004;44:24-38.
- Vermeerbergen L, Van Hootegem G, Benders J. A comparison of working in small-scale and large-scale nursing homes: a systematic review of quantitative and qualitative evidence. Int J Nurs Stud 2017;67:59-70.
- Brown Wilson C. Developing community in care homes through a relationship-centred approach. Health Soc Care Community 2009;17:177-86.
- Watson J. Developing the Senses Framework to support relationship-centred care for people with advanced dementia until the end of life in care homes. Dementia 2019;18:545-66.
- Colomer J, de Vries J. Person-centred dementia care: a reality check in two nursing homes in Ireland. Dementia 2016;15:1158-70.
- Carpenter J, Thompson SA. CNAs’ experiences in the nursing home: ‘It’s in my soul’. J Gerontol Nurs 2008;34:25-32.
- Skovdahl K, Kihlgren AL, Kihlgren M. Different attitudes when handling aggressive behaviour in dementia – narratives from two caregiver groups. Aging Ment Health 2003;7:277-86.
- Vassbø TK, Kirkevold M, Edvardsson D, Sjögren K, Lood Q, Bergland A. The meaning of working in a person-centred way in nursing homes: a phenomenological-hermeneutical study. BMC Nurs 2019;18:1-8.
- Barry TT, Brannon D, Mor V. Nurse aide empowerment strategies and staff stability: effects on nursing home resident outcomes. Gerontologist 2005;45:309-17.
- Carryer J, Hansen CO, Blakey JA. Experiences of nursing in older care facilities in New Zealand. Aust Health Rev 2010;34:11-7. https://doi.org/10.1071/AH09679.
- Cherry B, Ashcraft A, Owen D. Perceptions of job satisfaction and the regulatory environment among nurse aides and charge nurses in long-term care. Geriatr Nurs 2007;28:183-92.
- Bourgeault IL, Atanackovic J, Rashid A, Parpia R. Relations between immigrant care workers and older persons in home and long-term care. Can J Aging 2010;29:109-18. https://doi.org/10.1017/S0714980809990407.
- Fläckman B, Hansebo G, Kihlgren A. Struggling to adapt: caring for older persons while under threat of organizational change and termination notice. Nurs Inq 2009;16:82-91. https://doi.org/10.1111/j.1440-1800.2009.00434.x.
- Adra MG, Hopton J, Keady J. Constructing the meaning of quality of life for residents in care homes in the Lebanon: perspectives of residents, staff and family. Int J Older People Nurs 2015;10:306-18. https://doi.org/10.1111/opn.12094.
- Fossey J, Garrod L, Tolbol Froiland C, Ballard C, Lawrence V, Testad I. What influences the sustainability of an effective psychosocial intervention for people with dementia living in care homes? A 9 to 12-month follow-up of the perceptions of staff in care homes involved in the WHELD randomised controlled trail. Int J Geriatr Psychiatry 2019;34:674-82.
- Hunt SR, Corazzini K, Anderson RA. Top nurse-management staffing collapse and care quality in nursing homes. J Appl Gerontol 2014;33:51-74. https://doi.org/10.1177/0733464812455096.
- Backhaus R, Beerens H, van Rossum E, Verbeek H, Hamers JPH. Rethinking the staff-quality relationship in nursing homes. J Nutr Health Aging 2018;22:634-38.
- Powell C, Blighe A, Froggatt K, McCormack B, Woodward-Carlton B, Young J, et al. Family involvement in timely detection of changes in health of nursing homes residents: a qualitative exploratory study. J Clin Nurs 2018;27:317-27.
- Karsh B, Booske BC, Sainfort F. Job and organizational determinants of nursing home employee commitment, job satisfaction and intent to turnover. Ergonomics 2005;48:1260-81.
- Kjøs BO, Botten G, Gjevjon ER, Romøren TI. Quality work in long-term care: the role of first-line leaders. Int J Qual Health Care 2010;22:351-7. https://doi.org/10.1093/intqhc/mzq035.
- McGilton KS, Boscart VM, Brown M, Bowers B. Making tradeoffs between the reasons to leave and reasons to stay employed in long-term care homes: perspectives of licensed nursing staff. Int J Nurs Stud 2014;51:917-26.
- Swagerty DL, Lee RH, Smith B, Taunton RL. The context for nursing home resident care: the role of leaders in developing strategies. J Gerontol Nurs 2005;31:40-8.
- Scalzi CC, Evans LK, Barstow A, Hostvedt K. Barriers and enablers to changing organizational culture in nursing homes. Nurs Adm Q 2006;30:368-72.
- Leedahl SN, Chapin RK, Little TD. Multilevel examination of facility characteristics, social integration, and health for older adults living in nursing homes. J Gerontol B Psychol Sci Soc Sci 2015;70:111-22.
- Mallidou AA, Cummings GG, Schalm C, Estabrooks CA. Health care aides use of time in a residential long-term care unit: a time and motion study. Int J Nurs Stud 2013;50:1229-39. https://doi.org/10.1016/j.ijnurstu.2012.12.009.
- Vandrevala T, Samsi K, Rose C, Adenrele C, Barnes C, Manthorpe J. Perceived needs for support among care home staff providing end of life care for people with dementia: a qualitative study. Int J Geriatr Psychiatry 2017;32:155-63.
- Kontos PC, Miller KL, Mitchell GJ. Neglecting the importance of the decision making and care regimes of personal support workers: a critique of standardization of care planning through the RAI/MDS. Gerontologist 2010;50:352-62.
- Jones C, Moyle W. Staff perspectives of relationships in aged care: a qualitative approach. Australas J Ageing 2016;35:198-203.
- Puurveen G, Baumbusch J, Gandhi P. From family involvement to family inclusion in nursing home settings: a critical interpretive synthesis. J Fam Nurs 2018;24:60-85.
- Chenoweth L, Jeon YH, Stein-Parbury J, Forbes I, Fleming R, Cook J, et al. PerCEN trial participant perspectives on the implementation and outcomes of person-centered dementia care and environments. Int Psychogeriatr 2015;27:2045-57. https://doi.org/10.1017/S1041610215001350.
- Backhaus R, Hoek L, Van Haastregt J, Verbeek H, De Vries E, Hamers J. Increasing family inclusion in nursing homes for people with dementia: a literature review. Innov Aging 2018;2:537-.
- Irving J. Beyond family satisfaction: family-perceived involvement in residential care. Australas J Ageing 2015;34:166-70.
- Gjerberg E, Førde R, Pedersen R, Bollig G. Ethical challenges in the provision of end-of-life care in Norwegian nursing homes. Soc Sci Med 2010;71:677-84. https://doi.org/10.1016/j.socscimed.2010.03.059.
- Bauer M, Fetherstonhaugh D, Tarzia L, Chenco C. Staff–family relationships in residential aged care facilities: the views of residents’ family members and care staff. J Appl Gerontol 2014;33:564-85.
- Tjia J, Lemay CA, Bonner A, Compher C, Paice K, Field T, et al. Informed family member involvement to improve the quality of dementia care in nursing homes. J Am Geriatr Soc 2017;65:59-65.
- Forbes-Thompson S, Leiker T, Bleich MR. High-performing and low-performing nursing homes: a view from complexity science. Health Care Manage Rev 2007;32:341-51.
- Scott-Cawiezell J, Main DS, Vojir CP, Jones K, Moore L, Nutting PA, et al. Linking nursing home working conditions to organizational performance. Health Care Manage Rev 2005;30:372-80.
- Estabrooks CA, Morgan DG, Squires JE, Boström AM, Slaughter SE, Cummings GG, et al. The care unit in nursing home research: evidence in support of a definition. BMC Med Res Methodol 2011;11. https://doi.org/10.1186/1471-2288-11-46.
- Kuo HT, Yin TJC, Li IC. Relationship between organizational empowerment and job satisfaction perceived by nursing assistants at long-term care facilities. J Clin Nurs 2008;17:3059-66.
- Jack K, Tetley J, Chambers A. The education of nurses working in care homes for older people: an appreciative inquiry. Int J Older People Nurs 2019;14.
- Rapaport P, Livingston G, Murray J, Mulla A, Cooper C. Systematic review of the effective components of psychosocial interventions delivered by care home staff to people with dementia. BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2016-014177.
- Zeller A, Müller M, Needham I, Dassen T, Kok G, Halfens RJ. Dealing with aggressive behaviour in nursing homes: caregivers’ use of recommended measures. J Clin Nurs 2014;23:2542-53.
- Gillham D, De Bellis A, Xiao L, Willis E, Harrington A, Morey W, et al. Using research evidence to inform staff learning needs in cross-cultural communication in aged care homes. Nurse Educ Today 2018;63:18-23. https://doi.org/10.1016/j.nedt.2018.01.007.
- Yeatts DE, Cready CM. Consequences of empowered CNA teams in nursing home settings: a longitudinal assessment. Gerontologist 2007;47:323-39.
- Cammer A, Morgan D, Stewart N, McGilton K, Rycroft-Malone J, Dopson S, et al. The hidden complexity of long-term care: how context mediates knowledge translation and use of best practices. Gerontologist 2014;54:1013-23.
- Rokstad AM, Vatne S, Engedal K, Selbæk G. The role of leadership in the implementation of person-centred care using Dementia Care Mapping: a study in three nursing homes. J Nurs Manag 2015;23:15-26.
- Chenoweth L, Forbes I, Fleming R, King MT, Stein-Parbury J, Luscombe G, et al. PerCEN: a cluster randomized controlled trial of person-centered residential care and environment for people with dementia. Int Psychogeriatr 2014;26:1147-60.
- Tong M, Schwendimann R, Zúñiga F. Mobbing among care workers in nursing homes: a cross-sectional secondary analysis of the Swiss Nursing Homes Human Resources Project. Int J Nurs Stud 2017;66:72-81.
- Jacobsen FF, Day S, Laxer K, Lloyd L, Goldmann M, Szhebehely M. Job autonomy of long-term residential care assistive personnel: a six country comparison. Ageing Int 2018;43:4-19.
- Caspar S, O’Rourke N. The influence of care provider access to structural empowerment on individualized care in long-term-care facilities. J Gerontol B Psychol Sci Soc Sci 2008;63:S255-65.
- Rondeau KV, Wagar TH. Nurse and resident satisfaction in magnet long-term care organizations: do high involvement approaches matter?. J Nurs Manag 2006;14:244-50.
- Cramer ME, High R, Culross B, Conley DM, Nayar P, Nguyen AT, et al. Retooling the RN workforce in long-term care: nursing certification as a pathway to quality improvement. Geriatr Nurs 2014;35:182-7. https://doi.org/10.1016/j.gerinurse.2014.01.001.
- Etherton-Beer C, Venturato L, Horner B. Organisational culture in residential aged care facilities: a cross-sectional observational study. PLOS ONE 2013;8. https://doi.org/10.1371/journal.pone.0058002.
- Hafford-Letchfield T, Simpson P, Willis PB, Almack K. Developing inclusive residential care for older lesbian, gay, bisexual and trans (LGBT) people: an evaluation of the Care Home Challenge action research project. Health Soc Care Community 2018;26:e312-e20.
- Lea EJ, Goldberg LR, Price AD, Tierney LT, McInerney F. Staff awareness of food and fluid care needs for older people with dementia in residential care: a qualitative study. J Clin Nurs 2017;26:5169-78. https://doi.org/10.1111/jocn.14066.
- Donaldson WV, Vacha-Haase T. Exploring staff clinical knowledge and practice with LGBT residents in long-term care: a grounded theory of cultural competency and training needs. Clin Gerontol 2016;39:389-40. https://doi.org/10.1080/07317115.2016.1182956.
- Sion KYJ, Verbeek H, de Boer B, . How to assess experienced quality of care in nursing homes from the client’s perspective: results of a qualitative study. BMC Geriatr 2020;20:1-12.
- Curtis LA. Unit Costs of Health and Social Care 2013: Personal Social Services Research Unit. Canterbury: University of Kent; 2013.
- Tonkin JD, Heino J, Altermatt F. Metacommunities in river networks: the importance of network structure and connectivity on patterns and processes. Freshw Biol 2018;63:1-5.
- Ward H. Prevention strategies for sexually transmitted infections: importance of sexual network structure and epidemic phase. Sex Transm Infect 2007;83:ii43-9.
- Reagans R, McEvily B. Network structure and knowledge transfer: the effects of cohesion and range. Adm Sci Q 2003;48:240-67.
- Dearing JW, Beacom AM, Chamberlain SA, Meng J, Berta WB, Keefe JM. Pathways for best practice diffusion: the structure of informal relationships in Canada’s long-term care sector. Implement Sci 2017;12:1-13.
- Byrnn D. The Attraction Paradigm. New York: Academic Press; 1971.
- The Federation of European Social Employers . Staff Shortages in Social Services across Europe 2022. https://socialemployers.eu/files/doc/Staff%20shortages%20in%20social%20services%20across%20Europe.pdf (accessed 14 April 2022).
- National Care Forum . Just Grim, Difficult and Relentless 2022. www.nationalcareforum.org.uk/ncf-press-releases/just-grim-difficult-and-relentless/ (accessed 14 April 2022).
- Chambers N, Jane T. Policy Issues and Management Challenges in the Nursing Homes Sector. Manchester: University of Manchester, Manchester Centre for Healthcare Management; 2002.
- Orellana K, Manthorpe J, Moriarty J. What do we know about care home managers? Findings of a scoping review. Health Soc Care Community 2017;25:366-77.
- Legislation Gov UK . The Health and Social Care Act 2008 (Regulated Activities) Regulations 2010 2010. www.legislation.gov.uk/uksi/2010/781/contents/made (accessed 14 April 2022).
- Breiman L. Statistical modeling: the two cultures. Stat Sci 2001;16:199-215.
- Castle NG, Engberg J. The influence of staffing characteristics on quality of care in nursing homes. Health Serv Res 2007;42:1822-47.
- West M, Dawson J, Admasachew L, Topakas A. NHS Staff Management and Health Service Quality Results from the NHS Staff Survey and Related Data: Department of Health and Social Care 2011. www.gov.uk/government/publications/nhs-staff-management-and-health-service-quality (accessed 14 April 2022).
- INVOLVE N . Briefing Notes for Researchers – Public Involvement in NHS, Health and Social Care Research 2021. www.nihr.ac.uk/documents/briefing-notes-for-researchers-public-involvement-in-nhs-health-and-social-care-research/27371 (accessed 14 April 2022).
- Staley K, Barron D. Learning as an outcome of involvement in research: what are the implications for practice, reporting and evaluation?. Res Involv Engagem 2019;5:1-9.
- Tulloch J, Green R, Tunnah C, Coffey E, Ashton M, Ghebrehewet S. COVID-19 outbreaks in care homes during the first wave: are Care Quality Commission ratings a good predictor of at-risk homes?. J Hosp Infect 2021;111:96-101.
- Netten A, Trukeschitz B, Beadle-Brown J, Forder J, Towers AM, Welch E. Quality of life outcomes for residents and quality ratings of care homes: is there a relationship?. Age Ageing 2012;41:512-7. https://doi.org/10.1093/ageing/afs050.
- Barber N, Alldred DP, Raynor D, Dickinson R, Garfield S, Jesson B. Care homes’ use of medicines study: prevalence, causes and potential harm of medication errors in care homes for older people. BMJ Qual Saf 2009;18:341-46.
- Cross R, Kaše R, Kilduff M, King Z. Bridging the gap between research and practice in organizational network analysis: a conversation between Rob Cross and Martin Kilduff. Hum Resour Manag 2013;52:627-44.
- Huerta TR, Dandi R. Advances in Health Care Organization Theory. San Francisco: Jossey-Bass; 2014.
Appendix 1 Five questions the Care Quality Commission ask of all care servicesa
| Are they safe? | Safe: you are protected from abuse and avoidable harm. |
| Are they effective? | Effective: your care, treatment and support achieve good outcomes, helps you to maintain quality of life and is based on the best available evidence. |
| Are they caring? | Caring: staff involve and treat you with compassion, kindness, dignity and respect. |
| Are they responsive to people’s needs? | Responsive: services are organised so that they meet your needs. |
| Are they well-led? | Well-led: the leadership, management and governance of the organisation make sure it’s providing high-quality care that’s based around your individual needs, that it encourages learning and innovation, and that it promotes an open and fair culture. |
Appendix 2 Deviations from original study protocol due to coronavirus disease 2019 pandemic
| WP | Original planned work | Work undertaken due to impact of COVID-19 on care home staff and/or restrictions imposed on research team |
|---|---|---|
| WP1 | Surveys with: (1) care home staff to understand roles of the nursing and support workforce; (2) care home managers to understand recruitment and retention challenges. |
(1) We completed a systematic review of research studies focusing on the roles and responsibilities of RNs and CAs linked with promoting quality of care and quality of life; (2) A separate review funded by NIHR (which commenced August 2021) is being undertaken to understand what strategies are effective (and ineffective) for attracting, recruiting and retaining RNs and care workers in the long-term care sector (https://fundingawards.nihr.ac.uk/award/NIHR131016). |
| WP3 | Management practice survey (SCREC ethics approval as an amendment to 17/WM/0232). | We were not able to administer this survey due to COVID-19 pandemic. This impacted on plans for follow-on discussions with the care provider; these discussions did not occur. |
| WP4 | In-depth exploration of care processes using case studies (n = 6). | Documentary analysis of a purposive sample of CQC reports with ratings of outstanding or inadequate (n = 30). However, due to the ongoing COVID-19 situation, we were unable to undertake follow-up focus groups and interviews to share findings to understand whether these resonated with different care home contexts. |
| WP5 | SNA | Partially completed but impacted data collection plans and follow-up. We planned follow-up interviews with care home managers’ but all but 3 (or 11 managers) had left the care home. |
Appendix 3 Example search strategy for work package 1i review
Database: APA PsycINFO <2002 to February Week 3, 2021>
Search strategy:
-
exp nursing homes/ (5701)
-
“home* for the aged”.tw,id. (343)
-
nursing home*.tw,id. (8184)
-
“care home*”.tw,id. (1612)
-
residential care institutions/ (5589)
-
long term care/ (4573)
-
((long-term or longterm or long-stay or longstay) adj5 (facilit* or institution* or setting* or resident* or care)).tw,id. (9751)
-
institutionalization/ (1734)
-
((residental or residence? or institution* or facility or facilities) adj5 (elder* or geriatric* or seniors or older or aged)).tw,id. (2758)
-
((residential or long-term or longterm or long-stay or longstay or dementia) adj5 (facilit* or institution* or setting* or resident* or institution?)).tw,id. (23542)
-
((residential or retirement*) adj2 (facilit* or home?)).tw,id. (2489)
-
assisted living/ (698)
-
assisted living.tw,id. (1213)
-
(life care cent* or continuing care cent* or extended care facility or extended care facilities).tw,id. (32)
-
((residential or long-term or longterm or long-stay) adj5 (care or facility or facilities or ward? or institution*)).tw,id. (13,333)
-
((skilled or intermediate) adj2 (nursing facility or nursing facilities)).tw,id. (455)
-
retirement communities/ (278)
-
or/1–17 [care homes] (40,152)
-
((care or worker*) adj2 (staff or professional* or personnel or assistant*) adj4 (experience* or expectation* or satisfaction or view* or opinion* or perception* or perspective* or attitude* or preference* or belief* or perciev* or feeling* or idea*)).tw,id. (1278)
-
((support worker* or healthcare assistant* or service provider* or carer* or staff or care provider* or nurse* or nursing or healthcare professional* or physician* or general practitioner* or care worker* or healthcare attendant* or care assistant* or care home manage* or health facility administrator* or nursing home manager* or activit* co ordinator* or healthcare worker) adj4 (experience* or expectation* or satisfaction or view* or opinion* or perception* or perspective* or attitude* or preference* or belief or perciev* or feeling or idea*)).tw,id. (28,083)
-
((interview* or qualitative or theme* or survey* or questionnaire* or focus group*) adj5 (support worker* or healthcare assistant* or service provider* or carer* or staff or care provider* or nurse* or nursing or healthcare professional* or physician* or general practitioner* or care worker* or healthcare attendant* or care assistant* or care home manage* or health facility administrator* or nursing home manager* or activit* co ordinator* or healthcare worker)).tw,id. (20,910)
-
exp health personnel attitudes/ (17,195)
-
employee attitudes/ (11,820)
-
“work (attitudes toward)”/ (3061)
-
exp qualitative methods/ or exp Interviews/ or exp questionnaires/ (37,562)
-
(((care or worker*) adj2 (staff or professional* or personnel or assistant*)) or (support worker* or healthcare assistant* or service provider* or carer* or staff or care provider* or nurse* or nursing or healthcare professional* or physician* or general practitioner* or care worker* or healthcare attendant* or care home manage* or health facility administrator* or nursing home manager* or activit* co ordinator* or healthcare worker)).tw,id. (205,520)
-
25 and 26205 (3849)
-
19 or 20 or 21 or 22 or 23 or 24 or 27107 (68,357)
-
(role* or responsibili* or workload*).tw,id. (517606)
-
exp professional role/ (1180)
-
role expectations/ (653)
-
role perception/ (936)
-
professional standards/ (4073)
-
“professional credential*”.tw,id. (102)
-
exp responsibility/ (14,979)
-
Professional Competence/ (6731)
-
work load/ (2043)
-
professionalism/ (3568)
-
professional competence/ (6731)
-
or/29–3932 (533,425)
-
18 and 28 and 40 (937)
-
limit 41 to (english language and yr=“2010-Current”) (630)
Appendix 4 Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow diagram for work package 1i review
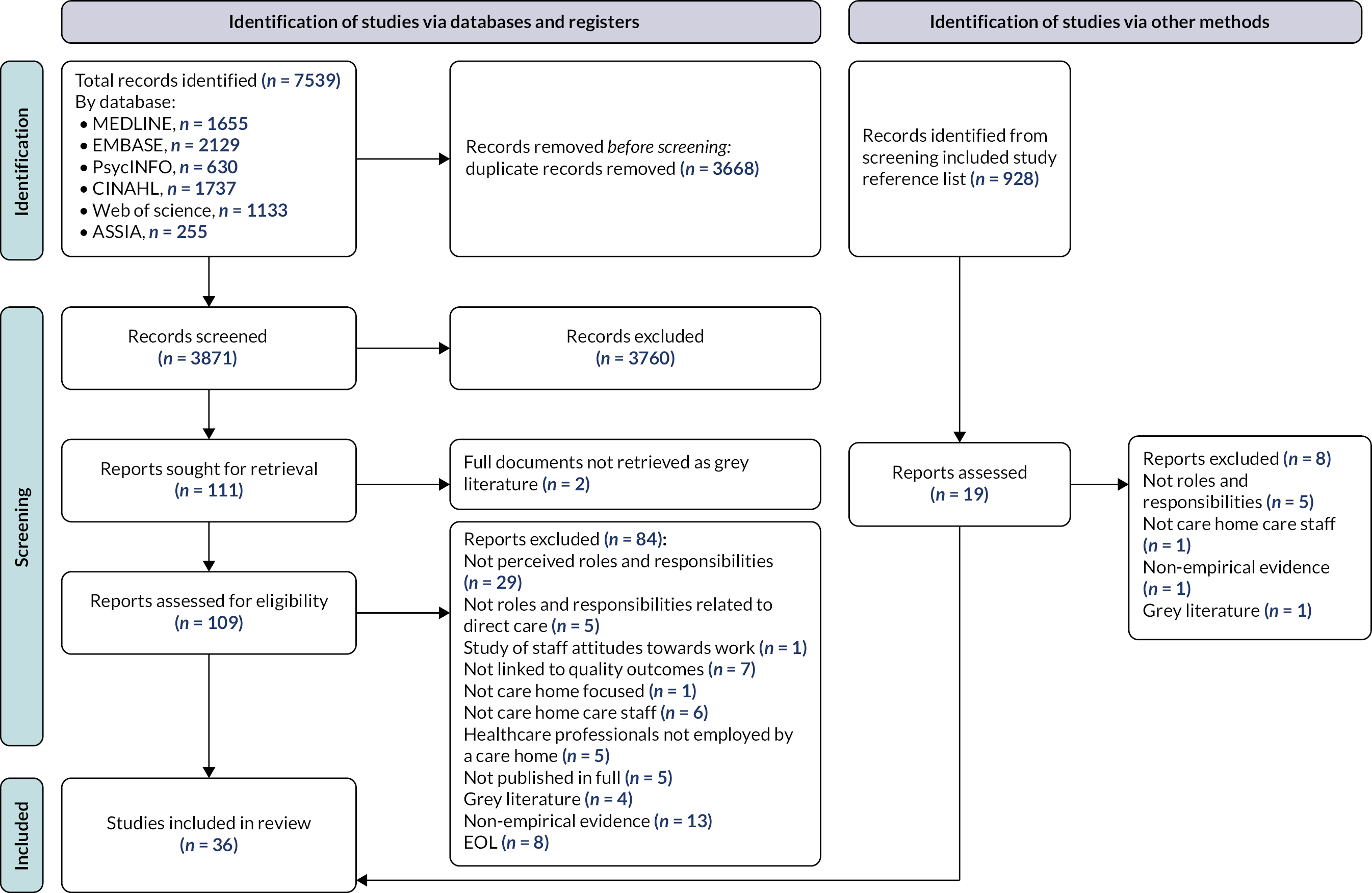
Appendix 5 Quality assessment of included studies using Mixed Methods Appraisal Tool for work package 1i review
| Qualitative included studies |
Quality checklist criteria for qualitative studies | ||||||
|---|---|---|---|---|---|---|---|
| Screening questions | Qualitative studies | ||||||
| Are there clear research questions/aims? | Do the collected data allow to address the research questions/aims? | Is the qualitative approach appropriate to answer the research question/aim? | Are the qualitative data collection methods adequate to address the research question/aim? | Are the findings adequately derived from the data? | Is the interpretation of results sufficiently substantiated by data? | Is there coherence between qualitative data sources, collection, analysis and interpretation? | |
| Abrahamson, 2020 100 | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Andersen, 2016 108 | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Backhaus, 2018 117 | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Banerjee, 2015 109 | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Bedin, 2013 122 | Yes | Yes | Yes | Yes | Cannot be determined | Cannot be determined | Cannot be determined |
| Cho, 2020 125 | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Chung 2010 101 | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Craftman, 2016 113 | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Daly, 2012 135 | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Ellis, 2012 110 | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Ellis, 2015 131 | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Forss, 2018 114 | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Halifax, 2018 102 | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Heath, 2010 119 | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Johansson-Pajala, 2016 115 | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Kusmaul, 2017 103 | Yes | No | Yes | No | Yes | Yes | Yes |
| Laging, 2018 133 | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Liu, 2014 128 | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Lung, 2016 129 | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Marshall, 2020 112 | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Medvene, 2010 104 | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Odberg, 2018 123 | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| O’Doherty, 2013 124 | Yes | Yes | Yes | Yes | Yes | No | Cannot be determined |
| Olsson, 2014 116 | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Ostaszkiewicz 2016 134 | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Park, 2018 126 | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Sun-Young, 2020 127 | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Talbot, 2016 120 | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Vandrevala, 2017 121 | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Vogelmeirer, 2011 106 | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Vogelmeirer, 2014 107 | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Yektatalab, 2012 130 | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Screening questions | Quantitative studies | ||||||
| Are there clear research questions/aims? | Do the collected data allow to address the research questions/aims? | Is the sampling strategy relevant to address the research question/aim? | Is the sample representative of the target population? | Are the measurements appropriate? | Is the risk of nonresponse bias low? | Is the statistical analysis appropriate to answer the research question? (or study aim?) | |
| Knopp-Sihota, 2015 111 | Yes | Yes | Yes | Yes | Yes | Cannot be determined | Yes |
| Kuk, 2017 118 | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Mueller, 2012 105 | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Screening questions | Mixed methods | ||||||
| Are there clear research questions/aims? | Do the collected data allow to address the research questions/aims? | Is there an adequate rationale for using a mixed-methods design to address the research question/aim? | Are the different components of the study effectively integrated to answer the research question/aim? | Are the outputs of the integration of qualitative and quantitative components adequately interpreted? | Are divergences and inconsistencies between quantitative and qualitative results adequately addressed? | Do the different components of the study adhere to the quality criteria of each tradition of the methods involved? | |
| Hunter, 2010 132 | Yes | Yes | Yes | No | Cannot be determined | Cannot be determined | Yes |
Appendix 6 Review process for work package 1ii realist review
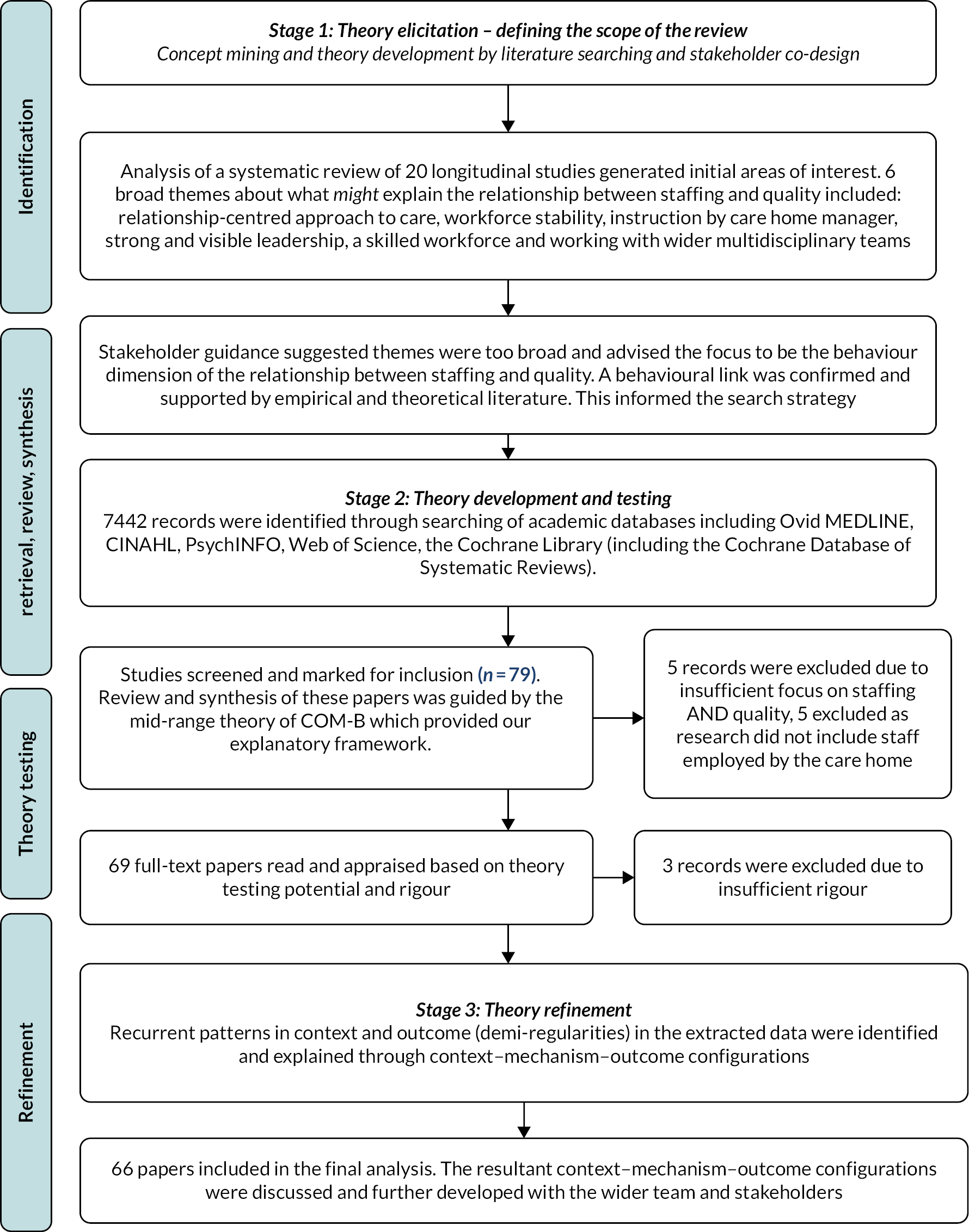
Appendix 7 Theory elicitation through if–then statements for work package 1ii
| Title | If | Then |
|---|---|---|
| Relationship-based approach to care | If the long-term care facility’s approach to care promotes relationships and connections (familiarity) between long-term care facility staff and residents | then long-term care facility staff will know the person and are more able to detect a change in the resident’s physical, psychological, emotional and social status and provide early and timely intervention |
| Workforce stability | If the long-term care facility has a stable workforce and there is regular ongoing contact between residents and long-term care facility staff over time | then this helps establish routines for care delivery which leads to enhanced confidence for (1) residents due to an established and trusting relationship with long-term care facility staff and (2) long-term care facility staff for assessing and monitoring residents |
| Instruction by the long-term care facility manager | If long-term care facility staff are directed by a visible, skilled and competent manager with a strong vision of the overarching philosophy of care for the home | then the manager will have clear oversight of what care is being delivered, why and how and long-term care facility staff will understand what is expected of each team member which will enable monitoring and maintaining of care standards that contribute to quality |
| Strong and visible leadership throughout the home | If there is strong and visible leadership throughout the long-term care facility | then this will provide direction and support for the long-term care facility staff team about the ethos of care in the home and open communication between team members which leads to enhanced clarity of roles and expectations of how and in what way different members of the team contribute to resident care |
| Skilled workforce | If the long-term care facility has a workforce who are a good fit – that is those who practice empathy, kindness and compassion, or who are willing and trained to adopt empathy, kindness and compassion. and a level of competence and skill developed through education, training and/or experience and | then the long-term care facility can deploy its workforce appropriately, long-term care facility staff who are a good fit in terms of attitudes and are equipped with the knowledge, understanding and expertise to assess and evaluate residents. Long-term care facility staff also have the confidence to be able to delegate and offer direction to other members of staff in the team which leads to appropriate deployment and use of skills in the team and early and timely detection of changes in residents’ status to prompt action for intervention |
| Working with the wider multidisciplinary team | If there are ways for long-term care facility staff to access and establish relationships with the wider multidisciplinary team | then this will promote confidence for long-term care facility staff to approach and engage with other members of the multidisciplinary team to raise concerns about a resident in a timely manner to ensure appropriate investigation for the management and/or interventions to promote the best care for residents |
Appendix 8 Search terms and databases for work package 1ii realist review
| There were no limitations on dates. Searches were from inception up to November 2019. Search alerts scanned up to April 2020. Language restricted to English. Databases included: Ovid MEDLINE (n = 1760 records), PsycINFO (n = 1548 records), CINAHL (n = 4859 records), Web of Science (n = 1276 records), Cochrane Database of Systematic Reviews (n = 6 records), Cochrane Central Register of Controlled Trials (n = 241 records). Number of records after de-duplication were n = 7442 records. |
Search terms
|
Appendix 9 Purposive sampling of care homes for documentary analysis of Care Quality Commission inspection reports
Care home ownership and size of the provider organisation
Not-for-profit organisations
We included:
-
Three outstanding care homes, ranging in size, were included from the largest not-for-profit organisation in the UK. This provider had 91 care homes in their portfolio, none of which were rated as inadequate.
-
Two care homes from a medium-sized not-for-profit organisation (which had 21 care homes) were included: one was rated as outstanding and the other as inadequate.
-
One care home rated as inadequate from another medium-sized not-for-profit organisation (which owned 11 care homes in total). All care homes owned by this organisation varied in their CQC quality rating: none were rated as outstanding.
-
One care home rated as inadequate from a small not-for-profit organisation.
-
There were no outstanding not-profit care homes from a single provider.
For-profit organisations
We included:
-
Four care homes from the largest for-profit provider in the UK were represented in our sample: two were rated as outstanding and two as inadequate.
-
Three care homes from three medium-sized for-profit providers (which owned 14 care homes, 6 and 9, respectively).
-
Four independent single care home providers: two care homes were rated as outstanding, and two inadequate.
Local authority
-
Two care homes owned by the local authority and rated as outstanding were included in our sample. There were no local authority care homes rated as inadequate at the time of sampling.
Geographical location
We ensured we sampled the care homes (as described above) to represent geographical location, urban and rural. Care homes of the large provider (stage 1) revealed gaps in geographical location that we were able to address in stage 2 sampling. Care homes sampled in this second stage were located in the North East of England (n = 2), Yorkshire and Humber (n = 3), the North West (n = 3), East Midlands (n = 2), West Midlands (n = 1), the East of England (n = 2), London (n = 1), the South East (n = 4) and the South West (n = 2).
Individual size of the care home
The size of each individual care home ranged from 9 beds to 149 beds. We ensured there was a good spread of care home size in both the outstanding and inadequate categories of care homes in this second stage of sampling.
Appendix 10 Social network analysis concepts
| Concept | Description |
|---|---|
| #Advice Relationships | The number of relationships in the advice network. This gives a way to compare networks and the more relationships there are, the more likely advice flows through the network. |
| %Reciprocal Advice Relationships | Percentage of relationships expressing reciprocity. Reciprocity in this case is where person A says she goes to Person B for advice and Person B independently says that she goes to Person A for advice. This is one of the measures for reciprocity used in the hypothesis test. |
| #Influence Relationships | The number of relationships in the influence network. This gives a way to compare networks and the more relationships there are, the more likely influence flows through the network. |
| %Reciprocal Influence Relationships | Percentage of relationships expressing reciprocity. In this case, Person A says she is influenced by Person B and Person B independently says that she is influenced by Person A. This is one of the measures for reciprocity used in the hypothesis test |
| #Advice Cliques | Number of groups of at least three people who are all connected to each other in the advice network. Implied is that there are stronger ties within the group than outside which makes cliques fruitful ground for seeding innovations. |
| #Influence Cliques | Number of groups of at least three people who are all connected to each other in the influence network. Implied is that there are stronger ties within the group than outside which makes cliques fruitful ground for seeding innovations. |
| Overall Advice Clustering Coeff% (×100) | The tendency of the advice network to form clusters. Clusters are densely connected group of nodes which helps enable the spread of innovations. The more clusters in a network, the higher the probability of innovation spread. |
| Overall Influence Clustering Coeff% (×100) | The tendency of the influence network to form clusters. Clusters are densely connected group of nodes which helps enable the spread of innovations. The more clusters in a network, the higher the probability of innovation spread. |
| Advice Density | Density of the advice network. Density is the percentage of possible network ties that are being used. The denser the network, the more paths available for innovations. |
| Influence Density | Density of the influence network. The denser the network, the more paths available for innovations. |
| Highest Advice Betweenness | The people who most often serve as a bridge in the advice network with the betweenness centrality score in parentheses. The higher the score, the more likely advice travels from one side of the network to the other over these bridges. |
| Highest Influence Betweenness | The people who most often serve as a bridge in the influence network with the betweenness centrality score in parentheses. The higher the score, the more likely advice travels from one side of the network to the other over these bridges. |
| Highest Advice Out Degree Centrality | The people who give out the most advice in the care home with the number of advisees in parentheses. |
| Highest Influence Out Degree Centrality | The people with the most influence in the care home with the number of people influenced in parentheses. |
Glossary
- Capabilities, opportunities, motivation – behaviour model
- The capabilities, opportunities, motivation – behaviour model proposes that there are three components to any behaviour (B): Capability (C), Opportunity (O) and Motivation (M).
- Care Quality Commission
- The national health and social care regulator in England.
- Context–mechanism–outcome configurations
- The unit of analysis (in realist reviews) used to synthesise across studies to build and refine programme theory. [Programme Theory: describes how the intervention is expected to generate effects and under what conditions (usually expressed as context–mechanism–outcome configurations). Context: the conditions constituting the setting for the intervention. Context influences the way resources are perceived to generate outcomes. Mechanism: the resource the intervention provides and the impact it has on the reasoning of staff. Outcome: the expected or unexpected result.]
- National Minimum Data Set for Social Care
- An online workforce data collection system for the social care sector. It is the leading source of robust workforce intelligence for adult social care. National Minimum Data Set for Social Care was replaced by the Adult Social Care Workforce Data Set in August 2019.
- Skills for Care
- The strategic workforce development and planning body for adult social care in England.
List of abbreviations
- ASC-WDS
- Adult Social Care Workforce Data Set
- CA
- care assistant
- COM-B
- capabilities, opportunities, motivation – behaviour
- CQC
- Care Quality Commission
- ICC
- intraclass correlation
- KLOE
- key lines of enquiry
- LPA
- latent profile analysis
- NMDS-SC
- National Minimum Data Set for Social Care
- NoMAD
- Normalisation MeAsure Development questionnaire
- NPT
- normalisation process theory
- OLS
- ordinary least squares
- RN
- registered nurse
- SNA
- social network analysis
- StaRQ
- Staffing Relationship to Quality
- UTI
- urinary tract infection
- WP
- work package
