Notes
Article history
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as project number HSDR NIHR130298. The contractual start date was in January 2021. The final report began editorial review in January 2023 and was accepted for publication in April 2023. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
Copyright © 2024 Glasby et al. This work was produced by Glasby et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2024 Glasby et al.
Chapter 1 Introduction
Policy context
Transforming care so that people with learning disabilities and/or autistic people can receive support at home rather than in inpatient units, secure settings or assessment and treatment units (ATUs) is a key priority, which has significant implications for people’s quality of life as well as for public finances. Over the last decade, there have been a series of abuse scandals and significant public anger at such service models, often provided out-of-area and in the commercial sector at significant expense and with poor outcomes. A key aim of the ‘Building the Right Support’ and ‘Transforming Care’ programmes was to enhance community capacity, thereby reducing inappropriate hospital admissions and length of stay. 1,2 Despite this, some 2185 people with learning disabilities and/or autistic people were hospital inpatients at the end of January 2020, 58% of whom had a hospital stay of over 2 years. 3 In spite of significant policy pledges, progress has been painfully slow, with multiple missed deadlines. In 2012, the Department of Health4 was clear that:
By 1 June 2014 we expect to see a rapid reduction in the number of people with challenging behaviour in hospitals …. By that date, no-one should be inappropriately living in a hospital setting. (p. 22)
This was accompanied by a ‘concordat’ signed by the Department and some 50 partners:5
The abuse of people at Winterbourne View hospital was horrifying. Children, young people and adults with learning disabilities or autism … have for too long and in too many cases received poor quality and inappropriate care …. Too many people are ending up unnecessarily in hospital and they are staying there for too long …. [Our] actions are expected to lead to a rapid reduction in hospital placements for this group of people by 1 June 2014. People should not live in hospital for long periods of time. Hospitals are not homes. (p. 5)
When this target was not met, NHS England (NHSE) and partners2 (2015, p. 6) re-iterated their commitment to driving real change:
In February 2015, NHS England publicly committed to a programme of closing inappropriate and outmoded inpatient facilities …. Overall, 35–50% of inpatient provision will be closing nationally with alternative care provided in the community …. In three years we would expect to need hospital care for only 1300–1700 people where we now cater for 2600. This will free up money which can be reinvested into community services, following upfront investment.
As part of these national programmes, there have been a series of linked developments, including a national service model, a new financial framework, guidance for commissioners, model service specifications and the creation of 48 ‘Transforming Care Partnerships’ to re-shape services and reduce inpatient beds by up to 50% (www.england.nhs.uk/learning-disabilities/care/). Independent panels also conduct Care and Treatment Reviews (CTRs), with guidance suggesting that reviews should take place every 6 months for people in non-secure hospitals, every 12 months for people in secure hospitals, and every 3 months for children and young people in hospital. 6 More recently, the Department of Health and Social Care (DHSC)7 announced a series of additional measures:
All 2,250 patients with learning disabilities and autism who are inpatients in a mental health hospital will have their care reviewed over the next 12 months …. As part of the review, the government will commit to providing each patient with a date for discharge, or where this is not appropriate, a clear explanation of why and a plan to move them closer towards being ready for discharge into the community …. The government is also committing today to a further reduction of up to 400 inpatients to be discharged by the end of March 2020. For those in long-term segregation, an independent panel … will be established to oversee their case reviews to further improve their care and support them to be discharged back to the community as quickly as possible.
Despite all this, long-standing challenges remain (see Box 1). Moreover, many more recent actions seem very similar to previous initiatives, with no indication as to how these might be expected to achieve different outcomes second time round. As Hatton8 argues:
So what do I think are the lessons we can learn from the kind of ‘push’ that has already happened at least once, towards the end of Transforming Care in March 2019, and that policy announcements say are going to happen again?
Based on this evidence, the new initiatives announced … are unlikely to have the transformative effect claimed for them.
This has provoked widespread concern from disability rights campaigners:9
Measures introduced … to address the scandalous treatment of autistic people and people with learning difficulties in mental health hospitals are strikingly similar to failed government measures announced seven years ago …. [This] drew a furious response from disabled activists, who called for an end to meaningless government apologies and promises that fail to stop abuse in institutions.
In 2020, the Equality and Human Rights Commission (EHRC) announced that it was launching a legal challenge in response to alleged breaches of the European Convention of Human Rights (ECHR):10
Today we have launched a legal challenge against the Secretary of State for Health and Social Care over the repeated failure to move people with learning disabilities and autism into appropriate accommodation. We have longstanding concerns about the rights of more than 2000 people with learning disabilities and autism being detained in secure hospitals, often far away from home and for many years …. We have sent a pre-action letter to the Secretary of State for Health and Social Care, arguing that the Department of Health and Social Care (DHSC) has breached the ECHR for failing to meet the targets set in the Transforming Care program and Building the Right Support program … Following discussions with the DHSC and NHSE, we are also not satisfied that new deadlines … will be met. This suggests a systemic failure to protect the right to a private and family life, and right to live free from inhuman or degrading treatment or punishment.
Despite a subsequent government action plan,11 the EHRC have remained highly critical, with a subsequent press release (2022)12 reiterating long-standing concerns:
Every day a person is detained in hospital unnecessarily is a day too many. It is therefore unacceptable, more than a decade after action was first promised, that hundreds of people with autism and learning disabilities are still being kept as in-patients when they could be receiving community care. In too many cases, patients are also subject to restraint and segregation, which can worsen their conditions and make it increasingly hard for them to go home. In extreme cases, there could be significant violations of human rights. The DHSC’s plan to address these concerns has been delayed two years by Covid, and we are pleased it has finally been published. However, it does not go far enough …. The EHRC is exploring how best to use its legal powers to help patients and their families. This may include action in the courts.
There have also been similar debates in other nations of the United Kingdom (UK), with the publication of Scotland’s ‘Coming Home’ Implementation report,13 and critical responses from organisations such as Inclusion Scotland and C-Change Scotland:14
In February of this year the Scottish Government published the Coming Home Implementation Report detailing the proposed response to the critical issue of learning disabled and autistic people spending long periods of time in hospitals and inappropriate out of area placements.
Whilst we appreciate the Government’s focus on this issue and the intention to address it, we are gravely concerned about the process for compiling the report, and the proposals outlined within it ….
In 2022 it is not enough to write the words ‘nothing about us without us’ and publish a report that did not engage with disabled people. It is not good enough to cite human rights based approaches and fail to ensure the participation of the very people the report is about …. We believe the Scottish Government can and should do better. A critical first step would be ensuring real and meaningful engagement of disabled people and their families in any proposals to resolve these, and the other concerns, detailed.
Why this research is needed
All this matters because:
-
Hospitals, although potentially needed by some people for specific periods of time, are not designed to support people to lead an ordinary a life, and few people would want to live there if they could genuinely choose.
-
There has been a series of horrific care scandals in such settings, from Panorama investigations at Winterbourne View/Whorlton Hall to the death of Connor Sparrowhawk and the Justice for Laughing Boy campaign. 15–17 The distress that this has caused to individual people and families is immeasurable, and there are harrowing accounts of abuse, neglect, deaths and widespread deprivation of human rights. 18–20 These stories have been told in the mainstream media (see e.g. Birrell21–23), but with families also increasingly taking to social media (e.g. the 7 Days of Action campaign,24 #CloseATUs, or Bethany’s Dad). This has led to a raft of official reviews; an investigation by the Parliamentary Joint Committee on Human Rights;25 a highly critical report by the Children’s Commissioner for England;26 campaigns and policy recommendations by groups such as Mencap,27 the National Autistic Society,28 the Voluntary Organisations Disability Group (VODG)29 and the Centre for Welfare Reform;30 highly critical research (e.g. Brown et al. 31); and widespread criticism from voluntary and advocacy organisations such as Autistic UK, People First and Changing Perspectives (see e.g. Pring9).
-
Such services are very expensive, with average weekly and annual costs of £3500 and £180,000 per person. 32,33 This creates a vicious circle whereby funding is sucked into institutional forms of care, leaving less money for community services and leading to even more people being admitted.
While we focus on England, similar issues have been highlighted by the Mental Welfare Commission for Scotland,34 with one-third of patients waiting for discharge, sometimes for months or years. In Wales, a national review on behalf of the Chief Nursing Officer identified 256 people in long-stay settings, many of whom had ‘spent significant periods of their lives in hospital care, with some having been inpatients since reaching adulthood’ (Mills et al. 35, p. 179). Hatton36 also provides further cross-UK analysis.
Mencap32 warns of ‘a domestic human rights scandal’, pointing to:
-
‘Almost 2300 children and adults with a learning disability still detained in inpatient units.
-
Over 2500 restrictive interventions e.g. physical restraint in one month – over 820 of which were against children.
-
Average time in an inpatient unit away from home … is almost 5 and a half years.
-
8 years after Winterbourne View …, Government has not delivered on promise to “Transform Care”’.
The Care Quality Commission (CQC)37 suggests that
Thirteen of the 39 people that we visited were experiencing delayed discharge from hospital, and so prolonged time in segregation, because there was no suitable package of care available in a non-hospital setting …. Three of the people had been discharged from hospital previously but then readmitted when the placement could not meet the person’s needs. Staff and advocates have told us that the cost and question of who will fund an alternative placement can delay discharge. In one example a suitable property in the community, that would meet the person’s needs, could not be found for the budget available. Members of the expert advisory group have suggested that there may be conflicting incentives in the system for commissioning care and treatment for this group of people. (p. 20)
The Children’s Commissioner for England26 (pp. 1–2) concludes:
I am concerned that the current system of support is letting many children down and does not meet obligations under the United Nations Convention of the Rights of the Child …. Hospital admission may rarely be the right thing to do for children …. But it must always be in a child’s best interests and as part of a managed process with clear timescales and a focus on keeping the length of stay as short as possible. This is clearly not happening at the moment and we have a system which is costing millions, yet is letting these children down.
The House of Commons/House of Lords Joint Committee on Human Rights (p. 3)25 sets out a ‘pathway to detention’ which is entirely ‘predictable’:
It begins from before diagnosis. A family grows worried about their child. They raise concerns with the GP, and with the nursery or school. It takes ages before they get an assessment and yet more time passes before they get a diagnosis of autism. All that time they struggle on their own with their worries and without help for their child. This pattern continues throughout childhood as families are under-supported and what little help they have falls away when the child reaches the age of 18. Then something happens, perhaps something relatively minor such as a house move or a parent falls temporarily ill. This unsettles the young person and the family struggles to cope. Professionals meet to discuss what should happen, but parents are not asked for their views. Then the child is taken away from their home and the familiarity and routine which is so essential to them. They’re taken miles away and placed with strangers. The parents are desperately concerned. Their concerns are treated as hostile and they are treated as a problem. The young person gets worse and endures physical restraint and solitary confinement – which the institution calls ‘seclusion’. And the child gets even worse so plans to return home are shelved. The days turn into weeks, then months and in some cases even years. This is such a grim picture, yet it has been stark in evidence to our inquiry …. We have lost confidence that the system is doing what it says it is doing and the regulator’s method of checking is not working. It has been left to the media … to expose abuse. No-one thinks this is acceptable.
How this fills gaps in the literature
Despite significant national debate, very little previous research has engaged directly with people with learning disabilities and/or autistic people or their families to understand the issues from their perspective (see Chapter 3). In research into older people’s hospital admissions and discharge, there has been a similar failure to consider the lived experience of older people and families – and a previous National Institute for Health and Care Research (NIHR) study (‘Who Knows Best’)38–40 is believed to be the first research to meaningfully consider these issues from the perspectives of older people themselves. Whilst professionals often see the individual at a particular point in time (often in a crisis), it is only the person and their family who have a longitudinal sense of how their story has unfolded: their informal networks; their contacts over time with formal services; their experience of hospital; the different options considered; and what has ultimately helped/hindered in securing desired outcomes. Failing to take into account this lived experience is not only morally wrong, but also deprives us of a major source of expertise with which to improve services. Similarly, there has been little consideration of the perspectives of front-line staff, who are being asked to practise in very different ways in a difficult environment, arguably without the support needed to do this well. Again, this mirrors much of the literature around older people’s hospital admissions/discharge, where the tacit knowledge/practice knowledge of front-line staff is largely overlooked (see Chapter 7 for discussion of insights from the broader hospital discharge literature).
Seeking to make a similar contribution in services for people with learning disabilities and/or autistic people, this study addresses four main gaps in the literature (see Chapter 3 for further discussion):
-
While older people’s delayed discharges are frequently debated,41,42 the large numbers of people with learning disabilities and/or autistic people in long-stay settings when they no longer need to be is seldom framed as a ‘delayed transfer of care’ in the same way, is not counted as such in national datasets and is not researched to the same extent. This means that insights from other user groups are not applied to services for people with learning disabilities and/or autistic people, and that we lose an opportunity to improve policy/practice.
-
Most literature on older people’s delayed discharges neglects the lived experience of older people and their families, and most studies in learning disability services focus on information from ward censuses or researchers/clinicians working from medical notes. Even where agencies have sought to review services from multiple perspectives, they have seldom been able to involve people with learning disabilities and/or autistic people in meaningful ways, often lacking the time to get to know people well or to find ways to work effectively with people who do not communicate verbally. Elsewhere, there are powerful stories from family members, but some reports seem to fail to talk to the person themselves (e.g. National Autistic Society28). This is now starting to change, with agencies such as the CQC citing the stories of Adam, Jane, Rachel and John in their review of segregation (p. 20)37 or NHSE setting out Martin’s story (www.youtube.com/watch?v=VC1kQUkVUzM), and with a growing understanding of the importance and power of collating local learning about personal journeys in other service settings (see e.g. CQC43). However, this remains the exception rather than the norm, and has struggled to penetrate many aspects of long-stay settings.
-
Previous research neglects the tacit knowledge of front-line staff, and says little about how workers experience their roles, how delays impact upon them, what support they need and practical steps forward from a staff perspective. While our main aim is to better understand and value the lived experience of people with learning disabilities and/or autistic people and their families, an important secondary aim is to understand and value staff experience.
-
Much of the debate is essentially negative in nature (identifying problems, but seldom proposing practical ways forward). In contrast, this study will produce good practice guidance written from the perspective of people with learning disabilities and/or autistic people and their families and will develop a free online training video, so that our contribution is more solution-focused.
Aims and objectives
Against this background, the University of Birmingham and the rights-based organisation Changing Our Lives conducted a joint study to better understand the experiences of people with learning disabilities and/or autistic people in long-stay hospital settings, their families and front-line staff – using this knowledge to create practice guides and training material to support new understandings and new ways of working. Our aims were to:
-
review the literature on the rate/causes of delayed hospital discharges of adults with learning disabilities and/or autistic people from specialist inpatient units, NHS campuses and ATUs (referred to as ‘long-stay hospital settings’ as a shorthand);
-
more fully understand the reasons why some people with learning disabilities and/or autistic people are unable to leave hospital, drawing on multiple perspectives (including the lived experience of people with learning disabilities and/or autistic people and their families, and the tacit knowledge of front-line staff);
-
identify lessons for policy/practice so that more people can leave hospital and lead a more ordinary life in the community.
Achieving these aims in such service settings required in-depth work, and a unique set of skills and experiences. The University of Birmingham provides expertise around national research into health and social care policy priorities (including working to evaluate the national Building the Right Support programme), commissioning, people’s experiences of health and social care, and the implementation of new service models. Changing Our Lives brings extensive experience of working alongside people with learning disabilities and/or autistic people in long-stay and other settings to help them leave hospital and lead an ordinary life. They are also experts in working with people with a label of ‘challenging behaviour’ and people who do not communicate verbally.
In 2021, the NIHR asked us to consider extending the original research to include additional perspectives from social care (provided this was achieved within the timescales of the initial study). When our proposal was accepted in early 2022, we were able to supplement the original design by including the experiences of social workers, advocates and social care providers who support people as they leave hospital.
Chapter 2 Methods
Literature review
We conducted a formal review of the literature, identifying rates of delayed discharge for people with learning disabilities and/or autistic people in long-stay hospital settings, the methods used to identify such rates and the solutions proposed. This adopted the approach used in previous Department of Health/NIHR research into delayed transfers of care44 and the appropriateness of emergency admissions. 45 Studies were included if they reported original empirical data on rates of delayed discharge and were published from 1990 onwards (the year of the passage of the NHS and Community Care Act). An initial search was conducted by literature-searching specialists at the Health Services Management Centre (HSMC) Knowledge and Evidence Service (so that our search drew on detailed knowledge of the specific search terms utilised in each database and was therefore as broad and inclusive as possible at this initial stage). We searched the following databases (see Box 2 for sample search terms):
-
Applied Social Sciences Index and Abstracts
-
Health Management Information Consortium
-
MEDLINE
-
Scopus
-
Social Policy and Practice (including CareData, Social Care Online and AgeInfo)
-
Social Science Citation Index
-
Social Services Abstracts
The reference lists of articles included in this study were also searched, and an additional search of the ‘grey’ literature was undertaken via the websites of:
-
CQC
-
Centre for Welfare Reform
-
Challenging Behaviour Foundation
-
Children’s Commissioner for England
-
Department for Health and Social Care
-
EHRC
-
Health and Social Care Scotland
-
House of Commons/House of Lords Joint Committee on Human Rights
-
Learning Disability England
-
Learning Disability Wales
-
Mencap
-
Mental Welfare Commission for Scotland
-
National Audit Office
-
National Autistic Society
-
NHSE
-
Northern Ireland Assembly
-
Northern Ireland Audit Office
-
Scottish Commission for Learning Disability
-
Scottish Government
-
Scottish Learning Disability Observatory
-
Social Care Wales
-
Tizard Centre
-
UK Parliament
-
VODG
-
Welsh Audit Office
-
Welsh Government
-
Welsh Parliament
This also included a general Google search, using variants of terms such as ‘learning disabilities’, ‘delayed discharge’ and ‘hospital’, scanning at least 10 pages of search results for each of these combinations.
All abstracts identified were read independently by two members of the team (Glasby, J./Ince) and discussed in team meetings before inclusion. Alongside research studies, we included the most recent formal review for each of the four nations of the UK (rather than include all bulletins in an ongoing series of reports, for example, we included the most current reviews at the time of the search).
Included studies were summarised using the criteria for assessing the quality of material generated from diverse study designs proposed by Mays et al. ,46 extracting data on: rates of delayed discharge; the methods used to calculate these; the extent to which there has been engagement with people with learning disabilities and/or autistic people and their families, and with front-line staff; and the barriers/solutions identified. Specifically excluded were: material published and/or based on data collected prior to 1990; local inspections where findings had been summarised in a national report; additional articles reporting findings from studies already included in the review; admission to non-long-stay settings; and the admission of people with mental health problems (unless the person had learning disabilities and mental health problems). This initial review was designed to set the scene for the subsequent study, summarising the rate of delayed discharge identified in previous studies; the methods used to calculate such rates; the extent to which there has been engagement with people with learning disabilities and/or autistic people, families and front-line staff in conducting such research; the causes of delays; and potential solutions put forward.
Learning disabilities – People with learning disabilities; Learning disability; Learning disabilities; Learning disorders; Learning difficulties; Intellectual disability; Intellectual development disorder; Mental disorders; Mental impairment; Developmental disabilities; Autism; Autism Spectrum Disorder; Child & adolescent mental health; Autistic spectrum; Language development disorder; Mental handicap
Long-stay hospitals – Long-stay hospitals; Long stay patients; Mental health hospitals; Long stay units; Secure settings; Secure units; Medium secure units; Forensic; Psychiatric secure units; Segregation; Secure accommodation; ATUs; Assessment and treatment units; Treatment facilities; Hospitalization/hospitalisation; Hospitals; Hospital units; Hospitals, special; Hospitals, psychiatric; NHS in-patient; Child and adolescent mental health; CAMHS; Psychiatric units; Custodial institutions; Patient institutionalization; Assessment units; Inpatients; Institutionalization/institutionalization; Forensic psychiatric units; Hospital patients; In patients; Learning disability hospitals; Intellectual disability in patient units
Delayed discharge – Delayed discharge; Delayed hospital discharge; Delayed transfer of care; Appropriateness of stay; Blocked beds; Hospital stay duration; Discharge planning; Patient discharge; Hospital discharge; Timely discharge; Treatment duration; Length of stay; Hospital patients; Bed availability; Patient transfer; Long term care; Bed availability; Future plan; Shift of care
Case-study research
We worked with three long-stay hospital sites from across the country in order to conduct (see Figure 1 for an overview and Appendices 2 and 3 for all research materials):
-
in-depth work with up to 10 people with learning disabilities and/or autistic people and their families to understand their journey through services over time, their experience of long-stay hospital provision, the kinds of lives they would like to be living, and the barriers that are preventing them from leaving hospital;
-
focus groups with hospital staff (one group per site), with scope for individual interviews if a key person could not attend the focus group;
-
interviews with commissioners working with the people with learning disabilities and/or autistic people taking part in the research.
FIGURE 1.
Why are we stuck in hospital? (Overview).
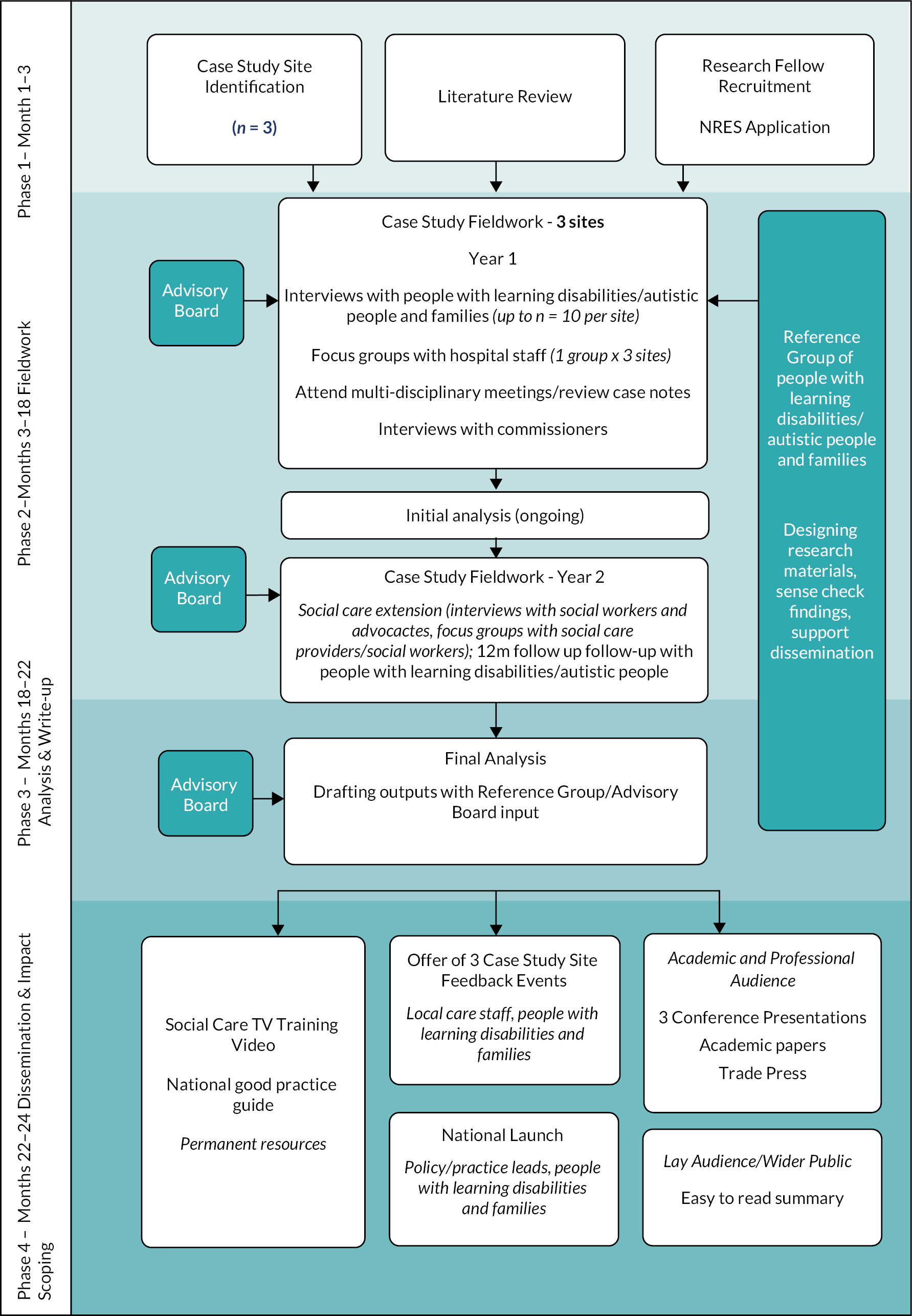
As part of a social care extension funded by NIHR part-way through the study, we supplemented our initial study with interviews/focus groups with the social workers supporting our participants and/or from the networks of advisory board members, as well as national focus groups with social care providers and interviews with advocacy organisations who support people in hospital.
Topic guides and a sample introductory letter/information sheet/consent form are set out in Appendices 2 and 3. While the latter had very minor changes in wording for the different groups taking part (e.g. a ‘declaration form’ rather than a ‘consent form’ for consultees), they were all written in an accessible style, and we have included the materials for people with learning disabilities as an example, rather than include all documents with only minor variations.
Inclusion/exclusion criteria
The study focused on people with learning disabilities and/or autistic people (aged 18 or over) in long-stay hospital settings (and included a family member, hospital staff and a commissioner for each person with a learning disability and/or autistic person who agreed to take part). With our subsequent social care extension, we later included a social worker for each person, as well as broader groups of social workers, advocacy organisations and social care providers who support people coming out of long-stay hospital (either working on a regular basis with our case-study sites or via partners’ national networks). While the definitions of ‘learning disability’ and ‘autism’ are seldom set out in national policy documents, we adopted definitions provided by the Valuing People White Paper (p. 14)47 and the National Autism Society (www.autism.org.uk/about/what-is.aspx):
-
‘Learning disability’ includes the presence of: ‘a significantly reduced ability to understand new or complex information, to learn new skills (impaired intelligence), with; a reduced ability to cope independently (impaired social functioning); which started before adulthood, with a lasting effect on development. This definition encompasses people with a broad range of disabilities’.
-
‘Autism’ is ‘a lifelong developmental disability which affects how people communicate and interact with the world’.
When defining ‘long-stay settings’ for people with learning disabilities and/or autistic people, our study followed the technical guidance issued by NHS Digital (https://digital.nhs.uk/data-and-information/data-collections-and-data-sets/data-collections/assuring-transformation) to define the long-stay settings which are the subject of its monthly statistical reports (as part of the Transforming Care programme):48
The collection will consider in-patients receiving treatment/care in a facility registered by the Care Quality Commission as a hospital operated by either an NHS or independent sector provider. The facility will provide mental or behavioural healthcare in England. Record level returns will reflect only in-patients or individuals on leave with a bed held vacant for them. This should include patients of …:
People not included:
The guidance from NHSE’s National Clinical Director for Learning Disability, regarding whether a patient should be included if they have a ‘primary diagnosis of Learning Disability’ only, is as follows: ‘For our purpose whether or not a person is recorded as having a primary diagnosis of LD is not relevant, and should not be used as a criterion for inclusion in this data collection. If a person is in specialist hospital bed (either MH or LD) and that person has a Learning Disability or Autism, then that person should be included in the Assuring Transformation data return.’
Our sample was therefore up to 30 people with learning disabilities and/or autistic people, with additional interviews/focus groups undertaken with a family member, care staff, a social worker and a commissioner relating to each person, and advocacy organisations and social care providers working to support people coming out of long-stay hospitals (either working with our three case-study sites, or recruited national via the networks of membership organisations such as VODG, Care England and Learning Disability England). There were no additional inclusion/exclusion criteria for these groups, other than that hospital staff and commissioners are closely involved in the care of the 30 people taking part, and that advocacy organisations/social care providers/social workers are either active in our case-study sites, working directly with our participants or volunteered to take part via national networks of Advisory Board members.
Case-study selection
Case studies were selected to include each of the main current service models and sectors (at least one ATU, one forensic unit, one NHS inpatient unit and one independent provider). These sites also included people with experience of long-term seclusion and segregation, and people with experience of the criminal justice system. While choice of sites was to some extent opportunistic (depending in part on willingness to grant access), we sought sites from different areas of the country and based in different localities in terms of factors such as affluence, ethnicity and rurality. Participating wards included a mix of male/female provision and a mix in terms of levels of security. Participants included a mix of people with learning disabilities and autistic people, some people with experience of the criminal justice system, and some people with experience of long-term seclusion and segregation. People also came from different health and social care systems across the country, and many had been in a number of different hospitals over many years (see below for further details). While all participants were aged 18 or over, some were young adults who were also reflecting on some experiences from before the age of 18. While some people came from minority ethnic communities, our sample was largely from a white UK background (see Chapter 7 for further discussion).
Clinical engagement
Having secured NHS research ethics and local approvals, we worked with lead clinicians in each site to seek their professional opinion as to who could consent to take part, and who might need a ‘consultee’ (usually a family member) under the Mental Capacity Act. This is an approach which we adopted in our ‘Who Knows Best’ research into older people’s experiences of emergency hospital admissions, and it was helpful in ensuring local ownership of the research and providing additional clinical expertise and insight (above and beyond the clinical experience of the research team). These leads gave our introductory letter to everyone on the ward, so that only members of the direct care team initially approached potential participants in the first instance. The introductory letter had a reply slip to confirm that the person was interested in finding out more and potentially exploring participation, and this was returned to the research team by the local lead.
Working with people and families
We chose a research team which is skilled at working with people with learning disabilities and/or autistic people and their families in long-stay settings, at working sensitively and ethically with issues of capacity/consent, and at designing accessible information. Making sure that we followed local/national COVID guidance around hospital visitors, we based ourselves in one or two wards/units per site, interviewing all people with learning disabilities and/or autistic people (or consultees) who agreed to take part. Subject to permission and depending on family circumstances, we also carried out an online interview of a family member. Our research team was experienced at working in situations where the person and their family have different views about what is best, or where there are tensions between families and care staff – and we made sure that our interviews enabled people to tell their stories and share their experiences, rather than our having to agree one single version of ‘the truth’ (thus allowing for multiple perspectives, rather than one person’s viewpoint potentially dominating).
Our approach differed according to the ward and people we were working with. In some sites, we were able to base ourselves on the ward for several days, getting to know the service in question, minimising potential disruption and allowing people to approach us if and when they felt comfortable to do so. People could then talk to the researcher direct and agree a time when they felt able to be interviewed. Where it was not possible/permitted to have such open access to the ward, a more formal approach to organising the interviews was adopted (e.g. working with care staff who would work with people on the ward to agree times to meet). People living on one ward also wanted to invite us to their regular ‘patients’ council’ before individuals decided whether or not to take part. In all instances, we were extremely aware of the difficult circumstances people were experiencing and were as flexible as possible to ensure we spoke to people at a time that worked best for them, often returning to see someone on multiple occasions if they did not feel like speaking to us on a given day. We also spoke to ward staff, familiarising ourselves with people’s preferred style of communication before beginning conversations.
During these interactions, which sometimes took place over several visits, we asked people about why they thought they are in hospital/still in hospital; how they felt about it; what they wanted their life to be like/why they thought their life isn’t currently like that; and what would help them, or others, leave hospital more quickly. Where we had spoken to people early enough in the project, we then repeated this 12 months later to get a sense of what had changed (or not) over time. Where people did not communicate verbally, we used other forms of communication, such as ‘talking mats’ (see Box 3) and art, utilising whatever communication mechanisms the person preferred. With permission from the participant, we also interviewed their family, attended multidisciplinary review meetings and reviewed hospital case notes.
We designed a ‘talking mat’ to be used in the discussion around what was helpful in moving people on. First of all, people from our Reference Group talked about what had helped them leave hospital. These suggestions were then incorporated into the talking mat, with each suggestion represented in a picture. People taking part in the research were offered each picture in turn and asked to place it on a different place on the mat, depending on whether they thought that element helpful for moving on, not helpful or not sure. There were also some blank cards so that people could add their own suggestions.
The talking mat worked particularly well in capturing the views of a participant with selective mutism. Here, the researcher sat on the floor with the mat and the pictures. As each one was held up in turn, the person used their foot to point to where they wanted it to be put on the mat.
For those who did not wish to use pictures, the same ideas were presented in words and the person sorted them into piles, according to what they found helpful and not helpful.
Even where people communicated verbally and were felt by staff to be fully able to take part in interviews, we found that the use of talking mats could help people structure their thoughts, express clear views and preferences and take a more active part in the discussion.
For practical examples from our research, see section What helps below. For information on talking mats more generally, see www.talkingmats.com/.
Staff perspectives
Hospital staff
For staff perspectives, we carried out a focus group of hospital staff in each site. These explored how staff experience their work; how delays impact upon them; what support they would like; key causes of delays; and practical steps forward from a staff perspective. When engaging with staff, we sought to include front-line members of the immediate ward/care team (e.g. support workers and nurses on the unit), as well as members of the wider clinical team (psychologists, psychiatrists, physios, OTs, social workers etc.). Focus groups were particularly helpful here, as they enabled people from different professional backgrounds to interact and, wherever possible, reach a degree of consensus around key issues. To guard against the dangers of front-line staff feeling unable to speak freely, we also offered the opportunity to have an individual interview if this would help them to feel more comfortable contributing their views and experiences. While we were intending to carry out focus groups face-to-face, COVID restrictions meant that these took place online.
In addition to these focus groups/interviews, we also reviewed each person’s case file and observed a series of multidisciplinary decision-making meetings relating to as many of our participants as possible. These were designed to help us better understand people’s journey through services and the local context – so were more for background/preparatory purposes, than to collect or report new data.
Interviews with commissioners
Once the person with a learning disability had consented to take part, the hospital care team contacted commissioners with an introductory email, information sheet and consent form. Interviews took place by telephone or online (Teams/Zoom).
Interviews/focus groups with additional social care participants
Having received agreement from NIHR that we could extend the study to include additional social care perspectives, we carried out online interviews with social workers allocated to each of our participants. In one site, the provider had in-house social care staff who helped co-ordinate discharge from the hospital perspective, so we interviewed them as well as social workers based in local authorities. We also carried out online interviews/focus groups with advocacy organisations and social care providers supporting people to leave hospital (recruiting both those active in our case-study sites, and from organisations which are part of our Advisory Board/their memberships). Because of the diverse nature of our Advisory Board, this meant that we included a range of organisations providing statutory advocacy (e.g. Independent Mental Health Advocates) to a whole ward, site or geographical area; potentially smaller organisations that work with particular individuals in a very person-centred and bespoke way; and a mix of local, regional and national providers across the voluntary, community and private sectors. Our interviews with social workers were also supplemented by national focus groups with social workers connected to the British Association of Social Workers (BASW) work around ‘homes not hospitals’.
Data analysis
Interviews/focus groups were recorded using an encrypted recorder (after obtaining security clearance to use such devices in locked settings) and transcribed by a professional transcription company. The research team also kept detailed records of their time on the ward, insights from case notes and observations from review meetings, building up an in-depth picture of what the person’s life was like, what kind of outcomes they were seeking, what sort of support might work best for them, barriers to leaving hospital, and possible ways forward. These notes were hand-written and were made as soon as possible after each visit (given that pens were not allowed in some sites). Where the person taking part did not want the interview recorded or the discussion could not be transcribed due to the nature of the person’s speech/communication, we drew in detail on such notes (making sure that these were much more extensive than in situations where notes were only really accompanying the formal transcript of the interview).
Data were analysed using the framework approach,49 identifying key themes from the data and constantly checking back to refine emerging themes and to ensure that these continued to represent the data. 50 Initial codes were developed (by Ince, in discussion with Glasby, J./Glasby, A.) after team meetings to share emerging informal themes (which were also sense-checked with our Advisory Board and Reference Group). Final codes were then agreed by consensus in regular team meetings, with two members of the team (Ince and Konteh) each independently coding the same initial six interviews and meeting to compare their experiences and the outcomes of this process. After this was found to be yielding a consistent approach, the remaining transcripts/notes were coded by one researcher only (Ince or Konteh), but with regular team meetings and a half-day analysis workshop to take stock of key themes and compare back with the original data. In later chapters, we label each quote with a letter for the case-study site (A, B, C) and according to whether the participant was a person with a learning disability (‘PLD’), family member, commissioner, social worker or advocate. Thus, for example, A6 PLD would be the sixth person with a learning disability and/or autistic person we interviewed in site A. Focus groups with hospital staff, care providers or social workers are labelled as ‘Provider focus group 1’ etc.
While we were sensitive to the possibility of very different views being expressed by different professionals in our hospital focus groups in particular, the overall themes that emerged tended to be very consistent, with the focus groups easily reaching a shared consensus. The main exception to this was around rates of delayed hospital discharges (see Different professional perspectives). Thus, quotes reported from focus groups are similar to quotes from interviews, typically representing a shared view from participants.
In our main findings chapters (see Chapters 4–6), we tend to highlight a key finding, then provide more detailed quotes to illustrate the issues at stake. Because we are focused on people’s lived experience and the practice knowledge of staff, we include longer quotes than may sometimes be the case in other types of research to maintain the richness and detail of people’s responses.
Drawing on lived experience and working with policy/practice partners
To ensure that our research was informed by lived experience, we worked with a Reference Group of people with learning disabilities and/or autistic people and their families to co-design our approach, sense-check findings and support dissemination. We recruited this group from initiatives such as the Sandwell Learning Disability Parliament (people with learning disabilities working together to improve local services), people with previous experience of leaving long-stay hospitals and people from previous Changing Our Lives projects such as Sky’s the Limit (supporting young people with complex needs to lead ordinary lives away from institutional settings). To make sure that this was a diverse group, we also built on a leadership development programme which Changing Our Lives runs on behalf of young adults with learning disabilities and from black and minority ethnic communities. Reference Group members were reimbursed for any expenses, paid for their time at INVOLVE rates, and received appropriate support for the tasks in which they were involved.
While we had initially intended to facilitate a national group on a face-to-face basis, COVID restrictions meant that we started by working with people one-to-one. Although this had not been our original plan, it enabled people from all across the country to take part (including from some very isolated health and social care communities, who might have found it difficult to be a member of the group if it was meeting in a single, central location). After starting one-to-one, we later brought a series of smaller groups together in order to begin moving from individual to more collective perspectives, with a mix of online and face-to-face meetings. Early on, our focus was on how we could describe the aims of the research to people in an accessible manner, and ways of making sure that people really understood that their participation might not mean that they themselves could leave hospital – but might benefit others. Later on, the role of the Reference Group was to sense-check emerging findings, and to help explain key themes in ways that would be as accessible as possible to people with learning disabilities and/or autistic people. Members of the Reference Group also contributed directly to our policy and practice outputs (e.g. being interviewed as part of our training video, helping to design an easy-read summary, narrating video summaries etc.).
We also worked with a national Advisory Board, chaired by a disabled person, to help secure access to case-study sites, advise on the development of policy/practice outputs and support dissemination. This included senior representation from the Social Care Institute for Excellence (SCIE), Think Local Act Personal (TLAP), NHS England/Improvement (NHSE/I), Learning Disability England, VODG, the Association of Directors of Adult Social Services (ADASS) and the Challenging Behaviour Foundation, as well as senior clinical, legal and academic experience (see Appendix 1). As we extended the study to include additional social care perspectives, representatives joined from BASW and Care England. Advisory Board members were also offered the opportunity to jointly badge our proposed outputs in order to maximise impact.
Dissemination and anticipated impact
We sought to plan how we would work with our findings and embed them in policy/practice from the outset, committing to:
-
hold a national launch, inviting key national policy/practice leads, people with learning disabilities and/or autistic people and families to an event which sets out findings/explores key implications;
-
summarise findings in an easy read version for people with learning disabilities and/or autistic people;
-
offer a feedback event to each case-study site, involving local staff, people with learning disabilities and/or autistic people and families;
-
create a short but attractively produced guide to tackling delayed discharges, drawing in particular on the experiences of people with learning disabilities and/or autistic people and their families; this may be jointly badged with partners from our Advisory Board, and will be sent to every Director of Adult Social Services/NHS Chief Executive in England;
-
produce a free training video for ‘Social Care TV’ (online resources used by SCIE to reach care staff who may not otherwise have access to formal training opportunities);
-
disseminate via articles in the trade press, academic papers and relevant academic/practice conferences.
Part-way through the project, we won additional funding from the University of Birmingham’s ESRC Impact Accelerator Account to work with a local gallery (The Ikon) to commission a leading artist to produce an original installation/exhibition to amplify the voices of people with learning disabilities and/or autistic people from our study (Murray;51 see also www.ikon-gallery.org/exhibition/why-are-we-stuck-in-hospital and our project webpage for more details).
Ethical issues and approvals
We sought research sponsorship from the University of Birmingham’s Social Sciences Research Ethics Committee, ethical approval from a Health Research Authority Research Ethics Committee, and local R&D approval from case-study sites. The research team was experienced at conducting complex health and social care research in difficult environments, at working sensitively and ethically with issues of capacity/consent in ways which enable people who are seldom heard to take part in research, and at working at the pace of individuals with particular communication needs. We conducted the research in a way that valued the voices and experiences of people with learning disabilities and/or autistic people, their families and front-line staff, whilst also recognising the need to minimise potential distress, be respectful of the complexities of life in long-stay settings and ensure safety for everyone involved (e.g. in situations where people may have behaviour that is labelled as challenging services).
All participants were given information about the research (including in accessible formats) and we regularly checked that they understood the aims of the study, consented to take part and were clear on key rights. In particular:
-
participation is voluntary, with no negative consequences from not taking part;
-
people may withdraw at any time prior to the completion of our final report without giving a reason – if they choose to withdraw, their data will not be used;
-
we would have to contact social services if we had any safeguarding concerns (NB this did not transpire in practice).
We did this on an ongoing basis in situations where capacity might fluctuate, checking back over previous conversations, understandings and agreements each time we met. After completing an initial reply slip to signal potential willingness to take part, participants received a more detailed information sheet, and were asked to sign a consent form at the time of interview. Where a lead clinician assessed someone as unable to consent to take part in the research, they approached a consultee on the person’s behalf. In the case of families, consultees, care staff and commissioners, the introductory letter, information sheet and consent form were given by the local lead clinician or a relevant member of the care team, and people who wanted to take part replied to the research team. Part way through the study we sought an amendment to our ethical approval for the research team to contact commissioners directly, given that invitations from hospital staff had not yielded many responses and mindful of the fact that these were senior managers who we felt would feel comfortable declining to participate if they did not wish to take part.
To make sure our research was safe, we:
-
completed university risk assessments;
-
ran training for the research team around being safe in long-stay settings, handling difficult conversations, behaviours that can escalate/de-escalate anger/frustration, and principles of safe practice;
-
consulted with case-study sites around any individuals or parts of the ward we should avoid and any known ‘triggers’ for people on the ward, taking any advice given (e.g. it may not be appropriate for a female researcher to be with a particular person on their own);
-
ensured we were inducted into local procedures around how to respond if there is a serious incident and where exits are and how to exit a locked area safely;
-
spent time on the unit/ward so that people got to know us gradually and are not made nervous by the presence of ‘strangers’ asking questions;
-
undertook ‘managing aggression’ training (which was a requirement for access to one of the sites).
Any recordings were made with an encrypted recorder, with data transferred to password-protected university computers and uploaded to university servers at the earliest opportunity. The recording was then deleted from the audio recorder. Interviews and focus groups were transcribed by a professional transcription company from a list of approved university suppliers, with a confidentiality agreement in place. Where an interview was not audio-recorded (e.g. if the person did not communicate verbally), we made detailed hand-written notes, transferred these to a password-protected computer as soon as possible and destroyed the notes. All data were kept on password-protected university laptops, on university servers or (for manual files) in a locked office at the University. When Changing Our Lives staff made any computer notes or were working on draft reports, they were working with anonymised data and transferred any materials to university servers at the earliest opportunity, deleting these files. Data transfer took place using secure university systems (known as ‘BEAR Data Share’). Personal data were destroyed at the end of the project (24 months), with any other data to be destroyed after 10 years. The document linking personal data to anonymised findings was kept on a password-protected university computer.
Success criteria and potential barriers
In designing this research, we were mindful of potential risks/barriers (many of which are reasons why similar research has not previously been undertaken) and had active plans in place to mitigate these (see Tables 1 and 2). In both tables, the nature and experience of the research team, the complementary nature of the skills of Changing Our Lives and the University of Birmingham, senior support from members of our Advisory Board and our prior experience of the NIHR ‘Who Knows Best’ study were key aspects of our approach.
| Selected (top 5) risks/barriers | Mitigating factors/steps |
|---|---|
| Difficulty recruiting case-study sites in challenging policy/practice context | Active support of Advisory Board (especially NHSE and Learning Disability England); strong profile and links of research team; ability to work in challenging/sensitive settings; anonymisation of case-study sites to prevent reputational risks |
| Difficulty recruiting people with learning disabilities and/or autistic people and families | Experience of working with people with learning disabilities and/or autistic people and families in long-stay settings; strong networks/practice links; support from active and senior Advisory Board; ability to work in sensitive, ethical ways, taking time to build trust and relationships; support of Reference Group in designing appropriate materials |
| Difficulty recruiting care staff/commissioners | As above |
| Complexities of engaging people with learning disabilities and/or autistic people in research (especially where people do not communicate verbally or have behaviour that challenges services) | Skilled/experienced research team. Changing Our Lives in particular has been selected as a partner for this research due to its long-standing/in-depth track record in this regard |
| Risk of violence/aggression towards research staff | See above (under ‘ethical approvals’) for practical steps around ensuring safety |
| Success criteria | How these will be delivered/met |
|---|---|
| Identification of skilled/experienced research team | Already assembled/set out in the initial proposal |
| Appointment of high-quality Research Fellow with experience of working with people with learning disabilities and/or autistic people | Successful track record of research team in previous studies; networks of applicants/Advisory Board |
| Securing research sponsorship (UoB), ethical approval (HRA) and local R&D approval | Experienced team comfortable working with issues of capacity/consent and in long-stay settings, with strong track record of securing ethical approval in timely fashion in previous studies |
| Creation of high-profile/influential Advisory Board (chaired by a skilled facilitator who is also a disabled person) and Reference Group of people with learning disabilities and/or autistic people and families | Advisory Board already assembled, with senior commitment from key national bodies, chaired by Siraaj Nadat BEM. Reference Group to be assembled from the Sandwell Learning Disability Parliament, people with previous experience of leaving long-stay hospitals and people from previous Changing Our Lives projects such as Sky’s the Limit (supporting young people with complex needs to lead ordinary lives away from institutional settings) |
| Three case-study sites signed up to the research, achieving the proposed number of participants | See above for approach to recruiting case-study sites and working with people/families/staff |
| Collection of proposed data within project timescales | See above for details of project management, roles and responsibilities, as well as online CVs (for details of prior successful delivery) |
| Quality of data analysis | See above for approach to data analysis, and see online CVs for prior track record of research team |
| Launch of high-quality outputs (academic and policy/practice) | See above/online CVs for practical examples of impactful policy/practice outputs and high-quality academic outputs |
| Delivery of project on time/to budget | See online CVs for details of prior successful delivery |
Chapter 3 Literature review
Overview of included studies
There were a very limited number of outputs which met the inclusion criteria (see Figure 2 and Table 3). Considering this is such a long-standing policy priority, this topic seems to be significantly under-researched, with existing claims to knowledge limited to a handful of very context-specific studies and national monitoring exercises (many of which have a number of methodological limitations). Overall, 13 research studies met our criteria (of which one – Thomas et al. 52 – came from the reference list of a study that had been identified in the initial searches – Beer et al. 53), together with five national reviews (see Figure 2). Of the 13 studies, 11 were based on bed census or retrospective case-note analysis and did not include qualitative data. Three of the 13 tested a hospital discharge protocol54–56 and often dealt with delays in a more indirect/implicit manner (e.g. the protocol seemed to significantly reduce delays, hence implying that there were significant delays before the project). Only five of the research studies involved front-line practitioners such as nurses or doctors in the research. Settings included both open and secure wards, large hospitals, small rehabilitation units, ATUs, whole Trusts, single wards and national overviews.
FIGURE 2.
Overview of included studies.

| Authors and date | Population/setting | Length of stay or delay (where included) | Rate of delayed discharge |
|---|---|---|---|
| Alexander et al. (2011)60 | 138 patients in a 64-bed forensic service over a 6-year period | Median length of stay for the discharged group was 2.8 years (1025 days), 75% staying for less than 5 years | Of 61 patients who were still inpatients, 36 (59%) were considered ‘difficult to discharge long-stay’ patients |
| Beer et al. (2005)53 | 200 inpatients across 20 low secure units (8 were for people with learning disabilities) in the South Thames region | 66 (33%) people were inappropriately placed; of these, 60 needed less security | |
| CQC (2020)61 | In-depth reviews of 66 people as part of inspection visits to a wide range of mental health and learning disability services | Discharge prevented due to lack of community services for 60% of the 66 people they met | |
| Cumella et al. (1998)57 | 21 patients admitted for more than 3 months to an acute admissions facility in North Warwickshire | Mean length of stay beyond treatment needs estimated at approximately 6 months | 18 out of 21 people (86%) |
| Devapriam et al. (2014)54 | 16-bed specialist learning disability inpatient unit for people with learning disabilities | 29% (14 out of 49 people) | |
| Dickinson and Singh (1991)62 | Specialist ‘mental handicap hospital’ in London | Average length of stay for ‘new long-stay’ cohort was over 2 years | 57 (55%) of 104 admissions were deemed ‘new long-stay’ patients (resident for over 12 months) |
| Kumar and Agarwal (1996)63 | ‘Mental handicap hospital’ in south of England | 68.4% (188/275 people) considered suitable for discharge to a small home with minimal supervision; 72 (26%) suitable for discharge, but some difficulties in management likely | |
| MacDonald (2018)64 | All but one Health and Social Care Partnerships in Scotland | More than 22% over 10 years; 9% for 5–10 years. Many people didn’t answer, but 13 people were delayed for 1 year+, and 10 people who were delayed had placements costing over £150,000 p.a. Only 51% had active discharge plans | 67 people |
| Mental Welfare Commission for Scotland (2016)34 | All 18 hospital units in Scotland – 104 people’s records (half of those in Scottish services) | 50% over 3 years; just over 20% over 10 years | Nearly one-third of current inpatients (32%) across Scotland were delayed discharges |
| Mills et al. (2020)35 | 256 patients with learning disabilities in units managed directly by, or commissioned by, NHS Wales (across 55 units) | Mean (all patients) – 5.2 years current admission; 53% over 2 years; 19% over 10 years. 18% of current costs (5.994 million) could be reinvested in community services if all people who could be transitioned were transitioned | 80 (54%) people could be considered for transition |
| Nawab and Findlay (2008)55 | Small nine-bed ATU in Lanarkshire | 74% of all admissions = 1 week to 3 months; 20% = more than 3 months; 5% = more than a year | 11% (18) considered delayed discharge |
| Oxley et al. (2013)58 | Two small inpatient units (total of 12 beds) in London (1999–2001 vs. 2009–2011) | Mean length of stay: period 1 = 198.6 days (6 months); period 2 = 244.6 days (9 months) | 67% (40/60) in period 1; 59% (24/41) in period 2 |
| Palmer et al. (2014)65 | All of Northern Ireland’s learning disability hospital inpatient population, mostly at Muckamore Hospital Belfast | Average length of stay 6.2 years (includes short stays of days or weeks – so some must be very long) | No rate of delay reported, but on 31 March 2014, 24 of 30 people from the Delayed Discharge List (people admitted for assessment and treatment) devised in 2011 were still not resettled; and in March 2015, 49 people on the Priority Transfer List (long-term inpatients over 12 months) still required resettlement |
| Perera et al. (2009)66 | All 15 Health Boards in Scotland (range of settings) | Nearly half (47.9%) had been inpatients for more than 5 years | 68 (17.52%) had delayed discharges |
| Taylor et al. (2017)56 | Offenders with learning disabilities in an 18-bed locked rehabilitation unit in Northeast England | See ‘rate of delayed discharge’ column for changes in length of stay | This is an evaluation of a discharge protocol, so no rate of delay given. However, the mean length of stay reduced by over 60% from 39 months (3 years 3 months) to 14 months (1 year 2 months) during the project (implying a degree of delay). The rate of discharge was 7, 6 and 8 people over the first 3 years of the study, jumping to 16 discharges following use of the protocol (again implying previous delays) |
| Thomas et al. (2004)52 | 102 offenders with learning disabilities in all high-security hospitals in England | Mean = 10.26 years; median = 8.5 years | 32 (31%) did not need this level of security (different professionals disagreed on another 16 patients) |
| Washington et al. (2019)59 | Two 21-bed ATUs in North England | Mean admission length = 151 days | Just over 50% (36/70) experienced delayed discharge |
| Watts et al. (2000)67 | Learning Disability Trust in Northeast England | At follow-up 16 months later, 23 of the 44 patients identified as delays remained in hospital | 44 (18%) out of 247 patients were delayed |
Rates of delay
Rates of delay varied significantly depending on location, setting, population studied and methods adopted (see Table 3). However, it is impossible to compare rates between different studies, given a wide range of definitions of ‘delay’, as well as a number of implicit definitions and/or proxy measures (see Table 4).
| Authors (date) | Definition |
|---|---|
| Alexander et al. (2011)60 | ‘Difficult to discharge long-stay’ group = stay longer than median for discharged group (2.8 years) |
| Beer et al. (2005)53 | Being in an ‘inappropriate’ placement – i.e. needing different levels of security |
| CQC (2020)61 | No formal definition: implied in relation to length of stay, length in segregation, readiness for transition |
| Cumella et al. (1998)57 | ‘Bed blockage’ – appropriate for discharge but not able to be discharged |
| Devapriam et al. (2014)54 | Medically fit for discharge but they are unable to leave hospital because arrangements for continuing care have not been finalised (p. 211) |
| Dickinson and Singh (1991)62 | ‘New long-stay’ patient – resident over 12 months |
| Kumar and Agarwal (1996)63 | Nurses asked whether ‘the patients could be discharged and managed in the community with minimal support or were likely to require prolonged inpatient treatment’ (p. 64) |
| MacDonald (2018)64 | A hospital inpatient who is clinically ready for discharge from inpatient hospital care and who continues to occupy a hospital bed beyond the ready for discharge date (p. 11) |
| Mental Welfare Commission for Scotland (2016)34 | We regard them as being kept in hospital when this is recognised as no longer the best place for them to be living (p. 18) |
| Mills et al. (2020)35 | Implied: readiness for transition |
| Nawab and Findley (2008)55 | Clinically fit for discharge but cannot move on from the unit for other reasons (p. 91) |
| Oxley et al. (2013)58 | A delayed transfer occurs when a patient is ready for transfer from a general and acute hospital bed but is still occupying such a bed (p. 37) |
| Palmer et al. (2014)65 | Identified as ready for discharge but there is nowhere for them to go (p. 35) |
| Perera et al. (2009)66 | When a patient, clinically ready for discharge, cannot leave the hospital because the other necessary care, support or accommodation for them is not readily accessible and/or funding is not available (p. 167) |
| Taylor et al. (2017)56 | Inpatients that are clinically fit to leave hospital (p. 144) |
| Thomas et al. (2004)52 | Implied as people who could move to a lower level but remain at higher security than needed |
| Washington et al. (2019)59 | When the original aims of the admission had been met and the length of stay exceeded the recommendations of the Learning Disability Senate (p. 28). The Learning Disability Professional Senate (2016) stipulated specifically that 75 per cent of admissions should be discharged within 3 months and 90 per cent should be discharged within 6 months (p. 25) |
| Watts et al. (2000)67 | Ready for discharge and able to cope in the community with appropriate support, but could not be discharged (p. 179) |
The highest rate of delay was 86% (18 of 21 patients) reported by Cumella et al. 57 in an acute admissions unit intended for shorter stays. Similarly, Oxley et al. 58 and Washington et al. 59 found almost 63% and over 50% of patients delayed in similar ATU settings. These very high rates are due to the expectation that these settings are not intended for stays of longer than a few months, but often ended up with people resident for years, sometimes becoming de facto long-stay settings. On the other hand, Nawab and Findley55 reported only 11% of patients as being delayed.
This was also an ATU, but here 74% of people stayed less than 3 months, suggesting considerable variation, either in service model and/or performance.
In studies of secure settings, rates of delay were reported differently – often based on the appropriateness of the setting or level of security for the patient’s needs. These rates were still very high: for example, 32% of patients in a low-security unit needed less security,53 while a similar proportion of people could be considered for transfer in a high-security setting. 52 In the medium-secure setting explored by Alexander et al. ,60 59% of people were considered ‘difficult to discharge long-stay patients’ (i.e. with a longer median length of stay than those discharged).
In studies based in general wards or a range of different service settings, rates of delay were still significant, ranging from around 18%66,67 to 29%54 and 32% in one of the reviews conducted in Scotland. 34 In CQC’s review across England, 60% of discharges were delayed due to problems finding community placements:
A lack of suitable care in the community prevented discharge for 60% of people we met. Most people in long-term segregation needed bespoke packages of care in the community, but this was difficult to achieve.
(CQC, 2020, p. 29)61
Those reporting proxy measures of delayed discharges identified even higher rates: Kumar and Agarwal63 found 68.4% of people were considered ‘suitable for discharge’ (but still in hospital), while Mills et al. 35 found 54% of people across Wales ‘could be considered for transition’.
A small number of studies also report the extent of delays: MacDonald64 found 67 people in ‘out of area’ placements (i.e. not within the local authority where they lived) across Scotland were considered to have delayed discharges, one-third of them for over a year. In Northern Ireland, Palmer et al. 65 found that of 30 people on a delayed discharge list, only 6 had been discharged between 2011 and 2014, leaving 24 people still delayed in hospital (and a further 25 new admissions since 2011 also delayed). Devapriam et al. 54 also noted the extent of delays at different stages of the discharge process, with the majority of people being delayed for an average of 4 months – but for one patient over 2.5 years – at the first stage of assessment and identifying a suitable placement.
Throughout these studies, there is no consistency as to how delays are defined (see Table 4), making it impossible to meaningfully compare results and gain an overview of delayed discharges across the UK. The majority of studies adopt either an explicit or an implicit definition that sees a ‘delayed discharge’ as occurring when a person stays in hospital after they have no clinical need to remain. However, studies in secure settings often focus on whether someone could be transferred to a less-secure setting (even if they remain an inpatient), and national reviews suggest that some people discharged from hospital are actually transferred to other hospitals (not really a ‘discharge’ at all in lay terms). Some studies use the terminology ‘difficult to discharge’60 or assume that lengths of stay exceeding a particular limit indicate a delay by default. 59,60,62,67 These varying interpretations generate important questions about subjectivity and perspective: in whose view is a person ready to move on? Who assesses whether the level of restriction is appropriate or what length of stay is excessive for different settings, and on what basis (see below for further discussion)?
Broader length of stay
Lengths of stay are sometimes reported either as context or as a proxy for delays, and in different ways. Some studies report the proportion of people staying for different lengths of time, while others report mean or median lengths of stay, and some a combination (see Table 4). Oxley et al. 58 also reported a longitudinal change in length of stay, with median stays increasing from 6 to 9 months across 4 years. Length of stay ranged significantly between settings – for example, ATUs or similar settings had shorter lengths of stay than secure settings, ranging from weeks55 to median stays of 3–6 months. 58,59 What is notable, however, is the large proportions of people staying for many years: secure settings reported a large number of people staying more than 5 years, including 42% of people staying over 5 years and 11% over 10 years in a medium-secure setting,60 mean lengths of stay in a locked rehabilitation unit of over 6 years (for those now discharged, Taylor et al. 56) and mean lengths of stay of over 10 years in a high-security setting. 52 In studies reporting across a range of settings, more than half of people were often staying more than 5 years. 35,65,66 In Scotland, the Mental Welfare Commission for Scotland34 found around 70% of people staying longer than 3 years. Where lengths of stay are reported as an average, of course, the inclusion of a number of short-stay settings means that some people experience very lengthy inpatient stays, sometimes reaching into decades.
‘Explaining’ delayed discharge
The range of reasons given for delayed discharges are shown in Table 5, and cover those associated with individual characteristics as well as those pertaining to the discharge process and wider system. In many ways, this is similar to Glasby’s41 review of delayed hospitals discharges from general hospitals, which explored individual, organisational and structural issues at stake, and argued for the need to work across multiple levels at the same time.
| Authors (date) | Reasons for delayed discharge – characteristics | Reasons for delayed discharge – process/system issues |
|---|---|---|
| Alexander et al. (2011)60 | More criminal sections and restriction orders; history of fire-setting; having suffered abuse; diagnosis of personality disorder; history of substance misuse | |
| Beer et al. (2005)53 | Factors that might predict a delay were being young, being admitted on an informal basis, and not having ‘overactive’ as a reason for admission | May be knock-on effects at different levels of security: ‘discharge problems at lower levels of security fail to free up low secure beds, creating discharge problems at higher levels of security’ (p. 635) |
| CQC (2020)61 | Re-traumatising and increased needs after failed community placements | Funding – availability, complexity and accessing, disputes over responsibility; commissioners’ fears over high levels of risk and cost in community; lack of appropriate care in the community |
| Cumella et al. (1998)57 | One person’s parents had left the country | Lack of places in suitable specialist accommodation or day care (13 people); funding disputes between NHS and local authority (4 people) |
| Devapriam et al. (2014)54 | Awaiting assessment of future needs and identifying suitable placement – 7 people (50%); awaiting social services funding or agreement – 4 people; the remaining 3 people were delayed due no suitable placement available or legal issues | |
| Dickinson and Singh (1991)62 | Psychiatric factors (increased previous admissions, family history and diagnosis of psychosis and dementia) and social factors (deceased parents and an inability to be discharged back to place of admission, particularly if admitted from home) | |
| Kumar and Agarwal (1996)63 | Of those suitable for discharge but who might be difficult to manage in the community, reported reasons/needs were: aggressive behaviour (24.5%), violent behaviour (8%) and self-injury (6.4%) | Staff attitudes; previous experiences of the successes/failures of resettlement |
| MacDonald (2018)64 | Primarily male; 40% had mental health problems (most commonly bipolar disorder, anxiety, depression, schizophrenia); nearly 75% currently had challenging behaviour, over two-thirds including physical aggression | Lack of accommodation (51%); lack of service providers (15%); other factors included legal/funding/geography issues |
| Mental Welfare Commission for Scotland (2016)34 | Complex needs requiring specially commissioned service (e.g. 24/7 care with 1 : 1 or more staff); deterioration in the person’s mental or physical health; needs escalate/incompatibility with other residents/placement becomes unsuitable | Funding (41%); housing (74%); no appropriate care provider (62%) (not mutually exclusive). Other reasons include lost places due to timing of available local authority funding with available appropriate placement; or delays in adaptations to properties, allocating a social worker, assessments, recruitment and training of support staff, and legal issues (e.g. guardianship) |
| Mills et al. (2020)35 | Factors in readiness for transition include: professional judgement; patient’s opinion; safety/risk to self/others; level of need and complexity etc. | |
| Nawab and Findley (2008)55 | Difficulty with placements – funding issues or lack of appropriate resources in the community (13/18); physical health – needing transfer to appropriate services (5/18); introduction of discharge/admission protocols saw shorter stays/more discharges | |
| Oxley et al. (2013)58 | Lack of identification of suitable placement – 69% of delayed discharges in 2009–2011, 44% in 1999–2001 | |
| Palmer et al. (2014)65 | Small number of new services and bed spaces created; lack of coordination between health, housing and social services; misalignment of funding streams; absence of an overall resettlement plan (e.g. monitoring, procurement); weak engagement by Trusts with patients and families; difficulty commissioning individual complex needs across health, social care and housing programme | |
| Perera et al. (2009)66 | 47% (32) – due to social care reason (people awaiting assessment, or waiting for commissioning of services); 5% – due to healthcare reason; 47% (32) – no suitable facility available in the community/service development needed | |
| Taylor et al. (2017)56 | No reasons given but positive feedback on protocol suggests issues in: - Clarity of process and roles, dedicated pre-discharge planning meetings - Partnership working – bringing departments together - Risk management training for staff (especially in community) - Extra clinical support post-discharge |
|
| Thomas et al. (2004)52 | Factors associated with continued need for high security: being younger, higher treatment and security needs, recent violent conduct, nature of initial offence | Most delays transferring to lower security were because a suitable placement did not seem to exist; others were due to funding issues, no bed available or not accepted (unsuitable services) or Home Office issues |
| Washington et al. (2019)59 | Individual characteristics acting as a barrier to discharge were only identified for 3% of delays (continuing mental (and physical health) difficulties) | For 83% of patients, delay was due to failure to source funding or find an alternative care provider. The remainder were delayed due to: placement/accommodation not ready; new trigger to mental health difficulties; finding a specialist bed; recruiting support staff to the provider |
| Watts et al. (2000)67 | Delayed patients tended to be older, admitted informally, having a more severe learning disability and a longer hospital stay. Those still delayed on follow-up needed high levels of care (e.g. 24-hour care, very experienced staff and high levels of staffing) | Lack of suitable accommodation (34 people); insufficient funding (10 people); carers unable to cope (17 people); insufficient clinical support (11 people); lack of suitable educational placement (13 people) |
Personal characteristics (individual factors)
Many studies reported reasons for delay/excessive lengths of stay which may relate to particular characteristics of the people who are delayed (see Table 5), seeking to find statistical associations between length of stay/rates of delay and patient characteristics such as age, gender, behaviour, level of disability, co-existing diagnoses and criminal record. For example, Washington et al. 59 found that 61% of inpatients with ‘barriers to discharge’ had a secondary diagnosis of autism, while 41% had other mental health diagnoses (e.g. bipolar disorder, depression and anxiety). In general, ‘challenging behaviour’, psychiatric diagnoses and a higher degree of intellectual disability are seen as some of the main predictors of a longer length of stay/difficulty discharging or transferring. 52,53,59,60,62,64,67 This is largely linked to risk, with those perceived as higher risk to themselves or others seen as being more likely to be delayed. ‘Social’ factors such as a poor home environment or a lack of home support were also mentioned,62 along with the patient having a high level of physical care needs or ‘complex needs’ such as mobility issues, needing 24-hour care, waking night staff or 1 : 1 (and more) care. 34,52,67 Interestingly Beer et al. 53 and Watts et al. 67 both found that being admitted informally (i.e. not formally admitted under the MHA) was associated with being delayed or needing a higher level of security, suggesting that being detained under the MHA can be a positive factor in a timely discharge or transfer, possibly because it is linked to a statutory process of regular reviews which includes continuous reassessment of the appropriateness of the setting.
While it seems likely that people with particularly significant needs might need a very bespoke response (which might take longer to arrange than more routine care), a number of authors recognise that each individual has a unique set of characteristics and needs: the groups being studied are very heterogeneous and everyone has a particular story or profile. 54,58,60,67 As a result, basic demographics were rarely found to be useful predictors of longer lengths of stay or being delayed. As Oxley et al. (p. 38)58 observe:
It is important to keep in mind that individuals with intellectual disabilities accessing specialist inpatient services are more likely to present with complex clusters of symptoms and behavioural problems that may span several diagnostic categories.
Moreover, highlighting individual characteristics feels problematic for a number of reasons. First, many studies report associations and possible links between characteristics, implying but not stating a causal relationship between the characteristics and the length of stay or delay. In some cases these statistical analyses have been conducted on small samples, arguably making techniques such as regression analysis less useful for exploring reasons for delays than other approaches (see below for further discussion). Second, it can lead to an over-simplification: for all the statistical calculations linking potential delayed to particular factors associated with the individual, there is a risk that much of this literature ultimately concludes that working with people with multiple, complex needs is essentially ‘complex’ – which does not feel a very earth-shattering observation. Finally, in the literature on older people delayed in general hospitals, there has been a concerted attempt to avoid labelling people as ‘bed blockers’, as this implies the delay is somehow their ‘fault’. In practice, the vast majority of older people would rather be at home, and the delay is usually due to system issues rather than any fault of the individual. In other areas of social policy, indeed, focusing on personal characteristics would be seen simply as ‘victim-blaming’, and might be considered offensive.
Process (organisational) and system (structural) issues
Many of the papers included also give reasons for delays that are related to the process of discharge, such as administrative issues, funding and the availability of suitable placements. In most studies, these factors are identified from case notes and so vary significantly, often dependent on the local context and on some of categories used by specific sites, members of staff or service providers at the time the notes were made. Some of the reasons given are also fairly speculative and tend to lack further explanation (e.g. a statement that there would be fewer delays if there were more suitable placements available in the community, without any real attempt to define what ‘suitable’ means, consider what kinds of placements are available or reflect on whether more or different placements really would make a key difference – and certainly no attempt to test any of this).
Lack of appropriate placement/services post-discharge
A significant number of papers suggest that a key issue is a lack of community placements appropriate to the person’s needs. Watts et al. ,67 Nawab and Findley55 and Cumella et al. 57 all report more than 70% of people delayed due to a lack of suitable accommodation or day care, Perera et al. 66 (p. 169) ascribe 47% of delays to there being no suitable facility available in the community and Thomas et al. 52 found that clinicians in a secure unit believed the vast majority of delayed transfers were due to the fact that alternative placements simply did not exist or beds were not available. Similar themes also emerged from national reviews, with the Mental Welfare Commission for Scotland34 in Scotland finding that 74% delays were due to a lack of suitable housing and 64% due to a lack of suitable service provider. MacDonald64 similarly reported that 51% of those delayed and in hospital out of area were delayed due to a lack of accommodation, with 15% due to a lack of service providers (not just accommodation). In Northern Ireland, Palmer et al. 65 highlight the small number of new community placements (referred to as ‘bed spaces’) as a factor in the slow progress made in discharging those still delayed in long-stay hospitals after many years.
However, it is sometimes difficult to know what this means: is it an absolute absence of placements, a lack of placements which are sufficiently specialised, a lack of fit between what providers can offer and what individuals need, and/or do hospital-based staff reflecting on what might ease delays not necessarily know enough about what is actually available in the community? As an example, both Devapriam et al. 54 and Oxley et al. 58 report that the majority of delays – 50% and 69% respectively – were not due to the lack of placements per se, but to difficulties in the process of identifying and/or starting a suitable placement:
Surprisingly, only one patient was delayed due to lack of availability of an appropriate placement in the community; the rest had existing community placements identified and only one other patient had to wait for a bespoke placement to be commissioned. This reiterates that the reason for delay in most cases is a system issue rather than a lack of available placements for complex care in the community.
(Devapriam et al., p. 213)54
Where studies have explored these issues in more detail, they tend to point to missing elements of current community placements – for example, a perceived lack of specialist staff, a lack of specialist training or an inability to support patients with particularly complex needs. 34,59,64,67 For a small minority, the reasons for delays included not being able to go back home or back to an original placement, either because the patients’ needs had changed and staff or family were no longer able to cope,55,58 the placement had become unavailable (bed filled), or family circumstances had changed. For example, one person’s parents had died and another’s family was in another country. 62 Together, a ‘lack of placement’ seems to indicate all or some elements of a future placement being missing, whether this relates to family circumstances, housing, the level of care needed and the specialism/training of staff. In one sense, all delayed discharges are caused in part by the ‘lack of a suitable placement’ (almost as if this category is so broadly/loosely defined that it loses all meaning).
Funding
‘Funding’ was the second most commonly reported reason for delays in transfer to lower levels of security according to Thomas et al. 52 The Mental Welfare Commission for Scotland34 also found that 41% of people were delayed due to ‘funding issues’, while Watts et al. 67 saw ‘insufficient funding’ as contributing to 23% delays. Funding issues obviously affect the availability and suitability of a placement and even where funding and placement issues have been reported separately, it is clear that these categories are not mutually exclusive – with many patients delayed for both reasons. 54,57,66,67 Sometimes, the process of agreeing funding seemed to be the issue (rather than necessarily the amount of money available), with Cumella et al. 57 finding that nearly a quarter of patients were delayed due to funding disputes between local authorities and (former) health authorities, and Devapriam et al. 54 reporting a similar proportion of people waiting for funding decisions to be made. Without giving rates or statistics, the CQC61 identified funding availability, disputes, access and complexity as major issues contributing to excessively long stays in hospital, and Palmer et al. 65 noted significant difficulties with commissioning individual complex packages across health, social care and housing. As with labels such as ‘lack of suitable placements’, it is difficult to tell what delays due to ‘funding’ actually mean in practice. After all, people are often delayed in very expensive hospital settings, suggesting not an absence of funding per se, but perhaps that existing funding is in the wrong place: difficulties moving funding create difficulties moving people.
Discharge process issues
Broadly, the literature highlights two areas of the discharge process that seem particularly problematic: waiting for assessments and a lack of proactive discharge planning, often not using tools or following protocols that are already available. Devapriam et al. 54 found 50% of discharges were delayed whilst awaiting a social care assessment, while Perera et al. 66 found 47% of people delayed for the same reason. In relation to discharge planning, Mills et al. 35 reported 82% of patients having no future placement identified, MacDonald64 found that around half of people in the Scottish services under review had no active discharge plans, and in England the CQC61 found that 60% of people had no good-quality discharge plan in place. These process-based issues indicate problems for discharges occurring at multiple stages of the inpatient journey, including at the point of admission, which Devapriam et al. 54 explored by identifying delays at different stages:
-
Stage 1: Assessment of needs and identifying an appropriate placement.
-
Stage 2: Awaiting funding decisions from local authority/NHS (including resolving disputes over responsibility).
-
Stage 3: Awaiting authorisation of funding from responsible authority.
-
Stage 4: Waiting for package to be made ready (e.g. staff trained, accommodation adapted).
Nearly half – and the largest proportion of patients – were delayed at the first stage for the longest period of time: an average of 4 months, with the longest delay around 2.5 years. The Mental Welfare Commission for Scotland34 also identified timing issues with the discharge process: for some patients, waiting for funding decisions at different stages resulted in potential placements being filled by someone else, indicating there were appropriate services but potentially not enough spaces in them, or a lack of mechanisms to prioritise who should get the next available bed.
Changing service structures, policy and governance
Oxley et al. ,58 Devapriam et al. ,54 Mills et al. ,35 MacDonald,64 the Mental Welfare Commission for Scotland34 and the CQC61 also note a wider shift towards the use of private/independent providers in an increasingly multi-sectoral mix of services – particularly in residential care. They suggest this influences delays for a number of reasons: concerns over the transparency of the offer, questions about quality and appropriateness of the care provided in some settings (particularly private providers), and the intersection of multiple agencies and providers potentially making co-ordinating care harder and processes slower. Naturally, there are challenges in governing a complex, multi-sectoral system that directly impact discharge processes, although it is hard to see how these issues might apply only to the independent sector, rather than any situation where there are multiple stakeholders with different roles and accountabilities.
One issue with the variability of reported rates of delay is the absence of legislation obliging authorities and services to collect, monitor and report such data:
The Department of Health published its good practice guidance on delayed discharges [from general hospitals] in 2003 and this was followed by the Community Care (Delayed Discharges etc.) Act 2003. However, this legislation did not extend to mental health or intellectual disability services (also known as learning disability services in the UK) and therefore delayed discharges in these services are not monitored or scrutinised, as they are in acute hospitals.
(Devapriam et al., p. 211)54
Furthermore, a number of studies identify a lack of clarity around overall responsibilities, communication between different partners, and the roles of all stakeholders involved in dealing with discharges overall, let alone those who are delayed. In Northern Ireland, Palmer et al. 65 attributed a lack of progress in discharging delayed patients to fundamental misalignments of funding streams and lack of co-ordination between health, housing, social services and social development departments. They also noted the absence of an overall resettlement plan, including monitoring and procurement and weak engagement by Trusts with patients and families. The CQC61 also highlight how disputes between different local and national commissioners, and between health and social care, can lead to a lack of agreement over responsibility for funding the person’s care – especially during transition periods.
All these issues may influence the nature of commissioning, with the CQC61 noting the influence of commissioners’ fears on the limited development of community services, reporting that commissioners perceived higher risks in community services than in hospitals with 24-hour care, and some incorrectly assuming community packages are more expensive than hospital beds. Cumella et al. 57 also identified three different commissioning approaches that influenced the extent of delays:
-
A ‘devolved’ approach where local teams organise transition process and placements, then commissioners approve funding.
-
‘No strategy’ – reviewing patients’ suitability for discharge and transfers is case-by-case and ad hoc.
-
The ‘clinical approach’, in which a resettlement officer liaises between providers and community teams throughout the process.
Of these, the third approach was found to be the most successful in reducing delays to discharge, alongside specific discharge protocols and CTRs. This literature is from the late 1990s and refers to a period shortly after a significant effort at deinstitutionalisation, so relates less to recent policy efforts and service structures. However, the range of issues it uncovers suggests that there are – and have been for some time – multiple parts of different UK health and social care systems where roles, responsibilities and processes relating to discharging patients with learning disabilities from hospital are poorly co-ordinated.
Perspectives and voices
A key argument of this study is that the perspectives and voices of people using services, their families and front-line care staff are often overlooked when we debate the issue of delayed discharge (see Thwaites et al. 68 for a similar argument with regard to older people in general hospitals). In our review, most of the data derive from bed censuses, case notes and the views of the individual researchers (often a medical practitioner). Remarkably, no academic journal articles we included were able to assess a rate of delay, suggest reasons for those delays and include the voices of service users, families and front-line care staff. Whilst patient and family voices were entirely absent from the academic literature (see Table 6), they were sometimes present in the national reviews included (which were usually authored by or in collaboration with a third-sector organisation or a national health and social care body). Even professionals’ voices (nurses, doctors, ward managers etc.) were only found in five of the 13 academic research articles included. These were included either to assess the appropriateness of the level of security for patients,52,53 give further detail as to the reasons for delay57,63 or, in one case, give feedback on a new discharge protocol. 56 However, even these sometimes felt like something of an ‘add on’ to what seemed to be the ‘main’ finding – the overall rate of delays (usually defined via bed census/case notes and based ultimately on the opinion of a lead researcher, usually a medic).
| Authors and date | Perspectives included: people using services, families, front-line staff |
|---|---|
| Alexander et al. (2011)60 | No |
| Beer et al. (2005)53 | Unit manager assessed ‘appropriateness of placement’ for each patient; data completed by a clinical lead who knew the patient rather than by the patient themselves |
| CQC (2020)61 | Yes – patients, carers, frontline staff and commissioners interviewed; questionnaires by service managers; visits |
| Cumella et al. (1998)57 | Nurses, consultants and staff responsible for purchasing learning disability services |
| Devapriam et al. (2014)54 | No |
| Dickinson and Singh (1991)62 | No |
| Kumar and Agarwal (1996)63 | Nurses in charge of each ward completed the questionnaire, usually charge nurse/ward sister |
| MacDonald (2018)64 | Yes – meetings with health and social care providers and with Health and Social Care Partnerships; individual case studies considered, supplied by Partnerships and by family carers |
| Mental Welfare Commission for Scotland (2016)34 | Yes – questionnaires to clinical service managers and nurses, spoke to nurses, spoke to individual patients, involved carers via meetings and questionnaires |
| Mills et al. (2020)35 | Practitioners (multiple, including therapy staff, nursing team); service users – advocates worked with 17 patients directly |
| Nawab and Findley (2008)55 | No |
| Oxley et al. (2013)58 | No |
| Palmer et al. (2014)65 | Consultations with policymakers, programme planners, service commissioners and senior manager; sister report on patient experiences of resettlement includes service users and carers |
| Perera et al. (2009)66 | No |
| Taylor et al. (2017)56 | 13 stakeholders (commissioners, nursing staff, clinicians, care staff, social workers etc.) gave feedback on protocol |
| Thomas et al. (2004)52 | Responsible medical officers and primary nurses identified the appropriateness of security level for each patient |
| Washington et al. (2019)59 | No |
| Watts et al. (2000)67 | No |
In contrast, the national reviews included from each of the four nations of the UK tried to include perspectives from a range of stakeholders – service users, carers, frontline staff, managers and commissioners. They did this using a range of methods such as questionnaires, focus groups, observations and interviews designed to delve deeper into the experiences and quality of care and practices involved, and the reasons behind delays. For example, Mills et al. 35 included multiple perspectives at each visit:
Information was gathered, during site visits to each unit, from the patient, therapy staff, nursing team, clinical notes and prescription charts. It was not possible to have a discussion with the patients’ families and carers ….
(Mills et al., p. 21)35
Palmer et al. 65 also sought views on the effectiveness of the policy programme overall, using:
Consultations with policymakers, programme planners, service commissioners and senior managers involved in resettlement, and in the delivery of housing and support services to resettled people, to explore their views and perceptions of: the pace of and influences on the rate of resettlement; standards and issues in the provision of housing, care and support services; views about the aims of the resettlement programme and the extent to which they have been or are being achieved. (p. 8)
Implications for research and practice raised in the previous literature
In general, the range of recommendations made fall into three broad types. Firstly, several studies stress the general principle of better provision, such as more and better services in the community for people with learning disabilities and/or autistic people. 52,53,57,62,64 Many also see closer joint working and co-ordination of services between social services and the NHS as an overall priority,35,54,55,58,61 including suggestions such as joint development of a greater range of community services or packages of care for complex needs. 61,64 Secondly, there are specific recommendations for changes to the governance, delivery and management of services for people with learning disabilities, and specific calls for improved discharge processes. Finally, a number of studies make recommendations in terms of knowledge and information, in relation both to services and to research – building understanding, gathering and reporting data and monitoring progress. Thus, almost all of the papers included call for more high-quality research, with some authors highlighting the need for research comparing different sites, settings and approaches rather than standalone studies of one site or intervention. 56,60 In particular, a number of studies call for a standard monitoring and reporting system for delayed discharge (see e.g. Mental Welfare Commission for Scotland34; Perera et al. 66; CQC61) – which, after all, exists with regard to discharges from general hospitals.
Many making recommendations about the discharge process itself call for more streamlined processes, earlier and better discharge planning with greater involvement of service users and families54,55,57,61 and consistent use of available tools, protocols and legal frameworks such as CTRs, the Care Programme Approach (CPA), the MHA and existing discharge protocols. 35,55,57,67 This includes one study calling for greater use of a specifically developed decision-making tool for addressing delayed discharges. 54 Other recommendations relate to responsibilities, governance and relationships between stakeholders at different scales, ranging from suggesting an overall national commissioner responsible for reducing delayed discharges61 to a designated professional within services whose remit is to manage and streamline discharges, such as the resettlement officer or responsible person role proposed by Cumella et al. 57 and Devapriam et al. 54 respectively. Linking to the purported lack of suitable placements in the community, some recommendations centre on changes to existing community provision. For example, Washington et al. 59 focused on specific training and skills for those working in the community in supporting people with the complex combination of learning disabilities or autism, mental health needs and challenging behaviour. MacDonald call for specific training in positive behaviour support (PBS), specialist support for co-existing autism and specific support for families and carers in times of crisis, located in the community. Others call for dedicated rehabilitation spaces for the transition period. 56,57
Summary
This review of the literature has explored the extent of delayed discharges for people with learning disabilities from long-stay hospitals across the UK, the reported reasons behind these delays, the range of recommendations made to address the problem and the extent to which service users, families and front-line care staff have been engaged in previous research. Overall, a very significant proportion of people across various long-stay settings are considered to be delayed or experiencing excessively long stays – some for decades. The reasons for this are broadly reported to be because of the extent or complexity of the individual’s needs, or because of system issues such as a lack of appropriate services in the community, disputes and issues with funding, poorly designed or implemented discharge or transfer processes, and wider problems with governance, commissioning and inter-agency relationships. However, the literature has a number of limitations:
-
Proxy indicators of delayed discharge such as length of stay or number of people with discharge plans, coupled with a general lack of precision/standardisation in terms of definitions, mean that data cannot be aggregated and that the extent of the issue cannot be fully understood. Beyond the rate of delay, there is also insufficient understanding of the amount of time different people are delayed, what this feels like and the impact it has on subsequent outcomes.
-
The use of statistical analysis to link particular demographics of individuals with delays or longer stays is generally unhelpful and lacks explanatory detail, running the risk of ‘blaming the victim’.
-
Explanations such as ‘funding’ or ‘lack of suitable placements’ provide a broad-brush sense of what might be needed, but often lack detail and may well over-simplify more complex realities and conflate a number of underlying issues.
-
The range of solutions proposed to improve the situation around delayed discharges often appear overly generalised, such as calls for more development of specialist community services and clarity over who has political and financial responsibility for the problem, issues which have already been the focus of many policy programmes and debates over a number of decades.
Above all, any further research in this area must include the lived experience of people living in long-stay hospitals and their families, as well as the practice knowledge of front-line staff. These perspectives are the most notable absence in the literature and this inevitably results (at best) in a partial picture of why people are stuck in hospital and what might help to make a difference. Such perspectives represent a key form of expertise that we neglect at our peril, and it is difficult to see how we might produce genuine solutions to these long-standing issues without drawing more fully on these insights. Despite widespread and long-standing official commitment to enabling people with learning disabilities and/or autistic people to come out of long-stay hospitals and lead more ordinary lives in the community, too many people are still ‘stuck’ in hospital – and we still do not know enough about why this is or what would genuinely make a difference (hence the need for the present study).
Chapter 4 Findings I: the perspectives of people and families
After a brief description of our case-study sites and an overview of participants, this chapter focuses on the experiences of people with learning disabilities and/or autistic people who took part in our study, as well as the experiences of their family. Although this chapter is mainly about people’s stories and situations, there are occasional quotes from a practitioner/commissioner to provide additional background and context, or to add missing details to the person’s account (particularly where the professional/system is in clear agreement with the person and their family).
Overview of case-study sites
Our three case-study sites were two NHS Trusts and one independent provider of inpatient services, all of which deliver both forensic and non-forensic services. These range from ATUs to low- and medium-secure wards, both for men and for women – although Site B only has male wards for people with learning disabilities and/or autistic people. Sites A and B are large hospital sites providing other mental health services, whereas site C is a smaller, specialist hospital just for people with learning disabilities and/or autistic people. We have deliberately kept this description broad-brush to make sure that we do not identify the sites concerned.
Overview of participants
Table 7 provides brief details of the people who took part. To make sure that we do not identify individual participants we have provided broad details of age (20s, 30s etc.) rather than an exact age, and have broken lengths of stay down into broader bands rather than citing an exact number of days in hospital at the time of interview.
| Participant (our internal code) | Sex | Age (as recorded in case file) | Ethnicity (as recorded in case file) | Length of stay (continuous inpatient stay at interview date, including other wards in the same service – i.e. time since not being in this hospital) | Forensic pathway (Y/N) | Setting (ATU, low secure, medium secure) |
|---|---|---|---|---|---|---|
| A1 | M | Late teens | ‘White (any other)’ | Nearly 1 year | Y | Low secure |
| A2 | M | 20s | Not given | Nearly 4 years | Y | Low secure |
| A3 | M | 30s | White British | Nearly 3 months | Y | Low secure |
| A4 | M | 40s | Not stated | Nearly 1 year | Y | Low secure |
| A5 | M | 30s | White British | Over 10 years | Y | Low secure |
| A6 | F | 40s | White British | Nearly 2 years | Y | Low secure |
| A7 | F | 30s | White British | Over 3 years | Y | Low secure |
| A8 | F | 40s | White British | Nearly 2 years | Y | Low secure |
| A9 | F | 20s | White British | Over 2 years | N | Medium secure (long-term segregation) |
| A10 | F | 30s | White British | Over 4 years | N | Medium secure |
| B1 | M | 40s | White British | Nearly 2 years | Y | Low secure |
| B2 | M | Late 50s | White British | Nearly 2 years | Y | Low secure |
| B3 | M | 40s | White British | Nearly 2 years | Y | Low secure |
| B4 | M | 40s | White British | Over 10 years | Y | Medium secure |
| B5 | M | a | a | (approx. 2–3 years)a | Y | Low secure |
| B6 | M | 20s | White British | Nearly 6 years | Y | Low secure |
| B7 | M | 20s | White British | Just over 1 month | N | ATU |
| B8 | M | 20s | White British | Nearly 2 years | N | ATU |
| C1 | M | 30s | White British | Just over 2 years | Y | Low secure |
| C2 | M | a | a | 4–5 years | a | Low secure |
| C3 | M | 30s | White British | Over 1 year | N | Medium secure |
| C4 | M | 40s | White British | Around 18 months | Y | Medium secure |
| C5 | M | 20s | White British | Nearly 4 years | Y | Medium secure |
| C6 | F | a | a | a | a | Low secure |
| C7 | M | a | a | Just over 2 years | a | Low secure |
| C8 | M | 30s | ‘Any other mixed’ | Just over 18 months | Y | Low secure |
| C9 | M | 20s | White British | Just over 2 years | Y | Low secure |
Of the 27 participants, 21 were male and 6 were female. The vast majority were recorded as being ‘White British’. While one person was in their late teens and one person in their late 50s, most people were in their 20s, 30s or 40s. We found it difficult to summarise people’s length of stay, and in the end chose to record continuous inpatient stays in the current hospital (that is, the length of time people had been in this particular hospital at the time of interview, including in other wards or other parts of the same organisation). However, lots of people had experienced multiple admissions as young people and/or as adults, may have transferred from other hospitals and/or had very complex journeys through services (see Admission to hospital for further discussion). Using this definition, people’s lengths of stay ranged from someone who had been in an ATU for just over 1 month at the time of interview, to two people who had each been in hospital for over 10 years. However, the majority of people had been in hospital for between 1 and 2 years.
Most people had a formal diagnosis of a learning disability, either as an adult or as a child. Some had a diagnosis of autism or Asperger’s syndrome without a learning disability, others alongside it. The majority of participants also had a diagnosis of a mental health or neurological condition – usually a personality disorder, but also including other conditions such as bipolar disorder, schizophrenia and/or attention deficit hyperactivity disorder (ADHD).
Of our 27 participants, 19 were on a forensic pathway (i.e. they had committed a criminal offence and came to hospital under a forensic section of the Mental Health Act). Only five people for whom we have information were not admitted on a forensic pathway, although one was later transferred to a forensic ward from an ATU (albeit this seemed to be due to a perceived need for greater security, rather than the origins of the person’s initial route into hospital). This has implications for the rest of our findings, as the majority of our participants had been involved in the criminal justice system as well as receiving NHS care and treatment. We do not know how typical this is of all the people still living in long-stay settings, but the government’s ‘Assuring Transformation’ data suggest that around 50% of people are in secure settings (www.england.nhs.uk/learning-disabilities/care/atd/), albeit some people on general wards or in psychiatric intensive care units may presumably have committed previous offences and had some involvement with the criminal justice system (see Chapter 7 for further discussion).
Admission to hospital
Admitted from prison for treatment
Some people came to hospital directly from prison under a forensic section of the MHA:
I come to hospital two times in my past prison sentence, I was in prison, then hospital, then back to prison, then hospital and then I stayed in hospital.
(A2 PLD)
At times, the person and their family had slightly different accounts of why they were transferred, although the conclusion was still the same – that hospital was seen as a better setting for that person than prison:
I got arrested and I was in prison for two years and they said it will be better if I do my course and I’ll be better in the hospital ward than I would in a prison, I learn better in a hospital than I would in a prison.
(A3 PLD)
He was admitted to hospital because he was referred – when he was in prison obviously he had quite a few issues mental health wise, so I think the mental health team came into it while he was in prison and I think that’s how he’s got referred because of obviously his mental health and I don’t think he was coping in prison.
(A3 Family)
Transferred from other hospitals or services
Some people came to one of our sites for very specific and structured programmes around sex offending or arson. In other cases, people were transferred because a previous setting was felt to be unable to meet their needs. In the case of the person below, a transfer was necessary because of a series of incidents in a previous setting, leading to admission to a medium-secure ward. However, commissioners had found it very difficult to identify anywhere that was appropriate in terms of security and in terms of gender – and eventually the current hospital was the only provider willing to admit her:
She one night absolutely destroyed the hospital – she broke out of seclusion – long term segregation – she put through something like 36 windows – she took doors off – all the doors to the patients’ apartments all had to be locked – staff barricaded themselves in the office and called the Police – that happened on two occasions. I ended up holding a provider event – I invited national providers – NHS and the independent sector – to a venue … because I still hadn’t secured a provider … and what happened was, bless her, the … clinical director from [Site A] came and she went ‘I’ll have a go’, put her hand up in this – and to be fair it was very poor uptake – I think there was only about five providers that turned up and I presented the case.
(A7 Commissioner)
Breakdown of family support or community placement
For the participants not on a forensic pathway, reasons for admission tended to relate to a deterioration or crisis in the person’s mental health, a particular incident or an increase in ‘challenging behaviour’ – which meant that a previous setting was no longer able to provide the necessary support. For example, one person had assaulted multiple staff at a previous community placement, as well as a police officer. Here, a staff member describes how that a crisis may have been triggered by a bereavement:
So he was admitted I think three or four years ago and then got discharged because he improved with his behaviour, he was taking medication, he was following a routine. Then he’s been readmitted following discharge. He’s displayed more … challenging behaviours which [are] deemed to be from his mother passing which he was quite close to, so we feel like his behaviours have escalated further from his mother’s passing away which has made him deteriorate a lot more. That’s how he’s ended up with us again.
(B7 Staff member who knew the person well commenting in the absence of family)
Multiple services over the years
Many participants had been previously assessed and diagnosed with a learning disability and/or as being autistic at a young age, and the most recent hospital stay was one in a long line of admissions. Other people were assessed and diagnosed while in prison, and this resulted in their being transferred to a long-stay hospital setting. Over time, most people had received a range of different services from different parts of the system, including community health and social care, specialist learning disability services, other hospitals, other wards on the same hospital site, mental health services, services for people with special educational needs and the criminal justice system. Examples of these complex journeys are set out in Box 4.
He’s had a really protracted admission because he was in low secure, we had him in low secure originally back in 2010, and then in 2012 he was admitted to medium security and he was there for seven years to the end of 2019.
(B1 Commissioner)
The first time I was here was nine years ago before I came back. And I was in there for six and a half years. And on here I was like three or four years. Then I’ve been on this ward, came back a second time for two years.
(C8 PLD)
Altogether, I’ve been locked up about 14 years, 15 years. I’ve done about, maybe, about six in hospital and stuff like that. Yes, been locked up quite a long time.
Interviewer: So, about six in hospital, and was the rest of the time …
In prison … started off when I was 18, and I’m just in and out of different prisons, yes. I got diagnosed with schizophrenia and then [they] said that you need to come to hospital, so that’s why I’m here now.
(C1 PLD)
Every night for 13–14 weeks, he ran away from home … and he used to kick off with the police …. Eventually they said they were going to take him to the General to have him checked out. So they said there were nothing wrong with him, he ran away from there, then they took him to [Place 1], 16 he was.
Interviewer: What sort of ward was he on when he was there at [Place 1]?
Adolescent psychiatric unit.
Interviewer: Right, so why did he move to [Site B]?
Because he was 18.
(B8 Family)
(This person was then moved from general mental health services to two different learning disability wards within the same site.)
History of offending, alongside long-term health and social issues
It was common for people on a forensic pathway who had been in multiple services over a long period to have long history of committing criminal offences and of being in and around the criminal justice system for many years:
So with [A7], she’s had a really complex, difficult time in managing to stay in the community due to her offending behaviour. So she’s got prolific history of both sexually offending, arson, behaviours that change into personal violence to others. She’s been in all levels of – she’s not been in high security but she’s been in low, medium, she’s been in locked rehab services. She was in the community and was offending, she had a Mental Health Act assessment and she was admitted to a locked rehab service, she was preparing for discharge – this is some years ago – she was preparing for discharge and sabotaged the discharge planning really because she went into the village and set fire to the local bin outside the post office, which didn’t go down very well, and she was smashing windows in the village and it was quite a conservative village, as you can imagine.
(A7 Commissioner)
In some cases, family members and professionals felt that the types of offences and the person’s ability to change those behaviours (or not) – that is, the reason they had kept offending – were directly linked to their learning disability and unlikely to change:
Personally, that behaviour’s not going to change. That is part of her, you know, she decides ‘That’s my person. That’s my carer’ and unfortunately in the past, in previous places … I’ve reiterated to the staff that, well they should already know, that you don’t give out phone numbers, don’t do this, don’t do that. ‘Oh yeah, but she’s so lovely’ and they do, and then we have a problem, then she’s found their houses. And she always does it.
(A6 Family)
B4’s primary offending risk was his paedophile behaviour … and as B4 had received psychological input and services over the years, it was evident that that risk had not reduced, and the reason why that risk had not reduced was because of B4’s intellectual functioning, not because of any disturbed, mental disorder, psychosis or psychiatric cause or mental ill health, it was primarily his learning disability.
(B4 Social Worker)
(Despite these views, it should be noted that both person A6 and B4 were discharged to the community during the course of the project, albeit with high levels of support, perhaps suggesting that it is sometimes important to find ways of managing particular behaviours and risks, rather than necessarily being able to stop them altogether.)
Many people’s stories illustrate ongoing patterns of struggling with transitions and moving between services, deteriorating in certain environments, the distress and upheaval of moving within sites, and ongoing difficulties finding services to meet more specialist needs. A1’s story in Box 5 illustrates some of this complexity.
Due to his mental health and ‘challenging behaviour’, A1 was under the care of children’s services until he was 18, at which point the transition to adult services seemed to happen in a rushed manner, and he moved between multiple services over a short period. He was at risk of being incarcerated for a criminal offence but after a lengthy process of being assessed as not having capacity, then a change to his legal status in his home country and a number of failed placements, he was transferred to hospital in the UK.
So in hospitals I’ve been in two years …. Across six, seven hospitals …. Because in three or four I was only there for a few weeks.
(A1 PLD)
He’s been in different residential units over the past three years, well literally nobody wanted him because they knew the history and everything – so it was very hard to get something …. Then he got granted a placement in [Site A] like, we were waiting for a place for a couple of months, but when it happened, you know, I was delighted and I was kind of hoping that it will help him. Now I have to say the first couple of months were very bad, OK, because he was first in [a different unit on the same site] for about four/five weeks I would say, but the hospital closed down, so he was brought to the unit where he’s in right now. He was supposed to go originally to [a] medium secure unit but because there was no place, they actually suggested that they might try it with a low secure unit first and it kind of wasn’t really working out, he was struggling, … and until about May there was incident after incident.
(A1 Family)
Interaction with other aspects of people’s lives and identities
Two participants on forensic pathways were diagnosed with ‘gender dysphoria’ alongside additional mental health diagnoses and were undergoing gender transition. Participant A7’s story, for example, demonstrates how this affected her journey, and how challenging it had been to find a hospital placement that met her needs as a transgender person, on a forensic pathway, with a diagnosis of a personality disorder – long before she could be considered for discharge:
I think it’s also important to note that … when there was the high levels of violence and aggression … was [when] her hormone medication was reviewed. And what is apparent is that at that time she had an increase in testosterone. So the hormone programme that she’s on … – there was obviously spikes in the testosterone levels – so there’s a view that that may have contributed to the antisocial behaviour that was being witnessed …. The access assessment was undertaken and medium security was required – because of the transgender – could I find a provider? I couldn’t …. So I could have got her into a medium PD [personality disorder] service no problem. The medium female PD services were saying ‘we are not equipped to take a transgender female’.
(A7 Commissioner)
A small but significant number of our participants also had long-term physical health conditions such as multiple sclerosis, diabetes and/or mobility issues which needed to be managed alongside their hospital treatment, and sometimes had implications for the kinds of services that might be suitable after hospital.
Life in hospital
Many people expressed negative views about being in hospital, including frustration, boredom, difficult relationships with some staff and concerns about the behaviour of other people on the ward (see Box 6). Given that many people had little choice as to where they might be for the foreseeable future, however, their response was often to ‘keep my head down’ and ‘keep myself to myself’ – hoping that they may one day be able to leave if they could ‘stay out of trouble’.
Interviewer: Do you prefer hospital or prison, would you say?
Honestly, I think prison.
(C4 PLD)
To be honest with you, I’ve had enough of being here now. I want to move on to another hospital, but I think … my psychiatrist, wants me to stay here.
(C1 PLD)
I get bored so easily, and it gets my hair off as well, and it’s not fair on the OT when you’ve got put on obs nearly all the time. We have to try to keep ourselves active, and the bedrooms where we’re saying, why are keeping … why are you staying in your bedrooms all the time? I said, well, you lot are not occupying us, so why should we occupy you?
(C2 PLD)
Obviously I don’t like it [here] but sometimes it’s alright if you kind of start realising that you stick to yourself and just behave yourself basically.
(A1 PLD)
If someone’s breaching the peace and breaking rules at night time, keeping people awake, they don’t put them in seclusion and separate them away from the ward like you would do in the community, they allow them to carry on breaching the peace all night until that person will spit at the manager … We were disturbed all night.
(A5 PLD)
Interviewer: And what about now, what’s your life like now?
Rubbish.
Interviewer: Why is it rubbish?
Because I’m in here.
(A7 PLD)
It was common for people to describe their life in hospital in terms of the restrictions on them and their activities, and a dependency upon permission and/or assistance from staff. For example:
It’s timed, you get allocated a certain amount of hours. So basically, my main nurse sent off my form which was agreed in MDT [multidisciplinary team], to go to the [de-identified place] with my parents. So obviously the first time I go, I have to go with one member of staff. After that, they will then say okay, now we’ve done our test run, your family can now pick you up …. Obviously, you have to stay within your time, so like … I’ve got two and a half hours at the moment, so obviously as soon as you leave, you have to be back within two and a half hours.
(C7 PLD)
Others were particularly aware of the restrictions placed on their care due to limited capacity of the staff in relation to the number of people receiving treatment:
At the moment, because I’ve only been here for two months, it’s a bit slow, because they’ve got a thing in place that it takes time to get everything sorted out, because it’s not just me here, so that stuff, they have to do everything for different people, so at the moment it’s going slow, I’m not allowed out, but I cope by [making models to pass time] or I come in here on the computer, so I do fill my time.
(A3 PLD)
Being around other people who are unwell
Many people described at length their experiences of being around other people who were unwell, and the effects of disruptive or violent behaviour towards them:
To be honest with you, I just keep to myself, in my room, just keep away from everyone, because they’re always bickering and people kicking off. I don’t want nothing to do with this, feel like the best thing I could do is just keep to myself.
(C1 PLD)
[Some of the other people here are] thieves, scumbags and people who obviously ought to be in high secure …. If you can prove you’re not a risk in this environment, you’ve done well.
(A5 PLD)
It’s OK [here] but I think it’s getting worse because like the other week three people kicked off. I put a complaint form in to have more staff on the ward.
(B1 PLD)
At one site during a follow-up visit, staff explained that the person we came to see was currently in a different part of the unit, as another patient was causing significant environmental damage on a daily basis, effectively meaning that some of the ward could not be accessed by other patients.
Some participants described the effects of repeated incidents of the ‘challenging behaviours’ of others on their own mental health, and the implications this had on their ability to move on:
You reach a peak of your health, so say like I’m well and I’m surrounded by unwell people, the behaviour of those unwell people would influence my well behaviour till I’m unwell, because the unwell people are more likely to be getting more attention and my progression – like going out and stuff – is being cut because people are kicking off and staff is needed …. So then that’s just going to agitate you and then you’re going to come from your peak to working downwards to being unwell again, then you’re going to have to start from the beginning …. So now you’re being prolonged in hospital.
(A2 PLD)
The same issues were described as a concern by various family members. In the example below, this related to other people’s reactions to the person’s offence:
I just think obviously that you’ve got other people in there with problems and I think that’s the only thing that’s getting him down is obviously that a couple of them, I think to what he’s said, have found out why he’s in there and obviously his offence and I think they’re giving him a hard time of it.
(A3 Family)
Potential positives
When asked what their life was like now, a number of participants compared their lives in hospital to what it was like in previous settings – either other hospital wards or prisons:
I’d say it has its perks, like, I would say … the atmosphere in prison is different to here and the progress here is different to prison, so it has its ups and downs.
(A2 PLD)
Interviewer: Out of all the places you’ve been, which have you preferred?
Here …. Because they weren’t nice to me …
Interviewer: So the staff support you better where you are now?
Yeah, miles better.
(A10 PLD)
Since I’ve come here I’ve got all the help I needed …. This is the best step ever.
(C6 PLD)
This was a particular focus for family members who often said that the current setting was the best for their family member so far:
She’s been in quite a few hospitals and I haven’t been impressed …. But the one she’s in now seem to work with her better.
(A7 Family)
Some family members added that they had worried for their family member’s safety and/or mental health in previous settings:
We used to go onto the ward sometimes and there were residents and patients on the ward just on the corridor, just laid there, not even in their bedrooms and whatever, on sleeping bags …. If he hadn’t have come out when he did he would have died because he were that bad when he went over to [Place 3], the drugs he were put on was unbelievable.
(B8 Family)
Despite the negatives described above, some people talked about activities, interests and going out on leave as positive features of what their life was like in hospital (see Box 7).
Well you see, I’ve done a lot of things, like I went to college for catering, I’m a level 3 qualified baker, I’m also a good cook. I do a lot of volunteering work. I worked for the RSPCA volunteering, I’m working down at the local café volunteering as well … I’ve got good skills, you know, so but I’m just happy to get a job.
(B6 PLD)
It is nice though, the activities.
Interviewer: Yeah, does it help pass the time?
It does, because I mean, I’ve spent a couple of months making a planter, for a lady who passed away in 2020, who was a psychiatrist, and she did my first part of treatment and started my second part, and then she went off ill. And sadly she passed away, so I did a planter for her, which is now outside.
(C7 PLD)
However, people also felt that the availability of these activities was often significantly limited by staff availability and other events and situations on the various wards:
It’s OK – I mean we don’t get to do a lot because there’s no staff.
(C6 PLD)
People who do a runner … – it just causes everyone else a problem when the ward clamp down on everyone.
(A5 PLD)
Interviewer: So how often do you do horticulture and woodwork and things like that?
Monday to Friday mostly, but we have a team … and yeah, I mean, we normally, Monday to Friday we normally aim to go up there every day, either woodwork … or we go in the garden on the unit. But this week, they’ve had to do other jobs, because, like, assessments for all the units, so we haven’t had as much this week.
(C7 PLD)
Other positive elements were the social bonds that people formed with others:
Me and my friend last Saturday, we went out together. I was one on one, she was one on one and we went to Primark together, two charity shops, McDonalds and Poundland and this week or next week we’re meant to be going to the zoo together. So I’m really getting on well. I like the girls now, I’ll miss them but we’ve all got to move on, you know what I mean? But I’m going to miss them, I will keep in contact with them …. They’re all nice girls. We struggle but we have to be there for one another. Everyone struggles. But I’m pleased the way they support me, the staff.
(A10 PLD)
While seemingly small in their own right, these acts of humanity made a major difference to people in a setting where they felt that so many of their rights and autonomy had been removed.
Wanting an ordinary life
When talking about how they wanted their life to be in future, most people just wanted an ordinary, meaningful life, with family, work or study, a partner and/or friends and opportunities to pursue their interests. Above all, people wanted to have some independence, to live in their own place and, in general terms, to ‘get on with life’ (see Box 8).
Basically I want this to be the last hospital or care home or prison – so I’m trying to get it right this time round, whatever. Hopefully in a few months I’ll be out of here for good and I can just live life.
Interviewer: So what would you like your life to be like moving forwards, what would you like to be doing?
Um … try and progress with my life and start working, family, stuff like that.
Interviewer: So do you want to be living in your own place or …
Yeah, definitely.
(A2 PLD)
Living on me own, having a job, settling down.
(C6 PLD)
Just being able to go out in nice weather, I like nice weather. You know, go for a bike ride around the park.
(C7 PLD)
I just hope, because I’m not like a fussy person, I don’t see myself living in a five or six bedroom [****] mansion or anything like that. If I’m still single – I haven’t found myself a girlfriend or anything yet which obviously will take time – but I’m happy enough with just a single room, try and find a part-time job. As long as I have my smokes, tobacco, I’m happy.
(A1 PLD)
So that’s what I want to do, I want to learn … to look after myself and eat at proper times and stuff.
(A3 PLD)
I would love to be as back to normal as possible, safely as I can …. Going college at night, going work in the day, doing some hobbies, so go out dining. I can go out cinemas, go partying, playing ball, shooting, cycling, fishing. So, that’s normal for me, gaming as well.
(C2 PLD)
Family and relationships
People often mentioned family when they talked about what they wanted their lives to be like, either in terms of spending more time with their existing family, or in terms of having a family of their own in the future. Although some participants had difficult family relationships, many wanted to be near their family when they left hospital (see Box 9).
Yeah, but I’d like a place in [ … ] then it’s not far. My brother lives in [….]. And if I move to by [….] my brother will be happy.
(B1 PLD)
Well, my niece is three and my brother wants me to see her, and I want to see her as well. I just want to get out and just be with my family.
(C1 PLD)
What I want now is I want to not be here, independent living I want, near my Mum.
(A10 PLD)
I want a family as well.
(C5 PLD)
Many people also mentioned wanting a partner in the future, although some also had concerns that this might be difficult as a result of their time in hospital or offences that some people had committed:
I want a, like, missus kind of thing …. A girlfriend kind of thing. It’s just I don’t think I’ll be able to get one, anyway where now I’ve got like the regulations and stuff it’s going to be harder …. Because I don’t think women – I don’t think anybody’s going to want to date me – but you never know.
(A3 PLD)
Work
Lots of people wanted to have a job – either with a specific career in mind or just in general terms:
[I want to] go into the construction business … I grew up around construction and stuff like that and carpentry, it’s in the family traits and stuff like that so … yeah.
(A2 PLD)
Equally, some people were aware that their options might be limited as a result of their time in hospital or offences that some people had committed:
I like outdoor stuff, I like gardening, I like animals, but with my regulations it would be hard to get a job, that’s the only problem.
(A3 PLD)
Studying
Many people talked about studying or training as a part of their life outside of hospital – either returning to something they had studied before or starting something new:
[I want to] go to college … I want to be a qualified chef. My uncle’s is a qualified chef. So, I want to follow in his footsteps.
(C8 PLD)
[I want to spend my time] like going out to places and stuff …. College and things like that. [I want to do] English and Maths.
(A7 PLD)
Well, I was thinking maybe I might go not exactly an HCA [healthcare assistant] but I want to do something, study in college or whatever, see if I can come back as like a care mentor or something like that.
(A1 PLD)
Probably going to college or uni or something, I want to be a social worker.
(A10 PLD)
Interests and activities
Almost all of the people we spoke to had particular interests and activities they liked to do which were an important part of their identity and their future life. Some of these people had been able to pursue in hospital or prison (such as films, woodwork or animal care), while others were interests and activities people had engaged in prior to hospital (such as watching sport, baking, day trips, fishing or paintballing).
Just like what I said about getting out, see my niece, my brother and all them, watch films and stuff, go to bodybuilding competitions … I like things with the Queen, Breakfast Club and all that, Harry Potter. Go to Harry Potter World and get out with my family.
(C1 PLD)
So he’s from […] – and he absolutely loves […] football club and every day he rings […] radio, so he’s got a friend who’s the DJ and they talk to him and sometimes they put him on air and he’ll talk about […] football, but […] football team really – they know him – he knows the manager – he knows the team.
(B1 Commissioner)
In particular, many people talked about wanting a pet or to work with animals:
And then I’d have a little dog, so the dog could run around. Or a rabbit. I’d like a rabbit because you can train a rabbit. I’m having a rabbit when I leave.
(C7 PLD)
[I’d like a job] helping animals … – dogs or go to the zoo and help out.
(C6 PLD)
Volunteer work outside in a kennel or I like my animals, that’s what I want to do.
(A3 PLD)
Keep myself busy. And do voluntary work, like work with horses.
(C8 PLD)
Location and setting
All participants were generally very clear about where they wanted to live in future. Some people had a clear idea of the type of specialist placement they wanted to live in or about a particular geographical location, often relating to other elements of their lives described above, such as their hobbies or their family:
[I want to] live in a place in […], I can go fishing every day, I can work on the lifeboat again.
(B1 PLD)
Many people were also clearly aware of their own needs in terms of environment, company and support, and specified what they felt was appropriate for them. Some people wanted to live alone, some with others, and some with specific levels or types of support:
I’d like to live in independent living near my Mum. I want to live on my own, staff on my site and have my own place … and then there’s staff that live in and support you because I take a lot of meds.
(A10 PLD)
One participant had considered every detail of what they might need and how they wanted their future property to look and be laid out. They communicated this by drawing the house during their interview. This person had also considered their emotional needs, risks and behaviour and how their property could be adapted to manage that:
And also I would like a room just full of sensory stuff so when I’m upset or anything, I can go in that room. Instead of smashing my house up I can go in that one room and just throw everything around.
(C7 PLD)
Some of the people who worked with our participants had a detailed understanding of the person and were aware of their hobbies, interests and aspirations. Often, this aligned with what the person said they wanted:
He’s very clear he wants his own flat, he doesn’t mind if it’s in a shared house but as long as he’s got his own front door kind of thing.
(B1 Commissioner)
He wants a place of his own …. He wants to live where he lives in his apartment, he wants to have a drink at the weekends, make his meals, meet a girl, settle down and have some children and such. That’s his dream, nothing really special. That’s just what he wants, is just the normal life I suppose.
(A1 Social Worker)
Family members also often had clear views about the kind of life their relative would like:
[A3] is very… he just wants an easy life. I’ll tell you now, he doesn’t like drama. He admits, you know, he’s put himself in there, he admits he knows what he’s done is wrong …. So he likes everything straightforward. He likes to have a plan, if you know what I mean.
(A3 Family)
Some participants, like A3 above, also had long-term health conditions which were a concern to them and their family in terms of how their life might be, and a factor that needed to be considered when they leave hospital:
I would like to live on my own and have my own property. Because I have MS it’s going to be hard to live on my own and things – because, you know, if it gets worse – but I would like to … rely on myself.
(A3 PLD)
In some cases, however, what the person wanted their life to be like and what others thought was realistic or feasible were different:
And, again, in terms of what she wants for the future, she wants a relationship, she’s desperate to meet somebody. But, again, in the past relationships have been a trigger to antisocial behaviour and interpersonal violence.
(A7 Commissioner)
She’s not happy anywhere, she just wants a place of her own again – well she’s not going to get that.
(A6 Family)
He’s met a friend who’s a patient in [Place 7] who fits his victim profile and they’re going out on unescorted leave for walks together. This patient’s being discharged to […] – [so] he wants to be discharged to […]. We’re all saying ‘hang on a minute, you’re not going to […]’!
(B1 Commissioner)
Overall, while there were some significant differences in opinion and expectations about what might be possible in future, most of the people we spoke to had what appeared to be very modest, ordinary aims for their future lives.
Barriers to leaving hospital
Behaviour, incidents and risk
When asked what needed to happen for them or others to be able to leave hospital, many people talked about the importance of their own behaviour and the need to be seen to be ‘behaving’ well enough on the ward to be perceived as low enough risk to move to the next stages of discharge. While some people spoke about their own behaviour, other people talked about the behaviour of others:
Maybe their behaviour. They’re always kicking off. That would keep them in, I reckon.
(C1 PLD)
Their behaviour. Saying stuff like, stupid stuff, keeping them back. Getting into trouble. Not sticking to the rules.
(C8 PLD)
Basically what happened was I was causing a lot of …, and a lot of staff had to come and support the ward at night mainly, and some staff had been assaulted, some night staff and basically they said I’m a bit too much of a risk for low secure unit. So I got put on long-term seclusion. I was in there for 8 or 9 days and I was told by the doctors if I don’t improve when I get out, because obviously they were trying to get me into medium secure with the assessment and everything – so basically they gave me the last chance and I used it to turn things round. Then I got community leave. I should be coming off the constant obs this week as well.
(A1 PLD)
Some people also felt that previous incidents, even some time ago, could delay their discharge. In the example below, one person felt that a previous incident had been used unfairly to deny them opportunity for additional leave, which they saw as an important part of being able to prove that they were ready to leave hospital:
I know for a fact that Tribunals supported my leave, the doctors supported it, but the Ministry of Justice turned round and said ‘no’, and when they were asked why: ‘he had an incident a couple of months ago’ – and that was all, they held the incident against us. ‘But that was a mental incident where a patient had come in and disturbed him and [****] him off and he went for him, like anyone would in the community’. But that’s enough to lose your leave. I was like ‘this is diabolical’. It’s like they expect you to behave in a medical environment. It’s like they expect you not to be [****] off by another patient who’s had a mental episode.
(C5 PLD)
Completing treatment
While behaviour was the main barrier that people mentioned, they also talked about some people’s eligibility for discharge being conditional on completing particular therapies. This was particularly the case for people on forensic pathways who needed to do psychology courses relating to their index offence (such as around sexual thoughts and feelings, or fire-setting), and a number of people had done or said that they still needed to do anger-management courses. Others said that they needed to complete specific tasks (via occupational therapy) in order to build life skills such as cooking, self-care, budgeting or relating to others:
Yes, it was very helpful. That was very helpful. How to speak to women. I know I don’t like women, but I’ve got my reasons for that, but … I know I need to start behaving myself, really, because I’m putting myself in that situation now where I’m … stopping me moving on.
(C2 PLD)
So they started with anger management therapy which is now finished. He had I think all together 18 sessions – but it was spread, you know, every week. I was unhappy with that, sad, but they have to do it this way, they can’t do all of it, you know, they need him to kind of think about it and have some time to process, you know …. Now then he started to work on, I don’t know what was it called? What he did was he set a fire, OK, two years ago. So he’s getting a therapy for this, something to do with fire …. So now this course goes every couple of weeks again, so when that’s finished, you know, that’s kind of it …. That’s how I understood it from everything, you know. He needs to do this before he will be released and that’s it.
(A1 Family)
Some people were undergoing treatment which might be spread over weeks, months or years. While the family member above was clear that this kind of phasing was needed to enable the person to reflect and for the intervention to be effective, other people wondered whether the greater availability of psychological support might enable some more intensive approaches in situations where this was clinically appropriate.
On other occasions, there were delays for other reasons. Sometimes it was difficult to offer and start courses, because people were still being assessed or settling into hospital. For the family member below, disputes about the person’s diagnosis delayed the start of proper treatment:
In one of those reports was that his IQ is below 70 which is very, very low. But in hospital they said ‘that’s not true, he is like around 90, he is like one of the others’, you know, like, his IQ is not that low as they expected, so they needed to observe him for a couple of months before they actually started with something. I was actually unhappy about that because I felt they’re doing nothing, like, he had absolutely no structure, you know, he was sleeping in the day, he was up during the night and everything, I was actually questioning, like, whether this is a good idea.
(A1 Family)
Sometimes people were aware of issues with staff capacity, and that it takes time to assess people and arrange/start treatment for multiple patients at once, with some people having to wait:
At the moment, because I’ve only been here for two months, it’s a bit slow, because they’ve got a thing in place that it takes time to get everything sorted out, because it’s not just me here, so that stuff, they have to do everything for different people. So at the moment it’s going slow, I’m not allowed out.
(A3 PLD)
People and their families also were aware that engaging in activities and therapies were key to being seen as ‘behaving’, and often described feeling as if they would be less eligible for discharge if they did not take up what was offered. While the person below did not feel they needed speech therapy, for example, they decided it was best just to do what he felt he had been told:
They want me to have it and [I’m] not allowed to … to refuse stuff. I am allowed to refuse stuff but it looks bad on me because I’m refusing stuff … I don’t think I’ve got – I can’t say my ‘Rs’ very good … but a lot of it is because I’m from […], pit village – so I’ve got a different accent …. But if it helps me get out it would be helpful – but I’m not sure if it’s going to be helpful or not, because … it’s not because my speech is what I’m in here for.
(A3 PLD)
Trialling leave outside the ward
People felt that how they coped and behaved whilst on leave (whether in the hospital grounds or in the community, and whether escorted or unescorted) was a key measure of whether they were ready to leave or not. However, getting access to (or increasing) leave was not straightforward – and could lead to significant delays. For leave within the hospital grounds, one MDT could agree and implement increases quickly, sometimes on the same day. However, for people on forensic pathways and subject to particular legal restrictions, the Ministry of Justice (MoJ) had to give permission for leave in the community, and for any changes to the amount or duration of leave and the level of support required. This could be a lengthy and frustrating process, and the people whom this affected felt that decisions were made without proper consultation or a detailed knowledge of their circumstances, sometimes in opposition to their clinical team:
They have written off for unescorted local now about four, maybe six times and been turned down for every one of them …. Because I’m sectioned, it has to go through Ministry of Justice so they’ve turned me down and hopefully I’ve just done a piece of psychology work which the Ministry of Justice asked for and so once that’s done, they’re going to write back off again and hopefully this time with that information, fingers crossed, definitely they might just say ‘yeah’. Because they’re just going to get bored with turning me down at one point.
(B6 PLD)
All they [MoJ] do is read reports – they don’t come to see me, they don’t talk to me, they don’t know me.
(A5 PLD)
Another person described how they were ready to leave hospital and looking for a place in a locked rehabilitation service. However, they feel that the MoJ intervened and said that this would not be possible until the person had undertaken more unescorted leave in the community, and so they were taken off the list of people to be discharged. When they requested unescorted leave, this was denied on three separate occasions on the grounds that there was a risk of assaulting other people and a risk of substance misuse. However, the person was already having unescorted leave in the hospital grounds (where they point out they would be perfectly able to assault staff, visitors, families and other patients if this was a genuine risk). They also feel that they cannot prove they will not misuse substances unless they have unescorted leave, so are effectively stuck. More generally, they wonder why being able to be out unescorted needed to be a stipulation to move to another locked setting.
In addition to the MoJ, some people felt that the involvement of other external bodies, such as Mental Health Review Tribunals, could be a sticking point, and not always in agreement with hospital staff:
It’s a test, so my Mum said it’s a test, and I agree. It is a test at the end of the day. They want to know what my actions are going to be. I took it all right. I rang my solicitor and said …, look, they want to keep me in, and all this, which I disagree, I really … but like he said, he’s not the boss, the psychiatrist. He’s not the boss, it’s down to the judges.
(C2 PLD)
Other people felt that their ability to complete leave was compromised by the availability of staff to support them to whatever level of leave they were currently entitled:
But sometimes trouble with staffing, so staff [are a barrier] sometimes …. It’s not good at all.
(B3 PLD)
Well, [leave] that’s a big problem, that is, because it’s … the lack of staff and that on here. Sometimes some patients can’t get out, because of the lack of staff.
(C2 PLD)
Person B5 did not have their interview recorded, but said that there is a lot of bank and agency staff, and this affects when he can go out. Recently, there was the right amount of staff – but not regular staff – and he needs people who know him to support him when he is out. He also said that people are more likely to ‘kick off’ when regular staff are not there.
This left some people feeling in something of a ‘Catch-22’ situation where they felt they needed to successfully complete unescorted leave to prove they can be discharged, but might not be given permission or be able to take leave – leaving them stuck.
Perceived lack of suitable placements
For many people who were ready for discharge, it seemed that the main reason for delay was around identifying and organising a community placement. The most frequently mentioned issues were simply that there did not seem to be any existing providers with placements that were:
-
appropriate for them in terms of the environment and location;
-
where the provider had space or was able to create a placement;
-
where the provider was willing to accept the person – that is, they were deemed ‘suitable’.
Because both people’s specific needs and providers’ criteria varied so much, each time a person was referred to a provider, a separate process of checking availability, assessing the person, visiting and scoping the potential place needed to happen. If the ultimate answer was ‘no’, then this complex and lengthy process – which could take weeks – needed to begin again. For some people, this might happen multiple times before they were finally able to leave.
[A key barrier is] places not being able to accept …. There aren’t enough places.
(B3 PLD)
This person then asked their support worker to step in to help explain their specific situation and plans in place. They both explained that B3 had been referred to four different places with different reasons for not being accepted – two due to concerns about the person re-offending, and two due to the person’s mobility (they also had a long-term health condition):
We have various plans in place. We are just stuck with finding a placement …. We’ve got the conditional discharge from the Tribunal, we’ve got all the assessments done, we’re just struggling to find a placement that will accept [B3]. So it’s an ongoing process, isn’t it? So – and the Parole Board’s in place as well – so everything’s in place barring a placement.
(B3 Support worker)
Given that identifying and making referrals to a potential placement could take weeks or months due to the complexity of the process and the very limited capacity of hospital staff, providers and other professionals such as commissioners and social workers to write reports, complete assessments and undertake visits, it is easy to see how this process could add months or even years to the length of a person’s stay in hospital.
Inappropriate placements
In the example above, one of the placements explored was up several flights of stairs, despite the person saying that this was completely impossible for them to access due to their disability. However, this did not seem to become fully apparent until significant time had elapsed waiting to see if the person would be accepted by the provider, and the process had to begin again. Other people were offered placements that turned out to be inappropriate due to conditions on their discharge relating to their index offence. In the example below, a family member recounted discovering that their relative – whose original offence was a sexual offence against a child, and who was still deemed a risk without appropriate support – had been given a potential placement next to a school. This person had been deemed ready for discharge 4 years prior to the interview and, at the time of the interview, was only just starting to move into a community placement:
First, obviously somebody had to go and find this place what would be equipped for him and then I’d say even before … it took about 18 months …. There were a few places, so we had a place potentially at […] and we were going through the motions, then at the very last minute this bungalow, at the very last minute, we’d never seen this bungalow, it came about that it were next to a school or next to a walkway to a school, so whoever … had suggested it in the first place – I would love to have that conversation with them. And I think it was the commissioners that must have gone and saw that it were next to a school …. So that was off the table immediately.
(B4 Family)
Another person was offered a placement in a location they had previously lived in where they had struggled with their mental health, anti-social behaviour and substance abuse. A family member felt it would be potentially very damaging for them to return to that environment. However, after weeks of assessment, this meant that the process of trying to find a suitable placement had to start again:
I mean they got her one place in […] but she can’t go to [there]. She’s had too much trouble there … I had to stop her going. She’s barred from the centre of […] and she’s known and she would have got a lot of trouble, so I got in touch with the social worker and explained it and they stopped that. Because that would have been a no-no.
(A7 Family)
Delays setting up placements
For many other people, a suitable community placement or provider had been identified, but the process was delayed due to the logistics involved when setting up an individual package. Once a provider was identified, properties sometimes had to be purchased and, in some cases, modified. Staff then needed to be recruited and trained – all before they could even start preparing the person for their transition out of hospital:
The delay is that [the provider], whilst they’ve offered, they don’t have the building yet and they don’t have the core team …. So we need this meeting next week to take place so that they can then be informed, so they can start looking – I don’t think there’ll be a delay around the property – I think the delay will be the recruitment of the core team.
(A7 Commissioner)
On top of this, some people experienced delays due to disputes over funding and who was responsible for what – some of which were witnessed directly by people and their families. This was universally a source of significant anger and frustration:
I think when they [the community provider] did say ‘yeah’, then there were a bit of toing and froing and who were responsible for the funding …. So nobody could agree on that and that went on for months, just I can’t … I really … this is a person’s life we’re dealing with.
(B4 Family)
I think the biggest thing is there’s too many cracks in the services and it’s easy for people to say, ‘It’s not for my team’… I think people use diagnosis as a way of excluding people now.
(B6 Commissioner)
In the example in Box 10, one person was stuck because of a dispute about their diagnosis, which then affected which community team would be responsible for them and which providers would accept them. This person went into hospital with a diagnosis of a learning disability but had repeatedly been assessed and found to be ‘borderline’, and their childhood diagnoses of ADHD and autism were disputed. To the person’s family, the label given to their relative does not directly affect the specific nature of their needs – which, in their view, should be the focus.
I’ve had about four places that have come to assess me but they’ve all turned me down. They turned me down because I don’t have a learning difficulty so I don’t fit a criteria and because I don’t fit a criteria, the commissioners won’t accept me.
(B6 PLD)
It’s been the biggest thing that’s held him back since the diagnosis was changed because we’ve not been told anything, any information as to why this was, you know, what this was based on. He has an existing diagnosis of ADHD he has from eight years old, whether he’s taking the medication or not to me is irrelevant, they didn’t seem to believe that he also had a diagnosis of ASD and asked if I could find the paperwork for that. I did say that you’re his doctor, it should be on his NHS records. I was just dumbfounded as to why I would be asked to prove the medical diagnosis that he should have access to …. The biggest stumbling block that we’ve come across – things were moving on slowly but they were moving on, until the diagnosis was changed and then more problems have arisen …. He’s borderline LD because of the ADHD. The autistic spectrum disorder has just been left behind, it doesn’t get mentioned …. But now they’ve decided he’s borderline, so how you can be borderline ADHD I do not know …. It’s affected [discharge] a lot because he’s not fitting anywhere. They did start looking at places for him to move on to go rehab, another down step sort of thing. But the social worker he had couldn’t do anything for him because … he didn’t meet the criteria. Other people have said he didn’t meet the criteria, he got turned down for funding because he didn’t fit into any of these groups anymore.
(B6 Family)
A similar issue was also noted by hospital staff:
I’ve also had disputes from the clinical team that there was a forensic team that could only work if they were supported by a CMHT [community mental health team] as well, and then the CMHT wouldn’t pick up this person because they didn’t feel that they were set up to deal with someone with not just an ASD, [but] a personality disorder. So, there was a lot of dispute about them picking them up, because they didn’t feel that they had that expertise to look after that person. But that was the only reason they had to accept in order for the forensic team to pick them up. So, there’s those local disputes, it’s not clear if they will accept the case, they also take time as well.
(Hospital staff, site A)
What helps
While most people highlighted a series of barriers that made it difficult to come out of hospital, some people identified things or people that they felt were helping them to get ready to leave hospital. This could be quite an abstract conversation to have with someone with a learning disability, and some people found it easier to identify what helped via a talking mat (see Box 3 in Chapter 2), placing words/pictures under different headings (‘helpful’, ‘not helpful’ or ‘not sure’) and building up a visual representation of the overall factors at play (see Figure 3 for examples).
FIGURE 3.
Examples of talking mats.
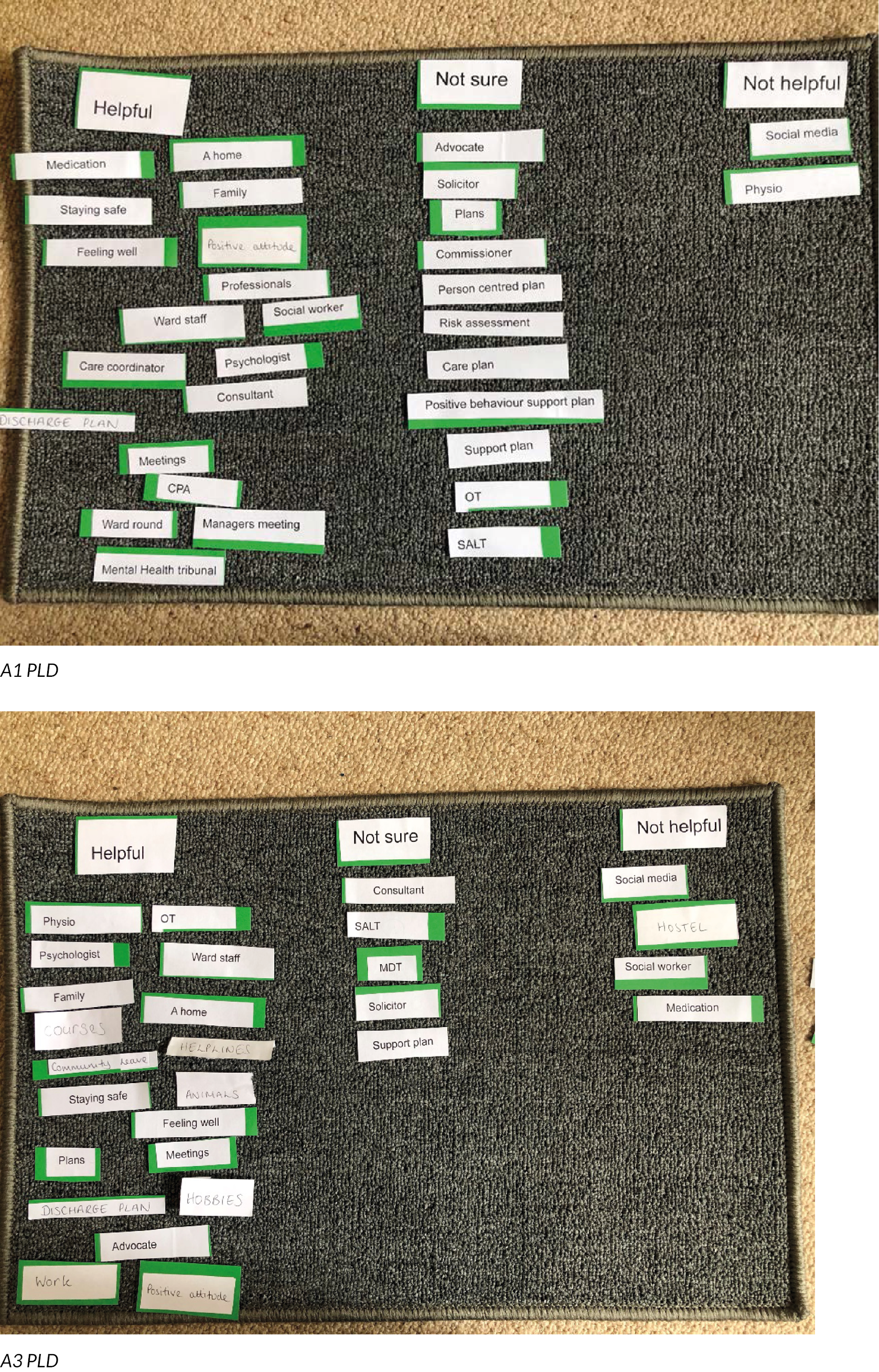
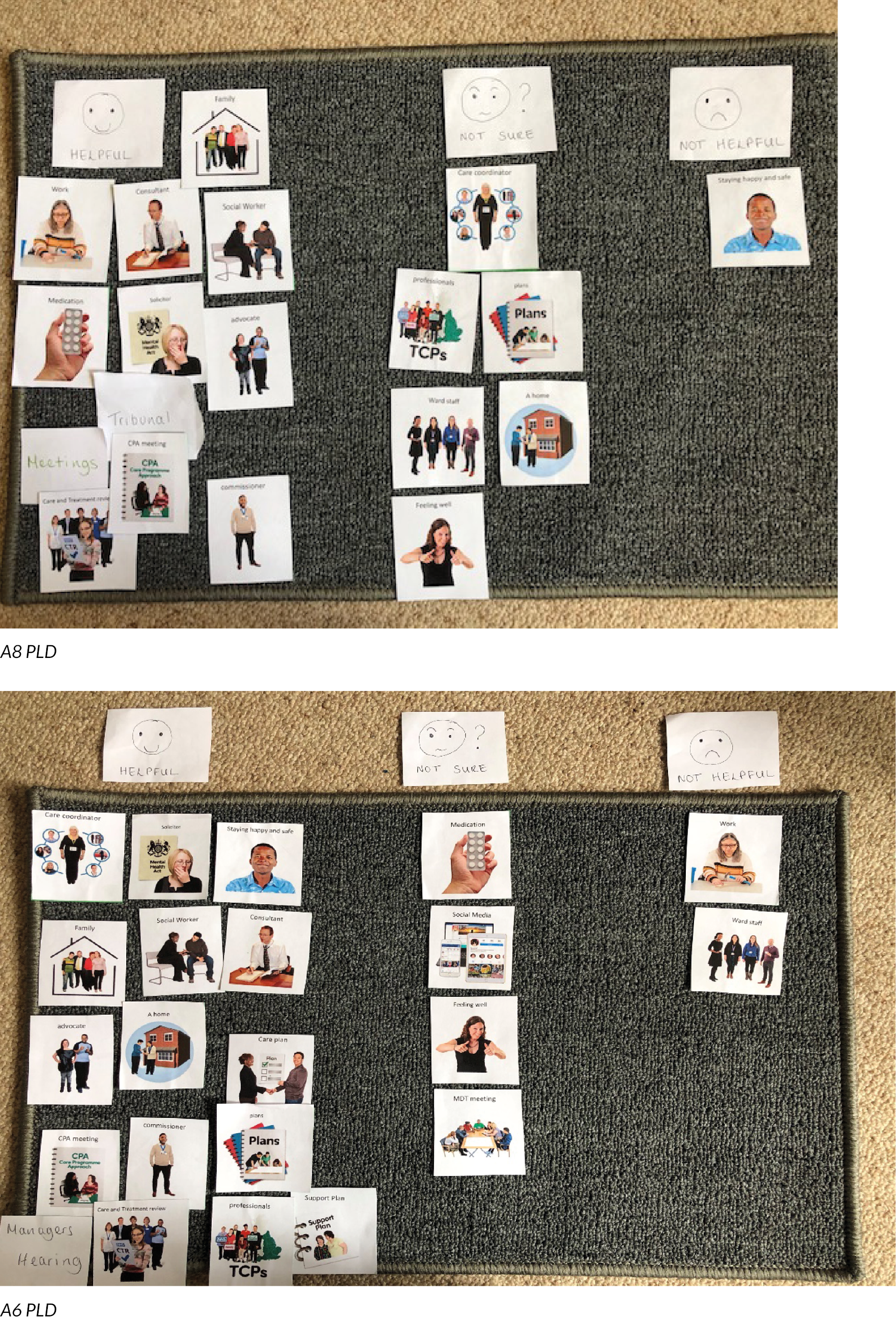
The role of specific professionals and supports
People’s views on which professionals were helpful (or not) varied significantly, depending on their individual circumstances and relationships. While person A1 did not feel that they had needed physiotherapy and so had listed it as ‘unhelpful’, person A3 described a bad experience with their social worker not being available or present most of the time. Person A8 had mixed views as to whether the various professionals involved in their care had been helpful (hence placing them under ‘unsure’), while person A6 did not find ward staff helpful at all in moving them closer to discharge.
Most people who mentioned specific professionals found their consultant, their solicitor and their advocate helpful. Family members gave similar responses, particularly around the role of solicitors in fighting for their family member to be able to come out of hospital:
I don’t ask [the hospital] any more, I ask the social worker or I actually email his solicitor and find stuff that way, because I find stuff’s easier to get that way. It’s wrong, but I’ve found that’s the way to do it …. He is a criminal law and mental health law solicitor and he obviously knew something that they didn’t, but certainly things started shifting. Maybe they realised, [****] hell, he’s got a solicitor, we’d better get our backsides moving here like, you know.
(B3 Family)
However, there were also some notable exceptions, including some people and families who felt the consultant was working against them to prevent discharge:
I’m sure that [****] psychiatrist is trying to keep my son locked up forever.
(B3 Family)
In addition to the role and contribution of specific individuals, people spoke about the value of specific treatments and broader activities that they felt had helped them progress towards discharge. These ranged from hobbies that helped occupy people’s time in a meaningful way (see Life in hospital), to services and interventions such as psychology, occupational therapy and physiotherapy (see below). People also spoke positively about speech and language therapy, courses about forming relationships, and courses about dealing with drug and alcohol issues – where specific needs could be met via a professional intervention or a specific programme that the person could undertake as part of getting ready to leave hospital. Several people also spoke about the importance of positive relationships with wider hospital support staff, rather than just the lead clinicians who might mainly see the person in formal meetings.
Psychology
A number of people highlighted input from psychology as particularly beneficial, especially where they were on a forensic pathway and in terms of helping people cope with the implications of their offences:
The courses what we’ve been talking about doing will help me to learn about what I’ve done and how to cope with it on the outside and to cope with it in the public eye.
(A3 PLD)
The psychology ones …. He’s doing quite a few courses with them which obviously in prison he wouldn’t have done …. More likely to help him move on when he gets out because he obviously can’t come back to [place X] and he can’t go back to where he was born. So wherever he’s going to be, it’s going to be by himself. I mean I’ll go and visit and do what I can but he’s going to be by himself.
(A3 Family)
When I started [a particular type of therapy] I didn’t want to do it, I was quiet, refused to talk to anybody, but then I got into it and I enjoyed it. But it’s turned my life around completely. I look at things a little bit differently. Some days, yeah, I do scream but I don’t hit anybody any more … I think [the therapy’s] a good thing for anybody …. [When I’m in the community] I’m going to see if they do something like that and carry it on because I think that’s really good for people who are in my situation and feel like self-harming and everything else.
(C6 PLD)
Occupational therapy
Occupational therapy was also seen as helpful in terms of preparation for living in the community, supporting people with life skills such as self-care, cooking, budgeting and personal safety:
I just need to show that, show them that I can cook, not cook but make meals, so I can show them that I can drink tea, make a microwave meal, so I need to show that I can do that.
(B3 PLD)
They’ve been asking for help when they need it, kept on doing sessions and things like that to help them move on and to living on their own and to save. The biggest part I need to do is save because when they’ve got a bit of money, they spend it like that.
(A10 PLD – talking partly about other people, hence ‘they’)
Meetings and plans
Although most people stated that most or all of the meetings about their care were helpful, some were seen as more helpful than others. More legally binding meetings such as Mental Health Review Tribunals and Manager’s Hearings tended to be talked about more positively, possibly because there were clear and immediate decisions arising from them:
So the Tribunal have said why is he still here? Why haven’t you moved him on? …. So if they don’t move me they might say ‘right, what’s he still doing here?’ and they might put a discharge to somewhere, to find somewhere for me from here.
(A2 PLD)
Although not many people seemed to know when they might be leaving hospital, some people said they had a plan in place and valued regular meetings, not least because these helped to provide short-term feedback on progress and gave people a sense of where their hospital journey was going:
I would say if you have stepping stones for people to be obliged to like, stick to them …. So like being on the Asperger’s spectrum … – I like to plan my steps ahead … – so if I do this then I’m going to get more time out or if I behave in this manner then I’m looking forward to home leave and stuff like that. But then if they start adding things in just there and then it starts messing up everything and people will start to get agitated and stuff like that and it will affect their health because you’re adding things in that wasn’t originally on their plan …. So if there’s stepping stones – keep to the stepping stones –… don’t just add [extra things] there and then.
(A2PLD)
Well what I like about mine [discharge plan] is I’ve got a date when I’m getting out … but I’ve got to do all this to try and get out …. So, like, a plan, so we’ve got something to work towards …. Everybody’s head works different, but I like to plan and then I’ve got something to work towards.
(A3 PLD)
For many people, what helped (in time) was a person’s ability to manage themselves without too many ‘risky’ incidents whilst on leave – firstly in the grounds and then in the community. This was seen as a key way of proving your ability to cope with being in the community and therefore your eligibility for discharge:
I would say … that some people that are willing to work with the system, do the courses and stuff, they, like I say, like the managers and staff, like they provide more – so like more leave and try and encourage you to get out more. So it’s like starting you off again in the community – getting out in the community and stuff like that is basically our first step to getting out.
(A2 PLD)
Establishing a life and a support network outside hospital
People talked a lot about the support available beyond hospital being vitally important. This was partly in practical terms (e.g. the simplest and most common helpful factor on talking mats being ‘having a home to go to’). However, it was also important to have a support network in case the person started to struggle:
We need a support group for him. We need, I don’t know, it’s hard to say. We need something in place where if he [thinks …] that he’s in danger he can call someone straight away.
(A3 Family)
At least he’s got a nurse with him because my biggest worry was they’d let him go into town on his own … I thought if they let him go into town, because of the way he is, he doesn’t understand if they say things and stuff, you know people talking …. Also he’ll talk over you as well and some people don’t like that. I thought, I could just see someone start to argue and shout at him and then he’s going to get all flustered and … I’m bothered about him getting hurt at that point, but I’m also bothered about what that’s going to do, what he’s going to do later on because of that, if you see my meaning …. He might be living away, but he has a carer with him at all times. He’s not allowed anywhere on his own, which I’m really pleased about, even to the local shops.
(B3 Family)
More broadly, some people talked about the importance of building a meaningful life with enough going on to motivate them to keep going and stay well:
It’s easier to stay on benefits but I think a job and working or something is better than just working voluntary. To stay on disability living allowance, you’ve got nothing to fight for then, you’ve got nothing to keep – you need to keep your job, you need to keep that animal, you need to keep a roof over your head, instead of just going on benefits and just getting everything paid for you. You need something to fight, fight for – I need this, putting in place a house, putting in place any job and stuff.
(A3 PLD)
A few people mentioned inappropriate housing – one specifically mentioning hostels – as being very unhelpful for a successful discharge because of the lack of support in such settings, and the risks that might arise if there were people with mental health and substance abuse problems.
Values and approach
People in hospital, their families and professionals alike all spoke about the underlying values and approaches that underpinned a good discharge. Many of the professionals we spoke to felt that one of the most important principles that helped to make a smooth transition or a quicker discharge was seeing the person beyond their labels and immediate needs – as a human being – instead of focusing on the risk they might pose to themselves or the community, or on the cost of their care package:
I think fundamentally if this was a member of your family how would you want their discharge and their pathway into the community to be – what would you want for them?…. And to see the person that we’re talking about as an individual with a right to live their life.
(B1 Commissioner)
It’s about being inclusive. It’s about working with people. It’s about helping [B4], for example, with his hopes and his aspirations. It’s about supporting service users to take responsibility and be accountable …. Say, if an incident occurred. What happened at the time? Maybe [B4] hit out at another …. Threatened a member of staff. So, to explore … what was happening at the time, how he was feeling? Helping people to reflect on that, and together as a community, to try and put things right and create that sense of community. So, those are the things that I’m trying to promote, but never minimising at all the risk to others and the public and the very nature of why people are in here. So, it’s that balance.
(B4 Social Worker)
Family members also talked about how a person-centred approach helped their family member progress towards discharge more quickly. In the example below, the person needed to improve their self-care skills, partly to get closer to discharge, but also to improve their overall well-being and quality of life:
I just think that they treat her like a person, whereas before I’ve tended to believe she’s more of a number. Yeah, they take her out more, you know, and at the moment they’re teaching her how to look after herself which is, she’s never done …. Cleaning, washing and things like that, brushing her teeth and stuff.
(A7 Family)
Understanding the person – personalised transition support
Related to this, a strong theme emerging from all participants was the importance of understanding the individual person and their unique personality, needs and challenges. They also noted the importance of assessing this properly, communicating these needs adequately between the hospital and community services – especially to the provider to which they might be discharged – and building this understanding into structured, personalised support for that person around their transition:
He needs the service specification that’s written for him, that he was part of writing. He needs that going out to the providers and for providers to actually read it and listen to what he’s saying he needs, because I think sometimes providers go out, do the assessments and they think ‘oh we know what you want’, when actually you’ve not listened to the person that you’re assessing.
(B1 Commissioner)
The … the community forensic outreach and liaison service … – they’ve been really proactive and supporting [A7] in her preparation for a transition. She has weekly contact with the caseworker from the … team – that’s been consistent I would say for the last eighteen months – personnel have changed but the two girls she had previously and the current worker, you know, they’ve maintained real high levels of contact with her.
(A7 Commissioner)
I think on the plus side, I think [the manager], where she is today, and a member of staff from the home who I think would become her key worker possibly, they visited the hospital and they had a sit down meeting with all the clinicians that was involved with her. I think they’ve got a pretty good handle at the home about what to expect, so that communication was good, so [the manager] and this other lady went to [deidentified placement] – psychiatrist, psychologist, clinical nurse, the social worker, whoever, there was a big on site meeting and they were – I think cards were laid on the table – and because I said something to [the manager] and she said ‘oh don’t you worry, I know all about it’, so I got the impression that – so I think that would be a good starting point for somebody coming out is that the person who is going to be looking after them needs to be – needs background – needs to know – the good and the bad.
(A6 Family)
To help build these relationships, many people talked about the importance of family involvement – both as a motivator for people to complete other necessary steps towards discharge, but also for supporting the person more generally:
[Family] – yes, that’s a big part of me wanting to get out for them …. My Mum said to me, we need you, and I’d say I need her, I need my family.
(C1 PLD)
It is helpful when my Mum’s here ’cos I find it hard to explain stuff over the phone, so it’s like it’s helpful for my family and stuff, yeah, I’d put it in helpful. We’re going to start having them in that ward round, because we need to talk about my health issues, so she said she’s going to bring it to ward round, so we need to have a talk about it.
(B3 PLD)
For one person, family were also crucial in managing complex finances when moving to a new property after over two decades in secure hospitals. Without family support (which came at significant personal cost), this person would likely have been delayed even further:
Right, okay, so we need to get this house some furniture, so we had to go through a process where we had to follow [deidentified place]’s rules/policies to get three quotes for each item … – anything over £200. So at this meeting I said, I had breast cancer last year, so I was off work at that moment in time, I were having chemotherapy treatment …. So I collated all the quotes, sent them to [case worker] and then … because again he’s got this substantial amount of money, believe it or not, he went over the threshold – so he had to pay for his own legal fees. I know, it’s mad. They’d had him build this money up in hospital for 27 years.
(B4 Family)
What happened next
Of the 27 participants, 21 were recruited in sufficient time to allow for a follow-up after 12 months (see Table 8). Of these, 15 were still on the same ward as at their original interview, 4 had been discharged from hospital and 2 had been transferred to different wards in the same hospital. Of the latter, one person had moved from low to medium secure, and one person from an ATU to a low-secure ward. Of the four people who had been discharged, the hospital was unable to provide new contact details for one person.
| Person | Initial location | Location 12 months later | Additional information |
|---|---|---|---|
| A1 | Low secure | In seclusion | Same ward (in seclusion) |
| A2 | Low secure | Low secure | |
| A3 | Low secure | Low secure | |
| A4 | Low secure | Low secure | Being discharged that week (Council flat) |
| A5 | Low secure | Medium secure | Same hospital |
| A6 | Low secure | Discharged | Discharged to residential home |
| A7 | Low secure | Low secure | |
| A8 | Low secure | Discharged | Supported living – own flat |
| A9 | Low secure | Late recruit – no follow-up | |
| A10 | Low secure | Late recruit – no follow-up | |
| B1 | Low secure | Low secure | |
| B2 | Low secure | Low secure | Place identified – waiting for MoJ, DoLS and funding |
| B3 | Low secure | Low secure | Discharged but readmitted |
| B4 | Low secure | Supported living | Discharged straight from medium secure |
| B5 | Low secure | Low secure | Likely to be extended stay |
| B6 | Low secure | Low secure | Place identified in residential care – waiting for someone else to move out |
| B7 | ATU | Low secure | Same hospital |
| B8 | ATU | ATU | |
| C1 | Low secure | Low secure | Declined follow-up |
| C2 | Low secure | Discharged | Hospital unable to locate |
| C3 | Medium secure | Medium secure | |
| C4 | Medium secure | Medium secure | Moving to low secure the following week |
| C5 | Medium secure | Medium secure | Accepted for low secure (different hospital) – waiting for MoJ decision |
| C6 | Low secure | Discharged | No details – late recruit |
| C7 | Low secure | Late recruit – no follow-up | |
| C8 | Low secure | Late recruit – no follow-up | |
| C9 | Low secure | Late recruit – no follow-up |
When following-up people who had left hospital, it could be difficult to make contact with a new service provider and re-establish contact with the person (usually care staff who were under significant pressure, who had not been involved in the original research and who sometimes acted as informal ‘gatekeepers’ on the person’s behalf). However, with perseverance, we were able to overcome these barriers for all the people for whom we had subsequent contact details.
Of the people who were still in hospital, some people had a better sense of what might happen next – either a clearer plan for discharge or a planned step down from a medium- to low-secure ward:
The bed’s there. It’s just getting more staff in, got to put [Deprivation of Liberty Standards] in place … and [organisation X] have got to fund it.
(B2 PLD)
I’ve signed a contract for some accommodation now.
(A4 PLD)
Yeah, I’m moving out. I am going to local secure on, next Tuesday.
(C4 PLD)
I know for a fact I’m being assessed for a low secure … and then two weeks later I got told they’ve accepted me.
(C5 PLD)
However, other people were facing continued uncertainty, and some felt as if they were genuinely stuck, with little sense of what might help to resolve their situation:
I’m stuck …. They should have a plan B then I wouldn’t be stuck.
(A7 PLD)
For some people, this was relating to the remaining sentence that they needed to serve after their treatment in hospital was complete. One of these people said that they would rather have been in prison than in hospital, as there would be a definite release date:
I’d rather go back to prison.
(A3 PLD)
One person had left hospital after we had spoken to them originally, but returned after a couple of weeks when the placement broke down. While we do not have any details, the person mentioned being left alone by staff that they feel should have been with them one-to-one, and some sort of ‘incident’ occurring:
They sent me to [a new place] but that didn’t work out.
(B3 PLD)
The three people who had left hospital and agreed to a follow-up interview (see Box 11) came from two different sites. Notably, one person was discharged directly from a medium-secure ward (typically people here transition to low secure, then a subsequent discharge). It is also interesting that three of the people who were discharged were women, given that most of our sample were male – and it may be that there are additional barriers in terms of leaving hospital for some men. While it was lovely to see a small number of people thriving in new homes, and while some people were closer to leaving hospital than when we first met them, the fact that so many people were still in hospital 1 year later (and two people possibly further away from discharge than when they were first interviewed) simply highlights the scale of the challenge that this research is seeking to address.
B4 was living in his own house with support from staff. He showed us his house, garden and new possessions, including his DVD and Star Wars collections. He spoke about the places he enjoys visiting, and was heading off to a local nature reserve. He had a photo on the wall of him and his family at the nature reserve, and his life felt very different to when we met him a year ago.
One person [A6] had wanted to move into their own flat, but was currently living in a small residential home. They were feeling unhappy and wanted to be back in hospital – although when we first met them a year previously they had been unhappy in hospital and wanted to leave. They were awaiting a further court case, so it is possible that their current arrangements were linked to this in some way, or were temporary until they received a verdict.
A8 had been discharged recently to her own flat, with support from staff. She said the discharge went well, in spite of feeling nervous – and she’d had lots of visits to her new flat before moving (including overnight stays). She put her progress down to her own behaviour (‘I was good’) and said that all her team from the hospital had helped her move on. She enjoys going to bingo, the cinema and shopping, and is keeping a close eye on the fortunes of her favourite football team. She does this via her phone, which typically are not allowed in hospital. She wants a pet tarantula, but does not have one yet.
Chapter 5 Findings II: systems issues from the perspective of hospital staff and commissioners
Whereas Chapter 4 focused mainly on the experiences of people with learning disabilities and/or autistic people and their families (but with some supporting quotes from health and social care staff where these were consistent with people’s/family perspectives), this chapter focuses on systems issues arising from observations of multidisciplinary meetings and insights from hospital staff and commissioners (but with some supporting quotes from people and families, where these back up professional perspectives).
Overview of participants/data
This chapter is based on data from several sources:
-
Across our sites, a range of different hospital staff took part in focus groups and individual interviews. They were working across a variety of settings, from ATUs to locked rehab wards, and from low to medium secure (see Table 9).
-
A total of eight commissioners were interviewed across sites A and B, with one commissioner taking part on behalf of two of people with learning disabilities and/or autistic people, as they were both part of the commissioner’s caseload (A4, A5, A7, A8, A9, A10, B1, B4, B6). However, all of the commissioners who participated were NHSE or regional specialist NHS case managers, not local authority commissioners (none of whom agreed to take part). Commissioners’ details were obtained largely from people’s case files or from local sites. For many of our participants, their commissioner had changed and notes had not always been updated. In some cases, we were put in touch with the most recent commissioner either by ward staff or by the previous commissioner, who had now moved on. In other cases, we were unable to identify or contact the person’s most recent commissioner. We received no responses to contacts made with the local authority commissioners listed on people’s notes, which could also have been partly due to incorrect or out-of-date details – or may relate to the amount of pressure that different stakeholders are facing and their subsequent willingness to take part in research.
-
To help familiarise ourselves with local contexts and service-specific issues, we observed 12 multidisciplinary meetings across sites A and B (despite ongoing negotiation, site C did not facilitate access). These were mostly regular MDT ward rounds, but also included one CPA review and two CTRs. In Site A, we observed six people’s meetings, comprising five MDT ward rounds (A1, A2, A3, A4 and A5) and one CTR (A7). In Site B, we observed six people’s meetings, comprising four MDT ward rounds (B1, B3, B7, B8), one CPA review (B2) and one CTR (B6). We were not able to secure an invitation to observe meetings in site C.
-
To gain an overview of people’s journeys through services, we reviewed 23 people’s case files (some were very extensive, and ran to the equivalent of several volumes). This included notes for all 10 people in site A, 7 of 8 people in site B and 6 people in site C. Some people did not give consent, while some people in one site had moved on and their records had been archived, meaning that we were unable to access them.
| Site A: five professionals | Focus group Nurse/ward manager (mixed settings) Psychologist (mixed settings) Forensic social worker (low and medium secure wards) |
| Individual interviews Consultant psychiatrist (mostly low secure) Peer support worker (mixed settings) |
|
| Site B: five professionals | Focus group Nurse/ward manager (medium secure) Psychologist (medium secure) Occupational therapist (mixed settings) Consultant psychiatrist (ATU) |
| Individual interviews Regional admissions and discharge co-ordinator (mixed settings) |
|
| Site C: three professionals | Focus group Psychologist (mixed settings) Psychologist (mixed settings) Consultant psychiatrist (mixed settings) |
Different professional perspectives
At the start of hospital focus groups, we asked people how many of the patients with whom they worked did not really need to be in hospital. In one sense, the actual percentage cited is not very meaningful when the question is asked in isolation, but we have found in previous research that this is a good way of getting different professionals to compare and contrast their different experiences. If one person thinks that everyone they work with needs to be in hospital, and the next person thinks that only half do – then the fact that two colleagues who work in the same setting have such different views is important, irrespective of the actual ‘guestimate’ they each make.
In site A, a psychiatrist felt that around 5% of people on low-secure wards did not need to be in hospital, while a psychologist felt that 100% of the people they worked with (6/6) did not necessarily need to be there. A ward manager felt that 20% did not need to be in hospital. When reflecting on medium-secure wards, the general consensus was perhaps one person out of 15 could be discharged, but that three or four could step down to a lower level of security.
In site B, some 60–80% of people in ATUs could be seen as having a delayed discharge:
So, the standards are that … 75% of people admitted to an ATU should be fit for discharge within three months. 90% of people should be fit for discharge within six months. They are stretch targets, I would say, clinically, but it’s not a million miles away from that in practice, and ours are the same as others nationally. So, typically, we’re probably around 50% within three months and 75% within six months. So, we’re not a long way off that, but the length of stay is over a year, with those people becoming delayed transfers of care because they tend to require provision which isn’t available within the community, within the market.
(Site B hospital focus group)
In medium-secure settings, a ward manager saw delayed transfers as ‘rare’, but said that there had been two ‘very protracted’ discharges in the last year. In contrast, a regional discharge coordinator found this difficult to answer, but did mention a number of people in secure services who (in their view) could be discharged. They also felt that all but two people in the ATU were considered delayed transfers because they had stayed beyond the stipulated 12-week period explained above. This was borne out when we followed people up 1 year later, as our two participants from the ATU were still in hospital.
In site C, there was a consensus that around 50% of people in men’s services and 20% of people in women’s services were delayed.
Timing and inertia
The most common issue raised by participants of all types was that everything involved in organising and preparing for a person’s discharge simply takes too long. This was the experience described by people in hospital and their families in the previous chapter, but was also noted by almost all health and social care workers involved in the study (whether they were providers, assessors or strategic commissioners). This was despite a number of national efforts to tackle this issue:
I think there’s a bigger ownership on the Transforming Care agenda …. There’s a lot of scrutiny and reporting up around the pathways. If I look back at my caseload for learning disability/autism it’s vastly reduced, but it takes such a long time, such a long time to move a patient through a discharge pathway.
(B1 Commissioner)
Another commissioner noted a sense of inertia for people on forensic pathways or with needs perceived to be complex or out of the ordinary in some way. Once a person had already been in hospital for a significant period of time, it was almost expected that they would remain as a long-stay patient and the urgency to progress their discharge diminished:
If somebody’s not well understood, people don’t have that consistency, they haven’t got the person in their head. And indeed probably there’s been a bit of inertia ‘oh we’ve got this patient, we’re quite used to having them for 1, 2, 3, 4, 5+ years’.
(A8 Commissioner)
Complexity and multiple stakeholders
Time and time again, hospital staff and commissioners talked about the sheer complexity involved in organising next steps for people leaving their current ward, whether this be to a less restrictive hospital environment or into a community placement. The range of organisations, teams and individual workers, coupled with the preparation needed for people to feel comfortable moving to new settings, created added time at every stage of the process, even with all the right people seemingly on board:
There’s lots of people involved in the discharging of the patients. So, you have the case manager, you have the CCG and all the funding being sorted out, and a number of processes that take place. So we often refer to a six-months’ period that we would say that actually, this patient might be discharged within six months, and then at that time we start linking them up for discharge and saying, actually, let’s start that process, because it might well take that length of time to actually find a place, if you’re funding, and then to move into it, and that’s even with the placement, you know, being in existence already. The staff and everybody in there – so there’s something in the system, once we flag it up, it’s taken some time for them to get into it, you know.
(Site A hospital staff focus group)
This experience was shared by the Consultant below, who described some of the delays that can easily creep into or even derail the discharge process where someone has ‘non-standard’ needs (almost by definition, this will be everyone involved in this study and perhaps most of the Transforming Care cohort):
So, providers are now saying that they will need typically nine to 18 months to set up a specialist package …. Even if there’s a property available, the model of provision now tends to be that people will recruit a bespoke team. So, they will recruit staff specific to an individual, and that’s tricky. So, as an example, we had a young woman admitted to us …. She got told that she was moving into a new property and the placement that she was in broke down, so she came into hospital, which of itself is an inappropriate admission, and we were told it’d be two to four months for them to complete recruiting staff. She was only discharged last week for no reason other than the provider couldn’t recruit the staff. We could say that that was in some part due to COVID and recruitment and issues like that, but it’s not unusual. So, people who are fit for discharge, and then other people are needing single occupancy – and care providers, rather than having properties, will then go to the market and buy a property specific for an individual, which obviously takes time, and then there’s usually environmental changes, a wet room and handrails or fencing for the garden, whatever it might be, or in the most extreme, complex-end people will be building bespoke properties. So, that tends to be the pattern for the non-secure end of assessment and treatment. People will come in, some of that’s appropriate, will be fit for discharge, typically, in three to six months, and then wait another, anything from 9 to 18 months, so on average another year waiting for that property to be available.
(Site B hospital staff focus group)
Similarly, the social worker below anticipated potential delays, even before the decision had been made about where the person should go next (particularly if the decision was to go to a community placement rather than another hospital setting):
If there’s locked rehab and there’s a bed available, that process could be a couple of months, couldn’t it? By the time funding’s agreed and you’ve allowed for some transition work, that could be a number of weeks to months. If it’s a community package, then that’s going to be more complicated, because that will depend on if the property’s already purchased, or if they’ll be looking at purchasing a property. Whether the staff team are already in existence or whether they would recruit specifically a staff team to support [person’s name]. So, it’s really going to depend on where that lands. It could be a community service that already has a set-up property and support team and they’re discharging somebody and [the person] can move into that service, which again, would just be weeks. If they’re talking about creating something more for [them], then yes, you’re talking about potential environment, property and staffing. So honestly today, I don’t think we could put a reasonable timeframe on it.
(A9 Social Worker)
Of course, this begs the question as to whether more could be done to plan for discharge on admission, as is meant to be the case in other settings (e.g. when older people are being admitted to/discharged from general hospitals). If someone is going to need a property to be purchased and their own staff team to be recruited, then it makes no sense to wait till they are ready to be discharged before starting such processes (see Chapter 7 for further discussion of insights from the broader hospital-discharge literature).
Processes and tools
Many participants described particular tools and processes surrounding both admission and discharge as being ineffective, unhelpful or actively hindering people’s ability to move on in different ways. This ranged from legal tools and policies at a national level to the specific assessment tools and processes used by providers.
In the example below, a psychiatrist described the multiple steps involved in the discharge process, with each assessment adding at least weeks to a discharge timeline. With community providers all using different assessment tools, which do not necessarily correspond to the ones used by the hospital, doing this repeatedly could create significant periods of delay after the point at which the person is deemed ready for discharge:
So we go to the case managers and we say, look, I think this patient could move into supported accommodation, that’s what I say, 24-hour support accommodation, and I think we should start looking for that, and then it takes time for them to find that. So, I don’t know, it might take three weeks for them to identify those ones, and then I think there’s … because I don’t know exactly what goes [on], I just experience the periods of delay. Then they come back and they send us an assessment form, and then it takes a while to write the assessment form, to fill it out properly. Then we send that off and they take three weeks or so to read through the form and see whether it’s done appropriate[ly]. Then they come and see the patient, they think about their provision, ‘do I have to make some adaptations?’, and that takes some time, and then they do some joint working, and yes, that whole process, and then the other bit is agreement of funding ….
(Site A hospital focus group)
Other hospital staff felt that risk assessments could conflate behaviours arising from a reaction to the hospital environment or behaviours which might arise out of someone’s learning disability, with what they called ‘intentional violence’ and a future risk of offending. This could then raise the person’s ‘risk’ profile, especially in relation to decisions by the Ministry of Justice about leave, or community placements’ assessments of suitability – resulting in the person being deemed ‘too risky’ for the next stage of leave or unsuitable for a place at a community provider:
There’s a poor differentiation between challenging behaviour and understanding that as different from instrumental violence, and yet the risk assessments that are prescribed by the NHS for inpatient services such as the [name of risk assessment] makes no differentiation between challenging behaviour – which is a mainstay of a hundred years’ worth of working with people with neuro-developmental disorders – and the forensic issues of things like unlawful killing and arson and murder and some of the other stuff. Whilst those two things are all jumbled up together, what it forces people like [my colleague] and other very sensible people to do, is to count problematic behaviour …. So one of the problems that everybody runs up against is this idea that somebody shouting because the lights are too bright or it’s too noisy on the ward is a risk indicator for still doing wicked things to children. Huh? How does that work then? Well it doesn’t, does it?
(Site A hospital focus group)
Legal status
Various practitioners talked about how the legal status of a person detained or treated under different sections of the Mental Health Act meant different things in terms of the support they might get after discharge, with a series of potential pros and cons to this. The social worker below expressed concern that people with learning disabilities who have committed offences might not get the same support to reintegrate into society and avoid reoffending as someone who has come out of the criminal justice system with support from probation and other agencies:
So for anybody coming out of the criminal justice system you have probation, you have all these safeguards in place … we have the conditional discharge options and things like that. But often they skip that because they’ve got a learning disability so we’ll make that exception and they’ll come on a Section 3 – perhaps, I’m generalising – but they’ll come on a Section 3. They haven’t been sentenced or properly convicted of the crimes that they’ve committed, so they don’t have … the luxury of being supported through probation, proper discharge things, and then they re-offend and you’re just going round in these circles. And actually they get missed because they’ve got a learning disability and you’ve made an exception for them because ‘oh bless him’, and that’s not OK because actually that’s the opposite of what you want to achieve. But it becomes the default.
(Site A hospital focus group)
However, it was not always seen as ‘better’ for a person to be detained under a forensic section. Often, when a person’s legal status required the Ministry of Justice to give permission for leave, discharge or transition visits, this added significant delays to the process (as described in the previous chapter), simply through waiting for decisions to be made.
Others wondered whether current mechanisms such as Care and Treatment Reviews (CTRs) had enough ‘teeth’ (legally or in terms of expertise/status) to be effective, particularly compared to the statutory powers of Mental Health Review Tribunals:
Unfortunately, in my experience so far, I haven’t been to a CTR … where it does something which … wouldn’t have happened before, that then results in the patient being discharged …. The CTR, I don’t know, they tend to … they make suggestions that might optimise a patient’s treatment pack, but it hasn’t been linked to them being discharged … I don’t think the people who are involved in that are necessarily the right individuals, the right group. They don’t have the power, necessarily, to discharge someone. They’re not able to challenge greatly the view of a consultant …. So, you could say the function of the CTR seems to be better served by a Tribunal which isn’t set up for that purpose necessarily.
(Site A hospital focus group)
Providers also noted they often felt as if hospital staff did not trust them to comply with the different legal frameworks, restrictions and reporting requirements of people detained under particular sections of the MHA:
I think legal frameworks often play a massive part and I think, you know, there’s a lack of understanding across our sector about what’s the best legal framework for people to come out [on]. But fundamentally I think it’s about, you know, people’s understanding about what the community can do …. [We have] RCs and people in hospitals going ‘we don’t even know you. So until we’ve got a relationship with you, why would we want to send somebody out into your package of support?’ and therefore you’re in this vicious circle.
(Social care provider)
Disputes over responsibility, next steps and funding
Participants described a number of situations in which multiple stakeholders and complex legal requirements led to disputes over clinical responsibility for the person in the community, as well as disputes between health and social care, and between different geographical areas, as to who should be responsible for funding the person’s subsequent care and support:
There’s an application that goes through to the local council and they sit around a board and discuss whether the funding’s approved, … and then there’s a debate whether it’s more social or health, and then, so sometimes that can take some time, and actually, they might come back with a decision, we have to challenge the decision, and then, we say, actually, this patient in the community, they need a forensic team to support them, in order to manage them properly, and then there’s disputes locally over which team it is that looks after them, and then there’s … say if they’re forensic, then they need a both clinical team and a social supervisor. Their social supervisors, depending on where they are, may dispute that a patient falls within their category.
(Site A hospital focus group)
In one multidisciplinary team meeting, staff described delays finding a consultant who would be prepared to take responsibility for a person (B2) once they left hospital. In other meetings (B3 and B6), the team discussed disputes over which community mental health team would be responsible for the person, relating to both the geographical area and the specialisms of the teams (whether it should a forensic team, learning disability team or mental health team). One commissioner clearly described multiple discussions behind the scenes about which community team might be best to support a person:
She’s ready for discharge, the CCG have now got an identified placement, they’ve approved the placement, but where we’re at is the meeting next week is to talk about which community team will pick her up because … she’s always been under learning disability services and myself and the [learning disability] team were adamant that’s where she should remain, as is the CCG. The Trust are saying ‘well actually does she need the SCFT team’, which is the Specialist Community Forensic Team – and we’re saying ‘no, she needs the learning disability … team’. So there’s a meeting next week to talk around that and who will be the appropriate [responsible clinician].
(A7 Commissioner)
A similar observation was made by a provider during a MDT meeting for a person due to move into one of their properties:
It just feels like it is … money orientated, and then you get the health and social care thing that goes on, you know. I sat in a meeting a couple of weeks ago and I can’t tell you how many commissioners and local authorities, and they were literally ‘this man’s being held like this and you’re arguing over …’ and [unidentified place] have never even – he wasn’t even born there, but they’re having to fork out all the money because they’ve got the values, do you know what I mean?
(Provider 1)
The broader impact of policy and austerity
Some people felt that funding issues had become less of a problem since the Transforming Care policy agenda, which was perceived to have created a strong impetus to discharge people experiencing lengthy stays in hospital. However, many people felt the longer-term impacts of austerity and budget cuts to local Councils had led to lack of staff and specialist provision available in the community:
We’re all strapped for staff – nursing, medical staff, local authority – and I know budgets are being cut – and I know the care managers – their hands are often tied – they’re working within tight remits – it’s not always them – it’s the bigger and the wider organisation structures and budget restrictions.
(B1 Commissioner)
Historically, I’ve faced challenges with funding, although I have to say, in recent months, the funding is less of an issue …. But there is still, obviously, money is always going to be money, isn’t it? So, there remain funding issues at times, especially in community provision.
(B1 Social Worker)
Community provision
In addition to disputed responsibilities for people’s care and support after hospital, another barrier was perceived to be the difficulty of finding suitable community services. Sometimes, there was perceived to be a shortage of appropriate services; at other times, some hospital-based staff were seen as not being fully aware of the range of services available in the community or the complexity that many community-based staff manage on a regular basis. This issue of understanding what was available was even harder when a hospital was working with people from all over the country – while they might have an awareness of local services, it was often impossible to know what was available in a large number of other areas. It is thus hard to tell whether the gaps identified in this section represent actual shortages and/or perceived issues – albeit we took away a strong sense that both these factors might be at play at once.
Lack of appropriate placements
A wide range of different professionals felt that there were simply not enough placements available that met the needs of people leaving hospital (see Box 12). Other staff identified particular gaps in terms of community services for people who have a learning disability and a personality disorder, for people who are transgender, and for some women:
We don’t have the balance between the inpatient expensive hospital forensic provision versus the corresponding step down in the community that adequately meets the needs of service users when they’re discharged, and particularly female service users with autism for instance.
(A8 Commissioner)
This was also the case for discharges that might involve a step-down in the level of security or restrictiveness of the setting (i.e. a person moving from medium- to low-secure, or a person moving from low-secure to locked rehab):
I would probably say it’s around the flow and the movement of patients between hospitals …. So, for example, we might have an influx of people from medium needing low, but low haven’t got any movement their end. That’s one of the …. Certainly historically, that’s one of the main ones. There’s a lot of people sitting around waiting for low secure beds.
(Site B hospital focus group)
So, there are some patients whose local area are further developed with specialist provision, and there are others who don’t have that. So, again, discharging into the community when we feel someone’s ready, finding a care provider can be a real challenge.
(B1 Social Worker)
The main issue … is the amount of places available in the market, or the slow stream of those. So, that people will often offer a placement, and so it’s there on paper, but practically, being able to move someone into it can take six to 12 months, I would say …. And the challenges relating to that are resourcing, paying for vacancies. If you want placements to be available, then there have to be vacancies in these providers, and they are typically all independent businesses – then why would they have vacancies if they don’t need them?
(Site B hospital focus group)
I can think of two very complex discharges that have been really long-winded and have kept people in hospital for probably up to a year longer than would have been ideal. Some of that has been impacted on by the pandemic, and by difficulties in terms of accessing transition visits and things like that, and others have just been about finding that right environment and that right placement that can meet the needs of people with a learning disability, a mental health condition and some complex forensic issues …. There’s not many that do it.
(Site A hospital focus group)
The issue what we have is people who have been in long-term care and who are ready to be discharged, say from a secure service like this, we’re ready to go at our end. It’s the community-based help and team and support who we’re having issues with …. Like I’ve spoken to a patient and the patient said to me ‘Well I’m being discharged’ and I’m like ‘That’s great. That’s fantastic’ …. And they’re like ‘Yeah, I’m just waiting for my social worker to get in touch with me because I’m waiting on a house placement.’ And then fourteen months later we’re still having the same conversation.
(Site A hospital focus group)
Lack of staff (hospital and community)
There was a widely held view – from hospital and community services – that one of the main issues contributing to a lack of suitable and readily available community placements was a struggle to find and recruit qualified and adequately trained staff. Almost everyone talked about how strained services were across the board, best captured by the following comment from a commissioner who was in the process of leaving the sector:
People are so tired. There’s not enough staff in, and I know I’m contributing to that by leaving, but you know, there’s not enough to be able to do this, at the moment. We need something to help us, because health and social care are going to implode otherwise.
(B5 Commissioner)
This view was supported by other participants, including a ward manager who described issues with staff shortages shared by the hospital and community services:
It’s the pool of people, the numbers of staff, it’s a national shortage isn’t there? They physically don’t exist. I think we run on low numbers every day. I don’t think there’s ever a day that where our numbers with regards to what would be our ideal staffing levels and I think we’re not alone, you know, the community services are faced with the same challenges.
(Site A hospital focus group)
In one multidisciplinary meeting, person B8 was hoping to be discharged to a community placement. While the identified provider had been trying to recruit staff, only two had been appointed and seven people were needed for a core team. The regional care co-ordinator directly attributed this to a ‘national staffing crisis’ and the team agreed that there was a widespread problem with recruitment to the sector. The same person had still not been allocated a social worker since his admission months before, and so had no social care representation at the meeting.
Some staff talked specifically about a lack of staff in community mental health or learning disability teams, in this case the local intensive support team for people with learning disabilities:
They’ve only got three nurses in that team currently and they’re operating over seven days …. So when somebody’s in crisis and you want that intensive, robust planning that we’ve just talked about …. Our intensive support team are really struggling – they’re all fantastic – they’ve got a wealth of knowledge – they’re really good – but they’re just spread too thin.
(Site B hospital focus group)
In addition to general staffing pressures, many hospital staff and commissioners alike expressed concerns about community providers having staff with the right skills and expertise to support people with complex needs, and about the difficulty of ensuring consistent, familiar staff who know the person well and can support a successful transition (see Box 13).
Some of them are down to not having enough staff and the staffing recruitment and retention crisis is a factor. But also things like making sure they’ve got – not just the numbers of staff but the right staff – they’ve got psychology discipline in place, etc. And they’re not running on agency staff who don’t know the patients – and of course this would be a big factor in slowing down somebody’s pathway.
(A8 Commissioner)
There’s definitely challenges, enormous challenges here, but on the whole we do have the people that know the patients and that can back up, in a team of 10–12 people you’ve got at least a couple of stables that can hold things together. If you’re in a community provision, it’s not as easy and you’re kind of reliant – there’s so many times when they’re talking to us about kind of relief support and kind of using an agency and things and it’s like ‘no, she can’t come to you if that’s the option because that’s not going to keep her safe, that’s not what’s going to be protective’.
(Site A hospital focus group)
And in the community there are fantastic examples of how to do services for people with autism and learning disabilities. I mean there are some superb examples of really caring and knowledgeable services that are set up with all the correct adaptations and in lovely parts of the country and they’re all over England, Scotland and Wales, you know, scattered about. One of the crucial things is a stable staff team, you know, and the investment in those staff that come on and that’s great. There’s just not enough of them!
(Site A hospital focus group)
This was perceived to be a particular issue when someone had committed a serious offence:
When patients are in secure services, these are people that have had really complex trauma, got really complex and high-risk offending behaviours, you know – to work with these people in the community it is challenging, it’s really challenging. And in terms of the skillset, I’m not convinced – and I know colleagues and partners and stakeholders aren’t convinced – that there’s the right skillset in the community to make sure these people don’t come back into hospital and to make sure they have got a quality of life that’s safe for themselves and the public.
(B1 Commissioner)
There was also a widespread impression that staffing and service pressures were preventing front-line staff from accessing training on fundamental issues such as safeguarding and communication. For example, participants in the site A hospital focus group said that:
I think, you’re just in essence taking people off the street and then expecting them to just go and work with these really complex patients …. And we’re surprised and disappointed with them when they don’t do it right …. So there really isn’t, well there have been some attempts to get some standardised training packages for autism and learning disability over the years, but they’ve not made it to the shop floor.
People haven’t been able to be freed up to attend [training]… I think I delivered the ‘Need to Know’ safeguarding that hadn’t been delivered for 18 months, so you’re thinking [it’ll be to] like huge amounts of people and I think it was to two people in the end. It’s [****].
Safeguarding is not even specific to this special venue is it? It’s just safeguarding, everybody ought to know safeguarding. So trying to get some even what I consider to be fairly basic training about how to moderate your language when talking to a patient with intellectual disability or autism and how to make those necessary, we don’t do that, we don’t deliver that training.
Limited awareness of community options and step-down processes
While they experienced numerous difficulties discharging people to community services, some hospital staff and other participants felt that there can also be a lack of awareness from within the hospital of what was actually possible or available in the community (in terms of the range of providers, the types of services available and/or the complexity with which some community services work). This was particularly the case in medium-secure settings which had previously tended to ‘step people down’ into low-secure, then to locked rehab or to the community. Over time, and often because of difficulties accessing low-secure services, a number of medium-secure wards were finding themselves holding on to people until they were ready to be discharged direct to community services – only to find that they need new knowledge and new relationships in order to be able to do this well:
What I find happens from a medium secure point of view is, we admit people who are quite poorly, need to be here, and then there’s a bit of a delay getting them to low secure, for whatever reason, whether that’s to do with their bed capacity and their movement, and then they end up here almost too long, that they don’t need low secure any more, and then we’re in a position that we’re having to find these really complicated placements that we’re not in the habit of doing …. So, then we’re having to set up links from scratch and go out there and find places that ordinarily low secure deal more with …. [Historically, someone would go from medium to low secure, before a subsequent discharge]. In the more recent years, it’s been less like that, and we have had some more creative ways of discharging people …. But typically and traditionally, that’s how the forensic pathway has worked, which means we’re not as au fait with what’s out there in the community as our low secure colleagues probably are, and we’re having to become more familiar with that, but it does take longer, and therefore people are here longer.
(Site B hospital focus group)
Although providers’ perspectives are explored further in the next chapter, it is worth noting here that they shared the view that there was an issue with a lack of awareness of what was possible or available in the community:
One of the first meetings I had was in [place X] with various representatives from then the CCG, now the ICBs or whatever, but they were saying ‘we don’t really understand what supported living is. We don’t understand what community-based placements are’.
(Provider 3)
I think there’s a lack of education within the hospital staff about the regulated activities as well, you know, when somebody says ‘we want residential for this person’, what actually does that mean? You know, if you’re a creative community provider you can provide the same service under whatever regulated activity is required and yet they still want residential! There was a consultant psychiatrist in a regional secure unit up in [place Y] who insisted that the conditions of the discharge should be a residential service and we were trying to say ‘but actually a residential service has got an element of communal living’, and what he was actually talking about was restricted environments and he thought that could only be achieved in a residential service …. But yeah, it’s about what people imagine – a lot of people can’t conceptualise what a particular service will look like. We’ve got supported living services that are a bit more like residential. We’ve got residential services that are individual flats under the same roof and if a person’s needs change and the commissioners decide that supported living is a much better option, they can actually change regulated process without changing their house.
(Provider 2)
Poor communication and collaboration
Lack of involvement of key professionals
Underpinning issues with timing, disputes about funding and the complexity of the process were also problems with getting different teams and individuals to, firstly, communicate effectively with each other in order to agree a discharge process and move it along; and secondly to individually complete the necessary actions needed to progress the person’s discharge. Many participants expressed particular frustration at the absence or lack of engagement of key professionals at CTRs and other meetings, lack of follow-up or a lack of information-sharing:
The other thing that jumps out is about getting the right people around the table. We’ll have meetings after meetings after meetings about the more complex discharges and the more creative discharges, but an individual isn’t present to say yes or no or take responsibility for something, then that whole meeting becomes pointless, and we’re waiting again. So, sometimes the more complex the discharge, the more people need to be involved, it becomes like a personnel difficulty.
(Site B hospital focus group)
Care managers not attending reviews, not keeping people up to date even if it’s to say they’ve been unsuccessful [with finding a placement], it’s that constant chasing for information.
(B1 Commissioner)
The frustrations from the MDT are such that it’s taken such a long time for the CCG to actually listen to what they’ve been saying and we’ve had numerous meetings … so I would say from the end of 2020 we were looking for a positive discharge by December 2021. I think it’s fair to say that the CCGs – I think time might have run away with them – so in my head at the MDT we were working to that discharge timeline and it did take quite a while to get the CCG to get providers to go out to be assessing her.
(A7 Commissioner)
Often, people identified the presence of a ‘responsible clinician’ from the community as being fundamental for decision-making and clarity around how best to support that person post-discharge:
I think one of the stumbling blocks we certainly feel in forensics is a lack of a medical representation. So, the bottom line with a detained service user is that that responsible clinician is, in fact, that responsible clinician, and decisions can be discussed and can be agreed, but they can’t be made without their input and their agreement. So, if they’re not there, that can be problematic. Not necessarily throughout the process of discharge, but certainly at any point where decisions are being made, we need medical representation, particularly from the RC or a delegate. And I guess, depending on what we’re talking about in terms of the discharge place, the environment, you need the representation from that area that is able to similarly make decisions, give all the correct information …. Without those two sides there, it feels like a big chat that we can have, and we can all have these nice ideas, but there’s no sense of achievement from it.
(Site B hospital focus group)
Many also noted issues in terms of the absence or turnover of social workers, and some people in hospital said that they had never even met the person’s social worker. This was different in one site, who employed their own in-house social workers. However, in around half the remaining meetings observed, there was no social worker present.
Poor communication by and between professionals
As well as the absence or lack of engagement of key professionals, many participants also noted persistent communication issues, in terms of either infrequency or inconsistency of contact, or the manner in which people communicated. In the example below, a commissioner described a situation in which they felt communication had been poor and decision-making almost unilateral:
The one patient I’m thinking about, he’s had an unsuccessful discharge into the community, so we had him out on Section 17 leave [leave authorised by the clinician in charge of the person’s care under the Mental Health Act]. There was an incident and he was brought back in and frankly he was forgotten about. Comms from the MDT outward were really restricted. We were going in, trying to work out what’s happening – we need to get this back on the pathway. The [community] team, they also actually for a period seemed just to – wasn’t important to pick him up again – and then I find out – they were there asking for discharge planning meetings to be scheduled – and I get an email yesterday to say that the RC has referred into a locked rehab service. No consultation with myself as the case manager, no consultation with the CCG … it just beggars belief. So I email her and say ‘I’ve just heard you’ve done this’ and she emails back and said ‘yeah, I’ve done it’. I was like ‘we’re looking for a community pathway, not another inpatient stay, he’s already been in hospital'.
(A5 Commissioner)
Other people described repeatedly having to give the same information during the referral process, which added time to an already potentially lengthy assessment:
All these services are so individual, and … they all seem to have their own different processes and refer to things in different ways. So, they may be requesting the same information, but asking it in a way that’s very different from the last service that we’ve dealt with. So, it feels like sometimes we’re duplicating work. They’re asking for an assessment or an understanding of someone’s needs, but you’re almost having to seek out, well, what is it that you actually want from us?
(Site B hospital focus group)
Poor communication with the person and family
People in hospital and their families were also aware of the risk of poor communication:
Well, there’s lack of communication, so they don’t tell you anything anyway. But when they do tell you, it’s the last minute. Definitely a lack of communication anyway …. They’re not giving us or saying stuff to us to help us to move on properly. So, they are telling us, but on the last minute, and it’s no point them telling us on the last minute. It needs to be well prepared and put it in our diaries as much as they can put it in theirs, and they’re not doing that.
(C2 PLD)
Below, a peer support worker reflected on his experiences of poor communication during his time in hospital, and how this created a lack of trust:
My medication got changed when I was in secure service. Two weeks after, I sat down with my psychiatrist to have like a ward round, and he didn’t even remember that he’d changed my medication and he didn’t even have the decency to open up his laptop, get my own file up to see the changes what have happened in the past couple of weeks. This is the person who gets to say if I stay in hospital or if I get discharged.
(Site A hospital focus group)
In the situation below, two family members discussed their brother’s situation and the absence of the local commissioner from important meetings. They went on to describe how they felt excluded from future meetings after challenging the team on their poor communication:
Family member 1: I’ve never seen such poor multi-agency working, not connecting, not information sharing, it’s dire, absolutely dire, and they should be held over hot coals for it.
Family member 2: Yeah, because basically the hospital were saying, ‘We’re ready to move him on, now we need you to do your bit.’ He [commissioner] never turned up for meetings and then ….
Family member 1: He did one.
Family member 2: He did do one didn’t he, yeah. I said to him, ‘I don’t think we’ll ever see you again.’ And, ‘Oh no, I will be at the next meeting.’ And I’ve never seen him since. It was at that meeting that I said, ‘I can’t believe, I’m a professional myself, I work in similar services, albeit it’s children’s, and I can’t believe that you don’t hold yourselves accountable for your information sharing,’ you know they don’t chain the email and add the people into the groups, I was just appalled, absolutely appalled. I said, ‘You’re all accountable, you’re paid to do a job, you’re all accountable for …’ and we’ve never been invited, that was the last big meeting I was ever invited to.
(B4 Family)
This was not the only situation in which family members felt they were excluded from communication after they challenged professionals. Below is an example that one family member cited from a previous setting to illustrate the power that professionals have:
Apparently she’d broken something in her room, well she’d even wrecked her room. They had her in a room for three weeks with just a mattress on the floor. Now to me, that’s not right. I was in the meeting and I said to them, I said ‘I challenge any one of you to stay in a room for three weeks on your own and not come out with some kind of mental health problem’. And they were like ‘Yes but she wrecked the room’. I said ‘Oh so it’s all about money this then is it?’ and after that they didn’t want me in their meetings.
(A7 Family)
Risk, labels and decision-making
Deep down, many of the disputes and delays described above seemed to relate to different conceptions of risk between professionals, and how to make decisions balancing the person’s needs for independence with managing any risks of harm to themselves or to the public.
From outside the hospital, both commissioners and providers described clinical staff as being ‘risk averse’ or ‘risk naïve’, particularly referring to hospital-based RCs whom they sometimes saw as not wanting to take responsibility for discharging someone who might go on to offend or harm themselves (please note: many participants also noted positive risk-related decisions made by RCs and other clinical staff, so this only related to some hospital staff):
The RC, you know, who we’re led to believe is the all-singing word of wisdom, can sometimes be extremely risk naïve.
(Provider 3)
I think part of the problem is that the staff are really good at keeping people in hospital and keeping people safe, if you like, but not having a life. And I think that when they’re asked what the person needs when they move into the community, all their reports and their recommendations are about recreating what’s provided in the hospital.
(Provider 4)
We had a community LD provider, a very experienced LD provider …, and the local authority were brilliant, the Social Worker, […] County Council was brilliant, very supportive. And the provider accepted him, the local authority agreed the funding, they were going to 100% fund it and then discuss the health part with the CCG later – and it was blocked by the RC …. My view is that he was risk averse and wasn’t prepared to discharge [B1] and just be accountable for that – and he didn’t want that accountability …. He just wanted him to go from medium to low secure then into the community. He didn’t want to discharge him from medium …. And I was trying to say to him … ‘give me the evidence that he needs to be in low secure, what are you expecting him to do, he’s been in hospital eight years, what more do you want him to do’? And he was just saying ‘there are risks.’ I said ‘there will always be risks lifelong, it’s how we help him manage to live with his profile’ … – it was like talking to a brick wall’.
(B1 Commissioner)
Even though this was the view of some professionals outside hospital, many hospital staff wanted to make more risk-positive decisions, but felt hampered by processes around them. One hospital-based RC described how it felt to be in the position of balancing different risks and the requirements of all the agencies involved:
I think sometimes we’re viewed as being difficult or punitive or unhelpful in the movement of people when really, a lot of the time, our hands are tied by legal things, such as the Ministry of Justice …. But we’re the people they know best and we’re the people that they speak to the most, so it can create some friction between the relatives and the clinical team as well.
(Site B hospital focus group)
This issue was made worse by the tendency to log (and communicate to community providers) people’s historical offences or incidents of ‘challenging behaviour’ – with people essentially acquiring a series of ‘labels’ which affected their perceived suitability for placements. However, some of these labels and behaviours might in part be the product of the stresses of being in a hospital environment – and might be less likely to occur in community settings where the person might feel less distressed and agitated:
A lot of our population are the challenging behaviours, the people that have probably been made worse from being here ultimately and not having the right support in the community that’s led to their admission. And the nature of what we do is that they’ve exhausted all the services around the country possibly before coming to us – so that’s impacted significantly on their behaviours in regard to challenging behaviours, but also in regard to self-harm, risk towards others and things like that. It actually makes it really tricky to then find the right place for them because the history precedes themselves, if that makes sense, so then they look quite scary on paper, but actually the reality is when they’re in the community there was no acute risk.
(Site A hospital focus group)
Community providers in a focus group agreed, describing the same issue of a historical reputation preceding the person, creating a sense of risk that they felt was at times unjustified:
We were just talking to a colleague in [place Z] where actually the area would have been perfect but there’s just this blanket approach so ‘actually we’re not doing semi-detached houses because people who have come from forensic settings are likely to expose themselves in the garden’ and I’m like ‘is there anything in the history that kind of talks about that or have you just made an assumption that everybody who’s got a forensic history is going to strip themselves in the garden?’ So there’s loads of things around talking up risk without looking at that person’s history and if somebody’s done something 10 or 15 years ago and there’s no demonstration of actually doing that again, is that a current risk or is that something that’s happened and over time has been resolved? So I think there’s lots of things around risks that stop people from being discharged in the first instance, before you even have that conversation about what kind of home is appropriate, etc.
(Provider 5)
What helps
When professionals were asked what they had experienced as good practice, or what they felt helped people to move on more quickly (despite the issues outlined above), a number of clear themes emerged.
Focusing on the person
Successful discharges seemed always to be underpinned by a genuine understanding of the person’s individual needs and by person-centred support plans:
What would help is … to see the person that we’re talking about as an individual with a right to live their life.
(B1 Commissioner)
[What would help is] having substantive case managers who sit in post who get to know their service user very well and his or her needs.
(A8 Commissioner)
This could be particularly powerful when someone senior and/or in a central co-ordinating roles had these values and could practise in this way:
So the RC that I’m thinking of who is doing it well …, she sees the person at the centre of every meeting, every meeting is person-centred, you know. There is a monthly discharge planning meeting for this lady and has been for the last, I don’t know, seventeen months since she came into post, maybe longer, eighteen months. She brings people to account in the meeting, she expects people to come with progress and an update, so she advocates for her, she sends out really clear minutes with an action plan. So the 12 point discharge plan is updated and circulated. The patient knows throughout where things have been in terms of the planning. She’s been involved in the discussions when it’s been difficult and explained, and she always explains to the patient and checks out with her does she understand what’s been said – and I think that speaks volumes about inclusion.
(B1 Commissioner)
This was also seen as more likely to occur when there is consistency of staff:
What they were doing behind the scenes was they were looking at an … extra package of care where she would be on the main ward, where she could be safe, where the other women could be safe, and she would have an improved quality of life …. So we initially had her on a 2 to 1 package, so she had two nurses with her throughout and then she has slowly transitioned – the whole ward moved from [Place X] to [Place Y] last year some time – but what’s been consistent is her care team’s been consistent, the RC cover’s been consistent and they understand her, they understand her really well.
(A7 Commissioner)
Co-ordination and communication
Basic co-ordination and communication were seen as fundamental – albeit this could sometimes be aided by specific additional roles to handle areas of particular complexity or tension:
Well … we had a re-settlement lead, and it really helps me to be able to hand over to a re-settlement lead – case manager – because they have a lesser caseload and they can keep going where I have a caseload that’s a real mix, and trying to do the discharge and the delays and everything is really hard. Yes, having a re-settlement lead has done wonders.
(A4 Commissioner)
Now the way that they looked at it is they thought they’d bring on-board a business development officer to look at accommodation and provision and the needs and to match the needs, so the CCG employed, she’s called [….], and I wish we could photocopy her and put her everywhere else because she’s fantastic and she works really closely with the local authority around need.
(Site B Focus Group)
We do have quite a robust group of very experienced case managers actually, all of whom have been in management/leadership roles and clinical roles, and the meeting I’m about to go to, we do look at – we do think about themes – we are developing new services, including community services, which are more local and which will, if people use them, gradually create local – more demand in the community when people are discharged. So that’s in parallel.
(A8 Commissioner)
In the last team I worked in, we created our own little ‘out of area cell’. Our team took on that and we created our own out of area cell, we took co-ordinators …, psychiatrists, psychologists and our team manager were all involved in that to try and find ways to move people back from locked rehab into the community. We had close working relationships with the housing, we were a regular part of the complex housing meetings, I offered supervision to a number of hostels and stuff. So there’s lots of good stuff that we did, a lot of stuff I did outside my job because I enjoyed all that stuff.
(B6 Commissioner)
Appropriate capacity
Finally, commissioners in particular talked about the importance of having manageable caseloads and being able to access support with particularly difficult cases – recognising that this could often be a key bottleneck:
If you try and do the maths and you look at one case worker …: 26 patients – CTRs, at least one a year; 26 CPAs at least twice a year; … eight weekly reviews, bi-monthly reviews, six times 26; and that’s before one gets into any other – anything else …. We have had an away day recently, …where we looked at what is ideal case management capacity to enable the follow up – the follow through of actions to be undertaken. We reckon it’s about 12. So … we’re putting in applications for re-banding of the admin so they can become business support managers and they’re going to work with us – we’re going to ringfence them – we’re going to look at case management capacity.
(A8 Commissioner)
I mean, we have a monthly [regional] surgery where the patients get – where the people get discussed – and we have a strategic case manager who works straight for NHS England … – and she will help me. I’d be happy to do it myself to negotiate with the medical director, but I’m happy that she’s around to do that because I probably run out of time. But having somebody where we can say, ‘what are the options open, where there are challenges in the pathway, so what might we be able to do …’.
(A8 Commissioner)
Chapter 6 Findings III: social care perspectives
In this chapter we consider the perspectives of social workers supporting the people with learning disabilities who took part in our study, advocates working with people in hospital settings and care providers who support people after they come out of hospital.
Overview of social care participants
As shown in Table 10, we recruited a total of 36 social care participants, including 13 social workers (7 from our case-study sites, and 6 via a national focus group), 18 social care providers and 5 advocates. For a topic that might be perceived by some as more of a health than a social care issue, we were very pleased with this response.
| Type of respondent/nature of data collection | Number of participants |
|---|---|
Interviews with social workers:
|
7
|
| National focus group (social workers) | 6 |
| Provider focus group | 18 (3 groups, each of 6 people) |
| Interviews with advocates | 5 |
| Total | 36 |
Different social care roles
Social workers
Social workers described their role as interacting with the person and their family, trying to co-ordinate discharge processes and documentation, and liaising with partner agencies:
I’d say my role is, at the moment, is very much gathering the information from (Place X) and reporting it back to the high court so that they understand and see how (A1) is in relation to return to [home country]. I would see my role also as advocating for him… and also feeding back information from the high court to [A1] and [hospital] staff as well about questions that they may ask or situations that they may have as well – so it’s a bit of a go-between at the moment.
(A1 Social Worker)
I guess whilst there’s not an appropriate placement identified, and whilst that work’s ongoing, there is an increased reliance on us to support assessments …. With every assessment comes a new document. Each service wants a different piece of paperwork completing …. We’ve probably completed about ten different pieces of paper, and they’re not short reports, across the last few months, and supported [A9] with actual face to face assessments. It’s part of our job, but I guess, whilst … we’re going through a number of different services, it increases workload in that regard.
(A9 Social Worker)
And I think that’s the same across all learning disability cases is if they’ve got a good case manager or a good social worker, things seem to move. If they haven’t, things don’t.
(A8 Commissioner)
Good social work is about promoting well-being generally. Good social work in my role here as a forensic social worker, equally important, it’s about public protection. All the patients in this hospital here, bar a few, have probably committed a crime that’s punishable by a minimum of a year in prison. There are some mitigating circumstances. They’re in hospital, perhaps, because of mental ill health. So, I think fundamentally, that’s the cornerstone of my approach. It’s about being inclusive. It’s about working with people. It’s about helping [B4] for example, with his hopes and his aspirations. It’s about supporting service users to take responsibility and be accountable.
(B4 Social Worker)
Where social workers were able to get involved early on and remain part of the person’s journey, it could provide a number of benefits, in terms of really understanding the person, being there to fight for them and really caring about what happens next. However, such continuity was very much the exception:
So, when he turned 18 it was pretty much [his] 18th birthday, special care is over, you’re an adult, you’re out, that’s it. There was no transition period or anything like that. It was very much we have to rush through this because when I got to know him, we had to find the housing, the support services, the funding, everything like that so very much no transition, nothing like that. It was just out from one place to another …. And of course, the problem you have with private organisations is when you send in a referral, they say we can’t do that. We can’t provide what is being recommended. We see a psychiatric assessment that says secure hospital, we can’t give that. We’re not going to risk or anything so he ended up staying in prison which isn’t very good for him at all just because no-one else will provide something. You’ll probably hear a bit of the bitterness within my voice.
(A1 Social Worker)
In such instances a relationship evolves and a level of trust develops. In the case of person A1, for example, when asked whom they would want supporting their discharge, they were quick to say, ‘Social worker, the one back in [Place 1]’. However, not all interviewees were complementary about the contribution of social workers. Alongside concerns regarding continuity and sometimes rapid turnover in social workers, participants raised issues about some social workers’ overall knowledge and skills when working in such complex service settings.
And so people like [A5] and that will have somebody that knows the systems to push the buttons to get them moving to discharge, and usually a delayed discharge [happens when the] social worker can’t find anywhere. It’s the provision, but also … some of the social workers don’t know …. They’re not up to speed, to say the least.
(A5 Commissioner)
So we submitted all the quotes, we got things sorted and we were like, ‘What’s happening, are the funds going to be released? There’s been talk about [B4] maybe going next week for an overnight stay, there’s nothing in the house.’ Well it were carpeted because that’s what they do with these houses, they carpet them and they do put [in a] fridge-freezer, all white goods were in, but no bed, no curtaining, no blinds. His social worker … couldn’t give me an answer.
(B4 Family)
Advocacy
Some people saw advocacy as helpful in identifying/addressing some of the barriers to leaving hospital. Among other things, advocacy roles were perceived as helping to make sure that family members are more involved in the person’s care and helping to repair, or manage, relationships between the person and their family where these are strained (see Box 14).
Advocates are brilliant …. They come every Friday to speak to us and that. They come to every meeting. They have their own views and stuff like that on you know how you progress and – yeah, they are really amazing people. They’re independent, they’re not tied to [the] NHS.
(B6 PLD)
A good advocate is like gold dust. I’ve had the pleasure of working with some incredible advocates in my time … I think actually being a good advocate is a tough task. I think there’s issues in terms of how it’s delivered … about people really understanding … – it’s not a friendship, it’s not a personal thing. It’s about standing up to families, to stand up to the institutions around people etc.
(Provider focus group 1)
She’s brilliant – so she works with families and she helps families plan and work out what they want and she does that really well.
(Provider focus group 1)
Our focus is very much on getting to know the individual and spending time with the individual, understanding their current situation and who they’ve got around them in terms of family, friends and professionals and then really developing quite a bespoke approach to working with them, with the goal of moving them towards an ordinary life in the community. So we will certainly use advocacy skills and we certainly do advocate for the person or support them to advocate for themselves, speaking for themselves, but we do more than that because we look at the whole situation that the person is in and we aim to kind of fill the gaps if you like that are stopping the person moving forward …. We do a lot of kind of facilitation work with the team around the person so that includes family where family are involved, so we will liaise with family if that’s going to help the situation change for the person and so in one example, a colleague worked with a family member who’d completely disengaged with services and really with her child as well, her young person, but our input helped to sort of repair some of those relationships.
(Advocate 3)
We’ve had no contact with family. He has got a brother but I think the contact with the brother is very sporadic. I think the only person who really maintained contact with him was a previous advocate that he had or a befriender that he had, but that, during COVID she wasn’t able to visit but did maintain telephone contact.
(B2 Social Worker)
Whenever we’ve been into this particular ward, ward staff are quite nervous as to why we’re there and what we’re doing and I understand that, you know. But once they see what we’re doing and that we’re starting to draw pictures or we’ve got photographs that could stimulate conversations, once people see what we’re doing, and then we start signing if we need to and little chats about some different things, then they calm down a bit, you know, and in a way, you can see the staff then almost learning how to be advocates themselves, although you’ve got to be careful with that because you can’t really advocate your own service but even so, but it’s just a way of upskilling the staff really, in a way, but also, you know, making sure that the people you’re talking to, when they see you writing things down, it makes them feel that you’re valuing what they’re saying or what they’re offering you.
(Advocate 2)
However, not everyone agreed. Some people stated outright that they did not have an advocate while others said they did not even know whether this was an option. In some cases, in the absence of a formal advocate, close family members or a member of staff played a more informal advocacy role. Most people had a solicitor, some of whom were also felt to perform some elements of an advocacy role. However, whilst they could have influence, solicitors were sometimes seen as less effective as an advocate in representing the best interests and views of the person. One commissioner also talked about the input of ‘senior intervenors’, recently introduced and being piloted:
The people that we’re supporting at the moment are fortunate enough to have family members that they’re happy to advocate on their behalf. But when someone does have that family member who’s actively involved, it automatically sometimes disqualifies them from actually getting an advocate …. It’s not always a given that someone’s entitled to an advocate.
(Provider focus group 2)
I think one of the concerning things … was sometimes people didn’t have any family involved. But then they also didn’t have an advocate. They had nobody.
(A9 Commissioner)
I’ll be honest here, the issue I have especially when I get like a letter from someone like [Name X] or whatever else, all I ever think about is it’s a money trail. So it’s a very candid response. Quite often what I tend to see is meddling from lawyers and solicitors that actually doesn’t do advocacy for the person.
(Provider focus group 3)
And so, if I ever face any challenges, she [senior intervenor] can advocate for me. She doesn’t just advocate for me. She advocates for [A9]…. Without a senior intervenor I would say we have found challenges with people coming to the table. We have found challenges with understanding how the system works.
(A9 Commissioner)
One person has got the nurse in charge … who is an absolute advocate for this person, you know you don’t often meet nurses who are that determined. On the same site there’s another person where the team has virtually given up, I think, and it just to me shows the importance of having that strong on-the-ground lead.
(Advocate 3)
However, much of the potential impact of advocacy depended on getting access to an advocate in the first place, and the advocate having the right skills – neither of which was necessarily a given:
We have to fight to get people advocates and then it’s pot luck as to whether you get an advocate who can do the job or not, put bluntly.
(Provider focus group 1)
When it comes to being in the community it’s really hard to get an advocate.
(Provider focus group 2)
I think we’ve had very mixed experiences. So I think where people have needed help from advocates, it’s hit and miss depending on the skills of the advocate really.
(Provider focus group 1)
Care providers
The role of care providers who support people after hospital featured prominently in many of our interviews and focus groups. As explored in previous chapters, it was rare for the right arrangements to be in place for people in a timely way, and demand rarely matched supply:
At the moment, the providers are saturated with referrals, so they’re picking and choosing and it’s getting somebody to come and do the assessment, then it’ll be about – well it’s not funding – that doesn’t delay things any more – it’ll be about can they assess and accommodate straightaway and then we’re looking at a transition period so that he can start building up some leave, they’re getting to know the service, yeah, and will he accept, will he buy in if it’s not in [Place X] – that’s the other new equation.
(B1 Commissioner)
If you’re going to offer a supportive living package to somebody with autism and a dual diagnosis, I don’t know, of antisocial personality disorder, then you need to make sure your staff understand what those diagnoses are … understand what a PBS [positive behaviour support] plan is, understand, you know, training around [particular risk assessment tool].
(A1 Commissioner)
From the providers’ perspective, things work best when the provider is involved at an early stage, contributing to the person’s assessment and discharge plan, agreeing on the person’s needs and liaising with community services:
I think that’s key, making sure it’s the right environment including the layout, but also the staff that are recruited. Getting the community links in place prior to the person being discharged so you’ve got that additional support from the off …. Luckily our local MDTs actually do pick the person up before they’re discharged and it makes it a lot easier. Transition, obviously depending on that person’s need, that’s really important for the person to feel comfortable in their new home with a new staff team, and for the staff team to get to know them …. And actually completing assessments into why the person’s behaving that way because it might be completely different from when they’re in hospital to when they move into that new home, to make sure that the strategies for supporting them are right – and if that all goes well, the risk of them being recalled to hospital just reduces significantly.
(Provider focus group 2)
Social care perspectives on barriers to timely discharge
Social care participants identified similar issues to hospital staff and commissioners, and expressed widespread frustration about the amount of time that people are delayed in hospital. For some people, this was heightened by a sense of helplessness and self-recrimination, which came from being unable (no matter how hard they tried) to help the situation by securing an early discharge (see Box 15).
It amazes that when people are … detained in hospital … there seems to be no idea that people are ever going to come out …. We’re talking about the most vulnerable people with … all the issues and problems that they’ve had, trauma, whatever, that has led to that situation – and you find people, you know, months and years into their hospital stay and suddenly people are talking about ‘well yeah, we need to get him out by six months time’ sort of thing and, you know, the housing market’s against that. It takes six months to get a good team, train them and put them in and do the transition work if you’re going to do all that properly.
(Provider focus group 2)
It’s awful, because he’s absolutely ready for discharge …. Sometimes I find it really, really difficult, I’ll be honest with you. I think it’s quite, quite upsetting. In terms of getting people out, yes, it can be incredibly, incredibly difficult.
(B1 Social Worker)
I personally found a lot of the processes very frustrating.
(B4 Social Worker)
Siloed or inflexible pathways
As with hospital staff and commissioners in the previous chapter, social care participants felt that some people faced such extended stays because of complex circumstances and/or diagnoses which makes it difficult for them to fit into narrowly defined pathways:
I guess she doesn’t fit into a natural pathway in that her risk has decreased to point where she doesn’t require our service, but some of the risk is untested, based on the intensity of the care she receives here, because of being in [long term segregation]. So, there’s quite a jump between that and locked rehab or community packages …. We’re working with her and community and commissioning teams at the moment to look at bespoke packages or specialist locked rehab and to do a thorough assessment to see what would next best suit [A9].
(A9 Social Worker)
I guess people need to make a decision as to whether [B4] is going to remain in hospital forever and a day because he’s going to present a high risk and an ongoing risk, and a statical risk towards harming children, or we look at other alternatives, and somewhere, somewhere along the line.
(B4 Social Worker)
[The] main blocks in regard to discharge have been that he was, his risk is still there. It’s more of a predictable risk now. The consultant wanting him discharged under DoLS, however I’ve assessed him as having capacity to decide where to live so DoLS wouldn’t be appropriate. So we’re at a bit of a stalemate at the moment …, which is really frustrating for him and all the professionals involved. Where it’s going to go to next I’m not a hundred percent sure. I’m waiting for the hospital to confirm whether they’re going to disagree with my capacity assessment in which case it will go through the Court of Protection to make a … decision on his capacity. If they are not wanting to disagree with my capacity assessment then we need to look at alternative legal frameworks for him to be discharged safely into the community.
(B2 Social Worker)
Appropriate accommodation and/or support
As with other chapters, a common barrier was a perceived lack of a suitable placements for the person awaiting discharge (see Box 16), especially when the person’s needs were seen as particularly complex.
The biggest issue right now is identifying the exact placement option for her. So, at the moment, that net is a bit wider, and those assessments have occurred for both locked rehab and for specialist community providers. So, I think it’s, as I was saying earlier, I’m getting feedback from those providers, so that we can identify what options are available to [A9] and being really clear about that, for having an option agreed to work toward. So, that’s the current, most important need, I guess, to actually establish what service, where, and how.
(A9 Social Worker)
So, what we get is when you get autism lumped in with intellectual disability, you have your standard intellectual disability services providing residential homes, your traditional residential home that doesn’t suit [A1] because that’s not him. That’s not where he should be and then we have this middle ground of people with high functioning autism, but also with an offending forensic background. It really isn’t, the services just don’t exist for those people really but you get these services that we do refer to which they’re just not set up to provide for these people.
(A1 Social Worker)
Not having the facilities in the community to accept the patients we’ve got …. There are people stuck in the system because they’re so complex and nobody can take them, or there is no provision that can support their care in any bespoke packages, which again, take time and a lot of funding. So, there’s lots of blockages by really complex care needs and not having community provisions to support them.
(A4 Social Worker)
Linked to this is the issue of ‘geography’, in terms of where the person would like to move to (bearing in mind the key factors that could support their transition) versus the location in which a suitable placement is available:
You could find a really good placement that you’d think could meet the needs of a number of the women that you work with, and they’re in the wrong parts of the country …. So, I’m working to support somebody else to leave medium secure, and she is funded by one area, because that’s where she was living years back, when she first became involved in services. Her family re-located to another area, quite significantly further away from that area. She’s placed with us, which is a different area, and we’re looking for her next locked rehab placement. So, her commissioning team said that they would look where her Mum’s moved to, because that’s what’s most important to her, and they did that, but no services exist. So, they’ve found a service for her that they believe meets her need, and it sounds like it really does, but that’s further away from Mum than even we are. So, it’s almost like she has to choose. Stay in medium secure to be closer to Mum, or move to locked rehab, but be even further away from your Mum …. And I’m not saying that to be critical of her commissioners, because they’ve looked, they’ve searched for services. It’s not that they weren’t willing to do it, it’s just a lack of service provision for them to commission …. So, we’re not getting that right for her, but it just doesn’t exist. You have a team willing to look in that area, willing to fund it, willing to be creative about how they supported her, it just doesn’t exist.
(A9 Social Worker)
In the example below, the opposite was true – with a possible placement seen as being too close to a family that were perceived as being exploitative:
The person who held the case before me had identified a place …, but the person didn’t want to move there. I think there was some fears around, I suppose, bits of exploitation from family, so he opted not to move to a placement. So, we’re now looking to try and source alternative accommodation for him to move to.
(B1 Social Worker)
It could also be difficult to identify the right environment for someone who might not be able to live alongside other people using that service:
It’s actually the physical environment that commissioners find difficult to find. Obviously getting the skills with the right support is also as important, but actually getting the right physical environment for somebody, especially when they will struggle to live with others and may have behaviours that cause damage, can be what leads to people staying in hospital longer than they need to be.
(Provider focus group 2)
Several participants also found it difficult to place someone because of a negative (historical) reputation or series of labels that they might be carrying:
Something needs to happen in terms of providers because that can really badly delay things as well – so once people have, you know, got a certain history attached to them, then it becomes harder and harder to find providers. I think that is a major issue.
(Advocate 3)
I think what happens is people have a crisis and then instead of people recognising that’s a crisis and that’s a temporary thing, that becomes the person’s reality really, and it’s that reputation that just follows the person wherever they are.
(Provider focus group 1)
Sometimes, providers felt that they received referrals which were more to do with other professionals trying to show that they had tried their best, rather than because this was the right placement for the person. At the same time, there was a perception that hospitals sometimes present stringent conditions, making it extremely difficult for a provider to accept the referral:
I get a lot of traffic from people who want me to say no to things because they want to justify sending them to another hospital. So, you know, I had a, let’s call it a referral for argument’s sake, the other week for a guy who needed 5:1 support. Well apart from ethically I won’t do that because for a guy in his own home and living in his own community, you shouldn’t need 5 people sitting on you to remain safe in your own home. Ethically we just don’t do it, we do de-escalation, we don’t do restraints, you know, so that’s an obvious line. I’ve never known a situation in the community with 5 staff which has been successful because there’s too many people and … there’s so many things that are wrong with that. So I’m obviously going to say no, then the commissioner says ‘well we asked the provider, they said no so therefore we’re going to move him to wherever’.
(Provider focus group 2)
I think part of the problem is that the staff are really good at keeping people in hospital and keeping people safe, if you like, but not having a life – and I think that when they’re asked what the person needs when they move into the community, all their reports and their recommendations are about recreating what’s provided in the hospital. So … the assessment process right from the beginning point of discharge is really flawed because actually you get all this stuff about this person needs a house that’s sound-proofed, they need to not have any neighbours, you know, all this stuff that’s about reputation, which people genuinely believe.
(Provider focus group 1)
On other occasions, delays took place because key actions were left till too late on in the process (particularly when thinking about housing-based approaches):
Sometimes it can be when it’s done at the last possible point, so then you’re kind of contacted as a provider to say ‘this person is ready for discharge’ but then actually that process only just begins then and we all know that if you’ve got to purchase a house that can be four, five months down the line and obviously you then can’t recruit until after that so you almost need to be at the beginning stage of trying to look at what is needed. And I think some services are getting better at that, but I think it’s all these delays add [up] – and we know that people then struggle so then that means they go backwards, which then some consultants say they’re no longer ready for discharge because they’ve now begun presenting with more behaviour than what they were six months ago when they were ready.
(Provider focus group 2)
Lack of staff
Part of not having the right services available when needed was the difficulty in recruiting and retaining the right number of staff with the right skills. This was partly due to a lack of social workers with specialist skills and/or to rapid turnover of social work staff:
Ten years ago … we had 12 specialist learning disability social workers working in a team for the borough; there’s 2 now. So obviously most cases are only open to review if they’re open at all.
(Provider focus group 1)
So then you’ve got to go through all that referral process and there’s a shortage of social workers still, so you’re still in that revolving cycle of not getting to the bottom of it.
(Provider focus group 2)
There’s a slow but very significant eradication of social workers. So most of the social workers I’ve either managed in the past or worked with have gone, they’ve left and quite a lot of them have gone to other local authorities. So they felt a kind of purge in terms of what’s happened really over the kind of austerity years and stuff. But what I’ve encountered now is there’s been shifts in the way that [place X] for instance puts out those care managers, that rather than have them in specialised teams, they put them into localities. So you might have people working, say, with significant complex needs for discharge from an ATU but their background is older people. So straight away they really don’t have a handle on what they’re managing in terms of those complexities and they may well have never even heard of supported living …. It’s detrimental to them and to their ability to meet the needs of the people that they’re actually trying to advocate for when their own experience and knowledge is so lacking.
(Provider focus group 3)
Many social care providers were also struggling with recruitment:
An example of receiving a referral from somebody who was classed as ready for discharge … and it took us 9 months to recruit a staff team, a suitable staff team, which obviously then led to issues with that person in hospital …, increases in behaviours, increases in incidents and self-harm and things like that. But the difficulty that I think a lot of social care providers are facing at the minute in terms of recruitment is just exaggerated when you are looking for specific staff to work in complex or forensic environments.
(Provider focus group 2)
One of the massive, massive barriers at the moment is the general recruitment situation …. You see there’s an advert for the NHS, ‘go and join the NHS’, they tend to pick the cream of the crop if you like from the candidates but you’ve got Aldi up the road paying £15 an hour, you’ve got Lidl paying 15 quid an hour, and then you’ve got the commissioners saying ‘but we only want it to cost this’…. Support work is no longer seen as sexy or anything exciting … and actually it’s a phenomenal role to come into and actually the people that are on our frontlines do – I don’t want this to sound cheesy in any way – but do an incredible job and they’re just not recognised for it. That’s what we really need, you know, pay them what they’re worth because they keep us all safe, they do an extremely difficult job and we don’t talk about how soul-destroying and lonely 1:1 support in the community setting can be sometimes, and we expect people to keep going … and they do and we try and look at creative ways to keep people engaged – but it’s not seen as that desirable job that I so wish it was.
(Provider focus group 3)
You know, I wouldn’t want to do it for £11 an hour …. You know, some of the level of support that people need, week in, week out, there’s so many challenges across the board with recruitment. Social care needs a massive injection of an incredible amount of money, just to be okay, and we find ourselves in a position where every provider you speak to, they don’t have enough staff …. They can’t meet the need, or you might need somebody of a specific sex to work with a person, and they can’t recruit males or females …. There isn’t enough people available to any service, and because of that, staff retention’s difficult as well. That’s a bigger picture.
(B1 Social Worker)
Funding
Providers were unanimous that funding issues were a major barrier to timely discharge. This ranged from the macro (including inadequate investment in the sector) to the micro (including arguments over who pays for what) (see Box 17).
I think this is about money. I’ve worked in the independent sector, there’s some people making an awful lot of money … I think when it suddenly blows that someone’s kept in a seclusion room like [Y] was, then suddenly it’s all blown. The last couple of weeks since [a TV programme], suddenly money is bursting out of everywhere …. It just feels like it is money, it is money orientated.
(Provider focus group 1)
It wasn’t until they got ready for discharge they then suddenly said ‘oh actually, at some point he was detained under a different local authority so we’re not going to foot the bill’.
(Provider focus group 2)
We’ve agreed a provider but actually we can’t go any further now until the funding has been agreed and there’s meeting after meeting, people are off sick, and this individual remains in hospital and I think it’s a 2 year delayed discharge …. We can’t go any further, I can’t recruit a team until that funding has been agreed. We’ve had a few examples of that where it’s just delayed it for several months because it’s between the local authority and health [deciding] who’s going to pay which part.
(Provider focus group 2)
In many of these examples, providers were absorbing significant costs and financial risks, particularly if a subsequent placement broke down. In the example below, a house had been purchased and a dedicated staff team recruited, with a potential lack of clarity as to who might manage these financial risks and around hidden costs:
I’ve just been working on a project where I was actually engaged with a person in the hospital for nearly three years and that was going through the legal frameworks that were required. It was a particularly complex and high-profile public case and I was working for three years before the police agreed on a premises in the first place. So the police then agreed on a premises, we had probation, the person on trial leave then started six months ago and that’s three years of no pay …. So it’s only me at this point, then we’ve got to do the house searches, we get agents involved. The company decided on purchasing a house so we did purchase the house – that took a little while, it had to be agreed by the police. So we purchased the house and … once the transition started, technically the person became on our books and started to experience some community living. So that’s how it started and then we started receiving payments only for the hours that were being provided at that point in time, so none of the research, none of the building modifications, none of any of that was sorted out. As it happened, the placement’s broken down.
(Provider focus group 3)
Risk averseness
Behind some of the different perspectives of health and social care staff was a series of different approaches to risk – which was sometimes seen as being ‘risk averse’ by a number of social care participants, often arising out of a perceived lack of knowledge about the nature of community services:
I think there’s such a different perception about risk … I think people from the best of intentions in the hospital treatment world, they’ve no understanding of community.
(Provider focus group 1)
We also can come up against some really restrictive MDTs that are like ‘this person isn’t ready for discharge’. But when you ask why, ‘well because they need a lock on their kitchen, they run this risk of …’. Actually I think it’s their understanding of … what can be done and what can be developed in the community collaboratively to discharge somebody into the community. We recently supported somebody after 22 years because every provider kept saying ‘it’s too risky, it’s too risky’. They moved into the community really successfully but actually if you’re not giving people a chance then you are just going to go round that same cycle day in, day out, month after month, and those years mount for them.
(Provider focus group 2)
What helps
In reflecting on what helps people to come out of hospital, social care participants identified a number of key factors – none of which are very dramatic when read in isolation, but which could be very powerful and meaningful when carried out in the right way and with the right values.
For many social care participants, the key is to be truly person-centred, working at the pace of the individual to achieve aspirations that are important to them:
So I’ll talk about my supported living accommodation that we … predominantly use for people with learning disabilities coming out of hospital, and we take the people that are risky, you know, that are in seclusions or that are aggressive to people. And through our assessment we will go and we will meet them, it’s not a sit-down assessment it’s like ‘let’s get to know you’ and then from that we would look at ‘what your goals and aspirations are, what don’t you like about the ward?’ and we take the person as a whole, you know. We look at it from an occupational therapy point of view, we look at it from sensory things and we do a whole package around them. We ask them what they would like their house to look like, what they want from [us], so they’re really in charge of their care and we then around them create a package. They’re involved in their homes, they’re involved in what staff work with them, they’re involved in looking for jobs if they want jobs, we have regular review meetings with them, so really it’s them leading us, that’s how we do it and we have some really, really good outcomes from that. We’ve got a gentleman who spent years and years of his life in hospitals and in prisons but we’ve had him now for – well, he moved in with us a year ago and he’s travelling the country going to gigs, he’s volunteering, he’s working with [national charity] and he’s got a job …. He really inspires me actually. I think he’s amazing and he’s just like ‘I was listened to and I was getting the care that I want’ rather than, you know, if he shouts and swears, he shouts and swears, but his history would be if he did that he would get secluded.
(Provider focus group 1)
I think having the person at the centre of it and letting them almost kind of plan their move into the community. The ones that I think have been the most successful is where that person has been able to verbalise and articulate what they want in a community, how they want that transition plan to go, if they want family involved, if they don’t, and almost kind of doing their own kind of workshop about ‘this is who I am and this is how I want you to look after me, even on a bad day’. Because I think staff then take it from a different perspective when it’s coming from the person they’re going to be supporting and looking after in the community. They can see it from a very different angle rather than a professional telling them …. Because actually that person knows how best to deal with their support … I think we found that [the] person being at the forefront of it and almost kind of leading that discharge into the community themselves rather than it being MDT led and what they think that person needs or should be having.
(Provider focus group 2)
With one person that I’m working with, we’ve done it by having person-centred planning meetings but for that individual, he’s never been to any other kind of meeting for more than about five minutes before and he usually refuses to go, so what we did was have a very small group of us, myself, the hospital advocate and his social worker and one member of staff came together with him, and we had a very, very loose agenda, lots of paper, lots of pens, a TV and the meeting kind of took place over about two and a half, three hours which was the longest he’s ever spent doing anything like that. But what we did was you know if he wanted to put Knight Rider on the TV then we watched that for five minutes, then we went back to talking about his future and what he wanted his house to look like, what he wanted to do when he moved, his hopes and dreams for the future, all those types of things. So it was very much free flowing, very much led by him and we created a person-centred plan out of that and we’ve had several meetings, three or four meetings since to update it as he moves closer.
(Advocate 3)
I think a good social worker is about the person-centred skills, building the relationship with the person, having an honest and transparent relationship with a person. Knowing what services are available in your area, bringing that expertise that you have for people and working together. And for me honesty is just the best thing that you could ever do for a person, for the service, for yourself, for cohesive relationships. And for a social worker, it’s also about working with that wider MDT and acknowledging that everybody brings something to the table, and you’re not an expert in all areas.
(B2 Social Worker)
Others felt that it is important to involve the subsequent care provider at an early stage, so that they can be more actively involved in shaping what happens next:
So I think there needs to be a better way of providers who are working in the community with quite tricky people, actually doing more of the assessment process in the hospital because what tends to happen is you get asked ‘will you support this person’ and they give you this big wish list and then you have to try and figure out ‘well which of the bits that we need will keep this person safe and which bits they can probably do without really’.
(Provider focus group 1)
Above all, social care participants emphasised the importance of education, relationships and collaboration to help navigate the system and enable more people to leave hospital:
I think it’s the educational piece that needs to happen with the clinical MDT teams but also maybe help with some community based teams, because I think again you can sometimes come across some community teams that are a bit hesitant to accept somebody moving into the community because of their risk history, so I think a huge educational piece around, you know, what can be done in the community to meet somebody’s needs now … rather than what that consultant who last worked in the community 25 years ago.
(Provider focus group 2)
The places that tend to work well are where the commissioners have been around for a long time and you have that relationship with them …. The ones that don’t are the ones where you’ve got constant churn. So, you know, again I’m going to give you an example, with [place X] we had a fantastic relationship with commissioners:… they understand, they get good outcomes, it’s going to cost money and they’re happy to do that because they see the bigger, strategic picture and that’s the emphasis here. Short term planning will not lead to long-term goals, it just doesn’t work out that way.
(Provider focus group 3)
From a practice perspective, I think it’s really important in order to manage risk, promote people’s health and well-being, that we look at it from a multidisciplinary perspective, because if something goes wrong and people go into the community, people with a mental illness or a mental disorder, all those questions are raised by, often the media and members of the public, but here it’s about the nursing staff, the doctors, psychologists, occupational therapists and social workers having a good working relationship and committing to that.
(B4 Social Worker)
Chapter 7 Discussion and conclusion
This study has sought to contribute to current debates about the best way to support people to leave long-stay hospitals by exploring the experiences and perspectives of people currently in hospitals and their families, as well as of health and social care staff. Despite so many previous policy commitments over the last decade or so, we believe that future solutions must be informed by lived experience and by practice knowledge if they are going to stand any chance of being effective.
Key themes
There is a well-known saying that ‘every system is perfectly designed to get the results it gets’ – and the experience of people with learning disabilities and/or autistic people in long-stay hospitals seems a classic example of this maxim. Whilst people in hospital, families and staff might sometimes have very different experiences and perspectives, there was marked similarity in how they described the system in overall terms:
-
People in hospital report widespread frustration, feel that hospital environments are not conducive to getting and staying well, and face all kinds of barriers to leaving hospital – with an overriding sense of people’s lives being on hold while services try to find ways to support people in the community. Without someone to really fight for them, people struggle to overcome the inertia built into our current systems and processes, and continue to experience very long hospital stays and very significant delays.
-
Hospital and community staff are equally frustrated and describe a complex and seemingly dysfunctional system which they find almost impossible to navigate. When people do come out, it seems to happen almost in spite of the current system rather than because of it.
-
Hospital staff from different professional backgrounds do not have a shared sense of who really needs to be in hospital or not – suggesting that different definitions, world views and professional judgements might be at play.
-
Hospital staff describe the difficulties they perceive when trying to discharge people into community services, while community services see some hospital staff as risk-averse and lacking up-to-date knowledge of what is possible to achieve in the community.
-
Despite over a decade of policy attempts to resolve these issues, very significant barriers remain.
Insights from the broader hospital discharge literature
In reflecting on these issues, we are struck by how many of these findings resonate with the broader literature around hospital discharge (which usually focuses on the experiences of older people being discharged from general hospitals). This is summarised in various accounts and reviews (see e.g. Glasby41; Glasby et al. 44; Cadel et al. 69) and in a series of policy documents (see e.g. DHSC70). Despite the different context and treatments that people might receive, this broader literature contains a series of principles and frameworks which might be useful when thinking about delays in people with learning disabilities and/or autistic people leaving long-stay settings.
Some key messages from this literature are that:
-
Hospital is not a good place for people to be if they do not really need the services provided there – and too many people unable to leave hospital causes all kinds of problems for broader health and social services (not least because this is very expensive and consumes resources that could arguably be better used keeping people healthy and well in the community).
-
Once someone comes to hospital, they may start in an emergency department or get moved to a medical assessment unit. However, the further they get into the hospital, the harder it can be to get out again in a timely fashion. This was described in a previous study as getting admitted into ‘the deeper hospital’, building in a series of extra delays with every move (Glasby et al., p. 27). 38
-
Delays should not be seen as ‘bed blocking’ (which tends to blame the individual, even though delays usually derive from the inability of the system to find ways to support people in the community), or even as ‘discharges’ (which implies that the hospital is ending its involvement and simply passing people to community services). Instead, recent policy focuses on ‘delayed transfers of care’, as a way of trying to more accurately describe the nature of the transitions that leaving hospital should entail.
-
Hospitals are encouraged to plan for discharge on admission and to work with patients to make sure that everyone is aware of an ‘estimated date of discharge’. More recently, policy has sought to encourage a ‘discharge to assess’ model, whereby people stay in hospital for short spells to resolve an immediate medical emergency, but are then transferred to other settings where longer-term assessment and planning can take place.
-
Over time, there has been lots of work to agree definitions and measure the extent of delays. While data are less than perfect, some of this work has helped build a shared understanding of the issues at stake and provides something of a baseline against which to measure attempts to develop new ways of working.
-
Different health and social care partners often find it hard to reconcile competing notions of good practice, with hospital services often based on a ‘throughput’ model (getting people in, treating them, getting them out again – freeing up the bed for people who may need it more), while social care in particular is often focused on an ‘empowerment’ model (supporting people in crisis to take their time to be the best they can be and to make potentially fundamental decisions about the long term). It is not necessarily that one of these notions of what success looks like is ‘right’ and the other ‘wrong’ – just that they are different, and potentially incompatible.
-
While policy and the media talk about delays and about the risks of ‘cost shunting’, it is not just the ‘cost’ that is passed backwards and forwards between different agencies and professionals – but the person that the cost represents. It can be incredibly disempowering to be argued over in this fashion – not because everybody wants you, but because everyone sees you as a drain on their scarce resources and wants to pass you off on someone else.
-
Although all the focus is usually on delays, premature and poorly co-ordinated discharges can be just as problematic, and it is just as important (if not more so) to prioritise preventive action to stop people being admitted to hospital in the first place.
Although the list above focuses on the discharge of older people from general hospitals, some of these issues also apply in terms of delays leaving mental health inpatient services. 71,72 While this is just a brief summary of key debates in the broader hospital-discharge literature, there are remarkable similarities with the situations of people with learning disabilities and/or autistic people in our study – and a greater sharing of evidence and experiences across different user group/service settings can only be positive.
Ten ‘top tips’ for helping people come out of long-stay hospitals
Working with our Advisory Board and Reference Group, we have sought to move from some of the barriers and challenges identified in this study to practical guidance for health and social services trying to do things differently. This will be published as ‘ten top tips’, sent to every health and social care leader in England – as well as in easy-read format, as an accessible video for people with learning disabilities, and via a free training video for care staff who might struggle to access training budgets. These take the key themes from this research, but turn them into more direct/tangible statements/pointers for future practice. These will be set out in more detail in each of these individual resources, but are also briefly summarised in Box 18.
-
Our lives are on hold – do your jobs and get some ‘oomph’
People spoke of their lives being on hold while arrangements were put in the place to support them after hospital. While there were some very complex situations, some delays seemed to be the result of widespread and engrained inertia – essentially just waiting for stuff to happen. In response, people called for the professionals involved in their care to simply do their jobs, highlighting the importance of people believing that they could leave hospital and fighting on their behalf to make this happen.
-
See the person behind the labels
People in our study felt that some community services didn’t really seem to know them as people – and perhaps deep down don’t really believe that they were capable of leaving hospital. Instead, they felt that labels – some of which they’d acquired a long time ago and which might no longer be relevant – stay with you forever and can be the main way in which some people try to understand your needs (and could often be used as a reason to say ‘no’ when asked to support people after hospital). Instead, people wanted to be seen just as people, and for the focus to be on the need to be met, not on the diagnoses or labels that that the person might come with.
-
Don’t make me jump through more hoops than is really needed
People recognised that getting everything in place for someone to leave hospital is complicated and needs lots of careful planning. However, there seemed to be a widespread belief that the way you persuade people that you’re well enough to come out is through basic compliance: if a professional suggests you do something, then you do it – otherwise you might be seen as ‘not co-operating’ or ‘lacking insight’. Sometimes people felt that they had to jump through more hoops than was really needed in order to prove they could leave hospital, and they asked for professionals to be clearer on what was a ‘must do’ and what was a ‘nice to have’.
-
Make sure the criminal justice system is on board
People called for much closer joint working between health/social care and the criminal justice system in order to prevent delays and speed up decision-making.
-
Help hospital staff know what’s available in the community
Some staff had worked in a long-stay setting for many years, and might not always have a detailed knowledge of what services are available in the community or what needs community services can meet. While they have a responsibility to find out more about the community, community services also have a duty to help hospitals know what is available – communication is ultimately a two-way process.
-
Don’t put us into boxes or ‘scatter-gun’
For all the talk of people’s needs being highly individual, people often seemed to be put in ‘boxes’, with some service responses feeling as if they had been developed from a fairly standard template. On other occasions, a worker might send out multiple referrals at once (perhaps through a desire to be seen to be doing something rather than because this might actually work). Instead, people wanted to be treated as individuals with support tailored to their needs (With this in mind, we were staggered that no one mentioned the potential of direct payments/personal budgets – this seemed a major oversight).
-
Give me the chance to try life outside
People asked not to be put in a ‘Catch 22’ position where they can’t come out of hospital until they prove that they’re ready, but can’t persuade the system to give them the opportunity to try.
-
Please help me with the trauma I’ve experienced
Lots of people had experienced significant trauma either before and/or during their hospital stay. They wanted practical support to help to overcome these experiences, including from trained psychologists.
-
Don’t let us fall through the cracks
People asked for health, social care and other workers to communicate and collaborate with each other, so that they did not fall between the gaps in existing services and get lost.
-
Don’t set us up to fail
People were keen to leave hospital, but also recognised that this needed to happen at the pace of the individual – rushing or working to artificially imposed timescales could jeopardise the chances of success.
The importance of involvement and engagement
National Institute for Health and Care Research guidance asks all reports to reflect on the importance of and approach to involvement and engagement. Since this was the ‘raison d’être’ of the current study, it is difficult to include a specific section on this, as it is embedded throughout the whole research. However, a key strength of the current project has undoubtedly been the focus on lived experience and practice knowledge, the perseverance, skills and prior relationships needed to gain access to long-stay settings, and the commitment to hearing and valuing seldom-heard voices. This contrasts strongly with a number of previous studies (Ince et al. 74; see also Chapter 3), which mainly take the form of bed censuses or reviews of case notes, without seeking meaningful engagement from the people most affected by the issues at stake. In an era where health and social care policy tries to proclaim a commitment to principles of ‘nothing about me without me’, this feels an important counterbalance to some previous research, providing much-needed expertise by experience in order to contribute to current policy and practice debates. While the very detailed and labour-intensive nature of the research (particularly during COVID) has meant that our sample is inevitably small, the extent to which such different stakeholders all identify common themes and issues is striking.
Potential limitations
In reflecting on the strengths/limitations of our approach, there are three issues of which we are particularly mindful:
-
People on forensic pathways: a significant proportion of our sample were on forensic pathways, and it is difficult to tell how similar to/different from the national picture this may be. However, drawing on insights from the ‘Assuring Transformation’ data collected on a monthly basis by NHS Digital, there are a number of potential clues (see Box 19). Overall, it seems likely that our sample includes more people who have had contact with the criminal justice system than might be the case for the overall group of people who are in long-stay settings at any one time. However, this in itself provides some additional nuance to previous policy and media debates, which often seem to talk about the 2000 or so people living in hospital as a single, homogeneous group, without perhaps explaining or exploring potentially significant differences between different people with different conditions and different journeys through services. Overall, we did not detect any differences in responses from people on forensic and non-forensic pathways, and our findings are very consistent with previous literature and our prior experience – so we do not think that this has led to significantly different results. However, future research could usefully explore these issues in more detail, perhaps including perspectives from the criminal justice system as well as from health and social care.
-
Equality and diversity: our study is based on hearing seldom-heard voices, and our attempts to promote equality, diversion and inclusion are therefore embedded throughout the report rather than solely explored in a single section. However, while our study including a number of different people with different protected characteristics, most of the people in our sample were recorded in their case files as being white. Time and time again, this prompted us to ask where people who are not white might be. For example, are some Afro-Caribbean people more likely to remain in prison rather than be diverted to hospital? Do some communities find current services so culturally inappropriate that people are less likely to seek support in the first place? Were people from minority ethnic communities less likely to take part in research? Is it a good thing that we did not find lots of people from black and minority communities in the wards we visited (as people are leading more ordinary lives in other settings), or is it a bad thing (people may not get the same access to health and social care services in the first place)? This was not a focus of the current study – but the fact that we have not been able to find answers to these questions seems significant, and worthy of further exploration.
-
The importance of recognising good practice: our study focused on engaging with people while they were still in hospital to understand their experiences and their sense of the barriers and potential success factors. While this is important in its own right, future research may be needed to follow people up over time to understand more about longer-term outcomes. As part of this, we still know relatively little about what good practice looks like in terms of supporting people to stay out of hospital (or indeed to avoid hospital in the first place). In one sense, it was lovely to see the small number of people who had come out of hospital again, and we will always remember the person now in supported living who showed us round his new home, his garden, his lawnmower (of which he is very proud), his DVD collection and his Star Wars figures. However, it was only possible to follow up with people with learning disabilities and/or autistic people themselves, so we sometimes lacked other perspectives. Some people also found it hard to say what had contributed to their discharge, so we know that they are out of hospital but not necessarily why. For example, the person who left hospital and then was readmitted made reference to being left on his own (when he should have had one-to-one support), leading to some sort of incident. Hardly surprisingly, he felt very uncomfortable talking about this, and so we only have a potential snapshot of what may have happened. As a follow-up to this study, our intention is to explore scope for a longer-term project which follows people through up to 5 years after hospital to explore what happens to people next, the extent to which people are leading ordinary lives and what kinds of support seem to maximise the chance of a positive outcome.
The data below are based on the NHS Digital report from July 2022 (https://digital.nhs.uk/data-and-information/publications/statistical/learning-disability-services-statistics/at-july-2022-mhsds-may-2022-final), and we are grateful to Professor Chris Hatton and Catherine Nolan from our Advisory Board for helping us piece together these insights.
Table 2.2 from the NHS Digital report sets out the reason for admission to inpatient services. Across August 2021–July 2022, a consistent 32–33% of people have a reason of admission of ‘assessment and/or treatment for offending’ (660 out of 1990 people in July 2022). In terms of sources of admission, for nearly half of people (47%) it is ‘acute beds’, for 10% of people it is a ‘penal establishment’, for 7% of people it is ‘secure beds’, and for a further 7% of people it is an ‘other hospital’.
Table 2.3 records inpatient bed type. For the 1690 adults in July 2022, 435 people (22%) were in low-secure, 270 (14%) were in medium-secure, 60 (3%) in high-secure, with a further 35 (2%) in low-secure/locked rehabilitation, 40 (2%) in high-dependency rehab and 150 (7%) in long-term rehabilitation/continuing care.
In terms of legal status, Part III of the MHA perhaps maps most closely onto reasons for being in hospital connected to offending. There were 220 people (12%) on an MHA Part III section with no restrictions, and 545 people (27%) on an MHA Part III section with Ministry of Justice restrictions in July 2022.
Drawing on some of the crosstabs (starting at Table 4.1), it is clear that people in secure inpatient services have longer total lengths of stay than people on general wards. People under an MHA Part III section with restrictions also have longer stays.
Essentially, this suggests that there are a significant number of people who may have committed offences or had various contacts with the criminal justice system, who are now in long-stay hospital. It seems likely that our sample includes a higher proportion of people from forensic pathways than may be the case in the more general ‘Assuring Transformation’ population – perhaps because people are in hospital for longer or are more likely to become stuck, because people might be bored in secure settings and keen to do anything to relieve this frustration (and so more likely to volunteer to take part in research) and/or because some people on forensic pathways might find it easier to take part in interviews than some people with more severe learning disabilities or people who are in more of an immediate crisis in an ATU. Equally, this research points to people having complex lives and backgrounds, moving between multiple services and ending up in hospital for multiple, inter-connected reasons, potentially ending up as being categorised in different ways and/or on different types of ward. There may also be people who have done similar things who are in prison rather than hospital, people who move back and forward between hospital and prison, people who have done similar things that did not reach the criminal justice system and people in secure settings who have not committed a formal offence – so most people’s situations remain difficult to categorise in a meaningful way.
Summary
This was a difficult and often distressing study to conduct – although nowhere near as difficult and distressing as life often is for people with learning disabilities and/or autistic people living in long-stay settings, or for health and social care staff trying to support people to leave hospital and lead more ordinary lives in the community. Throughout we have been struck by an overwhelming sense that this is a situation that no one planned, that no one really wants and that no one really knows how to resolve. Despite this, we remain convinced that we will struggle to make further and long-lasting progress unless we draw more fully on lived experience and practice knowledge, recognise these as valid and important ways of knowing the world, and work with the people who are most affected and – by definition – are expert in their own lives to develop better, more inclusive solutions in future.
Acknowledgements
Funder: this project was funded by the National Institute for Health and Care Research (NIHR) Health and Social Care Delivery Research (HSDR) programme (NIHR award ref: NIHR130298). The views expressed are those of the authors and not necessarily those of the NIHR or the Department of Health and Social Care.
Research team: the research team is grateful to Rhiannon Morgan and Becki Orleans (project managers) and their line manager (Rachel Withey), to Rachel Posaner and Christian Bohm (HSMC Knowledge and Evidence Service) for support with our literature review, to members of our Advisory Board and Reference Group (see Appendix 1), to our case-study sites and to all participants.
Contributions of authors
Jon Glasby (https://orcid.org/0000-0003-3960-7988) (Principal Investigator and Professor of Health and Social Care) led the overall study.
Robin Miller (https://orcid.org/0000-0003-2646-5589) (Professor of Collaborative Learning in Health and Social Care) managed the social care extension which we received part-way through the initial study.
Anne-Marie Glasby (Senior Development Officer, Changing Our Lives) worked with people with learning disabilities and/or autistic people.
Rebecca Ince (https://orcid.org/0000-0002-0725-7912) (Research Fellow) conducted interviews with families and commissioners.
Fred Konteh (https://orcid.org/0000-0002-8612-0323) (Research Fellow) conducted interviews/focus groups with social workers, advocates and social care providers.
All members of the research team contributed to research design, data collection, analysis and drafting written outputs.
Data-sharing statement
This is a qualitative study and therefore the data generated are not suitable for sharing beyond those contained within the report. Further information can be obtained from the corresponding author.
Ethics statement
This research is sponsored by the University of Birmingham, and has been granted Health Research Authority (HRA) and Health and Care Research Wales (HCRW) Approval via Wales Research Ethics Committee 5 (IRAS project ID: 290750; Protocol number: RG_20-144; REC reference: 21/WA/0059) – approval received 19 February 2021.
Information governance statement
The University of Birmingham is committed to handling all personal information in line with the UK Data Protection Act (2018) and the General Data Protection Regulation (EU GDPR) 2016/679. Under the Data Protection legislation, the University of Birmingham is the Data Controller, and you can find out more about how we handle personal data, including how to exercise your individual rights and the contact details for our Data Protection Officer here: www.birmingham.ac.uk/privacy/index.aspx.
Please note: Chapter 3 of this report forms the basis of an early output from the study: Ince R. et al. ‘Why are we stuck in hospital?’ Understanding delayed hospital discharges for people with learning disabilities and/or autistic people in long-stay hospitals in the UK. Health Soc Care Community 2022. https://doi.org/10.1111/hsc.13964.
Policy and practice resources from the study, including accessible versions, are available via: www.birmingham.ac.uk/schools/social-policy/departments/social-work-social-care/research/why-are-we-stuck-in-hospital.aspx.
Disclaimers
This report presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care.
References
- NHS England and Partners . Transforming Care for People With Learning Disabilities – Next Steps 2015.
- NHS England and Partners . Building the Right Support: A National Plan to Develop Community Services and Close Inpatient Facilities for People With a Learning Disability and Or Autism Who Display Behaviour That Challenges, Including Those With a Mental Health Condition 2015.
- NHS Digital . Learning Disability Services Monthly Statistics: Data from the Assuring Transformation Collection – January 2020 2020.
- Department of Health (DH) . Transforming Care: A National Response to Winterbourne View Hospital 2012.
- Department of Health (DH) and Partners . DH Winterbourne View Review Concordat: Programme of Action 2012.
- NHS England . Care and Treatment Reviews: Policy and Guidance 2017.
- Department of Health and Social Care . All inpatients with learning disability or autism to be given case reviews 2019. www.gov.uk/government/news/all-inpatients-with-learning-disability-or-autism-to-be-given-case-reviews (accessed 15 February 2023).
- Hatton C. One more heave? Autistic people, people with learning disabilities and inpatient units (again) 2020. https://chrishatton.blogspot.com/2020/01/as-report-afrer-report-documents.html (accessed 15 February 2023).
- Pring J. Anger as Hancock offers string of seven-year-old policies on institutional care. Disability News Service 2019. www.disabilitynewsservice.com.
- Equality and Human Rights Commission (EHRC) . Health Secretary faces legal challenge for failing patients with learning disabilities and autism 2020. www.equalityhumanrights.com/en/our-work/news/health-secretary-faces-legal-challenge-failing-patients-learning-disabilities-and (accessed 15 February 2023).
- HM Government . Building the Right Support for People With a Learning Disability and Autistic People: Action Plan 2022.
- Equality and Human Rights Commission (EHRC) . Health Department’s plan for detained patients falls well short of what’s needed 2022. www.equalityhumanrights.com/en/our-work/news/health-department%E2%80%99s-plan-detained-patients-falls-well-short-what%E2%80%99s-needed?s=03#.YuE3c0ITeH8.twitter (accessed 15 February 2023).
- COSLA/Scottish Government . Coming Home Implementation: A Report from the Working Group on Complex Care and Delayed Discharge 2022.
- Inclusion Scotland/C-Change Scotland . Submission in Response to the Coming Home Implementation Report 2022 2022. https://c-change.org.uk/wp-content/uploads/2022/08/Letter-to-Ministers-Coming-Home-Implementation-Report.pdf (accessed 15 February 2023).
- Café R. Winterbourne View: abuse footage shocked nation. BBC 2012. www.bbc.co.uk/news/uk-england-bristol-20084254 (accessed 15 February 2023).
- Ryan S. Justice for Laughing Boy: Connor Sparrowhawk - A Death by Indifference. London: Jessica Kingsley; 2017.
- Triggle N. Whorlton Hall: Hospital ‘abused’ vulnerable adults 2019. www.bbc.co.uk/news/health-48367071 (accessed 15 February 2023).
- Salman S. Seven years on from Winterbourne View, why has nothing changed?. The Guardian 2018. www.theguardian.com/society/2018/may/30/seven-years-winterbourne-view-learning-disabled-people-abuse (accessed 15 February 2023).
- Salman S. You can’t rehabilitate someone into society when they’re locked away. The Guardian 2019. www.theguardian.com/society/2019/jan/16/rehab-centre-learning-disabilities-secure-units-community (accessed 15 February 2023).
- BBC . People with learning disabilities ‘trapped’ in hospitals as target missed. BBC 2019. www.bbc.co.uk/news/health-47965894 (accessed 15 February 2023).
- Birrell I. I have seen so many horrors… but this is barbarism. Mail on Sunday 2018. www.dailymail.co.uk/news/article-6523805/IAN-BIRRELL-seen-horrors-barbarism.html (accessed 15 February 2023).
- Birrell I. Young people are being locked away for years because they have autism and learning disabilities. Some never make it out. The I 2018. https://inews.co.uk/opinion/the-care-system-remains-twisted-incarcerating-people-with-learning-disabilities-is-inhumane-235247 (accessed 15 February 2023).
- Birrell I. Profiteers of misery: parents slam health fat cats in UK and US who are raking in as much as £730,000 annually for every autistic child they ‘lock up’ in secretive secure psychiatric units. Daily Mail 2018. www.dailymail.co.uk/news/article-6375895/Parents-slam-health-fat-cats-getting-730-000-annually-autistic-child-lock-up.html (accessed 15 February 2023).
- James E, Neary M, Hatton C. Report on the First 7 Days of Action 2016.
- House of Commons/House of Lords Joint Committee on Human Rights . The Detention of Young People With Learning Disabilities and Or Autism 2019.
- Children’s Commissioner for England . Far Less Than They Deserve: Children With Learning Disabilities or Autism Living in Mental Health Hospitals 2019.
- Mencap . Winterbourne View: The Scandal Continues 2014.
- National Autistic Society . Transforming Care: Our Stories 2017.
- Voluntary Organisations Disability Group . Transforming Care: The Challenges and Solutions 2018.
- Duffy S. Close Down the ATUs: Submission to the Joint Committee on Human Rights by the Centre for Welfare Reform. Sheffield: Centre for Welfare Reform; 2019.
- Brown M, James E, Hatton C. A Trade in People: The Inpatient Healthcare Economy for People with Learning Disabilities and/or Autism Spectrum Disorder. Lancaster: Centre for Disability Research; 2017.
- Mencap . Government Due to Miss Deadline for Releasing People With a Learning Disability Locked Away in Inpatient Units, Mencap Warns 2019.
- National Audit Office . Local Support for People With a Learning Disability 2017.
- Mental Welfare Commission for Scotland . No Through Road: People With Learning Disabilities in Hospital 2016.
- Mills S, French M, Clarke A. Improving Care, Improving Lives: Chief Nursing Officer’s National Care Review of Learning Disabilities Hospital Inpatient Provision Managed or Commissioned by NHS Wales. Cardiff: National Collaborative Commissioning Unit; 2020.
- Hatton C. Specialist inpatient services for people with learning disabilities across the four countries of the UK. Tizard Learn Disabil Rev 2016;21:220-5.
- Care Quality Commission (CQC) . Review of Restraint, Prolonged Seclusion and Segregation for People With a Mental Health Problem, a Learning Disability or Autism: Interim Report 2019.
- Glasby J, Littlechild R, Le Mesurier N, Thwaites R, Oliver D, Jones S, et al. Who Knows Best? Older People’s Contribution to Understanding and Preventing Avoidable Hospital Admissions. Birmingham: School of Social Policy/NIHR Research for Patient Benefit programme; 2016.
- Glasby J, Littlechild R, Le Mesurier N, Thwaites R. Who Knows Best? Top Tips for Managing the Crisis – Older People’s Emergency Admissions to Hospital (Good Practice Guide Sent to Every English Hospital, Social Services Department and Clinical Commissioning Group). Birmingham: School of Social Policy/NIHR Research for Patient Benefit programme; 2016.
- Glasby J, Littlechild R, Le Mesurier N, Thwaites R. Who knows best? Older people’s and practitioner contributions to understanding and preventing avoidable hospital admissions. Health Econ Policy Law 2019;15:225-46.
- Glasby J. Hospital Discharge: Integrating Health and Social Care. Abingdon: Radcliffe Medical Press; 2003.
- National Audit Office . Discharging Older Patients from Hospital 2016.
- Care Quality Commission (CQC) . Beyond Barriers: How Older People Move Between Health and Social Care in England 2018.
- Glasby J, Littlechild R, Pryce K. Show Me the Way to Go Home: Delayed Hospital Discharges and Older People. Birmingham: Health Services Management Centre/Institute of Applied Social Studies (on behalf of the DH Policy Research Programme); 2004.
- Thwaites R, Glasby J, le Mesurier N, Littlechild R. Room for one more? A review of the literature on ‘inappropriate’ admissions to hospital for older people in England. Health Soc Care Community 2015;25:1-10.
- Mays N, Roberts E, Popay J. Studying the Organisation and Delivery of Health Services. London: Routledge; 2001.
- Department of Health . Valuing People: A New Strategy for Learning Disability for the 21st Century 2001.
- NHS Digital . Assuring Transformation 2016. https://digital.nhs.uk/data-and-information/data-collections-and-data-sets/data-collections/assuring-transformation (accessed 8 December 2023).
- Ritchie J, Spencer L. Analyzing Qualitative Data. London: Routledge; 1994.
- Miles MB, Huberman MA. Qualitative Data Analysis. London: SAGE; 1994.
- Murray J. Thousands with learning disabilities trapped in hospital, some for years. The Guardian 2023. http://theguardian.com/society/2023/mar/14/thousands-learning-disabilities-trapped-long-stay-hospitals (accessed 20 March 2023).
- Thomas S, Leese M, Dolan M, Harty M-A, Shaw J, Middleton H, et al. The individual needs of patients in high secure psychiatric hospitals in England. J Forensic Psychiatry Psychol 2004;15:222-43.
- Beer D, Spiller MJ, Pickard M, Gravestock S, Mcgovern P, Leese M, et al. Low secure units: factors predicting delayed discharge. J Forensic Psychiatry Psychol 2005;16:621-37.
- Devapriam J, Gangadharan S, Pither J, Critchfield M. Delayed discharge from intellectual disability in-patient units. Psychiatric Bull 2014;38:211-5.
- Nawab K, Findlay L. A survey of the use of an assessment and treatment unit for adults with learning disability in Lanarkshire over a six year period (2001–2006). Bri J Dev Disabil 2008;54:89-9.
- Taylor J, Breckon SE, Rosenbrier C, Cocker P. Development and implementation of a discharge pathway for detained offenders with intellectual disabilities. J Intellect Disabil Offending Behav 2017;8:144-54.
- Cumella S, Marston G, Roy A. Bed blockage in an acute admission service for people with a learning disability. Br J Learn Disabil 1998;26:118-21.
- Oxley C, Sathanandan S, Gazizova D, Fitzgerald B, Puri BK. A comparative review of admissions to an intellectual disability inpatient service over a 10-year period. Br J Med Pract 2013;6.
- Washington F, Bull S, Woodrow C. The transforming care agenda: admissions and discharges in two English learning disability assessment and treatment units. Tizard Learn Disabil Rev 2019;24:24-32.
- Alexander R, Hiremath A, Chester V, Green F, Gunaratna I, Hoare S. Evaluation of treatment outcomes from a medium secure unit for people with intellectual disability. Adv Mental Health Intellect Disabil 2011;5:22-3.
- Care Quality Commission (CQC) . Out of Sight: Who Cares? A Review of Restraint, Seclusion and Segregation for Autistic People, and People With a Learning Disability and Or Mental Health Condition 2020.
- Dickinson MJ, Singh I. Mental handicap and the new long stay. Psychiatric Bull 1991;15:334-5.
- Kumar A, Agarwal M. Discharge prospects of a mental handicap population: a survey of nursing perceptions. Br J Dev Disabil 1996;42:63-9.
- MacDonald A. Coming Home: A Report on Out-of-Area Placements and Delayed Discharge for People With Learning Disabilities and Complex Needs 2018.
- Palmer J, Boyle F, Wood A, Harris S. The Hospital Resettlement Programme in Northern Ireland After the Bamford Review Part 1: Statistics, Perceptions and the Role of the Supporting People Programme (a Report for the Northern Ireland Housing Executive) 2014.
- Perera C, Simpson N, Douds F, Campbell M. A survey of learning disability inpatient services in Scotland. J Intellect Disabil 2009;13:161-71.
- Watts RV, Richold P, Berney TP. Delay in the discharge of psychiatric in-patients with learning disabilities. Psychiatric Bull 2000;24:179-81.
- Thwaites R, Glasby J, Le Mesurier N, Littlechild R. Interviewing older people about their experiences of emergency hospital admission: methodology in health services research. J Health Serv Res Policy 2019;24:124-9.
- Cadel L, Guilcher SJT, Kokorelias KM, Sutherland J, Glasby J, Kiran T, et al. Initiatives for improving delayed discharge from a hospital setting: a scoping review. Br Med J Open 2021;11. https://doi.org/10.1136/bmjopen-2020-044291.
- Department of Health and Social Care . Hospital Discharge and Community Support Guidance 2022.
- Glasby J, Lester H. Delayed hospital discharges and mental health: the policy implications of recent research. Soc Policy Adm 2004;38:744-57.
- Lewis R, Glasby J. Delayed discharge from mental health hospitals: results of a postal survey. Health Soc Care Community 2006;14:225-30.
- Glasby J, Miller R, Glasby A-M, Ince R, Konteh F. ‘Why Are We Stuck in Hospital?’: A Guide to Overcoming the Barriers to People with Learning Disabilities and/or Autistic People Leaving ‘Long-Stay’ Hospital. Birmingham: University of Birmingham/Changing Our Lives; 2023.
- Ince R, Glasby J, Miller R, Glasby A‐M. ‘Why are we stuck in hospital?’ Understanding delayed hospital discharges for people with learning disabilities and/or autistic people in long-stay hospitals in the UK. Health Soc Care Community 2022;30. https://doi.org/10.1111/hsc.13964.
Appendix 1 Advisory Board and Reference Group
Advisory Board
-
Siraaj Nadat, Senior Quality of Life Facilitator, Changing Our Lives (Chair).
-
Samantha Clark, Chief Executive, Learning Disability England.
-
Vivien Cooper, Founder, Challenging Behaviour Foundation.
-
David Harling, Head of Leaning Disability Nursing, NHS England/Improvement.
-
Chris Hatton, Department of Social Care and Social Work, Manchester Metropolitan University.
-
Ewan King, Deputy Chief Executive, Social Care Institute for Excellence (later Chief Executive, Shared Lives Plus).
-
Oliver Lewis, Barrister, Doughty Street Chambers.
-
Andy McDonnell, Director/Consultant Clinical Psychologist, Studio III Training Systems and Psychological Services.
-
Catherine Nolan, Regional lead (people with learning disabilities and autism), Association of Directors of Adult Social Services.
-
Tim Parkin, Senior Policy Advisor, Think Local Act Personal.
-
Steve Scrown, Chief Executive (Dimensions) and Chair (Voluntary Organisations Disability Group). After Steve’s retirement, Pippa Foster, Director of Lived Experience and Clinical Practice (Dimensions) became a member.
Having received an extension to the project to include additional social care perspectives, the Board was joined by:
-
Liz Howard, British Association of Social Workers (‘Homes not Hospitals’ campaign).
-
George Appleton, Policy Manager, Care England.
Reference Group
-
Zeze Sohawon
-
Matthew Dolton
-
Mandy Warner
-
Roxy Begum
-
Ami-Lea Jones
-
Brandon Lee Jamie
-
Andrew Wright
-
Rebecca Wright
-
Catherine Carrington
-
Charlie Jerrison
-
Jeremy Harris
-
Monique Mehra
Appendix 2 Topic guides for interviews/focus groups
Background to the study (aide memoire for research team)
In recent years, there has been growing concern about the number of people with learning disabilities and/or autistic people living in long-stay hospitals. Although the UK decided to close asylums for people with learning disabilities from the 1960s onwards, there has been a growth in people admitted to so-called ‘assessment and treatment units’, with allegations that some people stay here for far too long, with little ‘assessment’ or ‘treatment’ that could not be provided elsewhere. Other people live in secure units or in an NHS campus where the previous hospital is still in the process of closing. Over 2100 people live like this at the moment (despite repeated policies to help people leave hospital and live in the community). This is a real problem as these services struggle to help people to lead ordinary lives, are very expensive, can be a long way from people’s homes and families, and have seen a number of abuse scandals – just as was the case with the asylums of the 1960s.
Despite this, there has been little research on why people with learning disabilities are delayed in such settings. In particular, previous debates have often failed to talk directly to people with learning disabilities, their families and front-line staff about their experiences of living or working in such settings, what they see as the main barriers and what would help more people to leave hospital. In other research with older people, we have looked at these issues from the perspective of older people themselves, their families and care staff, as each group has a unique view on what is happening and might make a difference. Unless we listen to these voices we will not find solutions to these problems, and too many people will remain in hospital unnecessarily. Our aim here is to do the same with people with learning disabilities, their families and care staff, so that their voices are heard too. This will increase the chance that people can leave hospital in a timely way and lead more ordinary lives in the community.
This is sensitive work, requiring skills in working with people who may not communicate verbally, where there is a risk that some people can be violent (as all of us can when we’re scared and distressed), and where there can be tensions around what is best. We have therefore included a skilled, experienced team who can carry out such in-depth work in a way that suits the needs of the individual. We also have strong relationships with local services, national policy and voluntary agencies working with people with learning disabilities in long-stay hospitals – and these will be crucial for the study’s success.
We will produce a report and articles so that people can read what we have found. We will also produce a good practice guide (based on the experiences of people with learning disabilities and their families) and send this to every health and social care leader in the country. We will also produce a free training video for care staff who may not have access to as much training/support as they need. We will ensure our research is conducted well and produces helpful findings by working with a group of national advisors, chaired by a person with a learning disability. We will design our research materials with a group of people with learning disabilities and families, so that the questions we ask, how we get to know people and how we share our findings work really well for people with learning disabilities and their families.
People with learning disabilities and/or autistic people
Note to research team:
-
This topic guide sets out the questions that we wish to explore with all participants – but we will adapt the process of data collection according to individual circumstances and needs. For some people, this may be a one-off traditional ‘interview’. However, many people may not communicate in this way or find it comfortable to take part in a one-off interview, so we will need to build up this information over time in a series of shorter conversations, via other forms of communication (such as pictures, talking mats, art or music), utilising whatever communication mechanisms the person prefers, and/or via insights from a family member/care staff/case file.
-
We will also test and refine this topic guide with our Reference Group of people with learning disabilities and/or autistic people and their families.
-
If the person seems to be upset or distressed, please stop the conversation, move away and check with care staff to make sure that the person is supported.
-
If you have concerns that someone isn’t safe or is being abused or neglected, then please contact the Principal Investigator immediately.
-
During the research, everyone’s safety is paramount – we shouldn’t be collecting data until we’ve attended team meetings on how to be safe in long-stay settings, handling difficult conversations, behaviours that can escalate/de-escalate anger and frustration, and key principles for safe practice; consulted with case-study sites around any individuals or parts of the ward we should avoid and any known ‘triggers’ for people on the ward, taking any advice given; ensuring we are inducted into local procedures around how to respond if there is a serious incident and where exits are and how to exit a locked area safely; and spending time on the unit/ward so that people get to know us gradually and do not feel nervous by the presence of ‘strangers’ asking questions.
Questions to cover:
-
Why was the person admitted to hospital?
-
Why are they still in hospital?
-
How do they feel about this?
-
What might need to happen for them to be able to leave hospital?
-
Why hasn’t this happened yet? When might it happen?
-
What does the person want their life to be like?
-
To what extent is their life currently like this, and what might need to happen for them to be able to lead a chosen lifestyle?
-
Are there any common policy or practice barriers that seem to be getting in the way of people leaving hospital, or any good practice that could be shared with others?
-
If we produce national guidance to help people leave hospital, what key messages should we include?
(At 12 month follow-up):
-
What has happened since the initial interview?
-
If the person is still in hospital, why is this? How close are they to leaving? What are the barriers? How do they feel about this?
-
If the person has left hospital, where are they living now? What support are they getting? How did their discharge go? How do they feel about this?
-
Are they closer to the chosen lifestyle that they talked about in the initial interview?
Interviews with family members
Note to research team:
-
Sometimes the person with a learning disability and/or autistic person and their family might have different views about what has happened and about what would be best for the person. If both people are being interviewed together, we will need to ensure that both people can share their views and experiences, without one person dominating or feeling unable to speak. We will explore how to manage these potential tensions in team meetings.
-
Some family members can feel very guilty or upset, so we will need to conduct the interview in a sensitive manner, and make sure that we do not leave people distressed after the interview has finished.
Questions to cover:
-
Why was the person admitted to hospital?
-
Why are they still in hospital?
-
How do they feel about this? How does the family member feel?
-
What might need to happen for them to be able to leave hospital?
-
Why hasn’t this happened yet?
-
When might it happen?
-
What does the person want their life to be like? What does the family member think?
-
To what extent is their life currently like this, and what might need to happen for them to be able to lead a chosen lifestyle?
-
Are there any common policy or practice barriers that seem to be getting in the way of people leaving hospital, or any good practice that could be shared with others?
-
If we produce national guidance to help people leave hospital, what key messages should we include?
Focus groups with care staff
Note to research team:
-
Focus group of 10–12 people, including front-line members of the immediate ward/care team (e.g. support workers and nurses on the unit), as well as members of the wider clinical team (psychologists, psychiatrists, physios, OTs, social workers etc.).
-
Time focus groups to be as convenient as possible for participants (e.g. to coincide with existing team meetings, reviews or MDTs where appropriate).
-
To guard against the dangers of front-line staff feeling unable to speak freely, we will also offer the opportunity to have an individual interview if this would help them to feel more comfortable contributing their views and experiences.
Questions to cover:
-
Nationally, there is a belief that a potentially large number of people with learning disabilities and/or autistic people live in long-stay hospitals much longer than they need to. How much do you feel this is an issue here?
-
Of all the people currently in this hospital/on this ward, what approximate % would you think could be discharged if appropriate alternatives were in place?
-
How does it affect the person with a learning disability and/or autistic person if they have to stay in hospital for longer than is necessary?
-
How does it affect care staff? Is there any support that might help you?
-
What are the main reasons why people are delayed in hospital?
-
What practical steps could be taken to help people leave hospital and live more independently in the community?
-
If we produce national guidance to help people leave hospital, what key messages should we include?
Interviews with Commissioners
-
Why was the person admitted to hospital?
-
Do they need to be there/why are they still in hospital?
-
What might need to happen for them to be able to leave hospital?
-
Why hasn’t this happened yet?
-
When might it happen?
-
What do we know about what the person might want their life to be like? To what extent is their life currently like this, and what might need to happen for them to be able to lead a chosen lifestyle?
-
Where someone is delayed in hospital, what impact does this have on the commissioner? Is there any support that would help them?
-
Are there any common policy or practice barriers that seem to be getting in the way of people leaving hospital, or any good practice that could be shared with others?
-
If we produce national guidance to help people leave hospital, what key messages should we include?
Interview/focus groups with social workers, advocates and social care providers
(As above – for focus interviews with commissioners – but with a small number of specific prompts by group)
-
[For social workers] – what skills, training and experience do social workers have to be able to undertake this work; how much work is entailed and what impact does this have on other aspects of their caseload; what professional/organisational support do they receive; what does good social work look like and what difference can it make; what is their experience of current discharge/review processes; and do they have any recommendations for future policy/practice/training?
-
[For social care providers] – what is their experience of working with people discharged from long-stay settings; what makes a good discharge; what is their experience of current discharge/review processes; what impact does this have on staff and other residents/service users; are there any financial implications; and do they have any recommendations for future policy/practice?
-
[For advocacy organisations] – what is their experience of providing advocacy support; how is this received by ward staff/other professionals; and how can the role of advocates can be strengthened?
Appendix 3 Sample introductory letter and information sheet/consent form




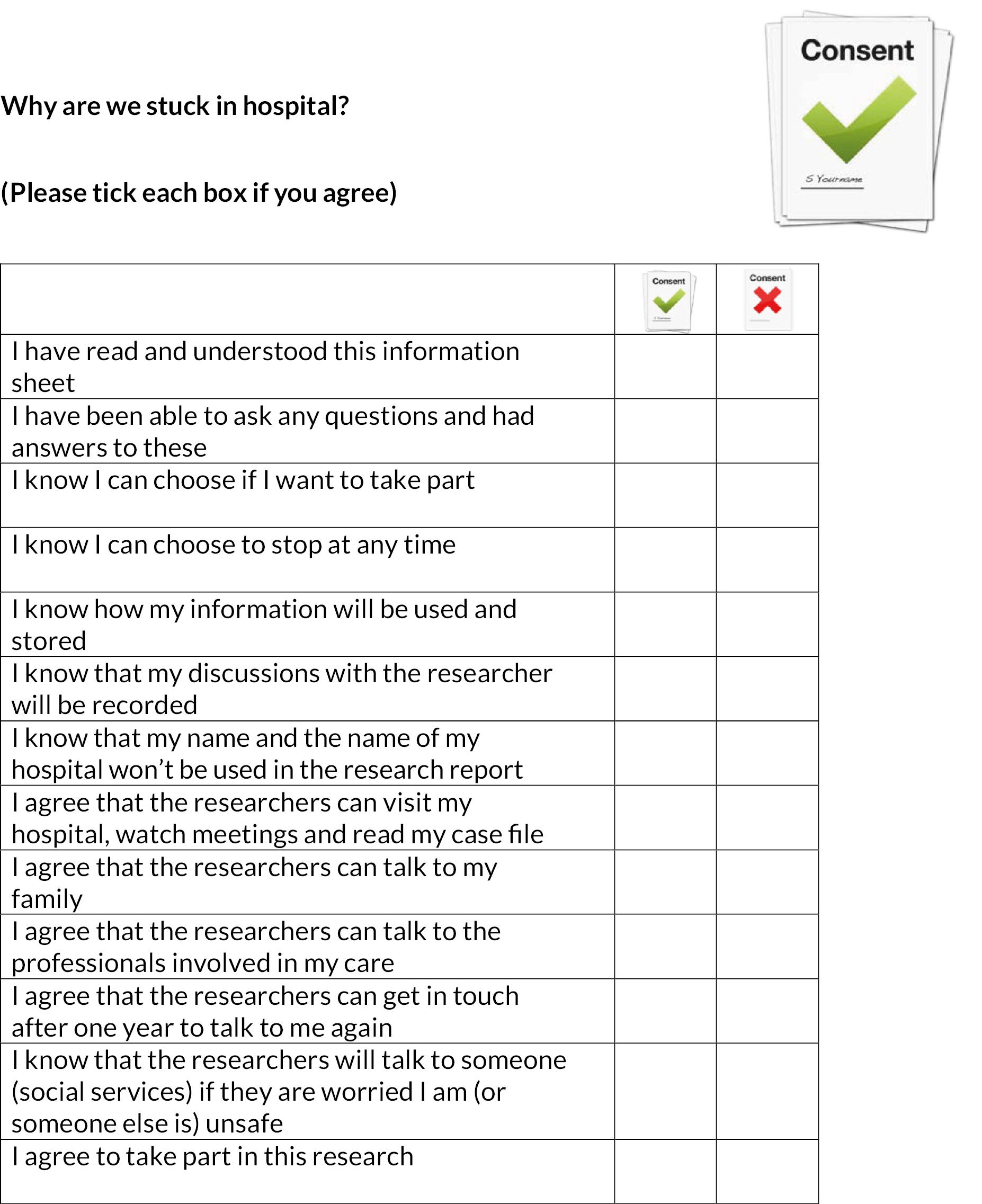
Appendix – your information
How will we use information about you?
-
We will use the information you provide in our research project (in reports, articles, online, on social media, in guides and in training material).
-
People will use this information to do the research or to check your records to make sure that the research is being done properly.
-
We will write our reports in a way that no-one can work out that you took part in the study. We will not use your name or contact details. Your data will have a code number instead (for example, ‘Person 1’).
-
We will keep all information about you safe and secure.
-
Once we have finished the study, we will keep some of the data so we can check the results.
What are your choices about how your information is used?
-
You can stop being part of the study at any time (up until we start writing our report), without giving a reason.
-
If you choose to stop taking part in the study, we would like to continue collecting information from your family, care staff, commissioner, hospital meetings and case files. If you do not want this to happen, tell us and we will stop.
-
We need to manage your records in specific ways for the research to be reliable. This means that we won’t be able to let you see or change the data we hold about you.
Where can you find out more about how your information is used?
You can find out more about how we use your information:
-
by asking one of the research team;
-
by sending an email to dataprotection@contacts.bham.ac.uk.
List of abbreviations
Please note: sometimes participants used abbreviations that the research team would not choose to use themselves. However, we have included them here so any abbreviations used in quotations make sense to the reader.
- ADASS
- Association of Directors of Adult Social Services
- ADHD
- attention deficit hyperactivity disorder
- ASD
- autistic spectrum disorder
- ATU
- assessment and treatment unit
- BASW
- British Association of Social Workers
- CAMHS
- Child and Adolescent Mental Health Service
- CCG
- Clinical Commissioning Group
- CPA
- care programme approach
- CQC
- Care Quality Commission
- CMHT
- Community Mental Health Team
- CTR
- care and treatment review
- DH/DHSC
- Department of Health/Department of Health and Social Care
- DoLS
- deprivation of liberty safeguards
- EHRC
- Equality and Human Rights Commission
- ESRC
- Economic and Social Research Council
- GDPR
- General Data Protection Regulations
- HCA
- healthcare assistant
- HCRW
- Health and Care Research Wales
- HRA
- Health Research Authority
- HSDR
- Health and Social Care Delivery Research programme
- HSMC
- Health Services Management Centre
- ICB
- integrated care board
- LD
- learning disability
- MHA
- Mental Health Act
- MoJ
- Ministry of Justice
- MDT
- multidisciplinary team
- MHRT
- Mental Health Review Tribunal
- NAO
- National Audit Office
- NHSE/I
- National Health Service England/Improvement
- NIHR
- National Institute for Health and Care Research
- OT
- occupational therapist/therapy
- PBS
- positive behaviour support
- PD
- personality disorder
- PLD
- person with a learning disability
- RC
- responsible clinician
- RSPCA
- Royal Society for the Prevention of Cruelty to Animals
- SCIE
- Social Care Institute for Excellence
- TLAP
- Think Local Act Personal
- VODG
- Voluntary Organisations Disability Group
