Notes
Article history
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as project number 15/145/06. The contractual start date was in June 2017. The final report began editorial review in November 2020 and was accepted for publication in June 2021. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Disclaimer
This report contains transcripts of interviews conducted in the course of the research and contains language that may offend some readers.
Permissions
Copyright statement
Copyright © 2022 Benger et al. This work was produced by Benger et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaption in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2022 Benger et al.
Chapter 1 Introduction and objectives
Overview
In this chapter, we set out the background, context and aims of the general practitioners working in or alongside the emergency department (GPED) study. We show how GPED has developed in response to increasing emergency department (ED) demand and how it relates to previous initiatives, drawing on a range of published literature. A taxonomy of GPED models, developed with the other research team undertaking related work and supported by the same funding call, is described, and this has also been published. 1 By considering the key determinants of GPED, we identify a lack of clarity and consistency regarding the expectations of GPED and the effects it will have on patients, staff, the ED and the wider health-care system. The central roles of streaming and governance are briefly considered before we set out the aims and objectives of the research, the expertise of the study team and the structure of this report.
Background and policy context
Health-care systems across the globe are facing unprecedented challenges. This is particularly apparent in urgent and emergency care, which is experiencing steadily increasing demand. 2 In 2019, attendances at EDs in England reached record levels; 2018–19 saw an increase of 4.4% compared with 2017–18, and an increase of 21% since 2009–10. 3
Although attendance numbers decreased dramatically in March 2020 because of the COVID-19 pandemic (decreasing by 29.4% in March 2020 compared with March 2019), the proportion of patients requiring admission reached its highest ever level. 4 COVID-19 required the NHS to change its approach to managing demand, for example by reducing capacity in EDs to accommodate social distancing on the assumption that all patients might have COVID-19. 5 Despite an uncertain future, the Royal College of Emergency Medicine (RCEM) and other authors have stated that EDs need to be transformed to avoid returning to previous experiences of crowding and to provide the best care for patients. 6,7
High levels of attendance result in high occupancy, which is often referred to as ‘crowding’. Crowding occurs when there are insufficient resources to adequately meet patient demand. 8 ED crowding can undermine patient safety, clinical outcomes and quality of care because of increased waiting times9–11 and delayed service delivery,12 with associated increased mortality13 and reduced patient and clinician satisfaction. 14
Waiting times to be seen and treated in England also reached record levels during 2019. Only 79.8% of patients were seen and discharged, admitted or transferred within 4 hours of arrival in December 2019, which was the lowest recorded performance since the ‘4-hour target’ was introduced in 2004. 15
Alongside an acknowledgement that overall ED attendances are increasing, one hypothesis is that more patients are attending the ED either ‘inappropriately’ (i.e. with medical conditions that are not sufficiently urgent to require ED care) or for routine care that could be better delivered elsewhere. It has been estimated that between 15% and 40% of patients attending the ED could be treated in general practices,16–18 particularly children17,19 and those aged 16–44 years. 20,21 However, the lack of a standardised definition of ‘inappropriate’ can be problematic. Using criteria developed by a panel of experts from the RCEM, Morris et al. 22 found that the proportion of avoidable attendances was 19.4%, lower than previously reported. 16
Explanations for avoidable ED attendances include the convenience of access, a sense of anxiety on the part of a patient or carer about the severity of the patient’s condition, a lack of self-care skills,23 the availability of prompt and effective care and access to hospital-based investigations within the ED, a lack of awareness of alternatives to the ED,18 patient dissatisfaction with their own primary care provider24 and a belief that the ED is the correct place to source health care. 25 In a qualitative metasynthesis, Vogel et al. 26 identified four reasons that patients visit the ED over primary care:
-
perceived urgency of the medical condition
-
barriers to accessing primary care
-
advantages of the ED
-
fulfilment of medical needs and quality of care in the ED.
Similarly, a team from the University of Sheffield27,28 identified six mechanisms that explain why patients make clinically unnecessary use of emergency and urgent care:
-
need for risk minimisation
-
need for speed
-
need for low treatment-seeking burden
-
compliance
-
consumer satisfaction
-
frustration in accessing general practitioner (GP) appointments.
Some authors believe that this is exacerbated by reduced access to primary care. 2 However, others report that poor access to GP services does not appear to influence patient attendances to the ED29 and this issue remains unresolved.
Many initiatives have been introduced in the UK to address this challenge, including telephone advice and guidance (NHS Direct/NHS 111) and the provision of alternative facilities, such as walk-in centres and urgent treatment centres, at which patients can access primary care for non-urgent conditions. 2 In addition, over the past decade, EDs across the UK and Europe have implemented a range of new models of care co-locating general practice services in or alongside the ED. By 2015, some form of general practice co-location existed in 43% of UK EDs. 18
Rationales for introducing GPs in or alongside the ED, in addition to addressing the rising demand in attendance, include bringing vital primary care skills and expertise into the ED, reducing admission and investigation rates, improving patient care and reducing costs. 30 However, there is a lack of clarity regarding the mechanism(s) through which these benefits might be achieved, and the hypotheses that underpin the deployment of GPs in the ED are often vague and unclear. 31
In 2014, four Medical Royal Colleges produced 13 recommendations to improve urgent and emergency care. 32 The first of these was that ‘Every emergency department should have a co-located primary care out-of-hours facility’ (copyright © The Royal College of Emergency Medicine, Royal College of Physicians, Royal College of Paediatrics and Child Health and Royal College of Surgeons). 32 This recommendation was echoed in 2015, when a review of urgent and emergency care in the NHS in England proposed that selected patients should be directed or ‘streamed’ to an alternative health-care provider who could better meet their needs to reduce ED attendances. 33 However, the RCEM reported in 2015 that ‘less than half of EDs in the UK have fully implemented co-located primary care out-of-hours facilities and a third have no co-located primary care facility at all’ (copyright © The Royal College of Emergency Medicine). 34
In 2017, these recommendations were translated into policy. In March 2017, the Next Steps on the NHS Five Year Forward View was published and set out a ‘comprehensive plan to reduce the growth in minor cases that present to A&E [accident and emergency] departments’ (contains public sector information licensed under the Open Government Licence v3.0.; URL: www.nationalarchives.gov.uk/doc/open-government-licence/version/3/). 35 An accompanying statement said that ‘[e]xperience has shown that onsite GP triage in A&E departments can have a significant and positive impact on A&E waiting times’. 36
To support this intervention, the UK government announced a capital fund of £100M in the Spring Budget 201737 to which hospitals in England could apply to support or introduce GPED. 36,38 This announcement occurred at the same time as our team was awarded funding to complete the research that is reported here, and this initiative has influenced our study and our findings significantly.
Although the UK government and NHS leaders have proposed the adoption of front-door streaming and co-located care, data to support the benefits of GPED are limited.
Some evaluations of early adopters in the UK and Europe suggested that situating GPs in the ED has the potential to be a promising innovation39 that may reduce resource use40,41 and increase patient satisfaction. 42 Carson et al. 30 reported that the proportion of cases seen by GPs varied and that clinical and operational governance was often disjointed. In a survey of patients, Bickerton et al. 43 found that, although co-located care offered patients a greater range of health-care provision, it also increased the risk of duplication of services and repeat attendance. Similarly, evaluations of nurse-led walk-in centres co-located with the ED found ‘no evidence of any effect on attendance rates, process, costs or outcome of care’. 44 More recently, in a relatively small study, Uthman et al. 45 found that GPs who saw patients in the ED used fewer resources without increasing reattendance and referred more patients to follow-up services. In addition, service users appreciated simplified health-care provision from a single point of access, although this required clear communication between health service staff and patients. 46
Critiques of GPED’s ability to address high levels of ED occupancy include the arguments that eligible patients are often quick and easy to manage, do not breach the ‘4-hour target’ and do not contribute to crowding. 30,47 A recent realist review concluded that, despite GPs in ED being associated with a reduction in process time for non-urgent patients, this does not necessarily increase capacity to care for the sickest patients. 48 The main cause of ED crowding was perceived be because of congestion in the flow of sicker patients into the hospital and a lack of beds, rather than absolute attendance numbers. 49 In addition, GPED may encourage patients to present to the ED with a primary care problem, thereby increasing attendance numbers. 47,50
Several recent reviews have examined GPED in more detail. In a rapid review, Fisher et al. 51 concluded that there was insufficient evidence to support policy or local system design. In an update of Fisher et al. ’s51 rapid review, Turner et al. 52 reported that ‘the evidence base to support development of this model of care was weak and based on poor quality studies’ (contains public sector information licensed under the Open Government Licence v3.0). These findings were supported by a narrative review by Ramlakhan et al. ,50 which recommended a robust evaluation to inform future policy.
A 2012 Cochrane review53 concluded that there was insufficient evidence regarding GPED to make recommendations for policy or practice. However, the review was based on three non-randomised studies that did not assess patient safety or outcomes and were judged to be of low quality. An updated review54 in 2018 still found insufficient evidence from which to draw conclusions for practice or policy.
Based on current evidence, the most recent guidance55,56 from the National Institute for Health and Care Excellence (NICE) concluded that there was insufficient evidence to reach a recommendation on co-located GP units. NICE found inconclusive evidence that such units reduce the demand on the ED or improve clinical or economic outcomes. 55,56
Providing a reliable solution that applies across the complex range of ED services is challenging and requires adaptation to the specific context. Nevertheless, co-location of GPs in or alongside the ED (i.e. the GPED intervention) remains a preferred option. 57
To date, the consequences for the NHS workforce, both GPs and hospital staff, have not been well considered. It is not clear what the impact is for GPs, who are already under considerable pressure, and GPED may not be the best use of their time and skills. It is also unclear how GPED might have an impact on existing primary care services that are themselves experiencing a steadily increasing demand, with particular challenges in recruitment and retention, and how the additional costs of employing GPs, which may exceed the employment costs of other types of staff, will be met. 58–61
Some of the apparent impact of GPED on EDs may simply be relabelling of the same work, with no real benefits for patients or the NHS. Furthermore, any improvements reported may be attributable to employing additional senior medical staff rather than the fact that they are specialist primary care practitioners. 62 Co-located GP services may stimulate an increase in demand at hospital sites, transferring the problem of overcrowding from EDs to co-located GP urgent care centres (UCCs).
In response to these challenges, and the lack of reliable evidence, this study is one of two commissioned by the National Institute for Health and Care Research (NIHR) [the other being Health and Social Care Delivery Research (HSDR) project 15/145/04; URL: https://fundingawards.nihr.ac.uk/award/15/145/04 (accessed October 2021)] to evaluate the clinical effectiveness, safety, patient experience and system implications of the different models of GPED.
Taxonomy of GPED models
Departments that were early adopters of GPED were pioneers in the design and execution of co-located GP services. These EDs provided a blueprint for those that followed, with some used as exemplars. Foremost among these was Luton and Dunstable Hospital (L&D) (for more information on the L&D model, which was included as one of our case study sites, see Chapter 3).
There are several models currently in use without any evidence regarding which is the most effective and efficient model of care. 30 An evaluation of 13 EDs in the north of England found that sites varied considerably with regard to their models of care. 59
In 2010, three types of service were identified in a published taxonomy: off-site GP services, a service co-located with the ED and GPs fully integrated with the ED team. 30 It should be noted that the primary purpose or intention of these models may differ; for example, off-site and co-located services may be implemented to move a cohort of patients with problems suitable for general practice out of the ED altogether (potentially reducing the recorded number of ED patients) and integrated GPs may be intended to improve the care and experience of ED patients.
In 2017, in a study of 13 EDs in the north-west of England, Ablard et al. 59 described three distinct models: primary care services embedded within the ED, co-located UCCs and GP out of hours (OOH). In a concept paper published jointly by our study team and the other NIHR-funded team described above,1 a four-model taxonomy was described (Figure 1).
FIGURE 1.
Taxonomy of GPED. (a) Inside – integrated; (b) inside – parallel; (c) outside – on site; and (d) outside – off site. Reproduced with permission from Cooper et al. 1 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The figure includes minor additions and formatting changes to the original figure.

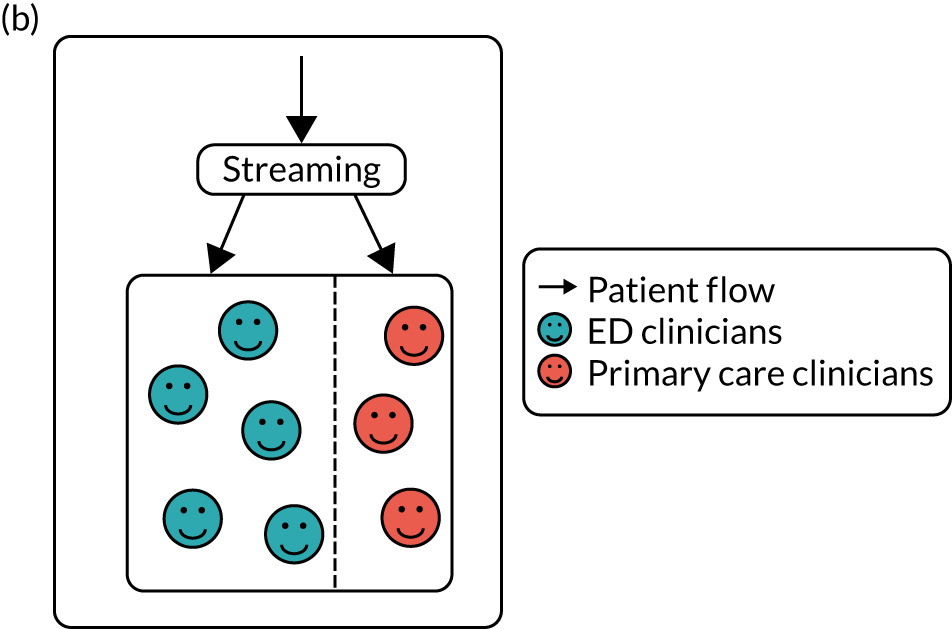
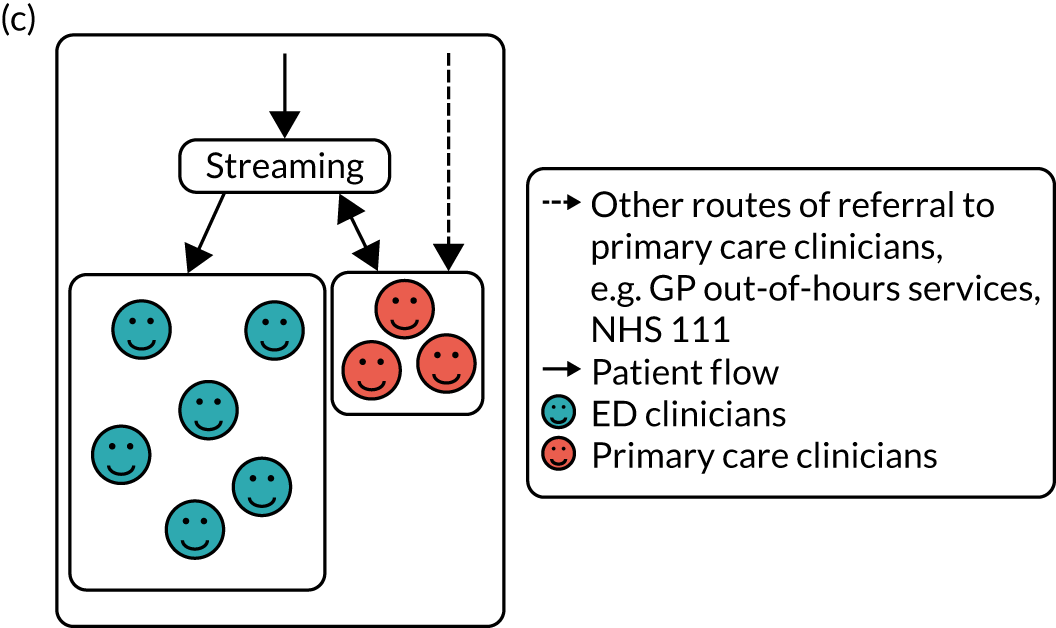

The four models are based on whether access to the GP service is inside the ED (patients access a primary care service within the ED) or outside the ED (patients access a primary care service that is distinctly separate from the ED). GP services located on a hospital site with no links to an ED are not included in this taxonomy:
-
Inside – integrated: the primary care service is fully integrated with the emergency medicine service.
-
Inside – parallel: there is a separate primary care service within the ED for patients with primary care problems.
-
Outside – on site: the primary care service is elsewhere on the hospital site.
-
Outside – off site: the primary care service is off site (may include telephone advice via NHS 111, or pharmacies, dentists, opticians, UCCs or registered in-hours or OOH primary care services).
Although this describes the structural location of the GPED service, there is still considerable variation in the way that GPED models operate across sites.
Factors influencing the implementation of GPED
This study was designed to examine the impact of GPED and the relative clinical effectiveness of the most common models of GPED currently in use. It is therefore important to recognise that these models can differ quite substantially. This might reflect the rationale for introducing GPED; local demands from both service users and community health-care provision; and practical issues, such as geographical space, financial constraints, and governance and managerial responsibilities.
Expectations and hypotheses of the use of GPED
There appear to be several implicit hypotheses that underpin GPED initiatives, including the following potential benefits: (1) reduced pressure on the ED, freeing resources to concentrate on those patients who are the most ill and injured and reducing waiting times; (2) improved outcomes for patients, assuming that the treatment of less seriously ill patients by GPs rather than hospital doctors will be associated with better risk management, reduced resource use and a lower chance of unnecessary hospital admission; (3) improved efficiency; and (4) redirection of patients into more appropriate services, improving patient experience, providing patient education and reducing future ED attendances for those patients with less serious conditions, thereby allowing EDs to concentrate on those with serious and urgent conditions. 31 However, little is known about whether or not these hypotheses are shared across different stakeholder groups or individuals and what underpins these beliefs.
Streaming of patients suitable for GPED
Central to the effective implementation of GPED services is the identification of patients suitable for redirection. Despite the promotion of ‘front-door clinical streaming’ to address increasing demands on urgent and emergency care,35 limited accompanying guidance has been provided. Initially, the NHS circulated advice based on the model used by L&D hospital,63 which is an ‘outside: on-site’ model with a primary care service on the hospital site, but distinctly separate to the ED. This was followed by a brief additional document,64 building on guidance produced by the RCEM. 65
This guidance emphasises the importance of a high-quality assessment and identifies three main objectives:
-
improving safety
-
identifying ‘acuity’ (the severity and urgency of a patient’s illness) to ensure that the most time-critical patients are treated by the right service within appropriate time frames, and that appropriate prioritisation occurs for the remaining patients
-
improving efficiency in the system to ensure that patients do not wait unnecessarily for investigations or diagnostic decision-making.
Clearly, patient safety is paramount, and this requires a trained clinician to enact clear streaming protocols. This can be undertaken by a range of personnel, such as senior ED nursing staff, emergency nurse practitioners (ENPs), primary care nurse practitioners and GPs.
Selecting patients who are appropriate for redirection can occur via streaming or triage. Streaming is described as a brief assessment of the patient, often based on strict protocols, and may occur either prior to or following registration (the point at which demographic information is collected and the patient is identified). Streaming seeks to identify which specific service or practitioner group (stream) best meets the patient’s needs. Triage is a more comprehensive assessment and is usually completed post registration. It seeks to determine the patient’s acuity and, therefore, the order of priority in which patients should be seen. Both processes require an experienced member of clinical staff. The choice as to whether streaming and/or triage is employed is likely to depend on the availability of non-ED services, demand and case mix. Patients suitable for GP care are more likely to be streamed to this service, whereas patients waiting for treatment in an ED are more likely to undergo triage. Limited assessment followed by direction off site may increase clinical risk; a more thorough assessment is required when longer delays to reassessment or definitive care are anticipated. Differences in the choice of triage or streaming, and in the type of clinician undertaking these roles, further complicate the different GPED models in operation, in addition to the four structural location types described in the taxonomy (see Figure 1).
GPED governance
Although the RCEM recommends that the ‘front door’ of the ED is managed by the ED,65 the implementation of GPED requires providers of primary care and secondary care to work together. The method of GPED governance varies considerably and can include GPs employed by a primary care provider, GPs employed by a Clinical Commissioning Group (CCG) and GPs employed by the acute hospital trust.
These differing governance systems can influence decisions relating to when the service runs, who decides how it is run, and the risk assessments and thresholds that are deemed acceptable. As such, the employing agency will be responsible for who they recruit and the relevant training that is provided. To our knowledge, the influence of GPED governance has not been explored to date.
Study aim
We aimed to explore the effects of GPED on patient care, the primary care and acute hospital team, and the wider urgent care system, and to determine the effects of different service models of GPED.
Study objectives
Ascertaining the current provision of GPED
Objective 1
Objective 1 was to map and describe current models of GPED in England by drawing on multiple sources, such as survey data, interviews and routinely available information.
Exploring the impact of GPED on emergency department performance
Objective 2
Objective 2 was to use the retrospective analysis of routinely collected ED attendance data [from the Hospital Episode Statistics (HES) data set66], collection of local data and non-participant observation to determine the impact of GPED on patient processes and outcomes, including overall attendances, attendances in different components of the local urgent care system, waiting times, emergency admissions, reattendances and mortality.
Objective 3
Objective 3 was to use the retrospective analysis of HES data66 to assess the impact of GPED on the case mix of admitted patients by exploring admission rates, including the number and proportion of short-stay and zero-day admissions, subject to an examination of coding behaviour by hospital trusts, and any changes that may undermine the reliability of this measure.
Exploring the impact of GPED on the local workforce
Objective 4
Objective 4 was to use a mixed-methods approach, including workforce surveys (WFSs) and interviews, to explore the impact of GPED on GPs, including turnover, absence, satisfaction, well-being and attitudes to and scope of practice.
Objective 5
Objective 5 was to use a mixed-methods approach, including WFSs and interviews, to explore the impact of GPED on the working patterns and roles of other health-care professionals (HCPs) in the ED, including training, workload, skill-mix and expertise.
Exploring the impact of GPED on the local community
Objective 6
Objective 6 was to use a mixed-methods approach, involving secondary data analysis and qualitative techniques, to explore the impact of GPED on local urgent care services; the wider system, including primary care (e.g. demand for in-hours and OOH GP appointments); and the interface between services, including patient flow.
Exploring the impact of GPED on service users
Objective 7
Objective 7 was to use interviews and non-participant observations to assess the impact of GPED on patients and carers.
Resource utilisation and costs of care
Objective 8
Objective 8 was to explore the costs and consequences of care at ED sites with and without GPs in or alongside the ED, and compare the costs of different service models.
Objective 9
Objective 9 was to use interviews with managerial and clinical leaders, the analysis of HES data66 (where available) and a prospective mixed-methods case study to prospectively evaluate the current promotion of GPED models of care through collaboration with sites that received capital funding to implement GPED. This objective was added after project initiation in response to the capital funding initiative announced by the UK government in spring 2017. 37
Report structure and overview of study plan
This was a mixed-methods study, comprising three work packages (WPs).
Work package A mapped, described and classified current models of GPED in all EDs in England. This classification was based on an updated taxonomy (see Figure 1) created in collaboration with the other NIHR-funded study to ensure consistency of terminology and, therefore, the comparability of findings. Our research team interviewed key national and local system leaders, staff and patients to identify the domains of influence and hypotheses underpinning GPED, and the potential mechanisms for benefit and disbenefit. We examined these further through WPs B and C.
Work package B used a retrospective analysis of routinely available HES data. 66 This was complemented by a detailed mixed-methods analysis in 10 case study sites. Our primary outcome measure was originally planned to be the number of ED attendances; however, in practice, this proved impossible and the changes that we made to the protocol as a result of this and other challenges arising during the study are considered further in the Chapter 2. Additional outcome measures included waiting times, admission rates, zero-day admission rates, reattendances, patient satisfaction and mortality.
In WP C, we reported a detailed mixed-methods analysis in 10 case study sites that were about to implement (six sites) or had already implemented (four sites) a new GPED model of care. In each of the 10 case study sites, we used survey and interview techniques to collect and synthesise quantitative and qualitative data to ascertain the views and experiences of GPED from staff working across the case study sites and from patients and carers attending the service.
The findings of all study WPs are reported in Chapter 3 and discussed in Chapter 4. The conclusions and implications for future research and policy are mapped out in Chapter 5.
Summary
In this chapter, we have set out the background of and context for GPED initiatives in England. We have described an underpinning taxonomy of GPED models of care and noted uncertainty regarding the anticipated impact of GPED at all levels of the system. ED streaming and models of GPED governance are identified as key determinants of success. We have stated our study aims and objectives and described the structure of the report that will follow.
Chapter 2 Methods
Overview
In this chapter, we set out our research methods and show how these addressed each of the nine study objectives. We describe the protocol changes that were required as the research progressed, and the reasons for these modifications. Of particular note is the fact that we found GPED to be more widely adopted than we had anticipated, highly variable within and between sites, and extremely sensitive to local context. For each of the three WPs, we describe our approach to data sampling/recruitment, collection and analysis. GPED has effects across multiple levels of the health-care system and, therefore, we have adopted an approach that recognises macro levels, meso levels and micro levels of influence. The chapter concludes with a description of our approach to mixed-methods data synthesis, the ways in which patient and public involvement (PPI) have contributed to and enhanced this research and our approach to knowledge mobilisation.
Study design
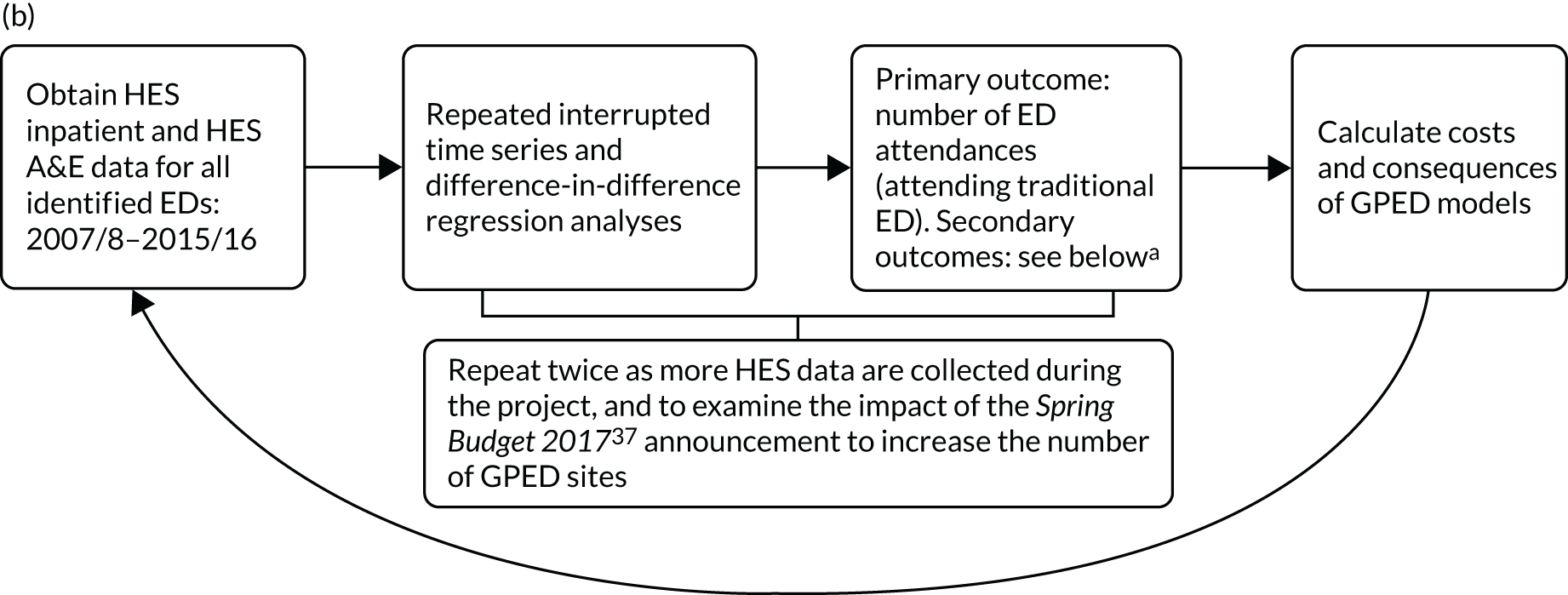
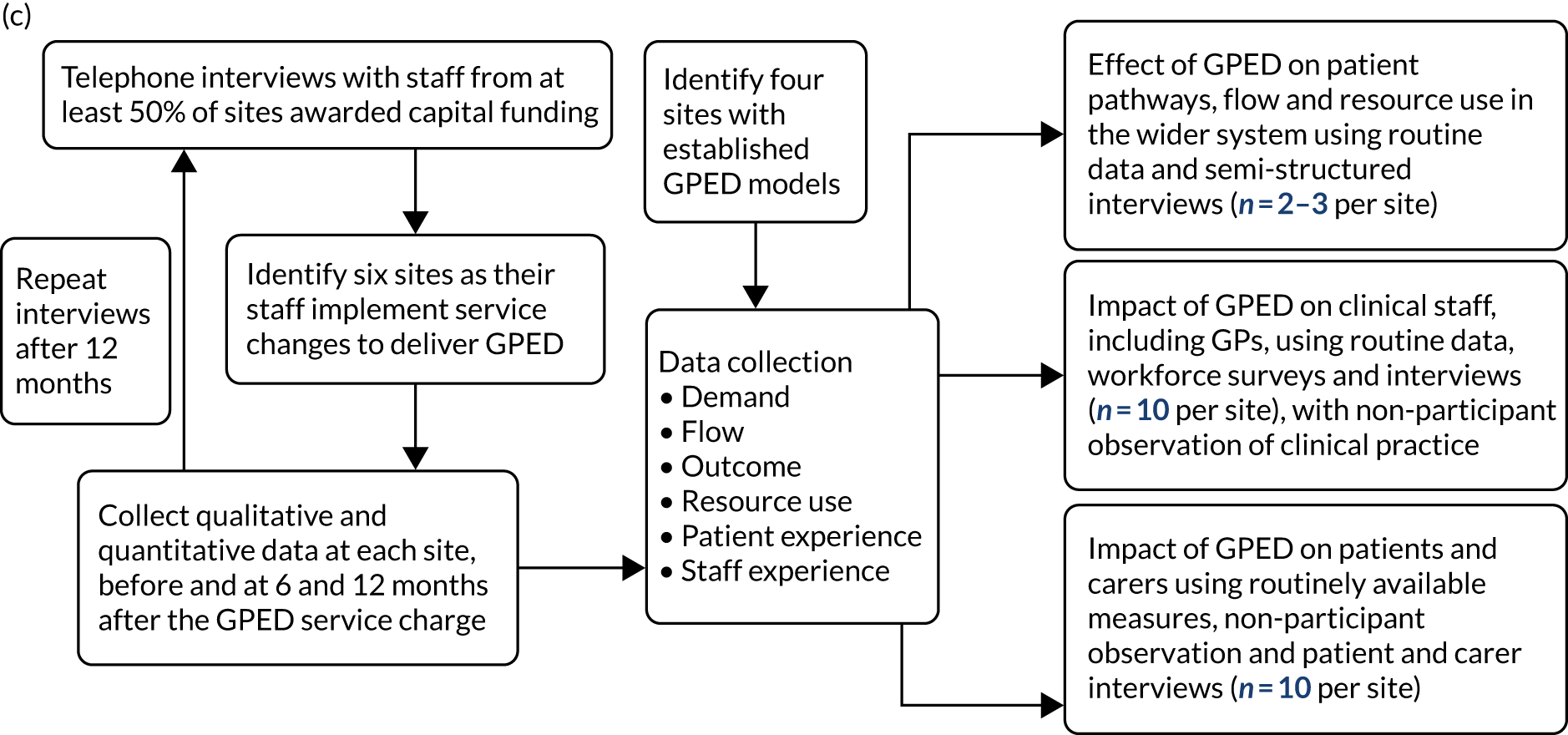
As described in Chapter 1, this study adopted a mixed-methods approach with three WPs. The links between the nine study objectives and the three WPs are shown in Table 1. Each WP is described in more detail below and is illustrated in Figure 2.
| Objective | WP |
|---|---|
| 1: to map and describe current models of GPED in England (drawing on multiple sources in WP A) | A |
| 2: to determine the impact of GPED on patient processes and outcomes, including overall attendances, attendances in different components of the local urgent care system, waiting times, emergency admissions, reattendances and mortality (from retrospective analysis of HES data66 in WP B, collection of local data in WP C and non-participant observation in WP C) | B and C |
| 3: to assess the impact of GPED on the case mix of admitted patients by exploring admission rates, including the number and proportion of short stay and zero-day admissions, subject to an examination of coding behaviour by hospital trusts, and any changes that may undermine the reliability of this measure (from retrospective analysis of HES data66 in WP B) | B and C |
| 4: to explore the impact of GPED on GPs, including turnover, absence, satisfaction, well-being and attitudes to, and scope of, practice (through a mixed-methods approach, including WFSs and interviews in WP C) | C |
| 5: to explore the impact of GPED on the working patterns and roles of other HCPs in the ED, including training, workload, skill-mix and expertise (through a mixed-methods approach, including WFSs and interviews in WP C) | C |
| 6: to explore the impact of GPED on local urgent care services; on the wider system, including primary care (e.g. demand for in-hours and OOH GP appointments); and on the interface between services, including patient flow (through a mixed-methods approach using secondary data analysis and qualitative techniques in WP C) | B and C |
| 7: to assess the impact of GPED on patients and carers (through interviews and non-participant observation in WP C) | C |
| 8: to compare resource utilisation and costs of care at ED sites with and without GPs in or alongside the ED, and to compare the costs of different service models (through economic analysis in WP B) | B |
| 9: to prospectively evaluate the current promotion of GPED models of care through collaboration with sites that have bid for capital funding to implement GPED, conducting interviews with identified system leaders and measuring changes in the above parameters over time and as implementation proceeds (through the baseline and 12-month interviews in WP A; the analysis of HES data,66 where available, in WP B; and a prospective mixed-methods case study approach in WP C) | A, B and C |
FIGURE 2.
General practitioners working in or alongside the ED: efficient models of care – flow diagram. (a) WP A: mapping different models of GPED in England; (b) WP B: retrospective quantitative analysis of national data – costs and consequences; and (c) WP C: prospective and retrospective mixed-methods evaluation in 10 case study sites. a, Includes 4-hour performance, unplanned ED reattendance within 7 days, patients leaving the ED without being seen, emergency hospital admission, zero-day admission, length of stay, re-admission to hospital within 28 days and in-hospital mortality. CQC, Care Quality Commission.

Ethics and research governance permissions
This research study was approved by:
-
East Midlands – Leicester South Research Ethics Committee (reference: 17/EM/0312)
-
University of Newcastle Ethics Committee (reference: 14348/2016)
-
Health Research Authority (HRA) (Integrated Research Application System: 230848 and 218038).
Changes to the study protocol
The study protocol has been published previously. 31 However, some important changes were required as the study progressed in response to ongoing research activity and the emerging findings.
Work package A
The WP A database (WP A1) proved much more challenging to construct than had been anticipated. We agreed with colleagues leading the complementary study, based at Cardiff University, that we would pool the information collected by both teams regarding service provision at each ED site. However, the data that our team collected were not always consistent with the Cardiff team’s survey findings. Different data sources sometimes conflicted, and it could be difficult to be certain regarding the type of model that was in place. Furthermore, key informants found it hard to recall previous service models or dates of change, and this was exacerbated by a rapid turnover in the managerial staff responsible for GPED in participating hospitals.
As the research progressed it became apparent that, contrary to previously published literature,34,67 almost every ED in England had some sort of pre-existing GPED service, and that the models in place tended to vary quite considerably over time and in response to service developments, local initiatives and workforce availability. Even within a single site, GPED usually operated for part of the working week only, and the nature of the service could vary over weeks and months or even within a single day. This made it hard to align sites with the agreed taxonomy or complete an analysis based on the type of GPED model in place. To address this, we created a three-level hierarchy of information sources (level 1, direct observation or interview; level 2, survey return; level 3, documentary or publicly available information), and included sites in our quantitative analysis only if we were confident regarding the type of model that was in use. As a result, the maximum number of sites that we could include in the WP B HES analysis was 40, when we had hoped to exceed 100.
We had originally intended to construct a series of hypotheses underpinning GPED from the initial interviews with system leaders (WP A2) to identify a set of expectations of GPED that could be tested in our research. However, it became apparent that by interviewing system leaders we risked overlooking the views of more local managers, as well as health-care staff, patients and carers. Therefore, we combined WP A2 with the interviews conducted in WP C to generate a fuller range of hypotheses from the perspective of all stakeholders across the system. This approach, however, highlighted that, for any specific issue, views regarding the likely effect of GPED could be profoundly contradictory, with some respondents postulating ‘positive’ effects but others predicting ‘negative’ outcomes. We therefore revised our approach to identify eight core ‘domains of influence’, alongside the anticipated effects of GPED on each, accepting that the predicted effects were sometimes contradictory.
Work package B
Our original aim, as outlined in the study protocol,31 was to compare the clinical effectiveness of different GPED models identified in WP A with a no-GPED model, and then to explore associated costs and consequences. Routinely collected hospital data do not identify the treating physician, and it is therefore not possible to compare outcomes for patients treated by GPs with those treated by usual ED staff. Furthermore, a successful GPED service may improve patient flow, which has positive effects on patients who are not seen by a GP but attend a hospital with GPED services. We had therefore planned two statistical analyses at hospital level: (1) a repeated interrupted time-series analysis of monthly hospital-level data that compared outcomes before and after the introduction of a GPED service, and (2) a difference-in-difference regression approach, with closely matched non-GPED sites as controls. Both methods rely on a clearly defined intervention point for all hospitals that have implemented a GPED service.
As described above, following completion of the initial mapping of different GPED models (WP A1), we found our planned analytical approach to be impossible for two reasons. First, it became clear that the vast majority, if not all, of type 1 EDs already included some form of GP care. It was therefore not possible to use a matched-control difference-in-differences approach. Second, we found that hospitals could not identify a reliable ‘intervention point’, which ruled out an interrupted time-series approach. GP services in EDs have evolved over time, and hospitals were unable to provide detailed retrospective information about the initial recruitment of GPs working in an ED setting, including the date on which a specific arrangement became operational.
These factors necessitated an early reconsideration of our analysis plans and, in consultation with the Study Steering Committee (SSC), we decided to implement a cross-sectional approach rather than a longitudinal approach. Therefore, we analysed data from hospitals with a well-established and clearly defined GPED service (level 1 in our WP A1 hierarchy) during the financial year April 2018 to March 2019. Instead of comparing GPED and control EDs over time, we used the presence of a GP in the ED as the intervention. A total of 40 of these hospitals were able to provide information about the hours (during weekdays and weekends) that a GPED service was (in principle) available, and there was substantial variation in operating hours among hospitals. This facilitated two different analytical approaches that involved comparing outcomes between patient groups who (1) attended the same ED, but at slightly different hours of the day, so were/were not exposed to GPED; or (2) attended different EDs at the same hour of the day which operated/did not operate a GPED service at that time. Both approaches have different strengths and weaknesses; however, by triangulating the results obtained under different approaches, we were able to increase our confidence in the validity of the observed results.
In our protocol,31 the planned primary outcome of WP B was intended to be the volume of patients attending the ED of each hospital. This reflected an assumption that GPED would ‘stream’ patients away from traditional ED attendance. WP A1 and early exploration of HES A&E data66 established that this is not necessarily the case; depending on hospital data-recording practices, the model of GPED and other local factors, it became apparent that GPED patients are often still entered into HES A&E data. 66 Therefore, we were unable to differentiate between patients seen by a GP and those seen by usual ED staff; as a result, our rationale for volume being a primary outcome did not hold. We considered adopting an alternative primary outcome, for which performance against the ‘4-hour wait standard’ was the most promising candidate. However, as this was not specified in our protocol, and to avoid any risk of bias from post hoc decision-making, we present the results of our quantitative analyses ranked equally, without an identified primary outcome. Nevertheless, we have retained volume of attendances in our indicator list, in case GPED affects the overall volume of patients attending the ED. 47,50
The issues with our primary outcome measure also changed our approach to the costs and consequences analysis. Again, as we had anticipated that GPED systems would redirect patients from ED to primary care interventions, we had planned to attach unit costs to any reductions in ED attendances and compare these with estimated costs of a GPED service (mainly the salary costs of GPs). As GPED and traditional ED attendances are not separately coded, this is not possible with routine data. Our exploration of costs and consequences was therefore adjusted to assess whether or not there are resource consequences of the range of performance indicators we observed, and to value any significant changes using Unit Costs of Health and Social Care 2019. 68 This was supplemented by a qualitative exploration of resource use and costs.
Work package C
Originally, it was our intention to explore the impact of GPED at 10 case sites. These sites were to be purposively selected to ensure that our analysis included ‘established’ sites, where GPED had been embedded for some time, and ‘prospective’ sites where the ambition was to use capital funding to introduce GPED. As described in our published protocol,31 10 case sites were purposively selected on this basis. However, it became clear during data collection that a GPED service had been implemented to some extent at all sites for some time. Therefore, we have not classified sites as prospective or established in our analysis, as any distinction on this basis would be artificial. Instead, we have explored the history of GPED at each site, which provided important context for understanding how the service was operationalised. This has also offered insights into national variation, as well as developed an understanding of how context had an impact on the perceived ‘success’ of each GPED model.
We had planned to use the taxonomy that was developed through WP A1 to not only structure our analysis, but also to allow us to compare the clinical ‘effectiveness’ of different GPED models. However, substantial heterogeneity in terms of both the length of time that sites had been operating a GPED model and the way that the policy was interpreted resulted in a wide range of implemented models. These complex contexts did not always fit easily into the broad categorisations outlined in the WP A1 taxonomy, limiting the value of any comparisons across and within the taxonomy.
We visited each ‘prospective’ case site at three time points, and had originally planned to treat the data as a longitudinal qualitative data set, from which we would explore how GPED was implemented at sites that had received capital funding and the impact of these changes on patient care, urgent care and the wider health-care community over time. However, the fact that GPED had been introduced in some form at all sites for different lengths of time meant that any changes resulting from capital funding were generally more gradual and subtle, making it difficult to analyse our data longitudinally. This finding was further reinforced in the findings from WP A3, in which interviews with staff from sites that had received capital investment to implement GPED often identified less change than expected over the 12 months following a funding award.
As a result of the different GPED models and time periods for which they had been in use, it could be argued that we were, in effect, evaluating the impact of different ‘interventions’ across an unknown time frame. This made any comparison of GPED by site or time point irrelevant. For transparency and to highlight the complexity associated with analysing our data at the case-site level, we have created a series of pen portraits for each of the 10 case sites that were included in the WP C analysis. These are detailed accounts of the GPED model and key findings at each site. We will refer to these pen portraits throughout this report. (The pen portraits for each site and for each time point are included in Appendix 3. This allows readers to explore each of our key qualitative themes by case site should they wish to do so.)
We had originally planned to collect data from the primary and urgent care systems surrounding our WP C case study sites to quantitatively evaluate the effect of GPED on the wider health-care system. However, it proved exceptionally difficult to obtain primary and community data, even with the assistance of the SSC. After considerable effort, we were able to obtain some quantitative data from four of our case study sites; however, these data were found to add little to the HES data that were already available. As a result, our views on wider system effects are largely based on the qualitative data collected from each case study site in WP C.
The difficulties that we encountered in distinguishing established case study sites from prospective ones also had implications for the analyses of the WFS in WP C. It was initially planned that analyses of established and prospective sites would be conducted separately and, in the case of prospective sites, there would be repeated administrations of the survey to staff members to determine whether or not perceptions of the new service changed over time and in the context of implementation. However, following our recognition of the lack of distinction between prospective and established sites, we decided that it would be preferable to combine data from surveys of established sites, as well as data from the baseline time point for prospective sites, which were viewed as comparable and appropriate for cross-sectional analyses. For example, the same survey items regarding work pressures, job satisfaction and turnover intentions were included in surveys administered to staff in both established and prospective sites, and data from these survey respondents could be readily pooled. This approach mirrors the protocol changes that were required in WP B in that we opted to convert our approach from a longitudinal to a cross-sectional design.
Summary of changes to the study protocol
Overall, we found that the reality of GPED was much more complex and variable than we had anticipated. Models varied between and within sites and changed frequently in response to a variety of factors, of which national policy and funding represented only one component. This made classification and comparison particularly challenging, both within and between sites. We adapted our data collection, analysis and interpretation to reflect this reality, moving away from a longitudinal approach towards a more cross-sectional one. We explore the implications of this observation further in the later sections of this report.
Work package A: mapping different models of GPED and interviews with key informants to understand the hypotheses that underpin GPED and the experience of implementing these models of care
Introduction
Before commencing the mixed-methods evaluation of the impact of GPED and the differential impact of alternative GPED models, it was necessary to develop an understanding of current practice and the rationale that underpins GPED initiatives. WP A was designed to (1) map and classify current models of GPED (WP A1) and (2) understand the rationale that underpins GPED (WP A2). With the announcement of £100M in capital funding to support the implementation of GPED in all EDs in England,37 we added a third objective: (3) identify how a sample of EDs planned to implement GPED and determine the extent to which these plans were realised over the subsequent 12 months (WP A3).
Work package A had four main purposes:
-
to map, classify and report the current models of GPED, describe how these changed following the provision of capital funding and examine whether or not the implemented models were associated with observable characteristics of the EDs
-
to understand the hypotheses that underpin GPED implementation (in combination with data from WP C)
-
to support the analysis of routinely available (HES) data66 that was required in WP B
-
to identify potential case study sites for WP C.
Work package A addressed objectives 1 and 9.
Database population (work package A1)
Data were collected regarding the GPED model(s) used (if any) in all 177 type 1 EDs (consultant-led 24-hour services with full resuscitation facilities) in England. Sources included a combined interview study (described below), an online survey conducted by our research team at the University of the West of England (UWE) and an online survey conducted by Cardiff University [the parallel research team funded by NIHR; URL: https://fundingawards.nihr.ac.uk/award/15/145/04 (accessed October 2021)]. This was supplemented by data sourced from public websites and NHS England, direct enquiry to individual sites and relevant data available from other researchers with an interest in this subject area, as well as data collected in WP C (from case study sites). The team assigned a level of confidence to each piece of information according to the three-level hierarchy described previously (see Work package A).
Data were collected at two time points, September 2017 and December 2019, and collated in a single database. Models were classified into one of four types according to a taxonomy developed iteratively with the team led by Cardiff University and funded by the same research call: inside – integrated; inside – parallel; outside – on site; and outside – off site (see Figure 1). 1
Alongside data classifying these GPED services in accordance with the agreed taxonomy, details of the service configuration (e.g. the times GPED was active and the number of GPs present) and the date of commencement of any service change(s) were also collected. This was supplemented by routinely available HES data66 and hospital site demographics, including annual ED attendances, the percentage of the area served by the ED that was classified as rural and the associated deprivation score. 69
We conducted a simple comparison of group means analysis to identify significant differences in hospital site demographics by the type of model used.
Interviews with national-level system leaders (work package A2)
Sampling and recruitment
Senior policy-makers and service leaders in selected commissioner and provider organisations, as well as NHS England, the Department of Health and Social Care (DHSC) and RCEM, were contacted by e-mail on up to two occasions inviting them to participate in a semistructured telephone interview.
Data collection
Detailed study information was provided and verbal consent was obtained. The aim was to explore the participant’s views of GPED, the potential advantages and disadvantages of this service configuration, and the mechanisms and hypotheses that underpin it.
Semistructured interviews, supported by a topic guide (see Appendix 1), provided some flexibility in the questions that were asked, allowing the interview to be adapted to the background and knowledge of the participant. During these interviews, participants were asked about their current role and its relation to GPED; the background to GPED and its main aims; perceptions of GPED and stakeholder involvement; models of GPED and likely effects on the ED, general practice, patient care and experience; and potential unintended consequences. When permission was given, the interview was audio-recorded and the researcher took notes. The interview recording was then transcribed verbatim by an independent transcription service. Interviews were conducted between December 2017 and January 2018.
Interviews with site-level system leaders (work package A3)
Sampling and recruitment
We identified the sites at which it was planned and not planned to implement GPED with capital funding provided by the Chancellor’s Spring Budget 2017 announcement. 37 For all 177 type 1 ED sites (defined as a consultant-led 24-hour service with full resuscitation facilities and designated accommodation for the reception of A&E patients) that were awarded capital funding to support the introduction of GPED, we sent an e-mail invitation to a managerial or clinical leader to participate in a structured telephone interview. We anticipated that recruitment of service leaders would be challenging, so to maximise our response rate each ED was sent three reminder e-mails by the project manager and/or the chief investigator.
Data collection
To ensure a systematic approach to data collection, structured telephone interviews were carried out with ED managers or clinical leads. Detailed study information was provided and verbal consent was obtained. Interviews were supported by a topic guide (see Appendix 1), designed to identify the local context and determine their planned model, expected benefits and wider impacts. Participants were asked a range of questions relating to hospital site demographics (e.g. annual attendance), the interviewee’s role in implementing GPED, challenges in the ED, perception of GP buy-in, barriers to and risks of GPED, patient perception of GPED, expected impact of GPED on ED and patient care, the current and proposed GPED model, the background to GPED introduction, the expected impact of GPED and perceptions of whether or not staff value GPED. In addition, the interviewees were asked what models of GPED had been adopted previously in their ED; the model of GPED they were using currently (when relevant), according to the described taxonomy; the times that GPED was active; and the number of GPs working at any given time. This information was then added to the WP A1 database. When permission was given, the interview was audio-recorded and the researcher also took notes. These interviews were not transcribed; instead, the researchers produced a matrix in which details of the responses were recorded.
All of those who received capital funding and were interviewed were contacted again 12 months later to review progress against their originally stated expectations, assess how successful the implementation of GPED has been and understand the extent to which the aims of the new GPED model had been achieved. For the repeat interviews, the approach to data collection was identical to that described above.
Analysis of work package A data
We conducted a simple descriptive analysis on the provision of GPED according to the three-level taxonomy and a comparison of group means analysis to identify significant differences in hospital site demographics by the type of model used.
The interview data from WPs A2 and A3 were combined with relevant WP C data and analysed collectively. (For further details of this analysis, see Work package C: detailed mixed-methods case studies of different GPED models, consisting of non-participant observation of clinical care; semistructured interviews with staff, patients and carers; and workforce surveys with emergency department staff.)
Work package B: quantitative analysis of national data to measure the clinical effectiveness of GPED using retrospective analysis of Hospital Episode Statistics
Introduction
The purpose of the quantitative analysis was to provide empirical evidence on the impact of GPED on patient flow in EDs and patient health outcomes using routinely collected health-care records for hospitals in England. WP B addressed objectives 2, 3, 6, 8 and 9.
Data sampling
This section describes the data sources and the steps that were taken to define the analysis samples.
Hospital Episode Statistics
The HES A&E data set66 contains routinely collected electronic health records for all attendances at type 1–4 EDs in England. We extracted data on all patients attending type 1 (i.e. 24 hours, 7 days per week, consultant led) EDs during the study period 1 April 2018 to 31 March 2019. Each observation pertains to an individual attendance and there may be more than one attendance for a given patient. The HES A&E data set66 provides information on the sociodemographic characteristics of the patient, including their unique (encrypted) NHS number, age, sex, ethnicity and the level of deprivation in their residential neighbourhood [as measured by The English Index of Multiple Deprivation (IMD) 201569 score]. It also records the reason for attendance and which, if any, treatments or diagnostic procedures were performed by ED staff. Because the reason for attendance was found to contain limited diagnostic information, this variable was not used in the analysis. For each attendance, the HES A&E data include the hospital code, as well as the exact date and time of arrival and discharge from the ED. 66 Finally, we extracted information on the discharge destination and used this to flag patients who were admitted to a hospital ward from the ED.
More detailed information on the clinical and sociodemographic characteristics of patients admitted to a hospital ward are available in the HES Admitted Patient Care (APC) data set. 66 We extracted information on all patients admitted to an English NHS hospital as an emergency [i.e. the variable ADMIMETH (admission method) takes on one of the following values: 21–28, 2a–c] during the study period. For each patient, we recorded the encrypted NHS number, as well as the dates of admission and discharge.
The two samples were combined to create a single data set, in which each observation pertains to a full care episode (i.e. from arriving at the ED to discharge from either the ED or the hospital ward). This was achieved in several steps. First, the data samples were merged using the patients’ encrypted NHS numbers as a key. Any admission records without at least one corresponding ED attendance record were excluded from the data set. This situation may arise if, for example, a patient is admitted directly to the hospital ward at the request of their community GP (i.e. the patient bypasses the ED and is therefore not subject to GPED). Second, in some cases, a unique merge could not be achieved because the same patient attended the ED more than once or was admitted to hospital on multiple occasions on the same day. To identify the relevant pairs of observations that comprised a care episode, we excluded any matches where
We did not enforce an exact match in dates (i.e. a difference of zero) because of issues around recording in instances in which the patient left the ED shortly before midnight and was admitted after midnight. When a patient was identified as being transferred to a different provider from an ED and a matching inpatient record was observed (in terms of encrypted NHS number and date), outcomes were attributed to the ED that the patient attended.
Mortality data
Information on the date of death for all patients who attended the ED during our study period was obtained from the Office for National Statistics (ONS). We used these data to construct indicators of 30-day mortality, calculated from the day of ED attendance.
GPED model and opening hours
Information on GPED opening hours and the type of GPED model that was operational in hospitals during the study period was collected during WP A (see Data collection). For each hospital, we established the start and end time of the GPED service on each day of the week as some hospitals operate their GPED model on different schedules during the week than on weekends. Complete data were available for 40 hospitals where we were confident which GPED model was in place (level 1 in our WP A1 information hierarchy). Hospitals with missing GPED hours information were excluded from the analysis; a comparison of all hospitals with the 40 analysed in our sample is shown in Appendix 2, Table 23.
Outcome measures
We investigated the impact of GPED on a range of different measures of ED performance and patient outcomes. All outcome measures are defined at the patient level except volume of activity, which was measured at the provider level. Detailed specifications for each outcome measure, as well as the relevant HES variables used in their calculation, are shown in Table 2.
| ID | Outcome | Definition | Level of measurement | Missing (%)a |
|---|---|---|---|---|
| 1 | Attendance < 4 hours | = 1 if the time from admission to discharge (depdur) in an ED was < 4 hours | Patient | 0.79 |
| 2 | No unplanned reattendance | = 1 if the patient does not reattend an ED within 7 days of discharge or that reattendance is planned (aeattendcat = 2) | Patient | 4.18 |
| 3 | Treated | = 1 unless the attendance was unplanned (aeattendcat = 1 or 3) and the patient left before being treated (aeattenddisp = 12) | Patient | 14.43 |
| 4 | Necessary attendance | = 1 if an attendance was ‘necessary’, defined as not meeting any of the following criteria for being unnecessary:
|
Patient | 0.00 |
| 5 | 30-day survival | = 1 if date of death of the patient was at least 30 days after ED attendance | Patient | 1.42 |
| 6 | Admission to ward | = 1 if patient was admitted as an inpatient following ED attendance (aeattenddisp = 1 or 7 and admimeth = 21–28, 2a–d) | Patient | 1.48 |
| 7 | Attendance not ending in same-day discharge | = 1 if patient attendance ended in discharge home or admission overnight (admitted = 0 or admitted = 1, and dischargedate – admissiondate > 0) | Patient | 0.00 |
| 8 | Volume of activity | Count of attendances per hour of day and day of week | Provider | 0.00 |
Statistical analysis
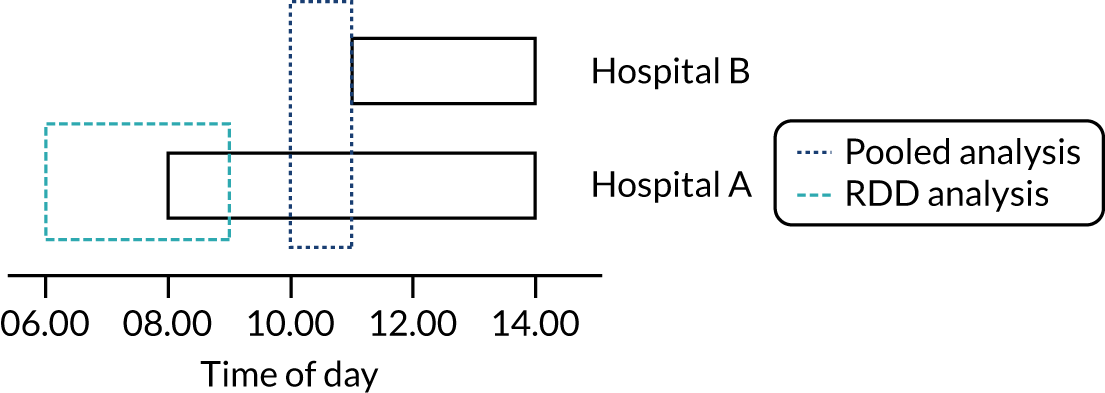
Each outcome was analysed separately and two alternative methodological approaches were considered: (1) a pooled analysis of all ED attendances to hospitals reporting GPED start and end times, in which differences in GPED opening hours across hospitals were used to separate the effect of GPED from the general effects of time of day; and (2) a regression discontinuity design (RDD) in which outcomes for patients attending the same ED shortly before or after the GPED service starts are compared to identify hospital-specific effects of GPED. Figure 3 provides a stylised representation of these analytical approaches.
FIGURE 3.
Stylised representation of alternative methodological approaches to quantify the impact of GPED using variation in GPED service opening hours.
All analyses use a critical value of α = 0.05 to determine statistical significance. No adjustment was made for multiple testing.
Pooled analysis
Our main approach was to pool data on all patients treated in English NHS hospitals in a single regression model and to use differences in GPED service availability across hospitals and times of day to identify the impact of GPED on outcomes. Nearly all hospitals for which we had data from WP A operated a GPED service for a specific, continuous subset of hours within each day, but the specific hours differ across providers. For example, a service might begin at 08.00 and end at 23.00 in one hospital, but run from 12.00 to 18.00 in another hospital. We quantified the effect of GPED by comparing outcomes for patients arriving at a given hour of the day in hospitals that (1) operate a GPED service at that time (the ‘treatment group’) or (2) do not operate the GPED service at that time (the ‘control group’).
We estimated separate ordinary least squares (OLS) (outcomes 1–7, i.e. linear probability models) and Poisson (outcome 8) panel data regression models for each outcome. Our main variable of interest was a binary indicator for whether or not the hospital operated a GPED model at the hour of the day when the patient attended the ED (yes/no). We also analysed the impact of different GPED models (inside –integrated, inside – parallel, and outside – on site; these models are referred to as ‘integrated’, ‘parallel’ and ‘on site’, respectively, in the rest of the report) by including a set of interaction terms between the GPED model and the binary indicator of service availability. All models controlled for hospital and hour-by-day of week fixed effects, month of year and, in the case of the OLS models, additional patient characteristics, such as their age (in 5-year bands), sex and socioeconomic deprivation profile, which may have acted as confounders. The hospital fixed effects captured time-invariant differences in performance across EDs that reflect hospital-specific factors, such as management quality, building infrastructure and the quality and availability of substitute health-care services within the local health economy. The hour-by-day fixed effects captured difference in service availability and patient acuity over the course of the day that follow a common pattern across all hospitals in England. For ease of interpretation, all regression coefficients are presented as average marginal effects on the original scale of the outcome variable. The estimates’ quantities refer to either percentage point changes in the likelihood of an event (for OLS models) or changes in the counts of events (for the Poisson model).
The scope of this pooled analysis was limited to hours of the day when there was variation in GPED service availability across hospitals. Patients attending EDs during hours of the day when all/none of the hospitals operated a GPED service contributed to the identification of hospital fixed effects and the influence of case-mix characteristics, but did not contribute to the statistical identification of the effect of GPED services on outcomes.
Regression discontinuity design
The pooled analysis estimated the average effect of GPED, calculated over all hospitals and hours of the day in our sample. To explore potential heterogeneity in the clinical effectiveness of GPED services across hospitals, we used a RDD that permits estimation of hospital-specific effects. In each hospital, there are some patients who attend the ED while the GPED service is in operation, whereas other patients arrive before or after those core hours and, therefore, are not treated by a GP. Patients attending at markedly different times of the day are likely to be systematically different in terms of their observed and unobserved characteristics, which precludes a direct comparison of outcomes for patients attending when the GPED service is operational with outcomes for patients attending at other times. However, we assumed that the exact arrival time of patients at the ED is exogenously determined (e.g. by the time of onset of their medical problem) and is not affected by the availability of GPED services. This implies that patients arriving shortly before or shortly after the time GPED starts are, in effect, randomly allocated to the control and treatment groups within the same hospital. The same principle holds for patients arriving shortly before (treatment group) and after (control group) the end of GPED each day. Consequently, we expect patients in both groups to have, on average, similar observed and unobserved characteristics so that any differences in outcomes between groups are unlikely to be biased by confounding. Put another way, the GPED start/end times create discontinuities in treatment allocation that the RDD exploits to obtain hospital-specific estimates of the effect of GPED on the relevant set of outcomes.
Under random allocation, the difference in outcomes between patients in the treatment and control groups can, in principle, be established using appropriate statistical tests (e.g. two-sample t-tests for continuous variables). However, residual imbalances in observed patient characteristics across treatment groups may remain, in which case inference can be further improved through regression adjustment. We therefore estimated the effect of GPED on outcomes 1–6 using logit regression models that include an indicator for treatment status and adjust for a set of observed patient characteristics. The volume of activity was not analysed with the RDD approach, as ED demand is known to fluctuate rapidly over the course of the day, so comparisons of volume across adjacent time intervals are not valid. As same-day discharge (outcome 7) is defined as discharge from an inpatient setting on the same calendar day as admission, time of ED attendance is strongly related to the probability of same-day discharge. Therefore, this outcome was also not analysed, as results would provide a partial picture only, strongly driven by the distribution of times when GPED starts and ends. We estimated separate models for each hospital and for each outcome around the start and end of GPED under the assumption that the effect of GPED may be partly driven by the hour of the day it was in operation, that is the effect at the start and end of the service may not be symmetrical. This resulted in up to 80 hospital- and time-specific estimates per outcome. We then summarised these estimates, with associated measures of uncertainty, using forest plots and random-effects meta-analysis, with subgroups defined by the type of GPED model in place (integrated, parallel and on site).
Some patients who arrive outside GPED opening hours may still be treated by a GP, for example because they are required to wait in the ED before being seen and a GP begins their shift in the meantime. These patients would be misclassified as belonging to the control group rather than the treatment group. We therefore excluded patients arriving during the hour before the start of GPED. Similar adjustments were applied around the GPED end time. These adjustments (described as 1-hour ‘doughnut holes’) may weaken the argument of random allocation and we tested for differences in observed characteristics of treated and control patients with a series of logit models, in which treatment status is used as the outcome variable and patient characteristics are used as covariates. Assuming that patients in both groups are similar in terms of observable variables, we would expect the overall explanatory power of these models, represented by the R-squared statistic, to be low. A cut-off value of 0.05 was used to exclude hospitals that showed poor balance, and, therefore, evidence of non-random treatment allocation, from the analysis. Based on this rule, three hospitals were excluded, leaving a sample of 37 hospitals.
Exploring the potential for cost savings
We explored the potential net cost savings from GPED using a simple and conservative approach. We used results from the WP A1 survey of EDs to ascertain the average hours that a GP service is in operation in English EDs and (if possible) the number of GPs present. We used salary and associated costs and the Personal Social Services Research Unit (PSSRU) Unit Costs of Health and Social Care 2019 to value GPs’ time. 68 These figures constitute the cost of operating a GPED service to the average hospital. We assumed that GPs are an addition to the existing workforce, rather than a replacement for ED staff, such as consultants. This assumption is based on our research results, in that we found GPs were almost universally engaged as an extra workforce. In a small number of sites, particularly where an integrated model was in place, GPs occasionally filled a gap in the ‘middle grade’ (registrar) ED roster, but in no cases were GPs specifically employed to replace ED consultants, and we did not identify settings where the number of ED staff had been reduced as a direct result of GPED.
To calculate the cost savings to commissioners resulting from the availability of GPED services, we used national tariffs for hospital care and multiplied these by the estimated changes in relevant outcomes obtained as part of the quantitative analysis of routine hospital data. Specifically, we focused on outcome measures that have resource implications (i.e. changes in attendances, reattendances and emergency hospital admissions, including zero-day admissions). We did not cost changes in the number of patients who left without being seen, as these would still trigger payments to providers.
These relatively crude quantitative estimates of the costs of operating a GPED service and the cost savings resulting from it were then compared to establish a net impact on NHS costs. For ease of interpretation, we express all figures as costs and cost savings per calendar year. Our costing study was further supplemented by qualitative data from our case study sites, where cost implications were considered in interviews with GPs, ED managers and other staff.
Our calculations constitute a cost–consequence analysis. We did not attempt to perform a formal economic evaluation that compared costs and health benefits of GPED as information on changes in patients’ health-related quality of life are not routinely collected in ED settings and the impact of GPED on mortality was found to be negligible.
Work package C: detailed mixed-methods case studies of different GPED models, consisting of non-participant observation of clinical care; semistructured interviews with staff, patients and carers; and workforce surveys with emergency department staff
Introduction
GPED has effects across multiple levels of the health-care system. Therefore, we completed a multimethods study consisting of interviews with policy-makers (macro level), service leaders (meso level) and health professionals and patients (micro level); and observations of clinical practice, as well as the distribution of quantitative surveys to the GPED workforce (Table 3). WP C addressed objectives 2, 4–7 and 9.
| Macro level | Meso level | Micro level | ||||
|---|---|---|---|---|---|---|
| National-level leaders | Site-level system leaders – time 1 | Site-level system leaders – time 2 | Time 1 | Time 2 | Time 3 | |
| Total number of participants | 10 | 57 | 26 | 124 health professionals; 94 patients/carers | 20 health professionals (13 had participated at time 1) | 82 health professionals (24 had participated at time 1/time 2); 54 patients/carers |
| Period of data collection | December 2017 to January 2018 | August 2017 to September 2018 | February 2018 to February 2019 | November 2017 to December 2019 | June 2018 to October 2018 | November 2018 to December 2019 |
| Number of EDs represented | N/A | 64 | 30 | 10 | 5 | 10 |
| Interview type | Semistructured telephone interviews | Structured telephone interviews | Structured telephone interviews | Semistructured face-to-face and telephone interviews | Semistructured face-to-face and telephone interviews | Semistructured face-to-face and telephone interviews |
| Other data collected | 83 periods of observation; 373 WFSs completed | No other data collected | 59 periods of observation; 87 WFSs completed | |||
| Aim | In-depth understanding from key informants | Broad perspective from a wide range of emergency settings | Broad perspective from a wide range of emergency settings | In-depth understanding from a small number of case sites | In-depth understanding from a small number of case sites | In-depth understanding from a small number of case sites |
| Job roles represented | NHS England, DHSC, CCGs, GPs, NHS trusts, NHS Improvement, RCEM | Chief executives, chief operating officers, clinical leads, lead nurses and ED managers | Chief executives, chief operating officers, clinical leads, lead nurses and ED managers | GPs, ED doctors (juniors, registrars, consultants) and nurses (streaming, triage, minor injuries) | GPs, ED doctors (juniors, registrars, consultants) and nurses (streaming, triage, minor injuries) | GPs, ED doctors (juniors, registrars, consultants) and nurses (streaming, triage, minor injuries) |
The macro level refers to national policy and wider social norms and in this report is based on interviews conducted with 10 key informants (WP A2) that aimed to gain detailed insights as to why GPED was implemented from a carefully targeted group of policy-makers. The meso level is the organisational level and involved a large number of structured interviews with ED managers and clinical leads (combined with the system leader interview data collected in WP A3) to gain a broad service-wide understanding of what EDs throughout England expected from GPED. Lastly, the micro level refers to the individual level and is based on semistructured interviews, along with a WFS, administered during in-depth visits to 10 selected ED case sites throughout England. The interviews and the WFS were intended to obtain a detailed understanding of health professional and patient perceptions of the impact of GPED. Adopting a macro-level, meso-level and micro-level approach enabled us to gain a detailed, but also service-wide, understanding of the impact of GPED on the urgent care system, primary and acute hospital teams, and patient care. 70–73
Sampling and recruitment
Macro level
Key informants were identified strategically, as described in Interviews with national-level system leaders (work package A2).
Meso level
Managerial or clinical leads were identified and invited to interview. Further details are given in Interviews with site-level system leaders (work package A3).
Micro level
Data were collected from 10 case study sites, which were selected purposively to ensure maximum variation according to GPED model, duration of using GPED, geographical location, deprivation index and ED volume (A&E attendances).
Sampling of staff, patients and their families was opportunistic by the research team, occurring while the team were undertaking on-site data collection. Care was taken to ensure that a range of health professionals representing different staff groups and grades, who had varying levels of involvement in introducing GPED and who undertook different roles within GPED models, were interviewed. Key informants at each site, such as ED leads and/or medical directors, were also interviewed.
We invited staff members at WP C case sites to complete a WFS and adopted multiple strategies to maximise recruitment. For example:
-
We prioritised survey distribution when conducting on-site data collection for WP C, which allowed the research team to promote the survey while on site. Paper and electronic versions of the survey were distributed to account for staff preference and local variation.
-
Key members of staff (e.g. research nurses, ED consultants, service managers) were also involved in survey distribution, and we invited service managers and clinical leads to promote the survey by e-mail and at team meetings, while the research team was on site and for up to 3 months after data collection.
-
At sites where initial response rates were particularly low, members of the research team returned with paper copies of the questionnaire and, in some cases, distributed paper questionnaires in person at departmental meetings, following permission from service leads.
-
E-mails from the study chief investigator were also sent to service leads at case sites, emphasising the importance of the survey and associated data collection.
Data collection
Macro level and meso level
Interviews with policy-makers and service leaders were conducted by telephone for pragmatic reasons. Further details on the macro level and meso level data collection are described above in Interviews with national-level system leaders (work package A2) and Interviews with site-level system leaders (work package A3).
Micro level
Interviews with health professionals, patients and carers were semistructured and followed a topic guide (see Appendix 3). We opted for a semistructured format for case site interviews because the purpose was to gain an in-depth understanding of how health professionals, patients and carers viewed GPED and its potential impact, but to still allow flexibility to explore issues specific to each site. During interviews, health professionals were asked about their current role in the ED and if they had a role in implementing GPED. They were also asked for details of the local GPED model and about the expected impact of GPED. Patients and carers were asked about their reasons for attending the ED, to describe their pathway through the ED, about awareness of issues with demand in the ED, about their views on the introduction of GPs in the ED and about the potential impact of GPED.
Interviews with patients and health professionals were largely conducted face to face at hospital sites during data collection for WP C. However, some interviews were conducted by telephone after on-site visits had finished at the request of the participant. Written informed consent was taken from all participants and all interviews were audio-recorded.
Non-participant observations of clinical practice were also used to gain insight into how the GPED service model was working at each case site. Observations consisted of up to 2-hour blocks, covering different parts of the day and evening, and different activities (e.g. clinical and non-clinical work, streaming, informal interactions and clinical consultations). Field notes were used to document everyday working practices, paying particular attention to the nature of the GPED model, how it was operationalised and the response from patients and clinicians.
The survey of ED staff (see Appendix 3) incorporated the Normalisation MeAsure Development (NoMAD) survey instrument,74 along with standardised measures of work-related experiences and attitudes, including job satisfaction and turnover intentions. This was designed to explore the impact of GPED on staff, including job satisfaction; specific work pressures; and the perceived impact of GPED on work patterns and the roles of HCPs and teams in the ED, including training, workload, skill-mix and expertise.
Surveys incorporated measures of background characteristics including sex and age (18–24, 25–34, 35–44, 45–64 and ≥ 65 years), length of service with the current employer (< 1, 1–5, 6–10 and > 10 years) and job category. Response options for job category included ED specialist (e.g. ED consultant, ED staff or associate specialist, ED registrar or equivalent); GP (e.g. GP, GP registrar); nursing staff (senior nurse, junior nurse, nurse practitioner, nursing assistant); doctors in a training grade [e.g. foundation training year 1 (F1) trainee, foundation training year 2 trainee, core training year 1 or core training year 2 doctor]; and other (e.g. advanced care practitioner, other).
Self-reported measures of work pressures, job satisfaction and turnover intentions were derived from the Ninth National GP Worklife Survey. 75 The work pressures scale comprised 12 items that were selected from a longer battery of questions, and asked respondents to indicate how much pressure they experienced in reference to domains such as increased demands from patients, long working hours and unrealistically high expectations of the role by others. Response options for each item were scored from 1 (no pressure) to 5 (high pressure). A 10-item measure was used to rate job satisfaction and asked how satisfied respondents were with multiple dimensions of their job, such as physical working conditions, remuneration and level of variety. Response options for these items ranged from 1 (extremely dissatisfied) to 7 (extremely satisfied). Turnover intentions were measured using four items asking about the likelihood of making work–life changes within 5 years, which were rated from 1 (none) to 5 (high). Potential work–life changes included leaving direct patient care, leaving medical work entirely, continuing medical work but with a different provider and continuing medical work but outside the UK.
The NoMAD survey instrument is based on normalisation process theory (NPT) and is designed specifically to gauge the perspectives of people directly involved in the implementation of health-care interventions. 76 It can be used for a variety of purposes and in a range of settings to support the evaluation of complex interventions. We incorporated this into the survey to gain perspectives on GPED across the whole ED/GPED team and applied the concepts of NPT in our mixed-methods data synthesis (see Mixed-methods data synthesis).
Data analysis
Qualitative data
Macro-level and micro-level data were transcribed verbatim and analysed using NVivo (QSR International, Warrington, UK), version 12. Because of the structured nature and range of meso-level data, comprehensive notes of salient themes were documented in an accompanying Microsoft Excel® (Microsoft Corporation, Redmond, WA, USA) spreadsheet. When available, data from the second interview were compared with data from the first interview to establish how often the original aims had been realised, along with common issues and challenges, and the barriers to and facilitators of change. Field notes were completed by the researchers during observations documenting everyday working practices, focusing specifically on the nature of the GPED service. These were included in the NVivo data file.
All data were initially analysed thematically and individually at the macro level, meso level and micro level. 77 Because of the large number of data collected at the micro level and the number of researchers involved in data analysis, a coding framework (see Appendix 3) was developed by the research team, after initial familiarisation, through a series of round-table discussions; this was refined and revisited during fortnightly researcher meetings on an ongoing basis throughout data collection and analysis. This framework was then used to produce a series of summaries and pen portraits to describe each case site. 78
At all stages of analysis, coding and interpretation were discussed by the relevant members of the research team. All participants were allocated unique personal identifiers (IDs), rather than a specific role, to protect anonymity and confidentiality. For transparency, it should be noted that we use the term ‘staff’ to refer collectively to GP and ED staff throughout Chapter 3, unless specified otherwise.
Workforce survey
For the WFS, data file preparation was completed using IBM SPSS (IBM Corporation, Armonk, NY, USA), version 25, and all subsequent analyses were conducted using R (The R Foundation for Statistical Computing, Vienna, Austria), version 3.4.3. These analyses addressed objectives 4 and 5.
The survey analyses were predominantly descriptive in nature and focused on describing the extent and distribution of survey-based measures of specific work pressures, job satisfaction domains and turnover intentions. These were considered for the sample of hospital workers involved with GPED as a whole, and across four readily discernible groups of employees: ED specialists, GPs, nursing staff and doctors in a training grade. Given the small numbers of employees within these groups, no inferential analyses were conducted and results are presented descriptively.
For the purposes of comparison, relevant data on equivalent measures from the Ninth National GP Worklife Survey75 are also presented. This survey was completed in 2017, and involved a random sample of GPs, including GP providers, salaried GPs and GP retainers, drawn from the General Medical Practitioners Prescribing Database for England and Wales. A total of 996 GPs participated in the 2017 iteration of the survey, through the completion of paper-based questionnaires. This was equal to 24.9% of GPs who were invited to participate (4000 GPs were approached to take part in the study).
Mixed-methods data synthesis
In addition to the individual analyses that were conducted for each of the GPED project’s three main WPs, we conducted a higher-level synthesis to integrate the study findings. This mixed-methods approach was pivotal to answering our research questions and for understanding and describing the complexity of GPED.
Integrating our findings was an iterative process that was undertaken throughout the GPED study, requiring regular discussion and sharing of findings between members of the research team. For example, the qualitative coding framework, pen portraits and WP A database were shared with the WP B team and were used to inform their knowledge of GPED models at sites that were included in their analyses. In some cases, this led to sites not being included in the WP B analysis because of uncertainty surrounding GPED operating hours.
In addition to this, we held three formal ‘mixed-methods’ roundtables, which were conducted during the final stages of the WP B and WP C data analysis. These meetings were held virtually as restrictions were in place because of the COVID-19 pandemic. The purpose of the meetings was to agree on how findings from each of the WPs could be integrated to demonstrate the impact of GPED from a mixed-methods perspective. Discussions were therefore centred around exploring complementary and divergent themes across each of our data sources. For example, how could our qualitative data be used to provide explanation and context to our quantitative findings? The inter-related nature of our findings meant that instead of presenting our results using separate chapters for each WP, we have chosen to report our study findings by theme in Chapter 3.
We then used NPT79 to reframe the overall data synthesis to understand the adoption of GPED into routine practice. NPT conceives making changes in established routines as a complex and dynamic enterprise, and proposes a model that explains the way in which new practices are adopted and absorbed by individuals into existing behavioural conventions and routines. The theory views implementation as a turbulent and unpredictable process that NPT, through its four core constructs (i.e. coherence, cognitive participation, collective action and reflexive monitoring), seeks to understand. NPT provides a theoretical framework that supports the integration of our qualitative and quantitative data and highlights the extent to which GPED has become a part of routine practice. Therefore, it is used to summarise and interpret our findings at the start of the Chapter 4.
Patient and public involvement
Patients and members of the public were involved throughout the development and delivery of the GPED research project. This began with an initial group of public contributors that was formed to provide input on the development of the grant proposal. This group formed the nucleus of the public involvement group that has worked with us since that time.
The group consisted of 10 public contributors with a wide variety of experiences of using ED services. Some had interacted with ED services as carers for children, partners or older parents, and others had used ED services as patients in their own right. Our public contributors came from a diverse range of social backgrounds and were of white British ethnicity.
Throughout the study, the group was kept informed of progress and was involved in regular workshops and meetings. Two members of the group were also full members of the SSC.
Early public involvement in the study focused on the preparation of data collection instruments and the ethics committee applications.
Workforce survey
The group reviewed the WFS. Their feedback emphasised the importance of making it clear to potential respondents why certain data were being collected. The group felt that doing so would improve uptake of the survey by addressing any sensitivities about the information requested.
Qualitative data collection
Topic guides, patient information sheets and consent forms were reviewed by the group as part of applying for research governance approvals. The group provided feedback that improved the clarity and readability of these documents.
Mixed-methods workshops
A major area of work was the involvement of the group in the interpretation of both quantitative and qualitative findings through a series of workshops that were facilitated by the public involvement lead and members of the qualitative and quantitative research teams, as appropriate. The public involvement lead and the relevant researchers worked with the patient and public contributors to make their involvement in the research process as easy and supported as possible. Public involvement in the interpretation of qualitative data is relatively common, but involvement in the interpretation of quantitative data and mixed-methods data synthesis is rarer.
Qualitative data interpretation
We held two workshops, one during the day and one in the evening, to maximise attendance.
Before the workshops, public contributors were given copies of anonymised interviews with a nurse, patient and GP, along with pen portraits of two of the study sites, to provide context for the interviews. Public contributors were asked to read the transcripts in advance and to note any major themes and/or issues that were relevant to the GPED research questions. In the first part of the workshop, public contributors discussed their varying interpretations of the interview data. In the second part of the workshop, the public contributors looked at how the data had been analysed by the qualitative research team using the developed framework. They then discussed the degree to which the analysis of the team resonated with the public contributors’ interpretation of the data, as well as examining any areas of apparent divergence, disagreement or overlap.
The workshop highlighted key issues related to patient knowledge of the ED system, the organisational implementation of the GPED system, the degree of GP embeddedness in the ED service and the central role played by the streaming nurse.
The themes raised in the workshop were reported back to the qualitative research team. The themes broadly fitted the analysis framework developed by the team, but also raised specific issues that were explored further in a subtheme analysis.
Quantitative data analysis
Our public contributors were involved in an initial preparatory workshop to explain to them how the quantitative data had been analysed and how to interpret the forest plots that were used to display the data. Examples of the forest plots of the marginal effects for the 1- and 2-hour GPED windows and patient ED attendance graphs were circulated in advance of the workshop.
A second workshop was then jointly facilitated by the PPI lead and quantitative research teams. During this workshop, the public contributors explored the forest plots in detail for each of the key outcome measures reported in WP B.
Knowledge mobilisation
Stakeholder analysis
A stakeholder analysis was conducted to identify key target stakeholders, guide the main knowledge mobilisation approaches and design an effective strategy for catalysing change. This stakeholder analysis, mapped into an assessment of power and interest in the study’s findings, is shown in Appendix 4, Table 33.
Ability to influence change
Knowledge mobilisation is about sharing knowledge between different communities to catalyse change. To understand the potential knowledge mobilisation opportunities for the study to bring about change and create impact, a force-field analysis was conducted. 80 This is described further in Appendix 4, Figure 16, along with the theoretical basis for our knowledge mobilisation approach.
Knowledge mobilisation strategy
A thorough knowledge mobilisation strategy considers mechanisms that both inform target audiences (breadth approaches) and actively engage them in the research and findings (depth approaches) in a two-way process. It was anticipated that by incorporating the multiple perspectives of stakeholders as the study progressed, this could increase both the relevance of the research and its use in practice. 81–83
Breadth approaches (dissemination)
These approaches focus on disseminating the key knowledge findings to target audiences and other stakeholders. Breadth approaches were chosen to target each stakeholder group and assume a more linear approach to the way knowledge is shared. However, these approaches have the advantage of reaching a far larger number of individuals than depth approaches.
Policy-makers
All outputs, both academic and non-academic, are publicly available on the study website. 84 Peer-reviewed academic outputs and research reports, together with associated summaries and key findings, will be produced for funders, policy-makers and NHS audiences and held on the website. Social media will be used to drive traffic to the website, which will act as a repository for materials. Blogs will also be used to generate interest and to increase the accessibility of the study’s findings.
Clinicians
Our findings are being shared nationally and internationally, through conferences, meetings, workshops and peer-reviewed publications, as described above. Associated summaries will be produced specifically for NHS audiences, as well as peer-reviewed publications.
Academic
Academic outputs will include a range of papers, submitted to high-impact, peer-reviewed journals. One academic publication has already been published and six others are currently being drafted. Presentations have already been given at the Health Services Research UK conference and a poster was given at the Society for Academic Primary Care. 85 We are using e-mail lists and Twitter (Twitter, Inc., San Francisco, CA, USA; www.twitter.com) to publicise and encourage active commentary on our outputs, and to generate debate within the academic field.
Hospital managers, service providers and members of the general public
In the dissemination phase, we are seeking opportunities for press releases and media interviews and exploring the use of digital stories, blog posts by staff members and Academic Health Science Network (AHSN) dissemination (via the network of networks). Other user-friendly, innovative ways of packaging and disseminating findings are being adopted, such as animations and video presentations.
Depth approaches (knowledge mobilisation)
Depth approaches are targeted at the key stakeholders identified as having high levels of power in the stakeholder analysis in terms of future impact on policy and practice. As described above, previous research has illustrated the importance of personal relationships and face-to-face interactions with clinicians and policy-makers to maximise knowledge sharing and mobilisation. Depth approaches aim to target individuals and key organisations to achieve the maximum number of opportunities to share and co-produce knowledge with stakeholders. We have started these on a small scale and at the local level, but intend for this learning to be used to inform breadth approaches with a wider reach at a later stage.
Collaboration with commissioning organisations
A collaboration with local urgent care commissioners was formed and members of the research team attended commissioning steering groups for urgent care and presentations at relevant events. Through the chief investigator’s links, these included national commissioning conferences and national commissioners’ attendance at study events. Existing relationships with CCGs were utilised and the networks built during the study were extended to other CCGs nationally. This could maximise opportunities to influence future commissioning decisions in relation to the study findings.
Knowledge broker
An experienced knowledge broker was a collaborator with the study team and had a role in the local commissioning organisation. Drawing on learning from the theoretical basis of communities of practice and the socialisation, externalisation, combination and internalisation (SECI) theory, the knowledge broker sought to understand the tacit organisational knowledge within the field of urgent care to identify opportunities to bring in and share knowledge generated by the study. The communities of practice and SECI theories explain how knowledge is shared, exchanged and transformed through social processes in a non-linear way (see Appendix 4 for a detailed explanation of both theories). The knowledge broker attended core business Urgent Care Control Centre meetings and established working relationships with project managers, transformation leads and strategy leads for urgent care in the organisation. The knowledge broker was also able to arrange meetings at key occasions when policy decisions were being made and arrange for members of the research team to share early findings that might assist local policy-makers. Related service development meetings with clinicians and health service managers in the local trust were also attended by the knowledge broker so that they could share related research findings that might have had relevance to decision-making.
Mid-way stakeholder meeting
The policy-making environment changes at a fast pace, which means that changes occur during the time taken to conduct a large-scale research study of this type. To ensure that the knowledge generated from the study was fed into practice while it was relevant to clinicians, commissioners, health service managers and service providers, a mid-study dissemination event was held. This was an opportunity for stakeholders to engage with the early findings of the study and to comment on and influence the direction of the final stages of the research to ensure its utility for practice. The first part of the 1-day event involved a series of presentations outlining the findings of the study at the mid-way point. The second part of the event was a round-table discussion in small groups to consider two key questions: ‘how should we judge the success of a GPED model of care?’ and ‘what outputs from the research will inform practice, and what more do we need to know?’. Approximately 50 clinicians, policy-makers, health service managers, public contributors and academics attended the event from the local and regional area. From the round-table discussion, a wide range of knowledge was shared from multiple perspectives that was then summarised as the following key points for the research team to consider as the study progressed:
-
key areas the stakeholders identified in judging the success of a GPED model of care –
-
safety and appropriate clinical risk management
-
cost-effectiveness
-
patient flow
-
the 4-hour target
-
-
key findings from the research that could most inform practice –
-
the most appropriate model for a specific setting
-
the sort of patients (demographic/condition) who are attending and why (education/availability/system factors)
-
the benefits and the unintended consequences.
-
These key areas identified by the stakeholders were then highlighted to be addressed in the dissemination of results at the end of the study.
Barriers to impact and mitigation
Barriers to change may occur at the individual, organisation or system level. The knowledge mobilisation approach for the study sought to identify these barriers from the outset to reduce their ability to block potential change.
Individual-level barriers
An example of this would be an individual with particularly strong views who was unreceptive to the study findings and had the power and/or influence to reduce the impact of knowledge on practice at a local or national level. We did not encounter any evidence of this happening at an individual level at the chosen research sites, or at a national or local level of policy-making. The knowledge mobilisation intervention to reduce the risk of this barrier was to form collaborative relationships with commissioning organisations from the outset. In addition, it became clear as the study progressed that the relationships that the core research team built with staff at the research sites were reducing the potential barriers at an individual level.
Organisational barriers
We anticipated barriers to change at an organisational level owing to the well-documented disconnect between academia and policy-making in terms of communication,86,87 differing priorities,87,88 different timescales89,90 and different ways of using and obtaining information. 91 It was intended that by involving a knowledge broker (as the knowledge mobilisation intervention) to work directly within commissioning organisations at a local level, wider learning on how to work with policy-makers in this area could be achieved. Key evidence in this area has highlighted the importance of relationship building, personal contact and conversation in communicating with policy-makers. 86,92,93 The support that the knowledge broker received from the commissioning organisations in terms of invitations to relevant meetings, discussions and conversations suggested that this intervention reduced these barriers.
System-level barriers
A major potential barrier to the acceptance of the study findings at a national level arose at the outset of the study, with the release of a national policy directive offering financial support for investment in GPED models of care. 37 The timing of this encouraged CCGs and hospital trusts to introduce these models within the first 6 months of the study set-up. Fortunately, the national role of the chief investigator encouraged national policy-makers’ involvement in the study’s progress and early-stage findings, despite this initial commitment to GPED models. This was further supported by the relationships that were built by the knowledge broker with local commissioners and a wider network of clinicians and service providers. Early stage dissemination and stakeholder events were the knowledge mobilisation interventions designed to reduce system-level barriers and ensure national policy-making involvement in the study. Through an ongoing collaboration with the research team based at Cardiff University and funded through the same call, it was possible to run three of these events at different stages in the study (two hosted by the Cardiff team and one by the Bristol team), which ensured several opportunities to mobilise and share the knowledge of research and practice in a two-way process. A final dissemination event hosted by the Bristol team and supported by the Cardiff team was held on a virtual platform in October 2020.
Proposed evaluation
It is good practice to evaluate the impact of knowledge mobilisation on further learning and clinical practice. However, all of these activities may not be possible within given resources and it is likely that any impact achieved will be recognised only after the study has ended. For these reasons, it may be prudent to gather evaluation information within the study time frame for review and revision for 1–2 years following completion of the main study. Relevant evaluation information includes:
-
Quality – is an accurate message reaching the key audiences? Are policy-makers, clinicians, patients and families receiving the intended message about the study findings?
-
Method – build a pop-up window into the study website that displays two brief questions asking visitors to clarify their current knowledge.
-
Outcomes – are the target audiences acting on the information? Are there any changes in the way services are being delivered in terms of GPED models?
-
Method – review models of GPED used in practice after 12–24 months to see if changes have occurred in line with the findings of the study.
-
Summary
This chapter has described our research methodology, showing how the three WPs combined to address the nine objectives of the project and explaining the protocol changes that were required as the research progressed. We have set out our approach to data analysis and synthesis, described the central role that PPI played throughout and described our approach to knowledge mobilisation.
Chapter 3 Results
Overview
In this chapter, we describe our research findings. We begin by reporting elements of data collection from all three WPs, individually, and then prepare for our mixed-methods analysis by considering the policy context and describing eight ‘domains of influence’ identified during WP A and WP C. The main section of the results then considers each of these domains in turn, combining quantitative and qualitative data from all three WPs to understand the potential effects of GPED and the factors that influence these.
Data collection from work package A
From our WP A database, we attempted to determine the GPED model(s) provided by all 177 type 1 EDs (consultant-led 24-hour services with full resuscitation facilities) in England at two time points: September 2017 and December 2019. Models were classified according to our iteratively developed taxonomy: inside – integrated; inside – parallel; outside – on site; and outside – off site (see Figure 1).
Data were obtained from 163 out of 177 (92%) of all the type 1 EDs in England:
-
149 out of 177 (84%) at September 2017
-
160 out of 177 (90%) at December 2019
-
139 out of 177 (79%) at both time points.
The GPED models in place in September 2017 and December 2019 are shown in Table 4. Capital funding was awarded to 87% (142/163) of the participating EDs.
| Model | Time point, n (%) | |
|---|---|---|
| September 2017 (N = 149) | December 2019 (N = 160) | |
| Inside – integrated | 38 (26) | 15 (9) |
| Inside – parallel | 44 (30) | 78 (49) |
| Outside – on site | 33 (22) | 55 (35) |
| Outside – off site | 5 (3) | 2 (1.3) |
| No GP streaming | 28 (19) | 8 (5) |
| Use of two models | ||
| Parallel and off site | 1 (0.7) | – |
| Integrated and on site | – | 1 (0.6) |
| Integrated and parallel | – | 1 (0.6) |
Between September 2017 and December 2019, 23 sites commenced and four sites ceased GPED provision. Three of the sites that ceased provision chose to discontinue an inside – integrated model. The most common service change (20 sites) was from an inside – integrated model to an inside – parallel model. In addition, 11 sites moved from an outside – onsite to an inside – parallel model.
We found no significant difference between group means by the type of GPED model adopted and the observable characteristics of included EDs (e.g. annual number of new attendances, deprivation, rurality, receipt of capital funding).
Data collection from work package B
The hours of operation for sites included in the WP B analysis are shown in Table 5.
| ED | Start time | End time | Duration (hours) |
|---|---|---|---|
| Integrated | |||
| RM3 | 08.00 | 20.00 | 12 |
| RRV | 08.00 | 22.00 | 14 |
| RXR | 08.00 | 23.00 | 15 |
| RBA | 08.00 | 23.00 | 15 |
| RMP | 10.00 | 20.00 | 10 |
| RXC | 10.00 | 22.00 | 12 |
| RCX | 12.00 | 20.00 | 8 |
| Mean hours | 12.3 | ||
| Median hours | 12 | ||
| Parallel | |||
| RFR | 08.00 | 22.00 | 14 |
| RVR | 09.00 | 17.00 | 8 |
| RKE | 09.00 | 21.00 | 12 |
| RAP | 09.00 | 24.00 | 15 |
| RTP | 10.00 | 22.00 | 12 |
| RNQ | 10.00 | 22.00 | 12 |
| RJ6 | 10.00 | 22.00 | 12 |
| REM | 10.00 | 22.00 | 12 |
| RQM | 10.00 | 24.00 | 14 |
| RBN | 10.00 | 01.00 | 15 |
| RTE | 12.00 | 22.00 | 10 |
| RQ8 | 12.00 | 22.00 | 10 |
| RXH | 14.00 | 22.00 | 8 |
| RX1 | 15.00 | 19.00 | 4 |
| RHM | 18.00 | 22.00 | 4 |
| Mean hours | 10.8 | ||
| Median hours | 12 | ||
| On site | |||
| RXQ | 08.00 | 23.00 | 15 |
| RC9 | 08.00 | 23.00 | 15 |
| RD3 | 09.00 | 20.00 | 11 |
| RAX | 09.00 | 23.00 | 14 |
| RTH | 10.00 | 22.00 | 12 |
| RGT | 11.00 | 23.00 | 12 |
| RTK | 12.00 | 19.00 | 7 |
| RMC | 12.00 | 24.00 | 12 |
| RHW | 12.00 | 24.00 | 12 |
| RD8 | 14.00 | 22.00 | 8 |
| RH8 | 18.00 | 22.00 | 4 |
| RCD | 18.00 | 23.00 | 5 |
| Mean hours | 10.6 | ||
| Median hours | 12 | ||
| Overall mean hours | 11.1 | ||
| Overall median hours | 12 | ||
Appendix 2, Table 24, summarises the main findings of our pooled analysis. The table reports results from all sites for which data were available, and separates these by GPED service type (integrated, parallel and on site). This pooled analysis uses the fact that GPED services operate at different times of the day, so the overall effect is identified by comparing the outcomes of patients arriving at a given hour of the day to hospitals operating or not operating a GPED service at that time. These results are considered further in Mixed-methods synthesis.
Data collection from work package C
Researchers collected data at three time points (0, 6 and 12 months) from six sites, and at two time points (0 and 12 months) from the other four sites. This reflected our original plan to divide these sites into ‘prospective’ and ‘established’ categories; however, as described in Chapter 2, this distinction was not identified in practice (Table 6).
| Type | Site | Region | Annual attendance (n) | IMD score | Rurality (%) | Date started/time 1 | Date revisited/time 2 (6 months) | Date revisited/time 3 (12 months) |
|---|---|---|---|---|---|---|---|---|
| Prospective | Juniper | South | 127,063 | 11.62 | 0.29 | November 2017 | June 2018 | December 2018 |
| Hawthorn | North | 46,544 | 10.74 | 0.27 | December 2017 | October 2018 | December 2018 | |
| Poplar | South | 96,108 | 10.24 | 0.02 | December 2017 | June 2018 | January 2019 | |
| Rowan | North | 123,481 | 28.00 | 0.08 | February 2018 | September 2018 | February 2019 | |
| Chestnut | London | 72,106 | 25.26 | 0.00 | June 2018 | Combined with time 3 data collection | October 2019 | |
| Birch | Midlands and East | 108,181 | 32.35 | 0.02 | March 2019 | Unable to arrange a return visit so data collection incomplete | ||
| Established | Linden | Midlands and East | 95,259 | 22.63 | 0.10 | October 2017 | November 2018 | |
| Teak | London | 143,062 | 29.50 | 0.01 | May 2018 | November 2019 | ||
| Redwood | North | 76,869 | 30.19 | 0.07 | November 2018 | December 2019 | ||
| Nutmeg | Midlands and East | 173,532 | 24.96 | 0.10 | February 2019 | October 2019 | ||
A total of 10 interviews were conducted at the macro level and 57 interviews (representing 64 EDs) were conducted at the meso level. Ten EDs were recruited as case study sites at the micro level. See Table 3 for a summary of our data collection and participant characteristics. To protect the anonymity and confidentiality of sites and participants, we have summarised our data collection in a combined characteristics table. The qualitative data reported here were collected during WP A and WP C (see Figure 2).
A total of 472 WFS responses were received across the 10 GPED case study sites. We endeavoured to determine the response rate to our WFS in each site; however, this was complicated by the fact that the survey was disseminated through both paper and electronic media on several occasions. In three out of our 10 case study sites where we were able to reliably determine a denominator, the response rates from staff were 9.4%, 25.5% and 36.4%, giving an average of 24%. A small number of surveys (n = 23) could be matched to individuals using a unique identifying code. However, given the limited number of these longitudinal data, and the decision to abandon any distinction between prospective and established sites, the analyses focused on cross-sectional data derived from surveys obtained from (1) established sites and (2) the baseline time point at prospective sites. These data were viewed as the most comparable and readily combined, producing a total analytic sample of 383 surveys.
Characteristics of the cross-sectional analytic sample are displayed in Appendix 3, Table 26. The majority of survey respondents were female (64.8%, n = 248), with the largest proportion of respondents being aged 18–34 years (41.8%, n = 160) and reporting having worked for their current NHS employer for 1–5 years (36.6%, n = 140). The largest proportions of respondents reported being nursing staff (41.3%, n = 158) or ED specialists (26.4%, n = 101), and indicated that they delivered care in the ED (67.1%, n = 257). Eleven per cent of the respondents (n = 42) indicated that they delivered care in the GP service related to the ED and 4.7% (n = 18) reported being GPs. The small number of GPs in the survey sample is arguably proportional to the number of GPs employed in EDs under the GPED model.
A summary of the WFS results and NoMAD findings can be found in Appendix 3. For the purposes of this primary report, a limited range of survey results is reported and selected according to mixed-methods considerations. That is, survey results were prioritised for reporting if they either aligned with or provided a potential contrast with findings from the qualitative data (thus allowing a form of triangulation between the data sources) and are incorporated into the mixed-methods synthesis below.
Mixed-methods synthesis
Introduction
This study was designed on the basis that GPED had been implemented in only a limited number of ‘established’ sites, with capital funding being the mechanism for the policy’s introduction nationally. However, while conducting interviews for WP A and WP C, it became apparent that GPs have been present in the vast majority of EDs throughout England, using a range of different models and initiatives, for some time. This posed various challenges for the GPED study, and changes to the protocol that we have described in Chapter 2. Therefore, we will first use qualitative data from interviews with national policy-makers and local service leaders (WP A2 and WP A3), health professionals, patients and carers (WP C) to describe how the national policy was developed and implemented. This provides important context for understanding why there is so much variation in how the policy has been interpreted and introduced throughout the NHS in England, which is crucial to the interpretation of our study findings.
GPED policy context
GPED: ‘a case of bias to action’
All stakeholder groups were critical of how GPED policy had been developed, describing GPED as a case of ‘bias to action’ and implemented ‘only because the government were under pressure to be doing something’. The national roll-out of GPED was perceived as rushed, with local service leaders sceptical about having to implement an initiative that had limited evidence supporting its clinical effectiveness and cost-effectiveness. These doubts were exacerbated by the lack of clinical and patient consultation that occurred during GPED’s design and implementation. Local service leaders also discussed how the policy originated largely from discussions between the Secretary of State for Health and Social Care and NHS England as a direct response to the rising pressure being placed on the government regarding poor ED performance:
I think it adds to the mix. I think that it was not a very well thought through policy decision . . . It was never part of the urgent, the care, the Keogh review16 of urgent emergency care, to have GPs in ED. Now, that review focused much more on NHS 111 and also trying to create consistency . . . So having GPs in ED was outside of that policy strand. So, and it was dropped in a very, at very great speed and without a great deal of thought.
Local service leader 01
The Luton and Dunstable model
The decision to introduce GPED on a national level was based largely on the perceived success of a GPED service that had been implemented at L&D. 63 This provided an ‘urgent care GP centre’ close to the ED on the L&D hospital site. The centre accepted only referrals of an agreed patient cohort from the ED, and operated daily between 08.00 and 23.00. 63 Patients arriving at the ED were greeted by an experienced nurse, who used a checklist and algorithm to support a streaming decision. Trauma patients, including those with head injuries, were not referred to the urgent care GP centre.
However, across all levels, participants criticised the process of and rationale for choosing L&D as the basis of a national initiative. First, local service leaders perceived the L&D model to have been ‘pushed out’ following what they perceived as conflicting guidance from NHS England on standards for urgent treatment centres. Although it was acknowledged that subsequent, more general, guidance was released regarding GPs at the ‘front door’ of the ED, local service leaders questioned why the previous Monitor report58 had not been used to inform GPED. The report concluded that six of the top 10 performing EDs were in north-east England and so these sites were considered a more appropriate foundation for informing national policy. 58 In addition, although the L&D GPED service was reported to have resulted in the successful delivery of the national ‘4-hour’ ED target, participants recognised difficulties disaggregating the cause of this success from other initiatives that had been introduced in L&D at the same time:
You know, it isn’t a sufficient evidence base to work from. You could have looked at the North East of England, I’m taking this call just now and said, you know, ‘six of the top 10 performers nationally sit in the North East, all right, and that tells us something about the system’ . . . and I think that, if we’re going to use examples as a way of developing policy, that would have been a better way of looking at it.
National policy-maker 05
GPED: a one-size-fits-all approach
Despite a number of local service leaders discussing the importance of local context and how a ‘one-size-fits-all’ approach was not intended for GPED, the majority of site staff viewed GPED as a top-down, generalised strategy that had been imposed on them and an example of national issues driving service-wide change. Consequently, local service leaders hypothesised that whether or not GPED would be ‘effective’ depended on the local context and key service issues in the sites where it was implemented. For example, the main focus of activity at one site was on moving patients who require admission from the ED to other parts of the service, and GPED was not considered likely to address this. For other EDs, the population they served was perceived to have higher health literacy and a limited number of primary care presentations, which tended to result in a reduced impact and relevance of GPED. There was, therefore, little perceived need for the service in some areas, where it was felt that the potential impact of GPED would be negligible because a good service and/or staff mix was already in place:
A small department, not a massive issue with primary care patients, but still have to comply with the directive on streaming into primary care. Would be welcome to see similar push in social care funding – to have impact on bed shortages, which are not due to minors numbers, lack of detail in social care funding plans.
Service leader 01
Some of this uncertainty and lack of enthusiasm surrounding GPED may be attributed to the fact that various attempts to introduce GPs into the ED have been made over the last decade, and most of the sites in our sample had a GP service and streaming in place when the capital funding was announced. Ultimately, variations in local context, ED demand and existing service provision meant that it was often not considered possible or necessary to introduce a new GPED initiative, with an expectation that ‘a proliferation of different models’ would be implemented, leading to considerable variation in service delivery and performance across the UK:
Whilst we started with a very clear ‘here’s the Luton model’, it became, obviously when trusts came to implement it locally, that due to various circumstances that were very specific to their trust and their community, the Luton model just wasn’t appropriate. So I think what we’ve ended up with is a range of different models. So you couldn’t look at GP streaming and say what we’ve got in place now is the same in every trust in the country because there’s almost certainly . . . there’s huge variation in practice around how they’re running.
National policy-maker 07
GPED: a sticking-plaster solution
There was scepticism that a single initiative could fix complex problems in the health-care system. Consequently, several local service leaders felt that GPED was ‘patching gaps in the system’ rather than addressing issues such as holistic care and mental health provision, which were seen to contribute more substantially to ED pressure. Annual growth in ED workload was also anticipated to mask the ‘visibility’ and impact of GPED. Suggestions for alternative approaches for improving ED performance and system-wide clinical effectiveness included adopting a ‘whole system approach’ and pathway planning post streaming. In addition, ‘upstream interventions’ that are aimed at managing patients before they become acutely unwell were perceived as potentially more beneficial than those aimed at controlling ED volume. This was highlighted by one participant who remarked that for GPED to lead to improved performance, efficiency and patient care, it would have to be a ‘phenomenally effective policy’ and would require ‘everything to be perfect’.
GPED domains of influence
We present our main results according to eight domains of influence, or areas that participants felt would be affected by the introduction of GPED. From the outset of the study, we were aware of a lack of consensus as to the desired or anticipated effects of GPED and, therefore, we sought to identify a series of hypotheses that could be tested in our research. However, as the work progressed it became apparent that in many areas even the direction of the effect was contested; thus, rather than establishing unidirectional hypotheses, we have chosen to identify more general domains of influence. These domains were identified through analysis of 228 semistructured interviews with national policy-makers, local service leaders, health professionals, patients and carers (WP A and WP C), and were developed through a series of roundtable discussions undertaken by the research team. The domains were refined and revisited during researcher meetings on an ongoing basis throughout the data collection and analysis, and are used as a framework for structuring our discussion of the impact of GPED.
In our WFS, most participants understood the potential value of GPED in principle: 78% of staff (n = 299) who responded agreed or strongly agreed with the statement ‘I can see the potential value of GPED for my work’, and 65.5% (n = 251) agreed or strongly agreed that participation in GPED was a legitimate part of their role. The overwhelming majority agreed or strongly agreed that they were open to working with colleagues in new ways to use GPED (91.6%, n = 351). However, reflecting the varying local needs and contexts and the different ways in which GPED had been introduced, there was disagreement at the individual, stakeholder and organisational levels about the purpose and anticipated impact of GPED. For example, only half (54%) of staff agreed or strongly agreed with the statement ‘the staff have a shared understanding of the purpose of GPED’.
In the subsequent sections, the impact of GPED on each domain will be explored using quantitative and qualitative data, as available. However, evidence for some domains will be either solely qualitative or quantitative because of the data that are available and the nature of the domain. This is summarised in Table 7.
| Domain of influence | Qualitative data | Quantitative data |
|---|---|---|
| Performance against the 4-hour target | Qualitative interviews with policy-makers (WP A), health professionals, patients and carers. Non-participant observation (WP C) | HES data:66 percentage of patients discharged within 4 hours of arrival |
| Use of investigations | Qualitative interviews with policy-makers (WP A), health professionals, patients and carers. Non-participant observation (WP C) | |
| Hospital admissions | Qualitative interviews with policy-makers (WP A), health professionals, patients and carers. Non-participant observation (WP C) |
HES data:66 admitted HES data:66 non-same-day discharge attendance |
| Patient outcome and experience | Qualitative interviews with policy-makers (WP A), health professionals, patients and carers. Non-participant observation (WP C) |
HES data:66 left without being seen HES data:66 unplanned reattendance within 7 days HES data:66 30-day mortality |
| Service access | Qualitative interviews with policy-makers (WP A), health professionals, patients and carers. Non-participant observation (WP C) |
HES data:66 unnecessary ED attendance HES data:66 volume of attendances |
| Workforce (e.g. recruitment, retention) | Qualitative interviews with policy-makers (WP A), health professionals, patients and carers. Non-participant observation (WP C) | Case site survey data: WFS and NoMAD questions |
| Workforce (e.g. behaviour, experience) | Qualitative interviews with policy-makers (WP A), health professionals, patients and carers. Non-participant observation (WP C) | Case site survey data: WFS and NoMAD questions |
| Resource use | Qualitative interviews with policy-makers and service leaders (WP A), health professionals, patients and carers. Non-participant observation (WP C) | Case site survey data: NoMAD questions |
Table 8 summarises the arguments that stakeholders posed regarding the potential impact of GPED, with most domains including arguments for positive, negative or no effects. Further details of how the domains of influence were identified and descriptions of the anticipated effect of GPED on each domain have been published separately. 94
| Domain of influence | Positive effect | Negative effect | No change |
|---|---|---|---|
| Performance against the 4-hour target/waiting times | |||
| Preventing primary care patients from waiting in lengthy ED queues |
GPED patients could prevent those with higher acuity being seen in a timely manner Diverting people with minor conditions will increase the acuity of ED work – more complex patients will occupy more time and increase the number of patients who wait > 4 hours |
The number of primary care ‘4-hour breaches’ that would need to be prevented is too large to see improvements in performance indicators | |
| Use of investigations | |||
| Reduced testing of lower-acuity patients when seen by a GP | Patients attend the ED because they want investigations and/or referral | GPs acculturate and order investigations in the same way as ED staff | |
| Hospital admissions | |||
| Streaming lower-acuity patients to a GP reduces admission rates in low-acuity patients | If the ED is left with high-acuity patients only, there is a likelihood of observing an increase in admission rates |
Admission rates would not be affected as the population being targeted are not those that would be admitted from the ED GPs acculturate and make unnecessary admissions Annual growth in ED workload and admission rates may mask the impact of GPED |
|
| Patient outcome and experience | |||
| Patient flow | Concerns that patient flow could be negatively affected and a backlog created by requiring patients to disclose clinical information on multiple occasions before seeing a GP |
Problems with specialties cause delays to GPED – the willingness of individual doctors to accept patients directly to specialties is variable Flow also depends on the number of beds available |
|
| Patient experience |
Improvements to patient experience are expected because of the improved flow and efficiency Experience improved by treating GP acuity patients immediately in GPED, rather than sending them elsewhere |
GPED patients could prevent those with higher acuity from being seen in a timely manner Models that required GPs to acculturate were thought to ask GPs to work beyond their clinical competency; they may not recognise higher-acuity patients, who would then be managed in the same way as in primary care, with the risk of poorer outcomes |
GP acculturate and order investigations in the same way as ED staff |
| Service access | |||
| Patient demand on EDs |
Long waiting times at GPED Patients indifferent about seeing a GP or ED clinician Patients accept waiting time for guaranteed consultation |
Difficulty accessing primary care GPED may worsen primary care staffing issues; primary care is less able to respond to surges in demand, leading to increased ED attendances Potential access to investigations/referrals increases ED attendance Guaranteed access to a clinician during that visit Replacement primary care service |
Lack of advertising and low patient awareness of GPED and how it operates Infrequency of visits ED generally perceived as a high-acuity service |
| Complexity of service navigation | GPED could simplify service navigation by offering a single point of access, potentially streamlining patient decision-making and providing an opportunity to educate patients |
GPED could add to an already complex health-care system and make navigating between existing services (e.g. UCCs, the ED, primary care and GP hubs) more difficult Patients will not be happy to see a GP |
|
| Workforce (e.g. recruitment, retention) | |||
| Likelihood of filling GPED GP vacancies |
GPED is attractive for portfolio, working to expand GP knowledge and skills Flexible hours associated with GPED: this flexibility makes it easier to fill rotas Ensure that GPs feel valued, supported and appropriately remunerated Use locums to mitigate GP staffing issues |
GPs are in limited supply; this may draw staff away from primary care and worsen the workforce crisis Working ‘beyond the walls of the surgery’ would not have universal appeal Shift working goes against one of the main reasons why people choose to become a GP GPs feel underqualified for the role GPED encourages GPs to become ED doctors and may cause deskilling |
|
| Likelihood of filling GPED nursing vacancies | Experienced nursing staff may prefer to work in GPED sites because of ‘better’ working hours and the perception that this is an easier job | Streaming is perceived to be a waste of clinical skills, taking nurses away from their central role and leaving the ED short staffed | |
| Workforce (e.g. behaviour, experience) | |||
| Likelihood of improved ED staff experience |
GPED has training and educational benefits for junior doctors (confidence in discharging patients and enhancing their primary care knowledge) Diverting patients with minor conditions to GPED has benefits for ED juniors and trainees by exposing them to more acutely ill patients |
Inconsistency in workforce supply could prevent GPED from integrating with the ED because of the frequent changes in staff (e.g. locums) Minor illnesses would be streamed to GPED, which could result in the deskilling of the ED workforce |
|
| ED workload | ED staff can focus on higher-acuity patients, alleviating pressure on ED staff from treating minor conditions | ||
| Resource use | |||
| Costs |
Reduction in hospital admission rates and patient investigations Streaming patients to the appropriate clinician may result in cost savings through the more effective use of staff resources |
GPs are a costly resource and GPED may not be an efficient use of their time Reliance on locums and agency staff |
|
| Infrastructure | Training and IT set-up and management | ||
In the following sections, we consider each of the eight domains of influence in turn.
Domain of influence 1: performance against the 4-hour target
There was considerable uncertainty regarding the expected impact of GPED on the ‘4-hour target’, that is that 95% of ED patients should be admitted, discharged or transferred within 4 hours of arrival. Although this was quoted as one of the potential benefits of GPED, not all stakeholders were convinced of the likely impact, given the site-specific patient mix, the selected GPED model and significant uncertainty as to whether or not GPED-streamed patients should be included in ED performance measures such as the 4-hour standard.
If GPED patients are counted in the ED group, then the premise on which GPED is based predicts that GPs in the ED will process these patients more efficiently and quickly (e.g. less testing, fewer unnecessary admissions) than ED staff. However, it was noted that annual growth in ED workload may mask the visibility of any improvements. If GPED patients were not included in the ED count, then this would reduce the number of ED patients, with the potential to reduce the number of patients exceeding the 4-hour standard. However, by diverting people with minor conditions, the acuity of those patients remaining in the ED is likely to increase. These more complex patients may require longer management, which could negatively affect performance against the target.
In our pooled analysis of HES data66 (WP B), we found no impact of GPED on the overall 4-hour performance (Table 9).
| 4-hour performance | All EDs | GPED model | Number of patients | ||
|---|---|---|---|---|---|
| Integrated | Parallel | On site | |||
| Waited less than 4 hours | |||||
| Coefficient | –0.002 | –0.011 | 0.006 | 0.018 | 4,278,180 |
| p-value | 0.803 | 0.267 | 0.587 | 0.097 | |
Figure 4 shows a forest plot derived from our RDD analysis of 4-hour performance in 35 EDs, reflecting ED throughput and some aspects of patient experience. It illustrates 4-hour performance in these 35 EDs around the times that GPED services start and finish, excluding a 1-hour period before and after the start and finish time (‘doughnut hole’), as described in Regression discontinuity design. Effects to the right of the line indicate better performance (shorter waits), whereas those to the left of the line indicate worse performance. In all forms of GPED, the start of the service each day is not associated with any significant change in the percentage of patients who stay in the ED for > 4 hours. Following the end of the service each day, there appears to be a slight reduction in the proportion of patients remaining in the ED for > 4 hours, but considerable heterogeneity remains. It is also important to note that, although the results of the RDD analysis (see Figure 4) are helpful in demonstrating the degree of heterogeneity that exists, the RDD summary measures are considered less reliable than the pooled analysis (Table 10) for the reasons described in Chapter 2.
FIGURE 4.
Forest plot illustrating the effect of GPED on 4-hour performance. Percentage discharged within 4 hours of arrival, with 1-hour doughnut hole at (a) GPED start; and (b) GPED end. REML, restricted maximum likelihood.


| Analysis | All EDs | GPED model | Number of patients | ||
|---|---|---|---|---|---|
| Integrated | Parallel | On site | |||
| Admitted | |||||
| Coefficient | –0.004 | –0.009 | 0.007 | 0.004 | 4,244,663 |
| p-value | 0.352 | 0.195 | 0.463 | 0.677 | |
| Non-same-day discharge attendance | |||||
| Coefficient | –0.002 | –0.003 | –0.002 | 0.005 | 4,241,954 |
| p-value | 0.422 | 0.599 | 0.839 | 0.568 | |
It is perhaps unsurprising that no clinically significant change was observed in performance against the 4-hour target in our pooled analysis. Differing approaches to counting patients across sites and the factors influencing time spent in the ED are likely to be working against each other, drawing any potential differences towards the null. In addition, the flow of patients through the ED is heavily influenced by factors other than GPED, such as the availability of inpatient beds, and diagnostics and timely reviews by specialist inpatient teams:
The complicated factors because we refer a lot of patients to specialty, some of the breaches are actually not due to us, but due to waiting long times to see specialties.
GP (Teak) 040, time 3
In the Linden case study site, a reduction in the 4-hour wait had been noted; however, this was due to additional steps being taken to ensure that complex patients who were not eligible for GPED were taken out of the ED system within the 4-hour target period:
That’s one of the reasons why we’re successful, and we’re talking about KPIs [key performance indicators], we are successful at the 4-hour target. Because we look at it from a quality perspective rather than a process perspective, rather than just the target. We’ve got to get them out, we’ve got to get them out. It’s about, it’s about the entire process. It’s about streaming, it’s about seeing patients within the first hour. It’s about diagnostics in the second hour, it’s about decisions in the third hour, by the fourth, between the third and the fourth hour the bed must be allocated. There must be a direction for where they’re going.
ED system lead (Linden) 031, time 1
The 4-hour target was also considered a blunt tool for evaluating impact; clinical indicators such as time to CT or time to receiving antibiotics were suggested as more relevant measures of good clinical practice.
Domain of influence 2: use of investigations
There was a lack of consensus as to whether or not GPED models should give GPs access to investigations and diagnostic tests, such as radiographs and blood tests. These differences in opinion were a source of tension and disharmony between staff working in EDs and GPED, and had implications for what people considered to be the purpose and impact of GPED. To this end, decisions regarding GPs’ access to investigations and diagnostic tests were often made during the design of GPED models at a given site, and were related to the service configuration and system of governance in place.
A number of site staff perceived giving GPs access to investigations as crucial to the model’s clinical effectiveness and worried that the potential scope of GPED would be limited if GPs were not able to undertake investigations and refer to specialties. Participants also felt that not giving GPs access to investigations reduced the clinical effectiveness of GPED by limiting the range of presentations that GPs could treat:
So, some people with abdomen pain and things, we sometimes do a little bit of the investigations as well . . . Try to take the pressure off the guys in majors really . . . So we don't do all the investigations, we don't do all the bloods, we don't wait for the results.
Locum GP (Birch) 016, time 1
In contrast, others believed that GPs should work in the same way as they believed that GPs to work in a community setting. These beliefs were based on perceptions that giving GPs access to investigations and diagnostic tests requires GPs to work outside their clinical competency and encourages a ‘hospitalisation of GPs’, which causes them to become middle-grade ED or ambulatory care doctors and lose their unique GP skills. However, there was a sense that, even if investigations were available, these were not used by GPs to the same extent as, perhaps, they would be in the ED and that the risk of acculturation was minimal:
But my thought would be while ever I’m organising a blood test and keeping a patient here that doesn’t need to be here because they’ve not got an urgent or emergency care need, they have got something that could go back to their own GP, I’m causing delays for other patients. I’m also reinforcing the behaviour of ‘if you go there they will do it today, you’ll not have to wait’. I’m also creating an unseen risk because, OK, I might do somebody’s blood test for their full blood count today and it might be just below the normal range and I’d say that’s probably alright. But without the context of having been to your own GP and got a trend of results that actually this has fallen over the last four blood tests and I’m worried about other stuff now. You’ve took that . . . that patient has got no awareness at risk and actually the clinician might be blind to that risk as well.
GP lead (Redwood) 013, time 3
Similarly, some ED staff felt that GPs did not possess the skills required to interpret investigations, particularly radiographs and scans. These concerns were heightened by fears that GPs may not be supported to use diagnostics and so would feel pressured to undertake ED work and/or be unable to recognise higher-acuity patients, with a consequent risk to patient safety and outcomes:
Actually looking at X-rays and ECGs [electrocardiograms] is, it becomes a bit of a, a dying art in general practice, if you’re not looking at those sorts of things on a daily basis, and what we provide again is allowing GP’s the ability to keep those sort of clinical skills up and running, when I think that, and I think that’s the attractiveness about doing this.
UCC clinical lead (Teak) 017, time 1
It was acknowledged that giving GPs access to investigations and diagnostic tests may provide a more convenient and efficient process for patients. However, patients may choose to inappropriately attend GPED as opposed to traditional general practice to gain access to further investigations and tests, thereby increasing the department’s workload and ED service pressures:
I suppose a bit more than a, than a clinic, because we are able to do these things [investigations]. That’s probably another reason why people do come here as opposed to, um, go elsewhere.
Band 5 ED nurse (Teak) 013, time 1
The potential for patient confusion when accessing a GP in the ED was noted, relating to the extent of the service that patients expect and the crossover of the general practice and ED. GPs were often faced with patients who did not understand why they could not access investigations that were available on site. It was considered that there needed to be clarity and consistency about the services on offer, which should then be communicated with patients. However, sometimes GPs themselves were unclear about which investigations were available to them and whether or not it was appropriate to use these investigations:
People turn up at a hospital and if you say ‘right, I’m a GP, but I can’t get an MRI [magnetic resonance imaging] scan for you’ [they say] ‘but you’re in a hospital, why can’t you?’, you know . . . in their heads, they can’t understand that. So people don’t turn up in the GP surgery requesting an MRI scan. Why? Because they know there are no MRI scans there, there’s no X-rays there, you know, so you can say to them ‘look, we don’t do that here’ and they can really accept it, and you come here, there’s a different thing. You have to work out what it is you want to do with your service, and then figure a way to keep it right; if you don’t want people coming in unnecessarily, then you, it mustn’t pay, it mustn’t benefit them to do that . . . I work here as a GP pretty much the way I work in surgery.
GP (Chestnut) 003, time 1
Domain of influence 3: hospital admissions
Staff at Linden highlighted that diverting people with minor conditions, which are, theoretically, quick to resolve, to GPs had screened minor issues out of the ED and resulted in ED admission rates that were now above the national average:
Obviously, with us streaming a proportion of our minor patients away it does make our admission percentage look a lot higher than the national average, um, because, obviously, we haven’t got those patients in our denominator, um, so that has been, that has been a, a query that we’ve had to answer on a, a number of occasions, though I think everyone’s got the message now.
ED system lead (Linden) 032, time 1
This respondent identified that the apparent change in admission rate is due only to reclassification and a consequent change in the denominator used in reporting statistics, rather than being a genuine effect.
When looking at our case sites more broadly, the impact of GPED on admissions was considered variable and, to some extent, associated with the different approaches to risk demonstrated by GPs and ED staff, and also individual views on whether or not GPs should have access to investigations and diagnostic tests when working in the GPED model. GPs were perceived to frame health and illness in a different way from ED staff, with the ‘wait and see’ culture of primary care leading many to view GPs as more ‘risk tolerant’ and more appropriately qualified to care for lower-acuity patients than their ‘risk-averse’ ED colleagues. This, in turn, was thought to be beneficial for GPED because GPs were viewed as less likely to admit or refer lower-acuity patients, order investigations and admit a patient unnecessarily. GPs were, therefore, perceived to be better placed to deal with lower-acuity patients or those with long-term conditions who need skilled holistic management rather than specialist investigations. Although some ED staff exhibited caution about what presentations to refer to GPED, ED staff were criticised for overinvestigating through fear of missing something important. GPs’ risk behaviour was generally viewed as beneficial; however, several GPs and ED staff expressed frustration that they were unable to order investigations and treat a wider range of patient presentations:
But what we are good at doing as GPs is identifying risk thresholds of, ‘this is something I can sort out and I’m happy to take that risk’. This is something why it’s beyond the risk that I’m willing to accept as something that I’m going to manage. What the A&E consultants struggle to grasp or chose not to, I’m not sure which it is, is that if I’m out there in a GP surgery and I see a patient is very poorly whether it’s because I don’t know what to do next or because I’ve decided you’re really unwell and need to go to A&E is never questioned. I can pick up a phone and I can dial 999 and somebody comes along in an ambulance and deposits them in the A&E department, at which point somebody sorts them out. When that threshold is met by a GP or an advanced clinical practitioner working here in the department, some ED consultants will not accept that transfer without a barrier to that by wanting to know all the ins and outs of what’s wrong with the patient. Trying to suggest helpful things that you might do to manage this patient as opposed to just accepting that.
GP lead (Redwood) 013, time 3
Our pooled analysis showed no effect of any GPED model on patient admission or non-same-day discharge attendance from the ED (see Table 10):
Figure 5 shows a forest plot derived from our RDD analysis. It shows the proportion of patients admitted from 32 EDs around the times that GPED services start and finish, excluding a 1-hour period before and after the start and finish time (a ‘doughnut hole’), as described in Regression discontinuity design. It confirms substantial heterogeneity but no overall or consistent effect of GPED on hospital admissions from the ED.
FIGURE 5.
Forest plot illustrating the percentage of ED attendances admitted as inpatients. Percentage of ED attendances admitted, with a 1-hour doughnut hole at (a) GPED start and (b) GPED end. REML, restricted maximum likelihood.
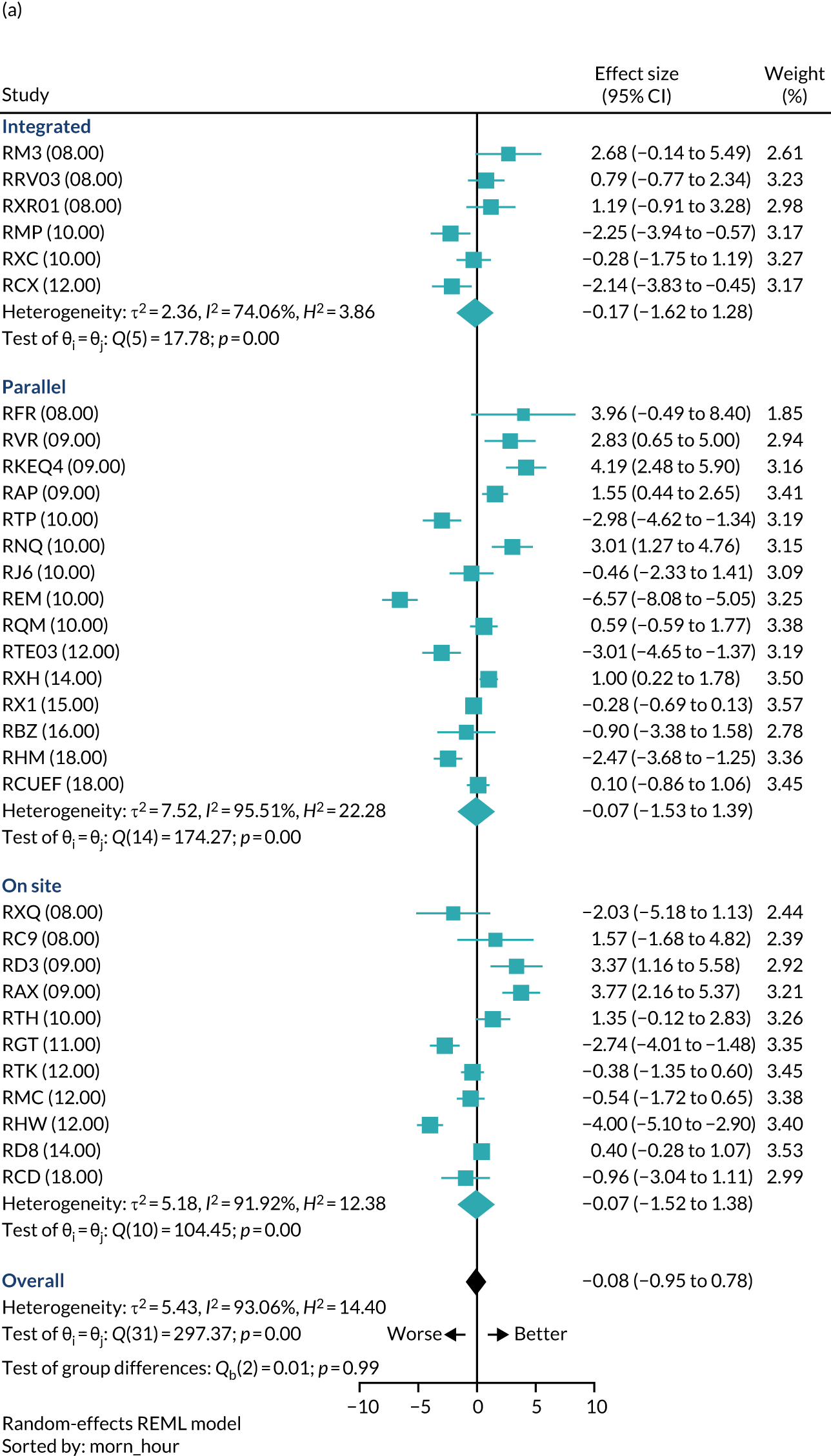
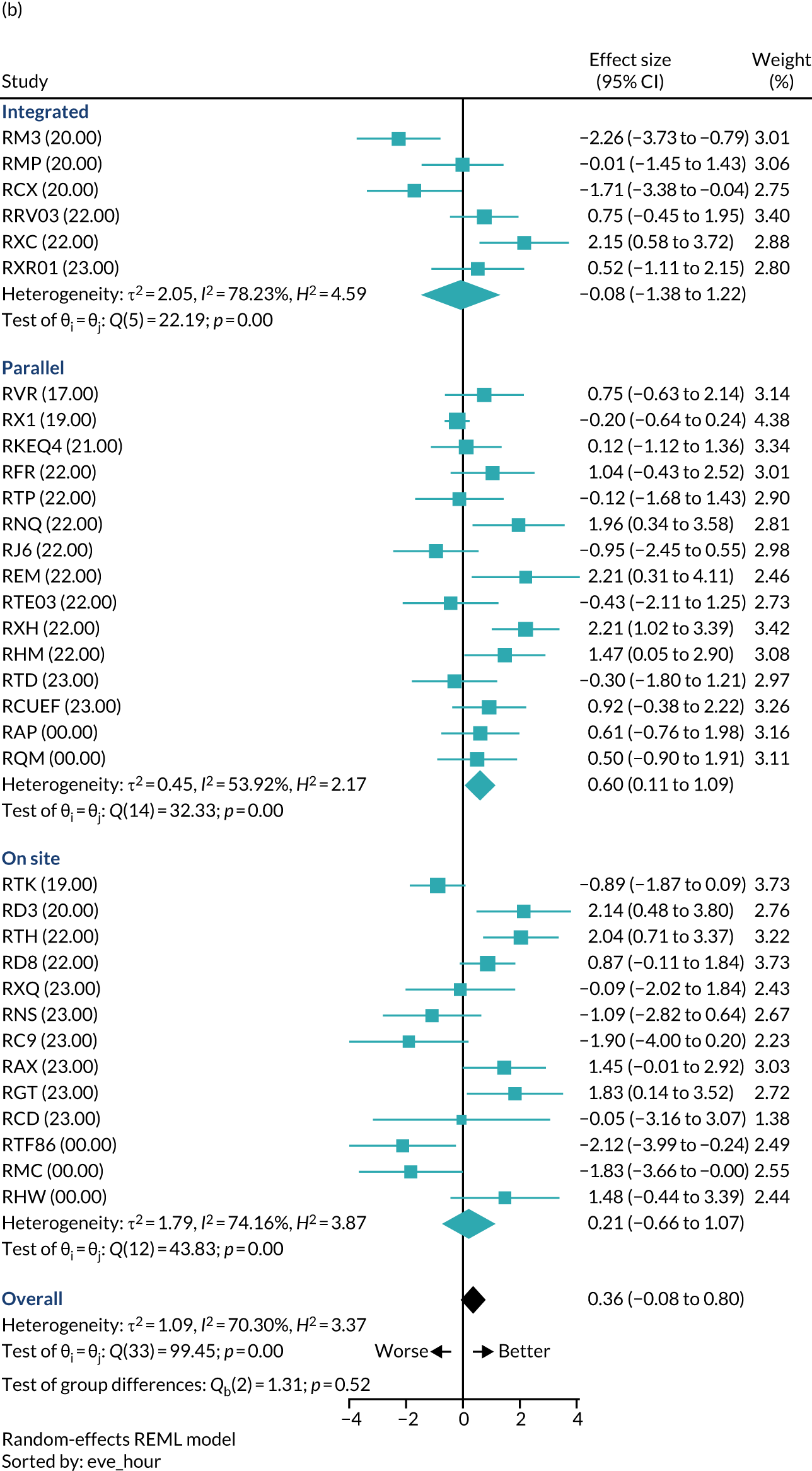
Domain of influence 4: patient outcome and experience
Overall, our patient interviews found that a positive patient experience of GPED was more likely if a patient was seen in a timely manner and if they felt that their complaint was taken seriously and was addressed in a reassuring and professional manner. Some staff expressed concern that patients would prefer to be seen by an ED doctor and reported feeling that they were in ‘the firing line’ when patients objected to seeing a GP. However, there was variation in patients’ opinion and knowledge of the expertise of GPs: some were happy to see a GP as they regarded them as having more experience than ED doctors, whereas others felt that ED doctors were the more senior and experienced staff. Some patients were aware of the role of other health-care practitioners [e.g. advanced nurse practitioners (ANPs)] and were happy to be seen by them, if appropriate. Indeed, many patients did not appear to know the type of clinician they had seen:
No. All I get told is it’s a doctor. That’s all you get told.
Patient (Rowan) 16, time 3
Patient expectations were potentially harder to meet when patients were aware of GPED within the department. Staff experienced both sides of the coin: patients unhappy about being sent to a GP because they felt that their condition was serious enough for ED and/or they wanted investigations, and patients who did not want to be sent to the ED because they believed that the waiting times for the GP would be shorter and it was less chaotic than the ED.
In general, however, patients were positive about GPED, with the majority of patients we interviewed being indifferent to the type of health professional they saw as long as they received appropriate care. Equally, most patients were happy to consult with a GP and, potentially, wait longer to be seen as they recognised that this was because their symptoms were not considered to be too serious. Patients therefore valued GPED and believed that it was beneficial to have GPs in the ED to enable less unwell patients to be seen and ‘relieve the pressure on the emergency doctors to actually be dealing with the real emergency cases’ [Patient (Poplar) 015, time 1]. It made sense to patients to have GPs in EDs as they were doctors, just with a different specialty.
Patients were also of the opinion that GPs in EDs could offer better care and a more thorough service than a patient’s own primary care GP. Patients felt that it was an easy option in terms of accessing care and guaranteed that they would be seen in a more timely manner than traditional general practice. The 4-hour target was not a high priority to patients; although they appreciated being seen more quickly, when possible, they were also happy to wait longer knowing that they would be seen at that visit. This arbitrary indicator was of far greater relevance to hospital managers than to patients:
Yeah, I think that’s really important, I think given the way the hospital performs with the government’s 4-hour target, I think it’s a source of pride for the hospital, for the Chief Exec[utive].
ED consultant (Linden) 029, time 1
Although patients were largely receptive to GPED, there were concerns from staff that patient flow could be negatively affected and a backlog created by requiring patients to disclose clinical information on multiple occasions before seeing a GP. Some staff reported that patients presented inconsistent medical information during their ED/GPED journey. Patients who attended for a second opinion after seeing their primary care GP or those who were referred to the ED by their primary care GP were less satisfied with GPED:
Because I was sent, I went to the GP, then it’s referred to the hospital, so in the circumstances today, I think I would prefer to see a specialist then, rather than a GP.
Patient (Poplar) 23
Some patient safety issues were also identified. The NHS requires urgent (‘2-week wait’) referrals for potential cancers to be provided by the patient’s own GP. 95 Therefore, patients may not be appropriately referred to secondary services or delays may occur if the GPED service advises them to go back to their own GP. Across sites, GPED had no review or follow-up system, so there was no way of checking whether or not patients had attended their own GP. Referring back to the patient’s own GP for onward referral was also considered highly inefficient by staff, given the unnecessary doubling of health-care attendances. Although it went against policy, some GPED staff did provide urgent referrals to prevent patients from slipping through gaps in the system. Likewise, GPED GPs gave ‘safety-net’ advice to patients, explaining what they should do if their condition deteriorated but, again, systems were not in place to follow up patients. This was mitigated somewhat by the production of electronic discharge letters to inform the patient’s own GP of GPED attendances and any follow-up/safety net advice given.
Although staff were concerned that knowledge of GPED was leading to an increase in patients attending the ED to see a GP specifically, most patients stated that they would still use their primary care GP as their first port of call and use the ED in an emergency only. However, they did voice concerns that other patients might use the ED more often to see a GP if they knew that the service was available.
Our pooled analysis identified no effect of GPED on the proportion of patients who leave the ED without being seen or who die within 30 days of attendance (Table 11). There was, however, a very small but statistically significant reduction in the rate of unplanned reattendances at the same ED within 7 days (–0.3%; p = 0.015) for patients attending during GPED service hours, but the clinical significance of this was judged to be negligible. This finding appears to be driven by integrated GPED services (–0.6%; p = 0.028), with estimated nil effects for the parallel and on-site GPED services (see Table 11). Note that these results may still reflect chance findings owing to the large number of tests conducted. Using a more conservative critical value of α = 0.0016 (based on the Bonferroni adjustment procedure and allowing for 32 tests), the results of the outcome of unplanned reattendance would not be considered statistically significant.
| Analysis | All EDs | GPED model | Number of patients | ||
|---|---|---|---|---|---|
| Integrated | Parallel | On site | |||
| Left without being seen | |||||
| Coefficient | –0.001 | –0.006 | 0.005 | 0.008 | 3,689,903 |
| p-value | 0.793 | 0.251 | 0.338 | 0.153 | |
| Unplanned reattendance within 7 days | |||||
| Coefficient | –0.003 | –0.006 | 0.003 | 0.005 | 4,140,340 |
| p-value | 0.015 | 0.028 | 0.252 | 0.060 | |
| 30-day mortality | |||||
| Coefficient | 0.0003 | 0.001 | –0.001 | –0.001 | 4,302,347 |
| p-value | 0.255 | 0.215 | 0.469 | 0.362 | |
This is further illustrated by the forest plots arising from our RDD analysis, which are shown in Figures 6–8.
FIGURE 6.
Forest plot illustrating the percentage of patients attending the ED who leave without being seen, with a 1-hour doughnut hole at (a) GPED start and (b) GPED end. REML, restricted maximum likelihood.

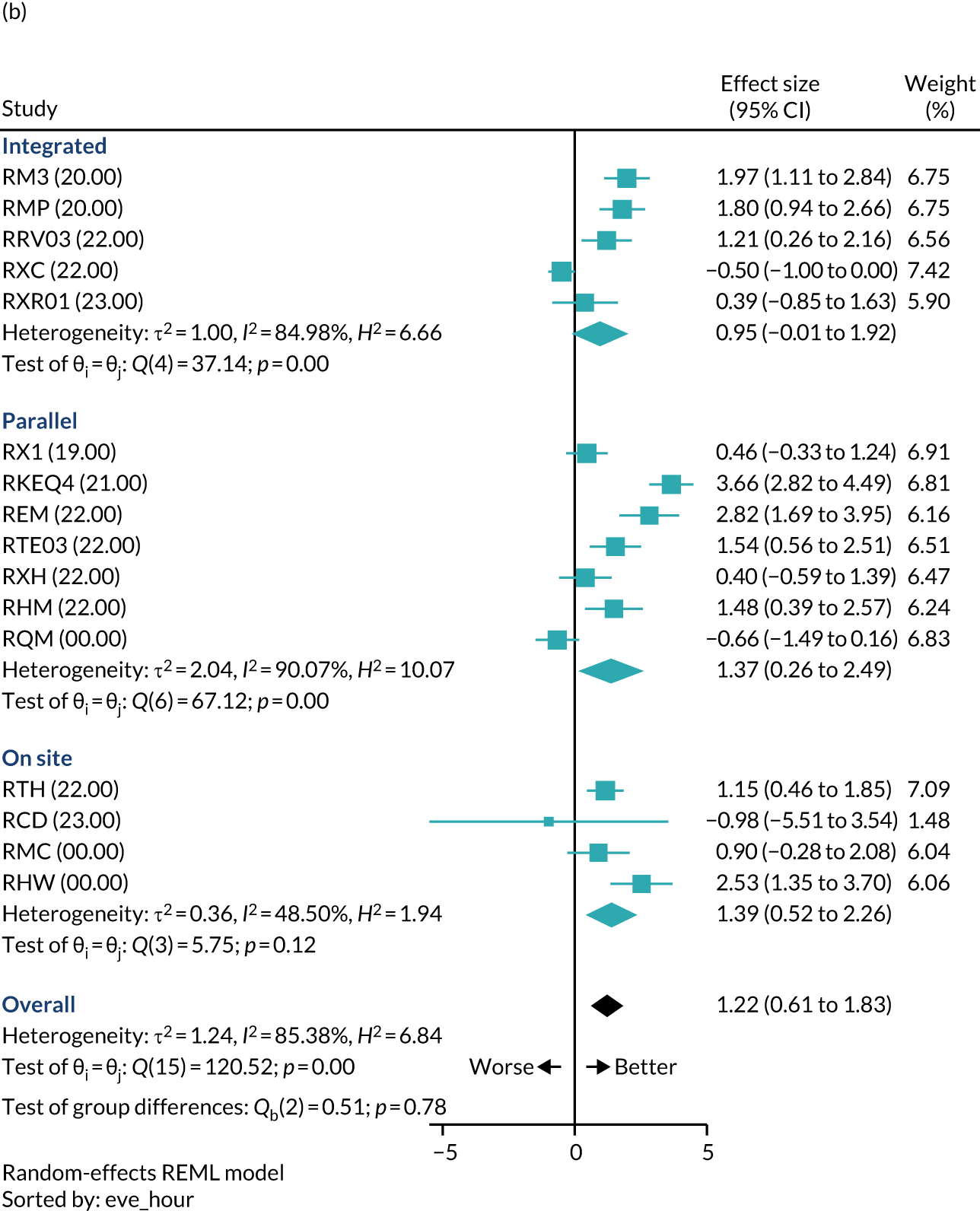
FIGURE 7.
Forest plot illustrating the percentage of patients attending ED who have an unplanned reattendance to the same ED within 7 days, with a 1-hour doughnut hole at (a) GPED start and (b) GPED end. REML, restricted maximum likelihood.
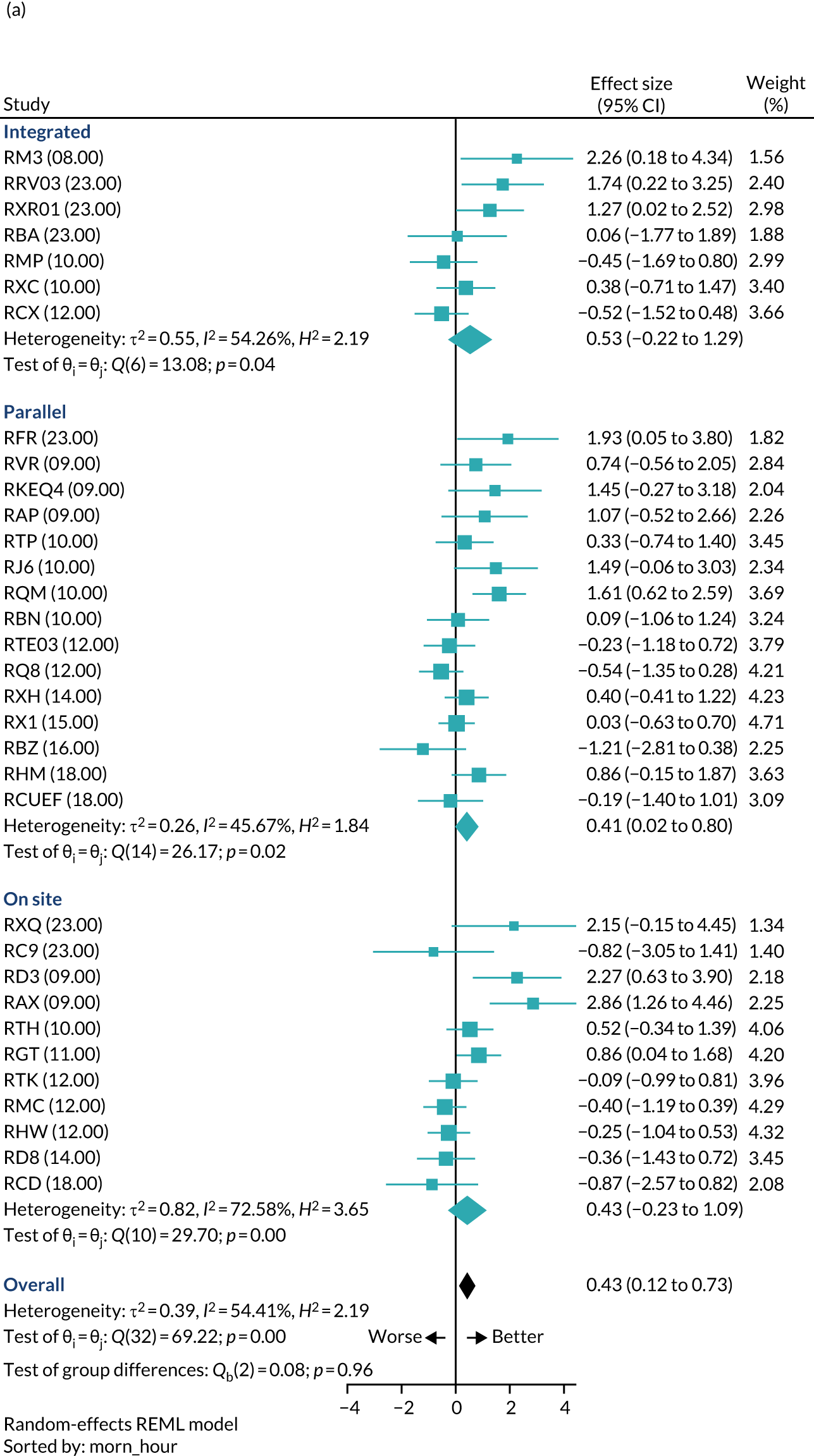
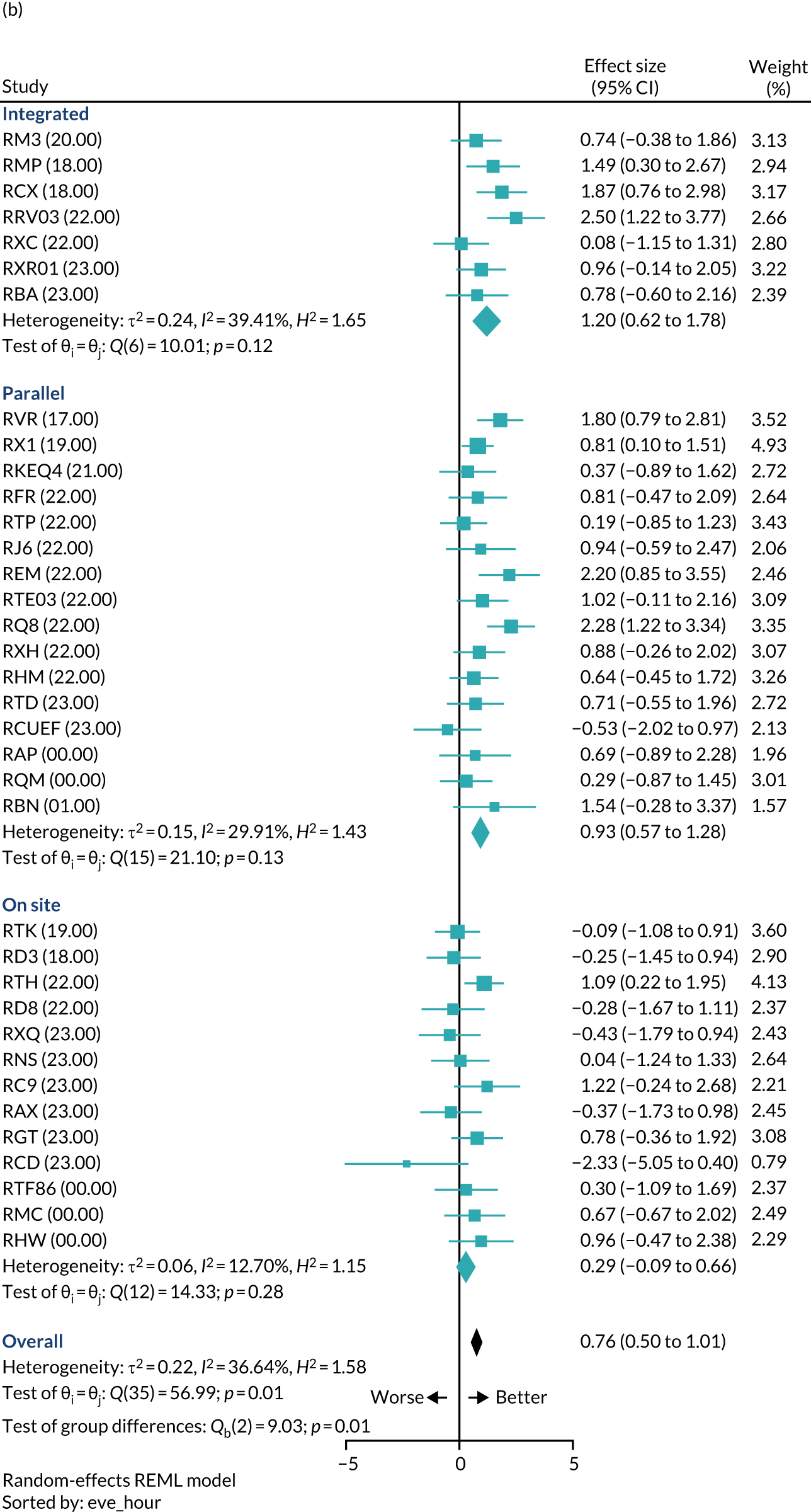
FIGURE 8.
Forest plot illustrating the percentage of patients who die within 30 days of an ED attendance, with a 1-hour doughnut hole at (a) GPED start and (b) GPED end. REML, restricted maximum likelihood.
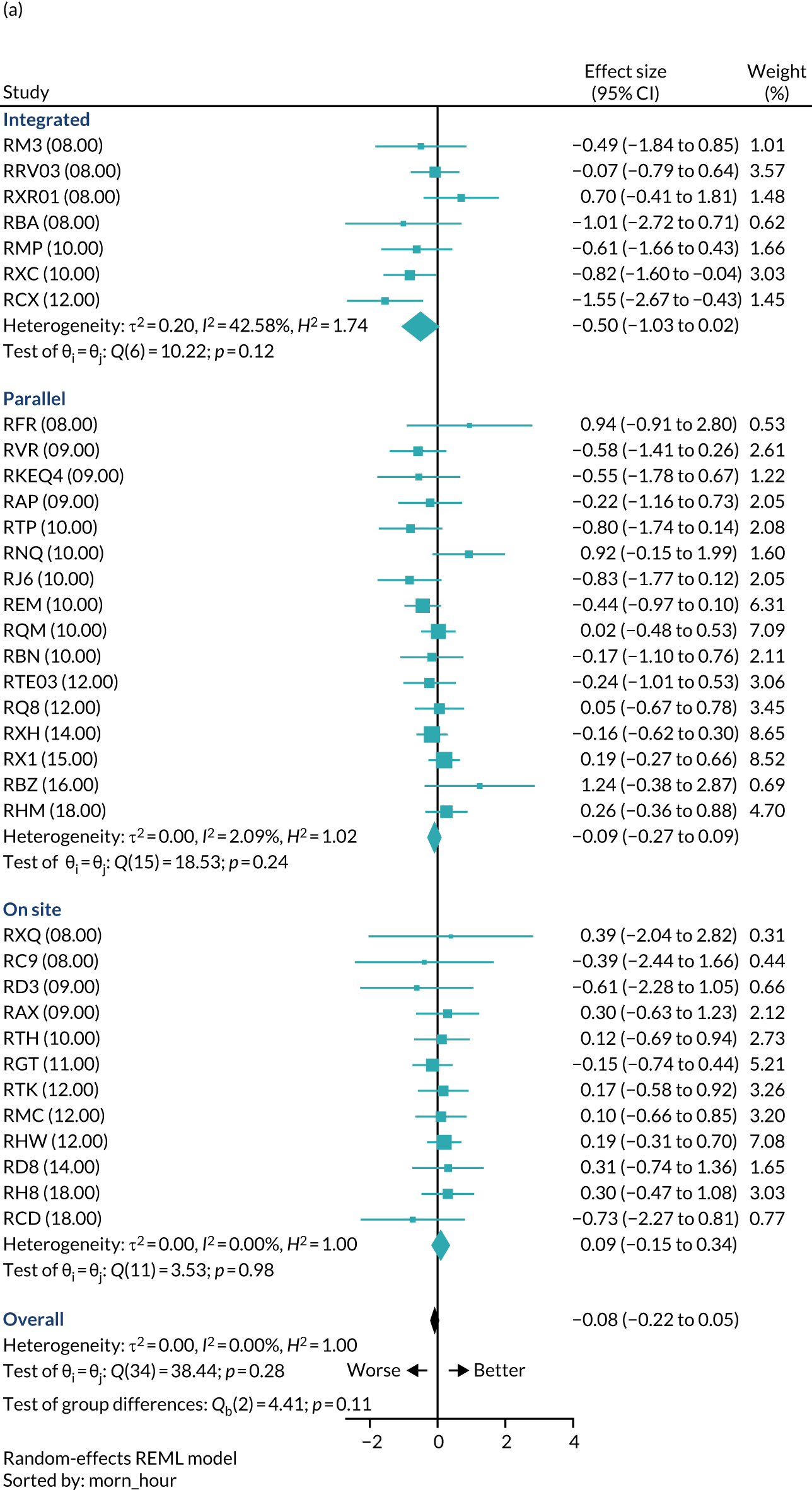

Figure 6 shows considerable heterogeneity at GPED start, with no consistent overall effect. At GPED end, there is a more consistent trend towards an improvement (i.e. decrease) in the proportion of patients who leave the ED without being seen; however, the effect is very small, and not confirmed in the more reliable pooled analysis (see Table 11).
Figure 7 confirms a statistically significant reduction in the rate of unplanned ED reattendance to the same ED within 7 days, which is associated with GPED. However, the clinical significance of this difference (< 1% change in 7-day unplanned reattendance rate) is negligible. This is considered further in Chapter 4.
In keeping with Table 11, Figure 8 shows no statistically significant effect of GPED on patient mortality at 30 days. The pooled estimates for both GPED start and finish are extremely close to zero, with very narrow confidence intervals. This is reassuring from a patient safety viewpoint, but is also expected, as there is no reason to anticipate that GPED would affect patient mortality.
Domain of influence 5: service access
Increasing use of emergency departments
There was variability with regard to patients’ knowledge of the health-care and ED systems. Reflecting the different stages of GPED implementation, patients from only a small number of case study sites reported having previously used the ED and expected to be streamed to GPED. Indeed, even those with prior knowledge of the system expressed uncertainty as to how the service worked or who it was aimed at. Some patients knew that they could see a GP in the ED, but the majority of those interviewed did not, which is perhaps surprising given that most sites had been implementing a form of GPED model for some time:
I think, from what I’ve found working in A&E for the last 4 years, there are still quite a lot of patients in the area that don’t know the service exists. When I’m assessing patients in triage and saying, ‘I’m going to send you to the out of hours’ they say ‘I didn’t realise you had that service.’ I explain ‘if you call 111, they can, if needs be, send you to us or if they feel it’s appropriate they can book a GP out-of-hours appointment’. A lot of patients don’t realise the service . . . They just come straight here. They don’t realise there’s an out-of-hours service, which is quite surprising, really, because it’s been here quite a few years.
ED nurse (Hawthorn) 010, time 3
Staff were worried that easy access to a GP through the ED would encourage further attendance and that the greater the supply, the more the demand would increase (i.e. supply-induced demand). There was also a perception that, if GPs refer to the ED patients who are subsequently seen in GPED, patients will then start to attend GPED directly, rather than their own primary care GP. Staff were anxious that GPED would become a ‘victim of its own success’, with patients attending frequently; hence, they did not want patients to be aware of the GPED service:
Do you know [what] I mean? But ED’s frightened to send anything away, so everything comes in. So I don’t blame the public for attending if they can see a GP within 3 hours, rather than having to wait 6–7 days or 2 weeks for an appointment. But I just wonder if it’s made a demand for it, because you get people coming back to see the GP again in ED.
ED nurse (Rowan) 037, time 2
At most sites the service was not advertised to avoid encouraging attendance for GP-type presentations:
We’re not shouting it from the rooftops because the minute you start shouting from the rooftops that you’re going to have a GP service within the ED then people are gonna be already camping outside waiting with their, you know, verrucas and things.
ED senior nurse (Juniper) 003, time 1
Staff perceived there to be an increase in the number of patient attendances at the ED both generally and between our research team’s site visits. Interviews with patients and carers suggested a number of reasons as to why individuals present at the ED, such as not being able to get a GP appointment or not being registered with a GP, wanting further investigations they knew would not be available at a primary care general practice or simply finding the ED more convenient than a primary care GP appointment. These reasons are summarised in Table 12.
| Reason for ED attendance | Summary | Quotation |
|---|---|---|
| Difficulty accessing GPs in the community | Most patients stated that they attended the ED because they could not get a timely GP appointment with their primary care GP. There was variability as to whether or not patients had tried, on this occasion, to get a primary care GP appointment. Some patients were not registered with a primary care GP because they were a temporary resident in the area or did not need medical care previously | Just because I’ve been to my GP before and they’re not very helpful and it’s a long waiting list and it’s now, I’m not sleeping at night. I can’t function at work properly and the past couple of days it has been unbearable and so I needed something like a quick relief rather than waiting for another appointment at the GPP (Nutmeg) 013, time 3Um, my daughter phoned the doctors ’cos she was feeling unwell. It’s been going on for a little while. But the doctor said ‘there are no appointments available’. So he suggested we either ring 111 or come up to you here at the [general practice] clinic and be seen here, so that’s what we decided to doC (Linden) 009, time 1 |
| Advised or sent to the ED by other urgent care service | Patients were advised to attend the ED by NHS 111, GPs and other health-care specialists. GPs advised ED attendance if they felt that the problem was outside their remit or if they had no available appointments. NHS 111 referrals were a cause of frustration for staff, who often felt that patients were referred unnecessarily | I have got a really bad toothache with an abscess on my tooth, which is coming up next week. The pain got a lot worse so much it spread up to the right-hand side. And I tried to persuade the dentist to drain the abscess to, sort of, relieve the pain. And the dentist told me that they don’t do that surgery. And they referred me, they said I should go down to A&EP (Juniper) 056, time 3I went to the GP about 10 past 10 because I’d fell over in the garden about 4 weeks ago. She had a look and she thought, well, it’s best if I come to the Birch for an X-rayP (Birch) 002, time 1 |
| Attending the ED as it is convenient |
GPED was easier than booking a primary care GP appointment and was seen as more beneficial than walk-in centres that were nurse led Although most patients did not know it was possible to see a GP in the ED, those that attended the ED frequently often knew this was possible; it was these patients who were more likely to attend the ED as they knew they would be seen and, for some patients, because they knew it was a convenient way to be seen by a GP specifically |
Because my GP is overcrowded. Never get appointments and I know if I come here, if I need anything, I’ll be able to go to hospital straightaway instead of going there and back all the time. I can just get seen hereP (Chestnut) 014, time 3OK, just because of history and the familiarity of it, I know that I can get my issue resolved here. They’ve got my records so it’s a lot easier for them just to see what’s going on and be able to direct me from thereP (Teak) 007, time 1 |
| Patient expectations | Some patients bypassed their GP or ringing NHS 111 because they expected a certain level of care/investigations that they believed that only the ED could provide. This was often because they believed that further tests or radiographs would be required | I mean, I don’t think, I hardly come in to A&E and the only reason I’ve come here is because I know that if I went to the GP they would have told me to come here, so it’s saved me the trip, so I just came straight here . . . To be honest, with me, I look tired but kind of made that deduction myself that I should actually come here rather than go to the GP and save myself timeP (Nutmeg) 011, time 3Yes. I think I need an X-ray, is why I came. Just to rule out not having fractured or broken my wristP (Hawthorn) 03, time 1 |
| Poor relationship with GP and obtaining a second opinion | A number of patients attended the ED because they did not feel valued by their primary care GP (e.g. they felt rushed and not listened to). Others did not agree with what the primary care GP had said or their symptoms had worsened since their primary care consultation | So, when I saw my GP yesterday I was, I came away feeling reasonably reassured, we had quite a long conversation, but [sighs] come lunchtime afternoon the pain got worse and worse and worse and by the time I got home it was, you know, it was making me weep, and then I suddenly thought actually he hasn’t, at no point has he actually examined me, you know, and because we’re going away at the end of the next week, I thought I can’t wait to go through the whole process of going back to see him again and, you know, asking for a more thorough consultation or even for a referral or something and that’s why I, and I was just so distressed last night I thought the only way I can do this is, to get something immediate is to come up hereP (Juniper) 054, time 3 |
Our quantitative analysis did not identify an association between the absolute and relative volume of attendances and GPED (Table 13).
| Volume of attendances | All EDs | GPED model | Number of patients | ||
|---|---|---|---|---|---|
| Integrated | Parallel | On site | |||
| Absolute volume | |||||
| Coefficient | 0.001 | –0.015 | 0.034 | –0.0002 | 336,882 |
| p-value | 0.970 | 0.673 | 0.414 | 0.996 | |
| Relative volume | |||||
| Coefficient | 0.001 | –0.018 | 0.039 | –0.001 | 336,882 |
| p-value | 0.931 | 0.635 | 0.380 | 0.972 | |
Health service literacy
Staff believed that patients lacked health service literacy and required more education about the purpose of ED services. However, they acknowledged that the constantly changing organisation of the systems and services at which patients could seek care would be confusing for patients and have a negative impact on their working knowledge of the optimal use of available services. This was witnessed at some sites, with patients thinking that they were attending a walk-in centre rather than an ED. Frequently, these patients had been misinformed or directed to the ED by NHS 111, or the service provided had changed since their last attendance. As we have shown, this confusion could be compounded by sites consciously not making it clear what types of services were available, with the intention being to reduce the perceived risk of generating additional demand. Indeed, Table 13 indicates that concerns relating to an increase in demand caused by the introduction of GPED services had not come to fruition, possibly because of a combination of these factors. There was very little evidence from the qualitative data to suggest that patients were presenting to the ED with the specific intention of seeing a GP.
Opinion was divided, particularly among GPs, on whether or not staff should ‘educate’ patients about appropriate attendance. Some felt that this was not their role and were uncomfortable with this suggestion, whereas others happily told patients that they should not have gone to A&E:
. . . or their perceived importance of their condition, that they need to be seen urgently. When, in fact, it’s a routine thing, and they can wait 3 days to see their own GP or even 2 weeks to see their own GP. We are seeing cohorts of patients that shouldn’t be going to A&E in the first place. How to square all of that and educate the patients, well, we’ve tried to do that for 30 years, haven’t we? [Laughter] It’s a bit of a tricky one.
GP (Rowan) 040, time 2
Although staff did recognise that it was often difficult for patients to know the severity or acuity of their complaint and, therefore, which service to access, they remained prepared to criticise the decisions that patients made regarding ED attendance. Local demographics also influenced what was perceived as an ‘inappropriate’ attendance. There was a view that this was more of a problem when the population surrounding the hospital had a lower socioeconomic status, if it was a tourist area or if it had a high population of immigrants or students. However, it is interesting to note that even highly experienced nurses did not always find streaming patients between GPED and the ED straightforward, yet expected patients to be able to make these decisions:
I think it’s down to, obviously, your training, but also how risk averse you are, and some people are very risk averse and will just have a much lower threshold for streaming people into ED and then also the urgent care centre, rather than directing appropriately, you know, taking that risk.
Paramedic (Chestnut) 022, time 1
The decision to use the label ‘urgent care’ was thought to legitimise a patient’s attendance and create further confusion about the difference between ED ‘minors’ and urgent care. A couple of local service leaders remarked that they are not ‘a fan of just putting a GP in an A&E department’. Although GPED was considered a good idea on paper, a single access system for unscheduled care with OOH provision in the ED was considered a more effective approach that would respond to consumer culture by ensuring that all services were accessible at one site. It was felt that a clearer distinction between unscheduled health-care demand and emergency care was needed, along with services responding to patients’ behaviours and expectations rather than expecting patients to fit into the needs of service providers.
Equally, the failure of previous national initiatives to encourage patients to attend elsewhere, coupled with the fact that, historically, patients have always attended the ED for primary care, meant that some local service leaders saw the solution as placing GPs where patients attend and investing in EDs rather than in primary care. Patients commented that GPED provision gives out mixed messages: on the one hand, patients are encouraged to use their own GP, but, on the other hand, GPED makes access easier and may promote ‘inappropriate’ attendance at the ED.
For some patients, GPED was thought to alleviate some of the anxieties around navigating services as they did not feel that they were taking up valuable emergency resources and were happy to consult with a GP. Despite staff acknowledging that navigating existing services was complex, staff accused patients of ‘playing the system’ to access care more quickly by bypassing their own GP. Staff felt that patients believed that by going to the ED they would be seen more quickly and could have an instant referral rather than having to wait for their own GP to make the referral from primary care. This perception was fuelled by those patients who arrived at the ED expecting or requesting further tests or investigations:
. . . they [patients] don’t tell you the same story. So they, and patients are savvy as well, so they’ll tell you what they think they want you to hear in order to get them into the service they want to be seen by.
Band 6 ED nurse (Linden) 006, time 3
Many patients, before attending the ED, had sought advice from other health services, such as NHS 111, a pharmacy or their own primary care GP. Often these patients were still viewed as ‘inappropriate attenders’ and streamed to see a GP. ‘Inappropriate’ referral by NHS 111 to the ED was a significant cause of frustration for staff. Furthermore, NHS 111 was believed to give patients the impression that the ED was expecting them, that they would be seen within a certain time frame and that the hospital would have their medical records. This led to expectations on the patient’s part and heightened tensions when these expectations were not met. This highlights the point that NHS services themselves can have different understandings of the roles of other services.
Despite these perceptions, our pooled analysis of patients who could potentially be seen in other health-care settings (i.e. ‘unnecessary attendances’) did not show any association with GPED (Table 14). This was confirmed in a RDD analysis forest plot of the same parameter, which showed no consistent association with GPED model, or GPED overall (Figure 9). In common with the other RDD analyses, however, considerable heterogeneity was observed between sites.
| Analysis | All EDs | GPED model | Number of patients | ||
|---|---|---|---|---|---|
| Integrated | Parallel | On site | |||
| ‘Unnecessary attendance’ | |||||
| Coefficient | 0.003 | 0.0003 | 0.009 | –0.004 | 4,302,347 |
| p-value | 0.497 | 0.964 | 0.291 | 0.525 | |
FIGURE 9.
Forest plot illustrating the percentage of ED attendances identified as ‘unnecessary’, with a 1-hour doughnut hole at (a) GPED start and (b) GPED end. REML, restricted maximum likelihood.
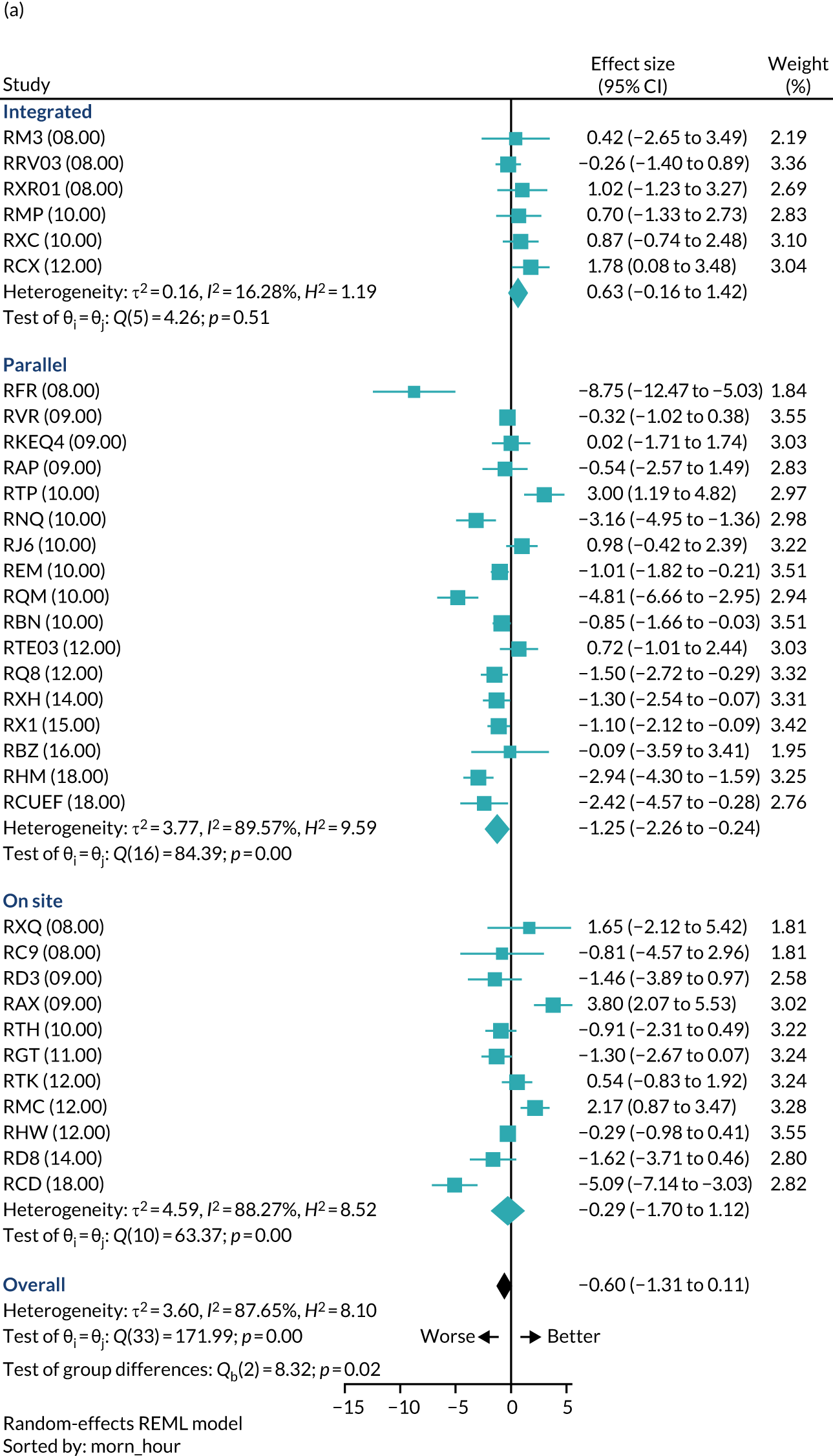
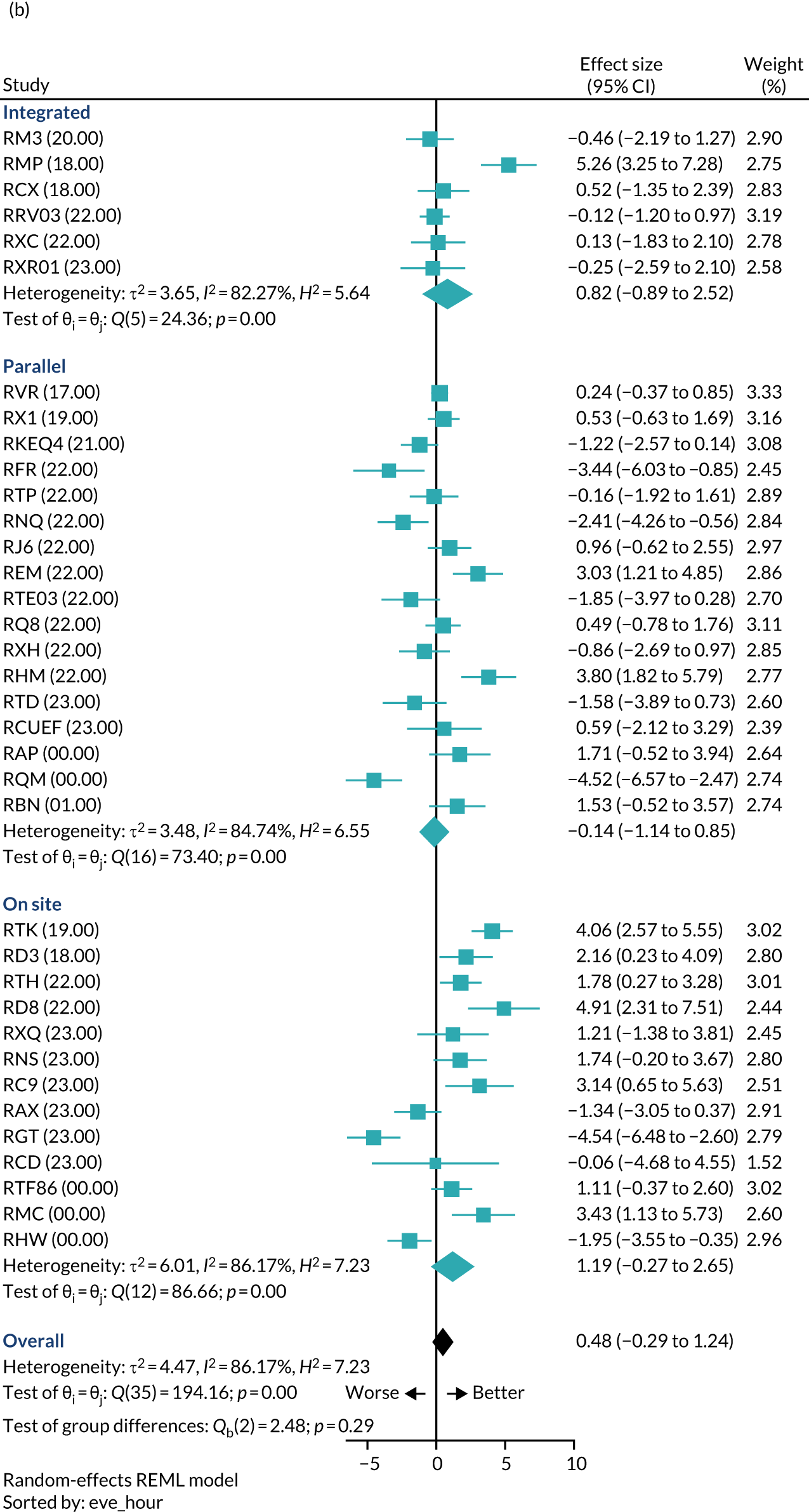
Domain of influence 6: workforce recruitment and retention
Staffing issues dominated discussions about the impact of GPED and posed a major threat to its success. Local services leaders and site staff expressed concern that GPED could draw GPs away from primary care and cause competition for GP staff. Consequently, GPED was perceived to have the potential to worsen primary care staffing issues:
Primary care is in crisis, there are not enough GPs and asking every ED in the country to hire GPs will make the existing situation worse. Somewhat strange policy for these reasons. The danger is that we are over resourcing this for the return that we get back from it and that we ship out GPs from primary care and put them into hospital, feeling that in this area not enough demand for this type of service.
Local service leader 01
It is important to note that this is occurring in the context of staff shortages more generally in both EDs and general practices; for many participants, this was identified as a key issue that had an impact on patient flow and waiting times. Several sites highlighted difficulties in the recruitment and training of doctors, and populating the middle-grade positions and the consultant rota alongside the financial restrictions on this:
I’m four doctors down due to people ringing in sick and they are in key pathway and middle-grade level, has an impact, short of doctors and also short of nurses despite repetitive recruitment drives, still have same number of nurse vacancies as when I started.
Service leader 31
GPED was considered an attractive prospect for GPs who were seeking portfolio careers and wished to expand their practice, knowledge and skills. Traditional primary care practices were seen as more stressful and less attractive workplaces than newer service models. This was because of several pressures, including the increasing volume and complexity of the workload and depleted community and social care provision. These findings were consistent with the results from GPED GPs who responded to the WFS, and the findings can be compared with those from all GPs that were reported in the Ninth National GP Worklife Survey. 75 These findings should be interpreted cautiously, and in the context of the relatively small numbers of GPED GPs who completed the WFS (n = 18). However, relevant comparisons indicated that GPED GPs were substantially less likely to report high or considerable pressure as a result of factors including ‘having insufficient time to do justice to the job’ (GPED GPs, 27.8%; all GPs, 85.3%), ‘long working hours’ (GPED GPs, 27.8%; all GPs, 82.6%) and ‘increasing workloads’ (GPED GPs, 33.3%; all GPs, 92.3%).
There was some debate as to how the flexible hours associated with GPED would have an impact on job satisfaction. For example, some participants found that this flexibility made it easier to fill rotas, whereas others felt that shift working goes against one of the main reasons that people choose to become a GP:
What appeals to me is that I can do a bit of acute general medicine, trauma, etc., and I’m trained in that, but, equally, I can also lapse into what was my comfort zone. I mean, some days if I’m feeling a bit tired then, actually, it’s much less stressful for me to go into my normal comfort zone and just go through stuff that I’m really competent with and, you know, I can sit down and I can bang through lots of info and that works really well, whereas when I’m feeling a bit more, sort of, ‘right, come on, you know, I can get into resus and I can learn a new thing’ and I really enjoy that.
GP (Juniper) 024, time 1
Some GPs used GPED as a form of semiretirement, enjoying the continued clinical role without the complexity of partnership arrangements and ongoing practice responsibilities. In this way, GPED enabled experienced GPs who would otherwise have left the workforce altogether to continue to contribute to medicine. Many actively chose locum work over salaried GPED positions, which were seen as less flexible, and some felt that moving to salaried positions would result in less experienced GPs being utilised, which might prove detrimental to the service. However, some GPs preferred salaried working and recognised the need for a consistency of provision within GPED:
What attracts many of us is that it is flexible. We really like that. Actually, not that many of us would particularly want to do it and be salaried, but that may make headaches for people in that, probably, the hospital would like people to [have a salaried post]. At the moment, many of us have done 25+ years in medicine. Yes, most of us were saying that we wouldn’t actually want to do this. If they made this salaried, we don’t know if we would do it. It’s that whole flexibility. Some of them are doing it in addition or they’re taking semiretirement and doing it and, actually, it’s having that flexibility. I don’t know, but if you went to a salaried model, you might end up with some of the people who were just coming out of medicine and into general practice, rather than actually, it might be then very different, because a lot of us have got a lot of experience and so are quite confident.
GP (Rowan) 003, time 1
There were several reasons why GPs thought that GPED was unattractive to GPs. As well as the pace of work, risks associated with the ED, and potentially sicker and more acutely unwell patients, practical issues such as travel, parking at the hospital and the pay scale were identified:
I’ve got to, I’d have to ask myself ‘why do I commute an hour when I could commute 20 minutes and do that job?’ . . . and I’m financially, you know, financially, I’m being paid on a sort of middle-grade salary, sort of fairly low, low pay rate . . . I don’t think that they would attract anyone to the role unless they did up the funding for it.
GP (Juniper) 024, time 1
These findings were potentially consistent with results from the small number of GPED GPs who completed the WFS. For example, only 38.9% (n = 7) of these GPs reported being ‘satisfied’ with the opportunity to use their abilities (with item scores ranging from 5 to 7, which was above the neutral mid-point on each scale), relative to 66.6% of all GPs who reported satisfaction with the same question in the Ninth National GP Worklife Survey. 75 Furthermore, only 55.6% (n = 10) of GPED GPs reported being satisfied with the amount of variety in their job, relative to 71.7% of all GPs in the Ninth National GP Worklife Survey. 75
Additional barriers to effective employment and GP working included IT and enforced contractual breaks arising from funding issues, which led to negative working practices:
So one of the problems, I had to take 2 weeks’ break in contract because they don’t want to employ me permanently in case the funding runs out, I guess. And it’s a 6-month contract that’s renewed every 6 months, which is a real pain because then when I come back my IT stuff doesn’t work, and my cards don’t work, my passwords don’t work, it’s just a pain in the arse. That’s what I’ve spent most of this morning doing until you rang. So I’ve seen one patient in the past 2 hours, it’s really annoying.
GP (Birch) 018, time 1
Of additional concern was the perceived lack of suitably qualified GPs with the necessary skills and experience. Site staff placed importance on making GPED an attractive place to work and ensuring that GPs felt valued, supported and appropriately remunerated for effective implementation. However, conflict was noted around the recruitment and retention bonuses that were sometimes required to encourage GPs to fill positions compared with the salaries that could be afforded for ED staff, which were described as ‘a slap in the face’.
Emphasis was also placed on ensuring that GPs felt protected and supported to work within their scope of practice. As a result, some participants felt that GPs needed to be upskilled or would require extra training. To compensate for this, some participants emphasised the importance of recruiting experienced GPs who had previously worked in the ED or employing GPs who were trained at their site as juniors. GPs felt supported when they had a sense of belonging and contributing to the wider team. Practical issues such as trusts contributing to GP indemnity were seen as facilitative, as previous arrangements in which GPs paid their own indemnity meant that costs were prohibitively high for OOH work:
Indemnity has changed now. A lot of out-of-hours requests by us is high risk, obviously, then it would be too expensive to do out-of-hours. As from April this year, it’s changed so NHS is taking over the indemnity side of things. Yeah, you still pay, like, you know, a fair amount, but like the big thing has been taken over by the NHS.
Locum GP (Birch) 016, time 1
Many staff perceived GPED to provide training and educational benefits for junior doctors, whom it was felt would, in some models, become more confident about discharging patients and build up their primary care knowledge. Equally, diverting patients with minor conditions to GPED was seen to have benefits for ED juniors and trainees by exposing them to more acutely ill patients.
Emergency department streaming and workforce
There was strong agreement across sites that the seniority and experience of the nurse had a positive impact on the clinical effectiveness and safety of streaming patients to GPED. However, there were not always enough suitably experienced nurses available to stream safely and effectively. This was considered to be because there was a limited pool of such experienced and qualified nurses, and also because streaming was not an attractive role to some senior nurses. This has implications for recruitment, retention and planning future streaming services:
The GP feels that one of the problems with the model is that there is a need for experienced triage nurses in order for it to work, but the department has a high turnover of nursing staff and has difficulty retaining staff. There are only a couple of appointed nurses who have the experience required.
ED consultant (Redwood) 001, time 1
Concerns about the implications of GPED for nurse retention were not necessarily substantiated by the results of the WFS, with relevant findings shown in Table 15. The survery found that, although 45.6% of nurses reported high or considerable intent to leave their current employer in the next 5 years (for a range of reasons), this rate was similar to that of GPs (44.4%) and only modestly higher than that of ED doctors (36.6%).
| Likelihood of leaving direct patient care within 5 years | Number of respondents (%) | Number of respondents (%) to Ninth National GP Worklife Survey75 | |||
|---|---|---|---|---|---|
| ED specialist | GP | Nursing staff | Trainee | ||
| None | 52 (55.4) | 6 (33.3) | 65 (41.1) | 27 (60.0) | 27.8 |
| Slight | 23 (22.8) | 8 (38.9) | 47 (29.7) | 13 (28.9) | 20.3 |
| Moderate | 8 (7.9) | 2 (11.1) | 26 (16.5) | 0 (0.0) | 12.9 |
| Considerable | 7 (6.9) | 1 (5.6) | 7 (4.4) | 5 (11.1) | 11.4 |
| High | 7 (6.9) | 2 (11.1) | 12 (7.6) | 0 (0.0) | 27.7 |
Streaming was seen to place staff in a vulnerable position in which they felt physically and psychologically unsafe. This was sometimes related to the physical location of the streaming desk (which was either isolated from the rest of the department or on full view in the ED waiting room) or because they felt that policies to protect them were either not in place or not followed:
He was just getting irate, just really angry. He was riling everyone else up, because he was like ‘we’ve been waiting too long, haven’t we? Don’t you think we‘ve been waiting too long?’. Everyone was glaring at me and I felt like I was in a goldfish bowl, it was awful, I had people kind of kicking off. So it can be a bit overwhelming at times, and you’ll get people that will say ‘no, I’m not going’, they’ll say point blank, ‘I’m not going to the GP, I want to be seen here, I’m not going to the GP’.
Band 6 ED nurse (Linden) 005, time 1
The WFS found that only 43.7% (n = 69) of nurses reported satisfaction with physical working conditions, but this figure was comparable with those reported by ED doctors (45.5%) and GPs (44.4%). By contrast, the proportion of respondents reporting high or considerable pressure from dealing with problem patients was higher among nurses (81.6%, n = 129) than among ED doctors (67.3%, n = 68) and GPs (61.1%, n = 11). This suggests that, although concerns about the physical context of work were shared across occupational groups, staff had different experiences in practice, which may, in part, be attributable to the streaming role of nurses in the ED.
Streaming was considered both physically and mentally challenging because of the volume of patients and the requirement to make quick, accurate and safe decisions. Streamers were conscious of the safety-critical nature of their role and the requirement to stream patients effectively. Consequently, streaming was considered a stressful and highly responsible position, leaving nurses feeling professionally vulnerable:
I think it will remain to be seen, how supported the nursing team are from the medical team as to, with regards to streaming patients . . . And at the end of the day, if we make that decision that the patient goes to a different facility, be it the GP or something else, and something happens to the patient, you know, are we going to be supported as a nursing team, making that [decision]?
Band 6 ED nurse (Juniper) 008, time 1
In the WFS, only one-third of nurses (34.8%, n = 55) reported ‘satisfaction’ with the amount of recognition they received for good work (relative to ED doctors: 46.5%, n = 47).
It was also identified that streaming was not appealing to senior nurses because it was seen as a diversion from ‘proper’ nursing and core ED work. Some staff felt and were observed to display signs of stress and burnout, including negative behaviour towards patients. Attempts were made at some case study sites to ameliorate this by rotating streaming staff to other areas of work. However, this option was limited because of a lack of experienced streaming staff. These issues have implications for ensuring that there are sufficient nurses to stream safely and effectively and for the future sustainability of streaming:
I’ve once streamed for 12 hours and it was like . . . I was ready to kill anyone that walked through the door, I can assure you [laughs] . . . And it takes away our autonomy, our years and years and years of experience by having to deal with people that don’t need to be here. So it’s kind of demoralising as well, isn’t it? Because you’re just, like, you come in every day and it’s the same [tasks], different day . . . we kicked off so much because we were just being dragged in there all the time and we couldn’t get on and do what we were supposed to be doing. And we’ve got a lot of experience, we’ve got a lot of skills and at the moment, the way this department is run, all we do is stream and triage, which is a waste of our skills.
Band 7 ENP (Linden) 002, time 1
Domain of influence 7: workforce behaviour and experience
Most staff could see how GPED differed from their usual ways of working (68.9%, n = 264) and felt that they were able to easily integrate GPED into their existing work (68.4%, n = 262). The clinical effectiveness of GPED services largely depended on effective communication, trust and confidence between streamers and GPs. Streamers were confident streaming to GPs whom they knew and trusted. Similarly, it was important for GPs to trust streamers and have confidence in their abilities to direct patients appropriately and safely. However, there was significant variation between both individual GPs and streamers in terms of what presentations streamers were prepared to refer to GPs and what presentations GPs were prepared to accept. Practices such as a dependency on locums and part-time GPs and the rotation of the streaming nurses were seen to reduce consistency and limit trust. This was reflected in the NoMAD survey, in the responses to which only 60% of staff strongly agreed or agreed that they had confidence in other people’s ability to conduct their roles in GPED (59.5%, n = 228) or that work was being assigned to those with skills appropriate to the role (58.0%, n = 222). Proactive behaviour on the part of both GPs and streamers was viewed as beneficial in enhancing working relationships and increasing the clinical effectiveness of the service:
We are familiar with probably two or three GPs who we would consider very well trained and able to deliver what it says on the tin. And that’s great when they’re on. The others are an unknown quantity and, to be honest, we have such a huge volume of locums through, they’re often an unknown quantity.
ED consultant (Chestnut) 024, time 1
However, tensions between GPs and streamers were identified at all sites. GPs were seen to ‘pick and choose’ their patients – ‘they’ll only see what they choose to see, you know, they won’t see this or they won’t see that’ [Streaming nurse (Birch) 001, time 1] – whereas nurses were criticised for streaming patients inappropriately. This increased when the ED was busy. Similarly, GPs were seen to pass patients back to the ED to reduce GPED workload. There was clear dissonance between the types of patient that ED staff and GPs perceived as being ‘GPED appropriate’. In this way, the relevant workforces acted to protect their own working environment:
There were some obvious frustrations around communication, and rejection of patients perceived as suitable for streaming to the UGPC [urgent general practice centre]. This included, for example, phone calls back and forth between the ED front desk and the primary care centre explaining/questioning the rationale for streaming certain patients.
Band 7 ED nurse (Linden) 001, time 1
As a consequence, and later in the study, one case site had developed plans to respond to excessively busy workloads from a broader perspective:
. . . it’s out-of-hours escalation plan that if we have an increase in workload that we might have to look at the activity that comes through ED and consider ‘have we got the capacity to take the streaming patients?’ and it’s part of the escalation plan. So we would review the activity as a bigger picture in terms of what’s the activity going through ED, what’s the activity coming through 111 and look at the kind of pathways, managing the levels of demand in line with acuity and everything else.
Band 5 nurse (Hawthorn) 015, time 3
However, individual streamers’ and GPs’ tolerance of risk and clinical ambiguity also had an impact on the clinical effectiveness of GPED and affected streaming decisions. This was linked to concerns regarding patient safety and was associated with not only the characteristics and behaviour of staff at an individual level, but also broader organisational and professional support:
Here in Hawthorn, we’re very risk averse, so not as many go to out-of-hours GP as they could. If I’m honest, it’s because the wider NHS complaints and concerns system will nearly always appear to take the patients’ position.
Band 5 nurse (Hawthorn) 018, time 1
Protocols had been developed in case study sites, with the aim of standardising both streaming decisions and GPED acceptance criteria. However, these protocols were disseminated and utilised with varying clinical effectiveness, and streamers and GPs adhered to these to differing degrees:
It should be fixed, but, as I said, depending on who you speak to, it does waver slightly on what practitioners and GPs are willing to see. So, it’s a bit of a grey area really. It depends who you’re working with really. I don’t . . . yes. So, it’s not fixed. It should be really.
ANP (Redwood) 002, time 1
Effective working relationships were also hindered by divergence in ways of working between primary and secondary care. Culturally, GPs and ED clinicians worked in different ways and this had an impact on the working relationships and integration between the clinical silos. Although there was physical integration, ED staff often felt that GPs lacked collegiality:
So, the GP will, sort of, arrive, go straight into their room and then stay in the room unless you call them out for huddle or something like that, whereas A&E nurses and all of our doctors are all quite social. We’re a team; we’re really visible to each other.
Band 6 nurse (Nutmeg) 015, time 1
However, findings from the WFS indicated similar rates of ‘satisfaction’ with colleagues and fellow workers among GPs (83.3%, n = 15), compared with ED doctors (84.2%, n = 85) and nurses (79.7%, n = 126). Likewise, very few staff indicated in the NoMAD survey that GPED disrupted their working relationships (13.3%, n = 51). Initially these data appear at odds with the qualitative findings; however, this is likely to reflect strong intra-ED staff and intra-GP staff collegiality, which was apparent from the interviews and observations.
Table 16 presents item-level descriptive analyses of the 10-item measure of job satisfaction for the sample as a whole and in comparison with relevant findings from the Ninth National GP Worklife Survey;75 Table 17 presents a further breakdown by job category. These tables include mean ratings for each job satisfaction item, as well as the number and proportion of respondents who provided a response above the neutral mid-point on the scale (item scores ranging from 5 to 7), which were, therefore, classified as ‘satisfied’.
| Satisfaction domain | Total | Ninth National GP Worklife Survey75 | |||
|---|---|---|---|---|---|
| Mean rating | Satisfied | Mean rating | Satisfied | ||
| n | Percentage | Percentage | |||
| Physical working conditions | 4.21 | 169 | 44.1 | 5.15 | 74.5 |
| Freedom to choose your own method of working | 4.24 | 147 | 38.4 | 4.71 | 60.4 |
| Your colleagues and fellow workers | 5.54 | 301 | 78.6 | 5.71 | 86.0 |
| Recognition you get for good work | 4.06 | 150 | 39.2 | 4.37 | 51.2 |
| Amount of responsibility you are given | 4.90 | 246 | 64.2 | 4.79 | 62.9 |
| Your remuneration | 3.72 | 122 | 31.9 | 4.22 | 48.3 |
| Opportunity to use your abilities | 4.63 | 209 | 54.6 | 4.92 | 66.6 |
| Your hours of work | 4.28 | 171 | 44.6 | 3.57 | 33.9 |
| Amount of variety in your job | 5.23 | 275 | 71.8 | 5.11 | 71.7 |
| Taking everything into consideration, how do you feel about your job? | 4.77 | 242 | 63.2 | 4.25 | 49.9 |
| Satisfaction domain | ED specialist | GP | Nursing staff | Doctor in training | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean rating | Satisfied | Mean rating | Satisfied | Mean rating | Satisfied | Mean rating | Satisfied | |||||
| n | Percentage | n | Percentage | n | Percentage | n | Percentage | |||||
| Physical working conditions | 4.21 | 46 | 45.5 | 4.06 | 8 | 44.4 | 4.19 | 69 | 43.7 | 4.24 | 22 | 48.9 |
| Freedom to choose your own method of working | 4.24 | 43 | 42.6 | 4.44 | 8 | 44.4 | 4.20 | 59 | 37.3 | 4.22 | 18 | 40.0 |
| Your colleagues and fellow workers | 5.47 | 85 | 84.2 | 5.44 | 15 | 83.3 | 5.54 | 126 | 79.7 | 5.71 | 38 | 84.4 |
| Recognition you get for good work | 4.21 | 47 | 46.5 | 4.28 | 8 | 44.4 | 3.94 | 55 | 34.8 | 4.36 | 23 | 51.1 |
| Amount of responsibility you are given | 5.00 | 72 | 71.3 | 4.72 | 10 | 55.6 | 4.83 | 102 | 64.6 | 4.91 | 31 | 68.9 |
| Your remuneration | 4.15 | 51 | 50.5 | 3.83 | 8 | 44.4 | 3.34 | 33 | 20.9 | 3.84 | 14 | 31.1 |
| Opportunity to use your abilities | 4.48 | 52 | 51.5 | 4.22 | 7 | 38.9 | 4.65 | 92 | 58.2 | 5.07 | 35 | 77.8 |
| Your hours of work | 4.34 | 54 | 53.5 | 4.33 | 8 | 44.4 | 4.09 | 62 | 39.2 | 4.24 | 20 | 44.4 |
| Amount of variety in your job | 5.15 | 75 | 74.3 | 4.67 | 10 | 55.6 | 5.20 | 118 | 74.7 | 5.34 | 33 | 73.3 |
| Taking everything into consideration, how do you feel about your job? | 4.74 | 68 | 67.3 | 4.61 | 12 | 66.7 | 4.68 | 96 | 60.8 | 4.96 | 31 | 68.9 |
As shown in Table 16, when compared with the national sample of GPs, hospital staff involved with GPED generally reported lower levels of job satisfaction in relation to physical working conditions, freedom to choose their own method of working and remuneration. By contrast, our sample of hospital staff reported higher levels of job satisfaction associated with work hours and overall ratings of job satisfaction.
Comparisons conducted across employee groups (see Table 17) indicated that job satisfaction was generally highest among ED specialists; the small number of GPs in this sample reported levels that were typically either similar to or lower than those of ED specialists. With some exceptions, the lowest levels of job satisfaction were typically reported by nursing staff.
Although the majority of staff understood how GPED had affected the nature of their own work (78.1%, n = 299), a far smaller number strongly agreed or agreed that they valued the effect that GPED had had on their work (56.7%, n = 217). Despite this ambiguity, most staff (across all staff groups) stated that they would continue to support GPED (86.4%, n = 331).
Domain of influence 8: resource use
Respondents could generally see the potential for overall cost savings associated with GPED, in principle, if all of the assumptions were met [i.e. having a positive impact on hospital admissions, reduction in patient investigations and more effective use of ED staff resources (seeing more unwell patients)]. However, much scepticism remained around whether or not these goals would be achieved by GPED alone, and it was often felt that broader investment in the number of acute beds and enhanced social care would also be necessary:
So the problem is not latching GPs onto here, it’s further back, it’s much, much closer to the root of the problem that they need to start looking, really, but they know that, but they’re not going to do it because it costs them too much money.
Band 7 ENP (Linden) 002, time 1
Staff and patients predicted that GPED would incur higher costs because of the cost of GP employment, and placed importance on ensuring that staffing and resources are carefully matched. As ED staff and local service leaders considered GPs a costly resource, they felt that GPs needed to demonstrate their clinical effectiveness and they would require that GPs saw adequate volumes of patients in a timely manner and were also on shift when demand was at its peak:
Eventually, I suppose, it would be to look at, are there days and times of the days where it’s not cost-effective? I think that has to be taken on board for the future.
GPED system lead (Rowan) 031, time 1
Staffing issues, such as struggles to recruit to GPED and the need for senior nurses to stream, also dominated discussions about the potential impact of GPED on resources. The employment of locums and agency staff to fill these positions led to higher costs. Some argued that the money could be better spent improving primary care provision, resulting in a reduction in the number of primary care patients attending ED in the first place.
It was also noted that in situations in which a GPED-streamed patient needed to be referred back to their own GP, an additional cost to the broader NHS would be incurred, as the patient was being seen more than once for the same illness episode. This was viewed as both being costly and generating additional unnecessary workload. For GPs, there was also a tension between service policies and associated funding and effective and safe patient care. As described in Domain of influence 4: patient outcome and experience, an example of this was ‘2-week wait’ for possible cancer referrals. For GPs, patient safety was paramount and this over-rode funding decisions. Consequently, GPED GPs would refer patients directly to the 2-week wait service, rather than back to their own GP, regardless of the cost implications:
I think it’s really important that we, again, it’s all about efficiency, that, actually, if we’ve picked up that the patient’s having palpitations, we should just send them to the cardiologist from here. It’s ridiculous to be sending them back to the GP, who then sends them, and there’s all sorts of excuses that everyone uses in here, it’s all to do with the funding and no one will pay for it . . . So, I think that those are the sorts of things that just really wind me up about the health service that actually, just because of the funding it means that actually there’s a really inefficient pathway in there and we need to try and change that. So, I think GPs have a role of being here and standing up for general practice and saying ‘hang on a minute, that’s not efficient, let’s refer him then go back to the GP for ongoing care’, why can’t we do that, it’s crazy, you know? It’s just making work that doesn’t need to be made.
GP (Juniper) 024, time 1
General practitioners felt that initiatives to broaden access to health care were, in reality, often confusing for patients and actually created a duplication of workload, resulting in increased costs. Although patients were often aware of traditional routes to care, such as primary care and the ED, they were less sure about other ways to access care. This led to patients using tried-and-tested access routes, only for them to then be signposted to different services. GPs saw this as a waste of resources:
I think there are a lot of resources out there that patients don’t use and don’t know about; so, for example, the minor eye condition service where patients with minor eye conditions can actually be treated by their optician and get payment rather than coming to their GP for their dry eyes or conjunctivitis or painful eye, but patients have no idea about that so they present to the GP anyway. That uses up an appointment, just being told ‘well you can go to [service name]’. So, you know, NHS Choices [now nhs.uk; www.nhs.uk (accessed 28 November 2021)], brilliant, it’s a fantastic website, but no one knows about it. 111 people are starting to know about, it’s taken a long time, I think we need to have some sort of national programme that really educates people about what services are available in their community and where to look for it.
GP (Juniper) 024, time 1
Incidental costs, such as paying for training and the set-up and management of new IT systems, constituted added expenses and time burdens that staff felt had not always been taken into consideration. Staff reported receiving little training when joining GPED and there were continued frustrations with IT and the lack of integration between GPED and ED systems. Findings from the NoMAD survey indicated that only one-third of staff felt that sufficient training was provided to enable staff to implement GPED (33.4%, n = 128) and that sufficient resources were available to support GPED (32.6%, n = 125).
Staff at case study sites described several different approaches to how capital funding had been used. These included structural changes, whereby new structures were created or existing spaces were adapted; governance and contractual changes that often included working in new partnerships across commissioners and providers of health and care; the integration or introduction of multiple IT systems; and operational changes, such as revised patient pathways or the reconfiguration of existing services. Changes made with this funding were, in some cases, minimal, but could also include physical changes, such as building a purpose-built UCC or dedicated waiting area, or alterations to management and governance. This was exemplified at one site, where staff were unclear how the new GPED service would differ from their established GP OOH service, apart from providing additional funding or new triage rooms. Table 18 summarises the key issues raised in relation to GPED resource use.
| Resource use | Summary | Quotation |
|---|---|---|
| Staff costs |
Extra staff were employed for GPED: GPs, specialist staff (e.g. physiotherapists) and streaming nurses (i.e. senior nurses) A shortfall in GPED staff meant that locum and agency staff were required to cover, which added extra salary costs There was variability in pay scales for GPs and within regions, and this was often higher than the pay of the ED consultant |
Capital funding does not pay for staffing which is the biggest cost. Might have to sacrifice middle-grade doctors to give us the funding to get the GPs into EDLocal service leader 16, time 1Costs had a massive factor in it. Staffing, we kind of have to work around the cost. So, sometimes it’s, painfully, not for how many you should have to be able to run the department, it’s how many can we afford to have to run the department safelyStaff (Chestnut) 023, time 1I don’t necessarily think it is a bad thing to have it, but it provides marginal gains and those marginal gains are happening at a very high capital cost and an ongoing staffing cost and, looking at the NHS budget as a whole, I think it’s a shocking waste of moneyStaff (Juniper) 050, time 3 |
| Financial loss/risk |
GPs were seen as an expensive resource and there were concerns that GPED may lead to financial difficulties for sites Tariff payments may be insufficient to cover the costs |
There’s already concern that the GP extended hours is not being filled and the cost of GP and EDStaff (Rowan) 030, time 1I’m not sure that the future of the service is necessarily 100% assured because it is, as once the funding, the central funding has, dries up we will be funding this service . . .Staff (Juniper) 047, time 3I suppose, with emergency physician and an emergency doctor, as opposed to a GP, is the flexibility to work across all areas of the department when the needs of the department change whereas if there’s no primary care workload then there’s no primary care workloadStaff (Juniper) 047, time 3 |
| Economic viability |
Concerns over whether or not GPED offered good value for money. This was exacerbated by the high cost of employing GPs GPs need to see enough patients and be on shift when demand is highest Negative impact of patients being sent back to the ED from GPED Would the money be better spent improving primary care, which may lead to the same outcome (reduced ED attendances and admission rates)? |
We don’t want an expensive asset like a GP to be just seeing very easy earaches; we want them to be seeing complex primary care patientsLocal service leader 39, time 1I would get more value for money from a primary care nurse practitioner or a good-quality, middle-grade doctor. It’s an expensive way to manage patients who are generally pretty straightforwardLocal service leader 43, time 1I would rather that more money was spent on training GPs, and recruitment and retention of GPsLocal service leader 48, time 1We‘re aware that if we send them back to ED, there are cost implications because they’re double charged or whatever and things, so it’s of no benefit to the whole model, if you like, if we send things back to ED, but that’s not meaning to say that we shouldn’t do itStaff (Rowan) 03, time 1If they’re acting like the SHOs [senior house officers] and they’re ordering tests and whatever, well, actually, it doesn’t really save anythingStaff (Linden) 007, time 1 |
| Governance |
There was variation in the source of funding for GPED and the contracts held by staff Governance structures were complex, with GPs often being self-employed |
Yeah [employed by the trust]. So I’ve got my own indemnity, they’ve got, they, they have indemnity, their own indemnity, but I’ve got personal indemnity as wellStaff (Juniper) 049, time 3The GPs themselves are employed through the trust. They’re not employed by a community provider. They are employed directly through the trust bank of the hospital. So the GPs, when they work in urgent care at [name] they effectively, they’re being GPs, but they’re employed by the emergency department and therefore part of their clinical governance structureStaff (Teal) 040, time 3 |
| Other costs | Other incidental costs were a burden to arrange and provide for, such as training, system changes and IT | Need for integrated IT system, but difficult to achieve; currently, GP, ED and ambulance trust all use different IT systems. It is currently difficult to envisage how this would work. This not only has implications for clinical work (i.e. 111 patients through ambulance service, booking patients through ED system), but also for measuring impact of service and generating data for key performance indicatorsLocal service leader 27 ,time 1The training was, I have to say, on the computer system, not great. I tried to get some IT training on the system. The IT department said there wasn’t any training available, but they’d let me know when there wasStaff (Redwood) 007, time 1 |
| Cost saving | GPED seen to offer cost savings through reduced admission rates a better use of resources, more staff and fewer tests | Having an extra doctor in the evening has helped with targetsLocal service leader 39, time 1It allows them to optimise their staff, it’s not costing them any more money, and also gives them a baseline from which they can operateLocal service leader 40, time 1I don’t get a sense that we are creating a monster, and, so I’m told, we‘re being cost-effectiveStaff (Rowan) 03, time 1 |
GPED costs and savings
The average time of operation of a GPED service in our quantitative sample of 34 EDs (see Table 5) was 11.1 hours per calendar day, or 4054 hours per year. Many hospitals were unable to report the exact working patterns of GPs in their service, which appeared to vary substantially over time. We therefore assumed that only one GP was present in each hospital for each GPED shift, which is likely to be an underestimate. We also did not consider any associated cost relating to support staff, building/refurbishment or estate maintenance. Given that all hospitals had a GPED service in place at the time of study, we did not judge it feasible to disentangle the associated costs that were specific to the GPED service rather than general to the ED.
The hourly cost of a GP is assumed to be £112, which is taken from the Unit Costs of Health and Social Care 2019 report. 68 This figure includes on-costs and various overheads, but excludes costs that are likely to arise in the traditional primary care setting only (e.g. other direct care staff, travel to visit patients), as well as qualification costs. For comparison, the hourly cost of a GP is very similar to the cost of a hospital consultant (£109–111 per hour) and twice the cost of a band 6 nurse (£47 per hour). The total cost of operating a GPED service is, therefore, on average, £454,048 per hospital per year (total cost = 4054 hours × £112 per hour).
The outcomes chosen to test the effects of GPED include several indicators with resource consequences (in particular, admissions and attendances). However, only unplanned reattendances to the same ED within 7 days showed a statistically significant reduction of –0.3% per patient. The sample of EDs included in our analysis treated, on average, 107,558 patients per ED (or 4.3 million patients in total) during the financial year 2018/19. Thus, the analysis suggests that GPED services may have helped to avoid ≈ 320 reattendances per hospital per year; however, the significance of this from a clinical and service delivery perspective is marginal at best.
Appendix 2, Table 25, illustrates the tariff costs of ED attendances, ranging from £63 for an attendance with no investigation or treatment to £328 for the highest-category emergency treatment. Our quantitative analysis of reattendances is not informative about the care needs of patients who reattend. However, it seems unlikely that the presence of GPs in the ED would reduce the probability of a high-acuity reattendance. We therefore decided to value the reduction in the rate of reattendances using the Healthcare Resource Group (HRG)’s tariff costs of category 1 investigations (VB06Z and VB09Z), which vary from £93 to £115. 96 This implies a cost saving from possible reduced reattendances of ≈ £30,000–7,000 per hospital per year.
Overall, and considering the cost of hospital reattendances only, it would appear that any cost savings attributable to the presence of a GPED service (≈ £30,000–7,000) are far exceeded by the salary cost of the GPED service alone (£454,000), which is also likely to be an underestimate of the total cost of the GPED service.
Patient and public interpretation
During the workshops held towards the end of the study, public contributors noted that many factors influenced the performance of GPED, making it difficult to attribute cause and effect. They further noted that any general pronouncement on the clinical effectiveness of GPED might not adequately take account of the potential benefits of GPED in specific circumstances. However, they felt that the quantitative data were ‘strongly suggestive of no effect’, which, in turn, led the public contributors to question whether or not GPED represented a good use of public money and GP time.
Data synthesis
A final workshop was held, at which both quantitative and qualitative data were jointly presented to the public involvement group. Owing to the large number of qualitative data collected, we asked the group in advance what qualitative data they would like to see. It was agreed that we would present a summary of the qualitative data on staff views regarding the clinical effectiveness of GPED and compare this with the quantitative findings. The public contributors concluded that GPED is not effective and should be used only when specific circumstances indicate that it may play a positive role.
The outcomes of this work were fed back to the research team and the SSC.
Summary
This chapter has used a mixed-methods synthesis to present our research results within the overarching policy context and eight identified ‘domains of influence’. We have found considerable heterogeneity and complexity, combined with a high degree of local variability, which makes it impossible to identify any consistent or sizeable effect or any evidence of general cost-effectiveness. We will consider the implications of this further in Chapter 4.
Chapter 4 Discussion
Overview
In this chapter, we summarise and interpret our research findings using NPT79 and discuss each of our nine objectives in context. We then consider the ‘success factors’ that influence the implementation of GPED, and the implications for clinical practice and local service delivery. A description of the strengths and limitations of our study is followed by our recommendations for future research.
Summary of research findings using normalisation process theory
Coherence: do stakeholders understand why GPED has been implemented?
For a health policy to be implemented and adopted into routine practice, there needs to be a shared sense of its purpose. Findings from WPs A and C suggest that many stakeholders understood that introducing GPs in the ED was a direct response to rising pressure on EDs and was seen as a potential mechanism for reducing ED attendances, thereby improving waiting times and other key performance indicators (KPIs). However, stakeholders criticised GPED for being a rushed, top-down policy that was based on limited evidence and conflicting guidance. There was also scepticism around the decision to choose L&D as the ‘blueprint’ for GPED, which, when combined with concerns that GPED did not consider local variations in demand for ED services, population needs and pre-existing GPED service delivery models, caused many to question whether or not the policy was universally applicable. As a result, GPED was interpreted differently throughout the NHS in England and this heterogeneity led to different anticipated impacts of GPED across each of the eight domains of influence that we identified. Ultimately, the challenges of applying a national solution to a local problem resulted in a lack of buy-in from key stakeholders at all levels of the health-care system and a feeling that GPED had been ‘forced’ on them. This, in turn, led to substantial heterogeneity in the measured effects of GPED across participating EDs, and no clear or consistent effect on ED attendance and routinely reported measures of ED performance. The findings on coherence are summarised in Table 19.
| NPT construct | Theme | Explanation |
|---|---|---|
| Coherence: do stakeholders understand why GPED has been implemented? | ||
| Does GPED have a clear purpose and do participants have a shared sense of its purpose? | The L&D model | The implementation of GPED was considered to be rushed and based on conflicting guidance. The anticipated effects of GPED and the direction of these effects were unclear or contested. There was uncertainty as to why L&D had been selected as the exemplar trust for GPED; participants were sceptical that their success was due to GPED, as opposed to other ED initiatives that were introduced simultaneously |
|
Will GPED fit with the overall goals and activity of the organisation? Is it clearly distinct from other interventions? |
A one-size-fits-all approach |
Stakeholders agreed that the potential benefits of GPED would depend on the local context in which it was implemented. There was some resistance towards GPED among those that viewed it as another ‘top-down, generalised, national policy’. This had a negative impact on the level of commitment (i.e. cognitive participation) that stakeholders were prepared to invest to ensure that GPED was a success Some stakeholders had difficulty understanding how GPED differed from previous unsuccessful attempts to introduce GPs into the ED. In addition, it was not always clear how GPED or the capital funding initiative differed from previous and existing interventions, particularly in EDs where GPs had been working for some time |
| What benefits will the intervention bring and to whom? Do people have a shared sense of GPED’s purpose? |
Domains of influence: expectations Data collection from WP A |
Variations in local context, ED demand and existing GP services in the ED resulted in GPED being interpreted differently (WP A); GPED is difficult to describe and distinguish from other interventions, and participants do not have a shared sense of its purpose. This resulted in stakeholders disagreeing on the potential effects of GPED, with positive, neutral or negative effects predicted for the majority of the eight identified domains of influence |
| Does it have a clear purpose for all relevant participants? | Health service literacy | GPED was considered confusing for patients. It was felt that, in some cases, patients use the ED inappropriately: GPED encourages patients to visit their own GP, but also makes accessing a GP easier and so facilitates ‘inappropriate’ ED attendance. The term ‘urgent care’ was believed to add to the confusion and make the difference between ED ‘minors’ and urgent care unclear. Despite staff criticisms of how patients use services, experienced streaming nurses, GPs and staff from other services (e.g. pharmacy, NHS 111) were often unclear about what constitutes a ‘GPED-appropriate’ patient |
Cognitive participation: are people committed to using GPED and what are the factors that promote and/or inhibit this commitment?
Stakeholder buy-in is not only important during initial policy development and implementation; it is also pivotal to ensuring that people remain committed to embedding a policy into routine practice. In addition to concerns that the introduction of GPED was rushed and based on little supporting evidence, there were significant doubts that a single initiative could provide the solution to complex problems in the health-care system. Representing a potential lack of support for the policy, alternative approaches to GPED, such as focusing on ‘upstream interventions’ that would prevent patients from becoming acutely unwell, along with a greater investment in mental health and social care services, were proposed and considered potentially more effective than GPED.
The lack of consensus as to the purpose of GPED, which varied according to the local context, was reflected in the types of GPED models that were implemented nationally. Whether or not GPED models should give GPs access to investigations was a particularly polarising issue that was grounded in perceived differences in the approach to risk between ED staff and GPs. Although some felt that giving GPs access to investigations would have a positive impact on hospital admissions, others felt that this invited GPs to work outside their clinical competency. However, whether or not GPs were given access to investigations varied and this heterogeneity was reflected in our quantitative analysis, which showed no significant effect of GPED on hospital admissions. The findings on cognitive participation are summarised in Table 20.
| NPT construct | Theme | Explanation |
|---|---|---|
| Cognitive participation: are people committed to using GPED and what are the factors that promote and/or inhibit this commitment? | ||
| Will stakeholders be prepared to invest time, energy and work in GPED? | GPED: a case of bias to action | Participants criticised the way in which GPED policy had been developed, and considered it to have been based on little evidence or patient/clinical consultation (see Table 19). GPED was, therefore, viewed as a rushed response from the government to rising ED pressures. This reduces the commitment to ensuring that it is embedded into routine practice |
| Will they be prepared to invest time, energy and work in it? | Use of investigations and hospital admissions | Although some participants felt that giving GPs access to investigations would improve the clinical effectiveness of GPED, others considered it a barrier and something that encouraged GPs to work beyond their clinical competency. The lack of consensus as to whether or not GPED models should give GPs access to diagnostic investigations created tension among GP and ED staff and may, depending on their views and the model at their site, make staff less likely to invest their time and energy into ensuring that GPED is a success. These differences in opinion were also, to some extent, related to people having different perceptions on the purpose of GPED (see Table 19). Differences in risk management between GPs and ED staff were considered to affect not only their use of investigations, but also the likelihood of patients being admitted to hospital unnecessarily |
| Will stakeholders see the point easily? | GPED: a sticking-plaster solution | There was doubt that GPED, as a single initiative, could fix complex problems in the health-care system. Suggestions for alternative approaches, which were perceived to have a greater potential impact on ED performance, were proposed |
Collective action: are people using GPED and what are the factors that promote and/or inhibit them from using GPED?
Opinion was divided regarding the potential impact of GPED on how patients access and use the ED. Local service leaders and site staff were particularly concerned that one of the unintended consequences of GPED could be that, by guaranteeing same-day access to a GP, GPED would become a replacement primary care service and increase ED attendance. Staff also felt that patients lacked health literacy and used the ED inappropriately. However, the reasons that patients provided for attending ED were complex and, although it was felt that some patients deliberately ‘play the system’, it was acknowledged that the constantly changing organisation of systems and the range of services available (e.g. GP hubs, urgent treatment centres, NHS 111, EDs) make navigating services difficult. Interestingly, despite heavy criticism of patients for perceived ‘inappropriate attendance’, our qualitative data provided examples of situations in which experienced nurses and services such as NHS 111 were unable to determine whether a patient’s complaint should be treated by primary care or at the ED. Despite concerns that GPED may increase ED attendance, no association was found between the absolute and relative volume of ED attendances and the proportion of ‘unnecessary attendances’.
Our findings also identified several factors that may promote or inhibit how staff use GPED, and the extent to which it becomes embedded in routine practice. These were categorised as factors relating to workforce recruitment and retention (e.g. staffing issues, training and educational benefits, and the impact of GPED on professional roles), workforce behaviour and experience (e.g. communication, trust, role-based cultural differences), and streaming and implementation issues (e.g. streaming protocols, interprofessional relationships and structural support). Although some of these factors, such as streaming, are unique to the adoption of GPED, many factors, such as staffing issues, communication and interprofessional relationships, are well established and have been regularly identified as barriers to implementing health policy. 98,99 It is essential that these issues are considered when developing future health policy and that service managers and health professionals work together to develop locally tailored implementation strategies that will support successful adoption. The findings on collective action are summarised in Table 21.
| NPT construct | Theme | Explanation |
|---|---|---|
| Collective action: are people using GPED and what are the factors that promote and/or inhibit them from using GPED? | ||
|
What effect will GPED have on ED and the health service? How will the intervention affect the work of user groups? |
Service access | Despite reports that GPs have been working in ED for some time, only a small number of patients reported having used GPED previously and expecting to be streamed to GPED. However, staff were concerned that by creating ‘easy access to a GP’ GPED may encourage people to attend the ED, that is GPED may become a victim of its own success and become a replacement primary care service |
| Health service literacy | Perceived poor health literacy of patients was considered by staff to affect how patients use GPED, with patients criticised for inappropriately attending the ED. Staff felt that patients required more education around ‘appropriate’ ED attendance, but whether or not this should be considered part of the GP’s role was debated | |
|
What impact will it have on division of labour, resources, power and responsibility between different professional groups? Will staff require extra training? How will the intervention affect the work of user groups? |
Workforce (e.g. recruitment and retention) |
Staffing issues posed a major threat to the successful implementation and adoption of GPED. This was in relation to both the potential for GPED to draw GPs away from primary care, worsening workforce shortages, and ED staff vacancies creating issues in the recruitment of ED and GPED staff. Site staff also felt that there was a lack of GPs with the skills and experience required to work in the GPED model, with some suggesting that GPs may require extra training for GPED to run efficiently. Staff emphasised the importance of ensuring that GPED is viewed as an attractive place to work and that GPs should feel valued, supported and appropriately remunerated to overcome issues with recruitment. In addition, nursing shortages and a limited pool of experienced nurses made the staffing of streaming services challenging The training and educational benefits that junior doctors may receive from working alongside GPED models were felt to be valuable, making them more committed to ensuring that GPED was embedded into routine practice. Conversely, in some cases, streaming was perceived to change the role of nurses and divert them away from proper nursing and core ED work, making GPED less attractive. For some participants, the psychological and physical impact of streaming was thought to negatively affect their work and willingness to invest energy and time in GPED (see Table 20) |
| What impact will it have on division of labour, resources, power and responsibility between different professional groups? | Workforce (e.g. behaviour, experience) |
The clinical effectiveness of GPED was perceived to depend on effective communication, trust and confidence between streamers and GPs. Different perceptions of what was considered a ‘GPED-appropriate’ patient and reliance on locums, part-time GPs and the rotation of streaming nurses limited this trust Tensions between GPs and streamers were common and were due to different attitudes towards risk, as well as staff members (ED and GPED) protecting their own working environment: staff streamed patients to GPED or back to the ED during busy periods to ease their respective workloads. Streaming protocols were developed to try to standardise streaming decisions and GPED acceptance criteria. However, these were disseminated and followed to varying degrees. Cultural differences in the way that GPs and ED clinicians work had an impact on working relationships, with ED and GPED staff achieving varying levels of cohesion, despite some GPED models physically integrating teams within the same department |
|
How will the intervention affect the work of staff? Will it promote or impede their work? Will staff require extensive training before they can use it? |
Success factors for introducing GPED: streaming and implementation issues | Streaming was critical to the success of GPED. Key factors that were pivotal to ensuring effective streaming and, therefore, GPED included structural support, streaming personnel, streaming protocols, negotiating primary and secondary care boundaries, interprofessional relationships and safety. A number of other implementation issues also affected the extent to which staff were able to embed GPED into their routine practice. These included structural support within the site; ensuring that there were integrated IT systems between the ED and GPED; and influencing factors relating to the GPs’ roles, such as ensuring a positive working environment and giving GPs access to investigations, when appropriate |
Reflexive monitoring: have people appraised GPED and its impact on practice?
GPED is a complex intervention that has been introduced through a range of different models into a complex and changing environment. Our mixed-methods evaluation was also affected by widespread uncertainty regarding GP operating hours and different governance arrangements, which, on a practical level, made it unclear for our analysis whether patients streamed to GPED were counted within or outside ED statistics at any given site. Therefore, although our analysis showed no statistically or clinically significant impact on the majority of performance indicators (e.g. 4-hour performance, patients leaving without being seen, ‘unnecessary’ attendances, hospital admissions, mortality at 30 days and reattendance to the same ED within 7 days), our qualitative analysis highlights the range of factors that influence whether or not a complex intervention such as GPED is embedded into routine practice.
Our study also explored the cost-saving potential of GPED and concluded that any cost savings that could be attributed to a GPED service are very modest when compared with the extra cost of employing a GP, and may not take into account other costs that potentially arise when implementing GPED, such as those relating to additional staff, training and IT systems. Given the significant capital investment of public money that was committed to supporting the implementation of GPED, our patient collaborators did not feel that GPED represented value for money when allocating NHS funding. The findings on reflexive monitoring are summarised in Table 22.
| NPT construct | Theme | Explanation |
|---|---|---|
| Reflexive monitoring: have people appraised GPED and its impact on practice? | ||
|
Will it be clear what effects the intervention has had? How are users likely to perceive the intervention once it has been in use for a while? |
WPs B and C: analysis of performance against the 4-hour standard, hospital admissions, patient outcome and experience, service access, reattendance within 7 days and resource use | Variations in site-specific patient mix, GPED models and whether patients streamed to GPED are counted within or outside ED statistics, combined with other factors that influence ED performance, meant that there was no significant impact on the majority of performance indicators (i.e. 4-hour performance, patients leaving without being seen, ‘unnecessary’ attendances, hospital admissions and mortality at 30 days). There was a small and statistically significant reduction in the rate of reattendance to the same ED within 7 days; however, the clinical and economic impact of this was limited |
| Is it likely to be perceived as advantageous for patients or staff? | Patient outcome and experience |
Although there were reports from staff that patients may prefer to be seen by an ED clinician and can object to seeing a GP, most patients were unaware of the type of clinician they had seen and did not mind who they saw, as long as they received appropriate care. In general, patients saw the value of GPED and viewed it as beneficial to ensure that the ED can focus on higher-acuity patients Concerns around patient safety were raised in situations in which patients may not be appropriately referred to further services and/or may encounter referral delays. Particular concern surrounded referring patients back to their own GP and the safety implications of this given that there is no formal follow-up mechanism |
| Will it be clear what effects the intervention has had? | Resource use/cost |
Most people could see the potential for GPED to result in cost savings if all assumptions were met (i.e. reduced hospital admissions, reduction in investigations, more effective use of ED staff resources). However, there was doubt as to whether or not this would be possible through GPED alone and without broader investment in the number of acute beds and enhanced social care Higher costs of GPED were predicted because of the cost of GP employment, the requirement for senior streaming nurses and the reliance on locums and agency staff to fill positions. In addition, the NHS costs of GPED patients being streamed back to their own GP were raised. This caused some participants to argue that capital funding could be better spent on different or alternative approaches to enhanced service delivery Any cost savings that are directly attributable to a GPED service were found to be very modest when compared with the extra cost of employing a GP. In addition, the incidental costs of training, management and the installation of IT systems were all seen to inhibit the effective running of GPED (see Table 22) |
Discussion of research objectives
Objective 1
Objective 1 was to map and describe current models of GPED in England by drawing on multiple sources, such as survey data, interviews and routinely available information.
We were able to map and describe the current models of GPED in England and, working with colleagues supported through the same funding call, we published a new taxonomy that divides the configuration of GPED services into four distinct categories. 1 In 2010, three types of service were identified in a published taxonomy: GP services off site, a service co-located with the ED and GPs fully integrated with the ED team;30 in 2017, a study of 13 EDs in north-west England also described three models: primary care services embedded within the ED, co-located UCCs and GP OOH services. 59 Our inside – integrated model reflects the ‘fully integrated’ or ‘embedded’ models described in 2010 and 2017, whereas our outside – off site model can be aligned with the previously described ‘GP services off site’ and ‘GP OOH’ designations.
The main area of distinction in our new taxonomy is to subdivide the ‘co-located’ model of both 2010 and 2017 into inside – parallel and outside – on site. We made this distinction for two reasons. First, there is a clear difference in patient experience between attending the ED and seeing a GP in a dedicated space within that ED, and attending the ED and being redirected to a physically separate and distinct facility on the same hospital site. Second, we observed that physically separate GPED services tended to have a different model of governance and clinical philosophy that was more aligned with general practice than the model in those GPED services that were physically integrated with the ED, which were more likely to be aligned with emergency medicine.
Once this taxonomy had been established, however, it was not always easy to identify and classify the model in place at a particular site, particularly when this was described in a written survey response or during a telephone interview. Furthermore, the GPED model could change quickly, sometimes within a single week or day (e.g. different service configurations operating in the evening or at weekends), as well as in response to service developments and staff availability. Therefore, the taxonomy proved to be of less value than we had anticipated and, although we analysed our results according to the GPED model in place, we did not find a strong association between model type and performance in our quantitative analysis. The reasons for this are clear from our qualitative data: the factors that govern the operation and success of GPED are far broader and more context specific than physical configuration alone.
Our findings indicate that the vast majority of EDs in England include a co-located general practice service, most commonly in parallel with ED provision. During the study period, fully integrated models tended to be replaced by a more distinct general practice service component, possibly as a result of capital funding allocations that allowed structurally separate facilities to be established. However, we found no association between the adopted GPED model and the observable characteristics of an ED.
Previous research reported that 43% of EDs had a GP service in 2015;18 therefore, the increase in adoption in the 2 years before our study (from 43% to 81% of EDs) exceeded the increase in the 2-year period following the capital funding allocation (from 81% to 95%). 100 Nevertheless, after the NHS policy announcement and associated capital funding, GPED became almost universally established. Despite encouragement from service commissioners at some sites, we found little appetite among clinicians for an outside – off-site model of GPED, which was viewed as carrying additional clinical risk. Therefore, the number of sites using this model dwindled from five to two during our study period, and we excluded these sites from our analysis.
Objective 2
Objective 2 was to use the retrospective analysis of routinely collected ED attendance data (from the HES data set66), collection of local data and non-participant observation to determine the impact of GPED on patient processes and outcomes, including overall attendances, attendances in different components of the local urgent care system, waiting times, emergency admissions, reattendances and mortality.
Objective 3
Objective 3 was to use retrospective analysis of HES data66 to assess the impact of GPED on the case mix of admitted patients by exploring admission rates, including the number and proportion of short stay and zero-day admissions, subject to an examination of coding behaviour by hospital trusts, and any changes that may undermine the reliability of this measure.
In WP B, we used routinely available HES data66 to estimate the impact of GPED services on seven KPIs: unnecessary attendance, waiting > 4 hours, leaving without being seen, reattendance within 7 days, admission to hospital, same-day discharge and 30-day survival. We also assessed effects on the total volume of attending patients, although we could not identify which patients were seen by a GP. We took two approaches in our analysis:
-
a pooled analysis across hospitals comparing patients attending hospitals where GPED was operational with patients attending, at the same time, hospitals where GPED was not operational
-
a regression discontinuity analysis within hospitals comparing patients attending the hospital immediately before and after the start and finish times of GPED services.
Overall, we found little or no difference in the volume of attendances, ED performance or outcomes between patients attending EDs during periods when GPED was operational and those attending at other times. For the pooled analysis, the only statistically significant finding was a marginal reduction in the rate of reattendance for patients attending during GPED (–0.3% per patient). For the RDD analysis, there were different findings depending on whether GPED was starting or finishing. When comparing patients attending shortly before the start of GPED with those attending shortly after, there was no significant difference for any indicator except reattendance within 7 days, for which there was a slight improvement (i.e. a lower reattendance rate) for patients attending during GPED hours, but the clinical significance of this was judged to be negligible. When comparing patients attending shortly before the finish of GPED with those attending shortly after, patients attending during GPED hours were less likely to wait > 4 hours, leave without being seen or reattend within 7 days. However, the differences were marginal and may reflect rapid changes in demand at the end of core working hours. There were slight variations in outcomes for different GPED models (i.e. integrated, parallel or on site), but no model consistently outperformed the others and none was associated with substantially improved performance or patient outcomes compared with normal services.
Early research examining GPED suggested that it had the potential to be a promising innovation that could reduce the rates of investigations, prescriptions, referrals and hospital admissions, and also increase patient satisfaction. 39–42 However, later researchers began to question these benefits, and also pointed to variable effects, disjointed governance, and the risks of confusing and inefficient service provision. 30,43 We have found no convincing evidence of benefit at an aggregate level; however, our RDD analysis and the resulting forest plots indicate considerable heterogeneity in effect, and this is supported by the qualitative data from our case study sites, showing substantial variability according to local context and circumstances. The potential ‘success factors’ that we identified during this study are considered in more detail in Success factors for introducing GPED.
Objective 4
Objective 4 was to use a mixed-methods approach, including WFSs and interviews, to explore the impact of GPED on GPs, including turnover, absence, satisfaction, well-being and attitudes to and scope of practice.
Objective 5
Objective 5 was to use a mixed-methods approach, including WFSs and interviews, to explore the impact of GPED on the working patterns and roles of other HCPs in the ED, including training, workload, skill-mix and expertise.
In keeping with objectives 2 and 3, we identified a complex and mixed picture regarding workforce effects. Workforce was a prominent issue in the data collected from our case study sites, in particular the challenge of ensuring that rosters were populated consistently with suitably qualified staff.
For ED doctors, GPED had the potential to enhance work experience by reducing ED demand, allowing ED clinicians to focus on patients with emergency needs and reducing the number of patients whom they considered to be using the ED ‘inappropriately’. There was also the possibility of valuable learning and information exchange between the knowledge bases of general practice and emergency medicine. However, the fact that GPs were often paid more than ED consultants and were perceived to be able to ‘pick and choose’ their workload led to resentment at some sites.
For GPs, work in the ED was an active choice and had the benefits of enhanced control over working hours and fewer of the responsibilities associated with traditional general practice. GPED GPs tended to be more recently qualified, often with previous experience in the hospital in which they were working, or approaching the end of their career and seeking change and control. In both cases, there tended to be a stated interest in maintaining and/or broadening emergency care skills. However, practical issues tended to be a source of irritation for GPs; these issues included the working environment, contracts, parking, IT difficulties and, in some cases, concern that their income would be greater in other settings, particularly in view of a relatively high demand for GPs across the health-care system. These qualitative reports from interviews with GPs were also reflected in the WFS. GPs were more likely to be satisfied and effective if they felt that they were part of the team and were valued for their contribution. In our WFS, GPED GPs were substantially less likely to report high levels of pressure relating to time and workload than in the same survey previously administered to GPs in traditional roles. This suggests that GPED may be a less pressured environment for GPs than general practice, though it is also possible that GPs who are less likely to be negatively affected by workforce pressures choose to work in GPED settings.
Some of the most complex workforce effects of GPED were observed within the nursing workforce, in particular more senior nurses who interact with GPs when working in a streaming role. Nursing staff found streaming to be isolating and physically and emotionally exhausting, and many reported that it diverted them from a traditional ED nursing role. We observed conflict with GPs in relation to patients suitable for GPED, and the re-referral of patients from one service to another. In some sites, attempts had been made to address this by agreeing formal protocols; however, the implementation and clinical effectiveness of these protocols was variable. In the WFS, ED nurses reported substantially reduced levels of job satisfaction compared with those of ED doctors, and were less likely to see value in the effect that GPED had on their work.
Furthermore, streaming nurses were unsure how effectively they would be supported by colleagues, the wider organisation and their profession. This indicates that future models of GPED should actively consider how streamers can be supported by colleagues, employers and professional bodies to feel physically, psychologically and professionally safe in their work. These and other support measures, such as stakeholder involvement in service development, appropriate training, clinical supervision, effective protocols and policies, were identified as facilitators that enable nurses to stream effectively and that support nurses in this challenging role.
The premise that ED staff and GPs have inherently different approaches to risk was central to the concept of GPED; however, objective evidence to support this is limited. GPs were perceived to frame health and illness in a different way to ED staff, with the ‘wait-and-see’ culture of primary care leading many to view GPs as more ‘risk tolerant’ and more appropriately qualified to care for lower-acuity patients than their ‘risk-averse’ ED colleagues. This, in turn, was thought to be beneficial for GPED by making GPs less likely to order unnecessary investigations, or admit or refer lower-acuity patients unnecessarily, thereby reducing the time spent in the ED and enhancing patient flow. Despite this general articulation of potential performance benefits, there was significant uncertainty about the impact of GPED within the local systems included in our case studies. One of the main areas of disagreement among site staff and service leaders was the implications for patient safety and risk management, and this resulted in variations in GPED models across sites. Individual views largely varied according to the degree of integration and the specific role of GPs within the system, making it difficult to identify generalised predictions relating to the potential impact of GPED.
Several participants raised concerns that GPs working in GPED services would acculturate and start to behave like ED doctors in their approach to risk, diagnostic investigations and hospital admissions. However, we found no evidence to support this concern. Decision-making around whether or not investigations are required for a specific patient is more complex than simply having access to the investigation, and GPs can access investigations and admit patients to hospital from the community as well as from an ED. In reality, these decisions require a balancing of clinical risk and it is, potentially, this risk that should be discussed with the patient, rather than whether the investigation or admission is readily available or not. Therefore, systematic differences between GPs and ED doctors may be small in comparison to within-group variation (i.e. the differences in risk tolerance and behaviour that exist between individual GPs or individual ED doctors). 101 As a result, any theoretical difference in risk management between GPs and ED doctors as a professional group may be overstated. 102
There is very little published literature that considers the impact of GPED on the staff who deliver it; therefore, to the best of our knowledge, we have completed the first comprehensive mixed-methods study of this policy on all elements of the GPED workforce.
Objective 6
Objective 6 was to use a mixed-methods approach, involving secondary data analysis and qualitative techniques, to explore the impact of GPED on local urgent care services; the wider system, including primary care (e.g. demand for in-hours and OOH GP appointments); and the interface between services, including patient flow.
For the reasons described in Chapter 2, we were unable to obtain meaningful quantitative data on the impact of GPED on local urgent care services and the wider system; however, given that we found no effect on ED attendances and a range of ED performance measures (with the exception of a minimal effect on unplanned reattendance within 7 days), it seems unlikely that the wider effects of GPED are substantial. This view was supported by our qualitative analysis, in which most of the patients who we interviewed were unaware of GPED and, therefore, had not changed their behaviour. Furthermore, because ED staff frequently expressed concern that GPED services would lead to increased demand these services were not advertised locally, reducing the likelihood of wider impacts. We observed confusion among patients, staff and other NHS services as to the availability and purpose of GPED, and the main drivers of ED attendance did not appear to be related to the presence or absence of ED services. This is in keeping with other evaluations of service initiatives in urgent and emergency care; for example, walk-in centres were introduced with the aim of shifting demand from EDs and urgent primary care, but were found to have a limited impact at best. 103 These centres were also found to be highly varied and sensitive to local context, with many subsequently closing. A report published in 2014 found that ‘commissioners who have closed [walk-in] centres often cited concerns that the centres were generating unwarranted demand for services; that they led to duplication . . . [and] caused confusion among patients (contains public sector information licensed under the Open Government Licence v3.0; www.nationalarchives.gov.uk/doc/open-government-licence/version/3/). 58 Concerns were also raised that commissioners were paying for general practice and the new service simultaneously. Parallels with GPED services are apparent.
Objective 7
Objective 7 was to use interviews and non-participant observation to assess the impact of GPED on patients and carers.
In general, we found patients to be accepting and understanding of GPED, and content to receive GPED care if they did not perceive their problem to require specific emergency skills, and if they had not been referred from a GP or other service with the express intention of accessing ED care. Service configuration and the specialty background of the treating practitioner were less important than other factors (e.g. timeliness, communication and problem resolution), and many patients were not clear as to whom they were seen by when attending the ED. We found no objective evidence that patients received better or worse care from GPED than from traditional ED services.
In a recent and relatively small study, Uthman et al. 45 found that GPs who saw patients in the ED used fewer resources, without increasing reattendance, and also referred more patients to follow-up services. This is in keeping with our finding that unscheduled reattendance to the same ED within 7 days was very slightly less likely for those patients who attended when a GPED service was in operation. We were not able to measure differences in follow-up arrangements in our study as these data are not collected routinely; however, if GPED services tended to arrange more follow-up appointments, this would be expected to reduce the frequency of unscheduled reattendance. This also has implications for resource use as if more follow-up appointments are arranged by GPED services, then this is likely to be associated with additional costs.
Both patients and staff indicated that a potential benefit of GPED is the provision of a unified service and access point to urgent care, with the potential to reduce confusion and repeat visits to different providers. This was also identified by Ablard et al. ,46 who found that service users appreciated simplified health-care provision from a single point of access.
Objective 8
Objective 8 was to explore the costs and consequences of care at ED sites with and without GPs in or alongside the ED, and compare the costs of different service models.
The improvements we found in reattendance rates under GPED equate to 0.88 reattendances avoided each day for the average study ED. If this was reproduced at the national level, it would result in around 47,000 reattendances avoided each year, without any apparent change in unnecessary attendances, admission rates or mortality. This is an appreciable reduction, generating a cost saving for the NHS of £4.4M–5.4M per year, depending on tariff costs and assuming no change in the case mix of reattendances. This is vastly outweighed, however, by the cost of running GPED services, which we crudely estimate at £66.7M per year.
It should be noted, however, that the salary cost of GPED services was based on national average figures,68 rather than the actual salaries paid to GPs working in GPED. These are likely to be negotiated individually, and are potentially higher than the national average. Furthermore, there are likely to be additional costs associated with GPED, such as support staff, training and IT costs, as well as the possibility that GPED leads to additional follow-up appointments, as discussed in Objective 7. Therefore, the calculated cost of GPED services is likely to be an underestimate, further undermining any possibility of cost-effectiveness.
Previous considerations of the costs and consequences of GPED have been theoretical, rather than based on research data. 59 Although our approach is very straightforward, the lack of any consistent evidence of measurable benefit makes it hard to anticipate a situation in which GPED is found to be generally cost-effective. However, given the degree of heterogeneity in our data, this overall finding does not preclude the possibility that GPED could prove to be cost-effective in individual sites if the factors to achieve this exist. This view was supported by the participants interviewed in our case study sites, who could understand and describe circumstances in which GPED had the potential to be cost saving, although this was acknowledged to require an unusual alignment of circumstances.
Objective 9
Objective 9 was to use interviews with managerial and clinical leaders, the analysis of HES data66 (where available) and a prospective mixed-methods case study to prospectively evaluate the current promotion of GPED models of care through collaboration with staff from sites that received capital funding to implement GPED.
Although high-level goals, including improvements in performance because of reductions in patient waits, were shared at both the macro level and meso level, the implementation of GPED was mainly influenced by micro-level factors, particularly the impact on front-line staff. The capital funding provided by central government was used to support operational, structural and organisational changes, and the reality of introducing GPED was very varied.
Some of the sites awarded funding were already using a GPED model, and this funding enabled further development, whereas other sites were introducing GPED for the first time. This was reflected in the taxonomy changes that occurred: the number using an integrated model reduced, whereas the number of parallel and on-site GPED models increased. This is likely to reflect the use of capital funding to build, extend or refurbish new facilities in which GPED services were then provided.
Experiences of GPED were also mixed. Some reported that the initiative had realised their expectations, resulting in positive outcomes. However, others reported several challenges, in particular issues in governance and staffing, with little impact on performance. Some abandoned GPED altogether.
Warwick104 indicates that the trajectory from policy to reality is rarely linear. Our findings suggest that the implementation of this national policy initiative was tempered by local needs, alongside available resources. 104 Warwick also argues that national policies are often driven by political agendas that differ from those featured in the policy. 104 GPED could be seen as a public response to rising demand in EDs with declining ‘4-hour’ performance, but with little evidence to support GPED as an effective solution. Similarly, Mee105 explores the disparity between government expectations related to funding provision for services local planning and decision-making; this was reflected in the some of our responses.
Framing the findings at the macro level, meso level and micro level was a useful way of studying the evolution of a policy from high-level idea to practice. 72 Our findings demonstrate that policy developed at a governmental level does not always translate into health-care provision locally. In addition, attributing the origin of outcomes is challenging. A top-down approach would suggest that any outcomes are associated with the governmental policy; however, taking a more bottom-up approach recognises the role of local actors and influences, and that outcomes are often the result of the implementation process. 73
Much of the progress and desire to change practice that we observed in our interviews was driven at the meso level and micro level, whereby the local system leaders and the front-line staff felt the need to change. Although stakeholders may push for policy changes at a macro level, it is the pull from the meso level/micro level that has the greatest effect in practice. 71
Furthermore, we found that interviewees often described quite different and complex approaches to GPED that contrasted with the simple high-level policy messages that accompanied the provision of capital funding. Pope et al. 70 report the complexities of translating a concept into practice and that the consequent local adaptations may result in a very different innovation from what was proposed. Our findings support this view.
Success factors for introducing GPED
This section identifies a series of ‘success factors’ that may inform how services choose to implement future GPED models. Examples of these success factors include streaming, staff training and IT access.
Streaming
Streaming was considered fundamental to the success of GPED. Several key factors that support streaming were identified across the case sites. These factors were structural support, streaming personnel, streaming protocols, negotiating primary/secondary care boundaries, interprofessional relationships and safety.
There are several factors that would be integral to implementing any service design, for example engaging staff in the planning and organisation of the service, visible leadership, addressing training needs and regularly auditing the service to evaluate clinical effectiveness. Practical issues such as functioning and integrated IT systems and adequately covered work rotas are also important. However, at several case study sites, these fundamental issues had been overlooked and the GPED service was weakened substantially as a result.
Although a flagship model (the L&D model) of GPED and streaming was recommended at a national level, case sites found this problematic and had developed streaming based on the perceived requirements of the local population, and also in response to the availability and skills of their staff. Streaming did not necessarily reflect national or professional definitions of streaming; instead, there were often a variety of streaming and triage processes that were based on previously established ways of working. It was often unclear to both staff and researchers what form of streaming was being used and whether patients were being streamed, triaged or both. Consequently, it was difficult to identify specific models that were more beneficial. There were, however, a number of factors that were identified across sites that influenced the clinical effectiveness of streaming. These can be used to develop and enhance future working practices.
The experience and seniority of streaming nurses
All streamers observed across all case sites were registered nurses, and there was significant agreement that the experience and seniority of the nurse was fundamental to safe and effective decision-making. This is because streaming is a safety-critical role that requires a high level of clinical knowledge and skill, as well as critical thinking and clinical decision-making, and tolerance to making decisions around clinical risk.
However, it was also clear that there was a lack of suitably qualified and experienced nurses, and that streamers often found streaming a stressful and unattractive role in which they sometimes felt unsupported in their streaming decisions. Consequently, it is necessary for streamers to be and to be seen to be systematically supported in their role and for policy-makers to develop strategies to support the training and development of streaming clinicians in a sustainable way. One case site had developed the role so that the streaming nurse also assessed and managed some patients. This allowed the streaming nurse to remain engaged in ‘hands-on’ clinical work that was commensurate with their level of skill and knowledge, as well as supporting the development of a close working relationship with GPs, which aided the appropriateness and clinical effectiveness of streaming.
The skills, confidence and abilities of general practitioners
The characteristics of GPs differed not only between case sites, but between individual clinicians, with GPs varying in skills, confidence and willingness to manage patients presenting with different conditions. GPED services across case sites depended on locum and part-time GPs, who varied in their levels of experience and scope of practice, so standardisation was difficult to achieve. Streamers were often unclear about which patients different GPs would accept, and proactive and experienced GPs were welcomed.
It was important to standardise GP practice and develop clarity on which presentations were considered appropriate to be seen by a GP within case sites. Some case sites had implemented policies and protocols to address this. This gave streamers guidance, and also redress when there were conflicting views between streamers and GPs about which presentations should be referred to GPED. However, it was acknowledged that there needs to be inbuilt safeguards to ensure that GPs can safely refer patients that they are not comfortable managing in GPED. Similarly, streaming nurses were more effective when they were able to exercise elements of their professional discretion. As a result, a careful balance needs to be struck between protocolised pathways and clinical expertise.
Emergency department and general practice culture
Streamers often had little understanding of primary care practice and worked in a way that reflected the cultural working practices of EDs and secondary care. This contrasted with GPs, who were used to working in a more autonomous and isolated way; this led to tension between primary and secondary care colleagues. ED staff expected GPs to assimilate into their established ways of working and communicating, yet, at the same time, they expected these individuals to bring their unique general practice skills to bear.
Staff often behaved in a way that protected their own working environment at the expense of other parts of the department. As a result, both the ‘inappropriate’ streaming of patients to GPED and the ‘inappropriate’ return of patients from GPED to the ED increased when the departments were busy. It was also felt that there was a lack of reciprocity between the ED and GPED, which encouraged resentment. In this way, the lack of cohesive working negatively affected both the ED and GPED. This links to trust between streamers and GPs, which was found to be a significant issue. Effective working relationships were based on streamers and GPs knowing and trusting each other, and being confident in their competence to carry out their role.
However, it cannot be assumed that co-location or integration of GPED within the ED is sufficient to promote or achieve collaborative working, generate trust or address cultural differences between different groups of clinicians, and we visited sites that were physically integrated but culturally divided. Therefore, it is necessary to actively work to enhance collaborative working; increase understanding of professional and primary/secondary care roles; and culturally integrate GPED staff, enabling them to feel less isolated and part of the wider team.
Streaming safety
Safety concerns were common and limited the clinical effectiveness of streaming and GPED more broadly. Streamers were less likely to stream patients to GPED if they had safety concerns.
Strategies are required to address the concerns of staff and to provide reassurance so that streaming can be implemented safely. For streamers, support to use their clinical judgement to deviate from protocols and procedures when appropriate helped to mitigate their concerns.
Streamers were usually senior nurses, so they often had an additional role of overseeing safety in the wider ED. This had an impact on their focus on effective streaming, but was seen as important in maintaining safety more broadly. Despite this dual focus, streamers were concerned by any changes that led to a reduction in their oversight of the ED as a whole. Consequently, it is necessary for staff to continue to have input into ongoing service development and for their concerns regarding safety to be taken into consideration.
Implementation issues
Issues surrounding implementation were largely related to structural support within the site, interprofessional relationships between staff, safety concerns and influencing factors related to the GP’s role within the ED. Staff mainly discussed negative aspects of implementation that they had faced; however, some facilitators of implementation were highlighted.
Structural support was variable between sites and was facilitated by effective, on-the-ground management and leadership. Where this was not present, staff tended to express frustration at being managed in a top-down way by those not on the ‘shop floor’. Daily huddles were seen as a positive for implementation, as were regular staff meetings. However, GPs were often criticised for not attending daily huddles and, at some sites, only senior staff were invited to regular meetings to feedback about the department, which made more junior staff feel alienated and ignored.
Positive interprofessional relationships were often evolving (i.e. relationships between ED and GPED staff were developing as time progressed); however, an ‘us and them’ atmosphere was still mentioned frequently, with the two departments often viewed as not well integrated and as having poor communication. This could be exacerbated by a high turnover of GPs and where there was high variation in what types of patients a GP would see. A good working relationship was fostered by cross-service working, strong communication and a shared working environment.
A lack of IT integration between ED and GPED systems was viewed as a safety risk by staff as it hindered the sharing of patient information between departments and required the same information to be entered twice. This could lead to errors during imputation or issues around patients providing slightly different information to staff.
Space was another safety issue, with staff at some sites stating that the waiting area was too small for the volume of patients, leading to overcrowding. Furthermore, in some instances, the configuration of the waiting room and department meant that patients were isolated from staff while they were waiting and GPs could be isolated from the rest of the department.
Regarding positives of implementation, GPs reported satisfaction with the GPED role and enjoyed the flexible working hours, the rates of pay, and the opportunity to treat different types of patients and to spend longer treating them than in primary care. Inadequate facilities were sometimes reported, such as small rooms and no access to a kitchen, with a feeling of being separated from the rest of the department.
Implications for clinical practice and service delivery
Following from the previous sections, we offer a summary of the key implications of our work for clinical practice and GPED service delivery:
-
GPED services are highly context specific and could be planned and implemented in a way that is sensitive to local circumstances, service provision, workforce and demand. One size does not fit all.
-
It is essential to be clear as to the intended benefits and outcomes that will follow GPED implementation; these benefits should be actively monitored and measured to understand the extent to which they have been achieved over time.
-
Clear governance and oversight arrangements could be established from the outset, in particular the expected scope of practice of those clinicians providing the GPED service. Access to diagnostic investigations, specialist reviews and hospital admissions could be agreed and consistent for all GPs.
-
GPED services are most likely to be successful in circumstances where significant numbers of eligible patients attend the ED, where a stable GPED workforce can be recruited and retained, and where the physical environment allows the planned service to be delivered successfully.
-
Effective streaming is central to an effective GPED service. Streaming staff are usually experienced nurses, and could be trained and supported to ensure that they are able to deliver a clear, safe, consistent and rewarding streaming process.
-
Staff engagement is required from the outset, at all levels and across all professions. Strong and visible management and clinical leadership are required over an extended period of time, and particular efforts could be made to foster effective communication and develop positive interprofessional relationships and a spirit of team working.
-
Care could be taken to ensure that supporting IT and administrative systems are put in place.
-
The GPED service should be subject to regular multidisciplinary audits and reviews, including a review of service performance and clinical incidents.
-
Enduring service change takes time, and results will not be realised immediately; commitment and perseverance are required from all parties.
Strengths and limitations
To the best of our knowledge, this is the most complete and detailed study of GPED provision in England to date. Our analysis used robust modelling approaches and individual patient data from type 1 EDs linked to in-patient and mortality data to assess the differences in hospital performance and patient outcomes between GPED services and normal services. The HES data set66 allowed us to adjust for a range of potential confounders, including age, sex, ethnicity, level of deprivation and arrival method. Crucially, given the strong associations between time of attendance and patient volume and acuity, we were also able to take account of the time of attendance in relation to the different timings of GPED services.
We used two different statistical approaches to quantify the impact of GPED on outcomes, which rely on different sources of variation in the availability of GPED services across hospitals or time. Both methods yielded similar findings, which greatly increases our confidence in our estimates. Our telephone interviews were conducted prospectively and through these we were able to collect the views of national policy-makers and local system leaders, based on their recent experiences. The ‘domains of influence’ that we have identified in this report were generated from a large evaluation that used ‘big qualitative data’ (n = 228 interviews) and the views of multiple stakeholders. This provided a rich and nuanced understanding of the complexity surrounding a current national policy: GPED. Our 10 case studies included participants from a wide range of EDs in terms of size, location and existing use of GPED, and we collected a very large number of interview, observation and survey data to provide a comprehensive understanding of GPED provision and address our study aims.
However, our study has a number of limitations. These are:
-
The reliability of the data sources used to populate our database (WP A) varied and required some interpretation by the research team. In addition, data collection relied on self-reporting and respondents’ ability to accurately describe their model of service provision. As a result, we included a smaller sample of EDs in our quantitative analysis than we had planned.
-
We were unable to complete our quantitative analysis as intended, and were required to adjust our analysis plan and exploration of the costs and consequences of GPED accordingly. We were also limited in our ability to collect data from the primary and urgent care systems surrounding our WP C case study sites, which significantly limited our ability to quantitatively evaluate the effect of GPED on the wider health-care system as planned. (This is considered further at the beginning of Chapter 2.)
-
There were several limitations to the quantitative analysis of the data –
-
We relied on data that were routinely collected by ED staff and were, therefore, dependent on the complete and accurate recording of patient episodes. Different key variables had different levels of missingness within the data set and between hospitals, and there is the potential for missingness not at random if, for example, GPs record information in different ways from ED staff or if ED staff change their recording behaviour in response to GPED.
-
There is the potential that patient episodes may be misclassified as GPED/not GPED, as streaming activity and GP availability may not have corresponded exactly to official GPED start and finish times, particularly for patients arriving close to these times or undergoing extended waits. Related to this, our analysis assumes that GPED was always operational during designated hours and, therefore, does not account for physician absence. To reduce the risk of misclassification, we excluded patients arriving in the hour before GPED start/finish times in our RDD analysis. Including these patients in a sensitivity analysis produced similar results, tending slightly more towards zero impact.
-
We lacked detailed cost data for GPED services, so we used crude estimates based on average GP salaries and estimates of hours of operation. Therefore, associated costs are missing from our analysis, as are any offsetting costs relating to compensatory reductions in other forms of staffing. Related to this, we were not able to assess ‘role substitution’ (i.e. whether GPs were directly added to normal services or they replaced another member of staff). In addition, we did not assess the full opportunity costs of GPED in terms of alternative uses of GP salaries by EDs (e.g. employing additional consultants and/or nurses) and reductions in GP availability in the community, which is already characterised by shortages.
-
Because of the national roll-out of GPED services and the lack of information on implementation dates, we were unable to conduct our intended analyses that would have provided a cross-sectional comparison across hospitals with and without GPED services (i.e. ‘intervention’ vs. ‘control’ hospitals) or a within-hospital comparison over time, using an interrupted time series (before and after) approach. Instead, for hospitals where a GPED service was already in place, we compared patients arriving at times when GPED was operational with patients arriving when GPED was not operational. Therefore, we could not account for any broader effects of GPED on hospital procedures and patient outcomes that occur outside the operational hours of the service.
-
-
In our interviews with system leaders who were implementing GPED initiatives with capital funding support, we were able to interview representatives from only 36% of all eligible EDs and the respondents may not have been representative of all EDs. This weakness was compounded by the fact that follow-up interviews were completed in only 47% of the EDs in which staff we were able to interview initially.
-
Our case study sites were purposively selected to be as representative as possible; however, the participation of all 10 sites, and of the staff and patients within those sites, was voluntary. We could interview only those who agreed to take part and, although our data span a very wide range of individuals and views, they are unlikely to be exhaustive.
-
In particular, staff choosing to complete the WFS may not have been representative of all of the staff involved in GPED at that site. The WFS return rate was 24%. This is at the lower end of the range reported from a meta-analysis of 59 methodological studies106 designed to estimate the magnitude of non-response bias in statistics of interest. This lower level of return reflects the challenges of engaging a wide range of staff and the relative length of the survey. In some sites, local concerns regarding information governance limited our ability to disseminate the survey effectively. Although the low response rate is a potential study weakness, it should be noted that response rate is not necessarily predictive of non-response bias validity and, therefore, low response rates should not be cited routinely as a reason to disregard survey results. 107 Given the close alignment between the results of the survey and our other approaches to data collection, we believe that the survey provides a valuable and complimentary contribution to the other study findings.
-
The analyses of data from the WFS involved comparisons that should be interpreted cautiously, for the following reasons –
-
Comparisons with data from the Ninth National GP Worklife Survey75 should be considered in relation to the very small number of GPED GPs who were represented in the survey sample.
-
As far as we are aware, comparable items from the Ninth National GP Worklife Survey75 (e.g. regarding job satisfaction) have not been widely administered to other staff groups (e.g. nurses).
-
This report presents a selection of results from the WFS that were chosen on the basis of mixed-methods considerations (i.e. they reported survey findings that either aligned or contrasted with qualitative data to provide a form of methodological triangulation). However, this approach means that some results from the WFS are not included in the main report, and these can be found in Appendix 3.
-
-
Our data apply to England only, so they may not be generalisable to other countries and health-care settings.
-
It could be argued that the data we present here represent the inherent uncertainty and resistance to change that most health-care policies encounter prior to or during early implementation, so the data are representative of typical ‘teething problems’. However, although there is evidence that it takes 2–6 years to achieve lasting service change and it is, therefore, assumed that such issues will improve over time,108 recent research suggests that issues that are identified early in the implementation process often persist long after establishment. 109
Recommendations for future research
This is a comprehensive mixed-methods evaluation of GPED in England and, when combined with the study that was commissioned under the same funding call (HSDR project 15/145/04; URL: https://fundingawards.nihr.ac.uk/award/15/145/04; accessed October 2021), which we anticipate will examine cost-effectiveness in more detail, it seems unlikely that further similar research will yield substantial additional knowledge. We therefore offer the following recommendations for future research, listed in priority order:
-
As identified in Strengths and limitations, although some forms of GPED have existed for decades, a co-ordinated national initiative is relatively new and expected to develop over time. If these service models continue, further research after a period of 3–5 years could be considered to understand the longer-term effects and implications.
-
We identified particular ambiguity and uncertainty in relation to streaming in the ED; further research to better understand streaming and clarify the optimal approach to streaming in terms of patient outcome, safety and experience, and associated staff experience is recommended.
-
Part of the underlying premise of GPED rests on assumptions regarding differing attitudes to risk tolerance and risk management between GPs and emergency physicians; however, empirical evidence to support this hypothesis is limited. Additional research to explore attitudes to risk and how these vary between and within medical specialties, and the impact that this has on practical clinical decision-making, could help to ensure that staff are trained, deployed and supported in ways that maximise clinical effectiveness, efficiency and patient safety.
-
Research addressing the ways in which national policy initiatives should be developed, piloted and implemented in the most clinically effective and cost-effective manner is surprisingly limited, with a lack of consensus across the health and care system. We have considered this issue in our report, and believe that further research is required to explore and understand the contrasting views of stakeholders, and provide empirical evidence as to how national health-care initiatives should be implemented (rather than whether or not a particular initiative is effective).
-
Following on from the above, comprehensive evaluations of new models of service delivery often lag behind practical implementation. This undermines the purpose of evaluation as by the time commissioned research has been completed the change has been enacted. This is a particular problem if the evaluation does not support the new model of service delivery. We, therefore, recommend that a set of standards is developed for health policy implementation, including an outline evaluation protocol to ensure that the necessary data are available and the necessary design is feasible. This should be supported by methodologies that allow rapid and ‘real-time’ evaluation of new models of workforce and service delivery in health and social care.
-
The relationship and interface between primary and secondary care within the wider context of the health and care system remains central to the future delivery of urgent and emergency care. Further research is required to understand this relationship and guide future models of service development and delivery in the context of rising health-care demand.
Summary
In this chapter, we have summarised our findings using the framework of NPT and discussed each of our nine objectives. We have considered the practical implications of our findings, described the strengths and weaknesses of our study and listed our recommendations for future research. A short conclusion chapter now follows (see Chapter 5).
Chapter 5 Conclusion
We set out to explore the effects of GPED on patient care, the primary care and acute hospital team, and the wider urgent care system, and to determine the differential effects of different service models of GPED.
The vast majority of EDs in England have a GPED model in place. Central direction supported by capital funding resulted in an increase in parallel GPED models and a corresponding reduction in integrated approaches. We found no relationship between the type of GPED model adopted and the receipt of capital funding or other observable characteristics of the ED.
Although high-level goals for the implementation of GPED were shared between national policy-makers and local system leads, there was a lack of agreement as to the anticipated effects of GPED and, in some cases, even the direction of effect was contested. We identified eight domains of influence in which GPED was expected to act: performance against the ‘4-hour target’, use of investigations, hospital admissions, patient outcome and experience, service access, workforce recruitment and retention, workforce behaviour and experience, and resource use. The policy context in which GPED was implemented nationally, and the use of L&D as a national blueprint, was seen as potentially problematic at a local level.
GPED had no effect on ED performance or patient outcomes, aside from a very slight reduction in the rate of reattendance at the same ED within 7 days, equivalent to 320 fewer reattendances per ED per year, which was judged to be of negligible clinical significance. There were minor differences in outcomes for alternative GPED models and at different times of operation, but no model consistently outperformed the other models. There was, however, a substantial degree of heterogeneity within these findings. This is explained by the considerable variation observed in our case study sites, and the sensitivity of GPED implementation to local site factors. The lack of overall effect on ED performance and outcome could be explained by the fact that these indicators are subject to a wide range of influences, of which GPED is a minor component only.
The effects of GPED on the workforce were complex: the effects were often positive for ED doctors and GPs, but less so for ED nursing staff. This effect on ED nursing staff was closely related to the process of streaming patients to GPED services, which generated stress and conflict. GPs were more likely to be satisfied and effective if they felt that they were part of the team and valued for their contribution; GPs generally reported levels of pressure that were lower than those of their peers working in traditional general practice settings.
Patients and carers were understanding and accepting of GPED services, and we found no evidence that staff concerns regarding GPED’s potential to create additional ED demand were justified. The main determinants of patient experience and outcome were not significantly influenced by GPED models of care.
Possible cost savings associated with reduced reattendances (£30,000–7,000 per ED per year; £4.4M–5.4M per year nationally) were heavily outweighed by the cost of GPED services which, even including salary costs of the GP alone and potentially a substantial underestimate, amount to (£454,000 per ED per year, £66.7M per year nationally). As a result, current GPED models do not appear to be an efficient use of health-care resources.
The implementation of GPED was highly subject to local context and micro-level influences. Key success factors were adequate staffing and training, streaming, infrastructure and support. Interprofessional working supported by effective processes and systems was a key determinant of success.
Even when a policy change is made mandatory and supported by dedicated funding to encourage and support adoption, subsequent success is not always assured. We found GPED to be highly sensitive to, and dependent on, local context, with no consistent evidence of improvement to patient outcome, experience or cost-effectiveness, and no significant difference between the various types of service model adopted.
Acknowledgements
We would like to acknowledge:
-
the research participants –
-
interviewees in national-level system leader interviews
-
interviewees in site-level system leader interviews
-
principal investigators at each of our 10 case study sites
-
all staff and patients who either participated in an interview or agreed to be observed in our case study sites
-
-
Dr Jason Scott, the qualitative researcher involved in data collection
-
Dr Hayley Dash, who provided administrative support for the study
-
all of the members of the SSC –
-
Professor Suzanne Mason (chairperson)
-
Professor Daniel Lasserson
-
Professor Matthew Sutton
-
Professor Catherine Pope
-
Mrs Adele Webb
-
Mr John Thompson
-
-
all of our public contributors
-
the sponsor/host –
-
Paul Roy, who provided contract management on behalf of the sponsor, Bristol, North Somerset and South Gloucestershire Clinical Commissioning Group (BNSSG CCG)
-
Alison Diaper, who provided project support on behalf of the sponsor, BNSSG CCG
-
Olena Doren, Associate Dean at the Research Faculty of Health and Applied Sciences, UWE
-
Katalin Bagi, who provided financial management on behalf of the sponsor, BNSSG CCG.
-
Contributions of authors
Jonathan Benger (https://orcid.org/0000-0001-6131-0916) (Chief Investigator) took responsibility for the integrity of the data and the accuracy of analysis, was involved in the study conception and design, interpreted the data, and drafted and critically revised this manuscript. He is the guarantor.
Heather Brant (https://orcid.org/0000-0001-9608-7451) (Project Manager) collected and interpreted the data, provided project co-ordination and support, and drafted and critically revised this manuscript.
Arabella Scantlebury (https://orcid.org/0000-0003-3518-2740) (Qualitative Researcher) was involved in the data collection, analysis and interpretation, and critically revised this manuscript.
Helen Anderson (https://orcid.org/0000-0002-6945-0590) (Qualitative Researcher) was involved in the data analysis and interpretation, and critically revised this manuscript.
Helen Baxter (https://orcid.org/0000-0002-3320-2915) (Knowledge Mobilisation Expert) was involved in the study conception and design, supported knowledge mobilisation and dissemination, and critically revised this manuscript.
Karen Bloor (https://orcid.org/0000-0003-4852-9854) (Statistician and Expert in the Analysis of Routine Health Data) was involved in the study conception and design, supervised data collection and interpretation, and critically revised this manuscript.
Janet Brandling (https://orcid.org/0000-0003-3352-7979) (Qualitative Researcher) was involved in the data collection, analysis and interpretation, and critically revised this manuscript.
Sean Cowlishaw (https://orcid.org/0000-0002-8523-3713) (Statistician with Expertise in Cross-Sectional and Longitudinal Observational Studies) was involved in the study conception and design, supervised data collection and interpretation, and critically revised this manuscript.
Tim Doran (https://orcid.org/0000-0001-7857-3704) (Statistician and Expert in the Analysis of Routine Health Data) was involved in the study conception and design, supervised data collection and interpretation, and critically revised this manuscript.
James Gaughan (https://orcid.org/0000-0002-8409-140X) (Data Analyst) undertook statistical data analysis and interpretation, and critically revised this manuscript.
Andrew Gibson (https://orcid.org/0000-0002-4641-2583) (PPI Expert) was involved in the study conception and design, supported PPI and critically revised this manuscript.
Nils Gutacker (https://orcid.org/0000-0002-2833-0621) (Statistician and Expert in the Analysis of Routine Heath Data) was involved in the study conception and design, supervised data collection and interpretation, and critically revised this manuscript.
Heather Leggett (https://orcid.org/0000-0001-8708-9842) (Qualitative Researcher) was involved in the data collection, analysis and interpretation, and critically revised this manuscript.
Dan Liu (https://orcid.org/0000-0002-1891-9352) (Data Analyst) undertook the statistical data analysis and interpretation, and critically revised this manuscript.
Katherine Morton (https://orcid.org/0000-0003-2413-8867) (Project Manager) collected and interpreted the data, provided project co-ordination and support, and critically revised this manuscript.
Sarah Purdy (https://orcid.org/0000-0002-3445-986X) (Expert in Primary and Urgent Care Research) was involved in the study conception and design, involved in the data analysis and interpretation, and critically revised this manuscript.
Chris Salisbury (https://orcid.org/0000-0002-4378-3960) (Expert in Primary and Urgent Care Research) was involved in the study conception and design, involved in the data analysis and interpretation, and critically revised this manuscript.
Anu Vaittinen (https://orcid.org/0000-0001-8471-9204) (Qualitative Researcher) was involved in the data collection, analysis and interpretation, and critically revised this manuscript.
Sarah Voss (https://orcid.org/0000-0001-5044-5145) (Researcher in Emergency Care) was involved in the study conception and design, supported data collection, interpreted the data and critically revised this manuscript.
Rose Watson (https://orcid.org/0000-0003-4549-3462) (Qualitative Researcher) was involved in the data collection, analysis and interpretation, and critically revised this manuscript.
Joy Adamson (https://orcid.org/0000-0002-9860-0850) (Expert in Mixed Methodology and Ethnographic Approaches) was involved in the study conception and design, supervised the data collection and interpretation, and critically revised this manuscript.
Publications
Morton K, Voss S, Adamson J, Baxter H, Bloor K, Brandling J, et al. General practitioners and emergency departments (GPED) – efficient models of care: a mixed-methods study protocol. BMJ Open 2018;8:e024012.
Cooper A, Edwards M, Brandling J, Carson-Stevens A, Cooke M, Davies F, et al. Taxonomy of the form and function of primary care services in or alongside emergency departments: concepts paper. Emerg Med J 2019;36:625–30.
Brant H, Voss S, Morton K, Cooper A, Edwards M, Price D, et al. Current provision of general practitioner services in or alongside emergency departments in England. Emerg Med J 2021;38:780–3.
Scantlebury A, Brant H, Anderson H, Leggett H, Salisbury C, Cowlishaw S, et al. Potential impacts of general practitioners working in or alongside emergency departments in England: initial qualitative findings from a national mixed-methods evaluation. BMJ Open 2021;11:e045453.
Scantlebury A, Adamson J, Salisbury C, Brant H, Anderson, H, Baxter H, et al. Do general practitioners working in or alongside the emergency department improve clinical outcomes or experience? A mixed-methods study. BMJ Open 2022;12:e063495-e063495.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care.
References
- Cooper A, Edwards M, Brandling J, Carson-Stevens A, Cooke M, Davies F, et al. Taxonomy of the form and function of primary care services in or alongside emergency departments: concepts paper. Emerg Med J 2019;36:625-30. https://doi.org/10.1136/emermed-2018-208305.
- Berchet C. Emergency Care Services: Trends, Drivers and Interventions to Manage the Demand. Paris: Organisation for Economic Co-operation and Development; 2015.
- NHS Digital . Hospital Accident &Amp; Emergency Activity 2018–19 2019.
- Royal College of Emergency Medicine . Performance Figures for February March 2020 2020. www.rcem.ac.uk/RCEM/News/A_E_Performance_Figures.aspx?WebsiteKey=b3d6bb2a-abba-44ed-b758-467776a958cd (accessed 1 March 2021).
- Edwards N. Here to Stay? How the NHS Will Have to Learn to Live with Coronavirus. London: Nuffield Trust; 2020.
- O’Dowd A. Emergency departments must not return to pre-covid days of overcrowding and lack of safety, says college. BMJ 2020;369. https://doi.org/10.1136/bmj.m1848.
- Royal College of Emergency Medicine (RCEM) . RCEM Position Statement COVID-19: Resetting Emergency Department Care 2020.
- Pines JM, Griffey RT. What we have learned from a decade of ED crowding research. Acad Emerg Med 2015;22:985-7. https://doi.org/10.1111/acem.12716.
- Bernstein SL, Aronsky D, Duseja R, Epstein S, Handel D, Hwang U, et al. The effect of emergency department crowding on clinically oriented outcomes. Acad Emerg Med 2009;16:1-10. https://doi.org/10.1111/j.1553-2712.2008.00295.x.
- Collis J. Adverse effects of overcrowding on patient experience and care. Emerg Nurse 2010;18:34-9. https://doi.org/10.7748/en2010.12.18.8.34.c8152.
- Morley C, Unwin M, Peterson GM, Stankovich J, Kinsman L. Emergency department crowding: a systematic review of causes, consequences and solutions. PLOS One 2018;13. https://doi.org/10.1371/journal.pone.0203316.
- Rasouli HR, Esfahani AA, Nobakht M, Eskandari M, Mahmoodi S, Goodarzi H, et al. Outcomes of crowding in emergency departments; a systematic review. Arch Acad Emerg Med 2019;7.
- Richardson DB. Increase in patient mortality at 10 days associated with emergency department overcrowding. Med J Aust 2006;184:213-16. https://doi.org/10.5694/j.1326-5377.2006.tb00204.x.
- Higginson I. Emergency department crowding. Emerg Med J 2012;29:437-43. https://doi.org/10.1136/emermed-2011-200532.
- Triggle N. ‘Misery’ for A&E patients facing record-long waits. BBC News 2020. www.bbc.co.uk/news/health-51046616 (accessed 1 March 2021).
- NHS England . Transforming Urgent and Emergency Care Services in England. Urgent and Emergency Care Review End of Phase 1 Report 2013.
- Thompson MI, Lasserson D, McCann L, Thompson M, Heneghan C. Suitability of emergency department attenders to be assessed in primary care: survey of general practitioner agreement in a random sample of triage records analysed in a service evaluation project. BMJ Open 2013;3. https://doi.org/10.1136/bmjopen-2013-003612.
- Murphy K, Mann C. Time to Act – Urgent Care and A&E: The Patient Perspective. London: Royal College of Emergency Medicine and The Patients Association; 2015.
- Foster S, Bisset C. Prescribing the remedy: co-located out-of-hours GP – what would this actually mean for a paediatric emergency department?. Arch Dis Child 2015;100:A43-A4. https://doi.org/10.1136/archdischild-2015-308599.99.
- Gnani S, McDonald H, Islam S, Ramzan F, Davison M, Ladbrooke T, et al. Patterns of healthcare use among adolescents attending an urban general practitioner-led urgent care centre. Emerg Med J 2014;31:630-6. https://doi.org/10.1136/emermed-2012-202017.
- O’Keeffe C, Mason S, Jacques R, Nicholl J. Characterising non-urgent users of the emergency department (ED): a retrospective analysis of routine ED data. PLOS One 2018;13. https://doi.org/10.1371/journal.pone.0192855.
- Morris T, Mason SM, Moulton C, O’Keeffe C. Calculating the proportion of avoidable attendances at UK emergency departments: analysis of the Royal College of Emergency Medicine’s Sentinel Site Survey data. Emerg Med J 2018;35:114-19. https://doi.org/10.1136/emermed-2017-206846.
- Greenfield G, Ignatowicz A, Gnani S, Bucktowonsing M, Ladbrooke T, Millington H, et al. Staff perceptions on patient motives for attending GP-led urgent care centres in London: a qualitative study. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2015-007683.
- Cowling TE, Cecil EV, Soljak MA, Lee JT, Millett C, Majeed A, et al. Access to primary care and visits to emergency departments in England: a cross-sectional, population-based study. PLOS One 2013;8. https://doi.org/10.1371/journal.pone.0066699.
- Sancton K, Sloss L, Berkowitz J, Strydom N, McCracken R. Low-acuity presentations to the emergency department: reasons for and access to other health care providers before presentation. Can Fam Physician 2018;64:e354-e360.
- Vogel JA, Rising KL, Jones J, Bowden ML, Ginde AA, Havranek EP. Reasons patients choose the emergency department over primary care: a qualitative metasynthesis. J Gen Intern Med 2019;34:2610-19. https://doi.org/10.1007/s11606-019-05128-x.
- Coster JE, Turner JK, Bradbury D, Cantrell A. Why do people choose emergency and urgent care services? A rapid review utilizing a systematic literature search and narrative synthesis. Acad Emerg Med 2017;24:1137-49. https://doi.org/10.1111/acem.13220.
- O’Cathain A, Connell J, Long J, Coster J. ‘Clinically unnecessary’ use of emergency and urgent care: a realist review of patients’ decision making. Health Expect 2020;23:19-40. https://doi.org/10.1111/hex.12995.
- Hull SA, Homer K, Boomla K, Robson J, Ashworth M. Population and patient factors affecting emergency department attendance in London: retrospective cohort analysis of linked primary and secondary care records. Br J Gen Pract 2018;68:e157-e167. https://doi.org/10.3399/bjgp18X694397.
- Carson D, Clay H, Stern R. Primary Care and Emergency Departments: Report From the Primary Care Foundation. Mar 2010 2010.
- Morton K, Voss S, Adamson J, Baxter H, Bloor K, Brandling J, et al. General practitioners and emergency departments (GPED) – efficient models of care: a mixed-methods study protocol. BMJ Open 2018;8. https://doi.org/10.1136/bmjopen-2018-024012.
- Royal College of Surgeons . Acute and Emergency Care: Prescribing the Remedy 2014.
- Emergency Care Intensive Support Team . Transforming Urgent and Emergency Care Services in England. Safer, Faster, Better: Good Practice in Delivering Urgent and Emergency Care. A Guide for Local Health and Social Care Communities 2015.
- Royal College of Emergency Medicine (RCEM) . Ignoring the Prescription 2015.
- NHS England . Next Steps on the NHS Five Year Forward View 2017.
- Iacobucci G. NHS gets £100m budget ‘sticking plaster’ to help manage emergency demand. BMJ 2017;356. https://doi.org/10.1136/bmj.j1248.
- HM Treasury . Spring Budget 2017 2017. www.gov.uk/government/publications/spring-budget-2017-documents (accessed 1 March 2021).
- Department of Health . A&E Departments to Get More Funding: Funds for Next Winter Will Ease Pressure on Accident and Emergency (A&Amp;E) Departments in England 2017. www.gov.uk/government/news/ae-departments-to-get-more-funding#:∼:text=The%20Department%20of%20Health%20has,in%20time%20for%20next%20winter (accessed 1 March 2021).
- Kool RB, Homberg DJ, Kamphuis HC. Towards integration of general practitioner posts and accident and emergency departments: a case study of two integrated emergency posts in the Netherlands. BMC Health Serv Res 2008;8. https://doi.org/10.1186/1472-6963-8-225.
- Dale J, Green J, Reid F, Glucksman E, Higgs R. Primary care in the accident and emergency department: II. Comparison of general practitioners and hospital doctors. BMJ 1995;311:427-30. https://doi.org/10.1136/bmj.311.7002.427.
- Wang M, Wild S, Hilfiker G, Chmiel C, Sidler P, Eichler K, et al. Hospital-integrated general practice: a promising way to manage walk-in patients in emergency departments. J Eval Clin Pract 2014;20:20-6. https://doi.org/10.1111/jep.12074.
- Boeke AJ, van Randwijck-Jacobze ME, de Lange-Klerk EM, Grol SM, Kramer MH, van der Horst HE. Effectiveness of GPs in accident and emergency departments. Br J Gen Pract 2010;60:e378-84. https://doi.org/10.3399/bjgp10X532369.
- Bickerton J, Davies J, Davies H, Apau D, Procter S. Streaming primary urgent care: a prospective approach. Prim Health Care Res Dev 2012;13:142-52. https://doi.org/10.1017/S146342361100017X.
- Salisbury C, Hollinghurst S, Montgomery A, Cooke M, Munro J, Sharp D, et al. The impact of co-located NHS walk-in centres on emergency departments. Emerg Med J 2007;24:265-9. https://doi.org/10.1136/emj.2006.042507.
- Uthman OA, Walker C, Lahiri S, Jenkinson D, Adekanmbi V, Robertson W, et al. General practitioners providing non-urgent care in emergency department: a natural experiment. BMJ Open 2018;8. https://doi.org/10.1136/bmjopen-2017-019736.
- Ablard S, Kuczawski M, Sampson FC, Mason SM. What does the ideal urgent and emergency care system look like? A qualitative study of service user perspectives. Emerg Med J 2020;37:200-5. https://doi.org/10.1136/emermed-2019-208921.
- Blunt I, Edwards N, Merry L. What’s Behind the A&E ‘Crisis’?. London: Nuffield Trust; 2015.
- Cooper A, Davies F, Edwards M, Anderson P, Carson-Stevens A, Cooke MW, et al. The impact of general practitioners working in or alongside emergency departments: a rapid realist review. BMJ Open 2019;9. https://doi.org/10.1136/bmjopen-2018-024501.
- Oliver D. David Oliver: Why force GP streaming on NHS emergency departments?. BMJ 2020;368. https://doi.org/10.1136/bmj.m992.
- Ramlakhan S, Mason S, O’Keeffe C, Ramtahal A, Ablard S. Primary care services located with EDs: a review of effectiveness. Emerg Med J 2016;33:495-503. https://doi.org/10.1136/emermed-2015-204900.
- Fisher J, Salman B, Cooke M, Carson D, Clay H, Stern R. Primary Care and Emergency Departments. London: Primary Care Foundation; 2010.
- Turner J, Coster J, Chambers D, Cantrell A, Phung V-H, Knowles E, et al. What evidence is there on the effectiveness of different models of delivering urgent care? A rapid review. Health Serv Deliv Res 2015;3. https://doi.org/10.3310/hsdr03430.
- Khangura JK, Flodgren G, Perera R, Rowe BH, Shepperd S. Primary care professionals providing non-urgent care in hospital emergency departments. Cochrane Database Syst Rev 2012;11. https://doi.org/10.1002/14651858.CD002097.pub3.
- Gonçalves-Bradley D, Khangura JK, Flodgren G, Perera R, Rowe BH, Shepperd S. Primary care professionals providing non-urgent care in hospital emergency departments. Cochrane Database Syst Rev 2018;2. https://doi.org/10.1002/14651858.CD002097.pub4.
- National Institute for Health and Care Excellence (NICE) . Emergency and Acute Medical Care in Over 16s: Service Delivery and Organisation. Recommendations n.d. www.nice.org.uk/guidance/ng94/chapter/Recommendations#emergency-and-acute-medical-care-in-hospital (accessed 16 October 2021).
- National Institute for Health and Care Excellence (NICE) . Chapter 17 GPs Within or On the Same Site As Emergency Departments. Emergency and Acute Medical Care in Over 16s: Service Delivery and Organisation n.d. www.nice.org.uk/guidance/ng94/evidence/17gps-within-or-on-the-same-site-as-emergency-departments-pdf-172397464604 (accessed 16 October 2021).
- Van den Heede K, Van de Voorde C. Interventions to reduce emergency department utilisation: a review of reviews. Health Policy 2016;120:1337-49. https://doi.org/10.1016/j.healthpol.2016.10.002.
- Monitor . Walk-in Centre Review: Final Report and Recommendations 2014.
- Ablard S, O’Keeffe C, Ramlakhan S, Mason SM. Primary care services co-located with emergency departments across a UK region: early views on their development. Emerg Med J 2017;34:672-6. https://doi.org/10.1136/emermed-2016-206539.
- Wickware C. Nearly 420 extra GPs needed across country to deliver A&E streaming service. Pulse 2017. www.pulsetoday.co.uk/news/uncategorised/gpnews-labour-welcomes-snap-election-chance-to-sort-out-the-nhs/ (accessed 1 March 2021).
- Wickware C. ‘No long-term evidence’ backing GP streaming in A&E, says leading GP. Pulse 2017. www.pulsetoday.co.uk/news/politics/no-long-term-evidence-backing-gp-streaming-in-ae-says-leading-gp/ (accessed 1 March 2021).
- Purdy S. Avoiding Hospital Admissions: What Does the Research Evidence Say?. London: The King’s Fund; 2010.
- NHS England . Primary Care Streaming: Roll Out to September 2017 2017.
- NHS England . Clinical Streaming in the A&Amp;E Department 2017.
- Royal College of Emergency Medicine (RCEM) . Initial Assessment of Emergency Department Patients 2017.
- NHS Digital . Hospital Episode Statistics n.d. https://digital.nhs.uk/data-and-information/data-tools-and-services/data-services/hospital-episode-statistics (accessed 18 November 2021).
- Royal College of Emergency Medicine and Urgent Health UK . The Royal College of Emergency Medicine and Urgent Health UK Call for the Colocation of Urgent Care Services With A&Amp;E Departments 2015.
- Curtis L, Burns A. Unit Costs of Health and Social Care 2019 2019.
- Ministry of Housing, Communities & Local Government . The English Index of Multiple Deprivation (IMD) 2015 – Guidance 2015. www.gov.uk/government/statistics/english-indices-of-deprivation-2015 (accessed 1 March 2021).
- Pope C, Robert G, Bate P, Le May A, Gabbay J. Lost in translation: a multi-level case study of the metamorphosis of meanings and action in public sector organizational innovation. Public Administration 2006;84:59-7. https://doi.org/10.1111/j.0033-3298.2006.00493.x.
- Travaglia JF, Nugus P, Greenfield D, Westbrook J, Braithwaite J. Contested innovation: the diffusion of interprofessionalism across a health system. Int J Qual Health Care 2011;23:629-36. https://doi.org/10.1093/intqhc/mzr064.
- Caldwell SE, Mays N. Studying policy implementation using a macro, meso and micro frame analysis: the case of the Collaboration for Leadership in Applied Health Research & Care (CLAHRC) programme nationally and in North West London. Health Res Policy Syst 2012;10. https://doi.org/10.1186/1478-4505-10-32.
- Sausman C, Oborn E, Barrett M. Policy translation through localisation: implementing national policy in the UK. Policy &Amp; Politics 2016;44:563-89. https://doi.org/10.1332/030557315X14298807527143.
- Finch TL, Girling M, May CR, Mair FS, Murray E, Treweek S, et al. NoMAD: Implementation Measure Based on Normalization Process Theory. [Measurement Instrument] 2015. www.normalizationprocess.org (accessed 16 October 2021).
- Gibson J, Sutton M, Spooner S, Checkland K. Ninth National GP Worklife Survey. Manchester: Policy Research Unit in Commissioning and the Healthcare System, Manchester Centre for Health Economics, University of Manchester; 2018.
- Finch TL, Girling M, May CR, Mair FS, Murray E, Treweek S, et al. Improving the normalization of complex interventions: part 2 – validation of the NoMAD instrument for assessing implementation work based on normalization process theory (NPT). BMC Med Res Methodol 2018;18. https://doi.org/10.1186/s12874-018-0591-x.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77-101. https://doi.org/10.1191/1478088706qp063oa.
- Sheard L, Marsh C. How to analyse longitudinal data from multiple sources in qualitative health research: the pen portrait analytic technique. BMC Med Res Methodol 2019;19. https://doi.org/10.1186/s12874-019-0810-0.
- May CR, Mair F, Finch T, MacFarlane A, Dowrick C, Treweek S, et al. Development of a theory of implementation and integration: normalization process theory. Implement Sci 2009;4. https://doi.org/10.1186/1748-5908-4-29.
- Lewin K. Resolving Social Conflicts; Selected Papers on Group Dynamics. Oxford: Harper; 1948.
- Batalden M, Batalden P, Margolis P, Seid M, Armstrong G, Opipari-Arrigan L, et al. Coproduction of healthcare service. BMJ Qual Saf 2016;25:509-17. https://doi.org/10.1136/bmjqs-2015-004315.
- Buick F, Blackman D, O’Flynn J, O’Donnell M, West D. Effective practitioner-scholar relationships: lessons from a coproduction partnership. Public Adm Rev 2016;76:35-47. https://doi.org/10.1111/puar.12481.
- Heaton J, Day J, Britten N. Collaborative research and the co-production of knowledge for practice: an illustrative case study. Implement Sci 2016;11. https://doi.org/10.1186/s13012-016-0383-9.
- University of the West of England Bristol . General Practitioners and Emergency Departments (GPED): Efficient Models of Care n.d. www.uwe.ac.uk/research/gped (accessed 16 October 2021).
- Brant H, Voss S, Adamson J, Vaittinen A, Morton K, Benger J. Implementing Primary Care Services in or Alongside EDs: Qualitative Analysis of a Policy Initiative n.d.
- Kothari A, MacLean L, Edwards N, Hobbs A. Indicators at the interface: managing policymaker-researcher collaboration. Knowledge Management Research &Amp; Practice 2011;9:203-14. https://doi.org/10.1057/kmrp.2011.16.
- Wye L, Brangan E, Cameron A, Gabbay J, Klein JH, Pope C. Evidence based policy making and the ‘art’ of commissioning – how English healthcare commissioners access and use information and academic research in ‘real life’ decision-making: an empirical qualitative study. BMC Health Serv Res 2015;15. https://doi.org/10.1186/s12913-015-1091-x.
- Frenk J. Balancing relevance and excellence: organizational responses to link research with decision making. Soc Sci Med 1992;35:1397-404. https://doi.org/10.1016/0277-9536(92)90043-p.
- Oliver K, Innvar S, Lorenc T, Woodman J, Thomas J. A systematic review of barriers to and facilitators of the use of evidence by policymakers. BMC Health Serv Res 2014;14. https://doi.org/10.1186/1472-6963-14-2.
- Kerr EA, Riba M, Udow-Phillips M. Helping health service researchers and policy makers speak the same language. Health Serv Res 2015;50:1-11. https://doi.org/10.1111/1475-6773.12198.
- Checkland K, Harrison S, Snow S, Coleman A, McDermott I. Understanding the work done by NHS commissioning managers: an exploration of the microprocesses underlying day-to-day sensemaking in UK primary care organisations. J Health Organ Manag 2013;27:149-70. https://doi.org/10.1108/14777261311321752.
- Wye L, Cramer H, Beckett K, Farr M, le May A, Carey J, et al. Collective knowledge brokering: the model and impact of an embedded team. Evidence &Amp; Policy: A Journal of Research, Debate and Practice 2020;16:429-52. https://doi.org/10.1332/174426419X15468577044957.
- Wye L, Cramer H, Carey J, Anthwal R, Rooney J, Robinson R, et al. Knowledge brokers or relationship brokers? The role of an embedded knowledge mobilisation team. Evidence &Amp; Policy: A Journal of Research, Debate and Practice 2019;15:277-92. https://doi.org/10.1332/174426417X15123845516148.
- Scantlebury A, Brant H, Anderson H, Leggett H, Salisbury C, Cowlishaw S, et al. Potential impacts of general practitioners working in or alongside emergency departments in England: initial qualitative findings from a national mixed-methods evaluation. BMJ Open 2021;11. https://doi.org/10.1136/jech-2021-SSMabstracts.86.
- National Institute for Health and Care Excellence . Suspected Cancer: Recognition and Referral n.d. www.nice.org.uk/guidance/ng12 (accessed 28 November 2021).
- Higginson I, Guly H. Payment by results: a guide for emergency physicians. Emerg Med J 2007;24:710-15. https://doi.org/10.1136/emj.2007.050906.
- Murray E, Treweek S, Pope C, MacFarlane A, Ballini L, Dowrick C, et al. Normalisation process theory: a framework for developing, evaluating and implementing complex interventions. BMC Med 2010;8. https://doi.org/10.1186/1741-7015-8-63.
- Maruthappu M, Hasan A, Zeltner T. Enablers and barriers in implementing integrated care. Health Syst Reform 2015;1:250-6. https://doi.org/10.1080/23288604.2015.1077301.
- Dixon-Woods M, McNicol S, Martin G. Ten challenges in improving quality in healthcare: lessons from the Health Foundation’s programme evaluations and relevant literature. BMJ Qual Saf 2012;21:876-84. https://doi.org/10.1136/bmjqs-2011-000760.
- Brant H, Voss S, Morton K, Cooper A, Edwards M, Price D, et al. Current provision of general practitioner services in or alongside emergency departments in England. Emerg Med J 2021;38:780-3. https://doi.org/10.1136/emermed-2020-210539.
- Platts-Mills TF, Nagurney JM, Melnick ER. Tolerance of uncertainty and the practice of emergency medicine. Ann Emerg Med 2020;75:715-20. https://doi.org/10.1016/j.annemergmed.2019.10.015.
- Coates D, Rawstorne S, Benger J. Can emergency care practitioners differentiate between an avoided emergency department attendance and an avoided admission?. Emerg Med J 2012;29:838-41. https://doi.org/10.1136/emermed-2011-200484.
- Chalder M, Sharp D, Moore L, Salisbury C. Impact of NHS walk-in centres on the workload of other local healthcare providers: time series analysis. BMJ 2003;326. https://doi.org/10.1136/bmj.326.7388.532.
- Warwick E. Policy to reality: evaluating the evidence trajectory for English eco-towns. Build Res Info 2015;43:486-98. https://doi.org/10.1080/09613218.2015.1012821.
- Mee A. E-learning funding for schools: a policy paradox?. Br J Educ Technol 2007;38:63-71. https://doi.org/10.1111/j.1467-8535.2006.00596.x.
- Groves RM, Peytcheva E. The impact of nonresponse rates on nonresponse bias: a meta-analysis. Public Opin Q 2008;72:167-89. https://doi.org/10.1093/poq/nfn011.
- Meterko M, Restuccia JD, Stolzmann K, Mohr D, Brennan C, Glasgow J, et al. Response rates, nonresponse bias, and data quality: results from a national survey of senior healthcare leaders. Public Opin Q 2015;79:130-44. https://doi.org/10.1093/poq/nfu052.
- Clarke G, Pariza P, Wolters A. The Long-term Impacts of New Care Models on Hospital Use: An Evaluation of the Integrated Care Transformation Programme in Mid-Nottinghamshire. London: The Health Foundation; 2020.
- Anderson H, Birks Y, Adamson J. Exploring the relationship between nursing identity and advanced nursing practice: an ethnographic study. J Clin Nurs 2020;29:1195-208. https://doi.org/10.1111/jocn.15155.
- Advanced Life Support Group . Manchester Triage System (2017) n.d. https://www.triagenet.net/classroom/ (accessed 31 December 2021).
- Gabbay J, le May A. Practice-based Evidence for Healthcare: Clinical Mindlines. Oxford: Routledge; 2010.
- Wenger E. Communities of Practice: Learning, Meaning, and Identity. Cambridge: Cambridge University Press; 1999.
- Wenger E, McDermott RA, Snyder W. Cultivating Communities of Practice: A Guide to Managing Knowledge. Boston, MA: Harvard Business School Press; 2002.
- Gabbay J, le May A. Evidence based guidelines or collectively constructed ‘mindlines?’ Ethnographic study of knowledge management in primary care. BMJ 2004;329. https://doi.org/10.1136/bmj.329.7473.1013.
- Nonaka I. A dynamic theory of organizational knowledge creation. Organization Science 1994;5:14-37. https://doi.org/10.1287/orsc.5.1.14.
- Nonaka I, Takeuchi H. The Knowledge-Creating Company: How Japanese Companies Create the Dynamics of Innovation. Oxford: Oxford University Press; 1995.
Appendix 1 Work package A
Topic guide for national-level system leaders interview
What is your current role and what has your role been regarding the introduction of GPs into EDs?
Tell us the background to the concept of introducing GPs into EDs as you see it:
-
Who have been key stakeholders in the idea?
-
What do they hope to achieve?
-
Where did it originally come from?
-
How does it fit with other services, e.g. walk-in centres, 111, out-of-hours GP?
-
Have lessons learnt from the experience of introducing other services been incorporated?
What is your sense of the ‘buy-in’ from GPs?
-
Sustainability (lack of GPs).
-
Desirable role for GPs.
-
What are the challenges/benefits for GPs in this role?
-
Terms and conditions (e.g. employer, indemnity).
Why do you think the government has decided to invest in GPED?
Describe the different models of GPED care that you are aware of having been/going to be implemented:
-
Have you got a sense of which might work better (according to what outcomes)?
-
What do you think patients think about the idea in general?
What do you think the likely impact will be (do you have evidence for this)?
-
On ED care delivery from perspective of ED department.
-
On primary care delivery across the community.
-
On patient care.
-
Have you considered unintended consequences (e.g. it will increase demand)?
Topic guide for site-level system leaders initial interview
ED context:
-
How many new adult patients does your ED see each year?
-
How many new paediatric patients does your ED see each year?
What model of working with GPs/primary care operates in your ED currently (if any)?
Tell us about the GPED model you are planning to implement.
Can you tell us the background to that decision?
-
What are hoping to achieve?
-
What discussions took place?
-
What options were considered?
-
What major factors impacted on decision-making?
-
(If do not mention might want to prompt on waiting time, cost, numbers.)
How is it different from the model you have in place now (is it clearly distinct)?
-
Structural requirements for proposed model.
-
Organisational requirements for proposed model.
-
How will changes (if any) be achieved?
-
Timetable for change (date).
Do you think this model makes sense/is the right thing for your department?
Do you think staff value the proposed model of service provision?
What do you think the impact will be to your department on?
-
Performance (4 hours, hospital admission rate).
-
Staff (which staff in particular, in what ways).
-
Division of labour.
-
Interaction between different professional groups.
-
Resources.
-
Consultations with patients.
Will staff require additional training before implementation?
-
Which staff and what training is planned/available?
-
How will you judge the success/impact of the new mode of service delivery?
-
What data might be available for research purposes?
-
Mechanism for staff feedback about the intervention.
-
Can the intervention be adapted on the basis of experience?
What are your thoughts on the decision to fund these models of service delivery?
-
Does the idea of GPs in ED make sense in general?
Any other comments to add about GPED?
Topic guide for site-level system leaders follow-up interview
What model of working with GPs/primary care is now operating in your ED (if any)?
Tell us what has happened over the last 12 months in relation to GP working in or alongside your ED:
-
What structural and organisational changes have occurred?
-
Is it running as initially planned or were changes made – if so, why?
-
What was the final timetable for implementation?
-
Did the changes require any training, if so, what form, was it sufficient?
-
What changes have you noticed in your day-to-day practice?
-
What were your expectations regarding the change, have they been met?
Do you think the current model is better or worse than where you were 12 months ago? Why do you think this?
Is the model that you now have in place the right thing for your department?
Do you think staff value the new model of service provision?
Do you think patients value the new model of service provision?
What has the impact of this change been on?
-
Performance (4 hours, hospital admission rate).
-
Staff (which staff in particular, in what ways).
-
Division of labour.
-
Interaction between different professional groups.
-
Resources.
-
Consultations with patients.
Do you have any evidence of these impacts (figures or case studies)?
What are the main enablers and barriers that you have encountered to GPs working in or alongside your ED?
What are your thoughts on the decision to fund these models of service delivery?
-
Does the idea of GPs in ED make sense in general?
Any other comments to add about GPED?
Appendix 2 Work package B
Pooled model
Table 24 reports results from all sites for which data were available, and separates these by GPED-service type (integrated, parallel and on site). This pooled analysis uses the fact that GPED services operate at different times of the day so that the overall effect is identified by comparing the outcomes of patients arriving within a given hour of the day at hospitals operating or not operating a GPED service at this time.
We found no statistically significant effect of GPED on the volume of attendance, nor was a statistically significant effect apparent for most performance indicators, including 4-hour waits, patients leaving without being seen, unnecessary attendances, hospital admissions or mortality at 30 days. Our analysis did, however, identify a very small, but statistically significant, reduction in the rate of reattendance within 7 days, and this is discussed further in Chapter 4, Discussion of research objectives, Objective 3.
| Characteristic | Trusts | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| All | Analysed | |||||||||
| Mean | Standard deviation | Minimum | Maximum | n (in millions) | Mean | Standard deviation | Minimum | Maximum | n | |
| Wait < 4 hours | 0.813 | 0.390 | 0 | 1 | 16.6 | 0.838 | 0.368 | 0 | 1 | 793,907 |
| No unplanned reattendance within 7 days | 0.914 | 0.280 | 0 | 1 | 16.2 | 0.912 | 0.283 | 0 | 1 | 766,781 |
| Treated | 0.978 | 0.147 | 0 | 1 | 15.2 | 0.973 | 0.162 | 0 | 1 | 684,703 |
| Necessary attendance | 0.890 | 0.313 | 0 | 1 | 16.6 | 0.882 | 0.323 | 0 | 1 | 800,196 |
| Not admitted | 0.812 | 0.391 | 0 | 1 | 16.4 | 0.835 | 0.372 | 0 | 1 | 788,863 |
| Patient not admitted or admitted overnight | 0.956 | 0.205 | 0 | 1 | 16.3 | 0.953 | 0.211 | 0 | 1 | 788,330 |
| 30-day survival | 0.983 | 0.127 | 0 | 1 | 16.6 | 0.985 | 0.120 | 0 | 1 | 800,196 |
| Patient age (years) | ||||||||||
| 1 | 0.025 | 0.157 | 0 | 1 | 16.6 | 0.028 | 0.165 | 0 | 1 | 800,196 |
| 2 | 0.019 | 0.136 | 0 | 1 | 16.6 | 0.020 | 0.140 | 0 | 1 | 800,196 |
| 3 | 0.015 | 0.122 | 0 | 1 | 16.6 | 0.016 | 0.126 | 0 | 1 | 800,196 |
| 4 | 0.012 | 0.108 | 0 | 1 | 16.6 | 0.013 | 0.112 | 0 | 1 | 800,196 |
| 5 | 0.010 | 0.100 | 0 | 1 | 16.6 | 0.011 | 0.103 | 0 | 1 | 800,196 |
| 6–10 | 0.043 | 0.203 | 0 | 1 | 16.6 | 0.047 | 0.211 | 0 | 1 | 800,196 |
| 11–15 | 0.047 | 0.211 | 0 | 1 | 16.6 | 0.049 | 0.216 | 0 | 1 | 800,196 |
| 16–20 | 0.058 | 0.234 | 0 | 1 | 16.6 | 0.059 | 0.236 | 0 | 1 | 800,196 |
| 21–25 | 0.069 | 0.254 | 0 | 1 | 16.6 | 0.070 | 0.255 | 0 | 1 | 800,196 |
| 26–30 | 0.070 | 0.255 | 0 | 1 | 16.6 | 0.071 | 0.256 | 0 | 1 | 800,196 |
| 31–35 | 0.062 | 0.241 | 0 | 1 | 16.6 | 0.063 | 0.242 | 0 | 1 | 800,196 |
| 36–40 | 0.054 | 0.226 | 0 | 1 | 16.6 | 0.055 | 0.228 | 0 | 1 | 800,196 |
| 41–45 | 0.048 | 0.214 | 0 | 1 | 16.6 | 0.048 | 0.215 | 0 | 1 | 800,196 |
| 46–50 | 0.052 | 0.223 | 0 | 1 | 16.6 | 0.052 | 0.223 | 0 | 1 | 800,196 |
| 51–55 | 0.053 | 0.224 | 0 | 1 | 16.6 | 0.053 | 0.224 | 0 | 1 | 800,196 |
| 56–60 | 0.048 | 0.213 | 0 | 1 | 16.6 | 0.047 | 0.211 | 0 | 1 | 800,196 |
| 61–65 | 0.042 | 0.200 | 0 | 1 | 16.6 | 0.040 | 0.197 | 0 | 1 | 800,196 |
| 66–70 | 0.042 | 0.201 | 0 | 1 | 16.6 | 0.040 | 0.197 | 0 | 1 | 800,196 |
| 71–75 | 0.046 | 0.209 | 0 | 1 | 16.6 | 0.044 | 0.205 | 0 | 1 | 800,196 |
| 76–80 | 0.043 | 0.204 | 0 | 1 | 16.6 | 0.040 | 0.197 | 0 | 1 | 800,196 |
| 81–85 | 0.043 | 0.202 | 0 | 1 | 16.6 | 0.040 | 0.195 | 0 | 1 | 800,196 |
| 86–90 | 0.034 | 0.180 | 0 | 1 | 16.6 | 0.032 | 0.176 | 0 | 1 | 800,196 |
| 91–95 | 0.016 | 0.126 | 0 | 1 | 16.6 | 0.015 | 0.123 | 0 | 1 | 800,196 |
| 96 + | 0.035 | 0.184 | 0 | 1 | 16.6 | 0.038 | 0.191 | 0 | 1 | 800,196 |
| Male | 0.493 | 0.500 | 0 | 1 | 16.6 | 0.491 | 0.500 | 0 | 1 | 800,115 |
| IMD score | ||||||||||
| 0–20 | 0.456 | 0.498 | 0 | 1 | 16.6 | 0.522 | 0.500 | 0 | 1 | 800,196 |
| 21–40 | 0.330 | 0.470 | 0 | 1 | 16.6 | 0.299 | 0.458 | 0 | 1 | 800,196 |
| 41–60 | 0.150 | 0.357 | 0 | 1 | 16.6 | 0.119 | 0.324 | 0 | 1 | 800,196 |
| 61–80 | 0.043 | 0.202 | 0 | 1 | 16.6 | 0.033 | 0.178 | 0 | 1 | 800,196 |
| 81–100 | 0.001 | 0.038 | 0 | 1 | 16.6 | 0.001 | 0.023 | 0 | 1 | 800,196 |
| Arrival by ambulance | 0.290 | 0.454 | 0 | 1 | 16.6 | 0.278 | 0.448 | 0 | 1 | 800,196 |
| Day of attendance | ||||||||||
| Monday | 0.156 | 0.363 | 0 | 1 | 16.6 | 0.158 | 0.364 | 0 | 1 | 800,196 |
| Tuesday | 0.144 | 0.351 | 0 | 1 | 16.6 | 0.149 | 0.356 | 0 | 1 | 800,196 |
| Wednesday | 0.142 | 0.350 | 0 | 1 | 16.6 | 0.147 | 0.354 | 0 | 1 | 800,196 |
| Thursday | 0.141 | 0.348 | 0 | 1 | 16.6 | 0.145 | 0.352 | 0 | 1 | 800,196 |
| Friday | 0.139 | 0.346 | 0 | 1 | 16.6 | 0.143 | 0.350 | 0 | 1 | 800,196 |
| Saturday | 0.134 | 0.341 | 0 | 1 | 16.6 | 0.127 | 0.333 | 0 | 1 | 800,196 |
| Sunday | 0.142 | 0.349 | 0 | 1 | 16.6 | 0.131 | 0.338 | 0 | 1 | 800,196 |
| Month of attendance | ||||||||||
| January | 0.086 | 0.280 | 0 | 1 | 16.6 | 0.085 | 0.279 | 0 | 1 | 800,196 |
| February | 0.079 | 0.270 | 0 | 1 | 16.6 | 0.079 | 0.270 | 0 | 1 | 800,196 |
| March | 0.088 | 0.283 | 0 | 1 | 16.6 | 0.088 | 0.284 | 0 | 1 | 800,196 |
| April | 0.079 | 0.270 | 0 | 1 | 16.6 | 0.078 | 0.269 | 0 | 1 | 800,196 |
| May | 0.086 | 0.280 | 0 | 1 | 16.6 | 0.087 | 0.282 | 0 | 1 | 800,196 |
| June | 0.083 | 0.276 | 0 | 1 | 16.6 | 0.084 | 0.278 | 0 | 1 | 800,196 |
| July | 0.087 | 0.282 | 0 | 1 | 16.6 | 0.089 | 0.284 | 0 | 1 | 800,196 |
| August | 0.080 | 0.271 | 0 | 1 | 16.6 | 0.080 | 0.272 | 0 | 1 | 800,196 |
| September | 0.081 | 0.273 | 0 | 1 | 16.6 | 0.080 | 0.272 | 0 | 1 | 800,196 |
| October | 0.084 | 0.278 | 0 | 1 | 16.6 | 0.084 | 0.277 | 0 | 1 | 800,196 |
| November | 0.083 | 0.277 | 0 | 1 | 16.6 | 0.083 | 0.276 | 0 | 1 | 800,196 |
| December | 0.083 | 0.276 | 0 | 1 | 16.6 | 0.082 | 0.274 | 0 | 1 | 800,196 |
| Performance indicators | All EDs | GPED model | n | ||
|---|---|---|---|---|---|
| Integrated | Parallel | On site | |||
| Waited more than 4 hours | |||||
| Coefficient | 0.002 | 0.011 | –0.006 | –0.018 | 4,278,180 |
| p-value | 0.803 | 0.267 | 0.587 | 0.097 | |
| Reattended within 7 days | |||||
| Coefficient | –0.003 | –0.006 | 0.003 | 0.005 | 4,140,340 |
| p-value | 0.015 | 0.028 | 0.252 | 0.060 | |
| Left without being seen | |||||
| Coefficient | –0.001 | –0.006 | 0.005 | 0.008 | 3,689,903 |
| p-value | 0.793 | 0.251 | 0.338 | 0.153 | |
| Unnecessary attendance | |||||
| Coefficient | 0.003 | 0.0003 | 0.009 | –0.004 | 4,302,347 |
| p-value | 0.497 | 0.964 | 0.291 | 0.525 | |
| Admitted | |||||
| Coefficient | –0.004 | –0.009 | 0.007 | 0.004 | 4,244,663 |
| p-value | 0.352 | 0.195 | 0.463 | 0.677 | |
| Non-same-day discharge attendance | |||||
| Coefficient | –0.002 | –0.003 | –0.002 | 0.005 | 4,241,954 |
| p-value | 0.422 | 0.599 | 0.839 | 0.568 | |
| 30-day mortality | |||||
| Coefficient | 0.0003 | 0.001 | –0.001 | –0.001 | 4,302,347 |
| p-value | 0.255 | 0.215 | 0.469 | 0.362 | |
| Volume of attendances | |||||
| Absolute volume | |||||
| Coefficient | 0.001 | –0.015 | 0.034 | –0.0002 | 336,882 |
| p-value | 0.970 | 0.673 | 0.414 | 0.996 | |
| Relative volume | |||||
| Coefficient | 0.001 | –0.018 | 0.039 | –0.001 | 336,882 |
| p-value | 0.931 | 0.635 | 0.380 | 0.972 | |
| HRG code | HRG name | Tariff (£) | |
|---|---|---|---|
| Type 1 and 2 departments | Type 3 departments | ||
| VB01Z | Emergency Medicine, Any Investigation with Category 5 Treatment | 328 | 63 |
| VB02Z | Emergency Medicine, Category 3 Investigation with Category 4 Treatment | 299 | 63 |
| VB03Z | Emergency Medicine, Category 3 Investigation with Category 1–3 Treatment | 216 | 63 |
| VB04Z | Emergency Medicine, Category 2 Investigation with Category 4 Treatment | 196 | 63 |
| VB05Z | Emergency Medicine, Category 2 Investigation with Category 3 Treatment | 164 | 63 |
| VB06Z | Emergency Medicine, Category 1 Investigation with Category 3–4 Treatment | 115 | 63 |
| VB07Z | Emergency Medicine, Category 2 Investigation with Category 2 Treatment | 144 | 63 |
| VB08Z | Emergency Medicine, Category 2 Investigation with Category 1 Treatment | 133 | 63 |
| VB09Z | Emergency Medicine, Category 1 Investigation with Category 1–2 Treatment | 93 | 63 |
| VB10Z | Emergency Medicine, Dental Care | 82 | 63 |
| VB11Z | Emergency Medicine, No Investigation with No Significant Treatment | 63 | 63 |
| VB99Z | Emergency Medicine, Patient Dead On Arrival | 227 | 63 |
Appendix 3 Work package C
Topic guides
Topic guide for patients
What brought you to the ED on this occasion?
Tell us about what happened after you arrived?
-
Who did you see first/what happened next?
-
Description of being selected to be seen by the GP.
Did you know it was possible to be sent to a GP after coming to ED?
-
Was this communicated to you?
-
Did you understand the process/reason you were selected for the GP?
-
How did you feel about being seen by a GP?
-
Have you any previous experience of this service (give example)?
Explore reason behind attendance at ED for this consultation – why did they use ED over other potential services (walk-in centres, GP surgery)?
-
Knowledge of different ways to access health services and what they consider the ‘appropriate’ ways to use them.
-
Would their experiences on this visit change their consultation choice in the future?
Explore awareness of increased demand on EDs/government funding made available to increase GPs in EDs:
-
Do they think GPs in ED good idea in principle?
-
What impact do they think it might have on reducing pressure on EDs?
-
Do they think it will change what patients do?
How does practice within GPED compare to other GP services?
How satisfied are they with the visit?
-
How long did you have to wait?
-
How satisfied are you with the outcome?
-
Can you think of any ways you could improve the service?
-
Opportunity to provide feedback.
Any other comments to add about GPED.
Topic guide for staff in emergency departments: before introduction of GPED
Personal
What is your current role in the ED?
Do you have a role in relation to the introduction of GPED? If so, what is it?
GPED model
Tell us what you understand about the GPED model that will be implemented in your department.
Do you feel that many of the patients you see are ‘inappropriate’ for ED and should be in primary care (give examples)?
Are you aware of the background to the decision to introduce GPED?
-
What it is hoped that GPED will achieve?
-
What discussions took place?
-
What options were considered?
-
What major factors impacted on decision-making (if do not mention might want to prompt on waiting time, cost, numbers)?
-
Was there (describe) consultation process with staff/patients?
How is it different from the model you have in place now (is it clearly distinct)?
-
Structural/organisational requirements for proposed model.
-
Training requirements.
-
Timetable for change (date).
-
Knowledge/views on the process for selection of patients to be seen by the GP.
What are your thoughts on the decision to fund these models of service delivery?
-
Does the idea of GPs in ED make sense in general for your department?
-
Are you aware of other types of GPED models being implemented elsewhere?
Do staff have a shared understanding of the purpose of the proposed model of GPED?
-
Do staff feel they have had sufficient buy-in?
-
What are your concerns (if any) regarding implementation?
-
Do you think there are any potential safety issues?
-
How supported do you feel by management going into the change?
Expected impact
What are your expectations of the impact of the new service on your own everyday working?
-
Clinically (type of patients/presenting conditions).
-
Working relationships with other staff (e.g. staff selecting patients to be seen by the GP, the GP staff).
-
Administratively/organisationally.
-
For the service provided to patients.
What you think the impact will be to your department on:
-
Performance (4 hours, hospital admission rate).
-
Resources.
-
How patients use the ED.
What do you think will be the key barriers/facilitators to the introduction of GPEP?
What do you think would be deemed to be successful outcomes?
How do you think patients will respond to the new service (satisfaction, ability to feedback, change in behaviour)?
Any other comments to add about GPED?
Topic guide for general practitioners in emergency departments: before introduction of GPED
Personal
What is your current role in the GPED?
What was your previous (or concurrent) role in primary care?
Did you have a role in relation to the introduction of GPED/how did you become aware of the new service model?
Explore decision around taking the role as GP in ED context.
Discussion around who is employer, professional indemnity, clinical supervision/support around clinical decision-making in role as GP in ED.
GPED model
Tell us what you understand about the GPED model that is being implemented.
Are you aware of the background to the decision to introduce GPED?
-
What it is hoped that GPED will achieve?
-
How the service came about?
-
Consultation process with CCG/other primary care forums.
What are your thoughts on the decision to fund these models of service delivery?
-
Does the idea of GPs in ED make sense in general?
-
Aware of other types of GPED models being implemented elsewhere.
Do staff (from GP component of service) have a shared understanding of the purpose of the proposed model of GPED?
-
Do staff feel they have had sufficient buy-in?
-
What are your concerns (if any) regarding implementation?
-
Do you think there are any potential safety issues?
-
How supported do you feel by management going into the change?
Expected impact
What are your expectations of the impact of the new service on your own everyday working?
-
Clinically (type of patients/presenting conditions).
-
Working relationships with other staff (e.g. staff selecting patients to be seen by the GP, the ED staff).
-
Administratively/organisationally.
-
For the service provided to patients.
What you think the impact will be to your ED department on:
-
Performance (4 hours, hospital admission rate)?
-
Resources?
-
How patients use the ED?
What do you think will be the key barriers/facilitators to the introduction of GPED?
What do you think would be deemed to be successful outcomes?
How do you think patients will respond to the new service (satisfaction, ability to feedback, change in behaviour)?
Any other comments to add about GPED?
Topic guide for all staff in EDs: after introduction of GPED
Personal
What is your current role in the GPED?
What has been your role in the implementation of GPED?
GPED model:
Tell us about GPED as it is currently running (any differences from original plan/reasons for any changes).
Describe the process of implementation
-
Key staff involved.
-
Structural/organisational changes.
-
Any training.
-
Communication with staff/patients.
-
Feedback from staff/patients.
-
Timetable.
What was expected to be achieved by the change?
What were the key barriers/facilitators?
What were the key issues for staff?
What was the attitude/approach to change from management?
Impact
How do you think the GPED model is working?
-
Process of selecting patients to be seen by the GP/getting the ‘right’ patients/transfer of patients.
-
Any safety concerns.
-
Key advantages/disadvantages.
How has it impacted on overall workings of the ED?
-
Has there been any impact on performance (e.g. 4 hours, hospital admission rate)?
-
Resources
Have you been able to feedback experiences of GPED (changes in response to feedback)?
Do you think any improvements could be made to the GPED model (aware of different service configurations in other places)?
What feedback have you had from patients about the GPED model?
Do you think the availability of this GPED model is likely to change the way the public make decisions about how, when and where to seek care?
Any other comments to add about GPED.
For emergency care staff:
How has GPED impacted on your own everyday working?
-
Clinically (type of patients/presenting conditions).
-
Working relationships with other staff (e.g. the staff selecting patients to be seen by the GP/ the GP staff).
-
Service provided to patients.
-
Administratively/organisationally.
-
Any surprises.
For general practice staff in GPED:
How is care organised within GP component of GPED?
How does practice within GPED compare to other services (general practice, walk-in centres):
-
Clinically (types of patients/presenting conditions).
-
Patient ‘outcomes’ (e.g. referrals, requests for testing, transfer back to ED).
-
Interaction with other professional groups within GP component/ED staff.
-
Workload.
-
Any surprises.
Discussion around who is employer, professional indemnity, clinical supervision/support around clinical decision-making in role as GP in ED.
Do you feel you act differently as a practitioner following time in ED (probe – both back in primary care and over time within ED)?
Satisfaction with role of GP in ED
-
Met with expectations.
-
Plan to continue in role.
-
Career plans.
How do you think patients have responded to the service?
-
Why they came to AE rather than general practice.
-
Satisfaction with GPED.
Workforce survey
| Characteristic | n | % |
|---|---|---|
| Sex | ||
| Female | 248 | 64.8 |
| Male | 120 | 31.3 |
| Age (years) | ||
| 18–34 | 160 | 41.8 |
| 35–44 | 113 | 29.5 |
| ≥ 45 | 95 | 24.8 |
| Job category | ||
| ED specialist | 101 | 26.4 |
| GPs | 18 | 4.7 |
| Nursing staff | 158 | 41.3 |
| Trainee | 45 | 11.7 |
| Other | 45 | 11.7 |
| Length of service with current trust (years) | ||
| < 1 | 62 | 16.2 |
| 1–5 | 140 | 36.6 |
| 5–10 | 70 | 18.3 |
| > 10 | 94 | 24.5 |
| I am involved in . . . | ||
| Overseeing the introduction of GPs into ED | 11 | 2.9 |
| Delivering care in ED | 257 | 67.1 |
| Delivering care in GP service related to the ED | 42 | 11.0 |
| Triage of patients between GP service and the ED | 22 | 5.7 |
| Likelihood of leaving direct patient care within 5 years | WFS | Ninth National GP Worklife Survey75 | |||
|---|---|---|---|---|---|
| Age (years), n (%) | Age (years), % | ||||
| 18–34 | 35–44 | ≥ 45 | < 50 | > 50 | |
| None | 77 (48.1) | 65 (57.5) | 37 (38.9) | 45.2 | 12.2 |
| Slight | 48 (30.0) | 26 (23.0) | 26 (27.4) | 27.6 | 13.8 |
| Moderate | 15 (9.4) | 12 (10.6) | 13 (13.7) | 13.7 | 12.2 |
| Considerable | 12 (7.5) | 4 (3.5) | 7 (7.4) | 7.7 | 14.7 |
| High | 7 (4.4) | 6 (5.3) | 12 (12.6) | 5.8 | 47.1 |
| Considerable/high intention to . . . | WFS, n (%) | Ninth National GP Worklife Survey,75 % | |||
|---|---|---|---|---|---|
| ED specialist | GP | Nursing staff | Trainee | ||
| Continue with medical work but with a different health-care provider | 26 (25.7) | 6 (33.3) | 47 (29.7) | 12 (26.7) | – |
| Continue with medical work but outside the UK | 23 (22.8) | 4 (22.2) | 29 (18.4) | 6 (13.3) | 8.7 |
| Leave direct patient care | 14 (13.9) | 3 (16.7) | 19 (12.0) | 5 (11.1) | 39.0 |
| Leave medical work entirely | 9 (8.9) | 2 (11.1) | 18 (11.4) | 2 (4.4) | 35.9 |
| At least one of the above | 37 (36.6) | 8 (44.4) | 72 (45.6) | 14 (31.1) | – |
| Job stressor | WFS total | Ninth National GP Worklife Survey75 | ||
|---|---|---|---|---|
| Mean rating | Considerable/high pressure, n (%) | Mean rating | Considerable/high pressure, % | |
| Increased demands from patients | 4.22 | 291 (76.0) | 4.29 | 85.8 |
| Dealing with problem patients | 4.08 | 271 (70.8) | 3.96 | 69.9 |
| Dealing with earlier discharges from hospital | 3.35 | 142 (37.1) | 3.90 | 66.5 |
| Worries about patient complaints/litigation | 3.30 | 159 (41.5) | 3.63 | 53.5 |
| Having insufficient time to do justice to the job | 3.82 | 230 (60.1) | 4.38 | 85.3 |
| Unrealistically high expectation of the role from others | 3.23 | 148 (38.6) | 3.77 | 63.7 |
| Insufficient resources within the practice | 3.44 | 158 (41.3) | 3.69 | 58.0 |
| Long working hours | 3.41 | 179 (46.7) | 4.11 | 73.7 |
| Paperwork | 3.39 | 179 (46.7) | 4.32 | 82.6 |
| Changes to meet requirements from external bodies | 3.38 | 160 (41.8) | 4.30 | 81.1 |
| Adverse publicity from the media | 2.97 | 106 (27.7) | 3.56 | 54.0 |
| Increasing workloads | 4.16 | 262 (68.4) | 4.58 | 92.3 |
| Job stressor | ED specialist | GP | Nursing staff | Trainee | ||||
|---|---|---|---|---|---|---|---|---|
| Mean rating | Considerable/high pressure, n (%) | Mean rating | Considerable/high pressure, n (%) | Mean rating | Considerable/high pressure, n (%) | Mean rating | Considerable/high pressure, n (%) | |
| Increased demands from patients | 4.18 | 77 (76.2) | 3.94 | 12 (66.7) | 4.44 | 134 (84.8) | 3.80 | 30 (66.7) |
| Dealing with problem patients | 3.94 | 68 (67.3) | 3.94 | 11 (61.1) | 4.29 | 129 (81.6) | 3.80 | 28 (62.2) |
| Dealing with earlier discharges from hospital | 3.52 | 48 (47.5) | 3.27 | 8 (44.4) | 3.32 | 61 (38.6) | 3.42 | 17 (37.8) |
| Worries about patient complaints/litigation | 3.44 | 49 (48.5) | 3.50 | 8 (44.4) | 3.30 | 63 (39.9) | 3.33 | 21 (46.7) |
| Having insufficient time to do justice to the job | 3.77 | 60 (59.4) | 2.94 | 5 (27.8) | 4.10 | 117 (74.1) | 3.50 | 23 (51.1) |
| Unrealistically high expectation of the role from others | 3.32 | 44 (43.6) | 2.65 | 5 (27.8) | 3.49 | 73 (46.2) | 2.56 | 8 (17.8) |
| Insufficient resources within the practice | 3.59 | 45 (44.6) | 3.07 | 5 (27.8) | 3.42 | 71 (44.9) | 3.08 | 13 (28.9) |
| Long working hours | 3.49 | 52 (51.5) | 2.75 | 5 (27.8) | 3.70 | 94 (59.5) | 2.98 | 14 (31.1) |
| Paperwork | 3.47 | 50 (49.5) | 3.00 | 5 (27.8) | 3.54 | 91 (57.6) | 3.00 | 15 (33.3) |
| Changes to meet requirements from external bodies | 3.60 | 49 (48.5) | 2.64 | 2 (11.1) | 3.46 | 77 (48.7) | 3.10 | 15 (33.3) |
| Adverse publicity from the media | 2.90 | 32 (31.7) | 2.50 | 3 (16.7) | 3.10 | 46 (29.1) | 2.79 | 13 (28.9) |
| Increasing workloads | 4.15 | 76 (75.2) | 3.13 | 6 (33.3) | 4.40 | 125 (79.1) | 3.77 | 24 (53.3) |
| Implementation measure | Total, n (%) | Occupational group, n (%) | |||
|---|---|---|---|---|---|
| ED specialist | GP | Nursing staff | Trainee | ||
| I can see how the GPED differs from usual ways of working | 264 (68.9) | 75 (74.3) | 14 (77.8) | 97 (61.4) | 34 (75.6) |
| Staff in this organisation have a shared understanding of the purpose of GPED | 208 (54.3) | 45 (44.6) | 10 (55.6) | 99 (62.7) | 26 (57.8) |
| I understand how GPED affects the nature of my own work | 291 (76.0) | 76 (75.2) | 14 (77.8) | 124 (78.5) | 34 (75.6) |
| I can see the potential value of GPED for my work | 299 (78.1) | 75 (74.3) | 14 (77.8) | 126 (79.7) | 40 (88.9) |
| There are key people who drive GPED forward and get others involved | 222 (58.0) | 60 (59.4) | 10 (55.6) | 91 (57.6) | 26 (57.8) |
| I believe that participating in GPED is a legitimate part of my role | 251 (65.5) | 59 (58.4) | 13 (72.2) | 115 (72.8) | 26 (57.8) |
| I am open to working with colleagues in new ways to use GPED | 351 (91.6) | 94 (93.1) | 16 (88.9) | 144 (91.1) | 43 (95.6) |
| I will continue to support GPED | 331 (86.4) | 82 (81.2) | 16 (88.9) | 139 (88.0) | 42 (93.3) |
| I can easily integrate GPED into my existing work | 262 (68.4) | 66 (65.3) | 13 (72.2) | 110 (69.6) | 34 (75.6) |
| GPED disrupts working relationships | 51 (13.3) | 17 (16.8) | 0 (0.0) | 20 (0.1266) | 3 (6.7) |
| I have confidence in other people’s ability to conduct their role in GPED | 228 (59.5) | 53 (52.5) | 13 (72.2) | 98 (62.0) | 32 (71.1) |
| Work is being assigned to those with skills appropriate to their role | 222 (58.0) | 50 (49.5) | 14 (77.8) | 94 (59.5) | 30 (66.7) |
| Sufficient training is provided to enable staff to implement GPED | 128 (33.4) | 32 (31.7) | 7 (38.9) | 60 (38.0) | 14 (31.1) |
| Sufficient resources are available to support GPED | 125 (32.6) | 29 (28.7) | 3 (16.7) | 60 (38.0) | 17 (37.8) |
| Management adequately supports GPED | 214 (55.9) | 56 (55.4) | 9 (50.0) | 87 (55.1) | 32 (71.1) |
| I am aware of reports about the effects of GPED | 149 (38.9) | 40 (39.6) | 6 (33.3) | 61 (38.6) | 16 (35.6) |
| The staff agree that GPED is worthwhile | 216 (56.4) | 46 (45.5) | 11 (61.1) | 97 (61.4) | 30 (66.7) |
| I value the effects that GPED has had on my work | 217 (56.7) | 55 (54.5) | 11 (61.1) | 95 (60.1) | 25 (55.6) |
| Feedback about the GPED model can be used to improve it in the future | 322 (84.1) | 88 (87.1) | 15 (83.3) | 130 (82.3) | 39 (86.7) |
| I can modify how I work within GPED | 228 (59.5) | 62 (61.4) | 11 (61.1) | 93 (58.9) | 27 (60.0) |
| National context | National: policy, pressures |
| Local context | Local: service landscape and population/specific local needs/considerations |
| Trust ED and UC culture | Respond or resist: whether staff are actively redirecting patients away from the ED to resist the flow or providing a service in response and recognition that patients have attended with health concerns. Where staff feel that they must see patients and responsibility rests with them to provide health care. UCC/GP in ED vs. primary care (differences to traditional primary care role) |
| Pen portrait data | Explanation of current system, patient journey through the ED, layout, history of GPED, future plans |
| Patients reasons for attending ED | Patient and staff explanations of why patients attend ED/previous use of services (e.g. have they seen/contacted service before ED?) |
| Service literacy | Any discussions around appropriate/inappropriate attendances, perceived impact of service literacy and actual patient service literacy on use of GPED/ED |
| Implementation | Perceived challenges and facilitators of implementation |
| Perceived impact | Perceived impact of GPED on patient safety, workforce and skills mix, staff interactions, performance/targets, views of GPED |
| Expectations of GPED (T1) | ‘Hypothesis’ from stakeholders at all levels regarding their expectations of what would be the outcome of the introduction to GPED. From T1 data only |
| Other/miscellaneous insights | Potential emerging insights that are outside the current framework, reviewed at regular meetings of the WP C team |
Pen portraits
Birch pen portrait
FIGURE 10.
Birch pen portrait. ENT, ear, nose and throat.
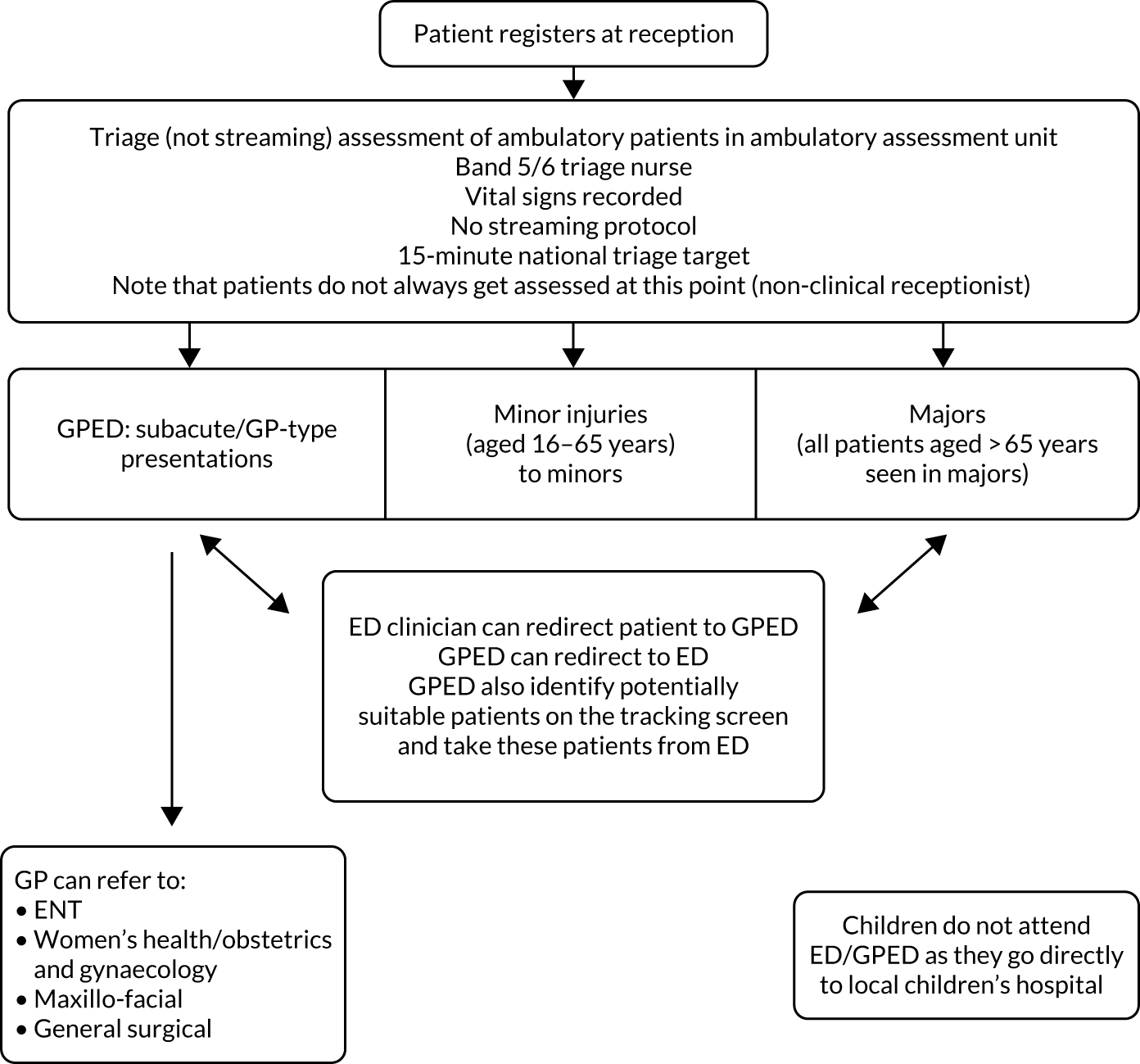
GPED service times unclear
Currently, patients register at the ED reception and, if ambulatory, they are sent to the ambulatory assessment unit for triage to a number of clinical streams, including GPED. Patients are triaged, rather than streamed, by a band 5/6 nurse and vital signs are recorded. There is no specific protocol for identifying which patients are suitable for GPED; instead, the process is based on an established triage assessment. Patients with ‘GP-type’ presentations or subacute problems are directed to GPED. A card is put in the GPED tray (or another appropriate clinician/majors, tray), which is then picked up and the patients are seen. However, the indication is that this process does not always take place and the times/staffing of GPED is unclear. GPs can redirect patients whom they assess to be inappropriate for GPED back to the ED and they can refer patients on to a number of specialities. GPs are expected to see an average of two patients per hour and between 22–25 patients per shift. The total number of patients attending the ED is approximately 300–380. If GPED is quiet, GPs may identify patients that they think are suitable for GPED on the tracking screen and see these patients (after discussion with an ED consultant). GPs have no access to patients’ primary care records, but they are able to order investigations such as radiographs and blood tests; this is seen as a hybrid GP/ED role. There is no designated GPED area or room.
There is one salaried GP and three or four GPs undertake regular locum shifts to cover the service. However, it is unclear what the established GPED service hours are and the service is patchy and sporadic. There appears to be a 07.30–18.00 shift (although some say it is 08.00–16.00/17.00), but sometimes the service runs from 10.00–18.00 and sometimes there is no service at all. There may be one or two GPs covering a shift. It is unclear whether or not the service runs at weekends:
Erm, [hesitantly] it’s, at the moment we are supposed to have our target or the common target, we are supposed to have a GP service to allow us a day for 7 days a week, so – no, at the moment we have one GP who basically is employed by us . . . so he mainly worked 08.00–16.00, 08.00–17.00, I think it’s 5 days, 9 days out of 10 days, so he takes every tenth day as an off day. And, in addition to him, we have some GPs who come and do basically GP locum work for us. So, at the moment, the person who’s working with us is a fully qualified GP who’s been a GP for years and years . . . So there might be a day we might have fully diverse coverage, or 12 hours coverage, but usually only Wednesday, Thursday. Some weekends we do not have any GPs, so . . .
Staff (Birch) 14, time 1
The current model has been in place for around 1–2 years. Previously, the service was run by a private company/CCG GP collective and its target was to see a preagreed number of patients per day. This target was not met and the service ceased. It was felt that the service remit and acceptance criteria were too narrow. There was then a gap during which the trust had no contracted service, but had an ad hoc arrangement with locum GPs instead. However, the trust saw value in a GP service and decided to take it in house, employing GPs directly (rather than employing a company to provide GPs as before). The new GPED model involved various stakeholders, including ED clinicians and nursing staff, as well as input from the wider trust. GPs are audited by the trust. The next stage in the process is to embed the service and increase coverage.
National context
Staff contextualised the GPED service against the backdrop of a highly challenged primary care service. However, they also felt that improvements could be made to general practice more broadly and that the nature and organisation of primary care was challenging, with the traditional ways of running practices not matching modern demands. In addition, patient behaviour and expectations were seen as a challenge, with patients’ expectations of the service increasing and demands for free prescriptions influencing patient behaviour. The ageing population was also seen to contribute to ED and secondary care problems, with poor community service provision failing to keep elderly patients out of hospital and in their own homes.
Local context
Staff felt that the ED is under pressure and struggling to meet targets against the backdrop of the high volume of patients. Variability among general practices meant that although some practices could accommodate patients, others struggle to offer appropriate appointments. Staff compare their service to other local hospitals that are seen to be better resourced, with GP availability 7 days per week and nurse practitioners available 10.00–22.00. Because there is a local childrens’ hospital, no patients aged < 16 years are seen at this hospital. Local commissioning groups have acted to address patients attending for free prescriptions by limiting the prescriptions that can be bought over the counter, which is something that staff seem to approve of:
But luckily some of the, the, err, Commissioning Groups have said ‘we won’t pay for over-the-counter medications, so you can’t prescribe it’. I said that to patients ‘you need to get some paracetamol, ibuprofen’, 25p in any supermarkets, round about, and they go ‘can you not prescribe it?’, ‘I’m not allowed, I’m afraid, I’m not allowed’.
Staff (Birch) 1, time 1
Trust emergency department and urgent care culture
Staff can be actively redirecting patients away from the ED, to resist the flow of arriving patients, or providing a service in response to, and recognition of, the fact that patients have attended with health concerns that need to be addressed. Staff may feel that they must see patients and that the responsibility rests with them to provide health care.
No patient interviews were carried out at this site as there were no GPs available at time 1 data collection.
Staff saw the cultures of the ED and GP as being quite separate, with the ED seen as working from the starting point that the patient is sick until proven otherwise, whereas for GPs it was seen as the opposite way around. This affected risk management. Staff recognised and valued the different roles and skills of ED and GPED clinicians. GPs were seen as better placed to deal with longer-term, lower-acuity presentations that required clinical reasoning rather than specialist investigations:
A&E likes what A&E likes. If it’s acute and it’s new, and it’s something which, you know, which can be dealt with, it can be really sick or it can be really well, but we like it to be new. And we like it to be something which requires immediate help. For long-term chronic conditions, actually, and conditions where decision-making can be done without high-tech investigations and where you can use your experience to say ‘it’s this, go home’, GPs are invaluable.
ED Staff (Birch) 8, time 1
The system worked particularly well with one GP, who was seen as proactive in seeking out patients and who staff felt was embedded in the ED team. However, GPED as a service was seen as being very selective about which patients/presentations would be accepted and there was an ‘us and them’ feeling, despite the departments recently becoming more integrated, with some staff unsure as to what GPED does and the rationale for the service. Some staff were concerned that patients were becoming increasingly aware of GPED, which could encourage attendance. When this happened, staff felt that they could not turn patients away or tell them that they had attended inappropriately. There was a feeling that, at a societal level, patients’ expectations had changed and the wider service needed to accommodate this.
Patients’ reasons for attending the emergency department
Patients attended for a number of reasons. Some stated that they could not get an appointment with their own GP or that the wait for an appointment was too long. Some patients had been advised by someone else to attend the ED (e.g. a carer who called an ambulance, a GP who thought that the patient needed a radiograph). One person attended for a second opinion after being seen in their own primary care practice. Although most patients had attended the ED previously, two had not.
Presentations included sore leg, burn, foot swelling, blocked ear and worsening headache, and a fall 4 weeks ago (for which the GP advised the patient to attend the ED for a radiograph).
Staff thought that patients may attend because they either could not get a GP appointment, or had failed to get an appointment previously and so had stopped trying to book GP appointments and instead came directly to the ED. They had the expectation that the ED would not turn them away and that their problem would be addressed that day. Staff felt that primary care should be the first point of contact, but decreased funding and increased patient volume led to GPs behaving in ways that helped to manage their workload, but had a negative impact on patients and the workload of the ED. For example, primary care GPs can refer patients directly for radiographs or to specialties, but are thought to send patients to the ED instead as this is a quicker process for GPs.
Staff felt that there were variations in what patients perceived as an emergency, but acknowledged that it is sometimes difficult for patients to know the level of severity/acuity and which services to access:
It’s easier for us ’cos we’re health-care professionals and, you know, like, ‘well, actually, I feel a bit ill, but it’s not that serious because I’m A, B, C, D and E’, whereas most people haven’t got that, have they?
Staff (Birch) 4, time 1
GPED patients were considered to be between acute ED patients, who need to attend the ED, and more chronic primary care patients, who probably attend their own general practice and have a good relationship with their GP. GPED caters for those who do not fall into either group. Some staff felt that patients from abroad used services differently and would attend ED if they could not get a GP appointment. Staff also implied that service efficiency encouraged patients to attend, sometime repeatedly, which was something they actively worked to prevent:
So it’s being recorded anyway but I don’t see anyone in less than an hour unless they’re ill because if you see them too quickly . . . we had one lady, she came back three times in a day, err, and that’s when we thought we really need to, err, we need to stop this somehow. We had a few keep coming back because it’s quicker to come here than it was to see their GP.
Staff (Birch) 18, time 1
Service literacy
The majority of patients were unaware of the GPED service, with only one having prior knowledge, although they lacked certainty about how the service worked and who it was aimed at. Because of this, there was no expectation that they would see a GP in the department.
Staff felt that patients had different expectations of primary and secondary care, so that although they may have been happy to wait for investigations in primary care, the expectation was that secondary care would provide this immediately. Consequently, patients were also perceived to attend the ED as a way of circumventing the system and being seen more quickly. Although staff had some sympathy with the difficulties patients faced in getting primary care GP appointments, they also felt that patients did not try to book a GP appointment and this was made worse by the availability of GPED:
I mean, we all know how difficult it is to get in and see your GP or to get and go and queue up at the walk-in centre and things like that, but I do believe that sometimes now it’s got to the point where people don’t even try because they know they can come and see a GP up here. Yeah ’cos I’m sure that that’s why people were coming what we used to call ‘inappropriately’ . . .
Staff (Birch) 4, time 1
There were undercurrents of frustration at this behaviour and although some staff challenged patients’ behaviour and tried to catch patients out by contacting the patients GP to check, others did not see this as their role:
And a lot of people say they can’t get hold of their GPs. I’m not very argumentative, but I’m not stupid either, if they say something I will double check it. So I normally ring their surgery and find out whether they did really have an appointment or not, usually they haven’t and they haven’t even bothered trying, they just turn up here because it’s easier.
Staff (Birch) 18, time 1
It was also considered that patients would attend the ED for a second opinion after seeing their GP. GPs themselves were sometimes reported to be the cause of a patient's ED attendance:
I’ve had a guy this morning that’s had a 2-year history of a cyst on his head and he’s come today to get it drained because his GP said ‘you’ll get it done quicker if you come to A&E’. So, people will come to A&E with the expectation that we can fix any chronic problem, and that’s what happened there.
Patients were seen to require education around appropriate ED attendance, and it was felt that it was the GPED GP’s role to do this. Staff also felt that patients were attracted to the Birch ED as it was well known and well regarded in the local area and, as a consequence, sometimes patients attended from outside the ‘catchment’ area.
It was highlighted that patients often used internet resources to research their problem prior to attending the ED. This was something one clinician found beneficial as they felt that it meant they could spend less time explaining differential diagnoses to patients.
Implementation
No patient views were available. Members of staff at all levels were involved in devising the GPED service, ranging from ED clinicians (including nurses) to trust- and executive-level leaders. Implementation was limited by staffing difficulties related to the lack of suitably qualified GPs and other clinicians, as well as a perception that GPs do not want to regularly staff GPED, but would rather work on a locum or ad hoc basis. This inconstancy in workforce supply reduced the ability of GPED to integrate with the wider ED system. The aim was for GPED to cover 12 hours per day for 7 days per week, but 12-hour cover was usually achievable only on Wednesdays and Thursdays, with patchy cover at other times. Some weekends had no GP cover. This inconsistency in service provision meant that the ED did not always send patients to GPED as they were unsure when it was staffed. There was a lack of integration between the ED and GPED, which staff felt was problematic. ED staff appreciated how beneficial GPED was, but only really noticed when it was understaffed:
When it’s here it works well, but when it’s not we miss it. It’s sporadic at the moment, and it’s too ad hoc. There needs to be a bit more of a structure and there needs to be a bit more integration with working. We’ve got one GP that we work with who’s amazing. He will pull, he will filter, he will be like ‘just come to me, just come to me.’ But, then others tend to be quite sedentary, sort of, working alone and we don’t even know if there’s a GP on or not.
Staff (Birch) 3, time 1
There were also practical implications for GPED staff working as locums. The model is that GP locums are employed on 6-month contracts, which are renewed after a short break between contracts (i.e. 2 weeks) to prevent invoking a permanent contract as funding is for a finite period only. This break in contract had unintended consequences, such as IT access and passwords no longer working.
It was suggested that, for effective implementation, and to increase the number of GPs, GPED needed to work reciprocally, that is GPs needed to feel valued, supported and appropriately remunerated. The lack of a designated space for the GPED service was seen as contributing to the lack of value placed on GPED. Although the relationship between GPED and the ED was generally considered to be good, some staff who were interviewed were unclear of the remit of GPED, the IT system that GPED runs from and whether or not GPED has access to primary care records. However, some staff did feel that the ED could learn from GPED GPs. They considered GPs to frame health and illness in a different way, which resulted in a difference in managing and tolerating risk. This was seen as beneficial in reducing inappropriate admission rates:
As I said, I think the GPs in A&E are a very good service. They could probably teach our doctors a lot regarding risk management and regarding long-term condition management and changing the boundaries. As a trainee ACP [advanced care practitioner], I am still at the point in my naive career where I see every patient as a ‘why can’t I send you home?’, whereas every GP sees a patient as ‘do I really have to send you to hospital?’ and I think getting the mindset of ‘you’re well until proven sick’, as opposed to ‘you’re sick until proven well’, and primary care is all well until proven sick and A&E is all sick until proven well. I think that would be very helpful, I think you could probably actually cut a lot of admissions by having a higher level of balls, which GPs have to have in their community role. Does that make sense?
Staff (Birch) 8, time 1
The lack of consistency in the streaming process was challenging. As well as variation in the presentations that individual GPs were comfortable with, there was no streaming pathway or protocol. This was seen as more problematic when the triage nurse was more junior. The streamers’ lack of general practice knowledge also made streaming more difficult in these circumstances. Although staff could feed back any concerns to the matron, the effectiveness of this was limited as the matron was not responsible for clinical staffing. There was also inconsistency in the clinical effectiveness of GPs. GPED sees 20–25 patients per day, but there is no specific/designated consultation time and there is an implication that GPs could see a greater number of patients. Some staff felt that there is not enough GP-appropriate work at Birch because there is a separate children’s hospital.
Perceived impact
For patients, being seen quickly and by an appropriate practitioner was key and they were not concerned whether that practitioner was an ED doctor or a GP.
Staff considered that patients were happy to be seen at GPED and their priority was to be seen quickly. It was thought that patients perceived GPED as different from their primary care GP service and thought that ED doctors were consultants and, therefore, senior to GPs (although it was also acknowledged that some patients were unaware of the difference between ED doctors and GPs). Staff also thought that patients saw GPED as a way of speeding up referrals to specialties.
Some staff considered GPED a positive addition to the ED in that it filtered patients who did not need to be seen in ED majors, improving waiting times for both patients with GP-type presentations and patients with major illness and injury. However, staff were sceptical that GPED would reduce patient volume and felt that it did not reduce the ED workload, but, instead, encouraged more people to attend with conditions that were seen as inappropriate for the ED. It was felt that GPED would change the way patients seek care and GPED was seen as encouraging patients to bypass their own GP and attend the ED instead. It was predicted that this may extend to patients presenting with chronic and acute problems. GPED was also thought to cause confusion for patients by providing a mixed message that encourages non-emergency attendance. The associated likely increase in footfall in the ED was seen as potentially reducing the pressure on primary care GPs, but conversely increasing ED attendance numbers. Patient confusion about the service was also demonstrated in reports of patients attempting to register with GPED as the patient’s own GP.
The filtering/triaging of patients depended on the experience of the nurse carrying out this role. The Birch GPED model had no formal streaming process or established protocols, but more junior staff could seek support from senior members of the team. Staff had seen the benefit of GPED models elsewhere and were aware of other models where streaming staff could redirect patients away from the hospital; however, this was not the policy at Birch.
GPED was seen as providing a more appropriate service to those patients suitable for GP management and, consequently, was thought to free up ED clinician’s time to see more seriously/acutely ill patients. GPs were considered to order fewer investigations for lower-risk patients and appropriately refer patients to the ED if they required more extensive work-up. It was expected that the planned co-location of GPED in its own purpose-built area would be beneficial to the ED as it could then concentrate on accommodating majors. GPs felt that GPED was already more merged with the ED than other departments in which they had worked. One GP enjoyed working with the ED team as they felt that it expanded their scope of practice, knowledge and skills. Similarly, ED staff considered GPs a valuable teaching and learning resource. However, the level at which GPs integrated with the ED was variable and this had an impact on working relationships. Although GPs could not quantify the impact of GPED, they felt that they were contributing to meeting the 4-hour KPI. They were also aware that GPED activity was audited and GPED patient outcomes were tracked.
Although there were some positives and GP input was valued, staff generally felt that GPED did not work as effectively as it should. For example, the service would benefit from greater consistency between GPs and the capacity to cover all required shifts, which was not possible all the time. When on duty, GPs were considered to see a reasonable number of patients and their clinical effectiveness was demonstrated by the service being missed when no GPs were available. The lack of consistency and the variance in GPs’ willingness and proactivity with regards to seeking out GP-type work were seen as major factors in reducing the impact of GPED. Some staff had worked at other trusts with a more comprehensive GP service and associated this consistency of service with a reduction in the amount of GP-type patients seen in the ED.
Expectations of GPED (time 1)
No patient stakeholder feedback was gained.
Staff felt that greater commitment to a fully staffed, consistent service was necessary to increase service impact. It was felt that GPED would increase the numbers attending the ED and reduce the pressure on primary care GPs. Staff were unsure whether or not moving GP resources from primary care to the ED would make any difference as it would not actually increase the resources, but simply redistribute ED and GP provision.
Chestnut pen portrait
FIGURE 11.
Chestnut pen portrait. HCA, health-care assistant.
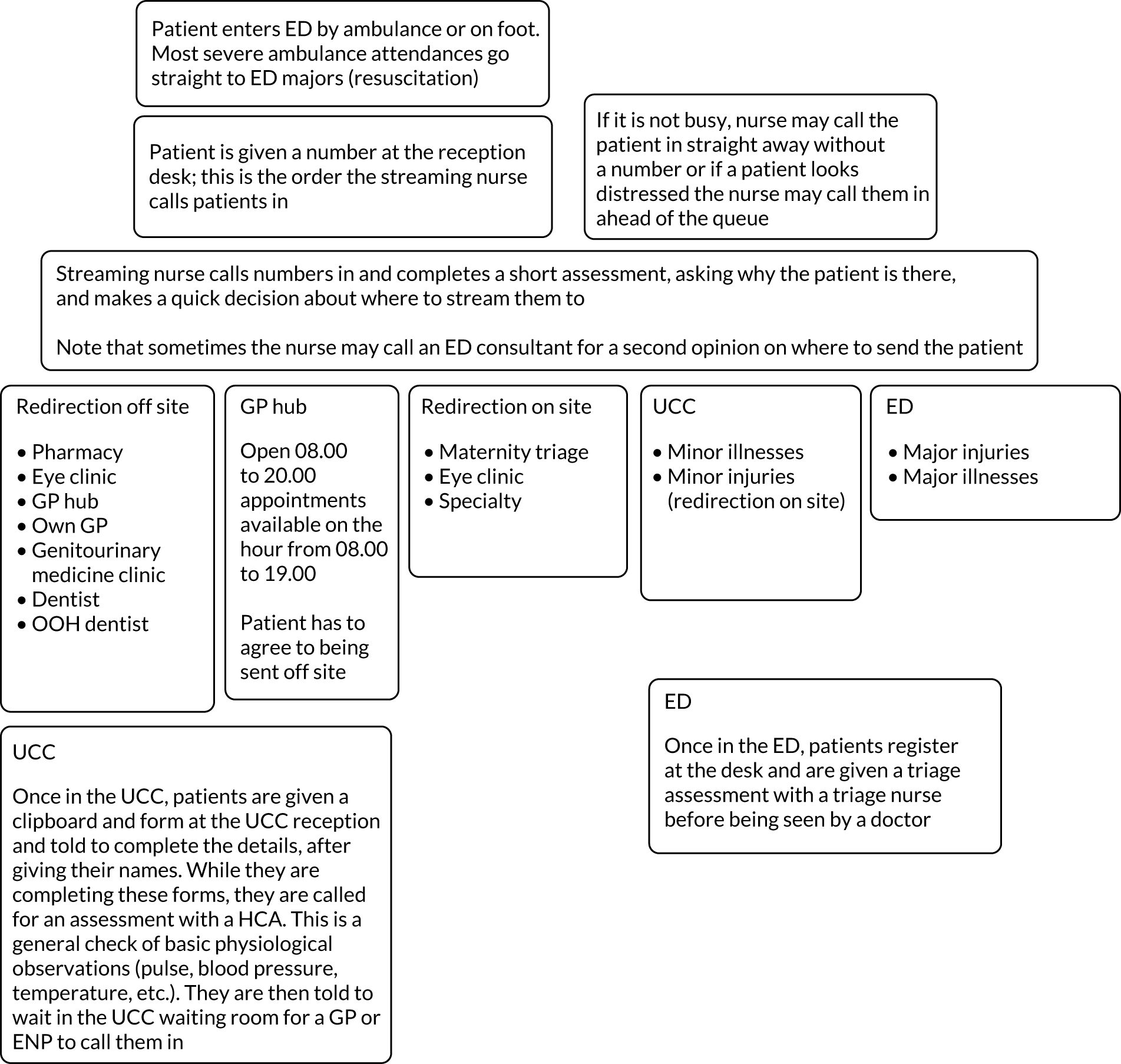
Current model
-
All patients are streamed at the front door. There is a quick assessment by a streaming nurse before they sign into the department; the streaming nurse also takes some very basic observations, that is oxygen saturation, blood pressure and heart rate (but no blood samples are taken).
-
UCC deals with minor illnesses and minor injuries:
-
It has access to radiographs.
-
It is staffed by GPs, health-care assistants (HCAs), nurse practitioners, usually one or two GPs at a time and ENPs. Issues identified around this include GPs generally not being trained enough to deal with injuries – nurse practitioners mainly deal with these injuries.
-
-
Majors in the ED deals with major illnesses and major injuries.
-
There is a separate paediatric ED; the UCC staff see suitable paediatric patients in the paediatric ED.
-
The OOH general practice is co-located in the UCC, but this is a separate system based on appointments. OOH GPs also do home visits and telephone consultations; these are not done as part of the UCC. They are funded separately, but both are funded by the same CCG. If the UCC gets really busy some patients can be transferred to OOH GPs if there is capacity, but the UCC and OOH general practice run on separate computer systems so this can be challenging.
-
Some staff move between departments; in particular, nurses and HCAs might move between the ED and UCC.
-
Some difficulties in getting enough GPs to staff the UCC were reported; the UCC is currently staffed from a local GP collaborative, with locums but not many permanent ED GP staff.
-
There were some issues with ED staffing as well: it was often short staffed and this was further exacerbated by needing to send staff from the ED to support the UCC when they were short staffed or too busy.
-
After streaming, patients sign in with reception in either the ED or UCC:
-
If it is the ED, they are then triaged by a nurse before seeing a doctor.
-
If it is the UCC, they are then assessed, usually by a HCA, before seeing a doctor.
-
Streaming/patient flow
-
All patients are streamed via the streaming nurse opposite main reception.
-
Patients can be streamed to:
-
On site – majors, UCC.
-
Redirection on site – maternity triage, eye clinic (on site), specialty or ambulatory care.
-
Redirection off site – pharmacy, eye clinic, own GP, genitourinary medicine clinic (off site or on site), dentist, OOH dentist, GP hub or another hospital with an ear, nose and throat (ENT) specialty.
-
GP hub – open 08.00–20.00, appointments available on the hour from 08.00–19.00 (note that patients can also be sent here from UCC after streaming to UCC).
-
-
Patients get frustrated when they have to go to another location on site or off site, and when they have to repeat their symptoms to different staff members.
-
There are strict streaming criteria; however, experienced and higher bands of nurses were reported as being better at streaming.
-
Streaming nurses occasionally call on ED staff to provide a second opinion on where to appropriately stream patients.
-
Patients can be referred to tertiary departments from the ED or UCC:
-
Issues were reported with patients from the UCC being referred to, for example, fracture clinics, but with no fractures.
-
-
NHS 111 referrals are made to the OOH GP service, but sometimes they get referrals from out of area. When this happens, the UCC duty manager has to call the patient and tell them not to come to the ED and make an appointment at the appropriate OOH service for them, as well as calling the NHS 111 service to let them know.
Future plans for GPED
-
A new purpose-built centre for the ED and UCC is being built.
-
Construction was not completed by the predicted end date and staff seem unsure about when it will actually happen.
-
The new building will see the ED and UCC located together without so much distance between them.
-
The new building will also have more space for the ED and more beds.
History of GPED
-
The UCC was previously operated by a private provider (2012–17) that did not renew their contract. It then came back under trust management. This history has caused some tension between the ED and UCC staff historically.
Physical environment
-
The ED and UCC have been in ‘temporary accommodation’ for around 2 years.
-
The reception and ED are in Portakabins® (Portakabin Ltd, Huntington, UK), with limited space. The UCC is also in a temporary building down the corridor, with limited space.
-
The streaming booth is opposite the main reception desk and it has a shoulder-height wall/small divider. It is a very small space, with room for a small desk with a computer, a chair for the streaming nurse, a chair for the patient and a small sink. There is limited privacy as the waiting area seats are directly behind the low wall.
-
Staff point out places where the floor is coming away and has been taped up or where temporary desk legs are loose. One nurse explains that they feel sorry for the cleaners as it does not matter how clean they make it, the building still looks shabby.
-
There is a shortage of space to see patients in the ED; sometimes there are discussions with patients in corridors and, when it is busy, there are patients in beds in the corridors.
-
The UCC is a couple of minutes’ walk from the ED, and there are green footprint stickers on the floor to direct people from reception.
-
This ‘geographical dislocation’ (C.S.022.int) was highlighted as a potential patient safety issue as if a patient needs to be transferred to the ED, a bed must be used to transport them from one location to another.
-
-
The paediatric ED is along the corridor and there are blue footprint stickers on the floor to direct people from reception.
-
Patients can get frustrated at being sent around the site and off site.
Time 3 summary
Pen portrait
The urgent treatment clinic (UTC) was run by a private provider until April 2019; it is now dual run by the GP collaborative and the hospital. Since the change in provider, two GPs now work in the UTC. In general, there is a GP present 7 days per week. The two GPs split the shifts, working either 11.00–19.00 or 4.00–13.00. In addition to the GPs, there are four permanent nurses present in the UTC from 20.00/20.30–22.00/22.30. Overnight, the UTC is staffed by junior doctors rather than GPs and ANPs, partly because of difficulties in recruiting GPs for OOH shifts. Staff reported this change to the rota as a significant change at this site since time 1 (or, possibly, time 2). GPs in the UTC can order tests at this site, if required, but they are considered part of standard clinical practice for GPs working at this site.
Since December 2018, the ED/UTC has been co-located in a new building. For > 12 months prior to this, the UTC and ED were housed in a temporary set-up in which they were physically separated (this was when time 1 interviews took place). The new building was designed/built when the ED/UTC was run by a private provider. It is noted by staff that there is less space (i.e. treatment rooms) in the new-build department. Its design may have been different (i.e. to facilitate cohesion and partnered working between the EDD/UTC) had it been known at the time that the trust would take over from the previous provider.
Patients arrive via either an ambulance or the walk-in entrance and are streamed by the nurse (band 6 or 7) at the main reception; brief clinical details are taken to determine where the patient will receive the most appropriate care and the receptionist checks the patient in. The streaming system is based on the Manchester triage. 110 A low score would indicate that a patient could be suitable to be seen by the UTC. Previously, streaming was conducted by a non-clinician and, because of this, the system was incredibly rigid, so that any hint of acuity would be seen by the ED.
Patients are seen in order of their arrival. The UTC/ED at this site has permanent HCAs who complete vital signs checks with patients within 15 minutes of rotations being booked. These checks help to quickly identify if a patient is seriously ill. A nurse then triages all patient (e.g. observations, urine, blood samples) to assess the urgency of the illness or injury. Triage is conducted on the basis of perceived urgency. Patients are then signposted to the most appropriate care:
-
resuscitation for people with life-threatening illness or injury
-
majors for people with urgent illness or injury
-
the UTC for people with an illness or injury that can be treated in one step
-
seen by an ACP and then directed off site to either the GP hub or their own GP.
From there, patients may be required to stay in hospital or may be discharged from the ED. Patients are treated here if they are aged > 17 years; younger patients are directed to the paediatric ED, whether or not they need to see the UTC/primary care staff. Both the ED and UTC share the same computer system; however, the system is designed for the ED, so it is not a good fit for the UTC.
Local context
There is an assumption among some patients that the health services in this locality are poor because they are based in the south of England. There is a strong acknowledgement from patients (and staff) that the GP service and wait-time is no better, and, perhaps, worse, than attending the ED/UTC. There is also recognition that the health service needs more financial resources for patients to receive medical care quicker.
National context
. . . it is interesting to go around the country and see the different units and see the way they cut the cake if you like in terms of who sees what and how we decide who sees what. The problem I generally have with that is the complexity of the rota and how these units work in the way that, you know, sometimes there’s a GP available to see these things and sometimes there is not and then they run two entirely different service models depending on who’s around that day or now, oh because Dr Smith has gone home, oh well in that case we’ll do it this way. I just do not like that whole set-up.
S 009, time 3
Trust culture
Team working was apparent at this site. It appeared to be common for GPs to be approached by other staff members (e.g. F1 doctors, ANPs) and asked for their opinion on the most appropriate course of care for patients who presented as complex cases. Some patients appeared to be resistant to ANPs’ diagnosis and requested to see a GP for a second opinion when the ANP did not give the patient the antibiotics they were expecting (i.e. because there was no infection present). In such cases, the GP felt that it was important not to undermine the diagnostic decisions of their colleagues. The new build, which had physically merged the ED and UTC, was perceived by most staff to have facilitated the interaction and integration of staff.
Staff appeared frustrated by patients’ need to be seen by a medical practitioner for non-urgent care whenever patients felt that this was required.
Interviews with both staff and patients identified a number of scenarios in which patients were using the ED/UTC services inappropriately. A prominent reason was patients being unable to get a timely appointment at their own GP, which meant that people often used the ED/UTC as a first port of call, rather than attempting to get an appointment with their GP. Staff noted that they would ask patients whether or not they tried to get an appointment at their GP before attending the ED/UTC if the staff did not feel that the patient’s issue was urgent. Although staff were aware of the protocols of redirecting patients away from the service when required, they did not necessarily agree with them. This was, in part, because staff felt that the service was there to be used, and it was considered more efficient to treat patients there and then, particularly when their issues could be resolved within minutes, rather than redirecting them away from the ED/UTC to another service in the community. It was also recognised that most patients were right to attend the ED/UTC when they did, as they required a responsive primary care service, a service that many GPs can no longer provide because of the lack of timely appointments.
The integration of the UTC within the ED and the implementation of the 4-hour wait target appealed to patients and, in turn, increased the number of attendances at the ED/UTC.
Service literacy
Most patients expected to have to wait a few hours to be seen at the ED/UTC; however, they anticipated this and it did not appear to be an issue. This was primarily because they knew that they would be seen on the day, whereas they would probably not be able to get an appointment at their GP surgery for days or weeks. In most cases, patients were seen by a clinician quicker than they anticipated.
Some patients attended the UTC knowing that they would be seen by a GP; others were not aware that GPs were now located in the ED. Nevertheless, most patients were satisfied with being seen by any medical practitioner at the UTC, whether that be a doctor or an ANP, as long as it meant they would receive the medical attention/treatment they felt that they needed.
However, some patients were dissatisfied with the practitioner they saw if it did not result in the outcome they were expecting, such as receiving antibiotics. In such cases, if the initial examination was completed by an ANP, patients were more likely to request to see a GP for a second opinion. Although staff facilitated this, GPs noted that it was vital that they were not seen to be undermining the decisions of their colleagues.
Patients attended the ED/UTC for reasons such as it was closer to their home than their own GP surgery, they were attending for very minor issues that did not require urgent/immediate attention (‘I see people come in with a cut finger . . . another had a bad splinter. Splinter! It’s not like its life-threatening’ Chestnut, Patient 012), being unaware of the standard pathways of referrals, and incorrectly using the ED/UTC in an attempt to be referred quicker. Several patients also attended the ED/UTC in an attempt to gain information about test results that had been requested by either their GP or private health services. One patient explained that they visited the ED/UTC for a practitioner to interpret test results, as they felt that ED/UTC staff were more ‘qualified’ than their own GP. It was noted by staff that some patients made an assumption that primary and secondary care is a fully integrated health service; however, this is not the case. For example, the ED/UTC do not have access to GP-based medical records.
It was perceived by some patients to be less strain on the NHS to visit the ED/UTC rather than their own GP surgery.
Patients’ reasons for attending the ED/UTC were as follows:
-
finger injury, mallet injury, male patient
-
injured wrist, female patient
-
lethargy, described as a complex case, male patient
-
suspected bronchiolitis, male patient
-
finger injury due to attack, female patient
-
injured wrist, male patient
-
painful back, requiring report of back scan to be read
-
broken finger
-
back pain
-
hip pain.
A recurrent reason for patients attending the ED/UTC was that they could not get an appointment with their own GP. Some patients did not attempt to get an appointment with their own GP before attending the ED/UTC, as it would be days/weeks before one would be available. For many patients, this was not their first time attending the ED/UTC. Some patients noted they would rather attend the ED/UTC than their own GP surgery for convenience, because it was closer to home or because attending the ED/UTC meant that they could have tests completed immediately that their own GP would have had to refer them for (e.g. radiograph), essentially ‘cutting out the middle man’.
Staff commented that some patients had replaced their own GP with the ED/UTC and that patients knowing that GPs were present in the ED/UTC encouraged its use.
One patient perceived that, regardless of whether patients were seen at the GP surgery or in the ED/UTC, the need for any medical care put a strain on the NHS.
Implementation
Facilitators
The UTC, including the nurses, GPs and ED doctors, worked closely and the service felt altogether more integrated in terms of daily working. The GPs’ varied skillset made them well placed to work within the ED/UTC to deal with patients who present with primary care issues. Their skill set meant that they could balance risk, they tended to order fewer tests and discharged people home quicker than ED doctors.
Barriers
The hospital struggles to recruit locum GPs owing to changes to rotas that now see the shifts run through the day. As a result, the GPs who would usually work OOH after spending the day in their own practices are unable to pick up the shifts. Having to use temporary staff and being unaware of their skill set proved problematic when trying to rota a multiskilled team. As a result, the UTC is staffed with junior ED doctors overnight.
Although it was felt that a GP’s skillset was ideal for treating minor illness, not all GPs had the correct knowledge to treat minor injuries. This was noted to be because GPs see very few minor injuries on a daily basis in their own surgeries, as patients with injuries are more inclined to seek medical care from the ED. Staff noted that in other UTC departments around the country GPs are responsible for treating patients with minor illness and ANPs are responsible for treating those who present with minor injuries. However, there was a reluctance at this site to rota staff in such a way because of the planning and logistics involved. It was the department’s preference to employ multiskilled staff, such as GPs, who can deal with both minor illness and injuries, although this was not always possible when having to cover shifts with locum staff whose skill sets were unknown.
Staff did not respond well to the transition from the ED/UTC being ran by a private provider to the trust, and some are still adjusting. When ran by the private provider, the ED and UTC were more autonomous and less integrated; this ethos is noted to be particularly prevalent among staff who have been at the site for many years and is seen to be a barrier to the full integration of the UTC/ED as a department. By encouraging staff to be more integrated in their thinking, the UTC can more effectively alleviate pressure from the ED. For instance, staff discussed how tests were not part of UTC care when it was run by the private provider. Now, tests (e.g. blood tests, ECGs, radiographs) can be requested if practitioners in the UTC believe that it will give them greater certainty regarding the correct treatment and care within the UTC and a timely discharge for the patient. However, some staff have not adjusted to these changes.
The trust would like to increase the number of patients seen by the UTC to further reduce the demand on the ED. To do this, an alternative streaming system would need to be put in place (currently, band 6 or 7 nurses are responsible for clinical streaming). GPs are cautious that this would increase the number of patients incorrectly streamed to them when the patients actually need emergency care.
Perceived impact
The new building has facilitated better integration and multidisciplinary working between the ED and UTC in comparison to previous set-ups where the ED/UTC were located much further apart. It has also helped to refine the streaming process and transfer patients from the UTC to the ED if needed.
The UTC was seen by both staff and patients to alleviate pressure on ED.
Changes to the rota in April saw the UTC being covered by ED doctors rather than GPs overnight, which reduced the department's compliance with the national 4-hour standard until staff adjusted to the set-up.
Patient safety was considered to have improved since the non-clinical streaming had been taken over by band 6 and 7 nurses.
Expectations
That’s the question. Because the question is, what are the GPs here to do? And the answer is no one is actually sure, as far as I can see, because I have sat in, you know, NHS England meetings where the argument is both. It’s only people who turn up with primary care issues that it would be far more sensible to put GPs in there to deal with those primary care issues because they’re the most skilled at doing that. They’re the most experienced. They know the pathways. They’re the ones who are able to deal with comorbidities and complex medical conditions, etc., the old party line and that’s fine. But then, on the other hand, you’ve got the same or similar level of seniority people saying that you need to be redirecting these people away, they shouldn’t be using secondary care, it’s an expensive way of doing it. So they’re turning up with a primary care problem, you should be redirecting them more appropriately to which to me, is two completely opposing things. As I say, it depends who you ask which answer you get and the answer is, at the moment, for example, we’re still commissioned to redirect an awful lot of stuff, you know, a lot of people would suggest it’s probably a lot more efficient to just see them at the point of care. Try and educate them for next time, although good luck with that! But, really, just see them and deal with the problem they’ve got, but we’re commissioned to send them away. So someone comes in asking for a repeat prescription, as long as it’s not an emergency, you know, if they’ve run out of insulin, they’re type 1 diabetic, then fine. But if they want their routine blood pressure medication then we just don’t give it to them. We’re commissioned to send them away, but it would take me 2 seconds to do that, but I’m not allowed to and I’m not supposed to. I mean, you can start talking about the fact that a lot of prescriptions are embargoed because the patient hasn’t come for their blood pressure check and if we start handing them out then they’re bypassing the system. But there are other drugs they come for where they just, you know, people just vote with their feet. In [place] there’s about a 3-week wait for a GP appointment. They come here. They know it’s going to take usually a 2.5-hour wait, on average, so they take their choice.
Chestnut, Staff 009, time 3
Hawthorn pen portrait
Current model
-
GPs are in operation Monday–Friday, 18.00–08.00 the following day. There are two GPs 18.00–23.00, one GP between 19.00 and 23.00 and one GP 23.00–08.00. There is coverage by GPs 24 hours per day at weekends. There is currently a HCA who undertakes patient observations in the OOH service at weekends.
-
GPs are part of an OOH service and so patients can be triaged from the ED, or they can book telephone or face-to-face appointments via NHS 111. GPs also perform home visits. The majority of patients who GPs see are booked via NHS 111. Patients who have a booked appointment through NHS 111 receive priority over ED-streamed patients or patients who ‘drop in’. Patients who arrive at the OOH service without an appointment are told that they are not supposed to do this and are seen, but have to wait for a time to become available. The analogy given by a GP was that ‘it is an OOH [service] with streaming tagged on.’
-
In the ED, there are two rooms dedicated to triaging patients. One has been purpose built as a result of the capital funding and was in place at our 6-month visit; the initial plan was to have two nurses triaging at all times, but, despite employing two nurses for this purpose, staffing issues have not allowed this to happen. However, there is usually one nurse triaging patients, with the other room used for a minor injuries nurse or ENP. During very busy periods or when the demand for triage is too high for one nurse, a second nurse may be called from the ‘shop floor’ and will start triaging from the second triage room. Sometimes an ED doctor may also sit in with the nurse who is triaging to try to discharge patients at this point when possible.
-
After booking in at reception, a card with the patient’s chief complaint is placed in a box by reception; the triage nurse uses this card to call patients for triage. Patients are seen in chronological order. The minor injuries nurse will either see patients after triage or select patients from the box who have presented with a minor injury, and so some patients may not be triaged.
-
There is also now an investigation and treatment room, which is staffed by a HCA and nurse. Patients who need further observations, for instance an ECG, will be sent here before being seen by a doctor, who will decide that the patient is either fit to wait in the waiting room or needs to be admitted to a cubicle. Patients can be sent to the investigation and treatment room for assessment/monitoring from either an ambulance or triage. For instance, patients who present with chest pain at triage may be sent for an ECG at investigation and treatment.
Streaming patient flow
-
The triage nurse was able to perform ECGs, but this has recently been removed from the triage room.
-
Observations at triage are limited to blood pressure, temperature and blood sugar.
-
There are no strict streaming criteria.
-
When a GP is not in operation, patients can be streamed to ED minors or majors. When a GP is in operation, patients can be streamed to minors, majors or the OOH service.
-
The triage nurse is not able to see how busy the OOH GPs are or the number of GPs who are on duty. This is a particular problem as the majority of GP patients are booked through NHS 111. If the GP is unable to see any ED patients because they are on a home visit or too busy, the only way to inform the ED is to physically go around to the ED.
Future plans for GPED
-
There are no further plans to expand the hours for GP service beyond or outside the GP OOH that is currently in place.
-
There are no immediate plans for any structural changes to the ED and the GP OOH set-up in terms of consultation rooms/layout of the service.
History of GPED
-
Prior to the GP OOH service being located around the corner from the main ED, the GP OOH service was located further down the corridor.
-
In terms of hours of service over the past 12 months, the service has not changed from what was described above, with the exception of the new paediatric/child waiting area and additional streaming rooms.
-
At one point, the service had a GP in the ED, but the staff felt that this did not work, which is part of the problem now because they want to keep the services separate and feel that it did not work last time.
Layout
-
The space used for GPs is not purpose built. GPs are based in the fracture clinic, with the same reception, rooms, etc. GPED is in operation when the fracture clinic is closed.
-
Since the GPED capital bid funding, a new paediatric ED has been built.
-
There are two rooms for triage in the ED. One has been purpose built since our first visit. This was to have two nurses streaming patients to the GP. However, currently, there is one nurse triaging and one room is used for an ENP/minors nurse.
-
The OOH service is managed by the trust, but there is a different manager for the ED and OOH service.
-
There is nothing in either the GP OOH service or the ED that states the number of GPs who are on duty or which GPs are on duty. Staff commented that this is problematic as some GPs will not see certain types of patients. The GPs also do not usually come to the ED and introduce themselves to the streaming nurse at the start of their shift.
FIGURE 12.
Hawthorne flow diagram. Black text indicates the baseline visit, dark-blue text indicates the 6-month follow-up and light-blue text indicates the 12-month follow-up.

Juniper pen portrait
This hospital changed from one system to another during the GPED project.
Time 1
The department had a large waiting area for ambulant patients, with a separate entrance for patients conveyed by ambulance. This ambulance entrance can allow access to either minors or majors.
Patients register at reception and take a seat in the waiting room. Although there is a paperless mechanism that notes and observations are entered straight into, there are still paper notes that follow the patient to the area in which they are seen. Patients are called for triage in a room next to the waiting room. The nurse conducts a rapid assessment, taking observations and making online notes. The nurse decides which area the patient should go to. Paediatrics enter the same waiting room, but when they are called they go into a separate area for assessment and treatment. GPs are integrated into the department as staff members and see patients who have conditions that could be dealt with by primary care. To enhance their skills, they also see other conditions such as injuries. They are also able to become involved in cases that go to majors and ambulatory majors, should they wish to do so. GPs are not available on every shift or all night. However, they do work some weekends and evenings.
Times 2 and 3
The department had invested in a new building in the car park for the redirection of GP-suitable patients.
The UTC was staffed by regular staff members. The usual nurse is newly qualified (band 5). They work most of their shifts in the UTC; the remainder are worked by the manager, other ED nurses or bank staff. There is usually a HCA who works in the department as well. The shift starts in the main ED and then they set up the department to open at 10.00. They keep an eye on the patient list and collect patients from the ED chairs area if they feel that they could be seen by a GP. They have tried to take more patients from this majors area, but it has not been successful as a registrar has not been available to work alongside the GP.
If GPs take blood samples and perform radiographs, they have to be coded as majors chairs, despite the fact that they have been seen in the UCC.
There is a suggested ‘variable risk appetite’ in the different GPs. Some work in both the ED and the UTC.
The process is that the reception staff take notes to the streaming zone in minors. The reception staff notify someone if they are concerned about a patient. There is a cubicle designated for streaming at present; however, the old triage room has recently been reconfigured and will soon be used for streaming.
Only one nurse is streaming at any one time. They sometimes come over to the UTC to ask for advice about whether or not patients are suitable to be seen by the GP. The UTC staff will collect patients prior to streaming if they look suitable on the ED list.
The UTC is open from 10.00 to 22.00, depending on staff levels. Nurse shifts are 07.30–20.00. They come to the UCC at 10.00 and stay until the end of their shift. At this point, if a doctor is working until 22.00, they will move over to the main department. At weekends, the department is open 13.00–20.00. They have just employed a GP to work from 10.00 to 22.00 on a Sunday.
There do not appear to be any protocols in place about which patients will be seen by a GP in the UTC. However, they have agreed that they will not take GP referrals, as this would be a GP-to-GP transfer.
They can see about 30 patients per day. Each consultation lasts about 30 minutes. The nurse walks between the departments frequently during the shift.
Training to undertake streaming is feasible after a newly qualified practitioner has been employed for 3 months, although streaming staff are mainly band 7. There is a training day available, but not all the nurses have completed this training. Streaming should last about 3–4 minutes. They usually take a brief history and undertake observations; it can take longer if they take a comprehensive history. The UTC nurse will undertake observations if they have not already been performed.
The nurse estimates that 4% of patients are streamed to the UTC.
Linden pen portrait
This ED has been streaming patients to GPs when they attend the ED for a considerable time (> 7 years, although it is difficult to get an exact timescale).
Patients attend the ED and go to a set of reception windows marked to indicate that they should go to one and then the next. At the first window, they see the streaming nurse, who is a band 7 nurse, very experienced and usually an ENP. The nurse asks a few questions to establish the condition that the patient is presenting with, its seriousness or otherwise, and gives them a slip of paper indicating where they should sit. There is a well-established protocol for which patients should and should not be sent to the general practice department. The nurse indicates that they need to go to the next receptionist window, where they will be entered into the ED patient-logging system. From there, they sit in the waiting room to go into the minors or majors department, or walk to the general practice department, which is a 5-minute walk, but is on the hospital site. Once inside the GP building, they tell reception that they have arrived and wait to be seen by the GP. The receptionist marks the patient list to indicate their arrival.
General practitioners are not permitted to undertake investigations, apart from a urinalysis. If any other investigations are required or the patient’s condition requires being seen by the ED or specialisms, they are sent back to the ED. Sometimes patients are told to return and, unless they announce their arrival, they can be overlooked. Similarly, if patients arrive and see the streaming nurse but do not register with the receptionist, they can go unnoticed in the waiting room.
The waiting room is very small and the tension about waiting often rises. When it is extremely busy, the GP service manager will announce the waiting times and invite people to go to their own GP instead. GPs tend to see patients for ≈ 20 minutes before they have completed the appointment and patients leave.
Some patients are sent to the GP department for dressings, for example postoperative dressing changes. This is possible when a nurse is on duty in the GP area, but if a nurse is not on duty the patient is returned to the ED.
There is some emphasis on the right to obtain treatment in the UK, with many posters displaying the process for obtaining treatment and providing identification.
The system is well established and has a regular governance procedure. The two teams meet monthly and discuss any issues that arise, including cases when clinical risk has been identified. There are varying views of the patients and sometimes there appears to be a resistance to patients who are believed to be ‘misusing’ services. Some staff are more tolerant than others with patients who have evidently not attempted to use their own GP or are not registered with a GP. Furthermore, the GP service becomes overwhelmed and attempts to discourage patients from using the service are based on the long waiting times.
Nutmeg pen portrait
The GPED/UCC service was very recently (in December 2018) relocated on site to an area integrated with the ED, which is where the fracture clinic was previously located (i.e. connected to the ED), and this is where the service was operating during the time 1 data collection. The walk-in entrance opens to the large waiting area, with a corridor leading to the majors department to the left of the entrance.
FIGURE 13.
Nutmeg layout.
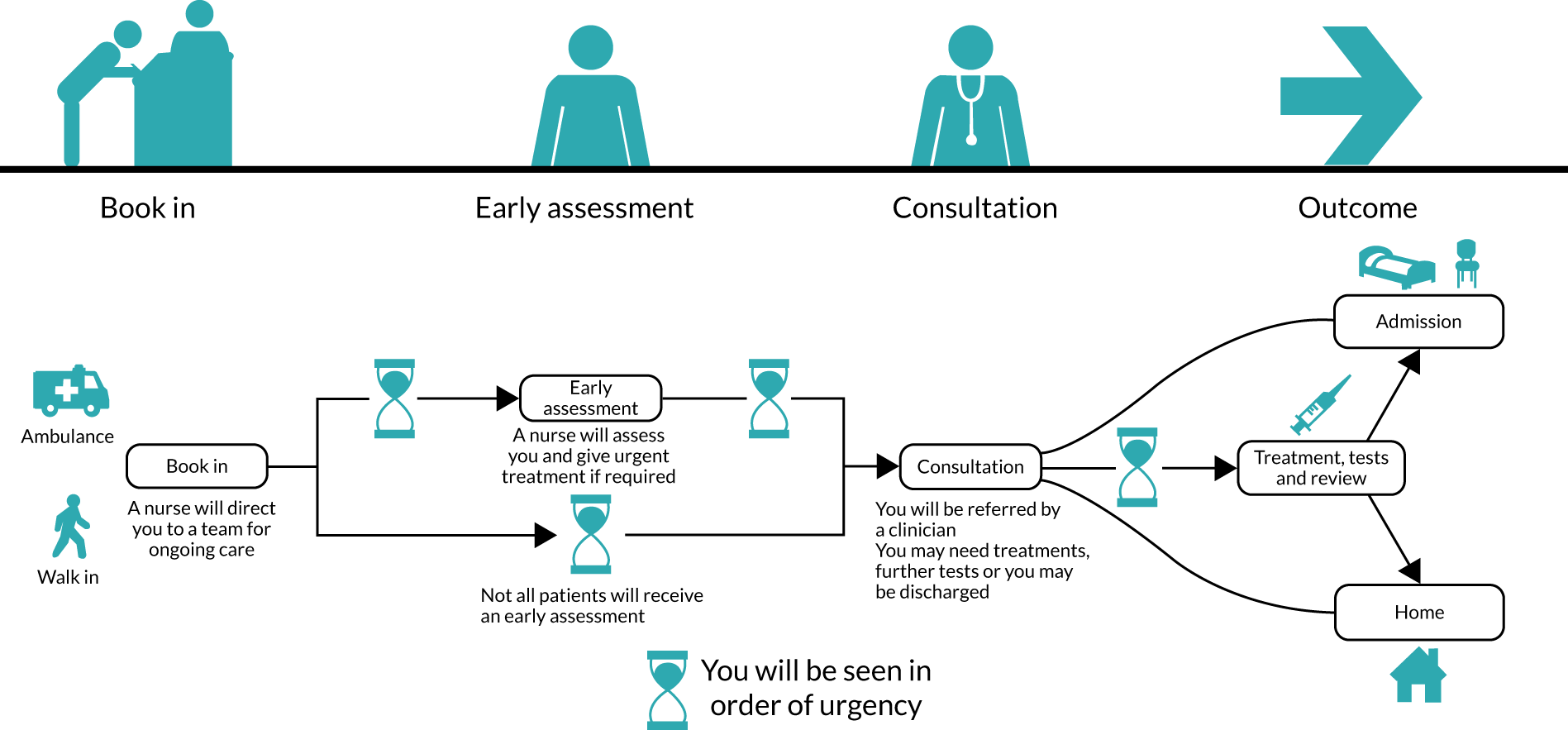
Service times
Although there is an aspiration to operate an ‘all-hours’ service, this is not being achieved currently owing to a shortage of GPs. A GP normally arrives at the urgent treatment unit at 08.00 or 09.00 and sees selected patients until the end of their shift, which is of variable duration.
Model and patient flow through GPED
This is a joint-led service for ambulatory patients. From 8.00 until 12.00 the GP service provides staff to look after, or to see and treat, appropriate primary care presentations. Outside of these times, the ED looks after this group of patients in conjunction with the GP service. The ED sees the patients that are unsuitable for the GP service, for instance those that are injured.
Interviewees described the service as changing from co-located to an integrated/embedded model. The primary care service in the UCC is provided by a private provider [the same provider as was involved in the previous co-located service (see Linden Pen Portrait)]. The site has a protocol which the band 6 and 7 nurses use to stream people from the front door if they meet the protocol to wait to see the GP. This means that some patients are not seen by an ED nurse through first contact; they are instead taken straight to chairs to wait to be seen. Subsequently, one of the GPs (or HCAs) will take the patient in to complete observations and a short assessment to check that they are suitable to wait in the queue. Then the GP will see and assess them. The ED staff have little contact with these patients, except at night when the GPs and other primary care staff are not present. If a patient brought in by ambulance is not considered suitable for the ‘majors’ area of the ED by the ambulance crew, they can be reassessed and directed to the GP service.
Poplar pen portrait
This hospital is located away from the local towns and thus is accessed by public or private transport, but rarely on foot.
The ED is currently split by a road across the site. On one side is the paediatric and majors department, and on the other is the UCC and reception for ‘walk-in’ patients. The main ED is connected to the main hospital, whereas the UCC is a much older, low-level building that has been cosmetically improved, but is periodically troubled by water and electrical supply difficulties. Each has a waiting area. The UCC has an immediate area, leading from the reception and waiting room, which has the consulting rooms used by the ED doctors, ENPs, triage nurses and GPs. There is another area further from the entrance that has recently been refurbished with consulting rooms, but it does not appear to be in use. Plans to move the GPs into this area seem to be afoot.
Ambulance-conveyed patients can be taken to either department, but it is unusual for them to be taken to the UCC. All children are seen by paediatrics. Paediatric patients enter the majors reception and then they continue on to the paediatric waiting area. There is sometimes confusion when patients are redirected between the two buildings as they have attended the incorrect place. There is reputed to be a plan to build a new unit (i.e. an urgent treatment centre) attached to the main department and a subsequent redesign.
At the initial data collection visit, patients booked in at the reception desk and moved to another desk next to it to speak to the streaming nurse (who was a band 6 or 7). The proximity means that patients can be overheard telling the receptionist what their complaint is and so the conversation is continued at either desk by the senior nurse. Sometimes the senior nurse will take observations as well. Once the nurse decides the most suitable route for the patient, they complete the paperwork and put it in a tray marked for the attention of the GP, ENP or ED doctor. Patients are seen in their order of arrival unless they have a priority need. As they become available, the triage nurse, ENP or doctor take a set of notes. These staff will rifle through the notes to check that patients are being seen by the correct person, and change the position of notes according to priority. There are also some direct referrals by the streaming nurse, on behalf of the doctors, to specialist areas (e.g. psychiatry, medicine, surgery). In addition, there are redirections to services such as the early pregnancy service. As well as streaming patients, the nurse manages the department, fielding queries, taking calls and making referrals to other departments. The patients sit in a waiting area that is quite small and cold. When it is busy, the waiting are soon fills up and people have to stand. There is no separation of patients at different stages and they frequently come up to the reception desk to ask when they will be seen. There are limited displays of waiting times. If the waiting times are extending, a laminated card is stuck to the wall to indicate this to waiting patients and relatives.
There is usually a triage nurse, two ENPs and an emergency care assistant working in the department, as well as the senior streaming nurse/co-ordinator. Doctors come over from the main department to work sections of the shift. The lead consultant comes to have a huddle several times a day. If the demand is higher in one area than another, staff are redirected to work until the volume of patients decreases.
The UCC opens at 08.00 and stays open until 22.00, then staff and patients transfer across to the main ED. For OOH GP-suitable patients, there are two small consulting rooms inside the waiting room.
Patients seen by the GP have approximately 20–30 minute appointments. The GP takes a comprehensive history because they do not have access to the primary care patient database. They are able to order investigations as deemed suitable and refer widely. Once seen, the GP would write a doctor’s letter to the patient’s own GP. As part of the consultation, the GP enquires whether or not the patient had seen their own GP, perhaps asking why not if they have not done so. There is a modicum of patient education to indicate whether or not seeing their own GP or some other community service, such as pharmacy, would have been appropriate. Referring to other specialties seems to be tricky, with there being some difficulty tracking down someone to take the referral. This was of particular difficulty when the referral was to another hospital, for instance for ENT referrals. Considerable time was taken to do this.
A GP had been employed by the trust already and was working to develop the protocol for streaming. They were aware of the L&D model and had seen other ED services streaming patients. There was no specific or formal training for the streaming activity and streaming was undertaken by band 6 staff with considerable experience and they were given informal direction by senior staff. The staff did not often refer to the protocol because of its complexity and comprehensiveness.
During the project, a small, glazed room was built in the UCC waiting area for the streaming nurse to work in. By the 6-month data collection visit, this was in situ. This meant that the nurse who was streaming was not also managing the department because they are removed from the central area and the locus of activity. In addition, patients were asked to take a numbered ticket to ensure that they were seen in order. There was an initial waiting area where people waited to book in and were seen to be streamed. Once streamed, they moved to the next waiting area. This was the same waiting area as before, but with a new partition wall separating the before- and after-streaming patients. Several more GPs were also employed to cover 10.00–22.00 and weekends. The general view of staff and management was that the service was attracting more patients and GPs were creating additional costs through their investigation requests and long appointments. Discussions were being held to decide how to move forward.
By the 12-month visit, the UCC had been taken over by a private company that was commissioned by the hospital to run the primary care service for 12–18 months. The service had taken on nursing staff through secondment arrangements to continue running the department. However, the lead nurse of the new service had been appointed by the new organisation, having previously worked in the ED as a senior sister. The GPs were on a locum rota and it was not always filled, although there was an intention to have two GPs on the shop floor at the busiest periods. The GPs were no longer able to order investigations and their appointment times were limited to 15 minutes, which was enforced by the service manager. The arrangements for patients remained the same: being streamed by a band 6 nurse, who had been trained thoroughly to do this by the new company. The parts of the building were being utilised more completely.
Redwood pen portrait
Layout
The UCC/GPED service is co-located in the same area of the hospital as the ED. They share the walk-in reception with the ED and minors department, and the waiting areas for all of these services were within the same space opposite the reception. The receptionists sit behind a glass screen when registering patients. Along the perimeter of the room, to the left of the reception area, there are three to four ANP/ENP consultation rooms where the patients have their observations taken before seeing the ED or GPED service. There is a corridor leading to more consultation rooms in the far left corner of the waiting room/reception area for the ED and GPED. There are consultation rooms situated along this corridor where the ANP/primary care nurses and GPs are located when the service is available. The paediatric waiting area is located further along this corridor. The entrance to the majors department and the ambulance entrance are on the other side of the reception from the walk-in entrance.
Service times
Currently, the GPED/primary care service is available between 08.00 and 22.00, 7 days per week. There is an OOH GP service that accepts patients through NHS 111 outside the GPED service times.
Model and patient flow through GPED
The patient arrives and they go straight to the reception (ED/GPED), where they report their reason for attending, are registered and then take a seat while they wait to see a triage nurse (Manchester triage). It is then determined whether they are a primary care, majors or minors patient.
During fieldwork data collection, the trust were piloting a ‘navigator’ role at reception. The navigator was a senior nurse practitioner who kept an eye on patients arriving and, when needed, conducted further questioning/symptom taking from patients, with the aim of ensuring that they were appropriately directed to the ED/GPED/minor injuries and identifying patients who may need to be escalated or could go directly to primary care without needing observations/blood samples taken. Previously, the service operated a ‘see-and-treat’ approach in which a GP sat at reception.
As noted above, the waiting area covered both the ED, minors and GPED. Paediatric patients waited in a separate children’s waiting area along the corridor, rather than in the main waiting area. The triage nurse called them in and then the triage nurse decided whether they needed to go to primary care, minors or majors. If they were to be sent to primary care then a GP (or GP and ED doctor) or an ANP would pick them out of a stream and assess them accordingly. The GPs work on the same computer system as the ED staff and have access to referrals to specialists within the hospital and to diagnostic tests. During fieldwork observations, the GPs generally did not utilise these referrals, but the ED doctors who had a dual role used the referrals during GP shifts when they were needed more readily. ANPs do not see children under a certain age.
Staff/workforce
The primary care service was generally staffed by at least one GP and one ANP at a time. However, during time 1 fieldwork observations, sometimes two clinicians were performing GP work (one GP and one ED doctor undertaking the GP shift). In terms of implementation, the staff integration had been somewhat challenging and there were a lot of initial tensions in bringing the ED and primary care staff to work together in the same space; some interviewees also suggested that this stemmed in part from how the ED and primary care staff are paid (e.g. some felt that the primary care staff received higher financial rewards, but did not have the same responsibility as members of staff on substantive contracts). Other challenges were that most of the primary care service staff were not on substantive contracts and that most were locums.
Future plans
Future plans include developing a primary care team with staff on substantive contracts, and making the navigator role part of this team.
Rowan pen portrait
FIGURE 14.
Rowan flow diagram.
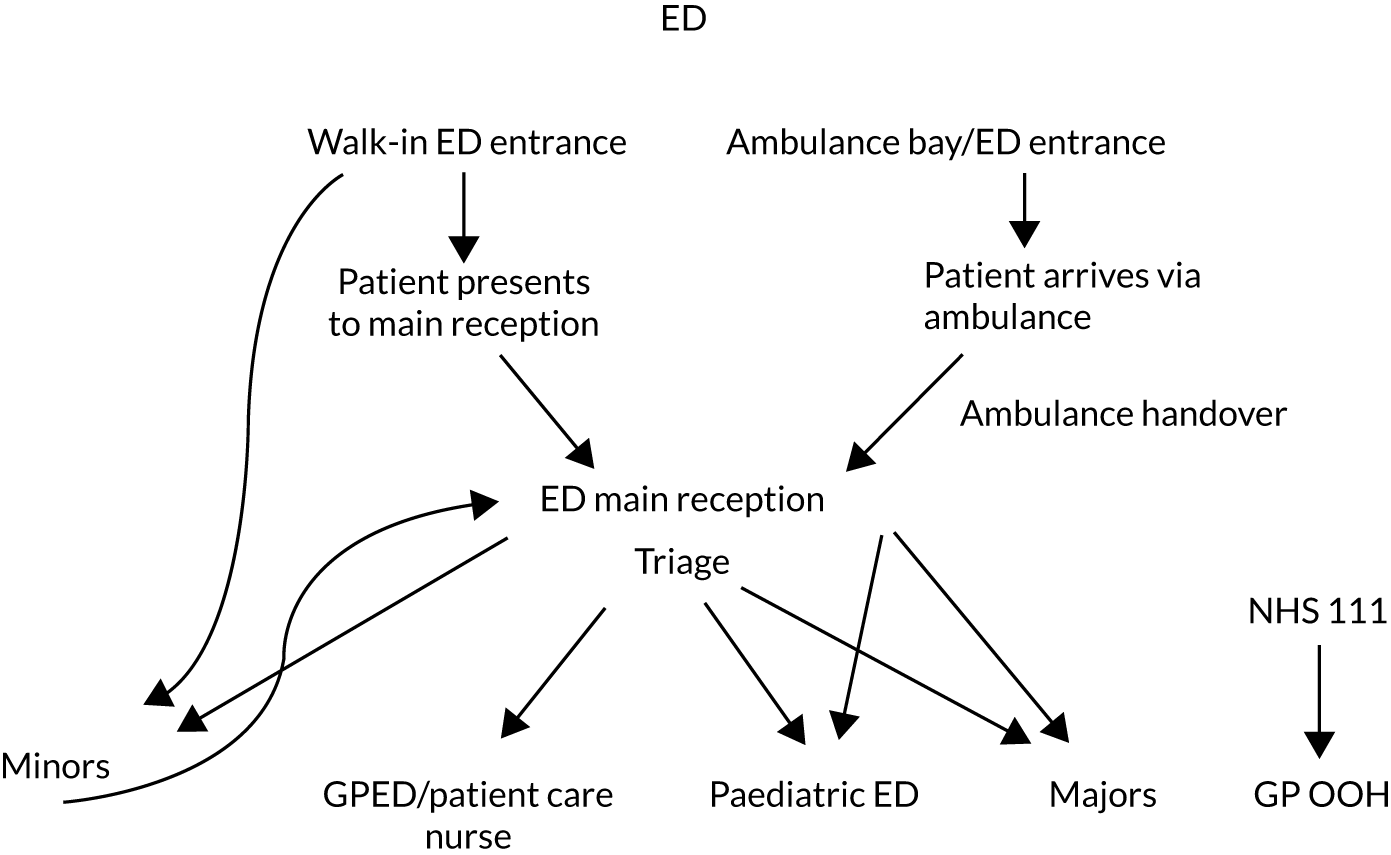
Baseline
Layout
The GPED service is co-located within the ED and operates from the same area as the ED minor injuries unit.
Service times
The GPED service is available 7 days per week from 08.00 to 23.00 and there is one GP available at any one time. The OOH GP service operates from the same area outside the GPED times (this service is accessible by appointment only).
Model and patient flow through GPED
Patients walk in through the main ED reception (they may also have been directed to the ED by NHS 111). Generally, patients report to main reception, where a triage nurse queries their reason for attending, asks additional questions and, subsequently, directs the patients to the main ED waiting area or to the GP or minors service. If they are directed to the GP service, the patient is given a GPED sticker. For main ED patients, the clerk registers the patient on the system at the main ED reception, whereas for GP or minors the patient is registered at the GPED/minors reception. Frequently during data collection patients presented at the minor injuries reception with GPED-appropriate concerns and the clerk had to direct them back to the main ED reception for triage. If they were triaged for the GP then they would return to be registered at the GPED reception, where the clerk would query whether or not they would allow the GP in the ED to access their GP notes. The patients were then asked to wait to be seen by the GP. If the GP deems it necessary, they can redirect patients back to the main ED queue. The GPs do not have access to any routine specialist referrals; patients who require this need to see their own GP to get an appropriate referral. Paediatric patients who register at the main ED reception after being triaged are asked to wait in the specialist paediatric ED waiting area whether they are waiting to see the paediatric ED or the GP.
Staff/workforce
The triage is undertaken by the band 6/7 ED nurse located at the main ED walk-in reception; currently there is only one primary care specialist nurse in post to work within the GPED service. There is one GP on shift at any one time and, during baseline data collection, there were some days when the patient care specialist nurse and GP were unable to get to the ED either entirely or for part of their shift because of the weather. There is currently a large pool of GPs (> 50) from the GP federation, which the trust works with in delivering the GPED service, who are undertaking shifts for GPED. The GP shifts are released on a certain day each month/at a certain time and GPs access this system and choose the shifts they would like to work. In addition to this, the GPs who saw the most patients each month were allowed to pick their shifts before other GPs.
Future plans
No major structural changes are planned, but there are plans for the development of the service and more coverage for the primary care specialist nurse.
Six months
Layout
There were no changes to the layout of the GPED service, but screens had been assembled at the main ED reception and the minors’ reception.
Service times
Service times were the same as at baseline.
Model and patient flow
The model and patient flow had not changed from baseline and the process had remained the same.
Staff/recruitment
There were no changes at this time; however, the site was in the process of recruiting more band 7 nurses to work as primary care specialist nurses within the GP service.
Future plans
There were no major future plans indicated at this stage, apart from the plans outlined above to recruit more primary care specialist nurses to share the work of the primary care nurse specialist.
Twelve months
Layout
There were no major changes to the existing layout structurally; however, in terms of the space from which the GPED service operates, there had been some minor changes. The service is still located in the same place as it was previously, but, at baseline and at the 6-month check-in, the primary care specialist nurse worked from a consulting room opposite the main ED waiting area, whereas at the 12-month check-in the nurse was more permanently located in one of the consulting rooms in the minor injuries unit area, which is also where the GPED service and GP consultation room were situated. This meant that the minor injuries nurses had one fewer consultation room to use when the GPED service was operating.
Service times
There were no changes in service times from baseline and the 6-month check-in, and the service is available 7 days per week, 08.00–23.00. There is still only one GP available at any one time and the daily service is generally divided into three GP shifts, albeit GPs sometimes work double shifts.
On a limited number of occasions during the winter, there had been two GPs on shift simultaneously, but this was not something the site is looking to adopt long term as it is not considered cost-effective and it is difficult to consistently predict the times when there will be a high volume of patients. The project manager did note that they were considering potentially starting the service a little later to provide a period of overlap between the two GPs, but this had not taken place yet.
Model
There were no major changes from baseline or the 6-month check-in, and the site continues to utilise the Manchester triage. There had been a few minor changes to the triage criteria (e.g. the conditions for which the GP does not see patients) at the 12-month check-in.
Patient journey and flow
The patient journey and flow through the service were the same as at previous data points. In observations, it was noted that patients still often presented directly to the minor injuries unit reception, from where they were directed to the main ED reception to be triaged first. After this, they were asked to return to the minor injuries unit/GPED reception if they were appropriate for either of the services. GPED stickers continued to be given to the patient, which they were to hand to the reception clerk.
In terms of patient journey, the only difference was that patients who required observations or urine tests prior to seeing the GP (or being directed back to the main ED, if required) now see the primary care specialist nurse, who completed these observations and then liaised with the GP when required. After this has taken place, the results were given to the GP and the patient went back to the waiting area and were seen by the GP in the ED in due course. If there were any issues regarding observations or urine tests that indicate that the patient needs further tests or their condition is more acute, then the patient care specialist nurse could move them into the main ED queue and direct them to the main ED waiting area to wait to be seen.
Staff/recruitment
Since baseline and the 6-month check-in, there were now four primary care specialist nurses, instead of one single nurse, working the primary care specialist shifts alongside the GP. There were no more nurses on shift at any one time, but the shifts were shared across the four nurses, who also work in the minor injuries unit as part of their role.
Future plans
No significant further changes to the system were planned.
Teak pen portrait
The Teak ED has been operating their model for > 12 years. The department was refurbished and reopened for use in March 2018.
Patients walk in and present to the front desk. Here, they are streamed by a nurse (band 6 or above). The streaming nurse is able to stream to a number of different places within and outside the department. The department is split into these areas, but all are in close proximity to each other. Inside the department, patients are able to go to the UCC, paediatrics, triage, majors or resuscitation. External directions for patients include the patient’s own GP, the GP hub or the pharmacy. The OOH GP service, which is on site but external to the department, is offered presently. This is via an external provider and has been in place for the last 2 weeks (i.e. early November 2018), operating between 18.00 and 22.00. This provides 20 appointments, but the maximum number filled so far has been 13.
Once a patient has been streamed into the department, they are given a number. When their number is called, they go to a registration desk to book in and, afterwards, they are directed to the appropriate seating area.
The UCC operates 24 hours per day, 7 days per week. Most staff rotate through the department, except for the GPs and ENPs. There are a number of GPs who are regular providers and are well known to the team. Other shifts are filled by locum doctors. The GPs are employed by the trust on a 0-hour contract basis.
Once a patient goes to the UCC, they are seen by a nurse, who conducts an initial assessment. They then wait to see either a GP or an ENP. ENP nurses see patients with injuries, whereas GPs see patients with minor illnesses and work within a protocol. This means GPs do not provide extended investigations.
FIGURE 15.
Teak flow diagram.
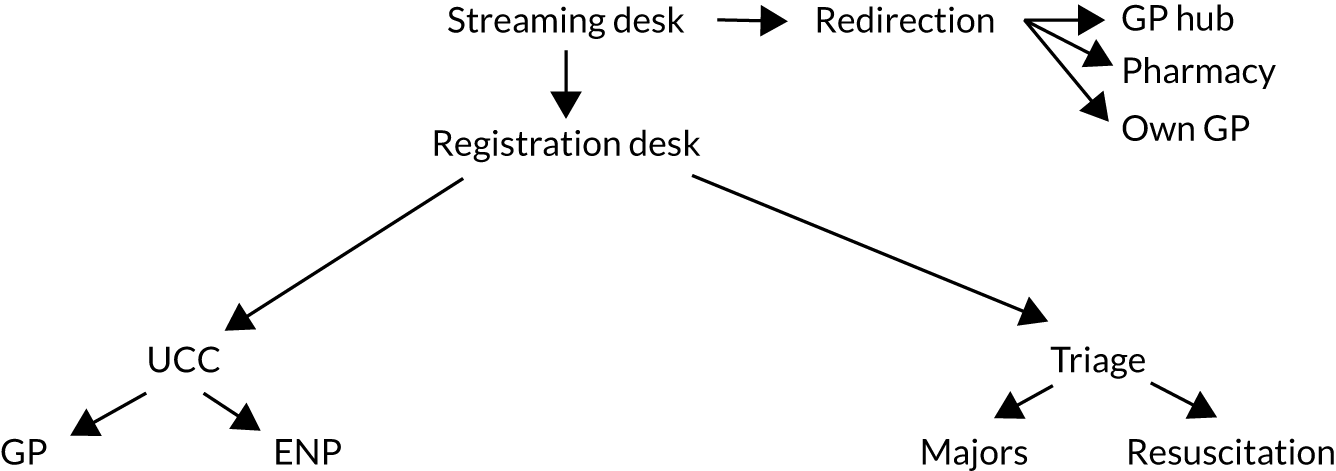
Appendix 4 Knowledge mobilisation
| Power | Interest | ||
|---|---|---|---|
| Low | Medium | High | |
| High | ED clinicians
|
National and local policy-makers
|
|
| Medium | General practice clinicians
|
Hospital managers
|
Academics
|
| Low | General public
|
||
Force-field analysis
A force-field analysis80 is conducted to identify the forces that drive change and those that resist change to understand the current state of equilibrium (Figure 16). For change to occur, the driving forces must be strengthened or the resisting forces weakened. It was intended that the findings of the study, if shared effectively, could become an additional driving force for change.
FIGURE 16.
Knowledge mobilisation force-field analysis.
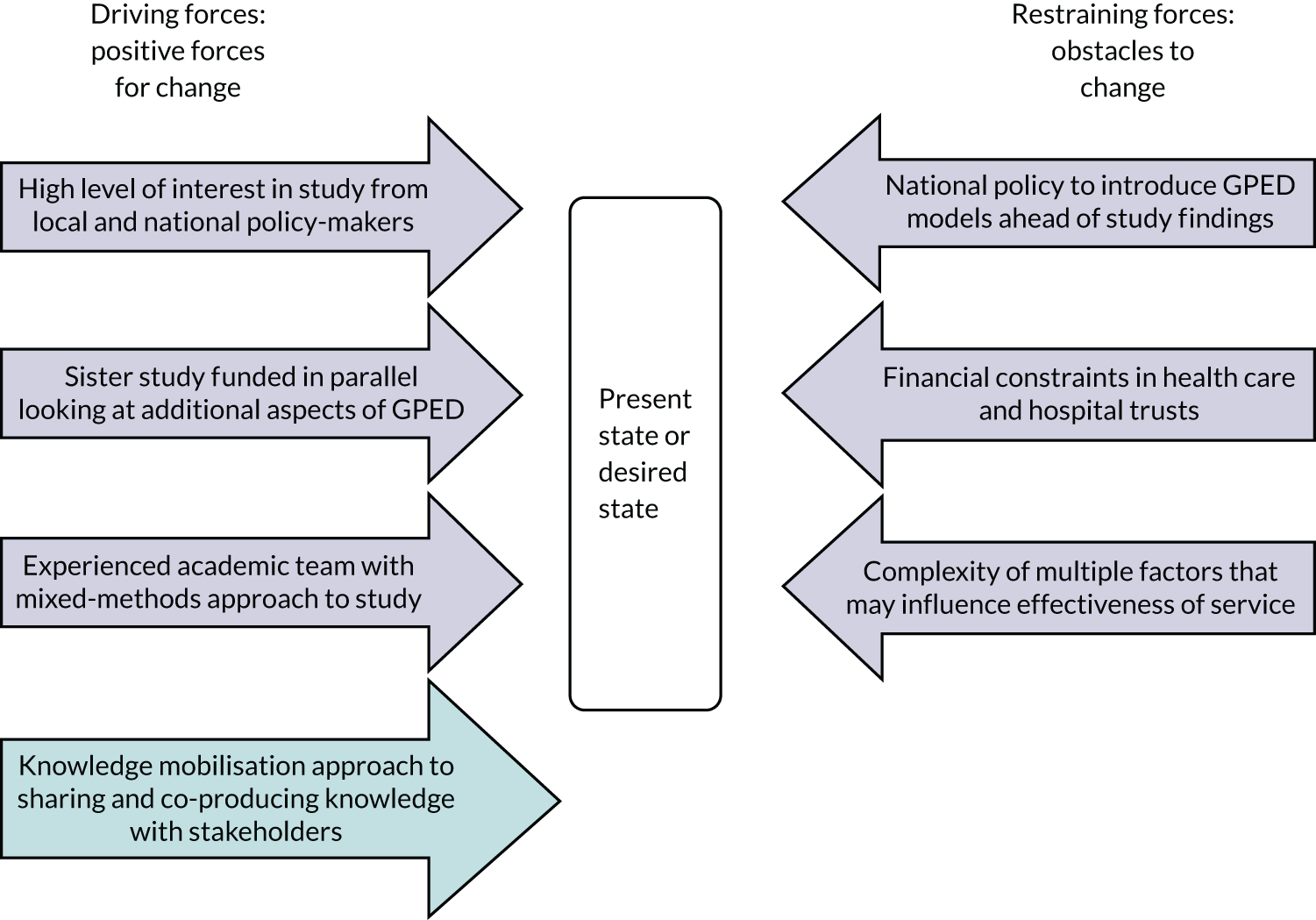
Theoretical basis for the knowledge mobilisation approach
Two theories of knowledge mobilisation were drawn on to inform the approach and strategy for the study. Both theories explain how knowledge is shared through everyday interaction and highlight where opportunities to introduce new knowledge may lie. By adopting the knowledge mobilisation approaches that are likely to be the most effective for the key stakeholder groups identified (i.e. clinicians and policy-makers), the impact of the study findings on practice could be maximised, as well as the opportunities for practice to influence the potential study outputs. Previous research looking at how policy-makers and clinicians share and mobilise knowledge have highlighted the importance of personal relationships, face-to-face interactions and trustworthy sources of information. 87,92,93,111
Communities of practice
The theory of communities of practice112,113 describes how groups are naturally formed of individuals who share a concern or a passion for something that they do. Additional learning occurs among this group from regular interaction, which is not necessarily intentional. A related body of work is that of Gabbay and le May on mindlines. 111,114 This examines the way that clinicians in general practice share and develop their learning through ad hoc social interactions in the form of a community of practice. The theory of communities of practice is relevant in informing the knowledge mobilisation approach for this study because of the growing body of research looking at how policy-makers and clinicians (i.e. the key target audiences) normally share and increase their knowledge. These studies have highlighted the importance of relationships, face-to-face communication and trusted sources, as well as highlighting the barriers to communication of written and academic information.
Socialisation, externalisation, combination and internalisation
The SECI theory115,116 provides some explanation of the processes involved in knowledge sharing in organisations. In their explanation of clinician mindlines, Gabbay and le May111,114 used the SECI theory to explain the processes that they observed between the clinicians in their community of practice. The four stages of the SECI theory describe a process of tacit knowledge being transferred into explicit knowledge and back again. The first stage (socialisation) takes place through observation and imitation, which then moves to the second stage (externalisation), in which knowledge is shared through stories and anecdotes. Explicit knowledge is exchanged during meetings and documents in the third stage (combination) and, in the final stage, explicit knowledge is transformed back into tacit knowledge in everyday practice (internalisation). The work of Gabbay and le May111,114 on mindlines highlighted two important aspects of this theory that are key to understanding how best to share academic knowledge. First, it is normally during the third stage, combination, that research evidence is shared as knowledge, although often without success. Second, the stages are not linear, as the authors often observed the stages to occur at different times in a different order.
List of abbreviations
- A&E
- accident and emergency
- ANP
- advanced nurse practitioner
- BNSSG CCG
- Bristol, North Somerset and South Gloucestershire Clinical Commissioning Group
- CCG
- Clinical Commissioning Group
- DHSC
- Department of Health and Social Care
- ECG
- electrocardiogram
- ED
- emergency department
- ENP
- emergency nurse practitioner
- ENT
- ear, nose and throat
- F1
- foundation training year 1
- GP
- general practitioner
- GPED
- general practitioners working in or alongside the emergency department
- HCA
- health-care assistant
- HCP
- health-care professional
- HES
- Hospital Episode Statistics
- HRG
- Healthcare Resource Group
- HSDR
- Health and Social Care Delivery Research
- IMD
- Index of Multiple Deprivation
- IT
- information technology
- KPI
- key performance indicator
- L&D
- Luton and Dunstable
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health and Care Research
- NoMAD
- Normalisation MeAsure Development
- NPT
- normalisation process theory
- OLS
- ordinary least squares
- OOH
- out of hours
- PPI
- patient and public involvement
- RCEM
- Royal College of Emergency Medicine
- RDD
- regression discontinuity design
- SECI
- socialisation, externalisation, combination and internalisation
- SSC
- Study Steering Committee
- UCC
- urgent care centre
- UTC
- urgent treatment clinic
- UWE
- University of the West of England
- WFS
- workforce survey
- WP
- work package
