Notes
Article history
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as award number NIHR132269. The contractual start date was in October 2020. The draft manuscript began editorial review in June 2022 and was accepted for publication in March 2023. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ manuscript and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this article.
Permissions
Copyright statement
Copyright © 2024 Varese et al. This work was produced by Varese et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2024 Varese et al.
Chapter 1 Introduction
What is the problem being addressed?
Responding to major incidents that impact on health and social care services is a challenging area in which to deliver services and evaluate outcomes, but guidance indicates the importance of pre-planning for these incidents, including a mental health response. 1 The ‘Resilience Hub’ approach is an innovative service model, originally developed in response to the 2017 Manchester Arena bombing,2 that could also address the urgent mental health needs of keyworkers affected by the coronavirus disease 2019 (COVID-19) pandemic. This system of care was designed not only to respond to the immediate needs of young people, adults and emergency response workers affected by the bombing, but also as an adaptive system of response that could be redeployed when the situation demanded, ensuring that expertise in large-scale mental health screening and trauma management could be sustained and expanded for responding to future crises. This adaptable service initiative can be flexed as needed, and while each large-scale trauma event will bring its own challenges and nuances, certain principles and understanding of processes to manage large-scale trauma can be vital to manage the system-wide challenges that emerge in the face of such emergencies. 3 Therefore, when the COVID-19 pandemic arose, local expertise and infrastructure were in place in Greater Manchester to provide large-scale mental health screening and support, and the Hub was adapted to support NHS, social care, ambulance service staff and some COVID-specific staff teams within fire and police services throughout the COVID-19 crisis. Broadly informed by the Greater Manchester Resilience Hub approach, similar services (i.e. variedly known as ‘Resilience Hubs’ or ‘Staff Mental Health and Well-being Hubs’) has been since set-up across various UK regions to respond to the mental health impact of the pandemic in these keyworker groups. As yet, no research has been conducted to evaluate the support offers of these novel NHS services.
Why is this research important?
During previous pandemics, mental health complaints have been found to be a common response, both within the general public4 and especially among health and social care keyworkers. 5 Previous work has also indicated the impact of a pandemic on front-line staff such as those found during the Severe Acute Respiratory Syndrome (SARS) outbreak where 549 respondents reported symptoms of post-traumatic stress disorder (PTSD) over a 3-year time frame. 6 Findings for the current pandemic are no different. Recent systematic reviews and meta-analyses which looked at the prevalence of mental health difficulties amongst front-line health care workers during COVID-19 found high levels of stress, anxiety and depression, highlighting the need for urgent action. 7–10 While the literature consistently finds evidence of immediate mental health impacts,11 the more long-term impacts such as burnout still require further attention. 12
Observational studies from countries most affected in the early stages of the pandemic were quick to highlight that keyworkers were at significant risk of adverse mental health outcomes due to a range of distinctive risk factors, including long working hours, risk of infection and fear of infecting family members, shortages of personal protective equipment, loneliness, physical fatigue and separation from families. 13 A meta-analysis14 found that at least 20% of keyworkers reported symptoms of depression and anxiety. Certain professional and demographic groups were highlighted as being disproportionately affected, for example, female keyworkers and nursing staff. 13 There is also recognition that keyworkers who belong to ethnic minorities may have been particularly affected,15 as well as keyworkers exposed to work circumstances conducive to ‘moral injury’, that is psychological distress that results from actions, or lack of, that violate a person’s moral or ethical code; for example, having to make difficult decisions about which patients can access life-saving equipment in times of critical shortage. 16
The large-scale impacts of policy to manage the pandemic, such as lockdowns, led to significant changes in healthcare utilisation. Despite considerable variation, research and official data suggested significant reductions in healthcare utilisation across a wide range of physical healthcare services. 17–20 Evidence also suggested that secondary mental health services experienced a reduction in service utilisation during lockdown,21 with reduced admissions observed for all service types, except children and adolescent mental health services, psychiatric intensive care units (ICUs) and intellectual disability acute beds. Other studies highlighted the reductions in referrals to primary care mental health services, psychological therapy and all secondary care mental health teams apart from early intervention in psychosis (EIP) services. 22 These reductions are a plausible result of public health messages (e.g. ‘stay home, save the NHS, save lives’) and policies required in order to ensure that the increased demand in other parts of the system, most notably ICUs,23 could be sustained at the height of the pandemic.
At an early point in the pandemic, the NHS Clinical Leaders Network24 issued an urgent call for action to ensure that NHS organisations prioritise initiatives to enhance mental health resilience and support provision for staff involved in patient care during the COVID-19 pandemic. In response to this, funding was announced to support the mental health of these staff, aiming to provide a proactive approach, rapid clinical assessments and onward referral and care navigation. As highlighted by other commentators, support was needed for everyone who had a direct clinical or caring responsibility,25 and the importance of supporting the social care sector in such initiatives was recognised, given the likely deleterious impact of the pandemic on this broad keyworker group (e.g. nursing homes staff). This is a sector where low pay and zero hours contracts have left that part of the system struggling with staff shortages and an estimated vacancy rate in 2019–20 of 7.3%, thereby in an already weakened state heading into the pandemic. 26
UK mental health services offer evidence-based psychological therapies, but what was missing was a way to identify keyworkers who most need support from these services, and help them to access support in a timely manner. 3 Consequently, both nationally and internationally, there were numerous recommendations to establish, scale-up and evaluate effective and timely systems for monitoring the mental health impacts of the COVID-19 outbreak among keyworkers, and facilitate access to appropriate psychosocial support for those who most need it. These recommendations, informed by extensive research in disaster mental health,27 particularly highlighted that response efforts should include: (1) proactive outreach approaches to encourage open communication about and disclosure of the mental health difficulties, therefore addressing possible reluctance amongst certain professional groups about disclosing vulnerability even when experiencing significant distress; (2) timely early detection and screening for mental health problems; (3) the importance of identifying and effectively treating milder mental health presentations before they evolve into more complex and enduring mental health issues; (4) the provision of tailored support according to individual needs, including ‘lower intensity’ support (e.g. psychoeducation; access to support hotlines and remote advice/support) as well as direct provision of psychological support to any healthcare workers who might need higher-intensity interventions. 27–32
The model described earlier and developed in Greater Manchester was highlighted as a potential exemplar of how this mental health support might be achieved. Several Hubs began set-up in 2020. While there was some variation in terms of how these Hubs operated, their central functions were aligned to the proactive approach, and rapid clinical assessments and onward referral were defined as being key characteristics of service delivery.
In autumn 2020, 38 further Hubs (also known in some regions as ‘Staff Mental Health and Well-being Hubs’) were commissioned by NHS England and established as pilots across England. NHS England provided guidance for Hubs,33–35 detailing, for example, expectations around the service model, such as proactive outreach, team-based working, rapid clinical assessment and ensuring access to evidence-based psychological care where required.
Research objectives
This research distils the learning from our evaluation of four Resilience Hubs in the North of England. To better protect the anonymity of Hub clients and staff considered in this project, the participating Hubs are here referred to as Site A, Site B, Site C and Site D. The research primarily pertains to two central functions of the ‘individual support’ offered by Resilience Hubs that were either already operational or at an advanced stage of set-up at the time of commencing the research (i.e. October 2020): (1) the provision of mental health screening to in-scope keyworkers; (2) facilitation of access to psychosocial support for NHS, social care and emergency response keyworkers. The exact support offers provided by these Hubs considerably evolved over the course of the pandemic in response to both local needs, ongoing learning and national guidance. One of the most significant changes was the expansion of the reach and volume of ‘team-based support’ provided to teams and organisations in their geographical footprint. While this offer is described in several components of the research (e.g. our health economic analyses), the project did not aim to formally evaluate team support offers.
As the project was set up and funded as part of an urgent National Institute for Health and Care Research (NIHR) call issued in early stages of the COVID-19 crisis to maximise ‘recovery and learning’ from the pandemic, a full clinical and cost-effectiveness evaluation of the Resilience Hub model using a controlled design was deemed unviable. Rather, the project employed a mixed-method approach combining observational quantitative, qualitative and health economic data to address the four main objectives listed below. After outlining the patient and public involvement and engagement (PPIE) work that underpinned our research in Chapter 2, and a detailed ‘service mapping’ exercise to better contextualise the support offers provided by the four participating Hubs and the processes needed to deliver the services in Chapter 3, we describe the methods and findings of research activities addressing the principal aims of the project in Chapters 4–7.
The four principal objectives of the project are summarised in Figure 1 and described below.
FIGURE 1.
Research objectives.
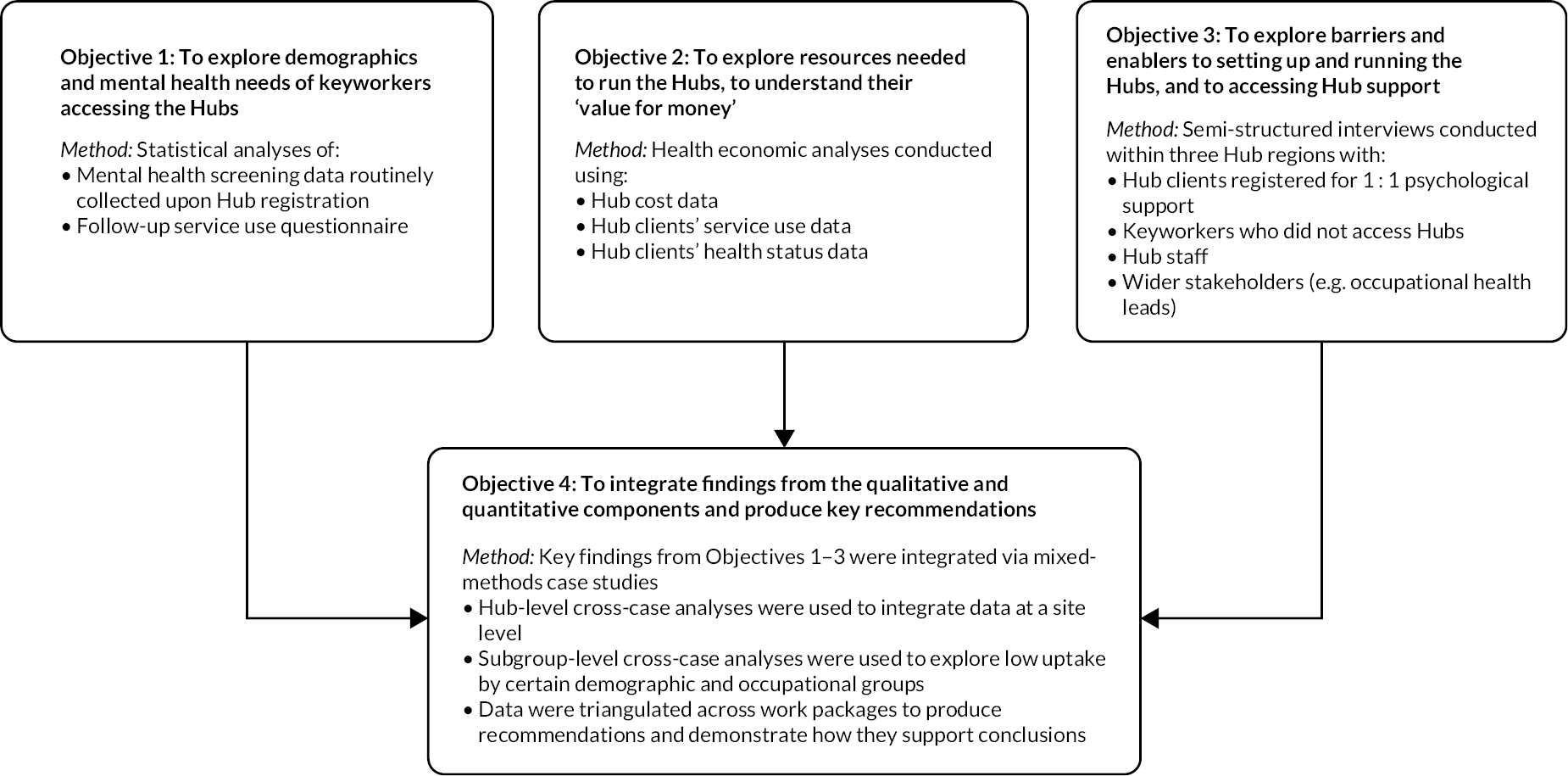
Objective 1: To provide findings to model service demand and guide future adaptations to the Resilience Hub approach to suit contextual needs and inform evidence-based commissioning, we aimed to conduct a quantitative analysis of routine demographic, occupational, and mental health screening data collected by the Hubs for keyworkers who accessed individual psychological support. These analyses aimed to consider:
-
sociodemographic and other keyworker characteristics associated with mental health presentations requiring higher levels of support
-
sociodemographic and other keyworker characteristics associated with lower levels of support access and uptake
-
specific exploration of points 1 and 2 for different keyworker groups, for example, different occupational and professional groups, and people from ethnic minority groups.
To address Objective 1, in Chapter 4, we report the findings of quantitative analyses conducted on routine screening data collected by the Hubs on a combined sample of 1973 Hub clients, alongside analyses of service use data collected from a subsample of Hub clients (N = 299) as part of a survey deployed approximately 5–8 months following Hub screening.
Objective 2: Conduct a health economic analysis, to explore the cost and health benefits associated with the set-up, use and management of Resilience Hubs.
To address Objective 2, in Chapter 5, we report analyses of costing data provided by the participating Hubs as well as analyses of health status and service utilisation data from Hub clients who completed the abovementioned service use survey, alongside a logic model developed to illustrate the potential benefits associated with Hub support.
Objective 3: To identify barriers and enablers relevant to the repurposing of the Hub model to respond to novel crises, and the implementation of the Resilience Hub model, we aimed to conduct a qualitative interview study with multiple relevant stakeholder groups at three sites (A, B and D).
To address Objective 3, in Chapter 6, we report the findings of in-depth qualitative interviews guided by normalisation process theory (NPT) and Sekhon’s Acceptability Framework, conducted with 14 members of Resilience Hub staff, 19 Hub clients who accessed individual Hub support, 20 keyworkers who had not accessed Hub support, and 10 wider stakeholders who were involved in the provision of support for staff within the health and care system (e.g. occupational health leads; HR directors).
Objective 4: To integrate and triangulate findings from the above qualitative and quantitative components, we aimed to produce mixed-method case studies.
These are presented in Chapter 7, and a combined discussion of the findings of all components of the research, alongside key clinical, service and research recommendations emerging from this programme of work are outlined in Chapter 8.
Chapter 2 Stakeholder/patient and public involvement and engagement
Overview
This chapter describes the PPIE activities for the study. In this research, ‘members of the public’ involved in stakeholder engagement were health and social care staff who either had accessed Hub support or did not access Hub support but would have been eligible to do so. This chapter aims to describe the PPIE activities while considering the recommendations of transparent reporting of PPIE in health service research. 36 In developing this project, the research team consulted front-line staff and Hub staff from two sites (Sites A and D) about the research teams’ proposed and PPIE strategy.
Methods
Definition of patient and public involvement and engagement and stakeholder engagement
PPIE in research is defined as an active partnership between researchers and patients and potential patients of health and social care services. 37 While there is typically a distinction made between the perspectives of the public and those who have a professional role in services, the nature of this study meant that we involved the perspectives of health and social care staff who would have been eligible for Hub support. To diversify the perspectives, we received through PPIE consultations, we carried out wider stakeholder engagement with health and social care staff in addition to consulting our formal staff consultation group.
Staff consultation group
In the first 2 months of the project, Hub clients at Site D who had given consent to being contacted for research purposes were e-mailed an invitation to be a part of the advisory group for the study. Further invitations were sent to clients and healthcare staff of Sites A and B to invite new members to join the group.
A core advisory group was set up, and around six members regularly attended the meetings. The group preferred to be called a ‘Staff Consultation Group’ rather than a PPIE group, as members considered themselves to be staff who care for patients, not the patients themselves. The Staff Consultation Group met virtually every 2 months, for on average 90 minutes, with frequent additional tasks (e.g. feedback on research materials, findings) also taking place between meetings. During the final 6 months of the study, the group agreed to meet monthly to review and discuss emerging study findings.
Meetings were arranged and chaired by the research team’s PPIE lead (KM). Members of the research team who attended the meetings included the study’s project manager (KA), and a research assistant (RA). The study’s health economist (GS), and health economics research associate (AR) and other RAs also attended meetings on an ad hoc basis to discuss specific aspects of the research with the group.
Efforts to diversify the staff consultation group
After the first meeting, a short, anonymous demographics form was sent to group members. While the group was diverse in terms of some characteristics (e.g. job role, sector, age and disability), all group members identified as being white women, although not all White British. This was most likely a result of initially approaching those accessing a Hub for support, amongst whom men and people from ethnic minority communities were under-represented (see Chapter 4).
The staff consultation group and the research team worked to diversify the group. Actions taken included targeted emails to Hub clients in under-represented groups, specifically highlighting that we sought to involve people who identified with a range of different demographic groups. RAs from each site also contacted local NHS Trusts’ ‘BAME Networks’ and equality, diversity and inclusion (EDI) leads, who provided advice around the wording of invitation e-mails. RAs attended network meetings for consultation, advice and promotion of the study.
For example, as part of this work, the RA at Site B also attended local BAME Network and EDI network meetings. At this meeting the RA introduced the Hub offer, the research study, and the need to diversify the Staff Consultation Group. These networks sent out information and invitations to be a part of the group via network meetings during online sessions and through the network mailing list. Other engagement included informal virtual meetings and e-mail correspondence with colleagues in EDI positions and NHS staff with a passion for reducing health inequality. The RA attended five BAME Network meetings and met informally with others outside the BAME Network (three monthly meetings with a smaller group of three stakeholders from December 2021 to February 2022; additional individual meetings with potential stakeholders who were interested in the research; meeting with champions in the community who worked with voluntary, community and social enterprise (VCSE) organisations to seek advice around engaging with under-represented communities).
Following these engagement efforts, two new regular members joined the Staff Consultation Group, one being from a white non-British background, and other from a minority ethnic group. However, the group nevertheless remained all women. Much of the involvement from people from minority ethnic communities was conducted in an informal manner due to the barriers with research engagement discussed in Equality, diversity and inclusion.
Other stakeholder engagement
Various stakeholders were also invited to make suggestions for the best ways to gather, interpret and disseminate research findings from the study. Stakeholders consulted included the study’s Project Steering Committee, and a regional BAME Network, and Site D’s Expert Reference Group, comprising of primary care, social care, VCSE and well-being leads from across the system. These groups shared several innovative methods that could be used, which were incorporated into the study’s impact and dissemination plan.
Involvement of the Staff Consultation Group across the research
Throughout the study, the Staff Consultation Group advised the research team on crucial aspects of the research from study set-up to data collection, to reviewing study findings. Further details of how the Staff Consultation Group contributed to the research at various stages can be found in subsequent chapters for each research objective. At the end of the project, the Staff Consultation Group reviewed and commented on study findings and two members of the group reviewed and amended the Plain language summary.
Chapter 3 Service mapping
Overview
The aim of this chapter was to describe, compare and contrast the models used by the Hubs, the interventions they provide, and detail an in-depth categorisation of the processes needed to deliver the services. 38
Methods
A service mapping template was developed from four different tools to capture relevant elements of service provision (available from the authors upon request). These tools included:
-
Section A (introductory questions) and Section D (service inventory) of the European Service Mapping Schedule,38,39 a widely used service mapping tool. Sections B and C were not included as these sections relate to counting large numbers of services, so were not informative for the current project.
-
The template for intervention description and replication (TIDieR) checklist,40 to provide an in-depth explanation of the interventions provided by the Hubs.
-
A checklist for describing health service interventions41 to provide additional contextual information, including organisational information, patient group, workforce and staffing.
Procedure
The template was completed by Hub RAs at each site. Sources of information included business cases, Hub websites and meetings with clinical leads and managers within each Hub. Information from each Hub was then integrated to compare and contrast features across the sites. The document was then reviewed by site leads (i.e. individuals with leadership or management responsibilities within each Hub) for accuracy. Data were collected between March 2021 and March 2022, capturing a snapshot in time of the Hubs’ services, while recognising possible future change.
Results
Geographical regions
The four Hubs were based in different geographical regions within England. Table 1 gives estimates of the number of eligible staff within each site region.
| Site | Health and social care staff within site regions (excluding staff from private organisations) |
|---|---|
| Site A | 126,000 |
| Site B | 165,000 |
| Site C | 129,000 |
| Site D | 180,000 |
The Hubs were set up as collaborations between several NHS trusts within their respective localities. Each site is hosted by one NHS Trust, with some local variations.
Goals
The initial goal of the Hubs was to offer timely psychological support to health and social care staff who had been psychologically affected by the pandemic. The aim was to support individuals, teams, organisations and the wider health and care system. This aim was operationalised through the provision of psychological support for individuals, and individual and team-based support for managers, leaders, and staff teams. The function of the Hubs continued to evolve, broadening beyond the pandemic, for example, providing support following local incidents.
Funding
Each of the Hubs was funded by NHS England and Improvement (NHSE and I), with some variation in local funding arrangements.
Target population
All Hubs opened to NHS and social care staff who lived or worked within the respective Hub regions; variations are described below. Some variations to Hub eligibility included staff outside of the NHSE and I national scope for Hubs, including education staff, and emergency services staff other than ambulance staff. Eligibility as defined by NHSE and I also changed over time, whereby Hubs were initially set up to support staff affected by the pandemic. Latterly, this remit changed to include all staff within in-scope groups, regardless of the cause of difficulties. 33 Table 2 details groups in scope at each site.
| Site A | Site B | Site C | Site D | |
|---|---|---|---|---|
| Over 18 (health and care staff) | ✓ | ✓ | ✓ | ✓ |
| 16–17 years (health and care staff) | ✓ | Not in scope | ✓ | ✓ |
| Family membersa | ✓ | Not in scope | ✓ | ✓ |
| Ambulance service | ✓ | ✓ | ✓ | ✓ |
| Police/fire | ✓ | ✓ | ✓ | ✓ (if involved in specific COVID-related health and care duties) |
| Education | ✓ | Not in scope | Not in scope | ✓ (if responsible for well-being) |
| 3rd sectorb | ✓ | ✓ | ✓ | ✓ |
| VCSE | ✓ | ✓ (if local authority commissioned) |
✓ | ✓ |
Site D was also open to staff who work in the VCSE sector, family members (including direct, extended or chosen family members from any region in the UK), ambulance staff and fire service and police officers involved in COVID-19-specific duties. Different workstreams were available for emergency services personnel and individuals working within complex safeguarding teams.
Sites A and C were open to all emergency services and VCSE staff, and immediate family members of healthcare staff who live or work in the respective Hub region. Site A also supported staff from education. Site B was also open to all emergency services, third-party organisations and voluntary organisations who had been commissioned by local authority. Although the Hubs were predominantly set up for people who had been affected by COVID-19, Site C and Site D opened to staff regardless of the cause of their difficulties. In contrast, Sites A and B supported staff whose difficulties were caused by or exacerbated by COVID-19.
Several of the Hubs opened to different occupational groups in a phased approach to avoid overwhelming Hub services. Site A opened to all staff in December 2020; Site C did not have a staged offer; however, a reduced version of the service opened in November 2020 to enhance existing occupational health and psychology services. Site C was opened on a larger scale to support individuals and teams in February 2021. Site B opened initially to NHS critical care staff in February 2021, broadening to all NHS staff in March 2021, followed by social care in July 2021 and emergency services in August 2021. Site D initially opened to screening and referrals from managers/leaders for health and care staff and targeted groups (e.g. staff working on COVID wards and care home staff) in May 2020, and was advertised to all health and social care staff, and their families in November 2020.
Model summary
All Hubs operated an outreach and screening model to support clients, although there were variations in the implementation of this overarching model. Each of the Hubs had an online self-referral system. Self-referral forms include mental health screening, demographic and occupational information, which inform subsequent clinical assessment. Subsequent psychological support differed across the Hubs and is outlined below (see Services offered by the Hubs).
The Hubs discharged clients following completion of support or treatment. Clients could re-refer to these Hubs if needed, and there was no limit on how many times a client could re-refer. Initially most of the support was provided virtually, but due to demand and easing of restrictions, all Hubs expanded their offer to provide face-to-face support when appropriate. At the time of data collection, the Hubs were open Monday–Friday, but offered some evening appointments if required.
Staffing
Staffing skill mix was similar across the Hubs, representing a ‘top-loaded’ model with a higher number of senior clinicians compared with non-qualified staff such as assistant psychologists (APs). Table 3 illustrates the breakdown of staff at the time of data collection, according to agenda for change (AfC) banding, demonstrating this staffing model. Band six members of staff correspond generally to qualified clinicians. Common skill mix across the Hubs’ teams included: clinical psychologists (CP); psychological therapists; mental health practitioners; cognitive–behavioural therapists; APs and administrators. Most staff was employed via secondment from their usual employment, or via fixed-term contracts.
| Service | Percentage of Band 6 staff or higher |
|---|---|
| Site A | 78.51% |
| Site B | 67.04% |
| Site C | 73.96% |
| Site D | 74.17% |
Similar rationales underpinned this staffing model across Hubs. More senior staff were employed due to an anticipated need for organisational working, for example, working with teams, as well as a need for staff experienced and accredited in trauma-focused interventions, to deliver NICE-recommended trauma therapies such as eye movement desensitisation and reprocessing (EMDR). 42 Furthermore, clients who required therapeutic input and presented with a range of difficulties and more complex needs required more senior clinicians. Finally, each Hub’s triage assessment and treatment planning was led by psychological formulation; ensuring a collaborative approach to explain difficulties and make sense of them while acknowledging the individual’s strengths and resources,43 necessitating experienced clinicians skilled in psychological formulation. However, Site B’s staffing was based on a ‘two-pronged model’, which included a high number of senior therapists as well as APs. In addition to the above need for senior staff, the sizeable workforce of APs was responsible for low+intensity interventions (see Self-help and psychoeducation and Low-intensity interventions), co-facilitating workshops, developing resources, regional mapping of available services and outreach.
Staffing numbers, AfC banding and roles across the Hubs as whole-time equivalents (WTEs) in post at the time of data collection are outlined in Table 4. Of note, this information does not necessarily reflect the staffing levels originally planned in the business cases of the Hubs (e.g. due to difficulties in appointing certain NHS posts) and may therefore underestimate the staffing resources forecasted to deliver planned Hub support at each site.
| Role | AfC banding | Site A | Site B | Site C | Site D | Staff group44 | Role code44 |
|---|---|---|---|---|---|---|---|
| Clinical leadership | 9 | 0.4 | – | – | – | STT | S2L |
| Clinical leadership | 8d | – | – | – | 0.45 | STT | S2L |
| Clinical leadership | 8c | 0.8 | 0.8 | 1.0 | 0.5 | STT | S2L |
| Clinical leadership | 8b | – | 1.8 | – | 0.9 | STT | S2L |
| Service lead | 8b | – | – | – | 0.3 | A and C | G1 |
| Clinical/principal psychologist | 8b | – | 1.2 | 2.0 | – | STT | S2L |
| Operational/service manager | 8a | 0.4 | 0.7 | 1.0 | 1.5 | A and C | G1 |
| Clinical psychologist/psychological therapist/practitioner | 8a | 4.4 | 3.2 | 1.0 | 2.9 | STT | S2L |
| Strategic engagement lead | 8a | – | 1.0 | – | – | A and C | G2 |
| Pharmacist/non-medical prescriber | 8a | 0.6 | – | – | – | STT | S2P |
| Assistant service manager | 7 | – | – | 1.0 | – | A and C | G2 |
| Clinical psychologist/psychological therapist | 7 | 3.3 | 6.3 | 2.9 | 1.9 | STT | S2L |
| Advanced practitioner | 7 | – | – | 2.0 | – | STT/N | S1U/N4D |
| Business manager | 6 | – | 1.0 | – | – | A and C | G2 |
| Research associate | 6 | 0.4 | – | – | – | A and C | G2 |
| Trainee clinical/counselling psychologist | 6 | – | 1.8 | 0.6 | – | STT | S8L |
| Mental health nurse | 6 | – | – | – | 0.6 | N | N4D |
| Research assistant | 5 | 1.0 | – | 1.0 | – | A and C | G2 |
| Trainee assistant psychological practitioner | 4 | 1.0 | – | – | – | STT | S8M |
| Assistant psychologist | 4/5 | – | 7.0 | 5.6 | 2.1 | STT | S5L |
| Pathways advisor | 4 | – | 0.8 | – | – | A and C | G2 |
| Administrator | 5 | – | – | – | 0.5 | A and C | G2 |
| Administrator | 4 | 0.4 | – | 1.0 | – | A and C | G2 |
| Administrator | 3 | 1.2 | 1.0 | 0.8 | 0.5 | A and C | G2 |
| Total WTEs | – | 13.9 | 26.6 | 19.9 | 12.15 |
Staff training and induction was arranged according to staff needs. Staff at each of the Hubs received training in electronic patient records systems, ongoing continuing professional development training and sessions on specific areas of concern, such as Long COVID, working with critical care staff, or specific mental health difficulties.
Services offered by the Hubs
Outreach
Each of the Hubs used outreach to promote the services and increase uptake of individual and team support. The Hubs offered presentations to staff teams to promote Hub support, how to self-refer and invite staff to ask questions. The Hubs’ team-based interventions were also used to disseminate to staff teams, regular meetings with acute trusts, stakeholders, social care and local authority, and through e-mail contacts between organisations. Common methods of outreach included distribution of flyers, banners and business cards, information packs distributed throughout care homes and meetings with leads of partner organisations. Other methods of promotion included social media (Site B), promotional items (e.g. branded stationery, well-being pack; Site B and D) and slots on local media platforms (all sites).
Site D used a locality system whereby Hub clinicians were assigned to specific workforces/areas within the region. Site A launched a branding and communications campaign across a wide range of partnership organisations.
Site B employed a full-time Strategic Engagement Lead to direct and manage communications and outreach across the region. Stakeholders were invited to a monthly Partnership Engagement Forum to gain stakeholder engagement and support targeted outreach. A monthly newsletter was disseminated across the region’s networks at the local and strategic levels to reach as many staff as possible. Site D and B’s critical care leads participated in close planning with the regions critical care network to direct critical care specific outreach and promotion.
Outreach activities were conducted by each Hub to target specific staffing and demographic groups that had lower uptake of Hub support. Targeted outreach included visiting and providing materials to care homes (Sites B, C and D), producing information for care homes (Sites A and D), gathering direct e-mail addresses for care home staff, ambulance staff and hospices to promote the offer (Site C; Site D), developing bespoke social media graphics for different groups (Site B; Site D), promoting workshops or facilitated peer support (FPS) sessions for care home staff (Sites B, C and D) and men’s mental health (Site C; Site D). Meetings with NHS Trusts Equality Leads took place to promote the Hubs and target health and care staff from minority ethnic backgrounds (Site C; Site D), as well as creating links with race equality networks (Sites B, C and D). A race equality campaign was implemented to attempt to reach more staff within this group (Site B). Webinars were also conducted with the local Council of Mosques (Site A). Face-to-face check-ins were delivered with critical care staff within the region (Site D) and links made with the ambulance service Suicide Prevention Lead to attempt to increase the uptake from this group (Site B). Meetings with representatives from emergency services also took place (Site A), and further meetings were held with representatives from critical care units to identify how best to spend specific funding to support critical care staff (Sites A and D).
Website resources
Each Hub had a website, providing information about services, eligibility, psychoeducation materials and downloadable self-help resources and short webinars. The websites also provided details of other mental health services/charities available to staff, as well as crisis helplines for emergencies. Individuals could self-refer on each Hub’s website. Site A’s website also included testimonials from Hub clients to promote and normalise the service. Staff accessing Site B’s website could book onto peer support groups and well-being workshops, as well as sending feedback, testimonials and suggestions to the Hub.
Self-referral and mental health screening
At each Hub, prospective clients were encouraged to self-refer online, although other options were available. Mental health screening formed a part of the self-referral process, although this process varied across Hubs. Screening at each Hub included measures of post-traumatic stress [International Trauma questionnaire (ITQ) or PTSD Checklist for the DSM-5 (PCL-5)],45,46 depression Patient Health Questionnaire-9 items (PHQ-9),47 anxiety Generalised Anxiety Disorder-7 (GAD-7)48 questionnaire and social and occupational functioning [work and social adjustment scale (WSAS)]. 49 Sites A, C and D also included a measure of problematic alcohol use alcohol use disorders identification test (AUDIT). 50 Each Hub collected demographic and occupational information from prospective clients, and on occasions additional screening measures not covered at other Hubs. The use of specific screening measures across Hubs is summarised in Table 5, and the measures are described in detail in Routinely collected measures.
| Site A | Site B | Site C | Site D | |
|---|---|---|---|---|
| Demographic and occupational questions | ✓ | ✓ | ✓ | ✓ |
| PHQ-9 | ✓ | ✓ | ✓ | ✓ |
| GAD-7 | ✓ | ✓ | ✓ | ✓ |
| WSAS | ✓ | ✓ | ✓ | ✓ |
| AUDIT | ✓ | No | ✓ | ✓ |
| ITQ | No | No | ✓ | ✓ |
| PCL-5 | ✓ | ✓ | No | No |
| Smoking/drug use | ✓ | ✓ | ✓ (since September 2021) |
✓ (since May 2021) |
| Questions around the impact of COVID-19 | ✓ | ✓ | ✓ | ✓ |
At Site A, online mental health questionnaires were presented as a tool for keyworkers to assess their own mental health and receive immediate feedback on their score, with the option to self-refer to the Hub after feedback. In contrast, completion of mental health screening within Sites C and D acted as a self-referral into the service, with immediate feedback provided via e-mail. Within Site B, individuals completed a brief self-referral form, and following acceptance of the referral by the Hub, clients were sent the mental health screening measures to complete prior to clinical assessment.
Assessment
Self-referral and mental health screening data were used to inform subsequent clinical assessment of keyworkers’ difficulties, to determine support and interventions offered by the Hubs.
At the time of data collection, Sites C and D offered an assessment phone call following the completion of screening questionnaires. Clients at Site C were offered either a rapid or a full assessment, dependent on the outcome of an initial review of screening scores. Within Site D, dependent on the initial presentation of the individual’s needs, the assessment was provided by any member of the clinical team, typically lasting between 30 and 60 minutes. The aim of this assessment was to gather information about the individual’s difficulties, construction of a collaborative formulation and quickly ascertain how the service could offer evidence-based support to manage those difficulties. Clients at Sites A and B were offered a full 60–90-minute formulation-based clinical assessment from a qualified clinician [a cognitive–behavioural therapy (CBT), therapist or CP] via video consultation as standard.
All Hubs offered an in-depth formulation-led assessment. Where Hubs offered shorter assessments as standard, in-depth assessments were offered dependent on clinical need. The aim of the in-depth assessment (60–90 minutes, with the potential to extend to a further session) was to develop a psychological formulation-led characterisation of individuals’ difficulties, and to inform support and treatment planning. For example, at Site D, a panel was used to decide whether a full assessment was clinically necessary or would expedite access into therapy. Site D also provided facilitated assessments into services where an agreement had been made, to prevent clients from re-telling their story. These assessments follow a pre-determined clinical framework developed by the Hub and are conducted by senior clinicians. If risk was a concern (e.g. a score of 2 or 3 on item nine of PHQ-9), duty clinicians at the Hubs ascertained the level of distress and facilitated support and/or access to appropriate services.
Onward referrals
There was variation across sites in the extent to which onward referrals were made following screening and assessment, versus direct provision of therapy within the Hubs. As one of the earlier sites to set up, the aim of Site D’s staff well-being work was to be proactive and preventative. As such, there was a focus on team and system support to reduce the number of clients requiring individual intervention. If deemed clinically necessary, onward facilitated referrals were typically made to maximise usage of already commissioned services, and fewer clients seen within the Hub for formal therapeutic work. Site D therefore facilitated a high number of outward referrals into other appropriate services, in addition to psychosocial support. When mainstream commissioned services were exhausted, or there was a clinical rational the Hub utilised its own therapy resource for those with complexity and clinical risk otherwise unmet. The site used an outreach and clinical advocacy model to ensure individuals received appropriate levels of support and offered evidence-based psychologically informed advice, self-help support and psychoeducation. Site C adopted these same principles and at the time of data collection facilitated approximately 60% of referrals to other services. Site B adopted the same principles, utilising regional mapping and waiting time check-ins to establish whether locally commissioned offers could be considered ‘timely’ to ascertain the most appropriate source of psychological support for that client, taking into account timeliness of available local support against risk of deterioration. As a result, Site B had an approximately even split between in-house intervention and onward referral.
By contrast, upon set-up of Site A, a scoping exercise of local services concluded that during the start of the COVID-19 pandemic, waiting times were significant; therefore, their intervention model was designed to provide in-house therapy provided directly by the Hub. Therefore, a small number of onward referrals were made to other services where appropriate.
Site B also provided a pastoral care pathway involving engagement with community, charity and third-sector organisations to offer an alternative model of care for interest-based support. A dedicated pathways advisor signposted keyworkers to appropriate support groups and activities, such as therapeutic singing, martial arts or music groups.
Interventions for individuals
Self-help and psychoeducation
Self-help and psychoeducation were offered at each Hub to provide support for low-level mental health needs. This involved providing materials, explanations of difficulties and signposting to other services. Self-help and psychoeducation were used to help the individual to manage their difficulties and offer advice on how to access further support if required. If an individual’s needs or levels of distress were significant, they may have been offered an alternative intervention to address those needs.
Sites C and D offered supported self-help and psychoeducation following every referral into the Hub. This was offered via telephone by APs or qualified clinicians, where required. Site C predominantly offered an assessment with a further two supporting phone calls to agree the treatment pathway, with the potential for further self-help and psychoeducation offered subsequently. However, within Site D, there was no maximum number of sessions of self-help and psychoeducation offered as this was dependent on the individual’s needs and goals at that time. Site B had a heavily front-loaded website containing substantial self-help and psychoeducational resources. These were signposted during assessment, or clients could be allocated to a low intensity in Hub intervention (see Low-intensity interventions).
Low-intensity interventions
Sites A, B and C provided a lower-level intervention for less complex difficulties, which was more formally structured than the self-help and psychoeducation offered at Site D. Low-intensity interventions typically involved a specific number of sessions based on low-intensity CBT principles, for example, guided self-help/psychoeducation, skill-building and relaxation exercises. At Site A, these were delivered by qualified psychological practitioners, APs and trainee associate psychological practitioners, typically over 6 sessions, with a maximum of 12 sessions. Individuals could be ‘stepped up’ to high-intensity therapy if clinically necessary. In addition, low-intensity sessions were used to support individuals waiting on the high-intensity waiting list at Site A. At Site B, low-intensity interventions were delivered by APs. These consisted of manualised, semistructured, psychoeducational and CBT skills-based sessions on topics such as sleep, anxiety, or panic, usually offered for four to eight sessions. Following low-intensity interventions, clients were subsequently offered higher-intensity interventions if required, signposted to other services, referred elsewhere, or discharged from the Hub.
Therapy
Direct therapy was offered by all Hubs. The rationale for providing direct therapies was similar across Hubs, including, for example, significant waiting times at local services; particular types of complexity (e.g. concerns around confidentiality; previous negative experiences in services) and circumstances in which clients’ presentations fell between gaps in services [e.g. difficulties that were too complex for improving access to psychological therapies (IAPT) services, but not sufficiently complex or enduring for community mental health team, support].
High-intensity therapy was delivered by CBT Therapists, EMDR therapists and consultant practitioners and CPs, and modalities included, for example, CBT; cognitive analytic therapy (CAT); compassion focused therapy; acceptance and commitment therapy (ACT); and trauma-focused interventions such as trauma-focused CBT and EMDR. This usually consisted of approximately 12 sessions at each Hub, but could greatly exceed this.
One difference across Hubs was that, at Sites B and D, the delivery of high-intensity therapies was further divided into ‘Step 3’ and ‘Step 4’ interventions (with Step 2 representing lower-intensity interventions), dependent on the complexity of the client’s difficulties. Step 3 therapy (usually 8–12 sessions) consisted of ‘straightforward’, single modality, problem-specific interventions, for example, CBT for low mood, EMDR for single-incident trauma. Step 4 therapy (20+ sessions) consisted of integrative, formulation-driven therapy or EMDR for complex difficulties. Both were delivered by CBT or EMDR therapists, CPs, or other similar qualified clinicians.
Two Hubs also offered group-based interventions. Site C’s 7-week bereavement support group helped individuals dealing with loss and grief in the workplace, delivered by clinicians trained in bereavement support or group analysis. A 6-week mindfulness group was also offered to help reduce stress and learn new skills, delivered by a Mindfulness-Based Cognitive Therapist. Site C also provided a nine-session peer support group for people experiencing Long COVID.
Pharmacological intervention
Individuals could receive pharmacological advice or support following psychological assessment at Site A. Pharmacological intervention was delivered by pharmacists, and included, for example, psychoeducation around medication, new prescriptions relating to mental health and medication reviews. Individuals could attend an initial appointment to discuss medication advice, follow-up appointments if medication was prescribed, and monthly medication reviews. Following discharge from the Hub, prescriptions were continued with the client’s GP. Site C offered support around medication from an associate nurse consultant, which included offering psychoeducation, advising individuals regarding non-medical prescribing and liaison with GPs.
Support for teams
A wide range of team-based interventions was offered across the Hubs, developed to support to the needs of managers, team leaders and help support the psychological safety of the health and social care system. Clinical leads, CPs or other psychological practitioners delivered team-based support across Hubs. Team-based interventions were bespoke to teams’ needs as determined through an initial consultation and formulation, and could be made up of a combination of different interventions.
While there were variations across sites, all sites provided consultation with managers and team leaders to help identify difficulties faced by teams and provide bespoke solutions. Team-based work incorporated trauma-informed approaches, signposting to supportive resources, reflective and resilience-based sessions, self-care workshops, training for teams and organisational strategy support, as well as direct support for managers as needed.
Workshops were provided virtually and face-to-face where appropriate across the Hubs. These were delivered by qualified clinicians with experience in supporting teams and organisations, and focused on different emotional well-being, self-care, psychological first aid and validation of the team’s difficulties. Examples included sessions on burnout, ‘containing the containers’, moral injury and psychological self-care. Furthermore, FPS was also offered by some Hubs to provide a safe reflection space for teams to come together to discuss relevant topics/difficulties.
Teams could engage with multiple aspects of team support provided by the Hubs, determined through initial and ongoing consultation with managers and teams. An example of this is outlined in Box 1.
A team manager contacted the Hub for support, and details of the Hub offer were sent to all services within the remit in the Hub’s region (promotion of the offer). An initial discussion was offered to the team manager, and discussion was had around support offered by the employer to identify the current difficulties (consultation). The manager provided the Hub with e-mail addresses of their employed staff, who were sent information on screening/self-referral and the Hub’s offer (outreach).
Face-to-face workshops were offered to this and other teams within the region to offer solutions and build psychological safety (workshops). The Hub joined the team’s ‘diversity and inclusion group’ to ascertain potential barriers that may have prevented some staff groups from accessing the Hub. A group of ward managers then requested a facilitated peer support session to provide validation of experiences and an opportunity for reflection (facilitated peer support).
Following this, the team experienced a death within their service, which resulted in the Hub re-promoting the offer and providing an explanation on colleagues re-engaging with the Hub without having to ‘re-register’ or complete questionnaires. Staff members were signposted to a bereavement service to provide more specialised support in this area (onward referral). Further consultation, promotion of the offer and a face-to-face workshop were provided. The team were also able to contact the Hub for support for additional difficulties.
Additional support for critical care staff
Critical care departments experienced high demand and were exposed to high numbers of patient deaths in the pandemic. Critical care staffs were therefore identified as a group likely to have been significantly impacted by the COVID-19 pandemic and all Hubs offered support by senior clinicians to this client group. Three of the Hubs utilised additional available funding to provide and co-ordinate support for this group, determined according to the number of ICU beds taken up with COVID-19 patients. The Hubs co-ordinated to provide broadly similar support across the services, differences in their methods of input are described below.
Within Site D, enhanced support was offered, including team and individual support, consultation, training and support for Professional Nurse Advocates to develop their skills, promotion of the general offer and more enhanced resources and ‘check-ins’ for Band 7 and Band 6 staff to help reflect and resolve difficulties. Each critical care unit had a senior clinician as an account manager and had the opportunity for onsite presence.
Site A similarly offered team well-being sessions for ICU staff as well as contributing to training consultations and supervision for key staff members. Site A also planned to assist these staff groups to enhance their well-being packages for example, team rooms and garden units.
Site B developed bespoke well-being resources for critical care staff and focused on promoting the offer to ICU staff. Drop-in sessions were also provided to some hospital sites to provide space to identify difficulties and access initial support with signposting.
Site B and Site D also joined a new critical care forum, which aimed to share learning and updates from supporting critical care staff to further improve the level of support.
Chapter 4 Quantitative analyses (Objective 1)
Overview
The analyses presented in this chapter considered screening data collected by the participating Hubs (N = 1973) as well as mental health service use data collected via an online survey in a subsample of Hub clients (N = 299). The aims were to identify keyworker characteristics associated with greater likelihood of mental health and functional difficulties that may benefit from mental health support, evaluate the extent to which keyworks accessed mental support following Hub input, explore keyworker characteristics associated with differential access to mental health support following Hub input, and gather data on keyworkers’ satisfaction with the support received by the Hubs.
Method
Participants
One thousand nine hundred and seventy-three individuals were included in the analyses of Hub screening data. All participants (1) were over 18 years of age, (2) completed screening at one of the Hubs and (3) consented for their data to be used for research purposes. Out of this sample, 900 participants had consented to be contacted for research purposes and were eligible for completing the follow-up survey deployed 5–8 months following the completion of the Hub screening measures. In total, 299 individuals completed the service use questionnaire that is 33.2% response rate across sites, with 77 participants in Site A (40.5%), 29 (29.9%) in Site B, 46 (27.5%) in Site C and 147 (33.0%) in Site D.
Routinely collected measures
Despite local variation in the screening information collected (see Chapter 3), the four Hubs routinely collected comparable data on the following domains.
Depression
Symptoms of depression were measured using the 9-item version of the PHQ-9. 47 This questionnaire asks participants to rate on a four-point Likert scale (0 = ‘not at all’ to 3 = ‘nearly every day’) the extent to which they have struggled with common symptoms of depression in the previous 2 weeks. PHQ-9 scores are added to compute a total score ranging from 0 to 27, with scores between 0 and 4 indicating ‘no depression’, 5–9 indicating ‘mild depression’, 10–14 ‘moderate depression’, 15–19 ‘moderate-to-severe depression’ and 20–27 ‘severe depression’. For the purposes of the present analyses, ‘caseness’ on the PHQ-9 was defined as scores suggestive of at least moderate depression.
Anxiety
Symptoms of anxiety were measured using the brief GAD-7,48 a self-administered tool that is frequently asking participants to rate on a four-point Likert scale (0 = ‘not at all’ to 3 = ‘nearly every day’) the extent to which they were bothered by common symptoms of anxiety in the previous 2 weeks. The total score can range between 0 and 21, with scores between 0 and 4 indicating ‘no anxiety’, 5–9 ‘mild anxiety’, 10–14 ‘moderate anxiety’ and scores ≥ 15 indicating ‘severe anxiety’. GAD-7 ‘caseness’ in the present analyses was defined as scores suggestive of at least moderate anxiety.
Post-traumatic stress symptoms
At two of the Hubs (Sites A and B), post-traumatic symptoms were assessed using the PTSD Checklist for the DSM-5 (PCL-5),46 a self-report questionnaire comprising 20 items corresponding to the DSM-5 symptom criteria for PTSD. Each item is rated on a five-point Likert scale (0 = ‘not at all’; 4 = ‘extremely’). A total PTSD severity score (ranging between 0 and 80) can be obtained by summing the items’ scores, and used to identify individuals with probable diagnosis of PTSD (i.e. individuals with severity scores ≥ 31). At the remaining Hubs (Sites C and D), post-traumatic symptoms were assessed using the ITQ. 45 The ITQ is a self-administered questionnaire assessing PTSD symptoms and additional features of complex PTSD (CPTSD) known as ‘disturbances in self-organisation’ (DSO) experienced by respondents in the previous month. It comprises 18 items rated on a five-point Likert scale (0 = not at all; 4 = extremely). The ITQ was scored to provide both a dimensional PTSD symptom score (i.e. a total post-traumatic stress score computed using six items assessing core PTSD symptoms including avoidance, hyperarousal and intrusions) and according to the standard ITQ diagnostic algorithm to identify probable International Classification of Disease – 11th Revision diagnosis of PTSD or CPTSD (via endorsement of specific PTSD and DSO items in conjunction with self-reported impact of symptoms on the person’s functioning). 45 For the purposes of the reported caseness analyses, any individual meeting ITQ criteria for PTSD on the PTSD subscale, irrespective of their CPTSD status, were regarded as having a probable diagnosis of PTSD.
Problematic alcohol use
Three Hubs (Sites A, C and D) collected data on harmful alcohol use using the AUDIT,50 a self-report questionnaire comprising 10 items rated on a five-point Likert scale (0–4). The AUDIT total score can range between 0 and 40, with scores between 0 and 7 indicating ‘low risk’, 8–15 indicating ‘hazardous drinking’, 16–19 ‘harmful drinking’ and scores ≥ 20 indicating ‘possible dependence’. In our analyses, AUDIT ‘caseness’ was defined as scores suggestive of at least hazardous drinking.
Social and occupational functioning
The WSAS49 is a brief measure comprising five items rated on a nine-point Likert scale (0 = ‘not at all’; 8 = ‘very severely’) to assess impact of mental health difficulties across multiple day-to-day tasks/domains. The total score can range between 0 and 40, with scores between 0 and 10 indicating functioning levels expected in non-clinical populations, between 11 and 20 indicating ‘significant’ impairment in functioning, and scores > 20 indicating ‘moderately severe or worse’ functional impairment. For the present analyses, WSAS ‘caseness’ was defined as scores suggestive of at least significant functional impairment.
The Hubs also collected data on a range of Hub clients’ characteristics relevant to the planned analyses, including the following.
Demographic data
Information was available on Hub clients’ age, gender, ethnicity, disability status (i.e. whether they self-reported having a disability) and sexual orientation.
Occupational and work environment characteristics
Although there was considerable variance across sites, the Hubs routinely collected information pertaining to Hub clients’ work setting, for example, whether the person worked in hospital settings (ICU/Critical care, Nightingale, A and E, Other Ward/Service, Across Hospital Site) or other setting (Primary care including GP Practices, Education, Emergency Services, Residential Care, Community Care, Local Authority, Voluntary/Charitable Sector, Other), and in what role.
Pre-pandemic mental health concerns
All Hubs collected information on whether the person was concerned about their emotional well-being/mental health before COVID-19.
Impacts of COVID-19
All Hubs collected information on common impacts of COVID during the acute phase of the pandemic. These covered whether the person had been impacted by COVID-19 in any of the following ways: (1) seconded to a different post; (2) moved to work in a different location; (3) undertaking new tasks within usual role; (4) been ill with confirmed COVID-19 (recovered at home); (5) been ill with confirmed COVID-19 (including being in hospital); (6) family member been ill with confirmed COVID-19 (recovered at home); (7) family member been ill with confirmed COVID-19 (included being in hospital); (8) experienced family/close friend bereavement; (9) suffered financial loss within the household.
Service use questionnaire
A service use questionnaire (SUQ) adapted from previous health economic research by the project team51 was developed to capture information on: (1) what level of support participants received from the Hubs, and their overall satisfaction with the support provided by the Hubs; (2) which mental health support services (if any) keyworkers accessed or were currently on waiting-list for following their registration with the Hubs; (3) to what extent keyworkers accessed these services as a result of Hub support. Additional health economic information collected as part of the SUQ is described in further detail in Chapter 5. A copy of the SUQ is available in Report supplementary material 1.
Procedures
All individuals screened by the Hubs were routinely asked to provide consent for their anonymised data to be used for research purposes, and whether they would like to be contacted for further follow-up research. Relevant data for all consenting Hub clients were extracted from the Hubs’ electronic patient records systems, cleaned, and anonymised by RAs based at each Hub. The data were compiled into a central database managed by the study statisticians, who performed quality checking and relevant re-coding/cleaning ahead of the planned analyses.
All keyworkers who consented to be contacted regarding follow-up research were sent an e-mail invitation to complete the SUQ (and additional measures relevant to the planned health economic analyses reported in Chapter 5) via a bespoke online survey deployed between 5 and 8 months following their Hub registration. Participants received up to four reminders over a 2-month period until they declined involvement or completed the survey. To minimise the impact of digital inequality, keyworkers who reported not having reliable access to an e-mail at Hub screening or completed the Hub screening measures over the phone were contacted by their respective Hub RAs using an alternative contact method (e.g. mobile phone) and given the opportunity to complete survey using alternative means (e.g. over the phone with support of the Hub RA). Data collected via the survey underwent data cleaning and recoding in preparation for statistical analysis by researchers based at the University of Manchester Biostatistics Collaboration Unit and in the Manchester Centre for Health Economics.
Analysis
For each site, and across sites, we numerically summarised data on participant demographic and occupational characteristics, and reported COVID-19 impacts and pre-pandemic emotional well-being concerns. Due to considerable differences in how occupational and work environment data were recorded across sites, occupational information was recoded so that data from all sites could be compared. Participants were allocated to seven mutually exclusive occupational categories: NHS; Primary care; Social care; Emergency services; Education; VCSE; Local authority; and other. We further defined a subgroup of NHS workers, namely those working in ICU or Critical Care (including Nightingale workers) and those in clinical and non-clinical roles, to explore the potential relative risk associated with these more specific NHS keyworker groups.
Data from mental health screening questionnaires were summarised numerically as total scores and used to determine the number of participant meeting threshold for clinically significant difficulties across the assessed domains. A series of logistic regression models, adjusted for site due to the multisite nature of the data, were conducted to examine the association between each candidate predictor and ‘caseness’ on each mental health screening outcome variables. In addition, for all scales, we conducted a series of supplementary analyses using linear regression to examine the associations between candidate predictors and mental health screening data using the scales’ dimensional/continuous scores (the findings of these analyses are available in Appendix 1, Part 3, Tables 37–57 and are broadly consistent with the caseness analyses reported in the main body of the report).
To evaluate whether these relationships varied across the sites, all models were refitted with an interaction between predictor variables and site. The interaction was assessed using a Likelihood Ratio Test for logistic regression models, and a F-test corresponding to an analysis of variance in linear regression models in our supplementary analyses. Owing to the large number of tests performed, p-values should be considered nominal; significant associations are best interpreted as exploratory. To offer some protection against spurious findings arising from multiple testing, we used a significance threshold of p < 0.001 for interaction analyses to identify potential differences across Hubs. A final set of analyses was conducted using proportional odds ordinal logistic regression analyses, adjusted for site, to identify potential predictors of an aggregate measure of ‘overall severity’ (low, moderate, high) across the various standardised screening measures collected by the Hubs. This was defined by the highest severity categorisation received on any of Hubs screening questionnaires (see Appendix 1, Part 1, Table 29 for further detail on this derived variable).
For the analyses of SUQ data, access to mental health support following screening and satisfaction with support were summarised numerically by Hub. Logistic regression models, adjusted for site, were used to examine the relationship between screening questionnaires and whether an individual accessed mental health support because of the Hubs. Due to the low numbers, these relationships were not compared across sites.
Results
Demographic and occupational characteristics
The demographic characteristics of included Hub clients are displayed in Table 6.
| Site A (n = 475) |
Site B (n = 367) |
Site C (n = 400) |
Site D (n = 731) |
Total (N = 1973) |
|
|---|---|---|---|---|---|
| Age (years) | 40.6 (10.6) 0% missing |
38.8 (11.4) 3.0% missing |
42.3 (11.2) 0% missing |
41.9 (11.4) 0% missing |
41.1 (11.2) 0.5% missing |
| Ethnicity | |||||
| White British | 433 (91.4) | 327 (91.6) | 367 (92.4) | 586 (88.5) | 1713 (90.6) |
| Other white | 12 (2.5) | 13 (3.6) | 11 (2.8) | 29 (4.4) | 65 (3.4) |
| Black | 1 (0.2) | 1 (0.2) | 4 (1.0) | 7 (1.1) | 13 (0.7) |
| Asian | 20 (4.2) | 10 (2.8) | 6 (1.5) | 29 (4.4) | 65 (3.4) |
| Mixed | 6 (1.3) | 4 (1.1) | 6 (1.5) | 8 (1.2) | 24 (1.3) |
| Other | 2 (0.4) | 2 (0.6) | 3 (0.8) | 3 (0.5) | 10 (0.5) |
| Missing/not stated | 0.2% missing | 2.7% missing | 0.8% missing | 9.4% missing | 4.2% missing |
| Gender | |||||
| Woman | 401 (84.4) | 309 (86.3) | 331 (82.8) | 612 (84.2) | 1653 (84.3) |
| Man | 73 (15.4) | 47 (13.1) | 63 (15.8) | 96 (13.2) | 279 (14.2) |
| Identified in another way | 1 (0.2) | 2 (0.6) | 2 (0.5) | 19 (2.6) | 24 (1.5) |
| Missing/not stated | 0% missing | 0% missing | 1% missing | 0.4% missing | 0.6% missing |
| Sexual orientation | |||||
| Heterosexual | 420 (90.1) | 307 (89.0) | 318 (94.6) | 587 (92.3) | 1632 (91.5) |
| Identified in another way | 46 (9.9) | 38 (11.0) | 18 (5.4) | 49 (7.8) | 151 (8.5) |
| Prefer not to say/left blank | 1.3% missing | 6.0% missing | 16.0% missing | 13.0% missing | 9% missing |
| Disability status (Yes) | 64 (13.5) | 30 (8.2) | 72 (18.0) | 29 (4.0) | 195 (10.9) |
Overall, the demographic characteristics of Hub clients were similar across Hubs. The average age of clients was 41.1 years [standard deviation (SD) = 11.2], ranging from 38.8 years at Site B to 42.3 years at Site C. The available ethnicity data indicated that clients were predominantly from White British backgrounds (between 89% and 92%), with only 5–6% of participants being from ethnic minority backgrounds; 1–2% White Irish and 2–3% from other white backgrounds. In terms of gender and sexual orientation, between 83% and 86% of Hub clients identified as women, and between 80% and 88% identified as straight/heterosexual. Self-reported information on disability status was more variable, ranging between 4% at Site D and 18% at Site C. Of note, these differences may be artefactual and due to variances in how questions on disability status were framed at different Hubs. In particular, at Sites B and D, items to confirm lack of a disability (i.e. ‘none’) were embedded within an extensive, alphabetically ordered list of potential disabilities, which may have led to high levels of missingness (80.4% and 67%, respectively). It is therefore considered likely that nearly all the missing responses at these sites are from people without a disability, and disability data were analysed accordingly in subsequent analyses.
In terms of occupational background (Table 7), NHS employees represented the largest occupational group. A sizable minority of these NHS employees (30% of all NHS participants at Site A, 18% at Site D, 12% at Site B Hub and 10% at Site C) worked in ICUs, including the decommissioned Nightingale hospitals. Only a relatively small proportion of Hub clients reported working in social care settings (between 4% at Site B and 8% at Site D) or in ‘blue light’ services (between 1% at Site B and 12% at Site C).
| Site A (n = 475) |
Site B (n = 367) |
Site C (n = 400) |
Site D (n = 731) |
Total (N = 1973) |
|
|---|---|---|---|---|---|
| NHS | 289 (60.2) | 315 (87.0) | 222 (57.8) | 312 (44.0) | 1138 (58.9) |
| Primary care | 31 (6.5) | 15 (4.1) | 20 (5.2) | 66 (9.3) | 132 (6.8) |
| Social care | 18 (3.8) | 13 (3.6) | 26 (6.5) | 59 (8.3) | 116 (6.0) |
| Emergency services | 20 (4.2) | 3 (0.8) | 45 (11.7) | 30 (4.2) | 98 (5.0) |
| Education | 14 (2.9) | 0 (0) | 1 (0.2) | 9 (1.3) | 24 (1.2) |
| VCSE | 2 (0.4) | 0 (0) | 13 (3.4) | 36 (5.1) | 51 (2.6) |
| Local authority | 17 (3.5) | 0 (0) | 4 (1) | 15 (2.1) | 36 (1.9) |
| Othera | 84 (17.5) | 16 (4.4) | 54 (14.1) | 182 (25.7) | 336 (17.4) |
| Missing | 0% missing | 1.4% missing | 4% missing | 3% missing | 2.1% missing |
Impact of coronavirus disease 2019 and pre-pandemic mental health concerns
Table 8 shows a breakdown of the COVID-19 impact questions included in the Hubs’ screening tools.
| Question | Site A (n = 475) |
Site B (n = 367) |
Site C (n = 400) |
Site D (n = 731) |
Total (n = 1973) |
|---|---|---|---|---|---|
| Have you been impacted in any of these ways by COVID 19? | |||||
| Ill with COVID-19 (recovered at home) | 147 (30.9) 0% missing |
84 (23.2) 1.4% missing |
144 (36.8) 2.3% missing |
204 (28.7) 2.9% missing |
580 (29.9) 1.5% missing |
| Ill with COVID-19 (including being in hospital) | 19 (4.0) 0% missing |
10 (2.8) 1.4% missing |
23 (6.0) 4.8% missing |
12 (1.7) 5.2% missing |
64 (3.3) 2.9% missing |
| Family member ill with COVID (recovered at home) | 119 (25.0) 0% missing |
68 (18.8) 1.4% missing |
136 (35.0) 2.8% missing |
187 (26.77) 4.2% missing |
511 (26.5) 2.1% missing |
| Family member ill with COVID (including being in hospital) | 37 (7.8) 0% missing |
14 (3.9) 1.4% missing |
39 (10.1) 3.8% missing |
60 (8.7) 5.3% missing |
150 (7.8) 2.7% missing |
| Suffered financial loss within the household | 84 (17.7) 0% missing |
33 (9.1) 1.4% missing |
84 (21.4) 2.0% missing |
152 (21.5) 3.3% missing |
353 (18.2) 1.6% missing |
| Undertaking new tasks within usual role | 245 (51.63) 0% missing |
173 (47.8) 1.4% missing |
193 (49.1) 1.8% missing |
409 (58.3) 4.1% missing |
1021 (52.7) 1.9% missing |
| Seconded or redeployed to a different post | 116 (26.2) 6.9% missing |
46 (12.7) 1.4% missing |
48 (12.2) 1.8% missing |
109 (16.2) 8.1% missing |
319 (17.0) 5.2% missing |
| Moved to a different work location | 153 (34) 5.3% missing |
61 (16.9) 1.4% missing |
105 (26.7) 1.8% missing |
253 (36.4) 4.9% missing |
572 (30.1) 3.7% missing |
| Bereavement | 71 (14.9) 0% missing |
44 (12.2) 1.4% missing |
65 (17.1) 4.8% missing |
168 (23.8) 3.3% missing |
348 (18.0) 2.2% missing |
| Were you concerned about your emotional well-being before COVID? | |||||
| Yes | 170 (36.3) | 169 (46.9) | 136 (34.0) | 276 (38.3) | 754 (38.6) |
| Unsure | 102 (21.8) 0% missing |
57 (15.8) 1.9% missing |
64 (16.0) 0% missing |
124 (17.2) 1.5% missing |
347 (17.8) 1.0% missing |
Mental health and functional screening data
Table 9 displays descriptive statistics pertaining to the mental health and functioning screening tools used by the Hubs.
| Site A (n = 475) |
Site B (n = 367) |
Site C (n = 400) |
Site D (n = 731) |
Total (n = 1973) |
|
|---|---|---|---|---|---|
| PHQ-9 score | 14.4 (5.5) | 13.8 (5.9) | 13.2 (5.9) | 11.4 (6.3) | 12.9 (6.1) |
| None | 21 (4.4) | 15 (4.6) | 27 (6.8) | 117 (16.0) | 180 (9.3) |
| Mild | 73 (15.4) | 76 (23.3) | 94 (23.6) | 185 (25.3) | 428 (22.2) |
| Moderate | 141 (29.7) | 94 (28.9) | 117 (29.3) | 186 (25.4) | 538 (27.9) |
| Moderately severe | 149 (31.4) | 78 (23.9) | 94 (23.6) | 159 (21.8) | 480 (24.9) |
| Severe | 91 (19.2) | 63 (19.3) | 67 (16.8) | 84 (11.5) | 305 (15.8) |
| Missing | 0% missing | 11.1% missing | 0% missing | 0% missing | 2.1% missing |
| GAD-7 score | 12.3 (4.9) | 12.6 (5.4) | 16 (5.5) | 10.2 (6.1) | 11.4 (5.7) |
| None | 28 (5.9) | 17 (5.2) | 44 (11.0) | 153 (20.9) | 242 (12.5) |
| Mild | 121 (25.5) | 91 (28.0) | 102 (25.6) | 207 (28.3) | 521 (27.0) |
| Moderate | 146 (30.7) | 84 (25.8) | 124 (31.1) | 164 (22.4) | 518 (26.8) |
| Severe | 180 (37.9) | 133 (40.9) | 129 (32.3) | 207 (28.3) | 649 (33.6) |
| Missing | 0% missing | 11.4% missing | 0.3% missing | 0% missing | 2.2% missing |
| PCL-5 score | 36.6 (16.6) | 34.3 (16.7) | – | – | 35.6 (16.7) |
| PTSD present | 293 (61.7) | 180 (55.4) | 473 (59.1) | ||
| Missing | 1.0% missing | 11.4% missing | – | – | 5.0% missing |
| ITQ score | – | – | 8.8 (6.3) | 8.2 (6.5) | 8.4 (6.4) |
| PTSD present | 40 (10.0) | 56 (7.7) | 96 (8.5) | ||
| Missing | – | 0.3% missing | 0% missing | 0.1% missing | |
| CPTSD present | – | – | 97 (24.5) | 147 (20.4) | 244 (21.6) |
| Missing | 1.0% missing | 1.6% missing | 1.4% missing | ||
| AUDIT score | 5.7 (5.8) | – | 5.0 (5.1) | 5.2 (5.0) | 5.3 (5.3) |
| Low risk | 351 (73.9) | 322 (80.5) | 564 (77.2) | 1237 (77.0) | |
| Hazardous | 88 (18.5) | 63 (15.8) | 131 (17.9) | 282 (17.6) | |
| Harmful | 18 (3.8) | 5 (1.3) | 23 (3.1) | 46 (2.9) | |
| Possible dependence | 18 (3.8) | 10 (2.5) | 13 (1.8) | 41 (2.6) | |
| Missing | 0% missing | – | 0% missing | 0% missing | 0% missing |
| WSAS score | 18.9 (8.3) | 17.5 (7.9) | 17.9 (9.5) | 15.1 (9.3) | 17.0 (9.0) |
| Subclinical | 65 (13.7) | 55 (16.9) | 77 (19.3) | 213 (29.1) | 410 (21.2) |
| Significant | 213 (44.8) | 152 (46.6) | 170 (42.5) | 311 (42.5) | 846 (43.8) |
| Moderately severe or worse | 197 (41.5) | 119 (36.5) | 153 (38.3) | 207 (28.3) | 676 (35.0) |
| Missing | 0% missing | 11.2% missing | 0% missing | 0% missing | 2.1% missing |
| Overall severity | |||||
| Low | 24 (5) | 23 (6.3) | 29 (7.3) | 128 (17.5) | 204 (10.3) |
| Moderate | 104 (21.9) | 71 (19.3) | 128 (32.0) | 230 (31.5) | 533 (27.0) |
| High | 347 (73.1) | 232 (63.2) | 243 (60.8) | 373 (51.0) | 1195 (60.6) |
| Missing | 0% missing | 11.2% missing | 0% missing | 0% missing | 2.1% missing |
A large proportion of Hub clients struggled with significant mental health and/or functional difficulties. The proportion of participants presenting PHQ-9 scores above the cut-off for moderate depression was 69% at Sites C and D, 72% at site B and 81% at Site A. In terms of anxiety, 51% of participants at Site D had scores above the cut-off for moderate anxiety; the corresponding figures for other Hubs were 63% for Site C Hub and 69% for Sites A and B. In Hubs that used the PCL-5 (Sites A and B), 55% and 62% of Hub clients had scores suggestive of probable PTSD. Conversely, a lower observed prevalence of possible trauma-related disorders (PTSD and CPTSD) was observed when the ITQ was used (34% at Site C and 28% at Site D). The proportion of participants presenting AUDIT scores above the cut-off for hazardous alcohol use was 20% at Site C, 23% at Site D and 26% at Site A. Most Hub clients presented WSAS scores above threshold for significant impairment in functioning (86% at Site A, 83% at Site B, 81% at Site C and 71% at Site D).
In terms of overall severity, 60% of Hub clients scored in the most severe range of scores at least one mental health screening measure (51% at Site D, 61% at Site C, 63% at Site B and 72% at Site A), and only 10% of users presented scores in the lower range of scores across all measures. Across all mental health domains assessed by the screening measures, most participants had scores suggestive of multiple comorbid difficulties. Specifically, 60% of the sample met caseness criteria on at least three different screening measures (see Appendix 1, Part 4, Table 55).
Predictors of depression
The regression analyses to identify predictors of PHQ-9 caseness (see Appendix 1, Part 2, Table 30) found that having a disability [OR = 1.71, 95% confidence interval (CI) 1.19 to 2.53; p = 0.005], identifying as any sexual orientation other than heterosexual (OR = 1.89, 95% CI 1.23 to 2.94; p = 0.004), suffering a financial loss (OR = 1.48, 95% CI 1.14 to 1.95; p = 0.004), and having pre-pandemic emotional well-being concerns (OR = 2.03, 95% CI 1.62 to 2.53; p < 0.001) were associated with higher likelihood for caseness. Undertaking new work-related tasks was also associated with greater likelihood of caseness (OR = 1.23, 95% CI 1.01 to 1.51; p = 0.038), with interaction analyses indicating more pronounced PHQ-9 caseness risk at Site D relatively to other sites (p < 0.001).
Predictors of anxiety
The GAD-7 analyses (see Appendix 1, Part 2, Table 31) found evidence of decreased likelihood of caseness with older age (OR = 0.98, 95% CI 0.97 to 0.99; p < 0.001). Suffering a financial loss (OR = 1.28, 95% CI 1.00 to 1.64; p = 0.049), having had a bereavement (OR = 1.38, 95% CI 1.07 to 1.77; p = 0.012) and reporting pre-pandemic emotional well-being concerns (OR = 2.05, 95% CI 1.66 to 2.53; p < 0.001) were associated with higher likelihood for caseness.
Predictors of post-traumatic stress symptoms
The results of the regression analyses to identify predictors of PTSD caseness based on PCL-5 and ITQ data are displayed in Appendix 1, Part 2, Tables 32 and 33. Working in ICU/critical care and having a disability was associated with higher likelihood of having PCL-5 scores suggestive of probable diagnosis for PTSD (OR = 2.23, 95% CI 1.45 to 3.52; p < 0.001). Undertaking new tasks (OR = 1.71, 95% CI 1.31 to 2.25; p < 0.001), moving to a new work location (OR = 1.49, 95% CI 1.13 to 1.95; p = 0.004) and suffering a bereavement (OR = 1.91, 95% CI 1.41 to 2.58; p < 0.001) were associated with higher likelihood of PTSD caseness on the ITQ. In both the PCL-5 and ITQ analyses, pre-pandemic emotional well-being concerns (OR = 1.95, 95% CI 1.42 to 2.70; p < 0.001 and OR = 1.59, 95% CI 1.20 to 2.11; p = 0.001, respectively) and suffering a financial loss (OR = 1.72, 95% CI 1.12 to 2.69; p = 0.015 and OR = 1.57, 95% CI 1.16 to 2.13; p = 0.003, respectively) were associated with increased likelihood of probable PTSD.
Predictors of problematic alcohol use
The AUDIT caseness analyses are displayed in Appendix 1, Part 2, Table 30. Identifying as a man (OR = 2.35, 95% CI 1.74 to 3.16; p < 0.001) and undertaking new tasks (OR = 1.38, 95% CI 1.09 to 1.76; p = 0.008) were associated with increased risk for problematic alcohol use. Conversely, identifying as from an ethnic minority group (OR = 0.24, 95% CI 0.09 to 0.51; p = 0.001), having a disability (OR = 0.65, 95% CI 0.41 to 0.98; p = 0.049), having experienced a hospitalisation because of COVID (OR = 0.20, 95% CI 0.05 to 0.54; p = 0.006) and moving to a new work location (OR = 0.71, 95% CI 0.55 to 0.93; p = 0.001) were associated with lower risk for problematic alcohol use.
Predictors of functional difficulties
The analyses to identify predictors of significant impairments in functioning are displayed in Appendix 1, Part 2, Table 35. Identifying as any sexual orientation other than heterosexual (OR = 2.44, 95% CI 1.45 to 4.35; p = 0.002), having a disability (OR = 1.93, 95% CI 1.23 to 3.15; p = 0.006), having a family member recovering from COVID at home (OR = 1.62, 95% CI 1.24 to 2.14; p = 0.001), suffering a financial loss (OR = 1.59, 95% CI 1.17 to 2.19; p = 0.004) and pre-pandemic emotional well-being concerns (OR = 2.29, 95% CI 1.77 to 2.97; p < 0.001) were associated higher likelihood of presenting with WSAS scores indicative of significant impairment in functioning.
Predictors of overall severity
The results of the proportional odds ordinal logistic regression analyses to identify predictors of greater overall severity across the various mental health screening measures used by the Hubs are displayed in Appendix 1, Part 2, Table 36. In these analyses, ORs relate to the odds of being in a higher severity category (moderate, high) in presence of the putative risk factor (or, for age, for each 1-year increase).
Age was negatively associated with severity rating, such that people with higher age tended to have lower overall severity ratings (OR = 0.99, 95% CI 0.98 to 1.00; p = 0.05). Identifying as any sexual orientation other than heterosexual was associated with higher rating (OR = 1.75, 95% CI 1.22 to 2.63; p = 0.004). Presence of a disability (OR = 1.70, 95% CI 1.21 to 2.41; p = 0.003), a family member having COVID-19 and recovering at home (OR = 1.31, 95% CI 1.06 to 1.63; p = 0.01), suffering financial loss (OR = 1.84, 95% CI 1.43 to 2.39; p < 0.001), and pre-pandemic emotional well-being concerns (OR = 2.11, 95% CI 1.72 to 2.59; p < 0.001) were associated with higher ratings. We did not find evidence that associations varied across Hubs.
Service use questionnaire data on mental health support access
Table 10 displays the demographic characteristics of participants who completed the SUQ (N = 299). Mean time between screening and SUQ completion at each site was 7.3 months at Site A, 5.4 months at Site B, 7.7 months at Site C and 8.2 months at Site D.
| Site A (n = 77) |
Site B (n = 29) |
Site C (n = 46) |
Site D (n = 147) |
Total (N = 299) |
||
|---|---|---|---|---|---|---|
| Age (years) | 43.4 (9.6) 3% missing |
41.9 (11.6) 0% missing |
46.5 (9.4) 4% missing |
43.7 (11.0) 0% missing |
43.9 (10.5) 1% missing |
|
| Ethnicity | ||||||
| White British | 64 (83.1) | 26 (89.7) | 43 (93.5) | 125 (85.0) | 258 (86.3) | |
| White Irish | 0 | 0 | 0 | 1 (0.7) | 1 (0.3) | |
| Other white | 4 (5.2) | 1 (3.5) | 0 | 5 (3.4) | 10 (3.3) | |
| Black African | 0 | 1 (3.5) | 0 | 0 | 1 (0.3) | |
| Black Caribbean | 1 (1.3) | 0 | 0 | 0 | 1 (0.3) | |
| Other black | 0 | 0 | 0 | 1 (0.7) | 1 (0.3) | |
| Chinese | 0 | 0 | 0 | 0 | 0 | |
| Indian | 1 (1.3) | 0 | 0 | 1 (0.7) | 2 (0.7) | |
| Bangladeshi | 0 | 0 | 0 | 0 | 0 | |
| Pakistani | 3 (3.9) | 0 | 0 | 2 (1.4) | 5 (1.7) | |
| Other Asian | 1 (1.3) | 1 (3.5) | 0 | 0 | 2 (0.7) | |
| White and Asian | 0 | 0 | 1 (2.2) | 0 | 1 (0.3) | |
| White and Black Caribbean | 1 (1.3) | 0 | 0 | 0 | 1 (0.3) | |
| White and Black African | 0 | 0 | 0 | 0 | 0 | |
| Other mixed | 0 | 0 | 0 | 1 (0.7) | 1 (0.3) | |
| Other | 0 | 0 | 0 | 0 | 0 | |
| Missing/not stated | 3% missing | 0% missing | 4% missing | 7% missing | 5% missing | |
| Gender | ||||||
| Woman | 60 (77.9) | 25 (86.2) | 34 (73.9) | 128 (87.1) | 247 (82.6) | |
| Man | 14 (18.2) | 4 (13.8) | 9 (19.6) | 16 (10.9) | 43 (14.4) | |
| Identified in another way | 1 (1.3) | 0 | 1 (2.2) | 2 (2.0) | 5 (1.7) | |
| Prefer not to say | 0 | 0 | 0 | 0 | 0 | |
| Missing | 0% missing | 0% missing | 0% missing | 0% missing | 0% missing | |
| Sexual orientation | ||||||
| Heterosexual | 65 (84.4) | 26 (89.7) | 39 (84.8) | 117 (79.6) | 247 (82.6) | |
| Identified in another way | 9 (11.7) | 2 (6.9) | 2 (4.4) | 14 (9.5) | 27 (9.0) | |
| Missing | 3 (3.9) | 1 (3.5) | 5 (10.9) | 16 (10.9) | 25 (8.4) | |
| Disability | ||||||
| Yes | 13 (16.9) | 1 (3.5) | 12 (26.1) | 4 (2.7) | 30 (10.0) | |
| No | 58 (75.3) | 1 (3.5) | 32 (69.6) | 16 (10.9) | 107 (35.8) | |
| Prefer not to say/not stated | 6 (7.8) | 27 (93.1) | 2 (4.4) | 127 (86.4) | 162 (54.2) | |
As displayed in Table 11, 73.2% of respondents reported having had further contact with Hub staff (e.g. in the form of e-mails support, telephone contact or access to psychological therapy) following the completion of screening (ranging between 67.4% at Site D and 80.5% at Site A). Across all Hubs, 57.2% reported receiving some form of mental health support since screening (including both completed support as well as ongoing support), and 11.4% reported to be on a waiting list for such support. Most respondents who had accessed mental health support since screening did so because of their involvement with the Hubs: 55.6% accessed support that was provided directly by Hub staff, and an additional 18.7% accessed other support that that was first accessed because of Hub support and advice.
| Site A (n = 77) |
Site B (n = 29) |
Site C (n = 46) |
Site D (n = 147) |
Total (N = 299) |
||
|---|---|---|---|---|---|---|
| Further contact with Hub staff | ||||||
| Contact of any kind | Yes | 62 (80.5) | 21 (72.4) | 37 (80.4) | 99 (67.4) | 219 (73.2) |
| No | 14 (18.2) | 7 (24.1) | 6 (13.0) | 42 (28.6) | 69 (23.1) | |
| Don’t know | 1 (1.3) | 1 (3.5) | 1 (2.2) | 6 (4.1) | 9 (3.0) | |
| Missing | 0% missing | 0% missing | 4% missing | 0% missing | 1% missing | |
| Telephone | Yes | 62 (80.5) | 21 (72.4) | 32 (69.6) | 91 (61.9) | 206 (68.9) |
| No | 0 | 0 | 4 (8.7) | 8 (5.4) | 12 (4.0) | |
| Don’t know | 0 | 0 | 1 (2.2) | 0 | 1 (0.3) | |
| Missing | 19%missing | 28% missing | 20% missing | 33% missing | 27% missing | |
| Yes | 33 (42.9) | 13 (44.8) | 30 (65.2) | 56 (38.1) | 132 (44.2) | |
| No | 25 (32.5) | 6 (20.7) | 6 (13.0) | 39 (26.5) | 76 (25.4) | |
| Don’t know | 3 (3.9) | 2 (6.9) | 0 | 4 (2.7) | 9 (3.0) | |
| Missing | 21% missing | 28% missing | 22% missing | 33% missing | 27% missing | |
| Access to mental health support | ||||||
| Via any route | Yes | 63 (81.8) | 20 (69.0) | 23 (50.0) | 65 (44.2) | 171 (57.2) |
| No | 13 (16.9) | 8 (27.6) | 20 (43.5) | 72 (49.0) | 113 (37.8) | |
| Missing | 1% missing | 3% missing | 6% missing | 7% missing | 5% missing | |
| Provided by the Hub | Yes | 51 (81.0) | 13 (65.0) | 15 (65.2) | 16 (24.6) | 95 (55.6) |
| No | 11 (17.5) | 7 (35.0) | 6 (26.1) | 45 (69.2) | 69 (40.4) | |
| Missing | 2% missing | 0% missing | 9% missing | 6% missing | 4% missing | |
| Provided by employer | Yes | 5 (7.9) | 1 (5.0) | 2 (8.7) | 13 (20.0) | 21 (12.3) |
| No | 13 (20.6) | 8 (40.0) | 10 (43.5) | 37 (56.9) | 68 (39.8) | |
| Missing | 71% missing | 55% missing | 48% missing | 23% missing | 48% missing | |
| Non-Hub support that was accessed by direct support of the Hub | Yes | 5 (7.9) | 4 (20.0) | 4 (17.4) | 19 (29.2) | 32 (18.7) |
| No | 51 (81.0) | 13 (65.0) | 15 (65.2) | 16 (24.6) | 95 (55.6) | |
| Missing | 11% missing | 15% missing | 17% missing | 46% missing | 26% missing | |
| Waiting list for mental health support | ||||||
| Via any route | Yes | 12 (15.6) | 1 (3.5) | 9 (19.6) | 12 (8.2) | 34 (11.4) |
| No | 62 (80.5) | 25 (86.2) | 32 (69.6) | 121 (82.3) | 240 (80.3) | |
| Missing | 4% missing | 10% missing | 11% missing | 9% missing | 8% missing | |
| Provided by the Hub | Yes | 2 (16.7) | 0 | 6 (66.7) | 0 | 8 (23.5) |
| No | 9 (75.0) | 1 (100) | 2 (22.2) | 12 (100) | 24 (70.6) | |
| Missing | 8% missing | 0% missing | 11% missing | 0% missing | 6% missing | |
| Provided by employer | Yes | 0 | 0 | 0 | 2 (16.7) | 2 (5.9) |
| No | 9 (75.0) | 1 (100) | 2 (22.2) | 8 (66.7) | 20 (58.8) | |
| Missing | 25% missing | 0% missing | 78% missing | 17% missing | 35% missing | |
| Non-Hub support that was accessed by direct support of the Hub | Yes | 3 (25.0) | 1 (100) | 0 | 6 (50.0) | 10 (29.4) |
| No | 2 (16.7) | 0 | 6 (66.7) | 0 | 8 (23.5) | |
| Missing | 58% missing | 0% missing | 33% missing | 50% missing | 47% missing | |
Satisfaction with Hub support and onward referrals
Despite relatively high levels of missingness in this section of the SUQ (approximately 30% of responses across various Hub satisfaction questions), respondents reported high levels of satisfaction with the support received from the Hubs (Table 12). The median rating of perceived helpfulness of the support provided by the Hubs was 92 (on a 0–100 scale), ranging from 85 at Site D to 97 at Site A. Most survey participants reported that the Hub either fully (46.5%) or partially (18.1%) met their needs, whereas only 4.4% reported that the Hubs did not meet their needs. In terms of onward referrals, approximately a third of participants reported they did not require support from services other than the Hubs, either because they received all the support they needed from the Hub (22.4%) or because no further mental health support was required from the Hub or other services (11%). Approximately 28% of respondents reported that the Hub helped them to access other beneficial services, whereas 6% reported that the Hubs helped them to access other services, but these proved to be insufficient for them. Only 5% reported of participants reported they did not receive sufficient support to access the support they needed.
| Site A (n = 77) |
Site B (n = 29) |
Site C (n = 46) |
Site D (n = 147) |
Total (N = 299) |
||
|---|---|---|---|---|---|---|
| How helpful was your contact with the Resilience Hub? | Median (IQR) | 97 (80–100) | 94 (81–100) | 89.5 (69–97) | 85 (63–98) | 92 (69–100) |
| Min, max | 2, 100 | 61, 100 | 0, 100 | 0, 100 | 0, 100 | |
| n | 58 | 20 | 34 | 90 | 202 | |
| Did the Resilience Hub meet your needs? | Yes, fully | 43 (55.8) | 16 (55.2) | 23 (50.0) | 66 (44.9) | 148 (46.5) |
| Yes, partially | 12 (15.6) | 5 (17.2) | 12 (26.1) | 25 (17.0) | 54 (18.1) | |
| No | 5 (6.5) | 0 | 1 (2.2) | 7 (4.8) | 13 (4.4) | |
| Missing | 22% missing | 27% missing | 22% missing | 33% missing | 28% missing | |
| Did the Resilience Hub refer you to any other services/help you to access any other services? | 1. Yes – the Hub helped me to access other services that I found beneficial | 23 (29.9) | 8 (27.6) | 18 (39.1) | 34 (23.1) | 83 (27.8) |
| 2. Yes – the Hub helped me to access other services but it wasn’t quite the right service for me | 2 (2.6) | 1 (3.5) | 6 (13.0) | 8 (5.4) | 17 (5.7) | |
| 3. No – I didn’t get enough help to access the support that I needed | 5 (6.5) | 0 | 1 (2.2) | 9 (6.1) | 15 (5.0) | |
| 4. No – they didn’t need to help me access other services as I got all the support I needed directly from the Hub | 26 (33.8) | 10 (34.5) | 7 (15.2) | 24 (16.3) | 67 (22.4) | |
| 5. No – I did not need any support from the Hub or referrals elsewhere | 5 (6.5) | 2 (6.9) | 4 (8.7) | 22 (15.0) | 33 (11.0) | |
| Missing | 21% missing | 28% missing | 22% missing | 34% missing | 28% missing |
Severity of mental health difficulties and access of mental health support as a result of the Hub
Of the 299 participants who completed the service use questionnaire, only 166 (55.5%) provided data on access to mental health support as a result of the Hubs: 129 (43.1%) had accessed support, 36 (12.0%) had not. The results of the logistic regression analyses found that none of the screening questionnaires, nor the combined measure of overall severity, was associated with mental health support access (Table 13).
| Odds ratio | 95% CI | p-value | ||
|---|---|---|---|---|
| Screening questionnaires | ||||
| PHQ-9 | 0.98 | 0.91 | 1.05 | 0.537 |
| GAD-7 | 0.96 | 0.89 | 1.03 | 0.225 |
| PCL-5 | 0.99 | 0.95 | 1.03 | 0.622 |
| ITQ | 1.01 | 0.94 | 1.08 | 0.819 |
| AUDIT | 1.03 | 0.94 | 1.12 | 0.545 |
| WSAS | 0.99 | 0.95 | 1.04 | 0.767 |
| Overall severity | ||||
| Moderate vs. low | 0.41 | 0.04 | 3.91 | 0.437 |
| High vs. low | 0.58 | 0.06 | 5.20 | 0.623 |
Discussion
The analyses indicated that most of Hub clients who completed the Hub screening offer worked in NHS settings, with considerably smaller proportions of respondents working for other in-scope sectors. Hub clients included in these analyses predominantly identified as women and from a white background. Only 14% of keyworkers identified as men and 9% as belonging to ethnic minority groups. These figures are in contrast with workforce demographics across health and social care sector, whereby men typically make up 18% and 23% of the workforce for social care and the NHS, respectively. 52,53 People identifying as from an ethnic minority background typically make up 21% and 22.1% of the workforce for social care and the NHS, respectively. 52,54 It is unlikely that the observed difference between the demographics of our sample and those of the broader NHS and social care workforce could be entirely attributable to self-selection for the present analyses (i.e. as participants consented for their anonymised data to be used for research purposes) or geographical variances. The findings are therefore suggestive that Hub clients may under-represent specific demographic and occupational groups, including individuals from ethnic minority groups, men and keyworkers from social care and ‘blue light’ services. While some of these differences may be due to restrictions of support to certain groups as per evolving national guidance during the study, for example, around inclusion of emergency service workers, as well as phased opening of offers that prioritised certain occupational groups (see Chapter 2), these findings highlight possible issues with the visibility and/or accessibility of Hub support for certain in-scope occupational and demographic groups, which could be addressed as part of future initiatives to better target these under-represented groups.
Participants presented with considerable mental health needs across all domains assessed. The incidence of mental health difficulties was broadly comparable across Hubs, but with slightly lower observed figures for Site D but also marked differences in PTSD caseness between sites that used different instruments to assess post-traumatic stress that is ITQ was associated with lower detected caseness relatively to PCL-5. Approximately 80% of Hub clients had scores suggestive of significant impairments in functioning. Furthermore, 60% of Hub clients scored in the most severe range of scores on at least one of the screening measures, while only 10% had subclinical scores across all measures. These figures are generally congruent with the findings of other research highlighting elevated mental health needs amongst the keyworkers during the COVID-19 pandemic as well as elevated pre-pandemic mental health risk in certain occupational groups (e.g. healthcare workers). 10,55–59 Nonetheless, the observed incidence of significant difficulties in this study is striking, and likely due to the help-seeking nature of this sample. These findings, alongside data indicating that a considerable proportion of Hub clients reported being concerned about their emotional well-being prior to the pandemic, suggest that the Hub clients presented with a degree of complexity, characterised by multiple ‘comorbid’ mental health difficulties which impacted functioning, as well as difficulties that may be long-lasting, that is they may precede (but may be aggravated by) the COVID-19 pandemic. While our analyses did not account for temporal trends, it is possible that levels of ‘caseness’ may have varied, and potentially increased, over the course of the pandemic. This would be consistent with the relatively lower incidence of difficulties observed at sites that became fully operational in earlier phases of the pandemic (i.e. Site D).
A series of regression analyses were conducted to explore characteristics associated with clinically significant mental health concerns in this sample. Interaction analyses to examine site differences in these associations used a conservative statistical significance threshold (p < 0.001) to protect against potential spurious findings arising from multiple testing, which would negatively affect accuracy of conclusions drawn in subsequent components of this project (i.e. the triangulation of findings via mixed-method case studies using individual Hubs as the unit of analysis; see Chapter 7). All other analyses were exploratory, and therefore were not adjusted for multiple testing; their findings should not be regarded as definitive and must be interpreted in the light of broader research literature on the mental health impacts of the COVID-19 pandemic and the health and social care workforce more generally.
Older age was found to be associated with reduced risk for anxiety and overall severity of presentations. Participants who described their ethnic background as white were at higher risk for problematic alcohol use. Individuals who identified as men had elevated risk for alcohol-related problems. Hub clients who identified as any sexual orientation other than heterosexual were at elevated risk for depression, alcohol misuse, functional impairment and higher overall severity. Having a disability was associated with increased risk for depression, post-traumatic stress, functional impairment, and higher overall severity, but also a reduced risk for alcohol-related problems compared to participants who did not report any disability on the screening questionnaires. These findings are consistent with those of prior studies focusing on the association between these individual characteristics and mental health difficulties in both specific keyworker groups eligible for Hub support (e.g. healthcare workers) and the general population. 58,60–63
While fine-grained analyses considering the relative risk of specific occupational characteristics were unviable (due to the heterogeneity in which this information was collected across sites), our analyses focusing ICU/critical care workers (a particular ‘high risk’ group due to their high level of disease exposure during the pandemic)64 found evidence suggestive of particularly elevated risk for post-traumatic stress. This finding is consistent with recent UK research reporting high levels of probable PTSD and other mental health difficulties in this group. 63 The caseness analyses found no evidence of differential risk between clinical and non-clinical NHS staff, but our supplementary analyses focusing on dimensional outcomes (see Appendix 1, Part 3) found some indication of lower WSAS scores (i.e. functional difficulties) and higher AUDIT scores (i.e. alcohol problems) amongst clinical staff. Other occupational variables potentially predictive of higher risk included specific stressful circumstances experienced during the pandemic. While being seconded or redeployed into different work roles was not associated with increased risk, moving to a new work location (a closely related variable) was associated with increased risk for PTSD, whereas undertaking new tasks was associated with increased risk for depression, post-traumatic stress and problematic alcohol use.
In line with findings from other research,8,65 other stressful life circumstances experienced during the pandemic also had an impact on the mental health difficulties reported by the present sample. Suffering a financial loss during the pandemic was (together with having pre-pandemic emotional well-being concerns) the most consistent predictor of caseness across all the domains assessed by the Hub screening measures. Having recovered from severe COVID illness which involved hospitalisation and/or having a family member undergoing a similar adverse experience was associated with increased risk for post-traumatic stress. Conversely, having family members who recovered at home from COVID was associated with higher anxiety risk as well as greater functional impairment. Suffering a bereavement was associated with increased risk for anxiety and post-traumatic stress.
In relation to the support navigation offer of the Hubs, the SUQ data collected from a subsample of 299 Hub indicated that most respondents (73%) reported having had some form of contact with Hub staff following the completion of their initial screening. Across all Hubs, 57% of respondents reported receiving some form of mental health support since screening (including completed support as well as ongoing support they continued to access at the time of survey completion), and 11% were on a waiting list for mental health support at the time they completed the survey. Approximately 75% of respondents who had accessed mental health support since screening did so because of their involvement with the Hubs (i.e. they accessed support that was provided directly by Hub staff or other services that were first accessed as a result of Hub support and advice). Survey respondents reported high levels of satisfaction with the support they received from the Hubs, with many participants reporting that the Hubs either fully (47%) or partially (18%) met their needs, and with only a small minority reporting that the support provided did not meet their needs (4%). Approximately a third of participants reported they did not require support from services other than the Hubs, either because they received all the support they needed from their local Hub or because no further mental health support was required from the Hubs or other services. A further 28% reported that the Hub helped them to access other beneficial services. Only 5% of participants reported they did not receive help to access the support they believe they needed. We did not find any evidence suggesting that the mental health and functional difficulties reported at screening predicted whether Hub clients accessed mental health support or not. This could be interpreted as consistent with the ‘universal support’ approach utilised by the Hubs, that is, all individuals who completed screening and/or self-referred to the Hubs are contacted and offered support, irrespective of the severity of their presenting difficulties.
Chapter 5 Health economic analyses (Objective 2)
Overview
The aim of the health economic analysis was to explore the financial costs and health benefits associated with the set-up, use and management of Hubs. Key objectives for this work were to
-
estimate the cost of Hub support, including one-off/set-up and ongoing costs of delivery;
-
summarise the health status of keyworkers accessing Hub support; and
-
summarise the health and social care service use and associated costs of keyworkers accessing Hub support.
If feasible, a further objective aimed to synthesise data collected from keyworkers accessing Hub support, and the wider published evidence, to explore whether Hubs are potentially cost-effective compared to usual care. However, it was determined that an economic model using the current evidence base would not be robust and might lead to misleading results. Work to explore the feasibility of economic evaluation is reported in Appendix 2, Part 1. A problem-orientated conceptual model of Hub service and care pathways is illustrated in Appendix 2, Part 1, Figure 6.
Methods
Costing Hub support
This work aimed to provide an overview of the potential resources required and cost of setting up and delivering Hub support, to assist commissioners and for future research/economic evaluation. The set-up and ongoing costs of implementing and providing Hub support were estimated from data collected via Hub teams and reflected Hub design and the number of keyworkers supported.
Example Hub business cases were reviewed to identify relevant categories of resource use related to Hub provision. This informed the development of a costing questionnaire (see Report supplementary material 2, Table 1). Hub teams completed the questionnaire between November 2021 and January 2022, with data representing a single time point (the time of completion). The questionnaire aimed to comprehensively capture the inputs required for Hub delivery, including staff time (management, leadership, clinical and administrative) and other costs (e.g. estates/overheads, stationery, information and technology equipment). To prevent underestimating Hub support costs, where data were not provided, Hub teams were either prompted to resolve the missing data or asked to provide a best estimate which could be used. Resource costs were provided by Hub teams for non-staff inputs (including estates/overheads, stationery, etc.). For staff costs, teams provided data (number of staff, banding and full-time equivalent) which were then multiplied by published staff costs. 66 As the published staff costs included some categories which overlapped with Resilience Hub data (e.g. overheads), these were excluded to prevent double counting. If Hubs provided support to other groups, only the costs related to providing keyworker support were requested and used for the costing exercise. The questionnaire also included fields related to Hub set-up (i.e. whether the Hub was newly established or expanded), number of keyworkers supported and the proportion of activity related to providing individual and team support to keyworkers.
One-off costs which related to the set-up of Hubs were summarised. Ongoing costs were summarised and used to estimate a cost per keyworker reached by Hub support, reflecting the proportion split between individual and team activity, as well as the number of keyworkers accessing Hub support. Costs are reported using simple descriptive statistics. Recognising the challenges of collecting this data, we also report uncertainties in the data and gaps in reporting. Sensitivity analyses to test the impact of changing key parameters are outlined in Appendix 2, Part 2, Tables 58 and 59.
Analysis of Hub client/keyworker data
This analysis used additional data collected as part of the SUQ online survey introduced in Chapter 4.
Health status
The EQ-5D, a generic measure of self-reported health status, was completed as part of the SUQ survey. The EQ-5D is used globally and allows for the comparison of health status across different disease areas and population groups. 67 The 5-L version of EQ-5D used in the present study captures five domains of health status: mobility, self-care, usual activity, pain/distress and anxiety/depression. Each domain is rated on a five-point Likert scale (no problems, slight problems, moderate problems, severe problems and extreme problems). Also included is the EuroQol visual analogue scale (EQ-VAS), a visual analogue scale in which participants rate their health on a scale between 0 (worst health imaginable) and 100 (best health imaginable).
The data from the surveyed keyworkers were analysed according to recommended methods. 67 The level of missing data was summarised, including: (1) missing altogether (i.e. participants failed to return any part of the EQ-5D questionnaire) and (2) missing in part (i.e. participants partially completed the EQ-5D questionnaire). Participant responses across the domains and levels of the EQ-5D were reported (number and percentage reporting at each level, and summarised for no problems vs. some or more problems by level). EQ-5D values (also known as utility values), which are summary scores traditionally anchored between 0 (dead) and 1 (full health), were calculated using value sets which reflect preferences for health states. In the absence of a value set for the EQ-5D-5L, the crosswalk algorithm which was recommended by NICE until February 2022, was used. 68–70 NICE recently revised their recommendation to the mapping function developed by the Decision Support Unit (DSU) using the ‘The National Institute for Health and Care Research’s Policy Research Unit in Economic Methods of Evaluation of Health and Care Interventions (EEPRU) data set’ for future appraisals. 71,72 Subsequently, health status profiles were converted to EQ-5D values using the methods recommended by NICE at the time of the study initiation and data collection (i.e. the crosswalk algorithm). However, the results using the new DSU algorithm are also reported. EQ-5D values are reported using simple descriptive summary statistics. A preliminary linear regression was conducted to assess whether participant characteristics were associated with participants EQ-5D values. A significance level of 0.05 was used to interpret the results. Variables for inclusion in the regression were first identified using stepwise linear regression (forward and backward) and were supplemented with common characteristics associated with the EQ-5D and characteristics that were important in this population. Participant responses to the EQ-VAS were summarised using simple descriptive statistics (Ms, SDs, minimum, maximum and frequencies).
The EQ-5D values were compared to population norms to assess how the health status of our participants compared to the norms for a similar age group. Population norms were taken from other published data, though it should be noted that this source used the three-level version of the EQ-5D. 73 A targeted review was conducted to identify publications focusing on utility and/or health and social care use among health and social care staff (keyworkers). However, no publications were identified for comparison. A comparison was made to Health Survey for England (HSE) 2018 data, as the EQ-5D(-5L) and occupation variables were collected. 74 HSE 2018 interviewed 8178 adults, capturing demographic and health data. The data and methodology are described elsewhere. 75 HSE reported two occupation categories which are highly relevant to our study; health professionals (n = 311) and health and social care associate professionals (n = 72). Data from these participants were combined and used to provide a sample of EQ-5D data for comparison, which reflected health and social care workers (keyworkers) before the COVID-19 pandemic. The HSE interview weight was applied to account for selection and non-response biases. 75
Service use and associated costs
SUQ participants were asked to provide data on both mental health support (including current, completed, discontinued/incomplete and waitlist), and any wider service use (including inpatient care, A and E, hospital visits and primary, community and social care) since completing screening with the Resilience Hub. Wider healthcare use is important due to interactions between mental and physical health. Furthermore, understanding total health and social care use can help to judge the level of access/engagement with services across the group. Participants entered service use descriptions as free text, which were categorised by the research team (e.g. ‘CBT’ and ‘cognitive–behavioural therapy’ were collapsed into CBT).
Service use data were costed using published standard national unit costs. 66,76 Unit costs are presented in Report supplementary material 2, Table 2. Assumptions to clean and cost the data were based on published sources (e.g. academic literature, or NHS sources) and/or expert opinion (e.g. discussion with clinical experts from the research team and/or Hub staff). For the present analyses, only the costs of services already used were estimated. The currency is Great British pounds, and the price year was 2021. The completion of the service use data is reported. The frequency of participants reporting accessing key mental health supports is reported across three categories; current support, completed support and discontinued/incomplete support. Use of key service use categories and total cost by category (as well as total NHS and social care cost) is summarised using descriptive statistics. An exploratory regression analysis was conducted to assess whether measured participant characteristics were associated with participants total NHS and social care costs. A significance level of 0.05 was used to interpret the results.
Logic model
A logic model was developed to illustrate the resources required, activities performed and potential outcomes related to providing Hub support. The logic model originally aimed to support ideas and focus for any future economic evaluation but was expanded to summarise Hub support more comprehensively. Note that while the economic components of the work focus on individual support, efforts were made to highlight and incorporate the benefits of team support for keyworkers and its role in increasing awareness and engagement with individual support within the logic model. The logic model aims to broadly summarise and illustrate how the Hubs produce outcomes. The draft logic model was developed using a prior published logic model developed for the Greater Manchester Resilience Hub77 as well as discussion with the research team, Staff Consultation Group and expert reference group feedback. The draft model structure and inputs were refined in collaboration with members of the immediate research team and Hub stakeholder review. Key changes to the draft included adding additional activities, services and types of outcomes to the model. For example, several stakeholders highlighted the importance of ‘feelings of validation and normalisation’ as key immediate outcomes. It should be noted that stakeholder groups did find it challenging to identify and define other potential relevant key health states which may be useful to either the logic model or economic modelling, due to the range in possible outcomes and variation in the rationale for seeking Hub support. Additional details, such as examples of services or resources, were also included and text was streamlined to the language used by Hubs (e.g. ‘clinical assessment’ became ‘clinical assessment and formulation’). The revised final logic model was shared with the research team and key stakeholders, to ensure agreement.
Patient and public involvement and engagement
The Staff Consultation Group provided important feedback on the development and refinement of the SUQ and development of the logic model.
Over the course of two meetings, the Staff Consultation Group provided feedback on how the SUQ could be improved. Key changes were made to the SUQ, in particular to make the questionnaire more user friendly (e.g. adding logic so that relevant follow-up questions only showed if participants selected particular responses; simplifying the language). The group was also consulted regarding the number and wording of e-mail reminders sent to potential participants about completing the SUQ.
Furthermore, the Staff Consultation Group provided input on the potential approach to economic modelling (reported in Appendix 2, Part 1) and the development of the logic model. Over the course of two meetings, the group was firstly introduced to the topic of economic evaluation and then asked to discuss several questions to help inform the potential economic evaluation approach, which included: (1) what are the key health states and events that might need to be reflected in an economic model; (2) what are the key outcomes related to Hub support; and (3) in the absence of a Hub what would the target population access. Following the meetings, an online survey was distributed to group to obtain additional responses to key questions. The group identified several Hub client key outcomes for inclusion in the logic model, including feelings of reassurance, risk of burnout, reducing the use of unhelpful or unhealthy coping mechanisms (e.g. alcohol use, smoking) and confidence at work. Outcomes related to friends and family, such as the quality of relationships and ability to conduct caring responsibilities, were noted. There was also an emphasis placed on outcomes of interest to employers, including productivity, staff retention, workplace incidents (e.g. accidents in the workplace, which are related to patient care) and workplace complaints. Furthermore, it was discussed that the presence of a Hub may have an impact on the wider culture of well-being in the health and social care/keyworker landscape.
Results
Hub intervention costs
In these analyses, it should be noted that there is considerable variation across Hubs (e.g. in terms of their remit, design and populations served), which limits the transferability of this evidence. Cost data were provided for three Hubs established to predominantly or specifically support keyworkers, and one existing Hub which serves other populations, alongside keyworkers. The broad budgets reported for the newly established Hubs ranged from £1,009,145 to £1,848,438, with an average of £1,346,527 across Hubs. Due to the varied populations served by the existing Resilience Hub, it was not possible to report the budget relating exclusively to keyworker support. As noted in Chapter 3, the four Hubs were funded by the NHS, though specific sources of funds varied across Hubs and over time. Hub funding is based on population size and weighted mental health need. NHS England provides guidance to Hubs which includes delivery of the key functions, such as proactive outreach, clinical assessment and supporting onward referrals to other services as well as care navigation.
All sites provided data on the number of keyworkers reached through individual support, while only three sites (A, C and D) provided data for team support. On average across the Hubs, 857 (range 573–1338) keyworkers were supported through individual support, and 1786 (range 900–2672) through team support. However, it was noted that Hubs are pragmatic services and can tailor support to maximise capacity (e.g. offering reduced length sessions to accommodate more keyworkers). The number of keyworkers supported varied across the Hubs, which would be expected due to the variations in design, time since set-up and populations served. While estimates have been provided for the number of keyworkers accessing team support, these figures likely underestimate those who benefit from such offer, for example, keyworkers who may receive support through knowledge transfer and resource sharing following team support. This was noted by Hub teams who reported that sessions delivered indirectly using online platforms are frequently shared to wider audiences (e.g. via recording), but these data are not captured.
Hub set-up costs
Hubs provided one-off costs associated with the set-up (or expansion) of Hub support for keyworkers. These are reported in Table 14. Site D, an existing service which expanded its provisions to include keyworkers, reported no one-off set-up costs as the service was already established with staff and equipment, and all staff and equipment were ongoing costs throughout the project. Therefore, the reported costs represent the set-up of new Hubs.
| Cost breakdown | Site A | Site B | Site C |
|---|---|---|---|
| Estates/overheads | ✓ | ✓ | |
| IT infrastructure | ✓ | ✓ | ✓ |
| Equipment | ✓ | ✓ | ✓ |
| Workshops/conferences | ✓ | ✓ | |
| Promotional material/advertisement | ✓ | ✓ | |
| Training | ✓ | ✓ | |
| Travel | ✓ | ||
| Printing/stationery | ✓ |
The average set-up cost was £111,713 (SD £53,471). It should be noted that set-up costs are challenging to collect retrospectively, and the teams noted some issues around this (e.g. a need to estimate costs). None of the Hubs reported any temporary staff set-up costs (e.g. staff hired on a temporary basis solely to set-up the Hub). Costs associated with staff recruitment were not considered, therefore potentially underestimating set-up costs. However, some Hubs reported that a percentage of their overheads would account for some of the associated recruitment cost. Across the remaining sites, the reported other costs were variable. All newly established Hubs reported set-up costs relating to IT infrastructure, equipment and staff training. Estates and overheads, reported for two sites, accounted for most cost and were also the most variable. These were noted by Hub teams to vary according to COVID-19 regulations (i.e. for a period one Hub needed to rent more space as per social distancing guidelines). One Hub did not report estate/overheads as they were virtual at the time of questionnaire completion. Training costs showed the least variability. Some ad hoc costs, such as printing, were not reported and estimates have been used where exact cost data are unavailable. The set-up costs are sunk costs (already spent and non-recoverable) and therefore any variability or uncertainty in the reported estimates will not impact the ongoing intervention cost estimates which follow in the next section.
Ongoing costs
The categories of ongoing resource use/costs related to providing Hub support and level of information reported by Hubs are reported in Table 15.
| Cost breakdown | Site A | Site B | Site C | Site Da |
|---|---|---|---|---|
| Staff costs | ||||
| Management | ✓ | ✓ | ✓ | ✓ |
| Clinical leadership | ✓ | ✓ | ✓ | ✓ |
| Clinical staff (to provide support) | ✓ | ✓ | ✓ | ✓ |
| Administrative support | ✓ | ✓ | ✓ | ✓ |
| Other staffb | ✓ | ✓ | ||
| Other non-staff costs | ||||
| Estates/overheads | ✓ | ✓ | ||
| IT infrastructure | ✓ | ✓ | ✓ | ✓ |
| Equipment | ✓ | ✓ | ✓ | ✓ |
| Workshops/conferences | ✓ | ✓ | ||
| Promotional material/advertisement | ✓ | ✓ | ✓ | |
| Training | ✓ | |||
| Travel | ✓ | ✓ | ✓ | |
| Printing/stationery | ✓ | ✓ | ✓ | |
| Other non-staffc | ✓ | |||
Staff costs were well reported across sites and accounted for the majority (86%) of ongoing costs. Management and administrative costs showed the least variation, while clinical staff and clinical leadership showed the most. Variation in clinical staff costs was expected due to capacity differences in the services provided directly by Hubs. Some variability was observed with how job roles were categorised. For instance, RAs were listed under ‘other’ by two sites and ‘clinical staff’ by one, contributing to greater differences between categories. However, due to variability in the level of detail provided (e.g. role description), it was not possible to standardise job roles across categories. While Site C reported two temporary staff members, employed for 6 months, these were excluded from ongoing costs as the funding for these roles was not continuous.
Other costs accounted for 14% of ongoing costs and were variable across Hubs. Estates/overheads accounted for the greatest share of non-staff costs. Promotion/advertisement (e.g. producing merchandise and promotional materials) and equipment costs demonstrated a large variation. However, this can largely be attributed to differences in how costs were reported. For instance, one site reported all ‘non-pay’ costs (including travel, supplies and consumables) as a single equipment estimate, as opposed to reporting these separately across categories.
Costs per keyworker reached
Across all four Hubs, the cost per keyworker given individual support ranged from £577 to £1481, with an average of £1011 (SD £409). The observed variability across Hubs was largely due to differences in the number of keyworkers supported, and given the unpredictable nature of the pandemic, it is likely that numbers of keyworkers requiring support will be challenging to predict. Additionally, some of the variation in cost per keyworker is very likely due to differences in service delivery (e.g. some Hubs provide complex interventions in house, while others facilitate more outward referrals for complex interventions). For instance, Hubs who make more outward referrals, as opposed to delivering support directly, would be capable of supporting (outwardly referring) more individuals, thereby reducing the cost per keyworker, but increasing the caseload and costs for other services. Producing an average cost per keyworker masks variability between keyworkers according to their need for services/support and engagement with the Hub. For instance, costs will be higher for those with greater mental health needs, or those with greater engagement, compared to those with lesser needs, or those who do not engage with support (e.g. those who are screened but do not access any support).
Team support estimates were based on data from three sites (A, C and D). The costs per keyworker accessing team support were less than for individual support, as would be expected, and ranged from £99 to £429, with an average of £272 (SD £165) across Hubs. Data on the number of whole team referrals were more variable (e.g. some based on actual figures, and some based on estimation etc.) and were therefore not used to produce a cost estimate as this may have impacted the accuracy of results. Furthermore, as noted earlier, the number of people who might benefit from team support is likely to be an underestimate. Therefore, these figures only provide an indication of costs.
Analysis of Hub client data
Health status
Summary of missing data
The EQ-5D was well completed, with 10% (29/299) missing, including 9% missing altogether (27/299) and 1% missing in part (2/299). Complete data (n = 270) were used for the analyses below.
Summary of EQ-5D profiles
Table 16 reports the frequency and proportion of participants reporting problems by dimension and level. Note that many of the participants had already received some form of support from the Resilience Hubs at the time of completion. The most affected domain is anxiety/depression, for which a minority of participants report experiencing no problems. Around half of participants reported problems with pain and discomfort. A minority of participants (16%) reported that they were in the best possible health state (no problems on any dimension).
| Level | Mobility | Self-care | Usual activities | Pain and discomfort | Anxiety and depression |
|---|---|---|---|---|---|
| 1 | 205 (76%) | 238 (88%) | 149 (55%) | 132 (49%) | 76 (28%) |
| 2 | 36 (13%) | 21 (8%) | 73 (27%) | 75 (28%) | 102 (38%) |
| 3 | 24 (9%) | 11 (4%) | 33 (12%) | 46 (17%) | 75 (28%) |
| 4 | 5 (2%) | 0 (0%) | 11 (4%) | 15 (6%) | 13 (5%) |
| 5 | 0 (0%) | 0 (0%) | 4 (1%) | 2 (1%) | 4 (1%) |
| Total (%) | 270 (100%) | 270 (100%) | 270 (100%) | 270 (100%) | 270 (100%) |
| Number reporting no problemsa (%) | 205 (76%) | 238 (88%) | 149 (55%) | 132 (49%) | 76 (28%) |
| Number reporting some problemsb (%) | 65 (24%) | 32 (12%) | 121 (45%) | 138 (51%) | 194 (72%) |
EQ-5D values
The mean EQ-5D value was 0.755 using the crosswalk method (SD 0.202, 95% CI 0.731 to 0.779). Using the alternative mapping function developed by the DSU, the mean EQ-5D is 0.750 (SD 0.206, 95% CI 0.725 to 0.775).
Relationship between EQ-5D values and participants characteristics
An exploratory multivariate linear regression (see Report supplementary material 2, Table 8) was conducted to assess whether participant characteristics were associated with participants EQ-5D values. Identifying as from an ethnic minority background was associated with lower EQ-5D values versus identifying as white (coef. −0.181, p = 0.001), as was having a disability versus no disability (coef. −0.120, p = 0.008). Related to the impact of COVID-19, having experienced a bereavement (coef. −0.070, p = 0.026), and having had a prior COVID hospitalisation (coef. −.0.238, p < 0.001) were also associated with lower health status. Finally having a high overall symptom severity at screening was associated with reduced health status (versus low overall symptom severity) (coef. −0.135, p < 0.001).
EQ VAS scores
The mean VAS score was 66.41 (SD 19.22, 95% CI 64.11 to 69.71) and the median was 70. Figure 2 displays the frequency of VAS scores, which shows the most commonly selected VAS scores were 50 (n = 32/270), 70 (n = 20/270) and 75 (n = 19/270).
FIGURE 2.
EuroQol visual analogue scale scores by frequency.
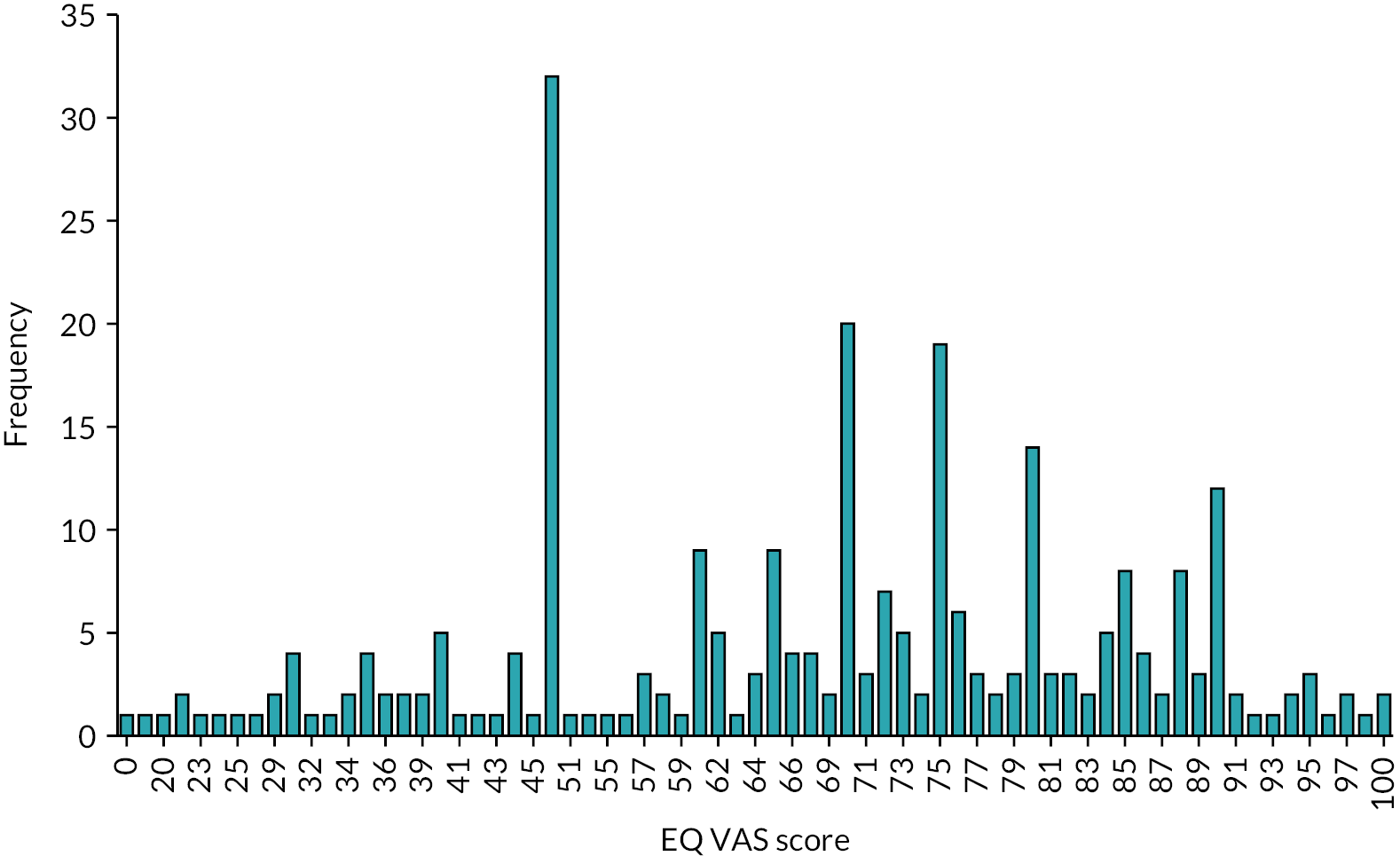
Comparison to population norms
It is challenging to compare Hub clients to the wider literature based on mental health concern, as Hub clients’ health status was measured approximately 5–8 months after Hub screening and because the Hubs target several well-being and mental health needs (i.e. not one single group). While the Hub clients mean EQ-5D score is higher than typically reported by publications focusing on the broader population with mental health concerns, this would be expected as they have been screened by Hubs and offered support. 78,79 Accordingly, the focus of the comparison is to the general population norms and pre-pandemic sample of health and social care workers included in the HSE 2018.
The mean age of participants who provided EQ-5D data was 44.24 (SD 10.45) and the majority were female (84%). The population norms for the UK (England) for an age group of 35–44 is 0.893, and for 45–54 the norm is 0.855. 73 Subsequently, the estimated mean for our sample of Hub clients is lower than would be expected based population norms. Compared to the 2018 HSE sample of health and social care staff participants, the sample of Hub clients were more likely to report having some problems across EQ-5D domains (despite being a slightly younger group). A full breakdown is reported in Report supplementary material 2, Table 3. The difference is particularly striking for the anxiety and depression domain and usual activities, as would be expected during the pandemic and for a group who have accessed mental health support services. It is important to consider that the HSE sample is before the COVID-19 pandemic. Accordingly, it is not clear from the data whether any differences are due to the pandemic or other factors. Reflecting the EQ-5D scores (see Report supplementary material 2, Table 4), the Hub client sample have a lower health status (mean EQ-5D 0.755, 95% CI 0.731 to 0.779; n = 270) in comparison to the pre-pandemic HSE health and social care worker sample (mean EQ-5D 0.870, 95% CI 0.853 to 0.888; n = 348). The total scores across the two groups (Hub clients and HSE health and social professionals) are statistically significantly different (p < 0.001, two-sided).
Service use and associated costs
Completion
The SUQ was split into two sections: (1) mental health support and (2) other support. Two hundred and thirteen (71.24%) participants reported sufficient detail to cost mental health support. For other health support (i.e. inpatient care, A and E, hospital visits, primary, community and social care), 237 (79.26%) reported details sufficiently for costing. In total, 182 (60.87%) participants reported sufficient data across both sections to estimate total service use costs between screening and follow-up. The sections below report service use and costs for participants with complete data (n = 182). The mean time between screening with a Hub and questionnaire completion was 7.85 months (SD 1.78, 95% CI 7.59 to 8.11).
Some factors were found to be significantly associated with whether a participant had complete cost data. This included the Hub accessed (chi-squared test, p = 0.001), having a disability (chi-squared test, p = 0.002), and whether a participant had experienced a COVID hospitalisation prior to Hub screening (chi-squared, p = 0.024). Two screening measures were significantly related to whether complete cost data were available: the PHQ-9 (two-sided t-test, p < 0.001) and the WSAS (two-sided t-test, p < 0.001). Participants with missing cost data had higher scores on these measures, perhaps suggesting that higher levels of depression and functioning impairment at screening resulted in challenges reporting service use at a later date. There are several ways this could be explained, for example, participants may have had accessed more services due to greater need, and therefore struggled to remember them.
Key mental health services used
A summary of key services reported in the mental health section of the service use questionnaire is presented in Table 17 for participants with complete service use/cost data (for all available cases, see Report supplementary material 2, Table 5). This reports the number of participants accessing each type of intervention and what percentage of the total sample this number represents. However, some participants reported using no mental health support while others reported accessing multiple types of support (across categories and within a category). The reported percentages do not equate to 100%. Note that reflective of the questionnaire, support is split into current (i.e. ongoing), complete and incomplete.
| Key mental health service types | Number of participants reporting (%) | ||
|---|---|---|---|
| Current | Complete | Incomplete | |
| Bereavement support | 1 (1%) | 2 (1%) | 0 (0%) |
| Counselling | 11 (6%) | 5 (3%) | 1 (1%) |
| COVID-specific supporta | 1 (1%) | 2 (1%) | 0 (0%) |
| Digital interventions and support | 0 (0%) | 1 (1%) | 0 (0%) |
| GP support | 2 (1%) | 1 (1%) | 0 (0%) |
| Occupational health assessment and support | 1 (1%) | 1 (1%) | 0 (0%) |
| Other third-sector offer (charity) | 1 (1%) | 0 (0%) | 0 (0%) |
| Other well-being support provided by the Hubb | 4 (2%) | 5 (3%) | 1 (1%) |
| Peer support | 1 (1%) | 1 (1%) | 0 (0%) |
| Pharmacological support | 18 (10%) | 2 (1%) | 0 (0%) |
| Psychological therapy/supportc | 25 (14%) | 26 (14%) | 4 (2%) |
| Secondary care mental health support | 1 (1%) | 2 (1%) | 0 (0%) |
| Well-being support | 1 (1%) | 1 (1%) | 0 (0%) |
Participants reporting an incomplete service were asked to give a reason; three participants commented on the format of support (e-mail/telephone and internet connection problems), two reported difficulties with scheduling appointments, two had specific complaints about the contents (e.g. input given) and a single participant commented about wanting to reduce the pressure on the services by trying alternatives instead.
Summary of costs
For participants with complete data, costs by category are reported in Table 18. In the mental health section, participants were asked to specify whether support was delivered by the Hub or accessed due to Hub support. In the wider sections on health and social care use participants were asked whether services were accessed due to Hub support. In the first cost column in Table 18, all services reported have been costed as typical (using standard unit costs). In second column, where participants indicated that services were Hub-delivered, support costs have been excluded (due to overlap with the Hub support costing exercise). In the final column, to illustrate the impact of Hub support on service use, services delivered by the Hub or accessed due to Hub support have been excluded.
| Category | Participants using a service (%) | Cost (95% CI) | ||
|---|---|---|---|---|
| Total | Excluding services delivered by the Huba | Excluding services delivered by the Hub and services accessed due to Hub supportb | ||
| Mental health care | ||||
| Current | 52 (29%) | £204 (£141 to £268) | £96 (£55 to £136) | £54 (£25 to £82) |
| Complete | 44 (24%) | £164 (£108 to £220) | £62 (£27 to £98) | £24 (£3 to £44) |
| Incomplete | 5 (3%) | £8 (£0 to £17) | £7 (< £1 to £15) | £7 (< £1 to £15) |
| Total mental health care | £376 (£294 to £459) | £165 (£108 to £221) | £84 (£47 to £121) | |
| Wider health and social carec | ||||
| Inpatient | 2 (1%) | £34 (< £1 to £80) | £34 (< £1 to £80) | £34 (< £13 to £80) |
| A and E | 9 (5%) | £10 (£3 to £18) | £10 (£3 to £18) | £10 (£3 to £18) |
| Hospital outpatient/day case | 21 (12%) | £42 (£20 to £65) | £42 (£20 to £65) | £42 (£20 to £65) |
| Primary care | 61 (34%) | £47 (£19 to £74) | £47 (£19 to £74) | £47 (£19 to £74) |
| Community and social care | 2 (1%) | £5 (< £1 to £11) | £5 (< £1 to £11) | £5 (< £2 to £11) |
| Total wider health social care | £138 (£73 to £202) | £138 (£73 to £202) | £129 (£64 to £193) | |
| Total | £514 (£410 to £618) | £302 (£219 to £386) | £213 (£140 to £286) | |
Table 18 demonstrates that mental health support was the greatest contributor to cost, as would be expected in this group. Confidence intervals indicate a moderate level of variation in the average costs per person, especially in relation to mental health support services. The services delivered or accessed as a result of Hub support make up over half of the total service costs. Of note, there was no indication that the average cost per participant differed between complete case and all available data (see Report supplementary material 2, Table 6).
An exploratory linear regression was conducted to assess whether participant characteristics were associated with participant total costs of health and social care. Two separate models were run with mental health support costs and total costs as outcomes, with the model for mental health cost having a greater adjusted R-squared (0.235 vs. 0.103). This suggests that wider health and social care are more likely to be affected by unmeasured covariates. Subsequently, the regression focused on mental health care (see Report supplementary material 2, Table 7) explored the relationship between mental health support costs and participant demographics demonstrates that being concerned about emotional well-being prior to the pandemic was statistically significantly associated with greater mental health support costs (coef. 213.76, p = 0.035). In addition, the Resilience Hub accessed was associated with mental health support costs (Hub A vs. Hub D; coef. 632.19, p < 0.001). However, it should be noted that this is likely to reflect other issues (e.g. potential interactions with other variables such as symptom severity, geographical heterogeneity in the availability of services and differing length of follow-up). Two variables were close to significance; age and overall symptom severity at screening, suggesting, as would be expected, that increased age and severity of symptoms were associated with higher costs.
Logic model
To aid future research, a logic model was developed. The aim was to describe how the implementation of Hub support for keyworkers will lead to various outcomes of interest (including key economic outcomes). Given the design constraints of the current project, the logic model can help to explain potential outcomes that cannot be analysed due to data limitations (e.g. productivity losses) and provides a starting point for future research in terms of highlighting the range of outcomes available. This is particularly helpful for future economic evaluation, as it demonstrates the complexity between activities and outcomes, and delays related to time as economic outcomes often take longer to occur (e.g. as health status is likely to only affected only once mental health symptoms change).
The logic model (Figure 3) summarises the key resources needed to deliver Hub support, the activities performed as part of Hub support and subsequently, the potential short, medium, and long-term outcomes. The resource section describes what is needed for Hub delivery. These were captured in the Hub support costing section where possible, but this gives an overview for future Hubs drafting business cases. The resources are used for three key activities (outreach and promotion, referral/screening for individual support and team support). There are also interactions between these, for example, a keyworker identified through outreach may self-refer, while similarly, a keyworker reached by team support may self-refer for further individual support. The relationship between team and individual support is likely to be bidirectional (e.g. individuals may be less likely to require individual support if their needs are sufficiently addressed through team initiatives). These interactions/relationships are demonstrated by arrows on the model diagram. Individual and team support can take several forms, which are presented on the diagram. It should be noted that some Hubs have very specific offerings (e.g. on pastoral care or pharmacological intervention), but as these are unique to Hubs, they have not been included in the logic model which summarises typical Hub support only. Following activities, keyworkers reached by Hub support will experience related outcomes, which are split into immediate, short term, and medium/long term. As previously discussed, the evidence base is limited, and more research would help to define the time period in which these outcomes would be achieved. External factors which may influence any part of the logic model are included. For example, the impact of stigma, which may affect resources (i.e. as Hubs think about how to effectively use social media to target groups likely more impacted by stigma), activities (e.g. if fewer keyworkers self-refer for support) and outcomes.
FIGURE 3.
Logic model. a, The impact of Hub support is not only likely to affect the Hub user, but also friends/family, colleagues and the healthcare system.
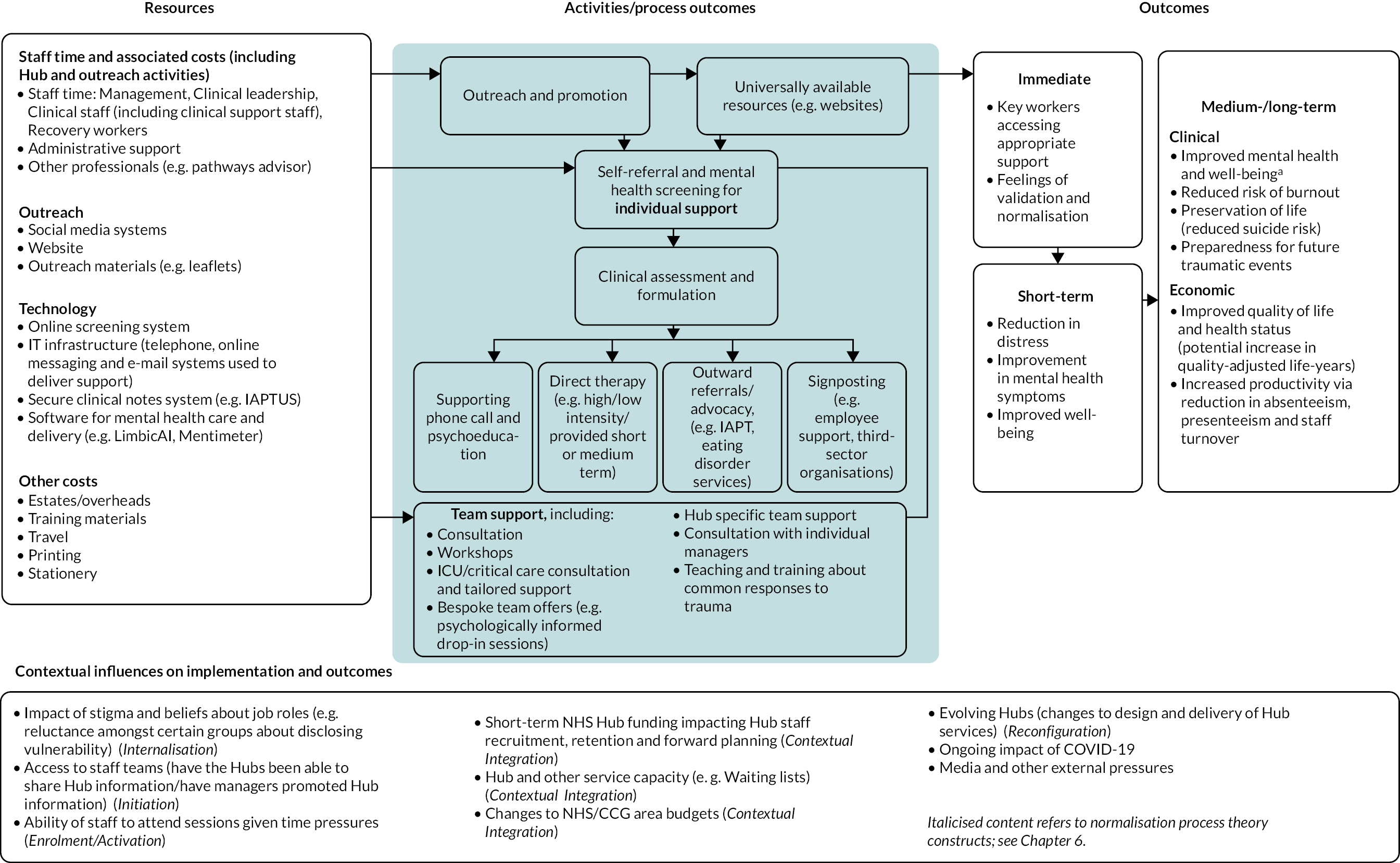
Discussion
In relation to Hub delivery costs, there was variability across the Hubs in terms of set-up and ongoing costs, as well as variability in the numbers of keyworkers reached. This would be expected given the differences in populations served by the Hubs and different designs (see Chapter 3). One Hub (Site D) was in existence prior to the pandemic, and this demonstrated that once the service is set up it can be expanded to meet the needs of new populations (avoiding some set-up costs and potentially reducing financial complexity). Staff costs accounted for most ongoing costs of Hub provision. Hub teams commented that they have a need for highly trained staff, due to the mental health needs of the population served (as highlighted by the analyses reported in Chapter 4). Promotional costs were variable; however, they were noted as being central to increasing engagement with Hubs and ensuring that keyworkers access the required support.
It should be noted that Hub delivery costs reflect their budgets. An average is reported; however, costs will vary considerably by user depending on the need/level of support required by the individual. Furthermore, Hub costs are not static and will be subject to change as both services and the COVID-19 landscape evolve (e.g. ongoing fluctuations in service demand as the pandemic progress, including a change in the breakdown of individual/team support and the complexity of presentations, will impact the estimated costs). As services develop, capacity may increase as services become streamlined, and new operational developments unique to each Hub may impact delivery costs and capacity (e.g. one Hub is considering a change to deliver more therapy in-house rather than referring to appropriate external services). Therefore, it should be noted that any cost estimates reported can only be used to provide an indication of costs.
It should be stressed how the cost of mental health services varies according to need. For examples, two economic evaluations reporting the total cost of IAPT support in the UK found a substantially higher estimate for more complex presentations, such as psychosis, bipolar and personality disorders (ranging from £1255 to £1634), relative to service users presenting with anxiety and depression (£599). 80 As shown in Chapter 4, Hub clients often had complex needs (often meeting the cut-offs for multiple mental health measures), and hence a higher cost for the provision of appropriate mental health support would be expected.
In 2021–2, 40 Resilience Hubs across England received £37 million in investment. 81 In 2021–2, the total NHS planned spend on mental health was £14,846.3 million. 82 Therefore, the Hubs costs are a very small proportion of the total planned spend on mental health (0.25%). Additionally, there is a substantial economic burden associated to mental health conditions in the UK, with a reported cost of £117.9 billion (£, 2019) (equivalent to 5% of GDP),83 with nearly three-quarters of this (72%) related to lost productivity. 84 The literature notes that investment is required to improve health emergency preparedness worldwide. 85 Hubs are an option for investment that could provide an adaptable service which can be tailored to the mental health needs of the population in new emergencies (e.g. trauma associated with terrorist attacks, pandemic, wars, etc.). However, adaptions would be required to ensure that additional population needs are effectively met (e.g. expanding the staffing model to include children and young people clinicians if offering support to younger age groups). This research provides an initial estimate of the cost of Hub, which will be useful for potential Hubs developing business cases and further research around Hub support.
Our study is the first known published EQ-5D data related to a sample of keyworkers and provides an exploratory comparison between the participants surveyed in the Hubs project and a pre-pandemic general sample of health and social care workers. In line with Chapter 4 findings, the analysis of the EQ-5D data demonstrates that most participants struggled with anxiety and depression. The mean EQ-5D was lower than the population norms for a similar age group and pre-pandemic samples of health and social care workers. This finding perhaps suggests that the pandemic is having an ongoing negative effect on the health status of keyworkers, which also aligns with more general research findings that COVID-19 has had a negative mental health impact among adults in the UK. 86 Furthermore, evidence suggests that not feeling protected against the pandemic had a strong negative association with mental well-being, which may have particularly affected keyworkers. 87 There is published evidence of delayed dysfunction (in which symptoms present later) following disasters, which suggests that mental health needs may increase further in the future (reducing health status over time). 88 Additionally, despite current Hub support, many staff were unsupported prior to the pandemic, and subsequently there remains a need to address the outstanding reduced health status within this group (e.g. with further intervention). It should also be noted that some of the participants are currently receiving mental health support which may have subsequently increased their health status.
The service use data describe how a sample of keyworkers accessed a range of NHS and social care services during the pandemic, and comprehensively covers inpatient, A and E, outpatient, primary, community and social care services. The analysis of costs related to health and social care service use demonstrates that services delivered or accessed as a result of Hub support make up over half of the total health and social care service costs. In a group with a high mental health need, this might suggest that the Hubs have had a positive impact in relation to ensuring users access to services. While it cannot be concluded with certainty (as we do not have a comparator arm), given the impact of COVID-19 on existing mental health services, it is very unlikely that in the absence of these Hubs service use cost would have been similar. Again, it should also be noted that some of the participants are currently receiving mental health support or on waiting lists which will result in higher service use costs.
Previous estimates of costs in mental health populations are available from RCTs conducted in the UK. 80,89–94 While differences in the populations covered, time frames and categories of service use (and cost) reported make a comparison challenging, these do suggest that the health and social care costs for the Hub keyworkers appear low given the need demonstrated at screening. Limited service use reflects feedback received in the qualitative interviews (see Barriers to valuing support: keyworkers’ beliefs about self and job roles), in which participants demonstrated they were wary of putting pressure on both the health service and their colleagues. This is also supported by previous research which identified both an ‘awareness of burden on colleagues and patients’ and being ‘worried about imposing on another busy doctor’ as barriers to physicians accessing appropriate care,95 which highlights the importance of supported outreach. Further, post-disaster evidence highlights that many keyworkers do not seek appropriate support due to concerns surrounding being seen as ‘unfit to work’ or ‘not coping’. 96 While it is common for keyworkers to forgo seeking psychological support, research has also identified this as more common among staff who may feel less justified in their help-seeking behaviour. 97 Reduced service use also likely reflects employment status, as scheduling service use may come with problems (as discussed by the Staff Consultation Group). Additionally, throughout the pandemic, reductions in both mental and physical health service availability and use have been reported. 17 In the UK, evidence showed reductions in adult mental health services, including a significant reduction in referrals to core adult mental health services. 21 Further, an increase in mental health service use (including referrals, admissions and caseloads) was reported following the easing of lockdown restrictions, which indicates that the timing of questionnaire completion may have an important impact on the reported resource use. 21
The work undertaken to assess the feasibility of economic evaluation (see Appendix 2, Part 1) highlighted that this was unfeasible; using the current evidence base (see Appendix 2, Part 1, Table 56) would not be robust and would risk leading to spurious results. Key challenges are outlined in Appendix 2, Part 1, Table 57. However, this work also outlined the vast potential economic impact of the Hubs and suggests some key avenues for future research. As illustrated in our logic model, the potential benefits associated with Hub support are not restricted to health impacts for keyworkers alone, but extend to productivity gains, potential improvements in patient care and the improved health of friends and family. Due to these wide-ranging impacts, we recommend that any future economic evaluation takes a societal perspective, as has been encouraged for economic evaluations in the context of the pandemic. 98
Chapter 6 Qualitative analyses (Objective 3)
Overview
In this chapter, we report the findings of 63 in-depth qualitative interviews guided by NPT and Sekhon’s Acceptability Framework conducted with Hub clients, keyworkers who did not register with Hub support, Hub staff, and wider stakeholders who were involved in the provision of support for staff within the health and care system. Qualitative data were collected across three of the Hub sites. The principal aims were to explore the barriers and facilitators to (1) the implementation of the Hub model and (2) keyworkers’ access to Hub support.
Theoretical frameworks
Interviews with keyworkers were based on Sekhon’s Acceptability Framework,99 to explore the extent to which Hub clients consider the Hubs to be effective, based on their experience and perceptions of the support they have received. Sekhon’s theoretical framework of acceptability consists of seven constructs: attitude towards the intervention, burden (e.g. reasons for dropout/discontinuation/non-engagement), perceived effectiveness, ethicality (extent to which the model fitted with participants’ value systems), intervention coherence (extent to which the participants understood the Hub model and how it works), opportunity costs (extent to which benefits or values had to be given up to the engage with the Hub) and self-efficacy (participants’ confidence that they could do what was required in order to engage with the Hub offer). Additional questions were drawn from two theoretical frameworks relating to behaviour change, the Theoretical Domains Framework100 and the Behaviour Change Wheel. 101 These frameworks provide a method for theoretically assessing implementation problems within a health context, addressing constructs such as: beliefs about consequences; social influences; social/professional role and identity; capability; motivation; and opportunity. Both frameworks have been used to understand barriers and facilitators of uptake of health-related interventions. 102
Interviews with Hub staff and wider stakeholders were based on NPT, a widely used theory to explain the processes by which an intervention becomes, or fails to become, embedded into routine practice. NPT offers a framework for assessing the conditions under which interventions become practically workable in health care. 103,104 NPT comprises four main constructs (sense-making, relational work, operational work and appraisal), which each have four subconstructs. ‘Sense-making’ identifies the ways in which participants understood and made sense of, or failed to make sense of, the Hub model, and subsequently the extent to which they placed value on the Hubs and what they offered. ‘Relational work’ describes the work needed to build and sustain the Hubs, such as the extent to which people drove forward the model, whether keyworkers referred themselves to the service, and what was needed in order to sustain engagement with the Hub services. ‘Operational work’ refers to what was required to enact the Resilience Hub model, transferring it from paper into practice, for example, the interactional work required between colleagues, with local and system-wide processes and practices, and with other parts of the health and care system to put the Hub model into practice. Finally, ‘appraisal work’ explores the methods participants used to evaluate the Hubs, individual and group appraisals of their support, and ways in which the Hubs could be improved or developed.
These constructs were used to explore Hub providers’ perceptions, expectations, attitudes, challenges and unintended consequences of using the Resilience Hub model.
Methods
Qualitative interviews were conducted at Sites A, B and D. Participants were purposively sampled for maximum variation from each site region, with consideration of a range of key characteristics, including professional background, employing organisation, gender and ethnicity.
-
Hub clients who had: accessed individual psychological support from a Hub; were over 18 years of age; and gave consent to be contacted for research purposes. Participants were sampled according to demographic and occupational groups (e.g. ethnicity, gender, professional/non-professional groups), and severity of mental health symptoms and risk indicators identified from the quantitative data, as well as on other relevant characteristics that might influence offer uptake and service access.
-
To provide a dissonant view, interviews were conducted with keyworkers over 18 years of age who did not register with the Hubs, despite being eligible and reporting struggles with their mental health and well-being during the pandemic. These participants were identified through: (a) e-mails to keyworkers via organisations through which the Hub advertised their screening offer; (b) e-mails to participants in the relevant Hub regions who took part in a study led by members of the research team (The COVID-19 Resilience Project, IRAS ID 282827), who gave consent to be contacted about other research opportunities; (c) e-mails to keyworkers who completed Hub screening but did not self-refer to a Hub; (d) social media. Groups who appeared to be under-represented (see Chapter 4) were specifically targeted for recruitment to understand why they may be under-represented. Methods included study information sent out to care homes, BAME Networks and staff groups that typically include more men, such as estates and facilities.
-
Hub providers were sampled according to different aspects of the Hubs’ commissioning, set-up, and delivery of clinical offers, for example, service managers, clinical team managers and wider professional stakeholders. These included both Hub staff directly employed by the three Hubs and wider professional stakeholders involved in work relating to the set-up of the Hubs or staff well-being initiatives in the three regions (e.g. commissioners, representatives from partner organisations and provider Trusts, HR directors or organisation well-being/occupational health leads).
Data collection continued until data saturation was thought to be satisfactorily achieved. Within each participant group, coded data and participant characteristics were examined to ensure that a wide range of perspectives were reflected, and that responses across NPT constructs had reached thematic saturation. Further recruitment was conducted to gather additional data in areas that were felt to be lacking (e.g. the final six non-Hub keyworker interviews targeted participants who identified within under-represented demographic and occupational groups, including men, people from ethnic minority groups, and emergency services). In addition, towards the end of data collection for Hub client interviews when it was felt the data set was nearing saturation, further review of coded data revealed that the majority of Hub clients interviewed had reported relatively positive experiences; therefore a further round of recruitment was conducted towards the end of data collection to specifically invite Hub clients who had dropped out of or discontinued their support from the Hubs, to try to better understand barriers to sustaining engagement with the Hubs.
Procedures
Semistructured, one-to-one interviews were conducted by telephone or video call. Topic guides were based on the above theoretical frameworks and updated according to preliminary findings of the previous objectives, new published literature and PPIE feedback, and can be found in Appendix 3, Topic guides. Minor amendments were made to topic guides according to participants being interviewed, for example, for Hub clients who disengaged from Hub support, and non-Hub keyworkers who had not heard of the Hub or had not accessed any alternative sources in of support. Interviews were audio-recorded using encrypted dictaphones and transcribed verbatim.
Interviews were conducted by graduate RAs and a qualitative researcher (KA, PhD), who supervised all RAs. Hub staff interviews were conducted by a RA between April 2021 and January 2022. Keyworker interviews, including Hub clients and non-Hub keyworkers, were conducted by RAs at Site A, B and D between October 2021 and January 2022. Wider stakeholder interviews were conducted by KA between January and March 2022.
Hub clients
Hub clients were invited by e-mail or telephone. Interviews explored in-depth the acceptability, enablers and barriers of the Hubs’ outreach approach; the acceptability of screening and self-referral processes; and reasons for engaging or disengaging. Interviews also explored (1) barriers and facilitators of support access and (2) whether Hub clients were considering or would have considered accessing other services in the absence of the Hub. This information helped to consider how keyworkers’ service use and health may have varied had the Hub support not been available, and inform the health economic analyses.
Keyworkers who did not engage with a Hub
Interviews explored whether participants had heard of their regional Hub, and if so, the reasons for choosing not to engage with the service. Participants were asked about whether they received any support from other services, and the types of difficulties for which they sought support. Participants were asked to complete a modified version of the SUQ used in Chapters 4 and 5, which avoided explicit reference to the Hubs’ involvement in the processes of accessing services as this is not relevant for this group. SUQ responses were used to elicit further qualitative information on how participants negotiated access to services, whether they met their needs, and whether they considered them to be helpful.
Hub staff and wider stakeholders
Interviews explored Hub clinicians’ perceptions and experiences of working at the Hubs, the feasibility and appropriateness of the model for supporting keyworkers, and how the Hub model was embedded into routine practice. Interviews explored clinicians’ perceptions of the enablers and barriers to outreach, supporting keyworkers, and helping them to access onward care via facilitated referrals and clinical advocacy. Contextual factors and implementation aspects were explored, including clinicians’ experiences of the set-up and structure of the Hubs, such as staffing and integration with other services.
Patient and public involvement and engagement
The Staff Consultation Group provided extensive feedback on various aspects of the qualitative objectives, including topic guides, recruitment, and interpretation of analysis.
The group reviewed topic guides for Hub client and non-Hub keyworker interviews to ensure that questions were meaningful and understandable by participants. Topic guides were refined based on the group’s feedback, such as breaking down complex questions into several easier to understand questions. In addition, each of the study RAs completed a practice interview with PPIE consultants as part of their training and received feedback on their interview style and further feedback on topic guides.
Group members reviewed the study’s recruitment materials (poster, invitation e-mails) and made suggestions for improvements, such as adding QR codes, using a range of images, and producing different versions with slightly different wording tailored for each participant group, and wording to address potential concerns about confidentiality. To improve recruitment of under-represented groups, the group recommended reaching out to local NHS Trust networks such as BAME Networks. These networks advised to name particular under-represented groups in invitation e-mails, and to highlight the potential benefit of the research to these communities, such as improving future access to services.
Towards the end of the project, emerging findings were presented to the group. Group members felt that findings were similar to their own experiences. Interestingly, a wide range of experiences (e.g. enablers and barriers) found across interview data were represented within the Staff Consultation Group, and group members could particularly understand some of the barriers interview participants had experienced.
Analysis
The National Centre for Social Research ‘Framework’ analysis approach105 was used. Themes of a priori interest related to NPT constructs and subconstructs. Rather than coding the data to all the theoretical frameworks used to shape interview topic guides, NPT was used deductively to form the coding tree for all interviews.
This was to enable a more streamlined approach to identifying the implementation barriers and enablers within and across participant groups, and to create an efficient narrative in an already multifaceted project.
Coding and analysis were completed by a RA and KA, who independently coded a sample of the transcripts, before conferring with each other and DH to resolve discrepancies in coding. Analysis took place in the latest version of NVivo. The consolidated criteria for reporting qualitative research (COREQ) guided the reporting of this chapter. 106
All interviewers identified as women and were non-clinical research staff, although all had had experience of working within mental health settings in non-qualified roles. KA had prior working relationships with teams at two Hub sites, having worked on other evaluations of Hub services, however she did not complete any interviews with Hub staff. Therefore, due to the way in which interviews were conducted, there were no prior relationships between interviewers and participants. A small number of Hub staff participants had been involved in facilitating the evaluation at their sites and so had had some contact with the research team prior to participation. Two of the RAs identified as from ethnic minority communities, including the RA who had been involved in the PPIE work described in (see Efforts to diversify the Staff Consultation Group). As reflected upon in (see Equality, diversity and inclusion), this was likely to have shaped both participant recruitment and the collection of data itself. Subsequent discussion during group supervision also brought to the fore discussion around equality, diversity and inclusion when raised in interviews. While these factors will have shaped analysis, particularly of interviews with participants from ethnic minority groups, care was taken during analysis to seek evidence that would disconfirm hypotheses around barriers to Hub access and use to ensure fair interpretation of the data.
Results
Interviews were conducted with 19 Hub clients, 20 keyworkers who did not register with Hub support, 14 Hub staff and 10 wider stakeholders (N = 63). Details of participants can be found in Tables 19–21. Mean interview duration was 62 minutes (ranging from 21 to 101 minutes).
| Participant ID | Occupation | Clinical or non-clinical | Organisation type | Gender | Ethnicity |
|---|---|---|---|---|---|
| Hub client 01 | Clinical laboratory lead | Non-clinical | NHS | Male | White other |
| Hub client 02 | Consultant anaesthetist | Clinical | NHS | Male | White British |
| Hub client 03 | Healthcare assistant | Clinical | NHS | Male | White British |
| Hub client 04 | Manager/senior leader quality and compliance team | Non-clinical | NHS | Female | Black British |
| Hub client 05 | Nurse, ICU | Clinical | NHS | Female | White British |
| Hub client 06 | Clinical research nurse | Non-clinical | NHS | Male | White British |
| Hub client 07 | Adult social worker | Non-clinical | Local Authority | Female | Pakistani |
| Hub client 08 | Adult social worker | Non-clinical | Local Authority | Female | White British |
| Hub client 09 | Nurse, stroke ward | Clinical | NHS | Male | White British |
| Hub client 10 | Ward manager, acute cardiology ward | Clinical | NHS | Female | White British |
| Hub client 11 | Pharmacist, ICU | Clinical | NHS | Female | White British |
| Hub client 12 | Deputy pharmacy manager | Clinical | NHS | Female | Mixed – White and Afro Caribbean |
| Hub client 13 | Consultant anaesthetist | Clinical | NHS | Male | White British |
| Hub client 14 | Teacher | Non-clinical | Education | Male | White British |
| Hub client 15 | IT system administrator | Non-clinical | NHS | Male | White British |
| Hub client 16 | Patient advice and liaison services (PALS) | Non-clinical | NHS | Female | White British |
| Hub client 17 | Nurse, advanced clinical practitioner, ICU | Clinical | NHS | Female | White British |
| Hub client 18 | Employment services | Non-clinical | NHS | Female | White British |
| Hub client 19 | Occupational therapist, mental health | Clinical | NHS | Female | Black |
| Non-Hub keyworker 01 | Organisation development manager | Non-clinical | NHS | Male | Mixed – White and Black African |
| Non-Hub keyworker 02 | Counsellor, IAPT | Clinical | NHS | Male | White British |
| Non-Hub keyworker 03 | Care home manager | Clinical | Social Care | Male | White British |
| Non-Hub keyworker 04 | Student nurse | Clinical | NHS | Female | White British |
| Non-Hub keyworker 05 | Equality, diversity and inclusion lead | Non-clinical | NHS | Male | Pakistani |
| Non-Hub keyworker 06 | Emergency medical technician | Clinical | NHS | Female | White British |
| Non-Hub keyworker 07 | Healthcare assistant | Clinical | NHS | Male | Black African |
| Non-Hub keyworker 08 | CBT practitioner, IAPT | Clinical | NHS | Male | White British |
| Non-Hub keyworker 09 | Administrator, cancer services | Non-clinical | NHS | Female | White British |
| Non-Hub keyworker 10 | Vaccinator | Clinical | NHS | Female | White British |
| Non-Hub keyworker 11 | Civilian investigator | Non-clinical | Police Service | Male | White British |
| Non-Hub keyworker 12 | Administrative assistant | Non-clinical | NHS | Female | Indonesian |
| Non-Hub keyworker 13 | Dietician, diabetes | Clinical | NHS | Female | White British |
| Non-Hub keyworker 14 | Senior carer in residential home | Clinical | Social Care | Female | White British |
| Non-Hub keyworker 15 | Manager, chemotherapy services unit manager | Clinical | NHS | Female | White British |
| Non-Hub keyworker 16 | Police support staff/systems analyst | Non-clinical | Police Service | Female | White European |
| Non-Hub keyworker 17 | Firefighter | Non-clinical | Fire Service | Male | White British |
| Non-Hub keyworker 18 | Police officer | Non-clinical | Police Service | Female | White British |
| Non-Hub keyworker 19 | Administrator, safeguarding | Non-clinical | NHS | Female | Somali British |
| Non-Hub keyworker 20 | Staff engagement and inclusion practitioner | Non-clinical | NHS | Female | Bengali British |
| Participant ID | Occupation |
|---|---|
| Hub staff 01 | Psychological therapist |
| Hub staff 02 | Clinical lead |
| Hub staff 03 | Senior clinical psychologist |
| Hub staff 04 | Clinical pharmacist |
| Hub staff 05 | Clinical lead |
| Hub staff 06 | Non-clinical manager |
| Hub staff 07 | Assistant psychologist |
| Hub staff 08 | Non-clinical staff member |
| Hub staff 09 | Psychological therapist |
| Hub staff 10 | Counsellor |
| Hub staff 11 | Clinical psychologist |
| Hub staff 12 | Assistant psychologist |
| Hub staff 13 | Senior practitioner |
| Hub staff 14 | Clinical lead and psychological therapist |
| Participant ID | Occupation |
|---|---|
| Wider stakeholder 01 | Director mental health services |
| Wider stakeholder 02 | Senior HR personnel |
| Wider stakeholder 03 | Occupational health lead |
| Wider stakeholder 04 | Senior HR personnel |
| Wider stakeholder 05 | Commissioner |
| Wider stakeholder 06 | Non-executive director |
| Wider stakeholder 07 | Clinical psychology lead |
| Wider stakeholder 08 | Regional lead |
| Wider stakeholder 09 | Occupational health lead |
| Wider stakeholder 10 | Well-being practitioner |
Table 22 outlines the thematic structure of the following Results section, which uses the structure of the constructs within the NPT framework. Figures 4 and 5 further illustrate these constructs and how they are linked. Example quotes are provided throughout the following Results section, alongside each theme/construct. Further quotes relating to NPT constructs can be found in Appendix 3, Part 2. To protect participants’ confidentiality and prevent participants from becoming identifiable, site identifiers were removed from this chapter.
| NPT construct | NPT subconstruct |
|---|---|
| Sense-making | Differentiation |
| Communal specification | |
| Individual specification | |
| Internalisation | |
| Relational work | Initiation |
| Enrolment | |
| Legitimation | |
| Activation | |
| Operational work | Interactional workability |
| Relational integration | |
| Skillset workability | |
| Contextual integration | |
| Appraisal work | Systematisation |
| Communal appraisal | |
| Individual appraisal | |
| Reconfiguration |
FIGURE 4.
Enablers to successful implementation of the Hubs.
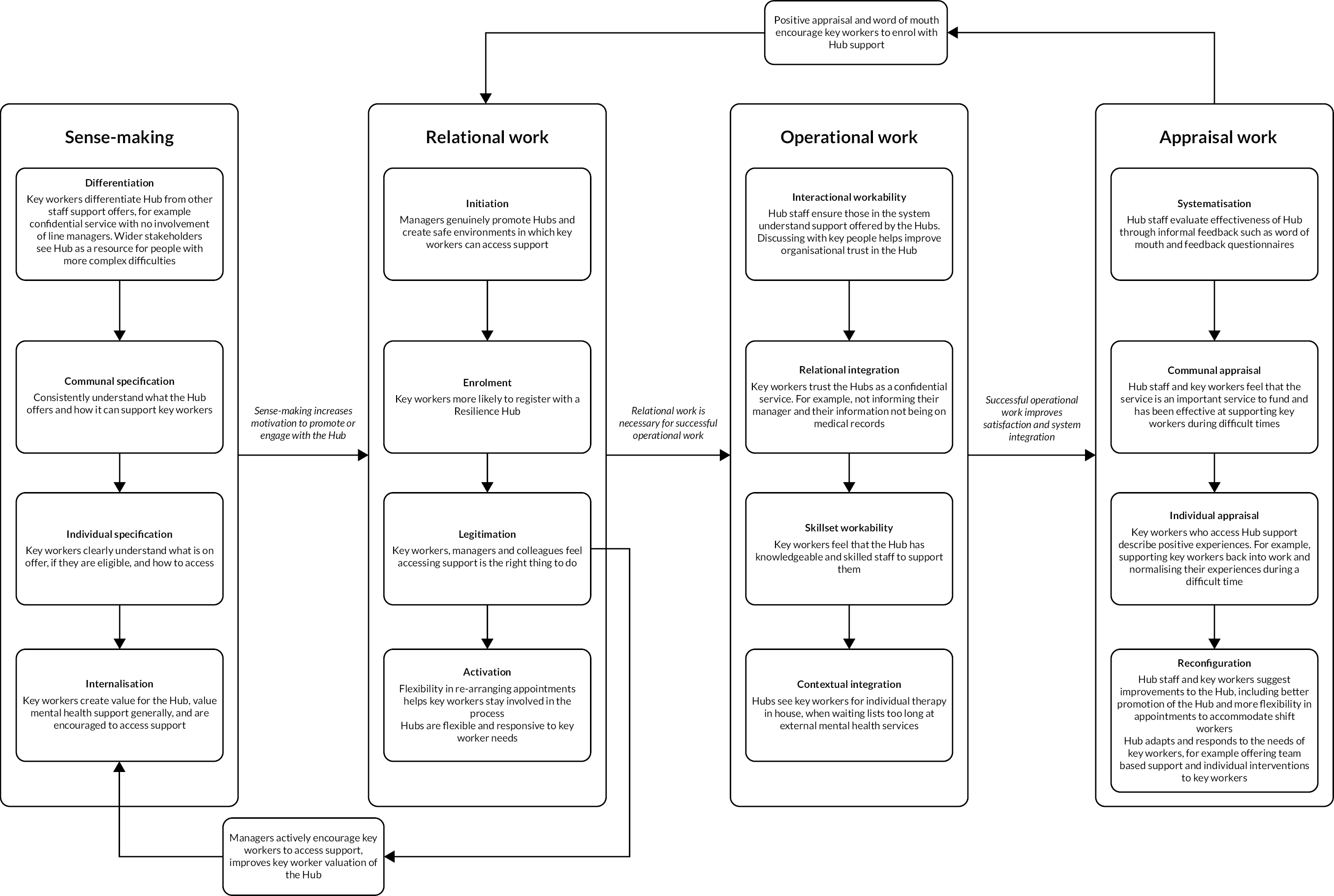
FIGURE 5.
Barriers to uptake and implementation of the Hubs.
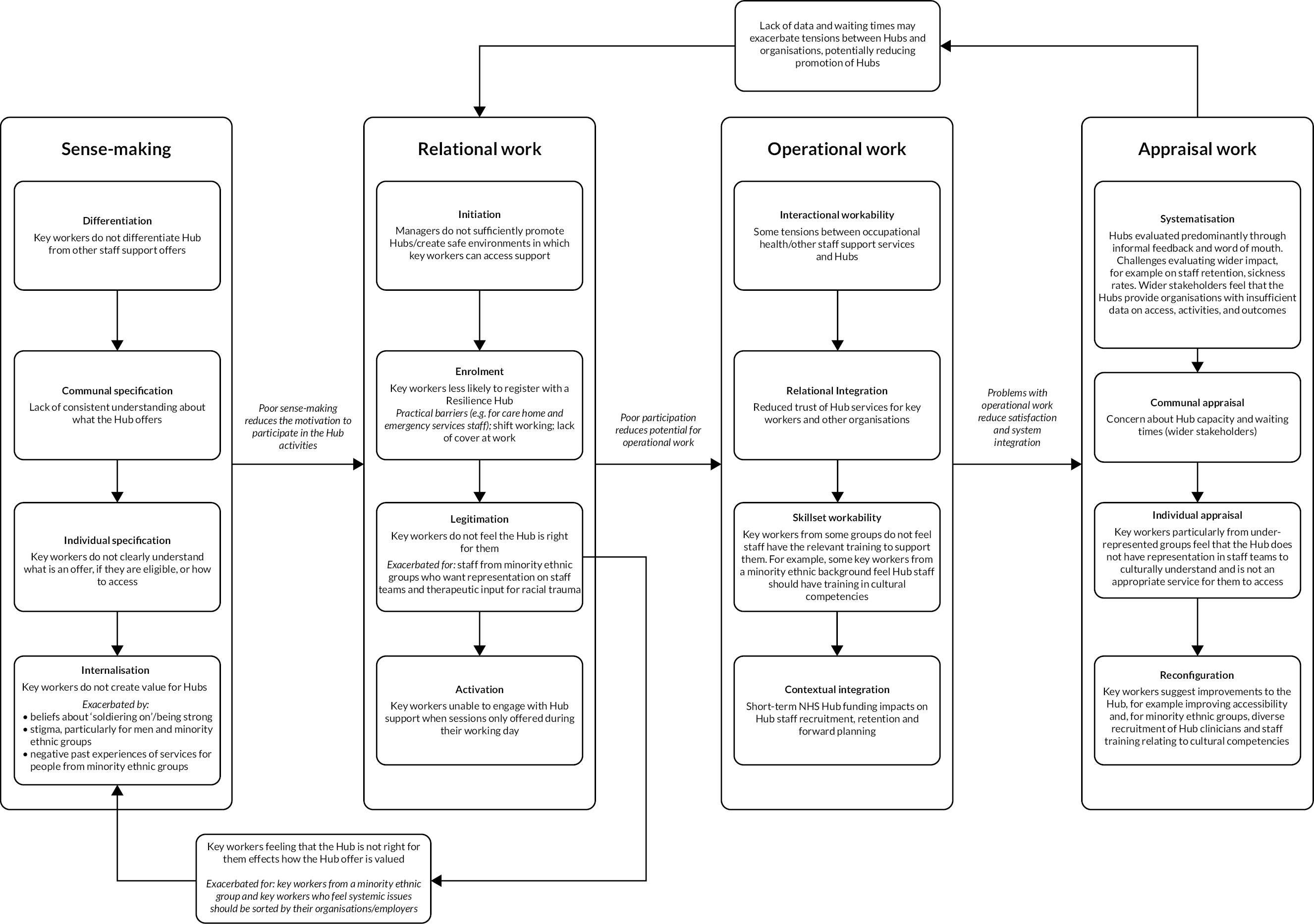
Sense-making
Understanding the ways the Hubs differ from other types of staff support (differentiation)
Hub staff across sites clearly distinguished the Hub model from other mental health services across several aspects including proactive outreach; timely assessment and intervention; team-based work; and responsiveness and flexibility according to need. They saw the Hubs as different from routine staff support in terms of confidentiality and separation from keyworkers’ employing organisations (differentiation):
the Hub is something that’s separate from all the Trusts and separate from all the local authorities … it’s neutral ground and it’s a place where the clients can come and feel a little bit more reassured of confidentiality.
Hub staff 05
Staff from one Hub described the Hub approach as having fewer constraints on session numbers compared with other services, whereby clinicians could work more flexibly, providing more supportive calls and containment prior to formal therapy, enabling a more comprehensive, holistic approach.
Wider stakeholders saw the Hubs as having more specialist mental health staff with the ability to see more complex presentations than standard organisational staff support offers:
[the Hub] was providing access to more specialist, higher-end support, which wouldn’t normally be provided to a normal organisational health and well-being service.
Wider stakeholder 04
lots of Trusts didn’t have psychology for staff health and well-being in existence. While there was a pathway and an offer through to talking therapies, some of this stuff was so much more specialist than that.
Wider stakeholder 03
Stakeholders from NHS Trusts that already provided different staff support offers, including high-intensity psychological therapies, felt that the Hubs were not significantly different from their own offer:
there’s a fair amount of overlap, we do offer some of the similar interventions, such as EMDR. We don’t offer the team interventions in the same way the Resilience Hub do … But a lot of it … is whether someone would like to be seen in house, or whether that’s uncomfortable for them.
Wider stakeholder 07
Keyworkers also positively differentiated the Hubs from occupational health in terms of simplicity of self-referral without involvement of managers, and speed of access. Keyworkers who had turned to private therapy valued the Hubs being free of charge:
the process of actually getting into the service can put you off sometimes, but the Resilience Hub seemed a lot more straightforward, not lots of paper filling in and lots of line manager involvement.
Hub client 12
Other keyworkers did not want to access occupational health due to potential negative consequences within work:
it’s all supportive and then it turns into ‘well is it going to become a performance issue here? Is this person going to be able to manage?’ … all they’re focused on is statistics and getting through the cases … there’s no room … for allowing real support for a staff member that’s unwell.
Hub client 07
Hub staffs were concerned that keyworkers may not always understand how Hub support differs from other initiatives being advertised:
they might perceive it as duplication of role like ‘why would I need the [Hub] because we’ve already got a staff well-being service’.
Hub staff 13
This concern was borne out amongst some keyworkers:
There were so many things about where you could go for help, you could ring this number, you could use that app … I almost felt I couldn’t see the wood for the trees … because I wasn’t feeling well, there was almost too much choice.
Non-Hub keyworker 10
Where keyworkers did not differentiate Hub support from occupational health, some were mistrustful of the Hubs (relational integration) and concerned that their managers would find out they had accessed support. Hub staff described having to work to build up this trust:
Initially, it was quite difficult to engage with the staff because there was a mistrust. There was a feeling that, maybe, anything that was said in confidence would be carried back to management or HR. So, it took a long time, a lot of listening, a lot of patience and a lot of cooperation to gain the trust.
Hub staff 10
Individual and system understandings of the Hubs (individual and communal specification)
Hub staff felt that amongst Hub teams, there was a consistent, shared understanding of the model, and a shared sense of the purpose of the Hubs as supporting and containing individuals and teams directly providing or supporting access to timely intervention; promoting well-being; and supporting staff in a way that prevented the need for individual psychological intervention. Hub staff and wider stakeholders acknowledged challenges in getting this message out to keyworkers:
I would say there is no consistent understanding … I don’t think that we have effectively been able to reach everybody within the Integrated Care System, to, first of all, help them have an awareness of the service, and then specifically what the service is about.
Hub staff 02
I think [communication is] an ongoing issue … I think for desk-based staff not so much, because it’s easy to communicate by e-mail and communicate about the different options; when we’re trying to reach ward staff who don’t spend a lot of time at the computers it’s difficult to convey complex messages, so it’s definitely not clear to everyone what the different options are, and that’s definitely an ongoing challenge.
Wider stakeholder 07
Keyworkers who had not accessed mental health support or the Hubs before, and had not accessed the Hubs, at times did not know where to start when looking for support. Where keyworkers were aware of their local Hub, they did not always understand the full extent of what was on offer (individual specification):
I just thought it was more of a resources website where people can get a little bit of general information about how to avoid burn-out and how to keep well when you’re stressed. So I feel like I didn’t really know the potential that it has to offer.
Non-Hub keyworker 13
Others were not sure how to access the Hubs, or thought they were only for front-line clinical staff:
I didn’t really know how to access it and then my supervisor wasn’t sure either how to access that and it’s just a case of when you get so busy, things get pushed aside, and you think I’ll look at that later.
Non-Hub keyworker 09
Misunderstandings around eligibility may have been exacerbated by limitations of other staff support offers:
I did the online triage [for a non-Hub service], and then I got an e-mail back saying that … they were unable to help me at that time, ‘cause they were prioritising critical care workers … it made me feel like … other people obviously needed help and services more than I did, and I thought, oh well, you know, I’m alright, I’ll manage … So, I didn’t actually go anywhere else at that point.
Non-Hub keyworker 10
Creating value for the Hubs and support in general (internalisation)
Hub staff strongly agreed about the value of the Resilience Hubs and the support they provided (internalisation), for example, in providing a separate, confidential service:
staff who don’t want to seek support from their colleagues … want to seek support from an outside service that’s not linked at all to occupational health, not linked to the team they work within or their management structure, and that’s very much a role the Hub fills.
Hub staff 09
Several keyworkers spoke of valuing mental health, and feeling comfortable about seeking support:
there was an element of that self-acknowledgement that, yeah, I’m struggling here and whatever I’m doing isn’t helping me, so I need somebody else to help me.
Hub client 19
However, prioritisation of mental health support was not universal amongst keyworkers.
Barriers to valuing support: keyworkers’ beliefs about self and job roles
Examples were given at individual, team, and organisational levels of mental health and well-being support not being sufficiently prioritised. At an individual level, Hub staff felt that keyworkers often struggled to seek support:
[it’s] really difficult for care providers, care givers to acknowledge their own difficulties and needs, because there’s often a lot of feelings of shame and guilt … where people then felt ‘I cannot prioritise my own needs and difficulties, I have to be a resource for others’.
Hub staff 02
Wider stakeholders from across Hub regions acknowledged long-standing issues of stigma and persuading keyworkers to access support:
I think we are dealing with the fact that people are still nervous about openly talking about mental health … in case it affects their job … So it isn’t necessarily the fault of the Resilience Hub, but we are still dealing with a consensus where mental health is still viewed with a level of suspicion.
Wider stakeholder 06
Many keyworkers confirmed Hub staff’s concerns. Participants described not wanting to create additional work for colleagues if they took time out to seek support:
I was aware of the effect on my colleagues because if I got sick they’ve got to cover me … I don’t want to be a burden on anyone.
Hub client 02
Managers felt the need to be strong for others:
I think sometimes leaders at that point needed to be leaders, and it wouldn’t help me lead if they saw that I was struggling with other things … you want to stay strong for them … you have to be like a buffer to them, and you have to absorb their problems, not the other way.
Hub client 17
When keyworkers did acknowledge that they needed support, some described concern that colleagues would not believe they were struggling, because they were still at work:
it was quite emotional for me to realise how … COVID and the whole pandemic, bereavement, my own illness … how that was impacting on me … and [on the other hand] whether people believed that I was still ill because I was going to work and managing work each day, even though I wasn’t performing to the level that I expect of myself.
Hub client 19
Keyworkers frequently spoke of not feeling they were struggling enough to merit support. They did not want to ‘waste people’s time,’ or take the place of someone who might have greater needs. Keyworkers in non-clinical roles particularly shared this concern:
I didn’t feel like I warranted that support … how can I honestly say that I’m feeling acutely stressed or anxious about something the same as a clinical member of staff or somebody who was shielding.
Non-Hub keyworker 01
These concerns were often shared within the context of staff knowing that mental health services were already stretched. The likelihood of long waiting lists was also a barrier:
from what little I know about mental health services … it’s very, very difficult … there’s no way that I could phone a doctor now and say, please could I speak to a counsellor next week? … It’s just not going to happen.
Non-Hub keyworker 11
Consequently, many keyworkers waited until things had become very difficult before acknowledging that they needed support:
you keep going, just keep going and it’s not until … everything just went bang, that I thought I need some help.
Non-Hub keyworker 06
Keyworkers across multiple roles and sectors felt that dealing with stressful or traumatic experiences was part of the job, and described beliefs within their professions that they had to cope with that:
I’ve been in acute care now for ten years so I know what it involves. If I didn’t like it then I could have left or I could have gone to a different area in practice … something less traumatic. So it’s kind of expected that if you’re choosing that as your speciality that you can cope with the mental side of it … I would hold that getting help is still seen as a sign of weakness rather than coping.
Hub client 17
These beliefs may have contributed to the perception of some Hub staff that some keyworkers, or teams, were initially resistant to support or input from the Hubs, ‘we don’t want anybody [the Hub] meddling with our well-being’ (Hub staff 14, paraphrasing a well-being lead). Hub staff felt that team-based work, and a gradual increase in keyworkers’ understanding of the Hubs (communal specification), increased the value keyworkers saw in the Hubs (internalisation) and built trust (relational integration):
I think they were just like, ‘… what is this and why would I need it anyway’ … It’s almost like, as a few people have come through, they understand us a bit more or we’ve done a few face-to-face team sessions now with ICU staff or teams of staff who were redeployed into ICU. I think, as those team sessions happen, people [think] ‘oh yes this makes sense, they do know what they’re talking about’, so they’re perhaps opening up to the potential that psychological therapy could be helpful to them.
Hub staff 01
Barriers to valuing support: organisational and systemic issues
At an organisational level, Hub staff and keyworkers felt that senior management and leaders within the care system did not always place sufficient value in mental health and well-being support for staff, and the offer of the Hubs:
I do think there could be more support from the system. I think there could be more buy-in.
Hub staff 14
As a result, keyworkers themselves did not always value the support on offer (internalisation).
Several keyworkers felt that their employers did not genuinely care about mental health or well-being support, and were just paying ‘lip service’ by sharing information about the Hubs or other support offers (internalisation/initiation);
it’ll be a forwarded e-mail. The e-mail will be, ‘see below’, it won’t be, ‘I’d really like you to try and access it’ … they won’t engage with it, it feels like they’re doing their job, like they’re ticking a box, as opposed to genuinely being behind it.
Hub client 17
Some keyworkers described a work culture that did not encourage speaking about well-being or accessing support, or a culture of just ‘crack on’ or ‘soldier on’ (internalisation). Others did not feel safe, or described experiences of bullying:
I think there’s very much a culture in the NHS of, this is your job, and you just deal with it and you just get on with it.
Non-Hub keyworker 15
I don’t feel like the organisation’s a psychologically safe organisation at this moment in time … there is still that idea of, we need to be stoic, we need to be brave.
Non-Hub keyworker 01
Some keyworkers described feeling resentful that their managers or organisation were suggesting employees sought support, improved their own resilience, or coped better, when they felt that employers should be resolving wider systemic issues, which they saw as the root cause of their stress (internalisation/legitimation):
I have complicated reasons for not accessing [the Hub]. I wanted [my] organisation to … step up and acknowledge what they do to damage people’s mental health and do something about that … rather than put a plaster on something. Why don’t [they] acknowledge that putting people under this amount of pressure isn’t good for them?
Non-Hub keyworker 08
Hub staff and some wider stakeholders acknowledged that the term ‘resilience’ was sometimes off-putting to keyworkers, by implying that workplace stress was the responsibility of individuals:
people really don’t like the word ‘resilience’ … I think people are feeling sometimes really negative about the word, that it feels like an expectation that they need to do more versus their employers looking after them and their working environment.
Hub staff 11
[Staff] were saying that they feel they’re being gaslighted. So it’s all this around … you need to be resilient. Everything’s getting pushed towards them as though this is their fault if they’re feeling tired or they’re not managing and they’re not coping.
Wider stakeholder 09
These concerns were also flagged within the context of keyworkers feeling that they had not been sufficiently consulted about what types of support would be most beneficial for them:
I think sometimes people thought what people needed, but when you actually spoke to people, maybe, it was slightly askew, … I think a lot of our ‘shopfloor’ workers were very angry that they didn’t see a lot of management. And the managers were making decisions almost [over] their heads, but they were living with it every day.
Wider stakeholder 10
Relational work
The role of managers in influencing engagement with Hubs (initiation and enrolment)
Within the Hubs, staff believed that the right people were involved in setting up and driving forward the services (initiation); key determinants were said to be extensive experience in mental health and trauma, seniority, contacts and positions of influence. However, Hub staff felt that senior managers in the care system were not always spreading the message of the Resilience Hubs to help promote the service to staff:
[organisations have] had challenges in terms of the senior managers, [maybe they] have been dealing with a crisis … perhaps they’ve had other priorities in the service, and if you don’t get in at a high level then it doesn’t happen.
Hub staff 13
Wider stakeholders felt that generally appropriate routes had been taken in promoting the Hubs at a senior level within organisations, although it was suggested that early involvement of Chief Medical Officers and Chief Nurses could have helped to establish further buy-in.
Some keyworkers agreed that managers and leaders within their organisations could be doing more to promote mental health and well-being support for staff, and encourage staff to access services including the Resilience Hubs. Some participants felt that management should be more strongly advocating support access, so that it became an expected or standard thing for staff to do:
it’s not coming from the powers that be that everybody has to … It needs to be said that, you know, everybody needs to access the support … I think everyone should, not be made to access it, but it needs to be really drilled down to people that, you know, this service is here for you.
Hub client 06
Hub staff described doing considerable groundwork such as establishing and maintaining new relationships with organisations and teams, and developing communication strategies to try to engage the right people within organisations. Keyworkers agreed that it was essential to make in-roads with senior management:
We try and find the right person in the system to engage with, who actually can make things happen … That’s often the workforce lead or the well-being lead or the staff well-being psychologist.
Hub staff 14
Hub staff and keyworkers both acknowledged that managers were under their own considerable pressures, and that this impacted the extent to which they promoted mental health and well-being services to their staff:
We talk about well-being and things. There isn’t an awful lot that is done about it though … And I do wonder whether, sometimes, managers are disinclined because it might reflect badly on them if their staff are needing to seek support. And then of course it’s going to affect their numbers [if I go off sick].
Non-Hub keyworker 08
The above challenges of understanding the Hub offer, how to access the Hubs, and barriers to prioritising mental health and well-being support all contributed to keyworkers’ decisions around whether or not to access support (enrolment). Managers also had an important role in encouraging keyworkers’ engagement with Hubs when they were involved and actively promoting the Hubs or mental health and well-being support in general (enrolment):
we so desperately want to engage these people and we so desperately want to support them and it almost feels that this manager level almost feels more key than the individual staff.
Hub staff 13
when I first asked for help in this job, it was as a direct result of my line manager saying … ‘I think it would be helpful for you to talk to Occupational Health and get some counselling’ … And she sort of pushed that quite hard, in a nice way, which was good.
Non-Hub keyworker 10
leaders in the organisation talking about their vulnerabilities I think has really helped more people come forward with stuff.
Wider stakeholder 03
Wider stakeholders echoed these views; one described how managers may not always proactively promote staff access to well-being support:
I think [managers promote well-being services] almost when it’s got to bubbling point rather than going to that proactive kind of thing … we should be looking after our staff slightly better than we are and … I’m not bashing the managers because they also need looking after as well.
Wider stakeholder 10
Hub staff and keyworkers found that managers sharing their own experiences of accessing support played an important role in personally promoting the Hub to others and creating safe spaces to talk about well-being (enrolment):
If managers are really well engaged in our service and then they manage somebody who’s struggling, they’re far more likely to actively encourage them to, you know, seek support.
Hub staff 13
if a senior leader said, oh, I accessed the Resilience Hub to get some support with A, B and C and they supported me in C, D and F, that would almost give people permission to say … ‘so it’s okay if he has done it, so it must be okay if I can access it as well’.
Non-Hub keyworker 20
The extent to which Hubs were seen as the ‘right’ way of supporting staff (legitimation)
Wider stakeholders generally agreed that the Hub model had utility and legitimacy as a service to support staff (legitimation). Particular aspects of the model were highlighted, including team-based and preventative work, and the Hub being part of an offer within the health and care system. It was felt that existing in-house support within organisations were vital, but that the Hub had an important external role:
[The Hub is] part of an offer and I don’t think it would be the right thing if it was the only offer … I think for us it’s good because it’s the end of a process, it’s the highest level of support and, therefore, it has to be accessed in a different way.
Wider stakeholder 02
One wider stakeholder from a VCSE organisation, however, felt that the Hubs should not have been hosted by NHS Trusts as they were not separated from the NHS system. They also felt that by virtue of being led by clinicians, the Hubs over-medicalised distress:
The Resilience Hub does pathologise because it’s a clinical system run by the NHS … by NHS clinicians … I think The Resilience Hub is far too clinical … it defaults into that person needs to have treatment with a clinical thing, whether that be CBT, whether that be counselling.
Wider stakeholder 06
Others, however, felt that the Hubs were less medicalised or diagnostic than other NHS mental health services.
However, Hub staff felt that at times they struggled to persuade management that the Hubs were legitimate, commissioned, services (legitimation). One Hub staff member felt that this would have been an easier task if organisations were encouraged or mandated at a system level to engage with the Resilience Hubs:
I think that some systems need to be told they have to engage with us. So we have got some areas that have not engaged [but] we know full well they’re not alright.
Hub staff 14
One wider stakeholder, however, felt that top-down national approaches to engagement would not work, and that the impetus to engage with the Hubs needed to come from the organisations themselves:
I think the evidence over a number of years, whether it’s been through strategic health authorities or whatever form the higher-level NHS took it, is that the NHS has at various points tried to push that kind of model onto organisations and make it happen. And actually, that’s never really worked. Because, if organisations are not willing to support it then it doesn’t happen. That’s why I attach so much importance to the information and the story telling, because I think that just starts to build that groundswell of bottom-up opinion that actually this is a really good thing and we need to support it.
Wider stakeholder 04
Problems of legitimation for groups under-represented amongst keyworkers accessing the Hubs
Groups that were under-represented within the Hubs also described problems relating to legitimacy. These groups include ethnic minority communities and care home staff.
Staff from each of the Hubs acknowledged that amongst Hub clinical teams there was limited representation of people from ethnic minority communities:
We don’t have a big BAME representation in the therapists … So there’s a potential that we’re unintentionally being excluding of certain populations and groups.
Hub staff 09
One wider stakeholder felt that by providing a service that was open to all, the Hubs would necessarily exclude some groups by virtue of not having specific culturally appropriate services:
[The Hub] worked on a very open access bid, which immediately by being open access you are then, by default, alienating to groups where open access is not appropriate. So, it’s very much about actually what was that specific offer around specific community groups.
Wider stakeholder 06
These concerns were echoed by some keyworkers, who felt that having representation of minority ethnic communities on Resilience Hub clinical teams was of central importance, particularly due to the disproportionate impact of the pandemic on these staff groups:
The fact that when I asked for a representative therapist they didn’t have any … I found that strange. Especially if they were set up due to COVID, and COVID was showing that BAME people were disproportionally affected, so who did they think was going to …? Just white staff? … I don’t mean to be pedantic. But it just doesn’t make any sense to me.
Hub client 04
Others did not share this view, as long as Hub clients were treated equally:
culturally, I don’t think it necessarily has a big place really, because again I would expect that it wouldn’t matter what culture [or] background somebody comes from and should be dealt with as just on an equal footing.
Hub client 12
One participant described others’ preferences for a therapist from the same cultural background as themselves, but this would not suit them personally:
from my perspective, I wouldn’t want somebody from a BAME background … I think someone from a BAME background understands the cultures too much, and I want someone to be completely impartial.
Non-Hub keyworker 05
The difference between participants may relate to the focus of support for which they had contacted the Hubs. Participants who specifically wanted support around experiences of racism, discrimination and the impact of such experiences had felt that the lack of representation and clinical skills on Hub staff teams was problematic as they felt that clinicians not from a minority ethnic group would not be able to understand their experiences. As a result, Hub client 04 had declined further support from the Hub with which they had registered:
I wouldn’t want to have to explain myself, which is what I usually do in work when people ask me questions and I try to explain how the experiences are. They say well, that could happen to anyone, how can you say it’s racism? So I didn’t want that to come into it … That’s why I wanted someone representative there.
Hub client 04
I wanted an Asian counsellor … it’s not something that I look for all the time, but … I just felt I wanted someone who could actually genuinely culturally understand … I was that vulnerable with what was going on with my symptoms and my mental health was really bad … there was all that Black Lives Matter stuff going on … that brought [up] a lot of stuff that had happened to me, that I’d experienced institutional racism … it’s like post-traumatic … I know it’s hard in the service to meet every single need, however, I think you do need somebody there whose got that background and that real cultural understanding sometimes, just for those 0.1 per cent that want it.
Hub client 07
For keyworkers who had not accessed a Resilience Hub, negative past experiences had already led to reduced trust in the system:
It’s … one of the reasons I’m very, very mindful of who I will go to support for … now that I know about [the Hub], if you were to say to me would you access it, I would say not really unless they [gave me] information to say we’ve got people trained in race-related stuff or this is inclusion or we will never release your data to anywhere without your explicit consent … I would need a lot of information because I don’t trust the system … my story is just one of many, many stories of structural inequality that impacts on experience, that then reinforces mistrust of the system.
Non-Hub keyworker 20
One wider stakeholder discussed the need for conversations to try to understand and resolve barriers to accessing support:
[Low support uptake amongst men and people from Black, Asian and minority ethnic groups] tends to be our overall experience as well … I think a lot of it is to do with just trying to bring … Some of it is suspicion, isn’t it? We did a piece of work around the vaccine … and we were only on 73 per cent uptake and we actually got it up to 94 per cent, just by calling … and having a conversation just to understand what the hesitancy was … you do have to reach out to those particular groups.
Wider stakeholder 09
Another wider stakeholder highlighted other systemic issues around perceptions of structural inequality:
the stuff I was hearing about in the context of COVID was around ethnic minority staff feeling a bit discriminated against in terms of where and when they were rostered. I think in our organisation there’s something about ethnic minority staff not being well represented at the highest levels. And I think there’s kind of learned experiences around not being listened to and nothing changing, or at least it seeming that way.
Wider stakeholder 07
The need for training around cultural competencies, and promotion of this training to prospective clients, was highlighted by several keyworkers:
[Their white colleagues] wouldn’t have race-related negative experiences on top of whatever other experiences they’ve had … So actually you have to be very culturally sensitive and race sensitive in your information and dialogue that you have with these individuals in order to create safe spaces.
Non-Hub keyworker 20
Other potential barriers shared by keyworkers who identified as being from ethnic minority group included stigma within their communities around accessing mental health support, and language barriers:
My extended family … very much have that view that mental health is non-existent really. If somebody has poor mental health, then they’re possessed or it’s that kind of … those superstitions start to come in and it’s not that they’re ill, they’re either making it up, they’re attention-seeking, it’s some sort of spirit, they’ve done something in a past life and all of those residual cultural kind of things come into play that actually really, really affect that individual accessing.
Non-Hub keyworker 01
Because obviously they could have a culture, or they have the community shame, like what people will say. Their own family or their own unit where somebody could say, well if you’re seeking help it means you can’t cope … Or there is a language barrier … they may think … what is it about, how is that useful?
Non-Hub keyworker 19
Wider stakeholders who were involved in the care sector felt that the Hubs were an important source of support for care home staff:
we were asking and expecting an awful lot of … low-paid staff in terms of supporting very vulnerable residents. And I think the hub’s been able to step into that space quite well … Some of the providers probably do provide a level of support for their employees but I don’t think it would include the sort of support that the Hub was able to offer.
Wider stakeholder 04
However, they acknowledged the challenges of promoting support offers to care homes:
because [care homes are] very often independent contractors they don’t have the wraparound that an NHS organisation would have. So, I think they’ve probably been left to struggle. I’m not sure that they’re in the loop as much in terms of understanding what’s available in the system and kind of getting the comms out because they are all independent and there never seems to be one conduit where you can … offer how you can access support. So, I think certainly with those that are in formal organisations, like, you know, the county council or an NHS trust, it works fairly well getting messages out there, but as for the wider system I’m not really sure that that’s the same. They feel inaccessible sometimes.
Wider stakeholder 02
Likewise, staff from across the Hubs described struggling to share information about the Hubs with care home staff and managers, including receiving small numbers of referrals following outreach at care homes, and relying on managers to share information rather than speaking to care home staff on the ground:
when we’ve gone to care homes a couple of times we’ve only been able to meet with the senior team, so the manager, the deputy manager … We are then reliant heavily, and solely really, on them cascading that information down, because we don’t have access to each individual staff e-mail address … we’re not actually speaking to everyone on the ground, which is where the help is probably needed the most.
Hub staff 07
Hub staff and keyworkers acknowledged that part of the challenge was due to extreme work pressures on care home managers:
I think it’s for the managers to really feed down the importance of accessing the Hub. Sometimes the managers over overwhelmed. They’re running around doing the reports, medication … and they simply don’t have the time to push the Hub.
Hub staff 08
There’s no time, that’s the problem … Obviously at some of these really big care homes maybe they do because they have quite a few managers in post. But particularly for the smaller ones these days, they’ve got all the extra stuff now with PPE, tests … And then … there are so many different risk assessments and things with visiting. These are all extra to what they had two years ago. And then all the time there’s more and more paperwork being put on, through the [Care Quality Commission] and safeguarding … So making [access to support] as simple as possible, I’ll be honest.
Non-Hub keyworker 14
Another challenge may have been due to managers expressing concerns about the consequences of an NHS service getting involved with their staff:
there are some care home companies who [we suspect] won’t pass our information on because they feel it’s suspicious, they feel we’re going to … support their staff to go off sick.
Hub staff 11
one of the care home owners (said) they were really concerned that we were coming in as the NHS and were going to pick up poor practice and … report that.
Hub staff 14
One keyworker who worked in a care home described the challenges of scheduling appointments around shift patterns, and differences in staffing, occupational health and sick leave between the care home sector and the NHS, which were all seen as barriers to accessing support:
we’ve got the shift patterns which can be difficult … we don’t use agencies or anything in our place … If you are sick at all, you don’t get paid … If you have a bereavement, you might get your manager understand and say, right, you can have a day off, but any longer than that you usually have to use your holiday for.
Non-Hub keyworker 14
One wider stakeholder suggested that there may be a different culture of help-seeking amongst organisations that do not typically have extensive occupational health services:
I think it’s maybe a bit of a cultural issue as well. If you’re not used to having that kind of support being available, and there’s also a little bit of a stigma attached to it anyway, you’re possibly going to be more reluctant to, or less inclined to, take up the offer.
Wider stakeholder 04
Sustaining engagement in the Hubs: flexibility and availability of services (activation)
Keyworkers who had accessed the Hubs found that Hub staff were flexible in terms of rearranging appointments. This flexibility helped some keyworkers to stay engaged in the process (activation):
If I’ve had to move anything around, there’s been a couple of times when I’ve been called into work and had to cancel last minute, but … [Hub clinician]’s been understanding and just rescheduled. So, it’s been quite noticeable that they’ve, sort of, worked around me and been really helpful as well.
Hub client 01
However, Hubs’ ability to offer out of hours or face-to-face appointments was limited, and having to fit in sessions while on site at work had caused one participant to stop attending. Other participants also described this as a barrier, or had had to disclose the support to their managers to arrange time off. Other keyworkers felt fortunate to be working from home due to COVID, as they would not otherwise have been able to engage with the Hub’s support.
Keyworkers described having a consistent clinician to speak to for each appointment as a strength of the Hubs. Where this had not been possible, inconsistency of Hub staff was described as a limitation. One participant had discontinued their support from the Hub in part due to speaking to multiple different Hub staff members, in favour of face-to-face support accessed through work.
Hub staff and wider stakeholders felt that the flexibility of the Hub model was an important strength that sustained the Hubs (activation), responding to the needs of keyworkers and the health and care system as the pandemic evolved.
[it] feels like there’s enough flex to move and adapt … So, the fact that it’s something that’s been allowed to evolve naturally, I think it’s doing its job quite nicely really.
Hub staff 01
I like that it’s flexible … I think it’s great that there’s a kind of responsiveness to what the need is and there’s ongoing change.
Wider stakeholder 07
Operational work
Integration of Hubs within the wider health and social care system (interactional workability)
Wider stakeholders identified some early tensions between the Hubs and organisations whose staff they supported, in part due to overlapping offers (interactional workability):
probably we could have done better at the outset in terms of getting a common view and a common understanding and a sign-up to that across all partners to what the Hub would offer … for quite a while I thought there was a little bit of tension playing out between organisational employee health and well-being services and what they were offering staff and what the Hub was offering.
Wider stakeholder 04
Where organisations such as NHS Trusts did not particularly differentiate the Hubs’ support from their own in-house staff support because they already provided high-intensity psychological interventions, several wider stakeholders reported not needing the Hubs’ services to a significant extent, particularly where waiting lists were longer than in local services:
I think we have probably not used the Hub as much as some organisations because we have our own staff psychology service and Clinical Psychologists. So, whilst we have referred some of our most difficult cases where they really need significant psychological support, we have dealt with a lot of it ourselves.
Wider stakeholder 02
I think my only reservation … is that if somebody comes through to the Hub, and it’s for something quite low level … they’ve had to wait quite a while for that [at the Hub], but actually the Trust has a commissioner provider service with a local talking therapies service where we can get them in within a week.
Wider stakeholder 03
Hub clinicians acknowledged that variations in the support offered by organisations’ occupational health or employee assistance programme (EAPs) created challenges for the Hubs in terms of identifying support available and referring on Hub clients (interactional workability).
Wider stakeholders suggested that Hubs and organisations could work together more closely in terms of information sharing so that Hubs could identify where to prioritise their efforts:
I think the Hub needs to work out where it needs to spend its time most, I think it needs to see some information from organisations to make those prioritisation decisions.
Wider stakeholder 04
Building trust and confidence in the Hubs (relational integration)
Work was required across the system to build confidence and trust in the Resilience Hubs and the support they provided (relational integration). Subsequent to the tension described above, Hub staff described anxiety and even suspicion of the Hubs at a senior level within some organisations, particularly from existing staff support services. Staff across the Hubs described having to be careful to complement other staff well-being offers to avoid duplication particularly where there was some overlap between the Hub offer and other staff well-being initiatives:
there was a lot of anxiety to start with [within some organisations], we’ve, kind of, dispelled that and helped people realise that we’re here to help them and here to, you know, to fill in the gaps in provision rather than to nick the stuff that they’re doing … by us engaging with their staff and seeing their staff and getting good feedback from those staff groups, that will, hopefully, give them more confidence to be able to engage with us at a strategic level when the time is right.
Hub staff 05
Extensive work was done by Hub staff to ensure that those in the system had a clear, shared understanding of what support is offered by the Hubs (communal specification); they reported having conversations with key people (activation) to improve trust and confidence within organisations (relational integration):
we are continuously trying to ensure that we have a voice around certain tables, to tell people more about us, to help people have a clear understanding of the offer from the Resilience Hub, and about our transparency with regards to activity outcomes … I think if it wasn’t for that, things might have been a lot trickier with certain organisations and referral numbers coming from those organisations. What’s actually happening now is those organisations, those specific services are actually active referrers to our service who would signpost their own staff members to us, because there’s a clear understanding of our offer, where historically they might have held onto those people within their services, and those people might have been on extensive waiting lists.
Hub staff 02
At an individual level, Hub staff recognised that some health and social care keyworkers did not trust the Hubs (relational integration), perhaps due to the previously described confusion about whether the Hubs would share information with employers. Concerted efforts were required to help to build keyworkers’ trust in the Hubs and clarify these points.
Most keyworkers who had accessed the Hubs’ support felt they could trust the Hubs and, crucially, saw them as a safe space to discuss their difficulties without fear of repercussions or negative implications:
I think everyone in the NHS to some extent has got a fear of judgement, but once I got to know [Hub therapist] better … I quite quickly realised I’m not going to be judged here for what I’m saying. He’s there to help me … So I can say things that other people might be shocked at, where he’s not going to be, he’s going to understand that and try and help me deal with those things rather than saying well, perhaps you shouldn’t have done that. So I probably took one or two sessions to properly relax and I felt I could say anything.
Hub client 02
Many NHS staff who had accessed the Hubs felt strongly that Hub staff understood what they were going through, and valued this understanding:
they understood what it was like being on critical care … And then the secondary bullying issue that I had, they’re very familiar with dealing with … that as well … I immediately had confidence that they understood what I was talking about … I think that was the most important thing, that this wasn’t a generic service where you had to explain everything about why you were where you were. They’re like, right we know you’ve been working in critical care, we know what that’s like.
Hub client 13
By contrast, one emergency services keyworker preferred to access support from within their own organisation, as they felt that they would better understand the unique challenges of their role:
I don’t think your everyday person will understand what we go through … there’s domestics, there’s [road traffic collisions], there’s sudden deaths, hangings … unless you’ve done that and been to those incidents, I don’t think you can ever understand what that person’s going through … I think if I spoke to a GP about that … they don’t understand the stress of the job … Whereas I think more work-related, they get it, they’ve had that experience, they’ve spoken to number of other people who’ve probably experienced the same thing.
Non-Hub keyworker 18
Trusting that nothing would go on their occupational or GP records was vital for keyworkers; participants who had not accessed a Hub flagged this as a key concern:
if I came to you and said, I’ve got suicidal thoughts, for example, would that be on my NHS record? Would that appear on my GP records? … I know, as an organisation, we can access people’s medical records in certain circumstances.
Non-Hub keyworker 11
Participants’ concerns were not just about employers finding out; some keyworkers described damaging past experiences in their personal lives that affected their trust in services. One keyworker described their experiences of mental health records causing problems getting insurance, another told of their mental health records being revealed in court, impacting on custody for their child.
Skills and experience of Hub staff (skillset workability)
Hub staff felt that the Hubs had a good mix of clinical skills and experience (skillset workability). This was felt to be important for several reasons linked with this client group, including engaging and maintaining engagement of Hub clients, particularly given the reluctance around help-seeking already described (internalisation). Hub staff felt that senior clinicians with experience in managing complex mental health difficulties were important, owing to the range of difficulties with which keyworkers presented.
Furthermore, clinicians’ ability to effectively support staff teams using experience in organisational working was seen as an important part of the Hub’s support offer. Hub staff felt that recruitment of staff with a variety of clinical skills, combined with availability of additional training and continued professional development to support development of clinical skills for specific and emerging difficulties (e.g. Long COVID) had appropriately helped the Hubs manage these more complex support offers.
Likewise, keyworkers typically described Hub staff as knowledgeable and skilled in relevant areas, such as trauma and burnout:
this is what people are suffering from, we’ve all got trauma. So, it’s having … people focusing on that specialism for us, that burnout and then branching out in those little areas around that. It’s so needed … For us caring helping services … you’ve got to keep us going, because there’s never ever been real good welfare or help for us, generally.
Hub client 07
Hub resources and linking Hubs with other resources in the mental health system (contextual integration)
Wider stakeholders acknowledged that the Hubs were an effective way of making available the expertise of a limited number of specialist staff to a wide range of keyworkers and organisations (skillset workability/contextual integration):
what the Hub can offer is targeted support from trained specialists, who are thin on the ground. So, it makes sense to provide that across organisations rather than to do it within each organisation.
Wider stakeholder 04
In addition to making available their resource of specialist clinicians, the Hubs were also integrated within the wider mental health system, and supported clients to take up support provided by other services (contextual integration). Where clients were facilitated into other mental health services by the Hub, such as IAPT services, staff across the Hubs described making follow-up enquiries to ensure that these referrals were actioned by services, due to pressures and demands on IAPT:
it’s like a point of practice now … if I do a referral, I will be calling that service to check that they’ve got it, because otherwise it just falls through the gaps.
Hub staff 12
When referrals were accepted by other services, Hub staff expressed concern at the long waiting lists for therapy due to immense pressure within overwhelmed mental health services:
I think [services] are becoming increasingly overwhelmed … they often don’t offer any kind of priority for staff members … it’s probably a symptom of the demand on services throughout the country.
Hub staff 13
Keyworkers similarly described the value of the Hubs’ work following up referrals and ensuring they were taken on:
I contacted IAPT, … I got told you don’t qualify for help. Which is not easy to hear. I spoke to the mental health nurse at the Hub about it, really upset. And she intervened and wrote a report … So she amplified that … And while I was waiting for [IAPT treatment] she was really knowledgeable about [trauma] and she was sending me booklets and things … she sent me lots of information about it and exercises to do while I was waiting for therapy to start. So it was a lot more than just talking to someone.
Hub client 08
Regarding funding within the Hubs, Hub staff flagged concerns around the lack of certainty of funding for the Hubs going forward, both for staff recruitment and retention within the Hubs, and for keyworkers’ perceptions of the Hub:
I think there’s a fear amongst staff and amongst people who access the Hub around the longevity of it, so I think improvement might come with a bit of certainty around this model not just going as quickly as it arrived. I think that would help with people trusting in the service and it being here not for a short time.
Hub staff 09
One wider stakeholder flagged the enduring impact of trauma, and the time it may take keyworkers to come forward for support, being incongruent with the duration of Hub funding.
Appraisal work
Means of evaluating the Hubs (systematisation)
Hub staff shared that within-Hub evaluation was predominantly through informal feedback, word of mouth and feedback questionnaires (systematisation). Engagement and Hub activity was monitored through key performance indicators, session activity, and engagement with the website and online screening tools by potential clients. Hub staff described very positive informal feedback from clients. Hub staff and wider stakeholders both described a challenge of more formally evaluating the Hubs’ work and producing evidence that justifies their funding, particularly regarding some of the higher-level goals of the Hubs, including reducing staff sickness absences:
I know we’re doing a good job in what we’re doing, but it’s how we capture that and prove that it’s worthwhile financially. So it’s really hard to prove that we’re stopping staff going off sick because it’s a really hard thing to measure.
Hub staff 11
Wider stakeholders universally felt that there were insufficient data being fed back from Hubs to organisations and the health and social care system. Some implied that this exacerbated some of the initial tensions between the Hubs and other organisations. Access, activity and outcome data, it was felt, would help to reassure organisations of the value of the Hubs:
I think we [HRDs] need to see some information about what’s been going on, to provide that reassurance about the levels of activity and how they’ve changed. I know it’s very personal but sometimes people consent to give their own story about how that’s helped. I think it’s useful to see all of that information because it just provides a bit of evidence.
Wider stakeholder 04
Some stakeholders from NHS Trusts were also keen to identify patterns of staff accessing the Hubs so that they could do more in-house to support staff:
I think, for me, in occupational health, we’ve got massive gaps around we don’t know who’s accessing it, so I don’t know whether we should be putting additional support in … because if we’re not getting any feedback, then we can’t be proactive.
Wider stakeholder 09
Individual, team and system appraisals of the Hubs (communal and individual appraisal)
Staff at each of the Hubs described coming together frequently as a team to discuss and feedback on Hub support and processes (communal appraisal). Hub staff across sites valued the ability to reflect on and fine-tune the ways in which the Hubs worked to support staff:
the beauty of the Hub and having a group of clinicians who are all enthusiastic and really invested in wanting to help staff, dilemmas like that, it’s helpful to have all of our heads together.
Hub staff 03
Some keyworkers described sharing positive experiences of the Hubs with colleagues, or deciding to access their local Hub after they had heard positive feedback from others:
I think it’s been a really beneficial service. I know a few other people that have engaged with it, both short-term and a bit more on a long-term basis, so, I think it’s been a really valuable resource, especially to people within the NHS that have been, and still are, going through a pretty rough time in a lot of instances.
Hub client 01
From a systems perspective, however, some wider stakeholders were concerned about capacity issues at the Hubs as waiting lists for formal interventions grew:
I’m significantly concerned about the waiting times, which seem long for the amount of money that’s been invested.
Wider stakeholder 02
I’ve had conversations about … support for staff members with complex needs; … when the Resilience Hub was first set up it had capacity to support staff members in that kind of situation, and not surprisingly that’s changed over time; so I think that does leave unmet need in that area.
Wider stakeholder 07
Nevertheless, from the feedback they had available from Hub clients, wider stakeholders valued the positive impact of the services. Team-based interventions were particularly valued, despite some initial disappointment that not all Hubs were able to provide on-site support due to infection control:
I think the outreach has worked really well. Once they’ve come on-site they’ve been really engaging. The staff have been quite receptive.
Wider stakeholder 09
Hub staff viewed the Hubs as generally very effective (individual appraisal) for those who have accessed them, but acknowledged that promoting the Hubs widely and persuading staff to engage had been two of the biggest challenges:
I think it’s been as effective as it can be as a new service that has hit the ground running. I feel like probably we’re in our prime now, I think we’re probably most effective now, because the word is out there, and people are understanding what we’re for and are accessing us and realising that we are there. I think it took time for that message (a) to get out there and (b) to be received.
Hub staff 01
Keyworkers who had accessed the Hub services typically described very positive experiences:
I got more out of it than I expected, because I expected just to fix the short term. I didn’t expect it to give me some long-term strategies to help prevent it happening again … I feel it’s an invaluable service. I do hope it continues. I think it’s a hugely neglected area of the NHS and of workers in the NHS, because the sort of stresses we’ve all suffered in the last two years, they’ve always been there to a certain extent.
Hub client 02
Sometimes it got me through the week knowing that that phone call was coming. It got me out of bed … At the end of every session I felt enlightened. I might have had a good cry all the way through. I might feel purged of all the anxiety that I’d been clogging up all week. But I did feel inspired at the end of it. I felt like there was something I could do. I had … not just tasks to do, but I had ideas that would help me stay well or stay less ill.
Hub client 08
Once exception to this positive feedback was around the previously described limitations around EDI:
The gaps are there … I asked for a culturally … somebody who’s on my background, you didn’t have that person, it’s not available … Your staff representation is not there of what’s on the outside, the diversity. Your wording of the assessments you use is not open.
Hub client 07
Adapting and developing the Hub model (reconfiguration)
Staff across the Hubs and wider stakeholders agreed that the flexibility of their service models, and adapting these to the changing needs of keyworkers and the system as a whole were strongly valued aspects of the services (reconfiguration):
I think we always try and do things differently. So, the beauty of the hub is that we’re always reassessing and re-evaluating and reviewing what we do.
Hub staff 14
Key adaptations that had been made to the Hub models (reconfiguration) in response to arising needs included offering team-based interventions, and the provision of individual therapy within one of the Hubs to meet increased demand alongside extensive waiting lists in local services:
[we started] looking at the impact of COVID on the teams and how to build across the team, resilience, and well-being. So, that approach changed as well, flexing with the need because initially I think we just thought we were going to do one-to-one work and then it became apparent that whole teams were struggling.
Hub staff 01
Suggested improvements to the Hub model
Hub staff and wider stakeholder-suggested improvements to the Hub model included better promotion and description of what is offered to improve understanding (individual and communal specification) and therefore encouraging better uptake (enrolment); collaboration with more senior stakeholders in terms of integrating the Hubs into strategic level planning (activation); provision of permanent funding for the Hubs (contextual integration); and greater feedback of data into the health and care system (systematisation).
Keyworkers offered suggestions for (1) improvements to the way the existing Hub model works and (2) potential expansions to the existing support provided (reconfiguration). Each addressed potential barriers outlined in the constructs above.
Keyworkers’ suggestions for improvements to the current Hub model were centred around: promotion; accessibility; and EDI.
Keyworkers felt that genuine promotion of the Hubs through organisations’ senior management, and embedded within NHS Trusts’ agendas would improve uptake:
[Promotion of staff well-being] needs to come from the hierarchy in the Trusts. It really needs to be. You know, it needs to come on … your Trust’s agenda for the next five years.
Hub client 06
A more personal, engaging approach to promotion of the Hubs was felt by keyworkers to be a more effective method of appealing to staff than e-mails. Suggestions included short videos, testimonials by staff who had accessed the Hubs, Hub outcomes or other evidence, and methods that allowed staff to put a face to the Resilience Hub services, which were seen to increase trust around the services:
promotion of [Hubs] … where somebody actually speaks, not just this is available and this is what they offer, somebody with passion, enthusiasm, perhaps talking about what it is, a short 30 second video … Because you don’t get anybody face to face obviously now.
Hub client 15
if there’s any sort of little anecdotal case studies or quotes from people that, you know, said that it was fabulous, I came feeling this, and by the end it was that. It was quite easy to access … they were confidential, you know, I felt safe. Any quotes like that on stuff in the future, promotional stuff.
Non-Hub keyworker 03
Keyworkers gave practical suggestions for improving accessibility. Some keyworkers described the length of the online screening questionnaires as off-putting, and potentially a barrier for those less able to access, or less familiar with, digital technology. Participants suggested alternative ways of self-referring to the Hubs, or clearly advertising options to complete the questionnaires with someone over the telephone:
you had too many questions to be honest … I just hated them … when you’re in that state of mind the last thing I want is someone asking me a thousand questions. I didn’t like that process at all because I just wasn’t in the right place for it.
Hub client 07
we still have a huge amount of healthcare support workers, estates and facility staff, domestics, porters … who will not access any form of corporate communications that are electronic. So, I think we miss those groups of staff, not just for the Resilience Hub, but for lots of other things as well, and I think we have to be more meaningful with the way we engage with those groups of staff, which actually takes more effort, because it’s often on the ground stuff.
Wider stakeholder 03
Once keyworkers accessed the Hubs, despite the difficulty of restrictions due to COVID-19, many described a preference for online face-to-face or in person appointments. Keyworkers described Teams or other online platforms also being preferable to telephone calls:
they took their time to speak to me and listen to me and things, but … because I couldn’t see their face, or, you know, what they looked like, it just didn’t work in my head.
Hub client 10
As described above (activation), while the flexibility of appointments within Hubs helped some people, many keyworkers were only able to access the Hubs while they were at work, or not at all due to their shift patterns:
because I was still sat in work, I was then sort of in that working environment. I wasn’t able to fully walk away from it.
Hub client 18
Out-of-hours appointments were suggested to accommodate keyworkers who felt they could not discuss taking time out of work with their managers, or for those working night shifts:
all of these things are only offered during working hours. And that’s not good to people that work full-time. It’s not good for NHS staff that work shifts. It needs to be completely flexible. So, there needs to be maybe a, you know, eight-till-five service and a five-till-ten service.
Hub client 06
Following Hub support, a few participants valued the idea of a follow-up call from Hubs to check how they were getting on, whether they needed any further support, and to check in to see whether they had utilised any of the support to which the Hub signposted them. Some participants also flagged that they would have been keen to know what else the Hubs provided so that they could request to access it, such as further high-intensity support following intensity work:
So, it’s almost like when you start treatment and you stop to do a six-month follow-up call or, you know, a three-month follow-up call to say, did you feel as though that went okay, then is there anything you’d like in the future.
Hub client 06
One participant who struggled with Long COVID valued the idea of an action plan, provided at some Hubs, to refer back to in:
I would have liked to have got a discharge letter with some things that we talked about, that this works for me kind of thing, so I could refer back to … my cognition is not as good as it was, so that’s something that I would have liked, an end letter … I’m under the post-COVID clinic and that’s something that we’ve sort of put together, like a care plan and a relapse plan, if you will, things that trigger and what can I do.
Hub client 19
Finally, participants from minority ethnic groups suggested improvements to help Hubs better support people from minority ethnic groups. These suggestions predominantly centred around more diverse recruitment of Hub clinicians, and training around cultural understanding and racism, as well as wider measures within psychological professions more generally to facilitate greater representation within mental health teams:
Employ more BAME therapists please … I think there should be some positive action with training. We all know the psychological studies are really middle class, white, mostly women as well who get through. But they could do a positive action, in a class of 30 maybe five could be ring fenced just to get that in there … that could be a starting point, but I know that’s a long time coming.
Hub client 04
One participant suggested co-produced services:
recruit different diversity, males, females, age, everything, disability as well. I think it’s so important that you’ve got people there that do actually have some physical or mental disability … they’ve got a greater, deeper understanding and empathy, so when they respond and what they’re saying to that other person … or have more service user involvement … I know it’s hard to recruit anyway, but … you need to have that co-production within your model.
Hub client 07
A further suggestion was around the interpretation of mental health screening measures for people from minority ethnic communities:
I guess this is new for people looking at ethnic minorities and the outcome measures. I don’t know if there’s something around looking at the outcome measures, and not expecting people to be in dire distress to access it. Because that might not happen … Perhaps it could be positive action that if anyone BAME comes through that you see them.
Hub client 04
Keyworkers’ suggestions for other types of support that the Hubs could provide typically focused on team-focused and systemic working. Some keyworkers encouraged more Hubs to have a physical presence in workplaces and amongst teams, albeit they also recognised the challenges of implementing this type of support:
there’s perhaps an argument for being present at work … for example there was a night shift where there was a man who was I think he was only, like, 45, and he had a cardiac arrest, it was horrid, and I know I just came out of it and … I hit a wall … And it would have been nice if there’s someone to go right there and talk to … I don’t know how you would do that, but to be able to have that support available perhaps within a few hours or something.
Hub client 17
Other keyworkers spoke of the potential benefits of regular reflective practice and peer support, where this was not already provided by Hubs:
psychological supervision … that was about your mental well-being, stuff that you’d experienced in your cases … If that was a regular … monthly or bimonthly thing that was offered to people that they could book in, I’d probably use that.
Hub client 08
instead of … just one-to-one therapy, maybe having a forum of people who are happy to meet on Teams with other members of staff who are going through a similar thing or just feeling stressed or just feeling overwhelmed … Even if it’s once a month it helps for people to offload and say, well, I coped with that in this way.
Hub client 12
One care home manager suggested that training for managers would be beneficial:
I think training for managers. I think one of the key things for a spin off from the Hub could be consultancy services going out to organisations, you know, there’s a lot of private care providers of social care these days … it’s around consultancy and training them in well-being and support.
Non-Hub keyworker 03
Finally, suggestions were made around addressing workplace culture generally to enable staff to feel safe to seek mental health or well-being support:
I think it’s a culture change that needs tackling within nursing, which is I don’t know whether part of your remit, but that there is a lot of stiff upper lip and ‘we’re all fine’, and yeah, it’s still not okay to cry.
Hub client 17
Hub staff suggested wider expansions to the role of the Hubs. Going forward, Hub staff and wider stakeholders across the regions agreed that the Hubs should continue to evolve according to local and national needs:
it’s been suggested that a lot of our healthcare professionals don’t necessarily ask for help at the right time and they go into crisis before asking for help. So, I don’t see it as being anything that we can stand down any time soon. I think it needs to continue because … the outcomes of the pandemic for people’s individual welfare and emotional well-being are going to go on for a long time.
Wider stakeholder 01
Some supported broadening the model to support to staff that are experiencing challenges not resulting from COVID, and responding to other traumatic incidents, as well as playing a preventative role through training and consultation:
I think it’ll be broader than just the impact of COVID. I think that the Resilience Hubs could potentially be really well placed to be a public and integrated care system resource, so for example, if there is a major incident, that they can be mobilised and do an effective outreach to people affected by that … I think there’s a lot of opportunities for Resilience Hubs to be more proactive in informing, educating, training, supervising, providing consultation, both within organisations and the public … And just to be a specialist resource, to support the wider trauma-informed agenda, which is being rolled out across the wider Public Health domain. I think, the Resilience Hub has an option to kind of swing and become specialised in supporting a certain need, as and when required.
Hub staff 02
Discussion
Hub staff clearly differentiated Resilience Hub support from other mental health or staff support services. Keyworkers were more likely to access Hub support when: they could see how it was different to other support offers (differentiation); they understood how to access it and what it offered (individual specification); and they felt supported by their managers and their organisation (initiation) to access it (enrolment). Hub staff described difficulties in helping the care system to understand what was on offer and how it was different from other services. Consistent with these concerns, some keyworkers felt overwhelmed by different support offers (differentiation), were unclear about their eligibility, or what the Hubs offered. Confusion may have arisen from other support offers being limited to front-line staff (individual specification). These challenges lead to some keyworkers not seeing the Hubs as relevant (internalisation) nor signing up (enrolment).
Keyworkers who valued mental health support (internalisation) often felt that well-being was an organisational priority (internalisation/initiation). Managers and organisations genuinely valuing and promoting mental health support were seen as key to persuading staff to come forward to access support (initiation). Hub staff expressed concern that well-being support was not always valued, and relational work was required to build trust and confidence in the Hubs (relational integration), and persuade keyworkers of the value, and managers of the legitimacy, of Hub support (internalisation; legitimation).
Key barriers identified in this study that may have prevented or deterred staffs from accessing support during the pandemic, including beliefs about professional role, stigma, and workplace and systemic issues (internalisation), are consistent with pre-pandemic and COVID-related literature. The post-disaster literature demonstrates that professionals may take a long time to seek help, if at all,107 and that being professionally affected by incidents compared with personal involvement has a negative impact upon whether healthcare staff subsequently seek support. 97 Pre-pandemic literature demonstrates that stigma and healthcare staff’s beliefs around their job roles as a barrier to help-seeking is not a new issue. Concerns identified in the current study, including stigma and fears around letting down colleagues and patients, have been demonstrated amongst a survey sample of medics. 108 A more recent qualitative study conducted prior to the pandemic echoes similar themes identifying a culture of ‘invincibility’ amongst medics, and beliefs that managing distress and traumatic incidents were considered ‘part of the job’. 109 A qualitative study conducted during the pandemic highlights sources of work-related stress that are consistent with the barriers identified in this study, including toxic work cultures, such as bullying, sexism and racism, alongside stigma and a perception of needing to appear invulnerable. 110 Furthermore, it has been suggested that the traditional focus of individual interventions, reduction of distress and mental health symptoms, may be at odds with important organisational challenges that contribute to staff distress. 111 This and other literature are consistent with study findings that some keyworkers did not access Hub support as they felt that their organisations were demanding that individuals ‘cope better’, rather than addressing important workplace stressors, such as workload, staff shortages (internalisation/initiation/legitimation),112 and disconnection between front-line staff and senior management. 113 Within this organisational context, individual support and well-being-focused interventions in the absence of systemic changes112,114 have been seen to be resisted and even resented by staff. 109
Barriers to service access for people from ethnic minority communities, lack of culturally appropriate services or insufficient staff training in cultural competencies, were recognised by study participants as a system-wide rather than a Hub-specific issue. Indeed, these concerns are well-documented within the literature across multiple types of mental health services. 115–118 Limitations on Hub staff recruitment described in this chapter may also have had a negative impact on the ability of Hubs to recruit clinical staff from diverse backgrounds. Structural inequalities within the health and care system were identified by some participants as a further contributing barrier for people from minority ethnic communities. This finding is consistent with literature exploring the experiences of minority ethnic NHS staff during the pandemic,119 who described experiences of racial inequality, cultural insensitivity, and the exacerbation of systemic racism due to COVID. Likewise, while the Commission on Race and Ethnic Disparities denied that structural race inequality was a major factor impacting upon the lives of people from minority ethnic communities, the British Medical Association120 has refuted these findings, suggesting that the report was a missed opportunity to tackle race inequalities in the UK and within the NHS. In relation to barriers for other under-represented groups, further research has demonstrated that men and people identifying as from a minority ethnic community are disproportionately affected by stigma. 121 Furthermore, accessibility of appointments for psychological support may be exacerbated for care home staff, 24% of whom are on zero hours contracts, thus less likely to be able to take sick leave or attend appointments during work hours. 122 Barriers may be further compounded by intersectionality across groups; for example, 21% of the care home workforce are from ethnic minority groups. 52
Chapter 7 Mixed-method case studies (Objective 4)
Overview
Integration between study components conforms most closely to a sequential explanatory model, in which we connect earlier quantitative and service mapping findings with qualitative data and health economic analyses. 123 Screening data and follow-up service use data informed the health economic evaluation, and both quantitative and health economic data informed purposive sampling for qualitative interviews with Hub clients and non-Hub keyworkers. Qualitative data were then used to explain key quantitative and health economic findings. This chapter integrates findings from each component to further explore barriers and enablers to support access and implementation of the Hub model across sites, with an additional focus on groups under-represented amongst keyworkers accessing Hub support. This will inform recommendations made in the following chapter for resolving barriers and maximising enablers for implementation of Resilience Hub services and for the wider health and social care system for supporting the mental health and well-being of keyworkers.
Methods
Multisite cross-case comparison displays were produced to integrate key findings from different study components across sites at which all components of the study were conducted (Sites A, B, D). These were used to inform the recommendations and conclusions discussed in the following chapter. Four embedded units of analysis were used:
-
service mapping data detailing the Hub model at each site (see Chapter 3)
-
routinely collected mental health, demographic and occupational data from each Hub (see Chapter 4)
-
service use data (see Chapter 5)
-
analyses of Hub staff, wider stakeholder and keyworker interviews using NPT (see Chapter 6).
Service mapping data included: outreach activities; eligibility; interventions offered; and staffing at each Hub. Routinely collected quantitative data for keyworkers who registered with a Hub included: occupational group; demographics (ethnicity; gender); proportion of keyworkers meeting caseness on screening measures. Service use data included proportion of Hub-registered keyworkers: accessing services directly delivered by the Hubs; accessing services outside of the Hub, facilitated by the Hubs; accessing services provided by their workplace; reporting that the Hub with which they registered met their needs. Health status data were also included at a Hub level. Figures for service use data for under-represented groups were too low to reliably report; descriptors of these figures can be found in Appendix 4, Part 1, Tables 60 and 61. Likewise, health status data were not included for under-represented groups; these data were examined but the figures were too low to reliably report.
Cross-case analysis was used to identify similarities and differences among the cases. Case descriptions were developed using pattern-matching against the propositions of NPT and explanation-building. 124,125 Hub-level, cross-case analyses were used to merge and integrate data from the four embedded units of analysis. Cross-case analyses were conducted at the level of keyworker subgroups. Two cross-case analysis tables are presented, whereby qualitative data were used to explain and expand upon quantitative findings concerning low uptake by (1) under-represented demographic groups (keyworkers identifying as men, and keyworkers identifying as from minority ethnic communities) and (2) occupational groups (care home and emergency services staff). Finally, a generalising themes joint display table is presented to triangulate data sets to demonstrate how they support conclusions. 123 Assessment of fit of integration was rated as: ‘confirmation’ (data sets confirm the others’ findings); ‘expansion’ (data sets expand upon the others’ findings by describing complementary aspects or insights); or ‘discordance’ (inconsistent or contradictory findings). 126
To protect participants’ confidentiality and prevent participants from becoming identifiable, site identifiers were removed from under-represented groups tables and quotes were not included where they would have made participants identifiable.
Patient and public involvement and engagement
Towards the end of the project, emerging and key findings were presented to the Staff Consultation Group. The group felt that the findings for under-represented groups were particularly important, and that meaningful engagement would be required to improve access for these groups.
Results
Hub-level cross-case analyses
Although Site C was not included in the cross-case analyses as there was no qualitative data collection at this site, quantitative and health economic findings were consistent with other sites (see Chapters 4 and 5).
Impact of Hub models
The cross-case analysis display in Table 23 demonstrates that despite differences to the service model across Hubs, the demographic and occupational groups accessing services were broadly consistent. The proportion of Hub clients allocated to the ‘other’ category at Site D was likely due to lack of sufficient information to categorise into more specific groups, therefore does not represent a true difference (see Chapter 8, Limitations). Differences in the types of interventions offered appear to have impacted on the proportion of keyworkers accessing support directly from the Hubs, as would be expected. Site A, for example, delivered a higher percentage of services directly, while Site D’s model was more based on facilitating client access to existing services, and therefore had a smaller percentage of keyworkers accessing services delivered directly by the Hub (24.6% at Site D compared with 81% at Site A) (see Chapter 3, Onward referrals).
| Site A | Site B | Site D | |
|---|---|---|---|
| Service mapping – staffing | |||
| Proportion of senior Hub staff (Band 6+) | 78.51% | 67.04% | 74.17% |
| Proportion of therapy/formal psychological interventions provided directly by Hub | Majority provided directly by Hub | Approx. 60% provided directly by Hub – remainder referred on to local services where clinically indicated | Where therapies are clinically indicated, most clients are facilitated into appropriate services and supported to access non-Hub interventions |
| Screening data | |||
| NHS | n = 475 | n = 367 | n = 731 |
| 60.2% | 87% | 44% | |
| ICU/critical care | (30%) | (12%) | (18%) |
| Other NHS | (70%) | (88%) | (82%) |
| Primary care | 6.5% | 4.1% | 9.3% |
| Social care | 3.8% | 3.6% | 8.3% |
| Emergency services | 4.2% | 0.8% | 4.2% |
| Education | 2.9% | 0% | 1.3% |
| VCSE | 0.4% | 0% | 5.1% |
| Local authority | 3.5% | 0% | 2.1% |
| Other | 17.5% | 4.4% | 25.7% |
| Mental health screening data | |||
| Depression caseness (PHQ-9) | 81% | 72% | 69% |
| Anxiety caseness (GAD-7) | 69% | 69% | 51% |
| PTSD caseness (PCL-5 or ITQ) | 62% | 55% | 28% |
| Impairment in functioning caseness (WSAS) | 86% | 83% | 76% |
| Problematic alcohol use caseness (AUDIT) | 26% | – | 23% |
| Service use | |||
| Keyworkers accessing services delivered by Hub | 81% | 65% | 24.6% |
| Non-Hub support that was accessed by direct support of the Hub | 7.9% | 20% | 18.7% |
| Keyworkers accessing services provided by employer | 7.9% | 5% | 20% |
| Keyworkers who agreed that the Hub met their needs | Yes fully – 55.8% | Yes fully – 55.2% | Yes fully – 44.9% |
| Yes partially – 15.6% | Yes partially – 17.2% | Yes partially – 17% | |
| No – 6.5% | No – 0% | No – 4.8% | |
| Missing 22% | Missing 27% | Missing 33% | |
| Health and social care costs | Complete costing data (n = 44) | Complete costing data (n = 20) | Complete costing data (n = 101) |
| As would be expected, costs differ across Hubs (reflective of service design and delivery), but that variation is complicated by several factors, for example potential interactions with other variables such as screening symptom severity, geographical heterogeneity in service availability, timing of recruitment to the questionnaire (which will impact other variables affected by the pandemic, such as access to non-Hub mental health services) and differing length of follow-up. | Mean total mental healthcare cost (95% CI) £763 (£554 to £971) | Mean total mental healthcare cost (95% CI) £512 (£228 to £797) | Mean total mental healthcare cost (95% CI) £164 (£104 to £223) |
| Mean wider health and social care cost (95% CI) £203 (£70 to £335) | Mean wider health and social care cost (95% CI) £30 (< £1 to £72) | Mean wider health and social care cost (95% CI) £147 (£46 to £247) | |
| Health status | |||
| EQ-5D | N = 73 | N = 26 | N = 131 |
| Values for all sites below general population values and HSE health and social care professional sample. | Keyworkers reporting no problems: Mobility – 66% Self-care – 81% Usual activities – 45% |
Keyworkers reporting no problems: Mobility – 92% Self-care – 96% Usual activities – 65% |
Keyworkers reporting no problems: Mobility – 79% Self-care – 89% Usual activities – 59% |
| Some variation across Hubs’ EQ-5D values (likely to be reflective of varying demographics/socioeconomic characteristics, mental health need and other factors); however these were not significant. | Pain and discomfort – 43% | Pain and discomfort – 65% | Pain and discomfort – 51% |
| Anxiety and depression – 18% | Anxiety and depression – 27% | Anxiety and depression – 33% | |
| Mean EQ-5D = 0.684 | Mean EQ-5D = 0.815 | Mean EQ-5D = 0.779 | |
| Mean EQ-VAS = 62.49 | Mean EQ-VAS = 70.88 | Mean EQ-VAS = 68.02 | |
| Qualitative (NPT) | |||
| Higher level of need | only some of the most serious and significant cases [are] referred to the Resilience Hub. Wider stakeholder 02 it’s renowned that healthcare staff wait to the point of crisis before they ask for help. Wider stakeholder 01 | these are people with complex psychological needs [being referred to Hubs]. Wider stakeholder 07 I probably should have accessed things earlier, but I accessed them when I [was] almost at breaking point. Non-Hub keyworker 16 | a lot of staff are still coming to us at points when they are in absolute crisis. Hub staff 13 you keep going, just keep going and it’s not until … everything just went bang, that I thought I need some help. Non-Hub keyworker 06 |
| Clarity of offer: When keyworkers positively differentiated the Hubs from other staff support and understood the support on offer/how to access it, they were more like to value the support and register with Hubs | if I’d have had to have referred through my line manager, I probably wouldn’t have accessed the service. Hub client 12 (differentiation → individual specification → internalisation → enrolment) | I didn’t have to ring anyone up, I could just do it on my computer in my own time. It just made it so much easier to take that first step. Hub client 02 (differentiation → individual specification → enrolment) | It took 12 weeks for [a colleague] to get the help [from Occupational Health], whereas the Resilience Hub, for me, I got it instantly. Hub client 06 (differentiation) [staff] from the Hub came onto my ward meeting the other day and … explained to my team. I think a couple of them have accessed through that. Hub client 10 (individual and communal specification → internalisation → enrolment) |
| Clarity of offer: When keyworkers did not differentiate the Hubs from other services and did not understand what was on offer or how to access it, they were less likely to value the support or register with the Hubs | There were so many things about where you could go for help … I almost felt I couldn’t see the wood for the trees … because I wasn’t feeling well, there was almost too much choice. Non-Hub keyworker 10 (differentiation) | … you don’t really know … what services you need for what … I didn’t think counselling was always necessarily right and what I was needing at the time, and then I didn’t know what else there was [on] offer. Non-Hub keyworker 15 (differentiation) | … the employer didn’t know much about it. The employer would just read out sentences from the booklet or leaflet that the Hub had given him. They didn’t have enough information about it, and it made me think, well, if you don’t know about it, then should I really be accessing it. Non-Hub keyworker 05 (individual and communal specification → internalisation → enrolment) |
| Beliefs about accessing mental health support: When keyworkers valued mental health support and felt that their managers/employers valued and promoted well-being support they were more likely to access Hub support | We do see horrible things and upsetting things, and we should look after our staff, and that’s part of it. Hub client 17 (internalisation) it was my line manager that said to me, well, you’ve got [the Hub] and I decided to register myself. Hub client 16 (internalisation → initiation → enrolment) | [mental health] is a big priority of course, it’s something that I’ve got to understand and deal with and get through. Hub client 03 (internalisation → enrolment) | It’s word of mouth … the manager saying there’s this Resilience Hub … They’re there for you if you want. Take time out of work to do that. It’s anonymous. Hub client 08 (internalisation → initiation → enrolment) |
| Beliefs about accessing mental health support: Some keyworkers had wider concerns around accessing mental health support, including beliefs around their job roles. Further barriers included issues around workplace culture and wider organisational/systemic issues, and not feeling support by their managers, leading to not being as likely to register with the Hubs (enrolment) | you just feel that you shouldn’t have to be as worried as the front-line staff … you shouldn’t be having any mental health issues because … you’re not in such stressful situations. Non-Hub keyworker 09 (internalisation) it’ll be a forwarded e-mail … it won’t be, ‘I’d really like you to try and access it’ … it feels like they’re doing their job, like they’re ticking a box, as opposed to genuinely being behind it. Hub client 17 (internalisation → initiation) | The problem now is there’s just an expectation we’ll just crack on. … Trouble is, getting back to normal is not going back to normal, it’s carrying on. And it’s indefinite. Hub client 02 (internalisation → initiation → enrolment) to access the counselling again I’d have to go through my current manager … [but] I’ve been put off because I don’t have a good relationship with her. Non-Hub keyworker 15 (initiation → enrolment) | showing emotion and showing any kind of mental health issues was … a sign of weakness, we’re clinicians, we’re supposed to be stoic. Non-Hub keyworker 01 (internalisation) nurses are expected to be massively resilient, it’s part of the [Nursing and Midwifery Council] code, it’s what you’re signing up [to] – being resilient, having a cry, moving on. Non-Hub keyworker 04 (internalisation) |
Utilisation of Hubs as a resource for keyworkers with more severe or complex mental health difficulties
Each work package demonstrated that keyworkers accessing the Hubs tended to have severe and/or complex difficulties for which they needed support. Mental health screening data (see Chapter 4) suggested that most keyworkers accessing the Hubs had high mental health support needs, for example, 60% met criteria for clinically significant difficulties on at least three different screening measures, and approximately 80% had scores suggestive of clinically significant impairments in functioning. As noted in Chapter 4 (see Discussion), differences were seen in PTSD caseness between sites that used the ITQ compared with the PCL-5. Keyworkers reported lower health status in comparison with the general population and a pre-pandemic health and social care professionals’ sample (see Chapter 5, EQ VAS scores) suggesting unmet need and/or ongoing impact of the pandemic. Health status data also indicated that the most affected domain related to anxiety and depression, for which only a minority of participants reported experiencing no problems. Complexity of mental health presentations, in particular pre-pandemic mental health concerns and financial difficulties, predicted higher levels of distress across most measures, and across all Hub sites. Qualitative data may in part explain these findings. Wider stakeholders from NHS Trusts, including HR and occupational health leads, tended to view the Hubs as a means of providing specialist support to a small proportion of staff who had more severe or complex difficulties, rather than as an additional, parallel, pathway for lower-level support. It was suggested that NHS occupational health departments typically do not provide this level of specialist support, and that the Hubs meet this need. This may in part explain why keyworkers with these presentations tended to access the Hubs. The severity of presenting difficulties of keyworkers may also be explained by the qualitative data demonstrating that keyworkers typically waited until things were very difficult before seeking support (see Barriers to valuing support: keyworkers’ beliefs about self and job roles). The higher complexity of needs of keyworkers registering with the Hubs provide evidence for the Hub staffing model, whereby the Hubs were staffed by predominantly senior clinicians with the experience to work with this client group. This finding aligns with the cost of mental health services varying according to need, as is also the case in IAPT services (see Chapter 5, Discussion).
Barriers and enablers
Barriers and enablers to successful uptake and implementation of the Hubs were consistent across sites. Themes related to clarity of the Hub offer, and beliefs around accessing support. Valuing and taking up Hub offers were contingent on keyworkers understanding what was on offer and how to access it, as well as differentiating it from other offers (see Understanding the ways the Hubs differ from other types of staff support). Keyworkers who valued mental health support, and felt their managers valued and promoted well-being support, were more likely to access it. Keyworkers were inhibited from seeking support by beliefs about themselves and their role, which was exacerbated by negative workplace culture and perceived lack of management support.
Satisfaction with the Hubs
Across the sites, satisfaction with the Hubs reported on the SUQ demonstrated high median satisfaction scores, and a substantial proportion of clients reporting that the Hubs had met their needs (see Satisfaction with Hub support and onward referrals). Only a small proportion (4.4%) reported that the Hubs had not met their needs. These findings are supported by interview findings demonstrating that generally participants had very positive feedback regarding the support they had received from the Hubs (see Individual, team, and system appraisals of the Hubs).
Subgroup-level cross-case analyses
The following sections present cross-case analyses conducted at the level of keyworker subgroups found to have low uptake amongst those accessing Hub support. Table 24 presents demographic groups (keyworkers identifying as: from an ethnic minority community; men), and Table 25 presents occupational groups (care home and emergency services staff). Emergency services staff are included due to low uptake; however, this is also partly explained by not all Hubs being open to all emergency services staff, this exclusion is in line with NHSE guidance (see Target population and Chapter 4, Discussion). Furthermore, while the following sections atomise these keyworker characteristics, as demonstrated by some of the quotes in the tables below, intersectionality may well compound barriers to access for those who identify across multiple under-represented groups.
| Keyworkers identifying as from an ethnic minorities | Keyworkers identifying as men | |
|---|---|---|
| Service mapping | ||
| Targeted outreach by the Hubs | Webinar with Council of Mosques (Site A) Race equality campaign (Site B) Meetings with equality leads in all Trusts to promote the Hub via the workforce race equality group (Site D) Bespoke social media graphics for different groups (Site B and D) Created links with race equality networks (Site B and D) |
No data (Site A) Linked with external providers and regular tailored communication for men (Site B) Publicly promoted workshops and facilitated peer support sessions for men (Site D) |
| Staff training | No specific training received | No specific training received |
| Population statistics | ||
| National workforce statistics | 22.1% of NHS staff identify as from an ethnic minority community54 21% of adult social care workforce identify as from an ethnic minority community52 |
23% of NHS staff identify as men53 18% of adult social care workforce identify as men52 |
| Screening data | ||
| Hub keyworker demographics | White British: 89–92% Asian or Asian British: 1–2% Black or Black British: 0–1% Mixed: 0–1% Other: 0–1% |
Women: 84–86% Men: 13–15% Gender described in another way: 2–3% |
| Problematic alcohol use findings | Identifying as from an ethnic minority group associated with reduced reported problematic alcohol use | Identifying as male associated with increased reported problematic alcohol use |
| Qualitative (NPT) | ||
| Barriers to Accessing Support | Stigma (internalisation) → Negative past experiences (internalisation) → Culturally appropriate services (legitimation) → Alternative support/ways of coping (enrolment) I feel very let down by the system … in my previous experience of accessing occupational health, … the experience was very negative, if I’m being honest … You’re treated quite poorly in terms of being seen as a burden. Non-Hub keyworker 20 (internalisation) | Stigma (internalisation) → Alternative support/ways of coping (enrolment) something that I face quite a lot, is men are strong, men don’t cry, and that plays on my mind to fit that stereotype. I don’t want to be judged. I don’t want someone to think bad of me, or to think that I’m weak. Non-Hub keyworker 05 (internalisation) It can be perceived as being less manly, admitting weaknesses or failing, feels this is the way it has always been with society. Hub client 15 (internalisation) |
| Why would I go to them for support when I know that they don’t have any of the education required in order to support me effectively … I am not willing to put myself in a situation where I’m already feeling quite vulnerable and exhausted to then do the education work, educating the person that’s supposed to be supporting me. Non-Hub keyworker 20 (legitimation → enrolment → skillset workability → relational integration) | The alcohol thing became a big thing, that was our way of coping. And in particular, the drinking was something they did more than the women. Non-Hub keyworker 03 (enrolment – other coping methods) | |
| That support [from the Church] has been amazing because I found myself confessing a lot of my social problems or my personal issues with the pastor. Non-Hub keyworker 19 (enrolment) | ||
| Stigma (internalisation) → Negative past experiences (internalisation) → Culturally appropriate services (legitimation) → Limited representation among Hub staff (legitimation) → Lack of staff training in cultural competencies (skillset workability) → reduced trust in the Hub service (relational integration) | ||
| There was all that Black Lives Matter stuff going on. … that brought a lot of stuff that had happened to me, that I’d experienced institutional racism. … The main thing that put me off from seeking support, if I’m being honest … it feels better if you’re in a community of people who understand you, and that’s why I wanted a representative therapist. Hub client 04 (internalisation → enrolment → skillset workability) | ||
| I think people need to have training, if they don’t already … cultural competency, cultural bias, but also conscious and unconscious bias. And this Black Lives Matter stuff does matter to a lot of people … you do need to learn to know how it feels for them. Hub client 07 (skillset workability) | ||
| Care home staff | Emergency staff | |
|---|---|---|
| Service mapping | ||
| Targeted outreach by the Hubs | Visited care homes to provide Hub information (Sites B and D). Direct e-mail addresses used for care home staff to promote Hub offer (Site D). Publicly promoted workshops or facilitated peer support sessions for care home staff (Sites B and D). |
Promotion via ambulance Trust communications (Site D). Made links with the ambulance service Suicide Prevention Lead to increase the uptake (Site B). |
| Screening data | ||
| Percentage of keyworkers accessing the Hubs | Social care 4–8% | Emergency services 1–4% |
| Qualitative (NPT) | ||
| Barriers to accessing support | There were barriers to getting Hub information out to care homes and care home staff (communal specification), and there may not be the same expectation of seeking support through work as care homes do not tend to have occupational health departments (internalisation). Staff reported not wanting to be a burden on colleagues if they took time off (internalisation). Due to work pressures/lack of staff cover, there were also practical barriers to accessing support (enrolment). | Emergency services staff had often not heard of the Hub in their area; just advertising the services may not be sufficient (individual and communal specification). Barriers included beliefs about job role, feeling that one should be strong enough to handle the job (internalisation) and wanting support from someone who understood their specific job role (internalisation). Practical barriers due to shift work, consequently keyworkers tended to access in-house support at their own organisation (enrolment). |
| I’m not sure that [care homes are] in the loop as much in terms of understanding what’s available in the system … They feel inaccessible sometimes. Wider stakeholder 02 (communal specification) | for a poster or flyer, I’m just going to put it in the bin … I’d never heard of it [the Resilience Hub] before, didn’t even know that was open to us, so it’s good to know that. Non-Hub keyworker 18 (individual and communal specification) | |
| Shift patterns … can be difficult … we don’t use agencies or anything in our place … If you are sick at all, you don’t get paid. Non-Hub keyworker 14 internalisation → enrolment) | You can’t join the police or the ambulance or the fire or whatever and then think, well, I’m never going to see somebody who’s been killed … you need to be mentally strong enough that, for you to deal with things like that. But if the first time you see it … it affects you for the rest of your career then you’re probably in the wrong job. Non-Hub keyworker 11 (internalisation) | |
| Whereas I think more work-related [support within the police force], they get it, they’ve had that experience, they’ve spoken to number of other people who’ve probably experienced the same thing, whereas … the GP is quite broad, … they don’t understand the stresses of our job completely. Non-Hub keyworker 18 (internalisation → enrolment) | ||
Under-represented demographic groups
Ethnic minority groups
Table 24 shows that keyworkers from minority ethnic communities were under-represented amongst those accessing the Hubs, in comparison with the proportion of staff from these demographic groups living and working within the region. Interviewees from these communities often suggested that stigma around mental health from their own cultural and community beliefs may negatively impact upon the value placed on accessing well-being support, as did negative past experiences of mental health, health and/or social care services and a perception of system-wide structural inequality (internalisation). Although each of the Hubs conducted some outreach with these groups, the qualitative findings demonstrate that keyworkers felt that more needed to be done to make the Hubs more accessible to staff from ethnic minority communities, and culturally appropriate once engaged (legitimation).
Limitations of the Hubs included limited representation of people from minority ethnic groups within Hub teams, and inability to provide specific support around racial discrimination (skillset workability). For some keyworkers who did access the Hubs and wanted support around racial discrimination, the presence of a predominantly white workforce reduced trust in the service (relational integration). Representation within Hub teams may in part have been affected by difficulties in recruiting staff due to the temporary nature of Hub funding (see Hub resources and linking Hubs with other resources in the mental health system), thereby impacting the pool of staff applying for these roles. This finding was not consistent; other keyworkers who identified as from a minority ethnic community who accessed the Hubs for general mental health support did not feel that their care had been impacted by the absence of diversity amongst staff working at the Resilience Hubs. The finding that being from a minority ethnic group was associated with higher levels of depression (see Appendix 1, Part 2, Table 30) and lower health status (see Relationship between EQ-5D values and participants characteristics) may highlight an additional need to address mental health and well-being for keyworkers from these communities. These findings may also explain why those who did not access Hub support at times accessed alternative sources of support, including, for example, utilising community support such as their local church or mosque (enrolment).
These Hub-specific and system-wide barriers may explain the low proportion of staff from minority ethnic groups accessing the Hubs. This finding is also mirrored within Chapter 2, whereby alternative methods were needed to engage PPIE stakeholders from minority ethnic groups in the research.
Men
Keyworkers who identified as men were less likely to self-refer for individual Hub support compared to those who identified as women. Although the Hubs attempted to target outreach towards men, there was still limited uptake from this group across all sites. Men who had accessed the Hubs reported finding the practical process of registering straightforward, but there appeared to be other more complex barriers that prevent them from accessing support. This may be explained by qualitative findings, whereby stigma (internalisation) was repeatedly described as a barrier. Alternative support (enrolment) or ways of coping were used instead, including alcohol use. This finding was supported by screening data showing that greater problematic alcohol use was reported by men.
Under-represented occupational groups
Care home staff
Keyworkers from social care occupations were under-represented, making up 4–8% of those accessing the services. All Hubs conducted diverse, often intensive outreach to care home staff, none of which appears to have impacted uptake significantly.
Low uptake may be explained by interview data in Chapter 6, demonstrating that there were barriers to getting Hub information out to care home staff. Wider stakeholders and keyworkers flagged the differences in staff support available, for example, often care homes lacking an occupational health department and therefore having different expectations or cultures of work-based help-seeking (internalisation). Care home staff also described not wanting to be a burden on colleagues if they took time off (internalisation). Due to pressures of work and limited staff cover, there were also practical barriers to accessing support (enrolment). Practical barriers were seen as more problematic than within NHS services due to the care home context, and included very limited time to engage with support whereby staff and managers were busier than ever. Shift work and lack of cover by bank or agency staff made attending appointments difficult (enrolment). Therefore, staff appear to access more informal peer support (enrolment). It should also be noted that only two interviews with care home staff were conducted, therefore there is limited data for this group (for a detailed breakdown of participant interviews, see Chapter 6).
Emergency services staff
There was also low Hub uptake from emergency services staff, although it should be noted that Site D was only open to ambulance staff and a small number of emergency services personnel with specific roles/duties, in line with NHSE guidance, whereas the other sites had a wider scope (see Target population). These figures may be explained by interview data which demonstrated that emergency services staff often had not heard of the Hubs, and that simply advertising Hub services may not be enough to promote the offer amongst these groups (individual and communal specification). The phased approach to opening up the Hubs within some sites may also have impacted on the number of emergency services staff who had accessed the Hubs at the time of data collection (see Target population). Barriers to accessing support included beliefs about the job role, feeling that staff should be strong enough to handle the job (internalisation). Interviewees also described wanting support from someone who understood their specific job role (internalisation). Practical barriers due to shift work were also prevalent (enrolment). Consequently, interviewees described accessing in-house support at their own organisation (enrolment).
Integration of findings
A generalising themes joint display table (see Table 26) is presented to triangulate study data sets, demonstrating how the different study components were finally integrated to support our conclusions.
| Theme | Service mapping | Screening data | Health economics | Interviews | Assessment of fit |
|---|---|---|---|---|---|
| Staffing and use of Hubs | Hubs were predominantly staffed by senior and experienced clinicians. | Severe comorbid mental health needs across multiple domains. | Health status lower than population norms. Staffing was the central component of Hub cost. |
Keyworkers wait until they are finding things very difficult, or they are at ‘breaking point’ before seeking help. Wider stakeholders (e.g. HR and OH leads) describe that they have already low-intensity interventions, and that the Hub is useful for when needs are more intensive, justifying the costs. | Expansion |
| Uptake in general | Outreach and promotion conducted to increase uptake. | [Not addressed] | Service use accessed as a result of Hub support was a key component of total health and social care use. Compared to previous estimates of cost in mental health populations, it appears that health and social care costs for keyworkers are low. | Barriers to uptake may explain low health and social care costs, including confusion between Hubs and other support services; maladaptive beliefs about job roles, unsupportive managers, negative workplace cultures, and perception that systemic issues were the cause of difficulties. Some wider stakeholders had concerns around growing waiting times for Hub-provided therapy, and insufficient data on Hub usage and outcomes. Feedback was otherwise very positive. | Expansion |
| Under-representation | Some targeted outreach; no specific training. | Men, keyworkers from minority ethnic communities, care homes and emergency services staff under-represented. | [Not addressed due to small sample sizes] | Some keyworkers highlighted a perceived need for further diversity and cultural competency training to improve reach to under-represented communities. Other barriers for these groups included prior negative experiences of services, structural inequalities and stigma. | Expansion |
Chapter 8 Discussion
Summary of findings
The study had four key objectives:
-
to conduct quantitative analysis of routine demographic, occupational, and mental health screening data collected by the Hubs
-
to conduct health economic analysis to explore cost and health benefits associated with the set-up, use and management of Resilience Hubs
-
to conduct a qualitative interview study with multiple relevant stakeholder groups at three sites
-
to integrate and triangulate findings via mixed-method case studies integrating study findings.
Key findings of quantitative analyses (Objective 1)
Screening data were analysed for 1973 participants who completed the screening offer of the Hubs, of which the majority were NHS staff. Under-represented groups included clients identifying as men, members of minority ethnic communities, and care home and emergency services staff. Clients reported high mental health needs across multiple domains (anxiety, depression, post-traumatic stress, alcohol use, functioning). Difficulties were often comorbid and in a substantial proportion of keyworkers may have preceded the pandemic (but may have been aggravated by it). The most consistent predictors of higher need were financial loss during the pandemic and a history of pre-pandemic emotional well-being or mental health concerns, but other characteristics predicted ‘caseness’ across different mental health domains. Service use data collected from a subsample of participants indicated that many Hub clients accessed mental health support because of Hub support and advice, and reported high levels of satisfaction with the Hubs. There was no indication that individuals with more severe overall presentations were more likely to access mental health support following registration with Hubs, which may be consistent with the ‘universal support approach’ employed by the Hubs.
Key findings of health economic analyses (Objective 2)
The health status of Hub clients was lower than population norms and pre-pandemic data for health and social care staff. Commensurate with difficulties experienced by Hub clients, Hubs were predominantly staffed by senior clinicians with the experience to work with complex client groups and build strategic relationships with systems and teams, and staffing was the central component of Hub cost. Costs associated with health and social care use for Hub clients were low, which may be due to barriers to accessing support. This may indicate that the Hubs represent a valuable source of support for a population characterised by high need and low access to services. While the development of a full economic model was unviable, a logic model produced to guide this work suggested potential broad-reaching impacts of the Hub model, beyond mere amelioration of keyworker’s mental health and well-being, which should be evaluated more holistically in future.
Key findings of qualitative analyses (Objective 3)
Qualitative analyses identified a range of enablers to accessing Hubs, including having a clear understanding of the Hubs, how to self-refer, and personal promotion by managers. Barriers included confusion between Hubs and other support, and beliefs about job roles. Organisational barriers included managers not supporting help-seeking, negative workplace cultures and keyworkers feeling that systemic issues were the cause of their stress. Keyworkers from minority ethnic communities who wanted support around racism felt that representation within Hub teams and cultural competency training lacked visibility Other barriers for under-represented groups included prior negative experiences of services, structural inequalities and stigma. Some wider stakeholders had concerns around growing waiting times for Hub-provided therapy, and insufficient data on Hub usage and outcomes. Feedback was otherwise very positive. The responsiveness of the Hubs to local needs was strongly valued by all groups interviewed. Participants felt that the Hubs should continue to evolve according to local and national needs, including the continuation of staff support, and response to traumatic incidents.
Integration of study findings (Objective 4)
Findings were generally consistent across Hubs. The high proportion of Hub clients with considerable mental health needs was congruent with qualitative findings indicating that wider stakeholders viewed the Hubs as a resource for those with more severe or complex needs and many keyworkers typically waited until things were very difficult before seeking support. The demographic and occupational groups accessing services were broadly consistent, with low uptake from certain ethnic minorities being possibly explained by the desire for greater diversity and cultural competency amongst Hub staff. Low uptake of care home staff may have been due to less formalised routes of occupational support, leading to a different culture of help-seeking and practical barriers affecting social care and emergency services staff that may not have been experienced within the NHS (e.g. lack of cover by bank/agency staff to enable attendance of Hub support offers). Certain beliefs around one’s job role (e.g. feeling that they should be able to handle stressful or traumatic experiences as a routine part of their job) and related support preferences (e.g. wanting support from someone who understood their job) also represented significant barriers for some keyworkers.
Strengths and limitations
Strengths
The project involved ‘research supportive’ services who routinely included research consent questions in their screening offers. Our analyses considered routinely collected data from a relatively large proportion of keyworkers who completed the Hub screening offers (83.6% across the Hubs consented to have their anonymised data used for research purposes). Although the impact of self-selection cannot be ruled out fully, our findings may accurately reflect the overall level of mental health needs of individuals who accessed these services during the pandemic. Despite the observed under-representation of certain groups in our quantitative analyses, other key strengths of the study were our efforts to recruit individuals from minority ethnic communities and other under-represented groups. Other relative strengths include our efforts to interview keyworkers who did not engage with Hubs, which provided an understanding of the potential barriers to access and the reasons for not using Hub support. This sequential, explanatory mixed-methods approach was also designed to culminate in triangulation of the individual strands of work, bringing together mixed-methods findings across Hubs and across particular groups of interest. Our qualitative analyses and case studies also represent a rare example where an analytic framework relevant to the implementation of new services/interventions (NPT) has been applied in a highly time-critical and rapidly changing context characterised by accelerated implementation. The study therefore adds to the literature using theory-based approaches in rapidly changing situations, which is particularly valuable in the context of the NHS where change is constant. 127
Limitations
The evolving nature of the offers provided by the Hubs precluded our ability to comprehensively evaluate all Hub support offers to keyworkers and teams/organisations. For example, our research objectives did not consider in detail the evaluation of team-based support, as this grew substantially after the commissioning of this research. This component could not be evaluated to the same extent as individual offers as Hubs did not have the infrastructure to gather data from keyworkers who had received team-based support (e.g. consent for research contact).
Implications of our quantitative findings are limited by the lack of exact comparison data and potential self-selection bias, especially in relation to the SUQ survey. Self-selection might have affected a range of findings, most notably the reported satisfaction with the support provided by the Hubs, which may not be representative of all Hub clients. Furthermore, SUQ completion involved retrospective reporting, and is therefore subject to several sources of bias and error (e.g. participants might not remember accurately the extent to which they had contact with Hub staff, or discriminate between contact with Hubs and other support providers they might have accessed concomitantly). The self-completion, unassisted format of the SUQ meant that participants did not provide specific details that would more accurately allow an assessment of service use and costs for our health economic analyses. A range of practical factors could also bias the perceived level of contact with Hub staff following screening (as well as uptake of the SUQ survey deployed as part of this research), for example, reluctance to respond to phone calls from undisclosed numbers or e-mails being blocked by firewalls/spam filters. Additional clinical contact data extracted from Hub clinical records systems may have helped to corroborate and add to SUQ data, and allow further exploration of reported number of clinical contacts. This was not possible to collect in the current study due to lack of explicit participant consent but would be of interest to include in future research.
As many analyses relied on data routinely collected by the Hubs, our ability to define and examine certain demographic and occupational characteristics was constrained by the varied level of detail of the original screening measures. This might have led to error or imprecision in the definition of some of derived variables. More specifically, the definition of the occupational categories created for our descriptive analyses relied on the recoding of a very heterogeneous set of items across the Hubs, which might have let to imprecise categorisation of some participants, for example, Hub clients allocated to the ‘primary care’ group may be NHS workers, and many participants at Site D were allocated to the ‘other’ category (25% of clients at this Hub) due to lack of sufficient and/or unambiguous information to enable a more precise classification. Mindful of these limitations, this variable was only analysed descriptively. Finally, the lack of diversity in the sample (e.g. low numbers of participants who identified as belonging to ethnic minority communities in general, and very low numbers in specific ethnic minority categories) might have led to imprecision in analyses which explored the impact of certain individual characteristics in our quantitative and health economic analyses, and inability to conduct robust analyses focusing on specific under-represented groups.
There were challenges, and therefore potential error, in separating Hub set-up and support costs across categories (e.g. the split between time spent on individual and team support and figures for keyworkers reached, differed monthly). Our analyses provide only a static estimate, whereas costs and output are likely to fluctuate over time, and it was not possible to evaluate whether the implementation of Hub support may offset other health costs (e.g. by referring keyworkers in the first instance to most appropriate support and potentially avoiding unhelpful services). Our EQ-5D analyses would have benefited from baseline data prior to Hub support or pre-pandemic, and the pre-pandemic sample used for comparison analyses was more occupationally homogeneous relatively to our Hub sample (which included additional keyworker groups, e.g. education). The health and social care cost analyses relied on unit costs selected using nationally published sources; however, there is uncertainty around these estimates, especially related to the delivery of psychological therapies. Furthermore, there are other economic costs associated with mental health conditions that were not captured by this study, for example, productivity losses related to absenteeism and presenteeism. 128 This is the first known UK study of health and social care use/costs, specifically in a keyworker population. Further research comparing to non-keyworker populations would illustrate whether more should be done to ensure keyworkers are accessing required services.
The qualitative interviews conducted were cross-sectional, therefore unable to capture change across individual participants’ experiences of the Hubs or other support accessed. The different timepoints of interviews conducted for different participant groups demonstrate the rapidly changing nature of the Hubs, and longitudinal interviews may have better captured these changes. For example, Hub clients interviewed typically reported being seen quickly by the Hubs, whereas wider stakeholders interviewed later reported some concerns around waiting times for Hub-provided interventions. Likewise, the service mapping describes Hub models during a particular snapshot of time, and so could not account for further evolution of the Hubs after data collection, for example, changing approaches adopted by the Hubs to try to reduce waiting times.
Finally, while the impact of short-term Hub funding on staff retention was acknowledged in Chapter 6, the ability of Hubs to recruit staff via secondment or on a temporary basis was not explored in detail. The service mapping exercise did not collect information on staff vacancy rate or retention as this was not highlighted in our study protocol, however this information would be useful to collect in future as part of identifying challenges to service implementation.
Patient and public involvement and engagement
Patient and public involvement and engagement was incorporated at all stages of the study. A core Staff Consultation Group of Hub clients was established at the project onset. More informal consultations were also conducted with other stakeholders, predominantly with NHS staff from minority ethnic communities. Further detail on PPIE consultants and methods can be found in Chapter 2. As reported in the PPIE sections of Chapters 4–7, the Staff Consultation Group played an important role in refining data collection processes, study materials and data collection tools. The input of the Staff Consultation Group for these activities was invaluable in terms of ensuring that survey and interview questions were meaningful and understandable for participants. Likewise, the group provided crucial input in research staff training and the interpretation of data and review of emerging findings. This was vital for sense-checking study findings with a group of health and care staff directly affected by the pandemic, and who had had experience of the Hubs’ support. The group’s input also helped to shape the recommendations made to both Hubs and the wider health and care system for enabling better access to staff support.
The Staff Consultation Group has been consulted on key figures and groups with whom to share study findings, and the most effective methods of study dissemination. The group will support dissemination through involvement in preparation of lay summaries of findings, accessible dissemination materials, and dissemination amongst their networks.
Equality, diversity and inclusion
In general, there was a broad range of experience and expertise across the research team. Early career researchers and more junior members of the team were given opportunities to develop, such as involvement in project management (KA), and facilitated to attend training relevant to their roles, including qualitative research methods and analysis, management of risk, and training around race and racial trauma.
As described in Impact of Hub models quantitative methods were limited by lower numbers of people identifying as men and as from minority ethnic groups. However, purposive sampling was used for qualitative interviews, with efforts made to recruit interview participants from these groups, including engagement with local BAME Networks and EDI networks to seek advice on inclusive wording of targeted recruitment e-mails and posters for recruitment to both research interviews and the study’s Staff Consultation Group, and to support study advertising.
The research team was broadly representative of health and social care keyworkers across several demographic and occupational characteristics, including the involvement of Hub staff and health and social care keyworkers. The research team was predominantly comprised of white researchers; however, the involvement of a British Asian RA in PPIE and participant recruitment was strongly valued by some research participants and stakeholders from other minority ethnic communities, and allowed conversations to take place that stakeholders reported they may otherwise have found more difficult to have with a white researcher as they felt people often did not understand or could not fully empathise. Representation of diverse groups (broadly speaking, but especially of minority ethnic communities) on both mental health teams and research teams was an issue that was highlighted by interview participants and during stakeholder engagement. This is consistent with literature suggesting that engagement with people from minority ethnic communities should not focus solely on the willingness of participants to engage with research or clinical teams, but on building the trustworthiness of research teams themselves, through diversification of teams and meaningful stakeholder engagement. 129
Our stakeholder engagement activities highlighted several barriers to engagement in research, as well as avenues for improving PPIE in future research. Barriers included questioning the motives for the research, and the engagement of minority ethnic communities in research; the emotional effort of engagement; and prior negative experience of involvement in services and research. In terms of the motives for the research, it was felt by those involved in PPIE that where the research team’s genuine desire to have meaningful collaboration from the diverse communities the Hubs were set up to serve was clearly communicated, it was far better received. Where this was communicated well, this led members to promote the research, volunteer to take part and engage with the research more informally.
In smaller informal meetings, stakeholders discussed the emotional effort involved in some EDI work, and the importance of having a safe space to reflect on the impact of racial discrimination where it was relevant to the research. Stakeholders described feeling tired of doing the ‘education work’ for white professionals and therefore were hesitant in joining the Staff Consultation Group. Some stakeholders discussed mental health services not being set up to support minority ethnic communities and were therefore not keen on being involved in mental health research. Stakeholders also described past experiences of supporting projects and initiatives which then ended with limited acknowledgment of their effort, therefore they felt that previous work they had supported was done in a tokenistic way. Stakeholders communicated their disappointment that their involvement in prior initiatives, and others’ papers and reports had not led to any significant change. They felt this led to people not wanting to engage in this type of work.
These barriers were particularly described within the wider context of the Black Lives Matter (BLM) movement, and the disproportionate impact of COVID-19 on minority ethnic communities. Stakeholders reported that there had been additional strain on staff BAME Networks, as they supported different projects and EDI initiatives as part of efforts to reduce discrimination in the workplace and encourage and promote diversity. Stakeholders had already been asked by their NHS Trust to do a considerable amount of EDI work in light of the BLM movement, work which was at times felt to be emotionally draining, particularly when stakeholders felt that they had not seen significant change as a result.
The involvement of a more diverse participant group provided an important perspective that would not otherwise have been highlighted regarding the accessibility of the Hubs, and of health services in general. Furthermore, the perspectives of these participants brought to the fore the impact of the pandemic for these communities, and the additional EDI work asked of some staff, experiences of racial discrimination at work, and the need to support staff around these issues.
All the members of the research team involved in recruiting Staff Consultation Group members and interview participants were women, and it is logical to assume that if having research staff from a minority ethnic community aided engagement from other members of these communities, than having men involved in leading engagement would also have been beneficial. This highlights the importance of diversity within research teams that can further enhance diversity within research participants and PPIE.
Research and clinical teams should in future seek to better represent a diverse range of groups and communities, beginning from training courses and staff recruitment processes. Earlier and more extensive engagement and relationship-building with stakeholders from minority ethnic communities and other demographic groups, including involvement in research design and service development from the earliest stages is recommended, as well as clear communication about the reasons for consulting stakeholders, and the ways in which their contributions would be utilised meaningfully. Further research is needed with communities that may otherwise be excluded from services to identify and resolve barriers to access.
Implications for patients, clinicians and policy-makers
Resilience Hub recommendations
Table 27 summarises recommendations for Resilience Hubs.
| Recommendation | Description |
|---|---|
| Continuation of mental health screening, outreach and provision of direct/indirect support | The model has been shown to be sufficiently adaptable to different contexts, and Hubs should continue provision of their offer, including individual and team-based support |
| Promotion of Hubs | Suggestions are made to improve the clarity and impact of Hub promotion |
| Access in relation to equality, diversity and inclusion | Recommendations to facilitate access for under-represented groups, including keyworkers from minoritised ethnic communities |
| Collection of data on Hub access, mental health screening, Hub activities and outcomes | Routine collection of a standard set of screening questionnaires upon self-referral, and exploration of feasibility of collecting outcome data to further evidence Hub activities and contribute to future research and evaluation |
| Management of Hubs’ specialist resources | Information exchange between organisations so that Hubs can prioritise those that have less staff support available |
| Ensuring preparedness of the Hubs for responding to future crises | Ensure that Hubs are able to maintain a framework for responding to large scale incidents in the future so that lessons learnt can be quickly implemented |
Continuation of mental health screening, outreach and provision of direct/indirect support
The current study highlighted the potential value of the Hub model of outreach, screening, support navigation and provision of direct support, as well as ability of the Hubs to work flexibly in terms of responding to clinical need within staff groups. The model has been shown to be sufficiently adaptable to different contexts, including a new target population, and across multiple regions, and allowed targeting of Hub resources and monitoring of service access. The delivery of high-intensity interventions was particularly supported by study findings demonstrating the heightened mental health needs of Hub clients, and associated levels of complexity, necessitating the Hubs’ staffing of senior clinicians with the experience to work with individuals with these difficulties, as well as providing team-based support. The satisfaction levels of Hub clients were high across both quantitative and qualitative data, but consideration of selection bias needs to be taken into account. Although the Hubs’ team-based work was not directly evaluated by this study, our interviews demonstrated the value placed on these interventions by the wider system. Team-based interventions and prevention of mental health difficulties, rather than a solely reactive approach, were seen as unique and valuable additions to staff support within the health and care system. Wider stakeholders acknowledged that Hubs may not be able to provide that level of support or training for every team/organisation, but that prioritisation decisions could be made if there were greater information flow between the two. This recommendation is also supported by other research and NICE guidance for mental well-being at work. 130,131 Further evaluation will be required to further understand the potential clinical benefit of the Hubs (see Research and evaluation recommendations).
Promotion of Hubs
Hubs involved in the study had variable methods of outreach and promotion the research did not identify whether any particular methods of promotion used by the Hubs were more or less effective (see Chapter 7). Nevertheless, methods of promotion valued by keyworkers and wider stakeholders included testimonials and feedback from those who have been supported by the Hubs, and presentation of research evidence of the utility of the Hubs’ support. A personal approach was particularly valued, including face-to-face contact, team presentations and visibility of Hub staff within teams. Clarity of what is offered by the Hubs, and how to access support would be beneficial. Promotion should cover key areas of uncertainty/concern identified in our work, such as eligibility of staff groups (e.g. non-clinical staff) and not needing to be at crisis point to access support. Confidentiality of Hub support, specifically around self-referral and the Hubs’ use of standalone clinical systems (i.e. with no reporting back to occupational health, but nevertheless within the parameters of usual NHS systems, e.g. response to risk) was strongly valued by keyworkers, and could be emphasised within promotional materials.
Access in relation to equality, diversity and inclusion
The study was hampered by the same issues of recruitment of keyworkers under-represented groups as experienced by clinical teams. As such, recommendations are limited, however it is clear that simply providing information to particular staff groups is insufficient. It is important to understand and resolve barriers to access, and to understand the specific needs and reservations of different staff groups, which may in turn lead to more meaningful engagement with under-represented groups. Improvements are suggested to facilitate greater access by certain groups. Earlier and more extensive engagement with stakeholders identifying as men and from minority ethnic communities is recommended to design appropriate support offers that meet the specific needs of these groups. Representation of these communities on Hub clinical teams was recommended, as well as staff training, experience and understanding of how to support keyworkers with the impact of racism and discrimination, and promotion of how the Hubs can meet these needs. Ability to provide out of hours appointments was suggested to better support shift workers. Options to complete fewer questionnaire measures, or complete measures by telephone were valued to increase access for those in severe distress and/or less able to access digital technology.
Collection of data on Hub access, mental health screening, Hub activities and outcomes
This study demonstrated the value of the use of a standard set of screening questionnaires for understanding and triaging individuals who self-referred to the Hubs. The primary parameters of the screening offer of the four Hubs included in this evaluation (e.g. mental health domains assessed) are broadly consistent with those employed by the Greater Manchester Resilience Hub following the Manchester Arena incident, and therefore demonstrate sufficient adaptability to different contexts, populations and regions. It is recommended that screening initiatives continue at the study sites and is extended to other Hubs across England. It is also recommended that Hubs explore the feasibility of implementing standardised means of routinely gathering follow-up or outcome data following clients’ use of the Hubs. The value of routinely collected screening and outcome data should be balanced against the recommendations made in Resilience Hub recommendations to facilitate ease of access to the Hubs, such as options to omit questionnaires or complete them via telephone. In addition to their clinical value, the collection of standardised screening and outcome data has significant potential for further service evaluation/research and to address concerns related to sharing data with other organisations (see Data sharing and reporting). We elaborate further on how these measures could be used for research and evaluation purposes in Research and evaluation recommendations.
While it was acknowledged that granular data sharing that may identify staff members would be inappropriate, wider stakeholders reported that their ability to evaluate the Hubs’ effectiveness was impeded by insufficient high-level data shared across organisations on access and clinical activities provided by the Hubs. Some implied that this exacerbated tensions between Hubs and other organisations. Both wider stakeholders and Hub staff acknowledged the difficulties in evaluating the impact of the Hubs on higher-level concerns, including staff sickness and staff retention. That said, this is a wider issue affecting many NHS mental health services; services such as IAPT and EIP services are the exception in publishing activity and outcomes data. The Hubs were not set up to provide specific outcome or data metrics (unlike IAPT services) and have not yet had the time to develop appropriate metrics (unlike EIP services). The need for data collection and sharing should be balanced against the potential burden on clients, the importance of collecting information that is clinically valuable for the support of Hub clients, and the ‘ethos’ of the Hubs (e.g. protection of keyworkers’ confidentiality in light of specific barriers to access affecting these occupational groups). In addition, the Hubs evaluated in the study flagged the extensive Hub systemic and team-based activities which, while recommended in Hub guidance,33 were not currently systematically reported to NHSE. These data may usefully provide further evidence of some of the core activities of the Hubs.
Management of Hubs’ specialist resources
Interviews with wider stakeholders demonstrated the variability across organisations in terms of their own in-house staff well-being offer. There is a potential for greater information exchange with organisations so that Hubs can prioritise those that have less staff support on offer. For example, some NHS Trusts already had psychology provision separate to occupational health that could for example, offer specialist interventions (e.g. EMDR) or see more complex presentations, whereas many did not. Detailed mapping of services within regions may be appropriate to better allocate Hub resources. This should, however, be balanced against the need for organisations to have an adequate staff support provision, with Hubs providing an external offer to allow clients choice of access.
Ensuring preparedness of the Hubs for responding to future crises
Participants from all groups interviewed felt strongly that the pandemic had shone a light on staff well-being, as well as highlighting and exacerbating pre-pandemic issues in this area. Evidence suggests that keyworkers may take years before seeking support, if at all (Chapter 6, Qualitative Analysis), and our research corroborates a need for ongoing mental health and well-being support for health and care staff, which could be fulfilled, at least in part, by Hub support. Hub staff and wider stakeholders also saw a valuable potential role of the Hubs in trauma-informed system responses, and responses to traumatic incidents and emergencies. The literature also supports these recommendations in terms of the positive impact of staff health and well-being on patient outcomes. 132–134 Data collected as part of this study clearly suggest that Hubs that were already operational at early stages of the pandemic managed to reach and support a larger number of affected individuals. Having an existing Hub infrastructure in readiness for future incidents is therefore a vital part of the country’s emergency preparedness and response planning.
Organisation/systemic recommendations
Engagement in staff support is needed across the range of the health and care system, from smaller services, such as general practices and care homes, to large organisations such as acute hospitals, councils, and NHS Trusts. Recommendations are made across the system to address staff mental health and help resolve barriers to accessing staff support, summarised in Table 28.
| Recommendation | Description |
|---|---|
| Creation of psychologically safe environments | Organisations have a responsibility to address workplace stressors that may be psychologically damaging. Individual support offers should be offered as an adjunct to, not a replacement for, resolutions to systemic challenges |
| Genuine promotion of mental health and well-being support | Leaders and managers should be involved in cultivating positive workplace cultures to reinforce help-seeking, and genuinely promote the support available |
| Data sharing and reporting | Information sharing between organisations and the Hubs would facilitate better management of specialist resources, and sharing data such as staff sickness and retention would support evidencing Hubs’ impact |
Creation of psychologically safe environments
Some study participants felt strongly that their employing organisations were relying on individuals to seek support or ‘cope better’, rather than addressing systemic and workplace issues that keyworkers felt caused their difficulties. These findings demonstrate the importance of the psychological health and safety agenda in helping to prevent the development of staff mental health difficulties within health and social care organisations. Organisations should attend to aspects of job roles which may be psychologically damaging. Hubs have a role to play in helping organisations to do this (e.g. team-based recommendations; see Management of Hubs’ specialist resources); however, ultimately the responsibility lies with organisations themselves. Consistent with recent NICE guidance130 for supporting mental well-being in the workplace, individual support offers should be offered as an adjunct to, not a replacement for, resolutions to systemic challenges.
Actively addressing structural inequalities and workplace discrimination/racism would contribute to the creation of psychologically safe environments for staff from minority ethnic communities. Participants and PPIE consultants from these communities described often feeling unheard. These stakeholders had often been asked to do additional EDI work due to their ethnicity, but that this was typically unpaid. Many were passionate about this work, but felt it went unrewarded, particularly due to lack of change seen. Staff who worked in supportive roles (e.g. working with Trust BAME Networks) felt the burden of holding others’ distress and experiences of racism. Greater support offered to keyworkers from minority ethnic groups may be valuable within organisations.
Genuine promotion of mental health and well-being support
Health and social care organisations should share the responsibility of promoting the Hubs and other well-being or mental health support offers. The study demonstrated that involvement of managers and leaders was central to encouraging keyworkers to access support from the Hubs. The influence of workplace culture was also found to be important in encouraging staff to take up support offers. Well-being conversations between managers and staff to genuinely promote help-seeking were valued, particularly where managers promote and discuss support offers with teams and individual staff members, rather than simply forwarding e-mails or relying on organisation-level communications.
Data sharing and reporting
Further to the above Hub recommendation to share more data where possible, wider stakeholders also acknowledged that greater collaboration from both sides of the table would be beneficial. Hub leads suggested that greater clarity of where best to share Hub data, and who with, would strengthen this work, particularly within the context of changing Integrated Care Board structures. Organisations should share information with Hubs about their own support offers for staff, so that Hubs are facilitated to make prioritisation decisions about how to allocate time and resources. Information sharing across organisation should also play a role in evidencing the Hubs’ impact on staff sickness and retention; the research demonstrated that this is a key outcome of importance to Hubs and wider stakeholders that was not currently captured at the time of the research.
Research and evaluation recommendations
Certain strands of research emerging from our findings cut across multiple areas of the health sector, including the provision of culturally appropriate services, in line with NIHR EDI principles,135 and workplace barriers to help-seeking such as organisational culture, beliefs around professional roles and organisational promotion of well-being. These barriers offer general principles towards which future research could be oriented, for example, co-production136 approaches to: (1) intervention development with high-level NHS leaders to overcome the barriers identified in our study and (2) culturally appropriate services for ethnic minority communities. In addition, uncertainty remains around the short- and longer-term effects of certain interventions that are often embedded within Hub support, for example, team-based interventions. Further research is recommended to further consolidate the evidence base of these approaches (e.g. via high-quality evidence syntheses as well as further primary research).
Other research strands relate more specifically to the evaluation of the Hub model, which we outline in more detail below.
National service mapping of Hub services
The present study highlighted that, despite common core functions and close collaborations amongst the geographically neighbouring Hubs evaluated as part of this research, considerable heterogeneity exists between the exact offers, designs and interventions implemented by each Hub. While this is arguably a service strength valued by various stakeholders (i.e. ability to flexibly adapt to local needs and make best use of available resources and expertise), this heterogeneity makes the precise evaluation of the Hub approach challenging. A national service mapping mirroring that conducted within this study is warranted to understand how Hubs differ across England in terms of service model and interventions offered. As a minimum, dimensions assessed as part of the national service mapping should considers key variances in Hub configurations and offers highlighted as part of this project (differences in in-scope populations; operationalisation of core offers around outreach, screening, assessment, support navigation and provision of individual and team-based support via local services and directly from the Hubs). In addition, the service mapping should consider how key Hub functions, as indicated by current national guidelines33 are operationalised locally.
Standardisation and generation of routine screening and outcome data collected at the Hubs
While a robust evaluation of the clinical and cost-effectiveness of the Hub approach will require a controlled design (see Clinical and cost-effectiveness evaluation of the Hub approach for its current intended purpose), the routine collection of screening and outcome data across Hubs could facilitate both initial, ongoing and future evaluations of the potential impacts associated with Hub support. This study has demonstrated the feasibility of deploying and analysing mental health screening data across multiple Hubs. Further research would be greatly facilitated through the standardisation of screening measures and approaches across the Hub sites in England, enabling generation of screening data on a much larger scale, which would provide opportunities to examine a range of clinically relevant questions (e.g. exploration client heterogeneity amongst those accessing support, to determine who should be prioritised for intervention in-house at the Hubs and better allocate resources). Based on the experience gathered by the Hubs included in this evaluation, screening should include both demographic and occupational data and standardised mental health questionnaires. It should also request consent for anonymous data use for research purposes and consent for contact for research purposes. Inclusion of brief measures conducive to health economic evaluations (e.g. EQ-5D), although of limited direct clinical value, would also strengthen opportunities to evaluate the potential benefits associated with Hub use. Furthermore, Hubs could also usefully explore the feasibility of implementing standardised means of routinely gathering follow-up or outcome data following clients’ use of the Hubs. Outcomes should be time-bound to clients’ registration with Hubs (e.g. 6 months after self-referral), at the end of interventions, or at discharge to enable meaningful and comparable pre-post evaluation. The implementation of these initiatives could build on the experience of the original Resilience Hub set up in Greater Manchester following the Manchester Arena bombing, which has already demonstrated the feasibility of conducting ‘re-screening’ offers that could be suitably for the collection of outcome data. 2 Consideration should be given to the likely high level of attrition/missing data amongst Hub clients (in the light of both the response rate for the SUQ follow-up survey used in the present project, and ‘re-screening’ data from the Manchester Arena incident,2 which could be partly address via outcome data collection systems informed by those successfully implemented by other NHS services nationally (e.g. IAPT).
Clinical and cost-effectiveness evaluation of the Hub approach for its current intended purpose (i.e. keyworker support) via a natural experiment
The current study has demonstrated the feasibility of implementing the outreach, screening, support navigation and direct support offer of the current Hub model at multiple sites in response to a crisis that required accelerated implementation. However, questions around the clinical and cost-effectiveness of the Hub approach remain. Addressing these uncertainties via a randomised trial would incur in considerable pragmatic and ethical challenges, given the already wide-spread implementation of Hub services across England. A large-scale naturalistic evaluation using a quasi-experimental design would enable a comparison of the outcome data for health and social care staff in regions where Hub support is available, compared with regions where Hub support is not available. The identification of suitable control sites/regions will require careful consideration, and might include the recruitment of a carefully matched sample of workers from health and social care organisation based within UK countries outside of England (i.e. where the Hub model has not been implemented as yet). Clinical and health economic measures should be utilised to determine the clinical and cost effectiveness of the approach. Assessment of clinical outcomes could be informed by the standardised measures used by the Hubs included in the current evaluation. Assessment of health economics outcomes could benefit from consideration of the logic model delivered as part of the current project, and utilisation of both service use data collected from study participants as the use of more objective electronic data sources, although consideration should be given to challenges involved in the use of such methods in the UK (e.g. delays to accessing data, cost and problems linking between care types). In light of remaining uncertainties around the wider systemic impact of the Hubs, key occupational outcomes should consider the Hubs’ impact on staff sickness and staff retention. The follow-up period should be of sufficient duration to capture meaningful changes across these varied outcomes (e.g. at least 1 year, with health economic modelling of the lifetime horizon) and appropriate statistical techniques to mitigate the biases inherent in observational data sets should be employed. Attrition is to be expected regarding the collection of outcome data, and it would be important for researchers to explore methods to minimise loss to follow-up, for example, collection of outcome data via ‘outreach’ RAs in addition to service-based systems, and via implementation of emerging recommendations for maximising retention in clinical trials. 137–142
Hibernated trial to evaluate the implementation and effectiveness of the repurposing of the Hubs in response to future crises
The need for carefully conducted trials in the context of disaster research has been highlighted by others. 143 These are difficult to design and implement post hoc. The abovementioned recommendations for further standardised collection of screening and outcome data and the set-up of a natural experiment to evaluate the clinical and cost-effectiveness of the Hub could serve as springboards for the design and set-up of a hibernated clinical study (i.e. a study that is awaiting activation following a specific set of conditions) to evaluate the implementation and repurposing of the Hubs in the face of a new crisis. The study (i.e. a natural experiment comparing regions with and without Hub support provision) would be activated should the country face a novel, large-scale challenge that may require the repurposing of the Hubs (e.g. a new pandemic event or other non-viral unexpected crises likely to affect the mental health of large sections of keyworkers and/or the general population). The use of hibernated clinical trials has already been proposed as a potentially useful model for supporting research on future pandemic events, in the light of their successful deployment in the context of the UK hibernated pandemic influenza research portfolio, triggered for COVID-19. 144 Consideration would need to be given to the exact situation or magnitude of a crisis that would activate the trial, but this is likely to necessitate a cross-regional event or crisis to enable a meaningful evaluation.
Conclusions
This mixed-methods evaluation conducted across four Hubs has led to the production of a range of recommendations for ongoing and future Hub practice, and for organisations that interface with the Hubs, as well as research recommendations to better evaluate the clinical and cost-effectiveness of the Hub approach as a system for supporting the mental health needs of keyworkers, and as a possible flexible approach to respond to other crises and large-scale traumatic incidents in the future. While the system in the UK responded at pace to the mental health and well-being support for staff exposed to these increased pressures, it was reactive rather than proactive. In the short term, there will continue to be ongoing issues in relation to the challenges brought about by the COVID-19 pandemic. In the longer term, the country might be faced with other crises affecting large proportions of the population as well as the mental health and social care workforce, such as new pandemics, war conflicts or crises related to climate change. While no two large-scale trauma incidents will be the same and there will be important subtleties that require adaptation, a ‘clinical memory’ on how to manage those incidents is vital to hold onto. The overarching emphasis of this research suggests that a mental health response is built into the planning for future events and should be seen as important as stockpiling PPE with the potential for specialist national or regional units that can ensure a mental health response is embedded into future incident planning to ensure that updated evidence is appropriately utilised to manage those incidents. 145
Additional information
Acknowledgements
The research team would like to thank all the participants who took part in this study for generously giving their time to be interviewed or complete follow-up questionnaires, and to all the Resilience Hub clients who gave consent for us to use their screening data, which made this research possible. We would also like to thank the Resilience Hub teams who supported this project and provided essential data to conduct this programme of work.
We would like to thank the members of our Staff Consultation Group and other stakeholders with whom we consulted about the research, whose insights, openness and enthusiasm were invaluable throughout the project.
We are incredibly grateful to the study’s research assistants who worked tirelessly to collect and process both qualitative and quantitative data; site RAs Priscilla Chung, Alysha Hassan, Sally-Anne Wright, and Ellie Young, and particularly our central team RA Hannah White who as well as collecting data has been an invaluable support to the project throughout, including involvement in the preparation of the final report.
We would also like thank members of our Project Steering Committee for their support and guidance throughout the course of the project.
Contributions of authors
Filippo Varese (https://orcid.org/0000-0001-7244-598X) (Professor of Clinical Psychology, Principal Investigator) led the design of the study and co-ordination of the project, contributed to quantitative data analysis and interpretation, and is lead author of this report.
Kate Allsopp (https://orcid.org/0000-0002-5093-0404) (Research Fellow, qualitative research) was co-Investigator, contributed to the conceptualisation and design of the study, was responsible for day-to-day management of the project, the supervision of all research support staff, led qualitative data collection and analysis, and was involved in the preparation of this report.
Lesley-Anne Carter (https://orcid.org/0000-0002-1193-8681) (Lecturer, Biostatistics) was co-Investigator, led the statistical analysis for the quantitative component of the study, contributed to the interpretation and write-up of quantitative analyses findings and reviewed the final report.
Gemma Shields (https://orcid.org/0000-0003-4869-7524) (Lecturer, Health Economics) was co-Investigator, co-led the design of the health economics component, and led the health economics data collection, analysis, and write-up.
Daniel Hind (https://orcid.org/0000-0002-6409-4793) (Professor of Evaluation, School of Health and Related Research) was co-Investigator, led the design of the qualitative and case studies component, and contributed to the preparation and review of the report for these components.
Linda Davies (https://orcid.org/0000-0001-8801-3559) (Professor, Health Economics) was co-Investigator and co-led the design of the health economics component of the study.
Alan Barrett (https://orcid.org/0000-0002-9003-2422) (Strategic Clinical Lead – Adults, Greater Manchester Resilience Hub) was a co-Investigator and site lead for one of the Hubs considered in this evaluation, made a significant contribution to the design and conception of the study, critically revised the work for important intellectual content and reviewed the final report.
Gita Bhutani (https://orcid.org/0000-0002-2732-6479) (Director, Lancashire and South Cumbria Resilience Hub) was a co-Investigator and site lead for one of the Hubs considered in this evaluation, made a significant contribution to the design and conception of the study, critically revised the work for important intellectual content and reviewed the final report.
Katherine McGuirk (https://orcid.org/0000-0002-1229-7820) (PPIE lead and Operational Manager for staff well-being, Greater Manchester Resilience Hub) was co-Investigator, contributed to the design of the PPIE consultation, and led associated PPIE activities, as well as critically revised the work for important intellectual content and reviewed the draft final report.
Fay Huntley (https://orcid.org/0000-0003-0642-4368) (Clinical Lead, Cheshire and Merseyside Resilience Hub) was co-site lead for one of the Hubs considered in this evaluation, critically revised the work for important intellectual content and reviewed the draft final report.
Joanne Jordan (https://orcid.org/0000-0002-6141-5096) (Clinical Lead, Humber and North Yorkshire Resilience Hub), was co-site lead for one of the Hubs considered in this evaluation, critically revised the work for important intellectual content and reviewed the draft final report.
Aleix Rowlandson (https://orcid.org/0000-0002-9513-7821) (Research Associate, Health Economics) supported data collection and analyses of the health economic component of the study, contributed to the write-up of all health economics findings, and reviewed the final report.
May Sarsam (https://orcid.org/0000-0002-0506-0227) (Service Lead, Cheshire and Merseyside Resilience Hub), was co-site lead for one of the Hubs considered in this evaluation, critically revised the work for important intellectual content and reviewed the draft final report.
Hein Ten Cate (https://orcid.org/0000-0002-3394-7968) (Clinical Lead, Lancashire and South Cumbria Resilience Hub) critically revised the work for important intellectual content and critically revised the final report for important intellectual content.
Holly Walker (https://orcid.org/0000-0001-8863-569X) (Service Manager, Humber and North Yorkshire Resilience Hub) was co-site lead for one of the Hubs considered in this evaluation, critically revised the work for important intellectual content and reviewed the draft final report.
Ruth Watson (https://orcid.org/0000-0001-6950-1426) (Deputy Clinical Lead, Adults, Greater Manchester Resilience Hub), critically revised the work for important intellectual content and reviewed the draft final report.
Jack Wilkinson (https://orcid.org/0000-0003-3513-4677) (Research Fellow, Biostatistics) supported data management and analyses of the routinely collected Hub data, contributed to the interpretation and write-up of quantitative analyses, and reviewed the final report.
Jenni Willbourn (https://orcid.org/0000-0002-4965-4123) (Clinical lead, support to professionals, Greater Manchester Resilience Hub) critically revised the work for important intellectual content and reviewed the draft final report.
Paul French (https://orcid.org/0000-0003-4300-387X) (Reader in Nursing, Co-Principal Investigator) contributed to the design of the study and co-ordination of the project, the interpretation of data across all methodological streams, and contributed to the drafting and finalisation of the report.
All authors were involved in the final approval of the version to be published. All authors agree to be accountable for all aspects of the work in ensuring that questions relating to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Disclosure of interests
Full disclosure of interests: Completed ICMJE forms for all authors, including all related interests, are available in the toolkit on the NIHR Journals Library report publication page at https://doi.org/10.3310/HGQR5133.
Primary conflicts of interest: Paul French has previously been a member of NIHR HTA Prioritisation Committee and is a current member of NIHR HTS Clinical Evaluation and Trials funding Committee. Daniel Hind has previously been a member of NIHR Research for Patient Benefit, Yorks and NE Regional Advisory Committee, and is a current member of NIHR Health Technology Assessment Clinical Evaluation and Trials Funding Committee (2019–24). Linda Davies is a current member of DMC/TSC for NIHR funded projects in mental health, but unrelated to Resilience Hub service. Lesley-Anne Carter is a current member of the NIHR Research for Patient Benefit North West Committee. Filippo Varese has received an NIHR Advanced Fellowship in a clinical research area unrelated to the Resilience Hubs. Filippo Varese, Paul French, Daniel Hind, Linda Davies, Gemma Shields, Gita Bhutani, Lesley-Anne Carter and Jack Wilkinson are Investigators/Co-investigators in several other NIHR projects funded by various funding streams (RfPB, HTA, EME, HS and DR).
Alan Barrett is an honorary member of the National Mental Health and Well-being expert reference group at NHS England and NHS Improvement. Alan Barrett, Jenni Willbourn, Katherine McGuirk, and Filippo Varese are members of the Greater Manchester Psychosocial Board, and Jenni Willbourn, Ruth Watson and Katherine McGuirk are members of the Greater Manchester Expert Reference Group. Linda Davies is a member of an expert advisory board for Public Health England. Gita Bhutani is Interim co-chair of the National Institute of Health and Care Excellence (NICE) Quality Standards Advisory Committee. Paul French is clinical advisor to National Clinical Audit of Psychosis at Royal College of Psychiatry and Board member of International Early Psychosis Association.
Gita Bhutani, Alan Barrett, Hein Ten Cate, Katherine McGuirk, Fay Huntley, Joanne Jordan, May Sarsam, Holly Walker, Ruth Watson, and Jenni Willbourn have all held senior clinical and/or operational roles at the Hub sites involved in this study. Paul French has previously led research to evaluate the original Resilience Hub service set up to support those affected by the 2017 Manchester Arena bombing, in which Daniel Hind and Kate Allsopp were also involved. Kate Allsopp has also held a research and evaluation role at a second Hub involved in this project.
Patient data statement
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it is important that there are safeguards to make sure that they are stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review in consultation with broader study team and Sponsor.
Ethics statement
Ethical approval was granted for this study through North West – Preston Research Ethics Committee IRAS Project ID 290375 REC Reference 20/NW/0462 on 19th January 2021. Health Research Authority (HRA) approval was granted on 20 January 2021.
Information governance statement
Greater Manchester Mental Health NHS Foundation Trust is committed to handling all personal information in line with the UK Data Protection Act (2018) and the General Data Protection Regulation (EU GDPR) 2016/679. Under Data Protection legislation, Greater Manchester Mental Health NHS Foundation Trust is the Data Controller, and you can find out more about how we handle personal data, including how to exercise your individual rights here. The Greater Manchester Mental Health NHS Foundation Trust Data Protection Officer can be contacted at dpo@gmmh.nhs.uk.
Disclaimers
This article presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care.
References
- NHS England . Responding to the Needs of People Affected by Incidents and Emergencies: A Framework for Planning and Delivering Psychosocial and Mental Health Care 2021.
- French P, Barrett A, Allsopp K, Williams R, Brewin CR, Hind D, et al. Psychological screening of adults and young people following the Manchester Arena incident. BJPsych Open 2019;5:1-6.
- Allsopp K, Brewin CR, Barrett A, Williams R, Hind D, Chitsabesan P, et al. Responding to mental health needs after terror attacks. BMJ 2019;4828:4-7. https://doi.org/doi:10.1136/bmj.l4828.
- Xiong J, Lipsitz O, Nasri F, Lui LMW, Gill H, Phan L, et al. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J Affect Disord 2020;277:55-64. https://doi.org/10.1016/j.jad.2020.08.001.
- Phiri P, Ramakrishnan R, Rathod S, Elliot K, Thayanandan T, Sandle N, et al. An evaluation of the mental health impact of SARS-CoV-2 on patients, general public and healthcare professionals: a systematic review and meta-analysis. EClinicalMedicine 2021;34. https://doi.org/10.1016/j.eclinm.2021.100806.
- Wu P, Fang Y, Guan Z, Fan B, Kong J, Yao Z, et al. The psychological impact of the SARS epidemic on hospital employees in China: exposure, risk perception, and altruistic acceptance of risk. Can J Psychiatry 2009;54:302-11.
- Salari N, Khazaie H, Hosseinian-Far A, Khaledi-Paveh B, Kazeminia M, Mohammadi M, et al. prevalence of stress, anxiety and depression within front-line healthcare workers caring for COVID-19 patients: a systematic review and meta-regression. Hum Resour Health 2020;18:1-14. https://doi.org/10.1186/s12960-020-00544-1.
- Crocamo C, Bachi B, Calabrese A, Callovini T, Cavaleri D, Cioni RM, et al. Some of us are most at risk: systematic review and meta-analysis of correlates of depressive symptoms among healthcare workers during the SARS-CoV-2 outbreak. Neurosci Biobehav Rev 2021;131:912-22.
- Li Y, Scherer N, Felix L, Kuper H. Prevalence of depression, anxiety and posttraumatic stress disorder in health care workers during the COVID-19 pandemic: a systematic review and meta-analysis. PLOS ONE 2021;16:1-19. https://doi.org/10.1371/journal.pone.0246454.
- Varghese A, George G, Kondaguli S V, Naser AY, Khakha DC, Chatterji R. Decline in the mental health of nurses across the globe during COVID-19: a systematic review and meta-analysis. J Glob Health 2021;11.
- Cenat C, Kokou-Kpolou C, Noorishad P, Mukunzi J, McIntee S, Dalexis R, et al. Prevalence of symptoms of depression, anxiety, insomnia, posttraumatic stress disorder, and psychological distress among populations affected by the COVID-19 pandemic: a systematic review and meta-analysis. Psychiatry Res 2021;295.
- Sharifi M, Asadi-Pooya AA, Mousavi-Roknabadi RS. Burnout among healthcare providers of COVID-19; a systematic review of epidemiology and recommendations. Arch Acad Emerg Med 2020;9:1-17.
- Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease. JAMA Netw Open 2019;3.
- Pappa S, Ntella V, Giannakas T, Giannakoulis VG, Papoutsi E, Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav Immun 2020;88:901-7. https://doi.org/10.1016/j.bbi.2020.05.026.
- Razaq A, Harrison D, Karunanithi S, Barr B, Asaria M, Khunti K. Bame COVID-19 Deaths – What Do We Know? Rapid Data & Evidence Review: “Hidden in Plain Sight”. London: LSE Health; n.d.
- Greenberg N, Docherty M, Gnanapragasam S, Wessely S. Managing mental health challenges faced by healthcare workers during COVID-19 pandemic. BMJ 2020;368:1-4. https://doi.org/doi:10.1136/bmj.m1211.
- Moynihan R, Sanders S, Michaleff ZA, Scott AM, Clark J, To EJ, et al. Impact of COVID-19 pandemic on utilisation of healthcare services: a systematic review. BMJ Open 2021;11.
- Sandland-Taylor L, Jenkins B, Beckingham I. The impact of COVID-19 on bariatric surgery in England during 2020. Br J Surg 2021;108:19-20.
- Rutter MD, Brookes M, Lee TJ, Rogers P, Sharp L. Impact of the COVID-19 pandemic on UK endoscopic activity and cancer detection: a national endoscopy database analysis. Gut 2021;70:537-43.
- Flynn J, O’Connor L, Hanlon M, Bellani G, Contreras M, Doherty A, et al. The identification of needs and development of best practice guidance for the psychological support of frontline healthcare workers during and after COVID-19: a protocol for the FLoWS project. HRB Open Res 2021;3.
- Tromans S, Chester V, Harrison H, Pankhania P, Booth H, Chakraborty N. Patterns of use of secondary mental health services before and during COVID-19 lockdown: observational study. BJPsych Open 2020;6:1-6.
- Chen S, Jones PB, Underwood BR, Moore A, Bullmore ET, Banerjee S, et al. The early impact of COVID-19 on mental health and community physical health services and their patients’ mortality in Cambridgeshire and Peterborough, UK. J Psychiatr Res 2020;131:244-54. https://doi.org/10.1016/j.jpsychires.2020.09.020.
- Trentini F, Marziano V, Guzzetta G, Tirani M, Cereda D, Poletti P, et al. Pressure on the health-care system and intensive care utilization during the COVID-19 outbreak in the Lombardy region of Italy: a retrospective observational study in 43,538 hospitalized patients. Am J Epidemiol 2022;191:137-46.
- NHS Clinical Leaders Network . Enhancing Mental Health Resilience and Anticipating Treatment Provision of Mental Health Conditions for Frontline Healthcare Workers Involved in Caring for Patients During the COVID-19 Pandemic – A Call for Action 2020.
- Oliver D. Protecting healthcare workers in future pandemics. BMJ 2022;377.
- Parliament. House of Commons . Coronavirus: Lessons Learned to Date. Sixth Report of the Health and Social Care Committee and Third Report of the Science and Technology Committee of Session 2021–22 2021. https://publications.parliament.uk/pa/cm5803/cmselect/cmhaff/635/report.html (accessed 17 April 2024).
- Pfefferbaum B, North CS. Mental health and the COVID-19 pandemic. N Engl J Med 2020;383:510-12. www.nejm.org/doi/full/10.1056/NEJMp2008017 (accessed 13 July 2020).
- Nobles J, Martin F, Dawson S, Moran P, Savovic J. The Potential Impact of COVID-19 on Mental Health Outcomes and the Implications for Service Solutions: ARC West. NIHR Applied Research Collaboration West; 2020.
- Pappa S, Ntella V, Giannakas T, Giannakoulis VG, Papoutsi E, Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav Immun 2020;88:901-7. https://doi.org/10.1016/j.bbi.2020.05.026.
- Zaka A, Shamloo SE, Fiorente P, Tafuri A. COVID-19 pandemic as a watershed moment: a call for systematic psychological health care for frontline medical staff. J Health Psychol 2020;25:883-7. https://doi.org/10.1177/1359105320925148.
- Galbraith N, Boyda D, McFeeters D, Hassan T. The mental health of doctors during the COVID-19 andemic. BJPsych Bull 2020;45:93-7.
- Holmes EA, O’Connor RC, Perry VH, Tracey I, Wessely S, Arseneault L, et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiat 2020;7:547-60. www.thelancet.com/psychiatry (accessed 13 July 2020).
- NHS . Guidance for Staff Mental Health and Well-Being Hubs 2022–23 2022.
- NHS England, NHS Improvement . Guidance for Mental Health and Well-Being Hubs for Health and Social Care Staff 2020.
- NHS England . Staff Mental Health Support FAQs 2021.
- HSC R&D Division Northern Ireland . UK Standards for Public Involvement 2022. https://research.hscni.net/public-involvement-standards (accessed 17 April 2024).
- INVOLVE . Briefing Notes for Researchers: Public Involvement in NHS, Public Health and Social Care Research 2012. www.invo.org.uk/wp-content/uploads/2014/11/9938_INVOLVE_Briefing_Notes_WEB.pdf (accessed 17 April 2024).
- Johnson S, Kuhlmann R, Munizza C, Beecham J, Salvador-Carulla L, De Jong P, et al. The European Service Mapping Schedule (ESMS): development of an instrument for the description and classification of mental health services. Acta Psychiatr Scand Suppl 2000;102:14-23.
- Romero-López-Alberca C, Gutiérrez-Colosía MR, Salinas-Pérez JA, Almeda N, Furst M, Johnson S, et al. Standardised description of health and social care: a systematic review of use of the ESMS/DESDE (European Service Mapping Schedule/Description and Evaluation of Services and DirectoriEs). Eur Psychiatry 2019;61:97-110.
- Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014;348.
- Dorling H, White D, Turner S, Campbell K, Lamont T. Developing a checklist for research proposals to help describe health service interventions in UK research programmes: a mixed methods study. Heal Res Policy Syst 2014;12:1-8.
- National Institute for Health and Care Excellence . Post-Traumatic Stress Disorder 2018. www.nice.org.uk/guidance/NG116 (accessed 17 April 2024).
- British Psychological Society . Understanding Formulation: Working With a Psychologist 2019.
- NHS Digital . NHS Occupation Codes 2021.
- Cloitre M, Shelvin M, Brewin CR, Bisson JI, Roberts NP, Maercker A, et al. The International Trauma questionnaire: development of a self‐report measure of ICD-11 PTSD and complex PTSD. Acta Psychiatr Scand 2018;138:536-46.
- Weathers FW, Litz BT, Keane TM, Palmieri PA, Marx BP, Schnurr PP . PTSD Checklist for DSM-5 (PCL-5). Natl Cent Posttraumatic Stress Disord 2018;5. www.ptsd.va.gov/professional/assessment/documents/PCL5_Standard_form.PDF (accessed 17 April 2024).
- Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 2001;16:606-13.
- Spitzer RL, Kroenke K, Williams JBW, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med 2006;166:1092-7.
- Mundt JC, Marks IM, Shear MK, Greist JH. The Work and Social Adjustment Scale: a simple measure of impairment in functioning. Br J Psychiatry 2002;180:461-4. www.ncbi.nlm.nih.gov/pubmed/11983645 (accessed 30 April 2018).
- Saunders J, Aasland O, Babor T, De La Fuente J, Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption‐II. Addiction 1993;88:791-804.
- Davies G. The EQUIP Service Use Questionnaire 2018. www.dirum.org/instruments/details/111 (accessed 17 April 2024).
- Skills for Care . The State of Adult Social Care Sector and Workforce in England 2021. www.skillsforcare.org.uk/adult-social-care-workforce-data-old/Workforce-intelligence/publications/national-information/The-state-of-the-adult-social-care-sector-and-workforce-in-England.aspx (accessed 17 April 2024).
- NHS Employers . Gender in the NHS 2019.
- UK Government . NHS Workforce 2021.
- Adibi A, Golitaleb M, Farrahi-Ashtiani I, Pirani D, Yousefi K, Jamshidbeigi Y, et al. The prevalence of generalized anxiety disorder among health care workers during the COVID-19 pandemic: a systematic review and meta-analysis. Front Psychiatry 2021;12:1-7.
- D’ettorre G, Pellicani V, Ceccarelli G. Post-traumatic stress disorder symptoms in healthcare workers: a ten-year systematic review. Acta Biomed 2020;91:1-10.
- Salehi M, Amanat M, Mohammadi M, Salmanian M, Rezaei N, Saghazadeh A, et al. The prevalence of post-traumatic stress disorder related symptoms in coronavirus outbreaks: a systematic-review and meta-analysis. J Affect Disord 2021;282:527-38. https://doi.org/10.1016/j.jad.2020.12.188.
- Greenberg N, Weston D, Hall C, Caulfield T, Williamson V, Fong K. Mental health of staff working in intensive care during COVID-19. Occup Med 2021;71:62-7.
- Hill JE, Harris C, Danielle L. C, Boland P, Doherty AJ, Benedetto V, et al. The prevalence of mental health conditions in healthcare workers during and after a pandemic: systematic review and meta-analysis. J Adv Nurs 2022;78:1551-73.
- Wittgens C, Fischer MM, Buspvanich P, Theobald S, Schweizer K, Trautmann S. Mental health in people with minority sexual orientations: a meta‐analysis of population-based studies. Acta Psychiatr Scand 2022;145:357-72.
- UK Government . Harmful and Probable Dependent Drinking in Adults 2018.
- Weich RS, Stewart S, McBride R, Brugha O, Hassiotis T, Bebbington A, et al. Mental Health and Well-being in England: Adult Psychiatric Morbidity Survey 2014. Leeds: NHS Digital; 2016.
- Hall CE, Milward J, Spoiala C, Bhogal JK, Weston D, Potts HWW, et al. The mental health of staff working on intensive care units over the COVID-19 winter surge of 2020 in England: a cross sectional survey. Br J Anaesth 2022;128:971-9.
- De Brier N, Stroobants S, Vandekerckhove P, De Buck E. Factors affecting mental health of health care workers during coronavirus disease outbreaks (SARS, MERS & COVID-19): a rapid systematic review. PLOS ONE 2020;15. https://doi.org/10.1371/journal.pone.0244052.
- Uphoff EP, Lombardo C, Johnston G, Weeks L, Rodgers M, Dawson S, et al. Mental health among healthcare workers and other vulnerable groups during the COVID-19 pandemic and other coronavirus outbreaks: a rapid systematic review. PLOS ONE 2021;16. https://doi.org/10.1371/journal.pone.0254821.
- Jones AKB. The Unit Costs of Health and Social Care. Kent: Personal Social Services Research Unit; 2021.
- Devlin N, Parking D, Janssen B. Methods for Analysing and Reporting EQ-5D Data. Cham, Switzerland: Springer; 2020.
- Van Hout B, Janssen MF, Feng YS, Kohlmann T, Busschbach J, Golicki D, et al. Interim scoring for the EQ-5D-5L: mapping the EQ-5D-5L to EQ-5D-3L value sets. Value Heal 2012;15:708-15. https://doi.org/10.1016/j.jval.2012.02.008.
- National Institute of Health and Care Excellence (NICE) . Guide to the Methods of Technology Appraisal 2013 2013. www.nice.org.uk/process/pmg9/chapter/foreword (accessed 17 April 2024).
- National Institute of Health and Care Excellence (NICE) . NICE Health Technology Evaluations: The Manual 2022.
- Hernández-Alava M, Pudney S. Eq5Dmap: a command for mapping between EQ-5D-3L and EQ-5D-5L. Stata J 2018;18:395-41.
- Hernández-Alava M, Pudney S, Wailoo A. Estimating the relationship between EQ-5D-5L and EQ-5D-3L: results from an English Population Study. Pharmacoeconomics 2020;41:199-207.
- Szende A, Janssen B, Cabases J. Self-reported Population Health: An International Perspective Based on EQ-5D. Cham, Switzerland: Springer; 2014.
- National Centre for Social Research (NatCen), University College London, Department of Epidemiology and Public Health . Health Survey for England, 2018 2020. https://doi.org/10.5255/UKDA-SN-8649-1.
- NHS Digital . Health Survey for England 2018.
- NHS England and NHS Improvement . National Cost Collection 2019–2020 2021.
- Hind D, Allsopp K, Chitsabesan P, French P. The psychosocial response to a terrorist attack at Manchester Arena, 2017: a process evaluation. BMC Psychol 2021;9:1-20.
- Franklin M, Enrique A, Palacios J, Richards D. Psychometric assessment of EQ-5D-5L and ReQoL measures in patients with anxiety and depression: construct validity and responsiveness. Qual Life Res 2021;30:2633-47. https://doi.org/10.1007/s11136-021-02833-1.
- Lamers C, Bouwmans CAM, van Straten A, Donker MCH, Hakkaart L. Comparison of EQ‐5D and SF‐6D utilities in mental health patients. Health Econ 2006;15:1229-36.
- Mukuria C, Brazier J, Barkham M, Connell J, Hardy G, Hutten R, et al. Cost-effectiveness of an improving access to psychological therapies service. Br J Psychiatry 2013;202:220-7.
- UK Government . Major Reforms to NHS Workforce Planning and Tech Agenda 2021.
- NHS England . NHS Mental Health Dashboard 2022.
- The London School of Economics and Political Science . Mental Health Problems Cost UK Economy at Least £118 Billion a Year: New Research 2022. www.lse.ac.uk/News/Latest-news-from-LSE/2022/c-Mar-22/Mental-health-problems-cost-UK-economy-at-least-118-billion-a-year-new-research (accessed 17 April 2024).
- Mcdaid D, Park A-L, Davidson G, John A, Knifton L, Morton A, et al. The Economic Case for Investing in the Prevention of Mental Health Conditions in the UK. Mental Health Foundation; 2022.
- Clarke L, Patouillard E, Mirelman AJ, Ho ZJM, Edejer TTT, Kandel N. The costs of improving health emergency preparedness: a systematic review and analysis of multi-country studies. EClinicalMedicine 2022;44. https://doi.org/10.1016/j.eclinm.2021.101269.
- Chandola T, Kumari M, Booker CL, Benzeval MJ. The mental health impact of COVID-19 and lockdown related stressors among adults in the UK. Psychol Med 2020;52:2997-3006.
- Long D, Haagsma JA, Janssen MF, Yfantopoulos JN, Lubetkin EI, Bonsel GJ. Health-related quality of life and mental well-being of healthy and diseased persons in 8 countries: does stringency of government response against early COVID-19 matter?. SSM: Popul Heal 2021;15. https://doi.org/10.1016/j.ssmph.2021.100913.
- Goldmann E, Galea S. Mental health consequences of disasters. Annu Rev Public Health 2014;35:169-83.
- Hollinghurst S, Peters TJ, Kaur S, Wiles N, Lewis G, Kessler D. Cost-effectiveness of therapist-delivered online cognitive-behavioural therapy for depression: randomised controlled trial. Br J Psychiatry 2010;197:297-304.
- Richards DA, Ekers D, McMillan D, Taylor RS, Byford S, Warren FC, et al. Cost and outcome of behavioural activation versus cognitive behavioural therapy for depression (COBRA): a randomised, controlled, non-inferiority trial. Lancet 2016;388:871-80.
- Wiles NJ, Thomas L, Turner N, Garfield K, Kounali D, Campbell J, et al. Long-term effectiveness and cost-effectiveness of cognitive behavioural therapy as an adjunct to pharmacotherapy for treatment-resistant depression in primary care: follow-up of the CoBalT randomised controlled trial. Lancet Psychia 2016;3:137-44. https://doi.org/10.1016/S2215-0366(15)00495-2.
- Dixon P, Hollinghurst S, Edwards L, Thomas C, Foster A, Davies B, et al. Cost-effectiveness of telehealth for patients with depression: evidence from the Healthlines randomised controlled trial. BJPsych Open 2016;2:262-9.
- Green C, Richards DA, Hill JJ, Gask L, Lovell K, Chew-Graham C, et al. Cost-effectiveness of collaborative care for depression in UK primary care: economic evaluation of a randomised controlled trial (CADET). PLOS ONE 2014;9.
- Kuyken W, Hayes R, Barrett B, Byng R, Dalgleish T, Kessler D, et al. Effectiveness and cost-effectiveness of mindfulness-based cognitive therapy compared with maintenance antidepressant treatment in the prevention of depressive relapse or recurrence (PREVENT): a randomised controlled trial. Lancet 2015;386:63-7. https://doi.org/10.1016/S0140-6736(14)62222-4.
- Kay M, Mitchell G, Clavarino A, Doust J. Doctors as patients: a systematic review of doctors’ health access and the barriers they experience. Br J Gen Pract 2008;58:501-8.
- Smith EC, Burkle FM. Paramedic and emergency medical technician reflections on the ongoing impact of the 9/11 terrorist attacks. Prehosp Disaster Med 2019;34:56-61.
- Bentz L, Vandentorren S, Fabre R, Bride J, Pirard P, Doulet N, et al. Mental health impact among hospital staff in the aftermath of the nice 2016 terror attack: the ECHOS de Nice study. BMC Public Health 2021;21:1-17.
- Asukai Y, Briggs A, Garrison LP, Geisler BP, Neumann PJ, Ollendorf DA. Principles of economic evaluation in a pandemic setting: an expert panel discussion on value assessment during the coronavirus disease 2019 pandemic. Pharmacoeconomics 2021;39:1201-8. https://doi.org/10.1007/s40273-021-01088-5.
- Sekhon M, Cartwright M, Francis JJ. Acceptability of healthcare interventions: an overview of reviews and development of a theoretical framework. BMC Health Serv Res 2017;17:1-13. https://doi.org/10.1186/s12913-017-2031-8.
- Cane J, O’Connor D, Michie S. Validation of the theoretical framework. Implement Sci 2012;7.
- Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci 2011;6. www.implementationscience.com/content/6/1/42 (accessed 17 April 2024).
- Cassidy C, Bishop A, Steenbeek A, Langille D, Martin-Misener R, Curran J. Barriers and enablers to sexual health service use among university students: a qualitative descriptive study using the Theoretical Domains Framework and COM-B model. BMC Health Serv Res 2018;18:1-12.
- May C, Finch T. Implementing, embedding, and integrating practices: an outline of normalization process theory. Sociology 2009;43:535-54. http://journals.sagepub.com/doi/10.1177/0038038509103208 (accessed 30 March 2019).
- May C, Cummings A, Girling M, Bracher M, Mair FS, . Using Normalization Process Theory in feasibility studies and process evaluations of complex healthcare interventions: a systematic review. Implement Sci 2018;13:1-42.
- Ritchie J, Spencer L. The Qualitative Researcher’s Companion. Thousand Oaks, CA: SAGE Publications Inc; 1994.
- Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Heal Care 2007;19:349-57.
- Smith K, Bhui K, Cipriani A. COVID-19, mental health and ethnic minorities. Evid Based Ment Health 2020;23:89-90.
- Adams EFM, Lee AJ, Pritchard CW, White RJE. What stops us from healing the healers: a survey of help-seeking behaviour, stigmatisation and depression within the medical profession. Int J Soc Psychiatry 2010;56:359-70.
- Ladonna KA, Cowley L, Touchie C, Leblanc VR, Spilg EG. Wrestling with the invincibility myth: exploring physicians’ resistance to wellness and resilience-building interventions. Acad Med 2022;97:436-43.
- Riley R, Buszewicz M, Kokab F, Teoh K, Gopfert A, Taylor AK, et al. Sources of work: related psychological wide distress experienced by UK – foundation and junior doctors: a qualitative study. BMJ Open 2021;11.
- Himmels ME, Smedslund J, Flottorp G, Stensland G, Stroobants S, de Velde S, et al. The mental health impact of the COVID-19 pandemic on healthcare workers, and interventions to help them: a rapid systematic review. Psychiatry Res 2020;293.
- Scales SE, Patrick E, Stone KW, Kintziger KW, Jagger MA, Horney JA. A qualitative study of the COVID-19 response experiences of public health workers in the United States. Heal Secur 2021;19:573-81.
- Bennett P, Noble S, Johnston S, Jones D, Hunter R. COVID-19 confessions: a qualitative exploration of healthcare workers experiences of working with COVID-19. BMJ Open 2020;10.
- Berkhout SG, Sheehan KA, Abbey SE. Individual- and institutional-level concerns of health care workers in Canada during the COVID-19 pandemic: a qualitative analysis. JAMA Netw Open 2021;4.
- Prajapati R, Liebling H. Accessing mental health services: a systematic review and meta-ethnography of the experiences of South Asian service users in the UK. J Racial Ethn Heal Disparities 2022;9:598-619.
- Williams PE, Turpin G, Hardy G. Clinical psychology service provision and ethnic diversity within the UK: a review of the literature. Clin Psychol Psychother 2006;13:324-38.
- Islam Z, Rabiee F, Singh SP. Black and minority ethnic groups’ perception and experience of early intervention in psychosis services in the United Kingdom. J Cross Cult Psychol 2015;46:737-53.
- Kurtz C ZS. Mental health services for young people from black and minority ethnic backgrounds the current challenge. J Child Serv 2006;1:40-9.
- Jesuthasan J, Powell RA, Burmester V, Nicholls D. “We weren’t checked in on, nobody spoke to us”: an exploratory qualitative analysis of two focus groups on the concerns of ethnic minority NHS staff during COVID-19. BMJ Open 2021;11.
- Association BM . A Missed Opportunity BMA Response to the Race Report 2021. www.bma.org.uk/media/4276/bma-analysis-of-the-race-report-from-the-commission-on-race-and-ethnic-disparities-june-2021.pdf (accessed 17 April 2024).
- Clement S, Schauman O, Graham T, Maggioni F, Evans-Lacko S, Bezborodovs N, et al. What is the impact of mental health-related stigma on help-seeking? A systematic review of quantitative and qualitative studies. Psychol Med 2015;45:11-27.
- Skills for Care . The State of the Adult Social Care Sector and Workforce in England, 2022 2022. www.skillsforcare.org.uk/Adult-Social-Care-Workforce-Data/Workforce-intelligence/documents/State-of-the-adult-social-care-sector/The-state-of-the-adult-social-care-sector-and-workforce-2022.pdf (accessed 9 December 2022).
- Younas A, Pedersen M, Durante A. Characteristics of joint displays illustrating data integration in mixed-methods nursing studies. J Adv Nurs 2019;76:676-86.
- Trochim WMK. Outcome pattern matching and program theory. Eval Program Plann 1989;12:355-66. https://doi.org/10.1016/0149-7189(89)90052-9.
- Yin R. Case Study Research: Design and Methods. London: Sage; 2014.
- Fetters MD, Curry LA, Creswell JW. Achieving integration in mixed methods designs: principles and practices. Health Serv Res 2013;48:2134-56.
- Gilbert AW, Billany JCT, Adam R, Martin L, Tobin R, Bagdai S, et al. Rapid implementation of virtual clinics due to COVID-19: report and early evaluation of a quality improvement initiative. BMJ Open Qual 2020;9.
- Knapp M, Wong G. Economics and mental health: the current scenario. World Psychiatry 2020;19:3-14.
- Passmore SR, Kisicki A, Gilmore-Bykovskyi A, Green-Harris G, Edwards DF. There’s not much we can do … researcher-level barriers to the inclusion of under-represented participants in translational research. J Clin Transl Sci 2021;6.
- National Institute for Health and Care Research . Mental Well-Being at Work 2022. www.nice.org.uk/guidance/ng212 (accessed 17 April 2024).
- Tan L, Petrie K, Deady M, Bryant RA, Harvey SB. Systematic review of first responder post-deployment or post-incident psychosocial interventions. Occup Med 2022;72:160-9.
- Hall LH, Johnson J, Watt I, Tsipa A, O’Connor DB. Healthcare staff well-being, burnout, and patient safety: a systematic review. PLOS ONE 2016;11.
- Panagioti M, Geraghty K, Johnson J, Zhou A, Panagopoulou E, Chew-Graham C, et al. Association between physician burnout and patient safety, professionalism, and patient satisfaction: a systematic review and meta-analysis. JAMA Intern Med 2018;178:1317-30.
- Hall LH, Johnson J, Watt I, O’Connor DB. Association of GP well-being and burnout with patient safety in UK primary care: a cross-sectional survey. Br J Gen Pract 2019;69:e507-14.
- National Institute for Health and Care Research . Promoting Equality, Diversity and Inclusion in Research 2022. www.nihr.ac.uk/about-us/our-key-priorities/equality-diversity-and-inclusion/ (accessed 17 April 2024).
- O’Cathain A, Croot L, Sworn K, Duncan E, Rousseau N, Turner K, et al. Taxonomy of approaches to developing interventions to improve health: a systematic methods overview. Pilot Feasibility Stud 2019;5:1-27.
- Elfeky A, Treweek S, Hannes K, Bruhn H, Fraser C, Gillies K. Using qualitative methods in pilot and feasibility trials to inform recruitment and retention processes in full-scale randomised trials: a qualitative evidence synthesis. BMJ Open 2022;12.
- Finucane E, O’Brien A, Treweek S, Newell J, Das K, Chapman S, et al. The People’s Trial: supporting the public’s understanding of randomised trials. Trials 2022;23:1-12.
- Coffey T, Duncan EM, Morgan H, Lawrie L, Gillies K. Behavioural approaches to recruitment and retention in clinical trials: a systematic mapping review. BMJ Open 2022;12.
- Green SMC, Raine E, Hall LH, Collinson M, Mason E, Gillies K, et al. Developing theory-based text messages to support retention in clinical trials: a mixed methods approach. Res Methods Med Heal Sci 2022;3:22-31.
- Mitchell EJ, Sprange K, Treweek S, Nixon E. Value and engagement: what can clinical trials learn from techniques used in not-for-profit marketing?. Trials 2022;23:1-4. https://doi.org/10.1186/s13063-022-06417-3.
- Gillies K, Kearney A, Keenan C, Treweek S, Hudson J, Brueton VC, et al. Strategies to improve retention in randomised trials. Cochrane Database Syst Rev 2021.
- Litz BT, Gibson L. Interventions Following Mass Violence and Disasters: Strategies for Mental Health Practice. New York: The Guilford Press; 2006.
- Simpson CR, Thomas BD, Challen K, De Angelis D, Fragaszy E, Goodacre S, et al. The UK hibernated pandemic influenza research portfolio: triggered for COVID-19. Lancet Infect Dis 2020;20:767-9.
- Sutton L, Rowe S, Hammerton G, Billings J. The contribution of organisational factors to vicarious trauma in mental health professionals: a systematic review and narrative synthesis. Eur J Psychotraumatol 2022;13:1-21. https://doi.org/10.1080/20008198.2021.2022278.
- Kunzler AM, Helmreich I, Chmitorz A, König J, Binder H, Wessa M, et al. Psychological interventions to foster resilience in healthcare professionals. Cochrane Database Syst Rev 2020;2020.
- Noben C, Smit F, Nieuwenhuijsen K, Ketelaar S, Gärtner F, Boon B, et al. Comparative cost-effectiveness of two interventions to promote work functioning by targeting mental health complaints among nurses: pragmatic cluster randomised trial. Int J Nurs Stud 2014;51:1321-31.
- Noben C, Evers S, Nieuwenhuijsen K, Ketelaar S, Gärtner F, Sluiter J, et al. Protecting and promoting mental health of nurses in the hospital setting: is it cost-effective from an employer’s perspective?. Int J Occup Med Environ Health 2015;28:891-900.
- Schaar GL, Swenty CF, Phillips LA, Embree JL, McCool IA, Shirey MR. Nursing sabbatical in the acute care hospital setting: A cost-benefit analysis. J Nurs Adm 2012;42:340-4.
- Moran D, Wu AW, Connors C, Chappidi MR, Sreedhara SK, Selter JH, et al. Cost–benefit analysis of a support program for nursing staff. J Patient Saf 2020;16:E250-4.
- Hogan N, Knapp M, McDaid D, Davies M, Brewin CR. Cost-effectiveness of ‘screen-and-treat’ interventions for post-traumatic stress disorder following major incidents. BMJ Open 2021;11.
- NHS Staff Survey Coordination Centre . NHS Staff Survey 2021 National Dashboards 2021.
- Hudson B, Hardy B, Henwood M, Wistow G. In Pursuit of inter-agency collaboration in the public sector. Public Manag Rev 1999;1:235-60.
Appendix 1 Chapter 4 (Quantitative) supplementary information and analyses
Part 1: definition of the ‘overall severity’ variable
The measure of ‘overall severity’ used in our regression analyses was defined from the screening questionnaires as the highest severity grade received across the questionnaires using the categorisation system illustrated in Table 29. If the scores across all available measure were consistent with the mildest severity classification for each measure (as per Routinely collected measures), a person is categorised as presenting a ‘low’ severity profile. If the person’s highest severity grade was consistent with those listed in the moderate column, a ‘moderate’ severity category was applied. If the person scored in the higher tiers of severity in at least one measure, a ‘high’ severity classification was applied. Missing data was allowed on any measure, with overall severity being calculated from the available measures. Overall severity was set as missing if all measures had missing data for that individual.
| Overall severity | PHQ-9 | GAD-7 | PCL-5 | ITQ | AUDIT | WSAS |
|---|---|---|---|---|---|---|
| Low | None; mind | None; mild | No PTSD | No PTSD/CPTSD | Low risk | Subclinical |
| Moderate | Moderate; moderately severe | Moderate | N/A | N/A | Hazardous | Significant |
| High | Severe | Severe | PTSD present | PTSD/CPTSD present | Harmful; possible dependence | Moderately severe or worse |
Part 2: regression tables for the caseness and overall severity analyses included in Chapter 4
| Predictor | OR | 95% CI | p-value | Interaction p-value | |
|---|---|---|---|---|---|
| Demographics | |||||
| Age | 1 | 0.99 | 1.01 | 0.416 | 0.525 |
| Gender (man vs. woman) | 1.02 | 0.77 | 1.36 | 0.879 | 0.744 |
| Gender (identified in another way vs. woman) | 0.75 | 0.36 | 1.62 | 0.507 | – |
| Ethnicity (ethnic minority vs. white) | 0.66 | 0.43 | 1.03 | 0.063 | 0.044 |
| ICU/critical care | 1.14 | 0.81 | 1.64 | 0.458 | 0.466 |
| Clinical vs. non-clinical | 0.67 | 0.44 | 1.01 | 0.062 | 0.024 |
| Sexual orientation (identified in another way vs. heterosexual) | 1.89 | 01.23 | 2.94 | 0.004 | 0.969 |
| Disability | 1.71 | 1.19 | 2.53 | 0.005 | 0.264 |
| Impacts of COVID | |||||
| COVID illness (home) | 1.21 | 0.97 | 1.5 | 0.094 | 0.266 |
| COVID illness (hospital) | 1.32 | 0.74 | 2.48 | 0.364 | 0.483 |
| COVID family member (home) | 1.21 | 0.96 | 1.52 | 0.11 | 0.228 |
| COVID family member (hospital) | 1.06 | 0.74 | 1.54 | 0.763 | 0.995 |
| Financial loss | 1.48 | 1.14 | 1.95 | 0.004 | 0.489 |
| Undertaking new tasks | 1.23 | 1.01 | 1.51 | 0.038 | < 0.001 |
| Seconded or re-deployed | 0.93 | 0.71 | 1.23 | 0.616 | 0.661 |
| Moved work location | 1.22 | 0.98 | 1.53 | 0.076 | 0.211 |
| Bereavement | 1.26 | 0.97 | 1.64 | 0.089 | 0.242 |
| Pre-pandemic MH concerns | |||||
| Yes (vs. no) | 2.03 | 1.62 | 2.53 | < 0.001 | 0.085 |
| Unsure (vs. no) | 1.81 | 1.37 | 2.42 | 0.001 | – |
| Predictor | OR | 95% CI | p-value | Interaction p-value | |
|---|---|---|---|---|---|
| Demographics | |||||
| Age | 0.98 | 0.97 | 0.99 | < 0.001 | 0.576 |
| Gender (man vs. woman) | 0.95 | 0.73 | 1.25 | 0.725 | 0.726 |
| Gender (other vs. woman) | 0.78 | 0.37 | 1.64 | 0.507 | – |
| Ethnicity (ethnic minority vs. white) | 1.14 | 0.74 | 1.79 | 0.547 | 0.432 |
| ICU/critical care | 1.15 | 0.83 | 1.6 | 0.406 | 0.843 |
| Clinical vs. non-clinical | 0.98 | 0.67 | 1.41 | 0.899 | 0.689 |
| Sexual orientation (identified in another way vs. heterosexual) | 1.32 | 0.92 | 1.92 | 0.13 | 0.477 |
| Disability | 1.17 | 0.85 | 1.63 | 0.33 | 0.230 |
| Impacts of COVID | |||||
| COVID illness (home) | 0.9 | 0.74 | 1.1 | 0.311 | 0.003 |
| COVID illness (hospital) | 0.82 | 0.49 | 1.38 | 0.445 | 0.68 |
| COVID family member (home) | 1.13 | 0.91 | 1.4 | 0.272 | 0.001 |
| COVID family member (hospital) | 1.39 | 0.97 | 2.01 | 0.074 | 0.715 |
| Financial loss | 1.28 | 1 | 1.64 | 0.049 | 0.649 |
| Undertaking new tasks | 1.13 | 0.94 | 1.37 | 0.194 | 0.583 |
| Seconded or re-deployed | 0.92 | 0.71 | 1.19 | 0.521 | 0.494 |
| Moved work location | 1.21 | 0.98 | 1.49 | 0.074 | 0.192 |
| Bereavement | 1.38 | 1.07 | 1.77 | 0.012 | 0.613 |
| Pre-pandemic MH concerns | |||||
| Yes (vs. no) | 2.05 | 1.66 | 2.53 | < 0.001 | 0.399 |
| Unsure (vs. no) | 1.66 | 1.28 | 2.17 | 0.001 | – |
| Predictor | OR | 95% CI | p-value | Interaction p-value | |
|---|---|---|---|---|---|
| Demographics | |||||
| Age | 1 | 0.99 | 1.01 | 0.927 | 0.73 |
| Gender (man vs. woman) | 1.09 | 0.73 | 1.65 | 0.681 | 0.633 |
| Gender (identified in another way vs. woman)a | – | – | – | – | – |
| Ethnicity (ethnic minority vs. white) | 1.89 | 0.93 | 4.15 | 0.093 | 0.296 |
| ICU/critical care | 2.23 | 1.45 | 3.52 | < 0.001 | 0.536 |
| Clinical vs. non-clinical | 0.92 | 0.49 | 1.67 | 0.781 | N/Ab |
| Sexual orientation (identified in another way vs. heterosexual) | 1.59 | 0.99 | 2.63 | 0.062 | 0.627 |
| Disability | 1.79 | 1.12 | 2.94 | 0.018 | 0.384 |
| Impacts of COVID | |||||
| COVID illness (home) | 1.00 | 0.73 | 1.37 | 0.998 | 0.821 |
| COVID illness (hospital) | 2.56 | 1.09 | 7.02 | 0.044 | 0.436 |
| COVID family member (home) | 0.98 | 0.7 | 1.37 | 0.898 | 0.273 |
| COVID family member (hospital) | 1.27 | 0.7 | 2.38 | 0.445 | 0.227 |
| Financial loss | 1.72 | 1.12 | 2.69 | 0.015 | 0.019 |
| Undertaking new tasks | 0.97 | 0.73 | 1.29 | 0.826 | 0.004 |
| Seconded or re-deployed | 1.05 | 0.73 | 1.52 | 0.797 | 0.390 |
| Moved work location | 0.98 | 0.71 | 1.37 | 0.928 | 0.762 |
| Bereavement | 1.48 | 0.97 | 2.29 | 0.072 | 0.030 |
| Pre-pandemic MH concerns | |||||
| Yes (vs. no) | 1.95 | 1.42 | 2.7 | < 0.001 | 0.623 |
| Unsure (vs. no) | 1.29 | 0.87 | 1.91 | 0.205 | – |
| Predictor | OR | 95% CI | p-value | Interaction p-value | |
|---|---|---|---|---|---|
| Demographics | |||||
| Age | 0.99 | 0.98 | 1 | 0.191 | 0.923 |
| Gender (man vs. woman) | 1.17 | 0.82 | 1.67 | 0.381 | 0.818 |
| Gender (identified in another way vs. woman) | 1.13 | 0.46 | 2.55 | 0.783 | – |
| Ethnicity (ethnic minority vs. white) | 1.32 | 0.74 | 2.3 | 0.333 | 0.263 |
| ICU/critical care | 1.44 | 0.83 | 2.45 | 0.184 | 0.844 |
| Clinical vs. non-clinical | 1.1 | 0.69 | 1.8 | 0.686 | 0.239 |
| Sexual orientation (identified in another way vs. heterosexual) | 1.20 | 0.70 | 2.00 | 0.501 | 0.211 |
| Disability | 1.32 | 0.84 | 2.03 | 0.22 | 0.522 |
| Impacts of COVID | |||||
| COVID illness (home) | 0.83 | 0.62 | 1.09 | 0.187 | 0.504 |
| COVID illness (hospital) | 1.25 | 0.6 | 2.49 | 0.539 | 0.121 |
| COVID family member (home) | 1.27 | 0.96 | 1.67 | 0.097 | 0.639 |
| COVID family member (hospital) | 1.62 | 1.06 | 2.48 | 0.025 | 0.596 |
| Financial loss | 1.57 | 1.16 | 2.13 | 0.003 | 0.382 |
| Undertaking new tasks | 1.71 | 1.31 | 2.25 | < 0.001 | 0.713 |
| Seconded or re-deployed | 1.39 | 0.97 | 1.99 | 0.07 | 0.406 |
| Moved work location | 1.49 | 1.13 | 1.95 | 0.004 | 0.043 |
| Bereavement | 1.91 | 1.41 | 2.58 | < 0.001 | 0.314 |
| Pre-pandemic MH concerns | |||||
| Yes (vs. no) | 1.59 | 1.20 | 2.11 | 0.001 | 0.34 |
| Unsure (vs. no) | 1.07 | 0.73 | 1.55 | 0.72 | – |
| Predictor | OR | 95% CI | p-value | Interaction p-value | |
|---|---|---|---|---|---|
| Demographics | |||||
| Age | 1 | 0.99 | 1.01 | 0.909 | 0.553 |
| Gender (man vs. woman) | 2.35 | 1.74 | 3.16 | < 0.001 | 0.291 |
| Gender (identified in another way vs. woman) | 1.40 | 0.54 | 3.21 | 0.455 | – |
| Ethnicity (ethnic minority vs. white) | 0.24 | 0.09 | 0.51 | 0.001 | 0.151 |
| ICU/critical care | 1.43 | 0.98 | 2.08 | 0.061 | 0.009 |
| Clinical vs. non-clinical | 1.35 | 0.87 | 2.16 | 0.19 | 0.004 |
| Sexual orientation (identified in another way vs. heterosexual) | 1.47 | 0.95 | 2.22 | 0.072 | 0.167 |
| Disability | 0.65 | 0.41 | 0.98 | 0.049 | 0.214 |
| Impacts of COVID | |||||
| COVID illness (home) | 1.07 | 0.83 | 1.37 | 0.622 | 0.77 |
| COVID illness (hospital) | 0.2 | 0.05 | 0.54 | 0.006 | 0.329 |
| COVID family member (home) | 1.1 | 0.84 | 1.42 | 0.488 | 0.476 |
| COVID family member (hospital) | 0.74 | 0.46 | 1.15 | 0.2 | 0.568 |
| Financial loss | 1.17 | 0.87 | 1.55 | 0.291 | 0.807 |
| Undertaking new tasks | 1.38 | 1.09 | 1.76 | 0.008 | 0.627 |
| Seconded or re-deployed | 0.93 | 0.67 | 1.27 | 0.648 | 0.651 |
| Moved work location | 0.71 | 0.55 | 0.93 | 0.012 | 0.943 |
| Bereavement | 1.3 | 0.97 | 1.73 | 0.07 | 0.136 |
| Pre-pandemic MH concerns | |||||
| Yes (vs. no) | 1.18 | 0.90 | 1.53 | 0.226 | 0.018 |
| Unsure (vs. no) | 1.53 | 1.12 | 2.09 | 0.008 | – |
| Predictor | OR | 95% CI | p-value | Interaction p-value | |
|---|---|---|---|---|---|
| Demographics | |||||
| Age | 0.99 | 0.98 | 1 | 0.198 | 0.061 |
| Gender (man vs. woman) | 1.12 | 0.81 | 1.56 | 0.498 | 0.498 |
| Gender (identified in another way vs. woman) | 1.42 | 0.6 | 3.88 | 0.456 | – |
| Ethnicity (ethnic minority vs. white) | 0.87 | 0.54 | 1.45 | 0.568 | 0.481 |
| ICU/critical care | 0.85 | 0.59 | 1.26 | 0.409 | 0.674 |
| Clinical vs. non-clinical | 0.66 | 0.41 | 1.03 | 0.078 | 0.2 |
| Sexual orientation (identified in another way vs. heterosexual) | 2.44 | 1.45 | 4.35 | 0.002 | 0.189 |
| Disability | 1.93 | 1.23 | 3.15 | 0.006 | 0.190 |
| Impacts of COVID | |||||
| COVID illness (home) | 1.23 | 0.96 | 1.59 | 0.1 | 0.576 |
| COVID illness (hospital) | 1.26 | 0.66 | 2.67 | 0.513 | 0.882 |
| COVID family member (home) | 1.62 | 1.24 | 2.14 | 0.001 | 0.473 |
| COVID family member (hospital) | 1.06 | 0.71 | 1.64 | 0.772 | 0.628 |
| Financial loss | 1.59 | 1.17 | 2.19 | 0.004 | 0.912 |
| Undertaking new tasks | 1.13 | 0.9 | 1.41 | 0.295 | 0.129 |
| Seconded or re-deployed | 0.83 | 0.62 | 1.13 | 0.237 | 0.195 |
| Moved work location | 1.06 | 0.83 | 1.36 | 0.643 | 0.839 |
| Bereavement | 1.08 | 0.81 | 1.45 | 0.595 | 0.173 |
| Pre-pandemic MH concerns | |||||
| Yes (vs. no) | 2.29 | 1.77 | 2.97 | < 0.001 | 0.018 |
| Unsure (vs. no) | 1.71 | 1.25 | 2.37 | 0.001 | – |
| Predictor | OR | 95% CI | p-value | Interaction p-value | |
|---|---|---|---|---|---|
| Demographics | |||||
| Age | 0.99 | 0.98 | 1.00 | 0.05 | 0.91 |
| Gender (man vs. woman) | 1.07 | 0.82 | 1.40 | 0.62 | 0.83 |
| Gender (identified in another way vs. woman) | 1.07 | 0.52 | 2.25 | 0.86 | – |
| Ethnicity (ethnic minority vs. white) | 0.85 | 0.56 | 1.32 | 0.47 | 0.19 |
| ICU/critical care | 1.28 | 0.92 | 1.81 | 0.15 | 0.60 |
| Clinical vs. non-clinicala | 0.81 | 0.56 | 1.16 | 0.26 | Not computable |
| Sexual orientation (identified in another way vs. heterosexual) | 1.75 | 1.22 | 2.63 | 0.004 | 0.28 |
| Disability | 1.70 | 1.21 | 2.41 | 0.003 | 0.58 |
| Impacts of COVID | |||||
| COVID illness (home) | 1.18 | 0.97 | 1.45 | 0.11 | 0.19 |
| COVID illness (hospital) | 1.44 | 0.83 | 2.61 | 0.21 | 0.93 |
| COVID family member (home) | 1.31 | 1.06 | 1.63 | 0.01 | 0.13 |
| COVID family member (hospital) | 1.18 | 0.83 | 2.61 | 0.21 | 0.82 |
| Financial loss | 1.84 | 1.43 | 2.39 | < 0.001 | 0.92 |
| Undertaking new tasks | 1.19 | 0.99 | 1.44 | 0.06 | 0.04 |
| Seconded or re-deployed | 1.04 | 0.81 | 1.35 | 0.76 | 0.42 |
| Moved work location | 1.15 | 0.94 | 1.41 | 0.19 | 0.22 |
| Bereavement | 1.25 | 0.98 | 1.60 | 0.07 | 0.30 |
| Pre-pandemic MH concerns | |||||
| Yes vs. no | 2.11 | 1.72 | 2.59 | < 0.001 | 0.15 |
| Yes vs. unsure | 1.43 | 1.08 | 1.90 | 0.01 | – |
Part 3: supplementary linear regression analyses focusing on continuous outcomes/total scores
In these supplementary analyses, screening measure outcome scores were regressed on sociodemographic and keyworker features. As in our caseness analyses, each regression model was adjusted for site and a test of interaction between the feature and site was performed, to test whether there is evidence the association differs between Hubs.
The results of these supplementary linear regression analyses are reported below, and grouped according to the potential predictor/risk factor tested, alongside a brief summary of the finding of each group of analyses.
| Scale | Coefficient | 95% CI | p-value | Interaction p-value | |
|---|---|---|---|---|---|
| PHQ-9 | −0.01 | −0.04 | 0.01 | 0.323 | 0.756 |
| GAD-7 | −0.06 | −0.08 | −0.04 | < 0.001 | 0.888 |
| PCL-5 | 0.04 | −0.07 | 0.14 | 0.462 | 0.654 |
| ITQ | −0.02 | −0.05 | 0.01 | 0.248 | 0.946 |
| AUDIT | −0.01 | −0.03 | 0.01 | 0.477 | 0.515 |
| WSAS | 0 | −0.04 | 0.03 | 0.916 | 0.394 |
Summary: There was evidence of decreasing GAD-7 scores with increasing age.
| Scale | Coefficient | 95% CI | p-value | Interaction p-value | |
|---|---|---|---|---|---|
| PHQ-9 | −0.62 | −1.86 | 0.63 | 0.333 | 0.13 |
| GAD-7 | 0.1 | −1.07 | 1.27 | 0.869 | 0.44 |
| PCL-5 | 3.86 | −1.64 | 9.36 | 0.169 | 0.864 |
| ITQ | −0.77 | −2.5 | 0.97 | 0.387 | 0.830 |
| AUDIT | −3.4 | −4.57 | −2.23 | < 0.001 | 0.176 |
| WSAS | 0.82 | −1.03 | 2.67 | 0.386 | 0.303 |
Summary: There was evidence of decreased AUDIT score for individuals from ethnic minority groups compared to white individuals.
| Scale | Coefficient | 95% CI | p-value | Interaction p-value | |
|---|---|---|---|---|---|
| PHQ-9 | 0.54 | −0.37 | 1.46 | 0.244 | 0.807 |
| GAD-7 | 0.84 | −0.02 | 1.7 | 0.055 | 0.911 |
| PCL-5 | 5.95 | 2.71 | 9.2 | < 0.001 | 0.578 |
| ITQ | 0.83 | −0.74 | 2.40 | 0.302 | 0.974 |
| AUDIT | 1.05 | 0.15 | 1.95 | 0.022 | 0.006 |
| WSAS | −1.3 | −2.68 | 0.08 | 0.064 | 0.943 |
Summary: There was evidence of higher PCL-5 and AUDIT scores for ICU/critical care workers compared to other NHS participants. Interaction present for AUDIT: ICU working associated with greater increase in AUDIT at Site A.
| Scale | Coefficient | 95% CI | p-value | Interaction p-value | |
|---|---|---|---|---|---|
| PHQ-9 | 0.22 | −0.55 | 0.99 | 0.57 | 0.042 |
| GAD-7 | −0.22 | −0.94 | 0.5 | 0.555 | 0.698 |
| PCL-5 | 1.61 | −1.7 | 4.92 | 0.341 | 0.515 |
| ITQ | −0.10 | −1.18 | 0.99 | 0.862 | 0.686 |
| AUDIT | 1.95 | 1.23 | 2.68 | < 0.001 | 0.165 |
| WSAS | 0.94 | −0.2 | 2.08 | 0.107 | 0.18 |
Summary: There is evidence of increased AUDIT scores for male compared to female participants.
| Scale | Coefficient | 95% CI | Interaction p-value | |
|---|---|---|---|---|
| PHQ-9 | 0.01 | −2.15 | 2.18 | 0.99 |
| GAD-7 | −0.48 | −2.52 | 1.55 | 0.642 |
| PCL-5 | 23.94 | 5.07 | 42.82 | 0.013 |
| ITQ | 0.59 | −1.93 | 3.10 | 0.647 |
| AUDIT | 0.73 | −1.2 | 2.66 | 0.461 |
| WSAS | 0.92 | −2.26 | 4.1 | 0.571 |
Summary: No clear evidence of differences, although some estimates are clearly imprecise due to small numbers.
| Scale | Coefficient | 95% CI | p-value | Interaction p-value | |
|---|---|---|---|---|---|
| PHQ-9 | −1.25 | −2.25 | −0.25 | 0.014 | 0.148 |
| GAD-7 | −0.97 | −1.91 | −0.03 | 0.043 | 0.588 |
| PCL-5 | −3.88 | −7.68 | −0.07 | 0.046 | 0.9 |
| ITQ | −0.75 | −2.36 | 0.85 | 0.358 | 0.302 |
| AUDIT | −1.53 | −2.55 | −0.52 | 0.003 | 0.624 |
| WSAS | −2.21 | −3.7 | −0.71 | 0.004 | 0.349 |
Summary: Heterosexual participants presented reduced PHQ-9, GAD-7, PCL-5, AUDIT and WSAS compared to participants who identified in another way.
| Scale | Coefficient | 95% CI | p-value | Interaction p-value | |
|---|---|---|---|---|---|
| PHQ-9 | 1.39 | 0.49 | 2.29 | 0.003 | 0.685 |
| GAD-7 | 0.52 | −0.31 | 1.35 | 0.216 | 0.996 |
| PCL-5 | 6.76 | 2.84 | 10.68 | 0.001 | 0.36 |
| ITQ | 0.16 | −1.21 | 1.53 | 0.818 | 0.645 |
| AUDIT | −0.9 | −1.8 | 0 | 0.049 | 0.089 |
| WSAS | 3.14 | 1.77 | 4.51 | < 0.001 | 0.222 |
Summary: Evidence of increased PCL-5, PHQ-9, WSAS and of reduced AUDIT for persons who reported having a disability.
| Scale | Coefficient | 95% CI | p-value | Interaction p-value | |
|---|---|---|---|---|---|
| PHQ-9 | 0.46 | −0.12 | 1.05 | 0.122 | 0.249 |
| GAD-7 | −0.44 | −0.99 | 0.11 | 0.115 | 0.002 |
| PCL-5 | 0.08 | −2.5 | 2.65 | 0.954 | 0.178 |
| ITQ | −0.38 | −1.21 | 0.44 | 0.358 | 0.022 |
| AUDIT | −0.04 | −0.6 | 0.51 | 0.886 | 0.87 |
| WSAS | 1.02 | 0.15 | 1.89 | 0.022 | 0.509 |
Summary: Evidence of increased WSAS. There was a significant interaction for GAD-7 analysis, indicating that having COVID resulted in lower GAD-7 in Site C compared to other Hubs.
| Scale | Coefficient | 95% CI | p-value | Interaction p-value | |
|---|---|---|---|---|---|
| PHQ-9 | 1.53 | 0.03 | 3.04 | 0.046 | 0.346 |
| GAD-7 | −0.63 | −2.04 | 0.78 | 0.382 | 0.369 |
| PCL-5 | 5.94 | −0.35 | 12.22 | 0.064 | 0.189 |
| ITQ | 1.15 | −1.03 | 3.34 | 0.301 | 0.420 |
| AUDIT | −3.11 | −4.53 | −1.69 | < 0.001 | 0.398 |
| WSAS | 2.9 | 0.65 | 5.14 | 0.011 | 0.692 |
Summary: Evidence of increased PHQ-9 and WSAS scores, and reduced AUDIT scores.
| Scale | Coefficient | 95% CI | p-value | Interaction p-value | |
|---|---|---|---|---|---|
| PHQ-9 | 0.76 | 0.15 | 1.37 | 0.015 | 0.14 |
| GAD-7 | 0.47 | −0.1 | 1.05 | 0.107 | 0.003 |
| PCL-5 | −0.15 | −2.93 | 2.62 | 0.913 | 0.241 |
| ITQ | 0.89 | 0.05 | 1.73 | 0.038 | 0.686 |
| AUDIT | −0.1 | −0.67 | 0.48 | 0.738 | 0.214 |
| WSAS | 1.47 | 0.55 | 2.38 | 0.002 | 0.229 |
Summary: Increased PHQ-9, WSAS and ITQ. Having a family member with COVID-19 resulted in particularly elevated GAD-7 at Site D compared to other sites.
| Scale | Coefficient | 95% CI | p-value | Interaction p-value | |
|---|---|---|---|---|---|
| PHQ-9 | 0.74 | −0.27 | 1.74 | 0.152 | 0.346 |
| GAD-7 | 1.06 | 0.12 | 2 | 0.027 | 0.369 |
| PCL-5 | 2.56 | −2.28 | 7.4 | 0.299 | 0.189 |
| ITQ | 1.89 | 0.57 | 3.22 | 0.005 | 0.877 |
| AUDIT | −1.03 | −1.94 | −0.11 | 0.029 | 0.398 |
| WSAS | 1.52 | 0.03 | 3.02 | 0.046 | 0.692 |
Summary: Evidence of increased GAD-7, ITQ and WSAS scores, as well as reduced AUDIT scores.
| Scale | Coefficient | 95% CI | p-value | Interaction p-value | |
|---|---|---|---|---|---|
| PHQ-9 | 1.42 | 0.72 | 2.12 | < 0.001 | 0.954 |
| GAD-7 | 1 | 0.35 | 1.65 | 0.003 | 0.72 |
| PCL-5 | 4.97 | 1.62 | 8.31 | 0.004 | 0.181 |
| ITQ | 1.05 | 0.12 | 1.98 | 0.026 | 0.759 |
| AUDIT | 0.36 | −0.29 | 1.01 | 0.273 | 0.366 |
| WSAS | 2.58 | 1.54 | 3.62 | < 0.001 | 0.962 |
Summary: Evidence of increased PHQ-9, GAD-7, PCL-5, ITQ and WSAS scores.
| Scale | Coefficient | 95% CI | p-value | Interaction p-value | |
|---|---|---|---|---|---|
| PHQ-9 | 0.24 | −0.3 | 0.78 | 0.391 | 0.804 |
| GAD-7 | 0.46 | −0.05 | 0.96 | 0.079 | 0.816 |
| PCL-5 | 0.07 | −2.24 | 2.39 | 0.952 | 0.029 |
| ITQ | 1.52 | 0.76 | 2.29 | > 0.001 | 0.729 |
| AUDIT | 1 | 0.47 | 1.52 | < 0.001 | 0.259 |
| WSAS | 0.46 | −0.35 | 1.26 | 0.265 | 0.411 |
Summary: Evidence of increased ITQ and AUDIT scores.
| Scale | Coefficient | 95% CI | p-value | Interaction p-value | |
|---|---|---|---|---|---|
| PHQ-9 | −0.08 | −0.82 | 0.65 | 0.824 | 0.745 |
| GAD-7 | 0.14 | −0.55 | 0.83 | 0.687 | 0.508 |
| PCL-5 | 2.38 | −0.56 | 5.33 | 0.113 | 0.619 |
| ITQ | 1.34 | 0.25 | 2.44 | 0.016 | 0.787 |
| AUDIT | 0.37 | −0.32 | 1.07 | 0.294 | 0.793 |
| WSAS | −0.42 | −1.51 | 0.67 | 0.449 | 0.806 |
Summary: Evidence of increased ITQ scores.
| Scale | Coefficient | 95% CI | p-value | Interaction p-value | |
|---|---|---|---|---|---|
| PHQ-9 | 0.61 | 0.01 | 1.2 | 0.046 | 0.022 |
| GAD-7 | 0.67 | 0.11 | 1.23 | 0.019 | 0.015 |
| PCL-5 | 1.67 | −1.01 | 4.34 | 0.221 | 0.487 |
| ITQ | 1.12 | 0.30 | 1.93 | 0.007 | 0.191 |
| AUDIT | −0.41 | −0.96 | 0.15 | 0.148 | 0.735 |
| WSAS | 0.29 | −0.59 | 1.18 | 0.517 | 0.594 |
Summary: Evidence of increased PHQ-9, GAD-7 and ITQ scores.
| Scale | Coefficient | 95% CI | p-value | Interaction p-value | |
|---|---|---|---|---|---|
| PHQ-9 | 0.7 | 0.00 | 1.41 | 0.05 | 0.377 |
| GAD-7 | 0.92 | 0.26 | 1.58 | 0.006 | 0.813 |
| PCL-5 | 4.29 | 0.95 | 7.64 | 0.012 | 0.276 |
| ITQ | 2.18 | 1.26 | 3.11 | < 0.001 | 0.077 |
| AUDIT | 0.41 | −0.25 | 1.07 | 0.226 | 0.218 |
| WSAS | 0.82 | −0.23 | 1.87 | 0.125 | 0.108 |
Summary: Evidence of increased GAD-7, PCL-5 and ITQ scores. Weaker evidence of increased PHQ-9 scores.
| Scale | Coefficient | 95% CI | p-value | Interaction p-value | |
|---|---|---|---|---|---|
| PHQ-9 | 2.36 | 1.79 | 2.94 | < 0.001 | 0.049 |
| GAD-7 | 2.16 | 1.63 | 2.7 | < 0.001 | 0.18 |
| PCL-5 | 6.48 | 3.92 | 9.04 | < 0.001 | 0.668 |
| ITQ | 1.87 | 1.07 | 2.66 | < 0.001 | 0.038 |
| AUDIT | 0.87 | 0.31 | 1.43 | 0.002 | 0.266 |
| WSAS | 2.87 | 2.02 | 3.73 | < 0.001 | 0.007 |
Summary: Evidence of increased scores across all measures. Interaction analyses indicating that at Site D reporting pre-pandemic emotional well-being concerns was associated with particularly high WSAS scores.
| Scale | Coefficient | 95% CI | p-value | |
|---|---|---|---|---|
| PHQ-9 | 1.39 | 0.57 | 2.2 | 0.001 |
| GAD-7 | 1.52 | 0.75 | 2.28 | < 0.001 |
| PCL-5 | 1.69 | −1.48 | 4.87 | 0.296 |
| ITQ | 0.13 | −1.16 | 1.42 | 0.846 |
| AUDIT | 1.11 | 0.31 | 1.92 | 0.007 |
| WSAS | 1.44 | 0.22 | 2.66 | 0.021 |
Summary: Evidence of increased PHQ-9, GAD-7, AUDIT and WSAS scores.
Part 4: comorbidity analyses
The table below illustrates, for each site, a cumulative breakdown of the number of participants meeting ‘caseness’ criteria across multiple domains assessed via the standardised mental health and functioning screening tools administered at the four sites. Please note that Site B only administered four standardised tools (i.e. the AUDIT was not included in the screening offer of this Hub; see the Service Mapping chapter of the report) and therefore participants at this site could not meet caseness across five domains.
| Site A (n = 475) | Site B (n = 367) | Site C (n = 400) | Site D (n = 731) | Total (n = 1973) | |
|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | n (%) | |
| 0 | 24 (5.1) | 23 (7.1) | 29 (7.3) | 128 (17.5) | 204 (10.6) |
| 1 domain | 39 (8.2) | 41 (12.6) | 62 (15.5) | 121 (16.6) | 263 (13.6) |
| 2 domains | 64 (13.5) | 46 (14.2) | 73 (18.3) | 124 (17.0) | 307 (15.9) |
| 3 domains | 94 (19.8) | 91 (28) | 110 (27.6) | 153 (20.9) | 448 (23.2) |
| 4 domains | 185 (38.9) | 124 (38.2) | 95 (23.8) | 165 (22.6) | 569 (29.5) |
| 5 domains | 69 (14.5) | 0 (0) | 30 (7.5) | 40 (5.5) | 139 (7.2) |
| Missing | 0% | 10.2% | 0.3% | 0% | 2.2% |
Appendix 2 Chapter 5 (Health economics) supplementary information and analyses
Part 1: economic evaluation exploration
This appendix details the work undertaken to assess the feasibility of conducting an economic evaluation for Resilience Hubs. If it was decided that it was feasible, the objective was to synthesise the data (health status and service use) collected from keyworkers accessing Resilience Hub support, and the wider published evidence, within a decision-analytic model to explore whether Resilience Hubs are potentially cost-effective compared to usual care (no Resilience Hub provision).
Methods
To determine whether a robust and informative economic model would be viable, the work focused on the following key aspects: (1) whether a model structure could accurately reflect the service impact of varied Resilience Hub designs; (2) whether a comparator could be defined; and (3) whether the value of the Resilience Hub could be quantified using existing data sources. The methods applied to answer these questions are described below.
Review of prior economic evaluations
An electronic search of the Medline database was conducted in October 2021 to identify full economic evaluations of mental health interventions for health and social care workers, published in the last 15 years. Search terms for health and social care workers and mental health issues were taken from a published Cochrane review146 and were combined with search terms for economic evaluation. This review aimed to assess the current evidence base to determine whether interventions for health and social care workers have been found to be cost-effective, and to identify limitations of the existing evidence base.
Further targeted reviews were conducted to identify relevant and recent (published within the last 10 years) economic evaluations, conducted within the UK, of forms of support that were reported in the service use questionnaire. Terms relating to economic evaluation and the other study criteria (e.g. support type, such as CBT, IAPT, counselling, EMDR) were compiled to create search strings. These targeted reviews aimed to identify published evidence that may help to inform ideas for an economic model structure, or to provide supplementary data to feed into a potential economic evaluation for the Hubs.
Review of qualitative data
A key limitation of the evidence collected to date is the lack of data on a comparator arm. To help define what the counterfactual might be (i.e. what is the alternative to the Resilience Hub), the data from qualitative interviews with keyworkers were reviewed with a specific focus on questions related to this matter (e.g. ‘did you seek support elsewhere?’, ‘have you got support for you mental health or well-being in the past’, and ‘where would you normally get support for your well-being?’). Data were summarised descriptively. Note the qualitative research (Objective 3) is reported in Chapter 6 of the main report.
Service/care pathway review
Care pathways, processes and service offerings from Hubs were reviewed to aid ideas for a model structure. A problem-orientated conceptual model was drafted to reflect the decision problem and service pathways, probable complexities, and to aid discussion around the possible development of an economic model structure. It should be noted that development of the conceptual model focused on individual support alone, to reflect the data collected from this study (i.e. from keyworkers accessing individual support). While it is recognised that the team support offered by Hubs may have substantial benefits (e.g. increasing engagement with forms of support), these will likely remain unquantifiable without considerable data collection and may be difficult to accurately capture. For example, as the impact of team support will have a knock-on effect as people who attend may feedback their techniques and advise to their colleagues but without making a record of this. It is important to note that there is no standard design of service provision for the Hubs or alternative care services. Accordingly, the conceptual model is a simplification only. For example, it is understood that one Hub focuses on pastoral care, however as this was not common across Hubs, it has been excluded here.
Staff consultation and expert reference group feedback
Two meetings were held with the Staff Consultation Group, and Site D’s expert reference group in October and November 2021. Within these meetings, participants were firstly introduced to the topic of economic evaluation and then asked to discuss several questions to help inform the potential approach to economic evaluation, which included: (1) what are the key health states and events that might need to be reflected in an economic model; (2) what are the key outcomes related to Hub support; and (3) in the absence of a Resilience Hub what would the target population access. Following the meetings, an online survey was distributed to attendees to obtain additional responses to key questions with the feedback contributing to the development of the logic model.
Summary
It was determined throughout the project that a robust economic evaluation, which could adequately reflect the value of the Resilience Hub, was not feasible with the current evidence base. An overview of the challenges related to conducting an economic evaluation is reported in the Results section, with steps for future research.
Results
Review of prior economic evaluations
Following screening only four studies were identified as relevant (i.e. focusing on mental health intervention in populations of health and social care workers). 147–150 The identified studies are summarised in Table 56.
| Publication | Noben et al.147 | Noben et al.148 | Schaar et al.149 | Moran et al.150 |
|---|---|---|---|---|
| Study type and stated economic evaluation type | Pragmatic cluster randomised controlled trial with cost-effectiveness analysis | Pragmatic cluster trial with cost–benefit analysis | Hypothetical cost–benefit analysis | Markov model with cost–benefit analysis |
| Perspective | Societal | Employer | Employer | Employer |
| Population (sample size if applicable) | Nurse (n = 617) in the Netherlands | Nurses (n = 413) in the Netherlands | Nurses in the USA | Nurses in the USA |
| Intervention(s) | Mental health screening with feedback and consultation with occupational physician Mental health screening with feedback and enrolment on an e-mental health module |
Mental health screening with feedback and consultation with an occupational physician | 12-week nursing sabbatical (12 weeks) | Resilience in stressful events (RISE) support program – a peer support programme used in the John Hopkins Hospital |
| Comparator | Mental health screening without feedback | Mental health screening without feedback | No sabbatical | No support programme |
| Time horizon | 6 months | 6 months | 1 year | 1 year |
| Measure of benefit | Work functioning (Nurses Work Functioning Questionnaire) | Workforce productivity (absenteeism and presenteeism) | Staff retention | Loss of labour (staff retention) and workforce productivity (time off) |
| Included costs | Intervention, direct medical, and non-medical and lost productivity (presenteeism and absenteeism) | Intervention and productivity (absenteeism and presenteeism) | Nursing staff including salary, turnover, sabbatical and replacement | Nursing staff |
| Key study results | Occupational physician intervention was dominant (i.e. net cost saving and net health gains) versus control E-mental health intervention was €4054 (added costs) per treatment responder |
Intervention led to cost reductions related to absenteeism and presenteeism resulted in net savings | Intervention had a cost–benefit ratio of 1.7 compared to control, that is the cost of the sabbatical was more than offset by savings related to staff turnover | The RISE intervention was associated with a net monetary benefit saving of US $22,576 per nurse |
All four identified studies suggested that the implementation of mental health interventions could result in economic benefits, and it was also frequently reported that savings (related to productivity) could offset intervention costs. However, there are substantial limitations which limit the usefulness of the evidence base in practice. Most notably, the review identified a paucity of evidence, with only four studies identified (two of which were closely related) which all focused on nursing staff in only two countries. Two studies used data from a single RCT, which is a robust source of evidence, but reflective of a restricted population (one Dutch academic medical centre). 147,148 The modelling study by Moran et al (2020) took key parameters from a survey with only 36 nurse participants at a single hospital, which has not only a restricted population, but was also based on hypothetical questions, which may not reflect reality. 150 The earliest identified study was based on a hypothetical situation, driven by assumptions, and did not use any data from research studies. 149 The health and social care workforce are a diverse and varied group; hence the reliance of the evidence base on very limited (or no) evidence is a concern. No studies were identified for periods either during or closely after an epidemic or pandemic when the feasibility, costs and benefits associated with implementing support are likely to be very different. For example, the ability to roll out a sabbatical scheme during a global pandemic may be impossible when services are under increased pressure. Other notable limitations included restrictive perspectives, limited cost categories included across studies, time horizons and uncertainty in the evidence base. Unfortunately, none of these studies could be used to inform the economic model for the Resilience Hubs project as they were not generalisable to the specific study context. The review did, however, identify that there are substantial limitations in the current evidence base and that more research (e.g. on a range of interventions and across more settings) is needed.
Additional targeted reviews were conducted to identify relevant economic evaluations, in more general populations (i.e. not restricted to health and social care workers), to support ideas for model structures and possible supplementary parameters. Typically, model designs for interventions of this type focus on treatment completion, and subsequent response and remission. One particularly relevant study was identified, which evaluated the cost-effectiveness of a ‘screen-and-treat’ intervention for post-traumatic stress following major incidents was identified. 151 This is highly relevant to our study as one example of a service of this type is a Resilience Hub. Furthermore, the services included in this economic evaluation aim to identify a need for additional care and provide or refer participants to additional services, in the same way as the Resilience Hubs work for keyworkers affected by the pandemic. This study applied a simple decision tree structure to model patient outreach (which included screening) compared to no outreach (the comparator). In the outreach arm, patients were screened and could subsequently receive CBT. CBT uptake, completion and recovery rates were taken from the published literature, as was the rate of spontaneous remission. The comparator arm of the model was assumed to receive no treatment, unless they were identified through conventional routes (e.g. primary care). Due to a lack of available data, the authors were required to make assumptions around parameters (e.g. utility values chosen). While a useful example, the decision problem is more easily simplified when compared with Resilience Hubs as the population accessing the intervention are more heterogeneous.
Review of qualitative data
Across both groups (participants who accessed Resilience Hub support and those who did not), there were some common services or support cited, including friends and family (n = 29), counselling (n = 14), occupational health services (n = 10) and GP support (n = 8). Similarly, across both groups, multiple services and sources of mental health/well-being support were cited. For instance, respondents commonly cited accessing more formal sources of support, such as therapy or counselling, alongside more informal sources, such as discussions with friends and family. The sources of support cited were also highly varied, including things such as GP consultations, hobbies and exercise. Therefore, difficulties arise when attempting to identify a single resource or service to use as a comparator as people often access a multitude of services. To select a single service or resource as a comparator would mean that other forms of support are overlooked, reducing the accuracy of the analysis.
Keyworkers who did not access Resilience Hub support were asked to report on services which they had ever accessed previously, with counselling (n = 11), medication (n = 3), occupational health (n = 2), workplace well-being (n = 2) and GP (n = 2) being the most cited. In contrast, Hub keyworkers were asked to report any alternative services which they considered, during the pandemic, with occupational health (n = 8), GP (n = 6) and counselling (n = 5), being the most common. As some services may have been more difficult to access during the pandemic, the time of consideration for the questions may have had an impact on the alternative services cited by respondents. For instance, more Hub keyworkers cited occupational health, a service accessed through their employer, than non-Hub keyworkers. However, while this could be due to other services being unavailable or more difficult to access, the exact cause of the observed difference is difficult to determine and presents an additional challenge when attempting to select an appropriate comparator for analysis.
Both Hub (n = 7) and non-Hub (n = 4) keyworkers cited feelings of depression as a reason for seeking support. More Hub clients cited workplace stressors (n = 9) as the main reasons for accessing support, while more non-Hub clients cited experiencing a notable deterioration in their mental health (n = 9). These differences may be influenced by when support was last accessed. For instance, the Hub clients had generally more recently accessed services and may therefore have a better recall as to the specific reasons as to when and why they were accessing support.
Service/care pathway review
The conceptual model, which focuses on service pathways, is presented in Figure 6.
FIGURE 6.
Resilience Hub problem-orientated conceptual model for individual support.

The conceptual model demonstrates the possible routes for transitioning through the service pathway and subsequently, the complexity of Hub provision (and alternatives to Hub provision). The conceptual model illustrates (albeit in a simplified format) potential routes through service support. There are many stages within the model where a keyworker may be discharged from the service, or may remain in the service but progress to another support type, or be referred outwards for further support. The decision on whether support is needed will be based on interactions between staff and the keyworker and will likely be based on discussion and screening questionnaires. The treatments provided are variable, as is the length of treatment. Furthermore, waiting times are likely to differ across services accessed (Hubs, as well as wider NHS). It is assumed that in the absence of a Hub, keyworkers would transition through similar pathways (e.g. through an alternative service such as IAPT); however, in reality, the comparator is likely to be highly variable and may include a proportion of keyworkers accessing no support. Furthermore, keyworkers may access services through more direct routes (e.g. they may go straight to therapy if paying for this privately), although some more direct routes of access are likely to be less common (e.g. due to the financial costs typically associated with these options). It is also useful to note that while keyworkers are within a service, they may also access wider services (e.g. a keyworker accessing Hub support may also use wider materials or private therapy options). So, the conceptual model focuses on a limited range of service use. There is likely to be interaction between Hubs and wider NHS and private services (e.g. some Hubs commission private treatment for keyworkers if other options are unavailable to avoid long wait times), as well as interactions between the support offered or accessed initially and subsequent Hub access. This may suggest that a discrete event simulation (DES) or similar model structure is required. While more flexible in terms of capturing events (e.g. services accessed) over time, these models are data hungry.
In reality there is variation across the Hubs and any alternative services accessed, which adds complexity to this conceptual model. For example, for the Hub support, there is no standard service provision (e.g. some services may be offered internally in some Hubs, whereas other Hubs may instead focus on facilitating keyworker access to appropriate external services). It is anticipated that Hub support will affect the service pathway in multiple ways: (1) the proportion of keyworkers accessing support, (2) when keyworkers access support and time to receive support and (3) support/interventions received both in and out of the Hub. This will subsequently affect key costs and health outcomes included in any future economic evaluation.
Staff consultation and expert reference group feedback
The stakeholder groups found it particularly challenging to define key health states for any economic modelling, as people will have varied reasons for accessing Hub support and maybe find it difficult to clearly state a single reason (e.g. anxiety or trauma). Key events discussed included accessing Hub support, receiving a diagnosis (if relevant), proceeding with mental health care (including referral to different services), completion of activities and discharge. The groups also noted that the time taken from referral to treatment initiation was important, as well as accessing other services (e.g. if effective Hub services could prevent A and E visits and hospitalisations). Typically, economic evaluation focuses on quality-adjusted life-years, however a wider range of potential short-, medium- and long-term outcomes associated with Hub support were mentioned by the groups and it was also discussed that the outcomes affect a range of people/perspectives, not just the Hub client. Hub client key outcomes were commented to be reassurance, burnout, reducing the use of unhelpful or unhealthy coping mechanisms (e.g. alcohol use, smoking) and confidence at work. Outcomes related to friends and family, such as the quality of relationships and ability to conduct caring responsibilities, were noted. There was also an emphasis placed on outcomes of interest to employers; including productivity, staff retention, workplace incidents (e.g. accidents in the workplace, which are related to patient care) and workplace complaints. Furthermore, it was discussed that the presence of a Hub may have an impact on the wider culture of well-being in the health and social care/keyworker landscape. Feedback received was varied. In some instances, the groups thought no alternative services would be relevant (i.e. health and social care staff would not access services unprompted). Listed services included occupational health, employee programmes, therapy through the NHS and non-NHS services, and charity support (e.g. the Samaritans). To summarise, from the staff consultation and expert reference group feedback it was clear that any decision model would struggle to be able to reflect all outcomes and potential comparators to the Resilience Hubs.
Summary
The key challenges for any economic evaluation are outlined in Table 57.
| Challenge | Description |
|---|---|
| Access to baseline data | While screening data are available from the Hubs, there were no measures collected at screening (baseline) and follow-up. In particular, for any economic evaluation we do not have baseline EQ-5D data available to estimate a change in utility resulting from accessing Resilience Hub support. |
| Comparator definition | There is no clear comparator to the Resilience Hubs. Following a review of the qualitative data and feedback received by the staff consultation and expert reference groups, concludes that the alternative is likely to be highly variable (e.g. from talking to family and friends, to alternative services), and may include no support at all (e.g. people would not access support unless prompted). Discussion with Hub teams highlighted that prior to the Hub support staff/keyworker needs were not consistently met with defined care services. In addition, during the pandemic many mental health services faced disruption and subsequently may not have been accessible to this group (i.e. in reality the comparator is likely to include a proportion of the population not receiving support). One key advantage of the Hubs may be that they lead to people accessing care faster and better engagement with healthcare services, however, without more comprehensive data on a comparator arm this would not be quantifiable. This may lead to any economic evaluation work capturing the impact of Resilience Hubs on costs but not capturing the true associated impact on health benefit. |
| Variation in reasons for accessing Hub support | Hubs support different occupational groups, and the goal is to offer psychological support to any keyworker who requires it. This is a varied group; as there is no single defined mental health condition, and there will be a range of keyworkers accessing services with a range of different mental health conditions (and potentially multiple mental health needs), as well as a range of severity of symptoms. Additionally, while Hubs were initially funded to provide COVID-related support, some expanded their scope to offer more general psychological support to keyworkers. |
| Hub service model variation | As described in the service mapping chapter and partially reflection in the problem-orientated conceptual model, there is substantial variation across Hubs. This creates complexity for economic model as there are no common pathways of care and differences in Hub design (e.g. what is provided in house versus what is an outward referrals) would be reflected in different outcomes, however there is no data to model this. Furthermore, it may be unhelpful to suggest that Hub support is standardised for any economic modelling work as a key benefit of the Hubs is that they can adapt their design to meet the needs of their served population and the available services in the local area. |
| Range of key outcomes and data availability | As noted in the logic model and the feedback from the Staff Consultation Group and expert reference groups, there are a number of outcomes (related to workers accessing the Hubs and wider perspectives) that we are unlikely to find any data to support. An expert panel consensus publication introduces the need for economic evaluation to adapt during the COVID-19 pandemic.98 While noting that the key principles of economic evaluations remain the same, the authors discuss how for interventions related to COVID-19 several additional elements of value (outside of the traditional quality-adjusted life-year) may need to be reflected. While the paper focuses on interventions targeted towards COVID-19 some of which (equity, family spillover effects and a societal perspective) are highly relevant to the Hubs economic evaluation. However, data would not be available to quantify these within an economic evaluation for the Hubs. |
| Furthermore, there is no evidence to date which quantifies the impact of Hub support on the population served. While data from other services could be used, there is likely limited generalisability to this specific population and to the pandemic. While it could be assumed equal to published evidence for other services or treatments (e.g. CBT) this would reduce the validity of the work. Additionally, there may be a benefit to receiving support via a Hub as it is tailored to keyworkers (rather than via other services) which could be reflected in outcomes that would not be captured. | |
| Ongoing changes to services and the needs of the population | Hub services are evolving over time (e.g. changing methods for allowing keyworkers to register). As a further complication, due to the pandemic, the needs of the population are continuously changing. Therefore, the value of a static estimate of cost-effectiveness could be debated as it will be outdated immediately. The economic evaluation would also note capture the benefit of having Hubs organised to react in new disasters/emergencies for other populations (e.g. terrorism, wars, future pandemics). |
Reflecting on the key questions posed prior to the research
Can a model structure accurately reflect the service impact of varied Resilience Hub designs?
Simplifications could be made to a model structure to account for some of the variation in Hub design (i.e. to reflect the core components included across the majority of Hubs). However, it is unlikely that a model structure could reflect all of the differences between Hubs. Furthermore, as the Hubs evolve over time, it is likely that any modelling would become outdated (e.g. as services change how they allow keyworkers to self-refer to the services).
Can a comparator for the Resilience Hubs be defined and populated?
The range of support accessed in the absence of the Resilience Hub is likely to be varied (e.g. from something as minimal as support from family and friends to more intensive therapy options). Rather than being a simple case of comparing one intervention to another, it is likely that the Resilience Hub support impacts the proportion of keyworkers accessing support, the time taken to receive support, and the type/mix of support services received.
Can a model reflecting the value of the Resilience Hubs be parameterised using existing data sources?
The value of the Hubs is likely to be broad and to comprehensively reflect the value, outcomes included in an economic evaluation may need to extend outside of the typical outcomes considered in a UK cost-effectiveness study. For example, productivity and staff retention may be important. Furthermore, as keyworkers access the service for different reasons, an economic evaluation would need to reflect this (e.g. for some of the population the key health concern could be trauma, for others it could be stress, etc.). Any economic evaluation for the Hubs will be data-hungry due to the variation in Hub design and reasons for accessing support, as well as multi faceted impact of the Hubs on outcomes (including staff absences), inconsistencies in reporting outcomes, and the potential range of outcomes.
Due to the data limitations, an economic model would be unlikely to yield meaningful and robust results. Due to data availability, the key drivers of any cost-effectiveness results would need to be driven by assumptions. Furthermore, as the Hubs are evolving services and the pandemic results in continuous changes to service provision and health, any economic evaluation would become outdated quickly. In light of this, any economic modelling based on the current evidence base for Resilience Hubs would not be robust and would potentially lead to misleading conclusions. A particular concern is that the economic model would oversimplify Hub support and would be unable to accurately quantify the range of benefits of Hub support, which would be unsuitable for supporting decision-making. We recommend that the evidence is revaluated as the evidence base grows and a robust cost-effectiveness analysis may become feasible. This work provides a foundation for future research to build upon.
Part 2: sensitivity analysis of costing Hub support
This appendix details the work undertaken to assess the variability of the intervention cost estimates for the Resilience Hubs (see Chapter 5).
Methods
To reflect some of the uncertainty surrounding the inputs used to produce Hub cost estimates, sensitivity analysis was conducted (see Table 58). The sensitivity analysis focused on two key outputs; the cost per keyworker reached by individual support and the cost per keyworker reached by team support.
| Sensitivity analysis | Rationale |
|---|---|
| Staff time (and subsequently costs) increased to account for potential overtime.a | Staff in the Hubs commented that working overtime is a frequent occurrence. In the absence of Hub specific estimates of overtime. It was assumed staff work an average of 10.4 additional hours each week (6.3 paid and 4.1 unpaid), based on NHS staff survey 2020 results for participant’s reporting overtime.152 |
| Non-staff ‘other’ costs provided by the Hubs were excluded and replaced with the full PSSRU reported salary costs (including estates, overheads and other non-staff costs). | Overlap was identified between some of the PSSRU salary oncosts, and the costs reported by the Hub teams. To prevent double counting, the PSSRU salary oncosts were originally excluded from the initial costing exercise. However, as there was uncertainty in the cost estimates provided by the Hubs an analysis was performed which involved using the salary oncosts stated in by the PSSRU and excluding the ‘other’ non-staff costs reported by the Hubs. |
| Use of the upper estimates of Hub activity related to providing individual support (lower proportion of Hub activity relating to team support). | Hub teams were asked to provide an estimate of the proportion of Hub activity related to providing individual and team support. From the range (lower and upper) estimates provided, a midpoint was used for the initial analysis. A sensitivity analysis was conducted to investigate the impact that dedicating a higher or lower proportion of Hub activity to individual support would have on the cost per keyworker reached by individual versus team support. |
| Use the lower estimates of Hub activity related to providing individual support (higher proportion of Hub activity relating to team support). | |
| Use of predicted capacity estimates provided by Hubs (rather than data on the actual number of keyworkers supported) | As part of the intervention costing questionnaire, Hub teams were asked to provide data on both the actual number of keyworkers supported through individual and team support, and the predicted capacity (the estimated maximum number of individuals able to be supported through Hub provisions). The average predicted capacity was 1029 (range 613–1338) for individual support and 1548 (range 900–2672) for team support. As the predicted capacity estimates were often higher than the actual number of keyworkers supported through the Resilience Hubs, a sensitivity analysis was conducted to investigate the impact that Hubs running at maximum capacity would have on the intervention cost. |
Results
The outputs from the sensitivity analyses are provided in Table 59.
| Analysis | Description | Range | Average cost per keyworker reached (SD) |
|---|---|---|---|
| Individual support | |||
| Primary | Actual number of keyworkers supported (individual support) | £577–1480 | £1011 (£409) |
| Sensitivity analysis 1 | Staff overtime | £697–1855 | £1257 (£453) |
| Sensitivity analysis 2 | PSSRU oncost | £738–2281 | £1439 (£571) |
| Sensitivity analysis 3 | More individual support | £612–1481 | £1062 (£331) |
| Sensitivity analysis 4 | More team support | £542–1481 | £959 (£383) |
| Sensitivity analysis 5 | Predicted capacitya | £577–1568 | £769 (£313) |
| Team support | |||
| Primary | Actual number of keyworkers supported (team supportb) | £99–429 | £272 (£165) |
| Sensitivity analysis 1 | Staff overtime | £120–532 | £337 (£120) |
| Sensitivity analysis 2 | PSSRU oncost | £127–636 | £380 (£208) |
| Sensitivity analysis 3 | More individual support | £81–321 | £222 (£102) |
| Sensitivity analysis 4 | More team support | £116–536 | £322 (£171) |
| Sensitivity analysis 5 | Predicted capacity | £99–292 | £195 (£136) |
Assuming staff work 10.4 hours overtime each week, the cost per keyworker given individual support increased to £1257, and the cost per keyworker reached by team support to £337. Based on the revised staff costs, the costs per keyworker given individual support increased to £1439, while the cost per keyworker reached by team support increased to £380. Using the higher estimates of the proportion of activity related to individual support, the cost per keyworker increased to £1062 and reduced the cost per keyworker reached by team support to £222. Using the lower estimates of the proportion of activity related to individual support reduced the cost per keyworker given individual support to £959 and increased the cost per keyworker reached by team support to £322. Using predicted capacity data (which is uncertain), the average cost per keyworker reduced to £769 for individual support and £195 for team support, demonstrating that if Hubs reached their potential capacity, the cost per keyworker reached reduces. From the sensitivity analysis, adjusting staff costs in line with the full PSSRU estimates was found to have the largest impact. The sensitivity analyses highlight how existing uncertainty and changes to assumptions can impact cost estimates.
Appendix 3 Chapter 6 (Qualitative)
Part 1: topic guides
Hub staff topic guide
About you
-
I would like to start with a little background on you: Please could you tell me briefly about the role that you were doing before you came to work at the Hub?
-
And what role is it you are doing at the Hub?
-
-
How many days a week do you do at the Hub?
-
Depending on response to how many days – Do you work at the Hub full time? If not, where else do you work and in what role?
-
-
Have you been seconded to the Hub?
-
How’s that gone? Have there been any difficulties?
-
-
Did you receive any specific training or induction when you started at the Hub? (Not mandatory training but more specific training, e.g. trauma etc.)
Normalisation process theory
1 of 4 COHERENCE – how people make sense of what is new and what they have to do with it. Sense-making. Individuals’ clarity regarding the purpose of the intervention.
| Is the Resilience Hub a new way of working for you? How does the Resilience Hub way of working differ from your usual practice or ways of working in other mental health services? |
Coherence/differentiation
How do people come to understand the new thing is different from what was happening? What is different about it? What work do people have to do to see that and how do they come to understand these differences? |
| Do you understand what it is that you need to do within your role at the Hub? Could you tell me what that is? | Coherence/individual specification
How do people come to understand what it is they need to do individually to implement a change? |
| Does everyone involved agree about the purpose of the Resilience Hub? What do you see as its purpose? |
Coherence/communal specification
How people work together to build a shared understanding? What are the processes by which the team are making sense of what needs to happen to implement this? |
| Does everyone involved grasp the potential benefits and value of the Hub? What do you see as its value and benefits? |
Coherence/internalisation
Valued benefits. How do we understand the value of this? What is showing us that this is worth doing? What processes do we come to understand this is a worthwhile activity? |
2 of 4 COGNITIVE PARTICIPATION – relational work – building relationships, working out the work that people have to do around building and developing relationships. Work that individuals and organisations necessarily do in order to enrol individuals to engage with the intervention.
| Could you tell me who was involved in the set-up and driving forward of the Hub’s work? |
Cognitive participation/initiation
Who do we need to get this going? Who is in a position to get new things happening and what do they have to do to do it? Who are the people placed to do his work and what work do they have to do? |
What were the key factors or skills and experience that they had that helped with the Hub’s set-up?
|
|
Do you think the set-up of the Hub came at the right time?
|
|
| Have you needed to reorganise the Hub team or the ways in which you work together in order to accommodate changes to the model along the way? |
Cognitive participation/enrolment
How are we going to enact what it is we have made sense of? (moving from more sense-making to more practical aspects) The work people do to rethink their individual and group relationships and to work out how those new ways or working with each other are going to work. |
Are you or have you recruited any new staff over time?/ Has the Resilience Hub recruited any new staff over time?
|
|
Some people have mentioned that there is more demand for teams-based consultation work compared with individual work, do you agree, and in what ways has the Hub had to adjust its models to adapt to that?
|
|
Do you feel that the Hub model is the best way of supporting health and social care staff?
|
Cognitive participation/legitimation
The processes by which people being bought into this come to see this as an appropriate thing for them to do and something they can make a valid contribution to. |
When Hub staff speak to other teams and organisations, has work been needed to build credibility with health or social care staff who might access the Hub?
|
|
What were the actions and procedures that were necessary to put in place the right support for keyworkers, and how easy were these to come up with, put into practice, and keep them going?
|
Cognitive participation/activation
What are the procedures and work people need to do to bring this together as a whole body of work? Getting it going and making sure it keeps going, what is the relational work that needs to happen to keep the behaviours happening? |
How did the Hub break into the existing system of staff support? (e.g. Trust leads, HR leads, occupational health, staff well-being services) – e.g. so that people know what the Resilience Hub is, help get the word out to staff about the Hub, keep the Hub information visible etc., sharing staff contact details with the Hub, this is who we are, this is what we do to sell themselves as a service to get referrals
|
|
| How has the Hub team gone about defining what the Hub offer is? | |
How much involvement have you had personally in this?
|
3 of 4 COLLECTIVE ACTION – The operational work involved in the implementation itself. The work that individuals must do to make the intervention function.
Have you experienced any challenges with translating the Hub’s model from ‘on paper’ into everyday practice?
|
Collective action/interactional workability
Interactional work people do with each other are facts and other elements of a set of practices when they seek to operationalise them in everyday settings. |
| Have you met any (other) obstacles or barriers that have limited your (or the Hub’s) clinical effectiveness? | |
Do you think there are any aspects of the Hub model or the way the Hub works that might create barriers or accessibility issues for people from different demographic groups/cultural backgrounds?
|
|
Do you feel that you have the right skills and training needed for your role?
|
Collective action/skillset workability
Allocation work – who does what and who should do what? |
| Are you confident in how your team is delivering the Hub model? |
Collective action/relational integration
Knowledge work that people do to build accountability and maintain confidence in a set of practices and in each other as they use them. |
Are there any areas in which you’re less confident in the Hub? As a team, how have you helped build confidence in the Hub model?
|
|
Do you have confidence in the onward referrals that you are making to other services or organisations, that patients are being picked up and receiving the treatment that they need? (In what ways have you been able to improve connections with other services/negotiate referrals?)
|
|
| Does the Hub in general and the Hub team have sufficient resources? For example, are parts of the Hub model and its implementation held up because certain resources aren’t available? |
Collective action/contextual integration
Resource work – who gets what and who needs what? Are parts of implementation held up because certain resources aren’t available? It is contextual how you integrate what you are doing into the wider context of the organisations set of resources and relationships that are going on so that allocation work can happen. |
Hub team and Hub model:
|
|
| Have the resources been made available for you personally to do your work at the Hub? | |
Own role and personal:
|
|
| Could anything have been done better? |
4 of 4 REFLEXIVE MONITORING – The appraisal work people do to assess and understand the ways a new set of practices affect them and others around them. Appraisal work throws up what is going well/not so well and looks at does something need to change which feeds into reconfiguration.
In what ways do you judge the effectiveness of the Hub model?
|
Reflexive monitoring/systematisation (getting the data to support this kind of work) how effective and useful something is and collecting information (formal/informal) |
How effective do you think the Hub model has been in supporting keyworkers access mental health support during the pandemic?
|
Reflexive monitoring/individual appraisal
Work experientially as individuals to appraise its effects on them and the contexts in which they are set. Individuals might place different emphasis on different parts which might affect how they evaluate it. |
| Based on your evaluation and experience how do you think the impact/effectiveness of the Resilience Hub could be improved? | |
| Do you come together with other people to talk about how effective the Hub is? (Either formally or informally) |
Reflective monitoring/communal appraisal
Working together both formally and informally to evaluate the worth of a set of practices. The work people do and the processes |
Do you think it would be helpful?
|
|
Other people could be:
|
|
| Has the Hub model been redefined or changed in any way in response to any of the things that we have been talking about? |
Reflexive monitoring/reconfiguration
Appraisal work may lead to attempts to redefine procedures or modify practices and even change the shape of the new technology itself. |
Based on your evaluation and experience how do you think the impact/effectiveness of the Resilience Hub (either yours specifically, or the Resilience Hub model in general) could be improved?
|
|
| What might the Resilience Hubs look like in future? | |
| From your experience, what do you think would be the most important factors to consider in order for Resilience Hubs to be sustainable in the future? |
That concludes the interview, thank you. Do you have any questions for me? Or is there anything else you would like to add?
Wider stakeholder topic guide
As we are interviewing a range of people, some of the questions I will ask you in this interview may not be relevant to your job role. Please answer according to your experience and role, and if there are any questions you’re not able to answer that’s fine, just let me know.
About You
-
I would like to start with a little background on you: Please could you tell me briefly about your job role and organisation, and whether this has changed at all in light of the pandemic?
-
In what ways were you involved in the provision of support for staff who had been affected by their work during the pandemic?
Normalisation process theory
1 of 4 COHERENCE – how people make sense of what is new and what they have to do with it. Sense-making. Individuals’ clarity regarding the purpose of the intervention.
| At the start of the pandemic, what were the perceived needs, priorities and ‘drivers’ for supporting the mental health/well-being needs of health/social care staff in your area/organisation? Was there agreement across the care system about that? |
Coherence/communal specification |
What is your understanding of what the Resilience Hub is, and how it works?
|
Coherence/individual specification
How do people come to understand what it is they need to do individually to implement a change. |
| Does the Resilience Hub model differ from usual ways of working in other mental health services or staff support offers? In what ways? What, if anything, is the Hub providing that is different from what would otherwise be available for staff [in your organisation?] To what extent do you think other individuals or other parts of the system understand how the Hub differs from usual staff support provision? |
Coherence/differentiation
How do people come to understand the new thing is different from what was happening? What is different about it? What work do people have to do to see that and how do they come to understand these differences? |
What have been the facilitators or barriers that may have helped or hindered yours or others’ understanding of what the Hub does?
|
|
| In what ways does the concept of the Resilience Hub fit into the identified needs/priorities for supporting health and social care staff? To what extent do people agree about the specific purpose of the Resilience Hub(s) in supporting health and social care staff? Has that changed over time at all? What do you see as its purpose? |
Coherence/communal specification
How people work together to build a shared understanding. What are the processes by which the team are making sense of what needs to happen to implement this |
| Does everyone involved grasp the potential benefits and value of the Hub? Has that changed over time? What do you see as its value and benefits? |
Coherence/internalisation
Valued benefits. How do we understand the value of this? What is showing us that this is worth doing? What processes do we come to understand this is a worthwhile activity? |
If you felt you could benefit from some support, would you consider using your local Resilience Hub?
|
2 of 4 COGNITIVE PARTICIPATION – relational work – building relationships, working out the work that people have to do around building and developing relationships. Work that individuals and organisations necessarily do in order to enrol individuals to engage with the intervention.
| Do you think the right people were involved in the set-up and driving forward of the Hub’s work? Looking back, do you think there should/could have been anyone else involved in facilitating the Resilience Hub’s set-up? (either key individuals or roles; or whole departments/organisations) |
Cognitive participation/initiation
Who do we need to get this going? Who is in a position to get new things happening and what do they have to do to do it? Who are the people placed to do his work and what work do they have to do? |
Do you think the set-up of the Resilience Hub(s) came at the right time?
|
|
| How have you been able to get people on board with the Resilience Hub model? What work have you had to do to get people involved and help set up and drive forward the Resilience Hub? |
Cognitive participation/enrolment
How are we going to enact what it is we have made sense of? (moving from more sense-making to more practical aspects) The work people do to rethink their individual and group relationships and to work out how those new ways or working with each other are going to work. |
In what ways have you/your organisation collaborated with the Hub as part of its set-up/on an ongoing basis?
|
|
| What worked well in terms of collaboration between the organisations/services, and have there been any challenges? In what ways has this collaboration (or lack of) helped/hindered Hub’s set-up/the work of the wider system? Was it difficult to collaborate? 153 Were there any barriers to inter-agency collaboration? 153 From your organisation in particular? |
|
Do you feel that the Hub model is the best way of supporting health and social care staff?
|
Cognitive participation/legitimation
The processes by which people being bought into this come to see this as an appropriate thing for them to do and something they can make a valid contribution to. |
| Does the Resilience Hub as a model and a service fit with the aim of supporting professionals within the NHS access mental health support? Does the Resilience Hub fit with other organisations and services? | |
What were the actions and procedures that were necessary to put in place the right support for keyworkers, and how easy were these to come up with, put into practice, and keep them going?
|
Cognitive participation/activation
What are the procedures and work people need to do to bring this together as a whole body of work? Getting it going and making sure it keeps going, what is the relational work that needs to happen to keep the behaviours happening? |
| How did the Hub break into the existing system of staff support? (e.g. Trust leads, HR leads, occupational health, staff well-being services) – e.g. so that people know what the Resilience Hub is, help get the word out to staff about the Hub, keep the Hub information visible etc., sharing staff contact details with the Hub, this is who we are this is what we do to sell themselves as a service to get referrals | |
Hub staff have told us how much outreach has been needed to try to convince staff to come forward to seek support
|
3 of 4 COLLECTIVE ACTION – The operational work involved in the implementation itself. The work that individuals must do to make the intervention function.
How well do you think the Hub integrates with the existing system of staff support, Employee Assistance Programmes, or other mental health services across health and social care organisations in your region?
|
Collective action/interactional workability
Interactional work people do with each other are facts and other elements of a set of practices when they seek to operationalise them in everyday settings. |
| In what ways has the Hub’s integration with other services (or lack of) helped/hindered the work of the wider system? In what ways do you think the Hubs help (or don’t help) to meet unmet support needs within the system? What do you think are some of the benefits and challenges of the Hub’s position within this existing system of staff support?, |
|
Do you think there are any aspects of the Hub model or the way the Hub works that might create barriers or accessibility issues for people from different demographic groups/cultural backgrounds?
|
|
| Has there been sufficient availability of people with the right expertise (management; clinical skills) to work within the Hub/staff support in general (staffing/recruitment)? | Collective action/skillset workability
Allocation work – who does what and who should do what |
To what extent do you think local Trusts, organisations and individual staff members have confidence in the Resilience Hub services?
|
Collective action/relational integration
Knowledge work that people do to build accountability and maintain confidence in a set of practices and in each other as they use them. (Confidence – how well you think the Hub model works and how well the team works together) |
Some people have suggested that there are challenges in terms of persuading people to access support services, do you think this is the case, and if so why?
|
|
Any potential barriers?
|
|
Issues around under-represented groups?
|
|
(If relevant) Have the funding and resources been made available for you to be able to support the implementation of the Resilience Hub?
|
Collective action/contextual integration
Resource work – who gets what and who needs what? Are parts of implementation held up because certain resources aren’t available? It is contextual how you integrate what you are doing into the wider context of the organisations set of resources and relationships that are going on so that allocation work can happen. |
| Has the funding been made available for staff support in general in your organisation/the wider system? How does the Hub fit into that? |
4 of 4 REFLEXIVE MONITORING – The appraisal work people do to assess and understand the ways a new set of practices affect them and others around them. Appraisal work throws up what is going well/not so well and looks at does something need to change which feeds into reconfiguration.
What methods do you use for judging the effectiveness of the Hub model?
|
Reflexive monitoring/systematisation (getting the data to support this kind of work) how effective and useful something is and collecting information (formal/informal). |
How effective do you think the Hub model has been in supporting keyworkers access mental health support during the pandemic?
|
Reflexive monitoring/individual appraisal
Work experientially as individuals to appraise its effects on them and the contexts in which they are set. Individuals might place different emphasis on different parts which might affect how they evaluate it. |
| In what ways do you think the impact/effectiveness of the Resilience Hub could be improved? | |
Do you come together with other people to talk about how effective the Hub is? (Either formally or informally)
|
Reflective monitoring/communal Appraisal
Working together both formally and informally to evaluate the worth of a set of practices. The work people do and the processes |
Other people could be:
|
|
| Post-pandemic, do you see the Resilience Hubs as sitting within a range of services? And if so, where? | Reflexive monitoring/reconfiguration |
In terms of sustainability, beyond the pandemic, what do you see as the most useful role for the Resilience Hubs? For example.
|
Appraisal work may lead to attempts to redefine procedures or modify practices and even change the shape of the new technology itself. |
What do you see as the key aspects of the Hubs that are most valuable to the existing system of mental health/well-being services? For example.
|
That concludes the interview, thank you. Do you have any questions for me? Or is there anything else you would like to add?
Hub client topic guide
Context/about you
Did you register or sign up with the Resilience Hub in your area?
-
If yes – which Hub?
What help or support did you receive from the Hub?
Prompts –
-
Screening
-
Phone/e-mail support
-
Support navigation
-
Direct therapy/other intervention
Context questions for all participants
Please could you tell me briefly about the job that you were doing (at the time that you signed up with the Resilience Hub/during the COVID pandemic?)
-
Has your job changed at all between March 2020 and today? (e.g. redeployment)
Are you still doing the same job now?
[If not] What were the reasons for you changing roles/leaving?
-
Redeployment
-
Left as a result of COVID etc.
Could you tell me a little about the impact that the COVID pandemic had on you?
-
Job role
-
Redeployment?
-
Relocation?
-
Impact on self, mental health
-
Impact on family, other responsibilities (e.g. caring)
| Sekhon’s Acceptability Framework (2011) | Michie et al. COM-B (2011) | TDF domain | |
|---|---|---|---|
| Could you tell me a little about the impact that the COVID pandemic had on you, and how you came to access support from The Resilience Hub? If participant accessed a Resilience Hub: When did you first have contact with the Resilience Hub, and what made you get in touch? |
|||
Did you seek support anywhere else or consider any alternatives to the Hub, and if so, could you tell me a bit about that?
|
|||
| What are the main things that you were seeking support for? Did you hear about the Resilience Hub or other types of well-being support through your place of work? What would be the best way to promote these services/where would you expect to see them promoted? |
|||
Are you aware of what support is offered at the Hub?
|
Intervention coherence | Capability Opportunity Motivation (automatic) |
Knowledge Physical and social environment Reinforcement |
| Are there any aspects of the Hub that you don’t understand/don’t make sense to you? In what ways has the Resilience Hub worked for you/been beneficial for you? What is it about the Resilience Hub that works or doesn’t work for you? |
|||
How did you first get in touch with the Resilience Hub?
|
Burden | Capability (physical) | Beliefs about capabilities |
| How straight forward or difficult was that process for you? Were there any problems that you encountered when you accessed the Resilience Hub? |
Motivation (automatic and reflective) | Emotion Intention Physical skills |
|
Once you signed up/registered with the Hub, what was your experience of getting support/accessing the Hub and trying to get support?
|
|||
| Do you think that has changed over time? (depending on response/if appropriate) | |||
| Considering all the things that we have just discussed, how confident were you that you would be able to take part/participate with the support offered at the Resilience Hub? (How confident were you that you were able to do things asked of you at the hub?) |
Self-efficacy | Motivation (reflective) Capability (psychological) |
Beliefs about capabilities Cognitive and interpersonal skills |
Did you feel confident that you were able to do what the Hub asked of you? For example, complete tasks they have set for you, take on advice they have given, complete an intervention etc.
|
|||
| Overall, did it feel manageable? | |||
| What were you hoping to get out of the Hub’s support/psychological support in general? How confident were you that the Hub would provide the right support for you? In what ways do you think the Resilience Hub provided the support you needed? Was the support that you received from the Resilience Hub what you were expecting? Was there anything that you wanted help with that wasn’t addressed by the Hub? |
Perceived effectiveness | Motivation (reflective and automatic) | Goals Optimism Reinforcement |
Was there anything the Resilience Hub could have done differently in order to support you better?
|
|||
Could you tell me about any compromises you had to make in order to get support from the Resilience Hub?
|
Opportunity costs | Motivation (reflective) | Beliefs about consequences |
| Were there any downsides or issues that occurred from using the Resilience Hub? What do you think the impact would have been on you if you hadn’t have got support from the Hub? |
|||
| How do you feel about the Resilience Hub in general? | Affective attitude | Motivation (automatic) Capability (psychological) |
Reinforcement Emotion Behavioural regulation |
Do you feel comfortable talking about mental health?
|
Ethicality | Opportunity (social) | Environmental context and resources |
| Personal | Capability (psychological) Motivation (reflective) |
Skills Knowledge Memory, attention and decision process Social influences Social/professional role |
|
Where would you normally get support for your well-being?
|
|||
What sorts of things would be important to you when getting support in general?
|
|||
[Men/minority ethnic groups/care home staff/emergency services] are currently under-represented amongst those seeking support, have you personally experienced any barriers when seeking support?
|
|||
Would you say that what you have been offered from the Resilience Hub is a good fit with what is important to you?/Do you feel that the support you were offered from the Resilience Hub fits with what is important to you?
|
|||
Is there anything else in your life that is important to you that the Resilience Hub didn’t account for?/ could be better addressed?
|
|||
Other prompts/things to think about tapping into:
|
|||
|
|||
| Work Do you think that getting support is compatible with your professional role/identity? Do you know others/colleagues who have accessed support and how was it received by other people? Do you feel others/colleagues have the knowledge and resources to be able to access support? |
|||
Is it something that is encouraged in your workplace and in your role in particular?
|
|||
How often do your managers and colleagues talk about well-being or getting support?
|
|||
| In what ways could the Resilience Hub model be improved or better meet the needs of health and social care staff? Finally, was there anything else outside of the Hub that might have made a difference to how well the Hub could support you/your accessing further support? |
|||
| That concludes the interview, thank you. Do you have any questions for me? Or is there anything else you would like to add, or anything you feel that I have missed? | |||
Non-Hub keyworker topic guide
Context questions for all participants
Clarify any questions you may have already asked from the initial recruitment contact.
Demographics
-
Gender they identify with
-
Ethnic group
-
Age range
Please could you tell me briefly about the job that you were doing/during the COVID-19 pandemic?
-
Staff group/Job role
-
Department/Service type
-
Has your job changed at all between March 2020 and today? (e.g. redeployment)
Are you still doing the same job now?
[If not] What were the reasons for you changing roles/leaving?
-
Redeployment
-
Left as a result of COVID-19 etc.
Could you tell me a little about the impact that the COVID-19 pandemic had on you?
-
Job role
-
Redeployment?
-
Relocation?
-
Impact on self, mental health
-
Impact on family, other responsibilities (e.g. caring)
| Sekhon’s Acceptability Framework (2011) | Michie et al. COM-B (2011) | TDF domain | ||
|---|---|---|---|---|
| Could you tell me a little about the impact that the COVID pandemic had on you? | ||||
|
How do you feel about getting support in general?
|
Affective attitude | Motivation (automatic and reflective) Capability (physical and psychological) Policies, e.g. communication/Marketing – the approach of services |
Intention Emotion Knowledge Beliefs about consequences Behavioural regulation |
|
|
Where would you normally get support for your well-being?
|
||||
|
Have you got well-being and/or mental health support in the past?
|
||||
| Are you aware of (any other) local mental health/well-being services that you may be able to access? | ||||
|
What sorts of things encourage you, or make it more likely for you to seek support?
|
Ethicality | Motivation (reflective and automatic) Opportunity (social and physical) |
Memory, attention and decision process Social influences Behavioural regulation Reinforcement Skill Social/professional role Environmental Contact and resources |
|
|
What sort of things might put you off or prevent you from getting support?
|
||||
|
Stigma
|
||||
|
What is it about (these factors) that makes it difficult?
|
||||
| At work | ||||
|
Is accessing well-being support encouraged at your workplace?
|
||||
| In what ways do you think this has impacted your decision to seek support? | ||||
|
What sort of things would be important to you when getting support in general?
|
||||
|
[Men/minority ethnic groups/care home staff/emergency services] are currently under-represented amongst those seeking support, Have you personally experienced any barriers when seeking support?
|
||||
| If they have accessed other forms of support | If they have accessed no support | |||
At what point did you seek support for your mental health?
|
You’ve mentioned that you haven’t accessed any other forms of support, could you say a little bit about the reasons why not?
|
Burden | Capability (psychological and physical) Opportunity (social and physical) Motivation (automatic and reflective) |
Skill Reinforcement Beliefs about consequences |
|
How did you go about getting support for your mental health?
|
How confident are you that mental health or well-being support would be helpful for you? | |||
Would you consider getting support from any NHS mental health services?
|
||||
How easy or difficult was it to get the right support?
|
||||
| How confident were you that it would be the right support for you? How helpful did you find this support? |
||||
To what extent do you feel the service met your needs?
|
||||
| Did other people know you were getting support, and what was their response? | ||||
| Questions about the Hub | ||||
|
Were you aware of the Resilience Hub in your area?
|
||||
| It would be really helpful for us to understand a bit about why you didn’t end up getting support from the Resilience Hub, and if there is anything the Hub could have done differently that might have led to you using their service. | ||||
| Could you tell me about why you didn’t sign up/refer yourself to the Resilience Hub? | ||||
| What influenced your decision not to get support from the Resilience Hub? | ||||
| [The following questions will then be used as prompts, as appropriate, as to why the person may not have engaged with the Resilience Hub]: | ||||
| Sekhon’s Acceptability Framework (2011) | Michie et al. COM-B (2011) | TDF domain | ||
| What would be the best way to promote these services/how would you expect to see them promoted? | ||||
|
Are you aware of what support is offered at the Hub?
|
Intervention coherence | Opportunity (social and physical) – Motivation (automatic and reflective) |
Knowledge | |
| Do you know of anyone else who has used the Hub? What was their experience of the Hub? | ||||
|
How did you feel about the Resilience Hub when you first heard about it?
|
Affective attitude | Motivation (automatic and reflective) Capability (physical and psychological) |
Reinforcement Social/professional role and identity Optimism Intentions Goals Beliefs about consequences |
|
| I asked you earlier about any barriers, were any of these relevant for you in terms of accessing Hub support?a a[Men/minority ethnic groups/care home staff/emergency services] are currently under-represented amongst those seeking support, have you personally experienced any barriers when seeking support? |
||||
|
Did you think that the Hub could provide what you wanted/needed at the time?
|
Perceived effectiveness | Capability (physical and psychological) Motivation (reflective) Opportunity (social and physical) |
Knowledge Goals Social influences |
|
|
In what ways could the Resilience Hub provide better support?
|
||||
| Is there anything else that you think could be improved? | ||||
| How straightforward or difficult did you think it would be for you to access the Hub? Are there any problems you think you may encounter when trying to access the Resilience Hub? |
Burden | Capability (psychological and physical) Opportunity (physical and social) |
Skill Beliefs about capabilities Emotion |
|
|
Could you tell me about any compromises you felt that you would have to make in order to get support from the Hub?
|
Opportunity costs | Capability (psychological and physical) Motivation (reflective and automatic) Opportunity (physical) |
Beliefs about consequences | |
| Do you think there would be any downsides or issues that could occur when getting support from the Resilience Hub? | ||||
| Conversely would there be any downsides from not getting support from the Hub? | ||||
|
What sort of things do you think a service like the Resilience Hub might ask you to do?
|
Self-efficacy | Capability – psychological or physical ability to enact the behaviour Motivation |
Skill Beliefs about capabilities |
|
|
Are there certain aspects that you felt would have taken more effort than others?
|
||||
| When you first heard about the Resilience Hub, how confident were you that you would be able to do these things and participate with the support? For example, if you were accessing Hub support for anxiety and they gave you some strategies to practice outside of sessions, do you think you’d have the confidence to be able to do these things that the Hub is asking? |
||||
|
Break down the question to reflect types of support the Hub offers, if needed:
|
||||
| From what you know about the Resilience Hub, how do you think the support it offers fits with what is important to you? | Ethicality | Motivation (reflective) | Cognitive and interpersonal skills Memory, attention and decision processes |
|
|
Are there any factors that you felt the Resilience Hub may not have addressed?
|
||||
|
In what ways could the Hub have been described differently to make you feel more confident that it would have addressed these things? (if relevant)
|
||||
| Is there anything else that you can think of that could be improved or changed to better support staff? | ||||
| That concludes the interview, thank you. Do you have any questions for me? Or is there anything else you would like to add, or maybe is there anything important that you feel I have missed? | ||||
Part 2: additional interview quotes
| NPT construct | Participant quote |
|---|---|
| Sense-making (coherence) | |
| Differentiation | my understanding again has never been that this is a kind of free for all … if you’ve got a worry about the smallest thing you can go, or if you feel you need the least bit of support you can go. It’s always been it’s much more about the higher-level psychological support is how I’ve understood it. Wider stakeholder 02 |
| Communal specification | there was a lot of coming together and very open discussion, so I think, yeah, there was broad agreement. Wider stakeholder 07 |
| Individual specification | I think I just thought it was for front-line staff. I didn’t think it would be for non-clinical staff. Non-Hub keyworker 09 |
| Internalisation | you never think your way out of a mental health issue. The only way it gets better is by talking and sharing, and listening to other people’s experiences and things like that. So yeah, there’s mountainous amounts of downsides to not accessing help and finding help. Non-Hub keyworker 17 if I’m taking up somebody’s time, somebody else is having to wait in the queue. Non-Hub keyworker 11 I’ve had a very varied experience of how nurses can be negative towards other team members’ health and well-being from their mental health perspective. And they’ve not been aware of it what they’ve been doing or been saying has been damaging towards me … to be honest with you, when I left the health service about six months ago, I’ve got no regrets. Hub client 09 |
| Relational work (cognitive participation) | |
| Initiation | I think my line manager should be saying to me, listen, I hear of all the stuff that you’re going through at the moment, this is an offer, we can make sure that on Monday mornings that you can access some support around this. I think it should be a proactive thing. It shouldn’t be me needing to negotiate for my health and well-being because that just adds more pressure on me, and I don’t want to do it. Non-Hub keyworker 20 I think having a supportive work environment and work supervisor, makes it so much easier … the number of managers who … say ‘I can’t talk about that, that’s mental health … rather than saying, ‘well how are you feeling today, what’s going on for you, is there anything I can help with?’ Non-Hub keyworker 03 |
| Enrolment | We sent loads of e-mails out and expected loads of people to just ring in, but they didn’t because they either didn’t have the information or they were working in the thick of it, so perhaps didn’t have time or didn’t think that they needed it. Hub staff 11 staff have not been up for looking at things related to work out of hours … it’s that dilemma that there’s no time while at work, and there’s a want to escape from it when not at work. Wider stakeholder 07 |
| Legitimation | None of the people that I come across [in other services] are trained to [work with racism and discrimination], and I am not willing to put myself in a situation where I’m already feeling quite vulnerable and exhausted to then do the education work, educating the person that’s supposed to be supporting me … Even though I was offered to go to [occupational] health for support, I didn’t take up the offer. Non-Hub keyworker 20 I think in-house stuff is essential, … to be fully integrated with the other services. But I think an external hub is essential as well, so I do think the model we’ve got is absolutely vital. Wider stakeholder 07 |
| Activation | I needed to fit it within my working week, because that’s when obviously the therapist was working during those times, so I had to make time in a very, very full diary … it’s not the fault of the therapy or the therapist if that makes sense or the Resilience Hub, it’s the fact that there isn’t much breathing space within my working week to do things like this. Hub client 12 I had the same person who really knew me, week-by-week. She understood me. So it got easier … I didn’t have to explain who the people were I was talking about … I could just start off where I was right now. Hub client 08 |
| Operational work (collective action) | |
| Interactional workability | it felt like an additional string to the bow, and I think it was very complementary. I didn’t feel like it was stepping on any toes, or a duplication … we were trying to be as inclusive as possible, knowing that people will choose different options as well. Wider stakeholder 03 |
| Relational integration | would this go on my record, my occupational health record? … I suppose that’s another thing that might put people off accessing support through NHS, if they think it might somehow end up on their record. Non-Hub keyworker 13 I would definitely trust it as a service … you know it’s through work, you know that they’ve got your best intentions at heart … compared to other services I’ve used in the past for mental health, they’ve been very understanding. And, I think, very caring … So, I would definitely put my trust in them, and I’ve even said it to my colleagues that, if they ever needed any form of help to definitely seek help from the Resilience Hub. Hub client 18 |
| Skill-set workability | The chap that initially called me was very quick at identifying that I needed something more. The therapist I got was incredibly skilled and knowledgeable and got it straight away. Hub client 08 |
| Contextual integration | this is a difficult solution to find, but I think if there was money for permanent posts …, people would be prepared to do those … But if it’s a temporary job of 12 months, you can’t … take that gamble and just take a year-long post and leave another permanent post behind … It’s just difficult to get that funding long-term. Hub staff 11 |
| Appraisal work (reflexive monitoring) | |
| Systematisation | I think if it were possible to get the outcome data for our Trust, I think that would be really interesting and really helpful … We get the data about who is accessing, or the numbers, but we don’t get specific data on outcomes. Wider stakeholder 07 I don’t think it particularly feels well promoted … what are they doing … how are they supporting the system? … I think we just all get on with doing the do rather than proving what we’re doing … So, it’s not really a criticism of them but it’s probably just not helpful for them from a reputational point of view either. Wider stakeholder 02 |
| Communal appraisal | my colleague … was in contact with the Resilience Hub as well so her experience was a good experience which she said to me, yes, it’s good. So I think, yes, it was just before I contacted them so that again was talking between your friends and they’d had a good experience as well. Hub client 16 And one of them has shared the detail with me … but he was singing the praises of the service when he accessed the Hub, so that was interesting … you know, the member of staff concerned, he had no criticisms, and he was quite shocked how quick and easy it was to get in. Non-Hub keyworker 03 every time I’ve made enquiries, the waiting times have been too high so we would always go to our EAP services [instead]. Wider stakeholder 09 |
| Individual appraisal | It was excellent for me, truthfully … I was able to contact [therapist at Hub] if I needed him more urgently, there was always availability, we had about an hour a week, and it carried on till I didn’t need it any more … I can’t say anything negative. Hub client 17 I think, perhaps I’m a little bit cynical working in the NHS, but I think my experience with the Hub has exceeded expectations. Hub client 01 |
| Reconfiguration | I think word of mouth by a line manager is probably the most impactful … [it should be] reinforced through their [senior leaders] …, actively creating a safe space for it … I don’t think e-mails really work. I don’t think newsletters on e-mails really work … Picking it up as part of health and well-being conversations through appraisals or one to ones would probably be very impactful as well. Non-Hub keyworker 20 I think as time goes on we’re going to see less acute trauma and we’re going to see more burnout, you know, we’re maybe going to see people who kind of think they’ve got through the pandemic unscathed and then something triggers them further down the line. So I think that that responsiveness and flexibility is going to be key. Wider stakeholder 07 I would hope for this model where a Resilience Hub might maintain a core group, a smaller core group of staff who were doing the business of well-being or being part of that within the Trust … Then that could have the flexibility and the flex, should other crises occur … we could then respond to those in a timely manner. Hub staff 01 |
Appendix 4 Chapter 7 (Case studies)
Part 1: under-represented groups
Under-represented groups’ access to services
The following table summarises the demographic information of certain under-represented groups’ access to services. These are people who classified as accessing mental health services ‘via any route’ as defined in Table 11. Out of the 299 people returning SUQ data, 171 reported accessing mental health support via any route, percentages for the categories below are expressed out of this total. Results must be taken in context – these are only representative of the people screened who gave consent to be contacted who then provided SUQ data.
| Total (n = 171) | ||
|---|---|---|
| n (%) | ||
| Ethnic minority groups | Yes | 8 (4.7) |
| No | 156 (91.2) | |
| Missing | 7 (4.1) | |
| Men | Yes | 27 (15.8) |
| No | 141 (82.5) | |
| Missing | 3 (1.8) | |
| Social care | Yes | 5 (2.9) |
| No | 159 (93.0) | |
| Missing | 7 (4.1) | |
| Emergency services | Yes | 5 (2.9) |
| No | 159 (93.0) | |
| Missing | 7 (4.1) | |
| Site A | Site B | Site D | Ethnic minority groups | Men | Care home staff | Emergency staff | |
|---|---|---|---|---|---|---|---|
| N (with complete costing data) | 44 | 20 | 101 | 11 | 28 | 6 | 7 |
| Mean total mental healthcare cost (95% CI) | £763 (£554 to £971) | £512 (£228 to £797) | £164 (£104 to £223) | £383 (£56 to £710) | £492 (£235 to £749) | £346 (£12 to £680) | £321 (£5 to £637) |
| Mean wider health and social care cost (95% CI) | £203 (£70 to £335) | £30 (< £1 to £72) | £147 (£46 to £247) | £232 (< £1 to £600) | £105 (< £1 to £238) | £0 (NA) | £164 (£51 to £277) |
Glossary
- Caseness
- Meeting cut-off scores for clinically significant difficulties in the mental health screening measures used by the Hubs (i.e. generalised anxiety disorder 7-item questionnaire, patient health questionnaire 9-item questionnaire, International Trauma questionnaire/post-traumatic stress disorder checklist for Diagnostic and Statistical Manual of Mental Disorders, 5th edition, alcohol use disorders identification test, work and social adjustment scale).
- Employee assistance programme
- Health benefit provided to employees, offering non-work-related advice and information, and may provide access to brief interventions, such as counselling. Often but not always provided by an external provider; employees can contact EAPs directly and confidentially.
- Hub clients
- Keyworkers who registered with a Resilience Hub for individual psychological support.
- Hub staff
- Staff working within one of the Resilience Hubs involved in the study, including clinical staff (e.g. therapists, psychologists) and administrative staff.
- Improving access to psychological therapies
- National Health Service services offering short-term psychological therapies to people struggling with mild to moderate common mental health difficulties.
- Keyworkers
- Keyworkers from health, social care, emergency services and any other staff groups eligible for Resilience Hub support in their respective regions. See Chapter 3 for variances in eligibility across Hubs.
- Non-Hub keyworkers
- Keyworkers who did not register with a Resilience Hub for individual psychological support.
- Normalisation process theory
- A widely used theory to explain the processes by which an intervention becomes, or fails to become, embedded into routine practice.
- Occupational health
- Service supporting work-related physical and emotional health. Typically: not confidential from managers; requires a manager to refer the employee for support; reports back to managers; have the authority to sign employees off work.
- Sekhon’s acceptability framework
- A theoretical framework for assessing the acceptability of healthcare interventions.
- Sites A, B, C, D
- Site labels refer to the four anonymised Resilience Hubs that contributed data to this study.
- Wider stakeholders
- Professional stakeholders involved in work relating to the set-up of Hubs or staff well-being initiatives in local organisations within Hub regions. Examples include commissioners, representatives from partner organisations and NHS Trusts, HR directors and organisation well-being/occupational health leads.
List of abbreviations
- AfC
- agenda for change
- AP
- assistant psychologist
- AUDIT
- alcohol use disorders identification test
- BAME
- Black, Asian and minority ethnic
- BLM
- Black Lives Matter movement
- CAT
- cognitive analytic therapy
- CBT
- cognitive–behavioural therapy
- CP
- clinical psychologist
- DSM-5
- Diagnostic and Statistical Manual of Mental Disorders (5th edition)
- EAP
- employee assistance programme
- EDI
- equality, diversity and inclusion
- EIP
- early intervention in psychosis services
- EMDR
- eye movement desensitisation and reprocessing (therapy)
- EQ-VAS
- EuroQol visual analogue scale
- FPS
- facilitated peer support
- GAD-7
- Generalised Anxiety Disorder-7
- HR
- human resources
- IAPT
- improving access to psychological therapies
- ICU
- intensive care unit
- ITQ
- International Trauma Questionnaire
- NHSE and I
- NHS England and Improvement
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health and Care Research
- NPT
- normalisation process theory
- PCL-5
- post-traumatic stress disorder checklist for DSM-5
- PHQ-9
- Patient Health Questionnaire-9 items
- PI
- principal investigator
- PPIE
- patient and public involvement and engagement
- PTSD
- post-traumatic stress disorder
- RA
- research assistant
- SD
- standard deviation
- VCSE
- voluntary, community and social enterprise sector
- WSAS
- work and social adjustment scale
- WTE
- whole-time equivalent
Notes
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/HGQR5133).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
