Notes
Article history
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as project number 17/09/31. The contractual start date was in November 2018. The final report began editorial review in February 2021 and was accepted for publication in October 2021. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
Copyright © 2022 Wilson et al. This work was produced by Wilson et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaption in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2022 Wilson et al.
Chapter 1 Introduction
Background
Borderline personality disorder (BPD) is a serious mental health condition characterised by a pervasive pattern of emotional instability, interpersonal dysfunction, disturbed self-image and impulsive behaviour, including self-harm. 1 BPD is associated with severe and persistent functional impairment2,3 and a suicide rate 50 times higher than that of the general population. 4 It is estimated that up to 80% of individuals with BPD self-harm and 75% attempt suicide,5 and BPD symptoms are among the best prospective predictors of self-harm in young people. 6
Borderline personality disorder is a developmental disorder, with symptoms usually first evident during adolescence. 7 Approximately 3% of children and young people present with BPD symptoms. 8,9 Left untreated, the symptoms of BPD adversely affect the young person’s capacity to meet developmental milestones, such as establishing independent social networks, forming stable relationships and developing academic, occupational and independent living skills, precipitating lifelong disability. BPD is predictive of poor educational achievement,10 unemployment and dysfunctional employment. 11
Growing research interest in adolescent BPD10 has spurred the development of the first wave of evidence-based treatments for BPD symptoms in young people: cognitive analytic therapy (CAT), dialectical behaviour therapy for adolescents (DBT-A) and mentalisation-based treatment for adolescents (MBT-A). These interventions have been demonstrated in randomised controlled trials (RCTs) to result in improvements in clinically important symptom domains, including self-harm, suicidal ideation and mood disturbance. 11–13 However, despite these promising findings, BPD treatment is still not routinely accessed by young people and the availability of evidence-based treatments for BPD in adolescents is poor. 10
Implementation of evidence-based treatments for adolescent BPD in routine clinical practice has been hindered by the expensive, highly specialised nature of the clinical resources required to deliver these treatments. 14 Furthermore, current mental health service models often require young people to meet institutional requirements to receive treatment rather than provide treatment in a way that suits the needs of young people. 15 Consequently, those experiencing the most severe and complex mental health difficulties are both less likely to access services16 and less likely to receive evidence-based interventions when they do. 17 The severe and complex nature of BPD makes this group particularly vulnerable to the barriers to treatment such service models impose.
Therefore, late intervention is currently the norm, with specialist treatments being offered to only a small minority of individuals with a chronic disorder. Young people with BPD symptoms often access treatment only once they reach a state of chronic psychosocial dysfunction and frequent mental health crises. 18 This late intervention model comes at substantial personal, social and economic cost, both to young people and their families and to health services. 19
Therefore, there is an urgent need for interventions that are more accessible to facilitate early access to treatment for young people presenting with BPD symptoms. The nature and severity of BPD symptoms mean that interventions that rely on regular clinic attendance or self-directed digital delivery are likely to have low uptake and completion rates. 14 Instead, utilising opportunities to deliver early interventions in contexts that are accessible to young people through working in partnership with universal services is a promising strategy.
Study rationale
As outlined above, there is a pressing need for accessible interventions to address the growing prevalence of BPD symptoms, including self-harm, among young people. 20–22 Currently available evidence-based interventions for adolescent BPD symptoms are not able to be delivered at scale within the NHS context because of their high clinical resource requirements. CAT for adolescents with BPD symptoms comprises 16 individual sessions delivered over approximately 26 weeks. DBT-A comprises twice-weekly sessions (individual therapy and a multi-family skills training group) delivered over a period of 12–16 weeks, with between-session telephone coaching. MBT-A involves weekly individual sessions and monthly family sessions over a 1-year period. CAT, DBT-A and MBT-A must all be delivered by qualified mental health professionals with additional specialist training and supervision. As a result of the relatively long treatment durations and the highly trained practitioners needed to deliver these therapies, few young people with BPD symptoms can access appropriate treatment at present.
The challenge of delivering early intervention for BPD can be met only by moving away from complex, resource-intensive psychotherapies towards brief interventions that can be delivered by non-specialists in accessible settings. 14 The Brief Education Supported Treatment (BEST) intervention has been designed to overcome these barriers to implementing early intervention for BPD symptoms through an innovative, cross-sector approach. Based on a treatment package developed by the Norfolk Youth Service,15 the intervention distils key elements of existing evidence-based interventions for adolescent BPD into a brief practicable format. The package promotes understanding difficulties using a mentalising approach and the development of self-care strategies to enable young people to manage distress.
Prior to the current study, this treatment package was delivered in secondary mental health services only. Owing to limited funding for children and young people’s mental health services and high and increasing demand, thresholds for access to secondary care were high. As a result, few young people with BPD symptoms were able to access the treatment package, and often only after they had been experiencing symptoms for many years. Therefore, we aimed to adapt the treatment package to enable it to be delivered within schools and colleges to facilitate earlier intervention.
Schools and colleges can play an important role in the emotional health and well-being of young people and are well placed to identify those with mental health problems. 16 Increased recognition of the potential of schools and colleges as settings for early intervention has led to an expansion of school-based mental health interventions in many high-income countries. 17 In the UK, mental health provision has traditionally been delivered within the health service. However, recent policy developments23,24 have led to an increased role of schools and colleges in the provision of mental health services for young people.
It is critical that the development of these new services is evidence informed to ensure that the maximum benefit is gained from scarce public resources. Many studies have found school-based interventions to have positive effects on young people’s mental health. 17,25 A recent network meta-analysis26 found little evidence that school-based interventions for the prevention of anxiety and depression are effective. However, a meta-analytic review of indicated school-based interventions found some evidence that these interventions are effective in reducing elevated depression and anxiety symptoms,27 although there is considerable variability in effect sizes reported.
At present, education and health services are too often disconnected, and schools and colleges report receiving inadequate support to meet the needs of pupils experiencing mental health problems. 28 A 2017 survey29 found that a majority of secondary teachers felt they needed further support to identify mental health issues (62%) and provide appropriate support (68%). Similarly, in a survey of 105 colleges in England,30 only 18% reported that referrals to secondary mental health services were responded to in a timely manner and 74% had referred pupils with mental health problems to accident and emergency (A&E) during the previous academic year.
Maximising opportunities for joint working between education and mental health services is vital if we are to meet the needs of the most vulnerable young people. This approach is in line with Children and Young People’s Improving Access to Psychological Therapies (CYP IAPT) and THRIVE principles, which advocate applying psychological approaches in a range of settings and contexts. 29,31 Public and patient involvement (PPI) work during the development of the study indicated that school and college staff and young people would like to be able to access mental health interventions within educational settings.
Since the conception of this study, the UK government has committed to providing access to mental health support within schools and colleges through funding the creation of new mental health support teams (MHSTs). 32 Signalling a commitment to the expansion of school- and college-based mental health provision initially proposed in a 2017 Green Paper,23 the key priorities for the NHS in England set out in the NHS Long Term Plan24 included the roll-out of MHSTs to between one-fifth and one-quarter of the country by the end of 2023.
The BEST intervention model involves training members of a school or college’s pastoral team to deliver an adapted version of the treatment package developed by the Norfolk Youth Service. School and college staff members then work alongside a mental health professional to co-deliver the intervention to young people enrolled at their school or college who have been identified as experiencing BPD symptoms. This co-delivery model was intended to maximise engagement and facilitate continuity of care by utilising the young person’s existing support networks. Furthermore, we hypothesised that working alongside a mental health professional to deliver the intervention would reduce the anxiety often experienced by education staff supporting young people with BPD symptoms by empowering them with the tools to offer effective support.
At the commencement of the study, the adapted treatment package had yet to be delivered in a school or college setting. Therefore, an intervention piloting and refinement phase was needed before commencing the feasibility trial to enable us to ensure that the intervention was suitable to be implemented within the context of schools and colleges. Following this intervention refinement phase, we planned to conduct a feasibility RCT to assess the feasibility of a future trial of the clinical effectiveness and cost-effectiveness of the refined intervention. This feasibility RCT was also intended to inform the design of any future effectiveness trial by answering questions about the suitability of the proposed outcome measures and the extent to which contamination of the control arm could be limited in an individually randomised study. A cluster randomised design was initially considered because of the possibility of contamination occurring with schools and colleges. However, owing to concerns about our ability to retain the engagement of schools and colleges randomised to treatment as usual (TAU), and the increased sample size and thus resources a cluster randomised trial would require, establishing the feasibility of limiting contamination in an individually randomised design was an important objective.
If proven effective in a future definitive trial, the BEST intervention could be implemented nationally, transforming the treatment of BPD symptoms by making early intervention the norm. This has the potential to produce substantial long-term benefits to individuals, society and the NHS by reducing the number of young people who develop entrenched psychopathology associated with chronic functional disability. As the intervention is designed to be delivered by non-specialists in BPD, the existing mental health workforce could be upskilled to deliver the intervention, supervised by a relatively small number of more specialist practitioners, making the intervention potentially highly scalable.
Aim and objectives
The aim of the study was to finalise the BEST intervention and inform the design of a future trial of its clinical effectiveness and cost-effectiveness. To meet this aim, we planned to achieve the following objectives.
Objective 1
To refine the BEST intervention to maximise the likelihood that it can be successfully implemented within the context of educational settings (schools and colleges).
Objective 2
To assess the feasibility of evaluating the clinical effectiveness and cost-effectiveness of the refined BEST intervention in a future RCT.
The factors we planned to consider in assessing feasibility were:
-
our ability to recruit participants to time and target
-
our ability to retain participants in the trial post randomisation
-
the acceptability and suitability of the proposed outcome measures and feasibility of identifying all costs and resource use that are relevant to the intervention
-
the ability of staff to deliver the intervention with fidelity to the model
-
the degree of contamination of the control arm (i.e. the extent to which participants randomised to the control arm received elements of the trial intervention)
-
the acceptability of the intervention from the perspective of staff and young people.
Research overview
The study was reviewed by Yorkshire & The Humber – South Yorkshire Research Ethics Committee (18/YH0416) and confirmation of Health Research Authority approval was received on 7 November 2018. The study was conducted in two stages, corresponding to the two objectives outlined above.
Stage 1: intervention refinement
The first stage of the study was intended to allow for refinement of the intervention and study processes to maximise the likelihood of their successful implementation. This preliminary stage of the study comprised two components: (1) a rapid evidence synthesis of barriers to and facilitators of the implementation of indicated mental health interventions within schools and colleges, and (2) a pilot of the intervention within three educational settings (one school and two colleges). Learning from the evidence synthesis and findings from the pilot were combined to enable us to finalise the intervention manual and resources, refine the practitioner training workshop and amend study procedures in preparation for the feasibility RCT.
Stage 2: feasibility randomised controlled trial
This second stage of the study comprised a feasibility RCT in which eligible young people were randomised in a 1 : 1 ratio to receive either BEST plus TAU or TAU alone. Participants were assessed pre-randomisation and followed up at 12 and 24 weeks using a battery of validated self-report and interviewer-rated measures. The feasibility RCT was accompanied by a detailed mixed-methods process evaluation exploring the acceptability of the intervention, fidelity of implementation across educational settings and contamination of the control arm.
Patient and public involvement
Three young people with relevant lived experience and one parent/carer representative acted as advisors to the study. Our advisors reviewed all participant-facing study documents to ensure that the format and language used were appropriate. Based on the feedback of our young advisors, rather than preparing separate participant information sheets for young people under 16 years and those over 16 years as originally intended, we created an ‘easier to read’ and a ‘detailed’ version of the information sheet, both of which were provided to all young people. Our parent-carer representative gave feedback on the information provided to the parents or carers of potential participants, and our protocol for approaching parents/carers to gain informed consent was based on her advice.
Our young advisors were influential in refining the intervention in preparation for the feasibility trial, providing feedback on the proposed amendments and suggesting changes to the wording and format of the manual worksheets. For instance, rather than referring to tasks to be completed in between sessions as ‘homework’, we presented these as suggestions of things to practice.
A young advisor also contributed to the training workshop for practitioners, sharing his personal experience as a young person with BPD symptoms and how he felt he could have been better supported within school. Furthermore, young advisors provided valuable advice on the recruitment strategy and helped to prepare promotional materials. One young advisor and our parent-carer advisor were members of the Trial Steering Committee (TSC) to ensure that PPI perspectives were represented in study oversight.
Chapter 2 Evidence synthesis
This chapter is adapted with permission from Gee et al. 33 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
Aim and research question
It has been suggested that the fidelity of implementation of school-based interventions may be crucial to their effectiveness. 34 Furthermore, effective mental health interventions are often not successfully adopted and sustained, in part because of insufficient consideration of compatibility with the organisational contexts in which they will be used. 35 Therefore, it is important to understand factors influencing the implementation of mental health interventions within schools and colleges to create a final intervention that can be successfully implemented and sustained.
To maximise the relevance of the findings to the implementation of the BEST intervention and facilitate a meaningful synthesis, we focused the review on indicated interventions for adolescents experiencing symptoms of an emotional disorder within high-income countries. Emotional disorders (e.g. anxiety, mood, post-traumatic stress) are the most prevalent mental health conditions during adolescence and, although rates of behavioural disorders (e.g. hypokinetic, conduct) have remained broadly stable, rates of emotional disorders among young people in England have increased by around 50% since 2004. 36 ‘Indicated’ interventions refer to those interventions delivered only to pupils identified as experiencing symptoms of a disorder.
The aim of the rapid evidence synthesis was to bring together the available evidence on barriers to and facilitators of successful implementation of indicated interventions within schools and colleges. The evidence synthesis intended to address the following research question: ‘What are the barriers to and facilitators of to the implementation of indicated psychological interventions for adolescent emotional disorders delivered within schools and further education or sixth form colleges located in high-income counties?’.
Methods
Design
A rapid evidence synthesis is a type of systematic review in which components of the systematic review process are simplified, omitted or made more efficient to produce the information required for a specific purpose within a limited time period. 37 To ensure completeness and quality, we retained core features of the systematic review process, including publication of the protocol, a comprehensive literature search, and duplicate study selection and data extraction. The key simplification we made to the review process was the omission of formal assessment of the scientific quality of the included studies. This was considered less relevant to the aims of the review because the transferability of findings related to barriers to and facilitators of implementation of an intervention is not necessarily dependent on the validity of the study design used to examine its effectiveness, risk of bias or other factors commonly assessed as part of determining study quality. In addition, we limited the scope of the review by including only English-language publications and studies conducted in high-income countries.
The protocol was registered with the PROSPERO registry prior to implementation of the search strategy (CRD42018102830).
Search strategy
We searched eight electronic databases [EMBASE, MEDLINE, PsycInfo®, Cumulative Index to Nursing and Allied Health Literature (CINAHL), British Nursing Index, Applied Social Sciences Index and Abstracts (ASSIA), Education Resources Information Center (ERIC) and British Education Index] from inception to 15 November 2018. To identify potentially eligible articles missed by the electronic search, we hand-searched a list of records retrieved as part of a recent related systematic review27 and contacted key experts in the field.
Eligibility criteria
Studies were included if they met the following criteria: (1) the study had an interventional design; (2) participants were aged 10–19 years at the time of recruitment; (3) all participants were presenting with elevated mental health symptoms or psychological distress; (4) the intervention studied was a psychological intervention (i.e. based on psychological theory as evidenced in a manual or other supporting material) designed to reduce symptoms of an emotional disorder; (5) the intervention studied was delivered wholly or partly within an institution whose primary function was education; (6) the study was conducted in a high-income country (as defined by the World Bank38); and (7) the report included information on barriers to and/or facilitators of the implementation of the intervention.
We included studies with any interventional design, that is any study that involved the implementation of an intervention. Purely observational studies of interventions that were already part of routine practice were excluded. Studies of universal interventions delivered to all pupils were outside the scope of this review. Studies of integrated indicated–universal approaches were eligible for inclusion only if separate findings were reported on the implementation of the indicated component. The focus of this review was on the implementation of interventions in schools and (sixth form/further education) colleges; therefore, studies of interventions delivered within universities or other higher education institutions were excluded.
Study selection
Study selection was carried out with the aid of Covidence systematic review software (Melbourne, VIC, Australia). After duplicate records were removed, the titles and abstracts of all articles identified by the literature search were independently reviewed by two reviewers. All disagreements between reviewers were discussed as a team and consensus decisions were reached. The full texts of articles deemed potentially relevant were obtained and assessed for eligibility by two researchers. Reviewers assessed eligibility independently and all disagreements regarding eligibility or conflicts in criteria for exclusion recorded were discussed by the two reviewers concerned and, if consensus not reached, resolved by a third reviewer. A flow diagram of the selection process was maintained as per Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidance. 39
Data extraction
Data were independently extracted by two reviewers and cross-checked to ensure accuracy. Contextual information was recorded using a piloted data extraction spreadsheet. The following information regarding the study sample was recorded: lower and upper age, gender (percentage female) and criterion for elevated mental health symptoms or psychological distress. In addition, the following information about the intervention was recorded: name, brief description, planned contact hours, whether parents or carers were involved and whether the intervention was delivered by staff members internal to the school or external facilitators. Included articles were imported into NVivo software version 12 (QSR International, Warrington, UK) where barriers and facilitators were synthesised as described below. Post hoc, we extracted details of the participant identification and referral processes employed in each study.
Data synthesis
A thematic synthesis40 of factors reported to affect intervention implementation was conducted with the aid of NVivo (version 12) qualitative data analysis software. Included papers were imported into NVivo and sections of the text describing barriers to or facilitators of implementation, including both quoted original data and author interpretation, were coded using an inductively developed coding structure. Coding of all included studies was completed by Briony Gee and independently by one other member of the review team. Discrepancies in coding were discussed by the two reviewers concerned and consensus interpretations were researched in all cases.
Codes generated inductively were first organised into descriptive themes that aimed to summarise the barriers and facilitators reported, staying close to the primary studies. The next stage of the analysis involved developing analytic themes by structuring and interpreting the descriptive themes according to the selected theoretical framework. This stage of the analysis aimed to ‘go beyond’ describing the findings of the included studies to generate new understandings of the factors influencing successful implementation of indicated school-based mental health interventions. A suitable framework was selected a posteriori with the aid of Nilsen’s taxonomy of implementation science theories, models and frameworks. 41 The theoretical framework was selected only after the generation of initial descriptive themes to ensure that, as far as possible, the analytic themes developed were data driven rather than reflecting the review team’s prior assumptions.
Durlak and Dupre’s ecological framework for effective implementation42 is premised on the view that a multilevel ecological perspective is necessary for understanding successful implementation. It is a determinant framework41 that aims to understand influences on implementation outcomes by specifying individual, organisational and community-level factors that act as implementation barriers and enablers. This framework was deemed to be an appropriate organising concept for the current review because schools and colleges are dynamic and complex social organisations, and thus the implementation of new practices within them is influenced by factors on multiple interacting levels. 43
A sensitivity analysis was conducted in which only studies of interventions found to be effective were retained. Studies in which there was no evidence that the intervention was effective in improving the primary outcome or that did not report a group-based statistical analysis of intervention effectiveness were removed from the thematic synthesis to explore whether or not implementation issues differed by study outcome.
Results
Characteristics of included studies
Our electronic searches returned 2559 unique study records. In addition, 10 studies were identified through hand-searching and correspondence with experts. The study selection process is illustrated in Figure 1.
FIGURE 1.
The PRISMA diagram illustrating study selection process.
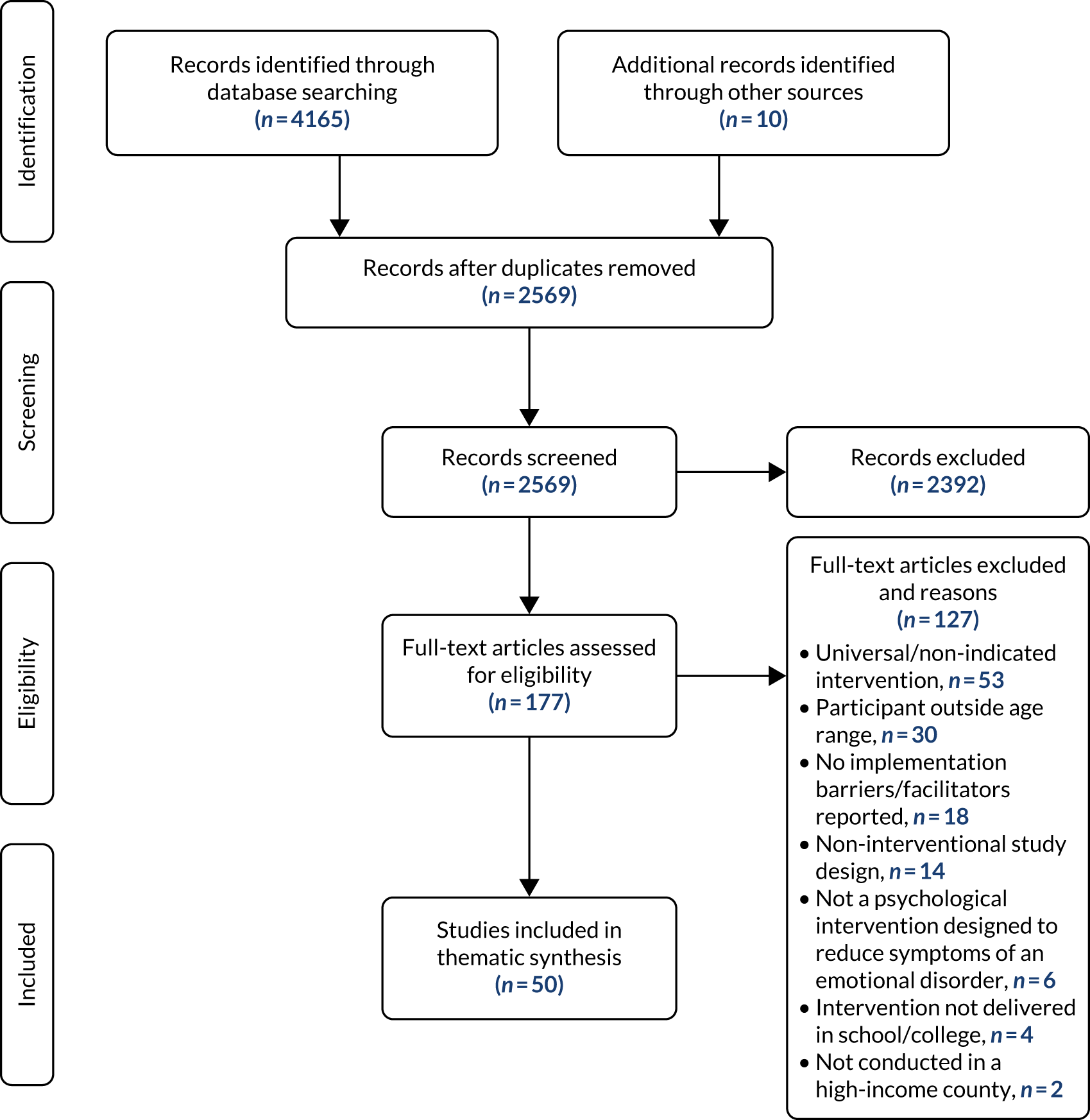
We identified 50 unique papers that met the inclusion criteria (Table 1).
| Author(s) | Year | n | Lower age (years) | Upper age (years) | % female | Presenting problem | Identification methoda | Intervention type | Parental involvement | Internal/external delivery |
|---|---|---|---|---|---|---|---|---|---|---|
| Bei et al.44 | 2013 | 10 | 13 | 15 | 100 | Sleep problems | A | Mindfulness | No | Both |
| Bernstein45 | 2010 | 4 | 11 | 18 | 100 | Anxiety | C | CBT | Yes | Internal |
| Berry and Hunt46 | 2009 | 46 | 12 | 15 | 0 | Anxiety | C | CBT | Yes | External |
| Burke et al.47 | 2017 | 7 | 10 | 11 | – | Anxiety | C | CBT | Yes | Unclear |
| Butler-Hepler48 | 2013 | 59 | 11 | 14 | 71 | Depression | A | CBT | No | Both |
| Chu and Weissman49 | 2009 | 35 | 12 | 14 | 60 | Either depression or anxiety | C | BA | No | External |
| Chu et al.50 | 2016 | 35 | 12 | 14 | 71.4 | Either depression or anxiety | A | BA | No | Both |
| Cooley et al.51 | 2004 | 10 | 10 | 11 | 80 | Anxiety | A or C | CBT | No | External |
| Cooper et al.52 | 2010 | 27 | 13 | 15 | 77.8 | Depression | A | Humanistic counselling | No | External |
| Crisp et al.53 | 2006 | 27 | – | – | 74 | Depression | C | CBT | No | External |
| Drmic et al.54 | 2017 | 44 | 13 | 15 | 14 | Anxiety | C | CBT | Yes | Both |
| Ehntholt and Smith55 | 2005 | 26 | 11 | 15 | 34 | Psychological difficulties as a result of trauma | C | CBT | No | External |
| Feldman56 | 2007 | 29 | 11 | 13 | 44.8 | PTSD | A | CBT | Yes | Both |
| Fitzgerald et al.57 | 2016 | 127 | 15 | 18 | 57.5 | Anxiety | A | Attention bias modification | No | Unclear |
| Gartenberg58 | 2017 | 2 | 15 | 15 | 50 | Anxiety | C | CBT | No | External |
| Ginsburg and Drake59 | 2002 | 12 | 14 | 17 | 83.3 | Anxiety | A | CBT | No | External |
| La Greca et al.60 | 2016 | 14 | 13 | 18 | 79 | Either depression or anxiety | A | IPT | No | External |
| Hunt et al.61 | 2009 | 260 | 11 | 13 | 43 | Anxiety | A | CBT | Yes | Internal |
| Jaycox et al.62 | 2009 | 76 | – | – | 51.3 | PTSD | A | CBT | No | Internal |
| Kaplinski63 | 2007 | 49 | 14 | 18 | 63.3 | Depression | C | CBT | No | External |
| Lamb et al.64 | 1998 | 41 | 14 | 19 | – | Depression | A | CBT | No | External |
| Liberman and Robertson65 | 2005 | 33 | 15 | 17 | – | Schizotypy | A | CBT | No | Unclear |
| Listug-Lunde et al.66 | 2013 | 16 | 11 | 14 | 37.50 | Depression | A | CBT | No | Both |
| Livheim et al.67 | 2014 | 98 | 12 | 18 | 82.70 | Depression | C | ACT | No | Both |
| Masia et al.68 | 2001 | 6 | 14 | 17 | 50 | Anxiety | C | CBT | No | External |
| Masia-Warner et al.69 | 2005 | 35 | 13 | 17 | 74 | Anxiety | A or C | CBT | Yes | Both |
| Masia-Warner et al.70 | 2016 | 138 | 14 | 16 | 68 | Anxiety | A or C | CBT | Yes | Both |
| McCarty et al.71 | 2011 | 67 | 12 | 13 | 55.6 | Depression | A | CBT | Yes | Unclear |
| Melnyk et al.72 | 2014 | 16 | 14 | 17 | 56 | Anxiety | C | CBT | No | External |
| Messinger et al.73 | 2011 | 8 | 11 | 13 | 62.5 | Anxiety | A | CBT | No | External |
| Morsette et al.74 | 2012 | 57 | 10 | 15 | 56 | PTSD | A | CBT | Yes | Internal |
| Mowatt75 | 2017 | 16 | 13 | 15 | 68.80 | Depression | C | CBT | No | External |
| Mufson et al.76 | 2004 | 63 | 12 | 18 | 84 | Depression | A | IPT | No | Internal |
| Oros77 | 2016 | 6 | 14 | 17 | 100 | BPD | A | DBT | No | External |
| Pass et al.78 | 2018 | 32 | 11 | 18 | 68.75 | Depression | B or C | BA | Yes | External |
| Pearson79 | 2017 | 3 | 11 | 12 | 0 | Anxiety | C | CBT | Yes | External |
| Rickard et al.80 | 2016 | 47 | 11 | 17 | 36 | General social/emotional problems | C | CBT | Yes | Internal |
| Riley81 | 2012 | 12 | 11 | 13 | 50 | Psychological distress as a result of loss/change | C | Grief education | No | External |
| Robinson et al.82 | 2015 | 21 | 14 | 18 | 81 | Suicidal ideation | B | CBT | No | External |
| Rohde et al.83 | 2014 | 378 | 13 | 19 | 68 | Depression | A | CBT | No | Internal |
| Ruffolo and Fischer84 | 2009 | 60 | 11 | 18 | – | Depression | B or C | CBT | No | Internal |
| Schoenfeld and Mathur85 | 2009 | 3 | 11 | 12 | 0 | Anxiety | C | CBT | No | External |
| Scotti86 | 2014 | 7 | 14 | 18 | 100 | Eating disorder | C | DBT | No | External |
| Stasiak et al.87 | 2014 | 34 | 13 | 18 | 41 | Depression | A | CBT | No | External |
| Stein et al.88 | 2003 | 126 | – | – | 56 | PTSD | A | CBT | No | Both |
| Stein89 | 2011 | 126 | – | – | 56 | PTSD | A | CBT | No | Internal |
| Stice et al.90 | 2011 | 306 | 14 | 19 | 100 | Eating disorder | A | Dissonance intervention | No | Internal |
| Woods and Jose91 | 2011 | 83 | 13 | 15 | – | Depression | A | CBT | No | Internal |
| Young et al.92 | 2010 | 57 | 13 | 17 | 59.7 | Depression | A | IPT | Yes | External |
| Young et al.93 | 2016 | 186 | 12 | 16 | 66.7 | Depression | A | IPT | Yes | External |
Included studies were published over a 20-year period between 1998 and 2018. Most included studies were of indicated interventions for young people with symptoms of depression (n = 17), anxiety (n = 16), post-traumatic stress disorder (n = 5) or either depression or anxiety symptoms (n = 3).
The majority of studies were of interventions described as cognitive behavioural therapy (CBT) or CBT based (n = 35). Half the included studies (n = 25) were of interventions delivered by an external facilitator, 11 were delivered by an internal school-based staff member and 10 by both internal and external personnel. The remaining studies (n = 4) did not report whether those delivering the intervention were internal or external to the school.
Although studies of interventions delivered within sixth form and further education colleges were eligible for inclusion, no such studies were identified. As all included studies were of interventions delivered within schools, the results of the thematic synthesis below are specific to school-based interventions.
Thematic synthesis
Eleven analytic themes were developed (Figure 2): two related to intervention characteristics (acceptability, practicality); three related to organisational capacity, that is practices, processes and culture of the structures through which the intervention is implemented (relationships between intervention facilitators and school staff, support of school leadership and school environment); two related to training and technical assistance (quality of training and ongoing supervision, and suitability of the intervention manual and other materials); two provider characteristics (ability of staff to deliver the intervention successfully and ability of staff to identify eligible students); and two community-level factors (stigma and mental health literacy, and priorities of health and education systems).
FIGURE 2.
Diagram of factors reported to influence the successful implementation of school-based indicated interventions for adolescents with symptoms of an emotional disorder.
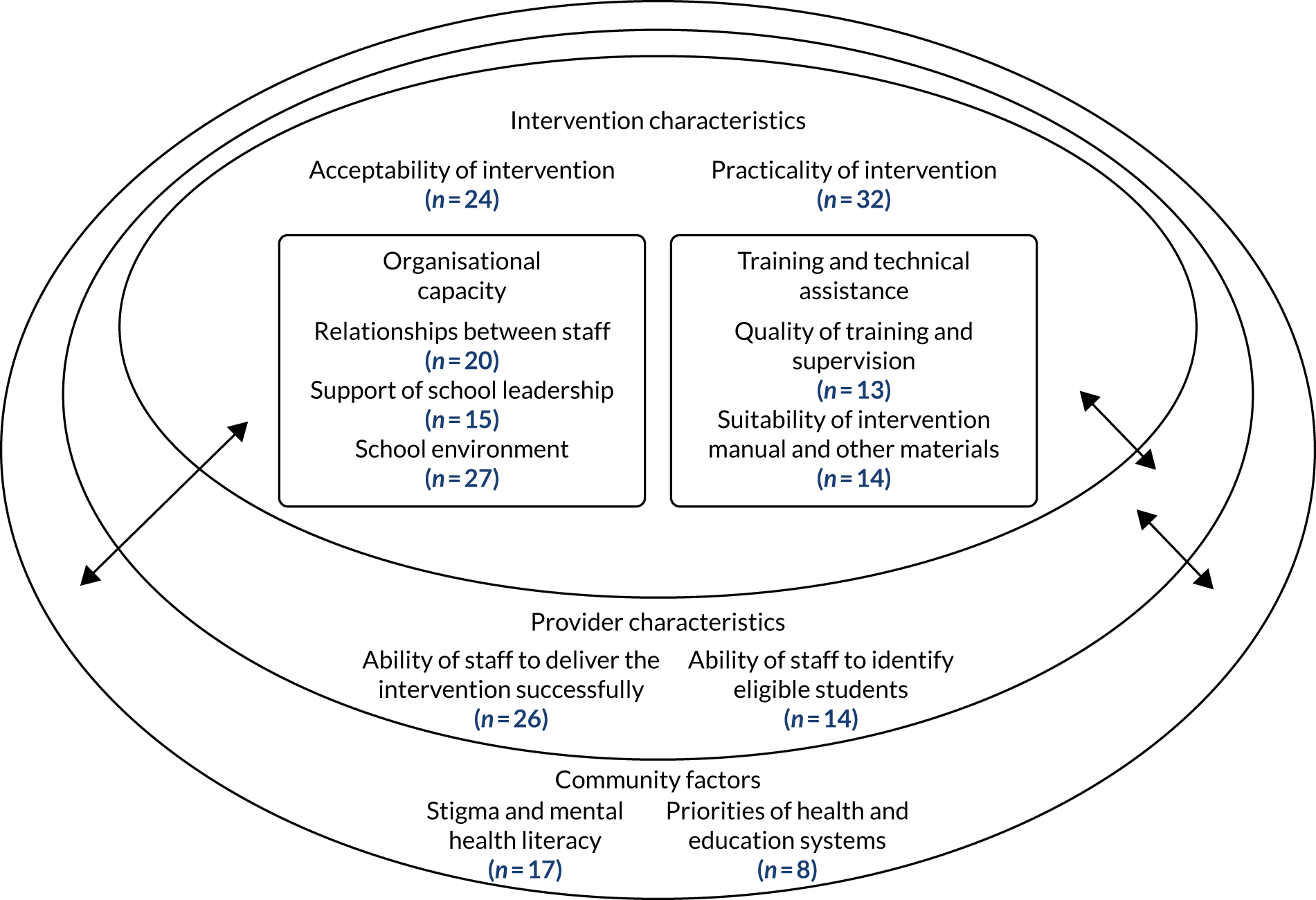
The number of the included studies that contributed to each analytic theme is given in brackets next to the name of each theme below. Quotations from primary papers to be presented alongside the findings were selected based on how clearly they exemplified the themes.
Intervention characteristics
Acceptability (24 studies)
Intervention acceptability was noted as important to attendance and engagement, and hence to successful implementation. Acceptability reflects the extent to which people delivering or receiving an intervention consider it to be appropriate, based on anticipated or experienced cognitive and emotional responses to the intervention. Characteristics identified as influencing the acceptability of interventions included whether or not it was experienced as helpful, enjoyable, developmentally appropriate and well designed, and the format of delivery. High acceptability was achieved through ensuring that the intervention matched the needs and preferences of participating adolescents by focusing on issues important to their lives and presenting material in an interactive, appealing and accessible but mature way.
Many of the school-based interventions studied were delivered in a group format. This was sometimes identified as contributing to high acceptability through capitalising on the developmental priority given to peer relationships during adolescence. Key perceived benefits of group delivery were the sense of belonging and mutual support, and the social connections fostered through participating in activities with other young people experiencing similar difficulties. For instance, Riley81 reported that ‘pupils favoured group over individual input due to feelings of reduced isolation, opportunities to make friends, normalisation of feelings, learning from others, building confidence and supporting each other’.
However, group delivery was also frequently identified as a barrier to implementation through contributing to a lack of acceptability for some students. A group was viewed as an unsuitable therapeutic setting for some young people, because of either behavioural issues (e.g. some groups included students who were unable to work appropriately in a group48) or young people not feeling comfortable disclosing personal experiences in front of peers (‘the group setting was inhibiting for some students, especially given that they knew one another relatively well’;66 ‘students did not want to talk about their fears in front of peers’54). This created problems conducting intervention sessions as planned and ensuring that the intervention was meaningful for all group members.
Practicality (32 studies)
The intervention feature most frequently reported as affecting the success of implementation was the extent to which the intervention could be flexibly deployed to cause minimal disruption to school routines. Restricting the length of sessions to single class periods, structuring the programme of sessions around the school term, scheduling sessions to minimise interference with academic activities and allowing for breaks in intervention delivery because of exam periods and other school events were commonly reported adaptations required for successful implementation within the school setting.
Certain intervention components were noted as being problematic to implement within a school setting. Parent/carer involvement was consistently noted as desirable but challenging to achieve. In some studies, components of the intervention involving parents/carers were noted to have been removed or reduced owing to resource limitations or concerns about the feasibility of organising sessions for parents/carers within the school setting. Studies that sought to involve parents/carers in sessions commonly reported disappointing attendance.
A further intervention component recurrently identified as posing challenges to implementation was exposure to feared activities, objects or situations. The school setting was noted to facilitate some types of exposure work; for instance, Masia et al. 68 in their study of an intervention for social phobia noted that the school setting enabled the intervention facilitators to set up in vivo exposure exercises within the schools. However, other researchers encountered barriers to conducting exposure therapy within a school setting. These included practical difficulties arranging exposure to infrequent, unpredictable or inaccessible events or objects; difficulties planning appropriately idiosyncratic exposure hierarchies in a group setting; resistance from adolescents; and lack of confidence among intervention facilitators not experienced in the use of exposure.
Some studies reported the group format as contributing to an increase in practicality through making more efficient use of available resources. This was recognised as particularly important in communities with limited access to mental health resources. 66 However, difficulty identifying a sufficiently homogenous group of students within a single school for group delivery to be appropriate was also discussed. Moreover, a study by Oros77 highlights the risk of iatrogenic harm as a result of inappropriate group composition. They recommend that participants are screened more carefully before being included, as they had observed that peer contagion may play a part in making some participants’ symptoms worse.
Organisational capacity
Relationships between intervention facilitators and school staff (20 studies)
Positive relationships between individuals delivering the intervention and other staff members were frequently cited as important facilitators of successful implementation. When the intervention was facilitated by staff external to the school, effective communication with school staff and efforts to integrate into school systems were seen as particularly important. Effective collaborations between external providers and school staff were sometimes supported by establishing a reciprocal partnership in which external staff members contributed their time and expertise to school activities beyond the intervention itself.
Maintaining positive relationships with teaching staff not involved in the implementation of interventions was sometimes cited as a challenge. For instance, Scotti86 reported that, although young people and their parents perceived a school-based intervention to be both acceptable and beneficial, teachers found that having students attend sessions during the school day was unacceptably disruptive. Scheduling sessions outside the normal school day minimised this disruption but it was more difficult to deliver the intervention with fidelity as attendance was sporadic and treatment adherence was poor. 86 Therefore, securing ‘buy-in’ from teaching staff and maintaining positive relationships between intervention facilitators and teachers is important to support successful implementation.
Support of school leadership (15 studies)
The support and involvement of senior school leaders were frequently cited as key facilitators of successful implementation. Support at the appropriate level within the school hierarchy ensured that necessary resources were made available, and positively affected support for implementation of the intervention within the wider school system. For instance, Drmic et al. 54 reported the vital importance of the involvement of a member of the school leadership team as an ‘opinion leader’ who was ‘intimately involved in all aspects of the implementation project’ and ‘was able to garner support/interest from key stakeholders’. Conversely, when interventions were implemented without the clear endorsement and direct input of a school’s senior leadership team, interventions were more difficult to implement and sustain. For instance, Pass et al. 78 reported that ‘we had to withdraw resources from one school where the senior leadership were not involved, and a major staff restructuring led to loss of pastoral leads who had been the main contacts for the therapy team’.
School environment (27 studies)
Logistical issues associated with delivering psychological interventions within the school environment were the most commonly reported barrier to implementation. Difficulties scheduling sessions within the constraints of school timetables were frequently reported. Kaplinski63 commented that they had not anticipated how regularly scheduled sessions would be interrupted or cancelled as a result of, for example, fire alarms and school assemblies. Lack of appropriate spaces within schools in which to conduct sessions was also a barrier.
The extent to which the wider school environment was conducive to good mental health and provided a suitable setting for therapeutic work was also noted as important to the successful implementation of interventions. For instance, Ehntholt et al. 55 reported that two schools participating in a study of a group intervention for children with post-traumatic stress symptoms ‘were far from ideal environments for the establishment of therapeutic groups . . . it was difficult for the children to genuinely relax during the sessions due to the school’s loud, chaotic environment’.
However, encouragingly, staff participants in a study by Butler-Hepler48 commented that, following the implementation of the intervention, the climate within the school appeared to be healthier, and teachers were more willing for students to have counselling, suggesting that the implementation of psychological interventions within schools has the potential to positively affect the school environment. Therefore, there is the potential for successful implementation to initiate a virtuous cycle.
Training and technical assistance
Quality of training and ongoing supervision (13 studies)
The need for high-quality training of intervention facilitators and supervision from appropriately experienced and qualified experts to support fidelity of delivery was emphasised in several studies. Although the importance of training and supervision was consistently endorsed, it appears that more intensive training and supervision are likely to be required for interventions delivered by staff with relatively little experience of delivering psychological interventions.
More informal support from others facilitating the intervention was also sometimes identified as important for successful delivery. For instance, Ruffolo and Fischer84 found that ‘the mentorship supervision model supported the school-based social workers in connecting with each other and providing each other ongoing support’. However, the authors noted that protecting staff time to participate in supervision was challenging and would require sustained funding and leadership support.
Suitability of intervention manual and other materials (14 studies)
The provision of an intervention manual that was clear and easy to follow, and good-quality supporting materials such as workbooks and resources to support homework exercises, was identified as a facilitator of successful implementation. Several authors suggested that well-structured, highly manualised interventions may be more easily mastered by novice facilitators, enhancing treatment fidelity. When interventions employed technology to facilitate delivery, it was important that these were well designed, with user-friendly interfaces to maximise acceptability and engagement.
Provider characteristics
Ability of staff to deliver the intervention successfully (26 studies)
Although some interventions studied were delivered by members of the research team or other external specialists, many of the interventions involved training existing school-based staff with diverse professional backgrounds to deliver a manualised programme. Skilled facilitation of interventions was noted as crucial to successful implementation and in all studies in which this was reported on, trained school-based professionals were found to be able to deliver the interventions with acceptable fidelity. However, the findings of some studies suggest that school-based professionals, who were often less experienced in delivering manualised interventions for emotional problems, were less able to implement the interventions as planned than specialist mental health staff. Although delivery of interventions by external specialist might therefore seem to be supported, some authors of studies of interventions that relied on external providers expressed concern about the sustainability and cost-effectiveness of this delivery model.
Ability of staff to identify eligible students (14 studies)
There were also some concerns raised about the feasibility of procedures used to identify students for whom interventions would be suitable. Although school-wide screening and other comprehensive recruitment strategies co-ordinated by the research team were reported to be successful in identifying eligible young people, these were acknowledged to be unlikely to be sustainable outside the research context. Although recruitment strategies relying on referrals from school staff members were often reported to be effective, the capacity of school staff to identify students who could benefit from an intervention was raised as a concern by some study authors. For instance, Pass et al. 78 described how ‘feedback from school staff suggested that many lacked confidence in identifying students with depression symptoms and had very little protected time to consistently manage the referral process’.
Community factors
Stigma and mental health literacy (17 studies)
The impact of stigma on implementation was considered by several study authors. The potential for stigma by peers within the school community was a concern for some young people and their parents. This finding might partially explain the lower than anticipated student uptake and difficulties obtaining parental consent for participation reported by many studies.
However, not all studies found stigma to be a barrier to implementation. For instance, Crisp et al. 53 asked participants to complete a self-report measure of their perceptions of barriers to treatment. Items assessing potential barriers related to stigma (e.g. ‘My friends thought I was stupid for going to therapy’ and ‘I felt uncomfortable about going to sessions at school’) were consistently rated as never or rarely a problem. Several authors reported that participating in a school-based intervention was viewed as less stigmatising than accessing conventional mental health treatment.
Priorities of health and education systems (eight studies)
The need to align the priorities of the health-care and education systems to facilitate successful implementation of school-based mental health interventions was alluded to by a number of studies. Lack of adequate resource allocation for services to support mental health and well-being within schools, arguably a symptom of low prioritisation of these issues, was also identified as a barrier to effective implementation.
Sensitivity analysis
Themes remained broadly similar when studies in which there was no evidence of effect on the primary outcome or that did not report statistical analysis of intervention effectiveness were removed. There was a change of more than 5% in the percentage of included studies that contributed to two of the themes: practicality was reported as affecting the implementation of fewer of the interventions found to be effective than the complete set of included interventions, and quality of training and ongoing supervision was reported as a facilitator of implementation by only the subset of studies of interventions found to be effective.
Discussion
The aim of this review was to identify and synthesise factors reported in the literature to influence the implementation of indicated interventions for adolescent emotional disorders delivered within schools and colleges. The thematic synthesis resulted in 11 analytical themes that brought together findings from 50 primary studies. Themes encompassed characteristics of the interventions, training and support, organisational factors and community-level factors that have been identified as affecting implementation.
The findings of this review support the view that delivering indicated mental health interventions within a school context presents many challenges and that implementation is influenced by factors on multiple interacting levels. The most frequently reported challenges were logistical in nature. Practitioners delivering interventions in a school setting must be aware of and prepared to work within the constraints imposed by school calendars, timetables and the physical school environment. It is important that those designing school-based mental health initiatives select interventions that can accommodate such constraints and consider whether or not all components of an intervention are feasible to deliver within the school context. However, which interventions can practicably be delivered within the school context will depend on factors at the organisation and community level.
Having intervention champions at an appropriately senior level within the school is crucially important if intervention delivery is to be prioritised and appropriate resources made available. Senior leadership support was reported to be influenced by the extent of competing priorities, and thus it is important that both the health-care and education systems maintain a shared focus on the emotional health of young people. UK schools have faced criticism for focusing on academic achievement at the expense of mental health and well-being. 94 However, recent proposals to include emotional and mental well-being in the education inspection framework95 might increase the priority given to mental health initiatives in future. Close collaboration between the Department of Health and Social Care and the Department for Education in the production of the Green Paper on transforming mental health provision for young people96 sets an important precedent of joint working with the potential to have an impact on implementation at the local level.
Studies included in the review evaluated interventions delivered by a wide variety of professionals, including external providers, and existing school-based staff. Although there is some evidence that external personnel can deliver interventions with higher fidelity than internal school-based staff, reliance on external facilitation was accompanied by some challenges. For instance, it was noted that external facilitators must make particular efforts to establish effective communication with school staff and to integrate into school routines. Authors also raised concerns about the sustainability and cost-effectiveness of reliance on external facilitators.
This potential tension between fidelity and sustainable implementation might be partially addressed by appropriate supervision and ongoing support. The quality of training and support is likely to be particularly important when intervention facilitators are less experienced in delivering evidence-based interventions. Furthermore, it appears that well-structured, highly manualised interventions may be easier for less experienced practitioners to implement with fidelity and so should be preferred within service models involving provision of interventions by practitioners with limited training in delivering psychological interventions.
For an indicated intervention to be successfully implemented it is important to have appropriate mechanisms to identify young people experiencing the symptoms targeted. As indicated in Table 1, the main identification strategies employed by studies included in the review were referral by school staff members, identification through screening or a combination of both strategies. A recent review97 of school-based identification methods concluded that universal screening may be the most effective method of identifying children experiencing mental health difficulties. However, studies included in the current review raised concerns about the sustainability of this approach for indicated programmes. Therefore, ensuring that school staff members who might act as ‘gatekeepers’ have appropriate training and capacity to identify students who could benefit from an indicated intervention is likely to be essential. This training must be ongoing to account for staff turnover and to ensure that knowledge and skills are maintained. As the feasibility of school-based identification of mental health difficulties was not the focus of this review, we direct interested readers to a review by Soneson et al. 98 for a fuller discussion of this issue.
Although there is evidence that targeted school-based interventions have larger and more durable effects on mental health outcomes than do universal approaches,25 concerns have been raised about potential stigma. A recent review of qualitative research found that some students are apprehensive about engaging with targeted school-based mental health interventions because of fear of negative stigma-related consequences. 99 Stigma has also been found to be one of the most commonly reported barriers to accessing school-based treatment in quantitative research. 100,101
Corroborating these concerns, the current review identified a number of studies that reported fear of potential stigma as a barrier to implementation. However, stigma was not universally viewed as a barrier: there was evidence that some young people view school-based interventions as less stigmatising than conventional mental health treatment and that acceptability of the indicated interventions was generally reported to be high. Studies directly exploring young people’s experiences of receiving school-based metal health support are scarce,99 and therefore there is a need for further research to fully understand acceptability.
Limitations
Although studies of interventions delivered within sixth form and further education colleges were eligible for inclusion, no such studies were identified. Therefore, we are unable to reach any conclusions about how to deliver mental health support in such colleges. In the UK, colleges educate and train more than two million people each year, and over two-thirds of all 16- to 18-year-olds are enrolled at a college. 102 There are substantial differences between schools and colleges that are likely to have an impact on the implementation of mental health interventions. For instance, colleges tend to be less formal environments than schools with less structured timetables and greater student independence. Therefore, there is a need for further research on the delivery of mental health interventions within this context to inform UK policy.
The scope of the current review was limited to studies conducted in high-income countries. This was necessary to facilitate meaningful synthesis as the factors affecting the implementation of interventions in low-resource contexts are likely to differ in important ways from the factors that affect the implementation of similar interventions in contexts in which greater resources are available. However, there are promising school-based mental health interventions delivered in low- and middle-income countries17 and understanding the factors that have an impact on the implementation of these interventions in these contexts is undoubtedly important.
The sensitivity analysis conducted post hoc was intended to provide an indication of whether or not the implementation barriers and facilitators reported differed according to the effectiveness of the interventions concerned. The results of this analysis indicate that the inclusion of studies of interventions not found to be effective did not have a substantial impact on the themes identified. However, there are several factors that complicate the interpretation of this analysis, including the use of inconsistent definitions of effectiveness across studies and the lack of systematic measurement and reporting of barriers and facilitators. Therefore, it is not possible to draw conclusions regarding whether or not implementation barriers and facilitators actually differed or to infer that the presence or absence of a particular factor is linked to effectiveness.
The findings of this review must be interpreted with some caution owing to the quality of the evidence regarding implementation synthesised. Although we did not formally assess the quality of included studies, because this would not necessarily relate to the quality of the information on implementation, we noted that most coded sections of the text describing barriers to or facilitators of implementation were from author interpretation rather than objectively collected process data. Implementation is a topic that has received relatively scant attention in comparison with effectiveness and, for this reason, it was rarely a primary focus of eligible studies. As a result, implementation factors were often captured informally and therefore the data lacked richness. Future research should employ formal process evaluation and implementation science designs. It has been argued that one of the most critical issues in mental health services research is the gap between what is known about effective treatment and what is provided in routine care. 35 If this gap is to be bridged, it is important that researchers give increased attention to factors affecting implementation and design studies accordingly, incorporating process evaluation and implementation science approaches.
Implications
The findings of this review have important implications for those with a role in planning and implementing school-based mental health initiatives (Box 1). Recent UK policy proposals23 include the creation of new MHSTs based within schools and colleges and the introduction of designated senior leads for mental health in each setting. MHSTs will offer direct support to young people experiencing mild to moderate mental health difficulties, supervised by NHS mental health professionals. There is the potential for this model to offer an effective solution to the tension between fidelity and sustainability highlighted by this review; learning from the current evidence will be important to realising this potential.
-
Involve young people and education professionals in the selection of psychological interventions to be delivered within schools to ensure that they are acceptable and practical to deliver in this context. Group interventions are efficient and often acceptable but do not meet the needs of all young people. Provision should be made for those who require individual support.
-
Carefully consider the best method of identifying young people who could benefit from indicated interventions. If whole-school screening is not feasible, staff will need training and support to enable them to identify and refer suitable students.
-
Ensure that those delivering interventions receive high-quality training and ongoing supervision.
-
Plan for the inevitable logistical challenges associated with the constraints of the school calendar, routines and environment.
-
Identify an (appropriately trained and supported) intervention champion at a senior level in each school to promote buy-in from other staff members and to develop a school culture that prioritises mental well-being.
-
Health and education policy should be designed to promote a shared focus on the emotional health of young people across sectors.
The findings of this review indicate the need to ensure that the curriculum for the workforce who will be trained to work as part of the new MHSTs is designed with input from young people and education professionals. This will help to ensure that the interventions this new workforce are trained to deliver are acceptable to young people and can practicably be delivered in educational settings. Interventions are more likely to be implemented successfully if they are well structured, manualised and delivered by staff who receive high-quality training and supervision.
Designated senior leads for mental health will be well placed to encourage genuine and committed ‘buy-in’ from all aspects of the system, including senior leaders, governors, teaching staff and parents/carers. However, changing whole-school culture is no small task. It will be important that leads are appropriately supported to fulfil this role. This might include the creation of forums for designated senior leads to share good practice, and the co-production of a school and college mental health charter to support cultural change.
There is a danger that the creation of new school-based services will add further complexity to a system that is already fragmented and which in turn could lead to the creation of more treatment silos. 103 We must avoid this and instead use these developments as an opportunity for greater joint working and system alignment.
Conclusion
Our findings suggest that those involved in the implementation of school-based mental health interventions should ensure that they select appropriate interventions, consider logistical challenges and provide high-quality training and supervision to enable staff to deliver interventions with fidelity. Furthermore, it is important to consider the structural and environmental support required for successful implementation to ensure that potential benefits are maximised.
Chapter 3 Intervention piloting and refinement
Description of prototype BEST intervention
Background
In Norfolk, following Future in Mind recommendations,22 child and adolescent mental health service (CAMHS) transformation and the development of local transformation plans (LTPs) encouraged services to develop innovative practices. Norfolk LTP priority areas included responding to the rise in reported self-harm and suicidal acts in young people and improving access to mental health support. It was recognised that mental health services for children and young people must be designed around their needs. Therefore, system leaders have been working to develop strong relationships between NHS mental health services and educational settings to facilitate improved collaboration.
The Norfolk Youth Service is a pragmatic, assertive and ‘youth-friendly’ service for young people aged 14–25 years that transcends traditional service boundaries between CAMHS and adult services. The service was developed in 2012 in collaboration with young people and partnership agencies and is based on an engaging and inclusive ethos. The service is recovery oriented and evidence based and aims to satisfy recent policy commitments to extend mental health provision for young people to those up to the age of 25 years. The challenges of engaging and supporting young people with early symptoms of BPD has been a key area of work for the Norfolk Youth Service. This work has been ongoing since the development of the youth service and has resulted in several innovative approaches to working with early symptoms of BPD in adolescence. This work has included collaboration with, and learning from, specialist services worldwide, including the Orygen (Orygen Youth Health, Parkville, VIC, Australia) service.
Part of the work of the Norfolk Youth Service has been to produce and deliver a treatment package for young people with BPD symptoms that distils fundamental elements of evidence-based interventions for adolescent BPD into a brief (three to six sessions) practicable format. This package was designed to be delivered within secondary mental health services. However, because of long waiting times and high thresholds for treatment as a result of increasing demand for mental health support, the team recognised that many young people with BPD symptoms did not access secondary services until they had reached crisis point. Therefore, the need to adapt the treatment package to enable it to be delivered outside specialist services to facilitate earlier intervention was identified.
Theoretical underpinnings
The BEST intervention was developed to address issues apparent in the delivery of evidence-based interventions for adolescent BPD symptoms, including difficulties of access to specialist services that provide such treatments, problems engaging young people in treatment, early treatment drop-out and lack of resources available to deliver lengthy interventions. Therefore, the intervention takes account of issues specific to engaging with an adolescent population and providing interventions tailored to this group.
The development of the intervention utilised knowledge from attachment theory, which identifies how patterns of relating are established in the context of early attachment relationships. In-depth psychological therapies that aim to identify unhelpful patterns of relating to others and work to establish new healthier patterns of relating (such as MBT-A or CAT) have been demonstrated as effective with young people. 1 However, as previously mentioned, there are also many difficulties in engaging young people in this form of treatment early enough and for a sustained period.
The BEST intervention draws from relational elements of attachment theory to support the young person to identify unhelpful patterns of relating and to work towards the development of more helpful strategies. This is supported through enhancing the relationship with an identified member of staff at the young person’s school or college, thus nurturing relationships that are already established and part of the young person’s everyday life, eliminating the need for additional specialist support from sources external to the young person’s current support network.
Drawing from MBT-A,2 the BEST intervention recognises that adolescents with BPD symptoms are those most vulnerable to mentalisation failure. Mentalisation refers to the ability to make sense of the subjective states and mental processes of self and others. It is known that a decrease in the ability to mentalise leads to an increase in emotional arousal. The initial phase of MBT-A involves formulation and crisis planning. The BEST intervention mirrors this phase and aims to develop a shared understanding of the presenting difficulties, identify difficulties of mentalisation and develop a crisis plan for managing periods of distress. The staff training element of the intervention aims to increase staff’s ability to mentalise during incidents of distress or conflict, thus supporting the young person to restore their own ability to mentalise. A recent systematic review of MBT interventions for children and families confirmed that these interventions support mentalising and reflective functioning skills. 104
The BEST intervention also incorporates elements from DBT-A. 4 This approach aims to support young people to achieve behavioural control and stabilisation through promoting the understanding of symptoms, the development of positive coping strategies and crisis planning. The BEST intervention makes use of resources for developing positive self-care coping strategies delivered within DBT-A.
Furthermore, the BEST intervention draws on theory from developmental psychology and neurodevelopmental research. Findings from neurodevelopmental research5,6 have informed current understanding of changes in emotional regulation and social cognition during adolescence. The intervention uses this evidence as the basis for educating professionals and young people about the difficulties they are experiencing, as well as to inform the structure and content of sessions.
Outline of prototype intervention
The BEST intervention is a brief, manualised treatment package designed to be co-delivered by a mental health professional working together with a member of staff from the young person’s school or college. Therefore, the intervention addresses several challenges faced by young people experiencing BPD symptoms and those working to support the young people. The approach is designed to:
-
tackle the confusion and anxiety experienced by the young person experiencing BPD symptoms by providing psychoeducation and strategies for the self-management of symptoms
-
contain the anxiety often experienced by educational staff supporting a young person with BPD symptoms by increasing their understanding of these symptoms and empowering them with tools to offer effective support
-
respond to evidence of the need for treatment strategies to focus on early intervention by providing support that, while drawing from existing evidence-based interventions, is delivered in a format that can be implemented consistently by staff without specialist training.
The BEST treatment package is delivered over up to six sessions lasting approximately 1 hour each, over a treatment window of 8 weeks. The sessions cover three manualised components delivered over the six sessions, supported by a resource pack (see www.journalslibrary.nihr.ac.uk/programmes/hsdr/170931/#/documentation; accessed 6 April 2022).
The first component of the intervention focuses on education about emotional instability: how it relates to early features of BPD, why it can happen and what helps with managing it. This component also looks in detail at typical early features of BPD and allows the young person to reflect on which of these symptoms are relevant to them and the ways in which they are affected by them. The key message in this component is one of education to reduce confusion and anxiety about distressing symptoms. This component is delivered by working through a psychoeducation leaflet about emotional instability and early features of BPD. This leaflet can then be taken away by the young person to be discussed further at the following session, with their reflections.
The second component of the intervention incorporates co-development of a maintenance cycle to help the young person understand what factors are maintaining the current difficulties, and thus identify areas for change. Feedback received from service users has indicated that they do not want to receive interventions that give the impression of ‘box ticking’ and that are not tailored to their unique individual experience. The formulation is used to validate the experience of the individual and provide a framework for the intervention, increasing its meaning and purpose for the young person. This individualised approach aims to encourage engagement and motivation.
The third component builds on areas for change identified in the development of the maintenance cycle. This incorporates the co-development of a crisis plan to support with managing periods of distress. Crisis plans will focus on the development and use of self-care strategies to support emotional regulation. This component introduces self-care distress tolerance strategies, including techniques for sensory self-soothing, grounding and distraction. Introduction of these strategies will be supported by completion of worksheets, which the young person can take away to support ongoing practice. Crisis plans will also incorporate the development of appropriate pathways for accessing additional support when needed to support the young person with managing their distress in a helpful way and to develop positive help-seeking behaviours.
The content of each of the six sessions is summarised in Table 2.
| Session | Objective | Key activities |
|---|---|---|
| 1 | For the young person to be able to recognise different emotions and their effects |
|
| 2 | For the young person to understand the concept of mentalisation |
|
| 3 | For the young person to be familiar with the features of emotional instability/BPD |
|
| 4 | For the young person to understand why the ability to mentalise sometimes breaks down and the consequences of this |
|
| 5 | To help the young person plan ways of managing difficult emotions |
|
| 6 | For the young person to reflect on their crisis plan |
|
Co-delivery
Every session is co-delivered by a trained member of pastoral staff from the young person’s school or college (referred to during the project and in this report as education practitioners) and a clinician working as part of local NHS-funded mental health services (referred to as mental health practitioners) working together. The role of the mental health practitioner is to support the education practitioner in maintaining adherence to the intervention and in monitoring and managing risk issues. The education practitioner was an ongoing point of contact for the young person between treatment sessions.
Co-delivery of the BEST intervention allows treatment to be delivered within a setting that is accessible to the young person and removes the need to access specialist services. As well as the benefits of a setting known to the young person, co-delivery also means that the intervention utilises an ongoing relationship that the young person has with school staff. Schools and college staff currently feel inadequately supported to meet the needs of pupils with mental health problems. 28 Leaving school and college staff to provide support to pupils experiencing BPD symptoms without professional advice is likely to result in suboptimal outcomes for young people and may build resistance to later interventions for those who go on to meet the thresholds for specialist CAMHS. Co-delivery of the intervention was intended to contain anxiety experienced by educational staff by reducing the confusion and anxiety that often surrounds young people with BPD who self-harm, increasing their understanding and empowering them with tools, knowledge and skills to offer effective support.
All staff (both education and mental health practitioners) attended a 1-day training workshop prior to delivering the intervention with young people. The purpose of the workshop was to prepare practitioners to co-deliver sessions and, in the case of education practitioners, provide ongoing support to participants from their institution. The 6-hour workshop introduced relevant theory, covered the practicalities of delivering sessions and equipped practitioners with skills to enhance their ability to mentalise during incidents of distress or conflict.
Supervision
Supervision for both education and mental health practitioners delivering the intervention was provided by supervisors trained in the delivery of MBT-A who had extensive experience of working with young people with early features of BPD within a CAMHS setting. Supervision was used to support the use of a mentalising approach within sessions and to support adherence to the treatment package. Supervision was provided in group format at least fortnightly during the intervention phase. At the end of each session, the co-facilitators rated their adherence to the intervention using the fidelity checklist and completed session notes, which were reviewed by the supervisor.
Pilot methods
Design
The prototype BEST intervention was piloted across three educational settings. This phase of the study was non-randomised; all referred participants who met the study eligibility criteria were offered the intervention. Process evaluation methods were used to identify potential barriers to successful delivery, enabling the team to refine the intervention and study procedures in preparation for the next phase of the study.
Setting
Three educational settings, two further education colleges and one secondary school, were selected to take part in the pilot phase of the study. Settings were selected from among those whose staff had expressed an interest in participating during the PPI work undertaken to inform protocol development. In selecting settings to participate in the pilot, we aimed to maximise variation in type of setting (school or college), geographical area (urban or rural) and levels of deprivation among the community served.
Participants
We aimed to recruit a convenience sample of two young people from each of the three pilot settings. Young people who met the following criteria were eligible to participate.
Inclusion criteria
-
Aged 13–18 years (school years 9–13).
-
Enrolled at a participating school or college.
-
Have a score of > 34 on the Borderline Personality Features Scale for Children (BPFSC), 11 item version.
-
Current self-harm assessed using the self-harm subscale of the Risk Taking and Self Harm Inventory for Adolescents (RTSHI-A). Current self-harm defined as having intentionally harmed him/herself more than once and at least one incident of self-harm occurred during the past month.
-
Able to provide written informed consent or, for those aged under 16 years, written informed assent and parent/carer consent.
Exclusion criteria
-
Currently receiving inpatient treatment or a specific psychological intervention.
-
Moderate/severe learning disability.
-
Current psychotic disorder or substance dependence requiring specialist care-planned treatment.
Recruitment procedure
Potentially eligible students were identified through liaison with school and college pastoral staff teams. Pastoral staff members were asked to consider the young people in their school and college and approach those that they believed might meet the study’s eligibility criteria to ask whether or not they would be interested in taking part.
Verbal consent (of the young person and, for those aged under 16 years, their parent or carer) to be contacted by the research team and participate in the screening was recorded using an expression of interest form. Young people (and their parent or carer if they were under 16 years of age) who expressed an interest were sent a copy of the participant information sheets and contacted by a research assistant who explained the study in more detail and answered any questions. If, following this conversation, the young person remained interested in participating (and with the verbal consent of their parent or carer if under 16 years of age), then the researcher arranged to meet with the young person at a convenient venue (e.g. their home address or the school/college) to complete the screening process.
The screening process involved the young person being asked to complete two self-report measures, the BPFSC and the self-harm subscale of the RTSHI-A, and being asked by the research assistant about any treatment for mental health problems they were currently receiving or have received in the past. If this screen indicated that the young person would likely meet the study’s eligibility criteria, then written informed consent in the case of participants aged ≥ 16 years, or written informed assent and parental consent in the case of participants aged under 16 years was then sought. This included consent for the video-/audio-recording of sessions and use of both written quotations and anonymised audio-/video-clips of session recordings.
Staff participants
Staff at each of the three settings were asked to identify one or more members of staff willing to be trained to co-deliver the intervention to participants from their school or college. Mental health practitioners were recruited to participate in the pilot through an e-mail sent to all local CAMHS/Youth Service teams inviting expressions of interest. Those practitioners invited to take part from among the expressions of interest received were selected to maximise variation in professional background and banding. This was to enable us to begin to explore the impact of prior training and level of experience on the ability to deliver the BEST intervention as planned.
All potential staff participants were provided with a copy of the staff participant information sheet and had the opportunity to have their questions answered before being asked to complete a consent form to document their informed consent to participate in the study.
Data collection
Demographic data were obtained from participants for the purpose of describing the sample. Site profile questionnaires were completed by a member of staff for each setting to capture information on the composition and training of the pastoral team, the level of demand for mental health support, and the protocols and procedures for supporting pupils with mental health needs.
After the screening measures had been administered and informed consent obtained, the research assistant completed the remaining baseline assessment measures with the participant. These were the Difficulties in Emotion Regulation Scale (DERS),105 the Childhood and Adolescent Social Support Scale (CASSS),106 the Time Use Survey (TUS),107 the Childhood Interview for Borderline Personality Disorder (CI-BPD)108 and the psychosis, alcohol and substance abuse modules of the Kiddie Schedule for Affective Disorders and Schizophrenia (K-SADS). 109 The purpose of administering these measures was to enable eligibility to be established and to allow for any issues related to the acceptability or practicality of the assessment battery to be identified at an early stage.
With the participants’ permission, treatment sessions were either audio-recorded or video-recorded (according to the preference of the participant) to facilitate the process evaluation. Following completion of the pilot cases, focus groups and individual interviews were conducted to gather data on staff participants’ experience of delivering the intervention and their ideas about how the intervention and research processes should be modified to facilitate successful implementation in the next stage of the research.
Data analysis
Demographic, site information and baseline assessment measures
Information on participant demographics, characteristics of participating educational settings and scores on baseline assessment measures were collated and presented using tables to facilitate interpretation.
Session recordings
To understand how the prototype BEST intervention was implemented within the context of schools and colleges, a two-stage analysis exploring how practitioners delivered the intervention across settings was carried out. The aim of this analysis was to identify interactional patterns and strategies that influenced intervention delivery.
We had initially intended to take a thematic approach to analysis; however, preliminary analysis of the transcripts quickly revealed that a thematic analysis would be inappropriate for identifying how intervention sessions were delivered, as it would provide limited insight into the structure and delivery of intervention components and how delivery was situated within the wider context of schools. We therefore considered which analytical approach might be better at serving this purpose. Rampton’s linguistic ethnographic approach to institutional encounters110 has been used across a diversity of disciplines. It includes a two-stage activity and interaction analysis that provides a means of analysing interactions as socially structured activities, first by identifying the structure, order and purpose of different interactional activities, and second by using conversation analysis to examine the turn-by-turn sequence within activities. Given the linguistic ethnographic methodology adopted in this study, the approach set out by Rampton110 had clear advantages over a thematic approach.
The first stage involved an activity analysis in which broad patterns of delivery were identified. An activity can be defined as a unit of interaction that is culturally recognised. It should be identifiable by constraints on goals/purposes, roles activated in the activity, its structure, sequence and stages, and, to some degree, its participants and setting. 110 The nature and duration of activities taking place during each treatment session were coded by dividing each recording into 30-second segments using timesteps and noting the segment during which a discrete activity began and ended and summarising the nature of this activity (setting the agenda, reviewing home practice, explaining mentalisation, demonstrating a grounding exercise, etc.). We also coded who each activity was led by (education practitioner, mental health practitioner or the young person), which participants took a conversational turn during each 30-second segment, silences of ≥ 10 seconds and verbal acknowledgements of another participant’s contributions.
Coding was carried out by two members of the research team, who each independently coded 50% of the recordings. Another member of the research team independently coded 10% of these recordings. Discrepancies in coding were discussed among the analysis team and consensus interpretations were reached. Concordance between team members’ coding was high except for coding regarding who led each activity. In particular, there was often a lack of consensus regarding whether an intervention was singly or jointly led. This was resolved by distinguishing contributions that initiated a new activity or progressed the current activity from simple acknowledgements or reinforcements of contributions made by others. This process enabled the coding framework to be clarified and refined in preparation for the feasibility RCT.
In the next stage, the results of the activity analysis were used to purposively select excerpts of session recordings exemplifying patterns of delivery for more detailed examination. The selected excerpts were transcribed using Jeffersonian transcription conventions111 and analysed to explore interactional patterns and strategies used by practitioners and young people. The analysis team met regularly during the analysis process to discuss interpretations and reach consensus.
Focus group and interview data
Focus group interviews and individual interviews were audio-recorded and written summaries were produced to efficiently identify key points that would inform the refinement of the intervention and research procedures in the feasibility trial. Summaries aimed to capture views on the acceptability and practicality of the intervention and research procedures, and suggested modifications. We had originally planned to transcribe focus group interviews verbatim and conduct a detailed thematic analysis of transcripts. However, the initial analysis revealed that staff primarily focused on logistical issues of intervention delivery. We decided that detailed verbatim transcription would be time-consuming and unnecessary given this focus on logistics. Instead, written summaries were produced to efficiently identify key points that would inform the prototype intervention and research procedures in the feasibility trial.
Pilot findings
School and college characteristics
Three educational settings acted as sites for the pilot phase: they will be referred to in this report as site A, site B and site C.
Site A is a large further education college, and the main campus is located close to the city centre. The college had approximately 4000 students enrolled on its courses for young people aged 16–19 years, as well as a large number of adult learners and apprentices. The college’s overall Ofsted (Office for Standards in Education, Children’s Services and Skills, London, UK) rating at the time of the pilot was ‘Good’.
Site B is a large further education college with provision spread over two campuses, both located in coastal towns. The college had approximately 2500 enrolled on its courses for young people aged 16–19 years, in addition to a smaller number of adult learners and apprentices. The college serves coastal and rural communities with high levels of deprivation. At the time of the pilot the college had an overall Ofsted rating of ‘Requires Improvement’.
Site C is a secondary school for children aged 11–16 years located in a small market town, serving the town and surrounding villages. The school had approximately 1200 students enrolled. At the time of the pilot the school had recently opened as an academy; however, the preceding school of the same name received an overall rating of ‘Good’ at its last inspection.
Responses to the site profile questions completed by staff at each site are summarised in Table 3.
| Site characteristics | Site A | Site B | Site C |
|---|---|---|---|
| Staff members in pastoral role, n | 7 | 5 | 15 |
| Students with mental health needs supported by the pastoral team in the past academic year, n | 322 | 669 | 200 |
| Mental health training provided for pastoral team | Mind (London, UK) first aid training and NSCB (Norfolk, UK) safeguarding training | Various multiagency training; mental health first aid | Mental health training as a school. Specific members have been on courses such as mental health first aid, bereavement, etc. |
| Mental health training provided for wider staff team | Optional CPD twice per year | Duty team have received mental health first aid training; other staff have received informal training | Whole school focuses on mental health |
| Support currently offered to students with an identified mental health need | Classroom support; counselling; mental health advisors | Counselling; mentoring; referral to external agencies for specialist support | Mindfulness; mentoring by heads of house and form tutors; counselling; cards granting permission to leave the classroom when needed; reduced timetables and homework; referral to external agencies for specialist support |
Recruitment
Recruitment of young people began following confirmation of local capacity and capability on 2 January 2019. The first participant was consented on 21 January 2019. Five participants were recruited to the pilot. We planned to recruit two participants from each of the pilot sites: this target was met at sites A and B, but we were unable to identify a second eligible participant from site C within the pilot’s recruitment window. Two young people referred by site C did not meet the eligibility criteria: one scored > 34 on the BPFCS and one was 13 years old but was in school Year 8.
Participant characteristics
The characteristics of the five young people who consented to participate in the pilot phase are summarised in Table 4.
| Characteristic | P001 | P002 | P003 | P004 | P005 |
|---|---|---|---|---|---|
| Site | C | B | A | A | B |
| Age (years) | 14 | 17 | 17 | 18 | 17 |
| Gender | Male | Female | Male | Male | Female |
| BPFS-C | 43 | 40 | 36 | 35 | 37 |
Staff characteristics
Eleven staff members were consented to participate in the pilot and were trained to deliver the intervention. Five staff participants were school or college staff members: two from site A employed as mental health advisors, two from site B employed as safeguarding co-ordinators and one from site C employed as a school counsellor. Six staff participants were mental health professionals, employed in a range of clinical roles with Agenda for Change (AfC) bandings ranging from band 4 to band 8a. The characteristics of the staff members allocated to deliver the intervention to the participants recruited are presented in Table 5.
| Participant | Mental health practitioner | Education practitioner | ||||
|---|---|---|---|---|---|---|
| Gender | Professional background | AfC Band | Gender | Professional background | Pre-existing relationship with participant | |
| P001 | Male | Senior psychological therapist | 8a | Female | School counsellor, prior training in CBT | Yes |
| P002 | Female | Adult nurse | 7 | Female | Safeguarding lead, no previous therapeutic training | Yes |
| P003 | Female | Occupational therapist | 6 | Female | Mental health advisor, no previous therapeutic training | Yes |
| P004 | Female | Mental health nurse | 7 | Female | Mental health advisor, no previous therapeutic training | No |
| P005 | Female | Assistant practitioner | 4 | Female | Safeguarding lead, no previous therapeutic training | No |
Implementation of the prototype BEST intervention
Of the five young people recruited, three (P001, P003 and P005) completed the full intervention, one (P004) completed only the first session before disengaging and one (P002) was unable to receive any sessions because they were excluded from the college. No reason for disengagement was given by P004; however, during the session he attended, he expressed scepticism about whether or not he would find the intervention helpful based on his prior experiences of mental health support.
For those who completed the intervention, two received six sessions and one (P003) received seven sessions because the content of session 3 was delivered over two sessions. The mean duration of sessions was 64 minutes; however, session 3 (which focused on psychoeducation regarding the features of emotional instability/symptoms of BPD) took significantly longer to deliver than other sessions (mean duration 87 minutes). Owing to constraints imposed by the school or college timetable, it was generally not possible to extend the length of sessions significantly beyond 1 hour. Therefore, the content of session 3 was completed at the beginning of the next session (P001), divided over two sessions (P003) or left unfinished (P005).
Each session was observed to follow a similar sequence of activities, in line with the structure of the intervention manual. Sessions began with setting an agenda and introducing the topic of the session and ended with rating the session and agreeing a task for the young person to complete over the coming week. Most of each session was spent on activities involving (1) conveying information to the young person, (2) modelling a skill or demonstrating the application of information conveyed and (3) applying the information or skills introduced to the young person’s own experiences.
An example of the completed activity analysis coding completed for all session recordings is included as Figure 3. In this figure, the first row of each block shows the recording timestamp corresponding with each column. The second row denotes the nature and duration of each activity occurring and the colour indicates the individual who led the activity: light blue indicates that the activity was led by the education practitioner, orange that the activity was led by the mental health practitioner, purple that the activity was jointly led by both practitioners and dark blue that the activity was led by the young person. Rows 3–5 represent the conversational turns taken by practitioners and participants (coloured cells) and other actions such as writing and referring to the manual (represented in the figure by letters explained in the key provided). Silences of more than 10 seconds, when these occurred, were presented in the final row (as in for P005).
FIGURE 3.
Sample activity analysis coding. To facilitate comparison, coding relating to the same activity from across cases is presented in a stacked arrangement, therefore discontinuations in the timestamps are present, for example for P001 between 29:30 and 40:00.
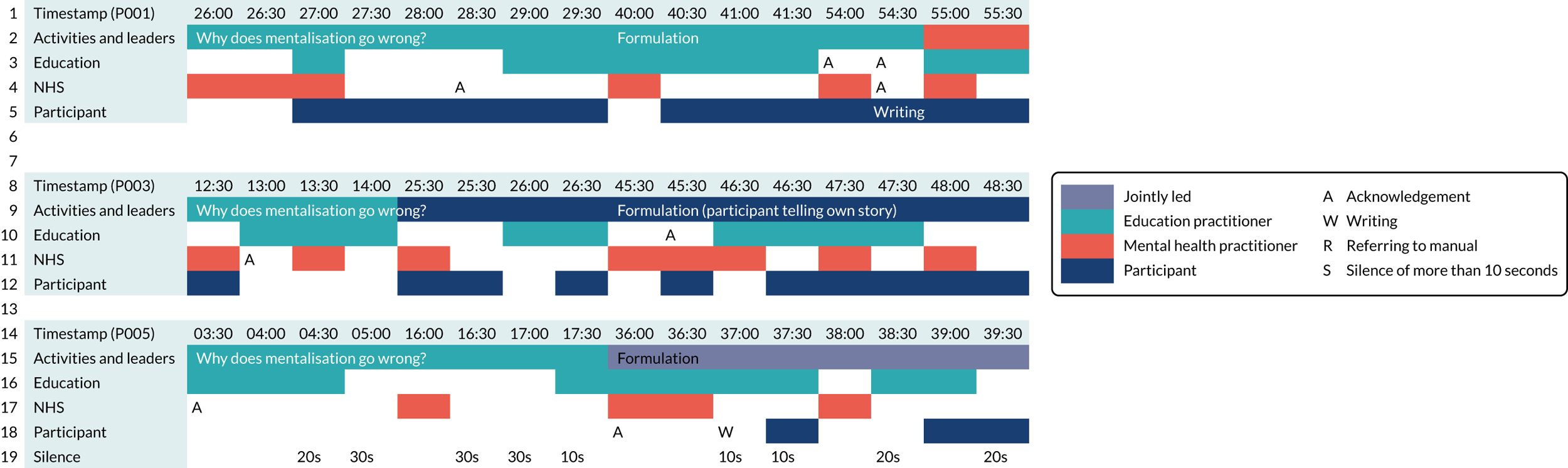
Completion of this coding allowed for broad patterns of delivery to be compared across cases and interactional patterns of interest to be identified for further analysis using conversation analysis techniques. For instance, in Figure 3 we see two patterns of delivery of the component of the intervention involving formulation of mentalisation failure. Across all three sessions, we see the activity being introduced and initially led by the education practitioner. The person coded as leading the activity was not necessarily the person who spoke most; for example, for P001, the explanation of mentalisation failure was led by the education practitioner. The activity commenced prior to the 26 minute timestamp, and, although at this point it is the mental health practitioner who is speaking, with contributions from the EP at 27 minutes, the EP continues to lead the activity, seen with utterances that demonstrate steering the activity (e.g. ‘so we’re just reading down on the er on the worksheet’).
As the activity progresses, we start to observe differing patterns of contributions from the young people. In the sessions with P001 and P003 we see consistent verbal contributions are made by the young people throughout the session. In addition, in the session with P003 we observe the young person taking the lead in the formulation activity by telling the story of an incident in their life when their ability to mentalise broke down. In contrast, the session with P005 is primarily characterised by frequent silences throughout the activity.
We, therefore, transcribed the relevant sections of these sessions to enable us to further examine how differing practices and patterns of delivery might lead to differences in the extent of the young person’s active participation and engagement in the session activities. Through this process, we identified patterns of delivery that appeared to be more successful in enabling the session objectives to be met to inform the development of the manual and content of practitioner training.
Patterns of co-delivery
On average, mental health practitioners were coded as leading session activities for longer during each session than education practitioners (mean duration of activities led by mental health practitioners was 21 minutes and 23 seconds per session vs. 13 minutes and 53 seconds for education practitioners). Education practitioners most often led activities involving conveying information to the young person. Activities involving modelling a skill or encouraging the young person to apply the content of the intervention to their own experiences were most commonly coded as being led by the mental health practitioner or led jointly by the mental health practitioner and education practitioner.
We often observed the practitioners signposting transitions between activity leads explicitly, suggesting that practitioners had agreed which of them would lead each activity prior to the session:
OK, so what I’m going to do is pass you to [name of mental health practitioner] and she’s going to tell you a little bit about mentalisation and then I’m going to take you through the exercises.
Education practitioner
When the same practitioner was leading consecutive activities, the practitioner would typically signal the conclusion of the activity by summarising the activity or asking the other practitioner or young person if they had anything further to add before proceeding:
What we’d like to do now, is it alright are you happy to move onto the next bit [name of mental health practitioner], yeah, any questions about that [name of participant]?
Education practitioner
This signposting acted to facilitate smooth transitions between session activities and activity leads. However, when session delivery was observed to diverge from prior arrangements, practitioners were able to negotiate the progression of activities and activity leads successfully within the session using less explicit practices. For instance, a statement of ‘I was just going to say we ran out of time a bit last week’ by an education practitioner was observed to function as a reminder for the mental health practitioner of the need to finish an activity left uncompleted at the end of the previous session (demonstrated by the mental health practitioner responding ‘oh yeah’). This utterance also served to signpost the start of a new activity and transition of lead to the young person.
We observed distinct approaches to delivering the components of the intervention, which raised hypotheses for further analysis in the subsequent feasibility study regarding which forms of communication successfully enact different components and engage young people. For instance, we identified two different ways practitioners conveyed the function of emotions to young people. In Box 2, from the first session with P001, the mental health practitioner begins the activity by reading from the manual (lines 1–14) and providing examples to explain the content (lines 15–19). The mental health practitioner then attempts to link the information contained in the manual to the young person’s experience by asking an open question: ‘Can you think of any ways in which your emotions help to motivate you to do things?’ (line 20). After a 3-second pause the young person replies, ‘not really’ (line 22), suggesting that, at this point in the interaction, they are not able to identify with the connection between motivation and emotions. However, the education practitioner follows this exchange with a question that is contextualised to the young person’s background and interests, enquiring about the motivational value of their football badges (lines 23 and 24). This strategy successfully elicits a response from the young person regarding how their emotions motivate them in a sporting context (lines 25–29). Beyond the extract the mental health practitioner subsequently uses a similar approach for the remainder of the activity, using examples personal to the young person to explain the concepts introduced.
MHP: .tch so >we’re just< (.) reading do::wn (0.6) on the e:::r (0.4) on the worksheet (0.4) so although some emotions can seem difficult, (0.4) emotions are actually very important, (0.6) and helpful to us (0.4) some reasons that we have them, (0.4) and (0.4) you’ve gone with the second one I think (you started) it said communication,
YP: .skuhHHHHHH[HH
MHP: [emotions (0.4) are to communicate with othe:r (0.4) other people (0.4) they help us to understand what is happening for someone e:lse, (0.4) and for other people to understand what is happening for us (0.6) a::h a:nd we’re gonna, (0.4) talk about this much more [(0.4) especially in the next session when =
YP: [.skuhhhhhhhh
MHP: = we (.) when we talk about mentalisation, (0.4).tch
YP: [.skuhhhh
MHP: [and the top one (0.4) protection (0.4) one of the basic functions of emotion (.) is to protect us if we feel threate:ned um we have an immediate response which se:rves to give the best chance of survival (0.4) so: >you know< that can even be::, (0.4) >if you< stepped out into a roa::d? (0.4) >and suddenly< there’s a car comi:ng and a massi:ve (0.4) er <anxious fea:r> (.) adrenalin (0.4) >kind of< reaction and that helps us to move really quickly to get out of the way (.).hhhh so it can be a really >kind of< basic function like tha:t in protecting us (0.6) u:::m (0.4) motivation? (0.4) so emotio:ns (.) encourage us to act to do something that will help relieve emotio:ns (.) you do not wa:nt or to create emotio:ns (0.4) that you do want(0.4) (0.6) an- can you think of any::? (1.0) any ways in which your emotio:ns help to motivate you to do things?
(3.0)
YP: mm:::: (1.0) not really,
EP: what about those badges on your (0.4) (thing?) (2.0) do you feel that motivation helps you:: (0.6) like (.) your emotions motivate you: (0.4) with spo:rt (.) and things like that?
YP: .hhh a little bi:t, (.) I mean like, (3.0) say if it was like that adrenalin I guess like say if it was li::ke, (0.6) a:: >final kick of a< football match or somethi:ng and you >sort of like< have feeling you’ve been under pressu:re been li:ke (.) >and stuff like< tha:t (0.6) but then li:ke (0.6) after you do it like sco:re or somethi:ng (0.4) it’s quite like (1.2) a relie:f, (0.6)
[that (feeling) (0.6) and like, =
EP: [(the relief)
YP: = (2.0) yea:h (0.6) °e::r°
EP, education practitioner; MHP, mental health practitioner; YP, young person.
This approach can be contrasted with the extract in Box 3, which is taken from the transcript of the same activity conducted with P005. In this extract, we see the education practitioner paraphrasing sections of the manual (lines 1 and 2) and linking the materials back to the mental health practitioner and participant’s previous contributions (lines 4–6). However, in contrast to the extract in Box 2, the language used by the practitioners directly mirrors the text of the manual. Therefore, information is presented using first-person plural pronouns (lines 7–33), for example ‘we have emotions for a reason’ or ‘we don’t think about that’. Furthermore, the practitioners draw on their own experience of completing the activities, reflecting on how they too found it difficult to identify specific emotions (lines 12–17), perhaps intending to normalise the difficulties being discussed. This requires little elaboration from the young person about how emotions make sense to them within their own experience, and instead we observe limited and ambivalent acknowledgement of the practitioners’ utterances, seen first with softly spoken laughter (lines 9 and 13) and then softly spoken acknowledgement [‘°°yeah°°’ (line 24)]. Consequently, it is not clear whether the young person has understood or is able to relate to the information presented.
EP: thinking that althou::gh, (0.8) emotions can be:, (0.6) really difficult thi:ngs actually: (.) we have emotions for a reason,
MHP: ↑mm::
EP: .hh u::::m, (.) and they play lots of differe:nt (0.4) ro::les and you just kind of (1.0) being a bit more aware o:f (.) of the different emotio::ns (0.4) u::m (0.6).hh and like MHP was saying one activity, (0.4) cleaning your roo:m can make you fee:l, (0.8) a whole range of differe:nt, (0.8) different emotions at different stages
MHP: um (.) but unfortunately in the proce:ss we don’t think about tha:t (.) so then when you’re sat in a chai:r and we’re going well what about this it feels really chalengi:ng doesn’t [it
YP: [hu:h huh >ha ha<
MHP: cos we:. (0.4) none of us take the ti::me (0.8) to break it do::wn and see things like tha:t (0.8) so we’ve only ever (>sort of<) (sitting right here) (?) well we were doing the ↓same [weren’t we
EP: [we were [doing the same =
YP: [°ha ha°
EP: = cos [↑we’ve (.) we’ve (.) ↑we’ve done this ↑ourse:lves
MHP: [ha ha ha ha ha ha ha ha [ha ha ha
EP: [so, (0.4) I understa:nd kind o:f (0.4) how tricky it can fee:l (0.4) cos ↑we’ve ↑had to do the ↑sa:me,
MHP: yea:h
EP: .hh u:::m, hh (1.4) yeah (2.6) OK.hhh so:::, (0.4) I think u::::m, (2.4) er a::nd (0.4) while emotions can kind of (0.4) always be changing some are >a little< bit easier, (0.8) to work with than others I thi:nk (0.4).hhhhhh (1.6) so if we: have a little loo:k (0.4) they’re different kind o:f, (0.6) some of the different reasons I think we ha:ve (0.6) the emotions that we have.hhhh u::m, (0.4) got protection,
YP: °°yeah°°
EP: so::: (0.6) someti:mes, (0.4) when we have the feelings’s we have it’s, (0.4) an insti:nct (0.4) fro:m if we felt we needed protection (0.4) >so sometimes< when we feel fea::r, (0.4) that type of thing, (0.6).hhh communications cos they ca::n, (0.4) help us communicate with other people, (0.4) °OK°.hhhh (0.4) um and we’ll look at that a little bit mo::re (0.4) next wee::k cos we’ll be learning abou::t um (0.4).hhh mentalisation so we’ll be looking at the mentalisation side of things and that’s a little bit more about.hhh communicating emotions and that type of thi:ng (0.6).hh.tch and we’ve already talked about motivation, (0.4) that someti:mes emot- emotions can help (0.4) motivate you to do things, (0.4) but other ti::mes (0.6) it can feel really hard (0.4) and you can feel really kind of.hhh (.) not motivated
MHP: and you: (.) you described that actually really well when we were looki::ng, (0.4) (back) bedroom (.) cos one of the words you did use was (0.4).hhhh that you kind of felt really motivated to start with wasn’t i:t,
EP: °hm::° (0.8).hh and perhaps sometimes when we kind of (.) reach barriers that kind of motivation can be harder to,
MHP: o::h ye::s
EP, education practitioner; MHP, mental health practitioner; YP, young person.
Although caution is required in using such evidence to link different interactional styles to young people’s responses, variation in the delivery of different intervention components generated hypotheses about how practitioners might best deploy and link the material presented in the manual to the young person’s personal experiences. These were that contextualising the materials within the young person’s everyday life might function to encourage better engagement, help activate the individual’s ability to reflect on their own emotions, and enhance and facilitate checking of their understanding. It also indicated that prior knowledge of the young person could be critical. The education practitioner who worked with P001 had a prior relationship with the participant and was able to use her knowledge of his interests to tailor the content of the intervention. The education practitioner who co-delivered the intervention to P005 had not worked with the young person previously and therefore would not have had knowledge of the participant going into the intervention.
Acceptability of prototype intervention and pilot research procedures
Acceptability of training and supervision and suggestions for improvement
Practitioners fed back via the interviews and focus groups that they enjoyed the training workshop and found it useful and informative. However, not all practitioners left the training with a clear understanding of co-delivery and how it would work. Specific suggestions for improvement made were:
-
be clearer on the division of roles when co-delivering the intervention and that school/college practitioners can bring up and use existing knowledge of participants
-
include video of someone with lived experience of BPD/emotional instability
-
include more practical examples of delivering components of the sessions (e.g. observing role plays)
-
include fuller explanations of research and medical terminology, which may be unfamiliar
-
cover sessions in chronological order during the training workshop instead of grouping by component covered.
Supervision was valued as an opportunity to seek guidance and support, but practitioners felt that it did not need to take place as frequently as every week; they felt that two to three supervision sessions over the course of the intervention would be adequate and reduce pressure on their time. Most practitioners told us that they would have been happy to receive supervision by telephone instead of face to face; none was enthusiastic about using video calls for supervision.
Acceptability of treatment sessions and suggestions for improvement
Practitioners were generally positive about the intervention and felt that the participants they worked with had benefited from it. They liked the manual and felt that most sessions worked well, but they made several suggestions regarding the content and format of specific sessions, and these suggestions are summarised below. Feedback on the process of co-delivering the intervention was also positive. Practitioners told us that they were able to work effectively with their partner to deliver the intervention and were surprised by how smoothly the sessions ran. The key challenge of co-delivery was co-ordinating the diaries of practitioners and the timetable of the young person. A suggestion was made to encourage practitioners to book the same time slot every week for the whole delivery window to minimise scheduling difficulties.
Session 1
-
Generally positive feedback.
-
Having slightly less content that later sessions allowed some time within the session for building rapport.
-
Include copies of the emotions wheel within every session as this was seen as a key tool that practitioners referred to frequently throughout the intervention.
Session 2
-
Again, feedback was generally positive.
-
It might be useful to include examples of mentalisation in the three boxes as well as a space to write what the situation was and who was involved in the situation.
-
Might need to support the practitioners and participants in having a stronger understanding of mentalisation (potentially through a training workshop, supervision or additional examples).
Session 3
-
Consistent feedback was that the content of this session was too long and quite heavy; it was suggested that this could be delivered over several sessions.
-
Add something at the end of the session that is more hopeful than the way it ends currently.
-
The format of boxes with symptoms felt repetitive and difficult to digest.
-
The leaflet was not very young person friendly and it was not in an ideal format.
-
A podcast in an interview style could be created.
-
The information from the leaflet could be included as part of the session content in smaller chunks.
Session 4
-
‘Emotional arousal’ sounded too clinical (e.g. instead use ‘feeling emotional’).
-
Include a worked example of the formulation diagram.
-
The three boxes felt repetitive of the formulation cycle.
-
Potentially include clearer headings (e.g. ‘Now let’s think about what you could have done to make this situation better’).
Session 5
-
The action plan (page 18, see www.journalslibrary.nihr.ac.uk/programmes/hsdr/170931/#/documentation; accessed 6 April 2022) felt repetitive and very similar to the boxes on page 17. Include numbers 1, 2, 3 in action plan on page 18.
-
Include a card to cut out and keep handy for when they are in crisis, or for participants to take a photo of their action plan.
-
Include examples of people whom a participant might contact for support, including apps.
-
Give additional examples of grounding and other stabilisation techniques to give the participant more choice.
-
Separate grounding and self-soothing strategies.
-
Suggestion made that participants could come up with their own example of stabilisation techniques.
Session 6
-
No suggestions specific to this session.
General
-
The scale used in the session review at the end of each session would be more helpful if it were a continuous scale instead of the thumbs up/thumbs down.
-
Several people mentioned that it would be beneficial to include suggested homework tasks at the end of each session and to add a standing agenda item to review last week’s homework task at the beginning of the next session.
-
Practitioners also suggested including one notes page at the end of each session, rather than only at the end of the booklet.
Acceptability of research procedures
Research procedures were generally viewed as acceptable; however, all education practitioners fed back that they found it challenging to identify eligible students, and this appears to have been a source of anxiety. Practitioners expressed that they were reticent to raise young people or their families’ hopes of participating by mentioning the study if they were unsure whether or not they would meet the eligibility criteria.
Practitioners experienced some difficulty using the video-recorder and in setting up the recorder to capture all three participants (it was observed that most often the camera was angled to focus on the young person rather than the practitioners). Practitioners also voiced some uncertainty about how the fidelity checklist should be completed, suggesting that further guidance would be useful.
All education practitioners fed back that they either had or intended to use aspects of the BEST intervention in their wider practice with other students. This alerted us to remain vigilant for possible contamination of the control arm in the feasibility trial phase.
Resulting amendments to intervention and study protocol
The findings of the evidence synthesis and pilot, together with input from our PPI advisors, allowed us to refine the intervention and research procedures in preparation for the feasibility RCT. Learning from the evidence synthesis that contributed to the refinement of the BEST intervention and influenced the conduct of the feasibility trial included (1) the need to consider how to maximise the ability of staff to identify and refer students likely to benefit from the intervention; (2) the importance of the intervention manual and supporting materials, as well as the quality of training and ongoing supervision, for the ability of staff to deliver interventions with fidelity; (3) the need to identify intervention champions at a senior level within settings to promote buy-in from other staff members; and (4) the inevitability of logistical challenges associated with the constraints of the school calendar, routines and environment. The findings of the pilot enabled us to identify specific changes within these broad domains to maximise the likelihood of successful delivery in the next phase.
Changes made to the intervention
Training and supervision
Key changes made to the training and supervision in response to learning from the pilot phase are summarised below:
-
Staff were provided with a preparatory slide deck prior to the training workshop, which introduced key topics (such as BPD and mentalisation) and research terminology (such as randomisation and contamination).
-
A glossary was added to the practitioner handbook provided at the workshop to explain research and medical terminology that might be unfamiliar.
-
Exercises and examples were added to the training workshop to support practitioners’ understanding and skills in successfully delivering session content.
-
A young person with lived experience of BPD symptoms was invited to contribute to facilitating the training workshop and share their experiences of coping with BPD symptoms while at school.
-
More information was included about the co-delivery model and division of roles, including clarifying that school and college practitioners are encouraged to use their existing knowledge of the young person to enhance intervention delivery.
-
Practitioners were encouraged to book weekly session slots throughout the intervention window in advance and confirm with the study team at the end of each session to reduce scheduling difficulties.
-
Frequency of supervision was reduced from weekly to at least twice during the intervention (e.g. after the first and fifth sessions). However, it was made clear to staff that more frequent supervision could be organised if needed. Telephone supervision was to be offered as an alternative to face-to-face meetings.
Manual and treatment sessions
Key changes made to the manual in response to learning from the pilot phase are summarised below. The final BEST intervention manual is included as an additional file (see www.journalslibrary.nihr.ac.uk/programmes/hsdr/170931/#/documentation).
-
Some language used within the manual was modified to make it less technical and more approachable, for example ‘emotional arousal’ was replaced with ‘feeling emotional’.
-
Further examples were added to the manual to strengthen participant and practitioner understanding of mentalisation and to clarify related exercises.
-
The content of session three was condensed to enable each session to be delivered within a 1-hour period. The psycho-education leaflet originally included as an appendix and referred to in the main manual was removed and key information from the leaflet was incorporated within the body of the manual.
-
Additional ideas for grounding and self-soothing techniques were added to session 5. The crisis plan template was simplified to avoid repetition and aid comprehension. Examples of sources of support were added to the crisis plan and the suggestion that the young person take a photograph of the completed plan to refer to was added.
-
The session review was revised to clarify the purpose of this activity. The prompt to rate the session was replaced with questions designed to promote discussion and reflection.
-
Suggested home practice tasks were added to each session. In accordance with the recommendation of our PPI representatives, we avoided referring to these tasks as ‘homework’ and presented each as a suggestion rather than a prescribed task.
-
A copy of the emotions wheel was added to the end of each session and practitioners were provided with a laminated emotions wheel as an additional resource to refer to during sessions. Flash cards providing information on each BPD feature were created for use as part of session 3.
Changes made to study procedures
We had initially planned to involve six to eight schools in the feasibility trial. However, our experience of recruitment in the pilot indicated that we may need to involve more schools and colleges to meet our recruitment targets. We therefore planned to increase the number of schools and colleges invited to participate from 6–8 to 12–16 settings. In response to the findings of the evidence synthesis, we approached all schools and colleges we invited to participate in the feasibility RCT via a member of the senior leadership team to ensure support for the study at an appropriately senior level within each setting.
Furthermore, to assist referrers in identifying young people potentially eligible to participate, we produced a brief pre-screening questionnaire for referrers to use to help them decide whether or not a potential referral was likely to be appropriate. Once a referral was received, we conducted the screening, informed consent and assessment process as original planned.
In line with the findings of the evidence synthesis regarding the logistical constraints imposed by the school environment, intervention piloting indicated that it was unlikely to be possible to complete the intervention within the 8-week time window originally proposed owing to school holidays and staff and student absences. Therefore, we increased the time frame for intervention delivery to 12 weeks and postponed the post-intervention follow-up to 12 weeks from randomisation (the final follow-up assessment remained at 24 weeks).
In line with feedback received, we updated the fidelity checklist to include further guidance on how to rate each item and added a space for practitioners to provide a brief justification of their rating. Furthermore, a section was added to allow staff delivering the intervention to record a session summary to be shared with the supervisor, including a prompt to note any risk issues and record actions taken to address any issues identified. To assess the extent of staff learning and development following training as a BEST practitioner as part of the process evaluation, we intended to administer an additional questionnaire assessing staff knowledge, skills and confidence pre training and after having co-delivered the intervention.
Chapter 4 Feasibility randomised controlled trial: methods
Design
We planned that the feasibility RCT would involve randomising 60 eligible young people in a 1 : 1 ratio to receive either BEST plus TAU or TAU alone. Participants were assessed pre randomisation and followed up at 12 and 24 weeks. A mixed-methods process evaluation was carried out alongside the feasibility RCT to explore how the intervention was implemented across education settings, to assess the acceptability of the intervention and monitor any contamination of the control arm.
Setting
We intended that 12–16 schools and colleges would act as research sites for the feasibility RCT. Staff at each participating setting were asked to identify one or more members of pastoral staff to be trained to co-deliver the BEST intervention to participants enrolled at their school or college who were randomised to the intervention arm. Identified staff members were invited to attend a 1-day training workshop prior to co-delivering treatment sessions with a mental health practitioner. The workshop was designed to prepare staff to deliver the intervention by introducing relevant theory, providing opportunities to practise delivering the content of each session and enhancing the ability of staff to mentalise during incidents of distress or conflict.
Eligibility criteria and recruitment procedure
Only young people who met the following eligibility criteria were randomised.
Inclusion criteria
-
Aged 13–18 years (school years 9–13).
-
Enrolled at a participating school/college.
-
Score of ≥ 34 on the BPFSC. 112
-
History of repeated self-harm assessed using the self-harm subscale of the RTSHI-A113 (has intentionally harmed him/herself more than once).
-
Able to provide written informed consent or, for those aged < 16 years, written informed assent and parent/carer consent.
Exclusion criteria
-
Currently receiving inpatient treatment or a specific psychological intervention.
-
Moderate/severe learning disability.
-
Current psychotic disorder (those with subthreshold psychotic symptoms were not to be excluded) or substance dependence (current substance abuse was not an exclusion criterion) requiring care planned treatment.
Potentially eligible young people were identified through liaison between the research team and staff from participating schools and colleges or local mental health services. Referrers were asked to consider the young people they worked with and approach those they believed might meet the study’s eligibility criteria to ask if they would be interested in finding out more about the study. Potential referrers were provided with an optional pre-screening questionnaire to complete with young people who expressed an interest to help determine whether or not a referral to the trial would be appropriate. The agreement of the young person (and a parent/carer for those aged < 16 years) to be contacted by the research team and participate in the screening was recorded using an expression of interest form.
Following a referral being made, young people (and their parent/carer if aged < 16 years) were contacted by a member of the research team who explained the study, answered any questions and provided copies of the approved study information sheets. If, following this, the young person remained interested in participating, the researcher arranged to meet with the young person at either their school/college or their home address to screen him or her for eligibility.
The screening process involved completing the BPFSC and the self-harm subscale of the RTSHI-A, and confirming any treatment for mental health problems they had received in the past or were currently receiving. If this screen indicated that the young person was likely to meet the study’s eligibility criteria, written informed consent (in the case of participants aged ≥ 16 years) or written informed assent and parental consent (for participants aged < 16 years) was sought.
After informed consent has been obtained, participants were asked to complete the remaining baseline assessment measures. Only young people who met all eligibility criteria outlined above were randomised. In recognition of their time and commitment, participants were given a £10 shopping voucher for each research assessment they completed (up to £30 in total across the three assessment points).
Sample size
The recruitment target for the feasibility RCT was 60 eligible young people. This sample size was selected with reference to published recommendations for feasibility studies114,115 and to enable rates of recruitment and retention to be estimated with reasonable precision. It was calculated that a sample size of 60 would allow us to estimate an attrition rate of 20% to within a 95% confidence interval of ± 10% and a recruitment rate of 50% of those eligible to within a 95% confidence interval of ± 9%.
Intervention and control arms
Participants were randomised to receive either the BEST intervention plus TAU or TAU alone. The BEST intervention and its refinement were described in detail in Chapter 3. To summarise, the intervention was delivered in up to six sessions lasting approximately 1 hour each, over a maximum treatment window of 12 weeks. Intervention delivery was supported by a therapy manual containing resources accompanying each session. Each session followed a set agenda and included interactive exercises that the practitioners completed together with the young person. Each session concluded with a review and choosing something to practise between sessions.
Session content was informed by two existing evidence-based treatments for adolescent BPD: MBT-A and DBT-A. Drawing from MBT-A, the intervention aimed to enhance the ability of participants to mentalise, that is to make sense of their own and other people’s behaviour using mental state concepts. Informed by DBT-A, the intervention aimed to promote understanding of symptoms, support the development of positive coping strategies and facilitate crisis planning.
All sessions were co-delivered by a mental health practitioner and a pastoral member of staff from the young person’s school or college working together. Co-delivery was intended to enhance continuity of care by equipping an individual within the young person’s existing support network with the knowledge and skills to provide effective ongoing support. In addition, the intervention was also intended to contain the anxiety of school and college staff, who often feel inadequately supported to meet the needs of pupils with mental health problems. 28
Supervision of education staff and mental health practitioners delivering the intervention was provided in a group format by qualified mental health professionals with extensive experience of working with young people with symptoms of BPD. Supervision was used to support the use of a mentalising approach during sessions, promote adherence to the intervention manual and ensure the appropriate management of risk and safeguarding concerns.
The control group received TAU, that is the standard care currently offered to young people with symptoms of BPD. Schools and colleges were instructed to follow their institution’s usual policies and protocols (including safeguarding policies and referral to external agencies) throughout the trial. Participants (whether allocated to the BEST plus TAU arm or the TAU-only arm) were not to be denied access to any service currently available, including specific psychological interventions offered as part of standard care pathways. Schools and college staff were encouraged to offer participants allocated to the TAU arm the usual pastoral support they would provide internally, as well as making referrals to external agencies as appropriate. However, to minimise contamination, schools and colleges were requested to plan for TAU participants to be supported by staff who have not been trained as BEST practitioners whenever practically possible.
Randomisation and blinding
Participants were randomised to treatment arms in a 1 : 1 allocation ratio using preset lists of permuted blocks with randomly distributed block size. Randomisation was stratified by school/college. The allocation sequence was generated by the Data Management Team at Norwich Clinical Trials Unit (CTU) and was not accessible by anyone outside of this team, including the research team, school and college staff, mental health practitioners or participants.
The allocation process was web based and managed by the Data Management Team at Norwich CTU. Following the completion and input of all baseline data for each individual participant, the study research assistant confirmed the participant’s eligibility and submitted the stratification information (participant’s school or college) to the web-based system. This generated an e-mail informing the research assistant that the participant had been successfully randomised without revealing their allocation. The system then generated a separate e-mail to the study co-ordinator and other nominated research team members informing them of the participant’s allocation to enable the allocation of treatment to be implemented.
Research staff collecting follow-up data remained blind to participant treatment allocations. Given the nature of the intervention, it was not possible for participants and those delivering the intervention to remain blind. All those informed of the allocation, including participants, intervention facilitators and the referrer, were asked not to reveal the treatment arm to which the participant has been allocated to blinded members of the research team. Participants were reminded at the beginning of each contact with a blinded member of the research team of the need to avoid disclosing their allocation. Any potentially unblinding data were stored in a separate database clearly labelled so as not to be inadvertently accessed by blinded team members. As the chief investigator and the participant’s responsible clinician were unblind to treatment allocation, no emergency unblinding procedures were required.
Data collection
Outcome measures
To assess the suitability and acceptability of the proposed outcome measures for a definitive RCT, participants were assessed pre randomisation (baseline) and at 12 and 24 weeks post randomisation with the following measures: BPFSC112 DERS,105 RTSHI-A (self-harm subscale),113 CASSS106 and TUS. 107 Data on school/college attendance and exclusions were also requested from the school or college with the participant’s consent. We also sought consent from participants (and their parent/carer if aged < 16 years) to access the information recorded about them on the National Pupil Database (NPD)116 to assess the feasibility of utilising these data in future research.
To enable us to describe the sample in terms of the number of eligible participants who meet research diagnostic criteria for BPD, we administered the CI-BPD108 at baseline only. We also administered the psychosis and substance abuse modules of the K-SADS109 at baseline only , to assist in determining whether or not a potential participant met the eligibility criteria. The scheule of enrolment, interventions and assessments in accordance with SPIRIT (Standard Protocol Items: Recommendations for Interventional Trials) guidelines is shown in Table 6.
| Assessment measure | Assessment schedule | |||
|---|---|---|---|---|
| Baseline (week–ta) | Randomisation (week 0) | Follow-up | ||
| 12 weeks | 24 weeks | |||
| Enrolment | ||||
| BPFSC | ✗ | ✗ | ✗ | |
| RTSHI-A (self-harm subscale) | ✗ | ✗ | ✗ | |
| Informed consent | ✗ | |||
| Allocation | ✗ | |||
| Interventions | ||||
| TAU | BEST or TAU | |||
| BEST plus TAU | ||||
| Assessments | ||||
| CI-BPD | ✗ | |||
| K-SADS psychosis module | ✗ | |||
| K-SADS substance abuse module | ✗ | |||
| DERS | ✗ | ✗ | ✗ | |
| CASSS | ✗ | ✗ | ✗ | |
| TUS | ✗ | ✗ | ✗ | |
| EQ-5D | ✗ | ✗ | ✗ | |
| Modified CSRI | ✗ | ✗ | ✗ | |
Health economic data
We recorded all resources required to implement the intervention, including providing training and supervision, staff time to deliver the intervention, consumables and materials required, and any other necessary expenditure. A modified version of the Client Service Receipt Inventory (CSRI)117 was administered at each assessment time point (baseline, 12 weeks and 24 weeks) to evaluate whether or not this measure was an appropriate tool for assessing use of health, pastoral and social care services in this group.
The CSRI was modified in accordance with discussions with the chief investigator to ensure that the instrument was relevant to individuals with BPD and to minimise the burden on individuals (see the Journals Library web page at www.journalslibrary.nihr.ac.uk/programmes/hsdr/170931/#/; accessed 6 April 2022). The CSRI collected data on several potential health and social care items of resource use. These included contacts in a person’s school or college, medicines, inpatient stays, outpatient and A&E visits, community-based health and social care contacts, overnight stays, and any health-care use by the participant’s family that was potentially connected to the participant’s BPD. The EuroQol-5 Dimensions, five-level version (EQ-5D-5L), was administered at all research protocol data collection time points to allow for its usefulness and likely sensitivity to adolescents with BPD symptoms to be assessed. Both the CSRI and the EQ-5D-5L were collected alongside other instruments using face-to-face interviews at baseline and face-to-face or telephone interviews at follow-up.
Process evaluation data
The process evaluation employed an ethnographic methodology118,119 to investigate how the wider context of schools and colleges shaped delivery of the intervention. A mixed-methods approach to analysing data was carried out, including site profile questionnaires; video-/audio-recordings of intervention sessions; staff log sheets to record contacts between participants and trained BEST practitioners; observational field notes of training workshops; workshop feedback forms; questionnaires assessing staff attitudes, skills and knowledge regarding work with young people with BPD symptoms; interviews with young people; and focus groups with staff (education and mental health practitioners) delivering the intervention.
All 45 available video-/audio-recordings were collected to describe intervention delivery and to assess implementation fidelity according to the study protocol. All young people participating in the RCT (from across both arms) were invited to take part in semistructured interviews. Young people who had consented to take part in a qualitative interview were approached about being interviewed by the research assistant by telephone following the 24-week assessment. Eleven interviews were conducted to understand participants’ perspectives on the acceptability of participating in the study. In the intervention arm this included eliciting their views on different intervention sessions and co-delivery with the educational and mental health practitioner; how and whether the intervention functioned to improve their understanding and skills for coping with mental health difficulties; perceived benefits or harms of taking part; completing outcome questionnaires; and asking for suggestions for improving intervention delivery. Interviews with young people allocated to the usual-care arm focused on forms of support obtained during the trial and views on completing questionnaires.
Six focus groups with a total of 19 staff members (nine education practitioners and 10 mental health practitioners) and one individual interview were conducted to obtain practitioner perspectives on delivering the intervention, contextual barriers to and facilitators of successful delivery, intervention sessions, potential contamination in the provision of usual support and additional work required to support the delivery of BEST, and to ask for suggestions for improvement.
At the conclusion of the study, a stakeholder feedback event was held to share key study findings and gather stakeholder views on the likely sustainability of intervention implementation and the future of the research programme.
Analysis
Statistical analysis
We initially intended that recruitment and retention rates would be estimated along with 95% confidence intervals and, if appropriate, time until dropout would be estimated using a reverse Kaplan–Meier curve. Analysis was based on the intention-to-treat principle, analysing each randomised patient in the arm they were allocated to regardless of compliance. Owing to the small sample size, formal hypothesis testing was not planned; instead, we intended that the analysis would focus on estimation. We planned that for the primary outcome measure, the BPFSC, the mean difference would be estimated using a linear model along with corresponding 95% confidence intervals. The rate of completion of each outcome measure would be given and, if appropriate, multiple imputation would be undertaken. A similar approach was planned for the secondary outcome measures.
The above plan was amended, prior to data analysis, owing to the early closure of the study with reduced sample size. Hence, the study team felt that the estimation plan above was too ambitious given the limited sample size, and that the analysis should report on the summary statistics of the relevant outcomes along with the completion rate and retention rate at each time point. Analysis was undertaken in Stata® (StataCorp LP, College Station, TX, USA).
Health economic analysis
As this was a feasibility study, it was not our intention to demonstrate the definitive cost-effectiveness of the intervention as part of this trial. This is because the study was not powered to demonstrate either clinical effectiveness or cost-effectiveness. This was further compounded by the need to stop the study early. However, we collected information to inform the economic evaluation alongside any future definitive trial. This will yield useful information, such as the likely cost of the intervention and key components of resource use. It will also inform the design of a future study by informing the best design of health economic data collection instruments. The focus in this evaluation was on three key pieces of information necessary to conduct an economic evaluation in any future study: resources required to provide the intervention, health and social care service use and health-related quality of life.
First, we collected data on the resources required to provide the intervention in this study. This included the costs associated with providing the two workshops required to train those providing the intervention. Resources used would relate to the time of those providing training and of those receiving it. We did not record time spent developing the training workshops. For the cost of providing intervention sessions, we recorded the number of sessions received by participants, the AfC band of the mental health practitioner providing the session and estimates of duration of sessions obtained from the pilot work. We were also able to estimate distance travelled to provide the intervention. We did not have a record of the type or grade of school/college staff so estimates of type staff were made based on those observed in the pilot study. The final element costed related to supervision received by those providing the intervention. Details were kept of the number of supervision sessions provided, the AfC band of those providing the supervision and the distance travelled to provide this supervision. Resources required to provide the intervention were combined with appropriate unit cost data to provide an estimate of the cost of providing the BEST intervention. Unit costs were obtained from a published source and relate to the cost year 2018/19. 120 As these costs were derived from a small sample, they were not reflective of costs applying to a large trial or to routine clinical practice. For this reason, we will conduct scenario analyses, which estimate the cost of provision if any assumptions about how the service is provided and who provides it are changed.
Second, we looked at health and social care resources used by the two study groups. This was carried out in three time periods: the 12 weeks prior to randomisation; the first 12 weeks of follow-up, when the intervention would be provided; and the final 12 weeks of follow-up. Owing to the small sample size, a formal costing of the service use by individuals was not undertaken; instead, analysis will focus on a description of the type of services used by individuals. In addition, we assessed the performance of the CSRI in terms of completeness. A key question would be whether the CSRI could be used in future studies or alternative methods of collecting resource use data would be needed.
Finally, we used the EQ-5D-5L121 to investigate health-related quality of life, to test whether or not this might be a suitable instrument to use in this population. The EQ-5D-5L was scored using the ‘crosswalk values’. 122 Again, this was limited by the small sample size in the study, particularly in follow-up periods. However, it was possible to look at response characteristics and correlations with other measures for the baseline sample.
Process evaluation analysis
Linguistic ethnography provides analytical tools for systematically analysing talk and behaviour within context. In process evaluations it can be used to search for how the implementation of the intervention ‘disrupts’ the complex system into which it is being introduced,123 exposing wider social forces structuring intervention delivery at the point of delivery: relationships that are otherwise hidden from view. Observational methods including using interactional data are central to a linguistic ethnography approach, and are often supported by interview data to triangulate perspectives with delivery in practice.
All recordings of individual sessions were independently rated against the fidelity checklist by members of the study team and subject to qualitative activity analysis using the same approach employed in the pilot study (see Chapter 3, Pilot methods) to identify patterns of successful delivery; interactional difficulties between staff and pupils in negotiating the content of the treatment sessions; and analysis of how the theories of adolescent development, attachment and mentalisation that underpin the BEST intervention are enacted within sessions.
Site profile questionnaires were completed by a member of staff from each school and college to enable us to identify characteristics of the participating settings that may have an impact on delivery. Practitioners were asked to complete log sheets of their contacts with participants to provide an audit trail of activities surrounding treatment sessions that either facilitate or constrain delivery and to allow us to assess the extent to which control participants may be receiving elements of the intervention.
All interviews and focus groups were transcribed verbatim and thematically analysed with the aid of NVivo software. The approach to the thematic analysis was informed by a critical realist stance, which holds that, although reality exists independently of our observation of it, our understanding of reality is filtered through our own past experiences and our particular social, cultural and historical position. Therefore, each individual occupies a unique vantage point from which they experience and interpret the world. Therefore, we sought to understand each participant’s individual experience of participation in BEST through close engagement with their language use.
The thematic analysis took an inductive approach, generating codes and themes based on the words used by participants themselves rather than an a priori framework. Coding was initially undertaken independently by authors Briony Gee and Jamie Murdoch, who then met to discuss the codes generated and develop provisional themes. Following this, Briony Gee revisited the data to ensure that each theme had sufficient empirical support, removing and collapsing themes where necessary, before defining each theme and naming it using a short quotation from the data set. Further verbatim quotations to be included in the presentation of the analysis were selected based on their suitability as stand-alone illustrations of each theme.
Although neither Briony Gee nor Jamie Murdoch was involved in the initial development of the BEST intervention, both played a role in its refinement in preparation for the feasibility RCT. Therefore, reflection on the impact that our investment in the success of the intervention had on our interpretation of participant experiences was an important part of the analytical process.
The analysis of qualitative data was iterative, moving between data collection and data analysis to test emerging theories, working laterally across data types. Care was taken to identify and follow up deviant cases that did not fit into emerging theories. By setting the analysis of intervention delivery within an understanding of the wider context of school and college environments, we were able to make the transition from the identification of routines and patterns of the use of BEST in specific schools and colleges to theoretical explanations of how different structural relations and mechanisms of the intervention organised moments of delivery, which then affected specific outcomes.
In drawing case comparisons across settings, we developed hypotheses about why the intervention was linked to outcomes, which we can test in a future definitive trial. This led us to identify factors that were plausibly and/or consistently related to successful or unsuccessful delivery of the components of the intervention. Emerging theories and the relationship of the data to the conceptual literature underpinning the intervention were discussed and refined at team meetings throughout the research.
Progression criteria
The primary output of the research was to be the design of a subsequent definitive trial. We planned to assess the outcomes of the feasibility trial against the following criteria to make recommendations regarding progression:
-
Recruitment rate is within 70% of the target.
-
At least 70% of those randomised to receive the intervention attended three or more treatment sessions within the 12-week treatment window.
-
Follow-up assessments were completed by at least 75% of participants at 12 weeks and 70% of participants at 24 weeks.
-
Contamination of the control arm was sufficiently limited for individual randomisation to be justified (informed by process evaluation findings).
The design of subsequent research will be informed by the results of the feasibility study, the views of participants in the stakeholder feedback event and Medical Research Council guidelines124 on developing and evaluating complex interventions. If the above progression criteria are met and a definitive RCT is judged to be a suitable and acceptable methodology, we intend to progress to a multisite, assessor-blind, superiority RCT of the effectiveness and cost-effectiveness of the intervention plus TAU in comparison with TAU alone. The proposed primary outcome measure is severity of borderline personality features measured using the BPFSC. 112 The primary analysis of effectiveness would be a multilevel comparison of BPFSC total score at 24 weeks, with treatment arm as the main effect, school as a random intercept and baseline BPFSC total score as a covariate. A definitive cost-effectiveness analysis would be conducted, informed by the results of the preliminary economic analysis conducted alongside the feasibility trial.
If one or more of the above progression criteria are met, we intend to discuss with the TSC whether or not the trial design proposed above is likely to be feasible given steps to overcome specific issues encountered during the feasibility trial. If it is not, alternative study designs will be considered; for instance, a cluster trial or stepped wedge design could be more suitable if the findings of the feasibility trial suggest that contamination of the control arm would threaten the validity of an individually randomised definitive trial. In the case that the results of the feasibility study suggest that substantial changes to the protocol are required prior to progression, we would incorporate an internal pilot with stop–go criteria within any future definitive trial.
Changes to protocol as a result of the COVID-19 pandemic
We experienced disruption to the trial from early March 2020 onwards owing to the impact of the COVID-19 pandemic, which led to staff absence and restrictions regarding external visitors to school and college sites. On 18 March 2020, the government announced that schools and colleges would be closed indefinitely to nearly all children. As a result, recruitment to the feasibility trial and intervention delivery were suspended. As delivery within the young person’s school or college is an integral part of the intervention and the feasibility of this mode of delivery is central to the research questions the study was designed to answer, it was not deemed appropriate to attempt to adapt the project for remote delivery.
Considering the prolonged and significant nature of the disruption caused by the pandemic and in discussion with the funder and study oversight groups, the decision was taken to conclude the study early. Only those participants who had reached the 12-week follow-up point before the project was suspended were followed up, and all follow-up assessments following suspension of recruitment were conducted remotely over the telephone. Qualitative interviews with participants were also completed by telephone and staff focus groups were conducted online using video conferencing software. As a result, the end date of study was brought forward by 3 months.
Our ability to carry out linguistic ethnography within the BEST study was compromised by this disruption and early closure as a result of the pandemic. Although we were able to collect and analyse some video- and audio-recorded intervention sessions, we were not able to collect key observations within schools or interview senior leaders, which undermined our ability to implement the approach as planned.
Chapter 5 Feasibility randomised controlled trial: results
Recruitment and retention
Recruitment of schools and college
Schools and colleges were approached about taking part via the research team’s existing contacts or through Educate Norfolk (Norfolk, UK), a local network of secondary school and college leaders. We presented an overview of the study at an Educate Norfolk forum and invited expressions of interest from school and college leaders in attendance.
Staff at 16 of the 21 schools and colleges that received details of the study and requirements for being involved gave their agreement for their school or college to take part. Reasons given for declining participation included that the study would place too great a burden on already stretched school staff members (n = 1) and an upcoming merger creating uncertainty about the structure of pastoral provision for the coming academic year (n = 1). Staff in other settings did not give a reason for declining.
Of the 16 schools and colleges that had staff who were willing to be involved, 12 went on to become sites for the feasibility trial. Staff at one school who had initially agreed to participate were unable to identify a member of staff able to attend one of the training workshops. Staff at a further three schools had confirmed their willingness to participate in the study and identified staff members to be trained to deliver the intervention just prior to the suspension of the trial.
School and college characteristics
An overview of the characteristics of the 12 schools and colleges that were sites is provided in Table 7.
| Site | Setting type | Approximate number of students (young people) | Location | Ofsted ratinga |
|---|---|---|---|---|
| A | Further education college | 4000 | City | Good |
| B | Further education college | 2500 | Costal | Requires improvement |
| C | State secondary school (no sixth form) | 1200 | Town | Good |
| D | State secondary school (no sixth form) | 499 | Village | Requires improvement |
| E | Alternative education provider for children unable to access mainstream schooling | 100 | City | Requires improvement |
| F | Sixth form college | 1600 | Costal | Good |
| G | State secondary school (with sixth form) | 1290 | Village | Good |
| H | State secondary school (no sixth form) | 937 | City | Good |
| I | State secondary school (with sixth form) | 1641 | Town | Good |
| J | State secondary school (with sixth form) | 1186 | Village | Good |
| K | State secondary school (with sixth form) | 1877 | Town | Outstanding |
| L | Independent secondary school (with sixth form) | 1003 | City | Excellentb |
Staff participants
In total, 30 school and college staff members and 21 mental health practitioners gave consent to take part in the feasibility trial, seven of whom had also participated in the pilot phase of the study. However, a proportion of these had been recruited and trained shortly before the suspension of the study as a result of the COVID-19 pandemic and so did not have the opportunity to deliver the intervention.
Practitioners who delivered the intervention to participants in the feasibility trial attended one of two training workshops. Workshop 1 was a full-day workshop attended by most trainees [15 school/college staff members and 15 mental health professionals (8 × band 4, 2 × band 5, 4 × band 6, 1 × band 7). Workshop 2 was a half-day workshop offered primarily as a refresher for those who had already attended training during the pilot phase [two school/college staff members and three mental health professionals (2 × band 4 and 1 × band 7)]. For those practitioners trained during the pilot phase who opted not to repeat the training workshop, a member of the team met with each practitioner individually to review the content of the intervention and provide updated training to reflect changes to the manual since the first phase.
Staff were asked to complete a questionnaire regarding their attitude, skills and knowledge in relation to working with young people experiencing BPD symptoms prior to the training workshop. Responses are summarised in Table 8.
| Item | Education practitioners, mean (SD) | Mental health practitioners, mean (SD) |
|---|---|---|
| Willingness to work with young people with symptoms of BPD | 1.19 (0.40) | 1.12 (0.33) |
| Optimism in working with young people with symptoms of BPD | 1.69 (0.70) | 1.47 (0.48) |
| Enthusiasm to work with young people with symptoms of BPD | 1.31 (0.62) | 1.12 (0.34) |
| Confidence in working with young people with symptoms of BPD | 2.47 (0.63) | 2.47 (0.62) |
| Theoretical knowledge about young people with symptoms of BPD | 3.06 (0.64) | 2.76 (0.72) |
| Clinical skills in working with young people with symptoms of BPD | 3.66 (0.82) | 2.53 (0.72) |
Participant flow
The flow of referrals and participants through the study is illustrated in Figure 4.
FIGURE 4.
Consolidated Standards of Reporting Trials diagram for feasibility trial.

Recruitment
We recruited and randomised 32 eligible participants prior to the suspension of the study. The overall rate of recruitment was slower than anticipated: on average four participants per month versus a target recruitment rate of 6.7 participants per month. The pattern of referrals suggests that staff at sites where more staff were trained as BEST practitioners may have been more able to refer suitable participants than sites where fewer staff were trained as BEST practitioners. Site J, at which four staff members were trained as BEST practitioners (the maximum number trained at other participating sites was two), referred considerably more students than any other setting: 16 students, of whom 12 were eligible.
This slower than anticipated recruitment rate was largely the result of very limited recruitment during school holidays. We had anticipated that we would receive a substantial proportion of our referrals from mental health teams. However, only five referrals (8%) were received from mental health services, with the majority received directly from schools and colleges. Consequently, we received few referrals at the start of the recruitment period, which coincided with the school summer break, and a pause in referrals over the Christmas break.
We encouraged referrals from mental health services through attendance at team meetings, distribution of promotional materials and contact with wait list co-ordinators and the single point of access (the central triaging function). A key barrier to recruitment via mental health teams was that the school or college attended was not routinely enquired about and recorded in young people’s medical records. Therefore, it was not possible for teams to easily identify service users who attended the schools and colleges participating in the trial. Potential referrers from within mental health services also reported that many of the young people on their caseload presenting with BPD features were nor currently engaging in education owing to the severity of their difficulties.
A further issue encountered was with the original inclusion criterion regarding self-harm, which required that self-harm had occurred within the past month. The rationale for including self-harm as an inclusion criterion in addition to BPD symptoms was to increase the predictive specificity for BPD. We also felt that including self-harm as an inclusion criterion may make it easier for school and college staff to identify potentially eligible young people because self-harm might be more visible/readily understood than BPD symptoms more generally.
However, the 1-month time frame selected as the index period for self-harm was not evidence based and was perceived by referrers as unduly restrictive. During the first 2 months of the recruitment period, we observed that help-seeking young people with BPD symptoms were not being referred or were excluded at the screening stage (the first five young people referred were excluded on this basis). We were also concerned about the potential for harm as a result of young people learning that they were not eligible to participate as a result of not having self-harmed recently enough. This criterion was therefore amended to include young people with a history of repeated self-harm regardless of the time period during which this had occurred. This substantial amendment received confirmation of favourable ethics opinion from the Research Ethics Committee on 17 October 2019. The number of young people recruited who would have met the original criterion is reported below.
The recruitment rate was also affected by the suspension of the study from mid-March, meaning that fewer participants were recruited in March that we would otherwise have anticipated. Planned screening assessments with seven participants who had been referred had to be cancelled as a result of the pandemic. The early closure of the study also affected the total number of recruits because the recruitment period was cut short.
From October, when the first participant was recruited, the average recruitment rate was 5.4 participants per month. To reach 70% of the target sample size a recruitment rate of 4.6 participants per month across the initially planned recruitment period would have been sufficient. The rate of recruitment is plotted alongside the projected recruitment rate and the rate of recruitment that would have enabled us to meet our progression criterion related to recruitment in Figure 5.
FIGURE 5.
Accrual curve for feasibility trail.
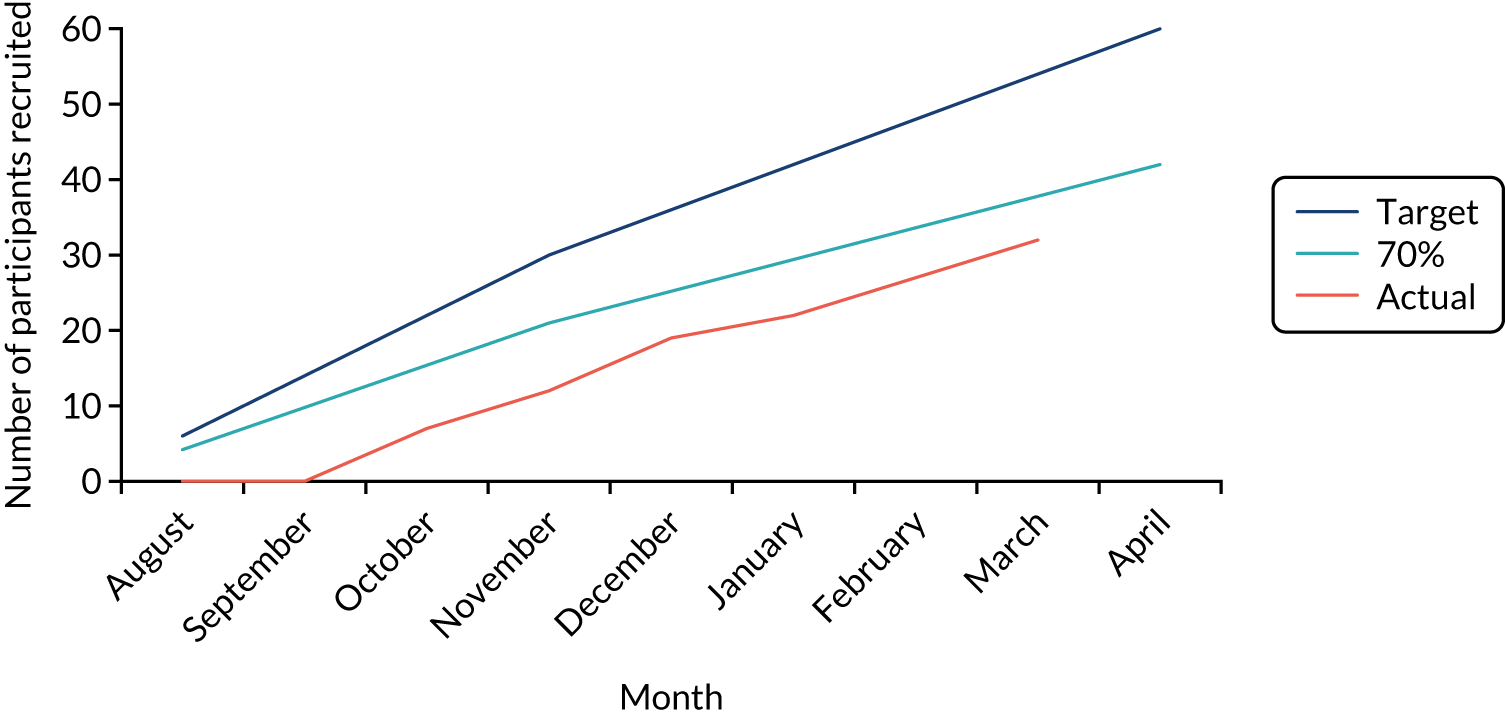
Retention
Only those participants who reached the 12-week time point prior to the suspension of the trial were followed up, because those randomised later did not have the opportunity to receive their allocated intervention (whether BEST plus TAU or TAU alone) owing to school closures. Of the 19 participants who had reached the 12-week follow-up before the suspension of the trial, 17 (89.5%) were followed up at 12 weeks and 14 (73.7%) at 24-weeks. Follow-up was more challenging at 24 weeks, as all assessments were completed remotely at a time when schools and colleges were closed to most students. As a result, schools and colleges were unable to assist in contacting participants and arranging appointments as they had at the 12-week time point.
Acceptability of recruitment and randomisation
The acceptability of research procedures, including recruitment and randomisation, was explored with practitioners and participants as part of focus groups and interviews.
Recruitment
Education practitioners were asked about their experience of identifying potentially eligible students and approaching them to participate in the study. There was some variation among staff in the experiences of identifying students for whom the study might be appropriate. Although practitioners from some settings reported experiencing considerable difficulty identifying potentially eligible students, those from other settings told us that they experienced this process as straightforward.
Staff at site J referred notably more eligible students to the study than staff in other participating settings. We explored with the practitioners from site J what they felt had facilitated the high rate of eligible referrals from their school. Practitioners from this school reflected on the importance of having a good knowledge of their students and of having several staff members trained as BEST practitioners working in different roles within the school:
We didn’t really have any problems at all identifying, did we? . . . I think that comes back to knowing your kids, you know, knowing the kids that you work with and having a good general knowledge of their backgrounds and, you know, I suppose being in safeguarding you get to know a little bit more about them as well, and just having that sort of mixed you know, [name of staff participant] from the classroom perspective, and [name of another staff participant] in the classroom, myself sort of in pastoral care, we have quite a good mix and, we just chatted about it and discussed and sort of agreed and, yeah, wasn’t an issue finding them.
Education practitioner
The accounts of practitioners from site J highlighted the important role played by relationships in facilitating the referral process; good relationships with students and parents, among school staff and with the research assistant were all seen as important factors in identifying and referring young people for whom the study was likely to be appropriate.
Practitioners from schools and colleges at which there was greater difficulty identifying potential participants identified the eligibility criteria as the key barrier. There appeared to have been some confusion regarding the exclusion criterion relating to interventions the young person was currently receiving. This exclusion criterion was intended to exclude only those currently receiving a specific psychological therapy (e.g. CBT, DBT-A). However, staff at some settings had interpreted this as excluding students who had already been referred for any type of mental health-related support. For instance, one practitioner commented:
I think for us we found that certainly before the criteria [regarding self-harm recency] changed our high-level students would be those that that would fit and they were, they are the ones that we have already got into other support, we wouldn’t, they’re students we wouldn’t have left to not have anything.
Education practitioner
Practitioners were positive about the change to the self-harm inclusion criterion as it allowed them to consider a broader range of young people as potential participants. One mental health practitioner spoke about feeling frustrated by the original criterion excluding young people for whom the trial would otherwise have been suitable:
. . . there was a few people that I’d assessed that I thought would be quite, you know, that would benefit from the project and because they hadn’t self-harmed within the time frame at that time, I know subsequently you changed the criteria because it was probably a bit narrow, but then there was a few people I felt missed out on the, on being part of the project . . . young people are impulsive aren’t they and they may self-harm and certainly report that at the assessment but then, you know, they might not do it for say 6 weeks or they might do it constantly for the next month and then not do it for 6 weeks, so I guess that time frame that you started with maybe that was a little bit rigid.
Mental health practitioner
Furthermore, practitioners felt that the intervention would be appropriate to a broader age range than specified by the inclusion criteria. Practitioners from schools felt that the study would have been appropriate for pupils in Years 7 and 8 (aged 11–13 years) and practitioners from colleges felt that some of their 19-year-old learners would have benefited from being involved. Some practitioners also believed that the intervention would potentially be helpful for young people with a broader range of difficulties than BPD symptoms, some commenting that aspects of the intervention would be helpful to all young people. However, another practitioner highlighted the potential for staff to refer young people for whom the project might not be right in the context of limited mental health support available to schools and colleges:
. . . it is about having the right participants to get the best out of the project . . . and I think that’s important, because I think if you just go into a school and say, ‘hi, we’ve got this all-singing, all-dancing project, would you like to be involved in it’, they’ll snap your hands off but they probably won’t give you the right people for the, you know, the project.
Education practitioner
Practitioners did not report any significant difficulties with the process of approaching young people or their parents about the research and reported that most of those they approached were happy to be contacted by the research team. Reasons mentioned for young people approached not being interested were already having support in place and concern about what peers would think about their involvement. Young people who participated in interviews did not report any concerns regarding the process of being approached about the project. When asked about their motivation for expressing an interest in participating, most replied that they thought it sounded interesting or believed that it might help them.
Complexities surrounding use of diagnostic language during recruitment
One practitioner expressed concern about using the term ‘borderline personality disorder’ when discussing the project with a parent, explaining she had ‘let it slip once and then sort of felt terrible’. In accordance with guidance from out PPI advisors, we advised referrers to explain the project in general terms when approaching young people and their families about the project. We suggested that they explain the sort of difficulties that young people for whom the study is appropriate might be experiencing (e.g. difficulties managing emotions, risky or impulsive behaviour) rather than using diagnostic language. Although it was not our intention to create a taboo around the term ‘borderline personality disorder’, there is clearly the potential for distress if the topic of BPD symptoms is not introduced to young people and their parents in the right way. This was illustrated by the experience of one parent who found information online about the study that referred to BPD, having been approached about the study by staff at her child’s school. The parent subsequently contacted the research team to express her concern that her child was being given a diagnostic label. Although we were able to reassure the parent that this was not the case and provided further information about the purpose of the study, it is likely that some distress was caused to the parent as a result of having learnt about the study in this way.
Randomisation
Most participants appear to have had a reasonable understanding of randomisation and expressed that they were happy to take part in the trial whether or not they received the BEST intervention. Education practitioners were accepting of the need for randomisation but expressed some disappointment that not all participating students were able to receive the intervention:
. . . because it was randomised people were going through that we were like, ‘oh they really need this intervention’ and they were getting rejected and we were like, ‘no!’
Education practitioner
The use of the word ‘rejected’ in this account to refer to a participant being allocated to the TAU-only arm conveys a lack of equipoise among practitioners regarding the relative benefits of the interventions. This is perhaps unsurprising given the difficulties in accessing specialist mental health support for students not involved in the trial.
One practitioner spoke about feeling that they were letting down students allocated to the TAU-only arm and believed that learning of their allocation had had a short-term negative impact on some TAU participants:
. . . it did feel like we were letting them down a little bit by sort of offering something it was almost sort of like, ‘here we are, have this, have this, oh no, sorry, we’re going to take it away,’ so it did feel a little bit unfair for one or two of us that . . . if I had had an influence over I would have said ‘can we make sure that one is randomised,’ you know what I mean and I do feel that for a couple of them, short term, it probably affected them quite a lot really when they were given the news that they hadn’t been selected.
Education practitioner
One young person, who was randomised to receive the BEST intervention, expressed a similar sentiment regarding the potential adverse effects of TAU participants not having access to the support they need:
. . . if someone who was also in my position and like sort of needed it and like wasn’t getting any help from anybody else and like they sort of like just had like the school or something because of the two groups then um yes I don’t think that’s completely fair but however I also understand to like actually see if it works like ‘cos it’s a trial so yes I completely understand that.
Young person
It was suggested that the control group should be offered some support in addition to TAU to minimise the potential for disappointment regarding allocation. Although TAU participants interviewed did not report any adverse impact of being allocated to the TAU arm, it is possible that this was because any participants who were negatively affected chose not to take part in a qualitative interview.
Participant demographic and baseline clinical characteristics
Baseline demographic and clinical characteristics of participants recruited to the feasibility RCT are presented in Tables 9 and 10.
| Characteristic | Number (%) of participants | |
|---|---|---|
| BEST plus TAU arm | TAU arm | |
| Gender | ||
| Female | 13 (72) | 11 (79) |
| Male | 5 (28) | 3 (21) |
| Year of education | ||
| 9 | 4 (22) | 7 (50) |
| 10 | 5 (28) | 3 (21) |
| 11 | 2 (11) | 0 (0) |
| 12/13/College | 7 (39) | 4 (29) |
| Ethnic group | ||
| Mixed: other | 1 (6) | 0 (0) |
| Mixed: white and Asian | 0 (0) | 1 (7) |
| Mixed: white and black African | 0 (0) | 1 (7) |
| White: British (English/Welsh/Scottish/Northern Irish/British) | 16 (89) | 12 (86) |
| White: other | 1 (6) | 0 (0) |
| Self-harm within the past month | ||
| Yes | 14 (78) | 9 (64) |
| No | 4 (22) | 5 (36) |
| Total, N | 18 | 14 |
| Item | Number (%) of participants | |||||
|---|---|---|---|---|---|---|
| BEST plus TAU arm (N = 18) | TAU arm (N = 14) | |||||
| Absent | Probably present | Definitely present | Absent | Probably present | Definitely present | |
| Inappropriate, intense anger or difficulty controlling anger | 3 (17) | 2 (11) | 13 (72) | 5 (36) | 3 (21) | 6 (43) |
| Affective instability owing to a marked reactivity of mood | 2 (11) | 2 (11) | 14 (78) | 3 (21) | 3 (21) | 8 (57) |
| Chronic feelings of emptiness | 3 (17) | 2 (11) | 13 (72) | 5 (36) | 2 (14) | 7 (50) |
| Identify disturbance, markedly and persistently unstable self-image of sense | 10 (56) | 3 (17) | 5 (28) | 9 (64) | 3 (21) | 2 (14) |
| Transient stress-related paranoid ideation or severe dissociative symptoms | 8 (44) | 3 (17) | 7 (39) | 10 (71) | 2 (14) | 2 (14) |
| Frantic efforts to avoid real or imagined abandonment | 12 (67) | 4 (22) | 2 (11) | 10 (71) | 2 (14) | 2 (14) |
| Recurrent suicidal behaviour, gestures, threats or self-mutilating behaviour | 0 (0) | 3 (17) | 15 (83) | 1 (7) | 3 (21) | 10 (71) |
| Impulsivity in at least two areas that are potentially self-damaging | 3 (17) | 0 (0) | 15 (83) | 4 (29) | 1 (7) | 9 (64) |
| A pattern of unstable and intense interpersonal relationships characterised by alternating between extremes of idealisation and devaluation | 10 (56) | 3 (17) | 5 (28) | 10 (71) | 2 (14) | 2 (14) |
| Number of criteria met for DSM-IV BPD | Three or fewer: 2 (11) | Four: 5 (28) | Five or more: 11 (61) | Three or fewer: 7 (50) | Four: 3 (21) | Five or more: 4 (29) |
Suitability of outcome measures
Rates of completion
Outcome measures were generally well completed. Of those successfully followed up at 12 weeks, 16 out of 17 (94.1%) completed all outcome measures, and of those successfully followed up at 24 weeks, 12 out of 14 (85.7%) completed all outcome measures. A study research assistant facilitated all assessments, and so they were able to check self-report measures for missing items and prompt the participant to complete those accidently missed. As a result, there were very few individual missing items within completed measures; missing item scores were present for only one participant who declined to complete the items missed.
Data on participants’ school or college attendance and exclusions were requested but complete data were received for only 26.3% of those followed up. However, this was requested at the end of the follow-up period when schools and colleges were closed to most pupils during the COVID-19 lockdown. We also sought consent to access the information recorded about participants on the NPD via an optional item on the consent form: 84.2% of participants agreed to these data being accessed by the research team.
Descriptive statistics for outcome measures collected
Descriptive statistics summarising the outcome measures collected are presented in Table 11.
| Measure | BEST plus TAU arm | TAU arm | ||||
|---|---|---|---|---|---|---|
| n | Mean score | SD | n | Mean score | SD | |
| BPFSC | ||||||
| Baseline | 18 | 42.3 | 5.3 | 14 | 40.43 | 5.9 |
| 12 weeks | 9 | 41.3 | 5.1 | 8 | 34.8 | 7.6 |
| 24 weeks | 6 | 35.0 | 7.0 | 7 | 32.3 | 7.2 |
| DERS | ||||||
| Baseline | 18 | 74.7 | 14.5 | 14 | 66.6 | 21.9 |
| 12 weeks | 8 | 68.0 | 15.8 | 8 | 62.0 | 26.9 |
| 24 weeks | 6 | 46.2 | 18.5 | 7 | 46.4 | 21.7 |
| CASSS total | ||||||
| Baseline | 18 | 214.4 | 44.9 | 14 | 227.1 | 43.1 |
| 12 weeks | 8 | 186.5 | 50.0 | 8 | 235.9 | 50.7 |
| 24 weeks | 6 | 226.2 | 52.1 | 7 | 205.5 | 35.8 |
| CASSS school | ||||||
| Baseline | 18 | 113.9 | 31.97 | 14 | 123.8 | 33.8 |
| 12 weeks | 8 | 106.3 | 32.8 | 8 | 127.6 | 37.2 |
| 24 weeks | 6 | 125.0 | 41.6 | 7 | 107.8 | 30.0 |
| TUS structured activity | ||||||
| Baseline | 18 | 43.7 | 28.8 | 14 | 44.0 | 20.2 |
| 12 weeks | 8 | 46.2 | 25.3 | 8 | 42.8 | 22.2 |
| 4 weeks | 6 | 30.7 | 19.4 | 7 | 19.7 | 16.4 |
Given that the objective of the study was to assess the feasibility of a future RCT, this study was not powered to detect any significant changes in outcomes. However, we were interested in any indication of whether or not the outcome measures would be likely to be able to detect any change as a result of the intervention in a future trial. Mean changes from baseline by allocated arm are presented for all continuous measures in Table 12, and data on change in self-harm in the past month is summarised in Table 13.
| Measure | BEST plus TAU arm (n = 18) | TAU arm (n = 14) | ||
|---|---|---|---|---|
| Mean score | SD | Mean score | SD | |
| BPFSC | ||||
| 12 weeks | –3.11 | 5.7 | –5.1 | 5.5 |
| 24 weeks | –7.8 | 5.6 | –7.1 | 3.5 |
| DERS | ||||
| 12 weeks | –14.4 | 16.6 | –3.13 | 12.6 |
| 24 weeks | –37.2 | 21.1 | –17.6 | 20.0 |
| CASSS total | ||||
| 12 weeks | –11.1 | 48.4 | 23.63 | 30.1 |
| 24 weeks | 31.0 | 29.51 | –18.7 | 33.9 |
| CASSS school | ||||
| 12 weeks | 1.4 | 26.7 | 20.3 | 25.6 |
| 24 weeks | 19.5 | 15.8 | –7.7 | 24.5 |
| TUS structured activity | ||||
| 12 weeks | –4.8 | 38.4 | –6.5 | 17.4 |
| 24 weeks | –27.6 | 48.9 | –27.6 | 25.5 |
| BEST plus TAU arm | TAU arm | ||||
|---|---|---|---|---|---|
| Participant ID | 12 weeks | 24 weeks | Participant ID | 12 weeks | 24 weeks |
| P007 | Yes → No | Yes → No | P006 | Yes → No | Yes → No |
| P008 | No change | Yes → No | P009 | No change | No change |
| P010 | Missing | Missing | P011 | No change | Missing |
| P012 | No change | No change | P013 | No change | Yes → No |
| P015 | No change | Missing | P014 | Missing | No change |
| P017 | Missing | No change | P016 | No change | Missing |
| P018 | No change | Missing | P020 | Yes → No | Yes → No |
| P019 | Yes → No | Yes → No | P021 | Yes → No | Yes → No |
| P022 | No change | No change | P024 | No change | No change |
| P023 | Yes → No | Missing | |||
| Yes → No, n (%) | 3 (38) | 3 (50%) | Yes → No, n (%) | 3 (38%) | 4 (57%) |
| No → Yes, n (%) | 0 | 0 | No → Yes, n (%) | 0 | 0 |
| No change, n (%) | 5 (63%) | 3 (50%) | No change, n (%) | 5 (63%) | 3 (43%) |
Acceptability of outcome assessments
Participants were asked about their experiences of completing research assessments as part of qualitative interviews. Most young people fed back that they found the process of completing the research assessments acceptable and did not recommend any changes to the outcome measures included in the assessments. Two young people commented that they had found completing the follow-up assessments beneficial as it had offered a chance to review how they were feeling and track their progress.
One young person fed back that the TUS did not feel relevant when she was asked to complete it during the lockdown, as it asked about activities that were not permitted at the time. Another participant commented that he found some questionnaires repetitive.
Only one participant told us that she had experienced discomfort completing the outcome measures, explaining that she had felt annoyed by how personal some of the questions were:
I knew you wouldn’t have to answer some of the questions if you didn’t want to but it’s just the fact that some questions were actually kind of so personal . . . they were kind of annoying.
Young person
When asked if there were any particular questions she found too personal, she replied, ‘the ones like the harming yourself ones and stuff like that’. She explained that she answered these questions, despite understanding that she did not have to answer any questions she was uncomfortable with, because she felt that she could trust the research team owing to their having the trust of the school:
Like it wasn’t way too personal for me to not answer but it was kind of personal but the fact that I knew I could probably trust you . . . ‘cos the school trust you.
Young person
Fidelity of intervention delivery
Fidelity of BEST intervention delivery
We encountered some practical and technical difficulties with recording equipment and file transfer, which meant that not all sessions could be reviewed. However, the majority of completed BEST sessions, 45 sessions with 10 participants (including two sessions with a participant who was not followed up owing to not reaching the 12-week time point before the study was halted because of the pandemic), were successfully recorded and available for analysis.
Fidelity ratings
All available session recordings for those who completed all six sessions of the intervention (n = 31) were rated against the fidelity checklist by members of the research team. Sessions were deemed adherent if they were rated 1 or 2 (component partially or fully present) on each of the core components for the session being delivered, which were as follows:
-
session 1 – engagement, emotion regulation
-
session 2 – engagement, formulation, mentalisation skills
-
session 3 – engagement, formulation, emotion regulation skills
-
session 4 – engagement, formulation, mentalisation skills
-
session 5 – engagement, emotion regulation skills, self-harm management, self-care skills
-
session 6 – engagement and at least one other component as appropriate.
A total of 29 of the 31 sessions (93.5%) were rated as adherent. The fidelity ratings are summarised in Table 14.
| Session | Adherent, n/N (%) | Engagement | Formulation | Emotion regulation skills | Self-harm management | Mentalisation skills | Self-care skills | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 0 | 1 | 2 | 0 | 1 | 2 | 0 | 1 | 2 | 0 | 1 | 2 | 0 | 1 | 2 | ||
| 1 | 3/3 (100) | 3 | 2 | 1 | 1 | 2 | 2 | 1 | 2 | 1 | 1 | 2 | |||||||
| 2 | 5/5 (100) | 5 | 4 | 1 | 4 | 1 | 3 | 2 | 1 | 4 | 5 | ||||||||
| 3 | 6/6 (100) | 6 | 4 | 2 | 5 | 1 | 4 | 2 | 5 | 1 | 5 | 1 | |||||||
| 4 | 5/5 (100) | 1 | 4 | 4 | 1 | 2 | 1 | 2 | 2 | 3 | 1 | 4 | 4 | 1 | |||||
| 5 | 4/6 (66.7)a | 1 | 5 | 3 | 2 | 1 | 1 | 4 | 1 | 2 | 4 | 4 | 2 | 1 | 5 | ||||
| 6 | 6/6 (100) | 3 | 3 | 4 | 2 | 2 | 4 | 5 | 1 | 5 | 1 | 6 | |||||||
Analysis of session structure and patterns of intervention delivery
An activity analysis identifying broad patterns of delivery across recorded sessions was conducted. Data summarising the recorded sessions and patterns of delivery derived from the activity analysis of recorded sessions are summarised in Table 15. In this table, we present the number of recordings corresponding to each of the six manualised sessions, the mean duration of each session and the mean number of cells corresponding to 30-second intervals during which each speaker was coded as taking a conversational turn.
| Activity | Session | Overall | |||||
|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | ||
| Number of recoded sessions | 8 | 8 | 9 | 8 | 6 | 6 | 45 |
| Mean duration (minutes) | 51.6 | 48.5 | 52.6 | 46.6 | 55.4 | 42.7 | 49.7 |
| 30-second intervals in which turns taken by (%) | |||||||
| Education practitioner | 64 | 66 | 54 | 56 | 57 | 65 | 60 |
| MH practitioner | 55 | 52 | 52 | 47 | 36 | 36 | 48 |
| Participant | 63 | 64 | 66 | 65 | 62 | 75 | 64 |
The activity analysis showed broad uniformity in the structure of session activities, corresponding to the structure of the manual’s content. Sessions began (except for session 1, which began with introducing the intervention) with reviewing the content of the previous session, reflecting on the period since the last session and discussing any home practice completed (often these activities were combined). Practitioners then gave the agenda for the session and worked through this agenda, which followed the prescribed session content. Each session ended with a discussion of how the participant had found the session and setting a home practice task.
Participants appeared actively engaged in the intervention, as evidenced by the high percentage of cells in which they took conversation turns across all sessions. There was variation across cases in how practitioners organised and divided delivery. However, we observed a broad pattern of mental health practitioners often initiating and maintaining focus on manualised activities, whereas education practitioners frequently conveyed information and supported the young person to relate session content to their own experiences. There was a reduction in the proportion of cells, on average, in which mental health practitioners took conversation turns over the course of the intervention. This pattern requires further exploration but may be indicative of mental health practitioners reducing their input as education practitioners gain confidence in delivering intervention content.
Drawing from the findings of the activity analysis, we looked for patterns of intervention delivery that provided initial evidence of potential mechanisms of change and potential tensions between context and implementation that may affect successful delivery. Our approach was informed by the activity analysis carried out in the pilot, as well as the initial activity analysis of sessions delivered in the feasibility study. These identified patterns in how mental health practitioners and education practitioners shared delivery of intervention sessions, as well as variations in how different intervention components (and mechanisms of the intervention) were communicated by practitioners and responded to by young people. Our approach was also informed by findings we identified in the analysis of interview and focus group data, which revealed that young people reported improved mentalisation skills, difficulties negotiating sensitive topics such as self-harm and the challenges of having confidential discussions in busy school and college environments.
Key topics of potential interest identified on the basis of this analysis included the impact of the pre-existing relationship (or lack thereof) between the participant and the education practitioner, strategies used to explain complex material (such as the concept of mentalisation) to participants, negotiating discussions of sensitive topics that the young person or practitioners may be reticent to explore (such as self-harm) and the impact on interaction of the location of the intervention within the school or college environment. These topics are explored further in Proposed mechanisms of change and factors affecting successful delivery.
Fidelity of treatment as usual (limiting contamination)
Compliance with the completion of practitioner contact logs was not high enough to offer useful information regarding contamination. However, findings from staff focus groups and interviews with participants allocated to the TAU arm did not suggest that any contamination occurred. Practitioner and participant accounts suggest that the support provided by school and college staff to those in the TAU arm was clearly distinct from the BEST intervention; support was typically provided on an ad hoc basis and centred around active listening, problem-solving and social activities. Participant reports suggest that TAU was less structured and less focused on emotions than the BEST intervention. For instance, one TAU participant reported that the support he was provided at school involved taking part in a ‘nurture’ group. When asked what happened in these group sessions, he replied, ‘we did an escape room and played Monopoly [Hasbro, Inc., Pawtucket, RI, USA]’. When asked whether he found these activities helpful, he replied, ‘yes ’cos I like Monopoly’.
Most TAU participants said that the support they received in school after consenting to participate in BEST was no different from the support they had received in school previously. However, one TAU participant said that she was offered more regular meetings with a member of the school pastoral team than had been the case before her BEST participation:
. . . support like in the past it was just like one thing like one thing and then not really caught up on, but this was like a more scheduled kind of thing that happened more than once.
Young person
However, when asked about the content of these sessions she replied, ‘we’d just catch-up on things and like asking questions [about my week]’. She also responded ‘no’ to a follow-up question about whether the sessions had involved using any worksheets or resources, suggesting that the support offered did not contain any BEST-specific components. When asked about what she liked about the support she received, the participant replied, ‘I liked that it was a familiar a familiar adult . . . I liked that it got me out of a couple of lessons’.
Although there was no evidence of BEST-specific components being used with TAU participants, some practitioners reported that they had used, or had intended to use, resources or strategies from BEST in their wider practice:
. . . the mentalisation section in particular is something that I want to do more with other students to get them to think about yes why other people might be behaving as they are and what might be going through their thought process.
Education practitioner
I have to be honest I have been using some skills from you guys with my current clinical practice because we also do like the relapse management plans but sometimes we have like difficulty and use different grounding skills that was quite helpful.
Mental health practitioner
Furthermore, some education practitioners reported that the experience of participating in BEST had changed how they viewed behaviours that may be symptoms of emotional instability (discussed further in Proposed mechanisms of change and factors affecting successful delivery). Therefore, although there does not appear to have been an issue with direct contamination of the control arm, it is possible that the implementation of BEST may indirectly have an impact on TAU over time through affecting wider practice.
Safety and adverse events
Four serious adverse events (SAEs) were recorded during the feasibility trial: three in the TAU arm and one in the BEST plus TAU arm. In the TAU arm, two participants were admitted overnight to an acute hospital ward following an overdose of medication and one participant was voluntarily admitted to a psychiatric inpatient unit having presented to the emergency department in a mental health crisis due to deteriorating mental health. The one SAE recorded in the BEST plus TAU arm was an overnight admission to an acute hospital ward following an overdose of medication. Details of all SAEs were reported to the sponsor’s participant safety subcommittee for independent review. None was deemed to be related to the study procedures.
There was one adverse event that the Data Monitoring Committee classified as an adverse reaction. This related to feedback received from a school referrer via e-mail that a participant had reacted negatively (reported feeling upset and disappointed, accompanied by a temporary deterioration in behaviour) in response to learning that he had been randomised to the TAU arm.
Health economic assessment
Estimated costs of providing the BEST intervention
The most important cost in providing this intervention was staff time. We did not have detailed information on the staff type and grade of participating school/college staff. However, staff type indicated in the pilot study had a mean annual salary similar to AfC band 4 NHS staff. Therefore, the cost per hour for AfC band 4 was used in the cost estimates presented here. We recorded the AfC grades for mental health practitioners co-providing the intervention sessions, providing supervision or facilitating the training workshop. Unit costs for these grades were obtained from a published source,120 and these relate to the cost year 2018/19. These unit costs include salary and on-costs (costs on top of salary e.g. employer pension contributions) as well as allowances for overheads. However, if any activities occurred outside the sessions or supervision, these would not be included in the costs reported here. Travel time, however, was included.
Training to provide the BEST intervention was provided in two workshops. Workshop 1 was a full-day event provided to 15 school/college staff members and 15 mental health professionals, delivered by four facilitators. A second workshop was provided primarily as a refresher for those who had already attended training during the pilot phase. Attendees at these workshops were recorded along with those facilitating. The cost of the workshop was calculated based on staff costs for all staff at the workshop, whether attending or facilitating.
There would have been some consumables (i.e. training materials, catering) but details of these costs were not included. Estimates for workshop costs are presented in Table 16. In terms of the feasibility study and estimating the cost of the intervention, these costs would be divided by the number of study participants who received the intervention. In this feasibility study this was nine participants, meaning that training would represent a very high proportion of the costs of the intervention. The training sessions were based on the original aim of recruiting 30 individuals and we have additionally estimated a cost per person based on this number; it is this estimate that will be used in the final per-person estimate of the BEST intervention. However, if this was rolled out to a larger study or to clinical practice then each person trained would likely provide sessions for a larger number of young persons and therefore the cost of training as a proportion of the cost the intervention is likely to be lower than the estimates presented here.
| Workshop | Cost of workshop (£) | Cost of workshop per person receiving the intervention (£) (n = 9) | Cost of workshop per person planned to receive the intervention (£) (n = 30) |
|---|---|---|---|
| 1 | 7982 | 887 | 266 |
| 2 | 867 | 96 | 29 |
| Total | 8849 | 983 | 295 |
We recorded the number of sessions received by participants in the BEST plus TAU arm. Each session was provided by one school/college member of staff and a mental health professional. We assumed that the average duration of sessions observed for the recorded sessions would be the same as the feasibility phase, hence assumed a duration of 50 minutes. We also recorded the AfC band of the mental health professional. In addition, we noted the distance from the school/college to the base of the mental health professional. This enabled an estimate of mileage costs (based on a cost per mile of £0.40) and travel time. An additional time of 10 minutes was estimated for parking and other activities. Again, school/college staff were costed using AfC band 4. 120 As part of the intervention, staff received ongoing supervision. Again, numbers of supervision sessions, the grade of staff providing the supervision and the distance from the supervisor’s base to the school/college were recorded. An average duration of supervision of 60 minutes was assumed. However, in one case supervision was provided by e-mail. In the absence of data on the time commitment involved, a value of 15 minutes was used for all practitioners involved with the supervision for writing and reading these e-mails. The cost of supervision included the time of those providing it as well as those receiving it.
Estimates of the cost of providing the intervention are given in Table 17. This is based on the nine individuals receiving the intervention. However, the cost per participant of training received is based on the cost of training the 30 participants who were originally planned to receive the intervention, as discussed above. This results in a total cost per participant receiving the BEST intervention of approximately £1000.
| Sessions | Total (£) | Cost per person (£) |
|---|---|---|
| Total cost of intervention sessions | 3700 | 411 |
| Total cost of supervision sessions | 2946 | 327 |
| Cost per participant of training | 295 | |
| Total cost per participant | 1033 |
There are some lessons from this costing exercise that could inform a future study. First, as carried out in this feasibility study, both training and supervision represent significant costs. Careful consideration should be given as to how these should be provided in a future study and whether or not these would be feasible and achievable in routine clinical practice. Second, the amount of information requested from individual practitioners was limited, such as details related to time spent in non-face-to-face activities. More details here could have affected cost estimates. However, there are likely to be limits to the amount of information that can be completed. A future larger-scale study is likely to be informed by more detailed surveys of a limited number of practitioners rather than taking information from all practitioners.
Resource use by participants
Question 1 of the CSRI related to individuals seen in the participant’s school or college in the last 3 months. The use of these resources can be seen in Table 18. This table shows the total number of participants at each time point in each arm who reported use of these services, as well as the total number of contacts reported. At baseline the type of contact that was most reported was welfare officer, with 8 out of 14 and 14 out of 18 participants reporting having used services provided by this contact in the TAU and BEST plus TAU arms, respectively. Service use appears highest in the BEST plus TAU arm, even at baseline. This illustrates the usefulness of having a baseline measure of resource use in any future study, as it allows for the analysis of costs in the follow-up period controlling for baseline costs. This table also shows total contacts and total contacts per person. Total contacts per person are slightly higher in the 12 weeks following randomisation than at baseline. Contacts per person are lowest in the final 12 weeks. Some individuals report quite high use of some services, for example one participant at the 24-week questionnaire reports 65 contacts with a school counsellor. The CSRI appeared to be well completed for this question with no reported missing data.
| Service | Baseline | 12 weeks | 24 weeks | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| BEST plus TAU arm (n = 18) | TAU arm (n = 14) | BEST plus TAU arm (n = 9) | TAU arm (n = 8) | BEST plus TAU arm (n = 6) | TAU arm (n = 7) | |||||||
| Used this | Contacts | Used this | Contacts | Used this | Contacts | Used this | Contacts | Used this | Contacts | Used this | Contacts | |
| Educational psychologist | 0 | 0 | 0 | 0 | 2 | 9 | 0 | 0 | 0 | 0 | 0 | 0 |
| Welfare officer/well-being officer/pastoral support worker/safeguarding lead | 14 | 157 | 8 | 66 | 4 | 48 | 4 | 55 | 3 | 17 | 3 | 8 |
| Classroom assistant | 4 | 77 | 1 | 5 | 1 | 30 | 1 | 9 | 1 | 1 | 1 | 2 |
| SEND co-ordinator | 2 | 10 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| School nurse | 5 | 20 | 6 | 20 | 3 | 47 | 2 | 8 | 0 | 0 | 2 | 4 |
| School counsellor | 3 | 8 | 2 | 2 | 1 | 2 | 1 | 2 | 2 | 77 | 0 | 0 |
| Other | 5 | 56 | 5 | 22 | 2 | 66 | 1 | 2 | 0 | 0 | 2 | 17 |
| Total contacts | 328 | 115 | 202 | 76 | 95 | 31 | ||||||
| Total contacts per person | 18 | 8 | 22 | 10 | 16 | 4 | ||||||
Questions 2 and 3 of the CSRI relate to the use of medicines. Question 2 relates to the use of specified medicines. These are fluoxetine, sertraline, melatonin, quetiapine, risperidone, mirtazapine, lorazepam and promethazine. Details of medicine use are given in Table 19. At baseline, 4 out of 18 individuals in the BEST plus TAU arm reported use of at least one of these medicines, with no reported use in the TAU-only group. At follow-up there was some reported use of these medicines in both groups. Again, these questions appeared to be well completed, with only one use of fluoxetine and one use of sertraline at the 12-week questionnaire potentially reported as missing. Question 3 relates to the use of any other medicines. This is reported in the last row of Table 19. Drugs here would include those not related to BPD, such as asthma medicines and antibiotics.
| Medicine | Baseline | 12 weeks | 24 weeks | |||
|---|---|---|---|---|---|---|
| BEST plus TAU arm (n = 18) | TAU arm (n = 14) | BEST plus TAU arm (n = 9) | TAU arm (n = 8) | BEST plus TAU arm (n = 6) | TAU arm (n = 7) | |
| Fluoxetine | 1 | 0 | 1 | 0 | 0 | 0 |
| Sertraline | 4 | 0 | 1 | 1 | 0 | 0 |
| Quetiapine | 0 | 0 | 1 | 0 | 0 | 0 |
| Risperidone | 2 | 0 | 1 | 0 | 1 | 0 |
| Promethazine | 0 | 0 | 0 | 1 | 0 | 2 |
| Any of the above | 4 | 0 | 3 | 2 | 1 | 2 |
| Other reported medicines | 11 | 9 | 3 | 4 | 0 | 6 |
Melatonin, mirtazapine and lorazepam were included in the CSRI but no use was indicated. At the 12-week follow-up, one individual (TAU arm) appeared to have a missing value for fluoxetine and 1 for sertraline.
Other health and community services are given in Table 20. There are some reported instances of inpatient stays, the majority being of short duration. However, one individual at the 24-week follow-up in the TAU arm reported a stay of 35 days for mental health reasons. There is also some reported use of CAMHS and A&E services. Total contacts per person for ‘other hospital services’ appear to show no clear pattern. Total contacts per person for ‘other services’ appear to be higher in the BEST plus TAU arm than in the TAU-only arm in the 3 months prior to baseline. Contacts for these services appear to decrease over time, being lowest at the 24-week time point. This may have been influenced by the introduction of lockdown in the UK.
| Services | Baseline | 12 weeks | 24 weeks | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| BEST plus TAU arm (n = 18) | TAU arm (n = 14) | BEST plus TAU arm (n = 9) | TAU arm (n = 8) | BEST plus TAU arm (n = 6) | TAU arm (n = 7) | |||||||
| Used this | Contacts | Used this | Contacts | Used this | Contacts | Used this | Contacts | Used this | Contacts | Used this | Contacts | |
| Question 4: inpatient stays | ||||||||||||
| Inpatient stay (days) | 3 | 4 | 1 | 2 | 1 | 1 | 1 | 4 | 0 | 0 | 1 | 35 |
| Question 5: other hospital services | ||||||||||||
| A&E | 2 | 2 | 2 | 5 | 2 | 2 | 1 | 4 | 0 | 0 | 1 | 1 |
| CAMHS department | 3 | 11 | 1 | 1 | 3 | 7 | 0 | 0 | 0 | 0 | 0 | 0 |
| Other outpatient appointment | 3 | 4 | 2 | 4 | 1 | 2 | 3 | 6 | 0 | 0 | 1 | 2 |
| Day hospital | 2 | 5 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 4 | 0 | 0 |
| Total contacts for question 5 | 22 | 11 | 11 | 10 | 4 | 3 | ||||||
| Total per person | 1.2 | 0.8 | 1.2 | 1.3 | 0.7 | 0.4 | ||||||
| Question 6: other services | ||||||||||||
| School nurse | 0 | 0 | 1 | 3 | 1 | 6 | 0 | 0 | 0 | 0 | 0 | 0 |
| Mental health nurse | 3 | 3 | 0 | 0 | 0 | 0 | 1 | 2 | 1 | 1 | 0 | 0 |
| GP | 10 | 31 | 2 | 5 | 6 | 9 | 3 | 7 | 0 | 0 | 1 | 2 |
| Paediatrician | 2 | 2 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Psychiatrist | 3 | 5 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Hearing specialist | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| OT | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Family therapist | 3 | 13 | 0 | 0 | 1 | 2 | 0 | 0 | 0 | 0 | 0 | 0 |
| Individual therapy | 5 | 23 | 0 | 0 | 2 | 7 | 0 | 0 | 0 | 0 | 0 | 0 |
| Social worker | 3 | 24 | 0 | 0 | 2 | 5 | 2 | 2 | 3 | 3 | 3 | 5 |
| Social services (fostering) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 |
| After-school club | 0 | 0 | 2 | 31 | 1 | 10 | 2 | 20 | 0 | 0 | 0 | 0 |
| Other | 2 | 26 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 16 |
| Total contacts for question 6 | 128 | 41 | 39 | 31 | 4 | 24 | ||||||
| Total per person | 7.1 | 2.9 | 4.3 | 3.9 | 0.7 | 3.4 | ||||||
Question 7 of the CSRI asks about overnight stays in a children’s home, with a foster carer or in other residential placement. One individual reported a stay of 14 days in the ‘other residential placement’ category. Finally, question 8 refers to any service use by the participant’s family that resulted from their behaviour or mental health. The BEST plus TAU arm had six contacts at baseline and four at the 12-week follow-up. There was also one contact for the TAU arm at the 12-week follow-up. Types of services contacted included a general practitioner (GP), family support, counselling and a social worker.
In general, the CSRI appears to have been completed well. Responses seem complete with little evidence of missing data, and feedback from the research assistants regarding the process of administering it was generally positive. However, question 8, which refers to any service use by the participant’s family that resulted from the participant’s behaviour or mental health, was experienced as challenging to ask in a sensitive manner. Given that the resource use here was comparatively low, this could be omitted from the modified version of the measure in a future study.
Performance of the EuroQol-5 Dimensions, five-level version
An important aim of the health economics assessment in the feasibility study was to inform the choice of health economics outcome measure in any future study. Hence, we wanted to evaluate the performance of the EQ-5D-5L in this feasibility study. To have a score for the EQ-5D-5L there needs to be a response for all five questions. In general, the completion rate for the EQ-5D-5L was very good. All 32 participants had a complete EQ-5D-5L instrument at baseline. At the 12-week follow-up, one person in the BEST plus TAU group did not complete the instrument and one person in this group did not give an answer to one of the five questions. Hence, there were two missing EQ-5D-5L scores at this time point. One person in the TAU group at the 24-week follow-up point did not complete the instrument. Therefore, we had EQ-5D-5L scores for 59 out of the 62 possible observations over the three time points. As well as the EQ-5D-5L instrument, there is also an associated visual analogue scale (VAS) in which participants rate their health that day on a scale between 100 (the best health you can imagine) and 0 (the worst health you can imagine). In total, there were 60 complete observations for this instrument over the three time points.
The responses for the EQ-5D-5L are shown in Figures 6 (baseline only) and 7 (all completed responses). For EQ-5D-5L responses for each dimension, possible responses vary from 1 (best case) to 5 (worst case). For both Figures 6 and 7, the majority of responses for the mobility and self-care dimensions show no or mild problems. In marked contrast, the anxiety and depression dimension shows respondents reporting responses across the whole range of possible responses, with few reporting no problems. The dimensions of ‘usual activities’ and ‘pain’ also had a wide range of responses. As three out of the five dimensions showed marked differences from full health, it offers encouragement that the EQ-5D-5L may be responsive to BPD and hence may show differences as a result of changes in BPD symptoms.
FIGURE 6.
Baseline EQ-5D-5L responses.
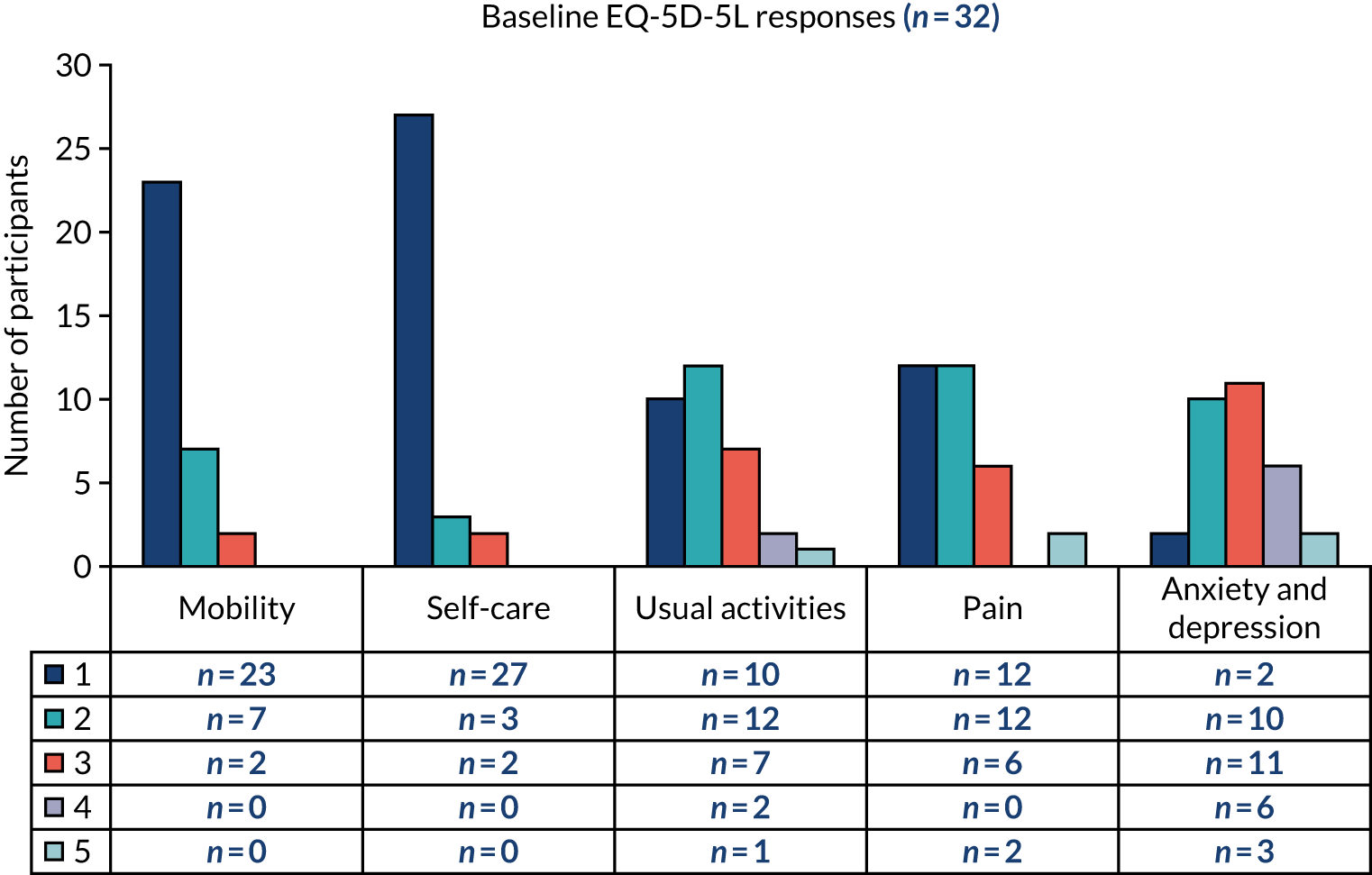
FIGURE 7.
The EQ-5D-5L responses for all time points.
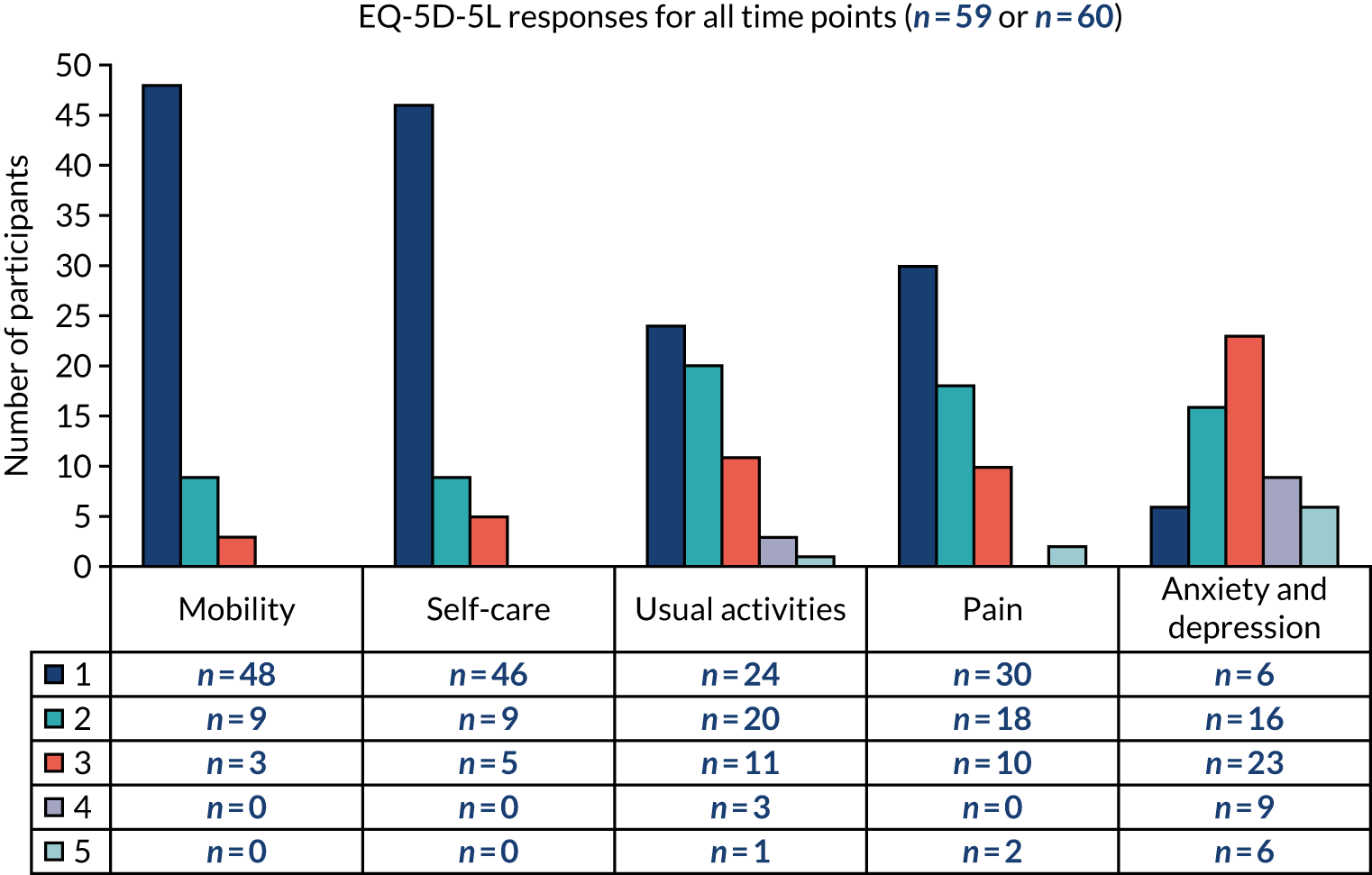
The EQ-5D-5L and EuroQol-5 Dimensions, visual analogue scale (EQ-5D-VAS) scores are shown in Table 21. For the EQ-5D-5L index score a value of one represents a health state considered equivalent to ‘full health’, a value of zero represents a health state of equative value to being dead. Negative scores are possible. Owing to the small sample size, we limited the analysis to a descriptive comparison between groups. One thing that immediately stands out is the low mean scores reported in this sample. Means of 0.59 and 0.67 at baseline indicate very large changes from a score of 1, which would be full health.
| Measure | BEST plus TAU arm | TAU-only arm | ||||
|---|---|---|---|---|---|---|
| n | Mean score | SD | n | Mean score | SD | |
| EQ-5D-5L | ||||||
| Baseline | 18 | 0.59 | 0.23 | 14 | 0.67 | 0.28 |
| 12 weeks | 7 | 0.59 | 0.29 | 8 | 0.74 | 0.24 |
| 24 weeks | 6 | 0.83 | 0.13 | 6 | 0.72 | 0.20 |
| EQ-5D-VAS | ||||||
| Baseline | 18 | 55 | 18 | 14 | 51 | 25 |
| 12 weeks | 8 | 52 | 21 | 8 | 62 | 21 |
| 24 weeks | 6 | 69 | 23 | 6 | 52 | 21 |
The EQ-5D-5L appears responsive in this sample as there are large changes from full health and it appears to be showing a range of responses in three out of the five dimensions. However, it would also be beneficial if the EQ-5D-5L was correlated with other, BPD-specific, scores. For this reason, Pearson correlations were performed against two other measures, the BPFSC and the DERS. For the 32 responses at baseline, there was a –0.720 and –0.595 correlation for EQ-5D-5L with the BPFSC and the DERS, respectively. Both were significant at the 0.01 level. When this was expanded to include all 59 observations at the three time points for which there were values for all three instruments, the correlations were –0.596 and –0.622 for the BPFSC and DERS, respectively. Again, both were significant at the 0.01 level. These results are also encouraging for the potential usefulness of the EQ-5D-5L in a future large study for individuals with BPD. The EQ-5D-5L is likely to be used in such a study as it enables the estimation of quality-adjusted life-years for use in economic evaluations.
Acceptability of the refined intervention
Adequacy of training and supervision
‘I don’t know how prepared I felt’
Most education practitioners expressed that they did not feel well prepared to deliver the intervention after completing the training workshop. They spoke about feeling overwhelmed by the amount of information covered during the workshop and uncertain about what they would be expected to do as part of co-delivering the intervention. As a result, they recalled feeling some apprehension before beginning to deliver the sessions. This contrasted with the experience of mental health practitioners, who fed back that the content of the workshop had been ‘pretty straightforward’, and that the manual was ‘fairly self-explanatory’. Consequently, most mental health practitioners felt that the training workshop had adequately prepared them to co-deliver the intervention. However, they raised concerns about how school and college staff might have experienced the workshop:
Having had previous training on mentalisation and knowing a bit about EUPD [emotional unstable personality disorder] or BPD it felt OK but I was quite aware that the people in educational settings that was probably the first time they had ever heard of mentalisation and or EUPD or BPD so for them it would be even more perhaps overwhelming and difficult to really absorb that knowledge in 1 day.
Mental health practitioner
Practitioners did feel that there were benefits to mental health practitioners and school and college staff attending the training workshop together, such as networking opportunities and ensuring that all practitioners were ‘on the same page’. However, practitioner feedback suggests that these benefits were probably outweighed by the difficulty of pitching material at the right level for those with differing professional backgrounds. One suggestion for overcoming this difficulty was to separate workshop content related to intervention delivery from content concerning research procedures. It was suggested that education and mental health staff could be offered separate training sessions on intervention delivery tailored to the prior knowledge of attendees, followed by a joint training session focusing on research procedures.
The timing of the workshop was also a factor that contributed to some practitioners feeling ill-prepared to co-deliver sessions. The workshop attended by the majority of practitioners was held in July, just before the school summer break. As a result of the delay in randomising the first participants (as discussed in Recruitment and retention), there was often a gap of many months between completing the training workshop and starting to deliver sessions. Practitioners recommended either that the timing of the workshop should be delayed or that a ‘refresher’ session should be offered just before practitioners begin working with their first participant.
Practitioners also suggested that it would have been helpful to know who they would be working with to deliver the intervention prior to the training workshop and, ideally, be paired with them for training exercises:
I think it would have been really nice to have kind of known who I was like what school I was paired with before the training and then perhaps kind of been paired off with them in the training and then kind of we could have both really kind of bounced of each other’s skills and helped each other in that way and started building that relationship from the beginning.
Mental health practitioner
‘We kind of just learnt as we went along, as we were delivering it’
The experience of delivering the intervention for the first time was seen as an important part of the training process. Practitioners spoke about the manual and the fidelity checklist as important resources for this learning. The manual was described as practical and easy to follow, enabling sessions to flow smoothly even when practitioners had little time to prepare in advance, which practitioners told us was very often the case. Completing the fidelity checklist at the end of sessions was viewed as a useful opportunity for practitioners to reflect together and ensure that they had covered the core components:
I found it [completing the fidelity checklist] really reassuring just to make sure we had covered everything so you can look back on the last session, OK, where do you focus on each session, what did you miss, so which areas do you need to focus more on the next session, it’s also like a good way to reflect on how you did it, like, on your own progress, how are your engagement skills, how is you how do you deliver, how well do you focus on, do you consider risks and safety planning and stuff, so it was actually good to have this discussion.
Mental health practitioner
Practitioners felt that, having delivered the sessions once, they would feel more confident delivering the sessions a second time. Owing to the early close of the study, few practitioners had the opportunity to deliver the complete intervention more than once. However, the experiences of those practitioners who did deliver the intervention more than once supports this growth in confidence, particularly in the case of education practitioners who often felt less confident initially:
. . . in the first one I did feel like a little bit of a spare part at times but I kind of was probably in myself I was probably not as confident . . . but then I had the confidence in the next one to kind of try and practice those skills and delivery so it was an interesting learning curve.
Education practitioner
‘We knew that the support was there if we needed it’
All practitioners reported feeling adequately supported to deliver the intervention and said that they were happy with the frequency and content of supervision sessions. Although most said that they did not feel the need for more supervision sessions than the two originally scheduled, they appreciated that they were available if needed:
We didn’t have that many [supervision sessions] but I think that was down to choice rather than kind of anything else, it didn’t feel like we were lacking and if we needed more there would have been more available should we have wanted some.
Education practitioner
Comparing the frequency of supervision in the pilot phase, during which supervision was offered every week, one practitioner commented:
The second time round in the actual phase [treatment phase] it was it really good because it was a little bit more as and when you needed it, it was spread out so I think [name of supervisor] was really good at saying, ‘we’ll have a supervision session on this day and this day and then if you need any in between’, and actually that was really useful ‘cos we could kind of pick and choose or just touch base with [name of supervisor] if we needed to.
Education practitioner
Some education practitioners raised that they were used to working with very little support, one jesting that ‘any support is better than nothing’. Two mental health practitioners mentioned that the education practitioners they were partnered with had limited prior experience of supervision and so were unsure what to expect from it:
I think my educational practitioner, I don’t think she’s got much experience of supervision so I didn’t think she really understood what it was about until we’d kind of had the first one and she was like, ‘oh but this is what we do’, sort of thing.
Mental health practitioner
This highlights a potential training need to ensure that practitioners who are unfamiliar with the supervision model can make use of it.
Practitioners received supervision in a variety of formats: face to face or by telephone and in group format or individually. Telephone supervision was viewed as more practical and less time-consuming, but not ideal for group supervision, as the lack of non-verbal cues led to participants not knowing who would speak next, creating some awkwardness. It was also raised that group supervision formats in which co-delivery partners were in the session together might have made it harder to openly discuss any difficulties in the co-delivery dynamic.
Overall acceptability
‘I really enjoyed it, she really enjoyed it’
The acceptability of the intervention was generally high. Practitioners who delivered the intervention, both school and college staff and mental health professionals, reflected that they enjoyed delivering the intervention and found it a useful learning experience. Practitioners also felt that the intervention was of benefit to the young people who received it; only one practitioner felt that it had not been of significant benefit to the young person they worked with. This was mirrored in the perceptions of the young people in that all but one (the same young person whom the practitioner did not feel had benefited) of the young people interviewed fed back that they had found the intervention valuable and believed that it had helped them make positive changes.
Acceptability from the perspective of practitioners and young people is explored in greater detail in the following sections, which address (1) the acceptability of the content and format of sessions and (2) the acceptability of the co-delivery model.
Views of content and format of sessions
‘it was very structured . . . you knew what you were doing’
The manualised nature of the intervention was appreciated by most practitioners and young people. For practitioners, having a manual to work from enabled them to feel more confident delivering the sessions than they might otherwise have been. For young people, the manual appears to have been helpful in maintaining focus during sessions and served as a reminder of content covered:
I liked the layout of it all the sheets and stuff I liked that, being organised.
What was kind of helpful about that being organised?
Um, it’s easy to focus on.
I liked filling in the book that was good ‘cos then you could visually see and it was like a reference that you could go back to as well.
Young person
I think even actually just having something tangible in his hand actually helped him when he wasn’t using it, it almost like helped him focus.
Education practitioner
Practitioners told us that the BEST intervention was more structured and focused than the support they usually provide. Mental health practitioners liked that the intervention had boundaries and was time limited, and that their remit was clearly defined. Reflecting on the difference between their usual practice and their experience of delivering the BEST intervention, one mental health practitioner commented:
. . . here in the community it’s like a bit it feels a bit cowboyish, it’s a bit like, maybe it’s the way I’ve been supervised a bit but and, you know, yes, the structure of it is really good and I think in I need to be more structured if I want to be a better clinician, decent clinician, then I probably need to be more structured so I, it suits me but it’s not what I’m used to.
Mental health practitioner
Although the structure imposed by the manual was largely viewed as positive, some mental health professionals expressed that they would have preferred to have more flexibility to be able to adapt the ways in which they delivered the intervention content to suit the needs of the individual young person:
. . . there were times that we had to kind of react to what was happening that following week or the previous week and perhaps kind of a different session would have fitted her slightly better, so for example there was one week where I think she was quite emotional and quite frustrated and then that was the week that we were kind of looking at emotional instability and it almost kind of felt quite cold and quite like we were just dismissing what had happened because we had to kind of go through that specific content of the session, so yes I personally would have preferred a bit of flexibility; however, I’m also aware that actually the point of it is that it’s easier to deliver for people who aren’t perhaps so familiar . . .
Mental health practitioner
Similarly, several practitioners spoke about finding it difficult to balance the need to be responsive to what the young person wanted to discuss during the session with the need to deliver the prescribed content:
I think also if it brings up something for the students you have to go with that you can’t say, ‘right we now need to, yes that’s not really, we haven’t got time for that let’s head back to the book’, it’s really good to allow that space, isn’t it.
Education practitioner
Practitioners attempted to manage this potential tension through allowing students time within sessions to talk about their concerns and then applying the content of the session to the issues raised by the young person. This strategy appears to have been successful as young people fed back that they felt heard and understood during sessions, sometimes contrasting this with previous experiences of not feeling listened to:
. . . they allowed me to say what I want they would allow me to like speak out but like others like before I had all this they were just like, ‘OK, ask me questions and now I want a specific answer’, and you have to have the specific answer for it . . . that was kind of really annoying because I didn’t have like [name of education practitioner] and [name of mental health practitioner] to ask me like, ‘oh so like we’re going to do this I would like you to explain your feelings about it’, and like your moods and everything . . . and they understood it so well.
Young person
‘The emotions wheel was really key’
The emotions wheel was experienced as a particularly helpful aspect of the intervention by both young people and practitioners. The version of this tool included in the manual contains six primary emotions each represented by a brightly coloured segment. Each segment presents a range of emotion words related to the primary emotion emanating from the centre of the circle, arranged in order of increasing nuance. Practitioners fed back that they had used this tool frequently during the intervention as a way of enabling the young person to verbalise emotions. Young people fed back that they had found the wheel helpful for enabling them to explain their experiences more clearly:
. . . when she couldn’t think of what the emotion was I’d kind of just push it towards her and be like . . . hint hint . . .
Mental health practitioner
I remember there was a, what is it, the little emotion wheel that was in there and I found that quite helpful because other than just like the broader terms of ‘oh I’m sad I’m happy’, I could then break it down into what it really was that I was trying to aim at to explain how my thoughts and feelings were working at, at that moment in time . . .
Young person
The increased emotional literacy promoted by use of the emotions wheel was seen to facilitate the successful delivery of other aspects of the intervention through increasing young people’s ability to label their emotions in a nuanced manner.
‘Something that makes it relevant to the tech that we have today’
Young people and practitioners felt that there would be benefits to creating a digital version of the manual as an alternative to the paper-based manual. Practitioners commented that this would offer the opportunity to incorporate multimedia content to make the manual more engaging, as well as offering practical benefits: young people would not be able to lose or forget their manual and the need for photocopying would be reduced:
I think something interactive would be really good, you know, we could use little film clips you could incorporate, all those kind of things into it couldn’t you, and then actually you’d know what you’re going to do session by session, you wouldn’t necessarily, I mean we’ve all talked about not having enough time to prepare but I guess those things would be on there, wouldn’t they, you could try and build them into the programme or whatever, into the website and I think young people like that kind of stuff don’t they? That’s my assumption though, generally, yeah. The person that I, that we did it with, so sometimes she wouldn’t bring the booklet and so I think there’s some of those practical obstacles, isn’t it. I guess if you could just log in, all the information is there.
Mental health practitioner
Greater use of technology was also seen as a way of potentially helping to encourage young people to complete home practice exercises. Most young people agreed that more use of digital tools would be a good idea but cautioned that there should still be the option of using a paper manual for those who prefer paper resources.
Experiences of co-delivery
‘It did just sort of flow’
Practitioners expressed that they were initially apprehensive about how delivering the sessions together with another practitioner would work, particularly as most partnerships did not have the opportunity to meet one another prior to delivering sessions. However, practitioners told us that they felt that co-delivery went smoothly and were unanimous in expressing that they valued this way of working. All practitioners expressed that they enjoyed working with their partner and were able to establish a working relationship that allowed them to deliver the intervention together in a way that felt natural:
. . . it actually flowed really well because I wasn’t sure of how it was going to flow you know, who was gonna say what, but we soon got into a kind of role . . . where the health professional would sort of introduce the topic and then I would sort of elaborate a bit, and then I could add some sort of personal details, like particular examples where the student had had to use some of the material. And we sort of bounced back and forward quite nicely.
Education practitioner
Practitioners spoke about valuing the skills and experiences one another brought to intervention delivery:
I just think it’s definitely worth having the two people because they just bring different skills to the mix, if it was just the mental health practitioner it would, it, yes, like you say, it would just be someone coming in and doing intervention and it would be really difficult to engage with that person ‘cos that educational person bridges that gap but also if the educational person did it on their own then they might not have enough knowledge around mental health to be able to, so I think the partnership is much better and it’s worth all the logistical problems.
Mental health practitioner
The experience of practitioners was mirrored in the feedback of most participants, who felt that their practitioners worked well together and played complementary roles.
‘It was great having someone . . . to make me feel a little bit more confident and be able to sort of follow her lead’
Education practitioners valued the clinical expertise of the mental health practitioners they were partnered with and told us that they acquired new skills by observing their partner during the co-delivery process:
I found like my listening skills improved as well when I was working with students and listening to what they had to say and actually repeating back, just taking the time to actively listen and respond to what they were saying and learning from the practitioner within that session and mirroring a little bit how they had proven that they were good at active listening and discussing topics, just using that kind of skill I found that really useful.
Education practitioner
Education practitioners also felt that the mental health practitioners they worked with were able to address mental health-related topics in greater depth than they would have felt able to:
I really enjoyed working with the practitioners, they were brilliant, really switched-on, like they were able to discuss more in-depth things that I didn’t fully understand or that I might have touched on but didn’t have the knowledge or expertise to take that discussion further, they were able to jump in and support me.
Education practitioner
[Talking about self-harm] that’s where I guess the professionals come in because they probably have much more of a professional view on how far you push that, how far you mention it, and I sort of feel that I would, in sessions that I was in if that was the discussion point I’d take a bit of a back step there and let the professional run with that bit.
Education practitioner
Most education practitioners told us that they would not have felt confident enough to deliver the intervention alone but were given confidence in their ability to do so successfully through being paired with a mental health professional. It was striking that, despite often having considerable experience in supporting young people experiencing emotional and behavioural difficulties, education practitioners appeared to see the mental health practitioners they worked with as the ‘expert’ in delivering the intervention. This was the case even when the mental health practitioner was relatively junior (e.g. band 4 practitioners without a core profession), and despite the fact that most mental health practitioners were also delivering the intervention for the first time.
Young people also valued the expertise of the mental health practitioner:
[Name of mental health practitioner] was like talking and she was doing most of the talking and she was like kind of like making it like make sense and she was like all the big words she’ll like, like say it so it’s more easier for me to understand.
Young person
I knew [name of education practitioner] before the project and I’ve known her for a while so it was good having someone that I know and knows me and also someone [referring the mental health practitioner] that knows how to do the proper therapy.
Young person
As suggested by the use of the phrase ‘proper therapy’ in the second quotation, it appeared that, for some young people, the involvement of a mental health specialist in delivering the sessions gave the intervention greater legitimacy than would have been the case if the intervention had been delivered by school or college staff members alone.
Although for most education practitioners, co-delivering the intervention with a practitioner perceived as having special expertise appears to have increased confidence, a comment from one practitioner highlights the potential for this perception to decrease education practitioners’ confidence in their abilities:
I was probably not as confident because I knew in my head, ‘oh I’m sitting here with the mental health like qualified practitioner I should probably be a little bit more quiet and listen and learn’.
Education practitioner
Practitioners also valued that they were able to share responsibility for risk management and safeguarding-related issues with their co-delivery partner. Whereas educational practitioners often looked to mental health practitioners for guidance on clinical issues, mental health professionals often looked to them to manage any safeguarding issues. Mental health practitioners expressed that they were confident that any safeguarding issues that arose could be managed appropriately by the school or college, which allowed them to focus on delivering the intervention:
I was very confident in, you know, how the person I was paired up with knew the student very well and would have been able to manage the situation if something hadn’t been right and, you know, they did do that, there was occasions when the person didn’t turn up, there’d been issues and, so that was quite nice, quite refreshing not to have to kind of jump in and do all the safeguarding.
Mental health practitioner
This collaborative approach clearly relies on good communication to ensure that each practitioner is clear of their responsibilities, to avoid a situation in which both practitioners believe the other is managing a particular issue.
‘Well she trusts her so I’ll trust her’
A key perceived benefit of co-delivery, from the point of view of both practitioners and most young people, was that, when the young person already had a good relationship with the education practitioner, the presence of the education practitioner helped the young person to feel at ease more quickly. For instance, when asked to explain why they liked that someone from their school co-delivered the sessions, one young person replied that ‘it made it a lot easier to talk because I know who the person is’. Similarly, one practitioner reflected:
. . . it was really good that you, you know, you had that relationship and there was that sort of initial ease. You didn’t spend the first two sessions sort of getting to know somebody I suppose is what I’m saying.
Education practitioner
Mental health practitioners also suggested that the trusting pre-existing relationship between the education practitioners they worked with and the young person appeared to carry over to their own relationship with the young person:
. . . because she [education practitioner] had that already built rapport with the participant that then kind of extended onto me so she kind of facilitated that rapport between me and the participant which was really helpful.
Mental health practitioner
This accelerated rapport building appears to have enabled the young person to feel more comfortable to speak openly about their experiences more quickly, enabling the relatively brief intervention period to be maximised.
Although in most cases the pre-existing relationship that education practitioners had with participants was seen as facilitative of the intervention, this was not true for all participants. The one young person interviewed who did not feel that she had benefited from the intervention explained that her previous interactions with the education practitioner who co-delivered the intervention had not been positive:
I’d spoken to the school counsellor before . . . however, yes that was not very helpful I tried to avoid him at all costs . . . I think it’s just more of like a personal connection like I had with him it just like I never wanted to like open up that much.
Young person
The mental health practitioner who worked with this young person together with the education practitioner expressed that he struggled to establish a rapport with her and felt that her reluctance to speak openly about her experiences ‘was sort of interfering with our ability to get the work done’. This suggests that, in the same way that a positive pre-existing relationship between the education practitioner and the young person might help the mental health practitioner to build rapport, a less positive prior relationship has the potential to interfere with the mental health practitioner’s ability to build rapport.
Several mental health practitioners expressed concern that it might be more daunting for a young person to work with two practitioners. The experiences of young people who took part in interviews suggests that this was not the case when the young person already had a good relationship with the education practitioner but may have had an impact when the young person did not.
‘That mental health worker cannot be in school all of the time whereas we are’
Practitioners and young people both spoke about the value of the education practitioner being based within the young person’s school or college. Three main benefits of this were discussed. First, education practitioners were able to use their prior knowledge of the young person they worked with and their behaviour at school or college to help participants to apply the content of sessions to their daily life:
. . . as I supported my student and I had known her for a couple of years, there was sometimes examples that actually happened that day that we could say, for instance, this morning when you came to me or the situation that happened last week, so that was good.
Education practitioner
I found it quite helpful obviously because I’d already known [name of education practitioner] before I walked into the sessions so it was quite helpful having someone else there who was aware of the things that I was struggling with so that then when I would just sort of go blank a bit she was there to prop me along, be like, ‘but you can use that to apply to that’.
Young person
Second, practitioners spoke about the value of the education worker being able to encourage young people to use the skills learnt both in-between sessions and after sessions had come to an end. Education practitioners also spoke about the sessions as providing an opportunity to strengthen their relationship with the young person so that they would be better placed to support the young person in school in future:
I felt all the way through these sessions that I was doing with my young person . . . I wanted to keep everything positive and her experience of what we were doing as a team as a positive to sort of almost put in more foundations for that relationship so that after the session is finished hopefully we would have enough of a relationship for her when she was being a bit of a liability struggling or doing something she shouldn’t be doing to have that trust in me to come and let me help her support her to deal with it.
Education practitioner
Third, it was mentioned that the involvement of a school or college staff member helped increase attendance at sessions. Education practitioners were able to remind young people of when sessions were taking place to encourage them to attend school on those days, as well as fetching participants who were on site but had forgotten about or were anxious about attending sessions:
. . . the type of young people we are working with are not the young people that turn up to school every day, they’re not the ones that are, you know, in every day on time . . . I was ringing home and saying to mum, ‘look, she’s definitely got a session tomorrow, can you make sure she is in’ and ‘you know, you know you’ve got a session tomorrow make sure you’re here, won’t you, sweetie?’.
Education practitioner
Although the involvement of a practitioner working within the young person’s school or college was valued for the reasons set out above, it also presented some challenges. Education practitioners spoke about sometimes having to consciously ‘switch role’ from member of school staff to BEST practitioner. For instance, one practitioner spoke about managing an incident in which the young person they were working with attended a session dressed in a way that contravened the school’s uniform policy:
I realised that I was having to switch from one role to another and I was very conscious of that at the time of the need to do that . . . it is an interesting dynamic that you’re having to move away from the those sort of innate ways of behaviour that we’ve learnt as we’ve worked in the schools and having to think about how that could be a really bad start to if you’re reprimanding the student that could be a really bad start to like work with them and gaining their trust and it’s not a natural, it certainly didn’t come naturally to back off and let him sit there like that but it felt like to be confrontational potentially would then ruin what we were trying to do.
Education practitioner
It was discussed that this need to switch roles was more likely to be an issue encountered by school-based practitioners than by college-based practitioners given that colleges typically have less restrictive behaviour and uniform policies than schools. Practitioners also suggested that young people might feel less able to speak openly about behaviours that contravene school or college behaviour policies with a school or college staff member present for fear of disciplinary action. However, this was not an issue raised by young people themselves; further, some young people were observed discussing issues such as use of alcohol and drugs openly within sessions, suggesting that they had confidence that disclosures would not lead to disciplinary action.
‘It took a bit of organising . . . a bit of juggling’
Nearly all practitioners reported that they found organising sessions to be the most significant challenge of the co-delivery model. The need to schedule sessions at a time both that the practitioners were available and that fitted the timetable of the young person proved a real logistical challenge:
. . . the frustration I had with working with college was . . . we had to then also work around the timetable, which was quite strict, you know, it started at a certain time and there was lessons that the teachers weren’t happy for them to miss . . . and then of course we hit half-terms and things like that so [the education practitioner] wasn’t working, so that was quite difficult to co-ordinate.
Mental health practitioner
The irregular school or college attendance of some participants further contributed to these logistical challenges. Despite education practitioners reminding participants about sessions as discussed under the previous theme in the previous section, several mental health practitioners experienced having to reschedule sessions after having travelled to the school or college because the young person was absent.
Despite these logistical challenges, there was consensus among practitioners that these challenges were outweighed by the benefits of co-delivery:
. . . having to kind of free up diaries and things like that it is difficult but actually the end result is worth that . . .
Mental health practitioner
Practitioners also discussed strategies that they had found helpful in minimising scheduling difficulties, including reminding the young person (and their parents, if appropriate) of session dates, and having a regular time slot for sessions each week:
I think the first session, the first couple of sessions she wasn’t there but then she got into the routine because it happened the same period hour on week 1 and the same hour on week 2 at the same time slot so as the sessions progressed she was there waiting for me.
Education practitioner
Proposed mechanisms of change and factors affecting successful delivery
Relevant sections of session recordings illustrating patterns of delivery of interest that were identified in the activity analysis described in Fidelity of intervention delivery were transcribed verbatim and presented to practitioners during focus groups. Each focus group was presented with the same set of transcripts, which were displayed on screen and voiced by the researchers. The aim was to elicit reflections on commonalities and differences between process issues occurring across implementation contexts. The reflections generated were used together with other qualitative data to identify possible mechanisms of change of the BEST intervention, that is key processes through which the intervention may lead to change in clinical outcomes. We also sought to identify factors that may help or hinder the action of these mechanisms.
Mechanisms of change
Taking together the perceptions of participants and practitioners expressed in the interviews and focus groups, and the processes observed to have occurred within sessions, we theorise that the mechanisms of change may operate on three interacting levels: the individual student, the education practitioner and the wider school or college. For the individual participant, the intervention was perceived to foster better self-understanding, enhance emotional and social literacy, and improve coping skills. For some participants, this appeared to have had a positive impact on their ability to regulate their emotions and their relationships with others. For the education practitioners involved in co-delivery, the perceived benefits of the intervention included increased confidence and skills in supporting young people experiencing emotional instability, equipping them to provide ongoing support to participants and informing their wider practice. Practitioners also perceived a potential benefit for the whole school or college, through enacting a change in attitudes towards behaviour that may be symptomatic of emotional instability. These proposed mechanisms are summarised in Figure 8 and discussed in more detail below.
FIGURE 8.
Possible mechanisms of change of the BEST intervention.
Individual participants
For individual students, a key perceived benefit of the intervention was their increased ability to manage their emotions. The intervention fostered increased understanding of the young person’s own emotions and the relationship with their behaviour, and developed their skills in recognising and reflecting on their emotions. This appears to have enabled participants to better regulate their emotions and behaviour:
I can still be a bit impulsive and reckless from time to time but in terms of managing emotions since taking part in the sessions that has definitely got a lot better for me, um, in terms of being able to manage it and being able to identify which emotion I’m struggling with at the time . . . because then I can, um, identify which emotion it is that I’m dealing with and then from there proceed with ‘OK, so how do I cope with this?’.
Young person
I don’t feel as sad as much, I do still get sad quite a bit but not as much and I know how to try and calm myself down from that now . . . because before I didn’t really know any good coping mechanisms to work with that but in some of the sessions we would go over coping mechanisms.
Young person
Participants commented on the value of the mentalisation skills taught in enabling them to better understand the behaviour of those around them:
. . . so say I could have been late for a class and I would be there thinking negative thoughts that other people might be having about me when in reality I need to be remembering that they might also have something going on that day and that it’s not that they have a negative thought towards me they’re just struggling in their own ways.
Young person
. . . it was kind of fun because like, I never thought of like thinking of that properly because like you don’t really think of what other people think you just know, OK they’ll say something about it or anything but you never really think, ‘oh they’re thinking that I’m happy’, or something in that way.
Young person
One participant who spoke about the experience of practising thinking about other people’s behaviours in terms of their mental states went on to speak about the positive impact of these new skills on her daily life:
. . . yes ‘cos obviously I’ve stopped self-harming, I have more friends and everything and they are always with me they help me . . . it’s a relief like getting people to like I trust you and like you trust me and I want you to put your belief into me and talk to me about everything don’t keep it away . . . my family problem at home, um, that got better, um, I haven’t had many fights with my parents, haven’t shouted at my parents yet, I haven’t hurt my brothers, I haven’t done, I haven’t stole anything or anything, um, my schoolwork is getting better . . .
Young person
Several participants spoke about the value of having the opportunity to speak about their experiences and feel heard, sometimes contrasting this with previous experiences of not feeling able to be open about their experiences or of feeling dismissed. The co-delivery of the intervention within the school setting by someone familiar to, and trusted by, the young person appears to have been key to participants feeling able to be open about their experiences. The opportunity to speak openly to trusted adults during the intervention appears to have had a positive impact on some participants’ ability to be open about their emotions with others around them:
. . . we received really good feedback from his mother who [tele]phoned the school and said it was brilliant: ‘I don’t know what you are doing with my boy but he’s more open, he talks more and he has stopped self-harming and he’s, he talks to us more.’
Mental health practitioner
One participant also spoke about how the delivery of the intervention within the school setting positively influenced his view of the school more generally:
. . . ’cos it’s like you’ll do it while you’re in school it’s just like it seems like the school wants to help a bit more . . . it’s just I’ve never really liked how the school copes with stuff . . . they would just have like a 5-minute conversation with you and then just leave it . . .
Young person
Education practitioners
Education practitioners expressed that co-delivering the intervention increased their confidence in their ability to support young people experiencing emotional instability and equipped them with a toolkit of strategies to use in future. This was viewed by practitioners as a key benefit of the co-delivery model, justifying the organisational challenges encountered:
I think also we’re, we’re helping the educational system to develop their skills so we’re giving them things so things have come up that my partner wouldn’t have even thought about you know and vice versa you know so I do think although it’s a bit of a pain trying to get us all together I do think the end result is better than doing individual stuff.
Mental health practitioner
I just feel that there are people in education that would also benefit from still being introduced to those sessions having some training around it and then because that mental health worker cannot be in school all of the time whereas we are and they need to pick up work with the student at any point, um, so it’s a, definitely tools that we would benefit from still having, um, given to us in some way.
Education practitioner
Furthermore, we observed that to co-deliver the intervention successfully, co-delivery partners had to remain cognisant of the mental states underlying one another’s communication. Therefore, the process of co-delivering the intervention required practitioners to model the mentalisation skills taught during the intervention.
Several education practitioners spoke about their intention to continue supporting the students they had worked with during BEST beyond the intervention:
. . . come September I would like to revisit with her and just sort of talk to her, regroup and maybe pick up some of the parts that could be helpful for her, you know, just to keep as strategies to help.
Education practitioner
. . . you need to revisit and revisit and revisit with the student because, OK, you get like 6 weeks of it and there’s a lot going in, so I want to take the stuff and I will take the stuff and go through it with her for the rest of her school experience.
Education practitioner
This upskilling of practitioners from participating school and colleges through the co-delivery model therefore has the potential to considerably extend the impact of a relatively brief intervention. Furthermore, it provides continuity for young people who, owing to the nature of their difficulties might otherwise find endings difficult. This was evident in the session recordings, in which education practitioners often discussed with the young person how they could continue to support them to use their crisis plan beyond the intervention. For instance, the following transcribed quotation is taken from the recording of a final session:
. . . and then we just try and keep putting things into practice and I guess if you found a particular session helpful and you weren’t sure and you wanted to you could come and see me and we could go through it again if you felt you needed to.
Education practitioner
Wider school or college
There was also some indication that the intervention may have positive impacts on participating schools or colleges more widely through enacting a change in attitudes towards behaviour that may be symptomatic of emotional dysregulation:
I think as well . . . having tolerance for other students that may be displaying signs of emotional dysregulation and thinking in my mind these are classic signs of emotional dysregulation even though there’s no formal diagnosis of having the tolerance and the patience and understanding due to the new knowledge that I’ve learnt to work with these students and say hang on a minute OK this is not you know a temper tantrum this is you know this has been ongoing for the student and maybe this is stuff that’s been undiagnosed and encouraging them to go and see their GP to, um, investigate more what’s going on with their moods and their behaviours and stuff so it’s been a really good thing.
Education practitioner
I think that also could then, you know, filter out onto the wider classroom-based, can’t it, because sometimes kids like that just get a reputation, don’t they or they didn’t come in today or, I don’t know. I think maybe you know trying to get the college or the school to see things slightly differently as well, I think you would lose that if it was just a mental health practitioner coming in, it would just another bit of work that you’d be doing.
Mental health practitioner
Potential barriers to and facilitators of successful delivery
We identified a number of factors that might help or hinder the effective activation of the proposed mechanisms discussed above.
Individual differences between participants
Practitioners discussed the impact of the individual characteristics of the young people they worked with on the process of intervention delivery. Practitioners observed that participants’ prior emotional literacy and willingness to talk openly about how they were feeling had an impact on their ability to engage with the content of the intervention:
I think the difference between participants is interesting in our first participant was very quiet and it took a lot to kind of get her to talk and engage and things like that whereas the second participant I felt was a lot more emotionally literate coming into it so actually she found the concept perhaps a little bit easier to grasp and to talk about because they were things that she’d had previously kind of heard about.
Education practitioner
This practitioner went on to speak about how this led her and her co-delivery partner to adapt their delivery, leaving more ‘quiet spaces for processing before rephrasing things’ when working with the first participant than with the second participant. This adaptation was also evident from the session recordings, with practitioners appearing to adapt the pace and style of delivery to match the young person with whom they were working.
Practitioners also commented on individual differences in participants’ motivation to put their learning into practice outside sessions, with some young people enthusiastic to complete home practice tasks and others very rarely doing so. Furthermore, the young person’s school/college attendance was noted as having significant impact on the extent of logistical challenges faced.
Individual differences between practitioners
The personalities and characteristics of individual practitioners was also considered a significant factor in successful delivery. All practitioners reported getting on well with their co-delivery partners and, as a result, did not experience any major challenges working together to co-deliver the intervention. However, it was hypothesised that a clash of personalities could compromise the success of this delivery model:
I mean luckily we all seem to have partnered with people we get on with but I think if you have a clash of people I think you know it probably wouldn’t work if the partnership wasn’t right.
Mental health practitioner
The practitioners’ personal characteristics and the impact of these on the ability to build a positive relationship with the young person were also considered important factors. Gender was a factor that practitioners speculated may play a role in this. One education practitioner felt that the fact that the mental health practitioner she was paired with was male had helped the male student they worked with to feel comfortable being open about his experiences. Another practitioner wondered whether or not the fact that he and his co-delivery partner were male might have affected their ability to connect with the female participant, with whom they struggled to engage. However, when asked about this, the young person did not believe that gender had played a role for her, although she acknowledged that it might do for others.
School or college environment
Several factors related to the school or college environment were identified as having an impact on the success of the intervention. It was observed in session recordings and reiterated within practitioner focus groups that consistent availability of appropriate spaces to deliver sessions varied across sites. Practitioners commented that it was often difficult to find an appropriate room within the school or college for sessions, and that sessions were sometimes interrupted by people walking in or by external noise:
. . . quite often it was difficult to get a room that was big enough, I think one time we were in a room off the kind of school gym so they had the dance class going on, it was really loud, it was kind of difficult for the young person to concentrate and for us to concentrate . . .
Mental health practitioner
. . . it was a constant issue, the room we were supposed to be in actually turned out to be a bit of a fish bowl, there was windows on every single side and I didn’t think it was really very appropriate, so we then moved to this other office which was quieter while lessons were going on but as soon as kind of people moving around it was absolutely horrendous.
Mental health practitioner
Young people did not comment on the environment in which sessions were conducted. Education practitioners expressed that space is always at a premium in schools, and so this is something they are used to working around.
I think it’s something that we just probably in schools we take for granted and we get used to, you know, to be fair we can be in a safeguarding meeting and you could put a note on the door to say, you know, meeting in progress and you can bet your life someone will still knock on the door and pop their head through and say, ‘we need to speak to say about something’, it is how it is.
Education practitioner
However, some practitioners expressed concern about the potential impact of the environment on the ability of young people to engage in sessions, and their own ability to concentrate on delivering the intervention:
I found the environment was a little bit chaotic . . . there would be people always coming to the office and lots of kids around, you know, obviously it’s a college it’s busy sort of in and I could understand that but actually I wonder if some of that was quite distracting for the young person at times.
Mental health practitioner
. . . we had one session where we had to use a different room just because the room we were using had been allocated for an exam so we had to use a different room in a part of the college they don’t usually go in, it was between the principal’s office and another member of senior leadership team’s office and actually on reflection afterward the session myself and the co-facilitator both felt the student was less comfortable . . . that impacted on actually perhaps how that session went I think.
Education practitioner
As touched on when discussing education practitioners’ switching of roles, practitioners described a several instances of perceived conflict between the academic priorities of the school or college and delivering the BEST intervention. For instance, one practitioner spoke about having had some complaints from teaching staff about a participant struggling to concentrate in lessons after attending a BEST session earlier in the day:
. . . we did the first session in the morning hours and then we had lots of complaints about other teachers because our student after our session he was going to attend other classes and he was struggling to concentrate . . . so we had some complaints from teachers that we should do this at the end of the day . . .
Mental health practitioner
Practitioners’ accounts suggest that the needs of academic lessons were generally viewed as having priority over intervention delivery by schools and colleges. However, interestingly, one participant discussed how prioritising engaging in the intervention over her academic work had led to an improvement in her academic performance:
I was like well if I’m going to get help then that means I have to like take part and listen in properly and do everything that I’ve been told and everything and like concentrate on that and obviously concentrating on that more than my work kind of helped with my work because like I guess like when you’re doing your work you have to feel your emotions to do it.
Young person
This suggests that there is not necessarily a zero-sum game between academic attainment and intervention delivery, which would demand prioritising one over the other.
Participants’ family context
The participant’s family context was identified as an additional factor with the potential to have an impact on intervention mechanisms. Difficult family relationships, particularly feeling unheard or misunderstood by their parents, was a topic frequently raised by participants within sessions. Although the intervention did not involve family members directly, several practitioners mentioned that participants had chosen, unprompted, to share the content of sessions with a family member:
. . . interestingly what was happening was when our student was going home and doing her little bit of homework she was actually rolling the sessions out to her mum, so that was quite interesting, hearing how she was doing that and I felt that she was really sort of taking it on forward you know . . .
Education practitioner
When participants chose to share the content of sessions with a family member, this was seen as a useful way of reinforcing the participant’s own understanding of skills and concepts covered in the intervention. For instance, one practitioner talked about how the young person had tried to explain mentalisation to her mother and that this had helped her gain a firmer understanding of the concept herself:
. . . actually my participant went home and delivered the session she’d had to her mum which I think kind of helped her really kind of firm up in her head what it was and then actually she came back and said she found it difficult to explain it to her mum but she kind of got it . . .
Mental health practitioner
Impact of mental health stigma
Education practitioners expressed that BPD was not something that they had much knowledge of prior to participation in BEST, and it was evident that some were uncertain about whether or not it was helpful to raise the topic with students:
I think the term borderline personality disorder was a bit scary . . . we have to make sure that we are not labelling them, that they don’t feel that they are going to be labelled because it does sound like a bit of a scary thing . . .
Education practitioner
I don’t think it’s something that’s discussed a great deal so usually we talk about depression and we talk about anxiety but conditions such as borderline personality disorder it’s certainly not something you would want to talk too much to the student about really if you don’t want to sort of plant ideas in their mind . . .
Education practitioner
Similarly, mental health practitioners spoke about being aware of the stigma that sometimes surrounds the diagnosis of BPD and controversies regarding the diagnosis of personality disorders in adolescents. Therefore, some chose not to explicitly mention BPD during the sessions to avoid ‘labelling’ the young person and minimise the potential for stigma:
I felt that it was enough to talk about the traits without necessarily mentioning BPD although it was there for her to read about . . . I wasn’t sure what would be the benefit to or what it would add to mention BPD as well as emotional regulation . . .
Mental health practitioner
. . . it’s really important to try and keep the stigma down as much as possible like especially when they’re adolescents as well and we don’t want to start like trying to label them at that age . . .
Mental health practitioner
Self-harm was a topic that practitioners told us they felt reasonably comfortable discussing but that some young people were reluctant to talk about:
. . . our student just refused to talk about self-harm she avoided it at all cost so if we kind of approached the subject she’d kind of say, ‘no I don’t want to talk about it’, and we’d have to kind of almost refer to it as a taboo subject so it was there but we weren’t talking about it . . .
Mental health practitioner
It was observed that young people sometimes expressed shame or embarrassment when prompted to discuss their self-harming behaviour. Practitioners observed that young people were often reluctant to name self-injuring behaviours as self-harm, perhaps reflecting stigma surrounding this particular term:
. . . he was more able to say, ‘OK I’m doing this to release my anger’, which is self-harm but we didn’t name it as self-harm we named it something else . . . like punching the wall or damaging my wrist . . .
Mental health practitioner
Education practitioners often saw discussion of self-harm as beyond their expertise, despite reporting that it was something they frequently encountered in their pastoral role. This may account for the relatively low adherence to the self-harm management component of the intervention observed: this was the only component not rated as fully present in any recorded session.
Unmet need for mental health support within schools and colleges
The high demand for mental health support and limited capacity within schools and colleges to provide this support is another factor we identified that would likely affect the implementation of the BEST intervention. Most education practitioners told us that, because of the high demand for support, they rarely have opportunities to work with a young person regularly over a number of weeks, instead signposting to external services or reacting to incidents as they arise:
. . . it’s always about kind of the queue at the door so actually we very much worked with see the student signpost on see the next student . . .
Education practitioner
Some mental health practitioners expressed a degree of surprise about the expectations placed on school and college staff members:
. . . they do have a really difficult job don’t they to do I think, because they literally have to do a bit of everything, I guess we are fortunate in some ways because we just focus on one thing whereas I guess when the young person is there for 8 hours of the day they literally you know just are everything to that person, particularly if they’ve got you know additional needs or if they’ve got some difficult behaviour, you know I guess, you know, I think that I kind of opened my eyes to that a bit more.
Mental health practitioner
. . . his job [the education practitioner] is so stressful and I just thought to myself, ‘well this guy never gets time to do this sort of stuff . . . a lot of the time he’s just firefighting . . .’
Mental health practitioner
This may have an impact on the sustainability of the intervention delivery model if the time commitment expected of school and college staff is too great to fit within already busy roles. However, education staff expressed that they appreciated this way of working and felt that it offered specialist external support that is rarely available to school and college staff members:
. . . you know something that we’ve asked for for years and years and years is supervision when we are dealing with safeguarding issues and you know traumatised young people and sometimes I mean not recently touch wood, but I remember having a really serious issue with a young person for months and months and months and months a few years ago and to be fair that nearly tipped me over the edge you know, but when you ever ask for supervision in a high-school setting it’s they’re very reluctant to invest in that and find the right person . . .
Education practitioner
In one focus group it was raised that senior leadership teams anticipated that demand for mental health support was likely to rise further in the wake of the COVID-19 pandemic. In this context, practitioners felt that any mental health support offered was likely to be welcomed by school and college leadership teams:
. . . they [the senior leadership team] want every piece of help they can get at the moment, especially with the lockdown and how it’s going to be when we come out of this you know, the message is anything that we can get to support our students we will take on board . . .
Education practitioner
Chapter 6 Discussion
Summary of findings
Although there is compelling evidence in support of early intervention for BPD, current evidence-based interventions for adolescent BPD are highly resource intensive, meaning few young people access timely treatment. The BEST intervention was designed to meet the need for accessible early interventions for young people experiencing BPD symptoms through a novel cross-sector approach involving mental health and education sectors working in collaboration. The intervention was adapted from a treatment package successfully delivered within secondary mental health services, but which had yet to be delivered in an educational setting prior to the current study.
The aims of this feasibility study were (1) to refine the prototype BEST intervention to maximise the likelihood of successful implementation within schools and colleges and (2) to inform the design of a future trial of the clinical effectiveness and cost-effectiveness of the refined intervention. As outlined in Chapter 1, Research overview, the study comprised two stages: an intervention refinement stage and a feasibility RCT. The key findings of each of these stages are summarised below.
Stage 1: intervention refinement
To inform the refinement of the prototype intervention, we carried out a rapid evidence synthesis to bring together the available evidence on what factors influence the successful implementation of indicated psychological interventions within schools and colleges. Fifty studies were identified for inclusion in the synthesis. All studies were of school-based interventions, highlighting a gap in the literature for studies involving implementing mental health support within further education and sixth form colleges.
A thematic synthesis of the factors reported by included studies to have an impact on implementation generated 11 analytical themes. These themes encompassed factors on multiple interacting levels, including intervention characteristics, organisational capacity, training and technical assistance, provider characteristics and community-level factors.
The findings of the evidence synthesis highlighted several important issues that contributed to the refinement of the BEST intervention and influenced the conduct of the feasibility trial. These included: (1) the need to consider how to maximise the ability of staff to identify and refer students likely to benefit from the intervention; (2) the importance of the intervention manual and supporting materials, as well as the quality of training and ongoing supervision, for the ability of staff to deliver interventions with fidelity; (3) the need to identify intervention champions at a senior level within settings to promote buy-in from other staff members; and (4) the inevitability of logistical challenges associated with the constraints of the school calendar, routines and environment.
Alongside the evidence synthesis, we piloted the prototype intervention with five participants from three education settings. Of the five young people recruited, three completed the full intervention, one completed only the first session before disengaging and one was unable to receive any sessions owing to being excluded from the setting. Analysis of 19 recorded treatment sessions suggested that the sequence of activities occurring during sessions closely mirrored the structure of the intervention manual. Both education practitioners and mental health practitioners were seen to play an active role in co-delivery of the intervention, although mental health practitioners were more frequently coded as leading activities. Analysis of the link between differing practices employed to deliver intervention activities and participant responses within sessions enabled us to generate hypotheses to be explored further in the second stage.
Practitioner feedback gathered through interviews and a focus group indicated that the intervention was generally positively received, and the co-delivery model was valued despite some logistical challenges. However, practitioners suggested several ways in which the training and supervision, content and format of treatment sessions, and research procedures could be improved.
Findings from the evidence synthesis and pilot were combined to enable us to finalise the intervention manual and resources, refine the practitioner training and amend study procedures in preparation for the feasibility RCT. Key refinements made to the intervention manual were to add further examples and replace technical language to improve comprehension, incorporating information originally provided as an appendix within the body of the manual, and reformatting one of the sessions to ensure that it was possible to deliver within the time frame of a typical school or college period. Key changes made to the training and supervision provided were providing staff with additional pre-training materials and enhancing the practitioner handbook, clarifying the co-delivery model and division of roles within the training workshop, and reducing the frequency of supervision sessions. In addition, several amendments were made to the planned study procedures. These included increasing the number of schools and colleges invited to participate and approaching all potential sites via the senior leadership team in the first instance, introducing a pre-screening questionnaire to assist staff to identify potentially eligible pupils, and increasing the intervention delivery window to allow for missed sessions owing to school holidays, staff and student absence, etc.
Stage 2: feasibility randomised controlled trial
Following the intervention refinement phase, we carried out a feasibility RCT to assess the feasibility of conducting a future trial of the clinical effectiveness and cost-effectiveness of the refined BEST intervention. The feasibility trial was disrupted because of the COVID-19 pandemic and resultant closure of schools and colleges. Consequently, the study was concluded early, reducing the window for recruitment and the number of data we were able to collect. However, the available data were sufficient to answer key research questions regarding the feasibility and acceptability of the intervention, and provide useful information to inform the most appropriate design for a future definitive trial.
Our findings on recruitment, retention and contamination are summarised below in relation to the criteria for progression to a definitive RCT, as set out in the study protocol (see https://journalslibrary.nihr.ac.uk/programmes/hsdr/170931/#/documentation; accessed 6 April 2022). Further factors that we planned to consider in determining the feasibility of evaluating the clinical effectiveness and cost-effectiveness of the refined BEST intervention in a future RCT were the acceptability and suitability of the proposed outcome measures, the ability of practitioners to deliver the intervention with fidelity to the model, and the acceptability of the intervention from the perspective of staff and young people.
The acceptability of the proposed outcome measures appears to have been satisfactory. Measures were generally well completed, and the qualitative feedback suggests that most young people did not find the experience of completing the measures unduly burdensome. However, one young person recounted experiencing some discomfort related to the personal nature of certain questions, particularly surrounding the topic of self-harm. This underlines the need to remain alert to the potential for distress and the importance of appropriate protocols to ensure that this is managed sensitively and in a way that minimises risk and maximises support.
Although the trial was not powered to detect any significant changes in outcomes in line with its aim, mean changes from baseline for continuous outcome measures suggest that they are sensitive to change and, if the intervention is effective, would be able to detect differences in a future trial. However, the BPFSC data, together with practitioner feedback regarding the framing of the intervention, promoted discussion with stakeholders regarding whether or not the severity of BPD symptoms would be the most appropriate primary outcome for a future effectiveness trial. This is discussed further in Stakeholder feedback event.
The health economic measures also appeared to perform adequately. The modified CSRI was well completed and generally acceptable, although we suggest that the final question concerning parental resource use could be omitted in a future study. Similarly, the EQ-5D appears to have performed acceptably in this population and so would be a good candidate for the health economic outcome measure in any future trial of the BEST intervention. Although the cost-effectiveness of the intervention would need to be established in a future trial, the estimated costs of delivering the intervention appear favourable compared with existing interventions for BPD. For instance, the cost of providing a DBT-A programme has been estimated at €10,511 (£9229). 125
Analysis of session recordings suggests that the ability of practitioners to deliver the intervention with fidelity to the model was very good. Of a sample of 31 session recordings rated for fidelity by intervention supervisors, 93.5% were rated as adherent to the manual. Unlike in the pilot phase, the majority of mental health practitioners who co-delivered the intervention in the feasibility RCT were AfC band 4 and band 5 practitioners without core professional training, such as assistant psychologists and children’s well-being practitioners. The high levels of fidelity we observed suggests that mental health practitioners without core professional training would be an appropriate workforce to train and to co-deliver the intervention in future research.
Acceptability of the intervention also appears to have been high. Excluding those who were unable to be offered the intervention as a result of the pandemic, 90% of those allocated to the intervention arm attended at least three sessions and the majority completed all six. Interview and focus group data indicate that the intervention was valued and seen to offer positive benefits both by practitioners and by the young people who received it.
The intervention was perceived to bring about positive benefits at three interacting levels. For the individual participant, the intervention was perceived to foster better self-understanding, enhance emotional and social literacy and improve coping skills. For some participants, this appears to have had a positive impact on their ability to regulate their emotions and on their relationships with others. For the education practitioners involved in co-delivery, the perceived benefits of the intervention included increased confidence and skills in supporting young people experiencing emotional instability, equipping them to provide ongoing support to participants and informing their wider practice. Practitioners also perceived a potential benefit for the whole school or college, through enacting a change in attitudes towards behaviour that may be symptomatic of emotional instability.
Factors identified as potentially facilitating or creating barriers to the activation of the hypothesised mechanisms of change spanned interacting contextual levels. In accordance with the socioecological model developed through the evidence synthesis, these findings underlined the likely impact of structural and environmental factors, interacting with intervention characteristics, in determining whether or not the intervention could be successfully implemented and sustained.
Qualitative analysis of audio- and video-recorded intervention sessions showed a close correspondence between the structure and delivery of sessions and the intervention manual. Analysis of interviews and focus groups revealed how both young people and staff found the intervention acceptable, appreciated the clear structure of sessions, and importantly, reported specific ways in which the intervention components functioned to improve young people’s capacity to mentalise. For example, it was reported that use of the emotions wheel improved how participants recognised and managed their emotions outside intervention sessions. These findings clearly enhanced our understanding of the quantitative finding that 93.5% of sessions were rated as adherent. They also offered important points of triangulations with the findings from Table 14 that showed that the relative contribution of both staff and young people was evenly distributed across session activities, indicating a high level of engagement. Taken together, we were able to conclude that the BEST intervention was not only feasible and acceptable to deliver in schools, but also possible to deliver with a high level of implementation and theoretical fidelity.
Progression criteria
Below we summarise our findings in relation to the prespecified criteria for progression to a multisite RCT of the effectiveness and cost-effectiveness of the BEST intervention plus TAU in comparison to TAU alone.
-
Recruitment rate was within 70% of the target.
Recruitment was slower than anticipated, largely owing to very limited recruitment during school holidays as nearly all referrals were received via schools and colleges as opposed to mental health services. However, prior to the suspension of recruitment owing to COVID-19, we had been confident that the total number of participants recruited by the end of the recruitment period would exceed 70% of the target. From October, when the first participant was recruited, the average rate of recruitment was 5.4 participants per month. The initially projected recruitment rate that would have enabled us to reach 100% of the target sample size within the recruitment period was 6.6 participants per month. To reach 70% of the target a recruitment rate of 4.6 per month across the recruitment period would have been sufficient. Furthermore, additional schools and colleges had agreed to participate in the project and there were a good number of pending referrals at the point of the COVID-19 lockdown, which we anticipated would have resulted in an increase in recruitment.
-
At least 70% of those randomised to receive the intervention attended three or more treatment sessions within the 12-week treatment window.
Of the 10 participants randomised to the BEST arm who had come to the end of the 12-week treatment window prior to suspension of intervention delivery, nine (90%) attended three or more treatment sessions.
-
Follow-up assessments were completed by at least 75% of participants at 12 weeks and 70% of participants at 24 weeks.
Of the 19 participants who had reached the 12-week follow-up before the suspension of the trial, 17 (89.5%) were followed up at 12 weeks and 14 (73.7%) at 24-weeks. All 24-week follow-up assessments were completed remotely at a time when schools and colleges were closed to most pupils because of COVID-19. As a result, staff were unable to assist in contacting participants and arranging appointments as they had at the 12-week time point.
-
Contamination of the control arm can be sufficiently limited for individual randomisation to be justified.
The data available to assess contamination were limited by poor compliance with completion of practitioner contact logs. However, findings from staff focus groups and interviews did not give any indication that direct contamination of the control arm through provision of the intervention or its components to those allocated to receive TAU had occurred. Although there was no evidence of the BEST intervention being used with TAU participants, some practitioners reported that they had, or intended to, use resources or strategies from BEST in their wider practice. Furthermore, some education practitioners reported that the experience of participating in BEST had changed how they viewed behaviours that may be symptoms of emotional instability. Therefore, it is possible that the implementation of BEST within schools and colleges may indirectly affect TAU over time through having an impact on wider practice.
Stakeholder feedback event
Following the conclusion of the feasibility RCT, a stakeholder feedback event was held to share key study findings and gather stakeholder views on the likely sustainability of intervention implementation and the future of the research programme. The online event was attended by stakeholders (n = 12) from across education and mental health services, all of whom had been involved in or supported the study in some capacity. The event began with a presentation of the study findings and opportunity for attendees to ask questions. The presentation of findings was followed by a group discussion on the topic of whether or not to continue to research the BEST intervention with a view to future widespread implementation. Last, break-out rooms were then used to facilitate small group discussions of the following questions:
-
What changes to the BEST intervention/approach would be needed for it to be sustainably implemented by schools and colleges?
-
What changes to the eligibility criteria or method of identifying young people who may benefit from the intervention might be needed?
-
What would be the most important outcomes to focus on in future research on the effectiveness of the BEST intervention?
The discussions were recorded with the consent of those in attendance, to enable stakeholder views to be captured and points of consensus and disagreement to be noted. Following the event, a recording of the presentation of findings was shared with those unable to attend and two further stakeholders provided written feedback on the topics discussed.
There was consensus among participating stakeholders that the programme of research is worth taking forward. The intervention was viewed as having value as a means of bringing the mental health and education sectors together, as well as in enabling schools and colleges to meet the needs of a group of students that they would otherwise feel ill equipped to support. It was raised that schools and colleges had seen a notable rise in the demand for mental health support in the wake of the COVID-19 pandemic; it was suggested that the intervention could potentially play a role in meeting this increased demand.
There was some debate as to whether or not the co-delivery approach would prove sustainable in the long term. However, most attendees agreed that co-delivery was a core component of the intervention and should be preserved. It was suggested that the sustainability of intervention delivery could be maximised by expanding the pool of staff members trained to deliver it. One attendee expressed that if there was evidence that provision of the BEST intervention would, in time, lead to decreased utilisation of specialist mental health services, this would justify diverting resources to its delivery.
The increased use of technology to facilitate intervention delivery was discussed. All were in favour of the creation of an electronic version of the manual. It was also suggested by some attendees that the mental health practitioner could participate in sessions via video call rather than in-person to reduce staff time required to deliver the intervention. However, stakeholders disagreed over whether or not the intervention could be successfully delivered in this format.
This is an issue that requires further exploration given the context created by the COVID-19 pandemic. To futureproof the intervention against the possibility of ongoing disruption, it would clearly be desirable to have the flexibility to accommodate remote delivery when needed. Therefore, this would be a pertinent issue to consider in future research, alongside exploring how trial procedures may need to be carried out in more innovative ways, including remote consent, randomisation and delivery processes.
Although they saw value in a targeted intervention, most stakeholders supported the widening of the inclusion criteria to encompass a broader range of young people who might benefit from intervention to improve their emotional regulation. However, it was raised that this would require a reframing of the intervention to avoid inappropriate pathologising. The prospect of allowing self-referrals or using school-/college-wide screening as a means of identifying young people to receive the intervention was not supported; it was felt that identifying potential recipients in this manner would risk overwhelming already stretched services.
Stakeholders suggested a range of outcomes that they felt would be important indicators of the success of the intervention: these included the young person having improved coping skills, relationships, behaviour and educational engagement, leading to better educational outcomes. It was also suggested that the confidence of school and college staff members in supporting students would be a valuable outcome to capture. There was consensus across groups that improved emotion regulation would be the most appropriate primary outcome for a future trial of the effectiveness of the BEST intervention.
Interpretation and implications
Taken together, the findings of the feasibility trial indicate that, following the refinements made during the piloting phase, the manualised BEST intervention co-delivered in school and college settings is broadly feasible to deliver and is acceptable to school and college staff, mental health practitioners and, most importantly, the young people who received the intervention. The study was not powered to assess the effectiveness of the intervention and, therefore, a further trial to establish whether or not the intervention leads to improved outcomes would be necessary before widespread implementation could be recommended. We believe that the results of this feasibility study provide support for progressing to a full trial of the BEST approach; however, it also identified a number of issues to be resolved and logistical barriers to overcome for a full trial to be successful.
Referral rates per school or college were low relative to the number of young people who might be expected to be experiencing BPD symptoms based on community prevalence studies. 9 As previously discussed, we received very few referrals from mental health services despite considerable efforts to promote the study. One barrier to recruiting from within mental health services was that the schools and colleges that were attended by service users were not routinely recorded, meaning it was not straightforward to identify service users who attended the settings participating in the trial. Furthermore, it was reported by potential referrers that many of the young people presenting with BPD symptoms who had met the threshold for access to secondary mental health services had disengaged from education. Therefore, nearly all referrals were received directly from schools and colleges.
In line with findings of the rapid evidence synthesis, this raises questions about the best way to identify young people in need of indicated mental health interventions within schools and colleges. To limit contamination, we trained only a proportion of each school and college’s pastoral workforce to enable a non-trained staff member to provide TAU whenever possible. However, responsibility for identifying possible participants appeared typically to fall to the BEST trained staff members only, rather than the wider team. Therefore, educational establishments who had a larger cohort of staff members trained to deliver BEST seemed better able to identify and recruit suitable participants. Although it would likely be beneficial to offer training to all school staff to enable them to identify patterns of behaviour that may warrant intervention, this would have implications for trial design that would require further consideration.
Referrers expressed frustration that young people who they felt would benefit from the intervention were ineligible for the trial. Although this frustration was lessened by the modification of the criterion regarding self-harm to include young people with a history of repeated self-harm at any time, it was not eliminated. There seems to be merit in considering broadening the criteria for participation for a future trial of BEST to enable more young people to benefit and to increase referrals. One way in which the criteria could be broadened is to increase the age range of eligible participants to include younger secondary school-aged pupils to facilitate earlier intervention. Furthermore, there may be benefits of reducing the severity of symptoms required to include those who do not meet a clinical threshold for BPD symptom severity. However, as the intervention specifically targets emotional instability and other BPD features, it is important that young people can identify with these features for the intervention content to be applicable to their experiences. Furthermore, it would be important to avoid the potential to pathologise what could be considered ‘normal’ teenage dysregulation. Therefore, there will be a need to balance potential benefits and harms of broadening the target group.
A related consideration is whether or not the initially proposed primary outcome (severity of BPD features as measured by the BPFSC) is the most appropriate focus for a future trial. Participants in the BEST intervention were, by design, presenting with complex difficulties, often experiencing significant distress and facing interpersonal challenges to successfully engaging in a therapeutic intervention. Furthermore, this group often cause considerable anxiety and disruption within educational settings and require a sophisticated approach to providing support. Given the severity and nature of participants’ difficulties, we would not expect instant resolution of symptoms. However, there were some indications of the potential for change at an individual level as a result of the intervention, for example a better ability to ‘name’ emotions and improved coping skills, including an enhanced ability to mentalise themselves and others. Therefore, individual pupil outcomes may be an appropriate primary focus, and it would facilitate an individually randomised trial design. However, improved emotion regulation skills or decreased emotional dysregulation may be preferred as a primary outcome over borderline personality symptoms.
The perceived benefits of the intervention extended beyond individual participants, suggesting that staff-focused and whole school or college outcomes are likely to be important secondary outcomes to capture. Educational practitioners reported developing a deeper understanding of the issues faced by young people presenting with behaviours associated with BPD, coupled with a framework on which to provide ongoing support and advice within the school or college setting. Practitioners reported relief at having a clear framework to work within and said that they felt that they could use future contact with the participant more productively as a result.
Reports of staff seeing poor behaviour not as ‘temper tantrums’ but as conveying meaning and requiring a more sophisticated response by the school or college were particularly encouraging. This increased ability of staff to mentalise the young people with whom they work would be of particular importance for young people with emerging features of BPD. It remains to be seen whether or not, if the intervention continued to be delivered, this would have an impact on culture within school and college settings; theoretically, such ongoing support may alter the responses experienced by pupils across the school or college in a positive way.
We faced many logistical challenges during the feasibility trial. Not least of these was schools and colleges being forced to close to most pupils during the COVID-19 lockdown. However, even prior to this, our experiences confirmed the conclusion of the rapid evidence synthesis: delivering indicated mental health interventions within educational settings is not without obstacles. Although co-delivery by an education and mental health practitioner working alongside one another appears to have been central to the perceived value of the intervention, it was also the source of many of the logistical challenges encountered.
Although this poses an apparent dilemma, a potential solution presents itself in the form of the new school and college-based mental health workforce currently being trained as part of a phased national roll-out. Following recent policy developments recognising the potential of schools and colleges as a setting for mental health early intervention,23,24 the government has committed to funding the creation of new MHSTs to work with children and staff in educational settings. These teams will be staffed primarily by education mental health practitioners (EMHPs), new members of the mental health workforce who will be trained to deliver evidence-based psychological interventions within schools and colleges. 126
At present, the training that EMHPs receive does not equip them to provide support to young people presenting with BPD symptoms. Therefore, under the currently proposed transformation model, young people requiring intervention for these types of difficulties, which are of such great concern to schools and colleges, will still require referral to secondary mental health services to receive intervention. However, given their training in delivering brief manualised psychological interventions, this new workforce looks to be extremely well placed to co-deliver an intervention such as BEST. Furthermore, their being based within schools and colleges has the potential to surmount many of the logistic barriers that CAMHS practitioners must overcome to deliver school-based interventions.
An issue the BEST approach shares with other interventions delivered within schools and colleges is that engagement with the intervention is inevitably closely correlated with the young person’s school or college attendance. Therefore, although delivery of interventions within schools and colleges may improve access to support for most young people, there are some young people who will not benefit from this approach. Given that this number is likely to include some of those most in need of support, it is important that the needs of young people not able to access school-based provision are not overlooked.
Beyond informing the future definitive trial of the BEST intervention, this study also suggests some boarder areas for further research. Research is required on the optimum model of school-based mental health provision, including thresholds of symptom severity amenable to intervention in a school setting, methods of identifying young people in need of intervention and adaptations needed to evidence-based interventions developed for use in clinical environments. Research on when and how to involve parents and carers and the wider community in school-based mental health services would also be beneficial. Furthermore, we identified a clear need for research focused on mental health support in sixth form and further education colleges, which differ in important ways from schools and have often been overlooked in prior research.
Strengths and limitations
We believe this feasibility study met its aim to refine the prototype BEST intervention in ways that maximises the likelihood of successful implementation within schools and colleges. The utility of the refined BEST treatment manual was evidenced by feedback from all stakeholders; the refinements made appear to have enabled the intervention to be implemented within educational settings with high levels of fidelity and acceptability. The study also provided much useful information to inform the design of any future trial of the clinical effectiveness and cost-effectiveness of the intervention.
A key strength of the study methodology was the use of multiple sources of information, enabling a range of factors that may have an impact on feasibility to be considered, and findings to be triangulated. Mixed-methods data capturing the experiences of a range of stakeholders reinforced learning from the systematic review and thematic synthesis, increasing our confidence in the transferability of findings to future work, despite the limitations we go on to discuss below. Another important strength of the study was strong stakeholder engagement throughout. We worked closely with individuals with relevant lived experience and those working with them within schools and colleges to shape the study throughout.
A major limitation of this research was that the second stage of the study (the feasibility RCT) faced considerable disruption because of the lockdown introduced to control the COVID-19 pandemic. As a result of the closure of schools and colleges to nearly all pupils in the wake of the pandemic, recruitment and intervention delivery were suspended in March 2020 and the study concluded 3 months earlier than initially planned.
This disruption and early closure affected the study in several ways. First, there was significant impact on the quantity of data we were able to collect, both through shortening the recruitment window and by reducing the number of young people who were able to be offered the intervention and followed up.
We planned to conduct observations of everyday encounters (e.g. meetings and informal conversations between teaching and pastoral staff) within schools to provide an understanding of relevant meso-contextual features (i.e. the organisation, norms, policies and practices affecting pastoral care) that would situate our analysis of recorded intervention sessions and interview data. However, after two periods of observations we found that it was very difficult to identify encounters in which staff discussed topics that were directly relevant to delivering the BEST intervention. We therefore decided that it would be more fruitful to interview senior leaders within schools, who would provide us with their perspectives of relevant meso-contextual features. We had planned to carry out these interviews during the feasibility study. However, the closure of schools and colleges in March 2020 meant that such interviews were extremely difficult to arrange with staff, and unfortunately these were not completed before the study closed.
Furthermore, we had intended to include an analysis of policy documents to support the ethnographic fieldwork within schools and colleges, in particular how wider macro-contextual features (e.g. mental health policy) was operationalised at a meso-contextual level as practices within schools and colleges and how this then shaped delivery of the BEST intervention at a micro-contextual level. However, as we were unable to complete our data collection of meso-contextual features (observations and interviews with senior school leaders), the analysis of policy documents would not have provided any meaningful insights into how schools operationalised such policy. As a result, we decided to prioritise our efforts on completing data collection and analysis of the process evaluation interview and focus group data.
The impact of the pandemic also reduced the likely transferability of some study findings. For instance, learning regarding likely retention of participants at 24 weeks was limited not only by the low number of participants eligible to be followed up, but also by the extraordinary circumstances in which follow-ups were conducted: remotely during a national lockdown. Although we believe that retention rates would likely have been at least as good if not higher had schools and colleges been able to assist in facilitating follow-up assessments, it is also plausible that they would have been lower had participants not been largely confined to their homes during this period. As a result, the conclusions drawn from the study are necessarily more tentative than they might otherwise have been.
Furthermore, we were unable to complete some of the planned analysis of process evaluation data within the available time frame. Therefore, the linguistic ethnography methodology originally proposed was not fully implemented and therefore caution is needed in interpreting some process evaluation findings. However, we believe that the analysis of the data provides a solid foundation for further planned analytical work. To enable us to more fully realise the potential of the data collected to answer important feasibility questions, we plan to (1) identify extracts of session recordings that exemplify areas identified as critical to optimising implementation of the intervention, (2) characterise communication patterns associated with differing approaches to delivery and (3) explore the interactional consequences for successful delivery of intervention components. We aim to publish these findings in Social Science & Medicine or another suitable peer-reviewed journal.
Conclusion
The refined BEST intervention represents a promising approach for providing timely support to young people experiencing BPD symptoms. The findings of this feasibility study suggest that it is feasible to deliver the intervention within schools and colleges and that it is acceptable to its intended users. However, we do not yet know whether or not, as a relatively low-intensity intervention delivered by non-specialists, the BEST intervention will prove sufficient to improve outcomes for young people. Therefore, a definitive trial of the clinical effectiveness and cost-effectiveness of the BEST intervention would be needed before widespread implementation could be recommended. Although the findings of the feasibility study provide support for progressing to a definitive trial, they also highlight several issues to be resolved and logistical barriers to overcome for a full trial to be successful.
We propose to use the learning from this study, in conjunction with further work to resolve remaining uncertainties, to design a future definitive trial, aiming to retain the core elements that have made the BEST intervention so well received. Questions that we will seek to address, through either PPI work or additional research, before finalising the protocol for the definitive trial include whether or not to broaden the inclusion criteria, the best way to identify eligible young people in schools and colleges, the most suitable primary outcome and whether or not the new EMHP workforce would be suited to co-deliver the intervention within schools and colleges.
Acknowledgements
Our heartfelt thanks go to the young people, school and college staff members, and mental health practitioners who participated in the research. We are extremely grateful for your time and commitment to the study. We would also like to sincerely thank the young people and parents who contributed to the development and conduct of the study as PPI representatives.
We gratefully acknowledge the central role in the delivery of the study played by Sophie Farthing, who worked as the BEST research assistant. We are also extremely grateful for the contributions of Christine Lowen and Adam Graham who acted as intervention supervisors and contributed to intervention refinement. Thanks also to Gabriel Abotsie, Helen Nicholls and Juan Herran-Alonso for their work completing outcome assessments. Thanks to Bhavna Sidhpara for her editorial assistance during the final stages of preparing this report.
We further acknowledge the contributions of Sophie Farthing, Ben Carroll, Christopher Jackson, Kahfee King, Helen Nicholls and Juan Herran-Alonso to the completion of the rapid evidence synthesis. We are grateful to staff of the Norfolk and Suffolk NHS Foundation Trust Frank Curtis and University of East Anglia libraries for their assistance refining the search strategy and accessing full texts.
We are extremely thankful to members of the study steering committee and data monitoring committee for contributing their time and expertise to oversee the study. We are also grateful for the advice and guidance of Professors Carla Sharp and Andrew Chanen and the International Global Alliance for Prevention and Early Intervention for BPD.
Finally, we thank the NIHR for supporting this work. Thanks especially go to Sue Pargeter and Jo Lunn (NIHR research managers) for their guidance and support.
Contributions of authors
Jon Wilson (https://orcid.org/0000-0002-5279-6237) (Norfolk and Suffolk NHS Foundation Trust) was the study’s chief investigator. He contributed to study conception and provided scientific and clinical leadership. He wrote the first draft of the discussion and read and edited other chapters.
Brioney Gee (https://orcid.org/0000-0003-0781-7753) (Norfolk and Suffolk NHS Foundation Trust) was the study co-ordinator. She managed the study, co-ordinating recruitment, data collection and data management, and contributed to intervention refinement and data analysis. She collated the contributions to the report of other authors and wrote the first draft of those sections not attributed to others.
Nicola Martin (Norfolk and Suffolk NHS Foundation Trust) co-developed the BEST intervention together with Dr Sarah Maxwell. She contributed to the training and supervision of practitioners and the monitoring of intervention fidelity, and wrote the description of the prototype intervention.
Sarah Maxwell (https://orcid.org/0000-0001-8399-3949) (Norfolk and Suffolk NHS Foundation Trust) co-developed the BEST intervention together with Nicola Martin. She contributed to training and supervision of practitioners and wrote the description of the prototype intervention.
Jamie Murdoch (https://orcid.org/0000-0002-9021-3629) (University of East Anglia) designed and oversaw the process evaluation components of the study and contributed to the data analysis and interpretation. He wrote sections of the report describing process evaluation data collection and analysis.
Tim Clarke (https://orcid.org/0000-0002-3901-9601) (Norfolk and Suffolk NHS Foundation Trust) played a key role in the design of the study and development of the protocol. He provided trial management oversight, supervised members of the study team and contributed to interpretation of findings.
Allan Clark (https://orcid.org/0000-0003-2965-8941) (University of East Anglia) was the study statistician. He wrote the statistical analysis plan and is responsible for the analysis presented in Chapter 5, Suitability of outcome measures.
David Turner (https://orcid.org/0000-0002-1689-4147) (University of East Anglia) was the study’s health economist. He designed the health economic component and conducted and reported the analysis presented in Chapter 5, Health economic assessment.
Caitlin Notley (https://orcid.org/0000-0003-0876-3304) (University of East Anglia) oversaw the rapid evidence synthesis and contributed to study selection and data analysis and interpretation.
Thando Katangwe (https://orcid.org/0000-0002-5450-412X) (University of East Anglia) contributed to the analysis of session recordings for the process evaluation and wrote the first draft of findings presented in Chapter 3, Pilot findings.
Peter B Jones (https://orcid.org/0000-0002-0387-880X) (University of Cambridge) provided scientific oversight and guidance as a non-independent member of the Trial Steering Committee.
Peter Fonagy (https://orcid.org/0000-0003-0229-0091) (Anna Freud Centre, University College London) was influential in study conception and protocol design. He acted in a mentorship role, providing guidance and support to the wider study team throughout the project, and contributed to interpretation of study findings.
Publication
Gee B, Wilson J, Clarke T, Farthing S, Carroll B, Jackson C, Notley C. Review: delivering mental health support within schools and colleges – a thematic synthesis of barriers and facilitators to implementation of indicated psychological interventions for adolescents. Child Adolesc Ment Health 2020;26:34–46.
Data-sharing statement
Following the publication of major outputs, we will make anonymised data available to the scientific community whenever possible within the constraints of relevant ethical principles. All data sharing requests should be submitted to the corresponding author for consideration by the Trial Management Group.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care.
References
- Diagnostic and Statistical Manual of Mental Disorders. Arlington, VA: American Psychiatric Association; 2013.
- Gunderson JG, Stout RL, McGlashan TH, Shea MT, Morey LC, Grilo CM, et al. Ten-year course of borderline personality disorder: psychopathology and function from the Collaborative Longitudinal Personality Disorders study. Arch Gen Psychiatry 2011;68:827-37. https://doi.org/10.1001/archgenpsychiatry.2011.37.
- Grant BF, Chou SP, Goldstein RB, Huang B, Stinson FS, Saha TD, et al. Prevalence, correlates, disability, and comorbidity of DSM-IV borderline personality disorder: results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry 2008;69:533-45. https://doi.org/10.4088/JCP.v69n0404.
- Leichsenring F, Leibing E, Kruse J, New A, Leweke F. Borderline personality disorder. Lancet 2011;377:74-8. https://doi.org/10.1016/S0140-6736(10)61422-5.
- Brickman LJ, Ammerman BA, Look AE, Berman ME, McCloskey MS. The relationship between non-suicidal self-injury and borderline personality disorder symptoms in a college sample. Borderline Personal Disord Emot Dysregul 2014;1. https://doi.org/10.1186/2051-6673-1-14.
- Glenn CR, Klonsky ED. Prospective prediction of nonsuicidal self-injury: a 1-year longitudinal study in young adults. Behav Ther 2011;42:751-62. https://doi.org/10.1016/j.beth.2011.04.005.
- Kaess M, Brunner R, Chanen A. Borderline personality disorder in adolescence. Pediatrics 2014;134:782-93. https://doi.org/10.1542/peds.2013-3677.
- Moran P, Coffey C, Mann A, Carlin JB, Patton GC. Personality and substance use disorders in young adults. Br J Psychiatry 2006;188:374-9. https://doi.org/10.1192/bjp.188.4.374.
- Zanarini MC, Horwood J, Wolke D, Waylen A, Fitzmaurice G, Grant BF. Prevalence of DSM-IV borderline personality disorder in two community samples: 6,330 English 11-year-olds and 34,653 American adults. J Pers Disord 2011;25:607-19. https://doi.org/10.1521/pedi.2011.25.5.607.
- Sharp C, Fonagy P. Practitioner review: borderline personality disorder in adolescence – recent conceptualization, intervention, and implications for clinical practice. J Child Psychol Psychiatry 2015;56:1266-88. https://doi.org/10.1111/jcpp.12449.
- Mehlum L, Tørmoen AJ, Ramberg M, Haga E, Diep LM, Laberg S, et al. Dialectical behavior therapy for adolescents with repeated suicidal and self-harming behavior: a randomized trial. J Am Acad Child Adolesc Psychiatry 2014;53:1082-91. https://doi.org/10.1016/j.jaac.2014.07.003.
- Rossouw TI, Fonagy P. Mentalization-based treatment for self-harm in adolescents: a randomized controlled trial. J Am Acad Child Adolesc Psychiatry 2012;51:1304-13. https://doi.org/10.1016/j.jaac.2012.09.018.
- Chanen AM, Jackson HJ, McCutcheon LK, Jovev M, Dudgeon P, Yuen HP, et al. Early intervention for adolescents with borderline personality disorder using cognitive analytic therapy: randomised controlled trial. Br J Psychiatry 2008;193:477-84. https://doi.org/10.1192/bjp.bp.107.048934.
- Chanen AM. Borderline personality disorder in young people: are we there yet?. J Clin Psychol 2015;71:778-91. https://doi.org/10.1002/jclp.22205.
- Wilson J, Clarke T, Lower R, Ugochukwu U, Maxwell S, Hodgekins J, et al. Creating an innovative youth mental health service in the United Kingdom: the Norfolk Youth Service. Early Interv Psychiatry 2018;12:740-6. https://doi.org/10.1111/eip.12452.
- Public Health England . Promoting Children and Young People’s Emotional Health and Wellbeing. A Whole School and College Approach 2015.
- Fazel M, Hoagwood K, Stephan S, Ford T. Mental health interventions in schools 1: mental health interventions in schools in high-income countries. Lancet Psychiatry 2014;1:377-87. https://doi.org/10.1016/S2215-0366(14)70312-8.
- Chanen AM, McCutcheon L. Prevention and early intervention for borderline personality disorder: current status and recent evidence. Br J Psychiatry Suppl 2013;54. https://doi.org/10.1192/bjp.bp.112.119180.
- Goodman M, Patil U, Triebwasser J, Hoffman P, Weinstein ZA, New A. Parental burden associated with borderline personality disorder in female offspring. J Pers Disord 2011;25:59-74. https://doi.org/10.1521/pedi.2011.25.1.59.
- Griffin E, McMahon E, McNicholas F, Corcoran P, Perry IJ, Arensman E. Increasing rates of self-harm among children, adolescents and young adults: a 10-year national registry study 2007-2016. Soc Psychiatry Psychiatr Epidemiol 2018;53:663-71. https://doi.org/10.1007/s00127-018-1522-1.
- Morgan C, Webb RT, Carr MJ, Kontopantelis E, Green J, Chew-Graham CA, et al. Incidence, clinical management, and mortality risk following self harm among children and adolescents: cohort study in primary care. BMJ 2017;359. https://doi.org/10.1136/bmj.j4351.
- Deighton J, Lereya ST, Casey P, Patalay P, Humphrey N, Wolpert M. Prevalence of mental health problems in schools: poverty and other risk factors among 28 000 adolescents in England. Br J Psychiatry 2019;215:565-7. https://doi.org/10.1192/bjp.2019.19.
- Department of Health and Social Care (DHSC), Department for Education (DfE) . Transforming Children and Young People’s Mental Health Provision: A Green Paper 2017.
- Department of Health and Social Care (DHSC) . The NHS Long Term Plan 2019.
- Werner-Seidler A, Perry Y, Calear AL, Newby JM, Christensen H. School-based depression and anxiety prevention programs for young people: a systematic review and meta-analysis. Clin Psychol Rev 2017;51:30-47. https://doi.org/10.1016/j.cpr.2016.10.005.
- Caldwell DM, Davies SR, Hetrick SE, Palmer JC, Caro P, López-López JA, et al. School-based interventions to prevent anxiety and depression in children and young people: a systematic review and network meta-analysis. Lancet Psychiatry 2019;6:1011-20. https://doi.org/10.1016/S2215-0366(19)30403-1.
- Gee B, Reynolds S, Carroll B, Orchard F, Clarke T, Martin D, et al. Practitioner review: effectiveness of indicated school-based interventions for adolescent depression and anxiety – a meta-analytic review. J Child Psychol Psychiatry 2020;61:739-56. https://doi.org/10.1111/jcpp.13209.
- Patalay P, Giese L, Stanković M, Curtin C, Moltrecht B, Gondek D. Mental health provision in schools: priority, facilitators and barriers in 10 European countries. Child Adolesc Ment Health 2016;21:139-47. https://doi.org/10.1111/camh.12160.
- Savanta ComRes . BBC School Report Mental Health Survey (Secondary School Teachers) n.d. https://comresglobal.com/polls/bbc-school-report-mental-health-survey-secondary-school-teachers/ (accessed 6 April 2022).
- Association of Colleges . Association of Colleges (AoC) Survey about Students With Mental Health Conditions in Further Education in England n.d. www.aoc.co.uk/sites/default/files/AoC%20survey%20on%20students%20with%20mental%20health%20conditions%20in%20Further%20Education%20-%20summary%20report%202015%20-%20FINAL.pdf (accessed 23 August 2021).
- Wolpert M, Harris R, Jones M, Hodges S, Fuggle P, James R, et al. THRIVE: The AFC–Tavistock Model for CAMHS n.d. www.annafreud.org/media/2552/thrive-booklet_march-15.pdf (accessed 6 April 2022).
- Parkin E, Long R. Support for Children and Young People’s Mental Health. London: House of Commons Library; 2020.
- Gee B, Wilson J, Clarke T, Farthing S, Carroll B, Jackson C, et al. Delivering mental health support within schools and colleges – a thematic synthesis of barriers and facilitators to implementation of indicated psychological interventions for adolescents. Child Adolesc Ment Health 2020;26:34-46. https://doi.org/10.1111/camh.12381.
- Paulus FW, Ohmann S, Popow C. Practitioner review: school-based interventions in child mental health. J Child Psychol Psychiatry 2016;57:1337-59. https://doi.org/10.1111/jcpp.12584.
- Proctor EK, Landsverk J, Aarons G, Chambers D, Glisson C, Mittman B. Implementation research in mental health services: an emerging science with conceptual, methodological, and training challenges. Adm Policy Ment Health 2009;36:24-3. https://doi.org/10.1007/s10488-008-0197-4.
- Vizard T, Pearce N, Davis J, Sadler K, Ford T, Goodman A, et al. Mental Health of Children and Young People in England, 2017: Emotional Disorders 2018. https://files.digital.nhs.uk/14/0E2282/MHCYP%202017%20Emotional%20Disorders.pdf (accessed 6 April 2022).
- Haby MM, Chapman E, Clark R, Barreto J, Reveiz L, Lavis JN. What are the best methodologies for rapid reviews of the research evidence for evidence-informed decision making in health policy and practice: a rapid review. Health Res Policy Syst 2016;14. https://doi.org/10.1186/s12961-016-0155-7.
- The World Bank . World Bank Country and Lending Groups n.d. https://datahelpdesk.worldbank.org/knowledgebase/articles/906519 (accessed 12 December 2022).
- Moher D, Liberati A, Tetzlaff J, Altman DG. PRISMA Group . Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLOS Med 2009;6. https://doi.org/10.1371/journal.pmed.1000097.
- Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol 2008;8. https://doi.org/10.1186/1471-2288-8-45.
- Nilsen P. Making sense of implementation theories, models and frameworks. Implement Sci 2015;10. https://doi.org/10.1186/s13012-015-0242-0.
- Durlak JA, DuPre EP. Implementation matters: a review of research on the influence of implementation on program outcomes and the factors affecting implementation. Am J Community Psychol 2008;41:327-50. https://doi.org/10.1007/s10464-008-9165-0.
- Zhao Y, Frank KA. Factors affecting technology uses in schools: an ecological perspective. Am Educ Res 2003;40:807-40. https://doi.org/10.3102/00028312040004807.
- Bei B, Byrne ML, Ivens C, Waloszek J, Woods MJ, Dudgeon P, et al. Pilot study of a mindfulness-based, multi-component, in-school group sleep intervention in adolescent girls. Early Interv Psychiatry 2013;7:213-20. https://doi.org/10.1111/j.1751-7893.2012.00382.x.
- Bernstein ER. Transportability of Evidence-Based Anxiety Interventions to a School Setting: Evaluation of a Modularized Approach to Intervention 2010.
- Berry K, Hunt CJ. Evaluation of an intervention program for anxious adolescent boys who are bullied at school. J Adolesc Health 2009;45:376-82. https://doi.org/10.1016/j.jadohealth.2009.04.023.
- Burke M, Prendeville P, Veale A. An evaluation of the ‘FRIENDS for Life’ programme among children presenting with autism spectrum disorder. Educ Psychol Pract 2017;33:435-49. https://doi.org/10.1080/02667363.2017.1367648.
- Butler-Hepler K. A Longitudinal Exploration of Factors Impacting Outcomes for Native American Students Participating in CBITS: Looking Beyond Quantitative Analysis 2013.
- Chu BC, Weissman AS. An initial description and pilot of group behavioral activation therapy for anxious and depressed youth. Cogn Behav Pract 2009;16:408-19. https://doi.org/10.1016/j.cbpra.2009.04.003.
- Chu BC, Crocco ST, Esseling P, Areizaga MJ, Linder AM, Skriner LC. Transdiagnostic group behavioural activation and exposure therapy for youth anxiety and depression: initial randomised controlled trial. Behav Res Ther 2016;76:65-7. https://doi.org/10.1016/j.brat.2015.11.005.
- Cooley MR, Boyd RC, Grados JJ. Feasibility of an anxiety preventive intervention for community violence exposed African-American children. J Primary Prev 2004;25:105-23. https://doi.org/10.1023/B:JOPP.0000039941.85452.ea.
- Cooper M, Rowland N, McArthur K, Pattison S, Cromarty K, Richards K. Randomised controlled trial of school-based humanistic counselling for emotional distress in young people: feasibility study and preliminary indications of efficacy. Child Adolesc Psychiatry Ment Health 2010;4. https://doi.org/10.1186/1753-2000-4-12.
- Crisp HL, Gudmundsen GR, Shirk SR. Transporting evidence-based therapy for adolescent depression to the school setting. Educ Treat Child 2006;29:287-309.
- Drmic IE, Aljunied M, Reaven J. Feasibility, acceptability and preliminary treatment outcomes in a school-based CBT intervention program for adolescents with ASD and anxiety in Singapore. J Autism Dev Disord 2017;47:3909-29. https://doi.org/10.1007/s10803-016-3007-y.
- Ehntholt KA, Smith PA. School-based cognitive-behavioural therapy group intervention for refugee children who have experienced war-related trauma. Clin Child Psychol Psychiatry 2005;10:235-50. https://doi.org/10.1177/1359104505051214.
- Feldman ES. Implementation of the Cognitive Behavioural Intervention for Trauma in Schools (CBITS) With Spanish-Speaking, Immigrant Middle-School Students: Is Effective, Culturally Competent Treatment Possible Within a Public School Setting? 2007.
- Fitzgerald A, Rawdon C, Dooley B. A randomized controlled trial of attention bias modification training for socially anxious adolescents. Behav Res Ther 2016;84:1-8. https://doi.org/10.1016/j.brat.2016.06.003.
- Gartenberg AS. School-Based CBT for Anxiety in Adolescents With High-Functioning Autism Spectrum Disorders: A Comparison of the Pragmatic Case Studies of Brian and Bridgette 2017.
- Ginsburg GS, Drake KL. School-based treatment for anxious African-American adolescents: a controlled pilot study. J Am Acad Child Adolesc Psychiatry 2002;41:768-75. https://doi.org/10.1097/00004583-200207000-00007.
- La Greca AM, Ehrenreich-May J, Mufson L, Chan S. Preventing adolescent social anxiety and depression and reducing peer victimization: intervention development and open trial. Child Youth Care Forum 2016;45:905-26. https://doi.org/10.1007/s10566-016-9363-0.
- Hunt C, Andrews G, Crino R, Erskine A, Sakashita C. Randomized controlled trial of an early intervention programme for adolescent anxiety disorders. Aust N Z J Psychiatry 2009;43:300-4. https://doi.org/10.1080/00048670902721152.
- Jaycox LH, Langley AK, Stein BD, Wong M, Sharma P, Scott M, et al. Support for students exposed to trauma: a pilot study. School Ment Health 2009;1:49-60. https://doi.org/10.1007/s12310-009-9007-8.
- Kaplinski HC. Client Characteristics and Barriers to Treatment in Cognitive-Behavioral Therapy for Adolescent Depression 2007.
- Lamb JM, Puskar KR, Sereika SM, Corcoran M. School-based intervention to promote coping in rural teens. MCN Am J Matern Child Nurs 1998;23:187-94. https://doi.org/10.1097/00005721-199807000-00005.
- Liberman RP, Robertson MJ. A pilot, controlled skills training study of schizotypal high school students. Verhaltenstherapie 2005;15:176-80. https://doi.org/10.1159/000087775.
- Listug-Lunde L, Vogeltanz-Holm N, Collins J. A cognitive-behavioral treatment for depression in rural American Indian middle school students. Am Indian Alsk Native Ment Health Res 2013;20:16-34. https://doi.org/10.5820/aian.2001.2013.16.
- Livheim F, Hayes L, Ghaderi A, Magnusdottir T, Högfeldt A, Rowse J, et al. The effectiveness of acceptance and commitment therapy for adolescent mental health: Swedish and Australian pilot outcomes. J Child Fam Stud 2015;24:1016-30. https://doi.org/10.1007/s10826-014-9912-9.
- Masia CL, Klein RG, Storch EA, Corda B. School-based behavioral treatment for social anxiety disorder in adolescents: results of a pilot study. J Am Acad Child Adolesc Psychiatry 2001;40:780-6. https://doi.org/10.1097/00004583-200107000-00012.
- Masia-Warner C, Klein RG, Dent HC, Fisher PH, Alvir J, Albano AM, et al. School-based intervention for adolescents with social anxiety disorder: results of a controlled study. J Abnorm Child Psychol 2005;33:707-22. https://doi.org/10.1007/s10802-005-7649-z.
- Masia Warner C, Colognori D, Brice C, Herzig K, Mufson L, Lynch C, et al. Can school counselors deliver cognitive-behavioral treatment for social anxiety effectively? A randomized controlled trial. J Child Psychol Psychiatry 2016;57:1229-38. https://doi.org/10.1111/jcpp.12550.
- McCarty CA, Violette HD, McCauley E. Feasibility of the positive thoughts and actions prevention program for middle schoolers at risk for depression. Depress Res Treat 2011;2011. https://doi.org/10.1155/2011/241386.
- Mazurek Melnyk B, Kelly S, Lusk P. Outcomes and feasibility of a manualized cognitive-behavioral skills building intervention: group COPE for depressed and anxious adolescents in school settings. J Child Adolesc Psychiatr Nurs 2014;27:3-13. https://doi.org/10.1111/jcap.12058.
- Messinger JW, Trémeau F, Antonius D, Mendelsohn E, Prudent V, Stanford AD, et al. Avolition and expressive deficits capture negative symptom phenomenology: implications for DSM-5 and schizophrenia research. Clin Psychol Rev 2011;31:161-8. https://doi.org/10.1016/j.cpr.2010.09.002.
- Morsette A, van den Pol R, Schuldberg D, Swaney G, Stolle D. Advances in school mental health promotion cognitive behavioral treatment for trauma symptoms in American Indian youth: preliminary findings and issues in evidence-based practice and reservation culture. Adv Sch Ment Health Promot 2012;5:51-62. https://doi.org/10.1080/1754730X.2012.664865.
- Mowatt HS. School-Based Implementation of a Prevention of Depression Program With Urban At-Risk Adolescents 2017.
- Mufson L, Dorta KP, Wickramaratne P, Nomura Y, Olfson M, Weissman MM. A randomized effectiveness trial of interpersonal psychotherapy for depressed adolescents. Arch Gen Psychiatry 2004;61:577-84. https://doi.org/10.1001/archpsyc.61.6.577.
- Oros E. The Effectiveness of Dialectical Behavior Therapy-Based Group Skills Training in a Traditional High School Setting 2016.
- Pass L, Sancho M, Brett S, Jones M, Reynold S. Brief Behavioural Activation (Brief BA) in secondary schools: a feasibility study examining acceptability and practical considerations. Educ Child Psychol 2018;35:10-2.
- Pearson KE. Effects of Anxiety Treatment Using Coping Cat on Problem Behaviors in the Classroom 2017.
- Rickard ED, Brosnan E, O’Laoide A, Wynne C, Keane M, McCormack M, et al. A first-level evaluation of a school-based family programme for adolescent social, emotional and behavioural difficulties. Clin Child Psychol Psychiatry 2016;21:603-17. https://doi.org/10.1177/1359104515603216.
- Riley A. Exploring the effects of the ‘Seasons for Growth’ intervention for pupils experiencing change and loss. Educ Child Psychol 2012;29:38-53.
- Robinson J, Hetrick S, Cox G, Bendall S, Yung A, Pirkis J. The safety and acceptability of delivering an online intervention to secondary students at risk of suicide: findings from a pilot study. Early Interv Psychiatry 2015;9:498-506. https://doi.org/10.1111/eip.12136.
- Rohde P, Stice E, Shaw H, Gau JM. Cognitive-behavioral group depression prevention compared to bibliotherapy and brochure control: nonsignificant effects in pilot effectiveness trial with college students. Behav Res Ther 2014;55:48-53. https://doi.org/10.1016/j.brat.2014.02.003.
- Ruffolo MC, Fischer D. Using an evidence-based CBT group intervention model for adolescents with depressive symptoms: lessons learned from a school-based adaptation. Child Fam Soc Work 2009;14:189-97. https://doi.org/10.1111/j.1365-2206.2009.00623.x.
- Schoenfeld NA, Mathur SR. Effects of cognitive-behavioral intervention on the school performance of students with emotional or behavioral disorders and anxiety. Behav Disord 2009;34:184-95. https://doi.org/10.1177/019874290903400401.
- Scotti JF. School-Based DBT Skills Groups for Adolescent Eating Disorders and Body Image Concerns: A Pilot Study 2014.
- Stasiak K, Hatcher S, Frampton C, Merry SN. A pilot double blind randomized placebo controlled trial of a prototype computer-based cognitive behavioural therapy program for adolescents with symptoms of depression. Behav Cogn Psychother 2014;42:385-401. https://doi.org/10.1017/S1352465812001087.
- Stein BD, Jaycox LH, Kataoka SH, Wong M, Tu W, Elliott MN, et al. A mental health intervention for schoolchildren exposed to violence: a randomized controlled trial. JAMA 2003;290:603-11. https://doi.org/10.1001/jama.290.5.603.
- Stein BD, Jaycox LH, Kataoka SH, Wong M, Langley AK, Avila JL, et al. Helping Children Cope with Violence and Trauma: A School-Based Program that Works. Santa Monica, CA: RAND Corporation; 2011.
- Stice E, Rohde P, Shaw H, Gau J. An effectiveness trial of a selected dissonance-based eating disorder prevention program for female high school students: long-term effects. J Consult Clin Psychol 2011;79:500-8. https://doi.org/10.1037/a0024351.
- Woods B, Jose PE. Effectiveness of a school-based indicated early intervention program for Māori and Pacific adolescents. J Pacific Rim Psychol 2011;5:40-5. https://doi.org/10.1375/prp.5.1.40.
- Young JF, Mufson L, Gallop R. Preventing depression: a randomized trial of interpersonal psychotherapy-adolescent skills training. Depress Anxiety 2010;27:426-33. https://doi.org/10.1002/da.20664.
- Young JF, Benas JS, Schueler CM, Gallop R, Gillham JE, Mufson L. A randomized depression prevention trial comparing interpersonal psychotherapy – adolescent skills training to group counseling in schools. Prev Sci 2016;17:314-24. https://doi.org/10.1007/s11121-015-0620-5.
- Turner C. Ofsted is considering new assessment to ensure schools look after pupils’ mental health and wellbeing. The Telegraph 2018. www.telegraph.co.uk/education/2018/12/22/ofsted-considering-new-assessment-ensure-schools-look-pupils (accessed 6 April 2022).
- Ofsted . Education Inspection Framework: Draft for Consultation 2019.
- Wormald C. Collaboration to Improve Mental Health Support for Young People n.d. https://civilservice.blog.gov.uk/2018/02/27/collaboration-to-improve-mental-health-support-for-young-people/ (accessed 6 April 2022).
- Anderson JK, Ford T, Soneson E, Coon JT, Humphrey A, Rogers M, et al. A systematic review of effectiveness and cost-effectiveness of school-based identification of children and young people at risk of, or currently experiencing mental health difficulties. Psychol Med 2019;49:9-19. https://doi.org/10.1017/S0033291718002490.
- Soneson E, Howarth E, Ford T, Humphrey A, Jones PB, Thompson Coon J, et al. Feasibility of school-based identification of children and adolescents experiencing, or at-risk of developing, mental health difficulties: a systematic review. Prev Sci 2020;21:581-603. https://doi.org/10.1007/s11121-020-01095-6.
- Gronholm PC, Nye E, Michelson D. Stigma related to targeted school-based mental health interventions: a systematic review of qualitative evidence. J Affect Disord 2018;240:17-26. https://doi.org/10.1016/j.jad.2018.07.023.
- Pella JE, Ginsburg GS, Casline E, Pikulski PJ, Drake KL. Children’s perceptions of barriers to session attendance in school-based treatment for anxiety. School Ment Health 2018;10:417-27. https://doi.org/10.1007/s12310-018-92.
- Rapee RM, Wignall A, Sheffield J, Kowalenko N, Davis A, McLoone J, et al. Adolescents’ reactions to universal and indicated prevention programs for depression: perceived stigma and consumer satisfaction. Prev Sci 2006;7:167-77. https://doi.org/10.1007/s11121-006-0035-4.
- Association of Colleges . Mental Health &Amp; Wellbeing: A Collection of College Case Studies 2018.
- Frith E. Children and Young People’s Mental Health: State of the Nation. London: Education Policy Institute; 2016.
- Byrne G, Murphy S, Connon G. Mentalization-based treatments with children and families: a systematic review of the literature. Clin Child Psychol Psychiatry 2020;25:1022-48. https://doi.org/10.1177/1359104520920689.
- Gratz KL, Roemer L. Multidimensional assessment of emotion regulation and dysregulation. J Psychopathol Behav Assess 2004;26:41-54. https://doi.org/10.1023/B:JOBA.0000007.
- Kerres Malecki CK, Kilpatrick Demaray MK. Measuring perceived social support: development of the child and adolescent social support scale (CASSS). Psychol Sch 2002;39:1-18. https://doi.org/10.1002/pits.10004.
- Hodgekins J, French P, Birchwood M, Mugford M, Christopher R, Marshall M, et al. Comparing time use in individuals at different stages of psychosis and a non-clinical comparison group. Schizophr Res 2015;161:188-93. https://doi.org/10.1016/j.schres.2014.12.011.
- Zanarini MC. Childhood Interview for DSM-IV Borderline Personality Disorder (CI-BPD). McLean Hospital; 2003.
- Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, et al. Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry 1996;36:980-8. https://doi.org/10.1097/00004583-199707000-00021.
- Rampton B, Bezemer J, Jewitt C, Lefstein A. Illustrations of linguistic ethnography in action: indicative analyses of a job interview. Ethnography Lang Comm 2007:1-28. https://eprints.ncrm.ac.uk/id/eprint/1481/1/LE%20illustrative%20analyses%20takehome%2012mar073.pdf.
- Jefferson G, Lerner G. Conversation Analysis: Studies from the First Generation. Amsterdam: John Benjamins Publishing Company; 2004.
- Crick NR, Murray-Close D, Woods K. Borderline personality features in childhood: a short-term longitudinal study. Dev Psychopathol 2005;17:1051-70. https://doi.org/10.1017/S0954579405050492.
- Vrouva I, Fonagy P, Fearon PR, Roussow T. The risk-taking and self-harm inventory for adolescents: development and psychometric evaluation. Psychol Assess 2010;22:852-65. https://doi.org/10.1037/a0020583.
- Julious SA. Sample size of 12 per group rule of thumb for a pilot study. Pharm Stat 2005;4:287-91. https://doi.org/10.1002/pst.185.
- Sim J, Lewis M. The size of a pilot study for a clinical trial should be calculated in relation to considerations of precision and efficiency. J Clin Epidemiol 2012;65:301-8. https://doi.org/10.1016/j.jclinepi.2011.07.011.
- Department for Education . National Pupil Database n.d. www.gov.uk/government/collections/national-pupil-database (accessed February 2022).
- Chisholm D, Knapp MR, Knudsen HC, Amaddeo F, Gaite L, van Wijngaarden B. Client Socio-Demographic and Service Receipt Inventory – European Version: development of an instrument for international research. EPSILON Study 5. European Psychiatric Services: Inputs Linked to Outcome Domains and Needs. Br J Psychiatry Suppl 2000;39:s28-33. https://doi.org/10.1192/bjp.177.39.s28.
- Rampton B, Tusting K, Maybin J, Barwell R, Creese A, Lytra V. UK linguistic ethnography: a discussion paper. UK Linguistic Ethnography Forum 2004:1-24. www.lancaster.ac.uk/fss/organisations/lingethn/documents/discussion_paper_jan_05.pdf (accessed 6 April 2022).
- Murdoch J. Process evaluation for complex interventions in health services research: analysing context, text trajectories and disruptions. BMC Health Serv Res 2016;16. https://doi.org/10.1186/s12913-016-1651-8.
- Curtis L, Burns A. Unit Costs of Health and Social Care 2019. Canterbury: PSSRU, University of Kent; 2019.
- Herdman M, Gudex C, Lloyd A, Janssen M, Kind P, Parkin D, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res 2011;20:1727-36. https://doi.org/10.1007/s11136-011-9903-x.
- van Hout B, Janssen MF, Feng YS, Kohlmann T, Busschbach J, Golicki D, et al. Interim scoring for the EQ-5D-5L: mapping the EQ-5D-5L to EQ-5D-3L value sets. Value Health 2012;15:708-15. https://doi.org/10.1016/j.jval.2012.02.008.
- Hawe P, Shiell A, Riley T. Theorising interventions as events in systems. Am J Community Psychol 2009;43:267-76. https://doi.org/10.1007/s10464-009-9229-9.
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing and Evaluating Complex Interventions. n.d. https://mrc.ukri.org/documents/pdf/complex-interventions-guidance/ (accessed February 2022).
- Murphy A, Bourke J, Flynn D, Kells M, Joyce M. A cost-effectiveness analysis of dialectical behaviour therapy for treating individuals with borderline personality disorder in the community. Ir J Med Sci 2020;189:415-23. https://doi.org/10.1007/s11845-019-02091-8.
- British Psychological Society . Mental Health Support Teams: How to Maximise the Impact of the New Workforce for Children and Young People 2019.
Glossary
- Co-delivery
- Joint delivery of intervention sessions by practitioners working alongside each other.
- Formulation
- A structured approach to understanding the factors underlying the development and maintenance of a person’s difficulties to inform a plan for intervention.
- Jeffersonian
- A system of transcription notation designed to enable the transcriber to capture speech patterns such as stress, intonation, pauses and overlap.
- Mentalisation
- The ability to make sense of the behaviour of oneself and others in terms of intentional mental states, for example thoughts and feelings.
List of abbreviations
- A&E
- accident and emergency
- AfC
- Agenda for Change
- BEST
- Brief Education Supported Treatment
- BPD
- borderline personality disorder
- BPFSC
- Borderline Personality Features Scale for Children
- CAMHS
- Child and Adolescent Mental Health Service
- CASSS
- Childhood and Adolescent Social Support Scale
- CAT
- cognitive analytic therapy
- CBT
- cognitive behavioural therapy
- CI-BPD
- Childhood Interview for Borderline Personality Disorder
- CSRI
- client service receipt inventory
- CTU
- clinical trials unit
- CYP IAPT
- Children and Young People’s Improving Access to Psychological Therapies
- DBT-A
- dialectical behaviour therapy for adolescents
- DERS
- Difficulties in Emotion Regulation Scale
- EMHP
- educational mental health practitioner
- EQ-5D-5L
- EuroQol-5 Dimensions, five-level version
- EQ-5D-VAS
- EuroQol-5 Dimensions, visual analogue scale
- GP
- general practitioner
- K-SADS
- Kiddie Schedule for Affective Disorders and Schizophrenia
- LTP
- local transformation plan
- MBT-A
- mentalisation-based treatment for adolescents
- MHST
- mental health support team
- NPD
- National Pupil Database
- Ofsted
- Office for Standards in Education, Children’s Services and Skills
- PPI
- patient and public involvement
- RCT
- randomised controlled trial
- RTSHI-A
- Risk Taking and Self Harm Inventory for Adolescents
- SAE
- serious adverse event
- SPIRIT
- Standard Protocol Items: Recommendations for Interventional Trials
- TAU
- treatment as usual
- TSC
- Trial Steering Committee
- TUS
- Time Use Survey
- VAS
- visual analogue scale
