Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its proceeding programmes as project number 09/1801/1026. The contractual start date was in May 2010. The final report began editorial review in August 2012 and was accepted for publication in January 2013. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors' report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Notes
For data confidentiality purposes, all figures are rounded to the nearest 5. Where there are fewer than five records for any breakdown, the number for that particular breakdown will be hidden but is still included in the rounded totals.
These data are taken from the Electronic Staff Record Data Warehouse, and as such represent only staff directly employed by NHS organisations. Two private provider organisations have recently been commissioned to provide community services: Serco in NHS Suffolk and Virgin Care in NHS Surrey. The figures reported relate to the PCT employees before transfer to private providers.
All qualified nursing staff were included, nursing assistants and auxiliaries as were, and health-care assistants who are recorded as working in an adult or general community setting.
Professionally qualified nursing staff:
-
N0H Community Services: nurse manager
-
N4H Community Services: nurse – district/community psychiatric nurse (CPN)/community learning disability nurse (CLDN) – first level
-
N5H Community Services: nurse – district/CPN/CLDN – second level
-
N6H Community Services: nurse – other first level
-
N7H Community Services: nurse – other second level
-
NAH Community Services: nurse consultant
-
NCH Community Services: nurse – modern matron
-
NEH Community Services: nurse – community matron.
Nursing and HCA staff:
-
N9H Community Services: nursing assistant/auxiliary
-
NFH Community Services: nursing AP
-
H2F Community Services: support workers
-
H1F Community Services: HCAs.
The following staff were excluded (as they are recorded as working in children's services, health visiting, learning disabilities or community psychiatry):
-
N0D Community Psychiatry: nurse manager
-
N0F Community Learning Disabilities: nurse manager
-
N1H Community Services: nurse qualified sick children's
-
N3H Community Services: health visitor
-
N4D Community Psychiatry: nurse – district/CPN/CLDN – first level
-
N4F Community Learning Disabilities: nurse – district/CPN/CLDN – first level
-
N5D Community Psychiatry: nurse – district/CPN/CLDN – second level
-
N6D Community Psychiatry: nurse – other first level
-
N6F Community Learning Disabilities: nurse – other first level
-
N7D Community Psychiatry: nurse – other second level
-
N7F Community Learning Disabilities: nurse – other second level
-
N8H Community Services: nursery nurse
-
N9D Community Psychiatry: nursing assistant/auxiliary
-
N9F Community Learning Disabilities: nursing assistant/auxiliary
-
NAD Community Psychiatry: nurse consultant
-
NAF Community Learning Disabilities: nurse consultant
-
NCD Community Psychiatry: nurse – modern matron
-
NCF Community Learning Disabilities: nurse – modern matron
-
NFD Community Psychiatry: nursing AP
-
NFF Community Learning Disabilities: nursing AP.
Permissions
Copyright statement
© Queen's Printer and Controller of HMSO 2013. This work was produced by Spilsbury et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Headline
Study describes the opportunities and challenges associated with the use of assistants to deliver care by the community nursing team. Study suggests that further attention at national and local levels is required to support and mediate the development of these roles in the future so as to promote the delivery of quality, safe and acceptable care. As provider organisations plan for delivering the future ambitious community services agenda, the role of the assistant is likely to have increasing importance.
Chapter 1 Introduction
Primary and community care services are the first point of contact within the NHS for most service users. 1 Public demand for these services is growing as a result of demographic changes, increasing public expectations of quality and choice, the changing nature of disease and disease management, continuing advances in technology and treatments, and the shifting focus from hospital- to community-based services. 2 The NHS review advocated primary and community care services that promote health, provide timely access for people experiencing ill health, are based on pathways of care, reflect the needs of service users and focus on promoting quality and safety. 1,2 The focus on service redesign to improve quality and efficiency requires the skills of the entire health-care team (both professionals and assistant staff) to be supported, developed and, crucially, deployed in the most efficient way. 3,4 However, the workforce planning and development that must accompany these changes has received minimal attention in primary and community care. 5
The assistant workforce
There are over 350,000 health-care assistants (HCAs) estimated to be working in the UK, of whom approximately 120,000 work in the NHS. 6 HCAs working with registered nurses (RNs) have been described by the Nursing and Midwifery Council (NMC)7 as:
Those who provide a direct service – that is they have a direct influence/effect on care and treatment to patients and members of the public and are supervised by and/or undertake health-care duties delegated to them by NMC registrants.
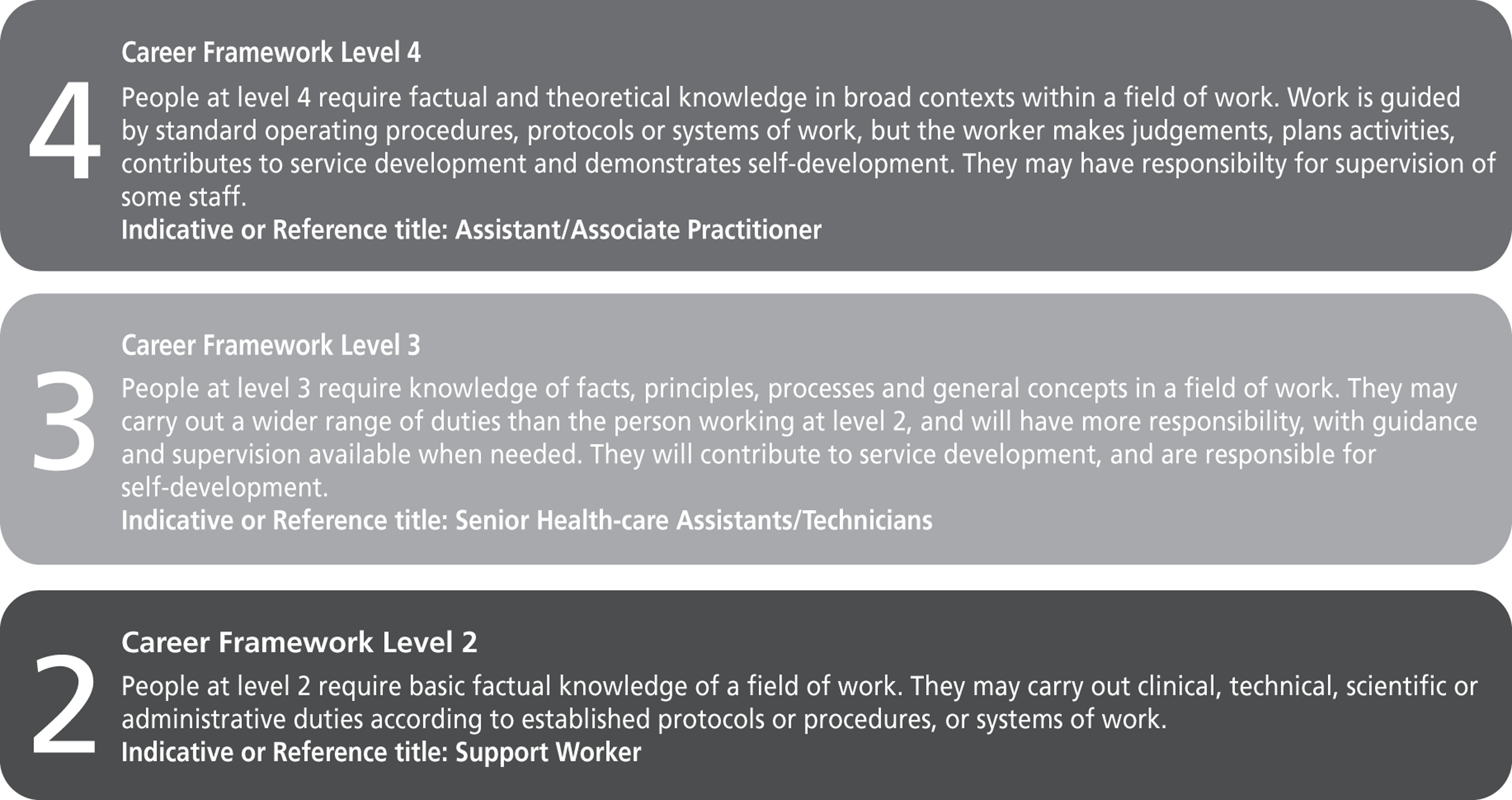
The national UK Skills for Health Career Framework8 describes the roles of all health-care staff in terms of level of competence. There are nine levels of competence, and assistant staff occupy levels 2, 3 and 4 (see Appendix 1). HCA is the role title applied to staff working at levels 2 and 3. Assistant or associate practitioner (AP) refers to staff at level 4. The expectations are that HCAs carry out protocol-based tasks that have been delegated to them by a registered practitioner (level 3 HCAs assuming more complex tasks and responsibility than level 2 HCAs) and APs are expected to deliver protocol-based clinical care and carry out assessments under the direction and supervision of a state registered practitioner. A definition of the AP role is offered by Skills for Health:9
An Assistant Practitioner is defined as a worker who competently delivers health and social care to and for people. They have a required level of knowledge and skill beyond that of the traditional health-care assistant or support worker. The Assistant Practitioner would be able to deliver elements of health and social care and undertake clinical work in domains that have previously only been within the remit of registered professionals. The Assistant Practitioner may transcend professional boundaries. They are accountable to themselves, their employer and, more importantly, the people they serve.
p. 1
There are no plans for the regulation of assistants in the NHS and they are currently not required to have any formal training or hold a recognised qualification. This has raised concerns about patient safety and quality of care. 10 However, the Career Framework for the NHS11 has emphasised a more structured approach to training and role competence for the entire health-care workforce. In theory, this more structured approach should mean that RNs (graded at level 5 and above) are supported by APs (level 4), and senior HCAs (level 3) and HCAs (level 2) trained to a level appropriate for their roles and levels of working. However, it is currently unclear how these different levels of worker are deployed in community nursing services and what aspects of nursing work they each perform. Our study aims to better understand the roles of community nursing assistants and their potential contribution to and impact on service delivery and patient care.
The report
First, the report presents the policy and literature context for the study (see Chapter 2), highlighting the limited evidence base about community nursing assistant roles. Chapter 3 presents the research objectives and the focus of Chapter 4 is to outline our research approach and methods. The study findings are presented in Chapters 5–7. Chapter 5 considers the changing landscape of community nursing and provides important context for the subsequent findings chapters; Chapter 6 scopes the roles of assistants in community nursing teams in England; and Chapter 7 explores in more depth the day-to-day use of assistants in providing community nursing services. Chapter 8 draws together the findings of the study, presenting main headlines and conclusions.
The study protocol is provided in Appendix 2. The study was supported by a National Institute for Health Research (NIHR) Service Delivery and Organisation Management fellowship. A senior NHS manager was seconded for 1 year to work alongside the research team. Further details about the fellowship are provided in Appendix 3.
Chapter 2 Background
It is a central part of our strategy … that we support the NHS and community clinicians in transforming these services and according them equal status to other NHS services.
NHS Next Stage Review,1 p. 43
Introduction
An international focus on more flexible working practices has led to changes in roles for the entire UK (and international) nursing workforce through role extension, expansion and redesign. 12 Such changes have potentially important implications for patient care and outcomes, as well as for service delivery and nursing teamwork. This study is concerned specifically with the introduction and development of assistant roles within adult community nursing services. This chapter defines the focus for the study – including what is meant by community nursing and assistant – and locates the study within existing policy and literature.
Defining community nursing
There are many definitions of community health services but they all share a number of key functions. These functions can all be linked to the following roles:
-
delivering treatment in a community or home setting and, where possible, avoiding unnecessary admission to hospital
-
supporting case management and disease management for those with complex long-term conditions and promoting independence
-
supporting rehabilitation
-
preventing disease and promoting health and healthy behaviours
-
providing palliative care
-
providing end-of-life care; and
-
supporting the health and well-being of carers.
A range of health-care staff are involved in the delivery of community health services, but nurses have an important role, accounting for about 70% of the community health-care workforce. 13 Understanding changes in skill mix within community nursing teams is therefore important for understanding potential impacts of these changes on service delivery, patient care and outcomes.
Community nursing refers, in its broadest sense, to any nursing care delivered outside the hospital setting, such as in patients' homes or health centres, or residential care. A wide variety of services and teams come under this banner, for example district nursing, intermediate care, falls prevention, tissue viability and community-based respiratory teams. Imison13 provided the following definition of district nursing:
District nurses work with teams of community nurses and support workers to provide advice and care to patients and their carers in the community in areas such as palliative care, wound management, catheter and continence care, and medication support; the work involves both follow-up care for recently discharged hospital inpatients, and longer-term care for chronically ill patients, as well as working to prevent unnecessary or avoidable hospital admissions.
p. 5
In a study of community nursing workload,14 the most common diagnostic categories for patients visited by district nurses included anaemia and other deficiencies, continence problems, cancer and health threats such as hypertension, diabetes, heart conditions, abscesses and ulcers, wounds, and mental health and addiction problems. The following services (in addition to assessment) were frequently provided by the community nurses: advice and support, phlebotomy, injection, wound care, monitoring and/or screening, continence management, pain control, pressure area care, administration of medicines, bowel care, percutaneous endoscopic gastrostomy (PEG) feeding (PEG feeding tubes are used to administer long-term enteral nutrition to patients in whom adequate nutrition cannot be maintained with oral intake), equipment, general nursing care, skin care and health education. 14 Other clinical work undertaken by community nurses includes prescribing, medication reviews, risk assessment, urinary catheterisation, intravenous therapy (including cancer chemotherapy), end-of-life care, bereavement care, interagency referral and patient advocacy. 15 There is also a growing recognition of the role that community nurses play in anticipatory care. 16 Our study aims to describe the roles and potential contributions that assistant staff play in supporting RNs in the delivery of care to patients in the community, including perceived impacts on patient experience and patient choice.
Opportunities for community health services and nursing
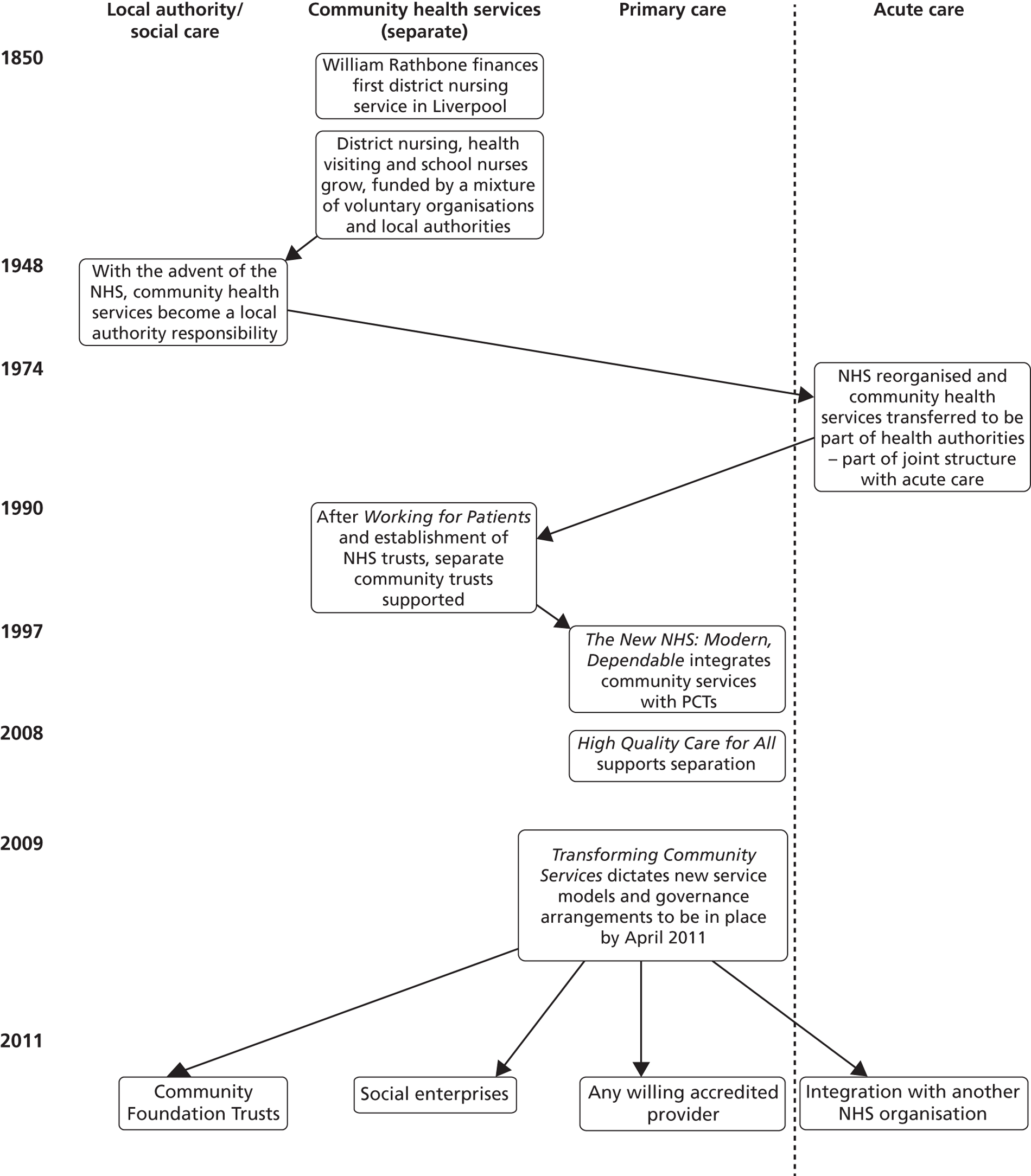
Community nursing (and health) services are faced with the growing challenge of caring for increasingly dependent patients with ever more complex needs as the disease burden shifts from acute to chronic conditions. This is further challenged by the emphasis on providing care and services closer to patients' homes rather than in hospital settings. Imison13 noted that, since the inception of the NHS in 1948, the pattern of provision of care has changed little: specialists are generally located in hospitals, general practitioners (GPs) in surgeries, and community health service staff are largely peripatetic, detached from both primary and secondary care. Community health services are considered to have had many years of inattention and underinvestment, which in turn is considered to have led to fragmented services17 and created variations in terms of the performance and productivity of community services. 13 However, these services have come under the spotlight during the last 5 years. Recent policies have created the opportunity for significant developments in the structure, organisation and provision of community health services. This includes the provision of local health-care systems to address the needs of the most vulnerable in their populations, particularly patients with chronic and disabling conditions. The reorganisations of community health services are captured in Imison's report13 and are represented here in Figure 1. It is these most recent changes that are of relevance to this report.
In 2008, Lord Darzi's review of the NHS2 signalled a shift in the focus of care from hospital to community settings. This marked the start of the separation of the commissioning and provider functions of primary care trusts (PCTs) in England, UK. PCTs were prompted to consider different forms of provision of community health services under the ‘any accredited willing provider’ model. The publication of Transforming Community Services18 set out the timetable for these changes to occur; by April 2011, PCTs were to have completed the transfer of services and governance arrangements to support new models of service provision. It is important to note here that these developments have led to turbulence and changes in the landscape of community health services, including community nursing. This policy context and the changes instigated are considered in further detail in Chapter 5 because these provide an important backdrop for understanding the findings of this study. In addition, it is important to highlight here the changes in commissioning because this is also impacting on community health-care provision.
Historically, UK NHS budgets were distributed from the Department of Health via regional and local health authorities, and community organisations received their funding through a block contract which was not related to the quality or volume of work delivered, but reflected their staffing commitments. PCT commissioning, introduced in 2005,19 involved moving away from contracts to a focus on service provision to meet the health needs of the local population. 20 A PCT's commissioning function included:
-
development of appropriate service specifications
-
defining measurable outcomes of care; and
-
ongoing monitoring and evaluation of service provision.
When developing a service specification, commissioners are expected to concentrate on care pathways and the outcomes of care delivery. In response, provider organisations have the freedom to shape their service provision to meet the expected service outcomes.
It is important to consider next the community nursing workforce, including the assistant workforce, and its contribution to the delivery of services.
Community nursing workforce
Community health services employ approximately 250,000 staff; this represents one-fifth of the NHS workforce in England. 1 These services employ an almost entirely non-medical workforce. More than 70% of the community services workforce (in its broadest sense) is made up of nurses and their support staff,13 with allied health professionals – such as physiotherapists, occupational therapists, speech and language therapists and community pharmacists – making up a further 20% of community staff. Therefore, the effectiveness of community services is largely dependent on the effectiveness of the (relatively predominant) nursing workforce:
The quality of experiences and outcomes of the people who use our services are almost entirely due to their interactions with our staff.
Lord Warner,21 p. 1
It is estimated that district nurses visit more than 2.6 million people per year, and the need for skilled home nursing is rising as the population ages, as more people live with long-term conditions, and as patients are discharged home earlier from hospital. 22,23 One in four people aged > 75 years, and one in two of those aged > 85 years, will receive care from a district nurse. 24 Community nursing services are delivered by both RNs (Agenda for Change band 5 and above) and their assistant staff (Agenda for Change bands 2, 3 and 4). 25 Securing a sufficient number of nursing staff with the appropriate skills across these levels, and deploying them effectively, is a highly complex challenge. Nonetheless, it is an increasingly important priority given the current economic climate and financial constraints in the NHS. The skills of the entire nursing workforce need to be deployed and used appropriately and efficiently. 26 The concerns of current government policy emphasise the importance of productivity, efficiency and quality. 4 The Queen's Nursing Institute23 is keen to ensure that the right nurse with the right skills provides care to people in their own homes; these patients tend to be among the most vulnerable in society, and the care they receive is delivered behind closed doors. This study was concerned specifically with understanding the contribution and potential impacts of community nursing assistants in the delivery of care by community nursing services. To provide context, it is important to consider the evolution of the community assistant role.
Evolution of community nursing assistants
The presence of assistants in nursing today has a history which has been well documented. 27–30 It is important to highlight that the shape of nursing practice today is the result of varied and complex sociopolitical interactions occurring over time, in a variety of social arenas and at differing policy levels. 31 Despite the introduction of a register for nurses, nursing care has continued to be delivered by a variety of workers, including assistants working at a range of levels with varied skills, knowledge and experience.
Assistants have been the focus of recent workforce reform in the UK, with polices supporting their growth in numbers and increasing scope of practice;32 assistant staff have been proposed as a means to meet future service demands. They are perceived to be an economically effective way to deliver care while enabling the registered workforce to upskill and provide more specialist services or meet the needs of more complex patients. The report of the Department of Health's Value for Money unit looked at district nurses' tasks in their daily work. 33 It recommended that more of this work could be delegated to other nurses and assistants, with higher grade district nurses becoming managers of care and fewer higher grade district nurses required in the future. 33 In the 20 years since this report was published, there has been an unprecedented increase in the numbers of assistants. The number of assistants in community nursing teams is reported to have increased by 118% to 16,968 over a 10-year period (1996–2006). 34 The number of qualified district nurses has fallen by around 23%, from 12,350 to 10,008, and the number of registered (but not necessarily community specialist) nurses in community services has increased by 38% to 35,179. 34 These changes in the composition of the community nursing workforce have diluted the skill mix and been accompanied by wide-ranging debates about role boundaries between RNs and assistant staff.
Determining the skill mix required to deliver health care is an important, but complex, issue. A number of drivers influence the health system and therefore the human resources required to deliver a service. Key drivers include skill shortages, cost containment, quality improvement, technological innovation, new medical interventions, new health sector programmes or initiatives, health sector reform and changes in the legislative or regulatory environment. 35 These are not mutually exclusive; more than one driver will often be acting on a health system at any one time, and a combination of these drivers has led to the increasing numbers of assistants in today's UK health-care workforce.
There are several factors influencing the demand and supply of nurses that are having an impact on community nursing services, as well as shaping the roles of community nurses and their assistant staff. These include:
-
demographic trends and the impact of an ageing population on future demands for health and social services
-
the changing acuity and complexity of patients being cared for in the community
-
changing public expectations of the health service
-
concerns with the delivery of evidence-based practice
-
technological changes that impact on training and staffing requirements
-
changes in workforce availability within the UK (and international) labour market; and
-
key policy changes and implications for the funding of health services.
These factors are influencing the profile of the community nursing workforce. This is occurring against the backdrop of an ageing community nursing workforce; more than 30% of the current district nursing and health visitor workforce are aged > 50 years, and could retire within the next 10 years. 36 Alongside this, the number of training places commissioned for district nurses is decreasing. 23 Much of the care delivered by nurses in the community may be considered routine. However, the growing number of more dependent patients with complex needs and the unpredictability of caring for someone at home mean that there is a need for an appropriate skill mix within community nursing teams. Such a skill mix includes RNs and nurses with extended and specialist skills but also incorporates assistants working at different levels.
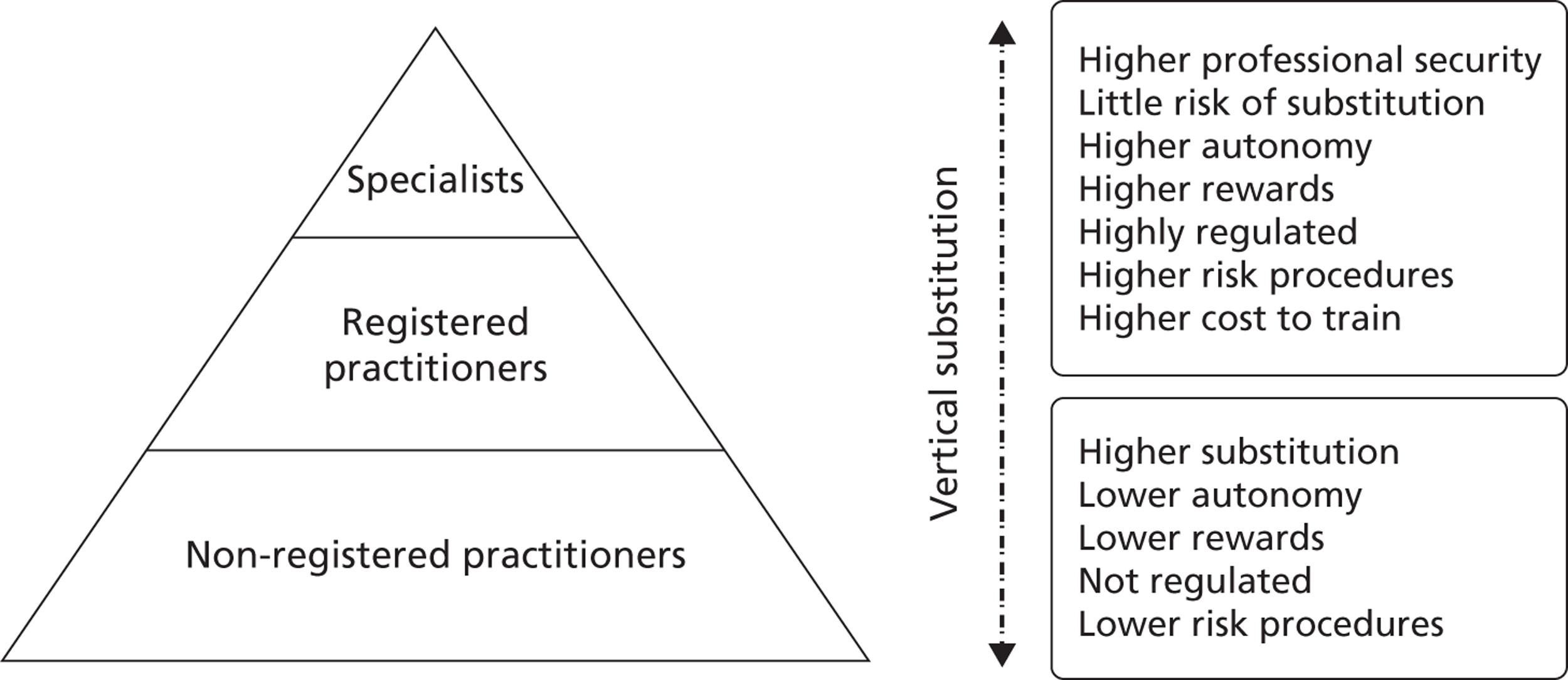
Nancarrow and Borthwick37 (p. 30) have provided a useful framework for understanding changing roles within the general health-care workforce (Figure 2). They identified movement of the workforce in four directions:
-
diversification: new work or new ways of performing work
-
specialisation: adoption of increasing levels of expertise
-
horizontal substitution: undertaking roles of another discipline by workers of a similar level of training and expertise
-
vertical substitution: delegation or adoption of tasks across disciplinary boundaries.
Within the community nursing workforce, there has been vertical substitution whereby some of the work of registered practitioners is being undertaken by assistant staff. The consequence of this substitution is that lower-risk work is being performed by unregulated staff with less autonomy and lower financial rewards. Moving work vertically among RNs and assistant staff raises a number of important issues that are located within the professional discourse on community nursing: boundaries and responsibilities of assistants, levels of supervision and regulation. Less is known about whether or not there is diversification or specialisation of roles for assistants in community nursing teams. These directions of change for assistant roles in community nursing teams are important considerations for our study.
The Royal College of Nursing (RCN)38 has developed definitions for the roles of HCAs and APs, and these provide a useful context for our study (Box 1). Assistants work at different levels to support the work of registered practitioners. The levels of work expected of assistants in community nursing teams can be linked with the levels of working described by Skills for Health in 2010 (Figure 3). 8 This indicates the levels of understanding, knowledge and skill required by assistants operating at these different levels, as well as levels of responsibility and required supervision. Importantly, assistant staff are not regulated and there are no plans for progressing this in the Health and Social Care Act 2012. 39 However, in response to wide-ranging debates on the issue of regulation and concerns about patient safety, the Department of Health has commissioned Skills for Health and Skills for Care, in consultation with unions, employers, support workers, regulators and education providers, to develop national minimum training standards and a code of conduct for health-care support workers reporting to registered practitioners in England (due to report in January 2013). 40 Similar work has been conducted in Scotland41 and Wales. 42 It is anticipated that this work will be delivered ahead of the establishment of a voluntary register for health-care support workers and adult social care workers in England.
Further understanding of the potential roles of assistants and how they relate to community nursing requires practical realisation, and it is to this that we now turn.
HCAs:
-
have their nursing tasks delegated to them and are supervised by registered professionals
-
are guided by protocols and act within these protocols at all times
-
perform tasks according to their competence levels (guided by Skills for Health Career Framework levels 2 and 3)
-
must demonstrate competence supported with the required level of knowledge before being delegated particular tasks. They have a duty to inform the delegating professional if they do not have competence to perform a task
-
should not be required to make stand-alone clinical judgements and plan the care of patients based on those judgements
APs:
-
have a level of knowledge and skill beyond that of the traditional HCA (guided by Skills for Health Career Framework level 4)
-
support the work of registered professionals and may transcend professional boundaries
-
make judgements requiring a comparison of options
-
plan straightforward tasks and work guided by standard operating procedures and protocols
-
may undertake the ongoing supervision of routine work of others
Existing evidence base on assistant roles in community nursing teams
There is ambiguity over the extent and nature of the contribution that assistant staff make to the delivery and outcomes of care. 26 In primary and community care, research efforts have tended to focus on the roles of registered health-care professionals. This research has dealt with issues such as the substitution of GPs with RNs,43–45 rather than the organisational, skill mix and workforce issues associated with the provision of community nursing services by a health-care team in its broadest sense. Changes to the roles of health-care professionals, through role expansion and redesign, have created specific opportunities for reviewing developments in assistant roles. 46 Assistants have been introduced across health-care settings to:
-
complement the work of professionals by carrying out activities alongside the professional, such as working with nurses to deliver fundamental care (co-produce)
-
carry out activities that do not require a professional, such as some administrative tasks (relieve) or
-
take on tasks and activities previously performed by professionals, such as phlebotomy (substitute). 47
Moran et al. 48 identified four core attributes of HCAs: the helper/enabler, the companion, the facilitator and the monitor. There follows an exploration of the evidence base for assistant roles in community settings.
Research on assistant staff in primary and community care is scant, comprising small-scale descriptive, localised projects which focus on assistant roles in GP practices rather than community nursing services. The Working in Partnership Programme (WiPP)49 was launched in 2004 to support general practice with capacity-building resources and strategies; one initiative was to develop a range of core principles and a practical toolkit to enable general practice to employ, train and develop HCAs. In general practice, assistant staff are commonly trained to undertake specific clinical and non-clinical procedures, such as blood pressure recording, new patient checks, urinalysis, weight and height recording, phlebotomy or ordering supplies. 50 However, assistant roles tend to evolve over time to meet the needs of individual practices leading to great variation in roles, responsibilities and tasks across these settings. 51 The lack of national guidance on the training, development and employment of assistants has led to a fragmented approach at the local level, with some unfortunate consequences including:52
-
wide variations in the structures and support available to assistant staff
-
local inequities in accessing training and support for assistants
-
the lack of a mechanism for sharing good practice with respect to training, employment practices or principles of delegation; and
-
the absence of a continuing and professional development culture for assistants, such as that which exists for other regulated primary care professionals.
We were unable to locate any published literature on the work of assistant staff (levels 2 to 4) in adult community nursing teams. Yet the consequences of introducing assistant roles in community nursing teams represent a fundamental rethink of who provides community care, in a way that has not been seen since the introduction of the new GP contract in 2003 or the rise of the practice nurse during the early 1990s. 53,54 Despite the introduction and development of assistant roles in community nursing teams, we still know little about their numbers, who they are and what they do. Distinguishing activities that could be performed by assistant workers has important implications for the entire health-care team and for patient care. 55,56 Over the last decade there have been increasing numbers of HCAs at levels 2 and 3 as well as the development of new higher-level (level 4) AP roles. 57 However, there are likely to be wide variations in the introduction, preparation and use of assistants across community nursing teams, with no obvious links between service need and their deployment.
It is likely that assistant roles in community nursing teams are being developed in an ad hoc manner in response to local need, but with wide variations in roles and training received, and possibly also in the competence of individuals to undertake the designated roles. It has been argued that more work could be delegated to assistant workers to better support health-care professionals, thus improving efficiency and effectiveness. 58 Lord Darzi's NHS review2 focused on the valuable role of frontline NHS clinical staff in driving improvements in the quality of care provided to patients. This review offered further opportunities for assistants to contribute to well-being and prevention services in the community with health-care professionals, and to ensuring that services promote access so that patients get ‘the right care, in the right place, at the right time’ (p. 62). 2
Summary
Our study focuses on community nursing, an area where there appears to be no evidence of the roles of assistants. We aim to describe numbers, types and roles of assistants in these settings and their potential contributions to service delivery patient experience and patient choice. To better understand the contribution of these staff in the delivery of community nursing care we will:
-
consider whether or not and why assistant roles have emerged and developed in community nursing services;
-
explore what roles and responsibilities assistant staff at different levels are undertaking and how they have been prepared for delivering quality and safe services; and
-
explore the potential impact of assistant roles on reducing health inequalities and their contribution to improving patient experience and patient choice.
Plans for the review and modernisation of services in this sector1,18 make an evaluation of current and potential developments for HCA and AP roles important. It is also timely so as to inform health service policy, decisions about commissioning, and workforce training and development, as well as decisions by service providers about the required workforce and skill mix to ensure safe and effective service delivery to patients and their families. An important starting point for a study of assistant roles in community nursing teams is identifying where assistant staff are employed, in what numbers and for what purposes. This is the focus of our study. It will provide the foundations for developing more detailed work on the roles of assistant staff in community nursing teams.
Chapter 3 Research objectives and questions
The previous chapter identified a lack of evidence on roles for assistants in community nursing teams. Our scoping study had the following research objectives:
-
Describe numbers, types and roles of assistant staff (at levels 2, 3 and 4) delivering services and care in community nursing services in England.
-
Explore how assistant roles affect the organisation of nursing work in these teams, particularly where new, integrated organisational models and ways of delivering services exist and innovative assistant roles are identified.
-
Explore how the use of assistants in community nursing teams impacts on (or has the potential to impact on) health-care professional workload, and patient experience and patient choice.
-
Report key findings and implications from the scoping study for policy, practice and research.
These objectives were addressed through the following research questions:
-
What have been the major influences (social, organisational, political/policy, historical, environmental and economic) on roles for assistant staff involved in delivering services and care in community nursing services?
-
What numbers of assistant staff work in community nursing teams and in what types of roles?
-
What tasks and activities are assistants undertaking in these settings and are there examples of innovative use of the roles?
-
How do assistant roles impact on the workload of health-care professionals in community settings?
-
What is the perceived impact of using assistants to deliver services on patient experience and patient choice?
We now turn to the research approach and methods deployed to address these objectives.
Chapter 4 Research approach and methods
Introduction
We adopted a three-stage approach for the scoping study to enable us to (1) present a national picture of assistant roles in community nursing teams at levels 2, 3 and 4; (2) reflect any regional variations in use of the roles at these levels; and (3) describe the type of work assistants undertake and their contribution to any innovative models of service delivery. These stages can be summarised as:
-
Stage 1: Establishing contact with senior managers (Director of Nursing or equivalent) to inform them about the scoping study and to determine (a) whether or not they employ assistants within community nursing teams and (b) if they would be interested in taking part in a short telephone interview.
-
Stage 2: Short telephone interview with all senior managers who indicate a willingness to participate, to scope the national use of community nursing assistant roles (at levels 2, 3 and 4), and use of the NHS iView data source (www.ic.nhs.uk/iview) from the Electronic Staff Record Data Warehouse (www.electronicstaffrecord.nhs.uk), to map numbers of assistant staff in community nursing teams across England.
-
Stage 3: In-depth telephone interviews with a purposive sample of service managers and team leads of services that use community nursing assistants in varied ways.
Appendix 4 provides an overview of the study.
Theoretical framework
Understanding the roles of community nursing assistants requires exploration of their work, the meanings attached to their work and their position within the division of labour in community nursing teams. Importantly, this understanding needs to be located within the context of nursing care delivery, health services and the wider social and policy arenas; these contexts were introduced in the previous chapter. It also requires a theoretical starting point, one that provides an analytical device through which to scrutinise and make sense of assistant roles in these teams. As such, this study of community nursing assistants is framed by the interactionist perspectives of Hughes59 and Abbott. 60
Hughes59 argued that the division of labour occurs in a social system and that the activities performed by individuals are social roles played out within the social system of which they are part. Abbott60 focused on the content, control and differentiation of work that gives rise to internal occupational divisions of labour and external conflict with other occupations over jurisdiction. He argued that work and jurisdictional claims take place within a system. Interactionism provides a useful framework for investigating the roles of assistants in community nursing teams in contemporary UK health care.
Stages 1 and 2: scoping community assistant roles
An important challenge for this study was managing data collection within the changing landscape of community nursing services. The study was conducted at a time of significant change resulting from the Transforming Community Services policy agenda. 18 This policy context and the challenges that this created for the study are the subject of Chapter 5. We considered the processes that we went through in describing this landscape to be of sufficient value to others to warrant a separate chapter (see Chapter 5). We outline here the methods used for stages 1 and 2.
The starting point was to locate and establish roles for community nursing assistants within the national context. At proposal stage there were 152 PCTs in England with a role in providing community nursing services. Following organisational and structural changes in service provision, this was reduced to 102 provider organisations (see Chapter 5). Our aim in stages 1 and 2 was to understand the configuration and use of assistant staff in community nursing teams within these provider organisations by mapping the role with the senior managers.
We recognised that the process of carrying out this scoping study would not be straightforward, owing to varied models of community nursing service provision across England and the locations of these community nursing teams. We therefore carried out some preliminary work both to refine our approach to the scoping study and to develop focused questions to capture the potential diversity in service provision. We consulted with individuals who had an understanding of the commissioning and provision of community nursing services [such as PCT Directors of Nursing, managers within strategic health authorities (SHAs), community nurses and individuals from professional organisations]. This consultation exercise helped to ensure the feasibility of our planned approach and ensured that our questions would enable us to scope the reality and diversity of assistant use in community nursing services in England.
Initially we proposed to conduct a survey with senior managers by administering the questionnaire by post and electronically. However, the piloting of the questionnaire revealed difficulties with administration and completion by busy senior managers. We were concerned that senior managers would not complete the survey and so changed the protocol to conduct this scoping work through telephone interviews. We restructured the questions accordingly and included both closed and open questions (see Appendix 5). Senior managers were invited to participate in a 15-minute interview, but many of the participants allocated 30 minutes for the interview. Further details of sampling and recruitment are provided below.
Telephone interviews were arranged for a time offered by the senior managers. Data collection was completed by KS, SP and RB. With the permission of participants, the interviews were audio recorded and notes were made throughout the discussion. Recordings were used to ensure that notes were comprehensive and to extract verbatim quotes to support the views of the senior managers. This process was carried out by the research interviewer as soon as possible after the interview. All senior managers who participated agreed to the interview being recorded. At the end of each interview we asked permission to contact the senior manager at a later date should we wish to include their organisation in stage 3. All participants agreed to be a point of contact for this stage. The processes for sampling and recruitment are described below.
At an early stage we recognised that while senior managers had an appreciation of the bandings and the types of roles assistants were undertaking, they were not always in a position to provide details about actual numbers of assistants and their banding within the community nursing teams. We therefore sought existing sources of secondary data so that we could establish numbers and banding of assistants in community nursing teams across England. In order to describe the numbers of assistant staff (at levels 2, 3 and 4) working in community nursing teams in England, we approached the NHS Information Centre to access NHS iView, which holds restricted data derived from the Electronic Staff Record. With the support of our local NHS acute trust (York Hospitals NHS Foundation Trust) we obtained permission to access this data source.
Stage 3: gaining depth of understanding about community assistant roles
Stages 1 and 2 supported the scoping of community nursing assistant roles nationally. Stage 3 aimed to gather further in-depth detail of these roles within organisations from the perspectives of managers who worked more closely with the assistants. For these purposes, stage 3 involved telephone interviews with service managers and team leads or caseload holders. These managers and leads were identified through the senior managers (see Sampling and recruitment). Data collection was completed by KS, SP and RB, and to promote in-depth understanding of an organisation the same interviewer conducted interviews across stages 2 and 3 for each organisation. In doing so the researcher could develop an understanding of the organisation and the roles of assistants in the community nursing teams from the different participants (both senior and service-level managers).
Service managers and team leads were invited to participate in a 30- to 40-minute telephone interview at a time most convenient for them. The aim of the interviews was to understand (in more depth) the day-to-day work of assistants, how they were managed and supervised, and the potential impacts of these roles on the community nursing team, service delivery and patients' experiences of care. Appendix 6 details the topic guide used for these interviews. With the permission of participants, the interviews were audio recorded and these recordings were then transcribed verbatim for analysis. All participants agreed to their interview being recorded.
Sampling and recruitment
The study had three sequential stages and the process for sampling and recruitment for each stage is described in further detail below. Stages 1 and 2 used a census approach because we wanted to establish contact with as many organisations as possible for initial scoping of the assistant roles. Stage 3 used purposive sampling to gain in-depth understanding of assistant roles across a range of services (see Stage 3, below). Figure 4 summarises the processes of recruitment for each stage.
FIGURE 4.
Recruitment to each stage of the study.
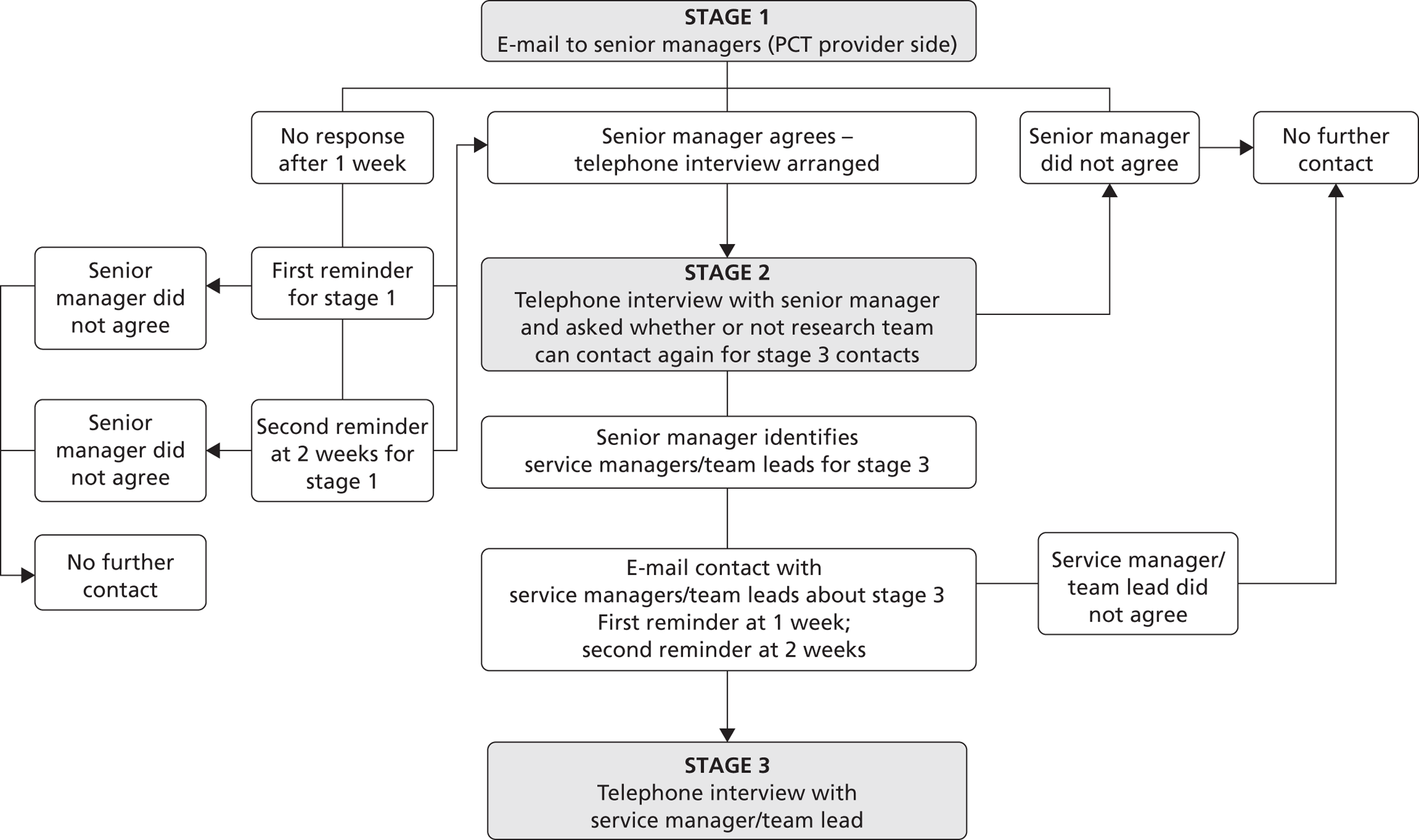
Stage 1
Stage 1 (and stage 2) used a census approach. All Directors of Nursing (or a senior manager in a position of equivalence) of organisations providing community nursing services in England, and for which we had successfully obtained research governance approval (see Ethical considerations, below), were contacted by e-mail (n = 76). This e-mail contact introduced the study. It included details of the funding body and independence of the research team from the NHS and aimed to determine (1) whether or not organisations employed assistants within community nursing teams, and (2) if the senior manager would be interested in taking part in a 15-minute telephone interview (stage 2). We requested that the senior manager replied to this contact e-mail to confirm the use of assistants and express their willingness to participate in an interview. We sent a maximum of three e-mails for this stage: one first e-mail, and two reminder e-mails at 1-week intervals after the initial e-mail (see Appendix 7). Thirty-seven senior managers (49%) of organisations where we had research governance approvals responded (n = 76). Directors who did not respond after two reminders were not contacted further (n = 39; 51%). A positive response to our e-mails implied consent to send further information about the interviews for stage 2. No senior managers who responded declined this further contact. We were unable to make contact with 26 organisations because we did not have the necessary approvals; these account for one-quarter (25%) of the total number of organisations providing community nursing services (n = 102).
Stage 2
On receipt of confirmation of a willingness to participate in a telephone interview, the senior managers were sent an e-mail (see Appendix 8) that contained information about the study (see Appendix 9) and a consent form (see Appendix 10). The preliminary consultation exercise and piloting revealed that senior managers prefer information to be covered in one page and so there were two versions of the information sheet: the one-page summary sent by e-mail which then referred to detailed information available on the study's web page, hosted by the University of York (see Appendix 11). At this stage, the senior managers were not committed to an interview; however, all of them agreed to participate. The sample is described in Chapter 6.
Prior to the interviews, we requested that the senior managers complete the consent form. We requested that if they completed this electronically it should be returned from their work e-mail address; this was considered equivalent to providing a signature on a hard copy of the form. However, for staff who preferred to sign the consent form and return it by post, we sent a paper copy with a stamped addressed envelope for its return to the research team. Informed consent (for stages 2 and 3) ensured that participants understood:
-
the purpose of the study
-
why they were being asked to participate and what would be involved if they agreed to participate
-
that they were able to withdraw from the study even after providing consent
-
that consent to participate, or not, would not affect their working position
-
how data would be stored, analysed and used; and
-
that the research team would respect the participant's anonymity and confidentiality.
On receipt of a completed consent form, we made an appointment to interview the participant on a day and time that best suited them. At the beginning of the interviews we also confirmed (and audio recorded) the senior mangers' willingness to participate in the interview. Further, we confirmed that they understood that the interview was being audio recorded for note-taking purposes. They were informed that this was to accurately transcribe and present any of their words that helped to illustrate points they made during the interview.
Stage 3
All participants in stage 2 agreed to be contacted again should we wish to interview service and team-level managers from their organisations for stage 3 of the study. Stage 3 aimed to gather further in-depth understanding from managers involved in the day-to-day management of community nursing services who would therefore have a service-level understanding of the assistant roles in the nursing teams. For stage 3, a purposive sample of 10 organisations was selected from stage 2. These organisations were selected to represent:
-
the range of types of organisations included in the scoping stage (e.g. community trusts, social enterprises, integrated services and other providers)
-
regions (by SHA cluster)
-
the banding of assistants (to include organisations with bands 2, 3 and 4 and to show differences in the configuration of these bandings); and
-
the range of services in which assistants were employed in community nursing teams.
For each of the sampled organisations, we re-established contact with the senior managers from stage 2 and asked them to identify service-level managers whom we could contact about this stage. We made contact with potential participants for stage 3 either directly or through the stage 2 participants. This was determined through correspondence with the stage 2 senior managers. The process for recruiting these participants was very similar to the recruitment of stage 2 participants. Our initial contact introduced the study (see Appendix 12) and provided one-page study information (see Appendix 13), which directed the potential participant to further study information on the study's web page (see Appendix 14). We emphasised in this initial contact that participation was voluntary, that we were seeking service and team-level managers to participate in an interview about community nursing assistant roles, and that this interview would last no more than 40 minutes. When these managers responded and indicated a willingness to participate, we requested that they provide written consent either electronically or by post (following the procedures we deployed for the senior managers in stage 2) (see Appendix 15). All of the service and team level managers approached agreed to participate (n = 20).
On receipt of a completed consent form, we made an appointment to interview the participant on a day and at a time that best suited them. We also provided a list of the questions that we would be asking the participants so that they could prepare for the interview if they wished (see Appendix 16). Piloting revealed that this would enable managers to find relevant information, consider their views and allay anxieties (many of these managers had never been interviewed for the purposes of research). At the beginning of the interviews we confirmed (and audio recorded) the senior mangers' willingness to participate in the interview and confirmed that they understood that the interview was being audio recorded. The sample recruited for stage 3 is described in Chapter 7.
Data analysis
Our strategy for analysing data was to use parallel mixed data analysis. 61,62 This involved separate processes for analysing qualitative data generated by the interviews in stages 2 and 3 and quantitative data provided by NHS iView. Although analyses of these data were independent, each provided an understanding of assistant roles in community nursing teams. These understandings from the different sources have been integrated to provide a description located within real-world contexts of health service delivery.
Qualitative data (from the interviews) were analysed for thematic content. 63 This approach is both inductive (data interrogated to answer research questions but themes allowed to emerge from the data) and iterative (data collection and analysis occurring simultaneously). Initially we understood each organisation and then we explored similarities and differences across the organisations. Throughout this process, comparative analysis was carried out; this method allowed data from different organisations to be compared and contrasted. In stage 3, these comparisons also established convergence and discrepancies in reports provided by participants operating at senior, service and team levels from within the same organisation. Deviant cases were actively sought throughout the analysis, and emerging ideas and themes modified in response. 64
Data analysis involved a process of organising the data, descriptive coding, interpretive coding, writing and theorising. We used an interactionist theoretical framework59,60 for writing up our study findings. As such, we focused on the ways in which roles of assistants were enacted within the broader teams and organisations and the ways in which the broader contexts influenced the roles of assistants. Interactionism provides a useful framework for investigating the roles of assistants in community nursing teams in contemporary UK health care. To promote quality, the following strategies were used: description of the participants to provide context (credibility and transferability), transparency of the research process and use of theory (transferability), evidence of consistency using multiple examples from data (dependability), and engagement of the wider research team, informants and participants with interim findings (confirmability). 65
Descriptive summary statistics were used to analyse quantitative data. Where appropriate, data from the stage 2 interviews were examined for proportions and patterns by organisation and region to promote the description and interpretation of national use of assistant roles in community nursing teams.
Using the iView data source, from the Electronic Staff Record Data Warehouse, we accessed data on staff in posts in NHS organisations. Data were extracted on the following:
-
Health-care organisations: these were restricted to those providing community services.
-
Occupation codes: these were restricted to nursing and assistant staff working in community settings and in adult services.
-
Staff in post: head count numbers, full-time equivalents and Agenda for Change bands.
These were analysed to describe numbers of assistant staff as a proportion of professionally qualified nurses working in community services. Subgroups were also explored including regions and types of provider organisations. Summary statistics were used to describe the community assistant workforce and to determine any differences between regions and provider types.
Ethical considerations
The study was reviewed by the Proportionate Review Sub-Committee of a Research Ethics Committee (REC)(REC reference number: 10/H0808/159) and received favourable opinion in December 2010 (see Appendix 17). At the same time, our study progressed through research governance procedures as a NIHR portfolio study. We were disappointed by the slow progress of obtaining research governance approvals. After 9 months, only two-thirds of these approvals had been received (n = 76). Approvals for this study have continued to come in up to 17 months after the application was submitted. The processes of seeking these approvals was further complicated by the changes in organisational structure and the location of community services; some of the initial approvals were withdrawn because the organisations were moving and therefore no longer came under the jurisdiction of the department that granted the original approval. We appreciated that this was out of the control of the departments providing research governance approvals. However, these lengthy procedures created considerable problems for the research team in establishing contact with organisations.
Approval was not granted for a large area of the north-east because of the amount of organisational change in Newcastle, North Tyneside and Northumberland. Research governance teams for these areas had spoken with Directors of Nursing who considered that the topic of our research may be too sensitive for staff to engage with due to the restructuring and relocation of services and staff.
Our main ethical considerations included:
-
the handling and storage of personal identifiable data
-
ensuring that informed consent was obtained from participants
-
maintaining confidentiality and anonymity; and
-
the use of participant quotes from interviews.
Our approach to managing these issues was negotiated and approved by the ethics committees and research governance departments. Consenting of participants has been described above. All data were stored on double-password-protected computers and accessed only by the research team. There was no electronic transfer of data. Data were stored separately from participant details to prevent linkage. Participants were given a study ID and organisations were presented at SHA level rather than being named. We have named organisations in Chapter 5 only when describing the changing landscape of community nursing services.
Summary
This chapter has outlined our broader methodological approach and described the methods deployed in meeting the study aims and objectives. Subsequent chapters present our findings. Chapter 5 focuses on the changing landscape of community nursing services. Chapter 6 provides findings of our scoping work to establish the extent and nature of community nursing assistant roles nationally, with Chapter 7 providing in-depth accounts of community nursing assistant roles in a sample of organisations considered representative of the national picture.
Chapter 5 The changing landscape of community nursing services
Introduction
Community health services encompass a broad and complex range of services. The focus of this study is on community nursing services as defined in the previous chapter. Importantly, this study was conducted at a time of significant change, when the structure and organisation of community services were being redesigned and relocated. Understanding this changing landscape is crucial for making sense of the findings presented in the subsequent chapters. This chapter presents this contextual detail.
Policy context
Over the past decade, significant UK policy initiatives have been introduced which have shaped the structure, organisation and responsibilities of primary and community care services, including community nursing services. These policies are wide ranging, but the central focus has been to promote the delivery of care closer to home for patients to better accommodate the changing health and care needs of the population. 18,66 A summary of the key UK policies affecting the development of community nursing services is provided in Table 1, culminating in the Transforming Community Services programme18 incorporated in the coalition government's plans for the NHS. 4 This programme of restructuring the provision of community services has had a significant recent impact.
Transforming Community Services18 recognised the lack of attention and years of underinvestment in community health services, and required PCTs to consider ways in which community health services could better meet the needs of the local populations, in particular those patients with long-term conditions. In 2009, PCTs started to identify strategies to split provider services from the commissioning functions of the PCT, with a government-imposed deadline of April 2011. A range of organisational models for community services were proposed. 18,77 Essentially, there were two main choices: the provider service could become a standalone organisation (community trust or social enterprise) or merge with another organisation (vertical integration with an acute or mental health trust). Alternatively, community services could be commissioned by the PCT from any PCT-accredited willing provider (named ‘any willing provider’ in earlier policies) to enable a plurality of providers (Table 2).
| Year | Policies |
|---|---|
| 1999 | PCGs formed to develop local primary and community care services67 |
| 2000 | NHS plan sets out measures to modernise the NHS with an emphasis on more choice and control for patients68 |
| 2000 | PCTs launched to purchase care for local communities from hospitals and other providers; provide community services; engage with local people; and tackle health inequalities and improve public health. There were initially 303 PCTs. Towards the end of 2002, the role of PCTs expanded to improve the health of the community and secure provision of services that encourage local integration of health and social care69 |
| 2002 | Payments by results led to remuneration for acute trusts for carrying out specific treatments70 |
| 2002 | Derek Wanless commissioned to evaluate NHS funding. He reported that the NHS was under-resourced by health-care staff across hospital and community services6 |
| 2003 | New GP contract introduced and resources allocated according to workload and patient population. GPs had more autonomy to provide a wider range of services to meet the needs of their practice populations71 |
| 2004 | The first NHS (hospital) Foundation Trusts emerged (not community focused)72 |
| 2005 | Creating a patient-led NHS required PCTs to introduce a choice of elective care73 |
| 2006 | Commissioning a patient-led NHS identified a need for step-change in the way services were commissioned. Under PBC, GPs took on responsibility for commissioning of services to meet the needs of their local populations74 |
| 2006 | PCTs and SHAs were reconfigured to strengthen commissioning and establish closer relationships between health, social care and emergency services. The number of PCTs was reduced from 303 to 152. The number of SHAs was reduced from 28 to 1075 |
| 2007 | Darzi set out the Government's 10-year plan for the NHS. The emphasis was on patient choice and the importance of services being provided close to the patient2 |
| 2008 | ‘Our vision for primary and community care’ set out plans to expand non-acute services and acknowledged that there had been a lack of focus on community nursing services1 |
| 2009 | PCTs established a contractual relationship with their provider services leading to internal separation between PCT commissioner and provider arms76 |
| 2009 | ‘Transforming community services’ suggested that all PCT community provider arms should be established as separate organisations with a deadline of April 201118 |
| 2010 | ‘Liberating the NHS’ set out the government's long-term vision with a focus on improving and innovating4 |
| Organisational model | Description |
|---|---|
| Community foundation trust | The provider services of the PCT separate from the commissioning arm and become an independent NHS organisation, called an autonomous provider organisation |
| Social enterprise | A business model that aims to combine market efficiency with social and environmental justice. There are several legal organisational forms, for example a CIC |
| Vertical integration with another NHS organisation | The provider services join another NHS organisation, such as a large acute hospital or mental health trust |
| Any willing PCT-accredited provider (originally called ‘any willing provider’) | Any provider accredited by the PCT commissioners which meets the specific requirements for meeting needs of the local population, for example a private company |
The processes by which provider services have been separating from the commissioning arm of PCTs (during 2010 to 2012), along with the change to PCTs themselves (PCTs are to be abolished in April 2013, with plans for clinical commissioning groups, the NHS Commissioning Board and local authorities to take over PCTs' commissioning and public health responsibilities), coincided with the data collection for our study and created a number of practical challenges. We present here our understanding of the provider organisations but recognise this is located in a particular time and subject to change. As such, it is a snapshot of how we developed our understanding of the contexts in which community nursing assistants are working.
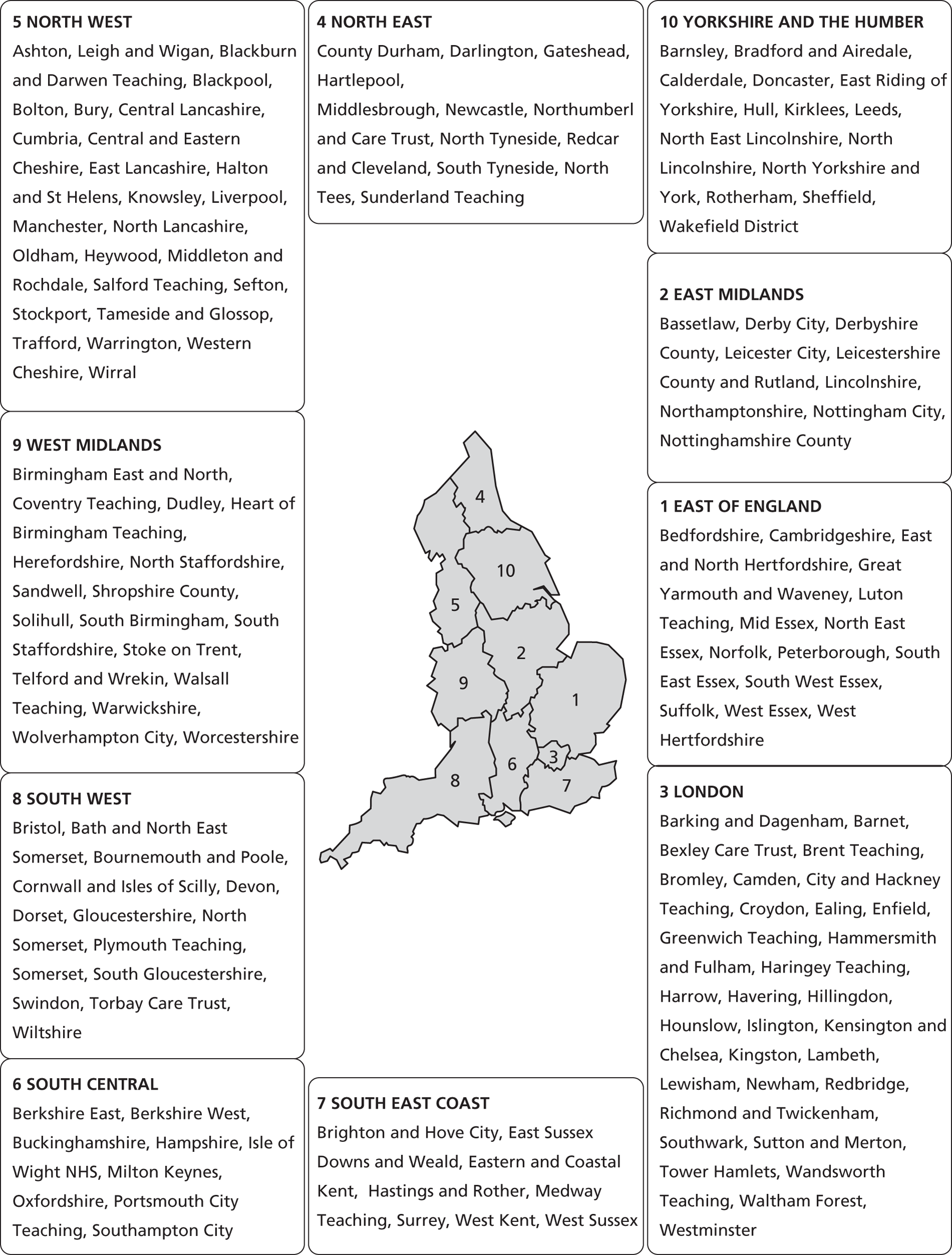
Practical challenges for the study
At the start of our study in 2010, there were 152 PCTs, operating under 10 SHAs, responsible for the provision of community health services (Figure 5). During the period of study the 152 PCTs became less meaningful because the provider services were being relocated, and the 10 SHAs were reconfigured into four SHA clusters: London, North, Midlands and South (Table 3).
A key challenge for the initial stages of the scoping study was to identify the most suitable senior manager (Director of Nursing or equivalent) to contact and, for later stages of our work, the types of new organisational structures for delivering community services (see Chapter 4). We therefore identified that it was important to:
-
establish where community nursing services were located following the split of the commissioning and provision of community nursing services; and
-
identify the emerging service models as a result of these changes in location.
Without this level of detail it would not be possible to describe the context within which our study of community nursing assistants has taken place. This is crucial for understanding the implications of the findings for practice and policy.
FIGURE 5.
Strategic health authorities (n = 10) and PCT providers of community services (n = 152) before Transforming Community Services.
| 10 SHAs | 4 SHA clusters |
|---|---|
| London | London |
| North East | North |
| Yorkshire and the Humber | |
| North West | |
| West Midlands | Midlands |
| East Midlands | |
| East of England | |
| South West | South |
| South Central | |
| South East Coast |
Shifting sands and needles in haystacks: establishing the location and models of community nursing services
Our starting point was the list of 152 PCT contacts that we identified with Binleys (www.binleys.com/About.asp). Early in 2011, we started making contact (by e-mail or telephone) with the senior managers who had been identified. However, it soon became apparent that we were making contact at a time of significant change and that our list of contacts was not always helping us make contact with the most appropriate senior manager, either because the organisation no longer existed or the manager was no longer in his or her post.
We were unable to locate a central source of the data we required and so we adopted a pragmatic approach: making contact with the original PCT provider services and tracking how the services were being transformed (including location, type of provider organisation and contact). This was a rather complicated and lengthy process as not all organisations responded to our request for information and we could not always rely on information that was provided. We sourced these data through web-based searches and e-mail or telephone contact with PCTs and SHAs. This mapping process was complicated further because we were trying to gather these data at a time when organisations were in the process of moving (this is apparent in the data presented below) and, as a result, the mapping of these changes extended into 2012. However, going through these stages of establishing the national picture of community nursing service provision enables us to describe our sample within the changing landscape of these services. Understanding this context will promote confidence in our findings.
Location and models of community nursing services
Following the transformation of community services, the community nursing services provided by the original 152 PCTs had been reorganised to be delivered by 102 provider organisations using the organisational models detailed in Table 2. The majority of organisations (n = 67; 66%) integrated with another NHS organisation: either an acute trust (n = 44) or mental health trust (n = 23). Similar numbers of organisations made the transition to a community trust, aspiring to foundation status (n = 15), or a community interest company (CIC) (n = 15). A small number of PCTs (n = 2) had tendered their community nursing services to an accredited willing provider/private company. We found a small number of organisations (all in the South SHA cluster) described as parked, with the PCT as an arms-length provider (n = 3) and the future of these services still being debated (Table 4). Table 5 presents the transitions by SHA cluster and shows that a higher proportion of PCTs in the North cluster integrated with another NHS organisation rather than using an alternative model for providing services. Alternatively, PCTs in the Midlands were proportionately spilt between integration with a NHS organisation and stand-alone organisations (including both community trust or community interest companies). It is not possible to determine reasons for these choices within this report. Exploratory data analysis was conducted but no clear patterns emerged with regard to factors that predicted the type of organisation that was created. Local discretion appears to have dominated the choice of organisational form. When reading organisations' web pages, the choices were all justified as promoting better services for the local populations.
| Organisational model | n (%) |
|---|---|
| Community trust | 15 (14.5) |
| Social enterprise | 15 (14.5) |
| Vertical integration with another NHS organisation | 67 (66) |
| Any willing PCT-accredited provider (originally called ‘any willing provider’) | 2 (2) |
| Parked with PCT | 3 (3) |
| Total number of organisations | 102 (100) |
The reduction in numbers of organisations (from 152 to 102) is due to the merged delivery of services into one organisation, where they were delivered by a number of original PCT. For example (and there are many), services delivered by Berkshire East PCT and Berkshire West PCT are now being delivered by Berkshire Healthcare NHS Foundation Trust (see Table 6). However, the services from one PCT could also be split across a number of new providers. Tables 6–10 provide detailed information about the original PCT and new provider organisations for community nursing services in England, considered up to date at the point of reporting (January 2013). These are presented to represent the main organisational models.
| SHA cluster | Integration, N (%) | Acute, N | FT, n | Non-FT, n | Mental health, N | FT, n | Non-FT, n | Community trust, n (%) | CIC, n (%) | Private company, n (%) | Parked (PCT), n (%) | Total, n |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| London | 14 (21.2) | 9 | 3 | 6 | 5 | 4 | 1 | 2 (13.4) | 2 (13.3) | 0 (0) | 0 (0) | 18 |
| North | 28 (42.4) | 21 | 16 | 5 | 7 | 6 | 1 | 4 (26.6) | 2 (13.3) | 0 (0) | 0 (0) | 34 |
| Midlands | 14 (19.7) | 8 | 2 | 5 | 6 | 1 | 5 | 7 (46.6) | 5 (33.4) | 1 (50) | 0 (0) | 27 |
| South | 11 (16.7) | 6 | 3 | 3 | 5 | 4 | 1 | 2 (13.4) | 6 (40) | 1 (50) | 3 (100) | 23 |
| Total | 67 (100) | 44 | 23 | 15 (100) | 15 (100) | 2 (100) | 3 (100) | 102 (100%) |
| SHA cluster | PCT | Provider organisation | Acute (FT) | Acute | Mental health (FT) | Mental health |
|---|---|---|---|---|---|---|
| North | North Yorkshire and York | Airedale NHS Foundation Trust | ✓ | |||
| Lancashire | ||||||
| South | Berkshire East | Berkshire Healthcare NHS Foundation Trust | ✓ | |||
| Berkshire West | ||||||
| North | Blackpool | Blackpool, Fylde and Wyre Hospitals NHS Foundation Trust | ✓ | |||
| North Lancashire | ||||||
| North | Bolton | Bolton NHS Foundation Trust | ✓ | |||
| North | Calderdale | Calderdale and Huddersfield NHS Foundation Trust | ✓ | |||
| North | Manchester | Central Manchester University Hospital NHS Foundation Trust | ✓ | |||
| North | County Durham | County Durham and Darlington NHS Foundation Trust | ✓ | |||
| Darlington | ||||||
| Midlands | Dudley | Dudley Group NHS Foundation Trust | ✓ | |||
| South | Wiltshire | Great Western Hospitals NHS Foundation Trust | ✓ | |||
| Bath and North East Somerset | ||||||
| London | Lambeth | Guy's and St Thomas' NHS Foundation Trust | ✓ | |||
| Southwark | ||||||
| North | North Yorkshire and York | Harrogate and District NHS Foundation Trust | ✓ | |||
| Midlands | Solihull | Heart of England NHS Foundation Trust | ✓ | |||
| London | City and Hackney | Homerton University Hospital Foundation Trust | ✓ | |||
| North | Newcastle | Newcastle on Tyne Hospitals NHS Foundation Trust | ✓ | |||
| North | Hartlepool | North Tees and Hartlepool NHS Foundation Trust | ✓ | |||
| North Tees | ||||||
| North | Northumberland Care Trust | Northumbria Healthcare NHS Foundation Trust | ✓ | |||
| North Tyneside | ||||||
| North | Rotherham | Rotherham, Doncaster and South Humber NHS Foundation Trust | ✓ | |||
| Doncaster | ||||||
| Bassetlaw | ||||||
| London | Sutton and Merton | Royal Marsden NHS Foundation Trust | ✓ | |||
| North | Salford | Salford Royal NHS Foundation Trust | ✓ | |||
| North | Middlesbrough | South Tees Hospitals NHS Foundation Trust | ✓ | |||
| Redcar and Cleveland | ||||||
| North | South Tyneside | South Tyneside NHS Foundation Trust | ✓ | |||
| Sunderland | ||||||
| Gateshead | ||||||
| Midlands | Warwickshire | South Warwickshire NHS Foundation Trust | ✓ | |||
| North | Stockport, Tameside and Glossop | Stockport NHS Foundation Trust | ✓ | |||
| South | Torbay | Torbay and Southern Devon Health and Care NHS Trust | ✓ | |||
| Devon | ||||||
| North | North Yorkshire and York | York Teaching Hospital NHS Foundation Trust | ✓ | |||
| London | Tower Hamlets | Barts Health NHS Trust | ✓ | |||
| South | Buckinghamshire | Buckinghamshire Healthcare NHS Trust | ✓ | |||
| North | Central and Eastern Cheshire | East Cheshire NHS Trust | ✓ | |||
| London | Croydon | Croydon Health Services NHS Trust | ✓ | |||
| London | Brent | Ealing Hospitals NHS Trust | ✓ | |||
| Ealing | ||||||
| Harrow | ||||||
| North | East Lancashire | East Lancashire Hospitals NHS Trust | ✓ | |||
| Midlands | East Sussex Downs and Weald | East Sussex NHS Trust | ✓ | |||
| Hastings and Rother | ||||||
| London | Lewisham | Lewisham Healthcare NHS trust | ✓ | |||
| South | Milton Keynes | Milton Keynes Community Health/Bedford Hospitals NHS Trust | ✓ | |||
| South | South Gloucestershire | North Bristol NHS Trust | ✓ | |||
| North | Bury | Pennine Acute Hospitals NHS Trust | ✓ | |||
| Oldham, Heywood Middleton and Rochdale | ||||||
| Manchester (north) | ||||||
| Midlands | Wolverhampton City | The Royal Wolverhampton Hospitals NHS Trust | ✓ | |||
| Midlands | Sandwell | Sandwell and West Birmingham Hospitals NHS Trust | ✓ | |||
| North | Sheffield | Sheffield Teaching Hospitals NHS Trust | ✓ | |||
| North | Sefton | Southport and Ormskirk Hospital NHS Trust | ✓ | |||
| West Lancashire | ||||||
| London | Wandsworth | St George's Healthcare NHS Trust | ✓ | |||
| Midlands | Walsall | Walsall Healthcare NHS Trust | ✓ | |||
| London | Haringey | The Whittington Hospital NHS Trust | ✓ | |||
| Islington | ||||||
| Midlands | Herefordshire | Wye Valley NHS Trust | ✓ | |||
| London | Camden | Central and North West London NHS Foundation Trust | ✓ | |||
| Hillingdon | ||||||
| North | Western Cheshire | Cheshire and Wirral Partnership NHS Foundation Trust | ✓ | |||
| North | Cumbria | Cumbria Partnership NHS Foundation Trust | ✓ | |||
| South | Bournemouth and Poole Dorset | Dorset Healthcare University NHS Foundation Trust | ✓ | |||
| London | Newham | East London NHS Foundation Trust | ✓ | |||
| North | Ashton, Leigh and Wigan Halton and St Helens Trafford Knowsley | Five Boroughs Partnership NHS Foundation Trust | ✓ | |||
| Warrington | ||||||
| North | East Riding of Yorkshire | Humber NHS Foundation Trust | ✓ | |||
| North | Central Lancashire | Lancashire Care NHS Foundation Trust | ✓ | |||
| Blackburn and Darwen | ||||||
| London | Waltham Forest Redbridge | North East London NHS Foundation Trust (NELFT) | ✓ | |||
| Barking and Dagenham Havering | ||||||
| South West Essex | ||||||
| South | Oxfordshire | Oxford Health NHS Foundation Trust | ✓ | |||
| London | Bexley Care Trust | Oxleas NHS Foundation Trust | ✓ | |||
| Greenwich | ||||||
| South | Somerset | Somerset Partnership NHS Foundation Trust | ✓ | |||
| Midlands | South East Essex | South Essex Partnership University NHS Foundation Trust | ✓ | |||
| South West Essex | ||||||
| Bedfordshire | ||||||
| Luton | ||||||
| West Essex | ||||||
| North | Barnsley | South West Yorkshire Partnership NHS Foundation Trust | ✓ | |||
| Wakefield | ||||||
| South | Hampshire | Southern Health NHS Foundation Trust | ✓ | |||
| North | Bradford and Airedale | Bradford District Care Trust | ✓ | |||
| Midlands | Coventry | Coventry and Warwickshire NHS Partnership Trust | ✓ | |||
| London | Enfield | Barnet, Enfield and Haringey Mental Health NHS Trust | ✓ | |||
| Midlands | Leicester City, Leicestershire County and Rutland | Leicestershire Partnership NHS Trust | ✓ | |||
| Midlands | Northamptonshire | Northamptonshire Healthcare NHS Foundation Trust | ✓ | |||
| Midlands | Nottinghamshire County | Nottinghamshire Healthcare NHS Trust | ✓ | |||
| South | Southampton City, Portsmouth City | Solent NHS Trust | ✓ | |||
| Midlands | Worcestershire | Worcestershire Health and Care NHS Trust | ✓ | |||
| 25 | 19 | 15 | 8 | |||
| Subtotals | 44 | 23 | ||||
| Total (all integration) | 67 | |||||
| SHA cluster | PCT | Provider organisation |
|---|---|---|
| Midlands | Birmingham East and North | Birmingham Community Healthcare NHS |
| Solihull | ||
| Heart of Birmingham | ||
| South Birmingham | ||
| London | Barnet | Central London Community Health Care Trust |
| Hammersmith and Fulham | ||
| Kensington and Chelsea | ||
| Westminster | ||
| Midlands | Cambridgeshire | Cambridgeshire Community Services NHS Trust |
| Peterborough | ||
| Luton | ||
| Midlands | Derby City | Derbyshire Community Health Services NHS Trust |
| Derbyshire County | ||
| Midlands | East and North Hertfordshire | Hertfordshire Community NHS Trust |
| West Hertfordshire | ||
| London | Hounslow | Hounslow and Richmond Community Health Trust |
| Richmond and Twickenham | ||
| South | Eastern and Coastal Kent | Kent Community Health NHS Trust |
| West Kent | ||
| North | Leeds | Leeds Community Healthcare NHS Trust |
| North | North Lincolnshire | Lincolnshire Community NHS Trust |
| North East Lincolnshire | ||
| North | Liverpool | Liverpool Community Health Trust |
| Sefton | ||
| Midlands | Norfolk | Norfolk Community Healthcare NHS Trust |
| Midlands | Shropshire County | Shropshire Community Health NHS Trust |
| Telford and Wrekin | ||
| Midlands | North Staffordshire | Staffordshire and Stoke-on-Trent Partnership NHS Trust |
| Stoke-on-Trent | ||
| South Staffordshire | ||
| South | West Sussex | Sussex Community NHS Trust |
| Brighton and Hove City | ||
| North | Wirral | Wirral Community NHS Trust |
| Total | 15 |
| SHA cluster | PCT | Provider organisation |
|---|---|---|
| Midlands | North East Essex | Anglian Community Enterprise |
| South | Bristol | Bristol Community Health |
| London | Bromley | Bromley Healthcare |
| North | Hull | City Health Care Partnership |
| Midlands | Mid Essex | Central Essex Community Health |
| Midlands | Great Yarmouth and Waveney | East Coast Community Healthcare |
| North | Kirklees | Local Community Partnerships |
| London | Kingston | Your Healthcare |
| Midlands | Medway | Medway Community Healthcare |
| South | North Somerset | North Somerset Community Partnership |
| Midlands | Nottinghamshire City | Nottingham City Care Partnership |
| South | Plymouth | Plymouth Community Healthcare |
| South | Cornwall and Isles of Scilly | Peninsula Community Health |
| South | Swindon | SEQOL |
| South | Bath and North East Somerset | Sirona Care & Health |
| Total | 15 |
| SHA cluster | PCT | Provider organisation (company name) |
|---|---|---|
| Midlands | Suffolk | Suffolk Community Health Care/Serco |
| South | Surrey | Surrey Community Health (Assura) |
| Total | 2 |
| SHA cluster | PCT | Provider organisation |
|---|---|---|
| South | Gloucestershire | NHS Gloucestershire Care Services |
| South | Isle of Wight | NHS Isle of Wight |
| South | Torbay, Devon | Torbay and Southern Devon Health and Care NHS Trust |
| Total | 3 |
Transitions or turmoil
In gathering these data, we have evidence that the majority of organisations were making the transition at the point when we were trying to make contact with a senior manager for the first stage interviews. During the period 1 April 2011 to 31 March 2012, 82% of organisations were transforming their services, with 11% doing so the year before (Table 11).
For the study, this created significant challenges in establishing contact with senior managers engaged in major reforms to their services. These transitions created turmoil for the research process, and this is reflected in the response rate we achieved for the first stage interviews, presented in Chapter 6. The barriers and challenges created by Research Governance have been discussed in Chapter 4, but again these added to the challenges for the research team when conducting what may appear a simple scoping study of the roles of assistants in community nursing services.
| Year | n (%) |
|---|---|
| Pre 31 March 2009 | 2 (2) |
| 1 April 2009 to 31 March 2010 | 1 (1) |
| 1 April 2010 to 31 March 2011 | 12 (11) |
| 1 April 2011 to 31 March 2012 | 83 (82) |
| Post 1 April 2012 | 2 (2) |
| Not planned yet | 2 (2) |
| Total | 102 (100) |
Summary
Understanding the changing landscape is important in providing the context in which community nursing assistants are working, and appreciating the challenges experienced in locating our findings within this context. We now go on to scope the community nursing assistant roles and the views of senior managers of these roles in terms of their potential impact on service delivery and care.
Chapter 6 Scoping the role of assistants in community nursing teams
Introduction
The previous chapter described the new organisational structures for community services. This chapter considers findings from interviews with senior managers about the roles of community nursing assistants in these organisations. First, it is important to provide detail of the participants and organisations involved in this stage.
Accessing senior managers
For the scoping stage of the study we recruited 37 senior managers of community nursing services for a telephone interview. This constitutes 36% of the total number of provider organisations (n = 102) and 49% of the organisations we had research governance permission to contact (n = 76). We consider this a reasonable recruitment rate, given the community services transformations going on at the time of data collection (described in Chapter 5). It is also comparable with that of other studies that have surveyed NHS staff at this level of seniority. 78–80
The senior managers were recruited from a range of organisations across SHA clusters (Table 12) and the diversity of models of care provision created through service transformations, including the provider organisations for community nursing services newly formed following the split from the PCTs (Table 13). The organisations also represented each of the original 10 SHAs, including London (n = 2), North East (n = 2), Yorkshire and the Humber (n = 7), North West (n = 4), West Midlands (n = 6), East Midlands (n = 3), East of England (n = 3), South West (n = 3), South Central (n = 3) and South East Coast (n = 4). We experienced particular difficulties recruiting organisations from London. In the north-east, permission was not granted to make contact with three organisations providing community nursing services to a significant proportion of the population in this SHA (see Chapter 4, Ethical considerations). Chapter 5 has indicated that the reasons for these difficulties relate to the organisational disruptions occurring at the time of data collection. In order to promote transparency and confidence in the representativeness of the sample and findings, the organisations sampled will be described.
| SHA cluster | Eligible provider organisations, n | Sample number (% of eligible organisations) |
|---|---|---|
| London | 18 | 2 (11) |
| North | 34 | 13 (39) |
| Midlands | 27 | 12 (44) |
| South | 23 | 10 (43) |
| Total | 102 | 37 (36) |
| Organisational model | Sample (%) | National sample (%) |
|---|---|---|
| Community trust | 7 (19) | 15 (15) |
| Social enterprise | 3 (8) | 15 (14) |
| Vertical integration with another NHS organisation | 24 (65) | 67 (66) |
| Any willing PCT-accredited provider | 2 (5) | 2 (2) |
| Parked with PCT | 1 (3) | 3 (3) |
| Total number of organisations | 37 (100) | 102 (100) |
We aimed to recruit senior managers at director level: for example, Director of Nursing. The senior managers recruited to the initial stage of the study had a range of titles (Box 2). This reflected the diversity of post holders considered to be the most senior person available to provide information about the role of assistants within organisations. These key informants represented either the senior manager e-mailed or a person they subsequently nominated to be interviewed. The level of responsibility of the participants determined their ability to answer certain questions, in particular those related to the strategic direction of nursing services, rather than the day-to-day operational management. However, difficulties with recruitment to this stage meant that we were keen to have a discussion with the most senior person put forward by the organisation.
Directors ( n = 14)
-
Assistant Director of Nursing (n = 2)
-
Associate Director of Nursing and Quality
-
Director of Community Nursing
-
Assistant Director of Operations
-
Deputy Director of Operations and Deputy Chief Nurse
-
Director of Nursing and Quality
-
Assistant Director of Adult Community Services
-
Assistant Director and Transformation Lead
-
Deputy Director of Community Services and Integrated Care for Provider Services
-
Company Director – Responsibility, Professions & Services
-
Director of Operations
-
Service Director
-
Associate Director of Clinical Standards
Professional leads/heads ( n = 8)
-
Interim Professional Head of Nursing
-
Head of Specialist Nursing
-
Professional Head Nurse
-
Head of Clinical Professional Leadership
-
Professional Lead for Nursing and Head of Clinical Effectiveness
-
Lead for Long Term Conditions, Community Nursing and Urgent Care
-
Head of Community Health Care Services
-
Head of District Nursing
Managers of clinical services ( n = 8)
-
Operations Manager Community Nursing
-
Community Nursing Manager (Adult Division)
-
Directorate Manager, Adult Community Services
-
Adult Service Manager
-
Neighbourhood Team Co-ordinator (Nursing and Therapy Services)
-
Locality Manager (n = 2)
-
Clinical Services Manager
Team leaders/managers ( n = 3)
-
Virtual Ward Team Leader (n = 2)
-
Integrated Team Manager of Community Services
Senior practitioner ( n = 1)
-
Community Matron
Other ( n = 3)
-
Senior Clinical Governance Lead
-
Workforce Development Lead
-
Generic Programme Co-ordinator
Defining community nursing: it includes a heck of a lot!
For the purposes of our study we described our definition of community nursing in Chapter 2. However, it was important to gather the views and definitions offered by senior managers as to what they considered community nursing to be and what services were delivered by their organisations under the label of community nursing. The main feature discussed in these definitions was the extent to which community services were delivered to patients who were housebound (a traditional feature of the work of district nurses) or whether or not services were delivered beyond the housebound to include care provided by clinics or community hospitals.
The ‘basket of goods’ (senior manager 37) delivered by organisations, and as reported by participants, varied enormously. This was due to the commissioning of services by the PCT. It is important to present the community nursing services being delivered nationally so that the roles of community nursing assistants can be understood within this complex picture of service commissioning and provision. These contexts have implications for the roles of assistants and the ways in which these roles may be used and developed to deliver community nursing services.
Unsurprisingly, all organisations described district nursing and community nursing services as delivering care to patients in their own homes. Not all reported their out-of-hours nursing services separately because this was often considered a continuation of the daytime nursing services offered. Over half (n = 21; 57%) of the organisations surveyed reported the role of community matrons as being included in community nursing service provision. This is related to the historical development of the role by different organisations. The role of community matrons was first proposed in the NHS Improvement Plan81 to focus on the case management of those with long-term conditions who may be at risk of unplanned hospital admissions. Following successful funding from the SHAs, community organisations put in place a range of models to introduce this service. This included integration with the district nursing team or as a central long-term conditions resource. This accounts for some organisations reporting community matron services being available but separate from community nursing services. Where organisations did not have community matrons they reported having nursing services with a focus on the management of care for older people (n = 2; 5%), long-term conditions or chronic diseases (n = 9; 24%). This remit often falls within the community matron role.
Specialist nursing roles were described by over half of the organisations (n = 19; 51%). These included the following: coronary heart disease (including heart failure), respiratory disease (e.g. chronic obstructive pulmonary disease), neurology (e.g. Parkinson's disease and multiple sclerosis), diabetes, continence, stroke, tissue viability, falls prevention, palliation and end-of-life care. Many organisations reported that there were specialist teams to support the early discharge of patients from hospital to home or to prevent the admission of patients from home to hospital (n = 24; 65%). However, these services had a range of titles including rapid response services, single point of care, intermediate care and rehabilitation; the last-named of these included the assessment of equipment for loan within the home. Some of these services and staff were funded jointly by the PCT and local authority. Other organisations called these services intensive care at home (senior manager 14) and enhanced recovery service (senior manager 9). In addition to specialist nursing services, two organisations reported the provision of practitioner-led services. This included services to manage minor injuries and anticoagulation therapy. Phlebotomy services were also highlighted and tele-health services were reported by two organisations. The extent to which these specialist- or practitioner-led services used assistant roles was variable, and this is discussed further later in this chapter (Community setting requires higher-level assistants).
Community nursing services delivered to patients who were not housebound included services in community hospitals (n = 7; 19%), clinics (n = 4; 11%) and walk-in centres (n = 2; 5%). When considering those patients who were housebound, organisations included patients living in their own homes, residential homes or care homes. When asked for a definition of community nursing services, one participant stated:
That was going to be one of my questions to you. We feel our community nursing is much more than district nursing. So it will encompass all of the nursing services. So it would be your community matrons, your community nurses for older people and all of your intermediate care services as well and there is a whole range of those services within intermediate care. So it covers any that deliver community services.
Senior manager, 4
By providing this contextual detail about how community nursing services are defined by senior managers across a range of organisations it is apparent that there is a lack of consensus with regard to definitions. This aspect is largely dictated by commissioning, and as such the variation is likely to increase owing to changes in the provision of community services and competitive tendering for services. This will mean that some organisations will be selective about the services that they have within their ‘basket of goods’. This contextual detail is crucial for understanding the subsequent sections; these sections aim to unpack the roles, contribution, potential impacts and future directions for assistant roles within these services.
The rise of the assistant
All respondents considered the numbers of assistants to have increased over the past decade, alongside an expansion of their roles and scope of practice. Senior managers perceived that the reasons for this included a range of national and international drivers.
Policy drivers, shifting the focus of care from secondary care to the community, have greatly influenced the demand for, and range of, services provided by community nursing teams:
I think we've had a gradual increase in the role for health-care assistants but that's come along as the business has come along. So it matches in line with the service that we require and the profile of that service. So it isn't sort of like, well I need to replace, you know, so many band 5s with health-care assistants. It's been something about where the new business has been created and how we've looked at that role. So I think that's been much more proactive in where the health-care assistants have come along.
Senior manager, 8
The demand for services (or ‘new business’) is coupled with the changing demands being placed on these services by the population now being cared for in the community; patients have an increasing complexity of needs and dependency and are living longer with long-term conditions:
I probably think that the complexity of the caseload of community nursing in general has increased. So I think that the type of patient has changed which has by necessity changed the type of patient, client, that the health-care workers would see, sorry, that the health-care assistant would see.
Senior manager, 15
The changes in the patient population have influenced the range of services now considered under the ‘community nursing’ banner (as described above) and the roles of the community nursing team.
An increasing focus has been placed on improving the productivity of teams delivering care across all health-care settings. 4 This is to ensure quality of care and the provision of services that are cost-effective. Over the past decade, this has led to shifts in the working practices of health-care teams: who does what, when, where and to whom. The emphasis from policy is ensuring that the worker with the appropriate level of knowledge and skill is providing care to the patient rather than continuing practices simply because that is the way things have always been done. These changes in roles across the workforce have led to developments at the assistant level. As RNs have expanded their practice to cover roles ‘traditionally’ associated with medicine, this has (in turn) created gaps in terms of who provides fundamental care to patients or undertakes ‘lower level’ nursing tasks and roles:
It's about having the right skills for the right tasks . . . A team wouldn't be a team if everyone was of the same band, it would be inappropriate. Some interventions require a very high level of specialist skill and some don't. Some require consistent, more routine interventions or some are of a less technical nature and so it seems entirely appropriate and right that any team should have a mixture of people and be able to service the needs of the community appropriately . . . Financially there is a driver there for less expensive workers but it's got to be based on the skills needed and on the risk, managing the risk.
Senior manager, 28
Assistants were viewed as having negotiated their way into these areas and, as social services have taken responsibility for providing personal care, the assistant role has taken on more technical aspects of care. The roles and activities of assistants are described in a later section of this chapter (Community setting requires ‘higher-level’ assistants).
There was recognition among senior managers of the importance of planning the workforce for delivering nursing care due to changes in its makeup and preparation for practice. Another important driver for considering the development of the responsibilities of the assistant role was the future projected shortage of nurses due to the ageing nursing workforce and a decrease in recruitment. The moves to an all-graduate profession for nursing were considered as limiting the caring potential for individuals who may not want, or are unable, to complete a degree. Organisations have developed the assistant role to support career development and progression for assistant staff and to ensure job satisfaction.
Having considered the drivers for increasing the numbers of assistants, and their scope of practice, the following sections examine the numbers and roles of assistants within community nursing teams.
Describing the assistant workforce using national secondary data sources
It was difficult to gather details about the numbers of assistants through the scoping study. Senior managers were not able to describe exact numbers in the workforce for their organisations but indicated that assistants constituted about one-third of the community nursing team. One participant (senior manager 18) thought the skill mix in the community nursing team was 40 : 60 (registered to non-registered). This was considered an extreme case when compared with the descriptions provided by other senior managers. However, this participant also indicated that the changing landscape of community nursing (and nursing generally) might lead to these sorts of ratios becoming more commonplace.
Assistants were also identified as working in smaller numbers as part of rapid response services, intermediate care and rehabilitation. Some assistants within these teams were delivering both nursing and therapies. Assistants were less likely to have a role within community matron or specialist nursing services.
To try and establish a clearer picture of the numbers of assistants in community teams in England we used NHS iView data, derived from the NHS Electronic Staff Record, on staff in posts in NHS organisations. Data were extracted on the following:
-
health-care organisations: these were restricted to those providing community services
-
occupation codes: these were restricted to nursing and assistant staff working in community settings and in adult services (see Appendix 18 for details)
-
staff in post: head count numbers, full-time equivalents (FTEs) and Agenda for Change bands.
Overall numbers of FTE HCAs in community provider organisations, and HCAs as a percentage of the overall nursing and assistant workforce, are reported by organisation in Appendix 18 and are summarised in Table 14. Overall, HCAs make up one-quarter of the nursing and assistant workforce delivering community services, so there is one HCA for every three professionally qualified nurses. One organisation (an acute trust in London) appeared to employ no HCAs in a community setting, but otherwise the range of HCAs as a percentage of the nursing and assistant adult community workforce was 13–40%.
| Mean (SD) | 25 (7) |
| Median | 25 |
| Minimum | 0 |
| Minimum excluding one outlier (with no assistants) | 13 |
| Maximum | 40 |
Data were explored to determine whether or not there were differences between the percentages of assistant staff in different regions and different provider organisations. As illustrated in Tables 15 and 16, and Figures 6 and 7, there were no apparent differences between regions or provider types in assistants as a percentage of the overall workforce.
| Region | n | Mean % (SD) |
|---|---|---|
| London | 16 | 23 (9) |
| Midlands | 26 | 27 (8) |
| North | 32 | 25 (7) |
| South | 20 | 23 (6) |
| Type of provider | n | Mean % (SD) |
|---|---|---|
| Community trust | 14 | 27 (8) |
| Mental health trust | 22 | 27 (6) |
| Acute trust | 42 | 24 (7) |
| CIC | 12 | 23 (8) |
| Othera | 4 | 24 (7) |
FIGURE 6.
Adult and general community HCA staff by region.
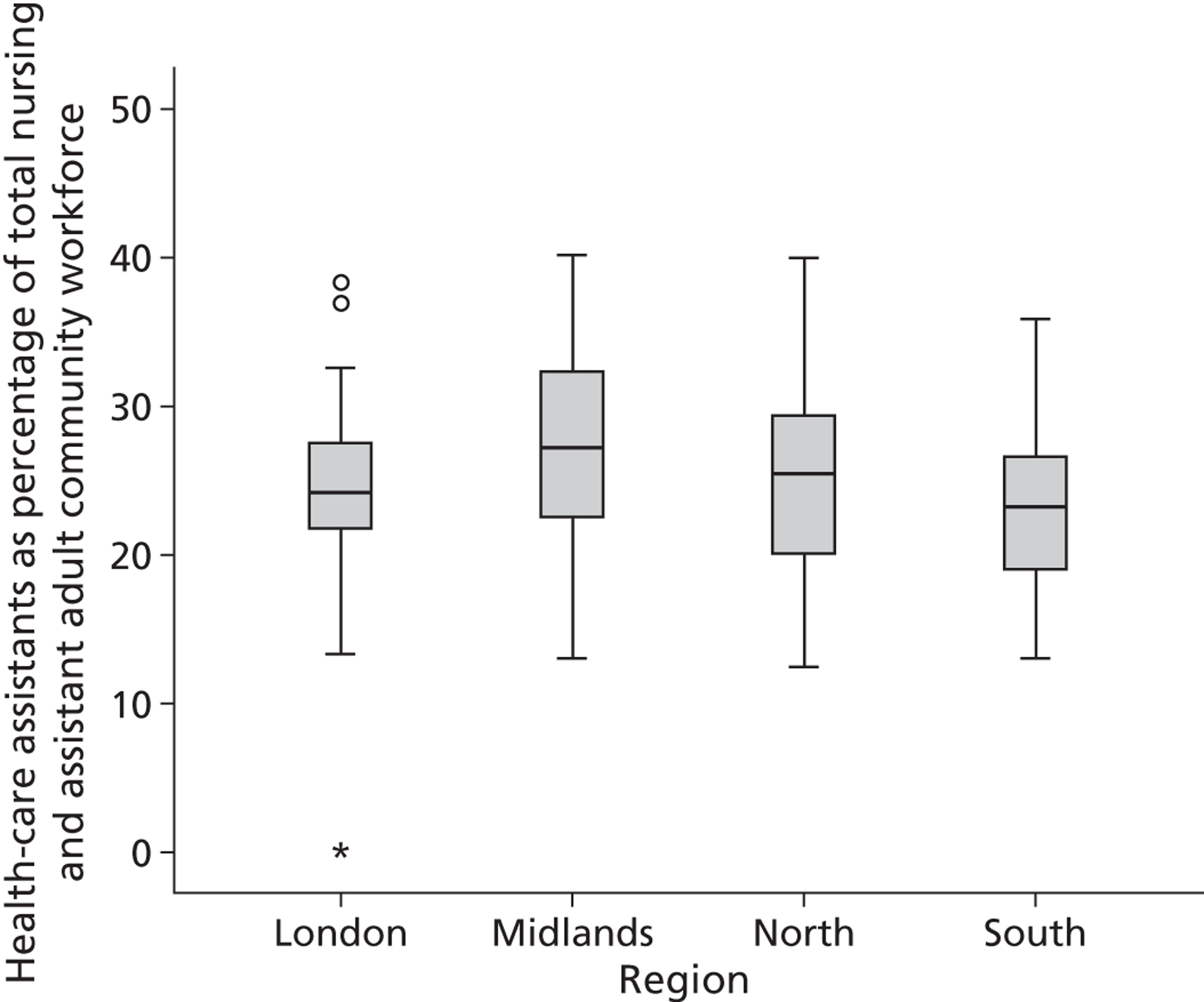
FIGURE 7.
Adult and general community HCA staff by type of provider.
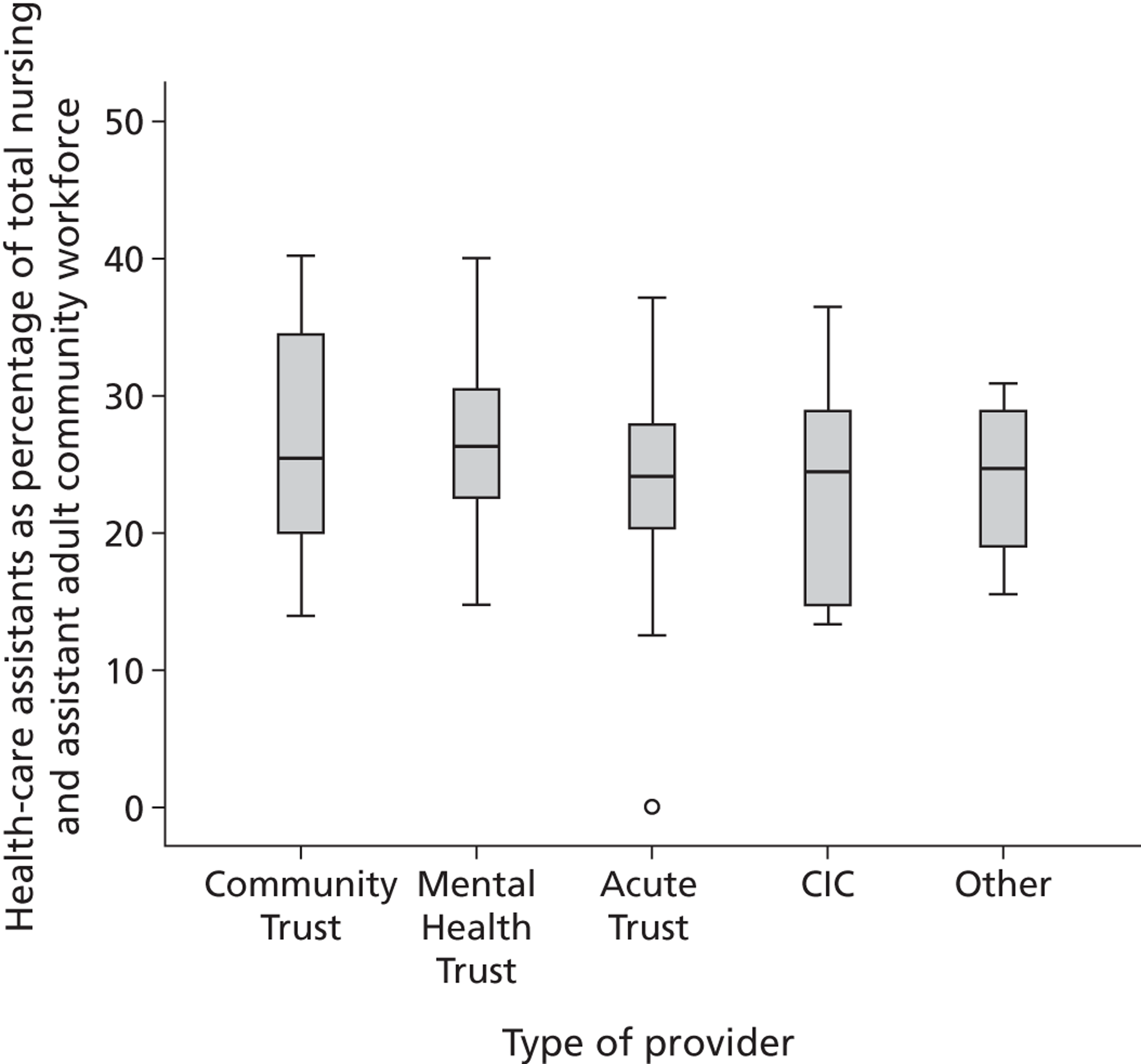
Community setting requires higher-level assistants
The majority of assistants in community nursing teams were reported to be employed at band 3 Agenda for Change25 or level 3 on the Career Framework. 8 This is consistent with the findings of iView analysis, where two-thirds of assistants were reported to be employed at band 3, with around 20% at band 2 and around 10% at band 4 (Table 17). The levels of working expected of assistants in community nursing teams can be linked with the levels of working described by Skills for Health (see Figure 3). 8
| HCA band | n | Mean (SD) | Median | Minimum | Maximum |
|---|---|---|---|---|---|
| Band 2 as % of all HCAs | 95 | 24 (18) | 20 | 0 (12 organisations) | 77 |
| Band 3 as % of all HCAs | 95 | 64 (19) | 67 | 9 | 100 (4 organisations) |
| Band 4 as % of all HCAs | 95 | 13 (14) | 10 | 0 (24 organisations) | 67 |
| Band 5+ as % of all HCAs | 95 | 1 (3) | 0 | 0 (81 organisations) | 13 |
Band 3 staff are expected to have increased responsibility compared with band 2 staff and to work independently if needed. Most band 3 staff have experience and qualifications [e.g. National Vocational Qualifications (NVQs)] associated with the work they perform. The focus on band 3 assistants in community nursing teams relates to the level of autonomous working and decision-making required of assistants when visiting patients in their homes:
Now the reason they are band 3 is, obviously because of their autonomous working. I mean they go out and see patients on their own, they have a level of, degree of competency, which we've looked at individually for each health-care assistant … within those teams.
Senior manager, 8
Roles for band 3 HCAs were wide ranging. Box 3 provides a list of tasks reported by participants that band 3 assistants are known to perform.
-
Personal care Assisting with hygiene needs; continence care (plus reassessment after initial assessment by RN); daily living support
-
Elimination care Bowel care; stoma care; inserting urethral catheters (female only)
-
Nutritional care Nutritional advice; dietary advice to patients with diabetes; blood glucose monitoring; PEG feeding
-
Rehabilitative care Movement/mobility; exercise sessions; fitting health-care equipment
-
Medicine administration Administering insulin (to stable patients only); administering eye drops; changing fentanyl patches (pain relief); reminding patients to take medications; ear syringing
-
Respiratory care Upper airway suctioning
-
Sample taking Venepuncture; testing specimens
-
Contribution to discharge planning
-
Clinical observations Systemic observations; electrocardiograms; pulse oximetry; bladder scanning
-
Long-term conditions care
-
Palliative/end-of-life care Supporting patient and relatives
-
Wound care Simple wound dressings (e.g. grade 1 or 2 pressure area care); assisting in leg ulcer clinic; compression bandaging
-
Administrative duties Record keeping: charting and reporting care delivery; entry of outcomes data
There was variation among participants, and so there was no consistency across organisations regarding what band 3 assistants can and cannot do. Equally, this list may not be fully representative of all tasks, but it usefully provides an overview of the range of activities being performed by this group of workers. Importantly, there was an emphasis on assistants at this level working with patients whose conditions were judged as stable, being involved in reassessments after a registered practitioner has completed the initial assessment, and working under the guidance of a registered practitioner who maintains overall responsibility for care delivery:
It may well be that [assistants] are supporting emollient regimes or they may well be supporting an element of a palliative care programme where the patient's not on complex drugs or they just need an intervention or, maybe very basic wound care or changing of compression hosiery. But all the time it's a, we're very mindful that it's a delegated task and actually, they have opportunity to come back after each, you know, during visits and they have a daily handover with staff. All of our staff have access to mobile phones so they have ongoing support throughout the day and ensuring that, you know, the unqualified staff have an opportunity to feed back issues and make sure that, as part of the cycle of visits, the patient that they're seeing is reviewed appropriately by qualified staff.
Senior manager, 15
Examples of when this might go wrong were provided. Take the following example where a senior manager was concerned about the ongoing assessment of the patient when patient care was broken up into tasks that were not closely supervised:
I am concerned that care delivery is being reduced to a series of tasks and not considering the whole person. We had a recent incident with a patient with diabetes developing a pressure wound. The HCA was administering insulin but not doing other activities to assess [the patient's condition].
Senior manager, 16
Despite the banding, there was an indication that banding did not always provide a good indication of what assistants at a specific banding (or level) could safely do. As a result of changes in the structure and organisation of community nursing services, some senior managers reported variations in practice. They also felt that this might be exacerbated by the history of the organisation and how this has shaped the contemporary practice of assistants in community nursing teams:
There's a lot of custom, practice and history that has gone on. Despite all [assistants] being paid at band 3 there is variation – some are developing and taking on additional tasks whilst others have not wanted to do that, have not been motivated to do that. So whilst paid the same they are working at different levels. But I personally feel there are two tiers of HCAs in the community at the moment.
Senior manager, 7
These variations in practice have led some organisations to consider ways in which they can promote consistency in service provision:
We've done a lot of work around clarifying and getting consistency across the service around what the roles and responsibilities are of the non-registered workforce because we found some inconsistency across different teams within the service so we did do a piece of work several years ago to clarify what they could do, what was reasonable for them to do and where they might develop their role further.
Senior manager, 36
Beyond community nursing teams, a small number of organisations reported band 3 assistants working as part of the specialist nursing services. This included roles for assistants as diabetes assistants, respiratory assistants, cardiac assistants, support workers in dementia support and stroke assistants (senior managers 3 and 29). Within rehabilitation teams the assistants are sometimes trained to deliver both nursing and therapies (senior manager 4).
When compared with band 3 assistants, those at band 2 are required to undertake fairly basic activities that are considered to require little or no experience or qualifications. However, some band 2 HCAs can end up taking on tasks associated with band 3, working beyond the roles originally intended for them. Senior managers discussed band 2 roles within their community nursing teams.
Band 2 HCAs were identified in the community nursing teams of 23 organisations (62%); one reported that the nursing teams inherited band 2 staff when the community hospitals closed in the area (senior manager 37). Four organisations (11%) identified band 2 assistants working only in the community hospitals. Ten organisations (27%) stated that they did not employ band 2 staff because the role was limited in the community setting; assistants in the community are expected to work with a level of autonomy.
Band 2 assistants were reported as being used as second workers, an extra pair of hands or a chaperone with the role of accompanying a registered professional on a home visit. As such, they were often part of the out-of-hours nursing teams for this purpose:
[These staff] tend to be used to ‘double up’. They are an extra pair of hands for the nurses when visiting dependent or complex cases.
Senior manager, 16
Other activities performed by the band 2 assistants were considered to (1) require basic knowledge in the field; (2) be delivered within established protocols or procedures; or (3) involve close supervision by a registered professional. For example, these included carrying out personal care (such as assisting someone to wash or dress or changing simple wound dressings), supporting end-of-life care or assisting within a supervised clinic (such as leg ulcer or continence clinic). Band 2 assistants had also been introduced to provide a phlebotomy service. The extent to which this was considered part of community nursing services varied among the participants. One organisation indicated that the introduction of a phlebotomy service using assistant staff was an innovation for their service delivery.
One organisation (senior manager, 32) reported employing a majority of band 2 assistants because they worked under the direct supervision of the district/community nurses. When describing the roles of these staff the manager reported that the assistants undertake activities such as ‘taking bloods, wound management, continence management, palliative care, diabetes care. They may have their own caseload. They do administration and ordering work’ (senior manager, 32). These activities were similar to the roles of band 3 staff in other organisations but this organisation stated that they did not employ any band 3 or band 4 assistants in the community nursing teams. Therefore, these band 2 staff may be working at a higher level, equivalent to a band 3 in another organisation.
The extent to which organisations had introduced band 4 assistants into adult community nursing teams varied, as did the services and ways in which roles had been introduced (Table 18). Almost half (n = 17; 46%) of organisations had introduced band 4 assistants. These staff were employed across a range of services including community/district nursing teams, supporting community matrons and care of patients with long-term conditions, rapid response teams, intermediate care teams, rehabilitation services and specialist teams (including stroke care, tissue viability and continence services). When supporting the district/community nursing teams, the role was recognised as being able to take on some of the lower-level responsibilities or work that is time consuming. This was to free up the RN to focus on more complex cases:
[APs] to take on some of the lower-level band 5 [registered nurse] work. So again they would be involved in simple dressings and may be able to run their own simple dressings clinic. We are currently skilling them up to give simple medications that don't require measuring . . .They would probably do some of the observations and support visits as well for patients who have got a palliative or terminal diagnosis.
Senior manager, 11
I think it's those additional skills around things like wound care. It's one of the biggest benefits because the majority of our district nursing workload is wound care and I think the assistant practitioners are able to do some of the more complex dressings.
Senior manager, 20
| Senior manager | Band 4 AP in adult community team? | Areas employing band 4/considering band 4 |
|---|---|---|
| 1 | Yes | Limited numbers across teams undertaking foundation degree |
| 2 | Yes | Support community matron |
| 3 | Yes | Assistants in provision of stroke care |
| 4 | Potential | To support community matrons/long-term conditions care |
| 5 | Yes | In specialist therapy services only |
| 6 | Yes | Recently introduced but not sure there are clear job descriptions |
| 7 | Planning | |
| 8 | Yes | Tele-health working with community matron |
| 9 | No | Considers organisation to lack structure and resources |
| 10 | Yes | But have left to do nurse training. Considering specialist roles for band 4 |
| 11 | Yes | District nursing teams |
| 12 | No | Walk-in centre only |
| 13 | Yes | Specialist teams – tissue viability and continence services |
| 14 | Yes | Community nursing teams |
| 15 | No | |
| 16 | Yes | Not sure where band 4 staff work but sure the organisation has them |
| 17 | No | Children's services only |
| 18 | No | |
| 19 | No | Children's services only |
| 20 | Yes | District nursing team |
| 21 | Yes | Inherited when organisations merged: considers staff not working at band 4 |
| 22 | Yes | Manage a caseload under supervision of community matron |
| 23 | Potential | |
| 24 | No | |
| 25 | No | |
| 26 | No | |
| 27 | Potential | To support community matrons/long-term conditions care |
| 28 | No | |
| 29 | Yes | Rapid response team and rehabilitation |
| 30 | Potential | Managing a caseload in tissue viability |
| 31 | No | Following skill-mix review redeployed to community hospital |
| 32 | No | |
| 33 | No | |
| 34 | Yes | Employed across services but some left to do nurse training, not replaced |
| 35 | Yes | Intermediate care, long-term conditions and rehabilitation |
| 36 | No | |
| 37 | No | Has an interest in developing roles but not supported by organisation |
There was support for the AP role because of its genericism; APs are able to work across traditional professional boundaries:
Certainly when you look at some of the new band 4 roles, actually the driver there is about the genericism of the role, so being able to have individuals that can work across professions.
Senior manager, 15
A number of organisations were employing APs to work in teams where the mix of nursing and therapy skills benefited service delivery, for example in rehabilitation teams. However, this can be contrasted with organisations that have introduced the role within specialist services, for example to develop the AP within a defined area of practice such as tissue viability or continence services. The shape of AP roles is determined by the organisational context in which they work and this creates variations across England in the ways in which these roles are being operationalised to support service needs. However, in determining suitable roles for APs, organisations expressed the importance of managing the risks associated with the work of the non-registered workforce and negotiating the scope of practice for these roles with registered practitioners:
We're having a debate with our tissue viability nurse about whether [APs] can do compression bandaging or not. There are kind of two schools of thought on that one. And that is part of the challenge, with some of the more complex tasks, is getting some of the specialist nurses to kind of think a little bit outside their box. And because assistant practitioners aren't registered, that raises people's anxieties, I think.
Senior manager, 14
Some organisations expressed a willingness to take a risk in substituting a registered practitioner with an AP and monitoring what happens:
So what we created was this role which we put an assistant practitioner in. Maybe with a little bit of degree of risk because did they need to be a qualified nurse? But that key role is a key focal point with tele-health direct and with the community matron.
Senior manager, 8
However, after taking a risk, some organisations paused to ensure that their staff were fully competent to undertake delegated tasks:
[APs] were doing four-layer bandaging but [senior staff] have pulled back on that at the moment because they want to make sure the competencies that they have in place are robust.
Senior manager, 22
In addition to those organisations with APs in post, a further four organisations were considering the potential for the role in their community nursing teams (within community matron and specialist services) and another was taking steps to introduce the role. A total of 15 organisations (41%) stated that they did not have and were not planning to introduce APs. This reflects a split in the ways in which assistant roles are being developed and deployed in organisations and community nursing services across England.
Increasing capacity for nursing care delivery or taking nursing work?
Senior managers reported the importance of ensuring that the ‘right person delivers the right care in the right place at the right time’, words echoed in a number of national strategy and policy documents. 2 In many ways, the rise of the assistant role has challenged managers to evaluate critically what different levels of staff are doing in community nursing teams and whether or not it is appropriate for them to be doing it. Appropriateness appears to relate to three key issues: (1) whether or not the skills of higher-level staff are being used in the best way possible and whether or not there is a demand for their level of skill elsewhere (e.g. focusing on more complex cases); (2) the costs; and (3) the risks and safety implications associated with what different levels of workers are doing. The range of activities and care being delivered by assistants was perceived as having increased over recent years, with assistants advancing their skills and taking over some of the work originally carried out by RNs.
Many senior managers reported assistants to be valued members of the nursing skill mix. They viewed assistants as meeting patients' needs and managing the range and volume of work covered by the community nursing services:
We could not deliver the service if HCAs were not involved.
Senior manager, 36
[Assistants] support the nursing team continually with day-to-day care so that qualified staff have more time to do the work they need to do, for example end-of-life care, complex wound management.
Senior manager, 27
Senior managers expressed the need for ensuring that the work delegated to assistants in the community nursing teams was risk managed, with suitable clinical governance arrangements in place. However, concerns were raised in three main areas:
-
the difficulties of supervising assistant staff who were delivering care in people's homes with a degree of autonomy
-
the lack of standardisation of work for assistants; and
-
the assistant workforce not being registered.
Senior managers felt that this was expressed through the reluctance of RNs to delegate, or let go of, certain areas of their work to assistants. There were descriptions of suspicion, threat and fear of assistant roles by RNs. Senior managers also expressed the importance of not diluting the skill mix in nursing teams too far. This was because there were activities that required a RN and comments were made about limitations to the scope of practice for assistants:
Band 3 [assistants] are cheaper than band 5 [registered nurses] but the staff nurse is more qualified and can do more. They have a higher level of skill and scope of practice.
Senior manager, 2
There are limitations to the assistant role. Registered nurses can act down but HCAs cannot act up.
Senior manager, 15
It wouldn't be sensible to have a team of just health-care assistants, because they are limited in what they can deliver compared to a trained nurse.
Senior manager, 31
More than one senior manager reported that care delivery was often based on custom, practice and history. This created future challenges for organisations to determine ways in which to support their nursing teams to consider different ways of delivering care, to maximise use of the entire workforce and offer potential benefits for patients in their care. Some organisations were working towards developing systems to promote confidence across the workforce, for example transparency of practice-based competence and systems to support delegation and reporting. In doing so, the aim was for assistants to be perceived as increasing the capacity of the nursing team to deliver care that benefited patients, rather than being viewed in a negative light as taking over the work of RNs. As one senior manager states:
Assistants are key to our future workforce and in moving forward but they will be working in very different ways compared to days gone by and will be much more skilled in the future.
Senior manager, 5
The visibility and approachability of assistants
Senior managers were asked about their perceptions of how assistant roles might be impacting on care delivery and the experiences of patients. This proved to be a difficult question for senior managers, with only a few able to provide examples of perceived impact on patient care and experiences. This may be because these staff are one level removed from the patients and care delivery. This issue was picked up in the next stage of interviews with service managers and team leaders. It was important to try and develop understanding about the potential impact of assistants on patient care and service delivery (see Chapter 7).
Senior managers focused on the closeness and stability of relationships that can develop between patients and assistant staff. Assistants were often described as going to see the same patients regularly and so were provided with opportunities for developing a rapport with patients. This regular contact was seen as an opportunity to promote patient confidence and trust in the assistants, whereas the RN was more likely to have competing commitments and be perceived as too busy to take the time to talk with patients:
Patients feel more comfortable, and aligned more, with the HCA. [Patients] feel they can talk to [assistants], and the [assistants] won't feel that the patient is daft.
Senior manager, 3
The trained nurse is running around being busy, delivering drugs and doing things that are far more important than talking to the patients. But the health-care assistant may stop and chat to the patient.
Senior manager, 9
I think [assistants] probably do pick up an awful lot of the softer intelligence, I think, that's going on [with patients] which maybe a qualified member of staff going in would be focused on, you know unfortunately, getting the notes done, the care plan written and all that kind of stuff and don't necessarily have the time to talk. But the health-care assistants often by their nature tend to be, you know, perhaps slightly more sociable and they have the opportunity to ask some of the softer questions in a less formalised way, I think.
Senior manager, 14
Health-care assistants have a very down-to-earth approach which is appreciated by our patients.
Senior manager, 31
There was also a sense in which assistants were perceived by patients as more approachable and (perhaps) on a level to be able to engage with their concerns. Senior managers implied the importance of this for patients, while also expressing the importance of the assistants in promoting stability and continuity of care for patients; assistants were often allocated the same patients each week. Perhaps more surprising was the perception among senior managers that the patients may not always recognise, or be concerned with, the difference between a RN and assistant:
Patients don't realise that some staff are HCAs. As long as the care they're getting is appropriate and safe and they're treated with respect and dignity.
Senior manager, 12
I don't think [the patients] mind who goes in to do the care as long as they feel that it's the right, the right care for them and that it's delivered by somebody who knows what they're doing and is competent to do it.
Senior manager, 20
Only one senior manager reported that patients clearly identified the difference between a RN and assistant. This manager described care delivery by nursing staff not in uniform and reported that patients could identify the district nurses because of ‘the way the nurse behaved or the information they had given to the patient’ (senior manager, 7). Further clarification of the behaviours displayed by the district nurse was not provided.
Providing specific examples of the impact of assistants on patient care was difficult for senior managers. In part, this was because they received feedback about the service delivery rather than the contributions of specific individuals. However, anecdotally, they reported not being aware of any complaints and noting generally good feedback (senior manager, 22) or compliments about assistants in certain areas of care. Significantly, valuing the time that assistants could provide to patients and carers was mentioned. Senior managers perceived assistants as playing an important role in throughput and ensuring that more patients were seen by community nursing services:
HCAs enable community nursing services to deliver a huge range of care within an affordable budget.
Senior manager, 29
[They're] allowing the trained nurses to do the role they're actually trained for. We can get our flow of patients and our throughput faster. . .If I've got a highly qualified nurse having to do a whole raft of interventions to that patient then that's not best use of their time. So, you know, the health-care assistant role is crucial to capacity really, meeting the demands and the capacity of the team.
Senior manager, 23
The assistant roles were also perceived to enhance services where the role crossed professional boundaries (e.g. nursing and therapies) or service boundaries (such as health and social care for end-of-life care).
Looking to the future: paralysis to stability and (some) development
As a result of the Transforming Community Services agenda,18 community nursing services have recently gone through an enormous change in terms of their organisation and structure. At the time of interview, many senior managers were just about to or had just gone through a significant change and so the focus for most was in securing stability for service delivery and their workforce. Therefore, given the timing of the interviews, the innovation and future of assistant roles was not always considered a priority. As such, there was a sense that the organisations and any plans that senior managers may have had for their workforce (including assistants) were in a state of paralysis. This was particularly the case where there had been integration of community services with acute or mental health trusts. Where developments were discussed, this related to types of services that the new organisations planned to deliver and the potential for reviewing the roles of staff for the delivery of these services.
Many organisations were exploring the education and training opportunities for the assistant workforce. They were aiming to implement competency frameworks and supervision for assistants to support the roles of these staff and their career progression. Concerns were expressed about the lack of national plans for the standardisation of education and training for these staff. They believed that variability would exist because organisations were implementing local arrangements in the absence of national support or guidance. As part of reviewing the competency of the assistant workforce, some organisations were exploring the potential for the introduction or development of higher-level AP roles within community nursing teams. Some senior managers indicated that they would look at ways in which these band 4 staff might substitute, or in some cases replace, band 5 community nurses.
Another priority for senior managers was looking at the integration of services when considering the future direction of community care. In particular, they envisaged integration across health and social care with assistants working across these boundaries. A small number of organisations were already doing this in their delivery end-of-life care. Social enterprises expressed innovation in assistant roles more clearly, and there was a sense in which their focus on business and new business was forcing them to consider new ways of delivering care within the competitive market for commissioning of future community services:
We need to make sure we are coming up with the competency frameworks for this up-skilling of assistants and in terms of what we will be delivering in the future. . .As a social enterprise we are looking at training needs and how these are changing as we go forwards. . .What key skill sets do we need, both district nurses and assistants.
Senior manager, 5
For other organisations, the main focus was on changing cultural and social expectations of staff to enable assistants to extend their roles; senior managers discussed the potential threat of the assistant roles for some registered practitioners and their reluctance to support development of assistant roles. However, senior managers discussed role developments for assistants, such as being able to administer insulin to patients with conditions categorised as stable, administer site pain relief patches or carry out compression bandaging. These activities are already performed by assistants in some organisations but not others:
I think you have to be cautious about what can be delegated safely, you know, so that you're not putting patients at risk . . .I mean the only one I have explored in the past, and we've drawn a blank, but I know some areas do it, is insulin. We have a fair number of elderly patients who can't give their own insulin. Even with exploring the devices with the diabetes team, we have to send a registered nurse in, literally, just to give the injection and that was something that we thought perhaps an HCA could do. But at this moment in time, it's not been deemed as the correct thing to do so we haven't pursued it.
Senior manager, 13
For others, the merging of organisations led to a questioning of the appropriateness of assistants undertaking particular activities and the lack of standardisation that may compromise quality of care:
Since merging with the Trust, questions have been raised about HCAs administering insulin.
Senior manager, 26
The merger of three organisations means that there is lack of standardisation in relation to assistant roles. That requires attention. There is some concern that [registered] staff shortages means that assistants will be delivering patient care with not as frequent reassessments by the trained nurse as there should be.
Senior manager, 10
The merger of three organisations is proving challenging for promoting equity across assistant roles due to differences in [assistant roles in] the 3 [original] organisations.
Senior manager, 18
The quotations above demonstrate the variability across organisations regarding what was deemed an acceptable task for assistants to undertake, driven on by sociopolitical influences. The merging of organisations means that some new services have to manage assistant roles that may have been influenced by more than one organisational context. This presents a significant challenge for these organisations in the short to medium term. Regardless of context, senior managers emphasised the need to ensure appropriate safeguards are in place to manage risks and balance this against the push to introduce change and innovation quickly:
We have to make sure the right safeguards are in place when assistants are delivering care. Quality and risk have to be balanced. . .Innovations can be pushed through quickly but it is important to take time to get things implemented. It needs to be done safely and this will take time.
Senior manager, 1
As organisations regain stability this may enable the focus to shift to innovation and development of the assistant workforce. Currently there are significant variations across organisations, and it will be interesting to see how this plays out in the competitive commissioning arena of future community nursing service provision.
Summary
This chapter has considered the national picture in relation to numbers and roles of community nursing assistants. It has relied on the views of senior managers and revealed variations in the levels of understanding about assistant roles among senior managers. The following chapter aims to develop depth of understanding of assistant roles in community nursing teams by gathering the perspectives of service-level managers who engage in the day-to-day work of assistants.
Chapter 7 Understanding community nursing assistant roles in practice
Introduction
The previous chapter considered the organisational perspective and vision on the role of assistants in community nursing teams. This chapter engages with the views of managers at the service level to present an in-depth understanding of the roles and responsibilities of assistants. It also addresses their potential impacts on service delivery and patient care at the operational level. First, we describe the participants for this stage.
Accessing service-level participants
For stage 3 of the research, we sampled 10 organisations from stage 2, which were representative of the range of organisations included in the scoping stage (e.g. community trusts, social enterprises, integrated services and other providers), regions (by SHA cluster), banding of assistants (to include organisations with bands 2, 3 and 4 and where there were differences in the configurations of these bandings) and range of services in which assistants were employed in community nursing teams.
We recruited a service manager and caseload holder from each of these organisations, or, where it was not possible to recruit a service-level manager, we recruited two caseload holders. However, there were variations in titles and responsibilities and so in many organisations our sample included a mix of band 8, 7 or 6 managers. By engaging two participants from each organisation we were able to gain different perspectives on roles for assistant staff within the sampled community organisations. The interviews for this stage of the research were conducted in the context of what we heard from the senior managers about the organisation and their strategies for the assistant roles. The total sample for stage 3 was 30 participants. This included six service managers (at bands 7 and 8a), 14 caseload holders (at bands 6 and 7) and 10 senior managers (from stage 2). Table 19 provides further details of the sampled organisations and interview participants.
| Organisation ID | Type of organisation | SHA cluster | Participant (and ID) | Comments about assistant role |
|---|---|---|---|---|
| 6 | Arms-length PCT provider moving to PCT-accredited provider | South | 6: senior manager | Band 3 assistants and developing band 4 roles |
| 6: service manager | About 20% of community nursing workforce | |||
| 6: caseload holder | Training on the job and NVQs/foundation degrees | |||
| Competency frameworks for assistants | ||||
| 8 | Social enterprise | North | 8: senior manager | Bands 2 and 3, and band 4 in specialist roles |
| 8: service manager | About 25% of community nursing workforce | |||
| 8: caseload holder | Training on the job and NVQs/foundation degree | |||
| Competency frameworks for assistants | ||||
| 10 | Vertical integration with NHS organisation | South | 10: senior manager | Band 2, band 3 and specialist band 4 assistants |
| 10: caseload holder A | About 20% of community nursing workforce | |||
| 10: caseload holder B | Training on the job and NVQs/foundation degrees | |||
| Competency frameworks for assistants | ||||
| 13 | Vertical integration with NHS organisation | Midlands | 13: senior manager | Band 3 assistants, specialist band 4 roles and band 2 phlebotomy |
| 13: service manager | About 20% of community nursing workforce | |||
| 13: caseload holder | Training on the job and NVQs | |||
| Competency frameworks for specific advanced skills | ||||
| 18 | Community trust | Midlands | 18: senior manager | Band 2, 3 and 4 assistants |
| 18: service manager | About 60% of community nursing workforce | |||
| 18: caseload holder | Training on the job and NVQs/foundation degrees | |||
| Competency frameworks for assistants | ||||
| 19 | Vertical integration with NHS organisation | Midlands | 19: senior manager | Band 2 and 3 assistants (no band 4) |
| 19: service manager | About 20% of community nursing workforce | |||
| 19: caseload holder | In-house training (as well as NVQs) | |||
| Competency frameworks for assistants | ||||
| 24 | Vertical integration with NHS organisation | North | 24: senior manager | Band 3 assistants |
| 24: caseload holder A | About 25% of community nursing workforce | |||
| 24: caseload holder B | Training on the job and NVQs | |||
| Competency frameworks for assistants | ||||
| 27 | Vertical integration with NHS organisation | London | 27: senior manager | Band 2, 3 and 4 assistants |
| 27: caseload holder A | About 25% of community nursing workforce | |||
| 27: caseload holder B | Training in-house and training for band 4 | |||
| Competency frameworks for assistants | ||||
| 30 | Vertical integration with NHS organisation | North | 30: senior manager | Band 2, 3 and 4 assistants |
| 30: service manager | About 20% of community nursing workforce | |||
| 30: caseload holder | Training on the job, NVQs and foundation degree | |||
| Competency frameworks for assistants | ||||
| 31 | Vertical integration with NHS organisation | North | 31: senior manager | Band 3 assistants and an inherited band 4 (redeployment) |
| 31: caseload holder A | About 20% of community nursing workforce | |||
| 31: caseload holder B | Training on the job with limited formal training | |||
| No written competency framework |
Changing roles to meet changing care demands on community nurses
Demands on the community nursing service were described as changing to meet the changing needs of the community nursing team caseloads. Policy influences and demographic changes described in Chapter 2 (such as the move from hospital to home-based care and the growing population of ageing patients with complex nursing needs) were viewed as influencing roles across all community nursing teams. Many participants described how all staff (registered and non-registered) were moving up in terms of the work and roles they performed:
Whereas the band 3s now some of their tasks, is probably what a band 5 was doing a few years ago. And like a band 5's moved on as well.
Caseload holder A, 31
I think the role of band 6s and band 5s have changed tremendously. We've got much more complex cases now with continuing care, the assessments and the auditing and there's so much to do, the caseload management, that I think that we need the health-care assistants for hands on clinical work which they're very good. So they do quite a lot of preventative work, for example, I mean you know skin care, leg care, preventing ulceration, all those things that are important to prevent leg ulcers developing and they're the ones that do those things.
Caseload holder A, 27
An important shift in the assistant role was perceived to have been instigated when personal care delivery was transferred to social services. This led to the demise of the bath nurse and a focus on developing the role for assistants to support health-care delivery by RNs:
I suppose we've always had them. We have always employed HCAs but I feel that role evolved so much over the years. I mean when I was a district nurse they were still bed-bathing patients. . .But that's no longer part of our community service and hasn't been for quite some time hence the role has changed and developed.
Senior manager, 24
Many participants described the caseloads that community nursing teams are now responsible for. Importantly, this was shifting to providing more care for older patients with more complex needs, as well as managing patients with long-term conditions:
Our demographics of people getting older – we've got far more volume and we perform far more, I suppose, what you would deem ordinary nursing care in the community, which can be delegated down to different grades of staff.
Senior manager, 13
About 50% are long term, with long-term conditions who we're managing – like bad ulcerated legs that are never going to heal, people who have got MS who we do support packages for. And the other 50% tend to be things like blood tests, routine bloods, removing of sutures, people who come on and off the caseload.
Caseload holder B, 24
Managers articulated a perceived need for assistants within the community nursing teams to manage these increasing caseloads. Assistants were viewed as having an important role in providing the more routine care so as to free up RNs' time to focus on patients with more complex care needs. This skill mix promoted better use of the available human resources within these teams:
I feel as though the health-care assistant's going to do more practical-based things and it frees up the qualified nurses to do the – to attend to the more complex patient needs, and we're getting more and more patients coming out [of hospital] early and we're doing lots more stuff we never ever did, or imagined we'd do, now in the community. . .I just think if [assistants] do the basic practical procedures – although they do have to have an understanding, and I think they do – I think it frees us to do the more complex patients.
Caseload holder B, 31
The right patient gets the right skill level really because I mean sometimes when you haven't got enough care assistant cover, you actually send in really experienced, skilled nurses to things that actually they don't really need to do. It's a waste of their skill really and taking them away from things that they do need to do. [Q: Can you give me an example of just that exact point where, you know, if you didn't have a care assistant and you're sending a nurse in that you think, actually it doesn't require. . .?] Yeah I can give you loads! Well bloods, catheter bag changes, really simple wound dressings, blood pressures, incontinence assessments, BM [blue glucose] monitoring, lots of basic visits that an auxiliary is quite capable of doing. And what happens in that scenario is, because it happens regularly, is that the nurse then has less time to spend on a really complex palliative patient which is really important now people are choosing to be cared for at home, you know, these visits are not quick visits but sometimes they have to be because you haven't got the time.
Caseload holder, 8
However, there was recognition of the importance of the RNs' role in the community teams and a concern that some organisations might start to replace the registered nursing workforce without thinking through the implications of care; this concerned participants for reasons we will return to. The RN role was described as important and one that cannot be replaced entirely by the assistant:
I wouldn't want a team to think, oh hang on a minute, I can have three health-care support workers instead of that trained nurse, let's do that. Forgetting that there are things that [assistants] won't be able to do.
Senior manager, 10
Assistants were described as plugging the gap in services and providing breadth to the nursing team. Some staff expressed concern about the developing two-tier system in nursing, and that development in roles for assistants was in many ways mirroring the past roles of the enrolled nurse (historically a second-level role in nursing27–31). For many participants, the rise in numbers of assistants and growth in their scope of practice was related to costs or the fact that organisations had a more business-like approach, recognising the future competitive nature of markets in the provision of community services:
From a skill-mix point of view, HCAs are a lot more cost-effective than what your staff nurse are sometimes because obviously if the health-care assistant can do the job instead of sending your staff nurse, you can send your staff nurse to a more complex situation.
Caseload holder, 13
I think we've had a gradual increase in the role for health-care assistants but that's come along as the business has come along, so it matches in line with the service that we require and the profile of that service. . .It's been something about where the new business has been created and how we've looked at that role, so I think that's been much more proactive in where the health-care assistants have come along.
Senior manager, 8
We had a new service-level agreement with the GP practices. . .So that altered the pressure of work for the band 2s really which is really when we had to pull quite an effort into the band 2s to get them up-skilled because a lot of the venepuncture work wasn't there any more, if that makes sense.
Service manager, 19
The numbers of assistants employed in community nursing teams was described with great variability. In many of the participating organisations, the assistants comprised 20–25% of the community nursing workforce (a ratio equivalent of 80 : 20 for registered to non-registered nurses). However, one organisation described their workforce as weighted towards assistants, making use of a range of assistant roles (banded 2 to 4):
We are about 60 : 40. So this means that we are about 60% HCAs, these are basically in the community units, you may get one or two trained staff on duty, so they have to ask the assistants to do more to support them and we have to look at the competency behind that.
Senior manager, 18
There was a suggestion that this more extreme case may become the norm over the next decade, particularly if roles for higher-level (band 4) assistants are developed. However, we note here that our analysis of NHS iView data did not reveal such extreme numbers. These secondary data sources supported the ratio of 25% cited by the majority of managers and revealed that the highest proportion of assistants in any of the organisations was 40%. The reliability of information provided by the senior manager quoted above should therefore be interpreted with caution.
The next section describes current roles and responsibilities for assistants in more detail.
The unrecognised workforce
Participants were largely positive about the contribution of assistants to the work of community nursing teams. Assistants were described as valuable or core members of the team, or the backbone of services. There was a sense in which care delivery would not be possible without the assistant staff and their level of commitment to service delivery. A number of managers commented on the work and attitudes of assistants:
The high level of care [provided by assistants], the high level of skill and the sort of joy and passion for it, it really made me feel humble. It really, really did. It was such an unrecognised workforce really, you know, and doing such a fantastic job and making such a difference to patients.
Service manager, 18
However, there was also a concern that despite being valued, assistant staff might become workhorses, allocated the mundane or repetitive or routine work. This could prevent assistants from being able to deploy their range of skills, lead to boredom among the workforce and create a culture in which the development and careers of assistants were not attended to:
They end up getting the boring jobs and then it's difficult then to try and make it interesting, you know, to give them the work that we need to give them but also make sure that they're not bored, that they're not getting fed up or that they're still a bit challenged and they feel that they're contributing to the team. . .I think sometimes it's difficult and you feel like you're the bottom of the pile if you're a HCA because you're the lowest band, whereas actually quite often you're holding everything together.
Caseload holder, 6
Organisational factors were also noted to influence the work allocated to assistants. So, for example, if the community nursing team was short staffed (i.e. not having enough RNs available) then this may place demands on assistants to undertake repetitive work:
I mean one of the problems we have is we have two leg ulcer clinics per week. . . and you know if you're a member of staff and you've got say five bilateral legs on a Monday morning and then you're going to be in the leg ulcer clinic all afternoon, you know that's sometimes very challenging and they would question the fairness of that. [Q: So is this something about a desire to have your workload mixed with different clinical skills, patients?] Yeah absolutely and certainly the band 3s felt that because they sort of undertake extra training, they feel that the work should reflect that. Which generally speaking, to be fair, the qualified nurses try but if you're short of staff somebody has got to pick it up at the end of the day and you can't always distribute work to the most appropriate band if there is nobody there.
Service manager, 19
Similarly, this could lead to differences in roles for assistants within the same organisation but working in different urban or rural locations:
I have to say she had more responsibility thrust on her shoulders than they do in the country areas. Do you understand what I mean? She was given – she was full time in [name area] and she had very, very little staff and she probably did more – she perhaps did things you know perhaps – she was trained because I trained her – I supervised, you know, but probably she wouldn't get the same duties in the country. Do you understand what I mean?
Caseload holder B, 31
The assistants were often described as experienced members of the community nursing teams with longevity of service. This created a stable influence within the community teams and assistants were described as providing emotional support or acting as motherly figures for younger RNs:
I often see the HCA as being quite a core member of the team. They don't tend to move about so much. They tend to stay and be a very stable influence within the team. Certainly within a lot of the teams that I've worked in, the HCA has often been quite a motherly figure within the team who looks after the members of staff within that team and it is relied on in a lot of ways to support the work of the other members of the team. But also support emotionally. I mean they often have great life experience that maybe some of the less experienced trained staff don't have and it's very important that you get that mix of not just of nursing skills but experience generally.
Service manager, 13
Individuals recruited to assistant posts in the community were often older with a life experience that enabled them to manage the nature of community nursing: lone working and going into people's homes. This experience seemed to support their ‘sixth sense’ of knowing when something may not be right with a patient, which helped to facilitate appropriate clinical input for patients:
We've got a lot of experienced [assistant] staff here who have worked in the community for a lot of years and have acquired skills in assessment and knowing that sixth sense when something is not quite right.
Service manager, 8
Many organisations discussed the recruitment of assistants to community nursing teams, valuing the experience and age of mature candidates. This was demonstrated by their recruitment policy to shortlist only candidates with previous nursing assistant experience and a NVQ qualification. However, one organisation also emphasised the importance of nurturing the future workforce by engaging younger individuals with community nursing as a potential career, and balancing this with ensuring an experienced assistant workforce. This model was not discussed by any other organisations:
So what we've started to do as well is, you know, sort of common with a lot of urban areas, we have got a large group of young people who are rudderless and not got opportunities, so I'm taking on apprentices to complex care and they do their NVQ 1 day a week and then they're supervised practice the other 4 days a week to try and start and they do numeracy and literacy testing, so we start nurturing. Start nurturing, get some enthusiastic youngsters. . .You sort of need youth and enthusiasm and you also need mature, clear heads and people that can respond to how complex it is in the community but people don't appreciate. I mean I certainly didn't. Definitely didn't, thought it was all about acute. I had such a surprise really. [Q: From the wide range of care that is delivered?] Absolutely and the level of skill and the specialist knowledge that you've got to have to nurse somebody in their own home.
Service manager, 18
We now move on to discuss the variability in assistant roles across, and even within, organisations and the ways in which assistants support the work of RNs.
It's not all routine: variability in the range of roles and complexity of work undertaken by assistants
Many participants initially described the assistant roles as providing care that was considered routine and for stable patients. Care was often delegated to assistants once a RN had assessed the patient and determined the most appropriate plan of care. This included making a decision about patients who should not be delegated to assistants because of their unstable conditions or potential for rapid deterioration:
We have some patients we wouldn't delegate to HCAs, for example, difficult diabetic foot ulcers. Even though our band 3 HCAs are trained quite thoroughly in using an aseptic technique, we would still try and keep that to a qualified nurse because they can deteriorate so rapidly, can't they, and I don't think it would be fair on the HCA to have the skills to pick up on that in the same way.
Caseload holder, 19
As such, the assistant role could be considered one of maintenance or monitoring of stable patients. However, further descriptions of assistant roles revealed that assistants may work beyond this level.
Many organisations considered that they required assistant staff to be of a certain level before they were deemed safe to go into people's homes. This safe level was described by managers as the band 3 assistant. Some organisations did employ band 2 staff, and the following description provides insight into the different levels and the work that they do:
We will be able to delegate [to a band 3] routine non-problematic care . . . recatheterisation, PEG feeds – commencing PEG feeds where we have a few patients with long-term neurological conditions who need, you know, a peg feed commencing in the morning and taking down again in the evening. The medication, this obviously all comes with proper training, but obviously you wouldn't delegate this to a band 2 at the minute. Evidence gathering, so continence assessments, the initial urine analysis and bladder scan. Helping patients fill the monitoring forms out, the forms that we need to gather the evidence for a qualified nurse to make a continence diagnosis if you like. Yeah after a qualified nurse has assessed a wound, a surgical wound, the band 3s will be able to remove clips. . . A band 2, we delegate quite a lot of responsible work for the band 2 but it's more around phlebotomy, taking blood in the patient's home or filling in for phlebotomy schedules when we don't have a phlebotomist on duty. A lot of wound care, again sort of stable healing wounds, not leg ulcers requiring compression. Taking blood, wounds, and so on.
Caseload holder, 19
Importantly, the nature of community work dictated this level. The unpredictability of what assistant staff may be faced with when visiting patients was considered to require this level of skill and experience:
You know, it can be quite daunting going into a patient's home even if it's somebody that you've visited previously because you never know quite what you're going to find at that time, you know, and often you have to deal with all sorts of things that might crop up either last time you visited or while you're actually in the house at that time.
Senior manager, 24
I do feel that health-care assistants in the community have to be trained to a certain level more than they would be say they were in a hospital setting because they are by themselves, because they do have to have some ability to react to patients when they see them if there is a problem but there will always be a time delay between them seeing there's a problem and someone getting to them, just because of the locality and how we work and where we are.
Caseload holder B, 24
To ensure that assistants were prepared for their lone working, organisations reported delivering a range of mandatory training including health and safety, governance and basic life support.
Activities carried out by assistants were sometimes described as simple but, on reflection, managers considered that they might actually be asking assistants to carry out more complex tasks. However, because they had confidence in the abilities of the individual assistant and a particular task was being undertaken by them on a regular basis, they often felt prepared to delegate tasks that may be considered to go beyond the role. Take the following example regarding wound care:
I'm saying simple dressings but they're probably not all that simple either, if you know what I mean. If we have a dressing that we're doing daily, and it was, say the wound was oozing or whatever, yes she would do the daily dressing as well. [Q: Right, so what would make you decide to delegate the wound dressing to the health-care assistant?] Because I suppose of her experience, I know what her capabilities are and what people, you know, because obviously – and it's quite hard answering these questions because I can think of some other ones perhaps you wouldn't delegate, whereas sometimes it's more a personality thing, isn't it, than actual job title as well.
Caseload holder A, 31
Variability in the roles and responsibilities of assistants employed at the same level was apparent, even within the same organisation. The following example highlights differences in practice between assistants within the same organisation (24) and at the same level (band 3), depending on the community nurse team they work with:
All three of them do bandaging, simple bandaging to two-layer, but they don't do compression bandaging. There's been major discussions over the years about whether health carers should actually do compression bandaging or not, but at the moment ours only do to two-layer.
Caseload holder A, 24
They do vary because the senior health-care assistant, as in NVQ, has been with us for about 15–16 years and she's developed her skills to be extended to do things like catheterisation and four-layer bandaging. . .The junior one has been with us for about 2 years is much more a task-orientated worker. . .So there is a skill mix between the two of them which is very different to what each one does even though they're on the same band.
Caseload holder B, 24
The merger of organisations as part of the transformation of community services was also exacerbating some of these discrepancies.
One area of practice where there seemed little agreement across organisations concerned the role of assistants in supporting medicine administration. Not all organisations approved this, but where this did occur it tended to involve prompting patients about their medications, and there was training and clear guidance on how assistants should perform this role. However, one organisation described a band 4 assistant's role in administering medicines:
She can give B12 injections, she can give insulin. We haven't had clarification on G-CFS [granulocyte colony-stimulating factor; the participant described what was meant by G-CFS: ‘It's simulating white blood cells for people that are having chemotherapy, so they're having their course of chemotherapy and it drops their white blood cells and they have these injections which just boosts it up and they have to have them for about 5 days just after each chemotherapy cycle, so we do that quite often’] so she hasn't been doing that. She can give Fragmin and Clexane and she can apply [opiate] patches, she can give eye-drops. She's got medication competencies that she's been through.
Caseload holder, 6
Some organisations described assistants as managing a caseload (this was presented in Chapter 6). We asked staff at the service level for examples of how assistants might manage patients. The following example was provided for a band 3 assistant; however, this perhaps reflects the different language used by different individuals, as case management in fact relates more to monitoring and seeking the input of the RN as required:
[The patient is for] INR monitoring [International Normalized Ratio (INR) is a measure of blood clotting most commonly used to monitor people on anticoagulant therapy] and she's for BP [blood pressure] – she's very elderly and she needs an ongoing – she's had an assessment by a qualified nurse but after that assessment, the health-care assistant would go in and deliver all the care. So she's really case-managed by a health-care assistant. [The assistant] goes in and does INR, her blood pressure, anything else – I think she needs continence care. And then she would, you know, if she had any problems with this person she would come back to us. But if she didn't, she would probably be carrying on dealing with this for quite a considerable length of time. If her condition changed because I suppose because by doing that as well, if the same person goes all the time, they can tell when the condition changes, can't they – really, much better than what we can – she would come back to us and ask us actually to go out and reassess.
Caseload holder A, 31
Assistants, particularly the band 2 staff, might also assist the RNs when required; this is often described as double-up care. Examples of this included visiting a patient to dress a large wound, where there was a considered safety risk associated with the visit, or providing palliative care and administering controlled medications:
Usually what we do is, if a patient who is palliative care has a syringe driver, we usually go in pairs because of controlled drugs policy that we need two nurses or a nurse and a health-care assistant to check the drugs. And usually what we do is the health-care assistant, as long as they can provide the personal care on their own and obviously we help if they need a second person, whilst the trained nurse sets up the syringe driver and then she checks the drugs afterwards.
Caseload holder B, 27
The characteristics of the assistant workforce, who tend to be older with a number of years' caring experience, mean that the assistants can have a lot of valuable knowledge and experience to share within the nursing team. In some situations, assistants advise RNs or make suggestions for patient care, but the decision to implement care was generally perceived to rely on the RNs' judgement:
When you've got [an assistant] that's been in the job for 10 years, for heaven sake, she will know an awful lot about the sorts of dressings that's likely to be or the type of treatment that might work and she'll come back and say, oh why don't we try a bit of this. And quite often I will say that's a great idea, yes we'll go for it but she has to check it out with [a registered nurse] first because, you know, we're the ones prescribing the treatment so therefore we will be prescribing the dressings and they don't actually prescribe.
Caseload holder, 18
However, there were some examples provided where an assistant had changed the care plan or decided on the care to provide following an assessment of a situation. Again, these situations arise because assistants are visiting patients in their own homes and there is a level of unpredictability as to what they may be asked by a patient. Importantly, there are mechanisms for the RNs to follow up these decisions:
If at a visit say a patient said that they had, they'd sort of like walked into the table yesterday, like they do, and got a skin flap, so that was like a new. . .[Q: A new injury or a wound?] [The assistant was] actually going into the house to do the bloods. It's nothing to do with that. So if that was – I suppose they would – they are assessing, aren't they? You know the health-care assistants probably do assess because they would be checking for if the wound was bleeding, if it was red, if it was hot, you know I suppose that is assessment. It's sort of like trained from us. So if this wound had none of them sort of symptoms and [the assistant] felt quite happy, she would either apply [a dressing or cream] and she would tend that herself. Then she would come back and so we would discuss that, but probably at the next visit I would make sure that one of us qualified would go just to check over. And then we would check it and then do the paperwork and dah, dah, dah. And then from that – so we've only seen the patient perhaps once and then [the assistant] would do, probably every visit after that.
Caseload holder A, 31
However, this raises important questions about when assistants do and do not make decisions about care, and how they develop an understanding of the boundaries for their own practice.
Authority, determining competence and monitoring the day-to-day work carried out by assistants
There was consensus that RNs manage the work of the assistants and have overall responsibility and accountability for the care that they delegate to these staff. The RN has to determine the competence of the assistants. However, there was variation across the organisations, and across teams within organisations, as to how this was best achieved. The preparation, training and development of assistants varied greatly; some organisations valued more formal structures and competency frameworks to support the work of assistants, whereas in other organisations, understanding the competence of assistants was achieved through informal mechanisms and knowing the individual assistants:
You know, it was from the introduction of competency-based frameworks, you know, where we can actually train people and then assess them and ensure that they're competent and that we can then delegate care down. . .[In the past] it was very much a case of someone watched you do it. You saw one, you were observed doing one and you did one. And that was it. But there was no formal training that I was aware of. You know, and I think we've probably much improved on how we support learning and assessment.
Senior manager, 13
We work with them and teach them how to do things and then we watch them several times over for us to know that they are safe to be able to carry on doing things and then we would allow them to go and, I know some team leaders are less kind of, you know, they don't let their HCAs do very much. However, in my team they do quite a lot really. I mean they do bandaging and things like that and I've now got them going out to new assessments and doing the beginnings of the new assessment to get some of the information ready for the trained nurse to then go in again afterwards.
Caseload holder, 18
These quotes highlight discrepancies in the ways in which assistants are deemed competent by different organisations or teams within organisations. Knowing the assistant was important in establishing trust between staff members; indeed, this was mentioned as being applicable to any new staff member, including RNs. In many cases, staff had developed an understanding about the individual assistants they worked with because of their length of service, and often because they would mentor them through formal qualifications, such as vocational qualifications. However, some organisations highlighted the variability in what this ‘knowing’ might mean and so, in striving for quality and consistency across services, they viewed competency frameworks as essential for ensuring that assistants across different community teams are taught skills in a similar way, and the nurses are supported in delivering this consistency:
In some teams there's been perhaps a nominated nurse to help a health-care assistant to reach her competencies. Teams have done it differently. It's been very much what has worked for them really and what's been manageable within those individual teams because teams are made up differently but it's just about ensuring that consistency and, you know, giving them that support as well really.
Senior manager, 24
I know we have NVQs, but there is something about standardisation of expectations, not only in our organisation but the NHS as a whole. . .I know there is a lot to be said for localising but we need a common core. . .It's almost as if you need a range of what your minimum expectations are going to be – and what your maximum expectation could be within that.
Service manager, 30
Some organisations reported having systems for recording the skills and competence of the assistants, to promote the delegation of tasks to assistants with appropriate skills. These systems were referred to as training logs, skills inventories or clinical passports:
We have, what we have, a skills inventory which is where the nurses, actually, it's got four shaded compartments and depending on their level of skill, the first one they shade in if they've had the training, the second one they shade in if they've had their training and practical and the third one is if they've had supervision and the fourth one is if they feel that they're competent. So the district nurse knows exactly what each of their individual staff are capable of doing and we also have a clinical passport which is about knowing what competencies somebody has, so the nurse allocating the work knows that they can undertake the dedicated work.
Service manager, 8
A number of mechanisms were also identified for RNs to be able to monitor the day-to-day work of assistants. An important mechanism reported by all organisations was the daily reporting of care delivery at a lunchtime handover between nursing staff, both registered and non-registered:
The caseload holder will meet with the team on a daily basis and there is an expectation that the team come back at 1 o'clock every day to the nursing office for a handover. So if they then encountered any problems, whichever band of staff, they can feed that back and certainly the unqualified have an opportunity to feed that back to a qualified nurse.
Service manager, 19
This also provided an opportunity for assistants to refer patients to a RN if they were at all concerned about the patient and care required:
Yeah just thinking back to yesterday, my band 2 colleague was concerned that a qualified nurse hadn't been to a certain patient over two visits and the wound wasn't progressing. She was quite concerned about it. She'd taken a swab anyway but she was concerned that the next visit would be a qualified nurse to pick up from there.
Caseload holder, 19
If an assistant required advice outside the handover period, all organisations reported having mobile telephones for urgent contact and many had administrative staff dedicated to the team who could support the locating of a RN for the assistants. One organisation (19) reported using a triage nurse, who could be on call to respond to any assistant queries about patient care and judge the need for a registered nurse to intervene. Assistants were generally described as having an awareness of the boundaries of their practice, and when a situation was different to that which they had expected, they would make a call to a RN for advice and support. Take the following example where a routine visit required action by an assistant:
It was with a diabetic patient who was normally on daily insulin, you know, quite stable and obviously the health-care assistant went to check the BM prior to giving the insulin and it was in his boots. She tried to get his insulin up, sorry get his BM up, but couldn't manage and I mean the first thing she did was to ring and say, look I can't give his insulin and his BM is really [low], can you come? Meanwhile while I was on my way there, she was then trying to get something into him and recheck on his BM, so she knew what she was doing but she had also made sure that she got somebody else there to cover, you know.
Senior manager, 31
The ability of assistants to know the boundaries of their practice was considered inherent to the individual but also an important quality of the responsible assistant:
I think there is a degree of responsibility for them that if they are asked to do anything that they feel in any way shape or form is outside the boundaries of what they've been trained to, they have a duty to respond back to that and tell you that. And I expect them to do that.
Caseload holder B, 24
Some caseload managers stated that they sometimes had concerns about how best to manage assistants' awareness of their boundaries, and an example of one occasion when reporting was not given in a timely fashion highlighted the importance of having systems and checks in place to ensure standards of care delivery:
I mean that doesn't tend to happen that much I've got to say. . .I can think of one example where I went recently to review somebody's wound because it was really chronic and again she's got a lot of really complex problems and is known to the vascular services and I did go and the wound had really got a lot bigger and nobody had really fed that back to me. I did sort of think, oh why hasn't this been fed back? But then again the health-care assistants don't tend to evaluate wounds by measuring them, that's really not their role. I mean it hadn't deteriorated a great deal, it had just got a bit bigger but I did sort of think I wonder why nobody had told me?
Caseload holder, 8
Many organisations also reported having systems in place [such as SystmOne electronic patient data and records system (www.tpp-uk.com)] to help identify visits to a patient by a RN. This supported the planning of visits by RNs to reassess patients on the caseload.
Most organisations reported using some form of clinical supervision or observed practice, where the team leader would organise joint visits with assistants to reassess their skills and discuss additional training needs that could then be incorporated into the annual performance appraisals of assistants. There were also more subtle techniques used by RNs to assess patient care delivery by assistants, including reading care documentation and receiving informal feedback from patients:
When I go into patients' homes myself, the patients talk to me. The patients love it when the sister goes in because they can tell, you know, they love to tell you stories about what the other team members are doing, so that's quite nice as well.
Caseload holder, 13
The structure and organisation of teams was also considered one of the ways in which the work of assistants could be better monitored. Although geographical working might be considered a good idea (assistants being shared across a range of community nursing teams), there was support for assistants being part of a team because this enabled RNs to ensure safe care delivery:
Other members of staff will follow in and obviously pick up on there being any issues. I think the fact that the band 3s are part of a regular team, that is the biggest probably safety net that we have for that. I mean there has been talk in the past about separating them off and having them in a big pool that they then go out and work geographically. But the thing about that that concerns me is that only by knowing your staff and working with your staff do you know what your staff are competent to be doing and as the caseload holder responsible for delegation of tasks, you need to have that level of assurance from the people that you're working with that you know them well enough and you know their work well enough to know what you can and can't delegate to them.
Service manager, 13
Even across one organisation there were differences in how assistants were used, and this appeared to have been influenced by the historical working of the organisations that merged. While in one part of the organisation assistants were attached to a district nursing team, in another area the assistants were shared across a number of teams to cover a geographical area. The manager of this area felt it would be better if they were attached to teams to promote better supervision of work:
I would personally like one nursing assistant per team. That they could just work in your little team, you know, they would see the same caseload of patients and would work more closely with the nurses because I think sometimes when there's only two per seven teams, they're not actually belonging to one particular little team and I think they would have more closer supervision and they would feel more part of a team. Obviously that's about numbers as well isn't it because there's only two of them, you would need more wouldn't you really. [Q: And so do you think there are real benefits of having that continuity of the same caseload and being part of the team for the assistants themselves?] I do because I think they'd be more closely supervised and I actually think as well, I think you would have more idea of their development needs as well and I think for another thing for the future for the nursing assistants is to go on more and more training really.
Caseload holder, 8
Only one organisation discussed ways in which it was trying to monitor quality and outcomes associated with the introduction of assistants in the workforce:
We measure with essential care indicators and also we start, we've just implemented a safety thermometer, so we can demonstrate it and the key performance indicators.
Service manager, 18
As roles for assistants within community nursing teams develop nationally, more organisations may wish to consider how they can demonstrate that the outcomes of care are not being compromised by the use of assistants.
Innovation in roles
We were keen to establish whether or not any organisations were using assistant roles in community nursing teams in ways which could be considered innovative. Innovation was considered as anything that organisations offered as new or different ways of using their assistant workforce. For this reason, there was great variability in what was considered innovative by our sampled organisations when discussing the range of tasks undertaken by assistants. With regard to those innovations that had changed the work of assistants, organisations recognised the shifts that had to occur in organisational cultures:
I don't think there is anything [innovative] particularly. I think the insulin was a massive one for us because we have an awful lot of patients, who are insulin dependent and cannot administer their own. That's been a really big issue for qualified staff and now that the health-care assistants have taken that on, it's made a big difference. I don't think it's particularly special because I think they do it in other areas as well but it has made a massive difference. . .[The assistants have] been doing it for such a while now and once [the nurses] realised the criteria was quite strict and [assistants] weren't going to be doing it willy nilly with everybody, then people felt a bit more comfortable with that.
Senior manager, 31
I mean the only one that we have explored in the past and we've drawn a blank, but I know some areas do it, is insulin. Because we have a fair number of elderly patients who can't give their own insulin, even with the devices with the diabetes team. And we go in. We have to send a registered nurse in literally just to give the injection, and that was something that we thought that perhaps an HCA could do, because there are devices that will only allow you to give X amount of – you know, for people who are partially sighted, you can set the dose, so it's very hard to give the wrong dose. But at this moment in time, you know, we can't – it's not been deemed that it's the correct thing to do. So we haven't pursued it.
Senior manager, 13
There were also structural factors that impacted on an organisation's willingness to take risks with assistant roles. For example, in some organisations covering more rural areas, caution was expressed regarding developing assistant roles because it would take longer for someone to get to a patient should something go wrong:
So there's all those sorts of things to be taken into account and because – obviously we've got a city, [name], but then it's extremely rural and you can't just ring up and get some help. It could be half an hour before somebody could there to help, so there are things like that to take into account as well.
Senior manager, 31
Some organisations identified roles for their assistants in helping to manage patients with long-term conditions:
One of our main drivers was because we were developing quite highly skilled nurses to do the management and long-term conditions and there was a lot of monitoring and support that needed underneath that which was looking at the holistic approach to patient care and it was felt that the health-care assistant was best placed for supporting that role and there is a lot of responsibilities that could be delegated, that didn't necessarily need a qualified member of staff to deliver on it, so that's where it came from really.
Senior manager, 19
For other organisations, innovation was about developing the roles of higher-level (band 4) assistants in helping with management of patients with long-term conditions or identifying a specialist role for these assistants where they could substitute for RNs. In other organisations, there was a focus on developing assistant roles to facilitate the integration of health and social care:
I also have within the health and social care end-of-life team a very strong band of health-care assistants and they deliver all aspects of health and social care under the guidance of senior practitioners to deliver that wrap-round care to patients in the community on a 24-hour basis.
Senior manager, 8
Analyses suggested that there was a difference across organisations in the ways in which they described innovation and their freedom in being able to develop assistant roles. The social enterprise appeared to be an example of an organisation that was prepared to think differently about assistant roles and to take risks with developing the role to enhance service delivery.
As well as considering innovation in terms of assistants' scope of practice, some organisations suggested that the roles of assistants were limited because of the lack of regulation for these staff. Hence, organisations were developing codes of practice to support the organisational development of such roles, but not innovation:
We also have the nursing charter and part of that now is how much we support the role of the health-care assistant and we have a code of practice but we also have the code with our nursing strategy where the health-care assistant is seen as a vital part of the work that we do, so they have a standard of conduct which is specific for them as well, which I think is really good.
Senior manager, 27
Many organisations were coming to terms with the recent major changes to the structure and organisation of their services. Areas for the future development of assistant roles were discussed, and included putting in place career structures for assistants and ensuring that assistants were able to continue to develop their roles to enhance service provision for patients. The future shape of community nursing is dictated by care that is being moved out of the hospitals and closer to home, and community organisations will have to consider how they can best deliver this in the future using their human resources:
So I think it's looking at that and it's looking at how wide we're looking at changing the hospitals and what happens here, you know, how much comes out into the community. Again the skill set will change then, you know, it's going to change for my nurses, so it's got to change for the assistant's role as well. So I think it's an open-ended book if I'm honest and we just need to keep it open and keep looking at the opportunities.
Senior manager, 27
Summary
This chapter has presented service managers' views of roles of assistants in community nursing teams. The final chapter brings the findings together by presenting main headlines from the research and considering the implications for policy, practice and research.
Chapter 8 Main headlines, conclusions and implications
Introduction
This scoping study was concerned with understanding the roles of community nursing assistants and their potential contribution and impact on service delivery and patient care. This involved scoping the numbers and types of assistant roles nationally, as well as trying to gain an in-depth understanding of service-level perspectives on the use of assistants. Quantitative and qualitative methods were employed to:
-
describe numbers, types and roles of assistant staff (at levels 2, 3 and 4) delivering services and care in community nursing services in England
-
explore how assistant roles affect the organisation of nursing work in these teams, particularly where new integrated organisational models and ways of delivering services exist and innovative assistant roles are identified; and
-
explore how the use of assistants in community nursing teams impacts on (or has the potential to impact on) health-care professional workload, patient experience and patient choice.
Previously we have described the findings from the study. Here we present the main headlines, conclusions and implications of these findings for policy, practice and research, and address the final objective of our study:
-
4. report key findings and implications from the scoping study for policy, practice and research.
The review of existing literature and policy highlighted that, to date, there has been very limited research into the roles of assistants in community nursing teams. Defining what is meant by community nursing was a key challenge, alongside keeping abreast of the pace of change in community services. We consider this scoping study important and timely, generating a useful grounding for any future studies in this area.
Main headlines
We used an interactionist theoretical framework59,60 for writing up our study findings. As such, we focused on the ways in which roles of assistants were enacted within the broader teams and organisations and the ways in which the broader contexts influenced the roles of assistants. Interactionism provides a useful framework for investigating the roles of assistants in community nursing teams in contemporary UK health care. We draw together here the range of findings from the different stages of this study by presenting the main headlines from the scoping study. In doing so, we aim to offer clear messages on the potential contribution of assistants and implications of their use within community nursing teams.
Assistants promote flexibility in the community nursing workforce so as to respond to changing demands on these services
The increasing workload and complexity of patients being cared for in the community is impacting on the roles of community nurses and assistants. Service-level managers agreed with their senior colleagues that assistants helped provide flexibility in a way that met the changing needs of community nursing team caseloads. Assistants were seen as especially valuable in supporting routine care, thereby enabling RNs to focus on the more complex cases. To varying extents, nurse managers agreed that assistants added breadth to the community nursing team and offered opportunities for a more efficient skill mix. Hence, managers felt that incorporating assistants into their services not only promoted better use of resources but also facilitated greater stability, while being sensitive to patient need. As care moves closer to patients' homes, demands on community nursing services are set to rise and this will impact on the roles of the entire nursing workforce (both registered and non-registered). As the nature of community nursing work changes, it will be important to consider the skills and competencies of assistants to deliver technical, as well as personal, care.
Lack of consensus in defining the roles of community nursing assistants has created inconsistencies in the ways these roles are deployed and are developing nationally
There is creeping role development for assistants determined at a service level. The scope of practice for assistants in community nursing teams appears to have been gradually developing in relation to local service needs. There was a lack of consensus about the appropriate roles for assistants, leading to role inconsistencies and confused responsibilities of assistants. This occurred through different Agenda for Change bandings, both across different organisations and within services in an organisation. Indeed, there appeared to be no fixed boundaries to demarcate how far some organisations were developing the roles of assistants at bands 2, 3 and 4. In addition, the roles of assistants appeared to be strongly influenced by local contextual factors, such as staff shortages, developmental opportunities, organisational changes or rurality. The consultation currently being undertaken by Skills for Health40 on minimum training standards and a code of conduct for assistants should go some way to addressing these national variations in deployment and development of assistant staff.
Ad hoc development of assistant roles has created variations in numbers, roles and preparation for practice
There was no consistent pattern in the ratio of RNs to assistants in community nursing teams and there was great variability between and within organisations. Participants also suggested that flexibility, discretion and unpredictability of the contexts in which care is delivered by assistants might mean that assistants work beyond their remit, banding or level. For these reasons, participants emphasised the importance of ensuring that assistants had sufficient competencies to ensure safe practice, particularly since they were expanding their scope of practice to take on more complex tasks. There was also a suggestion that different organisations experienced different levels of freedom in considering new ways of delivering services and new ways of working that involve development of assistant roles.
Assistants are core members of the community nursing team but there is a lack of clear structure for career development and progression
Participants were generally enthusiastic about the contribution of assistants, and their employment was regarded as fundamental to the ability of community nursing teams to deliver an acceptable and appropriate service. However, they did not want assistants to become workhorses, allocated only the more mundane tasks; they were concerned that this would hinder assistants' career progression and make the role unattractive. Participants from several organisations emphasised the general importance of making the assistants' roles a positive career choice. However, this was tempered by other managers who expressed concerns about the role (particularly at band 4) being developed as a substitute for that of the RNs. These national variations in support for assistant roles by managers reflect the more recent policy initiatives championing the need to develop minimum training standards and codes of conduct for assistant staff. These initiatives should (in theory) promote clearer role descriptions for community nursing assistants and support their career progression and development in ways that are not entirely locally driven.
Community nursing teams value the maturity and life experience of assistants
The majority of assistants bring a level of maturity and life experience to the role, which was recognised as being important for delivering care in this setting. Many managers reported taking this into consideration when recruiting assistants to community nursing teams because of the nature of community nursing work; assistants, in the main, are required to work on their own in patients' homes and the unpredictability of these situations was considered to be better managed by the more mature assistants. In addition, these assistants were described as motherly figures for the nursing team and as providing emotional support and stability to the community nursing workforce. Balancing the skills contribution of different members of the team, including the maturity of assistants in supporting other members of the team, is an important consideration for managers when recruiting and developing teams of community nursing staff.
Line management of assistants in community nursing teams is identified as creating challenges when trying to balance the management of risk while promoting innovation
Participants emphasised the importance of line management, responsibility and accountability in managing the work of assistants. However, there was little agreement across localities about how best to achieve this and a mix of formal and informal methods was evident. Generally, participants would have liked more guidance and advice on how best to manage the roles of assistants and to access examples of good practice. Systematic recording of competence, and proactive case management including (re)assessment of patient needs and defined team working, were identified as exemplary. Some participants would have liked better regulation of assistants and several organisations had developed codes of practice. Such codes of practice were seen as facilitating the roles of assistants, by giving clarity regarding what they could and could not do. This is important given that community nursing assistants are delivering care in patients' homes, unregulated, unsupervised, and to some of the most vulnerable members of our society.
Limitations of the research
This study was conducted at a time of significant change in the NHS. We were studying community nursing services during the implementation of the Transforming Community Services Programme,18 when community services were being redesigned and relocated. This inevitably had a significant impact on the study. Importantly, these structural and organisational changes to services created challenges when trying to identify provider organisations; over 80% of provider organisations were being reorganised at the time of the study (see Chapter 5). Alongside these organisational changes we encountered challenges with obtaining research governance approvals (see Chapter 4, Ethical considerations). In combination, these factors significantly impacted on the recruitment and participation rates for the study.
Our original proposal aimed to conduct a census (in stages 1 and 2) of senior managers from the 152 PCTs responsible for the provision of community health services. During the period of study the 152 PCTs became less meaningful because the provider services were relocated into 102 provider organisations (with different organisational models), and the 10 SHAs were reconfigured into four SHA clusters: London, North, Midlands and South. We successfully recruited 37 senior managers from these new provider organisations (n = 102). We obtained research governance approval for 76 of these new provider organisations and so our recruitment rate was 49%. This was considerably lower than we anticipated but we are confident that we took all steps to maximise recruitment during the study period, at a time of significant organisational change. Thus, we are confident that the sample includes different service models and organisations representing geographical areas across England.
There were variations in the organisational positions of participants recruited for stage 2, which included directors, professional leads, managers of clinical services, team leaders and managers, senior practitioners or staff with other positions (e.g. workforce development or governance leads). We accepted that these staff would have varying degrees of knowledge about the roles of assistants in community nursing teams within the participating organisations, based on their positions. However, given the practical difficulties of obtaining sufficient participants, we accepted this trade-off between standardisation of participants based on their positions in the organisations and further lowering the response rate. Despite this limitation, all participants were able to respond to our questions and impart their perspectives and understanding of assistant roles and responsibilities within their organisations. Participants in stage 3 (n = 20) were able to develop this understanding by offering a service-level perspective on community nursing assistants. We were not funded to interview assistants themselves or patients but recognise this is as an area for future research.
Despite the above challenges to the study, we are confident that it contributes to knowledge and understanding of assistants supporting the work of community nursing teams.
Conclusions
Our scoping study highlights the opportunities and challenges associated with the use of assistants to deliver care by the community nursing team. To the best of our knowledge, this is the first study to have explored the roles of these assistants in community nursing. Despite challenges encountered during the study, we have addressed our original research objectives. We have been able to describe numbers, types and roles of assistant staff (at levels 2, 3 and 4) delivering services and care in community nursing services in England. We have reported on how assistant roles are affecting the organisation of nursing work in community nursing teams, and ways in which assistants may be impacting on (or have the potential to impact on) health-care professional workload, patient experience and patient choice. This study relies on the description of assistant roles in community nursing teams by senior and service-level managers. Accepting this, we anticipate that the findings and implications are likely to be of value for organisations that are considering the contribution and future roles of assistant staff as part of their plans for delivering the ambitious community services agenda (we are establishing a web-based resource for the study to support practitioners and policy-makers in accessing our findings: www.york.ac.uk/healthsciences/research-information/support-matters/). It appears that the developing roles of assistants in community nursing teams have been relatively neglected. This may require further attention at national and local levels to support and mediate the definition and development of these roles in the future.
Policy and practice implications
Based on our findings, we offer the following implications for policy and practice. We consider the following areas to be key areas of consideration as the roles of assistants develop to deliver community nursing services:
-
developing clearer national guidance on the roles and responsibilities of assistants in community nursing teams to reduce local confusion and to highlight potential areas of benefit to organisations and patient care, while also allowing flexibility for local role development to meet the needs of the local patient population
-
supporting the development of national data sets that provide reliable information on numbers and roles of assistants in community nursing teams nationally
-
promoting clarity of role descriptions for assistants at different levels working in an organisation and good communication across the organisation so that assistant roles are valued and integrated within nursing teams
-
providing opportunities for national standardisation of the training and preparation of assistants to support the development of skills and competencies that are transferable within and across community nursing teams
-
promoting the importance of managing risk by organisations to ensure safe practice by assistants, but also promoting opportunities for innovation and new ways of working to meet the challenges of future community nursing service provision
-
encouraging organisations to learn from each other about the varied mechanisms available to clinically supervise and performance-manage assistants who are often lone workers going into the homes of vulnerable people
-
developing policies and processes for the recruitment and retention of the assistant workforce in organisations to ensure fairness and equity and to ensure future workforce planning
-
ensuring organisational support from managers and colleagues for assistants in practice to develop their clinical skills and competencies to meet the demands of their evolving workload
-
supporting organisational and national consideration of opportunities for continuing development for assistants to support their career progression and aspirations.
Future areas for research
-
Exploring the tasks and activities of community nursing assistants and how these roles are allocated, organised, managed and supervised from the perspectives of a range of stakeholders and by observing actual practice.
-
Understanding the impact of community nursing assistant roles on the practice, activities and workload of health-care professionals in community settings.
-
Understanding the effect of community nursing assistants on the quality and safety of patient care and patient outcomes.
-
Understanding the impact of community nursing assistants on patient experience, choice and quality.
-
Identifying the best standardised training packages for community-based assistants.
-
Evaluating the cost-effectiveness of innovation in assistant roles in community nursing services.
Acknowledgements
During the development, implementation and writing of this study, many people have been involved or contributed in some way. We make particular note of the study participants. We are very grateful for their time, their willingness to take part and their honesty. We also thank many of our colleagues for supporting this study along the way. In particular we would like to acknowledge the contributions of Liz Newbronner and Martin Baxter (Firefly Research and Evaluation, formerly Acton Shapiro Research and Consultancy) and Chris Bartlett (York Health Economics Consortium, formerly at Acton Shapiro Research and Consultancy). We are also grateful to Lynda Whincup (City Health Care Partnership CIC, Hull) for supporting Sue Pender to undertake the NIHR Service Delivery and Organisation (SDO) Management Fellowship associated with this study.
We would like to thank the following people for their invaluable guidance and support at different stages during the project: Rosemary Cook, Linda Bailey, Tannis Hand, Claire Goodman, Fiona Ross, Ian Wragg and Roger Thompson. We were also guided in our work by a range of senior managers of national Adult Services Community Nursing teams. We thank them for their time and support of our work.
Contributions of authors
Karen Spilsbury: conception and design of the study; analysis and interpretation of the data; drafting and revising the report; final approval of the report to be published.
Sue Pender: design of the study; analysis and interpretation of the data; drafting and revising the report; final approval of the report to be published.
Karen Bloor: conception and design of the study; analysis and interpretation of the data; drafting and revising the report; final approval of the report to be published.
Rachel Borthwick: analysis and interpretation of the data; revising the report; final approval of the report to be published.
Karl Atkin: conception and design of the study; analysis and interpretation of the data; revising the report; final approval of the report to be published.
Dorothy McCaughan: conception and design of the study; analysis and interpretation of the data; revising the report; final approval of the report to be published.
Ian Watt: conception and design of the study; analysis and interpretation of the data; revising the report; final approval of the report to be published.
Una Adderley: analysis and interpretation of the data; revising the report; final approval of the report to be published.
Ann Wakefield: conception and design of the study; analysis and interpretation of the data; revising the report; final approval of the report to be published.
Hugh McKenna: conception and design of the study; analysis and interpretation of the data; revising the report; final approval of the report to be published.
Disclaimer text
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- NHS next stage review: our vision for primary and community care. London: Department of Health; 2008.
- High quality care for all: NHS next stage review final report. London: The Stationery Office; 2008.
- A high quality workforce: NHS next stage review. London: Department of Health; 2008.
- Equity and excellence: liberating the NHS. London: The Stationery Office; 2010.
- Hurst K. Primary care and community care workforce planning and development. J Adv Nurs 2006;55:757-69. http://dx.doi.org/10.1111/j.1365-2648.2006.03966.x.
- Wanless D. Securing our future health: taking a long-term view. London: HM Treasury; 2002.
- The regulation of health care support workers: a scoping paper. London: NMC; 2006.
- The career framework. 2010.
- Core standards for assistant practitioners. Bristol: Skills for Health; 2009.
- McKenna HP, Hasson F, Keeney S. Patient safety and quality of care: the role of the health care assistant. J Nurs Manag 2004;12:452-9. http://dx.doi.org/10.1111/j.1365-2834.2004.00514.x.
- A career framework for the NHS. Discussion document – version 2. London: Changing Workforce Programme, NHS Modernisation Agency; 2004.
- Buchan J, Calman L. Skill-mix and policy change in the health workforce: nurses in advanced roles. Paris: OECD Working Papers No 17; 2004.
- Imison C. Shaping PCT provider services: the future for community health. London: King's Fund; 2009.
- 2020 vision: focusing on the future of district nursing. London: Queen's Nursing Institute; 2006.
- Barrett A, Latham D, Levermore J. Defining the unique role of the specialist district nurse practitioner: part 2. Br J Community Nurs 2007;12:522-6.
- Kennedy C, Elliott L, Rush R, Hogg R, Cameron S, Currie M, et al. Review of nursing in the community: baseline study. Edinburgh: Scottish Government Social Research; 2004.
- Wilkin D. Restructuring primary and community health services in four countries: from cottage industry to integrated provider?. Health Soc Care Community 2002;10:309-12. http://dx.doi.org/10.1046/j.1365-2524.2002.00374.x.
- Transforming community services: enabling new patterns of provision. London: Department of Health; 2009.
- Commissioning a patient-led NHS. 2005.
- Primary care trust commissioning responsibilities for general practice nursing. 2006.
- A national framework to support local workforce strategy development: a guide for HR Directors in the NHS and social care. Leeds: Department of Health; 2005.
- Patient care in the community. NHS district nursing: summary information for 2003–04 (England). London: Department of Health; 2004.
- 2020 vision: focusing on the future of district nursing. London: Queen's Nursing Institute; 2009.
- First assessment – a review of district nursing services in England and Wales. London: Audit Commission; 1999.
- Agenda for change: final agreement. Leeds: Agenda for Change Project Team; 2005.
- Buchan J, Ball J, O’May F. If changing skill mix is the answer what is the question?. J Health Serv 2001;6:233-8. http://dx.doi.org/10.1258/1355819011927549.
- Abel-Smith B. A history of the nursing profession. London: Heinemann; 1960.
- Baly M. Florence Nightingale and the nursing legacy. London: Croom Helm; 1986.
- Dingwall R, Rafferty AM, Webster C. An introduction to the social history of nursing. London: Routledge; 1988.
- Witz A. Professions and patriarchy. London: Routledge; 1992.
- Rafferty AM. The politics of nursing knowledge. London: Routledge; 1996.
- Saks M, Allsop J. Social policy, professional regulation and health support work in the United Kingdom. Soc Policy Society 2007;6:165-77. http://dx.doi.org/10.1017/S1474746406003435.
- The nursing skill-mix in the district nursing service. Leeds: NHS Executive; 1992.
- Position statement: nursing people in their own homes – key issues for the future of care. London: Queen's Nursing Institute; 2011.
- Buchan J, Dal Poz MR. Skill mix in the healthcare workforce: reviewing the evidence. Bull World 2002;80:575-80.
- Drennan V, Davis K. Trends over ten years in the primary care and community nurse workforce in England. London: St George's, University of London and Kingston University; 2008.
- Nancarrow SA, Borthwick AM. Dynamic professional boundaries in the health care workforce. Sociol 2005;27:897-919. http://dx.doi.org/10.1111/j.1467-9566.2005.00463.x.
- The nursing team: common goals, different roles. London: RCN; 2012.
- Health and Social Care Act 2012: chapter 7. London: The Stationery Office; 2012.
- Skills for health and skills for care set up focus groups for the code of conduct and minimum training standards. 2012.
- Healthcare support workers' toolkit: supporting role development in NHS Scotland. 2009.
- Code of conduct for healthcare support workers in Wales. 2011.
- Venning P, Durie A, Roland M, Roberts C, Leeses B. Randomised controlled trial comparing cost effectiveness of general practitioners and nurse practitioners in primary care. BMJ 2000;320:1048-53. http://dx.doi.org/10.1136/bmj.320.7241.1048.
- Kinnersley P, Anderson E, Parry K, Clement J, Archard L, Turton P, et al. Randomised controlled trial of nurse practitioner versus general practitioner care for patients requesting same day consultation in primary care. BMJ 2000;320:1043-8. http://dx.doi.org/10.1136/bmj.320.7241.1043.
- Shum C, Humphreys A, Wheeler D, Cochrane M, Skoda S, Clement S. Nurse management of patients with minor illnesses in general practice: a multi centre randomised controlled trial. BMJ 2000;320:1038-43. http://dx.doi.org/10.1136/bmj.320.7241.1038.
- Benson L, Venning P, Young R, Walshe K, Mullen C. Beginning to reinvigorate the workforce. Br 2004;10:274-9.
- Kessler I, Bach S, Heron P. Comparing assistant roles in education and social care: backgrounds, behaviours and boundaries. Int J Human Res Manag 2006;18:1648-65. http://dx.doi.org/10.1080/09585190701570726.
- Moran A, Enderby P, Nancarrow S. Defining and identifying common elements of and contextual influences on the roles of support workers in health and social care: a thematic analysis of the literature. J Eval 2011;17:1191-9. http://dx.doi.org/10.1111/j.1365-2753.2010.01505.x.
- HCA toolkit. 2006.
- HCA unit 2: good employment practice from a general practice employer's perspective. 2006.
- Vaughan P, Longbottom A, Celino G, Cross S. Reviewing the roles of nurses and health care assistants in general practice. Prim Health Care 2007;17:14-6.
- Bradford M. Health care assistants in general practice: an evaluation of trained health care assistants in general practice across 4 primary care trusts within the North Central London NHS sector. London: Department of Health Working in Partnership Programme; 2007.
- Hirst M, Lunt N, Atkin K. Were practice nurses distributed equitably across England and Wales, 1988–1995?. J Health Serv Res Policy 1998;3:31-8.
- Jenkins-Clarke S, Carr-Hill R, Dixon P. Teams and seams: skill mix in primary care. J Adv Nurs 1998;28:1120-6.
- Spilsbury K, Meyer J. Making claims on nursing work: exploring the work of health care assistants and the implications for registered nurses' roles. J Res Nurs 2005;10:65-83. http://dx.doi.org/10.1177/136140960501000104.
- Spilsbury K, Adamson J, Atkin K, Barlett C, Bloor K, Borglin G, et al. Evaluation of the development and impact of assistant practitioners supporting the work of ward-based registered nurses in acute NHS (Hospital) Trusts in England. Southampton: NIHR Service Delivery and Organisation programme; 2010.
- NHS hospital and community health services non-medical staff England 1997–2007. 2008.
- Richards A, Carley J, Jenkins-Clarke S, Richards DA. Skill mix between nurses and doctors working in primary care delegation or allocation: a review of the literature. Int J Nurs Stud 2000;37:185-97. http://dx.doi.org/10.1016/S0020-7489(00)00005-5.
- Hughes EC. The sociological eye. New Brunswick, NJ: Transaction Books; 1984.
- Abbott A. The systems of professions: an essay on the division of expert labour. Chicago, IL: University of Chicago Press; 1988.
- Cresswell JW, Plano Clark V. Designing and conducting mixed methods research. Thousand Oaks, CA: Sage; 2007.
- Greene JC. Mixing methods in social inquiry. San Francisco, CA: Jossey-Bass; 2007.
- Miles MB, Huberman MA. Qualitative data analysis. An expanded sourcebook. Thousand Oaks, CA: Sage; 1994.
- Silverman D. Interpreting qualitative data: methods for analysing, text and interaction. London: Sage Publications; 1993.
- Lincoln YS, Guba EG. Naturalistic inquiry. Newbury Park, CA: Sage Publications; 1985.
- Delivering care closer to home: meeting the challenge. London: Department of Health; 2008.
- Primary care groups: taking the next steps. Health Service Circular (HSC1999/246). London: Department of Health; 1999.
- NHS plan. A plan for investment. A plan for reform. London: Department of Health; 2000.
- The legacy of primary care trusts. London: Primary Care Trust Network NHS Confederation; 2011.
- Briefing: payment by results. London: King's Fund; 2007.
- Delivering investment in GP practice: implementing the new GMS contract. London: Department of Health; 2003.
- A short guide to NHS foundation trusts. London: Department of Health; 2005.
- Creating a patient-led NHS: delivering the NHS implementation plan. London: Department of Health; 2005.
- Practice based commissioning: practical implementation. London: Department of Health; 2006.
- Health reform. London: The National Archives; 2009.
- The standard NHS contracts for acute hospitals, mental health, community and ambulance services. London: Department of Health; 2010.
- The future for community services. London: Primary Care Trust Network NHS Confederation Briefing; 2009.
- Cowley S, Caan W, Dowling S, Weir H. What do health visitors do? A national survey of activities and service organisation. Public Health 2007;121:869-79. http://dx.doi.org/10.1016/j.puhe.2007.03.016.
- Mitchell N, Randell R, Foster R, Dowding D, Lattimer V, Thompson C, et al. A national survey of computerized decision support systems available to nurses in England. J Nurs Manag 2009;17:772-80. http://dx.doi.org/10.1111/j.1365-2834.2009.00986.x.
- Kessler I, Heron P, Spilsbury K. Nurse Support Workforce Survey: initial results. Oxford: Said Business School, University of Oxford; 2012.
- The NHS improvement plan: putting people at the heart of public services. London: Department of Health; 2004.
Appendix 1 Key elements of the UK Skills for Health Career Framework8

Appendix 2 Study protocol
Support Matters v1 Date: 17/11/10 REC Ref: 10/H0808/159

STUDY PROTOCOL
Full title of project
Support matters: Use of assistant staff in the delivery of community nursing services in England
Chief Investigator
Dr Karen Spilsbury, University of York
Co-Investigators
Professor Ian Watt,1 Professor Karl Atkin,1 Dr Karen Bloor,1 Ms Dorothy McCaughan,1 Professor Hugh McKenna,2 Dr Ann Wakefield3 (1University of York, 2University of Ulster, 3University of Manchester)
Background
Primary and community care services are the first point of contact with the National Health Service (NHS) for most service users [1]. Public demand for these services is growing due to demographic changes, increasing public expectations for quality and choice [2], the changing nature of disease and disease management, continuing advances in technology and treatments and the shifting focus from hospital to community-based services [3]. The NHS Review advocated primary and community care services that promote health, provide timely access for people experiencing ill health, are based on pathways of care, reflect the needs of service users and focus on promoting quality and safety [1,3]. To meet these demands and the modernisation agenda, the skills of the entire health-care team (both professionals and assistant staff) need to be supported, developed, and, crucially, deployed in the most efficient way [4]. As such, health-care role boundaries are being challenged through role enhancement (increasing the depth of a job, such as nurse-led primary care clinics), delegation (moving a task up or down a traditional uni-disciplinary ladder, such as specialist to non-specialist nurse or physician), substitution (expanding the breadth of a job, in particular by working across professional divides or exchanging one type of worker for another, such as nurse practitioners substituting for doctors) and innovation (introduction of ‘new’ roles, such as assistant practitioners) [5]. The workforce planning and development that must accompany these changes has received minimal attention in primary and community care [6]. There is a lack of international evidence to support policies on health-care staffing [7]. Research efforts have tended to focus on the roles of health-care professionals, such as substitution of General Practitioners (GP) with registered nurses [8–10] rather than the organisational, skill mix and workforce issues associated with the provision of primary and community care by a health-care team in its broadest sense. Research on assistant staff in primary and community care is scant, comprising small scale, descriptive localised projects which focus on assistant roles in GP practices rather than community nursing services.
Changes to the roles of health-care professionals, through role expansion and redesign, have created specific opportunities for reviewing developments in assistant roles [11–13]. Assistants have been introduced across health-care settings to:
-
complement the work of professionals by carrying out activities alongside the professional, such as working with nurses to deliver fundamental care (‘co-produce’);
-
carry out activities that do not require a professional, such as some administrative tasks (‘relieve’) or;
-
take on tasks and activities previously performed by professionals, such as phlebotomy (‘substitute’) [14].
The UK national career framework describes the roles of all health-care staff in terms of level of competence. There are nine levels of competence and assistant staff occupy levels 2, 3 and 4 [15]. Health-care assistant (HCA) is the role title applied to staff working at level 2 and 3, with staff achieving National Vocational Qualifications (NVQ) at level 2 and 3 respectively. Assistant practitioner (AP) refers to staff at level 4 who have probably studied for a foundation degree, BTEC higher or Higher National Diploma. The expectations are that HCAs carry out protocol-based tasks that have been delegated to them by a registered practitioner (level 3 HCAs assuming more complex tasks and responsibility than level 2 HCAs) and APs are expected to deliver protocol-based clinical care, carrying out assessment, under the direction and supervision of a state registered practitioner. We will use this framework to provide structure for understanding the roles of assistant staff (regardless of the varied assistant job titles) and to provide coherence to the study. We have found that assistant job titles can demonstrate considerable variations in ‘actual’ practice across workplace settings; assistant practitioners being ‘fully assistive’ to health-care professionals in some settings but ‘fully autonomous’ in others [16].
Assistants are a vital part of the care workforce, with over 350,000 HCAs estimated to be working in the UK [17], of which approximately 120,000 work in the NHS, the remainder working in the independent sector and within social care services. In primary and community care, assistants support clinic duties and provide care in patients' homes [18,19]. It is estimated that up to 6,500 assistants work in general practice in England [20]. An absence of data means that we do not know how many assistants work in community nursing teams, for example district nursing teams [21]. As health-care policies refocus on primary and community service provision, there will be an associated increase in the number of HCAs and APs employed in this health-care sector. Lack of understanding of the roles, training and development of assistant staff in this sector has raised concerns about their potential impact on care, safety and the quality of services provided to service users [22,23]. The lack of national guidance on training, development and employment of assistants has led to a fragmented approach at the local level with some unfortunate consequences [24]:
-
wide variations in the structures and support available to assistant staff;
-
local inequities in accessing training and support for assistants;
-
lack of mechanism for sharing good practice in respect of training, employment practices or principles of delegation;
-
absence of continuing and professional development culture for assistants that exists for other regulated primary care professionals.
The Working in Partnership Programme (WiPP) was launched in 2004 to support General Practice with capacity-building resources and strategies: one initiative was to develop a range of core principles and a practical toolkit to enable general practice to employ, train and develop HCAs [25]. In general practice, assistant staff are commonly trained to undertake specific clinical and non-clinical procedures, such as blood pressure recording, new patient checks, urinalysis, weight and height recording, phlebotomy or ordering supplies [26]. However, assistant roles tend to evolve over time to meet the needs of individual practices leading to great variation in roles, responsibilities and tasks of assistant staff across these settings [27]. The work of assistant staff (levels 2 to 4) in adult community nursing teams has not been studied. Therefore, our study will focus on community nursing; the area in greatest need of study.
‘Community nursing’ refers, in its broadest sense, to any nursing care delivered outside the hospital setting, such as patients' homes, or residential care or health centres. A wide variety of services and teams comes under this banner, for example district nursing, intermediate care, falls prevention, tissue viability, or community-based respiratory teams. We will seek to describe numbers, types and roles of assistant roles in these settings and their potential contribution to service delivery, and service-user experience and choice.
The consequences of introducing assistant roles in to health-care teams represents a fundamental rethink of who provides primary and community care in a way that has not been seen since the introduction of the new GP contract in 2003 and the rise of the practice nurse during the early nineties [28,29]. It is likely that assistant roles in community nursing teams are being developed in an ad hoc manner in response to local need but with wide variations in roles, training received and possibly variations in the competency of individuals to undertake the designated roles. It has been argued that assistant workers could be delegated more work to better support health-care professionals, improving efficiency and effectiveness [30,31]. Lord Darzi's NHS Review [3] offers further opportunities for assistants to contribute to wellbeing and prevention services.
Despite the introduction and development of assistant roles, we still know little about their numbers, who they are and what they do. Distinguishing activities that could be performed by assistant workers has important implications for entire health-care teamwork and service user care [32,33]. Over the last decade there have been increasing numbers of HCAs at level 2 and 3 and the development of new higher-level (level 4) AP roles [34,35]. However, there are likely to be wide variations in proportions of assistant workers in Primary Care Trusts (PCTs) and their introduction and use across community nursing teams, with no obvious links between service need and their deployment [36]. To better understand, and exploit, the public health contribution from this important group, we need to:
-
consider whether and why assistant roles have emerged and developed in community nursing services;
-
explore what roles and responsibilities assistant staff at different levels are undertaking and how they have been prepared for delivering quality and safe services; and
-
explore the potential impact of assistant roles on reducing health inequalities (for example outreach work or screening in poor areas), and their contribution to improving service-user experience and choice.
Plans for the review and modernisation of services in this sector [1,37], make an evaluation of current and potential developments for HCA and AP roles important and timely to inform health service policy, decisions about commissioning and workforce training and development, as well as decisions by service providers about the required workforce and skill mix to ensure safe and effective service delivery to service-users and their families. An important starting point for a study of assistant roles in community nursing teams is identifying where assistant staff are employed, in what numbers and for what purposes. This is the focus of the proposed scoping study. The scoping study will provide the foundations for developing more detailed work on the roles of assistant staff in community nursing teams.
Aims and objectives
The research objectives are to:
-
Describe numbers, types and roles of assistant staff (at levels 2, 3 and 4) delivering services and care in community nursing services in England.
-
Explore how assistant roles impact on the organisation of nursing work in these teams, particularly where new integrated organisational models and ways of delivering services exist and innovative assistant roles are identified.
-
Explore how use of assistants in community nursing teams impacts on (or has the potential to impact on) health-care professional workload, service user experience and choice.
-
Report key findings and recommendations from the scoping study for policy makers, service users, commissioners, providers, practitioners, managers and researchers.
These objectives will be addressed through the following research questions:
-
What have been the major influences (social, organisational, political/policy, historical, environmental and economic) on roles for assistant staff involved in delivering services and care in community nursing services?
-
What numbers of assistant staff work in community nursing teams and in what types of roles?
-
What tasks and activities are assistants undertaking in these settings and are there examples of innovative use of the roles?
-
How do assistant roles impact on the workload of health-care professionals in community settings?
-
What is the perceived impact of using assistants to deliver services on service user experience and choice?
Need
Workforce planning is central to the NHS Modernisation Agenda, and it is notoriously difficult and under-informed by good research evidence [7]. There is increasing emphasis on maximising the roles of assistant staff and their contribution to improving service user experiences and outcomes. An increasing number of studies focus on assistant roles in acute care settings (the research team have a portfolio of work in this area), and developments in GP practice settings. However, community settings have, thus far, been neglected, despite the growth in assistant roles over the past decade. Assistants in the community are more likely to be working on their own, and unsupervised, because they are delivering care in people's homes or outreach centres. This provides a completely different context for use of the assistant role than the acute care setting where the role is more likely to be working alongside health-care professionals. It is therefore important to consider assistant roles in these community settings. Our scoping study will contribute to the evidence-base on assistant roles (levels 2 to 4) in the community setting, provide examples of innovative use of assistant roles and offer recommendations of interest to policy makers, commissioners, provider organisations and practitioners. The findings will address the benefits to care and service delivery that may be gained by using assistant staff and how use of assistants might impact on service user experience and choice and flexibility in the delivery of primary and community care, in a way that is more appropriate to service user need and that addresses inequalities in access to provision and the provision of appropriate support. These factors are important for considering how care will be delivered to maximise the skills of the entire workforce in primary and community care to address future challenges in care delivery to best meet the needs of communities. In the future there may be more independent providers and they will need guidance on best ways to maximise the use of assistant skills in the delivery of quality and safe services [38]. Lack of regulation of the assistant workforce necessitates scrutiny of these roles. In summary, assistants are increasingly used in community nursing teams. The deployment, however, has tended to be ad hoc and we know little about who they are and what they do. We also know little about their impact on primary care and in particular how they can be best managed and used to improve patient outcomes.
Methods
We will carry out a scoping study to establish numbers, types and roles of assistant staff in community nursing teams. A comprehensive scoping review of the literature and policy on assistant roles in primary and community care will be carried out. The research team have already developed strategies for a review of assistant roles in acute care and will use similar search strategies and methods for this review. The review will inform the scoping study.
SCOPING STUDY OF ASSISTANT ROLES (LEVEL 2, 3 AND 4) IN COMMUNITY NURSING TEAMS (18 months)
The scoping study will establish numbers, types and roles of assistant staff working at levels 2 to 4 and delivering services and care in community nursing teams. Numbers of assistants will be placed in the context of overall team structures so that we can better understand assistant roles and where there are teams with no assistant staff. As well as describing numbers and use of assistants we will explore whether there are any innovative models of service provision using assistant staff. These data are not currently available. We will consult the Workforce Census in Primary Care for existing data and gaps in knowledge and understanding of assistants' roles and work will be collected through a census to scope the assistant role across England. There are 152 PCTs in England and our aim is to understand configuration and use of assistant staff in community nursing teams within each of these PCTs, with more detailed description of the roles from a purposive sample (10%) of identified community nursing teams. The sample would be comprised of nursing services which represent diversity in terms of location, numbers and types of assistant roles, roles for assistant staff, types of nursing services and innovative models of service delivery.
The process of carrying out this scoping study is not straightforward due to varied models of service provision across England and the location of these community nursing teams, particularly given the split of provider services from PCTs. Therefore, we have carried out some preliminary work to refine both our approach to the scoping study and to develop focused questions to capture this diversity. We have set up an advisory group consultation with individuals who have an understanding of the commissioning and provision of community nursing services (such as PCT Directors of Nursing, PCT Human Resource Directors, Community Nurses) to ensure feasibility of our planned approach and that the questionnaire will enable us to scope the reality and diversity of assistant use in community nursing services in England.
The preliminary consultation exercise has helped determine the best approach to capturing as complete a picture as possible of what is happening ‘on the ground’. This has ensured flexibility in our approach. Following these preliminary discussions and consultation, we have decided to pursue a 3-stage approach to this scoping study. [Note: We originally proposed a 2-stage approach to the scoping study: questionnaire to a Senior Manager (stage 1) and telephone interviews with Service Managers/Team Leads of a sample of these identified nursing services (stage 2). However, this approach was deemed unsuitable following discussions and consultation with the advisory group because of the time commitment required for completion of the questionnaire and current changes in primary and community care services and their location.] This approach will enable us to present a national picture of assistant roles in the community at levels 2, 3 and 4 and reflect any regional variations in use of the role at these levels and the type of work they undertake and their contribution to any innovative models of service delivery. Our approach will involve:
Stage 1 – Making contact: An email will be sent to a Senior Manager (PCT provider side and probably Director of Nursing or equivalent person) to inform them about the scoping study. The purpose of this email is to inform them about the study and to determine whether (a) they employ assistants within community nursing teams and (b) they would be interested in taking part in a 15 minute telephone interview (Stage 2). The Senior Manager will simply reply to the email to provide this information.
Stage 2 – Mapping assistant roles: We aim to carry out a 15-minute telephone interview with all Senior Managers that indicate a willingness to participate (Stage 1). We aim to gather as much detail as we can about use of assistants (please see topic guide). At the end of this interview we will ask whether they would be happy for us to contact them again in 4-months. This follow-up will be to establish potential contacts (most likely Service Managers/Team Leads of community nursing services) for a 30-minute telephone interview (Stage 3).
Stage 3 – In-depth interviews: We would carry out a 30-minute telephone interview with a purposive sample of Service Managers/Team Leads of services. Sampling will be based on data gathered in Stage 2.
Descriptive summary statistics will be used to present quantitative findings and open (qualitative) responses will be thematically coded [39].
Findings from the scoping study will:
-
contribute to the evidence-base on assistant roles (levels 2 to 4) in the community setting;
-
provide examples of innovative use of assistant roles; and
-
offer recommendations of interest to policy makers, commissioners, provider organisations and practitioners.
We anticipate that the scoping study will lead to the development of a ‘toolkit’ on the introduction and development of assistant roles in community nursing teams that will be useful to practitioners (assistants and professionals), commissioners and employers. We will seek further funds for development of this. We will liaise with the Centre for Reviews and Dissemination (CRD) (University of York) about the format of the research knowledge presentation and translation for practitioners and policy makers and with the Royal College of Nursing concerning production of a ‘toolkit’ for practitioners and employers. The scoping study will provide the foundations for the development of focused clinical and policy questions for future studies and we will submit further applications for research funding to develop the evidence-base in this area.
Contribution to collective research effort and research utilisation
We will use a multi-faceted approach in disseminating findings to different stakeholders (in addition to the expected refereed articles in academic journals and seminar presentations). The Research Team have an excellent track record of disseminating material in this way and have links with CRD to promote best practice in our dissemination efforts. In addition, the project team will exploit existing relationships with regional NIHR Collaborations for Leadership in Applied Health Research and Care (CLAHRCs). We will begin by preparing a summary of the research findings, which will specifically draw out the policy and practice implications of our work. These will be distributed to community nursing teams identified through the scoping review, commissioners of these services and professional and training bodies and trade unions. In forming relationships with statutory and government agencies, we hope they will formally endorse the summary, thereby giving our work greater credibility. We will liaise with managers to ensure our findings directly feed into their organisation's initiatives on use of assistant staff.
To further facilitate the dissemination of findings we will establish a web page on which the research findings are available for individuals to download. We will also liaise with the Royal College of Nursing (RCN) about potential for developing a ‘toolkit’ on assistant roles in community nursing teams that is useful for practitioners and employers. The RCN are a particularly useful partner because the organisation houses the Working in Partnership Programme toolkit on health-care assistants in GP practices (a Department of Health funded initiative). During the initial stages of the project we will explore other websites on which we can place links to our work. In doing so, we will explore the potential for developing broader relationships with the Royal College of General Practitioners and Community and District Nursing Association. On completion, we will ensure the findings are disseminated via national conferences and will seek advice of training bodies and NHS agencies about relevant key conferences to disseminate health-care workforce findings. In addition, as with all our research endeavours, findings from this study will be incorporated into our teaching.
We will ensure dissemination is timely. Reports will be prepared monthly for research team meetings and to monitor progress. Reports will also be prepared periodically for the Research Advisory Group; these will be relatively informal and will include provisional results or discussion papers for consultation. We will prepare formal project reports for the funder as requested in the form of interim and final reports.
Project management
We are aware that this project will require careful management and steering; particularly given the PI is responsible for day-to-day management and delivery of the project. The research team will meet monthly to ensure project milestones are being achieved. Karen Spilsbury will prepare summary reports for the monthly meetings so that progress can be monitored against project milestones. Karl Atkin will act as Chair for these meetings and contribute to SDO reports regarding study progress. Karen Spilsbury will be responsible for study management and will be engaged with data collection, analysis and ensuring the submission of reports (interim and final). She will work closely with the research consultancy (Acton Shapiro) and other researchers on the project. We will also form a Research Advisory Group, who will ensure that the project is being managed appropriately and provide advice on research issues at various stages of the project. The research team have been involved in complex organisational studies and so the study will be informed and guided by experience. Importantly, members of the research team have experience of working together on a number of successful collaborative projects. All finances will be managed by the University of York.
The study will be managed within the Department of Health Sciences (University of York). This is a large multi-disciplinary department, which specialises in high quality health services research. In the 2008 Research Assessment Exercise the Department achieved top rankings for Health Services Research (1st) and Nursing and Midwifery (4th). It has good international and national research links with universities, research centres and health service organisations. There are also close links with colleagues in other departments and research units in the University, including the Centre for Health Economics which has an international reputation for research activity on economic evaluation of health technologies, outcome measurement, resource allocation and health policy.
Approval by Ethics Committee
We will seek the necessary Research Ethics and Governance approvals for the study. The research team have considerable experience applying for ethics for studies using mixed qualitative and quantitative methods. We do not envisage any particular problems as our methods have been approved in the past.
Service users
The full proposal has been developed in consultation with a number of key stakeholders, including individuals who plan, manage, support and deliver services, such as Workforce Development and Design, Royal College of Nursing, Clinical Director of Community Nursing Teams and Assistant Workers. We plan to recruit additional stakeholders from policy, practice, education and research (including Primary Care Research Networks and Community and District Nursing Association). We will seek further clarification of any key stakeholders these individuals consider important to be involved in the development of the study. We note that one reviewer mentioned the Queen's Nursing Institute and so we will approach this organisation.
Expertise and justification of support required
The research team have a strong portfolio of successful management of national multi-disciplinary and multi-centre studies as well as extensive experience of using mixed methods for service evaluation. The methods presented in this study have been used successfully by the team before. Team members have considerable experience of researching the health-care workforce and role developments (in particular assistant roles), skill mix, work and organisational management and health service delivery systems. In addition, the research team have considerable experience in writing up research within the context of policy and practice concerns. The team also offer clinical expertise (GP, nursing) which is crucial to understanding the findings generated by this project. We will seek to recruit a community nurse manager from practice on to the research team. The research team have strong links with practice, education and policy. This proposal has involved a Workforce Modernisation Manager (Ian Wragg, Yorks and Humber SHA), Clinical Director Community Services (Alison Woodhouse, North Yorks and York PCT), Assistants (undertaking a Foundation Degree at University of York), Workforce Development Project Manager (Sue Beacock, Yorks and Humber SHA), HCA Advisor (Paul Vaughan, Royal College of Nursing) and Foundation Degree Programme Leads (Celia Grant, University of York). All these individuals are interested in the study and have agreed to be on the project advisory group (or nominate a colleague) if the study is funded.
Costings have been calculated for the scoping study and reflect the data collection and analysis which needs to occur. All staff are being costed at salary cost:
Dr Karen Spilsbury will oversee the entire project and has been costed at 100% fte throughout (18 months). She will manage negotiations for this complex study and ensure necessary applications for ethics approvals are submitted. She will manage data collection, with support from Acton Shapiro during the 10 months data collection, and be responsible for ensuring timely analysis and reporting. The study requires dedicated time of an experienced researcher to ensure its success. Karen has developed a portfolio of research on the assistant workforce in acute care and nursing home settings. Karen is also a registered nurse.
Acton Shapiro will support data collection and data management for a 10-month period, during the PCT provider census (telephone survey with Senior Manager) and telephone interviews of service managers/team leads of community nursing teams. Acton Shapiro have undertaken work on innovative health-care roles, such as Advanced Practitioners in primary and secondary care and intermediate care teams working in the community.
Professor Ian Watt (1% fte) has a portfolio of primary and community care research, with a particular focus on patient safety. He is also a practising GP. Ian will advise on the scoping study and will contribute to the literature and policy review.
Dr Karl Atkin (5% fte) has extensive research experience in primary care and has published widely on qualitative methodologies, workforce and more generally the organisation of health and social care, with particular reference to user accessibility and appropriateness. He will be primarily responsible for Chairing monthly research project meetings, reporting to SDO and advising on the scoping study, literature and policy review. Karl is a medical sociologist with considerable experience of research management.
Dr Karen Bloor (5% fte) will advise on the scoping study and data analysis. Karen is a health economist with a research focus on labour markets in health care.
Ms Dorothy McCaughan (1% fte) has been involved in large, national studies focusing on skill mix in nursing, nurses' roles and patient safety and has a wealth of research experience. She will advise on the scoping study and literature and policy review. Dorothy is also a registered nurse.
Professor Hugh McKenna (1% fte) has been researching and publishing on the role of assistants in health care for over a decade. He has been commissioned by governments to inform policy on the role of assistants. His input to the study will also take account of his experience in using mixed methods in this research area. Hugh is a registered nurse.
Dr Ann Wakefield (1% fte) has examined the boundaries of nursing work for over 10 years, from both an educational and policy perspective. She is a vice chair of a research ethics committee and will advise the team on ethical issues. She will advise on the scoping study and the literature and policy review. Ann is a registered nurse.
A community Nurse Manager (5% fte) will be approached to join the research team and offer support and guidance at monthly research team meetings, drawing on their clinical expertise and networks.
*Ms Sandi Newby (5% fte) will provide secretarial support for the duration of the study.
References
- NHS Next Stage Review: Our vision for primary and community care. London: Department of Health; 2008.
- The Case for User Choice in Public Services: Supplementary Evidence from Minister of State for Department of Health to Support Joint Memorandum from Minister of State for Department Of Health, Minister of State for Local and Regional Government and Minister of State for School Standards. 2007.
- High Quality Care for All: NHS Next Stage Review Final report. London: The Stationery Office; 2008.
- A High Quality Workforce: NHS Next Stage Review. London: Department of Health; 2008.
- Sibbald B, Shen J, McBride A. Changing the skill-mix of the healthcare workforce. Journal of Health 2004;9:28-3.
- Hurst K. Primary care and community care workforce planning and development. Journal of Advanced 2006;55:757-69.
- Bloor K, Maynard A. Planning Human Resources in Health Care: Towards an Economic Approach. An International Comparative Review. Ottawa: Canadian Health Services Research Foundation; 2003.
- Venning P, Durie A, Roland M, Roberts C, Leeses B. Randomised controlled trial comparing cost effectiveness of general practitioners and nurse practitioners in primary care. British Medical Journal 2000;320:1048-53.
- Kinnersley P, Anderson E, Parry K, Clement J, Archard L, Turton P, et al. Randomised control trial of nurse practitioner versus general practitioner care for patients requesting same day consultation in primary care. British Medical Journal 2000;320:1043-8.
- Shum C, Humphreys A, Wheeler D, Cochrane M, Skoda S, Clement S. Nurse management of patients with minor illnesses in general practice: a multi centre randomised control trial. British Medical Journal 2000;320:1038-43.
- Benson L, Venning P, Young R, Walshe K, Mullen C. Beginning to reinvigorate the workforce. British Journal of Health Care Management 2004;10:274-9.
- The changing workforce programme and continuing national role redesign projects. 2007.
- Agenda for Change: Final Agreement. Leeds: Agenda for Change project Team; 2005.
- Kessler I, Bach S, Heron P. Comparing assistant roles in education and social care: backgrounds, behaviours and boundaries. International Journal of Human Resource Management 2006;18:1648-65.
- The Career Framework. 2009.
- Wakefield A, Spilsbury K, Atkin K, McKenna H, . Assistant or substitute: Exploring the fit between national policy vision and local practice realities of assistant practitioner job descriptions. Health Policy 2009;90:286-95.
- Wanless D. Securing our future health: Taking a long-term view. London: HM Treasury; 2002.
- Hurst K. Primary Care Trust Workforce: Planning and Development. London: Whurr Publishers; 2005.
- Wright C. General Practice. In for the skill. Health Service Journal 2002;112:26-7.
- Andrews H, Vaughan P. Skill mix evolution: HCAs in general practice. Practice Nursing 2007;18:619-24.
- Storey C, Cheater F, Ford J, Leese B. Retention of nurses in the primary and community care workforce after the age of 50 years: database analysis and literature review. Journal of Advanced Nursing 2009;65:1596-604.
- Smith P, Young L. Facilitating the employment, training, development and integration of Health Care Assistants in traditional general practice. Department of Health Working in Partnership Programme; 2005.
- Hopkins S. Tasks and issues of accountability and responsibility in delegation to health care assistants. RCN Briefing Paper. 2005.
- Bradford M. Health Care Assistants in General Practice: An evaluation of trained Health Care Assistants in General Practice across 4 Primary Care Trusts within the North Central London NHS Sector. Department of Health Working in Partnership Programme; 2007.
- HCA Toolkit. 2006.
- HCA Unit 2: Good employment practice from a general practice employer's perspective. 2006.
- Vaughan P, Longbottom A, Celino G, Cross S. Reviewing the roles of nurses and health care assistants in general practice. Primary Health Care 2007;17:14-6.
- Hirst M, Lunt N, Atkin K. Were practice nurses distributed equitably across England and Wales, 1988-1995?. Journal of Health Services Research &Amp; Policy 1998;3:31-8.
- Jenkins-Clarke, Carr-Hill R, Dixon P. Teams and seams: skill mix in primary care. Journal of 1998;28:1120-6.
- Richards A, Carley J, Jenkins-Clarke S, Richards DA. Skill mix between nurses and doctors working in primary care delegation or allocation: a review of the literature. International Journal of Nursing 2000;37:185-97.
- Primary care workforce planning framework. 2002.
- Spilsbury K, Meyer J. Making claims on nursing work: Exploring the work of Health Care Assistants and the implications for Registered Nurses' roles. Journal of Research in Nursing 2005;10:65-83.
- Spilsbury K, Adamson J, Atkin K, Carr-Hill R, McCaughan D, McKenna H, et al. Evaluation of the development and impact of Assistant Practitioners supporting the work of ward-based registered nurses in Acute NHS (Hospital) Trusts in England. 2009.
- NHS Hospital and Community Health Services Non-Medical staff England 1997-2007. 2008.
- Selfe J, Roddam H, Cording H, Temple B, Bloor K, Green L, et al. Assistant Practitioner Foundation Degree Evaluation Project: Final Report. University of Central Lancashire; 2008.
- Meadows S, Levenson R, Baeza J. The Last Straw. London: King's Fund; 2000.
- Transforming Community Services: Currency and Pricing Options for. London: Department of Health; 2008.
- Transforming Community Services: Enabling new patterns of provision. London: Department of Health; 2009.
- Miles MB, Huberman MA. Qualitative data analysis. An expanded sourcebook. Thousand Oaks: Sage; 1994.
Appendix 3 Evaluation of the National Institute for Health Research Service Delivery and Organisation Management fellow
| Project title: | Support matters: use of assistant staff in the delivery of community nursing services in England |
| Project reference number: | 09/1801/1026 |
| Principal investigator: | Dr Karen Spilsbury |
| Organisation details: | Department of Health Sciences, University of York, York, UK |
| NIHR SDO management fellow: | Sue Pender, City Health Care Partnership CIC, Hull, UK |
| Secondment period: | 1 February 2011 to 31 January 2012 (1 year, part-time) |
Aims of the secondment
In 2010 the research team responded to a NIHR call to support funded research studies with a NIHR SDO Management fellow. The aim of these fellowships was to provide some additional resources, beyond those specified in the original proposal, to enable a practising NHS manager to become directly involved in the research project, assisting with the research and acting as a ‘knowledge broker’ between the research team and the local NHS. In the original application, the research team and City Health Care Partnership CIC proposed that the secondment of a senior manager from the provider organisations to the university would:
-
provide an opportunity to build an individual's capacity through direct experience of the research process
-
support engagement of a local organisation with the use of research evidence to support management decisions
-
promote dialogue with managers in the NHS to ensure wider dissemination of research evidence for service development
-
increase research capacity of NHS organisations, in both their ability to engage with research and their ability to use research in their day-to-day practice.
The fellowship was written to enable the secondment of Sue Pender, modern matron in end-of-life care, to become an integral member of the research team and to engage with the project throughout the research process by:
-
contributing to the practical application and operationalisation of the proposed research (this would involve contributing to development of the scoping questionnaire and topic guides for in-depth interviews with service managers);
-
supporting data collection and analysis activities for each stage; and
-
assisting with reporting and dissemination activities, with a particular focus on targeting practitioner-orientated journals so that our work is communicated to relevant NHS audiences.
The following summary provides an evaluation of the fellowship and its perceived contribution to the research study.
Personal background and aims
Sue has worked within the provision of health care in the community for over 25 years both as a practitioner and service manager. She has experience of service development and improvement initiatives, writing operational frameworks and job descriptions and person specifications. As a manager she has introduced new ways of working and new roles, such as the introduction of a HCA-only service, aiming to provide additional supportive care to patients with a life-limiting prognosis.
Sue openly admitted that she chose to take this secondment because of the appeal of the subject matter rather than a deep-rooted desire to move into research. Her expressed aim was to gain an opportunity for an added dimension to broaden out her understanding of examining evidence for health-care decisions.
Throughout the secondment Sue was given the opportunity to engage in a range of activities that supported the research and her own personal development, and promoted the opportunities for knowledge transfer within her employing health-care organisation. The activities associated with these aims and achievements to date are detailed below.
Research
-
Assisted in the development of the interview schedule for stage 3 interviews.
-
Conducted semi-structured telephone interviews with research participants.
-
Transcribed interview schedule in preparation for data analysis.
-
Participated in literature review and management of references.
-
Assisted in the management of REC approvals.
-
Developed topic guide for interviews with caseload holders/service managers.
-
Participated in reviewing and commenting on the project final report.
University/academic
-
Attended key research workshops/events, for example Department of Health Sciences Research Showcase, Health Inequalities Group.
-
Attended and participated in the Department of Health Sciences' team meetings.
-
Taught on the palliative and end-of-life care postgraduate modules.
Personal development
-
Learnt how to develop the sequence of questions used when interviewing (establishing rapport, questioning/probing techniques, managing process/time).
-
Developed interview transcribing skills.
-
Further developed literature searching and accessing skills (i.e. use of electronic databases and search engines, University of York library/interlibrary loans).
-
Applied EndNote (Thomson Reuters, CA, USA) training, through the use of the electronic software in managing the project’s references.
-
Gained knowledge of the REC process, and the ethical and governance standards required.
-
Completed Research Design Service online learning ‘Searching the Qualitative Research Literature’.
Sue has undertaken a variety of other developmental activities during the fellowship including:
-
Attended Health Services Research Network/SDO conference ‘Introducing research implementation and knowledge transfer in health services’ (July 2011).
-
Undertook ‘Introducing Research Implementation and Knowledge Transfer in Health Sciences at University of York. Submitted and passed written assignment (20 credits at Level 7).
-
Published article in Nursing Standard about own career and to promote fellowship (August 2011).
-
Established working relationship with Health Intelligence analyst from Public Health Observatory and commenced collaborative work to evaluate a Specialist Palliative Care Clinic (August 2011).
-
Good Clinical Practice in Research training (February 2012).
-
Joined the RCN Research Interest Group Forum.
The secondment was on a part-time basis. For 3 days each week Sue was based in the Department of Health Sciences at the University of York but she continued to work 1 day each week within City Health Care Partnership CIC; her role was to develop research capacity within the organisation (rather than her original role as modern matron).
Activities
-
Introduction of an Advancing Best Practice group within organisation established as a direct result of the fellowship. The aim of these meetings is to improve clinical effectiveness by applying the principles of best practice and to actively participate in clinical reviews and research. Sue acts as Chair for these meetings and organises the content.
-
Led and completed a review of the out-of-hours (OOH) nursing services and assisted in the development of the resulting action plan. Undertook a literature search to collate evidence around the use of non-medical out-of-hours services from around the country. The resulting report has been instrumental in supporting the reorganisation and reinvestment in OOH services within the organisation.
-
Led the evaluation of a community-based clinic, including developing a patient questionnaire, undertaking patient/carer semi-structured interviews, and reporting the evaluation findings.
-
Produced material for the organisation's intranet regarding research and development grants, funding and resources.
-
Reviewed CHCP CIC's Clinical Audit policy.
-
Represented Adult Services on CHCP CIC’s Clinical Effectiveness Committee.
-
Reviewed the single point of access service. Co-wrote article which has been accepted for publication in the Journal of Community Nursing, September 2012.
-
Completed an audit of Specialist Palliative Care Clinic attendees by designing, piloting and implementing a data capture tool.
-
Undertook telephone interviews with palliative care patients to elicit their experiences of services.
-
Reviewed the effectiveness of clinical nurse specialists within locality working. The report of this has been instrumental in the proposal for new service design for other nurse specialists in the community.
-
Developed data capture tool to review administrative services.
-
Undertook patient survey interviews as part of service review.
-
Acted as an advisor/support to others wishing to develop their clinical/service enquiry activities (e.g. psychological care service review of eating disorder service, Emergency Care Practitioner teams' exploration of the impact of their care, interagency reablement service).
Beyond completion of the fellowship
Although the 12-month secondment was completed at the end of January 2012, City Health Care Partnership CIC has allowed Sue to continue to work with the research team 1 day each week. This has been important to support the report writing and planned dissemination activities. This was agreed with the Director of Nursing in recognition of the two-way exchange of knowledge as well as her personal desire to see the project work completed. Sue has an honorary contract in the Department of Health Sciences.
Since returning to the organisation, Sue has been supported to continue to build the organisation's research infrastructure. She has successfully proposed a new research and development role for City Health Care Partnership CIC, which will incorporate elements of research, clinical effectiveness enquiry, governance and patient and carer engagement.
Appendix 4 Overview of the study
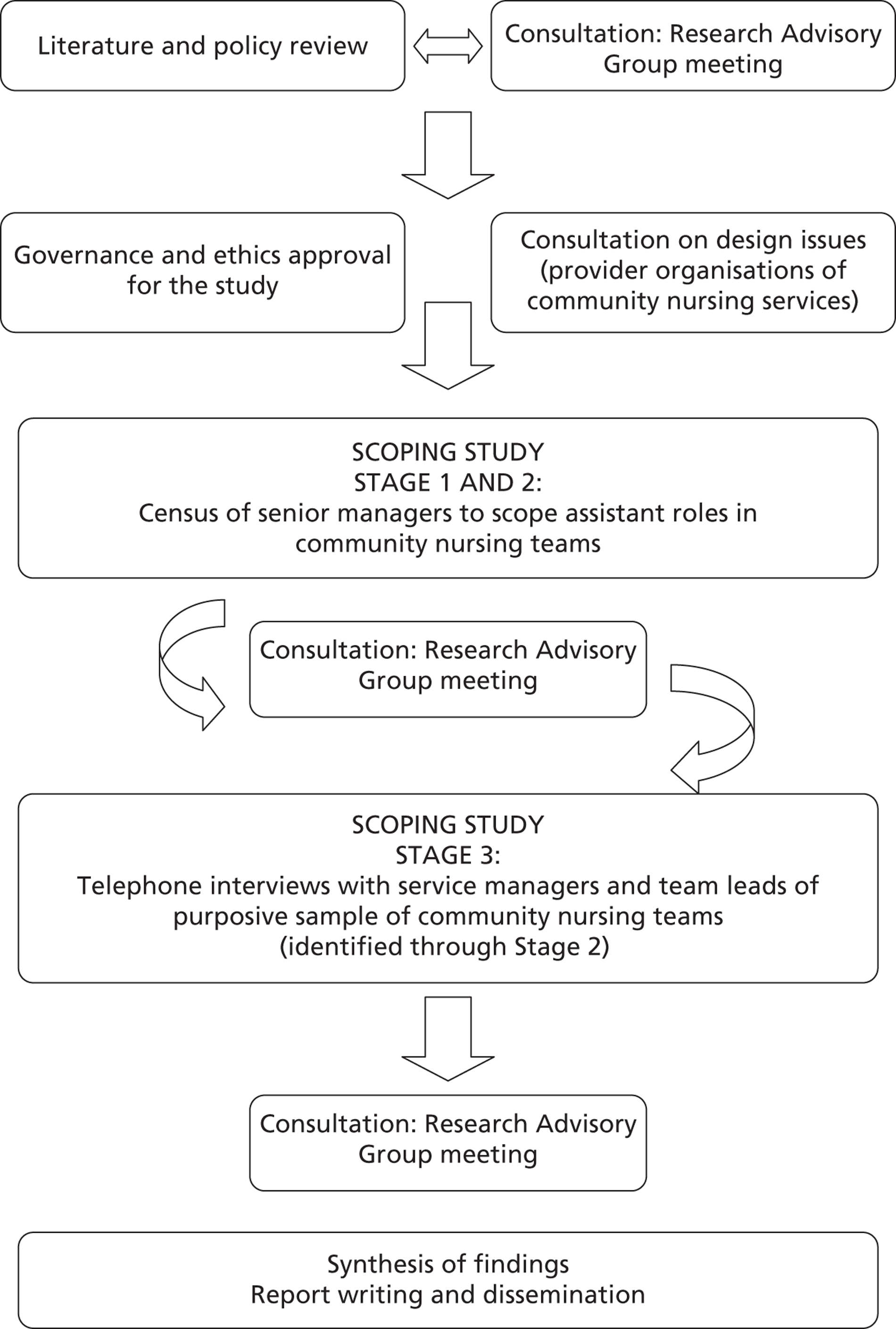
Appendix 5 Interview schedule for stage 2 interview with senior manager

Interviewer: Please take the time to go through information on this first sheet with the interviewee
Due to time pressure it would be good to get straight to the interview. Check whether the interviewee is clear with the purpose of the interview.
If yes ask permission to progress straight to the interview. You may wish to reiterate that any information shared is treated in confidence and will be anonymised. Take the time to clarify the amount of time that the individual has:
‘The interview will last approximately 15 minutes but will largely be dictated by how much you would like to tell us. Can I confirm that 15 minutes is still ok by you today? If the interview were to go on for slightly longer would that be ok?’
Ensure they are happy that the interview is being audio recorded – this is purely to ensure we capture the information they provide accurately.
If the interviewee would like further information then there are some prompts below to help.
PROMPTS
Why have you been approached to participate in this interview?
-
We are carrying out a national census to scope the roles of assistant staff in adult community nursing teams. In the last decade, numbers of assistants in community nursing teams have increased by 118%; yet little is known about their work and their potential contribution to service delivery.
-
This study is funded by the Department of Health (NIHR Service Delivery and Organisation Programme) and will generate important information to inform service delivery and national policy.
-
You have been approached to participate in an interview because you are a Senior Manager of an organisation responsible for the provision of adult community nursing services.
-
At this stage please confirm their job title and that they manage provision of community nursing services.
-
Also confirm, prior to progressing further with the interview, that they have assistant staff employed in these community nursing teams.
-
What is the interview about?
-
I would like to ask a series of questions about use of assistant staff (Agenda for Change Bands 2, 3 and 4) in the delivery of adult community nursing services by your organisation.
-
The questions are aimed at establishing detail about the numbers, types and roles of these assistant staff in your organisation.
-
There are no right or wrong answers. We would simply like to understand what currently happens in your organisation.
Who will see my answers?
-
The information you give is totally confidential. Only members of the research team will handle the data.
-
For accurate collection of data we would like to confirm that you are happy for this interview to be audio-recorded?
-
If interviewee happy with this, please reassure them that once you have inputted data into our database you will delete the interview.
-
If interviewee not happy, please reassure them that you are taking notes of the interview and will not record.
-
-
We have attached a reference number for this interview (rather than your name) for the purposes of data management.
-
When we report our findings they will be written in such a way that it is not possible for individuals or organisations to be identified.
-
The only exception may be where you would like your organisation to be acknowledged in the citation of examples of exploring the innovative use of assistants in the provision of services. In these circumstances, we would discuss this with you prior to any information being used and would check the draft reporting of this with you prior to any publication.
-
The findings from this census study will be made available to all organisations that participate but strictly in anonymised format, unless you indicate your willingness for us to do otherwise.
How long will the interview take?
-
The interview will last approximately 15 minutes but will largely be dictated by how much you would like to tell us. Can I confirm that 15 minutes is still ok by you today? If the interview were to go on for slightly longer would that be ok?
Do you have any questions before we begin the interview?
Bold text = questions
Non-bold text = prompts
Please start the interview with 3 points of clarification (unless you have done this as part of providing further information to the participant in the introduction)
You have been approached to participate in an interview because you are a Senior Manager of an organisation responsible for the provision of adult community nursing services.
-
Please can you confirm your job title and that you manage provision of community nursing services.
-
When was your organisation established as a provider organisation? [This should prompt interviewee to give us any details about change in location etc]
-
Also confirm, can you confirm that you have assistant staff/support workers employed in these community nursing teams.
Q1. Defining community nursing is challenging. Can I start by asking you to define what you mean or understand by the term community nursing services?
Q2. Our focus is adult community nursing teams, such as District Nursing or Community Matrons working with community nursing teams. With this definition in mind, what community nursing services does your organisation provide?
Q3. Of these services, can you describe assistant/support worker roles within the teams?
-
[Clarify where possible whether they have a sense of the numbers, banding, and roles]
Q4. Have the range of roles for assistants/support workers within these community nursing teams provided by your organisation increased over the past decade? It would be helpful to understand the range of titles you use for assistants/support workers.
-
[Clarify on what basis they have made this judgement]
-
[Explore whether they would be happy to share any data collected by HR about nursing workforce numbers that include assistant numbers. If yes, determine how we can obtain these data]
Q5. Would you say that your organisation has developed assistant/support worker roles in ways that may be considered innovative or present novel ways of working?
-
[If yes, explore and ask for examples. Check regarding reporting of these examples – would the organisation like to be named?]
-
[If no, determine whether there are any plans].
Q6. We would like to understand more about the work of assistants/support workers in community nursing teams. Can you describe their roles?
-
[Ask interviewee to expand upon anything said in response to Q3]
Q7. Would your organisation be happy to share job descriptions of these assistants/support workers?
-
[Use this as a strategy if Q4 is difficult for the Manager to answer].
-
[Offer to follow this up with a contact provided by the Manager if this would be easier].
Q8. Are assistant/support worker roles in your organisation supported by a competency framework?
-
Would you be happy to share copies of these? [Clarify how to obtain copies if the manager is happy to share]
Q9. What, in your opinion, have been the main drivers for introducing assistants/support workers within community nursing teams in your organisation?
Q10. What (if any) are your plans for future development of assistant/support worker roles in community nursing teams?
Q11. In what ways do you perceive assistant/support worker roles to be impacting on the wider nursing team?
-
[Explore organisation of nursing work and care delivery and workload issues].
Q12. In what ways do you perceive assistant/support worker roles to be impacting on patient experience?
-
[Where possible gather examples].
The next stage of our study involves gathering more in-depth information about assistant/ support worker roles from line managers of these workers. We will be selecting a sample of services to gather this level of detail. Can we approach you at a later stage to identify names of service managers that we could approach about taking part in this next stage of the study?
-
If yes, indicate this will be by July at latest.
-
[If they prefer, gather names at this stage, indicating we may/may not be including the services in the next stage].
That is the end of my questions. Is there anything you would like to ask me?
Take time to clarify how information provided will be used and reiterate about confidentiality and anonymity (taking into account any discussion regarding citing examples of innovative community assistant roles).
Remind them about website and that we will contact them with a summary of these first stage interviews after summer.
State that you will send a follow-up email to summarise this information.
Thank you again for your time.
Appendix 6 Interview schedule for stage 3 service managers/team leads

INTERVIEW SCHEDULE FOR CASELOAD HOLDERS/SERVICE MANAGERS – INTERVIEWER’S COPY
It would be helpful for us to understand a little about your experience and qualifications. Are you happy to share this information with us? (Remind that all responses will be anonymised and that they may opt out of answering these questions if they prefer)
-
What is your professional background?
-
When did you qualify?
-
How many years have you worked within the community?
-
When did you join the team that you are working in now?
-
What is your job title?
-
What band are you?
I hope that you have had the chance to look at the questions that we would like to ask you.
Ideally we would like to talk to you for 30–40 minutes, is this alright with you?
If you have less time available we can prioritise what we discuss.
CASELOAD
-
Q1 Can you describe you current caseload?
(Prompts – should get response about figures, referral, clinic responsibilities, locality/practice attachments, could prompt to ask how numbers change over the year? Whether all the patients on the caseload are ‘active’ i.e. receiving regular care, what are the types of patients/range of care needs)
TEAM
-
Q2 Can you describe your team?
(Prompts – should get a response that includes W.T.E and skill mix, do they have their ‘own’ dedicated nursing assistant or are these posts shared across teams)
DUTIES & RESPONSIBILITIES
-
Q3a Can you tell me the duties and responsibilities of the nursing assistants in your team?
(Prompts – should get responses that includes both patient and non patient care i.e. administrative duties, may be ‘link’ nurse or store room ‘monitor’)
-
Q3b Can you give me an example of patient care that you have recently asked your nursing assistant to deliver?
AUTHORITY
-
Q4 Who is considered the key worker or the person in charge of the nursing management of the patient?
(Prompt – wanting to hear about the lines of authority)
-
Q5a How does the key worker keep up to date with the care that has been delivered by the nursing assistant?
(Prompt – wanting to hear about mechanisms for updating or sharing patient care, When is the nursing care evaluated? How often are updates done? And how are they done? i.e. face-to-face, telephone, electronic patient records, message book? What is expected of the nursing assistant in terms of reporting to the key worker?)
-
Q5b Can you give me an example of a recent update from a nursing assistant?
IMPACT OF WORKING WITH NURSING ASSISTANTS WITHIN COMMUNITY TEAM
-
Q6a What are the benefits to you as a caseload holder of having nursing assistants within the team?
-
Q6b What are the challenges that you encounter in delegating work to nursing assistants?
-
Q6c What mechanisms does your organisation have in place to ensure that the assistant staff are competent to deliver patient care?
(Prompt – How confident do they feel about the care delivered by their nursing assistants? What is their perspective on accountability? Do they talk about ‘safe’ practice/quality care? Do they mention training and teaching activities?)
SUPPORTING ASSISTANTS
-
Q7 How do you know that your nursing assistant is capable of delivering the care that you have asked of them?
(Prompt – Should hear about mechanisms for monitoring and supporting such as supervision, supervisory rounds, observed practice, competency frameworks etc)
-
Q8 What are the most common issues that nursing assistants bring to you?
(Prompt – May hear about actual day to day issues around patient care/organisation/professional/team working )
FUTURE/VISION
-
Q9 What would you like to see in the future for nursing assistants?
(Prompt – May share how they would like to see the role develop or change? Whether they feel role should be regulated?)
-
Q10 Is there anything else that you would like us to know about your experience of working with nursing assistants?
That is the end of my questions.
-
Is there anything you would like to ask me?
Appendix 7 E-mail invitations for senior manager (stage 1)
Initial contact
Dear Colleague
An invitation to take part in a study about the use of assistant staff in the delivery of community nursing services in England
Over the last decade, there has been a significant increase in the numbers of assistants working in community nursing teams. Researchers at The University of York have been funded by the Department of Health to carry out a scoping study of these roles. This is the first national study of assistant roles in community nursing teams.
We would like to make contact with Senior Managers responsible for provision of community nursing services. If you are potentially interested in contributing to this study, please reply to this email to indicate whether:
-
You employ assistants in the community nursing services that you are responsible for; AND
-
You would be happy to take part in a short telephone interview (lasting no more than 15 minutes) to discuss the roles of community nursing assistants (or would like to nominate an alternative person for us to interview).
If you agree to participate in this study we will share with you findings from the study and resources on use of community nursing assistants.
We appreciate that you are very busy and thank you for taking the time to read this email. If you would be happy to consider our request to interview you, then we will send you further information about what would be involved. At this stage you simply need to reply to this ‘making contact’ email.
Kind regards
[Researcher name, position and contact details]
First reminder (after 1 week)
Dear Colleague
Reminder: An invitation to take part in a study about the use of assistant staff in the delivery of community nursing services in England
We recently emailed you about the above study to determine whether you would like to participate in a short telephone interview about use of assistants in community nursing teams.
Over the last decade, there has been a significant increase in the numbers of assistants working in community nursing teams. Researchers at The University of York have been funded by the Department of Health to carry out a scoping study of these roles. This is the first national study of assistant roles in community nursing teams.
If you are potentially interested in contributing to this study, please reply to this email to indicate whether:
-
You employ assistants in the community nursing services that you are responsible for; AND
-
You would be happy to take part in a short telephone interview (lasting no more than 15 minutes) to discuss the roles of community nursing assistants (or would like to nominate an alternative person for us to interview).
If you agree to participate in this study we will share with you findings from the study and resources on use of community nursing assistants.
We appreciate that you are very busy and thank you for taking the time to read this email. If you would be happy to consider our request to interview you then we will send you further information about what would be involved. At this stage you simply need to reply to this ‘making contact’ email.
Kind regards
[Researcher name, position and contact details]
Final reminder (2 weeks after initial invite)
Dear Colleague
Final reminder: An invitation to take part in a study about the use of assistant staff in the delivery of community nursing services in England
We have been trying to contact you about the above study to determine whether you would like to participate in a short telephone interview about use of assistants in community nursing teams Over the last decade, there has been a significant increase in the numbers of assistants working in community nursing teams. Researchers at The University of York have been funded by the Department of Health to carry out a scoping study of these roles. This is the first national study of assistant roles in community nursing teams.
If you are potentially interested in contributing to this study, please reply to this email to indicate whether:
-
You employ assistants in the community nursing services that you are responsible for; AND
-
You would be happy to take part in a short telephone interview (lasting no more than 15 minutes) to discuss the roles of community nursing assistants (or would like to nominate an alternative person for us to interview).
If you agree to participate in this study we will share with you findings from the study and resources on use of community nursing assistants.
This will be the last time we will try to contact you about this matter. We appreciate that you are very busy and thank you for taking the time to read this email. If you would be happy to consider our request to interview you then we will send you further information about what would be involved. At this stage you simply need to reply to this ‘making contact’ email.
Kind regards
[Researcher name, position and contact details]
Appendix 8 E-mail invitation for senior manager (stage 2)
Dear Colleague
An invitation to take part in a study about the use of assistant staff in the delivery of community nursing services in England
Thank you for replying to our earlier email and for expressing an interest in taking part in a short telephone interview (lasting no more than 15 minutes) about the use of assistant staff in the delivery of community nursing services. By participating in this study you will have an opportunity to inform future service provision and national policy.
This is the first national study of assistant roles in community nursing teams.
Please take the time to read the attached information sheet about the study and what would be involved. Then, when you have decided to take part, simply reply to this email and we will get in touch to discuss next steps.
Thank you for giving this your consideration. We hope to hear from you soon.
Kind regards
[Researcher name, position and contact details]
Appendix 9 E-mail study information sheet for stage 2 senior manager interview

1. What is the purpose of the study?
Researchers at The University of York have been funded by the Department of Health to carry out a scoping study of community nursing assistant roles. Over the last decade, there has been a significant increase in the numbers of assistants working in these settings. This is the first national study of assistant roles in community nursing teams and will provide important information to inform future service provision and national policy.
2. Why have you been chosen?
You have received this invite to participate in a short telephone interview because you are a Senior Manager responsible for community nursing services. You can obtain further information about our study and access resources about use of assistants in community nursing teams at http://www.york.ac.uk/healthsciences/research-information/support-matters/
3. Do you have to take part?
It is entirely up to you to decide whether to take part. If you would like to take part, then please confirm this by email or by returning the consent form by post. Once we have received your consent, we will arrange a suitable appointment time with you for the telephone interview.
4. What will happen if you choose to take part?
We will carry out a short telephone interview with you; no more than 30 minutes. We will ask your permission to audio record the interview. You will only be asked to take part in one interview.
5. What will happen to the information you provide?
The only people who will have access to your interview are members of the research team. When we report our findings they will be written in such a way that it is not possible for individuals or organisations to be identified. The only exception may be where you would like your organisation to be acknowledged in the citation of examples of innovative use of assistants. We will discuss this with you at the end of the interview. In the unlikely event that during the interview information is revealed which is considered by the research team to potentially threaten patient safety, then we will need to report this via routine incident reporting mechanisms.
6. What are the benefits of taking part?
There are no personal benefits to you for taking part. The findings of this study are of national importance for policy and services and we are happy to send you a copy of the findings.
7. What will happen to the results of this study?
The findings from the study will be published in a final report, in journal articles and at conferences.
8. Who is organising and funding the research?
The research is funded by the Department of Health. The research funding covers only the costs of undertaking the research; researchers will not receive payment for conducting the study.
9. Who has reviewed this study?
This study has been reviewed by the South East London Research Ethics Committee (3) and has been allocated reference number 10/H0808/159.
10. What if I have any questions or concerns?
Thank you for considering this study. If you have any questions about the study at any time, please contact the research team (contact details on the email).
Appendix 10 Consent form for stage 2 senior manager interview

Please read this form carefully and ask if there is anything that you do not understand.
| Please Initial Boxes | |
|---|---|
| 1. I have received and read the information sheet dated 17/11/10 (version 1) and understand what this study aims to do. I have had the opportunity to consider the information, ask questions and have had these answered satisfactorily. | □ |
| 2. I understand that I am being asked to participate in one interview carried out by a researcher from the University of York. | □ |
| 3. I understand that my participation is voluntary and that I am free to withdraw at any time without giving an explanation. | □ |
| 4. I understand that all information collected from me for the study will be kept confidential and that the only people who see this information are researchers at the University of York. | □ |
| 5. I understand that the information gathered will be used to write research articles and reports, but will not identify me by name, nor will it identify my organisation. The only exception is where I give permission for examples from my organisation to be used but the research team will discuss this with me. | □ |
| 6. I understand that if I disclose information that the research team feels compromises patient safety then the research team will need to report this via routine incident reporting mechanisms. | □ |
| 7. I agree to the interview being audio-tape recorded and that my words might be used anonymously in publications generated from this research. | □ |
| 8. I agree to take part in the above named study. | □ |
| ___________________________ | ____________ | _____________________ |
| Name of Staff member | Date | Signature |
| ___________________________ | ____________ | _____________________ |
| Name of Person taking consent | Date | Signature |
Appendix 11 Web-based study information for stage 2 senior manager interview

You are being invited to take part in a scoping study, which will gather information to inform future research. Before you decide whether to take part, it is important to understand why this work is being undertaken and what will be involved if you decide to participate. Please read this information sheet carefully. If there is anything you want to discuss in more detail or that is unclear please contact one of the people named at the end of this information sheet. Take as much time as you need to decide whether to take part. Your involvement is entirely voluntary.
1. What is the purpose of the study?
Nursing care is provided to patients in the community by both registered nurses and their assistant staff. Over the last decade, there has been a significant increase in the numbers of assistants working in community nursing teams. Community nursing (in this context) refers, in its broadest sense, to any nursing care delivered to patients in their own home. Researchers at The University of York have been funded by the Department of Health (NIHR Service Delivery and Organisation Programme) to carry out a scoping study to establish numbers, types and roles of assistant staff in community nursing teams and their potential contribution to service delivery, patient experience and patient choice. We are interested in gathering information about assistant staff working at Agenda for Change pay bands 2, 3 and 4 in teams that provide care principally to adults. An initial stage of this scoping work involves telephone interviews with Senior Managers responsible for community nursing service provision. You are being invited to participate in a short telephone interview (maximum of 15-minutes). You can obtain further information about our study and access resources about use of assistants in community nursing teams at http://www.york.ac.uk/healthsciences/research-information/support-matters/. This is the first national study of assistant roles in community nursing teams and will provide important information to inform future service provision and national policy.
2. Why have you been chosen?
You have received this invite because you are a Senior Manager responsible for the provision of community nursing services and responded to our email contact about the study, expressing your interest in participating in a short telephone interview.
3. Do you have to take part?
It is entirely up to you to decide whether to take part. If you have any questions or concerns about taking part, you should talk to a member of the research team (contact details overleaf). If you do decide you would like to take part, then we ask you to confirm this by email or returning the consent form by post. Once we have received confirmation that you would like to be interviewed then we will arrange an appointment for the interview which will be at a time and location best for you.
4. What will happen if you choose to take part?
We would like to interview as many Senior Managers as possible. If you would like to take part in the study, we will carry out a short telephone interview with you. The interview will take no more than 30 minutes. We will ask your permission to audio record the interview. You will only be asked to take part in one interview although we will ask if we can contact you at a later stage to gather names of Service Managers who may like to participate in a subsequent stage of our study. If you have decided you do not wish to take part in the study, we would like to take this opportunity to thank you for reading this information sheet and for considering this matter. Please email us (karen.spilsbury@york.ac.uk) if you would like to suggest another individual from your organisation who might be able to help us or to indicate that you do not want your organisation to be included in this scoping study.
5. What will happen to the information you provide?
The only people who will have access to your interview are members of the research team (the University of York are working with Acton Shapiro Consultancy). We will attach an identification number to your interview and will use this when reporting findings. When we report our findings they will be written in such a way that it is not possible for organisations to be identified. The only exception may be where you would like your organisation to be acknowledged in the citation of examples of innovative use of assistants in the provision of services. In these circumstances, we would discuss this with you prior to any information being used and would check the draft reporting of this with you prior to any publication. We will check this with you at the end of your interview.
The researchers are not employed by your Trust. All information collected from you will be kept strictly confidential and made anonymous. Your Trust will never see any individual's responses: only the research team will have access to any data. All information will be stored in accordance with the data protection act: your name and the name of your organisation will not be used in any publications or reports.
6. What are the benefits of taking part?
There are no personal benefits to you for taking part. However, the findings of this study are of national importance for policy and services. They will help to lead to a better understanding of the use of assistant staff in community nursing teams and their potential contribution to service delivery, patient experience and patient choice. We are happy to send participants a copy of the findings from this scoping study once complete.
7. What will happen to the results of this study?
The findings from the study will be used to inform a national report to the funding body, which will be relevant to practitioners, provider organisations, commissioners, policy makers and patients. In addition, we intend to publish the results in academic journals and via presentations at national and international conferences.
8. Who is organising and funding the research?
The research is funded by the Department of Health via their Service Delivery and Organisation programme of research. The research funding covers only the costs of undertaking the research; researchers will not receive payment for conducting the study.
9. Who has reviewed this study?
This study has been reviewed by the South East London Research Ethics Committee (3) and has been allocated reference number 10/H0808/159. (All research that involves NHS patients or staff, information from NHS medical records or uses NHS premises or facilities must be approved by a NHS Research Ethics Committee before it goes ahead. Approval does not guarantee that you will not come to any harm if you take part. However approval means that the Committee is satisfied that your rights will be respected, that any risks have been reduced to a minimum and balanced against possible benefits, and that you have been given sufficient information on which to make an informed decision to take part or not.)
10. What if I have any questions or concerns?
Thank you for considering this study. If you have any questions about the study at any time, please contact:
[Researcher name, position and contact details]
Appendix 12 E-mail invitations for service manager/team lead (stage 3)
Initial contact
Dear Colleague
An invitation to take part in a study about the use of assistant staff in the delivery of community nursing services in England
Over the last decade, there has been a significant increase in the numbers of assistants working in community nursing teams. Researchers at The University of York have been funded by the Department of Health to carry out a scoping study of these roles. This is the first national study of assistant roles in community nursing teams.
We would like to invite you to take part in a telephone interview that will last no more than 40 minutes. We would like to interview you because you are a Service Manager/Team Leader responsible for the day-to-day management of a community nursing team(s) that may or may not use assistant staff. By participating in this study you will have an opportunity to inform future service provision and national policy. We will also ensure you receive a copy of findings from this study and have access to resources on use of community nursing assistants.
If you are interested in the taking part, please read the attached information sheet about the study and what would be involved. Then, simply reply to this email and we will get in touch to discuss next steps.
Thank you for giving this your consideration. We hope to hear from you soon.
Kind regards
[Researcher name, position and contact details]
First reminder (after 1 week)
Dear Colleague
Reminder: An invitation to take part in a study about the use of assistant staff in the delivery of community nursing services in England
We recently emailed you about the above study to determine whether you would like to participate in a telephone interview about use of assistants in community nursing teams. We would like to interview you because you are a Service Manager/Team Leader responsible for the day-to-day management of a community nursing team(s) that may or may not use assistant staff. By participating in this study you will have an opportunity to inform future service provision and national policy. We will also ensure you receive a copy of findings from this study and have access to resources on use of community nursing assistants.
Over the last decade, there has been a significant increase in the numbers of assistants working in community nursing teams. Researchers at The University of York have been funded by the Department of Health to carry out a scoping study of these roles. This is the first national study of assistant roles in community nursing teams.
If you are interested in the taking part, please read the attached information sheet about the study and what would be involved. Then, simply reply to this email and we will get in touch to discuss next steps.
Thank you for giving this your consideration. We hope to hear from you soon.
Kind regards
[Researcher name, position and contact details]
Final reminder (2 weeks after initial invite)
Dear Colleague
Final reminder: An invitation to take part in a study about the use of assistant staff in the delivery of community nursing services in England
We have been trying to contact you about the above study to determine whether you would like to participate in a telephone interview about use of assistants in community nursing teams. We would like to interview you because you are a Service Manager/Team Leader responsible for the day-to-day management of a community nursing team(s) that may or may not use assistant staff. By participating in this study you will have an opportunity to inform future service provision and national policy. We will also ensure you receive a copy of findings from this study and have access to resources on use of community nursing assistants.
Over the last decade, there has been a significant increase in the numbers of assistants working in community nursing teams. Researchers at The University of York have been funded by the Department of Health to carry out a scoping study of these roles. This is the first national study of assistant roles in community nursing teams.
This will be the last time we will try to contact you about this matter. If you are interested in the taking part, please read the attached information sheet about the study and what would be involved. Then, simply reply to this email within 1-week of receipt and we will get in touch to discuss next steps. If you have decided you do not want to take part we would like to thank you for giving this matter your consideration.
Kind regards
[Researcher name, position and contact details]
Appendix 13 E-mail study information for stage 3 service manager/team lead interview

1. What is the purpose of the study?
Researchers at The University of York have been funded by the Department of Health to carry out a scoping study of community nursing assistant roles. Over the last decade, there has been a significant increase in the numbers of assistants working in these settings. This is the first national study of assistant roles in community nursing teams and will provide important information to inform future service provision and national policy.
2. Why have you been chosen?
You have received this invite to participate in a short telephone interview because you are a Service Manager or Team Lead responsible for day-to-day management of a community nursing team(s). You can obtain further information about our study and access resources about use of assistants in community nursing teams at http://www.york.ac.uk/healthsciences/researchinformation/support-matters/
3. Do you have to take part?
It is entirely up to you to decide whether to take part. If you would like to take part, then please confirm this by email or by returning the consent form by post. Once we have received your consent, we will arrange a suitable appointment time with you for the telephone interview.
4. What will happen if you choose to take part?
We will carry out a telephone interview with you that will last no more than 40 minutes. We will ask your permission to audio record the interview. You will only be asked to take part in one interview.
5. What will happen to the information you provide?
The only people who will have access to your interview are members of the research team. When we report our findings they will be written in such a way that it is not possible for individuals or organisations to be identified. In the unlikely event that during the interview information is revealed which is considered by the research team to potentially threaten patient safety, then we will need to report this via routine incident reporting mechanisms.
6. What are the benefits of taking part?
There are no personal benefits to you for taking part. The findings of this study are of national importance for policy and services and we are happy to send you a copy of the findings.
7. What will happen to the results of this study?
The findings from the study will be published in a final report, in journal articles and at conferences.
8. Who is organising and funding the research?
The research is funded by the Department of Health. The research funding covers only the costs of undertaking the research; researchers will not receive payment for conducting the study.
9. Who has reviewed this study?
This study has been reviewed by the South East London Research Research Ethics Committee (3) and has been allocated reference number 10/H0808/159.
10. What if I have any questions or concerns?
Thank you for considering this study. If you have any questions about the study at any time, please contact the research team (contact details on the email).
Appendix 14 Web-based study information for stage 3 service manager/team lead interview

You are being invited to take part in a study, which will gather information to inform future research. Before you decide whether to take part, it is important to understand why this work is being undertaken and what will be involved if you decide to participate. Please read this information sheet carefully. If there is anything you want to discuss in more detail or that is unclear please contact one of the people named at the end of this information sheet. Take as much time as you need to decide whether to take part. Your involvement is entirely voluntary.
1. What is the purpose of the study?
Nursing care is provided to patients in the community by both registered nurses and their assistant staff. Over the last decade, there has been a significant increase in the numbers of assistants working in community nursing teams. Community nursing (in this context) refers, in its broadest sense, to any nursing care delivered to patients in their own home. Researchers at The University of York have been funded by the Department of Health (NIHR Service Delivery and Organisation Programme) to carry out a scoping study to establish numbers, types and roles of assistant staff in community nursing teams and their potential contribution to service delivery, patient experience and patient choice. We are interested in gathering information about assistant staff working at Agenda for Change pay bands 2, 3 and 4 in teams that provide care principally to adults. We have established the national picture of use of assistants in community nursing teams and would now like to gain an understanding of their work and potential contribution to patient service delivery and care. You are being invited to participate in a telephone interview (lasting no more than 40-minutes). You can obtain further information about our study and access resources about use of assistants in community nursing teams at http://www.york.ac.uk/healthsciences/research-information/support-matters/. This is the first national study of assistant roles in community nursing teams and will provide important information to inform future service provision and national policy.
2. Why have you been chosen?
You have received this invite because you are a Service Manager/Team Lead responsible for the day-to-day management of a community nursing team(s). Your Senior Manager (who participated in an earlier stage of our study) suggested you as a suitable person for us to approach for this interview. However, your Manager does not know that we have made this approach to you.
3. Do you have to take part?
It is entirely up to you to decide whether to take part. If you have any questions or concerns about taking part, you should talk to a member of the research team (contact details overleaf). If you do decide you would like to take part, then we ask you to confirm this by email or returning the consent form by post. Once we have received confirmation that you would like to be interviewed then we will arrange an appointment for the interview which will be at a time and location best for you.
4. What will happen if you choose to take part?
If you would like to take part in the study, we will carry out a short telephone interview with you. The interview will take no more than 40 minutes. We will ask your permission to audio record the interview. You will only be asked to take part in one interview. If you have decided you do not wish to take part in the study, we would like to take this opportunity to thank you for reading this information sheet and for considering this matter. Please email us (karen.spilsbury@york.ac.uk) if you would like to suggest another individual from your organisation who might be able to help us or to indicate that you do not want to participate in the study.
5. What will happen to the information you provide?
The only people who will have access to your interview are members of the research team (the University of York are working with Acton Shapiro Consultancy). We will attach an identification number to your interview and will use this when reporting findings. When we report our findings they will be written in such a way that it is not possible for you to be identified.
The researchers are not employed by your Trust. All information collected from you will be kept strictly confidential and made anonymous. Your Trust will never see any individual's responses: only the research team will have access to any data. All information will be stored in accordance with the data protection act: your name and the name of your organisation will not be used in any publications or reports.
If during the interview information is revealed which is considered by the research team to potentially threaten patient safety then we will need to report this via routine incident reporting mechanisms.
6. What are the benefits of taking part?
There are no personal benefits to you for taking part. However, the findings of this study are of national importance for policy and services. They will help to lead to a better understanding of the use of assistant staff in community nursing teams and their potential contribution to service delivery, patient experience and patient choice. We are happy to send participants a copy of the findings from this scoping study once complete.
7. What will happen to the results of this study?
The findings from the study will be used to inform a national report to the funding body, which will be relevant to practitioners, provider organisations, commissioners, policy makers and patients. In addition, we intend to publish the results in academic journals and via presentations at national and international conferences.
8. Who is organising and funding the research?
The research is funded by the Department of Health via their Service Delivery and Organisation programme of research. The research funding covers only the costs of undertaking the research; researchers will not receive payment for conducting the study.
9. Who has reviewed this study?
This study has been reviewed by the South East London Research Ethics Committee (3) and has been allocated reference number 10/H0808/159. (All research that involves NHS patients or staff, information from NHS medical records or uses NHS premises or facilities must be approved by a NHS Research Ethics Committee before it goes ahead. Approval does not guarantee that you will not come to any harm if you take part. However approval means that the Committee is satisfied that your rights will be respected, that any risks have been reduced to a minimum and balanced against possible benefits, and that you have been given sufficient information on which to make an informed decision to take part or not.)
10. What if I have any questions or concerns?
Thank you for considering this study. If you have any questions about the study at any time, please contact:
[Researcher name, position and contact details]
Appendix 15 Consent form for stage 3 service manager/team lead interview

Please read this form carefully and ask if there is anything that you do not understand.
| Please Initial Boxes | |
|---|---|
| 1. I have received and read the information sheet dated 17/11/10 (version 1) and understand what this study aims to do. I have had the opportunity to consider the information, ask questions and have had these answered satisfactorily. | □ |
| 2. I understand that I am being asked to participate in one interview carried out by a researcher from the University of York. | □ |
| 3. I understand that my participation is voluntary and that I am free to withdraw at any time without giving an explanation. | □ |
| 4. I understand that all information collected from me for the study will be kept confidential and that the only people who see this information are researchers at the University of York. | □ |
| 5. I understand that the information gathered will be used to write research articles and reports, but will not identify me by name, nor will it identify my organisation. | □ |
| 6. I understand that if I disclose information that the research team feels compromises patient safety then the research team will need to report this via routine incident reporting mechanisms. | □ |
| 7. I agree to the interview being audio-tape recorded and that my words might be used anonymously in publications generated from this research. | □ |
| 8. I agree to take part in the above named study. | □ |
| ___________________________ | ____________ | _____________________ |
| Name of Staff member | Date | Signature |
| ___________________________ | ____________ | _____________________ |
| Name of Person taking consent | Date | Signature |
Appendix 16 Interview schedule sent by e-mail as information for stage 3 service managers/team leads

OUTLINE OF INTERVIEW SCHEDULE FOR COMMUNITY CASE-LOAD HOLDERS
ABOUT YOU
It would be helpful for us to understand a little about your experience and qualifications – all responses will be anonymised, although you may opt out of answering these questions if you prefer;
What is your professional background? and when did you qualify?
-
How many years have you worked within the community?
-
When did you join the team that you are working in now?
-
What band are you?
Listed below is the range of questions that we would like to discuss with you, depending upon the time that you have available. Ideally we would like to talk to you for 30–40 minutes, but if you have less time, just let us know at the beginning of the interview and we can prioritise what we discuss.
CASE LOAD & COMMUNITY NURSING TEAM
-
Can you describe your case load?
-
Can you describe your team?
DUTIES & RESPONSIBILITES
-
Can you tell me about the duties and responsibilities of the nursing assistants that you work with?
-
Can you give me an example of nursing care that you have recently asked a nursing assistant to deliver?
-
Who is considered the ‘key worker’ or person in charge of the nursing management of the patient?
-
How does the key worker keep up to date with the care of the patients that have been visited by the nursing assistants?
-
Can you give me an example of a recent update?
NURSING ASSISTANTS' IMPACT WITHIN THE COMMUNITY TEAM
-
What are the benefits to you as a case load holder of having nursing assistants working within your team?
-
What are the challenges that you encounter in delegating work to nursing assistants?
-
What mechanisms does your organisation have in place to ensure assistant staff are safe and competent to deliver patient care?
SUPPORTING ASSISTANTS
-
How do you know whether the nursing assistant is capable of delivering the care that you have asked of them?
-
What are the most common issues that nursing assistants bring to you?
FUTURE/VISION
-
What would you like to see in the future for nursing assistants?
-
How would you like to see the role develop or change?
Is there anything else that you would like us to know about your experience of working with nursing assistants?
Appendix 17 Letter of Research Ethics Committee favourable ethical opinion

National Research Ethics Service
This Research Ethics Committee is an advisory committee to London Strategic Health Authority. The National Research Ethics Service (NRES) represents the NRES directorate within the National Patient Safety Agency and Research Ethics Committee in England.
South East London REC 3
(formerly King's College Hospital Research Ethics Committee)
1st Floor Camberwell Building
King's College Hospital
94 Denmark Hill
London
SE5 9RS
Telephone: 020 3311 7227
Facsimile: 020 3311 7280
Dr Karen Spilsbury
Senior Research Fellow
The University of York
Department of Health Sciences
Area 2 Seebohm Rowntree Building
York YO10 5DD
15 December 2010
Dear Dr Spilsbury
| Study Title: | Support Matters: Use of assistant staff in the delivery of community nursing services in England |
| REC reference: | 10/H0808/159 |
| Protocol number: | 2 |
The Proportionate Review Sub-committee of the South East London REC 3 Research Ethics Committee reviewed the above application at the meeting held on 01 December 2010.
Ethical opinion
The Committee commented that the methodology wil combine qualitative and quantitative analysis.
The Committee also commented that the research questions are well defined and the methods of data analysis are sound.
The members of the Committee present gave a favourable ethical opinion of the above research on the basis described in the application form, protocol and supportng documentation, subject to the conditions specified below.
Ethical review of research sites
The favourable opinion applies to all NHS sites taking part in the study, subject to management permission being obtained from the NHS/HSC R&D office prior to the start of the study (see “Conditions of the favourable opinion” below).
Conditions of the favourable opinion
The favourable opinion is subject to the following conditions being met prior to the start of the study.
Management permission or approval must be obtained from each host organisation prior to the start of the study at the site concerned.
For NHS research sites only, management permission for research (“R&D approval”) should be obtained from the relevant care organisation(s) in accordance with NHS research governance arrangements. Guidance on applying for NHS permission for research is available in the Integrated Research Application System or at http://www.rdforum.nhs.uk . Where the only involvement of the NHS organisation is as a Participant Identification Centre, management permission for research is not required but the R&D office should be notified of the study. Guidance should be sought from the R&D office where necessary.
Sponsors are not required to notify the Committee of approvals from host organisations.
It is the responsibility of the sponsor to ensure that all the conditions are complied with before the start of the study or its initiation at a particular site (as applicable).
Approved documents
The documents reviewed and approved at the meeting were:
| Document | Version | Date |
|---|---|---|
| Protocol | 1 | 17 November 2010 |
| Letter of invitation to participant | 1 (Senior manager - stage 1) | 17 November 2010 |
| Letter of invitation to participant | 1 (Senior Manager - stage 2) | 17 November 2010 |
| Letter of invitation to participant | 1 (Service Manager - stage 3) | 17 November 2010 |
| Participant Information Sheet Senior Manager - Web | 1 | 17 November 2010 |
| REC application | 65856/166448/1/507 | 17 November 2010 |
| Participant Consent Form: Senior manager | 1 | 17 November 2010 |
| Letter from Funder | 02 February 2010 | |
| Participant Information Sheet: Senior Manager - Email | 1 | 17 November 2010 |
| Participant Consent Form Service Manager | 1 | 17 November 2010 |
| Investigator CV | 17 November 2010 | |
| Participant Information Sheet: Service Manager - Email | 1 | 17 November 2010 |
| Participant Information Sheet: Service Manager - Web | 1 | 17 November 2010 |
| Covering Letter | 17 November 2010 | |
| Summary/Synopsis | 1 | 17 November 2010 |
| Interview Schedules/Topic Guides | 1 (Senior manager) | 17 November 2010 |
| Interview Schedules/Topic Guides | 1 (Service Manager) | 17 November 2010 |
| Evidence of insurance or indemnity | 15 November 2010 | |
| Referees or other scientific critique report | 07 December 2009 |
Membership of the Proportionate Review Sub-Committee
The members of the Sub-Committee who were present at the meeting are listed on the attached sheet.
Statement of compliance
The Committee is constituted in accordance with the Governance Arrangements for Research Ethics Committees (July 2001) and complies fully with the Standard Operating Procedures for Research Ethics Committees in the UK
After ethical review
Now that you have completed the application process please visit the National Research Ethics Service website > After Review
You are invited to give your view of the service that you have received from the National Research Ethics Service and the application procedure. If you wish to make your views known please use the feedback form available on the website.
The attached document “After ethical review - guidance for researchers” gives detailed guidance on reporting requirements for studies with a favourable opinion, including:
-
Notifying substantial amendments
-
Adding new sites and investigators
-
Progress and safety reports
-
Notifying the end of the study
The NRES website also provides guidance on these topics, which is updated in the light of changes in reporting requirements or procedures.
We would also like to inform you that we consult regularly with stakeholders to improve our service. If you would like to join our Reference Group please email referencegroup@nres.npsa.nhs.uk.
| 10/H0808/159 | Please quote this number on all correspondence |
With the Committee's best wishes for the success of this project
Yours sincerely
Dr Mike Philpot
Chair
| Enclosures | List of names and professions of members who were present at the meeting and those who submitted written comments |
| “After ethical review - guidance for researchers” | |
| Copy to: | |
| Sponsor's Contact | Professor Christine Godfrey |
| Sponsor | Sue Final |
| R&D | Ms Caroline Mozely |
South East London REC 3
Attendance at PRS Sub-Committee of the REC meeting on 01 December 2010
Committee Members:
| Name | Profession | Present | Notes |
|---|---|---|---|
| Dr Nora Donaldson | Head of Clinical Research Statistics | Yes | |
| Mr John Fowler | Lay Member | Yes | |
| Dr Mike Philpot | Consultant Old Age Psychiatrist | Yes |
Also in attendance:
Appendix 18 Adult and general community nursing and assistant staff by organisation
List of abbreviations
- AP
- assistant/associate practitioner
- CIC
- community interest company
- CLDN
- community learning disability nurse
- CPN
- community psychiatric nurse
- FTE
- full-time equivalent
- GP
- general practitioner
- HCA
- health-care assistant
- NIHR
- National Institute for Health Research
- NMC
- Nursing and Midwifery Council
- NVQ
- National Vocational Qualification
- PEG
- percutaneous enteral gastrostomy
- PCT
- primary care trust
- RCN
- Royal College of Nursing
- REC
- Research Ethics Committee
- RN
- registered nurse
- SDO
- Service Delivery and Organisation
- SHA
- strategic health authority
All abbreviations that have been used in this report are listed here unless the abbreviation is well known (e.g. NHS), or it has been used only once, or it is a non-standard abbreviation used only in figures/tables/appendices, in which case the abbreviation is defined in the figure legend or in the notes at the end of the table.