Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 10/1007/22. The contractual start date was in July 2011. The final report began editorial review in April 2013 and was accepted for publication in August 2013. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
None.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2013. This work was produced by Tuffrey-Wijne et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Section 1 Introduction
Chapter 1 Background to the study
Introduction
The safety of patients with learning disabilities in NHS hospitals has been a subject of growing interest and concern in recent years. It follows a number of high-profile reports of poor care and avoidable harm, including avoidable deaths in this patient population. 1–3 This has resulted in a range of recommendations and strategies for promoting better and safer health-care delivery to people with learning disabilities. 4,5
This study explored the factors that affect the implementation of such strategies in six NHS acute hospitals in England; in particular, the cross-organisational, organisational and individual influences that have a bearing on this. It was not an audit or mapping of current practice, although the study included an investigation of the extent to which the six study sites had put relevant strategies in place. Rather, the aim of this study was to understand the systems and processes that either helped or hindered the implementation of these strategies. Through exploring examples of good practice, as well as examples of practice that could be improved or was suboptimal, the study aimed to identify both the key determinants and the key barriers to successful implementation. It aimed to understand how the degree of success with which the strategies were implemented may be linked to safer hospital environments for people with learning disabilities. It also explored to what extent this could be generalised to other vulnerable patient groups.
Definition and prevalence of learning disability
Definition
The term ‘learning disability’ covers a wide spectrum of impairments. In the White Paper Valuing People, the Department of Health6 states that learning disability means the presence of:
-
a significantly reduced ability to understand new or complex information and to learn new skills [impaired intelligence; intelligence quotient (IQ) below 70], with
-
a reduced ability to cope independently (impaired social functioning).
These impairments start before adulthood, with a lasting effect on development.
The White Paper points out that presence of a low IQ is not in itself a sufficient reason for deciding that an individual should be provided with additional health and social care support. An assessment of social functioning and skills should also be taken into account. Many people with learning disabilities also have physical and/or sensory impairments.
The definition covers adults with autism who also have learning disabilities. It does not include:
-
those with a higher-level autistic spectrum disorder, who may be of average or even above average intelligence – such as some people with Asperger syndrome
-
all people with ‘learning difficulties’, which is more broadly defined in education legislation
-
people whose impaired intelligence and/or impairments in social functioning (even if they are lifelong) have been acquired during adulthood, for example those with dementias or brain injuries.
Prevalence
There are no definitive figures for the prevalence of learning disabilities. The presence of learning disabilities is not recorded in the decennial census of the UK population, and no government department collects comprehensive information on the presence of learning disabilities in the population. The Department of Health6 estimated that around 2.5% of the population in England have learning disabilities, most of whom (85%) have mild learning disabilities. Emerson and Hatton7 suggest that 3% of children and 2% of adults have learning disabilities. The number of people with learning disabilities is set to rise by 1% per year. 6 It is estimated that, between 2011 and 2030, there will be a 14% increase in the number of people with learning disabilities aged ≥ 50 years using social care services, and a 164% increase of those aged ≥ 80 years. 8
Health inequalities
The health status of people with learning disabilities has been well described. They have poorer health than the general population, with a much higher prevalence of certain conditions and diseases, which often go undiagnosed. 9–13 These differences in health status are, to an extent, avoidable and can therefore be described as health inequalities. The health inequalities, as described in the following section, are substantial. 14–17
Access to health care
Most people with learning disabilities have greater health-care needs than the general population. Common health problems include respiratory and cardiovascular diseases, mental illness, epilepsy, physical and sensory disability, being underweight, obesity, oral health problems and cancer. 14,18 People with learning disabilities experience more admissions to hospital than the general population. 19
Valuing People Now,20 which sets out the government policy and a 3-year strategy for people with learning disabilities, specifies the objective that all people with learning disabilities should get the health care and support they need to live healthy lives.
The Disability Rights Commission,17 established by an Act of Parliament to stop discrimination and promote equality of opportunity for disabled people, carried out a formal investigation into the health inequalities experienced by people with learning disabilities. Focusing on primary care, the Commission found that there were several reasons for health inequalities, of which social deprivation was only one. People with learning disabilities were less likely to access health promotion or screening programmes. They also experienced ‘diagnostic overshadowing’, that is reports and symptoms of physical ill health were viewed as being inherent in the person’s learning disability and so not investigated or treated. 14 Primary care services often remained inaccessible and unresponsive to people with learning disabilities, as they had not put into place effective adjustments (including policies and procedures) to change this.
In a progress report, the UK government – in recognition of the finding by the Disability Rights Commission that people with learning disabilities often receive a poorer quality of service from the NHS – pledged that it would use progress in relation to this particularly vulnerable group as a way of testing whether its approach to tackling health inequalities was working. 21
Premature deaths
The Department of Health22 quotes figures drawn from Hollins et al.,23 estimating that people with learning disabilities are 55 times more likely to die prematurely than the population as a whole if they are < 50 years of age; for those > 50 years of age, the figure is 58 times more likely. Hollins et al. also found that the majority of deaths were due to respiratory disease, which accounts for only 15–17% of deaths in the general population.
Hoghton et al. 24 assert that:
. . . health inequalities are the result of the interaction of several factors including increased rates of exposure to common ‘social determinants’ of poorer health (e.g., poverty, social exclusion), experience of overt discrimination and barriers people with learning disabilities face in accessing health care.
p. 5. Reproduced with permission from Hoghton M, Turner S, Hall I. Improving the Health and Wellbeing of People with Learning Disabilities: An Evidence-Based Commissioning Guide for Clinical Commissioning Groups (CCGs). London: IHAL, Royal College of General Practitioners and Royal College of Psychiatrists; 2012
Issues around premature or avoidable death were highlighted poignantly in Mencap’s Death by Indifference report,1 detailing the case histories of six people with learning disabilities who died in hospitals from avoidable conditions. In the report investigating these deaths, the Health Service Ombudsman for England2 highlighted distressing failures in the quality of health and social care and found that patients with learning disabilities were treated less favourably than others, resulting in prolonged suffering and inappropriate care. When relatives complained, they were left drained and demoralised, and with a feeling of hopelessness. One of the cases investigated was that of Martin Ryan, aged 43 years, who had severe learning disabilities and no speech. Martin died after he went without food for 26 days while in hospital following a stroke; by the time staff realised what was happening, his condition had deteriorated and his life could not be saved. The Ombudsman concluded that:
. . . had service failure not occurred it is likely the patient’s death could have been avoided.
HC 203 I-VIII, p. 142
The Ombudsman recommended that all NHS care organisations in England should:
. . . review urgently the effectiveness of the systems they have in place to enable them to understand and plan to meet the full range of needs of people with learning disabilities in their areas.
HC 203 I-VIII, p. 12. 2 We acknowledge The National Archives as custodian of this document
A 3-year confidential inquiry into premature deaths of people with learning disabilities (CIPOLD), investigating the deaths of 247 people with learning disabilities within five primary care trusts (PCTs) in England, reported its findings during the final month of this study. 3 It found that people with learning disabilities died, on average, 16 years sooner than people in the general population. Twenty-two per cent of people with learning disabilities in CIPOLD were < 50 years of age when they died, compared with 9% of the general population. Forty-two per cent of the deaths were considered to be premature. The most common reasons for this were delays or problems with diagnosis or treatment, and problems with identifying needs and providing appropriate care in response to changing needs. A similar proportion of deaths in a control group of 58 adults without learning disabilities were premature, but these were largely due to lifestyle factors such as smoking or alcohol, rather than poor-quality health care.
Healthcare for All
The independent inquiry into access to health care for people with learning disabilities (2008)
The evidence from Mencap’s Death by Indifference report1 and other inquiries led to an independent inquiry into access to health care for people with learning disabilities, set up by the Department of Health. Its report, Healthcare for All, was published in 2008. 4 The inquiry found that the cases highlighted in the Death by Indifference report1 were by no means isolated. There was:
. . . convincing evidence that people with learning disabilities have higher levels of unmet need and receive less effective treatment, despite the fact that the Disability Discrimination Act and Mental Capacity Act set out a clear legal framework for the delivery of equal treatment . . . witnesses described some appalling examples of discrimination, abuse and neglect across the range of health services.
p. 7. 4 Reproduced with permission from Michael J. Healthcare for All: Report of the Independent Inquiry into Access to Healthcare for People with Learning Disabilities. London: Aldridge Press; 2008
Several reasons for such evidence of unsafe and unlawful treatment were highlighted, including cross-organisational, organisational and individual influences. The report concluded that:
. . . the evidence . . . suggests very clearly that high levels of health care need are not currently being met and that there are risks inherent in the care system. People with learning disabilities appear to receive less effective care than they are entitled to receive. There is evidence of a significant level of avoidable suffering and a high likelihood that there are deaths occurring which could be avoided.
p. 53. 4 Reproduced with permission from Michael J. Healthcare for All: Report of the Independent Inquiry into Access to Healthcare for People with Learning Disabilities. London: Aldridge Press; 2008
The report sets out 10 clear recommendations for service planners, providers and practitioners to improve this unacceptable situation.
Healthcare for All recommendations
Four out of the 10 recommendations fall within the responsibility of acute care service providers and are the focus of this study:
All healthcare organisations including the Department of Health should ensure that they collect the data and information necessary to allow people with learning disabilities to be identified by the health service and their pathways of care tracked.
Recommendation 2, p. 114
All trust boards should demonstrate that they have effective systems in place to deliver effective, ‘reasonably adjusted’ health services for those people who happen to have a learning disability. This ‘adjustment’ should include arrangements to provide advocacy for all those who need it, and arrangements to secure effective representation on PALS [Patient Advice and Liaison Service] from all client groups including people with learning disabilities.
Recommendation 10, p. 114
Family and other carers should be involved as a matter of course as partners in the provision of treatment and care, unless good reason is given, and trust boards should ensure that reasonable adjustments are made to enable them to do this effectively. This will include the provision of information, but may also involve practical support and service co-ordination.
Recommendation 3, p. 114
Section 242 of the National Health Service Act 2006 requires NHS bodies to involve and consult patients and the public in the planning and development of services, and in decisions affecting the operation of services. All trust boards should ensure that the views and interests of patients with learning disabilities and their carers are included.
Recommendation 9, p. 11. 4 The above quotations are reproduced with permission from Michael J. Healthcare for All: Report of the Independent Inquiry into Access to Healthcare for People with Learning Disabilities. London: Aldridge Press; 2008
Starting points for this study
This study was undertaken in response to a call from the then National Institute for Health Research (NIHR) Service Delivery and Organisation (SDO) programme, now the NIHR Health Services and Delivery Research (HS&DR) programme to investigate the factors affecting patient safety in health-care organisations. The starting points for the study were the above four Healthcare for All4 recommendations, as well as three particular patient safety issues for people with learning disabilities: medication errors, preventable deterioration and misdiagnosis.
Structure of the report
The report has four main sections: Introduction (see Chapters 1–3), Literature review (see Chapter 4), Results (see Chapters 5–11) and Conclusions (see Chapters 12–14).
Section 1: Introduction
Chapter 1 provides the background and rationale for the study, the national context, a definition of ‘learning disability’ and an overview of the structure of the report.
Chapter 2 sets out the study aims and theoretical framework.
Chapter 3 provides a description of the study methods, the participants and the research team. It also sets out the major challenges encountered in carrying out the research.
Section 2: Literature review
Chapter 4 provides an updated literature review, conducted during the course of the study, with a focus on the specific lines of inquiry in the study and in the light of national developments during the study period. This gives an important context for the study results.
Section 3: Results
Chapters 5–8 report on the findings in relation to the four recommendations of Healthcare for All,4 as follows:
-
Chapter 5 explores ways of identifying patients with learning disabilities in NHS hospitals and tracking their pathways of care.
-
Chapter 6 looks at providing reasonably adjusted hospital services.
-
Chapter 7 discusses the involvement of carers as partners in care.
-
Chapter 8 examines how patients and carers may be involved in service planning and development.
Chapters 5–8 each include an empirical subframework of the cross-organisational, organisational and individual factors that affect the safety of patients with learning disabilities in NHS hospitals.
Chapter 9 reports on the findings in relation to the learning disability liaison nurse (LDLN) role in NHS hospitals.
Chapter 10 reports on the findings in relation to specific patient safety issues faced by patients with learning disabilities.
Chapter 11 reports on the results of stage III of the study, which focused on the extent to which the study findings are generalisable to other vulnerable patient groups. This includes a brief review of the literature.
Section 4: Conclusions
Chapter 12 summarises the main findings and explores some of the main themes. It integrates the results and empirical subframeworks, resulting in an empirical framework of factors that promote or hinder a safer environment for patients with learning disabilities in NHS hospitals.
Chapter 13 discusses the implications of the study results for health-care services.
Chapter 14 provides recommendations for further research.
Chapter 2 Study aims and theoretical framework
Rationale for the aims and objectives
Knowledge gaps
As has been described (see Chapter 1), there have been a range of initiatives and examples of good practice with regards to implementing the changes recommended in Healthcare for All4 in order to promote the safety of patients with learning disabilities in NHS hospitals. However, it has been reported that such good practice examples are patchy. The extent to which these initiatives are effective in promoting safer care, and the factors that promote effective long-term change, are poorly understood. In particular, it is not clear:
-
which particular organisational and management structures contribute to the safer care of patients with learning disabilities
-
how effective ‘change agents’ (such as LDLNs) are in promoting safer care for people with learning disabilities in NHS hospitals
-
how patients with learning disabilities and their relatives can be effectively engaged in improving safety in hospitals
-
which contributions to patient safety can be effected within individual NHS acute hospitals, and which require a wider approach (for example through regulatory bodies).
Implementing the recommendations requires changes in both the organisation of systems and services, and staff practice. The examination of these issues at organisational, group and individual level is essential in order to understand how change may be facilitated with regard to learning disability practice. Without a clear understanding of these issues, improved safety for patients with learning disabilities in hospitals is likely to remain haphazard.
The purpose of this study was not to perform an audit of NHS acute trusts in relation to their performance against targets or the implementation of policies and systems to improve safe care of patients with learning disabilities. Rather, its purpose was to understand the processes of implementation and the factors that influence the effectiveness of the measures.
Healthcare for All4 concludes:
The evidence shows a significant gap between policy, the law and the delivery of effective health services for people with learning disabilities.
p. 53. Reproduced with permission from Michael J. Healthcare for All: Report of the Independent Inquiry into Access to Healthcare for People with Learning Disabilities. London: Aldridge Press; 2008
There is a lack of knowledge about how to translate hospital policy and guidelines into effective practice and improved services. This study was set up to address that knowledge gap. It aimed to understand the extent to which evidence of good practice in promoting safety for patients with learning disabilities is driven by (a) policy and its communication downwards through the health service organisation and/or (b) bottom-up initiatives originating from new patient/practitioner partnerships, innovative teams and charismatic leaders.
Defining cross-organisational, organisational and individual influences
In the context of this study, cross-organisational influences are those that affect the care of patients with learning disabilities across multiple NHS acute hospitals. This may include influences from primary care, secondary care and social care settings. They are imposed by the external policy context, by the structure and delivery of the NHS as a national organisation or by the interface between different health-care organisations and structures. They encompass decisions made at a regional or national level. Cross-organisational influences on patient safety issues cannot be addressed by NHS acute hospital trusts in isolation.
Organisational influences comprise the policies and systems adopted by individual NHS acute trusts which ultimately affect the resources available and local working conditions. It is at the level of organisational influences that NHS acute hospital trusts have a unique power to address patient safety issues within their organisations.
Individual influences are related to the way in which individual staff and staff teams can affect the care and safety of patients with learning disabilities. They are reflected, for example, in ward culture and staff attitudes. Individual influences also comprise factors inherent in the population profile of patients with learning disabilities and their carers, over which NHS hospitals will have little control.
Study aims
Aims
The primary aim was to describe the cross-organisational, organisational and individual factors in NHS hospitals that promote or compromise a safe environment for patients who have learning disabilities.
The secondary aim was to develop guidance for NHS acute trusts about the implementation of successful and effective measures for promoting a safer patient environment.
Research questions
-
What systems and structural changes have been put in place in NHS acute hospitals to prevent adverse outcomes for patients with learning disabilities, in particular with regards to specific safety issues (medication errors, misdiagnosis and preventable deterioration), and to recommendations 2, 3, 9 and 10 of Healthcare for All?
-
How successful have these measures been in promoting safe practice? In particular:
-
What cross-organisational, organisational and individual factors have been barriers and enablers in implementing the Healthcare for All recommendations for patients with learning disabilities in a sample of six NHS hospitals?
-
What are the examples of effective, replicable good practice at these six sites?
-
-
To what extent can the findings and learning from question (2) be generalised to other vulnerable patient groups?
With regards to the third question, the study aimed to identify which factors affecting patient safety are likely to be unique to the presence of learning disability, and which are due to general vulnerability and communication problems. This will enable the identification of findings that are transferable to other vulnerable patient groups.
Theoretical framework
This study took a systematic approach to an empirical identification of the factors that affect the implementation of strategies to promote a safer environment for patients with learning disabilities in hospitals, and in particular the implementation of recommendations 2, 3, 9 and 10 of Healthcare for All,4 as well as patient safety issues that had been identified in consultation documents by the Care Quality Commission (CQC)25 and the Department of Health26 (no longer available). A theoretical framework was developed for understanding the range of factors that might impact on such implementation in NHS hospitals. This framework was based on the literature summarised in Chapter 1, as well as the wide-ranging insights and experience of the multidisciplinary research team and the research advisory board.
The theoretical framework identifies potential barriers and facilitators to improving safety for patients with learning disabilities in NHS hospitals in a number of domains: cross-organisational, organisational and individual. Organisational and individual domains are indicated in boxes A, B and C of the theoretical framework (Figure 1). Each box contains a number of factors within each domain that might be anticipated to function as barriers to or facilitators of promoting a safe environment for people with learning disabilities in NHS acute hospitals.
FIGURE 1.
Theoretical framework identifying factors that affect the promotion of a safer environment for patients with learning disabilities. LD, learning disabilities.
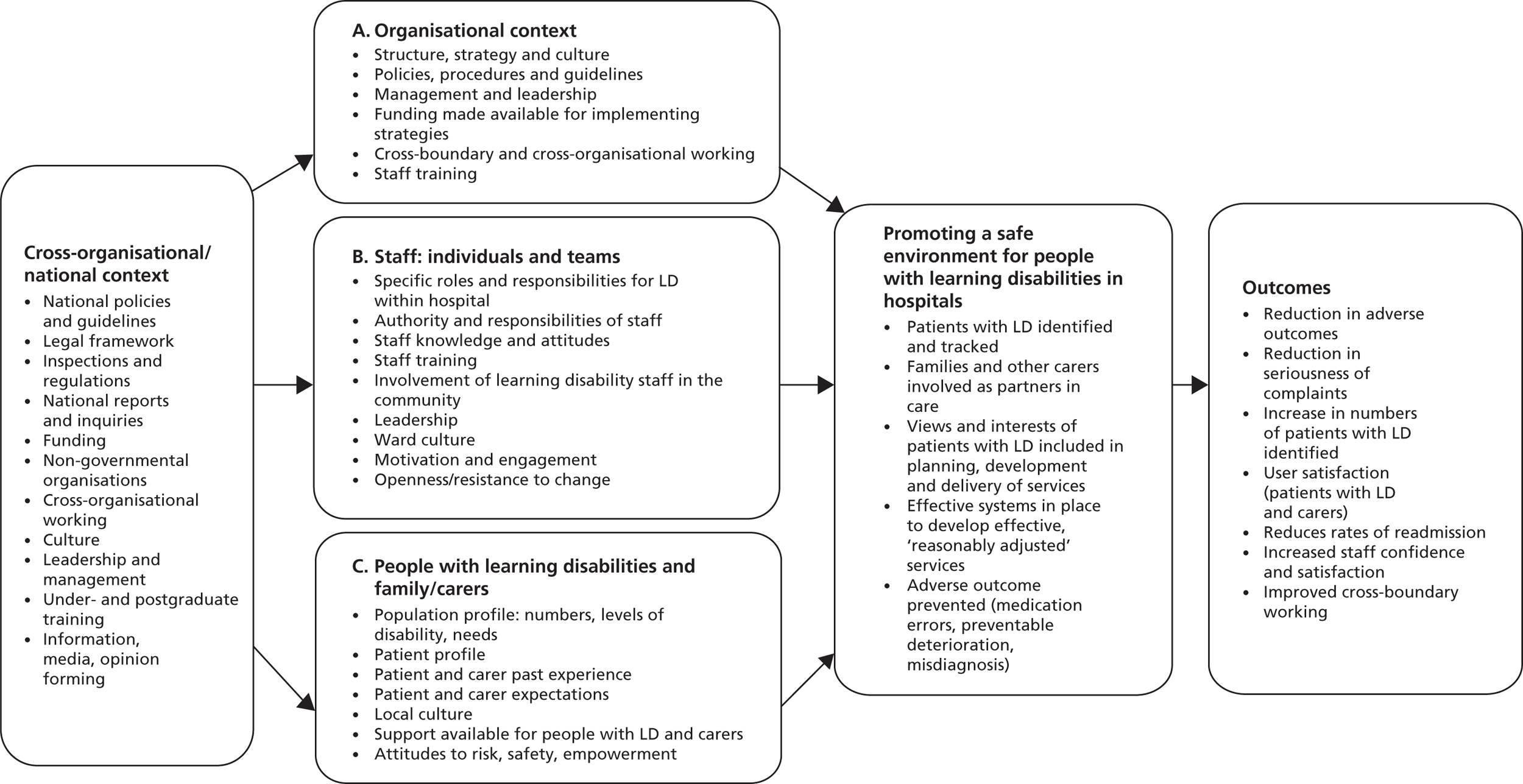
In addition, the framework identifies a number of outcomes that might be associated with effective patient safety measures for patients with learning disabilities in NHS hospitals. These outcomes are largely derived from the research team’s interpretation of Healthcare for All,4 and other reports and literature described earlier.
After testing and further developing the theoretical framework over the course of the study, it will be re-presented in Chapter 12 as an empirical framework for promoting the safety of patients with learning disabilities.
Research framework
From the theoretical framework flows the research framework (Table 1), where specific research questions are asked within each domain (A, B and C). The research methods, described in Chapter 3, are derived from this research framework.
| Research Focus | A. Organizational context | B. Staff individual and teams | C. People with LD and carers |
|---|---|---|---|
| Recommendation 3 | |||
| All health-care organisations, including the Department of Health, should ensure that they collect the data and information necessary to allow people with learning disabilities to be identified by the health service and their pathways of care tracked | A1. What are the policies, procedures and systems for identifying patients with LD? A2. On admission, what data and information are collected from patients with LD? A3. What are the policies, procedures and systems for tracking their pathways of care? A4. What do senior managers see as the barriers to and facilitators of collecting the necessary information? |
B1. Are staff on hospital wards aware of the need to identify and track patients with LD? B2. Do staff on hospital wards know the policies, procedures and systems for tracking patients with LD? B3. Do staff on hospital wards identify and track patients with LD? B4. How are staff on hospital wards alerted to the fact that a patient has LD? B5. Have LD staff (both within and outside the hospital) been asked to assist with providing the necessary information to enable people with LD to be identified and their pathways tracked? |
C1. Are patients with LD and their families/carers aware of the requirement for hospitals to identify their needs and track their care pathways? C2. Have patients with LD and their families/carers been asked to provide the necessary information? C3. Are patients with LD and their families/carers able and happy to provide the necessary information? |
| Recommendation 2 | |||
| Family and other carers should be involved as a matter of course as partners in the provision of treatment and care, unless good reason is given, and trust boards should ensure that reasonable adjustments are made to enable and support carers to do this effectively. This will include the provision of information, but may also involve practical support and service co-ordination | A5. What policies and reasonable adjustments are in place to enable and support families/carers to be involved as effective partners in care provision? A6. Does the hospital have guidelines on the provision of information for carers, practical support and service co-ordination? A7. Is there a culture among senior managers that encourages partnerships with families/carers? |
B6. Are staff on hospital wards aware of any policies or the need to make reasonable adjustments to enable and support families/carers to be involved as effective partners in care provision, including care and discharge planning? B7. In what ways are families/carers involved as partners in care provision by staff on hospital wards? (Is there provision of information, practical support and service co-ordination?) B8. Is there a culture among staff on hospital wards that encourages partnerships with families/carers? |
C4. Do families/carers feel that they have been supported and included as partners in care provision, including care and discharge planning? C5. Have families/carers been provided with information and practical support? C6. Are families/carers satisfied with the care provided by the hospital? |
| Recommendation 9 | |||
| Section 242 of the National Health Service Act 2006 requires NHS bodies to involve and consult patients and the public in the planning and development of services, and in decisions affecting the operation of services. All trust boards should ensure that the views and interests of people with learning disabilities and their carers are included | A8. What policies and systems have been put in place by the hospital to ensure that the views and interests of patients with LD and their families/carers are included in the planning, development and delivery of services? A9. Are people with LD and their families/carers represented on advisory and decision-making bodies within the hospital? A10. Is there a culture among trust board members and other senior managers that encourages inclusion of the views and interests of people with LD and their families/carers in the planning, development and delivery of services? |
B9. How are staff on hospital wards made aware of the views and interests of patients with LD and their carers? B10. Have LD staff (both within and outside the hospital) been invited to offer the necessary support to ensure that the views and interests of patients with LD and their carers are included? |
C7. How have the views and interests of people with LD and their carers been included? C8. Do people with LD and their families/carers believe that their views and interests are taken into account by the hospital? C9. If people with LD and their families/carers are represented on advisory/decision-making bodies, what has been their experience? |
| Recommendation 10 | |||
| All trust boards should demonstrate that they have effective systems in place to deliver effective, ‘reasonably adjusted’ health services . . . This ‘adjustment’ should include arrangements to provide advocacy for all those who need it, and arrangements to secure effective representation on PALS from all client groups including people with learning disabilities ‘Reasonable adjustments’ in this context are described in the literature and include:
|
A11. What systems have been put in place by the hospital to ensure reasonable adjustments are made? A12. What do senior managers understand by ‘reasonably adjusted services’? A13. What funding has been made available to ensure that reasonable adjustments are made? A14. What are the arrangements for provision of advocacy to all those who need it? A15. What partnerships are in place with other agencies who have a remit to support patients with LD? A16. Are there professionals within the hospital with a specific remit to promote the delivery of effective, reasonably adjusted health services? |
B11. What do individual staff members and teams understand by ‘reasonable adjusted services’? B12. How do individual staff members and teams ensure that they deliver effective, reasonably adjusted services? B13. Are individual staff members aware of the specific needs of patients with LD, and do they know how to ensure those needs are met? B14. Do individual staff members know how to arrange advocacy for patients who need it? B15. Have LD staff (both within and outside the hospital) been asked to assist with ensuring that hospital services are reasonably adjusted? |
C10. Do patients with LD and their families/carers feel that the patient’s individual needs have been met? C11. Was the patient given information in a way he/she could understand? C12. Did staff allow enough time in their care of the patient? C13. Were patients provided with advocacy when they needed it? |
| Safeguarding and safety: prevention of adverse outcomes | |||
With specific focus on:
|
A18. What measures are in place to ensure the safe administration of medication to patients with LD, including giving clear information about medicines to the patient? A19. What measures are in place to avoid preventable deterioration and misdiagnosis for patients with LD? A20. What systems are in place for monitoring adverse outcomes and complaints involving patients with LD? |
B17. Are individual staff and staff teams aware of the measures to ensure safe administration of medication to patients with LD? B18. Are individual staff and teams aware of the measures in place to avoid preventable deterioration and misdiagnosis for patients with LD? B19. Are individual staff and teams aware of the systems in place for reporting adverse outcomes? B20. Are adverse outcomes involving patients with LD reported by staff? |
C15. Do patients with LD and their families/carers think they have been given understandable information about medicines, including medicines to take home? C16. Do patients with LD and their families/carers think that preventable deterioration was avoided? C17. Do patients with LD and their families/carers feel they received an accurate and timely diagnosis? C18. Do patients with LD and their families/carers know how to make a complaint? C19. What adverse outcomes and complaints involving patients with LD or their families/carers have been recorded within the hospital during the data collection period? |
Chapter 3 Research design and methods
Study design
The theoretical and research frameworks posed a number of different research questions best addressed using a range of methods at a number of levels of enquiry. This was a complex study which integrated qualitative and quantitative methods and involved three stages, followed by a period of data synthesis. The study lasted 21 months (from July 2011 to March 2013).
Stage I consisted of mapping the systems and structural changes within each hospital site (related to research question 1).
Stage II (the main stage) was related to research question 2, and comprised a range of methods, including interviews, surveys and observation.
Stage III involved synthesis of the data, including synthesis with the literature on other vulnerable patient groups. In addition, structured feedback was gathered from clinical and patient safety leads in other vulnerable patient groups, to assess generalisability (research question 3).
The full research protocol can be found in Appendix 2.
Sampling
Selection of hospital sites
A purposive sample of six hospital sites was selected for the study. (The original research proposal and initial recruitment involved five study sites. Soon after the start of the study, site D was withdrawn and site F recruited. Site D was later re-included in the study, making a total of six sites.) A brief profile is shown in Table 2. Selection was made according to the following three criteria, which were likely to impact on the implementation of the strategies under investigation:
-
A range of urban/rural and sociodemographic environments were represented, and a range of hospital sizes (the number of staff per hospital was between 3000 and 6000; number of beds was between 450 and 900).
-
Hospitals selected had shown active engagement with issues around safety for patients with learning disabilities, based on the hospital’s record since 2008 in prioritising the safety of patients with learning disabilities. The selected study sites had a range of recent or more long-standing implementation plans for the recommendations in Healthcare for All. 4
-
Contrasting examples were sought of the use of a LDLN service. Three hospitals employed a LDLN; two hospitals worked closely with LDLNs based in primary care who had an explicit remit to provide a LDLN service at that hospital; and one hospital did not have a LDLN service. As terminologies and job titles for this role varied across study sites, for the sake of uniformity and anonymity the term LDLN is used throughout this report, and the gender of the LDLN has been assigned female in all quotes and descriptions.
| Hospital | Type | Area | Learning disability liaison nurse |
|---|---|---|---|
| A | Teaching | Urban | Hospital based |
| B | District general | Urban | Community based |
| C | District general | Urban | None |
| D | District general | Urban/rural | Hospital based |
| E | Teaching | Urban/rural | Hospital based |
| F | District general | Rural | Community based |
Collaborators
The research team worked with a collaborator at each site, whose role it was to promote and support the study within their organisation and to provide access to participants (staff, patients and carers). These initially consisted of two Directors of Nursing, two Deputy Directors of Nursing and two LDLNs. During the course of the study, four of these collaborators left their posts and new collaborators had to be found. In some cases, this caused delays to data collection.
The study site collaborators were an integral part of the study. The initial group of collaborators were involved in the design of the study protocol. Throughout the study period, the group of collaborators met five times in order to discuss progress and any difficulties with data collection, and provided advice on ways in which the protocol could be adapted in order to cope with any difficulties that had emerged.
Participants
A wide range of staff, patients and carers participated formally in the study through surveys, telephone and face-to-face interviews, participant observation and expert panel discussions (n = 1249 after exclusions). An overview of these participants is given in Table 3, and full details are given in Appendix 3. Sampling methods for each participant group are described under the relevant sections below (see Data collection). In addition, the researchers kept field notes of conversations and observations at the hospital sites, adding further informal participants.
| Data collection | Hospital site | Total | |||||
|---|---|---|---|---|---|---|---|
| A | B | C | D | E | F | ||
| Stage I informants (strategic managers) | 1 | 1 | 2 | 1 | 1 | 5 | 11 |
| Interviews with people with learning disabilities | 9 | 6 | 4 | 9 | 2 | 3 | 33 |
| Tracer patientsa | 4 | 4 | 0 | 1 | 5 | 5 | 19 |
| Carer survey | 35 | 12 | 2 | 19 | 8 | 12 | 88 |
| Carer interviews | 10 | 6 | 2 | 6 | 5 | 8 | 37 |
| Staff interviews | 12 | 9 | 8 | 14 | 10 | 15 | 68 |
| Staff survey | 253 | 76 | 81 | 133 | 296 | 151 | 990 |
| Panel discussion | 11 | 10 | 9 | – | – | 12 | 42 |
| Total | 335 | 124 | 108 | 183 | 327 | 211 | 1251b |
During the course of the study the researchers also spoke to staff, patients and carers involved in hospital trusts throughout England that were not part of the study. Whilst these are not specifically reported here, the insights gained from such ‘shadow hospital trusts’ informed the final analysis.
Data collection
Stage I
Stage I took place from August to September 2011. The aim of this stage was to map the systems and structural changes that had been put into place at the six hospital sites, with regards to research question 1. A questionnaire was developed and sent by e-mail to the collaborators at each site, who either filled it in themselves or nominated someone else within the trust who was well placed to answer the questions (n = 11). This was followed up by a telephone interview to clarify and complete the answers with some informants (n = 6).
Documents relating to all relevant policies, procedures and systems were examined. This included any systems for flagging or identifying patients with learning disabilities; any patient-held information documents currently being used at the trust; relevant carer policies; systems or arrangements in place to provide reasonable adjustments (specifically, whether trusts provided accessible information and met individual communication needs); and any specific arrangements in place to allow family and carers to make a complaint. Documents relating to particular patient safety issues including medication errors, preventable deterioration and misdiagnosis were also examined.
Stage II
Stage II was related to research question 2 and took place from October 2011 to September 2012. This stage formed the main part of the study and was concerned with examining the effectiveness of the measures identified in stage I. The wide range of methods, sampling strategies and data collection tools are set out below.
Survey for staff
An electronic questionnaire was distributed to all clinical staff. This was a deviation from the original research protocol, which stipulated that paper questionnaires would be distributed to all clinical staff on only three selected wards per hospital. The collaborators suggested that an electronic questionnaire to all staff would be easier to administer. The research advisory board agreed that this was an improvement on the protocol, as it would yield more a comprehensive data set. Questions were designed according to the theoretical framework within the study protocol, taking into account the findings from stage I, qualitative data gained from staff interviews conducted in the early part of stage II and with reference to existing literature. LimeSurvey software version 1.86 (open source) was used to design and host the electronic questionnaire. Details of the questions asked along with corresponding basic descriptive results are listed in Appendix 4.
Endorsement
A strategic manager at each collaborating site was asked to endorse the staff survey. At three sites this was the Director of Nursing or Deputy Director of Nursing and at three sites this was the Chief Executive. Links to the clinical staff electronic questionnaire were sent to all clinical staff via e-mail with the accompanying endorsement.
Inclusion and exclusion criteria
‘Clinical staff’ were defined as qualified or unqualified staff who care for or have a caseload of patients [e.g. nurses, health-care assistants (HCAs), doctors, allied health professionals (AHPs) and others]. The definition of ‘clinical staff’ acted as an initial screening question; participants were requested to exit the questionnaire if they indicated that they were not clinical staff. Where relevant to the interpretation of the results, only participants who indicated that they had cared for a patient with learning disabilities at their current hospital were included in the analysis; those who had never cared for a patient with learning disabilities, or who were not sure if they had cared for a patient with learning disabilities, were excluded (this information was supplied in answer to question 5 of the questionnaire). The exclusion criteria applied to the reporting of each question are documented throughout Appendix 4.
Survey response
A total of 1018 questionnaires were returned. Four of these responses were excluded as they had been completed by people who had indicated that they were not clinical staff. A further 24 questionnaires were returned completely blank and were therefore excluded from the analysis, leaving 990 usable questionnaires.
Response rate
Human resources departments at each site were requested to provide a breakdown of the numbers of clinical staff employed in each staff group (medical and dental, qualified nursing and midwifery, AHPs, HCAs, other support staff and other clinical staff) for the relevant time period. This allowed calculation of the percentage response rate from each site (Table 4). Differences in the response rates at each site are likely to be due to differences in the methods of distribution. For example: site E had a much more targeted approach to distribution; ‘clinical staff’ definition may differ between sites; and some figures exclude those on leave (sick/maternity) and those working 0-hours contracts, whereas others do not.
| Site | Number of questionnaires returned | Approximate % response ratea |
|---|---|---|
| A | 265 | 5.3 |
| B | 79 | 2.7 |
| C | 84 | 4.1 |
| D | 139 | 4.0 |
| E | 298 | 14.9 |
| F | 153 | 6.7 |
Survey representativeness
The survey response is likely to be biased towards those who have an interest in the subject matter; for example, almost a quarter (24.7%, 214 out of 866) indicated that someone in their family or close social circle had learning disabilities. It is also likely to be biased towards professionals who are comfortable with online surveys and who are able to spend some time completing the survey during work hours. The response rate seems low; however, there was a good spread of clinical staff groups across the six study sites, and using the online method, the number of questionnaires returned was higher than anticipated in the original protocol.
Interviews with staff
Semi-structured face-to-face interviews were held with hospital staff (n = 68). The interview schedule for ward staff included a tracer scenario27 designed to assess staff knowledge of policies, procedures, structures and issues related to learning disability. Interviews lasted between 30 and 60 minutes. They were audio recorded and transcribed verbatim.
Senior managers
For the purpose of this study, and throughout this report, the term ‘senior manager’ refers to managers with hospital-wide responsibilities for patient care. This includes, but is not limited to, (Deputy) Directors of Nursing, Medical Directors and Directors of Patient Safety. All Directors of Nursing and Medical Directors were invited to participate and to suggest one further senior manager with hospital-wide responsibilities (n = 27).
Clinical staff
At each hospital site, three wards were selected in which to conduct staff interviews. Selection criteria specified that these should be (1) a medical assessment ward or similar; (2) a ward selected by the collaborator as having a relatively high number of people with learning disabilities; and (3) the ward that had received the highest number of complaints (all complaints, not specifically related to people with learning disabilities), excluding accident and emergency (A&E) departments (which, at most sites, had the highest number of complaints). On each of these wards, the ward manager or sister was interviewed and asked to select two further ward nurses for interview (n = 31). This selection was partly purposive (to ensure a range of responsibilities and experience was included) and partly convenience (interviews were held with nurses available on the day of the researcher’s visit).
In addition, hospital staff with specific responsibilities for implementing learning disability policies were purposively selected for interview. This included, for example, the LDLNs and matrons who were responsible for a group of wards. Community learning disability nurses who had strong links with the hospital were also interviewed.
Sampling people with learning disabilities and carers
Inclusion criteria for people with learning disabilities were: (a) the presence of a learning disability, (b) age ≥ 16 years and (c) having been an in- or outpatient at the hospital during the 12-month stage II data collection period. Inclusion criteria for carers required being a family or paid carer of an adult (aged ≥ 16 years) with learning disabilities admitted to the hospital during the data collection period.
The theoretical definition of learning disability (see Chapter 1) is not easily operationalised in practice. Few people, for example, have a known IQ value. For the purpose of this study, we included any patient who had been identified by the hospital as having learning disabilities.
The extent to which patients and carers could be included in the study depended on the ability of the participating hospitals to identify patients with known learning disabilities. The sampling of patients with learning disabilities and their carers was further limited by the fact that many have never been formally identified as having learning disabilities and are unknown to health and social care services. The researchers’ efforts to identify patients and carers for the purpose of this study, and the lessons learnt, form part of the findings (see, in particular, Chapter 5).
The sampling strategy for people with learning disabilities and carers had to be adjusted during the study. The original protocol stated that all patients with learning disabilities identified within the hospital during the 12 months of stage II would be given information about the study and invited to contact the research team if they wished to take part in a face-to-face interview; their carers would be given a questionnaire and the option to take part in a telephone interview. The aim was to purposively select patients for face-to-face interview to ensure a range of abilities and hospital experiences, and to continue sampling until saturation of data had been reached (i.e. no new themes, issues or topics arising from the interviews). It was anticipated that this would be approximately 60 patients (10 per hospital). It was further estimated that around 600 carer questionnaires would be distributed and that around 50 carer interviews would be conducted.
The collaborators were asked to ensure that this happened. In practice, the task of distributing the study information sheets to carers (see below) and patients with learning disabilities fell to the LDLNs within the hospitals. They found this difficult to do, partly because they did not usually carry the study information sheets with them when seeing patients and carers, and partly because they felt that at the point of contact, the hospital experience was complicated and anxiety-provoking enough for the patient without any added information about a research study. To support recruitment of patients and carers, a flyer was distributed to a number of hospital wards. Five months into stage II, no patients had been recruited and only 18 carer questionnaires had been returned. The sampling strategy was changed in two ways: (1) following the patient’s discharge, carers were sent study information and a questionnaire, as well as study information to pass on to the person with learning disabilities (two people with learning disabilities were recruited in this way); and (2) a hospital open day was hosted at each study site, and people with learning disabilities living locally were invited to come and be interviewed. Information about these days was distributed among hospital staff, community learning disability teams and community residential and advocacy organisations. Twenty-three people with learning disabilities were recruited this way. Carers or supporters who came with the person were offered a carer questionnaire and an opportunity to be interviewed if they had supported a person with learning disabilities attending that hospital within the data collection period. Six carer interviews were held during the open days. One person with learning disabilities was interviewed during a stakeholder feedback conference.
In addition, the original protocol stated that all people with learning disabilities who were members of advisory/decision-making bodies or patient representation groups within the hospital, and all those who had made a formal complaint themselves, would be invited for face-to-face interview (estimated n = 15). In practice, only seven people with learning disabilities who were on advisory bodies were referred to the research team and invited to be interviewed (all took part). The research team was not aware of any patients with learning disabilities who made a formal complaint during the data collection period.
In total, 33 people with learning disabilities took part in an interview (32 face-to-face interviews and one telephone interview at the interviewee’s express request). Despite the collaborators and/or LDLNs being sent over 1000 carer questionnaires to distribute, only 94 questionnaires were returned.
The recruitment problems stemmed in great part from the difficulty all hospitals had in correctly identifying patients with learning disabilities (see Chapter 5). At one hospital with an active LDLN, 35 carer questionnaires were returned; at a hospital without a LDLN, only two carer questionnaires were returned.
Despite the carer and patient participant numbers being only around half the projected total, the research team and research advisory board believed that data saturation had been achieved by the end of the study.
Carer survey and carer interviews
Data collection tools for carers were developed with the support and advice of a carer representative on the research advisory board.
Survey
The carer questionnaire, including responses, can be found in Appendix 5. Six of the 94 completed carer questionnaires did not meet the inclusion criteria (four were concerned with people with learning disabilities aged < 16 years and two were completed not by carers, but by patients with learning disabilities themselves), leaving a total of 88 usable questionnaires. Of these, 54 (61.4%) were from paid carers and 34 (38.6%) were from family carers, mostly parents.
Interviews
All those who indicated that they were willing to be interviewed (n = 48) were contacted. A total of 37 semi-structured carer interviews were conducted, either by telephone (n = 26) or face to face (n = 11). Interviews were either audio recorded and transcribed verbatim (n = 18), or the interviewer wrote a summary of the interview immediately afterwards and sent it to the interviewee for verification, additions and approval (n = 19).
Interviews with people with learning disabilities
Interviews with people with learning disabilities were conducted by one of the two coresearchers who had learning disabilities themselves, with the support of one other researcher following several practice and training sessions. The coresearchers helped with the development of the data collection tools as well as the development of study information and consent sheets (see Appendix 6).
There were three different data collection tools:
-
Talking Mats™ (Talking Mats Ltd, Stirling, UK), a communication resource that helps people with communication difficulties to express their views. 28 Participants were asked to place specifically developed pictures on different sections of a mat to indicate ‘Like’, ‘Not sure’ or ‘Do not like’ (see Appendix 7). A set of neutral pictures was offered to start the session, in order to introduce the participants to the use of Talking Mats™ and to make them feel at ease.
-
An interview schedule using pictures and stories about other people attending hospital (see Appendix 8). Many people with learning disabilities find it easier to express their views through the use of story-telling. 29
-
An interview schedule consisting of a list of questions about the interviewee’s own hospital experiences (see Appendix 9).
The decision whether to use (b) or (c) in addition to (a) was taken by the supporting interviewer. Flexibility was used to allow for individual communication needs and comprehension. Interviewees could have their own supporter with them during the interview if they wished. Whether or not to use tape recording was agreed with each interviewee.
Tracer patients
‘Tracer patients’ were included with the aim of establishing how policies and procedures worked in practice, how the patients’ specific needs were met, and how their safety was ensured. The following data were collected: participant observational data (generally, two episodes of 2 hours); interview(s) with the patient if he/she had verbal understanding and ability; interview with a carer or carers; and interviews with hospital staff involved in the patient’s care. The patient’s hospital records and notes were studied. If the patient lacked the capacity to give informed consent, the research team identified and consulted someone who was not the patient’s professional care worker, to establish whether the patient should take part; this was in line with legislation in England under the Mental Capacity Act 2005. 30,31 Data consisted mostly of researchers’ field notes.
The original protocol stated that 30 tracer patients in total would be selected on the wards where staff interviews were held (see above). In practice, it proved extremely difficult to recruit tracer patients this way, for the following reasons: many wards did not have a suitable patient with learning disabilities within the data collection period; hospital staff (usually the LDLN nurse who was involved in selecting tracer patients) deemed the potential participant unsuitable for the study (for example, because the hospital stay was already stressful and complicated); or patients moved around the hospital or were discharged before researchers were able to complete information and consent procedures. The sampling base was extended to all inpatients, but despite much researcher effort, only eight tracer patients were recruited into the study.
Monitoring of records
The research team set out to monitor the following data throughout stage II:
-
the extent to which hospitals were able to identify and track patients with learning disabilities, by asking them to provide, as far as they were able, numbers of patients with learning disabilities accessing hospital services; where in the hospital the patient was admitted; length of stay; and readmissions to hospital within 7 days of discharge
-
all adverse incidents that involved patients with learning disabilities and/or their families/carers (not limited to serious incidents)
-
all complaints involving patients with learning disabilities and/or their carer(s).
The difficulties with these aims are set out in Chapter 5 (identifying and tracking patients) and Chapter 10 (monitoring adverse incidents and complaints).
Stakeholder feedback conferences
Towards the end of stage II, a stakeholder feedback conference was held at four of the six study sites (at the other two study sites, a convenient time when potential attendees were available could not be arranged). Stage ll participants at that site and local stakeholders were invited to attend; delegates included hospital staff, community learning disability staff, families, paid carers and people with learning disabilities. Attendance ranged from poor (with only two delegates) to moderate (around 30 delegates). The preliminary findings were presented by the research team and feedback was invited through discussion workshops. This was an additional way of testing the researchers’ interpretations around facilitators and barriers in promoting a safe environment for patients with learning disabilities in hospitals.
Stage III
Stage III was related to research question 3, and took place from November to December 2012. It was hypothesised that the factors associated with success and failures in dealing with patients with learning disabilities are likely to be similar for any vulnerable group with ‘non-standard needs’. A small number of questions on the differences and similarities in dealing with other vulnerable patient groups were part of the interview schedules in stage II.
At the end of stage II, the emerging findings were summarised in a discussion document alongside an emerging empirical framework.
Stage III consisted of synthesis of the emerging study findings with existing literature, which was searched for congruence with these findings in relation to other specific vulnerable patient groups, in particular patients with dementia and patients with mental health problems.
Expert panel discussions
Each hospital was invited to take part in an expert panel discussion, where the research team met with the hospital’s senior managers and senior clinicians who had a responsibility for patients with learning disabilities or for other vulnerable groups. Four of the hospitals were able to organise such a discussion, involving a total of 42 staff (see Appendix 3 for a breakdown of these participants).
The discussion document was presented to the panel by the principal investigator and a focused discussion was held to establish participants’ views on the generalisability of the emerging findings to other vulnerable patient groups. The discussions were audio recorded and transcribed verbatim.
Data analysis
This study consisted of six detailed local case studies followed by a stage of data synthesis and generalisation. A comparative case study approach enabled the identification of generic features of change as they were indicated across contrasting areas. Comparison between the six sites, in particular when taking differences between samples into consideration, provided insight into where the barriers to and facilitators of the safety of patients with learning disabilities have generic importance.
Qualitative analysis
All qualitative data (including face-to-face interviews, telephone interviews, ethnographic data from tracer patients and data from open-ended questionnaire questions) were collated and analysed together in order to aid data synthesis. All qualitative data were entered into NVivo 9 (QSR International, Southport, UK), a computer software programme for managing qualitative analysis. 32 The initial common analytical coding framework was based on the research framework (see Table 1). Data analysis took place throughout the data collection period and involved coding subsamples of the data and weekly discussions with the core research team about emerging findings and possible new analytical codes. Members of the wider research team (research advisors) joined these discussions approximately once a month. Data sets that did not fit into the framework, or were difficult to synthesise, were used to generate new themes and refine the coding framework throughout the data collection period. Themes emerging from all three levels of inquiry (organisational, staff, and people with learning disabilities/carers) were compared and accommodated within the framework, ensuring that any commonalities or differences (for example, between different stakeholder groups, wards or hospital sites) were highlighted in the analysis. Meetings were held with specific stakeholder representatives on the research advisory board to discuss emerging findings in relation to relevant topics. This included meetings with Vanessa Gordon (Associate Director of Patient Safety, NHS Commissioning Board), the family carers on the research advisory board (for the purpose of involving carers) and the coresearchers and advisors with learning disabilities. The emerging findings were also discussed with experts outside the research team and research advisory board, including Sir Jonathan Michael (chairperson of the independent inquiry and author of Healthcare for All4). A final analytical framework was agreed by the research team in the final month of stage II.
Quantitative analysis
The quantitative data in this study consisted of semi-structured questionnaires with carers and with clinical staff. Data were analysed using Statistical Product and Service Solutions (SPSS) Statistics 19 (SPSS, Inc., Chicago, IL, USA). Descriptive statistics have been used as follows: continuous data have been described with mean, standard deviation, minimum and maximum values, and categorical data with frequencies and percentages. The online staff questionnaire survey had some missing data as a result of people dropping out of the survey prior to completion. Where these data are presented, only the sample of people known not to have dropped out up to that specific question is included as the denominator in calculating the descriptive statistics.
Data synthesis
The number of qualitative and quantitative data generated by the study was extremely large. During the stage of data synthesis, the research team looked for congruence and incongruence between qualitative and quantitative findings. In particular, the team looked for instances of incongruence between policy and practice. Special attention was paid to specific examples of both good and poor practice in relation to the safety of patients with learning disabilities, and the identification of the specific cross-organisational, organisational and individual factors that had a bearing on these examples. This resulted in a final empirical framework of factors that affect the promotion of a safer environment for patients with learning disabilities.
It must be noted that in this report many examples of good and poor practice are highlighted. This does not reflect the quantitative incidence of such examples (which this study did not aim to elicit), but rather, it reflects the study focus of aiming to understand how and why good or poor practice occurs.
Ethical issues
Ethical approvals
The study was approved by the National Research Ethics Services (NRES). Three substantial amendments were submitted to NRES during the course of the study, to include the sixth study site and to reflect altered sampling strategies. All were approved (Research Ethics Committee reference 11/LO/0428). Local research approval was obtained at each participating trust.
Ethical issues
Vulnerability of people with learning disabilities
This study included data collection involving vulnerable adults. The research team had long-standing expertise in conducting research involving participants who have learning disabilities in sensitive areas including death, dying, bereavement and abuse, and have gained international recognition in this area. 33
The research team believed that ethical considerations for this study needed to be given attention above and beyond any requirements of research ethics committees. Therefore, a range of steps were taken in order to safeguard all informants from undue harm in accordance with the principal of beneficence. Particular attention was paid to obtaining informed consent from research participants with learning disabilities, using a range of accessible study information materials, and to ensuring sensitivity to the various ways in which people with learning disabilities may express withdrawal of consent.
Anonymity
It became clear during the course of the study that the sensitivity of the subject area was a major challenge. Both before and during the study period, a range of NHS trusts across England had been publicly ‘named and shamed’, in particular through Mencap’s Death by Indifference report and follow-up report. 1,34 It was important to emphasise to the participating sites throughout the study that the results would be reported anonymously and that confidentiality would be protected.
For this reason, the study sites are described in this report in general terms only, pseudonyms are used throughout, and identifying details altered where they do not affect the essence of the data. Unless it is necessary for understanding local differences, particular data have not been attributed to particular study sites.
Project management
The study was hosted by the Division of Population Health Sciences and Education at St George’s, University of London. It was conducted by a broad research team and supported by a research advisory board with a wide range of knowledge, skills, experience and expertise. This included investigators and advisors with academic skills, but also those with personal experience of having learning disabilities, caring for someone with learning disabilities, accessing NHS hospital services and working in NHS hospital settings including senior management. In order to ensure that the research was relevant to all informant and stakeholder groups, as well as academically sound, this collaboration between service users, clinicians and academics was crucial throughout the research process, from developing the original proposal to reporting its findings. All members of the research and advisory teams contributed in the areas where their expertise was most relevant, both in terms of topic area (for example: patient safety issues; organisational change; understanding the role of the learning disability nurse; other vulnerable patient groups) and in terms of research design (for example: design and administration of electronic and paper questionnaires; analysing and synthesising data from multiple sources; recruitment of participants).
The research advisory board had an independent chairperson, Sir Leonard Fenwick, an NHS trust Chief Executive, and met five times during the course of the study. Individual members of the research advisory board provided ad hoc expertise to the research team as needed. The role of the research advisory board included ensuring that the protocol was followed; ensuring that the project was kept within budget and that deadlines were met; and providing advice and support to the research team with regards to emerging barriers and ethical issues.
Full details of the members of the research team and research advisory board are given in Appendix 1.
Section 2 Literature review
Chapter 4 Literature review
Introduction
At the start of the study and throughout the study period, the initial literature review was updated and expanded to incorporate the specific issues addressed in the study. This chapter provides important context for the findings reported in Chapters 5–10. It presents an overview of national developments, inquiries and reports that affected the course of this study, as well as a more detailed literature review around the following aspects of the study: identifying patients with learning disabilities in NHS hospitals; providing reasonably adjusted services; involving carers as partners in care; and patient safety issues for people with learning disabilities.
Progress and national developments since Healthcare for All
The study follows four recommendations of Healthcare for All,4 but it was not conducted in isolation of events. Following another of Healthcare for All’s recommendations, the time-limited CIPOLD was set up and this published its final report in March 2013. 3 Furthermore, a learning disability public health observatory, the Improving Health and Lives Learning Disability Observatory (IHAL), was established as a 3-year project in 2010. 35 This has published a range of documents, data and reports on health inequalities and the progress that health and social care services are making in addressing these. 14,24,36 It includes a wide range of good practice examples, but also evidence that people with learning disabilities remain disadvantaged when accessing health services. The evidence from CIPOLD in particular is highly relevant in relation to this study; this is further discussed in Chapter 12.
In 2010, Mencap launched its campaign Getting it Right When Treating People with a Learning Disability, providing guidance for health care services. 5 It invited NHS hospitals to sign up to a charter of pledges to ensure that a range of reasonable adjustments were made (see Reasonable adjustments for people with learning disabilities in NHS hospitals). In 2012, over 200 health-care organisations had signed up, and Mencap reported excellent examples of good practice. However, Mencap claimed that the NHS continued to fail people with learning disabilities, leading to avoidable deaths, and in 2012 published a follow-up report in which it concluded that not enough progress had yet been made in addressing the health inequalities experienced by people with learning disabilities. 34
The issue of discrimination and abuse of people with learning disabilities within health and social care services was kept in the headlines through the disclosure in May 2011 of appalling criminal abuse practices at Winterbourne View, a care home for people with learning disabilities, and the subsequent Department of Health review. 37 This highlighted a widespread failure to design, commission and provide appropriate services for people with learning disabilities, and an unacceptable tolerance of people with learning disabilities being given the wrong care.
During the time this study was conducted, the NHS experienced one of the largest-scale structural changes in its history, with the transfer of commissioning responsibility from PCTs to clinical commissioning groups (CCGs) and the new NHS Commissioning Board, and responsibility for public health moving from the NHS to local authorities. Pressures on NHS services have increased. Although NHS funding has stayed broadly level in real terms since 2010, hospitals are dealing with a growing population, increasing numbers of older people, people with complex care conditions and people with dementia needing hospital treatment. The CQC reported that NHS services struggled to make sure they had enough qualified and experienced staff on duty at all times (with 16% of NHS hospitals being understaffed), and also struggled to make sure staff were properly trained and supervised. 38
It is important to remember that the first core value underpinning the NHS, as set out in its constitutions, remains a commitment to providing:
. . . a comprehensive service, available to all irrespective of gender, race, disability, age, sexual orientation, religion, belief, gender reassignment, pregnancy and maternity or marital or civil partnership status.
p. 3. 39 We acknowledge The National Archives as custodian of this document
Identifying patients with learning disabilities in NHS hospitals
Healthcare for All4 states that:
. . . chief among the obstacles to delivering and evaluating the effectiveness of health services for people with learning disabilities is a lack of information about them . . . it is difficult for services to prepare properly or make the necessary ‘reasonable adjustments’ if patients’ communication and other special needs are unknown.
p.36. Reproduced with permission from Michael J. Healthcare for All: Report of the Independent Inquiry into Access to Healthcare for People with Learning Disabilities. London: Aldridge Press; 2008
The report recommended that health-care organisations should ensure they collect the data necessary to allow people with learning disabilities to be identified by the health service. This was accepted by government and a pledge was made in the White Paper Valuing People Now to work towards better systems for general practitioners (GPs) to identify people with learning disabilities and share that information with other NHS sources. 20
General practitioner practices have been given guidance by the Department of Health to carry out annual health checks for people with learning disabilities, which come with financial entitlements. This has encouraged GP practices to identify their populations of patients with learning disabilities. However, despite investments in a major overhaul in NHS information technology (IT) systems,40 the aim to achieve effective sharing of patient information between different NHS services through fully integrated electronic patient records by 2010 has not been achieved. The implementation of summary care records is still under way; around one in three people in England have one. 41 Summary care records contain key medical information, such as medication and allergies, made available across England to NHS staff involved in treating the patient. Mencap supports the summary care records in principle, observing that there would be a benefit if people with learning disabilities were able to add key information about their needs that they wanted clinicians to know, for example, information about how they communicate, or contact details for their carer. 42
In 2012, IHAL published the report Have You Got a Learning Disability?,43 which considered the difficulties NHS services face in identifying and recording the presence of learning disability. The authors pointed out that learning disability is always relevant when caring for someone in hospital, so, where present, it should always be recorded as a comorbid condition. Without this information health services cannot adequately discharge their duties under equalities legislation or meet the requirements of registration legislation (see Equality legislation and reasonable adjustments). However, one fundamental difficulty with recording the presence of learning disability is that only an estimated 21% of people with learning disabilities in England are known to health and social care services. This means that even if communications with referring GPs are good, most people with learning disabilities will not have been flagged in the referrals. People with mild learning disabilities are most likely to be missed. This group of patients may have difficulty with written materials, keeping appointments, understanding consent procedures and complying with treatment regimes.
The authors argue that it is down to NHS services to identify this population at all care delivery points, but particularly at those points where patients enter care. They propose that all patients are asked questions to screen for disability, in the same way as they are asked questions about ethnicity; and they suggest specific ways in which NHS staff (in particular, nurses and administrative staff) can screen patients in this way. The implication is that such staff need training in learning disability.
Another way in which hospitals record patient characteristics is through clinical coding, used for statistical purposes to calculate how much the hospital should get paid for the care of each patient under the Payment by Results (PbR) system. Since March 2011, new minimum data sets from the NHS Data Standards Board have started to include a question about disabilities for statistical purposes. Glover and Emerson43 identified significant problems with the system. Current codes that can be used for learning disability are inadequate and misleading, with coding clerks commonly assigning the wrong code. The reasonable adjustments needed by people with learning disabilities are likely to require additional resources, but this is not reflected in the PbR system.
Providing reasonably adjusted health services
Equality legislation and reasonable adjustments
It is a legal requirement for public services to ensure that their services are accessible to people with disabilities. The Disability Discrimination Act44 came into force in 1995 and sets out the legal duties of service providers to make adjustments. Subsequent Acts have reinforced this legal requirement. 45,46
Where a provider of services has a practice, policy or procedure which makes it impossible or unreasonably difficult for disabled persons to make use of a service which he provides, or is prepared to provide, to other members of the public, it is his duty to take such steps as it is reasonable, in all the circumstances of the case, for him to have to take in order for him to change that practice, policy or procedures so that it no longer has that effect.
Part III, section 2144
Having due regard for equality means removing or minimising disadvantages suffered by people because of their protected characteristics, and taking steps to meet the needs of people from protected groups where these are different from the needs of other people. 47 There are three requirements that apply in situations where a disabled person would otherwise be placed at a substantial disadvantage compared with people who are not disabled:48
-
Changing the way things are done, where the disabled person is put at a substantial disadvantage by a provision, criterion or practice of the service provider (including written or unwritten rules). Reasonable adjustments could include changing or adapting the rules, or providing staff training. Barriers can include poor staff attitudes or a lack of knowledge and skills.
-
Altering physical obstacles or designs that put disabled people using a service at substantial disadvantage. The organisation must take reasonable steps to remove the feature, alter it, provide a reasonable means of avoiding it, or provide a reasonable alternative method of making the service available to disabled people. Physical features include steps and stairways, but also floor coverings, furniture, signs and toilet/washing facilities.
-
Providing extra aids and services like providing extra equipment or additional service (in law, these are called auxiliary aids). Examples include provision of accessible information, access to an interpreter, or offering a home visit when clients would usually come to the service premises.
Whether an adjustment is ‘reasonable’ depends on a range of factors, including whether it can actually be done, the cost, and the organisation’s resources and size. The guidance documents from the Equality and Human Rights Commission point out that ‘just because something is difficult does not mean it cannot also be reasonable’ (The copyright and all other intellectual property rights in the material to be reproduced are owned by, or licensed to, the Commission for Equality and Human Rights, known as the Equality and Human Rights Commission (‘the EHRC’). Reproduced with permission from Equality and Human Rights Commission. Your Rights to Equality from Health and Social Care Services. Equality Act 2010 Guidance of Your Rights, Volume 5 of 9. Manchester: Equality and Human Rights Commission; 2010, p.44.). 48 If an adjustment is costly, the organisation’s resources must be looked at across the whole organisation, not just the branch, section or ward that provides the particular service.
The legal requirement is for services to put reasonable adjustments in place even if they do not have any disabled clients at the time. In other words, organisations should not wait until disabled people try to use their service; rather, they should be proactive and anticipate the need for adjustments.
Reasonable adjustments for people with learning disabilities in NHS hospitals
Healthcare for All4 noted that, despite examples of good practice across the country, the lack of knowledge and information means that timely, appropriate and reasonable adjustments as defined by the disability legislation are not easy to make, even when services are keen to adapt their approach for people with learning disabilities.
Mencap’s Getting it Right charter (2010)49 listed nine pledges, all of which amount to reasonable adjustments, and several of which echo the Healthcare for All4 recommendations:
make sure hospital passports are available and being used
make sure that all staff understand and apply the principles of mental capacity laws
appoint a learning disability liaison nurse in hospital(s)
make sure every person with a learning disability can have an annual health check
provide ongoing learning disability awareness training for all staff
listen to, respect and involve family carers
provide practical support and information to families and carers
provide information that is accessible to people with a learning disability
display the Getting it right principles for everyone to see.
Reproduced with permission from Mencap. Getting it Right When Treating People with a Learning Disability. London: Mencap; 2010
Several of the study sites were among the first health-care trusts that signed up to this charter.
Following the Health Service Ombudsman report in 2009,2 the Department of Health published a progress report. 50 Having gathered evidence from a wide range of sources, the report stated that there were many good practice examples, but this was often dependent on individual staff and teams rather than embedded within organisational structures. Reasonable adjustments were less commonly mentioned in relation to acute care (compared with primary care). One frequently sighted adjustment was the provision of easy read information. The conclusion was that reasonable adjustments can hugely improve patients’ experiences and outcomes, and failure to make adjustments can have far-reaching negative consequences for patients; but there is a need for further work to ensure that reasonable adjustments are made within health-care settings.
The Chief Executive of the NHS, Sir David Nicholson, wrote to all Chief Executives of NHS trusts and NHS foundation trusts in England in 2008 and in 2010 (twice), reminding them of their legal obligation to make reasonable adjustments for people with learning disabilities, and to ensure that their staff are following the law in this respect. 51
A practical guide commissioned by the Department of Health presents a range of examples of NHS trusts that have made reasonable adjustments. 52 IHAL, set up by the Department of Health, has gathered data on the types and extent of reasonable adjustments made by NHS trusts. In its report,53 it summarises Giraud-Saunders’s comprehensive guidance,52 which:
. . . gives a very good sense of the wide range of systemic changes that are required for an NHS service to run a truly effective service for people with learning disabilities, including:
Information for people with learning disabilities
Working in partnership with families
Capacity, consent and advocacy
Service delivery (including making an appointment, initial attendance, receiving a service, discharge and follow-up)
Gathering, monitoring and reporting information about access and effectiveness of the health service by people with learning disabilities
Patient and public involvement
Employment of people with learning disabilities.
p. 12. 53 Reproduced with permission from Hatton C, Roberts H, Baines S. Reasonable Adjustments for People with Learning Disabilities in England: A National Survey of NHS Trusts. IHAL report 2011-03. London: IHAL; 2011
Improving Health and Lives reported findings collected from 119 trusts who responded to its survey, including 61 acute trusts (36% of all acute NHS trusts in England). The most commonly reported reasonable adjustment was the provision of accessible information, although the authors comment that it was not clear whether this information was specifically designed or comprehensible for people with learning disabilities, nor whether it was routinely available. Similarly, accessible information for carers was reported, but robust evidence for this was lacking. Other areas of reported reasonable adjustments included policies concerning mental capacity, staff training, having trust patients with learning disabilities who make use of an Independent Mental Capacity Advocate (IMCA), using patient-held information documents and health action plans. The authors found that:
. . . the most common solution for trusts concerning face-to-face contact with patients with learning disabilities and carers was to rely on staff with specialist learning disability training, skills or roles to act as liaison between the person with learning disabilities, the carer, the various parts of the trust and other learning disabilities services involved in the support of the individual.
p. 8. 53 Reproduced with permission from Hatton C, Roberts H, Baines S. Reasonable Adjustments for People with Learning Disabilities in England: A National Survey of NHS Trusts. IHAL report 2011-03. London: IHAL; 2011
Improving Health and Lives has now set up a public online database where NHS trusts can upload and share their good practice examples of making reasonable adjustments for people with learning disabilities. 54
Involving carers as partners in care
Definition of ‘carer’
Carers Trust55 defines a carer as:
. . . someone of any age who provides unpaid support to family or friends who could not manage without this help. This could be caring for a relative, partner or friend who is ill, frail, disabled or has mental health or substance misuse problems.
Reproduced with permission from Carers Trust. What is a carer? 2012. URL: www.carers.org/what-carer
Family carers of people with learning disabilities are unique among carers. Many have decades of caring experience and of negotiating the health, education and social care systems through infancy, childhood and adulthood. 55
Many people with learning disabilities rely on the support of paid care staff in their daily lives, including support staff working in the residential care, independent living arrangements and sheltered accommodation settings. Such care staff often provide support for people with learning disabilities when they attend hospital as inpatients or outpatients. Their expertise and knowledge of the person with learning disabilities may vary; whereas many may be highly experienced and trained, others are not. Paid carers range from experienced home managers who have known the person for many years to unskilled workers who do not know much about the person they support.
The Healthcare for All4 recommendation applies to these paid carers as well as unpaid family carers. For the purpose of this study and this report, a ‘carer’ is defined as any care giver who provides paid or unpaid support to someone with learning disabilities during their hospital episode, including both family carers and paid carers. There are overlaps but also distinctive differences in carer-related issues with regards to these two groups of carers, and where relevant, this report will differentiate ‘family carers’ (who provide unpaid help and support and have a relationship with the person with learning disabilities built on interaction and shared experiences) and ‘paid carers’ who are, by definition, paid to provide formal care. 56
Evidence on carer involvement from Healthcare for All
The independent inquiry gathered evidence from 79 family carers. The largest categories for comments were the importance of listening to carers (mentioned by 58% of carers), the need for staff education and training (55%) and the problem of communication (52%). In particular, they reported on the following issues:
-
poor staff attitudes, including ignorance, fear and unwarranted assumptions about the patient’s quality of life
-
difficulties in communicating effectively with carers
-
inconsistencies in the quality of information sharing with regards to the health and needs of the patient
-
carers’ needs not being taken into account
-
difficulties in accessing health services
-
difficulties in negotiating transition (for example, between child and adult services).
The roles and experiences of carers in hospitals
There are a number of studies focused on the roles and experiences of, and the problems faced by, carers of adults with learning disabilities while they are in hospital.
Carers report support roles that include providing direct support with personal care and mealtime assistance; providing communication support; providing emotional support and reassurance; providing information about the patient to hospital staff; and advocating for the patient’s needs. 56,57
Problems reported by carers of people with learning disabilities in hospital include ill-defined role boundaries, whereby hospital staff and carers (especially paid carers) are uncertain about what carers can and will do; not being supported to take a break from caring; and lack of recognition for carers’ expertise and advocacy role. 56,58 Several studies found that the family’s expert knowledge was rarely solicited by hospital staff,59 and that this had led to compromised safety or increased suffering and pain. 60
Other authors reported that carers felt they needed to be constantly present and vigilant, fearing that in their absence the patient’s needs, including basic care needs such as eating, drinking and toileting, would not be met and the patient could be harmed; this fear was often based on past experience. 57,59,61,62
Allen63 used ethnographic data from a study in a UK hospital to describe the different degrees to which family carers were involved with patient care. Her study was not focused on carers of people with learning disabilities, but the descriptions have relevance. Family members could act as ‘visitors’, ‘workers’ (undertaking care-giving tasks and being of help to the ward staff) or ‘expert carers’. Allen found that relatives and friends who adopted a worker role remained subordinate members of the nursing team. On the other hand, expert carers focused more on the needs of the patient, rather than the nurses. Allen noted that this presented a challenge to the ward nurses’ ability to control their work and their claims to expertise. As such, expert carers’ actions:
. . . could lead them to disrupt fundamental features of the social organisation of ward work . . . Thus, whilst other family members could be integrated into the ward caring division of labour with relative ease, the integration of expert carers was infinitely more problematic.
p.15563
Allen also noted that carers were reluctant to make a complaint about perceived poor standards of care, fearing a negative effect on their relationships with hospital staff.
The role of the learning disability liaison nurse
One key way in which the health inequalities and safety risks faced by people with learning disabilities in secondary health care has been addressed is through the development of new models, whereby nurses experienced in learning disability work in general hospital environments. They take on the specific role of supporting patients with learning disabilities and their families as well as the hospital staff these patients come into contact with. The term used most widely for such a role is that of LDLN. 64–67
The Department of Health has strategically advocated advanced nursing roles as a an effective way of overcoming problems facing the NHS. 68
There are different models for developing LDLN roles, including posts or teams working in general hospitals; learning disability community teams providing support to people with learning disabilities before, during and after their hospital admission; training hospital nurses to act as a resource (‘link nurse’) for other hospital staff; and creating city-wide nurse consultant posts to facilitate the provision of co-ordinated care across multisite hospitals. 69 A hospital-based learning disability nurse consultant post has also been described. 70
A national survey of reasonable adjustments made for people with learning disabilities in NHS trusts36 reported that 55 acute trusts (95%) made use of liaison staff with a specific role in providing health facilitation, such as LDLNs. However, this covered a wide range of models, not all of which included specific learning disability expertise. Nine acute trusts said that they employed LDLNs. Other models included engagement in partnership with community or PCT health facilitation staff; identifying health facilitation for people with learning disabilities, as part of the role of the trust’s clinical lead for safeguarding vulnerable adults and other non-learning disability-specific trust personnel; and employing health facilitators or acute liaison nurses.
Healthcare for All4 reported unanimous support among witnesses to the independent inquiry for LDLN roles, but found that the impact of such roles on health or service quality was difficult to measure. The inquiry reported on an informal survey that found only 20 securely funded staff in England with the liaison role as an explicit part of their job description.
The 2010 congress of the Royal College of Nursing supported the following resolution with 425 out of 476 votes (92%): ‘That this meeting of the RCN Congress asks Council to lobby for a learning disability liaison nurse in all hospitals’. 67,71 In its Getting it Right campaign, Mencap also called for an LDLN in all hospitals. 5
A literature search found only one research study focusing on the effect of the LDLN in acute hospital settings. Brown et al. 65,72 investigated the impact of LDLN services across four Scottish NHS boards. The authors found that the LDLN role was complex and had three key dimensions: clinical patient care, education and practice development, and strategic organisational development. Both carers and professionals viewed LDLNs as ‘credible ambassadors’ for people with learning disabilities and a positive driving force within the organisation.
Phillips73 observed that although there is evidence in the literature to support promotion of the role of the LDLN and implementation of such roles is generally considered to be good practice, liaison posts tend to be temporary and ad hoc.
Patient safety
Researching patient safety
Patient safety is concerned with any issue (separate to the natural progression of the patient’s illness or injury) experienced during a patient’s health care which could or did cause harm. 74 Examples include acquisition of a hospital-acquired infection, receiving the wrong medication or the wrong dose, or falling while under the care of the service provider. Studies conducted within health-care services in the developed world demonstrate that approximately 1 in 10 patients encounter harm as a result of the health care they receive. 75,76 It is estimated that around 50% of patient safety issues are preventable. 75 While this figure is well known and often quoted within the patient safety arena, it remains alarming and captivates audiences because of the widespread and often unfailing perception that ‘hospitals make people better’. However, all patients are at risk of being unintentionally and avoidably harmed during the process of their health care due to the impossibility of eradicating human error. 77
Reason78 highlights two approaches to understanding and ameliorating human error. The ‘person approach’ essentially blames the ‘aberrant mental processes’ of health-care professionals working at the ‘sharp end’ when an error is made (p. 768). 78 For example, if the wrong drug was administered to a patient, the health-care professional who gave the drug would be blamed and it would be assumed that their cognition was at fault. Conversely, the ‘system approach’ recognises that mental processes are flawed and seeks to adapt the error-producing conditions that are ever-present within the environment (known as latent conditions) rather than changing the individuals within the system. For example, if the wrong drug was administered to a patient, it would be important to look at all of the factors in the environment that may have contributed to this, such as the labelling on the medication, the physical location in which the medication was stored, the clarity of the method used to prescribe the medication, the level of training and working pattern of the health-care professional who administered the medication, etc. Changing the ‘systems’ that surround an error reduces the likelihood that another health-care professional will make the same error in the future. This approach acknowledges that there are often a number of different ‘contributory factors’, spanning cross-organisational, organisational and individual levels, which lead to adverse outcomes. Thus, there is a consensus within the patient safety arena that systems and underlying contributory factors can be studied and changed to make patient care safer.
Patient safety issues for people with learning disabilities
Although we do not know the incidence of adverse events experienced by patients with learning disabilities in NHS acute hospitals, a small number of reports have outlined the types of patient safety issues faced and have begun to describe contributory factors which underlie these issues. In 2004 the National Patient Safety Agency (NPSA) studied ‘patient safety priorities’ for people with learning disabilities. They concluded that ‘people with learning disabilities may be more at risk of things going wrong than the general population, leading to varying degrees of harm being caused whilst in general hospitals’ (p. 11, reproduced with permission from National Patient Safety Agency. Understanding the Patient Safety Issues for People with Learning Disabilities. London: National Patient Safety Agency; 2004). 79
Specific patient safety issues have been described surrounding: misdiagnosis or diagnostic overshadowing;1,3,4,34,79,80 inadequate treatment of pain;3,34,79 delayed diagnosis or treatment;3,6,34,80 inappropriate ‘do not attempt resuscitation’ (DNAR) orders;3,34 medication errors or omissions;3,81 over-reliance on psychotropic drugs to manage behaviour that is perceived to be challenging;6,80 inappropriate use of control and restraint;79,80 recognition of swallowing difficulties;82 lack of nutrition;1 pressure ulcers;18,83 and inconsistent personal care. 34,80
Within this literature, factors cited as contributing to safety issues comprise barriers to accessing NHS services and lack of reasonable adjustments to facilitate access;3,80 miscommunication of pain or symptoms;1,3,34 patients’ lack of understanding of their medical condition and medical interventions;79,80 patient non-compliance with treatment;3 a shortage of accessible information;79 inappropriate procedures for gaining patient consent, a lack of staff understanding of the Mental Capacity Act and flawed best interests decisions;1,3,34 reliance on carers to provide nursing care;34,79 poor communication between carers and hospital staff;1,34 poor record-keeping of patient observations (e.g. food and fluid intake) and patient preferences;3 failure to follow clear care pathways;3 lack of continuity of care within hospital and lack of after-care post discharge;3 a deficiency of hospital staff knowledge and skills to enable recognition of the specific needs of patients with learning disabilities;1,34,79 a lack of value placed on the lives of people with learning disabilities;1,34 insufficient advocacy;3 and an inaccessible complaints procedure within the NHS which compromises learning from previous adverse events. 1
At the outset of the research, an initial scoping review had suggested that preventable deterioration and, in particular, medication errors and misdiagnosis (due to problems with communication and comprehension), were particularly pertinent issues faced by patients with learning disabilities. 25,81 These safety issues were therefore incorporated within the initial theoretical framework and formed specific lines of enquiry during data collection. Additional patient safety issues and underlying contributory factors emerged during the course of the research and were subsequently integrated into the strategy for ongoing data collection and analysis.
Incident reporting
The information in this section was provided by Vanessa Gordon (Associate Director of Patient Safety for Learning Disabilities, NHS Commissioning Board, 2012, personal communication) and Noreen Gul [Analyst, National Reporting and Learning System (NRLS), 2012, personal communication].
The NRLS was established in late 2003 as a voluntary scheme for the reporting of patient safety incidents and focuses primarily on learning from these incidents in the NHS. The NRLS, therefore, does not provide the definitive number of patient safety incidents occurring in the NHS. In April 2010, it became mandatory for NHS organisations to report all patient safety incidents which result in severe harm or death to the NRLS. Over 99% of incidents in the NRLS are taken from local risk management systems.
The national picture of patient safety incidents in England and Wales is published quarterly by the NRLS. For the period April 2011 to March 2012, 1,250,206 patient safety incidents were reported as occurring in England, with 24,686 incidents (2%) reported in the care setting ‘learning disability’. The most common incident type reported from learning disability care settings was disruptive/aggressive behaviour (28%) followed by ‘patient accident’ (26%). 84
Identification of people with learning disabilities in acute care by means of incident reporting is particularly problematic as fields relating to any patient disability are poorly populated, and information contained within the free text description of an incident may not mention a patient’s disability or may be ambiguous. Phrases within an incident description, such as ‘a patient with complex needs’ or ‘a vulnerable patient’, can also mask a person with learning disabilities.
The reporting of incident types versus outcomes may be confusing to reporters and may result in the patient’s behaviour being recorded rather than a more appropriate incident type. The general taxonomies of reporting systems may also hinder appropriate reporting of patient safety incidents for specific types of patients, including those with learning disabilities. To reduce the burden on the NHS, the NRLS uses information from the individual organisation’s risk management system. If information regarding patient safety incidents and people with learning disabilities is not reported locally, it will not be collected nationally by the NRLS. Currently, the issue of identification of people with learning disabilities within reporting systems is a major barrier to analysis and to an understanding of patient safety for this group.
Organisational change
Following the report of the independent inquiry into widespread failings at one NHS acute hospital (the Francis Report),85 which identified lack of caring as an issue, discussions have tended to focus on measures to improve the attitudes and practice of individual staff, notably nurses. Less attention has been paid to the organisational structures and cultures that constrain or facilitate the adoption of good practice. Research suggests that successful implementation of the Healthcare for All4 recommendations will depend on changes in the organisational contexts that impact on individual behaviour, and that organisations vary in their ‘readiness’ or receptiveness to change. 86–88 Thus the development of best practice guidelines is only a first step in effecting change.
In terms of the organisational characteristics influencing the change process, the extent to which a proposed change ‘fits’ with the strategic goals, structure and culture of the organisation and the external environment with which it interacts has been identified as a major facilitating factor. 89,90 However, NHS trusts are set a wide range of performance indicators and are increasingly subject to resource constraints, so it is not clear how much strategic priority and resource is actually attached to dealing with learning disability. Moreover, alignment with government and trust strategy alone is not sufficient to bring about change: a number of studies have demonstrated how policies strongly supported by senior management can be undermined by the inability or unwillingness of line managers to implement policy and resources effectively. 91–94 Other constraints lie with the siloed nature of organisational structures, which may impede the transmission across organisational and departmental boundaries of information necessary to identify and respond to individual patients’ needs. Moreover, bureaucratic systems of rules, processes and procedures may act to facilitate better practice, but can also impede it by setting conflicting objectives or inhibiting initiative.
Changing service delivery to respond to individual need also depends on good interprofessional working, but professional groups, with their distinctive identities, training, knowledge bases and communities of practice, may have difficulty in agreeing how to implement policy, share information and work together. 95 Further, a number of studies have also documented the power of clinicians to block innovative practice. 96,97 This raises questions regarding whether or not health professionals have the skills and the motivation to deliver the changes required, and whether their reputed power may act as a barrier to or facilitator of new ways of working.
A final consideration is whether organisations have the leadership competence and capability to manage the change process. Several studies suggest that the charismatic and transformational leadership associated with innovation is absent in many health-care settings. 98–100 However, Balogun101 and Currie and Proctor102 concluded that, given discretion to act, middle managers in the NHS can play an important part in implementing strategic change.
All of this suggests that training and performance managing individuals, and putting in place dedicated professional posts such as that of the LDLN, though essential, may not be sufficient to bridge the gap between policy and practice. These changes will need the support of managers and professionals at all levels, and must be accompanied by changes in the organisational context, if they are to be effective.
Section 3 Results
Chapter 5 Identifying patients with learning disabilities in NHS hospitals
All healthcare organisations, including the Department of Health, should ensure that they collect the data and information necessary to allow people with learning disability to be identified by the health service and their pathways of care tracked.
Recommendation 2 (p. 11). 4 Reproduced with permission from Michael J. Healthcare for All: Report of the Independent Inquiry into Access to Healthcare for People with Learning Disabilities. London: Aldridge Press; 2008
Chapter summary
Most patients with learning disabilities remain invisible within the health-care system. The majority of patients with learning disabilities enter NHS hospitals without being identified as such. To various degrees, the hospitals in this study failed to identify patients with learning disabilities at the point of entry into the health-care system or during their patient journey. Hospital-based LDLNs were best able to provide lists and numbers of patients with learning disabilities who had used the hospital service, but even these were not comprehensive, with particular difficulties in identifying learning disabilities in outpatients. The failure to identify this patient population was due to:
-
a lack of patient record systems integrated with those of other NHS services, including primary care
-
a lack of effective flagging systems within the hospitals
-
a lack of staff knowledge and skill in identifying the presence of learning disability, leading to both underdiagnosis and misdiagnosis of learning disability
-
widespread staff reluctance to record the presence of learning disabilities in a routine and systematic way. There was a lack of understanding of the need for identifying learning disability, a fear of putting a negative label on people and a reluctance to ‘ask the question’.
The barriers and enablers that have emerged in this study in relation to identifying patients with learning disabilities in NHS hospitals are summarised in an empirical subframework (Figure 2).
FIGURE 2.
Empirical subframework: barriers and enablers in relation to identifying patients with learning disabilities in NHS hospitals.
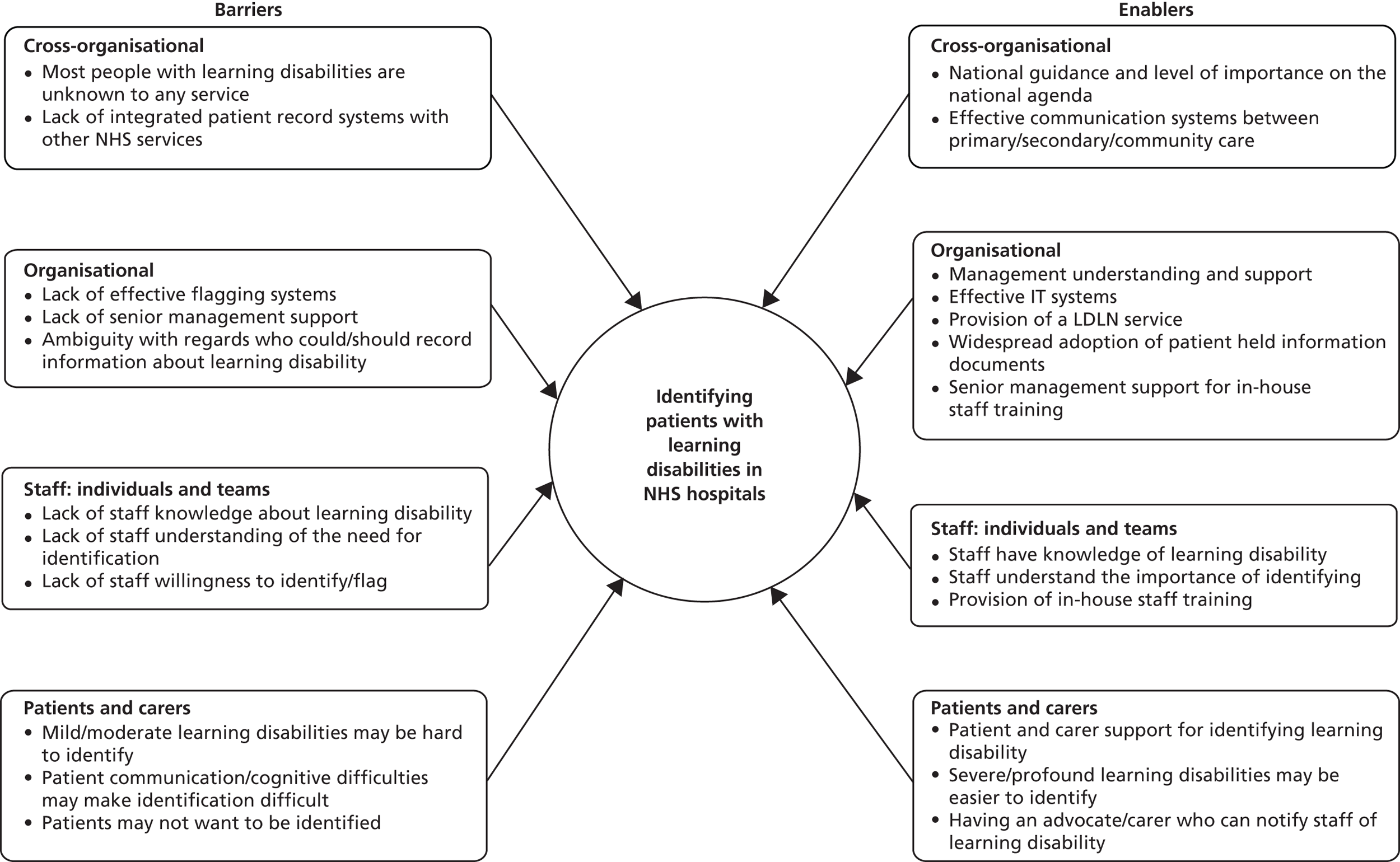
Identifying, flagging and tracking patients
There are two main reasons why health-care organisations should identify patients with learning disabilities: firstly, they need to be able to monitor their compliance with equality legislation, and secondly, if they are to implement adequate reasonable adjustments for people with learning disabilities, they need to be able to identify who needs them.
The importance of tracking patient care pathways is evident from the results presented in Chapter 6, which demonstrate the sometimes complex reasonable adjustments required by patients with learning disabilities. These may involve more than one ward or clinic (for example, a need to fast-track patients to a suitable ward environment or to limit the number of ward changes). Furthermore, people with learning disabilities are highly likely to have multiple medical conditions (CIPOLD found that 98% of people with learning disabilities had at least one long-term health condition or treatable medical condition, with a median of five conditions per person). This means that the co-ordination of care for people with learning disabilities is particularly important, and tracking the care pathway is part of this.
It is useful to differentiate between ‘identifying’, ‘flagging’ and ‘tracking’ patients with learning disabilities.
Identifying refers to the way in which the hospital and individual staff members recognise that a patient has learning disabilities. This could be through formal notification systems, or informally through handovers, GP letters, or through staff suspecting or noticing the presence of learning disability.
Flagging refers to a formal notification that the patient has learning disabilities. This can be done by adding a ‘flag’ or other notification to electronic patient records; using a system of marking patient notes (for example, using a coloured sticker); adding a mark against the patient’s name as displayed on the ward; having the patient carry a specific personalised information document; or through records kept by staff with specific responsibility for patients with learning disabilities (such as the LDLN).
Tracking refers to systems for monitoring the patient’s care pathway within the organisation, and the organisation’s ability to know where the patient is in their hospital trajectory at any given time. This ability is likely to depend on the presence of effective flagging systems.
These descriptions have emerged from reflections on the data. It has become clear that an organisation’s ability to monitor its overall performance in relation to patients with learning disabilities, including its compliance with equality legislation and the legal duty to provide reasonable adjustments, depends on the presence of effective flagging systems which retain information about current and prior users of the service. However, in order to identify and implement the necessary reasonable adjustments, simply flagging the patient is not sufficient; patients need to be identified by staff as having learning disabilities. It is possible to identify patients with learning disabilities (and put the necessary adjustments in place) without flagging them, but this is likely to lead to inconsistencies and a dependence on individual staff and teams. It is also possible to flag patients with learning disabilities without hospital staff identifying them as such, which may result in inadequate or absent reasonable adjustments.
Sometimes patients with learning disabilities are highlighted post admission through the clinical coding system. The real risk of miscoding43 and the fact that such flagging has no effect on the patient journey make this an inadequate method of identifying patients with learning disabilities.
How did the hospitals identify, flag and track patients with learning disabilities?
Policies, procedures and systems
Electronic flags
The participating hospital trusts used a variety of electronic patient record systems. Three hospitals were able to put a flag or alert on the patient’s electronic records to signal that the patient had learning disabilities; two were in the process of developing this possibility. These electronic systems relied on someone putting the flag on within the acute trust and often lacked integration with other systems in primary and secondary care. One hospital trust had tried to identify the local population of people with learning disabilities in order to enter the information proactively on the electronic hospital records, which had involved a laborious and inefficient process of writing to all patients identified by a local learning disability charity to obtain their consent. Towards the end of stage II, the trust had tried to overcome this problem by implementing a new flagging system where the need for specific reasonable adjustments was flagged, rather than the presence of learning disabilities.
Learning disability liaison nurse-kept records
Learning disability liaison nurses kept paper-based or electronic lists of patients with learning disabilities referred to them. Several trusts used this system as the principal way of knowing which patients had learning disabilities.
Ward checks
One trust had implemented a system whereby the bed manager visited each ward daily and specifically asked the ward managers whether or not any patients had learning disabilities; if so, details were passed on to the LDLN. Hospital-based LDLNs occasionally walked around the wards to see if they could ‘find’ any patients with learning disabilities, and found patients this way that had not been referred to them by staff.
If I found someone on the wards – ‘Well you didn’t tell me, why didn’t you tell me? They’ve clearly got Down syndrome.’
P9, LDLN
Identifying patients
Learning disability liaison nurses were often called upon by staff to assess whether or not a patient with suspected learning disabilities did indeed have learning disabilities. It was noted by the LDLNs that they were regularly called inappropriately to see patients who did not have learning disabilities but some other condition, such as mental health problems.
Tracking patients
Hospitals that were best able to track the care pathways of any patients with learning disabilities who had been identified through the hospital’s flagging systems were those that had allocated such responsibility to either the LDLN or a senior nurse manager, such as a matron or safeguarding lead. This member of staff would then make contact with the ward managers or clinical areas and follow the patient through the hospital system. Without such allocation of responsibility, hospitals were not able to track the patient’s hospital pathway in a meaningful way.
How effectively could study sites identify, flag and track patients with learning disabilities?
The collaborators were asked to provide the research team with the following data: numbers of patients with learning disabilities using the health-care service during the 12 months of stage II; which wards the patients were admitted to; lengths of stay; and numbers of readmissions within 7 days of discharge.
None of the hospital sites could provide the research team with comprehensive information. Three trusts could not provide any usable data. Two of these provided numbers obtained from clinical coding, which does not constitute identification of the patient during their hospital contact and is unreliable because of the high risk of miscoding. 43
Electronic systems, where used, were far from comprehensive or reliable, and there was evidence of patients with known learning disabilities not being identified in this way. At one trust, an intensive audit of inpatients with learning disabilities (which involved checking electronic flags as well as daily ward rounds to try and ‘find’ patients with learning disabilities) revealed only three such patients in three weeks.
We have a flagging system for identifying people with a learning disability . . . that can only be put on when a patient comes in. We recently did an audit and found that . . . we couldn’t find anyone within the trust with a flag on their computer records when there WERE people with learning disabilities.
P61, matron
The most comprehensive records came from the hospital-based LDLNs, who could give concrete numbers of patients with learning disabilities referred to their service and demonstrated that they were able to both flag and track patients with learning disabilities through their own recording systems. However, all LDLNs observed that their systems were limited by a reliance on hospital staff to refer patients to them, and by the fact that most patients with learning disabilities come into hospital without a notification of their learning disabilities. They particularly noted their inadequacy in identifying or flagging outpatients.
How did staff identify patients with learning disabilities?
Figure 3 shows staff response to the question of whether or not they are routinely informed of a patient’s learning disabilities. Less than 8% of all staff stated that they are rarely or never informed. This figure is 2.8% for inpatient staff but rises to 17.3% for outpatient staff.
FIGURE 3.
‘If a patient in your care has learning disabilities, are you routinely informed of this?’ Responses to staff survey question 6 [n = 783 (includes those who answered both survey question 6, ‘If a patient in your care has learning disabilities, are you routinely informed of this?’ and survey question 26, ‘Which clinical setting do you mostly work in?’)].
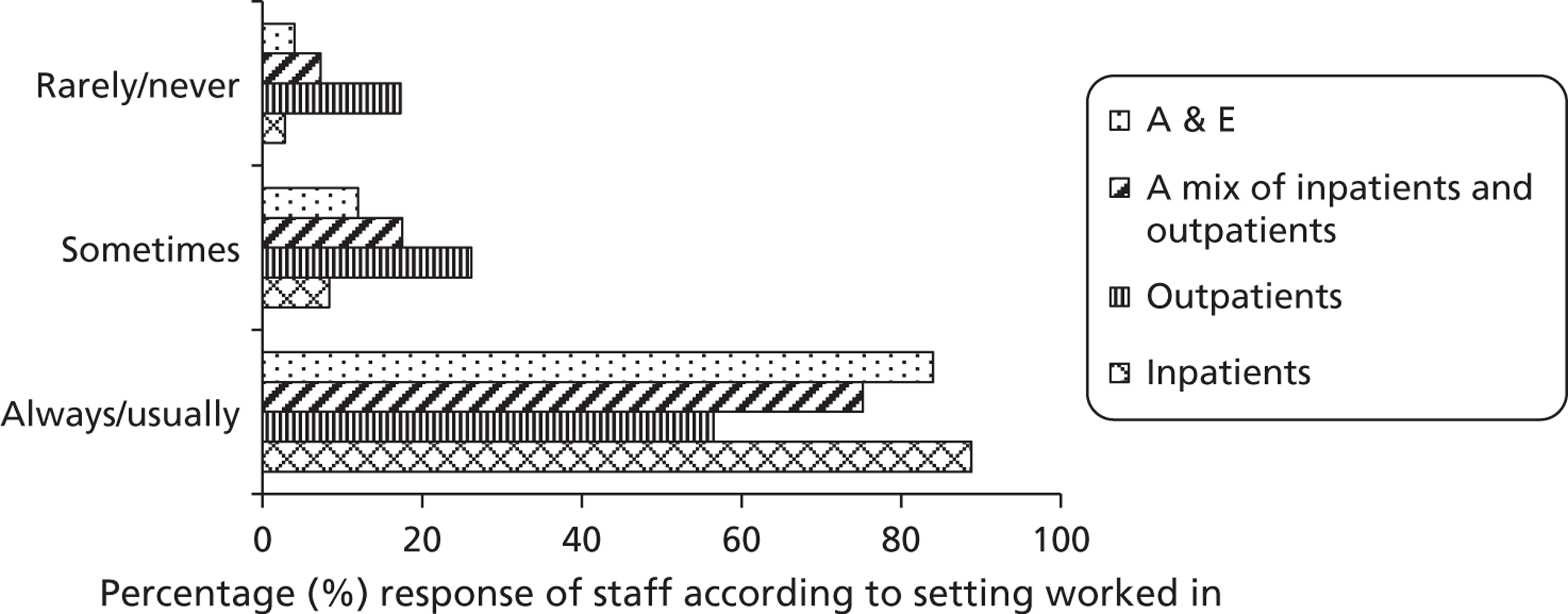
Figure 4 shows staff response to the question of how they usually find out that a patient has learning disabilities. This shows that the majority of staff did not identify the presence of learning disability through formal flagging systems, but rather through information obtained from colleagues within and outside the organisation (handovers and referral letters) or through direct assessment of the patient.
FIGURE 4.
‘How do you find out that a patient in your care has learning disabilities?’ Responses to staff survey question 7 (n = 987).
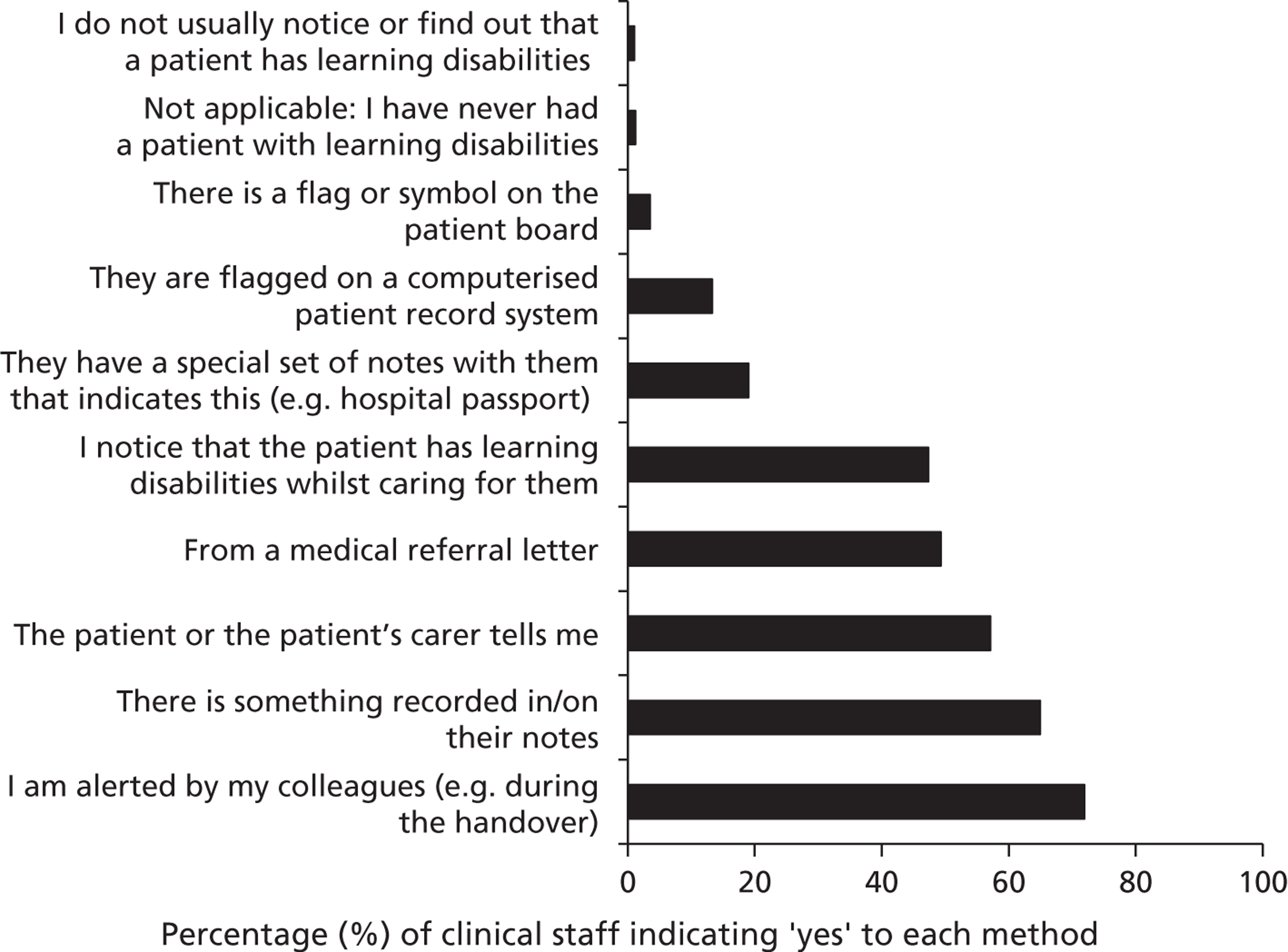
Figure 5 shows to what extent staff felt that they had been given sufficient background information about patients with learning disabilities to care for them in the best way. Although 69% of respondents (631 out of 915) felt that they were always or usually given sufficient clinical information, only 39.2% (359 out of 915) felt this way about information on the patient’s personal preferences.
FIGURE 5.
‘Are you given sufficient background information to enable you to care for patients with learning disabilities in the best way?’ Responses to staff survey question 8 (n = 915).
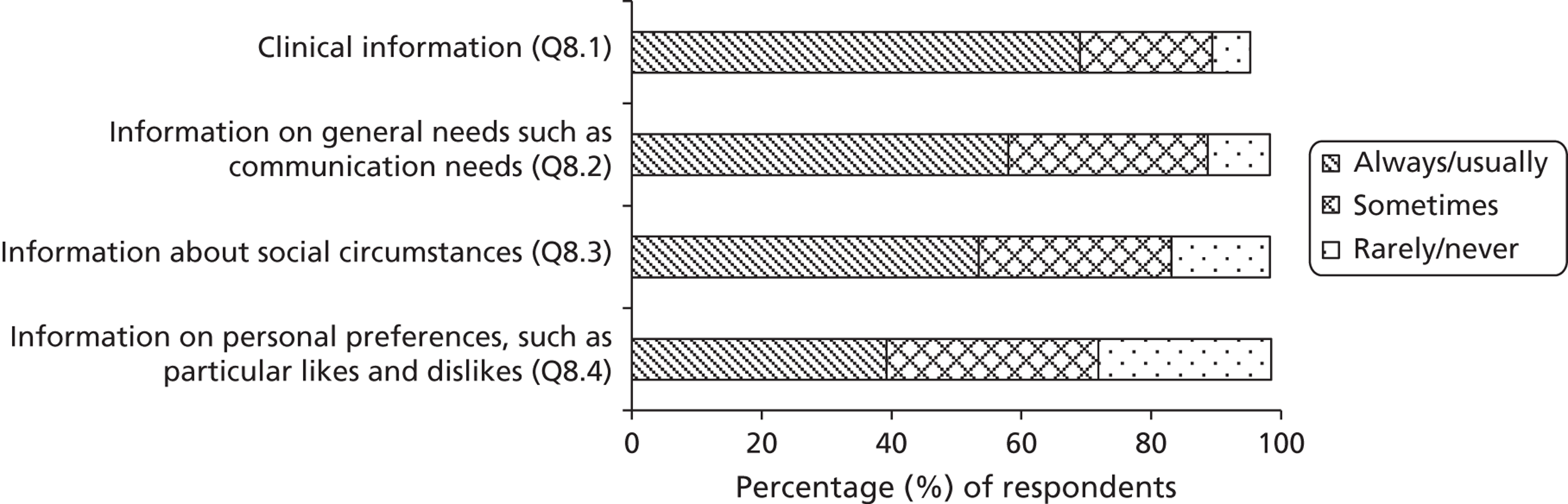
Several hospital trusts reported that one way of identifying or flagging patients with learning disabilities was through the use of special patient-held information documents which are owned and updated by people with learning disabilities and their carers to provide detail about important aspects of a person’s medical, nursing, social and emotional care needs. Patients and their carers are encouraged to bring these documents into hospital so that staff can use the information provided to modify and personalise their care of the patient (and hence make reasonable adjustments). These information documents have been given a variety of names, for example ‘patient passport’, ‘hospital passport’, ‘health action plan’ and ‘About Me book’. 103,104
The evidence from this study is that patient-held information documents are not a reliable way of identifying patients with learning disabilities. Patients do not always bring them in, particularly if the hospital admission is unplanned. Furthermore, many staff were unaware of such documents: although patient-held information documents had been introduced at all study sites, 61.1% of staff (601 out of 984) answered ‘no’ or ‘not sure’ to the question of whether or not their hospital used special patient-held information for people with learning disabilities (survey question 9).
Barriers to identifying patients with learning disabilities
It is clear that systems for identifying patients with learning disabilities are currently inadequate. Three key barriers were identified: lack of effective systems; lack of staff knowledge; and staff reluctance to flag patients with learning disabilities. There were also suggestions from staff that some people with learning disabilities may not want to be identified, although there was no evidence of this in the study sample of people with learning disabilities.
Lack of effective systems
The lack of effective systems for identifying people with learning disabilities stretches across and beyond organisations. The most significant barrier is the fact that the vast majority of people with learning disabilities (79%) have never been identified as such within any health or social care service system, and will therefore remain invisible within the hospital unless a system is implemented for screening and identifying this patient population. 43 Such screening systems are currently lacking, although LDLNs reported that they do occasionally get asked to assess patients with suspected learning disability. However, most unidentified patients will have mild to moderate learning disabilities, which are less likely to be suspected by staff.
Hospitals were further limited by a cross-organisational lack of integrated patient records. Over half of the respondents to the staff questionnaire (51.7%, 417 out of 815) said that they find out that a patient has learning disabilities from a medical referral letter; this rises to 78.4% (109 out of 139) for medical staff. Yet interview data and free-text questionnaire data showed that relevant information about learning disabilities is often not passed on by GPs. As a result, the hospital was not always aware of known learning disability, even for planned admissions or outpatient appointments.
Frequently when booking appointments, we are not informed that patients have learning disabilities and doctors will request [magnetic resonance imaging] scans which when the patient arrives to have, it is immediately clearly completely inadequate for such a patient to be able to cope with the scan requested and therefore has to be abandoned . . . Were it to be made known to the imaging staff that the patient had learning disabilities, allowances could have been made before the time of the appointment to cater for them.
P300, radiographer
Within some organisations, there was a lack of adequate electronic flagging systems, although those organisations were in the process of implementing such systems. Senior hospital managers noted the difficulties of correctly identifying the presence of learning disability. This raised questions about who could or should put the flags on. It was also frequently observed by managers at all trusts that the presence of a flag for learning disability is no guarantee that staff know what the implications of this are, causing them to doubt the benefit of such flags.
The lack of effective flagging systems made it difficult for LDLNs to ensure patients with learning disabilities received adequate support.
The only database is the one I keep and that’s relying on hospital staff informing me that the patient comes in. So I can’t go into a computer today and see how many learning disability patients are on these premises. I was at outpatients this morning and that’s only because the patient phoned me and told me they were coming and that they would like me to attend their clinic with them that I was there. Otherwise I wouldn’t know where any of my patients are.
P1272, LDLN
The lack of integrated flagging systems was not entirely cross-organisational. In one trust, patients with learning disabilities were flagged in A&E but this flag did not follow them through the hospital.
Lack of staff knowledge
As most patients with learning disabilities have never been identified as such,8 and many people with known learning disabilities who enter the health-care system are not flagged, whether or not they are identified as vulnerable patients in need of reasonable adjustments will depend on the ability of hospital staff to identify the presence of learning disabilities. There is strong evidence in this study that hospital staff lack the knowledge and skill to do so.
During the staff interviews, some staff demonstrated good understanding of what learning disabilities were, but this was not universal. Some staff gave examples of patients with dementia or dyslexia when asked about patients with learning disabilities. Even some senior nurses and consultants were not clear about what groups of patients fall within the definition. Most doctors and nurses admitted that they would find it extremely difficult to know whether or not a patient had mild learning disabilities, and they were therefore reluctant to consider undertaking the task of identifying learning disability.
Whereas with dementia [my colleagues] and I are very used to going along and making a new diagnosis, we would be feeling very, very uncomfortable on how to make a diagnosis of learning disability in someone who just passes through our system for the three weeks in their entire life.
P1249, consultant physician
I wouldn’t feel confident in actually saying that person has, and that person hasn’t.
P52, ward manager
Staff reluctance
Although senior managers understood the need for flagging in principle, there was a strong feeling of reluctance to flag patients with learning disabilities which pervaded all levels within the organisation, from the most senior hospital managers to junior ward staff. There were three main reasons for this, as follows.
A lack of understanding that identifying patients with learning disabilities is necessary
There was an underlying lack of staff understanding that patients with learning disabilities are at risk and in need of specific attention and adjustments. A common theme across staff interviews was the notion that all patients should be seen and treated as individuals, and that identifying ‘learning disability’ would not lead to care that was different or better suited to their needs. Interviewer:P25, staff nurse:
If you found out that a patient has a learning disability, is it compulsory on this ward for you to record it anywhere?
I don’t know . . . I don’t see how it would affect their nursing – how we give them their care. It wouldn’t make any difference if they’ve got a learning disability or not.
I don’t want patients with learning disabilities to have that title and a great big sticker put on them to say, ‘I’m a patient with learning disabilities, treat me very differently’ because I don’t want them to be treated very differently, I want them all to be treated as patients with individual needs.
P94, Director of Nursing
Concern about ‘labelling’ the patient
Many staff worried that any formal identification of the patient’s learning disabilities would lead to the patient being ‘put in a pigeon hole’. There was concern that this would lead to the patient receiving worse, not better, care due to potential negative staff attitudes towards learning disability; or that it would lead to staff making wrong assumptions about the patient’s abilities and needs.
If they are functioning quite well outside who am I to give them that label and say ‘Learning Disability’, because quite often there can be that stigma to it as well.
P211, consultant physician
I have to question why are we labelling people, whether it’s with a learning disability or with diabetes or with dementia – what is the purpose of us knowing?
P1270, Deputy Director of Nursing
Reluctance to ask the patient about their learning disabilities
Many nurses said that whereas noting severe and profound learning disabilities might be fairly straightforward, the picture was complicated if learning disabilities were mild. They were reluctant to ask the patient in case the question was insulting.
People can look very childlike and if people aren’t telling you they have a learning disability on arrival you’re not going to be judgemental and just say, ‘Look, you appear slow to me’. You’re not going to have that conversation. You’re going to treat them like you would anyone else.
P28, ward manager
Barriers to tracking patient care pathways
Although LDLNs in particular were good at tracking the hospital care pathways of patients with learning disabilities, there was a lack of organisational systems to ensure that all known patients with learning disabilities had their pathways tracked and their care co-ordinated. There was no effective cover for LDLN absence, for example (see also Chapter 9). In the absence of effective flagging systems and a general lack of staff understanding that flagging or tracking pathways might be important, it seemed that senior nurses who had been allocated responsibility for overseeing the care of patients with learning disabilities (such as matrons) were much less likely to be reliably informed about the presence of such patients within the hospital and to be able to track their hospital pathways.
Patient and carer views
Carers
Carers showed overwhelming support for the principle that patients with learning disabilities should be identified and flagged by the hospital. They recognised the need for adjusted health-care services and felt strongly that recording and noting information about learning disability was an important first step.
I think it should be on a computer system. Or maybe a note on her notes. I understand that some people might not want to be labelled in that way, but if there is some sort of note on the system, that could lead staff to having a quiet word with the family to find out more. I don’t think anyone would mind that.
P89, family carer
Patients
All study participants with learning disabilities who expressed their opinion on this issue were supportive of flagging the presence of learning disability within the hospital. It must be noted, however, that all people with learning disabilities interviewed for this study were self-selected. They had taken an active step to contact the research team or attend an open day. They therefore clearly identified themselves as having learning disabilities, and were probably less likely to oppose the notion of having their learning disability identified and flagged.
I think staff should be made aware of it so that they know and then they know how to deal with it.
P114, person with learning disabilities
Chapter 6 Providing reasonably adjusted health services
All trust boards should demonstrate that they have effective systems in place to deliver effective, ‘reasonably adjusted’ health services for those people who happen to have a learning disability. This ‘adjustment’ should include arrangements to provide advocacy for all those who need it, and arrangements to secure effective representation on PALS from all client groups including people with learning disabilities.
Recommendation 10 (p. 11). 4 Reproduced with permission from Michael J. Healthcare for All: Report of the Independent Inquiry into Access to Healthcare for People with Learning Disabilities. London: Aldridge Press; 2008
Chapter summary
This study found good examples of reasonable adjustments as well as examples where necessary adjustments were not made. Effective implementation of reasonable adjustments was affected by the following factors: (1) hospital structures, systems and policies that allow for the need for reasonable adjustments to be identified and acted upon; (2) funding and allocation of adequate resources; (3) management support for reasonable adjustments, and in particular support from ward managers; and (4) staff understanding of a wide range of potentially complex adjustments that may be needed.
The provision of extra aids or services (including, for example, patient-held information documents and the provision of a LDLN service) was often cited by hospitals as evidence that the trust provided reasonably adjusted services. However, although these were beneficial if used appropriately, there was strong evidence from all participant sources (and in particular from patients and carers) that ward culture and staff attitudes were crucial in ensuring hospital services were accessible to patients with learning disabilities.
Understanding of the need for reasonable adjustments was not uniformly present among staff, many of whom thought that ‘equal treatment’ meant ‘the same treatment’. Reasonable adjustments were often dependent on staff ‘common sense’ and flexibility. This points to the need for a culture where staff feel confident and able to make reasonable adjustments, with the support and supervision of senior colleagues.
The LDLN and the ward manager had key roles in the provision of reasonably adjusted services.
The barriers and enablers that have emerged in this study in relation to providing reasonably adjusted health services are summarised in an empirical subframework (Figure 6).
FIGURE 6.
Empirical subframework: barriers and enablers in relation to providing reasonably adjusted health services.
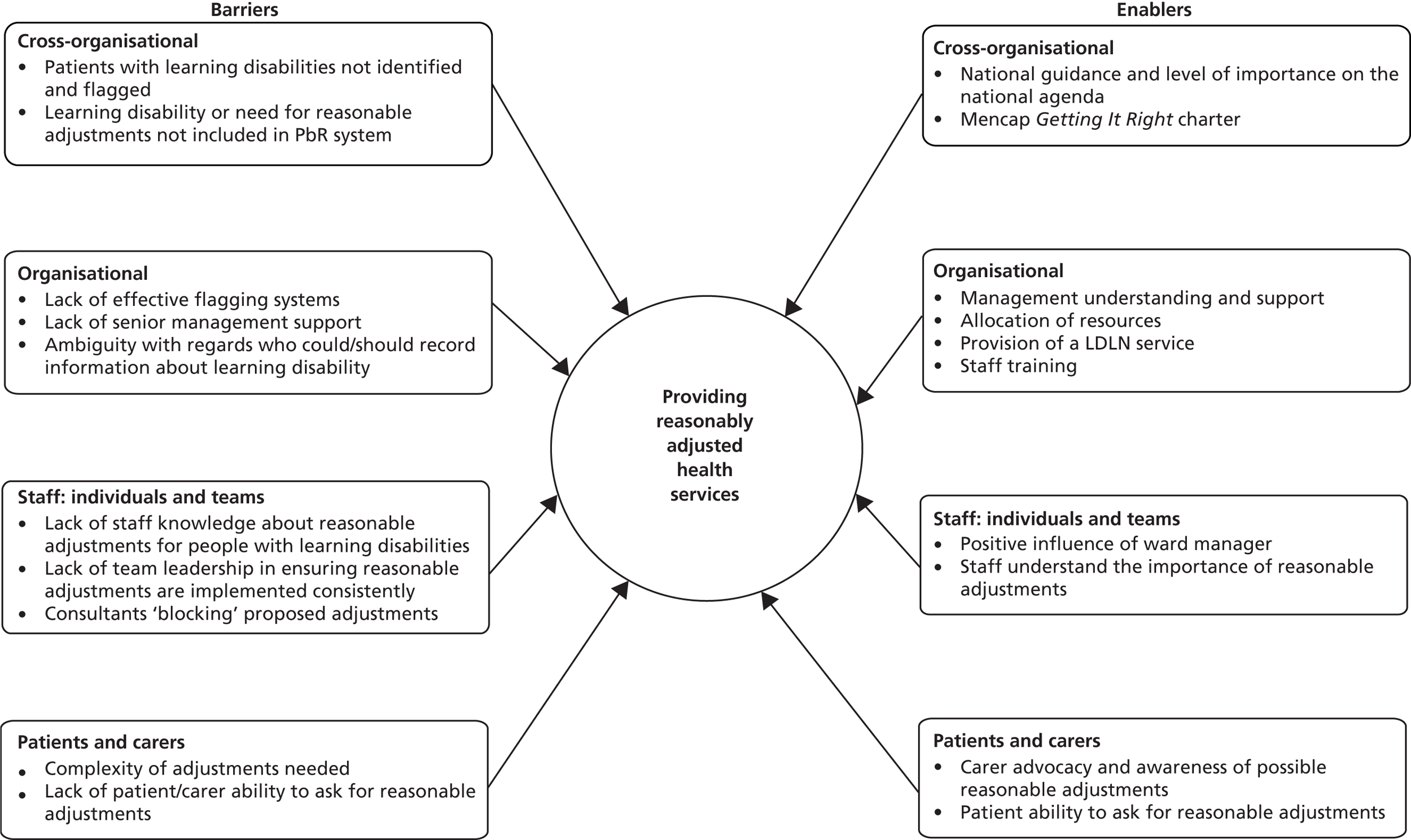
Reasonable adjustments implemented by the study sites
All six study sites had systems in place which aimed to facilitate the delivery of reasonably adjusted health services for people with learning disabilities. Senior hospital managers were aware of their legal duty and responsibility to provide reasonable adjustments and put resources into realising the provision of an equitable service. Flexible, lateral thinking was often evident and trusts endeavoured to enable patients with learning disabilities to access their services equitably. Table 5 gives some examples of a range of reasonable adjustments implemented by the study sites.
| Description of adjustment | Type of adjustmenta | |
|---|---|---|
| A. | Provision of an LDLN service by the hospital | Providing extra aids or services |
| B. | The LDLN provided training for hospital staff | Changing the way things are done |
| C. | Patients with learning disabilities were provided with patient-held information documents on which to record key information for the benefit of hospital staff, including likes and dislikes | Providing extra aids or services |
| D. | Patients with learning disabilities and their carers who attend outpatient appointments were provided with a bleep by the department’s receptionist, so they did not have to wait in the small waiting area | Providing extra aids or services |
| E. | Following lobbying by a hospital-based carer group, a disabled toilet was installed with sufficient space for changing the clothes of an adult | Altering physical obstacles or designs |
| F. | A patient with learning disabilities who needed dental treatment but could not bear to come into the hospital building was sedated in the car park (with his consent and his family’s support) | Changing the way things are done |
| G. | A patient with learning disabilities was offered a pre-scan visit to look around the scanning area | Providing extra aids or services |
| H. |
|
Changing the way things are done |
| I. | A patient with learning disabilities could not cope with tests and treatments. When he came in for dental surgery under general anaesthetic, several other necessary tests and treatments were carried out at the same time, involving a range of different clinicians | Changing the way things are done |
| J. | Carers were offered food, a bed and a parking permit | Providing extra aids or services |
| K. | A woman with learning disabilities liked her consultant and responded well to him. When she was offered her next appointment with a different doctor, her mother asked whether she could see the same consultant. The consultant rearranged his schedule so he would always be the doctor to see this patient | Changing the way things are done |
| L. | A medical assessment unit ensured that patients with learning disabilities were moved rapidly to the relevant ward | Changing the way things are done |
| M. | Another medical assessment unit allowed patients with learning disabilities who had become used to the staff and who only needed a few days in hospital to stay on the ward rather than be moved to a different ward | Changing the way things are done |
| N. | Patients with learning disabilities who had significant care needs were allocated additional care staff by the hospital | Providing extra aids or services |
| O. | Patients with learning disabilities were allocated a side room, or a quiet waiting area | Providing extra aids or services |
| P. | A staff nurse working in a busy bay of six patients took time between tasks to draw pictures for a patient with learning disabilities who liked colouring them in, and who may otherwise have found it hard to cope with the hospital day.
|
Providing extra aids or services |
| Q. | Patients with learning disabilities get a first appointment and/or a double appointment | Changing the way things are done |
| R. |
|
Changing the way things are done |
Facilitating factors necessary for successful implementation of reasonable adjustments
However, notwithstanding these positive examples, the application of reasonable adjustments ‘on the ground’ was not always consistent and evidence was gathered which demonstrated that good intentions at a policy level do not reliably translate to good practice.
It can be deduced from the examples in Table 5 that the implementation of reasonable adjustments requires a range of facilitating factors:
-
Hospital structures, systems and policies that allow for the need for reasonable adjustments to be identified and acted upon.
-
Additional funding and allocation of adequate resources (particularly for adjustments that involve provision of extra aids or services, or altering physical obstacles and designs).
-
Management support for reasonable adjustments (particularly where these adjustments represent a change to the way things are done). It is likely that many reasonable adjustments need to be instigated, encouraged and approved by the ward manager or the consultant, who in turn needs to be supported by senior management.
-
Staff understanding of a wide range of potentially complex adjustments that may be needed, and a ward culture where staff are willing to be flexible.
The following sections will examine examples of good and poor practice in the provision of reasonable adjustments, through consideration of these four influences on their implementation.
Hospital structures, systems and policies
Organisational systems for identifying learning disability
The ability of an organisation to make reasonable adjustments is in part dependent on recognition that an individual has additional needs and therefore requires, by law, adjustments to the care they receive. As discussed in Chapter 5, there were significant barriers to the trusts’ ability to identify patients with learning disabilities. This meant that reasonable adjustments, particularly those that require advance planning, could not be delivered as a matter of course.
The lack of advance communication of patients’ needs was not exclusively cross-organisational. Difficulties were also reported when inpatients were sent for tests in diagnostic departments, or when patients changed wards and crucial information was not passed on, demonstrating insufficient internal communication regarding patients’ needs.
I don’t think [staff] are prepared! But with our clients, it is usually quite obvious that they have learning disabilities . . . I don’t think our clients are flagged up on the computer. It would be good, because the staff could be prepared and adjust their approach.
P166, paid carer
There was also recognition that identification and flagging of learning disability is only helpful if it leads to the implementation of adequate reasonable adjustments. A number of participants questioned how that could be achieved, and how staff would know ‘what to do’ if their patient had a learning disability flag.
A flagging system with no learning disability expertise within the hospital is really a waste because you’re not going to be able to provide anything.
P2, LDLN
Provision of learning disability expertise
Trust boards may use the existence of a LDLN role as evidence that they have an effective system to ensure provision of reasonably adjusted services. The results of this study demonstrate that LDLNs can have a crucial role in ensuring that NHS hospital services are reasonably adjusted. They use their expertise to consider the reasonable adjustments that are required, to educate staff of the need to make appropriate reasonable adjustments and to ensure these are implemented successfully. Further evidence of the pivotal role of LDLNs is given in Chapter 9. The following quote summarises the rationale behind the need for a LDLN, with a focus on facilitating the implementation of reasonable adjustments:
. . . to break through barriers and not accept the rules and regulations that might be going in the trust. So if someone was saying, ‘You can’t have an appointment on a different day’, she could cut through some of that and say, ‘Well, actually I’m going to talk to the consultant and we’ll get a different appointment on a different day and we’ll do this’. Or if it was a ward issue, she’d have enough seniority to be able to say to a ward sister, ‘Well actually no, you need to change stuff, you need to let carers stay, you need to . . .’ or whatever, you know, ‘Visiting times might be visiting times but actually . . .’ – and would be able to sort those sort of things out.
P43, Director of Nursing
However, LDLNs could not be effective change agents and facilitate the changes suggested by this Director of Nursing unless they had the seniority and authority to do so, their posts had strong management support, and there was sufficient cover for post-holder absence. This is further explored in Chapter 9.
Planned versus emergency care
Service delivery within the NHS can be broadly divided into planned (elective) or unplanned (emergency) care. With planned appointments, tests or admissions, prior notification of patients’ needs is possible, which should make the provision of reasonable adjustments easier. A number of good practice examples were given which demonstrated the efficacy of advance planning.
Our patients are all elective so are screened in pre-assessment clinic. Any learning disability patients are flagged up to me as the senior sister prior to coming into hospital. One patient that was due for admission was cared for by his mother and we arranged prior to his admission to meet with his family and himself and during that visit familiarised him and his family with the ward and also talked about what his stay may include.
P269, senior sister (staff survey)
The importance of effective systems for identifying patients with learning disabilities is even more marked for emergency admissions, where the patient may be completely unknown to the hospital or where there is a delay in receiving information about a patient’s needs.
. . . if he was to be a planned admission, we’d have said, ‘he’s going to need to be able to be occupied during his day, etcetera’, that would have been part of the adjustments before admission. Because he’s been an unplanned admission, we’re chasing now to get it changed to what it needs to be.
P36, LDLN
Acute care in the NHS is often structured so that patients who require acute (emergency) medical or surgical care are assessed and monitored on admissions units and may subsequently be transferred to specialist wards for their ongoing care. Such a system may prove difficult for some patients with learning disabilities who find change and, indeed, busy environments difficult to cope with. Ward managers on admissions units frequently explained the considerations made in determining the most suitable clinical environment for their patients who have learning disabilities, hence making reasonable adjustments to their care (see examples L and M in Table 5). Some patients who needed frequent admissions were sometimes able to bypass this system, for example through the LDLN facilitating their immediate admission to the relevant ward, rather than the patient having to go through A&E.
Adoption of patient-held health records
One change adopted by all six hospital trusts was the introduction of patient-held health records such as ‘hospital passports’ as described in Chapter 5, How did staff identify patients with learning disabilities?. Trusts often suggested that this was an effective system to enable the delivery of reasonably adjusted services.
When patient-held records were used as intended, this system worked well. Of those staff respondents who did indicate that their hospital used such patient-held documentation, an overwhelming majority found it ‘very useful’ or ‘quite useful’ (97.6%, 321 out of 486).
I find that [with the patient-held health records] you get a lot more information for if they’re upset and the carer’s not there. And it’s just so helpful . . . Sometimes it can be things that we can deal with. It’s because we don’t put the lights out or because we do put the lights out. So we can deal with that here.
P31, HCA
However, many carers reported that the time and effort spent creating such a document was often unrewarded as hospital staff failed to look at or use the recorded information.
The nurse asked us to fill out a [patient-held health record] which was by our daughter’s bed – not one medical professional looked at it. It was a total waste of time completing it and appeared to be just for show.
P89, family carer
Some staff working on busy, fast-moving wards such as medical assessment units or A&E commented that reading patient-held documentation was not a priority. There was a perception that such documents contained information of a mostly social or emotional nature (including likes and dislikes), and that the nursing priorities lay with fast assessments of the patient’s medical condition.
Furthermore, many staff members reported not knowing about the existence of such documents. It seemed that the introduction, availability and use of patient-held health records was not consistent, and knowledge about their usage among staff was not universal. The evidence that such documents can contribute to patient safety is therefore very limited in this study.
Funding and resource allocation
Many reasonable adjustments require resources and therefore cost an organisation in terms of time and money. The amount of resource allocated to enable reasonable adjustments to be made depends upon a complex function of a number of factors. This may include the demographic make-up of the patient population to be served, the characteristics and expertise of staff working within the trust, the financial position of the trust, and the allocation of resources by the hospital’s management.
At present, NHS acute trusts do not receive additional funds for providing services to patients who have learning disabilities under the national PbR system.
There’s no additional funding. We’re putting in additional resources to make the reasonable adjustments but actually we’re not seeing any support in financial terms for that.
P1274, matron
In cases where relatively expensive reasonable adjustments are required, such as provision of a one-to-one nurse or care assistant, or indeed creation of a LDLN service, hospitals were required to allocate funds from within their existing budget. Over a quarter of respondents to the staff questionnaire (28%, 258 out of 914) agreed or strongly agreed with the statement ‘We do not really have the time or resources to cope with patients with learning disabilities properly’. However, when interviewed, some ward sisters did not question the need for extra resources and were willing to allocate the necessary resources if required.
We are never told we can’t get the resource because the money isn’t available . . . We absorb it within the costs, of the good budget management of a ward.
P1282, ward sister
In times of austerity, though, it is easy to surmise that scarcity of resources may impact negatively upon the ability of NHS acute trusts to provide reasonably adjusted services. Senior managers at one study site, which did not have a LDLN service, recognised the benefits of such a service but, as they had only been able to identify a very small number of patients with learning disabilities using the hospital, found it difficult to justify spending scarce financial resources on a LDLN.
Management support
Senior managers
Although the provision of reasonable adjustments is a legal requirement, the extent of their appropriate and timely execution, and the types of reasonable adjustment made within an organisation, depend in part upon decisions that are made at a managerial level and on the awareness of and consequent importance placed on the issue by senior managers and decision-makers. Their influence was felt in their drive to implement relevant policies and in the allocation of resources, such as the appointment (or not) of LDLNs or the provision of staff training. However, they could also be highly influential in their visible support for ‘changes in the way things were done’. Researcher field notes recorded the comment of one LDLN that if she found ward staff did not follow her suggestions for reasonable adjustments, she simply needed to alert the Director of Nursing, who would immediately request from the staff that these suggestions were carried out.
Unlike ward staff, senior managers had the oversight needed to enable the implementation of reasonable adjustments, in particular those that required resources or changes in the patient pathway that had implications beyond the individual ward. Some LDLNs also fulfilled the role of having this oversight.
Ward managers and junior staff
The data suggested that junior staff in particular may find it more difficult to adapt their usual practice and may require support from more senior members of staff in order to do so. It was proposed that such reticence on the part of junior staff is in fact an important safeguard; input from experienced staff who are able to understand the consequences of any actions is of great importance to the delivery of appropriate reasonable adjustments.
I guess a lot of the rigid rules are there for a reason, because we have this very pressured environment. They are actually to prevent mistakes happening . . . The concept that it’s more senior people making those decisions probably shouldn’t be thrown away lightly. Because I think those decisions need to be made by people who can actually see the wider ramifications of something that might at a junior level seem like an unnecessary rule.
P1265, clinical nurse specialist
Ward managers also have the oversight to take into account the needs of other patients on the ward and judge the effect of any reasonable adjustments on the functioning of the ward. It seems important, therefore, that ward managers support junior staff in the provision of reasonably adjusted care, either by directing them to implement appropriate adjustments, or by checking and approving adjustments suggested by junior staff. Without such leadership from ward managers, there is a danger that the provision of reasonable adjustments is inconsistent and (too) dependent on the knowledge and attitudes of individual staff members. An example of this is the common experience of carers that there is a discrepancy at ward level around which extra facilities or adjustments they are offered by staff.
Staff understanding and attitudes
Under- and postgraduate training
The provision of staff training around learning disability is an important reasonable adjustment; the need for this was highlighted in Healthcare for All. 4 It is clear from the examples, and it has been highlighted by the Equality and Human Rights Commission,48 that poor staff attitudes or a lack of knowledge and skills are a barrier to implementing reasonable adjustments, particularly if they involve a change to organisational systems and structures. This includes training on capacity issues.
All LDLNs in this study said that providing staff training was part of their remit, although some questioned how realistic it was to provide training for a very large number of staff across the hospital trust.
The staff questionnaire included questions on the training or guidance staff had received to help them care for patients with learning disabilities. Figure 7 summarises the results. It shows that significant numbers of staff had never received any such training, including over a third of all medical and dental staff and over half of all HCAs.
FIGURE 7.
‘Have you had any training to prepare you to care for patients with learning disabilities?’ Responses to staff survey question 8 (n = 875).
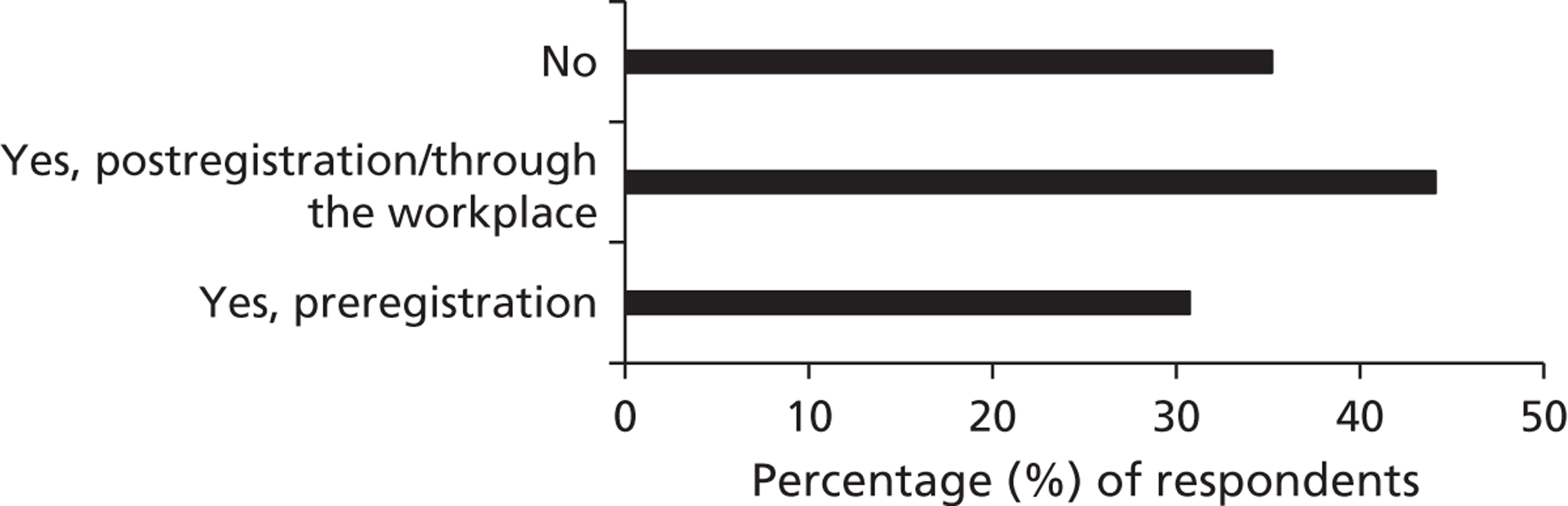
Staff attitudes and culture
As was demonstrated in Chapter 5, staff did not always recognise the need for identifying patients with learning disabilities. At the heart of this lies a lack of understanding that reasonable adjustments are necessary in order to provide people with learning disabilities with equal access to hospital services. One senior manager articulated this:
What we’ve found is that a number of staff have said, ‘Well, what we need to do is to treat everyone the same’, or ‘It needs to be individualised care’ . . . Actually it’s not doing the same, it is about recognising that there are individual needs and sometimes those needs are different and therefore, what adjustments are you going to make?
P43, Director of Nursing
Both individual staff members and staff teams working within an organisation have the ability to promote or hinder the adoption of reasonable adjustments. The provision of reasonable adjustments was often reported to vary between different hospital wards within the same organisation. This was particularly the case for the provision of reasonable adjustments which support carers.
On one ward a nurse was very abrupt with me. I asked for a parking permit and she said, ‘No-one gets a parking permit – unless she’s terminal you can’t have one – I have to pay for my parking too’, I asked another nurse on the same ward and she just said, ‘There you go,’ and she gave me one, and I have had one ever since. Parking is very expensive if you come every day.
P97, paid carer
Wards that were perceived as ‘good’ by carers and staff appeared to have a culture where staff felt confident and able to make reasonable adjustments, with the support and supervision of senior colleagues. Ward managers had an important role to play in ensuring that their staff understand the reasonable adjustments that are needed and implement them. There was a general agreement among staff and carers that ward managers and nurses at grass-roots level have the biggest influence on the hospital culture and the way patients with learning disabilities are cared for.
I don’t ever see a matron really knowing what’s happening on the ward, but nurses definitely.
P25, staff nurse
Staff on [ward] are brilliant. Everyone, from the cleaner to the senior consultant, is friendly, helpful and respectful. They all address the client every time, even if they know that the client can’t reply and it will be us who will reply for them. They treat the patients with total respect and dignity.
P166, paid carer
Interviewer:P166:
What do you think makes the staff so good on that ward?
I put it down to the ward manager. It affects the total attitude of all the staff.
Conversely, the following quote from a care home manager, who had sent in three of her staff members to ensure that a man with very high support needs could be supported to access hospital care, exemplifies a ward culture where reasonable adjustments are not routinely made for patients with such needs:
A registrar came out and he said, ‘Oh my God, three carers?’ and I said, ‘Yeah.’ And he said, ‘Well what was Dr [name] thinking about sending him here? How are we supposed to manage this boy? I’ve got one nurse to six beds. You know he’s very challenging, my staff team are scared of him.’
P184, care home manager
Perceptions of reasonable adjustments: ‘common sense’ or ‘breaking the rules’?
Many reasonable adjustments are dependent on staff ‘common sense’ and flexibility. Staff members’ perceptions of the actions required to make reasonable adjustments often lay on a spectrum ranging from ‘common sense’ to ‘breaking the rules’.
Sometimes we have to bend the rules. Things like even wheeling them down to the anaesthetic room. Don’t put them on a trolley, if they don’t want to go on a trolley. Just leave them in the wheelchair or walk down, whatever they want to do. And just bend the rules a bit and see what works best for them.
P53, staff nurse
The following extract from researcher field notes of a conversation with an LDLN demonstrates a ‘common sense’ attitude:
Someone with learning disabilities who needed a scan was shown around beforehand. The radiographer had suggested, without prompting, that if the patient feels OK during this tour, they actually do the scan there and then – ‘it only takes 5 minutes, we can always fit it in’ – rather than going home and having to come back for the planned appointment. LDLN thinks that such flexible thinking was a result of the training she gave to the radiography department.
Researcher field notes
Patient and carer views
Both patients and carers spoke repeatedly of their desire that hospital staff should be kind and patient, signifying the importance of a positive hospital culture in enabling patients with learning disabilities to access services. Selected comments of patients with learning disabilities are presented in Table 6. The views of carers are further discussed in Chapter 7.
| Quote | Type of reasonable adjustment |
|---|---|
|
Creating positive staff attitudes and culture |
|
Creating positive staff attitudes and culture |
|
Providing extra time |
|
Staff training, staff attitudes |
|
Reduce waiting times |
|
Involving carers as experts |
|
Open visiting times, positive staff attitudes |
The carer and patient interviews highlighted the importance of individual assessment of the necessary reasonable adjustments. For example, whereas providing a side room or a quiet waiting area may be essential for some patients with learning disabilities in order to cope with the hospital environment, for others the opposite is true.
I was upstairs in a ward with some people and then I went into a quiet room, they’ve put me into a quiet room . . . It was too quiet. And too lonely . . . It’s really hard when it gets really quiet and really lonely . . . And I didn’t have anybody to talk to.
P212, patient with learning disabilities
Chapter 7 Involving carers as partners in care
Family and other carers should be involved as a matter of course as partners in the provision of treatment and care unless good reason is given, and trust boards should ensure that reasonable adjustments are made to enable and support carers to do this effectively. This will include the provision of information, but may also involve practical support and service co-ordination.
Recommendation 3 (p. 11). 4 Reproduced with permission from Michael J. Healthcare for All: Report of the Independent Inquiry into Access to Healthcare for People with Learning Disabilities. London: Aldridge Press; 2008
Chapter summary
This study found that there are many positive examples of carer involvement, but this remains patchy and unpredictable. The most important factor contributing to the effectiveness of carer involvement was the degree to which staff understood the importance of carer expertise (rather than simply carer work) and welcomed it, and the degree to which the roles of both staff and carers were clarified on an individual basis. With regards to the latter, there were particular tensions and misunderstandings between hospital staff and paid carers.
A lack of staff understanding and acceptance of the role of carers as experts (i.e. staff not listening to carers) was a strong contributing factor in compromising patient safety.
Practical support for carers was essential in order to achieve effective carer involvement, as was a positive and welcoming staff culture. The ward manager had a pivotal role in this.
The lack of integration between health and social care funding was a barrier to active carer involvement; in particular, paid carers in the community are not funded to provide continued (and often necessary) support when the patient is in hospital.
The barriers and enablers that have emerged in this study in relation to involving carers as partners in care are summarised in an empirical subframework (Figure 8).
FIGURE 8.
Empirical subframework: barriers and enablers in relation to involving carers as partners in care. ICU, intensive care unit.
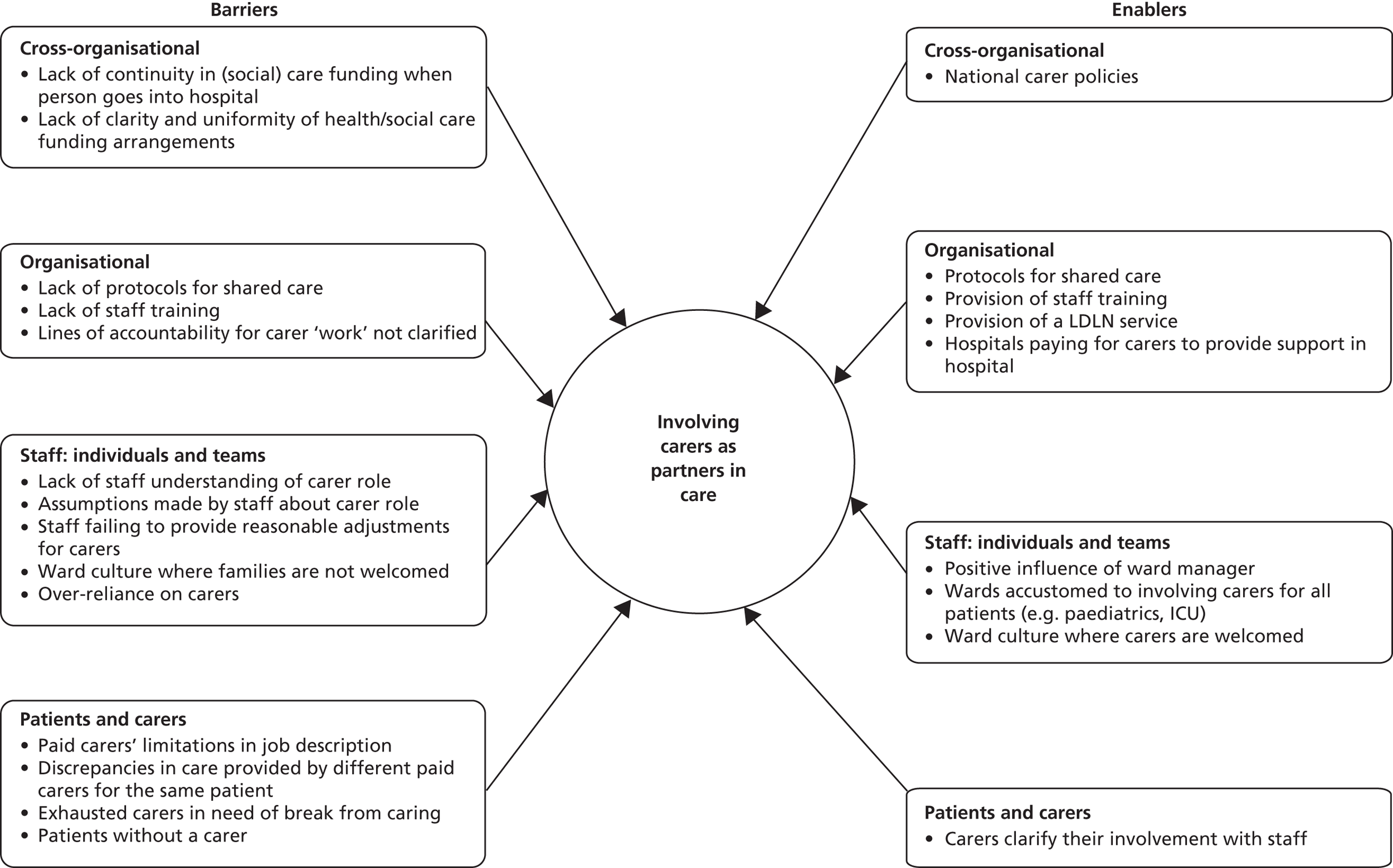
Carer policies
During stage I, two trusts had formal policies in place to support carers, and three trusts were in the process of developing such policies. These policies concerned carers of any hospital patient, not just carers of patients with learning disabilities. The policies included the provision of the necessary support and information for carers. One trust’s carer policy was detailed and extensive, directing staff to identify carers and involve (rather than just inform) them at all stages of the patient’s journey and to listen to carer expertise. One hospital trust had developed guidelines for the admission of patients with learning disabilities which included involving the carers.
During the course of the study, there was further development of carer policies, prompted in part by a national focus on the needs of patients with dementia. Several trusts had more detailed policies and support for carers in place during stage III. This included the provision of a special ‘carer badge’, designed to ensure that carers would not be questioned about staying with the patient outside visiting hours. Such badges came with an entitlement to parking permits and staff discounts in the hospital canteen. Evaluation of such schemes had not yet happened; for example, it was not yet clear how staff decided who could be issued with such badges.
Interviews with senior managers showed that there was a good understanding of carer involvement among Directors of Nursing and Medical Directors and strong support for welcoming carers as partners in care. Ward nurses were not always aware of the existence of policies but mostly understood the requirement to provide extra facilities for carers.
Carer and staff perspectives
Sources of bias
It must be borne in mind that the sampling strategy is a source of selection bias. As the principal method for questionnaire distribution was through the LDLN (particularly in the three hospitals with an on-site LDLN), it is probable that respondents were more likely to be carers who had received input from the LDLN. It is likely that this had a positive impact on their hospital experience (see Chapter 9).
Furthermore, there is the strong possibility of response bias, as those carers who hold particularly strong views on the care received (whether positive or negative) may be more likely to respond.
These limitations in the sampling strategy mean that the extent to which positive and negative carer experiences are representative of all carers cannot be determined. However, it does not negate the analysis of contributing factors to (in)effective carer involvement.
Carer perspectives
The full results of the carer questionnaire, including all free text comments, are listed in Appendix 5. Figure 9 gives an overview of the answers to questions 4–20, related to the hospital experience, ranked in order of the level of respondent agreement (highest first). It shows that a high proportion of carer respondents (85%, 75 out of 88) stated that staff were welcoming and supportive of them as the person’s carer.
FIGURE 9.
Carer feedback on the hospital experience, in response to carer survey questions 4–20 (n = 88). The data do not total 100%, taking into account missing data (respondents who did not answer the question).
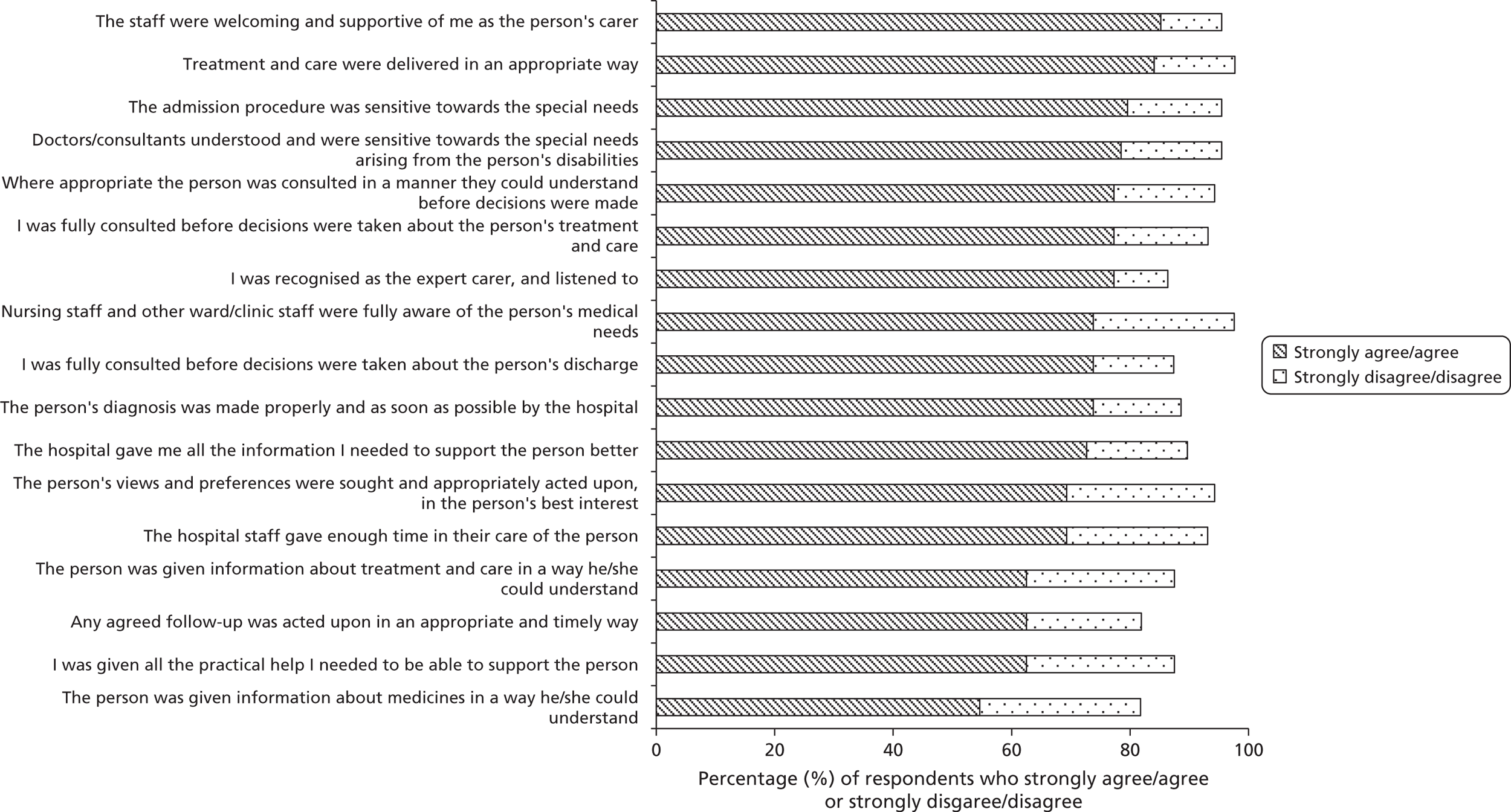
Carer respondents were asked ‘Overall, how satisfied are you with the standard of medical care provided to the patient by this hospital?’ and could give a rating between 1 and 10, where 1 was ‘not at all satisfied’ and 10 was ‘extremely satisfied’. The mean score was 7.3 (n = 84). Asked how satisfied they were with the ‘experience’ for the patient, the mean score was 7.0 (n = 83).
Carers were invited to provide ‘any other relevant comments’ in a free text box; 59 respondents did so. These comments were a mixture of positive and negative (summarised in Table 7), with some respondents describing both positive and negative experiences. Such ‘mixed’ comments were a result of opposing experiences on different wards, or differences in attitudes among staff, or one negative aspect of an overall good hospital experience.
| Carer perspectives | |
|---|---|
| Positive experiences | Negative experiences |
| Patient care | |
|
|
| Carer support | |
|
|
| Information sharing | |
|
|
| LDLN service | |
|
|
The issues raised in the questionnaire were further explored in the carer interviews. This confirmed that positive practice was present at each study site, but was not uniform within hospital sites or even within wards. For example, the following comments were made by two respondents from the same hospital:
I would like to thank hospital staff and especially [LDLN] for offering all support and recognition to carers from [residential care setting]. We had unlimited amount of time for stay with the patient, access to hospital staff and free parking permission during all period. Staff was friendly, professional and attentive, gave explanation when was asked and took their time with the patient to ensure she understands what they were doing.
P49, paid carer
Nurses/doctors need to listen to carers when they express concerns. We were not taken seriously on a number of occasions, leading to serious consequences for the person we support.
P97, paid carer
Staff perspectives
The staff survey (Appendix 4) contained a number of statements about involving carers; respondents were asked to rate their level of agreement with these statements. The responses to carer-related questions are summarised in Figure 10, ordered by level of agreement (highest first). This shows an overwhelming level of support among staff for carer involvement. One respondent commented in the free text box:
You can’t care for those patients or any patient without involvement of family and carers.
P94, Director of Nursing
FIGURE 10.
Staff views on carer involvement, in response to carer-related questions in the staff survey. Questions 10.5 and 10.7: n = 914; questions 11.1 to 11.11: n = 875.
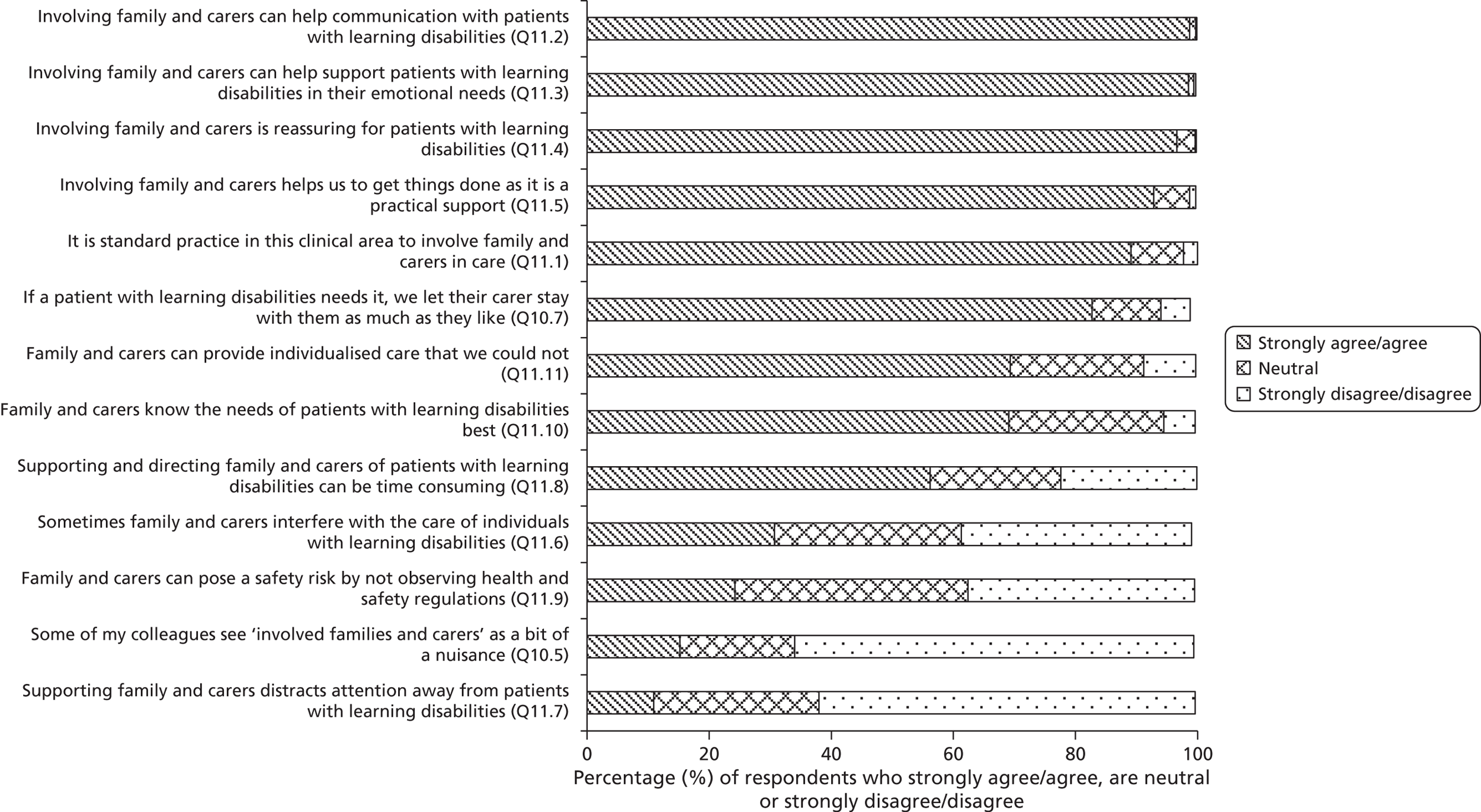
The interviews with clinical staff confirmed and expanded on the results of the staff questionnaire. Most nurses stated that they welcomed carers and that carers were offered practical support, in particular food and drink, unlimited visiting hours and facilities to stay with the patient. However, carer involvement was not always without problems or tensions. The positive and negative experiences of carer involvement from the perspectives of hospital staff are summarised in Table 8.
| Staff perspectives | |
|---|---|
| Positive experiences | Negative experiences |
| Carers provide important help | Who cares? |
|
|
| Carers need support | Under-involved carers |
|
|
| Over-involved carers | |
|
|
| Time | |
|
|
| Funding | |
|
|
Understanding carer roles and carer involvement
The positive picture emerging from the staff questionnaires and, to a lesser extent, the carer questionnaires is not entirely straightforward. There were persistent reports across all study sites of compromised patient care stemming from inadequate carer involvement, leading to compromised patient safety in a number of cases. Analysis of these reports showed that a major contributory factor was a lack of agreement on carer roles and diverse understanding of the concept of carer involvement. Conversely, where the carer role was well understood and supported, with carers’ concerns listened to and acted upon, reported outcomes were good and carer satisfaction was high.
In order to understand the barriers to effective carer involvement more fully, the following sections look in detail at the various aspects of the carer role, at staff perception of this role, and at the differences between family carers and paid carers.
Carer roles
Carers and staff described a range of tasks and roles that can be summarised as follows:
-
reassuring the patient
-
preventing ward disturbance
-
giving basic (nursing) care
-
providing communication support
-
contributing expert knowledge
-
participating in decision making
-
keeping the patient safe.
(a) Reassuring the patient
The presence of a familiar carer often helped patients to cope with the hospital environment.
Interviewer: Was it good having [Mum and Dad] there?
P115, patient with learning disabilities: Yeah. Because I felt safe with them around you see.
(b) Preventing ward disturbance
Staff and carers mentioned that some patients with learning disabilities coped better if they had someone with them who could keep them ‘occupied’. Without carer support, managing unconventional or challenging behaviour that could be disturbing to the ward and other patients could be difficult for staff.
It’s better to have the carer in, than have a complex patient with learning disabilities where we’re faced with really challenging behaviour because everything is strange and we’re all strangers.
P38, Director of Nursing
(c) Giving basic (nursing) care
Many carers supported the nurses’ tasks by assisting the patient with washing, dressing, feeding and toileting. These tasks could be time-consuming. Some patients with multiple disabilities needed one-to-one (or even two-to-one) support with basic nursing care when they were at home. In some cases, carers also offered to assist with the administration of medication.
(d) Providing communication support
Carers of patients who had communication difficulties acted as a ‘bridge’ between the patient and the hospital staff. They could interpret the patient’s communication and help hospital staff understand it, and they could ‘translate’ hospital staff’s communication and information about what was happening in a way the patient could understand and cope with. Doctors and nurses found communication support from carers invaluable in their assessment of the patient’s needs.
[The patient] was quite good at communicating but she was very repetitive in what she kept asking me . . . I really, really would have found it very difficult without the carer who was with her.
P84, Medical Director
(e) Contributing expert knowledge
Carers had in-depth knowledge of the patient and his or her needs, and could therefore advise and support staff in their attempt to understand the patient’s needs. This was important in providing timely treatment and care. Carers’ expert knowledge also meant that they could advise staff on providing appropriately adjusted care.
I looked after one gentleman and he would only have mustard with all his food, his drinks, his tablets, he would only have mustard and without mustard there’s no hope in getting anything in him. I only found that out by talking to somebody that knew him.
P33, staff nurse
(f) Participating in decision-making
Participating in decision-making around care and treatment, including discharge planning, goes beyond simply being informed by hospital staff of the care and treatment given.
I have found it invaluable to work closely with the patients’ family/carers and involve them with the plan of treatment. This encourages good communication and helps the family/carers feel their loved one is well cared for and in the right environment whilst they are being treated.
P803, senior staff nurse
(g) Keeping the patient safe
The role of the carer as someone who ensures that the patient is kept safe was described by a number of carers who felt that without their constant presence, the patient would be left anxious, poorly supported, lacking in basic nursing care and even at risk of harm.
I felt I couldn’t leave him. I stayed with him from 8 am to 7 pm every day, because the nurses were so clueless.
P17, family carer
Carers as ‘visitors’, ‘workers’ or ‘experts’
In analysing the tensions between carers and staff with regards to carer involvement, considering whether carers are seen as ‘visitors’, ‘workers’ or ‘experts’ as described by Allen63 (see Chapter 4, The roles and experiences of carers in hospitals) provides a useful framework. There is a certain degree of overlap between these three roles.
Carers as visitors
Despite carer policies that indicate the need for recognition of carers and provision of support for their role, there were examples where staff treated carers no differently from ordinary visitors. This was evident in reports of hands-on, involved carers who were asked to leave at the end of visiting hours. Such carers felt unwelcomed in their role as carer and unsure about the extent to which they could be involved with the patient’s care. There seemed to be a culture among some staff, and on some wards, of a strict adherence to hospital rules with little flexibility and support for the carer role and little understanding that carer involvement was a necessary ‘reasonable adjustment’ for many patients with learning disabilities. Several carers described a difference in attitude among different members of the same staff team, with some nurses treating them as part of the team and other nurses imposing the same restrictions as on visitors.
Carers as workers
Roles (a) to (c) and part of role (d) as described in Carer roles can be described as ‘worker’ roles, subordinate to the nurses. Carers performing worker roles relieved the staff (mostly nurses) of often time-consuming tasks that fell within the hospital staff’s remit. Both staff and carers recognised that carers were often better placed than hospital staff to fulfil these tasks effectively, as the carer knew the patient well and was trusted by the patient. The ‘worker’ roles helped the patient fit in with the routines of the clinical area and enabled staff to carry out their work in the usual way. Carers fulfilling roles (a) to (d) were greatly welcomed and appreciated by the hospital staff.
Carers as experts
Roles (e) to (g) and part of role (d) as described in Carer roles can be seen as ‘expert’ roles, different from and complementing the work of the hospital staff and thus making the carer an expert partner in care. Unlike most of the ‘worker’ roles, these ‘expert’ roles cannot be performed by hospital staff. In their role as experts, carers could help staff understand the reasonable adjustments needed for an individual patient. They often directed staff to a deviation from usual practice and routines in order to make hospital care acceptable and accessible to the patient. It is the ‘expert’ aspects of the carer roles that are particularly relevant in ensuring patient safety.
Discrepancies between staff and carer understanding of the carer role
The findings of this study suggest that ‘involvement in provision of treatment and care’ may be interpreted in a variety of ways by hospital staff. Many respected and appreciated carers as ‘workers’ but this did not necessarily extend to the inclusion of carers as ‘expert and involved partners’.
The staff and carer perspectives illuminate discrepancies in the way the concept of ‘carer involvement’ was understood. Staff mostly spoke about the importance of carers’ help in reducing the patient’s anxiety, ‘calming the patient down’, and providing help with basic nursing care – in other words, they spoke about carers as ‘workers’. Many carers, on the other hand, talked about the importance of sharing their expert knowledge of the patient with staff – they spoke about carers as ‘experts’. There were particular concerns if such expertise was not acted on by staff. Although some staff recognised, welcomed and sought carer expertise, carers acting as experts could also be seen as challenging by staff. Carers who reported that they felt they were not listened to usually referred to the fact that their expertise was dismissed and not acted upon – even if their role of workers was welcomed.
Difficulties arose in a variety of ways, and occurred mostly when staff and carers had different perceptions of the nature of the carer’s role, for example when:
-
carers viewed themselves as ‘experts’ and wished to contribute their expert knowledge, whereas staff viewed them as ‘workers’
-
carers wished to be seen as ‘workers’ whereas staff viewed them as ‘visitors’
-
staff thought the carers were experts, whereas the carers’ expectations were to be ‘workers’ (for example, short-term paid carers who had little expert knowledge of the patient)
-
staff thought the carers (usually paid carers) were ‘workers’ in the sense of being able to assist with basic nursing care, whereas the carers felt they could only assist with communication and providing reassurance.
Examples of some of these difficulties surrounding the carer’s role, as well as the factors that facilitate effective carer involvement, are given in Table 9.
| Examples of difficulties around carer involvement | Nature of barrier(s) | |
|---|---|---|
| A. | A mother told hospital staff that her adult son always had problems with diarrhoea when he was on antibiotics and therefore needed anti-diarrhoeal medication. She commented:
|
Carer expertise not taken into account |
| B. | The parents of a man who was in hospital for several weeks were not offered any food or drink. They felt that the patient needed one of his parents to support him 24/7, but found it difficult to afford meals and refreshments from the hospital canteen, which added up to over £10 per day | Lack of practical support for the carer ‘worker’ role |
| C. | A brother was asked by a ward nurse to feed the patient; the nurse then left. The brother had to leave, but the nurse did not check this | Lack of clarification of carer ‘worker’ role |
| D. | Paid carers noticed that the patient’s usual medication had not been administered in hospital. They were used to giving the medication at home and were not sure whether they could and should give it in hospital | Lack of clarification of the boundaries of carer ‘worker’ role |
| E. | Despite repeated explanations from a patient’s sister that the patient could not read and therefore needed literacy support, the patient was asked to sign her name on consent forms and received no help with filling in the menu forms | Carer expertise not taken into account |
| F. | A patient started to develop a pressure sore while in hospital. The nurses had left the carers to provide basic nursing care, and had not checked the patient’s pressure areas | Assumptions made about the extent of nursing care provided by carers |
| G. | A patient with severe learning disabilities, autism and challenging behaviour was accompanied to an emergency hospital admission by several members of his care staff team, who felt that without their support he would not cope with the hospital environment. The carer explained repeatedly to the ward staff that the patient needed a side room because of his autism and challenging behaviour; it would put other patients at risk if he was put on the ward. She was particularly concerned about the equipment and tubes used by other patients. The patient was moved into a bay, but ward staff decided to move him back into a side room when other patients’ families complained of the disturbance caused by his noises. The patient, who had presented with very high blood sugar levels, needed insulin injections but the ward staff refused to administer these as they could only be given if the patient was restrained or sedated – despite the carers’ willingness to support restraint in his best interest. Instead, they handed the injections over to be administered by the untrained care staff. Relationships between the ward staff and the carers were hostile. The carers felt that their role was to enable ward staff to do their job, and were exasperated that they were left to do all nursing tasks themselves, including some medical interventions that were beyond their skills | Staff expect carers to provide all nursing care, but do not welcome or act on carer expertise; lack of practical support for carer ‘worker’ role |
| H. | A paid carer was actively involved with basic nursing care for the patient. However, another paid carer from the same care team did not get involved with basic nursing care at all. This was frustrating and confusing for ward nurses | Lack of clarification of extent of ‘worker’ role |
| I. | One of the researchers, who had no background or expertise in health care, was observing a tracer patient she had only just met. She was asked by the nurse to assist with taking the patient’s blood. She refused and felt highly uncomfortable about this situation | Lack of role clarification |
| Examples of effective carer involvement | Nature of enabler(s) | |
| J. | Ward staff took the initiative to telephone paid carers with feedback and information, and were always forthcoming when information was requested | Active and effective information sharing by staff |
| K. | On arrival at an outpatient clinic, the paid carer accompanying the patient asked the nurses whether the patient could be fast-tracked. The nurses spoke to the doctor and fitted the patient in quickly. Carers reported that this was usually the case | Staff listen to carer expertise and are flexible in accommodating patient needs |
| L. | Following a poor experience where a client from a residential home was left without sufficient food and drink in hospital, the home’s manager set up a protocol with ward staff in order to manage mutual expectations and involve carers as part of the ward team | Structured and formal clarification of carer roles |
| M. | Ward nurses telephoned a patient’s mother every morning, asking for advice on how to look after the patient until such time as the mother could come on to the ward. When the nurses expressed concern about the patient’s drowsiness and poor eating in the mornings, the mother explained that this was normal for the patient. The ward team and the patient’s mother kept in regular telephone contact throughout the patient’s stay, giving updates and asking advice. New nurses would introduce themselves as the patient’s key nurse for the day. They checked when the patient’s mother would be able to come in and ensured that one-to-one patient support was available in her absence. The mother felt welcomed, able to care for her daughter without getting worn out, and reassured that her daughter was well cared for at all times | Good communication between the carer and all members of the ward team; carer expertise sought and acted upon; carer role clarified and supplemented appropriately every day |
| N. | A mother was concerned about the patient’s ability to cope with the environment on a day surgery ward. She asked if it was possible to have a separate room, but this facility did not exist; however, she was allocated a bed by the window. Together with the ward staff the mother was able to create an open space looking out of the window with the bed curtains drawn and the patient’s own possessions brought in | Carer’s expert advice welcomed and acted upon |
| O. | A ward sister was described by a carer as ‘running a tight ship’, ensuring that all staff communicated well with each other and with patients and carers. The carer felt that she was listened to by all staff at all times
|
Ward sister instrumental in creating positive ward culture |
Specific difficulties around paid carers
There were also some unique tensions around paid carers, who were not necessarily seen and supported as ‘carers’ in the same way as family carers. One hospital’s carer policy explicitly stated in its definition of a carer that ‘the carer we refer to is not employed to provide this help’. However, in many ways, the position and role of paid carers was similar to that of family carers. Tensions were related to limitations in paid carers’ job descriptions and (for some) limitations in their knowledge of the patient, and nurses’ perceptions of paid carer roles.
Role expectations
Hospital staff often made erroneous assumptions about the paid carer role. Not all nurses and HCAs were aware of the fact that some paid carers provided social care rather than support with basic physical care tasks. If carers provided intensive support at home, assisting the person with learning disabilities with all tasks of daily living such as feeding, washing and toileting – sometimes including skilled tasks such as the administration of percutaneous endoscopic gastrostomy (PEG) tube feeding – they often continued to perform these basic nursing care tasks when the patient was in hospital. In other cases, carers might simply be there because the patient could not navigate the hospital pathway alone; they would not expect to be involved in basic nursing care tasks.
This could lead to compromised safety if ward nurses assumed that paid carers were health workers like themselves, and left caring tasks to paid carers who could be ill-equipped (or even forbidden by their managers) to perform them. The following quotes, taken from different study sites, exemplify these tensions.
[The hospital staff] expected us to do things that we shouldn’t really be doing. They asked us to help with toileting, but we are not here to do that. We never help our clients with toileting . . . [The nurses] asked our support workers to go in for some quite intimate procedures, like helping with a groin wound: ‘Could you just come in and hold this or push this?’ Now that could be really awkward . . . It blurs the boundaries of your relationship with the client. You have to think about going back with the client into their house, and it would feel really awkward if you have done something so intimate with them . . . Personal care is just not our job. Our job is to get clients to appointments, things like that. So we give our staff quite clear boundaries about what they shouldn’t be doing. But our staff are made to feel uncomfortable on the ward if they are asked to assist and they say no.
P161, paid carer
If they’re a live-in carer or full-time carer of that patient then they should be fully involved in caring . . . here in hospital as well . . . I don’t think it’s any use to me or the patient for them just to be sat there . . . Why would you just need somebody to sit there in a chair, you know, not being involved in feeding?
P42, senior staff nurse
Ward staff further noted with frustration that the nature of paid carer support could vary even for the same patient, with some carers providing significant help with basic nursing care whereas others ‘just sit there’.
Paid carers as non-experts
Not all paid carers knew the patient well. Some were new or short-term agency staff who could not provide even the most basic information about the patient (including the patient’s name), which was difficult and frustrating for hospital staff.
Accountability
The issues of accountability and supervision of paid carers in hospital were not clarified. Ultimate responsibility for the care of a patient who is on acute trust premises lies with that trust. This is of relevance where ward staff leave basic nursing care to carers, or where paid carers perform their usual care tasks when their client is in hospital.
Barriers to and facilitators of carer involvement
The following were major factors contributing to effective care involvement:
-
protocols for shared care (including clarification of roles)
-
practical support for carers (including breaks from caring)
-
a staff culture where carers are welcomed as a matter of course
-
funding for high care needs.
Protocols for shared care
Many of the tensions between carers and staff arose simply because there was no clarity about mutual roles, in particular:
-
whether carers were experts or non-experts (or not carers at all, but simply a visitor)
-
to what degree carers would contribute to the ‘worker’ aspect of caring.
Carer involvement was most effective where there was good communication between the carer and the ward staff, and where ward staff were clear and explicit about responsibilities and roles, accommodated the contributions from carers and actively sought their expertise. Several trusts had become aware of the need to develop protocols for shared care, whereby the role of family carers (not limited to carers of people with learning disabilities) is made explicit and their contribution discussed. However, this was being trialled after the data collection period for this study.
We now have as part of our carers policy, a kind of negotiation that we have with the carers that says, ‘Okay, Joe’s in here, you normally do all of these things, while he’s in hospital what of those do you want to carry on doing, what of those do you want us to take up?’ I think we have a real responsibility around that and then we need to make sure we’ve documented that and we reflect on how that changes.
P65, Director of Nursing
Practical support for carers
In order to fulfil the role of ‘worker’, carers needed carer-related reasonable adjustments: facilities for carers that included food and drink, a bed and a parking space. The carers’ role became extremely difficult to fulfil if these were not given, either because they were not offered or because they were not available.
Most staff in this study understood this need. In some situations, carers reported that they were left by ward staff to carry out basic nursing care tasks, but were not afforded the same facilities as the nursing staff. This was particularly pertinent when carers were not given any relief from caring and were expected to stay with the patient for many hours without a break.
After the data collection period ended, two trusts initiated carer support programmes, whereby carers were given a ‘passport’ or ‘badge’ to indicate their status as carer.
A staff culture where carers are welcomed as a matter of course
The existence of carer policies, and senior hospital management support for these policies, did not necessarily translate into a culture of support for carers throughout the trust. There was a sense among both carers and staff that the ward manager had a pivotal role and a strong influence on ward culture. Ward managers could be role models in welcoming carers and demonstrating flexibility in the provision of reasonable adjustments.
Some nurses and parents highlighted the positive culture on children’s wards, where there is a much more ready recognition and acceptance of the role of the carer. Similar acceptance and support for carers was reported by carers in relation to intensive care wards. Conversely, example G in Table 9 exemplifies a ward culture where carer involvement is not welcomed. This team of paid carers not only offered support with basic nursing care, but also provided crucial knowledge about how such care provision could best be managed for this particular patient; both were received with hostility by the doctors and nurses.
Funding for paid carers
Many people with learning disabilities who are in hospital need a higher level of support than the average patient on the ward. This is particularly obvious for patients who receive social care support in the community setting. Difficulties arose from the lack of integration between health and social care provision.
There were local variations in the way in which these patients’ support needs were funded (if at all) when they were in hospital, and the rules about this were unclear. Hospitals tried to allocate extra staff to the ward when needed and when possible. Some hospitals paid for a member of the patient’s usual community care staff team to be with the patient while in hospital. There were also examples where the patient’s usual paid carers felt they were expected to provide continued support when their client was in hospital, but the social care payments did not always allow for this. Issues of responsibility and accountability were not always clear when hospitals paid for members of community care staff teams to provide part of the care while the patient was in hospital.
Model for clarifying carer involvement
Figure 11 represents a model for clarifying roles and carer involvement, developed as a result of this study’s analysis of tensions between carers and hospital staff.
-
Expertise: The involvement of carers who are ‘experts’ needs to be sought even if they are not physically present on the ward. This includes keeping carers informed, seeking their expert knowledge of the patient, taking their expert advice into account, and involving them in planning treatment and care.
-
Involvement in care and support tasks: The level of carer involvement in basic nursing care tasks, communication support and reassurance, through the carers’ presence with the patient in hospital, needs to be clarified and reviewed regularly.
FIGURE 11.
Model for establishing carer involvement and expertise.
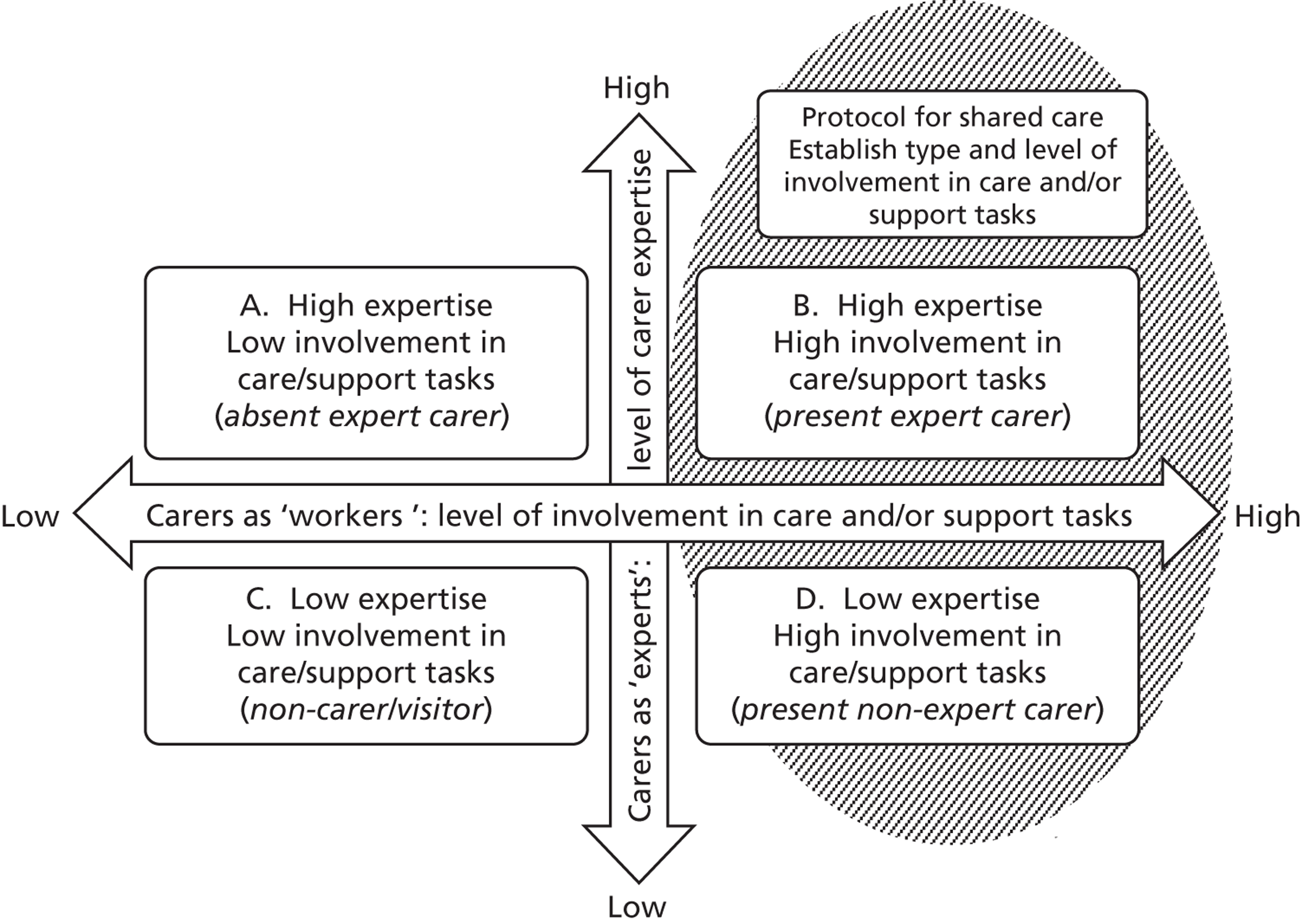
Below is a non-exhaustive list of examples of the different levels of involvement, all taken from examples within the study. Carers who fall within categories A and B should be included as expert care partners. If a carer falls within categories B or D, a protocol for shared care would be beneficial.
A. High expertise/low involvement in care tasks
-
Family carers who cannot be present with the patient in hospital.
-
Family carers who are with the patient in hospital but need breaks from active caring.
-
Paid carers who are highly involved in supporting the patient in the community but are unable to provide active care support in hospital.
B. High expertise/high involvement in care tasks
-
Family carers who provide intensive support to the patient at home and continue to do so in hospital.
-
Family carers of patients who have a degree of independence at home but need increased carer support in order to cope in hospital.
-
Paid carers who know the patient well, provide care in the community and provide the patient with care and support in hospital.
C. Low expertise/low involvement in care tasks (non-carers)
-
Visitors.
-
The researchers from this study.
D. Low expertise/high involvement in care tasks
-
Paid carers who do not know the patient well but who accompany the patient in hospital, providing a range of support tasks including communication support.
-
Extra care assistants provided by the hospital.
Chapter 8 Including patient and carer views in service planning and development
Section 242 of the National Health Service Act 2006 requires NHS bodies to involve and consult patients and the public in the planning and development of services, and in decisions affecting the operation of services. All trust boards should ensure that the views and interests of people with learning disabilities and their carers are included.
Recommendation 9 (p. 11). 4 Reproduced with permission from Michael J. Healthcare for All: Report of the Independent Inquiry into Access to Healthcare for People with Learning Disabilities. London: Aldridge Press; 2008
Chapter summary
Senior hospital managers understood the need for involving patient and carer views in the development of services and were supportive of it. Hospitals engaged with patient and carer views through formal structures, such as hospital user group meetings and forums, and through active engagement of hospital managers with external advocacy groups. There were some examples of successful implementation of tangible reasonable adjustments that were lobbied for or supported by user groups (including, for example, easy-read materials or accessible toilet facilities).
Effective inclusion of patient and carer views was facilitated by senior management support, and in particular by the LDLN who had a pivotal role in setting up and supporting user groups. Barriers included the sometimes difficult management of meetings involving patients and carers, the slow timetable for change, and the complexities of addressing less tangible issues around hospital structures and culture.
These are recent developments and it is therefore too early to evaluate the effectiveness of user involvement. The evidence for effective inclusion of patient and carer views at board level is currently limited. Early signs are that it is important to maintain awareness of learning disability issues, even if the effectiveness of involving patient and carer views is difficult to demonstrate.
The barriers and enablers that have emerged in this study in relation to including patient and carer views in service planning and development are summarised in an empirical subframework (Figure 12).
FIGURE 12.
Empirical subframework: barriers and enablers in relation to including patient and carer views in service planning and development.
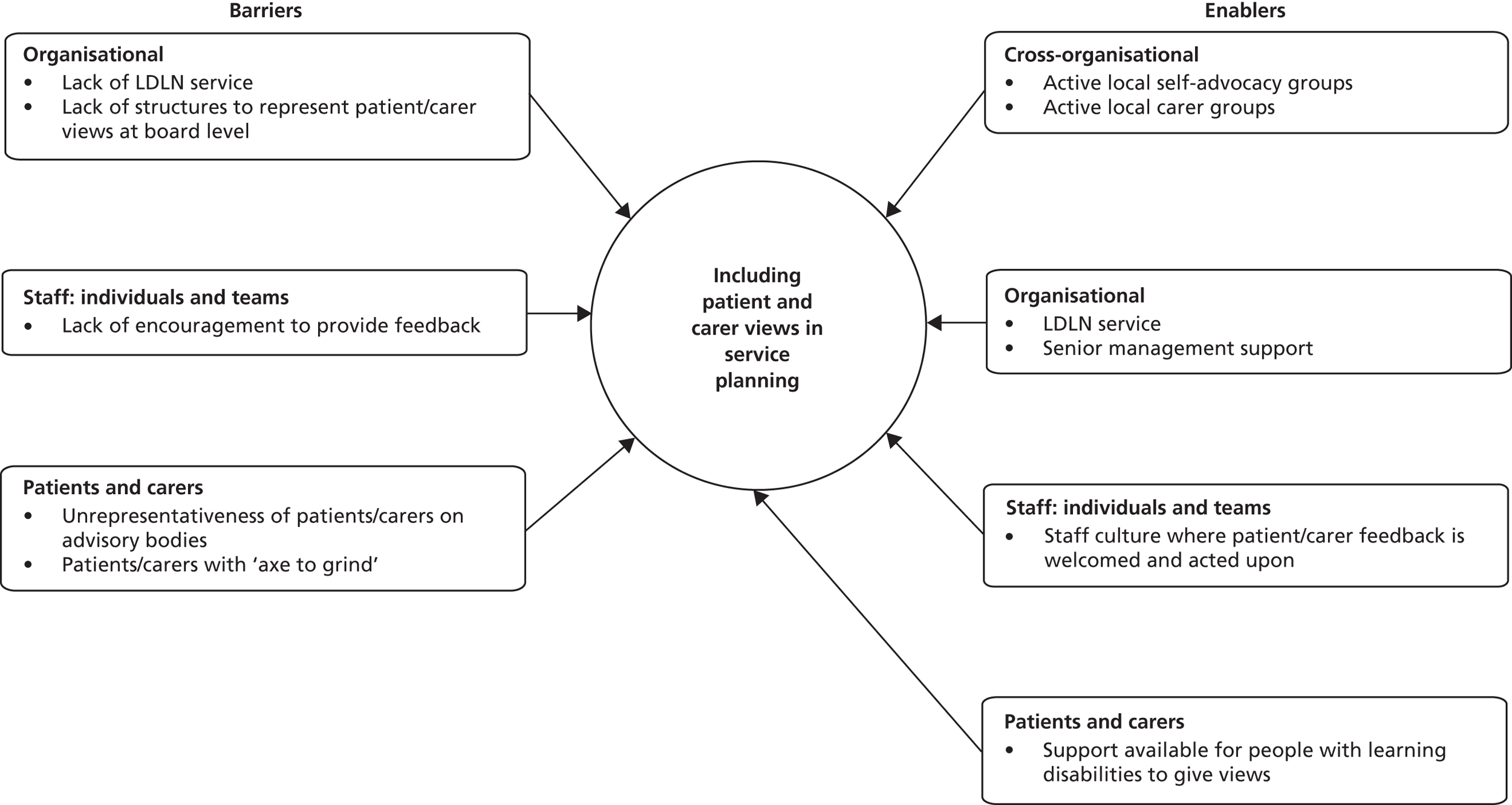
Accessing and including patient and carer views
Ways of accessing patient and carer views
All hospitals endeavoured to access patient and carer views, but there was a wide range of different ways of doing this. Most of these were in the early stages of implementation (some user groups had only just been established at the time of the participant interviews), and hospitals were still experimenting with the most beneficial formats.
Hospital advisory forums
The LDLNs at three hospitals had set up one or more hospital-based groups or forums with the specific remit of improving services for people with learning disabilities at the hospital. Membership of such groups varied, for example: people with learning disabilities only; family carers only; a mixture of people with learning disabilities and family carers; or a range of representatives (including hospital staff) as well as someone with learning disabilities.
Accessing local learning disability groups
Two hospitals accessed the views of people with learning disabilities through senior hospital managers attending established meetings of local service providers or learning disability advocacy groups.
Accessing patient views by proxy
One hospital reported that their main method of accessing patient and carer views was through contact with the community learning disability team if they had any questions or issues to be raised. At another hospital, the views of people with learning disabilities on their hospital experience were gathered by the community-based LDLN.
Senior management support
All senior hospital managers interviewed for the study were aware and supportive of the requirement to involve and consult patients and the public. Several Directors and Deputy Directors of Nursing were actively involved in attending local learning disability forums.
However, questions were raised about the best ways to access patient views. Some managers questioned the real contribution patients could make through patient representative bodies, and were concerned about the risk of including ‘token patients’ without any real influence.
The remit of patient/carer groups
A number of tasks were described by members of patient/carer groups, LDLNs and senior hospital managers, as follows.
Introduction of practical supportive measures
All groups had lobbied for and supported the introduction of practical measures to make hospitals more accessible for people with learning disabilities. These included:
-
the introduction of patient-held information documents
-
the production of easy-read hospital information leaflets and other easy-read materials
-
the acquisition of beds/chairs to enable carers to stay with the patient overnight
-
accessible toilets
-
hospital signs.
Providing consultation
All groups acted as a ‘sounding board’ by providing expertise for hospitals that were implementing new learning disability-related measures. Where hospitals did not have their own user group of people with learning disabilities, hospital managers consulted community-based learning disability groups. This included the development of any easy-read materials or of particular learning disability care pathways.
Providing feedback on hospital services
Whereas ‘consultation’ was hospital-directed (i.e. hospital managers requested feedback on issues they themselves raised), some groups also provided their own feedback. Examples included one hospital where people with learning disabilities attended nurses’ meetings to raise issues of importance to them.
An innovative way of providing feedback was through ‘secret shopper’ testing of hospital services. The LDLNs at two hospitals described how they had organised and supported people with learning disabilities to do a walkabout in the hospital in order to test the service and highlight any potential difficulties. In one hospital, this had demonstrated clinical areas where staff were helpful and respectful, but also an area where attitudes could be improved.
Lobbying for a learning disability liaison nurse service
People with learning disabilities at several hospital sites mentioned the importance of the LDLN service and had lobbied hospital managers for implementation or expansion of this service.
Teaching staff
At several hospitals, people with learning disabilities from local groups or hospital forums were invited to share their experience with hospital staff, for example through presenting at a conference, teaching students or attending a meeting with ward staff. The LDLNs who had supported this and the staff who had experienced it invariably reported to the research team that such patient and carer involvement was inspirational and memorable.
Raising learning disability awareness
Several groups had been involved in raising the profile and visibility of people with learning disabilities through the production of flyers promoting the LDLN service or organising ‘learning disability awareness events’ within the hospital.
Barriers and enablers
Enablers of effective inclusion of patient and carer views
Learning disability liaison nurse
The LDLN was instrumental in establishing patient and carer forums at the hospitals, in involving people with learning disabilities in staff training and in enabling people with learning disabilities to give feedback on hospital performance. One hospital’s learning disability lead (other than the LDLN) also facilitated the setting up of a patient forum.
Senior management support
The support of senior hospital managers was also important. Even if actual change achieved might be difficult to see, it appeared that the engagement of the Directors and Deputy Directors of Nursing with patient and carer groups kept the issue of learning disability in their consciousness, and it can be argued that this in itself is important for trust-wide recognition of learning disability issues.
Implementing practical measures
The effectiveness of patient and carer involvement was most clearly demonstrated through examples of the effective implementation of reasonable adjustments consisting of practical measures. In some hospitals, additional measures (such as extra beds for carers, toilets that are accessible for adults with profound or multiple disabilities, or easy-read information) were implemented following suggestions and direction from patients and carers. It is possible that the tangibility of such measures makes them easiest to understand – not just for people with learning disabilities but also for hospital managers – and their successful implementation easiest to measure, unlike less tangible changes such as those related to staff culture or hospital structures.
Barriers to effective inclusion of patient and carer views
Meetings and forums
The patient/carer meetings and forums were generally seen as a positive development, but there were also a number of challenges raised by people with learning disabilities, carers and staff.
People with learning disabilities enjoyed being part of such meetings and felt proud of their achievements. However, they also reported that the meetings could be difficult at times. Some forum members with learning disabilities (especially those in groups that also included carers and/or staff) found the meetings ‘not very accessible’, ‘not easy to understand’ and ‘hurried’.
Carers reported some frustration with the long time it took to achieve any changes and to become productive beyond ‘just talking’. There were challenges in managing meetings where some members may have their own strong agenda or (especially with meetings that included people with learning disabilities) some members could be easily distressed or lose focus. It was seen as important to draw up clear rules about this.
Hospital staff (in particular senior hospital managers), though supportive of the meetings in principle, expressed concern that such meetings might be tokenistic and could not include a representative group of patients and carers. There could also be different perceptions between patient groups and managers about priorities or possibilities for change:
Where they’ve got a really big issue and they really put it forward I think it works really well. Sometimes it’s a little bit frustrating when they get a bit stuck on a subject that you just can’t move them forward from and we’re just kind of saying, ‘We just absolutely recognise that’s an issue, but do you know what, we have to charge for the car park.’
P65, Director of Nursing
Complexity of change needed
It can be argued that the areas where patient and carer views are most important are in helping hospitals to understand what reasonable adjustments are needed, and in monitoring the effective implementation of reasonable adjustments. It is more difficult to see the impact of involving patient and carer groups on ensuring that hospital services are structured and delivered in a way that does not disadvantage people with learning disabilities. This includes staff attitudes, staff training, the co-ordination of care or the way hospital appointments are organised. Such changes are complex, and it may be more difficult to find effective systems to ensure that the needs of people with learning disabilities are consistently considered at board level in relation to this. A family carer on the research advisory board argued that trust boards should have at least one member whose role it is to consider the effect of new service developments and changes on patients with learning disabilities.
The positive examples of more complex issues being addressed did not involve meetings or forums with patients and carers, but rather more creative ways of listening to the patient and carer experience. The ‘secret shopper’ is one example of this. There were also cases where carers gave feedback to the hospital about poor care and the hospital listened and took action, for example by actively involving the carers in implementing changes.
A local advocacy service fed back some information that some clients had said that they felt they weren’t treated well . . . There was a specific project in A&E where work was done to make sure there was training for all staff and that that was ongoing. And we had positive feedback from [the local advocacy agency] at that stage that things were improving.
P43, Director of Nursing
Hospitals did listen to the patient experiences fed in by patient groups, including local advocacy groups. However, this appeared to be rather ad hoc, and there was a lack of structured ways to gather feedback or views from patients and carers who had used hospital services.
Chapter 9 The role of the learning disability liaison nurse
Chapter summary
The evidence from this study is that it is easiest for acute trusts with a LDLN service, particularly those with an on-site LDLN, to provide safe and good-quality health care for people with learning disabilities. The LDLNs were most effective if they had (a) a high level of expertise and understanding of the needs of people with learning disabilities and their carers; (b) authority to make decisions that change patient care pathways, as well as a good understanding of, and access to, all clinical areas within the acute trust structures; (c) high visibility and availability within the hospital; and (d) strong support from senior hospital managers.
The issues around patients with learning disability and the adjustments that may be needed were so complex that the support of a dedicated, highly skilled LDLN service was a key element of ensuring that preventable harm and preventable deaths were avoided in a number of cases. However, the effectiveness of the LDLN was often limited by a lack of cover for absence and by inadequate structures for senior management support and accountability, with a risk of the role being marginalised.
The learning disability liaison nurse roles at the study sites
Having a LDLN was a clear facilitator in every research question addressed in Chapters 5–8. This chapter reports on the study findings in relation to the LDLN role, the various elements of that role and the factors that made the role more or less effective at the study sites.
All LDLNs in this study were the first to occupy the post at each site, with several reporting that they wrote their own job description. At four of the trusts, the LDLN role was implemented in direct response to hospital inspections, national reports (including Death by Indifference1), inquiries (including Healthcare for All4) and recommendations. At one trust, the community learning disability nurses had successfully lobbied hospital management to implement the role. The roles varied, as follows:
-
Three trusts employed a LDLN who was based at the hospital. One of these worked part-time.
-
One trust was integrated with a PCT, which had one LDLN who was assigned to work at the hospital. Her base was in the community.
-
One trust worked closely with two LDLNs in the community, whose caseload consisted of patients within their catchment area who were in hospital.
-
One trust did not have a LDLN but worked with a number of learning disability community nurses, and was establishing the role of ‘link nurses’ on each ward.
Despite the praise that was heaped on the LDLN post holders by participants in this study, the continued existence of their posts was far from secure. Several LDLNs expressed concern that support for their post from senior managers and commissioners could wax and wane with changes in senior management positions and with the national profile of issues around health, safety, avoidable deaths and learning disabilities.
I’ve gone right down the pecking order because something else has come back up on the pecking order. And that’s so frustrating because it’s always on my agenda and in my head it’s the most important thing, but obviously in the Director of Nursing or Chairman’s head it isn’t.
P9, LDLN
Considerations of the cost of employing a LDLN, and the relatively low number of patients with learning disabilities identified within the hospital, led to some senior strategic managers concluding that implementing or maintaining a LDLN service was difficult to justify, particularly in an economic climate of funding cuts.
Elements of the learning disability liaison nurse role
Similar to the findings of Brown et al. ,65 the LDLN role was found by this study to comprise three key elements: clinical patient care; education and practice development; and strategic organisational development. In addition, the LDLNs had a role as champion for the needs of people with learning disabilities that straddled all these elements. The extent to which the LDLN was involved with each of the elements varied considerably between trusts.
Clinical patient care
All LDLNs had a caseload of patients with learning disabilities. They provided support for patients, carers and staff throughout the patient’s hospital journey. Referrals came either through the hospital (referrals from hospital staff, or the LDLN actively looking for patients within the hospital) or through the community, by carers and patients contacting the LDLN directly or by community staff making referrals.
The role was often extremely complex and required significant skills in communication and negotiation. Key aspects of the LDLN role included:
-
the provision of expertise around mental capacity assessments and individualised communication
-
communicating and liaising with carers, ensuring that the carers’ voices were heard and their needs were met
-
liaising with other services, in particular primary care services
-
co-ordination of care, which included ensuring a wide range of reasonable adjustments were in place (see Chapter 6).
Without [LDLN input] there is no sort of yardstick or benchmark. You know, a phone call: ‘Have you done this? Have you done that?’ Even if it’s ‘yes, yes, yes, yes’, that’s fine – but if it’s ‘no, no, no, no’, then she can either help, give advice. If you go and trawl through the intranet and it takes you half an hour to find the policy, you’re not likely to do it. And if the patient comes in on their own or there’s a problem with the relatives, then it also becomes problematic and [LDLN] can sometimes intervene.
P50, ward staff nurse
Education and practice development
The delivery of education and training to all hospital staff was an essential element of the LDLN role, although this was not straightforward in practice. Part of the challenge was finding effective ways of training a vast workforce. One LDLN had worked out that if she wanted to reach all the hospital’s staff in a formal training session across the year, it would mean training well over 100 staff members per week.
There was concern, in particular among senior managers, that having a LDLN could de-skill the workforce by ‘taking over’ patient care. However, there was no evidence in the study that the hospital staff were de-skilled by input from the LDLN. On the contrary, LDLNs ‘role modelled’ good practice, including possibilities for reasonable adjustments, that were then more likely to be taken up by hospital staff when the LDLN was absent. Interviewer:P79, Deputy Director of Nursing:
How do you think [employing a LDLN] has panned out in terms of staff being more skilled or not skilled?
Definitely more skilled . . . They see the different techniques that they can use, they then start to use those skills so she doesn’t get phoned to ask, ‘What do I do?’ She may well then get a contact which says, ‘I’ve done this, is that fine?’ The next step is then actually she doesn’t get called at all and it’s incorporated within the generalist care of the patient. And that is the end point, that’s what you want to achieve.
Strategic organisational development
The LDLNs, where there was one in place, were often a driving force behind the development of all policies, guidelines and resources related to learning disability. Several senior strategic managers indicated that they relied on the LDLN to be on top of relevant legislation and national recommendations as well as potential problem areas, as they themselves did not always have good understanding of the issues around learning disabilities.
Championing
Learning disability liaison nurses were enthusiastic advocates and champions of the needs of people with learning disabilities within the trust; this increased the effectiveness of the role. Some carers noted a positive change in staff attitude and hospital culture and thought that the LDLN was an important part of this change.
I’ve noticed a great sea change, it’s more an attitude on the part of the staff . . . [In the past] we were pretty much left to deal with things ourselves, you know, carrying trays whilst pushing a wheelchair. But now people help. [LDLN] has done a lot of work and I have seen the difference. Dealing with the staff, receptionists, doctors, they are more understanding of [my daughter]’s needs, even high powered consultants address [my daughter] now.
P157, family carer
Effective championing and awareness meant there was a greater likelihood that hospital staff considered the specific needs of individual patients with learning disabilities.
If I see those words [learning disability] come up [on the handover sheet] I think, ‘We must make sure that we let [LDLN] know they’re here’ . . . It just sort of clocks in my mind a little bit more.
P23, ward manager
Evaluation of the learning disability liaison nurse service
Although this study did not specifically address the levels of staff/carer/patient satisfaction with the LDLN service, it was clear from the qualitative data that such satisfaction was extremely high. Stakeholders reported improved communication, improved patient assessment (including capacity assessments) and improved patient pathways with good reasonable adjustments. Words such as ‘wonderful’, ‘brilliant’ and ‘amazing’ were frequently used to describe the individual post holders and their qualities.
We’ve got a [LDLN] and she’s absolutely brilliant. You can ring her with absolutely anything and she will endeavour to help you and always, always gets back to you. She’s really, really good.
P52, ward staff nurse
The only time that went well is when I saw [LDLN] . . .
P149, person with learning disabilities
Interviewer:P149:Interviewer:P149:
What was so great about her?
Because – brilliant.
What made her brilliant?
Because she take – she took time. To speak to you.
The degree to which the LDLN role contributed to patient safety and avoidance of potential harm is more difficult to measure and quantify (see Chapter 10). However, there were a range of examples within this study where the intervention of the LDLN undoubtedly contributed to the safer care of patients with learning disabilities, including examples where death was avoided. For instance, in a number of cases skilled mental capacity assessments led to ‘best interest’ decisions to deliver treatment that would, without the LDLN’s intervention, not have been given.
Although all Healthcare for All4 recommendations were difficult to achieve, synthesis of the evidence from this study, presented in Chapters 5–8, suggests that hospitals with a dedicated LDLN service (and particularly the three hospitals with an on-site LDLN) were best able to:
-
identify patients with learning disabilities throughout the hospital and track their pathways of care
-
increase awareness of, promote and support the role of carers as active and necessary partners in care
-
ensure that complex reasonable adjustments can be made, in particular those that involve changes to structures, rules and systems
-
develop appropriate policies, pathways and tools to support the needs of patients with learning disabilities and their carers.
Factors affecting the effectiveness of the learning disability liaison nurse role
The study results indicate that in order for the LDLN role to be effective, she must have:
-
a high level of learning disability expertise and credibility with hospital staff
-
authority to make decisions that change patient pathways
-
high visibility and availability within the hospital
-
strong support from senior trust managers.
Learning disability expertise
The LDLNs’ high level of learning disability expertise was clearly recognised and valued by hospital staff. They mentioned the LDLN’s expertise with communication, knowledge of the Mental Capacity Act, help with assessing the patient (including assessments of capacity) and skill in liaising with families. Physicians noted that they found it difficult to do mental capacity assessments for patients with learning disabilities and to keep up to date with legislation, and depended on the LDLN’s expert help.
Hospital staff admitted that they themselves lacked the necessary expertise to provide a good standard of care for patients with learning disabilities, and therefore needed expert help.
The ward link nurse model
Several hospitals had systems whereby ward nurses were allocated a role as ‘learning disability link nurse’. They would act as a resource or point of contact for other staff with regards to issues around learning disability. The evidence from this study suggests indeed that ward link nurses lack specific learning disability expertise and cannot therefore be relied upon to provide the necessary support for staff, patients and carers. In particular, they do not have sufficient understanding of the sometimes complex adjustments needed to ensure that patients with learning disabilities receive adequate health care.
Authority to change patient pathways
For patients and carers, the fact that the LDLN was able to affect and change the patient journey made a huge positive difference.
In the last admission we were blocked by a nurse at A&E, but within five minutes of a call to [LDLN] things went OK. When he came to A&E this time I phoned [LDLN] beforehand, and she and the GP told them he was coming and they were ready for him.
P11, family carer/parent
As has been shown in Chapter 6, the provision of reasonable adjustments can require complex changes to patient pathways involving trust-wide structures and systems. For the LDLN to be effective in her role, she needed to have an in-depth understanding of the organisation so that she could determine whether, and how, its structures and systems could be adapted to meet the patient’s needs. This included a consideration of the pressures and capacity on general hospital services as well as the needs of the patients. For this reason, senior managers and LDLNs at several trusts argued that it was important for LDLNs to be hospital based. There was indeed evidence within the study that the community-based LDLNs lacked the seniority and inherent authority within the hospital structures to be effective change agents. They also seemed much less well known by hospital staff, affecting the readiness of the hospital staff to make suggested changes to patient pathways. They were more dependent on the active backing of senior hospital management when giving specific advice around changes to individual patient pathways.
I have more freedom just to move within the hospital, so I can go into places like theatres . . . And it’s about knowing the people in the hospital and getting them to know and trust and respect what you say. I’ve got the back-up of the fact that we are all on the same team, whereas when I was a community nurse, outside . . . it sometimes felt like ‘you’re trying to drop us in it’.
P9, LDLN (hospital based)
Visibility, approachability and availability
Visibility
For the LDLN to be effective throughout the hospital, it was important that hospital staff knew who the LDLN was, understood her role and knew how to contact her. This was easiest to achieve if the LDLN had a physical base in the hospital. It was also important that the LDLN was known among community learning disability staff and carers, so patients that needed hospital tests or treatment could be flagged up to the LDLN directly – as has been described in Chapter 5, many patients with learning disabilities were not identified by hospital staff.
Knowledge of the LDLN post was good among hospital staff in the three hospitals where the LDLN had an on-site base. It was less widespread in trusts with community-based LDLNs, where the following quote comes from:Interviewer:P211, consultant physician:
Do you have any connection with the [LDLNs] at all?
Not that I’m aware of . . . There’s a Child Protection Officer and if it was an adult then clearly – I don’t know what I’d do actually – it’s an interesting point.
Approachability
The personal qualities and interpersonal skills of the LDLN post holders were important factors in their effectiveness and were commented on by many staff across study sites. When the researchers shadowed two of the hospital-based LDLNs, it was obvious that they were known, liked and trusted by hospital staff, and that staff recognised them immediately as being associated with patients with learning disabilities.
Availability
One of the key barriers to the LDLNs’ effectiveness was a lack of cover when the LDLN was absent. Many respondents mentioned the fact that they could not access the LDLN when needed. This lack of cover seemed to suggest a lack of recognition at board management level that the LDLN post was important to the organisation.
Senior management support
Learning disability liaison nurses who had direct and easy access to the (Deputy) Director of Nursing and were strongly supported in their role felt empowered and were able to perform well. This could include support for clinical decisions and implementation of specific adjustments to patient care. It was also reflected in the ease with which LDLNs could carry out their responsibilities, and the presence or absence of organisational barriers. One LDLN said:
For a while I wasn’t even included in the training programme. I had to do it ad hoc. I had to book my own rooms, I had to manage my own bookings.
P48, LDLN
The line management structure and lines of accountability for the LDLN post were important, not only for the support of the individual post holder but also for the implicit value placed on the role within the trust if the LDLN reported directly to a senior manager such as the Director of Nursing.
I’ve had no clinical supervision. I could be doing anything, I could do whatever I like, I could be absolutely rubbish and no-one would know. There’s a lot of lip service from the management but there is no understanding of my role and no support. It’s not valued internally.
P2, LDLN
Hospitals with strong management support for the LDLN role were more likely to have adopted a wider range of measures to improve the care and safety of patients with learning disabilities. This in itself was more likely to make the LDLN role effective. Senior management support for the LDLN role did not always seem to be embedded, but rather depended on the enthusiasm of individual senior managers or on how ‘high profile’ the issue of patient safety for people with learning disabilities was perceived to be.
Is appointing a learning disability liaison nurse the solution?
Based on the findings reported in this chapter, it may be tempting to see the implementation of hospital-based LDLN posts across NHS hospitals as a solution to the issue of compromised safety for patients with learning disabilities. Indeed, the evidence suggests that without such a role, it is much harder for NHS hospitals to achieve safer practice.
However, such roles cannot be seen as a quick or easy solution to the problem. Implementing the LDLN role ensures access to essential learning disability expertise, but without sufficient cover and without ongoing structural support and accountability for learning disability issues throughout the organisation, this is unlikely to have a sustainable impact. One LDLN clearly cannot achieve organisational change in isolation. Therefore, senior management support for the role has to be embedded within the hospital structures. This includes ensuring that there is sufficient cover and that the role carries sufficient authority and seniority.
This appeared to be the case at one study site, where the issue of learning disability seemed to be ‘owned’ by a much wider group of matrons and senior managers in liaison with the LDLN. There were regular learning disability meetings attended by senior clinical staff, annual trust-wide learning disability training days and clear lines of senior management support for the LDLN, who felt empowered by this support. This particular trust had set up systems for learning from poor practice. Conversely, the LDLN at another hospital reported that, since the departure of a highly supportive Director of Nursing, support for her post from senior management seemed to have waned; this LDLN felt disempowered and frustrated.
There was a sense at some study sites that any questions and difficulties related to learning disabilities were the remit of the LDLN only. If the LDLN was absent at such sites, it was difficult for the research team to obtain answers to questions, and some LDLNs felt that there was a lack of accountability for their work within the hospital structures. It also seemed notable that a role that was hailed as ‘wonderful’ and ‘important’ by staff throughout the hospital (including senior managers) would be left without effective cover for absence, or even be at risk of being discontinued.
Chapter 10 Patient safety issues
Chapter summary
The study results in conjunction with existing literature suggest that patients with learning disabilities are at risk of experiencing avoidable harm when using NHS acute services. The problems appear to be widespread and can occur at any time point during the patient pathway. However, the incidence of patient safety issues experienced by patients with learning disabilities has not been quantified.
Patient safety issues were commonly described surrounding the following: lack of basic nursing care, in particular in relation to feeding, hydration and pressure area care; misdiagnosis, often due to diagnostic overshadowing and communication difficulties; delayed investigations and treatment; non-treatment decisions and inappropriate DNAR orders, which may be due to assumptions about the patient’s quality of life; and misuse of the Mental Capacity Act, including a lack of staff knowledge and problems with capacity assessments. This is not an exhaustive list.
There is a common thread of delays and omissions of care and treatment which could lead to preventable deterioration. As acts of omission are more difficult to recognise, capture and monitor than acts of commission, it may be difficult for organisations to monitor the safety of patients with learning disabilities. At present, incident reports are an insufficient way to assess the types and number of patient safety issues experienced by patients with learning disabilities in NHS acute hospitals.
The research team noted few formal complaints. Carers indicated a desire to put negative experiences behind them, and voiced concerns that the future health care of the person with learning disabilities might be affected by complaining.
Patient safety issues
This chapter presents those results of the study that are concerned with the specific patient safety issues (those issues that may cause harm) faced by patients with learning disabilities in NHS acute hospitals. As described in Chapter 4 (see Researching patient safety), patient safety is concerned with any issue that could have or did cause harm to a patient as a result of the health care received. It is estimated that around half of all patient safety issues are preventable. 75
This chapter also reports on the findings concerning incidents and complaints involving patients with learning disabilities.
Examples of preventable deterioration
A number of examples of patient safety issues were recounted to the research team, some of which have already been described in this report. Further examples are given in Box 1.
A. An elderly, blind man with profound learning disabilities was admitted to hospital as his residential care home manager believed he was in pain. The cause of this pain was unknown. The medical staff initially refused to carry out a thorough assessment of his symptoms, stating that this patient was simply at the end of his life and that ‘the best thing is to let nature take its course and let him die’. The patient began to deteriorate rapidly and became malnourished and dehydrated due to lack of food and fluids. At the home manager’s insistence, investigations were eventually undertaken and simple treatment was provided. Treatment was successful and the patient returned home.
(Example provided by P44, paid carer.)
B. A woman with learning disabilities attended A&E with a carer. During the triage process, the patient was fiddling with the equipment used to take her observations. The observations were not within the ‘normal’ range and the nurse assumed that this may be because of the patient’s interference. The patient and her carer were requested to sit in the waiting room. The patient deteriorated rapidly during her wait and ultimately died.
(Example provided by P125, Director of Operations.)
C. A man with profound learning disabilities was admitted for an inpatient stay. The doctor requested him to remain nil-by-mouth but prescribed administration of fluids via a drip. The drip was not given for more than 16 hours as the nursing staff looking after this patient failed to note the request. The patient became dehydrated.
(Example provided by P124, paid carer.)
D. A man with learning disabilities attended A&E on his own as he had noticed blood in his underwear. He had difficulty articulating his symptoms and was sent home from A&E as staff incorrectly believed the man was drunk. Later on, a carer noticed the blood and the man returned to A&E. He had a rectal prolapse which required emergency surgery. While awaiting his theatre slot, the man was inappropriately given a hot drink. Because of this, the surgery was delayed.
(Example provided by P156, community learning disability nurse.)
E. A woman with learning disabilities and anorexia was admitted to hospital. Nutrition shakes were ‘left’ in front of her. She had no specialist help for her eating disorder while in the acute hospital. Her deterioration was so pronounced that she required a stay in intensive care.
(Example provided by P172, paid carer.)
F. A woman with learning disabilities needed an appointment for an endoscopy. The patient and her mother visited the department to make an appointment. They were told by the receptionist that the test could be done then, but they would need to wait for two hours in ‘recovery’ following the procedure. They scheduled the appointment for another day as they were short of time. At this pre-scheduled second visit, they were turned away as the department was too busy. On the third visit, the patient was accompanied by her brother. The department refused to conduct the endoscopy on the basis that the patient was unable to give consent and the brother did not have legal power of attorney. On the fourth visit, the mother was asked to sign a consent form for the procedure, which she did. (Note: the mother had no legal power of attorney either.) There was no 2-hour ‘recovery period’ following the procedure – the receptionist had misinformed them.
(Example provided by P95, family carer.)
G. A woman with learning disabilities was admitted to a ward. An air mattress was requested but this was not delivered for several days. The patient began to develop pressure sores on her heels.
(Example provided by P20, family carer.)
H. A man with learning disabilities needed a supra-pubic catheter fitted to help prevent urinary tract infections caused by urinary catheters. There were numerous delays in organising this procedure and the patient required a stay in intensive care when he developed urinary sepsis.
(Example provided by P97, paid carer.)
Difficulties in establishing preventable deterioration
These examples, taken from all six study sites, demonstrate a wide variety of ways in which preventable deterioration may occur in different clinical settings within acute hospitals, and show that patients across the spectrum of learning disability have been affected. However, attributing failures in care to the existence of a patient’s learning disability is extremely complex and usually requires a full and detailed investigation and analysis, as is demonstrated by the reports of the Health Service Ombudsman2 and CIPOLD. 3 Therefore, although many of the examples in Box 1 appear to demonstrate clear-cut service failure resulting in harm, the extent to which these failures are directly caused by discrimination against patients who have learning disabilities or lack of reasonable adjustment to accommodate their needs is difficult to assert with full confidence. Similarly, it is often the case that the ‘preventability’ of deterioration is difficult to define as, even with the best medical and nursing care, deterioration is often a natural consequence. For instance, it may be difficult to assert that the harm described in example E was indeed preventable.
Staff perceptions of patient safety and preventable deterioration
Most of the tangible examples of patient safety issues that had resulted in harm (rather than general descriptions of what might constitute a patient safety issue) were provided by carers. There may be a number of reasons for this. One issue was the apparent conscious or unconscious desire of hospital staff to paint their trust in a positive light and to focus on demonstrating the steps they had taken to improve the safety of care provided for people with learning disabilities. This may have been to the detriment of openly talking about any potential gaps in safety of care or areas for improvement. For example, within the clinical staff questionnaire, participants were asked whether patients with learning disabilities had deteriorated unnecessarily within the past 3 years. Just 2.9% of respondents (24 out of 825) indicated ‘yes’ in response to this question (see Appendix 4).
It also became clear throughout the interviews that a significant minority of clinical and managerial hospital staff did not think that patients with learning disabilities were at increased risk.
I think it’s the same as the safety for the rest of our patients, I don’t think that they are in any further risk than the rest of the patients that we see here.
P26, staff nurse
Your special need isn’t really going to kill you.
P54, ward manager
Analysis of patient safety issues identified in the study
Despite the difficulties described in Difficulties in establishing preventable deterioration and Staff perceptions of patient safety and preventable deterioration, the mixed-methods data gathered suggested that patients with learning disabilities are indeed at risk of experiencing patient safety issues in acute hospitals. A broad variety of safety issues were described. Synthesis of the data demonstrated that the following issues may be of particular significance to patients with learning disabilities (not in order of importance):
-
lack of basic nursing care
-
misdiagnosis
-
delayed investigations and treatment
-
non-treatment decisions and DNAR orders
-
misuse of the Mental Capacity Act.
Lack of basic nursing care
Several carers and hospital staff described a lack of basic nursing care provided for patients with learning disabilities, or an over-reliance on carers to carry out nursing tasks (see Chapter 7). Concerns relating to basic nursing care were frequently raised around feeding and hydration, and pressure area care.
Feeding and hydration problems
Examples A, C and E in Box 1 described situations where patients had become severely dehydrated or malnourished in hospital. Examples were also given by carers describing patients who were known to have swallowing difficulties and required soft foods but did not have this nutritional requirement met.
Most importantly, his food has to be pureed. It was so hard for us to get that message across. It was in his [patient-held information document] but they lost it, so we had to keep telling them. They kept giving him solid food. It took such a long time before it was sorted.
P161, paid carer
Among respondents to the clinical staff questionnaire, 6.3% (52 out of 825) said that within the past 3 years a patient with learning disabilities did not get sufficient food or drink (see Appendix 4). Further examples were provided in staff interviews, in free text responses to the staff questionnaire and within incident reports.
Identifying patients with deteriorating nutritional needs has gone unnoticed for several days. This adds an unnecessary delay in referral and then starting a nasogastric tube feed.
P539, AHP (free text on questionnaire)
One person with learning disabilities reported being regularly passed by when breakfast or coffee was served (see also Table 6). She thought this was because staff did not want to look after someone with learning disabilities.
Pressure sores
A number of hospital staff and carers stated that patients with learning disabilities may be at particular risk of developing pressure sores during an inpatient stay (see, for instance, example G in Box 1). The following reasons for this were suggested: clinical settings may lack the equipment needed to turn patients; there may be delays in implementing equipment such as special mattresses; nursing staff may be unfamiliar with turning methods for patients who have physical deformities; nursing staff may wrongly assume that carers are able to assess and take care of the patient’s pressure areas; and patients may not be compliant with pressure area care.
Misdiagnosis
Examples B and D in Box 1 illustrate diagnostic overshadowing leading to misdiagnosis. Participants with learning disability expertise suggested that this was a particular risk when hospital staff failed to engage carers or LDLNs who can provide background information and aid communication.
Difficulties in communicating with the patient about symptoms and medical history were described as being crucial in contributing to misdiagnosis or diagnostic overshadowing. Examples of misdiagnosis of patients with learning disabilities had led to varying outcomes, ranging from no known harm through to serious harm.
I once found it difficult to assess a young patient with learning difficulties who appeared agitated after a head injury. I had to rely on the information given to me by the mother which was not accurate. The patient was discharged and returned a few hours later with an inter-cranial bleed. This could have been prevented if I had been able to assess the patient better and more thoroughly.
P581, emergency care practitioner (free text on questionnaire)
However, it should be noted that a number of hospital staff did not feel that patients with learning disabilities were at increased risk of misdiagnosis in comparison with other patients. This finding could, in part, be due to the relative infrequency of misdiagnosis coupled with the relative infrequency of caring for patients with learning disabilities. This is perhaps reflected in the results of the clinical staff electronic questionnaire (see Appendix 4), where only 1.2% of staff (10 out of 825) indicated that, within the past 3 years, a patient with learning disabilities had been misdiagnosed within their clinical area.
It may be of interest to note here that the CIPOLD report3 stated that:
. . . a small number of problems with diagnosing a person’s illness were due to misdiagnosis (7%).
p. 58. Reproduced with permission from Heslop P, Blair P, Fleming P, Hoghton M, Marriott A, Russ L. Confidential Inquiry into Premature Deaths of People with Learning Disabilities (CIPOLD): Final Report. Bristol: Norah Fry Research Centre; 2013
These were mostly cases of cancer being misdiagnosed as another illness, or doctors not challenging a provisional diagnosis as symptoms developed.
Delayed investigations and treatment
Examples A, B, C, D, F and H in Box 1 all provide examples of compromised patient safety which resulted in harm to the patient as a result of delayed investigations and delayed treatment. Contributory factors underpinning these examples and others were wide-ranging. There could be difficulties in accessing hospital services (for example, non-attendance of outpatient appointments); failure to provide the reasonable adjustments needed to enable the patient to have the investigation or treatment (see Chapter 6); poor staff attitudes, including assumptions about quality of life (see Misuse of the Mental Capacity Act); and issues around the patient’s ability to give consent or the correct implementation of the Mental Capacity Act (see Misuse of the Mental Capacity Act).
Other examples in relation to delayed treatment included the timely recognition and treatment of pain, and problems with medication.
Recognising and treating pain
A number of participants (including people with learning disabilities, hospital staff and carers) suggested that recognising and appropriately treating pain had been problematic.
A couple of times on [the ward] I tried to get their attention, I was in pain and needed medication. I had to get my mum to speak to them and she had to complain, saying I need medication for my pain.
P64, person with learning disabilities
Several nurses talked about the difficulty of assessing pain when a patient is unable to communicate verbally and the reliance they have on close carers to establish this. Similarly, some expert carers acknowledged these difficulties.
Medication
Of respondents to the staff questionnaire, 2.1% (17 out of 825) indicated that within the past 3 years a patient with a learning disability had been given the wrong medication or the wrong dose, or did not receive their medication.
Omissions of medication were a particularly common patient safety issue.
On a number of occasions the care staff would come in and find that the patient’s medication remained untaken on the side. When they checked this with the ward staff they would claim that the patient had taken it because the medication chart had been signed.
P44, paid carer
It was proposed that some patients with learning disabilities may be less likely to challenge the omission of their medication with ward staff.
They’d be less likely to challenge the error . . . a patient with a learning disability would be much more vulnerable in that situation.
P194, Head of PALS
The degree of patients’ compliance with treatment was also cited as a possible cause of drug omissions for patients with learning disabilities.
Furthermore, it was proposed that some nursing staff working in acute hospitals may be unfamiliar with certain medications commonly taken by people with learning disabilities for their comorbidities (for example, anti-epileptics and mood stabilisers) and lack understanding of the importance of such medications, which may contribute to the increased likelihood of omission.
In addition, several examples were given by patients with learning disabilities and their carers who had experienced problems relating to medication following discharge, and a small number of incident reports had been filed in relation to this issue. Problems included insufficient communication with the carers about medication changes, or discharge medication not being issued in an appropriate format.
This patient with a learning disability who has support at home was discharged without being given a copy of his discharge letter. His insulin regime had been changed by the doctors here which was highlighted on the discharge letter. His carers were not informed of the changes.
Incident report
She has to have tablets in blister packs . . . and they had changed her medication, so that all had to be set up before she left the hospital. I explained all of this to them and they said ‘no don’t worry, that will all be set up’. I went to collect her and there were no blister packs. They gave her a bag and tablets in boxes and as much as I wanted to take her home because she was so fed up, I couldn’t because she cannot read or write. She can’t administer from boxes. And they then claimed it takes three days for them to get the pharmacist to do these blister packs.
P200, family carer
Non-treatment decisions and ‘do not attempt resuscitation’ orders
There were examples (including example A in Box 1) where carers felt that decisions about whether or not to provide active treatment for patients with learning disabilities were being inappropriately influenced by staff assumptions about quality of life or by staff members’ fear of treating patients whom they perceived to be challenging. In such examples, treatment was provided at the carers’ utmost insistence, and patients who may otherwise have died were able to return home.
[The doctor in A&E] took me to one side and he said, ‘What sort of quality of life is she going to have if we pull her through this?’ And I said, ‘She’ll have a fantastic quality of life, she’s got close family, she’s got excellent carers, she’s got lots of things to look forward to in her life’. And he said, ‘Well, it’ll be up to the ICU [intensive care unit] team whether or not they’ll treat her, you do realise that she isn’t going to survive if we don’t treat her?’
P128, family carer
If my staff had not supported [patient], he would either be in a coma or dead because they just wouldn’t have given him any medical intervention.
P184, paid carer
Similarly, in some cases nursing staff and carers felt that DNAR orders were inappropriately based on staff assumptions about the quality of life of patients with learning disabilities.
One thing, personally, which upsets me the most – I know they have learning disabilities and it’s not very severe sometimes – but they just put all of them when they come in, ‘Not For Resus’.
P57, ward manager
Misuse of the Mental Capacity Act
The study results revealed a number of problems that clinical staff working in acute hospitals have with understanding and correctly implementing the Mental Capacity Act. 30,31
Example F in Box 1 described incorrect use of the Mental Capacity Act. Other examples included patients being asked to sign a consent form (and obliging) without any explanation being given, despite staff having been told that the patient lacked literacy skills.
Furthermore, delays to investigation or treatment are often imposed while capacity is assessed or while a ‘best interest’ decision is being reached. One family carer described difficulties in trying to obtain a timely ‘best interest’ decision to enable her profoundly disabled son to have an urgent procedure to unblock his PEG feeding tube.
We literally ran round . . . What they should understand is that the PEG is his lifeline, the food, water, if that’s not working, he can’t swallow . . . and that’s where we run into trouble. People don’t always get it, they don’t understand that there’s urgency.
P123, family carer
Within the staff survey, 23.8% of clinical staff (196 out of 825) said that within the past 3 years certain tests or treatments were delayed because the patient was unable to give consent. Furthermore, 8.6% of clinical staff (71 out of 825) indicated that within the past 3 years certain tests or treatments were not given because the patient was unable to consent.
Many hospital staff appeared to misunderstand the Mental Capacity Act or lacked confidence in using it. Within the staff survey, staff were asked whether they felt confident in using the Mental Capacity Act; their responses can be found in Figure 13.
FIGURE 13.
‘Do you feel confident using the Mental Capacity Act?’ Responses to staff survey question 18 (n = 835).
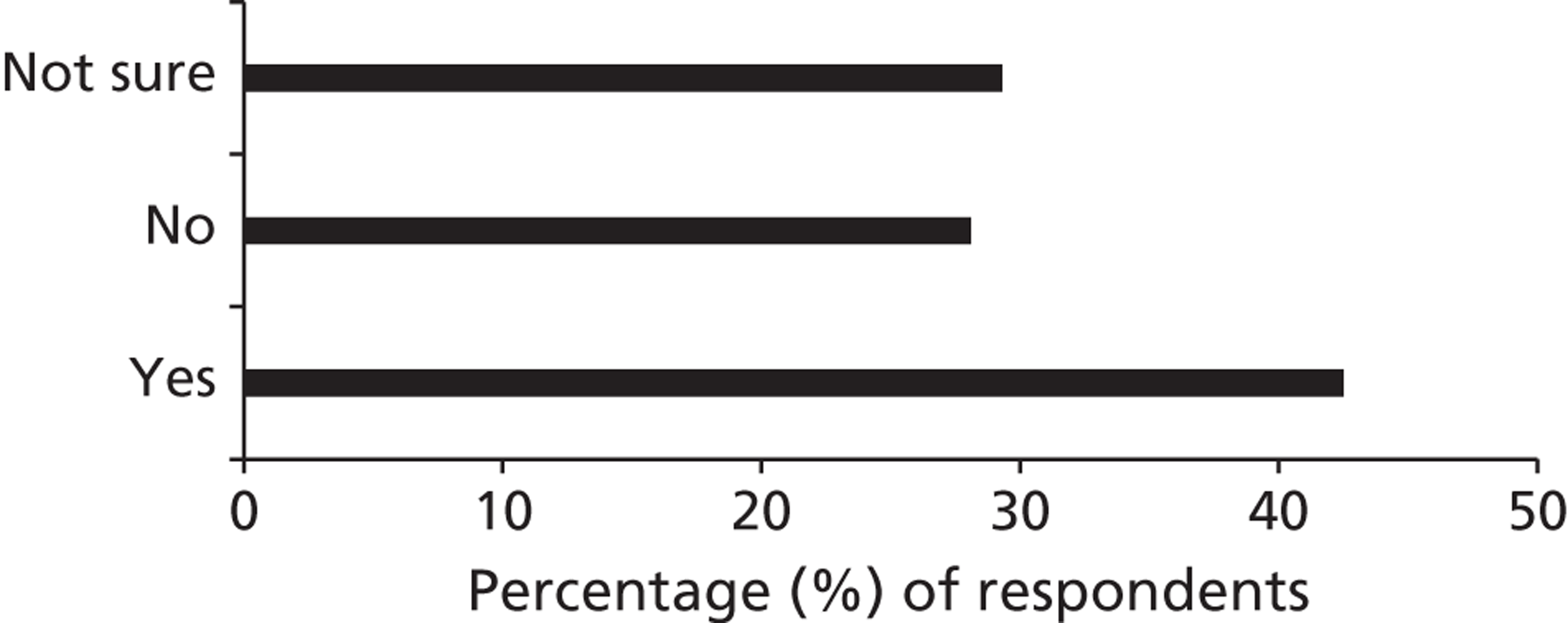
This uncertainty was not restricted to junior staff; during interviews a number of senior clinical staff highlighted difficulties in correctly following the Mental Capacity Act, which may result in harm or even patient death.
[The patient] had cancer and needed surgery. I didn’t realise that he didn’t have the capacity to say ‘no’ to the operation. He didn’t want the operation, and I just thought that was that. But [LDLN] came along and asked him, ‘What do you think will happen if you don’t have the operation?’ and he really didn’t know. He didn’t have the capacity. So it became a best interest decision, and we decided to do the operation.
P1289, consultant physician
Aside from the delays inherent in organising best interest meetings, where used these were generally thought to be productive. However, it appeared that the correct use of best interests meetings was still not ‘the norm’ in some settings.
Incident reports
Incident reports at the study sites
Incident report data were provided by five of the six study sites. Staff at the site that did not provide this information stated that they were unable to identify which incident reports involved patients with learning disabilities.
Qualitative analysis demonstrated that a wide range of incidents involving patients with learning disabilities had been reported. These spanned inappropriate management of perceived challenging behaviour; physical abuse towards hospital staff (sometimes resulting in injury and sometimes not); incorrect use of the Mental Capacity Act; delays to diagnostic tests; delays to treatment; drug errors and omissions; pressure sores; feeding problems; poor tracheostomy care; falls, accidents and injuries; hospital-acquired infections; safeguarding alerts; patients absconding/discharging against medical advice; treatment in an inappropriate clinical area; and unavailability of equipment.
Rudimentary assessment of the number of each type of incident reported revealed that staff often report tangible, physical patient safety issues (such as falls, pressure sores or medication errors), for which there may be a particular drive in favour of reporting at an organisational level. While this research did not seek to quantify the types of patient safety issues that are reported, cross reference to the other sources of data collated during the study may imply that important issues such as problems with feeding or hydration, or delays to patient care may be less readily identified than patient safety issues that require reporting.
Difficulties with using incident reports to monitor patient safety
It is known that incident reports tend to be biased towards certain patient safety incidents and the study results appear to concur with this. For example, some hospitals are excellent at reporting falls, as the need to do so has been widely promoted. There are, however, a vast number of potential reasons why some incident types may be under-reported. Acts of omission are a particular concern.
The study findings suggest that hospital staff are often unclear as to what the safety issues faced by people with learning disabilities are (see also Staff perceptions of patient safety and preventable deterioration). It can be suggested that this may make it difficult for staff to conduct thorough and appropriate risk assessments and safeguard against potential adverse events.
A further major difficulty in using incident reports to assess safety risks was the lack of effective systems for identifying patients with learning disabilities (as described in Chapter 5) and, therefore, accurately identifying all incident reports that involved patients with learning disabilities. Furthermore, discussions held throughout the course of the project revealed that hospital staff often felt that the person’s learning disability was not relevant to the incident and therefore failed to indicate the learning disability on the incident report.
For these reasons, incident reports which are specifically flagged as involving a patient with a learning disability are likely to be a small subset of the incidents that actually take place, and are consequently a poor method for monitoring patient safety issues in this group of people.
Complaints
Limited data were received on formal complaints made by people with learning disabilities or their carers. This is probably because of the sensitivity of this information, issues surrounding patient confidentiality, and the difficulty of identifying which complaints concern patients with learning disabilities. As a result of this, no complainants were directly invited to be interviewed for the study as was intended in the study protocol.
Of those formal complaints that the research team was notified of, one was made by a family carer who felt that the person’s personal hygiene needs had not been met and aggression had not been well managed; one was made by a family carer who felt that the person with learning disabilities had been inappropriately asked to sign a consent form which the patient did not understand; one was made by a family carer who reported a delay in A&E while waiting to see a specialist doctor; and one was made by a family carer with regards to a cancelled outpatient appointment. One trust was able to provide information about the number of complaints received but did not provide detail as to the type of complaints that were made. One trust described a process of ‘high flagging’ any complaints involving patients with learning disabilities, ensuring that a swift and thorough investigation was prioritised.
A small number of the carers and people with learning disabilities who were interviewed for the study suggested that they had previously made a formal complaint or that they may consider making a formal complaint in light of their recent hospital experience. The research team is unaware of whether or not the latter came to fruition. The outcomes of formal complaints were not always deemed satisfactory.
I put in a complaint to the hospital. They said they had investigated it, and I had a formal letter back from them. The outcome was – they have other patients to look after! (Transcriptionist note: participant doesn’t sound impressed with this).
P17, family carer
Carers indicated that they did not make complaints if they were dissatisfied with the hospital experience for two reasons: a desire to put the experience behind them and concerns that complaining might negatively affect the future health care of the person with learning disabilities.
It was just that this treatment of this lady – because her family and herself didn’t want to put in a complaint – I really felt that this is the only time that I could say anything for them on their behalf without making it too official; because they’re worried about repercussions basically. They’re worried that the hospital won’t want to treat them or the GP will strike them off.
P185, paid carer
Furthermore, the qualitative data demonstrate that a number of people raised concerns with hospital staff or with PALS about the care received by patients with learning disabilities which do not constitute formal complaints. In some cases this appeared to resolve concerns and in others it did not.
Chapter 11 Generalisability of the findings to other vulnerable patient groups
Chapter summary
Many of the study findings are likely to be echoed in other vulnerable patient groups such as patients with dementia and those with mental health problems. The lack of integrated records across NHS services, with information about vulnerabilities not consistently passed on by GPs, meant that the identification and flagging of vulnerabilities had to happen within the acute hospital itself. This posed challenges that were similar to those involving patients with learning disabilities.
Some issues around reasonable adjustments, including their cost implications and the lack of recognition of this through PbR, were also generalisable.
Although a lack of role clarification was an issue for carers of all patients, the challenges around carers of patients with learning disabilities were unique, in particular those concerning the involvement of long-term family carers with high expertise and the involvement of paid carers.
Meeting the needs of specific vulnerable groups calls for expertise. Mental health expertise was accessible through psychiatry liaison teams, and several hospitals had introduced expert dementia nursing posts. However, the complexity of the needs of patients with learning disabilities, and the lack of staff exposure to this group of patients, makes the need for a LDLN particularly acute.
Introduction to the stage III results
One research question was to examine whether the emerging findings, with regards to barriers to and enablers of safe care for patients with learning disabilities, were related to the nature of learning disability itself and the particular issues affecting this group, or to certain problems arising from the presence of learning disability, which may also be present in other vulnerable patient groups.
The method used for exploring the extent to which the study findings are generalisable to other vulnerable groups was a search of existing literature and expert panel discussions at the participating sites. The focus of the literature search and the panel discussions was on the key areas that emerged during stages I and II: identifying, flagging and tracking specific patient groups; providing reasonably adjusted services; involving carers as partners in care; and the role of a patient group-specific specialist nurse within the hospital.
For the purpose of this study, the focus was on patients with dementia and patients with mental health problems. Patients with communication problems due to other causes (including brain injuries and dysphasia) were also specifically included in the study protocol, but, as both the literature and the interview data were highly limited for these groups, there is no such focus in this chapter. Issues for additional vulnerable groups, including children and patients who are homeless, were raised briefly in the panel discussions.
It can be anticipated that the issues around other vulnerable patient groups are highly complex, as they are for patients with learning disabilities. The time frame for investigating the generalisability of findings in this study was relatively short (3 months), and therefore this could only be an exploration of relevant issues, rather than an in-depth investigation.
Literature review
Conducting the literature review
A vulnerable adult is someone who is ‘aged 18 or over, receives or may need community care services because of a disability, age or illness, and who is or may be unable to take care of themselves or protect themselves against significant harm or exploitation’. 105 Because of time constraints, this was not a comprehensive literature review, but rather an exploration of issues raised in this study, using web-based searches with a particular focus on relevant national policies and reports. Below is a brief summary.
Patient safety issues for other vulnerable patient groups
There is considerable evidence that vulnerable patients face health inequalities and safety risks in hospital, including a higher risk of medical error. Patient groups at increased risk include the elderly,85 patients with complex needs,106 patients with low socioeconomic status,107,108 patients with limited English proficiency or limited health literacy,109,110 minority populations and immigrant populations. 108
Patients with mental health problems have been reported to have poorer health and to die prematurely, caused in part by ‘diagnostic overshadowing’. 111 The term ‘treatment overshadowing’ has also been used in relation to this group. This includes an unwillingness to address possible barriers to appropriate care when making treatment decisions. 112
Dementia significantly increases the length of hospital admission113–115 and the risk of medical harm through the use of multiple medications. 116 Recent national reports and strategy documents117–119 have raised concerns regarding the quality of care received by people with dementia in acute hospitals. Carers of patients with dementia have reported how behavioural and psychological symptoms of dementia may worsen during hospital admission,117 although a systematic review found no studies on how hospital staff manage these symptoms and their impact on patients. 120
Identifying and flagging vulnerable patient groups
Literature on the subject of identifying and flagging vulnerabilities was found to centre mostly on identifying dementia. The CQC found that almost a third of hospital admissions involving people with dementia did not include a record of their dementia, despite the fact that it had been identified in the past, and called for better identification of dementia as well as comprehensive training for care staff. 121 It has been recommended that schemes are put in place to enable ward staff to identify patients with dementia,122 as in the case of the ‘butterfly scheme’. 123
However, as with people with learning disabilities, many people with dementia do not have a formal diagnosis. One study found that, in a cohort of 617 hospital patients aged > 70 years, 42.4% had dementia; less than half of these had been diagnosed before admission. 124 The routine screening for dementia proposed by the prime minister has not been universally welcomed by physicians, who fear it will not meet the criteria for screening and is not a good use of resources. 125
Providing reasonably adjusted health services
The national audit of dementia care in general hospitals,122 which involved 55 hospitals, found that there was a general lack of patient-centred care, with environments that were not dementia-friendly. Pockets of good practice were identified but there was no evidence of effective organisational systems for implementing person-centred care. The audit further found that carers were not systematically involved in patient care and discharge planning.
Specialist nursing roles
There has been recognition of the importance of training and appointing specialist nurses in order to ensure that the needs of particular vulnerable groups are met. In 1999, the National Service Framework for Mental Health stipulated that all A&E departments should have mental health liaison services to ensure appropriate and timely interventions for patients with mental health problems. This has since developed into a psychiatry liaison service in NHS hospitals that is much wider than just A&E departments. 126
Most recently (February 2013) the Francis Inquiry85 identified elderly patients as being particularly vulnerable in NHS hospitals and recommended that services consider introducing a registered older person’s nurse, in recognition of the special requirements needed to care for the elderly.
Results
Identifying vulnerable patients within NHS hospitals
Electronic flagging systems
The participating hospitals used electronic flagging systems for specific medical conditions or risks, such as diabetes, infections or an increased risk of falls. However, most hospitals did not have electronic flags for vulnerable patient groups such as those with dementia or mental health problems.
The difficulty of introducing flags for specific patient groups, whether electronic or otherwise, was related to the difficulty of identifying or diagnosing these particular vulnerabilities. As is the case for patients with learning disabilities, unless a patient enters the hospital with a clear diagnosis of dementia or a mental health condition, it can be difficult for staff to make a correct diagnosis. There is a significant risk of misdiagnosis and subsequent mislabelling, heightened by the risk that the symptoms of a patient’s presenting illness (such as confusion) may mimic those of dementia or mental ill health. It was further noted that the risk of diagnostic overshadowing is present for other vulnerable groups as it is for patients with learning disabilities.
Learning disability liaison nurses pointed out that they receive regular referrals for patients who turn out not to have learning disabilities at all, but another problem, including mental health problems.
It’s very difficult because it’s rare that you can just diagnose somebody with dementia. So there is a specific screening for them. But we’re having difficulty implementing that.
P201, Deputy Director of Nursing
The lack of integrated record systems between acute care, primary care and social care was noted as a problem for other groups as well, including patients with dementia and those on the End of Life Register, with information held by GPs not being passed on to acute hospitals.
Finally, some vulnerable patients might not want to have their vulnerabilities flagged for fear of negative attitudes or poorer treatment. This was noted particularly for patients with mental health problems.
Non-electronic flagging systems
Most hospitals were in the process of introducing non-electronic flagging systems for patients with dementia and cognitive impairments, by putting a specific symbol (a butterfly or a forget-me-not flower) by the patient’s name on the ward whiteboard or on their notes. The advantage of this was that it alerted not just the clinicians but the entire team, including porters and cleaners, to a need for adjustments. However, such schemes were still in their infancy; their use and impact had not yet been evaluated at the time of the study.
Should vulnerable patients be flagged?
There was disagreement about the desirability of flagging vulnerability, similar to the staff unease and disagreement around flagging learning disability.
Similar to concerns around flagging learning disability was the concern that by flagging vulnerable patient groups, too many flags could be introduced, confusing staff, causing staff to ignore the flags and rendering them useless.
Patient-held information documents
Some hospitals had introduced patient-held information documents similar to those used for patients with learning disabilities. The problems noted with these documents were also similar, particularly the experience that they are not used widely enough.
Now they get a [butterfly], you get out the [hospital passport], but what we’ve found is they fill it out and put it in the notes and then no-one uses it.
P1249, consultant physician
Reasonable adjustments
Flagging the need for reasonable adjustments
One hospital trust was moving away from flagging specific vulnerable patient groups and was in the process of introducing a system where it was the need for reasonable adjustments, rather than the patient’s vulnerability, that was flagged. This was designed to circumvent the problem of mislabelling and misdiagnosis, as well as the problem of staff not knowing what to do when a vulnerable patient is flagged. There was as yet no feedback about the use or effectiveness of this system.
Issues around reasonable adjustments are generalisable
Many staff members who were interviewed felt that the safety risks and issues involved for other vulnerable patients were very similar to issues faced by patients with learning disabilities.
I think all of those patients are at risk of not achieving basic standards of care because you . . . if they can’t ask for what they need or they won’t tell you if they’re hungry or they won’t eat or whatever – then yes it’s easy in an environment that’s got loads going on to leave them out.
P34, ward manager
However, there was a sense among panel discussion participants that patients with learning disabilities were one of the most difficult and vulnerable groups, and their care could be used as a yardstick for the care of all vulnerable patients.
It’s a small group but actually it’s quite representative of what goes on in the bigger scale . . . If it’s happening to people with learning disabilities, it’s going to be happening to people with dementia and it’s going to be happening to people with mental illness.
P36, LDLN
It was felt that the issues around implementing reasonable adjustments are not unique to learning disability. The skills required for recognising the need for reasonable adjustments and implementing them are transferable to all vulnerable patient groups. Participants noted that this was partly related to the culture of a hospital or ward: wards and staff who are willing and able to accommodate the different needs of patients with learning disabilities are likely to be able to do so for all their patients. Conversely, on wards where adjustments were not made for patients with learning disabilities, carers and LDLNs reported that the same was true for other vulnerable patients.
She says that whenever her care staff are with one of their residents in hospital, the care staff have to help and feed other patients on the ward because the ward staff don’t help them. P44 said: ‘They leave trays of food in front of people with dementia and don’t help them to eat it. Then they come round and clear the trays away.’
Transcription notes of non-tape-recorded interview with P44, paid carer
Cost implications of reasonably adjusted health services
There was strong agreement among participants (in particular strategic managers) that the implementation of reasonable adjustments for complex patients is costly, and that accounting for complexity of care through the PbR system would improve care delivery. This is the case for other vulnerable patient groups as well; for example, the care of someone with dementia who has a tendency to wander or to fall requires additional resources.
Involving carers
Protocols for shared care would be helpful for all patients who have carers. One hospital asked all patients on admission whether they relied on a carer or whether they had caring responsibilities themselves; this led to an assessment of the carers’ needs.
There was agreement that it would be helpful for all carers, not just carers of people with learning disabilities, to negotiate and agree the carer’s role and their support needs during the patient’s hospital stay, although some expert panel members felt that in some areas (such as ICUs), and for some patient groups, this was already being achieved. It was also recognised that any protocols or policies for shared care would have to allow for highly individual needs and focus on establishing the extent and boundaries of care.
The uniqueness of carers of people with learning disabilities
There was a consensus in the expert panel discussions that carers of patients with learning disabilities differed in some ways from carers of other vulnerable patients. Whereas carers of dementia patients were often spouses or children who were new to seeing themselves in the role of carer to their family member, and therefore needed a particular type of support and understanding, family carers of patients with learning disabilities had fulfilled the role for all of that patient’s life. Staff expectations of such carers were quite different.
If you know that somebody is coming in with a learning disability you’re almost expecting a carer to come with them. Whereas somebody with dementia your expectation isn’t necessarily that they’ll come in with a carer. They are coming in the hospital and you deal with the situation. [Sounds of agreement]
P1279, senior nurse
However, it was also observed that staff made assumptions about carers of other vulnerable patient groups, including children and people with dementia, providing basic care.
You make that assumption, don’t you: ‘Oh their daughter is here’, and you must work very hard not to assume and to go in and provide or offer the same care that you are giving to the patient next door.
P1248, consultant physician
Expert panel members felt, though, that it was more readily understood by ward nurses that while family carers of patients with dementia might be well placed to help calm the patient down, it could be inappropriate for them to provide personal care.
Panel members further thought that hospital staff were much less familiar with the care of patients with learning disabilities than with the care of other vulnerable patient groups, and more apprehensive; it was felt that they would therefore leave basic care to learning disability carers more readily.
Because staff are not always familiar with caring for people with learning disabilities, when they have carers they almost draw back a bit and think, ‘Well they know what they are doing’ [sounds of agreement] so – whereas if you had someone in a cubicle that was maybe on the Liverpool Care Pathway and they were dying, the nurse would still go in there because that person isn’t there for the expertise. I often think that they think the carers from learning disability homes will be the expert person that can take care of them.
P1243, matron
Having paid carers for people with learning disabilities is a unique feature; all four panels said that there were no other patient groups that routinely brought such carers with them to hospital. The panels also agreed that hospital staff had not found good ways of managing the relationship with paid carers; as one consultant physician (P1248) said: ‘We’ve not welcomed the paid carer in.’
Specialist nurses
Specialist nurses for other vulnerable patient groups
Specialist nursing roles within acute hospitals tended to focus on specific medical conditions (such as epilepsy, diabetes, multiple sclerosis or types of cancer). Discussions around the provision of specific expertise for vulnerable patient groups focused on dementia expertise. Some hospitals had dementia nurses; one hospital was in the process of appointing a dementia nurse. Other roles mentioned that covered specific patient groups were nurse specialist for older people and specialist palliative care teams.
Expertise in caring for patients with mental health problems was commonly provided by a liaison psychiatry team or hospital mental health nurse specialists.
The need for a specialist nurse
There was a sense in the panel discussions that the need for a specialist nurse was particularly acute for learning disability, perhaps more so than for any other vulnerable group. It was noted that other vulnerabilities (such as dementia) were more prevalent, and therefore staff were more aware of the issues involved and had a higher level of expertise. This led to a recognition that while the relatively small numbers of patients with learning disabilities may make it more difficult to justify the employment of a LDLN, their minority presence was in fact one of the reasons why such a nurse was needed.
Chapter 12 Discussion and empirical framework
Summary of the findings
This study found examples of good practice and a willingness to improve care for patients with learning disabilities across all six participating NHS hospitals. However, the study also found that, despite this willingness, and despite the implementation of strategies to achieve improvements, such good practice remained haphazard and people with learning disabilities remained at risk of suboptimal care and support within NHS hospitals. This study has not been able (and did not intend) to quantify this risk. With only six study sites and a large number of variables, it is not possible to say whether some hospitals were better than others at providing safe care for patients with learning disabilities, or to ascribe examples of good or poor practice to particular differences within organisations. However, there is sufficient evidence to suggest that the vulnerabilities of patients with learning disabilities can, and do, lead to compromised patient safety.
The most common safety issues were delays and omissions of care, ranging from delays and omissions of basic nursing care (for example, unmet nutrition needs) to delays and omissions of medical treatment (for example, treatment not given because of perceived inability to cope with or consent to treatment or because of staff assumptions about the patient’s quality of life). Although acts of omission (failing to diagnose or provide required care) are thought to be twice as prevalent as acts of commission (providing the wrong care),127 acts of omission are known to be more difficult to recognise, capture and monitor. 128
The strategies put in place by the hospitals’ management include the implementation of the LDLN role, carer policies, easy-read documentation (including patient-held information documents), staff training and the inclusion of people with learning disabilities and carers on advisory bodies. Overall, the situation appears to be improving somewhat. Many carers reported that hospital care for the person with learning disabilities is better than it was several years ago, with some wards and some staff described as excellent. However, most carers could also point to wards and staff where the opposite was true. Examples of poor practice were identified even where there appeared to be good policies and management support for learning disability issues. It seems, therefore, that policies and strategies do not reliably translate to better practice in the clinical areas. Furthermore, there was a lack of effective hospital structures to ensure that the pockets of good practice were consistently replicated hospital-wide.
Barriers
The study identified a number of major barriers to better and safer hospital care. The most significant of these appear to be:
-
invisibility of people with learning disabilities within the health-care system
-
widespread lack of staff understanding of learning disability, the vulnerabilities of people with learning disabilities and the reasonable adjustment they may need in order to access health-care services
-
lack of consistent and effective carer involvement
-
lack of clear lines of responsibility and accountability for ensuring that each individual patient with learning disabilities receives co-ordinated, appropriate and reasonably adjusted health care.
Invisibility of patients with learning disabilities
The fact that most people with learning disabilities are unknown to any health and social care services, and the current lack of effective systems for communicating information about known learning disability between primary and secondary health-care services, constitute significant cross-organisational barriers. Organisational barriers include a lack of effective systems for flagging learning disability and a considerable lack of staff expertise and staff willingness to identify and flag learning disabilities, encompassing not just junior but also the most senior staff.
Lack of staff understanding
Many of the staff interviewees were dedicated to improving care for people with learning disabilities and wanted to do the very best for their patients. However, there was a widespread and persistent lack of understanding across all staff groups and all levels of seniority of the ways in which the support needs of people with learning disabilities might differ from those of the general population. There was also a lack of staff understanding of the fact that delays in, or omissions of, care and treatment are a particular safety risk for people with learning disabilities, and of the reasonable adjustments that may be needed to ensure that they do not happen. Staff lacked understanding and skill in applying the Mental Capacity Act correctly to patients with learning disabilities. There were indications from all stakeholders that staff apprehension about caring for a patient with learning disabilities can lead to omissions of care.
Lack of consistent and effective carer involvement
Staff did not always understand the essential role of carers and the importance of including carer expertise. Although the study found some excellent practice, where carers were supported in their caring role and their expertise was sought and utilised by staff, many of the examples of compromised patient care involved carers that were not listened to. Carers were appreciated for the help they could give with patient care, communication and patient reassurance, but their crucial knowledge of the patient was often disregarded. Patients were put at further risk by staff making assumptions about the input of carers; at worst, there were examples of hospital staff failing to provide basic care.
Lack of clear lines of responsibility and accountability
Those with specific responsibility for the safe and reasonably adjusted health care of people with learning disabilities within the hospital, and for co-ordinating their care, varied across study sites and included the LDLNs, the trust’s clinical lead for safeguarding vulnerable adults, and hospital matrons. Most of these (and the LDLNs in particular) had learning disability expertise and demonstrated passion and drive to improve patient care. Their roles included co-ordination of care and ensuring that the needs of individual patients were met. However, patients with learning disabilities were not reliably referred to them, partly because of a lack of effective flagging systems. Several of these roles were part-time.
The lines of accountability and responsibility were not clear. It was not clear exactly what responsibility or accountability LDLNs had for the care of patients with learning disability, and who carried accountability, awareness and expertise in their absence.
At ward or clinic level, there was a lack of clear allocation of responsibility and accountability for ensuring that patients with learning disabilities had their care and treatment needs met. Carers reported seeing different members of staff on each shift. Given the significant lack of staff knowledge and understanding of learning disability and associated vulnerabilities, this led to good practice being haphazard throughout the organisation.
Enablers
Without board-level managers who are actively supportive of improving care for patients with learning disabilities, it will be difficult to sustain and replicate good practice. Supportive structures and policies are also important, including carer policies, the provision of accessible information and the implementation of flagging systems. Such policies and schemes were quoted by hospital managers to demonstrate commitment and effectiveness in providing reasonably adjusted health-care services.
However, the translation of such policies into practice at the point of patient contact was inconsistent and often depended on ward culture and the attitudes of individual staff. Therefore, the key enablers found in this study were the LDLN and the ward manager.
Learning disability liaison nurse
The LDLN role was pivotal in a number of areas. Hospitals with a LDLN were best able to identify patients with learning disabilities within their services. LDLNs identified individual needs for reasonable adjustments and were able to ensure their implementation. They were able to co-ordinate care that could be highly complex. They provided staff training and, possibly more importantly, they were a role model for staff and an effective advocate within the hospital, raising awareness and championing the needs of people with learning disabilities.
The lack of staff understanding of learning disability issues and associated patient safety risks, together with the invisibility of patients with learning disabilities within the health-care system, made the presence of on-site learning disability expertise particularly important in reducing patient safety risks. On-site LDLNs were better than community-based LDLNs at raising staff awareness, gaining staff trust and increasing the numbers of patients with learning disabilities identified within the hospital.
However, this enabling role could easily be undermined by a lack of resources (including a lack of cover), lack of senior management support, lack of clarity about the role and a lack of authority to act. The enabling role of the LDLN needed to be embedded and backed up by the hospital structures.
The ward manager
Wards that received the highest praise from carers, with reports of consistently positive staff attitudes and consistent provision of reasonable adjustments, were those where the ward manager ran ‘a tight ship’. LDLNs could pinpoint which wards were ‘good’ and which were less so; this was mostly dependent on a ward manager who understood the issues around learning disability, supported junior ward staff and called for learning disability expertise where needed. Front-line staff were key to delivering a better service to people with learning disabilities and their carers; ward managers were critical in ensuring that care was delivered well.
Generalisability to other vulnerable patient groups
The lack of integrated records across NHS services, with information about vulnerabilities not consistently passed on by GPs, poses challenges with identification and flagging that are likely to be similar for other vulnerable patient groups.
Issues around reasonable adjustments, including their cost implications and the lack of recognition of this through PbR, are also likely to be generalisable.
The challenges around carers of patients with learning disabilities were unique, in particular identifying the need for the involvement of long-term family carers with high levels of expertise as well as the involvement of paid carers.
The complexity of the needs of patients with learning disabilities and the lack of staff exposure to this group of patients makes the need for a LDLN particularly acute.
Putting the findings into context
During the final month of this project, two major inquiries reported their findings to parliament. The Francis Inquiry,85 which investigated the high numbers of patient deaths at Staffordshire Hospital, highlighted systemic failures and poor culture within the NHS, leading to severely compromised patient safety and, in particular, a lack of patient-centred care. The recommendations include an increased focus on a culture of compassion, better ward leadership and clear lines of responsibility for each patient’s care.
The CIPOLD report3 identified deficiencies in the quality and effectiveness of health care given to people with learning disabilities, contributing to premature deaths. This included a lack of identification of people with learning disabilities within the health-care system; delays in identifying, diagnosing and treating ill health in people with learning disabilities; a lack of systemic embedding of reasonable adjustments on a day-to-day basis, therefore disadvantaging people with learning disabilities at crucial stages of the care pathway; and a lack of co-ordination of care. There is a strong degree of coherence between the CIPOLD findings and the findings of the current study.
The CIPOLD recommendations3 include the following:
-
clear identification of people with learning disabilities on the NHS central registration system and in all health-care record systems
-
reasonable adjustments required by, and provided to, individuals to be audited annually
-
a named health-care co-ordinator to be allocated to people with complex or multiple health needs
-
Mental Capacity Act training and regular updates to be mandatory for staff involved in health-care delivery
-
patient-held records to be introduced and given to all patients with learning disabilities who have multiple health conditions.
The evidence provided by this current study is fully in line with most of these CIPOLD recommendations. The study findings also support the recommendations of the Francis Inquiry85 that there is a need for culture change, effective ward leadership and clear lines of responsibility for patient care.
One area where the study evidence is less strong is that of patient-held records. This study found no strong evidence that hand-held patient records made a significant difference to patient care and patient safety. This seemed to be mostly due to the fact that knowledge about and use of these documents was not sufficiently widespread, limiting their usefulness.
Study limitations
This study has added significantly to the current knowledge base. The evidence that patients with learning disabilities are vulnerable within health-care services and face safety risks that can be serious has been mounting through the publication of a range of reports, research studies and inquiries over the past decade, and this study adds to the evidence. The study has provided deeper insights into the reasons for hospital failures, and the barriers to be overcome for hospitals trying to ‘get it right’.
However, there are a number of study limitations. One was the limited number of study sites, which meant that any differences in study findings across sites could not be confidently attributed to differences between the study sites. In order to do so, a much larger sample is needed.
Another significant limitation was sampling bias. Although the sampling of staff was fairly straightforward and well facilitated by senior managers, sampling of patients and carers was much more difficult and was facilitated by the LDLN or learning disability lead at each hospital. This meant that the patients and carers sampled were more likely to have had LDLN involvement, and that it was more difficult to access the views and experiences of those who had not. It also meant that there was no access to a sample of patients who had not been flagged or identified as having learning disabilities; sampling through community contacts may have addressed this somewhat. In addition, the sampling strategy meant that large numbers of potential participants were not accessed as the LDLN was busy or absent.
However, saturation of data was achieved for these groups. The sample sizes of people with learning disabilities and carers in this study are large in comparison with existing published studies, and this study therefore adds significant insights.
The study was further limited by the sensitivity of the topic area and a desire by the participating trusts to be seen to be ‘doing well’ in caring for people with learning disabilities. A number of staff members were concerned about possible negative publicity for their hospital; this may have made staff try to present the hospital in a positive light.
The exploration of issues for other vulnerable patient groups was limited by the lack of scope within this complex study to investigate them in depth. This could only be an initial and fairly superficial exploration, highlighting areas for further investigation.
The empirical framework
The above is a summary of some of the most crucial barriers and enablers, but there was a very wide range of factors that affected the implementation of strategies to promote a safer environment for patients with learning disabilities in NHS hospitals. The empirical model (Figure 14) is a synthesis of all subframeworks given in Chapters 5–8.
FIGURE 14.
Empirical framework showing the factors that affect the promotion of a safer environment for patients with learning disabilities. LD, learning disabilities.
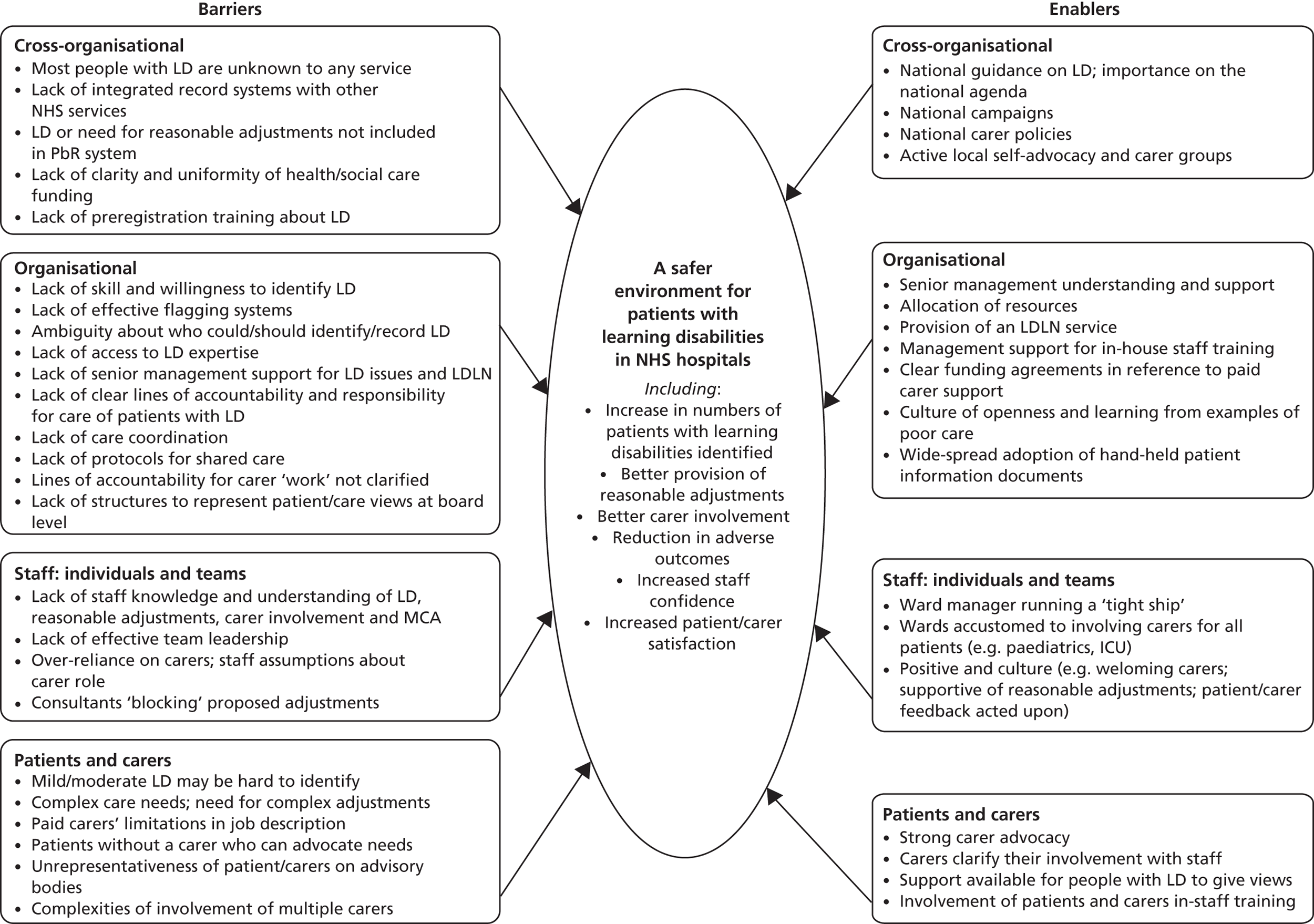
Chapter 13 Conclusions and implications for health-care services
The secondary aim of this study was to develop guidance for NHS acute trusts about the implementation of successful and effective measures to promote a safe environment for patients with learning disabilities. This chapter sets out the key implications of the study findings.
Following the summary of evidence in Chapter 12, we can draw out the following implications for NHS health-care services.
Identifying patients with learning disabilities within hospitals
This study found that many patients with learning disabilities are not identified as such at the point of entry into hospital services, and that staff across all levels of seniority lack the expertise, confidence and willingness to identify this group of patients.
The evidence suggests that the following may go some way in ensuring that patients with learning disabilities are identified within NHS hospitals: (1) the introduction of nationally integrated systems for sharing information about learning disabilities across NHS services, as well as with other organisations with responsibility for the care of people with learning disabilities; (2) the introduction of systems that enable GPs to identify patients with learning disabilities and pass on this information to NHS hospitals; and (3) the introduction of effective flagging systems at the point of referral or entry into hospital care.
Within the hospital, the utilisation of learning disability expertise (for example, through the LDLN and/or through targeted training of ward managers) may address staff inability to identify patients with learning disabilities correctly. General staff training and awareness raising may address the lack of staff willingness to identify patients in this group.
Responsibility and accountability
The evidence suggests that a clear allocation of accountability and responsibility for the co-ordination of the often complex health-care and support needs of patients with learning disabilities may reduce the patient safety risks for this group. There is a need to clarify where in the organisation the lines of accountability and responsibility lie, as well as the expertise. Currently, there is no clinician (whether a physician or a specialist nurse) in overall charge of the care of patients with complex needs.
The evidence suggests that ward managers are a critical part of the line of responsibility and accountability for meeting the needs of patients with learning disabilities, as they have direct responsibility for the behaviour of the front-line staff who are key to delivering reasonably adjusted health services at ward or clinic level. Allocating day-to-day accountability for the care of patients with learning disabilities to ward and clinic managers may address the current inconsistencies in providing reasonably adjusted health care.
It seems from the research evidence that both those with day-to-day accountability and those with ultimate accountability need to have ready access to learning disability expertise, as well as sufficient seniority and authority. Furthermore, accountability and awareness of learning disability issues needs to be present throughout the trust and not simply be ‘shifted off’ to an LDLN post that could be easily marginalised. In other words, there needs to be someone at every organisational level, from ward level to board level, ensuring that the needs of people with learning disabilities are met.
Learning disability liaison nurse
There is strong evidence to suggest that hospitals with an effective LDLN service are in the best position to ensure that the needs of patients with learning disabilities within their service are met. In order for this role to be effective, the LDLN had to be available and visible within the hospital and had to have the authority to change patient care pathways; this was more readily achieved by on-site LDLNs. By implication, the establishment of such roles across NHS hospitals, properly supported and resourced and with sufficient authority inherent in the role, could go some way in addressing issues of compromised safety for patients with learning disabilities.
However, as indicated above, it is important that the LDLN role is not isolated, and that there are clear lines of responsibility and accountability. The role authority of the LDLN needs to be well known and clear to all staff. The LDLN needs to work closely with ward managers and other staff responsible for vulnerable groups, as well as with senior hospital managers.
Protocols for shared care
The evidence suggests that the safety of patients with learning disabilities is compromised by a failure to involve and include carer expertise, as well as by a lack of clarity about carer roles and the extent of carer involvement for an individual patient. This issue may be addressed by the implementation of ‘protocols for shared care’, whereby the presence of carers is assessed for all patients with learning disabilities and the extent and nature of carer involvement is clarified and agreed with the carer(s) in each individual case. It should be clear that the hospital trust carries responsibility for ensuring that the patient receives basic care and treatment. Carer expertise should be sought to ensure that the care is given appropriately. Carer input into care tasks should be welcomed and supported, but not assumed.
Staff training and awareness raising
The evidence suggests that many of the barriers to the promotion of a safer hospital environment for patients with learning disabilities include a persistent hospital culture where staff lack knowledge, understanding and awareness of the specific vulnerabilities and needs of patients with learning disabilities. They also lack knowledge of the Mental Capacity Act, a problem which has not been sufficiently addressed by the implementation of policies. The implication is that hospital staff do not currently receive adequate pre- and post-registration training in these matters. Given the large numbers of hospital staff and the level of staff turnover, and considering the second implication described above (see Responsibility and accountability), in-depth training may best be targeted at those in overall charge of individual patient care, including ward managers.
There is further evidence that involving people with learning disabilities and carers in staff training may be particularly effective in raising awareness and changing perceptions.
Chapter 14 Recommendations for research
Introduction
This study has added significantly to the knowledge base around the safety of patients with learning disabilities in NHS hospitals. There is a remarkable and unprecedented degree of coherence and agreement between our study findings and the findings and recommendations arising from the work of past inquiries, research and reports. 3–5,14,34,50,129,130 The fact that people with learning disabilities face significant health inequalities within acute hospitals has now been well established. This study has added significantly to the insights into the nature of the problem.
Further research is now warranted into specific ways in which these problems can be addressed. Following on from this study, we offer the following key recommendations for research, in order of importance.
Providing reasonable adjustments
It is clear from the evidence obtained in this study that a lack of reasonable adjustments can lead to compromised patient safety. IHAL is collecting evidence about the types of reasonable adjustments currently implemented. 36,54 However, it is not clear what kind of reasonable adjustments are needed most in NHS hospitals, and what the resource implications of this are.
Research recommendation 1
Further research is needed to answer the following questions:
-
What reasonable adjustments are needed most frequently within the hospital care pathways of people with learning disabilities?
-
What knowledge, systems and structures are needed within the hospital to ensure that these reasonable adjustments are routinely made?
-
What are the cost implications of reasonable adjustments, and how can this be translated into the PbR system?
Such research might take the form of a large-scale multiple case study in which the hospital pathways of a large number of patients with learning disabilities are reviewed in depth, identifying and quantifying the barriers they face as well as the reasonable adjustments they need. This could also include an investigation of the facilitators of and barriers to (non-)provision of these reasonable adjustments.
Leadership and co-ordination of care
The evidence suggests that there is a need to allocate clear responsibility and accountability for the care of patients with learning disabilities, as well as for the overall co-ordination of their hospital care. This is in line with the Francis report,85 which recommends identifying a consultant or senior clinician and a nurse in charge of each patient’s care. However, it is currently not clear what the best structures are for allocating overall responsibility for the care of patients with learning disabilities throughout their hospital pathways, who should take responsibility for the complex care of people with learning disabilities, or whether ward managers are ready to take on day-to-day responsibility.
Research recommendation 2
Further research is needed to answer the following questions:
-
Who is best placed within acute NHS hospitals to take on overall responsibility and accountability for the care pathways of patients with learning disabilities, and what structures are needed to facilitate this?
-
How effective are ward managers in taking on day-to-day responsibility and accountability for the care of patients with learning disabilities?
-
How effective are ward managers in identifying patients with learning disabilities and their need for reasonable adjustments?
-
How effective are ward managers in ensuring that reasonable adjustments are consistently implemented, and in utilising specialist learning disability expertise?
-
What training and support do ward managers require in practice to enable them to achieve these goals?
Identifying patients with learning disabilities in NHS hospitals
The current inability of NHS hospitals to identify and flag the presence of learning disabilities is a major barrier to the provision of equitable and reasonably adjusted health care. IHAL has proposed a method of screening all patients for learning disabilities as they enter the health-care system and has suggested a script for administrative staff or nurses to enable them to ‘ask the question’. 43 The evidence from this study suggests that hospital staff currently lack both the expertise and the willingness to screen patients in this way.
Research recommendation 3
Further research is needed into practical and effective ways of flagging patients with learning disabilities in NHS hospitals, including the following questions:
-
What are the barriers to identifying and flagging people with learning disabilities within primary care, particularly GP practices, and to sharing this information consistently with NHS hospitals?
-
How can such barriers best be addressed across the NHS?
-
Within NHS hospitals, is it feasible to screen for learning disabilities? What expertise is necessary to do this effectively?
-
What are the views of patients with learning disabilities and their carers on identifying the presence of learning disability on NHS records?
Implementing and evaluating protocols for shared care
The importance of involving carers as partners in care was recognised and reported in Healthcare for All. 4 This study has provided further evidence that failure to involve carers and include carer expertise in care provision can lead to adverse patient outcomes. The lack of clarity around carer roles and carer involvement was a significant barrier to safe care delivery.
Research recommendation 4
There is a need to investigate, implement and evaluate models or protocols for shared care. This could be a protocol whereby the possible need for family or paid carer involvement is identified for all patients on arrival, with the specific individual contributions of carers to be clarified, agreed, monitored and recorded. As this constitutes an investigation of a change intervention that must be embedded and effective within the hospital setting, action research methods would be appropriate.
Evaluating learning disability liaison nurse posts
Although this study has clearly demonstrated the value of LDLN posts within hospitals, the evidence base for their effectiveness is currently limited, making specific NHS-wide recommendations for the implementation and development of such posts difficult. It is also unclear how LDLN posts can best be embedded within the hospital structures, what authority LDLNs have, and what the specific lines of responsibility and accountability are.
Research recommendation 5
Further research is needed to investigate (a) what different LDLN service models are available across the UK, and the advantages and disadvantages of these models; (b) what the comparisons are between hospitals with and without a LDLN; (c) how learning disability expertise can best be shared and accessed throughout the organisation; (d) what the best practice models are in relation to authority and lines of accountability for the care of patients with learning disabilities; (e) whether the LDLN service should be standardised or local differences are important; and (f) what the cost–benefit implications are of a LDLN service.
Investigating safety issues for other vulnerable patient groups
This study could only provide a superficial exploration of patient safety issues for other vulnerable groups. It has highlighted that difficulties around identifying and flagging vulnerabilities including dementia and mental health problems may cause care to be compromised. There are also strong indications that a failure to provide patient-centred, reasonably adjusted health services puts vulnerable patients at risk.
Research recommendation 6
Further research is needed into effective delivery of reasonably adjusted NHS health-care services to patients with dementia and patients with mental health problems. This needs to include an investigation of effective ways of identifying these patients within the health-care system (similar to research recommendation 3), and an investigation of the particular types of reasonable adjustments needed for these groups, together with their cost implications (similar to research recommendation 1).
Further implications and recommendations
The number of data collected for this study was vast. This report could only provide an overview. More detailed reports on specific aspects of this study will be disseminated through academic papers. This will include further implications for NHS services and further recommendations for research.
Acknowledgements
First and foremost, our thanks go to the six anonymous hospital trusts which have been extremely helpful and supportive of the research and committed considerable amounts of time and effort to it. Their commitment reflected, in all cases, a real desire to improve their services for people with learning disabilities and a desire to learn lessons from the study findings.
In particular, the authors would like to acknowledge the input of the collaborators at each study site. These consisted of Directors/Deputy Directors of Nursing and learning disability liaison nurses. They promoted the study throughout their trust, provided the research team with advice around participant recruitment and access to participants, and did a considerable amount of work supporting the recruitment of patients and carers. They also attended collaborator meetings with the research team to reflect on any difficulties encountered in conducting the study, and provided expert advice around possible solutions. This study could not have happened without their involvement and enthusiasm.
Secondly, our thanks go to all the anonymous participants (staff, carers and patients) who gave their time generously.
Specific contributions are listed below. More details on affiliations and expertise can be found in Appendix 1.
Contributions of authors
Irene Tuffrey-Wijne (Senior Research Fellow in Nursing, Learning Disabilities/Palliative Care) was the principal investigator. She undertook overall management and supervision of the project; was the major contributor to protocol development, study design and data collection tool development; supervised, and contributed to, data collection; contributed to data analysis; was the main contributor to data interpretation and synthesis; and drafted the manuscript.
Nikoletta Giatras (Research Fellow, Learning Disabilities) performed day-to-day management of the project and contributed to protocol development, study design and data collection tool development; carried out data collection (including a major contribution to collecting stage I data) and data analysis; and contributed to data interpretation, drafting of the manuscript and critical revision of the manuscript.
Lucy Goulding (Research Assistant, Patient Safety) contributed to data collection tool development; carried out data collection (including a major contribution to collecting and interpreting staff survey data), data analysis and data interpretation; contributed to drafting of the manuscript (including drafting Chapter 10); and critically revised the manuscript.
Elisabeth Abraham (Research Assistant, Learning Disabilities) contributed to data collection tool development; carried out data collection and data analysis; contributed to data interpretation; and critically revised the manuscript.
Leonard Fenwick (Chief Executive NHS Trust) chaired the research advisory board; contributed to study design and interpretation of data; and critically revised the manuscript.
Christine Edwards (Director, Institute of Leadership and Management in Health) contributed to protocol development, study design and interpretation of data, and critically revised the manuscript.
Sheila Hollins (Professor of Psychiatry of Disability, Member of the House of Lords and a family carer) supervised the principal investigator; contributed to protocol development, study design and interpretation of data; and critically revised the manuscript.
Acknowledgement of contributors
Paul Adeline (coresearcher) contributed to data collection tool development for people with learning disabilities, conducted interviews with people with learning disabilities and contributed to data interpretation in relation to people with learning disabilities.
Jim Blair (learning disability nurse consultant) contributed to protocol development.
Gary Butler (coresearcher) contributed to data collection tool development for people with learning disabilities, conducted interviews with people with learning disabilities and contributed to data interpretation in relation to people with learning disabilities.
Sara Christian (research fellow) contributed to staff questionnaire development.
Steve Gillard (Senior Lecturer, Mental Health) contributed to protocol development and study design, and advised on qualitative methodological issues and project management.
Vanessa Gordon (Associate Director of Patient Safety for Learning Disabilities, NHS Commissioning Board; member of research advisory board) contributed to interpretation of data around patient safety and incident reports, and critically revised the related parts of the manuscript.
Lloyd Page (self-advocate, Mencap) contributed to data collection tool development for people with learning disabilities.
Vicky Raphael (family carer, member of research advisory board) contributed to data interpretation in relation to carers, and critically revised Chapter 7 of the manuscript.
Monica Stannard (family carer, member of research advisory board) contributed to data collection tool development for carers and data interpretation in relation to carers, and critically revised Chapter 7 of the manuscript.
Sarah White (Statistician, Mental Health) contributed to survey development and data analysis, and advised on quantitative methodological issues.
Members of the research advisory board provided project governance and contributed to interpretation of data. In particular, and in addition to the contributors listed above:
Vikki Carruth, Deputy Director of Nursing.
Amanda Cresswell, self-advocate.
Alison Robertson, Director of Nursing.
Further acknowledgements
St George’s, University of London provided administrative support and support with IT, including the development of the e-questionnaire, and provided staff support for the coresearchers with learning disabilities.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- Death by Indifference. London: Mencap; 2007.
- Six Lives: The Provision of Public Services to People with Learning Disabilities. London: The Stationery Office; 2009.
- Heslop P, Blair P, Fleming P, Hoghton M, Marriott A, Russ L. Confidential Inquiry into Premature Deaths of People with Learning Disabilities (CIPOLD): Final Report. Bristol: Norah Fry Research Centre; 2013.
- Michael J. Healthcare for All: Report of the Independent Inquiry into Access to Healthcare for People with Learning Disabilities. London: Aldridge Press; 2008.
- Getting It Right: A Campaign Guide. London: Mencap; 2010.
- Valuing People: A New Strategy for Learning Disability for the 21st Century. A White Paper. London: Department of Health; 2001.
- Emerson E, Hatton C. People with Learning Disabilities in England. Lancaster: Centre for Disability Research; 2008.
- Emerson E, Hatton C. Estimating Future Need for Social Care Among Adults with Learning Disabilities in England: An Update. London: IHAL; 2011.
- Prasher V, Janicki M. Physical Health of Adults with Intellectual Disabilities. Oxford: Wiley-Blackwell; 2002.
- van Schrojenstein Lantman-de Valk H, Walsh P. Managing health problems in people with intellectual disabilities. BMJ 2008;337:1408-12. http://dx.doi.org/10.1136/bmj.a2507.
- O’Hara J, McCarthy J, Bouras N. Intellectual Disability and Ill Health: A Review of the Evidence. Cambridge: Cambridge University Press; 2010.
- Havenman M, Heller T, Lee L, Maaskant M, Shooshtari S, Strydom A. Report on the State of Science on Health Risks and Ageing in People with Intellectual Disabilities. Dortmund: IASSID Special Interest Research Group on Ageing and Intellectual Disabilities/Faculty Rehabilitation Sciences, University of Dortmund; 2009.
- Emerson E, Baines S. Health inequalities and people with learning disabilities in the UK. Tizard Learn Disabil Rev 2011;16:42-8. http://dx.doi.org/10.5042/tldr.2011.0008.
- Emerson E, Baines S, Allerton L, Welch V. Health Inequalities and People with Learning Disabilities in the UK: 2011. London: IHAL; 2011.
- Ouellette-Kuntz H. Understanding health disparities and inequities faced by individuals with intellectual disabilities. J Applied Res Intellectual Disabil 2005;18:113-21. http://dx.doi.org/10.1111/J.1468-3148.2005.00240.x.
- Krahn G, Hammond L, Turner A. A cascade of disparities: health and health care access for people with intellectual disabilities. Ment Retard Dev Disabil Res Rev 2006;12:70-82. http://dx.doi.org/10.1002/mrdd.20098.
- Equal Treatment: Closing the Gap – a Formal Investigation into Physical Health Inequalities Experienced by People with Learning Disabilities and/or Mental Health Problems. London: Disability Rights Commission; 2006.
- Glover G, Ayub M. How People with Learning Disabilities Die. London: IHAL; 2010.
- Treat Me Right! Better Healthcare for People with a Learning Disability. London: Mencap; 2004.
- Valuing People Now: A New Three-Year Strategy for People with Learning Disabilities. London: The Stationery Office; 2009.
- Health Inequalities: Progress and Next Steps. London: Department of Health; 2008.
- Improving the Health and Well-Being of People with Learning Disabilities. London: Department of Health; 2009.
- Hollins S, Attard MT, von Fraunhofer N, McGuigan S, Sedgwick P. Mortality in people with learning disability: risks, causes, and death certification findings in London. Dev Med Child Neurol 1998;40:50-6.
- Hoghton M, Turner S, Hall I. Improving the Health and Wellbeing of People with Learning Disabilities: An Evidence-Based Commissioning Guide for Clinical Commissioning Groups (CCGs). London: IHAL, Royal College of General Practitioners and Royal College of Psychiatrists; 2012.
- Quality and Risk Profiles of NHS Trusts in Early 2010. London: Care Quality Commission; 2010.
- Transparency in Outcomes: A Framework for the NHS. A Consultation of Proposals. London: Department of Health; 2010.
- Hornby P, Symon G, Cassel C, Symon G. Qualitative Methods in Organizational Research. London: Sage Publications; 1994.
- Murphy J, Cameron L. The effectiveness of Talking Mats™ with people with intellectual disability. Br J Learn Disabil 2008;36:232-41.
- Butler G, Cresswell A, Giatras N, Tuffrey-Wijne I. Doing it together. Br J Learn Disabil 2012;40:134-42.
- Mental Capacity Act 2005. London: The Stationery Office; 2005.
- Mental Capacity Act 2005: Code of Practice. London: The Stationery Office; 2007.
- Bazeley P. Qualitative Data Analysis with NVivo. London: Sage Publications; 2007.
- Tuffrey-Wijne I, Bernal J, Hollins S. Doing research on people with learning disabilities, cancer and dying: ethics, possibilities and pitfalls. Br J Learn Disabil 2008;36:185-90. http://dx.doi.org/10.1111/j.1468-3156.2008.00519.x.
- Death by Indifference: 74 Deaths and Counting. A Progress Report 5 Years On. London: Mencap; 2012.
- Public Health England . Improving Health and Lives Learning Disability Observatory 2013. www.improvinghealthandlives.org.uk (accessed April 2013).
- Hatton C, Roberts H, Baines S. Reasonable Adjustments for People with Learning Disabilities in England 2010: A National Survey of NHS Trusts. London: IHAL; 2011.
- Transforming Care: A National Response to Winterbourne View Hospital. London: Department of Health; 2012.
- The State of Health Care and Adult Social Care in England: An Overview of Key Themes in Care in 2011/12. London: The Stationery Office; 2012.
- The NHS Constitution. London: Department of Health; 2013.
- Delivering 21st Century IT Support for the NHS National Strategic Programme. London: The Stationery Office; 2002.
- NHS Connecting for Health . Summary Care Records 2013. www.nhscarerecords.nhs.uk (accessed April 2013).
- Publicservice.co.uk . Patient Groups ‘embrace Care records’ 2013. www.publicservice.co.uk/news_story.asp?id=17698 (accessed April 2013).
- Glover G, Emerson E. Have You Got a Learning Disability? Asking the Question and Recording the Answer for NHS Healthcare Providers. London: IHAL; 2012.
- Disability Discrimination Act 1995. London: The Stationery Office; 1995.
- Disability Discrimination Act 2005. London: The Stationery Office; 2005.
- Equality Act 2010. London: The Stationery Office; 2010.
- The Essential Guide to the Public Sector Equality Duty. Volume 1 of 5: Equality Act 2010 Guidance for English Public Bodies (and Non-Devolved Bodies in Scotland and Wales). Manchester: Equality and Human Rights Commission; 2010.
- Your Rights to Equality from Health and Social Care Services. Equality Act 2010 Guidance of Your Rights, Volume 5 of 9. Manchester: Equality and Human Rights Commission; 2010.
- Getting it Right When Treating People with a Learning Disability. London: Mencap; 2010.
- Six Lives Progress Report. London: Department of Health; 2010.
- Nicholson D. Letter from Sir David Nicholson 2010. www.ncuh.nhs.uk/about-us/trust-board/2010/november/letter-sir-dvid-nicolson.pdf (accessed April 2013).
- Giraud-Saunders A. Equal Access? A Practical Guide for the NHS: Creating a Single Equalities Scheme that Includes Improving Access for People with Learning Disabilities. London: Department of Health; 2009.
- Hatton C, Roberts H, Baines S. Reasonable Adjustments for People with Learning Disabilities in England: A National Survey of NHS Trusts. London: IHAL; 2011.
- IHAL . Reasonable Adjustments Database 2012. www.improvinghealthandlives.org.uk/adjustments (accessed April 2013).
- Carers Trust . What Is a Carer? 2012. www.carers.org/what-carer (accessed October 2013).
- Hemsley B, Balandin S, Worrall L. Nursing the patient with developmental disability in hospital: roles of paid carers. Qual Health Res 2011;21:1632-42. http://dx.doi.org/10.1177/1049732311415289.
- Webber R, Bowers B, Bigby C. Hospital experiences of older people with intellectual disability: responses of group home staff and family members. J Intellect Dev Disabil 2010;53:155-64. http://dx.doi.org/10.3109/13668250.2010.491071.
- Weiss J, Lunsky Y, Gracey C, Canrinus M, Morris S. Emergency psychiatric services for individuals with intellectual disabilities: caregivers’ perspectives. J Appl Res Intellect Disabil 2009;22:354-62. http://dx.doi.org/10.1111/j.1468-3148.2008.00468.x.
- Hemsley B, Balandin S, Togher L. Narrative analysis of the hospital experience for older parents of people who cannot speak. J Aging Stud 2007;21:239-54. http://dx.doi.org/10.1016/j.jaging.2006.12.001.
- Dinsmore A. A small-scale investigation of hospital experiences among people with a learning disability on Merseyside: speaking with patients and their carers. Br J Learn Disabil 2012;40:201-12. http://dx.doi.org/10.1111/j.1468-3156.2011.00694.x.
- Gibbs S, Brown M, Muir W. The experiences of adults with intellectual disabilities and their carers in general hospitals: a focus group study. J Intellect Disabil Res 2008;52:1061-77. http://dx.doi.org/10.1111/j.1365-2788.2008.01057.x.
- Iacono T, Davis R. The experiences of people with developmental disability in Emergency Departments and hospital wards. Res Dev Disabil 2003;24:247-64. http://dx.doi.org/10.1016/S0891-4222(03)00041-6.
- Allen D. Negotiating the role of expert carers on an adult hospital ward. Sociol Health Illn 2000;22:149-71. http://dx.doi.org/10.1111/1467-9566.00197.
- Foster J. Learning disability liaison nurses in acute hospitals: is there evidence to support the development of this role?. Learn Disabil Pract 2005;8:33-8. http://dx.doi.org/10.7748/ldp2005.05.8.4.33.c1622.
- Brown M, MacArthur J, McKechanie A, Mack S, Hayes M, Fletcher J. Learning Disability Liaison Nursing Services in south-east Scotland: a mixed-methods impact and outcome study. J Intellect Disabil Res 2012;56:1161-74. http://dx.doi.org/10.1111/j.1365-2788.2011.01511.x.
- Castles A, Bailey A, Gates B, Sooben R. Role of liaison nurses in improving communication. Learn Disabil Pract 2012;15:16-9. http://dx.doi.org/10.7748/ldp2012.11.15.9.16.c9379.
- Pearce L. Dedicated support in every hospital. Nurs Stand 2010;24:22-3.
- Modernising Nursing Careers: Setting the Direction. London: Department of Health; 2006.
- Backer C, Chapman M, Mitchell D. Access to secondary healthcare for people with intellectual disabilities: a review of the literature. J Appl Res Intellect Disabil 2009;22:514-25. http://dx.doi.org/10.1111/j.1468-3148.2009.00505.x.
- Holman A. In conversation with Jim Blair. Br J Learn Disabil 2012;40:166-8. http://dx.doi.org/10.1111/bld.12000.
- Royal College of Nursing . A Learning Disability Nurse in Every Hospital? (resolution) 2010. www.rcn.org.uk/newsevents/congress/2010/congress_2010_resolutions_and_matters_for_discussion/6._a_learning_disability_nurse_in_every_hospital (accessed April 2013).
- MacArthur J, Brown M, Hayes M, Mack S, McKechanie A, Fletcher J, et al. Learning Disability Liaison Nursing Services in South East Scotland: A Mixed Methods Impact and Outcome Research Study. Edinburgh: NHS Lothian, University of Edinburgh and Edinburgh Napier University; 2010.
- Phillips L. Improving care for people with learning disabilities in hospital. Nurs Stand 2012;26:42-8. http://dx.doi.org/10.7748/ns2012.02.26.23.42.c8933.
- World Health Organization . Patient Safety: What We Do 2013. www.euro.who.int/en/what-we-do/health-topics/Health-systems/patient-safety (accessed April 2013).
- Vincent C, Neale G, Woloshynowych M. Adverse events in British hospitals: preliminary retrospective record review. BMJ 2001;322:517-19. http://dx.doi.org/10.1136/bmj.322.7285.517.
- Design for Patient Safety. London: Department of Health; 2004.
- Kohn L, Corrigan J, Donaldson J. To Err is Human. Washington, DC: National Academy Press; 1999.
- Reason J. Human error: models and management. BMJ 2000;320:768-70. http://dx.doi.org/10.1136/bmj.320.7237.768.
- Understanding the Patient Safety Issues for People with Learning Disabilities. London: National Patient Safety Agency; 2004.
- Brown H. Safeguarding People with Learning Disabilities Within the NHS: An Agenda for the National Patient Safety Agency. London: National Patient Safety Agency; 2003.
- Transparency in Outcomes: A Framework for the NHS. London: Department of Health; 2010.
- National Patient Safety Agency . Ensuring Safer Practice for Adults With Learning Disabilities Who Have Dysphagia 2007. www.nrls.npsa.nhs.uk/resources/?entryid45=59823 (accessed April 2013).
- Ganesh S, Potter J, Fraser W. An audit of physical health needs of adults with profound learning disability in a hospital population. J Appl Res Intellect Disabil 1997;7:228-36. http://dx.doi.org/10.1111/j.1468-3148.1994.tb00128.x.
- NHS England . Quarterly Data Summaries 2013. www.nrls.npsa.nhs.uk/resources/collections/quarterly-data-summaries (accessed April 2013).
- Francis R. The Report of the Mid Staffordshire NHS Foundation Trust Public Inquiry. HC947. London: The Stationery Office; 2013.
- Cinate I, Duxbury L, Higgins C. Measurement of perceived organizational readiness for change in the public sector. Br J Manag 2009;20:265-77. http://dx.doi.org/10.1111/j.1467-8551.2008.00582.x.
- Pettigrew A, Ferlie E, McKee L. Shaping Strategic Change. London: Sage; 1992.
- Newton J, Graham J, McLoughlin K, Moore A. Receptivity to change in a General Medical Practice. Br J Manag 2003;14:143-53. http://dx.doi.org/10.1111/1467-8551.00271.
- Balogun J, Hailey V, Johnson G, Scholes K. Exploring Strategic Change. London: Prentice Hall; 2004.
- Mintzberg H, Ahlstrand B, Lampel J. Strategy Safari: A Guided Tour Through the Wilds of Strategic Management. London: Prentice Hall; 1998.
- Edwards C, Robinson O. Better quality part-time jobs? A study of part-time working in nursing and the police. Employee Relat 2001;23:438-53. http://dx.doi.org/10.1108/EUM0000000005898.
- Edwards C, Robertson O. An evaluation of the business case for flexible working among qualified nurses in the UK National Health Service. Br J Ind Relat 2004;42:167-83.
- Truss C. Enablers and constraints in the NHS. Int J Public Sector Manag 2003;16:43-61. http://dx.doi.org/10.1108/09513550310456418.
- McGovern P, Gratton L, Stiles P, Hailey H, Truss C. Human resource management on the line?. Hum Resour Manage J 1997;7:12-29. http://dx.doi.org/10.1111/j.1748-8583.1997.tb00286.x.
- Currie G, Finn R, Martin G. Spanning boundaries in pursuit of effecive knowledge sharing within healthcare networks in the NHS. J Health Organ Manag 2007;21:406-17.
- McNulty T, Ferlie E. Re-engineering Healthcare: The Complexities of Organisational Transformation. Oxford: Oxford University Press; 2002.
- Ferlie E, Pettigrew A. Managing through networks: some issues and implications for the NHS. Br J Manage 2005;7:81-99.
- Vera D, Crossan M. Strategic leadership and organisation learning. Acad Manage Rev 2004;29:222-40. http://dx.doi.org/10.2307/20159030.
- Bolden R, Gosling J, Casebeer A, Harrison A, Mark A. Innovations in Health Care: A Reality Check. Basingstoke: Palgrave Macmillan; 2006.
- Gilmartin M, D’Aunno T. Leadership research in health care: a review and roadmap. Acad Manage J 2007;1:387-438.
- Balogun J. From blaming the middle to harnessing its potential: creating change intermediaries. Br J Manage 2003;14:69-83. http://dx.doi.org/10.1111/1467-8551.00266.
- Currie G, Procter S. Exploring the relationship between HR and middle managers. Hum Resour Manage J 2001;11:53-69. http://dx.doi.org/10.1111/j.1748-8583.2001.tb00045.x.
- Blair J. Care adjustments for people with learning disabilities in hospitals. Nurs Manage 2011;18:21-4. http://dx.doi.org/10.7748/nm2011.12.18.8.21.c8841.
- Brodrick D, Lewis D, Worth A, Marland A. One-page patient passport for people with learning disabilities. Nurs Stand 2011;25:35-40. http://dx.doi.org/10.7748/ns2011.07.25.47.35.c8644.
- NHS Choices . Vulnerable Adults 2011. www.nhs.uk/carersdirect/guide/vulnerable-people/pages/vulnerable-adults.aspx (accessed April 2013).
- Weingart S, Wilson R, Gibberd R, Harrison B. Epidemiology of medical error. BMJ 2000;320:774-6. http://dx.doi.org/10.1136/bmj.320.7237.774.
- Asch S, Kerr E, Keesey J, Adams J, Setodji C, Malik S, et al. Who is at greatest risk for receiving poor-quality health care?. New Engl J Med 2006;354:1147-56. http://dx.doi.org/10.1056/NEJMsa044464.
- Glassman P. Health literacy. National Network of Libraries of Medicine 2012. http://nnlm.gov/outreach/consumer/hlthlit.html (accessed April 2013).
- Divi C, Koss R, Schmaltz S, Loeb J. Language proficiency and adverse events in US hospitals: a pilot study. Int J Qual Health Care 2007;19:60-7. http://dx.doi.org/10.1093/intqhc/mzl069.
- Mattox E. Identifying vulnerable patients at heightened risk for medical error. Crit Care Nurs 2010;30:61-70. http://dx.doi.org/10.4037/ccn2010102.
- Leucht S, Burkand T, Henderson J, Maj M, Sartorius N. Physical illness and schizophrenia: a review of the literature. Acta Psychiatr Scand 2007;116:317-33. http://dx.doi.org/10.1111/j.1600-0447.2007.01095.x.
- Jones S, Howard L, Thornicroft G. ‘Diagnostic overshadowing’: worse physical health care for people with mental illness. Acta Psychiatr Scand 2008;118:169-71. http://dx.doi.org/10.1111/j.1600-0447.2008.01211.x.
- Lyketsos C, Sheppard J, Rabins P. Dementia in elderly patients in a general hospital. Am J Psychiatr 2000;157:704-7.
- Fulop G, Strain J, Fahs M, Schmeidler J, Snyder S. A prospective study of the impact of psychiatric comorbidity on length of hospital stays of elderly medical-surgical inpatients. Psychosomatics 1998;39:273-80. http://dx.doi.org/10.1016/S0033-3182(98)71344-1.
- Zekry D, Herrmann F, Grandjean R, Vitale A, De Pinho M, Michel J, et al. Does dementia predict adverse hospitalization outcomes? A prospective study in aged inpatients. Int J Geriatr Psychiatry 2009;24:283-91. http://dx.doi.org/10.1002/gps.2104.
- Zekry D, Hermann F, Grandjean R, Meynet M, Michel J, Gold G, et al. Demented versus non-demented very old inpatients: the same comorbities but poorer functional and nutritional status. Age Ageing 2008;37:83-9.
- Lakey L. Counting the Cost: Caring for People with Dementia on Hospital Wards. London: Alzheimer’s Society; 2009.
- Living Well with Dementia: A National Dementia Strategy. London: Department of Health; 2009.
- Bourn J. Improving Services and Support for People with Dementia. London: The Stationery Office; 2007.
- Mukadam N, Sampson E. A systematic review of the prevalence, associations and outcomes of dementia in older general hospital inpatients. Int Psychogeriatr 2010;23:344-55. http://dx.doi.org/10.1017/S1041610210001717.
- CQC Care Update Issue 2. London: Care Quality Commission; 2013.
- Young J, Hood C, Woolley R, Gandesha A, Souza R. Report of the National Audit of Dementia Care in General Hospitals 2011. London: Royal College of Psychiatrists; 2011.
- The Butterfly Scheme . The Butterfly Scheme: Reaching Out to People With Dementia 2013. www.butterflyscheme.org.uk (accessed April 2013).
- Sampson E, Blanchard M, Jones L, Tookman A, King M. Dementia in the acute hospital: prospective cohort study of prevalence and mortality. Br J Psychiatry 2009;195:61-6. http://dx.doi.org/10.1192/bjp.bp.108.055335.
- Brunet M, McCartney M, Tomlinson J, Gordon P, Cosgrove J, Deveson P, et al. Open letter to the Prime Minister and the Chief Medical Officer regarding proposals to introduce screening for dementia. BMJ 2012;344.
- Harlow W. The Use of a Liaison Psychiatric Nurse to Promote Good Health, Treatment and Prevention of Mental Ill Health in a General Hospital Setting 2008. www.nice.org.uk/usingguidance/sharedlearningimplementingniceguidance/examplesofimplementation/eximpresults.jsp?o=185 (accessed April 2013).
- Wilson R, Runciman W, Gibberd R, Harrison B, Newby L, Hamilton J. The Quality in Australian Healthcare Study. Med J Aus 1995;163:458-71.
- Agency for Healthcare Research and Quality Patient Safety Network . Patient Safety Network Glossary 2013. http://psnet.ahrq.gov/popup_glossary.aspx?name=error (accessed April 2013).
- Meeting the Health Needs of People with Learning Disabilities: Guidance for Nursing Staff. London: Royal College of Nursing; 2006.
- General Medical Council . Learning Disabilities 2013. www.gmc-uk.org/learningdisabilities (accessed April 2013).
Appendix 1 Research team and research advisory board
| Core research team | ||
|---|---|---|
| Name | Position | Area of expertise |
| Dr Irene Tuffrey-Wijne (chief investigator) |
Senior Research Fellow, SGUL/Kingston University and Maastricht University (Netherlands) | Qualitative methodologies and mixed-methods research; clinical background in learning disability nursing and palliative care nursing; chairperson of the Palliative Care for People with Learning Disabilities Network; chairperson of the European taskforce on intellectual disability of the European Association of Palliative Care |
| Dr Niki Giatras | Research Fellow, SGUL; day-to-day project manager | Background in psychology, physical activity and mental health; qualitative methodologies |
| Dr Lucy Goulding | Research Assistant, SGUL | Patient safety in NHS hospitals; mixed-methods health services research |
| Ms Liz Abraham | Research Assistant, SGUL | Clinical background in occupational therapy; health services research |
| Mr Gary Butler | Coresearcher; Research and Training Advisor, SGUL | Doing inclusive research; experience of living with learning disabilities |
| Mr Paul Adeline | Coresearcher; Research and Training Advisor, SGUL | Doing inclusive research; experience of living with learning disabilities; member of independent inquiry (Michael 2008)4 |
| Extended research team | ||
|---|---|---|
| Name | Position | Expertise |
| Professor Baroness Sheila Hollinsa | Professor of Psychiatry of Disability, SGUL; Member of House of Lords; family carer | Learning disabilities, research; member of independent inquiry (Michael 2008);4 families/carers of people with learning disabilities |
| Professor Christine Edwardsa | Director, Institute of Leadership and Management in Health, Kingston University | Organisation/management research |
| Dr Steven Gillard | Senior Lecturer, Social Sciences and Mental Health, SGUL | Qualitative methodologies; managing collaborative research projects |
| Dr Sarah White | Senior Biostatistician, SGUL | Statistical analysis |
| Ms Sara Christian | Research Fellow, SGUL/Kingston University | Change management |
| Research advisory boarda | ||
|---|---|---|
| Name | Position | Expertise |
| Sir Leonard Fenwick (chairperson) |
Chief Executive of Newcastle upon Tyne Hospitals NHS Foundation Trust | Senior management; NHS hospitals |
| Professor Baroness Sheila Hollins | As listed above | |
| Professor Christine Edwards | As listed above | |
| Ms Vanessa Gordon | Associate Director of Patient Safety, NHS Commissioning Board | Patient safety; incident reporting |
| Ms Monica Stannard | Family carer | Families/carers of people with learning disabilities |
| Ms Amanda Cresswell | Research Assistant, SGUL; self-advocate | Experience of living with learning disabilities |
| Ms Vicki Raphael | Family carer | Families/carers of people with learning disabilities |
| Ms Vikki Carruth | Deputy Director of Nursing, St George’s Hospital | Nursing management, safeguarding |
| Ms Yvonne Connolly | Patient Safety Manager, St George’s Hospital | Patient safety, NHS hospitals |
| Dr Mark Cottee | Consultant and Senior Lecturer in Geriatric Medicine, St George’s Hospital | Elderly/dementia care; vulnerable groups |
| Ms Alison Robertson | Director of Nursing, St George’s Hospital | Professional leadership and quality improvement; management; NHS hospitals |
Two research advisory board members from Mencap (Beverley Dawkins and Helen Mycock) withdrew after the first meeting, when a conflict of interest with the study became obvious. One coresearcher with learning disabilities, Lloyd Page, who also worked for Mencap, withdrew simultaneously for the same reason and was replaced by Gary Butler.
Appendix 2 Research protocol
Appendix 3 Study participants
| Data collection | Hospital site | Total | |||||
|---|---|---|---|---|---|---|---|
| A | B | C | D | E | F | ||
| Stage I informants | |||||||
| Strategic managers | 1 | 1 | 2 | 1 | 1 | 5 | 11 |
| Staff interviews | |||||||
| Senior managers | 3 | 2 | 3 | 3 | 4 | 3 | 18 |
| Ward managers, matrons, senior sisters, senior nurses | 2 | 4 | 3 | 5 | 3 | 5 | 22 |
| Staff nurses | 4 | – | – | 3 | – | 2 | 9 |
| Physicians | 2 | – | – | 1 | – | 2 | 5 |
| LDLNs | 1 | 1 | – | 1 | 1 | 2 | 6 |
| Community LD nurses | – | – | 2 | – | – | – | 2 |
| Other | – | 2 | – | 1 | 2 | 1 | 6 |
| Total | 12 | 9 | 8 | 14 | 10 | 15 | 68 |
| Staff survey | |||||||
| Doctors | 37 | 25 | 4 | 19 | 49 | 25 | 159 |
| Nurses | 139 | 22 | 63 | 70 | 159 | 88 | 541 |
| HCAs | 10 | 6 | 5 | 10 | 40 | 12 | 83 |
| AHPs | 52 | 19 | 5 | 27 | 32 | 24 | 159 |
| Other | 15 | 4 | 4 | 7 | 16 | 2 | 48 |
| Not specified | 12 | 3 | 3 | 6 | 2 | 2 | 28 |
| Total before exclusions | 265 | 79 | 84 | 139 | 298 | 153 | 1018 |
| Excluded | −12 | −3 | −3 | −6 | −2 | −2 | −28 |
| Total | 253 | 76 | 81 | 133 | 296 | 151 | 990 |
| Carer survey | |||||||
| Family carers | 15 | 4 | 2 | 11 | 7 | 1 | 40 |
| Paid carers | 20 | 9 | – | 11 | 3 | 11 | 54 |
| Total before exclusions | 35 | 13 | 2 | 22 | 10 | 12 | 94 |
| Excluded | – | −1 | 0 | −3 | −2 | – | −6 |
| Total | 35 | 12 | 2 | 19 | 8 | 12 | 88 |
| Carer interviews | |||||||
| Family carers | 5 | 2 | 2 | 4 | 4 | 2 | 19 |
| Paid carers | 5 | 4 | – | 2 | 1 | 6 | 18 |
| Total | 10 | 6 | 2 | 6 | 5 | 8 | 37 |
| Tracer patients | |||||||
| Patient interviews/observation | 1 | 2 | – | 1 | 2 | 2 | 8 |
| Staff interviews | 3 | 1 | – | – | 2 | 2 | 8 |
| Carer interviews | – | 1 | – | – | 1 | 1 | 3 |
| Total | 4 | 4 | 0 | 1 | 5 | 5 | 19 |
| Interviews with people with learning disabilities | |||||||
| Total | 9 | 6 | 4 | 9 | 2 | 3 | 33 |
| Panel discussiona | |||||||
| Senior managers | 1 | 6 | 4 | – | – | 3 | 14 |
| Physicians | 1 | 2 | 2 | – | – | – | 5 |
| Matrons, ward managers, sisters, ward nurses | 3 | – | – | – | – | 8 | 11 |
| Clinical nurse specialists | 3 | 1 | 1 | – | – | 1 | 6 |
| LDLNs | 1 | 1 | – | – | – | – | 2 |
| Community LD nurses | 1 | – | 1 | – | – | – | 2 |
| Other | 1 | – | 1 | – | – | – | 2 |
| Total | 11 | 10 | 9 | – | – | 12 | 42 |
| Total | 335 | 124 | 108 | 183 | 327 | 211 | 1288 |
| Participants counted in more than one data set | |||||||
| Stage I participants already included as staff interviewees | – | −1 | – | – | – | −1 | −2 |
| Carer interview participants already included as carer survey participants | −6 | −6 | −2 | −4 | −4 | −6 | −28 |
| Panel discussion participants already included as staff interviewees | −2 | −2 | −3 | – | – | – | −7 |
| Total number of participants | 327 | 115 | 103 | 179 | 323 | 204 | 1251 |
Appendix 4 Staff survey
Distributed: Spring 2012
Original sample returned (n = 1018)
| Site | Number of questionnaires returned | Percentage of all questionnaires returned according to site |
|---|---|---|
| A | 265 | 26.0 |
| B | 79 | 7.8 |
| C | 84 | 8.3 |
| D | 139 | 13.7 |
| E | 298 | 29.3 |
| F | 153 | 15.0 |
| Total | 1018 | 100.0 |
Exclusion criteria
Four non-clinical staff members were excluded from all analyses as they did not meet the inclusion criteria.
A variable was created to indicate where participants dropped out of the electronic questionnaire. Twenty-four people out of 1018 did not complete any questions at all. These 24 cases were excluded from all analyses. The basic descriptive data presented for each question include only those participants who had not already dropped out. For example, if the last question that a respondent completed was question 6, their responses will be included in the analyses of questions 1–6 only and none of the questions thereafter.
| Last question completed by participants | ||
|---|---|---|
| Question number | Frequency | Percentage |
| 0 | 24 | 2.4 |
| 1 | 3 | 0.3 |
| 4 | 1 | 0.1 |
| 5 | 1 | 0.1 |
| 6 | 1 | 0.1 |
| 7 | 3 | 0.3 |
| 9 | 3 | 0.3 |
| 10 | 45 | 4.4 |
| 11 | 40 | 3.9 |
| 12 | 16 | 1.6 |
| 13 | 4 | 0.4 |
| 14 | 1 | 0.1 |
| 16 | 1 | 0.1 |
| 18 | 2 | 0.2 |
| 18 | 6 | 0.6 |
| 24 | 1 | 0.1 |
| 25 | 4 | 0.4 |
| 26 | 18 | 1.8 |
| 27 | 844 | 82.9 |
| Total | 1018 | 100.0 |
Where relevant to the interpretation of the results, people who had not cared for a patient with learning disabilities at their current hospital, who were not sure if they had cared for a patient with learning disabilities, or who did not answer the question to confirm whether or not they had cared for a patient with learning disabilities, were excluded from the analysis (these data were supplied in answer to question 5).
The exclusion criteria applied to the reporting of each question are documented throughout this appendix.
Q1. Are you clinical staff? (Qualified or unqualified staff who care for/have a caseload of patients)
[No exclusion criteria applied]
| Response | Frequency | Percentage |
|---|---|---|
| Yes | 990 | 97.2 |
| No | 4 | 0.4 |
| Missing | 24 | 2.4 |
| Total | 1018 | 100.0 |
Q2. What is your occupational group?
[Exclusion criteria: non-clinical staff, last question completed < 2]
| Response | Frequency | Percentage |
|---|---|---|
| Registered nurse/midwife | 539 | 54.4 |
| Auxiliary nurse or health-care assistant | 83 | 8.4 |
| Medical and dental | 159 | 16.1 |
| Allied health-care professional | 159 | 16.1 |
| Other | 48 | 4.8 |
| Missing | 2 | 0.2 |
| Total | 990 | 100.0 |
Q3. Which ‘Agenda for Change’ band are you? (Medical and dental staff/other staff who are not part of ‘Agenda for Change’ please select ‘not applicable’)
[Exclusion criteria: non-clinical staff, last question completed < 3]
| Response | Frequency | Percentage |
|---|---|---|
| Band 2 | 60 | 6.1 |
| Band 3 | 46 | 4.6 |
| Band 4 | 8 | 0.8 |
| Band 5 | 144 | 14.5 |
| Band 6 | 211 | 21.3 |
| Band 7 | 260 | 26.3 |
| Band 8A | 67 | 6.8 |
| Band 8B | 20 | 2.0 |
| Band 8C | 10 | 1.0 |
| Band 9 | 1 | 0.1 |
| Not applicable | 153 | 15.5 |
| Missing | 10 | 1.0 |
| Total | 990 | 100.0 |
SECTION A: IDENTIFICATION OF PATIENTS WITH LEARNING DISABILITIES
Q4. Is it part of your responsibilities to assess and screen patients (any patients) on admission/on arrival in your clinical setting and document this?
[Exclusion criteria: non-clinical staff, last question completed < 4]
| Response | Frequency | Percentage |
|---|---|---|
| Yes | 683 | 69.0 |
| No | 287 | 29.0 |
| Missing | 20 | 2.0 |
| Total | 990 | 100.0 |
Q5. Have you cared for a patient with learning disabilities at this hospital?
[Exclusion criteria: non-clinical staff, last question completed < 5]
| Response | Frequency | Percentage |
|---|---|---|
| Yes, regularly | 184 | 18.6 |
| Yes, occasionally | 735 | 74.3 |
| No, never | 53 | 5.4 |
| I’m not sure | 8 | 0.8 |
| Missing | 9 | 0.9 |
| Total | 989 | 100.0 |
Q6. If a patient in your care has learning disabilities are you routinely informed of this?
[Exclusion criteria: non-clinical staff; last question completed < 6; people who have never cared for a patient with learning disabilities, are not sure if they have cared for a patient with learning disabilities or did not answer the question to indicate this (in answer to question 5)]
| Response | Frequency | Percentage |
|---|---|---|
| Always/Usually | 708 | 77.1 |
| Sometimes | 142 | 15.5 |
| Rarely/Never | 64 | 7.0 |
| Missing | 4 | 0.4 |
| Total | 918 | 100.0 |
Q7. How do you find out that a patient in your care has learning disabilities? (Check any that apply)
[Exclusion criteria: non-clinical staff, last question completed < 7]
Number of respondents = 987
| Response | Yes (%) | Not selected (%) | Rank |
|---|---|---|---|
| They are flagged on a computerised patient record system | 131 (13.3) | 856 (86.7) | 7 |
| There is something recorded in/on their notes | 641 (64.9) | 346 (35.1) | 2 |
| There is a flag or symbol on the patient board | 35 (3.5) | 952 (96.5) | 8 |
| They have a special set of notes with them that indicates this (e.g. ‘hospital passport’) | 188 (19.0) | 799 (81.0) | 6 |
| I am alerted by my colleagues (for example, during the handover) | 710 (71.9) | 277 (28.1) | 1 |
| The patient or the patient’s carer tells me | 564 (57.1) | 423 (42.9) | 3 |
| From a medical referral letter | 487 (49.3) | 500 (50.7) | 4 |
| I notice that the patient has learning disabilities whilst caring for them | 467 (47.3) | 520 (52.7) | 5 |
| I don’t usually notice or find out that a patient has learning disabilities | 10 (1.0) | 977 (99.0) | 10 |
| Not applicable: I have never had a patient with learning disabilities | 12 (1.2) | 975 (98.8) | 9 |
| Other | [Qualitative data collected] | ||
Q8. Are you given sufficient background information to enable you to care for patients with learning disabilities in the best way?
[Exclusion criteria for all question 8 analyses: non-clinical staff; last question completed < 8; people who have never cared for a patient with learning disabilities, are not sure if they have cared for a patient with learning disabilities, or did not answer question 5 to indicate this]
Q8.1 Are you given sufficient background information to enable you to care for patients with learning disabilities in the best way? (Clinical information)
| Response | Frequency | Percentage |
|---|---|---|
| Always/Usually | 631 | 69.0 |
| Sometimes | 187 | 20.4 |
| Rarely/Never | 54 | 5.9 |
| Missing | 43 | 4.7 |
| Total | 915 | 100.0 |
Q8.2 Are you given sufficient background information to enable you to care for patients with learning disabilities in the best way? (Information on general needs such as communication needs)
| Response | Frequency | Percentage |
|---|---|---|
| Always/Usually | 531 | 58.0 |
| Sometimes | 281 | 30.7 |
| Rarely/Never | 88 | 9.6 |
| Missing | 15 | 1.6 |
| Total | 915 | 100.0 |
Q8.3 Are you given sufficient background information to enable you to care for patients with learning disabilities in the best way? (Information about social circumstances)
| Response | Frequency | Percentage |
|---|---|---|
| Always/Usually | 489 | 53.4 |
| Sometimes | 272 | 29.7 |
| Rarely/Never | 139 | 15.2 |
| Missing | 15 | 1.6 |
| Total | 915 | 100.0 |
Q8.4 Are you given sufficient background information to enable you to care for patients with learning disabilities in the best way? (Information on personal preferences such as particular likes and dislikes)
| Response | Frequency | Percentage |
|---|---|---|
| Always/Usually | 359 | 39.2 |
| Sometimes | 299 | 32.7 |
| Rarely/Never | 243 | 26.6 |
| Missing | 14 | 1.5 |
| Total | 915 | 100.0 |
Q9. Does your hospital use special patient-held information, such as a ‘hospital passport’, for patients with learning disabilities?
[Exclusion criteria: non-clinical staff, last question completed < 9]
| Response | Frequency | Percentage |
|---|---|---|
| Yes, always | 156 | 15.9 |
| Yes, occasionally | 217 | 22.1 |
| No | 116 | 11.8 |
| Not sure | 485 | 49.3 |
| Missing | 10 | 1.0 |
| Total | 984 | 100.0 |
Q9b. If ‘yes’ to Q9 . . . How useful do you think this patient-held information is?
| Response | Frequency | Percentage |
|---|---|---|
| Very useful | 268 | 27.2 |
| Quite useful | 88 | 8.9 |
| Not very useful | 8 | 0.8 |
| Not at all useful | 1 | 0.1 |
| Total of those who answered | 365 | 37.1 |
| Missing | 619 | 62.9 |
| Total | 984 | 100.0 |
Q10. Please indicate how much you agree or disagree with the following statements:
[Exclusion criteria for all question 10 analyses: non-clinical staff; last question completed < 10; people who have never cared for a patient with learning disabilities, are not sure if they have cared for a patient with learning disabilities, or did not answer question 5 to indicate this]
Q10.1 I often find it difficult to know whether or not a patient has learning disabilities
| Response | Frequency | Percentage |
|---|---|---|
| Strongly agree/Agree | 119 | 13.0 |
| Neutral | 193 | 21.1 |
| Disagree/Strongly disagree | 600 | 65.6 |
| Missing | 2 | 0.2 |
| Total | 914 | 100.0 |
Q10.2 I sometimes find caring for a patient with learning disabilities challenging
| Response | Frequency | Percentage |
|---|---|---|
| Strongly agree/Agree | 547 | 59.8 |
| Neutral | 190 | 20.8 |
| Disagree/Strongly disagree | 176 | 19.3 |
| Missing | 1 | 0.1 |
| Total | 914 | 100.0 |
Q10.3 We don’t really have the time or resources to cope with patients with learning disabilities properly
| Response | Frequency | Percentage |
|---|---|---|
| Strongly agree/Agree | 258 | 28.2 |
| Neutral | 215 | 23.5 |
| Disagree/Strongly disagree | 438 | 47.9 |
| Missing | 3 | 0.3 |
| Total | 914 | 100.0 |
Q10.4 I sometimes find communicating with patients with learning disabilities difficult
| Response | Frequency | Percentage |
|---|---|---|
| Strongly agree/Agree | 458 | 50.1 |
| Neutral | 200 | 21.9 |
| Disagree/Strongly disagree | 254 | 27.8 |
| Missing | 2 | 0.2 |
| Total | 914 | 100.0 |
Q10.5 Some of my colleagues see ‘involved families and carers’ as a bit of a nuisance
| Response | Frequency | Percentage |
|---|---|---|
| Strongly agree/Agree | 139 | 15.2 |
| Neutral | 172 | 18.8 |
| Disagree/Strongly disagree | 598 | 65.4 |
| Missing | 5 | 0.5 |
| Total | 914 | 100.0 |
Q10.6 Some of my colleagues don’t really understand what the specific needs of a patient with learning disabilities are
| Response | Frequency | Percentage |
|---|---|---|
| Strongly agree/Agree | 318 | 34.8 |
| Neutral | 214 | 23.4 |
| Disagree/Strongly disagree | 377 | 41.2 |
| Missing | 5 | 0.5 |
| Total | 914 | 100.0 |
Q10.7 If a patient with learning disabilities needs it, we let their carer stay with them as much as they like
| Response | Frequency | Percentage |
|---|---|---|
| Strongly agree/Agree | 756 | 82.7 |
| Neutral | 103 | 11.3 |
| Disagree/Strongly disagree | 44 | 4.8 |
| Missing | 11 | 1.2 |
| Total | 914 | 100.0 |
Q10.8 If a patient with learning disabilities needs it, we are able to give them extra time
| Response | Frequency | Percentage |
|---|---|---|
| Strongly agree/Agree | 547 | 59.8 |
| Neutral | 174 | 19.0 |
| Disagree/Strongly disagree | 184 | 20.1 |
| Missing | 9 | 1.0 |
| Total | 914 | 100.0 |
Q10.9 I know where to find easy-to-understand information for a patient with learning disabilities
| Response | Frequency | Percentage |
|---|---|---|
| Strongly agree/Agree | 373 | 40.8 |
| Neutral | 218 | 23.9 |
| Disagree/Strongly disagree | 317 | 34.7 |
| Missing | 6 | 0.7 |
| Total | 914 | 100.0 |
Q10.10 I sometimes feel it is inappropriate for a patient with learning disabilities to be cared for in my clinical setting
| Response | Frequency | Percentage |
|---|---|---|
| Strongly agree/Agree | 143 | 15.6 |
| Neutral | 178 | 19.5 |
| Disagree/Strongly disagree | 589 | 64.4 |
| Missing | 4 | 0.4 |
| Total | 914 | 100.0 |
SECTION B: INVOLVING FAMILY AND OTHER CARERS IN CARE
Q11. Please indicate how much you agree or disagree with the following statements around involving family and other carers in the care of patients with learning disabilities:
[Exclusion criteria for all question 11 analyses: non-clinical staff; last question completed < 11; people who have never cared for a patient with learning disabilities, are not sure if they have cared for a patient with learning disabilities, or did not answer question 5 to indicate this]
Q11.1 It is standard practice in this clinical area to involve family and carers in care
| Response | Frequency | Percentage |
|---|---|---|
| Strongly agree/Agree | 780 | 89.1 |
| Neutral | 75 | 8.6 |
| Disagree/Strongly disagree | 20 | 2.3 |
| Missing | 0 | 0.0 |
| Total | 875 | 100.0 |
Q11.2 Involving family and carers can help communication with patients with learning disabilities
| Response | Frequency | Percentage |
|---|---|---|
| Strongly agree/Agree | 864 | 98.7 |
| Neutral | 9 | 1.0 |
| Disagree/Strongly disagree | 2 | 0.2 |
| Missing | 0 | 0.0 |
| Total | 875 | 100.0 |
Q11.3 Involving family and carers can help support patients with learning disabilities in their emotional needs
| Response | Frequency | Percentage |
|---|---|---|
| Strongly agree/Agree | 862 | 98.5 |
| Neutral | 8 | 0.9 |
| Disagree/Strongly disagree | 3 | 0.3 |
| Missing | 2 | 0.2 |
| Total | 875 | 100.0 |
Q11.4 Involving family and carers is reassuring for patients with learning disabilities
| Response | Frequency | Percentage |
|---|---|---|
| Strongly agree/Agree | 845 | 96.6 |
| Neutral | 26 | 3.0 |
| Disagree/Strongly disagree | 2 | 0.2 |
| Missing | 2 | 0.2 |
| Total | 875 | 100.0 |
Q11.5 Involving family and carers helps us to get things done as it is a practical support
| Response | Frequency | Percentage |
|---|---|---|
| Strongly agree/Agree | 812 | 92.8 |
| Neutral | 52 | 5.9 |
| Disagree/Strongly disagree | 9 | 1.0 |
| Missing | 2 | 0.2 |
| Total | 875 | 100.0 |
Q11.6 Sometimes family and carers interfere with the care of individuals with learning disabilities
| Response | Frequency | Percentage |
|---|---|---|
| Strongly agree/Agree | 269 | 30.7 |
| Neutral | 268 | 30.6 |
| Disagree/Strongly disagree | 330 | 37.7 |
| Missing | 8 | 0.9 |
| Total | 875 | 100.0 |
Q11.7 Supporting family and carers distracts attention away from patients with learning disabilities
| Response | Frequency | Percentage |
|---|---|---|
| Strongly agree/Agree | 95 | 10.9 |
| Neutral | 237 | 27.1 |
| Disagree/Strongly disagree | 539 | 61.6 |
| Missing | 4 | 0.5 |
| Total | 875 | 100.0 |
Q11.8 Supporting and directing family and carers of patients with learning disabilities can be time consuming
| Response | Frequency | Percentage |
|---|---|---|
| Strongly agree/Agree | 492 | 56.2 |
| Neutral | 187 | 21.4 |
| Disagree/Strongly disagree | 195 | 22.3 |
| Missing | 1 | 0.1 |
| Total | 875 | 100.0 |
Q11.9 Family and carers can pose a safety risk by not observing health and safety regulations
| Response | Frequency | Percentage |
|---|---|---|
| Strongly agree/Agree | 212 | 24.2 |
| Neutral | 334 | 38.2 |
| Disagree/Strongly disagree | 325 | 37.1 |
| Missing | 4 | 0.5 |
| Total | 875 | 100.0 |
Q11.10 Family and carers know the needs of patients with learning disabilities best
| Response | Frequency | Percentage |
|---|---|---|
| Strongly agree/Agree | 605 | 69.1 |
| Neutral | 222 | 25.4 |
| Disagree/Strongly disagree | 45 | 5.1 |
| Missing | 3 | 0.3 |
| Total | 875 | 100.0 |
Q11.11 Family and carers can provide individualised care that we could not
| Response | Frequency | Percentage |
|---|---|---|
| Strongly agree/Agree | 606 | 69.3 |
| Neutral | 192 | 21.9 |
| Disagree/Strongly disagree | 74 | 8.5 |
| Missing | 3 | 0.3 |
| Total | 875 | 100.0 |
SECTION C: FLEXIBLE SERVICES FOR PATIENTS WITH LEARNING DISABILITIES
Q12. When caring for a patient with learning disabilities, is there flexibility in your clinical setting to:
[Exclusion criteria for all question 12 analyses: non-clinical staff; last question completed < 12; people who have never cared for a patient with learning disabilities, are not sure if they have cared for a patient with learning disabilities, or did not answer question 5 to indicate this]
Q12.1 Provide facilities for carers to stay if they wish to
| Response | Frequency | Percentage |
|---|---|---|
| Always/Usually | 351 | 41.7 |
| Sometimes | 158 | 18.8 |
| Rarely/Never | 121 | 14.4 |
| Not applicable | 136 | 16.2 |
| Don’t know | 71 | 8.4 |
| Missing | 5 | 0.6 |
| Total | 842 | 100.0 |
Q12.2 Accommodate visits out of visiting hours
| Response | Frequency | Percentage |
|---|---|---|
| Always/Usually | 416 | 49.4 |
| Sometimes | 120 | 14.3 |
| Rarely/Never | 48 | 5.7 |
| Not applicable | 196 | 23.3 |
| Don’t know | 54 | 6.4 |
| Missing | 8 | 1.0 |
| Total | 842 | 100.0 |
Q12.3 Provide ‘easy-to-read’ information
| Response | Frequency | Percentage |
|---|---|---|
| Always/Usually | 340 | 40.4 |
| Sometimes | 213 | 25.3 |
| Rarely/Never | 145 | 17.2 |
| Not applicable | 40 | 4.8 |
| Don’t know | 96 | 11.4 |
| Missing | 8 | 1.0 |
| Total | 842 | 100.0 |
Q12.4 Make special arrangements for health-care professionals to speak with carers
| Response | Frequency | Percentage |
|---|---|---|
| Always/Usually | 558 | 66.3 |
| Sometimes | 175 | 20.8 |
| Rarely/Never | 36 | 4.3 |
| Not applicable | 23 | 2.7 |
| Don’t know | 43 | 5.1 |
| Missing | 7 | 0.8 |
| Total | 842 | 100.0 |
Q12.5 Involve carers in planning treatment
| Response | Frequency | Percentage |
|---|---|---|
| Always/Usually | 649 | 77.1 |
| Sometimes | 106 | 12.6 |
| Rarely/Never | 20 | 2.4 |
| Not applicable | 28 | 3.3 |
| Don’t know | 29 | 3.4 |
| Missing | 10 | 1.2 |
| Total | 842 | 100.0 |
Q12.6 Involve carers in planning discharge
| Response | Frequency | Percentage |
|---|---|---|
| Always/Usually | 587 | 69.7 |
| Sometimes | 53 | 6.3 |
| Rarely/Never | 14 | 1.7 |
| Not applicable | 140 | 16.6 |
| Don’t know | 38 | 4.5 |
| Missing | 10 | 1.2 |
| Total | 842 | 100.0 |
Q12.7 Provide extra time for appointments
| Response | Frequency | Percentage |
|---|---|---|
| Always/Usually | 345 | 41.0 |
| Sometimes | 167 | 19.8 |
| Rarely/Never | 128 | 15.2 |
| Not applicable | 92 | 10.9 |
| Don’t know | 96 | 11.4 |
| Missing | 14 | 1.7 |
| Total | 842 | 100.0 |
Q12.8 Allow staff to have extra time to provide support that is required
| Response | Frequency | Percentage |
|---|---|---|
| Always/Usually | 334 | 39.7 |
| Sometimes | 202 | 24.0 |
| Rarely/Never | 228 | 27.1 |
| Not applicable | 26 | 3.1 |
| Don’t know | 42 | 5.0 |
| Missing | 10 | 1.2 |
| Total | 842 | 100.0 |
Q12.9 Provide first or last appointments of the day
| Response | Frequency | Percentage |
|---|---|---|
| Always/Usually | 202 | 24.0 |
| Sometimes | 158 | 18.8 |
| Rarely/Never | 117 | 13.9 |
| Not applicable | 161 | 19.1 |
| Don’t know | 190 | 22.6 |
| Missing | 14 | 1.7 |
| Total | 842 | 100.0 |
Q12.10 Provide special arrangements such as a quiet room
| Response | Frequency | Percentage |
|---|---|---|
| Always/Usually | 181 | 21.5 |
| Sometimes | 155 | 18.4 |
| Rarely/Never | 255 | 30.3 |
| Not applicable | 109 | 12.9 |
| Don’t know | 128 | 15.2 |
| Missing | 14 | 1.7 |
| Total | 842 | 100.0 |
Q12.11 Provide access to advocacy
| Response | Frequency | Percentage |
|---|---|---|
| Always/Usually | 363 | 43.1 |
| Sometimes | 138 | 16.4 |
| Rarely/Never | 91 | 10.8 |
| Not applicable | 50 | 5.9 |
| Don’t know | 187 | 22.2 |
| Missing | 13 | 1.5 |
| Total | 842 | 100.0 |
Q12.12 Provide access to an independent mental capacity advocate
| Response | Frequency | Percentage |
|---|---|---|
| Always/Usually | 305 | 36.2 |
| Sometimes | 109 | 12.9 |
| Rarely/Never | 115 | 13.7 |
| Not applicable | 57 | 6.8 |
| Don’t know | 242 | 28.7 |
| Missing | 14 | 1.7 |
| Total | 842 | 100.0 |
SECTION D: SAFEGUARDING AND SAFETY
Q13. Have you witnessed an incidence of abuse (verbal, physical or other), neglect or discrimination of a patient with learning disabilities by staff at your hospital in the past 3 years?
[Exclusion criteria: non-clinical staff, last question completed < 13]
| Response | Frequency | Percentage |
|---|---|---|
| Yes | 31 | 3.5 |
| No | 812 | 92.3 |
| Maybe – not sure if it was abuse/neglect/discrimination | 30 | 3.4 |
| Missing | 7 | 0.8 |
| Total | 880 | 100.0 |
If ‘yes’ or ‘maybe’ to Q13 . . .
Q13b. Was this abuse/neglect/discrimination reported?
[Exclusion criteria: non-clinical staff, last question completed < 13, answered ‘no’ or did not answer question 13]
| Response | Frequency | Percentage |
|---|---|---|
| Yes in all cases | 21 | 35.0 |
| Yes in some cases | 8 | 13.3 |
| No, not in any cases | 6 | 10.0 |
| Not sure whether it was reported or not | 25 | 41.7 |
| Total of those who answered Q13b | 60 | 100.0 |
Q14. Within your clinical setting, have any of the following occurred involving a patient with learning disabilities in the past 3 years? Check all that apply
[Exclusion criteria for all question 14 analyses: non-clinical staff; last question completed < 14; people who have never cared for a patient with learning disabilities, are not sure if they have cared for a patient with learning disabilities, or did not answer question 5 to indicate this]
The patient did not get sufficient food or drink
| Response | Frequency | Percentage |
|---|---|---|
| Not selected | 773 | 93.7 |
| Yes | 52 | 6.3 |
| Total | 825 | 100.0 |
Communication with the patient was not as good as it should have been
| Response | Frequency | Percentage |
|---|---|---|
| Not selected | 523 | 63.4 |
| Yes | 302 | 36.6 |
| Total | 825 | 100.0 |
Communication with the family or carers was inadequate
| Response | Frequency | Percentage |
|---|---|---|
| Not selected | 669 | 81.1 |
| Yes | 156 | 18.9 |
| Total | 825 | 100.0 |
Certain tests or treatments were delayed because the patient was unable to give consent
| Response | Frequency | Percentage |
|---|---|---|
| Not selected | 629 | 76.2 |
| Yes | 196 | 23.8 |
| Total | 825 | 100.0 |
Certain tests or treatments were not given because the patient was unable to give consent
| Response | Frequency | Percentage |
|---|---|---|
| Not selected | 754 | 91.4 |
| Yes | 71 | 8.6 |
| Total | 825 | 100.0 |
It was not possible to complete a full assessment of the patient’s needs
| Response | Frequency | Percentage |
|---|---|---|
| Not selected | 601 | 72.8 |
| Yes | 224 | 27.2 |
| Total | 825 | 100.0 |
It was not possible to obtain advice from a learning disability expert at the time this was needed
| Response | Frequency | Percentage |
|---|---|---|
| Not selected | 694 | 84.1 |
| Yes | 131 | 15.9 |
| Total | 825 | 100.0 |
The patient was given the wrong medication, the wrong dose, or did not receive their medication
| Response | Frequency | Percentage |
|---|---|---|
| Not selected | 808 | 97.9 |
| Yes | 17 | 2.1 |
| Total | 825 | 100.0 |
Staff avoided the patient because of unusual, different or challenging behaviour
| Response | Frequency | Percentage |
|---|---|---|
| Not selected | 722 | 87.5 |
| Yes | 103 | 12.5 |
| Total | 825 | 100.0 |
The patient was misdiagnosed
| Response | Frequency | Percentage |
|---|---|---|
| Not selected | 815 | 98.8 |
| Yes | 10 | 1.2 |
| Total | 825 | 100.0 |
The patient deteriorated unnecessarily
| Response | Frequency | Percentage |
|---|---|---|
| Not selected | 801 | 97.1 |
| Yes | 24 | 2.9 |
| Total | 825 | 100.0 |
Q15. Have you encountered any other problems in the past 3 years involving patients with learning disabilities that might have affected their health outcomes? If yes, please tell us about this in the box below
| [Free text box responses – qualitative analysis] |
Q16. Have you had any training to prepare you to care for patients with learning disabilities? (Check any that apply)
[Exclusion criteria: non-clinical staff, last question completed < 16]
Yes, pre registration/qualification
| Response | Frequency | Percentage |
|---|---|---|
| Not selected | 606 | 69.3 |
| Yes | 269 | 30.7 |
| Total | 875 | 100.0 |
Yes, post registration or through the workplace
| Response | Frequency | Percentage |
|---|---|---|
| Not selected | 489 | 55.9 |
| Yes | 386 | 44.1 |
| Total | 875 | 100.0 |
No
| Response | Frequency | Percentage |
|---|---|---|
| Not selected | 567 | 64.8 |
| Yes | 308 | 35.2 |
| Total | 875 | 100.0 |
Q17. Since working in this hospital have you received any of the following to help support you to care for patients with learning disabilities? (Check any that apply)
[Exclusion criteria: non-clinical staff, last question completed < 17]
Written guidance
| Response | Frequency | Percentage |
|---|---|---|
| Not selected | 521 | 59.6 |
| Yes | 353 | 40.4 |
| Total | 874 | 100.0 |
Oral guidance
| Response | Frequency | Percentage |
|---|---|---|
| Not selected | 552 | 63.2 |
| Yes | 322 | 36.8 |
| Total | 874 | 100.0 |
On-the-job guidance from a colleague
| Response | Frequency | Percentage |
|---|---|---|
| Not selected | 445 | 50.9 |
| Yes | 429 | 49.1 |
| Total | 874 | 100.0 |
Q18. Have you had any training on the Mental Capacity Act (MCA 2005)?
[Exclusion criteria: non-clinical staff, last question completed < 18]
| Response | Frequency | Percentage |
|---|---|---|
| Yes | 564 | 64.5 |
| No | 193 | 22.1 |
| Not sure | 82 | 9.4 |
| I don’t need to use the MCA | 27 | 3.1 |
| Missing | 8 | 0.9 |
| Total | 874 | 100.0 |
Q18b. If ‘yes’, ‘no’, or ‘not sure’ to question 18: Do you feel confident to use the Mental Capacity Act?
| Response | Frequency | Percentage |
|---|---|---|
| Yes | 355 | 42.5 |
| No | 235 | 28.1 |
| Not sure | 245 | 29.3 |
| Total of those who answered Q18b | 835 | 100.0 |
SECTION F: ABOUT YOU
Q19. Are you male or female?
[Exclusion criteria: non-clinical staff, last question completed < 19]
| Response | Frequency | Percentage |
|---|---|---|
| Male | 141 | 16.3 |
| Female | 724 | 83.6 |
| Missing | 1 | 0.1 |
| Total | 866 | 100.0 |
Q20. What is your age group?
[Exclusion criteria: non-clinical staff, last question completed < 20]
| Response | Frequency | Percentage |
|---|---|---|
| Under 21 | 1 | 0.1 |
| 21–30 | 118 | 13.6 |
| 31–40 | 205 | 23.7 |
| 41–50 | 285 | 32.9 |
| 51–65 | 253 | 29.2 |
| 66+ | 2 | 0.2 |
| Missing | 2 | 0.2 |
| Total | 866 | 100.0 |
Q21. Do you manage staff within the Trust?
[Exclusion criteria: non-clinical staff, last question completed < 21]
| Response | Frequency | Percentage |
|---|---|---|
| Yes | 421 | 48.6 |
| No | 438 | 50.6 |
| Missing | 7 | 0.8 |
| Total | 866 | 100.0 |
Q22. Do you have face-to-face contact with patients/service users as part of your job?
[Exclusion criteria: non-clinical staff, last question completed < 22]
| Response | Frequency | Percentage |
|---|---|---|
| Yes, frequently | 801 | 92.5 |
| Yes, occasionally | 52 | 6.0 |
| No | 7 | 0.8 |
| Missing | 6 | 0.7 |
| Total | 866 | 100.0 |
Q23. How many years have you worked for this Trust?
[Exclusion criteria: non-clinical staff, last question completed < 23]
| Response | Frequency | Percentage |
|---|---|---|
| Less than 1 year | 75 | 8.7 |
| 1–2 years | 106 | 12.2 |
| 3–5 years | 167 | 19.3 |
| 6–10 years | 157 | 18.1 |
| 11–15 years | 118 | 13.6 |
| More than 15 years | 241 | 27.8 |
| Missing | 2 | 0.2 |
| Total | 866 | 100.0 |
Q24. Does anyone in your family or close social circle have learning disabilities?
[Exclusion criteria: non-clinical staff, last question completed < 24]
| Response | Frequency | Percentage |
|---|---|---|
| Yes | 214 | 24.7 |
| No | 639 | 73.8 |
| Missing | 13 | 1.5 |
| Total | 866 | 100.0 |
Q25. Which of the following best describes your main area of clinical work?
[Exclusion criteria: non-clinical staff, last question completed < 25]
| Response | Frequency | Percentage |
|---|---|---|
| Accident & emergency | 23 | 2.7 |
| General medicine | 61 | 7.1 |
| General surgery | 47 | 5.4 |
| Audiology | 15 | 1.7 |
| Cardiology | 53 | 6.1 |
| Cardio-thoracic surgery | 21 | 2.4 |
| Care of the elderly | 21 | 2.4 |
| Child and adolescent psychiatry | 1 | 0.1 |
| Dermatology | 7 | 0.8 |
| Diabetes | 9 | 1.0 |
| Endocrinology | 2 | 0.2 |
| Gastroenterology | 17 | 2.0 |
| Haematology | 12 | 1.4 |
| Intensive care | 37 | 4.3 |
| Neurology | 25 | 2.9 |
| Neurosurgery | 5 | 0.6 |
| Nuclear medicine | 1 | 0.1 |
| Obstetrics and gynaecology | 79 | 9.1 |
| Occupational therapy | 22 | 2.5 |
| Orthopaedics | 34 | 3.9 |
| Paediatrics | 54 | 6.2 |
| Palliative medicine | 5 | 0.6 |
| Physiotherapy | 20 | 2.3 |
| Podiatry | 3 | 0.3 |
| Psychology | 2 | 0.2 |
| Radiology | 23 | 2.7 |
| Radiotherapy and oncology | 5 | 0.6 |
| Renal medicine | 18 | 2.1 |
| Respiratory | 9 | 1.0 |
| Rheumatology | 5 | 0.6 |
| Urology | 11 | 1.3 |
| Other | 121 | 14.0 |
| I work across a variety of settings | 90 | 10.4 |
| Missing | 7 | 0.8 |
| Total | 865 | 100.0 |
Q26. Which clinical setting do you mostly work in?
[Exclusion criteria: non-clinical staff, last question completed < 26]
| Response | Frequency | Percentage |
|---|---|---|
| Inpatients | 372 | 43.2 |
| Outpatients | 188 | 21.8 |
| A mix of inpatients and outpatients | 249 | 28.9 |
| Accident and emergency | 25 | 2.9 |
| Missing | 27 | 3.1 |
| Total | 861 | 100.0 |
Q27. What best describes your ethnic background?
[Exclusion criteria: non-clinical staff, last question completed < 27]
| Response | Frequency | Percentage |
|---|---|---|
| WHITE: British | 614 | 72.8 |
| WHITE: Irish | 38 | 4.5 |
| WHITE: Any other white background | 53 | 6.3 |
| MIXED: White and Black Caribbean | 3 | 0.4 |
| MIXED: White and Black African | 1 | 0.1 |
| MIXED: White and Asian | 2 | 0.2 |
| MIXED: Any other mixed background | 3 | 0.4 |
| ASIAN/ASIAN BRITISH: Indian | 41 | 4.9 |
| ASIAN/ASIAN BRITISH: Pakistani | 6 | 0.7 |
| ASIAN/ASIAN BRITISH: Bangladeshi | 1 | 0.1 |
| ASIAN/ASIAN BRITISH: Any other Asian background | 20 | 2.4 |
| BLACK/BLACK BRITISH: Caribbean | 9 | 1.1 |
| BLACK/BLACK BRITISH: African | 24 | 2.8 |
| BLACK/BLACK BRITISH: Any other black background | 2 | 0.2 |
| Chinese | 7 | 0.8 |
| Other | 19 | 2.3 |
| Total | 843 | 100.0 |
Optional
If you would like to tell us more about your experiences or thoughts, we would be very grateful to hear them. Please feel free to use the box below.
| [Free text box responses – qualitative analysis] |
Appendix 5 Carer survey
SECTION 1: ABOUT YOU
Q1. Are you:
| Response | Frequency (excluded) | Frequency after exclusions | Percentage after exclusions |
|---|---|---|---|
| Patient’s parent | 30 (2) | 28 | 31.8 |
| Patient’s sibling | 7 (2) | 5 | 5.7 |
| Patient’s husband/wife/partner | 0 (0) | 0 | 0.0 |
| Other relative of the patient (please specify) | 1 (0) | 1 | 1.1 |
| Patient with LD | 2 (2) | 0 | 0.0 |
| Patient’s support worker/care manager/other learning disability professional (please specify) | 54 (0) | 54 | 61.4 |
| Other (please specify) | 0 (0) | 0 | 0.0 |
| Total | 94 (6) | 88 | 100.0 |
Q2. How long have you known the patient?
| Response | Frequency | Percentage |
|---|---|---|
| Since birth | 31 | 35.2 |
| More than 20 years | 4 | 4.5 |
| Between 10 to 20 years | 6 | 6.8 |
| Between 5 to 9 years | 10 | 11.4 |
| Between 1 to 4 years | 18 | 20.5 |
| 6 to 12 months | 12 | 13.6 |
| Less than 6 months | 3 | 3.4 |
| Missing | 4 | 4.5 |
| Total | 88 | 100.0 |
Q2a. Your age
| Response | Frequency | Percentage |
|---|---|---|
| Younger than 25 | 2 | 2.3 |
| Between 25–60 | 30 | 34.1 |
| Between 61–74 | 8 | 9.1 |
| Older than 75 | 2 | 2.3 |
| Missing | 46 | 52.3 |
| Total | 88 | 100.0 |
SECTION 2: WHERE AND WHEN
Q3. The patient visited the hospital for treatment as an:
| Response | Frequency | Percentage |
|---|---|---|
| Outpatient | 15 | 17.0 |
| Inpatient | 40 | 45.5 |
| A&E patient | 7 | 8.0 |
| A&E plus inpatient | 17 | 19.3 |
| Outpatient plus A&E | 3 | 3.4 |
| Outpatient plus inpatient | 3 | 3.4 |
| Outpatient plus inpatient plus A&E | 2 | 2.3 |
| Missing | 1 | 1.1 |
| Total | 88 | 100.0 |
Q3a. In which month and year did the person come to hospital for treatment on this occasion?
All admissions were between June 2011 and September 2012. A breakdown of admissions by month can be seen below (valid = 61; missing = 27)
| Month and year | Frequency | Percentage |
|---|---|---|
| June 2011 | 1 | 1.1 |
| October 2011 | 10 | 11.4 |
| November 2011 | 3 | 3.4 |
| December 2011 | 3 | 3.4 |
| January 2012 | 2 | 2.3 |
| February 2012 | 2 | 2.3 |
| March 2012 | 12 | 13.6 |
| April 2012 | 7 | 8.0 |
| May 2012 | 3 | 3.4 |
| June 2012 | 4 | 4.5 |
| July 2012 | 7 | 8.0 |
| August 2012 | 4 | 4.5 |
| September 2012 | 3 | 3.4 |
| Total | 61 | 69.3 |
| Missing | 27 | 30.7 |
| Total | 88 | 100.0 |
SECTION 3: YOU AND THE PATIENT
Q4. The admissions procedure was sensitive towards the special needs
| Response | Frequency | Percentage |
|---|---|---|
| Strongly agree | 30 | 34.1 |
| Agree | 40 | 45.5 |
| Disagree | 8 | 9.1 |
| Strongly disagree | 6 | 6.8 |
| Missing | 4 | 4.5 |
| Total | 88 | 100.0 |
Q5. Doctors/consultants understood and were sensitive towards the special needs arising from the person’s disabilities
| Response | Frequency | Percentage |
|---|---|---|
| Strongly agree | 29 | 33.0 |
| Agree | 40 | 45.5 |
| Disagree | 11 | 12.5 |
| Strongly disagree | 4 | 4.5 |
| Missing | 4 | 4.5 |
| Total | 88 | 100.0 |
Q6. Nursing staff and other ward/clinic staff were fully aware of the person’s special needs
| Response | Frequency | Percentage |
|---|---|---|
| Strongly agree | 31 | 35.2 |
| Agree | 34 | 38.6 |
| Disagree | 15 | 17.0 |
| Strongly disagree | 6 | 6.8 |
| Missing | 2 | 2.3 |
| Total | 88 | 100.0 |
Q7. The person’s views and preferences were sought and appropriately acted upon, in the person’s best interest
| Response | Frequency | Percentage |
|---|---|---|
| Strongly agree | 20 | 22.7 |
| Agree | 41 | 46.6 |
| Disagree | 17 | 19.3 |
| Strongly disagree | 5 | 5.7 |
| Missing | 5 | 5.7 |
| Total | 88 | 100.0 |
Q8. Treatment and care were delivered in an appropriate way
| Response | Frequency | Percentage |
|---|---|---|
| Strongly agree | 28 | 31.8 |
| Agree | 46 | 52.3 |
| Disagree | 11 | 12.5 |
| Strongly disagree | 1 | 1.1 |
| Missing | 2 | 2.3 |
| Total | 88 | 100.0 |
Q9. Where appropriate the person was consulted in a manner they could understand (possibly through you) before decisions were made
| Response | Frequency | Percentage |
|---|---|---|
| Strongly agree | 28 | 31.8 |
| Agree | 40 | 45.5 |
| Disagree | 12 | 13.6 |
| Strongly disagree | 3 | 3.4 |
| Missing | 5 | 5.7 |
| Total | 88 | 100.0 |
Q10. The person was given information about treatment and care in a way he/she could understand
| Response | Frequency | Percentage |
|---|---|---|
| Strongly agree | 19 | 21.6 |
| Agree | 36 | 40.9 |
| Disagree | 18 | 20.5 |
| Strongly disagree | 4 | 4.5 |
| Missing | 11 | 12.5 |
| Total | 88 | 100.0 |
Q11. The person was given information about medicines, including medicines to take home (e.g. how/when to take the medicines) in a way he/she could understand
| Response | Frequency | Percentage |
|---|---|---|
| Strongly agree | 16 | 18.2 |
| Agree | 32 | 36.4 |
| Disagree | 20 | 22.7 |
| Strongly disagree | 4 | 4.5 |
| Missing | 16 | 18.2 |
| Total | 88 | 100.0 |
Q12. The hospital staff gave enough time in their care of the person
| Response | Frequency | Percentage |
|---|---|---|
| Strongly agree | 26 | 29.5 |
| Agree | 35 | 39.8 |
| Disagree | 15 | 17.0 |
| Strongly disagree | 6 | 6.8 |
| Missing | 6 | 6.8 |
| Total | 88 | 100.0 |
Q13. I, as a relative/carer/supporter, was fully consulted before decisions were taken about the person’s treatment and care
| Response | Frequency | Percentage |
|---|---|---|
| Strongly agree | 25 | 28.4 |
| Agree | 43 | 48.9 |
| Disagree | 10 | 11.4 |
| Strongly disagree | 4 | 4.5 |
| Missing | 6 | 6.8 |
| Total | 88 | 100.0 |
Q14. I, as a relative/carer/supporter, was fully consulted before decisions were taken about the person’s discharge
| Response | Frequency | Percentage |
|---|---|---|
| Strongly agree | 23 | 26.1 |
| Agree | 42 | 47.7 |
| Disagree | 9 | 10.2 |
| Strongly disagree | 3 | 3.4 |
| Missing | 11 | 12.5 |
| Total | 88 | 100.0 |
Q15. I was recognised as the expert carer, and listened to
| Response | Frequency | Percentage |
|---|---|---|
| Strongly agree | 30 | 34.1 |
| Agree | 38 | 43.2 |
| Disagree | 12 | 13.6 |
| Strongly disagree | 3 | 3.4 |
| Missing | 5 | 5.7 |
| Total | 88 | 100.0 |
Q16. The staff were welcoming and supportive of me as the person’s carer
| Response | Frequency | Percentage |
|---|---|---|
| Strongly agree | 31 | 35.2 |
| Agree | 44 | 50.0 |
| Disagree | 7 | 8.0 |
| Strongly disagree | 2 | 2.3 |
| Missing | 4 | 4.5 |
| Total | 88 | 100.0 |
Q17. Any agreed follow-up was acted upon in an appropriate and timely way
| Response | Frequency | Percentage |
|---|---|---|
| Strongly agree | 19 | 21.6 |
| Agree | 36 | 40.9 |
| Disagree | 10 | 11.4 |
| Strongly disagree | 7 | 8.0 |
| Missing | 16 | 18.2 |
| Total | 88 | 100.0 |
Q18. The hospital staff gave me all the information I needed to support the person better (for example, keeping me informed about what was happening to the person, information about tests, treatments, etc.)
| Response | Frequency | Percentage |
|---|---|---|
| Strongly agree | 20 | 22.7 |
| Agree | 44 | 50.0 |
| Disagree | 11 | 12.5 |
| Strongly disagree | 4 | 4.5 |
| Missing | 9 | 10.2 |
| Total | 88 | 100.0 |
Q19. I was given all the practical help I needed to be able to support the person (for example, refreshments, a space to be with the person)
| Response | Frequency | Percentage |
|---|---|---|
| Strongly agree | 23 | 26.1 |
| Agree | 32 | 36.4 |
| Disagree | 20 | 22.7 |
| Strongly disagree | 2 | 2.3 |
| Missing | 11 | 12.5 |
| Total | 88 | 100.0 |
Q20. The person’s diagnosis was made properly and as soon as possible by the hospital
| Response | Frequency | Percentage |
|---|---|---|
| Strongly agree | 23 | 26.1 |
| Agree | 42 | 47.7 |
| Disagree | 10 | 11.4 |
| Strongly disagree | 3 | 3.4 |
| Missing | 10 | 11.4 |
| Total | 88 | 100.0 |
SECTION 4: SOME FURTHER QUESTIONS
Q21. Hospital staff asked you to provide (additional) information about the patient’s disabilities and needs
| Response | Frequency | Percentage |
|---|---|---|
| Yes | 63 | 71.6 |
| No | 18 | 20.5 |
| Missing | 7 | 8.0 |
| Total | 88 | 100.0 |
Q22. Hospital staff asked the patient to provide (additional) information about the patient’s disabilities and needs
| Response | Frequency | Percentage |
|---|---|---|
| Yes | 23 | 26.1 |
| No | 51 | 58.0 |
| Not applicable | 3 | 3.4 |
| Missing | 11 | 12.5 |
| Total | 88 | 100.0 |
Q23. Details about the patient’s disabilities or special needs were recorded by the hospital (e.g. in the medical notes, in a hospital passport)
| Response | Frequency | Percentage |
|---|---|---|
| Yes | 45 | 51.1 |
| No | 9 | 10.2 |
| Not sure | 29 | 33.0 |
| Missing | 5 | 5.7 |
| Total | 88 | 100.0 |
Q24. If you wanted to make a complaint about any aspect of the care at the hospital, would you know how to go about it?
| Response | Frequency | Percentage |
|---|---|---|
| Yes | 56 | 63.6 |
| No | 25 | 28.4 |
| Missing | 7 | 8.0 |
| Total | 88 | 100.0 |
Q25. Overall, how satisfied are you with the standard of medical care provided to the patient by this hospital? Score 1 (least satisfied) to 10 (most satisfied)
| Score | Frequency | Percentage |
|---|---|---|
| 1.00 | 3 | 3.4 |
| 2.00 | 1 | 1.1 |
| 3.00 | 2 | 2.3 |
| 4.00 | 4 | 4.5 |
| 5.00 | 9 | 10.2 |
| 6.00 | 5 | 5.7 |
| 7.00 | 16 | 18.2 |
| 8.00 | 15 | 17.0 |
| 9.00 | 14 | 15.9 |
| 10.00 | 15 | 17.0 |
| Missing | 4 | 4.5 |
| Total | 88 | 100.0 |
Q26. Overall, how satisfied are you with the ‘experience’ for the patient at this hospital? Score 1 (least satisfied) to 10 (most satisfied)
| Score | Frequency | Percentage |
|---|---|---|
| 1.00 | 4 | 4.5 |
| 2.00 | 1 | 1.1 |
| 3.00 | 6 | 6.8 |
| 4.00 | 7 | 8.0 |
| 5.00 | 5 | 5.7 |
| 6.00 | 7 | 8.0 |
| 7.00 | 13 | 14.8 |
| 8.00 | 11 | 12.5 |
| 9.00 | 14 | 15.9 |
| 10.00 | 15 | 17.0 |
| Missing | 5 | 5.7 |
| Total | 88 | 100.0 |
SECTION 5: ABOUT THE PERSON (THE HOSPITAL PATIENT)
Q27. The person is:
| Response | Frequency | Percentage |
|---|---|---|
| Male | 49 | 55.7 |
| Female | 38 | 43.2 |
| Missing | 1 | 1.1 |
| Total | 88 | 100 |
Q28. At the time of the hospital visit, the person’s age was:
| Response | Frequency | Percentage |
|---|---|---|
| 16–19 | 3 | 3.4 |
| 20–25 | 9 | 10.2 |
| 26–35 | 12 | 13.6 |
| 36–45 | 18 | 20.5 |
| 46–60 | 27 | 30.7 |
| Over 60 | 18 | 20.5 |
| Missing | 1 | 1.1 |
| Total | 88 | 100.0 |
Q29. What is the person’s ethnic group?
| Response | Frequency | Percentage |
|---|---|---|
| White | 66 | 75.0 |
| Mixed/Multiple ethnic groups | 3 | 3.4 |
| Asian/Asian British | 6 | 6.8 |
| Black/African/Caribbean/Black British | 9 | 10.2 |
| Other ethnic group | 0 | 0.0 |
| Missing | 4 | 4.5 |
| Total | 88 | 100.0 |
Q30. How would you describe the person’s learning disabilities?
| Response | Frequency | Percentage |
|---|---|---|
| Mild | 14 | 15.9 |
| Moderate | 28 | 31.8 |
| Severe | 29 | 33.0 |
| Profound | 15 | 17.0 |
| Missing | 2 | 2.3 |
| Total | 88 | 100.0 |
Q31a. The person’s additional disabilities and health issues are: Down syndrome
| Response | Frequency | Percentage |
|---|---|---|
| Yes | 18 | 20.5 |
| No | 70 | 79.5 |
| Total | 88 | 100.0 |
Q31b. The person’s additional disabilities and health issues are: Epilepsy
| Response | Frequency | Percentage |
|---|---|---|
| Yes | 33 | 37.5 |
| No | 55 | 62.5 |
| Total | 88 | 100.0 |
Q31c. The person’s additional disabilities and health issues are: Autism
| Response | Frequency | Percentage |
|---|---|---|
| Yes | 10 | 11.4 |
| No | 78 | 88.6 |
| Total | 88 | 100.0 |
Q31d. The person’s additional disabilities and health issues are: Significant communication difficulties
| Response | Frequency | Percentage |
|---|---|---|
| Yes | 32 | 36.4 |
| No | 56 | 63.6 |
| Total | 88 | 100.0 |
Q31e. The person’s additional disabilities and health issues are: Other
| Response | Frequency | Percentage |
|---|---|---|
| Yes | 38 | 43.2 |
| No | 50 | 56.8 |
| Total | 88 | 100.0 |
Q31f. The person’s additional disabilities and health issues are: Please specify
The following were listed:
Angleman’s syndrome
Anxiety
Arthritis
Autistism [sic]
Benign ethnic neutropenia, schizophrenia
Blind
Cerebral palsy
Challenging behaviour, incontinence
Chest deformity
Congenital achondroplasia
Dementia
Depression
Diabetes
Diabetic – insulin dependent and emotional personality
Double incontinence wheelchair user
Enlarged heart
Fragile X [syndrome]
Gout
Hearing impairment
Hole in heart
Hydrocephalus
Hypoplastic lung
Impaired vision
Left hemiplegia
Microcephaly [2x]
Moderate anxiety
Mowat–Wilson syndrome
No speech
Non verbal
OCD [obsessive-compulsive disorder]
Pan-hypopituitorism [sic]
Paranoid schizophrenia, hypothyroidism
Paraplegic wheelchair user – No use of legs
PEG
Pica
Poor communication
Predisposed to urine infections
Registered blind
Rubinstein–Taybi syndrome
Schizophrenia
Scoliosis
Spastic quadriplegia
Spinal problems affecting walking
Spine fusion
Spine stenosis
Staphylococcul [sic]
Titanium rods
Type 2 diabetes
Under active thyroid, cataracts in both eyes
Q32a. The person’s main method of communication is: Normal speech
| Response | Frequency | Percentage |
|---|---|---|
| Yes | 40 | 45.5 |
| No | 48 | 54.5 |
| Total | 88 | 100.0 |
Q32b. The person’s main method of communication is: Limited words
| Response | Frequency | Percentage |
|---|---|---|
| Yes | 19 | 21.6 |
| No | 69 | 78.4 |
| Total | 88 | 100.0 |
Q32c. The person’s main method of communication is: Sounds
| Response | Frequency | Percentage |
|---|---|---|
| Yes | 9 | 10.2 |
| No | 79 | 89.8 |
| Total | 88 | 100.0 |
Q32d. The person’s main method of communication is: Written words
| Response | Frequency | Percentage |
|---|---|---|
| Yes | 2 | 2.3 |
| No | 86 | 97.7 |
| Total | 88 | 100.0 |
Q32e. The person’s main method of communication is: A signing system
| Response | Frequency | Percentage |
|---|---|---|
| Yes | 6 | 6.8 |
| No | 82 | 93.2 |
| Total | 88 | 100.0 |
Q32f. The person’s main method of communication is: Communication aids
| Response | Frequency | Percentage |
|---|---|---|
| Yes | 3 | 3.4 |
| No | 85 | 96.6 |
| Total | 88 | 100.0 |
Q32g. The person’s main method of communication is: Body language
| Response | Frequency | Percentage |
|---|---|---|
| Yes | 27 | 30.7 |
| No | 61 | 69.3 |
| Total | 88 | 100.0 |
Q32h. The person’s main method of communication is: Hand or limb movement
| Response | Frequency | Percentage |
|---|---|---|
| Yes | 13 | 14.8 |
| No | 75 | 85.2 |
| Total | 88 | 100.0 |
Q32i. The person’s main method of communication is: Facial expressions
| Response | Frequency | Percentage |
|---|---|---|
| Yes | 23 | 26.1 |
| No | 65 | 73.9 |
| Total | 88 | 100.0 |
Q32j. The person’s main method of communication is: Eye pointing
| Response | Frequency | Percentage |
|---|---|---|
| Yes | 6 | 6.8 |
| No | 82 | 93.2 |
| Total | 88 | 100.0 |
Q32k. The person’s main method of communication is: Other communication
| Response | Frequency | Percentage |
|---|---|---|
| Yes | 7 | 8.0 |
| No | 80 | 90.9 |
| None | 1 | 1.1 |
| Total | 88 | 100.0 |
Q32l. Other communication method: Please specify
The following were listed:
Degrees of ‘HAA’ sounds. High pitch if very distress to little whimpery sounds if in pain
Leads you to a particular object
Limited speech
Repeats what you say
Sign language BSL [British Sign Language]
Smiling or making loud high pitched noise
Q33a. Does the person have any sort of hospital information document which identifies such things as communication, medication and any special needs?
| Response | Frequency | Percentage |
|---|---|---|
| Yes | 63 | 71.6 |
| Yes, but the person didn’t have it with him/her (at home) | 6 | 6.8 |
| No | 10 | 11.4 |
| Don’t know | 4 | 4.5 |
| Unclear response | 2 | 2.3 |
| In process | 1 | 1.1 |
| Missing | 2 | 2.3 |
| Total | 88 | 100.0 |
Q33b. If yes, did the hospital staff use it?
| Response | Frequency | Percentage |
|---|---|---|
| Yes, mostly | 23 | 26.1 |
| Yes, occasionally | 20 | 22.7 |
| No | 13 | 14.8 |
| Don’t know | 10 | 11.4 |
| Not applicable | 7 | 8.0 |
| Missing | 15 | 17.0 |
| Total | 88 | 100.0 |
Q34. Please list up to 3 special needs or additional difficulties the person has
First additional need (27.3% left blank):
Anxiety
Anxious and agitated
Autism, needs to be explained to in a different way
Autistic tendancies [sic]
Behavioural issues – screams a lot. Difficult to understand why
Cannot talk but understands when somebody talking to [name]
Colostomy-bowel loops
Communicating the need for help
Communication
Communication skills
Communications – understanding complex information, needs to be delivered in basic terms and put in context for level of understanding e.g. visual
Crowded bay – too many people and not enough could understand her
Deaf
Diabetes
Difficulties to walk
Difficulty with communication with hospital staff – residential homes staff supported 24/7
Difficulty with movement as she is exhibiting stiffness
Dignity and privacy
Distressed by new environment
Eating/diet
Emotional due to death of close family members in [name of] hospital
Epilepsy
Extremely impatient; can’t wait in queue
Fussy eater. I was present at all times
Gout and staph problems
Hard of hearing
Having the LD [learning disabilities] team is a good thing to have
Hearing
Hoist
Incontinent
Is currently needing to be hoisted in and out of bed and onto a commode
Lack of understanding
Paraplegic wheelchair user
Medical intervention
Medication given PRN [according to need] for fluid balance ([medication] for diabetes insipidus) – hospital staff not involved as given by myself or carer
Mobility problems with walking
Needs assistance with personal care
Needs clear instructions
Needs ‘thinking’ time before answering a question. When this is not given she becomes upset and nervous (most people tried at least – some more consistently than others)
No verbal communication
Non mobile, uses wheelchair, sitting in/getting into wheelchair via hoist
PEG feed
Poor communication
Required a hoist. The staff did it with me as I was not insured to use this on their grounds
Short legs. This makes it difficult to get in and out of bed or off chairs
Speech and communication – not very well. The problems were not addressed to him
Understanding – communication
Very challenging behaviour
Vision problem
Visual impairment
Walking
Q34.1a How well did the hospital meet this need?
| Response | Frequency | Percentage |
|---|---|---|
| Very well | 24 | 27.3 |
| Quite well | 18 | 20.5 |
| Not very well | 15 | 17.0 |
| Not at all | 5 | 5.7 |
| Missing | 26 | 29.5 |
| Total | 88 | 100.0 |
Second additional need (40.9% left blank):
A proper cup of tea. Very simple – staff didn’t make it properly which ruined her stay then
Anxiety
Anxious/agitated/scared
Back
Behaviour that is challenging
Blind
Can be aggressive/physically/towards people who was around
Cerebral palsy quadruple
Communicating with him from certain angles
Communication [2x]
Diabetes
Difficulties to talk
Down’s syndrome
Eating while lying on back and after op
Epilepsy
Epilepsy – due to medication not being at the correct levels, client spends a lot of the time dazed, sleepy and confused
Feeding: excellent red tray and jug
Has had constipation since being in hospital. Was prescribed suppository but these weren’t consistently given as prescribed
Having staff as she needs 24 hour care
He is very slow in everything
Hearing
Hearing impairment
Helping with meal times (choking hazard)
His eyesight is poor. Needs to be shown closely to recognise
In wheelchair
Mobility – undressing/dressing – if I wasn’t with her she would struggle
Needs routine
Non communicating apart from noises
Nonverbal
Not understanding procedure
People, the family did not want to, see [name]
Person will refuse to eat, drink, take medication
Personal care
Personality disorder. Confidence/rejection emotional behaviour if needs not understood or met on demand
Poor communication/understanding skills
Reading-writing
Requires full support to consume food
Rubinstein–Taybi syndrome
Scoliosis
Self-injurious behaviour
She reacts badly to change, particularly if she is not warned beforehand. She can become very distressed and is likely to always remember any particular incident or event
Uncontrolled reflexes (banging arms on bed sides)
Understanding – explaining in simple form
Understanding what is going to happen. Especially when upset
Unsteady to walk
Visually impaired
Will answer even if she hasn’t understood the question
Q34.1b How well did the hospital meet this need?
| Response | Frequency | Percentage |
|---|---|---|
| Very well | 17 | 19.3 |
| Quite well | 15 | 17.0 |
| Not very well | 11 | 12.5 |
| Not at all | 6 | 6.8 |
| Missing | 39 | 44.3 |
| Total | 88 | 100.0 |
Third additional need (52.3% left blank):
24 hour care
Additional support from acute liaison nurse
Asthma
Clamping reflex with jaw (staff continually tried to use a mouth thermometer)
Communicating book/passport and his laptop communication aid
Communication
Communication – some nurses were very nice but some talked at her/over her. Didn’t like that
Diabetes poor management, needs support, waiting for food for hours causing distress. Cannot tell time or process passage of time very well
Fear of the dark
Got very nervous with tests, staff need to support all the way through the process
He can’t be on his own for a very long time
He could walk long distance at some time during attending the appointments
He understands more than he can express
Helping to maintain his personal hygiene
Left hemiplegia
Listening and understanding patients wants
Mild hearing problem
Missed messages from the doctors which made me angry
Mobility
Overall understanding of her learning disability
Person doesn’t like intrusive treatment, e.g. blood being taken
Personal care. I did not lift a finger. First class
Physical
Quadriplegic epilepsy
Refusing to eat
Requires own space e.g. own room due to dignity issues and challenging behaviour towards others
Returning to walk
Spine fusion, log rollover
Stubborn and un-cooperative at times
The need to take things slowly
Very sensitive skin. Although support workers consistently pointed this out when the wrong type of dressing was used the same type of dressing was used for a number of days
Vulnerable person
Walking
Wheelchair user
Q34.1c How well did the hospital meet this need?
| Response | Frequency | Percentage |
|---|---|---|
| Very well | 15 | 17.0 |
| Quite well | 8 | 9.1 |
| Not very well | 9 | 10.2 |
| Not at all | 4 | 4.5 |
| Missing | 52 | 59.1 |
| Total | 88 | 100.0 |
Appendix 6 Study information sheet for people with learning disabilities
All images in this appendix are reproduced with permission from Books Beyond Words, www.booksbeyondwords.co.uk.
Study information sheet for people with learning disabilities (PDF download)
Appendix 7 Talking Mats™
All images in this appendix are reproduced with permission from Books Beyond Words, www.booksbeyondwords.co.uk.
Appendix 8 Interview schedule for people with learning disabilities
All images in this appendix are reproduced with permission from Books Beyond Words, www.booksbeyondwords.co.uk.
Interview schedule for people with learning disabilities (PDF download)
List of abbreviations
- A&E
- accident and emergency
- AHP
- allied health professional
- CIPOLD
- confidential inquiry into premature deaths of people with learning disabilities
- CQC
- Care Quality Commission
- DNAR
- do not attempt resuscitation
- GP
- general practitioner
- HCA
- health-care assistant
- ICU
- intensive care unit
- IHAL
- Improving Health and Lives (Learning Disability Observatory)
- IQ
- intelligence quotient
- IT
- information technology
- LDLN
- learning disability liaison nurse
- NIHR
- National Institute for Health Research
- NRES
- National Research Ethics Service
- NRLS
- National Reporting and Learning System
- PALS
- Patient Advice and Liaison Service
- PbR
- Payment by Results
- PCT
- primary care trust
- PEG
- percutaneous endoscopic gastrostomy
- SPSS
- Statistical Product and Service Solutions