Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its proceeding programmes as project number 08/1819/221 The contractual start date was in August 2008. The final report began editorial review in August 2012 and was accepted for publication in December 2012. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2013. This work was produced by Mason et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Background
Introduction
There have been a number of changes made recently by the government to improve the working conditions of NHS staff based on evidence that improved working conditions can improve staff well-being and in turn improve the quality of patient care. However, the evidence of a direct link between the well-being of staff and the quality of patient care within health care is limited. More evidence is required about which characteristics of working in the NHS influence staff well-being and which aspects of well-being influence patient care.
This study aims to evaluate the well-being of foundation doctors and compare this with the quality of care provided to patients attending the emergency department (ED). Key aspects of well-being that may influence quality of care include motivation, job satisfaction and confidence. Measures of these factors will have the potential to be developed into a tool that may be utilised more widely for doctors throughout the NHS.
Policy context and literature review
NHS policy context
The health and well-being of NHS staff has been of great interest to policy-makers in recent years, with a growing acknowledgement that good levels of health and well-being are likely to have benefits for organisations and patients. The role of organisations in contributing to the health and well-being of staff is recognised as key, with support structures aimed at improving the health of staff likely to positively influence staff retention, sickness absence, productivity and also, potentially, patient satisfaction and quality of care. 1,2
The publication of two major reports has increased the focus on health and well-being in the UK workplace and NHS organisations. 3,4 The Black review3 examined the health of the UK working-age population with a focus on the large-scale problem of sickness absence and reduced productivity (including the role of common mental health conditions). There is evidence that reduced well-being is one of the major causes of reduced productivity for individuals in work. Alongside this, a growing literature links morale and job satisfaction with health outcomes and performance. Although individuals may differ in the importance they attach to issues such as salary or level of responsibility, this review identified key job-related characteristics that influence well-being at work, such as employee autonomy and adequate social support. Good management and leadership also play a vital role in promoting well-being and improving performance. 3
Following on from the Black review,3 the Boorman review4 examined issues of health and well-being in the NHS workforce. The focus on staff well-being is explained by the continuing high rates of sickness absence in the NHS, with over 10 million sick days lost annually, equivalent to 45,000 whole-time equivalent staff,5 with over one-quarter of absences caused by stress, depression and anxiety. The NHS review of health and well-being4 found links between the well-being of staff and key performance indicators such as patient satisfaction and trust performance, with trusts with lower rates of sickness absence and turnover more likely to score highly on indicators of patient satisfaction and quality of care. The report4 recommended that organisations develop strategies and provide services to NHS staff to prevent and treat sickness, including work-related stress, anxiety and depression, and that management be assessed on their contribution to staff health and well-being.
These reports are consistent with pledges made in Lord Darzi’s 2008 report6 regarding the need for a broader commitment to health and well-being in workplaces and the recognition that the health and well-being of NHS staff was an important component of the commitment of the NHS to provide high-quality care. National Institute for Health and Care Excellence (NICE) guidance has also been produced,7 which recommends a strategic approach by employers to the well-being of staff. This includes ensuring that job design, selection, recruitment, training and appraisal promote well-being and that assessment of the well-being of employees is undertaken to identify areas for improvement.
Although the link between staff development, motivation and well-being and patient care is recognised as important,8,9 the impact of staff stress, depression and other aspects of well-being on patient care has been generally under-researched. Evidence demonstrating a link between indicators of well-being and indicators of patient safety, experience and quality of care is rare and has primarily been collected in nurse settings in the USA. There is also a lack of good-quality evidence from data collected longitudinally. 10
Training doctors in the NHS
Training and appraisal have been identified in the literature as important elements of appropriate people management, impacting on knowledge and skills, job satisfaction and well-being, which in turn may influence patient outcomes. 11 Previous studies have demonstrated relationships between the quality and extent of training and appraisal and the well-being of staff and better patient care. 12–16 Recently, postgraduate medical training has undergone changes in response to long-standing criticism of its suitability in a modern, patient-centred NHS. A report by the Chief Medical Officer17 highlighted a number of perceived problems with the job structure, working conditions and training opportunities in postgraduate medical education, with the balance between medical training and service provision weighted too heavily in favour of providing for service delivery at the expense of a well-structured and well-planned training programme for postgraduate trainees [senior house officers (SHOs)]. SHO training placements were perceived as short term and stand-alone and not part of a clearly structured training programme.
These issues called into question whether doctors were being appropriately trained to meet the demands of a modern, patient-centred NHS. 18 Postgraduate training was also criticised for failing to provide more trained specialists for a consultant-led NHS. 2 The report recommended the introduction of a new programme-based system of postgraduate training [foundation training (FT)] that would provide broad-based specialty experience and flexible training arrangements.
Foundation training
The new model of FT was piloted in 2004 and introduced nationally in 2005. The model introduced a fixed 2-year Foundation Programme to address the perceived deficiencies of the previous postgraduate training grades (pre-registration house officer and SHO). Postgraduate training was structured around a formal programme with a national curriculum and structured assessment of clinical competencies (see Appendix 2).
The first year of FT (foundation year 1 or F1) focused on developing the skills and competencies learned during undergraduate medical training. The completion of core competencies was required during F1 to achieve full registration with the General Medical Council (GMC). The second year of FT (foundation year 2 or F2) was designed to enable doctors to become functioning members of the health-care team, competent in the management of the acutely ill patient and with key skills in team working, time management and communication with both professionals and patients.
Foundation training generally consisted of 4-month placements in a variety of specialties to give postgraduate doctors sufficient experience of different areas of medicine. Modernising Medical Careers (MMC) also provided a clear structure for post FT with ‘run-through’ specialist training following on from FT. 19
As well as introducing new structural arrangements, FT changed the delivery of training within placements. For the first time doctors were explicitly required to demonstrate competency to practise through the completion of a range of specific assessments (see Appendix 2). These assessments were based on a new Foundation Curriculum. 20 The Foundation Programme also required the designation of educational supervisors (ESs) and clinical supervisors (CSs), charged with ensuring that foundation doctors were meeting their educational and training goals.
The well-publicised problems with selection processes in the early stages of MMC reform led to an inquiry into MMC, which also examined FT. 21 The inquiry highlighted a number of areas of concern with the FT model, including the insufficient breadth of clinical experience in foundation placements; a lack of flexibility in programmes; and the length of programme placements. This contributed to a perception that foundation doctors were not reaching appropriate levels of clinical responsibility compared with their SHO predecessors. The report also recommended greater clarity about expectations of the role of F2 doctors in the health-care team and what their service contribution should be.
A more recent evaluation of the Foundation Programme reported improvements including a well-defined curriculum, trainees exposed to a wider range of medical specialties and implementation of a comprehensive programme of trainee assessment. 22 However, the report stated that the programme still lacked an articulated purpose, found that there was confusion over the role of the F2 doctor and questioned the ability of placements to accurately reflect the current and future needs of the NHS. Further, the assessment process placed excessive loads on ESs and there were safety and quality issues in the learning environment.
Reduced hours of working and the European Working Time Directive
As well as changes to the structure of postgraduate training, there has been a major change to the conditions of work for postgraduate foundation doctors. The New Deal for junior doctors, published in 1991,23 highlighted the need for improved working conditions for this workforce group primarily focused on working hours. It was widely acknowledged that excessive hours of practice amongst foundation doctors was a risk to patients. In 2003 the working week was limited to 56 hours and the European Working Time Directive (EWTD)24 further limited the hours that medical staff could work to a maximum of 48 hours. This was implemented in stages with the 48-hour limit enforced by law in 2012.
Health service staff motivation and well-being
High levels of stress among health-care professionals has been recognised as a problem for some time. A review of doctors’ stress levels found that between 28% and 30% of doctors had above-threshold levels of stress compared with about 18% of the general population. 16 A survey of over 11,000 NHS staff5 found staff reporting high levels of stress and that they did not consider that senior managers took a positive interest in their health. Some studies have also reported high levels of depression amongst doctors. 25,26
Studies have also reported higher levels of stress among doctors (both consultants and junior doctors) working in emergency medicine (EM), with above-threshold scores for around half of the respondents from each group. 27,28 These levels of stress are again higher than might be expected among the general population. 29 However, the impact of stress, depression and well-being on patient care has been generally under-researched. 10
Foundation doctor well-being
There is a limited literature examining the well-being of doctors in training. One study looked at levels of psychological distress in SHOs working in the ED. 27 SHOs were selected from six EDs in London and received questionnaires to measure psychological outcomes and coping strategies. Over half of respondents scored above the threshold for psychological distress on the General Health Questionnaire. 30 Higher levels of anxiety and depression were related to a venting style of coping (such as expressing negative feelings) whereas lower scores for these outcomes were associated with a more active coping style (such as devising strategies to cope with stressors). Another study followed junior doctors for 3 years after their graduation from medical school finding that first-year postgraduates reported levels of depression of 29%, dropping to 10% by their third postgraduate year. 26
Foundation doctors and quality of care
Studies evaluating the impact of foundation doctors on the quality of patient care have evaluated the following outcomes: (1) numbers of patients seen; (2) reattendance of patients in the ED; and (3) confidence and competence in managing conditions.
A prospective observational study compared the productivity (numbers of patients seen) of F2 doctors and SHOs working across two EDs in Scotland. 31 Both groups demonstrated a significant rise in productivity between the first and last months of their attachments. There were no significant differences in productivity between the two groups of doctors over the 12-month study period. However, there were concerns about a reduction in the percentage of patients seen by junior doctors overall and an increased need for senior review of patients. Further analysis by Armstrong et al. 32 investigated the number of patients seen by all junior doctors (SHO/F2) over a 3-year period. The study found a 4% decrease in the number of patients seen by junior doctors in this period. In addition, there was a significant reduction of 16.6% in the number of patients seen per hour (an indicator of work rate).
A study at an inner-city ED in England also found no significant differences in the mean number of patients seen by F2 doctors and SHOs over a 12-month period. 33 Individual doctor performance had a greater influence on the number of patients seen than type of doctor (either F2 or SHO), with a small number of F2 doctors seeing considerably more patients than their SHO colleagues.
A study by Whiticar et al. 34 compared reattendance rates of patients to the ED over a month in 2006 by grade of doctor assessing the first presentation. Junior doctors (SHOs and F2 doctors) had higher reattendance rates (2.83% vs. 2.32%; p = 0.52) than middle-grade doctors and nurse practitioners (although the result was not statistically significant).
Croft and Mason35 assessed levels of confidence in foundation doctors’ management of common minor clinical presentations in an inner-city ED. Foundation doctors’ confidence in treating minor injury patients was identified as a problem, and a lack of exposure to minor injuries during daytime hours was cited by doctors as a possible cause.
A further study36 evaluated junior doctors’ experience in performing practical procedures in an ED. Two cohorts were measured: trainee doctors in the ED in June 2005 and June 2006. The study found that doctors in the later cohort reported significantly less experience in each procedure.
One study37 measured SHO and pre-registration SHO knowledge of basic acute care in 12 topics. A total of 185 junior doctors from six UK hospitals were included in the study. This study found that knowledge was poor across a range of basic acute care topics and that junior doctors were poorly prepared to identify and treat critically ill patients.
Overall, these studies raise questions with regard to foundation doctors’ confidence and performance in the ED which require further investigation.
NHS staff motivation, well-being and patient care
There is limited evidence of a direct association between factors that affect performance and outcomes in health care, which would be important to take into account when studying a changing workforce. In one study,15 which sought associations between organisational practice and clinical outcomes, it was possible to demonstrate a linkage between good human resources practice (such as appraisal and training) and effective teamwork and reductions in measures of patient mortality. A further study in a non-health care setting demonstrated that organisational climate (e.g. skill development, concern for employee welfare) was significantly associated with productivity and profitability, and that the relationship was mediated by employee job satisfaction. 38 There is an increasing literature on links between patient safety and organisational culture and climate, with a range of tools and interview methods proposed. 39
The link between staff development, motivation and well-being and the influence of these factors on patient care is recognised as important. 8,9 In one review of the literature,10 a significant linear effect was found between levels of nurse stress and burn-out and patient outcomes (patient satisfaction, medication errors and patient falls). However, the cross-sectional designs of the studies and lack of control of confounding variables (such as doctor sickness absence)40 limits the usefulness of these findings. 10
Few studies have evaluated the consequences of well-being for foundation doctors in terms of confidence, competence or patient outcomes. A study of SHOs working in 27 hospitals evaluated the relationship between psychological distress and confidence in performing clinical tasks. 41 The questionnaire was administered four times during the 6-month rotation. Overall, confidence levels in carrying out a range of practical and clinical tasks (recorded on a visual analogue scale) increased significantly between the first and fourth months of the SHO training rotation. SHOs with higher psychological distress scores at the end of months 1 and 4 had lower confidence scores. Factors associated with greater psychological distress were organisational, such as workload, certain clinical presentations and consultation issues such as communication.
Summary
The changes to postgraduate medical training (including uncertainties over future direction) and restrictions on working hours impact directly on postgraduate foundation doctors in training. These changes have also occurred at a time of rising demand for health care, with greater demands on staff in terms of providing care in services that are increasingly performance driven. It is important to consider how these major changes have influenced the well-being and motivation of foundation doctors and also the consequent impact on quality of care.
Chapter 2 Aims and objectives
The study was conducted in two phases and used a mixed-methods approach across multiple sites to achieve the following aims and objectives.
Aims
-
To describe the current arrangements for the delivery of FT in England.
-
To identify how the experiences of F2 doctors training in EDs influence their well-being and motivation.
-
To evaluate how the well-being and motivation of F2 doctors in EDs is associated with the quality of patient care.
-
To identify key measures of F2 doctor well-being and motivation that are associated with quality of patient care. Key measures that are identified may underpin the development of a tool to monitor well-being and motivation during training.
Objectives
Phase 1
-
To conduct a national and regional consultation exercise with training stakeholders to:
-
describe the national strategic view of the aims of delivering FT, with a particular focus on the role of training in supporting the well-being of doctors
-
assess how the national view is implemented on a regional basis through the postgraduate deaneries and identify any regional variation to implementation within the specialty of EM
-
undertake a scoping exercise to identify factors contributing to the well-being of F2 doctors in training within up to four EDs to develop measures to inform a quantitative evaluation of foundation doctors in phase 2 of this study.
-
Phase 2
-
To undertake a longitudinal study using a structured survey to assess F2 doctors in terms of their well-being, motivation, confidence and competence at four time points over a 12-month period.
-
To conduct a survey at four time points (at the end of F1 and then after each F2 placement) to assess the level of and change in F2 doctor well-being, motivation, confidence and competence. One of these placements will be in EM and the impact of this placement can be assessed in relation to the study outcomes.
-
Assess patient safety and quality of care by F2 doctors by reviewing the clinical records of patients receiving emergency care from F2 doctors and evaluating routine ED data to link workload and mean time with the patient for each of the participating F2 doctors.
We will examine the findings from phase 2 to:
-
evaluate whether there is a relationship between F2 doctor well-being and motivation and patient care
-
identify best-practice models of F2 doctor training, which might be generalised and implemented across the NHS to promote a healthy and productive foundation doctor workforce
-
provide a starting point for the development of a tool that can be used to monitor the well-being, motivation and training of doctors in EM and other specialties.
Chapter 3 Phase 1: consultation exercise and scoping study
Introduction
A consultation exercise with national and regional postgraduate education stakeholders (PESs) and a scoping study with training leads (TLs) and F2 doctors in the ED were undertaken using qualitative methods to examine FT from multiple perspectives at the national, regional, trust and foundation doctor levels.
Aim and objectives
The aim of the consultation exercise and scoping study was to describe the current arrangements for the delivery of FT in England.
The objectives were to:
-
describe the national strategic view of the aims of delivering FT, with a particular focus on the role of training in providing for the well-being of F2 doctors
-
assess how the national view was implemented on a regional basis through the postgraduate medical deaneries (PMDs) and identify any regional variation to implementation within the specialty of EM
-
identify factors contributing to the well-being of F2 doctors within up to four EDs. The data collected were to inform the development of measures to be used in a quantitative evaluation of F2 doctors in the phase 2 longitudinal study.
Methods
Ethical and governance arrangements
Ethical approval for phase 1 was received in May 2009 (ref.: 09/H1307/27).
Approvals from non-NHS organisations and research governance approvals from participating NHS trusts were obtained between June and November 2009.
Consultation exercise
To understand the strategic aims, national structure and implementation of FT, national and regional stakeholders from key postgraduate educational organisations involved in the delivery and implementation of FT were interviewed by telephone or videoconference. A semistructured interview schedule was designed around the aims and objectives of the study, with a particular focus on identifying potential variation in the implementation of FT and provision within training of an appreciation of the well-being and motivation of F2 doctors (see Appendices 3 and 4 for interview schedules).
A letter of invitation and information sheet about the Evaluating the Impact of Doctors in Training (EDiT) study were given to interviewees in advance, along with the interview questions. Written, informed consent was received from each participant before the interview (see Appendices 6–8 for the letter of invitation, information sheet and consent form respectively).
Scoping study
A scoping study involving interviews with TLs and focus groups with F2 doctors was carried out in four EDs to evaluate the impact of training in the ED on both F2 doctors and other health-care staff. The four EDs were selected from 15 EDs recruited for the phase 2 longitudinal study. There was a particular focus on well-being and motivation of F2 doctors in order to develop measures to inform the quantitative evaluation in the phase 2 longitudinal study.
Interviews took place with TLs in EDs. A semistructured interview schedule was designed to assess the training role of doctors, the impact of training on staff, the well-being of training doctors and the quality of care (see Appendix 5). An Information sheet and interview questions were given to interviewees in advance (see Appendix 7). Written, informed consent was received from each participant before each interview.
Focus groups were held with four groups of foundation doctors in their ED placement (mainly F2 doctors, although some F1 doctors were present in two groups). A semistructured schedule (see Appendix 9) was also designed for the focus groups, which included issues around well-being, confidence, competence and ED training experiences. Written, informed consent was received from each individual before the focus groups.
Data analysis (consultation exercise and scoping study)
Three researchers were involved in the analysis of interview and focus group data in order to gain multiple perspectives and insights into the data collected and ensure inter-rater reliability. Interviews and focus groups were not recorded to maintain anonymity of the participants; however, data collected from all participants in the consultation exercise and scoping study comprised thematic accounts and reflections from each of the researchers,42 the content of which was validated with the participants to gain a full understanding of meaning. 43
One researcher produced templates for the four participant groups, aggregating themes at the group level for (1) national PESs, (2) regional PESs, (3) emergency department training leads (EDTLs) and (4) F2 doctors in the ED primarily by using the interview/focus group questions as a priori coding. 44,45 Each template was then examined by the other two researchers, checking for inter-rater reliability to reduce any potential bias. Agreement was high (92%), with issues of terminology being the main areas of correction; any areas of misunderstanding or possible bias were corrected on each template.
Individual templates derived from the interviews and focus groups were also reviewed by the three researchers for salience (agreement of themes across stakeholders) and difference (individual perspectives that add value to the enquiry) and key overall themes were derived for each group of participants. A summary template was then produced to bring together the similarities and differences between key themes across the groups (Table 1).
| National stakeholders | Regional stakeholders |
|---|---|
|
|
| TLs in NHS trusts | F2 doctors |
|
|
Results
Sample achieved
Consultation exercise
A total of 10 interviews were undertaken, three with national PESs and seven with regional PESs, between November 2008 and February 2009. Interviews lasted for approximately 60–90 minutes. The national PES interviews were with representatives of three national bodies involved with planning FT. The regional PESs were from four deaneries and foundation schools (FSs).
Scoping study
The scoping study took place between November 2009 and February 2010. Eight interviews with EDTLs were carried out across four EDs. The group comprised six consultants (two F2 TLs, four CSs or ESs) and two nurse practitioner tutors. The interviews lasted for approximately 60–90 minutes.
Four focus groups were held with F2 doctors in three EDs. Two focus groups were held within a teaching hospital site (with seven and four participants) and the other two focus groups were held in two separate large acute trust EDs (with eight and six participants). The focus groups lasted for approximately 90 minutes. A further planned focus group in a smaller district hospital was cancelled on two occasions because of staffing pressures.
National stakeholder interview findings
In the following sections the numbers in parentheses indicate the numbers of participants agreeing with a particular statement. Statements without a number are the comments of one participant only.
Number of trainees and sufficiency
Two of the three PESs agreed that there were 7000 Foundation trainees in England and a further 800 in Scotland (2). All participants felt that the volume was sufficient as there is open access for places between trainees from the UK and trainees from other European countries (3). Additional places are required to allow non-European trainees to access the programme.
Strategic aims and national structure
All participants described the aims of FT as delivering a structured programme to provide a range of experiences to foundation doctors (3). The outcomes of the programme were designed to be common to all foundation doctors but these could be achieved in a variety of ways.
A clear national structure was described consisting of (1) a National Curriculum, (2) a national structure of FSs headed by the UK Foundation Office, comprising the directors of FSs who met with education leaders to maintain an overall strategy, (3) an Assessment Framework and (4) a national conference to share best practice (with deanery, foundation doctor and organisational representatives present) and a Foundation Programme website containing guides and review papers.
Two participants described the regulator of medical education as having overall responsibility for training (2). At the time of our interviews there was joint responsibility for F1 training between the GMC and the Postgraduate Medical Education Training Board (PMETB), with F2 training regulated completely by the PMETB. Various review groups (such as the Curriculum Group) met with Academy of Medical Royal Colleges representatives to discuss standards and assessment tools and recommend changes to the PMETB in the form of review documents. Since completion of the interviews the PMETB has merged with the GMC and the latter is now responsible for the regulation of all stages of postgraduate education and training.
Participants described a variety of approaches that are currently being used to manage the implementation of F2 training, such as stakeholder conferences (with deanery, foundation doctor and organisational representatives present) (2) and a website containing guides and review papers.
Variation in implementing foundation training at the regional level
Placements
Participants agreed that foundation doctors have six 4-month rotations managed by the deaneries (3).
Two of the three participants concluded that a uniform national implementation of FT was difficult to achieve, mainly because of regional variation within the UK in terms of local population health needs and different operating structures (2). Some deaneries have placements of varying length (from 4 months to 1 year), combining a variety of roles (2), and participants noted that variation was encouraged within the national framework as a way of producing innovation and a variety of placements (3): ‘For example, combining GP and acute medicine placements with leadership development (was unpopular with F2 doctors at first) can produce a rounded programme’.
It was noted that up to 15 trainees per year worked their F2 placements outside the UK. Participants felt that foundation doctors were reluctant to try new learning opportunities that reflected current job opportunities, preferring placements reflecting a more traditional understanding of a doctor’s role in acute medicine. Some programmes offered good future career taster sessions whereas others did not (2). Overall, the innovative placements would seem to be in the minority and were often unpopular with trainees until they were established in their use. However, although the governing body (PMETB) encouraged varied training experiences, one participant felt that it did not evaluate outcomes.
Evaluation of the well-being of foundation year 2 doctors in foundation training
It was noted that, although support for trainees was ‘attempted and well meaning’, little systematic evaluation of trainees’ well-being or motivation appeared to occur in practice. Participants felt that a good deal of time was spent discussing the few ‘doctors in difficulty’ within the training system (1–2% in total) and little time was spent evaluating the well-being or motivation of the ‘average’ trainee.
The former PMETB trainee survey asks questions of the trainees about themselves and the programme (e.g. how often they were forced to cope with problems beyond their competence or experience; their concern about the reporting of medical errors) (2). Further placement feedback forms and multisource feedback may offer some insights into whether problems had occurred in the workplace. A participant noted that ‘medical training can be “over nurturing” and the idea of FT was to bring some sense of the reality to trainees about work’.
Assessments
A key part of achieving curriculum competencies is demonstrated by assessments (2) (e.g. observations, case-based discussions; see Appendix 2). Participants described the assessment of training outcomes as variable, from both the trainees’ and the supervisors’ perspectives. PESs’ concerns were that ‘deaneries vary in their understanding of the assessment process’ and ‘constructive feedback is not always being given’. PESs felt that the trainees found the assessments to be ‘just form filling’.
Several comments focused on the need to change, for example ‘Assessments need to be tightened up and not be so woolly’. In particular, it should be ensured that assessments ‘demonstrate[d] the achievement of competencies’, assessments ‘need[ed] to be refined and simplified for both the assessor and the trainee’ and they ‘need to be thoughtful; and focused’. However, it was noted that the ‘PMETB feel that work-based assessments are better than academic assessments’.
Evaluation of foundation training
Participants were asked how F2 training is evaluated and the following comments were made:
Deaneries are judged on how they meet their standards by QAFP [Quality Assurance of the Foundation Programme] assessments and visits.
Evidence of trainees completing their assessments in the electronic portfolio. (2)
Post placement questionnaires.
The Sign-off of the FY2 year.
In response to whether postgraduate training of doctors was ‘fit for purpose’, two participants felt that it was moving ‘in the right direction’ and one that ‘there are a lot of things in the FT that work better than the old system’. Much of this positive change was to do with ‘work-based assessments’ (2). FT has reduced the variability in training by setting a specific curriculum, which has been ‘the driver for learning’.
However, challenges were acknowledged with regard to FT. All participants agreed that it was difficult to ‘balance the F1 and F2 years’ (3), with F2 lacking in clarity in comparison to F1, which leads to GMC registration (2). Other issues were changing the view that ‘teaching sessions are the only learning opportunities’, ‘varying placements across deaneries and in particular getting enough community placements’. It was also noted that not all placements are filled by foundation doctors and that some F2 doctors are not employed after FT or ‘do not get the job they want’ (this comment would seem to refer to a greater number of generalist community roles available than specialty placements).
Career development of foundation year 2 doctors
As FT is the step between medical school and specialist training, we wanted to evaluate the level of support that existed for trainees to help them decide on their future career. Career development is also an important facet of job satisfaction,46 in particular ‘using your abilities’. 47
Participants described a variety of career support resources provided in various programmes: taster sessions, career management sessions, specialist training advisors and web resources. Recently, a National Education Advice Forum had been set up to improve careers advice. There was a comment that ‘more sideways movement should be made in programmes, offering change and more choice’. There was concern that trainees ‘were slotted into work and miss the bigger picture’. However, it was noted that ‘taster sessions are not well taken up by trainees, possibly because it is difficult to get release from their placements’. It was also noted that ‘career development should be done in medical training: FY2 is too late’ and that a more positive attitude was required of F2 doctors: ‘there is more that we can do; but the trainee has been in the NHS for five to six years at this point and they should be able to put some effort in themselves’.
Future development and changes
Foundation training had been under way for 3 years when this project started and there had been several challenges to its establishment, most notably the Tooke report. 21 We wanted to examine participants’ views on the future developments to this programme.
Although participants acknowledged criticisms of FT, they felt that there was political support for the training (and 4-month placements) and that it would remain relatively unchanged (2). However, participants acknowledged that there were opportunities for development:
There will be a curriculum review in 2009 and this will give the opportunity to refine and improve specific outcomes.
The review will give us chance to pull back and standardise things across the four countries.
There is a need to resource trusts and recognise training and learning time . . . we need to understand the issues of placements; while they should be less about service and more about learning. I do not want doctors to become supernumerary.
The next focus will be post FT; and this will need to be done flexibly.
Regional stakeholder interview findings
The seven regional PESs in our study were involved in programmes that offered places for between 200 and 550 postgraduate doctors. The smallest programme started in 2008 and worked with nine trusts, expecting to expand in the following year. The largest programme worked with 24 trusts and 19 community placements.
Regional implementation of Foundation Programmes
All regional stakeholder participants described a national structured programme for F2 (7), with three 4-monthly placements (2). Each region had its own pattern of committees and liaison groups that managed deanery and placement arrangements, for example ‘there are 16 individual programmes in the local “health economy” for two years’.
Participants (2) observed that trainees were employed by trusts while continuing in the privileged position of having deanery support to continue their medical education.
Most participants described three 4-month placements that were either ‘constructed from scratch’ or were developed ‘after some transition arrangements’ (2). A variety of placements were described involving primary care (2) and ED (but not in every rotation, 2). The use of primary care placements varied from being ‘in every track’ to descriptions of ‘GP placements that are poorly supported’ (2).
It was noted that the two foundation years were rarely considered concurrently: there is ‘no coupling of F1/F2 limiting choice and flexibility of the trainee if they want to do a different rotation that fits their career path’. One participant noted that ‘we have some FY2s who spend the whole year abroad’.
Involvement of placement organisations in the planning of training
Six out of seven participants commented on formal (and informal) meetings between PMDs and trusts regarding the planning of placements (6). In two cases FSs were based in the trusts and close working relationships were described. However, this was not true in all cases:
There is local design of the rotation against minimum standards; we visit every two years. We don’t handle this at all well; the education community is separate from service delivery distancing the Trusts.
Trusts need to be involved more: we try to listen to them; but this is often swept aside by demands of evaluation.
Poor transfer of information between departmental procedures and foundation school procedures; such as poor prescribing.
Quality assurance
A variety of mechanisms designed by the PMETB (e.g. end-of-placement trainee survey, annual report) and local mechanisms (e.g. trust reports, significant events) were described. Annual or biannual formal visits to trusts were carried out by postgraduate medical education representatives. A wide range of data were collected (e.g. induction, rotas, career outputs, job evaluation survey tool, end-of-placement survey, serious incident reporting). Most participants felt that these mechanisms were adequate but that little synthesis occurred with the information, commenting (4):
QA [quality assurance] systems are difficult.
Yes, the mechanisms exist but there is a danger of information overload.
If quality issues are indicated trusts produce an action plan.
Postgraduate assessments and supervision
Electronic portfolio (e-Portfolio) use was noted by five participants, with three commenting on widespread use and others noting difficulty in implementation – ‘needing to make them more user friendly’ – and ‘some trainees being more engaged with computer technology than others’. Their use as ‘a quality assurance tool allowing the deanery to track activity’ was welcomed.
There were mixed views about the value of formal assessments. On the positive side participants felt that the tools were effective [especially the mini-Peer Assessment Tool (mini-PAT)] but that they needed to be applied effectively and not used as ‘tick-box’ exercises (2). Difficulties were noted, such as getting ‘a full spectrum of procedures’ and ‘senior clinicians’ time’ (2). Trainee strategies were noted, such as ‘leaving all the assessments to the end of a rotation’ and ‘getting friendly staff member to sign-off competencies’ (2).
Participants recognised the important supervisory roles of the ES and CS (5), noting:
Consultants find it difficult to give their time as an ES as it is not recognised in their job plan. (2)
A good ES knows their trainees well; others have only one meeting.
We rely on CS assessments to know about problems with ill health or progress.
The ES is a key role; we are working on this but it is a poorly understood role. (2)
ES role needs to be close and special relationship with a trainee to build their competency – we need time and resources to build this capacity.
The quality of assessment and supervision varied:
e-Portfolios are only used by some and the role of the ES is poorly understood. (3)
Some trusts have difficulty providing ESs.
Trainees and assessors do not understand the importance of the assessment process.
Some areas are more engaged with computer processes than others.
Induction programmes were criticised (2) either as ‘lacking’ (not containing sufficient information, typically about how the hospital worked at night) or for being held at inappropriate times: ‘best in August and worse in December’.
Participants were asked what criteria were used to sign off the end of an F2 placement. Although participants (6) offered similar criteria, emphases were different. Criteria listed were teaching attendance levels of at least 70% (2), satisfactory appraisals, multisource feedback (2), completed e-Portfolio of competencies (2), good reports from all placements, deanery guidelines for assessment and end-of-year review.
Evaluation of well-being of foundation year 2 doctors in foundation training
Regional stakeholders described the formal process of defining a F2 doctor ‘in difficulty’ (3) when significant problems were noted and an action plan put in place to manage health issues (‘often going back to what was happening in medical school’). Others (2) noted an informal monitoring process (from the ES/CS). A majority of participants (5) felt that there could be ‘better ways to monitor trainees and check to see if they are reaching their potential’.
Regarding the question of who assessed well-being, no clear pattern emerged in the view of the participants. Two participants stated that the role of identifying issues lay with the CS and relevant medical team, who then needed to inform the ES at the deanery. Other participants felt that identification of well-being issues should rest at the deanery level, either with ESs or with postgraduate managers. There was a major concern regarding the degree to which problems could be kept hidden from supervisors in general, as serious issues of well-being known to a trainee’s GP or occupational health would not be routinely communicated to supervisors.
In terms of motivation the majority of participants believed that the foundation experience of practising medicine after a long undergraduate tenure was a motivating factor. Further, the opportunity to be part of a functioning team in the ED, making decisions (2) and being given timely feedback (3), was also a motivating factor for F2 doctors.
When asked which aspects of work F2 doctors struggle with a variety of examples were given: poor or little supervision (2); antisocial shift patterns; having to prioritise and make quick decisions (2); ED workload; not being involved in decision-making in some supernumerary roles; and work that involves a high level of communication and delegation.
One participant gave an example of a local patient safety group as a formal route by which an issue of F2 doctor well-being was identified, with the group identifying a ‘serious incident’ relating to a particular trainee. The majority of stakeholders (5) did not believe that the impact of F2 doctor well-being on patient care was evaluated formally:
Not sure if this is considered.
Currently we get indirect reports from staff saying when they are not good with patients.
Evaluation of foundation training
When asked about the extent to which FT was providing doctors who are fit for purpose there was a varied response from participants. Four of the seven participants believed that F2 was delivering training at the level required, ‘offering proof of certain competencies’ and ‘providing more rounded individuals who communicate well’, and was better at identifying doctors in difficulty than the previous model of training. Three participants had concerns about the variation in ‘active’ supervision and assessment in the workplace (2) and the ability of F2 to adequately prepare trainees for specialty training (2).
In terms of the EM context, there was widespread recognition among the participants that the ED was a tough training specialty for F2 doctors. However, the elements that made it difficult were also its strengths, requiring doctors to see large numbers of acutely ill patients and make decisions about whether to send them home or admit them to hospital (3).
Daunting for trainees, they have to work in a big team which is good, deals with a large numbers of ill patients; and they get a lot of peer support.
Training is very good in ED; they are consistently good at induction and teaching parameters.
This was not the type of experience offered by many other specialties. EDs were seen to have good induction processes for trainees, enabling them to understand what was expected of them (2).
The confidence levels of trainees were low at the beginning of their placements and they were likely to be exposed beyond their competence initially. For the process to work smoothly good levels of senior and middle-grade support (2) were required in departments.
Career development of foundation doctors
Participants noted that career development in FT was under further development in the regions where they were based (4). One region was investing heavily in career development, appointing an associate dean for careers, offering mandatory training in career development, having specialist careers advisors with open appointment times and offering podcasts about different specialties. Another talked about ad hoc taster weeks for trainees to experience different workplaces. However, most activities (3) were described as being ‘work in progress’ or ‘under discussion’.
Some limitations in terms of career choice were acknowledged (3) but it was felt that some F2 doctors needed to have more realistic aspirations based on their abilities. However, there was a sense that F2 was too late to begin careers training and that the process should begin at medical school (2).
There was disagreement between participants over whether F2 doctors were being asked to select specialist training posts too early in their careers. One participant felt that F2 doctors were old enough to make good decisions, whereas another felt that decisions to enter a particular specialty were being made without sufficient experience in that area. However, there was agreement that careers advice needed to be given at an early stage (2).
Future developments and changes
Participants were asked about any developments in FT that they thought would happen in the future. It was acknowledged that there was a lobby for change (2) – to put F1 into the medical school curriculum and extend FT for a third year. Both were felt to be unnecessary as it was thought that the system needs time to ‘bed down’ and that there was little need to change too much as FT will develop well over the next 4–5 years (2). However, participants agreed that more (and better-quality) supervision needs to be provided (2), assessments need to be improved and more work needs to be carried out around career development for F2 doctors.
Training lead interview findings
The interviews with the eight EDTLs elicited information about the implementation of FT in the ED, including the role of F2 doctors in the ED, changes in training provision, the evaluation of the well-being and motivation of F2 doctors, preparation for the delivery of patient care, and assessments.
Delivery of foundation training received in the emergency department
Participants described the experiences of FT with five to 24 students in their departments. One of the TLs from a department that took a higher number of students (both Foundation Programme and undergraduate) described an increase in numbers that had happened 2 years before: ‘there are too many trainees in the department; it is difficult to provide support for them all’.
Three of the eight participants described an induction to the ED lasting around 3 days. The purpose of the induction was to introduce F2 doctors to the way that the departments were run and their protocols and procedures. One participant described the support available for induction including posters and CDs with learning materials and protocols (additionally on the intranet). Most commonly, ED teaching was organised as 1- to 2-hour weekly sessions (4) focusing on specific aspects of ED work such as breaking bad news, dealing with domestic violence, trauma training and training in specific clinical conditions, sometimes using external speakers. One TL described a mandatory skills training day to learn specific procedures used in the ED such as intubation and the use of neck drains. Another TL described training that was supported with online modules tracking teaching sessions. A third TL stated that F2 doctors were encouraged to attend 3-day life support training courses (adult life support and advanced trauma life support).
In addition, two participants described generic teaching days (or deanery days) held twice a month delivering material from the Foundation curriculum. These sessions were usually consultant led and covered areas of clinical governance and audit and were described as ‘rather didactic, and not geared to the ED role’. Another TL described ongoing work in their centre to establish mandatory training for F2 doctors.
Role in the emergency department and day-to-day working
Training leads were asked about the role of F2 doctors in their EDs. F2 doctors were described as being part of the ED, gaining hands-on experience (2) and working with a wide range of patients (2), and with various degrees of autonomy to make decisions. Activities were described as watching and progressing patients’ treatment with support and feedback from senior medical staff (2). One TL noted that in the first 4 weeks of an F2’s placement every patient was seen by a senior doctor until the F2’s confidence increased. Another TL noted: ‘F2s may not be able to work to the standard of junior doctors – they are less confident now’.
A variety of departmental working arrangements were described by participants. ED work was considered as experiential learning (3) that was supported by discussion with middle grades (24 hours), senior registrars and consultants (2) and assisted with guidelines and by reading. Learning on the job was supported in one centre by an allocated CS who held appraisal meetings with F2 doctors at least twice in their training rotation. One participant described a nurse practitioner-led service in which F2 doctors assessed the diagnoses made by nurse practitioners to give them experience of minor injuries cases. One TL noted that all patients in the ED were seen by a consultant and that ‘there was a service tension between what was done in training and what was done as the job’.
Changes in the way that the emergency department has provided training in recent years
When asked about changes to training participants focused on teaching, supervision, increased workload, issues caused by the EWTD and the reduction of placement length from 6 months to 4 months.
Two TLs noted that training (teaching) was ‘no longer geared to ED specifically’ and that previously practical procedures had been taught more formally (on a one-to-one basis) followed by supervision until the trainee grew in confidence. It was noted that medical school training had changed its focus from teaching to problem-based learning; although this was thought to be better it was acknowledged that ‘there is a greater variation in learning as a result’. Gaps in trainee knowledge were noted (2) resulting in staff having to ‘offer more support and development in the ED than before’ (e.g. in anatomy and physiology). One TL commented that some F2 doctors had never been exposed to acutely unwell patients before and that the trainees found this difficult to cope with.
Central to these issues of training was the need to provide additional senior support to facilitate F2 doctor learning (5). Although some TLs noted that there were more consultants in the ED now (2), enabling all F2 doctors to have supervisors, others noted that there were not enough senior staff to support their students (2) or that other medical staff and nursing staff were undertaking supervision. For example:
There is insufficient senior staff for close supervision; we are not giving what we should be giving in terms of education and training.
increased strain on the team in ED to support trainees; this increases the stress on senior doctors.
Coupled with the issue of increased supervision for foundation doctors is the issue of increased workload (2). This is summarised well by the following quote: ‘We are incredibly busy; the workload just gets higher and we are not broken yet but it is not far off – we just need more senior staff’.
Changes in the working pattern of doctors to shift-based work (associated with the EWTD) were seen to be interfering with access to teaching and training opportunities for F2 doctors (3). For example:
Some training time is lost; many miss two or three (teaching) sessions as they are off shift or on holiday or study leave. They only attend sessions if they are interested and if they miss them this leaves gaps in their knowledge.
The TLs thought that career development also suffered from shift working, with trainees being asked to look at different work options when they are off duty.
Although it was noted that F2 doctors were on employment contracts, it was felt that there was little reward or monitoring of F2 doctor performance (2): ‘there is no clear system to reflect how well trainees work: good trainees get frustrated’.
One TL noted that the ED had productivity measures (noting the number of patients seen by a foundation doctor) so that staff were aware of the confidence levels of various trainees.
There were several negative comments about the change in rotation length (from 6 months to 4 months). The shorter rotation was perceived as not being enough time for the trainee to learn how to do the job well (2): ‘They are just becoming competent when they leave.’
Lack of confidence in the clinical setting was particularly evident if this was the first F2 rotation. One TL noted that the reduction in rotation length had required different ways of working with F2 doctors (supervising all of the patient episodes in the F2 doctors’ first 4 weeks of working, as noted above).
Evaluation of well-being and motivation
There was some divergence in TLs’ views on how effectively F2 well-being was evaluated in the ED. Some participants felt that well-being was poorly evaluated (2) as interviews were no longer used in placement allocation, whereas others believed that systems such as multidisciplinary team feedback (mini-PAT) or more informal feedback from staff (such as nurses) identified doctors who were ‘struggling’ or ‘in difficulty’ (2). However, it was clear that there was no formal system by which foundation doctor well-being and motivation were evaluated. Although this was the case, TLs felt that if there were issues then staff working with the F2 doctor would notice (3), through observation or by an incident occurring or unfavourable reports being given in the multisource feedback. It was felt that senior medical staff or ESs would become aware of issues of well-being (3) during assessments (such as the mini-PAT), when examining e-Portfolio progress or in supervisory meetings. If workload monitoring is used this would also offer a strong indicator of poor performance.
Motivation
The TLs were asked what aspects of ED work the F2 doctors are motivated by and about the areas in which they struggle. The profile of a ‘keen’ F2 who wants to progress was clearly described (2): ‘they have carried out audit projects, they turn up bright and early, and they are more flexible about working longer hours’. Motivated F2 doctors usually see acute medicine as part of their career plan.
Less motivated F2 doctors were the ones who did not enjoy working out of hours with really sick patients (2) or who found it difficult to work with non-medical management cases (such as with older frail patients). Some lack motivation because of poor clinical knowledge (‘this may be a long-standing problem’) or because their previous experience of ED (as a medical student or an F1) was poor and/or they did not see this rotation as part of their career plan.
The potential impact of poor F2 well-being on patient care was less considered. However, patient monitoring (e.g. waiting times) and workload monitoring (2) were thought to be useful in detecting issues.
Is foundation year 2 training adequate preparation for the delivery of patient care?
When asked whether F2 training adequately prepares doctors for service-level roles, TLs described variation in trainee performance and confidence (4), with some F2 doctors ‘able to meet the demands placed upon them’ but others ‘unprepared and lacking in confidence’. F2 doctors were perceived (in comparison with SHOs) to take longer to become independent fully functioning doctors, to be more reluctant to take decisions and to work at a slower rate.
When asked to evaluate the ED experience for F2 doctors there were rather more negative comments (16) than positive (5). From a positive perspective the ED offers problem-based learning, ‘an intense experience where trainees have to think for themselves and take decisions’, ‘broad exposure to a range of medical disciplines’ and ‘challenging shifts demonstrating service delivery’; in addition, ‘senior cover is always available’.
From a negative perspective, rotation patterns were often antisocial (5) and, coupled with the EWTD, there are issues of missed teaching and other learning opportunities (2); foundation doctors ‘have had little prior experience of acutely ill patients’ and ‘are less used to decision-making in their previous placements’; and they have had less ‘hands-on experience’ with practical aspects of training, reducing their confidence (2). Trainees are not well prepared for service delivery (3), having previously been encouraged to ‘do their best’, without taking into account how long this makes a patient episode (2). In addition, TLs felt that, as it was a busy environment, it was difficult to offer sufficient supervision in the ED (2), which the trainees were needy for.
When asked how the training could be improved, most TLs were mainly in favour of a return to 6-month rotations (5), whereas some could see that a balance between breadth and depth of experience was needed (3). For example: ‘A return to six months is needed, but this may have a negative impact on the breadth of understanding associated with less service delivery.’
Participants’ comments about improvements to training mainly focused on teaching (5), in particular the inclusion of more specific training related to each placement (2) and less generic training content. The change of emphasis to problem-based learning, requiring an active learner, was noted: ‘big change from passive formal learning to active trainee seeking learning. We need a marker for the “active learner”.’ However, this approach was criticised as ‘motivation to learn is not as high as in the past; they (trainees) expect to be taught’.
TLs wanted to offer more supervision (3) but this was felt to be impossible in a service-led specialty. In summary, TLs were aware of the difference in context between the various Foundation placements, in which many F2 doctors were not required to make decisions and were supernumerary to service delivery; however, in ED, ‘trainees are vital to service delivery and we have no control over our rotas’.
Assessments
Participants were asked about the contribution of FT assessments to ensuring that doctors provided good-quality patient care. Overall, half of the participants (4) felt that the assessments were an improvement in the evaluation of the delivery of patient care and half (4) felt that there were issues that needed to be addressed with the assessments before they would be of value. The strengths of the assessments included ‘providing the opportunity for observation of trainees undertaking practical procedures’ (direct observation of procedures or DOPs), for example suturing, and providing the opportunity for ‘trainees and supervisors to discuss elements of care that were worrying a trainee’ (case-based discussions) and for clinical assessments with direct feedback to the trainee (2). However, it was noted that the benefits were case dependent.
The issues limiting the use of assessments were the need for open-ended assessment of experience (and less ‘ticking boxes’ or mundane superficial questions) (2) and lack of confidence that assessments (such as multisource feedback in which the trainee chooses the assessors) reflected ability (2). It was felt that assessments were also limited in their ability to identify doctors who were struggling with service delivery.
Focus groups with foundation year 2 doctors
Focus groups were held with F2 doctors who were on placements in four of the EDs participating in this study (25 F2 doctors in total). The focus groups discussed issues of confidence and competence, anxiety and general experience in EM.
Foundation year 2 doctor competence and confidence
Participants were asked what gave them confidence to deliver good patient care. There was strong agreement across the focus groups that positive feedback on their performance from senior colleagues (consultants and registrars ‘affirming that the appropriate clinical process had been followed’), previous experience of the clinical situation (‘previously seeing how to manage a case like a Colles fracture’) and apparent patient satisfaction (‘patient saying that they feel better after treatment’) gave them confidence in their abilities.
Further, participants from three of the four focus groups agreed that good learning experiences, such as ‘learning from near misses’, and appropriate teaching, such as ‘acquiring knowledge that was specific and useful in ED, such as what to do when a patient presents with a headache’, increased their confidence.
In addition, participants from two of the four focus groups agreed that knowing that your skills work well, peer support (‘checking questions with peers before approaching seniors’), teamworking (‘working as part of a team when doing formal assessments’) and acknowledgement by the referral team that a correct referral was made all enhanced their confidence.
F2 doctors were asked what things they worried about when they finished their shift. There was agreement that the main worry was about sending a patient home: ‘was I right’, ‘should I have referred’, ‘I worry less if they are referred because the patient is safe’.
In addition, participants from two of the focus groups worried about making decisions within the 4-hour target (‘compared to other specialties there is a small space of time to make a decision whether to admit or discharge a patient’), their own self confidence (‘I am anxious about discharging patients; if I can discuss this with a consultant I am reassured’) and correctly diagnosing the condition (‘did I get it right’, ‘was my judgement correct’).
Improving training for foundation year 2 doctors
Participants from all of the focus groups agreed that teaching could be improved in terms of content (‘more clinically relevant topics rather than health and safety’) and their availability (‘EWTD cuts down teaching time’, ‘shift working does not allow me to complete the minimum teaching requirement’).
Participants from three of the four focus groups felt that it was important that there were review sessions (‘about patients that were seen on a shift after the event; talking about whether they discharged or not’), opportunities to address the poor work–life balance of working in the ED (‘some rotas are awful’, ‘doing a difficult shift every day is very demanding and I would have to consider the lifestyle implications if I took this job on as a career’) and consideration of specific difficulties of working in the ED (‘not having enough staff on at peak times like bonfire night’, ‘not having protocols to follow’, ‘repetition of the same questions: “is the patient going to breach” and “what drugs are needed”‘).
There were also varying views on teamworking in the ED. One group felt that the ED experience was improved by the teamworking of doctors and nurses, whereas another group noted that teamworking varied depending on the time of day: ‘teamworking was more likely out of hours when there were less seniors around’.
There were varying views of the appropriate length of the ED rotation: two focus groups agreed that they were ‘glad of the extra choice that a 4-month rotation gave within their FT’ and one group (with some participants doing a 6-month rotation) felt that the longer rotation was a good thing and that some trainees had made an active choice to do this length of rotation, saying ‘there was more opportunity to learn about acute care’ and ‘it would be considered a “badge of honour” completing a six-month rotation in ED’.
Value of assessments
Participants from three focus groups gave a balanced view of the positive (3) and negative aspects (3) of the formal assessment process.
From a positive perspective participants agreed that formal assessments build on the type of assessment used in the last 2 years of their undergraduate training (such as DOPs, which helped them begin to interact with senior medical staff); working as part of a multidisciplinary team facilitated assessment; and they enjoyed the mini-clinical evaluation exercise (mini-CEX) as it offered the best feedback on their progress.
Negative aspects were that assessments assume that ‘all junior doctors are the same’; the process is flawed as ‘you only put in the e-Portfolio things that you have done well; not where you may have learned more from something that you have done badly’; and there seems little point in doing DOPs as ‘these are done as part of everyday practice’.
Emergency department environment
When F2 doctors were asked whether they enjoyed the ED environment there was a positive ‘yes’ response (4) because ‘it is unpredictable work where you need to pick up clues to understand the patient’s condition’ (2); participants felt that it is a good teamworking environment where they did not feel isolated (as they did in some surgical rotations); and there are opportunities to carry out a large variety of different sorts of work enabling a fast rate of learning: ‘You learn so much by doing things at a fast rate – having to make decisions – it is great experience for the future.’ However, these views were balanced by the ‘rubbish’ working hours.
Chapter 4 Longitudinal study
Aims and objectives
Aims
-
To measure levels of (and change in) F2 doctor well-being, motivation, confidence and competence over the period of their F2 training.
-
To measure the impact of placements in EDs on F2 doctor well-being, motivation, confidence and competence.
Objectives
-
To undertake a 12-month longitudinal study to assess F2 doctors’ experiences of working in terms of their well-being, motivation, professional identity, confidence and competence.
-
To implement a survey at four time points during the longitudinal study (at the end of the F1 period and then after each of the F2 placements). One of these F2 placements will be in the ED and the impact of this placement on F2 doctors’ experiences of working will be assessed.
Methods
Ethical and governance arrangements
Ethical approval for the phase 2 longitudinal study was received in September 2009 (ref.: 09/H1300/80).
Approvals from non-NHS organisations and research governance approvals from participating NHS trusts were obtained between November 2009 and June 2010.
Survey design
We used a ‘closed’ online survey design because in the phase 1 focus groups F2 doctors expressed a preference for online surveys rather than paper versions. F2 doctors were eligible for this study if they had a placement in the ED during their F2 rotations. The online survey was accessible via a portal on the EDiT study website,48 with eligible doctors sent a link taking them to the appropriate part of the website to access the survey (see Appendix 13 for a screenshot of the website). The EDiT website provided information about the study, such as news and updates, and also included an interactive element (a medical casebook quiz). The website was designed to be informative and attractive to potential participants and thus increase recruitment and retention over the period of the survey. Visitors to the website could examine the information provided without being obliged to complete the survey itself.
Participants
As the focus of the study was examining the impact of placements in the ED on the FT experience of F2 doctors, the sampling frame (eligible doctors) for the survey was all F2 doctors in England who had a placement in the ED as part of their F2 training year. Eligible doctors were identified following discussions with PMDs and EDs.
Sample identification
In the first instance, (August–September 2008) we identified all type 1 EDs (defined as consultant-led 24-hour service with full resuscitation facilities and designated accommodation for the reception of emergency patients) in England from the Department of Health website. 49 We identified and contacted 176 NHS trusts in England with type 1 EDs for expressions of interest. After our approach, 45 trusts responded and expressed an initial interest in taking part in the study. Further contact took place with ED leads after the initial approach and more detailed discussions about the requirements of the study were held. Finally, 28 trusts with 30 EDs agreed to participate as the study sites. Study contacts, including lead consultants, foundation consultant leads and research nurses, were identified in the 30 participating EDs.
Deaneries and foundation schools
All 14 PMDs were contacted (December 2008–January 2009) to identify expressions of interest in participation. The postgraduate medical dean and the foundation school director (FSD) were contacted in the first instance. Details about the study were provided and agreement to participate in the study was sought from each deanery. Agreement to participate was obtained from nine deaneries. The FSD from each of these nine deaneries was asked to identify key contacts within the schools (foundation school administrators; FSAs) to assist the study team with the identification of F2 doctors who would have a placement in the ED within their F2 training (2010–11). EDs of NHS trusts were included in the study only when the deanery also agreed to participate.
Eligible participants
After recruitment of participating EDs and deaneries, our total eligible F2 doctor sample consisted of 654 F2 doctors, training between August 2010 and August 2011. Each of these F2 doctors had a placement in one of the 30 EDs participating in the study.
Participant contact
For data protection reasons and reasons stipulated by the approving ethics committee, we could not be given the names/addresses of the eligible F2 doctors by participating deaneries and FSs; instead, approaches to the doctors were made by study contacts in FSs and EDs on behalf of the study team.
The initial approach to inform the eligible F2 doctors of the study was made by the relevant FSAs. An e-mail with an attached letter of invitation and participant information leaflet (see Appendices 14 and 15 respectively) was sent to the F2 doctors before the start of the study (May 2010). The e-mail notified the doctors that they could opt out of the study at any stage and receive no further contact regarding the study.
Recruitment and consenting
In July 2010 a further e-mail was sent by FSAs to those eligible F2 doctors who had not opted out after the initial approach. This e-mail provided a link to and study password for the online survey. After accessing the survey, potential participants were required to enter their e-mail address and the study password to proceed any further (ensuring that only eligible F2 doctors completed the survey). Participants were asked to enter an e-mail address that would be current throughout the study time period to enable the accurate matching of participants’ responses at further time points. When participants entered the correct password an online survey consent form was generated (see Appendix 16). Participants were unable to proceed with the survey until they had completed the consent form (following consent, F2 doctors were able to access the survey proper with their e-mail address generating a unique study ID that would identify them throughout the study).
Following the initial recruitment e-mail in July, the sample of F2 doctors (with the exception of consenting participants or those who opted out) were contacted at two further time points (August and September 2010) by FSAs as a reminder to participate in the study. If F2 doctors had consented to take part at the first time point (T1) they were then contacted at subsequent time points directly by the study team. Participants could enter the study at T2 if they wished (and were coded accordingly) but not at later time points.
Development of survey measures
In the first instance a pilot questionnaire was designed to measure a range of work-related outcomes and job-related characteristics by adapting well-validated scales. The questionnaire was piloted with a small sample of F2 doctors and following feedback some minor amendments were made to the final questionnaire (see Pilot study of questionnaire). The pilot questionnaire and the final questionnaire are provided in Appendices 17 and 18 respectively.
The content of the final questionnaire is detailed in the following sections.
Background demographic information
Baseline information was collected on sample age, sex, place of qualification, year of qualification, ethnicity and description of Foundation placements (e.g. specialty undertaken, trust). Details of the placements (specialty and trust) were cross-checked with equivalent placement information from the nine participating deaneries to ensure accuracy of reported information.
Individual characteristics
Baseline background information was collected on personality and coping characteristics using validated scales:
-
Personality. A five-factor structure represents the most universal description of the dimensions of personality50 and from this the dimension of conscientiousness (feeling capable) is an important personality trait for F2 doctors to develop during their FT. Meta-analytic studies suggest that conscientiousness is a valid predictor of job performance. 51 The scale consisted of eight items (e.g. ‘Would you describe yourself as typically organised?’) rated by the participant from 1 (‘extremely inaccurate’) to 9 (‘extremely accurate’).
-
Coping. A coping scale consisted of 16 items (e.g. ‘When faced with a stressful situation I try to figure out how to resolve the problem’). This 16-item scale seeks to identify the strategies that individuals use to cope with difficult, upsetting solutions. Developed from the work of Tobin et al.,52 it examines a hierarchical structure of coping strategies stemming from problem-focused and emotional-focused higher-order categories of strategies. 53 The scale divides into four positive strategies:
-
personal proactivity (PPRO) – items a, e, i, m
-
seeking support (SSUP) – items c, g, k, o
-
not seeking revenge (NREV) – items d, h, l, p
-
not keeping things to self (NSLF) – items b, f, j, n.
-
Work-related outcomes
We were interested in how confidence and competence developed over the course of F2 training and this was measured using three scales. Two of the scales were adapted from a previous study. 35 The scale regarding confidence in decision-making was developed after discussions during the phase 1 focus groups with F2 doctors about influences on well-being.
-
Confidence in managing conditions. Participants were asked how they felt about managing 23 common acute medical conditions (such as elderly fall, chest pain, stroke, overdose and back pain). Participants scored their confidence on a nine-point scale from 1 (‘lowest level of confidence’) to 9 (‘highest level of confidence’). The 23 conditions were selected by an ED consultant and a consultant in acute medicine who were members of the project steering group. The conditions were selected as a comprehensive range of acute presentations that F2 doctors were expected to manage independently and competently during the course of their F2 training. Box 1 details the conditions included.
-
Experience in performing practical techniques. This scale aimed to measure experience in performing five common practical medical techniques. The five procedures were defibrillation, arterial blood gas analysis, suturing, electrocardiogram (ECG) interpretation and radiograph interpretation. Participants were asked how experienced they were in performing the techniques and they scored themselves from 1 (‘no/little experience’) to 9 (‘confident in performing alone’). The procedures were again selected by our steering group consultants as representing a comprehensive range of procedures that F2 doctors were expected to carry out independently and competently during the course of their F2 training and as part of their training curriculum.
-
Confidence in decision-making. Confidence in decision-making was one of the key issues raised by F2 trainees in our phase 1 focus groups. As there were no validated scales in this area, the study team developed a scale to examine the ability of trainees to make appropriate decisions. This consisted of three statements on elements of decision-making (e.g. ‘Thinking about the decision and judgements I made during the placement, I am confident I made the appropriate decisions’). Participants scored their agreement with the statements from 1 (‘strongly disagree’) to 5 (‘strongly agree’).
Diarrhoea and vomiting.
Shortness of breath.
Collapse – unknown cause.
Acute mental health problem.
Elderly fall.
Chest pain.
Back pain.
Cardiac arrest.
Palpitations.
Abdominal pain.
Acute painful joint.
Rectal bleeding.
Acute allergic reaction.
Left ‘side’ pain.
Acute stroke.
Overdose – paracetamol.
Diabetic ketoacidosis.
Acute confusion.
Headache.
Seizure.
Cellulitis.
Haematemesis.
Rash.
Well-being and motivation
We were interested in levels of and change in F2 doctor well-being and motivation during F2 and specifically the impact of their placement in the ED on well-being and motivation. Four well-established previously validated scales were used:
-
Anxiety and depression. These scales are derived directly from original measures of two dimensions of job-related well-being, from anxiety to contentment and from depression to enthusiasm. 54,55 The third dimension of well-being (from ‘displeasure’ to ‘pleasure’) is measured by the job satisfaction scale. These scales are used in preference to more general notions of well-being, for example the General Health Questionnaire,30 as they are specific to the work context, which may change over time with F2 doctor placements. These scales have been found to be sensitive for predicting absence,40 job demands56 and leader behaviour. 57 These scales use six items, three related to anxiety (e.g. ‘In the last month of your placement, how much of the time did your role make you feel worried’) and three to depression (‘In the last month of your placement, how much of the time did your role make you feel miserable’). There are five possible responses ranging from ‘not at all’ to a ‘great deal’. Responses are averaged across items with higher scores representing greater job-related anxiety or depression.
-
Job satisfaction. The questionnaire incorporated a 15-item job satisfaction scale. 46 The scale explores overall job satisfaction by combining subscales of intrinsic satisfaction (affective reactions to job features that are integral to the work itself) and extrinsic satisfaction (affective reactions to job features external to work). Items explored satisfaction with areas such as physical working conditions, freedom to choose own method of work, recognition for good work, clinical supervision and chances of career progression. The scale has been found to be a valid and reliable measure of job satisfaction and there is a large body of comparative data available (e.g. Mullarkey et al. ,58 Stride et al. 59). The wording of several of the original items was amended to make the scale more appropriate to the FT context. The 15-item job satisfaction scale has seven responses ranging from 1 (‘extremely dissatisfied’) to 7 (‘extremely satisfied’). An example item relating to intrinsic satisfaction is ‘How satisfied are you with the amount of responsibility you are given?’ An example item relating to extrinsic satisfaction is ‘How satisfied were you with your rate of pay’? Scale scores are derived by averaging item scores, with higher values representing greater satisfaction. A copy of the scale can be found in Appendix 18.
-
Motivation. In this study we wanted to explore what makes a motivating work environment for F2 doctors. Working with expectancy theory60 we assume that people have certain amounts of energy, which is used to satisfy our needs (such as achievement, safety), and motivation is the process which determines how that energy is used to satisfy needs. Motivation can be considered both as effort (the amount of time or energy put into work) and as direction (specific tasks that energy is applied to). One scale was included in the questionnaire. This scale focused on the effort that the participant would expend on his or her work placement. The scale included three items (e.g. ‘How would you rate the amount of effort you put into your job?’). Participants scored their effort from 1 (‘lowest effort’) to 5 (‘greatest amount of effort’).
-
Intention to quit. This refers to the individual’s intention to leave his or her role and was measured using three items61 including ‘It is very likely that I will actively look for a new job in the next year’. These items have previously been used with medical staff62 and were adapted to the FT context (e.g. ‘Thinking of your career in medicine so far, how true is the following statement: it is very likely that I will actively look for a new job outside the medical profession in the next year?’). Participants scored their agreement with the items from 1 (‘strongly disagree’) to 5 (‘strongly agree’).
Teaching and training
Teaching and training are important elements of a trainee doctors’ work placement and we included two scales related to teaching and training received and the knowledge acquired from the work placement. The two scales were developed after key issues were raised during our phase 1 focus groups about influences on well-being.
-
Impact of teaching and training on management of conditions. This included three items that measured how the management of medical conditions may have been improved during the work placement. Participants were asked if their management of the 23 acute conditions (see Box 1) would have been improved with clearer guidelines, better teaching or more supervision, with each item scored from 1 (‘strongly disagree’) to 5 (‘strongly agree’).
-
Development of professional knowledge. This examined the professional knowledge acquired over the course of F2 training. It was measured using three items (e.g. ‘Do you feel more able to work as part of a clinical team?’) and participants scored agreement from 1 (‘not at all’) to 5 (‘a great deal’).
Role characteristics
This section included three well-validated scales that examined the characteristics of the foundation placement roles.
-
Work demands. This scale was designed to measure the extent to which F2 doctors feel that they have the time and resources to carry out their job properly in their F2 placements. Studies have shown that time pressures and workload are major influences of well-being for health-care workers (e.g. Borrill et al. ,63 Borrill et al. ,64 Hipwell et al. ,65 Richardsen and Burke66). For example, a longitudinal study of health-care workers63,64 demonstrated medium to strong negative relationships between work demands and job satisfaction (r = −0.30). Based on a measure of subjective quantitative workload,67 the scale draws on the findings of Kahn et al. 68 This scale consists of six items with five responses ranging from 1 (‘not at all’) to 5 (‘a great deal’). An example of an item from this scale is ‘I could not meet all the conflicting demands made on my time at work’.
-
Task feedback. This scale explores the F2 doctors’ understanding of their own work performance and their colleagues’ perceptions of feedback. This is particularly relevant in the health-care context as there is a strong degree of interdependence with colleagues in the profession. Feedback is a core job dimension defining the salient properties of work69 and influencing outcomes such as work motivation, performance, satisfaction and attendance behaviour. 69–71 Feedback from various sources leads to knowledge of individual performance, role clarity and appropriateness of work behaviour. This measure was based on a subscale of the Job Diagnostic Survey: feedback from the job itself. 71 The scale has four items with five responses ranging from 1 (‘strongly disagree’) to 5 (‘strongly agree’). Two of these items refer to the individual’s understanding of his or her own work performance, for example ‘I usually know whether or not my work is satisfactory in this job’. Two further items explore the understanding of others’ perceptions of feedback, for example ‘Most people on this job have trouble figuring out whether they are doing a good or a bad job’.
-
Role clarity. This referred to how clear the individual felt in his or her role in terms of what was expected of him or her. This was measured using five items (e.g. ‘I had clear, planned goals and objectives for my job’), with agreement scored from 1 (‘not at all’) to 5 (‘a great deal’). A lack of understanding of the tasks that form a part of the individual job role is likely to be stressful. 72 Issues of role clarity are pertinent to the well-being of F2 doctors as their roles are often ill-defined and encompass a wide range of behaviours. Several large-scale studies of health-care staff have demonstrated that role clarity is related to job satisfaction. 63,64,73 For example, Borrill et al. 63 found strong positive relationships between role clarity and job satisfaction. These relationships were confirmed in a subsequent survey. 64
Relational characteristics
Social support
Two dimensions of social support have been described: the dominant characteristic of emotional/psychological support, which involves listening, caring, approval and sympathy, and instrumental support, which involves active behaviour. 74 However, social support is a complex phenomenon and may vary with different types of work. 75,76 Social support at work is provided by different people such as co-workers (peers) or colleagues, supervisors or managers and team members. In addition, there are non-organisational sources of support such as spouses, friends or relatives. A large-scale survey of NHS staff63 found strong positive relationships between social support and well-being, which was validated by a similar observation 2 years later. 64 In this study we examine two forms of support salient to F2 doctors:
-
Supervisor support. This referred to the availability of advice and support from supervisors and was measured by six items (e.g. ‘To what extent did your CS encourage you to give your best effort?’). Extent of support was scored from 1 (‘to a very little extent’) to 5 (‘to a very great extent’).
-
Colleague support. This referred to the availability of advice and support from colleagues and was measured by four items (e.g. ‘To what extent were you able to count on your colleagues to help you with a difficult task at work?’). Extent of support was scored from 1 (‘to a very little extent’) to 5 (‘to a very great extent’). The first item examines emotional support,74,77,78 asking the recipient about the extent to which colleagues ‘listen to you when you need to talk about problems at work’. The other three items focus on instrumental or tangible social support. 74,77,79 These ask the recipient the extent to which colleagues ‘back you up’, ‘help with a difficult task’ and ‘help in a crisis situation’.
Additional job-related characteristics.
Further job characteristic scales were derived from other potential determinants of well-being identified during our focus groups discussions with F2 doctors in phase 1. These were extent of teaching and training, hours of work in a working week and extent (hours) of contact with CSs.
-
Teaching and training received. This was measured by three items [e.g. ‘Thinking of your F2 roles did you have any formal teaching sessions arranged in your department (in addition to the external FT)?’]. Responses were rated from 1 (‘none’) to 5 (‘a great deal’).
-
Hours of work. Two questions addressed the issue of the number of hours of work that F2 doctors undertook in their different placements. The first question, ‘In a typical working week in your role how many hours did you work?’, had an open response to record number of hours. The second question, ‘In the last four weeks of your Foundation Role did you have a shift changed at short notice?’, had a dichotomous (‘yes’ or ‘no’) response.
-
CS contact hours. Two questions examined hours of contact with the CS and had open responses to record number of hours. (‘In a typical week how many hours of one-to-one contact did you have with your CS?’ and ‘In a typical week how many hours of close working contact, e.g. ward round managing a patient, did you have with your CS?’).
Survey free-text comments
The survey included a space for ‘further comments’, allowing participants to offer further commentary. Participants were able to highlight issues related to their working experiences that were not covered by our survey measures. They were also able to expand on elements in the survey measures that were of particular pertinence to them (a full description and results from this section are provided in Appendix 20).
Sample size
We planned to include a sample size of 210 F2 doctors from across EDs in England. We hypothesised that the job-related well-being of F2 doctors, measured using the six-item anxiety–contentment and six-item depression–enthusiasm dimensions of the Warr54 job-related well-being scale would change over the 12-month study period. Assuming a correlation of r = 0.4 between the baseline and 12-month test scores, a sample size of 210 cases was required to detect a 0.2-unit change in anxiety–contentment at the p < 0.05 level of significance with 95% power.
We envisaged an average of 24 F2 doctors in each participating ED during the 12-month period of the study. We assumed a 20% non-response rate within each ED and a further 20% loss of paired cases between pre- and post-placement surveys across the sample, giving us a final required sample of around 14 F2 doctors per ED. To satisfy the power analysis above we aimed to recruit doctors from at least 15 EDs.
Pilot study of the questionnaire
We conducted a pilot study in June 2010, primarily to test the reliability of the survey measures, particularly those developed by the research team, but also to examine:
-
the usability of the questionnaire (e.g. issues of length)
-
the feasibility of using FSAs to forward e-mails to F2 doctors on our behalf, with links to the online survey
-
the functionality of the online web-based platform for the questionnaire.
Participants
Three deaneries took part in the pilot study. These deaneries were selected on the basis that they had already identified a FSA who was able to forward the e-mails to F2 doctors, as proposed in the main study.
The three deaneries contacted a total of 57 doctors in seven EDs. The doctors were in their final F2 placement and therefore were not eligible to be part of the main study sample as they were leaving FT before the start of the study proper.
Analysis
We conducted a reliability analysis for all of the scale measures (sets of attitudinal items designed to measure a single construct) included in the questionnaire, using Cronbach’s alpha statistic to determine the internal consistency of each scale. We also assessed the item frequencies to check that a spread of responses was being collected (i.e. the full range of experiences was identified by each item) and the response rate for each item to check that all were understandable and relevant.
Results
Reliability
The reliability scores (Cronbach’s alpha) for the majority of the scales were > 0.7 (denoting acceptable reliability) (Table 2). Two motivation measures scored lower for reliability and were omitted from the final survey. These were motivation in terms of examining the direction (or prioritisation) of participants’ effort in the role, measured by three items (e.g. ‘I divide my time across tasks in the way that is most helpful to the organisation’), and motivation in terms of the level of reward that participants received for their effort, also measured by three items (e.g. ‘Working hard on this job is not rewarded’). For these two motivation scales participants rated agreement from 1 (‘strongly disagree’) to 5 (‘strongly agree’).
| Measure | Number of items | Reliability score (Cronbach’s alpha) |
|---|---|---|
| Job satisfaction | 15 | 0.92 |
| Depression | 3 | 0.92 |
| Anxiety | 3 | 0.92 |
| Intention to quit | 3 | 0.78 |
| Motivation (effort) | 3 | 0.92 |
| Motivation (direction of effort) | 3 | 0.77 |
| Motivation (need satisfaction) | 3 | 0.66 |
| Personality (conscientiousness) | 8 | 0.85 |
| Coping (personal proactivity) | 4 | 0.84 |
| Coping (seeking support) | 4 | 0.80 |
| Coping (not seeking revenge) | 4 | 0.71 |
| Coping (not keeping things to self) | 4 | 0.74 |
| Confidence in decision-making | 3 | 0.48 |
| Teaching/training received | 3 | 0.69 |
| Development of professional knowledge or learning | 3 | 0.88 |
Confidence in decision-making was found to have a lower scale reliability, but analysis showed that two items had good levels of reliability (‘I am confident that I made the appropriate decisions’ and ‘Considering the information available to me I made the best decisions possible’). A third item (‘I had sufficient time to make the number of decisions expected of me’) was introduced to the final survey scale to maintain it as a three-item scale. All other scales and items were retained for the main study.
Usability
The system for recruiting the F2 doctors worked well. E-mails were sent to them by the designated FSA in each deanery. This proved acceptable to both the deaneries and the doctors.
Twenty-four F2 doctors logged onto the survey via the website platform and did not report any problems with the usability/functionality of the questionnaire. A total of 21 F2 doctors completed the survey pilot and were included in the analysis. Three doctors did not complete any part of the questionnaire. These doctors were subsequently e-mailed to ask why they had not completed the questionnaire but they did not reply to the e-mail.
Survey implementation
Following the pilot study the final questionnaire was confirmed and administered identically at the four time points (T1–T4), with the exception of background information, which was collected at T1, and the development of professional knowledge scale, which was added at T4.
The survey utilised survey-design software (SurveyGizmo, Boulder, CO, USA) to enable online usage. The survey measures were grouped together in four sections, with the demographic data collected only the first time that a participant received the survey. The initial survey consisted of 31 items presented over eight pages. All items presented on one page had to be completed to proceed to the next page of the survey. A ‘back’ button allowed participants to go back through the survey and amend answers if they wished to do so.
Cohort sampling points
We aimed to administer the survey measures at up to four time points (T1–T4), capturing F2 doctors’ working experiences in four Foundation Placements, the final F1 placement and the subsequent three F2 placements (Table 3). Doctors were recruited initially at T1, although a small number did not join the study and respond to the survey until T2.
| Survey time point | Placement captured | Date of survey administration |
|---|---|---|
| T1 | Final F1 placement (April–August 2010) | July–September 2010 |
| T2 | First F2 placement (August–December 2010) | December 2010–February 2011 |
| T3 | Second F2 placement (December 2010–April 2011) | April–June 2011 |
| T4 | Final F2 placement (April–August 2011) | August–September 2011 |
Analysis
Using longitudinal multilevel modelling, the pattern of change in mean sample scores on each of our survey measures was assessed over the duration of the study. After the initial measurement of mean scores at the end of F1 (see Table 3), variation in mean sample scores on the survey measures, by time of placement in the ED, was also assessed by categorising each member of the sample as belonging to one of three groups, depending on whether they had completed their second-year placement in the ED as their first, second or final F2 placement (Table 4). Grouping the sample in this way allowed the measurement of the impact that a placement in the ED had on doctors’ role characteristics and work-related outcomes.
| ED group | F1 | F2 | ||
|---|---|---|---|---|
| T1 | T2 | T3 | T4 | |
| 1 | Placement in the ED | |||
| 2 | Placement in the ED | |||
| 3 | Placement in the ED | |||
Results
Response rate
Overall, 217/654 eligible F2 doctors completed/partially completed the questionnaire for at least one of the four time points, a response rate of 33.2%. Table 5 details the number (%) responding at each of the four time points.
| T1 | T2 | T3 | T4 | |
|---|---|---|---|---|
| No. (%) responding | 188 (86.6) | 154 (71.0) | 135 (62.2) | 108 (49.8) |
| No. (%) of non-responders | 29 (13.4) | 63 (29.0) | 82 (37.8) | 109 (50.2) |
| Total | 217 | 217 | 217 | 217 |
In total, 87 (40.1%) doctors completed the survey at all four time points, 26 (12.0%) completed the survey at three time points, 56 (25.8%) completed the survey at two time points and 48 (22.1%) completed the survey at one time point.
Sample characteristics
The mean age of our study doctors was 27 years, 58.2% were female and they had been qualified as a doctor for a mean of 1.5 years. A total of 68.7% were white British, 8.5% were black, 10.9% were South Asian, 6.0% were East Asian and 6.0% were of mixed race. UK-qualified (at undergraduate level) F2 doctors made up 83% of the sample.
Response by trust
Details of the number of F2 doctors recruited from each participating deanery and ED are provided in Appendix 19 (see Table 21).
Emergency department rotation groups
As detailed in the analysis section, we classified participants into three ED placement groups depending on the timing of their F2 placement in the ED (whether carried out as rotation one, two or three) (Table 6).
| ED group (time of ED training) | n | % |
|---|---|---|
| 1 (August–December 2010) | 90 | 41.5 |
| 2 (December 2010–April 2011) | 61 | 28.1 |
| 3 (April–August 2011) | 66 | 30.4 |
| Total | 217 | 100.0 |
In total, 26 participants (12.0%) also reported completing a placement in the ED as part of their F1 training. We analysed this subgroup to see whether they differed in any way from those without previous F1 ED experience.
There were no statistically significant differences between the three ED groups in terms of age, sex, length of time qualified as a doctor and scores on either the trait personality measures or the coping strategy measures (see Appendix 19, Tables 22 and 23).
Work-related outcomes
Confidence in managing common conditions
We measured levels of and change in mean sample scores for:
-
confidence in managing individual acute common conditions
-
overall confidence in managing acute common conditions (calculated across the 23 conditions).
Confidence was measured from 1 (lowest level of confidence) to 9 (highest level of confidence). Details of the 23 conditions are provided in Box 1.
Mean confidence scores for each of the 23 acute conditions varied significantly across the four time points, with a statistically significant increase in confidence for managing each condition between T1 and T4 (see Appendix 19, Table 24).
Mean overall confidence (across the 23 conditions) varied significantly across the four time points (F3,309 = 86.0, p < 0.005), with an increase in mean overall confidence found over the course of F2 training (Table 7).
| ED group | Time point of response | |||||||
|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | |||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| 1 | 5.96 | 0.96 | 6.80 | 0.78 | 6.80 | 0.73 | 7.10 | 0.78 |
| 2 | 6.25 | 0.80 | 6.30 | 0.86 | 7.24 | 0.62 | 7.33 | 0.49 |
| 3 | 6.10 | 0.90 | 6.41 | 0.87 | 6.63 | 0.89 | 7.36 | 0.71 |
Box 2 provides a quote from a free-text comment made by a F2 doctor on the questionnaire.
I really enjoyed this year; it was hard work but it helped me move on from stress of all the practical things to learn the bigger picture of patient-centred care and being part of a team.
T4 participant
Impact of placement in the emergency department
Participants were divided into three groups depending on the rotation in which they had completed their second-year placement in the ED (see Table 4).
For 14 of the 23 conditions (shortness of breath, collapse – unknown cause, acute mental health problem, elderly fall, chest pain, back pain, abdominal pain, acute allergic reaction, acute stroke, overdose – paracetamol, diabetic ketoacidosis, acute confusion, seizure and rectal bleeding) there was a statistically significant interaction between change in confidence and group (i.e. time of placement in the ED), with the biggest increase in mean confidence for each group of doctors associated with the placement in the ED compared with other placements (see Appendix 19, Table 24 for mean scores over time by condition and ED group).
There was a significant interaction between change in confidence and group (i.e. time of placement in the ED) when predicting mean overall confidence across the 23 conditions (F6,309 = 9.3, p < 0.005), with the biggest increase in confidence for each group of doctors associated with their placement in the ED compared with other placements (Figure 1).
FIGURE 1.
Interaction between time and time of ED placement and mean overall confidence in managing patients with different conditions.
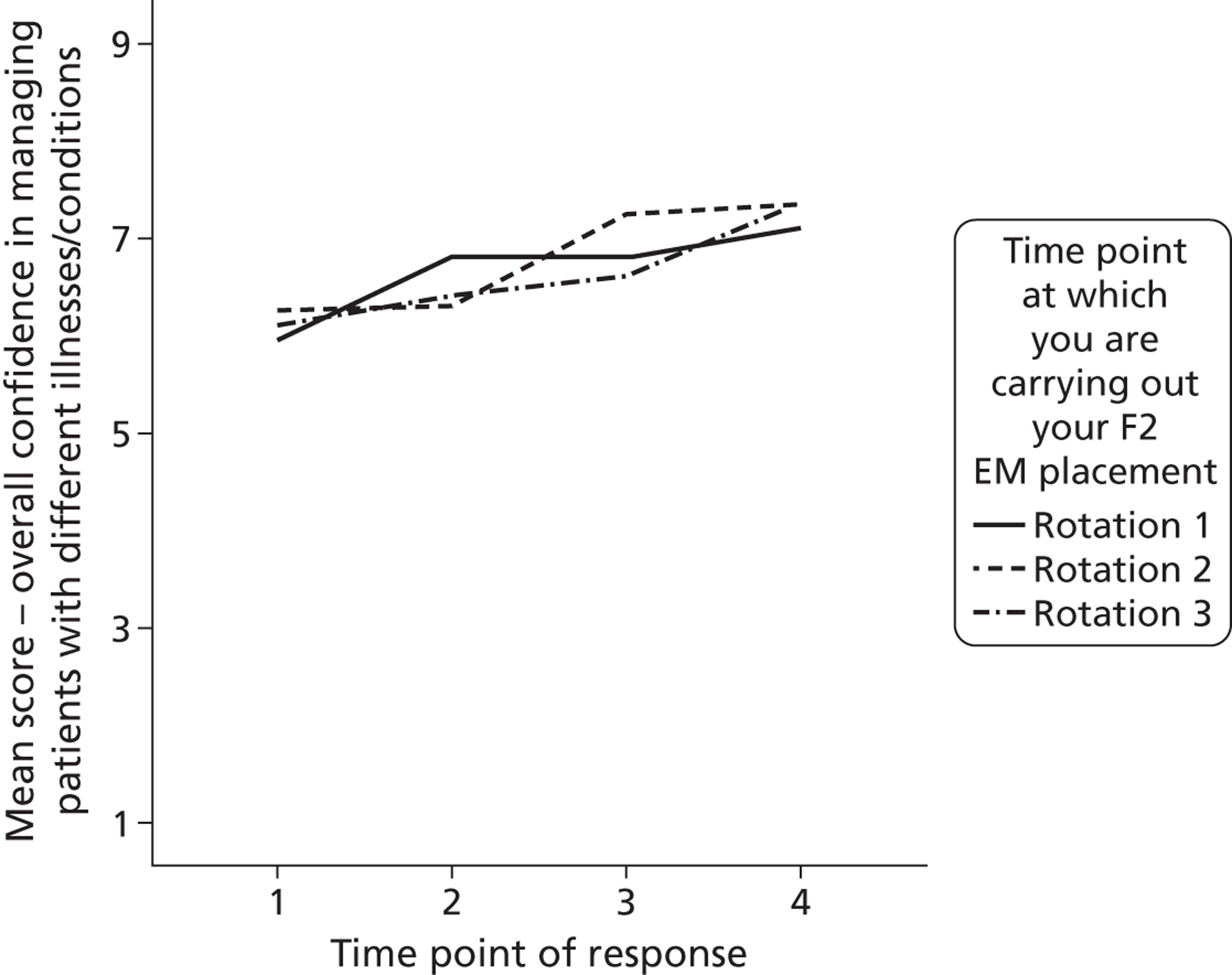
Box 3 provides some quotes from the free-text comments made by F2 doctors on the questionnaires.
A&E was a very good clinical experience, and I am glad that I had the opportunity to undertake this placement.
T4 participant
ED is an excellent training ground for F2s for any future field, given the sheer volume of patients, good support and regular teaching.
T4 participant
Experience in performing practical procedures
We assessed the levels of and change in mean sample scores for:
-
experience of doctors in performing five common practical procedures (defibrillation, arterial blood gas analysis, suturing, ECG interpretation and radiograph interpretation)
-
overall experience across the five common practical procedures.
There was a statistically significant increase in reported mean experience over time for defibrillation (F3,344 = 23.3, p < 0.005), suturing (F3,323 = 61.4, p < 0.005), ECG interpretation (F3,315 = 27.2, p < 0.005) and radiograph interpretation (F3,362 = 19.1, p < 0.005). Mean scores across the four time points for overall confidence are shown in Table 8.
| ED group | Time point of response | |||||||
|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | |||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| 1 | 5.96 | 0.96 | 6.87 | 0.96 | 6.35 | 1.55 | 6.99 | 1.05 |
| 2 | 5.96 | 0.95 | 6.29 | 1.19 | 7.28 | 0.81 | 7.44 | 0.72 |
| 3 | 5.72 | 1.20 | 5.77 | 1.46 | 7.18 | 0.76 | 6.02 | 1.40 |
The coefficient alpha for mean overall experience in performing practical procedures ranged from 0.60 (T4) to 0.80 (T3). Mean overall experience (across the five different practical procedures) varied significantly across the four time points (F3,367 = 61.1, p < 0.005), with a statistically significant increase in experience over the course of F2.
Impact of placement in the emergency department
There was a statistically significant interaction between change over time and group (i.e. time of placement in ED) when predicting the improvement in mean experience scores for arterial blood gas analysis, suturing, ECG interpretation and radiograph interpretation. For each of these techniques the biggest increase in mean experience was associated with the placement in the ED compared with other placements (see Appendix 19, Table 25 for mean scores over time for each procedure by ED group).
There was a significant interaction between change over time and group (i.e. time of placement in the ED) when predicting mean overall experience across the five practical procedures (F6,367 = 10.3, p < 0.005), with the biggest increase in perceived experience reported by each group of doctors associated with their placement in the ED compared with other placements (Figure 2).
FIGURE 2.
Interaction between time and time of ED placement and mean overall experience in performing practical procedures.
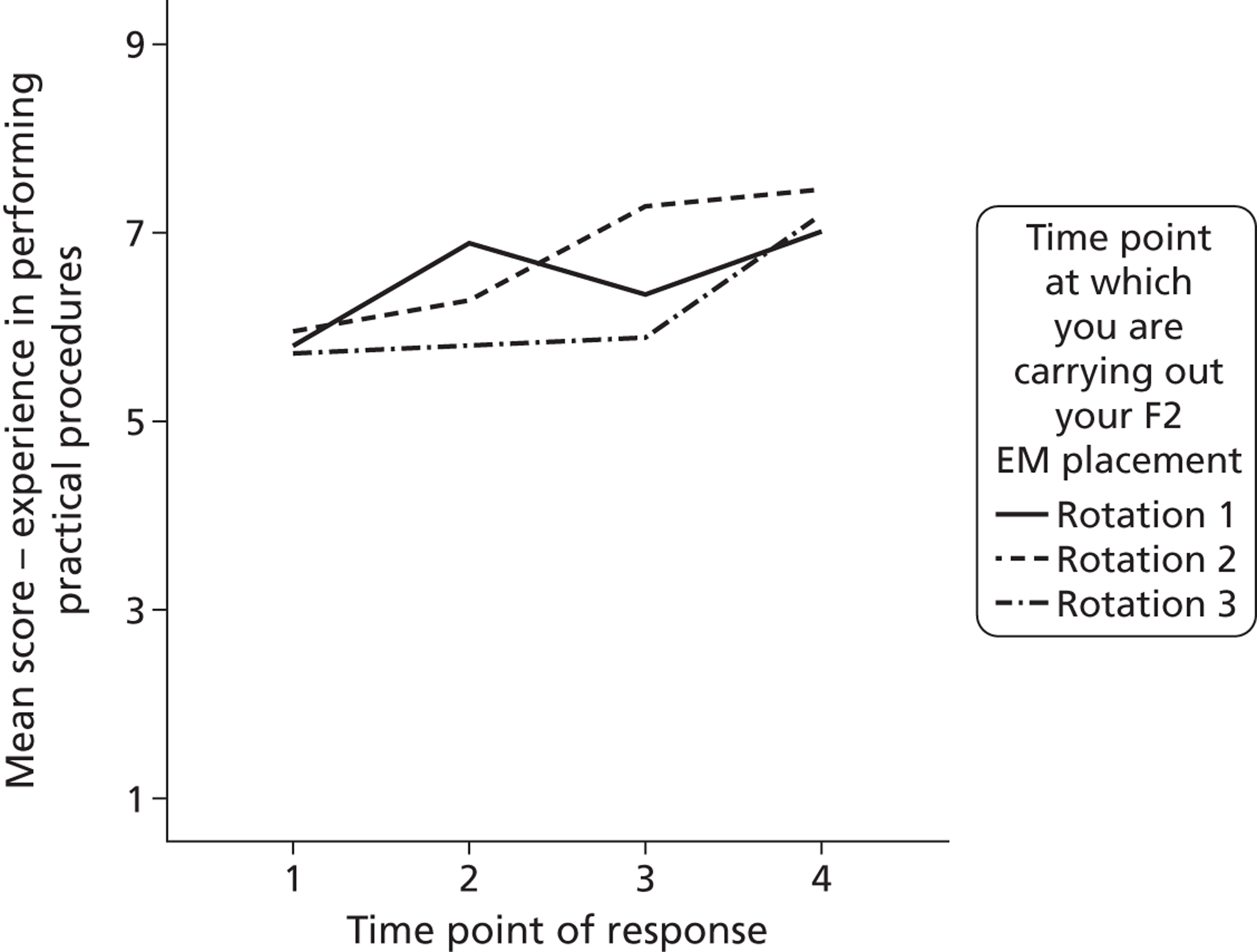
There were many positive free-text comments made on the questionnaires about the learning experience of working in the ED (Box 4).
I learned an incredible amount clinically in knowledge and practical skills.
T2 participant
Experience was rewarding as I gained skills and experiences that I could not have got elsewhere.
T2 participant
Going forward, I feel more confident clinically for the experience.
T3 participant
A&E was a very good clinical experience, and I am glad that I had the opportunity to undertake this placement.
T4 participant
Well-being
Anxiety and depression
Levels of and change in mean sample scores for anxiety and depression were calculated. Scores for each ranged from 1 (lowest level) to 5 (highest level). The coefficient alpha for anxiety ranged from 0.85 (T4) to 0.91 (T2) and for depression ranged from 0.87 (T1) to 0.93 (T3).
There were no statistically significant variations in mean sample scores for either anxiety or depression across the four time points. The mean scores for anxiety and depression over time are shown in Appendix 19 (see Table 26).
There was a significant interaction between time of placement in the ED and mean anxiety (F6,390 =7.9, p < 0.005) with all three groups of doctors showing the biggest rise in mean anxiety during their placement in the ED (Figure 3). There was no difference between ED placements and other placements for scores on depression. Mean scores for each ED group by time point can be found in Appendix 19 (see Table 26).
FIGURE 3.
Interaction between time and time of ED placement and anxiety.
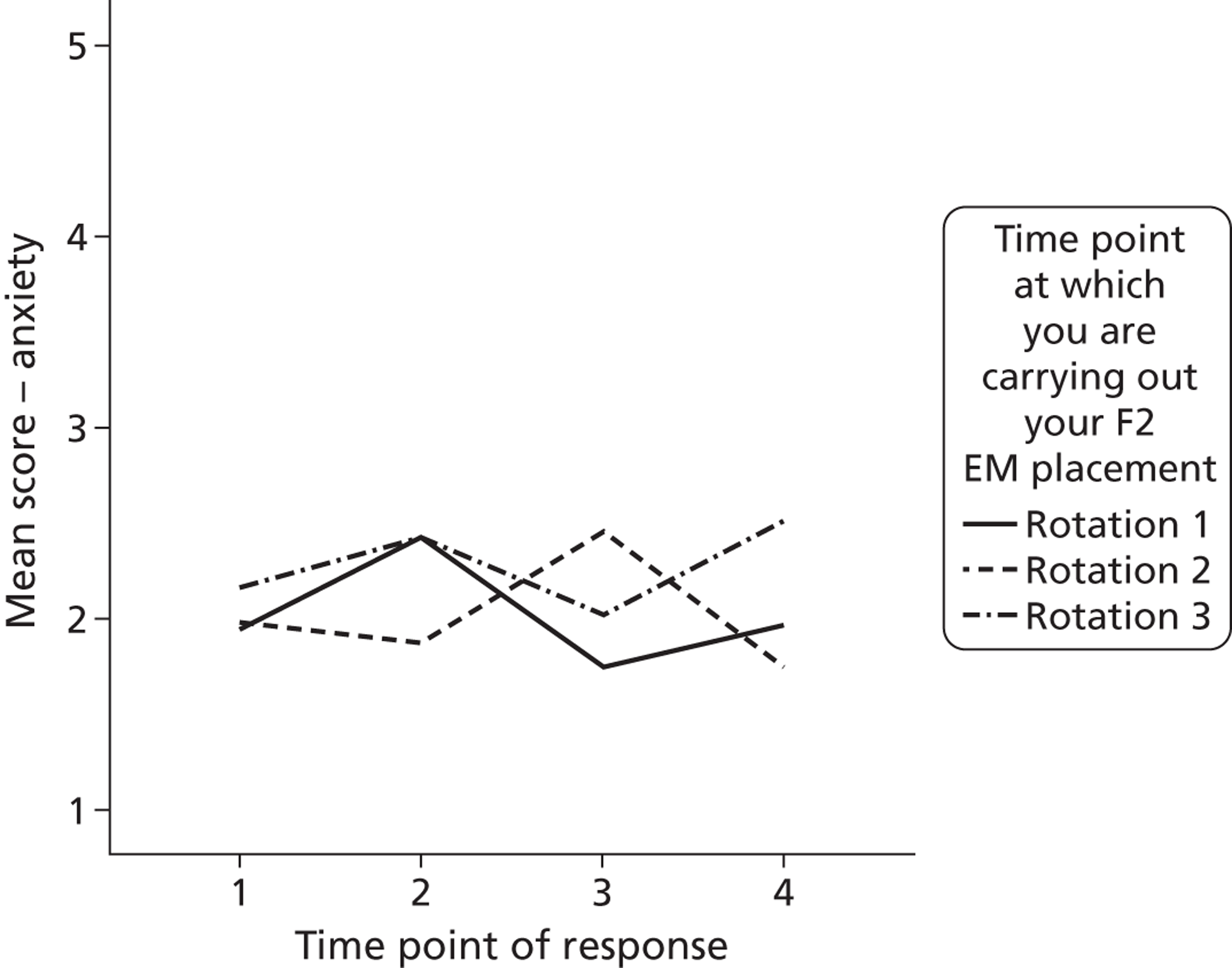
Several free-text comments were made about the nature of the ED experience and the impact on participants’ well-being, with examples provided in Box 5.
ED was stressful at the beginning.
T2 participant
A&E is a stressful job but the most rewarding I have done so far.
T3 participant
A&E is stressful and always very busy.
T3 participant
We compared F2 doctors’ mean levels of anxiety [mean 2.10, standard deviation (SD) 0.61] and depression (mean 1.68, SD.59) at each of the time points with those of a comparison group of 2909 professional and technical workers (mean anxiety 2.4, SD 0.83; mean depression 1.88, SD 0.87). F2 doctors reported significantly fewer anxious and depressive symptoms than the comparison group at T1, T3 and T4 and similar levels of symptoms as the comparison group at T2.
Job satisfaction
Levels of and change in mean sample scores for job satisfaction were calculated. As well as an overall mean job satisfaction score, the 15-item overall score was divided into two separate scale mean scores for intrinsic job satisfaction and extrinsic job satisfaction. All items on the job satisfaction scale were scored from 1 (lowest level) to 7 (highest level).
The coefficient alpha for mean overall job satisfaction ranged from 0.86 (T1) to 0.90 (T2), which compares favourably with the reliability of 0.87 obtained in a study of 20,694 NHS trust employees. 59 The coefficient alpha for mean intrinsic job satisfaction ranged from 0.80 (T1) to 0.86 (T2) and for mean extrinsic job satisfaction ranged from 0.72 (T1) to 0.78 (T2).
All measures of mean job satisfaction increased over the time period of the study; this was significant for overall job satisfaction (F3,397 = 7.2, p < 0.005) and intrinsic job satisfaction (F4,410 = 9.5, p < 0.05).
Mean scores for job satisfaction at each time point are shown in Appendix 19 (see Table 27).
Impact of placement in the emergency department
There was no statistically significant interaction between time of placement in the ED and mean sample scores for overall job satisfaction or intrinsic job satisfaction.
There was a statistically significant interaction between time of placement in the ED and mean extrinsic job satisfaction score (F6,380 = 3.72, p < 0.005), with two of the three ED groups reporting a decline in mean extrinsic job satisfaction immediately after their placement in the ED (Figure 4). Mean job satisfaction scores for each ED group at each time point are shown in Appendix 19 (see Table 27).
FIGURE 4.
Interaction between time and time of placement in the ED and mean extrinsic job satisfaction.
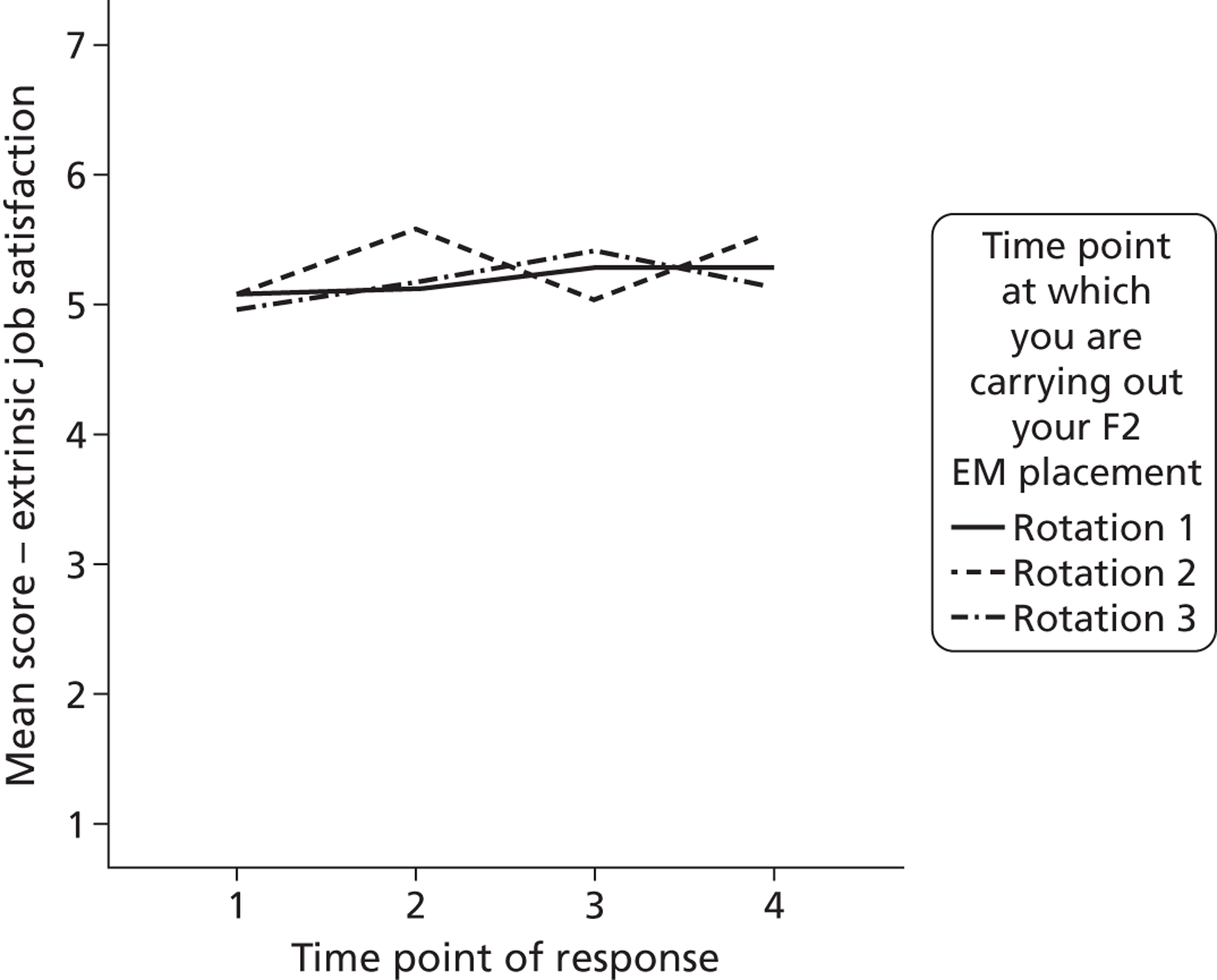
Several free-text comments were made about levels of satisfaction with working in the ED, with examples given in Box 6.
Thoroughly enjoyed.
T2 participant
I would thoroughly recommend this job to any FY2. Although very demanding it was very rewarding.
T2 participant
I thoroughly enjoyed my second placement and learned a great deal.
T3 participant
Thoroughly enjoyed my A&E placement, really grew up as a doctor.
T3 participant
However, participants were not happy with the shifts and working hours (extrinsic aspects of the role) (Box 7).
Objected to working 12 out of 16 weekends when others worked eight or nine.
T2 participant
Pretty antisocial shifts of mostly afternoon and evenings to cover service needs.
T3 participant
Excessive working hours.
T3 participant
Rota was tough and life was put on hold.
T3 participant
Shift work was difficult and work life balance was almost non existent.
T4 participant
Comparison with other occupational groups
We compared F2 doctors’ mean levels of job satisfaction (overall mean 5.13, SD 0.55) at each of the time points with those of a comparison group of 2616 doctors and NHS staff (mean 4.55, SD 0.80). F2 doctors were significantly more satisfied than the comparison group of NHS staff at all time points.
Motivation (effort)
Levels of and change in mean sample scores for motivation were calculated, with scores ranging from 1 (lowest level) to 5 (highest level). The coefficient alpha for motivation ranged from 0.83 (T1) to 0.91 (T3).
There was no statistically significant variation in mean motivation scores over the four time points of the survey (see Appendix 19, Table 28).
Impact of placement in the emergency department
There was a statistically significant interaction between time of placement in the ED and mean score for motivation (F6,384 = 4.1, p < 0.005), with all three groups of doctors showing the biggest rise in motivation during their placement in the ED compared with other placements (Figure 5). Mean motivation scores for each ED group at each time point are shown in Appendix 19 (see Table 28).
FIGURE 5.
Interaction between time and time of placement in the ED and motivation.
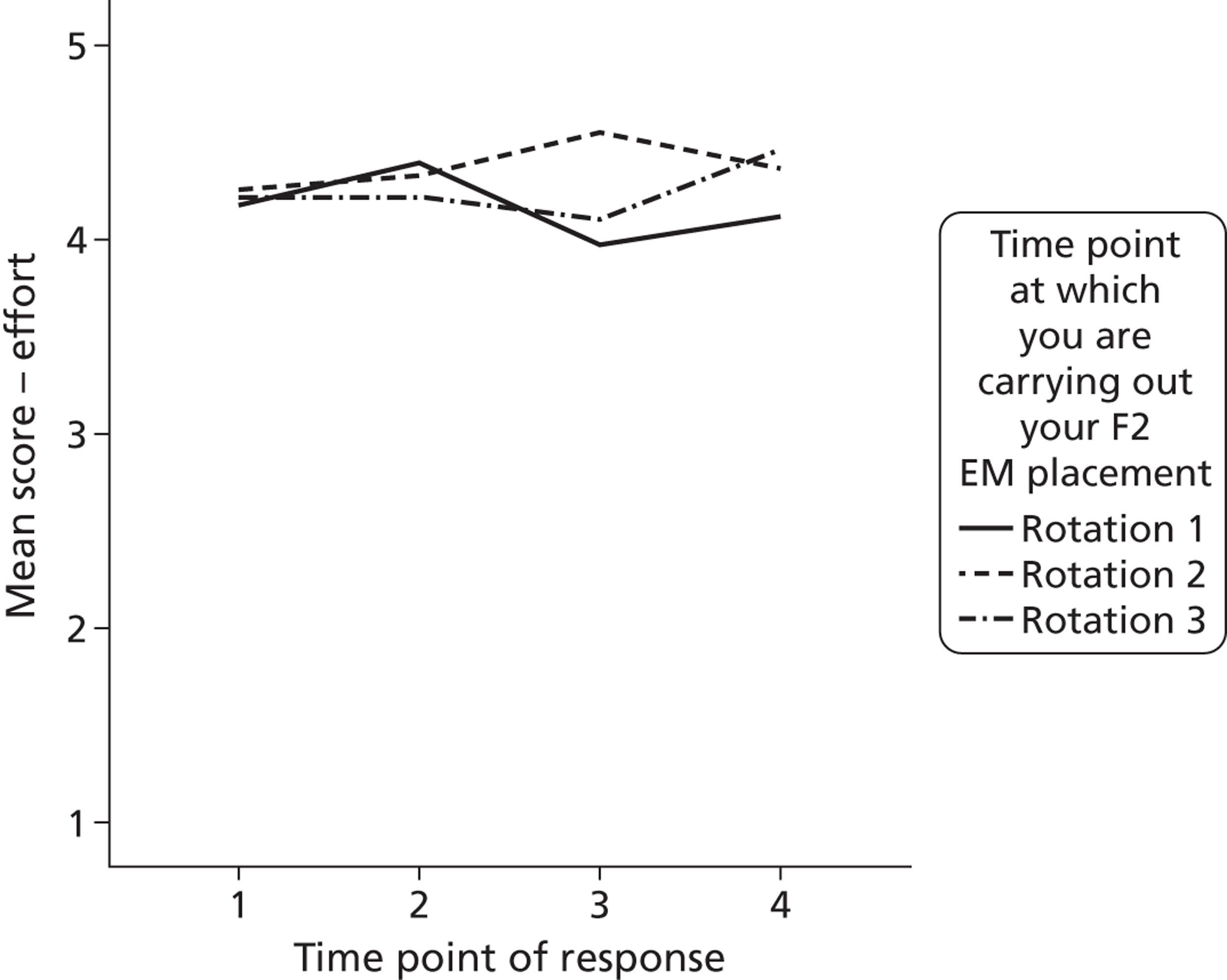
Several free-text comments were made about the effort that F2 doctors expended, with examples given in Box 8.
I worked very hard to fully clerk patients.
T3 participant
The pressure of 4 hour target made it difficult to feel you had completed everything before patient left dept.
T3 participant
Intention to quit
Levels of and change in mean scores for intention to quit were calculated, with scores ranging from 1 (lowest level) to 5 (highest level). The coefficient alpha for the current sample ranged from 0.79 (T2) to 0.86 (T4), which compares reasonably well with the reliability of 0.91 obtained in a study of 110 EM staff (including junior doctors, emergency care practitioners and paramedics). 62
There was no significant variation in mean intention-to-quit scores across the four time points and there was also no impact on intention to quit of placement in the ED (see Appendix 19, Table 29).
Comparison with other occupational groups
We found no difference between F2 mean scores for intention to quit (T1–T4) and scores from a previous study of 110 EM staff. 62
Job-related characteristics
Role characteristics
We measured levels of and changes in mean sample scores for work demands, role clarity and task feedback, with scores ranging from 1 (lowest level) to 5 (highest level). We also measured mean hours worked in a typical working week and shift changed at short notice in the last 4 weeks (‘yes’/‘no’).
The coefficient alpha for work demands ranged from 0.81 (T4) to 0.88 (T2), which compares well with the reliability of 0.80 quoted by Dwyer and Ganster. 80 The coefficient alpha for task feedback ranged from 0.82 (T1) to 0.90 (T3, T4). This compares well with the reliabilities of 0.80–0.87 with health-care samples in the study by Haynes et al. 81 The coefficient alpha for role clarity ranged from 0.85 (T1, T4) to 0.87 (T2). This compares well with the reliabilities of 0.76–0.90 with health-care samples in the study by Szilagyi et al. 82
There was evidence of statistically significant variation across the four time points in mean scores for both work demands (F3,393 = 10, p < 0.005) and role clarity (F3,389 = 6.5, p < 0.005).
There was no statistically significant variation in mean hours worked or shifts changed at short notice between placements. The mean scores at each of the four time points and overall for work demands, role clarity, task feedback, hours worked in a typical working week and shift changed at short notice in the last 4 weeks are provided in Appendix 19 (see Tables 30 and 31).
Impact of placement in the emergency department
There was a statistically significant interaction between time of placement in the ED and task feedback, with each of the doctor groups reporting the biggest decline in mean task feedback score after their placement in the ED (F6,371 = 3.24, p < 0.005) (Figure 6). Box 9 shows some free-text quotes from comments made by F2 doctors on the questionnaires.
FIGURE 6.
Interaction between time and time of placement in the ED and task feedback.
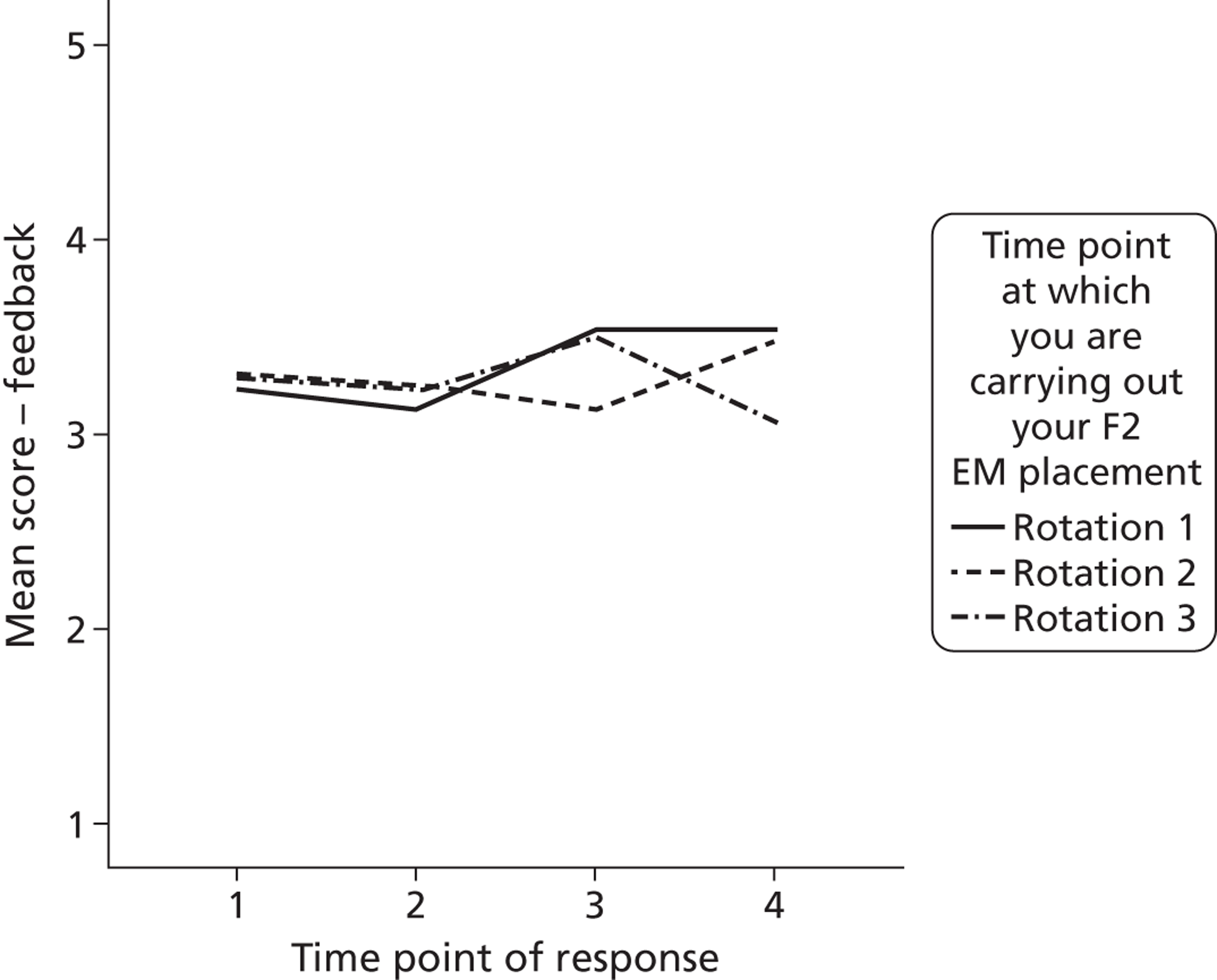
I tried to learn but lack of feedback on whether management of cases were satisfactory or not was the biggest problem.
T4 participant
A wealth of experience; did not get much feedback on what we were doing – I’m not sure the job can ever offer this.
T3 participant
There was also a significant interaction between time of placement in the ED and mean hours worked in a typical working week, with the biggest increase apparent for each group of doctors associated with their ED placement (F6,416 = 7.5, p < 0.005) (Figure 7).
FIGURE 7.
Interaction between time and time of placement in the ED and hours worked.
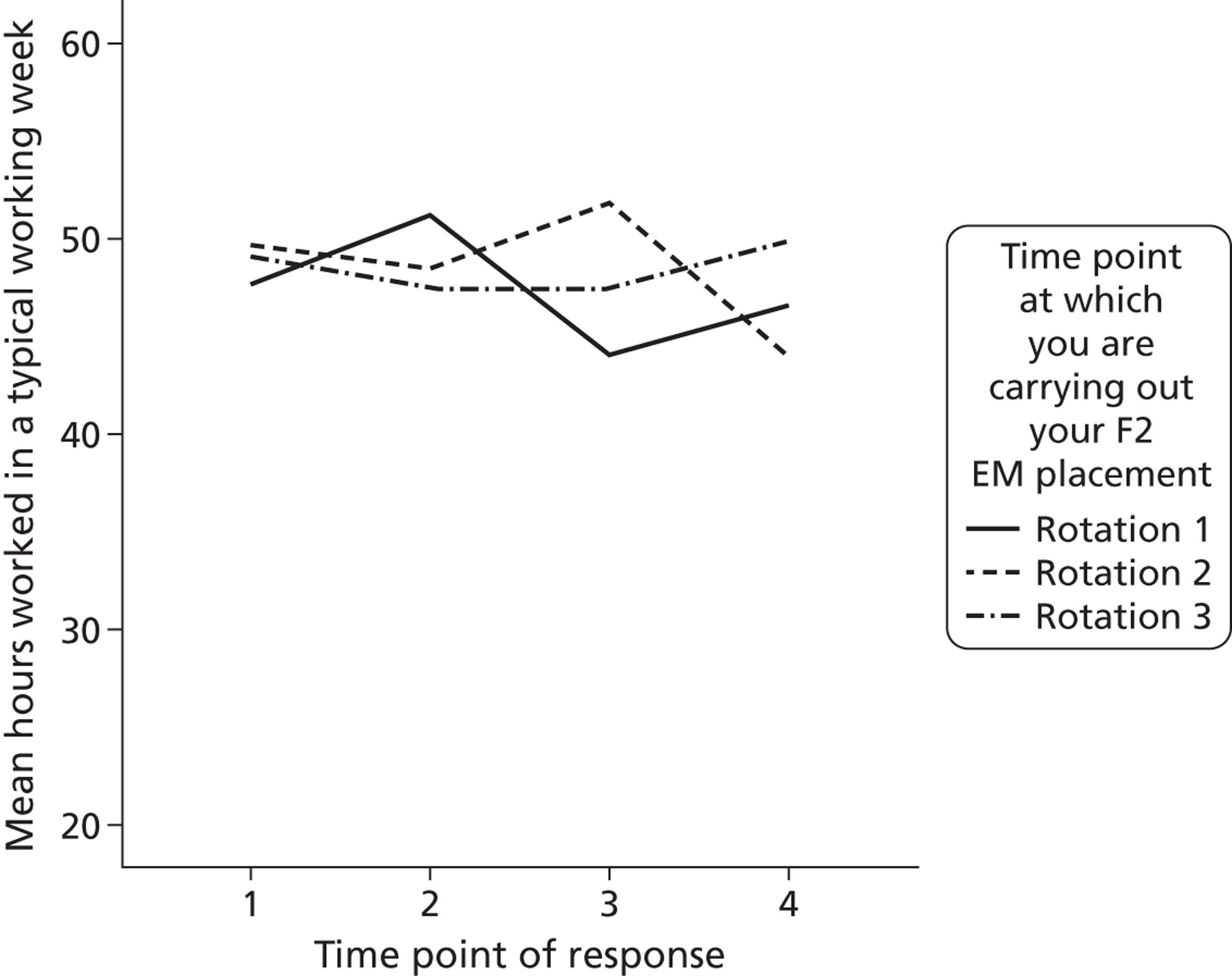
There were many free-text comments made on the questionnaires about working hours and shift patterns, with examples given in Box 10.
Long hours and close to EWTD limit of less 70 hours per week; but not taking ruling at its value of avoiding exhausted staff.
T2 participant
Pretty antisocial shifts of mostly afternoon and evenings to cover service needs.
T3 participant
Excessive working hours.
T3 participant
Shift work was difficult and work life balance was almost non existent.
T4 participant
Relational characteristics
Levels of and change in mean sample scores for support from CSs and colleagues were assessed on two scales. Extent of support on each scale was scored from 1 (‘to a very little extent’) to 5 (‘to a very great extent’).
The coefficient alpha for CSs support ranged from 0.90 (T1) to 0.94 (T2, T3, T4). The coefficient alpha for colleague support ranged from 0.90 (T1) to 0.94 (T2, T3). This compares well with quoted reliabilities for each relational scale of 0.90–0.92 with health-care samples. 81
There was no statistically significant variation in mean sample scores for reported support from either CSs or colleagues across the four placement periods (see Appendix 19, Table 32).
Impact of placement in the emergency department
There was a statistically significant interaction between time of placement in the ED and mean support from colleagues (F6,390 = 3.4, p < 0.005). This was mainly caused by a large increase in mean support from colleagues reported by one ED group immediately after their ED placement (Figure 8).
FIGURE 8.
Interaction between time and time of placement in the ED and colleague support.
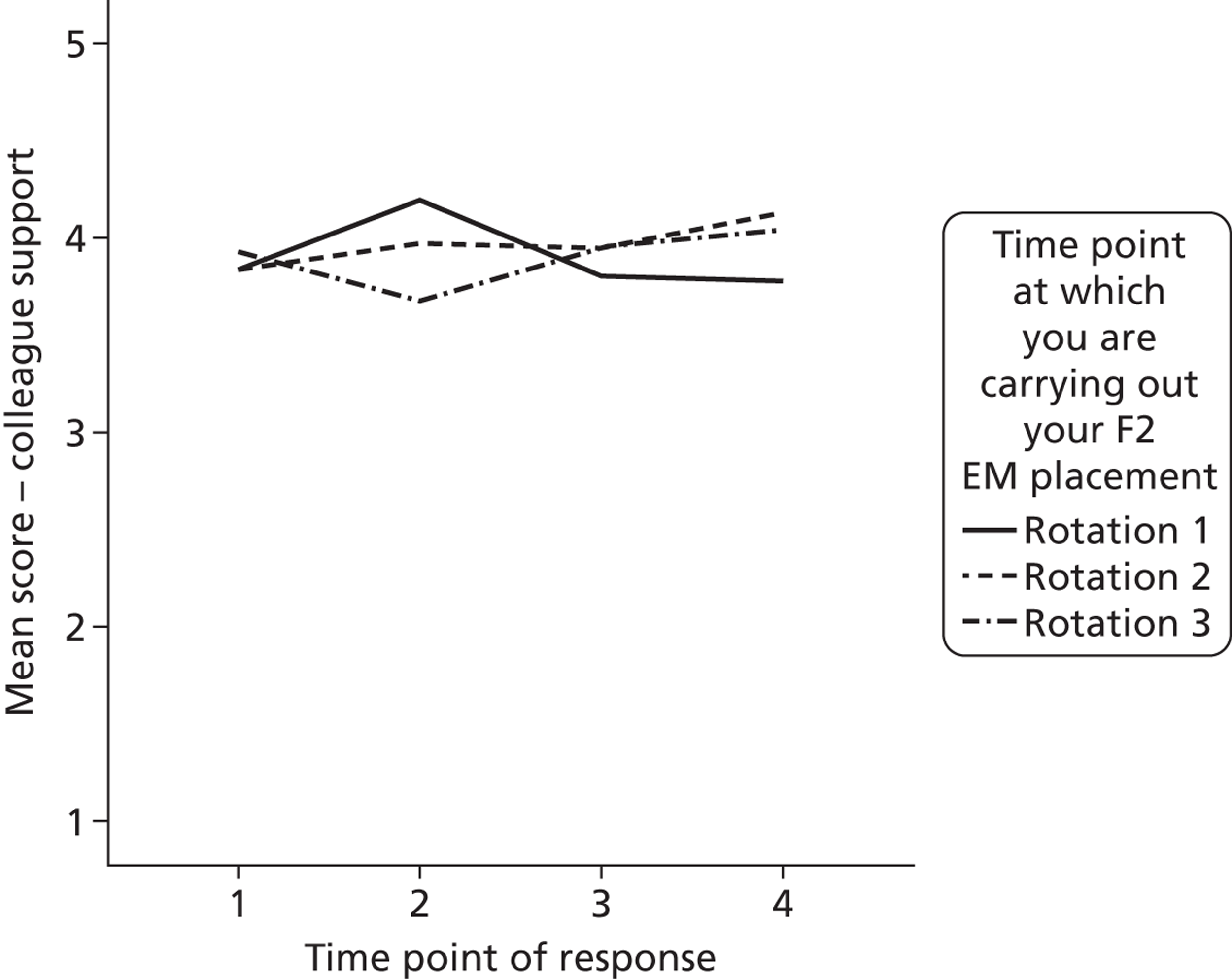
There were several free-text comments made about support during the ED placement, but mostly from staff and supervisors, with examples given in Box 11.
Fantastically supportive staff.
T2 participant
Medical staff were approachable and supportive.
T2 participant
Highly trained nurses who encouraged junior doctors a lot.
T2 participant
I always felt there was someone to ask if I needed to check a decision I made.
T3 participant
Well supervised.
T3 participant
Good support and regular teaching.
T4 participant
Emergency department-level comparison of role characteristics and work-related outcomes
We also investigated whether non-trivial variation existed in respondents’ role characteristics and work-related outcome measures across the participating EDs. This analysis was cross-sectional in nature as respondents’ role characteristics and work-related outcomes relative to the specific ED in which they did their ED training were typically measured just once, immediately after their ED placement (i.e. respondents did not typically do their other F2 placements in the same department).
The majority of the variables showed little or no variance that could be explained by the ED in which the F2 doctors were working during their ED placement. The percentage variance in scores for each of the role characteristics and work-related outcomes that existed at the ED level exceeded 10% for CS support, number of hours of one-to-one contact with supervisor, number of hours of close working contact with supervisor and job satisfaction.
Summary of results
-
F2 doctors reported a significant increase in confidence in managing 23 common acute conditions over the course of F2 training, with the biggest increase in confidence arising immediately after their ED placement.
-
Experience managing common procedures improved significantly over the four time points (with competence in interpreting arterial blood gases improving non-significantly between T1 and T4), with the biggest increase in competence in all five procedures arising immediately after the ED placement.
-
In terms of well-being, F2 doctors showed similar (T2 comparison) or better (T1, T3, T4) levels of anxiety and depression than a comparison group of professional and technical workers. Levels of anxiety and depression did not vary significantly over time but the biggest rise in anxiety was associated with an ED placement.
-
Job satisfaction is another aspect of well-being and F2 doctors reported significantly higher levels of job satisfaction than a large comparison group of doctors and other NHS staff. A significant improvement in overall and intrinsic job satisfaction was seen during F2. However, in two of the three groups studied the ED placement was associated with significantly lower scores for the extrinsic aspects of job satisfaction (e.g. pay, hours of work).
-
Motivation was examined in terms of effort and this did not vary significantly across F2. Reported levels of effort were similar to (T3) or lower than (T1, T2, and T4) those in a comparison group of managers. However, a steep increase in effort was associated with the ED placement.
-
Examination of work characteristics showed that there was significant variation in work demands and role clarity across the various placements. However, the ED placement was associated with a significant reduction in task feedback and an increase in social support from colleagues and hours worked in a typical week (work demands increased slightly and role clarity improved but not significantly).
-
There was some weak (cross-sectional) evidence of variation in work characteristics across trusts associated with variation in hours of one-to-one contact and close working contact with CS, work demands, job satisfaction, amount of teaching and support from CSs.
Chapter 5 A clinical case notes review of foundation year 2 doctors’ quality of care
Introduction
Reviewing quality of care as documented in patient records has become an established method for assessing the quality of care in health-care organisations. 83 This approach has been used in a variety of health-care settings, including emergency care. 84–88 The two main approaches currently used for retrospectively assessing quality of care as recorded in clinical records are (1) holistic review (also referred to as implicit review), whereby reviewers use their clinical knowledge and professional judgement to assess the quality of care, and (2) criterion-based review (also referred to as explicit review), in which there is a consensus or established standard of care that supports review against these explicit standards.
The advantages and disadvantages of these two review methods are identified in Brown et al. 89 Holistic review can be easier to conduct as it relies on professional judgements of ‘good’ and ‘poor’ care that can be applied to any condition. The subjectivity of these judgements is regarded as a weakness of implicit review compared with criterion-based assessments of care, which rely on more explicit criteria (e.g. those derived from national clinical guidelines) and have greater reproducibility. Structured methods for holistic review and for developing explicit review criteria that can be applied to assessing quality of care from case notes have been revised in the UK. 90 Evidence-based clinical guidelines published by NICE are now being accompanied by review criteria to support the assessment of clinical quality. The criterion-based review method has been criticised for not being sensitive enough to identify unexpected factors potentially influencing outcomes of care,91,92 whereas the relative advantage of holistic review is that judgements can capture the full extent of clinical decisions about care.
The issue of poor to moderate levels of inter-rater reliability is acknowledged as a problem with the use of case-note review, and findings from a systematic review of inter-rater reliability show higher reliability values for studies that used criterion-based review than for studies that used holistic review. 93 This might be expected given the subjective nature of implicit assessment in the latter approach and the review authors do highlight the potential drawback of this higher reliability being the possibility that predefined review criteria may omit elements of care that can be considered when using the holistic approach. On that basis, Lilford et al. 93 argue that the two methods may be regarded as complementary and advocate a mixed holistic and criterion-based approach.
A more recent study by Hutchinson et al. 94 aimed to determine which of the two methods provides the most useful and reliable information for assessing quality of care. The study entailed a large-scale review of case notes across several hospitals and reviewers using both holistic and criterion-based review methods. Their study found a reasonable level of agreement between the two methods and the individual reviewers. The findings in relation to inter-rater reliability were broadly consistent with those of other studies, showing lower scores for holistic reviews. The review methods used in this study are consistent with those employed by Hutchinson et al. 94
Aims
A review of the clinical records of patients treated by participating F2 doctors was undertaken to evaluate the quality of care and adherence to evidence-based guidelines.
The aims of this review were to:
-
assess the quality of care provided by all F2 doctors during their ED placement
-
provide a measure of quality of care that can be used to assess its relationship with job-related characteristics, well-being and motivation.
Methods
Quality of care provided by F2 doctors during their ED placement was assessed using a combination of criterion-based and holistic review methods. The study assessed quality of care delivered in relation to two clinical conditions: head injury and chronic obstructive pulmonary disease (COPD). Specialist registrars in EM were recruited from each of the participating EDs to act as reviewers in their own hospital, as would happen with clinical audit.
Recruitment of emergency departments/sites and reviewers
The aim was to recruit 12 EDs to the quality-of-care study with the expectation that this would provide access to 144 F2 doctors. Initially, all 30 participating EDs were contacted by e-mail in November 2010 to assess whether their ED information systems recorded the identifiers of the primary caregivers (in this case F2 doctors) for clinical episodes in the ED. Identifying ED episodes for which the F2 doctors were the primary caregiver was a necessity in the records review of F2 doctor quality of care. Nineteen of the 30 responded, detailing that their ED information systems had this facility. These 19 were then contacted by e-mail in March 2011 with an outline of the study and an invitation to take part. Fourteen of the 19 EDs contacted expressed interest in participating, but four of these were unable to complete the reviews within the required time frame for the project. A total of 10 EDs took part in the study and provided access to 74 F2 doctors. These 10 EDs represented six of the nine deaneries where F2 doctors carried out their placements in EM.
Recruitment of the EDs also relied on the recruitment of sufficient numbers of middle-grade doctors (specialist registrars) in EM to review the selected records at each site. Reviewers were recruited through the lead consultants at each site; a total of 28 reviewers were recruited across the 10 participating EDs. A copy of the reviewer information sheet is provided in Appendix 21.
Choice of clinical conditions for review
The choice of clinical conditions for review involved the initial identification of conditions that F2 doctors could be expected to see with reasonable frequency during their time in the ED, that are reasonably common in presentation, that present in adults, that will differentiate performance and that have well-defined clinical guidelines to support the criterion-based review. Following discussions between the project team and local ED consultants, six potential clinical conditions were identified:
-
overdose
-
head injury
-
COPD
-
asthma
-
back pain
-
gastrointestinal bleed.
The consultant leads at the 14 EDs that had expressed an interest in participating in the quality-of-care review were asked to rank the six conditions in relation to their suitability and likelihood that F2 doctors at their site would have responsibility for the care of patients with these conditions. In total, 10 of the 14 sites and two F2 doctors provided rankings for the provisional list of conditions. Three sites suggested chest pain as an additional condition but it was felt that there would be less scope for variation in practice. Taking an average of all ranks, overdose, head injury and COPD were ranked highest across all sites. COPD and head injury were the two conditions chosen for the study on the basis that they best met the criteria above. These two conditions also had the advantage that they were quite ED specific and different from the range of conditions included in the longitudinal study assessment of confidence in managing conditions across all placements.
Development of criterion-based review form
Criterion-based review requires the reviewer to identify and record specific items of care that are consistent with established guidelines on quality of care. The review criteria in this study were developed using established methods for developing explicit evidence-based review criteria from clinical guidelines as detailed in Hutchinson et al. 95 For each of the two conditions, the first drafts of the criteria were developed using relevant national clinical guidelines96,97 and local ED guidelines; these were subsequently validated by the project team and ED clinicians.
Clinicians in the project team in consultation with ED colleagues identified a subset of criteria that might be useful in the study. Refinement of the criteria involved three stages. Initially, the criteria were reviewed to consider whether the necessary information was likely to be available in the case notes. The draft lists of criteria were then sent to the consultant leads at participating EDs to classify the criteria as essential, desirable or non-essential and to elicit comments on the structure and wording of each item. A final review by the project team sought to ensure that all criteria were clear and logical. This process resulted in 15 head injury criteria and 20 COPD criteria. The criterion-based review items and scores for head injury and COPD are provided in Appendices 23 and 24 respectively.
Development of the holistic review form
The structured review form used for the holistic review was consistent with that in previous studies using this approach88,94 in providing a framework to structure implicit judgements with a view to maximising inter-rater reliability. Unlike the criterion-based approach, reviewers were not provided with any specific criteria for current best practice and were asked to use their professional judgement. The holistic review form provided reviewers with a limited structure to enable different levels of health-care quality to be identified – from excellent to poor care across different aspects of care (see Appendix 25). This approach has been used successfully by the study team in previous research examining quality in emergency care. 88
The reviewers were asked to rate the quality of care actually provided (as documented in the clinical notes) in relation to three key aspects of care (assessment of the clinical problem, investigations performed and patient management) and overall care on a numerical scale (1 = unsatisfactory, 6 = very best care). Reviewers were provided with written guidance to aid consistency in the interpretation of the numerical quality-of-care scale (Table 9). In addition, reviewers were asked to provide textual comments regarding the overall quality of care.
| 1 | Care fell short of current best practice in one or more significant areas resulting in the potential for, or actual, adverse impact on the patient |
| 2 | Care fell short of current best practice in more than one significant area but is not considered to have the potential for adverse impact on the patient |
| 3 | Care fell short of current best practice in only one significant area but is not considered to have the potential for adverse impact on the patient |
| 4 | This was satisfactory care, falling short of current best practice in more than two minor areas |
| 5 | This was good care, falling short of current best practice in one or two minor areas only |
| 6 | This was excellent care and met current best practice |
Assessing the quality of recording in the case notes
Assessing quality of care using case-note review is dependent on the extent to which information is recorded in the patient record, the quality of that information and the legibility of the record. Furthermore, the patient record is itself an indicator of quality of care, as information recorded in clinical notes underpins decisions about patient care and continuity of care. A study examining the relationship between quality of case notes and adverse events found that poor quality (completeness, readability and adequacy) of the available patient information was associated with higher rates of adverse events. 98 Reviewers were therefore asked to assess the quality of each record using a six-point rating scale (1 = inadequate, 6 = excellent) following the guidance in Table 10.
| 1 | The patient record contains gaps in three or more significant areas |
| 2 | The patient record contains gaps in two significant areas |
| 3 | The patient record contains gaps in one significant area |
| 4 | The patient record is satisfactory and contains gaps in only three or more minor areas |
| 5 | The patient record is good and contains gaps in only one or two minor areas |
| 6 | The patient record is excellent |
Assessing case mix: complexity
To assess the potential variation in case mix across the case notes a question was included to determine the complexity of each case, consistent with that used by assessors as part of clinical evaluation in the FT programme. Reviewers were asked to rate the complexity of the clinical presentation detailed in each patient record as low, average or high.
Developing the web-based data-collection tool
The project team developed a web-based data-collection tool using the same survey-design software (SurveyGizmo) as the longitudinal study. The data-collection website enabled reviewers to record responses to each of the assessment categories on the review form and submit their data directly to the study team (see Appendix 22 for screenshot of the data-collection website).
The presentation of the criterion-based and holistic review forms was consistent with the format outlined above. For each record, the reviewer was asked to identify the clinical presentation detailed in the patient record as either a head injury or COPD and was then directed to the relevant review form. Reviewers were required to complete the criterion-based form first, followed by the holistic form.
Selection of records
Much of the research on case-note review has focused on care provided at site level rather than individual doctor level, and Hofer et al. 99 recommend a relatively small sample of 5–10 reviews as sufficient to characterise care for a site where the condition has a good evidence base. The study aimed to select 10 case notes per F2 doctor over a specified period during their ED placement, to include a mix of five head-injury and five COPD cases. It was not always possible to obtain five records per condition for each F2 doctor and some sites selected > 10 records when they were available. Across the 10 participating sites, between six and 17 records were selected for each doctor during their ED placement. All personal identifiers were removed from the records. To minimise potential bias resulting from harshness or leniency of individual reviewers, the case notes for each F2 doctor were distributed amongst the individual reviewers at that site.
To assess inter-rater reliability at sites with more than one reviewer, a small subset of records was assessed by all reviewers within each site. As the records were accessible only to those staff within each site, it was not possible to assess reliability across the participating sites. The study team worked closely with research staff and administrators at each of the participating sites, who assisted in identifying suitable patient records for review, copying records and removing any personal identifying information. This included copying sets of common records required to assess inter-rater reliability.
Table 11 shows the numbers of F2 doctors, reviewers, records to assess quality of care and records to assess inter-rater reliability at each participating ED.
| Site (ED no.) | No. of F2 doctors | No. of reviewers | No. of records to assess quality of care per F2 doctor (total records) | No. of records to assess inter-rater reliability |
|---|---|---|---|---|
| 26 | 5 | 2 | 8–10 (48) | 12 |
| 67 | 2 | 1 | 10 (20) | NA |
| 70 | 4 | 1 | 9–10 (39) | NA |
| 121 | 15 | 5 | 6–11 (132) | 12 |
| 155 | 6 | 2 | 10–12 (63) | 12 |
| 165 | 8 | 3 | 11–17 (106) | 7 |
| 227 | 5 | 3 | 7–12 (49) | 10 |
| 230 | 8 | 6 | 8–10 (76) | 8 |
| 238 | 17 | 3 | 6–12 (172) | 9 |
| 285 | 4 | 2 | 9–11 (40) | 12 |
| Total | 74 | 28 | 745 |
Reviewer training
The study provided all reviewers with standardised training in case-note review during a 3-hour session delivered at various participating sites. The aim of the training was to provide guidance on how to complete the criterion and holistic review forms and the type of textual comments required, and to allow reviewers to practice conducting reviews with a set of anonymised case notes. The data-collection website was also demonstrated.
Reviewers were aware of the aims of the study. It was considered unlikely that the reviewers would know any of the F2 doctors because of rotation changes; however, the importance of making assessments solely on the basis of the information contained in the patient case notes was stressed.
At the end of the training the reviewers were sent an e-mail providing them with access to the data-collection website. The reviewers were also provided with a set of case notes for review, including any additional records to support the assessment of inter-rater reliability.
Data analysis
Data from the SurveyGizmo database were transferred to IBM SPSS version 19 (SPSS Inc., Chicago, IL, USA) for statistical analysis. Statistical analysis examined inter-rater reliability, the quality of care delivered by F2 doctors during their ED placements and the relationship between work characteristics, well-being and quality of care.
Scoring of criterion-based data involved calculating a total score for each head injury and COPD patient record based on the total criteria met per record (see Appendices 23 and 24 for criterion scores for head injury and COPD respectively). To compare mean criterion scores for the two conditions, a score for the proportion of the criteria met was also calculated by dividing the total score by the maximum potential score. Analysis of holistic scores for head injury and COPD cases used the actual ratings from each of the holistic rating scales, which are comparable across the two conditions. Mean criterion-based and holistic scores for the two conditions were calculated for use in assessment of the relationship between quality of care, job-related characteristics, well-being and motivation.
Intraclass correlations (ICCs) were calculated to assess the reliability of ratings between pairs or groups of reviewers within participating EDs. The ICC gives the correlation between reviewer ratings for the same set of case notes and is based on continuous data, unlike kappa statistics, which require the data to be categorical.
Descriptive statistics were calculated for criterion-based and holistic ratings to examine quality of patient care delivered by F2 doctors during their ED placements.
Mean scores were calculated for criterion-based and holistic ratings across three levels of case complexity (low, average and high) and statistical tests were conducted to assess the statistical significance of differences in scores [analysis of variance (ANOVA), t-test].
Pearson’s correlation coefficients were calculated to assess the relationship between criterion and holistic ratings.
Results
Inter-rater reliability
Table 12 provides the ICCs used to assess inter-rater reliability; these are based on the actual (absolute) scores rather than the ranked (consistency) scores as the actual ratings are used to examine performance. The single-measure ICCs are presented as the quality-of-care analysis uses ratings from single reviewers rather than averaging multiple ratings for each record. In general, these will be lower than the reliability that might be expected from using the average of several raters (Table 13).
| Records, reviewers and approach | Site (ED code)a | |||||||
|---|---|---|---|---|---|---|---|---|
| 26 | 121 | 155 | 165 | 227 | 230 | 238 | 285 | |
| No. of records | 12 | 12 | 12 | 7 | 10 | 8 | 9 | 12 |
| No. of reviewers | 2 | 5 | 2 | 3 | 3 | 6 | 3 | 2 |
| No. of F2 doctors | 5 | 15 | 6 | 8 | 5 | 8 | 17 | 4 |
| Inter-rater reliability: ICC (95% CI) | ||||||||
| Criterion – total | 0.94 (0.82 to 0.98) | 0.73 (0.52 to 0.88) | 0.65 (0.07 to 0.89) | 0.92 (0.62 to 0.98) | 0.69 (0.35 to 0.90) | 0.74 (0.49 to 0.93) | 0.94 (0.83 to 0.98) | 0.93 (0.57 to 0.98) |
| Holistic – assessment | 0.40 (−0.19 to 0.79) | 0.29 (0.07 to 0.61) | 0.43 (−0.09 to 0.79) | 0.21 (−0.25 to 0.75) | 0.38 (0.03 to 0.75) | 0.18 (−0.01 to 0.60) | 0.58 (0.21 to 0.87) | 0.30 (−0.14 to 0.71) |
| Holistic – investigations | 0.34 (−0.18 to 0.74) | 0.08 (−0.01 to 0.32) | 0.36 (−0.29 to 0.77) | 0.14 (−0.27 to 0.70) | 0.47 (0.10 to 0.80) | 0.19 (0.01 to 0.58) | 0.14 (−0.17 to 0.61) | 0.43 (−0.08 to 0.78) |
| Holistic – management | 0.31 (−0.33 to 0.74) | 0.11 (−0.01 to 0.37) | 0.39 (−0.18 to 0.77) | 0.10 (−0.06 to 0.53) | 0.66 (0.27 to 0.89) | 0.14 (−0.09 to 0.41) | 0.19 (−0.10 to 0.63) | 0.32 (−0.14 to 0.72) |
| Holistic – overall quality | 0.48 (−0.13 to 0.82) | 0.20 (0.00 to 0.39) | 0.35 (−0.16 to 0.74) | 0.11 (−0.11 to 0.60) | 0.60 (0.18 to 0.87) | 0.12 (−0.05 to 0.52) | 0.31 (−0.02 to 0.72) | 0.20 (−0.18 to 0.62) |
| Holistic – ED record | 0.65 (0.17 to 0.88) | 0.47 (0.22 to 0.75) | 0.32 (−0.16 to 0.72) | 0.56 (0.10 to 0.90) | 0.49 (0.09 to 0.82) | 0.30 (0.05 to 0.71) | 0.39 (−0.05 to 0.79) | 0.37 (−0.15 to 0.76) |
| Records, reviewers and approach | Site (ED code)a | |||||||
|---|---|---|---|---|---|---|---|---|
| 26 | 121 | 155 | 165 | 227 | 230 | 238 | 285 | |
| No. of records | 12 | 12 | 12 | 7 | 10 | 8 | 9 | 12 |
| No. of reviewers | 2 | 5 | 2 | 3 | 3 | 6 | 3 | 2 |
| No. of F2 doctors | 5 | 15 | 6 | 8 | 5 | 8 | 17 | 4 |
| Inter-rater reliability: ICC (95% CI) | ||||||||
| Criterion – total | 0.97 (0.90 to 0.99) | 0.93 (0.84 to 0.98) | 0.79 (0.07 to 0.89) | 0.97 (0.83 to 0.99) | 0.87 (0.61 to 0.97) | 0.94 (0.85 to 0.99) | 0.98 (0.94 to 0.99) | 0.96 (0.73 to 0.99) |
| Holistic – assessment | 0.58 (−0.48 to 0.88) | 0.67 (0.28 to 0.89) | 0.61 (−0.09 to 0.79) | 0.44 (−1.46 to 0.90) | 0.64 (0.10 to 0.90) | 0.58 (−0.06 to 0.90) | 0.81 (0.44 to 0.95) | 0.47 (−0.33 to 0.83) |
| Holistic – investigations | 0.51 (−0.43 to 0.85) | 0.31 (−0.08 to 0.70) | 0.53 (−0.84 to 0.87) | 0.32 (−1.79 to 0.88) | 0.73 (0.24 to 0.92) | 0.58 (0.07 to 0.89) | 0.32 (−0.78 to 0.82) | 0.60 (−0.17 to 0.88) |
| Holistic – management | 0.47 (−0.99 to 0.85) | 0.38 (−0.03 to 0.74) | 0.56 (0.45 to 0.87) | 0.26 (−0.21 to 0.77) | 0.85 (0.52 to 0.96) | 0.20 (−0.98 to 0.81) | 0.41 (−0.39 to 0.84) | 0.49 (−0.32 to 0.84) |
| Holistic – overall quality | 0.65 (−0.31 to 0.90) | 0.42 (0.01 to 0.76) | 0.52 (−0.38 to 0.85) | 0.27 (−0.43 to 0.82) | 0.82 (0.40 to 0.95) | 0.44 (−0.40 to 0.87) | 0.58 (−0.05 to 0.89) | 0.33 (−0.43 to 0.76) |
| Holistic – ED record | 0.79 (0.29 to 0.94) | 0.82 (0.59 to 0.94) | 0.49 (−0.37 to 0.84) | 0.80 (0.25 to 0.96) | 0.74 (0.23 to 0.93) | 0.72 (0.26 to 0.94) | 0.66 (−0.17 to 0.92) | 0.54 (−0.36 to 0.86) |
The correlations for the criterion-based reviews range from 0.65 to 0.94 and represent strong agreement. The correlations for the holistic review are lower and more variable (0.08–0.66) but are reasonably consistent with those from other studies. 93,94 These studies also report lower ICC statistics for holistic review than for criterion-based review.
Although an ICC of 0.8 is regarded as indicative of good agreement, this generally relates to data having a clear right and wrong answer and for which 100% agreement is possible. Higher levels of agreement are more achievable with criterion-based review using well-established criteria, whereas in the holistic review approach, based on subjective judgements, such a high level of agreement is less likely.
Appendix 26 provides ICC analyses based on the ranked review scores rather than the actual (absolute) scores (Tables 36 and 37).
Quality of care delivered by foundation year 2 doctors during emergency department placements
Table 14 presents the mean criterion-based and holistic scores for all F2 doctors. The mean scores for the different aspects of care assessed by holistic review are all > 4 on the six-point rating scale. There was a significant difference between the mean scores for ‘investigations’ [t(739) = 2.04, p = 0.04], with head-injury case notes scoring higher than COPD case notes.
| Review | Head injury (n = 382), mean (SD) | COPD (n = 359), mean (SD) |
|---|---|---|
| Holistic – assessment | 4.14 (1.15) | 4.30 (1.12) |
| Holistic – investigations | 4.61 (1.29) | 4.42 (1.23) |
| Holistic – management | 4.46 (1.21) | 4.33 (1.20) |
| Holistic – overall quality | 4.32 (1.24) | 4.28 (1.17) |
| Holistic – ED record | 4.17 (1.15) | 4.16 (1.15) |
| Criterion – total (% of criteria met) | 50.78 (14.60) | 54.88 (16.00) |
Appendix 27 provides details of the proportions of review criteria assessed as being met in the head injury and COPD patient case notes. This gives an indication of the relative strengths and weaknesses of F2 doctors’ performance and quality of care for these two conditions. Appendix 28 shows the distribution of holistic review scores for head injury and COPD case notes across the six-point rating scale.
The more detailed information on proportions of review criteria being met (see Appendix 27) highlights omissions in recording information. A common issue across both the head injury records and the COPD records appears to be the level of detail provided. Criteria relating to documenting the mechanism and details of head injury are met by 93% and 80% of case notes respectively; however, information is lacking in relation to loss of consciousness and the reason for organising a computerised tomography (CT) head scan. Similarly, for the COPD case notes, details about shortness of breath and respiratory rate were recorded by most but there was variable recording for other criteria.
Case mix
Table 15 shows the distribution of head injury and COPD case notes across the three categories of complexity of case presentation. The majority of cases across the two conditions were classified as ‘average’. A higher proportion of head injury cases than COPD cases were categorised as ‘low’ complexity and conversely a higher proportion of COPD cases than head injury cases were classified as ‘high’ complexity.
| Complexity | Head injury (n = 384), % (n) | COPD (n = 361), % (n) |
|---|---|---|
| Low | 32.6 (125) | 10.8 (39) |
| Average | 62.8 (241) | 77.0 (278) |
| High | 4.2 (16) | 11.6 (42) |
| Missing data | 0.5 (2) | 0.6 (2) |
A one-way ANOVA was carried out to test for differences in mean quality-of-care scores across the three complexity categories. No significant difference was found for head injury scores, but the COPD criterion scores were significantly higher for more complex cases (F2,356 = 8.55, p = 0.00). A post hoc Tukey test showed that the difference was specific to the ‘high’ complexity category, which had significantly higher scores than the ‘low’ or ‘average’ complexity categories (p < 0.05). A further t-test analysis was conducted to assess whether F2 doctors with more complex COPD cases achieved higher criterion scores than those with COPD cases of ‘low’ or ‘average’ complexity only. This analysis found no significant differences in COPD criterion scores between F2 doctors with ‘high’ complexity cases and those with ‘low’ and ‘average’ complexity cases only. Therefore, we are confident that any variation observed in the quality of care is not attributable to a variation in case mix.
Relationship between criterion-based and holistic quality-of-care ratings
Pearson’s correlation coefficients calculated to explore the relationship between criterion-based and holistic ratings for head injury and COPD case notes are presented in Tables 16 and 17 respectively. Associations between the various holistic measures are slightly stronger than those between the holistic and criterion-based measures.
| Aspects of care | Investigations | Management | Overall quality | ED record | Criterion – total | |
|---|---|---|---|---|---|---|
| Assessment | Pearson’s correlation | 0.682 | 0.714 | 0.791 | 0.837 | 0.638 |
| Significance (two-tailed) | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | |
| Investigations | Pearson’s correlation | 1 | 0.780 | 0.802 | 0.694 | 0.440 |
| Significance (two-tailed) | 0.000 | 0.000 | 0.000 | 0.000 | ||
| Management | Pearson’s correlation | 1 | 0.885 | 0.755 | 0.468 | |
| Significance (two-tailed) | 0.000 | 0.000 | 0.000 | |||
| Overall quality | Pearson’s correlation | 1 | 0.814 | 0.491 | ||
| Significance (two-tailed) | 0.000 | 0.000 | ||||
| ED record | Pearson’s correlation | 1 | 0.603 | |||
| Significance (two-tailed) | 0.000 | |||||
| Aspects of care | Investigations | Management | Overall quality | ED record | Criterion – total | |
|---|---|---|---|---|---|---|
| Assessment | Pearson’s correlation | 0.642 | 0.677 | 0.762 | 0.789 | 0.599 |
| Significance (two-tailed) | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | |
| Investigations | Pearson’s correlation | 1 | 0.800 | 0.833 | 0.701 | 0.504 |
| Significance (two-tailed) | 0.000 | 0.000 | 0.000 | 0.000 | ||
| Management | Pearson’s correlation | 1 | 0.927 | 0.765 | 0.531 | |
| Significance (two-tailed) | 0.000 | 0.000 | 0.000 | |||
| Overall quality | Pearson’s correlation | 1 | 0.821 | 0.558 | ||
| Significance (two-tailed) | 0.000 | 0.000 | ||||
| ED record | Pearson’s correlation | 1 | 0.611 | |||
| Significance (two-tailed) | 0.000 | |||||
Summary
Intraclass correlations calculated to assess inter-rater reliability showed a high level of agreement amongst reviewers for the criterion-based review (0.65–0.94). The holistic review ICCs were much lower (0.08–0.65) and varied across sites. Taking an average measure of quality across reviewers produced higher ICCs for criterion-based (0.79–0.98) and holistic (0.20–0.85) review.
Mean scores for the proportion of head injury and COPD criteria met were 50.78% and 54.88% respectively. Mean scores for the different aspects of care assessed by holistic review range from 4.14 to 4.61 on the six-point scale. Analysis of the criteria met identifies strengths and weaknesses in relation to quality of care, specifically the extent of information recorded in case notes.
Findings from an analysis of case mix for head injury and COPD cases found no significant differences in relation to quality of care and complexity of clinical presentation, indicating that any observed differences in quality of care are not attributable to case mix variation.
Correlations between criterion-based and holistic quality-of-care ratings show associations between all review measures, but the intercorrelations between the holistic measures are somewhat higher (0.64–0.93) than those between the holistic and criterion-based measures (0.44–0.64).
Chapter 6 Analysing the relationship between foundation year 2 doctors’ job-related characteristics, work-related well-being and motivation, quality of care and performance during (emergency department) placements
Introduction and aims
This part of the study aimed to explore possible associations between the well-being of F2 doctors and the quality of patient care being delivered. Therefore, data from the longitudinal study that related to the well-being of our cohort during their ED placement were extracted (see Chapter 4), as well as data from our clinical records review study relating to the quality of care provided (see Chapter 5). The new data set aimed to:
-
evaluate how the job-related characteristics, well-being and motivation of F2 doctors in the ED is associated with the quality of patient care
-
identify key measures of F2 doctor well-being and motivation that are associated with quality of patient care and which will underpin the development of a tool to monitor well-being and motivation during training.
Methods
As described in the previous chapter, quality-of-care data for two conditions (head injury and COPD) were retrospectively collected from the ED clinical records of 74 F2 doctors, from the time of their F2 placement in the ED. These 74 F2 doctors had participated in the longitudinal study of F2 doctors.
A subsample of 55 of the 74 F2 doctors from the clinical case notes review who also supplied data in the longitudinal study about their job-related and work-related outcomes during their placement in the ED were subsequently included in this analysis.
Analysis
Detailed information on how the work-related outcomes and job-related characteristics were calculated is contained in Chapter 4. In summary, measures of work-related outcomes (well-being and motivation, intention to quit, confidence in managing acute conditions) and job-related characteristics (e.g. work demands, task feedback, role clarity) were analysed for 55 F2 doctors from the time of their placement in the ED.
Detailed information on how the quality-of-care outcomes were calculated is contained in Chapter 5. In summary, two approaches were used, criterion-based review and holistic review. Criterion-based review involved calculating a total score for each head injury and COPD patient record based on the total number of criteria met per record. The holistic review provided reviewers with a numerical scale to rate the quality of care actually provided (1 = unsatisfactory, 6 = very best care). For this analysis we used four outcomes – two criterion-based scores for head injury and COPD and two holistic overall care scores for the two conditions. Holistic overall scores were calculated by combining holistic scores for assessment, investigations and management.
Correlations between mean scores for the work-related outcomes and job-related characteristics relating to the time point at the end of each respondent’s ED placement and the four quality-of-care outcomes were calculated using Pearson’s correlations. A statistically significant level of association was set at p < 0.05. The correlated variables are listed in Box 12.
Confidence in managing common conditions.
Improvement in management.
Work demands.
Role clarity.
Feedback.
CS support.
Colleague support.
Job satisfaction.
Depression.
Anxiety.
Intention to quit.
Motivation.
Professional knowledge/learning.
Teaching/training received.
Quality-of-care outcomesHead injury – criterion-based score.
Head injury – holistic overall care score.
COPD – criterion-based score.
COPD – holistic overall care score.
Results
Quality of care
The only statistically significant association at the p < 0.05 level was the association between task feedback and holistic overall care. However, there was a clear pattern of small- to medium-sized correlations between levels of motivation and two quality-of-care outcomes (head injury – holistic overall care and COPD – holistic overall care) such that higher levels of motivation were more likely to occur amongst those doctors with higher scores for these two quality-of-care outcomes.
A similar pattern of effects existed, albeit in the opposite direction, for work demands and these two quality-of-care outcomes such that respondents with higher work demands were more likely to have lower quality-of-care outcomes for head injury – holistic overall care and COPD – holistic overall care (with the latter approaching statistical significance, p < 0.051). Indeed, when we examined the association with the single holistic measure of overall care, the association between work demands and overall care was statistically significant.
The correlations between all job-related characteristics/work-related outcomes and quality-of-care outcomes are provided in Table 18.
| Job-related characteristic/work-related outcome (at single point in time post ED placement) | Pearson’s correlations | |||
|---|---|---|---|---|
| Head injury (criterion-based score) | COPD (criterion-based score) | Head injury (holistic overall care) | COPD (holistic overall care) | |
| Confidence in managing common conditions | 0.057 | −0.074 | 0.181 | 0.033 |
| Improvement in management | −0.175 | −0.105 | −0.140 | −0.040 |
| Work demands | −0.056 | −0.069 | −0.169 | −0.264 |
| Role clarity | 0.034 | 0.021 | 0.064 | 0.202 |
| Feedback | −0.177 | 0.017 | −0.314 | 0.061 |
| CS support | −0.172 | −0.038 | −0.204 | −0.071 |
| Colleague support | −0.162 | 0.059 | −0.192 | 0.049 |
| Job satisfaction | −0.115 | 0.166 | −0.112 | 0.157 |
| Depression | −0.140 | 0.000 | −0.057 | −0.219 |
| Anxiety | 0.156 | 0.174 | 0.154 | −0.075 |
| Intention to quit | −0.076 | 0.125 | 0.048 | −0.123 |
| Motivation | −0.030 | −0.176 | 0.204 | 0.146 |
| Profession knowledge/learning | −0.037 | 0.168 | 0.159 | 0.105 |
| Teaching/training received | 0.129 | 0.101 | 0.209 | 0.124 |
Routine performance data
Participants
To further explore links between well-being and care provided to patients in the ED, we aimed to collect performance data on their ED placements for all 217 F2 doctors who had participated in the longitudinal study. We approached the 30 participating EDs to provide the relevant data; data were supplied by 18 EDs (60%) on 116 F2 doctors (53.4%).
A subsample of 74 of the 116 (63.8%) F2 doctors had also supplied data in the longitudinal study about their work-related outcomes and job-related characteristics during their placement in the ED and they were subsequently included in this analysis.
Data collected
All data were routinely collected by the participating EDs. The following individual-level data were requested from all participating EDs:
-
The total number of patients seen by each F2 doctor during their ED placement.
-
The percentage of patients seen by each F2 doctor within the 4-hour ED performance target.
-
The number of unplanned patient reattendances within 7 days per F2 doctor.
-
The mean doctor episode time per F2 doctor (over placement in the ED). Episode time was defined as the time interval from when the patient first saw the F2 doctor to discharge/referral from the ED.
-
The mean total time per F2 doctor (over placement in the ED). Total time was defined as the time interval from patient arrival in the ED to discharge/referral from the ED.
In addition, data were collected at the ED level as follows:
-
Mean waiting time for each month during the period of the longitudinal study. Waiting time was defined as the time interval from when the patient arrived in the ED to when he or she left the ED.
-
The percentage of waiting times in the ED that were within 4 hours for each month during the period of the longitudinal study.
Analysis
Pearson’s correlations between mean scores for the work-related outcomes and job-related characteristics relating to the time point at the end of each respondent’s ED placement and performance outcomes were calculated. A statistically significant level of association was set at p < 0.05.
Results
As in the analysis of quality of care, no statistically significant associations existed between well-being and motivation and scores on the performance outcomes at the p < 0.05 level (Table 19). There was a clear pattern of small- to medium-sized correlations between both anxiety and depression and two of the performance outcomes such that:
-
respondents with reported higher levels of anxiety or depression had higher mean episode times and higher mean total waiting times
-
respondents with reported higher levels of anxiety or depression were more likely to see a smaller percentage of patients within the 4-hour ED performance target.
| Job-related characteristic/work-related outcome (at single point in time post ED placement) | F2 doctor mean episode time | F2 doctor mean total waiting time | % of F2 doctor patients seen within 4 hours | Mean ED waiting times | % of ED patients seen within 4 hours | |
|---|---|---|---|---|---|---|
| Confidence in managing common conditions | Pearson’s correlation | 0.019 | −0.040 | 0.126 | −0.150 | 0.023 |
| n | 74 | 69 | 60 | 57 | 74 | |
| Improvement in management | Pearson’s correlation | −0.215 | −0.060 | 0.042 | −0.223 | 0.091 |
| n | 74 | 69 | 60 | 57 | 74 | |
| Work demands | Pearson’s correlation | 0.059 | 0.200 | −0.178 | 0.099 | 0.112 |
| n | 74 | 69 | 60 | 57 | 74 | |
| Role clarity | Pearson’s correlation | −0.049 | −0.209 | 0.136 | −0.124 | 0.049 |
| n | 74 | 69 | 60 | 57 | 74 | |
| Feedback | Pearson’s correlation | 0.110 | −0.060 | 0.048 | −0.060 | 0.024 |
| n | 74 | 69 | 60 | 57 | 74 | |
| CS support | Pearson’s correlation | 0.026 | −0.120 | 0.136 | −0.100 | 0.055 |
| n | 73 | 68 | 59 | 56 | 73 | |
| Colleague support | Pearson’s correlation | 0.046 | −0.024 | −0.034 | 0.024 | 0.023 |
| n | 73 | 68 | 59 | 56 | 73 | |
| Job satisfaction | Pearson’s correlation | 0.131 | −0.040 | −0.034 | 0.079 | 0.027 |
| n | 72 | 67 | 58 | 55 | 72 | |
| Depression | Pearson’s correlation | 0.181 | 0.250 | −0.183 | 0.096 | 0.071 |
| n | 72 | 67 | 58 | 55 | 72 | |
| Anxiety | Pearson’s correlation | 0.227 | 0.286 | −0.227 | 0.203 | 0.068 |
| n | 72 | 67 | 58 | 55 | 72 | |
| Intention to quit | Pearson’s correlation | 0.174 | 0.256 | −0.120 | 0.001 | 0.060 |
| n | 72 | 67 | 58 | 55 | 72 | |
| Motivation | Pearson’s correlation | −0.190 | −212 | 0.211 | −0.235 | −0.136 |
| n | 72 | 67 | 58 | 55 | 72 | |
| Professional knowledge/leaning | Pearson’s correlation | 0.237 | 0.092 | −0.126 | −0.073 | 0.123 |
| n | 72 | 67 | 58 | 55 | 72 | |
| Teaching/training received | Pearson’s correlation | 0.030 | −0.075 | 0.040 | −0.049 | −0.110 |
| n | 72 | 67 | 58 | 55 | 72 | |
Summary
There was only one statistically significant association at the p < 0.05 level between work-related well-being and motivation and job-related characteristics and scores on either the quality-of-care outcomes or the performance outcomes. This was unsurprising given the small sample sizes in both of the analyses.
There was evidence of small- to medium-sized associations between motivation and two quality-of-care outcomes (with higher levels of effort associated with better quality-of-care scores). A similar strength of association was seen for anxiety and depression and two performance outcomes (with higher levels of anxiety or depression associated with poorer performance outcomes).
Further research is required to collect longitudinal data on measures of both well-being and quality/performance to further investigate the nature and strength of these relationships.
Chapter 7 Discussion
Introduction
We used a multiple perspective mixed-methods study to examine the current arrangements for the delivery of FT in England and to examine a group of 217 foundation doctors as they proceeded through their second year of training (F2, August 2010–August 2011) in 28 NHS trusts. We were particularly interested in exploring doctors’ confidence and competence during training as well as their well-being and motivation; the impact of an ED placement on their well-being and abilities; and the quality of care that they provided.
Principal findings
The main findings from our study are shown in Table 20. This chapter will explore these findings and discuss them in relation to evidence from other studies.
| Phase 1 – stakeholder study | Phase 2 – longitudinal study of F2 doctors |
|---|---|
|
|
Postgraduate medical training: the theory and the reality
Postgraduate medical training has changed from the previously unstructured and service-led experience of the ‘house officer’ years to a more structured programme of FT accommodating over 8000 trainees in England. Collins22 undertook an evaluation of this change and this report became available during the course of this study, allowing some comparisons. FT was established in 2005; our stakeholder study examined the position of the programme in its fifth year of operation and the longitudinal study examined the reality for the trainees in its sixth year of operation.
We found that there was a strong national framework for FT across England and Scotland which was well understood by national and regional stakeholders, demonstrating the successful change to a structured programme of postgraduate development and agreeing with the Collins evaluation. 22 However, examining the realities of implementation at regional and trust level revealed several differences in terms of placement quality and the amount of supervision and assessment available for trainees. There was evidence that the training programme had good quality-assurance processes in place and the regional and national stakeholder groups were aware of some of these differences, but issues of communication and involvement of NHS trusts in placement planning and delivery were highlighted as reasons for implementation difficulties. There was also concern expressed at the trust level in relation to the capacity of trainers to deliver the volume of training and assessments required by FT, and that this often conflicted with service delivery commitments.
We found that there was a variety of innovative placements being employed (such as general practice and palliative care or highly specialised roles such as medical biology and neonatal orthopaedics) and there was a slight variation in the length of ED placements, with some regions preferring the use of 6-month rotations to 4-month rotations; however, this variation occurred in a minority of cases. This agreed with the pattern reported in the Collins evaluation. 22
We found that one of the main areas of variation was the educational philosophy of the FT programme held by the educators and the programme implementers at trust level. National and regional stakeholders communicated a view of the programme that built on current problem-based medical education with experiential learning in the workplace, enabling development of the competency and confidence of junior doctors. By contrast, several TLs and some trainees emphasised the importance of ‘specific training sessions on ED-related topics’ to develop trainee competency and confidence. These differences would seem to undermine the purpose of FT, requiring the espoused needs of the programme to be fully and widely articulated and debated both at trainee and at trust level to move FT forward. This issue has been noted previously100 and would appear not to have been resolved. Collins22 concluded that the FT programme lacked an articulated and accepted purpose, especially in its second year, and we would contend that differences in educational philosophy and implementation of agreed learning outcomes are a major reason that the purpose of FT is not clearly understood.
This study shows that, according to the perceptions of F2 doctors, there is improvement in undertaking their work role throughout the F2 period. The time spent in the ED had the greatest impact on their perceived confidence and competence compared with all other placements that they experienced during the year. However, the influence of the FT programme itself is unclear given that we did not include any control areas not delivering FT for comparison. However, it is clear that, overall, F2 doctors perceived that their skills improved over time. Our study has moved the understanding of F2 doctors’ training forward by exploring development across a range of placements over time, in which F2 doctors experienced various work roles in diverse patterns (such as day, night, on-call or shift working). By looking at several cohorts of F2 doctors we have been able to enlarge the scope of enquiry of postgraduate medical education compared with studies considering only a single specialty or work pattern; this was called for in the review by Scallan. 101 In addition, we have developed a simple, self-report measure to assess perceived confidence and competence during training, called for by Miller and Archer. 102
Variation in implementation across organisations
Our study demonstrated cross-sectional evidence of variation between trusts in the number of hours of one-to-one and close working contact with CSs, work demands and amount of teaching and support from CSs. These findings validate the comments of regional stakeholders who noted variation in supervision and those of national stakeholders who were concerned that not all trainees were getting constructive feedback on their work. In their focus groups trainees demonstrated the importance of adequate supervision in enabling them to gain confidence in their decision-making abilities, especially early in a placement, and comments about the quality of support and supervision were frequently included in the questionnaires – with examples of excellent and poor supervision being given. These data build on reviews and studies (e.g. Scallan,101 Marteau et al. 103) offering clear support for the need for and value of close, supportive supervision, including feedback for trainees on their abilities, to enable them to develop confidence and competence as doctors. However, the study was not sufficiently powered to reveal any objective evidence that reduced supervisor support impacted negatively on the perceived clinical competence and confidence of the doctors when directly questioned.
It would appear that two factors stand in the way of developing a strong framework of supervision within the workplace. The first is the difference in educational philosophy between medical educators, supervisors and trainees that we have already discussed. Second, but probably the most important, is the fact that supervision and support are taking place in the workplace and supervisors have to find the time and opportunity to undertake these activities, often during periods of busy service delivery. This is particularly an issue in time-pressured specialties like EM. This is an important resource issue associated with workplace education that seems to rest solely with trusts, who are also responsible for service delivery. It is hard to ignore the comment made by a busy consultant looking at the impact that FT has had on his department: ‘We are not broken yet but it is not far off – we just need more senior staff.’
Clearly a more joined-up resource between medical training and service delivery needs to be explored, particularly with senior NHS trust staff, to enable the appropriate level of supervisory support to be delivered.
Assessment of competence
An obvious focus of the support and development of trainees is the completion of their e-Portfolio of competence. This study, along with the evaluation by Collins,22 shows the development of a national assessment programme. However, the stakeholder groups describe variation in implementation. National and regional stakeholders commented that the implementation of assessment was far from consistent across the regions and varied in quality between departments and assessors. Regional stakeholders noted that e-Portfolios were being used by most trainees, although there were some challenges with regard to the availability and use of information technology in various trusts. TLs recognised the importance of assessment in experiential learning but noted that feedback required delivery on a 24-hour basis, necessitating the involvement of senior and middle-grade medical staff along with senior and practitioner nursing staff. However, the value of actually being able to observe the trainee in structured situations was acknowledged. Trainees held a balanced view of the national assessment process: some saw the value of gaining direct feedback on their competence and the opportunity to discuss individual cases with their supervisor; others felt that the format was ‘too tick boxed’ and, although allowing the examination of routine clinical cases, did not allow discussion of complex cases that might provide greater opportunities for learning. These findings are supported by the study by Hrisos et al. ,104 which examined learning e-Portfolio use in one deanery between 2004 and 2005. Although direct comparisons with this study are difficult, it would appear that trainees and supervisors have developed a little more faith in the recording of experiential work-based learning in the e-Portfolio. Clearly more development work needs to be carried out with assessments to examine the balance between feedback and case discussion that is possible in a busy working environment.
One of the main criticisms of FT was the lack of a consistent framework to assess the completion of the F2 period of workplace training. Unlike the end of F1 training, which is marked by registration with the GMC, a strong outcome as it involves a shared responsibility between the deanery and the trusts,22 the end of F2 training relies on the ‘sign off’ by TLs. National stakeholders fear that this end stage lacks focus and is not a sufficiently significant milestone for the junior doctors. Regional stakeholders are concerned that there is not a consistent approach, as with assessment, and it is likely that different sign-off criteria are required by different assessors. Qualitative comments from trainees would encourage a view that they have self-evaluated their learning over the F2 period and have acknowledged the experiences that have benefitted their practice (see comments in The impact of the emergency department placement). There was little evidence from any of the stakeholder groups that F2 sign-off led to the identification of specific issues or ‘doctors in difficulty’. It would seem that more work is needed to develop a nationally agreed scheme that marks the end of F2.
Well-being and motivation of foundation doctors
National and regional stakeholders and TLs confirmed that there were no systems in place to identify and support periods of overwork and strain for F2 doctors in general but that there was provision for those few who had been designated as ‘doctors in difficulty’ during their training programme. Our study was the first to systematically examine a sample of trainees at the end of their F1 training and throughout the F2 programme.
On average, trainees reported levels of anxiety and depression that were similar to (T2) or better than (T1, T3, T4) those of a normative group of professional and technical workers. Levels of anxiety and depression did not vary significantly over time. Reported levels of job satisfaction were, on average, significantly higher than those of a normative group of doctors and other NHS staff, and overall and intrinsic job satisfaction (associated with aspects of work such as freedom to choose their own method of working and opportunity to use their abilities) were seen to increase over the period of their FT. Trainees reported lower levels of motivational effort than a group of general managers and this did not vary significantly across their training. This study has demonstrated that it is possible to systematically record levels of well-being of trainee doctors and compare these with levels found in other normative studies, enabling appropriate interpretation. It is likely that these measures could be incorporated within trainees’ e-Portfolios.
Robust and stable levels of well-being of foundation doctors from a number of NHS trusts are demonstrated in this study, describing a more positive picture of trainee well-being than has been found in previous single-centre or single-measure studies (e.g. Brennan et al. ,105 Yates et al. 106).
We examined various job-related characteristics associated with well-being across the F2 period and found that there was significant variation in work demands and role clarity across the various time points and, therefore, placements. These data were supported by qualitative comments from trainees who describe a variety of work roles: in some they are being stretched with a heavy workload (e.g. being on-call at night) whereas in others they have nothing to do and are not involved in decision-making about patients. For example:
I feel that my first F2 placement was not representative of my experiences as a doctor to date, as it was a particularly difficult job. As the SHO on ‘take’ for 3 busy admissions units I could take up to 40 referrals per 12 hour shift, and I spent a substantial amount of time doing paperwork, answering the bleep and organising the list rather than seeing patients. When the opportunity arose to learn a new skill (e.g. lumbar puncture) I was constantly being called away to do mundane tasks and training suffered as a result. The consultants, registrars and other SHOs on the unit were excellent – very approachable and supportive – it was just the nature of the job that ground me down – it was a relentless stream of clerking without any feedback as to whether your initial management was correct. This was not the fault of anybody, it was just the nature of the work, but I did find it very dispiriting. I did learn from the 4 months, but I felt that my job was 98% service delivery with very little training, hence why I have given quite negative feedback about it. By contrast, currently I am working on POSU [postoperative surgical] and my job is exactly what I hoped for. I am learning new skills, I have time to do tasks properly and give patients high quality care, the team are excellent, and I feel very well supported with plenty of teaching and other opportunities for development including ring-fenced training time.
T2 participant
I very much enjoyed my time in this placement, but the hours were just very unsociable. I think that more could have been learned if the department was not so busy – every patient that I saw, I felt I could learn something from, but there was not the time for much teaching on the shop floor.
T3 participant
I had a rotation in XX was quite frankly, dreadful. I had three consultants (one working 50% for the trust) who I would see for about an hour a day. I had no junior colleagues, hence no support. I had minimal teaching, certainly no formal teaching in the job. I was largely on my own, in a meaningless role (there is not much an F2 can do in a XX department and certainly very little responsibility or decisions you can take). I had no patients.
T2 participant
Similarly, in some placements trainees are clear about what is expected of them within their work whereas in other placements there is little direction as to what they are expected to do and ambiguity over whether or not they are part of the medical team responsible for service delivery. Examples show that some ongoing monitoring of the trainees’ work environment, as we have shown in this study, would identify issues of work demands and role clarity and, if measured at an appropriate time, enable changes to be made in placements reporting less than satisfactory learning outcomes.
From this we can conclude that the average junior doctor is likely to have comparable or better levels of well-being than other NHS workers and, on average, to expend a lower level of effort than those in managerial roles. However, before we conclude that trainees cope well with their FT, we should bear in mind that these are averaged data and within these groups there may be specific individuals who require additional support at specific times and/or in certain placements. A monitoring process using measures such as those within this study could be incorporated into the e-Portfolio, fulfilling recommendations made by Borman4 and Darsi. 6
Application of these findings would encourage regular monitoring and review of junior doctor well-being (we note that there is a general ‘job satisfaction’ survey within the trainee annual survey used by deaneries; however, this would seem to be concerned with specific training-related outcomes). We see the value in two levels of assessment: at the placement level associated with the e-Portfolio and at an organisational level within the NHS trust. This study has demonstrated an accurate and valid method of assessing trainee well-being and motivation, the outcomes of which are required by both supervisors and trainees in order to adapt and develop placements as appropriate learning experiences. Therefore, these data should not be kept at deanery level but communicated locally and swiftly to supervisors and trainees. A useful method of assessing well-being is the trust’s annual staff survey (provided by the National NHS Staff Survey Co-ordination Centre). By adapting this survey to include specific categories for F1 and F2 doctors, these doctors could be identified at trust level and their results compared with those of other doctors within that specific trust; in addition, national and between-trust comparisons would also be possible. Incorporating assessment of junior doctor well-being within the human resource framework of each trust may increase local ownership of FT.
The impact of the emergency department placement
We were particularly interested in the impact of ED placements on trainees’ competence and confidence and well-being and motivation. The longitudinal design of the study provided the opportunity to study a group of trainees who encountered the ED during their first, second or third F2 placement.
This study has shown that trainees display a significant increase in competence and confidence managing common conditions and performing routine procedures across F2, and the biggest increase in competence and confidence occurred immediately after their ED placement, regardless of when in the year the ED placement occurred and what other placements they experienced during the year. This finding was validated by qualitative comments from trainees who, although noting difficulties relating to the high work demands, long working hours and difficult shift patterns associated with the service delivery role of EM, also described the excellent supervision, fantastic learning experiences and excellent teamworking that increased their confidence as doctors. For example:
Despite how stressful I found A&E in the beginning, on the whole it was a fantastic experience and I am definitely glad to have done it. The consultants and SpRs [specialist registrars] at XX A&E are without exception brilliant doctors to work with.
T2 participant
A&E was a very good clinical experience, and I am glad that I had the opportunity to undertake this placement. It was difficult at times, particularly with regards to the rota/hours, but I have learnt a lot.
T4 participant
Emergency department placements were also associated with changes in well-being, motivation and the way that trainees worked. On average, the biggest increase in effort by trainees was shown in relation to their ED placement compared with all other placements during the year, indicating that they had to use up greater reserves from their energy pool during their ED placement. Further, although not significantly different, on average trainees’ biggest increase in anxiety was associated with their ED placement. Qualitative commentary in the questionnaires and material from trainees’ focus groups suggest that this anxiety stems from worry about making the right decision to admit or send home a patient, and it is this that trainees want the most feedback on and support for. In terms of work characteristics we found a significant reduction in task feedback during the ED placement, which was not matched by the trainee need for feedback on their decisions from senior staff. This reflects the busy and often unplanned nature of the workload in EM, which often makes planning one-to-one time with trainees challenging. Overall levels of job satisfaction and intrinsic job satisfaction were not seen to decrease during the ED placement whereas some participants reported a significant decrease in levels of extrinsic job satisfaction at this time. Extrinsic satisfaction is related to aspects such as pay, hours and conditions of work and these factors received a good deal of commentary from trainees, particularly with regard to long shifts and antisocial hours of work, supported by data revealing increased hours worked per week. The contrast between the demands of service delivery in EM and those in other placements is often great, with some trainees coming into EM having never experienced working night shifts, for example. It is, therefore, perhaps not surprising that there are some reported changes in job satisfaction as a result. Trainees clearly cope well with these difficulties as, with the exception of extrinsic satisfaction, there were no other significant differences in well-being, which remained favourably comparable with that of other health-care workers. Increased social support from colleagues during their ED placement would appear to help trainees, as would the clarity of their role in the ED, helping them know how to direct their efforts. Unfortunately, these factors would seem to go hand in hand with the nature of emergency working, which for some trainees would have been their first taste of service delivery and a contrast to their previous year of training.
This study has shown that there are considerable benefits of the ED placement in terms of competence and confidence gained by junior doctors. However, this does come at a cost of slightly increased anxiety and decreased extrinsic job satisfaction, although the levels of these are comparable to those of other doctors and health-care workers. Careful monitoring of trainees and good supervision with direct feedback on the quality of referral decisions are vital at this time. However, it should be noted that this burden will fall on hard-working staff with few additional resources to offer. If the ED is adopted as a fixed rotation for F2 training, additional senior resources in the ED should be carefully considered.
Quality of care provided by foundation year 2 doctors
The stakeholder study showed a level of disagreement with regard to the quality of care provided by F2 doctors. Regional and national stakeholders suggested that F2 doctors were able to provide adequate patient care and were better prepared in terms of their communication and procedural skills than postgraduates predating MMC. However, supervisors working in trusts found F2 doctors underprepared for service demands, having had little previous experience of decision-making with acutely ill patients. Trainees recognised their supervisors’ concerns, admitting to anxieties relating to decision-making, but agreed with the educational stakeholders that they were able to deliver adequate patient care at the end of their 4 months of training.
Given these varying views of the adequacy of the quality of care provided by F2 doctors we carried out a clinical case notes review of doctors involved in the longitudinal study for their ED placement. Following consultation, two conditions were selected for the case notes review: head injury and COPD.
Overall, the quality of care provided by the cohort of F2 doctors in this study during their ED placements appears good, with mean scores from holistic review ranging from 4.14 to 4.61 on a scale from 1 to 6. Examination of the spread of holistic ratings across all records does highlight some scope for improvement in a small proportion of cases. The mean score for the proportion of review criteria met was > 50% for both head injury and COPD cases. Examination of the proportions of review criteria met highlights aspects of care for which there is scope to improve the level of detail recorded in patient case notes. Given the importance of patient case notes for communication, audit and legal purpose, it is important that all relevant information is clearly documented.
Assessment of quality of care can focus on care outcomes or the process of care. Process measures such as case notes review are recommended as being more suitable for judging quality in health care. 83 The literature suggests that both criterion-based and holistic review methods have strengths and weaknesses and should be regarded as complementary. 93 The findings show stronger correlation coefficients for intercorrelations between the various holistic measures than for correlations between criterion-based and holistic review measures, despite the criterion-based review being carried out first for each record. This appears to support the view that holistic review is assessing aspects of quality not reflected in criterion-based review94 and a thorough assessment of performance should combine the two approaches. Furthermore, the inter-rater reliability results illustrate the benefit of enhanced reliability when using two reviewers and taking an average measure of quality of care. The web-based data-collection tool proved very efficient for collecting the review data such that the addition of automated data analysis and output functions could support performance review and feedback by CSs and potentially peer and even self-review by junior doctors.
When we examined the relationship between well-being and motivation and the quality-of-care outcomes there were no statistically significant associations found, although small- to medium-sized correlations were noted between motivation and work demands and holistic care of head injury and COPD cases. Junior doctors reporting greater effort during their ED placement were likely to have better quality-of-care outcomes for these two conditions. However, junior doctors who reported higher work demands were likely to have lower quality-of-care scores for these conditions. Detailed examination of performance data for 74 junior doctors working in the ED revealed no statistically significant associations with well-being; however, there was a suggestion of small- to medium-sized correlations between anxiety, time spent with patients and percentage of patients seen. This suggests a possible relationship between anxious F2 doctors and longer patient episodes and seeing fewer patients within their ED placement. Although none of these relationships is statistically significant, they are plausible in busy working conditions and are in keeping with the comments of the supervisors during phase 1 of the study. This study indicates that these relationships should be investigated in more depth in large-scale studies. However, these findings (length of patient episode and number of patients seen) may offer a useful and easy rubric for supervisors to use to identify trainees who are struggling with the EM working environment. There is already anecdotal evidence (S Mason, emergency medicine consultant, Sheffield Teaching Hospitals NHS Foundation Trust, 2011, personal communication) that such measures are already being used informally to chart trainees’ progress in the ED.
Limitations
-
The strength of this study is that it followed a group of foundation doctors throughout their F2 training. However, this group consisted of 217 doctors and this may be considered a small number considering the 8000 doctors currently undertaking FT. Our sample covered nine deaneries and 28 trusts in England. Because of confidentiality constraints deaneries self-selected to be part of this sample, which may preclude those that had particular difficulties in well-being and motivation. However, the study achieved its intended sample size of 210 doctors needed to address the primary outcome of the study (change in well-being over the year). The fact that these doctors were distributed over a range of EDs and NHS trusts probably strengthens this study in terms of reporting these findings as generalisable.
-
Participants explored the information about the study and self-selected to be involved. Therefore, it is possible that the group of participants who made themselves available for this study had robust levels of well-being when joining the study. Nevertheless, the study was able to track their well-being and motivation over a period of 12 months, exploring any changes that may have occurred during that time, and thereby fulfilling one of its key objectives.
-
The focus groups in the stakeholder study included F2 doctors from three large EDs, two of which were teaching hospitals. There may have been differences between the views and experiences of F2 doctors in this study and the views and experiences of F2 doctors from smaller trusts. Further, our sample of 10 PESs may be considered a small sample but it was sufficient for ‘saturation’ of information. Our sample of stakeholders from EDs mainly consisted of consultant TLs who were therefore at a senior grade and may have had specific work experiences. Further studies may benefit from including greater numbers of other staff who have a more informal role in supervising and supporting F2 doctors, such as senior nursing staff and nurse practitioners.
-
Assessing quality of care through case-note review is reliant on information being recorded in the notes, which may not reflect every detail of the care provided. Completeness of the record is itself a quality issue and in this study poor recording is reflected in lower quality-of-care scores. This part of the study did not achieve its intended sample of 144 doctors from 12 EDs. However, this is the first study of its kind to use case-note review to evaluate quality of care in the ED and also to try and link it with well-being and motivation amongst doctors.
-
The reliability analysis found a high level of agreement between reviewers in relation to the criterion-based review. The level of agreement for the holistic review of case notes was lower and was less consistent across sites. Establishing inter-rater reliability was challenging as ethics and research governance constraints meant that reviewers could review notes only within their own hospital. Therefore, it was possible to obtain a measure of inter-rater reliability only within sites with more than one reviewer, to give a broad indication of consistency across reviewers. The number of records for review was selected to ensure that the reliability analysis did not outweigh the main reviewing activity and was based on a previous study of quality in emergency care using holistic review that had achieved moderate to strong reliability (0.52–0.64) using 14 records. 88 The higher level of agreement in that study may have been achieved because the records examined were more concise than the ED records in this study.
Future study
-
Further examination of quality-of-care outcomes and junior doctors’ well-being and motivation. Future studies would need to be large-scale, multicentre studies to provide sufficient power to examine possible relationships.
-
More large-scale studies looking at assessment of competence, feedback and case discussion conducted by a range of health-care staff may yield further good practice that can be incorporated into the FT assessment programme.
Implications for practice
-
Disseminate the findings of this study to encourage more general support for work-based learning and assessment as part of postgraduate medical education, especially to organisations such as the UK Foundation Programme Board. We would seek national communication of the findings so that participating trusts can learn of the findings through conferences such as the Health Services Research Network annual symposium and the NHS Confederation conferences.
-
Trainees’ levels of well-being and motivation can be measured accurately over time and would form an appropriate part of the e-Portfolio, but this would require timely feedback to supervisors to enable appropriate work demands and role clarity to be determined within the placement period. If this service cannot be provided within a useful time frame a trainee report measure regarding their well-being, work demands and role clarity and use of their abilities should be communicated to the trainees and their supervisors, enabling local changes to be made to placements. There is a well-validated system for recording well-being amongst NHS staff (the National NHS Staff Survey107) and this would be utilised to specifically identify and benchmark the well-being of foundation doctors. However, it would need to be acknowledged that this is an annual review and not as accurate as placement measures.
-
This study offers clear evidence that all F2 doctors would gain in confidence and competence from an ED placement; however, this should be accompanied by additional support17 for senior staff to enable them to provide the level of support that trainees need during this intense learning period. In addition, more consideration needs to be given to work–life balance issues during this placement period.
-
The success of workplace learning depends on the provision of adequate levels of supervision and support of trainees. The exact level of senior support needs to be determined by working closely with senior staff and supervisors. 22 This by necessity will not be one-size-fits-all as it will depend on a number of factors associated with service delivery and requires consultation with both the Foundation Programme and the trusts involved.
-
Consideration should be given to debating the espoused educational philosophy of medical training (as problem-based education supported by workplace experiential learning) to articulate a clear and understood purpose of FT, enabling the implementation of agreed learning outcomes with supervisors and trainees.
-
Further studies should be carried out on work-based assessment, with close examination and development of specific criteria that lead to a national scheme marking the end of F2 training.
-
Careful consideration should be given to incorporating formal processes for careers advice at both the F1 and the F2 points in training to ensure that foundation doctors acquire the most appropriate training for their intended career track. Although the benefits of ED placements are acknowledged, this may not always be the case when intended career tracks involve service specialties such as laboratory medicine and radiology.
Acknowledgements
We would like to thank the following for their contribution to the research:
-
staff at the participating research sites, particularly staff at PMDs, FSs and EDs, who agreed to participate and provided assistance with contacting the study participants and their recruitment
-
the specialist trainee reviewers who took part in the clinical case notes review
-
the members of the steering group committee for their contribution to the management of the study.
Contribution of authors
Suzanne Mason, Colin O’Keeffe, Angela Carter, Rachel O’Hara and Chris Stride were the grant holders and managed the main parts of the study.
For phase 1, Angela Carter, Colin O’Keeffe and Suzanne Mason undertook the qualitative interviews and the analyses.
For phase 2, Colin O’Keeffe, Suzanne Mason, Angela Carter and Chris Stride designed and implemented the longitudinal study and Chris Stride undertook the analyses for the longitudinal study.
Rachel O’Hara, Colin O’Keeffe and Suzanne Mason designed and implemented the clinical case notes review and Rachel O’Hara and Chris Stride undertook the analyses for the clinical case notes review.
Colin O’Keeffe, Angela Carter and Rachel O’Hara wrote the drafts of the report and Suzanne Mason, Chris Stride and Angela Carter edited the final report.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- The NHS knowledge and skills framework (NHS KSF) and the development review process. London: Department of Health; 2004.
- The NHS plan. A plan for investment. A plan for reform. London: The Stationary Office; 2000.
- Black C. Working for a healthier tomorrow. London: The Stationary Office; 2008.
- Boorman S. NHS health and well-being review – final report. London: Department of Health; 2009.
- Van Stolk C, Starkey T, Shehabi A, Hassan E. NHS health and well-being, the Boorman review. London: Department of Health; 2009.
- A high quality workforce: NHS next stage review. London: Department of Health; 2008.
- Promoting mental wellbeing through productive and healthy working conditions: guidance for employers. London: NICE; 2009.
- Karasek R, Theorell T. Healthy work: stress, productivity and the reconstruction of working life. New York, NY: Basic Books; 1990.
- Parker S, Wall T. Job and work design: organizing work to promote well-being and effectiveness. Advanced topics in organizational behavior. Thousand Oaks, CA: Sage Publications; 1998.
- Hewitt C, Lankshear A, Maynard A, Sheldon T, Smith K. Health service workforce and health outcomes: a scoping study. London: National Co-ordinating Centre For Service Delivery and Organisation; 2003.
- Michie S, West MA. Managing people and performance: an evidence based framework applied to health service organizations. Int J Manag Rev 2004;5:91-111. http://dx.doi.org/10.1111/j.1460-8545.2004.00098.x.
- Grol R, Mokkink H, Helsper-Lucas A, Tielens V, Bulte J. Effects of the vocational training of general practice consultation skills and medical performance. Med Educ 1989;23:512-21. http://dx.doi.org/10.1111/j.1365-2923.1989.tb01577.x.
- Tharenou P, Burke E, Robertson I, Callinan M, Bartram D. Organisational effectiveness: the role of psychology. Chichester: John Wiley; 2002.
- West E. Management matters: the link between hospital organisation and quality of patient care. Qual Health Care 2001;10:40-8. http://dx.doi.org/10.1136/qhc.10.1.40.
- West MA, Borrill CS, Dawson J, Scully J, Carter M, Anelay S, et al. The relationship between staff management practices and patient mortality in acute hospitals: a longitudinal study. Int J Human Resource Manag 2003;13:1299-310.
- Wall TD, Bolden RI, Borrill CS, Carter AJ, Golya DA, Hardy GE, et al. Minor psychiatric disorder in NHS trust staff: occupational and gender differences. Br J Psychiatry 1997;171:519-23. http://dx.doi.org/10.1192/bjp.171.6.519.
- Donaldson L. Unfinished business: proposals for reform of the senior house officer grade. London: Department of Health; 2002.
- Clough C. Modernising Medical Careers: effect on NHS service delivery. Hosp Med 2005;66:139-41.
- National Health Service . Modernising Medical Careers n.d. www.mmc.nhs.uk/ (accessed 7 August 2013).
- Foundation programme curriculum 2012. London: Academy of Medical Royal Colleges; 2012.
- Tooke SJ. Aspiring to excellence: findings and recommendations of the independent inquiry into Modernising Medical Careers led by Sir John Tooke. London: MMC Inquiry; 2008.
- Collins JF. Foundation for excellence – an evaluation of the foundation programme. London: Medical Education; 2010.
- Junior doctors. The new deal. London: NHS Management Executive; 1991.
- Temple J. Time for training: a review of the impact of the European Working Time Directive on the quality of training. London: Medical Education; 2010.
- Firth-Cozens J. Emotional distress in junior house officers. Br Med J (Clin Res Ed) 1987;295:533-6. http://dx.doi.org/10.1136/bmj.295.6597.533.
- Reuben DB. Depressive symptoms in medical house officers. Effects of level of training and work rotation. Arch Intern Med 1985;145:286-8.
- McPherson S, Hale R, Richardson P, Obholzer A. Stress and coping in accident and emergency senior house officers. Emerg Med J 2003;20:230-1. http://dx.doi.org/10.1136/emj.20.3.230.
- Burbeck R, Coomber S, Robinson SM, Todd C. Occupational stress in consultants in accident and emergency medicine: a national survey of levels of stress at work. Emerg Med J 2002;19:234-8. http://dx.doi.org/10.1136/emj.19.3.234.
- Caplan RP. Stress, anxiety, and depression in hospital consultants, general practitioners, and senior health service managers. BMJ 1994;309:1261-3.
- Goldberg DP, Hillier VF. A scaled version of the General Health Questionnaire. Psychol Med 1979;9:139-45. http://dx.doi.org/10.1017/S0033291700021644.
- Armstrong PA, White AL, Thakore S. Senior house officers and foundation year doctors in emergency medicine: do they perform equally? A prospective observational study. Emerg Med J 2008;25:725-7. http://dx.doi.org/10.1136/emj.2008.059154.
- Armstrong PA, White AL, Thakore S. Reduced productivity among junior trainees in the emergency department and the impact on senior clinicians. Emerg Med J 2010;27:97-9. http://dx.doi.org/10.1136/emj.2008.071431.
- Eager R, Banks M. Transition to the foundation programme: does it affect the numbers of patients seen by SHOs?. Emerg Med J 2006;23:888-9. http://dx.doi.org/10.1136/emj.2006.038281.
- Whiticar R, Webb H, Smith S. Re-attendance to the emergency department. Emerg Med J 2008;25:360-1. http://dx.doi.org/10.1136/emj.2007.050617.
- Croft SJ, Kuhrt A, Mason S. Are today’s junior doctors confident in managing patients with minor injury?. Emerg Med 2006;23:867-8. http://dx.doi.org/10.1136/emj.2006.035246.
- Croft SJ, Mason S. Are emergency department junior doctors becoming less experienced in performing common practical procedures?. Emerg Med J 2007;24:657-8. http://dx.doi.org/10.1136/emj.2006.045302.
- Smith G, Poplett N. Knowledge of aspects of acute care in trainee doctors. Postgrad Med J 2002;78:335-8. http://dx.doi.org/10.1136/pmj.78.920.335.
- Patterson M, Warr P, West M. Organizational climate and company productivity: the role of employee affect and employee level. J Occup Organ Psychol 2004;77:193-216. http://dx.doi.org/10.1348/096317904774202144.
- Morey JC, Simon R, Jay GD, Wears RL, Salisbury M, Dukes KA, et al. Error reduction and performance improvement in the emergency department through formal teamwork training: evaluation results of the MedTeams project. Health Serv Res 2002;37:1553-81. http://dx.doi.org/10.1111/1475-6773.01104.
- Hardy GE, Woods D, Wall TD. The impact of psychological distress on absence from work. J Appl Psychol 2003;88:306-14. http://dx.doi.org/10.1037/0021-9010.88.2.306.
- Williams S, Dale J, Glucksman E, Wellesley A. Senior house officers’ work related stressors, psychological distress, and confidence in performing clinical tasks in accident and emergency: a questionnaire study. BMJ 1997;314:713-18. http://dx.doi.org/10.1136/bmj.314.7082.713.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77-101. http://dx.doi.org/10.1191/1478088706qp063oa.
- Bryman A, Bell E. Business research methods. Oxford: Oxford University Press; 2003.
- Carter A, Wood S, Goodacre S, Sampson F, Stables R. Evaluation of workforce and organizational issues in establishing primary angioplasty in England. J Health Serv Res Policy 2010;15:6-13. http://dx.doi.org/10.1258/jhsrp.2009.009019.
- King N, Symon G, Cassell C. Qualitative methods and analysis in organizational research: a practical guide. Thousand Oaks, CA: Sage Publications; 1998.
- Warr PB, Cook JD, Wall TD. Scales for the measurement of some work attitudes and aspects of psychological well-being. J Occup Psychol 1979;52:129-48. http://dx.doi.org/10.1111/j.2044-8325.1979.tb00448.x.
- Warr P, Clapperton G. The joy of work? Jobs, happiness and you. Sussex: Routledge; 2010.
- Health Services Research, School of Health and Related Research (ScHARR), University of Sheffield . The EDiT Study n.d. www.editstudy.org (accessed 12 July 2013).
- Department of Health . A&Amp;E Attendances n.d. http://webarchive.nationalarchives.gov.uk/20130107105354/http://www.dh.gov.uk/en/Publicationsandstatistics/Statistics/Performancedataandstatistics/AccidentandEmergency/DH_077485 (accessed 11 June 2013).
- Costa PT, McCrae RR. Revised NEO personality inventory (NEO PI-R) manual (UK edition). Oxford: Hogrefe; 2006.
- Ones DS, Dilchert S, Viswesvaran C, Judge TA. In support of personality assessment in organizational settings. Person Psychol 2007;60:995-1027. http://dx.doi.org/10.1111/j.1744-6570.2007.00099.x.
- Tobin DL, Holroyd KA, Reynolds RV, Wigal JK. The hierarchal factor structure of the Coping Strategies Inventory. Cognit Ther Res 1989;13:343-61.
- Lazararus RS, Folkman S. Stress, appraisal and coping. New York, NY: Springer; 1984.
- Warr P. Work, unemployment and mental health. Oxford: Oxford University Press; 1987.
- Warr PB. The measurement of well-being and other aspects of mental health. J Occup Psychol 1990;63:193-210. http://dx.doi.org/10.1111/j.2044-8325.1990.tb00521.x.
- Warr PB. Decision latitude, job demands, and employee well-being. Work Stress 1990;4:285-94. http://dx.doi.org/10.1080/02678379008256991.
- Van Dierendonck D, Haynes C, Borrill C, Stride C. Leadership behavior and subordinate well-being. J Occup Health Psychol 2004;9:165-75. http://dx.doi.org/10.1037/1076-8998.9.2.165.
- Mullarkeys WT, Warr PB, Clegg CS, Stride C. Measures of job satisfaction, mental health and job-related well-being: a bench-marking manual. Sheffield: University of Sheffield; 1999.
- Stride C, Wall TD, Catley N. Measures of job satisfaction, organisational commitment, mental health and job related well-being: a benchmarking manual. Chichester: John Wiley; 2007.
- Pritchard E, Ashwood EL. Managing motivation: a manager’s guide to diagnosing and improving motivation. New York, NY: LEA/Psychology Press; 2008.
- Cammann C, Fichman M, Jenkins D, Klesh J. The Michigan organizational assessment questionnaire. Ann Arbor, MI: University of Michigan; 1979.
- Mason SOKC, Coleman P, O’Hara R, Dixon S, Rick J. A multi centre community intervention trial to evaluate the clinical and cost effectiveness of emergency care practitioners. London: National Co-ordinating Centre for NHS Service Delivery and Organisation (NCCSDO); 2008.
- Borrill CS, Wall TD, West MA, Hardy GE, Shapiro DA, Carter A, et al. Mental health of the workforce in NHS Trusts. Sheffield: Institute of Work Psychology, University of Sheffield; 1996.
- Borrill CS, West MA, Wall TD, Shapiro DA, Haynes CE, Stride C, et al. Stress among staff in NHS trusts. Sheffield: Institute of Work Psychology, University of Sheffield; 1998.
- Hipwell AE, Tyler PA, Wilson CM. Sources of stress and dissatisfaction among nurses in four hospital environments. Br J Med Psychol 1989;62:71-9. http://dx.doi.org/10.1111/j.2044-8341.1989.tb02812.x.
- Richardsen AM, Burke RJ. Occupational stress and job satisfaction among Canadian physicians. Work Stress 1991;5:301-13. http://dx.doi.org/10.1080/02678379108257028.
- Caplan RD. Organizational stress and individual strain: a social-psychological study of risk factors in coronary heart disease amongst administrators, engineers and scientists. Ann Arbor, MI: University of Michigan, Institute for Social Research; 1971.
- Kahn RL, Wolfe DM, Quinn RP, Sneok JD, Rosenthal RA. Organizational stress: studies in role conflict and ambiguity. New York, NY: Wiley; 1964.
- Hackman J, Oldham GR. Motivation through the design of work: test of theory. Organ Behav Hum Perform 1976;15:250-79. http://dx.doi.org/10.1016/0030-5073(76)90016-7.
- Cordery JL, Wall TD. Work design and supervisory practice: a model. Hum Relat 1985;38:425-41. http://dx.doi.org/10.1177/001872678503800503.
- Hackman J, Oldham GR. Development of the job diagnostic survey. J Appl Psychol 1975;60:159-70. http://dx.doi.org/10.1037/h0076546.
- Rizzo J, House RJ, Lirtzman SJ. Role conflict and ambiguity in complex organizations. Admin Sci Q 1970;15:150-63. http://dx.doi.org/10.2307/2391486.
- Kelloway EK, Barling J. Job characteristics, role stress and mental health. J Occup Psychol 1991;64:291-304. http://dx.doi.org/10.1111/j.2044-8325.1991.tb00561.x.
- House J. Work stress and social support. Reading, MA: Addison-Wesley Publishing; 1981.
- Abdel-Halim AA. Individual and interpersonal moderators of employee reactions to job characteristics: a re-examination. Person Psychol 1982;32:121-37.
- Caplan RD, Cobb S, French JRP, Van Harrison RV, Pinneau SR. Job demands and worker health. Washington, DC: National Institute for Occupational Safety and Health; 1975.
- Caplan RD, Cobb S, French JRP, Van Harrison RV, Pinneau SR. Job demands and worker health. Ann Arbor, MI: University of Michigan, Institute for Social Research; 1980.
- Malakh-Pines A, Aronson E, Kafry D. Burnout. New York, NY: Free Press; 1987.
- Cohen S, Wills TA. Stress, social support, and the buffering hypothesis. Psychol Bull 1985;98:310-57. http://dx.doi.org/10.1037//0033-2909.98.2.310.
- Dwyer DJ, Ganster DC. The effects of job demands and control on employee attendance and satisfaction. J Organ Behav 1991;12:595-608. http://dx.doi.org/10.1002/job.4030120704.
- Haynes CE, Wall TD, Bolden RI, Rick JE. Measures of perceived work characteristics for health service research: test of a measurement model and normative data. Br J Health Psychol 1999;4:257-75. http://dx.doi.org/10.1348/135910799168614.
- Szilagyi AD, Sims HP, Keller RT. Role dynamics, locus of control, and employee attitudes and behavior. Acad Manag J 1976;19:259-76. http://dx.doi.org/10.2307/255776.
- Lilford RJ, Brown CA, Nicholl J. Use of process measures to monitor the quality of clinical practice. BMJ 2007;335:648-50. http://dx.doi.org/10.1136/bmj.39317.641296.AD.
- Hiatt HH, Barnes BA, Brennan TA, Laird NM, Lawthers AG, Leape LL, et al. A study of medical injury and medical malpractice. N Engl J Med 1989;321:480-4. http://dx.doi.org/10.1056/NEJM198908173210725.
- Wolff AM. Limited adverse occurrence screening: using medical record review to reduce hospital adverse patient events. Med J Aust 1996;164:458-61.
- Wolff AM, Bourke J. Detecting and reducing adverse events in an Australian rural base hospital emergency department using medical record screening and review. Emerg Med J 2002;19:35-40. http://dx.doi.org/10.1136/emj.19.1.35.
- Sari AB, Sheldon TA, Cracknell A, Turnbull A, Dobson Y, Grant C, et al. Extent, nature and consequences of adverse events: results of a retrospective casenote review in a large NHS hospital. Qual Saf Health Care 2007;16:434-9. http://dx.doi.org/10.1136/qshc.2006.021154.
- O’Hara R, O’Keeffe C, Mason S, Coster JE, Hutchinson A. Quality and safety of care provided by emergency care practitioners. Emerg Med J 2012;29:327-32. http://dx.doi.org/10.1136/emj.2010.104190.
- Brown C, Hofer T, Johal A, Thomson R, Nicholl J, Franklin BD, et al. An epistemology of patient safety research: a framework for study design and interpretation. Part 3. End points and measurement. Qual Saf Health Care 2008;17:170-7. http://dx.doi.org/10.1136/qshc.2007.023655.
- Hutchinson A, McIntosh A, Anderson J, Gilbert C, Field R. Developing primary care review criteria from evidence-based guidelines: coronary heart disease as a model. Br J Gen Pract 2003;53:690-6.
- Camacho LA, Rubin HR. Assessment of the validity and reliability of three systems of medical record screening for quality of care assessment. Med Care 1998;36:748-51. http://dx.doi.org/10.1097/00005650-199805000-00014.
- Mohammed MA, Mant J, Bentham L, Stevens A, Hussain S. Process of care and mortality of stroke patients with and without a do not resuscitate order in the West Midlands, UK. Int J Qual Health Care 2006;18:102-6. http://dx.doi.org/10.1093/intqhc/mzi081.
- Lilford R, Edwards A, Girling A, Hofer T, Di Tanna GL, Petty J, et al. Inter-rater reliability of case-note audit: a systematic review. J Health Serv Res Policy 2007;12:173-80. http://dx.doi.org/10.1258/135581907781543012.
- Hutchinson A, Coster JE, Cooper KL, McIntosh A, Walters SJ, Bath PA, et al. Comparison of case note review methods for evaluating quality and safety in health care. Health Technol Assess 2010;14.
- Hutchinson A, Coster JE, Cooper KL, McIntosh A, Walters SJ, Bath PA, et al. Assessing quality of care from hospital case notes: comparison of reliability of two methods. Qual Saf Health Care 2010;19. http://dx.doi.org/10.1136/qshc.2007.023911.
- Head injury. Triage, assessment, investigation and early management of head injury in infants, children and adults. London: NICE; 2007.
- Chronic obstructive pulmonary disease. Management of chronic obstructive pulmonary disease in adults in primary and secondary care. London: NICE; 2010.
- Zegers M, de Bruijne MC, Spreeuwenberg P, Wagner C, Groenewegen PP, van der Wal G. Quality of patient record keeping: an indicator of the quality of care?. BMJ Qual Saf 2011;20:314-18. http://dx.doi.org/10.1136/bmjqs.2009.038976.
- Hofer TP, Asch SM, Hayward RA, Rubenstein LV, Hogan MM, Adams J, et al. Profiling quality of care: is there a role for peer review?. BMC Health Serv Res 2004;4.
- O’Brien M, Brown J, Ryland I, Shaw N, Chapman T, Gillies R, et al. Exploring the views of second-year foundation programme doctors and their educational supervisors during a deanery-wide pilot foundation programme. Postgrad Med J 2006;82:813-16. http://dx.doi.org/10.1136/pgmj.2006.049676.
- Scallan S. Education and the working patterns of junior doctors in the UK: a review of the literature. Med Educ 2003;37:907-12. http://dx.doi.org/10.1046/j.1365-2923.2003.01631.x.
- Miller A, Archer J. Impact of workplace based assessment on doctors’ education and performance: a systematic review. BMJ 2010;341. http://dx.doi.org/10.1136/bmj.c5064.
- Marteau TM, Wynne G, Kaye W, Evans TR. Resuscitation: experience without feedback increases confidence but not skill. BMJ 1990;300:849-50. http://dx.doi.org/10.1136/bmj.300.6728.849.
- Hrisos S, Illing JC, Burford BC. Portfolio learning for foundation doctors: early feedback on its use in the clinical workplace. Med Educ 2008;42:214-23. http://dx.doi.org/10.1111/j.1365-2923.2007.02960.x.
- Brennan N, Corrigan O, Allard J, Archer J, Barnes R, Bleakley A, et al. The transition from medical student to junior doctor: today’s experiences of tomorrow’s doctors. Med Educ 2010;44:449-58. http://dx.doi.org/10.1111/j.1365-2923.2009.03604.x.
- Yates PJ, Benson EV, Harris A, Baron R. An investigation of factors supporting the psychological health of staff in a UK emergency department. Emerg Med J 2012;29:533-5. http://dx.doi.org/10.1136/emj.2010.099630.
- National NHS Staff Survey n.d. www.nhsstaffsurveys.com/Page/1010/Home/Staff-Survey-2013 (accessed 22 November 2013).
Appendix 1 Schematic of current postgraduate training in the UK following the Tooke report21
Schematic of current postgraduate training in the UK following the Tooke report 21 (PDF download)
Appendix 2 Summary of key components of the Foundation Programme
| Team assessment of behaviour | Multisource feedback given to trainee from a number of multiprofessional colleagues. Previously known as 360-degree feedback |
| CS end-of-placement report | A summary of the progress and achievements of the foundation doctor following a meeting to discuss these with the CS |
| ES end-of-placement report | Comprising information from both the CS’s end-of-placement report and the e-Portfolio |
| Mini-CEX | An evaluation of an observed clinical encounter |
| DOPs | An observation of a doctor’s interaction with a patient whilst they carry out a specific clinical procedure |
| Case-based discussion | A retrospective discussion between a supervisor and a trainee regarding a specific clinical case managed by the trainee |
| Developing the clinical teacher | An assessment tool to develop a trainee’s skills in teaching and presentation |
| Mini-PAT | The mini-PAT provides feedback from a range of co-workers across the domains of good medical practice. Using Portfolio Onlinea these can be mapped to the core objectives of the curriculum. The PMETB and the GMC have identified peer ratings as suitable for postgraduate assessment and revalidation evidence |
Appendix 3 National stakeholder interview schedule
Interview questions for national stakeholders in postgraduate medical education (phase 1)
Good morning/afternoon, my name is Angela Carter/Suzanne Mason. I would like to thank you for giving me some of your valuable time for this interview.
The interview is part of a national evaluation of FY2 doctor well-being. The study is being carried out over 3 years and is examining different arrangements for the emergency departments. In particular, we are interested in the influence of well-being and motivation on patient care.
We sent you an information sheet about the study when we arranged the interview – would you like to see this again? I have sent/will forward a consent form for you to sign and return to us. Are you happy to sign this?
This particular interview is one of a series we are conducting with stakeholders in postgraduate medical education at a national and regional level who are in a position to influence decision-making, particularly the FY2 training agenda. The aim of the interview is to explore your perceptions and experiences of FY2 training nationally.
I’d like to assure you that anything that you say to me/us today will be treated in confidence. NO individual will be identified. I only have your name to note that I have completed my interviews as planned.
The interview will take about 60 minutes and I have a copy of the questions for you to have a look at to help you. Is there anything you would like to ask before we begin? (5 minutes)
Background
1. Briefly describe your own role in relation to FY2 training? (3 minutes)
Prompt: Can you describe the input that you have in the planning and implementation of FY2 training.
Approach to postgraduate medical education
2. Can you describe to what extent there is a national strategic approach to FY2 training in England/Wales/Scotland? (5 minutes)
Prompt: Who is responsible?
Prompt: What mechanisms exist for implementing a national approach?
Prompt: Policies, policy documents, conferences and curriculum?
Prompt: Nationally how many trainees are there? Is this sufficient?
3. What are the challenges that exist in the implementation of a national strategic approach for FY2 training? (5 minutes)
Prompt: What are the likely successes? How are these measured?
Prompt: What are the likely failures? How are these measured?
Prompt: Issues specifically for the ED?
Variation in training
4. To what degree is there variation in the implementation of postgraduate training at the regional level? (5 minutes)
Prompt: Is there variation at foundation school level?
Prompt: What do you think are the causes of variation in implementing training?
Quality
5. What are the criteria for success for FY2 doctors’ training? (7 minutes)
Prompt: How are these measured?
Prompt: How well are these met? (in terms of patient care and performance)
Prompt: Are they sufficient? (in terms of patient care and performance)
Prompt: Is training providing FY2 doctors that are fit for purpose?
6. What quality assurance mechanisms exist for FY2 training at a national level? (5 minutes)
Prompt: e.g. Feedback from health organisations, doctors?
Prompt: Are these sufficient? If issues are noted what changes are made?
(35 minutes to this point)
(Sue takes over)
Well-being and motivation of FY2s
7. How is the well-being and motivation of FY2 doctors evaluated in their training? (8 minutes)
Prompt: How is this assessed, when and by whom? (Is it part of the assessment process?)
Prompt: If there are issues of well-being or motivation how are these addressed?
Prompt: Differentiate between local and strategic responses.
Prompt: Is the potential impact on patient care considered?
Career development
8. Do you feel there is sufficient career development built in to the training so that FY2s can build their careers on a firm basis? (7 minutes)
Prompt: Is there limitation of choice for doctors?
Prompt: Are they specialising too early?
Prompt: Are doctors ‘slotted in’ to operational arrangements and miss out on the bigger picture?
(50 minutes to this point)
Future developments
9. Can you describe any developments that will occur in the near future that may affect FY2 training? (5 minutes)
Prompt: Regional or national basis?
Prompt: Are there any changes you would personally like to see made to postgraduate medical training?
Ending
Is there any information you would like to add that would enable us to understand the current and planned future state of postgraduate medical training?
Thank you for your valuable time – we will be sending you a copy of our final report. (5 minutes)
Appendix 4 Regional stakeholder interview schedule
Interview questions for regional stakeholders in postgraduate medical education (phase 1)
Good morning/afternoon, my name is Angela Carter/Suzanne Mason/Colin O’Keeffe. I would like to thank you for giving me some of your valuable time for this interview.
The interview is part of a national evaluation of FY2 doctor well-being. The study is being carried out over 3 years and is examining different arrangements for the emergency departments. In particular, we are interested in the influence of well-being and motivation of the FY2 doctors on patient care.
We sent you an information sheet about the study when we arranged the interview – would you like to see this again? I have sent/will forward a consent form for you to sign and return to us. Are you happy to sign this?
This particular interview is one of a series we are conducting with stakeholders in postgraduate medical education at a national and regional level who are in a position to influence decision-making, particularly around the FY2 training agenda. The aim of the interview is to explore your perceptions and experiences of FY2 training regionally.
I’d like to assure you that anything that you say to me/us today will be treated in confidence. NO individual will be identified. I only have your name to note that I have completed my interviews as planned.
The interview will take about 55 minutes and I have a copy of the questions for you to have a look at to help you. Is there anything you would like to ask before we begin? (5 minutes)
Background
1. Briefly describe your own role in relation to FY2 training? (2 minutes)
Prompt: Can you describe the input that you have in the planning and implementation of FY2 training?
Planning and implementation (regional level)
2. How is FY2 training planned and implemented at the regional level? (5 minutes)
Prompt: Individuals responsible, policy?
Prompt: Is this approach consistent with the national strategic approach or does it differ in any way?
Prompt: How many trainees are there? How many trusts are involved? Is this sufficient for your regional area?
3. Are the placement organisations involved in the planning of training? (3 minutes)
Prompt: If so, how?
Prompt: Meetings, visits, joint bodies?
Variation
4. Is there variation in the implementation of foundation training across the regions? (5 minutes)
Prompt: What are the points of variation (e.g. placement length)?
Prompt: What are the causes of variation?
(20 minutes to this point)
Quality
5. What are the key training outcomes for FY2 doctors? (5 minutes)
Prompt: How useful is the mentor/educational supervisor role for you in making an assessment of the junior doctors?
Prompt: Is there variation in educational supervisors?
Prompt: Are these the same criteria for signing off the successful completion of a placement? If not, why not?
Prompt: Is the e-Portfolio used?
(Sue takes over)
6. To what extent is FY2 training providing doctors that are fit for purpose? (5 minutes)
Prompt: How useful are the formal assessments to assess FY2s’ ability?
Prompt: Are doctors ‘slotted in’ to operational arrangements and miss out on the bigger picture? This repeated later in career development?
Prompt: Are there any specific issues for the ED?
Prompt: What type of issues are you finding with FY2 doctor training? Did these happen before foundation training? (if a specific issue is mentioned ask them to describe the example fully)
7. What quality assurance mechanisms exist for foundation training in your region? (5 minutes)
Prompt: e.g. Feedback from health organisations, doctors?
Prompt: Are these sufficient? If issues are noted what changes are made?
(35 minutes to this point)
Well-being and motivation of FY2s
8. How is the well-being and motivation of FY2 doctors evaluated in their training? (10 minutes)
Prompt: How is this assessed, when and by whom? (Is it part of the assessment process?)
Prompt: In your experience what motivates FY2 doctors?
Prompt: What aspects of work do FY2s struggle with?
Prompt: How is the potential impact on patient care considered?
Career development
9. Is sufficient career development built in to the training so that FY2s can build their careers on a firm basis? (5 minutes)
Prompt: Is there limitation of choice for doctors?
Prompt: Are they specialising too early?
Prompt: Are doctors ‘slotted in’ to operational arrangements and miss out on the bigger picture?
(50 minutes to this point)
Future developments
10. What developments will occur in the near future that may affect foundation training? (5 minutes)
Prompt: Are there any changes you would personally like to see made?
Prompt: Changes that may influence patient care?
Prompt: Changes that may influence FY2s well-being and motivation
Ending
Is there any information you would like to add that would enable us to understand the current and planned future state of postgraduate medical training?
Thank you for your valuable time – we will be sending you a copy of the Executive Summary of our final report. (5 minutes)
Appendix 5 Trainer stakeholder interview schedule
Interview questions for consultants/training leads in emergency departments (phase 1)
Good morning/afternoon, my name is [Researcher]. I would like to thank you for giving me some of your valuable time for this interview.
The interview is part of a national evaluation of FY2 doctor training. The study is being carried out over 3 years and is examining different arrangements for the implementation of training in emergency departments. In particular, we are interested in the influence of well-being and motivation on patient care.
We sent you an information sheet about the study when we arranged the interview – would you like to see this again? I have sent/will forward a consent form for you to sign and return to us. Are you happy to sign this?
This particular interview is one of a series we are conducting with stakeholders in training at a regional and local level who are in a position to influence decision-making around postgraduate medical training, and particularly the FY2 training agenda. The aim of the interview is to explore your perceptions and experiences of FY2 training locally.
I’d like to assure you that anything that you say to me/us today will be treated in confidence. NO individual will be identified. I only have your name to note that I have completed my interviews as planned.
The interview will take about 60 minutes and I have a copy of the questions for you to have a look at to help you. Is there anything you would like to ask before we begin? (5 minutes)
Background
1. Briefly describe your own role in relation to FY2 training please? (3 minutes)
Prompt: How are you brought into contact with FY2s working in your department?
Training
2. Can you describe the training FY2 doctors receive in your ED? (4 minutes)
Prompt: What is the role of the junior doctors in the ED?
Prompt: How many trainees are there? Is this sufficient or is it too many?
3. Has there been any changes to the way training in the ED has been provided in recent years? (3 minutes)
Prompt: What is the impact of changes to training (e.g. changes to way you deliver care, workload and supervision)?
4. Do you think the FY2 doctor training is adequate preparation for them to deliver the care they are expected to provide? (5 minutes)
5. In what way do you think training can be improved? (5 minutes)
(25 minutes to this point)
Quality
6. How well do assessments measure the ability of FY2s to deliver good clinical care? (5 minutes)
7. How are FY2s assessed? (5 minutes)
(35 minutes to this point)
Well-being and motivation of FY2s
8. How is the well-being and motivation of FY2 doctors evaluated in their training? (10 minutes)
Prompt: How is this assessed, when and by whom? (Is it part of the assessment process?)
Prompt: In your experience what motivates FY2 doctors?
Prompt: What aspects of work do FY2s struggle with?
Prompt: Is the potential impact on patient care considered?
Prompt: Do FY2s integrate into the ED?
9. What clinical support or supervision do the FY2 doctors get in the ED? (5 minutes)
Prompt: Do you consider the clinical support to be adequate or is too much support/supervision required?
Prompt: What other types of support do FY2s receive (peers, occupational health)?
Prompt: What support should they receive?
Impact on care
10. To what extent do you feel FY2s in your ED contribute to the provision of a good quality service? (5 minutes)
Prompt: Issues such as workload, work rate, independent working.
Prompt: Are there any improvements that could be made to the way FY2s work in your ED? Give examples.
Ending
Is there any information you would like to add that would enable us to understand the current and planned future state of FY2 training?
Thank you for your valuable time – we will be sending you a copy of the Executive Summary of our final report. (5 minutes)
Appendix 6 Letter of invitation to postgraduate medical education stakeholders and emergency department consultants/training leads for participation in phase 1 interviews
Sent to staff via NHS service address or via e-mail.
Dear [name of individual],
Title of project: The EDiT Study: Evaluation of Doctors in Training (phase 1: consultation and scoping study)
I am writing to ask if you would kindly consider taking part in an interview for a national research study evaluating the experiences of foundation year 2 (FY2) doctors and how this impacts on their well-being, motivation and the quality of care they provide. I am contacting you because the organisation where you work is involved in the study and you have been identified because you are involved in FY2 training and may be interested in participating.
The study is funded for 33 months. Phase 1 lasts for 5 months and includes a consultation and scoping study in up to four postgraduate deaneries and EDs in England. Interviews with key stakeholders in these organisations are part of this consultation study and I am asking you to consider taking part in one of these interviews.
I am attaching some further information about the research and what agreeing to take part in the interviews may involve for you. I would be grateful if you could read this carefully. I hope this is clear but if you have any further questions please contact the project manager Colin O’Keeffe on 0114 222 0780 or email him at c.okeeffe@sheffield.ac.uk.
If after reading the information leaflet and discussing this with others you feel happy to participate then please email the project manager who will contact you regarding setting up the interview. If you would rather not take part then thank you for your time and we will not contact you again.
Yours sincerely
Signed
Suzanne Mason Lead Investigator
Appendix 7 Participant information sheet for phase 1 interviews
The EDiT study: Evaluation of Doctors in Training: phase 1 interviews with postgraduate medical education stakeholders/ED consultants (training leads)
Participant information sheet
We would like to invite you to take part in a research study. The study is evaluating the experiences of foundation year 2 (FY2) doctors and the impact on their well-being and the quality of care they provide. The evaluation is being carried out in England. Before you make any decision regarding participation you need to understand why the research is being done and what it would involve for you. Please take time to read the following information carefully. Talk to others about the study if you wish. If you have any further questions, please contact the project manager (contact details provided at the end of this leaflet).
What is the purpose of the study?
The purpose of the study is to understand the current arrangements for the implementation of FY2 training in England on a national and regional basis. We are particularly interested in how the planning and implementation of training at the national, regional and local level impacts on the well-being of FY2 doctors. A number of interviews are taking place in England in order to better understand these issues.
Who is conducting the study?
The work has been funded by the NIHR Service Delivery and Organisation (SDO) Research Programme. It is being undertaken independently by a research team, led by a senior medical doctor based at the University of Sheffield.
Why have I been selected?
You have been selected because the organisation where you work is involved in the planning and implementation of FY2 training. You have been identified as someone who delivers FY2 training and therefore may be interested in participating.
Do I have to take part?
A decision to take part in this study is entirely voluntary. Any decision regarding participation will be confidential between you and the research team. You are also free to withdraw from the study at anytime.
What does agreeing to take part involve?
Your involvement would be to participate in one interview with a member of the research team. The main topic of discussion will be how postgraduate medical education is planned and implemented by your organisation, particularly in regard to FY2s. The interview will take place at a convenient time for you, either at your place of work or over the telephone. The discussion will last for around an hour. Data collected from the interview will be analysed independently by the research team. If you agree to take part you would participate in the study for 5 months during the consultation phase of the project (phase 1). The research study is funded for 33 months in total.
What about confidentiality and data protection?
All information you may give will be treated in the strictest confidence. The interviewer will take notes on the discussion but any information you give during the interview will be fully anonymised and combined with the views and experiences of other participants who agree to take part. No individual will be identifiable at any stage in the publication or presentation of the findings. Data collected will be stored securely in a manner consistent with the data protection act.
What are the risks of participating?
We believe that the risks are minimal. We understand that there are many demands on your time and there is some inconvenience in taking part in the interview. You are free at any stage to withdraw from the interview or take time out if you wish.
How will I benefit from this study?
We hope you will find the experience of taking part in the interviews interesting and useful. You will have the opportunity to receive feedback from the study team in a short report of the overall interview findings if you wish to.
What will happen as a result of the study?
The data collected from you will be aggregated with the data from other participants in the interviews and this will be analysed and used to produce a report which will be made available for all participants. This report will be published by the funders of the study and will be available to inform policy decisions around postgraduate training.
Who has reviewed the study?
All research in the NHS is looked at by an independent group of people, called a Research Ethics Committee, to protect your safety, rights, well-being and dignity. This study has been reviewed and given a favourable opinion by ___________________ Research Ethics Committee. The study has also been scientifically reviewed by independent peer reviewers prior to funding being given.
What should I do now?
You should take enough time as you feel you need to consider whether to take part. If you do wish to take part, there is a contact email/number of the Project Manager to reply to below. The research team will then contact you to arrange a time for the interview and forward a consent form for you to sign. If you do not wish to take part then you are not required to do anything and we will not contact you again.
What will happen if I don’t want to carry on with the study?
If after consenting to take part in the interview you subsequently change your mind about participating, you can withdraw from the study at any time (including during or after the interview itself). Any data collected from you would not be included in the study.
Further contact
If you have any further questions then please feel free to contact Colin O’Keeffe, Project Manager.
Thank you for your time
Appendix 8 Consent form for phase 1 interviews
Appendix 9 Foundation year 2 doctors focus group schedule (phase 1)
Foundation year 2 doctors focus group schedule
As people come in ask them to complete the consent form.
Introduction (5 minutes)
Good morning/afternoon, my name is Angela Carter/Colin O’Keeffe and Suzanne Mason and we are researchers working on the EDiT study. Many thanks for your interest in this work.
I hope you will have seen the information sheet about the study. If not here is another copy. If you are happy to take part in this discussion I would be grateful if you could sign the consent form.
This is one of a planned series of focus groups and interviews to discuss with those involved in foundation training to find out what it is like to do this work and training and what contributes to a successful learning experience. The aim of the project is to appreciate the things that contribute to effective training and how this may be implemented elsewhere. We are interested in your ideas of how this training can be done in the best way; in particular what motivates you and gives you confidence when working with patients.
This is a supportive study; no one is here to criticise what you do. We will examine issues today and ask for your suggestions that will be put in our final report. Anything that you say to us today will be treated in confidence and NO individual will be identified. Identities will be protected and individuals will not be named. Further, no feedback will be given to anyone in the trust or other organisations about what we discuss today. The study will conclude next year and the findings will be made available.
It is intended that we work together for 55 minutes. Are you happy to continue? Let anyone leave who is not happy to contribute to the study. (5 minutes)
Start of group
First establish that the group are people who are FY2 doctors.
1. Think of an experience of working practice that gives you confidence in your competence to deliver good patient care.
Can you write down (for a few minutes keeping this to yourself) the things that give you confidence
Individual working for three or four minutes on successful and unsuccessful events. (5 minutes)
1a. What gives you confidence?
1b. What helps you feel competent?
Go round the group recording material on a flip chart exploring comments for specific detail. (10 minutes)
(20 minutes)
2. Think about when you finish a shift – what are the things that you worry about/keep you awake?
Can you write down (for a few minutes keeping this to yourself) the things that give you confidence
Individual working for three or four minutes on successful and unsuccessful events. (3 minutes)
Go round the group recording material on a flip chart exploring comments for specific detail and differences. (15 minutes)
Prompts: What clinical support do you get in your training? Who is this from (fellow doctors, nursing staff, AHPs)? What part does the formal assessment play in your training?
(35 minutes to here)
3. What could be done to improve your work experience as an FY2 doctor in the ED?
Can you write down (for a few minutes keeping this to yourself) the things that give you confidence
Individual working for three or four minutes on successful and unsuccessful events. (3 minutes)
Go round the group to get out ideas (encourage a debate and workable solutions looking for the resources that will be required). (15 minutes)
Consider length of attachment, supervision, order of placements; assessments, size of department, number of trainees; shifts; mentors; pressure of working environment; feedback on work performance.
(50 minutes to here)
4. We are keen to use a questionnaire to examine the issues the next intake of FY2s have in more detail – this would be at the beginning, middle and end of placements – do you think this is feasible and in what format would you best like to receive it – electronic via email, paper, other? (7 minutes)
(57 minutes to here)
Conclusion
We have reached the end of our time now and would like to thank you for your participation. Many thanks for your time. A copy of the Executive Summary of our report will be made available to all who have participated in this study. (3 minutes)
End
Appendix 10 Letter of invitation to foundation year 2 doctors for participation in phase 1 focus groups
Distributed at deanery training event.
Dear Sir/Madam,
Title of project: The EDiT Study: Evaluation of Doctors in Training (Phase 1: consultation and scoping study)
I am writing to ask if you would kindly consider taking part in a focus group for a national research study, evaluating your experiences as a foundation year 2 (FY2) doctor and how this impacts on your well-being, motivation and confidence. I am contacting you with the permission of the deanery and foundation school which organises your FY2 programme.
The study will last for 5 months and includes work in four deaneries in England. Focus group discussions with interested FY2 doctors are planned in each of the four deaneries.
I am attaching some further information about the research and what agreeing to take part in the focus groups may involve for you. I would be grateful if you could read this carefully. I hope this is clear but if you have any further questions please contact the project manager Colin O’Keeffe.
If after reading the information leaflet and discussing this with others you feel happy to participate then please email the project manager (see above) who will then contact you about taking part. If you do not feel as if you want to be involved in the study then thank you for your time and you will not be contacted again.
Yours sincerely
Signed
Suzanne Mason Lead Investigator
Appendix 11 Focus group participant information sheet
The EDiT study: Evaluation of Doctors in Training (Phase 1: focus group with foundation year 2 doctors)
Participant information sheet
We would like to invite you to take part in a focus group for a research study. The study is evaluating the experience of foundation year 2 (FY2) doctors in England and the impact on their well-being, motivation and confidence in their role. Before you make any decision regarding participation you need to understand why the research is being done and what it would involve for you. Please take time to read the following information carefully. Talk to others about the study if you wish. You may wish to speak with your FY2 representative about participating. Alternatively, if you have any further questions, please contact the project manager (contact details provided at the end of this leaflet).
What is the purpose of the study?
The purpose of the study is to understand what influences the well-being, motivation and confidence of FY2 doctors. There have been a number of policy initiatives aimed at improving the experiences of the NHS workforce (including postgraduate doctors) and evaluation of these initiatives is aimed to measure their successes and failures.
Who is conducting the study?
The work has been funded by the NIHR Service Delivery and Organisation (SDO) Research Programme. It is being undertaken independently by a research team, led by a senior medical doctor based at the University of Sheffield.
Why have I been selected?
You have been selected because your FY2 programme is organised by a deanery which has agreed for you to be approached regarding participation in the study.
Do I have to take part?
A decision to take part in this study is entirely voluntary and it is entirely your decision whether to take part or not. Any decision regarding your participation will be confidential between you and the research team. You are also free to withdraw from the study at anytime without any repercussions to yourself.
What does agreeing to take part involve?
Your involvement would be to participate in one focus group discussion with other FY2 doctors, facilitated by a member of the research team. The main topic of discussion will be what contributes to a successful learning and training experience. The focus group will take place at a convenient time for you. The discussion will last for around an hour. Data collected from the focus group will be analysed independently by the research team.
What about confidentiality and data protection?
All information you may give will be treated in the strictest confidence. The researchers will take notes during the discussion but any information you give during the focus group will be fully anonymised and combined with the views and experiences of other FY2 doctors who agree to participate. If an issue is raised by participants during the focus groups which is judged to have serious consequences for either the well-being of FY2 doctors, or serious implications for patients, then this issue may be discussed with senior staff in the postgraduate deanery and the ED. However, no individual FY2 doctor will be identifiable at any stage in discussions, publication or presentation of the findings. Data collected will be stored securely in a manner consistent with the Data Protection Act.
What are the risks of participating?
We understand that there are many demands on your time and there is some inconvenience in taking part in the focus group. We are also aware you may have concerns about taking part in further evaluation of your role along with your work-based assessments. The focus group will be organised at a time which is convenient to you and is likely to take place during teaching time organised by the deanery which runs your Foundation Programme. We will be asking you about both positive and negative experiences during your FY2 year. There is a very small chance you may become upset if you voluntarily disclose an experience that was particularly stressful or unhappy. You are free at any stage to withdraw from the focus group or take time out if you wish. The focus group is designed to be a supportive environment and the facilitator is an experienced researcher in this methodological approach. Only other FY2 doctors and the research team will be present at the focus group.
How will I benefit from this study?
We hope you will find the experience of taking part in the focus group interesting and useful. You will have the opportunity to receive feedback from the study team in a short report of the overall focus group findings if you wish to.
What will happen as a result of the study?
The data collected from you will be aggregated with the data from other FY2 participants and this will be analysed and used to produce a report which will be made available for all participants. This report will be published by the funders of the study and will be available to inform policy decisions around postgraduate training.
Who has reviewed the study?
All research in the NHS is looked at by an independent group of people, called a Research Ethics Committee, to protect your safety, rights, well-being and dignity. This study has been reviewed and given favourable opinion by Leeds West Research Ethics Committee. The study has also been scientifically reviewed by independent peer reviewers prior to funding being given.
What should I do now?
You should take enough time as you feel you need to consider whether to take part. If you do wish to take part, there is a contact email/number for the study project manager to reply to below. The research team will then forward a consent form for you to sign along with the details of when and where it is suggested the focus group will take place. If you do not wish to take part then you are not required to do anything and we will not contact you again.
What will happen if I don’t want to carry on with the study?
If you after consenting to take part in the focus group you subsequently change your mind about participating, you can withdraw from the study at any time (including during or after the focus group itself). Any data collected from you would not be included in the study.
Further contact
If you have any further questions then please feel free to contact Colin O’Keeffe, Project Manager.
Thank you for your time
Appendix 12 Focus group consent form
Appendix 13 Website information/screenshot
Appendix 14 Letter of invitation to foundation year 2 doctors for participation in phase 2
Distributed at deanery training event.
Dear Sir/Madam,
Title of project: the EDiT study: Evaluation of Doctors in Training (phase 2: longitudinal observational study of foundation year 2 doctors)
I am writing to ask you to consider taking part in a national research study evaluating the well-being of foundation year 2 (FY2) doctors and the quality of care they provide. The focus of this research is on the experiences of FY2 doctors in the emergency department (ED) and we are interested in your experiences in your ED placement in particular. I am contacting you with the permission of the deanery and foundation school which organises your FY2 programme.
Part of the national evaluation is a 12-month longitudinal observational study of FY2 doctors. It is this particular study I am asking you to consider taking part in.
I am attaching some further information about the research and what agreeing to take part may involve for you. I would be grateful if you could read this carefully. I hope this is clear but if you have any further questions please contact the project manager Colin O’Keeffe.
If after reading the information leaflet and discussing this with others you feel happy to participate then please sign and date the enclosed consent form and return this in the pre-paid envelope provided. If you wish to discuss participation further then please email the project manager (see above), who will then contact you again about taking part. If you do not want to be involved in the study and you want no further contact about it, then please email this request to the project manager.
Many thanks for your time
Yours sincerely
Signed
Suzanne Mason Lead Investigator
Appendix 15 Survey participant information sheet
The EDiT study: Evaluation of Doctors in Training (phase 2: longitudinal observational study of foundation year 2 doctors)
Participant information sheet
We would like to invite you to take part in a research study. The study is evaluating the experience of foundation year 2 (FY2) doctors in the emergency department (ED) and the impact on their well-being and the quality of care they provide. The evaluation is being carried out in a number of EDs in England. Please take the time to read the following information which explains why the research is being done and what it would involve for you. Talk to others about the study if you wish.
You may wish to speak with your FY2 representative (contact details to be included) about participating. Alternatively, If you have any further questions, please contact the project manager (contact details provided at the end of this leaflet).
What is the purpose of the study?
The purpose of the study is to understand what influences the well-being, motivation and confidence of FY2 doctors in the ED and how this is linked to the quality of care they provide. There have been a number of policy initiatives aimed at improving the experiences of the NHS workforce (including postgraduate doctors) and evaluation of these initiatives is aimed to measure their successes and failures.
Who is conducting the study?
The work has been funded by the NIHR Service Delivery and Organisation (SDO) Research Programme. It is being undertaken independently by a research team, led by a senior medical doctor based at the University of Sheffield. The research is being conducted independently by the research team.
Why have I been selected?
You have been selected because your FY2 programme is organised by a deanery which has agreed for you to be approached regarding participation in the study AND because you have an FY2 placement in the ED.
Do I have to take part?
We understand there are various expectancies placed upon you in your roles but please be assured there is no pressure on you to participate. A decision to take part in this study is voluntary and it is your decision entirely whether to take part or not. Any decision regarding your participation will be confidential between you and the research team. You are also free to withdraw from the study at any time without any repercussions to yourself.
What does agreeing to take part involve?
If you agree to take part you would participate in the longitudinal observational study for the full 12 months of your FY2 year. The research study is funded for 33 months in total.
-
Initially some limited contact details (name and email address) will be entered onto a database in order that we may contact you about the study when necessary to do so. A study ID will be assigned to each participating doctor which will substitute for these contact details as a means of ensuring anonymity of participants.
-
Your main involvement would be to complete a questionnaire up to a maximum of four times during your FY2 year. You will be contacted by email in order that a link to an electronic questionnaire can be provided at the appropriate time points. Alternatively you may receive a postal questionnaire if this is considered a more appropriate method in your department. The questionnaire will use validated measures to assess your well-being, confidence and motivation at key time points in your FY2 year. It will take in the region of around 15–20 minutes to complete.
-
In addition, a random selection of ED notes, in which you were the primary care giver during your ED placement, will be reviewed by experienced ED clinicians in order to assess the quality and safety of care provided. This process will take place retrospectively, after you have left the ED. This process will be carried out exclusively by the reviewers and the research team. A member of the clinical team in each ED will identify the relevant notes for all participating FY2 doctors in each participating ED. The research team will randomly select a small sample of these notes for each doctor. Each set of notes will be fully anonymised and the relevant doctor study ID assigned. In this way the reviewers will be blinded to who has carried out the care.
-
Data collected from you, from the survey and the notes review, will be analysed independently by the research team. All data collected will be entered onto a database which will be fully anonymised. Your personal details will not be stored on this database. Data collected from you will be aggregated with the data of the other participating trainee doctors in your department in order that relationships between well-being and quality can be measured at the department level and variation across participating EDs can be measured. In this way no individual doctor’s well-being or quality-of-care scores will be reported. There may be instances where a participating doctor’s research scores may need to be examined on an individual basis. The quality-of-care scores for an individual doctor may be such that there is evidence that patients are being put at serious risk. The processes to be followed in such instances are described below under confidentiality and data protection.
What about confidentiality and data protection?
All information you may give will be treated in the strictest confidence. It is possible that we will hold limited electronic information about you such as your name and email address. This information will be held purely for the means of contacting you about the study where necessary to do so. After the study is complete all names and email addresses will be deleted.
No individual FY2 doctor will be identifiable at any stage in the publication or presentation of the findings. Data collected will be stored securely in a manner consistent with the Data Protection Act.
Exceptional circumstances where breaching of confidentiality may be necessary
Unless exceptional circumstances demand otherwise, individual identifiable study data will be kept confidential at all times between yourself and the study team. There are instances where data confidentiality would have to be compromised and information disclosed to an individual outside the research team. They are as follows:
-
If included clinical notes were reviewed and detailed care which may have put a patient at serious risk, then the identity of the doctor who provided this care would be disclosed. The relevant ID number of the participating doctor would be disclosed to the lead consultant of the department by the doctor carrying out the case notes review. Any action taken would be at the discretion of this lead clinician, but may include contacting the relevant participating doctor to discuss the matter further and recommend any necessary support. The types of errors which may result in this course of action are as follows: serious medication errors and unidentified missed conditions such as a missed fracture.
-
If you were interested in receiving feedback regarding your scores on the well-being survey or the quality of care study then this could only be provided by accessing your personal identifiers in order to select the relevant data and send a summary to you.
What are the risks of participating?
We understand that there are many demands on your time and there is some inconvenience in completing surveys. As described above there may be instances when confidentiality has to be broken and your results from the study discussed with a third party.
How will I benefit from this study?
We believe there are benefits to taking part in this study. If you specifically request the information from the research team, you will be able to receive feedback on your individual scores from the well-being survey and the quality of care study. As stated above, in order to provide this information your confidentiality would have to be breached.
What will happen as a result of the study?
The data collected from you will be aggregated with the data from other FY2 participants and this will be analysed and used to produce a report which will be made available for all participants. This report will be published by the funders of the study and will be available to inform policy decisions around postgraduate training.
Who has reviewed the study?
All research in the NHS is looked at by an independent group of people, called a Research Ethics Committee, to protect your safety, rights, well-being and dignity. This study has been reviewed and given favourable opinion by Leeds East Research Ethics Committee on 30 September 2009. The study has also been scientifically reviewed by independent peer reviewers prior to funding being given.
What should I do now?
You should take enough time as you feel you need to consider whether to take part. If you do wish to take part, there is a contact email/number for the study project manager to reply to below. The research team will then forward a consent form for you to sign along with the details of when the study will begin.
What will happen if I don’t want to carry on with the study?
If you agree to participate but then decide to withdraw from the study, then there will be no repercussions for you. Any data we have collected will be analysed as planned but you will not receive any additional questionnaires nor will your notes be included in the review of quality of care.
Further contact
If you have any further questions then please feel free to contact Colin O’Keeffe.
Thank you for your time
Appendix 16 Survey consent form
Appendix 17 The EDiT study survey: pilot questionnaire
A survey on working as a foundation doctor
Once you have read the following information please enter the survey password and your email address (at the bottom of this page) and press ‘Next’ to begin the survey.
What is this survey?
This is a survey of your views and opinions of your current F2 PLACEMENT and of the department as a whole where you are undertaking this placement. This is not a test. There are no right or wrong answers.
We want to know your personal views on the issues raised in the questionnaire. You will have received an information sheet about why this questionnaire is being administered. If you want further information then please visit the study website at http://edit.group.shef.ac.uk/.
Who will see my answers?
The information you give is totally confidential. Findings will be made available to all who participate, but in such a way that it is not possible for individuals to be identified. The research team at the University of Sheffield will be the only organisation to have access to the questionnaires completed by individuals.
How do I fill in this survey?
Please complete the questionnaire for your current role. The survey will take about 15–20 minutes to complete.
How should I respond?
For each statement you are asked to select one response that best fits your views. Please answer all the questions as openly and honestly as possible. Respond according to your first reaction. Do not spend too long on one question.
Please enter your email address.*
____________________________________________
Consent form
Title of project: The EDiT Study: Evaluation of Doctors in Training (Phase 2: Longitudinal Observational Study of Foundation Year 2 Doctors)
Name of researcher: Ms Suzanne Mason, Principal Investigator
I confirm that I have read and understand the information sheet dated 29/09/2009 (version 5) for the above study. I have had the opportunity to consider the information, ask questions and have had these answered satisfactorily. *[ ] Yes
I understand that my participation in the study is voluntary and that I am free to withdraw at any time without giving any reason and without being affected in any way. *[ ] Yes
I understand that relevant data collected from me during the study may be looked at by authorised individuals such as regulatory authorities (for purposes such as monitoring the conduct of the research). I give permission for these individuals to have access to data collected during the study. *[ ] Yes
I agree to take part in the above study. *[ ] Yes
Your confidence in managing common conditions
The following section is designed to identify how confident you feel in managing common medical conditions, many of which you will come across throughout your Foundation Years.
(*Indicates that a question is compulsory and must be completed before moving to the next page.)
1. How do you feel about managing patients with the following presenting complaints?*
Select a response from 1–9 and mark below with 1 = lowest level of confidence and 9 = highest level of confidence.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
|---|---|---|---|---|---|---|---|---|---|
| Diarrhoea and vomiting | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Shortness of breath | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Collapse – unknown cause | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Acute mental health problem | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Elderly fall | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Chest pain | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Back pain | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Cardiac arrest | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Palpitations | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Abdominal pain | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Acute allergic reaction | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Left ‘side’ pain | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Acute stroke | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Overdose – paracetamol | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Diabetic ketoacidosis | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Acute confusion | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Headache | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Seizure | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Cellulitis | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Haematemesis | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Rash | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Acute painful joint | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Rectal bleeding | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
2. How experienced are you at performing the following practical techniques?*
1–2 = no/little experience, 3–4 = some experience with support, 5 = moderate experience, 6–7 = good experience, 8–9 = confident alone
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
|---|---|---|---|---|---|---|---|---|---|
| Defibrillation | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Arterial blood gas analysis | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Suturing | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| ECG interpretation | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Radiograph interpretation | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
3. Would your management of the conditions shown be improved with:*
| Strongly disagree | Disagree | Neither disagree nor agree | Agree | Strongly agree | |
|---|---|---|---|---|---|
| Clearer guidelines | ( ) | ( ) | ( ) | ( ) | ( ) |
| Better teaching | ( ) | ( ) | ( ) | ( ) | ( ) |
| More supervision | ( ) | ( ) | ( ) | ( ) | ( ) |
Your job
The following questions ask you to describe your job. Please answer all the questions ticking the answer which best describes your current role.
4. How often do you find yourself meeting the following problems in carrying out your job*
| Not at all | Just a little | Moderate amount | Quite a lot | A great deal | |
|---|---|---|---|---|---|
| I do not have enough time to carry out my work | ( ) | ( ) | ( ) | ( ) | ( ) |
| I cannot meet all the conflicting demands made on my time at work | ( ) | ( ) | ( ) | ( ) | ( ) |
| I never finish work feeling I have completed everything I should | ( ) | ( ) | ( ) | ( ) | ( ) |
| I am asked to do work without adequate resources to complete it | ( ) | ( ) | ( ) | ( ) | ( ) |
| I cannot follow best practice in the time available | ( ) | ( ) | ( ) | ( ) | ( ) |
| I am required to do basic tasks, which prevent me completing more important ones | ( ) | ( ) | ( ) | ( ) | ( ) |
5. How true are the following of your job?*
| Not at all | Just a little | Moderate amount | Quite a lot | A great deal | |
|---|---|---|---|---|---|
| I have clear, planned goals and objectives for my job | ( ) | ( ) | ( ) | ( ) | ( ) |
| I know what my responsibilities are | ( ) | ( ) | ( ) | ( ) | ( ) |
| I know that I have divided my time properly | ( ) | ( ) | ( ) | ( ) | ( ) |
| Explanation is clear of what has to be done | ( ) | ( ) | ( ) | ( ) | ( ) |
| I know exactly what is expected of me | ( ) | ( ) | ( ) | ( ) | ( ) |
6. The following statements concern the information you and others get about your work performance.*
| Strongly disagree | Disagree | Neither disagree nor agree | Agree | Strongly agree | |
|---|---|---|---|---|---|
| I usually know whether or not my work is satisfactory in this job | ( ) | ( ) | ( ) | ( ) | ( ) |
| I often have trouble figuring out whether I’m doing well or poorly on this job | ( ) | ( ) | ( ) | ( ) | ( ) |
| Most people on this job have a pretty good idea of how well they are performing their work | ( ) | ( ) | ( ) | ( ) | ( ) |
| Most people on this job have trouble figuring out whether they are doing a good or bad job | ( ) | ( ) | ( ) | ( ) | ( ) |
Working relationships
The following questions ask you about the relationships you have in your current role. Please answer all the questions, selecting the answer which best describes how you feel.
7. How much does your Clinical Supervisor:*
| To a very little extent | To a little extent | To some extent | To a great extent | To a very great extent | |
|---|---|---|---|---|---|
| Encourage you to give your best effort? | ( ) | ( ) | ( ) | ( ) | ( ) |
| Set an example by working hard him/herself? | ( ) | ( ) | ( ) | ( ) | ( ) |
| Offer new ideas for solving job-related problems? | ( ) | ( ) | ( ) | ( ) | ( ) |
| Encourage those who work for him/her to work as a team? | ( ) | ( ) | ( ) | ( ) | ( ) |
8. To what extent can you count on your Clinical Supervisor:*
| Not at all | To a small extent | Neither great nor small extent | To a great extent | Completely | |
|---|---|---|---|---|---|
| To listen to you when you need to talk about problems at work? | ( ) | ( ) | ( ) | ( ) | ( ) |
| To help you with a difficult task at work? | ( ) | ( ) | ( ) | ( ) | ( ) |
9. In a typical week how many hours do you have contact with your Clinical Supervisor?*
____________________________________________
10. To what extent can you:*
| Not at all | To a small extent | Neither great nor small extent | To a great extent | Completely | |
|---|---|---|---|---|---|
| Count on your colleagues to listen to you when you need to talk about problems? | ( ) | ( ) | ( ) | ( ) | ( ) |
| Count on your colleagues to back you up at work? | ( ) | ( ) | ( ) | ( ) | ( ) |
| Count on your colleagues to help you with a difficult task at work? | ( ) | ( ) | ( ) | ( ) | ( ) |
| Really count on your colleagues to help you in a crisis situation at work, even though they would have to go out of their way to do so? | ( ) | ( ) | ( ) | ( ) | ( ) |
Your well-being and motivation
The following questions ask you to describe things you like and dislike about your current role and your general well-being. Please answer all the questions, ticking the answer which best describes what you do most of the time.
11. The statements below concern how satisfied you feel with different aspects of your role. How satisfied are you with:*
| Extremely dissatisfied | Very dissatisfied | Moderately dissatisfied | Not sure | Moderately satisfied | Very satisfied | Extremely satisfied | |
|---|---|---|---|---|---|---|---|
| The physical work conditions? | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| The freedom to choose your own method of working? | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Your fellow workers? | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| The recognition you get for good work? | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Your Clinical Supervisor? | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| The amount of responsibility you are given? | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Your rate of pay? | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Your opportunity to use your abilities? | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Relations between doctors and other health-care professionals? | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Your chance of career progression? | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| The way the department is managed? | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| The attention paid to suggestions you make? | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Your hours of work? | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| The amount of variety in your job? | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Your job security? | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
The following questions ask you about your general well-being and motivation. Please answer all the questions. It is possible that completing some questions may draw your attention to problems you experience. If you are worried that these are serious, we would advise you to contact your GP.
12. In the last month, how much of the time has your current role made you feel:*
| Not at all | Just a little | A moderate amount | Quite a lot | A great deal | |
|---|---|---|---|---|---|
| Gloomy | ( ) | ( ) | ( ) | ( ) | ( ) |
| Uneasy | ( ) | ( ) | ( ) | ( ) | ( ) |
| Worried | ( ) | ( ) | ( ) | ( ) | ( ) |
| Tense | ( ) | ( ) | ( ) | ( ) | ( ) |
| Depressed | ( ) | ( ) | ( ) | ( ) | ( ) |
| Miserable | ( ) | ( ) | ( ) | ( ) | ( ) |
13. Thinking of your current role, how true are the following:*
| Strongly disagree | Disagree | Neutral | Agree | Strongly agree | |
|---|---|---|---|---|---|
| I often think about leaving medicine? | ( ) | ( ) | ( ) | ( ) | ( ) |
| It is very likely that I will actively look for a new job outside medicine in the next year? | ( ) | ( ) | ( ) | ( ) | ( ) |
| I am starting to ask my friends/contacts about other job possibilities outside medicine? | ( ) | ( ) | ( ) | ( ) | ( ) |
Please answer the following questions about your overall motivation in your current role by marking the most accurate answer.
14. How would you rate the amount of effort you put into your job?*
( ) Very low
( ) Low
( ) Moderate
( ) High
( ) Very high
15. I consistently put forth the maximum effort possible at work.*
( ) Strongly disagree
( ) Disagree
( ) Neutral
( ) Agree
( ) Strongly agree
16. How much of your total, maximum possible effort do you put into your job?*
( ) 50% or less
( ) 51–75%
( ) 76–85%
( ) 86–95%
( ) 96–100%
Please answer each question in relation to your current role by marking the most accurate answer.
17. It is not clear to me how much effort to put into different parts of my job.*
( ) Strongly disagree
( ) Disagree
( ) Neutral
( ) Agree
( ) Strongly agree
18. I divide my time across tasks in the way that is most helpful to the organisation.*
( ) Strongly disagree
( ) Disagree
( ) Neutral
( ) Agree
( ) Strongly agree
19. My supervisor and I agree on what tasks are most and least important.*
( ) Never
( ) Rarely
( ) Sometimes
( ) Usually
( ) Always
Please answer each question by marking the box that gives your opinion. We want to know how much effort in your role influences how good or bad your job outcomes are (such as criticisms, feelings of accomplishment, friendships).
20. I get better job outcomes if I increase my level of effort.*
( ) Never
( ) Rarely
( ) Sometimes
( ) Usually
( ) Always
21. There is a strong tie between how hard I work and how good my job outcomes are.*
( ) Strongly disagree
( ) Disagree
( ) Neutral
( ) Agree
( ) Strongly agree
22. Working hard on this job is not rewarded.*
( ) Strongly disagree
( ) Disagree
( ) Neutral
( ) Agree
( ) Strongly agree
23. Would you describe yourself as typically:*
| Extremely inaccurate | Very inaccurate | Moderately inaccurate | Slightly inaccurate | Not sure | Slightly accurate | Moderately accurate | Very accurate | Extremely accurate | |
|---|---|---|---|---|---|---|---|---|---|
| Careless | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Disorganised | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Efficient | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Inefficient | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Organised | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Practical | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Sloppy | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Systematic | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
24. People cope with difficult, stressful or upsetting situations in a variety of ways. Please read each statement and select the response that best indicates how much you tend to react in that way when faced with a difficult, stressful or upsetting situation. When faced with a difficult/stressful situation:*
| Never | Seldom | Sometimes | Often | Very often | |
|---|---|---|---|---|---|
| I try to figure out how to resolve the problem | ( ) | ( ) | ( ) | ( ) | ( ) |
| I act as though nothing happened, hoping it will go away | ( ) | ( ) | ( ) | ( ) | ( ) |
| I seek the support and guidance of other people | ( ) | ( ) | ( ) | ( ) | ( ) |
| I get upset or angry with the people who cause the problem | ( ) | ( ) | ( ) | ( ) | ( ) |
| I change something so the situation will improve | ( ) | ( ) | ( ) | ( ) | ( ) |
| I avoid the problem by sleeping, watching TV, engaging in diversionary activities more | ( ) | ( ) | ( ) | ( ) | ( ) |
| I ask someone I respect for advice | ( ) | ( ) | ( ) | ( ) | ( ) |
| I try to get back at those who created the trouble | ( ) | ( ) | ( ) | ( ) | ( ) |
| I come up with a couple of strategies to make the situation better | ( ) | ( ) | ( ) | ( ) | ( ) |
| I keep my concerns and emotions about the situation to myself | ( ) | ( ) | ( ) | ( ) | ( ) |
| I talk to friends or family about my circumstances | ( ) | ( ) | ( ) | ( ) | ( ) |
| I figure out who was responsible for what happened | ( ) | ( ) | ( ) | ( ) | ( ) |
| I double my efforts to correct the situation and achieve my objective | ( ) | ( ) | ( ) | ( ) | ( ) |
| I put off dealing with the matter | ( ) | ( ) | ( ) | ( ) | ( ) |
| I get sympathy and understanding from someone | ( ) | ( ) | ( ) | ( ) | ( ) |
| I make sure that those responsible for the problem receive their due punishment | ( ) | ( ) | ( ) | ( ) | ( ) |
Thinking of the decisions (or judgements) about patient care that you have made during your current role assess the following statements:
25. I am confident that I made the appropriate decisions.*
( ) Strongly disagree
( ) Disagree
( ) Neutral
( ) Agree
( ) Strongly agree
26. Considering the information available to me I made the best decisions possible.*
( ) Strongly disagree
( ) Disagree
( ) Neutral
( ) Agree
( ) Strongly agree
27. How much assistance did you need in making these decisions?*
( ) None at all
( ) Just a little
( ) A moderate amount
( ) Quite a lot
( ) A great deal
28. Thinking of your current role did you have:*
| None | Just a little | A moderate amount | Quite a lot | A great deal | |
|---|---|---|---|---|---|
| Any formal teaching offered in your department (in addition to the generic teaching)? | ( ) | ( ) | ( ) | ( ) | ( ) |
| Any informal training offered in your department (in addition to the generic training), e.g. one-to-one shop floor teaching from a senior member of the medical staff, informal mentoring by senior medical staff? | ( ) | ( ) | ( ) | ( ) | ( ) |
| Any feedback on the quality of your work? | ( ) | ( ) | ( ) | ( ) | ( ) |
29. Thinking about your current role:*
| Not at all | Just a little | A moderate amount | Quite a lot | A great deal | |
|---|---|---|---|---|---|
| Has your knowledge of medical conditions increased? | ( ) | ( ) | ( ) | ( ) | ( ) |
| Do you feel more able to work as part of the clinical team? | ( ) | ( ) | ( ) | ( ) | ( ) |
| Do you understand more about how health-care professionals work together? | ( ) | ( ) | ( ) | ( ) | ( ) |
Background details
It is important we know some of your background details to represent the views of different groups of people.
About your job:
30. Year of qualification:*____________________________________________
31. Place of qualification:*
( ) UK
( ) Non-UK
About you:
32. Age:* ____________________________________________
33. Are you:*
( ) Male?
( ) Female?
34. What is your ethnic background? (Please select the answer that best describes your ethnic background)*
( ) White – British
( ) White – Irish
( ) White – Other
( ) Black – British
( ) Black – Caribbean
( ) Black – African
( ) Any other Black background
( ) Asian – British
( ) Asian – Chinese
( ) Asian – Indian
( ) Asian – Pakistani
( ) Asian – Bangladeshi
( ) Any other Asian background
( ) Mixed – White and Black British
( ) Mixed – White and Black Caribbean
( ) Mixed – White and Black African
( ) Mixed – White and Asian
( ) Any other mixed background
( ) Any other ethnic group (please specify): _________________
Hours of work:
35. In a typical working week in your current role, how many hours are you contracted to work?*
____________________________________________
36. What is the total number of extra hours worked in a typical week?*
____________________________________________
37. In the last four weeks of your current role have you had a shift changed at short notice (less than five days)?*
( ) Yes
( ) No
Foundation training experience:
38. Please indicate your first, second and final F1 placements:*
| General practice | Hospital medicine | Hospital surgery | Emergency medicine | Obstetrics and gynaecology | Radiology | Psychiatry | Paediatrics and child health | Trauma and orthopaedics | Medical education | Academic based | Laboratory medicine | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Your first F1 placement: | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Your second F1 placement: | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Your final F1 placement: | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
39. Please indicate your first, second and final F2 placements:*
| General practice | Hospital medicine | Hospital surgery | Emergency medicine | Obstetrics and gynaecology | Radiology | Psychiatry | Paediatrics and child health | Trauma and orthopaedics | Medical education | Academic based | Laboratory medicine | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Your first F2 placement: | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Your second F2 placement: | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Your final F2 placement: | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
Future plans:
40. What do you plan to do after your F2 year?*
( ) Take a short-term contract in medicine
( ) Work abroad in medicine
( ) Take some time out from medicine
( ) Don’t know yet
( ) Go onto specialist training
What specialty will you be moving into?
( ) General practice
( ) Hospital medicine
( ) Hospital surgery
( ) Emergency medicine
( ) Obstetrics and gynaecology
( ) Radiology
( ) Psychiatry
( ) Paediatrics and child health
( ) Trauma and orthopaedics
( ) Medical education
( ) Academic based
( ) Laboratory medicine
( ) Other (please state): _________________
Further comments
41. If you have any further comments to make, please feel free to write them below.
__________________________________________________________________________
__________________________________________________________________________
Thank you for your co-operation.
Dr A Carter, Dr CB Stride, Ms S Mason, Mr C O’Keeffe
Copyright 2010 the Authors. All rights reserved.
Appendix 18 Final questionnaire
A survey on working as a foundation doctor
Once you have read the following information please enter the survey password and your email address (at the bottom of this page) and press ‘Next’ to begin the survey.
What is this survey?
This is a survey of your views and opinions of your current F2 PLACEMENT and of the department as a whole where you are undertaking this placement. This is not a test. There are no right or wrong answers.
We want to know your personal views on the issues raised in the questionnaire. You will have received an information sheet about why this questionnaire is being administered. If you want further information then please visit the study website at http://edit.group.shef.ac.uk/.
Who will see my answers?
The information you give is totally confidential. Findings will be made available to all who participate, but in such a way that it is not possible for individuals to be identified. The research team at the University of Sheffield will be the only organisation to have access to the questionnaires completed by individuals.
How do I fill in this survey?
Please complete the questionnaire for your current role. The survey will take about 15–20 minutes to complete.
How should I respond?
For each statement you are asked to select one response that best fits your views. Please answer all the questions as openly and honestly as possible. Respond according to your first reaction. Do not spend too long on one question.
Please enter your email address.*
____________________________________________
Consent form
Title of project: The EDiT Study: Evaluation of Doctors in Training (Phase 2: Longitudinal Observational Study of Foundation Year 2 Doctors)
Name of researcher: Ms Suzanne Mason, Principal Investigator
I confirm that I have read and understand the information sheet dated 29/09/2009 (version 5) for the above study. I have had the opportunity to consider the information, ask questions and have had these answered satisfactorily. *[ ] Yes
I understand that my participation in the study is voluntary and that I am free to withdraw at any time without giving any reason and without being affected in any way. *[ ] Yes
I understand that relevant data collected from me during the study may be looked at by authorised individuals such as regulatory authorities (for purposes such as monitoring the conduct of the research). I give permission for these individuals to have access to data collected during the study. *[ ] Yes
I agree to take part in the above study. *[ ] Yes
Your confidence in managing common conditions
The following section is designed to identify how confident you feel in managing common medical conditions, many of which you will come across throughout your Foundation Years.
(*Indicates that a question is compulsory and must be completed before moving to the next page.)
1. How do you feel about managing patients with the following presenting complaints?*
Select a response from 1–9 and mark below with 1 = lowest level of confidence and 9 = highest level of confidence.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
|---|---|---|---|---|---|---|---|---|---|
| Diarrhoea and vomiting | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Shortness of breath | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Collapse – unknown cause | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Acute mental health problem | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Elderly fall | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Chest pain | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Back pain | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Cardiac arrest | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Palpitations | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Abdominal pain | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Acute allergic reaction | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Left ‘side’ pain | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Acute stroke | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Overdose – paracetamol | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Diabetic ketoacidosis | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Acute confusion | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Headache | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Seizure | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Cellulitis | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Haematemesis | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Rash | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Acute painful joint | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Rectal bleeding | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
2. How experienced are you at performing the following practical techniques?*
1–2 = no/little experience, 3–4 = some experience with support, 5 = moderate experience, 6–7 = good experience, 8–9 = confident alone
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
|---|---|---|---|---|---|---|---|---|---|
| Defibrillation | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Arterial blood gas analysis | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Suturing | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| ECG interpretation | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Radiograph interpretation | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
3. Would your management of the conditions shown be improved with:*
| Strongly disagree | Disagree | Neither disagree nor agree | Agree | Strongly agree | |
|---|---|---|---|---|---|
| Clearer guidelines | ( ) | ( ) | ( ) | ( ) | ( ) |
| Better teaching | ( ) | ( ) | ( ) | ( ) | ( ) |
| More supervision | ( ) | ( ) | ( ) | ( ) | ( ) |
Your job
The following questions ask you to describe your job. Please answer all the questions ticking the answer which best describes your current role.
4. How often do you find yourself meeting the following problems in carrying out your job*
| Not at all | Just a little | Moderate amount | Quite a lot | A great deal | |
|---|---|---|---|---|---|
| I do not have enough time to carry out my work | ( ) | ( ) | ( ) | ( ) | ( ) |
| I cannot meet all the conflicting demands made on my time at work | ( ) | ( ) | ( ) | ( ) | ( ) |
| I never finish work feeling I have completed everything I should | ( ) | ( ) | ( ) | ( ) | ( ) |
| I am asked to do work without adequate resources to complete it | ( ) | ( ) | ( ) | ( ) | ( ) |
| I cannot follow best practice in the time available | ( ) | ( ) | ( ) | ( ) | ( ) |
| I am required to do basic tasks, which prevent me completing more important ones | ( ) | ( ) | ( ) | ( ) | ( ) |
5. How true are the following of your job?*
| Not at all | Just a little | Moderate amount | Quite a lot | A great deal | |
|---|---|---|---|---|---|
| I have clear, planned goals and objectives for my job | ( ) | ( ) | ( ) | ( ) | ( ) |
| I know what my responsibilities are | ( ) | ( ) | ( ) | ( ) | ( ) |
| I know that I have divided my time properly | ( ) | ( ) | ( ) | ( ) | ( ) |
| Explanation is clear of what has to be done | ( ) | ( ) | ( ) | ( ) | ( ) |
| I know exactly what is expected of me | ( ) | ( ) | ( ) | ( ) | ( ) |
6. The following statements concern the information you and others get about your work performance.*
| Strongly disagree | Disagree | Neither disagree nor agree | Agree | Strongly agree | |
|---|---|---|---|---|---|
| I usually know whether or not my work is satisfactory in this job | ( ) | ( ) | ( ) | ( ) | ( ) |
| I often have trouble figuring out whether I’m doing well or poorly on this job | ( ) | ( ) | ( ) | ( ) | ( ) |
| Most people on this job have a pretty good idea of how well they are performing their work | ( ) | ( ) | ( ) | ( ) | ( ) |
| Most people on this job have trouble figuring out whether they are doing a good or bad job | ( ) | ( ) | ( ) | ( ) | ( ) |
Working relationships
The following questions ask you about the relationships you have in your current role. Please answer all the questions, selecting the answer which best describes how you feel.
7. How much does your Clinical Supervisor:*
| To a very little extent | To a little extent | To some extent | To a great extent | To a very great extent | |
|---|---|---|---|---|---|
| Encourage you to give your best effort? | ( ) | ( ) | ( ) | ( ) | ( ) |
| Set an example by working hard him/herself? | ( ) | ( ) | ( ) | ( ) | ( ) |
| Offer new ideas for solving job-related problems? | ( ) | ( ) | ( ) | ( ) | ( ) |
| Encourage those who work for him/her to work as a team? | ( ) | ( ) | ( ) | ( ) | ( ) |
8. To what extent can you count on your Clinical Supervisor:*
| Not at all | To a small extent | Neither great nor small extent | To a great extent | Completely | |
|---|---|---|---|---|---|
| To listen to you when you need to talk about problems at work? | ( ) | ( ) | ( ) | ( ) | ( ) |
| To help you with a difficult task at work? | ( ) | ( ) | ( ) | ( ) | ( ) |
9. In a typical week how many hours do you have contact with your Clinical Supervisor?*
____________________________________________
10. To what extent can you:*
| Not at all | To a small extent | Neither great nor small extent | To a great extent | Completely | |
|---|---|---|---|---|---|
| Count on your colleagues to listen to you when you need to talk about problems? | ( ) | ( ) | ( ) | ( ) | ( ) |
| Count on your colleagues to back you up at work? | ( ) | ( ) | ( ) | ( ) | ( ) |
| Count on your colleagues to help you with a difficult task at work? | ( ) | ( ) | ( ) | ( ) | ( ) |
| Really count on your colleagues to help you in a crisis situation at work, even though they would have to go out of their way to do so? | ( ) | ( ) | ( ) | ( ) | ( ) |
Your well-being and motivation
The following questions ask you to describe things you like and dislike about your current role and your general well-being. Please answer all the questions, ticking the answer which best describes what you do most of the time.
11. The statements below concern how satisfied you feel with different aspects of your role. How satisfied are you with:*
| Extremely dissatisfied | Very dissatisfied | Moderately dissatisfied | Not sure | Moderately satisfied | Very satisfied | Extremely satisfied | |
|---|---|---|---|---|---|---|---|
| The physical work conditions? | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| The freedom to choose your own method of working? | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Your fellow workers? | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| The recognition you get for good work? | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Your Clinical Supervisor? | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| The amount of responsibility you are given? | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Your rate of pay? | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Your opportunity to use your abilities? | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Relations between doctors and other health-care professionals? | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Your chance of career progression? | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| The way the department is managed? | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| The attention paid to suggestions you make? | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Your hours of work? | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| The amount of variety in your job? | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Your job security? | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
The following questions ask you about your general well-being and motivation. Please answer all the questions. It is possible that completing some questions may draw your attention to problems you experience. If you are worried that these are serious, we would advise you to contact your GP.
12. In the last month, how much of the time has your current role made you feel:*
| Not at all | Just a little | A moderate amount | Quite a lot | A great deal | |
|---|---|---|---|---|---|
| Gloomy | ( ) | ( ) | ( ) | ( ) | ( ) |
| Uneasy | ( ) | ( ) | ( ) | ( ) | ( ) |
| Worried | ( ) | ( ) | ( ) | ( ) | ( ) |
| Tense | ( ) | ( ) | ( ) | ( ) | ( ) |
| Depressed | ( ) | ( ) | ( ) | ( ) | ( ) |
| Miserable | ( ) | ( ) | ( ) | ( ) | ( ) |
13. Thinking of your current role, how true are the following:*
| Strongly disagree | Disagree | Neutral | Agree | Strongly agree | |
|---|---|---|---|---|---|
| I often think about leaving medicine? | ( ) | ( ) | ( ) | ( ) | ( ) |
| It is very likely that I will actively look for a new job outside medicine in the next year? | ( ) | ( ) | ( ) | ( ) | ( ) |
| I am starting to ask my friends/contacts about other job possibilities outside medicine? | ( ) | ( ) | ( ) | ( ) | ( ) |
Please answer the following questions about your overall motivation in your current role by marking the most accurate answer.
14. How would you rate the amount of effort you put into your job?*
( ) Very low
( ) Low
( ) Moderate
( ) High
( ) Very high
15. I consistently put forth the maximum effort possible at work.*
( ) Strongly disagree
( ) Disagree
( ) Neutral
( ) Agree
( ) Strongly agree
16. How much of your total, maximum possible effort do you put into your job?*
( ) 50% or less
( ) 51–75%
( ) 76–85%
( ) 86–95%
( ) 96–100%
Please answer each question in relation to your current role by marking the most accurate answer.
17. It is not clear to me how much effort to put into different parts of my job.*
( ) Strongly disagree
( ) Disagree
( ) Neutral
( ) Agree
( ) Strongly agree
18. I divide my time across tasks in the way that is most helpful to the organisation.*
( ) Strongly disagree
( ) Disagree
( ) Neutral
( ) Agree
( ) Strongly agree
19. My supervisor and I agree on what tasks are most and least important.*
( ) Never
( ) Rarely
( ) Sometimes
( ) Usually
( ) Always
Please answer each question by marking the box that gives your opinion. We want to know how much effort in your role influences how good or bad your job outcomes are (such as criticisms, feelings of accomplishment, friendships).
20. I get better job outcomes if I increase my level of effort.*
( ) Never
( ) Rarely
( ) Sometimes
( ) Usually
( ) Always
21. There is a strong tie between how hard I work and how good my job outcomes are.*
( ) Strongly disagree
( ) Disagree
( ) Neutral
( ) Agree
( ) Strongly agree
22. Working hard on this job is not rewarded.*
( ) Strongly disagree
( ) Disagree
( ) Neutral
( ) Agree
( ) Strongly agree
23. Would you describe yourself as typically:*
| Extremely inaccurate | Very inaccurate | Moderately inaccurate | Slightly inaccurate | Not sure | Slightly accurate | Moderately accurate | Very accurate | Extremely accurate | |
|---|---|---|---|---|---|---|---|---|---|
| Careless | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Disorganised | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Efficient | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Inefficient | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Organised | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Practical | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Sloppy | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Systematic | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
24. People cope with difficult, stressful or upsetting situations in a variety of ways. Please read each statement and select the response that best indicates how much you tend to react in that way when faced with a difficult, stressful or upsetting situation. When faced with a difficult/stressful situation:*
| Never | Seldom | Sometimes | Often | Very often | |
|---|---|---|---|---|---|
| I try to figure out how to resolve the problem | ( ) | ( ) | ( ) | ( ) | ( ) |
| I act as though nothing happened, hoping it will go away | ( ) | ( ) | ( ) | ( ) | ( ) |
| I seek the support and guidance of other people | ( ) | ( ) | ( ) | ( ) | ( ) |
| I get upset or angry with the people who cause the problem | ( ) | ( ) | ( ) | ( ) | ( ) |
| I change something so the situation will improve | ( ) | ( ) | ( ) | ( ) | ( ) |
| I avoid the problem by sleeping, watching TV, engaging in diversionary activities more | ( ) | ( ) | ( ) | ( ) | ( ) |
| I ask someone I respect for advice | ( ) | ( ) | ( ) | ( ) | ( ) |
| I try to get back at those who created the trouble | ( ) | ( ) | ( ) | ( ) | ( ) |
| I come up with a couple of strategies to make the situation better | ( ) | ( ) | ( ) | ( ) | ( ) |
| I keep my concerns and emotions about the situation to myself | ( ) | ( ) | ( ) | ( ) | ( ) |
| I talk to friends or family about my circumstances | ( ) | ( ) | ( ) | ( ) | ( ) |
| I figure out who was responsible for what happened | ( ) | ( ) | ( ) | ( ) | ( ) |
| I double my efforts to correct the situation and achieve my objective | ( ) | ( ) | ( ) | ( ) | ( ) |
| I put off dealing with the matter | ( ) | ( ) | ( ) | ( ) | ( ) |
| I get sympathy and understanding from someone | ( ) | ( ) | ( ) | ( ) | ( ) |
| I make sure that those responsible for the problem receive their due punishment | ( ) | ( ) | ( ) | ( ) | ( ) |
Thinking of the decisions (or judgements) about patient care that you have made during your current role assess the following statements:
25. I am confident that I made the appropriate decisions.*
( ) Strongly disagree
( ) Disagree
( ) Neutral
( ) Agree
( ) Strongly agree
26. Considering the information available to me I made the best decisions possible.*
( ) Strongly disagree
( ) Disagree
( ) Neutral
( ) Agree
( ) Strongly agree
27. How much assistance did you need in making these decisions?*
( ) None at all
( ) Just a little
( ) A moderate amount
( ) Quite a lot
( ) A great deal
28. Thinking of your current role did you have:*
| None | Just a little | A moderate amount | Quite a lot | A great deal | |
|---|---|---|---|---|---|
| Any formal teaching offered in your department (in addition to the generic teaching) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Any informal training offered in your department (in addition to the generic training), e.g. one-to-one shop floor teaching from a senior member of the medical staff, informal mentoring by senior medical staff? | ( ) | ( ) | ( ) | ( ) | ( ) |
| Any feedback on the quality of your work? | ( ) | ( ) | ( ) | ( ) | ( ) |
29. Thinking about your current role:*
| Not at all | Just a little | A moderate amount | Quite a lot | A great deal | |
|---|---|---|---|---|---|
| Has your knowledge of medical conditions increased? | ( ) | ( ) | ( ) | ( ) | ( ) |
| Do you feel more able to work as part of the clinical team? | ( ) | ( ) | ( ) | ( ) | ( ) |
| Do you understand more about how health-care professionals work together? | ( ) | ( ) | ( ) | ( ) | ( ) |
Background details
It is important we know some of your background details to represent the views of different groups of people.
About your job:
30. Year of qualification:*
____________________________________________
31. Place of qualification:*
( ) UK
( ) Non-UK
About you:
32. Age:*
____________________________________________
33. Are you:*
( ) Male?
( ) Female?
34. What is your ethnic background? (Please select the answer that best describes your ethnic background)*
( ) White – British
( ) White – Irish
( ) White – Other
( ) Black – British
( ) Black – Caribbean
( ) Black – African
( ) Any other Black background
( ) Asian – British
( ) Asian – Chinese
( ) Asian – Indian
( ) Asian – Pakistani
( ) Asian – Bangladeshi
( ) Any other Asian background
( ) Mixed – White and Black British
( ) Mixed – White and Black Caribbean
( ) Mixed – White and Black African
( ) Mixed – White and Asian
( ) Any other mixed background
( ) Any other ethnic group (please specify): _________________
Hours of work:
35. In a typical working week in your current role, how many hours are you contracted to work?*
____________________________________________
36. What is the total number of extra hours worked in a typical week?*
____________________________________________
37. In the last four weeks of your current role have you had a shift changed at short notice (less than five days)?*
( ) Yes
( ) No
Foundation training experience:
38. Please indicate your first, second and final F1 placements:*
| General practice | Hospital medicine | Hospital surgery | Emergency medicine | Obstetrics and gynaecology | Radiology | Psychiatry | Paediatrics and child health | Trauma and orthopaedics | Medical education | Academic based | Laboratory medicine | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Your first F1 placement: | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Your second F1 placement: | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Your final F1 placement: | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
39. Please indicate your first, second and final F2 placements:*
| General practice | Hospital medicine | Hospital surgery | Emergency medicine | Obstetrics and gynaecology | Radiology | Psychiatry | Paediatrics and child health | Trauma and orthopaedics | Medical education | Academic based | Laboratory medicine | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Your first F2 placement: | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Your second F2 placement: | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| Your final F2 placement: | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
Future plans:
40. What do you plan to do after your F2 year?*
( ) Take a short-term contract in medicine
( ) Work abroad in medicine
( ) Take some time out from medicine
( ) Don’t know yet
( ) Go onto specialist training
What specialty will you be moving into?
( ) General practice
( ) Hospital medicine
( ) Hospital surgery
( ) Emergency medicine
( ) Obstetrics and gynaecology
( ) Radiology
( ) Psychiatry
( ) Paediatrics and child health
( ) Trauma and orthopaedics
( ) Medical education
( ) Academic based
( ) Laboratory medicine
( ) Other (please state): _________________
Further comments
41. If you have any further comments to make, please feel free to write them below.
____________________________________________________________________
Thank you for your co-operation.
Dr A Carter, Dr CB Stride, Ms S Mason, Mr C O’Keeffe
Copyright 2010 the Authors. All rights reserved.
Appendix 19 Expanded results tables
| Deaneries | Site (ED code) | No. of F2 doctor participants | No. of eligible F2 doctors in trust | Response rate (%) |
|---|---|---|---|---|
| North West | 26 | 9 | 15 | 60.0 |
| 230 | 10 | 33 | 30.3 | |
| 261 | 6 | 21 | 28.6 | |
| 285 | 4 | 10 | 40.0 | |
| Northern | 58 | 3 | 15 | 20.0 |
| 165 | 8 | 21 | 38.1 | |
| 171 | 2 | 15 | 13.3 | |
| 178 | 3 | 24 | 12.5 | |
| 187 | 8 | 25 | 32.0 | |
| 188 | 6 | 25 | 24.0 | |
| 249 | 1 | 9 | 11.1 | |
| 250 | 1 | 9 | 11.1 | |
| East Midlands | 67 | 2 | 15 | 13.3 |
| Yorkshire and Humber | 70 | 6 | 9 | 66.7 |
| 121 | 20 | 39 | 51.3 | |
| 139 | 4 | 33 | 12.1 | |
| 140 | 2 | 27 | 7.4 | |
| 238 | 18 | 34 | 52.9 | |
| London | 76 | 7 | 18 | 38.9 |
| 99 | 28 | 57 | 49.1 | |
| 123 | 11 | 24 | 45.8 | |
| 298 | 8 | 30 | 26.7 | |
| Mersey | 155 | 6 | 9 | 66.7 |
| 180 | 8 | 27 | 29.6 | |
| Severn | 227 | 5 | 12 | 41.7 |
| 304 | 2 | 14 | 14.3 | |
| West Midlands | 280 | 8 | 24 | 33.3 |
| 283 | 8 | 27 | 29.6 | |
| 312 | 10 | 21 | 47.6 | |
| Kent, Surrey and Sussex | 302 | 3 | 12 | 25.0 |
| Total | 217 | 654 | 33.2 |
| n | Mean | SD | SE | 95% CI for mean | Minimum | Maximum | |
|---|---|---|---|---|---|---|---|
| Age at start of study (2010) (years) | |||||||
| ED group 1 | 83 | 26.87 | 3.60 | 0.39 | 26.08 to 27.65 | 24 | 40 |
| ED group 2 | 55 | 26.78 | 4.10 | 0.55 | 25.68 to 27.89 | 24 | 44 |
| ED group 3 | 63 | 27.06 | 3.70 | 0.47 | 26.13 to 28.00 | 24 | 40 |
| Total | 201 | 26.91 | 3.70 | 0.26 | 26.38 to 27.43 | 24 | 44 |
| Log-age at start of study (2010) | |||||||
| ED group 1 | 83 | 3.30 | 0.12 | 0.01 | 3.26 to 3.31 | 3.18 | 3.69 |
| ED group 2 | 55 | 3.30 | 0.13 | 0.02 | 3.24 to 3.31 | 3.18 | 3.78 |
| ED group 3 | 63 | 3.30 | 0.12 | 0.02 | 3.26 to 3.32 | 3.18 | 3.69 |
| Total | 201 | 3.28 | 0.12 | 0.01 | 3.27 to 3.30 | 3.18 | 3.78 |
| Years before 2010 that respondent qualified | |||||||
| ED group 1 | 83 | 1.34 | 1.10 | 0.13 | 1.09 to 1.59 | 1 | 8 |
| ED group 2 | 55 | 1.73 | 2.68 | 0.36 | 1.00 to 2.45 | 1 | 17 |
| ED group 3 | 63 | 1.81 | 2.44 | 0.31 | 1.20 to 2.42 | 1 | 15 |
| Total | 201 | 1.59 | 2.09 | 0.15 | 1.30 to 1.88 | 1 | 17 |
| Log of years before 2010 that respondent qualified | |||||||
| ED group 1 | 83 | 0.15 | 0.42 | 0.05 | 0.06 to 0.24 | 0.00 | 2.08 |
| ED group 2 | 55 | 0.20 | 0.61 | 0.08 | 0.04 to 0.37 | 0.00 | 2.83 |
| ED group 3 | 63 | 0.27 | 0.63 | 0.08 | 0.11 to 0.43 | 0.00 | 2.71 |
| Total | 201 | 0.20 | 0.55 | 0.04 | 0.13 to 0.28 | 0.00 | 2.83 |
| n | Mean | SD | SE | 95% CI for mean | Minimum | Maximum | |
|---|---|---|---|---|---|---|---|
| Organisational skills/ability | |||||||
| ED group 1 | 83 | 7.5318 | 0.89390 | 0.09812 | 7.3367 to 7.7270 | 4.00 | 9.00 |
| ED group 2 | 56 | 7.7194 | 0.64233 | 0.08584 | 7.5474 to 7.8914 | 5.43 | 9.00 |
| ED group 3 | 63 | 7.5737 | 1.04396 | 0.13153 | 7.3108 to 7.8366 | 4.00 | 9.00 |
| Total | 202 | 7.5969 | 0.88383 | 0.06219 | 7.4743 to 7.7195 | 4.00 | 9.00 |
| Coping via positive strategies | |||||||
| ED group 1 | 83 | 3.7892 | 0.33639 | 0.03692 | 3.7157 to 3.8626 | 2.88 | 4.50 |
| ED group 2 | 56 | 3.8449 | 0.32443 | 0.04335 | 3.7580 to 3.9317 | 2.94 | 4.38 |
| ED group 3 | 63 | 3.8353 | 0.34017 | 0.04286 | 3.7496 to 3.9210 | 3.00 | 4.63 |
| Total | 202 | 3.8190 | 0.33361 | 0.02347 | 3.7727 to 3.8653 | 2.88 | 4.63 |
| Condition | Time point of response | |||||||
|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | |||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| ED group 1 | ||||||||
| TREAT1 Diarrhoea and vomiting | 6.68 | 1.18 | 7.27 | 1.09 | 7.34 | 0.90 | 7.71 | 0.88 |
| TREAT2 Shortness of breath | 6.66 | 1.05 | 7.39 | 0.92 | 7.34 | 0.86 | 7.63 | 0.92 |
| TREAT3 Collapse – unknown causes | 5.95 | 1.25 | 6.80 | 1.06 | 6.85 | 0.91 | 7.08 | 0.91 |
| TREAT4 Acute mental health problem | 4.25 | 1.63 | 5.58 | 1.54 | 5.83 | 1.40 | 6.10 | 1.55 |
| TREAT5 Elderly fall | 6.42 | 1.31 | 7.05 | 1.01 | 7.07 | 1.06 | 7.33 | 0.97 |
| TREAT6 Chest pain | 6.99 | 1.09 | 7.53 | 0.82 | 7.44 | 0.82 | 7.75 | 0.77 |
| TREAT7 Back pain | 5.46 | 1.33 | 6.52 | 1.18 | 6.75 | 1.25 | 7.20 | 1.06 |
| TREAT8 Cardiac arrest | 5.71 | 1.65 | 6.52 | 1.52 | 6.29 | 1.13 | 6.78 | 1.36 |
| TREAT9 Palpitations | 5.84 | 1.21 | 6.63 | 1.06 | 6.63 | 0.91 | 6.82 | 0.95 |
| TREAT10 Abdominal pain | 6.85 | 1.27 | 7.30 | 0.95 | 7.08 | 1.09 | 7.53 | 0.95 |
| TREAT11 Acute allergic reaction | 5.70 | 1.56 | 7.05 | 1.13 | 6.85 | 1.14 | 7.10 | 1.15 |
| TREAT12 Left ‘side’ pain | 5.49 | 1.43 | 6.39 | 1.20 | 6.51 | 1.07 | 6.96 | 1.04 |
| TREAT13 Acute stroke | 5.54 | 1.53 | 6.64 | 1.38 | 6.47 | 1.12 | 6.67 | 1.26 |
| TREAT14 Overdose – paracetamol | 5.66 | 1.73 | 7.36 | 1.23 | 7.02 | 1.09 | 7.31 | 1.09 |
| TREAT15 Diabetic ketoacidosis | 5.67 | 1.55 | 6.73 | 1.38 | 6.80 | 1.17 | 6.84 | 1.21 |
| TREAT16 Acute confusion | 6.04 | 1.31 | 6.64 | 1.20 | 6.78 | 0.89 | 6.94 | 1.16 |
| TREAT17 Headache | 5.82 | 1.37 | 6.52 | 1.30 | 6.63 | 1.00 | 7.08 | 0.89 |
| TREAT18 Seizure | 5.39 | 1.39 | 6.50 | 1.15 | 6.47 | 1.10 | 6.73 | 1.04 |
| TREAT19 Cellulitis | 7.01 | 1.29 | 7.45 | 0.91 | 7.37 | 1.00 | 7.75 | 0.77 |
| TREAT20 Haematemesis | 6.63 | 1.16 | 7.17 | 1.08 | 7.14 | 0.99 | 7.37 | 0.87 |
| TREAT21 Rash | 5.15 | 1.23 | 5.95 | 1.21 | 6.19 | 1.12 | 6.49 | 1.29 |
| TREAT22 Acute painful joint | 5.54 | 1.53 | 6.31 | 1.23 | 6.51 | 1.19 | 6.78 | 1.12 |
| TREAT23 Rectal bleeding | 6.59 | 1.24 | 7.19 | 1.05 | 7.00 | 1.02 | 7.41 | 0.92 |
| ED group 2 | ||||||||
| TREAT1 Diarrhoea and vomiting | 6.94 | 1.29 | 7.20 | 1.09 | 7.69 | 0.72 | 7.86 | 0.59 |
| TREAT2 Shortness of breath | 6.92 | 0.87 | 7.02 | 0.88 | 7.80 | 0.68 | 7.64 | 0.62 |
| TREAT3 Collapse – unknown cause | 6.24 | 1.14 | 6.45 | 1.02 | 7.31 | 0.99 | 7.39 | 0.79 |
| TREAT4 Acute mental health problem | 4.55 | 1.70 | 4.66 | 1.36 | 6.26 | 1.22 | 6.32 | 1.25 |
| TREAT5 Elderly fall | 6.78 | 1.14 | 6.66 | 1.12 | 7.60 | 0.77 | 7.64 | 0.68 |
| TREAT6 Chest pain | 7.18 | 0.95 | 7.16 | 1.14 | 7.91 | 0.70 | 8.04 | 0.58 |
| TREAT7 Back pain | 6.22 | 1.38 | 6.25 | 1.18 | 7.09 | 0.89 | 7.14 | 0.93 |
| TREAT8 Cardiac arrest | 5.90 | 1.70 | 6.11 | 1.59 | 7.09 | 0.82 | 7.43 | 0.74 |
| TREAT9 Palpitations | 6.20 | 1.23 | 6.39 | 1.19 | 6.94 | 1.00 | 7.14 | 0.89 |
| TREAT10 Abdominal pain | 6.98 | 1.19 | 6.95 | 1.10 | 7.57 | 0.81 | 7.54 | 0.96 |
| TREAT11 Acute allergic reaction | 5.61 | 1.59 | 5.98 | 1.56 | 7.03 | 1.04 | 7.07 | 0.90 |
| TREAT12 Left ‘side’ pain | 5.90 | 1.33 | 6.27 | 1.15 | 7.06 | 0.87 | 7.11 | 0.92 |
| TREAT13 Acute stroke | 5.84 | 1.42 | 5.89 | 1.56 | 7.26 | 1.17 | 7.32 | 0.86 |
| TREAT14 Overdose – paracetamol | 5.86 | 1.27 | 5.89 | 1.51 | 7.83 | 0.86 | 7.89 | 0.79 |
| TREAT15 Diabetic ketoacidosis | 5.90 | 1.19 | 5.91 | 1.34 | 7.23 | 1.03 | 7.29 | 0.81 |
| TREAT16 Acute confusion | 6.31 | 1.12 | 6.16 | 1.24 | 7.11 | 0.93 | 7.36 | 0.83 |
| TREAT17 Headache | 6.33 | 1.32 | 6.32 | 1.14 | 7.03 | 1.04 | 7.21 | 0.79 |
| TREAT18 Seizure | 5.49 | 1.41 | 5.89 | 1.38 | 6.94 | 1.06 | 6.86 | 0.97 |
| TREAT19 Cellulitis | 7.31 | 0.97 | 7.14 | 1.11 | 7.60 | 0.81 | 7.82 | 0.61 |
| TREAT20 Haematemesis | 6.88 | 1.07 | 6.66 | 1.38 | 7.43 | 0.92 | 7.54 | 0.96 |
| TREAT21 Rash | 5.71 | 1.40 | 5.59 | 1.42 | 6.29 | 1.27 | 6.46 | 1.04 |
| TREAT22 Acute painful joint | 5.82 | 1.20 | 5.89 | 1.28 | 6.97 | 1.20 | 6.93 | 1.02 |
| TREAT23 Rectal bleeding | 6.78 | 1.01 | 6.57 | 1.35 | 7.60 | 0.85 | 7.57 | 0.74 |
| ED group 3 | ||||||||
| TREAT1 Diarrhoea and vomiting | 6.90 | 1.24 | 7.20 | 0.96 | 7.27 | 0.95 | 8.00 | 0.83 |
| TREAT2 Shortness of breath | 6.67 | 1.05 | 6.98 | 1.00 | 7.32 | 0.85 | 7.83 | 0.79 |
| TREAT3 Collapse – unknown cause | 5.83 | 1.40 | 6.39 | 1.24 | 6.59 | 1.38 | 7.60 | 0.86 |
| TREAT4 Acute mental health problem | 4.09 | 1.69 | 4.65 | 1.65 | 5.29 | 1.72 | 6.60 | 1.25 |
| TREAT5 Elderly fall | 6.52 | 1.31 | 6.76 | 1.25 | 6.66 | 1.20 | 7.70 | 0.92 |
| TREAT6 Chest pain | 6.97 | 1.09 | 7.09 | 1.24 | 7.15 | 1.04 | 7.83 | 0.75 |
| TREAT7 Back pain | 5.76 | 1.50 | 6.57 | 1.38 | 6.39 | 1.20 | 7.27 | 1.17 |
| TREAT8 Cardiac arrest | 5.72 | 1.63 | 6.37 | 1.51 | 6.59 | 1.47 | 6.93 | 1.26 |
| TREAT9 Palpitations | 6.12 | 1.34 | 6.33 | 1.25 | 6.66 | 1.35 | 7.43 | 0.94 |
| TREAT10 Abdominal pain | 7.07 | 1.14 | 6.76 | 1.12 | 6.98 | 0.94 | 7.73 | 0.74 |
| TREAT11 Acute allergic reaction | 5.74 | 1.48 | 6.41 | 1.36 | 6.54 | 1.36 | 7.43 | 0.97 |
| TREAT12 Left ‘side’ pain | 6.03 | 1.24 | 6.24 | 1.23 | 6.85 | 1.01 | 7.33 | 1.15 |
| TREAT13 Acute stroke | 5.62 | 1.50 | 5.98 | 1.54 | 6.27 | 1.61 | 7.17 | 1.34 |
| TREAT14 Overdose – paracetamol | 5.71 | 1.69 | 6.02 | 1.57 | 6.49 | 1.66 | 7.47 | 1.20 |
| TREAT15 Diabetic ketoacidosis | 5.67 | 1.67 | 6.17 | 1.55 | 6.49 | 1.25 | 7.00 | 1.49 |
| TREAT16 Acute confusion | 6.24 | 1.22 | 6.22 | 1.32 | 6.41 | 1.28 | 7.27 | 0.98 |
| TREAT17 Headache | 6.07 | 1.11 | 6.41 | 1.31 | 6.51 | 1.14 | 7.07 | 1.28 |
| TREAT18 Seizure | 5.36 | 1.54 | 5.72 | 1.52 | 6.05 | 1.60 | 7.13 | 1.28 |
| TREAT19 Cellulitis | 7.21 | 1.25 | 7.46 | 0.89 | 7.51 | 0.71 | 8.20 | 0.61 |
| TREAT20 Haematemesis | 6.71 | 1.28 | 6.70 | 1.28 | 7.07 | 1.15 | 7.67 | 0.92 |
| TREAT21 Rash | 5.40 | 1.65 | 5.80 | 1.53 | 5.85 | 1.53 | 6.37 | 1.54 |
| TREAT22 Acute painful joint | 5.91 | 1.71 | 6.52 | 1.35 | 6.39 | 1.53 | 6.87 | 1.70 |
| TREAT23 Rectal bleeding | 6.97 | 1.15 | 6.74 | 1.34 | 7.12 | 1.21 | 7.43 | 1.25 |
| Practical technique | Time point of response | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | Total | ||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| ED group 1 | ||||||||||
| EXPT1 Defibrillation | 3.35 | 2.01 | 3.81 | 2.42 | 3.71 | 2.24 | 4.37 | 2.33 | 3.76 | 2.26 |
| EXPT2 Arterial blood gas analysis | 8.05 | 1.11 | 8.58 | 0.79 | 7.78 | 1.96 | 8.27 | 1.04 | 8.17 | 1.31 |
| EXPT3 Suturing | 4.77 | 2.44 | 7.39 | 1.84 | 6.47 | 2.39 | 7.31 | 1.77 | 6.34 | 2.42 |
| EXPT4 ECG interpretation | 6.52 | 1.24 | 7.33 | 1.10 | 7.02 | 1.57 | 7.49 | 1.17 | 7.04 | 1.33 |
| EXPT5 radiograph interpretation | 6.29 | 1.13 | 7.25 | 0.94 | 6.78 | 1.74 | 7.51 | 1.01 | 6.89 | 1.32 |
| ED group 2 | ||||||||||
| EXPT1 Defibrillation | 2.90 | 1.91 | 4.18 | 2.23 | 4.97 | 2.08 | 5.64 | 2.23 | 4.20 | 2.32 |
| EXPT2 Arterial blood gas analysis | 8.53 | 0.83 | 7.95 | 1.40 | 8.43 | 0.78 | 8.54 | 0.64 | 8.35 | 1.01 |
| EXPT3 Suturing | 4.80 | 2.50 | 5.91 | 2.18 | 7.83 | 1.67 | 7.86 | 1.27 | 6.32 | 2.43 |
| EXPT4 ECG interpretation | 6.76 | 1.21 | 6.73 | 1.56 | 7.63 | 0.69 | 7.68 | 0.67 | 7.11 | 1.23 |
| EXPT5 radiograph interpretation | 6.80 | 1.18 | 6.68 | 1.41 | 7.54 | 0.89 | 7.50 | 0.84 | 7.06 | 1.20 |
| ED group 3 | ||||||||||
| EXPT1 Defibrillation | 3.19 | 1.83 | 3.54 | 2.36 | 4.15 | 2.12 | 4.27 | 2.33 | 3.69 | 2.16 |
| EXPT2 Arterial blood gas analysis | 7.91 | 1.29 | 7.65 | 1.85 | 7.83 | 1.88 | 8.60 | 0.56 | 7.94 | 1.55 |
| EXPT3 Suturing | 4.67 | 2.47 | 4.41 | 2.53 | 4.07 | 2.53 | 7.50 | 1.63 | 4.95 | 2.64 |
| EXPT4 ECG interpretation | 6.36 | 1.27 | 6.76 | 1.75 | 6.90 | 1.87 | 7.97 | 0.85 | 6.87 | 1.59 |
| EXPT5 radiograph interpretation | 6.45 | 1.23 | 6.50 | 1.64 | 6.51 | 1.89 | 7.57 | 1.01 | 6.67 | 1.53 |
| Total | ||||||||||
| EXPT1 Defibrillation | 3.18 | 1.93 | 3.84 | 2.35 | 4.17 | 2.21 | 4.67 | 2.36 | 3.86 | 2.25 |
| EXPT2 Arterial blood gas analysis | 8.14 | 1.12 | 8.12 | 1.41 | 7.96 | 1.72 | 8.43 | 0.84 | 8.15 | 1.32 |
| EXPT3 Suturing | 4.75 | 2.45 | 6.08 | 2.48 | 6.10 | 2.68 | 7.50 | 1.62 | 5.92 | 2.57 |
| EXPT4 ECG interpretation | 6.54 | 1.24 | 6.99 | 1.47 | 7.14 | 1.52 | 7.67 | 0.99 | 7.01 | 1.39 |
| EXPT5 radiograph interpretation | 6.48 | 1.19 | 6.86 | 1.35 | 6.90 | 1.65 | 7.52 | 0.96 | 6.87 | 1.36 |
| Time point at which F2 ED placement carried out | Time point of response | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | Total | ||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| ED group 1 | ||||||||||
| Depression | 1.71 | 0.77 | 1.82 | 0.98 | 1.56 | 0.87 | 1.59 | 0.69 | 1.68 | 0.84 |
| Anxiety | 1.94 | 0.77 | 2.42 | 1.15 | 1.74 | 0.59 | 1.95 | 0.68 | 2.02 | 0.86 |
| ED group 2 | ||||||||||
| Depression | 1.59 | 0.79 | 1.55 | 0.88 | 1.72 | 0.95 | 1.49 | 0.67 | 1.59 | 0.83 |
| Anxiety | 1.97 | 0.82 | 1.88 | 0.76 | 2.46 | 1.05 | 1.74 | 0.62 | 2.02 | 0.86 |
| ED group 3 | ||||||||||
| Depression | 1.66 | 0.86 | 2.00 | 0.99 | 1.63 | 0.74 | 1.92 | 1.00 | 1.79 | 0.90 |
| Anxiety | 2.15 | 0.90 | 2.42 | 0.87 | 2.01 | 0.81 | 2.51 | 1.10 | 2.25 | 0.92 |
| Total | ||||||||||
| Depression | 1.66 | 0.80 | 1.80 | 0.97 | 1.62 | 0.85 | 1.65 | 0.79 | 1.69 | 0.86 |
| Anxiety | 2.01 | 0.82 | 2.27 | 1.00 | 2.01 | 0.85 | 2.05 | 0.85 | 2.09 | 0.89 |
| Time point at which F2 ED placement carried out | Time point of response | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | Total | ||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| ED group 1 | ||||||||||
| Job satisfaction | 4.81 | 0.68 | 5.14 | 0.70 | 5.23 | 0.78 | 5.22 | 0.81 | 5.08 | 0.75 |
| Extrinsic job satisfaction | 5.06 | 0.65 | 5.12 | 0.69 | 5.28 | 0.75 | 5.30 | 0.74 | 5.17 | 0.70 |
| Intrinsic job satisfaction | 4.53 | 0.86 | 5.18 | 0.80 | 5.18 | 0.92 | 5.12 | 0.97 | 4.97 | 0.93 |
| ED group 2 | ||||||||||
| Job satisfaction | 4.93 | 0.79 | 5.41 | 0.77 | 4.98 | 0.89 | 5.40 | 0.57 | 5.15 | 0.80 |
| Extrinsic job satisfaction | 5.08 | 0.81 | 5.56 | 0.68 | 5.03 | 0.83 | 5.56 | 0.49 | 5.28 | 0.77 |
| Intrinsic job satisfaction | 4.76 | 0.89 | 5.23 | 0.96 | 4.92 | 1.03 | 5.22 | 0.84 | 5.01 | 0.94 |
| ED group 3 | ||||||||||
| Job satisfaction | 4.86 | 0.78 | 5.01 | 1.06 | 5.33 | 0.70 | 5.14 | 0.80 | 5.06 | 0.86 |
| Extrinsic job satisfaction | 4.96 | 0.80 | 5.16 | 1.03 | 5.39 | 0.71 | 5.12 | 0.86 | 5.14 | 0.87 |
| Intrinsic job satisfaction | 4.74 | 0.88 | 4.85 | 1.18 | 5.26 | 0.78 | 5.16 | 0.81 | 4.97 | 0.95 |
| Total | ||||||||||
| Job satisfaction | 4.86 | 0.74 | 5.18 | 0.85 | 5.19 | 0.79 | 5.24 | 0.75 | 5.09 | 0.80 |
| Extrinsic job satisfaction | 5.03 | 0.74 | 5.25 | 0.82 | 5.25 | 0.77 | 5.32 | 0.73 | 5.19 | 0.77 |
| Intrinsic job satisfaction | 4.66 | 0.88 | 5.09 | 0.98 | 5.13 | 0.92 | 5.16 | 0.89 | 4.98 | 0.94 |
| Time point at which F2 ED placement carried out | Time point of response | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | Total | ||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| ED group 1 | ||||||||||
| Effort | 4.18 | 0.54 | 4.39 | 0.56 | 3.98 | 0.73 | 4.11 | 0.64 | 4.17 | 0.63 |
| ED group 2 | ||||||||||
| Effort | 4.25 | 0.63 | 4.33 | 0.65 | 4.54 | 0.59 | 4.36 | 0.54 | 4.36 | 0.61 |
| ED group 3 | ||||||||||
| Effort | 4.21 | 0.66 | 4.20 | 0.57 | 4.10 | 0.71 | 4.45 | 0.57 | 4.22 | 0.64 |
| Total | ||||||||||
| Effort | 4.21 | 0.60 | 4.32 | 0.59 | 4.16 | 0.72 | 4.27 | 0.61 | 4.24 | 0.63 |
| Time point at which F2 ED placement carried out | Time point of response | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | Total | ||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| ED group 1 | ||||||||||
| Intention to quit | 1.66 | 0.82 | 1.57 | 0.74 | 1.63 | 0.73 | 1.53 | 0.69 | 1.60 | 0.75 |
| ED group 2 | ||||||||||
| Intention to quit | 1.54 | 0.69 | 1.37 | 0.65 | 1.40 | 0.62 | 1.33 | 0.70 | 1.42 | 0.66 |
| ED group 3 | ||||||||||
| Intention to quit | 1.79 | 0.90 | 1.99 | 0.97 | 1.76 | 0.79 | 1.83 | 1.06 | 1.84 | 0.92 |
| Total | ||||||||||
| Intention to quit | 1.67 | 0.82 | 1.64 | 0.83 | 1.61 | 0.73 | 1.56 | 0.82 | 1.63 | 0.80 |
| Time point at which F2 ED placement carried out | Time point of response | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | Total | ||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| ED group 1 | ||||||||||
| Work demands | 2.34 | 0.83 | 2.39 | 0.83 | 1.90 | 0.63 | 1.91 | 0.67 | 2.16 | 0.78 |
| Role clarity | 3.42 | 0.61 | 3.68 | 0.53 | 3.52 | 0.74 | 3.69 | 0.66 | 3.56 | 0.64 |
| Feedback | 3.23 | 0.75 | 3.13 | 0.89 | 3.53 | 0.83 | 3.52 | 0.77 | 3.33 | 0.83 |
| ED group 2 | ||||||||||
| Work demands | 2.47 | 0.79 | 2.12 | 0.81 | 2.23 | 0.75 | 1.98 | 0.63 | 2.23 | 0.78 |
| Role clarity | 3.54 | 0.68 | 3.76 | 0.76 | 3.88 | 0.72 | 3.90 | 0.65 | 3.74 | 0.72 |
| Feedback | 3.29 | 0.79 | 3.26 | 0.84 | 3.13 | 0.89 | 3.48 | 0.79 | 3.28 | 0.83 |
| ED group 3 | ||||||||||
| Work demands | 2.56 | 0.85 | 2.68 | 0.90 | 2.10 | 0.90 | 2.27 | 0.70 | 2.43 | 0.88 |
| Role clarity | 3.38 | 0.81 | 3.57 | 0.81 | 3.71 | 0.88 | 3.76 | 0.62 | 3.57 | 0.81 |
| Feedback | 3.31 | 0.71 | 3.22 | 0.82 | 3.49 | 0.74 | 3.06 | 1.04 | 3.29 | 0.81 |
| Total | ||||||||||
| Work demands | 2.44 | 0.83 | 2.40 | 0.87 | 2.05 | 0.76 | 2.02 | 0.68 | 2.26 | 0.82 |
| Role clarity | 3.44 | 0.69 | 3.67 | 0.69 | 3.67 | 0.79 | 3.76 | 0.65 | 3.61 | 0.72 |
| Feedback | 3.27 | 0.75 | 3.19 | 0.85 | 3.41 | 0.83 | 3.39 | 0.87 | 3.30 | 0.82 |
| Time point at which F2 ED placement carried out | Time point of response | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | Total | ||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| ED group 1 | ||||||||||
| Hours worked | 47.71 | 4.79 | 51.21 | 7.43 | 44.05 | 8.33 | 46.54 | 10.71 | 47.52 | 8.13 |
| ED group 2 | ||||||||||
| Hours worked | 49.65 | 5.78 | 48.41 | 9.60 | 51.80 | 6.82 | 44.18 | 6.82 | 48.80 | 7.74 |
| ED group 3 | ||||||||||
| Hours worked | 49.09 | 5.04 | 47.43 | 6.57 | 47.45 | 6.46 | 49.83 | 5.66 | 48.39 | 5.95 |
| Total | ||||||||||
| Hours worked | 48.65 | 5.18 | 49.31 | 7.99 | 47.14 | 8.01 | 46.81 | 8.81 | 48.12 | 7.45 |
| Time point at which F2 ED placement carried out | Time point of response | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | Total | ||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| ED group 1 | ||||||||||
| CS support | 3.22 | 0.84 | 3.69 | 0.83 | 3.75 | 0.85 | 3.59 | 0.99 | 3.54 | 0.89 |
| Colleague support | 3.85 | 0.76 | 4.19 | 0.65 | 3.81 | 0.84 | 3.78 | 0.80 | 3.91 | 0.77 |
| ED group 2 | ||||||||||
| CS support | 3.46 | 0.92 | 3.78 | 0.94 | 3.63 | 0.90 | 3.95 | 0.73 | 3.67 | 0.90 |
| Colleague support | 3.83 | 0.94 | 3.97 | 0.74 | 3.95 | 0.72 | 4.13 | 0.63 | 3.95 | 0.79 |
| ED group 3 | ||||||||||
| CS support | 3.49 | 0.84 | 3.50 | 1.04 | 3.52 | 1.11 | 3.59 | 1.03 | 3.52 | 0.98 |
| Colleague support | 3.92 | 0.76 | 3.69 | 1.11 | 3.95 | 0.87 | 4.04 | 0.80 | 3.89 | 0.90 |
| Total | ||||||||||
| CS support | 3.37 | 0.87 | 3.66 | 0.93 | 3.65 | 0.95 | 3.68 | 0.95 | 3.57 | 0.92 |
| Colleague support | 3.87 | 0.81 | 3.98 | 0.86 | 3.89 | 0.82 | 3.94 | 0.77 | 3.92 | 0.82 |
| Time point at which F2 ED placement carried out | Time point of response | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | Total | ||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| ED group 1 | ||||||||||
| One-to-one contact hours with CS | 0.60 | 0.65 | 0.55 | 0.69 | 0.87 | 0.70 | 0.67 | 0.63 | 0.67 | 0.68 |
| Close working contact hours with CS | 1.38 | 0.82 | 1.02 | 0.87 | 1.25 | 0.84 | 1.15 | 0.77 | 1.21 | 0.84 |
| ED group 2 | ||||||||||
| One-to-one contact hours with CS | 0.50 | 0.66 | 0.71 | 0.67 | 0.44 | 0.41 | 0.76 | 0.61 | 0.59 | 0.61 |
| Close working contact hours with CS | 1.58 | 0.89 | 1.38 | 0.81 | 1.18 | 0.89 | 1.28 | 0.89 | 1.38 | 0.87 |
| ED group 3 | ||||||||||
| One-to-one contact hours with CS | 0.60 | 0.63 | 0.72 | 0.63 | 0.60 | 0.66 | 0.48 | 0.45 | 0.61 | 0.61 |
| Close working contact hours with CS | 1.60 | 0.72 | 1.29 | 0.91 | 1.32 | 0.85 | 1.16 | 0.88 | 1.37 | 0.84 |
| Total | ||||||||||
| One-to-one contact hours with CS | 0.57 | 0.64 | 0.65 | 0.67 | 0.68 | 0.65 | 0.64 | 0.59 | 0.63 | 0.64 |
| Close working contact hours with CS | 1.50 | 0.81 | 1.20 | 0.87 | 1.26 | 0.85 | 1.18 | 0.83 | 1.31 | 0.85 |
Impact on management of conditions for teaching and training
We included a three-item scale on impact of teaching and training to assess whether F2 doctor management of the 23 medical conditions may have been improved by clearer guidelines, better teaching or more supervision (e.g. ‘During you most recent training period would your management of the conditions have been improved with clearer guidelines?’) Responses to the three items were on a five-point scale ranging from ‘strongly disagree’ to ‘strongly agree’. The reliability of the scale ranged from 0.67 (T1) to 0.82 (T4). There was no significant variation across the four time points for any of the improvement in management variables.
| Time point at which F2 ED placement carried out | Time point of response | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | Total | ||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| ED group 1 | ||||||||||
| Clearer guidelines | 3.51 | 0.90 | 3.45 | 0.92 | 3.22 | 0.77 | 3.37 | 0.94 | 3.40 | 0.89 |
| Better teaching | 3.73 | 0.83 | 3.59 | 0.97 | 3.47 | 0.82 | 3.69 | 0.78 | 3.63 | 0.86 |
| More supervision | 3.72 | 0.80 | 3.33 | 0.98 | 3.12 | 0.71 | 3.53 | 0.81 | 3.45 | 0.86 |
| ED group 2 | ||||||||||
| Clearer guidelines | 3.69 | 0.81 | 3.39 | 0.99 | 3.37 | 1.00 | 3.21 | 0.74 | 3.45 | 0.91 |
| Better teaching | 3.86 | 0.78 | 3.86 | 0.98 | 3.57 | 0.88 | 3.68 | 0.82 | 3.77 | 0.87 |
| More supervision | 3.69 | 0.93 | 3.48 | 1.02 | 3.26 | 0.95 | 3.54 | 0.88 | 3.51 | 0.96 |
| ED group 3 | ||||||||||
| Clearer guidelines | 3.55 | 1.03 | 3.61 | 0.91 | 3.56 | 0.92 | 3.47 | 1.14 | 3.55 | 0.99 |
| Better teaching | 3.91 | 0.86 | 4.09 | 0.86 | 3.68 | 0.99 | 3.70 | 1.15 | 3.87 | 0.95 |
| More supervision | 3.79 | 0.93 | 3.87 | 0.81 | 3.37 | 1.09 | 3.57 | 1.04 | 3.67 | 0.97 |
| Total | ||||||||||
| Clearer guidelines | 3.57 | 0.92 | 3.48 | 0.94 | 3.36 | 0.89 | 3.36 | 0.95 | 3.46 | 0.92 |
| Better teaching | 3.82 | 0.82 | 3.82 | 0.96 | 3.56 | 0.89 | 3.69 | 0.90 | 3.74 | 0.89 |
| More supervision | 3.73 | 0.87 | 3.53 | 0.96 | 3.24 | 0.90 | 3.54 | 0.89 | 3.53 | 0.92 |
Appendix 20 Qualitative analysis of survey text comments
Included in the survey was a space for ‘further comments’ and a number of participants took the opportunity to offer further commentary. The proportion of F2 doctors providing comments at each time point is shown in Table 35.
| T1, n/N (%) | T2, n/N (%) | T3, n/N (%) | T4, n/N (%) |
|---|---|---|---|
| 35/188 (18.6) | 31/154 (20.1) | 41/135 (30.4) | 27/108 (25) |
These comments were analysed using template analysis with the researcher blind to the quantitative findings of the survey.
Comments made at the end of the foundation year 1 training period
Participants made slightly more negative than positive comments on the overall F1 experience. Positive comments were mainly about the good supervision and support and the opportunities for learning, for example:
An excellent year, I enjoyed all my rotations.
ED was the hardest but the most rewarding placement; it was the most varied and supportive one of the year.
Some participants commented that they had had ‘an unpleasant time’ or that placements made them feel ‘miserable’. A poor environment for learning (because of either dysfunctional dynamics within the team or the environment being isolated from mainstream medicine), poor supervision (remote CS, having to make decisions alone), the heavy workload or the lack of resources to support their work within the trust were the main reasons cited by participants for lack of enjoyment.
A couple of participants described mixed positive and negative experiences and only one described a pattern of working (four placements) that was not the regular three placements within a year. Two further participants described career choices that they were able to make at the end of the F1 training period.
Comments made at the end of the first foundation year 2 placement
Comments were made about both ED and non-ED rotations. The ED was described fairly equally as a challenging and a rewarding experience, for example ‘I felt miserable most of the time because of the time pressure and antisocial working hours’, ‘it was a fantastic experience and I am glad that I have done it’ and ‘I gained skills and experiences that I could not have got elsewhere’. In fact, many of the comments considered both the challenging and the rewarding aspects of the ED placement.
Positive experiences were mainly the result of good support and supervision, good learning opportunities, supportive teaching, excellent teamworking and learning that increased participants’ confidence in their clinical practice.
Challenging aspects of the ED were the hours of work and rotas that included shifts that left little time for life outside the ED, the high work demands and feeling stressed, with some (a minority) finding the teaching poor and a lack of support from consultants.
A variety of placements other than the ED were described, such as general practice and palliative care or specialised roles such as medical biology and neonatal orthopaedics. Several participants commented that their placement was not what they had thought it would be from the advertisement or that changes had occurred since their application (e.g. a department closing). Experiences were seen as negative mainly because of poor support and supervision, little training or teaching and having to carry out what were considered to be mundane or administrative tasks. General practice rotations were seen positively, for example ‘I have learned valuable skills in being able to identify problems in short periods of time’. This rotation was seen as being a good match with an ED rotation.
Only one participant described a pattern of working that was not the regular three placements within a year (two placements).
Comments made at the end of the second foundation year 2 placement
Most of the comments about ED and non-ED placements were made at this time point. The ED was described as being rather more challenging than rewarding, but many of the negative comments were balanced with positive aspects of the role/learning. For example, ‘A&E is a stressful job but the most rewarding I have done so far’ and ‘a good experience with plenty of independence; much better than when I was here as an F1’.
Comments about the challenging experiences in the ED mainly related to the high work demands, rotas that included unsocial hours of work, less than good supervision and difficulties in attending training because of shift working. Positive experiences included excellent supervision and good learning experiences that increased trainees’ confidence in their clinical practice.
The placements other than those in the ED varied from academic placements to those in general medicine, with critical care and general practice placements being enjoyed and offering excellent training opportunities. Positive and negative experiences were described fairly equally, although there were rather more factors associated with negative experiences than with positive experiences. Negative non-ED experiences were associated with poor support and supervision with little feedback, high levels of expected service provision (sometimes in excess of their work experience to date) and little teaching. Positive experiences were associated with a good level of supervision and support with an emphasis on training.
One participant commented on the stresses of applying for future jobs during the second placement.
Comments made at the end of the third foundation year 2 placement and at the end of foundation training
Unsurprisingly, this was the time point with the least commentary; however, some participants did describe their ED and non-ED experiences. Again, there was a mixed pattern of commentary regarding the ED placement and, although more challenges than rewards were mentioned, the comments showed maturity. For example, ‘ED is an excellent training ground for F2 doctors for any future field, given the sheer volume of patients, good support and regular teaching’.
Negative comments described high work demands, difficult rotas and limited supervision and teaching. Positive comments described excellent learning experiences and plenty of support, although the opportunity to reflect on the quality of referral was sometimes requested but rarely available.
Comments about non-ED placements were more positive than negative. A range of placements was described and some participants took the opportunity to reflect on their F2 Year. Positive experiences were characterised by good learning opportunities, being supported by a range of supervisors and a positive working environment. Less positive experiences were associated with a range of work demands, from having to organise one’s own time to having little to do, and training being provided out of step with learning opportunities.
Reflections over the F2 Year noted the effort required – ‘I really enjoyed this year but it was hard work (A&E, Acute med, POSU [paedriatic observation unit])’ – and the overall value – ‘helped me move on from stress of all the practical things to learn to the bigger picture of patient-centred care and being part of a team’.
Only two participants commented on their future work, with one staying on in a department that they had enjoyed working in and the other withdrawing from patient care to work in pathology. What was remarkable about this was how few participants commented about the next steps in their medical careers.
Appendix 21 Reviewer information sheet
The EDiT study: evaluation of doctors in training: a notes review study evaluating the quality of care of junior doctors in the emergency department
Reviewer information sheet
We would like to invite you to assist us in a research study. The study is evaluating the experience of foundation year 2 (FY2) doctors in the emergency department (ED) and the impact on their well-being and the quality of care they provide. The evaluation is being carried out in a number of EDs in England. Please take the time to read the following information which explains why the research is being done and what it would involve for you. Talk to others about the study if you wish.
What is the purpose of the study?
The purpose of the study is to understand what influences the well-being, motivation and confidence of FY2 doctors in the ED and how this is linked to the quality of care they provide. There have been a number of policy initiatives aimed at improving the experiences of the NHS workforce (including postgraduate doctors) and evaluation of these initiatives is aimed to measure their successes and failures.
Who is conducting the study?
The work has been funded by the NIHR Service Delivery and Organisation (SDO) Research Programme. It is being undertaken independently by a research team, led by a senior medical doctor based at the University of Sheffield.
Why have I been selected?
You have been selected because you are a middle grade doctor in a participating ED and have the required experience to undertake an assessment of the quality of care of junior doctors in your department. We understand there are various demands placed upon you in your role and a decision to take part in this study is entirely voluntary.
What does agreeing to take part involve?
If you agree to take part you would participate in a Quality of Care Notes Review Study over a 4- to 6-week period. Essentially you will review and rate the ED notes of selected FY2 doctors in your ED using a structured electronic proforma. This work is designed to be a learning opportunity which will enhance your career by participating actively in a research study and learning a useful technique which you can utilise in your daily practice in the future.
-
You will undergo training in all aspects of conducting a notes review. This will be a single day of training and will include demonstrations of the proforma software, how to review ED notes for quality of care including working through examples.
-
You will be allocated a number of ED notes to review. The review process is straightforward and we have experience of carrying out similar studies in this setting. Previous reviewers have found the task interesting and fairly straightforward.
How will I benefit from this study?
We believe there are benefits to taking part in this study:
-
It is an opportunity to take part in a national research study that may contribute to your continuing professional development.
-
This piece of research can form part of your study time and be added to your CV.
-
You will receive a certificate of participation in research which can be added to your portfolio.
-
Your involvement will be acknowledged on publications following on from the study.
-
You will be trained in a technique of notes review which will be of benefit to your future day-to-day practice in emergency medicine, especially in relation to handling complaints and undertaking notes review for assessing trainees.
What about confidentiality and data protection?
Your identity will not be disclosed during the research process nor the names of any other staff or the hospital where you work. All data collected will be fully anonymised.
What should I do now?
You should take enough time as you feel you need to consider whether to take part. If you do wish to take part, there is a contact email/number for the study project manager to reply to below. The research team will then contact you in order to take this work forward.
Further contact
If you have any further questions then please feel free to contact Colin O’Keeffe.
Thank you for your time
Appendix 22 Screenshot of quality data-collection tool: front page
Screenshot of quality data-collection tool: front page (PDF download)
Appendix 23 Head injury criteria and scoring
Part A: history
1. Was the mechanism of injury leading to this head injury documented?
(1) YES 1
(6) NO 0
2. Was the timing of the injury (e.g. 2 hours ago, yesterday) documented?
(1) YES 1
(6) NO 0
3. Was loss of consciousness (LOC) documented?
(1) YES with duration 2
(2) YES no duration 1
(3) No LOC 1
(6) Not recorded 0
4. Was the presence/absence of amnesia recorded?
(1) YES amnesia with duration recorded 2
(2) YES amnesia recorded but no duration 1
(3) NO amnesia present 1
(4) Not applicable (e.g. patient has hearing loss) 1
(6) Not recorded 0
5. Was the presence/absence of vomiting recorded?
(1) YES vomiting with duration recorded 2
(2) YES vomiting recorded but no duration 1
(3) NO vomiting present 1
(6) Not recorded 0
6. Was the presence/absence of headache recorded?
(1) YES headache with duration recorded 2
(2) YES headache recorded with no duration 1
(3) NO headache present 1
(4) Not applicable (e.g. patient has hearing loss) 1
(6) Not recorded 0
7. Are the details of current medication and medical history recorded?
(1) YES both recorded 2
(2) YES either current medication or medication history recorded 1
(6) Not recorded 0
Part B: examination
8. Is the Glasgow Coma Scale (GCS) score recorded?
(1) YES and the split between E, V and M given 2
(2) YES but no split between E, V and M 1
(6) Not recorded 0
9. Are any details of the injury recorded, e.g. wound, swelling, boggy swelling (depressed skull fracture), open fracture?
(1) YES 1
(6) NO 0
10. Has basal skull fracture been considered?
(1) YES and signs such as raccoon eyes, cerebrospinal fluid (CSF) leak, otorrhoea, battles sign, haemotympanum detailed 2
(2) YES but no signs detailed 1
(6) Not recorded 0
11. Has a neurological examination been recorded?
(1) YES 1
(6) NO 0
12. Has assessment for other injuries been recorded?
(1) YES 1
(6) NO 0
Part C: investigations
13. If CT head organised, was a reason recorded and was this appropriate?
(1) YES, CT reason given and appropriate 2
(2) YES, no reason given but appropriate 1
(3) YES, reason given but inappropriate 0
(4) NO CT done but should have been 0
(5) NO CT done but appropriate not to do it 1
(6) Not recorded 0
Part D: further management
14. Is there a record of a head injury advice card being given?
(1) YES 1
(6) NO 0
15. What is the record of the patient’s disposal?
(1) Discharged and details given re. responsible adult to care for 1
(2) Discharged with no details re. responsible adult to care for 0
(3) Admitted appropriately 1
(4) Admitted inappropriately 0
(6) Not recorded 0
Appendix 24 Chronic obstructive pulmonary disease criteria and scoring
Part A: history
1. Is shortness of breath recorded?
(1) YES and details given, e.g. duration 2
(2) YES but no details given 1
(3) Yes, no change 1
(6) Not recorded 0
2. Is the presence of cough recorded?
(1) YES and details given, e.g. worse than usual 2
(2) YES but no details given 1
(3) No cough present 1
(6) Not recorded 0
3. Is the presence of sputum recorded?
(1) YES and details given, e.g. amount and colour 2
(2) YES but no details given 1
(3) No sputum present 1
(6) Not recorded 0
4. Is the usual COPD treatment recorded?
(1) YES and details given, e.g. inhalers, home nebulisers, home oxygen 2
(2) YES, referred to only but no clear details 1
(6) Not recorded 0
5. Is the usual functional status recorded?
(1) YES and details given, e.g. exercise tolerance, activities 2
(2) YES, referred to only but no clear details 1
(6) Not recorded 0
6. Are previous admissions and treatment recorded?
(1) YES and details given, e.g. intubation, NIV 2
(2) YES, referred to only but no clear details 1
(6) Not recorded 0
Part B: examination
7. Is respiratory rate recorded?
(1) YES and rate recorded 2
(2) YES but no rate recorded 1
(3) Not recorded but appropriate as recorded elsewhere (e.g. nursing notes) 0
(6) Not recorded 0
8. Is there a record of using/not using accessory muscles?
(1) YES 1
(6) Not recorded 0
9. Is either conscious level/confusion or Glasgow Coma Scale (GCS) score recorded?
(1) YES 2
(2) Not recorded but appropriate as recorded elsewhere (e.g. nursing notes) 1
(6) Not recorded 0
10. Is ability to speak/complete sentences recorded?
(1) YES 1
(6) Not recorded 0
Part C: investigations
11. Was a chest radiograph done?
(1) YES and results recorded 2
(2) YES but no results recorded 1
(3) NO and appropriate not to do so 1
(4) NO but should have been done 0
(6) Not recorded 0
12. Was an ECG done?
(1) YES and results recorded 2
(2) YES but no results recorded 1
(3) NO and appropriate not to do so 1
(4) NO but should have been done 0
(6) Not recorded 0
13. Were arterial blood gases carried out (if Sats < 92% or decreased conscious level)?
(1) YES and results recorded 2
(2) YES but no results recorded 1
(3) YES but inappropriate given criteria above 0
(4) NO but should have been done 0
(5) NO but appropriate not to do 1
(6) Not recorded 0
14. Were bloods carried out?
(1) YES and details of which tests ordered recorded 2
(2) YES but details of tests not recorded 1
(3) NO and appropriate not to do so 1
(4) NO but should have been done 0
(6) Not recorded 0
Part D: management
15. Was oxygen given?
(1) YES and amount recorded, e.g. 28% 2
(2) YES but no amount specified 1
(3) YES but inappropriate to give 0
(4) NO but should have been given 0
(5) NO but appropriate not to give 1
(6) Not recorded 0
16. Were nebulisers given?
(1) YES and details of nebulisers given recorded 2
(2) YES but no details recorded 1
(3) YES but inappropriate to do so 0
(4) NO but should have been given 0
(5) NO but appropriate not to give 1
(6) Not recorded 0
17. Was prednisolone/hydrocortisone given?
(1) YES and details given, e.g. timings and dose 2
(2) YES but no details given 1
(3) YES but inappropriate to do so 0
(4) NO should have been given 0
(5) NO but appropriate not to give 1
(6) Not recorded 0
18. Was a senior asked to review if not responding to above management?
(1) YES 1
(2) NO but should have had senior review 0
(3) NO senior review needed 1
(4) Not recorded 0
19. Was IV aminophylline given if not improving with above treatment/deteriorating?
(1) YES and details given, e.g. timings and dose 2
(2) YES but no details given 1
(3) NO but should have been given 0
(4) NO but appropriate not to give 1
(5) Not recorded 0
20. What is the record of the patient’s disposal?
(1) Discharged with details of advice and/or treatments given 1
(2) Discharged with no details of advice and/or treatment 0
(3) Admitted appropriately 1
(4) Admitted inappropriately 0
(6) Not recorded 0
Appendix 25 Holistic review form
This section is relevant to every record you are completing – regardless of the condition. You will be asked to make a judgement on the quality of care detailed in the record. Please make this judgement based on what is recorded in the notes and on the understanding that if care is not recorded in the notes then it is considered not to have been provided.
1. Please rate the quality of the assessment of the clinical problem in terms of the assessment of the completeness of the history and examination and whether it was in accordance with current best practice (for example, your professional standards).
( ) Unsatisfactory
( )
( )
( )
( )
( ) Very best care
2. Please rate the appropriateness of any investigations undertaken for this patient in terms of the type of investigation carried out, whether it was in accordance with current best practice (for example, your professional standards) and whether there were any omissions.
( ) Unsatisfactory
( )
( )
( )
( )
( ) Very best care
3. Please rate the quality of care the patient received in terms of the management of the clinical problem, i.e. was the treatment given and their disposal appropriate in this case? Was the management in accordance with current best practice (for example, your professional standards)?
( ) Unsatisfactory
( )
( )
( )
( )
( ) Very best care
4. Please rate the quality of care the patient received overall. Was the overall care in accordance with current best practice (for example, your professional standards)?
( ) Unsatisfactory
( )
( )
( )
( )
( ) Very best care
5. Please comment on the quality of care the patient received overall including the assessment of the clinical problem, investigations performed, the patient management and anything else that you think is important or relevant that you wish to comment on. Was the overall care in accordance with current best practice (for example, your professional standards)? You may also wish to comment from your own professional viewpoint.
6. We would like to know about the complexity of this clinical presentation. How would you rate the complexity of the clinical presentation detailed in this record?
( ) Low
( ) Average
( ) High
7. We are interested in your view about the quality of the ED record as a marker of quality of care provided. Please rate the quality of the ED record.
( ) Inadequate
( )
( )
( )
( )
( ) Excellent
Appendix 26 Inter-rater reliability: consistency/rank scores
| Site (ED code)a | ||||||||
|---|---|---|---|---|---|---|---|---|
| 26 | 121 | 155 | 165 | 227 | 230 | 238 | 285 | |
| No. of records | 12 | 12 | 12 | 7 | 10 | 8 | 9 | 12 |
| No. of reviewers | 2 | 5 | 2 | 3 | 3 | 6 | 3 | 2 |
| No. of F2 doctors | 5 | 15 | 6 | 8 | 5 | 8 | 17 | 4 |
| Inter-rater reliability: ICC (95% CI) | ||||||||
| Criterion – total | 0.95 (0.82 to 0.98) | 0.76 (0.56 to 0.91) | 0.75 (0.33 to 0.92) | 0.96 (0.85 to 0.99) | 0.67 (0.32 to 0.89) | 0.72 (0.46 to 0.92) | 0.94 (0.82 to 0.98) | 0.96 (0.85 to 0.99) |
| Holistic – assessment | 0.40 (–0.20 to 0.78) | 0.48 (0.22 to 0.76) | 0.46 (–0.13 to 0.81) | 0.20 (–0.22 to 0.73) | 0.45 (0.05 to 0.80) | 0.20 (–0.01 to 0.62) | 0.60 (0.21 to 0.88) | 0.41 (–0.19 to 0.78) |
| Holistic – investigations | 0.37 (–0.23 to 0.77) | 0.17 (–0.02 to 0.51) | 0.34 (–0.26 to 0.75) | 0.13 (–0.26 to 0.69) | 0.56 (0.21 to 0.86) | 0.25 (0.02 to 0.67) | 0.15 (–0.21 to 0.64) | 0.52 (–0.04 to 0.84) |
| Holistic – management | 0.30 (–0.31 to 0.73) | 0.22 (0.01 to 0.56) | 0.39 (–0.20 to 0.78) | 0.25 (–0.18 to 0.76) | 0.75 (0.45 to 0.92) | 0.04 (–0.10 to 0.43) | 0.23 (–0.15 to 0.69) | 0.41 (–0.18 to 0.79) |
| Holistic – overall | 0.46 (–0.12 to 0.81) | 0.25 (0.03 to 0.59) | 0.39 (–0.21 to 0.77) | 0.18 (–0.23 to 0.73) | 0.74 (0.42 to 0.92) | 0.12 (–0.06 to 0.54) | 0.40 (–0.01 to 0.79) | 0.29 (–0.31 to 0.73) |
| Holistic – ED record | 0.65 (0.15 to 0.89) | 0.54 (0.28 to 0.80) | 0.38 (–0.22 to 0.77) | 0.55 (0.08 to 0.89) | 0.47 (0.08 to 0.81) | 0.30 (0.05 to 0.70) | 0.36 (–0.05 to 0.77) | 0.40 (–0.19 to 0.78) |
| Site (ED code)a | ||||||||
|---|---|---|---|---|---|---|---|---|
| 26 | 121 | 155 | 165 | 227 | 230 | 238 | 285 | |
| No. of records | 12 | 12 | 12 | 7 | 10 | 8 | 9 | 12 |
| No. of reviewers | 2 | 5 | 2 | 3 | 3 | 6 | 3 | 2 |
| No. of F2 doctors | 5 | 15 | 6 | 8 | 5 | 8 | 17 | 4 |
| Inter-rater reliability: ICC (95% CI) | ||||||||
| Criterion – total | 0.97 (0.90 to 0.99) | 0.94 (0.87 to 0.98) | 0.86 (0.50 to 0.96) | 0.99 (0.94 to 1.00) | 0.86 (0.59 to 0.96) | 0.94 (0.84 to 0.99) | 0.98 (0.93 to 0.99) | 0.98 (0.92 to 0.99) |
| Holistic – assessment | 0.57 (–0.49 to 0.88) | 0.82 (0.58 to 0.94) | 0.63 (0.29 to 0.89) | 0.41 (–0.20 to 0.89) | 0.71 (0.14 to 0.62) | 0.59 (–0.09 to 0.91) | 0.82 (0.44 to 0.96) | 0.58 (–0.47 to 0.88) |
| Holistic – investigations | 0.54 (–0.59 to 0.87) | 0.51 (0.12 to 0.84) | 0.51 (–0.72 to 0.86) | 0.31 (–0.58 to 0.87) | 0.81 (0.44 to 0.95) | 0.67 (0.12 to 0.92) | 0.35 (–0.04 to 0.84) | 0.69 (–0.09 to 0.91) |
| Holistic – management | 0.46 (–0.89 to 0.84) | 0.58 (0.04 to 0.86) | 0.57 (–0.51 to 0.88) | 0.50 (–0.86 to 0.91) | 0.90 (0.71 to 0.97) | 0.21 (–0.13 to 0.82) | 0.48 (–0.63 to 0.87) | 0.58 (–0.45 to 0.88) |
| Holistic – overall | 0.63 (–0.28 to 0.89) | 0.63 (0.14 to 0.88) | 0.56 (–0.54 to 0.87) | 0.40 (–0.25 to 0.89) | 0.89 (0.69 to 0.97) | 0.45 (–0.47 to 0.87) | 0.67 (–0.04 to 0.92) | 0.45 (–0.92 to 0.84) |
| Holistic – ED record | 0.79 (0.26 to 0.94) | 0.85 (0.66 to 0.95) | 0.55 (–0.55 to 0.87) | 0.79 (0.20 to 0.96) | 0.73 (0.21 to 0.93) | 0.72 (0.24 to 0.94) | 0.63 (0.15 to 0.91) | 0.57 (–0.48 to 0.88) |
Appendix 27 Proportions of explicit review criteria met across all head injury and chronic obstructive pulmonary disease case notes
| Head injury criteria | % (n) |
|---|---|
| Part A: history | |
| 1. Was the mechanism of injury leading to this head injury documented? | |
| YES | 93.8 (360) |
| NO | 6.3 (24) |
| 2. Was the timing of the injury (e.g. 2 hours ago, yesterday) documented? | |
| YES | 56.5 (217) |
| NO | 43.5 (167) |
| 3. Was loss of consciousness (LOC) documented? | |
| YES with duration | 12.8 (49) |
| YES no duration | 73.2 (281) |
| Not recorded | 14.1 (54) |
| 4. Was the presence/absence of amnesia recorded? | |
| YES amnesia with duration recorded | 5.2 (20) |
| YES amnesia recorded but no duration | 46.1 (177) |
| Not recorded | 48.7 (187) |
| 5. Was the presence/absence of vomiting recorded? | |
| YES vomiting with duration recorded | 12.0 (46) |
| YES vomiting recorded but no duration | 64.1 (246) |
| Not recorded | 24.0 (92) |
| 6. Was the presence/absence of headache recorded? | |
| YES headache with duration recorded | 9.4 (36) |
| YES headache recorded with no duration | 42.2 (162) |
| Not recorded | 48.4 (186) |
| 7. Are the details of current medication and medical history recorded? | |
| YES both recorded | 67.4 (259) |
| Yes either current medication or medication history recorded | 13.0 (50) |
| Not recorded | 19.3 (74) |
| Part B: examination | |
| 8. Is the Glasgow Coma Scale (GCS) score recorded? | |
| YES and the split between E, V and M given | 21.9 (84) |
| YES but no split between E, V and M | 49.5 (190) |
| Not recorded | 28.4 (109) |
| 9. Are any details of the injury recorded, e.g. wound, swelling, boggy swelling (depressed skull fracture), open fracture? | |
| YES | 80.5 (309) |
| NO | 19.3 (74) |
| 10. Has basal skull fracture been considered? | |
| YES and signs detailed, e.g. raccoon eyes, cerebrospinal fluid (CSF) leak, otorrhoea, battles sign, haemotympanum | 20.1 (77) |
| YES but no signs detailed | 9.9 (38) |
| Not recorded | 69.8 (268) |
| 11. Has neurological examination been recorded? | |
| YES | 71.4 (274) |
| NO | 28.4 (109) |
| 12. Has assessment for other injuries been recorded? | |
| YES | 59.1 (227) |
| NO | 40.6 (156) |
| Part C: investigations | |
| 13. If CT head organised, was a reason recorded and was this appropriate? | |
| YES CT reason given and appropriate | 13.8 (53) |
| YES no reason given but appropriate | 75.8 (291) |
| Not recorded/inappropriate | 10.2 (39) |
| Part D: further management | |
| 14. Is there a record of a head injury advice card being given? | |
| YES | 54.9 (211) |
| NO | 44.8 (172) |
| 15. What is the record of the patient’s disposal? | |
| Appropriate disposal | 51.0 (196) |
| Inappropriate disposal/not recorded | 48.7 (187) |
| COPD criteria | % (n) |
|---|---|
| Part A: history | |
| 1. Is shortness of breath recorded? | |
| YES and details given, e.g. duration | 75.1 (271) |
| YES but no details given | 16.3 (59) |
| Not recorded | 8.6 (31) |
| 2. Is the presence of cough recorded? | |
| YES and details given, e.g. worse than usual | 52.9 (191) |
| YES but no details given | 30.2 (109) |
| Not recorded | 16.9 (61) |
| 3. Is the presence of sputum recorded? | |
| YES and details given, e.g. amount and colour | 49.0 (177) |
| YES but no details given | 29.6 (107) |
| Not recorded | 21.3 (77) |
| 4. Is the usual COPD treatment recorded? | |
| YES and details given, e.g. inhalers, home nebulisers, home oxygen | 57.9 (209) |
| YES referred to only but no clear details | 15.5 (56) |
| Not recorded | 26.6 (96) |
| 5. Is the usual functional status recorded? | |
| YES and details given, e.g. exercise tolerance, activities | 27.7 (100) |
| YES referred to only but no clear details | 15.2 (55) |
| Not recorded | 57.1 (206) |
| 6. Are previous admissions and treatment recorded? | |
| YES and details given, e.g. intubation, NIV | 23.1 (77) |
| YES referred to only but no clear details | 18.6 (67) |
| Not recorded | 60.1 (217) |
| Part B: examination | |
| 7. Is respiratory rate recorded? | |
| YES and rate recorded | 63.7 (230) |
| YES but no rate recorded | 1.7 (6) |
| Not recorded | 34.6 (125) |
| 8. Is there a record of using/not using accessory muscles? | |
| YES | 17.2 (62) |
| Not recorded | 82.8 (299) |
| 9. Is either conscious level/confusion or Glasgow Coma Scale (GCS) score recorded? | |
| YES | 46.5 (168) |
| Not recorded | 53.5 (193) |
| 10. Is ability to speak/complete sentences recorded? | |
| YES | 31.9 (115) |
| Not recorded | 68.1 (246) |
| Part C: investigations | |
| 11. Was a chest radiograph done? | |
| YES and results recorded | 44.9 (162) |
| YES but no results recorded | 42.7 (154) |
| Not recorded | 12.5 (45) |
| 12. Was an ECG done? | |
| YES and results recorded | 35.5 (128) |
| YES but no results recorded | 31.3 (113) |
| Not recorded | 33.2 (120) |
| 13. Were arterial blood gases carried out? | |
| YES and results recorded | 38.5 (139) |
| YES but no results recorded | 39.9 (144) |
| NOT recorded | 21.6 (78) |
| 14. Were bloods carried out? | |
| YES and details of which tests ordered recorded | 31.6 (114) |
| YES but details of tests not recorded | 54.0 (195) |
| Not recorded | 14.4 (52) |
| Part D: management | |
| 15. Was oxygen given? | |
| YES and amount recorded, e.g. 28% | 34.1 (123) |
| YES but no amount specified | 37.4 (135) |
| NOT recorded/inappropriate | 28.5 (103) |
| 16. Were nebulisers given? | |
| YES and details of nebulisers given recorded | 53.2 (192) |
| YES but no details recorded | 29.4 (106) |
| Not recorded/inappropriate | 17.5 (63) |
| 17. Was prednisolone/hydrocortisone given? | |
| YES and details given, e.g. timings and dose | 36.8 (133) |
| YES but no details given | 34.6 (125) |
| Not recorded/inappropriate | 28.5 (103) |
| 18. Was a senior asked to review if not responding to above management? | |
| YES | 74.8 (270) |
| Not recorded/inappropriate | 25.2 (91) |
| 19. Was IV aminophylline given if not improving with above treatment/deteriorating? | |
| YES and details given, e.g. timings and dose | 1.4 (5) |
| YES but no details given | 77.0 (278) |
| Not recorded | 21.6 (78) |
| 20. What is the record of the patient’s disposal? | |
| Appropriate disposal | 84.8 (306) |
| Inappropriate disposal/not recorded | 15.2 (55) |
Appendix 28 Distribution of holistic review scores across all head injury and chronic obstructive pulmonary disease case notes
| Aspects of care | Score, % (n) | ||||||
|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | Missing | |
| Assessment | 2.6 (10) | 8.4 (32) | 13.8 (53) | 28.4 (109) | 40.6 (156) | 5.7 (22) | 0.5 (2) |
| Investigations | 3.4 (13) | 6.3 (24) | 7.3 (28) | 15.9 (61) | 42.4 (163) | 24.2 (93) | 0.5 (2) |
| Management | 3.4 (13) | 4.9 (19) | 9.1 (35) | 24.0 (92) | 41.7 (160) | 16.4 (63) | 0.5 (2) |
| Overall quality | 3.9 (15) | 6.5 (25) | 9.4 (36) | 27.1 (104) | 39.1 (150) | 13.5 (52) | 0.5 (2) |
| ED record | 2.6 (10) | 7.6 (29) | 12.8 (49) | 31.8 (122) | 37.2 (143) | 7.6 (29) | 0.5 (2) |
| Aspects of care | Score, % (n) | ||||||
|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | Missing | |
| Assessment | 3.6 (13) | 4.4 (16) | 10.2 (37) | 27.7 (100) | 47.4 (171) | 6.1 (22) | 0.6 (2) |
| Investigations | 4.2 (15) | 4.7 (17) | 8.6 (31) | 24.4 (88) | 42.7 (154) | 15.0 (54) | 0.6 (2) |
| Management | 4.4 (16) | 4.4 (16) | 9.7 (35) | 27.4 (99) | 42.7 (154) | 10.8 (39) | 0.6 (2) |
| Overall quality | 5.0 (18) | 3.0 (11) | 10.8 (39) | 29.1 (105) | 43.2 (156) | 8.3 (30) | 0.6 (2) |
| ED record | 4.4 (16) | 5.0 (18) | 10.8 (39) | 35.5 (128) | 37.7 (136) | 6.1 (22) | 0.6 (2) |
Appendix 29 Protocol (phase 1)
The impact of foundation doctor training: impact on workforce well-being and patient care – phase 1 (The EDiT Study)
Scientific Summary
Aims
-
To describe the current arrangements for the delivery of foundation training in England.
-
To identify how the training experiences of foundation year 2 doctors (FY2) impacts on their well-being, motivation and job satisfaction.
Study type and setting
A consultation of Postgraduate education stakeholders and a scoping study in up to four English Postgraduate educational Deaneries and four emergency departments (EDs) using qualitative methods in order to gain a full contextual understanding of the issues contributing to the experiences of the FY2 doctors, with a particular emphasis on the speciality of emergency medicine.
-
Consultation exercise: up to 15 in-depth semi structured interviews will be carried out with national and regional stakeholders
-
Scoping study: Interviews with consultant training leads and focus groups with FY2 doctors in up to four Postgraduate Deaneries and four EDs.
Outcomes
-
Description of current variation in the organisation and delivery of training to FY2 doctors throughout England
-
Describe the provision for the well-being of FY2 doctors in the planning and implementation of their training
-
An understanding of the factors contributing to FY2 doctor, well-being, motivation and job satisfaction and patient care.
Lay Summary
There have been a number of changes made recently by the government to improve the working conditions and well-being of NHS staff as there is evidence that improved working conditions can improve staff well-being, and in turn patient care. However the evidence of a direct link between well-being of staff and quality of patient care within healthcare is limited. More evidence is required about which aspects of working in the NHS impact on staff and also which aspects of well-being influence patient care.
This study aims to evaluate the well-being of doctors in training (foundation year 2) and compare this with quality of care provided to patients attending the emergency department (ED). Key aspects of well-being such as motivation, job satisfaction, and confidence that may impact on quality of care will be considered.
The study comprises; 1) a consultation exercise to determine the current training arrangements for foundation year 2 doctors (FY2s) at the national and regional level and 2) a scoping study in a small sample of Postgraduate Medical Deaneries and EDs to understand how the organisational and training arrangements for FY2s impact on their well-being.
Information from the consultation exercise and scoping study will be analysed in order to identify those key factors that potentially impact on the well-being of FY2 doctors (e.g. length of training rotations, induction procedures, support and supervision). The aim of this study (phase 1) is to provide a full contextual understanding of the issues contributing to the experiences of FY2 doctors, with an emphasis on their experiences in the specialty of Emergency Medicine. It is also anticipated this phase will inform the subsequent phase 2 study (not part of this protocol).
Research Outline
Introduction
In 2005 all UK Deaneries introduced Foundation Programmes as the initial phase of Modernising Medical Careers (MMC). The foundation programmes were designed as 2 year holistic programmes for doctors in training, suited for medical graduates. Postgraduate training is now structured around a formal programme with a national curriculum and structured assessment of clinical competencies. The impact of these new arrangements is not well understood, particularly in terms of the impact on the well-being of the doctors in training and the impact on services and patients.
This study aims to evaluate the national and regional arrangements for the planning and implementation of foundation training with a particular emphasis on identifying variation in these arrangements and how this impacts on FY2 doctors. The study will also investigate the factors which contribute to the well-being, motivation and confidence of FY2 doctors at the local level, with an emphasis on the specialty of emergency medicine.
Aims
-
To describe the current arrangements for the delivery of foundation training in England.
-
To identify how the training experiences of foundation year 2 doctors (FY2) impacts on their well-being, motivation and job satisfaction.
Objectives
-
To conduct a national and regional consultation exercise with training stakeholders in order to
-
Describe the national strategic view of the aims of delivering foundation year 2 doctor training with a particular focus on the role of training in providing for the well-being of doctors
-
Assess how the national view is implemented on a regional basis through the Postgraduate Deaneries and identify any regional variation to implementation within the specialty of emergency medicine.
-
-
To gather information on the experiences of FY2 doctors, from the perspective of both those in training and those carrying out the training, particularly how these experiences impact on FY2 doctor well-being, motivation and job satisfaction. This will be carried out in up to four Postgraduate Deaneries and four EDs. Based on these findings we will develop a measure to inform a quantitative evaluation of FY2 doctors in a further proposed phase 2 study.
Background, including NHS context and relevant literature
NHS context
Recent initiatives have been introduced into the NHS designed to improve the organisation and conditions of work and hence workforce well-being. The impact on NHS staff of inadequate working conditions has been of increasing interest to policy makers, with issues such as poor recruitment and retention of staff negatively impacting on healthcare effectiveness. 1,2 These initiatives have highlighted the importance of support within organisations for the effective development of individuals, with clarity about what is required from a post, in order that they meet their potential.
Importance of training on doctor well-being and patient outcomes
The link between staff development, motivation and well-being and the impact on patient care is recognised as important. 3,4 Training and appraisal have been identified in the literature as an important element in appropriate people management, impacting on knowledge and skills, job satisfaction and well-being, which in turn may influence patient outcomes. 5 Previous studies have demonstrated relationships between the quality and extent of training and appraisal with psychological well-being of staff and better patient care. 6–10
There is limited evidence of direct association between factors which effect performance and outcomes in health care and that would be important to take into account when studying a changing workforce. In one study9 which sought associations between organisational practice and clinical outcomes, it was possible to demonstrate a linkage between good Human Resources practice (such as appraisal and training) and effective teamwork with reduction in measures of patient mortality. A further study11 demonstrated, in a non-health care setting, that organisational climate (e.g. skill development, concern for employee welfare) was significantly associated with productivity and profitability, and that the relationship was mediated by employee job satisfaction.
There is an increasing literature on links between patient safety and organisational culture and climate, with a range of tools and interview methods proposed. 12
Training doctors in the NHS
Recently doctor training has undergone change in response to policy initiatives to improve the quality of patient care. The introduction of Modernising Medical Careers (MMC) in 200513 was in response to perceived longstanding problems with the job structure, working conditions and training opportunities in Postgraduate medical education. Training posts were criticised for being short term, stand-alone and not part of a clearly identified training programme, while supervision and assessment was judged as variable. These issues called into question whether doctors were being appropriately trained to meet the demands of a modern, patient-centred NHS. 14
The first stage of MMC reform introduced a two year, Foundation Programme (Foundation years 1 and 2) to address these perceived deficiencies. Postgraduate training now is structured around a formal programme with a national curriculum and structured assessment of clinical competencies.
A recent inquiry into MMC15 has highlighted a number of areas of concern with the foundation training model; variability in the quality of the year 2 placements and doctors not reaching appropriate levels of clinical responsibility when compared with their SHO predecessors. These issues have the potential to impact on the well-being and motivation of doctors and also on quality of patient care provided by them.
The report recommended greater clarity about what role Foundation year 2 doctors are expected to play in the healthcare team and what their service contribution should be. A further period of re-structuring of Postgraduate training now seems possible and this may affect the Foundation Programmes and hence the first stages of a doctors career.
Importance of evaluation
There is a need for better quality research evidence to fully investigate the nature of causal links between doctor training, other aspects of people management and their impact on psychological aspects of this workforce and patient outcomes. Studies need to incorporate a longitudinal element into their design, need to be adequately powered and need to incorporate validated measures in order to better establish these causal links. 16
It is crucial that initiatives designed to improve the knowledge, skills and well-being of the workforce, are evaluated and monitored. There is also a need for the development of standardised measures of factors such as well-being and job satisfaction that impact on patient care, which can provide meaningful comparative data across organisations and to act as a baseline for future studies. 17
The ED is in a unique position to provide an excellent broad based experience for foundation doctors in a challenging, high profile environment where there is the need to demonstrate safe and effective care and decision making in the context of rising demand and scarce resources. This makes the ED an appropriate setting for this proposed evaluation.
It is proposed to use qualitative methods in a phase one study to understand the national, regional and local factors that contribute to the experiences of FY2 doctors. The focus of the qualitative evaluation will be to study the impact of these organisational and strategic factors on well-being, motivation and satisfaction of FY2 doctors. Data collected will contribute to the development of quantitative measures of doctor well-being.
Plan of investigation
The study will use a qualitative approach across multiple sites as follows:
-
Planning and preparation
-
Ethical approval will be sought via the National Research Ethics Service.
-
All EDs in England will be approached for participation in phase one and a proposed second phase of the study.
-
As EDs agree to participate in the study, applications for research & development approval will be instigated within each Trust.
-
-
Consultation exercise
-
Interviews will identify, compare and assess different strategies and organisational arrangements for the implementation and delivery of post-graduate medical education and training.
-
We will undertake a national, regional and local service level consultation involving stakeholders who will be consulted about the arrangements to deliver and monitor doctor training and determine the local context in which Postgraduate training is being implemented and delivered.
-
-
A scoping study is proposed in up to four Postgraduate Deaneries and four EDs selected to represent diversity in approach to training, organisation size and type, as well as urban and rural location.
-
To identify the range of factors that contribute to the well-being, motivation and satisfaction of FY2 doctors
-
To identify important data collection items for a survey instrument to be used in a proposed second phase of the study.
-
Methods (including the plan of analysis)
1. Consultation exercise
Up to 15 in-depth semi structured telephone or face-to-face interviews will be carried out with national and regional stakeholders. These may include representatives from the Postgraduate and medical education training board (PMETB), General Medical Council (GMC), the national Foundation Programme Office (www.foundationprogramme.nhs.uk), modernising medical careers (MMC), the MMC Inquiry team, Postgraduate deans and foundation school directors within English Postgraduate Deaneries. Topics will include; the current organisation of foundation doctor rotations, monitoring and assessment issues, criteria for success and planned developments in future training. Data will be collected on; arrangements for the implementation of the foundation training agenda, key initiatives and examples of best practice occurring nationally.
2. Scoping study in up to four Postgraduate Deaneries and four emergency departments
Up to four Postgraduate Deaneries and four EDs will be selected for a combination of interviews and focus groups. Selection of these Postgraduate Deaneries and EDs will be informed by data gathered in the consultation exercise and will include criteria such as variation in approach to the implementation of training, variation in size of organisation and geographical profile.
The main aspects of this work will include:
Foundation year 2 doctors
Views will be sought from FY2 doctor focus groups about the training programme, experiences in their working environment, peer support and mentorship, value of the job and opportunities for development.
Consultant trainers and training leads
Two interviews per site with emergency medicine consultants involved in the delivery of training at FY2 level will gather information on induction, monitoring, assessments and sign off. In addition, the impact that the new training arrangements have on other staff within EDs in terms of workload, motivation and job satisfaction will be explored.
Foundation year 2 doctor survey development
A survey for a proposed second phase study will be developed mainly using adaptations of previously validated scales that reflect the information gathered from themes identified during the scoping work. 18–23 It is felt that the use of pre-existing validated scales that have normative data on doctors within the NHS17 versioned to reflect the variables identified in phase one, will enable both contemporaneous and longitudinal comparative studies during the phase 2 study.
2. Data analysis
Qualitative analysis (scoping study of up to four Postgraduate Deaneries and four EDs)
Analysis of data collected from focus groups, interviews and ethnographic observations carried out in up to four Postgraduate Deaneries and four EDs will be analysed using thematic analysis (TA). This method is flexible and has the potential to identify, analyse and report themes within the data. 24 A broadly theoretical TA approach will be taken in order that analysis is driven by the research aim of identifying key themes related to well-being, motivation and job satisfaction in FY2 doctors.
Main Outputs
-
Description of current variation in the organisation and delivery of training to FY2 doctors throughout England
-
Describe the provision for the well-being of FY2 doctors in the planning and implementation of their training
-
An understanding of the factors contributing to FY2 doctor, well-being, motivation and job satisfaction and patient care.
Proposals for the involvement of stakeholders
Stakeholders have had a key role in the planning and writing of this proposal. The input from co-applicants GN (the UK Lead Dean for Emergency Medicine) and AF (an ex-local Foundation Programme Director, and current Training Programme Director for the Acute Care Common Stem) has proved invaluable in identifying existing organisations and processes for the phase one stakeholder consultation in this study. Our patient representative (BD) has attended meetings and commented on drafts and her input has ensured that the patient experience is incorporated into the design. The steering group also has representation from a Foundation School Director and two FY2 junior doctor representatives who will review and comment on relevant documentation and be consulted at each stage of the study regarding junior doctor involvement and provide feedback on the junior doctor perspective. It is expected that the consultation exercise in this phase one study will enable the views of stakeholders (from training, emergency medicine and patient perspective) to shape the format of a proposed second phase study, which will include a Foundation year 2 doctor survey and records review study. In addition, key stakeholders from medical education, emergency medicine and patient representation will form the steering committee for the study. Finally, participants at all levels will be invited to two workshops at the conclusion of the study, in order to disseminate and discuss the findings.
Plans for dissemination of results
The results will be disseminated as:
-
Final report to the NIHR SDO detailing the findings in relation to the aims and objectives.
-
Two workshops held at the end of the study to disseminate the findings from both phases.
-
The first will be for key stakeholders such as Deanery, PMETB, GMC and MMC representatives.
-
The second will be for participating Trusts, EDs and patients.
-
A report for distribution to policy makers, the College of Emergency Medicine and academy of Royal Colleges, the GMC, PMETB, MMC team and MMC Inquiry team, regional Postgraduate deans, foundation school directors and local training leads and trainers.
-
A series of research papers for publication in relevant peer reviewed journals.
-
Presentation of the findings at relevant health services research, medical education and emergency medicine meetings.
Steering Committee
The remaining applicants (GN, AF, JG, BD) will support the study through the formation of a steering committee that will be responsible for monitoring its progress. These individuals have extensive experience of doctor training and modernising medical careers, emergency care delivery and research in this field in the UK. The steering group also has representation from a Foundation School Director and two FY2 junior doctor representatives who will review and comment on relevant documentation and be consulted at each stage of the study regarding junior doctor involvement and provide feedback on the junior doctor perspective. Meetings will be held at 6 monthly intervals to; ensure safety of participants, monitor the study, ensure data protection and advise on the final report.
Team Expertise
The research team combines significant medical, clinical and HSR expertise and this study will build on local strengths and prior work in service evaluation. SM and AF have extensive clinical experience in emergency medicine. SM currently divides her time between clinical commitments in the ED, and HSR in emergency medicine at the University of Sheffield.
Previously and current commissioned projects involving SM and CO have evaluated the impact of paramedic practitioners on older people (The Health Foundation), assessed factors that affect ED waiting times (NIHRSDO) and evaluated the role of Emergency Care Practitioners (NIHRSDO).
The Institute of Work Psychology is dedicated to conducting applied research in work settings and is the leading centre for research in Work and Organisational Psychology in the UK. AC was the member of a team that undertook a large scale project for the Department of Health, examining the well-being of 193 secondary health care teams and 5,000 individuals in NHS Trusts in England. RO has extensive experience in risk management, patient safety and changing workplace behaviour. Relevant research projects include methods for assessing quality from hospital records, stakeholder consultations with UK rail companies, passenger representatives and health and safety regulators, and the contribution of organisational and individual factors to employee health status. GN is the National Lead Dean for emergency care and has extensive research experience in the field of Postgraduate medical education and a flexible healthcare workforce. JG is a member of the PMETB board and has worked for more than 30 years in medical education development and policy research, JG is Special Adviser to the World Federation for Medical Education. BD is a lay advisor who has experience as service user, but has also participated in previous research into organisational aspects of emergency medicine.
Project timetable
Phase one (months 0–12)
In the first 12 months of the project we will complete:
-
Planning and preparation of the study
-
Consultation exercise with key stakeholders
-
Scoping study of four Postgraduate Deaneries and four EDs
-
Development of the survey tool for phase one
-
Analysis and write up of phase one.
References
- The NHS knowledge and skills framework (NHS KSF) and the development review process. London: D of H; 2004.
- Improving working lives standard: NHS Employees Committed to Improving the Lives of People who Work in the NHS. London: Department of Health; 2000.
- Karasek R, Theorell T. Healthy Work: stress, productivity and the reconstruction of working life. New York, NY: Basic Books; 1990.
- Parker S. Advanced topics in organisational behaviour. Sage Publications; n.d.
- Michie S, West M. Managing people and performance: an evidence based framework applied to health service organizations. International Journal of Management Reviews 2004;5/6:91-111.
- Grol R, Mokkink H, Helsper-Lucas A, Tielens V, Bulte J. Effects of the vocational training of general practice consultation skills and medical performance. Medical Education 1989;23:512-21.
- Tharenou P, Burke E, Robertson I, Callinan M, Bartram D. Organisational Effectiveness: The Role of Psychology. Chichester: John Wiley; 2002.
- West E. Management matters: the link between hospital organisations and the quality of patient care. Quality in Health Care 2001;10:40-8.
- West MA, Shackleton VJ, Borrill CS, . The relationship between staff management practices and patient mortality in acute hospitals: a longitudinal study. Birmingham: Aston Business School Working Paper Series; 2003.
- Wall TD, Bolden RI, Borrill CS, . Minor psychiatric disorder in NHS trust employees: occupational and gender differences. British Journal of Psychiatry 1997;171:519-23.
- Patterson MG, Warr PB, West MA. Organisational climate and productivity. J Occupational and Organisational Psychology 2004;77:193-216.
- Morey JC, Simon R, Jay GD, . Error reduction and performance improvement in the emergency through formal teamwork training: evaluation: results of the MedTeams project. Health Serv Res 2002;37:1553-81.
- The National Health Service . Modernising Medical Careers n.d. URL: http://www.mmc.nhs.uk/pages/resources/keydocuments.
- Clough C. Modernising Medical Careers: effect on NHS service delivery. Hospital Medicine 2005;66:139-41.
- Aspiring to Excellence: Findings and Recommendations of the Independent Inquiry into Modernising Medical Careers Led by Sir John Tooke n.d. URL: http://www.mmcinquiry.org.uk/draft.htm.
- Yamey G. Promoting wellbeing among doctors. British Medical Journal Editorial 2001;322:252-3.
- Mullarkey S, Wall TD, Warr PB, Clegg CS, Stride C. Measures of job satisfaction, mental health and job-related well-being: A bench-marking manual. Sheffield, England: Sheffield Academic Press Ltd; 1999.
- Warr PB. Work, unemployment and mental health. Oxford: Oxford University Press; 1987.
- Warr PB. The measurement of well-being and other aspects of mental health. Journal of Occupational Psychology 1990;63:193-210.
- Pritchard RD, Payne S, Holman D, Wall T D, Clegg C W. The new workplace: people technology and organisation: a handbook and guide to the human impact of modern working practices. John Wiley; 2003.
- Warr PB, Cook JD, Wall TD. Scales for the measurement of some work attitudes and aspects of psychological well-being. Journal of Occupational Psychology 1979;52:129-48.
- Pratt M, Rockmann K, Kaufmann J. Constructing professional Identity. The role of work and identity learning cycles in the customization of identity among medical professionals. Academy of Management Journal 2006;49:235-62.
- Croft S, Mason S. Are Emergency Department junior doctors becoming less experienced in performing common practical procedures?. Emergency Medicine Journal 2007;24:657-8.
- Braun V, Clark V. Using thematic analysis in psychology. Qualitative Research in Psychology 2006;3:77-101.
Appendix 30 Protocol (phase 2)
The impact of foundation doctor training: impact on workforce wellbeing and patient care – Phase 2 (The EDiT Study)
Scientific Summary
Aims
-
To identify how the experiences of foundation year 2 (FY2) doctors training in EDs impacts on their well-being, motivation and job satisfaction.
-
To evaluate how the well-being and motivation of FY2 doctors in emergency departments (EDs) impacts on the quality of patient care.
-
To identify key measures of FY2 doctor well-being and motivation, which impact on quality of patient care and which will underpin the development of a tool to monitor well-being and motivation during training.
Study type and setting
Multi-site longitudinal observational study in at least 15 EDs. The study will evaluate the well-being of FY2 doctors, the quality of the care they deliver and investigate the relationship between these dimensions.
Methodology
-
Survey utilising validated measures carried out with three successive cohorts of FY2 doctors, measuring their well-being, motivation and job satisfaction. Professional identity, confidence and competence will also be measured. An overall well-being score for each doctor will be calculated from these measures. The survey will be carried out in at least 15 EDs, at up to four time intervals over the 12 months of the study. Surveying at four time intervals will allow measurement of FY2 doctors’ well-being over the whole foundation year and before and after their ED placement.
-
Quality of care provided by FY2 doctors will be measured by selecting a sample of clinical records for the three cohorts of doctors across the participating EDs. A holistic records review approach will be taken by trained middle grade doctor reviewers to provide a quality-of-care score for each FY2 doctor.
-
Routine data will be collected from each ED to measure the performance of FY2 doctors and the ED over the study period.
-
FY2 doctors’ scores on well-being and quality of care will be evaluated to explore the relationship between well-being and quality of care in this cohort.
Outcomes
-
Workforce Outcomes:
-
FY2 doctor, well-being, motivation and job satisfaction
-
Differences in FY2 doctor well-being, motivation and job satisfaction compared across EDs.
-
-
Patient Outcomes:
-
Score on safety and quality of clinical care provided by FY2 doctors following the records review
-
FY2 doctor performance, perceived confidence and competence over time.
-
-
Service outcomes:
-
ED performance measured by mean waiting times, 4-hour performance, workload and work rate of FY2 doctors.
-
-
Research outcomes:
-
Identification of measures of well-being and motivation that may be further developed into a validated generic tool for use in foundation training.
-
Lay Summary
There have been a number of changes made recently by the government to improve the working conditions and well-being of NHS staff as there is evidence that improved working conditions can improve staff well-being, and in turn patient care. However the evidence of a direct link between well-being of staff and quality of patient care within healthcare is limited. More evidence is required about which aspects of working in the NHS impact on staff and also which aspects of well-being influence patient care.
This study aims to evaluate the well-being of doctors in training and compare this with quality of care provided to patients attending the emergency department (ED). The relationship between well-being and quality of care aims to identify key aspects such as motivation, job satisfaction, and confidence that impact on quality of care. The measures will have the potential to be developed into a tool that may be utilised more widely for doctors in the NHS.
The study will comprise surveys of doctors in their second year of training (FY2 doctors) who are working in the ED as part of this year. The survey will collect data relating to doctor well-being, motivation, job satisfaction, professional identity, confidence and competence. These data will be compared with quality of care provided by these doctors through an examination of patient records detailing care given to patients.
It is anticipated that this study will identify key factors in the experiences of FY2 doctors that can improve well-being, motivation and job satisfaction and that directly link to improvements in the care of patients.
Research Outline
Introduction
This study aims to evaluate the well-being of doctors in training and explore the association with the quality of care provided to patients attending the ED.
In 2005 all UK Deaneries introduced Foundation Programmes as the initial phase of Modernising Medical Careers (MMC) for doctors in training as 2 year holistic programmes, suited for medical graduates.
The Emergency Department (ED) is a complex and challenging training environment for doctors. Specifically, it encompasses patients with a wide range of presenting clinical conditions, where doctors in training work autonomously and often act as the main decision makers in patient care. In this sense it is ideal as a study context to link doctor well-being with quality of patient care. In most other clinical specialties it would be hard to ascribe care solely to doctors in training as they more often work within a clinical team comprising a number of clinicians.
The study will comprise a longitudinal survey of doctors in their second year of training (FY2 doctors) who are working in the ED as part of this year. The survey will collect data relating to doctor well-being, motivation, job satisfaction, professional identity, confidence and competence. These data will be analysed along with the data collected on quality of care provided by FY2 doctors, by a clinical records review and analysis of routine performance data. Finally, measures of FY2 doctor well-being which are found to be strongly associated with patient care will be identified for future development into a validated tool that may be utilised more widely in the NHS.
Aims
-
To identify how the experiences of FY2 doctors training in EDs impacts on their well-being, motivation and job satisfaction.
-
To evaluate how the well-being and motivation of FY2 doctors in EDs impacts on the quality of patient care.
-
To identify key measures of FY2 doctor well-being and motivation, which impact on quality of patient care and which will underpin the development of a tool to monitor well-being and motivation during training.
Objectives
Undertake a longitudinal study within at least 15 English EDs to evaluate FY2 doctor well-being, motivation and job satisfaction and compare this with quality of patient care. The components of this phase will be to:
-
Use a structured survey to assess FY2 doctors working in the ED in terms of their well-being, motivation and job satisfaction. In addition, issues of professional identity, confidence and competence will be explored.
-
Assess patient safety and quality of care by FY2 doctors by:
-
a review of clinical records of patients receiving emergency care from these doctors
-
examining routine ED data to link workload, casemix, mean waiting times and four-hour performance between the EDs.
-
Examine the findings from the study in order to:
-
Evaluate the relationship between FY2 doctor well-being, motivation and patient care
-
Identify best practice models of FY2 doctor training which might be generalised and implemented across the NHS in order to promote a healthy and productive Foundation doctor workforce
-
Provide a starting point for the development of a tool that can be developed to monitor the well-being, motivation and training of doctors in emergency medicine and other specialities.
Background, including NHS context and relevant literature
NHS context
Recent initiatives have been introduced into the NHS designed to improve the organisation and conditions of work and hence workforce well-being. The impact on NHS staff of inadequate working conditions has been of increasing interest to policy makers, with issues such as poor recruitment and retention of staff negatively impacting on healthcare effectiveness. 1,2 These initiatives have highlighted the importance of support within organisations for the effective development of individuals, with clarity about what is required from a post, in order that they meet their potential.
Importance of training on doctor well-being and patient outcomes
The link between staff development, motivation and well-being and the impact on patient care is recognised as important. 3,4 Training and appraisal have been identified in the literature as an important element in appropriate people management, impacting on knowledge and skills, job satisfaction and well-being, which in turn may influence patient outcomes. 5 Previous studies have demonstrated relationships between the quality and extent of training and appraisal with psychological well-being of staff and better patient care. 6–10
There is limited evidence of direct association between factors which effect performance and outcomes in health care and that would be important to take into account when studying a changing workforce. In one study9 which sought associations between organisational practice and clinical outcomes, it was possible to demonstrate a linkage between good Human Resources practice (such as appraisal and training) and effective teamwork with reduction in measures of patient mortality. A further study11 demonstrated, in a non-health care setting, that organisational climate (e.g. skill development, concern for employee welfare) was significantly associated with productivity and profitability, and that the relationship was mediated by employee job satisfaction.
There is an increasing literature on links between patient safety and organisational culture and climate, with a range of tools and interview methods proposed. 12
Training doctors in the NHS
Recently doctor training has undergone change in response to policy initiatives to improve the quality of patient care. The introduction of Modernising Medical Careers (MMC) in 200513 was in response to perceived longstanding problems with the job structure, working conditions and training opportunities in Postgraduate medical education. Training posts were criticised for being short term, stand-alone and not part of a clearly identified training programme, while supervision and assessment was judged as variable. These issues called into question whether doctors were being appropriately trained to meet the demands of a modern, patient-centred NHS. 14
The first stage of MMC reform introduced a two year, Foundation Programme (Foundation years 1 and 2) to address these perceived deficiencies. Postgraduate training now is structured around a formal programme with a national curriculum and structured assessment of clinical competencies.
A recent inquiry into MMC15 has highlighted a number of areas of concern with the foundation training model; variability in the quality of the year 2 placements and doctors not reaching appropriate levels of clinical responsibility when compared with their SHO predecessors. These issues have the potential to impact on the well-being and motivation of doctors and also on quality of patient care provided by them.
The report recommended greater clarity about what role FY2 doctors are expected to play in the healthcare team and what their service contribution should be. A further period of re-structuring of Postgraduate training now seems possible and this may affect the Foundation Programmes and hence the first stages of a doctors career.
Importance of evaluation
There is a need for better quality research evidence to fully investigate the nature of causal links between doctor training, other aspects of people management and their impact on psychological aspects of this workforce and patient outcomes. Studies need to incorporate a longitudinal element into their design, need to be adequately powered and need to incorporate validated measures in order to better establish these causal links. 16
It is crucial that initiatives designed to improve the knowledge, skills and well-being of the workforce, are evaluated and monitored. There is also a need for the development of standardised measures of factors such as well-being and job satisfaction that impact on patient care, which can provide meaningful comparative data across organisations and to act as a baseline for future studies. 17
The ED is in a unique position to provide an excellent broad based experience for foundation doctors in a challenging, high profile environment where there is the need to demonstrate safe and effective care and decision making in the context of rising demand and scarce resources. This makes the ED an appropriate setting for this proposed evaluation.
Evaluating new ways of working requires new ways of measuring their effect. It is proposed therefore to use surveys and a quality records review using validated, relevant instruments to collect longitudinal data from doctors operating in a range of emergency medicine working environments, and also data from the patients they treat. These data will be analysed to evaluate the well-being and motivation of FY2 doctors and the quality of care they provide. The relationship between well-being and motivation and quality of patient care will also be evaluated. The identification of important measures of doctor well-being that can be linked with patient care may allow the further development of tools for wider use within the NHS to monitor and evaluate doctors in training.
Plan of investigation
A longitudinal observational study will explore and measure FY2 doctors’ experiences and the experiences of patients. Within the participating EDs the study will involve three successive cohorts of FY2 doctors. This will include:
1. FY2 doctor survey
A survey of all FY2 doctors to assess aspects such as well-being, motivation, job satisfaction, professional identity, confidence and competence;
-
prior to commencing year 2 of their training rotation
-
at the end of year 2 of their training rotation
-
at the beginning and end of each ED placement.
2. Quality of patient care
To assess patient quality of care we will undertake a safety and clinical records review to evaluate quality of care. In addition, we will collect routine data from each ED such as waiting times, four-hour performance, workload and work rate of the FY2 doctors
3. Identification of measures for future development
Analysis of these data over time will enable the relationship between quality of patient care and FY2 doctor well-being and motivation to be identified both within each ED and between them. Important measures will be identified that can be developed further into a validated tool for more widespread use in monitoring doctor performance throughout training.
Methods (including the plan of analysis)
Longitudinal study
All English EDs will be approached for participation in the study. It is anticipated that at least 15 EDs will participate. Three successive cohorts of FY2 doctors will be surveyed in order to ensure evaluation of these doctors at key stages in the FY2 year. This longitudinal study will analyse both the workforce well-being and motivation of FY2 doctors and the quality of patient care being provided by them in the ED setting. There are three main elements:
1. FY2 doctors:
Doctors eligible for this study are all those entering the second year of foundation training, where one of their four-month posts is in the specialty of emergency medicine.
All eligible doctors will complete a survey at the beginning and the end of their second year. Up to two further surveys will be completed by doctors to ensure each is surveyed at the beginning and the end of each four-month ED post (see Figure 1). Each survey will measure well-being, motivation, job satisfaction, professional identity, confidence and competence and therefore anticipated changes over time in these variables will be measured.
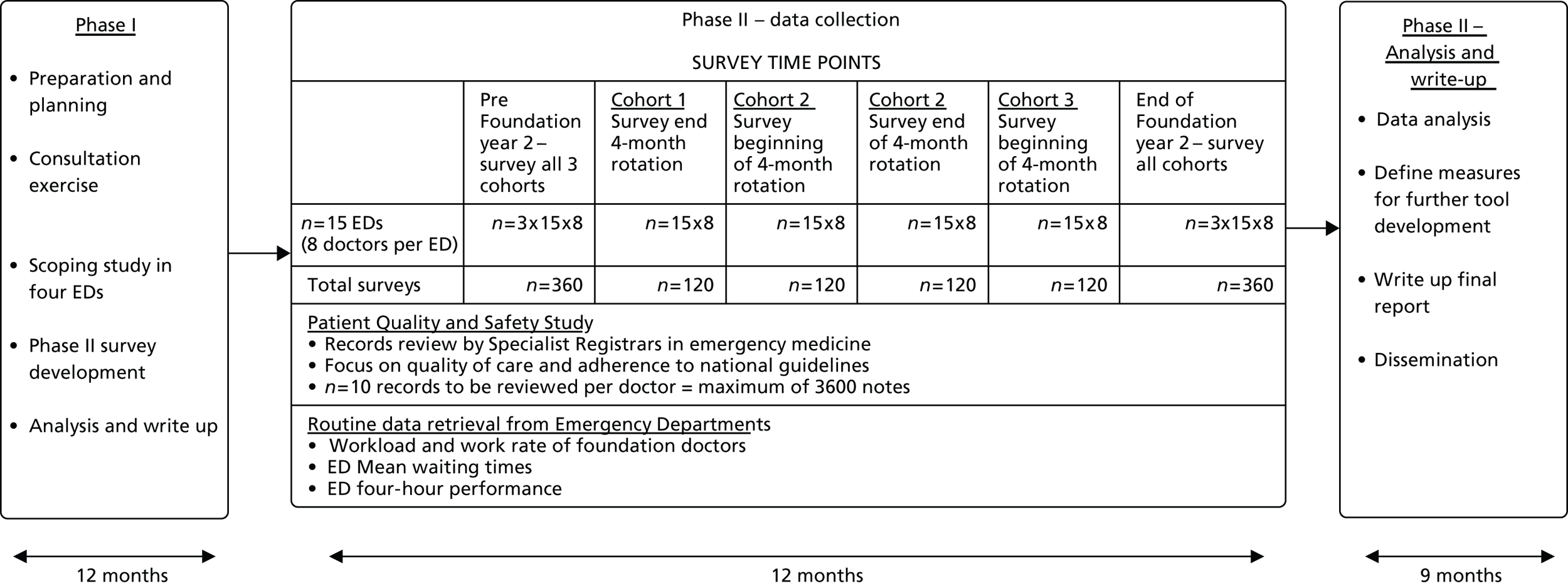
It is anticipated that the main headings of the survey will include:
-
Generic measures: Well-being,18,19 motivation,20 job satisfaction,21 professional identity,22 confidence in role23
-
Programme/training measures: Mentorship, formal teaching, formal assessments, feedback24
-
Emergency department measures: Environment – workload, casemix, peer support, competence in role, job characteristics.
The survey will be administered by post or electronically, depending on local preferences. Data will be analysed to provide understanding of the differences in job perceptions and attitudes that exist within and between participating EDs, between doctors and over time.
2. Patients:
Quality of care will be assessed using a clinical records review. Record review has become an established method of examining the quality of care provided by a health care organisation. 25 Members of the research team have refined these methods in a major study on the reliability of review methods. 26 The proposed study will use a combination of approaches to derive a quality and safety of care rating for each FY2 doctor. Middle grade doctors in emergency medicine will be recruited from each participating ED to act as reviewers in their own hospital as would happen with clinical audit. Ten clinical records per doctor will be randomly selected from a specified period during their time working in the ED. The records will be reviewed using the implicit approach method. 27,28
To assess reliability, two reviewers will independently assess the same set of records at one time point in six of the participating EDs. Training will be provided for all reviewers.
3. Service:
Routine data will be collected from each participating ED to assess service performance within EDs over the study time period and also compare across EDs on the proportion of patients seen within the four-hour target, mean waiting times, casemix, workload and work rate of FY2 doctors.
Statistical Issues
1. Sample Size
Foundation doctor sampling
We plan to include a sample size of 210 FY2 doctors from across EDs in England.
Firstly we hypothesise that the job-related well-being of FY2 doctors, measured by the 6-item anxiety-contentment and 6-item depression-enthusiasm dimensions of the Warr job-related well-being scale,18 will change over the duration of the training. Having employed surveys immediately pre- and post-training to capture this information:
-
Assuming a correlation of r = 0.4 between the pre- and post- tests scores, to detect a 0.2-unit change in anxiety-contentment, (which, given the estimated standard deviations of these measures from published benchmarking data29 on a comparable sample would be classified as a medium effect size), at the p < 0.05 level of significance, with 95% power, would require a sample size of 210 cases.
-
Assuming a correlation of r = 0.4 between the pre- and post- tests scores, to detect a 0.2-unit change in depression-enthusiasm, (which again, given the estimated standard deviations of these measures from published benchmarking data29 on a comparable sample, would be classified as a medium effect size), at the p < 0.05 level of significance, with 95% power, would require a sample size of 170 cases.
Secondly we hypothesise that the job satisfaction of FY2 doctors, measured by the 15-item, 7-point response scale Job Satisfaction scale,21 will change over the duration of the training. Assuming a correlation of r = 0.4 between the pre- and post- tests scores, to detect a 0.25-unit change in Job Satisfaction, (which, given the estimated standard deviations of these measures from published benchmarking data on a comparable sample,29 would be classified as a medium effect size), at the p < 0.05 level of significance, with 95% power, would require a sample size of 170 cases.
Finally, we hypothesise that both the well-being and the job satisfaction of FY2 doctors at the end of the study, and the change in these outcome variables will vary significantly across the EDs. The nested nature of our sample (i.e. a sample of doctors, within a sample of hospitals) will result in a multilevel data set, with two sample sizes to consider; that of doctors within each hospital, and that of the hospitals. The sample size of the higher level, in our case, hospitals, is almost always the restrictive element in such designs.
We envisage that there will be on average 24 FY2 doctors in each participating ED during the 12 month period of the longitudinal study. If we assume a 20% non-response within each ED, and a further 20% loss of paired cases between pre- and post-placement surveys across the sample, then this will give us a final sample of around 14 FY2 doctors per department. In order satisfy the most stringent of the power analyses above, this will mean recruiting at least 15 EDs.
2. Data analysis
Descriptive statistics and exploratory analysis of the outcome and predictor variables in the surveys will be summarised by tabulation of mean scores (or medians where their distribution makes this the more appropriate summary statistic), both for the whole sample and split by ED. Bar charts will be employed to illustrate differences between EDs. Where variables are measured at multiple time points summary statistics will be displayed for each time point, and graphically illustrated by line graphs showing the changes over time.
A variety of inferential statistical techniques will be used to test hypotheses, which will of course develop as the study progresses. Initially, to assess the impact of predictor variables on the final levels of our key outcomes, multiple regression will be used, with background and demographic variables entered into the model first, followed by the predictor variables of primary interest.
When assessing and predicting change in outcomes over the period of doctor training, a variety/number of different methods will be employed;
-
Paired t tests, or non parametric equivalent, to assess the extent of any change.
-
Repeated measures/mixed ANOVA to assess whether any change found differs by factors defining sub groups of the data (gender, age, previous placements).
-
Multiple regression, with the dependent variable being the end of training measure of the outcome, and with the time one measure of the outcome entered as the first predictor, followed by the predictors of primary interest, to see whether these latter predictors are related to the change over time.
Finally, to enable us to best describe the effect of departments on our outcome, (and on the relationship between these outcomes and our predictor variables), through partitioning the variants of outcomes into between – and – within- hospital portions, and modelling each portion appropriately; we will use hierarchical linear modelling (aka multi level modelling). Initially this will be via a 2 level model (doctors nested in hospitals), but may extend to a 3 level model (observations over time in doctors nested in hospitals), with the non-independence of the repeated measures of doctors modelled by an auto regressive correlation structure. Such a longitudinal hierarchical linear model will enable us to include data from those cases which have responded at only one time point thus boosting the power of the analysis.
Cases with missing data on one or more variables will most likely be deleted on an analysis by analysis basis, having first checked for the existence of non random and systematic missing data. Assumptions regarding the sample attrition over time have been built into our sample size calculation; note also that the hierarchical linear modelling techniques outlined above will enable us to include respondents who have not replied at all time points in our longitudinal analyses.
Main Outputs
-
1. Workforce Outcomes:
-
FY2 doctor, well-being, motivation and job satisfaction.
-
Differences in FY2 doctor well-being, motivation and job satisfaction compared across EDs.
-
-
2. Patient Outcomes:
-
Score on safety and quality of clinical care provided by FY2 doctors following the records review.
-
FY2 doctor performance, perceived confidence and competence over time.
-
-
3. Service outcomes:
-
ED performance measured by mean waiting times, four-hour performance, workload and work rate of FY2 doctors.
-
Recommendations for best practice regarding the implementation and delivery of FY2 training in acute NHS settings in order to optimise patient care.
-
-
4. Research outcomes:
-
Identification of measures of well-being and motivation that may be further developed into a validated generic tool for use in foundation training.
-
Plans for dissemination of results
The results will be disseminated as:
-
Final report to the NIHR SDO detailing the findings in relation to the aims and objectives.
-
Workshops held at the end of the study to disseminate the findings from the study.
-
The first will be for key stakeholders such as Deanery, PMETB, GMC and MMC representatives.
-
The second will be for participating Trusts, EDs and patients.
-
A report for distribution to policy makers, the College of Emergency Medicine and academy of Royal Colleges, the GMC, PMETB, MMC team and MMC Inquiry team, regional Postgraduate deans, foundation school directors and local training leads and trainers.
-
A series of research papers for publication in relevant peer reviewed journals.
-
Presentation of the findings at relevant health services research, medical education and emergency medicine meetings.
Project timetable
-
Planning and preparation of the study (months 1–5)
-
Data collection (months 6–18)
-
FY2 doctor survey over three cohorts of doctors in 12 EDs
-
A records review approach to assessing the quality and safety of care provided to patients by FY2 doctors
-
Collection of routine data from the 12 participating EDs.
-
-
In the final 6 months we will undertake:
-
Analysis of data
-
Writing up of the study results
-
Production of the final report
-
Dissemination of the results including workshops to feedback findings to participants.
-
References
- The NHS knowledge and skills framework (NHS KSF) and the development review process. London: D of H; 2004.
- Improving working lives standard: NHS Employees Committed to Improving the Lives of People who Work in the NHS. London: Department of Health; 2000.
- Karasek R, Theorell T. Healthy Work: stress, productivity and the reconstruction of working life. New York, NY: Basic Books; 1990.
- Parker S. Advanced topics in organisational behaviour. Sage Publications; 1998.
- Michie S, West M. Managing people and performance: an evidence based framework applied to health service organizations. International Journal of Management Reviews 2004;5/6:91-111.
- Grol R, Mokkink H, Helsper-Lucas A, Tielens V, Bulte J. Effects of the vocational training of general practice consultation skills and medical performance. Medical Education 1989;23:512-21.
- Tharenou P, Burke E, Robertson I, Callinan M, Bartram D. Organisational Effectiveness: The Role of Psychology 2002:115-33.
- West E. Management matters: the link between hospital organisations and the quality of patient care. Quality in Health Care 2001;10:40-8.
- West MA, Shackleton VJ, Borrill CS, . The relationship between staff management practices and patient mortality in acute hospitals: a longitudinal study. Birmingham: Aston Business School Working Paper Series; 2003.
- Wall TD, Bolden RI, Borrill CS, . Minor psychiatric disorder in NHS trust employees: occupational and gender differences. British Journal of Psychiatry 1997;171:519-23.
- Patterson MG, Warr PB, West MA. Organisational climate and productivity. J Occupational and Organisational Psychology 2004;77:193-216.
- Morey JC, Simon R, Jay GD, . Error reduction and performance improvement in the emergency through formal teamwork training: evaluation: results of the MedTeams project. Health Serv Res 2002;37:1553-81.
- The National Health Service . Modernising Medical Careers n.d. URL: http://www.mmc.nhs.uk/pages/resources/keydocuments.
- Clough C. Modernising Medical Careers: Effect on NHS Service Delivery. Hospital Medicine 2005;66:139-41.
- Aspiring to Excellence: Findings and Recommendations of the Independent Inquiry into Modernising Medical Careers Led by Sir John Tooke n.d. URL: http://www.mmcinquiry.org.uk/draft.htm.
- Yamey G. Promoting wellbeing among doctors. British Medical Journal Editorial 2001;322:252-3.
- Mullarkey S, Wall TD, Warr PB, Clegg CS, Stride C. Measures of job satisfaction, mental health and job-related well-being: A bench-marking manual. Sheffield, England: Sheffield Academic Press Ltd; 1999.
- Warr PB. Work, unemployment and mental health. Oxford: Oxford University Press; 1987.
- Warr PB. The measurement of well-being and other aspects of mental health. Journal of Occupational Psychology 1990;63:193-210.
- Pritchard RD, Payne S, Holman D, Wall T D, Clegg C W. The new workplace: people technology and organisation: a handbook and guide to the human impact of modern working practices. John Wiley; 2003.
- Warr PB, Cook JD, Wall TD. Scales for the measurement of some work attitudes and aspects of psychological well-being. Journal of Occupational Psychology 1979;52:129-48.
- Pratt M, Rockmann K, Kaufmann J. Constructing professional Identity. The role of work and identity learning cycles in the customization of identity among medical professionals. Academy of Management Journal 2006;49:235-62.
- Croft S, Mason S. Are Emergency Department junior doctors becoming less experienced in performing common practical procedures?. Emergency Medicine Journal 2007;24:657-8.
- Postgraduate Medical Education Training Board 2006 National Trainee Survey – Key Findings n.d.
- Lilford RJ, A Brown CA, Nicholl J. Use of process measures to monitor the quality of clinical practice. British Medical Journal 2007;335:648-50.
- Hutchinson A. Comparative Study Of Different Methods To Assess Quality Of Care/Safety. National Co-ordinating Centre for Research Methodology Project Code RM03/JH08/AH; n.d.
- British Thoracic Society (BTS) and Scottish Intercollegiate Guidelines Network . British guideline on the management of asthma. Thorax 2003;58:i1-94.
- Clinical Guideline N0234. National Institute of Clinical Excellence; 2003.
- Stride, Toby, Catley. Measures of Job Satisfaction, Organisational Commitment, Mental Health and Job Related Well-being: A Benchmarking Manual 2007.
Glossary
- Analysis of variance
- A psychometric test of the difference between two variables.
- Chronic obstructive pulmonary disease
- A collection of lung diseases including chronic bronchitis, emphysema and chronic obstructive airways disease.
- Clinical supervisor
- A consultant trained to supervise foundation doctors. A clinical supervisor is responsible for monitoring and ‘signing off’ those foundation doctors working in their department as part of their Foundation Programme.
- Comparative study
- A comparative study is one in which only a small body of evidence exists to benchmark the results of the study against.
- Conference of Postgraduate Medical Deans of the United Kingdom
- A quarterly conference of Medical Deans.
- Cronbach’s alpha
- A measure of reliability with a higher correlation suggesting a stronger reliability.
- Educational supervisor
- A medical practitioner trained to supervise foundation doctors during a specific specialty placement or through a number of placements across their Foundation Programme.
- Electronic portfolio
- An online record of progress maintained by all foundation doctors. Includes the recording of scores from the Foundation Programme assessments of competency.
- Emergency department
- Department within a hospital where emergency or acute patients are taken for initial assessment and management.
- Emergency medicine
- Refers to the specialty of emergency medicine (or choice of career).
- Evaluating the Impact of Doctors in Training (EDiT) study
- A national research study being undertaken by the Health Services Research section at the School of Health and Related Research (ScHARR), University of Sheffield. The study is funded by the Health Services and Delivery Research programme of the National Institute for Health Research as part of a programme of work examining the impact of staff motivation and well-being on patient care.
- Foundation doctor
- Generic term for all foundation doctors (foundation year 1 and foundation year 2).
- Foundation Programme assessments
- Assessments that must be completed by all foundation doctors to demonstrate competency against the Foundation Curriculum.
- Foundation school
- A body that administers the Foundation Programme within a locality within the deanery area.
- Foundation school administrator
- Administrative role within the foundation school.
- Foundation school director
- The head of the foundation school. This individual reports to the postgraduate dean.
- Foundation training
- The term for the new structure for postgraduate medical training, introduced in 2004. It consists of a 2-year programme-based training structure giving trainees (foundation doctors) experience of a wide range of medical specialties before they choose their career specialty.
- Foundation year 1 doctor
- A postgraduate doctor in his or her first year of training following graduation from medical school. At the end of this year doctors achieve full registration with the General Medical Council.
- Foundation year 2 doctor
- A doctor in the second and final year of his or her postgraduate training, now termed foundation training. Doctors at this level are usually expected to practice increasingly as independent and autonomous practitioners.
- General Medical Council
- The statutory body/regulator of undergraduate and postgraduate medical training in the UK.
- Intraclass correlation
- A measure of inter-rater reliability.
- Junior doctor
- Previous title of foundation doctor.
- Longitudinal study
- A type of research design in which participants are followed up for a specified period and data are collected at different time points.
- Normative data
- A substantial body of evidence or data on a specific variable (e.g. job satisfaction) that can be used to benchmark the results of a study.
- Placements
- The clinical specialties where foundation doctors obtain their training. Typically there are six placements in the 2-year Foundation Programme.
- Postgraduate education stakeholders
- A study term to describe those individuals who work in postgraduate medical education, such as postgraduate deans and foundation school directors.
- Postgraduate medical deaneries
- Administrative regional bodies responsible for the implementation of postgraduate medical training in the UK, in accordance with the standard set out by the General Medical Council.
- Postgraduate Medical Education and Training Board
- The authority for training throughout the NHS before its merger with the General Medical Council in 2010.
- Specialist training
- Period of specialised training leading to consultant recognition.
- Trainee
- Generic term for all doctors in training, including foundation year 1 and foundation year 2 doctors.
- Training leads
- Generic term in our study for all staff with responsibilities for training foundation doctors.
List of abbreviations
- ANOVA
- analysis of variance
- COPD
- chronic obstructive pulmonary disease
- CS
- clinical supervisor
- CT
- computerised tomography
- DOPs
- direct observation of procedures
- ECG
- electrocardiogram
- ED
- emergency department
- EDiT
- Evaluating the Impact of Doctors in Training
- EDTL
- emergency department training lead
- EM
- emergency medicine
- e-Portfolio
- electronic portfolio
- ES
- educational supervisor
- EWTD
- European Working Time Directive
- F1/FY1
- foundation year 1
- F2/FY2
- foundation year 2
- FS
- foundation school
- FSA
- foundation school administrator
- FSD
- foundation school director
- FT
- foundation training
- GMC
- General Medical Council
- ICC
- intraclass correlation
- mini-CEX
- mini-clinical evaluation exercise
- mini-PAT
- mini-Peer Assessment Tool
- MMC
- Modernising Medical Careers
- NICE
- National Institute for Health and Care Excellence
- PES
- postgraduate education stakeholder
- PMD
- postgraduate medical deanery
- PMETB
- Postgraduate Medical Education Training Board
- SD
- standard deviation
- SHO
- senior house officer
- TL
- training lead