Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its proceeding programmes as project number 10/1009/14. The contractual start date was in September 2011. The final report began editorial review in March 2013 and was accepted for publication in July 2013. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2014. This work was produced by Locock et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Background
Objective
To use a national video and audio archive of patient experience narratives to develop, test and evaluate a rapid patient-centred service improvement approach (‘accelerated experience-based co-design’ or AEBCD).
Improving patient experience
Measuring, understanding and improving patients’ experiences is of central importance to health care systems worldwide. 1 Health care policy frameworks in several countries describe ‘patient experience’ as a core component of health care quality. Recent evidence suggests positive associations between patient experience, patient safety and clinical effectiveness for a wide range of disease areas, and positive associations between patient experience and self-rated and objectively measured health outcomes. 2,3
Even in the best-funded health systems, patients may report less than satisfactory experiences. There have been persistent concerns about the quality of basic ward care, and the 2010 Commonwealth Fund International Health Policy Survey showed that the percentage of patients in 11 countries rating care from their doctor as excellent or very good ranged from 84% in New Zealand down to only 43% in Sweden (with the UK at 79% and the USA at 74%). 4
At a time of global recession, better quality patient experience may be seen as a luxury rather than a top priority. The recent scandal of poor care at Mid Staffordshire Hospital in the UK is a chastening example of what happens when a focus on financial and other performance targets displaces listening to and learning from patients and their views and experiences. 5 But the supposed conflict between managing the bottom line and providing good patient experience may be more imagined than real.
First, we know that many of the things patients say matter most to them are attitudinal rather than resource-driven – for example, affording patients dignity, courtesy and kindness. But internationally, there is also growing evidence linking patient-centred care with decreased mortality and lower hospital-acquired infection rates; patient feedback about hospital cleanliness is a positive predictor of staff participation in activities such as hand-washing, and of methicillin-resistant Staphylococcus aureus (MRSA) rates. Good patient experience is also linked to other organisational goals such as reduced malpractice claims, lower operating costs, increased market share and better staff retention. Patient adherence seems to improve, length of stay is shorter and fewer medication errors and adverse events occur in organisations where care is patient centred. 6–12
Since the late 1990s, there has been a step change in how health care organisations collect, share and reflect on patient experiences. In England, a recent government White Paper on NHS reform emphasises ‘putting patients and the public first’, or ‘no decision about without me’, as it has been characterised. 13 Ensuring that the way care and information are provided reflects what patients themselves think is thus a priority. Nonetheless, the White Paper notes that:
The NHS . . . scores relatively poorly on being responsive to the patients it serves. It lacks a genuinely patient-centred approach in which services are designed around individual needs, lifestyles and aspirations. Too often, patients are expected to fit around services, rather than services around patients.
Section 1.9
To address this, health care organisations need to draw on the experiences of those who have used services at first hand – but there is debate about the best methods for gathering and understanding patient experience information and then using it to improve care. 14–16 There is no shortage of general recommendations to health care organisations as to how to capture patient feedback and use it to improve patient experience,14,17 but still little systematic and responsive improvement work goes on to actually improve this important component of the quality of health care services.
Internationally, health care organisations tend to use questionnaire surveys to provide patients’ perspectives on how they are performing. Large-scale surveys across multiple organisations can play an important role in meeting broader policy agendas such as accountability and transparency. Much has been achieved through the rigorous development and sustained commitment to surveying patient views of their experiences. Yet surveys may be less effective at supporting local quality improvement if they lack clinical credibility, or are insufficiently timely or specific to guide action by senior leaders. A review of 41 research papers explored how the 600,000 patient responses to the national inpatient survey from 2002 to 2009 had been used;18 it concluded that ‘the inpatient survey is not in itself a quality improvement tool’ and that ‘simply providing hospitals with patient feedback does not automatically have a positive effect on quality standards’.
In England, acute hospital trusts are increasingly deploying a wider range of methods and approaches locally. A range of alternative methods and techniques have been devised including comment cards, self-completion/paper-based surveys, and Personal Digital Assistants (PDAs), delivered by either researchers, ward staff, audit teams and/or hospital volunteers. Different information technologies have been devised – such as Optimum Contact (Optimum Contact Ltd, Middlesex, UK), Picker Frequent Feedback (Picker Institute Europe, Oxford, UK), Snap (Snap Surveys, London, UK) and Dr Foster Intelligence Patient Experience Trackers (Dr Foster Intelligence, London, UK) – which can be used to reach large numbers of patients, but local clinical teams and middle management are not yet making consistent use of national patient survey data to monitor service quality and drive local quality improvement. Anecdotal evidence suggests that many clinicians do not believe that the generic outpatient or inpatient surveys reflect the experiences of ‘their patients’ and complain that the data are frequently out of date. 19 In a recent survey of hospital clinicians in Denmark, Israel, England and the USA, the current situation has been portrayed as a ‘chasm’ between senior leaders and front-line clinicians. The study found that only 9.2% of over 1000 respondents thought that their department had a structured plan for improving patient satisfaction and that 85.5% of clinicians thought that hospital management should take a more active role in conducting patient satisfaction improvement programmes. 20 Related to this latter finding, 41% of almost 150,000 staff in the English NHS in 2011 said they had not received patient experience training and 22% said it was not applicable to them. 21
Recent research with hospital board non-executive directors22 has demonstrated that patients’ experiences of care have become more of an interest and concern at board level, which can only have intensified since the publication of the Francis Report into poor-quality care and above average death rates at Mid Staffordshire,5 and the Care Quality Commission’s Dignity and Nutrition Inspection findings. 23 Strikingly, however, over 95% of the time, hospital boards’ minuted responses to patient experience reports were to note the report but take no further action. 22 Examples where patient experience data were used to spark debate and action were rare, as were examples of non-executive directors challenging performance. At organisational level, we do not know which national policy levers (incentives, penalties, targets, market competition or publication of information) work best to improve patient experience; this is a relatively ‘evidence-light’ zone in which to make policy decisions. 24 As Robert and Cornwell24 conclude, ‘current measures of patient experience are not being used meaningfully or systematically at the local level for a range of reasons but, not least, because they are not seen as clinically relevant at a service level, and are captured too infrequently’ (p. 9). These issues have been major barriers to patient experience being placed on an equal footing with clinical effectiveness and patient safety as a key dimension of health care quality.
Different methods of collecting patient experience data can also produce different results. All methods have their strengths and weaknesses,25 and organisations which rely solely on survey data may overlook important nuances of how patients reflect on their care experiences. To illustrate, as part of a previous study an elderly woman completed both a patient survey and a narrative interview exploring her experiences on an acute elderly care ward;26 in her response to the survey question ‘Overall, did you feel you were treated with respect and dignity while you were in hospital?’, she ticked the box ‘Yes, always’; similarly, in response to the survey question ‘Overall, how do you rate the care you received?’, she ticked the box ‘Excellent’. And yet the following is an extract from her narrative interview:
The other thing I didn’t raise and I should have done because it does annoy me intensely, the time you have to wait for a bedpan . . . elderly people can’t wait, if we want a bedpan it’s because we need it now. I just said to one of them, ‘I need a bedpan please’. And it was so long bringing it out it was too late. It’s a very embarrassing subject, although they don’t make anything of it, they just say, ‘Oh well, it can’t be helped if you’re not well’. And I thought, ‘Well, if only you’d brought the bedpan you wouldn’t have to strip the bed and I wouldn’t be so embarrassed’.
The contrasting quality improvement implications arising from these different methods of capturing this experience could not be starker. The results from the patient survey would not lead to any action and, indeed, the ward team could be commended for the excellent, dignified care it provided, whereas the narrative interview revealed how annoyed and embarrassed the person was as a result of an interaction that had clearly formed a lasting impression on her subjective experience.
A significant gap between rhetoric and management action still persists. Quantitative data provide little depth and detail, and can therefore be difficult to interpret in terms of identifying specific priorities for improvement. 27 The emerging policy context is one of a movement away from driving improvement through top-down performance management towards transparency, information for and accountability to the public, and information to support individual patients’ choice and ability to participate in decisions about their own care (‘nothing about me without me’).
So, given the shortcomings of existing (largely quantitative) methods, where should we look for alternative approaches that might hold the key to understanding and improving the relational aspects of patient experience? There is growing interest in the use of in-depth qualitative research to gain richer and more meaningful accounts of what it is like to be a patient,22 yet providers of health care struggle to make effective use of qualitative rather than quantitative experiential evidence to improve local services. Whichever particular approach is adopted, there are issues of the burden on staff of collecting additional patient information, issues of bias, neutrality, and providing support for the patient’s clinical needs rather than quality improvement tasks. Collecting in-depth patient experience data needs to be balanced with having both appropriate methods and resources to do so, to be able to evaluate change activities and, ultimately, to show evidence of quality improvement. Few organisations have adequate systems for co-ordinating data collection and assessing its quality, or for learning from and acting on the results in a systematic way. 14 Some NHS trusts may be focusing on collecting data rather than seeking to move to action as a result. The focus of this report is on enabling change at the local level through the use and evaluation of an accelerated quality improvement intervention with the explicit aim of improving patient experiences.
The value of narrative
Narrative persuasion is a well-established psychological theory. 28 Narrative and stories, oral or written, are far and away the most powerful and natural way of accessing human experience, and it is, therefore, no surprise to find them in rapidly growing professional use in contemporary medicine and medical research. Stories have the ability to transport us to another world or to see the world through another’s eyes. This in turn can bring about attitude change. Narratives are a powerful way to engage care providers in reflecting upon how services could be improved, through emotional impact. 29,30
Narratives are not gathered because they are assumed to be objective, accurate or verifiable but because they are uniquely human and subjective, describing not a fact or a reality but a recalled experience or set of experiences. 30 Detailed patient accounts of their experiences can nonetheless suggest priorities and solutions that may not occur to people who are immersed in day-to-day service delivery. 31,32 Through personal stories, users reveal what they like about a service (or health care in general), what they hate about it, what matters to them, what works well for them, and what sorts of things cause real anxieties or problems as well as comfort and reassurance. Many NHS organisations are now successfully experimenting with qualitative methods of gathering user views and using them to improve services. However, it is important that such work is based on rigorous research with a broad sample of users and a full range of different perspectives, rather than relying on a single representative on a committee or the collection of a few anecdotes. 33 Stories and storytelling are accessible and memorable; they are a rich source of learning about people’s experiences, and provide a direct route to a deep appreciative understanding of the strengths and weaknesses of a particular health care service and what is needed for the future.
Experience-based co-design
The development, implementation and evaluation of a narrative-based, participatory action research (PAR) approach known as experience-based co-design (EBCD)30,34 marks a significant contribution to involving patients in quality improvement efforts in health care. EBCD has been implemented in collaboration with patients, families and staff in quality improvement efforts in various settings, care pathways and countries. A survey undertaken in the summer of 2013 identified at least 57 EBCD projects which had been implemented in seven countries worldwide since 2005 (in a variety of clinical areas including emergency medicine, drug and alcohol services, a range of cancer services, paediatrics, diabetes care and mental health services); at least a further 24 projects were in the planning stage at the time of the survey. 35 Many of these projects involved implementing the approach in more than one clinical department; for example, the PATH project in Ontario, Canada encompasses 12 health-care organisations (source: www.changefoundation.ca/library/backgrounder-partners-advancing-transitions-healthcare-path-northumberland/, accessed 20 December 2013). Independent evaluations of recent implementations of the approach in both the UK and Australia36,37 have found that, as well as making specific changes to particular services, the projects also supported wider improvements across the health care system. A follow-up evaluation in Australia38 specifically explored the sustainability of the impact of EBCD 2 years after implementation and reported that:
Co-design has been shown to strengthen service provider-service user relationships . . . co-design harbours a collaborative principle that should be woven into how health services and health departments conceptualise and structure their communication with patients, families and the public.
pp. 2–3
Adams et al. 39 report on the outcomes – in terms of spread and sustainability – of implementing EBCD in a cancer centre that was formed across two large NHS trusts in 2006 with the aspiration of delivering internationally renowned cancer services – in the ‘top 10 globally’ – for patients in the region. In 2008 the centre began an action research project encompassing several work streams (such as the engagement and training of senior managers) to implement patient-centred care. The chosen quality improvement approach was EBCD and, as initially undertaken in two breast cancer and two lung cancer services, closely followed the traditional six-stage design process (see Figure 1). The approach was tailored in different ways as it was then formally disseminated in three other cancer services (two colorectal services and one gynae-oncology service) and informally diffused into three community mental health services (an addictions service, a psycho-social service, and supported housing).
The study found that two-thirds of the 56 quality improvements made across the four initial cancer services were sustained at 2-year follow-up. Unlike in the original four case studies, the planned dissemination of EBCD implementation in two colorectal services (leading to four co-designed solutions in one service and only one in the other) was undertaken without external project funding or research support, and clinical staff were marginal to the co-design work. In contrast, the relative success of EBCD in the gynae-oncology service (13 co-designed solutions) was enabled by the work of an ‘in service’ clinical lead champion – as well as a senior clinical nurse specialist (CNS) – and the alignment of the work with established structures [such as multidisciplinary team (MDT) meetings], as well as a recognition that patient experience survey results needed to improve. Overall, through the course of the spread of the EBCD in the cancer centre, there was notable slippage from a vision of co-design to ‘listening to patients’, highlighting the central importance of tailoring quality improvement approaches, including EBCD, to local contexts. The authors argue that such sensitive tailoring is, in itself, a dimension of co-design requiring those advocating and leading such projects to adopt an adaptable and flexible approach that listens to the concerns of front-line staff while retaining the core philosophy of approaches such as EBCD.
The informal diffusion of the EBCD approach into a neighbouring mental health organisation was enabled by particular factors: the ‘push’ of active support and ‘opinion leadership’ at a high level of an organisation; the ‘pull’ of active quality improvement teams on the ‘look out’ for new approaches; and the mediating effects of ‘outward-reaching’ quality improvement leaders to build potential relationships. The tailored implementation of EBCD in the three mental health services was managed and led by the same quality improvement team in the mental health organisation. Implementation of EBCD in this organisation was more focused and innovative than the formal dissemination of the EBCD in the cancer centre.
Previous implementations of EBCD – including the examples above – have, therefore, resulted in tangible improvements that have been felt by patients and staff, with many leaving a significant legacy in terms of patient-centred working, support groups, and information for patients, as well as cultural change and a recognition by staff and patients that its collaborative approach is radically different to other change initiatives. 40 EBCD is now also being adapted for use by commissioning organisations in England (‘experience-led commissioning’) and has recently been piloted in the context of end-of-life-care services in the West Midlands, where evaluation has shown similar positive impact. 41
The experience of family carers is a neglected area in quality improvement, but EBCD has also recently been used to develop and test an intervention for carers in the chemotherapy outpatient setting. 42 Through a facilitated EBCD process, carers and staff designed components of a carer intervention that took the form of a DVD and a leaflet. The delivery and impact of the intervention was then tested in a feasibility trial. Forty-three carers were recruited to the trial, randomised between the intervention (n = 21) and control (n = 22) groups. Standardised psychometrically sound measures, completed pre and post intervention, provided preliminary evidence of beneficial impact on carer experience; in particular, the feasibility trial results indicated an improvement in carers’ knowledge of chemotherapy and their perceived confidence with their care-giving situation. Staff and carer focus groups confirmed the feasibility and acceptability of the intervention. These preliminary data are encouraging and support the development of interventions, using a co-design process, to improve carer experience.
Four overlapping strands of thought have contributed to the development of the EBCD approach, namely:
-
PAR
-
user-centred design
-
learning theory
-
narrative-based approaches to change.
With its roots in social psychology and phenomenology and important influences from the likes of Kurt Lewin and Paolo Freire, participatory action research sets out – in contrast to a traditional, positivist, science paradigm – to recognise and directly address complex human and social problems. Although encompassing a wide range of research practices, McIntyre proposes four underlying tenets to the majority of PAR projects:43
(a) a collective commitment to investigate an issue or problem, (b) a desire to engage in self- and collective reflection to gain clarity about the issue under investigation, (c) a joint desire to engage in individual and/or collective action that leads to a useful solution that benefits the people involved, and (d) the building of alliances between researchers and participants in the planning, implementation and dissemination of the research process.
p. 1
Action research has not had a particularly distinguished record in the health care sector, or indeed in other policy areas. Much of the early action research in health care was criticised for poor design and lack of rigor, and it was often neither educative nor empowering for those involved. Proponents of PAR have since argued that the sacrifice of some methodological and technical rigor is worth the additional face validity and practical significance that is gained.
With similar roots to PAR, user-centred (or participatory) design draws its inspiration from a subfield of the design sciences (which include architecture and software engineering) whose distinctive features are (a) direct user and provider participation in a face-to-face collaborative venture to co-design services, and (b) a focus on designing experiences as opposed to systems or processes. Ethnographic methods such as observation and narrative interviews are thus preferred. 44,45 User-centred design makes two particular contributions to quality improvement thinking. Firstly, it offers a new lens, or frame of mind, through which to conceive approaches to improving patient experiences of health care; primarily, its pragmatic nature highlights the importance of ‘making sense’ of experience and finding solutions to poorly designed interactions. Secondly, it offers methods, tools and techniques (such as modelling and prototyping) which were little used in health care improvement work until very recently.
The influence of learning theory on the development of EBCD emerges from a wide variety of sources including Argyris and Schon46 and, more recently, Wheatley47 and Kerr. 48,49 The central argument is that, in contrast to traditional forms of management and clinical skills training, we should be training ‘reflective practitioners’, enabling staff to ‘draw back’, to pause, reflect and gather information, people, and insight. The implications for improving patient experiences of health care services are that we should (a) focus on what both groups (staff and patients) want, and (b) provide a ‘safe haven’ within which to rehearse and practise new ways of thinking, feeling, doing and relating. Emotional disclosure, in which discussion of emotions is constructed as a normal and healthy human activity, is an important part of this. 50,51
Finally, narrative approaches (see The value of narrative, above) are an important strand because ‘stories and storytelling are the basis of EBCD . . . [they] contain huge amounts of information, wisdom and intelligence about experiences that are waiting to be tapped as a rich source for future service development and design’ (pp. 66–7). 30 In keeping with PAR, user-centred design and learning theory, narrative-based approaches to change are premised on subjective, socially constructed stories that enable connections with ‘assumptions, values, expectations, cognitions and emotions’ (p. 65). 30
Taken together, these four strands of thought also relate to the increasing interest in what Bushe has termed ‘dialogic’ organisational development (OD) approaches. 52,53 Such approaches have turned away from traditional, top-down, leader-centric and diagnosis-led OD and towards practices that ‘assume organisations are socially co-constructed realities’ and have in common ‘a search for ways to promote dialogue and conversation more effectively’ as it is ‘by changing . . . conversations that normally take place in organisations that organisations are ultimately transformed’ (pp. 619–20). 53
Steps in experience-based co-design
A full description of the EBCD approach has been published elsewhere, accompanied by a case study of the pilot implementation in a head and neck cancer service. 30 Detailed materials are also available from The King’s Fund’s online EBCD toolkit. 54 Integral to the approach is that patient, carer and staff experiences are used systematically to co-design and improve services. To date, this has involved an intensive local diagnostic phase, using rigorous qualitative research, including video- or audio-recorded narrative interviews in which participants are invited to recount their experiences using a storytelling approach, highlighting concerns and priorities and identifying ‘touch points’ (key interaction points) along their journey. The methods used to collect these interviews are very similar to those used by the national archive described below. Trigger films based on these experiences are then used, firstly to enable patients and carers to share and discuss their experiences with each other, and then to stimulate discussion between local staff and patients, who can then jointly identify actions to bring about systematic, sustainable improvements.
Figure 1 details the six stages of the action research process that together make up the EBCD approach to improving patient experiences. Stage 1 involves establishing the governance and project management arrangements. The fieldwork underpinning an EBCD project typically then begins with a 4-month data collection period (stages 2 and 3). In stage 2 a wide variety of staff (from, for example, receptionists to lead clinicians) are interviewed about their experiences of working within a service using a semi-structured interview schedule; over multiple implementations of the approach we have found that the data from approximately 12–15 interviews provide sufficient insights for the purposes of being able to represent back and reflect on staff experiences. The staff interviews are transcribed and analysed thematically. Non-participant observation helps to contextualise and understand patient experiences from both patient and staff perspectives; for example, in a recent EBCD project, two researchers conducted a total of 219 hours of participant observation of clinical areas along the relevant patient pathway. 40 The specific aspects of care that are observed are not pre-determined and the observations focus on both functional and relational aspects of patient/staff interactions. Following the data collection, staff meet to review the themes arising from the staff interviews and observational data in order to identify their priorities for improving services.
FIGURE 1.
Steps in the EBCD process.
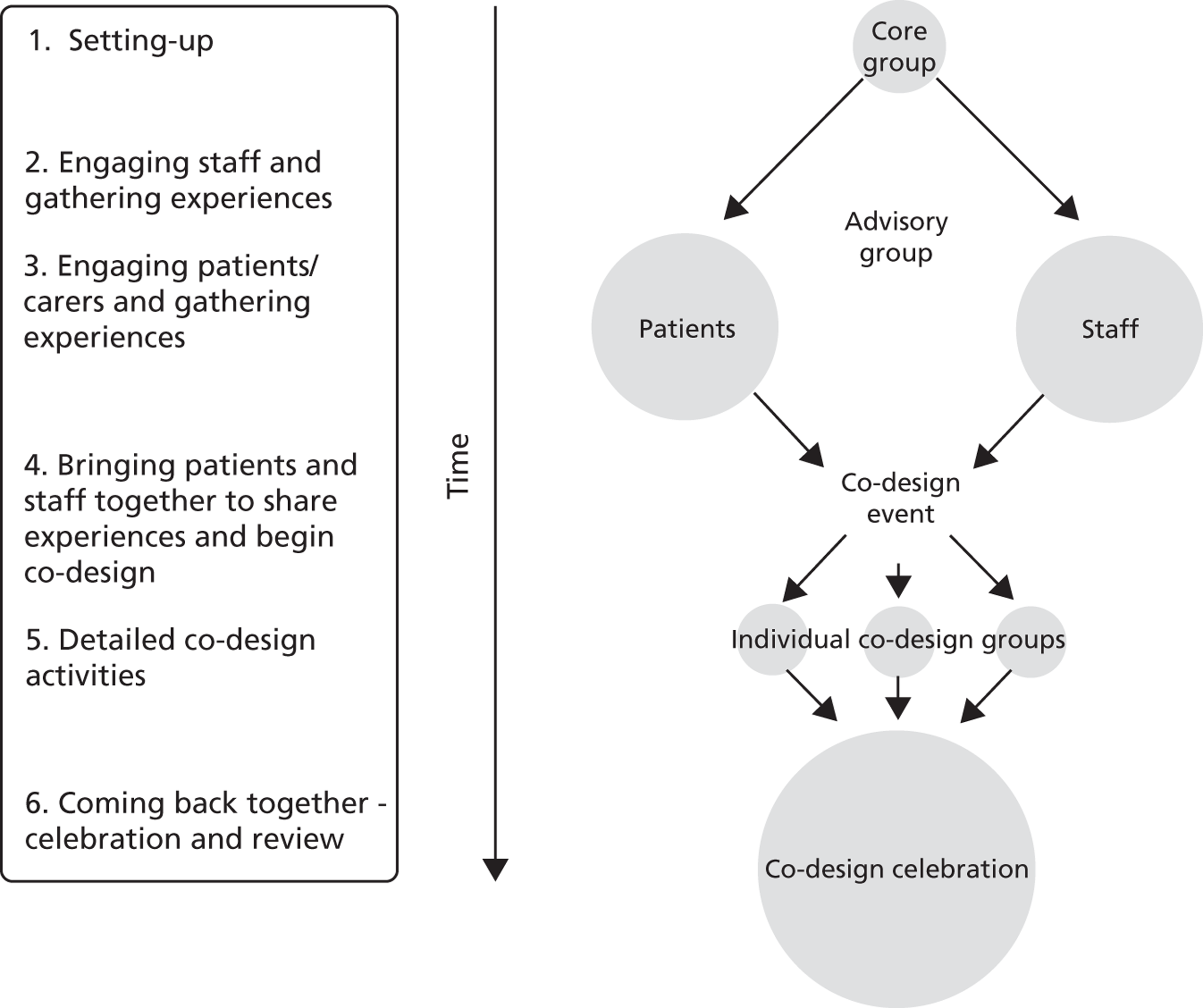
In stage 3 – which runs in parallel with stage 2 – patients and carers are recruited (e.g. through clinical nurse specialists in outpatient clinics) and an experienced qualitative researcher conducts filmed, narrative-based, unstructured interviews lasting, on average, 1 hour, in which patients describe their experiences of care since first diagnosis. Each patient is then sent their own film to view before deciding whether or not it can be shared with other patients and staff. Two researchers view the films independently to ensure analytical rigour and shared understanding of significant ‘touch points’. 55 ‘Touch points’ are the crucial moments, good and bad, that shape a patient’s overall experience; the concept originated in the airline industry and represent the key moments where people’s subjective experience of the service is shaped. Exemplar ‘touch point moments ‘ that emerged from the pilot implementation of EBCD in a head and neck cancer service included breaking of the bad news; percutaneous endoscopic gastrostomy (PEG) feeding tube; ‘waking up in an intensive care unit’ (ICU); the cancer ward; ‘looking in the mirror’; and radiotherapy and radiotherapy planning.
Films are then edited to produce one composite 35-minute film, representing all the key touch points in a service. In addition, audio recordings of the narrative interviews can be transcribed and the data analysed thematically. All of the patients and carers are invited to a showing of the composite film, following which a facilitated group discussion highlights any different or emerging issues. An emotional mapping exercise is then used to help patients reflect together on the emotional impact of the touch points. 30 Following this group work, patients vote on their shared priorities for improving services.
In stage 4 the staff and patient priorities are presented at a joint event at which staff view the composite patient film for the first time. Mixed groups of patients and staff use the issues highlighted in the film, together with the priorities from the separate staff and patient meetings, as a basis to identify joint priorities for improving services. Patients and a variety of medical, allied health professional and administrative staff then volunteer to join specific ‘co-design working groups’ (typically four to six groups) to design and implement improvements to services (stage 5), initially over a 3-month period. The majority of these groups are facilitated by quality improvement specialists from the participating health care organisation, and ground rules are established from the outset, ensuring that all participants have equal voices. At stage 6, these separate co-design working groups reconvene to discuss their work to date and plan the next stages of the improvement process.
The challenge
As noted above, independent evaluations have shown EBCD to be effective in improving the quality of health care services. However, the diagnostic phase before quality improvement can begin is undoubtedly lengthy and costly, and has been noted in evaluation as a barrier to uptake. 35,36 Replicating 5–6 months of qualitative interviewing on each pathway in each hospital is impractical. And yet – as explained elsewhere34 – crucial to the success of approaches such as EBCD are the discursive, narrative–based interactions between staff and patients that are enabled by the change process. 56 The filmed patient narratives are held to be key in triggering these interactions and fulfil several functions: they are a tool for reflective learning (for both patients and staff); they provide data to drive the co-design process; and they (re-)establish an emotional connection between the staff and patients. In the following quotation from the original head and neck cancer pilot, a staff member considers the impact of watching the patient film:57
When people watch the film they might think, ‘I remember that lady’, they know they’re our patients – they can’t get away from the fact – but it actually makes it more real for them. Whatever way they’re captured, it’s about capturing it so that people recognise these are patients I have cared for, nursed, met, who are saying this . . . and I think that’s what is so different from other improvement work in terms of things like discovery interviews and focus groups: it’s that direct connection between them.
Experienced-based co-design has, therefore, been found to result in improved service quality, but one of the major barriers to widespread implementation is the time and cost involved in the discovery phase (stages 2 and 3 in Figure 1). However, ‘accelerated’ approaches may not work as well if, for example, local staff and patient engagement in the change process is less forthcoming. Even if ‘accelerated’ forms of EBCD do not work as well as the traditional approach, they may work ‘well enough’ to be worth pursuing.
Our aim is to generate new knowledge by testing a potentially less costly, more efficient and therefore more feasible way of implementing EBCD locally, but one that still draws on rigorously conducted and analysed qualitative research, which has been one of the hallmarks of EBCD. The archive of patient narrative interviews held by the Health Experiences Research Group (HERG) in Oxford and disseminated through Healthtalkonline (see following section) offers a potential resource to make this a reality. 58 The need for the NHS to seek ways to improve patient experience is a political and ethical ‘given’, and so if this project can demonstrate a faster and less costly way to do it, there could be substantial gains for both clinical staff and patients.
The Health Experiences Research Group and Healthtalkonline – existing narrative evidence on what matters to patients
The Health Experiences Research Group at the University of Oxford collects and analyses video- and audio-recorded interviews with people about their experiences of illness. It now has an innovative national archive of around 3000 interviews, all collected between 2000 and the present and covering over 80 different conditions or topics, which provides a unique source of evidence on patient experiences and priorities. The interviews combine an unstructured narrative (elicited by the question ‘tell me your story’) followed by semi-structured prompting. For each condition approximately 40 interviews are collected, and coded and analysed thematically using the constant comparative method.
The HERG studies use purposive maximum variation sampling. This aims to get the broadest practicable mix of people (variation across different demographic characteristics such as age, gender, ethnicity and social class) and types of experience; Patton59 argues that the advantage of using a maximum variation approach is that ‘any common patterns that emerge from great variation are of particular interest and value in capturing the core experiences and central, shared aspects’ on a specific topic (p. 172). The different types of experience for which HERG studies sample vary by condition, and are determined with input from an expert advisory panel brought together for each condition-specific study. Typical factors for which variation may be sought include time since diagnosis; severity of condition; nature of local service provision; type of treatment; recurrence or not; degree of progression; and extent of lasting disability or symptoms.
The interviews are approved by participants for use in research, teaching, publication, broadcasting and dissemination on an award-winning patient experience website, www.healthtalkonline.org, one of the first health information sources to meet the Department of Health’s Information Standard. 60 A primary purpose of Healthtalkonline has always been to provide practical information and emotional support for other individuals going through the same experience, but the interviews are increasingly used in teaching health professionals and to inform health policy – for example, National Institute for Health and Care Excellence (NICE) guideline development now frequently incorporates evidence from Healthtalkonline, and it is the only source of patient experience evidence recommended in the NHS Evidence Process and Methods Manual. Recent General Medical Council (GMC) guidance on end-of-life care drew on a specially commissioned analysis of interviews from the archive. 61 This analysis for the GMC was subsequently compared with a local set of interviews on end-of-life care. This showed that very few themes were identified locally that could not have been anticipated from the national data set. 62 The archive thus has enormous potential as an evidence base of patients’ experiences to support service change. Indeed, for many participants, knowing that their experience may be used to help improve things for other people is an important motivator for agreeing to take part.
Using national narratives for local improvement
There is considerable similarity in the interviewing technique used by HERG and EBCD; when Bate and Robert30 were designing the initial head and neck cancer pilot in EBCD, they spent time with HERG discussing methods for conducting video patient experience interviews. Both use unstructured narratives followed by semi-structured prompting, collected by experienced social science researchers; both anticipate that the some or all of the data collected will be used and seen publicly rather than used purely as anonymised text for research purposes. Both projects offer people the opportunity to give an audio or written-only narrative as well as video, though in practice very few people take this option in EBCD, whereas most HERG collections include a proportion of audio or written-only narratives. (This may well be influenced by the internet dissemination route through Healthtalkonline which may prompt people to seek a greater level of anonymity.) Key differences are that HERG studies (a) are national rather than local and (b) generally use a larger sample but cover a wider range of issues, many of which are not directly relevant to quality improvement (such as the effect of illness on family relationships, on work and social life, and on body image and self-esteem). EBCD patient discovery interviews normally draw on a more focused sample and more targeted semi-structured prompting to understand experiences of care services in a particular locality.
Despite these differences we felt that there was enough common ground to test whether or not HERG interviews could be used to accelerate the EBCD cycle by reducing the discovery phase with local patients. At the outset, we recognised that the accelerated approach might not work as well as a traditional approach, if local engagement were less forthcoming. We hypothesised that staff might feel unconvinced that issues raised by patients in the film applied to them locally; that it might be easier to say ‘that never happens here’, and feel less moved by the narratives to think differently about the care they offer. On the other hand, we speculated that seeing a different sample of patients could defuse critical comments and make staff feel less defensive. The very fact that it is not local could enable a more collaborative approach.
As far as patients and families were concerned, we debated whether or not they would feel that the issues raised in the film did not resonate sufficiently with their own experiences or with specific local concerns – or whether or not it might in fact be easier for them to raise difficult issues with staff indirectly by appealing to what others in the trigger film have said rather than in potential direct confrontation.
This led us to formulate the following research questions:
-
Is the accelerated approach acceptable to staff and patients?
-
How does using films of national rather than local narratives affect the level and quality of engagement with service improvement by local NHS staff? Does this have implications for the overall impact of the approach?
-
From local patients’ perspectives, how well do they feel that national narratives capture and represent themes important to their own experiences?
-
Does any additional work need to be done to supplement the national narratives at the local level? If so, what form might this take?
-
What improvement activities does the approach stimulate and how do these activities impact on the quality of health care services?
-
What are the costs of this approach compared with traditional EBCD?
-
Can accelerated EBCD be recommended as a rigorous and effective patient-centred service improvement approach which could use common ‘trigger’ films to be rolled out nationally?
Chapter 2 Methods
This study involved two components: the intervention (adaptation and implementation of an accelerated form of EBCD) and an evaluation. For clarity, we document the methods of each of these in turn, though in practice they proceeded side by side.
The intervention – accelerated experience-based co-design
Sampling and setting
The two partner hospital sites were selected partly on the basis of senior clinical managerial commitment to the project, which has been shown to be an important enabling factor for change. 63,64 Our two hospital partners also provided a contrast between a tertiary specialist provider (Royal Brompton and Harefield NHS Foundation Trust) and a general hospital (Royal Berkshire NHS Foundation Trust) to demonstrate whether or not the approach was equally acceptable and practicable in both types of setting. Senior management team members from both organisations were co-investigators (CIs) in the study, and therefore they are not anonymised as overall partners in the research. However, elsewhere in the report we have explicitly anonymised our results. Our purpose was never to compare one site against another, but rather to compare AEBCD against EBCD.
In each of the two participating hospitals, a ‘site captain’ was identified – the senior individual in each organisation who had agreed to participate as a CI, negotiated site access and identified the service improvement facilitators who would take day-to-day responsibility for the project locally, including the identification and recruitment of participants.
Royal Brompton and Harefield’s early involvement in the planning of the study determined the selection of pathways relevant to their specialist heart and lung services, and in discussion with Royal Berkshire we settled on two exemplars: intensive care and lung cancer. Co-applicants Shuldham and Fielden brought not only senior management support but also directly relevant expertise in cardiac and intensive care nursing (Shuldham), and intensive care medicine (Fielden).
These two pathways offered interesting potential insights. One advantage was that lung cancer had already been the subject of a full EBCD project, which provided us with a good comparison with an accelerated version both in terms of process and in terms of costs and impact. Intensive care provided an example of a topic area which has not previously been subject to EBCD. In terms of generalisability, like many other serious health conditions, having lung cancer or requiring critical care impacts on many aspects of a person’s life and necessitates a range of interventions. The experience can be life changing, and in the immediate or longer term can have psychological effects. Cancer is one of the most common pathways in the NHS, accounting for 1.7 million finished consultant episodes (FCEs) in 2009–10, around 10% of all FCEs. 65 Many aspects of the lung cancer pathway are similar to other cancers and other acute conditions where symptom recognition (and delays in consultation), investigations, diagnosis, treatment choices, recovery, discharge, follow-up and medication are all important. In many cases, there will also be similarities with other serious long-term conditions, such as heart failure or chronic obstructive pulmonary disease, in which long-term management and deteriorating health may need to be managed. Lung cancer’s poor prognosis also means that this pathway has relevance for end-of-life care. The two hospitals were involved in different aspects of the care pathway; at Royal Berkshire, diagnostic services, outpatient care, chemotherapy and radiotherapy are provided locally but patients requiring surgery are transferred to a central London specialist hospital for that part of the pathway. Royal Brompton and Harefield, by contrast, take specialist referrals for surgery for lung cancer from many different parts of the country.
Intensive care provided an interesting setting because it is not one single condition, but rather focuses on a care system in a defined location, offering a range of treatments for a variety of conditions in the very acute phase of severe illness. It raises generalisable issues about co-ordination and handover between departments and disciplines, and about improving the care of people who may be unable to communicate at the time or take part in decision-making, and whose utter dependence on staff is a key feature of their experience. It is thus an area in which family carers are particularly closely involved, spending many hours in hospital helping to provide care and assisting in the person’s recovery, as well as taking responsibility for many decisions and interactions with staff, but often feeling helpless and potentially excluded from a specialised, high-tech, automated world. As noted earlier, family carer experiences are a neglected area in quality improvement. As with intensive care, the two hospitals’ intensive care services had different patient profiles, with Royal Brompton and Harefield seeing many planned admissions after complex heart or lung surgery, and Royal Berkshire having a mix of planned and emergency admissions with a range of diagnoses.
Within each pathway, all staff were invited to be part of the intervention, given that staff engagement was a fundamental aim of the intervention. Patients and carers were carefully and purposively selected in order to identify people who could participate effectively in the co-design process. In line with The King’s Fund’s EBCD toolkit,54 the local facilitators were advised to:
-
identify patients who had been through different aspects of the service, and who were beyond the critical point of their treatment, so that they could reflect on their experience
-
try to include a range of people – determined not only by age, gender and ethnicity but also in terms of the treatment types and services experienced and to make sure that participants’ experiences of the service had been quite recent, so that the aspects of the service that they reported were still current
-
try to avoid going to ‘the usual suspects’, and that if they recruited patients involved in existing patient support groups, to explain carefully that in this project they will need to focus on aspects of service delivery that could lead to improvements
-
not worry about finding the ‘perfect patient sample’ as the project was deliberately focusing on the views of a relatively small number of people, and so it was not intended to represent every detail about the service.
Particularly in the case of lung cancer, staff felt it was important that people nearing the end of life should have an opportunity to express their views, but at the same time we were mindful of people’s state of physical and emotional health and the possible burden of taking part. Potential participants were thus approached individually through members of the clinical team, especially consultants and nurse specialists, with closest knowledge of local patients/carers, either during their hospital episode or after they had left. A member of the clinical team made initial contact by mentioning the project to likely participants, and this was then followed up with a participant information sheet and invitation to participate, until sufficient numbers for the co-design process were obtained. All patients and carers approached were adults able to give informed consent, and were advised that they could withdraw at any stage. They or their relative had received care in one of the four participating services during the 6-month period of the fieldwork.
The number of staff and patients from each pathway was intended to be sufficient to give a broad range of views as to issues influencing staff well-being and patient experiences. Typical previous EBCD projects have recruited 12–15 patients/carers and 12–15 staff members per pathway. Across four pathways this would have meant 48–60 patients/carers and 48–60 staff. In fact, 159 people took part overall at one or more stages: 96 staff members and 63 patients. Information and consent materials are shown in Appendix 2.
Steps in the process
The design of our accelerated form of EBCD involved seven different stages, adapted from traditional EBCD as described in the Background section, above. These stages are:
-
secondary analysis of narrative interviews from the HERG archive
-
creation of trigger films
-
discovery and engagement work with staff, including staff feedback event
-
focus group workshop with local patients and carers
-
co-design workshop with local staff, patients and carers
-
co-design subgroups of staff, patients and carers
-
final event.
The detail behind each of these steps is set out below. During the first phase of the project (the two intensive care pathways), some of the events described below were filmed, with participants’ consent, in order to provide visual examples of the kind of work involved for dissemination of the method, and training for new facilitators and potential EBCD participants. We have also captured, on film, short interviews with the facilitators and others involved in the two hospitals, again to feed into training for new facilitators.
Secondary analysis
Secondary analysis of relevant patient narratives from the HERG interview archive was undertaken to identify ‘touch points’ along each care pathway (intensive care and lung cancer). This replaced much of the intensive local discovery phase (face-to-face interviews and ethnographic observation) normally used in EBCD. Secondary analysis66 involves reusing data collected for another prior purpose to answer a new or different question. The interviews in the HERG archive have all been collected to understand people’s experiences of particular illnesses or health topics, ranging widely across social, physical and emotional issues, but they also contain detailed accounts of diagnosis, treatment, discharge and follow-up, information, communication with professionals and decision-making, which we hypothesised would be well suited for identifying touch points, although the interviews were not specifically conducted for that purpose. Among many other collections, the archive contains 40 interviews with people who have been in intensive care, 38 interviews with relatives and close friends of people who have been in intensive care and 45 interviews with people with lung cancer; these were used as exemplar conditions for the project. (These are more interviews than would normally be collected in a local EBCD discovery phase; however, we felt it was important to include this larger sample to compensate for the fact that the interviews were not specifically designed to capture touch points.) The analysis included interviews available in audio and written-only format to identify themes, but only one audio extract was included in the trigger films (see Trigger films, below).
Secondary analysis was undertaken by two experienced qualitative researchers from the group, under the supervision of the principal investigator (PI) Locock and CI Ziebland. All interviews were reread and recoded, looking specifically for instances of touch points. The lung cancer interviews were reanalysed by the same researcher who had originally collected them. The intensive care interviews were reanalysed by a researcher who had not been involved in the original data collection but who was able to call on the original researcher for advice. CI Robert held a half-day workshop with the two researchers and the PI to demonstrate previous films used in EBCD projects, explain how they are used in practice, and discuss what to look for in identifying touch points. To test whether or not the touch points were similar to those which would be identified by a researcher experienced in EBCD, CI Robert took one of the lung cancer transcripts and coded it independently, then compared this with sections identified as touch points by the HERG researcher. This confirmed a high degree of consistency.
Trigger films
Trigger films were then created drawing on the secondary analysis, featuring video and, in one case, audio extracts from a range of individuals illustrating the touch points. The selection of illustrations was led by the researcher who conducted the secondary analysis, in discussion with the PI. This discussion resulted in some minor changes in clip selection (e.g. in the ICU film, a clip was added on the value of follow-up appointments and diaries of what happened to help people come to terms with their experience, and the number of clips on ‘dreams and nightmares’ and ‘hallucinations’ were condensed into one shorter section). Discussions at this stage explicitly included the need to offer a balance of positive and negative experiences. The draft films were then shared with CI Robert and the service improvement facilitators. At this point there was scope for some further minor adjustments to be made [see Chapter 3, Results (4)]. Each trigger film lasted approximately half an hour and was provided on DVD for the facilitators to use at local events. (The trigger films are copyrighted to the University of Oxford; they will be made available for free future use in health care service improvement through The King’s Fund’s EBCD toolkit website and on the ‘Improving care’ section of the Healthtalkonline website.)
Discovery and engagement work with staff
While the trigger films were being developed, local service improvement facilitators were identified in each trust and trained by CI Robert in co-design techniques. The role of the facilitators was to recruit staff and patients to the project, run the co-design process, collect data as appropriate (both for the evaluation and for quality improvement activities), and champion the approach within their organisations.
The facilitators used a combination of participant observation and one-to-one discovery interviews with staff to learn about their experiences of the two exemplar care pathways and staff views and expectations about what local patients experience. All staff who worked in the four participating services were invited to participate in the project, with no exclusion criteria. Staff were sent a covering letter in the internal post from the research team, together with the staff information sheet. An outline of the appropriate semi-structured interview schedule was also sent to each potential interviewee in advance of the proposed interview. Signed informed consent was sought from all staff who participated, whether as an interviewee or by attending meetings (see below). The staff information sheet and covering letter both made clear that participation was entirely voluntary and that staff could withdraw at any time without giving a reason. The facilitator took detailed notes during the discovery interviews and produced a summary of findings.
The facilitators also undertook observation of routine care in appropriate settings depending on the specific service (e.g. on wards or in outpatient clinics). Relevant members of staff were informed by the facilitator of his or her wish to observe routine day-to-day activities. Patients who might be directly observed were verbally informed of the presence of an observer and the purpose of the research. Again, the facilitator took notes of their observations.
Anonymised findings from both staff interviews and observations were presented to any staff member who wished to attend a staff feedback meeting. These were discussed and staff priorities for improvement were agreed. Although there was considerable overlap between staff who were interviewed and staff who attended the workshop, some staff who were interviewed were unable to attend, and staff who had not been interviewed were also welcome to bring new perspectives to the discussion. A total of 42 staff agreed to be interviewed across the four pathways and 46 people attended the staff feedback event. (See Sampling and setting for more detail on sampling for the intervention.)
Focus group workshops with local patients and carers
Patients and family members who were invited to take part were given or sent an information sheet describing the study and asked by the local service improvement facilitator to complete a consent form. The participant information sheet and covering letter both made clear that participation was entirely voluntary and that patients and carers could withdraw at any time without giving a reason. Travel expenses were reimbursed, and lunch and refreshments were provided at meetings.
The first step for patients and carers after consenting to take part was to attend a focus group workshop at the hospital in question around their particular pathway, facilitated by the local service improvement facilitators and observed by the ethnographer (see Evaluation, below) but otherwise not attended by staff. This was similar to the patient feedback event in traditional EBCD, but in EBCD the participants would be the patients already interviewed during the discovery phase and they would be watching their own interviews in the trigger film. In the accelerated form, participants instead watched the trigger film derived from analysis of the national archive, and then discussed how far the touch points identified reflected their own priorities and experiences. Participants were offered the opportunity to raise specific local issues of importance which may not have been captured. Other EBCD techniques (such as emotional mapping) were adapted from their traditional application and used at the workshops to enable participants to share their experiences and inform the selection of their priorities for improvement. Forty-nine patients and carers overall attended one of the four patient workshops across the different sites and pathways.
Co-design workshops with local staff, patients and carers
After the two separate events, one for staff and one for patients and carers, a multidisciplinary group of local staff, patients and carers were brought face to face in a co-design workshop to share their experiences of giving and receiving services. The trigger film was shown again to the whole group. Again, this is very similar to the same stage in traditional EBCD, except that the staff (who were seeing the film for the first time) were not watching their own patients. The film was used to stimulate group exercises to focus on key ‘touch points’ where systematic and sustainable improvements might be made. Patients, carers and staff shared their respective priorities for improvement and agreed which of these they would work on together in the co-design subgroups (see next section); these could be anywhere along the patient pathway, and were the priorities for improvement adopted by each of the pathway projects. Building a coalition for change between staff and patients is central to this stage in the process. Again, this work was led by local service improvement facilitators with training and support from CI Robert. Across the four workshops, a total of 93 people took part. Although there was considerable overlap in attendance from the previous staff feedback event and patient/carer focus group, people were free to dip in and out of the process at any stage and new participants were welcomed.
Co-design subgroups of staff, patients and carers
The co-design workshops led to the establishment of subgroups of patients, staff and carers working together in each partner organisation to respond to the agreed priorities for improvement by planning and implementing changes. A key feature of the approach is that the interventions are designed collaboratively by patients and staff, with continued support from local service improvement facilitators. The groups recorded their activities and fed this information into the evaluation. The choice of topics, the way in which meetings were organised and their frequency varied from site to site, and this is discussed in Chapter 3, Results (5).
Final event
As in traditional EBCD, the final stage is to bring participants from each pathway together to review and celebrate their achievements, and plan for further joint work. This is an opportunity for patients and carers to see that they have been involved as equal partners in achieving change, and that their ideas have been listened to and acted upon. Patients and carers often lead parts of the presentation. It is also an opportunity for wider dissemination, as staff from other parts of the hospital may be invited to see what has been achieved, and consider whether or not to adopt the approach in their own departments. In this study, 45 staff and 19 patients/relatives attended final celebration events overall.
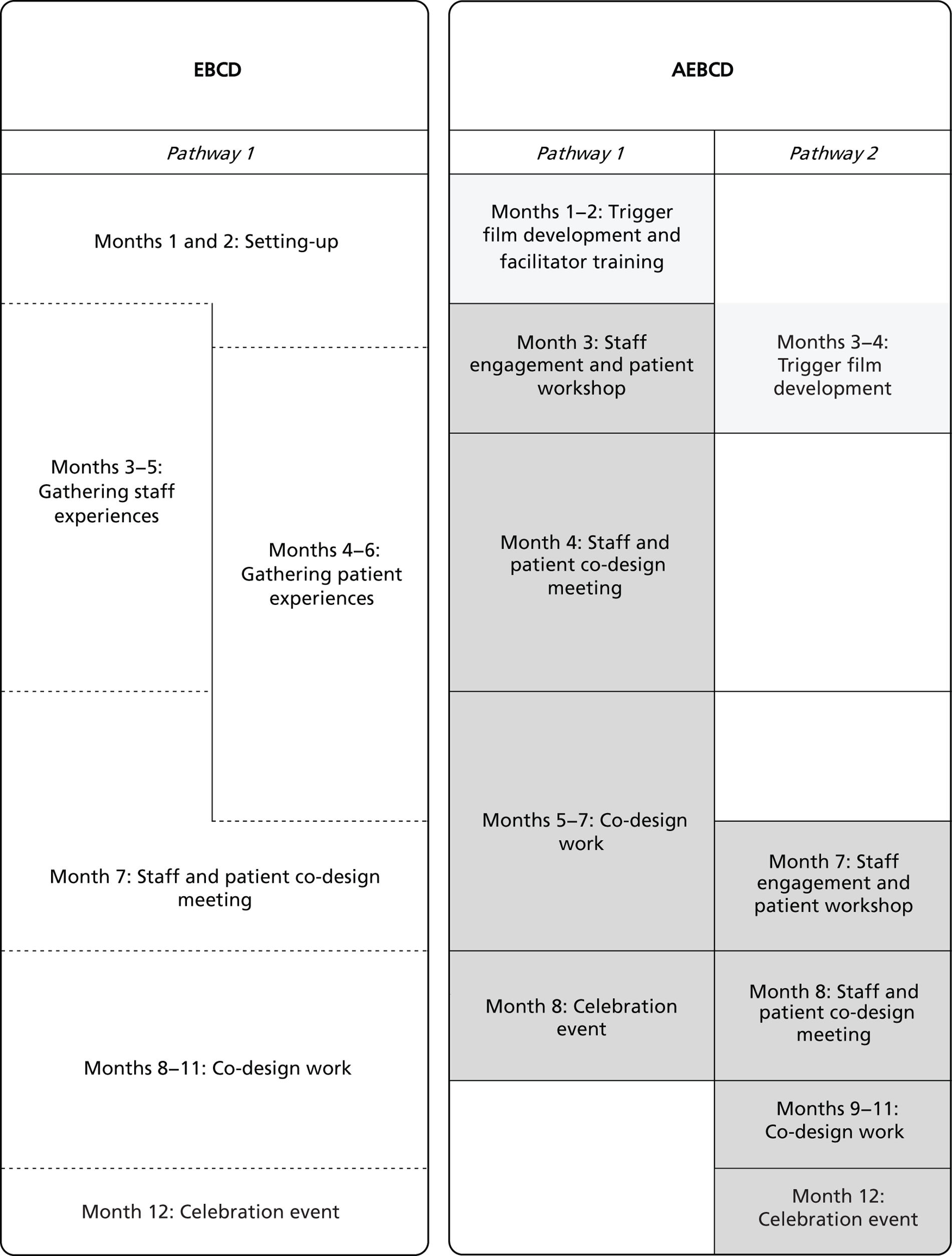
Shortening the experience-based co-design process
Figure 2 below compares the time frame for traditional EBCD with that for AEBCD. A traditional EBCD cycle typically takes around 12 months’ work in each trust to complete one pathway. In the accelerated version as described above, we set out to halve the cycle to 6 months per pathway (plus 2 months as a one-off set-up time to develop a trigger film around that pathway, which could then be reused in other trusts). Much of the shortening would be achieved by using national rather than local patient interviews, while still ensuring that the process was informed by rigorous patient-centred research. The amount of staff input would also be significantly lower. A traditional EBCD cycle involves a full-time researcher for 6 months and a half-time service improvement facilitator for 6 months (a total of 9 months of staff input). In the accelerated version, there would be a one-off staff commitment of 2 months to develop the trigger film. Within a given hospital, staff involvement would be reduced to a 40% facilitator for 6 months (= 2.4 months). The staff discovery phase was reduced and the time for co-design groups to meet shortened from 4 months to 3. (See also Chapter 3, Results, for a discussion of the impact and feasibility of shortening the process.)
FIGURE 2.
Comparison of EBCD and AEBCD timetables.
Evaluation
Design
The ethnographic evaluation aimed to observe the implementation process in both pathways in each trust and to evaluate the acceptability to patients and staff – and the impact – of this adapted approach to patient-centred quality improvement. The aim was not to evaluate EBCD per se, as there have been a number of previous studies of the approach,36,38,56 but to assess whether or not the accelerated approach provided a workable, affordable and acceptable alternative.
To assess the impact of the accelerated approach, we used a longitudinal comparative case study design and observational methods which are well suited to the study of complex change. 67,68 In effect, there were four ‘cases’: two different pathways in each of two trusts which were compared with EBCD. The evaluation used multiple data sources, including observation, interviews, questionnaires, group interviews with patients, documentary analysis and administrative data on costs. Members of the project team were also encouraged to keep reflective diaries of their experiences and to complete service improvement logs.
In order to place some distance between the intervention and the evaluation, the evaluation team was located in a separate department of King’s College London from CI Robert (and a different institution from PI Locock). While the wider team were involved in recruiting the ethnographer, she worked directly to the CI responsible for the evaluation (Boaz).
Ethnography can contribute to process evaluation by providing rich accounts of activities, projects and programmes. 69 The methodological design for this evaluation incorporated multiple methods and varied lines of inquiry to achieve ‘within research’ and ‘between method’ triangulation. 70 The ethnographer was in post throughout and was therefore able to observe all stages of the project.
At all stages of the evaluation, the ethnographer collected data to address the project’s research questions:
-
Is the accelerated approach acceptable to staff and patients?
-
How does using films of national rather than local narratives affect the level and quality of engagement with service improvement by local NHS staff? Does this have implications for the overall impact of the approach?
-
From local patients’ perspectives, how well do they feel national narratives capture and represent themes important to their own experiences?
-
Does any additional work need to be done to supplement the national narratives at the local level? If so, what form might this take?
-
What improvement activities does the approach stimulate and how do these activities impact on the quality of health care services?
-
What are the costs of this approach compared with traditional EBCD?
-
Can accelerated EBCD be recommended as a rigorous and effective patient-centred service improvement approach which could use common ‘trigger’ films to be rolled out nationally?
Evaluation participants and recruitment
Observations included staff, patients and friends at all four sites. Evaluation interviews were conducted with the facilitators and a sample of participants drawn from the events and the co-design groups. The principle of maximum variation sampling was used to ensure that a spread of different types of participants (staff, patients and friends) had an opportunity to participate. All patients who attended the celebration events in the ICU pathway were invited to take part in a group interview immediately after the event. Arrangements for staff and patient interviews, group interviews and questionnaire distribution were facilitated by the local service improvement facilitator, with support from the clinical lead at each site.
Data collection
Evaluation data collection took place between November 2011 and December 2012. To achieve an enhanced level of immersion required for an ethnography as well as a methodological triangulation, a wide range of formative and summative evaluation methods were employed, described in the following seven sections.
Observations
A total of 155 hours of observations took place between November 2011 and October 2012, including facilitator training sessions, staff and patient workshops, joint events, co-design group meetings and celebration events, project steering group and core group meetings. Furthermore, work-based observations in clinical settings and patient support activities were conducted to acquire a better understanding of the wider context of the intervention as well as the physical spaces and processes discussed during co-design group meetings. Observations were recorded as field notes and transcribed.
Evaluation interviews were conducted with the local facilitators, the PI, the project leads in the trusts, the CIs and the co-design group leads. The evaluation interviews were distinct from the staff discovery interviews (described as part of the intervention methods, above). A total of 30 interviews were conducted with 25 participants: 11 entry interviews were conducted between November and December 2011 and 18 exit interviews were conducted between November and December 2012. Most interviews were conducted face to face except four exit interviews that were conducted over the telephone to accommodate the interviewees’ workload. Interviews lasted between 30 minutes and 90 minutes. The topic guide for the entry and exit interviews was designed around the following themes: involvement in the project and perceptions of the process; project contribution to service delivery; and project sustainability and legacy. The exit interview questions were based on the summative evaluation interview questions used in the head and neck cancer EBCD project30 to generate comparable data. Additionally, 12 informal unstructured interviews were conducted with members of the project team and hospital staff members to capture personal insights into the implementation process and to catch up on emerging issues. These short interviews were conducted by telephone and were not recorded, but detailed notes were taken. Interviews and group interviews were audio-recorded and transcribed. Training sessions and events were audio-recorded to supplement field notes but were not transcribed. Brief conversations were recorded as field notes.
In addition, two evaluators of previous EBCD interventions observed ICU celebration events in the two trusts and contributed their own observation notes. They reflected, in particular, on similarities and differences between EBCD and AEBCD.
Group interviews
Two group interviews were conducted after the celebration events at the end of the first two projects on ICU at each trust. Each group interview was attended by four patient participants and lasted 1 hour. Participants were asked to discuss their involvement and perceptions of the process during each step of the intervention. Staff were not invited to attend group interviews in order to ensure that patient participants could express freely their views about participating in this project, watching the film and co-designing improved services.
Evaluation questionnaires
End-of-event evaluation questionnaires were distributed at the end of each patient, staff and joint event. The questionnaire topics included experiences of watching the film; engaging with other patients and staff; and participating in co-design (see Appendix 3). The content was based on the questions used in the evaluation questionnaires used in the breast cancer EBCD project to generate comparable data. 36 A total of 170 questionnaires were completed by patients and staff across all four sites. Feedback forms were also distributed during celebration events to capture post-hoc experiences of participation and perceptions of impact. A total of 53 celebration event forms were completed by participants at three events. A brief evaluation form was also distributed at the end of co-design group meetings to capture the participation experiences. Where co-design groups held multiple meetings, this form was distributed only at initial meetings to avoid repetition. A total of 166 co-design group evaluation forms were completed by patients and staff across four sites.
Reflective diaries
Reflective diaries provided a source of direct information from project participants on issues and concerns regarding the day-to-day running of the project. They included information on activities that took place, and reflections on personal practice, professional participation and the process as a whole. The main emphasis was placed on obtaining project diaries from the project facilitators (17 monthly diaries were received from two facilitators), although other project staff such as the PI and CIs and patients and co-design group leaders were given the opportunity to complete diaries. A further 5 monthly diaries were obtained from the PI (n = 1), a trust lead/CI (n = 1), a patient representative (n = 2) and co-design group leaders (n = 4).
Document analysis
The following key documents which were produced as part of this process were collated and analysed: 80 key documents such as activity summaries, clinical governance and conference presentations, meeting minutes and action plans, interview summaries and internal reports; 101 e-mails exchanged between the facilitators and patient, staff, management and academic partners; and service improvement logs and three cost spreadsheets for the co-design activities.
Cost data
A cost spreadsheet was developed by the evaluation team and sent to project facilitators to enable them to log directly incurred costs such as travel and catering expenses as well as indirectly incurred costs such as staff time. The cost spreadsheet aimed to address the hidden cost of participatory research in terms of staff time released from clinical duties. Comparable EBCD data were extracted from the breast and lung cancer project budget files and consisted of cost data on researcher time, film production, facilitation and other costs similar to AEBCD (though it was not possible to collect, retrospectively, the staff time involved).
Comparative experience-based co-design data
In order to be able to compare AEBCD to EBCD, the following materials were consulted: four articles,16,52,56,71 one book30 and seven working papers on past EBCD projects. 36–38,72–75 We were also given access to the 71 evaluation questionnaires completed during the independent evaluation of a breast cancer EBCD intervention. 36
Analysis
Transcripts, documents and e-mails were entered into a computer-assisted qualitative data analysis package (NVivo, QSR International, Warrington, UK). Coding was based on the seven research questions as well as emerging themes. Data were tabulated using framework analysis76 based on the themes linked to research questions: acceleration, service improvement and approaches to design; and constant comparison with EBCD. More specifically, data analysis involved the following stages:
The first stage involved familiarisation with AEBCD and EBCD data – alongside the ethnographic data, the evaluation team revisited reports of previous EBCD evaluations and the AEBCD protocol.
The second stage consisted of detailed coding of the qualitative data using NVivo. The quantitative questionnaire data from both AEBCD pathways and EBCD pathways in breast cancer, lung cancer and an emergency department were entered into Microsoft Excel (Microsoft Corporation, Redmond, WA, USA). Costing data were also collated in a series of tables.
As a third stage, the codes from the qualitative data analysis were indexed and used to develop a comparative framework based on three main themes: acceleration (film, facilitator and time frame), service improvement (performance, patient safety and patient experience) and implementation processes (enablers, barriers and legacy) to compare AEBCD and EBCD cases. The service improvement activities were also categorised based on a framework used by previous EBCD evaluators: grouping design ideas as small-scale changes, process redesign within teams, process redesign within teams, process redesign between services and process redesign between organisations.
As a fourth stage, quantitative data tables for the EBCD and AEBCD pathways were collated and used to generate graphical representations. The team also met with a health economist to support the analysis of the costing data for EBCD and AEBCD. Costs were estimated for each pathway based upon trust reported staff costs and these were combined with central project costs to estimate the average cost of implementing AEBCD. At this stage, the evaluation team met with the PI and CI Robert for a 2-day analysis meeting to consider the data collated and the emerging analysis. The discussion informed the further development of the analysis, mapping of key themes and interpretation of findings.
Patient, family and staff involvement
Patient involvement is a fundamental principle of both EBCD and AEBCD; patients and family carers were therefore an integral part of the intervention at all stages, and their views were central to the evaluation. At the heart of EBCD is also the creation of a coalition between patients and frontline staff as equal partners, and so staff involvement was also important.
The evaluation plan and proposed activities were discussed at the advisory group meetings where patients, support group representatives and staff from the two hospitals commented on evaluation design, methods (including data collection tools) and early findings. One of the patient representatives also checked the plain English summary of this report. The evaluation team found the opportunities to present emerging findings to the group meetings useful in developing their analysis, for example in helping to understand reported patient responses to the trigger films in the two pathways. Patients and staff in the two trusts were regularly informed and consulted about lines of enquiry, methods and tools during fieldwork visits. For example, drafts of the service improvement logs and costing tables were circulated for feedback.
The evaluation had a formative dimension, and so the evaluation team fed back key emerging issues to the wider project advisory group. For example, the ethnographer observed some confusion among participants at an early event when the trigger film was shown. As she had been reading the EBCD evaluations, she immediately saw a solution to this problem based on previous EBCD practice and shared her idea with the project team. The project team responded to the suggestion by producing a script to be read prior to showing the film, so that the purpose was clearer to patient participants [see Chapter 3, Results (4)].
Ethics and consent
Ethics approval was obtained by proportionate review from National Research Ethics Service Committee North West – Greater Manchester West, Research Ethics Committee (REC) reference number: 11/NW/0653. All staff and patients were given a participant information sheet explaining the study, and consented to be observed and interviewed (see Appendix 2 for the REC-approved documents). (It should be noted that EBCD itself, as a quality improvement activity rather than a research activity, does not normally require ethics approval. However, because of the evaluation component of this project ethical approval was required.)
Project management and governance
The project was managed by PI Locock with administrative project management support from the Thames Valley Health Innovation and Education Cluster (TVHIEC). An initial meeting of the CI team was held before the start of the grant to plan implementation. Thereafter, the CI team met every 4–6 months with the hospital service improvement facilitators and as a core management group. A wider project advisory group was also convened, comprising the core group plus representatives from The King’s Fund’s Point of Care Programme, the Department of Health Directorate of Public and Patient Experience and Engagement, and five lay representatives recruited from our hospital partners and voluntary organisations (Intensive Care National Audit and Research Centre, and the British Lung Foundation). The advisory group met on the same day as the core group, and was chaired by the director of TVHIEC (see Appendix 1).
As noted above, in order to place some distance between the intervention and the evaluation, the evaluation team was located in a separate department of King’s College London from CI Robert (and a different institution from PI Locock).
Chapter 3 Results
From the outset, the focus of the evaluation has been the extent to which AEBCD offers a feasible alternative to traditional EBCD. Although we present data on improvement activities in the processes of care associated with the intervention [see Results (5), below], we do so not to evaluate EBCD itself, but rather to assess whether or not the nature and extent of change achieved across the four pathways is similar to what we could expect from traditional EBCD – and if not, why not. Consistent with our seven research questions, we did not set out to make internal comparisons judging the ‘success’ of one case against another within the study and, as noted earlier, have anonymised in which hospital they took place.
Results (1): Is the accelerated approach acceptable to staff and patients?
A key focus of the evaluation was whether or not accelerating the experience based co-design process affected the acceptability of the approach to staff and patients. Previous evaluations of EBCD have found a high level of acceptability of the EBCD approach. 36,38,56 This section draws on observational data from events, questionnaires completed by staff and patients, qualitative interviews with staff, patients and project staff, and reflective diaries and service improvement logs completed by facilitators in the pathways. Further detail on staff and patient responses specifically to the trigger film is given in sections 2 and 3 of the results. Overall, the project was positively received; both patients and staff welcomed the notion of patient-centred design. The events and interviews featured many positive accounts of participating in the AEBCD process. The following sections discuss the views of staff participants and of patients and carer participants.
Staff participants
At the end of the staff events in each of the four AEBCD pathways, attendees were asked to complete an end-of-event questionnaire (see Appendix 3). Figure 3 shows the percentage of staff who rated their ‘overall impressions and feelings about the event’ as ‘excellent’, ‘good’, ‘average’ or ‘poor’. For comparison purposes, the figure includes responses to the same question from two historical EBCD projects. No staff members from any of the staff events ranked their impressions as ‘poor’. The majority of staff in both EBCD and AEBCD ranked their overall impressions as ‘good’ or ‘excellent’. A minority of staff ranked their overall impression as ‘average’ in one of the EBCD and two of the AEBCD projects.
FIGURE 3.
Staff responses to ‘What are your overall impressions and feelings about the event today?’ BC, breast cancer; LC, lung cancer.
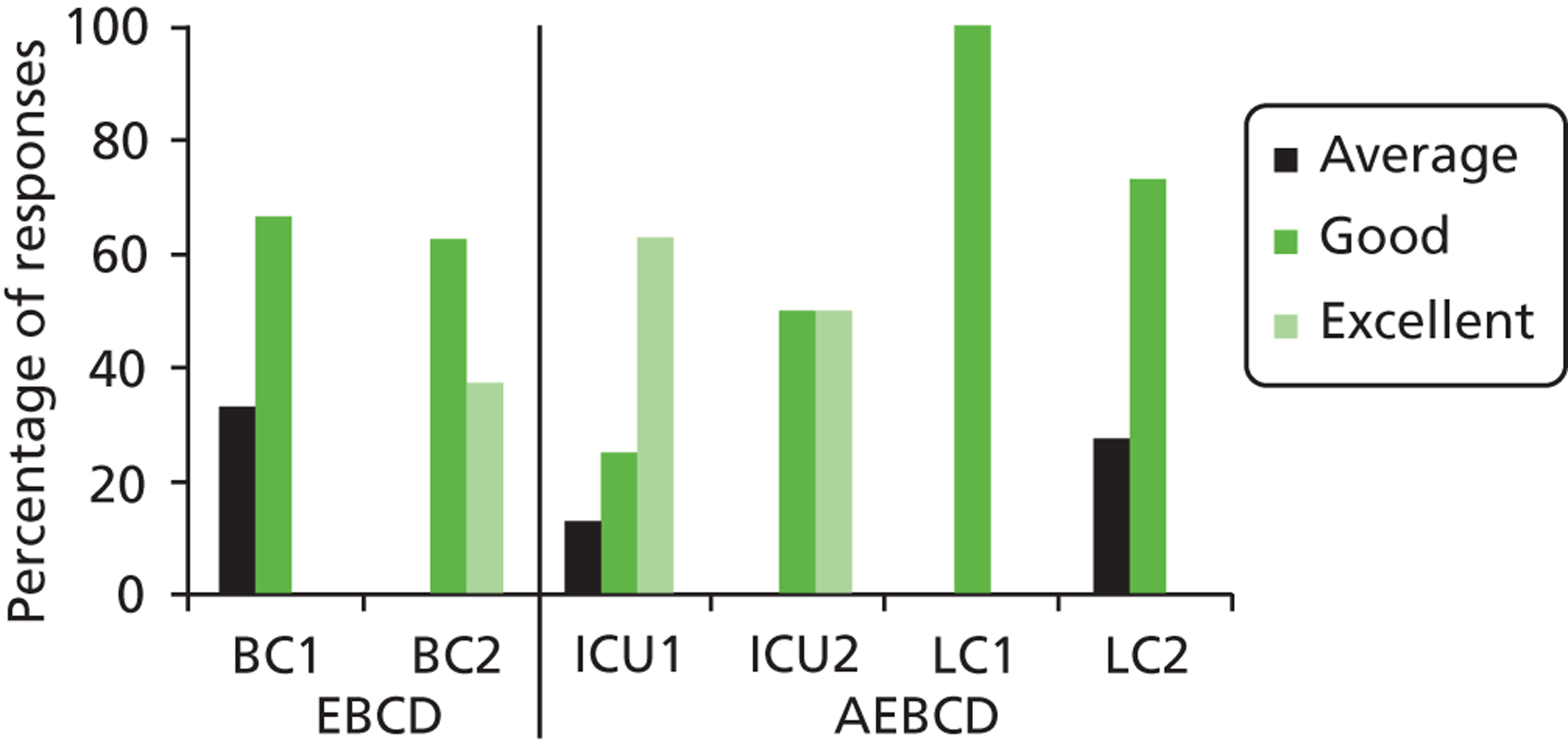
Members of staff also typically reported that this was a good or excellent way to reflect about their experiences at work in both EBCD and AEBCD projects (Figure 4).
FIGURE 4.
Staff responses to ‘What do you think of this event/process as a way to reflect upon your experiences at work?’ BC, breast cancer; LC, lung cancer.
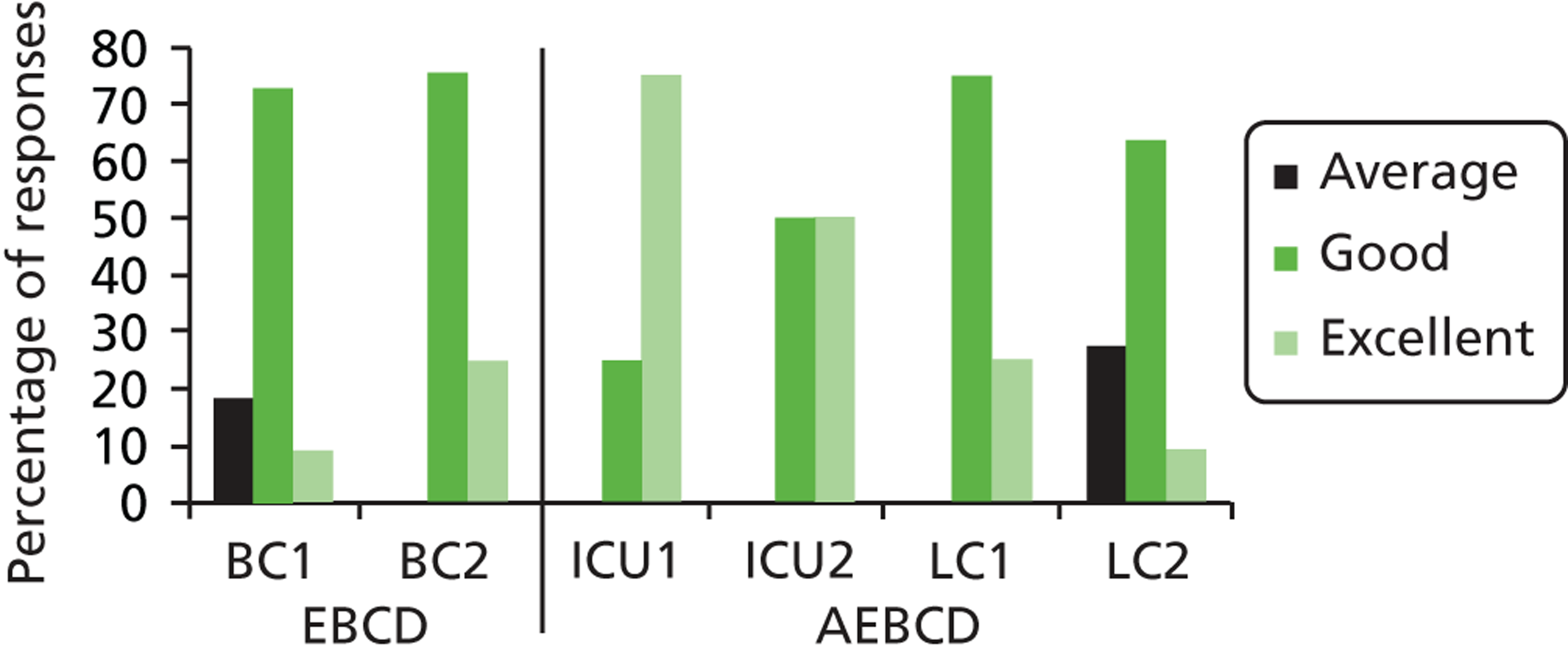
Anonymous open comments in the end-of-event questionnaires included:
Able to focus on things we do inefficiently.
AEBCD, intensive care
Excellent, helped me to reflect.
AEBCD, intensive care
Was fantastic to get involved with other staff members outside of radiotherapy in areas normally distanced from.
AEBCD, lung cancer
It is very good to know what patients reflect upon and how they view the staff.
AEBCD, lung cancer
These positive reflections were borne out by the observations of the staff events by the AEBCD ethnographer, and in interviews with the facilitators and others involved in the process. The staff-only events were just the start of a process, and the evaluation data suggest that the face-to-face encounters with patients often had a profound effect on staff in making them think differently about their practice and reconnect with their core professional values, resulting in a renewed sense of motivation. A senior manager in one site reported that a member of staff in intensive care had said it was the first time in more than 20 years of practice that he had sat down and talked to patients in this way. A senior lung cancer nurse (unprompted) told a meeting of the project advisory group that it was the most inspiring thing she had done in her professional career.
One of the co-design group leads described her experience of attending the AEBCD events:
It was very interesting. It was a light bulb moment, because you had four different groups, nurses, doctors, patients, and relatives. It was one of the first times I’ve sat down and talked about the same problem and how we all view it, and some of the things other people were concerned about I didn’t think anything of that, and then at the same time some of the things I thought were important, other people didn’t think they were important. It was very, very interesting. It may me realise what a crazy system we are working at the moment. People are doing their own things; they are assuming lots of things.
Interview with co-design group lead, intensive care
Critical aspects of the process identified included creating the space to think and to listen to others (both patients and other staff):
I think the most important things were that staff really appreciated the time to think about the experience. It became apparent that they perhaps didn’t have or make time to reflect on what they do in their daily workings, so I think they actually found it quite cathartic and therapeutic. It actually raised the thinking of experience, and I think the staff really appreciated that their point of view was being listened to because up until that point the political drive had always been patient experience and now all of a sudden we were interested in staff experience.
Facilitator, interview
The opportunity to hear directly from patients and carers had a transforming effect on some staff participants. One participant described herself on a co-design evaluation form as ‘a better nurse because of it.’ Here, a consultant and a nurse describe their personal experiences of AEBCD and how their views of patients as people had changed over the course of the project:
I think [AEBCD] is phenomenal . . . I see people not only in intensive care, but I see them in the outpatient department as well. . . . That patient is about more than just what you see in the form of the numbers or the clinical elements that you come into contact with. There are relationships involved in this whole scenario. There are feelings that are involved in this whole scenario. . . . [AEBCD] allows us to become more curious, rather than judgemental, okay, and I think that’s a very important lesson for most intensive care units. . . . We’re quick to judge, because we’re paid to do that. I have to make a quick decision, otherwise somebody is on the realms of life and death. But when it comes to patients – and I don’t have any idea, as a unit we don’t have an idea of what is beyond what I’m seeing. This informs that process. So I can see that this person is not only a human being, but he is also a father, he is a son, he is a brother, he is a friend, he is a cousin, he’s a plumber or an electrician, he is a sportsman, he has an interest in horse riding, whatever it happens to be. He has a dog, he has a budgie, he has plans, he has expectations, he has regrets, he has feelings. And as much as we possibly can, I would like to think that I just don’t judge the number, but I want to be able to provide a service that benefits all those processes.
Consultant, interview, intensive care
I have already changed the way I think and care for patients even though we haven’t started implementing changes yet. I have a better understanding now of how things are from the patients’ perspective.
Nurse, field note of conversation, intensive care
Similarly, one of the facilitators reflected on how the active involvement and presence of patients had galvanised staff – and now seemed an obviously better way to work.
Has this project been different to other improvement projects you’ve been involved in?
Yes, because the absolute core of it is the humanistic connections. Because of hearing patients’, relatives’ and staff experience it acts as a catalyst and gives you energy to keep going and make the change, and make sure it happens. It’s a real driver to keep going and it seems to be the only thing that makes sense.
The only thing that makes sense?
It is. So many people have echoed that without me saying anything. I have not had to convert people into this methodology now. People just get it and wonder why we have never done it before.
Facilitator, interview, ICU
As one participant observed in discussion with the ethnographer, it is easy for staff to make decisions for the patients without finding out more about the patients, their needs and choices:
So important that priorities are highlighted and worked on by both parties to gain a better understanding of needs. So easy for the health professional to tell the patient what is best for them without actually listening to their needs (and vice versa).
Staff member, lung cancer, field note of conversation
Finally, one of the facilitators described how the project led to a turn-around in attitudes on the part of one consultant who had initially felt quite threatened:
And I think with [consultant], in particular, he was frightened that if he got too near, too close to these patients and relatives, that it would dismantle his coping strategies. And I respect that, absolutely totally respect that. So, I think he felt very much that he was under the microscope, but he always rose to the challenge. So, even though it was disappointing that I had to fight the cause for the methodology, it was so rewarding. So that one instance is my disappointment, but my success if you like, because it changed him completely. And that’s not just me saying that, the two [co-design group facilitators] have just said, and the sisters on the ward say, how different he is, you know, he went the next day and changed the way he did the ward round. So, it wasn’t just lip service with him, he went out and carried out what he said he was going to do.
Facilitator interview, lung cancer
Of course, it is possible that some staff might feel unable to voice major concerns or disagreement with the process without appearing to lack empathy or to place low priority on patient experience. Staff were assured of anonymity in giving their feedback but in a defined service area people may not trust that this will be the case. However, our fieldwork observations suggest genuine enthusiasm rather than socially desirable compliance. There were some comments about the time commitment required, but overall the feedback suggested that staff felt it was a good investment of time compared with some other organisational activities, and one that was likely to improve morale rather than threaten it. This staff feedback was consistent with previous EBCD evaluations. If anything, staff commented that they would have liked more patients involved, especially in the co-design groups – again, however, observations by the evaluators of previous EBCD initiatives noted that the process and engagement of staff and patients (including the number of patients involved) were remarkably similar.
Patient and carer participants
Patients and carers found it most valuable meeting other people who had shared their experiences as part of the co-design process. Across all EBCD and AEBCD projects, a high proportion of patients and carers ranked the experience of meeting other patients and talking about their experiences as ‘excellent’; a small minority in AEBCD ranked the experience as ‘average’, which was not the case for EBCD (Figure 5).
FIGURE 5.
Patient responses to ‘meeting other patients and talking about your experiences’ during the patient event. BC, breast cancer; LC, lung cancer.
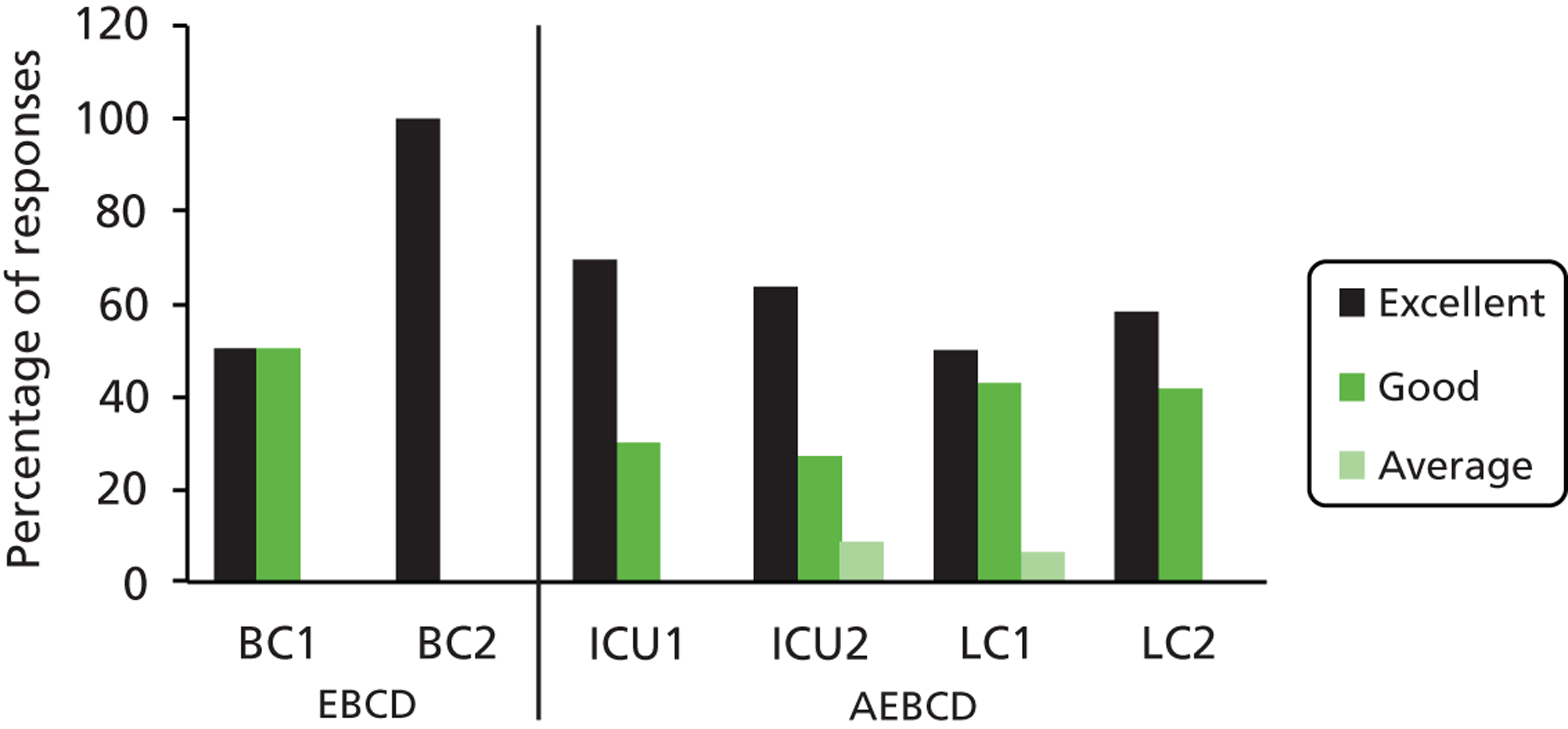
The majority of patients across EBCD and AEBCD projects ranked the activity of using ‘The touch points and emotional mapping exercise as a way to reflect on your experiences and identify priorities for improving the service’ as ‘good’. A minority of AEBCD participants reported the experience as ‘average’ (Figure 6). Observational data suggests that AEBCD participants were slightly unsure what to do during this process.
FIGURE 6.
Patient responses to the ‘touch points and emotional mapping exercise as a way of reflecting on your experiences and identify priorities to improve the service’ during the patient event. BC, breast cancer; LC, lung cancer.
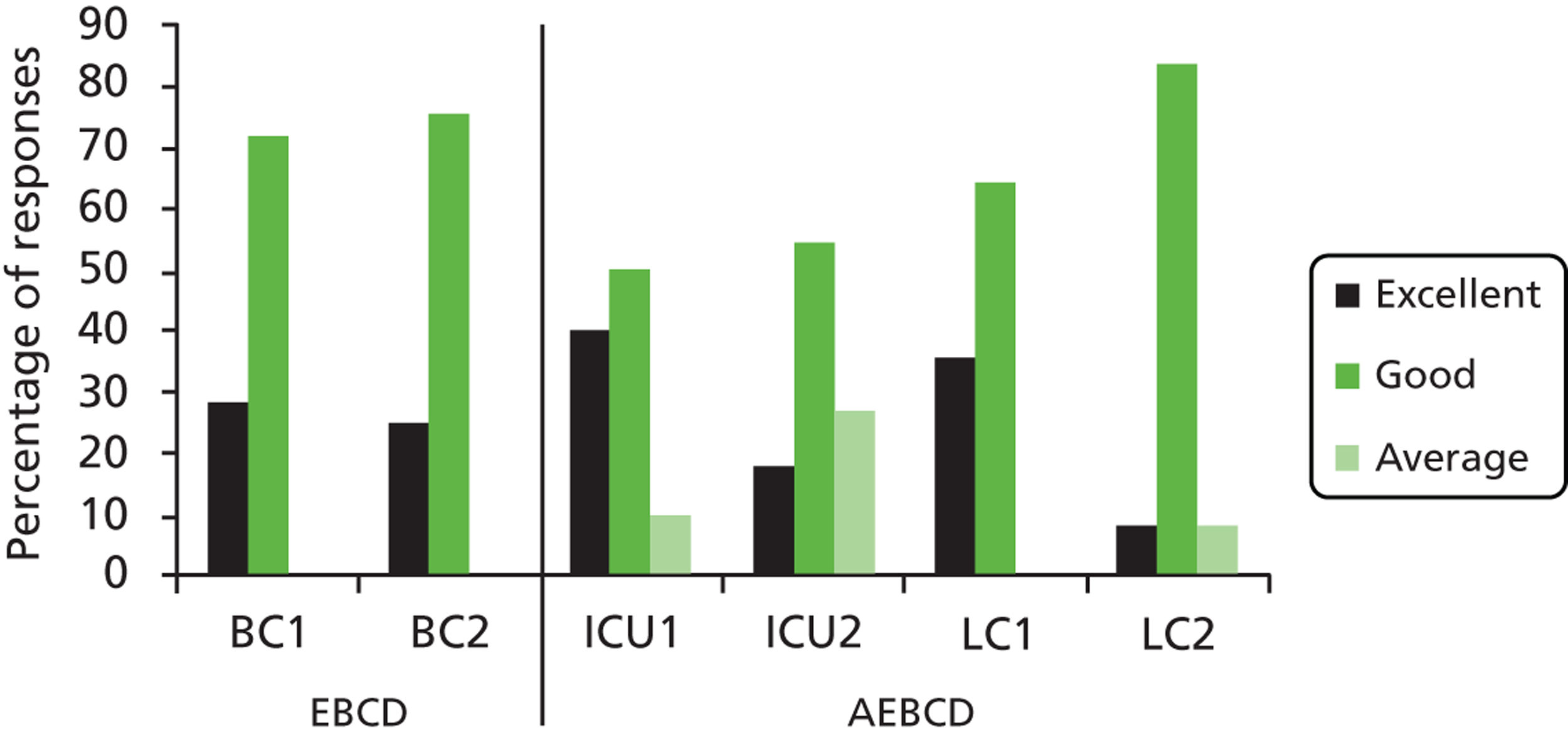
Patients are often invited to share their views as part of consultation processes within the NHS. Patients engaged in AEBCD spoke positively about their involvement in what they perceived to be a more active and meaningful approach to patient engagement in quality improvement, in a very similar way to past EBCD projects.
It was great to see you all at the ‘Patient Experience’ event this week, what a wonderful thing it will be if we can contribute to and change what is already an incredible service that the intensive care department already provide – it makes me feel humble to be part of such a cause. Sorry to be gushing, but [facilitator] you truly are a guardian angel. I also feel that this experience should be shared with other hospitals as it seems they could learn a lot.
Patient, intensive care, e-mail correspondence
One patient at a lung cancer joint event contrasted AEBCD with normal consultation in which ‘people say I’ll do this, I’ll do that, and nothing happens’. An intensive care participant said, ‘I feel I was really listened to’ and that it was ‘much better than expected’. Several expressed surprise that they had felt able to contribute as equal partners and that their views were taken seriously.
Group interviews were conducted with patients and carers following events in two of the pathways. Their responses were positive about the AEBCD process and their role within it:
So what did you think of the first event? The first event was when it was only patients and you were shown the film for the first time.
It was thought-provoking.
Well, it converted me because I was very sceptical as to whether I could give any contribution to it.
Group interview, intensive care
A theme within these interviews was a concern that their involvement would lead to little or no change and, as a consequence, the participants spoke positively about the actions arising from AEBCD:
I wondered what, if anything, will be taken on board. To be honest with you, everything has been taken on board, and that in itself was a complete surprise.
Patient interview
One facilitator agreed with this perspective, but felt that in that particular lung cancer pathway it was still a little early to be sure of real change:
I think the success is that the patients really, really engaged with this, they want to help and be involved, and they want to help improve things. And I think we don’t use them as a valuable resource, because they’ve been through it, they’ve been there, done it, and they know exactly what’s wrong, or what’s good. So I think the positive out of this is that we have now, kind of, a nice group of really engaged individuals, who can see there’s a benefit for them being engaged. And that, I think, is a big difference, a big improvement, and a massive positive for our service, that we’ve got such a group of engaging individuals. On the negative side of things, I suppose it’s probably a bit too early to see yet, because not all of the individual projects have yet, I suppose, finalised and come to fruition, so I think it’s probably a little bit too early.
Facilitator interview
Patients who presented at celebration events expressed strong support for the process and what had been achieved. One carer at an ICU celebration event made the following speech reflecting on his experience of engagement in AEBCD:
Thank you for the chance to take part in this study. We hope our contribution has been valuable – whether it has or not, it has certainly been very valuable to us. In both [co-design] groups we have participated in we have heard things that have helped us to come to terms with what happened. And it has been wonderful to know you all – staff and patients alike. I have learnt many things and even some new words – ‘wardable’ I think is my favourite . . . I am aware there is very little in a practical sense that either my wife or I can do from now on. But as this is the year of the Olympics it occurred to me that two of my favourite events – the 100 and 400 metre relay races – provide a good metaphor for what we have been discussing over the last few months. Even the same word is used – Transition – and while I wouldn’t want to describe [my wife] or any of the patients as a baton, there are some similarities.
The patient – as is the baton – is held securely until it is time to pass it on to other hands. It doesn’t matter how well the lap is run – or what progress is made – if when the baton is passed on to the next runner it is fumbled or even dropped. Then any good work is lost.
It happens three times in a relay race – and may only happen once in the hospital – but a practised and smooth transition can only speed up the process of healing and recovery, and be beneficial to the patient, the staff and in the end to the relative who hopefully will be last in this ‘real life’ relay race. And the baton and the patient will be passed securely into the waiting hands of their loved ones.
Carer, speech
The ethnographer also noted the following:
There was a comment from a patient within the event who said that everything that had been discussed had been taken forward into improvements . . . ‘our views were not dismissed, they were looked at and things changed.’ ‘Thank you for looking at the little things.’
Excerpt from ethnographer’s field notes at celebration event
Evaluation evidence also suggests that patients drew some direct personal benefits from taking part, as the comment above from the carer about coming to terms with his experience suggests.
I drew a picture of a tracheostomy on a patient on a ventilator, and I showed that to a patient to explain why they can’t talk while they are on a ventilator. So he’s framed it and he’s asked me to sign it and date it, and this picture took about ten seconds to draw.
Consultant interview
A patient today said it [AEBCD] had been ‘therapeutic’ for her as she realised that she was not the only one who had experienced hallucinations. It confirms you sometimes have to be bold and go with your instincts as to what is a good thing to do.
Excerpt from senior manager’s reflective diary
One question that has emerged from our study but which our study design was not intended to address is whether or not AEBCD brings less personal therapeutic benefit to individual patients involved. Although individual patients reported finding AEBCD a beneficial process, one of the former EBCD evaluators, who was in a position to compare the two approaches directly, suggested this as one possible ‘cost’ of using AEBCD:
I do think there is a therapeutic element to storytelling which AEBCD misses.
EBCD evaluator, observation notes from AEBCD celebration event
Thus, anecdotal evidence – from those who have previously led or facilitated EBCD implementations – would suggest that, at the level of the individual participating patient/carer, the impact of AEBCD is less as participants did not have the opportunity to tell their own stories, listen and potentially watch them back, hear stories of other patients who had been cared for in the same service as themselves, and then reflect together with them on their own shared experiences. However, the evaluation did not set out to explore the question of individual therapeutic benefit, and so confirming this assertion would require further research and a different study design.
One of the facilitators also identified a benefit in terms of mutual understanding between staff and patients, and described
. . . [a] paradigm shift in the patients and relatives. They gained an insight into the ‘real world’ of the NHS and healthcare professionals restraints and constraints and became ‘caring and protective’ of them – which was very evident in both pathways. They reported that it wasn’t just about them being listened to but that change was made possible because of their involvement and the tenacity and passion of staff.
E-mail observation, facilitator
Role of facilitation and impact on facilitators
The role of skilled facilitation is known to be a major influence on implementation;77 in this accelerated form of EBCD the facilitators took on some additional responsibility, which in traditional EBCD would usually have been led by an external researcher. They also exercised more independent leadership of implementation. In most previous evaluations, an external researcher has worked in the hospital setting alongside the facilitator, providing continued advice and support around the process as well as gathering and analysing patient and staff discovery interviews. However, this is an expensive way to achieve change and is one of the barriers to wider uptake,36 and so we designed the accelerated model on the basis of a more sustainable ‘real world’ approach of building internal capacity to facilitate improvement initiatives. Thus, the facilitators were trained at the beginning by CI Robert, and were able to contact him for advice and support whenever they wanted, but did not have continuing on-site support. They also used the EBCD ‘toolkit’ on The King’s Fund’s website to supplement their knowledge.
Each hospital organisation received funding for a 40% post for 6 months for a local facilitator for each pathway. The hospital partners chose their own approach to local facilitation. One appointed a single person to facilitate both pathways, while the other opted to appoint two different people. All three took on facilitation part-time alongside other continuing responsibilities; in practice, the extent to which they were able to back-fill their time to free up space for facilitation varied. All EBCD initiatives make significant demands on facilitators, in terms of both time and organisation, but also in terms of direct personal exposure to potentially distressing or challenging patient experiences as well as engaging staff colleagues who may feel demoralised, threatened or indifferent. However, a key difference in AEBCD was in the handling of the staff discovery component. In traditional EBCD, staff discovery takes place alongside the patient discovery interviews, over the course of 6 months. While the patient interviews, analysis and film editing are the major parts of the workload during this time, the extended time frame allows staff discovery to take place on a more relaxed timetable and allows momentum around staff engagement to build over several months. In AEBCD, because the patient discovery phase was removed, staff discovery and engagement were confined to a short time frame, which created substantial pressure on facilitators early on in the projects, at a time when they were also recruiting patients for the workshops, organising venues and invitations, and on a learning curve about how to do EBCD. As two of the facilitators themselves noted in successive reflective diaries:
We are both finding things a little difficult because we have been given very little time to do this, i.e. only 3/4 weeks.
Facilitator reflective diary entry
We had our training on 21st October and in that month you were trying to assimilate what had been said, or what it was all about, look at the King’s Fund website, recruit your patients, do your interviews, process the whole lot, organise the first event, and hold the first event, and that was one month. I think if we just stretch it a little bit longer, six weeks, or at least have your training day earlier so you’ve got – and a few key pointers – so you’ve got time to digest what you’re being told and what is being asked of you, and ask questions and things, rather than training and then straight into it.
Facilitator reflective diary entry
I have had to be very organised, forward thinking and think creatively with this project. I have felt quite anxious on occasion, particularly about the patient recruitment, and this led me to feel a little negatively about the project as a whole. Once I had finished the interviews and had recruited the patients I felt more positive about the project. I have received very good support from other people.
Facilitator reflective diary entry
The actual workload and intensity was huge and it required far more hours in a week than were scheduled for – but I have the flexibility to manage my own workload and I am committed to this process (therefore expected to work above and beyond the required hours). I worked hard to plan and prepare for the patient and carer event and it did pay off.
Facilitator reflective diary entry
We observed that the workload was ‘front-loaded’, which had not been anticipated in the way the posts were set up. Even in the case where the same facilitator moved from one pathway to the next, the fact that they were dealing with an unfamiliar and disparate group of staff in the second pathway created some of the same challenges second time around. The facilitators managed this pressure in various ways with the support of senior leaders in their organisations, including working extra hours at the beginning of the intervention, and drawing on other people in the organisation to help, but with hindsight more time for staff engagement would have been beneficial. In one case, the hospital had a nursing researcher who was interested in patient-centred improvement and provided additional support. The facilitators demonstrated that it was possible to work to this shortened timetable through sheer hard work and commitment, but this came at a personal and organisational cost.
This is a demanding project for the staff. [The facilitator] did extremely well at the staff event and the staff participated fully. The manager of the unit and an anaesthetist (not the consultant I had involved) were very involved. The atmosphere over lunch suggested the patient event went well too. The estimate of staff resources to facilitate this project were too conservative. [The facilitator] has effectively worked full time on this over the past few weeks and has had support from [internal trust research staff]. At the meetings [the facilitator] was assisted by [internal trust research staff] and the PPI lead and a staff nurse from the ICU. I should have made sure I knew more about the demands on the Trust staff and been even stronger about staff resources at the funding stage. That said I am really pleased we are doing this project and see that we should get benefits for patients.
Excerpt from senior manager’s reflective diary
A further unanticipated issue was how to record and analyse the content of staff discovery interviews. In past EBCD projects when this has been the responsibility of the external researcher, that person has recorded, transcribed and coded the staff interviews for a thematic analysis, to present to the staff feedback workshop. However, the primary purpose of staff discovery interviews is engagement and broad identification of important areas of concern, rather than in-depth research into staff perspectives. Internal staff facilitators are not trained to do qualitative data coding and thematic analysis and it was questionable whether or not this would be good use of their time. In consultation with the facilitators they were advised to take detailed notes during staff interviews rather than recording and transcribing, and to use the notes in a pragmatic manner to produce anonymised feedback which could be confirmed or challenged at the staff workshop.
In the event, both of the ICU facilitators chose to record the staff interviews so that they could listen back to the recordings if necessary when they compiled the staff feedback (although they did not transcribe them):
On the audio recording point, I understand that [co-investigator] suggested at the training morning at [hospital] that it would be better for facilitator 1 and facilitator 2 not to record the interviews (precisely because it makes the analysis so much more time-consuming, especially if you’ve never done it before) and just to use notes taken at the time, reflecting that this was meant to be an accelerated process, rather than the kind of intensive discovery phase normally used in EBCD. But facilitator 1 and 2 both felt they wanted to have recordings. This is certainly something we should note for the evaluation – perhaps the answer would be to rely on notes for the analysis but to know that the recording is there if they do decide they need to go back to it.
Co-investigator, e-mail correspondence
The facilitators stressed that while the burden of conducting a new quality improvement initiative was significant, they could also identify benefits which they have derived from their involvement. All reported that they were taking back to their pre-existing clinical or managerial roles a new insight into the gains for staff and patients of working together on quality improvement, and that they planned to continue using EBCD techniques in future. The hospital organisations have a legacy of new skills and experience, and two of the facilitators have already moved on to lead further EBCD projects within their organisations. The facilitators have been and will continue to be active in dissemination activities around the project, including co-authoring and lead-authoring papers for different audiences, submitting abstracts to and presenting at conferences, and cascading skills to colleagues. Importantly, they have contributed to an updated version of The King’s Fund’s EBCD toolkit to share their experiences to provide practical information and support to future facilitators.
Results (2): How does using films of national rather than local narratives affect the level and quality of engagement with service improvement by local NHS staff? Does this have implications for the overall impact of the approach?
A trigger film compiled from a series of narrative interviews conducted with local patients is used in the traditional form of EBCD, whereas a film made with footage from an existing national archive of patient experiences was used in our evaluation of AEBCD. EBCD and AEBCD films are similar in length (approximately 30–35 minutes) and introduced at the same stage of the change process with the same primary purpose: to stimulate individual and shared reflection among participants to inform the identification of shared improvement priorities for the co-design phase of the intervention. Watching and discussing the films is also a crucial mechanism for engaging both patients and staff, enhancing their commitment to working together in partnership to improve services. Patients were shown the film at the beginning of the patient event in each of our four pathways. Patients and staff together were also shown the film at the beginning of three of the four joint patient and staff events. (In the remaining pathway, the facilitator experienced technical problems and was unable to show any of the film at the joint event.)
Some minor changes were made to the content of the lung cancer film after a draft edition was shared with CI Robert and the service improvement facilitators, and before it was shown to staff and patients. For example, one clip was removed in which the person described having a plaster of Paris mask made for radiotherapy as being ‘like buried alive’; it was felt that this was no longer common practice for making masks and could be needlessly distressing. However, a decision was made to leave in a clip about CHART (continuous hyperfractionated radiotherapy); although local facilitators said this was not used in their hospitals, it was established that it is used in other centres. Given that the study aimed to test whether or not films made using the national archive would serve their purpose in a wide range of health care organisations, we explicitly did not want to tailor them to local contexts.
Staff (and patients – see below) were asked to rank their experience of seeing the film at the joint events in the three pathways where they were shown. Staff across the AEBCD pathways consistently ranked the film more highly than patients in the same sites, ranking it as good or excellent in all cases (Figure 7).
FIGURE 7.
Staff responses to ‘seeing the film’ at joint events. BC, breast cancer; LC, lung cancer.
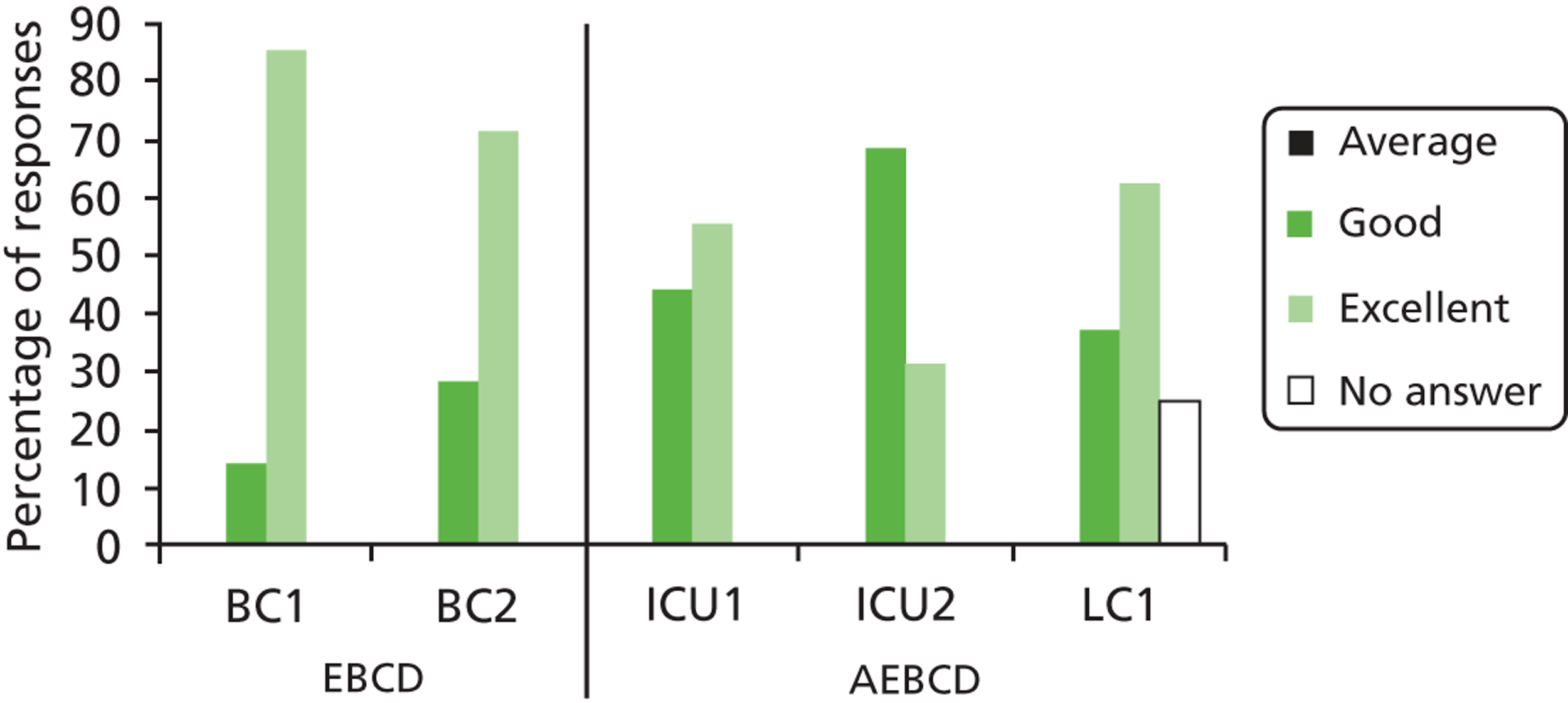
NHS staff rated the representation of the experiences presented in the film as more similar to their own observations than patients did. It was observed in one site that staff defended the film when patients said that they felt some aspects were too negative and therefore not an accurate reflection of care in the trust; staff felt able to challenge this perception, confirming that such things did indeed happen locally on occasion and sharing their experiences of witnessing suboptimal care. A staff member in intensive care felt the differences in perspective may have arisen partly because of the nature of the patients who took part, with a bias towards those who have been satisfied with their care and want to ‘give something back’.
Patients are very grateful for their treatment. It would have been good to have had more mixed experiences discussed i.e. the group wasn’t representative
Staff member, free-text comment on questionnaire
Accelerated experience-based co-design staff participant responses followed similar patterns to those of EBCD participants reported in previous evaluations. One of the evaluators of the EBCD breast cancer project was invited to observe an AEBCD celebration event for staff and patients and contributed her reflections as part of our observations. Her concerns about acceptability focused on the potential impact of using an external trigger film. However, observing the event she felt that there was no difference in acceptability for participants, observing that an external trigger film can still ‘get people talking.’ In her notes she commented:
Initially I thought that not having a [locally produced] film would mean that both patients and staff would not feel as engaged with the process. But this did not prove to be barrier to bringing about change. In fact it may have made staff more engaged since they perhaps did not feel as confronted as the staff in the EBCD project. Some EBCD staff felt threatened when they saw their own patients speaking about the difficulties they encountered when receiving care at the service.
Observation notes, EBCD evaluator
The observational data confirmed that the film achieved the goal of acting as a trigger to stimulate thought, discussion and plans for action, and that using national narratives seemed to allow staff to engage comfortably with patient experiences. They watched the film with great interest and showed a mixture of emotions as they listened to the patient stories, from amusement to astonishment and sadness. Seeing things through patients’ eyes was enlightening; as one lung cancer nurse commented, ‘What struck me was the loss of hope upon diagnosis. This really struck a chord with me’ (lung cancer joint event, observation notes). She joined the co-design group on diagnosis-giving in the next phase of the project.
One facilitator reflected in an interview at some length on staff reactions, and speculated that the use of national rather than local narratives may have helped staff feel less threatened by negative comments and able to externalise any criticisms of care. She had had to manage the anxiety of a consultant who was worried about seeing the film for the first time at a joint event and wanted to see it beforehand to prepare.
It is arguable that to gain the most from a co-design process, a certain amount of unsettlement among staff can be productive, and that if they are too comfortable with the views expressed by patients there will be fewer opportunities for deep emotional reflection and self-challenge. At the same time, a genuine coalition between staff and patients is an important component of EBCD, and may be easier to achieve if staff do not feel personally criticised.
Because the aim is to get people talking about their own, and feeling comfortable, with describing their experience. So having sat in a room with staff, hearing both positive and negative things about a service, it almost gives the patients permission to discuss those sorts of things.
And how did you feel the other members of staff found it, not only being in the same room with all the colleagues they didn’t know, and patients as well, and being asked to do a film, and the emotional mapping?
Yeah. I think that they really liked being with patients, and on this equal footing, because often they are with patients, you know, perhaps because there’s a complaint being made, and I noticed that there were several things in the meetings. So for instance, one of the patients would say, ‘Oh come here, we’ll look after you,’ so the relationship between patients and staff became equal, with occasions where patients were taking responsibility for staff.
Interview with lung cancer co-design group lead
In practice, the use of the national trigger films did not seem to have an adverse impact on the co-design phase, and the range and type of improvement activities compared with previous EBCD projects [see Results (5), below]. It may even be an advantage to use non-local films.
Results (3): From local patients’ perspectives, how well do they feel national narratives capture and represent themes important to their own experience?
After the patient event in each of the four pathways, attendees were asked to complete an end-of-event questionnaire (see Appendix 3). Figure 8 shows the percentage of patients from each of the four pathways who rated the film based on the national archive as an ‘excellent’, ‘good’, ‘average’ or ‘poor’ representation of what it was like to be a patient in each respective service. For comparison purposes we used the same questionnaire as had been used in two historical EBCD projects which used a film of locally collected patient interviews. Figure 8 includes responses to the same question from these two projects as well as AEBCD.
FIGURE 8.
Percentage of patient responses to ‘seeing the film today – did you think it was a good representation of what it is like to be a [breast cancer/lung cancer/intensive care] patient with at X NHS Trust?’ BC, breast cancer; LC, lung cancer.
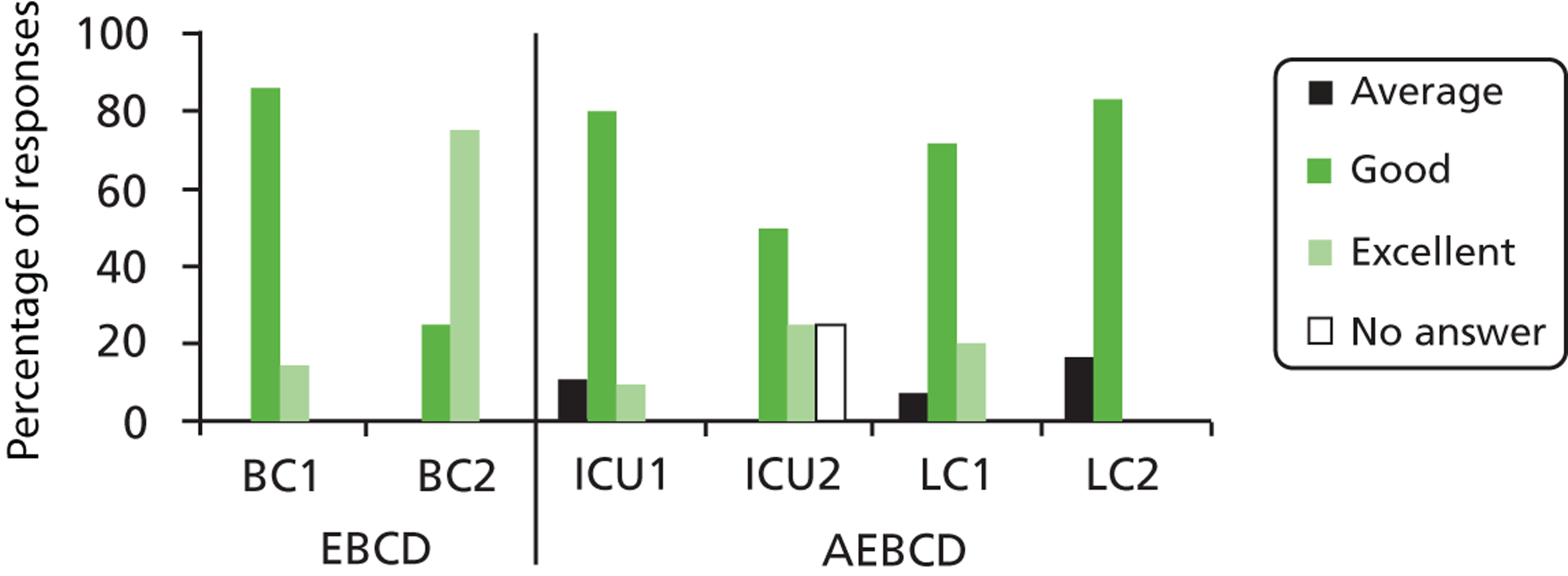
The fact that we were using the previous EBCD questionnaire for comparison and that this question was therefore not designed specifically for AEBCD may have affected the responses. One would not necessarily expect a nationally derived film to be able to represent what it is like at one particular trust, even though it might (in the words of our own research question) ‘capture and represent themes important to [your] own experience’. Despite the wording of the question, no patients from any of the four AEBCD pathways rated the film they saw as a ‘poor’ representation of their experience, just as in EBCD. AEBCD elicited some ‘average’ responses, whereas EBCD did not, and some patients did not answer. Patients typically responded that the trigger films were a ‘good’ representation of what it is like to be a patient, with a smaller percentage answering ‘excellent’, except in one of the two historical EBCD projects where over 70% of respondents rated the film as ‘excellent’. In one of the four AEBCD pathways, no patients rated the film as ‘excellent’.
Free-text responses and interviews with patients shed further light on these responses. Patients and carers reported that, although their experiences were similar, those represented in the film were sometimes more negative than their own. Comments indicated a high level of variation; across the six EBCD and AEBCD pathways the films were variously reported as too negative, positive and similar to participants’ own experiences (including sometimes by the same individuals reporting that it was both similar and too negative). Some EBCD participants reported finding the film powerful and cathartic, but also ‘hard to watch’ – this may have been because they were watching extracts from their own interviews. Participants in EBCD reported finding the film less powerful when they watched it a second time at the joint staff/patient event.
Although patients in AEBCD did not say in questionnaires that they found the film hard to watch, in one case two patients who had watched the intensive care film (and also recently attended an intensive care support group meeting) experienced some distress later, recalling their own experiences. (It is clinically common for people to experience flashbacks and distressing memories after intensive care stays.) Both were given appropriate clinical support and counselling which the facilitator already had in place for such an eventuality, and both were very keen to stay involved in the process, opting to join a co-design group on hallucinations. The facilitator discussed the clinical response with the project team and it was felt this was part of normal recovery process after intensive care.
Concerns that the film was too negative seemed more common in intensive care than lung cancer. Some examples of the range of comments are given in Boxes 1 and 2.
Well-balanced response.
Pretty representative.
Well presented by seemingly ‘normal’ people.
More negative responses than expected.
The film gave a good cross-section of viewpoints and experiences.
Not what we experienced.
Patient experiences a true reflection.
I could relate to many of the issues raised.
Not the experience of a [local] patient!
Film more about patient experiences in general. Good film as every clip I could empathise with experiences.
Some good/some bad. I hope the Trust as a whole views it.
The film is harsh on doctors, they are humans too. The film criticised a doctor who did not smile. Medical staff work very long hours and they cannot smile all the time. Sometimes the patients expect too much. On the film another patient complained about a wide range of clinical staff coming in to see him but these people are there to help you. What is the reason to complain?
There are two kinds of people: those who see the glass half full and those who see the glass half empty. It seems that the people who chose to appear in this film are the people who see glass half empty, as if they are not grateful to be alive.
Not an accurate reflection of the care I received, which was excellent.
Film mostly negative, [hospital] was not.
Many similarities, film had too many negative points.
80% was a similar experience to mine.
Not representative of care I received.
Several possible explanations for why the intensive care film in particular might be perceived as too negative were suggested in evaluation interviews:
-
Both ICUs deliver high-quality specialist care and patient satisfaction is high relative to other units.
-
As many ICU patients have experienced near-death experiences, they are very grateful for the life-saving care they received and are not inclined to be critical of staff – which may be a particular issue when the facilitator is also a member of the clinical team.
-
As internal facilitators from the clinical service were responsible for participant recruitment, the high level of reported satisfaction might arise from a bias towards the inclusion of participants who were satisfied, although the facilitators worked hard to reach a wide range of people, for example sending out letters to a sample selected from a database of recent patients.
-
By the time the lung cancer films were shown, an additional ‘script’ had been developed for facilitators to use to explain the purpose and limitations of the film more clearly [see Results (4), below]. Although the facilitators were not observed to use the script exactly as prepared, they may have felt more comfortable introducing the film and leading the discussion arising from it.
However, it is worth noting that, even in one of the two previous EBCD projects, participants also reported finding the film too negative, even though it was their own experiences that were being shown. This may reflect concerns that in the editing process negative touch points had been unduly emphasised as a vehicle to trigger change. Alternatively, it may reflect something about the nature of working in a group and the constraints that this imposes on participants. There may be a difference between what people feel able to acknowledge in the one-to-one context of an in-depth interview and what seems appropriate in front of others, and specifically in a group setting where the emphasis is on improvement rather than complaint.
Two further points emerged from further observation and evaluation interviews. Firstly, after watching the film and getting into discussion, patients in both pathways gradually revealed more of the things that they felt had not gone well in their care, and began to reflect more on aspects of care which could have been better. One of the facilitators commented:
The DVD got everyone’s attention and helped focus on what was important to each individual.
Facilitator interview
In this sense it seems to have served a very similar role to the trigger film in other EBCD projects – triggering discussion. As we report in section 5 of the results, below, the range and type of resulting improvement activities was also remarkably similar.
Secondly, one facilitator was intrigued by the perception that the film was negative and watched it again with participants:
Whilst there has been feedback that the ICU DVD was negative, I have asked them to look at it again and count the positives – and this far outweighed the negatives – again interesting.
But the same facilitator also went on to comment that ‘it is the ‘negative’ feedback that energises any change’. Many of the negative experiences highlighted in the films ended up becoming improvement priorities (e.g. dealing with noise or managing hallucinations).
One person commented that in the intensive care film there were ‘not enough patients, same patients were reoccurring [sic]’. In fact, clips from 11 different people were included, which is not very different from current EBCD practice. The King’s Fund’s EBCD toolkit recommends conducting discovery interviews with 5–15 patients, and in its section on editing the trigger films suggests that conducting 11 or 12 interviews is typical. However, in the lung cancer film, clips from a much wider range of people were used (n = 23). The selection of clips was partly affected by the fact that a relatively high proportion of participants in the Healthtalkonline intensive care patient interviews did not consent to video recording: 16 out of 40 people, compared with only 9 out of 46 people in the lung cancer collection. The combination of fewer available videos and the fact that interviews were not focused specifically on collecting touch points constrained the range of material available.
In summary, our answer to the question ‘From local patients’ perspective, how well do they feel national narratives capture and represent themes important to their own experience?’ is that the films were not perfect, but were ‘good enough’ to start the process of co-design. The role of the films themselves (and therefore the patient discovery phase of traditional EBCD) came to seem less important than the co-design process from that point on. As one of the previous EBCD evaluators commented after observing an AEBCD celebration event:
I don’t think it’s so much the film that makes the difference, rather I think it relates to a few factors: Patients can watch any film about ‘experience’, it’s the discussion that occurs after this that is important. Therefore it needs good facilitation to recognise and understand the experience of those present, whether the film is an accurate representation, and if not, what is missing. I think it’s about dialogue where both patients and staff come out of their roles. The idea of the film is to simply get people talking.
EBCD evaluator, observation notes from AEBCD celebration event
Results (4): Does any additional work need to be done to supplement the national narratives at the local level? If so, what form might this take?
At the outset it was anticipated that additional local patient interviews might be required to ensure that the narratives reflected local patient experience. Participants responded well to the trigger films and no significant concerns were identified about the content. Given that patient responses to the trigger films were ‘good enough’ to get discussion going, and the DVD ‘helped focus on what was important to each individual’ (facilitator), it was felt that additional work to supplement national narratives at local level was unnecessary. People were able to use the local workshops and co-design group meetings to feed in aspects of their own local experiences.
However, during the first pathway it became apparent that some patients and carers were unsure of the purpose and content of the trigger film. Some presumed it was a NHS documentary (despite the absence of any NHS logos or identifiers). As the evaluation had a formative dimension, the ethnographer fed back these observations at an early project team meeting.
The trigger films produced for previous EBCD projects started with a brief description of when the film was made, how many participants took part and in which ward they were treated. While the last point would not be relevant for a national film, a similar preamble would be recommended for future AEBCD trigger films, and indeed is probably more important given that the participants have not themselves been part of the interviews in the discovery phase. In the meantime we developed a ‘script’ for facilitators to use in the second pathway, shown in Box 3.
The film has been put together from analysis of a national sample of 46 people who have had lung cancer. Researchers at the University of Oxford collected interviews with people all round the country, many on video, some audio or written only. They present findings from these interviews on the patient information website Healthtalkonline.org. The interviews are not just about NHS care but also much wider experiences, for example their emotional reactions to the diagnosis, deciding how to tell other family members about the diagnosis, how they coped at work, how they felt others reacted to them when they discovered they had lung cancer.
For this project, the original researcher looked again at the whole interview collection and this time pulled out specific themes around experiences of services and ‘touchpoints’ where people come into contact with the NHS.
Obviously these are not people at your trust and everybody has a different experience, though some patterns do start to emerge from looking at many stories. Some of the things they say you may think aren’t relevant to this hospital or what happened to you. But our hope is that listening to them will help you reflect on your own memories and spark some ideas for what could be done differently here.
There may be some where people are sad or angry, because being told you have lung cancer is never a nice experience. You will hear some negative comments, because we can learn a lot from looking at when things went wrong and what could have been done to make that a better experience. Even when patients are largely positive about the rest of their care, one damaging bad moment can colour the whole thing. But listen out for positive comments too, where people remember some small act of kindness or a particularly good moment that made all the difference to them.
This highlighted several points which we felt had not been adequately addressed in the first pathway:
-
The research behind the interviews.
-
The film may include experiences which do not seem relevant to a particular site.
-
It may include things patients locally disagree with or did not experience.
-
The aim is to stimulate further reflection on local services and experiences, not to provide all the answers.
-
We can learn from both negative and positive experiences.
-
It may be an emotional experience to watch it.
This last point was also felt to be an important way of preparing people who might find the film distressing if it stirred up difficult memories.
Results (5): What improvement activities does the approach stimulate and how do these activities impact on the quality of health care services?
Approaches to implementation in different pathways; managing and facilitating the co-design groups
As with traditional EBCD (and, indeed, any quality improvement initiative), implementation varied in style and outcome in the four different cases. As noted above, the hospitals took different approaches to the appointment of facilitators. One appointed a single person to facilitate both pathways. This individual had a clinical background in one of the pathways but not the other. The other organisation opted to appoint a different person from within each of the pathways: one from a clinical background and one from a service management role. Consistent with other evidence,77 experience in our study suggested that the appointment of skilled, experienced and trusted individuals to these roles made a vital difference; that someone who has built a reputation for EBCD in their own service area can successfully transfer these skills to a new area; and that quite different facilitation styles can work equally well (see also Identifying local facilitators, below).
When it came to the co-design phase of the project, one of the facilitators felt that The King’s Fund’s EBCD toolkit did not provide sufficient guidance and support on how to manage the co-design groups and the quality improvement process:
The King’s Fund EBCD website has been invaluable to this point but I found a lack of information in regard to how to manage this change process. As a result momentum was temporarily slowed down as I spent time considering the best process.
Facilitator, reflective diary, ICU
Working with a colleague, the facilitator identified an approach called Quality Circles (developed by the National Society of Quality through Teamwork) which had been used locally to bring about embedded and sustained change. It did take time to identify an approach, but the facilitator felt that this was valuable, as the Quality Circles method provided a detailed and stepped approach ensuring that the project stayed on track (with constant referencing to the process and the problem identified). 78 The other facilitators did not adopt a formal tool such as Quality Circles.
One facilitator attended all of the co-design groups but chose to involve other members of staff (and, in one instance, a patient) to help lead them. The aim was to promote and support individual learning about the research methodology as well as project management. The facilitator reported that this meant that spread and sustainability occurred and also that those project leads were enabled to build relationships with the patients, relatives and staff. It was felt that this increased their own emotional connection, which in turn increased their accountability and responsibility to drive forward and complete the co-design work, knowing that they would be facing those patients/relatives and staff at the next meeting and would be held to account – as the facilitator said, ‘there is nothing more powerful’. The project leads were briefed regarding the process, provided with literature and had open access to the facilitator and the support of the ICU nurse consultant, who became an influential ‘voice’ in the trust promoting the project.
The other facilitators chose to lead the co-design groups themselves. They retained control of the process, had a detailed knowledge of the proposals discussed and took the lead in putting the plans into action. In one case, the groups met twice, once following the staff and patient event to plan what needed to be done and again before the celebration event (3 months later) to check that the actions suggested by the group had been followed up. This was supplemented in between by continued virtual contact, for example communicating by e-mail about sourcing particular items such as clocks or electric toothbrushes, and patients going off to do their own research. The other facilitator held co-design group meetings immediately after the staff and patient event and took away a plan to work with colleagues to address the emerging issues, but had not made firm plans to bring the co-design group back together at the end of our fieldwork period. It was unclear how far this was a decision driven by lack of time; organisational practicalities (including a period of sick leave and the impact of the summer holiday period); or the potential burden on participants, many of whom were very ill and lived some distance from the hospital. In the same pathway, the trigger film was shown only once, at the patient event; plans to show it at the joint staff and patient event had to be abandoned because of technical problems. This meant that staff were not directly exposed to the patient narratives on film, though they had direct interaction with local patients.
These kinds of process decisions, adaptations and practical challenges are common across all attempts to make patient-centred quality improvement work, and are not unique to AEBCD.
Improvement activities
The four pathways generated a large volume of service improvement activities. The activities were captured in service improvement logs (completed by the facilitators), observations of co-design events, interviews with the facilitators and with other group members, minutes of co-design group meetings and the celebration events held for participants.
Fifteen different co-design working groups were established. The topics are summarised in Table 1 (individual hospitals are anonymised).
| Service area | Co-design groups topics |
|---|---|
| Intensive care | Enhancing basic care |
| Reducing noise and sleep deprivation | |
| Communication | |
| Patient–doctor communication on ward rounds | |
| Transition to the ward: ‘lost in translation’ | |
| Hallucinations | |
| Ventilation | |
| Individualised care | |
| Lung cancer | Pillows |
| Personal items | |
| Information | |
| Privacy | |
| Diagnosis-giving | |
| Support | |
| Information |
The improvement activities are summarised in Table 2. There are a number of different approaches to categorizing improvement activities. For example, Glouberman and Zimmerman79 have used the framework of simple, complicated and complex problems to categorise improvements in a Dutch implementation of EBCD. Their examples were following a recipe (simple); sending a rocket to the moon (complicated); and raising a child (complex). For this project, we adapted a framework used in a previous EBCD study by Adams et al. 39 Adams et al. suggest the following categories for improvement activities: ‘quick fix’ involving little or no change in everyday working practices (e.g. revisions of written patient information); process redesign within a service (e.g. new in-service procedures for patient consent); process and structural redesign spanning different services (e.g. improving access to pre- and post-operative physiotherapy care); process and structural redesign within the wider organisation [e.g. addressing delays in obtaining positron emission tomography (PET) scan results]. Here, we organise the activities under the following headings: small-scale changes; process redesign at the team level; and between services and between organisations.
| Service | Improvement activities | Type of improvement | |||
|---|---|---|---|---|---|
| Small-scale change | Process redesign within team | Process redesign between services | Process redesign between organisations | ||
| ICU | Sign created to enhance privacy and dignity | ✗ | |||
| ICU | Promoting the involvement of families in personal care via team news | ✗ | |||
| ICU | Promoting the washing of patients’ hair more regularly via team news. New wash basin to be trialled | ✗ | |||
| ICU | Encouraging wards to send patients wash bags to ITU – email to all sisters and managers. Infection control view sourced | ✗ | |||
| ICU | Sourcing appropriate clocks to aid patient orientation | ✗ | |||
| ICU | Encouraging nurses to brush patients’ teeth more regularly – via team news and through sourcing new toothbrushes to trial | ✗ | |||
| ICU | Promoting the correct application of CPAP (continuous positive airway pressure) masks. Creation of a guide and teaching on team days | ✗ | |||
| ICU | Informing patients about the potential for hallucinations – via rehab and therapies booklet | ✗ | |||
| ICU | Trialling washing patients in the evening rather than first thing in the morning. Feedback blog created. Staff opinion sourced | ✗ | |||
| ICU | Sourcing eye masks | ✗ | |||
| ICU | ITU buzzer being answered promptly during visiting hours | ✗ | |||
| ICU | Ensuring digital TVs bought into service | ✗ | |||
| ICU | Creating posters to promote quiet on ITU | ✗ | |||
| ICU | Creating a sign to indicate patient tired – did not sleep | ✗ | |||
| ICU | Delirium working group to be created | ✗ | |||
| ICU | Telephone with more sophisticated ring tone to be sourced | ✗ | |||
| ICU | Porters to remove waste outside the rest period. Whole process to be changed | ✗ | |||
| ICU | Quieter bins to be sourced | ✗ | |||
| ICU | Doctors to wear name badges | ✗ | |||
| ICU | Trialling set times for family meetings | ✗ | |||
| ICU | Critical care news to be sent to all MDT staff | ✗ | |||
| ICU | Nurses to be given training in communication skills | ✗ | |||
| ICU | Nurses in charge to be reminded to offer support to juniors | ✗ | |||
| ICU | Nurses to be informed of support mechanisms via critical care news | ✗ | |||
| ICU | Relatives information booklet to be updated with key contact numbers | ✗ | |||
| ICU | Orientation and ‘house rules’ booklet to be updated with key information | ✗ | |||
| ICU | Timing of ward rounds to be reviewed to ensure consistency | ✗ | |||
| ICU | Consultant surgeons to be informed that patients would like to see them post-op in ITU | ✗ | |||
| ICU | Information booklet to be updated explaining key doctors’ roles | ✗ | |||
| ICU | Mini ‘Schwartz rounds’ to be commenced on ITU | ✗ | |||
| ICU | Discharge summary redesigned with professionals from all teams involved and patients | ✗ | |||
| ICU | Developed information for staff: staff training | ✗ | |||
| ICU | Developed information for patients about ventilation | ✗ | |||
| ICU | Developed section of DVD for patients on experience of being voiceless while ventilated | ✗ | |||
| ICU | Developed information for staff and patients on the impact and experience of hallucinations | ✗ | |||
| ICU | Developed section of DVD for patients on experience of hallucinations | ✗ | |||
| ICU | Identified suitable tablet computer applications to assist ventilated patients communicate | ✗ | |||
| ICU | Developed guidelines for personalised care ‘person’ tab on ICU system for staff to log the patients’ personal information | ✗ | |||
| LC | Acquiring more comfortable V-shaped pillows for post-operative patients | ✗ | |||
| LC | A new process for effective transfer of patients belongings (including dentures and frames) from theatre to recovery ward | ✗ | |||
| LC | Improved patient information from admission to discharge to follow-up | ✗ | |||
| LC | New multidisciplinary lung cancer service development group established | ✗ | |||
| LC | Identified and modified private room for receiving support after the diagnosis | ✗ | |||
| LC | Better planning for diagnosis giving from medical team | ✗ | |||
| LC | Patient support group established | ✗ | |||
| LC | Patients made aware of support available through clinical nurse specialist | ✗ | |||
| LC | Improved information booklet for patients transferring to another site for surgery | ✗ | |||
| LC | Consultants agreed to send summary letter to patients after consultation | ✗ | |||
Forty-eight improvement activities were reported to be under way by the service improvement facilitators and are recorded in Table 2. It should be noted, however, that the number of activities is only a crude measure of the degree of change and the impact on quality; what looks like a tiny change can be of great significance to individuals, but, equally, focusing on one difficult process redesign rather than making many small changes can be important. As one facilitator noted:
Research can be done in the real world, if you are committed, enthusiastic, believe in it. The difference with this research is that it is relational and not a clinical trial, i.e. people matter and numbers don’t. Sometimes you cannot count what counts.
Facilitator, reflective diary, ICU
Similarly, the ethnographer observed:
The biggest and most sustainable improvement that took place, though, was the change in the attitude and behaviour of staff towards patients that cannot feature in an ‘improvement log’.
Ethnographer, observational notes
As in any quality improvement initiative, not all proposed changes will be acted upon, and at the time of writing some of the improvement activities were still being pursued, or had been partially implemented. For example, changing practice to encourage staff to brush intensive care patients’ teeth more regularly had taken place but the sourcing of new electric toothbrushes (which had been led by an enthusiastic patient) was on hold. In some cases, improvements may take place initially but then do not remain in place; it is too early for us to be able to identify examples of this kind. Again, however, this is common across AEBCD and EBCD; Adams et al.’s forthcoming study39 of the spread and sustainability of EBCD initiatives will provide evidence of the longer-term fate of EBCD improvement activities.
Comparing experience-based co-design and accelerated experience-based co-design
Table 3 lists the activities undertaken in a lung cancer and breast cancer pathway in a previous EBCD evaluation. The scale of the changes is similar. There were 28 activities across the two EBCD pathways, compared with 48 across the four AEBCD examples. There are similarities in terms of the co-design group topics. For example, two of the three EBCD lung cancer groups focused on the same overall topics as the AEBCD lung cancer groups: information and diagnosis giving. There are also identical activities in the EBCD and AEBCD lists. For example, name boards were introduced so that patients would know staff names and both groups identified the importance of a special, private room for diagnosis giving. Finally, the table shows a similar distribution of activities, with more small-scale changes and process redesign within teams than wider process redesign between services and between organisations. In the EBCD pathways, there were 12 small-scale changes, 12 process redesign within teams, two process redesign between services and two process redesign between organisations. In AEBCD there were 21 small-scale changes, 21 process redesign within teams, five process redesign between services and one process redesign between organisations.
| Service | Improvement activities | Type of improvement | |||
|---|---|---|---|---|---|
| Small-scale change | Process redesign within team | Process redesign between services | Process redesign between organisations | ||
| BC | Patients no longer separated from loved ones early in the process | ✗ | |||
| BC | Establishment of dedicated consultation room – offers more privacy and dignity | ✗ | |||
| BC | Lead for breast surgery reviewed information flow from pre assessment to post surgery | ✗ | |||
| BC | Physiotherapists identified best time to offer patients information about exercise | ✗ | |||
| BC | New, efficient appointment processes | ✗ | |||
| BC | All newly diagnosed patients agree the date of surgery and subsequent appointments on the day of their results | ✗ | |||
| BC | Much of the breast patient information reviewed and updated | ✗ | |||
| BC | All administrative staff receive customer-care training and are shown patients’ DVD | ✗ | |||
| BC | Health care assistants’ interpersonal skills assessed prior to recruitment | ✗ | |||
| BC | Managers and administrative staff use values based performance tool which can improve patients’ experiences | ✗ | |||
| BC | Changes to structure of clinics to reduce waiting times | ✗ | |||
| BC | Patients regularly updated about waiting times in clinic | ✗ | |||
| BC | All staff names displayed on noticeboard | ✗ | |||
| BC | Designated phlebotomist has reduced waiting times for blood tests | ✗ | |||
| BC | Patients receiving same chemotherapy treatment given option to receive information in a group | ✗ | |||
| BC | Enhancing processes for accessing support around hair loss | ✗ | |||
| LC | Establishment of second breaking bad news room | ✗ | |||
| LC | Guidance on diagnosis procedures including junior doctors’ induction | ✗ | |||
| LC | Improving links between patients and CNSs | ✗ | |||
| LC | Patients waiting in oncology outpatients encouraged to visit information office | ✗ | |||
| LC | Promotion of information and support centres at different sites (advertisement at the hospital entrance) | ✗ | |||
| LC | Patient information leaflets for specific points in the pathway | ✗ | |||
| LC | Patient DVD ‘welcome to cancer services’ for newly diagnosed and referred patients | ✗ | |||
| LC | Link nurse scheme to improve cross-site working | ✗ | |||
| LC | Quarterly CNS forum to facilitate development of service | ✗ | |||
| LC | Staff name board (with pictures) enables patients to identify staff easily | ✗ | |||
| LC | Cross-site visibility of test results, email and remote access for staff (IT systems) | ✗ | |||
| LC | Improved access to out-of-hours oncology services | ✗ | |||
Small-scale change
Thank you for looking at the little things.
Patient, observation field notes at celebration event, ICU
With mine [co-design group] it will be, ‘Make sure the mask fits. Be aware, make sure the mask fits’. All of it is very simple. The clocks, everything was simple. Nothing was rocket science here that people were asking.
Patient, patient and carer group interview, intensive care
We preferred the term ‘small-scale change’ to ‘quick fix’, as observation suggested that apparently small changes were not necessarily quick and could be quite complicated to implement – in some cases implementation extended beyond the immediate time scale of the project or was ongoing at the time fieldwork ended. They could also be changes that were highly valued by patients.
Under the theme of enhancing basic care, one site identified the following small-scale changes in intensive care: producing a sign to pin to bed curtains when personal care was under way to enhance privacy and dignity; promoting the correct application of breathing masks (supported by a written guide and teaching on team days); and sourcing ‘day and date’ clocks to aid patient orientation on the ward (given that patients may have long periods of being unconscious). The group planned to include information about hallucinations in the rehabilitation and therapies booklet produced for patients. Under a second theme of reducing noise and sleep deprivation, they identified the need for eye masks, making sure the ward entry buzzer was answered promptly and buying televisions that patients could watch using headphones. Also under this theme, the group set out to create posters to promote quiet on the ICU and signs to indicate that a patient was tired and needed to sleep. Finally, they aimed to source a telephone with a less intrusive ring tone and to purchase quieter bins. While some of the activities planned by this group were still ‘works in progress’ by the time of the celebration event in April, the group reported back that the porters were no longer emptying bins during rest periods. As part of the third theme on communications, a relatives’ information booklet was to be updated with key contact numbers, and doctors were to be asked to wear name badges. In the co-design group, a patient supported the idea of name badges, but suggested that they should be in a ‘nice, large font’ so that patients would be able to read them from their beds.
The group on doctor–patient communication on ward rounds set out to update the orientation and ‘house rules’ booklet and to update an information booklet for patients and families, adding explanations of key doctors’ roles in ICU. In one of the lung cancer pathways, acquiring comfortable pillows and the transfer of pillows, dentures and frames from theatre to the recovery ward were identified as potential small-scale changes, but ones which could make a profound difference to people’s experiences; being without one’s own dentures has the potential to undermine an individual’s sense of self and dignity.
Process redesign at the team level
A group looking at enhancing basic care group in ICU had a number of improvement activities at the process redesign within the team level. These were promoting the involvement of families in personal care and promoting the washing of patients’ hair more regularly (both via the team electronic newsletter). New washbasins and toothbrushes were to be trialled and nurses were to be encouraged to brush patients’ teeth more regularly (again via the team newsletter). In the noise and sleep deprivation group, the group set out to trial washing patients in the evening rather than first thing in the morning to prevent the exclusion of relatives and allow patients to sleep. A feedback blog was to be created to access staff opinions about the changes to working practices. In the communications group the following team level resigns were identified: trialling set times for family meetings, sending out critical care news to all multidisciplinary teams, training for nurses in communication skills, reminding nurses to offer support to junior staff and informing nurses of support mechanisms via the critical care news. The group working on communication between doctors and patients on ward rounds identified timing of ward rounds as an issue and suggested reviewing the timings to ensure consistency. Consultant surgeons were to be informed that patients would like to see them post-operatively on the intensive therapy unit. Finally, mini ‘Schwartz rounds’ were proposed to discuss emotional and social issues relating to patient care. At the celebration event in April, the co-design group announced that the first round was scheduled for 1 May.
The hallucinations group planned to develop information for staff and patients on hallucinations, including staff training, a patient leaflet and a DVD. A half-hour training session about hallucinations was planned, covering the theory behind hallucinations, patient experiences and how best to talk to patients about them. The ventilation group also developed a DVD about the experience of being voiceless while ventilated. Patients and staff were interviewed as part of the process of developing and applying the DVD.
The ventilation group also introduced an iPad application (Apple Inc., Cupertino, CA, USA) to help ventilated patients communicate. However, one of the consultants commented on how difficult it was to make this change:
We’ve got an iPad and we’ve got a program on there, that’s been a bit more difficult to get into place than I thought it would be. Yes I suppose the main thing is the time it’s taken to get things in place. That would be the main disappointment, but you could argue that I’m just being impatient.
Interview, consultant, ICU
The individualised care group set out to develop guidelines for a personalised care ‘person’ tab on the ICU system for staff to log the patients’ personal information. The group found that most staff knew the details of a patient’s condition and treatment, but very little about the patient as a person (in terms of hobbies, interests, job, etc.). Group members observed that experience and seniority seemed to have very little bearing on staff knowledge; it appeared to the group that the personality of staff members was the biggest factor affecting their ability to get to know their patient. In her reflective diary, the co-design group lead commented on the progress they were making to draw attention to the patients as people:
We decided to use a tool that is currently in use called a ‘spirituality assessment’. It is not being utilised very well at present and we plan to customise the tool and re-educate staff to promote its use and empower staff that are not gifted with the type of personality that facilitates getting to know their patients on a personal level.
Co-design group leader, reflective diary, ICU
Team-level improvements in lung cancer included identifying and modifying a private room for supporting patients after receiving their diagnosis as part of the privacy theme. The identification of a private room proved more challenging than anticipated. However, the facilitator observed that the loss of the room did not derail the project, and another room was found. She highlights the reasons why, focusing in particular on the contribution of an unexpected local ‘champion’:
The Out of Clinic room, it was the change in attitude, about when patients are given their diagnosis. Whereas, perhaps, it had become something that was an everyday occurrence, I think that the attitude, and there was a cultural change, and in her, she became a champion for making sure that patients are treated in the right way after they’ve been given their diagnosis. So she’s now given up half her office, which will be a room for people to go in. And the biggest thing with that is . . .
Was this when I took the photos of the room?
Yes.
And has this room been revamped now?
No.
No?
No, because then there were some other issues relating to, I don’t know what it was, but now another plan – so whereas she could have said, ‘oh it can’t be done,’ she went on to get another plan, so actually there’s another room that’s now going to be the area. But the way I would describe it is that, the whole project ignites fires in people who are not necessarily – you wouldn’t normally expect them to take the initiative, but it ignites the desire to, kind of, change, it changes the way people think. And so you end up with unlikely champions, you know, and that’s one of the really good things about it, is seeing people who you wouldn’t expect to, and that’s why it’s so powerful, it’s seeing the impact it has on people. Yeah, unexpected champions, I suppose, is the way we would put it.
Co-design group co-facilitator, Interview, lung cancer
A lung cancer co-design group addressing the theme ‘support’ aimed to set up a patient support group and promoted the role of the clinical nurse specialist in supporting patients. Following discussion, the co-design group felt that a ‘social’ group was the best approach to supporting patients and suggested meeting at a pub every couple of months. There was an agreement that this social group would be run by the patients and relatives. The co-design group decided that the way forward would be to have a one-off meeting in the evening at the trust to work out the details. Ideas for a name were discussed, and ‘Windbags’ was proposed. The group thought the name captured the focus on lungs and on providing a forum to chat. They agreed that everyone would be welcome, with the intention to break the isolation that patients sometimes feel. The facilitator noted that the set-up meeting was scheduled for October. However, the meeting did not happen. The co-design group facilitator commented that he was waiting for the patients to organise the group and would chase it up. The group had not yet met by the end of January 2013 (when the project team was writing this report).
Finally, a group on diagnosis giving focused on better planning for diagnosis giving from the medical team. The co-design group lead spoke very positively about the work of the group and the experience of working in a co-design group. She also provided examples of changes in diagnosis giving practice on the ward, while emphasising the time required for sustained changes in practice:
So for once, it is something that is just good to do, and feels good to do, rather than something that people are being told to do because.
I see what you mean, yes.
So it’s not to tick a box, it’s not because we have no money, it’s because, actually, all the people there wanted to make things better. So then seeing the changes, so seeing things, you know, for all the groups, they were different things. For the diagnosis group, actually, seeing somebody’s practice change is really exciting, you know, so seeing [doctor] influencing his colleagues. So we still haven’t solved the problems, and there is still work to be done, but the changes that you see in people . . . I suppose observing, reading in the notes that somebody had planned giving the news of diagnosis to a patient, whereas they wouldn’t have planned it before, they would have just gone in and told the patient, ‘These are the results,’ whereas actually, just reading that a junior doctor, influenced by the person involved in the project then. So it was, actually, seeing something real and tangible that had already impacted on a patient. At the same time, a disappointment is that, I suppose it’s not a quick fix, that project, the diagnosis project in particular, is something that is going to take a lot longer, and my concern is that after – it’s not my concern, it will be a challenge to maintain the impetus of keeping with the project, because a lot of the others, they’ve had quite clear outcomes. So the information booklet, that job is done, the support, you know, we’re nearly at the point where the letters will be going out. The diagnosis issue, because it’s an educational thing, it’s not going to be, [clicks fingers] right, that’s it we’ve sorted it all out, so it will need to be an ongoing project. So that’s how I see is that, I hope that we will be able to maintain that, and only time will tell.
Co-design group facilitator, interview, lung cancer
Process redesign between services and organisations
A much smaller number of improvement activities involved process redesign between services and organisations. The enhancing basic care theme in ICU looked at encouraging wards to send patients’ wash-bags to ICU. To promote this change, an e-mail was sent to all sisters and managers. The reducing noise and sleep deprivation theme set out to change the waste collection timings to have waste collected by porters from the ICU outside the patients’ rest period. In the other ICU pathway, the discharge summary was to be redesigned with professionals from all teams involved with discharge and patients.
So the biggest thing for this for me is that the three groups, the physiotherapists, the nurses and the doctors, all looked at the same thing, and so we just fill out one form as before it was, ‘This is your form, this is the nurses’ form, this is the doctors’ form.’ So it made it very much a patient focused document, which is very, very good and we need to do that a lot more so we will add the notes.
Consultant, interview, ICU
Between March and July 2012, the co-design group facilitator embarked on a consultation process with staff members in other wards to which ICU patients are discharged. Outside co-design group meetings, the group kept in touch via regular e-mail communication in which the contents and structure of a new discharge summary were discussed. Members of the co-design group noted how one of the consultant anaesthetists, in particular, had become much more patient-centred as a result of participating in the group. This change was also observed by the ethnographer in an e-mail from the consultant to other co-design group members in response to suggestions of clinically centred discharge-form categories:
Sorry to be a pain but I think this is hugely important! I don’t feel the final form should have sections divided by health care professional – it will mean that the docs don’t read the nurse bits, physios ignore docs bit, etc. I FEEL VERY STRONGLY THAT IT HAS TO BE A PATIENT CENTRED DISCHARGE DOCUMENT.
Consultant, e-mail correspondence, ICU
Only one change concerned service change between organisations: One of the lung cancer pathways sought to redesign an information booklet for patients being referred for surgery at another hospital. This involved accessing information for the booklet from the other hospital.
The information group was co-led by a patient. The ethnographer recorded in her notes that the patient took this role very seriously:
I notice that the patient who is a co-lead has a folder with his notes from each meeting, handouts and evaluation forms.
Ethnographer’s fieldwork notes, co-design group meeting, lung cancer
The group identified an existing leaflet but noted that it applied to all lung surgery and did not address particular issues for patients travelling to the hospital in question for surgery (e.g. where to park). The patient co-lead wrote directly to the consultant surgeon at the other hospital updating him on the progress of the information co-design group and explaining patients’ information needs when changing hospital.
The service improvement facilitator noted in an e-mail to the ethnographer that this letter had prompted the consultant to send letters to patients following their first consultation. This was something that local staff had been hoping to implement with the other hospital for some time, and so they saw this as a very important achievement.
The group co-lead commented on the impact of having a patient so actively involved in the group:
[The patient] was really happy to co-lead that [the co-design group], yes, I think that made such a difference. I think his feelings and experiences of having the surgery; I think that kind of gave us that drive really. All of them knew that there had to be a change, so it really inspired . . . I think it inspired the staff who were in the group to try and improve the information, because all of the patients . . . I think that was the powerful thing, they were all saying actually, ‘This needs to be changed’. It’s not really difficult to produce this information, but actually when the information is available to other patients, it will make a difference to them.
Co-design group leader, interview, lung cancer
Spread within the organisation
In both hospitals, senior managers report that experience-based co-design principles have been adopted in other areas and engagement in the project has given staff involved confidence in working with patients in a collaborative way. One hospital CI notes that:
AEBCD (and EBCD) provide a framework for staff to use which enables patients and staff to have a voice and make a commitment to improving services in the light of the experiences patients have of the service.
Co-investigator
In one trust, plans were in place to use the experience within the lung cancer pathway to implement an accelerated approach with another part of the lung cancer service. The trust also planned to train other staff in the AEBCD approach with a view to using it more widely in future service development activities. Two other projects were reported at this site, employing EBCD methodology. The first, a 1-year project, focused on the transfer process from intensive care to the high dependency unit. The team was looking at solving any problems for patients in the whole process of transfer. When the member of staff leading this project was interviewed at the end of AEBCD, the project was 2 weeks away from a co-design event. The second was a project with a patient experience evaluation which explored the experiences of patients referred to pulmonary rehabilitation for chronic obstructive pulmonary disease, where rehabilitation has been shown to be effective in increasing the quality of life of patients.
One of the hospitals is rolling out an EBCD approach to patient experience in the emergency department. This is supported by the College of Emergency Medicine, and has active commitment from a senior accident and emergency medicine consultant, who was inspired by involvement in the original intensive care project and by hearing the PI speak about AEBCD at a local emergency medicine conference. New local interviews are being scheduled, with consent for these to be used on Healthtalkonline in future. The same hospital is also a collaborator on a research grant application with members of the research team to explore the use of EBCD in the management of early labour (not yet funded).
Results (6): What are the costs of this approach compared with traditional experience-based co-design?
Cost savings between AEBCD and EBCD were, as expected, primarily in the discovery phase. Costs of the co-design phase were not anticipated to be different from those for EBCD, and will vary according to the investment that facilitators and hospitals wish to make: longer co-design phases technically cost more irrespective of whether they are part of EBCD or AEBCD. The definition of a ‘cost’, however, needs to be problematised, as participation in such an initiative could be taking place during staff development, training or education time allocated for NHS staff.
There are two elements to this economic evaluation: (i) the total cost of implementing AEBCD and (ii) the comparison with traditional EBCD. The cost of implementing AEBCD in this project in terms of NHS staff costs is detailed in Table 4. Of the four implementations of AEBCD over the two pathways (lung cancer and ICU), we have detailed expenditure data for three sites. For Trust 2 (ICU2 and LC2), the hourly wages of the actual staff attendees were provided by the trust, to which we added the employer national insurance and pension contributions to reach a total hourly staff cost. For ICU1, we were provided with the Agenda for Change band for the staff attendees and we used the mid-point on this band (for example, for entry-level nurses in Band 5 we used spine point 4 of 8). We calculated total cost to include employer national insurance and pension contributions, and London weighting (20% of basic salary for Royal Brompton staff, 15% of basic salary for Harefield staff and 5% for fringe staff in Reading). We divided the total annual salary by 52.14 to calculate weekly costs and divided by 37.5 to obtain hourly costs.
| AEBCD stage | ICU1 | ICU2 | LC2 | Mean |
|---|---|---|---|---|
| Staff interviews | 374 | 507 | 337 | 406 |
| Staff feedback event | 876 | 1235 | 696 | 936 |
| Patient feedback event | 407 | 168 | 38 | 204 |
| Staff/patient event | 1018 | 1839 | 1262 | 1373 |
| Co-design teams | 1832 | 94a | 716 | 881 |
| Celebration event | 825 | 554 | 385 | 588 |
| Catering | 1692 | 890 | 879 | 1154 |
In addition to the staff costs per pathway, the mean over the three pathways is also presented in Table 4. It is clear that the mean is influenced by outliers, for example LC2 in terms of the patient feedback event cost and ICU2 for the co-design event cost. The total cost for time spent by NHS staff and catering at AEBCD events was £7024 for ICU1, £5287 for ICU2 and £4313 for LC2, giving an average cost of £5541 over the sites. This figure is carried over to the total cost calculation reported in Table 6.
While the catering costs reported in Table 4 were directly incurred for the project the staff costs are measured in terms of the employment costs to the NHS but the true cost would be the opportunity cost of staff involvement (i.e. what could have been achieved with the time that was spent at the events). In many respects this is likely to be much higher for clinical staff.
As Table 5 illustrates, there is variability in both the number and composition of the attendees. The ICU1 pathway included vastly more staff than the other two pathways reported here, while Trust 2 appears to have included more expensive staff. For example, the chief medical officer attended events at an approximate cost of £153 per hour compared with a Band 5 nurse at one-tenth of this cost. This kind of variation in approach is to be expected in any quality improvement initiative. The data return from ICU2 was also missing some data on co-design teams, which affects the costing – see Table 5 footnote.
| AEBCD stage | Hours per person | Staff numbers | Cost per staff hour | ||||||
|---|---|---|---|---|---|---|---|---|---|
| ICU1 | ICU2 | LC2 | ICU1 | ICU2 | LC2 | ICU1 | ICU2 | LC2 | |
| Staff interviews | 1 | 1 | 1 | 18 | 18 | 11 | 21 | 28 | 31 |
| Staff feedback event | 2 | 2 | 2 | 20 | 16 | 11 | 22 | 39 | 32 |
| Patient feedback event | 5 | 4 | 2 | 3 | 2 | 1 | 27 | 21 | 19 |
| Staff/patient event | 2 | 3 | 3 | 19 | 17 | 14 | 27 | 36 | 30 |
| Co-design teams | Mixed | 1 | 1 | 59 | 4a | 27 | N/A | 24 | 27 |
| Celebration event | 1.5 | 1 | 1 | 21 | 13 | 10 | 26 | 43 | 39 |
In addition to the costs incurred by the trust for staff to attend the various events which make up an AEBCD implementation, there is a cost for facilitating the events (the costs of facilitating the event are taken from the NIHR budget and do not represent actual expenditure. However, as the vast majority of these costs relate to salary costs there will be high correlation between planned and actual expenditure in this area). The average cost for employing a facilitator for 6 months over the four sites on a part-time (0.4 full-time equivalent) basis was £11,935. This included two facilitators based in London and therefore these costs will be higher than the national average. In addition, an average of £2800 per site was incurred to facilitate the events including the travel and subsistence of patients and relatives who attended the event. These costs are all detailed in Table 6.
| Activity | Cost item | Cost (£) |
|---|---|---|
| Production of ‘trigger film’ | Researcher time | 5289 |
| Editing | 3000 | |
| AEBCD events | Facilitator | 11,935 |
| Travel | 300 | |
| PPI expenses | 500 | |
| NHS staff time | 4387 | |
| Event catering | 885 | |
| Consumables | 2000 | |
| Total | 28,565 |
If a trigger film already existed than the total cost of implementing AEBCD, on average, during this project was approximately £20,000. This would be a good estimate of the cost of implementing AEBCD in the future for lung cancer and intensive care at other trusts in the south-east of England. However, for this project and for future implementations that require a new trigger film to be produced, the total cost would be approximately £28,565.
The trigger film therefore represents a fixed cost (approximately 30% of the total per implementation cost) which could lead to trusts waiting until another trust implements a pathway of interest. If all trusts behave in this manner then perhaps none will implement AEBCD. It therefore raises questions about the most effective way of financing production of trigger films.
The trigger film has two main components. First, for each new pathway a researcher must analyse the interview collection thematically, looking for touch points, and select appropriate clips for the trigger film. On this project 36 days were spent by the researcher working on the ICU trigger film (which involved analysing two collections on both patients’ and relatives’ experiences) and 25 days by the researcher working on the lung cancer trigger film. In addition to the data analysis, editing costs of £3000 per film were incurred. For the purposes of this comparison, we are using the 25-day period as a reference point, as this is more typical for developing a trigger film from one interview collection. The total staff cost for these 25 days was £5289. This figure includes salary, national insurance and superannuation.
The stages followed by traditional EBCD and AEBCD are the same except for how the trigger film is produced, and the staff discovery stage (which we incorporated into the 6-month period of facilitator time). Therefore, the difference in the costs of the two interventions is in the production of the trigger film and not in the actual co-design events detailed in Table 4. Table 7 compares the differential costs of EBCD and AEBCD. In EBCD, a bespoke film is produced for every intervention, with a researcher spending a minimum of 6 months collecting and analysing patient narratives to produce the film. In comparison, AEBCD relies upon a pre-existing collection of patient narratives which require only analysis to identify and collate the narratives.
| Activity | EBCD per pathwaya | Cost (£) | AEBCD per new pathway | |
|---|---|---|---|---|
| Fieldwork to collect patient narratives and staff interviews (and non-participant observation) |
|
23,375 | Not applicable | 0 |
|
300 | |||
|
1000 | |||
| Production of ‘trigger’ films |
|
1100 |
|
5289 |
|
3000 | |||
| Total | 30,485 b | 8289 | ||
Therefore, for a new pathway, AEBCD is 73% cheaper than traditional EBCD in the production of the trigger film, and overall is 44% cheaper than EBCD (EBCD costs £30,870 for the trigger film plus £20,276 for the events, a total of £50,761 per implementation. In comparison, AEBCD costs a total of £28,565 or is 44% cheaper than EBCD). Further cost savings can be achieved in AEBCD through the reuse of existing trigger films. In these cases, AEBCD saves the entire £30,485 and is 60% cheaper than EBCD implementation overall.
Overall, AEBCD cost an average of £28,565 per site in this project, an estimated saving of nearly half over traditional EBCD. We have argued that this is a reasonable estimate of the future cost of implementing AEBCD for new pathways. However, implementing either lung cancer or intensive care AEBCD would cost approximately £20,000 in the future, a saving of almost 60% of traditional EBCD. As more trigger films are produced, more trusts can benefit from this significant cost saving. Given that AEBCD and EBCD produced similar outcomes, AEBCD represents good value for money.
Results (7): Can accelerated EBCD be recommended as a rigorous and effective patient-centred service improvement approach which could use common ‘trigger’ films to be rolled out nationally?
In simple terms, the answer to this final research question is ‘yes’, given the answers to the previous research questions. The need to improve patient experience is both a political and a moral imperative, and AEBCD has proven to be a feasible and effective patient-centred quality improvement approach which is welcomed by staff and patients. It maintains two key characteristics of EBCD but at reduced cost: (1) it draws rigorously on a wide range of carefully researched patient narratives, and (2) it fosters a meaningful partnership between patients and professionals, co-designing solutions as equals. As with EBCD, it has been transformative of attitudes; it leaves a legacy of individuals and organisations feeling empowered and energised to take patient experience seriously, as word spreads from patients, families and staff who have felt genuinely listened to, involved and trusted.
However, we have noted that the accelerated approach did entail a very high workload for the facilitators, particularly early on in each pathway, and would suggest that some additional time might be factored in in future for staff discovery work.
One question that has emerged from our study but which our study design was not intended to address is whether or not AEBCD brings less personal benefit to individual patients involved, in terms of the therapeutic benefit of telling their own story. However, important though personal benefit is, this is not the primary purpose of quality improvement initiatives.
Chapter 4 Conclusions
In our results we have demonstrated that:
-
Accelerated experience-based co-design is generally acceptable to staff and patients, and indeed has been greeted with enthusiasm.
-
Using national rather than local patient narratives did not significantly affect staff engagement.
-
National narratives were sometimes felt to be more negative than those of patient and carer participants, but captured sufficient important themes from their experience to trigger co-design discussions.
-
Formal additional work to supplement national narratives with local experiences was unnecessary; the workshops and co-design events gave sufficient opportunity for participants to feed in local issues.
-
The range and type of improvement activities varied across the four pathways but was similar to standard EBCD projects, and resulted in a mix of small-scale and wider process changes.
-
The costs of AEBCD are considerably lower than those of EBCD, particularly if the one-off costs of developing a national trigger film are excluded. Facilitator time may need to be more generous, but many trusts will already be spending this money on in-house quality improvement teams whose time could be reallocated. This may need a change of mind-set and reconsideration of how priorities are determined.
-
AEBCD and the use of nationally derived trigger films show strong potential to be rolled out nationally, in a variety of services.
However, there are several further practical and methodological issues to consider, which we go on to explore below.
Implications for health care
Identifying local facilitators
As in any quality improvement initiative, we have observed the central importance of the facilitator role. The hospital organisations chose their own approach to local facilitation. One appointed a single person to facilitate both pathways, who had a clinical background in one of the pathways but not the other. The other organisation opted to appoint two different people from within each of the pathways, one from a clinical background and one from a service management role. It was evident from our study that the appointment of skilled, experienced and trusted individuals to these roles made a vital difference; that someone who has built a reputation for EBCD in their own service area can successfully transfer these skills to a new area; and that quite different facilitation styles can work equally well.
Other hospitals might choose to use a central quality improvement team. There are advantages to both approaches; building a core team with facilitation skills reduces the need for repeated training and avoids the ‘learning curve’ problem of new facilitators. In the accelerated model of EBCD, this may be particularly important; there is no lengthy discovery phase in which to learn, plan and build up to the co-design phase. Hospitals which already fund a quality improvement team may find this a cost-effective route to adopting AEBCD, requiring no further expenditure but rather a change in existing routine work. A central facilitation team may also bring a fresh external perspective to staff discovery interviews, and become practised at identifying key themes. Their lack of identification with a particular service may make it easier for patients and carers to voice criticisms. On the other hand, facilitators who come from within the relevant service already have first-hand knowledge of local issues to help set the national trigger film in context, and have ready links to local staff and patients, which will enable swift co-ordination of co-design meetings. Their understanding of the area may enable them to spot and draw out relevant patient concerns and priorities which a central team might miss. They may be more trusted by their colleagues to understand staff feedback, especially if they come from a clinical background themselves. Using co-design within their own area may sensitise facilitators more generally to the patient’s experience of their service, which may lead to a more lasting impact. There is no right answer to this question; each hospital will need to assess its own resources and preferred approach, and this may differ from one pathway or service area to the next.
There are clear advantages in keeping momentum going during the co-design phase, in terms of enabling both patients and staff to see clear progress, maintaining enthusiasm and commitment, and minimising the burden of time commitment. The degree of acceleration we applied to the staff discovery and engagement phase, however, may not be essential. It is achievable, and the speed did not seem to affect staff engagement, but there is no reason why hospitals could not set themselves a more relaxed timetable for this (and indeed for the implementation phase) to reduce the pressure on facilitators, resources permitting.
Training and support for facilitators
The facilitators in our study were given training by CI Robert, one of the originators of the EBCD approach in health care. They were also encouraged to use The King’s Fund’s online EBCD toolkit. Despite this, they reported that when they began work on the first pathway (intensive care), they would have liked more opportunities to learn directly from the experience of other facilitators who had already used the approach, particularly around practical methods of supporting the co-design groups. The two facilitators working on intensive care shared experiential learning with each other and gave each other mutual support and encouragement.
Three implications for practice arise from this. Firstly, we have expanded The King’s Fund’s toolkit to include reflections from the facilitators in this study and other participants, including patients, so that future facilitators can benefit from their learning, feel more prepared for what to expect and be reassured that the process works, and that genuine staff and patient engagement is possible.
Secondly, we suggest that there would be benefits in providing more opportunities for EBCD and AEBCD facilitators to network, to cascade learning and provide a continuing source of information and support.
Thirdly, we identify a need for more regularly available face-to-face training alongside the EBCD toolkit. While the toolkit undoubtedly provides a valuable reference – in effect an online textbook – we know that deep learning is more likely to happen where there is a chance to interact and relate learning to one’s own context. New facilitators benefit from an opportunity to ask questions and share their doubts and fears. There is an opportunity for hospitals and other organisations which are already repositories of experience on EBCD and AEBCD to develop and run more training courses for other hospitals. This could be self-financing if a small course fee is charged.
Generating new trigger films
For this study, we conducted secondary analysis and produced two trigger films covering three of the interview collections in the HERG archive (lung cancer; patients’ experiences of intensive care; and relatives’ experiences of intensive care). At the time of writing, the archive contains collections on over 80 different conditions and topics, and 8–10 collections are added per year. This is an enormous body of work from which to create new trigger films. The financial model on which the research has been based has always included free dissemination of findings to patients, public and professionals through the Healthtalkonline website, but this analysis has been designed first and foremost on the basis of what may help individuals learning to live with their condition and seeking emotional support. Individuals may have a better experience of illness as a result, and professionals may gain insights which improve their personal practice and, thus, patient experience, but the purpose has not thus far been explicitly to analyse and improve the organisation of health care.
There are several options for how we might handle this, both looking back at previous collections and on a rolling basis as new studies are added. These various potential solutions may require further research (see Implications for research, below).
-
With new collections, cost some additional researcher and technical time into each HERG grant proposal to incorporate an additional EBCD-focused analysis and produce a trigger film to place on Healthtalkonline at the same time as doing the main analysis.
-
For previous collections, seek funding for a service improvement fellowship to work back through the archive to produce a series of trigger films.
-
For both new and existing collections, experiment with producing trigger films based on what is already on Healthtalkonline rather than conducting a full secondary analysis.
-
Use a forthcoming ‘scrapbook’ feature on the Healthtalkonline website to enable anyone using the site to create their own useful collections of clips for specific purposes and share these with others. EBCD scrapbooks created by NHS staff working on quality improvement could be specifically encouraged and shared.
-
Use online feedback on existing films to help identify where they may need updating in the light of new treatment developments.
-
Encourage local patients and carers in future EBCD projects to search the website for clips that they feel capture issues important to them and which they would like to show to local staff – this would be an interesting extension of co-design principles into a ‘co-discovery’ approach, thereby empowering patients to create their own trigger films.
-
Work with future EBCD projects collecting new local patient discovery interviews to share these online (through Healthtalkonline or The King’s Fund’s EBCD toolkit). If, as we believe we have demonstrated, a film developed from national experiences can work in a local setting, it may be equally effective to transfer a locally developed film from one setting to another. This wider use would need to be built into participant consent for being filmed at the outset. Previous EBCD projects could also be encouraged to make their trigger films more widely available (subject, of course, to participant consent).
Given the comment from one patient that too few patients were used in the intensive care film, it may be valuable to make a more conscious effort to use clips from a wider range of people in representing the themes found in the analysis of all the interviews. In collections where fewer people have consented to the use of video, the inclusion of some audio clips could be considered.
The fundamental importance of co-design
As the intervention progressed, it became apparent to the research team that the extent of agreement or identification with the content of the films was not really the central issue. It is important to remember that the purpose of the films is to ‘trigger’ discussion. In traditional EBCD, too, they are only the start of a process of sharing ideas and concerns, and then working together to redesign care. If the national trigger films are sufficient to initiate such conversations, then local specifics can be brought into discussion along the way, and even disagreement with the content can generate fruitful discussion. But the elements of the intervention that have left both staff and patients feeling energised and empowered is the direct encounter with each other, the active partnership in co-design groups to achieve change, and the sense of tangible results.
It is possible to implement quality improvements that are based on patients’ wishes and experiences but without involving them in the change process. Staff could be shown a trigger film or interview data previously collected from patients and then decide as a staff working group what needs doing. It is certainly true that just seeing patient narratives on film can have a powerful effect. But the evaluation data from this study suggest that the face-to-face encounters with patients have been even more transformative, inspiring and revelatory to staff in making them think differently about their values and their practice. Having patients involved throughout is also a way of ensuring that improvement activities really do address patient concerns, and of holding staff to account to see change through. Their involvement – their physical presence – acts as a constant reminder to staff of who change is for, and why it is so important compared with other potentially overwhelming pressures and demands in their working lives. When staff volunteer – as they did in this study – the information that this is the first time in 20 years that they have really talked to patients in this way or that it is the most rewarding thing they have ever done in their careers, the full potential of EBCD to reconnect staff with their fundamental values of care and compassion is striking. We are grateful to one of our anonymous reviewers for the comment that ‘far from being a burden, involvement in this work helped to lighten (in many ways) the emotional and other forms of labour in which people are engaged’. Patients too report a different level of appreciation for staff, a belief that they will be listened to and that change is possible, and a renewed sense of trust in local NHS services.
The fact that both of our partner hospitals have independently decided to invest staff time and funding to adopt a co-design approach more widely in their organisations demonstrates their view of its value as a quality improvement intervention that benefits the organisation as a whole.
Implications for research
Accelerated experience-based co-design as designed for this study has substantially reduced the cost of using co-design to improve patient experiences. No quality improvement work is cost free, and all NHS organisations are now required to make improving patient experience a top priority. However, spending on quality improvement may be highly cost-effective, given the growing evidence that improved patient experience is linked to various outcomes such as lower mortality and hospital-acquired infection rates, reduced lengths of stay, and improved staff morale and retention (see Chapter 1, Background).
Nevertheless, we believe there may still be scope for further economies in developing trigger films, while ensuring that they remain based on high-quality research into patient experience. In particular, we have identified the following additional research questions:
-
Would it be equally effective to develop trigger films from the national archive using clips already published on the Healthtalkonline website, rather than a new secondary analysis of full interview transcripts from the Oxford archive?
-
What would the advantages and disadvantages be of involving patients in ‘co-discovery’ as well as ‘co-design’ – selecting and presenting material for their own trigger films?
-
Would films developed from patient discovery interviews for one local EBCD project work in another local setting?
We would have material with which to test this last question. One of the hospitals involved in the current study is already conducting new local interviews on experiences of emergency departments for EBCD, and gaining consent for these to be used on Healthtalkonline.
Additionally, HERG has already been experimenting with using secondary analysis of the archive for other audiences and purposes. This includes an ongoing study with NICE to explore what the data can add to the development of clinical guidelines and quality standards; secondary analysis and trigger films to support commissioners redesigning services (experience-based commissioning); the development of training resources for health professionals to improve clinical practice (e.g. in life-threatening conditions in pregnancy); and analysis of patient-reported treatment uncertainties to contribute to James Lind Alliance Priority Setting Partnerships. An as yet unexplored question is:
-
To what extent can different policy and practice audiences make use of common secondary analyses and trigger films, or do they require separate tailored resources?
One question that has emerged from our study is:
-
Does AEBCD bring less personal therapeutic benefit to individual patients involved than EBCD?
It is possible that at the level of the individual participating patient/carer, the impact of AEBCD is less because participants did not have the opportunity to tell their own stories, and hear stories of other patients who had been cared for in the same service as themselves, and then reflect together with them on their shared experiences. However, the evaluation did not set out to explore the question of individual therapeutic benefit, and so confirming this assertion would require further research and a different study design.
There is very limited evidence on the costs and cost-effectiveness of patient-centred quality improvement. In working on the comparison between EBCD and AEBCD, this study has for the first time provided a detailed analysis of the costs of EBCD. The next stage is to understand more about cost-effectiveness, prompting the following research questions:
-
How should we measure the cost-effectiveness of patient-centred quality improvement initiatives?
-
Does patient-centred quality improvement translate into measurable longer-term changes in patient satisfaction rates and the quantity and content of patient ratings on sites such as NHS Choices and Patient Opinion?
-
Does patient-centred quality improvement impact on clinical and organisational outcomes such as length of stay, infection rates and medication errors?
-
Does patient-centred quality improvement lead to improved staff morale?
Chapter 5 Dissemination
During the life of the study, both the CIs and the facilitators have disseminated the project and emergent findings in a varied range of conferences, seminars, and practitioner journal items. An academic book chapter has also been accepted for publication in 2014 in a book of papers from the Organisational Behaviour in Healthcare Conference 2012. CIs have plans to continue dissemination through these routes and to prepare several articles.
In March 2013 a presentation was given to a TVHIEC partnership meeting on patient experience, and a concluding dissemination workshop was held in partnership with The King’s Fund. This was to an invited audience of approximately 50 practitioners, policy-makers, managers, EBCD specialists and patient support groups, and included presentations by the research team, the facilitators and patients who were involved.
For the longer term, our key dissemination routes are The King’s Fund’s EBCD toolkit and the Healthtalkonline website. The King’s Fund is updating the toolkit to feature an explanation of AEBCD and to link to the trigger films already produced as a resource for others. It will also include new contributions from the AEBCD facilitators explaining what to expect and giving the practical advice on running EBCD projects that they wished they had had when they started. The trigger films will also be made available on the ‘Improving care’ section of the Healthtalkonline website.
Acknowledgements
The co-authors would like to thank the following:
Royal Berkshire and Royal Brompton and Harefield NHS Foundation Trusts for taking part.
All the patients and staff at the two trusts who took part in the study.
All the members of our project advisory group (see Appendix 1).
Jocelyn Cornwell and Joanna Goodrich from The King’s Fund’s Point of Care Programme for advice and help in updating the online EBCD toolkit.
Michelle Farr from University of Bath, Vicki Tsianakas from King’s College London, and Catherine Dale from Guy’s and St Thomas’ NHS Foundation Trust, for their insights into comparisons with previous EBCD projects.
Cathy O’Sullivan, Richard Freeman and the VHIEC team for chairing and project management support.
Farasat Bokhari (now at University of East Anglia) for designing the cost data collection.
Graham Cookson from King’s College London, for additional health economics support to analyse costs.
Alison Chapple from University of Oxford and Joe Calabrese from University College London, for secondary analysis of interviews and clip selection for the trigger films.
The DIPEx Charity which runs the Healthtalkonline website, and particularly Adam Barnett and Wale Oyeleye, for editing the trigger films.
Abi Eccles and Sophie Pask from Primary Care Health Sciences, University of Oxford, for help with preparing references.
Nicola Small, Clare Wickings and team from Primary Care Health Sciences, University of Oxford, for financial and administrative support.
Sue Pargeter from the NIHR National Evaluation, Trials and Studies Coordinating Centre (NETSCC) for advice throughout the project.
Our NIHR Journals Library editors and anonymous peer reviewers for their encouragement and support.
NIHR Health Service and Delivery Research Programme for funding the study.
Department of Health, Macmillan Cancer Support and the Intensive Care National Audit and Research Centre for funding the original interview studies from which the trigger films were drawn.
Contributions of authors
Louise Locock (Deputy Research Director, Health Experiences Research): principal investigator – led the overall design of the study and the analysis of archived interviews, contributed to analysis and led final report writing.
Glenn Robert (Professor of Healthcare Quality and Innovation): contributed to overall study design, designed and led the intervention component, contributed to analysis and report writing, and gave final approval of manuscript.
Annette Boaz (Lecturer in Translational Health Care Research): designed and led the evaluation component, supervised analysis of evaluation data, contributed to report writing and gave final approval of manuscript.
Sonia Vougioukalou (Research Associate, Evaluation Ethnographer): conducted all data collection for evaluation, led analysis of evaluation data for report and gave final approval of manuscript.
Caroline Shuldham (Director of Nursing and Clinical Governance, NHS hospital): contributed to overall study design, supervised implementation of intervention, contributed to report writing and gave final approval of manuscript.
Jonathan Fielden (Medical Director, NHS hospital): contributed to overall study design, supervised implementation of intervention, contributed to report writing and gave final approval of manuscript.
Sue Ziebland (Research Director, Health Experiences Research): contributed to overall study design and supervised the analysis of archived interviews, contributed to report writing and gave final approval of manuscript.
Melanie Gager (service improvement facilitator, Royal Berkshire NHS Foundation Trust): played a major role in shaping the intervention, collected data, helped analyse and interpret emerging findings, drafted material for the report and gave final approval of the manuscript.
Ruth Tollyfield (service improvement facilitator, Royal Brompton and Harefield NHS Foundation Trust): played a major role in shaping the intervention, collected data, helped analyse and interpret emerging findings, drafted material for the report and gave final approval of the manuscript.
John Pearcey (service improvement facilitator, Royal Brompton and Harefield NHS Foundation Trust): collected data, helped analyse and interpret emerging findings, drafted material for the report and gave final approval of the manuscript.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- Garratt A, Solheim E, Danielsen K. National and Cross-national Surveys of Patient Experiences: A Structured Review. Oslo: Norwegian Knowledge Centre for the Health Services; 2008.
- Doyle C, Lennox L, Bell D. A systematic review of evidence on the links between patient experience and clinical safety and effectiveness. BMJ Open 2013;3. http://dx.doi.org/10.1136/bmjopen-2012-001570.
- Matthew P, Manary MSE, Boulding W, Staelin R, Seth W, Glickman MD. The patient experience and health outcomes. N Engl J Med 2013;368:201-3.
- International Health Policy Survey. New York, NY: Commonwealth Fund; 2010.
- Report of the Mid Staffordshire NHS Foundation Trust Public Inquiry. London: HMSO; 2013.
- Greaves F, Pape UJ, King D, Darzi A, Majeed A, Wachter RM, et al. Associations between Internet-based patient ratings and conventional surveys of patient experience in the English NHS: an observational study. BMJ Qual Saf 2012;21:600-5. http://dx.doi.org/10.1136/bmjqs-2012-000906.
- Meterko M, Wright S, Lin H, Lowy E, Cleary PD. Mortality among patients with acute myocardial infarction: the influences of patient-centered care and evidence-based medicine. Health Serv Res 2010;45:1188-204. http://dx.doi.org/10.1111/j.1475-6773.2010.01138.x.
- Jha AK, Orav EJ, Zheng J, Epstein AM. Patients’ perception of hospital care in the United States. N Engl J Med 2008;359:1921-31. http://dx.doi.org/10.1056/NEJMsa0804116.
- Murff HJ, France DJ, Blackford J, Grogan EL, Yu C, Speroff T, et al. Relationship between patient complaints and surgical complications. Qual Saf Health Care 2006;15:13-6. http://dx.doi.org/10.1136/qshc.2005.013847.
- Raleigh VS, Hussey D, Seccombe I, Qi R. Do associations between staff and inpatient feedback have the potential for improving patient experience? An analysis of surveys in NHS acute trusts in England. Qual Saf Health Care 2009;18:347-54. http://dx.doi.org/10.1136/qshc.2008.028910.
- Edgcumbe DP. Patients’ perceptions of hospital cleanliness are correlated with rates of meticillin-resistant Staphylococcus aureus bacteraemia. J Hosp Infect 2009;71:99-101. http://dx.doi.org/10.1016/j.jhin.2008.09.009.
- Charmel PA, Frampton SB. Building the business case for patient-centered care. Healthc Financ Manage 2008;62:80-5.
- Equity and Excellence: Liberating the NHS. London: HMSO; 2010.
- Coulter A, Fitzpatrick R, Cornwell J. The Point of Care: Measures of Patients’ Experience in Hospital: Purpose, Methods and Uses. London: The King’s Fund; 2009.
- Foot C, Cornwell J. Improving Patients’ Experiences: An Analysis of the Evidence to Inform Future Policy Development. Internal report to the Department of Health. London: The King’s Fund; 2010.
- Tsianakas V, Maben J, Wiseman T, Robert G, Richardson A, Madden P, et al. Using patients’ experiences to identify priorities for quality improvement in breast cancer care: patient narratives, surveys or both?. BMC Health Serv Res 2012;12. http://dx.doi.org/10.1186/1472-6963-12-271.
- Feeling Better? Improving Patient Experience in Hospital. London: NHS Confederation; 2010.
- DeCourcy A, West E, Barron D. The National Adult Inpatient Survey conducted in the English National Health Service from 2002 to 2009: how have the data been used and what do we know as a result?. BMC Health Serv Res 2012;12. http://dx.doi.org/10.1186/1472-6963-12-71.
- Mountford J, Shojania K. Refocusing quality measurement to best support quality improvement: local ownership of quality measurement by clinicians. BMJ Qual Saf 2012;21:519-23. http://dx.doi.org/10.1136/bmjqs-2012-000859.
- Rozenblum R, Lisby M, Hockey P, Levtzion-Korach O, Salzberg C, Efrati N, et al. The patient satisfaction chasm: the gap between hospital management and frontline clinicians. BMJ Qual Saf 2013;22:242-50. http://dx.doi.org/10.1136/bmjqs-2012-001045.
- Robert G, Waite D, Morrow E, Cornwell J, Maben J. Education and training to understand and improve patient experience: a national survey of higher education and healthcare sectors. Nurse Educ Today 2012;34:112-20.
- Intelligent Board 2010 – Patient Experience. London: Dr Foster Intelligence; 2010.
- Dignity and Nutrition Inspection Programme: National Overview. London: Care Quality Commission; 2011.
- Robert G, Cornwell J. What Matters to patients? Policy Recommendations – A Report for the Department of Health and NHS Institute for Innovation & Improvement. Warwick: NHS Institute for Innovation & Improvement; 2011.
- Ziebland S, Coulter A, Calabrese JD, Locock L. Understanding and Using Health Experiences: Improving Patient Care. Oxford: Oxford University Press; 2013.
- Maben J, Peccei R, Adams M, Robert G, Richardson A, Murrells T, et al. Patients’ Experiences of Care and The Influence of Staff Motivation, Affect and Wellbeing 2012.
- Coulter A. Can patients assess the quality of health care? Patients’ surveys should ask about the real experiences of medical care. BMJ 2006;333:1-2.
- Green MC, Brock TC. The role of transportation in the persuasiveness of public narratives. J Pers Soc Psychol 2000;79:701-21. http://dx.doi.org/10.1037//0022-3514.79.5.701.
- Greenhalgh T, Russell J, Swinglehurst D. Narrative methods in quality improvement research. Qual Saf Health Care 2005;14:443-9. http://dx.doi.org/10.1136/qshc.2005.014712.
- Bate P, Robert G. Bringing User Experience to Healthcare Improvement: The Concepts, Methods and Practices of Experience-Based Design. Oxford: Radcliffe Publishing; 2007.
- Locock L. Maps and Journeys: Redesign in the NHS. Birmingham: University of Birmingham, Health Services Management Centre; 1998.
- Iles V, Sutherland K. Organisational Change: A Review for Health Care Managers, Professionals and Researchers. London: National Co-ordinating Centre for NHS Service Delivery and Organisation; 2001.
- Daly J, Willis K, Small R, Green J, Welch N, Kealy M, et al. A hierarchy of evidence for assessing qualitative health research. J Clin Epidemiol 2007;60:43-9. http://dx.doi.org/10.1016/j.jclinepi.2006.03.014.
- Robert G, Ziebland S, Coulter A, Calabrese JD, Locock L. Understanding and Using Health Experiences: Improving Patient Experience. Oxford: Oxford University Press; 2013.
- Donetto S, Tsianakas V, Robert G. Experience-based Co-design for improving patient experience: mapping where we are now and establishing future directions. London: King’s College London; 2013.
- Farr M. Evaluation Report of the Patient Centred Care Project. London: The King’s Fund; 2011.
- Iedema R, Merrick E, Piper D, Walsh J. Emergency Department Co-design Stage 1 Evaluation – Report to Health Services Performance Improvement Branch, NSW Health. Sydney, NSW: Centre for Health Communication, University of Technology; 2008.
- Piper D, Iedema R. Emergency Department Co-Design Program 1 Stage 2 Evaluation Report. Sydney, NSW: Centre for Health Communication (UTS) and NSW Health; 2010.
- Adams M, Maben J, Robert G. Improving Patient-Centred Care Through Experience-based Co-design (EBCD). An Evaluation of the Sustainability and Spread of EBCD in a Cancer Centre. London: National Nursing Research Unit; 2013.
- Tsianakas V, Robert G, Maben J, Richardson A, Dale C, Wiseman T. Implementing patient centred cancer care: using experience-based co-design to improve patient experience in breast and lung cancer services. J Support Care Cancer 2012;20:2639-47. http://dx.doi.org/10.1007/s00520-012-1470-3.
- Cheshire A, Ridge D. Evaluation of the Experience-Led Commissioning in End of Life Care Project. London: University of Westminster; 2012.
- Ream E, Tsianakas V, Verity R, Oakley C, Murrells T, Robert G, et al. Enhancing the Role of Carers in the Outpatient Chemotherapy Setting: A Participatory Action Research Project. London: King’s College London; 2013.
- McIntyre A. Participatory Action Research. Los Angeles, CA: Sage Publications; 2008.
- Ziebland S, Ziebland S, Coulter A, Calabrese JD, Locock L. Understanding and Using Health Experiences: Improving Patient Experience. Oxford: Oxford University Press; 2013.
- Calabrese JD, Ziebland S, Coulter A, Calabrese JD, Locock L. Understanding and Using Health Experiences: Improving Patient Experience. Oxford: Oxford University Press; 2013.
- Argyris C, Schön DA. Organizational Learning: A Theory of Action Perspective. Reading, MA,: Addison-Wesley; 1978.
- Wheatley MJ. Turning to One Another: Simple Conversations to Restore Hope to the Future. San Francisco, CA: Berrett-Koehler; 2009.
- Kerr C, Lloyd C. Pedagogical learnings for management education: developing creativity and innovation. J Manage Organiz 2008;14:486-503. http://dx.doi.org/10.5172/jmo.837.14.5.486.
- Kerr C. Community engagement and artful academic staff development: a return on expectations through collaborative practice. Int J Work Organis Emotion 2010;3:384-99. http://dx.doi.org/10.1504/IJWOE.2010.035326.
- Howard C, Tuffin K, Stephens C. Unspeakable emotion – a discursive analysis of police talk about reactions to trauma. J Lang Soc Psychol 2000;19:295-314. http://dx.doi.org/10.1177/0261927X00019003002.
- Drew G. An Artful Learning Framework for organisations. J Manage Organ 2008;14:504-20. http://dx.doi.org/10.5172/jmo.837.14.5.504.
- Bate SP, Robert G. Towards more user-centric organisational development: lessons from a case study of experience-based design. J Appl Behav Sci 2007;42:41-66.
- Bushe GR, Rothwell WJ, Stavros JM, Sullivan RL. Practicing Organization Development a Guide for Leading Change. Hoboken, NJ: John Wiley & Sons; 2009.
- The King’s Fund . Online EBCD Toolkit 2013. www.kingsfund.org.uk/projects/point-care/ebcd (accessed 3 December 2013).
- Dewar B, Mackay R, Smith S, Pullin S, Tocher R. Use of emotional touchpoints as a method of tapping into the experience of receiving compassionate care in a hospital setting. J Res Nurs 2010;15:29-41. http://dx.doi.org/10.1177/1744987109352932.
- Iedema R, Merrick E, Piper D, Britton K, Gray J, Verma R, et al. Codesigning as a discursive practice in emergency health services: the architecture of deliberation. J Appl Behav Sci 2010;46:73-91. http://dx.doi.org/10.1177/0021886309357544.
- Robert G, Bate S. Piloting, Testing and Evaluating Experience-based Design (EBD): Key Findings and Lessons for the Future. London: University College London; 2006.
- DIPEx . Healthtalkonline 2013. www.healthtalkonline.org (accessed 3 December 2013).
- Patton MQ. Qualitative Evaluation and Research Methods. London: Sage; 1990.
- NHS England . The Information Standard 2013. www.theinformationstandard.org (accessed 3 December 2013).
- The Development of ‘Treatment and Care Towards the End of Life: Good Practice in Decision Making (2010)’. London: General Medical Council; 2010.
- Calabrese JD. A Comparison of Data on Patient Experiences of End of Life Care. Oxford: Green Templeton College; 2010.
- Dopson S, Locock L, Chambers D, Gabbay J. Implementation of evidence-based medicine: evaluation of the Promoting Action on Clinical Effectiveness programme. J Health Serv Res Policy 2001;6:23-31. http://dx.doi.org/10.1258/1355819011927161.
- Fitzgerald L, Ferlie E, McGivern G, Buchanan D. Distributed leadership patterns and service improvement: Evidence and argument from English healthcare. Leadership Qu 2013;24:227-39. http://dx.doi.org/10.1016/j.leaqua.2012.10.012.
- Hospital Episode Statistics Online 2012. www.hesonline.nhs.uk/Ease/servlet/ContentServer?siteID=1937 (accessed 28 February 2013).
- Heaton J. Reworking Qualitative Data. London: Sage; 2004.
- Pettigrew A, Ferlie E, McKee L. Shaping Strategic Change: Making Change in Large Organizations - The Case of the National Health Service. London: Sage; 1992.
- Fitzgerald L, Dopson S, Buchanan D, Bryman A. Handbook of Organizational Research Methods. London: Sage; 2009.
- Green J, Thorogood N. Qualitative Methods for Health Research. London: Sage; 2004.
- Denzin NK. The Research Act. Englewood Cliffs, NJ: Prentice Hall; 1989.
- Davies E, Madden P, Coupland V, Griffin M, Richardson A. Comparing breast and lung cancer patients’ experiences at a UK Cancer centre: implications for improving care and moves towards a person centred model of clinical practice. Int J Person Centred Med 2011;1:177-89. http://dx.doi.org/10.5750/ijpcm.v1i1.44.
- Cockram A, Mouat S, Gadd B. Redesigning Healthcare with Staff and Service Users. Experience-Based Co-design. Melbourne, VIC: NorthWestern Mental Health Service; 2008.
- Hodgkiss F, Barrie K, Sinclair C. Experience Based Design Cancer Pilots. Interim Reflection Report. Edinburgh: Better Together, Scotland’s Patient Experience Programme; 2011.
- Mulligan J. Chest Clinic Experience Based Design Project. London: Whipps Cross University Hospital NHS Trust; 2011.
- Experience Based Design Project. Sunshine Acute Adult Psychiatric Unit Internal Report. Melbourne, VIC: Northwestern Mental Health; 2008.
- Ritchie J, Spencer L, Bryman A, Burgess R. Analyzing Qualitative Data. London: Routledge; 1994.
- Kitson A, Harvey G, McCormack B. Enabling the implementation of evidence based practice: a conceptual framework. Qual Health Care 1998;7:149-58.
- Tear R, Scheuing ES, Atkinson C, Westwood C. Teamworking and Quality Improvement: Lessons from British and North American Organizations. London: Cassell; 1997.
- Glouberman S, Zimmerman BJ. Complicated and Complex Systems: What Would Successful Reform of Medicare Look Like?. Sasketoon, SK: Commission on the Future of Health Care in Canada; 2002.
Appendix 1 Original protocol
SDO Protocol – project ref: 10/1009/14
Version: 2
Date: 19th August 2011
Testing accelerated experience-based co-design: using a national archive of patient experience narrative interviews to promote rapid patient-centred service improvement
| Chief investigator Co-investigators |
Dr Louise Locock Listed in appendix A |
| Sponsor | University of Oxford |
| Funder | National Institute for Health Research Service Delivery and Organisation programme |
| NIHR Portfolio number | 10/1009/14 |
| ISRCTN registration (if applicable) | n/a |
Testing accelerated experience-based co-design: using a national archive of patient experience narrative interviews to promote rapid patient-centred service improvement
1. Aims/Objectives:
Aim:
To use a national video and audio archive of over 2,000 recently collected patient experience narratives to help develop, test and evaluate a rapid patient-centred service improvement approach (‘Accelerated experience-based co-design’).
Our objectives are to:
-
Identify common themes arising from the University of Oxford’s national patient narrative archive in each of two exemplar care pathways
-
Use these analyses to create ‘trigger films’ illustrating these themes which can be accessed and used by all NHS acute trusts
-
Test these films alongside techniques that are part of the existing experience-based co-design (EBCD) approach to stimulate service improvement work led by staff, patients and carers in two provider organisations (Royal Brompton and Harefield NHS Foundation Trust and Royal Berkshire NHS Foundation Trust) in each of the two pathways
-
Observe what happens in both pathways in each trust and evaluate the acceptability to patients and staff – and the impact - of this adapted approach to patient-centred service improvement
-
Measure the costs of this accelerated approach compared with traditional EBCD
-
Make recommendations for quality improvement practice in the NHS.
A traditional EBCD cycle typically takes around 12 months’ work in each trust to complete one pathway. In the accelerated version, we propose to halve the cycle to 6 months per pathway.
2. Background:
Improving patient experience is a key aim for the NHS. The new White Paper, ‘Equity and Excellence: Liberating the NHS’, emphasises ‘putting patients and the public first’, and ensuring that the way care and information are provided reflect what patients themselves think is important (Secretary of State for Health, 2010). To do this the NHS needs to draw on the narratives and experiences of those who have used and observed healthcare services at first hand, but there is considerable debate about the best methods for gathering and understanding patient experience information and then using it to improving the experience. Narratives are a powerful way to engage care providers at a deep emotional level in thinking how services could be improved (Greenhalgh et al 2005). Patient experiences can suggest priorities and solutions that may not occur to people who are immersed in service delivery (Locock 2001; Iles and Sutherland 2001). Many NHS organisations are now successfully experimenting with ways of gathering user views and using them to improve services. However, it is important that such work is based on rigorous research with a broad sample of users and a full range of different perspectives, rather than relying on a single representative on a committee or the collection of a few anecdotes (Dalyet al. 2007).
This project draws on and seeks to combine two existing initiatives that recognise the value of narratives: a national collection of 2,000 video and audio recorded narrative interviews with UK service users and a participatory action research approach to service improvement using patient experiences, Experience-Based Co-Design (EBCD).
The Health Experiences Research Group at the University of Oxford collects and analyses video and audio-recorded interviews with people about their experiences of illness. It now has an innovative national archive of over 2,000 interviews, all collected between 2000 and 2010, and covering 55 different conditions, which provides a unique source of evidence on patient experiences and priorities. The interviews are approved for use in research, teaching, publication, broadcasting and dissemination on the award-winning Healthtalkonline website, one of the first health information sources to meet the Department of Health’s new Information Standard. The interviews are increasingly used in teaching health professionals, and to inform health policy – for example, NICE guideline development now frequently incorporates evidence from Healthtalkonline, and the recent GMC guidance on end of life care drew on a specially commissioned analysis of interviews from the University of Oxford archive. The Oxford end of life care analysis has recently been compared with local interviews conducted by one PCT on end of life care. This showed that very few themes were identified locally that could not have been anticipated from the national dataset (Calabrese, 2010). The University of Oxford archive thus has enormous potential as an evidence base of patients’ experiences to support service change.
EBCD (Bate and Robert 2007a) has been implemented in collaboration with patients, families and staff in service improvement efforts in various settings, care pathways and countries. Integral to the approach is that patient, carer and staff experiences are used systematically to co-design and improve services. To date, this has involved an intensive local diagnostic phase, using rigorous qualitative research, including video or audio-recorded narrative interviews in which participants are invited to recount their experiences using a story-telling approach, highlighting concerns and priorities and identifying ‘touchpoints’ (key interaction points) along their journey. Trigger films based on these experiences are then used, firstly to enable patients and carers to share and discuss their experiences with each other, and then to stimulate discussion between local staff and patients, who can then jointly identify actions to bring about systematic, sustainable improvements. Building a coalition for change between staff and patients is central. The approach is being widely used in the UK, Australia and the Netherlands; The King's Fund is currently evaluating it as one of two improvement approaches in the Point of Care programme. There is evidence from independent evaluations that EBCD can bring about changes which significantly impact on patient experience, and are acceptable to a range of service users (Piper and Iedema, 2010).
Whilst EBCD may be effective, the diagnostic phase is undoubtedly lengthy and costly. Replicating 5 months of qualitative interviewing on each pathway in each trust is impractical at a time of recession. EBCD and the Oxford group use very similar narrative interview techniques. We will therefore develop and test a new accelerated form of EBCD by using the University of Oxford archive to provide the majority of the evidence on patients’ experiences and thereby scale up EBCD more efficiently across different settings. What we do not know is how far using national rather than local narratives will affect local credibility and buy-in, and whether anything else may need to be done locally to supplement national data. This project seeks to investigate the question of whether Accelerated EBCD can provide a rigorous and less costly alternative to conventional EBCD.
3. Need:
There is a clear and consistent high-level policy imperative to improve patient experience. But understanding what really matters to patients and how best to translate the policy rhetoric into real practical change remains a challenge. This project is supported by the newly formed Thames Valley Health Innovation and Education Cluster (TVHIEC) in South Central SHA. TVHIEC was funded to deliver an innovative skills development programme driven by a strong patient and client focus. The lead applicant (Louise Locock) is a member of the TVHIEC Partnership Board and its patient and public involvement sub-group, and will be the main link between the project and the HIEC.
Care which is redesigned around patient needs and preferences can improve:
-
acceptability (e.g. switching care to a more convenient location)
-
effectiveness (e.g. increased adherence to treatment regimes)
-
cost-effectiveness (e.g. combining previously separate activities or appointments)
-
targeting and equity (e.g. by challenging perceptions of particular patient groups, or by understanding and tackling what motivates some groups to resist or decline care)
-
quality of life (by developing care that responds to issues patients think are important).
Two provider organisations have already signed up as partners in the project. The Director of Nursing at the Royal Brompton and Harefield NHS Foundation Trust (Caroline Shuldham) had already approached the Health Experiences Research Group to enquire about possible ways of using the interview archive to support service change. The trust was enthusiastic to discover the application was planned and that they could become a partner. Since this, another trust within South Central, the Royal Berkshire NHS Foundation Trust, has committed to become a partner. This project comes at a time when trusts are facing severe financial difficulties, and offers a valuable way to keep the quality of patient experience at the heart of trust priorities despite cuts in staffing and other resources. An advisory group of patients will be established in each local site for each pathway.
4. Methods:
a. Setting
The two partner provider sites have been selected partly on the basis of senior clinical managerial commitment to the project, which has been shown to be an important enabling factor for change (Dopsonet al, 2001). Royal Brompton and Harefield’s early enthusiasm determined the selection of pathways relevant to their specialist services, and in discussion with Royal Berkshire we have settled on two exemplars: intensive care and lung cancer. Our co-applicants Caroline Shuldham and Jonathan Fielden bring invaluable expertise in cardiac and intensive care nursing, and intensive care medicine respectively.
These two pathways offer interesting potential contrasts. In intensive care, patients themselves are often unable to take part in decision making at certain stages and may have difficulties communicating, yet their utter dependence on staff is a key feature of their experience. Family carers have a different perspective, having to take responsibility for many decisions and interactions with staff, but often feeling helpless and potentially excluded from a specialised, high tech, automated world. The Health Experiences Research Group archive includes interviews with patients themselves (40 interviews) and with family carers and close friends (38 interviews), so we can identify touchpoints from both groups. By contrast lung cancer (45 interviews) offers a more traditional pathway through symptom recognition (and delays in consultation), investigations, diagnosis, treatment choices, recovery, short and long term management and medication. Given the often poor prognosis for lung cancer, it may also involve coping with progression and potentially end of life care. The Research Group also has an interview collection on end of life care which can shed additional light on this aspect of the pathway.
In recruiting a second provider site, we sought a trust with a more general hospital profile, within the catchment area of the Thames Valley Health Innovation and Education Cluster, again with senior clinical managerial commitment to the project (Royal Berkshire). The contrast between a tertiary specialist provider and a general hospital will help demonstrate whether the approach is equally acceptable and practicable in both types of setting.
b. Design
The evaluation will be a process evaluation and cost analysis, building on existing evidence already available about the effectiveness of patient-led service improvement approaches. Whilst we will document improvement activities that take place as a result of the intervention in each trust, our aim is not to evaluate EBCD in itself. Our starting-point is that it has already been shown to be an effective approach, and our aim with the evaluation is rather to demonstrate whether an accelerated version of it is a workable, cost-effective and acceptable alternative.
The evaluation will be led by an organisational ethnographer, supervised by Annette Boaz, using a longitudinal comparative case study design and observational methods which are well suited to the study of complex change. (Pettigrew, Ferlie, Mckee 1997; Fitzgerald and Dopson 2010). In effect we will have four ‘cases’: two different pathways in each of two trusts. The ethnographer will be in post throughout the project and will thus be able to observe the set-up period during which the Oxford research group will be creating the trigger films, as well as the implementation phase. The evaluation will use multiple data sources, including observation, interviews, documentary analysis and administrative data on costs. Members of the project team will also be encouraged to keep reflective diaries of their experiences.
c. Study participants and recruitment
All staff who work in the four participating services will be invited to participate in the project and a sample of these staff will be invited to participate in the staff evaluation interviews. All patients over the age of 18 and under the age of 65 who receive care in the four participating services during the 6 months period of fieldwork and who can give informed consent will be invited to participate in the project. A sample of these patients and/or the carers will be invited to participate in the patient/carer evaluation interviews. The role of carers in this action research project will be solely determined by the individual patients. We are unable to specify at this stage how many carers may or may not be involved as it is for the patients to decide whether they wish to invite carers to become involved by accompanying them to the workshop.
There are no exclusion criteria with regards to staff working in the four participating services. All patients who are unwilling or unable to give informed consent (as identified by staff) will be excluded (including for example patients with dementia or learning disabilities); any patients under the age of 18 or over the age of 65 will be excluded.
In each of the two participating NHS organisations a ‘site captain’ has been identified and will be asked to assist the research team in arranging staff interviews and other meetings (as necessary). The site captain is the senior individual in each organisation who has discussed the research in detail with the research team and agreed to participate as a coinvestigator (see appendix 1). In each service the site captain has helped identify a local service improvement facilitator who will take day-to-day responsibility for the project locally including the identification and recruitment of participants.
Potential staff interviewees will be identified through discussions between the local site captain, facilitator and other relevant managers of the selected services. A sample of patients who are cared for in each of the services will be identified through a combination of (a) discussions between the local facilitator and staff in each of the services, and (b) as a result of the nonparticipant ethnographic observation of routine care undertaken by the local facilitator.
Ethnographic observation (a) of routine care will take place in appropriate settings depending on the specific service (for example, on wards or in outpatient clinics) and (b) at the AEBCD meetings; the presence of the observer will be renegotiated with both staff and patients as required.
Staff will be sent a covering letter in the internal post from the research team, together with the staff information sheet, and an outline of the appropriate semi−structured interview schedule will be sent (or delivered by hand) to each potential interviewee at least 24 hours prior to the time of the proposed interview. The staff information sheet and covering letter both make clear that participation is entirely voluntary and that staff can withdraw at any time without giving a reason.
Patients will be invited to participate either through (a) a letter from the research team sent to patient's home address by the NHS organisation or by hand together with a patient information sheet, and outline of the semi−structured interview schedule to be used at least seven days prior to proposed interview taking place. The participant information sheet and covering letter both make clear that participation is entirely voluntary and that patients can withdraw at any time without giving a reason or (b) informal approach during observation of AEBCD meeting and leaving the patient with a patient information sheet and asking whether they agree to being telephoned by research team to arrange interview at a later date.
Relevant member(s) of staff will be informed by researcher of his/her wish to observe routine daytoday activities. Patients who may be directly observed will be verbally informed of presence of observer and the purpose of the research.
Informed consent will be obtained by the local service improvement facilitator in each of the two NHS Trusts prior to any individual participating in the project. Staff and patients will be given an information sheet describing the study and asked to complete the attached consent form.
The number of staff and patients from each pathway are intended to be sufficient to give a broad range of views as to issues influencing staff wellbeing and patient experiences, and to allow the research team to be able to qualitatively assess the impact of the Accelerated Experience-Based Co-Design approach. Typically this will mean 12–15 patients/carers and 12–15 staff members from each of the four services participating.
Patients and carers will be offered to have their travel expenses to meetings and/or an evaluation interview reimbursed. Lunch and refreshments will be provided at meetings.
d. Data collection
The intervention will not require substantial new data collection in the first instance, as we will be using secondary analysis of our existing interview archive to elicit the important themes for people experiencing lung cancer and intensive care. We will use a thematic analysis approach; the data will be coded using techniques of constant comparison and deviant case analysis, and looking specifically for ‘touchpoints’ in the care pathway. Trigger films will be created on the basis of this analysis.
In each trust, the local facilitators will use a combination of observation and one-to-one interviews with staff to learn about their own experiences of the 2 care pathways and their views and expectations about local patients’ experiences. Findings will be presented and discussed at a staff feedback meeting.
One of our key research questions is how well local users feel national narratives capture themes important to their experience, and whether anything else needs to be done to supplement them at local level. At this point, therefore, the trigger films will be shown to two specially convened focus group workshops of local patients and carers with experience of intensive care and lung cancer. Participants will discuss how far the analysis of the national archive has captured their own priorities and experiences, and whether there are specific additional issues they would like to raise about local services. Depending on the outcome of these discussions, some further local data collection may be undertaken by the service improvement team in each partner provider site to supplement the national dataset, with support and advice from Glenn Robert. This could include new interviews or further focus groups. Patients in intensive care are often given diaries recording details of their stay, and these could also contribute to local analysis, for example.
As the intervention progresses, local staff and patients/carers will be working together to map existing care pathways, and make changes agreed as part of the co-design process. Their records of their activities will be used both for their own service improvement processes and to feed into the evaluation (see below). All workshops of staff and patients will be filmed (with consent) to help document the process of the intervention and to help answer our evaluation questions about the acceptability and credibility of using nationally collected patient experience data. We will also use a brief post-event survey to gauge participant reactions to the style and content of the workshops. This informs the unfolding intervention but can also feed into the evaluation.
e. Data analysis
Observations and brief conversations will be recorded as field notes; interviews will be transcribed for framework analysis (Ritchie and Spencer, 2004). Framework analysis is a widely used matrix based approach to organising and analysing qualitative data. It can be used to generate descriptive accounts, identify themes and develop explanatory theories.
The cost analysis will draw on administrative records from previous EBCD projects to develop a list of cost items associated with EBCD. Detailed records will be completed throughout the study period of costs associated with AEBCD. In particular, any costs associated with additional activities conducted at the local level to supplement the national narratives will be recorded. Data on staff and non-staff costs and time input will be systematically collected through micro-costing procedures and compared to data collected in existing EBCD evaluations (including Jocelyn Cornwell’s work on the Point of Care Programme, a soon to be completed evaluation of a large-scale EBCD project in two London teaching hospitals), with the support of a health economist and local trust staff. We will keep a careful record of how much time is committed to the intervention by staff at different levels in each trust as part of this comparison. Those involved in the co-design process will also contribute to the evaluation their record of service improvement activities undertaken and changes made.
At all stages of the evaluation, the ethnographer will be collecting data to address our research questions:
-
Is the accelerated approach acceptable to staff and patients?
-
How does using films of national rather than local narratives affect the level and quality of engagement with service improvement by local NHS staff? Does this have implications for the overall impact of the approach?
-
From local patients’ perspective, how well do they feel national narratives capture and represent themes important to their own experience?
-
Does any additional work need to be done to supplement the national narratives at the local level? If so, what form might this take?
-
What improvement activities does the approach stimulate and how do these activities impact on the quality of health care services?
-
What are the costs of this approach compared to traditional EBCD?
-
Can accelerated EBCD be recommended as a rigorous and effective patient-centred service improvement approach which could use common ‘trigger’ films to be rolled out nationally?
5. Contribution of existing research:
EBCD and other patient-centred improvement techniques have already been widely adopted in practice settings. This research will add to our collective knowledge about how best to ensure patient perspectives are at the heart of service change, and to ensure this is done as quickly and cost-effectively as possible.
The archive of patient interviews collected by the Health Experiences Research Group has added significantly to our understanding of patient experiences across a range of conditions; their dissemination through the Healthtalkonline website already provides a resource for patients themselves, and around 80 peer review publications in social science and clinical journals have reached an academic and clinical audience. The interviews are also used in clinical education in a number of universities, and professional training packages have been produced in partnership with NHS Education South Central. Recently, a secondary analysis on end of life care has contributed to the new GMC guidance on end of life care. But there is considerable untapped potential to use this archive more effectively to support service change and to inform policy-makers, managers and practising clinicians, providing a high standard of qualitative research evidence and reducing the need to replicate local research into patient experience. Both EBCD and the work of the Health Experiences Research Group are fundamentally concerned with drawing on people’s accounts of their experiences to identify commonalities and potential improvements, as well as providing a channel for patients’ voices in what it is like to have their condition. All the health experiences interviews are copyrighted for use in teaching and learning, as well as research, publication and the website.
For many participants, knowing that their experience may be used to help improve things for other people is an important motivator. Each local provider site will have patients directly involved in helping us explore the important research question of how far nationally derived trigger films resonate with local patient concerns and what additional work needs to be done locally to identify additional issues. They will then be engaged in co-designing services with staff, and monitoring the results. The researchers involved in the bid all have a track-record of working at the interface between research and practice, and take seriously the need for knowledge transfer.
Within TVHIEC, the results of the project will feed directly into future plans for innovative staff development, and will be extended to other conditions and sites. The TVHIEC user panel will be closely involved throughout the project. Nationally, the HIECs are working together to share learning and new approaches. We anticipate that the project would result in the production of a wide range of trigger films and a supporting service redesign methodology which would be available to other provider organisations through a subscriber website, in partnership with TVHIEC and the DIPEx Charity, which runs the Healthtalkonline website. We propose to hold two major dissemination events, one led by TVHIEC and one led by The King’s Fund, to ensure findings and recommendations are widely shared. We will of course also publish in peer review journals and present at national conferences, especially the SDO joint annual conference with the Health Services Research Network and the Organisational Behaviour in Health Care Symposium.
6. Plan of Investigation:
As noted above, our accelerated EBCD model is expected to halve the amount of time spent per care pathway in each trust. The figure below provides an overview of how our proposed timetable compares to a traditional EBCD cycle.

MONTHS 1–2
A core group (chaired by the Chief Investigator, Dr Louise Locock) and advisory group (chaired by Catherine O’Sullivan, Thames Valley HIEC Chair) will be established. In each site, a local service improvement facilitator will be identified and trained (by Glenn Robert) to lead the intervention. The ethnographer will begin observations, collate costing data from previous EBCD studies and put in place systems for recording economic data for AEBCD. The Oxford-based researcher will conduct secondary analysis of relevant interviews from the Health Experiences Research Group’s archive and develop a ‘trigger film’ around the first pathway.
MONTHS 3–4
The first trigger film will be shown at a workshop with a local patient and carer advisory group in each site, to test for resonance with their concerns and identify specific local service issues not adequately captured in the about their own experiences of the first care pathway and their views and expectations about local patients’ experiences. Findings will be presented and discussed at a staff feedback meeting in each site. In month 4, the local facilitators (supported by Glenn Robert) will lead a workshop on the first pathway, including the trigger film, with patients, carers and staff to begin the process of co-design. Participants will share their experiences of giving and receiving care and identify priorities for improvement. The ethnographer will conduct interviews and observations during this period. Meanwhile, the Oxford-based researcher will continue secondary analysis of relevant interviews from the archive to develop a ‘trigger film’ around the second pathway.
MONTHS 5–7
Co-design subgroups for pathway one will be established to respond to the agreed priorities for improvement; these may occur anywhere along the patient pathway. The ethnographer will continue observations and interviews, and monitor co-design activities and impact. Staff and non-staff cost data will be collected. Once the co-design groups for pathway one are established, the local facilitators will start work in month 7 on the second pathway, conducting staff observation and engagement, and showing the trigger film to a workshop of local patients. In month 4, the local facilitators (supported by Glenn Robert) will lead a workshop on the first pathway, including the trigger film, with patients, carers and staff to begin the process of co-design. Staff and patients will share their experiences of giving and receiving care and identify priorities for improvement. Evaluation fieldwork will continue throughout.
MONTH 8
Patients, carers and staff involved in co-design in each trust around the first pathway will conclude their activities and come together as a group to celebrate and share achievements and lessons from the collaboration. The local facilitators (supported by Glenn Robert) will lead a workshop in each site on the second pathway, including the trigger film, with patients, carers and staff to begin the process of co-design.
MONTHS 9–11
Co-design subgroups for pathway two will be established in each site to take forward their own work programme, supported by their local facilitator. Evaluation fieldwork continues.
MONTH 12
Those involved in co-design around the second pathway will conclude their activities and come together for a celebration event in each trust.
MONTHS 13–15
Complete evaluation fieldwork and analysis (ethnographer and Annette Boaz), collect any further health economics data on costs, compare with existing cost data on EBCD. Make recommendations to TVHIEC.
MONTHS 16–18
Dissemination workshops with The King’s Fund and TVHIEC. Preparation of final report and peer review articles. Trigger films and supporting service redesign methodology will be made available through a subscriber website.
7. Ethics
Assurances will be given to participants that all discussions and interviews are entirely confidential. All interviews and field notes will be coded for anonymity and stored in a locked filing cabinet. Participants identities will be protected through anonymisation or pseudonymisation of data as required. It is intended that anonymous abstracts from the interviews may be used in publications arising from this research but any materials will not be used without the full permission of participants.
The study team will ensure that it adheres to the Research Governance Framework with respect to confidentiality. Any communication by email will not identify participants and their identities will be protected by identity codes. Publication of direct quotations from research participants may be included in project outputs, such as the final report, conference presentations and articles submitted to peer reviewed journals. However, all identifying information about participants will be removed to ensure their anonymity and to protect their identity.
8. Insurance
The University of Oxford maintains Public Liability and Professional Liability insurance which will operate in this respect.
9. Project Management:
Funding has been included to enable the Thames Valley HIEC to provide project management support throughout the project. The new HIEC Programme Manager, Richard Freeman, will take on this role and will liaise with team members in different institutions to ensure each stage of the project is completed on time. We will establish a core group and a project advisory group at the outset of the project.
The project manager will convene regular meetings of both groups. The core group will comprise the coapplicants and project manager, and will be chaired by Louise Locock as Principal Investigator. The project advisory group will comprise staff, patient and carer representatives from both our partner provider sites, representatives from the Department of Health Public Engagement and Patient Experience directorate, and core group members. It will be chaired by Cathy O’Sullivan, Interim Director of the HIEC.
The individual components of the project will be managed on a day-to-day basis by Louise Locock (analysis of interview archive and production of trigger films), Glenn Robert (development and implementation of accelerated EBCD intervention), and Annette Boaz (evaluation). Glenn Robert will work closely with service improvement facilitators at Royal Brompton and Harefield and Royal Berkshire Hospitals, who will also have day-to-day managerial support within their trusts from Caroline Shuldham and Jonathan Fielden.
The investigators will be involved in reviewing drafts of the manuscripts, abstracts, press releases and any other publications arising from the study. authors will acknowledge that the study was funded by the NIHR SDO programme. Authorship will be determined in accordance with the ICMJE guidelines and other contributors will be acknowledged.
10. Service users/public involvement:
Both EBCD and the work of the University of Oxford Health Experiences Research Group are fundamentally concerned with giving patients (and family carers) a voice as the experts in what it is like to have their condition or face a particular health situation. The project team do not believe that including patients as participants in research is sufficient in terms of PPI and we have used many other ways of involving patients and public, for example in guiding our research strategy, as members of steering groups, in helping to appoint new researchers, disseminating results, co-authoring articles and commenting on conceptual frameworks.
The Health Experiences Research Group has been primarily focused on using in-depth patient narratives to support other people going through a similar condition or facing similar health choices, through www.healthtalkonline.org, as well as providing insights for personal professional practice. EBCD has used similar narratives to stimulate service improvement. Both use in-depth interviewing, with an initial unstructured invitation to ‘tell me your story’, to give people space to elaborate on what matters to them, not driven by a professional or organisational agenda. Both use video recording to enable patients to give vivid and direct testimony. A key principle at the heart of both these existing workstreams is that we should base our understanding of what matters to patients and carers on rigorously conducted and analysed research with a broad range of people, rather than relying on a few anecdotes or the involvement of one or two representatives on daunting NHS committees. At the same time, this project seeks to address the problem that trying to replicate such research in each locality for each pathway is not only expensive but very demanding of patients and carers who may be facing an extremely difficult and emotional time in their lives. We have recently compared themes emerging from the University of Oxford archive on what matters to patients in end of life care with interviews on the same topic done locally by one PCT. This demonstrated that very few themes were identified locally that could not have been identified from the national dataset (Calabrese, 2010). We therefore feel confident that the archive has great potential to be used as an evidence base of patient experiences to support service change.
Once the trigger films have been developed, Glenn Robert will work with our two provider partner organisations and their service improvement teams to identify a group of local patients and carers with an interest in intensive care and lung cancer. Stage one of their involvement will be a focus group workshop at which they will view the trigger films and then discuss whether the films adequately capture the things that matter to them, and whether there are specific additional issues they would like to raise about local services. Depending on the outcome of these discussions, some further local data collection may be undertaken by the service improvement team to supplement the national dataset. Stage two will be to convene co-design working groups of both staff and patients/carers, to agree and implement specific service redesign projects. Building a coalition between staff and service users is central to this process. The project advisory group will include patient and carer representatives from both our partner provider sites.
References:
- Bate SP, Robert G. Bringing User Experience to Healthcare Improvement: the Concepts, Methods and Practices of Experience-Based Design. Oxford: Radcliffe Publishing; 2007.
- Calabrese J. A Comparison of Data on Patient Experiences of End of Life Care. Oxford: Green Templeton College; 2010.
- Daly K, Willis K, . A hierarchy of evidence for assessing qualitative health research. J Clin Epidem 2007;60:43-9.
- Dopson S, Locock L, Chambers D, Gabbay J. Implementation of evidence-based medicine: evaluation of the Promoting Action on Clinical Effectiveness programme (PACE). J Health Serv Res Policy 2001;6:23-31.
- Fitzgerald L, Dopson S, Buchanan D, Bryman A. Handbook of Organizational Research Methods. London: Sage; 2009.
- Greenhalgh T, Russell J, Swinglehurst D. Narrative methods in quality improvement research. QSHC 2005;14:443-9.
- Iles V, Sutherland K. Organisational change: a review for health care managers, professionals and researchers. London: SDO; 2001.
- Locock L. Maps and Journeys: Redesign in the NHS. Birmingham: University of Birmingham; 2001.
- Pettigrew AM, Ferlie E, McKee L. London: Sage; 1992.
- Piper D, Iedema R. Emergency Department Co-Design Program 1 Stage 2 Evaluation Report. Sydney: Centre for Health Communication (UTS) and NSW Health; 2010.
- Ritchie J, Spencer L, Bryman A, Burgess RG. Analyzing Qualitative Data. London: Routledge; 2004.
- Equity and Excellence: Liberating the NHS. London: HMSO; 2010.
This protocol refers to independent research commissioned by the National Institute for Health Research (NIHR). Any views and opinions expressed therein are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the SDO programme or the Department of Health.
APPENDIX A CO-INVESTIGATORS
Dr Glenn Robert
Senior Research Fellow, National Nursing Research Unit
PhD, MSc, BA (Combined Hons)
King’s College London
James Clerk Maxwell Building, 57 Waterloo Road, London, SE1 8WA
Sue Ziebland
Research Director, Health Experiences Research Group
BA, MSc
University of Oxford
2nd Floor, 23-38 Hythe Bridge Street, Oxford, OX1 2ET
Dr Vicky Harrison
Policy director, Health Experiences Research Group
BA, MA, DPhil
University of Oxford
2nd Floor, 23–28 Hythe Bridge Street, Oxford, OX1 2ET
Dr Annette Boaz
Lecturer in Translational Research, Division of Health and Social Care Research
BA, MSc, PhD
King’s College London
7th Floor, Capital House, 42 Weston Street, London, SE1 3QD
Dr Caroline Shuldham
Director of Nursing and Clinical Governance
MSc, PhD
Royal Brompton and Harefield NHS Hospital Foundation Trust
Sydney Street, London, SW3 6NP
Dr Jonathan Fielden
Chief Medical Officer/Director Clinical Standards
FRCP, FRCA, BSc, MB, ChB
Royal Berkshire NHS Foundation Trust
London Road, Reading, RG1 5AN
Dr Farasat Bokhari
Post Lecturer, Division of Health and Social Care Research
Qualifications PhD
Employer King’s College London
Work Address 42 Weston Street, London, SE1 3QD
Appendix 2 Information and consent materials approved by Research Ethics Committee
Letter of invitation to patients/carers
Patient/carer information sheet
Patient/carer consent form
Letter of invitation to staff (baseline discovery interview)
Letter of invitation to staff (evaluation interview)
Staff information sheet
Staff consent form (observation)
Staff consent form (interview)
Appendix 3 Evaluation data collection tools
Patient feedback event
Staff feedback event
Patient and staff event
Celebration event – patients and relatives
Celebration event – staff
AEBCD celebration event observation sheet
Reflective diary
Co-design event participant feedback
Co-design event summary
Service improvement log
| Area of improvement (co-design group focus) | Activity | No. of staff involved | Time taken (total) | Enablers to implementation | Barriers to implementation | Observed outcomes (including testimonials, observations, etc.) |
|---|---|---|---|---|---|---|
Participation interview topic guide
Name:
Role:
Date:
About yourself and the service
What is your role in the Trust?
What do you consider to be the main issues in your service?
This project
What made you get involved in AEBCD?
What are your hopes from this partnership?
EBCD uses an external professional researcher as process facilitator whereas AEBCD uses an internal clinical researcher for this role. What do you consider to be the advantages and disadvantages of the latter?
EBCD uses films made by patients in each participating hospital whereas AEBCD uses a national video archive of patient narratives. What do you consider to be the advantages and disadvantages of the latter?
Contribution to service delivery
How do you envisage the results of the project will feed directly into future plans for innovative staff development?
How is AEBCD addressing the priorities highlighted at the NHS White Paper ‘Equity and
Excellence: Liberating the NHS’ on ‘putting patients and the public first’?
How can AEBCD help maintain quality of patient experience despite cuts in staffing?
The future of this project
How do you see AEBCD contributing to sustainable service improvement?
How do you envisage AEBCD and footage of health experiences being promoted through a subscriber website to train staff in other wards?
Is there anything else you would like to add?
Exit interview topic guide
Could you briefly describe your role in the Trust?
Tell us the story of your involvement in this project:
Experience of being interviewed
Experience of attending events: patient, staff, staff and patient and/or celebration event
Experience of watching the film
Contribution of project participation to career development
Has this project been different to other improvement projects you have been involved in?
Tell us one successful story and one not so good or a disappointment
Do you think the service is more efficient now?
Do you think the service is safer now?
What has improved in terms of the patient experience?
What have been the most important parts of the project/process from your perspective? Why were they important?
Anything you should have done differently as part of the process (i.e. to make it better?)
How have you found working closely with patients/staff? Has working closely with patients/staff made a difference? Was it as you expected it to be?
Would you recommend this for other staff to get involved with? Can you give reasons as to why you might recommend it?
Are there any aspects of the service that you still think need to be improved urgently?
What do you think will happen now? Will the work continue? In what way/form? What is needed for change to continue?
Do you think the outcomes of the project can be measured through current methods of performance management? How might they best be measured?
If other parts of the hospital were interested in adapting the approach what advice would you give them?
Do you feel that these questions have covered your experiences? Is there anything else that you would like to add?
Thank you very much for all your thoughts and time.
Patient group interview topic guide
Experience of participating in the different stages of this project
Being invited to take part
Attending the patient event
Seeing the film
Attending the staff – patient event
Seeing the film again
Participating in co-design
Perceptions of co-design
Patient-doctor relationships
Service improvement process
Impact on self
Positive: confidence, engagement with services, recovery
Negative: time, travel
Cost data collection spreadsheet
| Participants | ||||||
| Activity types | ||||||
| Interview | ||||||
| Event (staff/patient/staff-patient) | ||||||
| Co-design group meeting | ||||||
| Meeting (facilitators training, advisory group meeting, internal meetings) | ||||||
| Other (please specify) | ||||||
| Participants | ||||||
| Nurse (Trainee, Sister, Matron) | ||||||
| Physiotherapist | ||||||
| Occupational Therapist | ||||||
| Speech and Language Therapist | ||||||
| Doctor (Trainee, Qualified) | ||||||
| Consultant | ||||||
| Administrator (Secretarial support) | ||||||
| Manager (ICU manager, PPI lead, Research Officer) | ||||||
| Patient/Relative | ||||||
| Other (please specify) | ||||||
| Expenses | ||||||
| Catering | ||||||
| Travel expenses | ||||||
| Materials (flipcharts, pens) | ||||||
| Other (please specify) | ||||||
| Facilitator | ||||||
| Activity | ||||||
| Interview | ||||||
| Event (staff/patient/staff-patient) | ||||||
| Co-design group meeting | ||||||
| Admin/communication | ||||||
| Meeting (facilitators training, advisory group meeting, internal meetings) | ||||||
| Teleconference | ||||||
| Other (please specify) | ||||||
| Participants | ||||||
| Date | Activity | Comments | Participants | Band | Time (minutes) | Hourly rate (£) |
| Expenses | ||||||
| Date | Activity | Comments | Cost | |||
| Facilitator | ||||||
| Date | Activity | Comments | Participants | Comments | Time (minutes) | Hourly rate (£) |
Appendix 4 Membership of project advisory panel
Cathy O’Sullivan, Chief Executive, Thames Valley Health Innovation and Education Cluster (chairperson).
Annette Boaz, Lecturer in Translational Research, School of Medicine, King’s College London (from January 2013: Reader, Health Care Research, St. George’s, University of London and Kingston University); co-investigator and evaluation lead.
Farasat Bokhari, Lecturer in Health Economics, King’s College London; co-investigator (until August 2012).
John Cain, Public and Patient Experience and Engagement Directorate, Department of Health.
Jocelyn Cornwell, Director, the Point of Care Programme, The King’s Fund.
Maureen Dalziel, Trustee, Intensive Care National Audit and Research Centre.
Jonathan Fielden, Medical Director, Royal Berkshire NHS Foundation Trust (from July 2012: Medical Director, University College London Hospitals NHS Foundation Trust); co-investigator.
Richard Freeman, Programme Manager, Thames Valley Health Innovation and Education Cluster; study project manager (until January 2013).
Melanie Gager, Senior Sister, Intensive Care, Royal Berkshire NHS Foundation Trust; service improvement facilitator.
Ashley Green, Support and Development Manager, British Lung Foundation.
Sharon Hegginbottom, lung cancer patient.
Louise Locock, Deputy Research Director, Health Experiences Research Group, Primary Care Health Sciences, University of Oxford, and Health Experiences Fellow, NIHR Oxford Biomedical Research Centre; principal investigator.
John Pearcey, Cancer Service Manager, Royal Brompton and Harefield NHS Foundation Trust; service improvement facilitator.
Glenn Robert, Professor of Healthcare Quality and Innovation, National Nursing Research Unit, King’s College London; co-investigator and intervention lead.
Caroline Shuldham, Director of Nursing and Clinical Governance, Royal Brompton and Harefield NHS Foundation Trust; co-investigator.
Alasdair Short, Trustee, Intensive Care National Audit and Research Centre.
Gordon Sturmey, intensive care patient.
Ruth Tollyfield, Senior Sister, Intensive Care, Royal Brompton and Harefield NHS Foundation Trust; service improvement facilitator.
Sonia Vougioukalou, Research Associate, School of Medicine, King’s College London; project evaluation ethnographer (from February 2013: Public Engagement Associate in Health Sciences, Centre for Public Engagement, University of Bristol).
Carl Waldmann, Consultant in Intensive Care, Royal Berkshire NHS Foundation Trust.
Jane Woodhull, Clinical Nurse Specialist, lung cancer, Royal Berkshire NHS Foundation Trust.
Sue Ziebland, Research Director, Health Experiences Research Group, Primary Care Health Sciences, University of Oxford; co-investigator.
List of abbreviations
- AEBCD
- accelerated experience-based co-design
- CI
- co-investigator
- CNS
- clinical nurse specialist
- EBCD
- experience-based co-design
- FCE
- finished consultant episode
- GMC
- General Medical Council
- HERG
- Health Experiences Research Group (University of Oxford)
- HIEC
- Health Innovation and Education Cluster
- ICU
- intensive care unit
- MDT
- multidisciplinary team
- NICE
- National Institute for Health and Care Excellence
- OD
- organisational development
- PAR
- participatory action research
- PI
- principal investigator
- REC
- Research Ethics Committee
- TVHIEC
- Thames Valley Health Innovation and Education Cluster