Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its proceeding programmes as project number 10/1007/26. The contractual start date was in April 2011. The final report began editorial review in January 2013 and was accepted for publication in May 2013. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
the University of Warwick received funding from NIHR in order to support this work; this money was provided to the institution and not to any of the authors, other than to cover relevant travel expenses.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2014. This work was produced by Sujan et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction
This report explores the risks to patient safety associated with failures of clinical handover within the emergency care pathway, and it investigates organisational factors that affect the quality of handover. Organisational factors relate to inner tensions within the activity of handover that require trade-offs, and to the management of the flow of patients across organisational boundaries and organisational cultures.
Findings are presented from a multidisciplinary qualitative study that investigated patient handover in three NHS emergency care pathways in England. The study was funded by the National Institute for Health Research (NIHR) Service Delivery and Organisation (SDO) programme, Department of Health. The study was led by a research team based at Warwick Medical School, University of Warwick, in collaboration with researchers from Hampshire Hospitals NHS Foundation Trust, Oxford University Hospitals NHS Trust, United Lincolnshire Hospitals NHS Trust, and Heart of England NHS Foundation Trust.
This research was justified by the broad agreement among relevant organisations, such as the British Medical Association (BMA), the Joint Commission and the World Health Organization (WHO) that clinical handover represents a crucial element in patient care, and that handover failures constitute considerable risks to patients. This is particularly true for the dynamic and time-critical emergency care pathway, where there is a recognised need for further research. 1–3
This project was designed in response to a call issued by the NIHR SDO on patient safety. The NIHR had previously funded research in patient safety that evidenced gaps in the existing knowledge base. In particular, the organisational dimension of patient safety was perceived to require further investigation. One of the highlighted areas for further research was around the safety problems when patients cross care boundaries, either interdepartmental or interorganisational. The study described in this report investigated the risks associated with failures of handover within the emergency care pathway, thus focusing on communication across organisations (ambulance services and hospitals), as well as across departmental boundaries [emergency department (ED), acute medicine]. The findings should be of use to practitioners and policy-makers as a basis on which to inform their decisions about possible improvements to the handover process.
Patient on a spinal board
The vignette below (Box 1) describes the case of a patient with suspected spinal injury, who was left in a cubicle in the ED without the nurse being aware. The ambulance crew (AC) had done a handover to the nurse co-ordinator, but were unable to do a handover to the nurse looking after the patient, as they needed to get back out on to the road in order to continue to deliver emergency response services in the community.
The project aimed to investigate systematically such risks arising from failed handover, and to describe the underlying organisational complexities that contribute to such failures.
The ED was busy due to of icy roads, and a large number of people being involved in road traffic collisions. The patient was the driver of a car involved in a low-speed collision, but had complained of neck and back pain at the scene. They were subsequently immobilised in a collar and head blocks, and put on a spinal board. On arrival in the ED, the patient was allocated to a bed space. The receiving nurse for that cubicle was not available to hand over to, so the crew independently transferred the patient on to a trolley, removed the spinal board, but left the patient immobilised. The crew then left. Shortly afterwards the patient was assessed by a doctor and nurse, and cervical spine radiographs were ordered. This necessitated the patient being on a firmer orthopaedic mattress to enable lateral transfer while maintaining spinal alignment. The crew had not been aware of the need for the patient to be on a special mattress, and in the absence of the nurse on transfer, and no handover having taken place, this important piece of equipment was missed initially. To resolve the issue, extra manual handling of the patient was required to get the patient on to another orthopaedic stretcher then lift them on to an orthopaedic mattress, with the consequences being increased staff time, delays in investigation for the patient and the clinical risks of increased handling of a potentially spinally injured patient.
Aims and objectives
The purpose of this study was to provide a systematic description of the risks associated with failures of clinical handover within the emergency care pathway, and to elicit and to describe staff perceptions on common organisational factors that impact on the quality of handover. The study focused on investigating interorganisational and interdepartmental handover.
The project addressed the following research questions:
-
R1 What is the potential risk of clinical handover failures along the emergency care pathway?
-
R2 What are common organisational deficiencies that affect clinical handover in the emergency care pathway, and what impact does the organisational model of emergency care delivery have?
The detailed objectives of the project were:
-
O1–1 To identify and to systematically describe clinical handovers within the emergency care pathway.
-
O1–2 To describe failure trajectories through the pathway and to systematically assess the potential risks of handover failures.
-
O1–3 To assess the frequency with which particular types of information are communicated, and the language forms that are used.
-
O2–1 To identify common organisational deficiencies that affect clinical handover in the emergency care pathway.
-
O2–2 To describe the impact on handover of the organisational model of care delivery within the emergency care pathway.
-
O3–1 To provide recommendations for improving clinical handover in the emergency care pathway.
Study design
Setting
Organisations participating in this study were two English NHS ambulance services and three English NHS hospitals [ED and acute medical ward or clinical decision unit (CDU)]. Each ambulance service provides emergency care in the catchment area of one particular study hospital and conveys patients there. The ambulance service providing transportation to the third study hospital felt unable to participate in this study. As a result, no observational, audio or interview data involving ambulance service staff were collected in the third pathway.
Participating organisations were chosen to reflect a range of characteristics in terms of the population they serve and their organisational structure (large inner city hospital; teaching hospital in an area with above average prosperity and life expectancy; district general hospital in a rural area with a large proportion of migrant workers). Below is a brief description of each of the five participating organisations.
Ambulance service A Ambulance service A serves a population of approximately 5.3 million people, and provides emergency transportation to the ED at hospital C. The population is ethnically diverse, and the area being served includes both deprived as well as prosperous areas, urban as well as rural. The ambulance service responds to approximately 800,000 emergency and urgent incidents annually. In 2011–12, the ambulance service achieved the targets for responding to category A calls [category A8 (CatA8) = 76.3%, category A19 (CatA19) = 98%].
Ambulance service B Ambulance service B serves a population of approximately 4 million people, and provides emergency transportation to the ED at hospital D. The population characteristics include wealthy areas with above-average life expectancy, as well as deprived areas. The ambulance service responds to approximately 500,000 emergency and urgent incidents annually. In 2011–12, the ambulance service achieved the targets for responding to category A calls (CatA8 = 75.9%, CatA19 = 95.3%).
Hospital C Hospital C is part of a large NHS Foundation Trust. The hospital provides services for a population of about 440,000. It provides local services to a very deprived community with ethnic diversity, as well as some specialist services for a wider population. The area has high infant mortality, teenage pregnancy and other markers of health inequalities. The hospital has a capacity of approximately 750 beds. The ED provides care for approximately 110,000 patients per year, with an admission rate of about 20%. The department has five resuscitation bays, with a dedicated paediatric resuscitation bay. The department has 25 other adult bays. There is an eight-bedded CDU that cares for 3500 patients a year. The ED has its own radiography department with the picture archiving and communications system (PACS). There is access to both computed tomography (CT) and magnetic resonance imaging scanning. There is mobile ultrasound within the ED. There is a fully separate children’s area within the ED, with eight cubicles and a separate waiting area. Approximate staffing levels within the ED for a 24-hour weekday are nine foundation-year doctors over five staggered shifts, seven to ten middle-grade doctors over six staggered shifts, three advanced clinical practitioners (ACPs) over three staggered shifts up to midnight only, and three or four consultants over two staggered shifts up to 22:00 only, as well as eight qualified nurses of different grades, three unqualified health-care assistants (HCAs), and two ED practitioners during both day and night. The acute medical ward is located some distance from the ED on the same floor, and has 24 beds.
Hospital D Hospital D is part of a NHS trust comprised of four teaching hospitals. The hospital provides services to a population of approximately 650,000 (including 150,000 city central). The population is slightly younger than the regional and national average, and it has above-average health and life expectancy. The hospital has a capacity of approximately 850 beds. The ED provides care for approximately 90,000 patients per year, and 25% of these attendances are children. There is a separate children’s area with seven cubicles and its own waiting room. In 2011–12 the ED met the 95% 4-hour total time indicator. The department has four resuscitation bays: three adult bays and one paediatric bay. The department has 16 other major cubicles and a geographically separate ambulatory area (minors), consisting of nine cubicles. Approximate staffing levels within the ED for a 24-hour weekday are 18 medical staff (comprising two or three consultants, seven middle-grade doctors and eight junior doctors), 11 or 12 qualified nurses, one HCA, one emergency nurse practitioner (ENP) and one paediatric nurse during the day and nine qualified nurses during the night. The emergency assessment unit (EAU) is located adjacent to the ED, on the same floor as the intensive care unit (ITU), on level 1 of the hospital. It has 29 single-sex beds catering for acute ED and medical patients. The short-stay ward (< 96 hours) has 36 beds and is located on level 6 of the main hospital, and the long-stay ward (> 96 hours) has 110 beds and is located on the seventh floor of the same block.
Hospital E Hospital E is a district general hospital forming part of a NHS trust comprising three hospitals. The hospital provides services to a population of approximately 300,000. The hospital has a capacity of approximately 400 beds. The ED provides care for approximately 49,000 patients per year. In 2011–12 the ED fell short of the 95% 4-hour total time indicator (83%). The department has three resuscitation bays. The department has 19 other bays. Approximate staffing levels within the ED for a 24-hour weekday are seven medical staff, seven qualified nurses, two HCAs, one ENP and nine qualified nurses during the night. The acute medical ward is located behind the ED and has 27 beds.
Table 1 provides a basic comparison of the participating EDs. Table 2 shows the accident and emergency (A&E) national quality indicator data for the corresponding trusts for July 2012 (a trust can comprise several hospitals, hence the data are for more EDs than the ones participating in the study).
| Hospital | Population | Beds | Annual A&E attendances | A&E bays |
|---|---|---|---|---|
| C | 440,000 | 750 | 110,000 | 30 |
| D | 650,000 | 850 | 90,000 | 36 |
| E | 300,000 | 400 | 49,000 | 22 |
| Trust | A&E attendances | Patient left before being seen (%) | Reattendance (%) | Time to initial assessment (median; minutes) | Time to treatment (median; minutes) | Total time in A&E (median; minutes) |
|---|---|---|---|---|---|---|
| C | 21,731 | 4.5 | 6.8 | 0 | 65 | 148 |
| D | 10,068 | 4.5 | 5.7 | 40 | 111 | 188 |
| E | 12,618 | 3.2 | 6.3 | 2 | 53 | 139 |
In the remainder of this report, the term ‘study site’ or ‘site’ refers to the pathway consisting of ambulance services bringing patients to ED, the ED, and the acute medicine ward in the respective hospital for ambulance service A/hospital C, and ambulance service B/hospital D, and the pathway consisting of ED and acute medicine ward at hospital E.
Methods
The study design utilised a multidisciplinary qualitative research approach organised into two research strands. The methods used within each research strand will be described in detail in the corresponding section for the two research strands (see Chapters 3 and 4). A summary is provided in Box 2.
The aim of this research strand was to describe the potential risk of clinical handover failures along the emergency care pathway. The main data sources used were:
Qualitative risk analysisInformal observations.
Nine focus-group-based risk analysis sessions.
Conversation analysis50 audio-recordings of handovers for resuscitation patients.
90 audio-recordings of handovers for patients with major injuries.
130 audio-recordings of patient referrals from ED to acute medicine.
Research strand 2: organisational factors influencing handoverThe aim of this research strand was to describe common organisational deficiencies that affect clinical handover in the emergency care pathway, and to describe the impact of the organisational model of emergency care delivery.
Thematic analysis39 semi-structured interviews conducted with a purposive convenience sample of stakeholders in pre-hospital and hospital-based emergency and acute care.
A stakeholder workshop was held at the College of Emergency Medicine, London, in July 2012, to validate findings and to provide input on recommendations generated by the research.
Project timeline
The study commenced in April 2011 and was completed in December 2012. A summary of the timeline for the different project activities is provided in Table 3.
| Activity | Duration |
|---|---|
| Ethics and institutional approvals | April 2011 to August 2011 |
| Research strand 1 | September 2011 to July 2012 |
| Research strand 2 | March 2012 to November 2012 |
| Recommendations and draft final report | November 2012 to December 2012 |
Some challenges occurred in the early phases of the project. One organisation withdrew from the study following an organisational merger prior to the start of the project. An additional organisation needed to be recruited and this incurred a delay of about 6 months until data collection could be started at this site. Prolonged unsuccessful negotiations with one ambulance service about institutional approvals delayed data collection at the corresponding hospital for about 4 months. The local Principal Investigator at one of the participating organisations had an illness-related absence for 4 months. This led to delays in data collection at this site. In light of these challenges a no-cost extension was requested and granted resulting in the revised end date of 31 December 2012 (the extension was for a period of 3 months from 1 October 2012 to 31 December 2012).
Research ethics
The study had full NHS research ethics approval from South Birmingham Research Ethics Committee (reference 11/WM/0087) as well as institutional approval at all participating organisations.
All study participants were staff of the participating organisations. Participants received a participant information leaflet, and provided written consent prior to their involvement. Participation was voluntary, and participants were free to withdraw at any time. Patient handovers were audio-recorded with the permission of participants, and the audio-recordings were subsequently transcribed and all identifiers removed from the transcript. The same process applied to the interviews. If participants did not consent to the audio-recording then the handover was not included in the data collection, and handwritten notes were taken during the interviews.
Report structure
The report is organised as follows:
Introduction Section just covered. Introduction to the research.
Background Background to the research and the relevant literature.
Risk analysis research strand Research strand 1: aims and objectives, detailed explanation of methods used for data collection and analysis, presentation and discussion of results.
Organisational factors research strand Research strand 2: aims and objectives, detailed explanation of methods used for data collection and analysis, presentation and discussion of results.
Discussion Findings of the two research strands and input received from the stakeholder workshop are brought together. Limitations of the study.
Conclusion Implications for health care and recommendations for research are described.
Appendices Additional data and materials.
Chapter 2 Background
Introduction
This chapter provides a brief overview to the background of the research and the relevant literature. A short section summarises the knowledge about the extent of preventable harm to patients (see Harm to patients). The following two sections describe key insights about risks posed to patient safety resulting from handover and communication failures in different care settings (see Handover as a risk to patient safety) and specifically in emergency care (see Handover and communication in emergency care). The chapter concludes with a description of identified research gaps (see The need for further research) that informed the development of the present study.
Harm to patients
It is now widely recognised that patients across all health-care systems may suffer preventable harm resulting from inadequate care provided. Since the publication of the landmark Institute of Medicine (IoM) report To Err is Human4 in the USA, and the UK Department of Health report An Organisation with a Memory,5 there has been a significant increase in research about patient safety and the factors that contribute to or adversely affect the delivery of safe care to patients. The IoM report included earlier findings of the Harvard Medical Practice Study6 that studied 30,000 discharges from 51 hospitals in New York State and concluded that around 3.7% of patients had suffered an adverse event during the course of their treatment. Around half of these were found to be preventable. The IoM report extrapolated these figures and estimated that there may be as many as 98,000 deaths in the USA resulting from medical error. Since, further studies in the USA as well as in other countries, including the UK, have found similar and often slightly higher figures. 7–12 There is now available a wealth of research from different medical specialties and different countries that indicates that health care is a high-risk domain where patients may be harmed, for example in surgery13,14 or medicines management and prescribing. 15,16
In addition to causing needless harm and suffering to patients, poor-quality health-care provision has significant financial implications for the health systems. In the UK, a study estimated that preventable adverse events could cost the NHS £1B annually in additional bed-days alone. 8 A report published by the Health Foundation compiles further evidence illustrating some of the costs associated with poor quality in health care. 17 For example, the costs to the NHS associated with adverse drug events are estimated to be around £0.5–1.9B annually.
Handover as a risk to patient safety
The purpose of handover
Handover denotes ‘the transfer of professional responsibility and accountability for some or all aspects of care for a patient, or group of patients, to another person or professional group on a temporary or permanent basis’. 18 Handover may occur between members of the same profession, for example during nursing shift change, or between individuals belonging to different medical professions or even different organisations, such as the ambulance service handover to the ED. Handover is a frequent and highly critical task in clinical practice, as it ensures continuity of care and provides clinicians with an opportunity to share information and plan patient care. 19
Handover is often regarded as a unidirectional activity, for example in analogy to sports as ‘passing the baton’ or similar. Ideally, however, handover should be thought of as a joint activity and a dialogue that creates shared awareness and provides an opportunity for discussion and error recovery as participants bring different perspectives and experiences to this interaction. 20–24 This includes not only the ‘telling of the story’ by the person giving the handover, but also interpretation and confirmation of the story, and the development of a mental model by the recipient of the handover, which allows seamless transition of care. 22 In addition, handover can serve further functions other than simple information transfer. These may include aspects of training, socialisation, and enhancing teamwork and group cohesion. 23,25
Handover failures contribute to patient harm
Communication failures are a recognised threat to patient safety. 4 In 2009, Johnson and Arora26 wrote that ‘the buzz generated by these [research, policy and improvement] efforts has resulted in handovers jostling for top position as one of the hottest topics in the global patient safety arena’. There is certainly now a large body of evidence, including a number of systematic reviews that suggest that inadequate handover practices are putting patients at risk. 27–31 Inadequate handover can create gaps in the continuity of care and contribute to adverse events. 32 A report prepared by the Joint Commission states that breakdown in communication was the leading root cause of sentinel events reported during 1995–2006. 33 The report further suggests that miscommunication during handover between medical providers contributed to an estimated 80% of serious medical errors. 33 A survey of 161 internal medicine and general surgery physicians in training in one US hospital found that 59% of respondents reported harm to one or more patients caused by inadequate handover, and 12% reported that the resulting harm had been major. 34 A survey of physicians in training on an acute paediatric ward found that in 31% of the surveys received the physician on call during the night reported that something happened for which they were not adequately prepared. The study suggests that these may have been linked to inadequate handover, as the quality of handover was rated below average on nights when something happened. 35
Some of the consequences and adverse events associated with inadequate handover include hospital complications and increased length of stay following multiple handovers,36 treatment delays,20,37 repetition of assessments,38 confusion regarding care,39,40 inaccurate clinical assessments and diagnosis and medication errors,41 and avoidable readmissions and increased costs. 33
Contributory factors leading to inadequate handover and communication
The existing literature on communication and handover in health care identifies a large number of contributory factors that may lead to inadequate handover. These include the following.
Lack of adequate standardisation
A frequently identified contributory factor is the absence of adequately structured handover processes. 26 Interviews conducted in an Australian hospital found that 95% of participants did not identify a formal procedure for shift-change handover. 38 A qualitative study comparing handover practices to pit stop practices in motor car racing concluded that handover had no clear procedures and was not supported by formal checklists. 42 A focus group-based study involving junior doctors found that shift handover was perceived as frequently being conducted in an ad hoc or chaotic fashion, and without obvious leadership. 43
Inadequate documentation and over-reliance on documentation
Another contributory factor discussed in the literature is missing and inaccurate documentation, or inadequate reliance on documentation. A study observing nursing handover of 12 simulated patients found that purely verbal handover resulted in information loss fairly quickly, whereas verbal handover supported by a typed handover sheet suffered only minimal information loss. 44 On the other hand, the use of such handover sheets may potentially make the handover more vulnerable by detracting from the focus on the most relevant items. 45 Over-reliance on medical records was reported in a study that investigated handover and communication between doctors and nurses. 46 This study found that often there was inadequate communication, and, as a result, there were disagreements on issues such as planned medication changes (42%), planned tests (26%) and necessary procedures (11%).
Non-verbal behaviour does not support building of shared understanding
Although the content of handover has been studied frequently, less is known about how non-verbal behaviour influences the quality of handover. A recent study in a number of US Department of Veterans Affairs (VA) medical centres investigated types of non-verbal behaviour in nursing and physician handover. The authors concluded that participants frequently adopted forms of non-verbal behaviour that may result in suboptional transfer of information. 47 Such forms of non-verbal behaviour included holding patient lists or other artefacts in such a way that they could not be seen by the other participant (‘poker hand’), not having a joint visual focus (‘parallel play’) and situations where the person giving the handover was standing while the other party was sitting, which resulted in hurried handovers with fewer questions (‘kerbside consultation’). The most productive form of non-verbal behaviour was reported to be the joint focus of attention, where both parties co-ordinate their verbal and visual attention jointly on an object.
Lack of organisational priority given to handover and absence of training
The literature suggests that a lack of organisational priority given to handover, and the absence of formal training in communication and handover both at universities as well as within health-care organisations are further barriers to the implementation of effective handover. 26 A recent interview study investigating transitions from primary care into hospital suggested that participants perceived handover as an administrative burden that took away time for their patient care duties. The study also found that handover and communication competencies were rarely taught, and that clinicians learned these skills ‘by being around and immersed in the clinical effort’. 48 A national survey of internal medicine training programmes in the USA found that 60% of these did not provide training in handover. 36 One study reports that junior doctors had not received any training in handover, and that, as a result, they had a narrow view of handover concerning only completion of outstanding tasks. 43 Arora et al. 49 present a competency-based approach to improving handover that entails the development of a standardised instructional approach to teach communication skills and the establishment of corresponding robust assessment systems.
Standardisation of handover communication
The most frequently encountered recommendation for improving handover communication is that of standardisation through procedures, checklists or mnemonics, and appropriate training in their use. 31,42,49,50 Standardisation may simplify and structure the communication, and create shared expectations about the content of communication between information provider and receiver. 51 The Joint Commission introduced in 2006 a requirement for organisations to implement a standardised approach to handover. 28,52 The specific communication protocol recommended is situation, background, assessment, recommendation (SBAR),53 which provides a general order to topics. 51 A review of different handover mnemonics found that SBAR was the most favoured approach in practice. 31 As part of a simulation study, final-year medical students were taught the SBAR approach. The study found that this improved their handover performance during the simulation compared with students who had not received this training. 54 In the UK, trauma guidelines often include now the use of the ATMIST (age, time, mechanism, injury, signs, treatments) handover tool. The NHS Litigation Authority Risk Management Standards 2012–13 require an approved documented process for handing over patients. 55 This requirement stresses in particular consideration of the out-of-hours handover process, and emphasises the need for monitoring of compliance.
Handover and communication in emergency care
The characteristics of emergency care create additional challenges for handover
In the ED, the risks arising from inadequate communication and handover may be even more significant than in other areas, and the environment may be more conducive to communication failures. EDs have been described as high-risk contexts characterised by overcrowding conditions that pose particular threats to patient safety, such as ambulance diversions, treatment delays owing to long wait times, and patients leaving the ED without being seen. 1,56
Handover and communication taking place in such settings of high patient acuity and overcrowding are particularly vulnerable and pose significant risks not only to the patients being handed over, but also to other patients requiring urgent care. 20,57 The IoM report states that ineffective handover has been identified as one of the leading causes of medical error in the ED. 1
Problems with shift handover in the emergency department
Several studies have investigated shift handover in the ED. 58 An ethnographic study in five EDs found that practices varied significantly, and that they lacked structure and standardisation. 24 An Australian study investigating doctors’ shift handover in three EDs using a post-handover questionnaire and a survey tool found that in around 15% of cases required information was not handed over. 39 The missing information related predominantly to aspects of management, investigations and patient disposition. Participants stated that this resulted in repetition of assessments and delay in management of the care. The study found that handover failures were particularly likely for patients with longer stays in the ED, who received multiple handover.
Handover across boundaries is of particular importance in emergency care
There has been less research investigating handover across organisations,59,60 although this is starting to change. This area is of particular importance because of cultural differences, often high levels of uncertainty and absence of clear diagnosis, pending test and investigation results creating opportunities for omission, and the more vulnerable state of the patient, for whom delays or other handover failures may have serious consequences. 60 A systematic review of the literature pertaining to handover from ambulance services to EDs published in 2010 identified eight relevant studies. 27 The studies included in the review describe a number of barriers to effective handover. These include the lack of common language, perceived lack of active listening skills, lack of clear leadership, multiple repeated handovers, and inadequate environmental conditions. A subsequent ethnographic study found that the quality of handover between ACs and ED nurses appeared to be dependent on staff expectations, prior experience, workload and working relationships. 61
Similar results were found by studies that investigated the transfer of patients from ED to the hospital. In a survey of ED and internal medicine physicians, around 30% of respondents reported that one of their patients had experienced an adverse event or a near-miss following transfer from ED. 60 The survey identified communication problems, unsuitable work environment, information technology (IT) issues, and unclear allocation of responsibility as contributory factors. Participants in an interview study referred to the communication between ED and hospital physicians as ‘grey zone’ characterised by information ambiguity. 20 The conflicting information expectations of physicians from the different specialties represented a particular barrier to efficient handover communication. Randell and colleagues62 developed a descriptive model of handover that links the strategies that the participants of the handover adopt to the different contexts within which handover may take place and to the different functions that handover can serve. They provide examples, taken from observations in eight different settings, including an EAU and Medical Admissions Unit, of how practitioners adapt their behaviour and provide flexibility to the handover in response to, for example, different workload and staffing levels or particular patient conditions.
Improving handover in emergency care
Suggestions for improvement of handover include the adoption of structured communication protocols,20,51,60,61,63,64 the creation of opportunities for interdisciplinary, interdepartmental and interorganisational collaboration,60,61 the introduction of IT across departmental and organisational boundaries,60 and the teaching of appropriate communication skills20 including shared training programmes across organisations. 61
The need for further research
A systematic review of the literature on handover in hospitals up to 2008 argued that many of the severe risks to patient safety could be found in handover across departments, and that efforts at standardisation that are confined to departments may even exacerbate the situation for interdepartmental handover. 28 The review concluded that there was no reliable body of evidence that standardisation of handover provided sustainable improvements in patient outcomes. This insight and the brief review above suggest that current research is limited by its predominantly narrow focus on transfer of clinical content and the adherence to a standardised communication protocol,26,50,65 and the equally narrow focus on shift handover or handover within a single department. 48,66 Further research is required that addresses the following:
-
The role of handover in the wider network of activities of each actor Further research is required that goes beyond consideration of the transfer of clinical content. This research should investigate the role that handover plays in the wider network of activities of each actor. The research should provide descriptions and models of the goals and motivations of the actors and their resulting needs and behaviours, and of the structural and organisational environment within which handover and the actors’ other activities take place. 60,65 This would enable better understanding of the risks that arise from handover failures and their underlying causes. Such a broader view might also contribute to understanding why standardisation of communication has not achieved its potential,47 and it may provide insights as to when and how standardisation could improve handover practice.
-
The embeddedness of handover in the activities and goals of actors across departments and organisations The second area where further research is required is in understanding handover across organisational boundaries. Different organisations have different goals and exhibit different local cultures and behaviours. 26 Handover across organisations implies that these differences have to be reconciled and overcome through negotiation and adaptive forms of behaviour. Further research should provide qualitative accounts and models that describe how handover is embedded in the activities and goals of actors across departments and organisations, and how the actors achieve the alignment of their different individual and organisational motivations and backgrounds. Such research could be particularly useful to understanding risks that arise from unclear allocation of responsibility for patient care across organisational boundaries, enabling organisations to develop necessary systems of collaboration, responsibility and escalation.
Chapters 3 and 4 describe in detail how the research project contributed to each of the two domains identified above.
Chapter 3 Systematic identification and analysis of the potential risks of clinical handover failures
Introduction
Research strand 1 was concerned with the identification and analysis of the risks associated with handover failures in the emergency care pathway, using methods from improvement science and safety engineering. This chapter summarises the aims and objectives of the research strand (see Aims and objectives) and then briefly describes the principles of systematic risk analysis (see Principles of risk analysis). Longer sections describe in detail the methods used (see Methods) and the results obtained (see Results). A discussion concludes the chapter (see Discussion).
Aims and objectives
The aim of this research strand was to identify and to analyse systematically the risks of clinical handover failures within the emergency care pathway.
Specific objectives were:
-
O1–1 To identify and to describe systematically clinical handovers within the emergency care pathway.
-
O1–2 To describe failure trajectories through the pathway and to systematically assess the potential risks of handover failures.
-
O1–3 To assess the frequency with which particular types of information are communicated, and the language forms that are used.
Principles of risk analysis
Undertaking a systematic risk analysis is a legal requirement in safety-critical industries. 67 The purpose of systematic risk analysis is to inform the risk management process on the ways in which harm can occur, the frequency with which these may occur, and the severity of the harm should it present itself. Risk analysis is a proactive approach, i.e. the analysis takes place before a harm event has occurred, and it may even be applied before a system or service is operational in order to demonstrate adequate safety and fitness for purpose.
Following risk analysis, the risk management process usually entails steps to determine appropriate risk controls (risk reduction measures), to implement the risk controls and to monitor their effectiveness. 68 These subsequent steps were outside the scope of the project.
In the safety engineering community there is the distinction between ‘hazard’ and ‘risk’. A hazard denotes a situation that may lead to harm. Risk is a description of the likelihood of occurrence of the hazard and the severity of the consequences. The Health and Safety Executive defines these terms as:67
-
Hazard ‘The potential for harm arising from an intrinsic property or disposition of something to cause detriment.’
-
Risk ‘The chance that someone or something that is valued will be adversely affected in a stipulated way by the hazard.’
Consequently, systematic risk analysis entails identification of relevant hazards and subsequent investigation of the risks posed by these. Risk analysis can be carried out in a number of ways. It becomes ‘systematic’ when there is a formal process describing and guiding how it is carried out. Risk analysis can be both qualitative as well as quantitative. In many high-risk industries both forms are used. There is a range of methods supporting the risk analysis process, such as failure mode and effects analysis (FMEA),69 hazard and operability studies,70 fault tree analysis71 and event tree analysis. 72 In practice, several of these are usually utilised in order to provide a broad and comprehensive characterisation of risk.
Increasingly, policy-makers in health care recognise the need for proactive assessments of threats to patient safety. In particular, the use of FMEA is now recommended widely in health care as an appropriate tool for proactive safety analysis. For example, the Joint Commission requires from participating organisations evidence that they carry out at least one proactive assessment of a high-risk process every year,52 FMEA being the approach recommended. The US VA has developed an FMEA version tailored to health care, health-care failure mode and effects analysis. 73 During the past few years, FMEA has been used in health care to assess the risks associated with, for example, organ procurement and transplantation,74 intravenous drug infusions,75 blood transfusion76 and communication in the ED. 77
The approach to risk analysis adopted in this project to identify and describe the risks associated with handover failures in the emergency care pathway follows largely the standard FMEA approach for qualitative hazard identification and risk analysis. This will be described in detail for this research strand in the next section.
Methods
Systematic description of clinical handover within the emergency care pathway
For the purpose of this study of handover, the emergency care pathway consists of handover from the ambulance service to the A&E department, handover within the A&E department, and handover (or referral) from the A&E department to the acute medical unit (AMU) or CDU, where the majority of patients that are admitted to hospital go to from A&E. The focus of the study was on handover involving patients with major injuries and resuscitation patients, as the risks arising from handover failures are greater for this category of patients.
Familiarisation with the pathway by the researcher at each site was achieved through process walks and informal observation. Together with process mapping these are widely adopted improvement science methods, and are recommended by bodies such as the Institute for Healthcare Improvement in the USA78 and the NHS Institute for Innovation and Improvement in the UK. 79 Process mapping was also a key tool for understanding the discharge process as part of the HANDOVER project funded by the European Union. 80 The purpose of the familiarisation phase was to enable the researcher to build an initial understanding of the flow of activities, and to identify suitable staff roles for participation in the subsequent process mapping session.
Process mapping is an improvement method based on the focus group approach. 81 It has been used traditionally as part of quality improvement initiatives, such as ‘Lean’. 82,83 The aim of process mapping is to provide a graphical representation of the process, which represents a shared understanding of all the stakeholders involved. Process mapping is a quick way of providing a relatively simple (compared with, for example, more resource-intensive ethnographic approaches) graphical representation of how work unfolds in practice. The group setting that is a characteristic feature of focus groups is useful for stimulating discussion among participants, where they can present their unique point of view, be made aware of possibly differing points of view of their colleagues and comment on their respective experiences. This is very relevant to process mapping, as each staff role or actor will have their own goals in addition to the overarching shared process goal, and each will usually see only part of the process and will thus be less familiar with the steps preceding or following their own.
For each pathway, a half-day process mapping session was held in order to produce a graphical representation of the process. The graphical representation used was a simple sequential flow diagram. Figure 1 illustrates the elements of the graphical notation used. Each session was held on the premises of the respective A&E department and involved a purposive convenience sample of participants from ambulance services (for ambulance service A/hospital C and ambulance service B/hospital D), the A&E department and the AMU or CDU. Two members of the project team with experience in conducting process mapping (NR and MS) facilitated the process mapping sessions together at each site. Table 4 provides a detailed breakdown of participants by role. The output of the process mapping session was a graphical representation of the process generated by the participants.
FIGURE 1.
Sequential process mapping graphical elements.
| Role | Ambulance service A, hospital C | Ambulance service B, hospital D | Hospital E |
|---|---|---|---|
| Paramedic | 2 | 1 | – |
| A&E senior nurse (co-ordinator) | 1 | 2 | 1 |
| A&E staff nurse | 1 | 1 | 1 |
| A&E consultant | 2 | 1 | 1 |
| A&E middle-grade doctor (registrar) | 1 | 1 | 1 |
| Acute medicine senior nurse | 1 | 1 | – |
| Acute medicine middle grade (registrar) | 1 | 1 | 1 |
| Total | 9 | 8 | 5 |
The sequential process map provides a description of the key steps of a process. It is an abstraction and simplification. The opposite extreme is represented by ethnographic approaches that provide a ‘thick description’ of human behaviour and the context within which it takes place. 84,85 Following such an in-depth approach was not part of the project design. In order to complement the sequential process map with some contextual description, participants were prompted to consider who is involved in each process step, what each actor’s respective goals are, what kind of external or cognitive tools the actors are using, and what kind of tacit knowledge is called upon in order to carry out the process step. The template used to represent individual process steps is shown in Table 5. The terminology is derived from Activity Theory, an approach rooted in cultural–historical psychology. 86,87
| Actor | Goal | Artefacts (external tools, cognitive tools) | Rules (tacit knowledge, social rules) |
|---|---|---|---|
| Staff roles involved in carrying out a particular activity | The goals of each of the actors | The external and internal (cognitive) tools that are used to accomplish the goals, e.g. documents, procedures | The informal rules and the knowledge that regulates how staff behave within the team/within their work place, e.g. knowledge of what is usually done |
Systematic risk identification and risk analysis
The identification and analysis of risks associated with failures of handover was achieved through the application of standard FMEA. 69 FMEA is a proactive, inductive, bottom-up approach for analysing systems in order to evaluate the main vulnerabilities and the potential for failures. 88 FMEA originated in the reliability engineering community as a tool to enhance the reliability of military equipment. It is now a widely adopted technique across industries.
Failure mode and effects analysis considers the possible failures of a system component (failure modes) and determines potential consequences of such a failure on the system. FMEA is systematic in that this process is repeated for every component and every failure mode. Failure modes are prioritised based on the risk they pose. The risk is described as a multiplicative combination of the likelihood of occurrence of the failure mode and the severity of the consequences. In some forms of FMEA a third parameter, the likelihood of detection of the failure, is included in the calculation. These values are usually based on expert judgement. FMEA is particularly useful for identifying single failures that could result in catastrophic consequences. Owing to its systematic approach, FMEA is considered very resource intensive. 68
Failure mode and effects analysis is usually utilised to contribute to the identification of hazards and the qualitative risk analysis of technical systems. As a result, there are often well-established lists of possible failure modes, sometimes with corresponding quantitative failure rates, on which the analyst can draw. Depending on the situation, FMEAs for technical systems are conducted by a single or a small number of engineers. For use in sociotechnical systems, the approach needs to be adapted. In health care, the application of FMEA typically is based on the focus group approach, similar to the process mapping described above. FMEA requires a ‘system description’ and this is usually derived from a process map in health care. In addition, one of the biggest benefits of the application of FMEA in health-care settings is the interaction created among stakeholders in the group setting. 89 The application of FMEA in health care commonly is not as detailed and not as exhaustive as for technical systems due to resource constraints.
One member of the project team (MS) with experience in conducting FMEA facilitated two half-day FMEA sessions at each site with the participants who had already contributed to the process mapping. At the start of the session, the facilitator explained the aims of the session and provided a brief introduction to FMEA. The process map produced during the preceding process mapping session was used as the basis for the analysis. A template sheet was used to record the results of each FMEA (Table 6). Discussion of process steps selected for analysis was restricted to 1 hour maximum per step in order to ensure broad coverage of the process given the time available for the risk analysis. Ratings for the likelihood of occurrence and the severity were determined according to the rating scheme described in Table 7. This rating scheme was developed and agreed during a project meeting. The descriptions have been chosen pragmatically through discussion with the aim of providing a spectrum of scores that would be used fully (i.e. all scores were deemed to be likely to be used during the FMEA). Conflicting views of study participants were resolved in discussion, where the aim was not to reach a consensus (e.g. an averaged risk score) – rather, the discussions were aimed at providing insights into the different assumptions and interpretations about the task at hand. Once participants had a common frame of reference, conflicts usually disappeared and led to the identification of additional failure modes or a differentiation of the consequences, rather than an averaged-out consensus risk score. For some of the highest-ranking risks, contextualised failure trajectories (described as ‘vignettes’ in this report) were produced subsequently in discussion with stakeholders. These are based on examples that participants provided during the FMEA sessions to illustrate the failure modes. The contextualised failure trajectories are, therefore, grounded in actual experiences, but should not be regarded as objective description of an actual case as they represent one or several individuals’ recollection of events that may have happened some time ago. The purpose of these failure trajectories is to provide a more realistic and contextualised description of risks to people who have not participated in the risk analysis sessions, and who may find reading an abstract template sheet difficult. Hence, factual accuracy is not necessary. The failure trajectories also enable better appreciation of the multiple contributory factors and underlying organisational complexities than is possible with the abstract tabular FMEA representation alone.
| Step | Failure Mode | Consequences | Likelihood | Severity | Risk Score | Causes | Mitigation |
| Value | Likelihood | Severity |
|---|---|---|
| 1 | Less than once a year | No harm or increased length of stay |
| 2 | Less than once a month | Non-permanent minor harm or increased length of stay |
| 3 | Less than once a week | Non-permanent major or permanent minor harm |
| 4 | Less than once a day | Permanent major harm |
| 5 | Once a day or greater | Death |
Assessment of the frequency of information types and language forms used
To provide an in-depth description of the verbal communication act of handover, three different types of handover that include the transfer of responsibility for patient care were selected for the study with a focus on interorganisational and interdepartmental handover. The three different types of handovers selected were (1) paramedic to A&E nurse (major injuries); (2) paramedic to senior A&E doctor (resuscitation cases); and (3) telephone referrals from A&E doctor to AMU (or CDU) doctor or senior nurse (major injuries).
Patient handovers were audio-recorded by members of the project team during daytime (0800–1800) for a period from November 2011 to July 2012, on days when the researcher was on site. Prior to the recording, participants were asked to provide verbal consent to ensure that they were still happy for the researcher to capture this particular episode. Participants had already provided written consent before the start of the data collection period. The audio-recordings were subsequently transcribed and all identifiers removed.
In the original research plan, the objective of this activity was to provide a frequency count of the types of content communicated during handover as a proxy measure for the reliability of handover compared with a core data set. It was intended to use this information as input to the systematic risk analysis to act as prompts for participants to consider. However, the data collection started later than anticipated, and the data collection process was slower than expected. In particular, collecting data for resuscitation cases proved to be difficult, as these are less frequent occurrences and, owing to their highly critical nature, asking for consent and audio-recording the episode was not always possible. As a result, the project team decided to complete the systematic risk analysis without the input provided from this activity. Instead, it was decided to extend the analysis of these handovers to consider both content as well as language forms used to communicate the content.
Conversation analysis (CA) was used to describe the content and the language form used for each handover. 81,90 CA is an approach to the study of social interaction based on the notion of turn-taking behaviour. The spoken utterances of each participant represent turns, which are both facilitated by and dependent on the behaviour and utterances of the other participant. Such sequences of turn-taking often exhibit stable and recurring patterns that are characteristic of particular types of social interaction. The notion of repair relates to behaviours that participants employ to deal with problems in the interaction.
Conversation analysis was chosen as analytic approach for two reasons. A previous study91 used discourse analysis to develop a handover assessment tool based on the analysis of a small sample of 15 handovers from ED physicians to hospital doctors. Following a similar approach would allow comparison of the findings. Secondly, CA is a useful tool to provide a better understanding of how difficult aspects of the handover communication are generated and dealt with, for example the transfer of responsibility or coping with situations of uncertainty.
The project team discussed the coding categories used in the previous study91 in a review meeting. Two small changes were introduced to the originally proposed coding categories. It was felt that the category ‘history’ was broad and may hide some of the issues of particular interest to the study, such as the social situation and background of patients. As a result, this category was split into two separate categories: ‘clinical history’ and ‘social history’. The second change was the introduction of the category ‘injury’, as this is an integral part of ambulance service handovers that follow the age, time, mechanisms, injury, signs, treatments (ATMIST) protocol and it may fall ambiguously between the original categories ‘history’ and ‘symptom’. No other changes were introduced in order to stay as close as possible to the coding categories of the reference study. The resulting coding scheme is shown Tables 8 and 9.
| Coding category | Definition |
|---|---|
| Patient presentation | |
| Patient identifiers | Statements that convey patient identifiers such as name, date of birth or hospital number |
| Clinical history | The patient’s past medical problems/conditions that are pertinent to the current diagnosis or clinical impression |
| Social history | The patient’s social circumstances describing, for example housing situation and existing care arrangements, family or friends accompanying, etc. |
| Injury | Statements that convey the mechanisms and the injuries sustained |
| Symptom | Descriptions and explanations that provide information about symptoms of concern |
| Procedure | Statements about pertinent laboratory data, pertinent test results, medications, and evaluation that already been performed to address the patient’s current condition |
| Assessment | |
| Treatment | Statements about future medical procedures to be taken to address the patient’s current problem |
| Clinical impression | Identification of the current clinical impression, naming the problem or reasons for the problem |
| Prognosis | Probabilistic statement about patient’s future condition based on completed or proposed treatments |
| Outcome | Definite utterances about the result of the handover, e.g. accept, not accept, wait and see |
| Transfer of responsibility | Statements about what was being asked of the recipient of the handover |
| Professional environment | |
| Logistic processes | Descriptive or evaluative talk about logistics or procedural issues in ED, hospital or health-care system |
| Courtesies | Statements such as ‘thank you’, greeting and closing remarks, etc., which provide a context of professional courtesy |
| Coding category | Definition |
|---|---|
| Information seeking | |
| Closed question | An utterance that is designed to solicit specific information |
| Open question | An utterance that is designed to solicit information in a manner that affords the respondent the opportunity to elaborate |
| Clarifying question/request | An utterance that is a question designed to seek clarification of another’s immediately preceding utterance; may take the form of a request |
| Information giving | |
| Description | Utterances that provide description about the patient and the patient’s past or present condition and circumstances |
| Explanation | Utterances that state the facts and make an inference about the patient |
| Rationale | A justification is offered to account for any medical procedures, tests, medications or recommendations concerning the patient; the intent is to justify why an action has been taken or will be taken in the future |
| Directive | Advisements, orders or recommendations that inform patient evaluation, treatment and disposition |
| Context talk | Talk about contextual issues in clinical environment such as logistics and procedures |
| Social amenities | Utterances in which physicians exchange courtesies and talk that tells the sender that the receiver is paying attention |
| Decision | Utterances in which the physician accepts or does not accept the patient; may be directly stated or implied |
| Information verifying | |
| Read-back | Statements that paraphrase or restate what the other has said |
Two members of the project team with a human factors and a clinical background (MS and PC respectively) coded an initial sample of 30 transcripts of audio-recordings collaboratively to allow familiarisation with the coding scheme. Ambiguities and uncertainties were resolved in discussion. One researcher (PC) subsequently coded the remaining audio-recordings independently. Simple frequency counts of handover content and language form were performed for each type of handover and for each study site.
Findings from existing literature, the reference study,91 and the output of the risk analysis informed the exploration of potentially problematic aspects of the communication, such as the transfer of responsibility. All transcripts were reread, and patterns of turn-taking were identified and described through examples.
Results
Systematic description of clinical handover within the emergency care pathway
A summary description of the emergency care pathway for each site is provided below. For each site, the pathways for resuscitation patients and patients with major injuries are described, from ambulance services into the ED and to the AMU (or CDU), with a particular focus on communication and handover (i.e. predominantly clinical steps such as ‘treat patient’ have been described at the highest, most abstract level). Further details about the different motivations or goals of the actors involved, and the tools and knowledge they may use can be found in Appendix 1. An in-depth analysis of the content and language forms of particular types of handover within the pathway is described in the Results section below (see Content and language form of handover). The interviews conducted as part of research strand 2 provide further insights into how people perceive these handovers.
Ambulance service A/hospital C
The graphical representation of the pathway for resuscitation patients is shown in Figures 2 and 3, and the representation for the pathway for patients with major injuries is shown in Figures 4 and 5. The complementary tabular descriptions are included in Appendix 1.
FIGURE 2.
Hospital C resuscitation pathway – part 1. DOB, date of birth; ETA, expected time to arrival; NIC, nurse in charge.
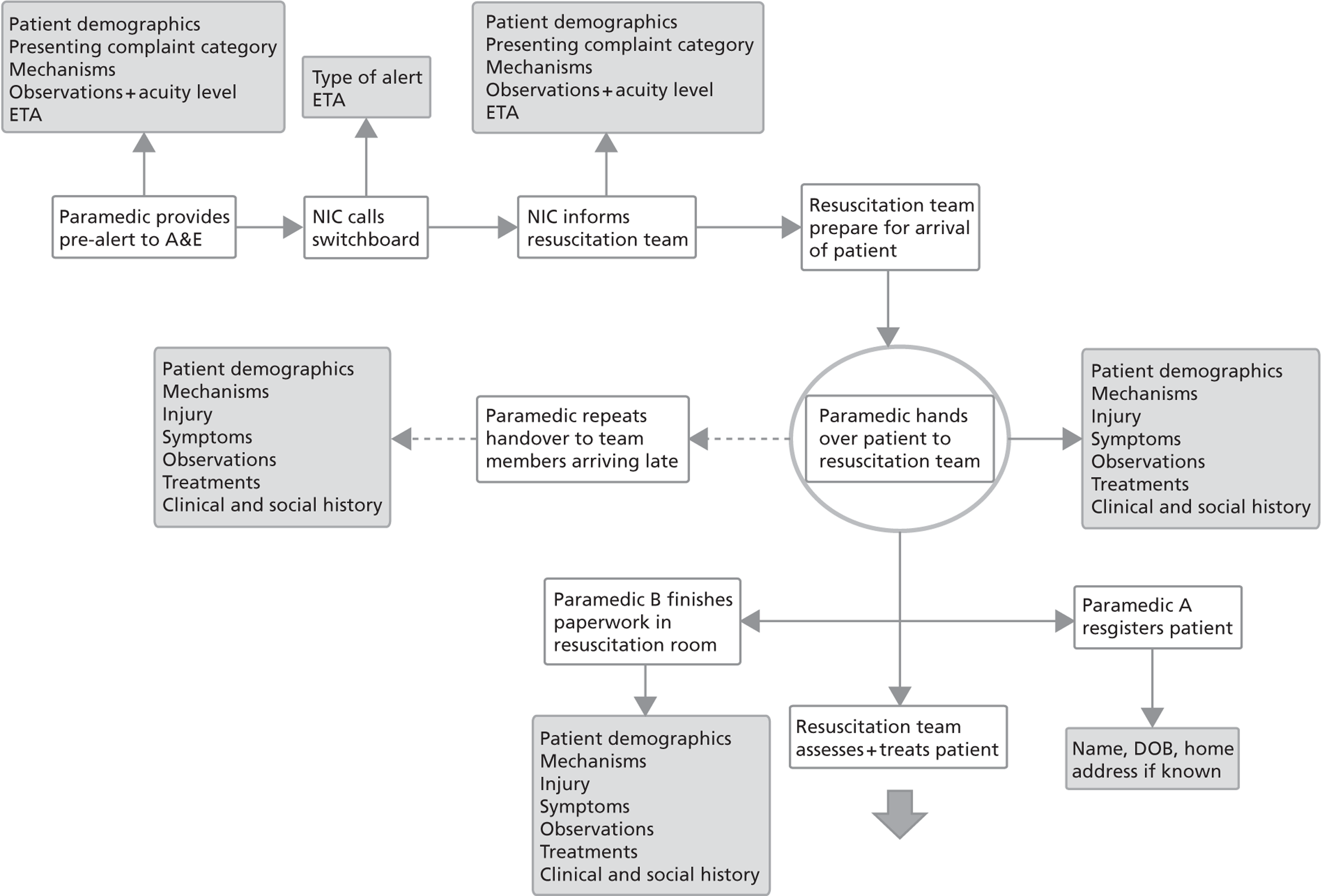
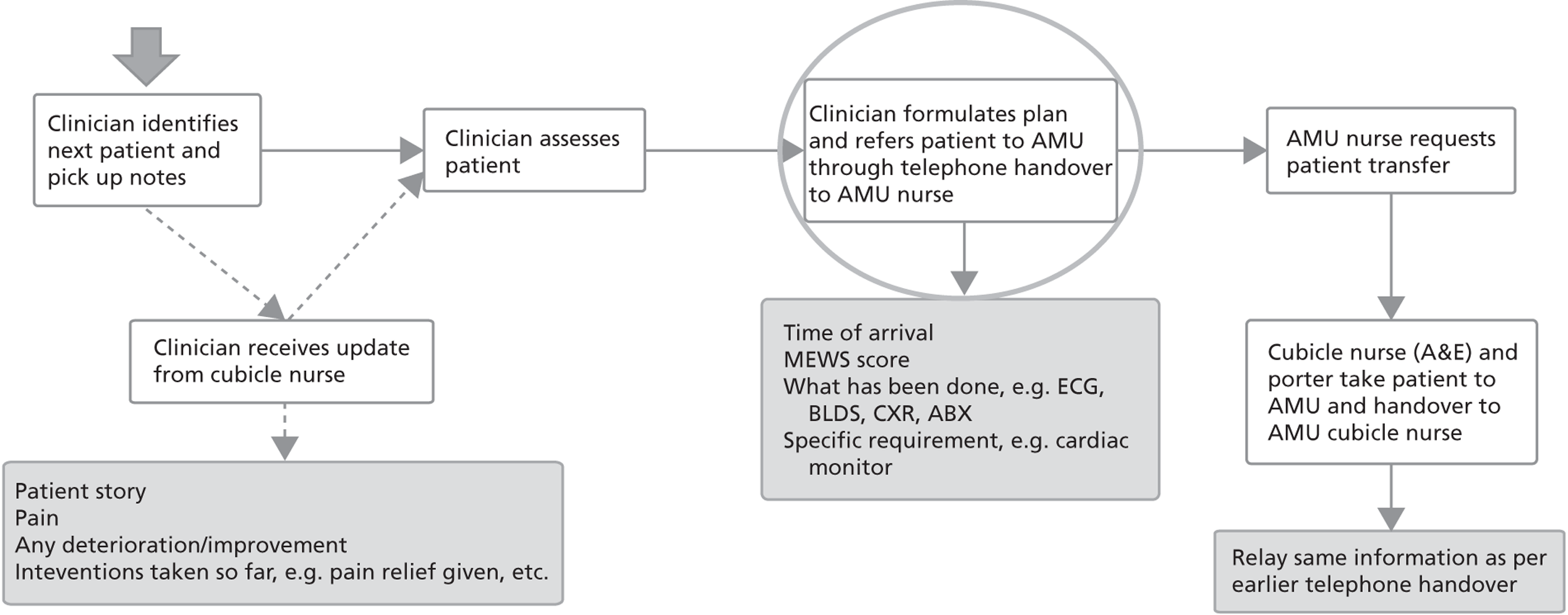
FIGURE 3.
Hospital C resuscitation pathway – part 2. ABX, antibiotics; BLDS, bloods (blood tests); CXR, chest X-ray; ECG, electrocardiogram; MEWS, Modified Early Warning Score.
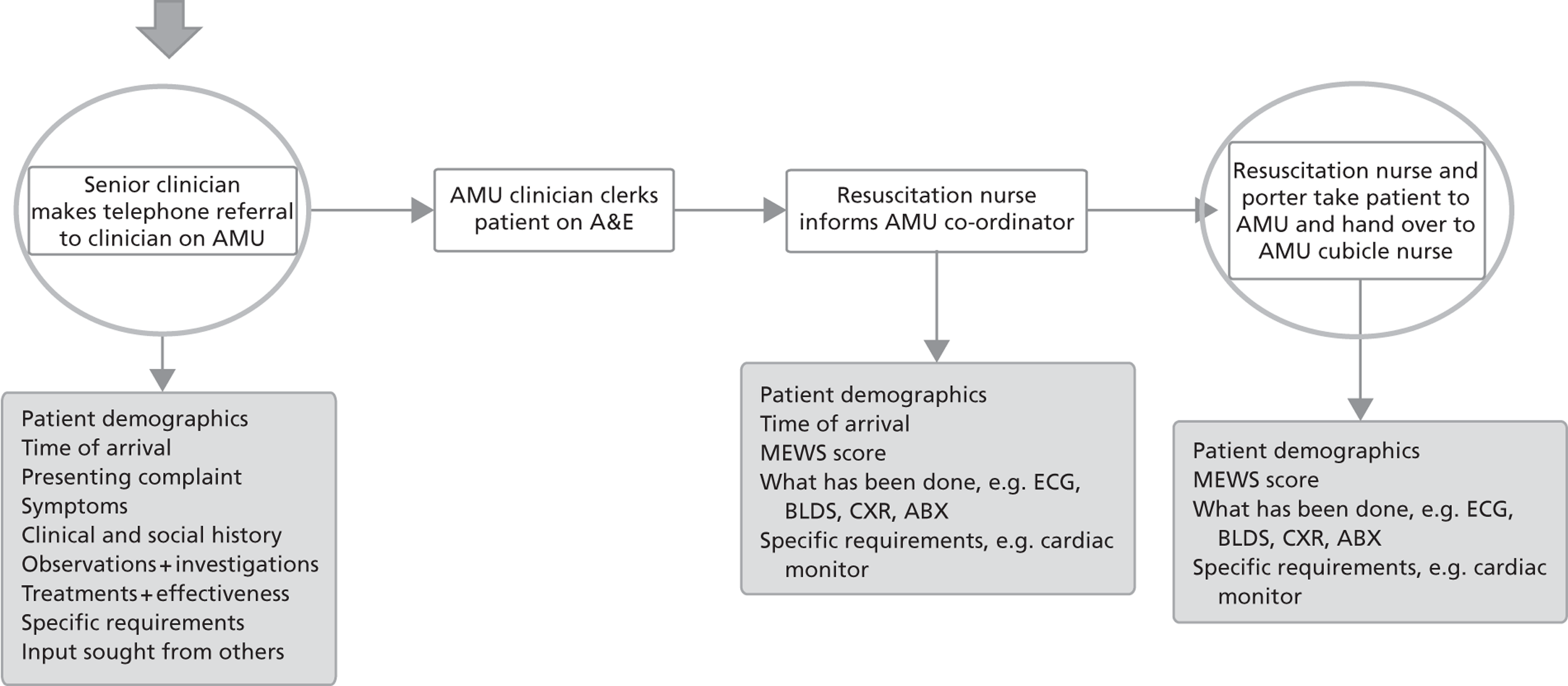
FIGURE 4.
Hospital C major injuries pathway – part 1. ACC, ambulance control centre; BLDS, bloods (blood tests); DOB, date of birth; ETA, expected time to arrival; MEWS, Modified Early Warning Score.
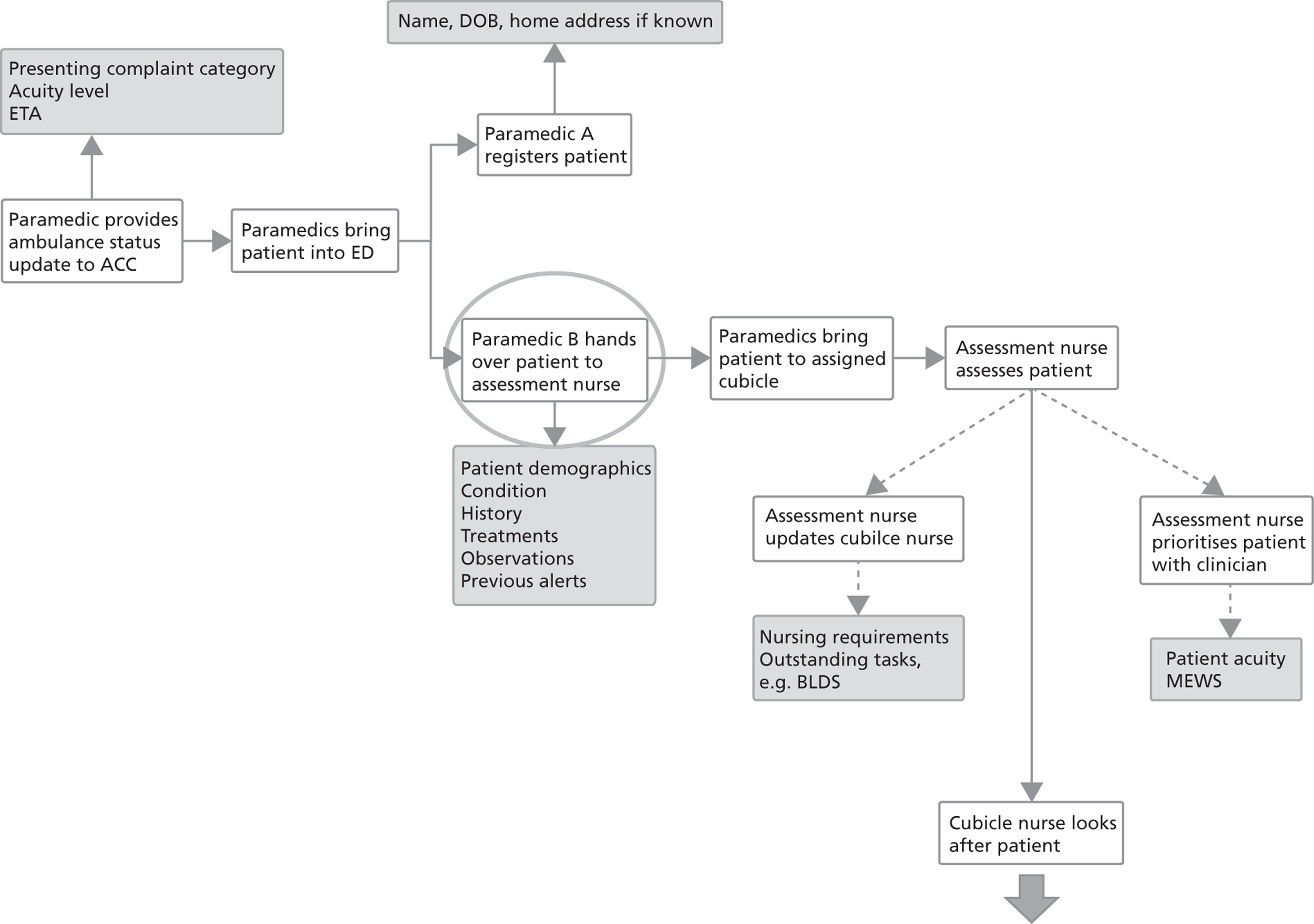
FIGURE 5.
Hospital C major injuries pathway – part 2. ABX, antibiotics; BLDS, bloods (blood tests); CXR, chest X-ray; ECG, electrocardiogram; MEWS, Modified Early Warning Score.
In the resuscitation pathway, the first type of handover may occur when the ambulance service [either the AC or the ambulance control centre (ACC) having received this information from the AC] provides a pre-alert to the hospital ED, providing initial information about patient demographics, presenting complaint category, patient acuity and expected time of arrival. This handover provides an anticipatory and logistic function. The A&E resuscitation team uses this information to inform and to assemble the appropriate staff members and other teams (e.g. trauma team), to prepare the resuscitation bay and to ensure that necessary equipment is available. The next type of handover occurs when the ambulance arrives at the ED and the patient is brought into the resuscitation room. One AC member hands over to the senior clinician (in this organisation the term clinician is used refer to roles that make decisions on the treatment of patients, such as doctors of different grades, ACPs and ENPs) information including patient demographics, clinical history, mechanisms and details of injury, assessments done by the AC, any treatments undertaken, and the known medication history. The social history is not usually handed over at this stage. The handover should follow the ATMIST communication protocol. Although the handover is to the senior clinician, other team members listen in, and they may have questions themselves. This handover is considered the main handover between the ambulance service and the ED. It serves the dual functions of communication of immediately relevant clinical information and of transfer of responsibility for patient care. Sometimes, aspects of the handover are repeated when team members arrive after the handover. The AC member remains in the resuscitation room during the first part of the assessment in order to finish the paperwork and to be available for further questions. The patient report form (PRF) is an important tool for the handover, as it documents all the information that was available to the AC, even if some of this was not verbally handed over (e.g. social history). It provides an archival function, enabling future access to information. The second crew member registers the patient at reception, where another secondary handover occurs including patient demographics. This handover provides a logistic function.
The next handover occurs when a decision to admit has been taken, and the senior clinician makes a telephone referral to a clinician on the AMU. This telephone handover includes patient demographics, presenting complaint, observations and investigations done, any treatments that have been done and their effectiveness, as well as a request for referral, either explicit or implicit. This telephone handover is considered as another point at which there is a transfer of responsibility for patient care, although practically the patient remains under the care of the ED. In addition to the referral, there are two further handovers between A&E and AMU. The resuscitation nurse gives a nursing handover to the AMU co-ordinator on the telephone. This involves the communication of information including patient demographics, Modified Early Warning Score (MEWS), assessments and treatments done, specific requirements, and the time of arrival of the patient in the ED. This handover provides both an anticipatory and logistic function. The second handover occurs face to face, when an A&E nurse and the porter take the patient to AMU. This handover communicates the same information as the previous telephone handover but this time the handover is to the nurse who will be looking after the patient. This handover entails a full transfer of responsibility for patient care.
For patients with major injuries there is not normally a pre-alert. The AC typically provides a brief status update to their control centre, communicating basic details about presenting complaint category, patient acuity and expected time of arrival to allow monitoring and oversight of ambulance activities. This information is also available to the hospital ambulance liaison officer (HALO), who is stationed in the ED. The first handover to the ED occurs when the AC arrive at the ED with the patient. This handover is a verbal handover to an assessment nurse at the rapid assessment triage (RAT) point, and it potentially includes all of the clinical and social information that the AC has gathered, for example patient demographics, clinical and social history, symptoms, and any assessments and treatments done. The PRF supports the handover. The assessment nurse triages the patient and instructs the AC to take the patient to a dedicated cubicle. This handover is perceived to include a transfer of responsibility for patient care, and this is documented by signing the PRF. In parallel to this handover, the second crew member registers the patient and does a basic handover to the receptionist, providing a logistic function. The assessment nurse then goes to do an in-depth assessment of the patient. There may be optional, additional handovers depending on the acuity of the patient and the workload and availability of the cubicle nurse. The assessment nurse may prioritise the patient with the physician or may instruct the cubicle nurse to undertake certain activities. The latter serves the purpose of delegation of aspects of patient care. A further optional handover may occur if the cubicle nurse provides an update on the patient to the clinician who comes assess the patient. The next handover occurs when a decision to admit is taken, and the clinician refers the patient to AMU through a telephone handover to the AMU nurse co-ordinator. On the AMU side, this handover is supported by a SBAR checklist. This is again perceived as a transfer of responsibility for patient care, providing both an anticipatory and logistic function. The final handover occurs when an A&E nurse takes the patient to AMU and hands over to the nurse looking after the patient. This handover entails a full transfer of responsibility for patient care.
Ambulance service B/hospital D
The resuscitation pathway is identical to hospital C as far as the basic steps are concerned. There are small variations in terms of tools used. For example, there is a dedicated ATMIST reporting form next to the telephone where pre-alerts are received. However, in most aspects the resuscitation pathway is standardised across organisations.
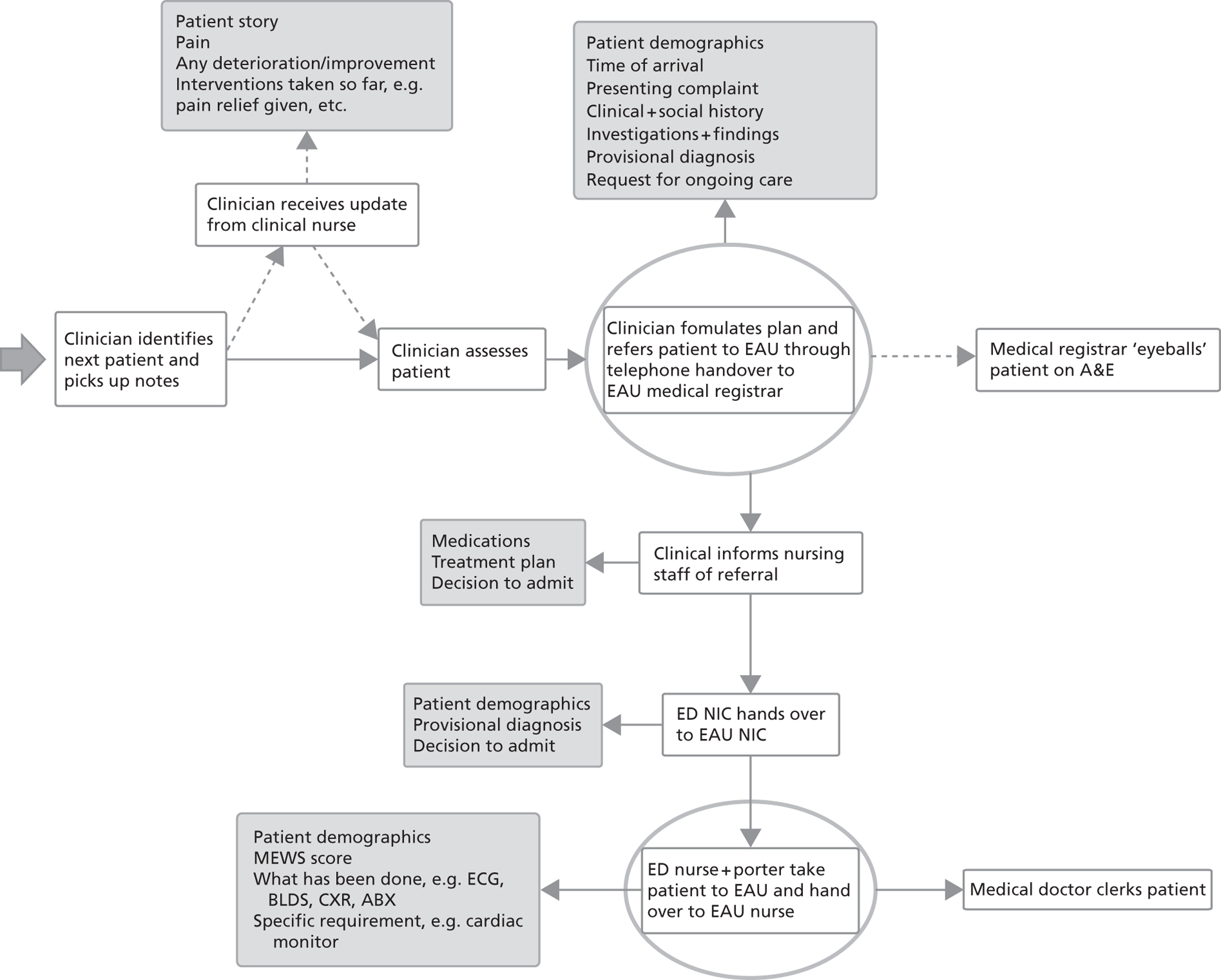
The pathway for patients with major injuries is shown in Figures 6 and 7. The model adopted at this site differs slightly from the model adopted at hospital C. This site does not normally have a dedicated HALO. A HALO is present in situations of high demand, only. The information displayed on the ambulance computer screen prior to the arrival of the ambulance is not commonly used. The handover from the AC is to a dedicated senior nurse co-ordinator and may include all information that the AC have gathered. The nurse co-ordinator records on a pro forma basic triage details, such as patient demographics and triage category. This sticker is given to the AC to take with the patient. This handover is perceived to include the transfer of responsibility for patient care, and also provides a logistic function enabling assessment of the impact on the resources in the department. In order to improve ambulance turnaround times, the AC is supposed to leave the patient in the assigned cubicle and return to their vehicle. In practice, there may be an informal secondary handover from the AC to the nurse who is going to look after the patient. This handover provides the function of highlighting aspects of the patient’s care that are of particular importance. Another difference is the referral from A&E to the EAU, which is a handover from the A&E clinician to a doctor on EAU. This is perceived to involve the transfer of responsibility for patient care. The clinician will then inform the A&E nursing staff of the decision to admit. This serves the purpose of delegation, prompting the senior A&E nurse to start to arrange the transfer of the patient to EAU. The senior nurse will liaise with the senior nurse on EAU. This handover provides an anticipatory and logistic function.
FIGURE 6.
Hospital D major injuries pathway – part 1. GP, general practitioner; NIC, nurse in charge.
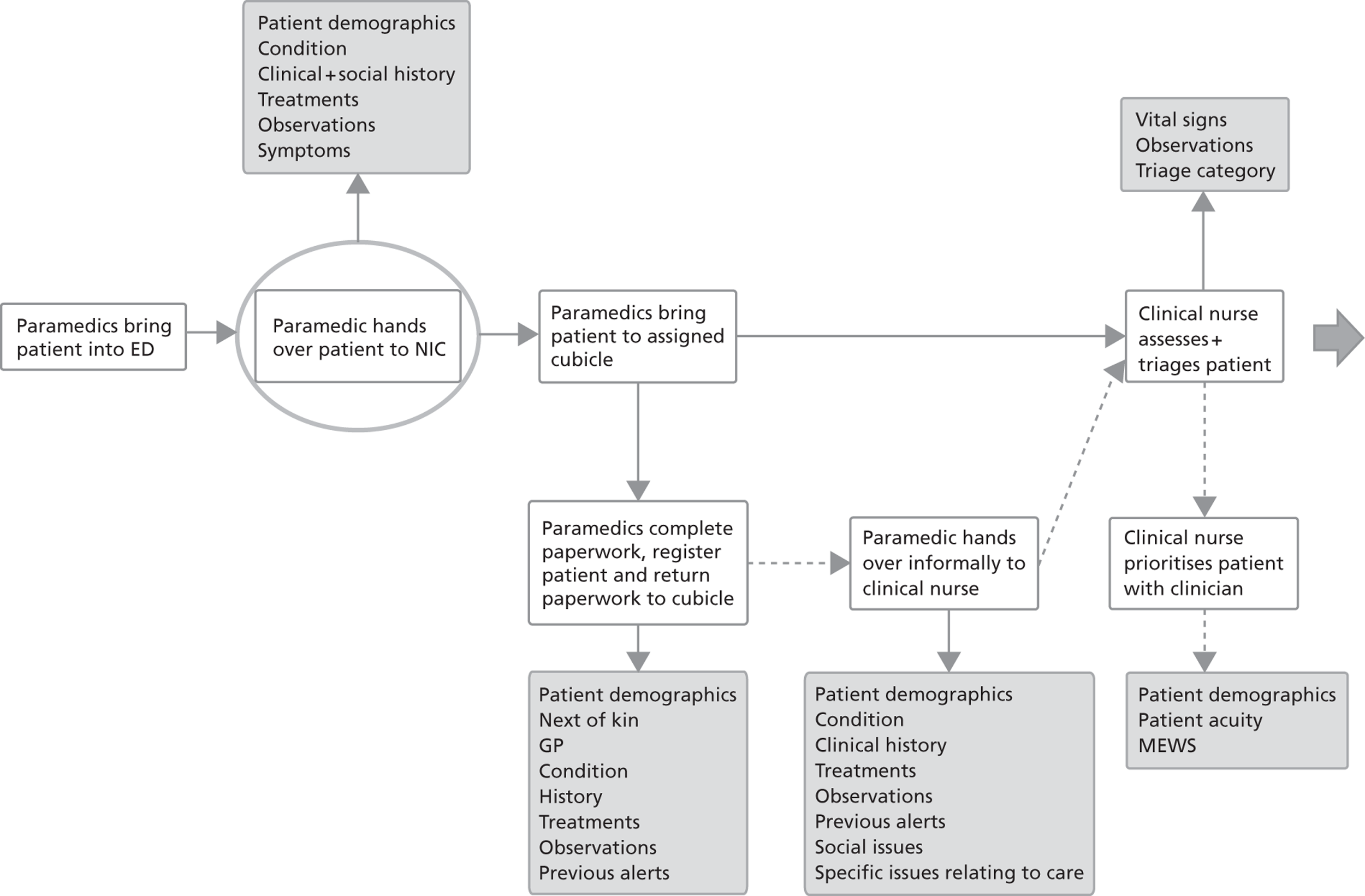
FIGURE 7.
Hospital D major injuries pathway – part 2. ABX, antibiotics; BLDS, bloods (blood tests); CXR, chest X-ray; ECG, electrocardiogram; NIC, nurse in charge.
Hospital E
The pathway for resuscitation patients follows the same general model as those at hospitals C and D.
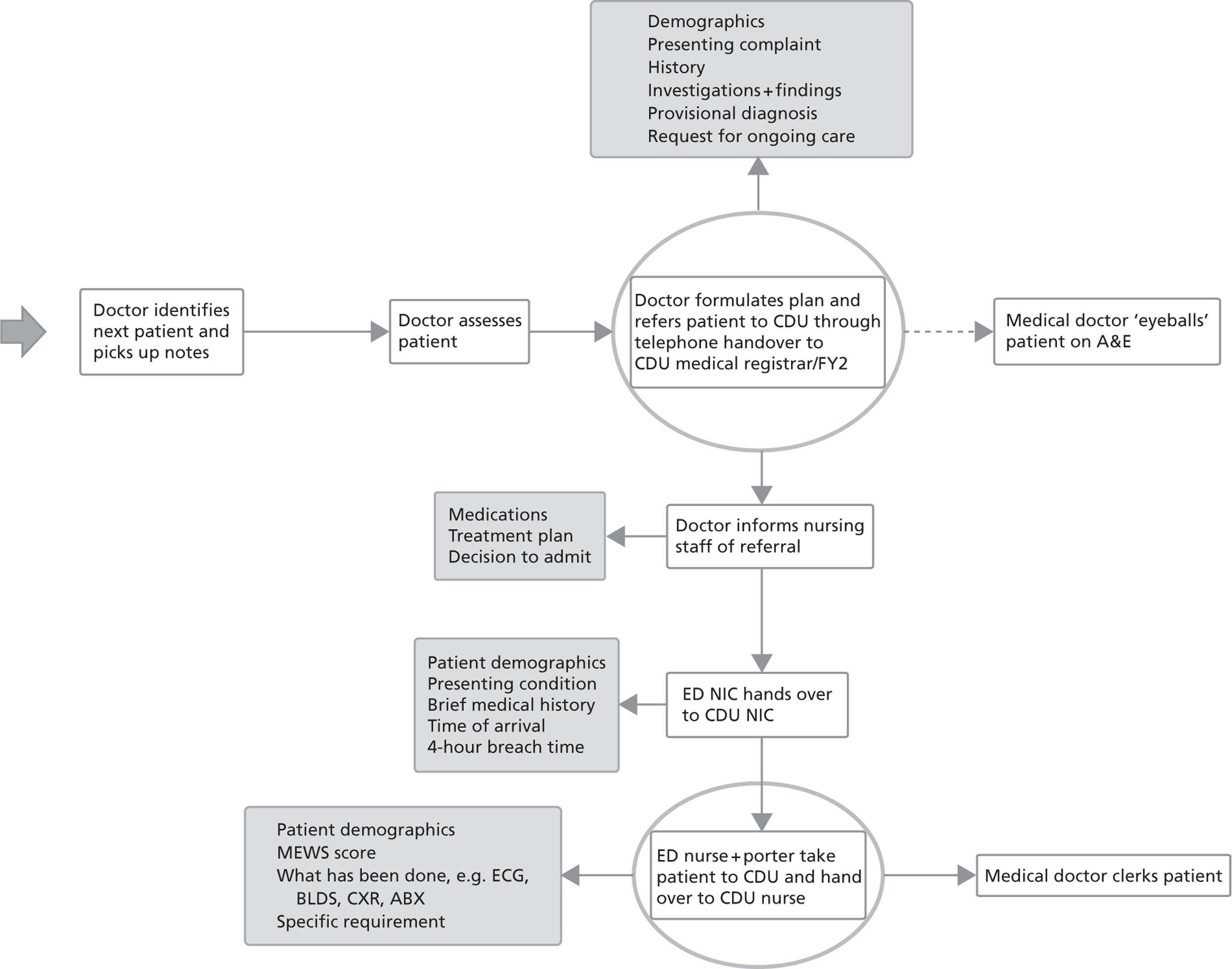
There are, again, some variations for the pathway for patients with major injuries. The pathway is represented in Figures 8 and 9. There is a handover from the AC to the senior nurse co-ordinator at the nurses’ station. This handover follows the same pattern as at the other sites, and it includes the transfer of responsibility for patient care and also provides a logistic function. At this site, there is a dedicated assessment room, and the AC transfer the patient to this room after the handover. There is an assessment team consisting of a qualified nurse and a HCA, who assess and triage the patient. There is not normally a handover to the assessment team. Following the assessment and depending on the acuity of the patient, there may be an optional prioritisation of the patient with the nurse co-ordinator, who, in turn, will prioritise the patient with the doctor. Upon the decision to admit, the referral takes place as at hospital D as a telephone handover between the A&E clinician and the clinician on CDU. This referral includes the transfer of responsibility for patient care. As before, there are subsequent handovers between the senior nurse on A&E and the senior nurse on CDU, as well as the face-to-face handover between the A&E nurse and the receiving CDU nurse.
FIGURE 8.
Hospital E major injuries pathway – part 1. DOB, date of birth; ETA, expected time to arrival; NIC, nurse in charge.
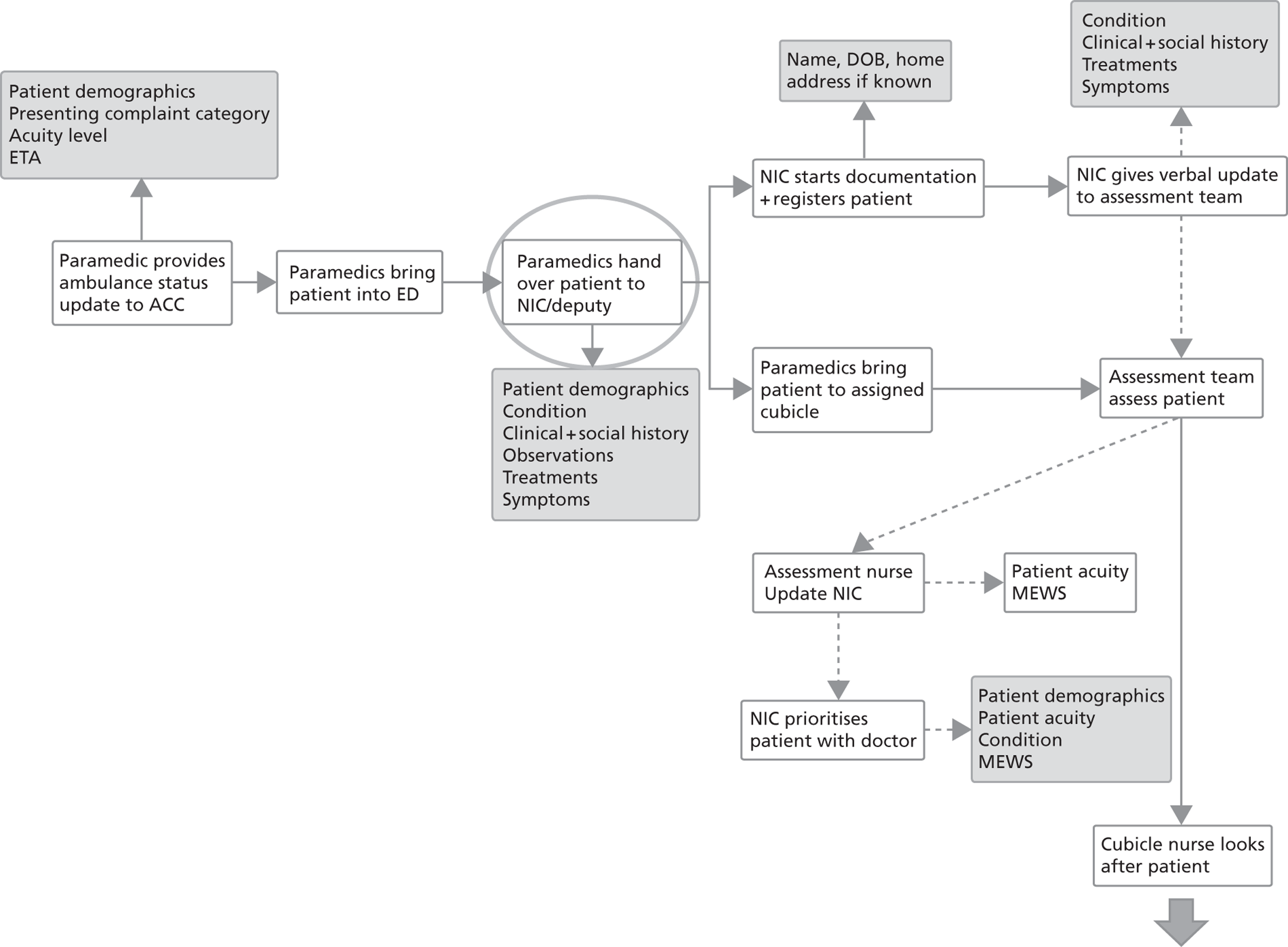
FIGURE 9.
Hospital E major injuries pathway – part 2. ECG, electrocardiogram; FY2, foundation year 2 doctor; NIC, nurse in charge.
Discussion
A summary of the findings of the pathway description is given in Table 10.
| Handover serves different goals and functions, e.g. | The people involved in handover may have different and not necessarily overlapping goals |
| Management of capacity and demand |
|
| Responsibility and delegation |
|
| Information transfer |
|
| Drawing attention to specific aspects |
|
| There can be uncertainty about who is responsible for the patient’s care | Pinpointing where the transfer of responsibility occurs is sometimes difficult. For example, when ambulances are in a queue and waiting to hand over the patient to the senior nurse, they are on the premises of the ED but have not formally handed over responsibility. Likewise, when a patient is referred on the telephone to acute medicine, the patient may remain on the premises of A&E for some time even after responsibility has been handed over |
| Resuscitation pathways exhibit a greater degree of standardisation | The resuscitation pathway is similar across sites and exhibits a higher level of standardisation than the pathway for patients with major injuries. Communication is often supported by protocols (e.g. ATMIST) and checklists for recording information. This may be due to the acuity of the patient, and the availability of national supporting guidelines and protocols |
| There are different models for receiving and giving handover of patients with major injuries | Different models are adopted at the different sites for receiving patients from the ambulance service, emphasising either the logistic function (understanding demand and capacity; speeding up ambulance turn-around) or the transfer of clinical and social information |
The process walks, observations and process mapping sessions provide a detailed representation and understanding of how handover is linked to clinical practice, and the different goals and functions it can serve. There are numerous situations where patient-related information is handed over, and this takes place between people with different backgrounds and potentially different goals. For example, the handover between paramedic and senior A&E nurse involves potentially conflicting goals. The goal of the paramedic is to communicate relevant clinical and social history. The goal of the receiving A&E nurse, on the other hand, is to assess the criticality of the patient and determine the impact on the resources available in the department.
Handover may involve only the communication of patient-related information or it may involve also the transfer of responsibility for patient care. Pinpointing where this transfer of responsibility occurs is sometimes difficult. For example, when ambulances are in a queue and waiting to hand over the patient to the senior nurse, they are on the premises of the ED but have not formally handed over responsibility. Likewise, when a patient is referred on the telephone, the patient may remain on the premises of A&E for some time, and will be cared for by A&E staff even after the handover has taken place and the patient is shown on the computer system as under care of another specialty.
The resuscitation pathway is similar across sites and exhibits a higher level of standardisation than the pathway for patients with major injuries. Communication is often supported by protocols (e.g. ATMIST) and checklists for recording information. This may be due to the acuity of the patient, and the availability of national supporting guidelines and protocols.
On the other hand, the pathway for patients with major injuries exhibits greater variation across sites, although not being completely dissimilar. Different models are adopted at the different sites for receiving patients from the ambulance service, for example handover to an assessment nurse who also looks after the patient or handover to the nurse co-ordinator, who is responsible primarily for managing the department and patient flows. The latter model is adopted to support the logistic function, i.e. in order to provide a better overview of demand and capacity, and to speed up ambulance turnaround times. There are also different models for referring patients from ED to acute medicine. An A&E clinician always gives the referral but it can be given to either a doctor or a nurse in acute medicine.
This systematic description of handover along the emergency care pathway embeds handover within the overarching patient journey, and illustrates the different types of handover that are present as well as the goals and motivations that may be involved. Such a representation is useful to investigate further both the risks that arise from handover failures (see Systematic risk analysis, below) and the way the verbal communication actually takes place (see Content and language form of handover, below).
Systematic risk analysis
The FMEA templates for resuscitation and major injuries pathways for each site are included in Appendix 2. Below, the highest-ranking risks from each site are discussed. A description and discussion of all significant risks is included in Appendix 3. During the FMEA sessions, participants described current and possible future mitigations. It is important to note that future mitigations should be regarded as ideas or starting points for possible exploration rather than as definite recommendations. Sometimes there may be good reasons not to pursue such ideas. This is in line with the purpose of a risk analysis, i.e. to identify and to describe risks. The definition of risk controls, their implementation and the monitoring of their effectiveness are subsequent steps of the risk management process, which are beyond the scope of this project.
Short vignettes of failure trajectories are included for selected risks to illustrate how handover failures may propagate through the system, and how they may align with other factors to produce the adverse outcome. Further vignettes are included Appendix 4. This section concludes with a discussion of risks across the three sites.
Ambulance service A/hospital C
At this site, 10 handover failure modes and associated risks were perceived to be of particular significance (risk scores of ≥ 12). These are discussed in more detail in Appendix 3. A brief list of the top five handover failure modes is shown in Box 3 for illustration.
Delay in handover from AC to assessment nurse.
Assessment nurse does not prioritise patient on computer system or verbally with clinician.
Patient referral not accepted by AMU medical registrar.
Inadequate verbal handover given during patient transfer to AMU due to unfamiliarity with patient.
Full patient story not communicated (either not given or not received) during paramedic to assessment nurse handover.
Participants related a number of these failure modes to a lack of capacity within the hospital, in terms of either staff or beds (but there may be other reasons too). For example, delays in handover of patients from AC to A&E staff may occur because of queues upon arrival; the fact that medical registrars on AMU do not accept patient referrals straightaway may be due to a lack of available beds on AMU and the resulting more stringent ‘gatekeeping’ behaviour; and the inadequate verbal handover of the nurse accompanying the patient during transfer to AMU owing to unfamiliarity with the patient is usually down to the fact that the nurse who had been looking after the patient is busy elsewhere and unable to accompany the patient. Overcrowding in the A&E department also means that nurses have to make more difficult decisions about whether or not to prioritise patients with the clinician, and a lack of experience may contribute to situations where patients are not prioritised adequately.
Further commonly identified contributory factors are described in the vignette below (Box 4) describing the risk arising from the failure to prioritise the patient with the clinician.
The patient is a 75-year-old man with known kidney failure. The AC told the triage nurse that he has been feeling unwell for a few days. Yesterday he thought he was developing flu and had two episodes of fever and shaking. This morning his wife thought he was a bit confused and called an ambulance. The AC told the nurse he had a pulse (p) of 100 beats per minute, a temperature of 36.0 °C and a normal BP.
The nurse placed the patient in a cubicle and then repeated his observations. They were p = pulse 110 beats per minute, BP = 96/70 mmHg, temperature 35.5 °C, respiratory rate = 9 breaths per minute, and oxygen saturation of 94% on air. NEWS was calculated as 6. She wrote all this information in his notes.
There was then another patient waiting to be handed over by the ambulance service, so she placed the note in the tray of patients waiting to be seen and carried on her work.
The department was busy so it was another hour before the patient was seen by the clinician. When he went in to the cubicle the patient’s wife was very anxious. He was mumbling and did not respond appropriately to questions. His clinical condition had deteriorated considerably. He was transferred to the resuscitation room, where treatment was started for his septic shock.
Contributory factorsThis patient’s condition deteriorated unnecessarily because of the failure to communicate his poor condition of arrival to the clinician and to prioritise his care. The department had a policy that any patient should be prioritised if their NEWS was ≥ 6, but this was forgotten because of the interruption of the nurse by another case arriving, the busyness of the department and the lack of visual alert to the patient’s condition on the notes or the IT system.
RecommendationParticipants suggested senior clinician input at triage, and a cultural shift that allows senior nursing staff to move patients to relevant clinical areas dependant on acuity and for doctors to follow the patient.
Ambulance service B/hospital D
At this site, nine failure modes and associated risks were perceived to be of particular significance (risk scores of ≥ 12). These are discussed in more detail in Appendix 3. A brief list of the top five handover failure modes is shown in Box 5.
Ambulance service does not give pre-alert for resuscitation patient.
Delay in handover from AC to NIC.
Full patient story not communicated (either not given or not received) during paramedic to NIC handover.
Criticality of patient not communicated adequately during paramedic to NIC handover.
Information not received during resuscitation handover when A&E staff get hands-on too quickly.
The lack of capacity and delays due to queues are perceived to contribute to risks identified at this site as at the previous site. In addition, handover for resuscitation patients was perceived to carry significant risks owing to the criticality of the patient condition, where even short delays could have severe adverse consequences. On the one hand, this makes the pre-alert an important step providing an anticipatory function as it allows the A&E department to prepare for the patient. Failure to give a pre-alert either because the ambulance is very close by or because the criticality of the patient may not have been recognised may lead to situations where there can be delays in getting the right people to the resuscitation room or freeing up space. On the other hand, owing to the perceived need to act quickly, A&E staff may get hands-on as soon as the patient arrives, which makes the handover from the paramedic more vulnerable as important information may not be heard or consciously processed.
Further commonly identified contributory factors are described in the vignette below (Box 6) describing the risk arising from delayed ambulance handover.
The ED was very busy, with two nurses off sick, and a higher than average attendance. At the time when the patient arrived there were four ambulances waiting to hand over, and there were no ED trolleys on which to put any new patients. The patient was already compromised physiologically when the ambulance first attended but had made a slight improvement with initial treatment. No pre-alert was made. From arrival in the ED to when a nurse formally assessed the patient there was an hour of delay. At the point when the nurse did eventually assess the patient, it was recognised that this patient was seriously ill and she was moved straight into the resuscitation room, where she suffered a cardiac arrest 20 minutes later. She subsequently died.
Contributory factorsNo pre-alert made although the patient was physiologically compromised on initial review.
Lack of capacity for patient to be seen within department.
Inadequate staffing levels to cover sickness.
Overworked small workforce that becomes sick.
RecommendationParticipants suggested that patients that are compromised initially might respond transiently to steps taken in the community. However, this can mask their underlying acuity unless a full and proper handover outlining the case is delivered promptly. If an ED has no capacity to properly assess patients, there needs to be a clear allocation of responsibility as to who is reviewing the stability of patients. If a patient is found to be deteriorating while awaiting a trolley, their acuity should be escalated appropriately. There should be clear guidance for this.
Hospital E
At this site, nine failure modes and associated risks were perceived to be of particular significance (risk scores of ≥ 12). These are discussed in more detail in Appendix 3. A brief list of the top five handover failure modes is shown in Box 7 for illustration.
No resuscitation bed available for patient.
Drugs given are not communicated during handover from A&E nurse to CDU nurse.
Ambulance service does not give pre-alert for resuscitation patient (or at short notice).
Patient referral not accepted by CDU medical registrar.
Information not received during resuscitation handover when A&E staff get hands-on too quickly.
As with the other two sites, the highest-ranking risks often relate to capacity and resource issues, such as the unavailability of resuscitation beds, the unfamiliarity of the nurse accompanying the patient with the patient’s story and the resulting inadequate verbal handover, possible gatekeeping behaviour owing to lack of capacity on CDU, and the missing of important information due to getting hands-on too quickly in situations of perceived urgency.
Further commonly identified contributory factors are described in the vignette below (Box 8) describing the risk arising from failed referral of a patient from A&E to acute medicine (medical registrar does not accept referral).
An 80-year-old woman who lives alone in her own warden-controlled flat was admitted to the ED via ambulance following a fall. She had mild dementia, osteoporosis and a previous total hip replacement. She had recurrent urine infections. She was unable to give a coherent history, as she was confused, disorientated, in pain and was unaccompanied.
The FY2 who assessed her was fresh from induction and had never practised Emergency Medicine, but had just finished a medical FY1 job, which she loathed. She had always wanted to be a surgeon. The nurse assessing the patient performed a 12-lead ECG, recorded vital signs, took blood tests and gave analgesia. The attending physician was made aware of these observations and tests but did not record that these observations and tests had been seen. She arranged a radiograph of the chest and femur in addition to this. She referred the patient to the medical registrar on call with limited history, no investigation results and no ongoing treatment plan. She did not have a working diagnosis and was not able to give a consistent story.
The medical registrar, who had just finished working with this doctor, had not enjoyed the placement and refused the patient until more information was known. A heated discussion took place on the telephone that was left unresolved. The patient moved to acute medicine under the care of ED, thought to be awaiting medical review.
The patient had indeed a periprosthetic fracture and urinary sepsis, and deteriorated on the ward while being nursed and monitored. ITU review was required. Invasive monitoring was required while she had anaesthetic review pending theatre, fracture stabilisation and antibiotics.
Contributory factorsPoor quality of handover.
Personality of stakeholders.
Unclear diagnosis.
Clinician story-changing.
RecommendationClear lines of communication and ownership are required. Participants suggested that ED physicians must be primarily responsible for the care of the patient until they are actually seen by the admitting specialty team. Immediate point-of-care investigations and radiographs that may change management must be seen by the ED team, and if any tests are outstanding these should be highlighted to the accepting team. Clear communication (both verbal and written) of what has been done and what is expected of the specialty team is fundamental, as is clear acceptance of the transfer of responsibility.
Discussion
A summary of the main lessons from the risk analysis is provided in Table 11.
| Many handover failure modes are linked causally to capacity and resource issues | Inadequate patient flow may give rise to several potential handover failures: delays in AC handover, more difficult prioritisation decisions, inadequate patient transfer handover owing to unfamiliarity with the patient, information loss resulting from different information needs, and refusal to accept patient referrals |
| FMEA provides qualitative insights into handover failures, the causes and possible consequences | The application of FMEA provided structure to the risk analysis. This resulted in a rich qualitative understanding of common handover failures, their causes and potential consequences. The estimation of risk scores is difficult and not necessarily consistent across sites |
The output of the risk analysis at each site shares many similarities with the other sites. The handover failure modes that have been identified apply across all three sites. There were no failure modes with significant associated risk that were particular to just one of the sites. The causes for the failure modes were also similar across the sites. This may be one of the most important lessons of the risk analysis. Many of the identified failure modes are linked causally to capacity and resource issues. As described, inadequate patient flow may lead to overcrowding in the ED, giving rise to several potential handover failures: delays in AC handover, more difficult prioritisation decisions, and inadequate patient transfer handover due to unfamiliarity with the patient. In addition, in order to manage patient flows better, handover from the AC may be taken by a senior nurse with an overview of capacity of the whole ED. The senior nurse has different information needs, which may result in information such as social history not being communicated or not being consciously heard. Inadequate patient flow into the hospital further contributes to overcrowding. This may be caused by resource constraints on the wards themselves. Appendix 3 provides a more in-depth description of the risks identified, the possible contributory factors, and mitigations that have been proposed during the FMEA sessions.
Differences existed in the assessment of risk associated with failure modes, i.e. in the estimation of the likelihood of occurrence and the severity of the consequences. This represents a limitation of FMEA when used for the risk analysis of sociotechnical systems. As described earlier, FMEA is traditionally used as one of several methods to conduct the risk analysis of technical systems. For such systems failure modes and corresponding failure rates are often sufficiently well documented to ensure consistency. For example, failure rates of computer processors or bit flips of memory chips are readily available. On the other hand, it is significantly more difficult to provide consistent estimation on the likelihood of a person not listening attentively during handover. The estimation of the severity of the consequences is difficult both for technical as well as for sociotechnical systems. However, in health care this is exacerbated by the need for consideration of the patient condition. Depending on the patient condition, one could actually look at radically different ‘systems’, in as much as the patient condition represents a major factor in determining the consequences of a failure. Participants repeatedly stressed that if a patient was sufficiently vulnerable, even the most insignificant delays or errors could be sufficient to trigger a catastrophic turn of events. The conversations that participants had when determining the severity of the consequences provided insights that their understanding and perception of the severity of consequences were fundamentally similar, even if they assigned a different risk score across sites.
Content and language form of handover
The preceding systematic descriptions of handover within the emergency care pathway, and the systematic risk analysis have taken a broad view of handover as a social (or sociotechnical) activity embedded in the wider activity network of each stakeholder. In this section, the unit of analysis is temporarily narrowed to the actual communication act, i.e. the types of information that people communicate and the ways in which they communicate. This will provide insights into how the handover communication is shaped by the interaction of the participants.
Frequency of handover communication content and language forms used
The three types of interorganisational and interdepartmental handover selected for analysis of the content and language forms used were (1) resuscitation handover from paramedic to senior ED doctor; (2) major injuries handover from paramedic to senior ED nurse; and (3) the telephone referral of patients from ED clinician to acute medicine doctor or senior nurse. At hospital E, only referrals were studied, as the ambulance service did not provide permission to involve their staff in the study.
Table 12 shows the number of audio-recordings that were collected for each type of handover at the three sites, and the number of audio-recordings included in the analysis. Table 13 shows the mean duration for the different types of handover at each site (low and high values shown in parentheses). Some audio-recordings could not be included owing to excessive background noise, poor recording quality or technical failures (technical failures refer to, for example, telephone handovers during which only utterances of one party could be heard due to problems with the in-ear microphone used to record telephone conversations). All suitable audio-recordings were included in the analysis. Suitable means that the conversation could be meaningfully reconstructed during the transcription process, with the exception of individual inaudible words or very short utterances.
| Study site | No. of audio-recordings: used (collected) | ||
|---|---|---|---|
| Resuscitation | Major injuries | Referral | |
| Ambulance service A/hospital C | 14 (25) | 40 (45) | 31 (45) |
| Ambulance service B/hospital D | 20 (25) | 39 (45) | 26 (40) |
| Hospital E | N/A | N/A | 33 (45) |
| Study site | Mean duration of handover in minutes (low–high) | ||
|---|---|---|---|
| Resuscitation | Major injuries | Referral | |
| Ambulance service A/hospital C | 1:39 (0:58–2:19) | 1:31 (0:30–6:01) | 2:39 (1:02–5:08) |
| Ambulance service B/hospital D | 2:18 (0:38–4:00) | 2:14 (1:02–4:35) | 3:31 (1:35–6:50) |
| Hospital E | N/A | N/A | 2:44 (1:15–6:03) |
Tables 14 and 15 provide overviews of the frequency with which particular content was communicated during each type of handover, and the frequency of the language forms used.
| Content | Percentage of utterances (total no.) | ||||||
|---|---|---|---|---|---|---|---|
| Resuscitation | Major injuries | Referral | |||||
| A/C | B/D | A/C | B/D | A/C | B/D | E | |
| Patient presentation | |||||||
| Patient identifiers | 5.5 (14) | 1.9 (12) | 4.7 (45) | 5.0 (69) | 8.9 (155) | 8.8 (124) | 13.6 (178) |
| Clinical history | 46.2 (117) | 25.5 (164) | 37.1 (354) | 42.0 (574) | 18.5 (322) | 16.7 (234) | 25.3 (330) |
| Social history | 3.2 (8) | 2.5 (16) | 3.5 (33) | 5.4 (74) | 2.8 (49) | 1.4 (20) | 2.5 (33) |
| Injury | 1.6 (4) | 3.1 (20) | 1.7 (16) | 0.0 (0) | 0.3 (5) | 0.0 (0) | 1.5 (19) |
| Symptom | 8.7 (22) | 13.0 (84) | 12.4 (118) | 10.6 (145) | 9.2 (161) | 11.5 (161) | 2.5 (33) |
| Procedure | 15.0 (38) | 32.3 (208) | 14.9 (142) | 11.5 (157) | 19.9 (347) | 14.8 (208) | 21.7 (283) |
| Assessment | |||||||
| Treatment | 0.0 (0) | 5.0 (32) | 1.7 (16) | 0.3 (4) | 8.1 (142) | 10.0 (140) | 4.0 (52) |
| Clinical impression | 4.3 (11) | 0.0 (0) | 6.5 (62) | 0.7 (9) | 3.2 (55) | 5.6 (78) | 6.5 (85) |
| Prognosis | 0.0 (0) | 0.0 (0) | 0.0 (0) | 0.0 (0) | 1.8 (33) | 1.9 (26) | 0.3 (4) |
| Outcome | 0.0 (0) | 0.0 (0) | 0.0 (0) | 3.1 (42) | 2.1 (37) | 2.6 (36) | 2.0 (26) |
| Transfer of responsibility | 0.0 (0) | 0.0 (0) | 0.0 (0) | 0.1 (1) | 4.6 (80) | 5.6 (78) | 2.5 (33) |
| Professional environment | |||||||
| Logistic processes | 4.3 (11) | 5.6 (36) | 2.9 (28) | 5.9 (81) | 4.6 (80) | 3.3 (46) | 1.0 (13) |
| Courtesies | 11.1 (28) | 11.2 (72) | 14.8 (141) | 15.4 (211) | 16.0 (279) | 18.1 (254) | 16.6 (217) |
| Form | Percentage of utterances (total no.) | ||||||
|---|---|---|---|---|---|---|---|
| Resuscitation | Major Injuries | Referral | |||||
| A/C | B/D | A/C | B/D | A/C | B/D | E | |
| Information seeking | |||||||
| Closed question | 3.5 (9) | 11.2 (72) | 4.8 (46) | 5.0 (68) | 8.9 (155) | 11.1 (156) | 11.6 (151) |
| Open question | 10.9 (28) | 1.2 (8) | 0.9 (9) | 1.0 (14) | 5.3 (93) | 5.1 (72) | 4.5 (59) |
| Clarifying question | 2.7 (7) | 3.7 (24) | 2.5 (24) | 3.8 (52) | 1.8 (31) | 3.3 (46) | 4.5 (59) |
| Information giving | |||||||
| Description | 61.3 (157) | 62.7 (404) | 66.0 (630) | 65.8 (900) | 48.2 (840) | 50.8 (714) | 45.6 (596) |
| Explanation | 5.5 (14) | 0.6 (4) | 1.3 (12) | 0.7 (10) | 4.9 (86) | 2.2 (31) | 4.6 (60) |
| Rationale | 3.5 (9) | 1.9 (12) | 6.1 (58) | 0.4 (5) | 2.1 (37) | 3.3 (46) | 2.5 (32) |
| Directive | 0.4 (1) | 5.6 (36) | 2.3 (22) | 2.3 (31) | 0.3 (6) | 1.1 (15) | 1.6 (21) |
| Context talk | 0.8 (2) | 1.2 (8) | 1.5 (14) | 5.4 (74) | 5.3 (93) | 1.4 (20) | 2.5 (33) |
| Social amenities | 11.3 (29) | 10.6 (68) | 14.7 (140) | 15.2 (208) | 16.0 (279) | 18.1 (254) | 16.6 (217) |
| Decision | 0.0 (0) | 0.0 (0) | 0.0 (0) | 0.1 (2) | 2.1 (37) | 2.2 (31) | 2.0 (26) |
| Information verifying | |||||||
| Read-back | 0.0 (0) | 1.2 (8) | 0.0 (0) | 0.2 (3) | 4.9 (86) | 1.4 (20) | 4.0 (52) |
Qualitative interpretation of frequency counts
Review of the frequency counts provided a number of qualitative insights.
Ambulance service handover is shorter than referral
Across the sites, resuscitation handovers lasted between 38 seconds and 4 minutes, handovers for patients with major injuries lasted between 30 seconds and 6 minutes, and referrals to acute medicine lasted between 1 minute and approximately 7 minutes. The shorter duration of ambulance service handover is not surprising, as this consists normally of a descriptive monologue by the AC, possibly followed by some clinical questioning at the end, for example around pain management or allergies.
Ambulance service handover is descriptive and focused on patient presentation
The frequency count demonstrates that around 80% of handover communication content for resuscitation patients and 75% of handover communication content for patients with major injuries is around patient presentation. Of the remainder, another 10–15% of handover communication serves the purpose of establishing a friendly and professional relationship. The language forms used support this view, with around 60–65% of utterances being purely descriptive. Questions, on the other hand, were used less frequently, with around 16–17% in resuscitation cases and only 8–10% for patients with major injuries. The difference in frequency of questions between these two types of handover may be down to the fact that in resuscitation the team leader often adds a number of focused questions, as treatment needs to start immediately. In actual practice, the information transfer is not necessarily finished with the conclusion of the handover, as the AC frequently stay in the resuscitation room to complete the documentation. In this way, they ensure that they are available during the initial stages of the assessment and treatment in case there are further questions. The use of questions in the handover communication for patients with major injuries is frequently centred on elicitation of specific information on a limited number of topics such as pain and allergy status.
Referrals entail discussion and can be forward looking
Referrals take place in a different context and this is reflected in the communication patterns. For handover from the ambulance service the transfer of responsibility is already decided when the ambulance arrives, and there is no negotiation required. Referrals, on the other hand, provide an opportunity to seek specialist advice and to reach a joint decision about what the best course of action should be for the patient. As a result, referrals tend to be slightly longer conversations than ambulance service handovers. These conversations are more of a dialogue, and the handover communication content is more forward looking than the ambulance service handover. Approximately 15–25% of handover communication content was concerned with consideration of the patient’s future journey, as opposed to 4–8% for ambulance service handovers.
Ambulance service handover may be standardised more easily, but referrals can also benefit from standardisation
The different nature of the ambulance service handover and the referrals to acute medicine suggests that it may be easier to standardise handover communication for ambulance service handover compared with referrals. However, this does not mean that standardisation of handover for referrals may not be useful. Structuring the initial parts of the conversation may support the communication partners in establishing a joint understanding as the basis for their subsequent discussion and negotiation.
Social issues are not communicated routinely
The data further showed that approximately 2–5% of ambulance service handover communication content related to the social circumstances of the patient, compared with 1.5–2.8% for referrals. This was surprising, as participants suggested that social issues were not as important during resuscitation handover, when the focus was on the immediately relevant clinical aspects. The data suggest that social issues are not discussed much during referrals, either. There may be an assumption that these issues are documented and will be consulted once the patient has been transferred.
Standardisation of handover communication
As described above, ambulance service handover may be standardised more easily than referrals. The ATMIST communication protocol had already been implemented by the participating ambulance services. Referrals may be more difficult to standardise but they may still benefit from a structured approach. This issue will be described in more detail with examples in this short section.
The AMU at hospital C had adopted a checklist-supported communication protocol for referrals from the ED. As a result, referrals at this site usually followed a particular pattern, often guided by the receiving AMU nurse:
(*PID, patient identifier.)
An experienced clinician in the ED can pre-empt what he or she is going to be asked, and therefore the handover may start with the clinician verbally filling out the AMU form for the AMU sister.
(*PID, patient identifier.)
At hospital E no standardised approach had been implemented. Below the full transcript of a referral from ED to CDU at hospital E is shown. The initial part of the transcript illustrates that the communication partners do not share an understanding of how the conversation should unfold. As a result a number of clarifying questions are used to repair the conversation flow. For the major part, the conversation is guided through questions from the registrar on CDU receiving the referral. There are several instances where the ED doctor is unsure what information is required and needs to revert to asking for clarification. Throughout the conversation it appears that the communication partners are navigating from utterance to utterance without being able to develop a shared understanding of what is going to be discussed next. The CDU registrar deduces and summarises the reason for admission only about two-thirds of the way through the conversation.
(*CRP, C-reactive protein; INR, international normalised ratio.)
The transcript also illustrates that the duration of the handover and the number of questions that are asked, are not necessarily markers of quality. Senior clinical decision-makers will often give a more detailed referral to a specialty team in less time. In addition, interruptions from the specialty can sometimes throw the inexperienced referrer off their tracks, and prolong and confuse the handover process. It is less likely that there are extended discussions about whether or not to accept the referral of a patient in a top-down hierarchical handover (ED consultant to medical registrar) than with an ED foundation year 2 junior doctor to a medical registrar.
Discussion
The aim of this research strand was to identify and to analyse the risks associated with handover failures in the emergency care pathway. This is a critical activity informing any subsequent improvement activities. 92 To this end, we produced detailed representations of how handover is linked to clinical practice, and the different goals and functions it can serve. Taking this as the basis, we subsequently performed a systematic risk analysis to identify the most significant risks and their possible causes at each site. This provided a number of interesting results:
-
Handover serves different goals and functions The people involved in handover may have different and not necessarily overlapping goals. These can relate to issues such as the management of capacity and demand, the transfer of responsibility and the delegation of aspects of care, the communication of different types of information, and the prioritisation of patients or highlighting of specific aspects of their care.
-
Many handover failure modes are linked causally to capacity and resource issues Inadequate patient flow may give rise to several potential handover failures: delays in AC handover, more difficult prioritisation decisions, inadequate patient transfer handover owing to unfamiliarity with the patient, information loss owing to different information needs, and refusal to accept patient referrals.
-
Similar vulnerabilities were identified across the three sites The vulnerabilities identified across the three sites were similar, and no failure mode with significant risk was particular to any one site. There existed differences in the evaluation of risk. This is a limitation of the application of FMEA in health-care settings.
During the CA of the different types of handover, the focus was temporarily narrowed to the actual communication act. The results of this analysis demonstrated that different types of handover have very different structures. Types of handover that are predominantly descriptive in nature and where the transfer of responsibility is unambiguous, may lend themselves to standardisation more readily than other types of handover that involve more dialogue and negotiation in order to reach a joint decision. Standardisation in the latter case may still be useful, but requires greater flexibility.
The findings of this systematic analysis of the risks associated with handover failures across the emergency care pathway provide useful insights to and form the basis for subsequent improvement efforts.
The next chapter describes research strand 2, which investigates in greater depth the perception of staff on issues such as their different goals and motivations, and the role that the different organisational and cultural background plays in shaping interdepartmental and interorganisational handover. This will be useful in providing an in-depth understanding of how the risks identified in this chapter are brought about and influenced by organisational behaviours.
Chapter 4 Staff perceptions on common organisational deficiencies and on the impact of the organisational model of emergency care delivery on clinical handover
Introduction
Research strand 2 was concerned with the identification and description of organisational factors that influence handover in practice. A qualitative approach using semistructured interviews for data collection and thematic analysis for data analysis was used. This chapter summarises the aims and objectives of the research strand (see Aims and objectives) and describes in detail the methods used (see Methods). The main part of this chapter is dedicated to the presentation of the results of this research strand (see Results). A discussion concludes the chapter (see Discussion).
Aims and objectives
The aim of this work stream was to elicit and to describe staff perceptions on common organisational deficiencies and the impact of the organisational model of care delivery on handover within the emergency care pathway.
The detailed objectives of this work stream were:
-
O2–1 To identify common organisational deficiencies that affect clinical handover in the emergency care pathway.
-
O2–2 To describe the impact on handover of the organisational model of care delivery within the emergency care pathway.
Methods
Participant recruitment
To elicit and to describe staff perceptions, a qualitative form of enquiry was adopted. An initial purposive convenience sample of 15 front-line staff (five per site) participated in semistructured interviews. Selection of participants was based on their role and actual involvement with handover in the emergency care pathway, and their availability for participating in an interview on scheduled dates. A second round of semistructured interviews was carried out subsequently with a purposive convenience sample of 24 additional staff. Selection of participants was again based on their role and availability but included also staff with managerial rather than hands-on duties.
Staff were approached by the site principal investigator or the site researcher. Prior to the interview, staff received a participant information leaflet. Interviews took place in a meeting room on the site of each organisation. Participation was voluntary, and all participants provided written consent. Table 16 provides a breakdown of participants by service/department and their role.
| Service | Role | Interview round 1 | Interview round 2 | Total |
|---|---|---|---|---|
| Ambulance service | 7 | |||
| Paramedic | 2 | 1 | 3 | |
| HALO | 1 | – | 1 | |
| Team leader (ambulance service) | – | 1 | 1 | |
| Area manager (ambulance service) | – | 1 | 1 | |
| Clinical director (ambulance service) | – | 1 | 1 | |
| ED | 23 | |||
| Staff nurse | 3 | 1 | 4 | |
| Senior nurse (co-ordinator) | 2 | 1 | 3 | |
| Nurse consultant | 1 | 2 | 3 | |
| Emergency practitioner | – | 2 | 2 | |
| Junior doctor | – | 1 | 1 | |
| Middle-grade doctor (registrar) | 1 | 1 | 2 | |
| Consultant | 2 | 3 | 5 | |
| Clinical lead (consultant) | – | 1 | 1 | |
| General manager emergency care | – | 1 | 1 | |
| Clinical director emergency care | – | 1 | 1 | |
| Acute medicine | 8 | |||
| Nurse | 1 | 1 | 2 | |
| Senior nurse | 1 | 2 | 3 | |
| Middle grade (registrar) | 1 | 2 | 3 | |
| Other | Medical education (directorate) | – | 1 | 1 |
| Total | 15 | 24 | 39 | |
Data collection
Data were collected through semistructured interviews during May 2012 to November 2012. One of three project team members (PC, PS, MS) conducted the interview. The interviews were held in a meeting room on site of the respective organisation. Each interview lasted between 20 and 50 minutes. Interviews were audio-recorded or, if the interviewee preferred, the researcher took written notes. The audio-recordings were subsequently transcribed, and during the transcription process all identifiers were removed to ensure anonymity.
Data analysis
Data collection and analysis followed an iterative approach, where the preliminary analysis of initial interviews informed the content of subsequent interviews. As shown in Table 16, the first set of interviews involved 15 participants. These initial interviews followed the topic guide shown in Table 17.
| Introduction | Background to the study and the interview |
| Professional background | Interviewee’s professional background and current role |
| Handover practices | Interviewee’s involvement with handover; factual description of how handover takes place; description of documentation used |
| Perceptions on current practices | Interviewee’s perceptions on handover practices; purpose of handover; impact of handover on patient care; common handover deficiencies; education and training for handover |
| Recommendations | Suggestions for improving handover both short term and longer term |
| Ending | Expression of thanks for contribution |
In the original research protocol included in the application document, the use of the London Protocol93 as a coding framework had been proposed. This is a simple framework that classifies factors contributing to adverse events and incidents into broad categories, such as patient characteristics, individual factors, team factors, task factors, organisational and institutional factors. This would have allowed classifying organisational deficiencies identified by participants accordingly. However, as the initial set of interviews was conducted, it became quickly apparent that this approach would not be able to adequately describe the richness of the data. In a project meeting, it was therefore decided to utilise an inductive qualitative analysis approach (thematic analysis) with greater explanatory power.
Following transcription of the interview data, one researcher (MS) conducted the thematic analysis. In a first step, all interviews were read in order to allow familiarisation with the data. Subsequently, each interview was coded using a mixture of descriptive, open and in vivo coding. 94 Table 18 provides a brief description of the three coding approaches. An analytic memo was produced for each interview summarising the researcher’s thoughts and issues of particular interest.
| Descriptive coding | Coding approach in which codes identify the topic of a passage of qualitative data |
| Open coding | Coding approach (often used in the early stages of grounded theory studies) for breaking down qualitative data into discrete parts, identifying concepts and comparing their properties and dimensions across the data |
| In vivo coding | Coding approach in which codes refer to a word or a short phrase from the participant’s own language |
Using the codes and the analytic memos major categories were identified through clustering of codes in meetings of the project team.
Subsequent interviews then followed a modified topic guide, shown in Table 19, for which participants were asked to comment on and to refine the identified categories. In addition, participants were asked to reflect on different handover practices that had been observed in the different sites, and to consider what impact these may have on patient care.
| Introduction | Background to the study and the interview |
| Professional background | Interviewee’s professional background and current role |
| Perceptions on current practices | Interviewee’s perceptions on handover practices; purpose of handover; impact of handover on patient care; common handover deficiencies; education and training for handover |
| Exploration of identified categories | Interviewee’s perception on identified categories; exploration of dimensionality; exploration of relationship between categories |
| Organisational differences | Exploration of organisational differences; reasons for adopting or not adopting certain practices; impact on patient care |
| Recommendations | Suggestions for improving handover both short term and longer term |
| Ending | Expression of thanks for contribution |
The additional interviews were then coded using the existing codes and additional codes where appropriate. Categories were constantly compared with the data and revised until new data added no further conceptual insights.
Stakeholder workshop
A stakeholder workshop was held at the College of Emergency Medicine on 16 July 2012. The programme and presentations of the workshop are available from: www2.warwick.ac.uk/fac/med/staff/sujan/research/echo/wp3_ws/. The aims of the stakeholder workshop were to:
-
provide external validation of the preliminary project findings
-
stimulate critical reflection among the project team
-
gather suggestions for and experiences of handover improvements in practice
-
provide a platform for practitioners to network and to share experiences.
The workshop was open to participants with an interest in handover in emergency care. The workshop call was distributed through professional and personal networks. Twenty-six external delegates and eight project team members attended the workshop.
The workshop format was as follows:
-
Project team presentations Presentation of project overview and preliminary project findings. Short discussions with delegates after each presentation.
-
Improvement experiences Two invited delegates gave presentations about particular handover improvement experiences they had been involved with (electronic PRF; electronic referrals from A&E).
-
Plenary discussion Delegates were invited during a longer plenary discussion to provide feedback on the preliminary project findings.
-
Group work Delegates split into small groups according to their interests in order to discuss one particular risk theme per group. Delegates were asked to think about particular handover improvement experiences they may have had and to provide suggestions for practice. Groups were reshuffled once after a set interval, but participants were free to join other groups at any time.
-
Feedback Delegates provided feedback from their group work supported by notes on a flip chart.
-
Concluding plenary discussion Delegates and project team members reflected on the outputs of the group work to identify themes of suggestions for improvement across the different groups.
After the close of the workshop, project team members held a review meeting to reflect on the workshop discussions. This review meeting was supported by the notes participants had made on the flip charts and notes team members had made during the delegate feedback session.
Results
Two main themes were identified during the thematic analysis – inner tensions within the activity of handover that require trade-offs, and management of the flow of patients across organisational boundaries (Table 20). Participants described a range of tensions inherent in handover that require dynamic trade-offs. These are related to documentation, the verbal communication, the transfer of responsibility, and the different goals and motivations that a handover may serve. Participants also described the management of flow of patients and of information across organisational boundaries as one of the most important factors influencing the quality of handover. This includes management of patient flows in and out of departments, the influence of time-related performance targets, and the collaboration between organisations and departments. The two themes are related. The management of patient flow influences the way trade-offs around inner tensions are made, and, on the other hand, one of the goals of handover is ensuring adequate management of patient flows. The evidence suggests that handover may be improved by providing individuals and organisations with the required skills to acknowledge and to manage the required trade-offs, and by fostering engagement and collaboration across organisations.
| Theme 1: inner tensions within handover require trade-offs | The elements of handover – documentation, verbal communication, the transfer of responsibility, and the goals of the actors have inner tensions that require trade-offs depending on the patient and the circumstances |
| Theme 2: management of patient flows across organisational boundaries affects handover | The management of patient flows across organisational boundaries is a key factor affecting the quality of handover; this includes the management of capacity, the influence of time-related targets, and the collaboration of actors from different organisations and of the organisations themselves |
Theme 1: inner tensions within handover require trade-offs
In relating their perceptions of how handover plays out in practice, participants described a range of tensions inherent in the activity. Depending on their professional background and the specific circumstances, different participants manage these tensions through different trade-offs. Below the main elements and their tensions are described in more detail. A summary is provided in Table 21.
| Documentation | Organisational push to document everything Practitioners cannot rely on documentation alone Lack of time and capacity leads to inadequate use of documentation |
| Verbal communication | Enables better care Highly dependent on individuals and their goals May not take place due to lack of time and capacity |
| Transfer of responsibility | Explicit transfer of responsibility ensures seamless transitions of care Difficult conversations may result in refusal to accept responsibility for patient care Lack of capacity may lead to situations with unclear allocation of responsibility and patients being stuck or lost in the system |
| Goals | Different actors have different motivations and information needs Staff from different departments and organisations have to work together and trust one another Trust among colleagues is put under pressure by time performance targets |
Documentation
The major tensions inherent in documentation described by interview participants are summarised in Table 22.
| Organisational push to document everything | There is an organisational push to document everything for legal and quality assurance purposes. There is also an assumption that with comprehensive documentation multiple handover can be avoided, as people can simply read the notes |
| Practitioners cannot rely on documentation alone | Practitioners feel they cannot rely on documentation alone. Documentation cannot convey subtleties and does not allow for questions. It is more difficult to determine and prioritise what is important. Documentation can be variable or inaccurate, and professional accountability requires that practitioners get a full picture |
| Lack of time and capacity leads to inadequate use of documentation | Producing comprehensive notes requires time. When the environment is busy, practitioners may write less, and those working off the notes may not read them |
The documentation of information is an important part of clinical handover and it contributes to the delivery of high-quality care. There is a drive at organisational level across organisations to document as much as possible (‘if it’s not documented, it didn’t happen’). This is both for legal as well as for quality assurance purposes. In addition, there is a perception at the management level that the number of verbal handovers can be reduced if everything is documented comprehensively (‘no point in them [AC] replicating handover several times’). This would save time and allow, for example, the ACs to get back out on to the road more quickly. On the other hand, there is the recognition, especially among practitioners directly involved in patient care, that one cannot simply rely on documentation. Documentation can be missing, temporarily unavailable, inaccurate and incomplete. Documentation may not highlight or prioritise the important bits of information, and subtleties or concerns may not be documented. Most importantly, documentation is unidirectional and, therefore, does not provide the opportunity to discuss and clarify areas of particular concern or interest. This is important to staff who take on responsibility for patient care. For professional and personal accountability, gathering accurate and up-to-date information in a dialogue is perceived as highly valuable (‘get things clear in my head’).
One participant from the ED describes this tension, where they also indicate the importance of experience in determining the amount and ultimately the quality of documentation. In this view, documenting everything is a naive and suboptimal approach. Experience provides people with the skills to determine and articulate what is important.
You’ve got an organisational system, which ideally should allow all these ports of transfer of information. So they should allow the actual chat between paramedic and the nurse or the paramedic and the doctor and should also allow the written conveying of that information. The formal part, the recorded part must be there for legal purposes. [. . .] In both my management and my clinical role, I would insist that both are always done. To be able to effectively do that is experiential. So the person with little experience is going to be required or going to have a necessity to record an awful lot of normal information. Because he or she, or the computer. Because computers are doing a lot of this sort of thing now which is a most dire system. You know, it really is. But it’s a computer. It’s a computer saying no! And it’s a very simplistic thing. Then you get an untrained person, they’re going to have a simplistic approach. And the simplistic medical or nursing practitioner, you take every single bit of information and you record it. The consultant’s approach, the senior person right at the end, is going to record the important positives and the important negatives. He or she can justify his clinical actions, justify the treatment and will hopefully represent exactly what the patient said.
The way documentation is used is also influenced by departmental capacity and workload. Writing comprehensive notes takes time, and people may write less when they feel that they are under time pressure. This may lead to omissions. Equally, the person taking on responsibility for patient care may not read the notes or only consult them superficially owing to the perceived pressure of seeing the patient quickly.
A second participant from the ED describes this trade-off, and also emphasises again the importance of experience over a simplistic standardised approach that may be inappropriate depending on the circumstances.
You can read stuff very quickly. I think you can probably read information quicker than you can hear it if someone’s speaking to you. So the quickest way would be to read what somebody’s written. But that then takes longer for the person who actually has to write it down because it takes longer to write than to say. So it’s really looking to all different time pressures because everybody is under a time pressure. You can’t have a standard formula for all the information because for a 21-year-old, otherwise fit and healthy person, you probably don’t want to know the social information you might need to know for someone who is house-bound with elderly relatives at home. So you can’t standardise and say this is what must be given. In many ways, it’s experience knowing what’s important and which is the information that you really do need to get.
Verbal communication
The major tensions inherent in verbal communication described by interview participants are summarised in Table 23.
| Enables better care | Verbal communication provides added value by conveying subtleties and extra information, and by allowing for questioning, feedback and education. The personal interaction fosters greater collaboration and effective relationships across departmental and organisational boundaries |
| Highly dependent on the individuals and their goals | Verbal communication relies on memory and the sender may filter information depending on perceived importance. The communication may be unstructured and confusing. Sender and receiver may have different goals and information needs. Interruptions, noise and lack of privacy may negatively affect verbal communication |
| May not take place due to lack of time and capacity | Verbal communication can be delayed or skipped owing to queues or unavailability of one party, or because the person giving the handover is unfamiliar with the patient |
Handover is usually conducted verbally, either face-to-face or over the telephone, even although there is now a trend to rely on documentation in order to reduce the number of handovers and the time required. Participants described many advantages of verbal communication that enables them to provide better care to patients. Verbal communication goes beyond documentation and provides added value by conveying subtleties and information that may not be immediately relevant to the patient’s acute condition, but which may be of importance later on (‘small things that may seem unimportant, but aren’t’), by allowing highlighting and prioritisation of the important pieces of information, and by providing information first hand (‘straight from the horse’s mouth’). As it is a dialogue, it also allows for questioning, feedback and education. Verbal communication also fosters collaboration between colleagues, and the resulting personal familiarity with colleagues is perceived as an important facilitator in providing high-quality care across departmental boundaries. On the other hand, participants also pointed out many problems they faced with verbal communication. It relies on memory and it usually conveys only what the sender perceives as the important issues. The communication can be unstructured, rushed, and jumping from topic to topic without providing a clear picture of what is required. Verbal communication often takes place in less than adequate locations, where there are frequent interruptions, high levels of noise and activity, and little privacy.
One participant from the ED describes the tension that is inherent in verbal communication when referring a patient by contrasting this with the alternative form of electronic referrals, pointing out the potential risks of not having the possibility of a discussion.
Then there’s the actual transmission of the information of course, which obviously there’s the amount of communication that you have, the method of it and the records of it, so our systems at the moment for instance, we’re trying to move with some of our referrals to an electronic system where we would be able to transmit information electronically, because what happens at the moment is a lot of the conversation that’s happening is just repetition of information that’s already available. Now, there are two sides to it. As the manager of this area I can say, yes this will smooth the process and make it much quicker. Looking at the system I would say, yes but that also means that the person, if there isn’t any element of discussion or challenge at the point of referral, potentially these inaccuracies won’t be picked up, so there’s kind of – that’s something that can improve systems, but also a risk can be accentuated by that as well.
Verbal communication is also strongly affected by departmental capacity and workload. On the one hand, verbal communication allows people to prioritise their work and manage flow and their own workload more efficiently. On the other hand, however, the lack of capacity and flow may mean that the communication is delayed (e.g. due to queues or unavailability of one party) or may even be skipped altogether. The lack of capacity can also lead to situations where the verbal handover is given by somebody who is not familiar with the patient, and who is thus unable to provide that added value. This may also lead to frustrations on the part of the receiving party (‘we can all read’). The verbal communication can also be perceived as taking away time that could be spent on actual patient care.
A second participant (from ED) describes how a trade-off could be made between relying on documentation only and having the verbal communication that allows providing added information. The trade-off, in this instance, relies on the subjective notion of ‘being worried’, i.e. on the clinical judgement by and experience of the person giving the handover about what is of importance.
If I’m seeing the patient first, I’m quite happy just to look at that initial documentation. When I want a verbal handover is when they’re worried about a patient because if they’re worried, I want to know and I want to know earlier. I don’t just want to happen to find it. So I like to know that if somebody is concerned, they will alert me otherwise I think it’s too much by chance that you find out that your patient is sick whereas if that’s already been recognised, then you go in then with a heightened sense of urgency and then heightened awareness.
Transfer of responsibility
The major tensions inherent in the transfer of responsibility described by interview participants are summarised in Table 24.
| Explicit transfer of responsibility ensures seamless transition of care | Verbal communication provides the opportunity to discuss, review treatment plans, and to ensure that the transfer of responsibility is appropriate and in the patient’s best interest. The feeling of personal accountability motivates both parties involved in handover to communicate all of the information that they feel is relevant |
| Difficult conversations may result in refusal to accept responsibility for patient care | Patient referrals from ED can be difficult conversations. This may be due to different professional cultures leading to perceptions that patients need to be sold or that one is creating work for the other. Poorly structured referrals may cast doubts on the appropriateness of the referral. There is a lack of pull for patients by the specialist wards |
| Lack of capacity may lead to situations with unclear allocation of responsibility and patients being stuck or lost in the system | Lack of capacity leads to queues or delays in handover and patient transfer. The allocation of responsibility in such situations is often implicit and may be unclear. This may lead to situations where patients are not progressing in the pathway or where they are lost in the system for a period of time |
Clinical handover entails both the communication of information and the transfer of responsibility for patient care. The explicit transfer of responsibility ensures that there are no gaps in the provision of care. Participants receiving handover described the transfer of responsibility in terms of personal accountability (‘it’s my patient’), and their desire and professional responsibility to gather all relevant information (see verbal communication). The same holds for the party giving the handover, who perceive it as their professional duty to communicate all the information they have gathered. When the transfer of responsibility involves verbal communication, this provides also the opportunity to have a discussion, review treatment plans, and to ensure that the transfer of responsibility is appropriate and in the patient’s best interest (‘ensuring the patient goes to the right place, first time’).
Participants from ED described the referral of patients from ED to other departments as ‘a difficult conversation’ and ‘not a handover, but a bargaining tool’, which may result in the transfer of responsibility for patient care being refused. Participants from ED and from acute medicine provided differing explanation for this experience. From an ED perspective the refusal to accept patients by specialists or the ‘selling of patients’ that they have to do may be caused by ‘boxing’ or ‘gatekeeping’ behaviour of specialist wards and their concern for their own work. Selling of patients in this context means that the person giving the referral perceives that they have to make the patient appear attractive to the specialist or highlight those aspects of the patient’s condition that make the patient particularly relevant to the specialty. They report that ‘A&E is seen to create work for others’ and that there is an absence of a pulling mechanism from wards. Such pulling mechanisms would entail that specialists highlight appropriate patients within the ED and will proactively organise the forward planning of their care. They also described situations where junior doctors receiving the referral were unfamiliar with organisational policies for admitting patients that provided clear guidelines. On the other hand, participants from acute medicine described the conversation around patient referral as an opportunity to discuss and to ensure that the patient goes to the right place. They also described situations where handover was poorly structured and confusing, which may cast doubts on the appropriateness of the referral. They also reported on a tendency of junior doctors in A&E to ‘medicalise’ reasons for admission even if the admission is primarily for social reasons or if there is a large degree of uncertainty.
One participant from ED describes the difficulties they experience when referring patients that may not fit a particular specialty unambiguously. This can lead to discussions and refusal to accept the patient, which ultimately leads to delays and situations of crowding. The solution they offer is being assertive and being backed by a formal trust policy on referrals and admissions into hospital.
The classic thing is medicine has become so boxed and every specialty in the hospital has made their box as small as possible and they put up as big a wall as they can around it, so we’ve got our upper GI [gastrointestinal] surgeons, we’ve got lower GI surgeons, we’ve got little finger toenail surgeons almost. It’s just ridiculous. We, as the attending clinicians, have to make a decision about who is most appropriate. And if we’re wrong, which we will be, they then send on to the next team that they think. But it’s classically patients who fall in between. So that GI bleed. Is it lower GI or upper GI? So should a surgeon take that or is it Medicine? So you can end up with patients waiting in the ED, and that’s what’s classically has happened across EDs, across the country. For hours and hours and hours, no one makes a decision. So we have to make a decision which way they should go. It’s still a problem but we try and force the issue by doing these techniques. The patient is coming in, I say they are coming in under you, that’s been agreed by the Chief Operating Officer of the Trust [name], and you need to come and see them now. Occasionally they fight back. Occasionally I have very difficult conversations with consultant colleagues. And they say ‘Oh, this is all about 4 hours’ and I say, ‘Yes, it is about 4 hours.’ But that’s really about quality of care of patients.
Participants described as problematic those situations where the transfer of responsibility was implicit and unclear. This can lead to situations of patients being ‘stuck or lost in the system’. Participants described several such scenarios. When ACs are queuing owing to a lack of capacity in the ED, there may be an unclear allocation of responsibility for the patient’s care. On the one hand, the patient is physically still on the ambulance stretcher. On the other hand, the patient is physically already in the ED. Handover may not have been given yet, but paramedics are not trained to provide extended care in the ED. This situation gets even more complicated when a rapid triage has been conducted, but no explicit transfer of responsibility has taken place. Similarly, the elimination of handover between paramedics and the cubicle nurse in favour of a single handover to the nurse co-ordinator or triage nurse, may lead to situations of patients being left in cubicles without the nurse realising and patients being left unattended (‘patient saying “is anybody going to come and see me?” ’).
The referral of patients from ED to other departments may also lead to situations of unclear allocation of responsibility. Participants described situations where patients had been referred by telephone, but remained in the ED for an extended period of time until a specialist was seeing them. Even more confusing situations arise when patients have been seen by the specialist (‘eyeballing’) but are waiting for a bed to become available on the ward or where they have been admitted on to a ward but remain under the care of the ED consultant.
A participant from an ambulance service describes the problem of allocation of responsibility when there are delays at the ED and ACs are queuing. For them, the responsibility for care should transfer as soon as the ambulance arrives at the ED. In their view, the solution to achieving this lies in clear guidelines, education and greater collaboration between organisations.
In fact, I’ve just come from a meeting with one of our hospitals in the region where we’ve been exploring the issues of ambulance delays, and one of the issues that I’m certainly now very comfortable with is that I think all acute hospitals are on the same page as us as an ambulance service and they understand that responsibility does commence as soon as patients arrive and that it’s the responsibility of all of us to work jointly to ensure that that handover process takes place as rapidly as possible to free the crews up so that they can get back out to the community and undertake their primary role. [. . .] Clearly potential tension lies at an operational level. My observations are that, at a strategic and tactical level within the organisation, there’s no issue. People understand the issues and responsibility. The reality, I think, where things break down, is there is failure in the operational plans or implementation of effective handover. That’s the level where things can break down. I think one of the things that contribute to that is a lack of understanding, particularly amongst emergency nursing staff, about where the duty of care begins and just simply ignoring a patient that’s arrived for half an hour, if they’re in the ambulance entrance or still on the vehicle, doesn’t offset their requirements in terms of responsibility. So I think, when people understand that at an operational level then there’s much better engagement. Clearly one of the things that I’ve been anxious about is to try and ensure as far as we’re able to make sure there isn’t tension at operational level and so this is where education and working together jointly becomes, I think, very important.
Goals
The major tensions inherent in the different goals that handover may serve are summarised in Table 25.
| Different actors have different motivations and information needs | Staff responsible for managing patient flows through the department require a short handover conveying the criticality of the patient. Staff giving handover and staff responsible for providing patient care require a more detailed handover that conveys subtleties and provides an opportunity for discussion |
| Staff from different departments and organisations have to work together and trust one another | Staff from different departments and organisations have to work together and trust one another in order to avoid duplication and to provide best possible care. Staff cannot rely uncritically on one another as the story they may get from the patient may be different, and because they have taken on the patient as their responsibility |
| Trust among colleagues is put under pressure by time performance targets | Time performance targets act as powerful motivation and may affect trust among staff negatively. People may use purposeful misinformation and particular keywords in order to force others to prioritise and accept patients. This may result in a degree of mistrust between individuals and departments |
Different actors have different motivations and these can create tensions in the handover process. Handover plays an important role in managing patient flows. Participants described the importance of identifying more seriously ill patients quickly, and of determining the impact on departmental resources and capacity. For example, the senior nurse receiving handover from paramedics prefers to have a quick handover in order to understand the impact on the department and to decide where the patient needs to go (‘I want to hear three words’). Handover to a single dedicated nurse co-ordinator ensures that the co-ordinator can construct and maintain this departmental overview, and thereby provide better management of patient flow. On the other hand, from a clinical perspective handover also helps staff in assessing their own workload and in prioritising their activities accordingly. In addition, both parties involved in handover are motivated by personal and professional accountability. In the case of paramedics this means, for example, that more information than the nurse co-ordinator wants to hear will be communicated or that the paramedics will seek out the nurse looking after the patient to convey this additional information (‘seeing the patient through’), even if from a managerial perspective this may be perceived as needlessly replicating handover. Similarly, the nurse looking after the patient would like to hear the full story to enable them to provide high-quality care, rather than having to rely on documentation only (‘it’s a responsibility you take on’).
A participant (from ED) reflected on the informal practice of paramedics giving a second handover, although this was discouraged at organisational level.
And I think that’s why you still do get the verbal handover to a certain point because I think the Paramedics want to know that somebody realises that their patient has arrived. So I think they want to know that they have completed that care. And I think it is just professionalism isn’t it, that you want to know.
Staff from different departments and organisations recognise that they have to work together and trust one another in order to provide best possible care. The party receiving handover has to work with the information that is provided, and the sender should describe subtleties, concerns and uncertainties (‘give an honest rundown’). Ideally, staff try to anticipate each other’s information needs and act accordingly, for example by doing all observations before transferring a patient. Participants described the need to understand the pressures and capacity limitations faced by other departments and organisations. There is a tension between having to trust one’s colleagues (‘take what the GP [general practitioner] says as gospel’) and avoiding duplication (‘patients don’t want to be asked the same things over and over’), but also knowing that the stories they can get from, for example, the paramedics may be quite different from the patient’s story (‘decisions cannot be based on information from ambulance service alone’). In addition, the patient’s condition may have changed over time. So, on the one hand, people have to trust each other, but on the other hand they are not relying on others uncritically.
A participant from ED describes this tension, and they provide a reflection of how they address the required trade-off in practice by verbally checking with the patient and adding to the documentation selectively, rather than simply copying what was documented before.
You can check the information verbally but, if it’s correct, you don’t need to write it out. I have literally seen people who have got my notes and copied them. That isn’t them being personally accountable. That’s them being good at copying. They are not actually necessarily checking what I’m doing, they are just copying. That is totally and utterly redundant and should not happen. [. . .] I will often go through and say, say an example of diabetes, ‘I believe you are diabetic. How long have you been diabetic?’ And add in the extra information I am getting. Or sometimes I’d say ‘It says that you’ve had a stroke.’ And they’d say ‘No, I haven’t’, in which case, then again, I will say that they haven’t. So it’s more that the time which you are really wasting is when you are documenting in writing information that is already in writing. It doesn’t mean that you can’t check it verbally. And, if you agree with what’s already been said verbally, you can just write ‘as above’. So then actually you can say that you agree with that. It doesn’t mean that you are no longer personally accountable. And then you can add in the extra information that you’ve added, your subtleties or whatever. And I think that everybody knows that a patient tells slightly different stories every time, so therefore you can actually put in your different subtleties. The pain that they’re describing. How they described it to the first person may be slightly different to the way they describe it so I would then document how they’ve described it to me. And that will all help to build up a picture. So that would be as far as people who say it shouldn’t happen because they’re not now personally accountable. You can still make yourself personally accountable by checking it verbally and documenting any discrepancies.
Trust among colleagues is put under pressure by time performance targets. Participants described situations where people may use purposeful misinformation and particular keywords in order to force others to prioritise and accept patients. As a result, there may be a degree of mistrust between individuals and departments, for example wards asking questions that appear inappropriate from an ED perspective or refusing to accept a patient. This was discussed above in relation to the transfer of responsibility during referral. The influence of targets will be discussed further below as part of the second theme, the management of patient flows across organisational boundaries.
Theme 2: management of patient flows across organisational boundaries
The management of patient flows across organisational boundaries was described by participants as a key factor affecting the quality of handover. This includes the management of capacity, the influence of time-related targets, and the collaboration of actors from different organisations and of the organisations themselves. These are described in more detail below. A summary is provided in Table 26.
| Capacity and patient flow | Handover is a tool for understanding and managing demand at the individual, departmental and organisational level Lack of capacity and patient flow negatively affects handover and contributes to tensions |
| Time-related performance targets | Time-related performance targets provide a strong organisational focus for quality improvement Pressures resulting from targets may negatively affect the quality of care and create risks for patients |
| Collaboration across departmental and organisational boundaries | Patient flow and patient safety need to be addressed by the whole system Greater collaboration across departments and organisations, and cultural awareness are possible ways of achieving this |
Capacity and patient flow
Handover contributes to the efficient management of capacity and patient flows. In situations where there is a lack of capacity or inadequate patient flow, there may also be a negative effect on handover. The relationship between patient flow and handover is summarised in Table 27.
| Handover is a tool for understanding and managing demand at the individual, departmental and organisational level | Handover allows individuals to manage their own workload and prioritise their activities Handover contributes to gaining an overview of demand on a department, and it supports prioritisation and patient disposition to maximise patient flow Ambulance services provide pre-alerts and status information to EDs, which enables EDs to anticipate and prepare for incoming demand |
| Lack of capacity and patient flow negatively affects handover and contributes to tensions | When patient flows break down and there is a lack of capacity, handover may be negatively affected on several levels Frequent problems are ACs queuing, leading to delayed handover or multiple and increasingly filtered handover; this also leads to unclear allocation of responsibility and affects the ability of ambulances to respond to emergencies in the community Many surges in demand may be predictable, but are not supported by adequate resources |
Participants related handover to capacity and patient flow issues by describing the purpose of handover as supporting the understanding of demand and capacity at a departmental level, as supporting the controlling of the flow of patients, and as enabling them to prioritise their own activities and patients (at an individual level). For example, a stated reason for having a dedicated senior nurse receiving all ambulance service handovers for patients with major injuries was that it provided an overview of ‘what’s coming in’ and allowed the creation of ‘awareness of the impacts on the rest of the department over the rest of the shift’. As described above, this goal of handover may be at odds with the goals of paramedics giving the handover, who may feel that ‘there’s so much more to tell’ than simply how sick the patient was. Even before ambulances arrive the provision of advance notification through pre-alerts or through the ambulance information system contributes to the anticipation of demand and the preparation for it in the ED in order to maintain patient flow.
The lack of capacity and inadequate patient flows may create multiple problems for handover. For example, participants described that problems occur when people are not answering their bleeps because they are in theatre (surgeons) or when the appropriate person is temporarily not around. In these situations handover cannot take place and the patient needs to remain in the ED or may be admitted without handover. In either case, this may lead to situations of unclear allocation of responsibility for patient care or delays in moving the patient onward. A similar problem can occur when handover has taken place, but the patient cannot be moved onward because there are no free beds. Another major problem described by participants is the situation where a nurse, who is not familiar with the patient, may need to transfer the patient and then give a handover that is perceived as simply reading off the notes and does not provide any added value. This occurs when the nurse who had been responsible for the patient’s care is busy with other duties and asks another nurse to take the patient in order to free up the bed and keep patients moving.
The lack of capacity also leads to ambulance queues. This is described as a potentially serious problem. On the one hand, ambulance queues may result in multiple and increasingly filtered handovers as one crew hands over their patient to another crew. This leads to situations where one crew may be handing over several patients with whom they are unfamiliar and where they cannot provide any additional verbal information. On the other hand, as crews are queuing, there may be situations of unclear allocation of responsibility, as already described above. Participants from the ambulance services described as the most serious problem resulting from queues the loss of capacity to respond to emergencies in the community as the ambulances are stuck at the ED.
A participant from an ambulance service describes the trade-off that needs to be made between potentially less than ideal handover and freeing up crews to get back out into the community based on a risk assessment of the patient’s condition.
So we’ll deploy an ambulance liaison officer, particularly if we’ve got multiple patients or multiple vehicles stacking and that is to support the management of those patients. To provide oversight, if necessary, to take over the care of those patients if necessary because one of the things we practice as an ambulance service when we’ve got stacking is to risk-assess those patients and see if we can free up those crews and get the crews to double up and monitor two patients, fully accepting that that’s less than ideal. We we’re in this situation we’re operating in a decompensated circumstance so, in other words, we need to modify. Essentially, we’re effectively managing patients as we would in a major incident where we are sort of streamlining processes but clearly we’re having to, out of necessity, to address unmet clinical need in the community. So of course, the other side of things that I’m very cognisant of is that the risks of having to accelerate clinical handover or to streamline the handover process and release crews back into the community. The risks of that, in my view, are far less than having a patient with chest pain or a potentially life-threatening issue with no clinician available to support or resuscitate them. So that’s the balance. But if the system is well resourced and well managed the key to this in terms of avoiding these systems, is having upstream management measures in place to prevent the queue occurring in the first place.
The same participant continues by describing that queues resulting from increased levels of demand are predictable, and that they should be accounted for by adequate resources in order to avoid having to make such trade-offs in the first place.
So, one of the things that I consider to be crucial in terms of risk mitigation is that, bearing in mind that these surges in demand are predictable, they occur at predictable times of day. Then the critical thing from my point of view is to make sure there’s an adequate nursing resource to be able to take responsibility for these patients as soon as they arrive. And I would suggest in the ratio of no more than five patients to one – probably three to one would be the right level. So modelling where there’s been a single Escalation Nurse may not be adequate if there are 10 or 15 patients waiting to be off-loaded and handed over and again, this is areas of practice that we’ve tried to share with colleagues.
Further problems resulting from a lack of capacity include poor documentation as people ‘write less when busy’, which contributes to the tension of people being asked to rely increasingly on documentation in order to avoid duplication of handover. The lack of capacity may lead to abuse of the handover process, for example certain keywords may be used during handover to force admission of a patient. This could set off the admitting team on a wrong path and lead to delays and complications in patient care. It contributes to tensions between the need to trust one’s colleagues and the knowledge that the system may be abused to ‘get the patient through the front door’. Familiarity with colleagues makes this tension manageable. However, this is threatened by high turnover of staff and the increasing reliance on agency staff, another capacity issue.
Time-related performance targets
Time-related performance target are an important quality improvement tool. However, the pressures created by the targets may introduce risks to patients and contribute to tensions between departments and organisations. The relationship between targets and handover is described in Table 28.
| Time-related performance targets provide a strong organisational focus for quality improvement | Time-related performance targets provide focus and are an important quality improvement tool The handover target for ambulances contributes towards ensuring that the ambulance service maintains its capacity to respond to emergencies The 4-hour target in the ED ensures that patients are seen within a reasonable amount of time and it contributes to patient flow |
| Pressures resulting from targets may negatively affect the quality of care and create risks for patients | Clinical processes may be designed around targets, and this may lead to dissatisfaction among frontline staff and create risks for patients Staff may adopt informal working practices in order to balance the need to meet the target and to deliver high-quality care Pressures from targets may lead to distrust between departments as well as poor patient experience |
Emergency departments, and more recently ambulance services, have to meet time-related performance targets to ensure that patients get seen in the ED within a reasonable amount of time and that ambulances can get back out on to the road in order to be able to respond to emergencies. Meeting targets acts as powerful motivation. Participants with management responsibility described targets as an important quality improvement tool that ‘provides significant corporate focus’.
Frontline staff also felt quite strongly about time-related performance targets, but cautioned against too many pressures. In combination with increasing patient numbers and more junior staff responsible for their care this poses additional significant challenges. Some participants even expressed significant negative attitudes towards the resulting system (‘I hate it!’). For example, the target introduced for ambulance services was described as leading to a process ‘designed entirely around the target’, which may threaten the quality of care and which people feel is inappropriate. This can lead to situations that create patient safety risks, such as when a patient is simply left in the ED and the nurse is unaware.
A participant from ED describes the tensions in perception between clinical and management staff, and between the ambulance service and the ED. They describe a situation from their clinical experience when the focus on targets led to a hazardous situation for the patient.
That is a problem. We know it’s a problem. They [ambulance service] just say ‘It’s your problem, why are you keeping our paramedics too long’. It’s not us, it’s them pressing their button and getting out there. So there are issues around timing, and there are organisational pressures, which I don’t think you should put too much pressure on, because actually they ensure quality. But the ambulance service is great. They do a superb service but they have managers who are pressing their guys to be back out on the road, back out on the road, back out on the road. Too much pressure inevitably will cause quality of care to drop. I’ve seen a patient two or three months ago who was just left on the spinal ward in a cubicle. Our nurse didn’t pick it up. We had put in nursing governance issues. The patient was left on the spinal ward but none of us knew about it except the handover people. That’s because the paramedics had been told to get out and leave the boards here. In the past, we would always have a policy where they were always logged off by the paramedics. So organisational pressures to achieve organisational targets, like paramedics attending to patients within 8 minutes or whatever, are pressures, which [inaudible] can impact on the quality of handover and have done. And will continue to do. We guard against that. The paramedics guard against that. But you may have some people sitting in offices upstairs here or sitting in offices in [ambulance service] who don’t appreciate our efforts.
Frequently participants described how they used their professional judgement in order to balance the tension of having to meet the target and delivering high-quality care to the patient they are responsible for. This can lead to the adoption of an informal working practice and a discrepancy between work-as-imagined (i.e. prescribed by policy) and work-as-is.
A participant from an ambulance service described how they perceive the time frame set by the target as the point by which they have to be back out on the road. They will use this time available according to their own judgement in order to ensure good care.
We’ve got 15 minutes from when we arrive to when we should handover. [. . .] And then 15 minutes from when we’ve handed over to when we’ve finished our paperwork and we’ve come clear. [. . .] So we’ve only got a 30-minute window here. [. . .] So I look at it as, OK as long as I press that button I will wait around and talk to the nurse, as long as I’ve cleared in 30 minutes, how I spend my time here is up to me.
Similar attitudes were expressed towards the ED breach target. This may lead to what are perceived inappropriate referrals in order to meet the target, and it may threaten trust among colleagues from different departments. Participants also described that it may create negative perceptions towards A&E and their staff (‘wards don’t welcome A&E nurses’), thereby threatening interdepartmental collaboration. Participants also cautioned that meeting the target can lead to poor patient experience and that their responsibility was to ‘provide quality experience for the patient, not just moving them quickly’.
Collaboration across departmental and organisational boundaries
The problems around handover and patient safety are frequently linked to inadequate patient flows and lack of capacity (see above). These cannot be addressed where they present themselves, alone. An approach supported by the whole system is required. Greater collaboration and communication across departments and organisations through engagement at all levels and through joint working may offer possible ways for achieving this. The relationship between collaboration across boundaries and handover is summarised in Table 29.
| Patient flow and patient safety need to be addressed by the whole system | The lack of collaboration and concern for the impact on each other’s work across departments and organisations may lead to inadequate patient flow and may create risks to the patient These problems cannot be left to be addressed where they manifest themselves. If a queue occurs, the system has already failed. An approach that includes the whole system is required Current drivers in the health system do not encourage greater collaboration between departments and organisations |
| Greater collaboration across departments and organisations, and cultural awareness are possible ways of achieving this | Communication at all levels and access to key decision-makers can foster greater collaboration across departments and organisations, and create greater cultural awareness at an operational level Joint working, shared staff and embedding staff in different services can support this collaboration Senior clinical input and discussions with GPs early may be one particular way of maintaining flow and reducing ambulance delays and ED overcrowding |
The actors involved in providing emergency care to patients belong to different departments and organisations. This means that they have their own respective concerns and pressures, as well as their respective local cultures. This can at times lead to very strong views about the perceived lack of concern or unwillingness to collaborate by the other parties. For example, ED staff described their frustrations with specialists from other disciplines whom they perceive to be only ‘interested in their own work’. The tensions that may arise from this have already been described in detail above when looking at verbal communication and the lack of patient flows. Similarly, participants described their dissatisfaction with general practitioner (GP) attitudes and the provision of out-of-hours service. This may lead to predictable peaks in demands in the ED, for example on a Monday when patients who had been feeling sick over the weekend are sent in large numbers to the ED. These in turn cause ambulance delays and flow problems. Participants described that the solution to such problems will probably not be found in increasing the numbers of staff or improved local handover practices. The problem would need to be addressed at a system level, by engaging with GPs, where the problem is created.
Closely related to this is the set-up of the health system and the drivers who are in place. One participant from the ED suggests that the drivers would need to be reconsidered and realigned in order to create appropriate incentives for engagement and collaboration at the system level.
The key thing that needs to change though in the NHS is the drivers. The drivers are all in the wrong place. The money has to follow the patient. It doesn’t at the moment. The money is given to the self-interest groups who use it in their own way, to the GPs at the moment and to the hospital doctors to an extent. It is going back to basic simple things. You know, we’re not going to improve the quality of care until we sort out what’s driving things. I have problems with handovers because things that my consultant colleagues are judged on are nothing to do with the quality of patients that arrive in the department. The only person that’s really judged on sorting out emergency care is the emergency department. So no one else is bothered. They do not give a toss about it. So they don’t do anything about it. GPs couldn’t care less if I have 200 patients arriving at half past whatever. You know our numbers have gone up 10% in the last 6 months. They are the largest number of patients in our department. No one gives a damn about it. It doesn’t bother them what’s happening here. [. . .] You’ve actually got to change the drivers in the system. So while the drivers are set up as they were, these issues, these pressure points, are going to get worse. And they’re going to get worse at the final deliveries of care.
Participants also described their own attempts at finding solutions to these problems. A participant from the ambulance service describes engagement with people at all levels as a key ingredient in fostering greater collaboration, and in developing whole system solutions.
In fact I’ve just come from a meeting with one of our hospitals in the region where we’ve been exploring the issues of ambulance delays and one of the issues that I’m certainly now very comfortable with is that I think all acute hospitals are on the same page as us as an ambulance service. [. . .] The challenge is managing surges in demand and trying to secure the cultural awareness that this is an issue and that we all do have a responsibility to ensure that our crews get back out into the community quickly. [. . .] This is why I have felt it’s been critically important to engage at the highest level within the organisation so we’ve had engagement at Chief Executive and Medical Director level. [. . .] The reason that that is critical is that, in order to maintain flow in these circumstances, you actually need the whole system supporting so it requires good operational management but also actually requires clinical buy-in from the in-patient team.
Joint working was proposed as an additional way of strengthening collaboration and creating a shared awareness of risks to patient safety. This could include joint, part-time appointments between the ambulance service and the ED, or ambulance service staff being integrated within the ED. This would create staff with experience of working both in pre-hospital as well as hospital-based care.
Participants described the need to tackle the problem where it arises, before it actually becomes a problem (‘if there’s a queue, the system has failed’). This requires communication and collaboration between all stakeholders involved in order to develop a system that is able to maintain flow. For example, one way of reducing ambulance queues at the ED and the resulting problems for handover and quality of care is to reduce the number of necessary conveyance to hospital. Participants from the ambulance service described protocols they had established with GPs for patients with a degree of uncertainty about their past medical history. The protocol ensures there can be a discussion with the patient’s GP, who may choose to take on responsibility for that patient or advise that they be escalated, admitted or they may choose to arrange an alternative care pathway. Similar arrangements have been proposed by participants from the ED in order to ensure senior clinical input prior to referral of a patient by their GP. One participant nicely summarised what was needed was ‘a systems approach – how do we provide emergency care services for people who live in this area’.
Stakeholder feedback
Preliminary research findings were presented to delegates at the stakeholder workshop. The comments received during the plenary discussion suggest that delegates were able to identify with the suggested categories and could relate these to their own practical experiences. Delegates provided examples of how they experienced certain tensions and how they dealt with these. Delegates also suggested, both during the plenary discussion as well as during the group work, that the management of patient flow was closely related to the quality of handover.
During the group work and the subsequent feedback and concluding plenary sessions delegates were invited to make suggestions for the improvement of handover. As a result of these interactions, delegates suggested the following main topics or domains (list in the order in which the topics were discussed) (Table 30):
| Management of patient flows | Delegates suggested that many of the problems with handover are the result of inadequate patient flows. Sorting out patient flows was regarded as a prerequisite to improving handover, but no concrete improvement suggestions were provided |
| Electronic tools | Following the presentations on electronic referrals and electronic PRFs, delegates suggested that, in general, the use of electronic support tools could be beneficial, but few delegates had practical experiences with these |
| Structured communication protocols | Delegates suggested that the adoption of structured communication protocols would improve handover. Several delegates reported positive experiences with structured communication protocols. Some delegates, although being positive about structured communication protocols as such, reported negative experiences with the way these had been introduced in their environments, e.g. unilaterally by one department |
| Personal relationships | Delegates described several situations where they managed problems or prevented problems with handover through personal relationships. Delegates suggested that being able to put a face to a name (or to a voice on the telephone), and having established a level of trust with colleagues from other departments or organisations, greatly facilitated their interactions. As a result, delegates cautioned that personal relationships need to be maintained when electronic tools, such as electronic referrals, are introduced |
| Geographic responsibility | A specific problem many delegates discussed concerned the allocation of responsibility for patient care across organisations and departments. The consensus among delegates was that responsibility should be allocated depending on geographic boundaries, e.g. if a patient is in the ED (e.g. waiting in a queue to be handed over), the responsibility for patient care needs to be with the ED |
| Training | Delegates suggested in-house training that involves different disciplines or different departments could lead to improvements in handover. Delegates felt that this provides both a basis for building personal relationships with your colleagues as well as a sense of shared goals in patient care |
Discussion
The results presented in this chapter, irrespective of the particular context or setting, make clear the inevitable tensions inherent in the undertaking of a complex task by multiple actors representing different roles, perspectives, priorities and indeed organisations. This is almost inevitable in any such complex, dynamic interactive process. However, recognising these subtleties is important in how the vulnerabilities of the handover process are understood, how some existing approaches to improvement have been framed and what type of future recommendations may be appropriate.
Typically there is a desire to describe the context of behaviour, i.e. what was said, in the hope that omissions will be identified and extended checklists of coverage devised. The approach subsequently leads to a desire to document more and more. However, the examples given in this chapter make clear the new dilemmas and pressures excessive documentation can create. A more sophisticated approach involves the recognition of handover as a dynamic interpersonal context and to recognise that the participants are not merely role representatives but bring into the exchange a mental model of what they understand the process to be, what they want out of it and what they need to do to ensure that their own needs and priorities are achieved. This notion of mental models has been explored in a range of contexts by Spurgeon et al. 95 in terms of use of information and by Flanagan et al. 96 in terms of how managers enact their role and achieve their goals.
A mental model is akin to the concept of organisational culture, except that it operates at an individual level. From experience and sets of assumptions and requirements individuals construct a model of how an interactive process will operate in order to allow them to achieve their desired outcomes. When multiple actors and thereby multiple mental models are involved there is a continuing, often unstated negotiation going on during the exchange. During a handover the tensions, strains and pressures observed here are these negotiations being played out in real time.
There are a variety of ways in which the interplay of these models can heighten the concerns around an effective handover:
-
A dominance of one individual’s model that imposes itself on the exchange, leaving another’s model suppressed and unsatisfactory.
-
An ill-formed model, often used by an inexperienced practitioner, may not achieve the necessary outcomes but the deficiency may not be recognised.
-
Competing models, especially under time pressure, may lead to compromises and a frustration with the outcome of the exchange.
The more explicit, rather than implicit, these models can be made to the various participants then the better chance there is of accommodating the different needs.
A second key conceptual finding is the need to ensure that handover is recognised as part of a whole system process, and not something completed to the satisfaction of a part of the system, whether a subpart of the organisation or different organisations. It is mentioned at the outset of the Results section (above) that the two themes identified (role tensions and patient flow) are related. As a consequence there is a danger that subsystem initiatives, i.e. by a part of the system and not involving the other elements, will exacerbate the problem of achieving the outcome of the handover process by prioritising ‘our’ goal above others. Subsystem initiatives will have an impact upon individual’s mental models and will alter priorities. This could well have the effect of reducing the likelihood of the handover partner achieving their objectives.
Chapter 5 Discussion
Introduction
In this chapter the findings of the different research activities are brought together and interpreted with a view to the existing evidence base. This introductory section provides a summary of the key research findings across the research strands (see Introduction). The following two sections discuss these findings in turn, and explore how they relate to and build on the knowledge available from the literature (see Handover is a sociotechnical activity and Capacity and patient flow across boundaries). The chapter finishes with a description of the limitations of the research (see Limitations of the research) and a short conclusion (see Conclusion).
We identified two key themes arising from the different research activities (Table 31):
| Handover is a sociotechnical activity embedded in clinical and organisational practice | Handover can serve different goals and motivations. Inner tensions give rise to observable disturbances or problems. Inner tensions are always present and cannot be eliminated. Practitioners deal with tensions by adapting their behaviour, thereby possibly creating new tensions. Understanding handover as a sociotechnical activity embedded in clinical and organisational practice means that improvement efforts should focus on providing flexibility to practitioners to make trade-offs in order to resolve tensions |
| The quality of handover is frequently linked to issues of capacity and patient flow across organisational boundaries | Lack of capacity and patient flow negatively affects handover and contributes to tensions. Time-related performance targets provide a strong organisational focus for quality improvement, but pressures resulting from targets may negatively affect the quality of care and create risks for patients. Patient flow and patient safety need to be addressed by the whole system. Greater collaboration across departments and organisations, and cultural awareness are possible ways of achieving this |
Handover is a sociotechnical activity
In research strand 1 we described handover as a sociotechnical activity, i.e. as an activity with different actors, different goals and motivations, and different supporting tools (external and cognitive tools). This activity is embedded in clinical and organisational practice, which serves both as context as well as providing goals for handover. This also means that in practice there is a range of different types of handover that may be very different in nature and may provide different functions. Taking this view allowed us to identify and to describe in research strand 2 a number of inner tensions that can be found in this sociotechnical activity. This approach may lead to a radically different view on the problems with handover and on how people create safety.
As described in the literature review in Chapter 2, there is evidence in the literature that handover may serve different functions other than the transfer of clinical information about patients. Other functions identified include aspects of training, of socialisation and of enhancing teamwork and group cohesion. 23,25 Some authors have highlighted the fact that handover is a dialogue that can create shared awareness between participants, and even provide an opportunity for error recovery. 20–24 Behara et al. 24 refer to handover as ‘exercises in building distributed cognition’. Although they do not provide further discussion of what they mean by this or what the underlying theoretical principles are, this is a view that is highly relevant to the interpretation of the findings produced by the present research.
The distributed cognition approach was made popular with the publication of Ed Hutchins’ seminal book Cognition in the Wild in 1995. 97 In the book, Hutchins provides a detailed ethnographic account of ship navigation. As its central premise, distributed cognition assumes that representations of knowledge are distributed both spatially and temporally over a network of actors and external artefacts. The appropriate unit of analysis thus becomes the cognitive system, for example the ‘cockpit system’ that provides functions such as remembering its speed through the interaction and transformation of representations distributed over people and artefacts. 98 The distributed cognition approach tends to produce detailed descriptions of human interaction with external artefacts, for which reason the approach has become particularly popular in the field of human–computer interaction. In addition, distributed cognition places emphasis on understanding co-ordination and alignment of actors within a distributed process. 99
Closely related in its concern for studying context in order to understand the relationships between people as individuals, the tools they use, and the societies (in terms of groups and their cultures) to which they belong, is Activity Theory,86,87,100 briefly alluded to in Chapter 3. Activity Theory is an approach to studying human behaviour that is rooted in the cultural–historic tradition of soviet psychology. A detailed account of the roots of Activity Theory is provided by Engestrom. 101 Activity Theory and cultural–historic psychology87 are broad philosophic forms of enquiry, and the description given here is necessarily brief and simplistic. In essence, the basic unit of analysis within the activity-theoretic framework is the activity – a form of doing directed to an object. 102 The relationship between the individual and their object is mediated by a third element, namely a tool or an artefact. Tools can be both internal, such as a plan or a strategy, as well as external. Tools are both enabling and limiting, i.e. tools extend human capabilities, but they also limit how the object is perceived. This is illustrated in the popular saying that ‘if all you have is a hammer, everything looks like a nail’. 103 However, this basic mediation triangle consisting of individual, object and artefact, is still too simple to describe fully the structure of an activity. The individual always acts as part of a community, which when added to the basic unit of analysis, gives rise to two further relationships. These are the relationship between the individual and the community, and the relationship between the community and the object of the activity. These relationships are mediated by rules of social interaction in the former case, and by a formal division of labour in the latter case. The resulting structure is known as extended mediation triangle,101 and forms the basic unit of analysis.
The reason for drawing on Activity Theory in the interpretation of the results of this research is to be found in its dialectical concept of inner contradictions of an activity. 101,104,105 The most famous application of the dialectical method is, of course, the analysis of capitalist society in Karl Marx’s Kapital. Inner contradictions are tensions inside of an activity. Kuutti102 explains that ‘Activity Theory uses the term contradiction to indicate a misfit within elements, between them, or between different developmental phases of a single activity’. Inner contradictions manifest themselves externally as disturbances or disruptions, i.e. as the undesired effects that we perceive. These undesired effects cannot simply be eliminated without addressing the underlying contradiction. However, the fundamental point of the application of dialectics in this case is that ‘contradictions are the driving force of transformation. The object of an activity is always internally contradictory. It is these internal contradictions that make the object a moving, motivating and future-generating target’. 104
Engestrom’s bold statement above101 has important implications for this research on handover. It means that the inner tensions that we identified in Chapter 4 as part of the thematic analysis are not only present and give rise to the disturbances and problems with handover that are so frequently observed, but also these inner tensions may well be inevitable. As a result, improvements in handover cannot simply aim to eliminate disturbances, such as missed information during handover; neither can they necessarily eliminate the corresponding inner tensions, for example the need to tell the full story conflicting with the need to determine the criticality of the patient and to assess the impact on the department. What this really means is that the inner tensions will drive the shape and form of the activity to different levels of development, which, in turn, may give rise to new tensions and disturbances as their outward manifestations.
This can be seen extremely well by considering the practice of the ‘secret’ second handover, taking place between paramedic and the nurse looking after the patient (described in Chapter 4). The official procedure foresees one handover only between the paramedic and the nurse co-ordinator. However, in those cases in which the paramedic is concerned or feels that there are important details they need to communicate, they may find reasons to stay in the department and thereby create the opportunity for a verbal handover to the nurse. The paramedic, therefore, adapts to the inner tension in order to resolve it, because it cannot be eliminated. By doing so, new tensions may be created, for example this practice may conflict with the need to get back into the community.
What we can observe is that practitioners use their experience and skill to make the required adjustments and necessary trade-offs in order to deal with these tensions. In the above example, the paramedic will decide on a case-by-case basis whether a second handover is required. This type of behaviour forms the basis for a different way of thinking about how people create safety in complex sociotechnical systems. It denotes a shift from thinking about safety as the avoidance of failure towards a perception of safety as the creation of success. This is the basic premise of the discipline of Resilience Engineering. 106,107
Resilience can be defined as ‘the intrinsic ability of a system to adjust its functioning prior to, during, or following changes and disturbances, so that it can sustain required operations under both expected and unexpected conditions’. 108 A fundamental principle of Resilience Engineering is the assumption that performance variability is the essential feature of individual and collective performance that makes it possible to adjust strategies and activities to changing demands and dynamic situations. 109 In this view, there is no fundamental difference between how things go right and how they go wrong – failures happen when the adjustments of an organisation (or team, individual) do not quite match the current conditions, but not because performance is variable in the first place.
The principles of Resilience Engineering are described in depth in the references provided. At this point, the implications of these theoretical deliberations for the present research should be reviewed. The research has made visible inner tensions within the activity of handover. These inner tensions manifest themselves as disturbances that we perceive as the problems with handover. Practitioners use their experience to adapt their behaviour in order to resolve the tensions, thereby possibly creating new tensions. Failure occurs when the adaptations are insufficient or inappropriate. Improvement efforts may try to resolve some of these tensions, but there will always be some tensions. As a result, improvement efforts need to consider how the system can provide flexibility and support to practitioners in making the required trade-offs. Isolated solutions and the measurement of compliance with a procedure or a standard protocol may have limited success if these considerations are ignored.
Capacity and patient flow across boundaries
The review of the literature described in Chapter 2 suggests that research on handover in emergency care has frequently focused on single-discipline shift handover, and that there was a need for further research investigating handover across departmental and organisational boundaries. 20,59–61 Studies that have considered handover across a departmental or an organisational boundary found that there are increased co-ordination costs between individuals from different specialties,60 and that the different information expectations and cultural backgrounds could lead to information ambiguity and situations of unclear allocation of responsibility,20 putting patients at risk of ‘falling between the cracks’. 60 Gobel et al. 48 suggest that these are risks created by ‘a fragmented health-care system in which there are many people involved each with ambiguously defined responsibilities’. It is a strength of the present research that we considered the pathway from ambulance services to ED and the patient’s onward journey to acute medicine. A recently published study investigating communication and handover across a surgical pathway takes a similar view, suggesting that ‘any strategy that aims to improve the system of surgery should involve identifying and improving information and communication processes across the pathway’. 92 The same most likely holds for improvements in emergency care.
Taking this view, we found as a result of the research conducted in research strand 1 that capacity issues and inadequate patient flows may give rise to many of the identified potential handover failures, thus contributing to threats to patient safety. Research strand 2 provided further in-depth understanding of the relationship between capacity and patient flow, and organisational and national targets on the one hand, and the problems that staff experience with handover on the other hand.
The flow of patients through the ED is already recognised as an important issue for patients. Delays in care can result in worse clinical outcomes110 (e.g. delay in antibiotics for septic patients or thrombolysis for stroke) and also impact on the patient’s experience. The resulting overcrowding is also associated with increased mortality111 but also increased errors, attributed to issues such as increased distractions, interruptions and decreased time per patient. To combat this, the English NHS introduced a target that all patients should have their episodes of A&E completed in < 4 hours, as part of the NHS Plan. However it is recognised that although it has decreased delays overall, it has, in some circumstances, led to actions designed to achieve the time target rather than having a primarily clinical improvement focus. The 2013 guidance Everyone Counts: Planning for Patients 2013/14112 has determined that the 4-hour time measure will continue to be a focus of performance management and that the ambulance turnaround time will have a similar focus. Failure to achieve these will be associated with significant financial penalties. Although study participants acknowledged that such targets are useful tools for providing a corporate focus on improvement, the research also provided evidence that this potentially has an impact on the quality and safety of handover as described in Chapter 4.
When an AC hand over a patient they have 15 minutes from the time they arrive at the ED until they have clinically handed over care. The NHS Confederation has recently issued guidance113 on how this can be achieved, recognising that ambulances lose their capability to respond to emergencies when they are stuck waiting in queues at the ED. However, there is a danger that such efforts are only concerned with speeding up the process and not necessarily about improving the quality of handover. The results of research strand 2 suggest that efforts aimed at achieving this target have contributed to tensions in handover, potentially resulting in processes that have been designed around the target to the exclusion of other considerations. In line with the above first theme, the research also provided evidence about how practitioners make flexible trade-offs in practice, taking into account the local circumstances in order to manage these tensions and to continue to provide safe care.
A similar situation was found with respect to referrals from the ED. Timely referral from the ED to the medical assessment unit will impact on the total time in the ED. If a patient is approaching the 4-hour limit then the referral may be hurried or ill prepared. In some cases the patient could be referred earlier than the clinically optimal, and there is evidence that admission rates increase when overcrowding occurs. 114 The research suggests that this may lead to distrust between individuals from different departments, as well as to poor patient experience.
A common feature of these two examples of time performance targets is that overcrowding and targets can contribute to tensions in handover. The findings of the research suggest that issues of patient flow, capacity and overcrowding on the one hand, and the quality of handover on the other hand should be considered and addressed together. This necessitates a collaborative effort of the whole system including greater collaboration between departments and between organisations.
In a recent publication, Horwitz et al. 115 report preliminary experiences of an institution-wide task force to standardise and to improve physician handover across Yale New Haven Hospital. They suggest that such a broad approach has already led to improvements in patient care. They argue that the development of an institution-wide written sign-out tool embedded in the electronic medical record system has resulted in nearly ubiquitous uptake, and has contributed to staff satisfaction with handover practices. They emphasise that such an institution-wide initiative was instrumental to establishing handover as an organisational priority, and that it provided opportunities for clinical educators as well as other staff to learn from each other and from other areas, and to pool ideas and resources to improve handover throughout the organisation. This may be in line with our own research findings, which suggest that greater collaboration across departments and organisations, and cultural awareness may be possible ways of achieving sustainable improvements, both of handover and of patient flows across organisational boundaries. This should include communication at all levels and access to key decision-makers, efforts at joint working across departments and organisations, and access to senior clinical input along the pathway as well as to other stakeholders such as GPs.
Limitations of the research
The research utilised qualitative methods. These produced rich accounts of participants’ experience with, and perceptions of, handover and the associated problems and risks. However, qualitative research methods have limitations that need to be understood.
The first limitation pertains to the generalisability of the study. Participants in this study came from five NHS organisations. The study sample was chosen to exhibit diversity in terms of size, geographical location and population served. Yet this was only a small sample and questions may be asked about how context specific the findings are. The risks that we identified and the perceptions of staff about organisational issues were similar across the sites. The findings should be of use to stakeholders within emergency care outside the study sample but this limitation needs to be borne in mind.
A second limitation pertains to the stakeholder perspectives that informed the study. We used a purposive convenience sample including staff from the ambulance service, the ED and staff from acute medicine, trying to ensure a broad representation of different perspectives. Often, only a small subset consisting of participants from a single specialty is considered, and the findings of this study, therefore, can draw on a much wider range of views and experiences. However, we acknowledge that this still represents only a partial view. The research has shown how intricately linked the problems with handover are to issues of patient flow across boundaries and the importance of interorganisational collaboration. With the benefit of this knowledge, we acknowledge that the inclusion of the views of GPs and other actors in the community may have provided interesting additional perceptions.
At one study site, we were unable to include participants from the ambulance service. This means that we were not able to include their perceptions in the systematic risk analysis and in the description of organisational factors affecting handover practices. As such, the findings at this site represent a partial view, which is biased towards perceptions of hospital staff. This is a limitation that should be acknowledged. However, the risks identified across study sites showed similarities, and one could argue that the qualitative findings are supported sufficiently by the perceptions of staff from the two participating ambulance services.
Another limitation of the study is the reliance on staff perceptions. Although staff are in a very good position to provide rich and detailed accounts of handover, their perceptions are subject to errors of recall or bias. Perceptions by their very nature are subjective views on the world. There are good reasons for exploring complex social phenomena through a diverse range of subjective views on the phenomenon, but one needs to bear in mind that the findings are subjective accounts of the participants and the researchers interpreting these.
A final limitation we would like to point out relates to the use of FMEA for the systematic identification and assessment of risk. The limitations of FMEA are often not properly understood in health care and, therefore, deserve special mentioning. The application of FMEA for the risk assessment in sociotechnical systems relies predominantly on expert judgement for the description of the likelihood of occurrence of a failure and the severity of the consequences. It is well known that people are often poor at estimating probabilities. In addition, the severity of the consequences in health-care systems is highly dependent on the condition of the patient. This makes consistent assessment across different groups of participants difficult, as they may have different frames of reference. We dealt with these limitations of FMEA by providing first and foremost qualitative descriptions of the risks identified, both through short summaries of the discussion around each significant risk, and through the use of contextualised failure trajectories, i.e. context-rich descriptions of how failures can manifest themselves, provided by the participants during the FMEA focus groups.
Conclusion
The research findings suggest that handover should be understood as a sociotechnical activity embedded in clinical and organisational practice. Capacity, patient flow and national targets, and the quality of handover are intricately related, and should be addressed together. Improvement efforts should focus on providing practitioners flexibility to make trade-offs in order to resolve tensions inherent in handover. Collaborative holistic system analysis and greater cultural awareness and collaboration across organisations should be pursued.
Chapter 6 Conclusions
In this concluding chapter, we identify a number of key implications from this research, which different health-care stakeholders may wish to consider (see Implications for health care). We also describe the implications for future research that we see (see Recommendations for research).
Implications for health care
This research, as well as previous research, provides evidence that handover has significant patient safety implications. The research has identified some of the organisational factors affecting efficient and effective handover, such as time pressures, departmental capacity, staff resource, patient flow and ED overcrowding. These factors are closely interrelated. Tensions have been highlighted resulting from differing agendas of different stakeholders. The findings suggest that improvements to handover require a collaborative effort across departmental and organisational boundaries. Joint working within health-care systems should replace traditional silo working patterns. Below we describe the implications of this research for health-care practice (Table 32):
| Collaboration between GPs, ambulance services, ED and hospital services may be a prerequisite for sustainable improvement of handover practice | The research has described and highlighted the major importance of considering handover along the emergency care pathway. Inadequate patient flows across departmental and organisational boundaries may lead to delays and problems with handover, including unclear allocation of responsibility for patient care, as boundaries for responsibility can be blurred in times of high bed occupancy, breach of capacity and queue formation |
| 1. Establish a culture of integrated, patient-centred care | Organisations should establish a culture of and clear commitment to integrated, patient-centred care. The research findings suggest that sustainable improvements may occur when leaders from all parts of the local health economy commit to work as partners to reduce delays with a view to improve patient safety, care and patient experience throughout the emergency care pathway. This could involve, for example, considering joint appointments between ambulance services and EDs at a senior level. Commissioning boards should mandate and monitor that organisations that regularly transfer patients across the interfaces of care ensure there are ongoing consultation, safety incident and improvement groups focusing on handovers and transitions of care |
| 2. Establish an interorganisational communication strategy | Organisations should formulate and implement in partnership an explicit communication strategy that addresses at least aspects such as: communication between ambulance services and GPs to inform the decision-making process for conveyance; communication between EDs and GPs to inform decisions around appropriate care; and communication between EDs, hospital services and GPs to communicate discharge information. The communication strategy should be disseminated to staff, and appropriate training and support systems should be implemented |
| 3. Establish clear systems of responsibility for patient care | Organisations should formulate and implement in partnership clear systems of responsibility for patient care across boundaries to avoid situations of ambiguity that pose a threat to patient safety. Such systems should address at least aspects of allocation of responsibility for patient care in case of: ambulance queues and delays; patients in ED waiting to be seen by specialist; patients in hospital still under the formal care of the ED physician |
| 4. Monitor and review the effectiveness of interorganisational collaboration | Organisations should determine and implement quality indicators to monitor the effectiveness of their interorganisational collaboration. These may include patient-focused outcome measures that reflect the whole pathway, as well as specific measures of process across boundaries. Such quality indicators should be regarded as jointly owned as the learning and suggestions for improvement they provide focuses on the patient rather than any individual organisation. Areas for improvement as well as successful collaboration should be reviewed during regular multidisciplinary meetings |
| Transitioning from a target-driven culture towards a culture of compassionate excellence may improve the quality of handover | The research provided evidence that national targets, such as ambulance turn-around times, may potentially lead to practices where these are regarded as over-riding principles, potentially affecting the safety of patients and the quality of the care they receive. Targets should be regarded as quality improvement tools, and should not have a negative impact on patient care. Care processes should be designed around the needs of the patient, not around targets |
| 5. Establish a culture of compassionate excellence | Organisations should establish and demonstrate a clear commitment to a culture of compassionate excellence. They should communicate, assess and feedback on values and expected and unacceptable forms of behaviour to staff |
| 6. Provide flexibility to practitioners in target-driven processes | Organisations should demonstrate commitment to meeting targets, but should also provide flexibility to practitioners to allow them to make judgements based on their expertise. The organisational commitment should shift to a culture of doing ‘what is right for the patient’ in the broadest sense, empowering staff to utilise their knowledge and experience in providing the best possible care to patients |
| 7. Adopt patient-centred process design practices that involve frontline staff and patients | Organisations should adopt design practices that ensure that processes are designed around patient needs, rather than around meeting targets. Such design practices need to draw on the expertise of frontline staff, who should be encouraged to contribute to the design. Crucially, this should also include the involvement of patients and their carers, and it should utilise a wide range of patient and staff feedback |
| Efforts at nurturing shop floor relationships in order to maintain trust and respect may contribute to sustainable improvements in handover | The research provided evidence to suggest that there may be conflicting perceptions on handover between ED staff and the admitting medical team. For example, ED staff may perceive the behaviour of the admitting team as ‘gatekeeping’, and the admitting staff may perceive referrals as inappropriate and not in the best interest of the patient. However, the research also suggests that these tensions are managed better when there is an established personal relationship between staff. This highlights the importance of interpersonal contact and its impact on handover quality and productive handover results |
| 8. Establish clear procedures for admitting patients | Hospitals should establish clear procedures for the decision-making process for admitting patients to the hospital. This reduces ambiguity and uncertainty such that there are clear lines of responsibility even in situations where patients fall between multiple specialties. Such procedures do not replace the need for personal negotiation, but should be regarded as facilitators of such interaction |
| 9. Adopt a system of shadowing | Departments should consider introducing systems of shadowing that allow staff from one department to spend time in another department observing the ways of working and the constraints in this environment. Shadowing may contribute to forming an understanding of each other’s goals and motivations, and to building a shared awareness around patient care. It presents an opportunity to respect and value the contribution to care by colleagues from other departments. Other and additional approaches that could be considered include secondments or staff rotations |
| 10. Institutionalise opportunities for personal contact across departments | Hospitals should institutionalise opportunities for nurturing shop floor relationships across departments, and they should be mindful of the possibly destabilising effect of frequent staff changes. This could include multidisciplinary review meetings (see recommendation 4) and multidisciplinary training (see recommendation 13), and should also consider the introduction of new members of staff to other departments as part of their induction process. This may contribute to building mutual confidence in the abilities of colleagues, and it may improve trust |
| Flexible approaches to standardisation may support handover practices | There is a large amount of research that suggests standardisation of handover as a way to improve practice. Our research provides further evidence that this may be a reasonable path to pursue. The research suggests that not every handover can be standardised in the same way or to the same extent. Some handovers require greater flexibility than others. The research provides some evidence that even in cases where flexibility is required, appropriate levels of standardisation can have a positive impact on handover practices |
| 11. Adopt formal systems for handing over patients from ambulance services to ED | Ambulance services and EDs should adopt in partnership formal systems for handing over patients. For resuscitation patients, structured protocols such as ATMIST should be considered both for the pre-alert as well as for the handover of the patient upon arrival in the ED. There should be a clear procedure for the conduct of handover in the ED, which identifies at least: when the handover takes place; to whom the handover takes place; how information is made available to team members arriving late. Adequate training and support systems should be implemented in order to ensure that all relevant stakeholders are familiar with the procedures and the structured communication protocol |
| 12. Adopt formal systems for handing over patients to the specialties | The ED should agree with the specialties formal systems for handing over patients. The use of structured communication protocols should be considered, possibly supported by checklists, but the adoption of such communication protocols needs to provide sufficient flexibility. Adequate training and support systems should be implemented in order to ensure that all relevant stakeholders are familiar with the procedures communication protocols |
| Stakeholders in education and training should consider establishing handover priority as a cultural norm | This research, as well as previous work, suggests that education and training are key factors in improving the practice of handover |
| 13. Adopt realistic, multidisciplinary training systems | Organisations should adopt training systems that capture the essence of real working practice, particularly by training multiprofessional groups of staff who actually work together using simulation and role play. Training scenarios should support the suggestions above including interorganisational communication, responsibility for patient care across boundaries, admission of patients to hospital, and use of structured communication protocols. The training should be designed to increase patient focus, and to prevent divergence of objectives and processes over time |
| 14. Develop a curriculum that includes non-technical skills | The College of Emergency Medicine, Royal College of Physicians, the College of Paramedics, Royal College of Nursing, other professional bodies and universities training registered health professionals should determine an appropriate curriculum that ensures that junior staff possess adequate non-technical and communication skills |
| 15. Include non-technical skills in competency assessments | Accrediting training bodies should adapt their competency assessments to include consideration of non-technical and communication skills, including aspects of multidisciplinary and interorganisational communication and collaboration |
Recommendations for research
This study has provided new qualitative insights into the risks associated with handover, their relationship to inner tensions within handover and their intricate link to organisational issues of capacity, patient flow and interorganisational collaboration. The research findings point to a number of areas that future research could seek to address. These are listed in the order of relevance to the NHS.
Evaluation of system-wide improvement efforts may provide insights about whether and how interventions lead to sustainable improvement of handover
This research provided qualitative insights into the risks associated with handover, and the links to organisational factors. We were able to formulate from this research implications for health-care practice. However, these conceptual recommendations – as well as findings generated by previous research – need to be rigorously evaluated in practice. The findings from the literature review suggest that there is a gap in the current evidence base about whether, through what kind of mechanisms and under which circumstances interventions lead to sustainable improvement of handover in practice. In this way lessons can be aggregated across individual studies and can be generalised to different settings. For example, research should investigate whether the introduction of electronic tools such as the electronic PRF or electronic referrals lead to sustainable improvements of handover practices, it should provide explanations grounded in empirical data of how any improvements are brought about by the use of the electronic tools, and it should identify the supporting organisational infrastructure (in terms of procedures, training, culture) that is necessary for any such improvements to be sustainable. A similar approach is recommended for other suggested interventions, such as the involvement of GPs in ambulance conveyance decisions, or the involvement of senior ED clinicians at the point of handover.
Understanding the role of general practitioners and the contribution they can make may provide useful insights for system-based improvements
The research findings suggest that the quality of handover is linked to patient flow across organisational boundaries. Many of the risks associated with handover failures related to inadequate patient flows, such as ambulance queues in the ED. The thematic analysis of study participants’ perceptions suggests that the role of GPs in this may be central, both by contributing to tensions in handover, and as a key resource in improving patient and information flow and thus the quality of handover. The involvement of GPs was not a focus of this research, but the findings clearly suggest that understanding their perceptions and their role may provide useful insights for system-based improvement efforts. Future research should extend the present study to involve GPs and other actors in the local health community in the safety assessment of handover within the emergency care pathway. Improvement interventions should be developed in collaboration with these actors, and any interventions should be evaluated appropriately (see above).
Understanding how staff make trade-offs in order to deal with tensions may provide novel insights about organisational resilience
The research provided examples of how staff make trade-off decisions based on their experience and the local circumstances in order to deal with inner tensions in their activities. For example, paramedics consider, depending on the situation, how to balance the need to get back out into the community with the need to hand over all relevant details to the nurse looking after the patient. This implies a considerable departure from the perception that the quality of handover is determined simply by adherence to a standard protocol. This view opens up an entire field of questions beyond the consideration of handover that require answers through future research: how do staff make such trade-offs in practice? To what extent can organisations used to ‘policing’ procedural compliance support staff in taking such context-dependent trade-offs? How can organisations assess and ‘measure’ the degree to which they exhibit such organisational resilience?
Novel methods for system-based risk analysis in health care may overcome the limitations of current techniques
Closely related to the above observation is the question about what methods are appropriate for systems-based risk analysis in health care. The risk analysis conducted as part of this research was based on standard techniques such as process mapping and FMEA. Although the application of these techniques provided valuable insights about the risks associated with handover failures, the research also provides evidence to suggest that there may be limitations to these techniques in a health-care context. From a methodological perspective there is clearly a need to develop novel methods for systems-based risk analysis in health care. Such methods should be capable of taking into consideration the finding suggested by this research that safety is the result of both prudent design as well as of the dynamic trade-offs taken by frontline staff in response to tensions inherent in their activities.
Acknowledgements
We would like to thank all the participants involved in this research for their time and contributions to the focus group activities and interviews. We are grateful to the study organisations for agreeing to participate in this study.
We thank the members of the project advisory group for their input and advice.
We would like to thank the participants of the stakeholder workshop for their interest and for providing lively and engaging discussions. We are particularly grateful to Dr Pamela Chrispin, Medical Director at East of England Ambulance Service NHS Trust, and to Dr Arne Rose, Emergency Medicine Consultant at Heart of England NHS Foundation Trust, for their guest presentations at the workshop.
We are also grateful to Dr Nick Rich (Montalt Enrich), who facilitated the process mapping sessions, Peter Morgan (AMPM Research & Consulting), who provided the economic commentary, and Sally Beer (Oxford Radcliffe University Hospitals NHS Trust), who assisted with the data collection for research strand 1.
Contributions of authors
Mark Sujan (Associate Professor of Patient Safety) was chief investigator and is guarantor for this study. He contributed to the design of the study, development of the application, data collection and data analysis for both research streams, synthesis of findings and writing of the final report. He also provided overall project management and chaired project team meetings.
Peter Spurgeon (Professor of Health Services Management) contributed to the design of the study, development of the application, data collection and data analysis for research strand 2, synthesis of findings and writing of the final report.
Matthew Inada-Kim (Lead Consultant in Acute Medicine) contributed to the design of the study, development of the application, synthesis of findings and writing of the final report. He also chaired the stakeholder workshop.
Michelle Rudd (Nurse Consultant in Emergency Care) undertook the data collection for research strand 1 at one study site, contributed to the analysis of these data, and contributed to writing of the final report.
Larry Fitton (Consultant in Emergency Medicine) oversaw the research at one study site, and contributed to the synthesis of findings and writing of the final report.
Simon Horniblow (Senior Nurse, Emergency Medicine) undertook the data collection for research strand 1 at one study site, contributed to the analysis of these data, and contributed to writing of the final report.
Steve Cross (Patient Safety and Quality Manager) oversaw the research at one study site, and contributed to the synthesis of findings and writing of the final report.
Peter Chessum (Nurse Practitioner, Emergency Care) undertook the data collection for research strand 1 at one study site. He also contributed to the analysis of data for research strand 1, the data collection and analysis for research strand 2, and to the synthesis of findings and writing of the final report.
Matthew W Cooke (Professor of Emergency Medicine) contributed to the design of the study and development of the application. He also oversaw the research at one study site, and contributed to the data analysis for research streams to the synthesis of findings and writing of the final report.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- Hospital-Based Emergency Care: At the Breaking Point. Washington, DC: The National Academies Press; 2007.
- Wong MC, Yee KC, Turner P. Clinical Handover Literature Review. Sandy Bay, TAS: University of Tasmania; 2008.
- Cheung DS, Kelly JJ, Beach C, Berkeley RP, Bitterman RA, Broida RI, et al. Improving handoffs in the emergency department. Ann Emerg Med 2010;55:171-80. http://dx.doi.org/10.1016/j.annemergmed.2009.07.016.
- Kohn LT, Corrigan JM, Donaldson MS. To Err Is Human: Building a Safer Health System. Washington, DC: The National Academies Press; 2000.
- An Organisation with a Memory. London: The Stationery Office; 2000.
- Brennan TA, Leape LL, Laird NM, Hebert L, Localio AR, Lawthers AG, et al. Incidence of adverse events and negligence in hospitalized patients. N Engl J Med 1991;324:370-6. http://dx.doi.org/10.1056/NEJM199102073240604.
- Thomas EJ, Studdert DM, Burstin HR, Orav EJ, Zeena T, Williams EJ, et al. Incidence and types of adverse events and negligent care in Utah and Colorado. Med Care 2000;38:261-71. http://dx.doi.org/10.1097/00005650-200003000-00003.
- Vincent C, Neale G, Woloshynowych M. Adverse events in British hospitals: preliminary retrospective record review. BMJ (Clinical Research Edn) 2001;322:517-19. http://dx.doi.org/10.1136/bmj.322.7285.517.
- Davis P, Lay-Yee R, Briant R, Ali W, Scott A, Schug S. Adverse events in New Zealand public hospitals I: occurrence and impact. N Z Med J 2002;115.
- Davis P, Lay-Yee R, Briant R, Ali W, Scott A, Schug S. Adverse events in New Zealand public hospitals II: preventability and clinical context. N Z Med J 2003;116.
- Sari AB, Sheldon TA, Cracknell A, Turnbull A, Dobson Y, Grant C, et al. Extent, nature and consequences of adverse events: results of a retrospective case note review in a large NHS hospital. Qual Saf Health Care 2007;16:434-9.
- de Vries EN, Ramrattan MA, Smorenburg SM, Gouma DJ, Boermeester MA. The incidence and nature of in-hospital adverse events: a systematic review. Qual Saf Health Care 2008;17:216-23. http://dx.doi.org/10.1136/qshc.2007.023622.
- McGuire HH, Horsley JS, Salter DR, Sobel M. Measuring and managing quality of surgery. Statistical vs incidental approaches. Arch Surg 1992;127:1960-7. http://dx.doi.org/10.1001/archsurg.1992.01420060113017.
- Vincent C, Moorthy K, Sarker SK, Chang A, Darzi AW. Systems approaches to surgical quality and safety: from concept to measurement. Ann Surg 2004;239:475-82. http://dx.doi.org/10.1097/01.sla.0000118753.22830.41.
- Dean B, Schachter M, Vincent C, Barber N. Prescribing errors in hospital inpatients: their incidence and clinical significance. Qual Saf Health Care 2002;11:340-4. http://dx.doi.org/10.1136/qhc.11.4.340.
- Lewis PJ, Dornan T, Taylor D, Tully MP, Wass V, Ashcroft DM. Prevalence, incidence and nature of prescribing errors in hospital inpatients: a systematic review. Drug Saf 2009;32:379-89. http://dx.doi.org/10.2165/00002018-200932050-00002.
- Ovretveit J. Does Improving Quality Save Money?. London: Health Foundation; 2009.
- Guidance on Clinical Handover for Clinicians and Managers. London: British Medical Association; 2004.
- Joint Commission . Strategies to improve handoff communication: implementing a process to resolve strategies. JT Comm Perspect Patient Saf 2005;5:1-12.
- Apker J, Mallak LA, Gibson SC. Communicating in the ‘gray zone’: perceptions about emergency physician hospitalist handoffs and patient safety. Acad Emerg Med 2007;14:884-94. http://dx.doi.org/10.1197/j.aem.2007.06.037.
- Jeffcott SA, Ibrahim JE, Cameron PA. Resilience in healthcare and clinical handover. Qual Saf Health Care 2009;18:256-60. http://dx.doi.org/10.1136/qshc.2008.030163.
- Perry SJ, Croskerry P, Cosby K, Schenkel SM, Wears RL. Patient Safety in Emergency Medicine. Philadelphia, PA: Lippincott, Williams & Wilkins; 2009.
- Patterson ES, Roth EM, Woods DD, Chow R, Gomes JO. Handoff strategies in settings with high consequences for failure: lessons for health care operations. Int J Qual Health Care 2004;16:125-32. http://dx.doi.org/10.1093/intqhc/mzh026.
- Behara R, Wears RL, Perry SJ, Eisenberg E, Murphy L, Vanderhoef M, et al. Advances in Patient Safety: From Research to Implementation (Volume 2: Concepts and Methodology). Rockville, MD: Agency for Healthcare Research and Quality; 2005.
- Horwitz LI, Moin T, Krumholz HM, Wang L, Bradley EH. What are covering doctors told about their patients? Analysis of sign-out among internal medicine house staff. Qual Saf Health Care 2009;18:248-55. http://dx.doi.org/10.1136/qshc.2008.028654.
- Johnson JK, Arora VM. Improving clinical handovers: creating local solutions for a global problem. Qual Safety Health Care 2009;18:244-5. http://dx.doi.org/10.1136/qshc.2009.032946.
- Bost N, Crilly J, Wallis M, Patterson E, Chaboyer W. Clinical handover of patients arriving by ambulance to the emergency department: a literature review. Int Emerg Nurs 2010;18:210-20. http://dx.doi.org/10.1016/j.ienj.2009.11.006.
- Cohen MD, Hilligoss PB. The published literature on handoffs in hospitals: deficiencies identified in an extensive review. Qual Saf Health Care 2010;19:493-7. http://dx.doi.org/10.1136/qshc.2009.033480.
- Patterson ES, Wears RL. Patient handoffs: standardized and reliable measurement tools remain elusive. Jt Comm J Qual Patient Saf 2010;36:52-61.
- Raduma-Tomas MA, Flin R, Yule S, Williams D. Doctors’ handovers in hospitals: a literature review. BMJ Qual Saf 2011;20:128-33. http://dx.doi.org/10.1136/bmjqs.2009.034389.
- Riesenberg LA, Leitzsch J, Massucci JL, Jaeger J, Rosenfeld JC, Patow C, et al. Residents’ and attending physicians’ handoffs: a systematic review of the literature. Acad Med J Assoc Am Med Coll 2009;84:1775-87. http://dx.doi.org/10.1097/ACM.0b013e3181bf51a6.
- Cook RI, Render M, Woods DD. Gaps in the continuity of care and progress on patient safety. BMJ (Clinical Research Edn) 2000;320:791-4. http://dx.doi.org/10.1136/bmj.320.7237.791.
- Improving Transitions of Care: Hand-off Communications. Oakbrook Terrace, IL: The Joint Commission; 2010.
- Kitch BT, Cooper JB, Zapol WM, Marder JE, Karson A, Hutter M, et al. Handoffs causing patient harm: a survey of medical and surgical house staff. Jt Comm J Qual Patient Saf 2008;34:563-70.
- Borowitz SM, Waggoner-Fountain LA, Bass EJ, Sledd RM. Adequacy of information transferred at resident sign-out (in-hospital handover of care): a prospective survey. Qual Saf Health Care 2008;17:6-10.
- Horwitz LI, Krumholz HM, Green ML, Huot SJ. Transfers of patient care between house staff on internal medicine wards: a national survey. Arch Int Med 2006;166:1173-7. http://dx.doi.org/10.1001/archinte.166.11.1173.
- Solet DJ, Norvell JM, Rutan GH, Frankel RM. Lost in translation: challenges and opportunities in physician-to-physician communication during patient handoffs. Acad Med J Assoc Am Med Coll 2005;80:1094-9. http://dx.doi.org/10.1097/00001888-200512000-00005.
- Bomba DT, Prakash R. A description of handover processes in an Australian public hospital. Aus Health Rev 2005;29:68-79.
- Ye K, McD Taylor D, Knott JC, Dent A, MacBean CE. Handover in the emergency department: deficiencies and adverse effects. Emerg Med Australas 2007;19:433-41. http://dx.doi.org/10.1111/j.1742-6723.2007.00984.x.
- Sexton A, Chan C, Elliott M, Stuart J, Jayasuriya R, Crookes P. Nursing handovers: do we really need them?. J Nurs Manag 2004;12:37-42. http://dx.doi.org/10.1111/j.1365-2834.2004.00415.x.
- Petersen LA, Brennan TA, O’Neil AC, Cook EF, Lee TH. Does house staff discontinuity of care increase the risk for preventable adverse events?. Ann Int Med 1994;121:866-72.
- Catchpole K, Sellers R, Goldman A, McCulloch P, Hignett S. Patient handovers within the hospital: translating knowledge from motor racing to healthcare. Qual Saf Health Care 2010;19:318-22. http://dx.doi.org/10.1136/qshc.2009.026542.
- Cleland JA, Ross S, Miller SC, Patey R. ‘There is a chain of Chinese whispers . . .’: empirical data support the call to formally teach handover to prequalification doctors. Qual Saf Health Care 2009;18:267-71. http://dx.doi.org/10.1136/qshc.2008.029983.
- Pithier D, Montero P, Mortar M, Shaw A. Pilot study to show the loss of important data in nursing handover. Br J Nurs 2005;14:1090-3.
- Philibert I. Use of strategies from high-reliability organisations to the patient hand-off by resident physicians: practical implications. Qual Saf Health Care 2009;18:261-6. http://dx.doi.org/10.1136/qshc.2008.031609.
- O’Leary KJ, Thompson JA, Landler MP, Kulkarni N, Haviley C, Hahn K, et al. Patterns of nurse–physician communication and agreement on the plan of care. Qual Saf Health Care 2010;19:195-9. http://dx.doi.org/10.1136/qshc.2008.030221.
- Frankel RM, Flanagan M, Ebright P, Bergman A, O’Brien CM, Franks Z, et al. Context, culture and (non-verbal) communication affect handover quality. BMJ Qual Safety 2012;21:121-8. http://dx.doi.org/10.1136/bmjqs-2012-001482.
- Gobel B, Zwart D, Hesselink G, Pijnenborg L, Barach P, Kalkman C, et al. Stakeholder perspectives on handovers between hospital staff and general practitioners: an evaluation through the microsystems lens. BMJ Qual Saf 2012;21:106-13. http://dx.doi.org/10.1136/bmjqs-2012-001192.
- Arora VM, Johnson JK, Meltzer DO, Humphrey HJ. A theoretical framework and competency-based approach to improving handoffs. Qual Saf Health Care 2008;17:11-4. http://dx.doi.org/10.1136/qshc.2006.018952.
- Manser T, Foster S, Gisin S, Jaeckel D, Ummenhofer W. Assessing the quality of patient handoffs at care transitions. Qual Saf Health Care 2010;19. http://dx.doi.org/10.1136/qshc.2009.038430.
- Iedema R, Ball C, Daly B, Young J, Green T, Middleton PM, et al. Design and trial of a new ambulance-to-emergency department handover protocol: ‘IMIST-AMBO’. BMJ Qual Saf 2012;21:627-33. http://dx.doi.org/10.1136/bmjqs-2011-000766.
- Joint Commission . Comprehensive Accreditation Manual for Hospitals 2012.
- Haig KM, Sutton S, Whittington J. SBAR: a shared mental model for improving communication between clinicians. Jt Comm J Qual Patient Saf 2006;32:167-75.
- Marshall S, Harrison J, Flanagan B. The teaching of a structured tool improves the clarity and content of interprofessional clinical communication. Qual Saf Health Care 2009;18:137-40. http://dx.doi.org/10.1136/qshc.2007.025247.
- NHS Litigation Authority . NHSLA Risk Management Standards 2012-13 for NHS Trusts Providing Acute, Community, or Mental Health &Amp; Learning Disability Services and Non-NHS Providers of NHS Care 2012.
- Derlet R, Richards J, Kravitz R. Frequent overcrowding in U.S. emergency departments. Acad Emerg Med 2001;8:151-5. http://dx.doi.org/10.1111/j.1553-2712.2001.tb01280.x.
- Wilson MJ. A template for safe and concise handovers. Medsurg Nurs 2007;16:201-6.
- Lawrence RH, Tomolo AM, Garlisi AP, Aron DC. Conceptualizing handover strategies at change of shift in the emergency department: a grounded theory study. BMC Health Serv Res 2008;8. http://dx.doi.org/10.1186/1472-6963-8-256.
- Beach C, Croskerry P, Shapiro M. Profiles in patient safety: emergency care transitions. Acad Emerg Med 2003;10:364-7. http://dx.doi.org/10.1197/aemj.10.4.364.
- Horwitz LI, Meredith T, Schuur JD, Shah NR, Kulkarni RG, Jenq GY. Dropping the baton: a qualitative analysis of failures during the transition from emergency department to inpatient care. Ann Emerg Med 2009;53:701-10. http://dx.doi.org/10.1016/j.annemergmed.2008.05.007.
- Bost N, Crilly J, Patterson E, Chaboyer W. Clinical handover of patients arriving by ambulance to a hospital emergency department: a qualitative study. Int Emerg Nurs 2012;20:133-41. http://dx.doi.org/10.1016/j.ienj.2011.10.002.
- Randell R, Wilson S, Woodward P, Galliers J. The ConStratO model of handover: a tool to support technology design and evaluation. Behav Inf Technol 2011;30:489-98. http://dx.doi.org/10.1080/0144929X.2010.547220.
- Hindmarsh D, Lees L. Improving the safety of patient transfer from AMU using a written checklist. Acute Med 2012;11:13-7.
- Farhan M, Brown R, Vincent C, Woloshynowych M. The ABC of handover: impact on shift handover in the emergency department. Emerg Med J 2012;29:947-53. http://dx.doi.org/10.1136/emermed-2011-200201.
- Jeffcott SA, Evans SM, Cameron PA, Chin GS, Ibrahim JE. Improving measurement in clinical handover. Qual Saf Health Care 2009;18:272-7. http://dx.doi.org/10.1136/qshc.2007.024570.
- Johnson JK, Barach P. Patient care handovers: what will it take to ensure quality and safety during times of transition?. Med J Aus 2009;190:110-12.
- Understanding Risk, Protecting People. London: HSE; 2001.
- Storey N. Safety-critical Computer Systems. Harlow: Pearson Prentice Hall; 1996.
- Analysis Techniques for System Reliability – Procedure for Failure Mode and Effects Analysis (FMEA). Geneva: IEC; 2006.
- A Guide to Hazard and Operability Studies. London: CIA; 1977.
- Fault Tree Analysis (FTA). London: BSI; 2007.
- Guidelines for Hazard Evaluation Procedures. London: John Wiley & Sons; 2011.
- DeRosier J, Stalhandske E, Bagian JP, Nudell T. Using health care Failure Mode and Effect Analysis: the VA National Center for Patient Safety’s prospective risk analysis system. Jt Comm J Qual Improv 2002;28:248-67.
- Steinberger DM, Douglas SV, Kirschbaum MS. Use of failure mode and effects analysis for proactive identification of communication and handoff failures from organ procurement to transplantation. Prog Transplant 2009;19:208-14.
- Apkon M, Leonard J, Probst L, DeLizio L, Vitale R. Design of a safer approach to intravenous drug infusions: failure mode effects analysis. Qual Saf Health Care 2004;13:265-71. http://dx.doi.org/10.1136/qhc.13.4.265.
- Burgmeier J. Failure mode and effect analysis: an application in reducing risk in blood transfusion. Jt Comm J Qual Improv 2002;28:331-9.
- Redfern E, Brown R, Vincent CA. Identifying vulnerabilities in communication in the emergency department. Emerg Med J 2009;26:653-7. http://dx.doi.org/10.1136/emj.2008.065318.
- Leonard M, Frankel A, Simmonds T. Achieving Safe and Reliable Healthcare: Strategies and Solutions. Chicago, IL: Health Administration Press; 2004.
- Improvement Leaders’ Guide: Process Mapping, Analysis and Redesign. London: NHS; 2005.
- Johnson JK, Farnan JM, Barach P, Hesselink G, Wollersheim H, Pijnenborg L, et al. Searching for the missing pieces between the hospital and primary care: mapping the patient process during care transitions. BMJ Qual Saf 2012;21:97-105. http://dx.doi.org/10.1136/bmjqs-2012-001215.
- Pope C, Mays N. Qualitative Research in Healthcare. Oxford: Blackwell Publishing; 2006.
- Womack JP, Jones DT, Roos D. The Machine that Changed the World. New York, NY: Free Press; 1990.
- Jones DT, Mitchell A. Lean Thinking for the NHS. Ross-on-Wye: Lean Enterprise Academy; 2006.
- Geertz C. The Interpretation of Cultures. New York, NY: Basic Books; 1973.
- Finn R, Waring J, Walshe K, Boaden R. Patient Safety: Research into Practice. London: Open University Press; 2006.
- Vygotsky LS. Mind in Society. Cambridge, MA: Harvard University Press; 1978.
- Cole M. Cultural Psychology: A Once and Future Discipline. Cambridge, MA: Harvard University Press; 1998.
- Maguire R. Safety Cases and Safety Reports. Aldershot: Ashgate; 2006.
- Dean Franklin B, Shebl NA, Barber N. Failure mode and effects analysis: too little for too much?. BMJ Qual Saf 2012;21:607-11.
- Sacks H. Lectures on Conversation, Volumes I and II. Oxford: Blackwell Pubishing; 1992.
- Apker J, Mallak LA, Applegate EB, Gibson SC, Ham JJ, Johnson NA, et al. Exploring emergency physician-hospitalist handoff interactions: development of the Handoff Communication Assessment. Ann Emerg Med 2010;55:161-70. http://dx.doi.org/10.1016/j.annemergmed.2009.09.021.
- Nagpal K, Arora S, Vats A, Wong HW, Sevdalis N, Vincent C, et al. Failures in communication and information transfer across the surgical care pathway: interview study. BMJ Qual Saf 2012;21:843-9. http://dx.doi.org/10.1136/bmjqs-2012-000886.
- Vincent C, Taylor-Adams S, Stanhope N. Framework for analysing risk and safety in clinical medicine. BMJ 1998;316:1154-7. http://dx.doi.org/10.1136/bmj.316.7138.1154.
- Saldaña J. The Coding Manual for Qualitative Researchers. London: Sage; 2009.
- Spurgeon P, Mazelan P, Barwell F. A management control approach to monitor large-scale change: an illustration in the context of reconfiguration. Health Serv Manage Res 2011;24:19-28. http://dx.doi.org/10.1258/hsmr.2010.010010.
- Flanagan H, Barwell F, Mazelan P, Spurgeon P, Spurgeon P, Burke RJ, et al. The Innovation Imperative in Health Care Organisations: Critical Role of Human Resource Management in the Cost, Quality, Productivity Equation. Cheltenham: Edward Elgar Publishing; 2012.
- Hutchins E. Cognition in the Wild. Cambridge, MA: MIT Press; 1995.
- Hutchins E. How a cockpit remembers its speed. Cogn Sci 1995;19:265-88. http://dx.doi.org/10.1016/0364-0213(95)90020-9.
- Nardi BA, Nardi BA. Context and Consciousness. Cambridge, MA: MIT Press; 1996.
- Nardi BA. Context and Consciousness. Cambridge, MA: MIT Press; 1996.
- Engestrom Y. Learning by Expanding. Helsinki: Orienta-Konsultit; 1987.
- Kuutti K, Nardi BA. Context and Consciousness. Cambridge, MA: MIT Press; 1996.
- Maslow AH. The Psychology of Science: A Reconnaissance. New York, NY: Harper & Row; 1966.
- Engestrom Y, Sannino A. Studies of expansive learning: foundations, findings and future challenges. Educ Res Rev 2010;5:1-24. http://dx.doi.org/10.1016/j.edurev.2009.12.002.
- Ilyenkov EV. Dialectial Logic: Essays on its History. Moscow: Progress; 1977.
- Hollnagel E, Woods DD, Leveson N. Resilience Engineering: Concepts and Precepts. Aldershot: Ashgate; 2006.
- Hollnagel E, Paries J, Woods DD, Wreathall J. Resilience Engineering in Practice: A Guidebook. Aldershot: Ashgate; 2010.
- Hollnagel E, Hollnagel E, Paries J, Woods DD, Wreathall J. Resilience Engineering in Practice: A Guidebook. Aldershot: Ashgate; 2010.
- Hollnagel E. The ETTO Principle: Efficiency-Thoroughness Trade-Off. Aldershot: Ashgate; 2009.
- McCarthy ML. Overcrowding in emergency departments and adverse outcomes. BMJ 2011;342. http://dx.doi.org/10.1136/bmj.d2830.
- Sprivulis PC, Da Silva JA, Jacobs IG, Frazer AR, Jelinek GA. The association between hospital overcrowding and mortality among patients admitted via Western Australian emergency departments. Med J Aus 2006;184:208-12.
- Everyone Counts: Planning for Patients 2013/14. Leeds: NHS; 2012.
- Zero Tolerance: Making Ambulance Handover Delays a Thing of the Past. London: NHS; 2012.
- Guttmann A, Schull MJ, Vermeulen MJ, Stukel TA. Association between waiting times and short term mortality and hospital admission after departure from emergency department: population based cohort study from Ontario, Canada. BMJ 2011;342. http://dx.doi.org/10.1136/bmj.d2983.
- Horwitz LI, Schuster KM, Thung SF, Hersh DC, Fisher RL, Shah N, et al. An institution-wide handoff task force to standardise and improve physician handoffs. BMJ Qual Saf 2012;21:863-71. http://dx.doi.org/10.1136/bmjqs-2011-000658.
- Electronic Patient Report Form System – Full Business Case. UK: South East Coast Ambulance Service; 2010.
Appendix 1 Systematic description of handover within the emergency care pathway
The complementary tabular description of the resuscitation pathway and the major injuries pathway for each site is shown below. The tabular description describes the actors, their goals, the artefacts that are used, and the knowledge that the actors rely on for each step. The graphical representations (process maps) are included in the main report, and are not repeated here.
Ambulance service A/hospital C: resuscitation pathway
| Actor | Goal | Artefacts (external + cognitive tools) | Rules (tacit knowledge, social rules) |
|---|---|---|---|
| AC | To ensure that senior team is ready upon arrival | Mobile telephone; electronic system | Current position + respective location of A&E; trauma networks |
| NIC | To know what needs to be done in order to get resuscitation area ready for arrival | Red telephone; form with set of questions | Knowledge of where senior team are; importance of red telephone |
| HALO | To maintain strategic awareness, management, logistics | Ambulance computer system | Awareness of status of the department |
| Actor | Goal | Artefacts (external + cognitive tools) | Rules (tacit knowledge, social rules) |
|---|---|---|---|
| NIC | To notify relevant staff to prepare for incoming patient | Telephone | |
| Switchboard Operator | To notify relevant staff to prepare for incoming patient | Telephone; bleep system; list of on-duty doctors + bleep numbers |
| Actor | Goal | Artefacts (external + cognitive tools) | Rules (tacit knowledge, social rules) |
|---|---|---|---|
| NIC | To alert resuscitation team as quickly as possible | Form | |
| Resuscitation nurse/clinician | To anticipate what kind of case is coming in; to set up the area | Form; trauma guideline | Knowledge about appropriateness of resuscitation cases |
| Actor | Goal | Artefacts (external + cognitive tools) | Rules (tacit knowledge, social rules) |
|---|---|---|---|
| Senior clinician (team leader) | To ensure that the space is ready and everybody knows what to do | Trauma pathway + booklet + checklist | Knowledge of skills of team members |
| Resuscitation team | To ensure that equipment and space is ready and individual roles are understood | Resuscitation equipment |
| Actor | Goal | Artefacts (external + cognitive tools) | Rules (tacit knowledge, social rules) |
|---|---|---|---|
| Paramedic | To communicate important issues quickly and comprehensively | Photos; items from the scene; ATLS; ATMIST protocol; ABCDE approach | Knowledge of information that may be relevant based on hunches |
| Team leader | To identify the major problems | ATLS guideline; ABCDE approach | |
| Resuscitation team members | To identify the major problems | ATLS guideline; ABCDE approach |
| Actor | Goal | Artefacts (external + cognitive tools) | Rules (tacit knowledge, social rules) |
|---|---|---|---|
| Paramedic A | To provide demographic information to reception | PRF | |
| Receptionist | To register patient and to print off notes and labels | Electronic information system; printer |
| Actor | Goal | Artefacts (external + cognitive tools) | Rules (tacit knowledge, social rules) |
|---|---|---|---|
| Team leader | To ensure there is a systematic approach to addressing the problem | A&E notes; PRF; guidelines (ABCDE; ATLS; trauma pathway) | Structure of hospital care pathways and patient disposition |
| Resuscitation team members | To fulfil their role in the patient’s care |
| Actor | Goal | Artefacts (external + cognitive tools) | Rules (tacit knowledge, social rules) |
|---|---|---|---|
| Senior clinician A&E | To inform the medical registrar and get them to attend resuscitation | Patient’s notes; resuscitation telephone; bleep system; MSS | Knowledge of what is expected in such cases (medical model) |
| Registrar on AMU | To ascertain criticality of the case | Bleep; AMU telephone; pieces of paper | Number signifies priority; knowledge of what is expected in such cases (medical model); capacity levels on AMU |
| Actor | Goal | Artefacts (external + cognitive tools) | Rules (tacit knowledge, social rules) |
|---|---|---|---|
| Registrar AMU | To clerk the patient | AMU admission document; patient’s notes; MSS; PACS | Structure of hospital care pathways and patient disposition |
| Resuscitation staff | To adapt to new specialist plan + deliver added care | MSS; AMU admission document; patient’s notes; scanner |
| Actor | Goal | Artefacts (external + cognitive tools) | Rules (tacit knowledge, social rules) |
|---|---|---|---|
| A&E nurse | To get the patient out of resuscitation, and to make AMU aware of patient | Telephone; MSS; patient’s notes | Departmental situation that may put added pressure on getting patient out |
| AMU co-ordinator | To schedule patient flows in and out of AMU; to prepare for arrival of patient | Telephone; protocol + checklist (SBAR); whiteboard | Capacity on AMU |
| Actor | Goal | Artefacts (external + cognitive tools) | Rules (tacit knowledge, social rules) |
|---|---|---|---|
| Resuscitation nurse | To accompany patient; to provide summary of important issues to AMU nurse | A&E notes | Knowledge of important bits of patient’s story |
| Cubicle nurse (AMU) | To ensure that all initial treatment steps have been done and to get as accurate a picture as possible | A&E notes | Knowledge of whether cubicle nurse (A&E) is familiar with patient; preconception about what should have been done |
| Senior nurse (AMU) | To maintain awareness of patient movements | Whiteboard | Capacity levels on AMU |
| Porter | To move patient; to get job done; to juggle other patients | Equipment for patient transfer | Knowledge of other requests for patient transfer |
Ambulance service A/hospital C: major injuries pathway
| Actor | Goal | Artefacts (external + cognitive tools) | Rules (tacit knowledge, social rules) |
|---|---|---|---|
| Paramedic | To alert ED; to keep control centre updated | Radio; laptop + computer system; Manchester Triage System, ambulance computer system | Presenting complaint interpretation |
| Control room staff | To maintain strategic awareness, management and logistics; to alert ED | Radio; laptop + computer system; Ambulance computer system | Importance of ambulance targets; status of other hospitals + ambulances |
| HALO | To maintain strategic awareness, management and logistics; to raise awareness on ED/AS side | Ambulance computer system | Awareness of status of the department (busyness); current status of assessment nurse (workload, movement), awareness of what’s happening at front door (ambulances queuing, coming in) |
| Actor | Goal | Artefacts (external + cognitive tools) | Rules (tacit knowledge, social rules) |
|---|---|---|---|
| Paramedics | To convey the patient’s story to the assessment nurse; to get handover done + get back on the road. | PRF; handover target | Distilling what information is important and what is not; keywords assessment nurse needs to hear |
| Assessment nurse | To get a first impression of criticality of patient in order to make appropriate decision of where to put the patient | PRF; handover target | Current level of demand on ED; ability to assess wider consequences for ED |
| HALO | To assist paramedics in the logistics of handover and their timely return to the road | Handover target | Awareness of where assessment nurse is; awareness of what else is happening |
| Actor | Goal | Artefacts (external + cognitive tools) | Rules (tacit knowledge, social rules) |
|---|---|---|---|
| AC member A | To provide demographic information to reception | PRF | |
| Receptionist | To register patient and to print off notes and labels | Electronic information system; printer |
| Actor | Goal | Artefacts (external + cognitive tools) | Rules (tacit knowledge, social rules) |
|---|---|---|---|
| Paramedics | To move the patient | PRF, rack for notes | Layout of department |
| Actor | Goal | Artefacts (external + cognitive tools) | Rules (tacit knowledge, social rules) |
|---|---|---|---|
| Assessment nurse | To determine acuity of patient to greater level than initial handover; reconfirm handover; meet time targets (e.g. ECG) | Target protocols; PRF; patient notes | Busyness of department |
| Actor | Goal | Artefacts (external + cognitive tools) | Rules (tacit knowledge, social rules) |
|---|---|---|---|
| Cubicle nurse | To make patient comfortable; to do observation | Patient’s notes; MEWS tool | Where clinician can be found in case of emergency; whom to call on for help/assistance |
| Actor | Goal | Artefacts (external + cognitive tools) | Rules (tacit knowledge, social rules) |
|---|---|---|---|
| Clinician | To diagnose the problem and formulate a plan | MSS; PRF + notes; racking system | Awareness of which patients to see first depending on targets, acuity |
| Cubicle nurse | To instigate treatment as soon as possible | Previous knowledge of the patient’s condition |
| Actor | Goal | Artefacts (external + cognitive tools) | Rules (tacit knowledge, social rules) |
|---|---|---|---|
| Clinician | To ‘sell’ patient to specialty, to get patient to appropriate place (convincing, justifying, selling, rather than clinical details) | Telephone; notes; computer screen | Personal knowledge of who is on the end of the telephone; breach times; awareness of breach time implication on AMU |
| Senior nurse AMU | To ensure that when patient arrives on ward initial steps are done to buy some time to be reseen by doctor; to optimise use of their resources | Protocol + checklist (SBAR); whiteboard | Personal knowledge of the person making the referral and their skills; awareness of how busy their own department is |
| Actor | Goal | Artefacts (external + cognitive tools) | Rules (tacit knowledge, social rules) |
|---|---|---|---|
| AMU nurse | To get bed managers off their back; to get patients in before breach time | Telephone, MSS | Breach time status; general busyness of department + A&E + hospital |
| Assessment nurse | Logistics of A&E (how quickly can patient go up and who can take the bed) | Telephone, MSS, scanner, notes | Breach time status |
| Actor | Goal | Artefacts (external + cognitive tools) | Rules (tacit knowledge, social rules) |
|---|---|---|---|
| Cubicle nurse (A&E) | To accompany patient; to provide summary of important issues to AMU nurse; to get back as quickly as possible | A&E notes | Knowledge of important bits of patient’s story |
| Cubicle nurse (AMU) | To ensure that all initial treatment steps have been done and to get as accurate a picture as possible | A&E notes | Knowledge of whether cubicle nurse (A&E) is familiar with patient; preconception about what should have been done |
| Senior nurse (AMU) | To maintain awareness of patient movements | Whiteboard | Capacity levels on AMU |
| Porter | To move patient; to get job done; to juggle other patients | Equipment for patient transfer | Knowledge of other requests for patient transfer |
Ambulance service B/hospital D: resuscitation pathway
| Actor | Goal | Artefacts (external + cognitive tools) | Rules (tacit knowledge, social rules) |
|---|---|---|---|
| AC | To alert the ED of the patient condition and ETA | Mobile telephone; pre-programmed ED ‘red telephone’ number; ATMIST; criteria for pre-alerting | The threshold for making a ‘pre-alert’ may vary depending on how busy the crew think the department might be |
| Clinical staff answering the call (commonly NIC) | To receive details in order to make a plan and be ready for the incoming patient | Red telephone; ‘pre-alert’ (ATMIST) sheet; pen; ambulance service computer screen | Current level of demand on ED; ability to assess wider consequences for ED |
| Actor | Goal | Artefacts (external + cognitive tools) | Rules (tacit knowledge, social rules) |
|---|---|---|---|
| NIC | To alert the appropriate medical and nursing staff of the imminent arrival of a critical patient | ATMIST form; criteria for trauma/specialist team call out; telephone; designated emergency switchboard number | Overview of all patients in ED, staffing, skill mix and workload; predicted needs of incoming patient based upon information given in pre-alert |
| Senior ED doctor | To anticipate the needs of the incoming patient; to balance the needs of the incoming patient with the needs of those already in the department | ATMIST form | Overview of all patients in ED, staffing, skill mix and workload; predicted needs of incoming patient based upon information given in pre-alert |
| Switchboard Operator | To receive information to alert appropriate staff | Telephone; bleep system |
| Actor | Goal | Artefacts (external + cognitive tools) | Rules (tacit knowledge, social rules) |
|---|---|---|---|
| NIC | To ensure that there is space for incoming patient | ATMIST form | Bed status within department/hospital; movements within department + out of department; availability of beds on wards; skill mix in case additional help is needed |
| Resuscitation nurse | To prepare the equipment and space to receive the patient | Monitor and accessories; ATMIST form; resuscitation bed; trauma guidelines/ATLS protocols; sticker labels with job roles | Predict what equipment is likely to be needed in the ‘worst-case scenario’ |
| Senior ED doctor | To anticipate the needs of the incoming patient; to balance the needs of the incoming patient with the needs of those already in the department | ATMIST form | Skill mix; acuity of patients in department |
| Actor | Goal | Artefacts (external + cognitive tools) | Rules (tacit knowledge, social rules) |
|---|---|---|---|
| Resuscitation nurse | To share information with the team about the incoming patient | ATMIST form; name and role labels | Knowledge of who should be present in the team called; knowledge of tasks to be allocated to specific roles; knowledge of individual preferences; how to source specialist equipment that may not be immediately available |
| Senior ED doctor (team leader) | To ensure that everybody understands what to expect in terms of their role, potential patient needs and the goal of the patient management | Anticipate patient needs; knowledge of performance indicators such as time to CT scan; awareness of experience of team members | |
| Resuscitation team | To know their role; to prepare appropriately for their role | Knowledge of other team members’ skills + competencies |
| Actor | Goal | Artefacts (external + cognitive tools) | Rules (tacit knowledge, social rules) |
|---|---|---|---|
| Paramedic | To communicate important (from the paramedic's point of view) information to the resuscitation team to enable them to take over the patient | PRF (often incomplete);observations or details written on hand or glove; ATMIST tool; ATLS | Urgency of situation; need to focus on clinically most relevant details |
| Team leader | To determine whether any steps need to be undertaken urgently; to understand the acuity and nature of injury in order to deliver fast and appropriate care | ATLS – national guideline) | |
| Resuscitation team members | To understand the acuity and nature of injury in order to deliver fast and appropriate care | ATLS |
| Actor | Goal | Artefacts (external + cognitive tools) | Rules (tacit knowledge, social rules) |
|---|---|---|---|
| Reception staff | To book patient into records system and generate notes and ID wristbands | Admission sheet; Smart card; computer/EPR; printer for notes; printer for wristband | Knowledge of where to get patient demographic details from (ambulance PRF) without disturbing patient assessment |
| AC | To complete written notes as medico-legal document | PRF; knowledge of audit data (e.g. three sets of patient observations, blood sugar level recorded); ambulance computer with timings of the call | Knowledge that rapid booking in of a patient on to the hospital system enables investigations to be ordered quickly; knowledge that more information may be required by different team members that was not delivered in the main handover |
| Actor | Goal | Artefacts (external + cognitive tools) | Rules (tacit knowledge, social rules) |
|---|---|---|---|
| Team leader | To ensure there is a systematic approach to addressing the problem | A&E notes; PRF; guidelines (ATLS; trauma pathway) | Structure of hospital care pathways and patient disposition |
| Resuscitation team members | To fulfil their role in the patient's care |
| Actor | Goal | Artefacts (external + cognitive tools) | Rules (tacit knowledge, social rules) |
|---|---|---|---|
| Senior clinician A&E | To refer the patient | Telephone, number to contact; results from patient history, findings of clinical examination, investigations; computer displaying chest radiograph or blood results; clinical notes to use as a prompt; observation chart; set referral criteria/trust guidelines or protocols | Knowledge of what is expected in such cases (medical model) |
| Registrar on EAU | To ascertain criticality of the case | Pager, telephone; computer to look at blood results or chest radiograph for themselves; 30-minute-window guideline | Number signifies priority; knowledge of other specialties and referral criteria; capacity levels on EAU |
| Actor | Goal | Artefacts (external + cognitive tools) | Rules (tacit knowledge, social rules) |
|---|---|---|---|
| Registrar EAU | To clerk the patient | EAU admission document; patient's notes | Situation of A&E (workload etc.), ways in which to communicate with A&E staff |
| Resuscitation staff | To adapt to new specialist plan + deliver added care | Patient's notes |
| Actor | Goal | Artefacts (external + cognitive tools) | Rules (tacit knowledge, social rules) |
|---|---|---|---|
| A&E NIC | To get the patient out of resuscitation, and to make EAU aware of patient | Telephone; patient's notes; EPR | Hospital bed state (availability of beds for EAU to move patients to, so that space is available for ED patients to move in); awareness of staffing and skill mix on EAU and ED |
| EAU co-ordinator | To schedule patient flows in and out of EAU; to prepare for arrival of patient | Telephone; EPR | Hospital bed state; awareness of staffing and skill mix on EAU and ED; number of GP admissions expected |
| Actor | Goal | Artefacts (external + cognitive tools) | Rules (tacit knowledge, social rules) |
|---|---|---|---|
| Resuscitation nurse | To accompany patient; to provide summary of important issues to EAU nurse | A&E notes | Knowledge of important bits of patient's story |
| Cubicle nurse (EAU) | To ensure that all initial treatment steps have been done and to get as accurate a picture as possible | A&E notes | Knowledge of whether cubicle nurse (A&E) is familiar with patient; preconception about what should have been done |
| Senior nurse (EAU) | To maintain awareness of patient movements | Capacity levels on EAU | |
| Porter | To move patient; to get job done; to juggle other patients | Equipment for patient transfer | Knowledge of other requests for patient transfer |
Ambulance service B/hospital D: major injuries pathway
| Actor | Goal | Artefacts (external + cognitive tools) | Rules (tacit knowledge, social rules) |
|---|---|---|---|
| Paramedic | To hand over responsibility for patient care; to transfer summary of relevant patient information; to get back on to the road | PRF; ATMIST protocol; ambulance telephone | Patient condition, observations, provisional diagnosis and interventions |
| Driver | To remain with the patient and to keep them informed of the process | Understanding of the sequence of events and the process of moving the patient into the ED | |
| NIC | To triage the patient; to make clinical and operational plans; to achieve handover target time | Pager; Sticky note to document triage and plan; clipboard with department/patient details; EPR; floor plan; documentation procedure (sign PRF, document time) | Staffing levels, skill mix, available space in ED, bed availability in EAU and rest of hospital |
| Actor | Goal | Artefacts (external + cognitive tools) | Rules (tacit knowledge, social rules) |
|---|---|---|---|
| NIC | To determine safe & appropriate placement of patient in department | EPR; clipboard with department/patient details; available trolley space in ED | Information from ambulance handover; skill mix, staffing levels, patient acuity; throughput of all patients in ED; operational issues, for example need for side room, need for security attendance |
| AC | To transfer patient on to ED trolley | Ambulance trolley; ED trolley moving and handling equipment | Knowledge of availability of equipment |
| Actor | Goal | Artefacts (external + cognitive tools) | Rules (tacit knowledge, social rules) |
|---|---|---|---|
| Paramedic | To ensure that all appropriate patient information is handed over to the clinical nurse that will be looking after the patient; to provide safe, individualised and good-quality care | PRF; patient medications; procedures or treatments carried out | Patient condition, observations, provisional diagnosis and interventions; social information about the patient or their family; anticipated ongoing needs of the patient (e.g. likely discharge home, so patient has a door key) |
| Clinical nurse | To meet the specific individual needs of the patient, both clinical, psychological and social | PRF | Patients have unique and individual needs that cannot be captured on a clinical PRF or on a triage sticker |
| Actor | Goal | Artefacts (external + cognitive tools) | Rules (tacit knowledge, social rules) |
|---|---|---|---|
| AC | To ensure accuracy of patient details to enable efficient booking in of the patient on the hospital system | PRF; ambulance service computer in ED | Previous attendances of the patient in the ED; turnaround times |
| Reception staff | To make a record of the patient's attendance in the ED; to access any old notes by cross-referencing details | PRF; computer/EPR access; printer; smart care to access EPR |
| Actor | Goal | Artefacts (external + cognitive tools) | Rules (tacit knowledge, social rules) |
|---|---|---|---|
| Clinical nurse | To assess the patient's nursing needs and make a safe plan of action | Ambulance PRF; monitor (ECG, BP, oxygen sturation), ECG machine; paperwork including ED notes, observation chart, blood bag; equipment for taking blood, blood gas machine; track-and-trigger tool; smart card access to EPR; understanding of Manchester triage tool; understanding of when to act upon results of VBG or ECG | Ability to prioritise tasks depending on patient's clinical need; knowledge of other patients in department and need to prioritise assessment by doctors |
| Actor | Goal | Artefacts (external + cognitive tools) | Rules (tacit knowledge, social rules) |
|---|---|---|---|
| Clinician | To make a safe and accurate diagnosis and treatment plan | EPR/computer; smart carded notes, observation charts, printout of VBG and ECG; clinical knowledge | Where clinician can be found in case of emergency; who to call on for help/assistance |
| Clinical nurse | To facilitate the safe and accurate diagnosis and treatment of the patient | Monitor, observation chart; track-and-trigger tool | Experience and pattern recognition from seeing previous similar presentations |
| Actor | Goal | Artefacts (external + cognitive tools) | Rules (tacit knowledge, social rules) |
|---|---|---|---|
| Clinician | To make a diagnosis and treatment plan | Results of history-taking, clinical examination and investigations; blood results/radiograph results | Time it takes for blood tests to be processed; presentation skills using the medical model |
| Senior clinician/consultant | To support clinical decision-making | Teaching needs of juniors |
| Actor | Goal | Artefacts (external + cognitive tools) | Rules (tacit knowledge, social rules) |
|---|---|---|---|
| Clinician (ED) | To refer the patient | Telephone, number to contact; results from patient history, findings of clinical examination, investigations; computer displaying chest radiograph or blood results; clinical notes to use as a prompt; observation chart; set referral criteria/Trust guidelines or protocols | How to make the referral sound appealing (significant words); understanding the purpose and role of the medical team |
| Medical registrar (EAU) | To accept appropriate referrals; to protect own workload and that of team by not accepting inappropriate referrals | Pager, telephone; computer to look at blood results or chest radiograph for themselves; 30-minute-window guideline | Knowledge of other specialties and referral criteria |
| Actor | Goal | Artefacts (external + cognitive tools) | Rules (tacit knowledge, social rules) |
|---|---|---|---|
| ED clinician | To communicate the plan for the patient to the clinical and operational nursing team | EPR/computer; drug chart; ED notes | How to find an ED nurse |
| ED clinical nurse | To deliver care in a safe and timely manner | ED notes; drug chart | Prioritisation of tasks and workload |
| ED NIC | To manage 4-hour target time for transfer or discharge of patients from the ED | EPR records of times and decision to refer patient | Advance planning for likely patient admission |
| Actor | Goal | Artefacts (external + cognitive tools) | Rules (tacit knowledge, social rules) |
|---|---|---|---|
| ED NIC | To move the patients from ED within 4 hours | EPR; KPI 4-hour target | How to find an ED nurse |
| EAU NIC | To have space to receive patients both from ED and the community (GP referrals) | EPR; KPI ED 4-hour target; EAU targets | Prioritisation of tasks and workload |
| Operational manager | To manage patient flow through the hospital | EPR; telephone | Hospital bed state, and staffing; awareness of number and timing of discharges from wards |
| Actor | Goal | Artefacts (external + cognitive tools) | Rules (tacit knowledge, social rules) |
|---|---|---|---|
| ED nurse | To accompany patient; to provide summary of important issues to EAU nurse | A&E notes | Knowledge of important bits of patient's story |
| Cubicle nurse (EAU) | To ensure that all initial treatment steps have been done and to get as accurate a picture as possible | A&E notes | Knowledge of whether cubicle nurse (A&E) is familiar with patient; preconception about what should have been done |
| Senior nurse (EAU) | To maintain awareness of patient movements | Capacity levels on EAU | |
| Porter | To move patient; to get job done; to juggle other patients | Equipment for patient transfer | Knowledge of other requests for patient transfer |
| Actor | Goal | Artefacts (external + cognitive tools) | Rules (tacit knowledge, social rules) |
|---|---|---|---|
| Medical doctor | To clerk the patient and ascertain care needs | EAU admission document; patient's notes |
Hospital E: resuscitation pathway
| Actor | Goal | Artefacts (external + cognitive tools) | Rules (tacit knowledge, social rules) |
|---|---|---|---|
| AC | To ensure that senior team is ready upon arrival | Mobile telephone; ATMIST | Current position + respective location of A&E; specialist services |
| ED nurse in charge | To know what needs to be done in order to get area ready for arrival | Dedicated telephone; ATMIST checklist | Knowledge of where senior team is; importance of resuscitation telephone |
| Actor | Goal | Artefacts (external + cognitive tools) | Rules (tacit knowledge, social rules) |
|---|---|---|---|
| NIC | To notify relevant staff to prepare for incoming patient | Telephone | |
| Switchboard operator | To notify relevant staff to prepare for incoming patient | Telephone; bleep system; list of on-duty doctors + bleep numbers |
| Actor | Goal | Artefacts (external + cognitive tools) | Rules (tacit knowledge, social rules) |
|---|---|---|---|
| NIC | To alert resuscitation team as quickly as possible | ATMIST pre-alert form | |
| Resuscitation nurse/doctor | To anticipate what kind of case is coming in; to set up the area | ATMIST pre-alert from; trauma guideline | Knowledge about appropriateness of resuscitation cases |
| Actor | Goal | Artefacts (external + cognitive tools) | Rules (tacit knowledge, social rules) |
|---|---|---|---|
| Senior ED doctor (team leader) | To ensure that the space is ready and everybody knows what to do | Trauma pathway + booklet + checklist | Knowledge of skills of team members |
| Resuscitation team | To ensure that equipment and space is ready and individual roles are understood | Resuscitation equipment |
| Actor | Goal | Artefacts (external + cognitive tools) | Rules (tacit knowledge, social rules) |
|---|---|---|---|
| Paramedic | To communicate important issues quickly and comprehensively | Photos; items from the scene; ATLS; ATMIST protocol | Knowledge of information that may be relevant based on hunches |
| Team leader | To identify the major problems | ATLS guideline | |
| Resuscitation team members | To identify the major problems | ATLS guideline |
| Actor | Goal | Artefacts (external + cognitive tools) | Rules (tacit knowledge, social rules) |
|---|---|---|---|
| Paramedic | To provide demographic information to reception | PRF | |
| Receptionist | To register patient and to print off notes and labels | Electronic information system; printer |
| Actor | Goal | Artefacts (external + cognitive tools) | Rules (tacit knowledge, social rules) |
|---|---|---|---|
| Team leader | To ensure there is a systematic approach to addressing the problem | A&E notes; PRF; guidelines (ATLS; trauma pathway) | Structure of hospital care pathways and patient disposition |
| Resuscitation team members | To fulfil their role in the patient's care |
| Actor | Goal | Artefacts (external + cognitive tools) | Rules (tacit knowledge, social rules) |
|---|---|---|---|
| Senior clinician A&E | To hand over responsibility for the patient | Telephone; notes; computer screen | Personal knowledge of who is on the end of the telephone |
| CDU medical registrar | To ensure that patient is an appropriate referral; to determine acuity of patient and necessary actions | Bleep; telephone | Personal knowledge of the person making the referral and their skills |
| Actor | Goal | Artefacts (external + cognitive tools) | Rules (tacit knowledge, social rules) |
|---|---|---|---|
| Registrar CDU | To clerk the patient | CDU admission document; patient's notes | |
| Resuscitation staff | To adapt to new specialist plan + deliver added care | Patient's notes |
| Actor | Goal | Artefacts (external + cognitive tools) | Rules (tacit knowledge, social rules) |
|---|---|---|---|
| ED NIC | To move patient onwards in their journey; to make space in ED | Telephone | |
| CDU NIC | To get an understanding of who is coming in | Telephone, referral sheet/referral book | CDU status |
| Actor | Goal | Artefacts (external + cognitive tools) | Rules (tacit knowledge, social rules) |
|---|---|---|---|
| Resuscitation nurse | To get back as quickly as possible; | A&E notes | |
| Cubicle nurse (CDU) | To find out bullet points; categorising acuity of patient | A&E notes | |
| CDU NIC | To identify where patient should go | ||
| Porter | To move patient; to get job done; to juggle other patients | Equipment for patient transfer |
Hospital E: major injuries pathway
| Actor | Goal | Artefacts (external + cognitive tools) | Rules (tacit knowledge, social rules) |
|---|---|---|---|
| Paramedic | To alert ED; to keep control centre updated | Radio; laptop + computer system; Manchester triage system, ambulance computer system | Presenting complaint interpretation |
| Control room staff | To maintain strategic awareness, management and logistics; to alert ED | Radio; laptop + computer system; ambulance computer system | Importance of ambulance targets; status of other hospitals + ambulances |
| Actor | Goal | Artefacts (external + cognitive tools) | Rules (tacit knowledge, social rules) |
|---|---|---|---|
| Paramedics | To convey the patient's story to the NIC; to get handover done + get back on the road | PRF; handover target | Distilling what information is important and what isn't; keywords NIC needs to hear |
| NIC | To get a first impression of criticality of patient in order to make appropriate decision of where to put the patient | PRF; A&E pro forma; Manchester Trial System; handover target | Current level of demand on ED; ability to assess wider consequences for ED |
| Actor | Goal | Artefacts (external + cognitive tools) | Rules (tacit knowledge, social rules) |
|---|---|---|---|
| NIC | To provide demographic information to reception | PRF | |
| Receptionist | To register patient and to print off notes and labels | Electronic information system; printer |
| Actor | Goal | Artefacts (external + cognitive tools) | Rules (tacit knowledge, social rules) |
|---|---|---|---|
| AC | To move the patient; to get back on to the road | Layout of department |
| Actor | Goal | Artefacts (external + cognitive tools) | Rules (tacit knowledge, social rules) |
|---|---|---|---|
| NIC | To provide a brief initial update to the assessment team, highlighting any issues the paramedics considered particularly important | Memory of prior handover; knowledge of what kind of information assessment team may look for | |
| Assessment team | To identify important aspects of the patient's care and circumstances |
| Actor | Goal | Artefacts (external + cognitive tools) | Rules (tacit knowledge, social rules) |
|---|---|---|---|
| Assessment team | To determine acuity of patient to greater level than initial handover | Target protocols; PRF; patient notes; A&E pro forma | Status of department in terms of workload + demand |
| Actor | Goal | Artefacts (external + cognitive tools) | Rules (tacit knowledge, social rules) |
|---|---|---|---|
| Cubicle nurse | To make patient comfortable; to do observations | Patient's notes. MEWS tool; whiteboard | Where doctor can be found in case of emergency. Acuity of patient; own busyness. Whom to call on for help/assistance. |
| Actor | Goal | Artefacts (external + cognitive tools) | Rules (tacit knowledge, social rules) |
|---|---|---|---|
| Doctor | To diagnose the problem and formulate a plan | A&E notes; ‘to be seen’ tray; red tray | Prioritisation rules for nurses |
| Actor | Goal | Artefacts (external + cognitive tools) | Rules (tacit knowledge, social rules) |
|---|---|---|---|
| Doctor (ED) | To hand over responsibility for the patient; to meet breach target | Telephone; notes; computer screen | Personal knowledge of who is on the end of the telephone; breach times |
| CDU medical registrar/junior doctor | To ensure that patient is an appropriate referral; to determine acuity of patient and necessary actions | Bleep; telephone | Personal knowledge of the person making the referral and their skills; awareness of how busy their own department is; awareness of breach time |
| Actor | Goal | Artefacts (external + cognitive tools) | Rules (tacit knowledge, social rules) |
|---|---|---|---|
| ED doctor | To communicate the plan for the patient to the operational nursing team | Drug chart; ED notes; sticker | |
| ED NIC | To manage 4-hour target time for transfer or discharge of patients from the ED | Drug chart; ED notes; sticker; whiteboard | Advance planning for likely patient admission; awareness of breach status |
| ED nurse | To prepare for patient admission and transfer | ED notes; photocopy machine |
| Actor | Goal | Artefacts (external + cognitive tools) | Rules (tacit knowledge, social rules) |
|---|---|---|---|
| ED NIC | To move patient onwards in their journey; to make space in ED; to meet breach targets | Telephone | Breach time status; general busyness of department + A&E + hospital |
| CDU NIC | To get an understanding of who is coming in; to meet breach targets | Telephone, referral sheet/referral book | Breach time status; CDU status |
| Actor | Goal | Artefacts (external + cognitive tools) | Rules (tacit knowledge, social rules) |
|---|---|---|---|
| Cubicle nurse (A&E) | To get back as quickly as possible | A&E notes | Knowledge of important bits of patient's story |
| Cubicle nurse (CDU) | To find out bullet points; categorising acuity of patient | A&E notes | Knowledge of whether cubicle nurse (A&E) is familiar with patient; preconception about what should have been done |
| CDU NIC | To identify where patient should go | Capacity levels on EAU | |
| Porter | To move patient; to get job done; to juggle other patients |
Appendix 2 Systematic identification of risk associated with handover failure
The FMEA sheets that were produced for the resuscitation and the major injuries pathway at each site are shown below. For each step, participants were asked to identify possible failure modes, estimate the likelihood of occurrence of those failure modes, describe the credible worst-case consequences, and think of possible mitigation means.
Ambulance service A/hospital C: resuscitation pathway
| Step | Failure mode | Consequences | Causes | Likelihood | Severity | Risk score | Mitigation |
|---|---|---|---|---|---|---|---|
| (1) Telephone pre-alert (AC or control centre to assessment nurse or ED staff closest to red telephone) | No pre-alert | There may be a delay of maximum 10 minutes in getting the right people, resuscitation bed; if criticality has not been recognised by paramedic, patient may have to wait in queue | Proximity to location; AC failed to recognise clinical need; patient deteriorates en route | 4 | 3 | 12 | Dedicated telephone line; HALO; ED starts treatments quickly |
| Clarity of message leading to misinterpreting information, numbers, abbreviations | E.g. paediatric patient instead of adult and hence resuscitation team composition not optimal | 3 | 2 | 6 | |||
| ACC makes call and cannot answer questions leading to fragmented information | Similar to (1b) | ACC not clinical and not familiar with patient | 1 | 2 | 2 | Digital radio link to ensure AC gets through to ED; cautious ED planning | |
| Inappropriate (unnecessary) pre-alert | Resources diverted away from patients who require them more urgently | ED overcrowding and queues may lead to more pre-alerts (jumping the queue) | 4 | 2 | 8 | ||
| (4) Resuscitation team prepares for arrival of patient | No resuscitation bed available | Less critical patient moved out of resuscitation; reduced monitoring; poor patient experience due to sudden move | Staffing; availability of resources | 4 | 2 | 8 | High-visibility cubicles |
| Less immediate access to equipment if patient cannot go to resuscitation | Staffing; availability of resources | 2 | 8 | ||||
| Ideal team not available | More junior staff involved; rest of department left less attended | Staffing | 4 | 3 | 12 | Calling specialist teams; move staff from other areas | |
| (5) Paramedic to resuscitation team handover | Not all team members present | Disruptions; additional communication | Staff busy with other patients | 3 | 1 | 3 | Repeat handover by paramedic to team members arriving late; paramedic remains in resuscitation until initial assessments completed |
| People not listening | Duplication of medications | People keen to start treatment; focusing on their own bit; inexperience | 2 | 3 | 6 | Training; experienced nurses; documentation | |
| Delay in handover | Similar to (5a) | Senior clinician arrives late (attended to other duties while waiting for ambulance to arrive) | 3 | 1 | 3 | Team will have attended to essential patient needs | |
| (10) Telephone referral, senior clinician to AMU registrar | AMU registrar reluctant to assist with decision, requesting further investigations | Delay in patient being seen; delay in seeing other patients | Possible alternative pathways; protocol-driven interaction; uncertainty about diagnosis; atypical patient; AMU busy; poor quality referral | 4 | 3 | 12 | Escalate to higher level; protocol of acceptance to avoid discussions; ‘eyeballing’ patients on A&E within 30 minutes; when referral could be made to two specialties both come down to A&E; training on making + receiving referrals |
| Cannot get AMU registrar on telephone | Short delay in handover | AMU handover time means registrar is unavailable for that period | 5 | 2 | 10 | ||
| (11) AMU registrar clerks patient on A&E | Delay in coming to see the patient after having accepted the referral | Unclear who is responsible for the patient during this period; patient takes up A&E space; delay in patient journey | Registrar busy elsewhere | 4 | 2 | 8 | A&E nurses/staff still looking after patient |
| (12) Resuscitation nurse informs AMU co-ordinator (telephone) | AMU co-ordinator unaware of referral | May not accept patient until confirmation from registrar received; delay in patient journey | Busy work environment, registrar forgets to inform co-ordinator | 3 | 3 | 9 | |
| (13) Patient transfer | Patient story not communicated | Inconvenience to patient and staff (need to find information; social issues, e.g. whether relatives have been informed); medication could be duplicated | Other resuscitation nurse is taking the patient | 4 | 3 | 12 |
Ambulance service A/hospital C: major injuries pathway
| Step | Failure mode | Consequences | Causes | Likelihood | Severity | Risk score | Mitigation |
|---|---|---|---|---|---|---|---|
| (4) Paramedic B hands over patient to assessment nurse | Mechanisms of injury not adequately communicated | Could miss significant injuries | 1 | 5 | 5 | ||
| Full story not communicated, information missed | Under triage; possible allergies | Interruptions; nurse not fully listening; nurse does not place confidence in paramedic handover; queue makes people haste; too much information given and important pieces not picked up; too little information given; busy + noisy work environment leads to shorter handover; no contact with clinician and no opportunity to ask questions | 5 | 3 | 15 | Handover assessment point away from noise + queues; HCA support for assessment nurse (high workload); senior clinician (rapid assessment consultant) available for handover | |
| Paramedic underestimates severity | Patient fall assumed to be due to alcohol, but may be due to acute disease, leads to delay in treatment | Wrong assumptions; lack of experience | 3 | 2 | 6 | ||
| Delay in handover | Pain; deterioration, e.g. septic patient; may require more intensive treatment | ED overcrowding and queues; observations not rechecked while queuing | 5 | 4 | 20 | ||
| (6) Assessment nurse assesses patient | PRF unavailable | Delay in treatment; less objective assessment | Paramedic leaves PRF at assessment point, then it gets misplaced | 5 | 2 | 10 | Electronic PRF |
| Information on CAS card not recorded properly | Replication of assessments later on | Busy department; lack of experience | 5 | 1 | 5 | Clinician asks important questions again | |
| Wider aspects not recorded | Safeguarding and social issues missed | 3 | 3 | 9 | |||
| Higher priority of patient not annotated on computer | Critically ill patient not being seen quickly, not escalated | Experience; distraction; MEWS not calculated; time pressure | 4 | 5 | 20 | Rapid assessment with consultant | |
| (10) Clinician identifies next patient + picks up notes | PRF unavailable | 2: see (6a) | See (6a) | 5 | 2 | 10 | See (6a) |
| PRF ignored/not consulted | Premature discharge; pre-hospital treatments not taken into account | Clinician not valuing PRF information; lack of experience (junior doctors) | 3 | 3 | 9 | ||
| Over-reliance on nurse documentation | Inappropriate discharge of elderly | Experience; busy work environment; lack of senior cover (time of day) | 3 | 5 | 15 | Senior clinician review before discharge | |
| (13) Clinician formulates plan and refers patient to MAU (telephone handover to MAU sister) | Referral delayed | Minor delay in moving patient | No telephone available; MAU telephone busy; multitasking | 4 | 1 | 4 | Breach target reminders; electronic referral (but telephone offers opportunity for dialogue) |
| Patient not accepted | Delay in treatment; sepsis; increased workload | Poor quality of handover; personality of people; unclear diagnosis; clinician changing story along the way | 5 | 4 | 20 | Escalation to higher level | |
| (15) Cubicle nurse (A&E) + porter take patient to MAU and handover to cubicle nurse (MAU) | Patient story not communicated | Inconvenience to patient and staff (need to find information; social issues, e.g. whether relatives have been informed); medication could be duplicated | Other nurse who is unfamiliar with patient does handover | 5 | 3 | 15 | Nurse who has looked after patient should do handover (e.g. NIC looks after patients while nurse is away) |
Ambulance service B/hospital D: resuscitation pathway
| Step | Failure mode | Consequences | Causes | Likelihood | Severity | Risk score | Mitigation |
|---|---|---|---|---|---|---|---|
| (1) Telephone pre-alert (AC or control centre to NIC or ED staff closest to red telephone) | No pre-alert | Delay in getting the right people, bed (trauma/airway patients); possibly inexperienced staff around rather than senior staff; other resuscitation patient may have to be moved unexpectedly from resuscitation area to free up space | Poor mobile telephone connection; ED telephone not working | 4 | 5 | 20 | Improved radio link; reduction in ED overcrowding; keep resuscitation bed free |
| Misinterpreting information, numbers, abbreviations | ED is prepared but may require different/additional resources when patient arrives | Inexperienced staff; communication comes from control centre who cannot answer clinical questions | 4 | 3 | 12 | Cautious ED planning; communication coming from ACs | |
| Fragmented information | Similar to (1b) | Similar to (1b) | 4 | 3 | 12 | Similar to (1b) | |
| Failure to notify of deteriorating patient condition | ED is prepared but patient may be a lot sicker than expected and right people may not be around | Too little time; failure to recognise deterioration | 3 | 5 | 15 | ||
| Failure to notify of improving patient condition | Resuscitation team/room needlessly prepared and not available for other patients | Failure to recognise improvement; lack of understanding of impact on ED | 4 | 2 | 8 | Increase awareness among ACs | |
| (5) Paramedic to resuscitation team handover | Not all team members present | Late comers will receive handover and instructions from team members who are already present; additional communication and distraction; information may be communicated in abbreviated fashion | Staff busy with other patients | 4 | 2 | 8 | |
| People not listening | Duplication of medications | People keen to start treatment; hierarchy; stress levels | 5 | 3 | 15 | Timeout for handover; clear leadership; patient remains on ambulance bed for handover and is moved to ED bed after handover to demonstrate that patient still ‘belongs’ to ambulance service during handover | |
| Paramedic forgets to provide certain information | For example, aspects of mechanisms of injury; paramedic is in the room while treatment starts and will fill in details as appropriate | Busy work environment; hierarchy/experience; information not regarded as essential | 3 | 2 | 6 | Paramedic remains in resuscitation room until initial assessments/treatments have started | |
| Team misunderstands information | Similar to (5c) | Busy work environment; stressful situation | 3 | 2 | 6 | Similar to (5c) | |
| Team comes with preconception and finds it difficult to adapt to actual patient/patient condition | For example, paediatric cases in which the patient is younger than expected and the dose of a particular drug may be inappropriate | Lack of experience | 3 | 4 | 12 | ||
| (10) Telephone referral ED doctor to admitting doctor | See Majors (11) | ||||||
| (11) Clerking by EAU doctor of patient on A&E | See Majors (12) | ||||||
| (13) Patient transfer | See Majors (15) |
Ambulance service B/hospital D: major injuries pathway
| Step | Failure mode | Consequences | Causes | Likelihood | Severity | Risk score | Mitigation |
|---|---|---|---|---|---|---|---|
| (2) Paramedic to NIC handover | Handover delayed | For example, delay in intravenous antibiotics administration for patients with sepsis | Queue (longer wait) | 5 | 4 | 20 | Queue nurse; RAT; education to public about A&E use (to reduce ED overcrowding); transfer to other departments; quicker discharge |
| AC unable to get to next patient quickly (impact on AC) | Nurse busy elsewhere (shorter wait) | 2 | 10 | ||||
| Missing/incomplete information/documentation | Medication may be duplicated | Distraction, interruption; nurse is focusing on assessing patient rather than on handover; access to PRF is delayed; takes longer to book in patients with EPR | 5 | 4 | 20 | Paramedic does a second handover to cubicle nurse; Section on sticker for paramedic to write notes; checkbox for PRF reviewed; third copy of PRF; second AC member can pick up and correct communication errors | |
| Failure to communicate criticality adequately | Patient may not be seen as quickly as would be required | Unclear handover, inadequate handover, paramedic unable to articulate criticality in terms that is expected by nurse | 4 | 4 | 16 | Assessment by nurse | |
| (11) Telephone referral ED doctor to admitting doctor | Patient not added on to admitting doctor's list of patients to be seen | Delay in patient being seen; increased length of stay | Admitting doctor not next to list | 3 | 2 | 6 | A&E nurses will take action to investigate why patient has not been seen |
| Incomplete/inaccurate handover due to unfamiliarity with patient | Pertinent information not communicated; criticality not adequately communicated; clinical intuition and tacit knowledge not communicated; patient may be seen with delay | Referral from doctor who had not originally seen the patient | 5 | 2 | 10 | Face-to-face handover and eyeballing of patient | |
| Patient not accepted | Delay in patient journey | Hierarchy; EAU full; unclear responsibility/process when patient could go on different pathways; unclear referral; patient should go to subspecialty rather than medical ward | 5 | 2 | 10 | Medical controller to oversee referrals and communicate with specialties | |
| (12) ‘Eyeballing’ + clerking of patient on A&E by EAU doctor | Patient not seen within allocated time frame | Delay in patient journey | Floating junior doctor; busy ward; patient elsewhere for assessments, tests, etc. | 4 | 2 | 8 | |
| (15) Patient transfer | Notes not available, lost | Patient arrives without care plan; delay in treatment | Patient moved after clerking on A&E, but notes not yet available; care plan not done | 5 | 2 | 10 | Patient safe to be moved; EAU nurse will ask what needs to be done |
| (16) Clerking of patient on admitting ward | Notes incomplete | DNR misplaced; ECG missing; drug list missing/incomplete; leads to delays in treatment and need for gathering data; false sense of security | Patient has been seen quickly and notes have not yet been completed; documents not appropriately copied; documents lost or scattered | 5 | 2 | 10 | |
| Clerking information gets lost | Delay in treatment; nurse time wasted; logistical implications | No dedicated place to go and do the notes, hence notes easily misplaced/not found | 5 | 2 | 10 | Dedicated place to do + store notes; nurse will look for notes; double checking procedure before administering high-risk drugs |
Hospital E: resuscitation pathway
| Step | Failure mode | Consequences | Causes | Likelihood | Severity | Risk score | Mitigation |
|---|---|---|---|---|---|---|---|
| (1) Telephone pre-alert (AC or control centre to assessment nurse or ED staff closest to red telephone) | No pre-alert | Delayed treatments (e.g. airways); impact on department puts pressure on ongoing care; right people may not be around, e.g. trauma team not ready; critical delay for stroke patients | AC assumes A&E is ready/‘buffer’ zone; AC do not recognise need for pre-alert | 3 | 5 | 15 | Include standard list of conditions to pre-alert in JRCALC + provide education to staff |
| Pre-alert at very short notice | Similar to (1a) in worst case; usually less severe as there is less delay | AC close by | 3 | 5 | 15 | ||
| ACC makes call and cannot answer questions leading to fragmented information | Observations can be wrong (or even opposite); cannot answer questions; time omitted for stroke patients and patient not thrombolised properly | ACC are not clinicians; unfamiliar with patient; urgency not recognised, not aware of need | 4 | 3 | 12 | Conservative/pessimistic planning on A&E side; ACC pro forma and standardisation of communication | |
| Patient deteriorates en route | Delay in treatment (minutes), but department is already expecting the patient | 3 | 1 | 3 | Staff have experience and are aware that patients may deteriorate | ||
| Information missing because right questions are not asked | Observations missing; planning of impact on department not optimal | Inexperienced staff | 2 | 3 | 6 | ||
| (3) Nurse informs resuscitation team | Resuscitation team not alerted immediately | Severity is already controlled, as somebody would be available, even if not senior doctor | Senior doctor is busy | 2 | 1 | 2 | Awareness of importance of red telephone calls |
| (4) Resuscitation team prepares for arrival of patient | No resuscitation bed available | Less critical patient moved out of resuscitation; reduced monitoring; poor patient experience due to sudden move | Staffing; availability of resources; multiple casualties | 4 | 2 | 8 | High-visibility cubicles in Majors |
| Less immediate access to equipment if patient cannot go to resuscitation, could trigger initiating events for later complications | Staffing; availability of resources; multiple casualties | 5 | 20 | Move less critical patients out of resuscitation; high-visibility cubicles in Majors | |||
| (5) Paramedic to resuscitation team handover | Information interpreted wrong (e.g. shortness of breath could be normal for this particular patient) | Increased diagnostic complexity | Patient history not communicated fully at this point | 5 | 1 | 5 | Paramedics usually around during initial assessment; PRF contains further information |
| Whole story not communicated/received | Vital pieces of information not communicated/received, e.g. medications already given, could lead to duplication | Resuscitation team focused on task | 4 | 3 | 12 | Paramedics usually around during initial assessment; PRF contains further information | |
| (6) Handover repeated to team members arriving late | Focus on few aspects rather than whole story | Extra communication can lead to distraction; other team members will fill in details as assessment/treatment progresses | 3 | 1 | 3 | Other team members are aware | |
| (7) Paramedic finishes paperwork | Delay in finishing the paperwork | Delay in progressing patient later on | Paramedic in resuscitation room in case further information is required | 5 | 2 | 10 | |
| (10) Telephone referral, senior doctor to CDU registrar | Referral not accepted | Delay of patient journey; may lead to complications | Possible multiple specialties; busy CDU | 2 | 3 | 4 | Resuscitation cases are recognised as important |
| Referral accepted, but patient condition not properly understood | Patient not seen quickly; patient may deteriorate with assumption on A&E side that patient has been referred and will be looked after | Poor quality handover; not asking questions for clarification | 2 | 5 | 10 | ||
| Referral to wrong specialty | Delay in getting patient to the right people; may lead to irreversible complications later | Wrong diagnosis | 1 | 5 | 5 | ||
| (12) NIC/resuscitation nurse informs CDU co-ordinator | CDU co-ordinator does not update whiteboard | Patient transfer from A&E delayed; blocking space in A&E | Busy work environment | 4 | 2 | 8 | |
| (13) Patient transfer | Notes incomplete | Delay in getting the full set of notes to CDU | Doctors take notes and may leave parts behind | 5 | 1 | 5 | |
| Drugs that have been given not communicated fully | Handover not comprehensive; may lead to complications; duplication of medication; medication given late | Assumption that information is in documentation and will be looked at; nurse transferring patient unfamiliar with patient | 4 | 4 | 16 | Specific drug card rather than A&E sheet |
Hospital E: major injuries pathway
| Step | Failure mode | Consequences | Causes | Likelihood | Severity | Risk score | Mitigation |
|---|---|---|---|---|---|---|---|
| (3) Paramedics hand over patient to NIC/deputy | Medications not communicated fully | Could lead to duplication of medications (e.g. morphine, paracetamol) | Documented, but not communicated | 2 | 3 | 6 | Handover should provide opportunity to ask questions; sticker with prompts; look at PRF |
| Social situation not communicated | Possible safeguarding issues missed | Not perceived as relevant at this point, reliance on documentation | 3 | 2 | 6 | Documented in PRF | |
| Important observations/information not handed over | Possible major complications later | Distraction; not believing what is communicated | 2 | 5 | 10 | Structured, uninterrupted handover | |
| (6) Assessment nurse assesses patient | PRF unavailable | Delay in treatment; less objective assessment | Notes in circulation, not yet ready | 5 | 1 | 5 | Notes arrive during assessment |
| (10) Doctor identifies next patient + picks up notes | PRF/notes unavailable | Delay in treatment | Notes in circulation, misplaced | 2 | 2 | 4 | See (6a) |
| Patient not seen quickly | Possible significant delay, e.g. septic patient | Workload | 4 | 3 | 12 | ||
| (13) Telephone referral senior doctor to CDU registrar | Referral not accepted | Delay of patient journey; may lead to complications, e.g. make surgery more difficult/complex | Possible multiple specialties; busy CDU | 4 | 3 | 12 | |
| Referral accepted, but patient condition not properly understood | Patient not seen quickly; patient may deteriorate with assumption on A&E side that patient has been referred and will be looked after | Poor-quality handover; not asking questions for clarification | 2 | 5 | 10 | ||
| Referral to wrong specialty | Delay in getting patient to the right people; may lead to irreversible complications later | Wrong diagnosis | 1 | 5 | 5 | ||
| (16) NIC/resuscitation nurse informs CDU co-ordinator | CDU co-ordinator does not update whiteboard | Patient transfer from A&E delayed; blocking space in A&E | Busy work environment | 4 | 2 | 8 | |
| (17) Patient transfer | Notes incomplete | Delay in getting the full set of notes to CDU | Doctors take notes and may leave parts behind | 5 | 1 | 5 | |
| Drugs that have been given not communicated fully | Handover not comprehensive; may lead to complications; duplication of medication; medication given late | Assumption that information is in documentation and will be looked at; nurse transferring patient unfamiliar with patient | 4 | 4 | 16 | Specific drug card rather than A&E sheet | |
| Wrong interpretation of information/information not taken on board | Delay in assessing/treating patient | Patient looks OK and is not taken as seriously as their condition requires | 5 | 2 | 10 |
Appendix 3 Description of identified risks
Below, the significant risks (risk score of ≥ 12) that have been identified across the three sites are described in more detail.
| ID | Failure mode | Description of risk |
|---|---|---|
| AC-01 | Ambulance service does not provide a pre-alert to A&E | The purpose of this pre-alert is to allow the A&E resuscitation team to prepare adequately for a time-critical patient. This involves getting the resuscitation bed ready, assembling the necessary equipment and alerting all relevant staff. Time permitting, there may also be a team brief to ensure that roles and activities are discussed. In cases where there is no pre-alert from the ambulance service, this preparation will not have taken place, and, as a result, there will be a delay of as much as 10 minutes in getting people and equipment ready. Reasons for not receiving a pre-alert include proximity of the ambulance to the A&E department, but also deterioration of the patient en route or a failure to recognise the criticality of the patient and the need for a pre-alert. This may happen frequently, at least once a week. The current mitigation in place is the ability of resuscitation staff to start treatment quickly to stabilise critical patients, even in the absence of required equipment and staff |
| AC-02 | Ideal resuscitation team not available | Even in cases in which a pre-alert has been received, there is a possibility that required staff are not available. In such cases, more junior staff may have to take responsibility for aspects of the patient's care, and other areas of the department may be left less attended as staff members attend to resuscitation. This may happen due to staffing and workload levels, and is a regular occurrence (at least once a week). The current mitigation in place is to move staff from less critical patients and areas or to request support from specialist teams and other wards |
| AC-03 | Full story not communicated during handover from paramedic to assessment nurse | The handover from paramedic to assessment nurse for patients with major injuries is the only opportunity for paramedics to communicate verbally not only the immediately relevant clinical history, but also social information and other issues that they feel require highlighting. It is also an opportunity for the nurse to ask clarifying questions and to seek additional information. If important information is not communicated successfully at this point, the nurse may underestimate the patient's acuity or may miss information, such as known allergies. The reasons for this may be numerous: there may be interruptions, the nurse may not be listening with full attention, queues may lead to rushed handover, there may be too much information given by the paramedic or too little, and the environment may be noisy and busy. This is a regular occurrence and is perceived to happen every day. Possible mitigations proposed were a dedicated handover point away from noise and queues (already in existence, but not always used for handover), HCA support to the assessment nurse, and a system that ensures availability of a senior clinician during handover (rapid assessment consultant) |
| AC-04 | Delay in handover from paramedic to assessment nurse | In those cases where the AC are queuing and waiting to hand over a patient to the assessment nurse, there may be the possibility that the patient deteriorates while in the queue, potentially requiring more intensive treatment later on, for example sepsis that is treated with delay. Causes for this are A&E overcrowding or observations that have not been re-checked in the queue, possibly because ACs have handed over to another crew who are now looking after several patients. Delays are perceived to happen every day |
| AC-05 | PRF unavailable when nurse or clinician assess patient | The PRF is perceived as a very detailed and comprehensive document that provides a lot of valuable, additional information to the A&E staff, which is not possible to communicate during the verbal handover. If this document is unavailable, there may be a delay in assessment and treatment while the nurse or clinician look for the form, or the assessment may not be based on all available evidence, and may therefore be less accurate. Reasons for this are that the PRF travels around the department and may get misplaced or lost as somebody picks it up but does not return it to the designated area. This is also perceived to be a daily occurrence. A possible mitigation proposed was the introduction of an electronic PRF |
| AC-06 | Assessment nurse does not prioritise critical patient with clinician | Some patients are more critically ill than others, and the assessment nurse has the opportunity to prioritise patients with the clinician through an annotation on the A&E computerised information system and through a verbal, informal handover. If this does not take place, the patient will get seen in order of arrival, which means there can be a significant delay until a critically ill patient is seen by a clinician, which may lead to possible deterioration of the patient's condition. Reasons for this include a lack of experience and time pressure, which prevents adequate assessment and calculation of MEWS score. This is perceived to happen at least once a week. The proposed mitigation is a system where there is a rapid assessment with a senior clinician when the ambulance service hands over the patient |
| AC-07 | Clinician overly relies on nursing documentation | A lot of information is recorded in the PRF and the A&E notes by the time the clinician assesses the patient. There is a trade-off that the clinician needs to make between starting each assessment with an open, unbiased mind and the need to get through many patients quickly, in part by relying on this prior documentation by colleagues. In cases where the clinician falsely relies on the documentation produced by a nurse, important medical information can be missed that may lead, for example, to the inappropriate discharge of an elderly patient where the underlying condition for the current episode was not correctly assessed. Reasons for this may be high levels of workload and a busy work environment, a lack of experience on part of the clinician and the absence of senior colleagues who could provide additional advise. This is perceived to occur with moderate frequency, between once a month and once a week. The proposed mitigation is a system of senior review before discharge to provide discussion and support, similar to those situations in which a decision to admit is taken |
| AC-08 | AMU registrar reluctant to assist with decision or requesting further investigations | The telephone referral between the A&E clinician and the AMU registrar provides an opportunity to discuss the patient and possible pathways for continuing care. If this conversation breaks down or fails to achieve its aims, there may be a delay for the patient to be seen by the appropriate specialty, and the patient takes up resources as they remain on A&E, which may have an impact on other patients. There are various reasons why this communication may be problematic: there may be possible alternative pathways and the AMU registrar tries to ensure that the patient goes to the right place; a protocol-driven communication that distracts from actually discussing the patient's needs; uncertainty about the diagnosis on part of the A&E clinician that may prompt the AMU registrar to request further investigations in order to ensure that the patient goes to the right place; a lengthy referral by the A&E clinician without proper articulation of the problem or of what is requested; and a busy AMU environment that may make it more difficult to accept patients with unclear diagnosis. Problems with this communication are a frequent occurrence (at least once a week). The current mitigation is referral to another specialty or escalation to a consultant. Possible suggested mitigations include a clear policy and protocol of acceptance to avoid discussions, a protocol that patients need to be ‘eyeballed’ on A&E within a 30-minute time window, a procedure that requires all specialties to come to A&E in those cases in which referrals to different specialties could be considered, and training in communication and handover |
| AC-09 | AMU nurse co-ordinator does not accept referral of patient | This situation is similar to the one above, but the difference is that for patients with major injuries the referral is to the nurse co-ordinator rather than to the medical registrar. If the patient is not accepted this may lead to delays in treatment, additional workload on A&E, and possible deterioration of the patient. Reasons for this are similar to the above, but for patients with major injuries as opposed to resuscitation patients, this is a more frequent occurrence, and is perceived to happen on a daily basis. The current mitigation is the escalation to a senior clinician |
| AC-10 | Patient story not communicated during patient transfer | When the patient is physically transferred from A&E to AMU there is a verbal handover between the A&E nurse and the AMU nurse. The purpose of this handover is to provide an in-depth description of important aspects of the patient's story, including not only the patient's current condition, but also, for example, social aspects that require highlighting. If this is not highlighted, there may be an inconvenience to the patient and the staff who need to trace the relevant information, or certain aspects may be overlooked. This may happen in those cases where the nurse who is accompanying the patient has not looked after the patient on A&E and is therefore unfamiliar with the patient's history. As possible mitigation, a system whereby the nurse looking after the patient always accompanies the patient was proposed |
| BD-01 | Ambulance service pre-alert not given; deteriorating patient condition not communicated; information inaccurate or fragmented | A number of high-risk failure modes were identified around the ambulance service pre-alert including not giving a pre-alert, failure to notify of deteriorating patient condition, and providing information or understanding information that is fragmented or inaccurate. This may lead to situations where they A&E are not prepared for the patient or they are expecting a patient of different condition or characteristics. Causes for these failure modes include poor mobile telephone reception in rural areas, too little time to provide a pre-alert, failure to recognise deterioration, and in the case of calls from the ACC, the fact that no clarifying questions are possible and information may have been misinterpreted. Such failures are perceived to be regular occurrences, happening at least once a week. Proposed mitigations include an improved, dedicated radio link, and a reduction in ED overcrowding such that one resuscitation bed can be kept free for unforeseen emergency arrivals |
| BD-02 | ||
| BD-03 | ||
| BD-04 | ||
| BD-05 | Resuscitation staff not listening attentively during paramedic handover | In the busy and time-critical resuscitation setting, A&E staff may engage in multiple tasks while receiving the handover from the paramedic. As a result, some information may be missed or misinterpreted, for example what kind of medications the paramedic had already given. This could potentially lead to a duplication of medications. Causes for this are stress levels and the perceived urgency within the resuscitation environment, which may lead staff to be keen to get ‘hands on’ quickly. Such behaviour is perceived to occur on a daily basis. Proposed mitigations include a procedure that consists of a time-out for handover and a protocol that the patient remains on the ambulance trolley until the handover has been given as a visible sign that the patient is still under the responsibility of the AC |
| BD-06 | Resuscitation staff fail to adapt their preconceptions to actual situation | The pre-alert may not convey all relevant information, for example it may only mention a paediatric case, without providing the age of the patient. The A&E staff may have certain preconceptions about important characteristics, such as age and weight, but the patient could be younger or more vulnerable than expected. Failure to adapt the mental model to the actual situation during handover could result in situations where inappropriate drug doses are given. The cause for this could be inexperience on part of the A&E clinician. Such failures are perceived to occur with moderate frequency, between once a month and once a week |
| BD-07 | Delay in handover from paramedic to nurse in charge | See AC-04. Additional mitigations that were proposed include: queue nurse, RAT and education to the public about appropriate A&E use to reduce overcrowding |
| BD-08 | Missing or incomplete information and documentation during paramedic to nurse in charge handover | See AC-03. When the paramedic hands over to the nurse in charge, some information may not be mentioned, or it may not be heard properly. This could, for example, pertain to treatments already provided by the paramedics en route. In such a case, there is a potential that medication may be duplicated. This was perceived to be happening on a daily basis. Additional mitigations proposed included a second handover from paramedic to cubicle nurse (currently this takes place informally), and a dedicated section on the sticker for the paramedic to write notes on (currently only the nurse writes on the sticker) |
| BD-09 | Failure to communicate criticality adequately | From the nurse's point of view, a key aim of the handover from the paramedic is to understand the criticality of the patient's condition in order to allocate resources appropriately. If the criticality is not communicated adequately, the patient may end up having to wait for an extended period of time thus delaying their treatment and potentially leading to a deteriorating situation. This was perceived to be a regular occurrence, happening at least once a week. Causes for this include an unstructured and inadequate handover, or the inability of the paramedic to articulate criticality in terms that is expected by nurse. The mitigation currently in place is the separate assessment by the nurse |
| E-01 | No pre-alert Pre-alert at short notice ACC makes call and cannot answer questions/provides fragmented information |
See AC-01 and BD-01 to BD-04. Additional mitigations proposed were the inclusion of a standard list of conditions to pre-alert in JRCALC and the provision of corresponding education to staff, and a standardised pro forma to support ACC staff in providing adequate and relevant information |
| E-02 | ||
| E-03 | ||
| E-04 | No resuscitation bed available | Even in cases where a pre-alert has been received, there may be situations where no resuscitation bed is available for the patient. The consequences include less immediate access to necessary equipment and more difficult monitoring of the patient's condition if the patient cannot go to resuscitation. This could trigger initiating events for later complications. Such a failure is perceived to occur regularly, at least once a week. Possible causes are the limited number of resources and staffing levels, as well as exceptional situations such as incidents with multiple casualties. The current mitigation in place is to assess whether resuscitation patients that are stable can be moved out of the resuscitation area. A proposed mitigation would be to have high-visibility cubicles in the major injuries area for such patients to facilitate the monitoring of their condition |
| E-05 | Whole story not communicated/received during resuscitation handover | See BD-05. The frequency was estimated to be at least once a week |
| E-06 | Drugs that have been given not fully communicated during handover from A&E nurse to CDU nurse (resuscitation patients; majors patients) | See AC-10. The concern here was particularly on drugs that have been given. Failure to communicate these was perceived to be a regular occurrence, happening at least once a week. A suggested mitigation was to have a dedicated drug card in addition to the A&E notes |
| E-07 | ||
| E-07 | Doctor identifies/sees next patient late | Patients with major injuries are usually seen in the order in which they present, unless they are prioritised due to their criticality. There can be significant delays until a patient is seen. A possible consequence of such delays is the possible deterioration of a patient while they are waiting to be seen. Such significant delays are perceived to be a regular occurrence, happening at least once a week. A possible cause is excessive workload for the doctor |
| E-08 | Referral not accepted by CDU registrar | See AC-08 |
Appendix 4 Additional failure trajectories
This appendix provides two further examples of contextualised failure trajectories for significant risks identified during the risk analysis (Boxes 9 and 10).
The patient throughout this vignette was an 86-year-old lady with a background of bullous pemphigoid, who was fully independent and still driving prior to admission. She had developed acute confusion at home, was seen by her GP the day prior to her admission, her urinalysis had had ‘everything in it’ and she had begun on oral trimethoprim. She was referred directly to the medical registrar and brought to A&E by a paramedic crew. There had been an outbreak of norovirus, meaning that lots of wards were closed, forcing lots of GP referrals that would normally go to the AMU being diverted to A&E. The GP had faxed a referral letter to the AMU as per protocol. The medical registrar had been extremely busy that day, and although the referral had been put on ‘her personal list’, it had not been added to the daily admission take list.
On arrival in A&E at 16:55, Mollie was confused (unable to comply with an abbreviated mental test score) and slightly drowsy (GCS score 14/15), her observations showed a BP of 94/60 mmHg, pulse was 42 beats per minute and a respiratory rate of 14 breaths per minute. Her capillary refill was 4 seconds and her temperature was unrecordable. She was taking regular prednisolone, 15 mg/OD once daily (for the pemphigoid).
Her examination was normal except for the widespread denuded skin lesions; these did not appear overtly infected. Initial bedside tests showed a normal urine dipstick, an and ECG showing showied sinus bradycardia (with normal QT interval and no J waves) and a normal capillary blood glucose (6.4 mmol/l). Her portable CXR did not demonstrate any pathology.
She was seen by the A&E junior staff, who prescribed fluids and a Bair Hugger®. The bloods were sent and the medical team informed of her arrival. She was initially assessed by the medical SHO on call. She did not have the faxed GP referral letter or any verbal/written handover from her registrar.
Mollie’s daughters arrived at 2030 and added that she had recently been started on trimethoprim by her GP, following a urinalysis at home that ‘had everything in it’.
The POD system (pneumatic air tube system, using pods) was under maintenance, meaning bloods had to be portered by hand to the laboratory in batches, delaying results. The results came back at 1830 and showed evidence of an inflammatory response – white cell count of 19, platelets of 545 and a CRP of 194. There was evidence of kidney injury (potassium 6.0 mmol/l, urea 12.4 mmol/l, creatinine 164 μmol/l).
There was still no available downstream bed on the AMU. The prescribing system in A&E was paper based for fluids and all drugs, in contrast with the downstream wards, which all used an electronic prescribing system.
At 2035, the medical SHO assessed the patient and wrote up hydrocortisone, piptazocin and gentamicin as stat doses on the A&E card and added a bag of fluid. The patient had not passed urine since arrival. The downstream AMU bed became available at 20:45 and she was hurriedly transferred to the AMU (just avoiding the ‘breach time’). A ‘blue light’ trauma was coming in in 3 minutes and the only available transfer nurse was a bank nurse (unfamiliar with the hospital), who had not been previously been involved in her care; he read the impression and plan directly from the medical SHO clerking documentation. The medical and nursing teams changed shifts at 2100 with ‘handover’ usually occurring between 2100 and 2130. The AMU nursing team and medical assessment team involved in her care were all ‘outgoing’ staff. The handover meeting had been delayed by 10 minutes due to the high activity and ended 10 minutes late owing to the large numbers of sick patients that needed discussion and frequent interruptions.
The night medical team finished the handover at 21:54, with an urgent call to review Mollie, whose observations now showed a still unrecordable temperature, BP of 76/40 mmHg, pulse 35 beats per minute, respiratory rate 10 breaths per minute and GCS score of 13. At 2210 an A&E ward clerk brought through some bits of paper that had been left in the resuscitation room in A&E, including the A&E clerking booklet. It was clear that the prescribed medication and fluids had not been signed for.
At 2225, Mollie was prescribed and given hydrocortisone, antibiotics and fluids but unfortunately did not improve, and intensive care review was sought, but she arrested peri-assessment and despite 45 minutes of rewarming and CPR, she died.
Contributory factorsGP referral information not collated centrally.
A/E staff not aware of the referral or the background information.
Non-standardised prescribing systems: written prescribing in one department vs. an electronic system everywhere else.
Insufficient medical handover.
Insufficient nursing handover.
Orientation issues for the bank nurse.
Non-optimised night handover: start/finish/non-sterile cockpit.
Poor recognition of a deteriorating patient, escalation and continuity of care.
Multitasking leading to confusion.
The patient throughout the vignette was a 72-year-old pensioner who was knocked over by a car on the way home from the shops; it was late afternoon around 1630. It was difficult to ascertain exactly what had happened, as the driver of the vehicle had failed to stop following the collision, and Frank remembered little of the events because it all happened so quickly.
At 16:42, at the scene, the paramedics found Frank sitting upright; he was a stoic kind type of gentleman who did not have time for fuss. A few of the passers-by stated that they heard the breaks screeching and the bang but none was sure of how fast the car would have been travelling or whether indeed Frank had lost consciousness directly after the incident.
Frank complained of some pain to his left hip and left leg; he felt that he could not walk because of the pain but had no recollection of being hit. He said repeatedly ‘I will be fine’ and ‘I just feel a little dizzy’. He said, ‘I think the car bumped me and I fell’. He was asked about medications but obviously had no prescription with him – he remembered that he was on some blood thinners but did not know the name of them or any of his other drugs. There was no significant blood on his clothes and only some grazing to his forehead; it was wet, cold and dark but his legs looked OK so the paramedics decided to scoop him up rather then than assessing him fully in the cold.
As Frank looked well, the ambulance crew did not call or activate the Trauma desk; they felt that his injuries were probably minimal – he was probably just clipped and fell, as he complained of so little pain and his observations were all normal. The crew elected to take him to the nearest ED department, in a small district general hospital, and no pre-alert was made.
When the paramedic crew arrived at the local hospital, as usual on a Friday, the ambulances were queuing up. Owing to poor bed availability, many patients had been waiting to be moved from the ED to the wards; consequently, with no outflow there was no space to review the patients that had been brought in by ambulance. An assessment nurse was working her way down the queue of patients still on ambulance trollies taking a quick history and doing an initial set of observations: Frank was seventh in line to be seen;, he was tucked away on a corridor adjacent to where the main stream of patients were was filtering into the ED Majors section. Initially, no member of the ED team spoke to Frank upon his arrival, but the paramedics booked Frank in at 1700 as a ‘fall with leg injury’ at the front desk.
After about 30 minutes the paramedic went to find where the assessment nurse had got to; he found the nurse dealing with walking wounded patients in- between taking handovers from crews when an ED cubicle became free. The assessment nurse was also involved with regular telephone calls to the bed manager about how many trolleys were now in the corridor and how many other ambulances were en route.
The paramedic explained that Frank had complained of more pain in his leg now – he was saying it was 9/10 and that he was uncomfortable on the trolley. The assessment nurse stated that Frank was her very next patient and that she would be with him in a minute – when she had assessed him, she would ask a doctor to prescribe some pain relief until he could be transferred to a bed.
Another 30 minutes passed, Frank had been in the queue to be seen for just over an hour; he was much quieter now, and he was not complaining of pain. The lighting on the corridor was poor but the paramedics observed that Frank was sweating, and had become paler. Since the initial incident, an hour and a half had passed; one paramedic had stayed with Frank while the other had gone for coffee. The paramedic went again to find the assessment nurse to express his concerns at leaving Frank alone in a corridor. It was at this time that Frank’s daughter arrived; the police had contacted her following the incident.
When the paramedic and assessment nurse returned Frank was now only moaning; the observations were done and his BP was dangerously low. It was clear to the assessment nurse that something was definitely wrong and that Frank should go to the resuscitation area. While all of the other cubicles were full, as per policy, one bed was kept empty in the resuscitation area just in case. The paramedics helped move Frank on to the resuscitation trolley and then wished him well; the nurse was scrabbling to get a blood pressure reading, and some ECG leads in situ. The crew took the point that she was flustered so merely handed the PRF handover form to the nurse. They had been standing around for over an hour and were anxious to leave, so took the immediate opportunity to go once the ‘handover’ had occurred.
Once Frank arrived in the resuscitation area the senior ED doctor was bleeped to review him. When the ED consultant arrived the crew had left and the assessment nurse was writing down the observations. The consultant asked ‘What’s happened?’. He was told ‘It says he’s fallen’. Overhearing the discussion through the paper curtains, Frank’s daughter added, ‘He didn’t fall at all, the police told me that he was a hit and run victim, how somebody is capable of running an old man over then speeding off is beyond me’. Snatching the rain-soaked PRF from the side the consultant read ‘pedestrian vs. car,?speed,?loc,?medications – pain to left hip’. . .
Frank lived. He had immediate radiographs that showed a fractured displaced pelvis, a fractured left neck of femur, and a left-head fibula fracture. The team in the emergency department started resuscitation with warmed fluids, and then subsequently emergency blood products. He had to wait for the CT scan that showed his abdominal injuries, as the radiographers had gone home at 1700; they had to have time to come in from home and re-start the scanner. Frank required emergency orthopaedic and general surgery that night; consultants having left for home, and their registrars already undertaking surgery at the time, also delayed these life-saving interventions.
Contributory factorsThe problem may have started with poor assessment, but genuinely the paramedics wanted to get Frank to somewhere warm. This initial misjudgement was compounded by a system pushed beyond safe functional capabilities. Frank waited over an hour to be seen and assessed owing to capacity issues. There was over an hour before a second pair of eyes, or further observations, were taken, highlighting his deterioration. The paramedics were desperate to stop hanging around and get on with their next job, they felt they did not know much so the PRF said all that they did know. The initial misjudgement became catalysed through a variety of poor handovers and delays in care into a near catastrophic incident.
Had Frank been ‘alerted’ into the ED by phoning ahead, even if it was just reported as a ‘pedestrian vs. car’ he would have been met by a receiving ED consultant, and resuscitation team, and the paramedic crew would have been able to describe what was seen to the lead clinician, and answer questions that would have been posed. The radiographers, radiologists, orthopaedic and general surgeons would have still been in the hospital, drastically reducing time to imaging and surgical interventions.
Appendix 5 Accountancy commentary
This appendix provides a brief commentary on the costs associated with some of the improvements suggested by participants. The majority of these recommendations have been costed on the basis of the additional costs or investment required. The research did not include a cost–benefit analysis, and financial implications of the benefits arising from improved handover – such as reduced length of stay, improved patient outcomes or savings elsewhere in the clinical pathway – have not been considered. Therefore, the majority of the financial implications detailed here represent the gross cost of making these benefits. As such any organisation would need to subject any of these areas for improvement in the handover process to the rigours of the business case.
In respect of staff, this is primarily around additional resource to either provide extra capacity or greater input into the handover process.
The introduction of a queue nurse is based on an 8-hour shift rota on a one-to-one basis as recommended by a recent publication. 115 To allow sufficient cover this shift pattern would require the employment of 7.18 whole-time equivalents. The costing is based on the mid-point for a Band 6 nurse plus additional of 26%. The annual cost would be £284,000.
The input of a senior clinician into the handover has been costed on the basis of 3.5 minutes. Equally allowing time for a more comprehensive handover that allows such things as social history, etc., to be shared has been based on an additional minutes from each of the key protagonists, namely nurse, paramedic and clinician. For both of these it has been shown as an additional cost, whereas there may be the possibility of it displacing other activity or fitted in around other activities.
The additional training has been based on the delivery and staff cost of three training sessions for 15 staff at each session. This provides a cost of £18,000.
The investment in an ERF is based on the recurring and non-recurring cost of introducing it across an ambulance trust. The costs have been based on the experience of an English ambulance trust that has introduced ERF. 116 There are implementation costs for staff training and project management of £760,000. The annual service costs and other non-pay costs of £365,000 are offset by estimated revenue savings (primarily staff costs) of £185,500 providing a net annual running cost of £464,000.
The provision of a dedicated telephone and telephone line for a pre-alert is a relatively small investment with one-off costs of £3500 for handsets and ongoing line rental and charges of £800–1000 per annum.
Two of the suggestions for improvement are providing dedicated physical space in the A&E department in the provision of high-visibility cubicles and a dedicated space for handovers. We have estimated the capital cost of remodelling to be £175,000–340,000 (dependent on size of department) and £30,000, respectively.
A general view that emerged from interviews and observations was that insufficient capacity, with respect to both staff and beds, contributed to handovers not being as efficient and effective as might be. The other was that of creating a organisational culture around patient safety and improved patient outcomes. Clearly, both of these factors have far reaching implications for quality management in the clinical process but are not able to be financially quantified within the confines of this research project.
A summary of the improvements suggested by participants during the FMEA sessions and the corresponding resource implications is provided below.
| Reference | Suggested improvement | Category | Resources implications | Cost implications | Commentary/assumptions | |
|---|---|---|---|---|---|---|
| Type | Level | |||||
| 1 | Queue nurse | Staff | Increased staff costs – research tends to indicate a requirement of 1–2–1, based on 8-hour shifts | High | £284,000 | Based on shift pattern of 1–2–1 requiring 7.2 whole-time equivalent |
| 2 | Increased senior clinician input into handovers | Staff | Staff resources | Medium | £50,000–90,000 (depending on size of department) | Based on attendance of consultant for 3.5 minutes at each handover |
| 3 | More comprehensive handover, e.g. routinely include social history | Staff | Increase staff resources | Medium | £18,000–39,000 (depending on size of department) | Based on one additional minute per handover |
| 4 | Electronic PRF | Technology | Capital investment/recurring maintenance | High | Implementation cost of £760,000 and net annual running costs of £464,000 | Based on costs where previously implemented South East coast and East Midlands |
| 5 | Dedicated telephone/telephone line for pre-alert | Technology | Capital investment/ongoing rental and charges | Low | One-off cost of £500 and annual running cost of £800–1000 | Based on two dedicated lines |
| 6 | Increased/further training | Development | Staff cover and cost of training sessions | Medium | Around £18,000 | Based on three training session per annum for 15 staff each time |
| 7 | High visibility cubicles | Built environment | Non-recurring remodelling cost | Low | Estimated capital cost between £175,000 and £340,000 (depending on size of department) | Estimated redesign costs – dependent on available space |
| 8 | Dedicated space for handovers/assessments | Built environment | Non recurring remodelling cost | Low | Capital cost of £30,000 | Based on refurbishment cost of 20 m2 – dependent on available space |
| 9 | Increased capacity – staff and beds | Staff | Insufficient evidence to determine | ? | Not possible to quantify | |
| 10 | Improved organisational culture focussed on quality and safety | Development | Insufficient evidence to determine | ? | Not possible to quantify | |
Appendix 6 Research protocol
1. Aims/objectives:
The project addresses the following Research Questions:
-
R1: What is the potential for harm of clinical handover failures along the Emergency Care pathway?
-
R2: What are common organisational deficiencies that affect clinical handover in the Emergency Care pathway and what impact does the organisational model of care delivery have?
The detailed objectives of the project are:
-
O1-1: To identify and to systematically describe clinical handovers within the EC pathway
-
O1-2: To assess the reliability of handovers within the EC pathway
-
O1-3: To describe failure trajectories through the pathway and to systematically assess the potential for harm of handover failures
-
O2-1: To identify common organisational deficiencies that affect clinical handover in the EC pathway
-
O2-2: To describe the impact on handover of different organisational models of care delivery within the EC pathway
-
O3-1: To provide recommendations for improving the reliability and quality of clinical handover in the EC pathway
Data will be gathered along Emergency Care pathways in three participating NHS health economies with different organisational models.
2. Background:
The project aims to contribute to the research on clinical handovers and patient safety in Emergency Care through the following specific contributions:
-
Study of the Emergency Care pathway considering inter-organisational and inter-disciplinary handover rather than a single type of handover
-
Systematic risk analysis and description of significant failure trajectories
-
Qualitative analysis of the system and organisational factors contributing to failure.
-
Consideration of the impact of different organisational models of the Emergency Care pathway by studying three health economies with different characteristics.
-
Recommendations for sustainable improvement by consideration of pathway and underlying factors
-
Contribution towards an organisational culture of proactive end-to-end patient safety risk management through the choice of methods which include traditional research methods as well as improvement science and safety science methods (Process mapping, Failure Mode & Effects Analysis).
Literature review:
-
Handover is a high-priority area: A recent Australian literature review concludes that clinical handover is a high-risk scenario for patient safety (Wong et al, 2008). In the US, the Joint Commission suggests that communication failures among clinicians are a major contributor to sentinel events and near-misses (WHO, 2007) and it requires from accredited organisations the adoption of standardised handover approaches (JCAHO, 2007). The World Health Organization Patient Safety Alliance High 5s initiative includes reduction in handover errors as one of its priorities (WHO)
-
Handover around emergency care poses particular threats to patient safety: Handovers between ambulance services and emergency care, and handovers within emergency care, are characterised as being particularly problematic (Wong et al, 2008). This is due to the fact that emergency care has unique characteristics such as multiple and overlapping patient encounters, unscheduled care, incomplete historical data, and handover often takes place in settings of high patient acuity and overcrowding (Bomba & Prakash, 2005; Wilson, 2007)
-
Few studies considering inter-organisational handover and emergency physician handover: A literature review on ambulance services to emergency department handover found only 8 studies relating to the topic (Bost et al, 2010). A paper on behalf of the American College of Emergency Physicians states that there is a lack of empirical evidence and that the study of handover in emergency care was still in its infancy (Cheung et al, 2009)
-
Reliability of handover in emergency care: There is little systematic evidence as to the actual reliability and potential of harm of clinical handovers. A survey in three large metropolitan emergency care departments in Australia (Ye et al., 2007) employed post-handover questionnaires and found that information was perceived to be lacking in 15.4% of handovers. A study looking at handover between ambulance services and emergency department at two sites found that ED staff retained only 56.6% of the information correctly (Talbot & Bleetman, 2007).
-
Our recently concluded WISER study looking at shift handover in three sites found that certain elements, such as tests awaiting results (18.1%), tests not done yet (16.7%) and ongoing treatment (16.7%) were communicated infrequently (Burnett et al, 2010).
-
Contributory factors: The absence of a standard approach is frequently identified as a contributory factor along with factors such as lack of training in communication skills, missing or inaccurate information, time constraints and frequent interruptions (Ye et al, 2007; Bomba & Prakash, 2005; Philibert, 2009; Wong et al, 2008).
-
Over-simplification of recommendations: Recommendations for improving handover frequently focus on standardisation. A recent literature review concludes that at present there is no evidence that demonstrates that standardisation leads to a measureable improvement in patient outcomes (Cohen & Hilligoss, 2010). A recent editorial in the Annals of Emergency Medicine emphasises that this may be due to extreme over-simplification of the problem and a poor understanding of underlying contributory factors (Patterson & Wears, 2008). The editorial also points out that the scope was too narrow with looking at only one particular handover instead of the pathway.
3. Need:
This will be the first study that systematically studies handover failure in the emergency care pathway from a systems perspective. There is broad agreement in the literature as well as among relevant organisations (e.g. BMA, JCAHO, WHO etc) that clinical handovers represent a crucial element in patient care and that failures constitute considerable risks to patients. This is particularly true for the dynamic and time-critical Emergency Care pathway. NPSA data (per comm., 2010) shows that the commonest causes of adverse events in A&E departments relate to misdiagnosis and mistreatment. Both of these are known to be influenced by information handover. Organisations such as the American College of Emergency Physicians or the Health Foundation and the NHS Institute for Innovation & Improvement in the UK acknowledge that research on clinical handovers is required in order to ensure the continuity of care and reduce patient harm. The recent review of the patient safety research programme highlighted the needs for a systems focus, with its view of latent and upstream factors rather than the individual focus and that the admission process was an important area of research.
Clinical handovers are currently of even more interest due to changes in the working hours of doctors, which lead to an increased number in shift handovers. Various changes such as those in rotas becoming EWTD compliant have resulted in a large increase in handovers, often from one per day to 3 per day for medical handovers alone.
As outlined above, there is little systematic evidence about the reliability and potential harm of clinical handovers, in particular in the UK. In addition, the studies often consider a single handover and proposed improvements usually do not consider the wider systems aspects. Checklists are often suggested as the means of reducing error, occasionally changes of environment to stop interruptions have been suggested, but rarely has any study been made of the broader organisational issues that create the atmosphere and approach that supports better handover. Undertaking the research will also promote a research based discussion after results are released which will assist in modifying underlying root causes at individual locations as well as inducing change by more formal routes.
The proposed project looks at the Emergency Care pathway and provides descriptions of the risks of failures in clinical handovers along the pathway. The Health Foundation’s Safer Clinical Systems programme, led by this team, has demonstrated wide variation on handover practice and has developed methodologies that will be utilised in this study to diagnose and analyse handover problems. It considers the influence of the organisational setup of care delivery. It also provides a demonstration of how organisations can assess risks proactively.
4. Methods:
The project will employ a multi-disciplinary mixed-methods approach consisting of both quantitative and qualitative research methods as well as methods drawn from safety and improvement science. The team includes individuals with clinical, human factors and safety engineering, improvement science and organisational behaviour backgrounds.
a. Setting
The project investigates handovers along the Emergency Care pathway, including the interfaces into and out of the emergency department (e.g. ambulance services, ward-based care). The three sites selected have been chosen because of their diversity. They differ in size of organisation, and include foundation and ordinary NHS trusts with a geographical spread. The communities they serve are very different including metropolitan, urban and rural with both multi-cultural and near uni-cultural populations. The styles of emergency care practised also differ with departments having many emergency medicine consultants and undertaking many investigations and treatments in the emergency department to small departments with few consultants where most investigation is undertaken by the admitting teams. The study also involves two different ambulance services with whom we have worked previously. The choice of study sites reflects common NHS Emergency Care pathways that a patient may encounter. By choosing diverse sites, the study will provide descriptions of the impact on handover of different models of Emergency Care, while at the same time providing a basis for drawing out common organisational deficiencies across sites. Focusing on three sites, represents a reasonable compromise with respect to cost and effort required and strength of the findings.
b. Design
The research is organised into three work streams as outlined below in detail.
WP1 looks at the entire Emergency Care pathway including the interfaces into and out of the Emergency Care department to identify the main vulnerabilities and opportunities for harm associated with handover failures. This includes handover from Ambulance services to A&E and from A&E to MAU (where the majority of patients requiring medical admission go). The handovers studied are related to progression along the pathway rather than shift handover. Handovers include a range of variables such as format, existence of guidance and checklists, urgency, environment and professional groups to ensure that systems issues are detected. We use improvement science methods, such as process walks and process mapping, to describe the pathway and the handovers along the pathway. There will be an element of quantitative data collection through observations and audio recording of handover in order to determine the reliability of handover. Data will be analysed using Communication Analysis and a tool developed for the assessment of handover (Apker et al, 2010). From safety science, we adopt a technique called Failure Mode & Effects Analysis (FMEA) to elicit proactively from staff their perceptions about vulnerabilities in the system and possible trajectories of handover failures through the system and its safety defences. WP1 will, therefore, provide a rich description of the Emergency Care pathway and the handovers, as well as a systematic and contextualised description of the major risks associated with handover failures, their possible causes and promising safety improvements.
WP2 looks at organisational factors that affect the quality of handover. This work stream utilises qualitative research methods based on the Grounded Theory approach (Strauss & Corbin, 1998). The interviews with staff will be coded and common organisational deficiencies identified through constant comparison with the data and theoretical comparison with the literature (e.g. Reason, 1997; Vincent et al, 1998). This work stream will also look at the differences between the sites in terms of their geography, patient population, Emergency Care pathway structure etc. and elicit from staff their perceptions about how these differences affect handover and the impact of handover failures on patient safety. WP2 will provide a qualitative description of common organisational deficiencies and a qualitative assessment of the impact of different ways of structurally organising the Emergency Care pathway. Our overall aim remains to examine how far day-to-day organisational factors may contribute to any deficiencies observed in the handover process. These are of course not deigned to be inadequate but can occur as a consequence of embedded, well-established work practices often acquired by role incumbents as part of the role socialisation process. Some authors (Bate 2000, Ham et al 2003, Waring et al 2007, Skipton et al 2008) would refer to such behaviour as reflecting the cultural practices of an organisation, indeed the safety culture of the organisation. It is not our intention to examine and assess factors by formal survey - relevant assessment tools exist - but through interviews and discussion with staff directly involved identify whether such cultural factors may be operating.
Our focus is initially the potential for organisational issues to shed light on deficiencies in handover. On a more positive note we would want the study to contribute to how change or improvement in practice might be achieved. In this sense we would wish to explore, albeit at a limited level given the scope of the study, how far the knowledge of behavioural implications can be captured and disseminated more widely within the whole organisation (Swan, Newell and Scarbrough, 2008). It may be difficult to generalise to the entire NHS from findings in three key hospitals, however we would hope to identify aspects of organisational practice (which may of course be site specific) which may influence handover practice and may be operating similarly in other contexts.
WP3 synthesises, summarises and prioritises the findings of the previous work streams to provide recommendations from a systems perspective to policy makers and managers for sustainable improvements of clinical handover within the Emergency Care pathway. The recommendations will be commented upon independently by an individual with expertise in NHS finances to provide an indication of the feasibility within the current NHS climate of the different recommendations. The recommendations will be documented in the final project report.
c. Methods
WP 1: Potential for harm of clinical handover failures along the Emergency Care pathway (Lead: Prof Matthew Cooke; 8 months)
This work package will:
-
describe the Emergency Care pathway and handovers at each site (WP 1.1; 3 months)
-
quantitatively assess the reliability of handovers (WP 1.2; 3 months)
-
systematically assess the potential for harm of handover failures and describe significant failure trajectories (WP 1.3; 2 months).
Methods:
The main methods used are:
-
WP 1.1: Process Walks, Process Mapping
-
WP 1.2: Observation and audio-recording of handover; post-handover questionnaire
-
WP 1.3: Failure Modes & Effects Analysis, Focus Group
Outputs:
-
WP 1.1: Process map detailing handovers along the EC pathway; structured description of each handover
-
WP 1.2: Reliability measure for each type of handover
-
WP 1.3: Systematic risk analysis (FMEA template)
WP 2: Common organisational deficiencies and the impact of organisational models of care delivery (Lead: Prof. Peter Spurgeon; 6 months)
This work package will:
-
identify and classify the main organisational deficiencies that impact the quality of handover (WP 2.1; 3 months)
-
describe the impact of organisational models of care delivery on handover (WP 2.2; 3 months)
Methods:
The main methods used are:
-
WP 2.1: Semi-structured interviews
-
WP 2.2: Comparative qualitative analysis
Outputs:
-
Qualitative description of common organisational deficiencies as perceived by staff
-
Qualitative description of structural differences between sites and their impact on handover
WP 3: Recommendation for improving the reliability and quality of handover (Lead: Dr Mark-Alexander Sujan; 1 month)
This work package will bring together in a final report the findings of the previous work and provide recommendations for enhancing the reliability and quality of handover from a system's perspective. The recommendations will be commented upon by an individual with expertise in NHS finances with a view to their feasibility within the current NHS climate.
5. Contribution to existing research:
This proposal is highly relevant to the present SDO agenda in that it addresses an important topic in an area not previously explored. Patient safety is considered a national priority and various initiatives are in place to reduce risk and harm, but currently this work has not included non-shift related handovers or the special circumstances of the emergency care pathway.
It will build on previous research on patient safety and reliability. Most existing research has looked at handover between shifts and primarily with ward-based teams. This research will extend that work to the emergency care setting and to inter-organisational, inter-departmental and inter-professional handover. It will have high impact on the 13 million emergency department attendances per year.
This project will ensure that the profile and importance of handovers is heightened in ambulance services, emergency departments and assessment units. Existing links with the NHS Institute, Health Foundation and Patient Safety First campaign will ensure that the findings are widely applied and consideration is given to the generalisable findings for other pathways. MWC will have the opportunity to link the findings with policy development and to have access to a wide emergency care audience. The findings will also be placed on NHS Evidence emergency and urgent care collection (managed by us) and included in their briefing series.
A copy of the final project report will be sent to the INVOLVE registry and key findings communicated to the public via The University of Warwick's very successful media office.
One of the stated objectives of the NIHR is that “research is needed to identify the most effective, value-for-money interventions and to ensure these are implemented quickly”. The intended output of this project would provide information required to reduce handover errors and improve safety in a sustainable manner because of the systems focus. The previous work of the group allows this project to use established and tested methods increasing the cost effectiveness. The systems focus of this work is highly relevant to managers as well as clinicians and it is expected that many of the latent conditions detected in the study will be implicated in many safety errors not just those of handovers.
6. Plan of investigation:
| Work Package | Start | Complete by (latest) | Deliverables | Staff |
|---|---|---|---|---|
| Project Management Objective: Provide ongoing project management; set up project web site; prepare interim and final reports |
01/04/11 | 30/09/12 | MAS, MWC, PS, Project Manager | |
| WP 0 – Ethics Objective: Finalise research protocol & obtain ethics approval |
Following positive indication of funding, no later than 01/04/11 | 30/06/11 | Research Protocol Ethics approval |
MAS, MWC, PS, Project Manager |
| WP 1 – Potential for harm of clinical handover failures Objective:
|
01/07/11 | 28/02/12 | MAS, MWC (WP Leader), MIK, SC, NR, Researcher | |
| WP 1-1: Description of pathways & handovers Process walks, process mapping sessions |
01/07/11 | 30/09/11 | Process map for each site Structured description of each handover |
MAS, MWC, MIK, SC, NR, Researcher |
| WP 1-2: Quantitative reliability assessment Collect quantitative data for 3 handovers at each site Conduct data analysis Produce reliability assessment report |
01/10/11 | 31/12/11 | Reliability assessment report for each site | MAS, MWC, MIK, SC, Researcher |
| WP 1-3: Potential for harm & failure trajectories Conduct 2 half-day FMEA workshops at each site Analyse data Produce final WP 1 report |
01/01/12 | 28/02/12 | Systematic risk assessment of handovers Qualitative description of failure trajectories through the emergency care pathway Final WP 1 report |
MAS, MWC, MIK, SC, Researcher |
| WP 2 – Common organisational deficiencies and the impact of organisational models of care delivery Objective:
|
01/03/12 | 31/08/12 | MAS, PS (WP Leader), SC | |
| WP 2-1: Common organisational deficiencies Cycles of:
|
01/03/12 | 31/05/12 | Qualitative analysis of common organisational deficiencies impacting the quality of handover | MAS, PS, SC |
| WP 2-2: Impact of organisational models of care delivery Perform comparative qualitative analysis Produce final WP 2 report |
01/06/12 | 31/08/12 | Qualitative description of differences in the organisational models of care delivery and their impact Final WP 2 report |
MAS, PS, SC |
| WP 3 – Recommendations Objective: Provide recommendations from a systems perspective for improving the reliability and quality of handover within the Emergency Care pathway |
01/09/12 | 30/09/12 | Final report | MAS (WP Leader), MWC, MIK, PS, SC, NR, Researcher, JN |
Gantt Chart
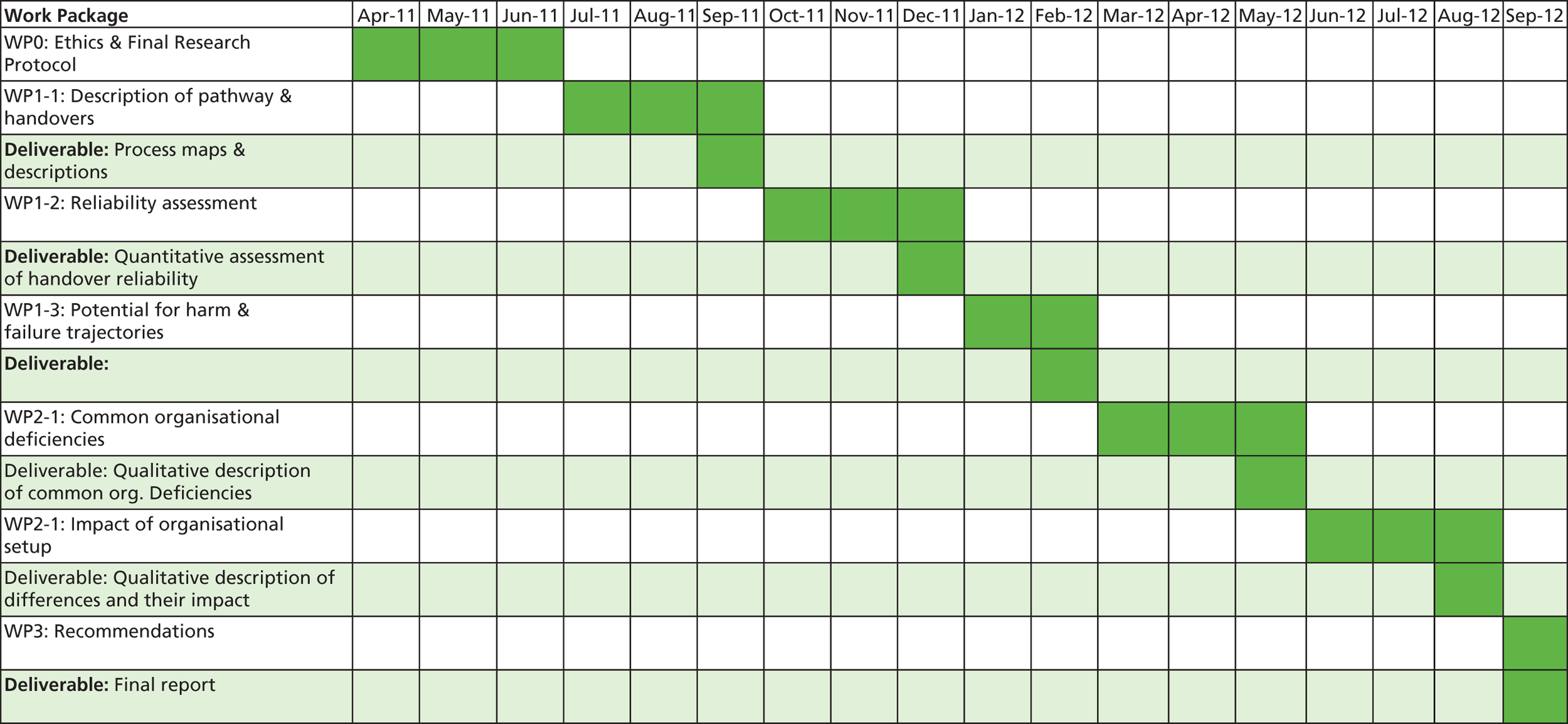
7. Project Management:
The project will be monitored and management by the Project Executive Team (Dr Sujan, Prof Cooke, Prof Spurgeon, Project Manager) under the overall leadership of Dr Mark-Alexander Sujan. As Chief Investigator, Dr Sujan will be responsible for overseeing relations with the study sites, general coordination and communication with the SDO programme, and for ensuring that deliverables and reports are produced according to the project plan. The Project Executive Team is based at Warwick Medical School and will hold fortnightly project meetings. This arrangement ensures that the experience of successfully managing a large number of projects by the co-applicants can be brought fully to this project, and that potential risks can be anticipated early and mitigated effectively.
Researchers at the sites will be supervised by local site leads. During the time of their involvement, local researchers will also participate in a fortnightly telephone conference.
A monthly project review meeting will be held involving all project members. We aim to make extensive use of telephone and video conferencing facilities considering the geographic spread of the study sites and participants. Dr Sujan will regularly visit the sites to maintain efficient face-to-face contact with all team members.
Each of the work streams has been allocated a designated lead with responsibility for ensuring the smooth and timely flow of activities within that work stream. Prof Cook will be leading on WP 1 (Potential for harm of handover failures), Prof Spurgeon on WP 2 (Organisational factors) and Dr Sujan on WP 3 (Recommendations).
A Project Advisory Group will be formed involving representatives from the Royal College of Emergency Medicine, Ambulance services, NPSA and INVOLVE. The Project Advisory Group will be chaired by Dr Jane Jones (Assistant Director, The Health Foundation). Throughout the course of the project, the Project Advisory Group will review the progress of the project through electronic communication and will hold a mid-term review meeting at Warwick.
8. Service users/public involvement:
The project will have a lay person on the Project Advisory Group. Geoff Aitcheson has been involved with Warwick Medical School as a lay research advisor for 8 years focussing on projects related to diabetes and emergency care. He will review the ethics and governance forms before submission and advice on improvements. He will actively participate in project management meetings. At the end of the project he will also ensure that findings are appropriately patient focussed. As with previous projects that he has been involved with, he will be a full member of the research team and will receive all appropriate documentation and invitations to all meetings as well as the key roles described above. He has undertaken extensive teaching of research staff and has worked with INVOLVE, so has a broad remit and experience.
9. References:
- Apker J, . Exploring emergency physician – hospitalist handoff interactions: development of the handoff communication assessment. Ann Emerg Med 2010;55:161-70.
- Bate P. Changing the culture of a hospital from hierarchy to networked community. Pub Admin 2000;78:485-512.
- Bomba DT, Prakash R. A description of handover processes in an Australian public hospital. Aus Health Rev 2005;29:68-79.
- Bost N, Crilly J, Wallis M, . Clinical handover of patients arriving by ambulance to the emergency department - A literature review. Int Emerg Nurs 2010.
- Burnett S, Cooke M, Deelchand V, . How safe are clinical systems?. London: The Health Foundation; 2010.
- Cheung DS, Kelly JJ, Beach C, . Improving Handoffs in the Emergency Department. Ann Emerg Med 2009;55:171-80.
- Cohen MD, Hilligoss PB. The published literature on handoffs in hospitals: deficiencies identified in an extensive review. Qual Saf Health Care 2010.
- Deming WE. Out of the crisis. MIT Press; 1986.
- Ham C, Kipping R, Mcleod H. Redesigning work processes in health care: lessons from the National Health Service. Milbank Q 2003;81:P415-439.
- JCAHO. 2008 . National Patient Safety Goals - Goal 2E. 2007. URL: www.jointcommission.org/PatientSafety/NationalPatientSafetyGoals/08_hap_npsgs.htm (accessed 29 June 2010).
- Leonard MS, Frankel A, Simmonds T, Vega KB. Achieving safe and reliable healthcare. Health Administration Press; 2004.
- NHS Institute for Innovation and Improvement . Quality and Service Improvement Tools – Process Mapping: An Overview n.d. URL: www.institute.nhs.uk/quality_and_service_improvement_tools/quality_and_service_improvement_tools/process_mapping_-_an_overview.html (accessed 14 July 2010).
- Patterson ES, Wears RL. Beyond Communication Failure. Ann Emerg Med 2009;53:711-12.
- Philibert I. Use of strategies from high-reliability organisations to the patient hand-off by resident physicians: practical implications. Qual Saf Health Care 2009;18:261-6.
- Reason J. Managing the Risks of Organisational Accidents 1997.
- Shipton H, Armstrong C, West M, Dawson J. The impact of leadership and quality climate on hospital performance. Int J Qual Health Care 2008;20:439-45.
- Storey N. Safety-Critical Computer Systems. Prentice-Hall; 1996.
- Strauss A, Corbin J. Basics of qualitative research: techniques and procedures for developing Grounded Theory. Sage Publications; 1998.
- Swan J, Newell S, Scarbrough H. “Why don’t (or do) organisations learn from projects?”. Manag Learn 2008;41:325-44.
- Talbot R, Bleetman A. Retention of information by emergency department staff at ambulance handover: do standardised approaches work?. Emerg Med J 2007;24:539-42.
- Vincent C, Taylor-Adams S, Stanhope N. Framework for analysing risk and safety in clinical medicine. BMJ 1998;316:1154-7.
- Waring J, Harrison S, McDonald R. A culture of safety or coping? Ritualistic behaviours in the operating theatre. J Health Serv Res 2007;12:s1-3.
- Wilson MJ. A template for safe and concise handovers. MedSurg Nurs 2007;16:201-6.
- Wong MC, Yee KC, Turner P. Clinical Handover Literature Review 2008.
- World Health Organization . Action on Patient Safety - – High 5s n.d. URL: www.who.int/patientsafety/solutions/high5s/en/index.html (accessed 29 June 2010).
- World Health Organization . Communication During Patient Hand-Overs 2007. URL: www.who.int/entity/patientsafety/solutions/patientsafety/PS-Solution3.pdf (accessed 29 June 2010).
- Ye K, Taylor D, Knott JC, . Handover in the emergency department: deficiencies and adverse effects. Emerg Med Australas 2007;19:433-41.
List of abbreviations
- A&E
- accident and emergency
- AC
- ambulance crew
- ACC
- ambulance control centre
- ACP
- advanced clinical practitioner
- AMU
- acute medical unit
- ATMIST
- age, time, mechanisms, injuries, signs, treatments handover tool
- BMA
- British Medical Association
- CA
- conversation analysis
- CatA8
- category A8
- CatA19
- category A19
- CDU
- clinical decision unit
- CT
- computed tomography
- EAU
- emergency assessment unit
- ED
- emergency department
- ENP
- emergency nurse practitioner
- ETA
- expected time to arrival (in clinical context)
- FMEA
- failure mode and effects analysis
- GP
- general practitioner
- HALO
- hospital ambulance liaison officer
- HCA
- health-care assistant
- IoM
- Institute of Medicine
- IT
- information technology
- ITU
- intensive care unit
- MEWS
- Modified Early Warning Score
- NIHR
- National Institute for Health Research
- PACS
- picture archiving and communications system
- PRF
- patient report form
- RAT
- rapid assessment triage
- SBAR
- situation, background, assessment, recommendation communication protocol
- SDO
- Service Delivery and Organisation programme
- VA
- Department of Veterans Affairs
- WHO
- World Health Organization