Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its proceeding programmes as project number 10/1008/35 The contractual start date was in June 2011. The final report began editorial review in January 2013 and was accepted for publication in July 2013. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2014. This work was produced by McCourt et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction
Aims and objectives
The aims of this study were to investigate how care is organised and provided in alongside midwifery units (AMUs), commonly called birth centres. We use the term ‘alongside midwifery unit’ to distinguish hospital-based birth centres from free-standing midwifery units (FMUs) (or free-standing birth centres) and to highlight that these are both midwifery-led services. AMUs provide midwife-led care for women who are deemed ‘low risk’ according to National Institute for Health and Care Excellence (NICE) intrapartum guidelines at the start of labour care on a hospital site that has a consultant-led obstetric unit (OU), either within the same building or in close proximity.
The need for this study arose out of questions emerging from the Birthplace in England study1,2 about the rationale for AMUs’ development. A number of factors may affect effective working within the units, including appropriate staffing models and their stability, training and preparation for midwife-led care, and interprofessional relationships and cultural and communication issues, particularly when escalation or transfer of care is required within a single site. The number of such services had risen rapidly, from 0% in 1995/6 to 7% of NHS trusts in 2005/6. 3 The Birthplace Mapping Study noted an increase in the percentage of NHS trusts with an AMU from 13.2% in 2007 to 25.7% in 2010. There has also been an increase in trusts with both an AMU and a FMU, from 3.3% to 8.8%. 4 Their development has aimed to enhance maternal choice and satisfaction and facilitate opportunities for ‘normal’ birth for women of low obstetric risk by providing a homely environment with a low-intervention philosophy. In addition, it was hoped to improve midwife job satisfaction and retention.
The primary research questions for this study were:
-
How are AMUs organised, staffed and managed in order to seek to provide safe and high-quality care on a sustainable basis?
-
What are the professional and service user perceptions and experiences of care in AMUs?
Objectives:
-
Exploration and analysis of potential unanticipated as well as intended consequences of AMU development, including system effects.
-
Analysis of models of organisation and staffing that addresses such aims and challenges and contributes to staff satisfaction and retention.
-
Analysis of how AMU development can respond to current policy directions, including provision of choice for service users, and safe effective and equitable care.
Background and literature
Current policy on place of birth in England
Over the last 10 years, there has been a clear policy direction on the importance of offering women choice in childbearing, and particularly on giving healthy women the choice of where they give birth. The National Service Framework (NSF) emphasised the importance of choice, continuity and control for women in maternity care and advocated more targeted approaches to ensure a safe and high-quality service. 5 The maternity standard of the NSF specified that service providers and trusts should ensure that ‘. . . options for midwife-led care will include midwife-led units in the community or on a hospital site.’ Care is to be provided in a ‘. . . framework which enables easy and early transfer of women and babies who unexpectedly require specialist care’ (© Crown copyright 2004, contains public sector information licensed under the Open Government Licence v2.0). 5 The related guidance Maternity Matters6 identified that all women should have a choice of place of birth by 2009, including birth in a local facility, including a hospital or under the care of a midwife. 6 Current NICE intrapartum care guidelines for healthy women provide information for women, health professionals and managers to inform decision-making on choice of place of birth. 7
Overarching NHS objectives inform the commissioning of maternity services. 8 Maternity services are specifically highlighted within the 2012/13 Operating Framework for the NHS9 with expectations that services will deliver improved continuity of care, choice, access and productivity:
Continuity in all aspects of maternity care is vital, from antenatal care through to support at home. Mothers and their families should feel supported and experience well-coordinated and integrated care.
Para 2.39, © Crown copyright 2011, contains public sector information licensed under the Open Government Licence v2.09
Choice is critical to giving patients more power in our systems. PCT [primary care trust] clusters should drive forward improvements in patient choice so there is a presumption of choice for most services from 2013/14. During 2012/13 this means continuing the implementation of choice about maternity care.
Para 3.22, © Crown copyright 2011, contains public sector information licensed under the Open Government Licence v2.09
In addition, the Outcomes Framework for the NHS 2012/1310 sets the high level nationally required outcome measures that commissioners should use to judge the quality and effectiveness of their services, including maternity services, as reflected in Table 1.
| Domain | Aim | Outcome |
|---|---|---|
| Domain 1 | Preventing people from dying prematurely | Perinatal mortality rates |
| Domain 4 | Ensuring that people have a positive experience of care | Patient-reported outcome measures using nationally determined survey questions to users |
| Did you get enough information from a midwife or doctor to help you decide where to have your baby? | ||
| Thinking about your antenatal care, were you involved enough in decisions about your care? | ||
| Were you (and/or your partner or companion) left alone by midwives or doctors at a time when it worried you? | ||
| Thinking about the care you received in hospital after the birth of your baby, were you treated with kindness and understanding? Did you feel that midwives and other carers gave you active support and encouragement? | ||
| Did you feel that midwives and other carers gave you active support and encouragement? | ||
| Domain 5 | Treating and caring for people in a safe environment and protecting them from harm | Percentage of term babies admitted to neonatal intensive care |
Finally, the Government’s mandate to the NHS Commissioning Board for the period April 2013 to March 201511 advised work with partner organisations to ensure that the NHS:
-
offers women the greatest possible choice of providers
-
ensures that every woman has a named midwife who is responsible for ensuring she has personalised, one-to-one care throughout pregnancy, childbirth and during the postnatal period, including additional support for those who have a mental health problem.
The Board is legally required to pursue the objectives in the mandate, and the way in which services are organised is an important factor in meeting these policy objectives to improve services. There is considerable variation within and between regions regarding what services are provided and inequalities in provision. Options for place of birth have improved since 2007,12 but almost half of women did not have a full range of choice in 2010. Currently 13% of women give birth outside an OU, in midwife-led units (AMUs or FMUs) or at home. 13
Maternity services offer a range of models of care, aimed at improving continuity14 and organisational configuration reflecting local needs, which include offering services in midwife-led settings of AMUs, FMUs and home. The number of AMUs has increased since 2007 compared with FMUs,4 and they are, therefore, increasingly relevant to the configuration of maternity services currently under consideration in England. They have the potential to deliver responsive and effective high-quality care, but there remains a paucity of evidence to inform these processes, and the ways in which AMUs operate requires greater scrutiny. AMUs are more likely to be developed than FMUs because of the political and financial climate, in which funds for rebuilds are scarce, and also because of concerns about transfer times and distances. 15
Additionally, changes to medical training, the European Working Time Directive,16 maternity staffing standards and neonatal service reconfigurations are all altering the configuration of maternity units, professional practice boundaries, skill mix and relationships. 17
Development of birth centres
Midwife-led birth centres have been developed in an effort to provide a better birth environment for women and their families and to tackle rising intervention rates, but they also aim to address the problem of midwife retention within the NHS. The most comprehensive survey to date on why midwives leave the profession found that, aside from retirement, the most common reason was because they were ‘unwilling to practise the kind of midwifery demanded of them by the NHS, despite their desire to continue working as midwives’. 18 Furthermore, the evidence suggests that this tension between how midwives would like to practise and how they are required to practise is a significant source of emotional difficulty for them. 19 Birth centres were developed in part as an attempt to resolve some of the discrepancy between the ideals of midwifery and the perceived reality of work within the NHS, by creating a separate space within which midwives could practise with a social model of care. 20
Environment and ‘home-like’ spaces
Midwifery scholars and social scientists have both addressed issues of space and place in birth. To date this interest has mainly been incidental to other concerns, such as women’s choice of place of birth21 or the development of midwife-led services outside OUs. 22–26 Other work in this area has focused on midwives rather than women and explored the effects on midwives of working in the community19,27 or in midwife-led units28–30 rather than in consultant-led units. In addition, much of the wider work in health care that has explored problems of space and place has done so while focusing on workplace relationships, for example health-care professionals’ relationships with managers31 and midwives’ relationships with junior doctors32 and support staff. 33,34
Shaw and Kitzinger35 and Davis-Floyd and Davis36 are among scholars who have suggested that women feel more in control of their birth at home or in home-like settings such as free-standing birth centres. One reason given for this feeling of control is that the woman has the higher status of ‘resident’ at home and the midwife is constructed as a ‘visitor’, whereas in hospital these roles are reversed. 37 Following this, Gilmour38 argued that transforming hospital spaces so they are more home-like challenges the dominance of biomedical values, a claim disputed by Fannin,39 who argued that it is presumptive to assume that making a hospital space more like a home will in itself fend off the controlling influence of biomedicine. Others have also been critical of the assumptions that underlie the discourses of pro-home birth academics and activists. The discourse of home equals control assumes that women have agency in their own homes, which is not always the case: ‘home does not signify autonomy and bodily control for all women, nor is domestic space always the safest place for women’. 40
The discipline of geography has put space and place more firmly into the social science agenda. There is little literature by geographers on maternity care, but the literature on geographies of nursing, like that of health and medicine, is growing rapidly. Andrews41–43 and Andrews and Shaw44 have written a number of introductory ‘manifestos’ for the geography of nursing, which explore the role of space in health-care organisations.
Hospital developers, fuelled by the drive to build new hospitals though private finance initiatives,45 have sought to design hospital environments that promote the healing and well-being of patients. Aside from the architecture of the hospital building itself, the introduction of visual art into hospitals (see Lankston et al. 46 for an evaluation of its benefits) is one example of the way in which designers have attempted to make hospitals into therapeutic landscapes. These interior designs have particularly focused on integrating ‘nature’47 and ‘home’38 into the institutional space because they are two arenas strongly imbued with the qualities of a ‘therapeutic landscape’. 48 Contemporary interest in the design of hospitals has applied the principle that a therapeutic landscape is not only one that is outside, but may also be brought into an institution and that ‘the hospital, rather than being a place of scientific inquiry removed from everyday life, is conceptualised as the home place for its inhabitants’. 38
This trend towards designing hospital wards as what are considered to be ‘home-like’ spaces assumes (problematically) that the home is a therapeutic landscape for all women, while also allowing them to birth within a hospital environment that is specifically away from the home, where those tools that are culturally assumed to improve safety, such as medicines, doctors and monitors, are readily available. This ‘hybrid space’38 is a manifestation of a wider cultural conception of childbirth as both a normal life event49 and inherently risky and in need of medical assistance (see Hausman50 for a discussion of the discourse of obstetric risk).
Efficacy and effectiveness
The evidence regarding efficacy and effectiveness with respect to birth settings is also increasing. A Cochrane review of AMUs compared with conventional hospital labour wards (or OUs) found increased likelihood of spontaneous vaginal birth, labour and birth without analgesia or anaesthesia, breastfeeding at 6–8 weeks post partum and satisfaction with care and decreased likelihood of oxytocin augmentation, assisted vaginal birth, caesarean birth and episiotomy. 24 Although no difference occurred in infant outcomes, substantial numbers of women were transferred to standard care, either before or during labour, because of maternal request, such as for epidural pain relief or because they no longer met eligibility criteria for the midwifery unit setting. 51 A similar pattern has been found with planned home birth for ‘low-risk’ healthy women.
The Birthplace in England study assessed outcomes by intended place of birth at the start of care in labour for women at low risk in AMUs, FMUs and home, compared with women planning birth in OUs. 1 For all women, the incidence of major interventions including intrapartum caesarean section was significantly lower and normal birth increased in all settings outside the OU. The overall incidence of adverse perinatal outcomes was low in all birth settings. For multiparae, no significant differences were reported in adverse perinatal outcomes between any settings. For nulliparae, no significant differences were reported in adverse outcomes between AMU or FMU and OU care. However, the risk of a composite adverse perinatal outcome was significantly higher for nulliparae who planned to give birth at home than for those who planned to give birth in an OU.
For all women, planning birth in any of the settings outside the OU significantly lowered the incidence of major interventions, including intrapartum caesarean section, and increased the rate of normal birth, relative to the OU (Table 2).
| Maternal outcome | OU (%) | AMU (%) | FMU (%) | Home (%) |
|---|---|---|---|---|
| Intrapartum caesarean section | 11.1 | 4.4 | 3.5 | 2.8 |
| Forceps | 6.8 | 4.7 | 2.9 | 2.1 |
| Use of oxytocin | 23.5 | 10.3 | 7.1 | 5.4 |
| Normal birthb | 57.6 | 76.0 | 83.3 | 87.9 |
| Immersion in water | 9.1 | 30.2 | 45.7 | 33.3 |
The study also found that the cost to the NHS of intrapartum and related postnatal care, including costs associated with transfers and clinical complications and admission to higher-level care, was lower for birth planned at home, in a FMU or in an AMU than for planned birth in an OU. 53
Women’s choice, information, access and experience of alongside midwifery units
Unlike women who plan to give birth at home or in FMUs, women who planned to give birth in AMUs were reasonably similar in demographics to women who planned to give birth in OUs in the Birthplace in England study. 1 Research into how women and their families make decisions about where to give birth has tended to focus on home and OUs, with the following factors being consistently important to women: finding a balance between safety and a satisfactory birth experience, the influence of friends, family and doctors, social class and cultural values,54,55 and the model of care on offer. 56 More recent work has found that women value birth centre care, particularly the environment, personal attention, calm ambience and close to obstetric support if needed,51,57–59 in essence what is often perceived as ‘the best of both worlds’. 58
Longworth et al. 60 found that women who chose a home birth valued continuity of care, a homely environment and the ability to make their own decisions regarding interventions. In contrast, hospital birth respondents placed a relatively high value on access to an epidural for pain relief and not needing to be transferred to another location during labour if a problem arose. 60
Transfers from midwifery units
Transfer from midwifery units to OUs both during and after labour is common, especially for first-time mothers and more common from AMUs than free-standing ones. In the Birthplace in England study, the overall intrapartum transfer rate ranged from 21% to 26% for all women, but was higher for nulliparae (36–45%).
The overall intrapartum transfer rate ranged from 21% to 26% for all women but was higher for nulliparae (36–45%), as shown in Table 3.
| Parity | OU (%)a | AMU (%) | FMU (%) | Home (%) |
|---|---|---|---|---|
| Primiparous | 1 | 40.2 | 36.3 | 45.0 |
| Multiparous | 0.4 | 12.5 | 9.4 | 12.0 |
| All | 0.7 | 26.4 | 21.9 | 21.0 |
In AMUs, the primary reason for transfer was failure to progress in labour, followed by request for an epidural. In FMUs or home birth cases, the primary reason was also failure to progress in labour, followed in this case by meconium staining. In both types of midwifery unit, compared with multiparous women aged 25–29 years, nulliparous women aged < 20 years had higher odds of transfer [FMU-adjusted odds ratio (OR) 4.5, 95% confidence interval (CI) 3.10 to 6.57; AMU-adjusted OR 2.6, 95% CI 2.18 to 2.06] and the odds of transfer increased with increasing age. Nulliparous women aged ≥ 35 years in FMUs had 7.4 times the odds of transfer (95% CI 5.43 to 10.10) and, in AMUs, six times the odds of transfer (95% CI 4.81 to 7.41). Starting labour care after 40 weeks of gestation and the presence of complicating conditions at the start of labour care were also independently associated with a higher risk of transfer. 61
A qualitative study drawn from the same cohort found that most women hoped for, or expected, a natural birth and so did not expect to be transferred. Transfer was disappointing for many, but sensitive and supportive care and preparation for the need for transfer helped women to adjust to their changing circumstances. A small number of women, often in the context of prolonged labour, described transfer as a relief. For women transferred from FMUs, the ambulance journey could be described as a limbo period. Women who were worried or fearful felt as though they were being transported rather than cared for. For many, this was a direct contrast with the care they experienced in the midwifery unit. After transfer, most women appreciated the opportunity to talk about their experience to make sense of what happened and help them plan for future pregnancies, but they did not necessarily seek this out if it was not offered. 62 Sensitive care and preparation can help women adjust to changing circumstances, as some apparently straightforward changes to practice have the potential to make an important difference to women’s experience of ambulance transfer and transfer or escalation of care. 2
Organisation of care
Previous research that has focused on AMUs has uncovered a number of questions about their function, particularly in the long term. The Health Care Commission review63 and the Birthplace Mapping Study4 highlighted the ad-hoc nature of the development of AMUs, challenges in developing usable data systems and lack of agreed definitions, eligibility, staffing or operational criteria.
Following on from its previous inquiry into the safety of maternity services, The King’s Fund commissioned further research to answer a fundamental question: can the safety of maternity services be improved by more effectively deploying existing staffing resources? The report Staffing in Maternity Units: Getting the Right People in the Right Place at the Right Time concluded that the key to improving maternity care is using midwives and other maternity staff more effectively. 17 The report considered the available evidence about the relationship between staffing levels and deployment practices and safety of care for mothers and babies, focusing specifically on labour and birth. It reviewed evidence particularly on the relationship between staffing levels and outcomes, the potential for shifting tasks between various health professionals and making use of new and extended roles, the effectiveness of different models of care and the impact of these on use of resources. 17
There is very little published evidence on how midwife units should be organised and staffed. While midwives are present at all births and are the main providers of antenatal and postnatal care, it has been difficult in the past to prescribe appropriate staffing levels because patterns of care vary between maternity services. Staffing needs in both hospital and community settings depend on service design, buildings and facilities, local geography and demographic factors, as well as models of care and the capacity and skills of individual midwives. Other significant variables with an impact on staffing levels include women’s choice and risk status. As maternity services develop different models of service delivery, such as home birth, caseload midwifery practices and FMUs, their staffing requirements may alter, particularly in the service development phase. The ratios of midwives to births recommended by the Royal College of Midwives (RCM)64 are designed to deliver a safe, high-quality maternity service, as described in the Maternity Matters report. 6
The Royal College of Obstetricians and Gynaecologists’ review entitled Safer Childbirth recommended staffing levels in recovery, theatre and high-dependency units. 65 The NHS Litigation Authority66 has published risk management standards for NHS organisations providing labour ward services. 67 The standards require staffing levels for all obstetric midwifery, nursing and support staff for each care setting, which should be calculated using the figures identified in Safer Childbirth. 65 The ratio recommended by Safer Childbirth, based on the expected national birth rate, is 28 births to one whole-time equivalent (WTE) midwife for hospital births and 35 : 1 for home births. Further specific recommendations are as follows:
-
Birth centres/midwifery-led units: the normal recommended ratio is 35 : 1 to reflect the generally low dependency of women accessing these services. However, separate assessment is needed when providing intrapartum care for women requiring transfer to hospital care, or providing ante- or postnatal care on an inpatient basis.
-
Obstetric units: the number of midwives allocated to each shift must enable a minimum of 1–1.4 midwives for each woman in established labour, depending on case mix.
Research on the development, implementation and sustainability of AMUs has found that wider institutional support and senior leadership are crucial. 68 There has been little research carried out to date on the organisation of midwifery units in the UK, both free-standing69 and alongside. 70,71 The Birthplace in England Organisational Case Studies2 also included three sites with AMUs and two with FMUs. There is evidence that such settings provide a space for the development of specialist midwifery skill and expertise in physiological birth and improved midwife job satisfaction and retention. 72 However, while midwifery units have provided midwives with a space that allows them some congruence between ideals and practice, an unintended consequence is that the philosophy and practice of the midwifery unit and their local OU, labour ward or delivery suite can become polarised. This can have a negative effect on the relationships between the midwives in the two clinical areas. 70
While few studies have been conducted of AMUs, enquiries into safety problems in FMUs and in OUs have indicated that even when formal systems, such as staffing levels and mix, appear well functioning, problems in the informal operation of those systems may arise. These may be as a result of factors such as poor inter-professional teamworking, management and training limitations, and failure to consistently implement agreed guidelines or the effect of economic and political concerns on clinical decision-making. These all lead to quality and safety concerns. 73,74 Additionally, little is known about the effect on the OU or on women with higher or intermediate levels of clinical risk factors of developing separate places with different philosophies of care.
There is a need for research that analyses not only the everyday function of midwifery units, but also their role within the rest of the maternity system and their effects, both intended and unintended, on the function of the OU. Although substantive literature on AMUs is very limited to date, the wider sources and the theoretical literature points to the importance of structural and systemic features of health-care systems, and organisational culture as well as formal organisation. They suggest that power play and local cultures may strongly affect risk and safety within health-care institutions and that interpersonal or professional issues may influence behaviour and decision-making amongst health-care professionals. 70,75,76 Vaughan’s study of health-care organisation, for example, posited ‘structural secrecy’77 – inherent barriers or resistance to communication – as an important source of danger in complex systems. Vaughan proposed that social organisation in itself (rather than merely the actions or omissions of individuals, or technical systems in isolation from social systems) forms a source of safety or danger. 77 The theoretical and substantive literature points to the need to examine the environment and processes of care, looking at different areas of activity and different professional groups as part of a complex system, rather than in isolation. 75
The factors that may influence effective transfer are of particular interest since the Birthplace Cohort Study found that 21% (95% CI 19.2% to 23.2%) of women were transferred from AMUs to OUs during or shortly after labour. Overall, local transfer guidelines were of poor quality. 26 Few studies of transfer have focused on the management of transfers within hospital sites, but a study of home birth transfers in two cultures indicated that organisational and attitudinal factors were a primary cause for concern, rather than the more technical transport issues. 78 This was also found in a Scottish audit of outcomes of community maternity units (FMUs). 79
A case study of an AMU, conducted as part of a wider study of implementation of protocol-based care, indicated that while benefits were observed in terms of satisfaction and midwifery teamworking within the birth centre, there were also unintended consequences – specifically, more negative relationships with obstetric and other midwifery colleagues – which could have an impact on overall quality of care. 80 This study also highlighted, but did not investigate, the key role of managers and management approaches in such developments.
However, a small-scale study by Huber and Sandall81 of intrapartum referral and transfer in an AMU identified a number of organisational issues to be addressed in further research. Rather than promoting safe and effective coworking and transfer, the physical proximity of the units appeared to engender competition around physical and human resources, confusion and conflict around responsibility. Clashes of philosophy, rather than shared understandings or protocols, also formed barriers to teamworking and effective communication. This study indicated the need to explore approaches to staff deployment, management and training, clear guidelines and interprofessional communication that can avoid such problems arising. It echoed findings of the few earlier studies of transfer indicating that organisational and staffing as well as cultural issues may be of major importance to quality and safety.
Questions from the Birthplace in England Research Programme
The Birthplace in England Cohort Study raised a number of questions with particular relevance for AMUs. Although AMUs had lower intervention rates for low-risk women than for those planning to give birth in OUs, the rates were higher than for women planning to give birth in FMUs. 1 This raised questions about the possible reasons for these differences. Apart from differences in the nature and background of women planning to give birth in these settings, are any features of organisation or professional practice contributing to this? The Birthplace Organisational Case Studies2 found that more attention is given to the training and support needs of midwives in FMUs than to the needs of community midwives and those working in AMUs. Are the approaches different between types of midwifery unit and what might the reasons for or implications of this be? The case studies also highlighted a major issue of proximity of the AMUs leading to blurring of spatial and professional boundaries, with potential implications for safety. Differences in equity of information and access were also found. 2 Given that the profile of women in England planning birth in AMUs is more like that of women planning birth in OUs than that of those planning home births or birth in FMUs, do the AMUs offer access to midwife-led care in labour to a more diverse range of women and what might this be based on?
The trend towards provision of AMUs raises important questions. What factors may adversely (or positively) affect the safety of care and experience for women and babies in such units? There is a need to explore the specific function of those midwifery units that are situated close to – usually in the same building, or at least on the same campus as – an OU.
Many of the everyday tensions described by NHS midwives stem from the conflicting demands of different metrics and measures. Therefore, there is value in a study such as this that explores the key performance indicators, financial constraints and local commissioning priorities that filter down to the birth centres and the rest of their local maternity service.
These policy initiatives and previous research findings from the Birthplace Organisational Case Studies raised a number of questions about the organisation and function of AMUs in order to inform service planners and managers developing and operating AMUs in the future. Therefore, this study aimed to clarify the experiences of existing AMUs that impact on their functioning through addressing two key research questions: (1) how are AMUs organised, staffed and managed in order to seek to provide safe and high-quality care on a sustainable basis? (2) What are the professional and service user perceptions and experiences of care in AMUs?
Design and methodology
Design and conceptual/theoretical framework
The study used an organisational ethnography approach. 82–84 Since there is very little prior research on this topic, small-scale but in-depth qualitative case studies are most appropriate and will also inform future larger scale development and research. The ethnographic approach is particularly suited to more exploratory phases of research. It can provide a rich description and analysis of service models, which can inform service managers, commissioners and practitioners about how to develop and provide care effectively in such settings. This approach includes a range of data collection methods.
Sampling
Our selection of case study sites involved a maximum variation sampling approach, with purposive selection. The purposive criteria were based on key research aims and questions that built on the emerging findings of the Birthplace Programme and questions that were raised by the work. Our key criteria were size of unit, geographical/regional location, age of unit, staffing model and deployment, management approach and leadership (formal arrangements and style). The site description table (see Table 4) shows how these criteria were operationalised to select an optimal mix of participating sites.
Methods of data collection
Documentary analysis: service delivery and configuration
Key documents relevant to the study were obtained and analysed, prior to site visits and interviews when possible, to provide:
-
an initial description of the background, configuration and organisation of the service
-
key questions and queries for discussion during site visits.
Key documents included service planning, consultation and reconfiguration documents, eligibility criteria for AMU care, any formal care pathways, algorithms or transfer protocols in use, and any safety and risk management tools in use.
Interviews with key stakeholders
Interviews (see Appendix 1 for details) were conducted with key stakeholders such as service managers, commissioners and user representatives, using a semistructured approach. These interviews were also used to collect key data on the background and history, as well as the current configuration of the service and its rationale and aims.
Questions and topics included:
-
service configuration history, including consultations, service reconfigurations or developments and reasons for these
-
details of current service configuration and organisation, including workforce arrangements, skill mix, models of care and escalation/transfer services and protocols
-
any plans for change or development and reasons for these.
Observation of key decision making points in the service
Observation of selected aspects of the service was conducted at key locations and times, including staff handover meetings, audit and risk meetings and everyday life of the AMU. The observations were mainly conducted before interviews with staff and service users took place and used to inform the interview questions. The observation data were audio-recorded in note form, transcribed and added to the NVivo database (QSR International, Warrington, UK).
Interviews with professionals
Interviews were conducted with a purposive sample of service providers in each case study, including midwives working in different settings, maternity care assistants (MCAs)/support workers, obstetricians and nurses.
The interviews were, in most cases, individual, but for certain staff groups it was more appropriate to arrange discussion meetings with a group of staff. The interviews used a semistructured approach, seeking unelicited views as well as responses to more focused questions developed through the earlier phases of the study and during the Birthplace study. The interview questions were also guided by the observations conducted by the researchers. In all sites (as appropriate to each interviewee), their views were sought on:
-
recent history of service configuration, including consultations, service reconfigurations or developments and reasons for these
-
service organisation, including workforce arrangements, skill mix, models of care and escalation/transfer services and protocols
-
facilitators and barriers to choice of place of birth in different settings for low-risk women
-
facilitators and barriers for professionals working in different birth settings
-
training provision and needs for staff working in different birth settings
-
management and staff support and development arrangements
-
any local, contextual or organisational factors impacting on quality of care and staff or user satisfaction.
All interviews were audio-recorded, with permission, and were transcribed in full, except in a few cases when recording was not practicable. In such cases, detailed notes were taken. Interviews were conducted in the venue chosen by the participant.
The team originally planned to use visual images within the staff interview process. Midwives were invited to take photographs of spaces and places and to bring these to the interview to trigger discussion of what matters to the staff and what different spaces and images mean to them. However, we found that this was not effective in practice as the busyness and unpredictability of current maternity service staffing meant that most midwives asked to be interviewed on the spot while they had quiet periods in the day (which were not predictable), or proved not to be available when the researcher returned on their next site visit. Additionally, we did not pursue this method following initial experience because the resulting narratives focused largely on the environment and less on other aspects of care and service organisation which were also of interest to the study.
Interviews with service users and their birth partners
Women’s experiences and pathways through care were explored using individual semistructured interviews with women and (when appropriate and available) their partners. Women were encouraged to tell the story of their maternity experience. However, to ensure that key study questions were addressed, an interview topic guide and prompts was used including:
-
pathways through care, including choices offered and made and any change of plans or referrals
-
experience of maternity care, with particular focus on the birth setting
-
experiences of birth complications and escalation or transfer of care.
Obtaining women’s, and their partners’, views and experiences is important to an understanding of the meanings of the choices available and taken, experiences of service provision, what works in practice and what they themselves define as important. The aim in this study was to understand how women came to access different types of care setting for birth and how these settings affected women’s perceptions and experience of care in labour and birth. Specifically, do AMUs succeed in providing women with the sense of autonomy, control, respect and privacy that research studies have suggested they value?85–88
Qualitative interviews were conducted with a range of women and, when possible, their birth partners, including those recruited from community centres in lower-income areas, with an emphasis on women who intended to give birth in AMUs at the onset of labour, or women who were offered the option of AMU care. The number of interviews was based on the theoretical sampling approach, using the principle of data saturation employed in grounded theory. The analysis of this sample built on the interviews conducted with women planning care in a range of settings conducted as part of the Birthplace programme, including women who required transfer or escalation of care during labour.
Data analysis
Qualitative and structural analytical approaches were employed according to data type and in order to facilitate exploration of process and structural as well as experiential aspects of the systems of care. Data were analysed using a framework approach. 89 A coding framework was developed based on the analysis and emerging questions from the Birthplace study and amended in the light of initial readings and discussion of the data collected and potentially emerging themes. This was done in a series of core study team, co-investigator and advisory group meetings, during the continuing data collection phase. This initial analysis was also used to guide further sampling and data collection decisions. In a framework approach, the prior coding frame is applied and tested by informing study questions and by mapping against the data, but a thematic approach is then incorporated using open coding to identify and explore newly developing themes and progressing to both axial and selective coding to identify key themes and categories. NVivo 10 qualitative data analysis software (QSR International, Warrington, UK) was used to facilitate systematic and rigorous analysis. Box 1 provides an illustration of this process, showing the nodes and codes used within the parent node referring to user experience.
-
Who uses AMUs?
-
Why and how women choose or end up birthing in AMUs.
-
Antenatal information.
-
Staff influence on choice of birthplace.
-
-
Users’ expectations for the AMU.
-
Opt-in and opt-out models.
-
-
Women’s and partners’ experiences of the AMU.
-
Features of care liked/not liked by users.
-
Features of environment liked/not liked by users.
-
Inclusion of partners and relatives.
-
Critical birth experiences.
-
-
Pain management.
-
Women’s perception of what is safe and risky.
-
Continuity of care and carer
-
Women’s observations about staff skills.
-
Negotiation of admission and being/not being sent home.
-
Women’s perceptions of staff relationships.
-
-
Transfers out of the AMU.
Structural approaches were also utilised to help explore the data. Process maps were used to focus particularly on mapping care pathways, transfer processes, staffing configuration and interprofessional teamworking and communication. While individual site descriptions were drawn up (see Case study site descriptions) subsequent analysis was largely on a cross-site basis. Strengths, weaknesses, opportunities and threats (SWOT)-type summaries for which respondents’ perceptions of advantages or drawbacks, opportunities or threats relating to AMUs were mapped onto tables.
In order to ensure that the process was both valid and trustworthy, preliminary coding and data analyses were commenced as early as possible. Feedback was given at regular intervals to co-investigator and advisory group meetings and discussed fully. The members of the advisory group in particular were asked to comment on whether or not the emerging findings rang true for them, whether or not anything particularly surprised them and whether or not any important issues appeared to be missing or overlooked. A participative meeting approach was used to discuss emerging issues in small groups, to identify and prioritise them and to highlight additional questions or queries. Analysis was primarily conducted by the four core team members (CM, JS, JR and SR) but co-investigators also independently read, coded and discussed the data in selected areas in which they had particular knowledge and interest. Although initially planned for sharing findings, further validation also took place during a series of regional practice-based workshops during the report drafting, in which participants discussed the issues in relation to their own service.
Ethical Issues
Ethical permission to conduct the study was obtained from the National Research Ethics Service Proportionate Review Committee (ref 11/LO/1028). Researchers were especially mindful of the need for continually negotiated consent when observing practice areas to ensure that staff and patients could exercise their right not to be included, and of the need to guard confidentiality when conducting research with small samples. Advisory group members were asked to read a draft of the report with particular reference to inclusion of any material that may lead to an inadvertent breach of confidentiality. Pseudonyms have been used for all people and places and some site details that may identify precise locations have been excluded. Professional and stakeholder respondents have been categorised very broadly to avoid identifying individuals with less common positions or work roles.
Chapter 2 Study findings
Case study site descriptions
In this section, we provide a summary description of the four case study sites to situate the findings and analyses. We focus on their history and organisational context, their locality and features of their formal organisation and practice. The experiences of staff and service users and the quality and safety of their care were shaped by the context in which this care took place. Table 4 presents some basic data on each of the sites. To maintain anonymity, pseudonyms have been adopted for these services and some figures have been rounded.
| Site (pseudonyms)/features | Westhaven | Northdale | Midburn | Southcity |
|---|---|---|---|---|
| Geography | Urban/suburban | Suburban/rural | Urban | Urban |
| Total number of births 2011/12 in trust (rounded) (including AMU) | 6200 | 6000 | 5700 | 5300 |
| Of which, AMU total | 620 | 830 | 800 | 700 |
| Service configuration, % of total births 2011/12 (rounded). Home includes BBAs | OU: 87% | OU: 73% | OU: 77% | OU: 86% |
| AMU: 10% | AMU: 14% | AMU: 14% | AMU: 13% | |
| FMU: 11% | FMU: 7% | |||
| Home: 3% | Home: 3% | Home: 2% | Home: 1% | |
| Year AMU opened (in current location) | 2005 | 2008 | 2010 | 2001 |
| Location to the OU | Adjacent | Different floor | Different floor | Different floor |
| Number of birthing rooms in AMU | 4 | 7 | 6 | 5 |
| Parity: primiparous/multiparous (rounded) | Data not available | Data not usable | ||
| Trust | 32%/68% | Data missing | ||
| AMU | 32%/68% | 46%/54% | ||
| Proportion of women transferred to OU in labour and immediate postnatal period | 32% | Data not usable | 27.5% | 26.5% |
| Top three reasons for transfer | 1. FTP | Data not usable | 1. Epidural | 1. FTP (first stage) |
| 2. Epidural | 2. Meconium | 2. Fetal distress | ||
| 3. Meconium | 3. FTP (first stage) | 3. Epidural | ||
| Trust normal birth ratea | 59% | 70% | 67% | 30%b |
| Instrumental delivery rate for trust | 14% | 9% | 9% | 18% |
| Caesarean section rate for trust | 27% | 21% | 23% | 29% |
| Epidural rate for trust | Data missing | 16% | Data missing | 56% |
| Level of multiple deprivation by PCT 2010 | Moderate | Moderate | Severe | Moderate |
| Ethnicity: trust/AMU (rounded) | Data missing | AMU only: white/mixed British 26%; Asian 39%; African/West Indian 20%; European 16% | ||
| White | 77%/83% | 56%/62% | ||
| BME | 23%/17% | 44%/38% |
We experienced difficulty in obtaining some figures for the services overall and for the AMUs. In addition, some data were not usable because of lack of clarity, obvious errors or inconsistencies in definitions. For example, in one case, there was apparent duplication of admission counting. Women sent home in early labour were counted twice, meaning that it was not possible to estimate transfer rates. For future research and audit purposes, an agreed, clearly defined and easily accessible dataset would be valuable.
Westhaven
Model of care
Westhaven AMU is located in city suburbs with varied levels of deprivation and affluence. The unit was opened in 2005 and since that time has continued to host, as planned, 10% of the trust’s births. This proportion has been maintained despite the increase from 5000 to over 6000 deliveries in the trust, with AMU births rising from 500 in 2005 to over 600 in 2011–12. In 2011/12, the AMU had a little over 900 admissions in labour with a total transfer rate of around 32%. The unit is situated on the same corridor as the OU delivery suite. It is run using an opt-in model, meaning that the OU is the default option and women have to make a specific choice and booking to attend the AMU. The AMU has a core staff of 9 (8.36 WTE): one band 7 midwife (0.6 WTE) and eight band 6 midwives. Support workers are not used on the AMU. The unit has four delivery rooms, all with birthing mats rather than beds, and one has a plumbed-in pool. There is a transitional room used by the AMU and delivery suite for women with some complications but who may not need transferred to the delivery suite. The trust has recently opened a midwifery unit a few miles away.
Alongside midwifery unit history and funding
The AMU was opened in 2005 in response to a public campaign and a trend that had seen a number of trusts opening birth centres at the time. It was funded with a bid won from a government competition. The work was delayed for 2 years by the trust’s financial difficulties, but the money was eventually used to undertake small renovations at one end of the delivery suite and to pay for some furnishing, mats and interior decoration.
Staffing model
While the delivery suite manager has overall responsibility for the AMU as well as the labour ward, the AMU has a designated part-time (band 7) manager who was appointed to lead and promote the unit. Individual shifts are co-ordinated across both areas by the on-duty delivery suite co-ordinator, but in practice the AMU and delivery suite remain quite distinct, with separate off-duties and a core group of midwives who work on the AMU. The AMU is staffed by one midwife per shift during the day and two at night, working 12-hour shifts. There has been a move to have two midwives on the AMU at all times, but this has not yet been implemented. The trust has introduced bespoke in-house training for maternity support workers (MSWs) on the delivery suite with protected study time. The trust plans to use these MSWs to support midwives on the delivery suite to release midwifery time.
Funding and future plans
There are plans to increase the number of midwives employed on the AMU and to increase the numbers of women using the service by making it the default birthplace for all low-risk women (i.e. an opt-out model) unless they request a birth at home, in the FMU or on the delivery suite. AMU staff expressed some concern that increasing their numbers would also increase the likelihood of them being ‘pulled’ (Southcity manager 2) to cover the delivery suite. The AMU is considered by the trust to be functioning well and there is no current threat to its future. This is in part because it is in high demand from women and in part because it is helping the trust achieve its Commissioning for QUality and Innovation targets to increase the normal birth rate by 1%. The trust is recruiting a senior midwife to manage the new FMU and to lead on normal birth across the trust.
Northdale
Model of care
Northdale is a town with moderate levels of deprivation. In 2011/12, the maternity service cared for a population of women consisting of 77% white and 23% BME. The population of women using the AMU was slightly different as 83% who used the AMU were white and 17% were BME. There were around 6000 births in the trust in 2011/12, with the AMU accommodating 14% of these and the local FMU 10%. Managers reported the transfer rate from AMU to OU in labour as approximately 16%, which is comparable to national averages. The AMU was opened in 2008 as part of a reconfiguration that included the merging of two local trusts. The two delivery suites were centralised at Northdale and the other delivery suite was converted into a FMU. The AMU is located two floors below the delivery suite and has seven en-suite delivery rooms. It is run on an opt-out model, meaning that the AMU is the default option for all women in the area who meet low-risk criteria, unless they request otherwise. The AMU has a core staff of 10.2 WTE midwives (1.2 at band 7 and nine at band 6), with two midwives and one MSW covering each shift. Additionally, on-call community midwives are encouraged to come in to attend births on the unit.
Alongside midwifery unit history and funding
The AMU commenced as a GP (general practitioner) unit in the 1970s, run by community midwives, with two labour rooms and around 250 births a year, which made up 10% of the total births in the trust’s maternity service. It remained a GP unit until the mid-1990s, when the service introduced midwife-led care following the Changing Childbirth91 report In 2001, Northdale Trust merged with another local trust and the obstetric services were centralised at Northdale. The old GP unit became a midwife-led unit next door to delivery suite in a newly built hospital. The head of midwifery drove a redevelopment of the AMU, and in 2008 the AMU opened in its current form. The old midwifery unit was moved to another floor in the hospital and increased in size from four to seven birth rooms, to cater for the increased birth rate.
Staffing model
The AMU has a full-time manager, who is responsible for its day-to-day running. The head of midwifery recently instigated some meetings to improve communication and teamwork between midwives on the AMU and the delivery suite. In the last year, the AMU has developed a core midwifery team headed by a new manager. There are two midwives and a midwifery assistant on duty for each shift and an on-call community midwife can be called in if needed. The AMU midwives are frequently also asked to cover shortages on the delivery suite.
There have been proposals to reintroduce the rotation of staff to improve working relationships between clinical areas. The trust has been using the Lean process ‘Visual Hospital’ to rationalise use of beds and staff92 (see Managing staff resources). This system is intended to facilitate placing midwives where they are most needed between the OU wards, the AMU and FMU.
Funding and future plans
Plans for the AMU are centred on the deployment of staff. Using Visual Hospital is seen by managers as helping them to deploy midwives where they are most needed although alternative plans for rotation or further integration of community midwives were also under consideration (see Managing staff resources). As with all the case study sites, Northdale is struggling with restricted spending and cost-saving measures, so managers aim to reduce the costs of bank staff by using their existing personnel more efficiently.
Midburn
Model of care
Midburn AMU opened in 2010 as part of the merging of two OUs that centralised at Midburn hospital, in an area of severe multiple deprivation. It is within the same building but on a different floor from the delivery suite. It hosts around 700 births a year, approximately 11% of the total births at the trust. Approximately 27.5% (2010–11) of the women are transferred during or shortly after labour, which is slightly below the national average. The AMU is organised on an opt-out model so that all women who meet low-risk criteria are booked for the AMU by default, unless they choose to birth at home, in the local FMU or in the OU.
The AMU received significant capital investment and a lot of attention was put into making it a comfortable, home-like space. There are six en-suite birthing rooms: two have plumbed pools, and inflatable birth pools are available for the other rooms. The unit has a kitchen that is shared between staff and patients, an aromatherapy room, a patient sitting room and staff room as well as the usual clinical stores and sluice.
Alongside midwifery unit history and funding
The AMU was conceived as part of a strategy to increase the capacity of Midburn maternity services following centralisation. It was proposed with the dual aim of improving facilities for women and attracting midwives to work at the trust, where recruitment had diminished in response to service quality problems that had been publicly observed. The AMU was developed quickly, with full support from the trust executives and an assigned budget to cover the development costs. The money was spent on adapting a ward, with a focus on interior design and decoration of the space.
The project was led by the consultant midwife who provided the brief, oversaw the building work and recruited the core staff team of midwives committed to working in a ‘low-tech’ birthing space that would promote normal birth. A FMU has since been opened nearby.
Staffing model
Midburn AMU has a dedicated manager who is responsible for the day-to-day running of the unit. She is supported by the consultant midwife, who continues to take a close interest in the unit and acts as its advocate both within the trust and by promoting it externally. The AMU midwives are core to that area, although they are frequently asked to cover for staffing shortages on the OU delivery suite. All community midwives are required to do one shift a month on the AMU to maintain their intrapartum skills. At each shift, there are three core AMU midwives, one on-call community midwife and a MSW. The three core midwives are on call for the FMU, which is opened on demand. Currently community midwives are not expected to work at the FMU.
Funding and future plans
A FMU was recently opened near the hospital and an effort is being made to increase the numbers of women using this service. A new manager has recently been appointed to oversee the AMU.
Southcity
Model of care
The AMU at Southcity was opened in 2001 and had approximately 750 births in 2011–12, which is around 13% of the total births at the hospital. There are plans to increase this to 1000 births a year (a level achieved in previous years), although some managers consider this to be unsustainable at current staffing levels. The unit has six delivery rooms that have delivery mats rather than beds. Approximately 20% of women admitted to the AMU are transferred to the OU delivery suite during or shortly after labour, which reflects the national average. Until recently, the AMU also cared for a proportion of postnatal women from the delivery suite, but this postnatal bay has now been closed. The trust has opened a triage centre to improve management of admissions in early labour and to divert more eligible women to the AMU, which is part of an on-going plan to increase the numbers of AMU births by changing from an opt-in to an opt-out model (AMU as default option for low-risk women unless they choose otherwise).
Alongside midwifery unit history and funding
The unit was opened to increase the capacity of the trust’s maternity services. Although there was some opposition from the trust’s obstetricians at the time, the AMU is now well established. Locally, the trust is known particularly for its obstetric care of higher-risk women. The trust recently merged with a neighbouring hospital, and this has brought challenges in finding consistent practices and guidelines across units with different histories and organisational cultures and a number of changes in management arrangements.
Staffing model
The AMU has two band 7 lead midwives who co-ordinate the everyday running of the unit. It is currently staffed by a core team of midwives but there are proposals for 6-monthly rotations for most midwives, which started to be introduced during the fieldwork period. The plans include keeping a core team on the AMU to ensure that midwives continue to practise according to its ethos of promoting normal birth. With a view to sustainability, the maternity service recently recruited a number of midwives at senior management level and the consultant midwife’s remit has been expanded to include the Southcity AMU.
Funding and future plans
The recent merger presented a number of difficulties for managers striving to create consistent working practices across both sites. The consultant midwife has implemented a number of changes to the AMU including closing the postnatal bay and adjusting AMU eligibility criteria to ensure that they are consistent with the trust’s AMU on its other site.
Summary
Although the case study sites were selected for maximum variation, each shared some key features. The AMUs catered for between 10% and 14% of births in their services, representing about one-third of the women eligible for such care. Although two operated an opt-in and two an opt-out booking system, there were no apparent differences in numbers or proportion of women using the AMU on this basis, although numbers overall were reported to be limited by staffing and room capacity and the basis for comparison is small. Despite having been open for different lengths of time, all AMUs had originated through some form of service reconfiguration that had provided an opportunity to develop the unit. The figures included in the summary data table indicate that these services were similar to the national picture for AMUs as reflected in the Birthplace study. 1 All four services were operating a core staffing model for the AMU, in three cases supported by MSWs. Two were in the process of integrating community midwifery teams and a third had operated with caseload midwifery group practices coming in to the AMU to attend births for women on their own caseloads. All were considering introduction of some form of midwifery staff rotation across areas in the future, and two were in a process of integrating community midwifery teams with the midwifery unit provision.
All the AMUs were said to be fully established within their service. They enabled midwife-led birth care for low-risk women within their trusts, and in two trusts the AMUs were considered to have helped enable the service to open a FMU. However, no plans were apparent for expanding the provision of the AMU itself to cater for a larger proportion of low-risk women in the four services. The numbers of women giving birth in the units had been maintained, on the whole, rather than increased over time.
Despite differing opportunities and funds for design or refurbishment of the unit, all had been designed to provide a low-intervention, homely and comfortable environment for women and their birth partners, in order to better facilitate normal, physiological birth. The rooms were mostly designed without birthing beds, to promote mobility and active birth, and all had birth pools plumbed in, or accessible, as well as various active birth aids. Beds were mostly intended for postnatal use and typically were either designed to pull down after birth or were hidden behind curtains. Attitudes towards the environment and use of beds are discussed in Chapters 4 and 5.
Two of the AMUs had a band 7 lead midwife (Westhaven and Southcity) while one (Northdale) had more senior leadership, with a consultant midwife as designated lead for the AMU or for normal birth care within the service. Across the units, there were between one and four midwives on each shift, and three of the AMUs also used some level of MSW. Westhaven had the lowest number of midwives on shift and did not use MSWs on the AMU, which, in addition to its small size, limited the numbers of births that could be catered for. However, Midburn, the newest unit, appeared to have more generous staffing, as we will discuss in Chapter 3, and these midwives also provided cover for the recently opened FMU from the AMU base.
Three of the AMUs were on different floors of the hospital from the OU delivery suite, while Westhaven was adjacent, having been converted from one end of the labour ward. As we will discuss, although preference was generally for a high degree of separation, we did not find clear evidence of differences between this and the other AMUs. However, this was a limited sample. On all four sites, midwives were ‘pulled’ to the OU delivery suite. In Westhaven, which was the adjacent unit and had only one midwife on shift during the day and two at night, midwives were reluctant to attend handover or transfer with women for fear of closing the AMU. This issue will be discussed in Chapter 4. Chapter 3 looks at management and stakeholder perspectives on the AMU and its place within its service, while Chapter 4 looks at staff perspectives and Chapter 5 looks at service user perspectives. Each section touches on the issue of relationships between service areas and professionals working them, in different ways.
Chapter 3 Organisation and management of the alongside midwifery units
This section addresses the first study aim: to explore how AMUs are organised, staffed and managed in the attempt to provide high-quality and safe care, on a sustainable basis. Here we discuss issues relating to provision of AMU care primarily from a management perspective, while following sections explore the perspectives of maternity care professionals, service users and families.
Our 136 interviewees (see Appendix 1) comprised 47 postnatal women and partners, 54 clinical staff members (midwives, obstetricians and support workers) and 35 managers and stakeholders (including midwifery and obstetric consultants with management roles, commissioners and user representatives). As there was not a clear line in practice between professionals in more senior roles and managers, this section draws on the perspectives of both. To conserve confidentiality, we do not give specific details of management roles. This section draws mainly on our interviews with managers and stakeholders such as commissioners.
The analysis in this section suggests that a number of key issues affect the capacity of services to provide high-quality and safe care across the range of birth settings, including lack of midwifery staffing resources and tensions around models or philosophies of care, which are often expressed in terms of place of care, and around professional skills, decision-making, teamwork and relationships. Providing choice of care settings creates new boundaries within the service that require careful management. Previous studies of quality and safety in health systems indicate that boundaries and discontinuities between different areas and professional groups in a service can present particular quality and safety challenges. 2,93 Our analysis in the Birthplace organisational case studies also indicated that the proximate nature of an AMU and the OU delivery suite to which it links can create particular tensions, with implications for quality and safety of care. 2 In this section, the development of AMUs is shown to present important opportunities to think differently in terms of service models and to provide a sustainable model of care, in a way that provides choice of birth setting for women and facilitates a more clinically appropriate level of birth interventions. However, a number of management and leadership challenges to maintaining safe and high-quality care in this distributed maternity care system are highlighted.
Drivers for service development and change
Pragmatic drivers
Key drivers for managers in respect of midwife units were economic and pragmatic, but also included a quality and safety aspect. Examining the history of these services revealed that the origins of their AMUs were predominantly pragmatic rather than ideological or philosophical, although practical considerations were embraced as opportunities to bring about desired service improvements, with anticipated benefits for service users and providers. In two services, Southcity and Northdale, creating the AMU had been part of a reconfiguration strategy to close a neighbouring OU and centralise services on one hospital site; in another, Midburn, it was a key element of a strategy to turn around what a senior manager described as a ‘failing’ service (Midburn manager 3). Westhaven was created by refurbishing rooms on an existing delivery suite, achieved opportunistically through a government fund for improving hospital environments. In Northdale, a GP unit that was run by community midwives had already been in existence on this hospital site, so that the reconfiguration enabled both continuity and renewal, in terms of offering midwife-led normal birth care.
In the Birthplace Organisational Case Studies, the view commonly expressed by managers, commissioners and many professionals was that midwife units were a luxury and an unaffordable drain on the overall service. 2 Therefore, we were interested to note that in the services included in the current study, finance had formed a key driver for the creation of these units. This was not only linked to reconfiguration of obstetric services towards a more centralised model. In Midburn, managers and senior professionals emphasised that the introduction of the AMU enabled them to provide more appropriate levels of care to women, thus using their resources more effectively to improve quality and safety:
[Before this change] There was no concept of low-risk care, higher-risk care, everybody was just managed poorly in the same way, whatever their risk
Midburn, manager 3
In Southcity, the AMU had been created to resolve an impending bed shortage with the merger of two OUs. When the new build of the maternity hospital proved insufficient, the AMU was designed through refurbishment of a disused ward in the adjoining older hospital building, to provide an additional 1000-birth capacity. Despite its pragmatic origins and support from a number of obstetricians, some saw the unit as a drain on resources in a service hard pressed by financial problems and insufficient midwifery staffing and as taking away from the low-risk birth experience of midwives on the labour ward:
Yeah, it does have an impact and this was a problem to us. It meant that you were sucking out very low risk deliveries from the labour ward and sending them off to a separate unit . . . And I come back to my point: if I were to design a unit I wouldn’t split my shop in two different places on the high street. It just doesn’t make sense to me. If you have everybody all in one place you don’t have those problems. You’ve got greater monitoring of everything that’s going on; you’ve got greater use of your resources, [it’s] more efficient
Southcity, consultant obstetrician 3
In contrast, some professionals – both obstetricians and midwives – talked of the removal of some low-risk women as lightening the workload of the OU:
We’ve got less [laugh] low-risk patients to be fair um [pause] (. . .) It’s made a positive impact that that they have . . . that it has lightened the load on us.
Midburn OU, midwife 8
While some concerns and anxieties were expressed regarding the levels and sensitivity of new tariffs to be shadowed in maternity services in the coming year, the shift from payment by results (measured in terms of interventions) to one based more on risk levels of those booking for care was seen as an opportunity to consolidate recent developments in midwife-led provision. Some obstetricians and managers in Southcity, in particular, commented on normal birth as being a ‘loss-making activity’ (Southcity manager 5) under the current commissioning system, and service managers and obstetric consultants in all services expressed concerns about service funding and midwife staffing levels:
. . . we are looking at, um, the bottom line, service line reporting of all of our services and looking at what makes a loss, what breaks even and what we can do at profit, and maternity, because of CNST [Clinical Negligence Scheme for Trusts], because of the costs of obstetricians and the costs of midwives against the current tariff is unquestionably loss-making. So it’s really difficult. With midwifery-led births, because the tariff is lower, you’ve got more costs to cover within a lower amount of income, so it’s cheaper to do but less profitable. Or rather, more loss-making.
. . . yes you have to make the risk argument, yes you have to make the safety argument, yes all of that has to be there, but you also need to think about how you are going to answer the questions about, well this is going to represent an increased spend on workforce, this, you’re not going to meet the cost reduction targets
Southcity, manager 6
The paradox here was that, although managers recognised that high intervention rates were expensive, leading midwife units to be more cost-effective than OUs,53 payment systems had not been not well matched to this and services in constrained financial situations received greater income for more interventionist approaches to care.
Commissioners explained the degree to which the tariff system had worked through targets and drivers, but despite introduction of specific targets to increase normal birth rates or reduce caesarean section rates, the general tariff system with differential rewards for normal or operative births had not facilitated this:
So you can use the, you know, the contractual levers and use performance as a good starting point really for looking at making the best use of resources. Sometimes it’s about service redesign, there’s not going to be more money so they’ve got to do things differently.
Southcity, commissioners 1 and 2
Midwifery units were seen as a key element in strategies to reduce unnecessary intervention, to contain costs as well as to improve health outcomes, while also enhancing the recruitment and retention of midwives, as reflected in this comment by one Southcity manager:
You know, we’re having to reduce Caesarean section rates, and it’s sad but since, you know, we’re having to save all this money finally even the most sort of, um . . . even the consultants that weren’t so supportive of the birth centre are realising that actually our normal birth rate here is double what it is upstairs [OU], so you know, we are a money-saving, um . . . entity.
Southcity, manager 2
The accounts of managers and obstetricians indicated that the development of a stable AMU service also increased confidence in the abilities of midwives to provide more autonomous care, to ensure escalation and transfer when needed, and in the likely cost-effectiveness of the service. Although each service experienced challenges in inter- and intraprofessional relationships relating to these issues, which will be described in Chapter 4, once embedded and accepted within a maternity service, the AMU appeared to increase confidence in midwifery-led and normal, physiological labour care. Although this was not, in any case, an easy process, it was reflected in decisions to develop FMUs. These had recently been opened in Northdale and Midburn, and one was being developed in Westhaven. These developments were also utilising opportunities created by wider service reconfigurations. A further key consideration was the need to recruit and retain a well-motivated midwifery workforce.
Philosophical drivers
Although the development of AMUs was generally achieved through pragmatic circumstances, managers on all sites had a clear view of the aims and philosophy of the unit to provide a more homely birth environment that would be woman and family centred and facilitate normal birth practices and midwife-led care for low-risk women:
If people are relaxed and in a relaxed environment their hormones and their body can work better than if they’re tense and they feel that they’re being imposed on in here. You know, we say to women as they come in, ‘Make yourself at home, go where you like, move things around, whatever you want to do,’ and it’s their area to do what they want in. And it’s been shown to improve outcomes and . . . I would say, I can’t say shorten labours but not prolong them by that fear aspect of changing, you know, if you’ve been at home and you’ve been relaxed and calm and then you come in and all of a sudden contractions go off, and that’s what we’re trying to avoid really. So they can relax and (pause) get on with their business.
Northdale, manager 2
Managers commented that, although it would be ideal to promote such care in all areas, this had not been achieved in practice previously and lack of progress in creating an environment to support normal birth and to establish midwife-led care on their labour ward had been a key motivator for creating a separate unit:
Part of what was very obvious at that stage, I kind of touched about midwifery performance, um, in the context of midwifery-led care it was virtually non-existent. Um . . . [name] was one of our consultant midwives, had been slaving away here for a few years and had tried to make inroads into providing low-risk/midwifery-led care, and at that point she had succeeded in having a couple of rooms assigned to that within the labour ward on [first hospital]: there was no such, I don’t think there was any such practical arrangement at [the other hospital] at the time. Um, but despite her best intentions it hadn’t really got anywhere because of the culture of the practice both by obstetricians and midwives . . . um . . . aligned to the performance issues that I’ve mentioned.
Midburn, manager 3
Therefore, although managers saw it as desirable to ensure that midwife-led care and supportive care for normal birth was available on OUs, challenges in achieving such aims in practice had formed key motivators for developing a separate space to facilitate such care.
Management and leadership
The histories and current status of these services illuminated the strategic importance of appropriate management and leadership, as well as their importance for quality and safety of care in a complex, distributed system of maternity care. This echoes the findings of the Birthplace organisational case studies2 and numerous wider safety and enquiry reports in maternity and health services. The qualities of leadership that had enabled the AMU to be developed and established were also those perceived as important for ensuring quality and safety in the service overall. Management respondents emphasised the importance of senior midwifery, obstetric and general managers working together to support and sustain the development.
Key issues were similar to those described in our earlier Birthplace organisational case studies, which looked across all birth settings within a maternity service, focusing on services which had scored as ‘better’ or ‘best’ performing in a recent Health Care Commission survey:63 good communication between professional groups and between hierarchical ‘levels’, and openness and involvement in monitoring and reviewing care and incidents, underpinned by clear and agreed guidelines and facilitated by the tone set by managers in both obstetrics and midwifery. 2 These features are arguably even more important in a situation in which new boundaries and discontinuities were being created in the service, such as the development of different units and distributed care, with the potential for interprofessional tensions and competition over resources, along with the need to ensure smooth and effective interactions and transfers between areas when needed. Service boundaries, such as those between a midwife unit and an OU, needed to be clear and established enough to maintain a stable system, supported by all, but permeable enough to ensure appropriate and smooth transfer across the boundaries.
Two contrasting cases illustrate this well. In Midburn, the AMU had been specifically developed as part of a strategy to turn around a service that had been perceived as failing. To achieve this, leadership and positive communication between senior managers and between obstetric and midwifery leaders was seen as central. While tensions and conflicts over resources were still present, the motivation to work together to overcome such challenges was apparent in the reports of a range of interviewees. In Southcity, the AMU had been opportunistically established as part of a reconfiguration that resulted in bed shortage. In a 10-year period of frequent changes in midwifery management and further service changes, a picture was described of an AMU that was not fully embedded within the overall service at a strategic level, with AMU midwives relatively isolated from their peers and lack of growth of interprofessional confidence and trust. Although none of our respondents suggested the AMU should be closed, and clear support was expressed by some senior obstetricians, the AMU was seen by others as a drain on resources and was clearly regarded with suspicion by some staff. There was little movement of midwives between units, and midwife-led and normal birth practices had not been replicated on the delivery suite, which midwives working in both areas described as medically dominated. Managers who had been appointed more recently were focused on encouraging all professionals to participate actively in service review and development, with staff development through planned rotation, clearer communication and integration of professionals across professional and unit boundaries.
Measures to support and promote safety
Use of guidelines and protocols
All the services had guidelines for low-risk or midwife-led care rather than guidelines developed specifically for the AMU. In the services that were now developing FMUs, it was interesting to note that focus on guideline development had increased, as staff and managers perceived a need for more specific guidelines when transfer would occur over a distance:
We started off really just focusing on criteria for [the FMU], but obviously in that process we decided we have to review the whole guideline and, and um . . . to be able to look at the sort of whole processes for antenatal risk assessment referral, um, for everywhere. And, er . . . so essentially, you know, it’s important sort of guidance for [the FMU], you know, because . . . because being a midwife-led centre, being a stand-alone centre we want to be able to make sure that women are appropriately selected for there, given that it’s half an hour away. Um . . . on a good day! [Laughs]
Westhaven, manager 4
Nonetheless, such guidelines had apparently not been in place for home births. Guidelines were drawn on in terms of eligibility for admission to an AMU and for decision-making around transfer to the OU in labour.
The key message from managers and professionals was that clear guidelines for admissions and transfers that were supported and adhered to by all were crucial, for the safety and well-being of the service and individual professionals as well for the women:
I think the other thing about success for AMUs is really don’t, really don’t blur those referral criteria.
Westhaven, manager 6
Midwifery units and midwives, as well as the women themselves, were perceived to be vulnerable without such guidelines, which also helped to create and protect a space for supporting physiological birth. In Westhaven, for example, managers emphasised the obstetric support for normal birth and midwife-led care but still saw guidelines as functioning to maintain confidence in this:
In some respects we have the guidelines in place because we want to maintain that confidence and, you know, there are times when things drift and et cetera et cetera, but um, on the whole they don’t want to know about them, but what we do need to know is that . . . that they are being managed in that unit according to what we’d expect, and er, so that you’re not creating any additional risks for the mother. And, um, so I think, I think it will . . . in terms of it being . . . er, you know, the whole idea about having sort of high risk and midwife-led is just to define the women they do need to know about, rather than intervene, interfere in those low-risk women that they don’t want to know about.
Westhaven, manager 4
The majority of managers and midwives stated that guidelines needed to be strictly adhered to for such reasons. However, in practice, there were many grey areas and cases needing consideration regarding low-risk criteria. Individualised assessment was seen as appropriate when maternal age and body mass index were borderline and in the cases of teenage mothers, women who had previously experienced postnatal depression and women around 37 or 42 weeks’ gestation:
They were really, really exclusive with mental illness. I think to begin with it was any mental illness. But that’s daft. If you’ve got somebody who had postnatal depression surely they’re going to be better off like having a nice birth experience. Now, this is the difference between me and some of my colleagues: I might be a bit like, oh . . . like I was, I went there the other day and, um, I accidentally let someone in who was 36 plus six, and they were like, ‘Transfer her!’ and I’m like, oh for God’s sake. You know, 36 plus six, really? One day?
Midburn, midwife 2
Maternal age being one, you know, because it’s ridiculous if you’ve had three children before. (. . .) Of course you’re not suddenly, suddenly high risk. Maybe if you were 42 and you’re having your first baby that’s something that you’d want to look at . . .
Southcity, midwife 4
Some managers also commented on pressures to accept higher-risk women because of service pressures and crowding on the labour ward, both in labour and postnatally:
I find, I think they find it hard to be a birth centre, totally birth centre, because they’re so close to the labour ward that they cannot help being involved with the fact that the labour ward would be full and phone them and say, ‘Well you’re only just downstairs, will you take this woman? Yeah she’s quite high risk but, you know, as you’re only downstairs.’
Northdale, manager 4
Pressures to take women outwith guidelines were strongly resisted because of safety concerns:
There’s a very clear line that we don’t take high-risk women, um, you know, women who are in labour who have got, who are high risk so that they don’t get moved round there because of space – occasionally it does have to happen I think just for the sake of it, so it’s a room, but it’s the excep—, real exception, if you’re desperate for a room you can, you know, you can move a bed, but I think we’ve just tried to keep it as a [pause] you know, the philosophy of the Birth Suite is for low-risk women.
Westhaven, manager 4
The Birthplace study identified that the proportion of higher-risk women planning birth at the start of labour care in an AMU is low, at 4.4%, although higher than for FMUs, at 2.5%. These figures compare with a higher rate of home births of 7.4%, for which, although professionals can advise women of evidence on safety, criteria for entry cannot be applied. 1
Consultant midwives and AMU managers reported experiencing some pressures to provide AMU care for women who did not fit the clinical criteria, but who may otherwise give birth at home. Most were not comfortable to support this because of perceived risks to the service, as well potential risks to the women, although the greater risk to the woman if she gave birth at home without care was acknowledged. This was also echoed by some consultant obstetricians:
I think it works reasonably well but I do get put under pressure at times as a consultant to be asked to OK it for someone to go to the birth centre when I’m a bit uncomfortable with it. And the truth is by the time they come to me they are already assuming they are going to deliver on the birth centre and it puts me in a difficult stroke impossible position. That does happen. People with gestational diabetes primarily.
Southcity, consultant obstetrician 3
One consultant midwife felt that such risks to the woman placed an onus on the service to provide more individualised care. In either case, written care plans with documentation of advice given and consultation with supervisors of midwives, senior obstetric and midwifery colleagues were recommended. This was in order to protect both the woman and the service and the professionals providing the care, while respecting women’s wishes. In a number of UK maternity services, consultant midwives are providing special clinics for women requesting care that did not fall within the guidelines (consultant midwife, Pauline Cooke, Imperial College Healthcare NHS Trust, 2012, personal communication). Such clinics were not mentioned in this study, but women requesting such care were referred to consultant midwives for individual care planning. Some midwives’ comments indicated a difference of view about accepting such women in AMUs as compared with FMUs, for which transfer distance was a concern:
We don’t get a lot of transfers really, but it’s, it’s because there is a real problem. I think they, you know, they’re selective about who goes there as well. You know, so their criteria . . . their criteria’s supposed to be the same as the [FMU] but they do tend to take a lot, a lot more . . . high-risk stuff on our birth centre [AMU] if a woman’s, may have had a previous section and she’s adamant to have a birth on the birth centre then she’d have had to see a consultant midwife, but then she would have had to, she would be able to go onto the birth centre as long as there’s some plan in place. So whereas at the other birth centre everything’s definitely low risk, . . . there’s got to be no need for a doctor.
Northdale, midwife 6
In one service, Westhaven, managers and professionals described the use of their intermediate room to care for such women. This room was formally part of the OU but lay between both as this AMU was immediately adjacent to the OU, separated only by double doors. This room had been set up to provide a homely environment supporting physiological birth, but with access to obstetric facilities if needed:
I think probably because the birth centre was popular option and women failed to understand why, because of their raised BMI [body mass index] tends to be the problem, the BMI cut-off I think is 30, isn’t it, and, um . . . [laughs] I suppose how many of us do have a BMI of under 30 through pregnancy? Um, and I suppose . . . women don’t necessarily, um . . . see themselves as high risk, so there was a need, particularly I think it was the VBAC [vaginal birth after caesarean] ladies where they’d had a first, they’d had a caesarean section first time, um, who wanted to have . . . encouraged and supported and wanted to have a trial, um, of labour for their next event, but likewise weren’t able to use the birth centre because of their previous caesarean, because of the closer monitoring, and so we try to sort of find a compromise.
Westhaven, manager 2
The use of such a transitional room raises questions around providing care to support physiological birth more routinely on OUs. The challenge of changing OU practices to ensure that such women felt more confident of receiving care to support physiological birth and a positive birth experience was not specifically raised with respect to women who fell outside the guidelines, but respondents referred to a general aim of improving care in OUs, which had not been realised in practice. The majority of managers firmly opposed blurring of boundaries around low- or high-risk care to maintain safety and the philosophy of the unit:
We’ve sometimes had women who want to have a home birth and they’re really not suitable for a home birth. They’ve (. . .) had three previous caesarean sections or . . . and then it’s been, they’ve been to see their consultant and then (. . .) the consultant might say, ‘Oh look, she really doesn’t want to, I don’t want her to deliver at home but could you let her deliver in the birth centre?’ Um, and we’ve been quite . . . we’ve said, ‘No, we can’t, we can’t let her deliver in the birth centre because it’s not . . . it’s not what she needs’ (. . .) The whole ethos there is non-intervention.
Westhaven, manager 6
However, one consultant midwife, when asked about the question of caring for women who had previously had a caesarean section on an AMU, argued that individual documented care plans and senior professional involvement would make this acceptable because the women would be more likely to be monitored closely and less likely to be subjected to potentially risky interventions, and would benefit from the short transfer time if transfer to an OU were required:
I say better place because we’re giving that one-to-one care, you’re not putting someone on a monitor and going out and looking after somebody else for a while, you’re listening and you’re watching and you’re listening in, and you’re there so closely with them, and they’re feeling what they’re feeling, and I think being upstairs on a monitor with an epidural you’re more likely to miss the signs than you are down here.
Northdale, manager 2
This lack of progress in changing care had formed part of the motivation for development of AMUs. Views about the impact of the AMU on practice in the labour ward are discussed in Chapter 6.
Maintaining clear and agreed eligibility guidelines, supported by timely risk assessments, was seen as protective for both the women and the professionals. The importance of good antenatal assessment by community midwives was highlighted, as was the value of effective triage before admission in labour:
What is inappropriate is to have a woman moved from our triage to [AMU] and then there be a discussion there, and say she’s suitable or not. That is not the place, if a woman isn’t suitable for [AMU] and she’s already touched base with our triage midwives, she needs to stay there until that decision’s made. I don’t want her to be in the middle of a discussion between two groups of professionals.
Midburn, manager 1
Management of transfers
While eligibility criteria for planning birth in an AMU were seen as important, guidelines for management of transfer were often cited as being of primary importance:
Transfer guidelines are more important than the guideline for excluding low risk, I feel, um, in terms of the midwives are – it’s very precise as to who can or what should or should not be looked after during or after delivery, um . . . and most of the time it’s followed.
Midburn, consultant obstetrician 1
Good management of transfers across unit boundaries is widely acknowledged to be important for safety and for the quality of women’s care. Managers in Northdale echoed the need for straightforward management in arguing that transfer should simply be about the most appropriate care and who can deliver it. This argument reflected a concern to avoid tensions and also to avoid issues such as territorialism or conflict over workloads that might undermine quality and safety of transfer decisions. We introduce the term ‘permeability’ in this report to capture the concept. This perspective seemed to implicitly emphasise the need to avoid territorial approaches or professional disputes and instead sought to advocate an approach in which different professional roles and areas are viewed as complementary and integrated rather than divided. 94
Given that many professionals and service users see the proximity of AMUs to OUs as a safety feature, what was most striking in our data analysis was the degree to which some AMUs appeared to be under pressure from the OUs to avoid transferring women. In some instances, OU staff perceived transfers to be unnecessary, reflecting AMU midwives’ lack of skills or lack of willingness to use interventions to speed up labour progress:
The main, I think the main reason why they, one of the main reasons they get transferred round is because, um, prolonged second stage, you know, they’re pushing for too long. But once they get transferred round here obviously we actually do get them pushing, because round there they kind of use this, what is it, surge, or . . . they don’t actually use the word . . .
No active pushing.
Yeah, not . . .
They let the body . . .
They just let the body and nature take its course. Well sometimes that’s not enough and you need to really encourage the women and get them to actively push.
Midburn OU, midwives and registrar
Conflict around transfer levels between OU and AMU staff appeared to be complicated by distance and lack of trust between staff groups and tension over resources and burden of care. Such conflict was mainly focused around OU perceptions of excessive transfer, rather than a perception of midwives on AMUs not being willing to transfer women:
When we very first opened you’d phone up and you’d say – and this happens downstairs on the other unit as well – what they’ll say is, ‘Oh, why are you transferring this woman?’ They start questioning why you’re transferring her. Um, you know, ‘Have you done a VE [vaginal examination]?’ ‘Oh, you know, oh leave her another hour,’ or you know, ‘Have you emptied her bladder? Have you done this, have you done that?’ And that’s very demeaning to the midwives. Um, lots and lots of little comments. And then when you do bring the woman over you get cold-shouldered a lot of the time, as though you’ve made a terrible mistake.
Northdale, manager 4
This manager expressed concerns around the impact of such tensions on the safety of transfer decision-making:
When we’re looking after women on here we do the utmost for those women to have a lovely birth on here; that is our aim. The very last thing we want is to transfer a woman from here. But you have to know when to stop. And obviously those transfers then, but we . . . comments are made to . . . within our hearing sometimes . . . you know like you’re doing the walk of shame as you walk up with your woman. And that can have two effects really: one, it makes you, it can make you not want to go upstairs, and perhaps you’ll make a slightly different decision. Hopefully we won’t, and we’ll still make that cut-off where we’re supposed to make it, but it’s got to be there at the back of your mind. And silly things like midwives in the morning have come on and they’ve saved inco-pads because in the past they’ve been questioned on things, their clinical judgement is questioned, it’s as if the midwives up there sometimes think we’re not quite as . . . like a second class of midwife if you like because we don’t do the high risk, we haven’t got those abilities.
Northdale, manager 2
This concern was also echoed by obstetricians:
Because clearly if a woman comes into the birth centre with a breech presentation, particularly as a primip, the appropriate thing is to send her up, the management was completely appropriate. Um, but I think because there can be that ‘them and us’ culture, clearly some of that had been communicated to the couple and they had got the impression that the midwife caring for them was reluctant to have to ring the labour ward to say that they thought she’d got a breech and she needed to come up.
Northdale, obstetrician 1
Such tensions appeared common, but were not universal. One manager defended transfers and argued that OU staff do not understand how vulnerable AMU midwives feel if they have any concern and their need to err on the cautious side regarding transfers. However, some OU staff did express understanding and trust in the skills and judgement of their AMU colleagues:
. . . generally people come up here for that reason [clinical issues mentioned] they don’t normally come up here because they can’t cope any more, which I think is good for the midwives down there because they are obviously doing their jobs properly by you know helping the women aren’t they, to cope.
Southcity OU, midwife
Interviews with a range of staff indicated that such trust and mutuality was more likely in settings where OU and AMU staff had worked together and knew each other well.
Managing transfers for pain relief or women’s choice
Midwives working on AMUs were prepared for the desire for some women to transfer for pain relief, even after preparation and encouragement. However, their accounts indicated feelings of pressure to avoid such transfers:
. . . just because they start here doesn’t mean they’ll deliver here, because you know, things happen, the baby might get distressed or the woman might want an epidural, you aren’t going to close the door and say, ‘No you can’t go and have one.’ You try and nurture her through the bit where she’s really feeling like she wants one, but you can’t stop a person, you know, you can only do your best. So you do have a transfer rate of around sort of 20% mark. So it’s unrealistic I think to think we can get any more than that until . . . we have, we have . . . more . . . um, women coming through the doors that are well educated about, um, a birth without an epidural, because at the end of the day we can only do as many as the women want to be here, you know . . .
Southcity AMU, midwife 1
. . . she thought I’d lied about ringing labour ward, she thought I was trying to pacify her, and I wasn’t. Well I probably was a little bit, at the beginning, but when she said, ‘No, I’ve had enough, the baby’s not coming right now so I want my epidural,’ I did ring labour ward and said, ‘Look, I have this multip, she’s not fully yet but she’s been hankering after epidural for a few hours, I’ve managed to put her off for a while but now she’s absolutely adamant,’ and they basically said no, they’re too busy. ‘They’re in theatre and if she wants an epidural she’d have to come up but you’d have to look after her.’ But that left me in a predicament because I couldn’t leave the other midwife because she had somebody in labour.
Northdale AMU, midwife 2
The accounts of managers and professionals indicated that, particularly in a busy overcrowded labour ward, the non-emergency transfers were not seen as a priority, despite their potential importance to the women:
The issue around epidural is I would think purely expediency. If you’re up on labour ward and you’ve asked for an epidural, anaesthetist’s in theatre, the second anaesthetist is maybe also in theatre or the second anaesthetist is doing something else, there is going to be a pecking order, and I do think the pecking order means that the birth centre is at the bottom of that pile. Do I agree with it? No I don’t. How do I change it? I’m not quite sure. Um . . . I think there’s more work to be done with supporting women in transition . . .
Northdale, manager 7
Typically, delays were related to lack of bed space or midwives, but there were also indications of a judgemental attitude from some OU-based staff:
Um . . . when whatever it is they do down in the birth centre doesn’t work they come up here and have their epidurals. So . . . I suppose we view them, well some of us view them, the ladies that come up they’re sort of refugees from birth centre, it hasn’t worked down there, all the chanting and whatever it is they do, er, hasn’t worked and they need the real thing, which we regard . . . you know, our fentanyl and other drugs.
Southcity, nurse 2
Managers in Northdale and Midburn felt that intrapartum transfer rates were initially too high, reflecting midwives’ lack of experience of midwife-led care, but had now settled to a more appropriate level of about 15%, although a Northdale manager noted that AMU rates remained higher than those for the FMU which had opened more recently within the service, potentially influencing a perception among OU staff of high transfer rates. As shown in Table 3, rates for intrapartum and early postpartum transfer in these four services were comparable to the national rate identified in the Birthplace study of 26.4% for AMUs. The national rate for AMUs was higher than found for home or FMU births, a figure potentially accounted for by higher rates of transfer for epidural request in AMU planned births. 1
Maintaining safety and quality
Audit, review and governance
As identified in the Birthplace organisational case studies,2 appropriate governance systems were seen as important dimensions of maintaining safe and high-quality care in a distributed system. Managers prioritised open and regular reviews of practice, with routine reviewing of transfers and any untoward incidents and an emphasis on interprofessional participation. However, several commented that this had been an unfamiliar and uncomfortable process for many professionals, needing a strong managerial steer until established as a norm:
[The audit meeting] looks at all the cases from the previous 24 hours where there have been any concerns or emergency sections or things like that, and we’ve made it all right for people to challenge other people’s decisions and practice and so on. . . . it was really difficult at first, you know, people felt really uncomfortable with it, um, but it’s just persistence, and managing those challenges in the right way. You know, this isn’t about being personal, this is about saying, ‘Right, why did you make this decision? Here’s the evidence that suggests x, y and z, so you know . . . would, next time . . .’ kind of almost like a reflective learning environment.
Midburn, manager 2
New managers in one service had worked particularly on its escalation of reporting policy and engendering a culture of participation and staff speaking up following a ‘whistle-blowing incident’ (manager, service X) reported directly to the Care Quality Commission. This simply threw into sharper relief the concerns of all managers to ensure that reporting and review were encouraged in order to learn from and prevent errors. The importance of documentation was also emphasised, although one midwife commented on the tendency to fall back on cardiotocograph (CTG) use in a busy risk-oriented environment:
You know and you’ve got the doctors saying, ‘Can you do this? Can you do that? Can you just go and get that for me? Can you..?’ you know. Too much . . . you know, I know litigation is hovering above us and that’s why but it’s too much really. It is too much. I use my CTG as my little diary because otherwise you literally would be writing going, ‘Hello,’ you know not even looking at the poor woman. So I just tend to ignore my paperwork towards the end and, and write everything quickly on the CTG you know if anything’s happened and use that afterwards as my reference for writing my notes up.
That’s if she’s on a CTG?
Hmm. Which she will be.
Southcity OU, midwife 7
Staff rotation as a safety measure
Managers in all sites were considering introduction of a system of rotation. The idea of midwife rotation as a safety measure encompassed two contrasting issues, which unit managers were constantly working to balance. Rotation of midwives around areas – community and hospital, high and low risk – was seen as a means to ensure and support midwives maintaining their birth skills and knowledge of both high- and low-risk care. It was also seen as a means to preserve good interprofessional relationships and integration across boundaries:
Rotation is the only way I can do it, but then there are service implications, they have a service to deliver, they have pressures, they have caseloads. It is easier said than done. Um, but unless we integrate them, unless they feel part and parcel of the same team, and also subject to the same governance . . .
Midburn, manager 3
However, it was also argued that, without careful management, rotation of midwives could undermine the safety of the AMU as a thriving and sustainable place of care, the development and maintenance of midwifery-specific skills to provide less interventionist care for low-risk women, and midwives’ morale and satisfaction in their work:
. . . we are aware that you can’t just suddenly rotate too many people, so you need to rotate on a slower pace so that you build their skill to be able to function to that area as the culture or environment or, you know, the . . . the guidelines and the principles should be for that place to function. (. . .) And actually major change has happened also, all the practice development midwives will be also doing 50% clinical work with those people, whether it is night shift, weekend shift, all that will happen. So all these works are happening to facilitate that.
Southcity, manager 3
Working to capacity
Although the AMUs were described by managers as mainly working to capacity, in terms of the numbers of women admitted and births per year, relating to unit size and their original targets, managers and professionals identified some issues which reduced the activity and capacity of AMUs, including midwife numbers and booking systems. Finance overall was cited by the majority of managers as a major challenge to maintaining quality and safety, as well as the operation of the AMU, even though they recognised the value of change to meet these challenges, such as introducing new ways of working:
I’ve got to find the, er, savings and, er, it’s quite a challenging time I think across the NHS, because the demand for care is increasing, the birth rate’s increasing significantly in [city], the capacity remains the same, and the establishments remain the same, because the government have said that we have to save 13 to 15 billion by the end of 2013, the NHS as a whole, and every trust has to play its part, and our part is bigger than others because we started with a deficit. And so, um . . . it’s quite challenging trying to deliver a service thinking of the quality and the safety agenda versus the, um . . . versus the fi—, the bottom line on the financial spreadsheet.
Southcity, manager 6
Therefore, although midwifery units were widely seen as a means to improve the clinical effectiveness and efficiency of the service, resource issues including lack of midwifery staff numbers were also cited as a barrier to these units working to capacity or in a fully effective way. These concerns are also discussed in the next section under staff relationships. Shortage of midwives was universally cited, with many accounts of midwives needing to be ‘pulled’ from the AMU to cover shortages on the delivery suite. Competition over midwifery resources was frequently referred to and formed a key source of tension between staff groups, with midwives describing being ‘pulled’ between areas to cover service gaps and conflicts engendered over who was working hardest:
I think the thing that most gets us down is, um . . . lack of support from other areas, and shortage of staff: we are, I feel that, you know, we’re always, or it’s a general feeling that we’re always called upon to help delivery suite out when they’re short-staffed and if, you know . . . I’m completely in agreement we should be helping them out if we’re sort of quiet and they’re busy, but it’s never really reciprocated, and, um . . . mostly because they can’t because they’re always busy, but there are moments. And, um . . . it just sort of . . . recently I’ve found it quite difficult because it’s had a knock-on effect and women actually have had not such good care down here because the second midwife’s been pulled upstairs. So that’s when it really started to upset me recently.
Southcity, manager 2
The worries around midwives being pulled to delivery suite could also have a negative impact on midwives’ willingness to maintain continuity of care by transferring with women:
I would say that when you’re dealing with teenagers they’re afraid of needles so they do tend to avoid the epidural and see how they’ll go, then if you promise that yeah, if they want the epidural you’ll go up, and unlike looking after somebody that comes in on the birth centre if they think they want an epidural, you know what, you don’t want to accept them because if you transfer up they keep you upstairs. That leaves the birth centre closed to other labourers, so you’ve just shut down the birth centre because somebody decides they want an epidural, and they won’t let you hand over care upstairs, because they’re always short-staffed. So you brought her up, you keep her. So there’s like a time clock running.
Southcity, midwife 2
Such conflicts appeared to compound ideological differences or lack of familiarity and trust between groups of midwives:
Sometimes round there, as you say, they get a bit cocky, don’t they? And the band 7s trying to tell them and give them advice, but you can tell by the way that the co-ordinator’s talking, the person on the other end of the phone is not listening and they just want to get them round here.
And then when they do, a lot of the time we say, ‘Yeah, you can bring her round but you’re going to have to stay with her.’ They don’t really like that, you know.
Midburn, OU midwives, group interview
Ruptures and conflicts within a service may have negative effects on quality and safety and also on user experience, as illustrated by this woman’s observations about staff relations during her transfer to Southcity OU:
When she [AMU midwife] was bringing us in and the woman on the [OU] desk said, ‘Oh has she been admitted?’ or ‘Have you admitted her?’ (. . .) . . . there wasn’t like an easy conversation that they had between them (. . .) It felt like oh, they’re bringing another one up and you know, and have they done the paperwork to go with it or something like that.
Southcity, woman 2
Midwives’ and managers’ accounts revealed complex views about the movement of midwives between areas, which reflected at times the perceived fragile nature of the AMU service. Most emphasised the importance and value of supporting each other and working together and acknowledged the benefits of maintaining all-round skills and insight into each others’ experiences:
. . . in an ideal world I’d like to see all the midwives who deliver intrapartum care rotating through different aspects of the care. There are advantages and disadvantages to that, um, but I always feel that unless we rotate midwives through high risk and low risk you end up with kind of a silo mentality, you end up with them and us, um, and that’s not conducive to, to good care, I think, especially when the two overarch, when you’ve got transfer rates that are 20, 25% intrapartum you want people who are comfortable with both. The counter-argument of course is that if you do that neither of them develop the skills that they should be to the right level, but I’d like to think that we would have better training to deal with that, and to me a midwife is a midwife, it’s not a low-risk midwife or a high-risk midwife.
Midburn, manager 3
However, managers and midwives also expressed great concerns about dilution of skills and teamwork in one area by movement of midwives between them in an ad hoc fashion:
. . . you can’t take a skilled member of the birth centre team away and put somebody who doesn’t know how we work down there to start giving advice to people and get involved in labours. (. . .) . . . if you just send somebody who doesn’t want to be there and doesn’t think they have anything to learn, and they practise like they do upstairs, then you’re actually asking for disasters.
And what was the thinking behind that?
To spread our skills. The idea was that we have low risk skills that aren’t recognised, and that people don’t have, and that if we went upstairs and . . . and the other thing is we couldn’t practise our low risk skills like water birth, and having babies off the bed if we didn’t have the equipment up there, and if we had to look after two or three people at once.
Southcity, midwife 2
Some midwives and managers expressed the fear that, without a core of AMU midwives, sufficient skills in normal birth and midwife-led care would not be maintained. Continuity of care or carer issues were less likely to be highlighted by staff and managers as a potential disadvantage of rotation, although continuity of care has been identified as important to women. 2
Managing staff resources
Midwives in AMUs were also concerned about the implications for keeping the unit functional, with typical staffing on any one shift of two midwives. There was a trade-off between size and ability to maintain a sufficient basic number of midwives on each shift: maintaining a limited size was seen as important for the homely and family-centred ethos of the unit, while sufficient numbers were sought to justify a sustainable number of midwives per shift. A dominant staffing model in which midwives staff areas rather than orienting around the women added to the challenges of maintaining the core staffing required to keep the AMU functional. The issue of more women-centred staff models, with community or caseload midwives working with women across boundaries, will be discussed further (see Staffing models).
In Northdale, an IT-based management system based on lean thinking called ‘Visual Hospital’ had been introduced with the aim of ensuring staff were available where most needed. This was welcomed to some extent as supporting efficient use of limited staff resources. However, it contradicted two key quality principles in practice: continuity of care for women and consolidation of working patterns and skills in the AMU. It also failed to overcome the perceived tensions between staff based in different areas:
With Visual Hospital . . . the idea is to be working closely together, working where the women are, and we do go up and work on there [the OU] for hours at a time. And again not always treated the same, they’re not offered drinks or breaks or . . . I don’t know, I can’t explain it. I can’t explain it. They’re just not . . . you know, they want our help but then they’re saying we’re not, you know, quite as good.
Northdale, AMU manager
Therefore, although using Visual Hospital was seen by some managers as helping them to deploy midwives where they are most needed, this had not been popular with staff and this is discussed further in Staff experiences and perspectives.
Two services had different approaches of integrating community midwifery with midwife-unit care, with the aim of enhancing skills as well as deployment of staff resources. In Northdale, community midwives had provided the care in the GP unit, which was the precursor of the current AMU. Community midwives were accustomed to providing such care and had maintained greater levels of experience in attending births as a result. They were motivated to work in the midwife units and the key limitation for this was staffing capacity, which had forced a reduction in their midwifery unit role. In Midburn, community midwives were required to work one shift per month on the AMU to develop and maintain their birth skills. Managers hoped this could be extended in future to the new FMU but considered that community midwives were not yet sufficiently experienced in birth care:
I think that it’s not just here, I think that nationally there is a problem. The model’s fine, but we haven’t found a way of integrating community midwives appropriately by way of development, professional development and training to satisfy ourselves that actually they . . . that they can do a good, that we’ve given them the tools to do a good enough job. I’m not talking about numbers and I’m not talking about how many caseloads and all of that, that, set aside that, I’m talking about having a professional midwife continue to practice safely, continue to be developed, continue to have access to education, to change, to updates, all of that, which I feel just is non-existent in . . . well, is very deficient in community midwifery.
Midburn, manager 3
Managers anticipated that integration with the AMU would facilitate the rebuilding of the community midwives’ birth skills and confidence:
In practice that’s what we’re doing. They are, we are organising some updates for them, some professional updates from a theory perspective. But the main bit of updating is on the ground. Our colocated birth unit is very busy, so actually what I’ve advised is that there are three midwives that actually work in our colocated birth unit and the community midwife is the fourth on each shift; when she comes into the unit she has an induction period, she’s then allocated to a woman to look after that woman with the help of another midwife that’s used to our unit. There has been a recommendation that they never move from [AMU] and they stay there. They don’t go to the ward if we need help, it’s our [AMU] midwives, our colocated midwives go out to the hospital if we need any help. The community midwife stays put.
Midburn manager 1
In contrast, in Westhaven, such integration with community midwifery had not been established and there was some evidence that community midwifery teams varied in informing women about the option of birth in the AMU. In Southcity, the original integrated model of a small core AMU staff supplemented by community midwives from caseloading group practices coming in to the unit with women on their caseload had not been maintained in a period of service instability and management changes, leaving the AMU midwives feeling relatively isolated within the service.
Northdale managers, in particular, cited the integration of community midwives as a positive strategy for future development, while managers in Midburn also referred to concerns about maintaining the birth skills and confidence of community midwives in a service context with very low home birth rates:
They need some intrapartum experience. And the intrapartum experience that we’re giving them is that we’re expecting all of the community midwives to rotate on a regular basis into our colocated birth unit, for probably a maximum of 3 weeks in a year, to update their skills. So from an intrapartum perspective they need to . . . to develop, and that’s what we’re doing at this present moment in time. That’s probably our biggest challenge.
Midburn, manager 1
Such lack of confidence had also been experienced among hospital-based midwives, and the AMU was seen as a stepping-stone to all midwives developing their skills and confidence in midwife-led care, as well as intrapartum care for community midwives:
There’s been a little bit of resistance from the staff that work in the colocated unit, and that’s probably because they’re really . . . they’re really happy to work in a colocated unit; working in a free-standing is probably a little bit more than they want to take on board. They’re coming on board, so from the staff from within [name of AMU] it’s fine. The midwives, the community midwives to take that on board is quite a challenge for us, because our birth rate in the home and in the community is very low. So we’ve got to do an awful lot of training of our community midwives so that they will be quite comfortable working in the colocated, in the free-standing .
Midburn, manager 1
In three of the four services, support workers were also used on the AMU, augmenting the level of staff cover per shift. Northdale, Midburn and Southcity each had one MSW on duty per shift. MSWs were not used in Westhaven AMU, although the trust had introduced in-house training for them on the delivery suite with protected study time. In Southcity and Midburn managers considered that there was a greater potential role for support workers, especially in postnatal care and breastfeeding support (Southcity manager 6, Midburn manager 3).
Support workers had generally been incorporated in OUs and community services, but they were still seen as a largely ‘untapped’ resource in AMUs (Midburn manager 3). A trainee assistant practitioner on one site said that she received encouragement from the head of midwifery and the local FMU had seemed to accommodate her role quite smoothly. However, in the AMU it was a new function and staff needed to be more informed about the role:
. . . nobody seemed to know anything about it, because it’s new, um, you know, and people say, ‘Well what is it? What is it to do?’ And I just feel that maybe somebody should have got, had a meeting with, especially the staff on here, a meeting with the midwives to tell them what it is really, not left for me to say, ‘Oh this is what they want me to do.’ Because nobody on here knows what I’m supposed to be doing.
Site X, support worker 1 – site pseudonym removed to protect confidentiality owing to small numbers of support workers
A Southcity midwife said that historically MSWs on the labour ward had been doing a lot of cleaning and stocking and were not getting as much patient contact as they had hoped. An associated problem was the lack of clear guidelines to differentiate between band 2 and band 3 support workers. This midwife felt that support workers were underutilised and that they needed guidelines for training and for their role. She saw a need for their role to extend, particularly given increasing pressures on midwives (Southcity midwife 9 – researcher field notes).
A MSW on one site described her function on the labour ward as being ‘sort of a general gopher’. She said that she sometimes felt underutilised and that support workers were undervalued and taken to be ‘glorified cleaners’ but that it had been easier to find a distinct role on the AMU:
. . . whereas here [AMU] I feel that I’m more valued in that I’m able to use my skills that I’ve picked up over the years, er, with breastfeeding, um . . . assisting mums with various things with bathing babies, looking after babies. Um . . . and also I have occasionally, depending on the midwife, been supportive to a labouring mother. If she’s on, if the midwife is on her own and she’s got another labourer that’s a bit more ahead than this one I go and just basically stay there as support if necessary. Um, but that depends on the midwife per se, not all the midwives feel it’s appropriate for us to do that.
Site Y, support worker 1
Referral systems: opt-in and out models of booking
Two of the services – Westhaven and Southcity – had an opt-in approach to booking women, while Northdale and Midburn, the more recently opened units, had opt-out approaches. In an opt-in approach, women need to specifically select care in the AMU whereas, in an opt-out approach, the AMU is established as the default intrapartum pathway for low-risk women, unless they prefer to give birth in an OU, at home or in a FMU. The opt-out approach was seen by managers as having three major potential advantages: to support working to capacity, equity of access for women and establishing midwife-led care as a norm for women with straightforward healthy pregnancies. For such reasons, both the opt-in units were planning a shift towards an opt-out approach, and Southcity had recently introduced a triage area and protocol to ensure that women were offered appropriate care level and to manage more effectively women arriving in latent or early labour. Conversely, the key potential advantage of an opt-in approach was considered to be women’s greater preparedness for giving birth in a midwife unit, having made a more active choice. The implications of these approaches for women and the wider issue of support and preparation for women to give birth physiologically are discussed further in the section on women’s and birth partners’ perspectives on care.
Midwife skills, competence and confidence
Evidence from the Birthplace Cohort Study indicated that AMUs are safe places for women to give birth. 1 Neonatal outcomes, especially for multiparous women, are similar to those found in OU planned births, with significant reductions in intervention rates, and no increase in adverse outcomes for mothers. This supports the premise that midwives practising in AMUs have sufficient competence and skill to maintain safety and even to improve safety for women in terms of reduced intervention rates. However, the Birthplace study found that intervention rates in AMUs were not as significantly reduced as those in FMU settings compared with OU care. Additionally, rates of transfer nationally were higher from AMUs than those from FMUs1 (see Introduction). Although the Birthplace analysis was adjusted for measurable differences in women planning birth in AMUs or FMUs, it is possible that less measurable differences between the women (such as confidence level or fear of pain) may account for differing intervention rates. This point is touched on further in Chapter 5. However, it is also plausible that differences in midwife skills and confidence in providing such care may also contribute to differences in intervention rates.
Managers and professionals argued that, when their AMUs were initially established, midwives lacked skills and confidence in supporting normal birth and in working more independently, as these had not been fostered in typical delivery suite environments. This was more than a matter of skills training, as it demanded practical experience and appropriate support from senior colleagues, along with positive relationships between different areas and professional groups to develop these skills. Managers reported that this grew with experience, as well as through training, and so could be undermined by high rates of staff movement or change. Several commented that training needs to be interdisciplinary to be effective – as in the PRactical Obstetric MultiProfessional Training or Advanced Life Support in Obstetrics training courses that were used regularly for emergencies training. One also commented on the need for such training to take place in the midwifery unit settings.
When asked about training provision, managers tended to emphasise that emergency drills and skills training was provided to all staff, but few commented on training to support normal birth skills:
. . . every year at our mandatory training, for 3 days – used to be 5 – um, so now it’s 3 days, we have skills drills of obstetric emergencies and haemorrhage and eclamptic fits and stuck babies and breech babies and all of that, and I always, and in the feedback I always write, ‘Where’s our midwifery skills training?’ You assume everybody is up to speed with physiological third stage and augmenting labour naturally and advice on postdates pregnancy etc., what to do in latent phase of labour, advice over the phone, good advice so people come in active labour: no. That’s just assumed as basic knowledge and it’s not given much value by the midwives themselves or by the people who train us or by the obstetricians.
Southcity, midwife 2
. . . they’re scared of low-risk midwifery. They’re scared of being in an environment where they haven’t just got, um, a buzzer to pull and a million people fly through the room. And I just think it’s simply that. And it’s not necessarily a bad thing it’s just that once they actually . . . if everyone got the opportunity to come down here for a month I think everyone would feel so much different, so much better about intermittently monitoring, pool births, low-risk midwifery, assessing women in labour, knowing when it’s safe to send women home, all these sorts of things.
Southcity, midwife 1
The provision of training for midwives was affected by staff shortages and managers expressed concern that this could impact on the range of skills needed for AMU care, both normal birth and emergency skills:
I think there needs to be something explored about how one maintains all the midwifery skills, or is that relevant? You know, complexity. You know, we have midwives on the birth centre that are fantastic, they’re highly skilled: if I had a huge peak and there was huge crises, and I pulled somebody to the labour ward, they would be able to say to me, ‘I’m going to be unsafe and therefore I can’t help,’ if they can’t read CTGs, if they can’t, you know, do more, you know, some of the complex care.
Southcity, manager 6
In this context of staff shortage and pressure, training often took place in a responsive rather than planned fashion:
. . . the midwife probably hadn’t had . . . they’d obviously had some training in, er, in management of shoulder dystocia, but clearly hadn’t had that recently, and didn’t go through in their mind, hm, maybe a large baby, what will we do with this? Will we have . . . I think one midwife initially started to deliver the woman without a second person in the room. Er . . . and obviously when she ran into problems she called for the second person, but one could have anticipated that she might have had shoulder dystocia, it might have been nice to start with the second person in the room. That sort of thing. (. . .) We do have these courses available, er, but it is very difficult for the midwives to be released to participate in them. That is a major failing and a big problem.
Northdale, manager 8
. . . the only way round I see it is unfortunately having, spending more money on midwives in . . . across the piece. And having a core of midwives who are, well not supernumerary but releasing midwives for meetings. (. . .) we have six perinatal mortality meetings a year, we do have other meetings to discuss CTGs . . . and things, so there are plenty of meetings that people can get to but they can’t get to them because of, um . . . difficulty, staffing difficulties and being released. But I think the trust has to bite the bullet and put in more money for that, that’s the only way round I think. And getting more money from the PCTs.
Northdale, manager 8
Obstetricians did not comment on implications of midwifery unit developments for their students or trainees unless questioned on this, and tended not to see this as an issue, although some had commented that a potential impact of having fewer low-risk women on the labour ward was that staff working there would begin to view labouring women only in terms of problems. This obstetrician, for example, felt that, despite his concerns about the AMU ‘sucking out’ (Southcity consultant obstetrician 3) low-risk women, the labour ward experience was sufficient:
I don’t think that matters very much because I think to be honest, if you are training as an obstetrician you’ll see enough of the low-risk aspect of birth on the delivery suite. I don’t think it’s a problem.
Southcity, consultant obstetrician 3
The picture regarding views of skills, confidence and training was complicated by what we observed to be a skills hierarchy operating in all the services, even when clear interprofessional support for midwifery units was apparent. Put simply, high-risk and high-technology skills were typically rated as more ‘skilful’ than the ‘traditional’ midwifery skills, such as intermittent auscultation, pain coping and support skills and wider skills to observe labour progress that are drawn on to support normal, physiological birth care. Therefore, although interdisciplinary training was utilised as a way of bringing different staff groups together to develop shared skills, this tended to be focused on high-risk skills and active management rather than active labour skills:
We do intrapartum study days, so we, the whole of the unit from receptionists, HCAs [health-care assistants], MCAs, midwives, student midwives, student doctors, junior doctors, consultants, anaesthetists, they all come and do the same day, we all have to do it annually, there are one each month. And we do fixed emergency procedures and any updating required from NICE and such like, and we do it all en masse so we all know what each other are getting.
Westhaven, midwife 6
I mean all the Pinards have been taken away and put on the side. Now actually they’re coming back because the keen midwives say no no, we need to learn the skill. But there are midwives here qualified who don’t know how to use it. (. . .) so never mind about not doing a Birthing Centre forever if the midwives don’t even have the basic skills to be a midwife. You know, the fact that a lot of midwives here cannot do vaginal examination in other positions. The fact that you might be taking on board a case and the midwife goes to you, ‘OK, um, I think I will have to examine, do you need to examine, shall I come out from the pool?’ And I ask them why. ‘Oh, because your colleague’s asked me to come out from the pool.’ Excuse me, you can do a VE under the water. And that’s how you discover that there is a lot of work to be done on the personnel, even before you put around the environment, the two need to be patched together. (. . .) We don’t have a clinical meeting. Our meeting is all . . . we need to do this and we need to do that, and we’re filling up a lot of, um, stats, audit of hand-washing, audit on this and the other. Midwifery – bye!
Southcity, midwife 3
However, this hierarchy was not uniform and when professionals worked across units, and from a more managerial perspective, skills and practice benefits for the OU were observed:
. . . every morning I attend the daily review, which is our clinical review of activity over the last 24 hours, that includes the birth centre. (. . .) and I bring midwifery into it, so I would challenge, um . . . dialogue around the medical model, um, and what [Clinical Director] does, and [Clinical Director] would always ask for a midwifery opinion from me if, um, for instance we have a breech, um, and I would advocate – obviously if it’s appropriate – but I would advocate vaginal birth of a breech, so he would ask for my input as that’s a passion of mine too. So I’m influencing medical care down on delivery suite.
Midburn, manager 4
Managers also highlighted the value of training in relational and interpersonal skills when establishing a new unit, and to deal with professionals’ anxieties and challenges in relation to teamworking:
. . . so we had these core midwives, we did a lot of team building work around, and I was, um, sort of privileged enough to be able to attend that training as well with [name], our head of midwifery, so we did a lot of work about team building, relationship building, transfer criteria et cetera.
Northdale, manager 6
Staffing models
As discussed above, midwifery managers in all services felt that a carefully managed model balancing a minimum core of sufficiently experienced and senior birth centre midwives, with some rotation of midwives through the service and integration of community midwifery cover for births was ideal. All had core midwife staffing models in place, since this was felt to have been essential to establishing and maintaining the AMU service but all reported the desire to increase staff rotation as a means to attend to midwifery skills concerns. The issue of intraprofessional relationships was also highlighted in this respect, with managers aware of the tensions between different midwife groups that we had observed. This tension was acknowledged as potentially impacting on staff morale but also on quality and safety, if allowed to influence decision-making and practices around transfer. The models adopted in these services are summarised in Table 5.
| Service | Current model | Past models | Future plans |
|---|---|---|---|
| Westhaven | 8.36 WTE core midwives on AMU (band 7: 0.6 WTE, band 6: 7.76 WTE) = 2.09 midwives/bed. One midwife per shift during the day, two at night. No support workers | No change | Introduce manager post |
| Births 620 | |||
| Birth rooms 4 | |||
| Northdale | 10.2 WTE core midwives plus some community midwife birth cover (band 7: 1.2 WTE, band 6: 9.0 WTE) =1.46 midwives/bed. Two midwives and an MSW per shift. MSW: 5.7 WTE. Ward clerk: 1.0 WTE | GP unit run by community midwives | More integration of community midwives. Rotation |
| Births 830 | |||
| Birth rooms 7 | |||
| Midburn | 17.22 WTE core midwives (band 7: 1 WTE, band 6: 18 WTE) = 2.87 midwives/bed, not including FMU beds covered. Four midwives (including one community midwife) and an MSW per shift; core midwives also provide staffing for the FMU. MSW: 8.13 WTE, all band 2 | Maternity services on two sites before merger | Rotation of all staff between units proposed, not yet agreed |
| Births 800 | |||
| Birth rooms 6 | |||
| Southcity | 13.76 WTE core midwives (band 7: 1.76 WTE, band 6: 12 WTE) = 2.75 midwives/bed. Two midwives and an MSW per shift. MSW: 4.5 WTE. Ward clerk: 0.8 WTE | Originally integrated with community based caseload practices | Rotation of midwives while maintaining band 7 core midwives |
| Births 700 | |||
| Birth rooms 5 |
Inter- and intraprofessional relationships
While it may be assumed that development of AMUs will introduce gaps in working relationships between midwives and obstetricians, we did not find evidence to support this view. With some exceptions among obstetricians who tolerated the role of AMUs, or who lacked confidence in midwife care except in cases for which individual midwives were known and trusted, obstetricians were generally supportive of the role of the AMUs and valued this within the service. Reasons included economy and practicality and a view that midwife-led care and normal birth are more difficult to achieve on the OU and that this is a more appropriate triage of women to levels of care. We experienced greater challenges in recruitment of obstetricians as study respondents as many did not consider the AMUs to be something for them to comment on, except for more senior obstetricians with a strategic role. In Midburn and Northdale, obstetricians saw the AMUs as providing more appropriate care for low-risk women and having contributed to rationalising the service overall. In contrast, obstetric views in Southcity were more divergent with some very supportive, some far less so, and some having quite mixed views set in a challenging context:
I would not . . . absolutely would not stop alongside midwifery unit, I think they are great and they take a lot of . . . not . . . absolutely the wrong word to use rubbish but things that we don’t need to get involved in. It’s busy enough on a high-risk unit, you want your low-risk women to go downstairs so that you can prioritise your attentions on the high-risk women. The problem is we can’t do that as effectively because they can’t take them so we have low-risk women up here diluting the staffing for what we should be doing. So you end up getting, of course you end up getting low-risk women on a monitor because there isn’t a midwife to look after her so it’s not favouring the woman either . . . to my mind, and I am very simple, it boils down to staffing numbers.
Southcity, consultant obstetrician 2
In contrast, another obstetrician in the same service indicated that the unit was tolerated rather than positively welcomed in a service with a reputation for its high-tech medical care:
Um, It was a kind of . . . OK, if we have to, provided we can make sure that things work safely and that the institution’s reputation isn’t harmed in any way by having the birth centre on site.
Southcity, consultant obstetrician 3
The main focus of concern regarding professional relationships was around relationships between groups of midwives. Dividing working spaces for labour and birth risked polarising views of midwifery work and roles. There was a tendency, in busy and hard-pressed services, for each group of midwives to typify the other as working less hard, as less skilled, or as either hanging onto women for ideological reasons, or transferring women too quickly, for practical or resource reasons. Alongside unit midwives were criticised, for example, for failing to use certain interventions, such as augmentation, to avoid transfers of women for slow progress in labour or for greater pain relief. In turn, alongside unit midwives tended to criticise OU midwives for over-medicalising care and for attempting to pass women with some risk factors over to the AMUs for organisational rather than women-centred reasons, such as overspill from postnatal care. This is discussed in more detail in Chapter 4.
Managers highlighted concerns around the impact of tensions among midwives on service quality and safety. Actions planned to address these concerns included shared training approaches, greater rotation of midwives between areas and management-led interventions to improve communication and understanding. In one service, a midwifery meeting to discuss tensions had proved difficult as staff felt either reluctant to give their views openly or misunderstood, while in another service, a meeting organised with external expert facilitation was considered to have been effective.
Summary
The key drivers for development of AMUs in all the case study services had been a combination of pragmatic (even opportunistic) decisions and moves towards service improvement. Managers were making decisions in a highly constrained environment with midwifery staffing challenges, while subject to a series of targets and financial drivers including cost reduction measures. Initial developments had usually come about through a service reconfiguration initiated for other reasons, such as centralisation or service improvement plans, but managers still sought to utilise reconfiguration to improve the quality of care and experiences for service users and professionals. The AMUs were intended to provide a more relaxing and comfortable environment for birthing women and their partners as well as for midwives’ work. The aims were also to improve midwife recruitment and retention, through enabling midwives to develop and maintain their all-round midwifery skills and to support normal physiological birth. The environment was also explicitly intended to support physiological processes of birth as well as to provide a homely and comfortable environment for women and their partners.
Although the commissioning environment and payment tariffs had been described as making normal birth a ‘loss-making’ (manager 6, Southcity) activity, managers and commissioners hoped that the development of a tariff centred more on assessment of women’s care needs would help to remove such perverse incentives. Midwifery units were seen as essentially cost-effective and positively contributing to service improvement. Three of the four case study services were developing FMUs, building on the experience of establishing the AMU, yet there was little evidence of plans to scale up provision of midwife-led care more widely across the service.
Ineffective past attempts to establish midwife-led care and to fully support normal physiological birth in the OU environment had led to a need for distinct midwifery units to support midwife-led care. Additionally, a skills hierarchy was observed by researchers and reported by midwives and managers, with a lack of attention to development of the ‘traditional’ skills for midwifery and active birth.
The importance of clear and appropriate leadership and management observed here, in terms of the sustainability and integration of the AMUs within its overall service, echoes the findings of previous studies on the importance of management and leadership for service quality and safety. 2 Of the four services included in these case studies, it was notable that the two services which lacked clearly assigned leadership for the AMUs above a band 7 midwife level were also those that were less integrated within their overall service, despite being the most long-standing units. Senior staff in all services faced considerable challenges in terms of balancing a range of priorities, for which imperatives such as targets or preparation for CNST may take precedence over supporting normal birth.
In terms of promoting quality and safety, managers highlighted the importance of the active participation of all staff across the service, rather than only certain sections, in audit and review. As in our previous organisational study of different birth settings, such activities were regarded as important to quality and safety particularly through underpinning a ‘learning culture’2 (© Queen’s Printer and Controller of HMSO 2011, contains public sector information licensed under the Open Government Licence v2.0) in which professional reflection, communication and learning from experience could be promoted. Similarly, guidelines for admission to, and transfers from, the AMUs were seen as vital to underpin the safety of the professionals and the service as well as that of the women and families.
Managers’ accounts highlighted a number of challenges and pressures that could impact on quality and safety of AMU care. These included professional skills and confidence, learning, communication and relationships. Tensions in relationships between midwives were highlighted as a potential consequence of AMU development that needed careful management. A number of measures to counter such problems were under consideration, including carefully planned and managed midwife staff rotation and integration of community midwifery teams with midwife units. In Chapter 4 we go on to discuss such issues from the perspectives and stories of professionals working in the service, including midwives working in different areas and obstetricians at different levels of seniority.
Chapter 4 Staff experiences and perspectives
In this section, we explore the experiences of the staff working on the AMUs and OUs and their views on the role and function of their AMU. This section is primarily based on the interviews we carried out with 52 frontline staff across the four sites, but also draws on the interviews with managers, many of whom also worked clinically. Quotes from staff are numbered according to staff type and unit, rather than consecutively from 1 to 52 and area of work is indicated when relevant but limited detail of staff respondents is given to protect confidentiality.
Here our analysis focuses on the trends within the interviews that we analysed as a core research team, in consultation with the co-investigator and advisory groups. This work elicited five key themes: (1) staff relationships with colleagues, (2) the autonomy of the AMU, (3) skill, (4) philosophy and models of care and (5) the environment. All of these were perceived by professionals to contribute to, or detract from, the unit providing high-quality and safe care for women.
Relationships with colleagues
Our interviews with staff across the four trusts were dominated by discussions about relationships. These relationships between groups of midwives, or between midwives and obstetricians, were at the heart of stories about the everyday function of the AMUs and their capacity to work within their maternity systems. The evidence we collected suggests that the relationships between staff working on the AMU and the OU were characterised by a lack of understanding of the nature of each other’s work. Furthermore, sometimes staff found it difficult to empathise with the experiences of the other midwives:
I would say it’s actually improving. The relation didn’t used to be, you know, good. There, I would say there was quite a bit of mis- . . . I wouldn’t say misunderstanding but, um, maybe . . . um . . . what’s the word I’m looking for? Um . . . maybe territorial, you know . . . each sort of unit or area functioned as if they were completely, you know, independent of the other. So you know, relations were a little bit difficult, I must say.
Southcity OU, midwife 5
By interviewing staff from all areas, we found that in some cases staff in single units had different interpretations of the same events. For example, in Northdale, the AMU midwives told us about longstanding problems with the transfer of women to the labour ward:
One of the midwives the other day was saying, ‘Oh, I transferred a woman up because I saw meconium-stained liquor there, and when I got up, I took the woman up and then they phoned back down and said, “Oh we didn’t see any meconium”.’ So she said now they’ve started to do things like save the pads so they can say, ‘Look, this woman did have meconium, look, this is what she had,’ instead of believing them. And all sorts of things happen like, um, you’ll examine a woman internally and say, ‘Oh she’s four centimetres,’ and . . . or five centimetres say, and then the labour ward will phone back and say, ‘Oh she was only two, she wasn’t even in labour.’ Very undermining, very undermining, you can never prove that, you can never prove that.
Northdale, manager 4
However, a senior OU midwife did not recognise that there was a problem:
I don’t know what you’re getting at but I don’t . . . we don’t have a trans- . . . we don’t have a problem with the midwives transferring patients. We don’t honestly perceive a problem, we don’t . . . we don’t think of it as, ‘they’re the birth centre midwives’. They just happen to be the midwife that’s looked after that lady. (. . .) We don’t see a difference between one of our midwives transferring, or from triage to us than from birth centre to us.
Northdale OU, manager 10
This scenario suggests a lack of communication between staff at Northdale that was mirrored by many interviewees in other sites. Although some midwives on the OU admitted that their view of the AMU was distorted by lack of experience of it, their language suggested that they were not so reflective during their everyday dealings with colleagues on the AMU:
You see on here, we only see the bad side of [the AMU], we only see the transfers, and I’ve said this before, they have hundreds and hundreds of babies born over the year what are all normal, but because we’re a labour ward we only see the transfers here, and we always look at the negative: oh they’ve done this, they’ve done that, they ain’t done this, why didn’t they do that? Because that’s how we are – that’s how we work.
Midburn OU, midwife 5
The difficulties groups of midwives had in respecting and empathising with each other meant that silos developed, and an ‘us and them’ culture persisted across all four trusts between midwives on the midwife-led and those on the OU. This ‘us and them’ culture was fertile ground for the circulation of myths about the ‘other’s’ work that were difficult to counteract:
I’m one of the integrated midwives that’s worked all over. Some midwives haven’t, or if they have it was a long, long time ago. So some of the midwives that work on delivery suite haven’t left there for 5 years. They don’t know what happens down here, so they think that the midwives down here are lazy because they look after one person, or they think the midwives down here don’t do anything, you know, because the birth numbers per month here versus upstairs are different. So there was a little bit of kind of . . . not . . . not nastiness per se, but ignorance. Like so if I heard colleagues of mine upstairs being like, ‘What do they even do down there? Like they just sit down there all the time don’t they, like what, looking after one lady all the time, what’s that?’ you know, like . . . I’d sort of say to them, ‘But have you ever worked down there?’
Southcity AMU, midwife 1
I’ve heard a couple of midwives say that we don’t, we just don’t examine women round here. Which obviously isn’t true, you know, we do vaginally examine women, you know, when we need to, but what we, because . . . when things are going very normally for a woman who’s had a baby before, for example, we tend to use a lot more signs of natural labour as our showing that she’s making progress.
Westhaven AMU, midwife 3
The relationships between staff on all four sites were not universally poor and they tended to be better between midwives and obstetricians than between different groups of midwives:
The doctors here are really good at accepting and trusting our judgement and asking our opinion, and bouncing ideas back, and we ask them to check our examinations, they’ll ask us to check theirs as well, and they’ll say if we transfer women round they’ll say, ‘Are you just asking us to sign to say she needs something or do you want us to make a plan that . . .?’ They really seem to involve us. I think we’ve got a really nice working relationship.
Westhaven AMU, midwife 6
Good relationships were founded on mutual respect for the others’ roles and their skill, and this was most likely when midwives and obstetricians knew each other and had worked together:
There’s always a difference when one of our midwives, one of our labour ward midwives, goes to work there [on the AMU]. Say for example, you know, there’s times when I say ‘who’s there? [on the AMU]’ she says, ‘Oh, it’s [so and so].’ ‘Oh, that’s all right then.’ You know (. . .) because she knows, obviously, she knows what she’s talking about. Or when, it’s the same as here, when a midwife comes and says, ‘Oh, will you come and see my CTG?’ you know, ‘Just come and have a look at it,’ oh, OK, I’ll come here, something must be wrong.
Midburn, obstetrician 5
The relationships between obstetricians and midwives were less harmonious at Southcity than at other sites. The few alongside unit midwives who had previously worked on the OU attributed this to the high vacancy rate, fast turnover of staff and slow rotation:
I had a great working relationship with doctors. I wasn’t, you know, um . . . sort of rude to them or dismissive of them or anything like that, and them me, because once you actually get to know one another and they trust you and you can have a great working relationship. (. . .) So on a ward round if I’ve written on the board ‘low-risk woman,’ they won’t come and interfere, and then they know if I’ve asked them for help it’s because it’s needed. Because they know you, they trust you, whereas sadly at the moment with staffing levels there’s a lot of agency and bank midwives, so there’s no working relationship there.
Southcity AMU, midwife 1
Although the trust between staff groups varied across the sites, with Southcity having particular problems, there were notable similarities between the experiences of staff at all four sites. No site had found a way to entirely resolve the tensions, in particular between different groups of midwives. Northdale and Midburn benefited from the advocacy of senior midwifery leaders who had achieved widespread support within the trust. These leaders helped to promote the AMU within the maternity services. These leaders, both consultant midwives for normal birth, were tasked with integrating practices to support normal birth within the rest of the service. They gave credibility to the philosophy of practice that was embodied by their midwifery units. The lower-ranking leaders at Westhaven and Southcity felt they were less able to assert themselves amongst the senior maternity professionals and managers.
The autonomy of the alongside midwifery unit
The AMU midwives at all four sites trod a fine line between pressing for autonomy from the OU and remaining close enough to feel supported during obstetric emergencies. The midwives on all sites brought up this tension by talking about the costs and benefits of a physical distance between their two units. AMU staff, when asked about the costs and benefits of their kind of unit, tended to contrast their experiences with those of FMUs, rather than of other AMUs that were located closer to or further from the OU than they were:
I think because we’re quite close in, um, you know, distance, it’s quite easy if something did happen, if the baby was in distress, then it’s quite quick to get them round to say theatre if we needed to, to help baby get, you know, delivered a bit sooner. Um, rather than if you were in a stand-alone birth unit, obviously then you’d have to ring up, get them sent in, it’s a lot more sort of hassle.
Westhaven AMU, midwife 2
If the emergency situation is one that we need people to come to us all we have to do is put out what we call a 2222 call, um, obstetric emergency, shoulder dystocia, Birth Centre Room 6, whatever, and they come flying down to us. Um, whereas if you’re, you know, in that scenario in a stand-alone unit you’ve got longer transfer times haven’t you before help arrives or you go to help.
Southcity AMU, midwife 1
The staff on the Westhaven AMU articulated the advantages and disadvantages of being directly next door to the OU in terms of a tension between the quality of their service (because it was separate from the OU) and its safety through being close to obstetric back-up:
I think it’s, it can be seen as good and bad, being alongside as we are. I think the good side to it is there’s always an element of safety obviously in birth, you know, we’re all very proud that we have very low rates of mortality and morbidity and everything (. . .) Therefore being through some double doors, when things do go wrong – and they do sometimes, it’s rare but you know, sometimes you have a bradycardia or whatever – and you’re quite grateful that you’re through a set of double doors! [Laughs] And you can whip round there and, you know, I’ve had a couple of instances like that and I’ve been really glad of that.
Westhaven AMU, midwife 3
I think location is really important, and it’s becoming more obvious to me, just the last couple of weeks of this business of, this suggestion that we should go up there [the delivery suite] for [handover]. If we were in another building, even on the site but in another building, even as close as the antenatal clinic which is just across the car park, that would make a difference (. . .) I would advise anybody setting up an alongside midwife unit not to do it just down the corridor. We’ve kept it going for 6 years but I can feel it being swallowed up, and I know it happens and I’m really worried that it’s going to happen here. So I would advise anyone to just get as far away as reasonably possible, but of course if it was the other side of the hospital it wouldn’t really be alongside, so somewhere in between would be best.
Westhaven AMU, midwife 1
It was not uncommon for maternity staff, like these midwives, to describe quality and safety as mutually exclusive and at odds with each other. This perceived tension was apparently more acute within AMUs than those that were free-standing. Other reported disadvantages to being colocated, as opposed to free-standing, included frequently being asked to care for higher-risk women when the OU was busy, being asked to provide care for women staying postnatally after more complex births on the OU and being asked to work on the OU when it was particularly short staffed. This manager of a FMU explained:
The manager over there [at the AMU] has very different problems than I have, and the alongside issues are very different to the free-standing issues. And the alongside issues are different in as much as . . . I find, I think they find it hard to be a birth centre, totally birth centre, because they’re so close to the labour ward that they cannot help being involved with the fact that the labour ward would be full and phone them and say, ‘Well you’re only just downstairs, will you take this woman? Yeah she’s quite high risk but, you know, as you’re only downstairs.’ Or, ‘This woman’s just had a forceps delivery, yes she’s got a drip up, yes she’s on IV [intravenous] antibiotics, but you’re only downstairs’.
Northdale FMU, manager 4
Skills and confidence for midwife-led care
Much of the talk about the ‘other’70 midwives revolved around their perceived skill, or lack of it, in caring for either higher-risk or lower-risk women. Midwives tended to contrast the skills needed to care for high-risk women with those of midwifery care or care of normal birth and see each as mutually exclusive of the other. This dichotomisation was not surprising within these services, which partitioned the care of the women according to a binary (high/low) risk status, but the hierarchies associated with such skills are perhaps indicative of wider attitudes towards labour and birth. Much of the debate about skill revolved around who had what skills and which skills were (more) important to have. The findings from all four sites suggest that skills in dealing with abnormal labour were held in higher esteem than the kind of traditional midwifery skills that were used during normal labour. Labour ward midwives were often concerned about birth centre midwives’ skill in detecting abnormality and their capacity to intervene when women developed complications during labour or in an obstetric emergency.
There were reports of alongside unit midwives transferring too soon:
There is animosity I think between the two, the birth centre and the labour ward; sometimes the labour ward will see that they’re transferring things up here too readily.
Northdale, manager 1
And too late:
Um . . . occasionally there have been cases where transfer of the women to labour ward has been slightly delayed. It has never led to an adverse outcome but it led to, it led to the woman being in a prolonged labour ending up on oxytocin for hours on end, because, um, there was this presumption that, oh it’s just the latent phase.
Midburn, obstetrician 1
As a consequence, AMU midwives sometimes felt that, whatever they did, they could not win. When their judgement about transfer was criticised, they felt that this could influence their decision to transfer, with potential implications for patient safety.
Midwives and obstetricians favoured the rotation of midwives between clinical areas to help develop midwives’ skills and to break down the silos that had developed between teams:
I feel they . . . the midwives, if they had a compulsory rotation in either places, would make things better on either side. It does become a ‘them and us’. I think anywhere is a core midwifery led it does become them and us. Like they sent the patient to us.
Midburn, obstetrician 1
I think the midwives on the consultant unit complain that the . . . women are transferred up for . . . not . . . reasons that they feel are not appropriate. Um, but . . . I’m not sure that there’s very much that can be done about that, other than again education and if the midwives from the alongside unit participated more in educational meetings they would get, they would get more used to discussing anything with medical staff. Because I think that’s one of the things that these meetings do, they just simply enable people to speak to other people and just get used to speaking to other people.
Northdale OU, manager 8
One midwife at Southcity, who was used to rotating between areas, explained how rotating helped her to understand how the whole maternity system was interconnected. Her description of the benefits that followed suggests that it may bring similar benefits to others:
So I’m actually quite lucky in that I do I will be happy to slot in wherever so even when my home ward isn’t here or hasn’t been there I’ve always been around and it makes me, genuinely makes me laugh the fact that each manager of each department honestly thinks that everyone else has it easier than them. And it’s like really they don’t. You know it’s like postnatal is working their arses off to clear their beds for delivery suite and delivery suite is just harassing postnatal ward, but then postnatal ward will have beds and they won’t ever tell and it’s like my god you know ‘guys can you not just communicate?’ and it is simply communication and I think some of its to do with um . . . a sense of ownership of the ward.
Southcity AMU, midwife 4
Although none of the sites currently had regular rotation for midwives, there were proposals at all sites to introduce it. Most staff that we spoke to supported the idea that midwives would gain better skills from rotating between the OU and the AMU:
I decided, although I loved it on there I asked if I could come out for a little while to consolidate some of the more, the other midwifery, the cannulation, suturing, theatre, everything else that I should be knowing, really, to make me a better midwife, if you like. So I thought I need to do that and then come back. So I did, I went . . . well I wasn’t out for long, I was out for about nine months the way the staffing worked, but it was enough and I did what I wanted.
Northdale AMU, manager 2
Midwives on both the OU and the AMU appreciated that the skill of identifying abnormality was important, but sometimes AMU midwives felt that the focus on training in obstetric skills took attention away from training for midwives in traditional midwifery skills. The proposals for training and the rotation of staff between labour ward and the AMU were concerned with ensuring that AMU midwives maintained their skills in dealing with obstetric emergencies. However, there was no equivalent training for OU midwives to learn skills in caring for women during normal birth. A few OU midwives saw, and explained, the benefits of having some regular exposure to ‘normal birth practices’ such as physiological third stage and water birth:
You know, we don’t tend to utilise that pool because of [the AMU].
Why not? What’s the connection?
Because we’ve got a water birth room, but because [the AMU]’s got five they, you know . . . And a lot of the issue is like a lot of the midwives [on the OU] aren’t competent really, are they, to . . . You know, I mean it does work both ways, perhaps we should rotate there once every six months or something just to see how they do the water births and things, and I think that is going to happen, you know, people are interested.
Midburn OU, midwife 5
Although the majority of participants at all sites favoured these proposals, some midwives expressed concern to their managers and in interviews that the security of the AMUs relied on them being staffed by midwives who were committed to a birth centre model of care. These concerns were more prevalent at Southcity than elsewhere, perhaps because the AMU at Southcity was the most culturally isolated from its OU and was not supported by all obstetricians. Some Southcity staff explained their concern:
What the birth centre midwives say is that . . . they get any old person coming in to work in the birth centre that doesn’t believe in normality, so the first sign of a bradycardia or a problem, they pull the emergency bell and the woman gets transferred out. And maybe we might be able to tease . . . look at that with regard to the transfer rates for those units that are truly colocated and those units that are on different floors.
Southcity, manager 6
They want to keep the philosophy of care here, about promoting normality. They don’t want midwives coming down here just because they want to see what’s going on; they want midwives down here because they want to be here and they want to promote normality, and they’re good, strong individuals that can make the right decisions.
Southcity AMU, midwife 1
Southcity managers had proposed one potential solution: to have a core of senior midwives working on the AMU, with the rest rotating to the OU or another area.
Philosophy and models of care
Staff at each site described a tension between the ideologies, or ‘philosophies’ as they sometimes described them, on the AMU and the OU. This tension was sometimes presented as a problem and sometimes as something to be celebrated. At most sites, both the benefits and disadvantages were well described. For example, at Westhaven, an AMU midwife described the particular difficulties experienced by the AMU:
I applied to go to the free-standing birth unit which I’m quite excited about if that comes off, if that happens, just because I do find there’s, um . . . I find there’s quite a battle that goes on between the philosophies that I’ve talked about, between the delivery suite and the birth centre, and I find that often you have to sort of fight your corner quite a lot, which I think can be quite exhausting and I think it’s just . . . I’m looking forward to working in a place where that philosophy is shared by everybody and there’s not the answering to people coming at you with a different philosophy, you know, with the medical model philosophy basically, and that sort of lack of understanding. It just does make your job that bit more difficult, I think, that you’re sometimes having to fight to keep things normal.
Westhaven AMU, midwife 3
The AMU manager at Westhaven also explained why keeping the ‘philosophies’ different could benefit the AMU:
At the base of it it’s about trying to keep the birth centre different from delivery suite, because we need to have a different environment and a different ethos, and a different way of practising, otherwise we won’t give the women a different service. And we now know from Birthplace that women get a good service from alongside midwife-led units; they get just as safe a service for themselves and the baby whether they’re primips or multips, and they get less intervention if they’re planning a birth in a midwife, and we know that now. So we have to . . . protect, or . . . what’s the word, keep them going basically.
Westhaven AMU, manager 1
At Westhaven, Northdale and Midburn, the introduction of the AMU had precipitated some diffusion of birth centre practices to the OU. In some cases, these were changes to the environment; for example, at Midburn, the murals that had been commissioned for the AMU were also added to walls in the delivery suite, and at Westhaven birthing balls were introduced to the delivery suite:
I think what’s changed is the . . . bringing more, well I’m hoping a bit more low risk up to the labour ward. So you know, things that we use down there, think oh well I’ll use it up here. So . . . you know, we do use the birthing stool, we do use it a lot more I feel, because, er, the staff see people using it and think, oh well I’ll use that.
Northdale OU/AMU, midwife 6
And also, things like CTGs were done quite routinely on women when they came in. . . . slowly we’ve started, to, move away from that now. Not doing traces on ladies that don’t need it or you know strapping them to the bed um, encouraging mobilisation. Let, giving them a chance, you know, let them try and do it themselves, I think that’s come across as well, you know, giving them a couple of hours let them walk around and if they’re not doing anything, take it from there.
Midburn OU, midwife 8
These were small practical changes, but they had a larger symbolic significance. Some staff, both managers and midwives, aspired to take these changes further:
I think that would be lovely, if we could have the birth centre really coming out more into delivery suite.
Westhaven, manager 5
This kind of influence of the AMU on the OU was often reported at Westhaven, but at Southcity there was less evidence that this was an agenda or an effect of having an AMU. The difference between these two AMUs’ capacity to influence their OUs could have been explained by their relative physical and cultural distance from the OU and how relatively embattled they felt within the service. Southcity had a reputation for being relatively medicalised and obstetric led, in contrast to the wider organisational culture at Westhaven.
Environment
All four of the sites aimed to give their AMUs what one midwifery manager called a ‘low-intervention look’ (Northdale manager 2). A particular ‘look’ was common across all the sites and included elements such as hiding medical equipment away, pushing the bed to one side or closing it into a cupboard, having adjustable low lighting, birth pools, soft furnishings, mats and other props. All four of the birth centres had received significant financial investment and careful interior design, either recently or some time ago. All four were created from former wards, so although their basic footprint could not have been chosen, a lot of thought had gone into how the space was used.
As the term ‘low-intervention look’ suggests, the environment was not only aesthetic, but was constructed to facilitate normal birth. This was geared towards three aims: (1) to promote the physiology of normal birth, (2) to emulate the home and (3) to distinguish the AMU from the delivery suite. Midwives in AMUs explained the connection, as they saw it, between the environment and the physiology of birth:
Everyone who walks into this room is like ‘Oh my gosh, it’s really nice,’ and they’re relaxed and there’s music and it’s calm and there’s no noise and . . . you know, there’s like normal furniture and normal pillows and a rocking chair, just normal stuff (. . .)
This is going to sound like a really silly question: why is that important?
Your oxytocin is what you need, you know, it’s your labour hormone, brings you on contractions, everything like that, and your oxytocin is hugely inhibited by your fear hormone, your cortisol and your stress hormones and all that.
Westhaven AMU, midwife 1
In addition, the beds were removed or hidden (by folding up to the wall or behind curtains) at some of the sites so that women were encouraged, just by the space they were in, to be more active in labour:
If you’re on delivery suite you’ve got, it is quite clinical, you’ve got your bed, you’ve got your resuscitaire and you’ve got all your equipment and, you know, everything’s there, whereas on the birth centre there’s no bed, you know, there’s a mat on the floor, a ball and a wedge and, you know, it’s all very dimly lit and all very homely looking. Um, so you’re more likely to say, ‘Right, you know, move around more, get on your hands and knees, try standing’.
Westhaven AMU, midwife 2
Not only did the space look different, but those who designed it hoped that it would promote different kinds of practices, both by the women and by the midwives. The distinctive ‘low-intervention look’ of the midwifery units in each trust contrasted with more conventional OU environments, despite the moves to introduce some elements, such as birthing balls or murals, into the OU. This difference demarcated not only the two types of physical space, but also, as the AMU environment was created to mirror and promote a certain kind of birth ‘philosophy’, the ideological differences at work in each space:
It really helps to have the toys to encourage women and make it comfortable. It’s also a sign for the doctors.
What kind of a sign do you mean?
I think it, I think it’s a . . . well they wouldn’t come down unless it’s an emergency, would they. That it’s not their normal territory.
Southcity AMU, midwife 2
Sometimes midwives described the AMU as a place that helped to soften the sharp contrast between a woman being at home and being in the OU, by bringing elements of the home into the hospital. As the home was a space within which women were assumed to have more control over their environment, a home-like space within the hospital would promote the same feelings of control over their labours. One midwifery manager at Midburn explained:
When I walk in there I see partners walking through the unit and it feels as if I’m walking into their home. It’s quite weird. (. . .) The funny thing about when you go into the midwifery-led unit is you walk in there and the women and the partners have almost, walking around as if, they don’t know you, and they shouldn’t know me. I’m walking into their environment. And it’s lovely. They go into the kitchen and they make their drinks and . . . they don’t, very often the partners aren’t wearing shoes. It’s a very, very relaxed feel about that unit, quite unlike any other unit I’ve been in.
Midburn, manager 1
Although supporting its principles, a few midwives challenged how far this idea could be implemented in practice within an institutional building. However, these analyses were few and far between, particularly at Midburn, which had the clearest commitment to the idea of the home within the hospital:
We call it ‘home-like’, I suppose, because we expect that the woman will feel most comfortable in her home, but of course it isn’t anything like her home. [Laughs] So perhaps it’s a misnomer. Perhaps we should find it something else to call it. Because I don’t think it’s anything like her home (. . .) I don’t know, I think it’s just a name, and what we really mean is a comfortable place. A little nest, really, where she’d feel at home but not in her own home.
Westhaven AMU, manager 1
So, for me, a home-like space would not for example have Entonox on the wall. But it does in a hospital, it does in a birth centre because it’s an easy way of doing it um . . . and there’s nothing wrong with that you know. A home-like space does not have a birthing pool in the middle um, it probably doesn’t have this kind of floor so you know it’s the it’s the little things but I think you know, it is actually the little things that do make a difference because um, for a woman, wherever, when she walks into that room it is inevitably going to be a medicalised space unless, you can do some sort of magic to it (. . .) I’m always telling people that they need they can bring whatever they want in but realistically you can’t, you know. I couldn’t bring in my big picture of Stonehenge, which is on my wall, you know, or I couldn’t bring in . . . I can’t bring in my cats [laughs] as much as I’d love to.
Southcity AMU, midwife 4
Some obstetricians were dismissive about what they saw as senior midwives’ unnecessary preoccupation with interior design:
I believe, really believe that if a woman is a, for want of a better way of describing it, a midwifery-led labour and delivery, then that midwifery care should be able to be provided anywhere and if that lady happens to be in one of the rooms which is nominally in the [labour ward] at the moment because say the birth centre is full, then why should her care be any different from what it would be if she were ‘round the corner?’ (. . .) Therefore the whole obsession with the curtains – having to have a curtain to put around any bit of machinery, all that sort of thing does seem a bit like nonsense to me.
Westhaven, obstetrician 3
The obstetrician above apparently felt that quality of care did not, and should not, depend on the environment of care per se and dismissed the impact of the environment on labour and birth, whether real or symbolic. This could be understood in terms of differing physiological theories of birth, or potentially in terms of gender concepts, or medical versus social models of birth. The decoration of the midwifery units reflected both the gendered and classed dynamics of the maternity unit. One midwife at Midburn said of her AMU that ‘it’s almost like a really white, middle-class concept, do you know what I mean? Put it in somewhere like [middle class area] or [middle class area] and people would be all over it’ (Midburn AMU, midwife 2). However, this belied its deprived, inner-city location and the fact that a socially and ethnically diverse range of women in this socioeconomically deprived community were giving birth in the AMU. As we discuss in Chapter 5, while it may be argued that concepts of a domestic space are gendered and/or class-based, the AMU environment was important to and valued by a diverse range of service users.
Working in an alongside midwifery unit
Notwithstanding these many challenges, midwives at all sites talked about working at the AMU as a positive experience. This was despite recognising the difficulties they faced, particularly in being an AMU:
I just thank my lucky stars that I came to this trust really, I know that sounds a bit sycophantic, but to have two working birth centres in one trust, and it does work. Yes there are trials and tribulations of the relationships, but it does work. Women come and they enjoy the services, in both places. And . . . we enjoy working in it. [Laughs] You know, it’s for the women but it’s for the midwives as well. That’s who we are, that’s what we want to do, and it’s difficult practising in the way we practise sometimes when you’re in a very medicalised environment.
Northdale, manager 2
It’s just, just completely the sort of midwifery that I love, I love to . . . to do, really, it’s how it should be. Unless it’s too busy that you can’t be with the woman, but you know, it’s such, so nice to strip it back and be in this sort of home environment, it’s really nice.
Westhaven AMU, midwife 5
It was lovely and it was nice to go sort of back to basics and back to normality, because a lot of the time on delivery suite obviously people are round there because there’s complications, so it’s nice to get back to lack of use of monitors and . . . and goodness knows, and trying to pre-empt everything that’s going to go wrong! And just let the women get on and do it themselves, which is really great.
Westhaven OU, midwife 2
The common thread in AMU midwives’ accounts was that the unit was a protected space in which they could do ‘the sort of midwifery that I love’ (Westhaven AMU, midwife 5). The AMU appeared to provide such a space for the midwives working on it and a break from a different kind of midwifery for those OU midwives who worked there occasionally. However, as we can see from the findings of the interviews with staff, this was not without cost in terms of intraprofessional relations.
Summary
A SWOT analysis is often used within organisations to identify the possible consequences of a change or intervention. In the analysis of qualitative research findings, it can be used to draw out the trends across a large number of interviews. We carried out a summary analysis, using similar techniques, focusing on the presence of a thriving birth centre to identify the SWOTs to the four birth centres from our analysis of the perspectives of the staff working there and their OUs. Analysing the data in this way showed how the comments different professionals made in interviews collectively formed a way of talking about the birth centre amongst and between the staff in the different clinical areas.
The perspective of the AMU midwives, unsurprisingly, was that the AMU was beneficial to both women and midwives. Women’s experiences of AMU care will be discussed in Chapter 5. It was a place where midwives had more professional autonomy than they had experienced within the OU setting, where they had a supportive team of colleagues with a shared philosophy and where they could provide care with fewer time constraints, in a quiet and relaxing environment that facilitated normal birth. Obstetricians were generally supportive of the AMU, but often midwives (and sometimes obstetricians themselves) spoke about keeping medical staff from ‘interfering’ with normal labour. The midwives tended to attribute their AMU’s weaknesses to factors outside their control, for example staff shortages, overwork, the OU, community midwives’ unwillingness to work on the unit and the privilege of medical over midwifery skills.
Most OU staff described the benefits of the AMU in terms of its relationship with the OU, rather than as having benefits in its own right. The AMU took pressure off the OU and AMU midwives were willing (at times) to provide cover. However, they attributed weaknesses of the model to the perceived attitude and clinical skill of the midwives working on the AMUs and what was perceived as their preoccupation with normal birth. A few commented on how their own lack of exposure to normal birth encouraged them to see birth as high risk and to view the AMU in this way. They also expressed some concern, therefore, that increasing numbers of women in AMUs might further increase this divergence of perspectives.
Midwives working in both settings gave insightful and helpful examples of opportunities that were open to the AMU. The AMU midwives focused on strategies to improve the numbers of women using the service, for example by becoming opt-out if they were not already, giving women better-quality information and instituting better triage for women who come to the labour ward in early labour. Similarly to the OU midwives, they emphasised the need for rotation to improve midwives’ familiarity and skill in different clinical areas, but also called for a good skill mix on birth centre shifts and the recruitment of staff whose values were congruent with what they considered to be a birth centre ethos.
The differences between groups of staff were more striking than any differences of experience between sites. Each group tended to view the characteristics of the AMUs from firmly within their own shoes. The disagreements focused particularly on midwives’ skills and the value of medical compared with midwifery skill. From the perspective of many OU staff, the skills hierarchy was topped by technical skills such as cannulation and suturing, whereas the alongside unit midwives tended to prioritise the benefits of active birth skills, birth environment, family-centredness and flexibility.
These rather stereotypical attitudes were not ubiquitous, and most professionals understood the issues from the other’s perspective, even if they did not necessarily use the reflexivity they demonstrated during interviews in their everyday work. However, the attitudes summarised here formed an evident collective trend among and between the two groups of staff.
The midwifery units were built to provide a physical space for a particular kind of midwifery practice. The physical wall(s) or doors between the AMUs and their OUs help to ensure that normal birth practice is protected from what is perceived as the influence of medicalised, high-intervention care of the OU. However, when a wall is built, there is an obligation to ensure that it can also be crossed safely by women who need to transfer to the labour ward and by staff who are accompanying them. The challenges faced by the AMU staff were predominately found before, during and immediately after these crossings. In Chapter 5, which focuses on the experiences of women using the service and their partners, we go on to describe how these crossings also form key points of potential disjuncture, which may affect women’s feelings of being safe and the quality of care they experienced.
Chapter 5 Women and partners’ experiences and perspectives
In this section we analyse the organisation of AMUs from the perspective of women’s and birth partners’ experiences at different stages of the pathway of care: antenatal including choice of birthplace, seeking admission, labour, delivery and postnatal care. Few of the women we interviewed had transferred so transfer is not a key feature of our analysis of the women’s interviews. Women’s experience of transfer has been addressed at length in other studies. 62,95
The flow chart in Figure 1 depicts the combined pathways through the services of the women we interviewed. The squares represent the formal or ideal pathway and the diamonds deviations from that pathway experienced by any of the participants. White diamonds represent deviations in which this system was functioning appropriately (for example, referring to obstetric care in cases of complications). Green diamonds show when the women’s pathways were adversely affected by organisational factors, such as booking processes or shortages of staffing or space. The flow chart reflects our finding that systems across the four sites often worked well for women in many aspects, but that there were notable exceptions. The chart helped to identify key flash points for our analysis. For example, the flow chart section on women’s admission to the AMU in labour is particularly complex indicating that this was an area of difficulty for many women, that requires further attention.
FIGURE 1.
Flow chart of women’s pathways through care.
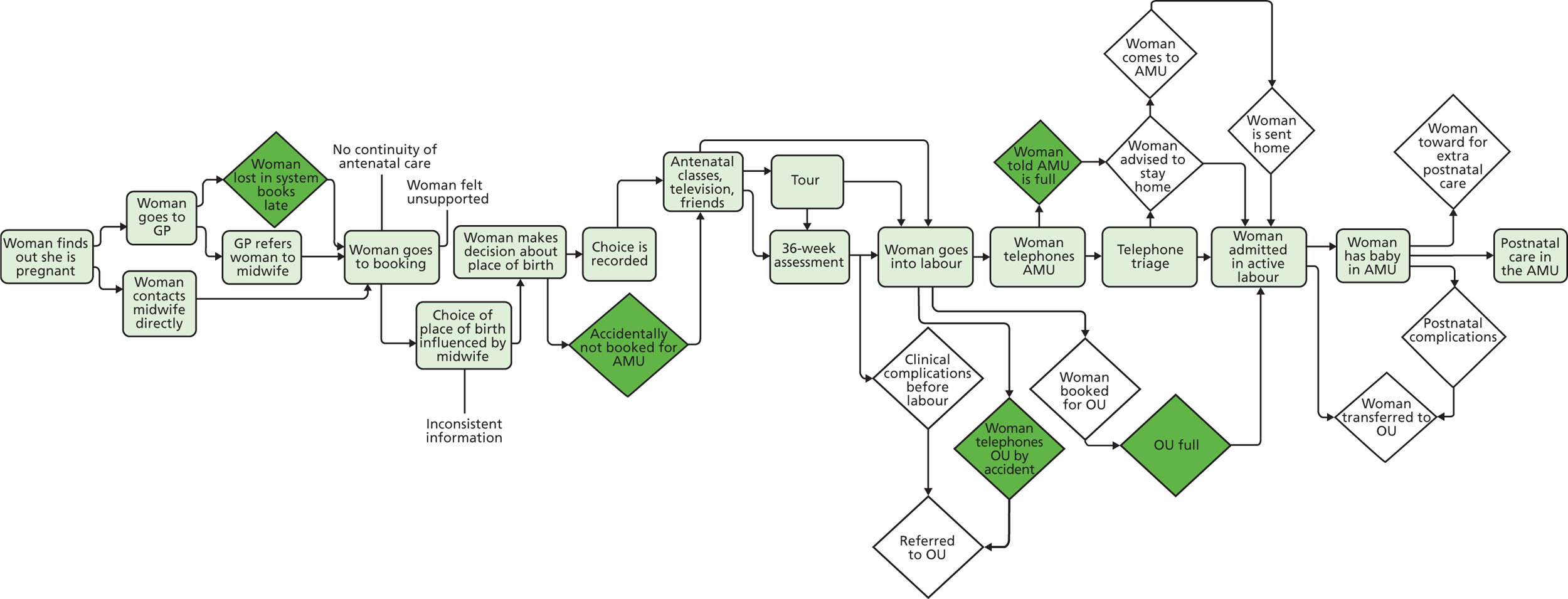
We interviewed 47 participants (35 women and 12 birth partners) about their experiences of birth. Quotes from women and partners are numbered sequentially for each study site, rather than consecutively from 1 to 47. The women ranged in age from 19 to 38 years and 12 out of the 47 participants were of BME origin. Twenty-eight out of the thirty-five women had planned to birth in the AMU and three had transferred to the OU during or shortly after labour. Two additional women were moved to the transitional room within the Westhaven AMU, but were not transferred to the OU. Almost all the women had a spontaneous vaginal birth, with no instrumental deliveries, and five births were by caesarean section. Most women who had a vaginal birth on the AMUs used water to help them manage labour pain and a third of them used nitrous oxide and oxygen. Opiates were available at all four sites but rarely used at most sites. Three of the women we interviewed had used pethidine, all on the Westhaven AMU. Table 6 shows sociodemographic characteristics of the women and partners interviewed.
| Fieldwork site | Women (partners) | Age range of women (years) | Parity | Ethnicity (women/partners) | Planned AMU? | Transfer | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Primiparous | Multiparous | White | BME | Unknown | No | Yes | No | Yes | |||
| Westhaven | 8 (1) | 24–32 | 4 | 4 | 8 | 1 | 0 | 4a | 4 | 8 | 0 |
| Northdale | 10 (2) | 22–37 | 5 | 5 | 10 | 1 | 1 | 0 | 10 | 9 | 1 |
| Midburn | 9 (5) | 19–35 | 6 | 3 | 6 | 7 | 1 | 2b | 7 | 9 | 0 |
| Southcity | 8 (4) | 26–38 | 3 | 5 | 8 | 3 | 1 | 1b | 7 | 6 | 2 |
| Total | 35 (12) | 19–38 | 18 | 17 | 32 | 12 | 3 | 7 | 28 | 32 | 3 |
Information and choice of birth setting
The majority of the women we spoke to had opted for labour and birth on an AMU. This decision was made during their antenatal period with the information they had available to them. In the case of those units in which women had to opt in to AMU care, they had followed the procedure to book their care on the AMU. The other sites, Midburn and Northdale, were opt-out. All clinically eligible women in these trusts were booked for the AMU by default unless they did not wish to give birth there, but the women we spoke to still tended to talk about making an active decision to plan their birth on the AMU. Many of women’s experiences of labouring or birthing on the AMU were informed by their expectations of the unit before they went into labour. For example, women who did not expect the birthing rooms to have beds were more comfortable with not finding beds there and women who were prepared for managing their labour pain using non-pharmacological strategies were less concerned about ease of access to epidural analgesia. Only Southcity AMU offered women antenatal appointments at the end of their pregnancy. This system was developed to help prepare women for a birth on the AMU and to familiarise them, to some extent, with the environment and the staff. Women valued this opportunity to visit the AMU in advance of their labour and also valued that these appointments involved less waiting time and they felt calmer than during their experiences at the hospital antenatal clinic:
This time around I actually went in and had a midwives appointment at the birth centre for antenatal . . . for one of the check-ups and I was quite worried because I went 11 days over this time around so um, so they’d actually made the appointment for my, for induction and I really didn’t want to have an induction. (. . .) I really appreciated that I was actually quite stressed about it at the time and when I walked out of the birth centre and I could have a little look around then again to remind myself, but um that really calmed me down and I was then happy with going to sit it out. I don’t need to, I don’t need to be induced if I don’t want to be but then I started labour the day before my induction date.
Southcity, woman 7
Pathways through care
Women’s pathways through antenatal care were influenced by their access to information about the birth options available, but also to adequate information and preparation for what different choices would entail. As identified in our previous organisational study of different birth settings,2 differences in women’s awareness of choice and access to detailed information could be compounded by service structures, professional attitudes and the ways in which they approached information provision. In this current study, however, we found that the opt-out approach to booking for AMUs had the potential to reduce differences in such access through establishing the AMU as the normal pathway for low-risk women. Figure 2 maps out the established antenatal pathways for women to book for AMU care and some deviations in the pathways of the women we interviewed.
FIGURE 2.
The antenatal care pathway.
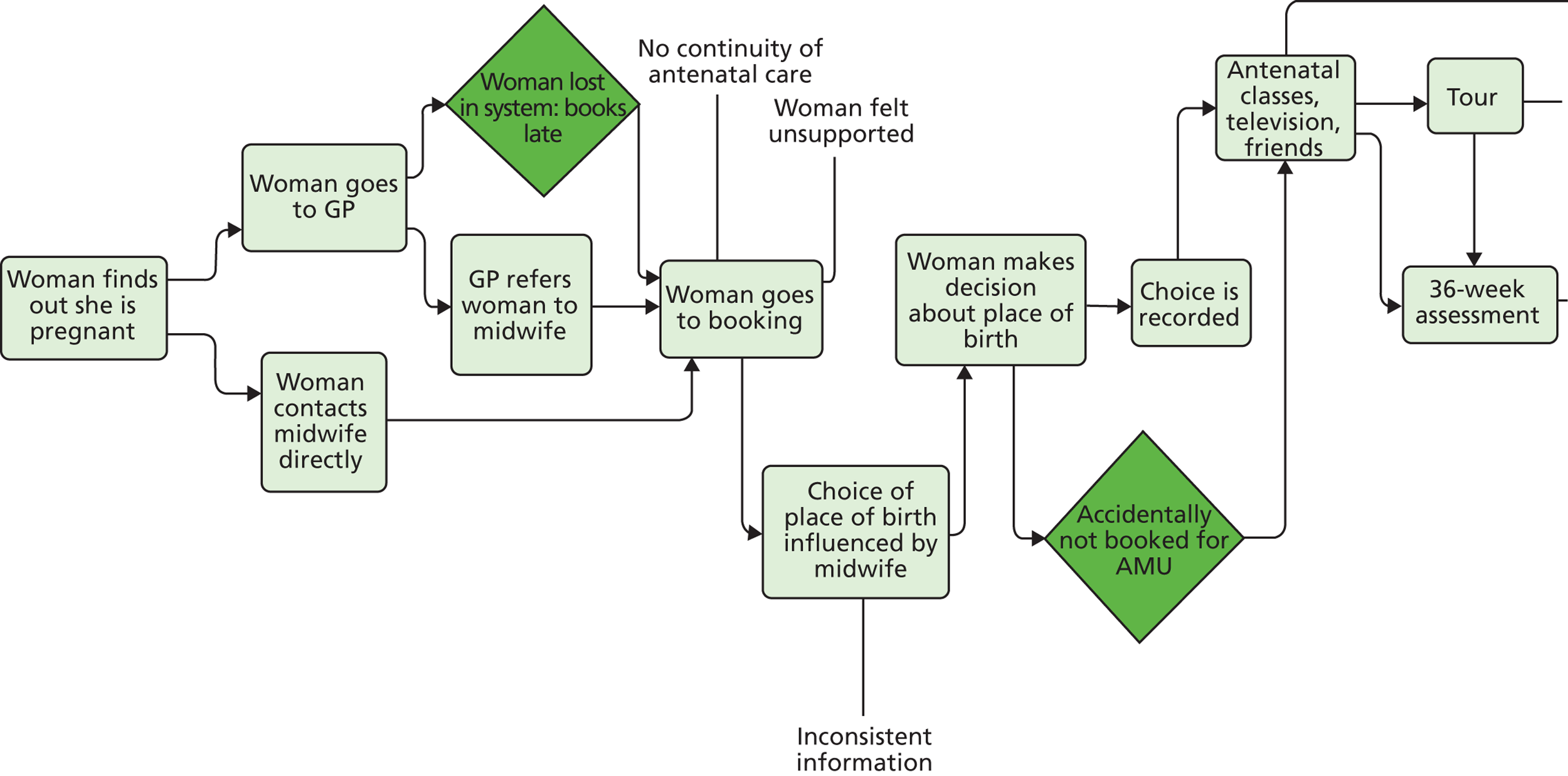
The formal pathway of care through maternity services relies on a number of factors to ensure that women have the best care possible and a choice of the available birthplaces in their area. Women needed to proactively contact the maternity services, attend midwifery appointments and midwives needed to give consistent and appropriate information to women about their options and make an effective assessment of their risk status and eligibility to plan a birth in the AMU. In practice, women interviewees’ pathways through care often deviated from the norm through the interplay of factors such as unequal access to information, their different priorities in selecting a hospital or unit, an AMU’s opt-in or opt-out policy, midwives’ influence on her decisions and the organisation of care under the pressure of shortages of staff and space.
Women chose to give birth in an AMU for a number of reasons, including the opportunity for partners to stay, the possibility of a water birth and a desire to avoid drugs and medical intervention. Sometimes women wanted to avoid the risk of a road transfer from a FMU or from home and expressed a wish to be in the AMU primarily because they felt safer being near doctors:
It’s very reassuring to know that there’s a great big medical world that’s right there that I don’t want to have anything to do with but if I needed it . . . You are committing to the natural route for so long as you are safe but then the moment it stops becoming safe you go the medical route.
Southcity, woman 9
The women we interviewed who deliberately opted for the AMU knew what to expect in terms of having a natural birth, being close to medical services and the differences between the AMU and the OU. This was the case in both opt-in and opt-out units. They received this information from a variety of sources. However, our evidence suggests that community midwives at all sites gave inconsistent information to women about the AMU. For example, they mentioned it to some women but not to others, as these women’s contrasting experiences illustrate:
There was a section in the [maternity] pack to fill in every week with the midwife. She did go through the choices. I had a clear vision. I didn’t want any drugs. But I tried to make it clear that if on the day I changed my mind that was OK. She said that was fine.
Northdale woman 10
I did a lot of my own home prep into having a birth centre birth and you know, and looked into hypno-birthing and all these kind of things and using a pool and all this. I did that myself; she didn’t provide me with any of that information (. . .) She didn’t really tell me about the birth centre or anything like that, she . . . I think she was very much a labour ward midwife.
Southcity, woman 2
One service manager commented that community midwives in her service tended to tailor the information they gave to their assumptions about different women.
Women and partners from different cultural backgrounds found tours of the AMU thorough and informative. In some cases, taking these tours during NHS antenatal classes gave them their first opportunity to hear about the AMU:
They show us every single detail of the ah . . . of, of the what is going to happen and we should be prepared in this way and explanation was very clear and also the hospital’s staff is very friendly but approachable so we ask as many questions as we could and we felt very confident as our first birth, my wife’s first birth and without knowing anyone, any friend who has given birth here and you see, without family members, so that was very important for us to get support.
Southcity, partner 3
Um, to be honest it were just not something that I even thought about, because you think it’s a million miles away, you know, you think you’ve got ages and ages. I didn’t really think about it (. . .) [At the antenatal class they] take you down to see where the delivery suite is, where the birthing centre is. So after I’d been for that visit I’d made my mind up I wanted to go to the birthing centre, because it just looked really calm.
Northdale, woman 4
Experiences of opt-in or opt-out models
Northdale and Midburn had an opt-out policy so that the normal pathway for low-risk women was into the AMU unless they requested another birthplace:
. . . what we was actually told when we phoned in was, was there any complications in the actual pregnancy or with the mother, and as we said no they said they’d advise us to like, for her to give birth, have the baby in this unit.
Midburn, woman 8
This arguably gave women a more limited choice of birthplace, although theoretically they could opt-out to the OU or choose home or FMU birth. At the same time, it could increase their opportunity to birth on the AMU, as a Northdale woman explained:
Now as it happened the birth centre was fine and it was all fine and dandy, but it nearly wasn’t, and that thought that they’re just pushing you into something that you’re not entirely comfortable with . . . is a bit distressing when you’re in your very early stages. (. . .) They just kind of went, ‘We’ll stick you down for birth centre,’ at that point, and it was just accepted throughout until, I think it was maybe 37 weeks when they said, ‘So you’re down for the birth centre, are you happy?‘ Well, I don’t even know if I was asked if I was happy about it, whether I had a choice, to be honest. Um, but because I was happy about it I just didn’t query it.
Northdale, woman 8
More women heard about the AMU from their community midwife at opt-out sites than at opt-in sites in which women had to specifically request the AMU. However, most women in opt-out sites still found out about the AMU first from friends or antenatal classes.
It was particularly important for women at Westhaven and Southcity, where they had to opt in to the service, to get consistent information from community midwives in order to make their choice. However, at these sites, very few of the women we interviewed had first heard of the AMU from their community midwife. Many women instead found out about it through chance encounters or conversations with friends or National Childbirth Trust (NCT) antenatal teachers, or through their own internet research:
At some point where it was explained about the differences between the different units, and I remember somebody explaining, maybe it was in an NCT class, (. . .) that like you go through one door and it’s the Delivery Suite and one, the other door and it’s the [AMU] and they’re just next door to each other. So I think it may have been NCT that explained exactly what the birth centre was. Um, but I always knew that I wanted to be in that if I could, because I wanted a water birth.
Westhaven, woman 4
Even when community midwives mentioned the AMU, some women found the information inadequate:
She just basically said, you know, ‘[Westhaven] has these options: a birth centre, a birthing pool, a delivery unit,’ you know, there were no, she never gave us an opportunity to ask questions as to what they might entail, she didn’t really elaborate. I think she just said like, ‘The birth centre’s a more natural setting,’ um . . . and I think that was pretty much about it.
Westhaven, woman 1
Overall, women’s access to information about their options for place of birth was variable. Although all women saw midwives for their antenatal appointments, not all women had access to antenatal classes or to friends who had knowledge of local maternity services. If community midwives were not giving consistent information, then only some women were able to exercise their choice. Our evidence suggests that midwives at Westhaven and Southcity were less likely to be the first source of information about the AMU and this unequal access to information could make it more difficult for women to have an AMU birth in an opt-in system.
Seeking admission in early labour
The second key potential flashpoint on the women’s pathway, once they were booked for AMU care, was admission to the unit in labour. Two key issues could affect their experiences, diverging from the smooth picture of the theoretical care pathway. First, women may experience prelabour transfer if complications developed or pregnancy became post term and, second, admission to the AMU could be affected by busyness of services or by the assessment of active labour. Figure 3 shows the formal care pathway, and ways in which some women’s pathways diverged from this.
FIGURE 3.
The pathway to admission.
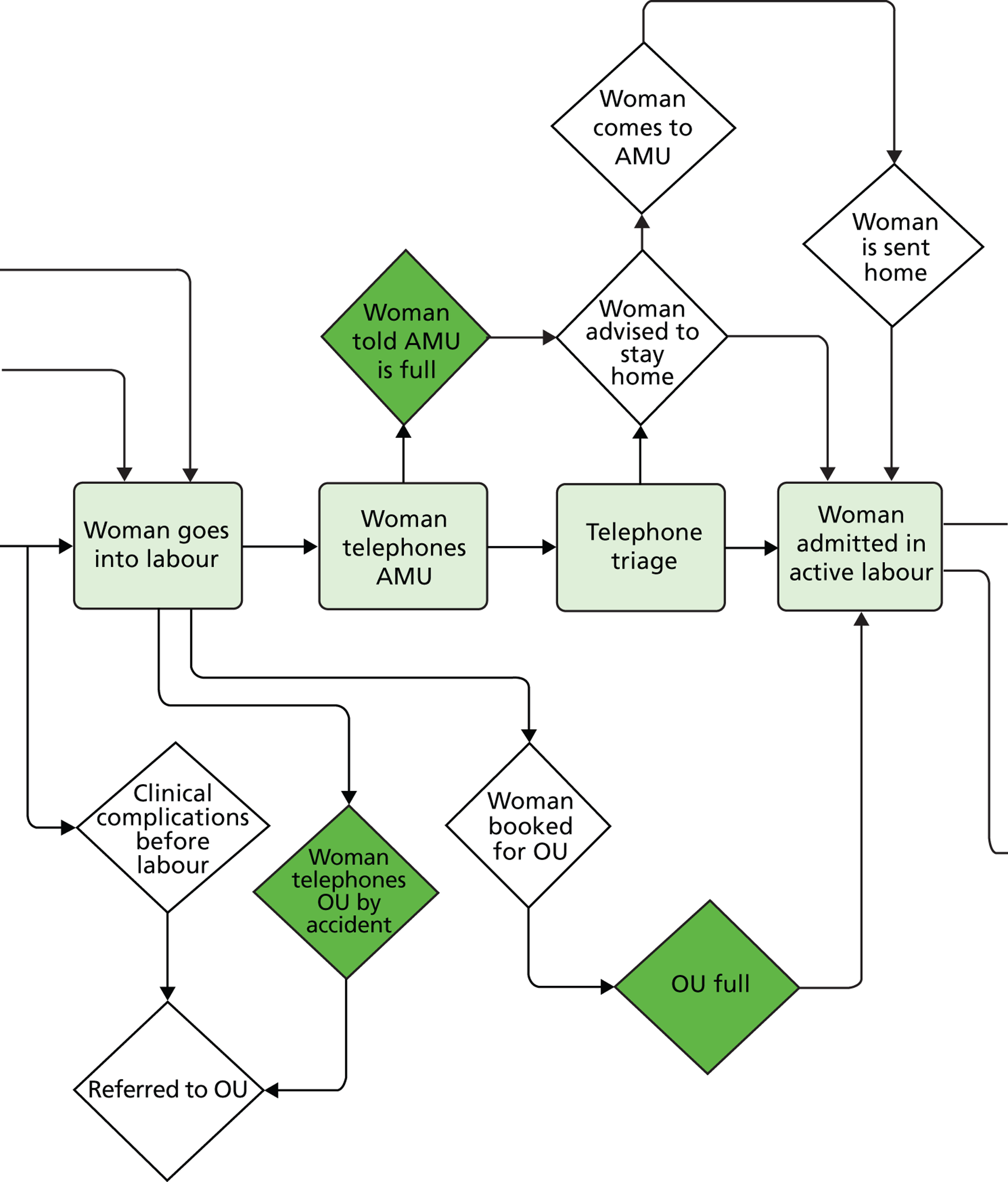
Most women reported knowing that coming into the hospital in early labour had to be carefully timed. They learned this from peers, from midwives at antenatal or NCT classes, or online, and from their previous experiences. Women made efforts to go through labour at home for as long as they could, to avoid coming to the hospital and being asked to go home to wait until their labour was further established:
. . . one of our concerns as well about you know the birth centre or any labour was arriving too early and being sent away then arriving and being sent away . . .
Southcity, woman and partner 2
When they arrived in the AMU, women felt calmed and encouraged if they encountered staff who listened, admitted them to the unit in a timely way and showed the woman from the start that she was expected and there was a room awaiting her. Women were often aware of the pressure on rooms, beds and staff and tolerated this busyness, as long as they felt valued as individuals:
[Midburn AMU] were absolutely fantastic, um, over the phone and in person. Really . . . made you feel like they wanted you to have your baby there rather than just you were a . . . I don’t know . . . a statistic or a number that comes through, which I imagine hospitals do become . . . that’s how they approach things because they do have a huge number of women to see, I suppose.
Midburn, woman 4
Half of the women we interviewed came to the unit and were admitted. In many cases, AMU midwives had reassured them during telephone assessments and encouraged them to stay home for as long as possible:
I think I phoned about three, and they said, ‘Call us back when they’re about three minutes apart and lasting for about a minute,’ I think they said, I can’t remember. (. . .) They were extremely relaxed, and they said to me, ‘You sound like you’re in control, you sound calm,’ they sort of reassured me in that sense that I didn’t need to rush in. And actually I was quite happy here [at home].
Westhaven, woman 5
The other half of the women we interviewed were sent home from the AMU in early labour, and most of those went willingly, if not happily. Sometimes these women were given the choice to stay or leave and opted to go home, but mostly they were advised to wait for their labour to progress at home and were not given the option to stay. Some women were advised by midwives that home was ‘the best place’ for them in early labour. Some observed that the AMU was short of rooms and women in more advanced labour were given priority. Units appeared to differ in their early labour policies. While women at Northdale and Southcity reported being given the option to stay in early labour, Midburn midwives encouraged all the women we interviewed who arrived in early labour to go home. Some Midburn women were happy to leave but three women were asked to go home when they did not want to:
And I was like, ‘Please, we’ve got to go back in, we’ve got to go back in.’ But again, it wasn’t because I wanted them to do anything, I just felt, I just needed to be there because I thought I’d feel safe.
Westhaven, woman 3
Two of them birthed very quickly on arrival back in the unit and reported feeling unsafe or even traumatised in consequence:
Horrible time for me was when they sent me back home. First pregnancy. According to me – home is not best place for me. Midwife advice, best position, they examine you again and again. Energy drinks. When they sent me home, confusing time for me. Go out, go in – painful time for your body, innit. They should keep the woman in [AMU] for the labour.
Why do you think they don’t keep you in?
I don’t know why. Because pain was stronger. They don’t tell me why.
Midburn, woman 7
She told me, ‘Unfortunately you’re only two centimetres dilated.’ And I was just like, oh, so defeated, I was like, ‘Oh no . . . please don’t send me home, please don’t tell me you have to send me home.’ And they’re like, ‘Unfortunately, because you’re only two centimetres dilated we’re going to have to send you home, because the policy here at [the birth centre],’ which I didn’t really know at the time, was you needed to be four centimetres dilated, that’s what they class as active labour, in order for you to stay at the [the birth centre]. (. . .) I think of the worst case scenario, you know, I could have, um . . . I could have laboured in the car park and then, you know, not knowing what was happening, no one was prepared, you know . . . he could have died.
Midburn, woman 2
Midburn woman 2 associated her postnatal depression with having had negative feelings about her birth during her experience of returning to the hospital in great pain in more advanced labour.
While midwives’ advice to women to stay at home in early labour was often argued in terms of a model of care intended to avoid medically unnecessary interventions, women’s experiences of admission also indicated to the women that busyness and lack of staffing were impacting on their ability to gain admission:
. . . when we got to the hospital (. . .) the first midwife we met was actually really quite rude and she was really abrupt and she was like, I’m really busy I’ve got three women in labour and um, I think she thought maybe I’d just started to have pains. I don’t think she’d obviously realised that I’d been in and come back . . .
Southcity woman 6
As in other situations they described, several women expressed understanding of NHS resource difficulties. Additionally, the ways in which professionals dealt with a difficult resource situation could make a considerable difference to the women’s experience:
. . . someone came and I explained who I was and they said, ‘Oh the birth centre’s full at the moment, but if you come up here we’ve got a room for you.’ (. . .) it was, it was a shame but (. . .) there was nothing I could do, if there was no room available. (. . .) And then about 20 minutes later . . . the midwife who actually ended up being with me the whole way through appeared and said, ‘I understand you want to give birth in the birth centre in a pool. It’s available now, would you like to come down?’ At which point I said, ‘Yes please. Definitely.’ And that was brilliant, at that point she took over my care. And she was fabulous.
Westhaven, woman 5
Traditionally, women have been encouraged to spend their early labour at home to avoid unnecessary medical intervention in hospital. The AMU midwives we spoke to gave this as one reason for encouraging women to go home, along with problems of capacity when caring for women during a potentially long latent phase. Our evidence suggests that the policy that home is the best place for all women in early labour was being continued in AMUs. Even though AMUs were presented as a home-like rather than a medical space, as midwives still had concerns about ‘the clock ticking’,96 they potentially felt pressure to intervene with women who appeared to be progressing slowly in labour. While few women were sent home against their will, some women were encouraged to stay at home for longer than they might have wished and feelings of uncertainty and worry around early labour care were evident across many of the women’s stories. This is something that has been frequently addressed in literature about care of women in an OU, but the issues around translating such a policy to AMUs deserve further attention.
Experiences in labour, delivery and postnatal care
Once women had been admitted to the AMU, their experiences were influenced by a number of factors, including their partner’s experience, the environment they laboured in, their choice of pain management strategies, whether or not they felt in control and, crucially, their previous expectations of what their labour and birth would be like. Figure 4 maps the established pathway from AMU care in labour to postnatal care and ways in which some women’s experiences deviated from this.
FIGURE 4.
Pathway from labour to postnatal care.
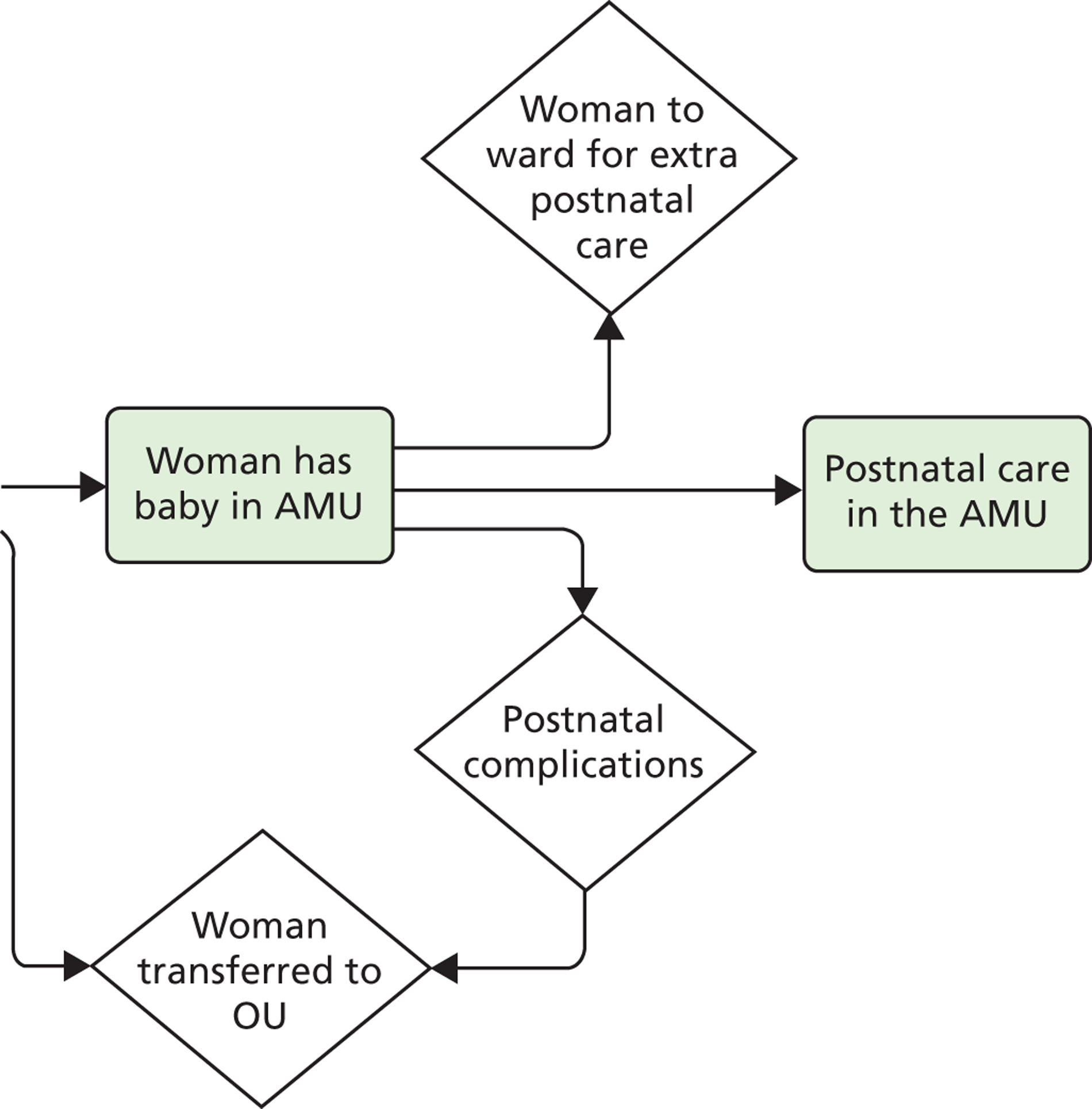
Family-centred care
A key factor in women’s well-being was support received from birth partners and midwives. Women who were accompanied by partners often valued the times of intimacy that were provided by midwives who knew when to leave them alone and when to come in and assist them with labour as a team, together. Women were often attracted to birthing in the AMU because it explicitly provided for partners and relatives, allowing them to stay over and support women during labour and postnatally. The AMUs prided themselves on putting families at the centre of care, and this was reflected in the furnishings, equipment and refreshments for birth partners’ comfort and use:
. . . this time they said, ‘[partner’s name] do you want a drink, do you want some toast?’ as well as me, whereas last time because we were on the proper ward [OU] where there’s, he didn’t get offered anything. Um, so this time, you know, it’s more about you as a couple, I think.
Northdale, woman 3
It’s nice to have your partner there and I found that a really nice touch that they pulled out the bed and (. . .) it felt like we were doing it together. Not like he goes home and then I’m stuck with a newborn for the first time by myself so that is, I think that is a nice touch to accommodate partners.
Southcity, woman 4
Effects of environment and care processes
Alongside midwifery units offered an environment that was markedly distinct from the medicalised OU setting. The birthing rooms were quiet and spacious, with adjustable lighting, nature-themed decoration and in some cases homely touches such as framed pictures, ornaments or soft furnishing, unlike a more familiar hospital environment. Women valued the exceptional setting in the AMU with every detail cared for in design and decor, sound and light:
I think it smells, I don’t know, I think it smells like in a spa, it’s, um . . . it’s just, yeah . . . I can’t explain the smell it’s just, it’s like being in a spa, it’s not like being in hospital with all that clinical smell, it’s a . . . completely change of atmosphere, not just visually but, you know, everything. (. . .) Um, well they’ve got the massive prints, um, which are in the corridor and in each room, which are like the flowers and things, um, which are lovely, again it’s that kind of spa atmosphere. Um, and all of the medical equipment is, is kept away.
Midburn, woman 4
. . . it felt, and again going back to that image of a love . . . a lovely big room with a pool and a ball and a hammock. It felt kind of, it felt expensive in a way that it probably isn’t compared to what actually goes on in the room but it felt like um . . .
It felt lush . . .
Yeah, it felt lush. That’s what it is (. . .) and that’s, that’s available on the NHS. That’s an NHS service.
Southcity, woman 9, partner 4
It was wonderful, wonderful and babies are healthy because they look after them. Very hygienic, no problem happened, food is excellent always as well so, very clean, never seen any spot. Can you believe that? No spot in the toilet, no, no, no.
Southcity, partner 3
As discussed under professionals’ perspectives, a few medical professionals viewed such aspects of the environment as unimportant and some saw them as based on class and gendered assumptions, geared to ‘white, middle class women’ (site 3 AMU, midwife 2). Conversely, the comments from women and partners from diverse social and cultural backgrounds suggest that the environment mattered to all women, even though some may not have felt such a sense of entitlement to choices in care. The comments of some women even suggested that they felt treated as special through the environment in a way that they did not normally experience. This also highlights that birth centre environments may offer choices to women whose circumstances and social situations are less conducive to a choice of home birth.
The design of the AMUs was also an integral part of natural birth philosophy and practice. Over half of the women interviewed chose the AMU explicitly to optimise their chances of having what they often termed a ‘natural’ birth, with minimal intervention or pharmacological pain relief. Many also chose it because they wanted the opportunity to labour or birth in water. This could work for those women who knew that the combination of environment and midwife-led care favoured a birth experience free of medical intervention, with space to move into different positions, and the best prospects for a smooth delivery:
. . . so they helped move me into whatever position, and we tried pretty much everything going, you know, we were standing up, over the bed, on my back, er, on the birthing stool, we tried that for a bit. (. . .) Um, they also had a rope hanging from the ceiling, which I chose not to use but, um . . . certainly a friend had said she found that really helpful, to swing on that, so the resources they had available, I mean there was a birthing ball as well I could have used if I’d wanted to, um, you know, I could have done pretty much anything I wanted to, and they were fine with that, so that was really good.
Northdale, woman 8
At all four sites, the AMUs were designed without delivery beds, to encourage women to adopt different birth positions. Most rooms had beds intended for postnatal rest but these were usually hidden behind curtains or pulled down from the wall. Women’s attitudes towards the absence of beds varied according to their expectations. Many women were well prepared for there to be no bed:
I think if there’d have been a bed in there I wouldn’t have gone anywhere near it, I just . . . maybe I would have leant on it, I don’t know, but . . . It didn’t faze me that there wasn’t a bed, I was relieved, I didn’t want one in there, there was no need for it. For me, I mean for some women, you know, maybe it would be completely different, would want the bed to feel safe, want to lie on it, but no, I didn’t want that at all.
Westhaven, woman 3
Others were more ambivalent, both about their commitment to an AMU birth, as well as being in a room without a bed:
And what did you think about that, having a room without a bed?
Er, I thought it was a bit weird, I’ve got to admit, it was a bit like, well . . . it’s comfy a bed, you know what I mean. And on the floor, why do you need somebody to get on the floor? But then I thought when it comes the time I was like, actually that’s quite practical because you can be on all fours then, or you can be squatting against the wall and it would be more comfortable, and um . . . when you think about it it’s like, well actually yeah, because this that and the other, positions and that.
Westhaven, woman 2
Considering that I ended up delivering her on a bed, I think that maybe they should [have beds in the birthing rooms], just because that way they wouldn’t have to necessarily move the room if they had the options that if they did need to change something you can still stay in the same room. (. . .) I decided ‘I’m not going to push, get the doctors, get the forceps, I’m not doing it, I need help, this isn’t going to happen’. Um, so obviously I needed to have been on a bed for that to have happened. That said, I’m not sure it wasn’t the change in environment that changed my head space so that I did just do it by myself.
Westhaven, woman 1
Managing pain
Most of the women we spoke to who had chosen the AMU knew that birthing in the AMU meant a greater possibility of an intervention-free birth and that epidural would not be available without transfer. Women weighed access to epidural, which many saw as an important as a back-up, against the opportunity for a quieter and more homely environment and care from midwives who were skilled in helping women manage pain:
[The midwife] kept me calm all the way through. (. . .) I really didn’t want any drugs, I wanted a natural birth and at one point I really thought, I can’t, I can’t do this, I can’t. And she just came in and said, ‘You’re doing it already, you’re doing it. You don’t have to, you know, worry about it, you’re doing it.’ You know, and then once I’d got in the pool I controlled it then and it was, I didn’t need anything then after that. And I’m so glad because she, because of her, I might, if it was somebody else who dealt with it in a different way I might have ended up having something which I would have probably regretted.
Northdale, woman 5
Some women explained their birthplace decisions in terms of a trade-off between the comfort of the birth centre environment and the availability of pain relief:
If you decide you want the relief, the pain relief, then you have to lose that relaxed atmosphere downstairs. So it’s almost like you put yourself through more pain because you want that . . . I mean because you know, you know when you go in there, I knew that [partner] could stay if we went downstairs [to the AMU], he couldn’t stay if we went upstairs [to the labour ward]. I knew that if I was downstairs there was less intervention but there’s also less pain relief.
Northdale, woman 3
In addition, several women spoke of the differences between the OU and the AMU in terms of the availability (or unavailability) of epidural:
I think um, people are afraid of the pain, that’s simply it I think and if the birth centre, you know if you, if you . . . if . . . if the place where you do have the epidural is up . . . is on the labour ward then that’s where you go . . .
Southcity woman 7
Additionally, the comments of some midwives about the issue of pain relief indicated that women might not be offered sufficient information and preparation around coping with pain. It appeared that the midwives’ knowledge of links between environment and care and the physiology of birth was not always communicated effectively to women to help them to understand the complexity of labour pain and the links between support and ability to cope better with pain:
. . . and also the attitude of the midwives like you can pick up . . . If someone’s really kind of, ‘It’s totally your decision,’ you know ‘Epidural is here if you want it but you but . . . You know you’re a woman, you are built for this, we think you can do it.’ Then they’re more likely to think about the birth centre. If you are really kind of well, ‘You know, birth centre is there but epidural you know, we’ve got the doctors and they’re just outside if anything goes wrong, we’ve got theatre around the corner,’ and you kind of big that up and they’ll see, they are going to want an epidural so . . . You can, you can tell which midwives . . . create more birth centre women and which create more labour [ward] women.
Southcity, midwife 6
Women made relatively little explicit reference to how the AMU environment might help them manage pain more effectively. Some did describe how midwives worked with them to get through difficult periods of labour, which reflected the midwives’ degree of comfort in working with pain rather than focusing on relieving it. All four AMUs offered women opiate pain relief, but at three of the sites it was used very sparingly. Three of the women we interviewed received pethidine, all at Westhaven. Two had previously decided that did not want to receive pethidine in labour, but were persuaded to try it in early labour by their midwives. They found it helpful to relax, but two found it had little effect on their pain:
I was adamant I didn’t want pethidine, and I didn’t actually think they’d give you pethidine in the birth unit, so I was really shocked when she offered it to me. (. . .) She just said, um, ‘I think it would be a really good idea for you to have it because, um, you’re exhausted, you need to sleep, if you want any chance of being able to push this baby out naturally you need to have energy, and if you don’t sleep now then you’re not going to be able to do it later on,’ and that was what made me change my mind because I thought, hang on a minute, I don’t really want to be able to, you know, end up saying, ‘I need help,’ at the later stage, after struggling all the way through
So in retrospect do you think pethidine was the right decision to make?
Yeah. Yeah because it made me sleep. Um, but I’ve heard obviously that every labour’s different, so I’m not saying that next time I’d say I definitely want pethidine because it did not help with the pain, it wasn’t . . . So I think like I said the midwives were clever, because for the way my labour was working they obviously knew that later on I was going to be tired so I needed to sleep then, they used it for me to sleep.
Westhaven, woman 3
As found in other studies on the management of labour pain, the most common strategies used in AMUs (water, nitrous oxide and oxygen, verbal support) reflected the units’ aims to promote physiological birth. Most of the women we spoke to who had planned a birth on the AMU were very clear about the link between the AMU and avoiding pharmacological pain relief. The availability of epidural was a practical manifestation of the ideological differences between the two different types of unit (the OU and the AMU).
Some women were aware not only of this practical difference but also of the underlying ideological differences. The subsequent tensions between staff working within different units filtered down to the women in their care:
And I burst straight into the [birth centre] and saw the same midwife who’d been in earlier, saying, ‘I’m so sorry, I can’t do it, I need an epidural!’ And I was, I think I was apologising to her because I knew that it meant that I’d need to go to the delivery suite if I had an epidural, so, so I was saying to her that I was sorry . . . because of that, because like . . . my perception is that the midwives are quite proud of their midwife-led units and things. So . . . so yeah, but I was just saying, telling her that I couldn’t do it and I had to have an epidural.
Westhaven, woman 4
We had talked so much about birth centres and potential tensions between labour wards I felt I picked up . . . see that’s just me . . . part of it was my view on it which wasn’t my main priority at the time but I felt there was tension and that kind of, ‘Oh, we’ve got another one who’s come up,’ not in a ni . . . not in an ideal sort of state and there wasn’t any sort of more direct criticism than that. Then there was the ‘au naturale’ comment then it kind of . . . that was the only really comment from the birth centre. I . . . there was just that comment, I’m sure there was a comment from someone of, ‘Oh another one from the birth centre,’ in kind of like an eyebrows raised sort of way.
Southcity, partner 2
Managing complications
Our study sample was not specifically focused on looking at transfers and it included only three women who needed to transfer from the AMU. It is not possible to generalise from these few cases. However, one woman who needed to be transferred to the OU for retained placenta emphasised the value of having the AMU midwife stay with her during the transfer:
. . . as she took me down to theatre I remember just crying when she weren’t allowed to come in, because she thought she would be allowed to come in but she were needed somewhere else. So . . . yeah, that were a bit upsetting as well, because you’d built that relationship and I wanted somebody with me to hold my hand and, you know. So . . . yeah, that were a good thing, but I think that she only came up from the birth centre because it was so busy on labour ward they didn’t have anybody else to look after me so she had to.
Northdale, woman 2
The value of interprofessional teamwork and co-operation between the AMU and the OU was also illustrated by a small number of cases in which obstetricians were consulted during the labour:
. . . it got to the point where she said she was contacting the unit upstairs for advice, because she wasn’t sure if I was going to need something to help the contractions come back stronger, or some other intervention. Um, and the obstetrician actually came down from upstairs, which apparently he never does (. . .) but in the end he said basically, ‘Yeah, I think she’ll do it,’ and he left the room and left it to the midwife and the assistant, and not long after we did manage to deliver him without too many problems.
Northdale, woman 8
Summary
Women’s pathways through care when planning birth in an AMU were often straightforward, but they were subject to several flash points relating to management of boundaries in care: obtaining information about birthplace options, gaining admission to the birth centre and the potential need for transfer. Our sample was targeted towards women who had received care in an AMU, whether or not they had transferred during labour and regardless of whether or not they had specifically planned for this form of care. Women in the sites with an opt-in approach were less likely to learn about the option earlier in pregnancy and often found out about it through a hospital tour or an antenatal class or through friends. This has potential implications for equity of access.
The quality of information given about birthplace options was also variable. Some women were aware of their choices but had only limited information about the differences between units and scant preparation for labour in a setting with a different approach to pain management. Most women chose birth-centre care because of the environment and a desire to have a natural birth, if possible, in a calm and comfortable, family-friendly setting, but some saw this choice as a trade-off with access to pain relief. Their accounts indicated that some midwives presented the options to them in this way. Nonetheless, none of the women in our sample required transfer for pain relief. Use of water immersion for pain management was common and often an attraction for women to use the AMU. The AMU environment and care was valued highly by the women who experienced it, and its more family-friendly nature was emphasised as a key benefit. The women in our sample were socially and ethnically diverse and the women’s and partners’ comments indicate that some were surprised to have access to an environment that they associated with luxury such as a hotel or spa.
Some women who did not need to be transferred were nonetheless moved around between rooms for organisational reasons. Some women who had been advised to return home in early labour were admitted late in the first stage. The women’s accounts indicate that these kinds of transitions can be very distressing and that women may feel unsafe if they do not have a secure and undisturbed space with sufficient support in which to labour and give birth.
Women’s difficulties in gaining admission to general maternity units in labour have been well documented. Our findings indicate that the concern can equally be applied to AMUs, despite their different environment and social model of care. While the rationale of midwives following a social model of care is evident, the AMUs themselves are developed as a more social than medical environment in which to birth. Additionally, the quality of information provision to women antenatally and in early labour appears to be limited and women who returned home unreassured about their labour progress could feel very anxious, unsupported and unsafe. As in the case of OUs, the issues concerning the most appropriate place to be in early or latent labour were compounded by staff shortages and crowded units. These factors could additionally reduce the quality of support and information-giving by midwives affecting women’s access to the unit.
Chapter 6 Discussion
In this section we first summarise our findings around intended or unintended consequences of AMU development, from the range of perspectives. We then draw together the themes arising in the analysis from the different perspectives of service managers, professionals, women and families using the services and other key stakeholders. This illuminates some of the key challenges of the development of AMUs as well as the benefits, intended or unintended consequences. Finally, we indicate some areas for service development and debate.
Intended and unintended consequences of alongside midwifery unit development
It is well documented that service changes and reconfigurations can have unintended as well as intended consequences, both positive and negative. 97,98 Even though the drivers for opening an AMU were pragmatic, linked to service reconfiguration and cost savings in three of the four services, the main aims of the unit in all cases had been to facilitate:
-
women- and family-centred care in a homely setting, including postnatal support
-
a space for midwife-led care, skills development and provision for normal birth
-
appropriate care pathways and use of resources aligned to women’s needs and choices
-
a comfortable and calm labour and birth environment.
The key intended, as well as unintended, consequences identified by managers and professionals in these case studies are summarised in Table 7.
| Intended positive | Anticipated negative |
|---|---|
| Community midwives’ improved experience in attending births (Northdale, Midburn) | Fear of drop in home birth rates (Westhaven, no evidence given of actual drop) |
| Improvement in triage: more appropriate use of medical and midwifery care | Two tier service for high/low risk (Midburn – now working to change this by bringing features back into labour Ward) |
| Creates a space for midwife-led care, improve rates of normal birth | Midwives on the OU had lost skills and confidence in normal birth and midwife-led care and can be anxious and reluctant to work on an AMU |
| Increase low-risk care approaches across service | Boundary can create mistrust among OU staff and tensions between midwives |
| Incentive for midwives: recruitment/retention/morale | |
| Greater choice for birthing women and families | |
| Comfortable birth environment in which women and partners feel valued and cared for | |
| Unanticipated positive | Unanticipated negative |
| Décor and equipment improved on labour ward, inspired by AMU (Midburn, Westhaven) | Normal birth practices not brought back to OU as much as hoped and differences mean negative impact for women who transfer during labour (Southcity) |
| Rethinking OU routine practices such as routine CTG monitoring; introducing active birth practices such as using pools (Midburn) | Midwives on OU losing low-risk birth experience, not picking up normal birth skills (as seen as remit of the AMU) and OU practice medically dominated (Southcity) |
| Potential greater equality of access to midwife-led environment, particularly in opt-out units, for more socially deprived women and families | Inequality: higher-risk women lose out on family-centredness, comfort, homeliness |
| Reputation of unit and staff morale have improved (Midburn) | Stressful for doctors if called down to AMU as an unfamiliar environment |
| Integration of community midwives with AMU increasing experience of attending births: perceived safety benefit for home births (Northdale, Midburn) | Staff on OU only see the problems, may affect view of normality of birth |
| Safety measure: AMU helped to achieve service reconfiguration overall, closure of ‘failing unit’ (Midburn, manager 2) and turnaround in staff practice plus triage. Now feel whole service is safer (Midburn) | Dilution of resources taken away from OU, tensions over resources (Southcity). Staff being pulled to and fro, being split |
| Increased confidence in midwife-units facilitated development of a FMU | Tensions between units impacting on transfer decisions and process |
The overall view in all the case study services was that having a midwifery unit with a distinct environment and specific objective of facilitating normal, physiological birth begins to change the practices of professionals and the expectations of women receiving care. Contradictory views were expressed regarding whether or not such changes in both care environment and practices could be achieved without creating a distinct space. While some professionals argued that they did not see why such care could not be provided within the same area as the OU, others argued that without a separate space midwife-led care that supports active, physiological birth could not have been established and would not be maintained:
I think we’ll just slip, slide back if we lose that unit.
Westhaven OU, midwife
This view was supported by comments from both midwives and obstetricians that midwife-led care on an OU site is not the same as care in a midwifery unit, owing to medical oversight and the tendency to fall back on routine use of interventions such as CTG, even for low-risk women. Analysis of the accounts of all our respondents suggests that processes and environment of care cannot be unpicked easily. The differing environments of care were considered to influence women’s physiological labour, but also to impact on professional feelings, attitudes and practices. This was also reflected in the comments of women and partners, who valued both the physical and psychosocial environment of care.
The introduction of AMUs was also explicitly intended to improve recruitment and retention of midwives through making the service a more satisfying place for midwives to work. The labour ward manager in Midburn, for example, commented on improved recruitment and retention in a previously struggling service, while a Southcity manager commented on the attraction for midwives in being able to practise a full midwifery role. Midwives also talked about the midwifery unit as a calmer and more satisfying environment in which to work and to provide care, contrasted with the atmosphere of the OU. Stresses and tensions occurred instead around the boundaries between different professional and physical spaces.
Looking at intended or unintended consequences highlighted a number of contradictions in our respondents’ accounts of the impact of AMUs on the service overall. While some apparent contradictions may represent the different perspectives of those with different standpoints, they were often seen as trade-offs within the everyday life of providing maternity services. For example, the aim of improving low-risk care overall was weighed against the risks of loss of low-risk care experience on labour wards. Some staff, managers and stakeholders also spoke of inequalities they feared would be generated by the comfortable and homely environment offered only to low-risk women and increasing focus on risk and intervention in the labour ward with loss of a proportion of low-risk women. Conversely, a number of professionals commented on the migration of homely touches such as murals into the labour ward. They spoke about increasing awareness that some practices, such as using immersion in water for pain relief, more selective use of CTG and encouraging more mobility and active birth approaches could also be used on the labour ward, with high- and low-risk women. It seemed that with greater awareness came an increase in confidence about introducing and supporting these changes in cultural practices.
Such changes suggest that what at first sight appeared to be a trade-off – the loss of low-risk women and hence fears of losing normal birth care skills on labour ward – might in fact be an overall gain, with more low-risk care in both settings, depending on the ways in which care was managed. The perceived risk of inequality of access between low- and high-risk women was also balanced against the potential equality gains of an AMU as the standard low-risk care pathway in increasing access to women-centred care for more socially disadvantaged women. A diverse range of women and families were giving birth in the AMUs in this study. Similarly, in the Birthplace study, 80.9% of women planning birth in AMUs were white compared with 81.7% in OUs, 91.6% in FMUs and 94.8% at home. 1 Additionally, since the cost-effectiveness of offering AMU care was generally recognised, taking away low-risk women from the labour ward was also seen by some as lightening the load so that obstetricians could give more focused care to high-risk women needing their input.
Accounts from a range of professionals of their general experiences and attitudes indicated a risk of developing divergent types and styles of midwifery, even separate categories of midwives, specialising in high- or low-risk care. Managers’ plans to introduce some forms of midwife rotation and integration of community or caseload midwifery were intended, in part at least, to address such perceived risks of professional division. As discussed above, a number of respondents also commented on practices from the AMU being brought back into the OU, triggering OU staff to think more about their practices and to increase use of active birth aids and facilities on the labour ward. A Westhaven manager expressed the view that such approaches will become more integrated over time. However, we gathered considerable data indicating that this is not automatically achieved, which illuminated the potential risk of divergence and conflict between midwife groups.
Alongside midwifery units were developed with an aim of providing an environment supportive to normal physiological birth, in which midwives can practise autonomously, providing midwife-led care for women with straightforward healthy pregnancies, as part of the wider maternity service and located close to the OU. They were equally intended to provide a space to meet women’s wishes for an environment and care to support a normal birth, when possible, and a positive birth experience. The AMUs in our study followed a social model of care intended to be family friendly and to support birth as a normal life process, and this was expressed in the design of the environment and care.
Women and their families valued AMU care highly, for its relaxed and comfortable environment in which they felt cared for and valued and for its support for normal birth. However, there were some unanticipated negative consequences. Key points of transition for women could pose threats to the equity of access and quality of their care: information and preparation for AMU care and gaining admission in labour and transfer out of the alongside unit. Midwives working in AMUs highly valued the environment, approach and the opportunity to exercise their greater professional autonomy, but relations between units could also be experienced as problematic and as threats to professional autonomy as well as to quality and safety of care. In the following sections we discuss the key emerging themes that pose potential challenges for the quality, safety and sustainability of AMU care: boundary work and management, professional issues, staffing models and relationships, skills and confidence and information and access for women.
Boundary work and management
The development of midwifery units creates new boundaries within the maternity service that must be managed and negotiated effectively to ensure good quality and safe care. In the case of AMUs, the proximity of the units makes for a very particular type of boundary. The concept of the AMU attempts to combine both distance and closeness. It brings together complex reasoning that potentially causes tension – that closeness to the OU creates safety, but also that separation is needed to protect a space for normal, physiological birth.
The boundaries between the obstetric and alongside units worked on several levels: philosophical, professional and practical as well as physical, and they were complicated, rather than simplified by proximity. Closeness to the OU was often viewed by service users and professionals as representing safety and there was a tendency to expect that transfer in a proximate situation would be smoother and safer than transfer over a distance, as in FMUs. This is not necessarily supported by evidence on health care, although the findings of the Birthplace study indicated that both alongside and FMUs in England are providing safe care, while also reducing obstetric intervention rates. 1 Nonetheless, our data suggests that such complex and close boundaries may pose challenges for quality and safety in settings characterised by inter- or intraprofessional tensions and power play. This requires skilled management and leadership. Professional boundary work, including pressure to avoid transferring women or to accept women outwith guidelines, may pose a particular safety challenge. This is discussed further in Staff experiences and perspectives. Such tensions were exacerbated in settings where resources, particularly staffing, were felt to be scarce and stretched thin.
The stated rationale for developing AMUs was largely shared between the different positions of professionals, managers and women using the service. The philosophical intention of supporting normal birth was underpinned from a professional viewpoint by physiological theory, and from professionals’, women’s and managers’ viewpoints by the desire to have obstetric interventions used when clinically appropriate rather than routinely. Managers’ viewpoints were also increasingly driven by pragmatic considerations: value for money, the desire to triage levels of care effectively, to respond to the new targeting and commissioning landscape and to improve the efficiency and effectiveness of the service as well as the satisfaction of service users and recruitment and retention of staff.
While some respondents questioned the need to develop distinct units to achieve such objectives, a greater number pointed to lack of progress of previous strategies to create a better birthing environment, to increase rates of normal birth and establish evidence-based practices on OUs. There was considerable support for this view from obstetricians as well as midwives. Nonetheless, most were aware from their professional experience of the potential quality and safety challenges presented by boundaries within health care. Continuity of care and carer – organisational, relational and informational – has been widely found in previous studies to be important for both quality and safety of care and boundaries may create disjunctures and breaks in continuity. 14,99,100 Boundaries need to be sufficiently permeable to ensure smooth transfer of information or care when needed, particularly when being escalated. In the Birthplace Organisational Case Studies,2 we observed considerable boundary work taking place, in the case of AMUs in particular, and this pattern was also observed in the current study, suggesting that these issues are widespread.
Although boundaries present challenges for quality, equity and safety of care, there is now accumulating evidence that the environment of care does matter. 101 Additionally, there is developing evidence to support the contention that the care environment has an impact on staff well-being, stress and burnout, which may further affect quality of patient care. 102 This literature supports the observations and reports in this study that the AMU environment was an important feature of the service provided. The accounts of professionals and service users suggest that these different aspects of the care environment cannot simply be unpicked as they are closely inter-related. Although some respondents regarded the design aspects of the environment, such as domestic touches, as superficial in relation to actual care processes, our study findings overall suggest that attempts to alter either processes or environment of care in isolation are less likely to be effective.
From the women’s and families’ perspective, the critical points that threaten their experiences of feeling safe and well cared for were generally focused on the boundaries, such as getting information and access to choice around birth settings, getting timely admission to the chosen place of care and how boundaries are handled when transfer of care is needed or desired.
As indicated in the introduction to this report, issues of power and established ways of working can have important implications for risk and safety in health care and interpersonal issues may influence behaviour and decision-making amongst health-care professionals. 70,75,76 This current study adds to previous findings on this issue, highlighting that intra- as well as interprofessional tensions and boundary work, related to attitudinal as well as resource factors, were impacting on decision-making and behaviour around admissions and transfers. Territoriality was reflected in defensiveness, lack of trust and lack of understanding of each others’ roles or sense of working together. Some managers argued that the service should simply be focused on the most appropriate care for each woman, with escalation or transfer responding to her needs. However, resource, professional and organisational factors limited the capacity for care to be designed fully and flexibly around patient need. This echoes Vaughan’s findings on inherent barriers or resistance to communication, rooted in social organisation, as an important threat to quality and safety of care. 77
Professional issues
We collected a considerable amount of data in this study, from managers, professionals and women and partners pointing to the importance of professional issues in the organisation of AMU care. Direct tensions between midwives and obstetricians were not common. Support and communication between midwives and obstetricians from the most senior level emerged as important for the development and sustainability of midwife units. This was found in three of the four case study units, and it set a tone for general support, effective communication and teamworking between midwives and obstetricians across the service boundaries. Southcity was an exception in this regard. This may have been due, in part, to a high level of service change and instability and a well-established obstetrically oriented culture. Here, the AMU appeared to be professionally isolated rather than integrated within the overall service. Current midwifery service leaders were strongly focused on developments to achieve a more widely supported and integrated unit status.
Considerable intraprofessional tensions between midwives were identified. The tensions expressed and described between midwives are perhaps indicative of the current state of midwifery within the UK. The development of midwife units could be posited as a professional project, with midwives attempting to re-establish occupational closure and distinction from obstetrics. This is following the lines of normal/abnormal pregnancy and birth that were established in the historical regulation of midwifery in the UK in 1902,103 although the sphere of normality has shifted in the intervening century. With this in mind, it was of interest that professional tensions were more apparent between different groups of midwives than between midwives and obstetricians. This highlights the risk of exacerbating or opening up of new divisions between forms of midwifery, with differing levels of professional autonomy. There was evidence that developing midwifery units can present new disjunctures between forms of midwifery practice and some respondents expressed fears or assumptions around the emergence of different types of midwives or forms of midwifery practice. Professionals and managers working in both areas expressed the view that working in separate areas can create lack of understanding, empathy or co-operation. This was of concern, since all women, whatever their level of risk, could benefit from a social midwifery model of care and managers in all four services were looking at strategies to resolve such concerns, particularly through staffing models, rotation and in-service training and review. 14
Such strategies and professional leadership may hold a key to a more positive and shared re-establishment of midwifery skills to support the optimum opportunities for a normal, physiological birth, for all women. There were indications of positive developments building on the establishment of an AMU. These included greater confidence in midwifery skills to underpin FMU development, re-establishing birth skills of community midwives and of active birth approaches and skills on the OU. However, such developments needed appropriate leadership to maintain positive staff relationships and promote mutual learning. Managers discussed the importance of providing training for skills in both high- and low-risk birth care for all midwives, and particularly those working in midwife units. However, in practice, an observed implicit skills hierarchy militated against giving priority to those working in midwife units. The study also highlighted the need for midwives to work across boundaries to maintain their skills, mutual understanding and a holistic sense of midwifery practice. Earlier studies of caseload midwifery suggest that such cross-boundary integrated working can be achieved safely in a way that enhances, rather than undermines, continuity of care. 104
The tensions observed between midwives, with reluctance and even hostility on the part of some midwives towards work in the AMU, reflected fears and lack of familiarity and confidence in such skills, as well as tensions produced by shortages of midwives and general resource constraints. Such conditions encouraged a tendency of separate spaces for birth to engender a sense of professional separation. While some professionals, obstetricians as well as midwives, spoke of trust in individuals they knew, across such service or professional boundaries, this sense of reliance on interpersonal familiarity to overcome more deeply held prejudices or structural boundaries may pose threats to quality and safety of care when interpersonal trust is not present.
Although professional tensions were more evident between midwives than between midwives and obstetricians, these took place in a context in which midwifery units had been developed, at least in part, to achieve changes in practice which had been found difficult within the OU setting. The higher rates of intervention experienced by low-risk women planning birth in OUs1 indicates that the obstetric environment is not meeting the care needs of women with straightforward, healthy pregnancy and births effectively. The tensions between midwives were set within a professional context, in which high-technology skills and medical work continue to be regarded as inherently more valuable than caring work or the more traditional low-technology skills of midwifery.
Staffing models and relationships
Staffing models and relationships were seen as an important key to the quality, safety and sustainability of AMUs. In addition to a greater integration of community midwifery teams with midwife units, managers and consultant midwives proposed carefully managed introduction of rotation to enhance quality and safety along the following lines:
-
Provide sufficient basic staffing of midwifery units to support effective rotation management.
-
Maintain a core of experienced and confident midwives on the midwifery unit to support its ethos and practice and midwives’ skills level.
-
Partner less experienced midwives with those more experienced in midwife-led care for mentorship and support.
-
Pay attention to continuity of care when planning rotation.
-
Provide sufficient community midwifery staffing to enable integration with midwifery units and allow community midwives to maintain birth skills.
-
Provide sufficient core staff to enable midwifery unit midwives to transfer with women during labour and continue to provide care for her birth on the OU, before returning to the AMU.
Skills and confidence
This strategy would be supported by attention to staff training, supervision and support. We found that the ‘skills hierarchy’ was reflected in training priorities, with greater emphasis on high-risk and emergency skills than on the more traditional midwifery skills also required to support physiological birth and care for women with straightforward pregnancy and labour. All professionals and managers recognised that emergency and high-risk skills are essential for midwife-led care and for appropriate transfer decision-making and emergency care, but there were concerns around the maintenance of all-round skills in midwifery and the impact this could also have on midwifery relationships and teamworking. The proposals for rotation of midwives were seen as means to address these concerns, but the need to maintain a core of skilled and confident midwives working on midwife units was also emphasised, as well as the need to consider continuity of care.
Alongside midwifery units present an opportunity for midwives and obstetricians to learn and consolidate skills in supporting normal birth. We found no evidence of midwifery units being used for medical training for students or qualified doctors, and it was not clear that all midwifery students had opportunities for placements on midwifery units. Several obstetricians and managers commented on unintended negative potential consequences of midwives and obstetricians failing to develop or losing normal birth skills and developing a distorted view of birth if many low-risk women do not labour and birth on the OU. We were surprised, therefore, that so few manager and senior professional comments addressed professional education and training. Experience on midwife units by students or trainees also has the potential to reduce conflict by increasing familiarity with working in different areas, but this issue was not raised by our respondents.
Information and access to birth in midwife units
Approaches to booking: opt-in or opt-out
The majority of NHS care in the UK is primary care based, yet maternity care has been based in acute services since the 1970s. A key model on which the efficiency and effectiveness of the NHS arguably rests is one in which primary care professionals assess health needs and refer to specialist care when clinically appropriate, continuing to provide a large proportion of care for their populations. 93 This secondary-based model of care is, therefore, unusual within the NHS context and has not changed fundamentally in a period of considerable and continuing policy focus on shifting services to a more primary-care base and orientation.
The AMUs in our study provided intrapartum care for between 11% and 13% of births in their services. The rates of birth in their OUs remained > 80% in all settings, even when home births and FMU births (recently opened in two services) were taken into account. This suggests that potentially a larger number of women could receive labour and birth care in midwifery units.
Two of the AMUs in our study operated a primarily opt-in model, in which women had to actively opt for AMU care, and two operated an opt-out model in which AMU care was the normal pathway of care for low-risk women. Our data suggest that the proportion of births booked for and taking place in AMUs did not appear to be affected by which of these two pathway approaches was used. However, other factors, such as age and capacity of the unit and staffing constraints, could also have an impact on numbers. In practice, there was convergence between models; some women in both types of model did not receive information about birthplace options. Under the opt-out model, some women were not clearly informed that they had been booked into the AMU. As has been documented before, in the opt-in model some women do not hear about the opportunity. In theory, an opt-out model of booking has the potential to increase equity of access to choice of birthplace, since less socially advantaged women may otherwise be less likely to be aware and informed about such options. However, without improvement in the consistency and quality of information-giving, these potential benefits may not be fully realised. There were indications in our data that some professionals were choosing not to inform women about the option of birth in an AMU, while some were said to be too busy to remember to do so. This suggests that AMUs are not always fully integrated into their service and that information-giving is not routine and is subject to professional tensions or lack of familiarity and comfort with the concept of birth in midwife units. As the number of services included in this qualitative study was small, no firm conclusions can be drawn about the potential impact of the opt-out model for increasing equity.
The key concern that may be raised with respect to an opt-out approach is one of informed choice. Current policy states that women should make an informed decision about their place of birth and, in the case of an AMU, they need to be aware that transfer may be needed for personal or clinical reasons. However, in practice we found that lack of, or poor quality, information-giving applied in some cases in either an opt-in or an opt-out model. Additionally, we found no evidence that professionals are informing women of any of the well-established maternal risks associated with OU care, such as that choosing an OU may make it more likely that they have more interventions. 1 Instead, the data from both women and midwives indicated that information is often presented as a simple trade-off between a ‘nice’ environment and access to pharmacological pain relief, or between a ‘nice’ environment and clinical safety. One service provided antenatal visits in late pregnancy on the AMU, and midwives felt this offered a better opportunity for information and preparation for giving birth in the unit, including managing labour pain, as well as an opportunity to meet the midwives working there. Midwives working in the other case study AMUs suggested that more information and preparation opportunities should be available. These professional observations were supported by the data from women and partners, which indicated they had received limited information about physiological labour, managing pain or about the risks and benefits of different options from midwives. In addition, we found that some women received information later in pregnancy and through more informal sources rather than from midwives. Equality of access may be strengthened by the adoption of approaches in which the midwifery unit, rather than the OU, is the default pathway for low-risk care, with women fully informed and offered preparation for physiological birth as well as being given alternative choices of birth setting.
Continuity of care has value from the women’s and partners’ viewpoint, as well as a service quality and safety perspective. Effective integration of the AMU within its service and appropriate arrangements for transfer can support continuity and quality of care. Movement across service boundaries was a potential difficulty for women and being admitted to, or transferred from the units were key points that could influence their experience and sense of well-being. The need for an integrated system from the women’s viewpoint mirrored the needs expressed by midwives for good working relationships across the boundaries.
Both a medical model of care and a social model of care may advocate for women to remain at home during early or latent phase labour. In a medical model, the view is that, until active labour is established, hospital care is not relevant, while a social model may regard the home environment as a more appropriate and relaxing place to be while labour becomes established. In either model, the view of the ‘clock ticking’ following formal admission may impact on professionals’ views of the appropriate place to be. 96 It was notable, therefore, that the policies used in these AMUs were essentially similar to those found nationally for OUs, despite the philosophy and environment designed and considered to be conducive to normal, physiological birth.
Limitations of the study
When considering the findings of this study, the limitations of the approach need to be borne in mind. This was a qualitative study with a sample of only four services in England. Although these were selected for maximum variation, they cannot be assumed to be a representative sample of services in England that include an AMU. In a study of this type, generalisation works on a conceptual and theoretical level and it cannot be assumed that other cases will share similar characteristics. Nonetheless, the services and the issues they raised appeared typical in that midwives and managers across the country in discussion workshops we have held about the study have confirmed that the themes ring true and engage with their own experiences and service challenges. While qualitative data analysis does not seek to achieve objectivity, but rather to understand the subjectivity and experiences of the case in hand, our approach, including checking of the analysis process within the core team, with co-investigators and the wider advisory group gives some confidence in the validity and reliability of the approach. While the study highlights the experiences and perspectives of those involved in these cases, and the researcher observations, the findings resonate strongly with the existing literature and with the findings of our prior Birthplace Organisational Case Studies.
Chapter 7 Conclusions and implications
The AMUs in this study were providing care for 10–14% of all births in their services (approximately 620–830 births per year), with two units having an opt-in and two an opt-out approach to referring women. Opt-in approaches sought to establish AMU care as the standard birth pathway for low-risk women, with women able to choose the OU, home birth or (when available) a FMU as alternatives. This was in line with an aim to normalise midwife-led care for low-risk women, which had been found difficult to establish in obstetrically led settings. With opt-in approaches, women needed to specifically opt to book their labour and birth care in the AMU. All four AMUs had core midwifery staffing, with between one and three core midwives per shift, supported in three cases by a MSW, and in one case also by on-call community midwives. One unit had also received cover by caseload midwives attending women on their personal caseloads, but this service was perceived as expensive and so had declined. All services were considering some form of rotation for midwives.
We did not find evidence in this study of impact of unit size but all were relatively similar in size, caring for between about 10% and 14% of births in their trust, around a quarter of the clinically eligible population. We similarly did not find any evidence that positioning of the AMU within the hospital makes a difference, as compared with quality of interprofessional relationships and ethos of care. However, this was a small sample with limited scope of comparison.
The development of AMUs has been intended to enable more appropriate and effective pathways for labour and birth care for women who are of low risk obstetrically, to support normal, physiological birth for low-risk women and to provide a home-like environment in which women and their families feel relaxed and comfortable. It is has also been intended to improve the professional satisfaction of midwives and enable them to practice their skills and role fully in caring for women with straightforward healthy pregnancies.
The concept of a care pathway ideally provides for the smooth and effective flow of people and resources through a complex system. The attempt to develop a low-risk pathway for birth arises in a service context, in the UK and internationally, in which birth had shifted towards an acute, secondary care model and base. However, the majority of women have straightforward, healthy pregnancies and so require a more primary-focused model of care. Additionally, concerns have been raised over a number of decades around the levels of obstetric intervention in childbirth and about dissatisfaction levels among providers as well as users of maternity care.
Developing midwifery units forms a key part of a strategy to provide a low-risk pathway for women throughout the maternity experience. Their development followed accumulated experience and evidence of the challenges to providing low-risk labour and birth care in OUs. Following this, the Birthplace in England study identified a relationship between type of unit and intervention rates, independent of women’s characteristics. 1
The aim in complex health-care systems is for professionals and patients to be located appropriately within this system and able to move across it without difficulty according to care needs. However, the development of a distinct unit involves the creation of a new set of boundaries that the care pathway needs to bridge. In the case of AMUs the service configuration brings together physical and organisational, philosophical and professional boundaries. Therefore, although the organisational intention is that the service boundaries should be permeable, with smooth flow across these according to agreed, evidence-based guidelines and patients’ preferences and needs, a range of factors may present challenges to this model.
A key challenge identified in this study was finance and its impact on staff resources, particularly in midwifery. Despite the philosophical aims of providing AMU care, most had been developed in the context of service reconfigurations involving centralisation and closure or merger of some services. The AMU was seen at management level as an effective use of limited resources, through more appropriate triage of women’s pathways of care according to level of risk. However, this understanding was not shared by all professionals and some midwives and obstetricians perceived the allocation of midwifery staff to the AMU as a drain on, or a dilution of, hard-pressed service resources. In all the services studied, lack of midwifery staff and feelings of pressure were observed at times to impact on decision-making around transfer of women between units. Accounts of professionals and some women indicated that admission and transfer could be influenced by service pressures and professional relationships as well as by clinical factors.
The context of constrained resources was also observed to interact with professional issues, and had the potential for development of tensions in relationships between different staff groups. The AMU was associated with a different philosophy of birth – a more social or ecological model as compared with a medical model. Managers, midwives and obstetricians talked of different types of midwives, and divergence of skills, while also maintaining the view that midwives in the UK are educated and professionally prepared to provide all-round care and to detect signs of complications or deterioration when caring for low-risk women. Interprofessional training was valued, but tended to focus on high-risk and emergency skills and protocols, without also giving attention to shared development of low-risk and normal birth skills. There was evidence from managers, midwives and obstetricians that some midwives used to working on an OU lacked confidence to work in an AMU; resistance to working across OU and AMU reflected some midwives’ lack of comfort with this, as well as reflecting staffing pressures. This pattern was also identified in Newburn’s in-depth study of an AMU,71 which, as in this current study, also highlighted an issue of lack of trust in the decision-making across midwives in obstetric and AMU settings, with less experienced midwives working in AMUs particularly affected by feelings of judgement from their OU peers.
The professional, service and philosophical boundaries were also expressed in the design of the AMU, both as a home-like space and as a space designed to facilitate more active, physiological labour and birth. The AMUs were also explicitly designed as family-oriented spaces, reflecting a social model of birth. This was reported to be a response to the difficulty of introducing such a model into OUs and in reducing intervention rates to a more clinically appropriate level. There were some indications in this study of spread of environmental and practice features from the AMU to the OU. This was a desired outcome, in the views of managers and professionals, rather than a formally developed strategy, but staff talked of homely touches and gradual familiarisation with and adoption of more active birth practices within the OU. This finding suggests that AMUs do have the potential to facilitate greater access to support for normal birth across all women, rather than dividing women in terms of risk and undermining normal birth practice on OUs. However, our findings indicate that good management is needed to foster and underpin this potential benefit.
From the women’s viewpoint as well as the management and professional perspective, smooth transfer across boundaries was important, and when this was not the case women and their partners were more likely to be distressed or dissatisfied with their care. Even with the AMU as the routine low-risk pathway, as in the case of opt-out models, women expressed some anxieties about being eligible for the AMU and being admitted at the appropriate time in labour. Additionally, some did not receive information about the option to labour and birth in the AMU and many only obtained this late in pregnancy, through more indirect means, rather than directly from midwives. Women and their partners were aware of the ethos of the unit, and valued this highly, and were aware of the potential need for transfer. However, their accounts indicated limited opportunities for preparation for giving birth in the AMU and particularly limited information and advice around the physiology and psychology of pain in labour and techniques for coping with pain. Few women in our study experienced transfer in labour out of the AMU, but most women regarded the short time and distance of transfer, if needed, as an advantage of AMU care. Nonetheless, the findings also highlighted that, while the transfer duration from AMU to OU is a potential benefit from the women’s viewpoint, inter- and intraprofessional tensions impacting on transfer decision-making could potentially lead to more hidden and less measurable delays and barriers to timely and smooth transfer of care.
Women who had experienced care within the AMU valued the care very highly, as well as the quality of the environment and its family-friendly aspect. The women we interviewed were very positive about having the choice to give birth in an AMU and felt it was an important option for those who would not contemplate a FMU or home. There is evidence that AMUs are caring for a more diverse range of women1 and our findings suggest that this is partly linked to being able to have an opt-out model, facilitating inclusion of women who have less particular information and confidence about alternative models of care. Nonetheless, there was some evidence that professionals, despite a rhetoric of choice and women-centred care, wanted to steer choices in terms of what they see as the women’s best interests, whether by avoiding giving information about choice of birth settings or by encouraging women to choose a particular option. Additionally, some women did not receive full and evidence-based information to support making choices or preparing for birth in different settings.
Midwives working in AMUs valued them highly, as did some OU midwives and those midwives who worked across areas. AMUs also represented, from the management viewpoint, an opportunity for community midwives to rebuild their experience of attending births and confidence in this, with a focus on normal birth skills as well as detecting abnormalities. There was some evidence of increased confidence in midwifery skills and midwife-led care across the whole service with the establishment of the AMUs. This was reflected in obstetricians’ views and in the moves to develop FMUs in three of the services, which managers felt would not have been achievable without the prior AMU development and experience. There was some, albeit limited, evidence of a shift towards adopting more normal birth practices across the service and managers were aware of the need to support this actively rather than assume this would occur.
Leadership was important for developing and sustaining the AMUs, to ensure integration within the service and for the AMU to be seen as a standard care pathway. This was also supported by guidelines and protocols that were agreed by all professionals, to counter tensions over skills and resources. Leadership steer across midwifery and obstetrics, between professional and trust leads, and between service and commissioners was important to this. Target driven care can support such developments but with a risk that managers are entrenched in targets in such a way that women-centred care or philosophy of care and public health considerations become secondary to these. Leadership roles were also important for establishing a learning culture and to set the tone for inter- and intraprofessional relationships, respect, communication and teamworking, and participation in service audits and reviews that are needed to underpin quality and safety.
All units had clear criteria for eligibility for AMU care, which guided admission and transfers. However, they commented that many individual women fall into grey areas when decision-making needs to be more individualised. At times, the AMU was treated as a compromise option for women at higher risk of complications who consultants feared might otherwise give birth at home, possibly without professional attendance. This raises questions for services about their capacity to offer more individualised care and to support normal birth for higher-risk women on the OU. Additionally, a number of organisational pressures were experienced that could impact on the application of guidelines, with pressures experienced to delay less urgent transfers, and questioning of midwives’ clinical judgement or management when transfer was requested. This indicates an area for further discussion around appropriate guidelines and the potential risks for service users and providers of pressures on use of guidelines in practice.
The development of AMUs brings together a set of key motivations and policies, which can be in tension with each other. Aims include increasing normal, physiological birth through providing a more facilitative environment and form of care, providing a more woman- and family-centred birth environment, improving the triage and effectiveness of care pathways and professional division of labour and improving, or re-establishing, the traditional normal birth skills of midwives, thus also improving midwife staff motivation and retention. Arguably, the development of AMUs is a professional project, intended to re-establish the full scope of midwifery practice and the normal-birth core of the midwife role, as well as a project to improve and increase choices for women and families. In our study, such a tension was illuminated in particular through boundary work and everyday conflicts between different groups of midwives, as well as more occasional conflicts with obstetricians.
Some initiatives for increasing integration of care were identified which could potentially mitigate the effects of creating new boundaries or discontinuities in the service. These could also support quality and safety of care, and the well-being of professionals as well as service users. They included a planned system of rotation for staff, with mentoring for midwives who are less experienced and skilled in caring for normal physiological birth and more integrated community-hospital models in which midwives based in the community attend the women on their caseload giving birth at home or in the FMU or AMU and transfer with them if required. The potential value of interdisciplinary training, situated in the FMUs and AMUs and covering both low-risk and emergency skills, was also proposed. Staffing models, supported by education and training, to enable midwives to move more easily between the midwifery unit and OU and provide continuity of care for women who transfer were highlighted as potentially more satisfying for midwives as well as women and their partners.
Recommendations for future research
As well as answering questions, studies such as this raise many new questions and refine existing ones. Additionally, ethnographic research approaches may often be important for generating hypotheses and for investigating in more depth the ‘how’ and ‘why’ questions posed in research around organisation of care.
This study raises a number of questions for future research including the following:
-
What is the most appropriate model for midwife staff rotation in a complex maternity service configuration to ensure continuity and quality of care, maintenance of professional skills and job satisfaction?
-
What is effective in increasing confidence and competence of hospital-based midwives and community-based midwives in normal birth and emergency skills, both of which include communication and escalation skills as well as clinical skills?
-
What is the potential of integration of community teams to enhance community midwives’ birth skills and confidence, in particular, and how can this be managed and supported?
-
What is the impact of the care environment on staff well-being and patient experience and outcome?
-
What is the impact of midwifery units on midwifery staffing recruitment and retention?
-
What are the facilitators and barriers to expansion of midwifery unit capacity, in order to attend a greater proportion of women who require low-risk care in labour?
This study highlighted possible factors to help explain the differences in outcomes identified in the Birthplace study between AMUs and FMUs, in terms of intervention rates and rates of normal birth. However, it is not able to provide definitive evidence on the significance or relative importance of factors such as staff skills, confidence and attitudes; women’s knowledge, confidence and attitudes; care processes; guidelines; ethos or physical design of the environment. In practice, this is difficult to discern because different factors are likely to be iterative but further work on this would be valuable. More work is also needed on the relationship of different aspects of the care environment to processes and outcomes of care, as well as to staff and user satisfaction.
In terms of women’s and partners’ experiences, research questions arising include:
-
How can information be provided more effectively to reduce inequities in access?
-
What is the most effective way prepare women and partners for labour and birth in a midwife unit, for normal, physiological labour and birth and for alternative approaches to pain management?
-
How can early labour/latent labour care be designed to ensure women feel supported and confident, while also avoiding risk of iatrogenic intervention?
Acknowledgements
We wish to thank all the women, families, professionals and other stakeholders who supported this study by responding in interviews, hosting the study observations or sharing their time and views with us. Thanks also particularly to our advisory group members who brought such a wealth of experience and commitment to improving maternity services to our meetings. Their ideas and discussions contributed greatly to the analysis.
This report was written by the authors on behalf of all the study co-investigators.
Co-investigator group members were: Sarah Beake – King’s College, London, UK, and Imperial College Health Care NHS Trust, London, UK; Susan Bewley – King’s College, London, UK and Guy’s and St. Thomas’s NHS Foundation Trust, London, UK; Peter Brocklehurst – University College London, London, UK; Pauline Cooke – Imperial College Health Care NHS Trust, London ,UK; Marie Macdonald – Guy’s and St. Thomas’s NHS Foundation Trust, London, UK; Mary Newburn – NCT, UK.
Advisory group members
Dr Narendra Aladangady, Neonatologist, Homerton University Hospital NHS Foundation Trust, Research lead for women’s and children’s health.
Sue Allen-Mills, Cambridge Maternity Services Liaison Committee (MSLC) chair, service user member.
Dr Ruth Deery, Professor in Maternal Health, University of the West of Scotland and NHS Ayrshire and Arran.
Liz Glenister, Head of Midwifery and Gynaecology, Southend University Hospital NHS Foundation Trust, replaced on retirement by Antoinette Walsh, Acting Matron for Postnatal and Antenatal Triage, Community Midwifery.
Barbara Kuypers, Local Supervising Authority Midwifery Officer, NHS West Midlands.
Dr Michele Mohajer, Consultant in fetal and maternal medicine and Lead Obstetrician, Shrewsbury and Telford Hospital NHS Trust.
Dr Mary Stewart, Senior Lecturer in midwifery, King’s College, London.
Janine Stockdale, RCM Research Fellow, RCM.
Dr Suzanne Tyler, Associate Director of Programmes, Maternity and Newborn, NHS South Central.
Hana Xassan, Chair Tower Hamlets MSLC, service user member.
Contributions of authors
Christine McCourt was principal investigator and was involved in the design, conduct, analysis and writing up of this project. She is Professor of Maternal and Child Health at City University, London, UK.
Juliet Rayment was a co-investigator and was involved in the design, conduct, analysis and writing up of this project. She was a full-time research associate for this project, based at City University, London, UK.
Susanna Rance was a co-investigator and was involved in the design, conduct, analysis and writing up of this project. She was a full-time research associate for this project, based at King’s College, London, UK.
Jane Sandall was a co-investigator and was involved in the design, conduct, analysis and writing up of this project. She is Professor of Social Science and Women’s Health at King’s College, London, UK.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- Birthplace Collaborative Group . Perinatal and maternal outcomes by planned place of birth for healthy women with low risk pregnancies: the Birthplace in England national prospective cohort study. BMJ n.d.;343.
- McCourt C, Rance S, Rayment J, Sandall J. Birthplace Qualitative Organisational Case Studies: How Maternity Care Systems May Affect the Provision of Care in Different Birth Settings. Birthplace in England Research Programme. Final Report Part 6 2011.
- NHS Maternity Statistics, England: 2005–06. London: The Information Centre; 2007.
- Redshaw M, Rowe R, Schroeder L, Puddicombe D, Macfarlane A, Newburn M, et al. Mapping Maternity Care. The Configuration Of Maternity Care In England. Birthplace in England Research Programme. Final Report Part 3 2011.
- Department of Health . National Service Framework for Children, Young People and Maternity Services: Maternity Standard 11. 2004.
- Department of Health Partnerships for Children Families and Maternity . Maternity Matters: Choice, Access and Continuity of Care in a Safe Service. 2007.
- Intrapartum Care Of Healthy Women And Their Babies During Childbirth. National Collaborating Centre for Women’s and Children’s Health. London: Royal College of Obstetricians and Gynaecologists; 2007.
- Tyler S. Commissioning Maternity Services: A Resource Pack to Support Clinical Commissioning Groups. London: NHS Commissioning Board, a Special Health Authority; 2012.
- Department of Health . The Operating Framework for the NHS in England 2012 13. 2011.
- Department of Health . The NHS Outcomes Framework 2012 13. 2011.
- Department of Health . The Mandate. A Mandate from the Government to the NHS Commissioning Board: April 2013 to March 2015 2012.
- Location, Location, Location: Making Choice of Place of Birth a Reality. London: National Childbirth Trust; 2009.
- Birthplace in England. Research Digest. London: NHS Confederation; 2012.
- Hatem M, Sandall J, Devane D, Soltani H, Gates S. Midwife-led versus other models of care for childbearing women. Cochrane Database Syst Rev 2008;4. http://dx.doi.org/10.1002/14651858.CD004667.pub2.
- Falconer T, Walker J, Richmond D, Kilby M. Perinatal and Maternal Outcomes by Planned Place of Birth for Healthy Women With Low Risk Pregnancies: The Birthplace in England National Prospective Cohort Study, Rapid Response. BMJ 2011. www.bmj.com/rapid-response/2011/12/01/re-perinatal-and-maternal-outcomes-planned-place-birth-healthy-women-low-r (accessed 16 January 2014).
- Working Conditions - Working Time Directive. n.d.
- Sandall J, Homer C, Sadler E, Rudisill C, Bourgeault I, Bewley S, et al. Staffing in Maternity Units: Getting the Right People in the Right Place at the Right Time. London: The King’s Fund; 2011.
- Ball L, Curtis P, Kirkham M. Why do Midwives Leave?: Report of the Women’s Informed Childbearing and Health Research Group. Sheffield: University of Sheffield; 2002.
- Hunter B. Midwifery 2004;20:261-72. http://dx.doi.org/10.1016/j.midw.2003.12.004.
- Walsh D, Newburn M. Towards a social model of childbirth Part 1. Br J Midwifery 2002;10:476-81.
- Young G, Hey E. Choosing between home and hospital delivery. BMJ 2000;320. http://dx.doi.org/10.1136/bmj.320.7237.798.
- Wax JR, Pinette MG, Cartin A. Home versus hospital birth-process and outcome. Obstet Gynecol Surv 2006;65:132-40. http://dx.doi.org/10.1097/OGX.0b013e3181d0fe5d.
- Walsh D, Downe SM. Birth 2004;31:222-9.
- Hodnett ED, Downe S, Edwards N, Walsh D. Home-like versus conventional institutional settings for Birth. Birth 2005;32. http://dx.doi.org/10.1111/j.0730-7659.2005.0359a.x.
- Mohajer M, Hughes A, Ghosh S. Midwifery-led birthing units. Obstet Gynaecol Reprod Med 2009;19:169-71. http://dx.doi.org/10.1016/j.ogrm.2009.03.003.
- Rowe RE. Local guidelines for the transfer of women from midwifery unit to obstetric unit during labour in England: a systematic appraisal of their quality. Qual Saf Health Care 2010;19:90-4. http://dx.doi.org/10.1136/qshc.2008.030239.
- Hunter B. Emotion Work in Midwifery: An Ethnographic Study of the Emotional Work Undertaken by a Sample of Student and Qualified Midwives in Wales 2002.
- Ledward A, Frith L. Ethics and Midwifery: Issues in Contemporary Practice. Oxford: Butterworth-Heinemann; 1996.
- Hunter M, Kirkham M. Birth Centres: A Social Model for Maternity Care. London: Books for Midwives; 2003.
- Kirkham M. Birth Centres: A Social Model for Maternity Care. London: Books for Midwives; 2003.
- Garelick A, Fagin L. The doctor–manager relationship. Adv Psychiatric Treat 2005;11:241-50. http://dx.doi.org/10.1192/apt.11.4.241.
- Pinki P, Sayasneh A, Lindow SW. The working relationship between midwives and junior doctors: a questionnaire survey of Yorkshire trainees. J Obstet Gynaecol 2007;27:365-7. http://dx.doi.org/10.1080/01443610701327529.
- Sandall J, Jill M, Mansfield A. Support workers in maternity services. J Fam 2007;17:191-2.
- Prowse J, Prowse P. Role redesign in the National Health Service: the effects on midwives’ work and professional boundaries. Work Employment Soc 2008;22:695-7.
- Shaw R, Kitzinger C. Calls to a home birth helpline: empowerment in childbirth. Soc Sci 2005;61:2374-83. http://dx.doi.org/10.1016/j.socscimed.2005.04.029.
- Davis-Floyd R, Davis E. Intuition as authoritative knowledge in midwifery and homebirth. Med Anthropol Q 1996;10:237-69. http://dx.doi.org/10.1525/maq.1996.10.2.02a00080.
- Halford S, Leonard P. Space and place in the construction and performance of gendered nursing identities. J Adv Nurs 2003;42:201-8. http://dx.doi.org/10.1046/j.1365-2648.2003.02601.x.
- Gilmour JA. Hybrid space: constituting the hospital as a home space for patients. Nurs Inq 2006;13:16-22. http://dx.doi.org/10.1111/j.1440-1800.2006.00276.x.
- Fannin M. Domesticating birth in the hospital: ‘family-centered’ birth and the emergence of ‘homelike’ birthing rooms. Antipode 2003;35:513-35. http://dx.doi.org/10.1111/1467-8330.00337.
- Michie H, Aiken SH, Brigham A, Marston SA, Waterston P. Making Worlds. Tucson, AZ: University of Arizona Press; 1998.
- Andrews GJ. Towards a more place-sensitive nursing research: an invitation to medical and health geography. Nurs Inq 2002;6:221-39. http://dx.doi.org/10.1046/j.1440-1800.2002.00157.x.
- Andrews GJ. Locating a geography of nursing: space, place and the progress of geographical thought. Nurs Philos 2003;4:231-48. http://dx.doi.org/10.1046/j.1466-769X.2003.00140.x.
- Andrews GJ. Geographies of health in nursing. Health Place 2006;12:110-18. http://dx.doi.org/10.1016/j.healthplace.2004.10.002.
- Andrews GJ, Shaw D. Clinical geography: nursing practice and the (re)making of institutional space. J Nurs Manag 2008;16:463-73. http://dx.doi.org/10.1111/j.1365-2834.2008.00866.x.
- Gesler W, Bell M, Curtis S, Hubbard P, Francis S. Therapy by design: evaluating the UK hospital building program. Health Place 2004;10:117-28. http://dx.doi.org/10.1016/S1353-8292(03)00052-2.
- Lankston L, Cusack P, Fremantle C, Isles C. Visual art in hospitals: case studies and review of the evidence. J R Soc Med 2010;103:490-9. http://dx.doi.org/10.1258/jrsm.2010.100256.
- Conradson D. Landscape, care and the relational self: therapeutic encounters in rural England. Health Place 2005;11:337-48. http://dx.doi.org/10.1016/j.healthplace.2005.02.004.
- Gesler WM. Therapeutic landscapes: medical issues in light of the new cultural geography. Soc Sci Med 1992;34:735-46. http://dx.doi.org/10.1016/0277-9536(92)90360-3.
- Foureur M, Davis D, Fenwick J, Leap N, Iedema R, Forbes I, et al. The relationship between birth unit design and safe, satisfying birth: developing a hypothetical model. Midwifery 2010;26:520-5. http://dx.doi.org/10.1016/j.midw.2010.05.015.
- Hausman BL. Risky business: framing childbirth in hospital settings. J Med Humanit 2005;26:23-38. http://dx.doi.org/10.1007/s10912-005-1050-3.
- Hodnett ED, Downe S, Walsh D. Alternative versus conventional institutional settings for birth. Cochrane Database Syst Rev 2012;8. http://dx.doi.org/10.1002/14651858.CD000012.pub3.
- Making Normal Birth a Reality. London: NCT/RCM/RCOG; 2007.
- Schroeder E, Petrou S, Patel N, Hollowell J, Puddicombe D, Redshaw M, et al. Cost effectiveness of alternative planned places of birth in woman at low risk of complications: evidence from the Birthplace in England national prospective cohort study. BMJ 2012;344:1-13. http://dx.doi.org/10.1136/bmj.e2292.
- Houghton G, Bedwell C, Forsey M, Baker L, Lavender T. Factors influencing choice in Birthplace: An exploration of the views of women, partners and professionals. Evid Based Midwifery 2008;6:59-64.
- Pitchforth E, Van Teijlingen E, Watson V, Tucker J, Kiger A, Ireland J, et al. ‘Choice’ and place of delivery: a qualitative study of women in remote and rural Scotland. Qual Saf Health Care 2009;18:42-8. http://dx.doi.org/10.1136/qshc.2007.023572.
- Hundley V, Ryan M. Are women’s expectations and preferences for intrapartum care affected by the model of care on offer?. BJOG 2004;111:550-60. http://dx.doi.org/10.1111/j.1471-0528.2004.00152.x.
- Newburn M. Culture, control and the birth environment. Pract Midwife 2003;6:20-5.
- Newburn M. The best of both worlds – parents’ motivations for using an alongside birth centre from an ethnographic study. Midwifery 2012;28:61-6. http://dx.doi.org/10.1016/j.midw.2010.10.014.
- Overgaard C, Fenger-Gron M, Sandall J. The impact of birthplace on women’s birth experiences and perceptions of care. Soc Sci Med 2012;74:973-81. http://dx.doi.org/10.1016/j.socscimed.2011.12.023.
- Longworth L, Ratcliffe J, Boulton M. Investigating women’s preferences for intrapartum care: home versus hospital births. Health Soc Care Community 2001;9:404-13.
- Rowe RE, Fitzpatrick R, Hollowell J, Kurinczuk JJ. Transfers of women planning birth in midwifery units: data from the birthplace prospective cohort study. BJOG 2012;119:1081-90. http://dx.doi.org/10.1111/j.1471-0528.2012.03414.x.
- Rowe RE, Kurinczuk JJ, Locock L, Fitzpatrick R. Women’s experience of transfer from midwifery unit to hospital obstetric unit during labour: a qualitative interview study. BMC Pregnancy Childbirth 2012;12. http://dx.doi.org/10.1186/1471-2393-12-129.
- Towards Better Births: a Review of Maternity Services in England. London: Commission for Healthcare Audit and Inspection; 2008.
- Staffing Standard in Midwifery Services. Guidance Paper No. 7. London: Royal College of Midwives; 2009.
- Safer Childbirth: Minimum Standards for the Organisation and Delivery of Care in Labour. London: Royal College of Obstetricians and Gynaecologists; 2007.
- Clinical Negligence Scheme for Trusts. Maternity Clinical Risk Management Standards. Version 1. 2012.
- Clinical Negligence Scheme for Trusts. Maternity Clinical Risk Management Standards. 2012.
- Deery RH, Kirkham M. Tensions and Barriers in Improving Maternity Care. Oxford: Radcliffe; 2010.
- Walsh D. Improving Maternity Services: Small Is Beautiful – Lessons From A Birth Centre. Abingdon: Radcliffe; 2007.
- Rayment J. Midwives’ Emotion and Body Work in Two Hospital Settings: Personal Strategies and Professional Projects. 2011.
- Newburn M. An Emerging Model for Maternity Care: an Ethnographic Pilot Study of an Inner-City Birth Centre. London: London School of Hygiene and Tropical Medicine; 2009.
- Kirkham M. Retention and return in the NHS in England. RCM Midwives 2007;10:224-6.
- Garland P, Cunningham S, Mander A, Sweeney J. Maternity Services at Wyre Forest Birth Centre 2004.
- Healthcare Commission . Investigation into 10 Maternal Deaths At, or Following Delivery At, Northwick Park Hospital, North West London Hospitals NHS Trust, Between April 2002 and April 2005 August 2006 2006.
- Silbey S. Taming Prometheus. Talk about safety and culture. Annu Rev Sociol 2009;35:341-69. http://dx.doi.org/10.1146/annurev.soc.34.040507.134707.
- West E. Sociological contributions to the study of adverse events: organisational sources of safety and danger. Qual Health Care 2000;9:120-6. http://dx.doi.org/10.1136/qhc.9.2.120.
- Vaughan D. The dark side of organisations: mistake, misconduct, and disaster. Annu Rev Sociol 1999;25:271-305.
- Davis-Floyd R. Home-birth emergencies in the US and Mexico: the trouble with transport. Soc Sci Med 2003;56:1911-31. http://dx.doi.org/10.1016/S0277-9536(02)00213-7.
- Hogg M, Penney G, Carmichael J. Audit of Care Provided and Outcomes Achieved by Community Maternity Units in Scotland 2005. Aberdeen: Scottish Programme for Clinical Effectiveness in Reproductive Health (SPCERH); 2007.
- Bick D, Rycroft-Malone J, Fontenla M. A case study evaluation of implementation of a care pathway to support normal birth in one English birth centre: anticipated benefits and unintended consequences. BMC Pregnancy Childbirth 2009;9. http://dx.doi.org/10.1186/1471-2393-9-47.
- Huber U, Sandall J. Mapping Women’s Journeys Through Care: Intrapartum Referral, Transfer and Handover from a Midwife Led Birth Centre to Tertiary Care. Poster presentation 2008.
- Hunter B. Final Project Report: A Policy Ethnography to Explore the Implementation of the All Wales Clinical Pathway for Normal Labour. Swansea: Institute of Health Research, Swansea University; 2007.
- Øvretveit J. Evaluating Health Interventions: an Introduction. Buckingham: Open University Press; 1998.
- Stake R, Denzin NK, Lincoln YS. Handbook of Qualitative Research. Thousand Oaks: Sage Publications; 1994.
- Creasy RK. Management of Labor and Delivery. Oxford: Blackwell Science; 1997.
- Green JM, Baston H, Easton S, McCormick F. Greater Expectations? Inter-Relationships Between Women’s Expectations and Experiences of Decision Making, Continuity, Choice and Control in Labour, and Psychological Outcomes 2003.
- McCourt C, Pearce A. Does continuity of carer matter to women in minority ethnic groups. Midwifery 2000;16:145-54. http://dx.doi.org/10.1054/midw.2000.0204.
- Walker J. Women’s experiences of transfer from a midwife-led to a consultant-led maternity unit in the UK during late pregnancy and labor. J Midwifery Womens Health 2000;45:161-8. http://dx.doi.org/10.1016/S1526-9523(99)00048-3.
- Ritchie J, Spencer L, O’Connor W, Ritchie J, Lewis J. Qualitative Research Practice: A Guide for Social Science Students and Researchers. London: Sage Publications; 2003.
- Latest UK Maternity Statistics. 2014.
- Changing Childbirth: Report of the Expert Maternity Group. London: HMSO; 1993.
- Making Hospitals Work. 2009.
- Jeffcott SA, Ibrahim JE, Cameron PA. Resilience in healthcare and clinical handover. Qual Saf Health 2009;18:256-60. http://dx.doi.org/10.1136/qshc.2008.030163.
- Mathers N, Hodgkin P. The gatekeeper and the wizard: a fairy tale. BMJ 1989;298:172-4. http://dx.doi.org/10.1136/bmj.298.6667.172.
- Christiaens W, Gouwy A, Bracke P. Does a referral from home to hospital affect satisfaction with childbirth? A cross-national comparison. BMC Health Serv Res 2007;12. http://dx.doi.org/10.1186/1472-6963-7-109.
- McCourt C, McCourt C. Childbirth, Midwifery and Concepts of Time. New York, NY: Berghahn Books; 2009.
- Fell G, Haroon S. Learning from a rapid health impact assessment of a proposed maternity service reconfiguration in the English NHS. BMC Public Health 2008;25. http://dx.doi.org/10.1186/1471-2458-8-138.
- Chew-Graham C, Slade M, Montâna C, Stewart M, Gask L. Loss of doctor-to-doctor communication: lessons from the reconfiguration of mental health services in England. J Health Serv Res Policy 2008;13:6-12. http://dx.doi.org/10.1258/jhsrp.2007.006053.
- Huber US, Sandall J. A qualitative exploration of the creation of calm in a continuity of carer model of maternity care in London. Midwifery 2009;25:613-21. http://dx.doi.org/10.1016/j.midw.2007.10.011.
- Leap N, Sandall J, Buckland S, Huber U. Journey to confidence: women’s experiences of pain in labour and relational continuity of care. J Midwifery Womens Health 2010;55:234-42.
- Ulrich RS, Zimring C, Zhu X, DuBose J, Seo HB, Choi YS, et al. A review of the research literature on evidence-based healthcare design. HERD 2008;1:61-125.
- Van Bogaert P, Meulemans H, Clarke S, Vermeyen K, Van de Heyning P. Hospital nurse practice environment, burnout, job outcomes and quality of care: test of a structural equation model. J Adv Nurs 2009;65:2175-85. http://dx.doi.org/10.1111/j.1365-2648.2009.05082.x.
- Witz A. Professions and Patriarchy. London: Routledge; 1992.
- McCourt C, Stevens T, Sandall J, Brodie P, Page L, McCandish R. The New Midwifery: Science and Sensitivity in Practice. Edinburgh: Churchill Livingstone; 2006.
Appendix 1 Interviewee numbers by group and site
| Fieldwork site | Total interviewees | Clinical staff | Managers and stakeholders | Postnatal women and partners | Fieldnote transcripts |
|---|---|---|---|---|---|
| Westhaven | 27 | 11 | 7 | 9 | 4 |
| Northdale | 33 | 10 | 12 | 11 | 7 |
| Midburn | 37 | 16 | 7 | 14 | 6 |
| Southcity | 39 | 17 | 9 | 13 | 3 |
| Total | 136 | 54 | 35 | 47 | 20 |
Appendix 2 Topic summaries
An organisational study of alongside midwifery units
Stakeholder interviews
The interview sample will be refined based on each case but is likely to include as a minimum:
-
clinical director and chief nurse
-
clinical lead obstetrics
-
clinical neonatology lead
-
head of midwifery
-
consultant midwife
-
supervisors of midwives
-
service commissioners
-
Maternity Services Liaison Committee members, including lay members
-
local consumer representatives
-
key managers or personnel involved with transfer services and risk management.
Questions and topics will include:
-
service configuration, including consultations, service reconfigurations or developments and reasons for these
-
details of service configuration and organisation, including workforce arrangements, skill mix, models of care and escalation/transfer services and protocols
-
any previous or current plans for change or development and reasons for these.
Interviews with professionals
Topics and questions will include discussion on the following:
-
experiences of working on, or in, relation to the AMU (using photos taken of the space as prompts for discussion)
-
service organisation, including workforce arrangements, skill mix, models of care and escalation/transfer services and protocols
-
facilitators and barriers to choice of place of birth in different settings for low-risk women.
-
facilitators and barriers for professionals working in different birth settings
-
training provision and needs for staff working in different birth settings
-
management and staff support and development arrangements
-
any local, contextual or organisational factors impacting on quality of care and staff or user satisfaction.
Interviews with women and their partners
Topics and questions will include the discussion of the following:
-
Women’s pathways through care, including choices offered and made and any change of plans or referrals.
-
(How) did they choose to give birth in the AMU?
-
Women’s experience of maternity care, with particular focus on the AMU birth setting.
-
Experiences of birth complications and escalation or transfer of care.
-
Experiences of any transfers of care or setting for organisational reasons, or personal choice.
-
Wishes for future births.
Glossary
- Alongside midwifery units
- These provide labour and birth care led by midwives for women categorised as at low risk. They provide a distinct service but are proximate to obstetric-led maternity units, most often within the same building.
- Advanced Life Support In Obstetrics
- An example of a multidisciplinary, practice-based course which has been shown to be effective in preparing maternity teams for working together in obstetric emergencies.
- Band 7 midwife
- Midwifery staffing in the UK at the time of publication was graded in bands, normally from band 5 (newly qualified midwife) to band 8 (usually more senior managerial roles). A band 7 midwife has some additional responsibilities such as co-ordination or shift leader roles. Some AMUs have a band 7 midwife in their specific lead role.
- Birth centre
- This is a more popular and widely used term for a midwifery unit, either alongside an obstetric unit or as a free-standing midwife unit, and is used interchangeably with these terms.
- Cardiotocograph
- A device used to monitor fetal heartbeat and uterine contractions during labour. The CTG can be used on admission, intermittently or continuously. Best clinical evidence indicates that routine use of CTG for women with straightforward healthy pregnancies does not confer benefits and may carry risks. However, routine use of continuous CTG is common in many obstetric units in the UK.
- Free-standing midwifery units
- These provide labour and birth care led by midwives for women categorised as at low risk. They provide a distinct service, on a separate site from obstetric-led maternity units, such that if transfer is required, it would be by car or ambulance. Midwifery units on the same site as community hospitals or clinics without an obstetric unit are categorised as free-standing.
- Low risk
- Women are normally categorised as at low risk in the UK if they do not have any of the conditions set out in National Institute for Health and Care Excellence Intrapartum Guidelines risk assessment regarding advice on planned place of birth. The term ‘low-risk’ is also sometimes used to refer to care pathways, guidelines or protocols designed for the maternity care of women at low obstetric risk.
- High risk
- Women in the UK are normally categorised as at increased risk of birth complications if they have any of the conditions set out in National Institute for Health and Care Excellence intrapartum guidelines risk assessment regarding advice on planned place of birth as warranting birth in an obstetric unit. In practice, the term high risk is more commonly used than at increased risk.
- Normal birth
- This term is in common use by professionals and the public to refer to labour and birth that takes place physiologically and without obstetric interventions. However, it is often used simply to refer to vaginal birth without instruments (use of forceps or ventouse). There is also a more restrictive definition of normal birth agreed by a UK National Consensus Working Party.
- Obstetric unit
- A labour ward within a hospital that provides obstetric services (facilities and doctors including obstetricians and anaesthetists) as well as antenatal and postnatal care. The ward for labour and birth is more commonly referred to as a ‘labour ward’, ‘delivery suite’ or ‘hospital birth centre’. Obstetric care is led at consultant level. A woman developing complications during labour or birth in an obstetric unit would not normally require transfer elsewhere, except in rare cases of more specialist maternal or neonatal care being required. Individual women who are ‘low-risk’ may receive care led by midwives within an obstetric unit, particularly those requiring epidural anaesthesia.
- Pinard stethoscope
- This is a low-technology instrument used mainly by midwives for intermittent monitoring of the fetal heartbeat during labour. Midwives may also use a Doppler fetal monitor (a ultrasonography device) as an alternative method of monitoring the fetal heartbeat intermittently.
- PRactical Obstetric MultiProfessional Training
- An evidence-based multiprofessional training package for obstetric emergencies.
- Strengths, weaknesses, opportunities and threats
- An analysis exercise which looks at strengths, weaknesses, opportunities and threats.
List of abbreviations
- AMU
- alongside midwifery unit
- BME
- black and minority ethnic (community)
- CI
- confidence interval
- CNST
- Clinical Negligence Scheme for Trusts
- CTG
- cardiotocograph
- FMU
- free-standing midwifery unit
- GP
- general practitioner
- MCA
- maternity care assistant
- MSLC
- Maternity Services Liaison Committee
- MSW
- maternity support worker
- NCT
- National Childbirth Trust
- NICE
- National Institute for Health and Care Excellence
- NSF
- National Service Framework
- OR
- odds ratio
- OU
- obstetric unit
- PCT
- primary care trust
- RCM
- Royal College of Midwives
- SWOT
- strengths, weaknesses, opportunities and threats
- VBAC
- vaginal birth after caesarean
- VE
- vaginal examination
- WTE
- whole-time equivalent