Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its proceeding programmes as project number 09/1816/1004. The contractual start date was in April 2010. The final report began editorial review in March 2013 and was accepted for publication in September 2013. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2014. This work was produced by Aspinal et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction
This research, funded by the National Institute for Health Research (NIHR) Health Services and Delivery Research (formerly Service Delivery and Organisation), built on previous research undertaken at the Social Policy Research Unit (SPRU) around integrated service provision and neurological conditions1 and outcomes. 2,3 It aimed to describe systems in which innovative models of integrated care for people with long-term neurological conditions (LTNCs) exist, identify the range of outcomes that people with LTNCs want to achieve and to consider how to assess these outcomes in integrated practice.
We undertook in-depth case study work in four primary care trusts (PCTs) in England, each with at least one community-based neurorehabilitation team (NRT), between 2010 and 2012. Data collection included reviewing local documentary evidence and interviewing different levels of staff to explore the context within which these teams worked; interviewing people with LTNCs to ascertain what types of outcomes they wanted to achieve; working with the teams to develop these service-user derived outcomes into an outcomes checklist (OC) that could be used in assessments; and evaluating the use of the OC in practice.
This document reports the methods, findings and conclusions of the research.
Background
Problems securing integration across health and social care boundaries for frail older people and those with long-term conditions have been evident since the early 1950s. 4 Similarly, concern about integration within service systems has been a consistent feature of evaluative research in both health and social care. This has become more so as increased specialisation, technological advances, and shifts in the place of care have accelerated. 5
There have been repeated attempts since the inception of the NHS to resolve these issues by changing policy and directing practice,4 and policy documents return continuously to the need to deliver ‘seamless’ care. Policy developments at the start of this research promoted integrated care provision ‘to enable partners to join together to design and deliver services around the needs of users rather than worrying about the boundaries of their organisations’. 6 It was assumed that these arrangements would help remove unnecessary gaps and duplication between services. 6
This emphasis on services rather than organisational structures was an important change, but left unresolved problems that impeded earlier attempts to encourage integrated provision. 7 Further, it takes for granted that we know that integrated care does make a difference, when the research literature is, at best, equivocal about this.
Our previous project on integrated care for people with LTNCs8 suggests three main reasons for this lack of clear evidence about outcomes of integration. The first relates to defining what integration means, the second to agreeing what integration should achieve, and the third to how we should measure the effects of integration.
What is integration? The literature contains examples of three main types of intervention described as ‘integration of health and social care’. 9 At the structural (macro) level, for example, ‘integration’ might be about bringing health and social care provision and/or commissioning into a single organisation. The second type of structural intervention relates to relationship issues (meso level); for example, facilitating joint planning, the exchange of information or budget sharing. Thirdly, the intervention may be about co-ordinating care at the level of the service user (micro level), for example via care/case management, single assessment processes or multidisciplinary teams.
What is integration for? Here, the literature shows that the aims of integrating health and social care can vary from enabling the closure of long-stay hospitals,10 through the reduction of acute hospital beds or nursing home use,11–13 to promoting user-directed services and empowerment,14,15 and most points between. In many cases, making better use of existing resources underpins these varied aims.
How should we measure the effects of integration? With little consistency in the literature (and indeed in policy) about the definition and aims of integration, it is perhaps not surprising that evidence about its impact for service users is limited. There is a substantial literature about organisational and professional issues involved in both structural integration and integration at the service level. 16–19 There is also some evidence about impact on process measures such as access, user satisfaction, and assessment. 20 However, evidence about effectiveness for service users and their families or carers – and, in particular, outcomes that are important to them, not just to service managers and professionals – is largely absent. 19–22
Our previous project underlined this lack of evidence about impact. The systematic review of integrated models of care (such as multidisciplinary teams, specialist nurses, integrated care pathways, and other services described as ‘integrated’) found little evidence of impact on physical function, health-related quality of life measures, clinical outcomes, mental health, and other outcomes reported in randomised controlled trials and controlled before-and-after studies. Other researchers, reviewing the wider literature on integration of health and social services for older people, have come to broadly similar conclusions about impact on these ‘conventional’ outcomes. 20–22
Yet people with LTNCs and their organisations argue that the experience of integrated provision is an important contributor to their quality of life. 23 The overwhelming view of people with LTNCs in our previous project who used integrated models of care was positive, particularly when compared with less integrated models. 1 However, the issues that concern them are rarely the outcomes about integrated provision reported in the research literature. For example, of the 50 studies included in the review, only 21 reported use of or contact with to services overall and 18 reported the users’ views of the model of care, both issues that service users themselves consider important. 24 Just three studies mentioned social outcomes such as housing, income, education or employment. Further, our evidence shows that issues such as a sense of empowerment or self-worth and the ability to make sense of one’s health condition can be very important to service users. However, these types of outcomes were totally absent from the evaluative literature we reviewed in that earlier project.
Integration and outcomes in national policy
Improving the integration of services across boundaries in order to deliver improved outcomes for service users, especially those with long-term conditions, has been a major concern of policy and system planning for some years.
Policy under the Labour government 1997–2010
Joint working and partnerships were central to the Labour administration’s reforms for public services. The Health Act 199925 removed some of the obstacles that had historically hindered joint working and these were formalised and consolidated in section 75 of the NHS Act 2006,26 providing mechanisms of pooled budgets and joint commissioning which might deliver integrated services more easily. The ‘NHS Plan’ in 200027 and the Health and Social Care Act 200128 explicitly encouraged structural integration of organisations providing health and social care services.
The importance of supporting people with long-term conditions was outlined in the NHS Improvement Plan,29 launched in June 2004. The subsequent Department of Health publication in 2005, ‘Supporting People with Long Term Conditions’30 set out the NHS and social care model for long-term conditions. In the same year, the National Service Framework (NSF) for LTNCs31 specifically addressed the needs of people with LTNCs. The need for an integrated approach to service provision was made clear, explicitly or implicitly, in all 11 quality requirements of the NSF.
Increasing interest in evidence-based policy and practice meant that monitoring service performance was increasingly important to commissioners and also focused attention on outcomes for users of services rather than just for the organisations delivering them. At the same time, the joint health and social care White Paper, Our Health, Our Care, Our Say: a new direction for community services, set a new strategic direction for community services. 32 It aimed to realign care in settings closer to home and introduce an outcomes-focused framework for commissioning health and well-being. Integration of services and support for people with long-term or complex needs, with a shift of resources away from secondary care to prevention, primary and community services, were the explicit aims. The Local Government and Public Involvement in Health Act33 and the Commissioning Framework for Health and Well-being34 went on to create a duty to design and deliver local area agreements and produce joint strategic needs assessments of the health and social care needs of local populations that would help inform and deliver a sustainable communities strategy.
The Integrated Care Pilot programme, introduced in the NHS Next Stage Review,6 focused on horizontal integration (i.e. between health and social care) and represented a ‘bottom-up’ approach to integrated care that was designed to explore the different ways health and social care could respond in an integrated way to address a particular local need. The national strategy ‘Transforming Community Services’35 helped to clarify relationships within community services and required a clear separation between commissioning and providing functions.
Despite such government initiatives, achieving effective integrated care remained elusive, or at best, patchy. Examples of joint financing across health and social care failed to be representative of a wider pattern. 36,37 In 2010, a report from the King’s Fund noted that there had been little significant shift in resources from acute care to the support of those with long-term conditions in the community. 38 The introduction of care trusts generally failed to result in comprehensively integrated structures39,40 and the evaluation of integrated care pilots highlighted specific problems in implementing large-scale organisational change. 41 Similarly, an evaluation of the NSF for LTNCs demonstrated how a policy can be overtaken by competing priorities when implemented with no new money and no firm targets in a culture of performance management. Despite the NSF, people with LTNCs struggled to access models of good practice for integrated care. 1,42 Moreover, the focus on outcomes had so far been framed primarily around organisational processes and performance management, with a lack of evidence around outcomes for individuals. 43
Policy under the coalition government since 2010
The persistent barriers to realising change were illustrated in the Nuffield Trust’s contribution to discussions about the possible direction of health reform under the incoming coalition government44. One concern that quickly arose was whether or not the interest in integrated care would continue despite a perceived greater emphasis being placed on choice and competition. 39,43,45 The new government’s health reforms were set out in the White Paper Equity and Excellence: Liberating the NHS46 and the initial draft of the Health and Social Care Bill focused on mechanisms to promote development of a competitive health-care market, with a key role in promoting competition for Monitor, the new economic regulator. However, the interim listening exercise before the Health and Social Care Act 201247 was passed, identifying integration as a neglected priority. 48
The NHS Future Forum reported a widespread concern and their ‘integration’ workstream report set out key recommendations to endorse and encourage integration ‘around the patient, not the system’. 48 The Health and Social Care Act, as it reached statute, placed new duties on the economic regulator Monitor, the new central NHS Commissioning Board, local Clinical Commissioning Groups (CCGs) and health and well-being boards to promote integration between health and social care. 47 To facilitate key changes, the NHS Commissioning Board was to host four new strategic clinical networks for up to 5 years from April 2013. 49 At the end of 2012, it was announced that one of the networks would specifically cover neurological conditions, dementia and mental health.
Concerns have been raised that in the major structural upheavals, existing partnerships are being dismantled and established collaborative networks and relationships threatened or lost. 43,50 Moreover, the ability of general practitioner (GP)-led commissioning groups to champion the sorts of services that work across boundaries in a more holistic way is unproven. 51 The emphasis given to performance management through national targets has been largely abolished, and the focus shifted to outcomes as the main mechanism by which government sets objectives and levels of performance for health and social care. At a clinical level, patient-reported outcome measures (PROMs), to assess the quality of care delivered to NHS patients from a patient perspective, currently covers four elective surgical procedures and have been collected by all providers of NHS-funded care since 2009. 52 PROMs for six long-term conditions – asthma, chronic obstructive pulmonary disease, diabetes, epilepsy, heart failure and stroke – are currently being piloted. 53 Three separate but inter-related outcome frameworks for the NHS, Adult Social Care and Public Health have been established. 54–56 The three frameworks are being increasingly aligned;57 shared and complementary indicators aim to reflect areas of joint responsibility and help provide a focus for joint-working and shared priorities.
Integration is likely to continue to be a significant policy theme. The Care and Support White Paper58 and accompanying draft bill59 affirmed the ambition that ‘everyone who uses health, care and support [will] experience joined-up services that meet their needs and goals’. 58 Aligning processes at an individual level via personal budgets (for social care) and the appointment of care co-ordinators to assist in navigating care systems are central proposals. However, a recent critique of social and health care integration views this more prominent role for care co-ordinators as accepting inherent fragmentation within services, without addressing the fundamental causes and, therefore, not necessarily enhancing integration. 60 Similarly, personal budgets could be viewed as a micro-level initiative that do not require change at a system level, at least until the results of pilots of health budgets are available and the feasibility of joint personal budgets for health and social care is established. Financial support for integration was pledged by enabling the transfer of £859M in 2013–14 from the NHS to local authorities via local agreements to support adult social care services that also have a health benefit.
The NHS Operating Framework 2012–13 illustrates the priority given to integrated care61 and supports a range of system levers to promote it. The management of long-term conditions remains a focus through the long-term conditions strategy: a cross-government initiative led by the Department of Health set up to look at how services such as health, social care, education, housing and others can work together to improve life chances and outcomes for people living with long-term conditions. 62 The Quality, Innovation, Productivity and Prevention (QIPP) programme, designed to achieve productivity savings within the NHS of £20B by 2015, includes a long-term conditions QIPP workstream, in which joint working is seen as an important strategy in tackling financial constraint. 63 More specifically, it describes a ‘Year of Care’ funding model that focuses providers on jointly delivering a ‘year of care’ based on a risk-adjusted capitation budget, and away from episodic, activity-driven funding. 64 There was a renewed focus on LTNCs in particular, in the concerns raised by the Public Accounts Committee. They drew attention to the failures so far to improve services and the need for better information about resource use, services and outcomes around LTNCs. 65
Assessing progress
Despite health and social care policy continuing to embrace integration and an outcomes approach, a mid-term assessment of health policy under the coalition government called for more to be done in evaluating innovative approaches to integrated care and the way long-term conditions are managed. 66 The impact of a parallel policy emphasising increased competition in health care on collaborative working has also yet to be felt and evaluated. Attributing outcomes to policy interventions demands a sound evidence base and an appreciation of the complexity of cause-and-effect reasoning. 67 Furthermore, government acknowledges the inherent difficulties in developing outcomes that measure service users’ experience of integration. 68 A recent review in 2012 called for an urgent need to improve the evidence base by developing studies that could not only provide an analysis of cost-effectiveness, but also assess the process of joint and integrated working from the perspective of service users and carers. 69 The Neurological Alliance recently emphasised the need for the current NHS Outcomes Framework to develop better measures, including disaggregated measures relevant to neurological conditions, that can deliver improved services for people with LTNCs, specifically, and those with long-term conditions, generally. Identifying the outcomes that matter most to people with LTNCs is seen as central to this aim. 70
Outcomes
As described earlier in this chapter, the policy around outcomes tends to focus on the outcomes of interventions by different care sectors, as witnessed in the assessment criteria included in the National Outcomes Frameworks (NOFs). 54–56 While these are likely to be of relevance to people using health and social care services, these measures are essentially defined in line with professional, service, sector and policy-makers’ priorities.
Our research does not focus on the outcomes of service provision per se but, rather, aims to discover what outcomes people using ‘integrated’ services want to achieve and whether or not these services are able to assess these outcomes in practice.
Social Policy Research Unit’s outcomes research
A substantial programme of research at York, using this conception of outcomes, explored conceptual issues and measurement challenges of assessing outcomes when needs are complex and changing and deterioration is more likely than recovery,2,71 and identified how these could be used to influence practice in social care services. 3
The work by Harris et al. 3 collated Qureshi’s2 findings into categories consistent with the social model of disability, which asserts that an individual’s impairment does not constitute disability but rather that society disables people with impairments through, for example, structural, ideological and material barriers. 72 It listed four main groups of outcomes: autonomy outcomes, personal comfort outcomes, economic participation outcomes and social participation outcomes. However, this work did not explain how these categories were determined, nor did it define their parameters, making it difficult to understand the origin and meaning attached to them. In addition, the research highlighted difficulties practitioners experienced in adopting a more ‘outcomes’ focused approach to assessment and service provision.
Our project built on this previous theoretical and empirical work. We wanted to understand what outcomes people with LTNCs wanted to achieve and, based on the views of people with a LTNC, to clarify the parameters of each of the outcomes outlined by Harris et al. 3 This approach to identifying outcomes follows a social model of disability that acknowledges that service users may view outcomes and outcome achievement differently from practitioners, commissioners and policy-makers. We also wanted to understand whether or not an outcomes-based approach to assessment could be implemented in practice and how this might influence practice in ‘integrated’ teams.
The need for research
At the time this research was commissioned, it was acknowledged that there was little evidence about how integrated care models are developed and implemented and about the effectiveness of integrated models of service delivery. 73 It would be easy to assume that the failure to demonstrate impact on conventional outcomes means that there is no impact to measure. However, it seems more likely to us that research has failed so far to measure the outcomes that might sensibly result from integrated health and social care and that actually matter to people with complex long-term conditions.
Our research aimed to improve understanding of the structures and mechanisms that allow integrated care delivery to work and the part that commissioning plays in enabling integration. This research was not intended to evaluate outcomes of integrated services or to result in a finished tool to assess the outcome of integrated care, but rather to address the need to develop ways of assessing outcomes that are important to people with LTNCs and that can be facilitated by integrated service provision. This research thus begins to fill the gap in evidence by exploring how user-desired outcomes can be incorporated in assessment processes in different micro-level models of integration, embedded within different meso- and macro-level structures.
Research questions and study aims
To address the gaps summarised above, we outlined four specific research questions:
-
What facilitates or impedes the development of innovative approaches to health and social care integration?
-
What outcomes do people with long-term conditions want from integrated health and social care?
-
Can these outcomes be assessed in everyday service delivery?
-
How can different models of integrated health and social care affect outcomes?
Associated with these were four main aims:
-
To describe innovative models of micro-level integrated care for people with LTNCs and the macro- and meso-level structures within which they are delivered.
-
To explore the relationship between models of care co-ordination and different structural approaches to health and social care integration. The focus was on what facilitates or impedes the delivery of integrated care, from the perspectives of service users, their families or carers, professionals who deliver care, and service managers and planners.
-
To work with those who use and those who provide innovative models of integrated care to develop and test ways of assessing outcomes that are meaningful to both.
-
To begin to understand if and how outcome assessment influences practice in integrated care, and whether or not this varies between different models, within different structures.
Long-term neurological conditions
We focused the research on adults with LTNCs because these clients pose complex challenges for effective health and social care integration. For example, with the exception of those who have Parkinson’s disease (PD), adults with LTNCs are younger than most long-term users of health and social care services. As a result, their roles as partners, parents, and economically active adults should be considered as part of their overall needs. The ‘boundaries’ that are important thus go beyond the conventional ones of health and even of social care, making the task of co-ordination potentially more complex.
Many LTNCs involve relative stability over long periods, interspersed with exacerbations that need rapid access to acute medical care or complex, community-based intervention. Unless people live close to specialist centres, their health needs during these periods are likely to be met via generalist services. Access to specialist advice, so that generalists can provide appropriate care for the specific LTNC, is a key boundary issue.
Some people with the same LTNC find that their condition changes slowly, while others experience rapid change and still others can experience both slow and rapid change at different stages. Responding to these differing trajectories and their unpredictability requires sophisticated management across boundaries within health care and between health and social care systems.
While innovations such as individual budgets can enable adults with health and social care needs to act as their own care co-ordinators,74 some people with LTNCs experience periods when their ability to do this will be seriously compromised. User-directed methods of integration thus introduce the potential of new boundaries to be negotiated from time to time.
For these and other reasons, we might expect that methods or mechanisms for integration that ‘get it right’ for people with LTNCs would also get it right for other adults with complex, long-term conditions. Using LTNCs as an exemplar thus generates knowledge that is transferable to other long-term conditions.
The research process
The research took place in four PCTs in England between 2010 and 2012. The evidence was collected using an in-depth case study approach, and included reviewing local documentary evidence and interviewing different levels of staff, people with LTNCs and their carers; developing an OC; and evaluating the use of the OC in practice. The research was undertaken in three stages.
Stage 1 – understanding the context and identifying outcomes
-
Documentary evidence was analysed and interviews were held with staff (e.g. PCT commissioners and senior managers, service-level managers and front-line staff) to help understand the context in which integrated teams were based.
-
Interviews were held with carers of people with LTNCs to help understand how they were included in integrated service provision.
-
Interviews were conducted with service users to identify outcomes.
Stage 2 – developing and implementing an outcomes checklist for use in practice
-
Service-user interview data were analysed to identify the outcomes that they wanted to achieve.
-
A summary list of outcomes was developed.
-
Working with the teams in each case site, the list of outcomes was developed into a checklist that they could use in practice.
-
Teams implemented the OC as part of their usual assessment processes.
-
Teams’ use of the checklist was monitored.
Stage 3 – evaluating the use of the checklist
-
Staff were interviewed about their views on the checklist and its utility in practice.
-
Service users were interviewed about their experience of the checklist being used in their assessment and about the items included on the checklist.
Service users, carers, representatives from voluntary sector organisations who sat on the project advisory group and the SPRU Adult Consultation Group (see Appendix 8, note a) advised on the research process for this study. Presentations and progress updates were given in meetings held regularly throughout the research and, as well as giving general advice throughout the period of research, they gave specific advice on documentation, recruitment, analysis and interpretation of findings. Between meetings, members of the project advisory group were also sent project newsletters to update them on progress and ask for advice on specific issues.
Ethical review
The research, and all associated documentation, was reviewed and approved by the University of York’s Humanities and Social Science Committee and was then reviewed and approved by the Research Ethics Committee (REC) for Wales in 2010 (see Appendix 8, note b). The Association of Directors of Adult Social Services also approved the research. PCTs and local authorities granted research governance approval prior to starting data collection.
Structure of the report
Chapter 1 has introduced the research. It has presented an overview of the study area and explained why this research is important. The introduction outlined the research context, research questions and the methods used for data collection.
Chapter 2 will present the case study methods. It will explain how the case study sites and participants were selected and recruited, and describe the methods used to collect data for each of the three stages of the research.
Chapter 3 will present case-by-case analysis of local demographics, commissioning arrangements and organisational and team profiles, providing a contextual backdrop for the rest of the findings. Team processes will be compared and service user and carer views about how processes could affect achievement of outcome will be reported.
Chapter 4 will report findings from staff, service users and carers about integration, how different elements of the organisation affect integration and how stakeholders are included. Cross-case comparisons, drawing together this evidence from across the four case sites, allowed us to identify some of the factors that might promote or inhibit integration at organisational and team level and help to answer the first research question: What facilitates or impedes the development of innovative approaches to health and social care integration? (See Appendix 8, note c for our working definition of ‘innovation’.)
Chapter 5 will draw service user data from across the four case sites together in order to answer the second research question: What outcomes do people with long-term conditions want from integrated health and social care? We will explain the key issues that people with LTNCs discussed, provide a comprehensive list of outcomes based on service user views, and the different levels of outcomes people with LTNCs will be discussed.
Chapter 6 will describe how, working with the teams in each case site, we developed the list of outcomes into a checklist. The way that the teams implemented the OC into their usual assessment processes will be reported and teams’ experiences of using the checklist in practice will be explored. Service users’ experience of the checklist being used with them, and their opinions about the topics included on the OC, will also be reported. This chapter, therefore, will answer the third research question: Can these outcomes be assessed in everyday service delivery?
Chapter 7 will draw together the findings from each stage of the research and from across the case sites to answer the final research question: How can different models of integrated health and social care affect outcomes? It will present an assessment of the strengths and limitations of the research and the implications of this research for policy and practice. The report will conclude with recommendations for future research in this topic area and plans for dissemination.
Chapter 2 Methods
In this chapter, we set out the methodological approach taken in this project, outline how we identified our case study sites and our samples, and describe the methods we used to collect data across the four case studies. We have summarised the rationale for the choice of methods, data collection techniques and adaptations that we needed to make. We will also describe the sample we achieved in each case site.
Reporting of the methods is organised around the three stages of the research, as outlined in the introduction: understanding the context and identifying outcomes; developing and implementing an OC for use in practice; and evaluating the use of the checklist in practice. Participation rates are discussed in the relevant findings chapters (see Chapters 4 to 6).
Justification for methods
The first section describes the different approaches to data collection that were adopted for this research and explains how we overcame some of the general limitations of the methods.
Case studies
The case study approach ‘focuses on the circumstances, dynamics and complexity of a single case or a small number of cases’. 75 A case is a single unit in a study and can be, for example, a person, a profession or an organisation. The case study approach is distinguished from other approaches, in that it does not attempt to control or exclude variables. Rather, it is a holistic approach that enables the complex nature of an issue to be explored. 76
As Yin notes, a case study is particularly useful when the study aims to investigate ‘a contemporary phenomenon within its real-life context, especially when the boundaries between phenomenon and context are not clearly evident’;76 for example, in circumstances where the relationship between organisational structure, approaches to practice or policy, and outcomes for people using those services, are unclear. The case study approach, therefore, is particularly suited to this research where the ability of people with LTNCs to achieve the outcomes they want may be determined by several factors. For example, having to deal with and navigate multiple services that are governed by many different policy directives might have as much impact as their level of ‘impairment’ or personal approaches to self-management.
Using a case study approach does not preclude any particular method of data collection, but for the purposes of this research, only qualitative methods were used. These comprised in-depth interviews with different stakeholders at the different stages of the research, group interviews, documentary analysis and field-note analysis.
Qualitative interviews
Qualitative interviews were used in two stages of the research: stages 1 and 3. They can be used to look below superficial and readily observable phenomena, allowing deep exploration of the study topic. 75 Interviews can provide information that is able to inform understanding of, for example, people’s opinions and preferences and also why they hold them. They allow for relationships between people, organisations and events to be explored and understood. 75,77
An ‘in-depth semistructured’ approach78 to interviews was used which allowed in-depth exploration of issues. During these types of interviews, the participant is allowed to talk through, or provide a narrative about, the issue being studied. This is important for this research, where we wanted to understand the things that were important to people with LTNCs, to explore reasons for their importance, and how they linked together. Furthermore, in using this method, we were able to explore the variety of factors that affect integration, service provision and outcomes.
Interviews were guided by a topic guide (all topic guides are included in Appendix 1), rather than by pre-set questions, which acted as an aide memoire for the researcher to ensure that relevant topics were addressed while a conversational style was maintained. Additional topics emerged from the dialogue during the interview. All topic guides were reviewed by our advisory group comprising commissioners, front-line professionals, service users and service user/carer representatives.
To counter the limitations of subject bias that can be associated with this method, we aimed to recruit a range of participants in each sample for each stage of the research. For views about the organisation and service structure, for example, we interviewed front-line professionals, commissioners and service managers across health and social care organisations and for views about outcomes people with LTNCs wanted to achieve, we aimed to hear the views of people representing different LTNCs, different condition trajectories and different points in that trajectory.
To counter interviewer bias, three researchers undertook interviews and reviewed each other’s interview transcripts at different points of the research. We also undertook some joint interviews so that feedback could be given on process and technique.
Focus groups
Focus groups use group discussion to generate qualitative data around a focused set of topics79 and, as with the in-depth interviews described above, they can be used not only to hear people’s opinions but also to understand why people hold these opinions. 75 Although focus groups can be used to explore dynamics of the group,80 for the purposes of this research we were only interested in understanding the views people had. Focus groups were thus used to gather views of staff who had used the checklist as part of their practice.
In stage 3, we offered staff in the NRTs the opportunity to take part in an individual interview or in a focus group with their colleagues. The topics covered in the individual interviews and focus group interviews were similar, but focus group interviews gave staff the opportunity to discuss issues as a team. We offered these choices for several reasons. First, focus groups would improve efficiency, reducing the time needed overall for staff to take part in interviews (i.e. 2 hours in all, rather than several interviews of approximately 1 hour each). Second, as this research addresses the feasibility of using the checklist in practice, a focus group provided the opportunity for staff to share experiences and learn from each other’s experiences. However, we also offered a choice of individual interviews so that NRT staff could express divergent views away from colleagues, if this is what they preferred.
One of the methodological concerns associated with focus group interviews is that divergent voices may not be heard in group discussion. To address this, the groups were facilitated by two experienced researchers who directed questions to participants who had not spoken, so that they were drawn into the discussion, and positively promoted discussion about views that were divergent from that expressed by the majority of participants.
Field notes
Field notes, an accepted approach in qualitative research to provide additional information to aid understanding of participants’ views, were made after interviews and focus groups, where appropriate, to record contextual information. For example, a person may express concern about leaving their home. For example, when a participant expressed concern about the safety of going out of their home, the researcher might make field notes about the participant's neighbourhood. Notes were also taken during meetings held with teams throughout the research process. Though these data have not been used to direct analysis, the information was used to provide contextual information and prompts for future interviews.
Documentary analysis
Analysis of documents is widely used in social research81 and also in health research75 and can draw on many documentary forms, including official demographic statistics and government department documents. 74 In this research, we wanted to learn about the local structures and processes for integrated service provision, the wider context in which these were based and to understand approaches to outcome assessment in services for people with LTNCs. Documentary analysis was thus well suited to this study.
Documentary accounts can be useful data sources, but as all documents are based on social constructions and judgements, it is important to be alert for inaccuracies and biases throughout the research process. 75 Documents from a variety of sources were triangulated to limit this and these were then triangulated, where appropriate, with staff interview data.
Non-participant observation of strategy meetings
Non-participant observation is a classic method that has been used extensively and is particularly useful for organisational analysis and evaluation. 75 It comprises observation of behaviour, actions, activities and interactions to inform understanding of complex situations and interactions. 75 As indicated above, the complexity of the systems being researched for this study made this approach potentially useful. Furthermore, non-participant observation is, by its nature, context specific. 77 Given that we were interested in understanding how local decisions were made around integration/co-ordination of services as well as who was involved in this decision-making, non-participant observation of meetings that focussed on integrating/co-ordinating services for people with LTNCs could provide interesting insight into how decisions about these issues were addressed.
Approach to analysis
We used the framework approach to data management and analysis. This is typically used in applied policy research where there are specific objectives or information needs. As such, frameworks can be data driven or led by a priori issues, or a mix of both. The approach also facilitates systematic data management and allows audit trails of the data management process.
Qualitative data are managed in a theme-by-case matrix, known as an ‘analytical framework’. 82 There are four stages of data management. First, researchers familiarise themselves with the data, and identify themes and key issues. Based on the identified themes and any other a priori issues, an index of themes is constructed, resulting in the analytical framework. Visually, this looks like a matrix or chart, with cases as rows and themes as columns. Data are then indexed according to which theme(s) in the framework they relate to. Finally, the indexed data from each case (e.g. participant, focus group) is summarised onto the chart under the relevant theme(s) (known as ‘charting’).
Where appropriate, we triangulated different sources of data. For example, in stage 1, we used both interview and documentary evidence to help understand organisational and wider contextual issues. When we took interview field notes, we also used these to help inform analysis of data from that interview.
Methods: in practice
Yin76 argues that carrying out multiple case studies increases generalisability of research data to other situations and contexts. We therefore undertook in-depth case studies in four PCT areas, including their associated local authorities.
We decided on four case studies because this research involved long-term in-depth work with the teams in each of the case sites. Having four cases would ensure we had enough time to manage each of the case studies, to develop and maintain relationships with the teams and to foster their interest and commitment throughout.
Ethical and research governance review
Before we undertook data collection, the research methods and all documentation were reviewed and approved by the appropriate ethical and research governance committees as outlined in Chapter 1.
Identifying and recruiting case sites
We invited PCTs to participate if they had a NRT that was based in a community setting. When we were planning the research, four PCTs, with whom we had worked in a previous study agreed, in principle, to take part in this study. These case sites reflected different approaches to integration at a strategic and/or commissioning level, different population profiles and different levels of rurality/urbanisation.
However, when the research was funded, one PCT was no longer able to take part because staff in the NRT did not have the capacity to be involved in long-term, in-depth research. In this site, health and social care was integrated at an organisational level, had a younger than average population with high deprivation and was classed as urban. To replace this case site, we wanted to include a site with similar characteristics, but the integrated structure of the PCT was our primary concern.
We identified several PCTs which had a NRT and integrated structural arrangements from benchmarking data that we had collected as part of a previous research study around LTNCS and integration. 50 We approached all of the sites with these characteristics (n = 11) and one of these agreed to participate in the research. Details of the four participating case sites are reported in Table 1.
| Organisation and population characteristics | Case site A | Case site B | Case site C | Case site D |
|---|---|---|---|---|
| Organisation integration arrangements (at start of research) | Standing joint commissioning board | Some joint commissioning posts | Standing joint commissioning unit | Integrated health and social care at operational level |
| Some joint commissioning posts | ||||
| Local authority type | Metropolitan | Borough | County | County |
| Urban/rural dataa | Major-urban | Major-urban | Significantly rural | Rural 50 |
| Populationb | 700,000 | 200,000 | 500,000 | 400,000 |
| Ethnic diversity | Low | Low | Low | Low |
| Deprivationc | Average | Very high | Low | Very low |
As Table 1 shows, we chose sites that had different population profiles, different organisational arrangements and different levels of rurality, so that we had possible factors on which to base comparisons. Further information about the case sites and associated structures are presented in Chapter 3.
Identifying and recruiting neurorehabilitation teams
As described earlier, we recruited PCTs with a NRT. This is because in previous research we had identified NRTs as one of the ‘gold standard’ models of integrated service provision for people with LTNCs. 85
In one case site, we involved two condition-specific services provided by the same NHS trust, one for people with multiple sclerosis (MS) and one for people who had experienced a brain injury (BI). This was because the local service manager felt that a single team would not be able to produce the maximum sample size of clients we hoped to achieve for the OC implementation and evaluation (stages 2 and 3). In addition, the two teams were expected to merge during the research period and the service manager wanted both teams to be using the same paperwork.
Our five NRTs, within our four case sites, represented different models of provision. For example, one of the teams was a joint health and social care team, three were based in the PCT but had semi-formal links with social care and one team had no links with social care. In this latter case site, the local authority (LA) declined to be involved with the research. The teams also differed in their relationships with acute services and how they involved service users and carers into their work. A detailed account of each of the teams is provided in Chapter 3.
Stages of research
The research took place in three stages and these are reported in turn.
Stage 1: understanding the service context and identifying outcomes
In this stage we had three aims:
-
to understand the models of integration for adults with LTNCs in each case site
-
to understand the relationship between NRTs and carers
-
to explore and identify the outcomes important to adults with LTNCs.
We used two forms of data collection for this stage of the research: documentary evidence and in-depth, semistructured interviews. We had also planned to collect data via observation of strategic meetings. Data collection for this stage took place between August 2010 and June 2011.
Documentary evidence
We collected three main documentary sources: national policy and population resources, local policy and strategy documents, and service-based assessment documents. Throughout the fieldwork period, new and additional documentary evidence was collected as we learnt about it.
National resources were used to identify official demographic statistics and national policy directives, providing a wider context to the research. Local documentary evidence included publications about local policies, services and strategies, such as PCT and public health annual reports and board discussion papers. These data were largely descriptive and were used to help develop a profile of integration and services for people with LTNCs within each of the case sites. We collected local documentary evidence via interview participants, key commissioning contacts and the NRTs and also accessed publicly available documents via local organisational websites. Where appropriate, we analysed these documentary data alongside interview data so that we could triangulate these in our analysis. This involved charting relevant documentary information into the analytical framework (as a separate ‘case’). We also used information in the documents for contextual purposes in describing the case sites. In addition, we collected examples of the ‘outcome’ and other assessment tools each of the NRTs used. This was to aid our understanding of the team’s general approach to assessment and to provide an insight into their current practice around ‘outcome assessment’.
Non-participant observation of meetings
As outlined earlier, we had intended to observe strategic meetings focusing on integrating/co-ordinating services for people with LTNCs. We were unable to do this in any of the case sites because there were no relevant meetings available for us to observe. Strategic teams including, for example, local implementation teams (LITs) that had developed in response to the NSF for LTNCs31 either had been disbanded or were suspended for the duration of the research. Further information about lack of strategic meetings is provided in Chapter 4.
In-depth semistructured interviews
We undertook interviews with commissioning and strategic staff, staff in the NRTs, people with LTNCs using the teams and carers of the people with LTNCs.
Interviews with organisational staff
To understand the structural integration arrangements of the organisations in the case sites, we conducted interviews with NHS and LA staff involved in commissioning and development of services for adults with LTNCs (hereafter referred to as ‘organisational staff’).
An initial interview was undertaken first with our key contact in each case study site. This person was typically a senior manager involved in service development. We then used a snowball approach to sampling,75 whereby our key contact identified other staff members involved in developing and/or commissioning services for adults with LTNCs. All subsequent interviewees were asked to identify any relevant individuals to approach. All of the relevant organisational staff identified were invited to participate in an interview. We assumed that all staff would be over 18 years old, be cognitively able to give informed consent and understand English well enough to take part in an in-depth interview.
All those invited to an interview were sent an invitation pack, either by e-mail or by post depending on the contact details we had for them. The pack contained a covering letter/e-mail, an information sheet, and a response form (see Appendix 1). Organisational staff were asked to return the response form directly to the research team, indicating whether or not they were willing to participate. Those who did not wish to be involved were given the opportunity to provide a reason, but were advised that this was entirely voluntary. Any reasons for not taking part were recorded. By using the response form, we were able to avoid recontacting people who did not wish to participate. Reminder packs were sent 3 weeks after the first invitation. If no response was received to this invitation, the person was not contacted again.
If a response was received indicating that a member of staff wanted to participate, they were contacted to clarify any issues, answer any questions and arrange a time for an interview. The interviews were conducted by telephone or in person, depending on the participant’s preference. Before telephone interviews were conducted, participants were sent a consent form to complete and return. The researcher signed the consent form, took a copy and sent it to the participant for their records. The original was stored securely by the research team. When conducting interviews in person, the consent from was completed in duplicate prior to the interview commencing and a copy given to the participant for their records. All participants were advised that they could ask questions, raise concerns or withdraw from the study at any point in the process.
Interviews focused on current structural arrangements, integration at different levels of the organisation, the factors that influenced integration, and future directions. Participants were also asked to provide, or direct us to, any documentation that might be relevant to the research. Participants were given the choice of a face-to-face or a telephone interview. Where participants consented, interviews were audio recorded and transcribed verbatim. Participants were given the option to view their transcript. All organisational staff agreed to allow audio recording and none asked to see their transcript. Interviews lasted between 30 minutes and 1 hour.
We were unable to set a target sample size for organisational staff interviews because the case sites had very different structures. It might be sufficient to interview one or two staff members in one case site, for example, while in another site we might need to interview several people to gather the same level of information. Thus, we intended to recruit and collect data until we achieved data saturation (see Appendix 8, note d) or, for stage 1 service information, until we had a map of local LTNC services and an understanding of how these worked together. A total of 15 organisational staff were recruited across our case sites. Table 2 summarises the number of organisational staff we approached for participation, and the number who agreed to participate, by case site. Further details of the sample are reported in Chapter 3.
| Site | NHS organisational staff | Social care organisational staff | ||
|---|---|---|---|---|
| Invited | Interviewed | Invited | Interviewed | |
| A | 3 | 1 | 2 | 1 |
| B | 6 | 3 | 4 | 1 |
| C | 6 | 3 | 2 | 2 |
| D | 6 | 4 | Social care in this site declined involvement in the research | |
| Total | 21 | 11 | 8 | 4 |
As Table 2 indicates, 14 staff who were invited did not take part. Six of these did not respond even after a reminder letter and the remaining eight people declined. Reasons for declining to take part were that they were too busy (n = 4), the interview was about issues outside their remit (n = 2) and that they were retiring (n = 1). One person did not provide a reason.
We struggled to recruit NHS commissioners, particularly in sites A and B. We continued to try to recruit organisational staff throughout the first 18 months of the research to get this information, without success. This thus creates a gap in our understanding of the NHS and/or joint commissioning arrangements in these sites. In site D, social care declined participation in the study and, as such, our understanding of organisational integration arrangements in this site relies upon documentary evidence and the accounts of NHS staff.
Interviews with neurorehabilitation team staff
To understand each NRT’s model of practice and their approach to general and outcome assessment, we conducted in-depth, semistructured interviews with NRT staff and other NHS and LA staff who worked closely with them. The process for recruitment, consenting and data collection followed that outlined above for organisational staff.
We asked NRT staff who we interviewed to identify professionals outside the team with whom they were ‘integrated’ and these staff were also invited to participate. For four of the teams, we invited all NRT staff to take part to ascertain different professional perspectives, but as the fifth team was large we invited a range of staff to represent the different professions within that team.
Interviews focused on the NRT’s structure and processes, including those around integration, relationships between the NRT and PCT, and factors affecting integration at practice level. Participants were also asked to provide examples of both their general and outcome assessment documentation. Using the same process as with organisational staff, interviews took place either in person or via telephone, were audio recorded and transcribed, and lasted approximately 1 hour.
We recruited staff in the team and practitioners who worked with the team. The size of NRTs differed across the case sites and this is reflected in the number of staff we could invite, and who agreed, to participate. Twenty-eight practitioners (team and non-team staff) were recruited across the four case sites. Table 3 summarises the number of team and non-team practitioners we approached and who were interviewed. Further details of the sample are reported in Chapter 3.
| Site | NRT staff | Non-NRT staff | ||
|---|---|---|---|---|
| Invited | Interviewed | Invited | Interviewed | |
| A | 5 | 5 | 2 | 2 |
| B | 9 | 9 | 0 | 0 |
| C | 7 | 6 | 2 | 2 |
| D | 4 | 3 | 1 | 1 |
| Total | 25 | 23 | 5 | 5 |
As Table 3 indicates, one team member in site C and one in site D who were invited did not take part. The person in site C had agreed to take part but had to withdraw due to work commitments and we did not receive a response from the person in site D.
Interviews with people with long-term neurological conditions
To explore and identify the outcomes important to adults with LTNCs, we conducted in-depth, semistructured interviews with clients using the NRTs in each case site. We ‘piloted’ interviews with four people with neurological conditions and their carers and adapted topic guides accordingly.
We aimed to recruit clients representing the range of conditions and different service needs that the NRTs covered. They were eligible if they had a LTNC, were existing clients or had been clients of the NRT within the previous 6 months, were aged 18 years or over, and were cognitively able to give informed consent and participate in an interview (as judged by the team using their usual cognitive assessment processes).
The NRTs identified clients who fulfilled these eligibility criteria and distributed invitation packs. We agreed to reimburse the cost of an independent advocacy agency to assist clients who required assistance to read the invitation documents and complete the response form but no client took this up. Packs contained an introductory letter and information sheet explaining the research and what taking part would entail, as well as response sheet, a demographic form and a freepost envelope (see Appendix 1). Clients were asked to complete and return the demographic form and the response form, indicating whether or not they were interested in taking part, directly to the research team.
Each pack was given a unique code and the NRTs kept a record of who received them. We contacted the teams regularly to find out which packs had been sent, and if we had not received a response with that code, we asked the NRT to send a reminder pack. Through this approach, the research team did not know the personal details of the NRT’s clients except those who agreed to take part and the NRT were not aware of clients’ decisions about participating, only that they had responded. Before interviews began we took consent following the procedures outlined for organisational staff interviews above.
The interviews focused on issues and outcomes that were important to the participant (using Harris et al. ’s3 outcomes framework to guide the discussion) and also whether or not, and how, the NRTs helped them to deal with their main concerns and to achieve the outcomes that were important to them. We also asked if they had a carer who we could invite to take part in a separate interview. People with LTNCs were given information about support organisations at the end of the interview.
As with the other types of participants, people with LTNCs were also offered the choice of in-person or telephone interviews. Interviews were audio recorded with the participant’s consent and transcribed. All service user participants chose to be interviewed in person and all agreed to audio recording of their interview; none requested to see their transcription. Interviews lasted between 30 minutes and 1.5 hours.
We intended to recruit a maximum of 10 people with LTNCs per site. This decision was based on experience in previous SPRU studies around LTNCs and around outcomes that indicated that this sample size would achieve data saturation across the dataset. A total of 35 people with LTNCs were interviewed across the four case sites. Table 4 gives details of the number of service users invited and that participated, by site. Further details of the participants are reported in Chapter 3.
| Site | Invited | Interviewed |
|---|---|---|
| A | 18 | 8 |
| B | 25 | 12 |
| C | 25 | 13 |
| D | 3 | 2 |
| Total | 71 | 35 |
As Table 4 indicates, approximately half of those invited agreed to take part. Of the other 36 people who were invited, one agreed to take part but had to withdraw due to an exacerbation of their condition, 26 did not respond despite being sent reminders and nine people declined to participate. Three people provided reasons for declining, all of which related to their neurological condition.
There were several occasions when we offered to contact participants’ NRTs about particular issues discussed during interviews but most declined, saying that they would discuss it with the team at the next visit. Even though we explained that doing so would mean that her involvement in the research would be disclosed, one participant asked that the researchers raise her issue with her NRT. A letter explaining the client’s concern was sent to the relevant NRT and a copy sent to the participant.
Interviews with carers
To explore integrated care from a carer perspective, we conducted in-depth, semistructured interviews with informal carers or family members that service users identified as providing them with significant support. Not all the service users we interviewed had a carer or wanted to nominate a carer.
The process for recruitment, consent and data collection with carers followed those outlined earlier. The aim of interviews with unpaid carers or family members (informal carers) was to explore their experience of integrated care and to relate these experiences to the different service models in the case study sites. All carers chose to be interviewed in person and all agreed that the interview could be audio recorded and transcribed. As with the other participants, none requested to see their transcription. Interview length ranged from 30 minutes to 1 hour. Carers were given information about support organisations at the end of the interview.
We intended to recruit a maximum of 10 carers per site (one carer per client), though we recognised that not all service users would have, or would want to nominate, a carer for us to contact. A total of 13 carers were interviewed across the four case sites. Table 5 gives details of the number of carers sent recruitment packs, and the number interviewed.
| Site | Invited | Interviewed |
|---|---|---|
| A | 7 | 0 |
| B | 10 | 6 |
| C | 6 | 5 |
| D | 2 | 2 |
| Total | 25 | 13 |
As Table 5 indicates, 12 of the carers we invited to take part in an interview did not do so. Of these, eight did not respond despite a reminder being sent, one agreed but then withdrew before the interview without providing a reason, and three others declined to participate, only one of whom provided a reason, citing that they did ‘not like interviews’.
Analysis of stage 1 data
Data collected from in-depth, semistructured interviews were managed and analysed using the framework approach. 82 Analytical frameworks were developed based both on the issues addressed in the topic guide and on key themes emerging in the data (see Appendix 2 for frameworks for each data set). Data from transcripts were charted onto the framework and the research team discussed entries throughout this process to ensure consistency and accuracy and to review the ‘fit’ of the data. Data within the framework were analysed thematically.
The service user framework underwent several iterations. To do this, an initial, a priori analytical framework was developed based on Harris et al. ’s3 outcomes, which had also formed the basis of discussion for data collection. This framework did not adequately reflect the nuances of the issues discussed by people with LTNCs and although some of the issues discussed were similar to those in Harris et al. ’s3 framework, the people we interviewed discussed them in different ways. We met several times to adapt the framework to better reflect the data and data were recharted accordingly. This reflective/recharting process continued until we arrived at a framework of outcomes that most accurately reflected the data. Each outcome identified in the final iteration of the framework constituted a framework ‘theme’. Data for each outcome were analysed thematically in the first instance, and diversity within themes was explored. Relationships and overlap between outcomes were then explored. This analysis assessed whether or not the outcomes were important and provided a description of the parameters of each outcome. Data from service users about the outcomes were analysed as one data set across the four case sites.
Stage 2: developing and implementing an outcomes checklist for use in practice
Between June 2011 and October 2011, we developed an OC based on stage 1 service user data. In stage 2, the NRTs used this OC as part of their usual assessment procedures.
Developing the outcomes checklist in partnership with the neurorehabilitation teams
We worked in partnership with the NRTs in each case site to develop the outcomes into a checklist that would work for them in practice. The outcomes included on the checklist were standard across the case sites. However, to complement local documentation and approaches to assessment and service provision, NRTs were able to determine the format of their checklist and the way it was to be used.
Meetings were arranged with each case study site to discuss their preferences. A standard list of discussion points was used and included preference for paper or electronic checklists and the need for action planning to be recorded on the checklist (see Appendix 3). A draft checklist was prepared for each NRT and a process of feedback and changes continued until we were able to finalise a checklist each NRT was satisfied with. However, the OC continued to be developed throughout the implementation phase. We contacted NRTs monthly to monitor their progress with the checklist, to see how many people they had used it with and to give staff an opportunity to discuss any difficulties or benefits they were experiencing. We also met with each of the NRTs on several occasions to discuss ways to maximise its use and user-friendliness in practice. We made field notes at these visits.
Implementing the outcomes checklist in practice
Electronic and hard copies of the checklist were given to each team, along with guidance for use, including the parameters of each outcome (see Appendix 4). We asked the NRTs to implement the checklist with new and re-referred clients as part of routine practice for an initial period of 6 months (October 2011 to April 2012).
We were not prescriptive about how the checklist should be used. Rather, we encouraged teams to use it in whatever way suited them, as long as it was with new and re-referred clients. To monitor how the checklist was working in practice, in addition to the regular contacts and meetings we outlined above we also conducted an audit of clients’ care records held by the NRT.
Care record audit
When the OC was used with a client, NRT staff gave the client an invitation pack if they fulfilled the eligibility criteria for the study; that is, they had a neurological condition, were aged 18 years or over, were new or re-referred clients, and were cognitively able to understand the research and give informed consent to participate. Using the same process as that outlined above for service user interviews in stage 1, NRTs recorded who received invitation packs alongside the unique number on the pack so that reminder packs could be distributed as necessary. Researchers contacted the team on a monthly basis to ascertain the number of assessments undertaken using the OC and the number of invitation packs passed to clients. (As reported in the previous section, we also asked about their experiences of using the OC in practice at these monthly contacts.) The number of these might differ, because NRTs could use the checklist with any of their clients, while we only wanted to invite people who fulfilled our eligibility criteria to ‘take part’ in the care record audit (CRA).
The invitation pack included a letter and two information sheets (one brief and one in more detail) explaining the research and what being involved would entail, a demographic form, a decline form, a consent form and a freepost envelope. The consent form asked clients to indicate their agreement to the CRA and to indicate their willingness to be contacted for an interview at a later stage. Because of this complexity, we included a short information sheet. This gave NRT clients a chance to quickly make a decision about not taking part without having to read all the information. The brief information sheet advised those considering agreeing to the CRA to read the full information sheet, and contact the research team if they had any questions or concerns, before they made their final decision (see Appendix 1 for examples of these documents).
Clients were asked to respond, with their consent or decline forms, directly to the research team. The decline forms gave clients the opportunity to provide a reason for not participating. When consent forms were received, the researcher contacted the NRTs and arranged to visit to access that client’s care records. As we did not want to see information about any clients who had not given consent, one of the NRT staff was advised which notes to prepare for our visit. As such, clients’ participation was not confidential from the NRTs and clients were informed of this on the information sheet.
When we visited the NRT offices to complete the CRA, we used a proforma (see Appendix 5) to guide the information we recorded. We recorded information about, for example, members of staff completing the checklist, level of detail recorded and recording of actions.
We hoped to recruit a maximum of 25 clients per case site but all sites had difficulties in achieving this number despite, as described earlier, teams’ reassurances that this was feasible. In an effort to increase checklist use and recruitment, and after approval from relevant ethical and research governance bodies, we revised eligibility for the CRA to include review clients (as well as new/re-referred clients). However, only two teams (those in sites C and D) used the checklist during reviews. We also asked the NRTs to extend the implementation period. Two of the teams agreed to this, and the implementation period for these two sites was 10 months (i.e. from October 2011 until August 2012). In addition, we clarified with NRTs that they could use the OC as part of their assessment with any and all clients. This was so NRTs had experience of using the OC as part of practice and would be able to contribute to the evaluation stage of the research.
Invitation packs were given to 45 eligible clients, meaning that an OC was used with at least 45 clients. We know from telephone contacts and the evaluation phase of the research that at least another seven OCs were used (four in site C, two in site D and one in site A). Twenty-four clients agreed that we could monitor the use of the checklist in their care records. Table 6 summarises the figures by site.
| Site | Invited | Consented to CRA |
|---|---|---|
| A | 7 | 3 |
| B | 19 | 9 |
| C | 16 | 10 |
| D | 3 | 2 |
| Total | 45 | 24 |
As Table 6 indicates, just over half of those invited agreed to the CRA. Of the 21 clients who did not take part, 18 did not respond despite being sent a reminder and three declined to take part, none of whom provided a reason.
We monitored the use of the OC throughout the implementation phase, we amended the methods in response to recruitment difficulties and we amended the format of the checklist in some sites following staff suggestions. The findings are reported in Chapter 5 alongside the evaluation data from stage 3.
Stage 3: evaluating the use of the outcomes checklist in practice
In stage 3 we evaluated the use of the checklist to assess its use in practice, and whether or not and how it affected practice. We also wanted to seek feedback from service users with whom the checklist had been used in order to assess its face validity and ascertain whether or not any changes had resulted from the checklist’s use.
Neurorehabilitation team interviews/focus groups
We offered NRT staff the choice of taking part in an in-depth, semistructured interview or a focus group to discuss their experiences of using the OC in practice.
We sent NRT staff an invitation pack including similar documents and following the procedures outlined in stage 1. The invitation packs for this stage, however, included two information sheets: one informing staff about an individual interview and what this would entail and one doing the same for focus groups (see Appendix 8, note e). For four of the teams we invited all NRT staff to take part so that we would be sure to include different professional perspectives and to hear views from those who had not managed to use the checklist in practice. In the fifth team, which was large, we invited a range of staff to represent the different professions within the team, as well as staff who had and had not used the checklist. NRT staff in sites B, C and D chose to have a focus group and staff from both teams in site A chose to be interviewed separately.
Interviews and focus groups explored how the checklist was used, views of the checklist, and its perceived impact. The analysis of the CRA data highlighted additional ‘prompts’ to cover if they did not arise as part of the discussion, such as perceived similarities between outcomes. Interviews were conducted in person or via telephone, depending on what suited the participant. They were audio recorded and transcribed in all but one case. They lasted approximately 40 minutes. Focus groups were held in the NRT’s office, were audio-recorded with all participants’ consent and were transcribed verbatim. They lasted around 1.5 hours. For the person who did not want the interview audio-recorded we took extensive field notes and analysed these data alongside transcripts. In addition, we invited social care colleagues who worked closely with the teams in sites A, B and C to give their views (via interview or in writing/e-mail) on the content of the OC and how it might relate to their practice.
To provide different perspectives on the checklist, we intended to recruit all those who had used the checklist as well as members of the team who had not. Again, as team structures and the number of staff per team differed (see Chapter 3), no sample size was set. A total of 21 NRT staff were recruited across the four case sites. Table 7 gives a breakdown of recruitment by case site.
| Site | NRT Staff | Non-NRT Staff | ||
|---|---|---|---|---|
| Invited | Participated | Invited | Participated | |
| A | 6 | 2a | 2 | 1 |
| B | 10 | 10 | 1 | 0 |
| C | 8 | 6 | 2 | 0 |
| D | 2 | 2 | Social care were not involved at this site | |
| Total | 26 | 20 | 5 | 1 |
Of the NRT staff who did not take part, two were ill on the day of focus group (C) and one in site A had agreed to take part in an interview but then withdrew due to scheduling conflicts. Of the three NRT members in site A who did not take part, one declined due to sickness and we did not receive a response from two people despite reminder packs being sent. The non-NRT staff invited were all social care practitioners who worked closely with the NRTs. (These relationships are explored in more detail in Chapter 3.) We received no response from three of them, despite reminders, and one declined because they had changed roles.
Evaluation interviews with people with long-term neurological conditions
We wanted to hear about service users’ experiences of having the checklist used as part of their assessment/review with the NRT, to hear about any resulting actions and to hear their views about the outcomes on the checklist.
In the invitation pack given to them in stage 2, service users were asked if they would be interested in taking part in an interview. We sent an interview invitation pack directly to those who had expressed interest (n = 21) after 3 months, enclosing further information and a response form to log their decision about participating. Response forms were returned directly to the research team. Although we were aware that some participants might not remember their assessment in detail given the cognitive issues that can accompany some neurological conditions, we wanted to give the NRTs time to implement any actions arising from the assessment. This was so that we could monitor whether the type of, or approach to, interventions were affected.
Before interviews began, we took consent following the procedures outlined in the organisational staff interviews in stage 1, emphasising a participant’s right to withdraw at any time without giving a reason. All service users agreed to in-person interviews and for these to be audio recorded and transcribed. None requested to see their transcription. Interviews lasted between 30 minutes and 1 hour. Participants were given information about support organisations at the end of the interview.
We aimed to recruit a maximum of five people with LTNCs per case site. A total of 12 were recruited across the four case sites. Table 8 gives a breakdown of recruitment by site. Further details of the participants are reported in Chapter 6.
| Site | Agreed to be contacted | Interviewed |
|---|---|---|
| A | 1 | 1 |
| B | 8 | 4 |
| C | 11 | 6 |
| D | 1 | 1 |
| Total | 21 | 12 |
As Table 8 shows, nine people who agreed in stage 2 that we contact them later for an interview did not take part. Seven did not respond to the invitation despite receiving a reminder and two declined because of poor health (n = 1) and confusion (n = 1).
Analysis of stage 3 data
Data collected from both service users and practitioner staff were managed and analysed using the framework approach. 82 For the practitioner data, an analytical framework was developed based on a priori issues addressed in the topic guide and key themes emerging from the data (see Appendix 2). Staff data were analysed thematically to understand the feasibility of using the checklist in practice, and identify the key barriers and facilitators to using the checklist. As the same topics were covered in the in-depth interviews and focus groups, and the sample included the same type of staff, we analysed interview and focus group data together. We did not find integrating these data problematic, most likely because they covered the same topics. We charted focus group data as one ‘case’, and we used a whole-group approach to analysis. This approach is most appropriate when there is homogeneity in the sample; however, we were careful to ensure that divergent voices were not lost in analysis. Service user data were analysed thematically to assess the validity of the checklist in addressing key concerns of the participant and overall views of the checklist. Researchers discussed charting throughout this process to ensure consistency and accuracy.
Reporting
Anonymity and identifiers
To maintain the anonymity of participants, each case study site was given a unique identification code (i.e. sites A–D) and no names of local organisations or locations are included. Where we have drawn on local documents, we have not referenced this material directly to protect anonymity.
Staff who participated in the research were also given a unique identification number. We include information about the type of organisation/service they worked for (e.g. social care or NRT) but, to protect anonymity, do not report designation. The site code is included only where this does not risk compromising individuals’ anonymity.
Service users and carers were assigned a unique identification number. In places, we have used plural pronouns to obscure a participant’s gender and thus ensure that their identity is not compromised. In general, where we have quoted a service user we have referred to them by their identification number, which includes a case site reference, and their condition. Where we have quoted a carer, we have used their identification number and their relationship to the person they support. However, where the combination of these could compromise a person’s anonymity, one or more of these labels have been removed.
As described earlier in this chapter, NRTs distributed invitation packs to service users for us and recorded their identification number and name. To ensure that NRT staff are not able to identify participants in this report, and to ensure consistency in format of identification number, we changed all participant identification codes.
Use of quotations
Quotations used within this report are not exhaustive of the issue being discussed but rather are used as illustrative examples of themes that emerged in interviews.
Chapter 3 Profiles and processes
Key messages
-
Integration structures vary between localities and are not stable over time within localities.
-
The ways in which NRTs work can affect whether or not service users’ desired outcomes can be assessed.
Introduction
This chapter presents findings from analysis of local documentary evidence and interviews with staff, service users and carers that were undertaken in stage 1 of the research. There are two sections; the first presents case site demographic, organisational and team profiles and provides a contextual backdrop for the rest of the findings. The ways the teams worked (processes) and the ways these processes might affect achievement of outcomes for people with LTNCs are presented in the second section.
As outlined in Chapter 2, we invited staff from different levels of the case PCTs and local authorities to take part in interviews about local structures and integrated working practices. Table 9 summarises the sample we recruited to the research and more details of these samples are provided, as appropriate, throughout this chapter.
| Participant type | Number of participants |
|---|---|
| NHS commissioners/strategic staff | 11 |
| Social care commissioners/strategic staff | 4 |
| NRT | 23 |
| Social care based practitioners | 5 |
| Total | 43 |
Case study profiles
Documentary evidence, including neighbourhood statistics and PCT annual reports, showed that the four case study sites, as described in Chapter 2, had different demographic profiles.
Demographic profiles
The data presented about these draw on the most recent available Neighbourhood Statistics for each of the case areas (PCTs), predominantly based on 2001 census figures (see Appendix 8, note f). 86 Rural/urban classification of the case study areas was based on the Department for Environment, Food and Rural Affairs (Defra) classifications of PCTs from 2009, which were the latest available statistics (see Appendix 8, note g). 83
Case study site A
Site A is a large PCT classified as ‘major urban’, indicating that at least half the population lives in urban areas. It has a resident population of close to three-quarters of a million, with the largest age groups being those in middle adulthood. The mean age of the population is slightly lower than the national average for England. It has relatively low levels of ethnic diversity compared with England as a whole but has several wards with large black and minority ethnic (BME) populations. It is ranked in the third quintile of deprivation, indicating medium levels of deprivation (see Appendix 8, note h). Around two-thirds of the population describe their health as good, and around one-tenth of the working-age population has a long-term limiting illness. Approximately one-tenth of the population is providing unpaid care, and of those, the majority provide between 1 to 19 hours per week while around one-fifth are providing more than 50 hours a week.
Case study site B
Site B is a small PCT comprising mainly towns and villages and is also classified as ‘major urban’. The largest age groups are those in early–middle adulthood and the mean age of the population is slightly lower than the national average for England. Overall, the area covered by the PCT has low levels of ethnic diversity, but there is a large BME population in the main town. The area is ranked in the first quintile of deprivation (very high). Around two-thirds of the population report good health but approximately one-fifth of the working age population have a long-term limiting illness. Unpaid care is provided by approximately one-tenth of the population. Just over 2% of the population are providing more than 50 hours of unpaid care a week.
Case study site C
Site C is a large PCT comprising towns and villages, and is classified as ‘significantly rural’, suggesting that more than one-quarter of the population live in rural settlements. It has a population of approximately half a million people, with the largest age groups being those in early–middle adulthood, followed by those in late adulthood, meaning that the case site age profile is similar to that of the national population. It is ranked within the fourth quintile of deprivation (low), and has very low levels of ethnic diversity. Just under 10% of the population are of working age with a lifelong limiting condition and the majority of the population rate their health as good. Over one-fifth of the population provides unpaid care, and of these, the majority are providing between 1 and 19 hours per week. Around one-fifth of those providing unpaid care provide over 50 hours a week.
Case study site D
Site D is a medium sized PCT comprising a small city, some towns and villages. It is classified as ‘Rural-50’, indicating that most of the population live in rural settlements and market towns. It has a population of just under half a million people, with the largest age groups being those in middle to late adulthood. The average age is slightly higher than the national average for England. It has low levels of ethnic diversity and is ranked within the fifth quintile of deprivation (very low). Around 10% of the working age population have a lifelong limiting condition and around three-quarters of the population rate their health as good. Just under 10% of the population are providing unpaid care and around three-quarters of them provide between 1 and 19 hours a week. Under one-fifth of those providing unpaid care provide more than 50 hours a week.
As is evident from these profiles, the PCTs and local authorities that made up our case study sites were dealing with populations that differed in, for example, age profile, deprivation levels and ethnic diversity. These demographic profiles are summarised in Table 10 for ease of comparison.
| Demographic characteristics | Site A | Site B | Site C | Site D |
|---|---|---|---|---|
| Mean agea | Lower | Lower | Similar | Above |
| Ethnic diversitya | Low | Low | Very low | Low |
| Deprivationb | Medium | Very high | Low | Very low |
| Population with good health (%)c | Over 60 | Over 60 | Over 70 | Over 70 |
| Working age population with a LTC (%)c | 10 | 20 | 10 | 10 |
| Population providing unpaid care (%)c | 10 | 10 | 20 | 10 |
Organisational profiles
The case sites also reflected different organisational structures at a commissioning and strategic level. To understand the structures, we interviewed 15 commissioning and strategic staff across the four case sites. Table 11 shows the organisational staff who were interviewed.
| Site | NHS commissioner/senior manager | Social care commissioner/senior manager | Total |
|---|---|---|---|
| A | 1 | 1 | 2 |
| B | 3 | 1 | 4 |
| C | 3 | 2 | 5 |
| D | 4 | NA | 4 |
| Total | 11 | 4 | 15 |
As described in Chapter 2, we had difficulty recruiting commissioning staff in two of the case sites, so the information provided here triangulates data from documentary evidence and interviews with commissioning, other strategic and NRT staff per case site. As we had worked with three of the case sites before, we were able to reflect on the changes that had taken place in these areas. Where we have done so, we have made it clear that evidence is from previous work.
Staff we interviewed described different mechanisms for working with other organisations, including joint posts and joint boards. Some posts, for example directors of public health, are required to be joint appointments between health and social care. In this chapter, when we refer to ‘joint posts’, we have not reported these statutorily required joint posts.
Case study site A
The PCT and LA are two separate organisations but have formal integration arrangements in the form of a joint commissioning board led by social care. This board focused on discrete topics but did not specifically cover neurological conditions. Indeed, no formal standing arrangements around neurology services enabling integration between health and social care were reported at either commissioning or strategic management level. From previous research undertaken in this PCT and LA, we know that formal structures used to exist around commissioning for neurology but when social care was reorganised, before the start of this research, these formal structures were lost.
A social care commissioner that we interviewed said that they regularly linked with the voluntary sector, user groups, the NHS provider trusts in the area, GPs, intermediate care and the PCT to commission and provide services to the local population. As we were unable to recruit any PCT commissioners in this area (see Chapter 2) we are not able to present views of integration arrangements from that perspective.
Case study site B
Formal integration existed between the PCT and social care for children’s services in case site B but, during the research, the organisations were not integrated around adult services. There were, however, several joint posts between health and social care, and staff from the PCT and LA would work together for particular projects. For example, at the time of the research, the PCT and social care strategic staff were working together on a project around deprivation.
A neurosciences network, which included this case study area, played a strategic role in developing neurology services across the region. Within the PCT there had been a joint forum for neurology services, which participants viewed as being a driver of integrated neurology services locally, but meetings for this no longer took place and a joint commissioner who had focused on services for neurology clients had recently retired, leaving no one to continue this focus.
Case study site C
The PCT and LA in site C were two separate organisations but formal integration structures existed between them in the form of a joint commissioning unit led by social care. This unit focused on specific work streams, none of which specifically included people with neurological conditions.
At the time that this research was undertaken, major organisational change was taking place in both health and social care sectors and, therefore, organisational arrangements were in flux. Although major restructuring included integration of statutory health and social care organisations, no one was able to say how services for people with LTNCs would fit into, or be affected by, the new structure.
Case study site D
Site D became a research site later in the research process, as described in Chapter 2. We invited this PCT to participate because we were aware from previous research that a joint operating structure between health and social care existed. However, this was dissolved before the research began. As a result, when we started the research in site D, no formal or informal arrangements to enable/promote integration between the PCT and the LA at practice or strategic level (except where mandated in legislation, such as public health) were reported. However, these organisations were in the process of developing a joint strategic commissioning board.
We were unable to interview any commissioners or senior strategic staff who had been in post throughout the transition and none of the people we interviewed felt confident enough about the reasons for the demise of the integrated arrangements to discuss it in detail during interviews. In addition, after initial interest in participating in the research was expressed by commissioners in the locale, social care services were unable to take part because of limited capacity.
The different arrangements for integrated working evident in the four case study sites are summarised in Table 12.
| Integration arrangements | Site A | Site B | Site C | Site D |
|---|---|---|---|---|
| PCT/LA integrated | No | No | No | No |
| Joint commissioning/strategic arrangements | Joint commissioning board | Some joint posts | Joint commissioning unit | None reported |
| Project-based groups | ||||
| Integrated working around neurology service provision | None reported | Part of neuroscience network | None reported | None reported |
As a result of ‘Transforming Community Services’,35 provider arms of PCTs had to separate from the commissioning arm of PCTs and tended to join with other provider organisations. The case sites followed different models: one joined with a mental health trust, one joined with the local acute trust, one became a community trust and one joined with other PCT and LA providers.
Neurorehabilitation team profiles
As described in the methods section, each case study PCT had at least one NRT. The teams in the case study areas were different sizes, covered different conditions and had different structures and processes. To understand these, we interviewed 24 staff in the NRTs and four social care professionals who worked closely with the team. Table 13 shows the designation of staff interviewed across the four case sites.
| Designation | Practitioners recruited and interviewed |
|---|---|
| Clinical manager | 3 |
| Occupational therapist | 9 |
| Nurse/nurse specialist | 5 |
| Physiotherapist | 3 |
| Rehabilitation support worker | 1 |
| Social worker | 3 |
| Speech and language therapist | 1 |
| Assistant physiotherapy practitioner | 1 |
| Social care assessor | 1 |
| Administrator | 1 |
| Total | 28 |
All teams talked about informal/referral links with other agencies including, for example, acute services, housing agencies, voluntary sector agencies and social care organisations. We have not included these ad hoc links in the descriptions of teams. A summary of each team is given below.
Neurorehabilitation teams in case study site A
Two community neurology services within the provider arm of the PCT were studied in site A: a BI team and a MS team. (As reported in Chapter 2, we worked with two teams in case site A to provide a population large enough for us to recruit up to 25 service users per case site for the implementation and evaluation of the OC in stages 2 and 3.) Both were part of a larger community neurology service that included several other specialist teams. They were based in a community hospital and were similar in their service models of integration, in that neither had a social worker employed as part of the team but they maintained close working links with neurology specialist social care practitioners.
The NRT specialising in BI comprised occupational therapists (OTs) (see Appendix 8, note i) and a neuropsychologist. One of the OTs worked as a family liaison officer within the team for some of their contracted hours. A BI specialist social worker, funded by adult social care, used to sit within this team but was no longer in place when we undertook this research. The arrangements between the team and the social worker were informal, with staff linking when they had clients common to both caseloads.
The team supported people within 5 years of their BI, meaning that the maximum length of time a client was supported by the team was 5 years. Clients could receive this ongoing support while they remained motivated to achieve goals. The BI NRT’s composition is summarised in Figure 1. (Dotted lines on figures summarising the teams denote informal working arrangements. Solid lines indicate disciplines that are core/formal parts of the teams.)
FIGURE 1.
Site A brain injury neurorehabilitation team.
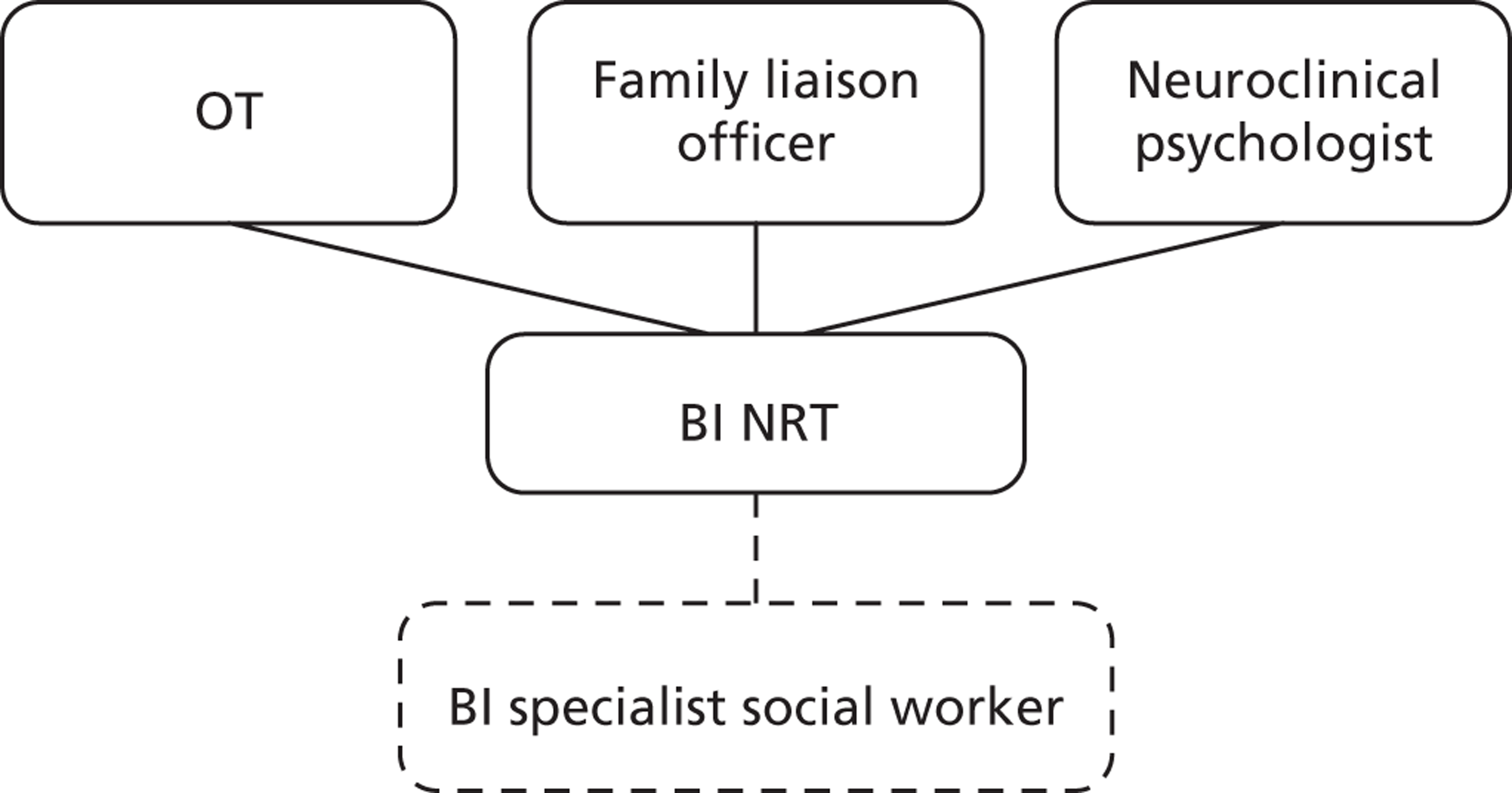
The NRT specialising in MS comprised an OT, an OT assistant and a clinical psychologist. The team used a goal-based approach and supported clients for the length of time it took for them to achieve their goals. Similar to the BI NRT, the MS NRT linked with a social worker specialising in MS, a post that was funded by adult social care. This social worker attended team meetings every 4–6 weeks to discuss clients’ social care needs and they also undertook joint visits with NRT practitioners, as appropriate. A MS nurse specialist from the local acute trust also attended these regular meetings. The MS NRT’s composition is summarised in Figure 2.
FIGURE 2.
Site A multiple sclerosis neurorehabilitation team.
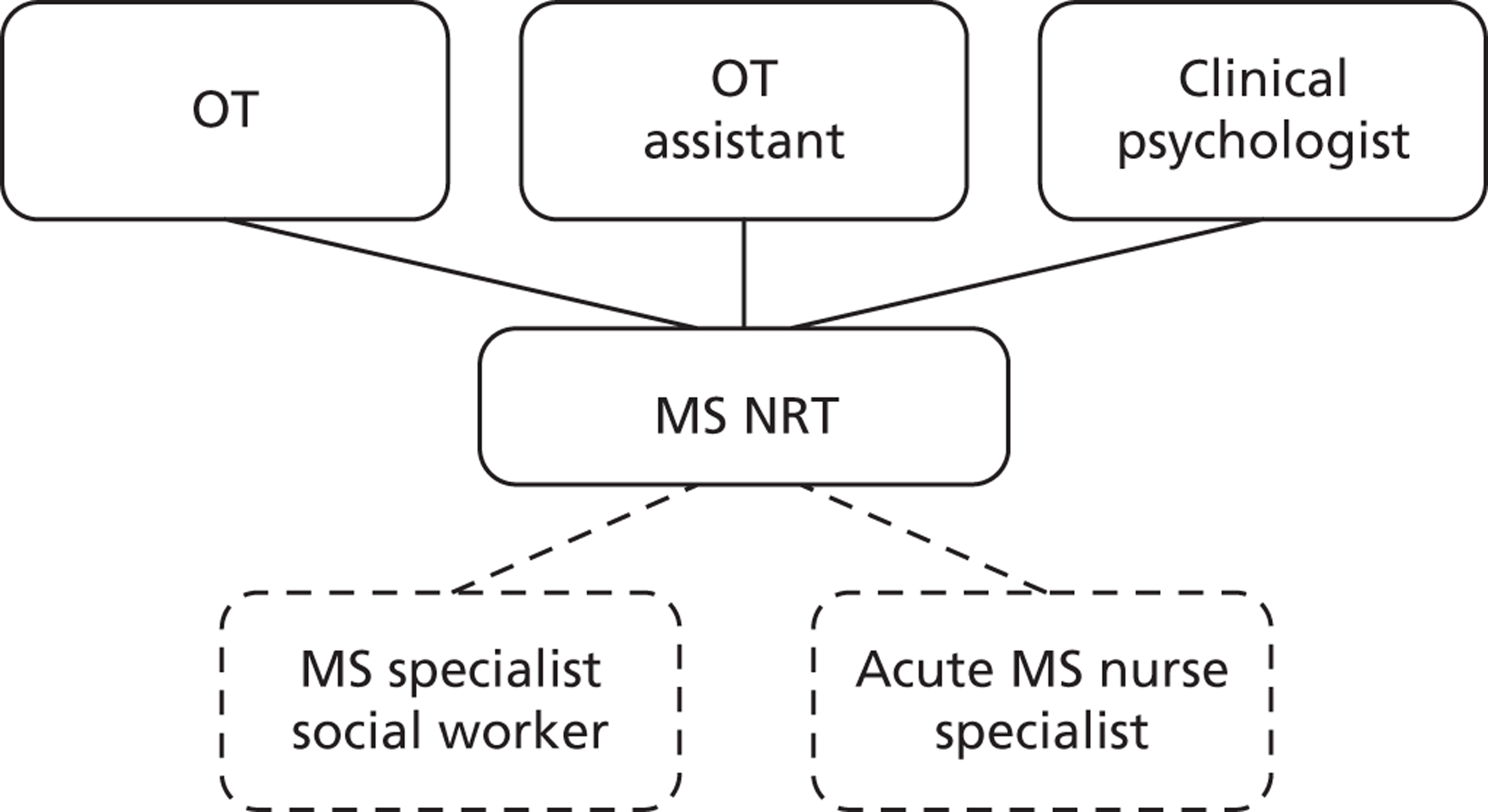
In the second year of the study, the community neurology services underwent phased reconfiguration. This resulted in the BI NRT and the MS NRT, along with other community neurology services, merging into a larger, community neurology team comprising OTs, psychologists, a senior nurse, a dietician and a rehabilitation consultant. After merging, the new team also had a designated administrator. Although the reconfigured community neurology services resulted in a non-condition-specific team, specialist pathways (e.g. for BI and MS) were retained. After the reconfiguration, the research team continued to work with those staff who previously comprised the BI NRT and the MS NRT and with service users with BI and MS.
Neurorehabilitation team in case study site B
The NRT in site B was a large interdisciplinary team and provided rehabilitation (up to approximately 12 weeks) for people with any LTNC and those who had experienced a stroke. Most posts within the team were funded by the PCT but one social worker post was funded jointly by the PCT and social care and three support workers were funded by social care. The team comprised a clinical lead, two nurse specialists (one for PD and the other for stroke), OTs, physiotherapists, a speech and language therapist, a social worker, support workers and a sessional dietician. The team also had a designated administration team. In the past, the team had contracts with the local acute trust but these had recently ended. Similarly, a previous service-level agreement for neuropsychology input to the team had ended. The composition of the NRT in site B is summarised in Figure 3.
FIGURE 3.
Site B neurorehabilitation team.
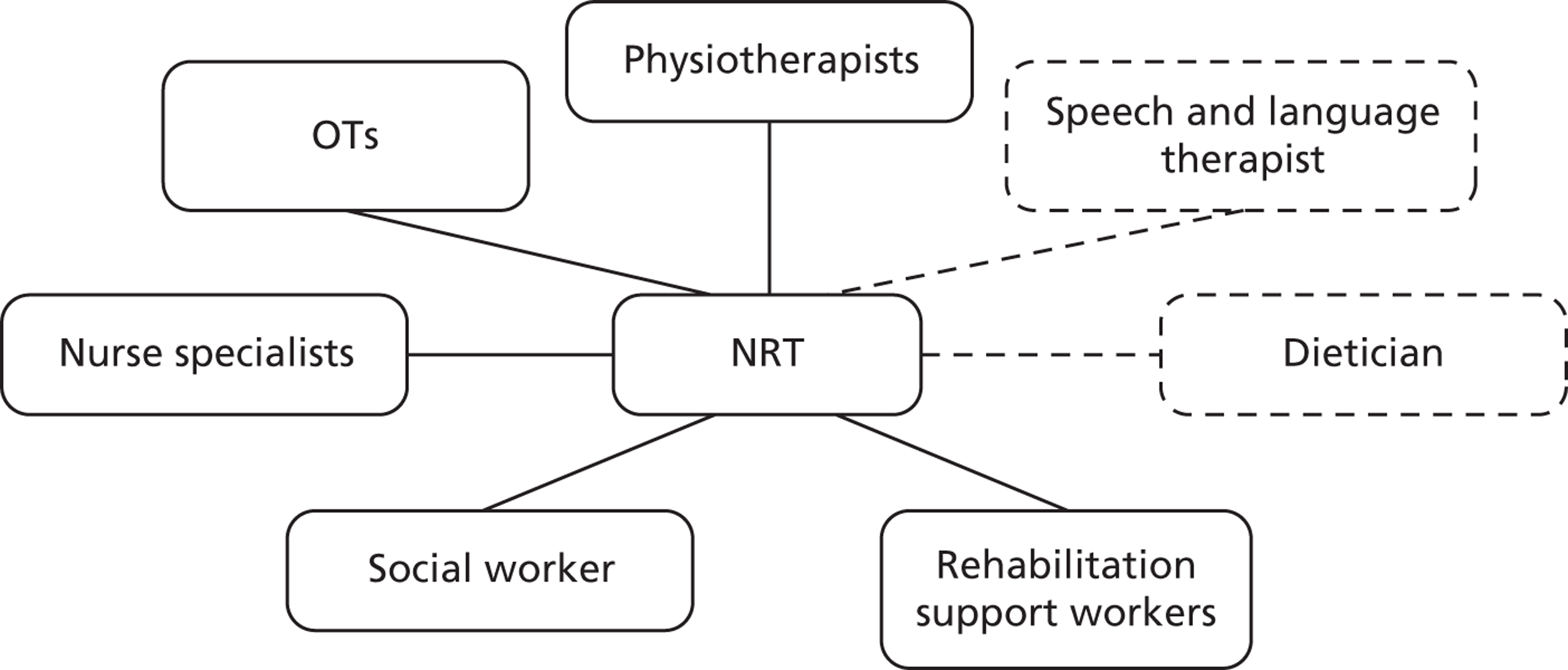
Neurorehabilitation team in case study site C
The NRT in site C was a medium-sized interdisciplinary community team funded by the PCT. It provided long-term support for adults with progressive neurological conditions. Disciplinary input included OTs, physiotherapists, a MS nurse specialist, a PD nurse specialist, a post-diagnostic counsellor and a designated administrator. The team also bought in sessions from a speech and language therapist based in a local acute trust and funded several respite beds in a local care centre.
Social care funded a social care assessor and an OT, both based in local social care services, to attend monthly team meetings to discuss the NRT’s clients and potential for ongoing social care input. NRT staff attended social care annual reviews for their clients and also undertook continuing health-care funding assessments with social workers, as appropriate. Some members of the team ran clinics at the local acute hospital, promoting links with acute staff. The team had also developed a computer-based alert system with the local acute trust so that they were able to provide timely specialist in-reach support and advice, including around discharge planning, when someone with a LTNC had been admitted. The composition of the NRT in site C is summarised in Figure 4.
FIGURE 4.
Site C neurorehabilitation team.
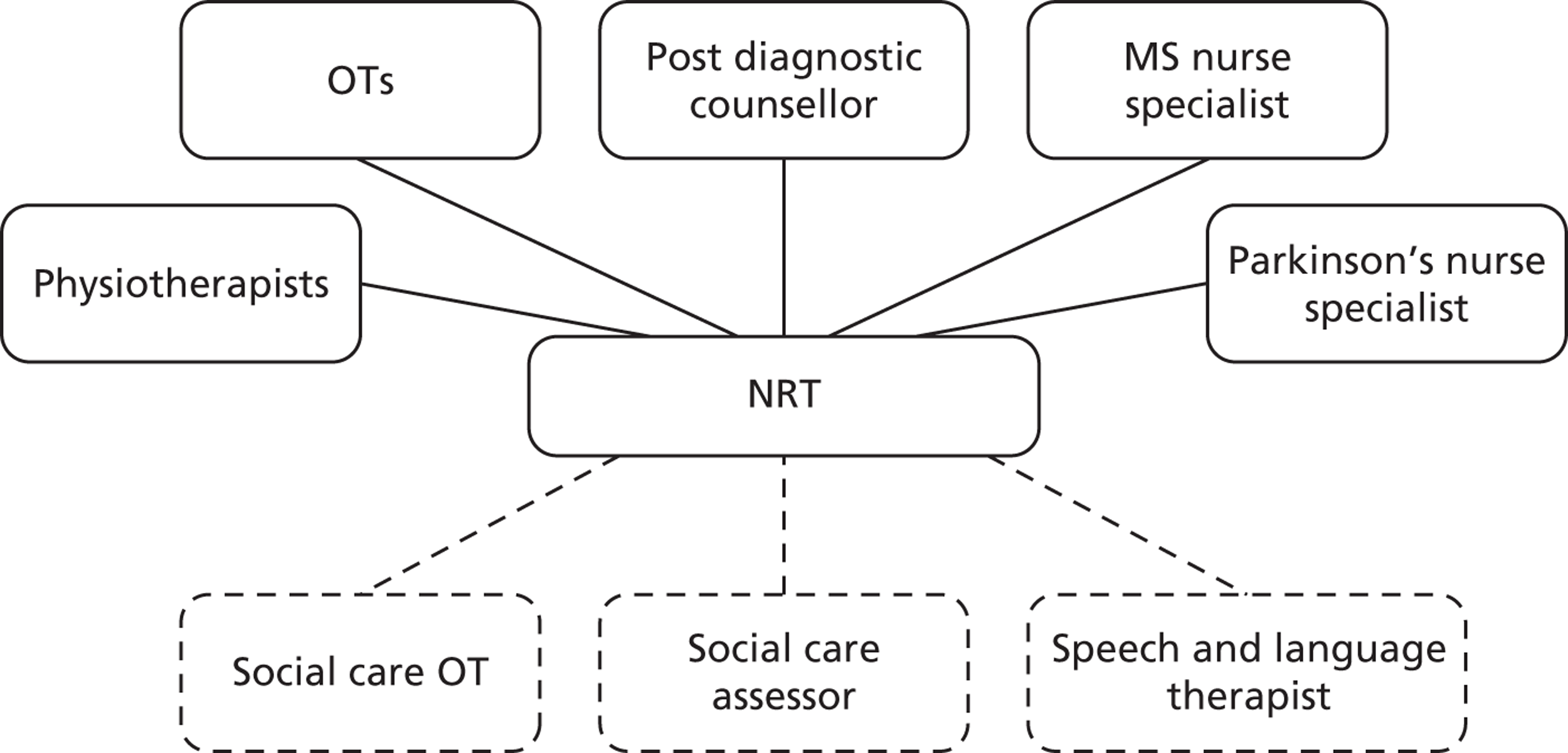
Neurorehabilitation team in case study site D
The NRT in site D was structurally different from those in the other three case sites. It was part of a larger community neurology service that comprised specialist nurses, physiotherapists, OTs, support workers and two care co-ordinators: one for MS and one for stroke.
This neurology service was split into smaller teams of up to four practitioners, covering the disciplines listed above, that were aligned with a generic (health-based) rehabilitation neighbourhood team. The neighbourhood teams provided rehabilitation to adults with any condition and the NRTs provided them with neuro-specific advice, support and training, meaning that NRT staff regularly undertook joint assessments and rehabilitation sessions with staff from the neighbourhood teams. In addition, the NRTs in each neighbourhood retained a client list including people who had experienced a BI and/or who presented particular challenges for service provision. Some staff from the NRT would also visit the local acute trusts on a weekly basis to help with discharge planning for people with LTNCs.
During the course of the research, the neurology service was restructured. Therapists based in the NRT were, after this point, line managed by the neighbourhood team manager and the nurse specialists were managed by the community nursing manager. Thus, after these changes, although members of the NRT were based in the same office, they had different line management structures.
Although social care staff used to be part of the neighbourhood teams, these were withdrawn before the research began and, during the research, there were no formal arrangements for integrating health and social care in practice. The composition of the neurology service/NRT in site D is summarised in Figure 5.
FIGURE 5.
Site D neurorehabilitation team.
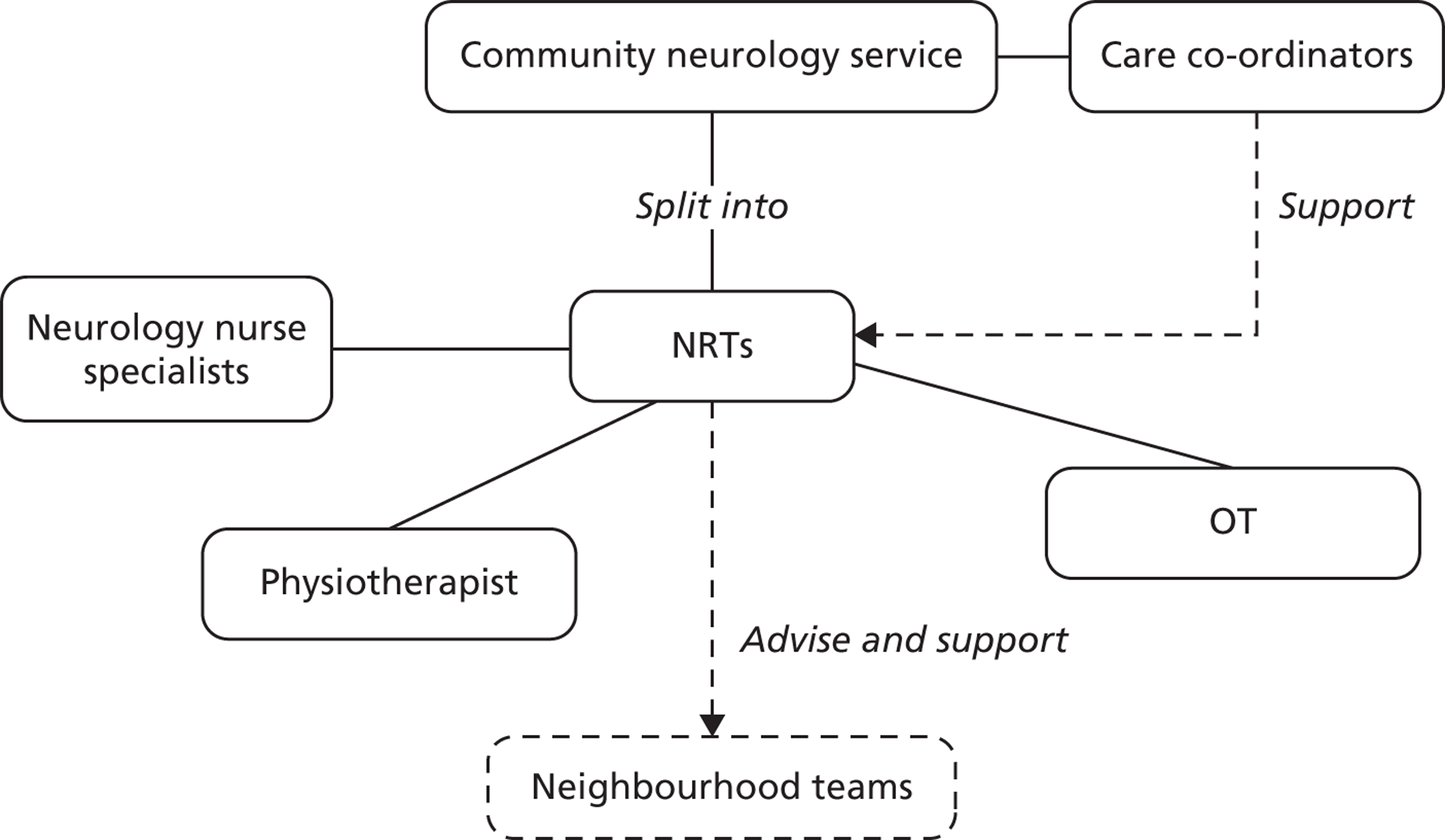
We interviewed staff at all levels of this arrangement, but we primarily worked with one NRT, based in a community hospital, which supported and advised two neighbourhood teams about neurorehabilitation and had their own client list of people with LTNCs with ‘complex needs’.
The NRTs, therefore, supported different client groups, had different staff composition, and represented different integration arrangements. Table 14 summarises the differences and similarities in the NRTs.
| Team characteristics | A1 | A2 | B | C | D |
|---|---|---|---|---|---|
| Conditions covered | BI | MS | All LTNCs (including stroke) | Progressive neurological conditions | BI and any complex LTNC client |
| Team base | Community hospital | Separate office | Separate office | Community hospital | |
| Number of staffa | 3 | 3 | 20–23 | 7–10 | 2–3 |
| Number of disciplinesa | 2 | 2 | 8 | 5 | 4 |
| Social care integration | When share a client | Formal – attendance at monthly meetings | Integrated into team | Formal – attendance at monthly meetings | None |
| Acute care integration | None discussed | Monthly meetings with MS nurse specialist | Recently ended | Acute-based clinic | Discharge assessments |
| In-reach work | |||||
| IT neuro-alert system | |||||
Team processes
As outlined in the previous section, NRTs in the case study areas were different sizes, covered different conditions and had different structures and processes. In this section, we compare team processes across the different case sites. We present service user and carer views to illustrate how these different processes can affect the degree to which outcomes are achieved.
All teams provided support from Monday to Friday. In site D, the neighbourhood teams continued rehabilitation input over weekends, as necessary. None of the other teams formally offered ‘out of hours’ rehabilitation, though some practitioners in the teams said that they would work later in the evening if that was the only time people with LTNCs were available to be seen.
Referrals to the teams were mainly from other health-care professionals, but could also be from social care staff and voluntary sector organisations, for example Parkinson’s UK in site B. The MS NRT in site A and the NRTs in sites B and C would accept self-referrals, as long as they had confirmation of the person’s neurological diagnosis from a professional. The other teams would only accept referrals from professionals.
All NRTs reported that clients received a holistic initial assessment and that they used a goal-based approach for guiding service provision and interventions. We obtained and compared copies of the initial assessment forms from each NRT and found that they covered similar issues, albeit in different ways (see Appendix 6 for more information). All teams assessed physical and emotional well-being and functioning, home and social circumstances, including relationships, and assessed risks. We asked teams if and how they assessed outcomes, and requested copies of documentation that was used. The teams described several tools they used for measuring ‘outcomes’ which were primarily physical, cognitive or emotional status measures, such as the Mini-Mental State Examination87 or the Timed Up and Go,88 or generic health outcome measures, such as the HowRU89 and the European Quality of Life-5 Dimensions (EQ-5D). 90 This illustrates NRTs’ everyday operational understanding and use of outcome assessment in practice. However, from our previous research, we know that these types of teams, which adopt a holistic, patient-centred approach, are able to provide much wider benefits to clients; benefits that are not necessarily captured by these types of assessment tools.
The maximum length of times that NRTs supported clients varied within teams as well as between teams. Some continued to support clients until they had achieved their goals (sites A and D), one NRT supported people for between 6 and 12 weeks, but this could be extended for a few additional weeks if clinically appropriate (site B), and one team kept people on their list indefinitely as either active or inactive clients (site C). With the exception of the BI NRT in site A, all teams that discharged clients once their goals were met allowed people to re-refer themselves to the team without having to go via a professional.
Although all the teams provided rehabilitation support in their clients’ homes, all, with the exception of staff in site D, described how they would also provide support in other locations to help achieve clients’ goals. For example, NRT staff visited workplaces with clients wanting to return to work and accompanied people in supermarkets and when travelling to help them regain confidence to continue with ‘mainstream’ social and practical activities. The NRT in site C also ran a multidisciplinary clinic with the local consultant neurologist at a local community hospital where clients could see any of the professionals they wanted/needed to at the same visit.
Service processes and outcomes
Interviews with service users for stage 1 of this research focused on desired outcomes. However, participants’ experiences of the NRTs and how the ways they worked helped clients achieve desired outcomes also arose during these interviews. Carer interviews focused on experience of NRTs, including the NRT’s approach to including carers.
A total of 35 people with a LTNC were interviewed across the four case sites. Table 15 provides demographic details of the people we interviewed.
| Sample characteristics | Number |
|---|---|
| Gender | |
| Male | 17 |
| Female | 18 |
| Primary diagnosis | |
| MS | 15 |
| BI | 6 |
| MND | 2 |
| PD | 4 |
| Stroke | 5 |
| Other | 2 |
| Prefer not to say | 1 |
| Age groups (years) | |
| 30–39 | 4 |
| 40–49 | 9 |
| 50–59 | 6 |
| 60–65 | 6 |
| 66–75 | 6 |
| 76–85 | 4 |
| Ethnicity | |
| Asian | 0 |
| Black/black British | 0 |
| White British | 35 |
| White other | 0 |
Thirteen carers were interviewed. Table 16 describes the carer sample.
| Sample characteristics | Number |
|---|---|
| Gender | |
| Men | 6 |
| Women | 7 |
| Age groups (years) | |
| 50–59 | 2 |
| 60–65 | 4 |
| 66–75 | 6 |
| 76–85 | 1 |
| 85+ | 0 |
| Ethnicity | |
| Asian | 0 |
| Black/British | 0 |
| Chinese | 0 |
| Mixed | 0 |
| White British | 13 |
| Relationship to service user | |
| Spouse/partner | 11 |
| Mother | 2 |
| Living with service user | |
| Yes | 10 |
| No | 3 |
| Service user’s neurological condition | |
| MS | 4 |
| MS and epilepsy | 1 |
| Stroke | 3 |
| PD | 2 |
| MND | 1 |
| Other | 2 |
The ways in which teams worked, or the way services were delivered, frequently affected service users’ perceptions of whether or how outcomes might be achieved.
A holistic approach to support, where people felt that the team saw the whole person, was highlighted as beneficial and was particularly evident in the accounts of service users in the BI NRT in site A and the NRTs in sites B and C. The ‘whole person’ ethos of these teams meant that they could apply their specialist knowledge to work in personalised, flexible ways that also promoted self-management in their clients.
Someone with MS in site C described how she had lost confidence before the NRT became involved and helped to sort out issues ranging from incontinence to mobility and housing issues. In site B several service users described how the team would identify functional and home-based issues, but these were broadened to the wider environment and the client’s personal goals, for example to provide help in accessing leisure activities and enabling psychological and employment support. One man with a BI, for example, described how memory loss had caused him anxiety and he saw overcoming this as the key to improving other areas of his life. The team had helped him with household tasks, such as cooking and shopping, and encouraged practical strategies for improving his memory in a variety of situations. Team support extended to benefits advice, helping him acquire new skills to improve future employment prospects via the job centre, and accompanying him to pursue leisure and exercise activities. Through the team being encouraging but not too directive, and demonstrating to him where and how he had made progress, he had regained confidence in himself, felt more in control and reassured that the NRT could offer support in new areas when, and if, necessary. This view was common across the teams that adopted a holistic approach to service user problems.
Linked to this, effective co-ordination of services and joined-up working within the team was often seen as key to finding solutions to problems which could be multifaceted. An interviewee in site A described how the BI team had arranged for a social care assessment, helped him find assistance with domestic tasks and assisted with his application for equipment. For someone with PD, living alone and with limited mobility, having the team in site C to help co-ordinate her care was key to maintaining her independence.
They really are good. They do fill a gap between a GP and a Consultant’s knowledge, and life in general, which can be very negative for people.
SU24C, PD
Providing information about services and support was fundamental to better care co-ordination and self-management and this was something that the specialist knowledge of team members enabled. Specialist knowledge included both knowledge about LTNCs and knowledge about services and support in a local area.
Once someone was accepted as a client, ease of contact with the NRT was a characteristic of all teams, and was particularly valued in promoting independence and confidence. Although an interviewee with motor neurone disease (MND) in site D saw the NRT relatively infrequently, he knew that he or his wife could contact them at any time if any concerns arose. A service user in site A particularly valued the way he could express his concerns to staff in the BI team and talk about his situation. Having someone who he felt understood his situation and condition to talk to, or to just listen, was important.
I think what it is, that you talk to people from the [BI Team] and you can talk to them about how you feel, what’s happened, what’s happening, what you want to do about the future, what’s gone wrong in the past and all that sort of stuff and just . . . and not get at all emotional about it.
SU7A, BI
A team’s positive attitude and encouragement could, in turn, generate confidence and self-esteem in service users themselves.
Because they believe in you. They give you that feeling that they believe I can do it, so, I can do it.
SU9B, condition withheld by participant
However, this was balanced by teams managing expectations around outcomes which helped service users remain realistic in their goals. Personalised discussions around goals, and teams offering practical strategies and solutions to help achieve these, were appreciated by service users. For example, the nurse specialist from the team in site C taught a service user with MS some useful techniques for dealing with complex mobility problems and how to break tasks down into smaller, more manageable components. In parallel, the OT accompanied her to view suitable new accommodation, relieving some emotional stress.
Having a responsive team that worked flexibly and accommodated individual and family needs as much as possible, helped carers as well as service users. The way teams were able to work in people’s own homes and the local environment was viewed as crucial in providing context to rehabilitation that had benefits for service users and carers. Where work around wider social and autonomy issues was incorporated, carers saw the benefits to service users in mood and confidence, but also in providing support to themselves. For example, accompanying service users to activities such as swimming provided carers with a break, and generated new topics of conversation.
Teams’ attitudes shaped the relationship with carers. In some instances, this could foster a supportive relationship that encouraged confidence in carers as well as service users. In contrast, one carer felt she was seen by the NRT in site D solely as someone to whom greater responsibility could be transferred while her own needs were ignored. Her feelings of emotional and social isolation were intensified and affected her capacity to cope with her caring role. However, this experience was seen as reflecting institutional rather than individual attitudes and the resource pressures the service was experiencing.
The time-limited input of most of the NRTs was also seen as a result of stretched resources and as a barrier to effectively monitoring changing needs or identifying new solutions. This was particularly relevant where LTNCs were fluctuating or progressive over time and carers needed advice and reassurance. Even an annual review would be helpful:
[about an annual review] . . . just to see and there may be nothing, but just that being aware that they are aware; that they still know we are here and that would be a nice feeling, I think.
Ca3B, husband of service user with MS
The ongoing contact with the NRT in site C was especially valued:
I think the thing that, sort of, helps you working with them is that you know, at the moment, they are available and you know that all it takes is a simple phone call. It’s not a long, protracted process of going to the GP, who then refers you onto somebody else. There are no gatekeepers to the service. They are freely available.
Ca2C, husband of service user with MS
Summary
This chapter showed how the profiles of the case study sites differed in terms of the population they supported, organisational structures and NRT structures. Having this variation across our sample meant that we could identify different factors that might influence innovation around integration and the feasibility of using an OC in practice. Furthermore, because of these differences, we might expect that when findings were similar across these divergent case sites, these similarities highlight a ‘real’ influence. However, as described, organisational and NRT structures were not static during the period of research and this created additional layers of complexity.
We compared the team processes, which showed differences in access, assessment and flexibility between the teams. It is clear that the way that services are provided can affect the degree to which outcomes can be assessed and addressed. Processes, in conjunction with the NRT structures, meant that these teams were able, to varying degrees, to fulfil the criteria that our previous research showed people with LTNCs valued. 1 These are inter-disciplinary team working; a holistic approach to service provision; specialist knowledge; provision of advice and information; and care co-ordination. People with LTNCs and their carers particularly valued services that were able to provide long-term support and were flexible, responding to changing needs over time. Service users and carers (further findings from carer interviews are provided in Appendix 7) we interviewed for this research described the teams positively, explaining how clients benefited from teams’ interdisciplinarity and knowledge of local services so that access to a range of service and professionals could be co-ordinated when they were needed. The holistic approach these teams adopted, which enabled service users’ role within families and carers’ roles to be understood and considered when planning support, was particularly valued and seen as central to desired outcomes being achieved.
Chapter 4 Exploring the mechanisms for integration in the case sites
Key messages
-
There is no single definition of integration or one single approach to integrated provision.
-
Developing and maintaining personal–professional relationships is key to making integration work.
-
Organisational and service restructuring can fragment integrated arrangements.
Introduction
This chapter presents findings from interviews with staff and carers that were undertaken in stage 1. The evidence presented here starts to answer the first of the research questions: ‘What facilitates or impedes the development of innovative approaches to health and social care integration?’ The way that teams talked about integration and the factors that affected integration arrangements are presented. The chapter concludes with a discussion of interview data from our case sites about the factors that facilitated or impeded innovation.
How did people talk about integration?
Staff talked about integration in different ways and this seemed to be related to the individual’s role and to be influenced by the local context. In general, commissioning and strategic staff described ‘integration’ in terms of organisational structural alignment, citing examples such as aligned budgets, jointly funded posts, joint commissioning units/boards and the merger of organisations in line with Transforming Community Services35 policy. They tended to focus on horizontal integration; that is, integration between the PCT and LA social care.
Practitioners, on the other hand, tended to focus on integration in service delivery and described integration in two ways: multiprofessional working within teams and working with front-line stakeholders in other organisations/sectors. In one case study site, as major structural changes got under way that would result in an integrated health and social care organisation, front-line staff started to use ‘integration’ to describe these structural changes and used ‘joint working’ to describe interdisciplinary practice inside and outside their team. Although front-line staff described the importance of vertical integration, such as working with acute care providers, they, like commissioners, tended to focus on horizontal integration, but they were more likely to discuss wider organisational integration, for example with the voluntary, housing and employment sectors.
Integration in commissioning and strategic planning
Formal working arrangements for commissioning and strategic decisions were most commonly described between PCTs and statutory social care organisations, though commissioners and service managers claimed that commissioning and strategic decisions were also informed via established links with GPs, service users, and professional expert groups.
Staff in both health and social care organisations viewed integration at a practice level as positive. In one case site, interviewees suggested that the organisations, particularly the PCT, had enabled integration at a service/practitioner level for many years. Commissioners and managers supporting of the NRTs’ approach to ‘integrated’ service delivery did enable continued service innovation and development, and was particularly evident in sites B and C.
Participants across the case sites described several ways that commissioners and senior managers worked across health and social care, including boards/groups with joint representation working around specific issues and advisory structures.
Two of the areas had joint commissioning groups. These were often led by one organization with representation from the other, rather than being equal partnership boards, and tended to focus on specific workstreams. In one case site (C), interviews with commissioning staff in the PCT and LA illustrated that this unit’s work was very much aligned with the priorities and models associated with the lead organisation in the group – the LA. In case site D, operational integration between health and social care had dissolved and there was no evidence of close working relationships between community health services and social care at the time this research was undertaken. Senior service managers tended to report integration at a neighbourhood level rather than at a higher strategic level. These local initiatives, like the joint commissioning boards, were likely to focus on specific pieces of work. Indeed, one participant suggested that at a time of organisational flux, multiagency working is ‘better when it’s around really specific pieces of work’ (OS1A).
Despite these systems and structures, our interviews revealed that a commonly held view was that there should be more integration or joined-up working between health and social care organisations. This was especially so in places where structures for joint working were in place but not necessarily utilised. For example, site B was part of a neurosciences network comprising commissioners and providers from the NHS (acute and community) and voluntary sector organisations. Our interviewees suggested that although invited to all meetings, LA representatives rarely attended.
Some structures that had promoted joint thinking, working and planning, such as the LITs (that had been introduced in line with the NSF for LTNCs recommendations), had been disbanded or no longer met due to reorganisations and the impact of cuts on staff capacity. Respondents felt that the progress that had been made in developing services that helped meet the needs of people with LTNCs had been lost or suspended as a result. Despite these difficulties and limitations, integration was viewed positively, and as a way of increasing inter- and intraorganisational efficiency, which could, in turn, improve service users’ experiences of care.
Integration between professionals and services
Participants described the links they had with other professionals. At a practitioner level, staff viewed working with practitioners from other organisations (health or social care) as a usual part of their role. However, similar to views about integration at a more strategic level, most felt that this could be improved. This was true for those sites with less integrated approaches and formal structures as well as for case study sites with more integrated approaches to commissioning and service provision.
Approaches to integration that practitioners described included networks of similar professionals either locally or nationally (e.g. national networks of neurology OTs or nurse specialists), interprofessional working within NRTs (e.g. joint visits and assessments undertaken by physiotherapists and OTs from the same team), working with other parts of their sectors (e.g. with the acute trust or GPs) and working with other sectors (e.g. working with social care or voluntary sector staff).
Neurorehabilitation team staff discussed their regional and/or national links with networks of other similar professionals, such as neurology nurse specialists. These networks often involved specialist training as well as providing a forum for practice-level discussion. They were considered a useful approach for fostering supportive relationships with professionals with similar interests, to stay up to date with current best practice and to provide an opportunity to share practice lessons and seek specialist advice from their peers.
Staff in the NRTs described how they worked in interdisciplinary ways within the teams and that although it was important to retain each profession’s key roles, the edges of these roles had to blur to ensure that an interdisciplinary approach was maintained. As one NRT practitioner explained:
I wouldn’t go in and try and advise somebody on their medications, because it’s the nurses that have got the specialist skills to be able to do that. But there are some things that are common within all of the different professions, such as posture and pressure. I think, you know, pressure, assessing for and providing equipment for pressure, is the job of a nurse, a physio[therapist], or an OT.
NRT1C
Across the case sites, within-sector relationships were described by social care and health care staff we interviewed. Social care staff described their work with other parts of the LA, for example housing and education services. Health-care staff described working relationships with other professionals in the community setting, such as district nursing teams, community physiotherapy services and with acute-based staff. Within-sector relationships in social care were more likely to be part of formal organisational strategies around particular work-streams. Conversely, in health, these types of relationships were commonly more informal and had been developed by front-line practitioners over time.
Neurorehabilitation teams reportedly had good links with local GPs in their area, but one team manager felt that the team’s relationship with GPs in the locality might have to adapt, given the move to GP commissioning. She suggested that the relationship would no longer be a care provision partnership but would become about the NRT marketing itself to GPs to ensure that the service for people with LTNCs continued.
Cross-sector working, for example between health and social care practitioners, could take several forms, such as social care staff attending NRT meetings, NRT staff undertaking annual reviews with social care staff and social care OTs and NRT OTs undertaking joint equipment assessments. Staff in the NRTs also described how professionals from other sectors, such as housing services, had worked in the team when they had been short-staffed, how the team regularly worked with voluntary sector staff, particularly when providing support for people with MND, and how they liaised with employers to assist people with LTNCs in returning to work.
Front-line practitioners, irrespective of different service sectors and different approaches, agreed that their main aim in developing integrated approaches to service provision was to enhance interprofessional service provision, meet clients’ holistic needs, and improve care experiences and quality of life for people with LTNCs and their carers.
Integration between neurorehabilitation teams and carers
Some NRTs viewed working with people caring for people with LTNCs as part of their integrated approach to service provision and ‘included’ carers in a variety of ways. Findings presented here are informed by staff and service user interviews, but are drawn primarily from carer interviews.
There was no expectation from the NRT in site B that carers would be directly involved in their interventions. Rather, the team took their cue from the attitudes of service users and carers, some of whom, our interview data showed, preferred that the carer was not too directly involved in team interventions. As such, this team was not necessarily proactive in engaging with carers, either as part of the rehabilitation team or as people requiring support in their own right.
None of the carers we interviewed had received a formal assessment of their needs by the NRT, although this would have been welcomed by those who were experiencing an increase in the intensity of their caring role. Some did not see themselves as needing support or see this as part of the NRT’s role. However, one carer said that he would be able to ask the team if he felt in need of support. Another carer felt that the NRT constantly assessed how she was coping with supporting her husband. She felt that her needs as a carer were being addressed because the team provided relevant and timely information and suggested how she might adapt her support. Having made the NRT aware that she wanted to be part of her husband’s rehabilitation, she felt that they had adapted their practice and co-opted her as ‘a willing helper’ (Ca2B). The relationship had evolved to be a close one that had benefits for both the service user and the carer.
I don’t think they realise, actually, how much support they give without saying an awful lot. It’s just intangible that. It – I just feel it all the time that, you know, they are aware of my problems.
Ca2B, wife of person with stroke
Carers in site C were more likely to be involved closely with the NRT as active participants in helping to support the team’s interventions with service users. Some saw themselves as an integral part of the team with their own valuable experience to offer or, as expressed by one carer, ‘their apprentice’ (Ca4C, husband, condition withheld to protect anonymity). Carers welcomed the opportunity for close involvement and the opportunity it provided to ask questions, gain information, and help them to be better able to give support. For example, the team would demonstrate ways of moving and handling, sharing skills and explaining reasons for decisions and courses of action. Moreover, carers’ relationships and ongoing contact with the NRT gave them a sense of being seen as a person, rather than defined by their caring or marital role. Even though they might not feel the need to discuss their own needs, several carers felt that support was available to them as well, by the team showing awareness of when they needed a break, relieving them from responsibilities of accompanying service users to hospital appointments, or sometimes ‘just [by] the fact of being there’ (Ca1C, wife of person with PD). One carer had initially encountered difficulties in her relationship with the NRT, but she described how the team manager had actively sought to resolve these. Furthermore, she had been offered a formal review of her needs and counselling, the latter of which she declined.
Only two carer interviews were completed in site D. Both carers felt that team resources were stretched and that the focus was entirely on the service user. In the event that carers’ views and opinions were sought, it was only in relation to the service user and there were not the resources to offer a wider range of support. Consequently, carers either felt neglected by the service and unsure of how the team viewed them, or felt they were seen as someone to whom greater responsibility could be transferred.
I think they start seeing you, not necessarily as a professional, but as someone who can do the task without it having to be someone from the healthcare area, and I think, again, that is possibly partly due to funding, you know.
Ca2D, wife (condition withheld to protect anonymity)
Not only did this bring about a shift in what she viewed as her primary role as a wife, but as a carer she did not feel best placed to monitor changes or make ‘professional’ judgements. Although both carers interviewed in site D felt an active responsibility for the care of their partners, a greater acknowledgement of their situation and pressures by the NRT would have provided welcome emotional support.
There were wide differences in the experiences of carers, not only across case study sites but also, at times, within areas, underlining the often complex relationship that evolves between service users, carers and formal services. Interviews showed how, if carers became involved with a NRT either by volunteering their services (site B) or by being included as a member of the team (site C), the ensuing relationship facilitated a process whereby carers’ needs were also addressed. Carers tended to feel more confident in their role, better informed and more confident about the parameters of potential problems and discussions, and more reassured about their ability to cope.
Perceived benefits and drawbacks of integration
Both practitioners and organisational staff tended to view integrated service provision as a positive approach to practice. Three main benefits were identified. First, staff felt that integration facilitated a better experience of care for service users. This was through reduced duplication, minimising contacts with professionals, speedy referrals to other staff within a team and taking a holistic approach to care. Second, these benefits of integration led to improved service efficiency, resulting in cost savings for services and improved support for service users and their families. Third, integrated service provision was thought to benefit service staff. It could facilitate professional development and interdisciplinary competence through role sharing and learning. Integrated provision also resulted in flexible staffing so that other members of the team could help cover staff absences (e.g. due to sickness). For staff outside the team, it meant being able to access a range of disciplines in one place as opposed to contacting individual professions separately. One practitioner, however, suggested that being the sole person from a particular profession within a multidisciplinary team could result in limited access to profession-specific peer support. In addition, as interviews with carers showed, when integration extended to include carers in NRT practice, the ensuing relationship could generate mutual benefits to service users, NRTs and carers.
Barriers and facilitators to integration
Participants in our case study sites identified several factors that affected integration at different levels of the case study organisations.
Participants were asked about the factors that influenced integrated ways of working. At senior levels, commissioners and NHS managers commonly described how national issues and policy were the main drivers of service structure and provision. For example, restructuring of community services as a result of ‘Transforming Community Services’35 meant that PCT provider arms were now integrated with, for example, acute trusts, mental health trusts and/or statutory social care. However, the impact of this on services, and on the staff providing these services, was not discussed by the senior staff in our interviews.
Organisational-level (macro) influences
Although organisational staff noted some factors that influenced integration in practice, they primarily discussed barriers and facilitators to organisational integration. Several factors were identified as affecting management and commissioning integration but the dominant themes were (a) the culturally distinct nature of health and social care, (b) the role of macro-level structures and processes, and (c) the motivations of individuals.
In sites A, C and D, organisational staff described the culturally distinct nature of health and social care as being a barrier to integration: different political agendas, different financial systems, different approaches to care, and different commissioning structures all made integration difficult. In site B, commissioning staff were not available for interview, which may have reflected the organisational upheaval in both health and social care at the time of our research. Therefore, it was difficult for us to ascertain whether or not organizational staff considered cultural distinctiveness an issue in this case study site. In sites A and C, there were joint commissioning units, both of which included senior staff from health and social care and oversaw joint commissioning streams. Despite this, commissioning staff in the joint units noted the cultural separateness of health and social care in relation to commissioning but also more broadly.
I think in the NHS there’s still this . . . sense of all commissioning is, is that you have some contracts with some providers and you manage those, and that’s commissioning, and then you decommission something and you buy something else. Whereas I’m always at pains to say, ‘well, that’s part of what we [local authority commissioning] do, but actually, in some ways, the bigger and more important bit of what we do is bring that . . . overall leadership to how we meet the needs of the people of [County]’.
OS4C, social care
This demonstrates that even where there is some structural integration at the commissioning level, this can be undermined by the cultural heterogeneity in how ‘commissioning’ is viewed between health and social care.
The role of structures and processes featured strongly in the accounts of many organisational staff of factors that influenced integration. Structures that hindered integration at the organisational level included separate finance and accountability systems. Structures that facilitated integration included joint posts between the PCT and the LA or neurology-specific commissioning networks. Collaborative commissioning and pathways were also valued as a means of promoting integration. In site B, for example, commissioning collaborations were well established across tertiary and secondary care. However, collaborative commissioning for primary care neurorehabilitation was weaker and tended to be provider led. Although there were aspirations for collaborative commissioning of community neurorehabilitation, this was hindered by slow development and difficulties in gaining commitment from others, particularly within the current climate of restructuring.
Organisational flux in both health and social care had negatively affected structural integration arrangements between organisations in sites A and B. Joint forums and structures that had previously facilitated integrated commissioning had ended following the latest NHS restructuring. This restructuring made it difficult to identify appropriate partners or left gaps in forums that had previously supported integration. For example, in site B, the LIT, originally set up to implement the NSF for LTNCs and provide a forum for integration, had been suspended:
Now those meetings have come to a grinding halt, again, because there’s so much crisis at the upper levels, and key personnel are missing. So all the personnel who I said would have absolute responsibility, and there were four of them, are no longer with us, so we have got this huge hole at a strategic level at the moment.
OS2B, social care
Participants also reported process issues that acted as barriers and facilitators to integration at the organisation level. For example, having clear, shared objectives and plans, and tangible outcomes to work towards were viewed as facilitating integration at the organisation level. Individual motivations and personal/professional relationships played a role in integration for some participants. Understanding the motivations, processes and structures of different organisations was noted by organisational staff in sites A, C and D as being important when working with other agencies.
Developing relationships, facilitated by colocation and regular meetings, was central to promoting and maintaining integrated working. Indeed, senior organisational staff in sites A and D suggested that relationships between agencies were a greater influence on joint working than were integrated structural arrangements such as contracts or pooled budgets. This partly reflects the sentiment expressed by practitioners in sites A and C, where good working relationships between agencies were argued to facilitate joint working across boundaries.
Practice-level (micro) influences
Neurorehabilitation team practitioners also outlined factors that helped or hindered integrated working. Evidence from practitioners can be grouped into service and person-level factors. Service-level factors are those that are rooted in how the service system is organised and delivered (e.g. referral pathways). Person-level factors are those that arise from motivations of individual people (e.g. developing good relationships).
In site A, aspects of the service system were often cited as facilitating or impeding integration. These included bureaucratic referral processes between health and social care, and waiting times for social care assessments, both of which created delays for people with LTNCs in getting access to services. Other factors that could create difficulties when clients were referred to other services were other services’ limited understanding of LTNCs, the wider service landscape for people with LTNCs, and the different roles and responsibilities that different services and professionals adopted.
The lack of integrated client notes, eligibility criteria for services in social care, different legal responsibilities and different approaches to care between health and social care staff were all seen to impede integrated working in this site. Building relationships with staff across sectors was seen as a way of countering these system limitations. Team meetings were viewed as useful opportunities to share information within teams and also, when staff from other sectors or agencies joined the meetings, between services. Being co-located could promote increased joint working, allowing longer-term integrated approaches to service provision to develop.
The NRT in site B was formally integrated between health and social care. Although based in the PCT, a social worker and several rehabilitation assistant roles were funded by social care, as described in Chapter 3. The social worker was the NRT lead for social inclusion and this role was seen to be essential in enhancing a holistic team perspective as well as providing a link with social care and other relevant services. However, despite the formal integration between health and social care in the NRT, staff still felt there was an absence of integration in other respects. For example, administration procedures and information technology (IT) systems remained separate and different contractual arrangements for health and social care staff within the team led to a perceived divide.
Practitioners also cited a number of factors that influenced the success of how this large, multidisciplinary team integrated within itself. For example, co-location, team meetings, open communication, supportive team culture and joint goal setting were helpful factors for team integration. Having a multidisciplinary clinic situated in a local health and social care centre was a valued integration arrangement, providing access to a range of disciplines for service users and practitioners alike. Similarly, having regular, interdisciplinary work-based training within the team was felt to facilitate integrated working by promoting a holistic view of care:
It’s very much presenting the whole person back [as] an individual case study, and how the individual elements affect the outcome of what we’re doing and the goals that we’re working towards and whether they’re achieved or not achieved.
NRT9B
Roles within the team reflected its integrated approach. For example, as well as the social worker role, the band 5 assistant practitioner/senior therapy assistant had competencies in a range of disciplines. The assistant practitioner worked alongside bands 3 and 4 rehabilitation support workers, employed by either the PCT or social care, in implementing integrated treatment plans. It was felt that having different employing organisations had not been a problem as posts were backed by what were believed to be robust service-level agreements and competency frameworks. However, team integration could be hindered when responsibilities to the team were restricted due to being line-managed outside the team, as in speech and language therapy and dietetics, or when heavy caseloads of individual therapists made it difficult to work actively alongside the team in an interdisciplinary way.
Negative factors influencing integration between the team and the wider service landscape were also highlighted. Sometimes these related to inadequate service provision with which the team could integrate. For example, neuropsychology input had been lost due to a service-level agreement ending and access was now dependent on funding approved by the treatment and advisory group on an ad hoc basis. Intermediate care services were primarily focused on older people and lacked capacity and expertise around people with LTNCs. Integration with other services was also argued to be influenced by poor information sharing between services, waiting lists, and time-limited input of service provision. It was felt that rotating staff between services (as had happened some years previously) could go some way to achieving a better understanding of different ways of working and approaches to rehabilitation. However, close working and good relationships with individual practitioners and services, established over time, facilitated integration with the wider service landscape.
Practitioners in the NRT in site C cited several barriers and facilitators to integration between health and social care, including having culturally different approaches to practice, a lack of resources in social care causing delays, having separate IT systems and paperwork, and not having a social worker in the team. Having good relationships with social care was seen as helpful, and the maturity of the team had facilitated this. In a similar way to site A (where formal service integration did not exist), joint working across boundaries by front-line practitioners had developed over time.
Practitioners in site C also referred to within-team integration. For example, practitioners described how adherence to different professional cultures within a team could pose difficulties in practice but that flexibility to go beyond one’s own professional role could promote integration.
I think you’ve got to appreciate that we all do work very different[ly] and we are different healthcare professions, and sometimes our roles will blur, but that is good, but it’s all about knowing in that team where they cross and you discuss that.
NRT3C
As in site B, one practitioner in site C was instrumental in promoting and maintaining a dynamic approach to integrated, interdisciplinary service provision. In line with data from the other case sites, this team argued that other services’ confusion about and/or poor knowledge of the wider service landscape for people with LTNCs hindered integration and co-location facilitated it.
Site D practitioners cited barriers and facilitators to integrated working in relation to social care and wider local services. A lack of clarity in the service pathway around roles and responsibilities between the locality team and the community neurology team was felt to cause delays in service provision and inhibit the development of integrated approaches to service delivery. One NRT practitioner described how visiting social care colleagues had promoted awareness of the NRT and what they could provide, which in turn had helped the two services to work together. Understanding each other’s responsibilities was also seen as important in building working relationships with social care, and NRT staff felt that this could be facilitated by joint visits.
Participants indicated that, when meeting with other services, it was important to have an independent chairperson, a strong agenda and a proactive approach to problem solving to ensure that all parties worked together. Clear communication between the NRT and neighbourhood teams was seen as essential to promoting integration more generally, as were being co-located, having case meetings with the clients, and maintaining regular e-mail contact across services and sectors.
In summary, common themes that influenced integrated provision in practice emerged across sites. The lack of an integrated IT system, different paperwork, lack of knowledge around LTNCs and services, and unclear roles and responsibilities all hindered staff on the front line from working as closely as many of them wanted. Factors that facilitated integrated provision included co-location, building of personal/professional relationships across boundaries of profession, service and sector, and having clinical/practitioner leaders around integration who could promote innovative means of overcoming barriers and developing systems for closer joint working.
Finally, while factors can be roughly grouped into ‘person level’ and ‘service level’, these were by no means independent of each other:
I think that’s important, ‘cause you can have your strategic level [integration], but if the ground force don’t speak to one another and work together and pull the stops out for one another, then you’ve got nothing.
NRT6B
Macro- and micro-level relationship influences
Relationships between different levels of the organisations could affect whether or not and how integration was achieved. Some team members felt that decisions made at senior levels, particularly around structural arrangements, did not really affect their practice; they just continued to try to provide the support that people with LTNCs needed and to work with colleagues across different services and sectors. However, it was acknowledged that some decisions did affect integrated working. For example, in one case site, health and social care organisations had had a partnership agreement in which social workers had been co-located with health-care staff. This had recently changed as a result of structural/commissioning decisions, meaning that the organisational and personal–professional relationships between health and social care staff were fragmented.
Furthermore, NRT staff discussed the how the impact of financial decisions (i.e. cuts) about other services might affect their work and the services that people with LTNCs were able to access. For example, in site A, statutory funding had been withdrawn from several resource centres that had provided day-opportunity services. This meant that these avenues to support were highly rationed, resulting in NRTs having to try to provide some of this support or clients having to go without.
Practitioners felt that senior managers/commissioners supported NRTs’ approaches to integrated service delivery. Indeed, senior managers and commissioners often identified the NRTs as examples of excellent service delivery models. Despite this, however, practitioners noted that no systems were in place to extend these models of integrated provision to the rest of the PCT or LA. Furthermore, practitioners felt that they had little real influence on decisions that were made at more senior levels, even when specific structures were in place to hear their views. Where it appeared that practitioners and existing integrated models had influenced wider service design and integration, practitioners argued that this was because these had simply been aligned with the PCT’s or LA’s existing priorities.
Innovation and integration: the impact of cost-containment and restructuring
During the course of the research, there were two key issues that interviewees discussed in relation to development and maintenance of integration arrangements: the priority given to cost-containment and current and future restructuring.
All four case sites were experiencing restructuring of some sort during the period of the research and this dominated discussions with staff. These changes were based at an organisational level and, as outlined in Chapter 3, also at the NRT level. Two of the teams experienced significant restructuring during the period of the research. In site A, condition-specific community neurology teams merged with the wider community neurology service. Teams, therefore, had to spend time adapting to their new working arrangements, finding their place in the service and dealing with different client groups. In addition to their usual clinical and administrative work, therefore, there was little time available or inclination for staff to try new ways of working.
Even where there were not specific team changes, some wider structural changes affected front-line services, and where this had not occurred, staff expressed concern or predicted that this would happen in the future. There was a feeling that constant restructuring made it increasingly difficult to work in an integrated way and for staff to be clear about how their service would fit into the new service landscapes. These factors, linked with ‘austerity’ measures, created job, role and team insecurity and inhibited front-line staff from continuing to develop services.
Front-line staff commented that working in an integrated way was becoming increasingly difficult. For example, staff in one team described how cuts to social care and voluntary sector budgets, in particular, had led to questions over availability and/or capacity of services in social care, which meant that service users might no longer be able to access some services or might have a very long wait. A senior social care manager explained that long-term input around joint commissioning was difficult because so many commissioners ‘had been lost’ from the PCT.
The foundations for moving towards CCGs47 were also being laid during the time this research was undertaken. Staff were concerned about the future of neurology services. This was, in part, because of the potential loss of neurological commissioning expertise. Existing commissioners were being made redundant and the commissioners who remained had to take on additional roles and responsibilities. In two of the case sites, practice-based commissioning was well established (sites C and D) but this did not alleviate concerns about new commissioning structures.
Interviewees were concerned about GPs’ limited interest in, and knowledge about, neurological conditions and their limited awareness about the range of providers that were part of the emerging economy of care. Given that lack of awareness of LTNCs and available services was identified as inhibiting integration, interviewees were concerned that this might impact negatively on service provision in the future. With a handover of responsibility for commissioning services, including neurology services, to GPs, practitioners and commissioners alike expressed concern that this might affect cross-boundary working, service availability and service quality.
Commissioners and practitioners felt vulnerable in relation to their jobs, their roles and the specialist neurology services they provided. Coupled with the organisational flux and a general feeling of unrest about changes to public services, resulting directly from restructuring and cost-containment policies, innovation to promote integration was inhibited and, in many people’s experiences, integrated arrangements for service provision had been fractured.
Summary
This chapter has reported findings from interviews with organisational, NRT and carer interviews and has provided an overview of the factors that they suggest affect integrated commissioning and service provision.
Integration was viewed positively, being seen as a key priority by strategic staff dealing with organisational integration and by practitioners dealing with care co-ordination issues with and for their clients. However, there was a feeling across all case sites, including those with integrated services and commissioning arrangements, that integration was not widespread enough. Barriers and facilitators to achieving integration could be at the person, service and structural levels but these factors were not mutually exclusive. Indeed, integration at a practice level, which was often instigated and maintained by practitioners, was facilitated by robust organisational structures supporting integration or by structures that promoted bottom-up innovation.
This research was undertaken at a time when service commissioners and providers had overseen structural changes and were faced with more major structural and financial change. Unsurprisingly, this dominated discussions at all levels of staff interviews. In general, commissioners and service managers seemed to have greater awareness of the developments, and what this might mean to staff and services, than did front-line staff. While front-line staff were aware of changes, several stated that they were unsure what impact the changes would have. This meant that staff at all levels were concerned about their jobs, their roles and the future of services that were provided to people with LTNCs. This insecurity, we suggest, made innovation towards increased and continued integration around LTNCs particularly difficult for practitioners, service managers and commissioners alike.
Chapter 5 What outcomes do people with long-term neurological conditions want from integrated health and social care?
Key messages
-
Outcomes described in earlier research in the SPRU were broadly relevant to people with LTNCs, but needed revision and additions.
-
Outcomes could be grouped into lower, intermediate and higher-level outcomes.
-
Outcomes were inter-related, both within and across levels.
Introduction
The research question ‘What outcomes do people with long-term conditions want from integrated health and social care?’ can be interpreted in two ways. First, it could be about the outcomes that can be achieved by services that are integrated. Second, it could be about the outcomes that people with long-term conditions want and how these might be achieved through health and social care integration. Building on the evidence presented in Chapters 1, 3 and 4, and the social model of disability, we chose the second interpretation, so that the outcomes we identified were those that were important to those using integrated services.
As noted in Chapter 1, previous research largely uses clinical and functional outcome measurement to assess the impact of services and of integration. 19–22 These outcomes may not be appropriate for people with long-term, complex conditions, as they do not easily account for the potential deterioration that can be associated with these conditions. Outcomes that go beyond the clinical and functioning aspects of health are likely to be equally, or more, important to people with LTNCs. As such, we adopted a wider approach to identifying and understanding the outcomes important to people with LTNCs. This chapter presents the results of using this wider approach to establish the important outcomes for people with LTNCs.
Our conceptualisation of outcomes intended to build on that put forward by earlier research completed at the SPRU under the Outcomes Research Programme, which focused on the identification of outcomes desired by users themselves. 2,91 The framework for understanding outcomes derived from this earlier work comprised:
-
Maintenance outcomes – for example, maintaining acceptable levels of personal comfort, social contact.
-
Change outcomes – for example, improving confidence, improving accessibility of the environment and ability to get about, reducing risk of harm, regaining self-care skills.
-
Process outcomes – the results of the way in which services are provided, for example whether people feel valued and respected, whether they feel they have a say over service provision, the ‘fit’ of the service with family and/or culture.
This framework was developed in the context of social care services for older people and those with disabilities. Harris et al. 3 then redefined the outcomes for younger adults with disabilities, based on the social model of disability, and gave a stronger focus to education, training and employment issues. They listed four main groups of outcomes for young adults with disabilities as shown in Figure 6.
FIGURE 6.
Themes in Harris et al. ’s outcomes framework.
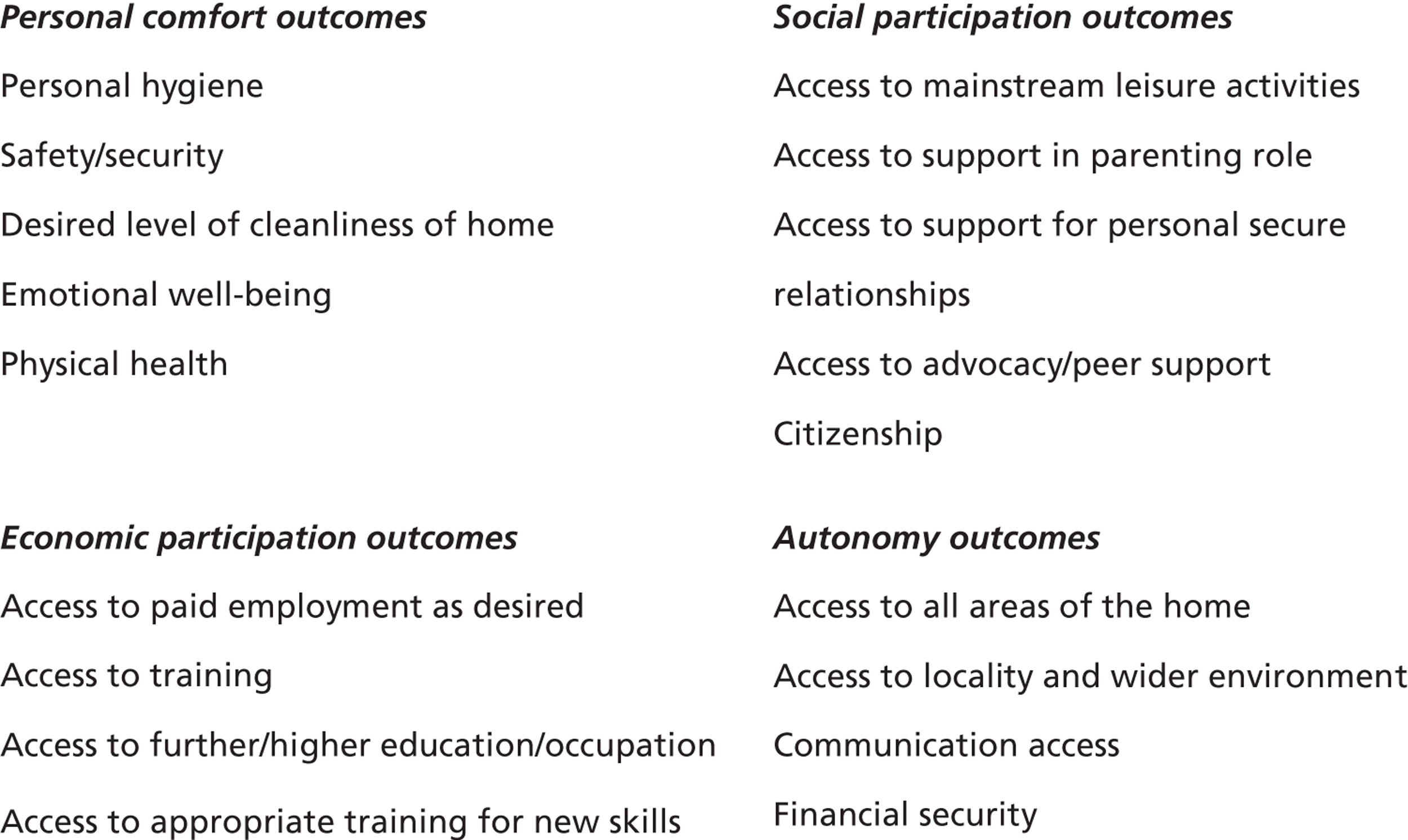
The current research applied this earlier thinking and conceptualisation to explore the sorts of outcomes people with LTNCs might want from integrated health and social care that could be used as an exemplar for long-term conditions generally.
Basing our understanding on the views of people with LTNCs, we aimed to clarify the parameters of each of these outcomes and assess whether or not these domains and outcomes were relevant for people with LTNCs. As outlined in Chapter 2, we carried out in-depth interviews, based around these outcomes, with 35 people with LTNCs.
Defining the outcomes
In-depth interviews asked service users to describe their main issues/concerns and explored the meanings people with LTNCs attributed to the outcomes presented by Harris et al. 3 We considered three main questions when addressing each outcome:
-
Is the outcome important and should it be retained on the checklist?
-
Should the name of the outcome be revised to better reflect the nature of the outcome?
-
What are the parameters of the outcome?
Through these interviews, we were able to identify what people with LTNCs understood by each of the outcomes. This enabled us to clarify definitions for each of the categories within the outcome domains. Where confusion about terms was evident or overlap existed between the different subcategories, we refined category names or merged categories (see Chapter 2) to better reflect the views of the people with LTNCs who we interviewed.
Personal comfort outcome domain
Outcomes within the personal comfort domain included a range of areas relating to functional capabilities and physical and emotional health. These were:
-
personal hygiene
-
safety/security
-
desired level of cleanliness of home
-
emotional well-being
-
physical health.
Personal hygiene
Personal hygiene was important to the majority of participants, but for some it was especially so. For example, one participant described it as ‘top of the list’ (SU26C, MS). Another described how the use of a urinary catheter meant that being clean was particularly important and referred to having a shower as something that ‘ought to be a human right’ (SU3A, MS). Many participants talked simply about the importance of being clean and maintaining care and hygiene routines while others emphasised how these tasks were accomplished.
The level of assistance required to achieve this outcome varied across the sample, with some being completely independent in their routines and others requiring varying levels of assistance. Regardless of a participant’s level of independence, well-being was often implicated in the importance that participants ascribed to personal hygiene. For example, some of those who were independent, or described being mostly independent in their care routines, talked about how being able to be independent in personal hygiene meant ‘maintaining control’ (SU12B, MS; SU15B, MS), ‘privacy’ (SU12B, MS) and avoiding a sense of ‘degradement’ (SU13B, stroke). For those who required assistance with personal care routines, there were reports of feeling ‘useless’ (SU9B), ‘helpless’ (SU11B), and that requiring assistance was ‘irritating’ (SU18B, stroke). For some, requiring assistance in personal hygiene routines was difficult but seen as something to which they had to adjust:
But you got to, you’ve got to face it, you’ve got to deal with it.
SU19B, condition withheld to protect anonymity
Adaptations often played a role in participants’ accounts of the importance of personal hygiene. This could be equipment (e.g. getting a shower stool) or home adaptations (e.g. installing grab rails) or adaptations to their routine (e.g. showering rather than bathing) to facilitate the maintenance of personal hygiene.
Although a small proportion of participants did not specifically discuss personal hygiene as something that was important to them, it is important to note that none of the participants actively described personal hygiene as not being important.
Safety and security
Issues of safety and security were discussed by most participants. Issues around personal safety were most commonly discussed, including personal safety both in one’s house and outdoors. Some described difficulties they had doing things safely around the house, for example moving around or preparing and cooking food. Some had adapted routines or developed strategies to counteract potential risks to personal safety, for example by having fire evacuation plans arranged. Participants commonly described house adaptations and use of equipment as a means of facilitating personal safety, and for some who lived alone and had mobility difficulties, care alarms were also used.
Participants also discussed issues of personal safety outside the home. There were concerns about getting around safely in manual wheelchairs, and about accidents or difficulties that had been experienced while outside. Difficulties with getting around safely outdoors could lead to people being reluctant to leave their homes. For example, one person described a tendency to stay indoors following an accident, while another described how safety problems with a manual wheelchair resulted in limited opportunities to go outdoors. Thus, personal safety issues overlapped with other outcomes, such as access to the wider environment.
Home security was important for some participants, although this was not as commonly discussed as issues of personal safety. Most of those who discussed this aspect of home security also discussed feeling secure in their home or described having some kind of security system in place.
It is important to note that while many people talked about issues of safety and security and indicated its importance in their lives, the accounts of some participants suggest that independence is more important than personal safety. For example, there were accounts of risk-taking, with people willing to take risks in order to maintain independence and control in their lives. The accounts of many participants indicated that being safe and secure was an important outcome to them but the specific issues it covers were diverse.
Desired level of cleanliness of home
The majority of participants in the sample discussed being able to maintain and clean the house to a desired standard and, for most, their accounts suggest that this was an important outcome for them. A few ascribed less importance to this outcome, but their accounts suggested that it still had some significance in their daily lives. For example, one participant described how it was important, but not as important as other things. For the majority of participants who indicated the importance of this outcome, only a few described being able to manage cleaning tasks without assistance. Assistance was in the form of either professional input (e.g. having a cleaner, professional carer or personal assistant) or informal help from family. Some of those with no formal support expressed a desire for support with household cleaning tasks.
In addition to the expressed importance of being able to clean one’s home, people also discussed the importance of doing this unassisted. Some talked about wanting to do specific tasks themselves because others did not clean to their standard. Others talked about disliking having to rely on others for house maintenance tasks or emphasised wanting to be as independent as possible. By contrast, two participants explicitly described being happy to let others take on these tasks, one of whom hinted that this was because it was a socially ‘normal’ thing to do:
I’m not that upset about it ‘cause there’s enough people who get cleaners in who, you know, just because they can’t be bothered to do it themselves.
SU23C, MS
Overall, the data suggest this was an important outcome to many people in the sample.
Emotional well-being
Participants’ accounts of issues relating to emotional well-being were diverse and complex. Such diversity was evident in two ways. First, there was the variety of terms that participants used. For example, while some participants chose to reflect the prompt of the interviewers and used the term ‘emotional well-being’, others talked about ‘psychological impact’, and ‘feeling’ various emotional states. Second, the diversity of this outcome is reflected in the varied experiences of emotional issues recounted by participants. Some talked about emotional well-being in general terms (i.e. without reference to specific concerns or issues), whereas some discussed experiencing specific emotional difficulties, often condition related, and how they coped in light of these. Some talked less about emotional difficulties and more about their personal resilience. Some also recounted experiences of longer-term mental health issues.
The accounts of all participants suggested that emotional well-being was important in some way; however, the significance and context attached to it differed across the sample. For example, there were accounts that reflected a sense of resilience to emotional difficulties, and an unconcerned rhetoric could imply that emotional well-being played a relatively minor role in life:
Yeah, it doesn’t affect me to that – I get down, don’t get me wrong, but it doesn’t – that’s all I do. I get down then I pick myself up. That’s the end of it.
SU14B, MS
In contrast, emotional well-being played a more prominent role in the lives of others, with many feeling it was a particularly important outcome:
So yeah, I think emotional, well I know emotional well-being is one of the key factors really that you’ve got to take into consideration.
SU31C, MS
The importance of emotional well-being was often implicated in the reported importance of other outcomes. That is, the outcome of emotional well-being was important but was achieved through the accomplishment of other outcomes that were also seen as important. For example, the importance of accessing leisure activities was emphasised by one participant who, when probed why this was important, responded: ‘For my well-being, peace of mind, really. It calms me down’ (SU6A, BI). Another participant, who had experienced communication difficulties following a stroke, noted that improving communication skills ‘makes me much, much happier’ (SU18B, stroke).
For another participant, the relationship between outcomes was more intricate, in that emotional well-being in the form of self-esteem was both an outcome of improved mobility and the driver of another desired outcome:
I suppose to improve me mobility and, so consequently that will give me more self-esteem to hopefully get into full-time employment.
SU27C, MS
This evidence demonstrates that emotional well-being was not only an important outcome to many participants, but also that its role could be intertwined with other desired outcomes.
Physical health
Nearly all participants spoke about their physical health or matters relating to physical health (e.g. diet or exercise), and indicated that it had an important role to play in their lives. It was evidently more important for some than others, particularly when there were concerns around specific health issues. In many instances, participants talked about physical functioning issues, as well as issues relating to physical health. Physical functioning issues were predominantly about walking, but included other issues such as being able to use their hands and difficulties with motor control.
The need for exercise and physiotherapy was also highlighted by some participants; this could be about maintaining strength in certain parts of the body or maintaining a desired level of ability in bodily functioning.
Sometimes the reasons why physical health was considered important went beyond physical health issues. For example, one participant, when asked why she felt physical health was important, indicated that the visible indicators of health facilitated a desired sense of ‘normality’:
I don’t like to look or seem any different to anybody else, you know, normal, that [I] haven’t got MS.
SU23C, MS
In the accounts of many participants, a clear relationship was demonstrated between physical health and other desired outcomes. Most commonly, poor physical health and functioning were perceived to affect social activities and outcomes, autonomy outcomes, employment and emotional well-being. The relationship could also be reversed, in that improving physical health and functioning was seen to contribute to other important outcomes. For example, one participant argued that increasing mobility would improve their self-esteem.
Cognitive skills
We identified an additional outcome in the personal comfort domain that people with LTNCs emphasised.
Some participants talked about cognitive difficulties they had experienced following BI, stroke or seizures. Difficulties were particularly around memory and attention, and could be frustrating and provoke anxiety. Others, particularly those with MS, recognised that fatigue could affect their cognition, particularly noting that memory and concentration deteriorated as fatigue increased.
Improving cognitive skills was seen as important, and some were being professionally supported in this. The importance of improving cognitive skills seemed linked to the impact such difficulties had on other areas of life. For example, cognitive difficulties could affect social elements of life, such as being able to maintain conversations or engaging in hobbies (e.g. knitting), daily activities (e.g. shopping), and also gaining employment.
Revisions to personal comfort outcome domain
Based on the material summarised above, we revised some of the outcomes included within this domain.
Personal hygiene
Although participants talked predominantly about hygiene routines such as washing and toileting, other issues about personal care were also discussed. For example, some participants talked about difficulties they had with dressing routines, or being able to shave. Therefore, ‘personal hygiene’ was revised to better accommodate these additional personal care routines and the outcome label was revised to ‘personal hygiene and care’.
Desired level of household cleanliness
Many of the participants who discussed their experiences of household tasks referred to cleaning and general household chores. However, participants also referred to garden maintenance and general house maintenance [e.g. do-it-yourself (DIY)]. To accommodate these additional household tasks, the name of the outcome was revised to ‘desired level of household cleanliness and maintenance’.
Emotional well-being
The evidence demonstrated the need for an outcome that encapsulated the variety of emotional issues identified in the interviews. As such, and despite the debate around the term ‘well-being’, we decided to retain the original outcome label of ‘emotional well-being’, because people with LTNCs appeared to understand it, but also to acknowledge the wide range of emotional issues that it covered in the parameters of the outcome.
Physical health
As participants often talked about physical functioning issues as well as physical health issues, we revised the label to ‘physical health and functioning’.
Cognitive skills
We identified cognitive skills as an additional outcome in this domain. The difficulties experienced by many of the people with LTNCs warranted its inclusion as a separate outcome. The label ‘cognitive skills’ was used to represent the broad range of cognitive issues that people with LTNCs discussed. They were not only concerned with cognitive ‘functioning’, but with learning, relearning and managing cognitive difficulties as and when they arose. However, the parameters of this outcome include both cognitive functioning and skills.
These outcomes reflect the range of issues that people discussed in relation to their personal comfort. Elements were frequently interlinked, both within this domain and with other outcome domains such as autonomy. Particular aspects – for example, personal hygiene and care – contributed to feelings of self-esteem and the way that they were addressed could affect people’s desire to exercise choice and control over their lives. Table 17 summarises the personal comfort outcomes we identified from service user accounts.
| Existing outcome | Revised outcome New outcomes are italicised |
Parameters |
|---|---|---|
| Personal comfort outcomes | ||
| Personal hygiene | Personal hygiene and care | Being able to maintain routines related to personal cleaning (e.g. washing hair, showering), toileting, and personal care (e.g. dressing, shaving); maintaining these with as much independence as possible (e.g. through adaptations) |
| Safety/security | Safety/security | General personal safety, personal safety in the home and outdoors, and home security [NB: personal safety issues in relation to getting around the house are likely to overlap with issues regarding accessibility of the home (e.g. adaptations). Personal safety issues in relation to getting around outdoors (e.g. wheelchair safety) may overlap with accessibility of wider environment] |
| Desired level of cleanliness of home | Desired level of household cleanliness and maintenance | All tasks relating to the maintenance of house (e.g. cleaning, bigger maintenance tasks such as painting) and garden |
| Emotional well-being | Emotional well-being | Maintaining general day-to-day well-being, being able to cope and maintain personal resilience, and dealing with specific and longer-term emotional difficulties |
| Physical health | Physical health and functioning | All aspects of physical health and related issues (such as accessing exercise opportunities), but also physical functioning issues, such as walking, balance, and motor control |
| Cognitive skills | Cognitive skills such as memory, concentration, and attention | |
| Economic and social participation outcomes (Economic and social participation outcomes have been combined to reflect better the close links between the two and the wide range of meanings people attributed to the former ‘economic’ outcomes) |
||
| Access to paid employment as desired | Access to paid employment as desired | Any activity that involves paid employment, full or part time, wherever based, and that may or may not be related to past activity |
| Access to training | Access to training or new skills | Any training, or acquiring of new skills that may be undertaken for a range of reasons, that may encompass personal, social, work-related or other reasons |
| Access to appropriate training for new skills | ||
| Access to further/higher education/occupation | Access to further/higher education | Any educational activity that is undertaken for personal, social, work-related or other reasons |
| Access to mainstream leisure activities | Establishing and maintaining social and recreational activities | Getting out (for a purpose, or for the sake of getting out); being able to start/maintain the social/recreational activities as preferred; adapting how activities are done or changing activities so person is able to continue to take part in social/leisure/recreational activities of their choice |
| Access to support for personal secure relationships + access to support in parenting role | Developing and/or maintaining intimate personal relationships and roles | To include sexual relationships, long-term partnerships, marriages, etc. |
| Developing and/or maintaining family relationships and roles | To include parenting/grandparenting relationships and roles, relationships, roles and support from siblings, children, and other wider family members | |
| Developing and/or maintaining social relationships and roles | Developing and maintaining activities and roles that promote friendships; developing and maintaining activities and roles that promote relationships with neighbours; developing and maintaining activities and roles that promote relationships with wider social groups | |
| Access to advocacy/peer support | Access to advocacy and peer support | That provided by voluntary organisations and other condition-specific groups |
| Citizenship | Contributing to wider community/ies | Voluntary work, providing advocacy for other people with LTNCs personally or via voluntary organisations, maintaining and developing political engagement |
| Autonomy outcomes | ||
| Access to all areas of the home | Access to all areas of the home | Being able to access different areas of the home and garden as independently as possible (NB: Issues relating to home accessibility may overlap with personal safety issues in the ‘Safety & Security’ outcome, and issues for the ‘Personal Hygiene and Care’ outcome] |
| Access to locality and wider environment | Access to locality and wider environment | Being able to get to desired destinations, as well as being able to get in and around buildings (other than one’s own home – covered in home accessibility); issues around shopping access are also included in this account, although this may extend beyond accessibility of shopping areas, and include general assistance (e.g. for packing/unpacking shopping) |
| Communication access | Being able to communicate | All aspects of functional communication (e.g. verbal, sign). This outcome does not include social communication skills (e.g. use of internet) – this is covered under the social participation outcomes |
| Financial security | Financial security | All aspects of financial security; disability benefits may play a role in facilitating this outcome |
| Personal decision-making | All aspects of being able to make decisions about one’s own life Including issues around timely access to equipment and adaptations (which may overlap with accessibility to all areas of the home, accessibility to locality and wider environment and personal hygiene and care and safety/security issues; issues around shopping (which may overlap with accessibility to locality and wider environment) and establishing and maintaining social and recreational activities; issues around being informed (which may overlap with other elements of autonomy outcomes) |
|
Social participation outcome domain
Social participation outcomes relate to all and any parts of a person’s social world, including their relationships inside and outside their families and their day-to-day activities.
There were originally five categories within this domain:
-
access to mainstream leisure activities
-
access to support in parenting role
-
access to support for personal secure relationships
-
access to advocacy and peer support
-
citizenship.
Access to mainstream leisure activities
Access to leisure activities was important across all the people we interviewed; everyone talked about this issue as something important in their life. However, people talked about many different sorts of leisure activities. These included:
-
continuing with or starting new hobbies, taking part in sporting activities and/or exercise, travelling, going on holidays and day trips, attending classes
-
socialising, including going to the pub and social events, eating out, visiting and meeting friends/neighbours, entertaining others and attending social groups (e.g. church)
-
everyday social activities, including shopping and cooking.
Some people talked about the importance of specialist activities for people with impairments, such as using a hydrotherapy pool and exercise classes for people who use a wheelchair. Though two people were averse to joining any leisure activities specifically for people with ‘disabilities’, some felt that support groups organised by voluntary organisations provided an enjoyable social activity.
Although everyone talked about leisure activities, the importance of this changed over time, as did the importance ascribed to different sorts of social activity. For example, some people no longer socialised, preferring to concentrate on their hobbies.
People talked about having to adapt to their impairment or their worsening condition. Some people with LTNCs had had to give up some activities while others had adapted how or when they did them so that they could continue to follow their interests. For example, some no longer took part in sporting activities but instead watched them live or on television. The fact that people tried different ways to be able to continue to take part in social activities supports the importance of this outcome.
Some participants were concerned that other people (e.g. family and friends) had to adapt their lives to accommodate supporting them. This was a particular concern when carers had had to give up their leisure activities to accommodate those of the person they supported.
Access to support in parenting role
The importance of maintaining a parenting role was important to participants with children whether or not the child was now an adult, though it was clear that this role changed as the child grew older. As well as parenting roles changing as children grew older, some participants discussed their role and the activities they had done with their child/grandchild having to change as a result of their condition worsening over time. Some described how the role of parent/child had now reversed to some degree with some expressing concern over these changing roles.
Parents also still wanted to be able to help adult children with practical things such as DIY or babysitting and emotional support, though not all those interviewed were in a position to be able to offer all, or some, of this type of support. Maintaining contact with children and grandchildren was very important and this was achieved in a variety of ways, such as visiting or being visited by family or, for those who lived some distance away or were unable to access their child’s home, by regular telephone or Skype contact.
Many participants talked less about their immediate parenting role and more about their grandparenting role, with two explicitly stating that their grandparenting role was now more important than their parenting role.
Only two people explicitly stated that they wanted, or had received, help with maintaining their family roles and three explicitly stated that they would not want help with this part of their lives.
Access to support for personal secure relationships
People talked about the importance of significant relationships in their lives, including spouse/partner relationships, relationships within families, friendships and other peer relationships via, for example, voluntary organisations (described in Access to advocacy and peer support, below). Most participants made some reference to important relationships in their life.
Spousal/partner relationships
Those with a spouse or partner who talked about this in the interview described the centrality of this relationship in their lives. While a spouse/partner provided emotional and practical support for them throughout their condition, participants also emphasised the importance of being able to maintain a ‘normal’ spousal role. This included being able to get out and socialise together and the spouse/partner not having to take on a full-time caring role for the participant or the participant not being completely dependent on their spouse/partner for support.
Family and spouse/partner relationships could be directly affected by the participant’s condition. Some people reported breakdowns in their marriages/partnerships, citing their condition as a direct cause of this. Support from services for maintaining spousal relationships was cited as important by three of the participants. Some participants, both with and without partners, raised particular concerns around initiating and/or maintaining romantic or sexual relationships. This was a particular concern for those with mobility difficulties because they found that they were less able to socialise, making it difficult to meet potential sexual partners. Participants also expressed concern that their physical limitations would affect their ability to engage in sexual and intimate relationships.
Family relationships
Participants talked about other roles and relationships within families, such as their role as a sibling, as son or daughter, son-in-law or daughter-in-law, and roles in the wider family, such as babysitting their nieces. Participants described wanting to maintain their ‘normal’ relationship with family members, whether or not this meant that they saw/contacted them regularly.
Some participants explicitly described the importance of their family and talked about the support that their families gave them. However, others made it clear that they did not want help from their family, at least not for practical things.
The importance of the reciprocal relationship between the participant and their family was highlighted by some, for example continuing to contribute to family life and to maintain (or reclaim) their role within their immediate and wider family. However, practical issues could impede this. Some participants described increased difficulty in being able to see family members; transport to family members’ houses could be problematic and their homes could be more difficult to get into or get around in. While some people made it clear that they did not want support from services with developing or maintaining their family relationships, input about how to deal with family roles changing over time would have been helpful.
Social relationships
People we interviewed also emphasised the importance of maintaining friendships and/or developing new ones and being able to maintain existing relationships with neighbours. They also emphasised the importance of being able to continue with activities that promoted/cemented these friendships. People we interviewed were keen for friendships to continue as they had always done as far as was possible, with activities such as going out together to shops, restaurants and pubs, going on holidays together and visiting each others’ homes. However, some interviewees acknowledged that both they and their friends had had to adapt their activities and roles in response to their changed/changing condition. The people we interviewed explained that, although it was more difficult for some of them to do so, it was important that they maintained regular contact with friends. For those who were not able to get out to meet friends as much as they would like, contact via e-mail, Skype and telephone was a very important means of maintaining existing friendships and helping new ones develop.
Many people described the supportive role friends took on, offering understanding, emotional support and social contact that was very important. For many people, peer support from friends was more important than that which could be accessed via condition-specific groups.
Some participants stated that their circle of friends had changed over the course of their condition. For some, this was because of changed circumstances such as no longer being in employment. Others described how no longer being able to participate in particular hobbies/activities had resulted in the loss of some friendships.
Several people we interviewed described difficulty in developing new friendships because their deteriorating physical health and functioning, made them less able to join in social activities. Two participants described how they viewed their personal assistants as friends and part of their social life, as well as people who assisted them in maintaining other social relationships and roles.
Access to advocacy and peer support
Peers were viewed as those who shared similar life experiences, beliefs and/or social activities and could include friends, neighbours and people who were part of the same social groups. Support and reassurance was seen as an integral element of these relationships.
Those who talked about receiving peer support via condition-specific voluntary organisations or groups described the type of support they received, including social and emotional support and understanding, and help in dealing and coming to terms with their condition. However, some people chose to use condition-specific voluntary organisations only for accessing information about their condition, and others, many of whom felt that they were getting all the peer support they needed from other sources, made it clear that they did not want ‘peer’ support via these groups.
Few people talked directly about the advocacy role played by anyone except their family members. Some interviewees did, however, talk about helping other people with the same condition, being advocates on their behalf and taking on voluntary roles with condition-specific organisations.
Citizenship
The outcome ‘citizenship’ was not clearly defined in previous work by Harris et al. 3 Pilot interviews and discussion with advisory groups led us to decide that if participants did not identify their own definition of citizenship, we would prompt them about being involved in different levels of decision-making and participating in their wider community/ies.
For some people we interviewed, ‘citizenship’ was simply about engagement with political processes; for others, it was about being engaged in their wider community/ies via social and economic structures.
People talked about being involved in political processes and said that it was important to be involved so that they could ‘have a say’. Processes in which participants reported being involved included volunteering for political parties around election time, voting in elections, and engagement around local planning proposals. However, some of the participants stated that they were not interested in being involved in these types of decision-making processes. These participants did, however, say that it is was important to be involved in decisions about their lives and the services they received. Two people were actively involved in influencing how services were provided in the local area, with one canvassing local councillors and MPs about services for people with a neurological condition.
Some of the people we interviewed felt it was important to ‘give something back’ and to be part of and/or to contribute to their community/ies. Undertaking voluntary work was seen, by some, as part of achieving this type of ‘citizenship’ though they were not always able to do this due their personal circumstances, and one person felt that employment was central to their sense of citizenship.
We identified some additional key issues that were important to participants: these were ‘getting out’ and ‘access to voluntary work’.
Getting out
‘Getting out’ was discussed by many people during interviews with people describing it as something of great importance to them. There were two strands to ‘getting out’: getting out with a purpose and getting out just for the sake of getting out.
Getting out with a purpose included going to shops, going to social events and leisure activities, meeting with friends and going to work.
The importance of getting out might fluctuate, but for many of the people with LTNCs that we interviewed, at times just being able to ‘get out’ was the most important thing in their life. In these cases, people did not talk about getting out for a reason, but some did add clarifications; it was important for one person that they could get out spontaneously and for another that they could get out independently, and this importance was related to feelings of freedom.
Access to voluntary work
Although voluntary work was not included on the original outcomes framework, its importance was discussed by several participants. The majority of interviewees in this sample were not in paid work and even where there was an aspiration to enter employment, their condition meant it may not be fulfilled. Access to voluntary work frequently performed several of the same functions as ‘paid work’ and also provided access to meaningful daytime activity. However, pressures of their deteriorating condition had forced some to withdraw from active engagement in voluntary work. People talked about voluntary work as providing a challenge or purpose and for some it helped to fill the gap left by the loss of paid work. Voluntary work generated social benefits of getting out, providing a focus outside the home and a sense of social inclusion.
It’s the social side of it as well, and I’ll be the first to admit, I would miss it because when I can’t get out of the house it’s still giving me something to do and it’s still giving me the contact with people other than my husband, other than my carers, so that is important.
SU21C, MS
Beyond this, people valued the opportunity to make a contribution and a difference to people’s lives, sometimes acknowledging the personal satisfaction gained from feeling appreciated and the sense of perspective that involvement in voluntary work gave them about their own circumstances. For example, when asked what was important about voluntary work, one participant said:
It gives, it gives me, it helps me to help them . . . It is important, to be, to be part of society, to me feels like I’m not just saying, ‘Ooh look at me, I’m disabled, I’m just going to sit back for now’. I, I don’t like that, and I’ve never been like that. So even if the volunteer work, maybe a little bit selfish as well, you know, it, it’s . . . helping other people . . .
SU19B, condition withheld to protect anonymity
Other comments were that voluntary work provided the chance to use skills previously acquired and for two people it was seen as a potential route into work, ‘an easy starter’ (SU7A, BI); a way to build confidence and skills to enable employment.
Revisions to social participation outcomes
We revised some of the outcomes included within this domain based on the material summarised above.
Access to mainstream leisure activities
Participants described many activities that would not usually be considered ‘leisure’ activities, such as ‘getting out’, and some wanted to use services that were specifically for people with impairments as well as mainstream services. The outcome, therefore, was renamed ‘establishing and maintaining social and recreational activities’ to better reflect the broad nature of this outcome and the way participants understood it in relation to their lives. We explicitly included ‘getting out’ in the parameters of this outcome.
Relationship-based outcomes
Asking participants about the two outcomes – ‘access to support in parenting role’ and ‘access to support for personal secure relationships’ – illustrated the importance of different types of relationships in people’s lives but also highlighted significant complexity and some confusion about what these outcomes covered. For clarity, we replaced them with three outcomes to ensure that we captured the different types of relationships and roles participants described.
To capture the broad nature of parenting and grandparenting, as well as wider family relationships and roles that participants described, we developed the outcome ‘maintaining and developing family relationships and roles’. We included issues about existing and prospective spousal and/or partner relationships in ‘maintaining and developing intimate personal relationships and roles’. Friendships and other social relationships were included in ‘maintaining and developing social relationships and activities’.
Access to advocacy and peer support
Many participants described the roles their partners, families and friends took in advocating for them. As such, and because this would now be covered in the three relationships outcomes described above, we redefined the parameters of this outcome to make it clear that it included only advocacy and peer support that was provided or arranged by condition-specific groups and other organisations.
Citizenship
Participants were often confused about the meaning of citizenship and what it meant in their lives and this resulted in participants describing a myriad of issues when asked about this outcome. Overall, people tended to discuss citizenship in terms of giving something back to their community. To limit confusion while capturing the range of issues discussed, we renamed the outcome ‘contributing to wider community/ies’. Given the importance participants placed on it, voluntary work was explicitly included within the parameters of this outcome.
The essential components that made up the social participation outcomes domain were, therefore, retained, but were expanded and redefined to capture the wider elements of people’s lives. These revised outcomes and the associated parameters better reflected the meanings that, during our in-depth interviews, people with LTNCs attributed to them, and overcame the confusion that participants expressed about the original outcomes. Table 17 summarises the social participation outcomes we identified from service user accounts.
Economic participation outcomes
This domain covered outcomes that were primarily framed around being able to work or acquire skills and education to enhance people’s economic positions. These were:
-
access to paid employment as desired
-
access to training
-
access to further/higher education/occupation
-
access to appropriate training for new skills.
Access to paid employment
Only a minority of interviewees were in paid employment. Those of working age held diverse views about the importance of paid work, while older people of retirement age, as would be expected, tended not to engage in this as an important outcome for discussion.
Whether in work or not, participants talked about the role work played in their lives. Its social function was cited, and this ranged from providing an opportunity to get out and participate socially to being an intrinsic ‘social good’. The latter was framed in terms of paying dues to society or giving something back. For some, perceived social expectations around the importance of paid work made this outcome particularly significant. Some felt a pressure from public attitudes to be in work and guilty either that it could not be a priority because of their condition or that by being out of work and claiming benefits, they were seen as ‘sponging off the government’ (SU19B, condition withheld to protect anonymity). The importance of being seen as the family breadwinner was also noted.
I know it sounds daft this, but you’re more of a man when you go out, work, earn money, come back . . . And I, I just, the fact that you’re, you’re normal if you’re going working and earning money and, and doing something good.
SU16B, BI
Access to paid employment also resonated with people’s personal goals and sense of fulfilment. Paid work not only gave a sense of purpose but contributed to self-esteem and feeling valued.
To get back to doing something, to put some worth back to your life. I am a doer. I’ve always been a doer. I’ve been – you know, I’ve achieved quite high things in my life so far.
SU11B, stroke
Views about the importance of access to paid employment generally went beyond narrow financial considerations. Although someone in work commented that it would be difficult financially if she was unable to work at all, paid work was generally viewed as important in wider ways.
The sample comprised, predominantly, people who were not in paid employment. Among those of working age, some talked of an overarching desire to return to work. This might be focused on a return to their previous employment or, if it was recognised that this might not be possible, any type of job would be acceptable. For others, their unemployed status was seen as something they were unable to change.
Unless participants were retired, the loss or change in the nature of possible paid work had often required considerable adjustment, which was highlighted by many. However, one woman acknowledged that she was happy as she was and another that her attitude towards her employment status had changed as her family circumstances and condition had changed. For those in work, the adjustments had been largely practical around the type of work that could be undertaken, or transferring their work to home-based activity. Others talked about the psychological adjustment that resulted from recognition of the limitations imposed by their LTNC. Some had come to an acceptance, but others struggled with the change and acknowledged associated depression or increased feelings of isolation and exclusion that the loss of paid employment precipitated.
Access to training
For the majority of participants, access to training was not important to them. Age-related reasons as well as cognitive problems resulting from their condition, such as poor memory or concentration, were cited as barriers to considering training. Where positive views were expressed, training was seen as able to enhance participants’ potential to work and part of adapting to changed circumstances, while for one man, who had taken early retirement due to his PD, keeping up with advances in IT was important.
Access to further/higher education
For the majority of participants, access to further and higher education was not felt to be relevant to them. Where views were expressed, cognitive problems, such as poor memory or concentration, were sometimes seen as barriers to undertaking any further or higher education. For others, access to further or higher education was a source of personal fulfilment, keeping motivated after stopping work or as a way of ‘just keeping the cogs going’ (SU17B, condition withheld to protect anonymity). Work-related or economic reasons were not mentioned by any interviewees in this sample.
Access to appropriate training for new skills
As with the last two outcomes, this outcome was important only for a minority of people in this sample. Where it was seen as important, the personal satisfaction and sense of purpose gained from learning a new skill or social dimensions were highlighted and several people specifically talked about gaining or improving IT skills. The importance of acquiring new skills in the context of work-related goals was less common, but for some it was viewed as important for adapting to changed circumstances and thereby enhancing employment potential. Again, cognitive barriers excluded some from considering this outcome as relevant to their lives.
Revisions to economic participation outcome domain
We revised some of the outcomes included within this domain based on the material summarised above.
Training-related outcomes
These outcomes were very closely linked in both content and the views they elicited. People did not distinguish between training and appropriate training for new skills in ways that inferred distinct activities, meanings or importance. There was no evidence in this sample to justify keeping these two outcomes separate. We therefore combined these two outcomes into ‘access to training or new skills’.
The other outcomes in this domain remained unchanged but we made the parameters of each clear, as is shown in Table 17. As participants emphasised the social importance of the ‘economic’ outcomes, we felt that the full meanings attributed to them would be better reflected by combining the social participation outcomes and economic participation outcomes into one domain. Table 17 shows these changes to the domains.
Autonomy outcomes
Outcomes within this domain incorporated issues around supporting autonomy:
-
access to all areas of the home
-
access to locality and wider environment
-
communication access
-
financial security.
Access to all areas of the home
The importance of being able to access all areas of the home as independently as possible was clear in the majority of participants’ accounts. A small number with few or no mobility difficulties ascribed low importance to the outcome because they had no difficulties with accessing areas of their home. Where this outcome was ascribed importance, there were three ways in which this was evident. First, the importance of accessing areas of the home was indicated through accounts of having home adaptations or use of equipment to facilitate getting around the house.
Second, long waiting times for services to fund adaptations to the home resulted in some participants self-funding adaptations in order to be able to have them sooner. This preference to self-fund rather than wait, in order to faster facilitate home access, indicates its importance as an outcome. Third, the importance of home accessibility was indicated through one participant’s account of moving home in order to live in a more accessible house and another envisaging a future move to a more accessible home. Moving home, however, was not always a desirable solution to accessibility problems. The perceived convenience of service users’ current homes could affect this choice.
The evidence also indicates that this outcome overlapped with two other outcomes. It overlapped with personal safety; for some participants, being able to access areas of the home was about being able to do so safely. It also overlapped with personal hygiene, with participants highlighting the importance of accessing the bathroom facilities (e.g. shower or toilet).
While house accessibility was, in most cases, discussed in terms of indoor areas of the home, some participants also highlighted the importance of accessing the garden, which could compensate for difficulties getting outdoors elsewhere:
It’s just nice to be able get out and – because – although I suppose, ‘cause it’s hard to get out of the house, it’s nice to be able to at home, you know, have some help and feel a bit more like you’re out and about.
SU3A, MS
Access to locality and wider environment
Being able to get out to the wider environment was a dominant theme in participants’ accounts. Two discourses of environmental accessibility were evident in the data – getting to places and getting in and around places. Getting to places was the most dominant of these discourses, with participants speaking about the difficulties of this as well as their actual and desired solutions. A range of solutions was discussed, most of which were about the use and importance of mobility equipment (e.g. manual and electric wheelchairs, mobility cars, automatic cars, wheelchair adapted vehicles and scooters). Some participants used taxis but this could be costly and, thus, could limit how often they were used. Use of blue badges for parking was described as being important in promoting wider accessibility. Other participants described having assistance from friends, family and carers to facilitate getting to places (e.g. the shops). Some participants used public transport but this was not always suitable. For example, buses might not go to useful places (e.g. where participants might shop) or there could be difficulties in getting a manual wheelchair on and off buses.
The second discourse, being able to get in and around buildings, mostly concentrated on accessibility of public buildings but also included private households of others (e.g. friends and family) or holiday accommodation. Some described positive experiences of being able to get in and around buildings, while others described difficulties:
But, now it’s really quite hard to get into – say to go round to a friend’s house; I can never get into their house and even those that maybe I can get in, then they’ve got an upstairs toilet or something and it’s impossible now. And so that’s ultimate – I feel like my life – I do feel like doors are closing a bit.
SU3A, MS
One particular issue that some participants referred to was the ability to get to, in and around shops and supermarkets. They described how they tended to use supermarkets because they were more accessible than local shops and had adequate parking, which meant that they did not have to carry shopping. Online shopping was a solution for avoiding fatigue. However, issues relating to shopping could also extend beyond accessibility issues, for example requiring assistance to pack and unpack shopping.
Communication access
The inclusion of this outcome in the previous framework was informed by data from a sample of deaf service users of social care and, thus, was about accessing specific communication aids. In the current research, communication issues were different, relating to speech difficulties for a small proportion of the sample. Regaining speech skills was important to most participants who had difficulties and this could contribute to emotional well-being.
While this outcome was relevant for only a small proportion of the sample, its importance was clearly demonstrated in participants’ accounts. For example, one participant described how, as she became tired, her voice became softer and this made it difficult for people to hear her. This resulted in frustration and affected her confidence in social situations. Sometimes, it was just important to able to communicate about what one wanted:
I wanted to get back to being OK and saying what I wanted to say.
SU16B, BI
Participants also talked about technological communication for social participation purposes, such as contacting friends or family by e-mail or Skype and using voice-activation software to dial telephone numbers.
Financial security
Financial security was important to many participants for a number of reasons. For many, it was linked with a sense of emotional ease and relief (e.g. being happier or avoiding anxiety) and such worries could be a distraction from focusing on improving health. Financial security was also important for facilitating social activities, paying for assistance to ease pressure on family carers, retaining one’s home and, for some, facilitating a sense of independence. While some participants described having few financial concerns presently, others described difficulties. Welfare benefits could play an important role in facilitating a sense of financial security.
Interviews with people with LTNCs identified other factors that were important in their day-to-day lives.
Shopping
Shopping was added as a key issue to the analysis chart (see Chapter 2) because it frequently arose in discussions around autonomy. Shopping was important to many participants and they made considerable efforts to continue to do their own shopping. Adapting where and how they shopped was a common feature: using large supermarkets that could provide scooters, help with packing, and accessible parking; using personal assistants, volunteers or friends to take them shopping; and shopping online. For these participants and those who were able to shop unaided, not only was shopping an important part of independence, in terms of personal decision-making and maintaining choice and control in their lives, but it also provided an important social outlet. Two people discussed how getting out to the shops was a benchmark of their rehabilitation progress – a part of getting back to normality.
Well it’s quite a lot important ‘cause I want to get back to me real self, what I used to be like. You know, like, just the fact to just go and shop when I want to, that’s what I was trying and I just want to do.
SU10B, stroke
Personal decision-making
Personal decision-making was also added as a key issue during analysis. Interviews illuminated the importance participants ascribed to being involved in and making decisions about different aspects of their lives.
This could be especially important when this element of autonomy was felt to have been curtailed or undermined by the impact of their condition. People talked about the importance of being the ‘instigator’ and ‘in control of [one’s] own destiny’ (SU18B, stroke) and how being in control may have been affected by the wider social and economic context. Hence, being involved in decisions about their care was particularly important, for example about the location of their care, the type and timing of equipment and adaptations, the timing of carers’ visits, or access to medication:
So I shall make sure that I get nursed and treated at home for as long as possible, ‘cos that really should be my right to.
SU29C, MS
The theme of adjustment as part of personal decision-making was also evident in discussions. This might be in the sense of it being important to adapt and develop solutions oneself to changed circumstances, in order to demonstrate that mental skills were not impaired, or because it was important to anticipate the future and maximise control over potential changes in one’s life.
Of those who discussed this area of their lives, a minority were happy to relinquish decisions to ‘professionals’, about either the type of care delivered or its management, for example by rejecting a direct payment even while acknowledging that there might be an associated erosion of choice.
Timely access to preferred equipment and adaptations
This was also identified during analysis as an issue that frequently arose in discussions. It was discussed in relation to personal safety and security and most importantly in terms of providing increased autonomy. Equipment and adaptations themselves were important, but for many people it was also important that they were able to exert choice in this significant area of personal decision-making. For some participants, this was about the type of equipment or adaptations that they felt they needed or that were acceptable, for example a lighter wheelchair or type of bathroom fittings. For others, choosing and self-funding equipment and adaptations were related to avoiding long waiting times for statutory provision and having control over the timings.
Being informed
This issue was also teased out during analysis and was a topic that arose in discussions in relation to a number of areas.
Participants discussed how they needed to feel informed about their condition. Having a better understanding of their LTNC might help them adjust to current or changing circumstances. This might lead to better self-management of their condition, or their having confidence in personal decisions they might make about the care and services offered, including medication options. In addition, knowledge about, for example, the availability of ‘end-of-life’ care, services more generally or the benefits system could contribute to feeling in control of decision-making or to financial security.
Revisions to autonomy outcome domain
Based on the material summarised above, we revised some of the outcomes included within this domain.
Access to all areas of home
Participants’ accounts of this outcome were relatively homogenous, but we included access to gardens explicitly in the parameters.
Communication access
This outcome was revised to distinguish the importance participants attached to being able to say what one wants to say from social communication that was covered by outcomes in the social and economic participation domain. Thus, we revised the label to ‘being able to communicate’.
Several additional categories, grounded in the data, arose during analysis of service user interviews. The importance of personal decision-making, as an aspect of people’s autonomy that in turn could contribute to a sense of choice and control in their lives and to their independence, warranted its inclusion as an additional outcome within this domain. Given the way participants discussed the other new issues – ‘shopping’, ‘timely access to preferred equipment and adaptations’ and ‘being informed’ – these were included as prompts within the newly created ‘personal decision-making’ outcome.
The revised outcome domains, constituent outcomes and outcome parameters are summarised in Table 17.
Levels of outcomes
During analyses of both individual teams’ assessment tools and of service user interviews around outcomes, it was apparent that desired outcomes could be defined and, therefore, assessed at different levels. We conceptualised outcomes at three different levels (Figure 7). Although they are described as lower, intermediate and higher-level outcomes, the relationships between them are not necessarily hierarchical and are often complex.
Lower-level outcomes
At their most basic, outcomes could address needs around, for example, functional mobility or washing and dressing, that, as reported in Chapter 3, were often captured in the functional-oriented outcome assessments that teams used in their current procedures. These may be viewed as the ‘building blocks’ on the basis of which the sorts of outcomes included in the three domains we identified can be achieved.
Intermediate-level outcomes
Interviews with people with LTNCs underlined that the outcomes, as envisaged by Harris et al. ,3 were important. By focusing them at the ‘intermediate level’, they were able to incorporate the lower-level outcomes and, at the same time, identify the ‘higher-level’, less tangible outcomes that people wanted to achieve.
Higher-level outcomes
We identified five higher-level outcomes in the accounts of people with LTNCs. These were independence, choice, control, normality and self-esteem.
Achieving independence was key for many people. It was an overarching outcome, to which aspects of autonomy in particular, but also elements of personal comfort and economic and social participation, contributed. For example, one service user described his independence as the most important thing to him and he had developed techniques in washing and dressing, or used aids and equipment, to prolong his independence as far and for as long as possible.
Maintaining his physical health so that he could continue to drive and do as much for himself as possible was important. Preserving this independence, in turn, underpinned his emotional well-being.
Choice and control were themes that ran throughout discussions of all categories of outcomes. For example, this could lead to people buying their own equipment so that they had greater choice, not only in the type but also in the timing of access to equipment. Financial insecurities and reliance on benefits could threaten people’s feelings of being in control or having choices in their lives. Maintaining control of available options in different spheres was important. Someone with MS talked about how being able to get out into her garden was really important to her, especially as she was limited in her opportunities to get out into the wider environment. Making the garden accessible, by installing a ramp and conservatory, had had a positive psychological impact on her feeling of exercising choice.
A recurring theme in narratives was the idea of feeling ‘normal’. This could refer to a sense of what felt ‘normal’ for them or ‘normal’ in terms of other people’s perceptions. Performing everyday household tasks, maintaining familiar family routines and relationships, driving, and returning to work were all bound up with a sense of who people once were and regaining ‘normality’. For many, it was also important how they appeared to other people. They did not want to appear ‘a fool’ or ‘a cabbage’ (SU35B, stroke) because of communication difficulties and wanted to walk well to avoid social embarrassment. For these people, there was a stigma attached to appearing different. In addition, maintaining their roles as parents and friends, or participating in mainstream leisure interests, were social activities seen by themselves and, they argued, by others, as defining normality:
So it’s getting used to, and I’m wanting to be the calm, casual, for someone to walk in and see me dealing with my kids ‘He’s normal, he’s all right, he can do that, he’s absolutely fine.’
SU16B, BI
Many of the outcomes discussed were an integral part of people achieving confidence in themselves and an associated feeling of self-worth or self-esteem. Personal care was important in this respect; being able to wash and dress one’s self was linked to personal dignity. For one man, his ability to wash and dress himself or go to toilet was variable, and on a bad day he felt that ‘all pride ha[d] gone out the window’ (SU19B, condition withheld to protect anonymity). It was important that he could make small steps in progress in his personal care. Employment, whether for its own sake and/or as a means of avoiding dependence on benefits, could also be a route to regaining people’s sense of self-worth. Participation in voluntary work provided similar support to those unable to contemplate paid work.
Exploring these different levels of outcomes throughout service user interviews helped to inform our understanding of meanings, hierarchies and inter-relationships. Figure 7 illustrates the complexity of the inter-relationships between the different levels of the outcomes.
FIGURE 7.
Example of inter-relationships between different levels of outcomes based on service user interviews.
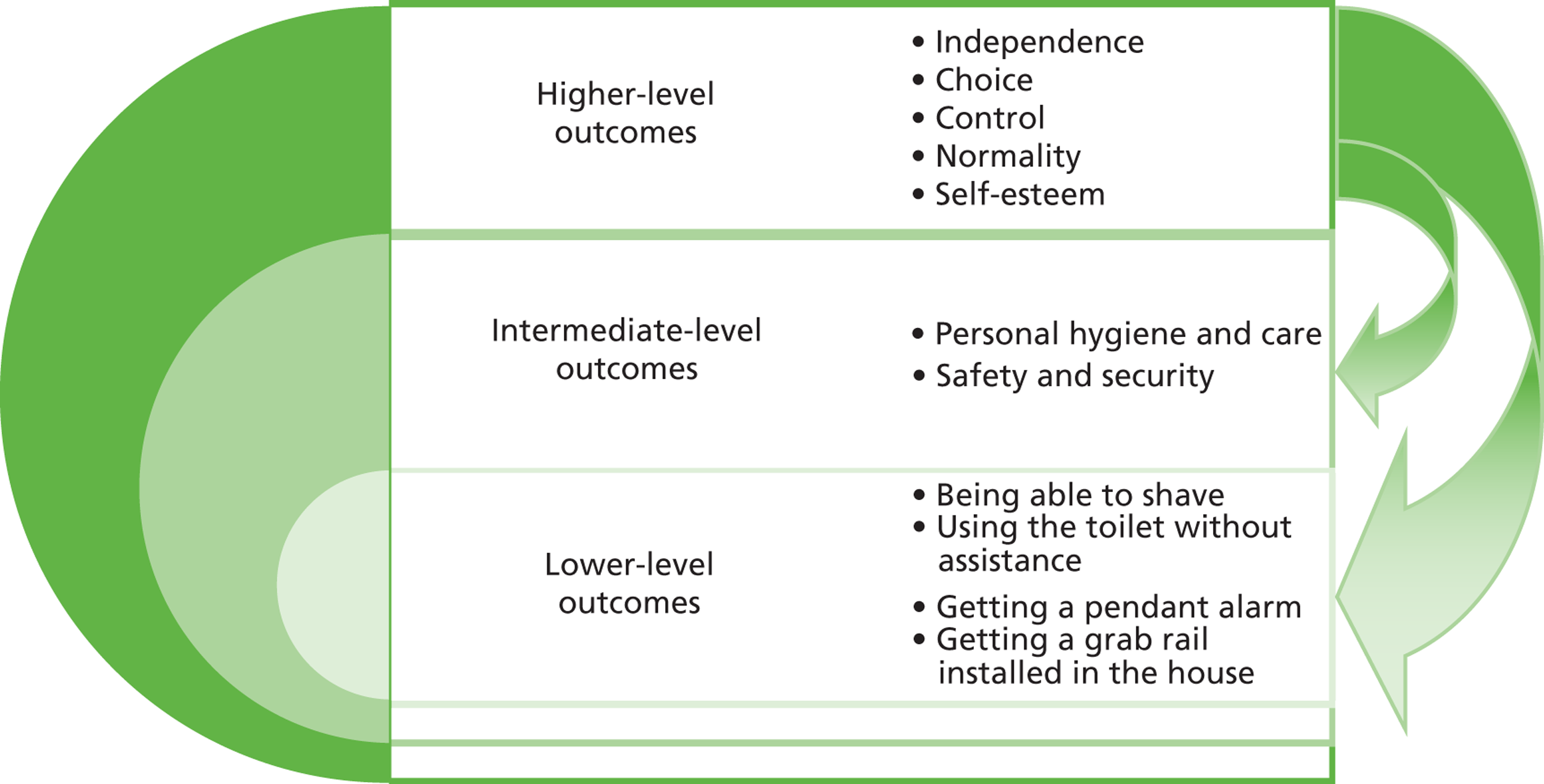
Summary
In this phase of the research, we sought to identify and define the types of outcomes people wanted to achieve in their lives and the ways in which having a LTNC influenced the meanings and priorities attributed to outcomes. Understanding these outcomes and their inter-relationships also informed our appreciation of the sorts of services people valued and what they expect from an integrated approach to their care. Teams’ views on the outcomes, including the most useful level at which to pitch outcomes in compiling a checklist that could be used in practice, and service users’ experiences of teams using the checklist, are discussed in the next chapter.
Chapter 6 Can these outcomes be assessed in service delivery?
Key messages
-
Organisational and service pressures affected the feasibility of using the OC.
-
Teams whose remit extended beyond an impairment-based approach were better able to use the outcomes in practice.
-
The OC held face validity and covered the issues important to those with LTNCs.
After identifying the outcomes in stage 1, the next stage was to develop the outcomes into a checklist and implement the checklist as part of NRTs’ practice. This chapter describes the process of developing the outcomes into the checklist, and then presents findings about its use by the teams. It goes on to present findings about whether or not the outcomes can be assessed in practice from the perspectives of staff and service users.
Developing the outcomes into a checklist
It is perhaps worth noting at this point that the level at which we focused the outcomes in the OC was guided by the earlier outcomes research. 2,3 However, it was also important to focus outcomes at the level that best suited NRTs’ practices. Focusing outcomes at the intermediate level meant that the constituent elements of higher-level outcomes would not be missed and also that NRTs and service users would still have the opportunity to discuss the lower-level outcomes during assessments. The research team also wanted to avoid the checklist replicating existing paperwork or becoming too long.
The content of the checklist was common across the five NRTs and was based on the outcomes in the three domains outlined in Chapter 5. However, the format and the way the teams used the checklist in practice could differ between teams to accommodate their different practices around assessment and service provision. We met with each team to discuss developing the outcomes into a checklist. We used a standard list of discussion points (see Appendix 3) to explore how teams wanted the checklist to look, what additional functions they wanted (e.g. space to record comments or actions), if and how they wanted to record that they had discussed the outcome with the client, and whether they would prefer a paper or an electronic version. Table 18 summarises each team’s preferences for how their checklist should ‘look’.
| Team | Client information | Paper/electronic | Functions | Appearance |
|---|---|---|---|---|
| A (BI) | The team use stickers containing client information that they attach to documents (name, date of birth and NHS number). A box where this sticker could be applied would be useful or, for when there are no stickers, a box where they can put this information | Prefer paper copies, but would like an electronic version | Three tick boxes to indicate whether or not the outcome is important to client (yes, no, not relevant at present – review later) | Would like the name of the team on checklist |
| Would like space to add details about referrals and when the outcome should be reviewed | Would like it to be in boxes or a grid that is consistent with their other documentation | |||
| Would like three columns to add in dates if and when the outcomes are reviewed | Would like it to be landscape | |||
| Do not want space to add in details about the outcome/need or actions taken as these are detailed in the assessment form | ||||
| Would like a space at the bottom to sign, initial and date each sheet | ||||
| A (MS) | Space to record name, NHS number and date of birth | Paper | Would like a way of recording which outcomes are and are not important to client | Would like name of new team on checklist, with MS added to it |
| Yes/no tick box to record this – having an explicit no reduces ambiguity for anyone else looking at the notes | Would like it in similar format to existing documentation | |||
| Would like space to summarise discussion had with client. They might refer to another document where they detail the goals they have set with the clients | Possibly landscape | |||
| Would like a way of recording which outcomes are in the remit of the team and which will be referred – possibly as part of the free-form text box | Were interested in distinguishing by colour, but not green | |||
| Would like to record intended actions in free-form text box | ||||
| Text box should have prompts for referral details, outcome of discussion, action | ||||
| B | Would like space for a label | Electronic template but paper version for use | Would like space for comments | Landscape |
| Would like ‘Does the client want help with this outcome’ as opposed to ‘Is this outcome important to the client’; would like yes/no tick box for indicating whether client wants help with outcome | Would like it in Ariel 11, on coloured paper | |||
| Would like a tick box for ‘referred on’ | ||||
| Would like space for signature, date and initials | ||||
| C | Space to record name, NHS number and date of birth | Paper | Three tick boxes to indicate whether the outcome is important to client (yes, no, not relevant at present – review later) | Landscape |
| Two columns for dates | ||||
| A space to write comments | ||||
| A tick box to indicate if a referral to another service is made | ||||
| A box to write down a review date | ||||
| Space to write name and designation of staff using checklist, and date of use | ||||
| D | This case site was recruited later in the research so we were able to show the team the checklists we had developed for the other teams. The NRT in site D chose the same format as that designed by the BI NRT in site A | |||
As can be seen from Table 18, the appearance and functions of the checklist were largely similar across all sites, but there were some minor differences. For example, sites B and C wanted to record referral information in the form of a tick box, while site A wanted to record this information in the comments box.
In line with the teams’ specifications and preferences, checklists were drafted and sent to each team for further comments and amendments. At this point, only minor amendments to formatting were requested. The OCs were then finalised and copies sent to each team, along with guidance for use and the parameters of each outcome (see Appendix 4).
Teams were asked how they wanted to use the checklist. Several different approaches were identified. For example, some teams initially discussed using it as a one-off assessment checklist, while others thought they might use it repeatedly with the same client over time to assess outcomes as an episode of care progressed. Some teams talked about using it simply as an aide memoire and others wanted to integrate it into their assessment processes. How this worked in practice is discussed later in this chapter.
The teams implemented the OC for a period of 6 to 10 months. We contacted them on a monthly basis to monitor the use of the checklist and to provide an opportunity for teams to report any difficulties they were having with checklist implementation. During this period, we also met with the teams to discuss progress and possible changes to the checklist to reflect NRTs’ needs. In site B, the team requested that the first question on their checklist (Was the outcome discussed with the client?) be replaced with ‘Is this outcome important to the client?’. In site C, the team requested that the first question on their checklist (Is this outcome important to the client?) be replaced with ‘Is this outcome a particular issue for you at this time?’, with a corresponding yes/no/referred to other professional or service tick-box option. The review date box was also amended at their request to include a way to record whether or not the outcome had been achieved.
Care record audit
During the implementation period, we undertook the CRA to help us monitor the use of the checklist in practice and any actions resulting from its use. As described in Chapter 2, we asked service users with whom the checklist had been used if we could monitor its use in their care records.
In site A, the checklist was used with at least (see Appendix 8, note j) seven clients during the implementation phase and three agreed to the CRA request. In site B, it was used with at least 19 clients and nine agreed to the CRA request. In site C, the checklist was used with at least 16 clients and 10 agreed to the CRA request. In site D, it was used with at least three clients, two of whom agreed to the CRA request. Thus, across the four sites, the checklist was used with at least 45 clients, 24 of whom agreed to a CRA. Table 19 gives demographic details of those for whom a CRA was completed.
| Demographica | Number in sample |
|---|---|
| Gender | |
| Male | 14 |
| Female | 8 |
| Primary diagnosis | |
| MS | 11 |
| Stroke | 8 |
| Other | 4 |
| Age (years) | |
| 30–39 | 1 |
| 40–49 | 7 |
| 50–59 | 6 |
| 60–65 | 4 |
| 66–75 | 4 |
| 76–85 | 1 |
| Ethnicity | |
| Asian | 1 |
| Black/black British | 2 |
| White British | 18 |
| White other | 1 |
Using the outcomes checklist
Not all members of staff in the NRTs used the checklist. Table 20 gives a breakdown of which staff used the checklist, by site.
| Site | Used with ‘at least’ . . . clients | Staff using checklist | |||||
|---|---|---|---|---|---|---|---|
| Psychologist | Nurse specialist | OT | Rehab-support worker | Physiotherapist | Social worker | ||
| A | 7 | 2 | NA | 1 | NA | NA | NA |
| B | 19 | NA | 0 | 1 | 1 | 4 | 3 |
| C | 16 | NA | 2 | 8 | NA | 0 | NA |
| D | 3 | NA | 1 | 1 | NA | NA | NA |
| Total | 45 | 2 | 3 | 11 | 1 | 4 | 3 |
Although these findings may reflect the different NRT compositions across the case sites, it is interesting to note that not all professions within the NRTs in sites A, B and C used the checklist. Possible reasons for this are discussed later in this chapter.
Evidence from the CRAs indicated that some of the outcomes were not discussed with clients during assessments. In particular, we found several checklists that did not record information about the ‘safety and security’ outcome in sites A and B, about the relationship outcomes in sites B and D and about the education and training outcomes in all case sites. In most cases, staff had noted on the checklist that these outcomes were not relevant for the client. It is not clear from the CRA alone whether clients or staff decided whether or not an outcome was relevant. In one instance, where the client had experienced a recent bereavement, the practitioner recorded that it was inappropriate to ask about relationship outcomes at the time of assessment (site B). Interviews and focus groups with NRT staff explored these issues in more detail and findings are reported later in this chapter.
All checklists allowed space for notes so that NRTs could include additional information. The depth and type of detail recorded varied across all checklists. Some checklists contained little or no detail, while others contained information about, for example, the client’s specific difficulties and concerns, goals set to help achieve outcomes, referral information, actions taken or planned, and further assessment that might be required. There were no discernible patterns to the depth and type of detail recorded by case site team.
Difficulties with using the outcomes checklist
From the CRAs, it appeared that staff and clients felt that some outcomes, particularly those in the social participation domain, were too similar to one another. For example, a member of staff in site C thought that the outcomes about social and recreational activities and about social relationships and roles covered the same issues, and a client in site D thought that the outcomes about intimate relationships and family relationships were similar. Findings from staff interviews about this issue are presented later in this chapter.
Summary of care record audit findings
The CRA demonstrated that use of the checklist varied across teams. All teams did use the checklist but some of the outcomes were listed as ‘not relevant’ and some outcomes were considered too similar. Interviews and focus groups with staff explored their use of the checklist and their views on its value and potential. The next section presents these findings.
Evaluation of the outcomes checklist: findings from staff interviews and focus groups
As outlined in Chapter 2, individual interviews were conducted in site A with three practitioners (two based in the NRT and one social worker). Focus groups were held with practitioners in the NRTs in sites B (n = 7), C (n = 6) and D (n = 2).
Following procedures
Initially, it had been agreed that the OC would be used with new clients and clients re-referred during the previous 6-month period. However, we modified procedures in response to pressures that teams were experiencing and the apparent difficulties in recruiting clients who met the research criteria. For example, during the first few months of implementing the checklist in site B, many clients attending the triage clinic did not need further input from the NRT or did not meet research eligibility criteria. To accommodate these challenges to recruitment, first, we offered all teams the option of also using the OC at review, or for new episodes of care with existing clients. One team in site A, and the teams in sites B and C agreed to this. However, only the site C team implemented this option. Although the site D team did not agree to using the checklist for reviews, it became apparent from data collected in stage 3 with service users that it had been used in review for one client. In site B, the team continued to use the checklist with new and re-referred clients. Second, we offered all sites the opportunity to extend the implementation period. Teams in sites B and C agreed to this, and the time period for using the checklist was extended for 4 months beyond the original 6-month recruitment period. The teams in sites A and D declined this extension.
Although there was an understanding that the checklist could be used more than once with each client, all sites limited its use to a single completion. However, it could act as an aide memoire to follow up additional needs with clients at future visits:
I think it made me think, ‘Oh, I haven’t really asked him about where he gets support from a peer point of view from.’ And I was able to ask him that, like, the second time I saw him, rather than it eventually coming up in conversation.
NRT2A(2)
Staff chose to use the checklist in different ways. Some dedicated a whole session with a client to using the OC and, in one case, this was reported to have taken 2 hours. It was more commonly reported that the checklist took 10 to 15 minutes to complete. The majority of staff used it alongside their existing tools, to supplement assessments, while on a few occasions it was completed after visiting a client.
Views on the process and format of the outcomes checklist
The teams in sites B and C seemed to find it easier to use the checklist than teams in A and D. In B and C, a factor cited as helping to facilitate use of the checklist was their team administrator, who reminded staff about the checklist before client visits. All teams commented how the compulsory paperwork for their initial assessments was already lengthy and had to be given priority. At one point, the site C team had to suspend their use of the checklist temporarily as they were forced to undertake other paperwork for the Commissioning for Quality and Innovation (CQUIN)-related commissioning exercise.
The format of the OC was modified slightly in sites B and C to reflect that, although an outcome might be important to someone, it might not be something they wanted help with at that particular time. Otherwise, the format was generally liked, found easy to use in practice and helped to take the service user through the process of discussing issues they might want to resolve. The comments box was useful in providing the opportunity to give more detail. The NRT in site C suggested that it might be used to record more explicitly whether and how service users wanted to address outcomes. The team felt that this would be more in-line with the self-management approach that underpinned the way outcomes were defined.
Some staff found it useful to use the commentary explaining the parameters of different outcomes when using the OC in practice. However, it became evident that not everyone referred to these parameters when undertaking assessments.
Views on individual outcomes
Discussions about individual outcomes focused on areas where outcomes on the checklist differed from current practice.
Personal comfort outcome domain
As part of the personal comfort outcomes, ‘safety and security’ generated debate in sites B and C, in particular. Site A saw ‘safety and security’ as covered by their existing assessment through asking about their clients’ environment and carrying out risk and falls assessments. In contrast, sites B and C, who also undertook risk and falls assessments, viewed this outcome as an important addition and something different from their usual way of assessing risk. They agreed that it had emerged as a key outcome to clients. It exposed people’s feelings of vulnerability and heightened an awareness of how the way in which the team might view the parameters of safety and security might be very different to clients’ conceptions. Rather than merely focusing on adapting or controlling people’s environments, using these wider conceptions of safety and security defined by service users, could help to generate discussions about people’s feelings of vulnerability and ways to help build their confidence.
If we feel that someone’s vulnerable, but they’re not necessarily highlighting it, then it gives you a bit of an inroad to discuss that, if you’re asking the question directly.
NRT14B(2)
Social and economic participation outcome domain
Nine separate outcomes were included in the social and economic participation domain on the checklist. Some staff felt that there was overlap and repetition in this section and that they would prefer to see outcomes condensed into fewer items. Others, again particularly in sites B and C, found it useful to highlight the different elements of social participation and encourage attention to detail, although they acknowledged that this might be a matter of professional perspective.
In site D, ‘access to paid employment as desired’ was seen as not relevant to most of their clients, while staff in site C liked the way that this outcome felt more holistic and put the person in control.
‘Developing and/or maintaining intimate personal relationships and roles’ was an outcome that generated much discussion. Some staff felt uncomfortable asking about this outcome at all. Others felt it appropriate to ask about relationships more broadly and allow the service user to choose how much they wanted to say. However, several staff across teams thought it was a neglected area that they ought to be addressing. In site B, some staff expressed the view that their discomfort was not about the topic, but rather around there being nowhere suitable they could refer people on to. There was general agreement across teams that timing could be difficult and it was not a topic that they could easily ask in an initial assessment. The team in site C commented that it was not an unusual topic to cover in their team’s remit; however, they preferred the way the topic was approached in the OC, rather than their usual way of addressing the issue through a direct a specific question about sexual problems. Teams suggested that having this outcome explicitly included on the assessment documentation used with every client, meant that service users were aware that they could return to the topic at a later date if they so wished:
But even if they don’t want to go further then, they know then that you are willing to go there, probably next visit, or the visit afterwards. So it does open the door, ‘cause it is an important thing to discuss it.
NRT7C(2)
‘Emotional well-being’ could also be a sensitive area and difficult for staff to discuss. It tended to be easier for people to focus on physical impacts. Clients, especially older people, often remained stoical about emotional issues.
‘Access to advocacy and support’ was another area where people commented that it was useful to explore more directly than their usual assessments allowed. A staff member in site A described how the use of the OC had led her to explore different support options for one young man at an earlier point in the assessment process than usual. Separating peer support from relationships with family members and significant others helped staff to question their assumptions about the type of support people might want.
Autonomy outcome domain
Within the grouping of autonomy outcomes, separating out ‘personal decision-making’ was highlighted as usefully extending the coverage of current assessments and prioritising an important outcome in a more forthright way. The team in site B commented that ‘self-management’ could be usefully incorporated in this domain. However, site C felt that ‘self-management’ was implicit throughout the checklist and was underlined in the way outcomes were phrased. Staff in site D found that asking clients about ‘financial security’ also required them to reassure clients that discussing these issues with them would not influence access to benefits.
Views on outcomes overall
While there were similarities between many of the outcomes on the checklist and those in teams’ existing assessments, it was generally felt that the checklist’s approach was different. Knowing that these outcomes were a formulation of what is important to people with LTNCs and were derived from service users themselves, was important. Teams in three of the four sites commented that the OC made them think more about outcomes than their current assessment process, limited the assumptions they made about people, their needs and their preferences, and helped them to ask more in-depth questions. The issues covered and the way outcomes were worded helped staff and service users open up discussions about otherwise difficult or neglected areas. Teams in sites B and C, in particular, commented on how they liked the phraseology, which encouraged a more person-centred style of questioning with an emphasis on self-management and how people felt about issues. For example, ‘desired level of household cleanliness’ reflected whether or not a person felt happy and in control of their household situation, rather that just that the house was clean.
The outcomes were viewed as comprehensive and relevant to the types of clients that the teams supported. However, some felt that having only one outcome explicitly covering physical functioning or cognitive skills did not enable detail about these issues to be recorded and did not match teams’ current assessments for achieving this. This research did not aim to replicate teams’ current functional assessment tools but rather a checklist to enhance current assessment processes. However, some staff reported that the overall emphasis of the checklist marginalized their professional input:
So you . . . you only give one question for physical health and functioning . . . And you think, oh, right, Physio, one question, okay, we know where we are [laughs] . . . But yeah, you’ve repeated quite a lot of social roles, family roles, community, in quite a lot of questions.
NRT5C(2)
In site D, management of medication was often a key reason for referral, and symptom and medication management inevitably were a priority. NRT staff expressed the need for more specific outcome measures around these areas, while in other teams it was felt that such outcomes could be inferred in the checklist’s ‘physical health & functioning‘ or ‘personal decision-making’ outcomes.
There was agreement that outcomes needed to be explored at all levels. Teams in sites B and C felt that the outcomes, as listed on the checklist, were addressed at the right level to start a useful discussion. Staff generally liked the way that they were not too prescriptive. Staff in site C felt that if the checklist had focused on higher-level outcomes, for example about choice and control or self-esteem, it might have been more difficult to achieve meaningful action, although they would have generated interesting discussions. In contrast, staff in site D felt that the outcomes as framed with the OC were more appropriate for use by social care teams during personal support planning. For them, outcomes as formulated in the checklist did not give the capacity to look at lower-level ways of building up functioning to achieve goals.
Fit of outcomes to professional practice
Where there was a divergence in overall views on outcomes, this generally reflected the differences between the teams. The teams in sites A and D experienced more challenges using the checklist than those in sites B and C. For example, the team in site D that practiced a more medical, clinically focused approach gave priority to detailed physical and psychological assessments. Although they tried to carry out holistic assessments with a wider focus, much of their work was around symptom and medication management. They felt that the checklist created a problem by giving the wrong impression of the type of support they could offer or, if acknowledging that support was outside their remit, a problem of signposting to other services when they were aware that clients would not meet eligibility criteria for social care. In addition, the OC encouraged the type of ongoing support that was difficult for the team to provide. Management pressures required them to discharge people from the service and deal with discrete episodes of care.
The BI NRT in site A had used the checklist on only two occasions, but felt that outcomes fitted in with their practice and could add value to their current assessments. However, it was difficult to justify the time needed to use it, especially when there were staffing pressures in the team. The MS NRT felt that their assessments already covered most of the outcomes and, if not directly, issues would probably come up in discussions. Hence, for them, the OC added nothing to their existing practice.
The teams in sites B and C were more open than teams in sites A and D to exploring how the checklist could add value to, and be used in, their existing practice. Interestingly, both site B and site C teams commented that they felt that more ‘impairment-based’ teams would struggle with using the checklist because of their narrower approach to assessment and care planning.
The way that individual practitioners within teams viewed the checklist also differed. Some practitioners thought that the outcomes were skewed towards social issues and that the checklist was, thus, irrelevant to their practice. Others felt that the OC, by capturing their team’s overall approach, was a valuable addition to assessments, even if some of the outcomes were outside their individual professional roles and skills.
Only site B employed a social worker as a member of the team whose remit was to work within the team and provide the lead on social isolation. This person was the only social care practitioner across all case sites to work with the team’s assessment paperwork and directly use the OC. In site A, a social care practitioner was interviewed to discuss her views on the checklist content and format, though she had not had the opportunity to use it in practice. Social care practitioners who worked closely with the NRT in site C were also invited to give their views on the checklist and explore how it might fit with their current practice, though none responded.
The social care practitioners we interviewed felt that the OC was comprehensive, reflecting the issues that should be covered from a social care perspective. They were concerned that some social workers might not understand the interconnectedness of some of the outcomes for people with LTNCs. They argued, for example, that cognitive problems tended to get overlooked and misunderstood by non-specialist social workers. Furthermore, funding in social care tended to dictate prioritising areas of ‘personal hygiene and care’ and ‘safety and security’, with a focus on critical need. Dealing with longer-term issues, such as family relationships or access to employment or training, demanded ongoing support but opportunities to provide this type of support were limited. Hence, to work towards the outcomes on the checklist, social care would need to liaise with or signpost to other agencies.
The differences we identified between teams in sites A and D and those in sites B and C may be explained by factors such as the degree of interdisciplinarity in the teams, staffing pressures and organisational changes experienced by teams.
Organisational and strategic factors affecting teams use of the checklist in practice
The current climate of financial constraints and reorganisation also influenced views about the outcomes and the ability of teams to help clients achieve outcomes and meet people’s needs. There was a discussion in site C about how OTs roles were changing, less time could be spent with clients and there was pressure to focus on the key elements of their role. As mentioned earlier, staff in site D commented on the way in which clients would not meet criteria for social care and this concern was echoed in other teams. Staff in all sites felt that the economic climate was driving the way services could respond to clients’ needs, not just within their own service and across social care but also in terms of benefits and employment. For example, being called for benefit reviews caused anxiety for clients because they were worried about the possibility of being forced into unsuitable employment. Service users and staff were concerned that information about service users striving to be positive about self-management and community involvement could be detrimental for service users in benefits claims. Furthermore, service users’ access to and participation in, for example, transport and exercise schemes was becoming increasingly difficult. Staff in site B described how all available exercise schemes incurred costs to clients that had to be a major consideration in discussions about what the team could facilitate. Moreover, funding of local transport schemes was becoming more problematic, especially in relation to specialised transport for people with mobility difficulties. Participation was curtailed and support from voluntary organisations experiencing cutbacks in their service meant that helping clients achieve outcomes was increasingly difficult.
Strategic-level reorganisations had had less impact on front-line practice in sites B and C than in sites A and D. In site A, amalgamating several teams was causing internal upheavals and staff changes created insecurity and a more inward focus on specific roles and responsibilities. These service changes created pressures that made it difficult to use the checklist:
But maybe in, kind of, 6 months’ time or a year’s time, when we’ve merged and things are more settled . . . [edited] this won’t seem as an extra imposition.
NRT2A(2)
In site D, the merging of the provider arm of the PCT with the acute trust had been accompanied by major reorganisation of the community neurology service. It was felt that the drive to develop community neurology services at a higher commissioning level had been lost and, coupled with a reduction in team staff, those remaining were forced to narrow their focus and felt under pressure to concentrate on what was perceived as core business:
All those things that would be lovely to do are just not going to happen now, are they, at all?
NRT1D(2)
Impact of using the outcomes checklist
All teams welcomed the evidence-based nature of the checklist and that outcomes were derived from service users’ views of what was important rather than being from a clinicians’ or organisational perspective. In addition, several staff felt that the way outcomes were framed helped teams achieve a more person-centred and holistic assessment:
It’s really very much their opinion on their health and life, rather than our opinion. And I think again, you know, some people are better at that than others, at seeing people holistically or seeing people in a box. And I think this really hands it back over to the patient to say, ‘What do you feel about that. I can see you are having problems with your hand, but how do you feel about it?’
NRT15B(2)
One person in site C commented that, although the team had worked hard in developing a generic, holistic assessment over the last 2 years, the OC had identified issues that had not been raised when using their usual assessment documents.
Staff suggested that the checklist could help service users to think about their lifestyle and understand how specific therapeutic input could be beneficial in the context of their life. In site B, where staff frequently worked with people recently discharged from hospital, using the checklist could help clients adjust and focus on the reality of functioning in their home and wider environment, and move on from the sorts of rehabilitation goals they would have worked towards in hospital.
Staff in site B also commented how, for them, using the OC made the whole assessment process smoother and fairer. The checklist made sure that everyone had an equitable assessment, each outcome had been addressed and all staff were aware whether the service user wanted something done, whether it could be done within the team, or whether they needed to signpost to another service.
Difficulties encountered in using the OC were often around time and capacity pressures, especially in sites A and D. Generally, it was felt that there was duplication in the issues covered within teams’ current assessment tools. For some, this made using the checklist a time-consuming chore that added little value, especially in site D where they felt that their main focus should be around clinical, functional and environmental adaptation issues. Others acknowledged some duplication but saw this as positive in that the checklist approached issues in a different, more holistic way.
All teams commented that the initial assessment was not always the most appropriate time to use the OC. This was partly due to time pressures but also because staff felt it might be important to establish a therapeutic relationship with their client before delving deeper into what might be considered sensitive areas. As discussed earlier, staff in site D felt that the OC gave the wrong impression of the type of the support they could offer and might raise unrealistic expectations, not just because the issues raised were outside their remit, but because no services were available to help.
The ways in which the OC could be used in the future were discussed with teams. It was agreed that it would require some changes to fit in with requirements of teams’ current paperwork. Interest in incorporating it into team practice varied across sites. This partly reflected differences in capacity or opportunity to establish and present a business case for developing their service. Teams in sites B and C viewed adapting the checklist as a potentially useful exercise in further developing their service in a direction that was consistent with the aims of their team and could influence commissioners. The teams in sites A and D viewed the outcomes they had to achieve as a service as being dictated by commissioners. Securing continued funding for their service was dependent on achieving these outcomes.
There were several common suggestions across the sites about how the checklist might be used in the future.
-
Assessment: Sites B and C saw it as a useful addition to a suite of assessment tools. Staff in site C suggested that a service user self-rated ‘before and after’ component, based on higher-level outcomes of, for example, self-esteem and choice and control, might help demonstrate an extra dimension to their team’s work.
-
Ongoing review: Staff in site B and from the BI NRT in site A felt that the checklist could be useful as a working document to be used throughout the team’s support of a client and in providing a final check of the team’s input.
-
Training: There was widespread agreement in sites A, B and C that it could be used in training junior and newer staff and could also help existing staff develop interview skills and a holistic approach to assessment. This was seen as potentially helpful for teams that were more impairment led, to prompt a wider personal and holistic approach. In addition, it was felt to be thought-provoking, to encourage reflection and to provide confidence in addressing issues: ‘I think it is really good for – maybe particularly for junior and newer staff members, because it does give you all these questions that, if you can’t answer, you haven’t asked the questions’ [NRT2A(2)].
-
Audit/benchmarking: One of the teams in site A and the team in site D saw the checklist as possibly working as an audit or benchmarking tool to check against whether or not their existing assessment paperwork was working on the issues rated as important to people with LTNCs.
Overall, as we have seen, sites A and D felt that the OC did not work for them. Although some staff in site A saw value in some of the outcomes that currently they did not cover (e.g. access to advocacy and peer support, and personal decision-making), changing their practice and assessment tools was not a priority at the current time. In both sites, there was a sense of multiple pressures (including staff pressures and organisational changes) on teams. This seemed to have an impact on their ability to contemplate innovation for current practice:
‘Cause I think, at the moment, this is just one other thing that we have to do, and we’re trying to meet these targets and we’re trying to fill in all these forms and we’re trying to get our waiting list down, when we’re under pressure for more clients because, you know, staff levels have reduced. I think this just came at the time when this was just another thing. Or that’s how it felt to me, anyway, and it just didn’t, unfortunately, register. However bad I felt for not doing it . . . it just didn’t register on my list of priorities.
NRT2A(2)
By contrast, the team in site B was keen to incorporate the checklist into their assessment process. Staff felt that they would need to keep their own more clinical sections, but saw value in integrating the checklist into their assessments to ensure equity and a focus on what service users wanted.
The NRT in site C was keen to see the OC developed as a validated assessment tool. Staff saw the potential to provide a good outcome measure that more effectively captured their work as a team and could thereby influence commissioners:
So we desperately, desperately need something that captures what we do, because nobody’s asking us, commissioners don’t really know what we do . . . And we were really hoping that this would carry on to be developed to do that.
NRT1C(2)
Summary of staff interview findings
Teams encountered a number of challenges using the checklist including staffing and caseload pressures, changes to service structures and remit, and competing demands of other compulsory paperwork. While it did not work for teams in sites A and D, teams in sites B and C felt that the checklist had potential and fitted in with their practice. Across all sites, it was felt to have value as a benchmarking and training tool. There were contrasting views about each individual outcome and whether they complemented, added to, or duplicated themes and issues in teams’ existing assessment paperwork. There was reluctance to raise certain outcomes with clients. This could be because it was not deemed to be within the staff member or team’s remit, because the outcome was a sensitive area, or because there was an absence of corresponding support and provision to help the client achieve the outcome. Some outcomes were viewed as particularly helpful and were seen to add to teams’ existing assessments.
Overall, a number of factors affected the extent to which these outcomes could be meaningfully assessed in practice. The next section describes service users’ view of the outcomes, and whether or not they capture the key issues they want to be addressed.
Service user interviews
During the third stage of the project, we invited service users (different individuals from those in stage 1) to take part in an interview if the team had used the OC with them. This interview aimed to discover service users’ experiences of the checklist being used as part of their assessment, to see if their key concerns were covered and to ascertain whether or not they were comfortable being asked about the topics included.
As reported in Chapter 2, we interviewed 12 people with LTNCs. Table 21 provides a demographic summary of the sample.
| Demographic | Number in sample |
|---|---|
| Gender | |
| Male | 7 |
| Female | 5 |
| Primary diagnosis | |
| MS | 6 |
| Stroke | 3 |
| Other | 3 |
| Age (years) | |
| 30–39 | 0 |
| 40–49 | 4 |
| 50–59 | 2 |
| 60–65 | 3 |
| 66–75 | 3 |
| 76–85 | 0 |
| Ethnicity | |
| Asian | 1 |
| Black/black British | 0 |
| White British | 10 |
| White other | 1 |
We initially asked interviewees if they were aware of the checklist and it being used as part of their assessment. Seven of the 12 people we interviewed did remember the checklist being used during their assessment/review with the teams. Three did not remember it being used but explained that this might be because their memory was poor. Three were unaware of the checklist being used.
As we had anticipated, then, not everyone remembered the teams using the checklist as part of their assessment. This might reflect the fact that some team members used the checklist as an aide memoire, completing it when they returned to the office as a way of checking if they had discussed all outcomes in assessments and for planning their next assessment with the client. However, as discussed in Chapter 2, memory limitations may also account for some of those who did not remember the checklist being used.
In most teams, as described above, the checklist was used as part of the initial assessment process. This might not be completed at the first meeting but over the first few client visits. Most of the participants who remembered the checklist being used as part of their initial assessment felt that the assessment was conversational. However, one commented that, while it had felt as though the OT was reading off a list, this was a good thing because it meant that everything was being covered.
In two case sites, the checklist was used for initial assessment and also as part of the review process. Those service users who remembered the checklist being used as part of a review process said that they did not think they discussed anything at their review meeting that they would not normally discuss with the team at other reviews/assessments. That is, that the checklist did not lead them to discuss any topics that they would not normally discuss with the team. However, one participant suggested that using the checklist ‘formalises what they were doing already’ (SU43C, MS).
Views on individual outcomes
Although some people could not remember their assessment, we showed all participants the checklist during their interview. This meant that they were able to comment on the relevance of the outcomes for them and their feelings about being asked about the outcomes.
Personal comfort outcome domain
Participants felt that the personal comfort outcomes were relevant to them and should be asked about as part of an assessment/review process, even if they were not necessarily relevant for them at the time we interviewed them.
Personal hygiene and care was an important issue in people’s lives, particularly with regard to being as independent as possible. However, people with LTNCs who we interviewed in this stage of the research not only viewed themselves as maintaining independence if they were able to achieve this outcome alone, with or without adaptations or equipment; they also described themselves as independent with this outcome where they received assistance with some aspects of maintaining their personal hygiene, toileting or personal care. Independence for some, therefore, might include, or indeed hinge on, some level of dependence. This was similar to the evidence collected in earlier interviews.
The importance placed on this outcome might change depending on the trajectory of the condition. Participants who had experienced a stroke suggested that ‘personal hygiene and care’ had been a more significant issue for them in the initial stages of their rehabilitation but that once they were able to achieve this outcome, whether with assistance or alone, other outcomes took priority. For people with other neurological conditions, the importance of this outcome might also change depending on deterioration or relapses/remissions over time.
As we found in interviews with people with LTNCs in stage 1 of this research, one of the main methods people described for maintaining independence with this outcome was to learn adaptive techniques. Some people might accept assistance from a ‘carer’, while others would learn different routines or use equipment to help them manage.
Safety and security was important for many of the participants and reflected what staff discussed in terms of this outcome. It was discussed in different ways. People described how their sense of safety and security was influenced by their functional status. To limit hazards such as falls, people had to adapt their homes, accept assistance or change the way they did things for themselves in and around their house and neighbourhood. They talked about having rails fitted to assist with getting around and maintaining usual activities such as being safe to shower, help around the house and go out:
. . . safety and security has got to be the first, probably, criteria first, because until all these things are all put in place here, in the house, like the banister, and the toilet thing that’s upstairs, and the chair things, and all that . . . I didn’t want that, but it’s the best thing that’s been done.
SU38B, stroke
However, for some, not being able to do things around the house, such as help with washing dishes, created feelings of insecurity about their role in the family and home.
People we interviewed talked about feeling safe in their neighbourhoods and their homes. As well as reflecting their functional ability and mobility levels, this could be affected by the area they lived in, how long they had lived there, whether or not they knew their neighbours and whether or not they felt that their house was secure from intruders.
Some of the people we interviewed had key-safe systems installed in their homes (see Appendix 8, note k) so that carers were able to enter the property, and this contributed to their feelings of safety because they knew that a carer could get in the house if they themselves were unable to get to the door. However, one person we interviewed regularly removed the key because they felt vulnerable when people could let themselves into her home. This shows that strategies which can make some people feel safe can have the opposite effect on others and shows, therefore, the importance of assessing and discussing these issues with each client.
As is evident from the range of issues described, what people think about when asked about their safety and security differs, and the level of safety and security someone feels may differ from how a carer/professional might assess this. For example, one participant with Huntington’s disease claimed to feel safe even though the people supporting the participant felt that they were at severe risk of falls. Staff working with people with LTNCs may, therefore, need to prompt people they are assessing to think about the whole range of meanings ascribed to safety/security, as well as the risks they are willing to accept.
Maintaining their desired level of household cleanliness and maintenance was viewed as important by some people, whether or not they were able to maintain their previous standards or do as much housework or maintenance as they used to do. One person remarked that ‘it [was] blooming awful’ (SU36A, MS) that he could no longer do maintenance work around his house. However, other people said that they had come to accept that they had to do less or had to lower their standards when it came to housekeeping and maintenance; they felt that this was just something that had to happen in order to maintain their safety.
Most of the people we interviewed described experiencing some degree of emotional difficulties related to their condition. Some were able to pinpoint particular reasons for their poor or fluctuating emotional well-being, such as changing roles as a result of their condition or specific physical issues. Others, however, just generally felt emotionally vulnerable but were aware that their LTNC influenced this. Unsurprisingly, therefore, emotional well-being was viewed as an important issue for most people we interviewed.
People described the strategies they had to help deal with these issues. Friends and family were key to maintaining or promoting emotional well-being for some of the people we interviewed, with, for example, one person describing her partner as her ‘emotional prop’ (SU47D, MS), therefore linking with outcomes around intimate, family and social relationships and roles. Being able to get out of the house was central to some in promoting their own emotional well-being. For example, one participant described how he decided to use a mobility scooter, something he had been reluctant to do, after the team working with him suggested it. As a result, he was able to continue with his social activities and meet with friends, and felt he could maintain his role as husband by being able to go and choose, for example, his wife’s birthday card rather than having to rely on others to choose for him. This outcome, therefore, links with outcomes around access to the wider environment, social and recreational activities, social and intimate relationships and personal decision-making.
As is clear from this second example, the team could play an important part in helping people through emotionally difficult times. They could help people to recognise the issue and see it as a usual consequence of their condition, suggest strategies or equipment that might help the person maintain or improve their emotional well-being, or help people to recognise when emotional issues were becoming more problematic and advise on (or refer to) medical or counselling support, where appropriate.
Given the sample, it is perhaps not surprising that ‘physical health and functioning’ was seen as very important by all participants. Some people talked about particular issues related to their health condition, such as continence and limited mobility (walking), but others talked about health in terms of general fitness and activity and the importance of taking exercise (within the constraints of their condition). However, some people saw physical health and functioning as important primarily because of how it affected their life more generally, and, in particular, their ability to get out of the house. At the same time, getting out for walks was seen as a way of maintaining physical health and functioning. Thus, this outcome links to that about access to the wider environment.
Although, as described in Chapter 2, people we interviewed were assessed by the teams as being cognitively able to give informed consent and take part in an interview, people who discussed cognitive skills did describe some degree of cognitive difficulty. These were mainly issues with memory, concentration, and intermittent confusion. Some people described how they became frustrated when they could no longer do things that they used to be able to, therefore linking this issue to emotional well-being. Participants described how they had developed strategies to help deal with some of these issues, often with advice and support from the team, and that the issue was important to include on a checklist.
Social and economic participation outcome domain
Most of the people we interviewed, many of whom were retired, explained that the outcomes around access to paid employment, training/new skills and further/higher education were generally not relevant for them. However, they agreed that it was important to ask about them to ensure that they were included for people to whom they were important.
Of the six people in the sample who were of working age, two had retired early and one was unable to work due to her condition and so they did not see these outcomes as important to them. The other three worked, but two of them had needed to stop working for some time when they first became ill. These two interviewees emphasised the importance of employment in their lives, with one claiming that the ‘main thing [for them] was to get back to work’ (SU39B). Work was important for several reasons: gaining financial security, maintaining status and roles in the family, and promoting a social life. These, in turn, helped to promote confidence.
Some of the people we interviewed explained how they were learning new ‘recreational’ skills, illustrating that this outcome links to social and recreational activities. The only person who reported being offered training to help with employment felt that it was not useful for him because it was not relevant to his job to which he wanted to return.
Many of the people we interviewed described the important of establishing and maintaining social and recreational activities and how these were affected by their condition. Some were able to adapt to these changes so that they were able to continue with hobbies and meet with friends/groups, while others felt that they were no longer able to continue with these pursuits because of their condition. The NRTs advised people on how to adapt or to access specialist equipment to continue with hobbies and activities, although, in general, people with LTNCs devised coping and management techniques themselves to try to maintain their social interests. The effort people with LTNCs put into working around their condition so that they were able to continue with social and recreational activities is testament to the importance of this outcome in participants’ lives. Most people acknowledged that if their condition deteriorated they would find it difficult to continue with social pursuits. Participants suggested that this would be a time when the team might be able to assist and thus it was important for this issue to be included on the OC.
As described in the previous chapter, importance was placed on maintaining different types of relationships and roles: intimate relationships, family relationships and social relationships. Despite some participants saying that they would not necessarily go into detail with the teams about maintaining intimate relationships, all participants felt that it was an important issue and so should be included on the checklist to enable issues to be raised, if desired. Participants could gain benefits from discussing this issue with their NRT. For example, one participant explained that when asked about this outcome in their assessment, the team had been able to reassure him that changes to his medication might help his sexual health.
While many of the people who discussed this outcome talked about the sexual side of intimate relationships, people also talked about holding hands with their spouse, buying presents for them, involvement in usual household tasks and emotional well-being as being central to maintaining these relationships. As such, this outcome links with outcomes included in the personal comfort outcomes (emotional well-being, household cleanliness and maintenance, physical health and functionality) and with autonomy outcomes [access to wider environment (getting out)].
Maintaining family relationships was also important for most of the people we interviewed in this stage; however, most of them felt that they were able to achieve this outcome themselves. People who talked about social relationships described them as very important and drew links between this outcome and the outcome about social and recreational activity. They also described how being able to achieve this outcome was dependent on several factors previously described, such as having the opportunity and being well, or functionally able enough, to continue meeting with friends. Although they acknowledged that social relationships might change, the importance of being seen as oneself rather than as a disabled person and not merging social relationships into ‘caring’ relationships was emphasised, as one participant explained:
Well, that’s one of the reasons why I ended up being divorced because the role changes, doesn’t it? And this is why I don’t want my friends to end up being involved in personal care and things . . .
SU42C, MS
Access to advocacy and peer support was not considered an important issue for this sample, with most of the people we interviewed not wanting to talk to people with the same condition about their experiences. Only two of the people we interviewed felt that advocacy was important to them – one said they would speak to their solicitor if they needed an advocate and another felt it important to have an advocate when applying for benefits – though neither necessarily saw these issues or that of accessing advocacy as being within the remit of their team. This contrasts with findings from our earlier work and data from staff interviews, and may reflect our sample for this stage of the research. Although most of the people in this stage of the research did not feel that this outcome was important for them personally, they nonetheless saw that it might have importance for others and thus should be included in assessments.
Few people talked about the ‘contributing to wider community/ies’ outcome, though a couple of people explained that they were involved in voluntary community work and one suggested that this might be something they would do in the future. The importance of this outcome, like others we have discussed, might therefore have different levels of importance at different points in people’s lives. As such, and given the importance people placed on this in earlier stages of the research, its inclusion on the checklist was valued.
Autonomy outcome domain
People felt that being able to access all areas of their home was an important outcome. Some participants were able to access everywhere in their home and gardens without specialist adaptations or equipment but some had made modifications to enable them to achieve this outcome as far as possible. These included having rails fitted throughout the house and using stair-lifts. Participants accepted, often reluctantly, that even if they could access all parts of their homes now, they might not be able to do so in the future and, therefore, made adaptations or installed equipment before it was a necessity. For example, one couple explained how they had converted part of a garage into a bedroom and a shower-room in preparation for the future. By including this outcome on the checklist, staff and clients could discuss current accessibility issues in the home as well as start to develop strategies together for dealing with issues that might arise in the future.
Accessing the locality and wider environment was also important to participants, irrespective of if they were currently able to do this as much as they wanted. Some people described how they were self-conscious about their gait, causing them to feel reluctant to go out in public. Teams worked with these clients to build their self-confidence, helping some to relearn walking skills and/or to relearn route planning to promote confidence, thus helping people to get out of the house again.
For those people who could only walk limited distances, access to transport was essential. Some described the importance of having their own transport in order for them to get to the places they wanted to go. Not everyone had this, and so public transport (with bus and/or rail passes) and voucher systems for taxis were essential. Being able to access the locality and wider environment was described as important for several reasons: it allowed people to continue with social and recreational activities (such as attending evening classes and going to local groups); it allowed people to continue with usual household roles (such as walking the dog and going shopping); and it allowed people to do things relevant to their roles in intimate, family and social relationships (such as choosing and buying presents for spouses, family and friends, or themselves). People described feelings of freedom associated with being able to get out of their homes and, indeed, out of the local environment. They talked about the importance this outcome had in promoting choice, control and feelings of ‘normality’.
Being able to communicate was important to people with LTNCs because it was viewed as essential to being able to express what was wanted and ensure that others ‘heard’ them. Those who discussed this outcome were primarily people who currently had, or had previously had, a speech or cognitive difficulty, making communication problematic for them. The teams helped people by facilitating access to or providing speech and language therapy or advising on exercise to help with memory, confusion and other cognitive issues.
Financial security was also viewed as important, including by those who saw themselves as financially secure at the time of the interview, thus underlining the importance of this outcome on the checklist. For those who were experiencing financial difficulties, this affected their family and intimate relationships and roles as well as other aspects of their lives. As one participant’s wife explained, not having a job, not qualifying for benefits, and the resulting financial insecurity affected the way he saw himself:
It’s like your pride, isn’t it? You know, being able to support his family, being the man of the house, the strength, which he always has been. And he doesn’t like it,. . .
SU39B, condition withheld to protect anonymity
Although people thought this outcome should be included on the checklist, some people were not sure if these issues were within the remit of the team or sat within the team’s area of knowledge. Others explained how the team in their area had assisted them with completing the forms to apply for benefits and it was suggested that, as completing the forms correctly is essential to qualifying for benefits in a timely way, the OC should expressly include a question about assistance needed with this.
Personal decision-making was important for everyone we interviewed, even if this meant that they were making decisions that made them potentially unsafe. It was particularly important for people to make decisions about things when they felt they had little control over that issue more generally. For example, the person who felt financially insecure (see above) emphasised the importance for him of making the financial decisions. The person who had carers visiting regularly emphasised the importance of controlling who could come into their home and when, and chose to remove the key from the key-lock system that had been installed to enable carer access.
Some people did not see personal decision-making as a sole decision. Instead, they described how they had always made, and wanted to continue to make, decisions with their spouse. Overall, this outcome was essential for maintaining independence.
Did the checklist cover participants’ main issues of concern?
We asked people what their main issues of concern were at the time of the interview and if they felt the checklist covered these issues.
The issues people reported covered a wide range of topics and reflected those identified in stage 1 interviews with service users and, therefore, the outcomes included on the checklist. When asked if they were able to place their issues within categories on the OC, people were able to find a category where they could fit the things that were important to them. However, some felt that their main concerns could fit into more than one category because these affected many areas of their life. Several people with MS, for example, explained that fatigue had an impact on whether or not they were able to achieve several of the outcomes and so could be included in any one, or all, of them, with one person suggesting that it should be a category of its own on the checklist. Outcomes people talked about explicitly also reflected the higher-level outcomes we described in Chapter 5, such as the importance of feeling ‘normal’ and being independent.
We also asked people if they were or would be happy for the team to raise the topics on the OC. Everyone we interviewed said that they were or would be happy for the team to raise any of the outcomes on the checklist with them because of their levels of expertise and one also suggested that it was because she felt she had developed a good relationship with the team over several years. However, as mentioned above, some people did express some hesitancy in talking about some of the issues, such as intimate relationships and financial security, unless the latter was about benefit entitlements. This was primarily because they viewed such outcomes as being outside the remit or expertise of the team. As described in Chapter 3, at least two of the teams (B and C) saw these issues as very much part of their remit and regularly assessed needs/goals around these issues.
Even where they felt reluctant to talk about an issue, the people we interviewed still felt it was important to include it on the checklist and in assessments because the issue might be important to other people with LTNCs. It was suggested that including these issues in assessments opened a door for clients who might want to talk about it later.
People we interviewed were happy to raise issues with the team or for the team to raise the issues. However, they thought it was useful if the team asked about areas clients might overlook, think were outside the remit of the team or miss because of poor memory. When asked whether she, or the team, raised issues during assessments, one client responded:
It’s half and half. If I don’t mention something that I’ve mentioned before, they’ll sort of ask how things are, which I think this is where the checklist is going to come in handy. If I’ll ask them to come, and it’s because I’ve got a specific problem, and then I’ll raise the issue, and so it’s, sort of, a mixture of both of us, really.
SU43C, MS
This, therefore, made the checklist useful for reviews. Those participants with whom the checklist had been used in reviews felt that many of the issues included on the checklist were similar to issues that they discussed in earlier meetings with the team. However, they felt that using the checklist would make certain that pertinent issues were raised at each assessment.
Impact of checklist use
The people we interviewed described the different interventions and actions the team took after their assessment. However, we are unable to attribute these to using the checklist in the assessment. These issues might already have been addressed, and the same actions might have resulted when using their usual assessment processes, albeit at different timescales (see staff analysis). Nonetheless, participants thought that it would be useful to use the checklist to ensure that all of clients’ key issues are sure to be covered in assessments.
Overall view on checklist
All those interviewed said that the OC would cover all of their concerns at the time of interview, with some going as far as to say that there was ‘nothing missing’ from the checklist (SU39B), that it ‘covers everything’ (SU36A, MS; SU45C, MS) and that it ‘covers life’ (SU47D, MS). One person we interviewed, who had worked in care services, suggested that the checklist covered all the things that were important to consider when planning care provision (identification number excluded to protect anonymity).
Participants agreed that the checklist covered the things that were important to them but that the importance or emphasis they placed on each of the outcomes might change over time, based on changes in their condition and/or other circumstances.
We specifically asked participants to identify anything missing from the checklist, and although they thought everything would be covered, two people suggested that some key issues for them should be made more explicit on the OC. They suggested, as is discussed above, that fatigue should be an explicit issue in the ‘physical health and functioning’ outcome and that assessing need for help in completing benefit application forms should be explicitly included in the ‘financial security’ outcome.
The way that the outcomes were worded were thought particularly relevant to service users, with one person saying that ‘. . . it seems like it’s been written for me’ (SU39B). Those who talked about the level at which the outcomes were pitched felt that it was appropriate; including the lower-level outcomes would increase detail and so would be ‘off-putting’, and using the higher-level outcomes would allow too much variation in how they were interpreted. However, some participants did suggest that the outcomes on the checklist, when viewed together, were all about promoting independence.
People with LTNCs who we interviewed in this stage of the research, therefore, not only understood the elements that contributed to the level of outcome that we used for the checklist, but were also able to see, unprompted, the contribution of these outcomes to those we identified as higher-level outcomes, such as independence, choice and control.
Some clients expressed confusion about who provided support or referred them on to other service providers. One person, who described being in contact with nine professionals from different service sectors, suggested that a more co-ordinated approach to service provision would be helpful:
. . . they are very good in their own ways, but you don’t necessarily know what everyone is doing . . . I would like to go to one person and say, ‘Right, you’re in charge of me,’ . . . they’re all doing their own thing, but if they co-ordinated it you might be able to improve the overall service.
SU36A, MS
Thus, clients recognised the important of professionals and services working together – an observation that supports more integrated provision for people with LTNCs.
One of the participants also suggested that the checklist could be used to improve communication and enhance co-ordination of care:
I think the checklist covers everything that people will be likely to want to discuss. I think it’s good to have it because you can – it focuses your mind on what you need to talk about. I think it’s good for the [NRT] to have a copy because, if somebody – if it’s not the same person coming out to you at the same time, every time, they will know what’s been discussed and what have been issues and what haven’t been issues before. So it gives better continuity, and if this was taken up nationally, if you moved to another area and you were working under another [NRT], you wouldn’t, in a way, be starting right from the word go with a new set of people, which would make it quite helpful.
SU43C, MS
Summary of service user interview findings
Although we cannot ascertain whether or not the checklist directly influenced care, those we spoke to about their experience of being assessed using the checklist demonstrated that it held face validity, and potentially could be a useful tool as part of assessing their care needs.
Discussions with people with LTNCs at this stage of the research reiterated the importance of most of the outcomes included on the checklist. For this sample, some of the outcomes in the social and economic domain did not have the same importance as they did for the sample in stage 1. Nonetheless, service users who we interviewed in this stage were keen for these to remain on the checklist because they recognised that they would be important for other people or, indeed, to themselves in the future.
It was clear from interviews with service users (at both stages of interviews) that although these outcomes were discussed separately, they were very much intertwined. Service user participants explained how the different outcomes affected each other. For example, physical health and functioning might be important for people because this allowed them to wash and dress themselves, feel safe, get into the wider environment and maintain their social and family relationships and roles. Meanwhile, maintaining social relationships might be an important outcome for people to achieve because this ensured that they were able to contribute to the wider community, maintain emotional well-being and financial security. Service users also described how the different levels of outcomes, as outlined in Chapter 4, were inter-related.
Summary
The outcomes we identified from service users at stage 1 were developed into a checklist and implemented as part of practice by the case site teams. This process demonstrated that a number of factors affected the feasibility of using this checklist in practice. Its use in practice was viewed positively in sites B and C, whereas in sites A and D, staff felt that it added little value. A number of factors may help to explain these differences and we discuss these in the next chapter by drawing together evidence from all stages of the research. The evidence also demonstrates that the OC held face validity as it reflected and covered the key issues that were important to those with LTNCs. However, there is a discrepancy between what issues are important to service users as part of their care and what issues teams were able to address in practice. The implications of this for policy and practice are discussed in the next chapter.
Chapter 7 Discussion
The main research questions that we aimed to answer in this research are:
-
What facilitates or impedes the development of innovative approaches to health and social care integration?
-
What outcomes do people with long-term conditions want from integrated health and social care?
-
Can these outcomes be assessed in everyday service delivery?
-
How can different models of integrated health and social care affect outcomes?
In this final chapter, we discuss the findings in relation to the key research questions. We draw on findings from Chapters 3 and 4 to answer question one, findings from Chapter 5 to answer question two and findings from Chapter 6 to answer question three. We address the final research question by drawing together findings from across the report. We then discuss the strengths and limitations of the research, and the implications of the findings for policy, practice and future research.
What facilitates or impedes the development of innovative approaches to health and social care integration?
Organisational and NRT staff viewed integration positively and agreed that more integration was needed. Several factors were identified that could help integration, many of which have also been reported elsewhere,69,92 for example co-location of services and or/practitioners,1,92,93 aligned administrative systems and financial arrangements;41,94–96 shared IT systems97,98 and shared outcome indicators. 97–99
The two staff groups who we interviewed described different types of integration and emphasised different benefits of integrated arrangements. During interviews, organisational staff – that is, those who worked at the commissioning/strategic level – tended to focus on formal integrated arrangements at organisational and commissioning levels. The primary benefit of integration they described was improved organisational efficiency but they also explained that this could lead to improved services and experience of care for people with LTNCs. Practitioners, however, focused on both formal and informal service-level and personal/professional integration arrangements, including interprofessional working within and across sectors and joint decision-making between professionals, people with LTNCs and their carers. For practitioners, the primary benefit of integrated working was improved service provision and a better experience of services for people with LTNCs and their carers, but they also acknowledged that service-level efficiencies could result from integrated service provision.
These different foci about the meaning and anticipated outcomes of integration could lead to misunderstandings and confusion when developments around health and social care integration were posited, thus inhibiting progress towards integration. The confusion around definitions and outcomes of integration is echoed in the findings of recent research on joint commissioning in health and social care. 100 As well as the factors outlined above, our research, therefore, suggests that developing integration between health and social care might also require a shared understanding of the process and aims of integration.
Our research found that although these other factors could influence development and maintenance of integrated service delivery, the most significant factors affecting integration at service and organisational levels were organisational change and the cost-containment agenda. Structural changes that had occurred in the PCTs, local authorities and NRTs often fractured both formal and informal integration arrangements and made maintaining or enhancing integration arrangements difficult. Staff at all levels were unsure of future structural arrangements and how they, or the NRTs, would fit within the new service landscape. This, as suggested by Ling et al. ,41 inhibited the continued development of integration.
Our research shows that integration at the service level was often informal, bottom-up and facilitated by professional relationships built-up over time. The importance of these bottom-up, relationship-based, local approaches in developing integrated services has been reported elsewhere. 41,99 As such, integration might best be achieved by health and social care organisations enabling practitioner-led innovation around integration. 1,99 In addition, it has been suggested that cost-containment policies can cause those working in health and social care organisations to be risk averse and stifle innovation. 101 Our findings show such factors at play in relation to integration. Cost-containment measures were in force throughout the period of this research and were being played out in the context of structural reorganisation in health and social care. These measures were perceived to have an impact on type, availability and capacity of services, within organisations and beyond, and were identified as a barrier, not only to better integration, but also to encouraging innovative practice.
The NRTs we worked with represented different models of integrated services. Service users and carers valued the teams and explained how they benefited from team interdisciplinarity and expertise so that access to a range of services and professionals could be co-ordinated when needed. Where it was provided, long-term, holistic and flexible support that ensured changing needs were responded to over time was particularly valued. The NRTs in this study, to varying degrees, fulfilled the criteria that our previous research showed people with LTNCs valued. 1 These are:
-
interdisciplinary team working
-
a holistic approach to service provision
-
specialist knowledge
-
provision of advice and information; and
-
care co-ordination.
What outcomes do people with long-term conditions want from integrated health and social care?
The current research applied earlier thinking and conceptualisations to explore further the sorts of outcomes people with LTNCs might want from integrated health and social care and that would provide an exemplar for long-term conditions generally. The outcomes service users wanted to achieve ranged from those focusing on health benefits and improvements to wider social outcomes concerned with more everyday aspects of life. Importantly, outcomes could be framed in the context of a deteriorating or fluctuating condition, such that they might be about maintaining a level trajectory rather than requiring specific improvements.
Many of the outcomes identified in earlier research resonated with our interviewees, but the current study provided the opportunity to redefine outcome categories and the meanings that people with LTNCs attributed to them. We identified additional outcomes, such as cognitive skills and personal decision-making. We also found that the way people characterised some outcomes meant that they did not fit in with the pre-existing outcomes framework. Definitions and parameters needed to be refined in relation to all outcome domains and their constituent categories, but especially for social and economic participation outcomes. These changes may have reflected the different client group in our research, the particular sample selected, or changes in service user expectations and lifestyles over time. Policy agendas and directives, for example around personalisation or choice and control, may also have influenced service user expectations.
We also noted some differences between the two samples of people with LTNCs that we spoke to in stages 1 and 3. ‘Advocacy and peer support’ and ‘contributing to wider communities’ did not seem as important to interviewees in stage 3 as they had to those interviewed in stage 1. They were retained on the final checklist because of the importance placed on them by stage 1 participants and because stage 3 participants recognised that these outcomes might be significant for other people or for themselves in the future.
Our data suggested that being able to achieve outcomes was a dynamic process that required awareness of the inter-relationships between different types of outcomes. Identifying the three levels of outcomes – lower, intermediate and higher level – reflected service user perceptions, as well as providing a useful framework on which to base discussions that could complement existing practice. Our findings suggested three domains – ‘personal comfort’, ‘economic and social participation’ and ‘autonomy’ – around which outcomes could be framed. Inter-relationships between outcomes, both within a particular domain and across domains, existed. For example, maintaining routines of personal hygiene and care, such as washing and dressing, also involved safety and security, which contributed to ‘personal comfort’. It also demanded consideration of issues relating to access and, hence, ‘autonomy’. Achieving higher-level outcomes such as independence or choice and control was dependent on recognising these potentially multiple and cross-cutting inter-relationships. Outcomes at lower and intermediate levels could work together to contribute to the higher-level outcomes in ways that were often complex and variable, depending on service user circumstances, as discussed in Chapter 5.
In addition, earlier research had suggested that the way in which something is done and the way in which services are delivered can undermine or contribute to quality-of-life outcomes. 2,102,103 Our findings confirmed that service processes were important to service users in achieving their desired outcomes. Moreover, from a carer perspective, the ways in which the service interacted with carers could critically affect experiences of support and had consequences for service user outcomes. Not merely the type of support offered but also the manner in which team members carried out their interventions was important to both service users and carers. For example, unless service users were given confidence and encouragement by the team, they were unlikely to build on the team’s input and move forward in their rehabilitation or adjust to changing circumstances in a sustainable way.
Can these outcomes be assessed in everyday practice?
Our findings show that some of the outcomes in our checklist were already being assessed to some degree by the NRTs taking part in this research. However, the checklist, with the accompanying list of parameters, did encourage some NRTs to discuss outcomes in more detail and guided them to prompt clients about additional outcomes and wider interpretations of the outcomes that clients might not otherwise have considered. Some of our outcomes added value to existing client assessment practices. In particular, ‘personal decision-making’, ‘access to advocacy and support’, and ‘developing and/or maintaining intimate personal relationships and roles’ were seen to extend the coverage of current assessment documentation for some teams.
However, some of the outcomes we identified proved difficult for some NRT staff to broach in client assessments, particularly ‘financial security’, ‘emotional well-being’, and ‘developing and/or maintaining intimate personal relationships and roles’. Perceptions of the outcomes being too sensitive to raise, or not being within the professional’s remit, partly accounted for this. Reluctance to raise outcomes in assessment was also linked to an absence of corresponding service support to address related issues.
For some of the teams, a holistic assessment was completed only as part of initial assessment processes. After this, ongoing reviews and assessments tended to focus on functional status ‘outcomes’, as is evident from the types of outcome measures that were used by the teams (see Appendix 6). Some of the NRT members discussed how no current validated outcome measures could capture the full effect NRTs could have, for example, on functional maintenance (rather than simply improvement), clients’ self-esteem, their perceptions of independence and their levels of choice and control over their lives. As outlined in earlier research,1,24 this could mean that NRTs were unable to demonstrate to commissioners the full range of work they did and the full impact that their work could have on quality of life for people with LTNCs and their carers.
Although the individual outcomes were valued differently across teams, and thus influenced the extent to which they were used, it is clear that these outcomes can be assessed as part of practice by NRTs. However, the use of the checklist was challenged by wider service pressures. As in other research,3,104 we found that time constraints, staffing pressures and heavy caseloads limited the ability of practitioners to use outcomes in practice. Other team structures and processes can also affect how the outcomes are assessed in practice, and we discuss this further in the next section.
How can different models of service delivery affect outcomes?
There are three ways that models of integrated care can affect outcomes: the way outcomes are interpreted, how outcomes are assessed and, ultimately, how outcomes are achieved. From the implementation and evaluation stages, we are able to understand how different models affect interpretation and assessment. However, we can draw tentative conclusions about whether or not teams are able to achieve these outcomes.
In site A, both NRTs were able to assess the range of outcomes we identified, as they both undertook a holistic approach to assessment. However, in practice, use of the outcomes was hindered by service changes and perceived duplication with their existing assessment processes. In site D, the NRT model was geared towards functioning and medication issues in discrete episodes of care. This limited their interpretation and assessment of outcomes to those that reflected these priorities. Outcomes beyond these (e.g. social participation outcomes) were felt to be outside their remit. Other reasons NRT staff cited for difficulties using the OC in practice included loss of team structure and strategic direction for neurology, changes in remit of the team, and line-management changes.
The NRTs in sites B and C were open to exploring the different outcomes and how they could be interpreted, assessed, and potentially achieved in practice. The holistic approach that these teams took to assessment and service provision meant that all of the service-user derived outcomes were within their remit. Interdisciplinarity appeared to give more scope to interpret and assess the outcomes and, possibly, to facilitate the achievement of outcomes through professionals working together and sharing expertise.
NRTs’ interpretations of outcomes in the checklist differed across case sites. For one team in site A and for the teams in sites B and C, staff were willing to think through individual outcomes and how they differed, added to and could be integrated into their practice. For the NRT in site D and one team in site A, there was more reluctance to engage with new ways of thinking about outcomes.
The NRTs in sites B and C were larger, meaning that that they were able to rely more on ‘in-house’ staffing and resources to deliver care. Originally, the teams in site A were small, and we know from stage 1 data that delivery of care had to rely more on joint working with, and referral to, outside services and sectors. It is possible that the same would apply to the achievement of the outcomes – bigger interdisciplinary teams may be better ‘equipped’ to help service users do this.
Strengths and limitations of the study
A social model of disability
Using a social model of disability as the theoretical underpinning for this research placed people with LTNCs at the centre of identifying important outcomes and allowed us to apply a progressive approach to the conception of outcomes. This service-user led, rather than professionally or organisationally driven, method was particularly useful because it highlighted issues of importance to people with LTNCs, some of which were not routinely asked about in assessments and many of which were not included in established outcome measures used to evaluate service provision. By taking a wider social view of outcomes rather than focusing on functional status outcomes, our work helped to illuminate a crucially important issue. It reinforced that by adopting a holistic, interdisciplinary approach to assessment and support, NRTs could promote desired outcomes (with, where necessary, the support of family, friends and services) despite the potential deterioration of service users’ physical and/or cognitive conditions.
However, this approach also highlighted some issues that were viewed as being outside the remit of some of the teams. As outlined in Chapters 3 and 4, there were different types and levels of integration across the NRTs and this influenced their ability or readiness to assess some of the outcomes included on the checklist. Some NRTs were required to focus on ‘core’ business as a response to organisational change and funding pressures. This meant that outcomes other than those about physical health and functioning and emotional well-being were not prioritised, which might be seen as antithetical to the concept of integrated service provision. As outlined in Chapter 6, two of the teams that adopted a particularly interdisciplinary approach to service provision felt that, although they might not be able to intervene around specific issues themselves, it was nonetheless important to assess the whole range of outcomes included on the checklist and to provide relevant information about referrals and to contact details for other services, as required. The importance of multidisciplinary teams in delivering good outcomes to service users is also highlighted by Petch et al. 103
We have shown how the different outcomes service users identified are inter-related; achieving one outcome can have a positive impact on achieving other outcomes and different levels of outcomes. Thus, commissioners need to understand these inter-relationships to be able to plan effective services for people with LTNCs.
Use of the case study approach
Case studies are useful for dealing with complexity in a ‘real-life context’,76 and their use here was a key strength of the study. This approach allowed us to explore, in-depth, the complexity of the organisations in which the services we studied were embedded. The diversity in each of our case sites was also a key strength. Diversity is important for quality in qualitative research,105 and our case sites were especially diverse in the models of NRTs and the approaches to integration. These differences meant that we were able to explore how the feasibility of using the checklist varied according to different models and approaches, and the influences these differences exerted.
Recruitment of organisational staff (stage 1)
We faced difficulties recruiting commissioning staff in some case sites, in both health and social care. In sites A and B, this resulted in a gap in our understanding of the NHS commissioning arrangements and structures. In site D, a similar gap in our understanding resulted due to adult social care declining involvement in the research. We have drawn on other sources of evidence (e.g. interviews with other organisational staff and documents) to redress this gap. However, we acknowledge that our understanding of the commissioning aspects of the organisations in case sites A, B and D might not be complete. As a result, the macro-level decision-making structures within which the teams operated might not be fully described.
Identifying the outcomes (stage 1)
In stage 1, we aimed to identify the outcomes important to those with LTNCs, and our approach to this was guided by earlier SPRU outcomes research. 3 However, an immediate challenge we faced was understanding the evidence behind these outcomes. First, it was not entirely clear how Harris et al. 3 had drawn upon the outcomes identified by Qureshi2 in order to produce their outcome framework. Second, there was little evidence about the meaning and parameters of the outcomes categorised within Harris et al. ’s3 outcomes framework.
At first, this presented difficulties as we had intended to use this framework as a guide when identifying the outcomes with our sample. However, it also presented us with the opportunity to develop the outcomes according to the meanings attached to them by participants in this study. Therefore, the outcomes identified were largely service-user driven and meaningfully rooted in their experiences of what they considered important in their lives. This is a major strength of the study.
NHS engagement with the research
Although all case sites and NRTs had agreed to take part, there was poor engagement from some of our case sites. This was mostly during the implementation stage, and was characterised by periodic non-response to telephone messages and e-mails, and a reluctance to try new ways of using the checklist. Non-response to telephone calls and e-mails was experienced across all sites at some point and we suspect that this partly reflected the issues of staffing pressures and service changes we discussed in Chapters 4 and 6.
The reluctance to use the checklist was most prominent in sites A and D. This was likely because they felt that it just did not work for them, along with other service pressures. In sites B and C, reluctance to use the checklist was episodic and appeared to be linked to service pressures. When these pressures alleviated, their engagement with the research resumed. They had a sense of ownership of the checklist and were keen to try different ways of using it.
Organisational change and instability at the service level may also have made it difficult to engage with the research. For example, in sites B and C, where engagement with the research was largely unproblematic, the teams were stable and experienced no changes to their service during the research period. In sites A and D, where engagement with the research was challenging, both teams were undergoing substantial change during the implementation stage of the research. It is possible that unstable periods of NHS reorganisations at the service level, among other issues, can create an environment that is not compatible with exploring new ways of working or engaging with research.
Similarities and differences between the teams suggest other factors that may also have influenced NHS engagement with the research. First, the teams in sites B and C were both large, whereas the team in site D was small, and the teams in site A were small before merging. Larger teams with more staff may facilitate interdisciplinarity (which was evident for teams in sites B and C), and enable them to deal with staff absences more easily than smaller teams. Second, the ‘closeness’ of the managers to the team may have played a role. The team managers in sites A and D played an overarching role, overseeing a number of teams. In sites B and C, the managers were part of the team and used the checklist. Teams in sites B and C also had designated administrators who were seen as integral members of the team. They played an important role in the day-to-day management of the research at the case sites; for example, they managed the documents and reminded staff to use the checklist and distribute invitation packs.
Recruitment of service users for the care record audit and stage 3 interviews
During the implementation phase, we intended to recruit up to 25 service users per site for the CRA. The purpose of the CRA was to monitor the use of the checklist and identify any difficulties in using it. The number of service users recruited for the CRA was much lower than we expected. Only two were recruited for site D, and the highest number we achieved was 10 for site C. The low numbers recruited in sites A and D (three and two, respectively) may reflect the difficulties they had in using the checklist, the limited number of times they were able to use it, and their generally low level of engagement with the research. The low numbers across all of the case sites may also reflect low numbers of eligible participants. Indeed, during the implementation phase, some teams noted that many of their referrals were clients with poor cognitive abilities who did not fulfil our eligibility criteria, and so they were not given an invitation pack.
We did attempt to maximise recruitment by asking teams to extend the implementation period and extend the sample by using the checklist in reviews as well during initial assessments. However, only the NRTs in sites B and C agreed to the former and sites C and D agreed to the latter. Neither of these methodological changes increased recruitment substantially enough to achieve the numbers we originally aimed for. Despite these difficulties, the CRA allowed us to monitor use of the checklist and enabled regular contact and meetings with the NRTs during implementation, which allowed us to explore any difficulties encountered in using it.
For the stage 3 interviews with service users, we had intended to recruit a maximum of five participants per site. Poor recruitment was again observed in sites A and D (n = 1 per site). We almost reached the target in site B (n = 4) and exceeded it in site C (n = 6). However, this did not affect our ability to explore the face validity of the outcomes. There were consistent messages in our data from those interviewed, suggesting that we achieved data saturation through the sample across the four case sites.
Recruitment of individuals from ethnic minority groups
Although one of our case sites had a large BME population in one area of the PCT, our recruited sample of staff and service users included few individuals from ethnic minority backgrounds. For the service user sample, it is possible that this reflected the NRT’s caseloads at the time of recruitment.
Implications for policy and practice
The findings from our research have several implications for policy and practice.
Understanding and assessing outcomes
Although working towards closer alignment, current NOFs remain separate, with one each for the NHS,54 adult social care55 and public health. 56 In identifying indicators that can measure improvement in services and reflect closer working, there have been efforts to move away from process measures. For example, the NHS and Adult Social Care NOFs have complementary indicators relating to quality of life for people with long-term conditions. However, the current NOFs are still seen as representing a hybrid of different levels of outcomes, some of which ‘are not outcomes themselves but rather outputs on the pathway to desired outcomes’. 67 This continued focus on improving the processes of care that are considered to be linked to health outcomes has been argued to undermine the professed aim, ‘to recalibrate the whole of the NHS system so it focuses on what really matters to patients and carers . . . the delivery of better health outcomes’. 106 Furthermore, the different types and levels of outcomes that constitute the NOFs make delineating cause-and-effect relationships between intervention/service and achieving outcomes, difficult. 67 Types of outcomes and relationships between services and outcomes need to be clear. Beginning with an understanding of what outcomes service users and carers want, underpins the task of designing and evaluating services around service user-driven outcomes.
Ways of gauging people’s experiences in relation to integrated care are widely recognised as problematic and underdeveloped. The NHS Future Forum report on integration recommended that new patient experience measures must be developed to evaluate patients’ experiences across whole journeys of care. 48 However, it was acknowledged in recent guidance that it would take time to produce a robust, long-term approach to measurement. 68
This research contributes to the development of that approach. Before commissioners and policy-makers can begin to assess service quality in relation to service users’ experiences of integrated care, there needs to be a clear understanding of the sorts of outcomes that people want and the types of service that are most effective in delivering those outcomes. In this project, we aimed to identify what people with LTNCs want and to see if those outcomes could be assessed in practice. Our research was set in a particular model of service delivery. In terms of contributing to unravelling cause-and-effect relationships, we were able to define outcomes derived from service user perspectives and definitions. It was also possible to draw conclusions around the feasibility of assessing outcomes of integrated care within these services, but inferences about how different models of integrated health and social care can affect outcomes are more speculative.
From both the current research and our earlier work on integrated services for people with LTNCs,1 we know that integrated NRTs frequently feel that they have difficulty in formally demonstrating to commissioners the ‘added value’ that their particular ways of working engender. Conventional outcome measures only partially reflect what such teams strive to achieve, tending to overlook broader social issues and the sorts of concerns, such as a sense of empowerment or self-worth, which are important to service users. Where teams work in an integrated way, identifying the outcomes that service users want and defining and formalising them into a checklist could help to reflect better what integrated teams do and offers the opportunity to develop an outcome tool for assessment.
The findings from this research suggested that:
-
Many of the outcomes that are important to service users with LTNCs are not addressed in validated ‘outcome measures’.
-
This has implications not only for service users’ experiences of the type and quality of care delivered, but also for those commissioning care in identifying priorities for investment.
Outcomes assessment in practice
All services endeavour to achieve equity in practice, but this may be compromised or interpreted in different ways. For example, we identified divergent approaches to exploring clients’ needs, and views differed about whose responsibility it was to identify clients’ needs beyond the strictly ‘clinical’. For some staff, identification of needs depended on clients assuming some responsibility for raising needs during assessment; they felt that staff should raise broad topic areas and then be led by the client. Other staff preferred to raise specific issues and directly ask clients if these were a particular concern for them.
Reluctance on the part of staff to raise particular issues was linked, in part, to concern about raising clients’ expectations when corresponding service support was absent. Staff across all case sites noted how services were contracting or disappearing and some saw discussions around, for example, exercise classes, skills training or relationship therapy as potentially raising service user expectations when there were no services available locally to offer support.
People with LTNCs also described these different approaches to raising concerns or problems in assessments; that staff sometimes raised issues directly and sometimes left it to clients to raise them. Although some service users were reluctant to discuss particular issues or saw some issues as being outside the team’s remit, there was, nonetheless, a consensus that staff should raise all outcomes on the checklist during assessment. This would help to limit the chance of outcomes being missed due to poor memory or service users’ lack of awareness of how the team might be able to help. Even if not every outcome was a priority for service users at the time of assessment, people with LTNCs suggested that raising every outcome opened a door to discussions that might be needed in the future.
We know that the outcomes on the checklist are important to service users because these were the key issues arising from our stage 1 interviews with people with LTNCs and are built on research undertaken by Qureshi2 and Harris et al. 3 with different groups of adults. It is important, therefore, that these outcomes are raised at assessment by staff so that clients’ needs are not missed and that clients receive an equitable assessment.
In the context of long-term conditions, support to maintain a level of functioning or participation is important. NRTs frequently worked with service users to maintain, rather than being able to improve, activities. Conventional outcome measurement tends to focus on pathways to recovery and rarely accounts for the potential deterioration associated with long-term conditions. Moreover, taking time to explore the range of meanings service users attribute to outcomes, rather than relying on service definitions and staff perceptions, is important. For example, although ‘safety and security’ might feature in NRTs’ assessments, in existing paperwork it has tended to be addressed in terms of limiting risk, falls assessment and providing aids and adaptations. The parameters of the service user-defined outcome were more wide-ranging and included feelings of vulnerability, as well as a need to balance safety and security against a desire for independence.
Our research indicated the following:
-
Equity of assessment can be compromised if practitioners do not raise each outcome.
-
Service availability may affect whether or not outcomes are assessed.
-
In the context of long-term conditions, assessment of service user outcomes must account for potential fluctuation and/or deterioration over time.
-
Understanding of and meanings attributed to individual outcomes by service users may differ from conventional staff or service-derived outcomes.
Innovation and integration
Services in health and social care have been required to respond to policy imperatives around innovation and integration promoted by successive governments. Evidence suggests that, most recently, commitment to such initiatives tends to have been overtaken by the demands of major structural reorganisation. Organisational change can lead to a loss of, or hiatus in, established professional roles and relationships that can affect attitudes to innovation and undermine the ability of front-line services to embrace change. This can have an impact on capacity to consider new ways of working within the immediate, and across the wider, service context.
The findings from our research suggested that:
-
Restructuring of health and social care services fractures existing integration arrangements.
-
Instability resulting from restructuring affects services’ scopes to innovate around integration.
Implications for future research
Evidence from our research has illustrated several areas that might require further research.
-
This research reinforced findings from previous work, suggesting that it is difficult to assess the full impact of integrated services, such as NRTs, on the lives of people with LTNCs. Developing the outcomes we identified into a measurement tool could go some way to addressing this problem. As well as assessing impact, a measurement tool could demonstrate the breadth of team activity, which would provide a useful way of assessing cost-effectiveness.
-
Evidence from this research showed that some staff and service user participants were reluctant to raise some of the outcomes during assessments, yet ensuring all outcomes are discussed is important in achieving equity in assessment. The evidence also shows how many of the outcomes are interdependent. Thus, it is possible that overlooking certain outcomes will limit the extent to which other outcomes can be achieved effectively. Further research may help to better understand the impact of this.
-
Some of the teams we worked with engaged with the research more than did others. Though we are able to infer what factors influenced this, we are not able to draw strong conclusions. Engagement from NHS and social care staff is vital to the conduct of high-quality research. Research should examine this issue to understand further what facilitates stakeholder engagement and to help in planning future research.
-
Teams who were involved in this research expressed concern about the future of local community-based specialist integrated services for people with LTNCs once commissioning arrangements were changed. Future longitudinal research could monitor any changes and assess their impact and cost-efficiency in community services for long-term complex conditions.
Plans for dissemination
Findings from this study will be fed back directly to all participants. We will disseminate our findings through SPRU Research Works, a series of publications providing easily accessible summaries of research undertaken by the unit and targeting a wide audience, including health and social care professionals, managers and policy-makers. This publication will be available on our website and will be sent out via all our dissemination channels: e-mail lists, blog, Twitter and RSS (rich site summary). We will use our working relationships with voluntary sector and other networks (including local and national Neurological Alliance contacts) to explore additional routes through which to disseminate findings to lay audiences. We will submit an abstract for a presentation at the forthcoming Health Services Research Network (HSRN) and the Health Care Interdisciplinary Research conferences. At least two academic papers in peer-reviewed journals are planned, one focusing on evidence from staff and one about service-user-derived outcomes.
Acknowledgements
This project was funded by the National Institute for Health Research Health Service and Delivery Research Programme (project number 09/1816/1004). Further information is available at: bit.ly/LTNCoutcomes.
The views and opinions expressed here are those of the authors and do not necessarily reflect those of the funders.
We are grateful for the co-operation of professionals in the four case study sites who made time to take part in interviews. Particular thanks are due to the neurology rehabilitation teams in each of the case sites who worked throughout the research to help us to understand how services were provided in each of the areas, to access people receiving their services and to develop and use the outcomes checklist – without them this research would not have been possible. We are especially grateful to all the people with long-term neurological conditions and their families who took time to engage with us in interviews. For everyone concerned, we hope that we have accurately reflected their views and experiences.
Our thanks and acknowledgements for advice and support go to:
-
The project advisory group. We benefited greatly from their commitment throughout the project.
-
The Social Policy Research Unit’s adults’ consultation group.
-
Those involved via the MS Society and Parkinson’s UK in discussing outcomes and helping us plan interview topic guides.
Finally, we are grateful for the hard work of Sally Pulleyn for the production of this report and administrative support throughout the project.
Contributions of authors
Fiona Aspinal (Research Fellow) co-developed the original proposal, managed the project, undertook data collection at all stages of the project, analysed data, developed the outcomes checklist and co-wrote the final report.
Sylvia Bernard (Research Fellow) undertook data collection at all stages of the project, analysed data, developed the outcomes checklist and co-wrote the final report.
Gemma Spiers (Research Fellow) undertook data collection at all stages of the project, analysed data, developed the outcomes checklist and co-wrote the final report.
Gillian Parker (SPRU Director) co-developed the original proposal, advised on methods and analysis and critically reviewed the final report for intellectual content.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- Bernard S, Aspinal F, Gridley K, Parker G. Integrated Services for People with Long-term Neurological Conditions: Evaluation of the Impact of the National Service Framework. York: Social Policy Research Unit, University of York; 2010.
- Qureshi H. Outcomes in Social Care Practice. York: Social Policy Research Unit, University of York; 2001.
- Harris J, Foster M, Jackson K, Morgan H. Outcomes for Disabled Service Users. York: Social Policy Research Unit, University of York; 2005.
- Lewis J. Older people and the health-social care boundary in the UK: half a century of hidden policy conflict. Soc Policy Adm 2001;35:343-59. http://dx.doi.org/10.1111/1467-9515.00238.
- Reid R, Haggerty J, McKendry R. Defusing the Confusion: Concepts and Measures of Continuity of Healthcare. Ottawa, ON: Canadian Health Services Research Foundation; 2002.
- Darzi A. High Quality Care for All: NHS Next Stage Review Final Report 2008.
- Hudson B. Interprofessionality in health and social care: the Achilles heel of partnership?. J Interprof Care 2002;16:7-17. http://dx.doi.org/10.1080/13561820220104122.
- Bernard S, Aspinal F, Gridley K, Parker G. Integrated policy-making in England for adults with long-term neurological conditions: some preliminary findings from a scoping study. Int J Integr Care 2008;8:1-8.
- Kodner D, Spreeuwenburg C. Integrated care: meaning, logic, applications, and implications – a discussion paper. Int J Integr Care 2002;2:1-6.
- Challis D, Darton R, Johnson L, Stone M, Traske K. An evaluation of an alternative to long-stay hospital care for frail elderly patients: II. Cost and effectiveness. Age Ageing 1991;20:245-54. http://dx.doi.org/10.1093/ageing/20.4.245.
- Landi F, Gambassi G, Pola R, Tabaccanti S, Cavinato T, Carbonin P, et al. Impact of integrated home care services on hospital use. J Am Geriatr Soc 1999;47:1430-4.
- Béland F, Bergman H, Lebel P, Dallaire L, Fletcher J, Contandriopoulos A, et al. Integrated services for frail elders (SIPA): a trial of a model for Canada. Can J Aging 2006;25:25-42. http://dx.doi.org/10.1353/cja.2006.0019.
- Bernabei R, Landi F, Gambassi G, Antonio S, Giuseppe Z, Vincent M, et al. Randomised trial of impact of model of integrated care and case management for older people living in the community. BMJ 1998;316:1348-51. http://dx.doi.org/10.1136/bmj.316.7141.1348.
- Glendinning C, Halliwell S, Jacobs S, Rummery K, Tyrer J. Bridging the gap: using direct payments to purchase integrated care. Health Soc Care Community 2000;8:192-200. http://dx.doi.org/10.1046/j.1365-2524.2000.00244.x.
- Plochg T, Klazinga N. Community-based integrated care: myth or must?. Int J Qual Health Care 2002;14:91-101. http://dx.doi.org/10.1093/oxfordjournals.intqhc.a002606.
- Johnson P, Wistow G, Shulz R, Hardy B. Interagency and interprofessional collaboration in community care: the interdependence of structures and values. J Interprof Care 2003;17:69-83. http://dx.doi.org/10.1080/1356182021000044166.
- Glendinning C. Breaking down barriers: integrating health and care services for older people in England. Health Policy 2003;65:139-51. http://dx.doi.org/10.1016/S0168-8510(02)00205-1.
- Hudson B, Hardy B, Henwood M, Wistow G. Working across professional boundaries: primary health care and social care. Public Money Manag 1997;17:25-30. http://dx.doi.org/10.1111/1467-9302.00088.
- Hudson B. Integrated care and structural change in England: the case of care trusts. Policy Stud 2002;23:77-95. http://dx.doi.org/10.1080/0144287022000011459.
- Kharicha K, Levin E, Illiffe S, Davey B. Social work, general practice and evidence-based policy in collaborative care of older people: current problems and future possibilities. Health Soc Care Community 2004;12:134-41. http://dx.doi.org/10.1111/j.0966-0410.2004.00482.x.
- Johri M, Beland F, Bergman H. International experiments in integrated care for the elderly: a synthesis of the evidence. Int J Geriatr Psychiatry 2003;18:222-35. http://dx.doi.org/10.1002/gps.819.
- MacAdam M. Frameworks of Integrated Care for the Elderly: A Systematic Review. Ottawa, ON: Canadian Policy Research Networks; 2008.
- In Search of a Service. London: Neurological Alliance; 2001.
- Parker G, Bernard S, Gridley K, Aspinal F, Light K. Rapid Systematic Review of International Evidence on Integrated Models of Care for People with Long-term Neurological Conditions. York: Social Policy Research Unit, University of York; 2010.
- Health Act 1999. London: The Stationery Office; 1999.
- National Health Service Act 2006. London: The Stationery Office; 2006.
- The NHS Plan: A Plan for Investment, A Plan for Reform. London: Department of Health; 2000.
- Health and Social Care Act 2001. London: Stationery Office; 2001.
- The NHS Improvement Plan: Putting People at the Heart of Public Services. London: Department of Health; 2004.
- Supporting People with Long Term Conditions: An NHS and Social Care Model to Support Local Innovation and Integration. London: Department of Health; 2005.
- The National Service Framework for Long-term Conditions. London: Department of Health; 2005.
- Our Health, Our Care, Our Say: A New Direction for Community Services. London: Department of Health; 2006.
- Local Government and Public Involvement in Health Act 2007. London: The Stationery Office; 2007.
- Commissioning Framework for Health and Wellbeing. London: Department of Health; 2007.
- Transforming Community Services: Enabling New Patterns of Provision. London: Department of Health; 2009.
- Means to an End: Joint Financing across Health and Social Care. London: Audit Commission; 2009.
- Joining Up Health and Social Care: Improving Value for Money Across the Interface. London: Audit Commission; 2010.
- Maybin J. A high-performing NHS? A Review of Progress 1997–2010. London: The King’s Fund; 2010.
- Curry N, Ham C. Clinical and Service Integration: the Route to Improved Outcomes. London: The King’s Fund; 2010.
- Wistow G. Still a fine mess? Local government and the NHS 1962 to 2012. J Integr Care 2012;20:101-14. http://dx.doi.org/10.1108/14769011211220517.
- Ling T, Brereton L, Conklin A, Newbould J, Roland M. Barriers and facilitators to integrating care: experiences from the English integrated care pilots. Int J Integr Care 2012;12.
- Winchcombe M. A Life More Ordinary - Findings from the Long-term Neurological Conditions Research Initiative. An Independent Overview Report for the Department of Health. London: Research Initiative for Long Term Neurological Conditions; 2012.
- Hudson B. Twenty years of health and social care joint working: a journey from Doctor Pangloss to Private Frazer?. J Integr Care 2012;20:115-24. http://dx.doi.org/10.1108/14769011211220526.
- Ham C, Smith J. Removing the Policy Barriers to Integrated Care in England. London: The Nuffield Trust; 2010.
- Hawkins L. Can Competition and Integration Co-exist in a Reformed NHS. London: The King’s Fund; 2011.
- Equity and Excellence: Liberating the NHS. London: Department of Health; 2010.
- Health and Social Care Act 2012. London: The Stationery Office; 2012.
- Alltimes G, Varnam R, Adebowale V, Bremner S, Bubb S, Christensen L, et al. Integration: A report from the Future Forum. London: Department of Health; 2012.
- The Way Forward: Strategic Clinical Networks. London: Department of Health; 2012.
- Bernard S, Aspinal F, Gridley K, Parker G. Benchmarking integrated care for people with long-term neurological conditions. J Integr Care 2012;20:152-63. http://dx.doi.org/10.1108/14769011211237492.
- Gridley K, Spiers G, Aspinal F, Bernard S, Atkin K, Parker G. Can general practitioner commissioning deliver equity and excellence? Evidence from two studies of service improvement in the English NHS. J Health Serv Res Policy 2012;17:87-93. http://dx.doi.org/10.1258/jhsrp.2011.010176.
- Devlin N, Appleby J. Getting the Most out of PROMS: Putting Health Outcomes at the Heart of NHS Decision-making. London: The King’s Fund; 2010.
- Department of Public Health: PROMs Background. Oxford: University of Oxford; 2011.
- The NHS Outcomes Framework 2013–14. London: Department of Health; 2012.
- The Adult Social Care Outcomes Framework 2013–14. London: Department of Health; 2012.
- The Public Health Outcomes Framework 2013–14. London: Department of Health; 2012.
- Improving Health and Care: the Role of the Outcomes Frameworks. London: Department of Health; 2012.
- Caring for our Future: Reforming Care and Support. London: Department of Health; 2012.
- Draft Care and Support Bill. London: Department of Health; 2012.
- Brand D. Social and health care integration: (1) The individual dimension. J Integr Care 2012;20:371-8. http://dx.doi.org/10.1108/14769011211285174.
- The Operating Framework for the NHS in England 2012/13. London: Department of Health; 2011.
- Long-term Conditions: Developing a Cross-government Strategy. London: Department of Health; 2012.
- QIPP Long Term Conditions Workstream. London: Department of Health; 2012.
- QIPP Long Term Conditions: Supporting the Local Implementation of the Year of Care Funding Model for People with Long-term Conditions. London: Department of Health; 2012.
- Services for People with Neurological Conditions. Seventy-second report of session 2010–12. London: The Stationery Office; 2012.
- Gregory S, Dixon A, Ham C. Health policy under the coalition government: a mid-term assessment. London: The King’s Fund; 2012.
- Bovaird T. Attributing outcomes to social policy interventions – ‘gold standard’ or ‘fool’s gold in public policy and management?. Soc Policy Administration 2012;48:1-23. http://dx.doi.org/10.1111/j.1467-9515.2012.00869.x.
- Interim Measures for Patient Experience at the Interfaces between NHS Services. London: Department of Health; 2012.
- Cameron A, Larch R, Bostock L, Coomber C. Factors that Promote and Hinder Joint and Integrated Working between Health and Social Care Services. Research Briefing 41. London: Social Care Institute for Excellence; 2012.
- Intelligent Outcomes: Applying the Health and Social Care Reforms to Improve Outcomes for People with Neurological Conditions. London: Neurological Alliance; 2012.
- Nocon A, Qureshi H. Outcomes of Community Care for Users and Carers. Buckingham: Open University Press; 1996.
- Oliver M, Barnes C. Back to the future: the World Report on Disability. Disabil Soc 2012;27:575-9. http://dx.doi.org/10.1080/09687599.2012.686781.
- Evaluating Innovations in Integrating Health and Social Care for Adults and Older People (Reference: IHS 240): Call for Proposals. London: National Institute for Health Research Service Delivery and Organisation; 2008.
- Glendinning C, Challis D, Fernandez J, Jacobs S, Jones K, Knapp M, et al. Evaluation of the Individual Budgets Pilot Programme. York: Social Policy Research Unit, University of York; 2008.
- Bowling A. Research Methods in Health: Investigating Health and Health Services. Maidenhead: Open University Press; 2002.
- Yin R. Case Study Research: Design and Methods. Thousand Oaks, CA: Sage; 2003.
- Sheppard M. Appraising and Using Social Rresearch in the Human Services: an Introduction for Social Work and Health Professionals. London: Jessica Kingsley; 2004.
- DiCicco-Bloom B, Crabtree B. The qualitative research interview. Med Educ 2006;40:314-21. http://dx.doi.org/10.1111/j.1365-2929.2006.02418.x.
- Morgan D. The Focus Group Guidebook: Focus Group Kit 1. Thousand Oaks, CA: Sage; 1998.
- Arksey H, Knight P. Interviewing for Social Scientists. London: Sage; 1999.
- Prior L. Using Documents in Social Research. Thousand Oaks, CA: Sage; 2003.
- Ritchie J, Lewis J. Qualitative Research Practice: A Guide for Social Science Students and Researchers. London: Sage; 2003.
- Rural Urban Classification and Other Geographies. London: Defra; 2013.
- Rural and Urban Statistics in England: Guidance Notes. London: Office for National Statistics; 2004.
- Gridley K, Aspinal F, Bernard S, Parker G. Services that promote continuity of care: key findings from an evaluation of the National Service Framework for Long-Term Neurological Conditions. Soc Care Neurodisabil 2011;2:147-57. http://dx.doi.org/10.1108/20420911111172738.
- Office for National Statistics . Neighbourhood Statistics 2013. www.neighbourhood.statistics.gov.uk (accessed 30 January 2013).
- Folstein MF, Folstein SE, McHugh PR. Mini-mental state. A practical method for grading the cognitive state of patients for the clinician. J Psychiatric Res 1975;12:189-98.
- Podsiadlo D, Richardson S. The timed ‘up & go’: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc 1991;39:142-8.
- Benson T, Sizmur S, Whatling J, Arikan S, McDonald D, Ingram D. Evaluation of a new short generic measure of health status: howRu. Inform Prim Care 2010;18:89-101.
- The EuroQoL Group . EuroQoL – a new facility for the measurement of health-related quality of life. Health Policy 1990;16:199-208.
- Nicholas E, Qureshi H, Bamford C. Understanding and Using outcomes in Social Care: Outcomes into Practice (Part 2). York: Social Policy Research Unit, University of York; 2003.
- Cameron A, Lart R, Bostock L, Coomber C. Factors that promote and hinder joint and integrated working between health and social care services: a review of research literature [published online ahead of print 11 June 2013]. Health Soc Care Community 2013.
- Parker G, Corden A, Heaton J. Synthesis and Conceptual Analysis of the SDO Programme’s Research on Continuity of Care. York: Social Policy Research Unit, University of York; 2009.
- Ware T, Matosevic T, Hardy B, Knapp M, Kendall J, Forder J. Commissioning care services for older people in England: the view from care managers, users and carers. Ageing Soc 2003;23:411-28.
- Glendinning C, Clarke S, Hare P, Kotchetkova I, Maddison J, Newbronner L. Outcomes-focused Services for Older People. SCIE Knowledge Review, 13. Bristol: Social Care Institute for Excellence; 2006.
- Elissen A, van Raak A, Paulus A. Can we make sense of multidisciplinary co-operation in primary care by considering routines and rules?. Health Soc Care Community 2011;19:33-42. http://dx.doi.org/10.1111/j.1365-2524.2010.00946.x.
- Goodwin N, Smith J, Davies A, Perry C, Rosen R, Dixon A, et al. Integrated Care for Patients and Populations: Improving Outcomes by Working Together. London: The King’s Fund and The Nuffield Trust; 2012.
- Humphries R, Curry N. Integrating Health and Social Care: Where Next. London: The King’s Fund; 2011.
- Darzi A, Howitt P. Integrated care cannot be designed in Whitehall. Int J Integr Care 2012;12.
- Dickinson H, Glasby J, Nichols A, Jeffares S, Robinson S, Sullivan H. Joint Commissioning in Health and Social Care: an Exploration of Processes, Services and Outcomes. Final report. London: National Institute for Health Research; 2012.
- Lewis R, Curry N, Dixon M. Practice-based Commissioning: from Good Idea to Effective Practice. London: The King’s Fund; 2007.
- Qureshi H, Henwood M. Older People’s Definitions of Quality Services. York: York Publishing Services; 2000.
- Petch A, Cook A, Miller E. Partnership working and outcomes: do health and social care partnerships deliver for users and carers. Health Soc Care Community 2013;21:623-33. http://dx.doi.org/10.1111/hsc.12050.
- Hughes R, Aspinal F, Addington-Hall J, Dunckley M, Faull C, Higginson I. It just didn’t work: the realities of quality assessment in the English health care context. Int J Nurs Stud 2004;41:705-12. http://dx.doi.org/10.1016/j.ijnurstu.2004.02.005.
- Flick U. Managing Quality in Qualitative Research. London: Sage; 2007.
- Liberating the NHS: Transparency in Outcomes – a Framework for the NHS. London: Department of Health; 2010.
Appendix 1 Research instruments
The original documentation was produced on headed paper.
Participant information sheets
Organisational staff interviews
You are being invited to take part in a research study being conducted by researchers from the Social Policy Research Unit at the University of York. This study is funded by the National Institute for Health Research. It has been reviewed and approved by [name of local PCT R&D office] Primary Care Trust Research and Development Office, the [name of REC] and the Association of Directors of Adult Social Services.
Before you decide whether you wish to take part or not, it is important for you to understand why the research is being done and what it will involve. Please read the following information carefully and take your time to decide whether you wish to take part.
What is the purpose of the study?
These interviews form part of a research project that focuses on levels and type of organisational and service integration. The research concentrates on the support provided by an integrated community team in your area and the outcomes that people who use this service expect from receiving this support. However, we are also interested in the wider context in which this team works and the mechanisms in place in your PCT area that enable services and practitioners to work together to provide continuity of care.
We are interested in learning about your experiences of working in [PCT name] and hearing your opinions about whether and how service integration is developing locally in general and for neurological services specifically.
Why have I been contacted?
You have been identified as playing a central role in services locally for people with long-term neurological conditions and/or in planning/delivering integrated approaches to service provision.
What are the benefits of this research?
The information you provide will be invaluable in identifying the issues, including facilitators and barriers, to the provision of a seamless service for people with long-term neurological conditions.
Will my taking part in this study be kept confidential?
Your involvement in the study, and the information that you provide, will be kept confidential. A personal identification number will be used throughout the research for each participant and all data will be anonymised. Data will be held in accordance with the 1998 Data Protection Act and University of York Ordinances.
There are rare circumstances where the researcher is required to disclose someone’s participation to a third party. However, this will only happen if the researcher is extremely concerned about the participant’s well-being. We will not tell the third party anything that was said in the interview unless it is directly related to the reason we were concerned.
Will taking part in this study affect my employment?
No, taking part in the research will not affect your employment in any way. Similarly, if you decide not to take part your employment will not be affected in any way. It is up to you whether or not you decide to take part and your decision will be kept completely confidential.
What will taking part involve?
If you would like to take part, you will need to complete the response form and return it to me in the enclosed freepost envelope. Please retain this information sheet.
I will then contact you to answer any questions you may have and to arrange a mutually agreeable time and place to conduct the interview.
On the day of the interview there will be further opportunity for you to ask questions and raise concerns. If you are still happy to go ahead, I will ask you to complete a consent form (a copy of which will be given to you for your records).
Note for the attention of REC – For telephone interviews, the following paragraph will replace the underlined paragraph above – it will not be italicised.
If you are happy to go ahead, I will send you a consent form. Please read and initial in the box after each of the four statements if you agree to them, then sign and date it and return it to us at the Freepost address: LTNC Team, Social Policy Research Unit, University of York, FREEPOST YO378, Heslington, York, YO10 1GY. Once we have received the form and signed it, we will return a copy to you and will contact you to conduct the interview. On the day of the interview there will be further opportunity for you to ask questions and raise concerns and if you are still happy to go ahead, the interview will be conducted.
The interview will take approximately 45 minutes and give you an opportunity to describe your views fully. It will be audio-recorded (with your permission). Recordings will be destroyed when the research is complete.
If you do decide to take part, you are still free to withdraw at any time and without giving a reason.
What if I choose not to take part?
Participation in this research is entirely voluntary. If you choose not to take part, just complete the top half of the response form indicating your choice and return it to me in the freepost envelope so that I do not contact you again. You do not have to provide a reason or complete the demographic form, but doing so would enable me to understand your reasons for declining to participate which might help when planning future studies. (Note: your reasons will be recorded anonymously. )
If you have any questions or would like more information, please contact [name of researcher] on [telephone number] email [email address].
Thank You.
NRT pre-implementation interview
You are being invited to take part in a research study being conducted by researchers from the Social Policy Research Unit at the University of York. This study is funded by the National Institute for Health Research. It has been reviewed and approved by [name of local PCT R&D office] Primary Care Trust Research and Development Office, the [name of REC] and the Association of Directors of Adult Social Services.
Before you decide whether you wish to take part or not, it is important for you to understand why the research is being done and what it will involve. Please read the following information carefully and take your time to decide whether you wish to take part.
What is the purpose of the study?
These interviews form part of a research project that focuses on levels and type of organisational and service integration. The research concentrates on the support provided by the [name of integrated community team] and the outcomes that people who use the [name of integrated community team] expect from receiving this support. However, we are also interested in the wider context in which this team works and the mechanisms in place in your PCT area that enable services and practitioners to work together to provide continuity of care.
We are interested in learning about your experiences of working [in/with] the [name of integrated community team] and hearing your opinions about whether and how service integration is developing in general and for neurological services specifically. We would also be interested to hear about the methods the team uses for monitoring outcomes for your clients.
Why have I been contacted?
You have been identified because you work with or in the [name of integrated community team].
What are the benefits of this research?
The information you provide will be invaluable in identifying the issues, including facilitators and barriers, to the provision of a seamless service for people with long-term neurological conditions and to help understand how the [name of integrated community team] works.
As you know, we will be talking to people who use the [name of integrated community team]. The information they provide will be used to develop an outcome checklist covering issues that people with neurological conditions tell us are important to them.
The information that you provide will be crucial when it comes to developing the outcome checklist for use within your everyday practice with new clients.
Will my taking part in an interview be kept confidential?
Your involvement in the study, and the information that you provide, will be kept confidential. A personal identification number will be used throughout the research for each participant and all data will be anonymised. Data will be held in accordance with the 1998 Data Protection Act and University of York Ordinances.
There are rare circumstances where the researcher is required to disclose someone’s participation to a third party. However, this will only happen if the researcher is extremely concerned about the participant’s well-being. We will not tell the third party anything that was said in the interview unless it is directly related to the reason we were concerned.
Will taking part in an interview affect my employment?
No, taking part in the research will not affect your employment in any way. Similarly, if you decide not to take part your employment will not be affected in any way. It is up to you whether or not you decide to take part and your decision will be kept completely confidential.
What will taking part involve?
If you would like to take part, you will need to complete the response form and return it to me in the enclosed freepost envelope. Please retain this information sheet.
I will then contact you to answer any questions you may have and to arrange a mutually agreeable time and place to conduct the interview.
On the day of the interview there will be further opportunity for you to ask questions and raise concerns. If you are still happy to go ahead, I will ask you to complete a consent form (a copy of which will be given to you for your records).
Note for the attention of REC – For telephone interviews, the following paragraph will replace the underlined paragraph above – it will not be italicised.
If you are happy to go ahead, I will send you a consent form. Please read and initial in the box after each of the four statements if you agree to them, then sign and date it and return it to us at the Freepost address: LTNC Team, Social Policy Research Unit, University of York, FREEPOST YO378, Heslington, York, YO10 1GY. Once we have received the form and signed it, we will return a copy to you and will contact you to conduct the interview. On the day of the interview there will be further opportunity for you to ask questions and raise concerns and if you are still happy to go ahead, the interview will be conducted.
The interview will take approximately 45 minutes and give you an opportunity to describe your views fully. It will be audio-recorded (with your permission). Recordings will be destroyed when the research is complete.
If you do decide to take part, you are still free to withdraw at any time and without giving a reason.
What if I choose not to take part?
Participation in this research is entirely voluntary. If you choose not to take part, just complete the top half of the response form indicating your choice and return it to me in the freepost envelope so that I do not contact you again. You do not have to provide a reason or complete the demographic form, but doing so would enable me to understand your reasons for declining to participate which might help when planning future studies. (Note: your reasons will be recorded anonymously. )
If you have any questions or would like more information, please contact [name of researcher] on [telephone number] email [email address].
Thank You.
Service user pre-implementation interview
Researchers from the Social Policy Research Unit at the University of York are conducting a study in your area. This study is funded by the National Institute for Health Research. It has been reviewed and approved by [name of case site] Primary Care Trust Research and Development Office, and the Research Ethics Committee for Wales.
Before you decide if you wish to take part, it is important for you to understand why the research is being done and what it will involve. Please read this information carefully and take your time to decide if you wish to take part.
What is the purpose of the study?
We are looking at services in your area that co-ordinate care for people with neurological conditions. We want to know how far they are able to meet people’s needs. The research is looking at the support provided by the [name of integrated community team] and what people who use the [name of integrated community team] expect from receiving this support.
We are interested to hear about the type of goals you might want to achieve and how the team supports you in working towards them.
Why have I been contacted?
You have been sent this pack because we understand you receive support from the [name of integrated community team].
What are the benefits of this research?
The information you provide will help us to understand what teams like the [name of integrated community team] can offer people with a neurological condition. This information will be used to develop a checklist of issues that staff need to think about when they are supporting you. The checklist will be about issues that people, who use community teams like the [name of integrated community team], have told us are important to them.
The checklist will be used by the team to make sure that they are thinking about the things that are important to their clients. We also hope that it can be used to show the benefits that teams like the [name of the integrated community team] can have on the lives of people with neurological conditions.
Will my taking part in this study be kept confidential?
Your involvement in the study, and the information that you provide, will be kept confidential. Everyone who takes part will be given a personal number so that they cannot be identified and all information provided will be anonymised. We will hold all data in line with the 1998 Data Protection Act and University of York Ordinances.
There are rare circumstances where the researcher is required to disclose someone’s participation to a doctor, nurse or other health care professional. However, this will only happen if the researcher is extremely concerned about the participant’s well-being. We will not tell the professional anything that was said in the interview unless it is directly related to the reason we were concerned.
Will taking part in this study affect my care?
No, taking part will not affect your care or the services you receive in any way. Likewise, if you decide not to take part, your care will not be affected in any way. It is up to you whether or not you decide to take part and your decision will be kept completely confidential.
What will taking part involve?
If you would like to take part, you will need to complete the response form and return it to me in the freepost envelope. Please keep this information sheet.
I will then contact you to answer any questions you may have and to arrange a time and place that suits you, to conduct the interview.
On the day of the interview, you will be able to ask more questions and raise any concerns. If you are still happy to go ahead, I will ask you to complete a consent form (and give you a copy of it to keep). The interview will take about 45 minutes and give you an opportunity to describe your views fully. It will be audio-recorded (with your permission). Recordings will be destroyed when the research is complete.
If you do decide to take part, you are still free to withdraw at any time and without giving a reason.
What if I choose not to take part?
Taking part in this research is entirely voluntary. If you choose not to take part, just complete the top half of the response form indicating your choice and return it to me in the freepost envelope so that I do not contact you again. You do not have to give a reason or complete the demographic form, but doing so would help me to understand why you did not want to take part, which might help when planning future studies. (Note: your reasons will be recorded anonymously. If you have decided not to take part, please do not give your name. )
If you have any questions or would like more information, please contact [name of researcher] on [telephone number] email [email address].
Thank You.
Carer interviews
Researchers from the Social Policy Research Unit at the University of York are conducting a study in your area. This study is funded by the National Institute for Health Research. It has been reviewed and approved by [name of local PCT R&D office] Primary Care Trust Research and Development Office, and the Research Ethics Committee for Wales.
Before you decide whether you wish to take part, it is important for you to understand why the research is being done and what it will involve. Please read the following information carefully and take your time to decide whether you wish to take part.
What is the purpose of the study?
We are looking at services in your area that co-ordinate care for people with neurological conditions. We want to know how successful they are at meeting people’s needs. The research focuses on the support provided by the [name of integrated community team] and what people who use the [name of integrated community team] expect from receiving this support.
We want to hear your views on how well you feel the [name of integrated community team] work with you and what things about the team are important to you.
Why have I been contacted?
You have been contacted because we understand you support someone who is a client of the [name of integrated community team]. This person has suggested that we contact you to hear your point of view.
What are the benefits of this research?
The information you provide will help us to understand what teams like the [name of integrated community team] can offer people with neurological conditions and those who support them. This information will be used to develop a checklist of issues that staff need to think about when they are supporting you and the person you provide care for. The checklist will cover the issues that people who use community teams like the [name of integrated community team] have told us are important to them.
The checklist will be used by the team to make sure they are thinking about the things that are important to their clients. We also hope that it can be used to show the benefits that teams like the [name of the integrated community team] can have on the lives of people with neurological conditions.
Will my taking part in this study be kept confidential?
Your involvement in the study, and the information that you provide, will be kept confidential. Everyone who takes part will be given a personal number so that they cannot be identified and all information provided will be anonymised. We will hold data in line with the 1998 Data Protection Act and University of York Ordinances.
There are rare circumstances where the researcher is required to disclose someone’s participation to a doctor, nurse or other health care professional. However, this will only happen if the researcher is extremely concerned about the participant’s well-being. We will not tell the professional anything that was said in the interview unless it is directly related to the reason we were concerned.
Will taking part in this study affect the support I, or the person I care for, receive?
No, taking part will not affect the support you, or the person you care for, receive in any way. Likewise, if you decide not to take part, the support that you or the person you care for receive will not be affected in any way. It is up to you whether you decide to take part and your decision will be kept completely confidential.
What will taking part involve?
If you would like to take part, you will need to complete the response form and return it to me in the freepost envelope. Please keep this information sheet.
I will then contact you to answer any questions you may have and to arrange a time and place that suits you, to conduct the interview.
On the day of the interview, you will be able to ask more questions and raise any concerns. If you are still happy to go ahead, I will ask you to complete a consent form (and give you a copy to keep). The interview will take about 45 minutes and give you an opportunity to describe your views fully. It will be audio-recorded (with your permission). Recordings will be destroyed when the research is complete.
If you do decide to take part, you are still free to withdraw at any time and without giving a reason.
What if I choose not to take part?
Participation in this research is entirely voluntary. If you choose not to take part, just complete the top half of the response form indicating your choice and return it to me in the freepost envelope so that I do not contact you again. You do not have to give a reason or complete the demographic form, but doing so would help me to understand why you did not want to take part, which might help when planning future studies. (Note: your reasons will be recorded anonymously. )
If you have any questions or would like more information, please contact [name of researcher] on [telephone number] email [email address].
Thank You.
Summary information sheet, care record audit
-
This study is looking at the support provided by the [name of team] and how the team meet the needs of their clients.
-
With help from [name of team] and their clients, we have developed a checklist of issues that teams need to think about when providing support to their clients.
-
As a client of the [name of team], the team will have used the outcome checklist with you as part of their assessment.
-
We would like to look at your care records held by the [name of team] to help us understand how it is being used. We will collect information about how the checklist has been used with you.
-
We will only collect information from your care record that is related to the checklist.
-
The information we collect will help us to understand how the checklist works in practice and if it covers the issues that are important to you.
-
Your involvement in the study, and the information that is collected, will be kept confidential.
-
Taking part in the study is voluntary, and if you decide to take part, you can still withdraw at any time.
-
Taking part will not affect your care or the services you receive in any way.
-
If you would like to take part, please complete the consent form and return it to me in the freepost envelope.
If you are interested in taking part, it is important that you read the full information sheet before making your decision. If you have any questions, you can contact us using the details in the full information sheet.
Participant information sheet – care record audit
Researchers from the Social Policy Research Unit at the University of York are conducting a study in your area. This study is funded by the National Institute for Health Research. It has been reviewed and approved by [name of local PCT R&D office] Primary Care Trust Research and Development Office, the Research Ethics Committee for Wales and the Association of Directors of Adult Social Services.
Before you decide whether you wish to take part, it is important for you to understand why the research is being done and what it will involve. Please read the following information carefully and take your time to decide whether you wish to take part.
What is the purpose of the study?
We are looking at services in your area that co-ordinate care for people with neurological conditions. We want to know how far they are able to meet people’s needs. The research is looking at the support provided by the [name of integrated community team] and what people who use the [name of integrated community team] expect from receiving this support.
The [name of integrated community team] and some of their clients have helped us to develop a new checklist that covers issues staff need to think about when supporting their clients. We have been working closely with the team to find out the best ways to use the checklist. They are now using it as part of their everyday work. The checklist is held in clients’ care records. As researchers, our role is to monitor how practical it is to use this checklist as part of the team’s everyday work. To do this, we are interested in looking at the care records held by the [name of integrated community team] to see how the checklist is being used. We also want to know what may need to change so that it works better and if using it affects how the team supports you.
Why have I been contacted?
You have been contacted because we understand you have recently been referred to the [name of integrated community team]. As a new client, the [name of integrated community team] will be using the checklist with you as part of their usual support and assessments. We would like to monitor your care records held by the [name of integrated community team] to help us assess how practical it is for the team to use the checklist as part of their everyday work.
What are the benefits of this research?
The checklist will be used by the team as part of their everyday work to make sure that they are considering things that are important to their clients. The information you provide will help us to understand how the checklist can work in practice and if it covers the issues that are important to you. We also hope that it can be used to show the benefits that teams like the [name of the integrated community team] can have on the lives of people with neurological conditions.
Will my taking part in this study be kept confidential?
Your involvement in the study, and the information that is collected, will be kept confidential. However, a member of the [name of integrated community team] will know you are involved because they will prepare your care record ready for us to look at when we visit the team’s headquarters. The person who prepares your records will be required to keep your involvement in the study confidential. We will ask a member of the team to prepare the care records for us so that we only see information about the checklist and we do not see any records of clients who are not involved in this research.
Everyone who takes part will be given a personal number so that they cannot be identified. All data will be anonymised. Data will be held in accordance with the 1998 Data Protection Act and University of York Ordinances.
Will taking part in this study affect my care?
No, taking part will not affect your care or the services you receive in any way. Likewise, if you decide not to take part, your care will not be affected in any way. It is up to you whether or not you decide to take part and your decision will be kept confidential.
What will taking part involve?
If you would like to take part, you will need to complete the consent form and return it to me in the freepost envelope. Please keep this information sheet.
This consent will only enable the researchers to see your care records held by the [name of integrated community team]. We do not need to see, and will not be able to access, your records held by any other organisation or professional, including for example, your GP notes, hospital notes and/or social care notes.
Once the researchers have received your consent form saying that we can access your care records held by the [name of integrated community team], the researchers will visit the team’s office and monitor the use of the checklist in your records every month for three months. We have a list of questions that we need to answer when we look at the checklist in your care records. We will only collect information from the checklist in your records that relates to these. These questions are included at the end of this information sheet.
Although we will do all we can to avoid it, it is possible that the research team may see information not relevant to the research while observing your records. Any information observed in this way will not be collected, recorded or used by the research team.
If you do decide to take part, and you have any questions or concerns during the time we will be looking at your care records, please do contact the research team using the contact details below. If you consent to take part, you are still free to withdraw at any time and without giving a reason. Just let us know, and we will stop reviewing your care records.
You will see that the consent form also asks if you are willing to be contacted in the future about taking part in an interview. This interview will be about your experience of staff using the checklist with you. If you say that you would be happy for us to contact you in the future about this, you will need to include some contact details but need do nothing more at this stage. We will not contact everyone who has agreed to this but if we do contact you, we will send you an information pack, similar to this one, that will explain what taking part in an interview will involve.
What if I choose not to take part?
Participation in this research is entirely voluntary. If you choose not to take part, just complete the decline form and return it to me in the freepost envelope. You do not have to give a reason or complete the demographic form, but doing so would help me to understand why you did not want to take part, which might help when planning future studies. (Note: your reasons will be recorded anonymously. If you have decided not to take part, please do not give your name. )
If you have any questions or would like more information, please contact [name of researcher] on [telephone number] email [email address].
Thank You.
NRT post-implementation interviews (INDIVIDUAL)
You are being invited to take part in a research study being conducted by researchers from the Social Policy Research Unit at the University of York. This study is funded by the National Institute for Health Research. It has been reviewed and approved by [name of local PCT R&D office] Primary Care Trust Research and Development Office, the [name of REC] and the Association of Directors of Adult Social Services.
Before you decide whether you wish to take part or not, it is important for you to understand why the research is being done and what it will involve. Please read the following information carefully and take your time to decide whether you wish to take part.
What is the purpose of the study?
We are interested in learning about the experiences of staff using the outcome checklist, developed earlier in this project and based on views of service users and carers, as part of routine practice with new clients in the [name of integrated community team]. We want to hear your opinions about how this worked in practice, barriers and facilitators to its use, and whether it has had any impact on your practice or the practice of the team more widely.
Why have I been contacted?
You have been identified as being a member of the [name of integrated community team] and as having experience of using the outcome checklist in practice.
What are the benefits of this research?
The information you provide will be invaluable in understanding the factors that influence the feasibility of using these types of checklists in practice and to identify factors that may make their implementation successful.
The information that you provide will be crucial when it comes to developing the outcome checklist for use in other community based teams that are co-ordinating care, within and across services and sectors, for people with neurological conditions.
Will my taking part in an interview be kept confidential?
Your involvement in the study, and the information that you provide, will be kept confidential. A personal identification number will be used throughout the research for each participant and all data will be anonymised. Data will be held in accordance with the 1998 Data Protection Act and University of York Ordinances.
There are rare circumstances where the researcher is required to disclose someone’s participation to a third party. However, this will only happen if the researcher is extremely concerned about the participant’s well-being. We will not tell the third party anything that was said in the interview unless it is directly related to the reason we were concerned.
Will taking part in an interview affect my employment?
No, taking part in the research will not affect your employment in any way. Similarly, if you decide not to take part your employment will not be affected in any way. It is up to you whether or not you decide to take part and your decision will be kept completely confidential.
What will taking part involve?
If you would like to take part, you will need to complete the response form and return it to me in the enclosed freepost envelope. Please retain this information sheet.
I will then contact you to answer any questions you may have and to arrange a mutually agreeable time and place to conduct the interview.
On the day of the interview there will be further opportunity for you to ask questions and raise concerns. If you are still happy to go ahead, I will ask you to complete a consent form (a copy of which will be given to you for your records).
NOTE for attention of REC – For telephone interviews, the following paragraph will replace the underlined paragraph above – it will not be italicised.
If you are happy to go ahead, I will send you a consent form. Please read and initial in the box after each of the four statements if you agree to them, then sign and date it and return it to us at the Freepost address: LTNC Team, Social Policy Research Unit, University of York, FREEPOST YO378, Heslington, York, YO10 1GY. Once we have received the form and signed it, we will return a copy to you and will contact you to conduct the interview. On the day of the interview there will be further opportunity for you to ask questions and raise concerns and if you are still happy to go ahead, the interview will be conducted.
The interview will take approximately 45 minutes and give you an opportunity to describe your views fully. It will be audio-recorded (with your permission). Recordings will be destroyed when the research is complete.
If you do decide to take part, you are still free to withdraw at any time and without giving a reason.
What if I choose not to take part?
Participation in this research is entirely voluntary. If you choose not to take part, just complete the top half of the response form indicating your choice and return it to me in the freepost envelope so that I do not contact you again. You do not have to provide a reason or complete the demographic form, but doing so would enable me to understand your reasons for declining to participate which might help when planning future studies. (Note: your reasons will be recorded anonymously. )
If you have any questions or would like more information, please contact [name of researcher] on [telephone number] or email [email address].
Thank You.
NRT post-implementation interviews (GROUP)
You are being invited to take part in a research study being conducted by researchers from the Social Policy Research Unit at the University of York. This study is funded by the National Institute for Health Research. It has been reviewed and approved by [name of local PCT R&D office] Primary Care Trust Research and Development Office, the [name of REC] and the Association of Directors of Adult Social Services.
Before you decide whether you wish to take part or not, it is important for you to understand why the research is being done and what it will involve. Please read the following information carefully and take your time to decide whether you wish to take part.
What is the purpose of the study?
We are interested in learning about the experiences of staff using the outcome checklist, developed earlier in this project and based on views of service users and carers, as part of routine practice with new clients in the [name of integrated community team]. We want to hear your opinions about how this worked in practice, barriers and facilitators to its use, and whether it has had any impact on your practice or the practice of the team more widely.
Why have I been contacted?
You have been identified as being a member of the [name of integrated community team] and as having experience of using the outcome checklist in practice.
What are the benefits of this research?
The information you provide will be invaluable in understanding the factors that influence the feasibility of using these types of checklists in practice and to identify factors that may make their implementation successful.
The information that you provide will be crucial when it comes to developing the outcome checklist for use in other community-based teams that are co-ordinating care, within and across services and sectors, for people with neurological conditions.
Will my taking part in a group interview be kept confidential?
The research team will keep your involvement in the study, and the information that you provide, confidential. Similarly, your colleagues involved in the group interview, will be required to keep your involvement in the study, and the information that you provide, confidential unless you decide between you that some information can be shared with other team members to aid learning and development.
There are rare circumstances where the researcher is required to disclose someone’s participation to a third party. However, this will only happen if the researcher is extremely concerned about the participant’s well-being. We will not tell the third party anything that was said in the interview unless it is directly related to the reason we were concerned.
A personal identification number will be used throughout the research for each participant and all data will be anonymised. Data will be held in accordance with the 1998 Data Protection Act and University of York Ordinances.
Will taking part in an interview affect my employment?
No, taking part in the research will not affect your employment in any way. Similarly, if you decide not to take part your employment will not be affected in any way. It is up to you whether or not you decide to take part and your decision will be kept completely confidential.
What will taking part involve?
If you would like to take part, you will need to complete the response form, indicating that you are happy to take part in a group interview, and return it to me in the enclosed freepost envelope. Please retain this information sheet.
I will then contact you to answer any questions you may have. I will contact all members of the [name of integrated community team] who have agreed to take part in a group interview and arrange the interview for a time that suits the most people.
On the day of the group interview there will be further opportunity for you to ask questions and raise concerns. If you are still happy to go ahead, I will ask you to complete a consent form (a copy of which will be given to you for your records).
The group interview will take approximately one and a half hours, but no more than two hours and give you an opportunity to describe your views fully and discuss your opinions with your colleagues. It will be audio-recorded (with the permission of everyone participating). Recordings will be destroyed when the research is complete.
If you do decide to take part, you are still free to withdraw at any time and without giving a reason.
What if I choose not to take part?
Participation in this research is entirely voluntary. If you choose not to take part, just complete the top half of the response form indicating your choice and return it to me in the freepost envelope so that I do not contact you again. You do not have to provide a reason or complete the demographic form, but doing so would enable me to understand your reasons for declining to participate which might help when planning future studies. (Note: your reasons will be recorded anonymously. )
If you have any questions or would like more information, please contact [name of researcher] on [telephone number] email [email address].
Thank You.
Service user post-implementation interviews
Researchers from the Social Policy Research Unit at the University of York are conducting a study in your area. This study is funded by the National Institute for Health Research. It has been reviewed and approved by [name of local PCT R&D office] Primary Care Trust Research and Development Office, the [name of REC] and the Association of Directors of Adult Social Services.
Before you decide whether you wish to take part or not, it is important for you to understand why the research is being done and what it will involve. Please read the following information carefully and take your time to decide whether you wish to take part.
What is the purpose of the study?
We are looking at services in your area that co-ordinate care for people with neurological conditions. We want to know how far they are able to meet people’s needs. The research has focused on the support provided by the [name of integrated community team] and what people who use the [name of integrated community team] expect from receiving this support.
In an earlier part of the research, people told us the most important things they want from a service like the [name of integrated community team]. The information was used to develop a checklist of issues that staff need to think about when they are supporting clients. Staff in the [name of integrated community team] have been using this checklist and we have been working with them to see how useful this is.
We are now interested in hearing the views of clients with whom the checklist has been used.
Why have I been contacted?
Some time ago, we contacted you about monitoring the use of the checklist in your care records held by the [name of integrated community team]. When you agreed to this, you also said that you might be willing to take part in an interview. We are contacting you now because we want to hear about your views about the team using the checklist with you.
What are the benefits of this research?
The information you provide will be helpful in understanding whether the checklist has covered the issues you feel are important and if you think the team dealt with these issues for you. We also hope that it can be used to show the benefits that teams like the [name of the integrated community team] can have on the lives of people with neurological conditions.
Will my taking part in this study be kept confidential?
Your involvement in the study, and the information that you provide, will be kept confidential. Everyone who takes part will be given a personal number so that they cannot be identified and all information provided will be anonymised. We will hold all data in line with the 1998 Data Protection Act and University of York Ordinances.
There are rare circumstances where the researcher is required to disclose someone’s participation to a doctor, nurse or other health care professional. However, this will only happen if the researcher is extremely concerned about the participant’s well-being. We will not tell the professional anything that was said in the interview unless it is directly related to the reason we were concerned.
Will taking part in this study affect my care?
No, taking part will not affect your care or the services you receive in any way. Likewise, if you decide not to take part, your care will not be affected in any way. It is up to you whether or not you decide to take part and your decision will be kept completely confidential.
What will taking part involve?
If you would like to take part, you will need to complete the response form and return it to me in the freepost envelope. Please keep this information sheet.
I will then contact you to answer any questions you may have and to arrange a time and place that suits you, to conduct the interview.
On the day of the interview, you will be able to ask more questions and raise any concerns. If you are still happy to go ahead, I will ask you to complete a consent form (and give you a copy of it to keep). The interview will take about 45 minutes and give you an opportunity to describe your views fully. It will be audio-recorded (with your permission). Recordings will be destroyed when the research is complete.
If you do decide to take part, you are still free to withdraw at any time and without giving a reason.
What if I choose not to take part?
Participation in this research is entirely voluntary. If you choose not to take part, just complete the top half of the response form indicating your choice and return it to me in the freepost envelope so that I do not contact you again. You do not have to give a reason or complete the demographic form, but doing so would help me to understand why you did not want to take part, which might help when planning future studies. (Note: your reasons will be recorded anonymously. If you have decided not to take part, please do not give your name. )
If you have any questions or would like more information, please contact [name of researcher] on [telephone number] email [email address].
Thank You
Example consent form, response form and demographic form
Example consent form
Example response form
Example demographic form
Topic guides
Organisational staff interviews
The interview will explore issues around:
Demographic information
-
Designation.
-
What their role involves.
Organisation
-
Organisational structure.
-
Organisational aims around.
-
Integration.
-
Long-term neurological conditions.
-
Integration
-
Integration strategy/policy.
-
Progress towards.
-
Integration.
-
Long-term neurological conditions.
-
-
Facilitators to integration.
-
Barriers to integration.
-
Suggestions for promoting service/organisational integration.
Service landscape (statutory and non-statutory organisations/services)
-
Organisations/services working in an integrated way.
-
Within sector.
-
Across sectors.
-
-
Organisations working towards integration locally.
-
Within sector.
-
Across sectors.
-
-
Levels of integration.
-
Which services.
-
Which staff.
-
Impact for service users of an integrated approach to service provision
-
Positive impact.
-
Negative impact.
Structures/processes that could improve integrated working
Identification of:
-
other key contacts
-
relevant meetings
-
documentation.
NRT pre-implementation interviews
The interview will explore issues surrounding:
Demographic information
-
Designation.
-
What their role involves.
What do they know of PCTs/Local Authorities
-
Integration strategy/policy.
-
Progress towards:
-
integration.
-
-
Facilitators to integration.
-
Barriers to integration.
-
Suggestions for promoting service/organisational integration.
Service landscape
-
How their service fits into the wider landscape for people with LTNCs and their carers.
-
Members of team:
-
disciplines.
-
-
The extent to which the team is integrated/promotes integrated working practices.
-
Work with other teams/services within the same sector.
-
Work with other teams/services and organisations on other sectors.
-
Nature of arrangements for integrated working (formal, informal arrangements, etc.)
-
Views on impact of integration
-
On their practice.
-
For their clients.
-
For carers/family members of their clients.
Current methods of assessing outcomes of their service
-
What processes are in place for assessing outcomes of their service?
-
Who is involved in assessments?
-
What assessment tools are used?
-
How often are they undertaken?
-
How are assessments stored?
-
Identification of:
-
other key contacts
-
relevant meetings
-
documentation.
Service user pre-implementation interviews
The interview will explore issues surrounding:
Outcomes generated by previous research (ask following questions about each outcome in the list below)
-
Is this important to you?
-
What kind of things are important about [the outcome]?
-
In what ways?
-
-
What other things about [the outcome] are important to you?
Personal comfort outcomes
-
Personal hygiene.
-
Safety/security.
-
Desired level of cleanliness of home.
-
Emotional well-being.
-
Physical health.
Economic outcomes
-
Access to paid employment as desired.
-
Access to training.
-
Access to further/higher education/occupation.
-
Access to appropriate training for new skills.
Social outcomes
-
Access to mainstream leisure activities.
-
Access to support in parenting role.
-
Access to support for personal secure relationships.
-
Access to advocacy/peer support.
-
Citizenship (being involved in decision-making).
Autonomy outcomes
-
Access to all areas of the home.
-
Access to locality and wider environment.
-
Communication access.
-
Financial security.
Does the [name of team] help you achieve these outcomes?
-
In what ways?
Prompt: Carer for interview?
Carer interviews
The interview will explore issues surrounding:
Demographic information
-
Relationship to service user.
-
Any other carers.
-
How long been a carer.
Role in supporting [service user]?
Experience of working with the [name of team] to support service user
-
How do you think the team sees you?
-
(e.g. recipient of support in their own right; integral team member; co-provider of services)
-
-
What is it about the way the team works that makes you think that?
-
(e.g. practical arrangements for working with team)
-
-
How would you like to be seen by the team?
-
Why?
-
What factors help/hinder working with a team like this?
NRT post-implementation interviews
The interview will explore issues surrounding:
Demographic information
-
Designation.
-
What their role involves.
Experience of using the outcome checklist
-
Have they completed it for any new/re-referred clients?
-
How often did they use it?
-
What types and level of information did they record?
Procedures
-
Were they able to follow procedures the team developed for use of the outcome checklist?
-
If not, why not?
-
What could be done to overcome these issues in future?
-
-
Was the format easy to use in practice?
-
If not, why not?
-
What could be done to overcome these issues in future?
-
-
Were there any other difficulties in using the outcome checklist?
-
What were these?
-
What could be done to overcome them in future?
-
-
Were there any benefits to using the outcome checklist?
-
For clients and/or their carers/family members?
-
For the interviewee?
-
For the team?
-
Impact
-
Did any actions arise as a result of using the outcome checklist?
-
If so, what were they? Why?
-
If not, why not?
-
-
Are they aware of any changes in practice related to integration/care co-ordination as a result of using the outcome checklist in routine practice?
-
In their practice?
-
In the practice of the team?
-
-
Would it be something you would recommend to other similar teams to use?
-
If yes, why?
-
If no, why not?
-
What would need to change?
-
-
Service user post-implementation interviews
The interview will explore issues surrounding:
Experience of receiving support from the Community Integrated Team
-
Benefits of receiving support from this particular team.
-
Reasons for this view.
-
-
Negatives of receiving support from this particular team.
-
Reasons for this view.
-
How they feel the Community Integrated Team works with?
-
Them.
-
Their carers/family members.
-
Other disciplines.
-
Other teams/services within the same sector.
-
Other teams/services and organisations on other sectors.
Level of integration evident in team’s practice
-
Within team.
-
Within sector.
-
Across sectors.
Whether they were aware of the staff using the outcome checklist
Whether the outcome checklist covered the issues they felt were important to them and to their families/carers
Appendix 2 Frameworks
Staff frameworks: stage 1
We had two frameworks to aid analysis of staff interviews: one focused on descriptions of NRTs and the other on organisational structures and integration.
Staff interviews: description framework
| Team disciplines | Team processes |
|---|---|
| Professions | Cover (24/7) |
| Funder | Area of PCT covered |
| Line management | Location of service delivery |
| Whole-time equivalent | Case loads |
| Location | Referral criteria |
| Notes | Waiting times (team/prof) |
| Referral routes in | |
| Discharge | |
| Re-referral | |
| Routine links with other profs/orgs (participant code) | |
| Evolution of team | |
| Team objectives/ethos |
Staff interviews: organisational structures and integration framework
| Organisational structures | High-level integration arrangements |
|---|---|
| Macro structure (e.g. networks, forums, voluntary sector) | Who links? (e.g. commissioner with commissioning or commissioner with provider) |
| PCT commissioning (including structure, policy drivers, priorities, cuts, etc.) | How do they link (meetings, board, etc.) |
| PCT provider (including structure, policy drivers, priorities, cuts, etc.) | Integration strategies |
| Acute (including structure, policy drivers, priorities, cuts, etc.) | Historical arrangements (if any) |
| Social care (including structure, policy drivers, priorities, cuts, etc.) | What led to changes? |
| Joint appt/pooled budgets (neuro) | |
| Joint appt/pooled budgets (other) | |
| GP commissioning | |
| Future organisational directions | |
| Integration | Barriers and facilitators |
| Terminology used to describe ‘integration’ | Barriers (commissioning) |
| Perception of integration (commissioning) | Barriers (operational management) |
| Perception of integration (operational management) | Barriers (practice) |
| Perception of integration (practice) | Facilitators (commissioning) |
| Benefits of integration on service users | Facilitators (operational management) |
| Benefits of integration on staff | Facilitators (practice) |
| Benefits of integration on other (costs) | |
| Drawbacks of integration | |
| What arrangements do teams have for integrated working (e.g. monthly meetings, joint assessments) | |
| Relationships and influence | Outcomes |
| Top-down influence | Approaches to outcomes (e.g. goal setting; priority given to different types of outcomes, etc.) |
| Bottom-up influence | Challenges of approach used |
| Horizontal influence | Outcome measures/tools used (describe tools – no detail needed re: functional status tools) |
| When used? | |
| How used? (Electronic?/format/with client/client gets copy? etc.) | |
| How do they store data? | |
| How do they data? | |
| Challenges to using outcome measure/tool and data in practice | |
| Additional notes |
Service user frameworks: stage 1
We had two frameworks to aid analysis of service user interviews: one provided a sample description and the other focused on the outcomes that people with LTNCs wanted to achieve.
Service user interviews: description framework
Neurological diagnosis
Age
Gender
Ethnicity
Level of mobility
Lives alone?
Service user interviews: outcomes framework
| Personal comfort outcomes | Economic participation outcomes |
|---|---|
| Personal hygiene | Access to paid employment as desired |
| Safety/security | Access to training |
| Desired level of cleanliness of home | Access to further/higher education/occupation |
| Emotional well-being | Access to training for new skills |
| Physical health | Voluntary work |
| Cognitive skills | Other |
| Sexual health | |
| Other | |
| Social participation outcomes | Autonomy outcomes |
| Access to mainstream leisure activities | Access to all areas of the home |
| Maintaining social relationships and activities | Access to locality and wider environment |
| Access to support in parenting role | Communication access |
| Access to support for personal secure relationships | Financial security |
| Maintaining family relationships and role | Shopping |
| Access to advocacy and peer support | Personal decision-making |
| Citizenship | Timely access to equipment and adaptations |
| Getting out | Being informed |
| Other | Other |
During the analysis process, we added additional charts for each of the higher-level outcomes we identified: (Independence, Choice, Control, Normality, Self-esteem) and for process-related outcomes.
Carer framework: stage 1
We developed one framework for analysis of carer interviews, which included a description chart.
| 1. Carer description | 2. Support role |
|---|---|
| Carer ID | Personal comfort outcomes |
| Gender | Social/economic outcomes |
| Age | Autonomy outcomes |
| Ethnicity | Other |
| SU’s neuro condition | |
| Relationship to SU | |
| Live with SU? | |
| Length of time as carer | |
| Any other carers | |
| 3. Impact of caring | 4. Carer’s needs |
| Relationship with SU | What are carer’s needs |
| Relationships with others | Carer’s needs assessed by NRT? |
| Physical health | Carer needs addressed by NRT? |
| Emotional well-being | NRT’s formal role for carer? |
| Employment | Other formal/informal support for carer |
| Financial issues | |
| Other | |
| 5. Experiences of NRT | 6. Perceptions |
| Support for SU’s needs | How carer sees self |
| Support for carer’s needs | Why do they see themselves this way? |
| How carer wants to be seen by team | |
| What helps/hinders NRT seeing them this way? | |
| How carer thinks team sees them? | |
| Why do they think the NRT sees them this way? | |
| 7. What helps/hinders carers working with NRT | |
| Attitudes | |
| Location of provision | |
| Ongoing/time-limited input | |
| Flexibility of input | |
| Practice | |
| Links to other services |
Frameworks: stage 3
We developed two frameworks in stage 3: one for charting data from interviews/focus groups with NRTs and one for charting service user data.
Staff framework: stage 3
| 1. Using the checklist | 2. Outcomes |
|---|---|
| Frequency of use | Views on individual outcomes |
| Who used it and why | Views on outcomes overall |
| Following procedures for use | Outcomes not covered by the checklist |
| Difficulties of process of using OC | Outcomes on checklist not covered on their assessment |
| Reasons for not using it (workload/capacity) | Outcomes beyond the reach/remit of the team |
| Reasons for not using it (time pressures) | Outcomes beyond the reach/remit of individual practitioners |
| Reasons for not using it (timing) | Overlap and repetition of outcomes within checklist |
| Reasons for not using it (duplication) | Overlap and repetition with existing assessment |
| Reasons for not using it (other) | Outcomes not asked about and why |
| Reasons for not using it (checklist) | Fit of outcomes to their practice |
| 3. Impact | 4. Other ways outcome checklist could be used |
| Benefits of using the outcome checklist | As assessment |
| Actions arising from using the checklist | For training |
| Would these actions arise from existing assessment? | Other |
| Impact on/changes to day-to-day practice | |
| Impact/changes (other) | |
| Future intentions for the checklist |
Service user framework: stage 3
| 1. Sample | 2. Views per outcome |
|---|---|
| Age | [column per outcome] |
| Gender | |
| Ethnicity | |
| Condition | |
| Other | |
| 3. Use of outcome checklist | 4. Checklist |
| Awareness of checklist being used | Are client’s key issues covered by outcome checklist? |
| How was the checklist used | Helpful outcomes |
| Views on how checklist was used | Unhelpful outcomes |
| Knowledge of actions arising from assessment more broadly | Outcomes client did not want to be asked about |
| Views on being asked about the outcomes | Preference for how outcomes are addressed (e.g. SU raising issue or team asking about it) |
| Other | Missing outcomes |
| Overall views | |
| Other | |
| 5. Key issues for SU | |
| Which outcomes (if any) would SU place their key issues under | |
| Which outcomes (if any) would WE place their key issues under |
Appendix 3 Development of outcomes checklist
Assessing outcomes of integrated care for long-term neurological conditions
Development of outcomes checklist: issues to discuss with teams
The outcomes checklist will consist of a list of ‘outcomes’ (i.e. issues which service users have told us are important to them). The same set of outcomes will be used in the checklist for the four case study sites, but the format of the checklist and how it is used can be tailored to meet the requirements of the team. Possible issues to consider when developing the outcomes checklist are described further below.
Client information
-
How much information do you want to include about the client on the outcomes checklist?
-
Name?
-
NHS Number?
-
Other demographic information?
-
Paper versus electronic
-
Would you prefer a paper version or an electronic version?
Functions
-
To indicate whether each outcome was discussed with the client, would you prefer a simple ‘tick box’ format or a ‘Yes/No’ format?
-
Would you like space on the tool to add detail about the discussion had with the client about the outcomes?
-
For example, space to add notes about outcome of discussion, or if client has highlighted anything in particular in relation to an outcome? Or, if an outcome wasn’t discussed, space to detail why this was?
-
-
It is possible that not all outcomes on the checklist may be important to the client. Do you want some way of recording which outcomes the client has indicated they would like help with? Do you want some way of recording which outcomes the client does not want help with?
-
Some outcomes that the client indicates they want help with may not be within the remit of the team. Do you want some way of recording which outcomes will be within the remit of the team, and which will be referred onto another agency/service where possible?
-
If no referral is made, would you like to have space to detail reasons for this?
-
-
Do you want to record the intended actions in response to outcomes that are the remit of the team, or is this covered in existing documentation within the team?
Who is using the outcomes checklist
-
We’d like to record which members of the team use the outcomes checklist. Do you have any preferences for how this is recorded?
Appearance
-
Do you want the name of the team on the outcomes checklist?
-
Do you want the appearance of the checklist to be consistent in style with other documentation you use?
-
Or, do you want to be able to distinguish the checklist from your existing documentation (e.g. by colour)?
-
Other
-
Is there anything else that you would like us to consider when developing the outcomes checklist?
Appendix 4 Instructions for using the checklist
Assessing outcomes of integrated care for long-term neurological conditions
Using the checklist and recruiting clients
The aim of this research is to develop an outcomes checklist and to explore the feasibility of using this in everyday practice.
Over the past year, we have been speaking to people with LTNCs, who use teams like yours, to find out what is important to them. From their accounts, we have developed a checklist of outcomes that people with LTNCs say are important. We are now asking you try out this checklist in practice. At the same time, the research team will monitor client records to see how the checklist is being used in practice.
We are asking you to:
-
Use the checklist in practice with your new/re-referred clients that fulfil the criteria listed below.
-
Pass out recruitment packs to these clients so that the research team can monitor their records and see how the tool is being used in practice. (We need to recruit up to 25 clients.)
This document tells you how to use the outcome checklist and recruit clients to the study.
In the week of the 17 October, you will receive a PDF copy and hardcopies of the outcomes checklist and client recruitment packs. We would like you to start using the outcomes checklist and handing out recruitment packs as soon as possible after you receive them. We will send you 25 recruitment packs and copies of the outcome checklist in the first instance. We will send you more later if needed.
Using the outcomes checklist
The checklist should be used in the initial assessment (at which point you should also give the client a recruitment pack). The checklist should be completed by a member of the team. It is not for completion by the client. It is up to you if you want to use the checklist again at later points with the same client.
The checklist is in the format agreed with your team. Each team’s version of the checklist includes some or all of the following functions:
-
Client details.
-
Recording if outcome was discussed with client, and date discussed.
-
Recording the importance of the outcome to the client.
-
Recording if the client wants help with the outcome.
-
Comments.
-
Recording referral actions.
-
Details of the team member using the checklist.
There are 20 outcomes on the checklist that are based around personal comfort, social and economic participation, and autonomy issues. We have described the outcomes and what each one includes in Appendix A.
Recruiting clients to the study
We would like to recruit up to 25 clients over a six-month period between October 2011–March 2012. You can stagger recruitment across this time (for example, recruitment may depend on how many new clients or re-referrals you get per month). If the research team get 25 positive responses for recruitment early in the six-month period, we will let you know, so that you do not need to continue handing out recruitment packs.
Each recruitment pack contains an invitation letter, information sheet (including a summary), consent form, decline form and a demographic form.
When you use the checklist with a client, please also give them a recruitment pack. However, please only pass on a recruitment pack if the client meets the following criteria:
-
S/he is a new or re-referred client.
-
Has a long-term neurological condition.
-
Is over 18 years of age.
-
Is cognitively able to read and understand the information sheet so that they can give informed consent.
When you pass on a recruitment pack to a client, please fill in the log sheet, which records the following:
-
Name of client.
-
Eligibility (tick box).
-
Study number (on the front of the recruitment pack).
-
Date recruitment pack given to client.
The client will respond directly to the research team indicating whether they are willing for us to monitor their care record held by your team.
The role of the research team in this phase of the study
We will contact you each month to find out how many clients have received recruitment packs, and their ID number. If we have not received a response from the client after three weeks, we will ask you to give that client a reminder recruitment pack. We will prepare and send this to you.
We will visit case sites each month, starting mid-November 2011, and monitor the records of those clients who have agreed for us to do this (see table below). We will let you know in advance whose records we will need to see when we visit. When we visit, it is important that we do not see details of clients who are not involved in the research.
| Clients recruited in: | Records monitored by research team between: (approximate timescales) |
|---|---|
| October 2011 | November 2011 – January 2012 |
| November 2011 | December 2011 – February 2012 |
| December 2011 | January 2012 – March 2012 |
| January 2012 | February 2012 – April 2012 |
| February 2012 | March 2012 – May 2012 |
| March 2012 | April 2012 – June 2012 |
Later, we’d like to talk to you about your experiences of using the checklist. We will be in touch with your team about this in Summer 2012.
If you have any questions or concerns about how to use the checklist or recruiting clients, please don’t hesitate to contact the research team.
[contact details removed]
APPENDIX A Outcomes on the checklist
| Outcome | Parameters |
|---|---|
| Personal comfort outcomes | |
| Personal hygiene and care |
|
| Safety/security |
|
| Desired level of household cleanliness and maintenance | All tasks relating to the maintenance of house (e.g. cleaning, bigger maintenance tasks such as painting) and garden. |
| Emotional well-being |
|
| Physical health and functioning |
|
| Cognitive skills | Cognitive skills such as memory, concentration, and attention. |
| Social and economic participation outcomes | |
| Access to paid employment as desired | Any activity that involves paid employment, full or part-time, wherever based, and that may or may not be related to past activity. |
| Access to training or new skills | Any training, or acquiring of new skills that may be undertaken for a range of reasons, that may encompass personal, social, work-related or other reasons. |
| Access to further/higher education | Any educational activity that is undertaken for personal, social, work-related or other reasons. |
| Establishing and maintaining social and recreational activities |
|
| Developing and/or maintaining intimate personal relationships and roles |
|
| Developing and/or maintaining family relationships and roles |
|
| Developing and/or maintaining social relationships and roles |
|
| Access to advocacy & peer support | That provided by voluntary organisations and condition specific groups. |
| Contributing to wider community/ies |
|
| Autonomy outcomes | |
| Access to all areas of the home | Being able to access different areas of the home and garden as independently as possible. |
| Access to locality and wider environment |
|
| Being able to communicate |
|
| Financial security | All aspects of financial security (including benefits). |
| Personal decision-making | Making decisions about all aspects of one’s life. |
Example outcomes checklist
Appendix 5 Proforma
Appendix 6 Assessment tools
Findings from comparison of assessment documents from each of the four case sites are reported here.
Approaches to assessment in the case site teams
Across all case sites, teams used a goal-based approach to assessment and care planning.
In sites A, B and C, staff described how their approach to assessment and care was patient defined and based on clients’ needs (site C), focused on facilitating quality of life, social and occupational participation, community integration, and independence (site A), and focused on social inclusion and participation (site B).
Initial assessment forms
For all sites, we obtained copies of the initial assessment forms used with clients, as well as additional documentation used. We provide a brief description below of each team’s initial assessment form. This description does not include the basic personal information prompts (e.g. diagnosis, consultant name, etc.) on the form, or issues/domains assessed through other documentation used by the teams (e.g. measures, quality-of-life scales, difficulty/ability checklists).
Site A
The domains covered in both teams assessment forms include perceptions of current problems and aims, medical condition, medication, living arrangements, occupational performance, food and nutrition, communication, nursing/physical, cognitive/psychological, carer issues, and immediate risks. A number of prompts are listed under each. The domain occupational performance covers a range of issues from personal care, through to household tasks, accessing the community and managing finances (among others).
Site B
The domains covered in the team’s assessment form include current medical status/health issues, investigations/appointments, past medical history/long-standing conditions or disabilities, current medications, social history, family/carer support, benefits, care package/other services involved, activity, participation, and well-being. Prompts are listed under all except investigations/appointments, social history, family/carer support, benefits, and care package/other services involved. Similar to site A, the activity domain covers a range of issues from domestic activities, to communication and mobility issues (among others).
Site C
The domains covered in the team’s assessment form include history of present condition, past medical history, medication/treatment, clients expectations of team’s care, social situation, mobility, transfers, activities of daily living, domestic, employment/benefits, hobbies and leisure, emotional health, cognition, general health, fatigue, pain, driving, carers issues, safety issues (environmental/social) and other health professionals involved. Prompts are included under all except history of present condition, medication/treatment, clients expectations of team’s care, employment/benefits, hobbies and leisure, fatigue, pain, driving, carers issues, safety issues (environmental/social) and other health professionals involved.
Site D
The domains covered in the team’s assessment form include: patient’s perception (daily activities and interests), physical health, communication, mobility, looking after yourself (health promotion and caring issues), mental health and emotional well-being, and safety, finances and relationships. A number of prompts are listed under each domain.
Grouping of prompts/issues
The assessment forms for teams in sites A, B and D are similar in that, compared with the team in site C, they have fewer domain groupings and more prompts under each domain. By comparison, site C has more overarching domains, with fewer prompts under each. In site C’s assessment form, pain, fatigue and driving are listed in their own right, whereas these issues are listed as prompts under the domains taking care of your health (site D), and occupational performance and physical function (site A). These issues are not listed as prompts in the site B initial assessment form, though they are referred to in another document used by the team.
All teams’ assessment forms cover similar issues, but are grouped differently. For example, sites A and B have domains labelled occupational performance and activity, respectively, which list similar prompts. These domains in both forms cover meal preparation, personal care, household/domestic tasks, and aids. The activity domain in site A also covers accessing the community, financial management, social and work prompts, which are covered under the participation domain in site B.
Similarly, ‘memory’ is covered by all the teams’ forms as a prompt, but under different domains. For example, it is listed under the domains well-being (site B) communication and well-being (site D), and cognition (A and C).
Issues of social contact, leisure and hobbies are covered in all the teams’ assessment forms, but under different domains. In site D, these are prompted for under the communication domain. In site C, ‘social situation’ and ‘hobbies’ are domains on the form, rather than prompts to domains. In site A, ‘social’ and ‘leisure’ are prompts in relation to ‘current daily routine’, which comes under the occupational performance domain. In site B, ‘social activities/leisure interests’ are prompted under the participation domain.
While the teams’ forms cover much of the same material (albeit in different ways), there are some obvious differences in assessment forms between sites, in terms of the issues that are covered. For example, employment is not covered as an explicit prompt in the assessment form for the site D team. By comparison, it is covered as a domain in the site C assessment form, and as a prompt in the site A assessment form (under occupational performance) and site B assessment form (under participation). ‘Family’ or ‘family relationships’ are covered as prompts in the assessment forms for sites C and D, but not A and B.
Other documentation used in assessment
In addition to the initial assessment form, we also obtained copies of other documentation used by the teams in clients’ assessments. Brief descriptions are given below for each site.
Site A
In addition to the initial assessment form, the teams also used the Modified Health Questionnaire, the Rehabilitation Complexity Scale, an assessment of difficulties from both the perspective of the client and carer (using a standard list of 33 items covering issues of mobility, physical and mental health, relationships, work, social activities, and cognition), the Care and Needs Scale, the MS Quality of Life Scale, the Mayo–Portland Adaptability Inventory, and the EQ-5D. The COPE Index is also used for carers.
Site B
In addition to the initial assessment form, the team also used a functional ability checklist (used by the OT), a four-item rating scale to be used for short-term clients (HowRU), the Patient Generated Index, a problem list, and outcome measures for physiotherapy, occupational therapy and speech and language therapy input.
Site C
In addition to the initial assessment form, the team also used a symptom profile, Timed Up and Go, Canadian Occupational Performance Measure, the Therapy Outcome Measure, cognitive assessments, MS specific screening tools, functional status assessments, bowel assessments, continence assessments, dietary assessments, FACE assessment tool, the Waterlow Score, the Berg Balance scale, the Lindop PD scale, and TINetti.
Site D
In addition to the initial assessment form, the team also used an environmental risk assessment tool, a record of medicines, a record of observations, a falls risk assessment, a manual handling care plan, a risk assessment for venous thromboprophylaxis, a nutritional screening record, a wound assessment tool, symptom management assessments, functional status assessments, the Modified Barthel Index, AMPS, the Mini-Mental State Examination, Addenbrooke’s Cognitive Examination, MS fatigue scale, and the Unified Parkinson’s Disease Rating Scale.
Appendix 7 Carers’ views
Findings from analysis of the 13 carer interviews that are not included in the main report are presented here.
Carers’ roles in supporting service users
Carers were providing high levels of personal care, assisting with washing, dressing, and toileting. Although for one person her involvement in her son’s personal care had reduced over time as he made improvements after a stroke, for most carers the progressive and deteriorating nature of conditions meant that their involvement had intensified over a number of years. Responsibilities extended to all tasks in the domestic domain. Carers took on cooking, cleaning, washing and maintenance of the house and garden, in some cases involving a sudden radical shift in former roles; in others a more gradual adjustment was negotiated over time, as conditions changed. Carers responded as circumstances demanded.
I do everything that needs to be done, from physical support to help her stand, sit down, use the toilet, shower, find things for her . . .
CCa03, husband of service user with MS
With fluctuating or deteriorating conditions, this also involved sensitivity to changes.
We steer a course around it . . . it’s accepting the inevitable . . . So, I don’t know, you try and, sort of, say, ‘Right, well that’s how [wife] is’ and we plan the day and what needs to be done accordingly.
BCa06, husband of service user with MS
Emotional support was seen as a key component of a carer’s role, in many cases carers feeling that they were the only person the service user could rely on for emotional support. Whether carers saw this as something explicitly discussed or more ‘unspoken’, staying positive, encouraging self-confidence, balancing the realities of deterioration with identifying possible support, being someone to offload on to and being responsive to change were all important elements of emotional support.
Support extended to outside the home, facilitating wider social contacts by providing transport and assisting with mobility problems, but also encouraging autonomy. For example, shopping together or encouraging and facilitating greater involvement in shopping activities could help people gain social confidence. The importance of promoting independence within the home where possible, for a person’s confidence and self-esteem, was also emphasised. Practical assistance extended to enabling partners to continue to do household tasks, even if they took longer or caused frustration. Judging when and how to enable greater autonomy was a key part of emotional support. Some carers adopted an advocacy role. For example, accompanying service users to hospital appointments involved extending beyond practical and emotional support to also take a more active role in acquiring information and participating in decisions about care.
Impact of caring role
The intensive experience of caring for someone with a LTNC had an impact on all areas of people’s lives, their relationships within and outside the family, physical and emotional well-being, employment and financial situation. Changes to their spouse/partner relationship frequently required considerable and ongoing adjustment. Spousal/partner carers talked of having worked as a team but felt that part of that reciprocal relationship was undermined by increased dependence:
We were sharing everything and that’s now just all mine. I just – I’ve got to do everything at the moment . . .
BCa05, wife of service user with stroke
It was recognised that this could lead to frustration both for the person with the LTNC who felt a ‘burden’ and for the carer who could not improve the situation. There was often a fine balance between being overprotective and encouraging independence. Where there had been slow deterioration over time, there had been more opportunity to negotiate, adapt and come to terms with changed roles.
For some couples, such issues in their relationship were discussed between them, but others acknowledged a tendency to withhold emotions more on both sides that had led to resentments and negative consequences for their relationship. Cognitive and emotional changes due to the LTNC could add further strain. One carer, despite feeling able to discuss things openly with her husband and able to sustain the essence of their interdependence, nevertheless experienced a subtle erosion of their relationship. Assumptions about her ability or willingness to undertake aspects of his care undermined their particular husband–wife relationship. Although caring for her husband was an intrinsic part of this, forced changes or expectations about performing certain tasks eroded its uniqueness.
It turns the wife much more into this carer, which you want to do naturally because, you know, you love your husband and you want to help them and you want to support them, but when you start to say, ‘Oh, well, your wife could clean your legs every day. Your wife could do the physio’, it actually turns you into a carer without, you know, it takes away the fact that you do it because you want to . . . And if it’s not something that you would have normally done in the husband-wife relationship, I feel that it’s not something that should be introduced, necessarily, because of need.
DCa02, wife of service user with MND
Two women who were supporting their sons with a LTNC both felt that the impact of their conditions (a stroke in one case and progressive MS in the other) had forced their sons to regress to childhood dependency and had put their mother–son relationship under strain. For both, there was ambivalence about the enforced closeness. Mixed emotions of supporting adult sons and no longer having an independent life were common to both and they felt, at times, that they received the backlash of their sons’ frustrations.
Impacts were felt on wider relationships within and outside the family. Social lives had changed. For some it may mean that more planning and consideration of accessibility was required; others acknowledged that restrictions means that both they and the person with the LTNC went out less and/or friendships changed.
So, it does change everybody’s lives, really, because our friends’ lives have been changed ‘cause they’re used to us doing certain things with them and going certain places and being able to play our part in the relationship, such as taking turns in driving when we’re going on holiday and now that’s all changed.
BCa05, wife of service user with stroke
However, maintaining friendships was also a source of support to carers. Feeling that people understood their situation and could offer practical and emotional support to both carers and their partners was important. Such friendships could help sustain a sense of ‘being normal’ and also provide a break to carers. Where carers expressed feelings of their own social isolation, their frustrations were tempered with feelings of guilt and helplessness in comparing or being unable to improve their partner’s situation.
I do want to look after him, but I need to get out because it’s cracking me up at home, ‘cause you’re with the same person 24/7 and I mean, I don’t mind doing anything for him, but it’s a strain.
BCa08, partner of service user with dystonia and spinal accident
Caring responsibilities took their toll physically and emotionally. The intensity of caring required was often exhausting and could involve hard physical work, such as manoeuvring wheelchairs and lifting. Some carers stressed the importance of keeping fit and active, so that they were better able to deal with situations. Others reported problems with sleeping and weight loss. The increased social isolation for some had led to frustration, increased stress and depression. There was a reluctance to seek support, such as counselling, or to prioritise their own needs generally. Although several carers were post retirement age, there were examples where people had left work prematurely due to changed circumstances, or reduced their hours in response to the level of care needed. Negative social and financial consequences arose from withdrawal from employment. Dependence on benefits and/or extra financial demands relating to the LTNC, such as house alterations and extra physiotherapy, put pressure on organising and maintaining family finances. The lack of autonomy and loss of independence experienced by people with the LTNCs was echoed by carers. Both of the mothers interviewed felt that they no longer had ‘a life’. Close partners also acknowledged such pressures and even when taking a break, carers often continued to worry about being away too long.
Carers’ needs
Carers and front-line practitioners gave priority to the needs of the person they with a LTNC, which created an unwillingness or delay in acknowledging carers’ support needs and shaped perceptions of the role of formal support services. In all cases, carers saw themselves as the main source of support, and responsible for responding to whatever was needed. This was a corollary of being husband, wife, partner or mother, and the role of carer was inextricably linked. Carers’ needs became secondary, and there was a tendency to underplay their own vulnerability. Some carers acknowledged the cumulative impact of caring as time went by, and that they would welcome practical assistance, opportunities for a break, or to work part-time. The importance of retaining external interests in order to maintain a balanced perspective was emphasised, although for some the constraints of their caring role made this difficult. At times they felt overwhelmed by their situation and at the same time unsure of sources of support, or what the legitimate parameters of discussion might be.
I, sort of, think, you know, ‘Help!’ no more, you know, ‘Help! Can’t someone do some of this for me?’, or something. I don’t know quite what, but then, it, sort of, evens out again, and it’s alright.
DCa01, wife of service user with PD
A need for better information about LTNCs and available support was highlighted, but again such issues were often framed in response to service user needs, rather than carer needs directly.
Appendix 8 Notes
-
A standing group of adult service users and carers who meet twice a year to identify key topics for research, help design projects and advise on existing projects.
-
The location of the REC (i.e. REC for Wales) was chosen because it reviewed a previous study to which this research was linked and does not necessarily reflect the location of case sites.
-
For the purposes of this research, we focused on innovation to promote integration. Innovation was used to describe the ways in which staff creatively adapted organisational, service and professional structures, processes and practice, in order to improve service integration.
-
That is, the points at which no new information or themes are being revealed. 74
-
The teams in site A were sent the interview information sheet only because they had previously indicated that they would prefer this option.
-
We have not included references per PCT because this would identify the case sites but the information was accessed via the Office for National Statistics’ Neighbourhood Statistics website. 86
-
Defra’s urban/rural LA classification was developed in 2005. There are six urban/rural classifications ordered from most urban (major urban, large urban, other urban) to most rural (significant rural, rural-50 and rural-80). Details of how PCTs are assessed for urban/rural classification are available either on the Defra website83 or on the Office for National Statistics website. 84
-
The Indices of Multiple Deprivation at PCT (n = 152) level was split into quintiles to represent levels of deprivation (first quintile = very high, second quintile = high, third quintile = medium, fourth quintile = low and fifth quintile = very low).
-
We have not reported whole-time equivalents of staff because this changed several times in all of the teams during the course of the research. Providing the range of disciplines gives an indication of team interdisciplinarity and the type of support each team was able to provide.
-
We use the term ‘at least’ because the checklist was used with additional clients who were not given an invitation pack. This was because clients did not meet the inclusion criteria or they declined to accept an invitation pack (see Chapter 2).
-
A combination-key box secured to the outside of the house for key storage. This allows carers (family members, friends and statutory carers) to access the house without the person with a LTNC having to come to the door.
List of abbreviations
- BI
- brain injury
- BME
- black and minority ethnic
- CCG
- Clinical Commissioning Group
- CRA
- care record audit
- Defra
- Department for Environment, Food and Rural Affairs
- DIY
- do-it-yourself
- EQ-5D
- European Quality of Life-5 Dimensions
- GP
- general practitioner
- IT
- information technology
- LA
- local authority
- LIT
- local implementation team
- LTC
- long-term condition
- LTNC
- long-term neurological condition
- MND
- motor neurone disease
- MS
- multiple sclerosis
- NOF
- National Outcomes Framework
- NRT
- neurorehabilitation team
- NSF
- National Service Framework
- OC
- outcomes checklist
- OT
- occupational therapist
- PCT
- primary care trust
- PD
- Parkinson’s disease
- PROM
- patient-reported outcome measure
- QIPP
- Quality, Innovation, Productivity, Prevention
- REC
- Research Ethics Committee
- SPRU
- Social Policy Research Unit